User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Boys may carry the weight, or overweight, of adults’ infertility
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
Fecal transplantation moves to the kitchen
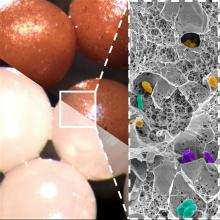
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
Fecal transplantation moves to the kitchen
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
Fecal transplantation moves to the kitchen
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
Mental health promotion
May is Mental Health Awareness Month, providing us a chance to go beyond discussing the screening, diagnosis, and evidence-based treatments for the mental illnesses of youth. The World Health Organization defines good mental health as “a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her own community.” While the science of mental health promotion and disease prevention in childhood and adolescence is relatively young, there are several discrete domains in which you can follow and support your patient’s developing mental health. This begins with the well-being of new parents, and then moves into how parents are helping their children to develop skills to manage their basic daily needs and impulses, their thoughts and feelings, their stresses and their relationships. With a little support from you, parents can confidently help their children develop the foundations for good mental health.
First year of life: Parental mental health
Perhaps the strongest risk factor for serious mental illness in childhood and adulthood is parental neglect during the first year of life, and neglect in the first several months of life is the most commonly reported form of child abuse. Infant neglect is associated with parental depression (and other mental illnesses), parental substance use, and a parent’s own experience of childhood abuse or neglect. Neglect is more common with teenaged parents and parents living in poverty. Pediatricians are uniquely connected to families during the first year of a child’s life. The American Academy of Pediatrics recommends screening new mothers for depression at 1-, 2-, 4-, and 6-month infant check-ups with the Edinburgh Postnatal Depression Screen. Even without a positive screen, new parents may need the fortifications of extra community support to adapt to the changes parenthood brings.
At checkups, ask (both) parents how they are managing the stresses of a new baby. Are they getting restful sleep? Do they have social supports? Are they connected to a community (friends, extended family, faith) or isolated? Are they developing confidence as parents or feeling overwhelmed? Simple guidance, such as “sleep when the baby sleeps” and reassurance that taking good care of themselves is taking good care of the baby is always helpful. Sometimes you will need to refer for treatment or to community supports. Have your list of online and in-person resources at the ready to provide parents with these prescriptions. Supporting parental mental health and adjustment in the first year of life is possibly the most important building block for their child’s future mental health.
Toddlers and up: Emotional literacy
Emotional literacy (sometimes called “emotional intelligence”) is the capacity to recognize, identify, and manage feelings in oneself and in others. This skill begins to develop in infancy when parents respond to their baby’s cries with attunement, feeding or changing them if needed, and at other times simply reflecting their feelings and soothing them with movement, singing, or quiet talking. As children grow, so does their range of feelings, and their (cognitive) capacity to identify and manage them. Parents support this development by being available whenever their young children experience strong emotions, calmly listening, and acknowledging their discomfort. Parents can offer words for describing those feelings, and even be curious with their young children where in their bodies they are feeling them, how they can stay patient while the feeling passes or things they might be able to do to feel better. Parents may want to remove their child’s distress, but staying calm, curious, and present while helping their child to manage it will build their child’s emotional health. Parents can nurture this development in a less intense way by reading books about feelings together and noticing and identifying feelings in other children or in cartoon characters.
School-age children: Adding mindfulness
While a child’s cognitive development unfolds naturally, school-age children can cultivate awareness of their thoughts. This becomes possible after awareness of feelings and parents can help their older children consider whether something they are experiencing is a thought, a feeling, or a fact. They do so in the same way they helped their child develop emotional literacy: By responding with calm, curiosity, and confidence every time their child comes to them in distress (especially mild distress, like boredom!) or with a challenge or a question. With a difficult situation, parents start by helping their child to identify thoughts and feelings before impulsively acting on them. Parents can help children identify what’s in their control, try different approaches, and be flexible if their first efforts don’t work. Children need to learn that failing at things is how we learn and grow. Just like learning to ride a bike, it builds their frustration tolerance, their knowledge that they can do difficult things, and that distress subsides. These are critical building blocks for adolescence, when the challenges become greater and they manage them more independently.
Learning “mindfulness” (a practice that cultivates nonjudgmental awareness of one’s own thoughts, feelings, and sensations) can help children (and parents) to cultivate quiet self-awareness outside of moments of difficulty. “Stop, Breathe, and Think” and “Mindful gNATs” are two free apps that are recommended by the American Academy of Child and Adolescent Psychiatry for children (and their parents) to use to practice this awareness of thoughts and feelings.
Early and later adolescence: Stress management skills
Building on this awareness of thoughts and emotions, adolescents develop adaptive coping skills by facing challenges with the support of their parents nearby. Parents should still be ready to respond to charged emotional moments with calm and curiosity, validating their child’s distress while helping them to consider healthy responses. Helping their teenager to describe their experience, differentiating feelings from thoughts (and facts), and considering different choices within their control is foundational to resilience in adulthood. Parents also help their teenagers by reminding them of the need for good self-care (sleep, exercise, nutrition), nourishing social relationships, and protecting time for rest and recharging activities. Sometimes, parents will think with their teenager about why they are engaged in an activity that is stressful, whether it is authentically important to them, and why. Adolescents should be deepening their sense of identity, interests, talents, and even values, and stressful moments are rich opportunities to do so, with the support of caring adults. Without intentionally building these skills, adolescents will be more prone to managing stress with avoidance or unhealthy coping, such as excessive eating, video gaming, drugs, or alcohol.
Infancy and up: Behavioral healthy habits (sleep, physical activity, nutrition, and screen time)
Healthy habits sound simple, but establishing them is not always easy. The idea of a habit is that it makes managing something challenging or important more automatic, and thus easier and more reliable. Many of the same habits that promote physical health in adulthood also promote mental health: adequate, restful sleep; daily physical activity; a nutritious diet and a healthy relationship with food; and managing screen time in a developmentally appropriate way. Infants depend entirely on their parents for regulation of these behaviors. As their children grow, parents will adapt these routines so that their children are gradually regulating these needs and activities more independently. In each of these areas, children need clear expectations and routines, consistent consequences and positive feedback, and the modeling and patient support of their parents. Educate parents about what good sleep hygiene looks like at each age. Discuss ways to support regular physical activity, especially as a family. Ask the parents about nutrition, including how they manage picky eating; how many family meals they enjoy together; and whether food is ever used to manage boredom or distress. Finally, talk with parents about a developmentally appropriate approach to rules and expectations around screen time and the importance of using family-based rules. Establishing expectations and routines during early childhood means children learn how good it feels to have restful sleep, regular exercise, and happy, healthy family meals. In adolescence, parents can then focus on helping their children to manage temptation, challenge, disappointment, and frustration more independently.
Infancy and up: Relational health
Children develop the skills needed for healthy relationships at home, and they are connected to all of the skills described above. Children need attuned, responsive, and reliable parenting to build a capacity for trust of others, to learn how to communicate honestly and effectively, to learn to expect and offer compassion and respect, and to learn how to handle disagreement and conflict. They learn these skills by watching their parents and by developing the emotional, cognitive, and behavioral healthy habits with their parents’ help. They need a consistently safe and responsive environment at home. They need parents who are attuned and flexible, while maintaining routines and high expectations. They need parents who make time for them when they are sad or struggling, and make time for joy, play, and mindless fun. While a detailed assessment of how the family is functioning may go beyond a check-up, you can ask about those routines that build healthy habits (family mealtime, sleep routines, screen time rules), communication style, and what the family enjoys doing together. Learning about how a family is building these healthy habits and how connected they are to one another can give you a clear snapshot of how well a child may be doing on their mental health growth curve, and what areas might benefit from more active guidance and support.
Dr. Swick is physician in chief at Ohana Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
May is Mental Health Awareness Month, providing us a chance to go beyond discussing the screening, diagnosis, and evidence-based treatments for the mental illnesses of youth. The World Health Organization defines good mental health as “a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her own community.” While the science of mental health promotion and disease prevention in childhood and adolescence is relatively young, there are several discrete domains in which you can follow and support your patient’s developing mental health. This begins with the well-being of new parents, and then moves into how parents are helping their children to develop skills to manage their basic daily needs and impulses, their thoughts and feelings, their stresses and their relationships. With a little support from you, parents can confidently help their children develop the foundations for good mental health.
First year of life: Parental mental health
Perhaps the strongest risk factor for serious mental illness in childhood and adulthood is parental neglect during the first year of life, and neglect in the first several months of life is the most commonly reported form of child abuse. Infant neglect is associated with parental depression (and other mental illnesses), parental substance use, and a parent’s own experience of childhood abuse or neglect. Neglect is more common with teenaged parents and parents living in poverty. Pediatricians are uniquely connected to families during the first year of a child’s life. The American Academy of Pediatrics recommends screening new mothers for depression at 1-, 2-, 4-, and 6-month infant check-ups with the Edinburgh Postnatal Depression Screen. Even without a positive screen, new parents may need the fortifications of extra community support to adapt to the changes parenthood brings.
At checkups, ask (both) parents how they are managing the stresses of a new baby. Are they getting restful sleep? Do they have social supports? Are they connected to a community (friends, extended family, faith) or isolated? Are they developing confidence as parents or feeling overwhelmed? Simple guidance, such as “sleep when the baby sleeps” and reassurance that taking good care of themselves is taking good care of the baby is always helpful. Sometimes you will need to refer for treatment or to community supports. Have your list of online and in-person resources at the ready to provide parents with these prescriptions. Supporting parental mental health and adjustment in the first year of life is possibly the most important building block for their child’s future mental health.
Toddlers and up: Emotional literacy
Emotional literacy (sometimes called “emotional intelligence”) is the capacity to recognize, identify, and manage feelings in oneself and in others. This skill begins to develop in infancy when parents respond to their baby’s cries with attunement, feeding or changing them if needed, and at other times simply reflecting their feelings and soothing them with movement, singing, or quiet talking. As children grow, so does their range of feelings, and their (cognitive) capacity to identify and manage them. Parents support this development by being available whenever their young children experience strong emotions, calmly listening, and acknowledging their discomfort. Parents can offer words for describing those feelings, and even be curious with their young children where in their bodies they are feeling them, how they can stay patient while the feeling passes or things they might be able to do to feel better. Parents may want to remove their child’s distress, but staying calm, curious, and present while helping their child to manage it will build their child’s emotional health. Parents can nurture this development in a less intense way by reading books about feelings together and noticing and identifying feelings in other children or in cartoon characters.
School-age children: Adding mindfulness
While a child’s cognitive development unfolds naturally, school-age children can cultivate awareness of their thoughts. This becomes possible after awareness of feelings and parents can help their older children consider whether something they are experiencing is a thought, a feeling, or a fact. They do so in the same way they helped their child develop emotional literacy: By responding with calm, curiosity, and confidence every time their child comes to them in distress (especially mild distress, like boredom!) or with a challenge or a question. With a difficult situation, parents start by helping their child to identify thoughts and feelings before impulsively acting on them. Parents can help children identify what’s in their control, try different approaches, and be flexible if their first efforts don’t work. Children need to learn that failing at things is how we learn and grow. Just like learning to ride a bike, it builds their frustration tolerance, their knowledge that they can do difficult things, and that distress subsides. These are critical building blocks for adolescence, when the challenges become greater and they manage them more independently.
Learning “mindfulness” (a practice that cultivates nonjudgmental awareness of one’s own thoughts, feelings, and sensations) can help children (and parents) to cultivate quiet self-awareness outside of moments of difficulty. “Stop, Breathe, and Think” and “Mindful gNATs” are two free apps that are recommended by the American Academy of Child and Adolescent Psychiatry for children (and their parents) to use to practice this awareness of thoughts and feelings.
Early and later adolescence: Stress management skills
Building on this awareness of thoughts and emotions, adolescents develop adaptive coping skills by facing challenges with the support of their parents nearby. Parents should still be ready to respond to charged emotional moments with calm and curiosity, validating their child’s distress while helping them to consider healthy responses. Helping their teenager to describe their experience, differentiating feelings from thoughts (and facts), and considering different choices within their control is foundational to resilience in adulthood. Parents also help their teenagers by reminding them of the need for good self-care (sleep, exercise, nutrition), nourishing social relationships, and protecting time for rest and recharging activities. Sometimes, parents will think with their teenager about why they are engaged in an activity that is stressful, whether it is authentically important to them, and why. Adolescents should be deepening their sense of identity, interests, talents, and even values, and stressful moments are rich opportunities to do so, with the support of caring adults. Without intentionally building these skills, adolescents will be more prone to managing stress with avoidance or unhealthy coping, such as excessive eating, video gaming, drugs, or alcohol.
Infancy and up: Behavioral healthy habits (sleep, physical activity, nutrition, and screen time)
Healthy habits sound simple, but establishing them is not always easy. The idea of a habit is that it makes managing something challenging or important more automatic, and thus easier and more reliable. Many of the same habits that promote physical health in adulthood also promote mental health: adequate, restful sleep; daily physical activity; a nutritious diet and a healthy relationship with food; and managing screen time in a developmentally appropriate way. Infants depend entirely on their parents for regulation of these behaviors. As their children grow, parents will adapt these routines so that their children are gradually regulating these needs and activities more independently. In each of these areas, children need clear expectations and routines, consistent consequences and positive feedback, and the modeling and patient support of their parents. Educate parents about what good sleep hygiene looks like at each age. Discuss ways to support regular physical activity, especially as a family. Ask the parents about nutrition, including how they manage picky eating; how many family meals they enjoy together; and whether food is ever used to manage boredom or distress. Finally, talk with parents about a developmentally appropriate approach to rules and expectations around screen time and the importance of using family-based rules. Establishing expectations and routines during early childhood means children learn how good it feels to have restful sleep, regular exercise, and happy, healthy family meals. In adolescence, parents can then focus on helping their children to manage temptation, challenge, disappointment, and frustration more independently.
Infancy and up: Relational health
Children develop the skills needed for healthy relationships at home, and they are connected to all of the skills described above. Children need attuned, responsive, and reliable parenting to build a capacity for trust of others, to learn how to communicate honestly and effectively, to learn to expect and offer compassion and respect, and to learn how to handle disagreement and conflict. They learn these skills by watching their parents and by developing the emotional, cognitive, and behavioral healthy habits with their parents’ help. They need a consistently safe and responsive environment at home. They need parents who are attuned and flexible, while maintaining routines and high expectations. They need parents who make time for them when they are sad or struggling, and make time for joy, play, and mindless fun. While a detailed assessment of how the family is functioning may go beyond a check-up, you can ask about those routines that build healthy habits (family mealtime, sleep routines, screen time rules), communication style, and what the family enjoys doing together. Learning about how a family is building these healthy habits and how connected they are to one another can give you a clear snapshot of how well a child may be doing on their mental health growth curve, and what areas might benefit from more active guidance and support.
Dr. Swick is physician in chief at Ohana Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
May is Mental Health Awareness Month, providing us a chance to go beyond discussing the screening, diagnosis, and evidence-based treatments for the mental illnesses of youth. The World Health Organization defines good mental health as “a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her own community.” While the science of mental health promotion and disease prevention in childhood and adolescence is relatively young, there are several discrete domains in which you can follow and support your patient’s developing mental health. This begins with the well-being of new parents, and then moves into how parents are helping their children to develop skills to manage their basic daily needs and impulses, their thoughts and feelings, their stresses and their relationships. With a little support from you, parents can confidently help their children develop the foundations for good mental health.
First year of life: Parental mental health
Perhaps the strongest risk factor for serious mental illness in childhood and adulthood is parental neglect during the first year of life, and neglect in the first several months of life is the most commonly reported form of child abuse. Infant neglect is associated with parental depression (and other mental illnesses), parental substance use, and a parent’s own experience of childhood abuse or neglect. Neglect is more common with teenaged parents and parents living in poverty. Pediatricians are uniquely connected to families during the first year of a child’s life. The American Academy of Pediatrics recommends screening new mothers for depression at 1-, 2-, 4-, and 6-month infant check-ups with the Edinburgh Postnatal Depression Screen. Even without a positive screen, new parents may need the fortifications of extra community support to adapt to the changes parenthood brings.
At checkups, ask (both) parents how they are managing the stresses of a new baby. Are they getting restful sleep? Do they have social supports? Are they connected to a community (friends, extended family, faith) or isolated? Are they developing confidence as parents or feeling overwhelmed? Simple guidance, such as “sleep when the baby sleeps” and reassurance that taking good care of themselves is taking good care of the baby is always helpful. Sometimes you will need to refer for treatment or to community supports. Have your list of online and in-person resources at the ready to provide parents with these prescriptions. Supporting parental mental health and adjustment in the first year of life is possibly the most important building block for their child’s future mental health.
Toddlers and up: Emotional literacy
Emotional literacy (sometimes called “emotional intelligence”) is the capacity to recognize, identify, and manage feelings in oneself and in others. This skill begins to develop in infancy when parents respond to their baby’s cries with attunement, feeding or changing them if needed, and at other times simply reflecting their feelings and soothing them with movement, singing, or quiet talking. As children grow, so does their range of feelings, and their (cognitive) capacity to identify and manage them. Parents support this development by being available whenever their young children experience strong emotions, calmly listening, and acknowledging their discomfort. Parents can offer words for describing those feelings, and even be curious with their young children where in their bodies they are feeling them, how they can stay patient while the feeling passes or things they might be able to do to feel better. Parents may want to remove their child’s distress, but staying calm, curious, and present while helping their child to manage it will build their child’s emotional health. Parents can nurture this development in a less intense way by reading books about feelings together and noticing and identifying feelings in other children or in cartoon characters.
School-age children: Adding mindfulness
While a child’s cognitive development unfolds naturally, school-age children can cultivate awareness of their thoughts. This becomes possible after awareness of feelings and parents can help their older children consider whether something they are experiencing is a thought, a feeling, or a fact. They do so in the same way they helped their child develop emotional literacy: By responding with calm, curiosity, and confidence every time their child comes to them in distress (especially mild distress, like boredom!) or with a challenge or a question. With a difficult situation, parents start by helping their child to identify thoughts and feelings before impulsively acting on them. Parents can help children identify what’s in their control, try different approaches, and be flexible if their first efforts don’t work. Children need to learn that failing at things is how we learn and grow. Just like learning to ride a bike, it builds their frustration tolerance, their knowledge that they can do difficult things, and that distress subsides. These are critical building blocks for adolescence, when the challenges become greater and they manage them more independently.
Learning “mindfulness” (a practice that cultivates nonjudgmental awareness of one’s own thoughts, feelings, and sensations) can help children (and parents) to cultivate quiet self-awareness outside of moments of difficulty. “Stop, Breathe, and Think” and “Mindful gNATs” are two free apps that are recommended by the American Academy of Child and Adolescent Psychiatry for children (and their parents) to use to practice this awareness of thoughts and feelings.
