User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Kleptomania: 4 Tips for better diagnosis and treatment
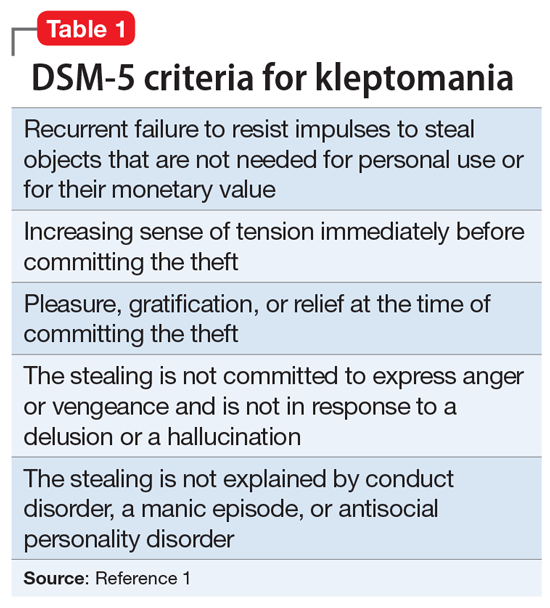
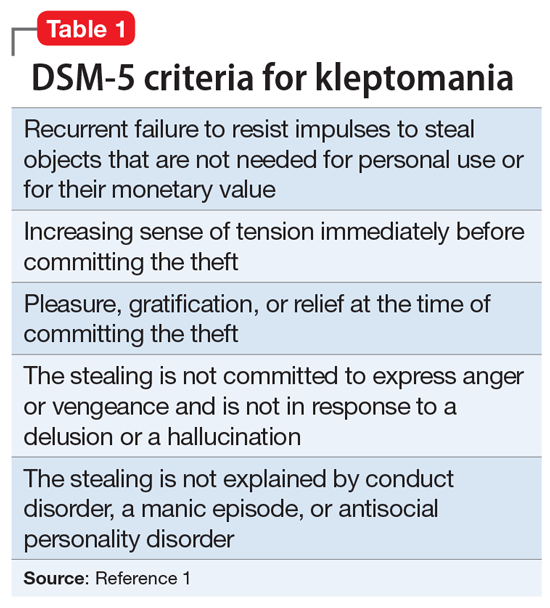
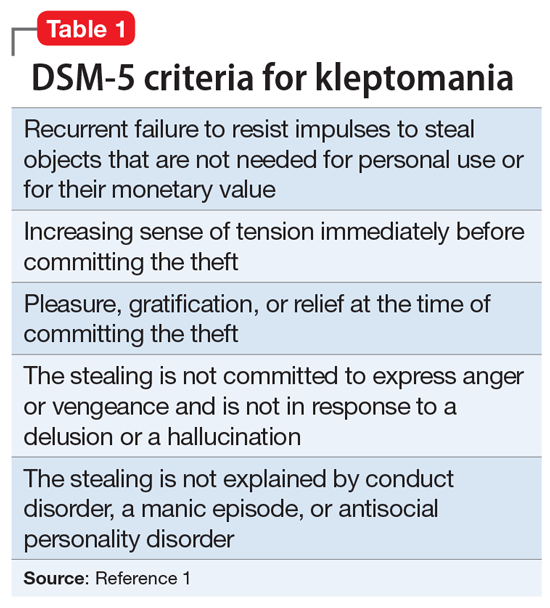
Kleptomania is characterized by a recurrent failure to resist impulses to steal objects that are not needed for personal use or their monetary value.1 It is a rare disorder; an estimated 0.3% to 0.6% of the general population meet DSM-5 criteria for kleptomania (Table 1).1 Kleptomania usually begins in early adolescence and is more common among females than males (3:1).1 Although DSM-5 does not outline how long symptoms need to be present for patients to meet the diagnostic criteria, the disorder may persist for years, even when patients face legal consequences.1
Due to the clinical ambiguities surrounding kleptomania, it remains one of psychiatry’s most poorly understood diagnoses2 and regularly goes undiagnosed and untreated. Here we provide 4 tips for better diagnosis and treatment of this condition.
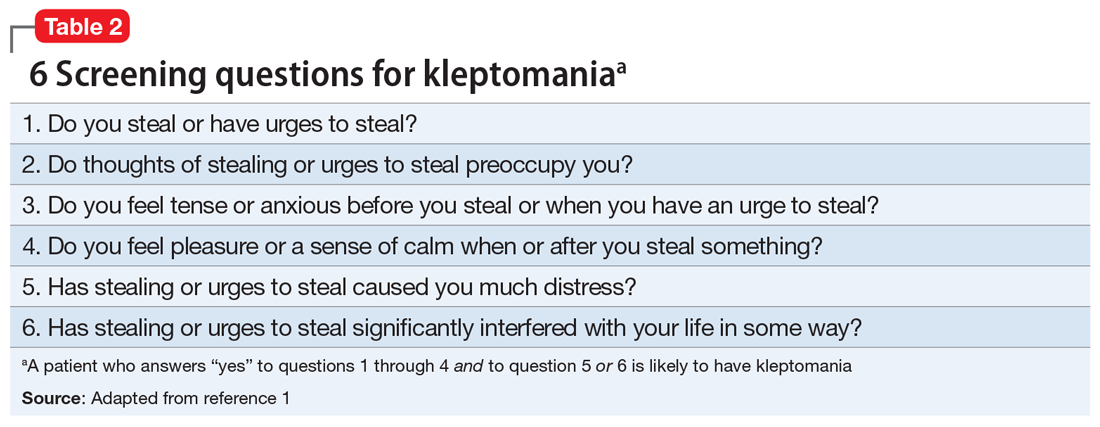
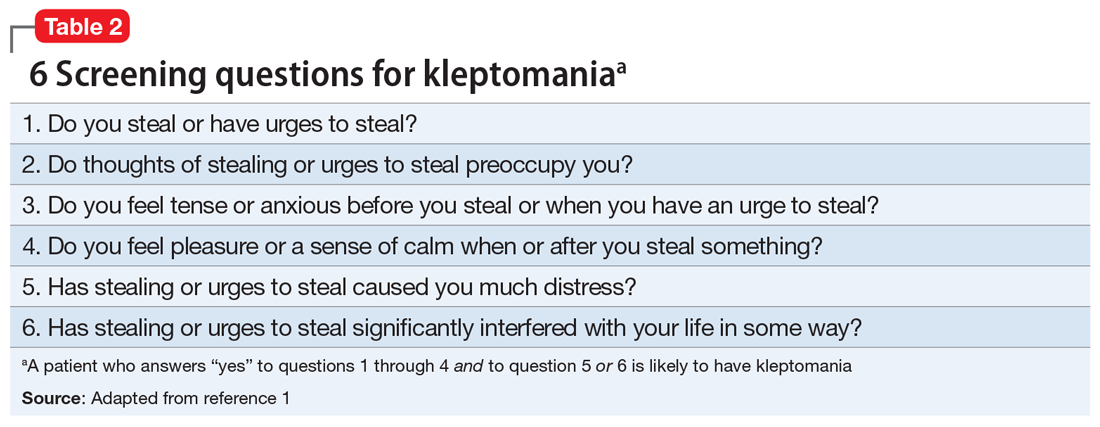
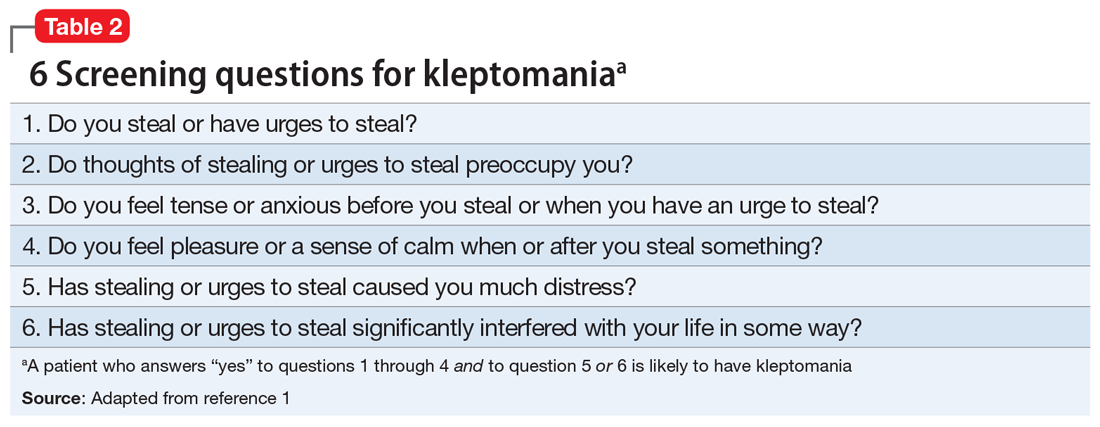
1. Screen for kleptomania in patients with other psychiatric disorders because kleptomania often is comorbid with other mental illnesses. Patients who present for evaluation of a mood disorder, substance use, anxiety disorders, eating disorders, impulse control disorders, conduct disorder, and obsessive-compulsive disorder should be screened for kleptomania.1,3,4 Patients with kleptomania often are reluctant to discuss their stealing because they may experience humiliation and guilt related to theft.1,4 Undiagnosed kleptomania can be fatal; a study of suicide attempts in 107 individuals with kleptomania found that 92% of the patients attributed their attempt specifically to kleptomania.5 Table 21 offers screening questions based on the DSM-5 criteria for kleptomania.
