User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Prioritize COVID-19 vaccination in both types of diabetes, say docs
The risk for increased COVID-19 severity in people with type 1 diabetes appears similar to that of type 2 diabetes, contrary to some official advice from the Centers for Disease Control and Prevention. The new finding indicates that people with both types should be priority for receiving a vaccine, investigators say.
The study is the first to prospectively evaluate both inpatients and outpatients and to examine COVID-19 severity factors in addition to death in people with type 1 and type 2 diabetes separately, and was published online Dec. 2 in Diabetes Care.
Among the patients, who were seen at Vanderbilt University Medical Center in Nashville, Tenn., between March and August of 2020, those with both type 1 and type 2 diabetes had between a three- and fourfold greater risk for COVID-19 hospitalization and greater illness severity compared with people without diabetes after adjustments for age, race, and a number of other risk factors.
This finding is important since as of Dec. 1, 2020, the CDC has classified the diabetes types differently in terms of underlying medical conditions that increase the risk for severe COVID-19.
Adults of any age with type 2 diabetes are considered “at increased risk of severe illness” from the virus that causes COVID-19 whereas the CDC says those with type 1 “might be at an increased risk.”
Lead author of the new paper Justin M. Gregory, MD, said in an interview: “I think this needs revision based on the current evidence. I think the data presented in our study and that of Barron et al. in Lancet Endocrinology 2020 indicate the need to place type 1 diabetes at parity with type 2 diabetes.
“These studies indicate both conditions carry an adjusted odds ratio of three to four when compared with people without diabetes for hospitalization, illness severity, and mortality,” he stressed.
Vaccines look promising for patients with diabetes
There were no phase 3 vaccine data available for the vaccine at the time that Dr. Gregory, of the Ian M. Burr Division of Pediatric Endocrinology and Diabetes, Vanderbilt University, Nashville, Tenn., and colleagues were writing their manuscript in late summer, so the article does not mention this.
But now, Dr. Gregory said, “Based on the initial press releases from Pfizer and Moderna, I am now optimistic that these vaccines might mitigate the excess morbidity and mortality from COVID-19 experienced by patients with diabetes.
“I am eager to see what we learn on December 10 and 17 [the scheduled dates for the meetings of the Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee to review the Pfizer and Moderna vaccines, respectively].”
But with the winter pandemic surge in the meantime, “Our investigation suggests that as COVID-19 hospitalizations rise, patients with both type 1 and 2 diabetes will comprise a disproportionately higher number of those admissions and, once hospitalized, demonstrate a greater degree of illness severity,” he and his colleagues said.
“In light of these data, we call on our colleagues to emphasize the importance of social distancing measures and hand hygiene, with particular emphasis on patients with diabetes, including those in the most vulnerable communities whom our study affirms will face the most severe impact.”
After adjustments, excess severity risk similar for both diabetes types
The new study data came from electronic health records at Vanderbilt University Medical Center, comprising 137 primary care, urgent care, and hospital facilities where patients were tested for SARS-CoV-2 regardless of the reason for their visit.
Between March 17 and August 7, 2020, 6,451 patients tested positive for COVID-19. Of those, 273 had type 2 diabetes and 40 had type 1 diabetes.
Children younger than 18 years accounted for 20% of those with type 1 diabetes and 9.4% of those without diabetes, but none of the type 2 group. The group with type 2 diabetes was considerably older than the type 1 diabetes and no-diabetes groups, 58 years versus 37 and 33 years, respectively.
Before adjustment for baseline characteristics that differed between groups, patients with type 1 diabetes appeared to have a risk for hospitalization and greater illness severity that was intermediate between the group with no diabetes and the group with type 2 diabetes, the researchers said.
But after adjustment for age, race, sex, hypertension, smoking, and body mass index, people with type 1 diabetes had odds ratios of 3.90 for hospitalization and 3.35 for greater illness severity, which was similar to risk in type 2 diabetes (3.36 and 3.42, respectively), compared to those without diabetes.
Deep dive explores COVID-19 severity risk factors in type 1 diabetes
The investigators then conducted a detailed chart review for 37 of the 40 patients with type 1 diabetes and phone surveys with 15 of them.
The majority (28) had not been hospitalized, and only one was hospitalized for diabetic ketoacidosis (DKA) within 14 days of positive SARS-CoV-2 testing.
This contrasts with a report from the T1D Exchange, in which nearly half of 33 patients with type 1 diabetes and COVID-19 had been hospitalized with DKA. The reason for the discrepancy may be that more severe patients would more likely be referred to the T1D Exchange Registry, Dr. Gregory and colleagues hypothesized.
Clinical factors associated with COVID-19 severity (P < .05) in their study included a prior hypertension diagnosis, higher hemoglobin A1c, at least one prior DKA admission in the past year, and not using a continuous glucose monitor (CGM).
Hospitalizations were twice as likely and illness severity nearly twice as great among those with type 1 diabetes who were Black versus White. Just 8% of those with private insurance were hospitalized, compared with 60% of those with public insurance and 67% with no insurance (P = .001).
“Whereas previous reports have indicated proportionally higher rates of hospitalizations from COVID-19 among Black patients and those with public insurance, this study is the first to show a similar finding in the population with type 1 diabetes,” Dr. Gregory and colleagues wrote.
Only 9% of patients using a CGM were hospitalized versus 47% who used blood glucose meters (P < .016). Similarly, hospitalizations occurred in 6% using an insulin pump versus 33% using multiple daily injections (P < .085).
“Our analysis cannot exclude the possibility that greater amounts of diabetes technology use are a surrogate for higher socioeconomic status,” they noted.
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases, JDRF, and the Appleby Foundation. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The risk for increased COVID-19 severity in people with type 1 diabetes appears similar to that of type 2 diabetes, contrary to some official advice from the Centers for Disease Control and Prevention. The new finding indicates that people with both types should be priority for receiving a vaccine, investigators say.
The study is the first to prospectively evaluate both inpatients and outpatients and to examine COVID-19 severity factors in addition to death in people with type 1 and type 2 diabetes separately, and was published online Dec. 2 in Diabetes Care.
Among the patients, who were seen at Vanderbilt University Medical Center in Nashville, Tenn., between March and August of 2020, those with both type 1 and type 2 diabetes had between a three- and fourfold greater risk for COVID-19 hospitalization and greater illness severity compared with people without diabetes after adjustments for age, race, and a number of other risk factors.
This finding is important since as of Dec. 1, 2020, the CDC has classified the diabetes types differently in terms of underlying medical conditions that increase the risk for severe COVID-19.
Adults of any age with type 2 diabetes are considered “at increased risk of severe illness” from the virus that causes COVID-19 whereas the CDC says those with type 1 “might be at an increased risk.”
Lead author of the new paper Justin M. Gregory, MD, said in an interview: “I think this needs revision based on the current evidence. I think the data presented in our study and that of Barron et al. in Lancet Endocrinology 2020 indicate the need to place type 1 diabetes at parity with type 2 diabetes.
“These studies indicate both conditions carry an adjusted odds ratio of three to four when compared with people without diabetes for hospitalization, illness severity, and mortality,” he stressed.
Vaccines look promising for patients with diabetes
There were no phase 3 vaccine data available for the vaccine at the time that Dr. Gregory, of the Ian M. Burr Division of Pediatric Endocrinology and Diabetes, Vanderbilt University, Nashville, Tenn., and colleagues were writing their manuscript in late summer, so the article does not mention this.
But now, Dr. Gregory said, “Based on the initial press releases from Pfizer and Moderna, I am now optimistic that these vaccines might mitigate the excess morbidity and mortality from COVID-19 experienced by patients with diabetes.
“I am eager to see what we learn on December 10 and 17 [the scheduled dates for the meetings of the Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee to review the Pfizer and Moderna vaccines, respectively].”
But with the winter pandemic surge in the meantime, “Our investigation suggests that as COVID-19 hospitalizations rise, patients with both type 1 and 2 diabetes will comprise a disproportionately higher number of those admissions and, once hospitalized, demonstrate a greater degree of illness severity,” he and his colleagues said.
“In light of these data, we call on our colleagues to emphasize the importance of social distancing measures and hand hygiene, with particular emphasis on patients with diabetes, including those in the most vulnerable communities whom our study affirms will face the most severe impact.”
After adjustments, excess severity risk similar for both diabetes types
The new study data came from electronic health records at Vanderbilt University Medical Center, comprising 137 primary care, urgent care, and hospital facilities where patients were tested for SARS-CoV-2 regardless of the reason for their visit.
Between March 17 and August 7, 2020, 6,451 patients tested positive for COVID-19. Of those, 273 had type 2 diabetes and 40 had type 1 diabetes.
Children younger than 18 years accounted for 20% of those with type 1 diabetes and 9.4% of those without diabetes, but none of the type 2 group. The group with type 2 diabetes was considerably older than the type 1 diabetes and no-diabetes groups, 58 years versus 37 and 33 years, respectively.
Before adjustment for baseline characteristics that differed between groups, patients with type 1 diabetes appeared to have a risk for hospitalization and greater illness severity that was intermediate between the group with no diabetes and the group with type 2 diabetes, the researchers said.
But after adjustment for age, race, sex, hypertension, smoking, and body mass index, people with type 1 diabetes had odds ratios of 3.90 for hospitalization and 3.35 for greater illness severity, which was similar to risk in type 2 diabetes (3.36 and 3.42, respectively), compared to those without diabetes.
Deep dive explores COVID-19 severity risk factors in type 1 diabetes
The investigators then conducted a detailed chart review for 37 of the 40 patients with type 1 diabetes and phone surveys with 15 of them.
The majority (28) had not been hospitalized, and only one was hospitalized for diabetic ketoacidosis (DKA) within 14 days of positive SARS-CoV-2 testing.
This contrasts with a report from the T1D Exchange, in which nearly half of 33 patients with type 1 diabetes and COVID-19 had been hospitalized with DKA. The reason for the discrepancy may be that more severe patients would more likely be referred to the T1D Exchange Registry, Dr. Gregory and colleagues hypothesized.
Clinical factors associated with COVID-19 severity (P < .05) in their study included a prior hypertension diagnosis, higher hemoglobin A1c, at least one prior DKA admission in the past year, and not using a continuous glucose monitor (CGM).
Hospitalizations were twice as likely and illness severity nearly twice as great among those with type 1 diabetes who were Black versus White. Just 8% of those with private insurance were hospitalized, compared with 60% of those with public insurance and 67% with no insurance (P = .001).
“Whereas previous reports have indicated proportionally higher rates of hospitalizations from COVID-19 among Black patients and those with public insurance, this study is the first to show a similar finding in the population with type 1 diabetes,” Dr. Gregory and colleagues wrote.
Only 9% of patients using a CGM were hospitalized versus 47% who used blood glucose meters (P < .016). Similarly, hospitalizations occurred in 6% using an insulin pump versus 33% using multiple daily injections (P < .085).
“Our analysis cannot exclude the possibility that greater amounts of diabetes technology use are a surrogate for higher socioeconomic status,” they noted.
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases, JDRF, and the Appleby Foundation. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The risk for increased COVID-19 severity in people with type 1 diabetes appears similar to that of type 2 diabetes, contrary to some official advice from the Centers for Disease Control and Prevention. The new finding indicates that people with both types should be priority for receiving a vaccine, investigators say.
The study is the first to prospectively evaluate both inpatients and outpatients and to examine COVID-19 severity factors in addition to death in people with type 1 and type 2 diabetes separately, and was published online Dec. 2 in Diabetes Care.
Among the patients, who were seen at Vanderbilt University Medical Center in Nashville, Tenn., between March and August of 2020, those with both type 1 and type 2 diabetes had between a three- and fourfold greater risk for COVID-19 hospitalization and greater illness severity compared with people without diabetes after adjustments for age, race, and a number of other risk factors.
This finding is important since as of Dec. 1, 2020, the CDC has classified the diabetes types differently in terms of underlying medical conditions that increase the risk for severe COVID-19.
Adults of any age with type 2 diabetes are considered “at increased risk of severe illness” from the virus that causes COVID-19 whereas the CDC says those with type 1 “might be at an increased risk.”
Lead author of the new paper Justin M. Gregory, MD, said in an interview: “I think this needs revision based on the current evidence. I think the data presented in our study and that of Barron et al. in Lancet Endocrinology 2020 indicate the need to place type 1 diabetes at parity with type 2 diabetes.
“These studies indicate both conditions carry an adjusted odds ratio of three to four when compared with people without diabetes for hospitalization, illness severity, and mortality,” he stressed.
Vaccines look promising for patients with diabetes
There were no phase 3 vaccine data available for the vaccine at the time that Dr. Gregory, of the Ian M. Burr Division of Pediatric Endocrinology and Diabetes, Vanderbilt University, Nashville, Tenn., and colleagues were writing their manuscript in late summer, so the article does not mention this.
But now, Dr. Gregory said, “Based on the initial press releases from Pfizer and Moderna, I am now optimistic that these vaccines might mitigate the excess morbidity and mortality from COVID-19 experienced by patients with diabetes.
“I am eager to see what we learn on December 10 and 17 [the scheduled dates for the meetings of the Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee to review the Pfizer and Moderna vaccines, respectively].”
But with the winter pandemic surge in the meantime, “Our investigation suggests that as COVID-19 hospitalizations rise, patients with both type 1 and 2 diabetes will comprise a disproportionately higher number of those admissions and, once hospitalized, demonstrate a greater degree of illness severity,” he and his colleagues said.
“In light of these data, we call on our colleagues to emphasize the importance of social distancing measures and hand hygiene, with particular emphasis on patients with diabetes, including those in the most vulnerable communities whom our study affirms will face the most severe impact.”
After adjustments, excess severity risk similar for both diabetes types
The new study data came from electronic health records at Vanderbilt University Medical Center, comprising 137 primary care, urgent care, and hospital facilities where patients were tested for SARS-CoV-2 regardless of the reason for their visit.
Between March 17 and August 7, 2020, 6,451 patients tested positive for COVID-19. Of those, 273 had type 2 diabetes and 40 had type 1 diabetes.
Children younger than 18 years accounted for 20% of those with type 1 diabetes and 9.4% of those without diabetes, but none of the type 2 group. The group with type 2 diabetes was considerably older than the type 1 diabetes and no-diabetes groups, 58 years versus 37 and 33 years, respectively.
Before adjustment for baseline characteristics that differed between groups, patients with type 1 diabetes appeared to have a risk for hospitalization and greater illness severity that was intermediate between the group with no diabetes and the group with type 2 diabetes, the researchers said.
But after adjustment for age, race, sex, hypertension, smoking, and body mass index, people with type 1 diabetes had odds ratios of 3.90 for hospitalization and 3.35 for greater illness severity, which was similar to risk in type 2 diabetes (3.36 and 3.42, respectively), compared to those without diabetes.
Deep dive explores COVID-19 severity risk factors in type 1 diabetes
The investigators then conducted a detailed chart review for 37 of the 40 patients with type 1 diabetes and phone surveys with 15 of them.
The majority (28) had not been hospitalized, and only one was hospitalized for diabetic ketoacidosis (DKA) within 14 days of positive SARS-CoV-2 testing.
This contrasts with a report from the T1D Exchange, in which nearly half of 33 patients with type 1 diabetes and COVID-19 had been hospitalized with DKA. The reason for the discrepancy may be that more severe patients would more likely be referred to the T1D Exchange Registry, Dr. Gregory and colleagues hypothesized.
Clinical factors associated with COVID-19 severity (P < .05) in their study included a prior hypertension diagnosis, higher hemoglobin A1c, at least one prior DKA admission in the past year, and not using a continuous glucose monitor (CGM).
Hospitalizations were twice as likely and illness severity nearly twice as great among those with type 1 diabetes who were Black versus White. Just 8% of those with private insurance were hospitalized, compared with 60% of those with public insurance and 67% with no insurance (P = .001).
“Whereas previous reports have indicated proportionally higher rates of hospitalizations from COVID-19 among Black patients and those with public insurance, this study is the first to show a similar finding in the population with type 1 diabetes,” Dr. Gregory and colleagues wrote.
Only 9% of patients using a CGM were hospitalized versus 47% who used blood glucose meters (P < .016). Similarly, hospitalizations occurred in 6% using an insulin pump versus 33% using multiple daily injections (P < .085).
“Our analysis cannot exclude the possibility that greater amounts of diabetes technology use are a surrogate for higher socioeconomic status,” they noted.
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases, JDRF, and the Appleby Foundation. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Demand for COVID vaccines expected to get heated – and fast
Americans have made no secret of their skepticism of COVID-19 vaccines this year, with fears of political interference and a “warp speed” timeline blunting confidence in the shots. As recently as September, nearly half of U.S. adults said they didn’t intend to be inoculated.