Early and later adolescence: Stress management skills
Building on this awareness of thoughts and emotions, adolescents develop adaptive coping skills by facing challenges with the support of their parents nearby. Parents should still be ready to respond to charged emotional moments with calm and curiosity, validating their child’s distress while helping them to consider healthy responses. Helping their teenager to describe their experience, differentiating feelings from thoughts (and facts), and considering different choices within their control is foundational to resilience in adulthood. Parents also help their teenagers by reminding them of the need for good self-care (sleep, exercise, nutrition), nourishing social relationships, and protecting time for rest and recharging activities. Sometimes, parents will think with their teenager about why they are engaged in an activity that is stressful, whether it is authentically important to them, and why. Adolescents should be deepening their sense of identity, interests, talents, and even values, and stressful moments are rich opportunities to do so, with the support of caring adults. Without intentionally building these skills, adolescents will be more prone to managing stress with avoidance or unhealthy coping, such as excessive eating, video gaming, drugs, or alcohol.
Infancy and up: Behavioral healthy habits (sleep, physical activity, nutrition, and screen time)
Healthy habits sound simple, but establishing them is not always easy. The idea of a habit is that it makes managing something challenging or important more automatic, and thus easier and more reliable. Many of the same habits that promote physical health in adulthood also promote mental health: adequate, restful sleep; daily physical activity; a nutritious diet and a healthy relationship with food; and managing screen time in a developmentally appropriate way. Infants depend entirely on their parents for regulation of these behaviors. As their children grow, parents will adapt these routines so that their children are gradually regulating these needs and activities more independently. In each of these areas, children need clear expectations and routines, consistent consequences and positive feedback, and the modeling and patient support of their parents. Educate parents about what good sleep hygiene looks like at each age. Discuss ways to support regular physical activity, especially as a family. Ask the parents about nutrition, including how they manage picky eating; how many family meals they enjoy together; and whether food is ever used to manage boredom or distress. Finally, talk with parents about a developmentally appropriate approach to rules and expectations around screen time and the importance of using family-based rules. Establishing expectations and routines during early childhood means children learn how good it feels to have restful sleep, regular exercise, and happy, healthy family meals. In adolescence, parents can then focus on helping their children to manage temptation, challenge, disappointment, and frustration more independently.
Infancy and up: Relational health
Children develop the skills needed for healthy relationships at home, and they are connected to all of the skills described above. Children need attuned, responsive, and reliable parenting to build a capacity for trust of others, to learn how to communicate honestly and effectively, to learn to expect and offer compassion and respect, and to learn how to handle disagreement and conflict. They learn these skills by watching their parents and by developing the emotional, cognitive, and behavioral healthy habits with their parents’ help. They need a consistently safe and responsive environment at home. They need parents who are attuned and flexible, while maintaining routines and high expectations. They need parents who make time for them when they are sad or struggling, and make time for joy, play, and mindless fun. While a detailed assessment of how the family is functioning may go beyond a check-up, you can ask about those routines that build healthy habits (family mealtime, sleep routines, screen time rules), communication style, and what the family enjoys doing together. Learning about how a family is building these healthy habits and how connected they are to one another can give you a clear snapshot of how well a child may be doing on their mental health growth curve, and what areas might benefit from more active guidance and support.
Dr. Swick is physician in chief at Ohana Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
Low disease state for childhood lupus approaches validation
MANCHESTER, ENGLAND – An age-appropriate version of the Lupus Low Disease Activity State (LLDAS) has been developed by an international task force that will hopefully enable childhood-onset systemic lupus erythematosus (cSLE) to be treated to target in the near future.
The new childhood LLDAS (cLLDAS) has been purposefully developed to align with that already used for adults, Eve Smith, MBChB, PhD, explained at the annual meeting of the British Society for Rheumatology.
“There’s a lot of compelling data that’s accumulating from adult lupus and increasingly from childhood lupus that [treat to target] might be a good idea,” said Dr. Smith, who is a senior clinical fellow and honorary consultant at the University of Liverpool (England) and Alder Hey Children’s NHS Foundation Trust Hospital, also in Liverpool.
Urgent need to improve childhood lupus outcomes
“We urgently need to do something to try and improve outcomes for children,” Dr. Smith said.
“We know that childhood lupus patients have got higher disease activity as compared to adults; they have a greater medication burden, particularly steroids; and they tend to have more severe organ manifestations,” she added.
Moreover, data show that one-fifth of pediatric patients with lupus have already accrued early damage, and there is much higher mortality associated with childhood lupus than there is with adult lupus.
“So, really we want to use treat to target as a way to try and improve on these aspects,” Dr. Smith said.
The treat-to-target (T2T) approach is not a new idea in lupus, with a lot of work already done in adult patients. One large study of more than 3,300 patients conducted in 13 countries has shown that patients who never achieve LLDAS are more likely to have high levels of damage, greater glucocorticoid use, worse quality of life, and higher mortality than are those who do.
Conversely, data have also shown that achieving a LLDAS is associated with a reduction in the risk for new damage, flares, and hospitalization, as well as reducing health care costs and improving patients’ overall health-related quality of life.
T2T is a recognized approach in European adult SLE guidelines, Dr. Smith said, although the approach has not really been fully realized as of yet, even in adult practice.
The cSLE T2T international task force and cLLDAS definition
With evidence accumulating on the benefits of getting children with SLE to a low disease activity state, Dr. Smith and colleague Michael Beresford, MBChB, PhD, Brough Chair, Professor of Child Health at the University of Liverpool, put out a call to develop a task force to look into the feasibility of a T2T approach.
“We had a really enthusiastic response internationally, which we were really encouraged by,” Dr. Smith said, “and we now lead a task force of 20 experts from across all five continents, and we have really strong patient involvement.”
Through a consensus process, an international cSLE T2T Task Force agreed on overarching principles and points to consider that will “lay the foundation for future T2T approaches in cSLE,” according to the recommendations statement, which was endorsed by the Paediatric Rheumatology European Society.
Next, they looked to develop an age-appropriate definition for low disease activity.
“We’re deliberately wanting to maintain sufficient unity with the adult definition, so that we could facilitate life-course studies,” said Dr. Smith, who presented the results of a literature review and series of Delphi surveys at the meeting.
The conceptual definition of cLLDAS is similar to adults in describing it as a sustained state that is associated with a low likelihood of adverse outcome, Dr. Smith said, but with the added wording of “considering disease activity, damage, and medication toxicity.”
The definition is achieved when the SLE Disease Activity Index-2K is ≤ 4 and there is no activity in major organ systems; there are no new features of lupus disease activity since the last assessment; there is a score of ≤ 1 on Physician Global Assessment; steroid doses are ≤ 0.15 mg/kg/day or a maximum of 7.5 mg/day (whichever is lower); and immunosuppressive treatment is stable, with any changes to medication only because of side effects, adherence, changes in weight, or when in the process of reaching a target dose.
“It’s all very well having a definition, but you need to think about how that will work in practice,” Dr. Smith said. This is something that the task force is thinking about very carefully.
The task force next aims to validate the cLLDAS definition, form an extensive research agenda to inform the T2T methods, and develop innovative methods to apply the approach in practice.
The work is supported by the Wellcome Trust, National Institutes for Health Research, Versus Arthritis, and the University of Liverpool, Alder Hey Children’s NHS Foundation Trust and the Alder Hey Charity. Dr. Smith reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MANCHESTER, ENGLAND – An age-appropriate version of the Lupus Low Disease Activity State (LLDAS) has been developed by an international task force that will hopefully enable childhood-onset systemic lupus erythematosus (cSLE) to be treated to target in the near future.
The new childhood LLDAS (cLLDAS) has been purposefully developed to align with that already used for adults, Eve Smith, MBChB, PhD, explained at the annual meeting of the British Society for Rheumatology.
“There’s a lot of compelling data that’s accumulating from adult lupus and increasingly from childhood lupus that [treat to target] might be a good idea,” said Dr. Smith, who is a senior clinical fellow and honorary consultant at the University of Liverpool (England) and Alder Hey Children’s NHS Foundation Trust Hospital, also in Liverpool.
Urgent need to improve childhood lupus outcomes
“We urgently need to do something to try and improve outcomes for children,” Dr. Smith said.
“We know that childhood lupus patients have got higher disease activity as compared to adults; they have a greater medication burden, particularly steroids; and they tend to have more severe organ manifestations,” she added.
Moreover, data show that one-fifth of pediatric patients with lupus have already accrued early damage, and there is much higher mortality associated with childhood lupus than there is with adult lupus.
“So, really we want to use treat to target as a way to try and improve on these aspects,” Dr. Smith said.
The treat-to-target (T2T) approach is not a new idea in lupus, with a lot of work already done in adult patients. One large study of more than 3,300 patients conducted in 13 countries has shown that patients who never achieve LLDAS are more likely to have high levels of damage, greater glucocorticoid use, worse quality of life, and higher mortality than are those who do.
Conversely, data have also shown that achieving a LLDAS is associated with a reduction in the risk for new damage, flares, and hospitalization, as well as reducing health care costs and improving patients’ overall health-related quality of life.
T2T is a recognized approach in European adult SLE guidelines, Dr. Smith said, although the approach has not really been fully realized as of yet, even in adult practice.
The cSLE T2T international task force and cLLDAS definition
With evidence accumulating on the benefits of getting children with SLE to a low disease activity state, Dr. Smith and colleague Michael Beresford, MBChB, PhD, Brough Chair, Professor of Child Health at the University of Liverpool, put out a call to develop a task force to look into the feasibility of a T2T approach.
“We had a really enthusiastic response internationally, which we were really encouraged by,” Dr. Smith said, “and we now lead a task force of 20 experts from across all five continents, and we have really strong patient involvement.”
Through a consensus process, an international cSLE T2T Task Force agreed on overarching principles and points to consider that will “lay the foundation for future T2T approaches in cSLE,” according to the recommendations statement, which was endorsed by the Paediatric Rheumatology European Society.
Next, they looked to develop an age-appropriate definition for low disease activity.
“We’re deliberately wanting to maintain sufficient unity with the adult definition, so that we could facilitate life-course studies,” said Dr. Smith, who presented the results of a literature review and series of Delphi surveys at the meeting.
The conceptual definition of cLLDAS is similar to adults in describing it as a sustained state that is associated with a low likelihood of adverse outcome, Dr. Smith said, but with the added wording of “considering disease activity, damage, and medication toxicity.”
The definition is achieved when the SLE Disease Activity Index-2K is ≤ 4 and there is no activity in major organ systems; there are no new features of lupus disease activity since the last assessment; there is a score of ≤ 1 on Physician Global Assessment; steroid doses are ≤ 0.15 mg/kg/day or a maximum of 7.5 mg/day (whichever is lower); and immunosuppressive treatment is stable, with any changes to medication only because of side effects, adherence, changes in weight, or when in the process of reaching a target dose.
“It’s all very well having a definition, but you need to think about how that will work in practice,” Dr. Smith said. This is something that the task force is thinking about very carefully.
The task force next aims to validate the cLLDAS definition, form an extensive research agenda to inform the T2T methods, and develop innovative methods to apply the approach in practice.
The work is supported by the Wellcome Trust, National Institutes for Health Research, Versus Arthritis, and the University of Liverpool, Alder Hey Children’s NHS Foundation Trust and the Alder Hey Charity. Dr. Smith reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MANCHESTER, ENGLAND – An age-appropriate version of the Lupus Low Disease Activity State (LLDAS) has been developed by an international task force that will hopefully enable childhood-onset systemic lupus erythematosus (cSLE) to be treated to target in the near future.
The new childhood LLDAS (cLLDAS) has been purposefully developed to align with that already used for adults, Eve Smith, MBChB, PhD, explained at the annual meeting of the British Society for Rheumatology.
“There’s a lot of compelling data that’s accumulating from adult lupus and increasingly from childhood lupus that [treat to target] might be a good idea,” said Dr. Smith, who is a senior clinical fellow and honorary consultant at the University of Liverpool (England) and Alder Hey Children’s NHS Foundation Trust Hospital, also in Liverpool.
Urgent need to improve childhood lupus outcomes
“We urgently need to do something to try and improve outcomes for children,” Dr. Smith said.
“We know that childhood lupus patients have got higher disease activity as compared to adults; they have a greater medication burden, particularly steroids; and they tend to have more severe organ manifestations,” she added.
Moreover, data show that one-fifth of pediatric patients with lupus have already accrued early damage, and there is much higher mortality associated with childhood lupus than there is with adult lupus.
“So, really we want to use treat to target as a way to try and improve on these aspects,” Dr. Smith said.
The treat-to-target (T2T) approach is not a new idea in lupus, with a lot of work already done in adult patients. One large study of more than 3,300 patients conducted in 13 countries has shown that patients who never achieve LLDAS are more likely to have high levels of damage, greater glucocorticoid use, worse quality of life, and higher mortality than are those who do.
Conversely, data have also shown that achieving a LLDAS is associated with a reduction in the risk for new damage, flares, and hospitalization, as well as reducing health care costs and improving patients’ overall health-related quality of life.
T2T is a recognized approach in European adult SLE guidelines, Dr. Smith said, although the approach has not really been fully realized as of yet, even in adult practice.
The cSLE T2T international task force and cLLDAS definition
With evidence accumulating on the benefits of getting children with SLE to a low disease activity state, Dr. Smith and colleague Michael Beresford, MBChB, PhD, Brough Chair, Professor of Child Health at the University of Liverpool, put out a call to develop a task force to look into the feasibility of a T2T approach.
“We had a really enthusiastic response internationally, which we were really encouraged by,” Dr. Smith said, “and we now lead a task force of 20 experts from across all five continents, and we have really strong patient involvement.”
Through a consensus process, an international cSLE T2T Task Force agreed on overarching principles and points to consider that will “lay the foundation for future T2T approaches in cSLE,” according to the recommendations statement, which was endorsed by the Paediatric Rheumatology European Society.
Next, they looked to develop an age-appropriate definition for low disease activity.
“We’re deliberately wanting to maintain sufficient unity with the adult definition, so that we could facilitate life-course studies,” said Dr. Smith, who presented the results of a literature review and series of Delphi surveys at the meeting.
The conceptual definition of cLLDAS is similar to adults in describing it as a sustained state that is associated with a low likelihood of adverse outcome, Dr. Smith said, but with the added wording of “considering disease activity, damage, and medication toxicity.”
The definition is achieved when the SLE Disease Activity Index-2K is ≤ 4 and there is no activity in major organ systems; there are no new features of lupus disease activity since the last assessment; there is a score of ≤ 1 on Physician Global Assessment; steroid doses are ≤ 0.15 mg/kg/day or a maximum of 7.5 mg/day (whichever is lower); and immunosuppressive treatment is stable, with any changes to medication only because of side effects, adherence, changes in weight, or when in the process of reaching a target dose.
“It’s all very well having a definition, but you need to think about how that will work in practice,” Dr. Smith said. This is something that the task force is thinking about very carefully.
The task force next aims to validate the cLLDAS definition, form an extensive research agenda to inform the T2T methods, and develop innovative methods to apply the approach in practice.
The work is supported by the Wellcome Trust, National Institutes for Health Research, Versus Arthritis, and the University of Liverpool, Alder Hey Children’s NHS Foundation Trust and the Alder Hey Charity. Dr. Smith reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT BSR 2023
Part-time physician: Is it a viable career choice?
On average, physicians reported in the Medscape Physician Compensation Report 2023 that they worked 50 hours per week. Five specialties, including critical care, cardiology, and general surgery reported working 55 or more hours weekly.
In 2011, The New England Journal of Medicine reported that part-time physician careers were rising. At the time, part-time doctors made up 21% of the physician workforce, up from 13% in 2005.
In a more recent survey from the California Health Care Foundation, only 12% of California physicians said they devoted 20-29 hours a week to patient care.
Amy Knoup, a senior recruitment adviser with Provider Solutions & Development), has been helping doctors find jobs for over a decade, and she’s noticed a trend.
“Not only are more physicians seeking part-time roles than they were 10 years ago, but more large health care systems are also offering part time or per diem as well,” said Ms. Knoup.
Who’s working part time, and why?
Ten years ago, the fastest growing segment of part-timers were men nearing retirement and early- to mid-career women.
Pediatricians led the part-time pack in 2002, according to an American Academy of Pediatrics study. At the time, 15% of pediatricians reported their hours as part time. However, the numbers may have increased over the years. For example, a 2021 study by the department of pediatrics, Boston Medical Center, and Boston University found that almost 30% of graduating pediatricians sought part-time work at the end of their training.
At PS&D, Ms. Knoup said she has noticed a trend toward part-timers among primary care, behavioral health, and outpatient specialties such as endocrinology. “We’re also seeing it with the inpatient side in roles that are more shift based like hospitalists, radiologists, and critical care and ER doctors.”
Another trend Ms. Knoup has noticed is with early-career doctors. “They have a different mindset,” she said. “Younger generations are acutely aware of burnout. They may have experienced it in residency or during the pandemic. They’ve had a taste of that and don’t want to go down that road again, so they’re seeking part-time roles. It’s an intentional choice.”
Tracey O’Connell, MD, a radiologist, always knew that she wanted to work part time. “I had a baby as a resident, and I was pregnant with my second child as a fellow,” she said. “I was already feeling overwhelmed with medical training and having a family.”
Dr. O’Connell worked in private practice for 16 years on Mondays, Wednesdays, and Fridays, with no nights or weekends.
“I still found it completely overwhelming,” she said. “Even though I had more days not working than working, I felt like the demands of medical life had advanced faster than human beings could adapt, and I still feel that way.”
Today she runs a part-time teleradiology practice from home but spends more time on her second career as a life coach. “Most of my clients are physicians looking for more fulfillment and sustainable ways of practicing medicine while maintaining their own identity as human beings, not just the all-consuming identity of ‘doctor,’ ” she said.
On the other end of the career spectrum is Lois Goodman, MD, an ob.gyn. in her late 70s. After 42 years in a group practice, she started her solo practice at 72, seeing patients 3 days per week. “I’m just happy to be working. That’s a tremendous payoff for me. I need to keep working for my mental health.”
How does part-time work affect physician shortages and care delivery?
Reducing clinical effort is one of the strategies physicians use to scale down overload. Still, it’s not viable as a long-term solution, said Christine Sinsky, MD, AMA’s vice president of professional satisfaction and a nationally regarded researcher on physician burnout.