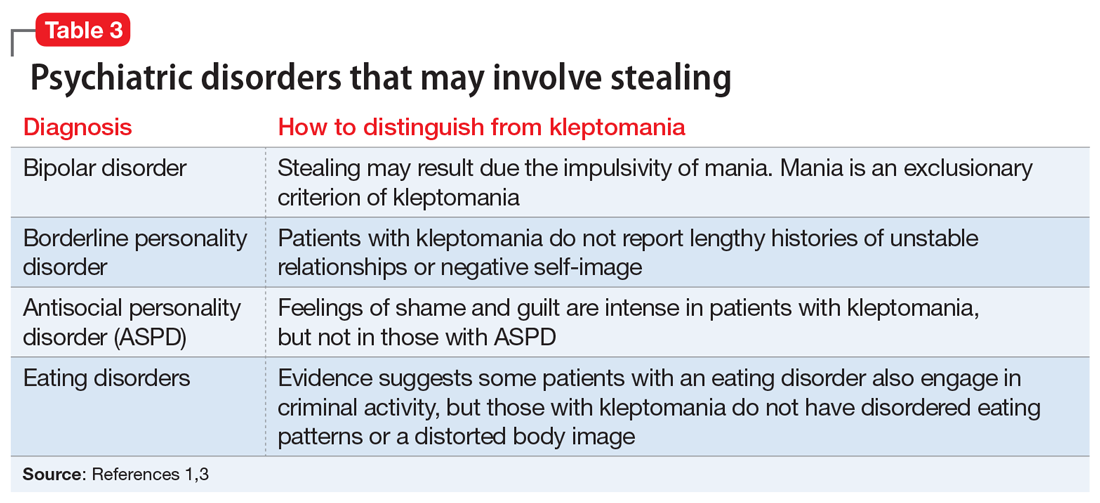
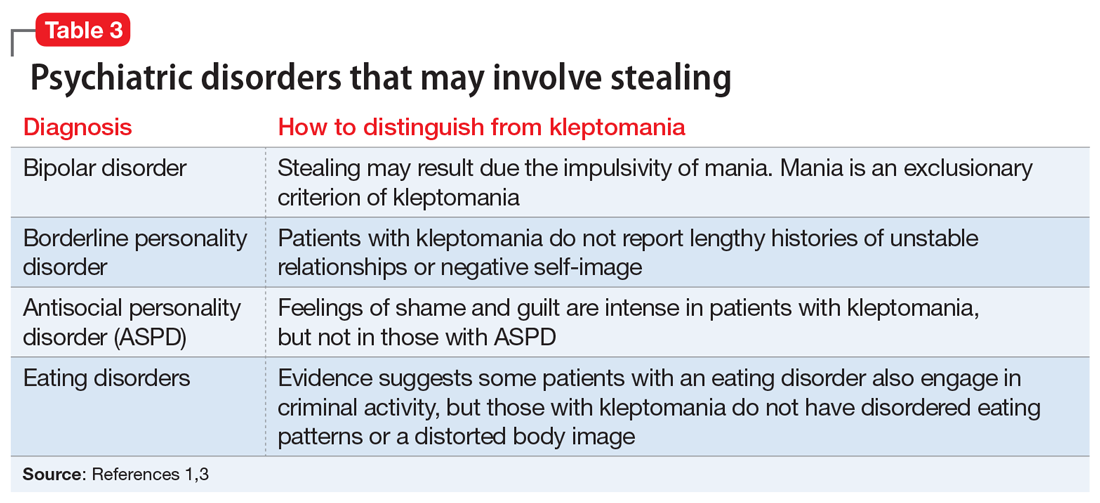
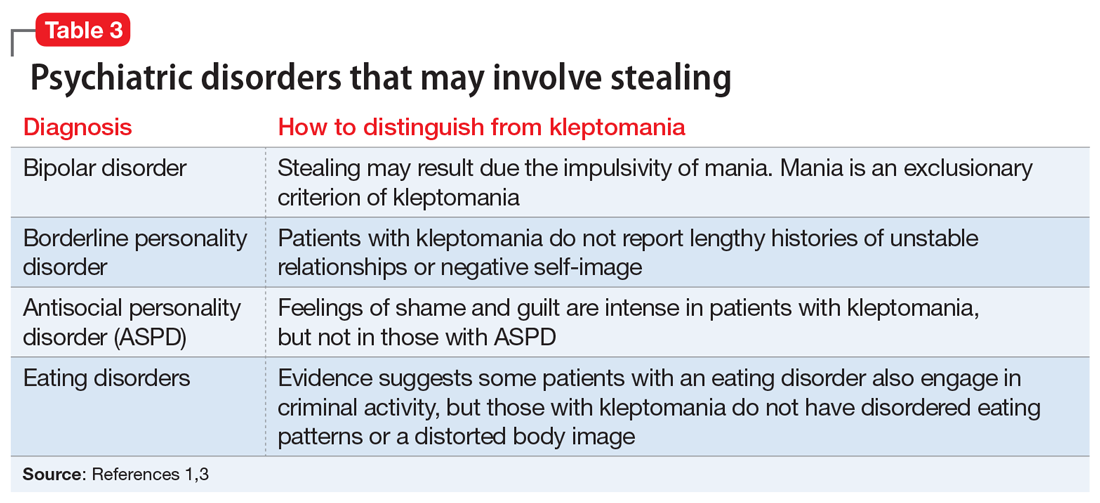
2. Distinguish kleptomania from other diagnoses that can include stealing. Because stealing can be a symptom of several other psychiatric disorders, misdiagnosis is fairly common.1 The differential can include bipolar disorder, borderline personality disorder, antisocial personality disorder, and eating disorder. Table 31,3 describes how to differentiate these diagnoses from kleptomania.