But with two promising vaccines primed for release, likely within weeks, experts in ethics and immunization behavior say they expect attitudes to shift quickly from widespread hesitancy to urgent, even heated demand.
“People talk about the antivaccine people being able to kind of squelch uptake. I don’t see that happening,” Dr. Paul Offit, MD, a vaccinologist with Children’s Hospital of Philadelphia, told viewers of a recent JAMA Network webinar. “This, to me, is more like the Beanie Baby phenomenon. The attractiveness of a limited edition.”
Reports that vaccines produced by drugmakers Pfizer and BioNTech and Moderna appear to be safe and effective, along with the deliberate emphasis on science-based guidance from the incoming Biden administration, are likely to reverse uncertainty in a big way, said Arthur Caplan, PhD, director of the division of medical ethics at New York University.
“I think that’s going to flip the trust issue,” he said.
The shift is already apparent. A new poll by the Pew Research Center found that by the end of November 60% of Americans said they would get a vaccine for the coronavirus. This month, even as a federal advisory group met to hash out guidelines for vaccine distribution, a long list of advocacy groups – from those representing home-based health workers and community health centers to patients with kidney disease – were lobbying state and federal officials in hopes their constituents would be prioritized for the first scarce doses.
“As we get closer to the vaccine being a reality, there’s a lot of jockeying, to be sure,” said Katie Smith Sloan, chief executive of LeadingAge, a nonprofit organization pushing for staff and patients at long-term care centers to be included in the highest-priority category.
Certainly, some consumers remain wary, said Rupali Limaye, PhD, a social and behavioral health scientist at the Johns Hopkins Bloomberg School of Public Health, Baltimore. Fears that drugmakers and regulators might cut corners to speed a vaccine linger, even as details of the trials become public and the review process is made more transparent. Some health care workers, who are at the front of the line for the shots, are not eager to go first.
“There will be people who will say, ‘I will wait a little bit more for safety data,” Dr. Limaye said.
But those doubts likely will recede once the vaccines are approved for use and begin to circulate broadly, said Dr. Offit, who sits on the Food and Drug Administration advisory panel set to review the requests for emergency authorization Pfizer and Moderna have submitted.
He predicted demand for the COVID vaccines could rival the clamor that occurred in 2004, when production problems caused a severe shortage of flu shots just as influenza season began. That led to long lines, rationed doses and ethical debates over distribution.
“That was a highly desired vaccine,” Dr. Offit said. “I think in many ways that might happen here.”
Initially, vaccine supplies will be tight, with federal officials planning to ship 6.4 million doses within 24 hours of FDA authorization and up to 40 million doses by the end of the year. The CDC panel recommended that the first shots go to the 21 million health care workers in the United States and 3 million nursing home staff and residents, before being rolled out to other groups based on a hierarchy of risk factors.
Even before any vaccine is available, some people are trying to boost their chances of access, said Allison Kempe, MD, a professor of pediatrics at the University of Coloradoat Denver, Aurora, and expert in vaccine dissemination. “People have called me and said, ‘How can I get the vaccine?’” she said. “I think that not everyone will be happy to wait, that’s for sure. I don’t think there will be rioting in the streets, but there may be pressure brought to bear.”
That likely will include emotional debates over how, when, and to whom next doses should be distributed, said Dr. Caplan. Under the CDC recommendations, vulnerable groups next in line include 87 million workers whose jobs are deemed “essential” – a broad and ill-defined category – as well as 53 million adults age 65 and older.
“We’re going to have some fights about high-risk groups,” Dr. Caplan said.
The conversations will be complicated. Should prisoners, who have little control over their COVID exposure, get vaccine priority? How about professional sports teams, whose performance could bolster society’s overall morale? And what about residents of facilities providing care for people with intellectual and developmental disabilities, who are three times more likely to die from COVID-19 than the general population?
Control over vaccination allocation rests with the states, so that’s where the biggest conflicts will occur, Dr. Caplan said. “It’s a short fight, I hope, in the sense in which it gets done in a few months, but I think it will be pretty vocal.”
Once vaccine supplies become more plentiful, perhaps by May or June, another consideration is sure to boost demand: requirements for proof of COVID vaccination for work and travel.
“It’s inevitable that you’re going to see immunity passports or that you’re required to show a certificate on the train, airplane, bus, or subway,” Dr. Caplan predicted. “Probably also to enter certain hospitals, probably to enter certain restaurants and government facilities.”
But with a grueling winter surge ahead, and new predictions that COVID-19 will fell as many as 450,000 Americans by February, the tragic reality of the disease will no doubt fuel ample demand for vaccination.
“People now know someone who has gotten COVID, who has been hospitalized or has unfortunately died,” Dr. Limaye said.
“We’re all seeing this now,” said Dr. Kempe. “Even deniers are beginning to see what this illness can do.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Americans have made no secret of their skepticism of COVID-19 vaccines this year, with fears of political interference and a “warp speed” timeline blunting confidence in the shots. As recently as September, nearly half of U.S. adults said they didn’t intend to be inoculated.
But with two promising vaccines primed for release, likely within weeks, experts in ethics and immunization behavior say they expect attitudes to shift quickly from widespread hesitancy to urgent, even heated demand.
“People talk about the antivaccine people being able to kind of squelch uptake. I don’t see that happening,” Dr. Paul Offit, MD, a vaccinologist with Children’s Hospital of Philadelphia, told viewers of a recent JAMA Network webinar. “This, to me, is more like the Beanie Baby phenomenon. The attractiveness of a limited edition.”
Reports that vaccines produced by drugmakers Pfizer and BioNTech and Moderna appear to be safe and effective, along with the deliberate emphasis on science-based guidance from the incoming Biden administration, are likely to reverse uncertainty in a big way, said Arthur Caplan, PhD, director of the division of medical ethics at New York University.
“I think that’s going to flip the trust issue,” he said.
The shift is already apparent. A new poll by the Pew Research Center found that by the end of November 60% of Americans said they would get a vaccine for the coronavirus. This month, even as a federal advisory group met to hash out guidelines for vaccine distribution, a long list of advocacy groups – from those representing home-based health workers and community health centers to patients with kidney disease – were lobbying state and federal officials in hopes their constituents would be prioritized for the first scarce doses.
“As we get closer to the vaccine being a reality, there’s a lot of jockeying, to be sure,” said Katie Smith Sloan, chief executive of LeadingAge, a nonprofit organization pushing for staff and patients at long-term care centers to be included in the highest-priority category.
Certainly, some consumers remain wary, said Rupali Limaye, PhD, a social and behavioral health scientist at the Johns Hopkins Bloomberg School of Public Health, Baltimore. Fears that drugmakers and regulators might cut corners to speed a vaccine linger, even as details of the trials become public and the review process is made more transparent. Some health care workers, who are at the front of the line for the shots, are not eager to go first.
“There will be people who will say, ‘I will wait a little bit more for safety data,” Dr. Limaye said.
But those doubts likely will recede once the vaccines are approved for use and begin to circulate broadly, said Dr. Offit, who sits on the Food and Drug Administration advisory panel set to review the requests for emergency authorization Pfizer and Moderna have submitted.
He predicted demand for the COVID vaccines could rival the clamor that occurred in 2004, when production problems caused a severe shortage of flu shots just as influenza season began. That led to long lines, rationed doses and ethical debates over distribution.
“That was a highly desired vaccine,” Dr. Offit said. “I think in many ways that might happen here.”
Initially, vaccine supplies will be tight, with federal officials planning to ship 6.4 million doses within 24 hours of FDA authorization and up to 40 million doses by the end of the year. The CDC panel recommended that the first shots go to the 21 million health care workers in the United States and 3 million nursing home staff and residents, before being rolled out to other groups based on a hierarchy of risk factors.
Even before any vaccine is available, some people are trying to boost their chances of access, said Allison Kempe, MD, a professor of pediatrics at the University of Coloradoat Denver, Aurora, and expert in vaccine dissemination. “People have called me and said, ‘How can I get the vaccine?’” she said. “I think that not everyone will be happy to wait, that’s for sure. I don’t think there will be rioting in the streets, but there may be pressure brought to bear.”
That likely will include emotional debates over how, when, and to whom next doses should be distributed, said Dr. Caplan. Under the CDC recommendations, vulnerable groups next in line include 87 million workers whose jobs are deemed “essential” – a broad and ill-defined category – as well as 53 million adults age 65 and older.
“We’re going to have some fights about high-risk groups,” Dr. Caplan said.
The conversations will be complicated. Should prisoners, who have little control over their COVID exposure, get vaccine priority? How about professional sports teams, whose performance could bolster society’s overall morale? And what about residents of facilities providing care for people with intellectual and developmental disabilities, who are three times more likely to die from COVID-19 than the general population?
Control over vaccination allocation rests with the states, so that’s where the biggest conflicts will occur, Dr. Caplan said. “It’s a short fight, I hope, in the sense in which it gets done in a few months, but I think it will be pretty vocal.”
Once vaccine supplies become more plentiful, perhaps by May or June, another consideration is sure to boost demand: requirements for proof of COVID vaccination for work and travel.
“It’s inevitable that you’re going to see immunity passports or that you’re required to show a certificate on the train, airplane, bus, or subway,” Dr. Caplan predicted. “Probably also to enter certain hospitals, probably to enter certain restaurants and government facilities.”
But with a grueling winter surge ahead, and new predictions that COVID-19 will fell as many as 450,000 Americans by February, the tragic reality of the disease will no doubt fuel ample demand for vaccination.
“People now know someone who has gotten COVID, who has been hospitalized or has unfortunately died,” Dr. Limaye said.
“We’re all seeing this now,” said Dr. Kempe. “Even deniers are beginning to see what this illness can do.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Americans have made no secret of their skepticism of COVID-19 vaccines this year, with fears of political interference and a “warp speed” timeline blunting confidence in the shots. As recently as September, nearly half of U.S. adults said they didn’t intend to be inoculated.
But with two promising vaccines primed for release, likely within weeks, experts in ethics and immunization behavior say they expect attitudes to shift quickly from widespread hesitancy to urgent, even heated demand.
“People talk about the antivaccine people being able to kind of squelch uptake. I don’t see that happening,” Dr. Paul Offit, MD, a vaccinologist with Children’s Hospital of Philadelphia, told viewers of a recent JAMA Network webinar. “This, to me, is more like the Beanie Baby phenomenon. The attractiveness of a limited edition.”
Reports that vaccines produced by drugmakers Pfizer and BioNTech and Moderna appear to be safe and effective, along with the deliberate emphasis on science-based guidance from the incoming Biden administration, are likely to reverse uncertainty in a big way, said Arthur Caplan, PhD, director of the division of medical ethics at New York University.
“I think that’s going to flip the trust issue,” he said.
The shift is already apparent. A new poll by the Pew Research Center found that by the end of November 60% of Americans said they would get a vaccine for the coronavirus. This month, even as a federal advisory group met to hash out guidelines for vaccine distribution, a long list of advocacy groups – from those representing home-based health workers and community health centers to patients with kidney disease – were lobbying state and federal officials in hopes their constituents would be prioritized for the first scarce doses.
“As we get closer to the vaccine being a reality, there’s a lot of jockeying, to be sure,” said Katie Smith Sloan, chief executive of LeadingAge, a nonprofit organization pushing for staff and patients at long-term care centers to be included in the highest-priority category.
Certainly, some consumers remain wary, said Rupali Limaye, PhD, a social and behavioral health scientist at the Johns Hopkins Bloomberg School of Public Health, Baltimore. Fears that drugmakers and regulators might cut corners to speed a vaccine linger, even as details of the trials become public and the review process is made more transparent. Some health care workers, who are at the front of the line for the shots, are not eager to go first.
“There will be people who will say, ‘I will wait a little bit more for safety data,” Dr. Limaye said.
But those doubts likely will recede once the vaccines are approved for use and begin to circulate broadly, said Dr. Offit, who sits on the Food and Drug Administration advisory panel set to review the requests for emergency authorization Pfizer and Moderna have submitted.
He predicted demand for the COVID vaccines could rival the clamor that occurred in 2004, when production problems caused a severe shortage of flu shots just as influenza season began. That led to long lines, rationed doses and ethical debates over distribution.
“That was a highly desired vaccine,” Dr. Offit said. “I think in many ways that might happen here.”
Initially, vaccine supplies will be tight, with federal officials planning to ship 6.4 million doses within 24 hours of FDA authorization and up to 40 million doses by the end of the year. The CDC panel recommended that the first shots go to the 21 million health care workers in the United States and 3 million nursing home staff and residents, before being rolled out to other groups based on a hierarchy of risk factors.
Even before any vaccine is available, some people are trying to boost their chances of access, said Allison Kempe, MD, a professor of pediatrics at the University of Coloradoat Denver, Aurora, and expert in vaccine dissemination. “People have called me and said, ‘How can I get the vaccine?’” she said. “I think that not everyone will be happy to wait, that’s for sure. I don’t think there will be rioting in the streets, but there may be pressure brought to bear.”
That likely will include emotional debates over how, when, and to whom next doses should be distributed, said Dr. Caplan. Under the CDC recommendations, vulnerable groups next in line include 87 million workers whose jobs are deemed “essential” – a broad and ill-defined category – as well as 53 million adults age 65 and older.
“We’re going to have some fights about high-risk groups,” Dr. Caplan said.
The conversations will be complicated. Should prisoners, who have little control over their COVID exposure, get vaccine priority? How about professional sports teams, whose performance could bolster society’s overall morale? And what about residents of facilities providing care for people with intellectual and developmental disabilities, who are three times more likely to die from COVID-19 than the general population?
Control over vaccination allocation rests with the states, so that’s where the biggest conflicts will occur, Dr. Caplan said. “It’s a short fight, I hope, in the sense in which it gets done in a few months, but I think it will be pretty vocal.”
Once vaccine supplies become more plentiful, perhaps by May or June, another consideration is sure to boost demand: requirements for proof of COVID vaccination for work and travel.
“It’s inevitable that you’re going to see immunity passports or that you’re required to show a certificate on the train, airplane, bus, or subway,” Dr. Caplan predicted. “Probably also to enter certain hospitals, probably to enter certain restaurants and government facilities.”
But with a grueling winter surge ahead, and new predictions that COVID-19 will fell as many as 450,000 Americans by February, the tragic reality of the disease will no doubt fuel ample demand for vaccination.
“People now know someone who has gotten COVID, who has been hospitalized or has unfortunately died,” Dr. Limaye said.
“We’re all seeing this now,” said Dr. Kempe. “Even deniers are beginning to see what this illness can do.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Rap music mention of mental health topics more than doubles
Mental health distress is rising but often is undertreated among children and young adults in the United States, wrote Alex Kresovich, MA, of the University of North Carolina, Chapel Hill, and colleagues.
“Mental health risk especially is increasing among young Black/ African American male individuals (YBAAM), who are often disproportionately exposed to environmental, economic, and family stressors linked with depression and anxiety,” they said. Adolescents and young adults, especially YBAAM, make up a large part of the audience for rap music.
In recent years, more rap artists have disclosed mental health issues, and they have included mental health topics such as depression and suicidal thoughts into their music, the researchers said.
In a study published in JAMA Pediatrics, the researchers identified 125 songs from the period between 1998 and 2018, then assessed them for references to mental health. The song selections included the top 25 rap songs in 1998, 2003, 2008, 2013, and 2018, based on the Billboard music charts.
The majority of the songs (123) featured lead artists from North America, and 97 of them were Black/African American males. The average age of the artists was 28 years. “Prominent artists captured in the sample included 50 Cent, Drake, Eminem, Kanye West, Jay-Z, and Lil’Wayne, among others,” they said. The researchers divided mental health issues into four categories: anxiety or anxious thinking; depression or depressive thinking; metaphors (such as struggling with mental stability); and suicide or suicidal ideation.
Mental health references rise
Across the study period, 35 songs (28%) mentioned anxiety, 28 (22%) mentioned depression, 8 (6%) mentioned suicide, and 26 (21%) mentioned a mental health metaphor. The proportion of songs with a mental health reference increased in a significant linear trend across the study period for suicide (0%-12%), depression (16%-32%), and mental health metaphors (8%-44%).
All references to suicide or suicidal ideation were found in songs that were popular between 2013 and 2018, the researchers noted.
“This increase is important, given that rap artists serve as role models to their audience, which extends beyond YBAAM to include U.S. young people across strata, constituting a large group with increased risk of mental health issues and underuse of mental health services,” Mr. Kresovich and associates said.
In addition, the researchers found that stressors related to environmental conditions and love were significantly more likely to co-occur with mental health references (adjusted odds ratios 8.1 and 4.8, respectively).