“If all the physicians in a community went from working 100% FTE clinical to 50% FTE clinical, then the people in that community would have half the access to care that they had,” said Dr. Sinsky. “There’s less capacity in the system to care for patients.”
Some could argue, then, that part-time physician work may contribute to physician shortage predictions. An Association of American Medical Colleges report estimates there will be a shortage of 37,800 to 124,000 physicians by 2034.
But physicians working part-time express a contrasting point of view. “I don’t believe that part-time workers are responsible for the health care shortage but rather, a great solution,” said Dr. O’Connell. “Because in order to continue working for a long time rather than quitting when the demands exceed human capacity, working part time is a great compromise to offer a life of more sustainable well-being and longevity as a physician, and still live a wholehearted life.”
Pros and cons of being a part-time physician
Pros
Less burnout: The American Medical Association has tracked burnout rates for 22 years. By the end of 2021, nearly 63% of physicians reported burnout symptoms, compared with 38% the year before. Going part time appears to reduce burnout, suggests a study published in Mayo Clinic Proceedings.
Better work-life balance: Rachel Miller, MD, an ob.gyn., worked 60-70 hours weekly for 9 years. In 2022, she went to work as an OB hospitalist for a health care system that welcomes part-time clinicians. Since then, she has achieved a better work-life balance, putting in 26-28 hours a week. Dr. Miller now spends more time with her kids and in her additional role as an executive coach to leaders in the medical field.
More focus: “When I’m at work, I’m 100% mentally in and focused,” said Dr. Miller. “My interactions with patients are different because I’m not burned out. My demeanor and my willingness to connect are stronger.”
Better health: Mehmet Cilingiroglu, MD, with CardioSolution, traded full-time work for part time when health issues and a kidney transplant sidelined his 30-year career in 2018. “Despite my significant health issues, I’ve been able to continue working at a pace that suits me rather than having to retire,” he said. “Part-time physicians can still enjoy patient care, research, innovation, education, and training while balancing that with other areas of life.”
Errin Weisman, a DO who gave up full-time work in 2016, said cutting back makes her feel healthier, happier, and more energized. “Part-time work helps me to bring my A game each day I work and deliver the best care.” She’s also a life coach encouraging other physicians to find balance in their professional and personal lives.
Cons
Cut in pay: Obviously, the No. 1 con is you’ll make less working part time, so adjusting to a salary decrease can be a huge issue, especially if you don’t have other sources of income. Physicians paying off student loans, those caring for children or elderly parents, or those in their prime earning years needing to save for retirement may not be able to go part time.
Diminished career: The chance for promotions or being well known in your field can be diminished, as well as a loss of proficiency if you’re only performing surgery or procedures part time. In some specialties, working part time and not keeping up with (or being able to practice) newer technology developments can harm your career or reputation in the long run.
Missing out: While working part time has many benefits, physicians also experience a wide range of drawbacks. Dr. Goodman, for example, said she misses delivering babies and doing surgeries. Dr. Miller said she gave up some aspects of her specialty, like performing hysterectomies, participating in complex cases, and no longer having an office like she did as a full-time ob.gyn.
Loss of fellowship: Dr. O’Connell said she missed the camaraderie and sense of belonging when she scaled back her hours. “I felt like a fish out of water, that my values didn’t align with the group’s values,” she said. This led to self-doubt, frustrated colleagues, and a reduction in benefits.
Lost esteem: Dr. O’Connell also felt she was expected to work overtime without additional pay and was no longer eligible for bonuses. “I was treated as a team player when I was needed, but not when it came to perks and benefits and insider privilege,” she said. There may be a loss of esteem among colleagues and supervisors.
Overcoming stigma: Because part-time physician work is still not prevalent among colleagues, some may resist the idea, have less respect for it, perceive it as not being serious about your career as a physician, or associate it with being lazy or entitled.
Summing it up
Every physician must weigh the value and drawbacks of part-time work, but the more physicians who go this route, the more part-time medicine gains traction and the more physicians can learn about its values versus its drawbacks.
A version of this article first appeared on Medscape.com.
On average, physicians reported in the Medscape Physician Compensation Report 2023 that they worked 50 hours per week. Five specialties, including critical care, cardiology, and general surgery reported working 55 or more hours weekly.
In 2011, The New England Journal of Medicine reported that part-time physician careers were rising. At the time, part-time doctors made up 21% of the physician workforce, up from 13% in 2005.
In a more recent survey from the California Health Care Foundation, only 12% of California physicians said they devoted 20-29 hours a week to patient care.
Amy Knoup, a senior recruitment adviser with Provider Solutions & Development), has been helping doctors find jobs for over a decade, and she’s noticed a trend.
“Not only are more physicians seeking part-time roles than they were 10 years ago, but more large health care systems are also offering part time or per diem as well,” said Ms. Knoup.
Who’s working part time, and why?
Ten years ago, the fastest growing segment of part-timers were men nearing retirement and early- to mid-career women.
Pediatricians led the part-time pack in 2002, according to an American Academy of Pediatrics study. At the time, 15% of pediatricians reported their hours as part time. However, the numbers may have increased over the years. For example, a 2021 study by the department of pediatrics, Boston Medical Center, and Boston University found that almost 30% of graduating pediatricians sought part-time work at the end of their training.
At PS&D, Ms. Knoup said she has noticed a trend toward part-timers among primary care, behavioral health, and outpatient specialties such as endocrinology. “We’re also seeing it with the inpatient side in roles that are more shift based like hospitalists, radiologists, and critical care and ER doctors.”
Another trend Ms. Knoup has noticed is with early-career doctors. “They have a different mindset,” she said. “Younger generations are acutely aware of burnout. They may have experienced it in residency or during the pandemic. They’ve had a taste of that and don’t want to go down that road again, so they’re seeking part-time roles. It’s an intentional choice.”
Tracey O’Connell, MD, a radiologist, always knew that she wanted to work part time. “I had a baby as a resident, and I was pregnant with my second child as a fellow,” she said. “I was already feeling overwhelmed with medical training and having a family.”
Dr. O’Connell worked in private practice for 16 years on Mondays, Wednesdays, and Fridays, with no nights or weekends.
“I still found it completely overwhelming,” she said. “Even though I had more days not working than working, I felt like the demands of medical life had advanced faster than human beings could adapt, and I still feel that way.”
Today she runs a part-time teleradiology practice from home but spends more time on her second career as a life coach. “Most of my clients are physicians looking for more fulfillment and sustainable ways of practicing medicine while maintaining their own identity as human beings, not just the all-consuming identity of ‘doctor,’ ” she said.
On the other end of the career spectrum is Lois Goodman, MD, an ob.gyn. in her late 70s. After 42 years in a group practice, she started her solo practice at 72, seeing patients 3 days per week. “I’m just happy to be working. That’s a tremendous payoff for me. I need to keep working for my mental health.”
How does part-time work affect physician shortages and care delivery?
Reducing clinical effort is one of the strategies physicians use to scale down overload. Still, it’s not viable as a long-term solution, said Christine Sinsky, MD, AMA’s vice president of professional satisfaction and a nationally regarded researcher on physician burnout.
“If all the physicians in a community went from working 100% FTE clinical to 50% FTE clinical, then the people in that community would have half the access to care that they had,” said Dr. Sinsky. “There’s less capacity in the system to care for patients.”
Some could argue, then, that part-time physician work may contribute to physician shortage predictions. An Association of American Medical Colleges report estimates there will be a shortage of 37,800 to 124,000 physicians by 2034.
But physicians working part-time express a contrasting point of view. “I don’t believe that part-time workers are responsible for the health care shortage but rather, a great solution,” said Dr. O’Connell. “Because in order to continue working for a long time rather than quitting when the demands exceed human capacity, working part time is a great compromise to offer a life of more sustainable well-being and longevity as a physician, and still live a wholehearted life.”
Pros and cons of being a part-time physician
Pros
Less burnout: The American Medical Association has tracked burnout rates for 22 years. By the end of 2021, nearly 63% of physicians reported burnout symptoms, compared with 38% the year before. Going part time appears to reduce burnout, suggests a study published in Mayo Clinic Proceedings.
Better work-life balance: Rachel Miller, MD, an ob.gyn., worked 60-70 hours weekly for 9 years. In 2022, she went to work as an OB hospitalist for a health care system that welcomes part-time clinicians. Since then, she has achieved a better work-life balance, putting in 26-28 hours a week. Dr. Miller now spends more time with her kids and in her additional role as an executive coach to leaders in the medical field.
More focus: “When I’m at work, I’m 100% mentally in and focused,” said Dr. Miller. “My interactions with patients are different because I’m not burned out. My demeanor and my willingness to connect are stronger.”
Better health: Mehmet Cilingiroglu, MD, with CardioSolution, traded full-time work for part time when health issues and a kidney transplant sidelined his 30-year career in 2018. “Despite my significant health issues, I’ve been able to continue working at a pace that suits me rather than having to retire,” he said. “Part-time physicians can still enjoy patient care, research, innovation, education, and training while balancing that with other areas of life.”
Errin Weisman, a DO who gave up full-time work in 2016, said cutting back makes her feel healthier, happier, and more energized. “Part-time work helps me to bring my A game each day I work and deliver the best care.” She’s also a life coach encouraging other physicians to find balance in their professional and personal lives.
Cons
Cut in pay: Obviously, the No. 1 con is you’ll make less working part time, so adjusting to a salary decrease can be a huge issue, especially if you don’t have other sources of income. Physicians paying off student loans, those caring for children or elderly parents, or those in their prime earning years needing to save for retirement may not be able to go part time.
Diminished career: The chance for promotions or being well known in your field can be diminished, as well as a loss of proficiency if you’re only performing surgery or procedures part time. In some specialties, working part time and not keeping up with (or being able to practice) newer technology developments can harm your career or reputation in the long run.
Missing out: While working part time has many benefits, physicians also experience a wide range of drawbacks. Dr. Goodman, for example, said she misses delivering babies and doing surgeries. Dr. Miller said she gave up some aspects of her specialty, like performing hysterectomies, participating in complex cases, and no longer having an office like she did as a full-time ob.gyn.
Loss of fellowship: Dr. O’Connell said she missed the camaraderie and sense of belonging when she scaled back her hours. “I felt like a fish out of water, that my values didn’t align with the group’s values,” she said. This led to self-doubt, frustrated colleagues, and a reduction in benefits.
Lost esteem: Dr. O’Connell also felt she was expected to work overtime without additional pay and was no longer eligible for bonuses. “I was treated as a team player when I was needed, but not when it came to perks and benefits and insider privilege,” she said. There may be a loss of esteem among colleagues and supervisors.
Overcoming stigma: Because part-time physician work is still not prevalent among colleagues, some may resist the idea, have less respect for it, perceive it as not being serious about your career as a physician, or associate it with being lazy or entitled.
Summing it up
Every physician must weigh the value and drawbacks of part-time work, but the more physicians who go this route, the more part-time medicine gains traction and the more physicians can learn about its values versus its drawbacks.
A version of this article first appeared on Medscape.com.
On average, physicians reported in the Medscape Physician Compensation Report 2023 that they worked 50 hours per week. Five specialties, including critical care, cardiology, and general surgery reported working 55 or more hours weekly.
In 2011, The New England Journal of Medicine reported that part-time physician careers were rising. At the time, part-time doctors made up 21% of the physician workforce, up from 13% in 2005.
In a more recent survey from the California Health Care Foundation, only 12% of California physicians said they devoted 20-29 hours a week to patient care.
Amy Knoup, a senior recruitment adviser with Provider Solutions & Development), has been helping doctors find jobs for over a decade, and she’s noticed a trend.
“Not only are more physicians seeking part-time roles than they were 10 years ago, but more large health care systems are also offering part time or per diem as well,” said Ms. Knoup.
Who’s working part time, and why?
Ten years ago, the fastest growing segment of part-timers were men nearing retirement and early- to mid-career women.
Pediatricians led the part-time pack in 2002, according to an American Academy of Pediatrics study. At the time, 15% of pediatricians reported their hours as part time. However, the numbers may have increased over the years. For example, a 2021 study by the department of pediatrics, Boston Medical Center, and Boston University found that almost 30% of graduating pediatricians sought part-time work at the end of their training.
At PS&D, Ms. Knoup said she has noticed a trend toward part-timers among primary care, behavioral health, and outpatient specialties such as endocrinology. “We’re also seeing it with the inpatient side in roles that are more shift based like hospitalists, radiologists, and critical care and ER doctors.”
Another trend Ms. Knoup has noticed is with early-career doctors. “They have a different mindset,” she said. “Younger generations are acutely aware of burnout. They may have experienced it in residency or during the pandemic. They’ve had a taste of that and don’t want to go down that road again, so they’re seeking part-time roles. It’s an intentional choice.”
Tracey O’Connell, MD, a radiologist, always knew that she wanted to work part time. “I had a baby as a resident, and I was pregnant with my second child as a fellow,” she said. “I was already feeling overwhelmed with medical training and having a family.”
Dr. O’Connell worked in private practice for 16 years on Mondays, Wednesdays, and Fridays, with no nights or weekends.
“I still found it completely overwhelming,” she said. “Even though I had more days not working than working, I felt like the demands of medical life had advanced faster than human beings could adapt, and I still feel that way.”
Today she runs a part-time teleradiology practice from home but spends more time on her second career as a life coach. “Most of my clients are physicians looking for more fulfillment and sustainable ways of practicing medicine while maintaining their own identity as human beings, not just the all-consuming identity of ‘doctor,’ ” she said.
On the other end of the career spectrum is Lois Goodman, MD, an ob.gyn. in her late 70s. After 42 years in a group practice, she started her solo practice at 72, seeing patients 3 days per week. “I’m just happy to be working. That’s a tremendous payoff for me. I need to keep working for my mental health.”
How does part-time work affect physician shortages and care delivery?
Reducing clinical effort is one of the strategies physicians use to scale down overload. Still, it’s not viable as a long-term solution, said Christine Sinsky, MD, AMA’s vice president of professional satisfaction and a nationally regarded researcher on physician burnout.
“If all the physicians in a community went from working 100% FTE clinical to 50% FTE clinical, then the people in that community would have half the access to care that they had,” said Dr. Sinsky. “There’s less capacity in the system to care for patients.”
Some could argue, then, that part-time physician work may contribute to physician shortage predictions. An Association of American Medical Colleges report estimates there will be a shortage of 37,800 to 124,000 physicians by 2034.
But physicians working part-time express a contrasting point of view. “I don’t believe that part-time workers are responsible for the health care shortage but rather, a great solution,” said Dr. O’Connell. “Because in order to continue working for a long time rather than quitting when the demands exceed human capacity, working part time is a great compromise to offer a life of more sustainable well-being and longevity as a physician, and still live a wholehearted life.”
Pros and cons of being a part-time physician
Pros
Less burnout: The American Medical Association has tracked burnout rates for 22 years. By the end of 2021, nearly 63% of physicians reported burnout symptoms, compared with 38% the year before. Going part time appears to reduce burnout, suggests a study published in Mayo Clinic Proceedings.
Better work-life balance: Rachel Miller, MD, an ob.gyn., worked 60-70 hours weekly for 9 years. In 2022, she went to work as an OB hospitalist for a health care system that welcomes part-time clinicians. Since then, she has achieved a better work-life balance, putting in 26-28 hours a week. Dr. Miller now spends more time with her kids and in her additional role as an executive coach to leaders in the medical field.
More focus: “When I’m at work, I’m 100% mentally in and focused,” said Dr. Miller. “My interactions with patients are different because I’m not burned out. My demeanor and my willingness to connect are stronger.”
Better health: Mehmet Cilingiroglu, MD, with CardioSolution, traded full-time work for part time when health issues and a kidney transplant sidelined his 30-year career in 2018. “Despite my significant health issues, I’ve been able to continue working at a pace that suits me rather than having to retire,” he said. “Part-time physicians can still enjoy patient care, research, innovation, education, and training while balancing that with other areas of life.”
Errin Weisman, a DO who gave up full-time work in 2016, said cutting back makes her feel healthier, happier, and more energized. “Part-time work helps me to bring my A game each day I work and deliver the best care.” She’s also a life coach encouraging other physicians to find balance in their professional and personal lives.
Cons
Cut in pay: Obviously, the No. 1 con is you’ll make less working part time, so adjusting to a salary decrease can be a huge issue, especially if you don’t have other sources of income. Physicians paying off student loans, those caring for children or elderly parents, or those in their prime earning years needing to save for retirement may not be able to go part time.
Diminished career: The chance for promotions or being well known in your field can be diminished, as well as a loss of proficiency if you’re only performing surgery or procedures part time. In some specialties, working part time and not keeping up with (or being able to practice) newer technology developments can harm your career or reputation in the long run.
Missing out: While working part time has many benefits, physicians also experience a wide range of drawbacks. Dr. Goodman, for example, said she misses delivering babies and doing surgeries. Dr. Miller said she gave up some aspects of her specialty, like performing hysterectomies, participating in complex cases, and no longer having an office like she did as a full-time ob.gyn.
Loss of fellowship: Dr. O’Connell said she missed the camaraderie and sense of belonging when she scaled back her hours. “I felt like a fish out of water, that my values didn’t align with the group’s values,” she said. This led to self-doubt, frustrated colleagues, and a reduction in benefits.
Lost esteem: Dr. O’Connell also felt she was expected to work overtime without additional pay and was no longer eligible for bonuses. “I was treated as a team player when I was needed, but not when it came to perks and benefits and insider privilege,” she said. There may be a loss of esteem among colleagues and supervisors.
Overcoming stigma: Because part-time physician work is still not prevalent among colleagues, some may resist the idea, have less respect for it, perceive it as not being serious about your career as a physician, or associate it with being lazy or entitled.
Summing it up
Every physician must weigh the value and drawbacks of part-time work, but the more physicians who go this route, the more part-time medicine gains traction and the more physicians can learn about its values versus its drawbacks.
A version of this article first appeared on Medscape.com.
Study of hospitalizations in Canada quantifies benefit of COVID-19 vaccine to reduce death, ICU admissions
A cohort study of more than 1.5 million hospital admissions in Canada through the first 2 years of the COVID-19 pandemic has quantified the benefit of vaccinations. Unvaccinated patients were found to be up to 15 times more likely to die from COVID-19 than fully vaccinated patients.
Investigators analyzed 1.513 million admissions at 155 hospitals across Canada from March 15, 2020, to May 28, 2022. The study included 51,679 adult admissions and 4,035 pediatric admissions for COVID-19. Although the share of COVID-19 admissions increased in the fifth and sixth waves, from Dec. 26, 2021, to March 19, 2022 – after the full vaccine rollout – to 7.73% from 2.47% in the previous four waves, the proportion of adults admitted to the intensive care unit was significantly lower, at 8.7% versus 21.8% (odds ratio, 0.35; 95% confidence interval, 0.32-0.36).