3. Select an appropriate treatment. There are no FDA-approved medications for kleptomania, but some agents may help. In an 8-week, double-blind, placebo-controlled trial, 25 patients with kleptomania who received naltrexone (50 to 150 mg/d) demonstrated significant reductions in stealing urges and behavior.6 Some evidence suggests a combination of pharmacologic and behavioral therapy (cognitive-behavioral therapy, covert sensitization, and systemic desensitization) may be the optimal treatment strategy for kleptomania.4
4. Monitor progress. After initiating treatment, use the Kleptomania Symptom Assessment Scale7 (K-SAS) to determine treatment efficacy. The K-SAS is an 11-item self-report questionnaire that assesses the severity of kleptomania symptoms during the past week.
1. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Goldman MJ. Kleptomania: making sense of the nonsensical. Am J Psychiatry. 1991;148:986-996.
3. Yao S, Kuja‐Halkola R, Thornton LM, et al. Risk of being convicted of theft and other crimes in anorexia nervosa and bulimia nervosa: a prospective cohort study in a Swedish female population. Int J Eat Disord. 2017;50(9):1095-1103.
4. Grant JE, Kim SW. Clinical characteristics and associated psychopathology of 22 patients of kleptomania. Compr Psychiatry. 2002;43(5):378-384.
5. Odlaug BL, Grant JE, Kim SW. Suicide attempts in 107 adolescents and adults with kleptomania. Arch Suicide Res. 2012;16(4):348-359.
6. Grant JE, Kim SW, Odlaug BL. A double-blind, placebo-controlled study of the opiate antagonist, naltrexone, in the treatment of kleptomania. Biol Psychiatry. 2009;65(7):600-606.
7. Grant JE, Odlaug BL, Kim SW. Kleptomania: clinical characteristics and relationship to substance use disorders. Am J Drug Alcohol Abuse. 2010;36(5):291-295.
Kleptomania is characterized by a recurrent failure to resist impulses to steal objects that are not needed for personal use or their monetary value.1 It is a rare disorder; an estimated 0.3% to 0.6% of the general population meet DSM-5 criteria for kleptomania (Table 1).1 Kleptomania usually begins in early adolescence and is more common among females than males (3:1).1 Although DSM-5 does not outline how long symptoms need to be present for patients to meet the diagnostic criteria, the disorder may persist for years, even when patients face legal consequences.1
Due to the clinical ambiguities surrounding kleptomania, it remains one of psychiatry’s most poorly understood diagnoses2 and regularly goes undiagnosed and untreated. Here we provide 4 tips for better diagnosis and treatment of this condition.
1. Screen for kleptomania in patients with other psychiatric disorders because kleptomania often is comorbid with other mental illnesses. Patients who present for evaluation of a mood disorder, substance use, anxiety disorders, eating disorders, impulse control disorders, conduct disorder, and obsessive-compulsive disorder should be screened for kleptomania.1,3,4 Patients with kleptomania often are reluctant to discuss their stealing because they may experience humiliation and guilt related to theft.1,4 Undiagnosed kleptomania can be fatal; a study of suicide attempts in 107 individuals with kleptomania found that 92% of the patients attributed their attempt specifically to kleptomania.5 Table 21 offers screening questions based on the DSM-5 criteria for kleptomania.
2. Distinguish kleptomania from other diagnoses that can include stealing. Because stealing can be a symptom of several other psychiatric disorders, misdiagnosis is fairly common.1 The differential can include bipolar disorder, borderline personality disorder, antisocial personality disorder, and eating disorder. Table 31,3 describes how to differentiate these diagnoses from kleptomania.
3. Select an appropriate treatment. There are no FDA-approved medications for kleptomania, but some agents may help. In an 8-week, double-blind, placebo-controlled trial, 25 patients with kleptomania who received naltrexone (50 to 150 mg/d) demonstrated significant reductions in stealing urges and behavior.6 Some evidence suggests a combination of pharmacologic and behavioral therapy (cognitive-behavioral therapy, covert sensitization, and systemic desensitization) may be the optimal treatment strategy for kleptomania.4
4. Monitor progress. After initiating treatment, use the Kleptomania Symptom Assessment Scale7 (K-SAS) to determine treatment efficacy. The K-SAS is an 11-item self-report questionnaire that assesses the severity of kleptomania symptoms during the past week.
Kleptomania is characterized by a recurrent failure to resist impulses to steal objects that are not needed for personal use or their monetary value.1 It is a rare disorder; an estimated 0.3% to 0.6% of the general population meet DSM-5 criteria for kleptomania (Table 1).1 Kleptomania usually begins in early adolescence and is more common among females than males (3:1).1 Although DSM-5 does not outline how long symptoms need to be present for patients to meet the diagnostic criteria, the disorder may persist for years, even when patients face legal consequences.1
Due to the clinical ambiguities surrounding kleptomania, it remains one of psychiatry’s most poorly understood diagnoses2 and regularly goes undiagnosed and untreated. Here we provide 4 tips for better diagnosis and treatment of this condition.
1. Screen for kleptomania in patients with other psychiatric disorders because kleptomania often is comorbid with other mental illnesses. Patients who present for evaluation of a mood disorder, substance use, anxiety disorders, eating disorders, impulse control disorders, conduct disorder, and obsessive-compulsive disorder should be screened for kleptomania.1,3,4 Patients with kleptomania often are reluctant to discuss their stealing because they may experience humiliation and guilt related to theft.1,4 Undiagnosed kleptomania can be fatal; a study of suicide attempts in 107 individuals with kleptomania found that 92% of the patients attributed their attempt specifically to kleptomania.5 Table 21 offers screening questions based on the DSM-5 criteria for kleptomania.
2. Distinguish kleptomania from other diagnoses that can include stealing. Because stealing can be a symptom of several other psychiatric disorders, misdiagnosis is fairly common.1 The differential can include bipolar disorder, borderline personality disorder, antisocial personality disorder, and eating disorder. Table 31,3 describes how to differentiate these diagnoses from kleptomania.
3. Select an appropriate treatment. There are no FDA-approved medications for kleptomania, but some agents may help. In an 8-week, double-blind, placebo-controlled trial, 25 patients with kleptomania who received naltrexone (50 to 150 mg/d) demonstrated significant reductions in stealing urges and behavior.6 Some evidence suggests a combination of pharmacologic and behavioral therapy (cognitive-behavioral therapy, covert sensitization, and systemic desensitization) may be the optimal treatment strategy for kleptomania.4
4. Monitor progress. After initiating treatment, use the Kleptomania Symptom Assessment Scale7 (K-SAS) to determine treatment efficacy. The K-SAS is an 11-item self-report questionnaire that assesses the severity of kleptomania symptoms during the past week.
1. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Goldman MJ. Kleptomania: making sense of the nonsensical. Am J Psychiatry. 1991;148:986-996.
3. Yao S, Kuja‐Halkola R, Thornton LM, et al. Risk of being convicted of theft and other crimes in anorexia nervosa and bulimia nervosa: a prospective cohort study in a Swedish female population. Int J Eat Disord. 2017;50(9):1095-1103.
4. Grant JE, Kim SW. Clinical characteristics and associated psychopathology of 22 patients of kleptomania. Compr Psychiatry. 2002;43(5):378-384.
5. Odlaug BL, Grant JE, Kim SW. Suicide attempts in 107 adolescents and adults with kleptomania. Arch Suicide Res. 2012;16(4):348-359.