The study findings were limited by several factors including the selection of songs only from the Billboard hot rap songs year-end charts, which “does not fully represent the population of rap music between 1998 and 2018,” the researchers said. In addition, they could not address causation or motivations for the increased mental health references over the study period. “We are also unable to ascertain how U.S. youth interact with this music or are positively or negatively affected by its messages.”
“For example, positively framed references to mental health awareness, treatment, or support may lead to reduced stigma and increased willingness to seek treatment,” Mr. Kresovich and associates wrote. “However, negatively framed references to mental health struggles might lead to negative outcomes, including copycat behavior in which listeners model harmful behavior, such as suicide attempts, if those behaviors are described in lyrics (i.e., the Werther effect),” they added.
Despite these limitations, the results support the need for more research on the impact of rap music as a way to reduce stigma and potentially reduce mental health risk in adolescents and young adults, Mr. Kresovich and associates concluded.
Music may help raise tough topics
The study is important because children and adolescents have more control than ever over the media they consume, Sarah Vinson, MD, founder of the Lorio Psych Group in Atlanta, said in an interview.
“With more and more children with access to their own devices, they spend a great amount of time consuming content, including music,” Dr. Vinson said. “The norms reflected in the lyrics they hear have an impact on their emerging view of themselves, others, and the world.”
The increased recognition of mental health issues by rap musicians as a topic “certainly has the potential to have a positive impact; however, the way that it is discussed can influence [the] nature of that impact,” she explained.
“It is important for people who are dealing with the normal range of human emotions to know that they are not alone. It is even more important for people dealing with suicidality or mental illness to know that,” Dr. Vinson said.
“Validation and sense of connection are human needs, and stigma related to mental illness can be isolating,” she emphasized. “Rappers have a platform and are often people that children and adolescents look up to, for better or for worse.” Through their music, “the rappers are signaling that these topics are worthy of our attention and okay to talk about.”
Unfortunately, many barriers persist for adolescents in need of mental health treatment, said Dr. Vinson. “The children’s mental health workforce, quantitatively, is not enough to meet the current needs,” she said. “Mental health is not reimbursed at the same rate as other kinds of health care, which contributes to healthy systems not prioritizing these services. Additionally, the racial, ethnic, and socioeconomic background of those who are mental health providers is not reflective of the larger population, and mental health training insufficiently incorporates the cultural and structural humility needed to help professionals navigate those differences,” she explained.
“Children at increased risk are those who face many of those environmental barriers that the rappers reference in those lyrics. They are likely to have even poorer access because they are disproportionately impacted by residential segregation, transportation challenges, financial barriers, and structural racism in mental health care,” Dr. Vinson added. A take-home message for clinicians is to find out what their patients are listening to. “One way to understand what is on the hearts and minds of children is to ask them what’s in their playlist,” she said.
Additional research is needed to examine “moderating factors for the impact, good or bad, of increased mental health content in hip hop for young listeners’ mental health awareness, symptoms and/or interest in seeking treatment,” Dr. Vinson concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Dr. Vinson served as chair for a workshop on mental health and hip-hop at the American Psychiatric Association annual meeting. She had no financial conflicts to disclose.
SOURCE: Kresovich A et al. JAMA Pediatr. 2020 Dec 7. doi: 10.1001/jamapediatrics.2020.5155.
This article was updated on December 21, 2020.
Mental health distress is rising but often is undertreated among children and young adults in the United States, wrote Alex Kresovich, MA, of the University of North Carolina, Chapel Hill, and colleagues.
“Mental health risk especially is increasing among young Black/ African American male individuals (YBAAM), who are often disproportionately exposed to environmental, economic, and family stressors linked with depression and anxiety,” they said. Adolescents and young adults, especially YBAAM, make up a large part of the audience for rap music.
In recent years, more rap artists have disclosed mental health issues, and they have included mental health topics such as depression and suicidal thoughts into their music, the researchers said.
In a study published in JAMA Pediatrics, the researchers identified 125 songs from the period between 1998 and 2018, then assessed them for references to mental health. The song selections included the top 25 rap songs in 1998, 2003, 2008, 2013, and 2018, based on the Billboard music charts.
The majority of the songs (123) featured lead artists from North America, and 97 of them were Black/African American males. The average age of the artists was 28 years. “Prominent artists captured in the sample included 50 Cent, Drake, Eminem, Kanye West, Jay-Z, and Lil’Wayne, among others,” they said. The researchers divided mental health issues into four categories: anxiety or anxious thinking; depression or depressive thinking; metaphors (such as struggling with mental stability); and suicide or suicidal ideation.
Mental health references rise
Across the study period, 35 songs (28%) mentioned anxiety, 28 (22%) mentioned depression, 8 (6%) mentioned suicide, and 26 (21%) mentioned a mental health metaphor. The proportion of songs with a mental health reference increased in a significant linear trend across the study period for suicide (0%-12%), depression (16%-32%), and mental health metaphors (8%-44%).
All references to suicide or suicidal ideation were found in songs that were popular between 2013 and 2018, the researchers noted.
“This increase is important, given that rap artists serve as role models to their audience, which extends beyond YBAAM to include U.S. young people across strata, constituting a large group with increased risk of mental health issues and underuse of mental health services,” Mr. Kresovich and associates said.
In addition, the researchers found that stressors related to environmental conditions and love were significantly more likely to co-occur with mental health references (adjusted odds ratios 8.1 and 4.8, respectively).
The study findings were limited by several factors including the selection of songs only from the Billboard hot rap songs year-end charts, which “does not fully represent the population of rap music between 1998 and 2018,” the researchers said. In addition, they could not address causation or motivations for the increased mental health references over the study period. “We are also unable to ascertain how U.S. youth interact with this music or are positively or negatively affected by its messages.”
“For example, positively framed references to mental health awareness, treatment, or support may lead to reduced stigma and increased willingness to seek treatment,” Mr. Kresovich and associates wrote. “However, negatively framed references to mental health struggles might lead to negative outcomes, including copycat behavior in which listeners model harmful behavior, such as suicide attempts, if those behaviors are described in lyrics (i.e., the Werther effect),” they added.
Despite these limitations, the results support the need for more research on the impact of rap music as a way to reduce stigma and potentially reduce mental health risk in adolescents and young adults, Mr. Kresovich and associates concluded.
Music may help raise tough topics
The study is important because children and adolescents have more control than ever over the media they consume, Sarah Vinson, MD, founder of the Lorio Psych Group in Atlanta, said in an interview.
“With more and more children with access to their own devices, they spend a great amount of time consuming content, including music,” Dr. Vinson said. “The norms reflected in the lyrics they hear have an impact on their emerging view of themselves, others, and the world.”
The increased recognition of mental health issues by rap musicians as a topic “certainly has the potential to have a positive impact; however, the way that it is discussed can influence [the] nature of that impact,” she explained.
“It is important for people who are dealing with the normal range of human emotions to know that they are not alone. It is even more important for people dealing with suicidality or mental illness to know that,” Dr. Vinson said.
“Validation and sense of connection are human needs, and stigma related to mental illness can be isolating,” she emphasized. “Rappers have a platform and are often people that children and adolescents look up to, for better or for worse.” Through their music, “the rappers are signaling that these topics are worthy of our attention and okay to talk about.”
Unfortunately, many barriers persist for adolescents in need of mental health treatment, said Dr. Vinson. “The children’s mental health workforce, quantitatively, is not enough to meet the current needs,” she said. “Mental health is not reimbursed at the same rate as other kinds of health care, which contributes to healthy systems not prioritizing these services. Additionally, the racial, ethnic, and socioeconomic background of those who are mental health providers is not reflective of the larger population, and mental health training insufficiently incorporates the cultural and structural humility needed to help professionals navigate those differences,” she explained.
“Children at increased risk are those who face many of those environmental barriers that the rappers reference in those lyrics. They are likely to have even poorer access because they are disproportionately impacted by residential segregation, transportation challenges, financial barriers, and structural racism in mental health care,” Dr. Vinson added. A take-home message for clinicians is to find out what their patients are listening to. “One way to understand what is on the hearts and minds of children is to ask them what’s in their playlist,” she said.
Additional research is needed to examine “moderating factors for the impact, good or bad, of increased mental health content in hip hop for young listeners’ mental health awareness, symptoms and/or interest in seeking treatment,” Dr. Vinson concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Dr. Vinson served as chair for a workshop on mental health and hip-hop at the American Psychiatric Association annual meeting. She had no financial conflicts to disclose.
SOURCE: Kresovich A et al. JAMA Pediatr. 2020 Dec 7. doi: 10.1001/jamapediatrics.2020.5155.
This article was updated on December 21, 2020.
Mental health distress is rising but often is undertreated among children and young adults in the United States, wrote Alex Kresovich, MA, of the University of North Carolina, Chapel Hill, and colleagues.
“Mental health risk especially is increasing among young Black/ African American male individuals (YBAAM), who are often disproportionately exposed to environmental, economic, and family stressors linked with depression and anxiety,” they said. Adolescents and young adults, especially YBAAM, make up a large part of the audience for rap music.
In recent years, more rap artists have disclosed mental health issues, and they have included mental health topics such as depression and suicidal thoughts into their music, the researchers said.
In a study published in JAMA Pediatrics, the researchers identified 125 songs from the period between 1998 and 2018, then assessed them for references to mental health. The song selections included the top 25 rap songs in 1998, 2003, 2008, 2013, and 2018, based on the Billboard music charts.
The majority of the songs (123) featured lead artists from North America, and 97 of them were Black/African American males. The average age of the artists was 28 years. “Prominent artists captured in the sample included 50 Cent, Drake, Eminem, Kanye West, Jay-Z, and Lil’Wayne, among others,” they said. The researchers divided mental health issues into four categories: anxiety or anxious thinking; depression or depressive thinking; metaphors (such as struggling with mental stability); and suicide or suicidal ideation.
Mental health references rise
Across the study period, 35 songs (28%) mentioned anxiety, 28 (22%) mentioned depression, 8 (6%) mentioned suicide, and 26 (21%) mentioned a mental health metaphor. The proportion of songs with a mental health reference increased in a significant linear trend across the study period for suicide (0%-12%), depression (16%-32%), and mental health metaphors (8%-44%).
All references to suicide or suicidal ideation were found in songs that were popular between 2013 and 2018, the researchers noted.
“This increase is important, given that rap artists serve as role models to their audience, which extends beyond YBAAM to include U.S. young people across strata, constituting a large group with increased risk of mental health issues and underuse of mental health services,” Mr. Kresovich and associates said.
In addition, the researchers found that stressors related to environmental conditions and love were significantly more likely to co-occur with mental health references (adjusted odds ratios 8.1 and 4.8, respectively).
The study findings were limited by several factors including the selection of songs only from the Billboard hot rap songs year-end charts, which “does not fully represent the population of rap music between 1998 and 2018,” the researchers said. In addition, they could not address causation or motivations for the increased mental health references over the study period. “We are also unable to ascertain how U.S. youth interact with this music or are positively or negatively affected by its messages.”
“For example, positively framed references to mental health awareness, treatment, or support may lead to reduced stigma and increased willingness to seek treatment,” Mr. Kresovich and associates wrote. “However, negatively framed references to mental health struggles might lead to negative outcomes, including copycat behavior in which listeners model harmful behavior, such as suicide attempts, if those behaviors are described in lyrics (i.e., the Werther effect),” they added.
Despite these limitations, the results support the need for more research on the impact of rap music as a way to reduce stigma and potentially reduce mental health risk in adolescents and young adults, Mr. Kresovich and associates concluded.
Music may help raise tough topics
The study is important because children and adolescents have more control than ever over the media they consume, Sarah Vinson, MD, founder of the Lorio Psych Group in Atlanta, said in an interview.
“With more and more children with access to their own devices, they spend a great amount of time consuming content, including music,” Dr. Vinson said. “The norms reflected in the lyrics they hear have an impact on their emerging view of themselves, others, and the world.”
The increased recognition of mental health issues by rap musicians as a topic “certainly has the potential to have a positive impact; however, the way that it is discussed can influence [the] nature of that impact,” she explained.
“It is important for people who are dealing with the normal range of human emotions to know that they are not alone. It is even more important for people dealing with suicidality or mental illness to know that,” Dr. Vinson said.
“Validation and sense of connection are human needs, and stigma related to mental illness can be isolating,” she emphasized. “Rappers have a platform and are often people that children and adolescents look up to, for better or for worse.” Through their music, “the rappers are signaling that these topics are worthy of our attention and okay to talk about.”
Unfortunately, many barriers persist for adolescents in need of mental health treatment, said Dr. Vinson. “The children’s mental health workforce, quantitatively, is not enough to meet the current needs,” she said. “Mental health is not reimbursed at the same rate as other kinds of health care, which contributes to healthy systems not prioritizing these services. Additionally, the racial, ethnic, and socioeconomic background of those who are mental health providers is not reflective of the larger population, and mental health training insufficiently incorporates the cultural and structural humility needed to help professionals navigate those differences,” she explained.
“Children at increased risk are those who face many of those environmental barriers that the rappers reference in those lyrics. They are likely to have even poorer access because they are disproportionately impacted by residential segregation, transportation challenges, financial barriers, and structural racism in mental health care,” Dr. Vinson added. A take-home message for clinicians is to find out what their patients are listening to. “One way to understand what is on the hearts and minds of children is to ask them what’s in their playlist,” she said.
Additional research is needed to examine “moderating factors for the impact, good or bad, of increased mental health content in hip hop for young listeners’ mental health awareness, symptoms and/or interest in seeking treatment,” Dr. Vinson concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Dr. Vinson served as chair for a workshop on mental health and hip-hop at the American Psychiatric Association annual meeting. She had no financial conflicts to disclose.
SOURCE: Kresovich A et al. JAMA Pediatr. 2020 Dec 7. doi: 10.1001/jamapediatrics.2020.5155.
This article was updated on December 21, 2020.
FROM JAMA PEDIATRICS
Phase 1 study: Beta-blocker may improve melanoma treatment response
Response rates were high without dose-limiting toxicities in a small phase 1 study that evaluated the addition of propranolol to pembrolizumab in treatment-naive patients with metastatic melanoma.
“To our knowledge, this effort is the,” wrote the two co-first authors, Shipra Gandhi, MD, and Manu Pandey, MBBS, from the Roswell Park Comprehensive Cancer Center, Buffalo, N.Y., and coauthors.
The need for combinations built on anti-PD1 checkpoint inhibitor therapy strategies in metastatic melanoma that safely improve outcomes is underscored by the high (59%) grade 3 or 4 treatment-related adverse event (TRAE) rates when an anti-CTLA4 agent (ipilimumab) was added to an anti-PD-1 agent (nivolumab), they noted. In contrast, a TRAE rate of only 17% has been reported with pembrolizumab monotherapy.
The phase 1b study was stimulated by preclinical, retrospective observations of improved overall survival (OS) in cancer patients treated with beta-blockers. These were preceded by murine melanoma studies showing decreased tumor growth and metastasis with the nonselective beta-blocker propranolol. “Propranolol exerts an antitumor effect,” the authors stated, “by favorably modulating the tumor microenvironment (TME) by decreasing myeloid-derived suppressor cells and increasing CD8+ T-cell and natural killer cells in the TME.” Other research in a melanoma model in chronically-stressed mice has demonstrated synergy between an anti-PD1 antibody and propranolol.
“We know that stress can have a significant negative effect on health, but the extent to which stress may impact the outcome of cancer therapy is not well understood at all,” Dr. Ghandi said in a statement provided by Roswell Park. “We set out to better understand this relationship and to explore its implications for cancer treatment.”
The investigators recruited nine White adults (median age 65 years) with treatment-naive, histologically confirmed unresectable stage III or IV melanoma and Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1 to the open-label, single arm, nonrandomized, single-center, dose-finding study. Patients received standard of care intravenous pembrolizumab 200 mg every 3 weeks and, in three groups, propranolol doses of 10 mg, 20 mg, or 30 mg twice a day until 2 years on study or disease progression or the development of dose-limiting toxicities (DLTs). Assessing the safety and efficacy (overall response rate [ORR] within 6 months of starting therapy) of pembrolizumab with the increasing doses of propranolol and selecting the recommended phase 2 dose were the study’s primary objectives.
Objective responses (complete or partial responses) were reported in seven of the nine patients, with partial tumor responses in two patients in the propranolol 10-mg group, two partial responses in the 20-mg group, and three partial responses in the 30-mg group.