“The good thing about waves five and six was we were able to show the COVID cases tended to be less severe, but on the other hand, because the disease in the community was so much higher, the demands on the health care system were much higher than the previous waves,” study author Charles Frenette, MD, director of infection prevention and control at McGill University, Montreal, and chair of the study’s adult subgroup, said in an interview. “But here we were able to show the benefit of vaccinations, particularly the boosting dose, in protecting against those severe outcomes.”
The study, published in JAMA Network Open, used the Canadian Nosocomial Infection Surveillance Program database, which collects hospital data across Canada. It was activated in March 2020 to collect details on all COVID-19 admissions, co-author Nisha Thampi, MD, chair of the study’s pediatric subgroup, told this news organization.
“We’re now over 3 years into the pandemic, and CNISP continues to monitor COVID-19 as well as other pathogens in near real time,” said Dr. Thampi, an associate professor and infectious disease specialist at Children’s Hospital of Eastern Ontario.
“That’s a particular strength of this surveillance program as well. We would see this data on a biweekly basis, and that allows for [us] to implement timely protection and action.”
Tracing trends over six waves
The study tracked COVID-19 hospitalizations during six waves. The first lasted from March 15 to August 31, 2020, and the second lasted from Sept. 1, 2020, to Feb. 28, 2021. The wild-type variant was dominant during both waves. The third wave lasted from March 1 to June 30, 2021, and was marked by the mixed Alpha, Beta, and Gamma variants. The fourth wave lasted from July 1 to Dec. 25, 2021, when the Alpha variant was dominant. The Omicron variant dominated during waves five (Dec. 26, 2021, to March 19, 2022) and six (March 20 to May 28, 2022).
Hospitalizations reached a peak of 14,461 in wave five. ICU admissions, however, peaked at 2,164 during wave four, and all-cause deaths peaked at 1,663 during wave two.
The investigators also analyzed how unvaccinated patients fared, compared with the fully vaccinated and the fully vaccinated-plus (that is, patients with one or more additional doses). During waves five and six, unvaccinated patients were 4.3 times more likely to end up in the ICU than fully vaccinated patients and were 12.2 times more likely than fully vaccinated-plus patients. Likewise, the rate for all-cause in-hospital death for unvaccinated patients was 3.9 times greater than that for fully vaccinated patients and 15.1 times greater than that for fully vaccinated-plus patients.
The effect of vaccines emerged in waves three and four, said Dr. Frenette. “We started to see really, really significant protection and benefit from the vaccine, not only in incidence of admission but also in the incidence of complications of ICU care, ventilation, and mortality.”
Results for pediatric patients were similar to those for adults, Dr. Thampi noted. During waves five and six, overall admissions peaked, but the share of ICU admissions decreased to 9.4% from 18.1%, which was the rate during the previous four waves (OR, 0.47).
“What’s important is how pediatric hospitalizations changed over the course of the various waves,” said Dr. Thampi.
“Where we saw the highest admissions during the early Omicron dominance, we actually had the lowest numbers of hospitalizations with death and admissions into ICUs.”
Doing more with the data
David Fisman, MD, MPH, a professor of epidemiology at the University of Toronto, said, “This is a study that shows us how tremendously dramatic the effects of the COVID-19 vaccine were in terms of saving lives during the pandemic.” Dr. Fisman was not involved in the study.
But CNISP, which receives funding from Public Health Agency of Canada, could do more with the data it collects to better protect the public from COVID-19 and other nosocomial infections, Dr. Fisman said.
“The first problematic thing about this paper is that Canadians are paying for a surveillance system that looks at risks of acquiring infections, including COVID-19 infections, in the hospital, but that data is not fed back to the people paying for its production,” he said.
“So, Canadians don’t have the ability to really understand in real time how much risk they’re experiencing via going to the hospital for some other reason.”
The study was independently supported. Dr. Frenette and Dr. Thampi report no relevant financial relationships. Dr. Fisman has disclosed financial relationships with Pfizer, AstraZeneca, Sanofi, Seqirus, Merck, the Ontario Nurses Association, and the Elementary Teachers’ Federation of Ontario.
A version of this article first appeared on Medscape.com.
A cohort study of more than 1.5 million hospital admissions in Canada through the first 2 years of the COVID-19 pandemic has quantified the benefit of vaccinations. Unvaccinated patients were found to be up to 15 times more likely to die from COVID-19 than fully vaccinated patients.
Investigators analyzed 1.513 million admissions at 155 hospitals across Canada from March 15, 2020, to May 28, 2022. The study included 51,679 adult admissions and 4,035 pediatric admissions for COVID-19. Although the share of COVID-19 admissions increased in the fifth and sixth waves, from Dec. 26, 2021, to March 19, 2022 – after the full vaccine rollout – to 7.73% from 2.47% in the previous four waves, the proportion of adults admitted to the intensive care unit was significantly lower, at 8.7% versus 21.8% (odds ratio, 0.35; 95% confidence interval, 0.32-0.36).
“The good thing about waves five and six was we were able to show the COVID cases tended to be less severe, but on the other hand, because the disease in the community was so much higher, the demands on the health care system were much higher than the previous waves,” study author Charles Frenette, MD, director of infection prevention and control at McGill University, Montreal, and chair of the study’s adult subgroup, said in an interview. “But here we were able to show the benefit of vaccinations, particularly the boosting dose, in protecting against those severe outcomes.”
The study, published in JAMA Network Open, used the Canadian Nosocomial Infection Surveillance Program database, which collects hospital data across Canada. It was activated in March 2020 to collect details on all COVID-19 admissions, co-author Nisha Thampi, MD, chair of the study’s pediatric subgroup, told this news organization.
“We’re now over 3 years into the pandemic, and CNISP continues to monitor COVID-19 as well as other pathogens in near real time,” said Dr. Thampi, an associate professor and infectious disease specialist at Children’s Hospital of Eastern Ontario.
“That’s a particular strength of this surveillance program as well. We would see this data on a biweekly basis, and that allows for [us] to implement timely protection and action.”
Tracing trends over six waves
The study tracked COVID-19 hospitalizations during six waves. The first lasted from March 15 to August 31, 2020, and the second lasted from Sept. 1, 2020, to Feb. 28, 2021. The wild-type variant was dominant during both waves. The third wave lasted from March 1 to June 30, 2021, and was marked by the mixed Alpha, Beta, and Gamma variants. The fourth wave lasted from July 1 to Dec. 25, 2021, when the Alpha variant was dominant. The Omicron variant dominated during waves five (Dec. 26, 2021, to March 19, 2022) and six (March 20 to May 28, 2022).
Hospitalizations reached a peak of 14,461 in wave five. ICU admissions, however, peaked at 2,164 during wave four, and all-cause deaths peaked at 1,663 during wave two.
The investigators also analyzed how unvaccinated patients fared, compared with the fully vaccinated and the fully vaccinated-plus (that is, patients with one or more additional doses). During waves five and six, unvaccinated patients were 4.3 times more likely to end up in the ICU than fully vaccinated patients and were 12.2 times more likely than fully vaccinated-plus patients. Likewise, the rate for all-cause in-hospital death for unvaccinated patients was 3.9 times greater than that for fully vaccinated patients and 15.1 times greater than that for fully vaccinated-plus patients.
The effect of vaccines emerged in waves three and four, said Dr. Frenette. “We started to see really, really significant protection and benefit from the vaccine, not only in incidence of admission but also in the incidence of complications of ICU care, ventilation, and mortality.”
Results for pediatric patients were similar to those for adults, Dr. Thampi noted. During waves five and six, overall admissions peaked, but the share of ICU admissions decreased to 9.4% from 18.1%, which was the rate during the previous four waves (OR, 0.47).
“What’s important is how pediatric hospitalizations changed over the course of the various waves,” said Dr. Thampi.
“Where we saw the highest admissions during the early Omicron dominance, we actually had the lowest numbers of hospitalizations with death and admissions into ICUs.”
Doing more with the data
David Fisman, MD, MPH, a professor of epidemiology at the University of Toronto, said, “This is a study that shows us how tremendously dramatic the effects of the COVID-19 vaccine were in terms of saving lives during the pandemic.” Dr. Fisman was not involved in the study.
But CNISP, which receives funding from Public Health Agency of Canada, could do more with the data it collects to better protect the public from COVID-19 and other nosocomial infections, Dr. Fisman said.
“The first problematic thing about this paper is that Canadians are paying for a surveillance system that looks at risks of acquiring infections, including COVID-19 infections, in the hospital, but that data is not fed back to the people paying for its production,” he said.
“So, Canadians don’t have the ability to really understand in real time how much risk they’re experiencing via going to the hospital for some other reason.”
The study was independently supported. Dr. Frenette and Dr. Thampi report no relevant financial relationships. Dr. Fisman has disclosed financial relationships with Pfizer, AstraZeneca, Sanofi, Seqirus, Merck, the Ontario Nurses Association, and the Elementary Teachers’ Federation of Ontario.
A version of this article first appeared on Medscape.com.
A cohort study of more than 1.5 million hospital admissions in Canada through the first 2 years of the COVID-19 pandemic has quantified the benefit of vaccinations. Unvaccinated patients were found to be up to 15 times more likely to die from COVID-19 than fully vaccinated patients.
Investigators analyzed 1.513 million admissions at 155 hospitals across Canada from March 15, 2020, to May 28, 2022. The study included 51,679 adult admissions and 4,035 pediatric admissions for COVID-19. Although the share of COVID-19 admissions increased in the fifth and sixth waves, from Dec. 26, 2021, to March 19, 2022 – after the full vaccine rollout – to 7.73% from 2.47% in the previous four waves, the proportion of adults admitted to the intensive care unit was significantly lower, at 8.7% versus 21.8% (odds ratio, 0.35; 95% confidence interval, 0.32-0.36).
“The good thing about waves five and six was we were able to show the COVID cases tended to be less severe, but on the other hand, because the disease in the community was so much higher, the demands on the health care system were much higher than the previous waves,” study author Charles Frenette, MD, director of infection prevention and control at McGill University, Montreal, and chair of the study’s adult subgroup, said in an interview. “But here we were able to show the benefit of vaccinations, particularly the boosting dose, in protecting against those severe outcomes.”
The study, published in JAMA Network Open, used the Canadian Nosocomial Infection Surveillance Program database, which collects hospital data across Canada. It was activated in March 2020 to collect details on all COVID-19 admissions, co-author Nisha Thampi, MD, chair of the study’s pediatric subgroup, told this news organization.
“We’re now over 3 years into the pandemic, and CNISP continues to monitor COVID-19 as well as other pathogens in near real time,” said Dr. Thampi, an associate professor and infectious disease specialist at Children’s Hospital of Eastern Ontario.
“That’s a particular strength of this surveillance program as well. We would see this data on a biweekly basis, and that allows for [us] to implement timely protection and action.”
Tracing trends over six waves
The study tracked COVID-19 hospitalizations during six waves. The first lasted from March 15 to August 31, 2020, and the second lasted from Sept. 1, 2020, to Feb. 28, 2021. The wild-type variant was dominant during both waves. The third wave lasted from March 1 to June 30, 2021, and was marked by the mixed Alpha, Beta, and Gamma variants. The fourth wave lasted from July 1 to Dec. 25, 2021, when the Alpha variant was dominant. The Omicron variant dominated during waves five (Dec. 26, 2021, to March 19, 2022) and six (March 20 to May 28, 2022).
Hospitalizations reached a peak of 14,461 in wave five. ICU admissions, however, peaked at 2,164 during wave four, and all-cause deaths peaked at 1,663 during wave two.
The investigators also analyzed how unvaccinated patients fared, compared with the fully vaccinated and the fully vaccinated-plus (that is, patients with one or more additional doses). During waves five and six, unvaccinated patients were 4.3 times more likely to end up in the ICU than fully vaccinated patients and were 12.2 times more likely than fully vaccinated-plus patients. Likewise, the rate for all-cause in-hospital death for unvaccinated patients was 3.9 times greater than that for fully vaccinated patients and 15.1 times greater than that for fully vaccinated-plus patients.
The effect of vaccines emerged in waves three and four, said Dr. Frenette. “We started to see really, really significant protection and benefit from the vaccine, not only in incidence of admission but also in the incidence of complications of ICU care, ventilation, and mortality.”
Results for pediatric patients were similar to those for adults, Dr. Thampi noted. During waves five and six, overall admissions peaked, but the share of ICU admissions decreased to 9.4% from 18.1%, which was the rate during the previous four waves (OR, 0.47).
“What’s important is how pediatric hospitalizations changed over the course of the various waves,” said Dr. Thampi.
“Where we saw the highest admissions during the early Omicron dominance, we actually had the lowest numbers of hospitalizations with death and admissions into ICUs.”
Doing more with the data
David Fisman, MD, MPH, a professor of epidemiology at the University of Toronto, said, “This is a study that shows us how tremendously dramatic the effects of the COVID-19 vaccine were in terms of saving lives during the pandemic.” Dr. Fisman was not involved in the study.
But CNISP, which receives funding from Public Health Agency of Canada, could do more with the data it collects to better protect the public from COVID-19 and other nosocomial infections, Dr. Fisman said.
“The first problematic thing about this paper is that Canadians are paying for a surveillance system that looks at risks of acquiring infections, including COVID-19 infections, in the hospital, but that data is not fed back to the people paying for its production,” he said.
“So, Canadians don’t have the ability to really understand in real time how much risk they’re experiencing via going to the hospital for some other reason.”
The study was independently supported. Dr. Frenette and Dr. Thampi report no relevant financial relationships. Dr. Fisman has disclosed financial relationships with Pfizer, AstraZeneca, Sanofi, Seqirus, Merck, the Ontario Nurses Association, and the Elementary Teachers’ Federation of Ontario.
A version of this article first appeared on Medscape.com.
1,726-nm lasers poised to revolutionize acne treatment, expert predicts
PHOENIX – When Jeffrey Dover, MD, addressed audience members gathered for a session on cutting-edge technologies at the annual conference of the American Society for Laser Medicine and Surgery, he reflected on a conversation he had with R. Rox Anderson, MD, almost 40 years ago, about eventually finding a cure for acne.
“Despite the fact that we have over-the-counter therapies, prescription therapies, and all kinds of devices available to treat acne, there are still barriers to care that get in the way of treatment,” said Dr. Dover, director of SkinCare Physicians in Chestnut Hill, Mass. “If we had a device based on innovative light science that could meet the needs of the acne patient to get rid of these barriers, wouldn’t that be something wonderful?”
The answer to this question, he said, is now “yes,” because of advances in lasers that target sebaceous glands.
In a seminal paper published in 2012, Fernanda H. Sakamoto, MD, PhD, Dr. Anderson, and colleagues demonstrated the potential for a free electron laser to target sebaceous glands . Following several years of refinement, Dr. Dover said.
“With the 1,726-nm laser, there is some selective absorption in sebum in skin, which beats out absorption in the other chromophores,” he said. “But it’s not a big difference like it is, for example, for pulsed-dye lasers and vascular targets. ... This means that the therapeutic window is relatively small and protecting the rest of the epidermis and dermis is crucial to be able to target these lesions or the sebaceous gland without unnecessary damage. If we can protect the epidermis and heat just the sebaceous glands, we should be able to get Accutane-like results if we get durability [by] shrinking sebaceous glands.”
Effective cooling, whether contact cooling, bulk cooling, or air cooling, is crucial to success, he continued. “It’s got to be robust and highly specific to protect the skin, so you don’t end up with side effects that are worse than the disease.”
The AviClear laser delivers seven 3-mm spots, which takes into account the thermal relaxation times of the sebaceous glands. The algorithm delivers a treatment imprint at roughly 0.3 Hz and a 1.5-mm depth of penetration, and the device relies on contact cooling. In pivotal data submitted to the FDA, 104 individuals with moderate to severe acne received three treatments with the AviClear 1 month apart, with follow-up at 1, 3, 6, and 12 months post treatment. They had no other treatment regimens, and the primary endpoint was the percentage of patients who achieved a 50% reduction in inflammatory lesion count 3 months after the final treatment. The secondary endpoint was an Investigator’s Global Assessment (IGA) improvement of 2 or greater.
Dr. Dover, who helped design the study, said that, at 3 months, 80% of those treated achieved a 50% or greater reduction in inflammatory lesion count (P < .001). As for secondary endpoints, 36% of individuals were assessed as having clear or almost clear skin; 47% achieved a 2-point or greater improvement in IGA score, compared with baseline, and 87% achieved a 1-point or greater improvement in IGA score, compared with baseline. By 6 months, 88% of individuals achieved a 50% or greater reduction in inflammatory lesion count; this improved to 92% by 12 months (P < .001).
“All of these procedures were done with no topical anesthetic, no intralesional anesthetic, and they tolerated these quite well,” he said. “There was no down time that required medical intervention after the treatments. All posttreatment erythema and swelling resolved quickly,” and 75% of the patients were “very satisfied” with the treatments.
The Accure Laser System features a proprietary technology that precisely controls thermal gradient depth. “So instead of guessing whether you are delivering the correct amount of heat, it actually tells you,” said Dr. Dover, a past president of the ASLMS and the American Society for Dermatologic Surgery. “It correlates surface and at-depth temperatures, and there’s an infrared camera for real-time accurate temperature monitoring.” The device features highly controlled air cooling and a pulsing pattern that ensures treatment of sebaceous glands of all sizes and at all depths. The clinical end marker is peak epidermal temperature.
In a study supported by Accure, the manufacturer, researchers evaluated the efficacy of the Accure Laser System in 35 subjects with types I to VI skin, who received four monthly treatments 30-45 minutes each, and were followed 12, 26, 39, and 52 weeks following their last treatment. To date, data out to 52 weeks is available for 17 study participants. According to Dr. Dover, the researchers found 80% clearance at 12 weeks following the last treatment, with continued improvement at 52 weeks. One hundred percent of subjects responded. Side effects included erythema, edema, crusting, blisters, and inflammatory papules. “None of these were medically significant,” he said.
As dermatologists begin to incorporate the AviClear and Accure devices into their practices, Dr. Dover said that he is reminded of the conversation he had some 40 years ago with Dr. Anderson about finding a cure for acne, and he feels a bit awestruck. “These 1,726-nm lasers are effective for treating acne. I personally think they are going to revolutionize the way we treat at least some of our patients with acne. They may both be effective for treating facial acne scars. Time will tell. Further study of both scarring and acne are needed to fully categorize the benefit and to optimize treatments.”