6. Grant JE, Kim SW, Odlaug BL. A double-blind, placebo-controlled study of the opiate antagonist, naltrexone, in the treatment of kleptomania. Biol Psychiatry. 2009;65(7):600-606.
7. Grant JE, Odlaug BL, Kim SW. Kleptomania: clinical characteristics and relationship to substance use disorders. Am J Drug Alcohol Abuse. 2010;36(5):291-295.
1. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Goldman MJ. Kleptomania: making sense of the nonsensical. Am J Psychiatry. 1991;148:986-996.
3. Yao S, Kuja‐Halkola R, Thornton LM, et al. Risk of being convicted of theft and other crimes in anorexia nervosa and bulimia nervosa: a prospective cohort study in a Swedish female population. Int J Eat Disord. 2017;50(9):1095-1103.
4. Grant JE, Kim SW. Clinical characteristics and associated psychopathology of 22 patients of kleptomania. Compr Psychiatry. 2002;43(5):378-384.
5. Odlaug BL, Grant JE, Kim SW. Suicide attempts in 107 adolescents and adults with kleptomania. Arch Suicide Res. 2012;16(4):348-359.
6. Grant JE, Kim SW, Odlaug BL. A double-blind, placebo-controlled study of the opiate antagonist, naltrexone, in the treatment of kleptomania. Biol Psychiatry. 2009;65(7):600-606.
7. Grant JE, Odlaug BL, Kim SW. Kleptomania: clinical characteristics and relationship to substance use disorders. Am J Drug Alcohol Abuse. 2010;36(5):291-295.
Improving your experience with electronic health records
The electronic health record (EHR) was introduced to improve how clinicians document patient information, contribute to medical research, and allow for medical records to be universally transferable.1 However, many clinicians find EHRs to be burdensome, time-consuming, and inefficient. Clinicians often spend multiple hours each day navigating their EHR system, which reduces the amount of time they spend interacting with patients and contributes to physician burnout.1-3 For example, in a study of 142 family medicine physicians, clinicians reported that they spent approximately 6 hours per work day interacting with their EHR.3
Clearly, the EHR needs a fundamental revision. In the meantime, how can we adapt to improve the situation? Here I suggest practical steps clinicians can take to improve their experience with their EHR system.4-8
Steps to take during patient visits
Because entering information into the EHR can be distracting, be prepared to multitask during each clinical encounter.1-7 Be ready to address pertinent inquiries and issues your patient raises, and provide instructions on therapies and interventions. Because interpersonal relations are important during clinical encounters, establish interaction with your patient by acknowledging them and maintaining frequent eye contact.7 Consider allowing your patient to view the EHR screen because doing so might increase his/her involvement in the visit.
So that you can pay closer attention to your patient, consider taking notes during the visit and entering the information into the EHR later. Consider improving your typing skills to increase the speed of your note-taking. Alternatively, using a voice-recognition recording tool to transcribe your notes via speech might help you spend less time on note-taking.3 Whenever possible, finish charting for one patient before meeting with the next because doing so will save time and help you to better remember details.7
In addition, lowering your overall stress might help reduce the burden of using the EHR.3-5 Adopt healthy behaviors, including good sleep, nutrition, exercise, and hobbies, and strive for balance in your routines. Attend to any personal medical or psychiatric conditions, and avoid misusing alcohol, medications, or other substances.
Optimize how your practice functions
With your clinical group and colleagues, create a comfortable environment, good patient-to-doctor interactions, and a smooth flow within the practice. Simplify registration. Ask patients to complete screening forms before an appointment; this information could be entered directly into their EHR.3 Consider using physician-extender staff and other personnel, such as scribes, to complete documentation into the EHR.3,8 This may help reduce burnout, create more time for clinical care, and improve face-to-face patient interactions.8 Employing scribes can allow doctors to be better able to directly attend to their patients while complying with record-keeping needs. Although scribes make charting easier, they are an additional expense, and must be trained.
Consider EHR training
EHR training sessions can teach you how to use your EHR system more efficiently.6 Such education may help boost confidence, aid documentation, and reduce the amount of time spent correcting coding errors. In a study of 3,500 physicians who underwent a 3-day intensive EHR training course, 85% to 98% reported having improved the quality, readability, and clinical accuracy of their documentation.6
Help shape future EHRs
Individual doctors and professional groups can promote EHR improvements through their state, regional, and/or national organizations and medical societies. These bodies should deliver EHR revision recommendations to government officials, who can craft laws and regulations, and can influence regulators and/or insurance companies. Clinicians also can communicate with EHR developers on ways to simplify the usability of these tools, such as reducing the amount of steps the EHR’s interface requires.5 With a more efficient EHR, we can better concentrate on patient care, which will reduce expenses and should yield better outcomes.
1. Ehrenfeld JM, Wonderer JP. Technology as friend or foe? Do electronic health records increase burnout? Curr Opin Anesthesiol. 2018;31(3):357-360.
2. Meigs SL, Solomon M. Electronic health record use a bitter pill for many physicians. Perspect Health Inf Manag. 2016;13:1d.
3. Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med. 2017;15(5):419-426.
4. Fogarty CT, Winters P, Farah S. Improving patient-centered communication while using an electronic health record: report from a curriculum evaluation. Int J Psych Med. 2016;51(4):379-389.
5. Guo U, Chen L, Mehta PH. Electronic health record innovations: helping physicians - one less click at a time. Health Inf Manag. 2017;46(3):140-144.
6. Robinson KE, Kersey JA. Novel electronic health record (EHR) education intervention in large healthcare organization improves quality, efficiency, time, and impact on burnout. Medicine. 2018;91(38):e123419. doi: 10.1097/MD.0000000000012319.
7. Fogarty CT. Getting your notes done on time. Fam Pract Manag. 2016;23(2):40.
8. DeChant PF, Acs A, Rhee KB, et al. Effect of organization-directed workplace interventions on physician burnout: a systematic review. Mayo Clin Proc Innov Qual Outcomes. 2019;3(4):384-408.
The electronic health record (EHR) was introduced to improve how clinicians document patient information, contribute to medical research, and allow for medical records to be universally transferable.1 However, many clinicians find EHRs to be burdensome, time-consuming, and inefficient. Clinicians often spend multiple hours each day navigating their EHR system, which reduces the amount of time they spend interacting with patients and contributes to physician burnout.1-3 For example, in a study of 142 family medicine physicians, clinicians reported that they spent approximately 6 hours per work day interacting with their EHR.3
Clearly, the EHR needs a fundamental revision. In the meantime, how can we adapt to improve the situation? Here I suggest practical steps clinicians can take to improve their experience with their EHR system.4-8
Steps to take during patient visits
Because entering information into the EHR can be distracting, be prepared to multitask during each clinical encounter.1-7 Be ready to address pertinent inquiries and issues your patient raises, and provide instructions on therapies and interventions. Because interpersonal relations are important during clinical encounters, establish interaction with your patient by acknowledging them and maintaining frequent eye contact.7 Consider allowing your patient to view the EHR screen because doing so might increase his/her involvement in the visit.
So that you can pay closer attention to your patient, consider taking notes during the visit and entering the information into the EHR later. Consider improving your typing skills to increase the speed of your note-taking. Alternatively, using a voice-recognition recording tool to transcribe your notes via speech might help you spend less time on note-taking.3 Whenever possible, finish charting for one patient before meeting with the next because doing so will save time and help you to better remember details.7
In addition, lowering your overall stress might help reduce the burden of using the EHR.3-5 Adopt healthy behaviors, including good sleep, nutrition, exercise, and hobbies, and strive for balance in your routines. Attend to any personal medical or psychiatric conditions, and avoid misusing alcohol, medications, or other substances.