While all patients experienced TRAEs, only one was above grade 2. The most commonly reported TRAEs were fatigue, rash and vitiligo, reported in four of the nine patients. Two patients in the 20-mg twice-a-day group discontinued therapy because of TRAEs (hemophagocytic lymphohistiocytosis and labyrinthitis). No DLTs were observed at any of the three dose levels, and no deaths occurred on study treatment.
The authors said that propranolol 30 mg twice a day was chosen as the recommended phase 2 dose, because in combination with pembrolizumab, there were no DLTs, and preliminary antitumor efficacy was observed in all three patients. Also, in all three patients, the investigators observed a trend toward higher CD8+T-cell percentage, higher ratios of CD8+T-cell/ Treg and CD8+T-cell/ polymorphonuclear myeloid-derived suppressor cells. They underscored, however, that the small size and significant heterogeneity in biomarkers made a statistically sound and meaningful interpretation of biomarkers for deciding the phase 2 dose difficult.
“In repurposing propranolol,” Dr. Pandey said in the Roswell statement, “we’ve gained important insights on how to manage stress in people with cancer – who can face dangerously elevated levels of mental and physical stress related to their diagnosis and treatment.”
In an interview, one of the two senior authors, Elizabeth Repasky, PhD, professor of oncology and immunology at Roswell Park, said, “it’s exciting that an extremely inexpensive drug like propranolol that could be used in every country around the world could have an impact on cancer by blocking stress, especially chronic stress.” Her murine research showing that adding propranolol to immunotherapy or radiotherapy or chemotherapy improved tumor growth control provided rationale for the current study.
“The breakthrough in this study is that it reveals the immune system as the best target to look at, and shows that what stress reduction is doing is improving a patient’s immune response to his or her own tumor,” Dr. Repasky said. “The mind/body connection is so important, but we have not had a handle on how to study it,” she added.
Further research funded by Herd of Hope grants at Roswell will look at tumor effects of propranolol and nonpharmacological reducers of chronic stress such as exercise, meditation, yoga, and Tai Chi, with first studies in breast cancer.
The study was funded by Roswell Park, private, and NIH grants. The authors had no disclosures.
SOURCE: Gandhi S et al. Clin Cancer Res. 2020 Oct 30. doi: 10.1158/1078-0432.CCR-20-2381
Response rates were high without dose-limiting toxicities in a small phase 1 study that evaluated the addition of propranolol to pembrolizumab in treatment-naive patients with metastatic melanoma.
“To our knowledge, this effort is the,” wrote the two co-first authors, Shipra Gandhi, MD, and Manu Pandey, MBBS, from the Roswell Park Comprehensive Cancer Center, Buffalo, N.Y., and coauthors.
The need for combinations built on anti-PD1 checkpoint inhibitor therapy strategies in metastatic melanoma that safely improve outcomes is underscored by the high (59%) grade 3 or 4 treatment-related adverse event (TRAE) rates when an anti-CTLA4 agent (ipilimumab) was added to an anti-PD-1 agent (nivolumab), they noted. In contrast, a TRAE rate of only 17% has been reported with pembrolizumab monotherapy.
The phase 1b study was stimulated by preclinical, retrospective observations of improved overall survival (OS) in cancer patients treated with beta-blockers. These were preceded by murine melanoma studies showing decreased tumor growth and metastasis with the nonselective beta-blocker propranolol. “Propranolol exerts an antitumor effect,” the authors stated, “by favorably modulating the tumor microenvironment (TME) by decreasing myeloid-derived suppressor cells and increasing CD8+ T-cell and natural killer cells in the TME.” Other research in a melanoma model in chronically-stressed mice has demonstrated synergy between an anti-PD1 antibody and propranolol.
“We know that stress can have a significant negative effect on health, but the extent to which stress may impact the outcome of cancer therapy is not well understood at all,” Dr. Ghandi said in a statement provided by Roswell Park. “We set out to better understand this relationship and to explore its implications for cancer treatment.”
The investigators recruited nine White adults (median age 65 years) with treatment-naive, histologically confirmed unresectable stage III or IV melanoma and Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1 to the open-label, single arm, nonrandomized, single-center, dose-finding study. Patients received standard of care intravenous pembrolizumab 200 mg every 3 weeks and, in three groups, propranolol doses of 10 mg, 20 mg, or 30 mg twice a day until 2 years on study or disease progression or the development of dose-limiting toxicities (DLTs). Assessing the safety and efficacy (overall response rate [ORR] within 6 months of starting therapy) of pembrolizumab with the increasing doses of propranolol and selecting the recommended phase 2 dose were the study’s primary objectives.
Objective responses (complete or partial responses) were reported in seven of the nine patients, with partial tumor responses in two patients in the propranolol 10-mg group, two partial responses in the 20-mg group, and three partial responses in the 30-mg group.
While all patients experienced TRAEs, only one was above grade 2. The most commonly reported TRAEs were fatigue, rash and vitiligo, reported in four of the nine patients. Two patients in the 20-mg twice-a-day group discontinued therapy because of TRAEs (hemophagocytic lymphohistiocytosis and labyrinthitis). No DLTs were observed at any of the three dose levels, and no deaths occurred on study treatment.
The authors said that propranolol 30 mg twice a day was chosen as the recommended phase 2 dose, because in combination with pembrolizumab, there were no DLTs, and preliminary antitumor efficacy was observed in all three patients. Also, in all three patients, the investigators observed a trend toward higher CD8+T-cell percentage, higher ratios of CD8+T-cell/ Treg and CD8+T-cell/ polymorphonuclear myeloid-derived suppressor cells. They underscored, however, that the small size and significant heterogeneity in biomarkers made a statistically sound and meaningful interpretation of biomarkers for deciding the phase 2 dose difficult.
“In repurposing propranolol,” Dr. Pandey said in the Roswell statement, “we’ve gained important insights on how to manage stress in people with cancer – who can face dangerously elevated levels of mental and physical stress related to their diagnosis and treatment.”
In an interview, one of the two senior authors, Elizabeth Repasky, PhD, professor of oncology and immunology at Roswell Park, said, “it’s exciting that an extremely inexpensive drug like propranolol that could be used in every country around the world could have an impact on cancer by blocking stress, especially chronic stress.” Her murine research showing that adding propranolol to immunotherapy or radiotherapy or chemotherapy improved tumor growth control provided rationale for the current study.
“The breakthrough in this study is that it reveals the immune system as the best target to look at, and shows that what stress reduction is doing is improving a patient’s immune response to his or her own tumor,” Dr. Repasky said. “The mind/body connection is so important, but we have not had a handle on how to study it,” she added.
Further research funded by Herd of Hope grants at Roswell will look at tumor effects of propranolol and nonpharmacological reducers of chronic stress such as exercise, meditation, yoga, and Tai Chi, with first studies in breast cancer.
The study was funded by Roswell Park, private, and NIH grants. The authors had no disclosures.
SOURCE: Gandhi S et al. Clin Cancer Res. 2020 Oct 30. doi: 10.1158/1078-0432.CCR-20-2381
Response rates were high without dose-limiting toxicities in a small phase 1 study that evaluated the addition of propranolol to pembrolizumab in treatment-naive patients with metastatic melanoma.
“To our knowledge, this effort is the,” wrote the two co-first authors, Shipra Gandhi, MD, and Manu Pandey, MBBS, from the Roswell Park Comprehensive Cancer Center, Buffalo, N.Y., and coauthors.
The need for combinations built on anti-PD1 checkpoint inhibitor therapy strategies in metastatic melanoma that safely improve outcomes is underscored by the high (59%) grade 3 or 4 treatment-related adverse event (TRAE) rates when an anti-CTLA4 agent (ipilimumab) was added to an anti-PD-1 agent (nivolumab), they noted. In contrast, a TRAE rate of only 17% has been reported with pembrolizumab monotherapy.
The phase 1b study was stimulated by preclinical, retrospective observations of improved overall survival (OS) in cancer patients treated with beta-blockers. These were preceded by murine melanoma studies showing decreased tumor growth and metastasis with the nonselective beta-blocker propranolol. “Propranolol exerts an antitumor effect,” the authors stated, “by favorably modulating the tumor microenvironment (TME) by decreasing myeloid-derived suppressor cells and increasing CD8+ T-cell and natural killer cells in the TME.” Other research in a melanoma model in chronically-stressed mice has demonstrated synergy between an anti-PD1 antibody and propranolol.
“We know that stress can have a significant negative effect on health, but the extent to which stress may impact the outcome of cancer therapy is not well understood at all,” Dr. Ghandi said in a statement provided by Roswell Park. “We set out to better understand this relationship and to explore its implications for cancer treatment.”
The investigators recruited nine White adults (median age 65 years) with treatment-naive, histologically confirmed unresectable stage III or IV melanoma and Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1 to the open-label, single arm, nonrandomized, single-center, dose-finding study. Patients received standard of care intravenous pembrolizumab 200 mg every 3 weeks and, in three groups, propranolol doses of 10 mg, 20 mg, or 30 mg twice a day until 2 years on study or disease progression or the development of dose-limiting toxicities (DLTs). Assessing the safety and efficacy (overall response rate [ORR] within 6 months of starting therapy) of pembrolizumab with the increasing doses of propranolol and selecting the recommended phase 2 dose were the study’s primary objectives.
Objective responses (complete or partial responses) were reported in seven of the nine patients, with partial tumor responses in two patients in the propranolol 10-mg group, two partial responses in the 20-mg group, and three partial responses in the 30-mg group.
While all patients experienced TRAEs, only one was above grade 2. The most commonly reported TRAEs were fatigue, rash and vitiligo, reported in four of the nine patients. Two patients in the 20-mg twice-a-day group discontinued therapy because of TRAEs (hemophagocytic lymphohistiocytosis and labyrinthitis). No DLTs were observed at any of the three dose levels, and no deaths occurred on study treatment.
The authors said that propranolol 30 mg twice a day was chosen as the recommended phase 2 dose, because in combination with pembrolizumab, there were no DLTs, and preliminary antitumor efficacy was observed in all three patients. Also, in all three patients, the investigators observed a trend toward higher CD8+T-cell percentage, higher ratios of CD8+T-cell/ Treg and CD8+T-cell/ polymorphonuclear myeloid-derived suppressor cells. They underscored, however, that the small size and significant heterogeneity in biomarkers made a statistically sound and meaningful interpretation of biomarkers for deciding the phase 2 dose difficult.
“In repurposing propranolol,” Dr. Pandey said in the Roswell statement, “we’ve gained important insights on how to manage stress in people with cancer – who can face dangerously elevated levels of mental and physical stress related to their diagnosis and treatment.”
In an interview, one of the two senior authors, Elizabeth Repasky, PhD, professor of oncology and immunology at Roswell Park, said, “it’s exciting that an extremely inexpensive drug like propranolol that could be used in every country around the world could have an impact on cancer by blocking stress, especially chronic stress.” Her murine research showing that adding propranolol to immunotherapy or radiotherapy or chemotherapy improved tumor growth control provided rationale for the current study.
“The breakthrough in this study is that it reveals the immune system as the best target to look at, and shows that what stress reduction is doing is improving a patient’s immune response to his or her own tumor,” Dr. Repasky said. “The mind/body connection is so important, but we have not had a handle on how to study it,” she added.
Further research funded by Herd of Hope grants at Roswell will look at tumor effects of propranolol and nonpharmacological reducers of chronic stress such as exercise, meditation, yoga, and Tai Chi, with first studies in breast cancer.
The study was funded by Roswell Park, private, and NIH grants. The authors had no disclosures.
SOURCE: Gandhi S et al. Clin Cancer Res. 2020 Oct 30. doi: 10.1158/1078-0432.CCR-20-2381
FROM CLINICAL CANCER RESEARCH
Air pollution linked to brain amyloid pathology
Higher levels of air pollution were associated with an increased risk for amyloid-beta pathology in a new study of older adults with cognitive impairment. “Many studies have now found a link between air pollution and clinical outcomes of dementia or cognitive decline,” said lead author Leonardo Iaccarino, PhD, Weill Institute for Neurosciences, University of California, San Francisco. “But this study is now showing a clear link between air pollution and a biomarker of Alzheimer’s disease: It shows a relationship between bad air quality and pathology in the brain.
“We believe that exposure to air pollution should be considered as one factor in the lifetime risk of developing Alzheimer’s disease,” he added. “We believe it is a significant determinant. Our results suggest that, if we can reduce occupational and residential exposure to air pollution, then this could help reduce the risk of Alzheimer’s disease.”
The study was published online Nov. 30 in JAMA Neurology.
A modifiable risk factor
Dr. Iaccarino explained that it is well known that air pollution is linked to poor health outcomes. “As well as cardiovascular and respiratory disease, there is also growing interest in the relationship between air pollution and brain health,” he said. “The link is becoming more and more convincing, with evidence from laboratory, animal, and human studies suggesting that individuals exposed to poor air quality have an increased risk of cognitive decline and dementia.”
In addition, this year, the Lancet Commission included air pollution in its updated list of modifiable risk factors for dementia.
For the current study, the researchers analyzed data from the Imaging Dementia–Evidence for Amyloid Scanning (IDEAS) Study, which included more than 18,000 U.S. participants with cognitive impairment who received an amyloid positron-emission tomography scan between 2016 and 2018.
The investigators used data from the IDEAS study to assess the relationship between the air quality at the place of residence of each patient and the likelihood of a positive amyloid PET result. Public records from the U.S. Environmental Protection Agency were used to estimate air quality in individual ZIP-code areas during two periods – 2002-2003 (approximately 14 years before the amyloid PET scan) and 2015-2016 (approximately 1 year before the amyloid PET scan).
Results showed that those living in an area with increased air pollution, as determined using concentrations of predicted fine particulate matter (PM2.5), had a higher probability of a positive amyloid PET scan. This association was dose dependent and statistically significant after adjusting for demographic, lifestyle, and socioeconomic factors as well as medical comorbidities. The association was seen in both periods; the adjusted odds ratio was 1.10 in 2002-2003 and 1.15 in 2015-2016.
“This shows about a 10% increased probability of a positive amyloid test for individuals living in the worst polluted areas, compared with those in the least polluted areas,” Dr. Iaccarino explained.
Every unit increase in PM2.5 in 2002-2003 was associated with an increased probability of positive amyloid findings on PET of 0.5%. Every unit increase in PM2.5 in for the 2015-2016 period was associated with an increased probability of positive amyloid findings on PET of 0.8%.
“This was a very large cohort study, and we adjusted for multiple other factors, so these are pretty robust findings,” Dr. Iaccarino said.
Exposure to higher ozone concentrations was not associated with amyloid positivity on PET scans in either time window.
“These findings suggest that brain amyloid-beta accumulation could be one of the biological pathways in the increased incidence of dementia and cognitive decline associated with exposure to air pollution,” the researchers stated.
A public health concern
“Adverse effects of airborne toxic pollutants associated with amyloid-beta pathology should be considered in public health policy decisions and should inform individual lifetime risk of developing Alzheimer’s disease and dementia,” they concluded.
Dr. Iaccarino noted that, although governments need to take primary action in reducing air pollution, individuals can make some changes to reduce their exposure to poor-quality air.
“Such changes could include not going out or using masks when pollution levels are very high (as happened recently in California with the wildfires) and avoiding areas where the air quality is known to be bad. In addition, there are activities which increase indoor air pollution which can be changed, such as certain types of cooking, cigarette smoking, use of coal fires,” he commented.
“Based on our findings, it would be reasonable to take action on these things, especially for individuals at higher risk of cardiovascular and respiratory disease or Alzheimer’s,” he added.
On a more optimistic note, Dr. Iaccarino pointed out that air quality in the United States has improved significantly in recent years. Meaningful improvements were found between the two periods in this analysis study (2002-2016), “so we are going in the right direction.”
The IDEAS Study was funded by the Alzheimer’s Association, the American College of Radiology, Avid Radiopharmaceuticals, GE Healthcare, and Life Molecular Imaging. Dr. Iaccarino has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Higher levels of air pollution were associated with an increased risk for amyloid-beta pathology in a new study of older adults with cognitive impairment. “Many studies have now found a link between air pollution and clinical outcomes of dementia or cognitive decline,” said lead author Leonardo Iaccarino, PhD, Weill Institute for Neurosciences, University of California, San Francisco. “But this study is now showing a clear link between air pollution and a biomarker of Alzheimer’s disease: It shows a relationship between bad air quality and pathology in the brain.
“We believe that exposure to air pollution should be considered as one factor in the lifetime risk of developing Alzheimer’s disease,” he added. “We believe it is a significant determinant. Our results suggest that, if we can reduce occupational and residential exposure to air pollution, then this could help reduce the risk of Alzheimer’s disease.”
The study was published online Nov. 30 in JAMA Neurology.