To date no direct clinical comparisons have been made between the AviClear and Accure devices.
Dr. Dover reported that he is a consultant for Cutera, the manufacturer for AviClear. He also performs research for the company.
PHOENIX – When Jeffrey Dover, MD, addressed audience members gathered for a session on cutting-edge technologies at the annual conference of the American Society for Laser Medicine and Surgery, he reflected on a conversation he had with R. Rox Anderson, MD, almost 40 years ago, about eventually finding a cure for acne.
“Despite the fact that we have over-the-counter therapies, prescription therapies, and all kinds of devices available to treat acne, there are still barriers to care that get in the way of treatment,” said Dr. Dover, director of SkinCare Physicians in Chestnut Hill, Mass. “If we had a device based on innovative light science that could meet the needs of the acne patient to get rid of these barriers, wouldn’t that be something wonderful?”
The answer to this question, he said, is now “yes,” because of advances in lasers that target sebaceous glands.
In a seminal paper published in 2012, Fernanda H. Sakamoto, MD, PhD, Dr. Anderson, and colleagues demonstrated the potential for a free electron laser to target sebaceous glands . Following several years of refinement, Dr. Dover said.
“With the 1,726-nm laser, there is some selective absorption in sebum in skin, which beats out absorption in the other chromophores,” he said. “But it’s not a big difference like it is, for example, for pulsed-dye lasers and vascular targets. ... This means that the therapeutic window is relatively small and protecting the rest of the epidermis and dermis is crucial to be able to target these lesions or the sebaceous gland without unnecessary damage. If we can protect the epidermis and heat just the sebaceous glands, we should be able to get Accutane-like results if we get durability [by] shrinking sebaceous glands.”
Effective cooling, whether contact cooling, bulk cooling, or air cooling, is crucial to success, he continued. “It’s got to be robust and highly specific to protect the skin, so you don’t end up with side effects that are worse than the disease.”
The AviClear laser delivers seven 3-mm spots, which takes into account the thermal relaxation times of the sebaceous glands. The algorithm delivers a treatment imprint at roughly 0.3 Hz and a 1.5-mm depth of penetration, and the device relies on contact cooling. In pivotal data submitted to the FDA, 104 individuals with moderate to severe acne received three treatments with the AviClear 1 month apart, with follow-up at 1, 3, 6, and 12 months post treatment. They had no other treatment regimens, and the primary endpoint was the percentage of patients who achieved a 50% reduction in inflammatory lesion count 3 months after the final treatment. The secondary endpoint was an Investigator’s Global Assessment (IGA) improvement of 2 or greater.
Dr. Dover, who helped design the study, said that, at 3 months, 80% of those treated achieved a 50% or greater reduction in inflammatory lesion count (P < .001). As for secondary endpoints, 36% of individuals were assessed as having clear or almost clear skin; 47% achieved a 2-point or greater improvement in IGA score, compared with baseline, and 87% achieved a 1-point or greater improvement in IGA score, compared with baseline. By 6 months, 88% of individuals achieved a 50% or greater reduction in inflammatory lesion count; this improved to 92% by 12 months (P < .001).
“All of these procedures were done with no topical anesthetic, no intralesional anesthetic, and they tolerated these quite well,” he said. “There was no down time that required medical intervention after the treatments. All posttreatment erythema and swelling resolved quickly,” and 75% of the patients were “very satisfied” with the treatments.
The Accure Laser System features a proprietary technology that precisely controls thermal gradient depth. “So instead of guessing whether you are delivering the correct amount of heat, it actually tells you,” said Dr. Dover, a past president of the ASLMS and the American Society for Dermatologic Surgery. “It correlates surface and at-depth temperatures, and there’s an infrared camera for real-time accurate temperature monitoring.” The device features highly controlled air cooling and a pulsing pattern that ensures treatment of sebaceous glands of all sizes and at all depths. The clinical end marker is peak epidermal temperature.
In a study supported by Accure, the manufacturer, researchers evaluated the efficacy of the Accure Laser System in 35 subjects with types I to VI skin, who received four monthly treatments 30-45 minutes each, and were followed 12, 26, 39, and 52 weeks following their last treatment. To date, data out to 52 weeks is available for 17 study participants. According to Dr. Dover, the researchers found 80% clearance at 12 weeks following the last treatment, with continued improvement at 52 weeks. One hundred percent of subjects responded. Side effects included erythema, edema, crusting, blisters, and inflammatory papules. “None of these were medically significant,” he said.
As dermatologists begin to incorporate the AviClear and Accure devices into their practices, Dr. Dover said that he is reminded of the conversation he had some 40 years ago with Dr. Anderson about finding a cure for acne, and he feels a bit awestruck. “These 1,726-nm lasers are effective for treating acne. I personally think they are going to revolutionize the way we treat at least some of our patients with acne. They may both be effective for treating facial acne scars. Time will tell. Further study of both scarring and acne are needed to fully categorize the benefit and to optimize treatments.”
To date no direct clinical comparisons have been made between the AviClear and Accure devices.
Dr. Dover reported that he is a consultant for Cutera, the manufacturer for AviClear. He also performs research for the company.
PHOENIX – When Jeffrey Dover, MD, addressed audience members gathered for a session on cutting-edge technologies at the annual conference of the American Society for Laser Medicine and Surgery, he reflected on a conversation he had with R. Rox Anderson, MD, almost 40 years ago, about eventually finding a cure for acne.
“Despite the fact that we have over-the-counter therapies, prescription therapies, and all kinds of devices available to treat acne, there are still barriers to care that get in the way of treatment,” said Dr. Dover, director of SkinCare Physicians in Chestnut Hill, Mass. “If we had a device based on innovative light science that could meet the needs of the acne patient to get rid of these barriers, wouldn’t that be something wonderful?”
The answer to this question, he said, is now “yes,” because of advances in lasers that target sebaceous glands.
In a seminal paper published in 2012, Fernanda H. Sakamoto, MD, PhD, Dr. Anderson, and colleagues demonstrated the potential for a free electron laser to target sebaceous glands . Following several years of refinement, Dr. Dover said.
“With the 1,726-nm laser, there is some selective absorption in sebum in skin, which beats out absorption in the other chromophores,” he said. “But it’s not a big difference like it is, for example, for pulsed-dye lasers and vascular targets. ... This means that the therapeutic window is relatively small and protecting the rest of the epidermis and dermis is crucial to be able to target these lesions or the sebaceous gland without unnecessary damage. If we can protect the epidermis and heat just the sebaceous glands, we should be able to get Accutane-like results if we get durability [by] shrinking sebaceous glands.”
Effective cooling, whether contact cooling, bulk cooling, or air cooling, is crucial to success, he continued. “It’s got to be robust and highly specific to protect the skin, so you don’t end up with side effects that are worse than the disease.”
The AviClear laser delivers seven 3-mm spots, which takes into account the thermal relaxation times of the sebaceous glands. The algorithm delivers a treatment imprint at roughly 0.3 Hz and a 1.5-mm depth of penetration, and the device relies on contact cooling. In pivotal data submitted to the FDA, 104 individuals with moderate to severe acne received three treatments with the AviClear 1 month apart, with follow-up at 1, 3, 6, and 12 months post treatment. They had no other treatment regimens, and the primary endpoint was the percentage of patients who achieved a 50% reduction in inflammatory lesion count 3 months after the final treatment. The secondary endpoint was an Investigator’s Global Assessment (IGA) improvement of 2 or greater.
Dr. Dover, who helped design the study, said that, at 3 months, 80% of those treated achieved a 50% or greater reduction in inflammatory lesion count (P < .001). As for secondary endpoints, 36% of individuals were assessed as having clear or almost clear skin; 47% achieved a 2-point or greater improvement in IGA score, compared with baseline, and 87% achieved a 1-point or greater improvement in IGA score, compared with baseline. By 6 months, 88% of individuals achieved a 50% or greater reduction in inflammatory lesion count; this improved to 92% by 12 months (P < .001).
“All of these procedures were done with no topical anesthetic, no intralesional anesthetic, and they tolerated these quite well,” he said. “There was no down time that required medical intervention after the treatments. All posttreatment erythema and swelling resolved quickly,” and 75% of the patients were “very satisfied” with the treatments.
The Accure Laser System features a proprietary technology that precisely controls thermal gradient depth. “So instead of guessing whether you are delivering the correct amount of heat, it actually tells you,” said Dr. Dover, a past president of the ASLMS and the American Society for Dermatologic Surgery. “It correlates surface and at-depth temperatures, and there’s an infrared camera for real-time accurate temperature monitoring.” The device features highly controlled air cooling and a pulsing pattern that ensures treatment of sebaceous glands of all sizes and at all depths. The clinical end marker is peak epidermal temperature.
In a study supported by Accure, the manufacturer, researchers evaluated the efficacy of the Accure Laser System in 35 subjects with types I to VI skin, who received four monthly treatments 30-45 minutes each, and were followed 12, 26, 39, and 52 weeks following their last treatment. To date, data out to 52 weeks is available for 17 study participants. According to Dr. Dover, the researchers found 80% clearance at 12 weeks following the last treatment, with continued improvement at 52 weeks. One hundred percent of subjects responded. Side effects included erythema, edema, crusting, blisters, and inflammatory papules. “None of these were medically significant,” he said.
As dermatologists begin to incorporate the AviClear and Accure devices into their practices, Dr. Dover said that he is reminded of the conversation he had some 40 years ago with Dr. Anderson about finding a cure for acne, and he feels a bit awestruck. “These 1,726-nm lasers are effective for treating acne. I personally think they are going to revolutionize the way we treat at least some of our patients with acne. They may both be effective for treating facial acne scars. Time will tell. Further study of both scarring and acne are needed to fully categorize the benefit and to optimize treatments.”
To date no direct clinical comparisons have been made between the AviClear and Accure devices.
Dr. Dover reported that he is a consultant for Cutera, the manufacturer for AviClear. He also performs research for the company.
AT ASLMS 2023
Interdisciplinary program reduced pediatric pain without pharmacology
WASHINGTON – A nonpharmacologic, interdisciplinary program significantly improved chronic pain in children and the quality of life for their families, based on data from 115 individuals.
Up to 40% of children experience chronic pain that affects their physical, psychosocial, and educational functioning, said Jessica Campanile, BA, a medical student at the University of Pennsylvania, Philadelphia, in a presentation at the Pediatric Academic Societies annual meeting.
Although interdisciplinary pediatric pain rehabilitation programs have shown positive outcomes, very few use only nonpharmacologic treatments, said Ms. Campanile. In addition, few studies have explored the effects of a hospital-based program on the patients and their families.
Ms. Campanile and colleagues conducted a retrospective cohort study of participants in an outpatient pain rehabilitation program at the Children’s Hospital of Philadelphia between April 2016 and December 2019. Patients were evaluated by a pediatric rheumatologist, psychologist, and physical and occupational therapists.
Patients engaged in 2-3 hours of physical therapy (PT) and 2-3 hours of occupational therapy (OT) in a 1:1 ratio at least 5 days a week. Physical activities included stepping into and out of a tub, carrying laundry, and desensitizing to allodynia as needed. Participants also received individual and group cognitive-behavior therapy interventions from psychologists, and psychological support during PT and OT sessions if needed. Parents/caregivers were invited to separate individual and group therapy sessions as part of the program. The median age at admission to the program was 15 years, and 79% of the participants were female. Patients participated the program for a median of 17 days, and 87% were outpatients who came to the hospital for the program.
Pain was assessed based on the 0-10 verbal pain intensity scale, energy was assessed on a scale of 0-100, and functional disability was assessed on a scale of 0-60, with higher scores indicating more pain, more energy, and more self-perceived disability, respectively.
Overall, scores on measures of pain, disability, allodynia, and energy improved significantly from baseline to discharge from the program. Verbal pain intensity scores decreased on average from 7 to 5, disability scores decreased from 26 to 9, the proportion of patients reporting allodynia decreased from 86% to 61%, and the energy level score increased from 70 to 77. The trend continued at the first follow-up visit, conducted 2-3 months after discharge from the program. Notably, pain intensity further decreased from a median of 5 at program completion to a median of 2 at the first follow-up, Ms. Campanile said. Improvements in allodynia also were sustained at the first follow-up.
Quality of life measures related to physical, emotional, social, and cognitive function also improved significantly from baseline to completion of the program.
In addition, scores on a quality of life family impact survey improved significantly; in particular, parent health-related quality of life scores (Parent HRQoL) improved from 60 at baseline to 71 at the end of the program on a scale of 0 to 100. The study findings were limited by several factors including the relatively short duration and use of a convenience sample from a retrospective cohort, with data limited to electronic health records, Ms. Campanile said. The study also was not powered to examine differential treatments based on psychiatric conditions, and any psychiatric conditions were based on self-reports.
However, the results support the value of a nonpharmacologic interdisciplinary program as “a robust treatment for youth with chronic idiopathic pain, for both patients and the family unit,” she said.
“This study also supports the need for and benefit of additional counseling for patients and their caregivers prior to and during enrollment in a pain rehabilitation program,” she concluded.
Study supports effectiveness of drug-free pain management
“The management of pain in any age group can be challenging, especially with current concerns for opioid dependence and abuse,” Cathy Haut, DNP, CPNP-AC, CPNP-PC, a pediatric nurse practitioner in Rehoboth Beach, Del., said in an interview.
“Chronic pain affects daily life for all populations, but for children, adolescents, and their families, it can have a long-lasting impact on growth and development, psychosocial and physical well-being,” Dr. Haut said. “Determining and testing nonpharmacologic alternative methods of pain control are extremely important.”
Given the debilitating effects of chronic pain, and the potential side effects and dependence that have been associated with use of pharmacologic modes of pain control, unique and creative solutions have begun to emerge and need further attention and study, she said.
However, “despite published research supporting the use of alternative and complementary approaches to pain control in children and adolescents, nonpharmacologic, collaborative, interprofessional approaches to pain control have not been widely shared in the literature,” she said.
“Barriers to this type of program include first and foremost a potential lack of financial and workforce-related resources,” Dr. Haut said. “Patient and family attendance at frequent health visits, daily or even every other day, may also hinder success, but opportunities for telehealth and family training to learn physical and occupational skills within this type of program may be beginning solutions.”
Additional research should be conducted at multiple children’s hospitals, with a larger number of children and adolescents at varying ages, with pain related to different diagnoses, and with the inclusion of collaborative methodology, said Dr. Haut. “The current study had some limitations, including the small sample size, predominantly female sex, and a short participation time frame utilizing retrospective review. Completing prospective research over a longer time frame can also yield generalizable results applicable to varied populations.”
The study received no outside funding. Ms. Campanile had no financial conflicts to disclose. Dr. Haut had no financial conflicts to disclose, and serves on the editorial advisory board of Pediatric News.
WASHINGTON – A nonpharmacologic, interdisciplinary program significantly improved chronic pain in children and the quality of life for their families, based on data from 115 individuals.
Up to 40% of children experience chronic pain that affects their physical, psychosocial, and educational functioning, said Jessica Campanile, BA, a medical student at the University of Pennsylvania, Philadelphia, in a presentation at the Pediatric Academic Societies annual meeting.
Although interdisciplinary pediatric pain rehabilitation programs have shown positive outcomes, very few use only nonpharmacologic treatments, said Ms. Campanile. In addition, few studies have explored the effects of a hospital-based program on the patients and their families.
Ms. Campanile and colleagues conducted a retrospective cohort study of participants in an outpatient pain rehabilitation program at the Children’s Hospital of Philadelphia between April 2016 and December 2019. Patients were evaluated by a pediatric rheumatologist, psychologist, and physical and occupational therapists.
Patients engaged in 2-3 hours of physical therapy (PT) and 2-3 hours of occupational therapy (OT) in a 1:1 ratio at least 5 days a week. Physical activities included stepping into and out of a tub, carrying laundry, and desensitizing to allodynia as needed. Participants also received individual and group cognitive-behavior therapy interventions from psychologists, and psychological support during PT and OT sessions if needed. Parents/caregivers were invited to separate individual and group therapy sessions as part of the program. The median age at admission to the program was 15 years, and 79% of the participants were female. Patients participated the program for a median of 17 days, and 87% were outpatients who came to the hospital for the program.
Pain was assessed based on the 0-10 verbal pain intensity scale, energy was assessed on a scale of 0-100, and functional disability was assessed on a scale of 0-60, with higher scores indicating more pain, more energy, and more self-perceived disability, respectively.
Overall, scores on measures of pain, disability, allodynia, and energy improved significantly from baseline to discharge from the program. Verbal pain intensity scores decreased on average from 7 to 5, disability scores decreased from 26 to 9, the proportion of patients reporting allodynia decreased from 86% to 61%, and the energy level score increased from 70 to 77. The trend continued at the first follow-up visit, conducted 2-3 months after discharge from the program. Notably, pain intensity further decreased from a median of 5 at program completion to a median of 2 at the first follow-up, Ms. Campanile said. Improvements in allodynia also were sustained at the first follow-up.
Quality of life measures related to physical, emotional, social, and cognitive function also improved significantly from baseline to completion of the program.
In addition, scores on a quality of life family impact survey improved significantly; in particular, parent health-related quality of life scores (Parent HRQoL) improved from 60 at baseline to 71 at the end of the program on a scale of 0 to 100. The study findings were limited by several factors including the relatively short duration and use of a convenience sample from a retrospective cohort, with data limited to electronic health records, Ms. Campanile said. The study also was not powered to examine differential treatments based on psychiatric conditions, and any psychiatric conditions were based on self-reports.
However, the results support the value of a nonpharmacologic interdisciplinary program as “a robust treatment for youth with chronic idiopathic pain, for both patients and the family unit,” she said.
“This study also supports the need for and benefit of additional counseling for patients and their caregivers prior to and during enrollment in a pain rehabilitation program,” she concluded.
Study supports effectiveness of drug-free pain management
“The management of pain in any age group can be challenging, especially with current concerns for opioid dependence and abuse,” Cathy Haut, DNP, CPNP-AC, CPNP-PC, a pediatric nurse practitioner in Rehoboth Beach, Del., said in an interview.
“Chronic pain affects daily life for all populations, but for children, adolescents, and their families, it can have a long-lasting impact on growth and development, psychosocial and physical well-being,” Dr. Haut said. “Determining and testing nonpharmacologic alternative methods of pain control are extremely important.”
Given the debilitating effects of chronic pain, and the potential side effects and dependence that have been associated with use of pharmacologic modes of pain control, unique and creative solutions have begun to emerge and need further attention and study, she said.
However, “despite published research supporting the use of alternative and complementary approaches to pain control in children and adolescents, nonpharmacologic, collaborative, interprofessional approaches to pain control have not been widely shared in the literature,” she said.