Optimize how your practice functions
With your clinical group and colleagues, create a comfortable environment, good patient-to-doctor interactions, and a smooth flow within the practice. Simplify registration. Ask patients to complete screening forms before an appointment; this information could be entered directly into their EHR.3 Consider using physician-extender staff and other personnel, such as scribes, to complete documentation into the EHR.3,8 This may help reduce burnout, create more time for clinical care, and improve face-to-face patient interactions.8 Employing scribes can allow doctors to be better able to directly attend to their patients while complying with record-keeping needs. Although scribes make charting easier, they are an additional expense, and must be trained.
Consider EHR training
EHR training sessions can teach you how to use your EHR system more efficiently.6 Such education may help boost confidence, aid documentation, and reduce the amount of time spent correcting coding errors. In a study of 3,500 physicians who underwent a 3-day intensive EHR training course, 85% to 98% reported having improved the quality, readability, and clinical accuracy of their documentation.6
Help shape future EHRs
Individual doctors and professional groups can promote EHR improvements through their state, regional, and/or national organizations and medical societies. These bodies should deliver EHR revision recommendations to government officials, who can craft laws and regulations, and can influence regulators and/or insurance companies. Clinicians also can communicate with EHR developers on ways to simplify the usability of these tools, such as reducing the amount of steps the EHR’s interface requires.5 With a more efficient EHR, we can better concentrate on patient care, which will reduce expenses and should yield better outcomes.
The electronic health record (EHR) was introduced to improve how clinicians document patient information, contribute to medical research, and allow for medical records to be universally transferable.1 However, many clinicians find EHRs to be burdensome, time-consuming, and inefficient. Clinicians often spend multiple hours each day navigating their EHR system, which reduces the amount of time they spend interacting with patients and contributes to physician burnout.1-3 For example, in a study of 142 family medicine physicians, clinicians reported that they spent approximately 6 hours per work day interacting with their EHR.3
Clearly, the EHR needs a fundamental revision. In the meantime, how can we adapt to improve the situation? Here I suggest practical steps clinicians can take to improve their experience with their EHR system.4-8
Steps to take during patient visits
Because entering information into the EHR can be distracting, be prepared to multitask during each clinical encounter.1-7 Be ready to address pertinent inquiries and issues your patient raises, and provide instructions on therapies and interventions. Because interpersonal relations are important during clinical encounters, establish interaction with your patient by acknowledging them and maintaining frequent eye contact.7 Consider allowing your patient to view the EHR screen because doing so might increase his/her involvement in the visit.
So that you can pay closer attention to your patient, consider taking notes during the visit and entering the information into the EHR later. Consider improving your typing skills to increase the speed of your note-taking. Alternatively, using a voice-recognition recording tool to transcribe your notes via speech might help you spend less time on note-taking.3 Whenever possible, finish charting for one patient before meeting with the next because doing so will save time and help you to better remember details.7
In addition, lowering your overall stress might help reduce the burden of using the EHR.3-5 Adopt healthy behaviors, including good sleep, nutrition, exercise, and hobbies, and strive for balance in your routines. Attend to any personal medical or psychiatric conditions, and avoid misusing alcohol, medications, or other substances.
Optimize how your practice functions
With your clinical group and colleagues, create a comfortable environment, good patient-to-doctor interactions, and a smooth flow within the practice. Simplify registration. Ask patients to complete screening forms before an appointment; this information could be entered directly into their EHR.3 Consider using physician-extender staff and other personnel, such as scribes, to complete documentation into the EHR.3,8 This may help reduce burnout, create more time for clinical care, and improve face-to-face patient interactions.8 Employing scribes can allow doctors to be better able to directly attend to their patients while complying with record-keeping needs. Although scribes make charting easier, they are an additional expense, and must be trained.
Consider EHR training
EHR training sessions can teach you how to use your EHR system more efficiently.6 Such education may help boost confidence, aid documentation, and reduce the amount of time spent correcting coding errors. In a study of 3,500 physicians who underwent a 3-day intensive EHR training course, 85% to 98% reported having improved the quality, readability, and clinical accuracy of their documentation.6
Help shape future EHRs
Individual doctors and professional groups can promote EHR improvements through their state, regional, and/or national organizations and medical societies. These bodies should deliver EHR revision recommendations to government officials, who can craft laws and regulations, and can influence regulators and/or insurance companies. Clinicians also can communicate with EHR developers on ways to simplify the usability of these tools, such as reducing the amount of steps the EHR’s interface requires.5 With a more efficient EHR, we can better concentrate on patient care, which will reduce expenses and should yield better outcomes.
1. Ehrenfeld JM, Wonderer JP. Technology as friend or foe? Do electronic health records increase burnout? Curr Opin Anesthesiol. 2018;31(3):357-360.
2. Meigs SL, Solomon M. Electronic health record use a bitter pill for many physicians. Perspect Health Inf Manag. 2016;13:1d.
3. Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med. 2017;15(5):419-426.
4. Fogarty CT, Winters P, Farah S. Improving patient-centered communication while using an electronic health record: report from a curriculum evaluation. Int J Psych Med. 2016;51(4):379-389.
5. Guo U, Chen L, Mehta PH. Electronic health record innovations: helping physicians - one less click at a time. Health Inf Manag. 2017;46(3):140-144.
6. Robinson KE, Kersey JA. Novel electronic health record (EHR) education intervention in large healthcare organization improves quality, efficiency, time, and impact on burnout. Medicine. 2018;91(38):e123419. doi: 10.1097/MD.0000000000012319.
7. Fogarty CT. Getting your notes done on time. Fam Pract Manag. 2016;23(2):40.
8. DeChant PF, Acs A, Rhee KB, et al. Effect of organization-directed workplace interventions on physician burnout: a systematic review. Mayo Clin Proc Innov Qual Outcomes. 2019;3(4):384-408.
1. Ehrenfeld JM, Wonderer JP. Technology as friend or foe? Do electronic health records increase burnout? Curr Opin Anesthesiol. 2018;31(3):357-360.
2. Meigs SL, Solomon M. Electronic health record use a bitter pill for many physicians. Perspect Health Inf Manag. 2016;13:1d.
3. Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med. 2017;15(5):419-426.
4. Fogarty CT, Winters P, Farah S. Improving patient-centered communication while using an electronic health record: report from a curriculum evaluation. Int J Psych Med. 2016;51(4):379-389.
5. Guo U, Chen L, Mehta PH. Electronic health record innovations: helping physicians - one less click at a time. Health Inf Manag. 2017;46(3):140-144.
6. Robinson KE, Kersey JA. Novel electronic health record (EHR) education intervention in large healthcare organization improves quality, efficiency, time, and impact on burnout. Medicine. 2018;91(38):e123419. doi: 10.1097/MD.0000000000012319.
7. Fogarty CT. Getting your notes done on time. Fam Pract Manag. 2016;23(2):40.
8. DeChant PF, Acs A, Rhee KB, et al. Effect of organization-directed workplace interventions on physician burnout: a systematic review. Mayo Clin Proc Innov Qual Outcomes. 2019;3(4):384-408.
COVID-19–related skin changes: The hidden racism in documentation
Belatedly, the disproportionate impact of COVID-19 on patients of color is getting attention. By now, we’ve read the headlines. Black people in the United States make up about 13% of the population but account for almost three times (34%) as many deaths. This story repeats – in other countries and in other minority communities.