A modifiable risk factor
Dr. Iaccarino explained that it is well known that air pollution is linked to poor health outcomes. “As well as cardiovascular and respiratory disease, there is also growing interest in the relationship between air pollution and brain health,” he said. “The link is becoming more and more convincing, with evidence from laboratory, animal, and human studies suggesting that individuals exposed to poor air quality have an increased risk of cognitive decline and dementia.”
In addition, this year, the Lancet Commission included air pollution in its updated list of modifiable risk factors for dementia.
For the current study, the researchers analyzed data from the Imaging Dementia–Evidence for Amyloid Scanning (IDEAS) Study, which included more than 18,000 U.S. participants with cognitive impairment who received an amyloid positron-emission tomography scan between 2016 and 2018.
The investigators used data from the IDEAS study to assess the relationship between the air quality at the place of residence of each patient and the likelihood of a positive amyloid PET result. Public records from the U.S. Environmental Protection Agency were used to estimate air quality in individual ZIP-code areas during two periods – 2002-2003 (approximately 14 years before the amyloid PET scan) and 2015-2016 (approximately 1 year before the amyloid PET scan).
Results showed that those living in an area with increased air pollution, as determined using concentrations of predicted fine particulate matter (PM2.5), had a higher probability of a positive amyloid PET scan. This association was dose dependent and statistically significant after adjusting for demographic, lifestyle, and socioeconomic factors as well as medical comorbidities. The association was seen in both periods; the adjusted odds ratio was 1.10 in 2002-2003 and 1.15 in 2015-2016.
“This shows about a 10% increased probability of a positive amyloid test for individuals living in the worst polluted areas, compared with those in the least polluted areas,” Dr. Iaccarino explained.
Every unit increase in PM2.5 in 2002-2003 was associated with an increased probability of positive amyloid findings on PET of 0.5%. Every unit increase in PM2.5 in for the 2015-2016 period was associated with an increased probability of positive amyloid findings on PET of 0.8%.
“This was a very large cohort study, and we adjusted for multiple other factors, so these are pretty robust findings,” Dr. Iaccarino said.
Exposure to higher ozone concentrations was not associated with amyloid positivity on PET scans in either time window.
“These findings suggest that brain amyloid-beta accumulation could be one of the biological pathways in the increased incidence of dementia and cognitive decline associated with exposure to air pollution,” the researchers stated.
A public health concern
“Adverse effects of airborne toxic pollutants associated with amyloid-beta pathology should be considered in public health policy decisions and should inform individual lifetime risk of developing Alzheimer’s disease and dementia,” they concluded.
Dr. Iaccarino noted that, although governments need to take primary action in reducing air pollution, individuals can make some changes to reduce their exposure to poor-quality air.
“Such changes could include not going out or using masks when pollution levels are very high (as happened recently in California with the wildfires) and avoiding areas where the air quality is known to be bad. In addition, there are activities which increase indoor air pollution which can be changed, such as certain types of cooking, cigarette smoking, use of coal fires,” he commented.
“Based on our findings, it would be reasonable to take action on these things, especially for individuals at higher risk of cardiovascular and respiratory disease or Alzheimer’s,” he added.
On a more optimistic note, Dr. Iaccarino pointed out that air quality in the United States has improved significantly in recent years. Meaningful improvements were found between the two periods in this analysis study (2002-2016), “so we are going in the right direction.”
The IDEAS Study was funded by the Alzheimer’s Association, the American College of Radiology, Avid Radiopharmaceuticals, GE Healthcare, and Life Molecular Imaging. Dr. Iaccarino has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Higher levels of air pollution were associated with an increased risk for amyloid-beta pathology in a new study of older adults with cognitive impairment. “Many studies have now found a link between air pollution and clinical outcomes of dementia or cognitive decline,” said lead author Leonardo Iaccarino, PhD, Weill Institute for Neurosciences, University of California, San Francisco. “But this study is now showing a clear link between air pollution and a biomarker of Alzheimer’s disease: It shows a relationship between bad air quality and pathology in the brain.
“We believe that exposure to air pollution should be considered as one factor in the lifetime risk of developing Alzheimer’s disease,” he added. “We believe it is a significant determinant. Our results suggest that, if we can reduce occupational and residential exposure to air pollution, then this could help reduce the risk of Alzheimer’s disease.”
The study was published online Nov. 30 in JAMA Neurology.
A modifiable risk factor
Dr. Iaccarino explained that it is well known that air pollution is linked to poor health outcomes. “As well as cardiovascular and respiratory disease, there is also growing interest in the relationship between air pollution and brain health,” he said. “The link is becoming more and more convincing, with evidence from laboratory, animal, and human studies suggesting that individuals exposed to poor air quality have an increased risk of cognitive decline and dementia.”
In addition, this year, the Lancet Commission included air pollution in its updated list of modifiable risk factors for dementia.
For the current study, the researchers analyzed data from the Imaging Dementia–Evidence for Amyloid Scanning (IDEAS) Study, which included more than 18,000 U.S. participants with cognitive impairment who received an amyloid positron-emission tomography scan between 2016 and 2018.
The investigators used data from the IDEAS study to assess the relationship between the air quality at the place of residence of each patient and the likelihood of a positive amyloid PET result. Public records from the U.S. Environmental Protection Agency were used to estimate air quality in individual ZIP-code areas during two periods – 2002-2003 (approximately 14 years before the amyloid PET scan) and 2015-2016 (approximately 1 year before the amyloid PET scan).
Results showed that those living in an area with increased air pollution, as determined using concentrations of predicted fine particulate matter (PM2.5), had a higher probability of a positive amyloid PET scan. This association was dose dependent and statistically significant after adjusting for demographic, lifestyle, and socioeconomic factors as well as medical comorbidities. The association was seen in both periods; the adjusted odds ratio was 1.10 in 2002-2003 and 1.15 in 2015-2016.
“This shows about a 10% increased probability of a positive amyloid test for individuals living in the worst polluted areas, compared with those in the least polluted areas,” Dr. Iaccarino explained.
Every unit increase in PM2.5 in 2002-2003 was associated with an increased probability of positive amyloid findings on PET of 0.5%. Every unit increase in PM2.5 in for the 2015-2016 period was associated with an increased probability of positive amyloid findings on PET of 0.8%.
“This was a very large cohort study, and we adjusted for multiple other factors, so these are pretty robust findings,” Dr. Iaccarino said.
Exposure to higher ozone concentrations was not associated with amyloid positivity on PET scans in either time window.
“These findings suggest that brain amyloid-beta accumulation could be one of the biological pathways in the increased incidence of dementia and cognitive decline associated with exposure to air pollution,” the researchers stated.
A public health concern
“Adverse effects of airborne toxic pollutants associated with amyloid-beta pathology should be considered in public health policy decisions and should inform individual lifetime risk of developing Alzheimer’s disease and dementia,” they concluded.
Dr. Iaccarino noted that, although governments need to take primary action in reducing air pollution, individuals can make some changes to reduce their exposure to poor-quality air.
“Such changes could include not going out or using masks when pollution levels are very high (as happened recently in California with the wildfires) and avoiding areas where the air quality is known to be bad. In addition, there are activities which increase indoor air pollution which can be changed, such as certain types of cooking, cigarette smoking, use of coal fires,” he commented.
“Based on our findings, it would be reasonable to take action on these things, especially for individuals at higher risk of cardiovascular and respiratory disease or Alzheimer’s,” he added.
On a more optimistic note, Dr. Iaccarino pointed out that air quality in the United States has improved significantly in recent years. Meaningful improvements were found between the two periods in this analysis study (2002-2016), “so we are going in the right direction.”
The IDEAS Study was funded by the Alzheimer’s Association, the American College of Radiology, Avid Radiopharmaceuticals, GE Healthcare, and Life Molecular Imaging. Dr. Iaccarino has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM JAMA NEUROLOGY
COVID-19 and risk of clotting: ‘Be proactive about prevention’
The risk of arterial and venous thrombosis in patients with COVID-19 has been a major issue throughout the pandemic, and how best to manage this risk is the subject of a new review article.
The article, by Gregory Dr. Piazza, MD, and David A. Morrow, MD, Brigham and Women’s Hospital, Boston, was published online in JAMA on Nov. 23.
“Basically we’re saying: ‘Be proactive about prevention,’” Dr. Piazza told this news organization.
There is growing recognition among those on the frontline that there is an increased risk of thrombosis in COVID-19 patients, Dr. Piazza said. The risk is highest in patients in the intensive care unit, but the risk is also increased in patients hospitalized with COVID-19, even those not in ICU.
“We don’t really know what the risk is in nonhospitalized COVID-19 patients, but we think it’s much lower than in those who are hospitalized,” he said. “We are waiting for data on the optimal way of managing this increased risk of thrombosis in COVID patients, but for the time being, we believe a systematic way of addressing this risk is best, with every patient hospitalized with COVID-19 receiving some type of thromboprophylaxis. This would mainly be with anticoagulation, but in patients in whom anticoagulation is contraindicated, then mechanical methods could be used, such as pneumatic compression boots or compression stockings.”
The authors report thrombotic complication rates of 2.6% in noncritically ill hospitalized patients with COVID-19 and 35.3% in critically ill patients from a recent U.S. registry study.
Autopsy findings of microthrombi in multiple organ systems, including the lungs, heart, and kidneys, suggest that thrombosis may contribute to multisystem organ dysfunction in severe COVID-19, they note. Although the pathophysiology is not fully defined, prothrombotic abnormalities have been identified in patients with COVID-19, including elevated levels of D-dimer, fibrinogen, and factor VIII, they add.
“There are several major questions about which COVID-19 patients to treat with thromboprophylaxis, how to treat them in term of levels of anticoagulation, and there are many ongoing clinical trials to try and answer these questions,” Dr. Piazza commented. “We need results from these randomized trials to provide a better compass for COVID-19 patients at risk of clotting.”
At present, clinicians can follow two different sets of guidelines on the issue, one from the American College of Chest Physicians and the other from the International Society on Thrombosis and Hemostasis, the authors note.
“The ACCP guidelines are very conservative and basically follow the evidence base for medical patients, while the ISTH guidelines are more aggressive and recommend increased levels of anticoagulation in both ICU and hospitalized non-ICU patients and also extend prophylaxis after discharge,” Dr. Piazza said.
“There is quite a difference between the two sets of guidelines, which can be a point of confusion,” he added.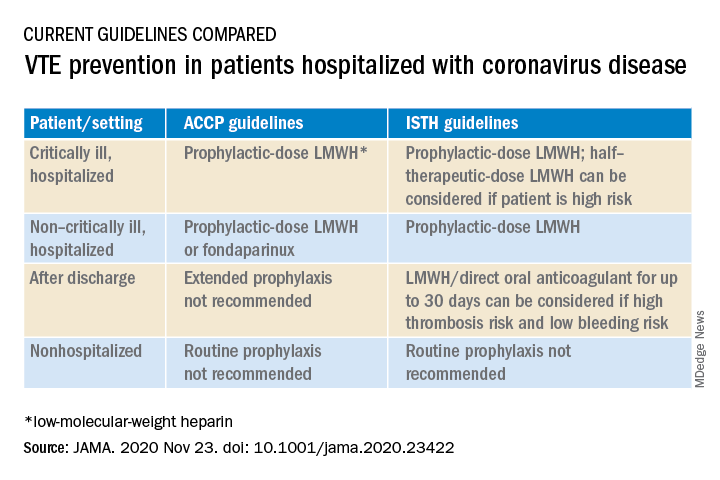
Dr. Piazza notes that at his center every hospitalized COVID patient who does not have a contraindication to anticoagulation receives a standard prophylactic dose of a once-daily low-molecular-weight heparin (for example, enoxaparin 40 mg). A once-daily product is used to minimize infection risk to staff.
While all COVID patients in the ICU should automatically receive some anticoagulation, the optimal dose is an area of active investigation, he explained. “There were several early reports of ICU patients developing blood clots despite receiving standard thromboprophylaxis so perhaps we need to use higher doses. There are trials underway looking at this, and we would advise enrolling patients into these trials.”
If patients can’t be enrolled into trials, and clinicians feel higher anticoagulation levels are needed, Dr. Piazza advises following the ISTH guidance, which allows an intermediate dose of low-molecular-weight heparin (up to 1 mg/kg enoxaparin).
“Some experts are suggesting even higher doses may be needed in some ICU patients, such as the full therapeutic dose, but I worry about the risk of bleeding with such a strategy,” he said.
Dr. Piazza says they do not routinely give anticoagulation after discharge, but if this is desired then patients could be switched to an oral agent, and some of the direct-acting oral anticoagulants are approved for prophylactic use in medically ill patients.
Dr. Piazza points out that whether thromboprophylaxis should be used for nonhospitalized COVID patients who have risk factors for clotting such as a prior history of thrombosis or obesity is a pressing question, and he encourages clinicians to enroll these patients in clinical trials evaluating this issue, such as the PREVENT-HD trial.
“If they can’t enroll patents in a trial, then they have to make a decision whether the patient is high-enough risk to justify off-label use of anticoagulant. There is a case to be made for this, but there is no evidence for or against such action at present,” he noted.
At this time, neither the ISTH nor ACCP recommend measuring D-dimer to screen for venous thromboembolism or to determine intensity of prophylaxis or treatment, the authors note.
“Ongoing investigation will determine optimal preventive regimens in COVID-19 in the intensive care unit, at hospital discharge, and in nonhospitalized patients at high risk for thrombosis,” they conclude.
Dr. Piazza reported grants from Bayer, Bristol Myers Squibb, Boston Scientific, Janssen, and Portola, and personal fees from Agile, Amgen, Pfizer, and the Prairie Education and Research Cooperative outside the submitted work. Dr. Morrow reported grants from Abbott Laboratories, Amgen, Anthos Therapeutics, Esai, GlaxoSmithKline, Takeda, and The Medicines Company; grants and personal fees from AstraZeneca, Merck, Novartis, and Roche Diagnostics; and personal fees from Bayer Pharma and InCarda outside the submitted work.
A version of this article originally appeared on Medscape.com.
The risk of arterial and venous thrombosis in patients with COVID-19 has been a major issue throughout the pandemic, and how best to manage this risk is the subject of a new review article.
The article, by Gregory Dr. Piazza, MD, and David A. Morrow, MD, Brigham and Women’s Hospital, Boston, was published online in JAMA on Nov. 23.
“Basically we’re saying: ‘Be proactive about prevention,’” Dr. Piazza told this news organization.
There is growing recognition among those on the frontline that there is an increased risk of thrombosis in COVID-19 patients, Dr. Piazza said. The risk is highest in patients in the intensive care unit, but the risk is also increased in patients hospitalized with COVID-19, even those not in ICU.
“We don’t really know what the risk is in nonhospitalized COVID-19 patients, but we think it’s much lower than in those who are hospitalized,” he said. “We are waiting for data on the optimal way of managing this increased risk of thrombosis in COVID patients, but for the time being, we believe a systematic way of addressing this risk is best, with every patient hospitalized with COVID-19 receiving some type of thromboprophylaxis. This would mainly be with anticoagulation, but in patients in whom anticoagulation is contraindicated, then mechanical methods could be used, such as pneumatic compression boots or compression stockings.”
The authors report thrombotic complication rates of 2.6% in noncritically ill hospitalized patients with COVID-19 and 35.3% in critically ill patients from a recent U.S. registry study.
Autopsy findings of microthrombi in multiple organ systems, including the lungs, heart, and kidneys, suggest that thrombosis may contribute to multisystem organ dysfunction in severe COVID-19, they note. Although the pathophysiology is not fully defined, prothrombotic abnormalities have been identified in patients with COVID-19, including elevated levels of D-dimer, fibrinogen, and factor VIII, they add.
“There are several major questions about which COVID-19 patients to treat with thromboprophylaxis, how to treat them in term of levels of anticoagulation, and there are many ongoing clinical trials to try and answer these questions,” Dr. Piazza commented. “We need results from these randomized trials to provide a better compass for COVID-19 patients at risk of clotting.”
At present, clinicians can follow two different sets of guidelines on the issue, one from the American College of Chest Physicians and the other from the International Society on Thrombosis and Hemostasis, the authors note.
“The ACCP guidelines are very conservative and basically follow the evidence base for medical patients, while the ISTH guidelines are more aggressive and recommend increased levels of anticoagulation in both ICU and hospitalized non-ICU patients and also extend prophylaxis after discharge,” Dr. Piazza said.