“Barriers to this type of program include first and foremost a potential lack of financial and workforce-related resources,” Dr. Haut said. “Patient and family attendance at frequent health visits, daily or even every other day, may also hinder success, but opportunities for telehealth and family training to learn physical and occupational skills within this type of program may be beginning solutions.”
Additional research should be conducted at multiple children’s hospitals, with a larger number of children and adolescents at varying ages, with pain related to different diagnoses, and with the inclusion of collaborative methodology, said Dr. Haut. “The current study had some limitations, including the small sample size, predominantly female sex, and a short participation time frame utilizing retrospective review. Completing prospective research over a longer time frame can also yield generalizable results applicable to varied populations.”
The study received no outside funding. Ms. Campanile had no financial conflicts to disclose. Dr. Haut had no financial conflicts to disclose, and serves on the editorial advisory board of Pediatric News.
WASHINGTON – A nonpharmacologic, interdisciplinary program significantly improved chronic pain in children and the quality of life for their families, based on data from 115 individuals.
Up to 40% of children experience chronic pain that affects their physical, psychosocial, and educational functioning, said Jessica Campanile, BA, a medical student at the University of Pennsylvania, Philadelphia, in a presentation at the Pediatric Academic Societies annual meeting.
Although interdisciplinary pediatric pain rehabilitation programs have shown positive outcomes, very few use only nonpharmacologic treatments, said Ms. Campanile. In addition, few studies have explored the effects of a hospital-based program on the patients and their families.
Ms. Campanile and colleagues conducted a retrospective cohort study of participants in an outpatient pain rehabilitation program at the Children’s Hospital of Philadelphia between April 2016 and December 2019. Patients were evaluated by a pediatric rheumatologist, psychologist, and physical and occupational therapists.
Patients engaged in 2-3 hours of physical therapy (PT) and 2-3 hours of occupational therapy (OT) in a 1:1 ratio at least 5 days a week. Physical activities included stepping into and out of a tub, carrying laundry, and desensitizing to allodynia as needed. Participants also received individual and group cognitive-behavior therapy interventions from psychologists, and psychological support during PT and OT sessions if needed. Parents/caregivers were invited to separate individual and group therapy sessions as part of the program. The median age at admission to the program was 15 years, and 79% of the participants were female. Patients participated the program for a median of 17 days, and 87% were outpatients who came to the hospital for the program.
Pain was assessed based on the 0-10 verbal pain intensity scale, energy was assessed on a scale of 0-100, and functional disability was assessed on a scale of 0-60, with higher scores indicating more pain, more energy, and more self-perceived disability, respectively.
Overall, scores on measures of pain, disability, allodynia, and energy improved significantly from baseline to discharge from the program. Verbal pain intensity scores decreased on average from 7 to 5, disability scores decreased from 26 to 9, the proportion of patients reporting allodynia decreased from 86% to 61%, and the energy level score increased from 70 to 77. The trend continued at the first follow-up visit, conducted 2-3 months after discharge from the program. Notably, pain intensity further decreased from a median of 5 at program completion to a median of 2 at the first follow-up, Ms. Campanile said. Improvements in allodynia also were sustained at the first follow-up.
Quality of life measures related to physical, emotional, social, and cognitive function also improved significantly from baseline to completion of the program.
In addition, scores on a quality of life family impact survey improved significantly; in particular, parent health-related quality of life scores (Parent HRQoL) improved from 60 at baseline to 71 at the end of the program on a scale of 0 to 100. The study findings were limited by several factors including the relatively short duration and use of a convenience sample from a retrospective cohort, with data limited to electronic health records, Ms. Campanile said. The study also was not powered to examine differential treatments based on psychiatric conditions, and any psychiatric conditions were based on self-reports.
However, the results support the value of a nonpharmacologic interdisciplinary program as “a robust treatment for youth with chronic idiopathic pain, for both patients and the family unit,” she said.
“This study also supports the need for and benefit of additional counseling for patients and their caregivers prior to and during enrollment in a pain rehabilitation program,” she concluded.
Study supports effectiveness of drug-free pain management
“The management of pain in any age group can be challenging, especially with current concerns for opioid dependence and abuse,” Cathy Haut, DNP, CPNP-AC, CPNP-PC, a pediatric nurse practitioner in Rehoboth Beach, Del., said in an interview.
“Chronic pain affects daily life for all populations, but for children, adolescents, and their families, it can have a long-lasting impact on growth and development, psychosocial and physical well-being,” Dr. Haut said. “Determining and testing nonpharmacologic alternative methods of pain control are extremely important.”
Given the debilitating effects of chronic pain, and the potential side effects and dependence that have been associated with use of pharmacologic modes of pain control, unique and creative solutions have begun to emerge and need further attention and study, she said.
However, “despite published research supporting the use of alternative and complementary approaches to pain control in children and adolescents, nonpharmacologic, collaborative, interprofessional approaches to pain control have not been widely shared in the literature,” she said.
“Barriers to this type of program include first and foremost a potential lack of financial and workforce-related resources,” Dr. Haut said. “Patient and family attendance at frequent health visits, daily or even every other day, may also hinder success, but opportunities for telehealth and family training to learn physical and occupational skills within this type of program may be beginning solutions.”
Additional research should be conducted at multiple children’s hospitals, with a larger number of children and adolescents at varying ages, with pain related to different diagnoses, and with the inclusion of collaborative methodology, said Dr. Haut. “The current study had some limitations, including the small sample size, predominantly female sex, and a short participation time frame utilizing retrospective review. Completing prospective research over a longer time frame can also yield generalizable results applicable to varied populations.”
The study received no outside funding. Ms. Campanile had no financial conflicts to disclose. Dr. Haut had no financial conflicts to disclose, and serves on the editorial advisory board of Pediatric News.
FROM PAS 2023
Integrating mental health and primary care: From dipping a toe to taking a plunge
In case anybody hasn’t noticed, the good ole days are long gone in which pediatric patients with mental health challenges could be simply referred out to be promptly assessed and treated by specialists. Due to a shortage of psychiatrists coupled with large increases in the number of youth presenting with emotional-behavioral difficulties, primary care clinicians are now called upon to fill in much of this gap, with professional organizations like the AAP articulating that .1
To meet this need, new models of integrated or collaborative care between primary care and mental health clinicians have been attempted and tested. While these initiatives have certainly been a welcome advance to many pediatricians, the large numbers of different models and initiatives out there have made for a rather confusing landscape that many busy primary care clinicians have found difficult to navigate.
In an attempt to offer some guidance on the subject, the American Academy of Child and Adolescent Psychiatry recently published a clinical update on pediatric collaborative care.2 The report is rich with resources and ideas. One of the main points of the document is that there are different levels of integration that exist. Kind of like the situation with recycling and household waste reduction, it is possible to make valuable improvements at any level of participation, although evidence suggests that more extensive efforts offer the most benefits. At one end of the spectrum, psychiatrists and primary care clinicians maintain separate practices and medical records and occasionally discuss mutual patients. Middle levels may include “colocation” with mental health and primary care professionals sharing a building and/or being part of the same overall system but continuing to work mainly independently. At the highest levels of integration, there is a coordinated and collaborative team that supports an intentional system of care with consistent communication about individual patients and general workflows. These approaches vary in the amount that the following four core areas of integrated care are incorporated.
- Direct service. Many integrated care initiatives heavily rely on the services of an on-site mental health care manager or behavioral health consultant who can provide a number of important functions such as overseeing of the integrated care program, conducting brief therapy with youth and parents, overseeing mental health screenings at the clinic, and providing general mental health promotion guidance.
- Care coordination. Helping patients and families find needed mental health, social services, and educational resources is a key component of integrated care. This task can fall to the practice’s behavioral health consultant, if there is one, but more general care coordinators can also be trained for this important role. The University of Washington’s Center for Advancing Integrated Mental Health Solutions has some published guidelines in this area.3
- Consultation. More advanced integrated care models often have established relationships to specific child psychiatric clinicians who are able to meet with the primary care team to discuss cases and general approaches to various problems. Alternatively, a number of states have implemented what are called Child Psychiatry Access Programs that give primary care clinicians a phone number to an organization (often affiliated with an academic medical center) that can provide quick and even immediate access to a child psychiatry provider for specific questions. Recent federal grants have led to many if not most states now having one of these programs in place, and a website listing these programs and their contact information is available.4
- Education. As mental health training was traditionally not part of a typical pediatrics residency, there have been a number of strategies introduced to help primary care clinicians increase their proficiency and comfort level when it comes to assessing and treating emotional-behavioral problems. These include specific conferences, online programs, and case-based training through mechanisms like the ECHO program.5,6 The AAP itself has released a number of toolkits and training materials related to mental health care that are available.7
The report also outlines some obstacles that continue to get in the way of more extensive integrative care efforts. Chief among them are financial concerns, including how to pay for what often are traditionally nonbillable efforts, particularly those that involve the communication of two expensive health care professionals. Some improvements have been made, however, such as the creation of some relatively new codes (such as 99451 and 99452) that can be submitted by both a primary care and mental health professional when there is a consultation that occurs that does not involve an actual face-to-face encounter.
One area that, in my view, has not received the level of attention it deserves when it comes to integrated care is the degree to which these programs have the potential not only to improve the care of children and adolescents already struggling with mental health challenges but also to serve as a powerful prevention tool to lower the risk of being diagnosed with a psychiatric disorder in the future and generally to improve levels of well-being. Thus far, however, research on various integrated programs has shown promising results that indicate that overall care for patients with mental health challenges improves.8 Further, when it comes to costs, there is some evidence to suggest that some of the biggest financial gains associated with integrated care has to do with reduced nonpsychiatric medical expenses of patients.9 This, then, suggests that practices that participate in capitated or accountable care organization structures could particularly benefit both clinically and financially from these collaborations.
If your practice has been challenged with the level of mental health care you are now expected to provide and has been contemplating even some small moves toward integrated care, now may the time to put those thoughts into action.
References
1. Foy JM et al. American Academy of Pediatrics policy statement. Mental health competencies for pediatric practice. Pediatrics. 2019;144(5):e20192757.
2. AACAP Committee on Collaborative and Integrated Care and AACAP Committee on Quality Issues. Clinical update: Collaborative mental health care for children and adolescents in pediatric primary care. J Am Acad Child Adolesc Psychiatry. 2023;62(2):91-119.
3. Behavioral health care managers. AIMS Center, University of Washington. Accessed May 5, 2023. Available at https://aims.uw.edu/online-bhcm-modules.
4. National Network of Child Psychiatry Access Programs. Accessed May 5, 2023. Available at https://www.nncpap.org/.
5. Project Echo Programs. Accessed May 5, 2023. https://hsc.unm.edu/echo.
6. Project TEACH. Accessed May 5, 2023. https://projectteachny.org.
7. Earls MF et al. Addressing mental health concerns in pediatrics: A practical resource toolkit for clinicians, 2nd edition. Itasca, Ill.: American Academy of Pediatrics, 2021.
8. Asarnow JR et al. Integrated medical-behavioral care compared with usual primary care for child and adolescent behavioral health: A meta analysis. JAMA Pediatr. 2015;169(10):929-37.
9. Unutzer J et al. Long-term costs effects of collaborative care for late-life depression. Am J Manag Care. 2008.14(2):95-100.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
In case anybody hasn’t noticed, the good ole days are long gone in which pediatric patients with mental health challenges could be simply referred out to be promptly assessed and treated by specialists. Due to a shortage of psychiatrists coupled with large increases in the number of youth presenting with emotional-behavioral difficulties, primary care clinicians are now called upon to fill in much of this gap, with professional organizations like the AAP articulating that .1
To meet this need, new models of integrated or collaborative care between primary care and mental health clinicians have been attempted and tested. While these initiatives have certainly been a welcome advance to many pediatricians, the large numbers of different models and initiatives out there have made for a rather confusing landscape that many busy primary care clinicians have found difficult to navigate.
In an attempt to offer some guidance on the subject, the American Academy of Child and Adolescent Psychiatry recently published a clinical update on pediatric collaborative care.2 The report is rich with resources and ideas. One of the main points of the document is that there are different levels of integration that exist. Kind of like the situation with recycling and household waste reduction, it is possible to make valuable improvements at any level of participation, although evidence suggests that more extensive efforts offer the most benefits. At one end of the spectrum, psychiatrists and primary care clinicians maintain separate practices and medical records and occasionally discuss mutual patients. Middle levels may include “colocation” with mental health and primary care professionals sharing a building and/or being part of the same overall system but continuing to work mainly independently. At the highest levels of integration, there is a coordinated and collaborative team that supports an intentional system of care with consistent communication about individual patients and general workflows. These approaches vary in the amount that the following four core areas of integrated care are incorporated.
- Direct service. Many integrated care initiatives heavily rely on the services of an on-site mental health care manager or behavioral health consultant who can provide a number of important functions such as overseeing of the integrated care program, conducting brief therapy with youth and parents, overseeing mental health screenings at the clinic, and providing general mental health promotion guidance.
- Care coordination. Helping patients and families find needed mental health, social services, and educational resources is a key component of integrated care. This task can fall to the practice’s behavioral health consultant, if there is one, but more general care coordinators can also be trained for this important role. The University of Washington’s Center for Advancing Integrated Mental Health Solutions has some published guidelines in this area.3
- Consultation. More advanced integrated care models often have established relationships to specific child psychiatric clinicians who are able to meet with the primary care team to discuss cases and general approaches to various problems. Alternatively, a number of states have implemented what are called Child Psychiatry Access Programs that give primary care clinicians a phone number to an organization (often affiliated with an academic medical center) that can provide quick and even immediate access to a child psychiatry provider for specific questions. Recent federal grants have led to many if not most states now having one of these programs in place, and a website listing these programs and their contact information is available.4
- Education. As mental health training was traditionally not part of a typical pediatrics residency, there have been a number of strategies introduced to help primary care clinicians increase their proficiency and comfort level when it comes to assessing and treating emotional-behavioral problems. These include specific conferences, online programs, and case-based training through mechanisms like the ECHO program.5,6 The AAP itself has released a number of toolkits and training materials related to mental health care that are available.7
The report also outlines some obstacles that continue to get in the way of more extensive integrative care efforts. Chief among them are financial concerns, including how to pay for what often are traditionally nonbillable efforts, particularly those that involve the communication of two expensive health care professionals. Some improvements have been made, however, such as the creation of some relatively new codes (such as 99451 and 99452) that can be submitted by both a primary care and mental health professional when there is a consultation that occurs that does not involve an actual face-to-face encounter.
One area that, in my view, has not received the level of attention it deserves when it comes to integrated care is the degree to which these programs have the potential not only to improve the care of children and adolescents already struggling with mental health challenges but also to serve as a powerful prevention tool to lower the risk of being diagnosed with a psychiatric disorder in the future and generally to improve levels of well-being. Thus far, however, research on various integrated programs has shown promising results that indicate that overall care for patients with mental health challenges improves.8 Further, when it comes to costs, there is some evidence to suggest that some of the biggest financial gains associated with integrated care has to do with reduced nonpsychiatric medical expenses of patients.9 This, then, suggests that practices that participate in capitated or accountable care organization structures could particularly benefit both clinically and financially from these collaborations.
If your practice has been challenged with the level of mental health care you are now expected to provide and has been contemplating even some small moves toward integrated care, now may the time to put those thoughts into action.
References
1. Foy JM et al. American Academy of Pediatrics policy statement. Mental health competencies for pediatric practice. Pediatrics. 2019;144(5):e20192757.
2. AACAP Committee on Collaborative and Integrated Care and AACAP Committee on Quality Issues. Clinical update: Collaborative mental health care for children and adolescents in pediatric primary care. J Am Acad Child Adolesc Psychiatry. 2023;62(2):91-119.
3. Behavioral health care managers. AIMS Center, University of Washington. Accessed May 5, 2023. Available at https://aims.uw.edu/online-bhcm-modules.
4. National Network of Child Psychiatry Access Programs. Accessed May 5, 2023. Available at https://www.nncpap.org/.
5. Project Echo Programs. Accessed May 5, 2023. https://hsc.unm.edu/echo.
6. Project TEACH. Accessed May 5, 2023. https://projectteachny.org.
7. Earls MF et al. Addressing mental health concerns in pediatrics: A practical resource toolkit for clinicians, 2nd edition. Itasca, Ill.: American Academy of Pediatrics, 2021.
8. Asarnow JR et al. Integrated medical-behavioral care compared with usual primary care for child and adolescent behavioral health: A meta analysis. JAMA Pediatr. 2015;169(10):929-37.
9. Unutzer J et al. Long-term costs effects of collaborative care for late-life depression. Am J Manag Care. 2008.14(2):95-100.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
In case anybody hasn’t noticed, the good ole days are long gone in which pediatric patients with mental health challenges could be simply referred out to be promptly assessed and treated by specialists. Due to a shortage of psychiatrists coupled with large increases in the number of youth presenting with emotional-behavioral difficulties, primary care clinicians are now called upon to fill in much of this gap, with professional organizations like the AAP articulating that .1
To meet this need, new models of integrated or collaborative care between primary care and mental health clinicians have been attempted and tested. While these initiatives have certainly been a welcome advance to many pediatricians, the large numbers of different models and initiatives out there have made for a rather confusing landscape that many busy primary care clinicians have found difficult to navigate.
In an attempt to offer some guidance on the subject, the American Academy of Child and Adolescent Psychiatry recently published a clinical update on pediatric collaborative care.2 The report is rich with resources and ideas. One of the main points of the document is that there are different levels of integration that exist. Kind of like the situation with recycling and household waste reduction, it is possible to make valuable improvements at any level of participation, although evidence suggests that more extensive efforts offer the most benefits. At one end of the spectrum, psychiatrists and primary care clinicians maintain separate practices and medical records and occasionally discuss mutual patients. Middle levels may include “colocation” with mental health and primary care professionals sharing a building and/or being part of the same overall system but continuing to work mainly independently. At the highest levels of integration, there is a coordinated and collaborative team that supports an intentional system of care with consistent communication about individual patients and general workflows. These approaches vary in the amount that the following four core areas of integrated care are incorporated.
- Direct service. Many integrated care initiatives heavily rely on the services of an on-site mental health care manager or behavioral health consultant who can provide a number of important functions such as overseeing of the integrated care program, conducting brief therapy with youth and parents, overseeing mental health screenings at the clinic, and providing general mental health promotion guidance.