Early detection is critical both to initiate supportive care and to isolate affected individuals and limit spread. Skin manifestations of COVID-19, especially those that occur early in the disease (eg, vesicular eruptions) or have prognostic significance (livedo, retiform purpura, necrosis), are critical to this goal of early recognition.
In this context, a recent systematic literature review looked at all articles describing skin manifestations associated with COVID-19. The investigators identified 46 articles published between March and May 2020 which included a total of 130 clinical images.
The following findings from this study are striking:
- 92% of the published images of COVID-associated skin manifestations were in I-III.
- Only 6% of COVID skin lesions included in the articles were in patients with skin type IV.
- None showed COVID skin lesions in skin types V or VI.
- Only six of the articles reported race and ethnicity demographics. In those, 91% of the patients were White and 9% were Hispanic.
These results reveal a critical lack of representative clinical images of COVID-associated skin manifestations in patients of color. This deficiency is made all the more egregious given the fact that patients of color, including those who are Black, Latinx, and Native American, have been especially hard hit by the COVID-19 pandemic and suffer disproportionate disease-related morbidity and mortality.
As the study authors point out, skin manifestations in people of color often differ significantly from findings in White skin (for example, look at the figure depicting the rash typical of Kawasaki disease in a dark-skinned child compared with a light-skinned child). It is not a stretch to suggest that skin manifestations associated with COVID-19 may look very different in darker skin.
This isn’t a new phenomenon. Almost half of dermatologists feel that they’ve had insufficient exposure to skin disease in darker skin types. Skin of color remains underrepresented in medical journals.
Like other forms of passive, institutional racism, this deficiency will only be improved if dermatologists and dermatology publications actively seek out COVID-associated skin manifestations in patients of color and prioritize sharing these images. A medical student in the United Kingdom has gotten the ball rolling, compiling a handbook of clinical signs in darker skin types as part of a student-staff partnership at St. George’s Hospital and the University of London. At this time, Mind the Gap is looking for a publisher.
Dr. Lipper is an assistant clinical professor at the University of Vermont, Burlington, and a staff physician in the department of dermatology at Danbury (Conn.) Hospital. He has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Belatedly, the disproportionate impact of COVID-19 on patients of color is getting attention. By now, we’ve read the headlines. Black people in the United States make up about 13% of the population but account for almost three times (34%) as many deaths. This story repeats – in other countries and in other minority communities.
Early detection is critical both to initiate supportive care and to isolate affected individuals and limit spread. Skin manifestations of COVID-19, especially those that occur early in the disease (eg, vesicular eruptions) or have prognostic significance (livedo, retiform purpura, necrosis), are critical to this goal of early recognition.
In this context, a recent systematic literature review looked at all articles describing skin manifestations associated with COVID-19. The investigators identified 46 articles published between March and May 2020 which included a total of 130 clinical images.
The following findings from this study are striking:
- 92% of the published images of COVID-associated skin manifestations were in I-III.
- Only 6% of COVID skin lesions included in the articles were in patients with skin type IV.
- None showed COVID skin lesions in skin types V or VI.
- Only six of the articles reported race and ethnicity demographics. In those, 91% of the patients were White and 9% were Hispanic.
These results reveal a critical lack of representative clinical images of COVID-associated skin manifestations in patients of color. This deficiency is made all the more egregious given the fact that patients of color, including those who are Black, Latinx, and Native American, have been especially hard hit by the COVID-19 pandemic and suffer disproportionate disease-related morbidity and mortality.
As the study authors point out, skin manifestations in people of color often differ significantly from findings in White skin (for example, look at the figure depicting the rash typical of Kawasaki disease in a dark-skinned child compared with a light-skinned child). It is not a stretch to suggest that skin manifestations associated with COVID-19 may look very different in darker skin.
This isn’t a new phenomenon. Almost half of dermatologists feel that they’ve had insufficient exposure to skin disease in darker skin types. Skin of color remains underrepresented in medical journals.
Like other forms of passive, institutional racism, this deficiency will only be improved if dermatologists and dermatology publications actively seek out COVID-associated skin manifestations in patients of color and prioritize sharing these images. A medical student in the United Kingdom has gotten the ball rolling, compiling a handbook of clinical signs in darker skin types as part of a student-staff partnership at St. George’s Hospital and the University of London. At this time, Mind the Gap is looking for a publisher.
Dr. Lipper is an assistant clinical professor at the University of Vermont, Burlington, and a staff physician in the department of dermatology at Danbury (Conn.) Hospital. He has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Belatedly, the disproportionate impact of COVID-19 on patients of color is getting attention. By now, we’ve read the headlines. Black people in the United States make up about 13% of the population but account for almost three times (34%) as many deaths. This story repeats – in other countries and in other minority communities.
Early detection is critical both to initiate supportive care and to isolate affected individuals and limit spread. Skin manifestations of COVID-19, especially those that occur early in the disease (eg, vesicular eruptions) or have prognostic significance (livedo, retiform purpura, necrosis), are critical to this goal of early recognition.
In this context, a recent systematic literature review looked at all articles describing skin manifestations associated with COVID-19. The investigators identified 46 articles published between March and May 2020 which included a total of 130 clinical images.
The following findings from this study are striking:
- 92% of the published images of COVID-associated skin manifestations were in I-III.
- Only 6% of COVID skin lesions included in the articles were in patients with skin type IV.
- None showed COVID skin lesions in skin types V or VI.
- Only six of the articles reported race and ethnicity demographics. In those, 91% of the patients were White and 9% were Hispanic.
These results reveal a critical lack of representative clinical images of COVID-associated skin manifestations in patients of color. This deficiency is made all the more egregious given the fact that patients of color, including those who are Black, Latinx, and Native American, have been especially hard hit by the COVID-19 pandemic and suffer disproportionate disease-related morbidity and mortality.
As the study authors point out, skin manifestations in people of color often differ significantly from findings in White skin (for example, look at the figure depicting the rash typical of Kawasaki disease in a dark-skinned child compared with a light-skinned child). It is not a stretch to suggest that skin manifestations associated with COVID-19 may look very different in darker skin.
This isn’t a new phenomenon. Almost half of dermatologists feel that they’ve had insufficient exposure to skin disease in darker skin types. Skin of color remains underrepresented in medical journals.
Like other forms of passive, institutional racism, this deficiency will only be improved if dermatologists and dermatology publications actively seek out COVID-associated skin manifestations in patients of color and prioritize sharing these images. A medical student in the United Kingdom has gotten the ball rolling, compiling a handbook of clinical signs in darker skin types as part of a student-staff partnership at St. George’s Hospital and the University of London. At this time, Mind the Gap is looking for a publisher.
Dr. Lipper is an assistant clinical professor at the University of Vermont, Burlington, and a staff physician in the department of dermatology at Danbury (Conn.) Hospital. He has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
‘Staggering’ increase in COVID-linked depression, anxiety
Since the start of the COVID-19 pandemic, there has been a dramatic increase in depression, anxiety, psychosis, and suicidality, new research shows.
The new data, released by Mental Health America (MHA), came from individuals who completed a voluntary online mental health screen.
As of the end of June, over 169,000 additional participants reported having moderate to severe depression or anxiety, compared with participants who completed the screen prior to the pandemic.
In June alone, 18,000 additional participants were found to be at risk for psychosis, continuing a rising pattern that began in May, when 16,000 reported psychosis risk.
“We continue to see staggering numbers that indicate increased rates in depression and anxiety because of COVID-19,” Paul Gionfriddo, president and CEO of MHA, said in a release.