“There is quite a difference between the two sets of guidelines, which can be a point of confusion,” he added.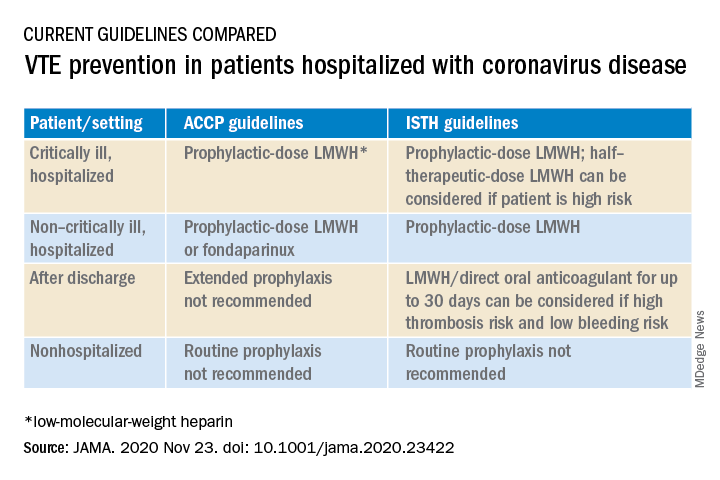
Dr. Piazza notes that at his center every hospitalized COVID patient who does not have a contraindication to anticoagulation receives a standard prophylactic dose of a once-daily low-molecular-weight heparin (for example, enoxaparin 40 mg). A once-daily product is used to minimize infection risk to staff.
While all COVID patients in the ICU should automatically receive some anticoagulation, the optimal dose is an area of active investigation, he explained. “There were several early reports of ICU patients developing blood clots despite receiving standard thromboprophylaxis so perhaps we need to use higher doses. There are trials underway looking at this, and we would advise enrolling patients into these trials.”
If patients can’t be enrolled into trials, and clinicians feel higher anticoagulation levels are needed, Dr. Piazza advises following the ISTH guidance, which allows an intermediate dose of low-molecular-weight heparin (up to 1 mg/kg enoxaparin).
“Some experts are suggesting even higher doses may be needed in some ICU patients, such as the full therapeutic dose, but I worry about the risk of bleeding with such a strategy,” he said.
Dr. Piazza says they do not routinely give anticoagulation after discharge, but if this is desired then patients could be switched to an oral agent, and some of the direct-acting oral anticoagulants are approved for prophylactic use in medically ill patients.
Dr. Piazza points out that whether thromboprophylaxis should be used for nonhospitalized COVID patients who have risk factors for clotting such as a prior history of thrombosis or obesity is a pressing question, and he encourages clinicians to enroll these patients in clinical trials evaluating this issue, such as the PREVENT-HD trial.
“If they can’t enroll patents in a trial, then they have to make a decision whether the patient is high-enough risk to justify off-label use of anticoagulant. There is a case to be made for this, but there is no evidence for or against such action at present,” he noted.
At this time, neither the ISTH nor ACCP recommend measuring D-dimer to screen for venous thromboembolism or to determine intensity of prophylaxis or treatment, the authors note.
“Ongoing investigation will determine optimal preventive regimens in COVID-19 in the intensive care unit, at hospital discharge, and in nonhospitalized patients at high risk for thrombosis,” they conclude.
Dr. Piazza reported grants from Bayer, Bristol Myers Squibb, Boston Scientific, Janssen, and Portola, and personal fees from Agile, Amgen, Pfizer, and the Prairie Education and Research Cooperative outside the submitted work. Dr. Morrow reported grants from Abbott Laboratories, Amgen, Anthos Therapeutics, Esai, GlaxoSmithKline, Takeda, and The Medicines Company; grants and personal fees from AstraZeneca, Merck, Novartis, and Roche Diagnostics; and personal fees from Bayer Pharma and InCarda outside the submitted work.
A version of this article originally appeared on Medscape.com.
The risk of arterial and venous thrombosis in patients with COVID-19 has been a major issue throughout the pandemic, and how best to manage this risk is the subject of a new review article.
The article, by Gregory Dr. Piazza, MD, and David A. Morrow, MD, Brigham and Women’s Hospital, Boston, was published online in JAMA on Nov. 23.
“Basically we’re saying: ‘Be proactive about prevention,’” Dr. Piazza told this news organization.
There is growing recognition among those on the frontline that there is an increased risk of thrombosis in COVID-19 patients, Dr. Piazza said. The risk is highest in patients in the intensive care unit, but the risk is also increased in patients hospitalized with COVID-19, even those not in ICU.
“We don’t really know what the risk is in nonhospitalized COVID-19 patients, but we think it’s much lower than in those who are hospitalized,” he said. “We are waiting for data on the optimal way of managing this increased risk of thrombosis in COVID patients, but for the time being, we believe a systematic way of addressing this risk is best, with every patient hospitalized with COVID-19 receiving some type of thromboprophylaxis. This would mainly be with anticoagulation, but in patients in whom anticoagulation is contraindicated, then mechanical methods could be used, such as pneumatic compression boots or compression stockings.”
The authors report thrombotic complication rates of 2.6% in noncritically ill hospitalized patients with COVID-19 and 35.3% in critically ill patients from a recent U.S. registry study.
Autopsy findings of microthrombi in multiple organ systems, including the lungs, heart, and kidneys, suggest that thrombosis may contribute to multisystem organ dysfunction in severe COVID-19, they note. Although the pathophysiology is not fully defined, prothrombotic abnormalities have been identified in patients with COVID-19, including elevated levels of D-dimer, fibrinogen, and factor VIII, they add.
“There are several major questions about which COVID-19 patients to treat with thromboprophylaxis, how to treat them in term of levels of anticoagulation, and there are many ongoing clinical trials to try and answer these questions,” Dr. Piazza commented. “We need results from these randomized trials to provide a better compass for COVID-19 patients at risk of clotting.”
At present, clinicians can follow two different sets of guidelines on the issue, one from the American College of Chest Physicians and the other from the International Society on Thrombosis and Hemostasis, the authors note.
“The ACCP guidelines are very conservative and basically follow the evidence base for medical patients, while the ISTH guidelines are more aggressive and recommend increased levels of anticoagulation in both ICU and hospitalized non-ICU patients and also extend prophylaxis after discharge,” Dr. Piazza said.
“There is quite a difference between the two sets of guidelines, which can be a point of confusion,” he added.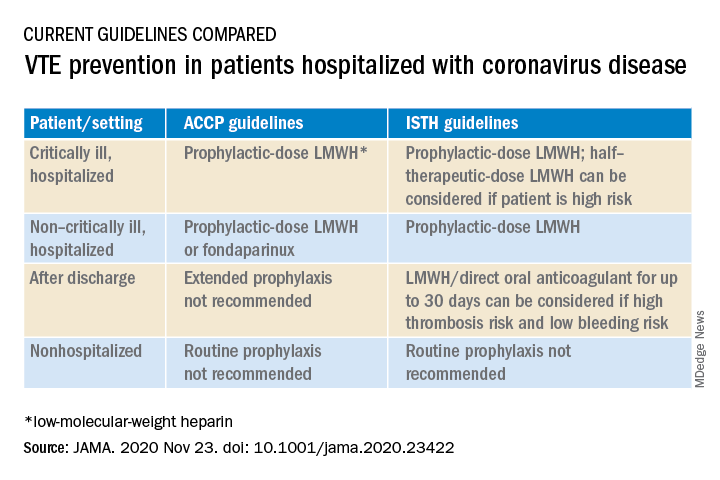
Dr. Piazza notes that at his center every hospitalized COVID patient who does not have a contraindication to anticoagulation receives a standard prophylactic dose of a once-daily low-molecular-weight heparin (for example, enoxaparin 40 mg). A once-daily product is used to minimize infection risk to staff.
While all COVID patients in the ICU should automatically receive some anticoagulation, the optimal dose is an area of active investigation, he explained. “There were several early reports of ICU patients developing blood clots despite receiving standard thromboprophylaxis so perhaps we need to use higher doses. There are trials underway looking at this, and we would advise enrolling patients into these trials.”
If patients can’t be enrolled into trials, and clinicians feel higher anticoagulation levels are needed, Dr. Piazza advises following the ISTH guidance, which allows an intermediate dose of low-molecular-weight heparin (up to 1 mg/kg enoxaparin).
“Some experts are suggesting even higher doses may be needed in some ICU patients, such as the full therapeutic dose, but I worry about the risk of bleeding with such a strategy,” he said.
Dr. Piazza says they do not routinely give anticoagulation after discharge, but if this is desired then patients could be switched to an oral agent, and some of the direct-acting oral anticoagulants are approved for prophylactic use in medically ill patients.
Dr. Piazza points out that whether thromboprophylaxis should be used for nonhospitalized COVID patients who have risk factors for clotting such as a prior history of thrombosis or obesity is a pressing question, and he encourages clinicians to enroll these patients in clinical trials evaluating this issue, such as the PREVENT-HD trial.
“If they can’t enroll patents in a trial, then they have to make a decision whether the patient is high-enough risk to justify off-label use of anticoagulant. There is a case to be made for this, but there is no evidence for or against such action at present,” he noted.
At this time, neither the ISTH nor ACCP recommend measuring D-dimer to screen for venous thromboembolism or to determine intensity of prophylaxis or treatment, the authors note.
“Ongoing investigation will determine optimal preventive regimens in COVID-19 in the intensive care unit, at hospital discharge, and in nonhospitalized patients at high risk for thrombosis,” they conclude.
Dr. Piazza reported grants from Bayer, Bristol Myers Squibb, Boston Scientific, Janssen, and Portola, and personal fees from Agile, Amgen, Pfizer, and the Prairie Education and Research Cooperative outside the submitted work. Dr. Morrow reported grants from Abbott Laboratories, Amgen, Anthos Therapeutics, Esai, GlaxoSmithKline, Takeda, and The Medicines Company; grants and personal fees from AstraZeneca, Merck, Novartis, and Roche Diagnostics; and personal fees from Bayer Pharma and InCarda outside the submitted work.
A version of this article originally appeared on Medscape.com.
Oral steroids benefit patients with cluster headache
Adjunctive oral prednisone appears to significantly reduce cluster headache attacks, new research shows. Results of the multicenter, randomized, double-blind trial show that patients who received the steroid had 25% fewer attacks in the first week of therapy, compared with their counterparts who received placebo.
In addition, more than a third of patients in the prednisone group were pain free, and for almost half, headache frequency was reduced by at least 50% at day 7 of treatment.
These findings provide clear evidence that prednisone, in conjunction with the use of verapamil, is effective in cluster headache, said lead author Mark Obermann, MD, director, Center for Neurology, Asklepios Hospitals Seesen (Germany), and associate professor, University of Duisburg-Essen (Germany).
The key message, he added, is that all patients with cluster headache should receive prednisone at the start of an episode.
The study was published online Nov. 24 in the Lancet Neurology.
‘Suicide headaches’
Cluster headaches are intense unilateral attacks of facial and head pain. They last 15-180 minutes and predominantly affect men. They are accompanied by trigeminal autonomic symptoms and are extremely painful. “They’re referred to as ‘suicide headaches’ because the pain is so severe that patients often report they think about killing themselves to get rid of the pain,” said Dr. Obermann.
The cause is unclear, although there is some evidence that the hypothalamus is involved. The headaches sometimes follow a “strict circadian pattern,” said Dr. Obermann. He noted that the attacks might occur over a few weeks or months and then not return for months or even years.
An estimated 1 in 1,000 people experience cluster headache, but the condition is underrecognized, and research is scarce and poorly funded. Previous research does show that the calcium channel blocker verapamil, which is used to treat high blood pressure, is effective in cluster headache. However, it takes about 14 days to work and has to be slowly titrated because of cardiac side effects, said Dr. Obermann. For these reasons, international guidelines recommend initiating short-term preventive treatment with corticosteroids to suppress, or at least lessen, cluster headache attacks until long-term prevention is effective.
Although some clinicians treat cluster headaches with corticosteroids, others don’t because of a lack of evidence that shows they are effective. “There’s no evidence whatsoever on what the correct dose is or whether it helps at all. This is the gap we wanted to close,” said Dr. Obermann.
The study included 116 adult patients with cluster headache from 10 centers who were experiencing a cluster headache episode and were not taking prophylactic medication.
The trial only included patients who had an attack within 30 days of their current episode. The investigators included this restriction to reduce the possibility of spontaneous remission, which is “a big problem” in cluster headache trials, he said. To confirm that episodes were cluster headache attacks, patients were also required to have moderate to severe pain, indicated by a score of at least 5 on a numerical rating scale in which 0 indicates no pain and 10 indicates the worse imaginable pain.
Participants were allowed to use treatments for acute attack, but these therapies were limited to triptans, high-flow oxygen, intranasal lidocaine, ergotamine, and oral analgesics.
Debilitating pain
Patients were randomly assigned to receive oral prednisone (n = 53) or placebo (n = 56). The study groups were matched with respect to demographic and clinical characteristics. Prednisone was initiated at 100 mg/d for 5 days and was then tapered by 20 mg every 3 days in the active-treatment group. All patients also received oral verapamil at a starting dose of 40 mg three times per day. The dose was increased every 3 days by 40 mg to a maximum of 360 mg/d.
All participants received pantoprazole 20 mg to prevent the gastric side effects of prednisone. An attack was defined as a unilateral headache of moderate to severe intensity. The study lasted 28 days.
The study’s primary outcome was the mean number of cluster headache attacks during the first week of treatment with prednisone versus placebo.
The mean number of attacks during the first week of treatment was 7.1 in the prednisone group and 9.5 in the placebo group, for a difference of –2.4 attacks (95% confidence interval, –4.8 to –0.03; P = .002). “This might not sound like much,” but reducing the number of daily attacks from, say, eight to six “really makes a difference because the attacks are so painful,” said Dr. Obermann.
The prednisone group also came out on top for a number secondary outcomes. After the first 7 days, attacks ceased in 35% of the prednisone group versus 7% in the placebo group.
‘Clear evidence’ of efficacy
About 49% of patients who took prednisone reported a reduction of at least 50% in attack frequency at day 7. By comparison, 15% of patients who received placebo reported such a reduction. The number of cluster attacks at day 28 was less in the prednisone group than in the patients who received placebo.
With respect to treatment effect, the difference between prednisone and placebo gradually lessened over time “in parallel to the verapamil dose reaching its therapeutic effect,” the investigators noted. “Therefore, attack frequency reduction slowly converged between groups,” they added.
The study results provide “clear evidence” and should reassure clinicians that short-term prednisone early in a cluster headache attack is effective, said Dr. Obermann.
Adverse events, which included headache, palpitations, dizziness, and nausea, were as expected and were similar in the two groups. There were only two severe adverse events, both of which occurred in participants in the placebo group.
Dr. Obermann said the investigators were surprised that so many patients in the study were taking analgesics. “Analgesics don’t work in cluster headache; they just don’t work in this kind of pain.”
He noted that prednisone exposure of study patients spanned only 19 days and amounted to only 1,100 mg, which he believes is safe.
The prednisone dose used in the study is “what most clinicians use in clinical practice,” although there have been reports of success using 500 mg of IV prednisone over 5 days, said Dr. Obermann. He added that it would be “interesting to see if 50 mg would be just as good” as a starting dose.
Potential limitations of the study include the fact that the majority of participants were White, so the findings may not be generalizable to other populations.
Long-awaited results
In an accompanying editorial, Anne Ducros, MD, PhD, professor of neurology and director of the Headache Center, Montpellier (France) University Hospital, said the study provides “strong and long-awaited evidence supporting the use of oral steroids as a transitional treatment option.”
The trial “raises many topics for future research,” one of which is the long-term safety of prednisone for patients with cluster headache, said Dr. Ducros. She noted that use of high-dose steroids once or twice a year for 15 years or more “has the potential for severe systemic toxic effects,” such as corticosteroid-induced osteonecrosis of the femoral head.
Other questions about corticosteroid use for patients with cluster headache remain. These include understanding whether these agents provide better efficacy than occipital nerve injections and determining the optimal verapamil regimen, she noted.
In addition, the risk for oral steroid misuse needs to be studied, she said. She noted that drug misuse is common among patients with cluster headache.
Despite these questions, the results of this new study “provide an important step forward for patients with cluster headache, for whom safe and effective transitional therapies are much needed,” Dr. Ducros wrote.
Dr. Obermann has received fees from Sanofi, Biogen, Novartis, Teva Pharmaceuticals, and Eli Lilly and grants from Allergan and Heel Pharmaceuticals outside of this work. Dr. Ducros has received fees from Amgen, Novartis, Teva, and Eli Lilly; grants from the Programme Hospitalier de Recherche Clinique and from the Appel d’Offre Interne of Montpellier University Hospital; and nonfinancial support from SOS Oxygene.
A version of this article originally appeared on Medscape.com.