- Care coordination. Helping patients and families find needed mental health, social services, and educational resources is a key component of integrated care. This task can fall to the practice’s behavioral health consultant, if there is one, but more general care coordinators can also be trained for this important role. The University of Washington’s Center for Advancing Integrated Mental Health Solutions has some published guidelines in this area.3
- Consultation. More advanced integrated care models often have established relationships to specific child psychiatric clinicians who are able to meet with the primary care team to discuss cases and general approaches to various problems. Alternatively, a number of states have implemented what are called Child Psychiatry Access Programs that give primary care clinicians a phone number to an organization (often affiliated with an academic medical center) that can provide quick and even immediate access to a child psychiatry provider for specific questions. Recent federal grants have led to many if not most states now having one of these programs in place, and a website listing these programs and their contact information is available.4
- Education. As mental health training was traditionally not part of a typical pediatrics residency, there have been a number of strategies introduced to help primary care clinicians increase their proficiency and comfort level when it comes to assessing and treating emotional-behavioral problems. These include specific conferences, online programs, and case-based training through mechanisms like the ECHO program.5,6 The AAP itself has released a number of toolkits and training materials related to mental health care that are available.7
The report also outlines some obstacles that continue to get in the way of more extensive integrative care efforts. Chief among them are financial concerns, including how to pay for what often are traditionally nonbillable efforts, particularly those that involve the communication of two expensive health care professionals. Some improvements have been made, however, such as the creation of some relatively new codes (such as 99451 and 99452) that can be submitted by both a primary care and mental health professional when there is a consultation that occurs that does not involve an actual face-to-face encounter.
One area that, in my view, has not received the level of attention it deserves when it comes to integrated care is the degree to which these programs have the potential not only to improve the care of children and adolescents already struggling with mental health challenges but also to serve as a powerful prevention tool to lower the risk of being diagnosed with a psychiatric disorder in the future and generally to improve levels of well-being. Thus far, however, research on various integrated programs has shown promising results that indicate that overall care for patients with mental health challenges improves.8 Further, when it comes to costs, there is some evidence to suggest that some of the biggest financial gains associated with integrated care has to do with reduced nonpsychiatric medical expenses of patients.9 This, then, suggests that practices that participate in capitated or accountable care organization structures could particularly benefit both clinically and financially from these collaborations.
If your practice has been challenged with the level of mental health care you are now expected to provide and has been contemplating even some small moves toward integrated care, now may the time to put those thoughts into action.
References
1. Foy JM et al. American Academy of Pediatrics policy statement. Mental health competencies for pediatric practice. Pediatrics. 2019;144(5):e20192757.
2. AACAP Committee on Collaborative and Integrated Care and AACAP Committee on Quality Issues. Clinical update: Collaborative mental health care for children and adolescents in pediatric primary care. J Am Acad Child Adolesc Psychiatry. 2023;62(2):91-119.
3. Behavioral health care managers. AIMS Center, University of Washington. Accessed May 5, 2023. Available at https://aims.uw.edu/online-bhcm-modules.
4. National Network of Child Psychiatry Access Programs. Accessed May 5, 2023. Available at https://www.nncpap.org/.
5. Project Echo Programs. Accessed May 5, 2023. https://hsc.unm.edu/echo.
6. Project TEACH. Accessed May 5, 2023. https://projectteachny.org.
7. Earls MF et al. Addressing mental health concerns in pediatrics: A practical resource toolkit for clinicians, 2nd edition. Itasca, Ill.: American Academy of Pediatrics, 2021.
8. Asarnow JR et al. Integrated medical-behavioral care compared with usual primary care for child and adolescent behavioral health: A meta analysis. JAMA Pediatr. 2015;169(10):929-37.
9. Unutzer J et al. Long-term costs effects of collaborative care for late-life depression. Am J Manag Care. 2008.14(2):95-100.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
Virtual care not linked with greater ED use during pandemic
Canadian family physicians’ increased use of virtual care during the first years of the pandemic was not associated with increased emergency department use among patients, a new analysis of data from Ontario suggests.
In a cross-sectional study that included almost 14,000 family physicians and almost 13 million patients in Ontario, an adjusted analysis indicated that patients with physicians who provided more than 20% of care virtually had lower rates of ED visits, compared with patients whose physicians provided the least virtual care.
“I was surprised to see that ED visit volumes in fall 2021 were below prepandemic levels,” study author Tara Kiran, MD, who practices family medicine at St. Michael’s Hospital of the University of Toronto, told this news organization.
“At that time, there was a lot in the news about how our EDs were overcrowded and an assumption that this related to higher visit volumes. But our data [suggest] there were other factors at play, including strains in staffing in the ED, hospital inpatient units, and in long-term care.” Dr. Kiran is also the Fidani chair in improvement and innovation and vice-chair of quality and innovation at the department of family and community medicine of the University of Toronto.
The study was published online in JAMA Network Open.
Embrace of telehealth
The investigators analyzed administrative data from Ontario for 13,820 family physicians (mean age, 50 years; 51.5% men) and 12,951,063 patients (mean age, 42.6 years; 51.8% women) under their care.
The family physicians had at least one primary care visit claim between Feb. 1 and Oct. 31, 2021. The researchers categorized the physicians by the percentage of total visits they delivered virtually (via telephone or video) during the study period, as follows: 0% (100% in person), greater than 0%-20%, greater than 20%-40%, greater than 40%-60%, greater than 60%-80%, greater than 80% to less than 100%, or 100%.
The percentage of virtual primary care visits peaked at 82% in the first 2 weeks of the pandemic and decreased to 49% by October 2021. ED visit rates decreased at the start of the pandemic and remained lower than in 2019 throughout the study period.
Most physicians provided between 40% and 80% of care virtually. A greater percentage of those who provided more than 80% of care virtually were aged 65 years or older, were women, and practiced in large cities.
Patient comorbidity and morbidity were similar across all categories of virtual care use. The mean number of ED visits was highest among patients whose physicians provided only in-person care (470.3 per 1,000 patients) and was lowest among those whose physicians provided greater than 0% to less than 100% of care virtually (242 per 1,000 patients).
After adjustment for patient characteristics, patients of physicians who provided more than 20% of care virtually had lower rates of ED visits, compared with patients of physicians who provided the least virtual care (for example, greater than 80% to less than 100% versus 0%-20% virtual visits in big cities; relative rate, 0.77). This pattern was consistent across all rurality of practice categories and after adjustment for 2019 ED visit rates.
The investigators observed a gradient in urban areas. Patients of physicians who provided the highest level of virtual care had the lowest ED visit rates.
Investigating virtual modalities
Some policymakers worried that inappropriate use of virtual care was leading to an increase in ED use. “Findings of this study refute this hypothesis,” the authors write. Increases in ED use seemed to coincide with decreases in COVID-19 cases, not with increases in virtual primary care visits.
Furthermore, at the population level, patients who were cared for by physicians who provided a high percentage of virtual care did not have a higher rate of ED visits, compared with those cared for by physicians who provided the lowest levels of virtual care.
During the pandemic, the switch to virtual care worked well for some of Dr. Kiran’s patients. It was more convenient, because they didn’t have to take time off work, travel to and from the clinic, find and pay for parking, or wait in the clinic before the appointment, she said.
But for others, “virtual care really didn’t work well,” she said. “This was particularly true for people who didn’t have a regular working phone, who didn’t have a private space to take calls, who weren’t fluent in English, and who were hard of hearing or had severe mental illness that resulted in paranoid thoughts.”
Clinicians also may have had different comfort levels and preferences regarding virtual visits, Dr. Kiran hypothesized. Some found it convenient and efficient, whereas others may have found it cumbersome and inefficient. “I personally find it harder to build relationships with patients when I use virtual care,” she said. “I experience more joy in work with in-person visits, but other clinicians may feel differently.”
Dr. Kiran and her colleagues are conducting a public engagement initiative called OurCare to understand public perspectives on the future of primary care. “As part of that work, we want to understand what virtual modalities are most important to the public and how the public thinks these should be integrated into primary care.”
Virtual care can support access, patient-centered care, and equity in primary care, Dr. Kiran added. “Ideally, it should be integrated into an existing relationship with a family physician and be a complement to in-person visits.”
The right dose?
In an accompanying editorial, Jesse M. Pines, MD, chief of clinical innovation at U.S. Acute Care Solutions, Canton, Ohio, writes, “There is no convincing mechanism consistent with the data for the observed outcome of lower ED use at higher telehealth use.”
Additional research is needed, he notes, to answer the “Goldilocks question” – that is, what amount of telehealth optimizes its benefits while minimizing potential problems?
“The right dose of telehealth needs to balance (1) concerns by payers and policymakers that it will increase cost and cause unintended consequences (for example, misdiagnosis or duplicative care) and (2) the desire of its proponents who want to allow clinicians to use it as they see fit, with few restrictions,” writes Dr. Pines.
“Future research would ideally use more robust research design,” he suggested. “For example, randomized trials could test different doses of telehealth, or mixed-methods studies could help elucidate how telehealth may be changing clinical management or care-seeking behavior.”
Equitable reimbursement needed
Priya Nori, MD, associate professor of infectious diseases at Montefiore Health System and associate professor at the Albert Einstein College of Medicine, both in New York, said, “I agree with their conclusions and am reassured about telehealth as a durable form of health care delivery.”
Large, population-level studies such as this one might persuade legislators to require equitable reimbursement for in-person and virtual visits “so providers have comparable incentives to provide both types of care,” she said. “Although only primary care was addressed in the study, I believe that virtual care is here to stay and can be applied to primary care, subspecialty care, and other services, like antimicrobial stewardship, infection prevention, et cetera. We need to embrace it.”
A similar study should be conducted in the United States, along with additional research “to ensure that visits done by telephone have similar outcomes as those done by video, as not all communities have adequate internet access or video conferencing technology,” said Dr. Nori.
The study was supported by ICES and grants from Ontario Health, the Canadian Institutes of Health Research, and the Health Systems Research Program of Ontario MOH. Dr. Kiran, Dr. Pines, and Dr. Nori have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Canadian family physicians’ increased use of virtual care during the first years of the pandemic was not associated with increased emergency department use among patients, a new analysis of data from Ontario suggests.
In a cross-sectional study that included almost 14,000 family physicians and almost 13 million patients in Ontario, an adjusted analysis indicated that patients with physicians who provided more than 20% of care virtually had lower rates of ED visits, compared with patients whose physicians provided the least virtual care.
“I was surprised to see that ED visit volumes in fall 2021 were below prepandemic levels,” study author Tara Kiran, MD, who practices family medicine at St. Michael’s Hospital of the University of Toronto, told this news organization.
“At that time, there was a lot in the news about how our EDs were overcrowded and an assumption that this related to higher visit volumes. But our data [suggest] there were other factors at play, including strains in staffing in the ED, hospital inpatient units, and in long-term care.” Dr. Kiran is also the Fidani chair in improvement and innovation and vice-chair of quality and innovation at the department of family and community medicine of the University of Toronto.
The study was published online in JAMA Network Open.
Embrace of telehealth
The investigators analyzed administrative data from Ontario for 13,820 family physicians (mean age, 50 years; 51.5% men) and 12,951,063 patients (mean age, 42.6 years; 51.8% women) under their care.
The family physicians had at least one primary care visit claim between Feb. 1 and Oct. 31, 2021. The researchers categorized the physicians by the percentage of total visits they delivered virtually (via telephone or video) during the study period, as follows: 0% (100% in person), greater than 0%-20%, greater than 20%-40%, greater than 40%-60%, greater than 60%-80%, greater than 80% to less than 100%, or 100%.
The percentage of virtual primary care visits peaked at 82% in the first 2 weeks of the pandemic and decreased to 49% by October 2021. ED visit rates decreased at the start of the pandemic and remained lower than in 2019 throughout the study period.
Most physicians provided between 40% and 80% of care virtually. A greater percentage of those who provided more than 80% of care virtually were aged 65 years or older, were women, and practiced in large cities.
Patient comorbidity and morbidity were similar across all categories of virtual care use. The mean number of ED visits was highest among patients whose physicians provided only in-person care (470.3 per 1,000 patients) and was lowest among those whose physicians provided greater than 0% to less than 100% of care virtually (242 per 1,000 patients).
After adjustment for patient characteristics, patients of physicians who provided more than 20% of care virtually had lower rates of ED visits, compared with patients of physicians who provided the least virtual care (for example, greater than 80% to less than 100% versus 0%-20% virtual visits in big cities; relative rate, 0.77). This pattern was consistent across all rurality of practice categories and after adjustment for 2019 ED visit rates.
The investigators observed a gradient in urban areas. Patients of physicians who provided the highest level of virtual care had the lowest ED visit rates.
Investigating virtual modalities
Some policymakers worried that inappropriate use of virtual care was leading to an increase in ED use. “Findings of this study refute this hypothesis,” the authors write. Increases in ED use seemed to coincide with decreases in COVID-19 cases, not with increases in virtual primary care visits.
Furthermore, at the population level, patients who were cared for by physicians who provided a high percentage of virtual care did not have a higher rate of ED visits, compared with those cared for by physicians who provided the lowest levels of virtual care.
During the pandemic, the switch to virtual care worked well for some of Dr. Kiran’s patients. It was more convenient, because they didn’t have to take time off work, travel to and from the clinic, find and pay for parking, or wait in the clinic before the appointment, she said.
But for others, “virtual care really didn’t work well,” she said. “This was particularly true for people who didn’t have a regular working phone, who didn’t have a private space to take calls, who weren’t fluent in English, and who were hard of hearing or had severe mental illness that resulted in paranoid thoughts.”
Clinicians also may have had different comfort levels and preferences regarding virtual visits, Dr. Kiran hypothesized. Some found it convenient and efficient, whereas others may have found it cumbersome and inefficient. “I personally find it harder to build relationships with patients when I use virtual care,” she said. “I experience more joy in work with in-person visits, but other clinicians may feel differently.”
Dr. Kiran and her colleagues are conducting a public engagement initiative called OurCare to understand public perspectives on the future of primary care. “As part of that work, we want to understand what virtual modalities are most important to the public and how the public thinks these should be integrated into primary care.”
Virtual care can support access, patient-centered care, and equity in primary care, Dr. Kiran added. “Ideally, it should be integrated into an existing relationship with a family physician and be a complement to in-person visits.”
The right dose?
In an accompanying editorial, Jesse M. Pines, MD, chief of clinical innovation at U.S. Acute Care Solutions, Canton, Ohio, writes, “There is no convincing mechanism consistent with the data for the observed outcome of lower ED use at higher telehealth use.”
Additional research is needed, he notes, to answer the “Goldilocks question” – that is, what amount of telehealth optimizes its benefits while minimizing potential problems?
“The right dose of telehealth needs to balance (1) concerns by payers and policymakers that it will increase cost and cause unintended consequences (for example, misdiagnosis or duplicative care) and (2) the desire of its proponents who want to allow clinicians to use it as they see fit, with few restrictions,” writes Dr. Pines.
“Future research would ideally use more robust research design,” he suggested. “For example, randomized trials could test different doses of telehealth, or mixed-methods studies could help elucidate how telehealth may be changing clinical management or care-seeking behavior.”
Equitable reimbursement needed
Priya Nori, MD, associate professor of infectious diseases at Montefiore Health System and associate professor at the Albert Einstein College of Medicine, both in New York, said, “I agree with their conclusions and am reassured about telehealth as a durable form of health care delivery.”
Large, population-level studies such as this one might persuade legislators to require equitable reimbursement for in-person and virtual visits “so providers have comparable incentives to provide both types of care,” she said. “Although only primary care was addressed in the study, I believe that virtual care is here to stay and can be applied to primary care, subspecialty care, and other services, like antimicrobial stewardship, infection prevention, et cetera. We need to embrace it.”
A similar study should be conducted in the United States, along with additional research “to ensure that visits done by telephone have similar outcomes as those done by video, as not all communities have adequate internet access or video conferencing technology,” said Dr. Nori.
The study was supported by ICES and grants from Ontario Health, the Canadian Institutes of Health Research, and the Health Systems Research Program of Ontario MOH. Dr. Kiran, Dr. Pines, and Dr. Nori have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Canadian family physicians’ increased use of virtual care during the first years of the pandemic was not associated with increased emergency department use among patients, a new analysis of data from Ontario suggests.
In a cross-sectional study that included almost 14,000 family physicians and almost 13 million patients in Ontario, an adjusted analysis indicated that patients with physicians who provided more than 20% of care virtually had lower rates of ED visits, compared with patients whose physicians provided the least virtual care.
“I was surprised to see that ED visit volumes in fall 2021 were below prepandemic levels,” study author Tara Kiran, MD, who practices family medicine at St. Michael’s Hospital of the University of Toronto, told this news organization.
“At that time, there was a lot in the news about how our EDs were overcrowded and an assumption that this related to higher visit volumes. But our data [suggest] there were other factors at play, including strains in staffing in the ED, hospital inpatient units, and in long-term care.” Dr. Kiran is also the Fidani chair in improvement and innovation and vice-chair of quality and innovation at the department of family and community medicine of the University of Toronto.
The study was published online in JAMA Network Open.
Embrace of telehealth
The investigators analyzed administrative data from Ontario for 13,820 family physicians (mean age, 50 years; 51.5% men) and 12,951,063 patients (mean age, 42.6 years; 51.8% women) under their care.
The family physicians had at least one primary care visit claim between Feb. 1 and Oct. 31, 2021. The researchers categorized the physicians by the percentage of total visits they delivered virtually (via telephone or video) during the study period, as follows: 0% (100% in person), greater than 0%-20%, greater than 20%-40%, greater than 40%-60%, greater than 60%-80%, greater than 80% to less than 100%, or 100%.
The percentage of virtual primary care visits peaked at 82% in the first 2 weeks of the pandemic and decreased to 49% by October 2021. ED visit rates decreased at the start of the pandemic and remained lower than in 2019 throughout the study period.
Most physicians provided between 40% and 80% of care virtually. A greater percentage of those who provided more than 80% of care virtually were aged 65 years or older, were women, and practiced in large cities.
Patient comorbidity and morbidity were similar across all categories of virtual care use. The mean number of ED visits was highest among patients whose physicians provided only in-person care (470.3 per 1,000 patients) and was lowest among those whose physicians provided greater than 0% to less than 100% of care virtually (242 per 1,000 patients).
After adjustment for patient characteristics, patients of physicians who provided more than 20% of care virtually had lower rates of ED visits, compared with patients of physicians who provided the least virtual care (for example, greater than 80% to less than 100% versus 0%-20% virtual visits in big cities; relative rate, 0.77). This pattern was consistent across all rurality of practice categories and after adjustment for 2019 ED visit rates.
The investigators observed a gradient in urban areas. Patients of physicians who provided the highest level of virtual care had the lowest ED visit rates.