“In fact, the problem is bigger than anyone imagined, making it clear how the pandemic is affecting people now and will continue to affect people who mourn loved ones and whose serious mental conditions are left untreated. So we need to take this very seriously,” Mr. Gionfriddo said in an interview.
Real-time data
MHA has been conducting online screenings for 6 years. To date, nearly 5.5 million screenings have been completed, making it the largest screening program of its kind in the United States, Mr. Gionfriddo reported.
“At the beginning of the pandemic, we were asked by a member of the media if we could offer any insight about how anxiety in particular was affecting people during the pandemic since we were the only ones with a database that could give quantitative detail,” he said.
The results of their screen could also help find that information “in real time,” he added.
More people are now undergoing mental health screenings, Mr. Gionfriddo noted.
At roughly 7,000 per day in May and June, the number of anxiety and depression screenings that were completed per day were 406% and 457% higher, respectively, than the number completed in January.
The youngest group of participants were those aged 11-17 years; the oldest age group consisted of individuals 65 years and older.
The Patient Health Questionnaire–9 was used to identify those at risk for depression, the General Anxiety Disorder–7 was used to identify those at risk for anxiety, and the Prodromal Questionnaire Brief Version was used to identify those at high risk for psychosis.
Current events
Roughly 90% screened positive for moderate to severe depression, and 80% screened positive for moderate to severe anxiety.
“Kids between the ages of 11 and 17 years have been the most stressed, but it seems to be easier to bear as you get older,” Mr. Gionfriddo said.
Loneliness and isolation were cited as contributors to depression and anxiety by the largest percentage of individuals with these conditions (74% and 65%, respectively).
In June, roughly one quarter of participants also cited grief or loss and financial concerns as contributors to anxiety (25.31% and 24.18%, respectively) and to depression (26.53% and 23.36%).
Current events were cited as an important contributor, leading to more mental health problems in June, compared with May (36.11% vs 29.41 for anxiety; 29.13% vs 21.77% for depression).
The June screen added the category of racism as a potential contributor. Close to 8% reported it as a reason for anxiety, and roughly 5% considered it a reason for depression.
“We will be releasing more data at the end of July, and it will be interesting to see how the racism category compares to data we collected at the end of June,” Mr. Gionfriddo noted.
Dramatic increase
The screen also showed a “dramatic increase” in the number of people who reported being at risk for psychosis, with 18,000 participants screening positive. This represented more than four times the baseline figures recorded through March.
“We were not surprised to see a spike in depression and anxiety, but why were we seeing a spike in psychosis in May/June?” Mr. Gionfriddo asked. He suggested that stress may play a role in driving this increased risk.
“These data, we hope, will get policymakers to pay attention, take it seriously, and intervene to prevent psychosis at an earlier stage before signs and symptoms emerge,” said Mr. Gionfriddo.
One of the most alarming findings was that in June, 25,498 participants who screened positive for depression reported thinking of suicide or self-harm on “more than half of days to nearly every day.” A total of 14,607 participants said they had these thoughts every day.
Overall, the results should reinforce the recommendations of the US Preventive Services Task Force to routinely screen for depression in any clinical setting on a regular basis, Mr. Gionfriddo said.
In addition, policymakers “need to balance reopening vs. quarantining and isolating, and we need to think about what the next 2-4 years look like in terms of balancing physical health risks and mental health risks,” he noted.
“We’ve been treating the pandemic like a sprint and now, 4 or 5 months into it, perhaps as a middle-distance run, when in fact it’s a marathon,” he added.
Advocates needed
The increase in anxiety and depression often centers on the changes and uncertainties in the college experience, such as whether classes will be held in person, online, or a hybrid of the two, said Dr. Ritchie, who was not involved with the research.
Additionally, some college students who have “left the nest” have been forced to “return to the nest,” which compounds stress, she said.
LGBTQ youngsters may be particularly affected because some have “come out of the closet” while away from home and now must negotiate going back to their home of record. They are uncertain whether or not “to go back into the closet,” added Dr. Ritchie, who is also vice chair of psychiatry at Georgetown University, Washington.
Psychiatrists and other mental health professionals should be advocates for “getting services to more people for the greatest good,” she noted.
For example, the MHA data “might be useful in advocating for keeping telehealth accessible and even promoting it,” she said.
The full report is available on MHA’s website.
Mr. Gionfriddo and Dr. Ritchie report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Since the start of the COVID-19 pandemic, there has been a dramatic increase in depression, anxiety, psychosis, and suicidality, new research shows.
The new data, released by Mental Health America (MHA), came from individuals who completed a voluntary online mental health screen.
As of the end of June, over 169,000 additional participants reported having moderate to severe depression or anxiety, compared with participants who completed the screen prior to the pandemic.
In June alone, 18,000 additional participants were found to be at risk for psychosis, continuing a rising pattern that began in May, when 16,000 reported psychosis risk.
“We continue to see staggering numbers that indicate increased rates in depression and anxiety because of COVID-19,” Paul Gionfriddo, president and CEO of MHA, said in a release.
“In fact, the problem is bigger than anyone imagined, making it clear how the pandemic is affecting people now and will continue to affect people who mourn loved ones and whose serious mental conditions are left untreated. So we need to take this very seriously,” Mr. Gionfriddo said in an interview.
Real-time data
MHA has been conducting online screenings for 6 years. To date, nearly 5.5 million screenings have been completed, making it the largest screening program of its kind in the United States, Mr. Gionfriddo reported.
“At the beginning of the pandemic, we were asked by a member of the media if we could offer any insight about how anxiety in particular was affecting people during the pandemic since we were the only ones with a database that could give quantitative detail,” he said.
The results of their screen could also help find that information “in real time,” he added.
More people are now undergoing mental health screenings, Mr. Gionfriddo noted.
At roughly 7,000 per day in May and June, the number of anxiety and depression screenings that were completed per day were 406% and 457% higher, respectively, than the number completed in January.
The youngest group of participants were those aged 11-17 years; the oldest age group consisted of individuals 65 years and older.
The Patient Health Questionnaire–9 was used to identify those at risk for depression, the General Anxiety Disorder–7 was used to identify those at risk for anxiety, and the Prodromal Questionnaire Brief Version was used to identify those at high risk for psychosis.
Current events
Roughly 90% screened positive for moderate to severe depression, and 80% screened positive for moderate to severe anxiety.
“Kids between the ages of 11 and 17 years have been the most stressed, but it seems to be easier to bear as you get older,” Mr. Gionfriddo said.
Loneliness and isolation were cited as contributors to depression and anxiety by the largest percentage of individuals with these conditions (74% and 65%, respectively).
In June, roughly one quarter of participants also cited grief or loss and financial concerns as contributors to anxiety (25.31% and 24.18%, respectively) and to depression (26.53% and 23.36%).
Current events were cited as an important contributor, leading to more mental health problems in June, compared with May (36.11% vs 29.41 for anxiety; 29.13% vs 21.77% for depression).
The June screen added the category of racism as a potential contributor. Close to 8% reported it as a reason for anxiety, and roughly 5% considered it a reason for depression.
“We will be releasing more data at the end of July, and it will be interesting to see how the racism category compares to data we collected at the end of June,” Mr. Gionfriddo noted.
Dramatic increase
The screen also showed a “dramatic increase” in the number of people who reported being at risk for psychosis, with 18,000 participants screening positive. This represented more than four times the baseline figures recorded through March.
“We were not surprised to see a spike in depression and anxiety, but why were we seeing a spike in psychosis in May/June?” Mr. Gionfriddo asked. He suggested that stress may play a role in driving this increased risk.