Adjunctive oral prednisone appears to significantly reduce cluster headache attacks, new research shows. Results of the multicenter, randomized, double-blind trial show that patients who received the steroid had 25% fewer attacks in the first week of therapy, compared with their counterparts who received placebo.
In addition, more than a third of patients in the prednisone group were pain free, and for almost half, headache frequency was reduced by at least 50% at day 7 of treatment.
These findings provide clear evidence that prednisone, in conjunction with the use of verapamil, is effective in cluster headache, said lead author Mark Obermann, MD, director, Center for Neurology, Asklepios Hospitals Seesen (Germany), and associate professor, University of Duisburg-Essen (Germany).
The key message, he added, is that all patients with cluster headache should receive prednisone at the start of an episode.
The study was published online Nov. 24 in the Lancet Neurology.
‘Suicide headaches’
Cluster headaches are intense unilateral attacks of facial and head pain. They last 15-180 minutes and predominantly affect men. They are accompanied by trigeminal autonomic symptoms and are extremely painful. “They’re referred to as ‘suicide headaches’ because the pain is so severe that patients often report they think about killing themselves to get rid of the pain,” said Dr. Obermann.
The cause is unclear, although there is some evidence that the hypothalamus is involved. The headaches sometimes follow a “strict circadian pattern,” said Dr. Obermann. He noted that the attacks might occur over a few weeks or months and then not return for months or even years.
An estimated 1 in 1,000 people experience cluster headache, but the condition is underrecognized, and research is scarce and poorly funded. Previous research does show that the calcium channel blocker verapamil, which is used to treat high blood pressure, is effective in cluster headache. However, it takes about 14 days to work and has to be slowly titrated because of cardiac side effects, said Dr. Obermann. For these reasons, international guidelines recommend initiating short-term preventive treatment with corticosteroids to suppress, or at least lessen, cluster headache attacks until long-term prevention is effective.
Although some clinicians treat cluster headaches with corticosteroids, others don’t because of a lack of evidence that shows they are effective. “There’s no evidence whatsoever on what the correct dose is or whether it helps at all. This is the gap we wanted to close,” said Dr. Obermann.
The study included 116 adult patients with cluster headache from 10 centers who were experiencing a cluster headache episode and were not taking prophylactic medication.
The trial only included patients who had an attack within 30 days of their current episode. The investigators included this restriction to reduce the possibility of spontaneous remission, which is “a big problem” in cluster headache trials, he said. To confirm that episodes were cluster headache attacks, patients were also required to have moderate to severe pain, indicated by a score of at least 5 on a numerical rating scale in which 0 indicates no pain and 10 indicates the worse imaginable pain.
Participants were allowed to use treatments for acute attack, but these therapies were limited to triptans, high-flow oxygen, intranasal lidocaine, ergotamine, and oral analgesics.
Debilitating pain
Patients were randomly assigned to receive oral prednisone (n = 53) or placebo (n = 56). The study groups were matched with respect to demographic and clinical characteristics. Prednisone was initiated at 100 mg/d for 5 days and was then tapered by 20 mg every 3 days in the active-treatment group. All patients also received oral verapamil at a starting dose of 40 mg three times per day. The dose was increased every 3 days by 40 mg to a maximum of 360 mg/d.
All participants received pantoprazole 20 mg to prevent the gastric side effects of prednisone. An attack was defined as a unilateral headache of moderate to severe intensity. The study lasted 28 days.
The study’s primary outcome was the mean number of cluster headache attacks during the first week of treatment with prednisone versus placebo.
The mean number of attacks during the first week of treatment was 7.1 in the prednisone group and 9.5 in the placebo group, for a difference of –2.4 attacks (95% confidence interval, –4.8 to –0.03; P = .002). “This might not sound like much,” but reducing the number of daily attacks from, say, eight to six “really makes a difference because the attacks are so painful,” said Dr. Obermann.
The prednisone group also came out on top for a number secondary outcomes. After the first 7 days, attacks ceased in 35% of the prednisone group versus 7% in the placebo group.
‘Clear evidence’ of efficacy
About 49% of patients who took prednisone reported a reduction of at least 50% in attack frequency at day 7. By comparison, 15% of patients who received placebo reported such a reduction. The number of cluster attacks at day 28 was less in the prednisone group than in the patients who received placebo.
With respect to treatment effect, the difference between prednisone and placebo gradually lessened over time “in parallel to the verapamil dose reaching its therapeutic effect,” the investigators noted. “Therefore, attack frequency reduction slowly converged between groups,” they added.
The study results provide “clear evidence” and should reassure clinicians that short-term prednisone early in a cluster headache attack is effective, said Dr. Obermann.
Adverse events, which included headache, palpitations, dizziness, and nausea, were as expected and were similar in the two groups. There were only two severe adverse events, both of which occurred in participants in the placebo group.
Dr. Obermann said the investigators were surprised that so many patients in the study were taking analgesics. “Analgesics don’t work in cluster headache; they just don’t work in this kind of pain.”
He noted that prednisone exposure of study patients spanned only 19 days and amounted to only 1,100 mg, which he believes is safe.
The prednisone dose used in the study is “what most clinicians use in clinical practice,” although there have been reports of success using 500 mg of IV prednisone over 5 days, said Dr. Obermann. He added that it would be “interesting to see if 50 mg would be just as good” as a starting dose.
Potential limitations of the study include the fact that the majority of participants were White, so the findings may not be generalizable to other populations.
Long-awaited results
In an accompanying editorial, Anne Ducros, MD, PhD, professor of neurology and director of the Headache Center, Montpellier (France) University Hospital, said the study provides “strong and long-awaited evidence supporting the use of oral steroids as a transitional treatment option.”
The trial “raises many topics for future research,” one of which is the long-term safety of prednisone for patients with cluster headache, said Dr. Ducros. She noted that use of high-dose steroids once or twice a year for 15 years or more “has the potential for severe systemic toxic effects,” such as corticosteroid-induced osteonecrosis of the femoral head.
Other questions about corticosteroid use for patients with cluster headache remain. These include understanding whether these agents provide better efficacy than occipital nerve injections and determining the optimal verapamil regimen, she noted.
In addition, the risk for oral steroid misuse needs to be studied, she said. She noted that drug misuse is common among patients with cluster headache.
Despite these questions, the results of this new study “provide an important step forward for patients with cluster headache, for whom safe and effective transitional therapies are much needed,” Dr. Ducros wrote.
Dr. Obermann has received fees from Sanofi, Biogen, Novartis, Teva Pharmaceuticals, and Eli Lilly and grants from Allergan and Heel Pharmaceuticals outside of this work. Dr. Ducros has received fees from Amgen, Novartis, Teva, and Eli Lilly; grants from the Programme Hospitalier de Recherche Clinique and from the Appel d’Offre Interne of Montpellier University Hospital; and nonfinancial support from SOS Oxygene.
A version of this article originally appeared on Medscape.com.
Adjunctive oral prednisone appears to significantly reduce cluster headache attacks, new research shows. Results of the multicenter, randomized, double-blind trial show that patients who received the steroid had 25% fewer attacks in the first week of therapy, compared with their counterparts who received placebo.
In addition, more than a third of patients in the prednisone group were pain free, and for almost half, headache frequency was reduced by at least 50% at day 7 of treatment.
These findings provide clear evidence that prednisone, in conjunction with the use of verapamil, is effective in cluster headache, said lead author Mark Obermann, MD, director, Center for Neurology, Asklepios Hospitals Seesen (Germany), and associate professor, University of Duisburg-Essen (Germany).
The key message, he added, is that all patients with cluster headache should receive prednisone at the start of an episode.
The study was published online Nov. 24 in the Lancet Neurology.
‘Suicide headaches’
Cluster headaches are intense unilateral attacks of facial and head pain. They last 15-180 minutes and predominantly affect men. They are accompanied by trigeminal autonomic symptoms and are extremely painful. “They’re referred to as ‘suicide headaches’ because the pain is so severe that patients often report they think about killing themselves to get rid of the pain,” said Dr. Obermann.
The cause is unclear, although there is some evidence that the hypothalamus is involved. The headaches sometimes follow a “strict circadian pattern,” said Dr. Obermann. He noted that the attacks might occur over a few weeks or months and then not return for months or even years.
An estimated 1 in 1,000 people experience cluster headache, but the condition is underrecognized, and research is scarce and poorly funded. Previous research does show that the calcium channel blocker verapamil, which is used to treat high blood pressure, is effective in cluster headache. However, it takes about 14 days to work and has to be slowly titrated because of cardiac side effects, said Dr. Obermann. For these reasons, international guidelines recommend initiating short-term preventive treatment with corticosteroids to suppress, or at least lessen, cluster headache attacks until long-term prevention is effective.
Although some clinicians treat cluster headaches with corticosteroids, others don’t because of a lack of evidence that shows they are effective. “There’s no evidence whatsoever on what the correct dose is or whether it helps at all. This is the gap we wanted to close,” said Dr. Obermann.
The study included 116 adult patients with cluster headache from 10 centers who were experiencing a cluster headache episode and were not taking prophylactic medication.
The trial only included patients who had an attack within 30 days of their current episode. The investigators included this restriction to reduce the possibility of spontaneous remission, which is “a big problem” in cluster headache trials, he said. To confirm that episodes were cluster headache attacks, patients were also required to have moderate to severe pain, indicated by a score of at least 5 on a numerical rating scale in which 0 indicates no pain and 10 indicates the worse imaginable pain.
Participants were allowed to use treatments for acute attack, but these therapies were limited to triptans, high-flow oxygen, intranasal lidocaine, ergotamine, and oral analgesics.
Debilitating pain
Patients were randomly assigned to receive oral prednisone (n = 53) or placebo (n = 56). The study groups were matched with respect to demographic and clinical characteristics. Prednisone was initiated at 100 mg/d for 5 days and was then tapered by 20 mg every 3 days in the active-treatment group. All patients also received oral verapamil at a starting dose of 40 mg three times per day. The dose was increased every 3 days by 40 mg to a maximum of 360 mg/d.
All participants received pantoprazole 20 mg to prevent the gastric side effects of prednisone. An attack was defined as a unilateral headache of moderate to severe intensity. The study lasted 28 days.
The study’s primary outcome was the mean number of cluster headache attacks during the first week of treatment with prednisone versus placebo.
The mean number of attacks during the first week of treatment was 7.1 in the prednisone group and 9.5 in the placebo group, for a difference of –2.4 attacks (95% confidence interval, –4.8 to –0.03; P = .002). “This might not sound like much,” but reducing the number of daily attacks from, say, eight to six “really makes a difference because the attacks are so painful,” said Dr. Obermann.
The prednisone group also came out on top for a number secondary outcomes. After the first 7 days, attacks ceased in 35% of the prednisone group versus 7% in the placebo group.
‘Clear evidence’ of efficacy
About 49% of patients who took prednisone reported a reduction of at least 50% in attack frequency at day 7. By comparison, 15% of patients who received placebo reported such a reduction. The number of cluster attacks at day 28 was less in the prednisone group than in the patients who received placebo.
With respect to treatment effect, the difference between prednisone and placebo gradually lessened over time “in parallel to the verapamil dose reaching its therapeutic effect,” the investigators noted. “Therefore, attack frequency reduction slowly converged between groups,” they added.
The study results provide “clear evidence” and should reassure clinicians that short-term prednisone early in a cluster headache attack is effective, said Dr. Obermann.
Adverse events, which included headache, palpitations, dizziness, and nausea, were as expected and were similar in the two groups. There were only two severe adverse events, both of which occurred in participants in the placebo group.
Dr. Obermann said the investigators were surprised that so many patients in the study were taking analgesics. “Analgesics don’t work in cluster headache; they just don’t work in this kind of pain.”
He noted that prednisone exposure of study patients spanned only 19 days and amounted to only 1,100 mg, which he believes is safe.
The prednisone dose used in the study is “what most clinicians use in clinical practice,” although there have been reports of success using 500 mg of IV prednisone over 5 days, said Dr. Obermann. He added that it would be “interesting to see if 50 mg would be just as good” as a starting dose.
Potential limitations of the study include the fact that the majority of participants were White, so the findings may not be generalizable to other populations.
Long-awaited results
In an accompanying editorial, Anne Ducros, MD, PhD, professor of neurology and director of the Headache Center, Montpellier (France) University Hospital, said the study provides “strong and long-awaited evidence supporting the use of oral steroids as a transitional treatment option.”
The trial “raises many topics for future research,” one of which is the long-term safety of prednisone for patients with cluster headache, said Dr. Ducros. She noted that use of high-dose steroids once or twice a year for 15 years or more “has the potential for severe systemic toxic effects,” such as corticosteroid-induced osteonecrosis of the femoral head.
Other questions about corticosteroid use for patients with cluster headache remain. These include understanding whether these agents provide better efficacy than occipital nerve injections and determining the optimal verapamil regimen, she noted.
In addition, the risk for oral steroid misuse needs to be studied, she said. She noted that drug misuse is common among patients with cluster headache.
Despite these questions, the results of this new study “provide an important step forward for patients with cluster headache, for whom safe and effective transitional therapies are much needed,” Dr. Ducros wrote.
Dr. Obermann has received fees from Sanofi, Biogen, Novartis, Teva Pharmaceuticals, and Eli Lilly and grants from Allergan and Heel Pharmaceuticals outside of this work. Dr. Ducros has received fees from Amgen, Novartis, Teva, and Eli Lilly; grants from the Programme Hospitalier de Recherche Clinique and from the Appel d’Offre Interne of Montpellier University Hospital; and nonfinancial support from SOS Oxygene.
A version of this article originally appeared on Medscape.com.
New residency matching sets record, says NRMP
beginning in 2021, the NRMP reported.
“Specifically, the 2020 MSMP included 6,847 applicants submitting certified rank order lists (an 8.9% increase), 2042 programs submitting certified rank order lists (a 4.3% increase), 5,734 positions (a 2.8% increase), and 5,208 positions filled (a 6.1% increase),” according to a news release.
The MSMP now includes 14 internal medicine subspecialties and four sub-subspecialties. The MSMP offered 5,734 positions this year, and 5,208 (90.8%) were successfully filled. That represents an increase of almost 3 percentage points, compared with last year’s results.
Among those subspecialties that offered 30 positions or more, the most competitive were allergy and immunology, cardiovascular disease, clinical cardiac electrophysiology, gastroenterology, hematology and oncology, and pulmonary/critical care. Each of those filled at least 95% of available slots. More than half of the positions were filled by U.S. MDs.
By contrast, the least competitive subspecialties were geriatric medicine and nephrology. Programs in these two fields filled less than 75% of positions offered. Less than 45% were filled by U.S. MDs.
More than 76% of the 6,847 applicants who submitted rank order lists (5,208) matched into residency programs.
The number of U.S. MDs in this category increased nearly 7% over last year, with a total of 2,935. The number of DO graduates increased as well, with a total of 855, which was 9.6% more than the previous year.
More U.S. citizens who graduated from international medical schools matched this year as well; 1,087 placed into subspecialty residency, a 9% increase, compared with last year.
A version of this article originally appeared on Medscape.com.
beginning in 2021, the NRMP reported.
“Specifically, the 2020 MSMP included 6,847 applicants submitting certified rank order lists (an 8.9% increase), 2042 programs submitting certified rank order lists (a 4.3% increase), 5,734 positions (a 2.8% increase), and 5,208 positions filled (a 6.1% increase),” according to a news release.
The MSMP now includes 14 internal medicine subspecialties and four sub-subspecialties. The MSMP offered 5,734 positions this year, and 5,208 (90.8%) were successfully filled. That represents an increase of almost 3 percentage points, compared with last year’s results.
Among those subspecialties that offered 30 positions or more, the most competitive were allergy and immunology, cardiovascular disease, clinical cardiac electrophysiology, gastroenterology, hematology and oncology, and pulmonary/critical care. Each of those filled at least 95% of available slots. More than half of the positions were filled by U.S. MDs.
By contrast, the least competitive subspecialties were geriatric medicine and nephrology. Programs in these two fields filled less than 75% of positions offered. Less than 45% were filled by U.S. MDs.
More than 76% of the 6,847 applicants who submitted rank order lists (5,208) matched into residency programs.
The number of U.S. MDs in this category increased nearly 7% over last year, with a total of 2,935. The number of DO graduates increased as well, with a total of 855, which was 9.6% more than the previous year.
More U.S. citizens who graduated from international medical schools matched this year as well; 1,087 placed into subspecialty residency, a 9% increase, compared with last year.
A version of this article originally appeared on Medscape.com.
beginning in 2021, the NRMP reported.