Investigating virtual modalities
Some policymakers worried that inappropriate use of virtual care was leading to an increase in ED use. “Findings of this study refute this hypothesis,” the authors write. Increases in ED use seemed to coincide with decreases in COVID-19 cases, not with increases in virtual primary care visits.
Furthermore, at the population level, patients who were cared for by physicians who provided a high percentage of virtual care did not have a higher rate of ED visits, compared with those cared for by physicians who provided the lowest levels of virtual care.
During the pandemic, the switch to virtual care worked well for some of Dr. Kiran’s patients. It was more convenient, because they didn’t have to take time off work, travel to and from the clinic, find and pay for parking, or wait in the clinic before the appointment, she said.
But for others, “virtual care really didn’t work well,” she said. “This was particularly true for people who didn’t have a regular working phone, who didn’t have a private space to take calls, who weren’t fluent in English, and who were hard of hearing or had severe mental illness that resulted in paranoid thoughts.”
Clinicians also may have had different comfort levels and preferences regarding virtual visits, Dr. Kiran hypothesized. Some found it convenient and efficient, whereas others may have found it cumbersome and inefficient. “I personally find it harder to build relationships with patients when I use virtual care,” she said. “I experience more joy in work with in-person visits, but other clinicians may feel differently.”
Dr. Kiran and her colleagues are conducting a public engagement initiative called OurCare to understand public perspectives on the future of primary care. “As part of that work, we want to understand what virtual modalities are most important to the public and how the public thinks these should be integrated into primary care.”
Virtual care can support access, patient-centered care, and equity in primary care, Dr. Kiran added. “Ideally, it should be integrated into an existing relationship with a family physician and be a complement to in-person visits.”
The right dose?
In an accompanying editorial, Jesse M. Pines, MD, chief of clinical innovation at U.S. Acute Care Solutions, Canton, Ohio, writes, “There is no convincing mechanism consistent with the data for the observed outcome of lower ED use at higher telehealth use.”
Additional research is needed, he notes, to answer the “Goldilocks question” – that is, what amount of telehealth optimizes its benefits while minimizing potential problems?
“The right dose of telehealth needs to balance (1) concerns by payers and policymakers that it will increase cost and cause unintended consequences (for example, misdiagnosis or duplicative care) and (2) the desire of its proponents who want to allow clinicians to use it as they see fit, with few restrictions,” writes Dr. Pines.
“Future research would ideally use more robust research design,” he suggested. “For example, randomized trials could test different doses of telehealth, or mixed-methods studies could help elucidate how telehealth may be changing clinical management or care-seeking behavior.”
Equitable reimbursement needed
Priya Nori, MD, associate professor of infectious diseases at Montefiore Health System and associate professor at the Albert Einstein College of Medicine, both in New York, said, “I agree with their conclusions and am reassured about telehealth as a durable form of health care delivery.”
Large, population-level studies such as this one might persuade legislators to require equitable reimbursement for in-person and virtual visits “so providers have comparable incentives to provide both types of care,” she said. “Although only primary care was addressed in the study, I believe that virtual care is here to stay and can be applied to primary care, subspecialty care, and other services, like antimicrobial stewardship, infection prevention, et cetera. We need to embrace it.”
A similar study should be conducted in the United States, along with additional research “to ensure that visits done by telephone have similar outcomes as those done by video, as not all communities have adequate internet access or video conferencing technology,” said Dr. Nori.
The study was supported by ICES and grants from Ontario Health, the Canadian Institutes of Health Research, and the Health Systems Research Program of Ontario MOH. Dr. Kiran, Dr. Pines, and Dr. Nori have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Studies suggest ways to refine neonatal hernia management
WASHINGTON – Congenital diaphragmatic hernia affects many areas of pediatrics. In a trio of posters presented at the Pediatric Academic Societies annual meeting,
Initial ventilation mode shows little impact on NICU outcomes
In one study, K. Taylor Wild, MD, and colleagues investigated whether high-frequency oscillatory ventilation (HFOV) as an initial mode of ventilation in the delivery room improved gas exchange and neonatal ICU (NICU) outcomes in infants with congenital diaphragmatic hernia (CDH), compared with conventional mechanical ventilation (CMV). In 2019, HFOV became standard practice at CHOP.
The researchers reviewed data on infants with severe CDH who were born at CHOP between 2014 and 2022. Of these, 75 were placed on HFOV and 114 on CMV. The mean gestational age at birth in both groups was approximately 38 weeks, and the mean birth weight was approximately 3 kg.
Compared with CMV, use of HFOV in the delivery room was associated with significantly higher pH (7.05 vs. 7.16, P = .03) and significantly lower CO2 (85.2 vs. 64.5, P = .005). However, after adjusting for CDH severity, no significant differences appeared in length of stay and overall survival to discharge. The higher rates of extracorporeal membrane oxygenation (ECMO) use in the HFOV group, compared with the CMV group (48% vs. 29.9%), may reflect more severe disease, the researchers noted.
Prenatal brain immaturity associates with developmental delay
In a second study, Sandy Johng, MD, and colleagues found a significant association between prenatal brain immaturity in babies with CDH and developmental scores at age 12 months and older. The researchers reviewed data from a single-center patient registry for 48 infants for whom prenatal neuroimaging results were available. Based on the imaging, a fetal Total Maturation Score (fTMS) was generated and used as a measure of prenatal brain immaturity.
Results from the Bayley Scales of Infant Development-III (BSID-III) – a composite of cognitive, motor, and language scores – were available for 26 neonates at ages 12 months and under as well as at 12 months and older.
In a linear regression model, the researchers found a significant association between difference in fTMS and BSID-III composite language scores in infants 12 months and older. After adjusting for ECMO treatment, an increase in fTMS of one unit was associated with a 6.5-point increase in language scores at age 12 months and older (P < .01). No significant differences were observed between fTMS difference and language scores in infants under 12 months, or in cognitive or motor scores at any age, the researchers noted. The findings were limited by the small sample size, but the study is the first to show an association between prenatal imaging and neurodevelopmental outcomes for infants with CDH. Results suggest that the risk for neurodevelopmental impairment in this population may start in utero, the researchers concluded.
Antibiotic use stays stable
In a third study, Sabrina Flohr, MPH, and colleagues reviewed antibiotic use among infants with CDH who are at increased risk for infection. In many cases, distinguishing between infection and inherent clinical illness is challenging and may lead to unnecessarily high rates of antibiotic use, the researchers noted.
They reviewed data from 381 infants with CDH born at CHOP between January 2013 and November 2022 who were treated and survived in the NICU. Overall, 97.1% of the newborns received antibiotics for a median of 13 days. Nearly two-thirds (63.5%) received antibiotics in the first 72 hours, and 98.1% received them after 72 hours. Ampicillin and gentamicin were the antibiotics used most often in the first 72 hours (approximately 50% for both). After 72 hours, the most commonly used antibiotics were cefazolin (91.6%), vancomycin (67.7%), and cefepime (65.7%).
The results show that antibiotic use among newborns with CDH did not change significantly over time, and the choices of later antibiotics likely reflect perioperative prophylaxis and broad-spectrum treatment, the researchers noted.
Studies show larger trends
“These are three interesting studies regarding congenital diaphragmatic hernia from a center that does a high volume of repairs,” said Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, in an interview.
“Each individual case can be consuming, but it is important to look for an aggregate of cases to see the larger trends in practices and outcomes,” said Dr. Joos, who was not involved in any of the studies.
The findings of the ventilation study surprised Dr. Joos. “Although high-frequency oscillatory ventilation improves initial gas exchange in the delivery room, compared with conventional mechanical ventilation, it was not associated with any larger NICU outcome,” he said. “This surprised me because my intuition would be that the HFOV would lead to less barotrauma and therefore better outcomes with the underformed lungs associated with this disorder.”
The imaging study demonstrates the need for more research on the association between CDH and neurologic outcomes, said Dr. Joos.
“Prenatal neuroimaging that shows delayed maturation with congenital diaphragmatic hernia correlates with lower language scores in early childhood, and suggests that this may be a predictor of neurologic outcome independent of the postnatal course,” he said.
Data from the antibiotics study reflect current trends, said Dr. Joos. “Antibiotics use is extremely common during the postnatal course of CDH and surgical repair,” he said. “The choice of antibiotics mirrors what we see in other neonatal conditions with regard to treatment for possible early neonatal sepsis, postsurgical prophylaxis, and later broad-spectrum empiric coverage,” he noted.
“I look forward to more studies to come out of large-volume centers like CHOP or aggregated results from many centers to help figure out best practices for this rare but very complicated and often devastating malformation,” he said.
The three posters received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose, but he serves on the Editorial Advisory Board of Pediatric News.
WASHINGTON – Congenital diaphragmatic hernia affects many areas of pediatrics. In a trio of posters presented at the Pediatric Academic Societies annual meeting,
Initial ventilation mode shows little impact on NICU outcomes
In one study, K. Taylor Wild, MD, and colleagues investigated whether high-frequency oscillatory ventilation (HFOV) as an initial mode of ventilation in the delivery room improved gas exchange and neonatal ICU (NICU) outcomes in infants with congenital diaphragmatic hernia (CDH), compared with conventional mechanical ventilation (CMV). In 2019, HFOV became standard practice at CHOP.
The researchers reviewed data on infants with severe CDH who were born at CHOP between 2014 and 2022. Of these, 75 were placed on HFOV and 114 on CMV. The mean gestational age at birth in both groups was approximately 38 weeks, and the mean birth weight was approximately 3 kg.
Compared with CMV, use of HFOV in the delivery room was associated with significantly higher pH (7.05 vs. 7.16, P = .03) and significantly lower CO2 (85.2 vs. 64.5, P = .005). However, after adjusting for CDH severity, no significant differences appeared in length of stay and overall survival to discharge. The higher rates of extracorporeal membrane oxygenation (ECMO) use in the HFOV group, compared with the CMV group (48% vs. 29.9%), may reflect more severe disease, the researchers noted.
Prenatal brain immaturity associates with developmental delay
In a second study, Sandy Johng, MD, and colleagues found a significant association between prenatal brain immaturity in babies with CDH and developmental scores at age 12 months and older. The researchers reviewed data from a single-center patient registry for 48 infants for whom prenatal neuroimaging results were available. Based on the imaging, a fetal Total Maturation Score (fTMS) was generated and used as a measure of prenatal brain immaturity.
Results from the Bayley Scales of Infant Development-III (BSID-III) – a composite of cognitive, motor, and language scores – were available for 26 neonates at ages 12 months and under as well as at 12 months and older.
In a linear regression model, the researchers found a significant association between difference in fTMS and BSID-III composite language scores in infants 12 months and older. After adjusting for ECMO treatment, an increase in fTMS of one unit was associated with a 6.5-point increase in language scores at age 12 months and older (P < .01). No significant differences were observed between fTMS difference and language scores in infants under 12 months, or in cognitive or motor scores at any age, the researchers noted. The findings were limited by the small sample size, but the study is the first to show an association between prenatal imaging and neurodevelopmental outcomes for infants with CDH. Results suggest that the risk for neurodevelopmental impairment in this population may start in utero, the researchers concluded.
Antibiotic use stays stable
In a third study, Sabrina Flohr, MPH, and colleagues reviewed antibiotic use among infants with CDH who are at increased risk for infection. In many cases, distinguishing between infection and inherent clinical illness is challenging and may lead to unnecessarily high rates of antibiotic use, the researchers noted.
They reviewed data from 381 infants with CDH born at CHOP between January 2013 and November 2022 who were treated and survived in the NICU. Overall, 97.1% of the newborns received antibiotics for a median of 13 days. Nearly two-thirds (63.5%) received antibiotics in the first 72 hours, and 98.1% received them after 72 hours. Ampicillin and gentamicin were the antibiotics used most often in the first 72 hours (approximately 50% for both). After 72 hours, the most commonly used antibiotics were cefazolin (91.6%), vancomycin (67.7%), and cefepime (65.7%).
The results show that antibiotic use among newborns with CDH did not change significantly over time, and the choices of later antibiotics likely reflect perioperative prophylaxis and broad-spectrum treatment, the researchers noted.
Studies show larger trends
“These are three interesting studies regarding congenital diaphragmatic hernia from a center that does a high volume of repairs,” said Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, in an interview.
“Each individual case can be consuming, but it is important to look for an aggregate of cases to see the larger trends in practices and outcomes,” said Dr. Joos, who was not involved in any of the studies.
The findings of the ventilation study surprised Dr. Joos. “Although high-frequency oscillatory ventilation improves initial gas exchange in the delivery room, compared with conventional mechanical ventilation, it was not associated with any larger NICU outcome,” he said. “This surprised me because my intuition would be that the HFOV would lead to less barotrauma and therefore better outcomes with the underformed lungs associated with this disorder.”
The imaging study demonstrates the need for more research on the association between CDH and neurologic outcomes, said Dr. Joos.
“Prenatal neuroimaging that shows delayed maturation with congenital diaphragmatic hernia correlates with lower language scores in early childhood, and suggests that this may be a predictor of neurologic outcome independent of the postnatal course,” he said.
Data from the antibiotics study reflect current trends, said Dr. Joos. “Antibiotics use is extremely common during the postnatal course of CDH and surgical repair,” he said. “The choice of antibiotics mirrors what we see in other neonatal conditions with regard to treatment for possible early neonatal sepsis, postsurgical prophylaxis, and later broad-spectrum empiric coverage,” he noted.
“I look forward to more studies to come out of large-volume centers like CHOP or aggregated results from many centers to help figure out best practices for this rare but very complicated and often devastating malformation,” he said.
The three posters received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose, but he serves on the Editorial Advisory Board of Pediatric News.
WASHINGTON – Congenital diaphragmatic hernia affects many areas of pediatrics. In a trio of posters presented at the Pediatric Academic Societies annual meeting,
Initial ventilation mode shows little impact on NICU outcomes
In one study, K. Taylor Wild, MD, and colleagues investigated whether high-frequency oscillatory ventilation (HFOV) as an initial mode of ventilation in the delivery room improved gas exchange and neonatal ICU (NICU) outcomes in infants with congenital diaphragmatic hernia (CDH), compared with conventional mechanical ventilation (CMV). In 2019, HFOV became standard practice at CHOP.
The researchers reviewed data on infants with severe CDH who were born at CHOP between 2014 and 2022. Of these, 75 were placed on HFOV and 114 on CMV. The mean gestational age at birth in both groups was approximately 38 weeks, and the mean birth weight was approximately 3 kg.
Compared with CMV, use of HFOV in the delivery room was associated with significantly higher pH (7.05 vs. 7.16, P = .03) and significantly lower CO2 (85.2 vs. 64.5, P = .005). However, after adjusting for CDH severity, no significant differences appeared in length of stay and overall survival to discharge. The higher rates of extracorporeal membrane oxygenation (ECMO) use in the HFOV group, compared with the CMV group (48% vs. 29.9%), may reflect more severe disease, the researchers noted.
Prenatal brain immaturity associates with developmental delay
In a second study, Sandy Johng, MD, and colleagues found a significant association between prenatal brain immaturity in babies with CDH and developmental scores at age 12 months and older. The researchers reviewed data from a single-center patient registry for 48 infants for whom prenatal neuroimaging results were available. Based on the imaging, a fetal Total Maturation Score (fTMS) was generated and used as a measure of prenatal brain immaturity.
Results from the Bayley Scales of Infant Development-III (BSID-III) – a composite of cognitive, motor, and language scores – were available for 26 neonates at ages 12 months and under as well as at 12 months and older.
In a linear regression model, the researchers found a significant association between difference in fTMS and BSID-III composite language scores in infants 12 months and older. After adjusting for ECMO treatment, an increase in fTMS of one unit was associated with a 6.5-point increase in language scores at age 12 months and older (P < .01). No significant differences were observed between fTMS difference and language scores in infants under 12 months, or in cognitive or motor scores at any age, the researchers noted. The findings were limited by the small sample size, but the study is the first to show an association between prenatal imaging and neurodevelopmental outcomes for infants with CDH. Results suggest that the risk for neurodevelopmental impairment in this population may start in utero, the researchers concluded.
Antibiotic use stays stable
In a third study, Sabrina Flohr, MPH, and colleagues reviewed antibiotic use among infants with CDH who are at increased risk for infection. In many cases, distinguishing between infection and inherent clinical illness is challenging and may lead to unnecessarily high rates of antibiotic use, the researchers noted.
They reviewed data from 381 infants with CDH born at CHOP between January 2013 and November 2022 who were treated and survived in the NICU. Overall, 97.1% of the newborns received antibiotics for a median of 13 days. Nearly two-thirds (63.5%) received antibiotics in the first 72 hours, and 98.1% received them after 72 hours. Ampicillin and gentamicin were the antibiotics used most often in the first 72 hours (approximately 50% for both). After 72 hours, the most commonly used antibiotics were cefazolin (91.6%), vancomycin (67.7%), and cefepime (65.7%).
The results show that antibiotic use among newborns with CDH did not change significantly over time, and the choices of later antibiotics likely reflect perioperative prophylaxis and broad-spectrum treatment, the researchers noted.
Studies show larger trends
“These are three interesting studies regarding congenital diaphragmatic hernia from a center that does a high volume of repairs,” said Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, in an interview.
“Each individual case can be consuming, but it is important to look for an aggregate of cases to see the larger trends in practices and outcomes,” said Dr. Joos, who was not involved in any of the studies.
The findings of the ventilation study surprised Dr. Joos. “Although high-frequency oscillatory ventilation improves initial gas exchange in the delivery room, compared with conventional mechanical ventilation, it was not associated with any larger NICU outcome,” he said. “This surprised me because my intuition would be that the HFOV would lead to less barotrauma and therefore better outcomes with the underformed lungs associated with this disorder.”
The imaging study demonstrates the need for more research on the association between CDH and neurologic outcomes, said Dr. Joos.
“Prenatal neuroimaging that shows delayed maturation with congenital diaphragmatic hernia correlates with lower language scores in early childhood, and suggests that this may be a predictor of neurologic outcome independent of the postnatal course,” he said.
Data from the antibiotics study reflect current trends, said Dr. Joos. “Antibiotics use is extremely common during the postnatal course of CDH and surgical repair,” he said. “The choice of antibiotics mirrors what we see in other neonatal conditions with regard to treatment for possible early neonatal sepsis, postsurgical prophylaxis, and later broad-spectrum empiric coverage,” he noted.
“I look forward to more studies to come out of large-volume centers like CHOP or aggregated results from many centers to help figure out best practices for this rare but very complicated and often devastating malformation,” he said.
The three posters received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose, but he serves on the Editorial Advisory Board of Pediatric News.
AT PAS 2023