“Specifically, the 2020 MSMP included 6,847 applicants submitting certified rank order lists (an 8.9% increase), 2042 programs submitting certified rank order lists (a 4.3% increase), 5,734 positions (a 2.8% increase), and 5,208 positions filled (a 6.1% increase),” according to a news release.
The MSMP now includes 14 internal medicine subspecialties and four sub-subspecialties. The MSMP offered 5,734 positions this year, and 5,208 (90.8%) were successfully filled. That represents an increase of almost 3 percentage points, compared with last year’s results.
Among those subspecialties that offered 30 positions or more, the most competitive were allergy and immunology, cardiovascular disease, clinical cardiac electrophysiology, gastroenterology, hematology and oncology, and pulmonary/critical care. Each of those filled at least 95% of available slots. More than half of the positions were filled by U.S. MDs.
By contrast, the least competitive subspecialties were geriatric medicine and nephrology. Programs in these two fields filled less than 75% of positions offered. Less than 45% were filled by U.S. MDs.
More than 76% of the 6,847 applicants who submitted rank order lists (5,208) matched into residency programs.
The number of U.S. MDs in this category increased nearly 7% over last year, with a total of 2,935. The number of DO graduates increased as well, with a total of 855, which was 9.6% more than the previous year.
More U.S. citizens who graduated from international medical schools matched this year as well; 1,087 placed into subspecialty residency, a 9% increase, compared with last year.
A version of this article originally appeared on Medscape.com.
COVID-19 fuels surge in overdose-related cardiac arrests
There has been a sharp increase in overdose-related cardiac arrests in the United States during the COVID-19 pandemic, a new analysis shows.
Overall rates in 2020 were elevated above the baseline from 2018 and 2019 by about 50%, the data show.
and efforts to combat the COVID-19 pandemic have not been effective at reducing overdoses,” Joseph Friedman, MPH, MD/PhD student, medical scientist training program, University of California, Los Angeles, said in an interview.
“We need to invest heavily in substance use treatment, harm reduction, and the structural drivers of overdose as core elements of the COVID-19 response,” said Mr. Friedman, who coauthored the study with UCLA colleague David Schriger, MD, MPH, and Leo Beletsky, JD, MPH, Northeastern University, Boston.
The study was published as a research letter Dec. 3 in JAMA Psychiatry.
Social isolation a key driver
Emergency medical services (EMS) data are available in near real time, providing a novel source of up-to-date information to monitor epidemiological shifts during the COVID-19 pandemic.
For the study, the researchers leveraged data from the National EMS Information System, a large registry of more than 10,000 EMS agencies in 47 states that represent over 80% of all EMS calls nationally in 2020. They used the data to track shifts in overdose-related cardiac arrests observed by EMS.
They found clear evidence of a large-scale uptick in overdose-related deaths during the COVID-19 pandemic.
The overall rate of overdose-related cardiac arrests in 2020 was about 50% higher than trends observed during 2018 and 2019, including a maximum peak of 123% above baseline reached in early May.
All overdose-related incidents (fatal and nonfatal) were elevated in 2020, by about 17% above baseline. However, there were larger increases in fatal overdose-related incidents, compared to all incidents, which may suggest a rising case fatality rate, the authors noted.
The observed trends line up in time with reductions in mobility (a metric of social interaction), as measured using cell phone data, they wrote.
“Many of the trends predicted by experts at the beginning of the pandemic could cause these shifts. Increases in social isolation likely play an important role, as people using [drugs] alone are less likely to receive help when they need it. Also shifts in the drug supply, and reduced access to healthcare and treatment,” said Mr. Friedman.
“We need to undertake short- and long-term strategies to combat the rising tide of overdose mortality in the United States,” he added.
In the short term, Mr. Friedman suggested reducing financial and logistical barriers for accessing a safe opioid supply. Such measures include allowing pharmacies to dispense methadone, allowing all physicians to prescribe buprenorphine without a special waiver, and releasing emergency funds to make these medications universally affordable.
“In the longer term, we should acknowledge that overdose is a symptom of structural problems in the U.S. We need to invest in making employment, housing, education, and health care accessible to all to address the upstream drivers of overdose,” he added.
The study had no commercial funding. The authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
There has been a sharp increase in overdose-related cardiac arrests in the United States during the COVID-19 pandemic, a new analysis shows.
Overall rates in 2020 were elevated above the baseline from 2018 and 2019 by about 50%, the data show.
and efforts to combat the COVID-19 pandemic have not been effective at reducing overdoses,” Joseph Friedman, MPH, MD/PhD student, medical scientist training program, University of California, Los Angeles, said in an interview.
“We need to invest heavily in substance use treatment, harm reduction, and the structural drivers of overdose as core elements of the COVID-19 response,” said Mr. Friedman, who coauthored the study with UCLA colleague David Schriger, MD, MPH, and Leo Beletsky, JD, MPH, Northeastern University, Boston.
The study was published as a research letter Dec. 3 in JAMA Psychiatry.
Social isolation a key driver
Emergency medical services (EMS) data are available in near real time, providing a novel source of up-to-date information to monitor epidemiological shifts during the COVID-19 pandemic.
For the study, the researchers leveraged data from the National EMS Information System, a large registry of more than 10,000 EMS agencies in 47 states that represent over 80% of all EMS calls nationally in 2020. They used the data to track shifts in overdose-related cardiac arrests observed by EMS.
They found clear evidence of a large-scale uptick in overdose-related deaths during the COVID-19 pandemic.
The overall rate of overdose-related cardiac arrests in 2020 was about 50% higher than trends observed during 2018 and 2019, including a maximum peak of 123% above baseline reached in early May.
All overdose-related incidents (fatal and nonfatal) were elevated in 2020, by about 17% above baseline. However, there were larger increases in fatal overdose-related incidents, compared to all incidents, which may suggest a rising case fatality rate, the authors noted.
The observed trends line up in time with reductions in mobility (a metric of social interaction), as measured using cell phone data, they wrote.
“Many of the trends predicted by experts at the beginning of the pandemic could cause these shifts. Increases in social isolation likely play an important role, as people using [drugs] alone are less likely to receive help when they need it. Also shifts in the drug supply, and reduced access to healthcare and treatment,” said Mr. Friedman.
“We need to undertake short- and long-term strategies to combat the rising tide of overdose mortality in the United States,” he added.
In the short term, Mr. Friedman suggested reducing financial and logistical barriers for accessing a safe opioid supply. Such measures include allowing pharmacies to dispense methadone, allowing all physicians to prescribe buprenorphine without a special waiver, and releasing emergency funds to make these medications universally affordable.
“In the longer term, we should acknowledge that overdose is a symptom of structural problems in the U.S. We need to invest in making employment, housing, education, and health care accessible to all to address the upstream drivers of overdose,” he added.
The study had no commercial funding. The authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
There has been a sharp increase in overdose-related cardiac arrests in the United States during the COVID-19 pandemic, a new analysis shows.
Overall rates in 2020 were elevated above the baseline from 2018 and 2019 by about 50%, the data show.
and efforts to combat the COVID-19 pandemic have not been effective at reducing overdoses,” Joseph Friedman, MPH, MD/PhD student, medical scientist training program, University of California, Los Angeles, said in an interview.
“We need to invest heavily in substance use treatment, harm reduction, and the structural drivers of overdose as core elements of the COVID-19 response,” said Mr. Friedman, who coauthored the study with UCLA colleague David Schriger, MD, MPH, and Leo Beletsky, JD, MPH, Northeastern University, Boston.
The study was published as a research letter Dec. 3 in JAMA Psychiatry.
Social isolation a key driver
Emergency medical services (EMS) data are available in near real time, providing a novel source of up-to-date information to monitor epidemiological shifts during the COVID-19 pandemic.
For the study, the researchers leveraged data from the National EMS Information System, a large registry of more than 10,000 EMS agencies in 47 states that represent over 80% of all EMS calls nationally in 2020. They used the data to track shifts in overdose-related cardiac arrests observed by EMS.
They found clear evidence of a large-scale uptick in overdose-related deaths during the COVID-19 pandemic.
The overall rate of overdose-related cardiac arrests in 2020 was about 50% higher than trends observed during 2018 and 2019, including a maximum peak of 123% above baseline reached in early May.
All overdose-related incidents (fatal and nonfatal) were elevated in 2020, by about 17% above baseline. However, there were larger increases in fatal overdose-related incidents, compared to all incidents, which may suggest a rising case fatality rate, the authors noted.
The observed trends line up in time with reductions in mobility (a metric of social interaction), as measured using cell phone data, they wrote.
“Many of the trends predicted by experts at the beginning of the pandemic could cause these shifts. Increases in social isolation likely play an important role, as people using [drugs] alone are less likely to receive help when they need it. Also shifts in the drug supply, and reduced access to healthcare and treatment,” said Mr. Friedman.
“We need to undertake short- and long-term strategies to combat the rising tide of overdose mortality in the United States,” he added.
In the short term, Mr. Friedman suggested reducing financial and logistical barriers for accessing a safe opioid supply. Such measures include allowing pharmacies to dispense methadone, allowing all physicians to prescribe buprenorphine without a special waiver, and releasing emergency funds to make these medications universally affordable.
“In the longer term, we should acknowledge that overdose is a symptom of structural problems in the U.S. We need to invest in making employment, housing, education, and health care accessible to all to address the upstream drivers of overdose,” he added.
The study had no commercial funding. The authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
From cradle to grave, alcohol is bad for the brain
There is “compelling” evidence of the harmful effects of alcohol on the brain.
The three periods are:
- Gestation (conception to birth), which is characterized by extensive production, migration, and differentiation of neurons, as well as substantial apoptosis.
- Later adolescence (aged 15-19 years), a period marked by synaptic pruning and increased axonal myelination.
- Older adulthood (aged 65 and beyond), a period associated with brain atrophy. Changes accelerate after age 65, largely driven by decreases in neuron size and reductions in the number of dendritic spines and synapses.
These changes in neurocircuitry could increase sensitivity to the neurotoxic effects of alcohol, Louise Mewton, PhD, of the Center for Healthy Brain Aging, University of New South Wales, Sydney, and colleagues said.
“A life course perspective on brain health supports the formulation of policy and public health interventions to reduce alcohol use and misuse at all ages,” they wrote in an editorial published online Dec. 4 in The BMJ.
Worrisome trends
Research has shown that globally about 10% of pregnant women drink alcohol. In European countries, the rates are much higher than the global average.
Heavy drinking during gestation can cause fetal alcohol spectrum disorder, which is associated with widespread reductions in brain volume and cognitive impairment.
Even low or moderate alcohol consumption during pregnancy is significantly associated with poorer psychological and behavioral outcomes in children, the investigators noted.
In adolescence, more than 20% of 15- to 19-year-olds in European and other high-income countries report at least occasional binge drinking, which is linked to reduced brain volume, poorer white matter development, and deficits in a range of cognitive functions, they added.
In a recent study of older adults, alcohol use disorders emerged as one of the strongest modifiable risk factors for dementia (particularly early-onset dementia), compared with other established risk factors such as high blood pressure and smoking.
Alcohol use disorders are relatively rare in older adults, but even moderate drinking during midlife has been linked to “small but significant” brain volume loss, the authors said.
Dr. Mewton and colleagues said demographic trends may compound the effect of alcohol use on brain health.
They noted that women are now just as likely as men to drink alcohol and suffer alcohol-related problems. Global consumption is forecast to increase further in the next decade.
Although the effects of the COVID-19 pandemic on alcohol intake and related harms remain unclear, alcohol use has increased in the long term after other major public health crises, they added.
Given the data, Dr. Mewton and colleagues called for “an integrated approach” to reducing the harms of alcohol intake at all ages.
“Population-based interventions such as guidelines on low-risk drinking, alcohol pricing policies, and lower drink driving limits need to be accompanied by the development of training and care pathways that consider the human brain at risk throughout life,” they concluded.
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
There is “compelling” evidence of the harmful effects of alcohol on the brain.
The three periods are:
- Gestation (conception to birth), which is characterized by extensive production, migration, and differentiation of neurons, as well as substantial apoptosis.
- Later adolescence (aged 15-19 years), a period marked by synaptic pruning and increased axonal myelination.
- Older adulthood (aged 65 and beyond), a period associated with brain atrophy. Changes accelerate after age 65, largely driven by decreases in neuron size and reductions in the number of dendritic spines and synapses.
These changes in neurocircuitry could increase sensitivity to the neurotoxic effects of alcohol, Louise Mewton, PhD, of the Center for Healthy Brain Aging, University of New South Wales, Sydney, and colleagues said.
“A life course perspective on brain health supports the formulation of policy and public health interventions to reduce alcohol use and misuse at all ages,” they wrote in an editorial published online Dec. 4 in The BMJ.
Worrisome trends
Research has shown that globally about 10% of pregnant women drink alcohol. In European countries, the rates are much higher than the global average.
Heavy drinking during gestation can cause fetal alcohol spectrum disorder, which is associated with widespread reductions in brain volume and cognitive impairment.
Even low or moderate alcohol consumption during pregnancy is significantly associated with poorer psychological and behavioral outcomes in children, the investigators noted.
In adolescence, more than 20% of 15- to 19-year-olds in European and other high-income countries report at least occasional binge drinking, which is linked to reduced brain volume, poorer white matter development, and deficits in a range of cognitive functions, they added.
In a recent study of older adults, alcohol use disorders emerged as one of the strongest modifiable risk factors for dementia (particularly early-onset dementia), compared with other established risk factors such as high blood pressure and smoking.
Alcohol use disorders are relatively rare in older adults, but even moderate drinking during midlife has been linked to “small but significant” brain volume loss, the authors said.
Dr. Mewton and colleagues said demographic trends may compound the effect of alcohol use on brain health.
They noted that women are now just as likely as men to drink alcohol and suffer alcohol-related problems. Global consumption is forecast to increase further in the next decade.
Although the effects of the COVID-19 pandemic on alcohol intake and related harms remain unclear, alcohol use has increased in the long term after other major public health crises, they added.
Given the data, Dr. Mewton and colleagues called for “an integrated approach” to reducing the harms of alcohol intake at all ages.
“Population-based interventions such as guidelines on low-risk drinking, alcohol pricing policies, and lower drink driving limits need to be accompanied by the development of training and care pathways that consider the human brain at risk throughout life,” they concluded.
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
There is “compelling” evidence of the harmful effects of alcohol on the brain.
The three periods are:
- Gestation (conception to birth), which is characterized by extensive production, migration, and differentiation of neurons, as well as substantial apoptosis.
- Later adolescence (aged 15-19 years), a period marked by synaptic pruning and increased axonal myelination.
- Older adulthood (aged 65 and beyond), a period associated with brain atrophy. Changes accelerate after age 65, largely driven by decreases in neuron size and reductions in the number of dendritic spines and synapses.
These changes in neurocircuitry could increase sensitivity to the neurotoxic effects of alcohol, Louise Mewton, PhD, of the Center for Healthy Brain Aging, University of New South Wales, Sydney, and colleagues said.
“A life course perspective on brain health supports the formulation of policy and public health interventions to reduce alcohol use and misuse at all ages,” they wrote in an editorial published online Dec. 4 in The BMJ.
Worrisome trends
Research has shown that globally about 10% of pregnant women drink alcohol. In European countries, the rates are much higher than the global average.
Heavy drinking during gestation can cause fetal alcohol spectrum disorder, which is associated with widespread reductions in brain volume and cognitive impairment.
Even low or moderate alcohol consumption during pregnancy is significantly associated with poorer psychological and behavioral outcomes in children, the investigators noted.
In adolescence, more than 20% of 15- to 19-year-olds in European and other high-income countries report at least occasional binge drinking, which is linked to reduced brain volume, poorer white matter development, and deficits in a range of cognitive functions, they added.
In a recent study of older adults, alcohol use disorders emerged as one of the strongest modifiable risk factors for dementia (particularly early-onset dementia), compared with other established risk factors such as high blood pressure and smoking.
Alcohol use disorders are relatively rare in older adults, but even moderate drinking during midlife has been linked to “small but significant” brain volume loss, the authors said.
Dr. Mewton and colleagues said demographic trends may compound the effect of alcohol use on brain health.
They noted that women are now just as likely as men to drink alcohol and suffer alcohol-related problems. Global consumption is forecast to increase further in the next decade.
Although the effects of the COVID-19 pandemic on alcohol intake and related harms remain unclear, alcohol use has increased in the long term after other major public health crises, they added.
Given the data, Dr. Mewton and colleagues called for “an integrated approach” to reducing the harms of alcohol intake at all ages.
“Population-based interventions such as guidelines on low-risk drinking, alcohol pricing policies, and lower drink driving limits need to be accompanied by the development of training and care pathways that consider the human brain at risk throughout life,” they concluded.
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.