“These data, we hope, will get policymakers to pay attention, take it seriously, and intervene to prevent psychosis at an earlier stage before signs and symptoms emerge,” said Mr. Gionfriddo.
One of the most alarming findings was that in June, 25,498 participants who screened positive for depression reported thinking of suicide or self-harm on “more than half of days to nearly every day.” A total of 14,607 participants said they had these thoughts every day.
Overall, the results should reinforce the recommendations of the US Preventive Services Task Force to routinely screen for depression in any clinical setting on a regular basis, Mr. Gionfriddo said.
In addition, policymakers “need to balance reopening vs. quarantining and isolating, and we need to think about what the next 2-4 years look like in terms of balancing physical health risks and mental health risks,” he noted.
“We’ve been treating the pandemic like a sprint and now, 4 or 5 months into it, perhaps as a middle-distance run, when in fact it’s a marathon,” he added.
Advocates needed
The increase in anxiety and depression often centers on the changes and uncertainties in the college experience, such as whether classes will be held in person, online, or a hybrid of the two, said Dr. Ritchie, who was not involved with the research.
Additionally, some college students who have “left the nest” have been forced to “return to the nest,” which compounds stress, she said.
LGBTQ youngsters may be particularly affected because some have “come out of the closet” while away from home and now must negotiate going back to their home of record. They are uncertain whether or not “to go back into the closet,” added Dr. Ritchie, who is also vice chair of psychiatry at Georgetown University, Washington.
Psychiatrists and other mental health professionals should be advocates for “getting services to more people for the greatest good,” she noted.
For example, the MHA data “might be useful in advocating for keeping telehealth accessible and even promoting it,” she said.
The full report is available on MHA’s website.
Mr. Gionfriddo and Dr. Ritchie report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Since the start of the COVID-19 pandemic, there has been a dramatic increase in depression, anxiety, psychosis, and suicidality, new research shows.
The new data, released by Mental Health America (MHA), came from individuals who completed a voluntary online mental health screen.
As of the end of June, over 169,000 additional participants reported having moderate to severe depression or anxiety, compared with participants who completed the screen prior to the pandemic.
In June alone, 18,000 additional participants were found to be at risk for psychosis, continuing a rising pattern that began in May, when 16,000 reported psychosis risk.
“We continue to see staggering numbers that indicate increased rates in depression and anxiety because of COVID-19,” Paul Gionfriddo, president and CEO of MHA, said in a release.
“In fact, the problem is bigger than anyone imagined, making it clear how the pandemic is affecting people now and will continue to affect people who mourn loved ones and whose serious mental conditions are left untreated. So we need to take this very seriously,” Mr. Gionfriddo said in an interview.
Real-time data
MHA has been conducting online screenings for 6 years. To date, nearly 5.5 million screenings have been completed, making it the largest screening program of its kind in the United States, Mr. Gionfriddo reported.
“At the beginning of the pandemic, we were asked by a member of the media if we could offer any insight about how anxiety in particular was affecting people during the pandemic since we were the only ones with a database that could give quantitative detail,” he said.
The results of their screen could also help find that information “in real time,” he added.
More people are now undergoing mental health screenings, Mr. Gionfriddo noted.
At roughly 7,000 per day in May and June, the number of anxiety and depression screenings that were completed per day were 406% and 457% higher, respectively, than the number completed in January.
The youngest group of participants were those aged 11-17 years; the oldest age group consisted of individuals 65 years and older.
The Patient Health Questionnaire–9 was used to identify those at risk for depression, the General Anxiety Disorder–7 was used to identify those at risk for anxiety, and the Prodromal Questionnaire Brief Version was used to identify those at high risk for psychosis.
Current events
Roughly 90% screened positive for moderate to severe depression, and 80% screened positive for moderate to severe anxiety.
“Kids between the ages of 11 and 17 years have been the most stressed, but it seems to be easier to bear as you get older,” Mr. Gionfriddo said.
Loneliness and isolation were cited as contributors to depression and anxiety by the largest percentage of individuals with these conditions (74% and 65%, respectively).
In June, roughly one quarter of participants also cited grief or loss and financial concerns as contributors to anxiety (25.31% and 24.18%, respectively) and to depression (26.53% and 23.36%).
Current events were cited as an important contributor, leading to more mental health problems in June, compared with May (36.11% vs 29.41 for anxiety; 29.13% vs 21.77% for depression).
The June screen added the category of racism as a potential contributor. Close to 8% reported it as a reason for anxiety, and roughly 5% considered it a reason for depression.
“We will be releasing more data at the end of July, and it will be interesting to see how the racism category compares to data we collected at the end of June,” Mr. Gionfriddo noted.
Dramatic increase
The screen also showed a “dramatic increase” in the number of people who reported being at risk for psychosis, with 18,000 participants screening positive. This represented more than four times the baseline figures recorded through March.
“We were not surprised to see a spike in depression and anxiety, but why were we seeing a spike in psychosis in May/June?” Mr. Gionfriddo asked. He suggested that stress may play a role in driving this increased risk.
“These data, we hope, will get policymakers to pay attention, take it seriously, and intervene to prevent psychosis at an earlier stage before signs and symptoms emerge,” said Mr. Gionfriddo.
One of the most alarming findings was that in June, 25,498 participants who screened positive for depression reported thinking of suicide or self-harm on “more than half of days to nearly every day.” A total of 14,607 participants said they had these thoughts every day.
Overall, the results should reinforce the recommendations of the US Preventive Services Task Force to routinely screen for depression in any clinical setting on a regular basis, Mr. Gionfriddo said.
In addition, policymakers “need to balance reopening vs. quarantining and isolating, and we need to think about what the next 2-4 years look like in terms of balancing physical health risks and mental health risks,” he noted.
“We’ve been treating the pandemic like a sprint and now, 4 or 5 months into it, perhaps as a middle-distance run, when in fact it’s a marathon,” he added.
Advocates needed
The increase in anxiety and depression often centers on the changes and uncertainties in the college experience, such as whether classes will be held in person, online, or a hybrid of the two, said Dr. Ritchie, who was not involved with the research.
Additionally, some college students who have “left the nest” have been forced to “return to the nest,” which compounds stress, she said.
LGBTQ youngsters may be particularly affected because some have “come out of the closet” while away from home and now must negotiate going back to their home of record. They are uncertain whether or not “to go back into the closet,” added Dr. Ritchie, who is also vice chair of psychiatry at Georgetown University, Washington.
Psychiatrists and other mental health professionals should be advocates for “getting services to more people for the greatest good,” she noted.
For example, the MHA data “might be useful in advocating for keeping telehealth accessible and even promoting it,” she said.
The full report is available on MHA’s website.
Mr. Gionfriddo and Dr. Ritchie report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Psychiatrists report rare case of woman who thinks she’s a chicken
LEUVEN, Belgium — A 54-year-old woman has suffered the delusion of thinking she is a chicken for 24 hours. This very rare condition, known as zoanthropy, in which people think they are an animal is often not recognised, say researchers from the University of Leuven.
Zoanthropy can include people believing they are, or behaving like, any kind of animal: from a dog, to a lion or tiger, crocodile, snake, or bee.
It’s important to recognise this as a potential symptom of something serious, say the researchers in the July issue of the Belgian Journal of Psychiatry, Tijdschrift voor Psychiatrie.
“Additional investigations with brain imaging and electroencephalogram are therefore advised,” say the authors.
Psychiatrists Need to Be Aware That Clinical Zoanthropy Exists
In their paper, they describe the case of the woman who briefly thought she was a chicken, which was followed by her having a generalized epileptic seizure.
“Clinically, we saw a lady who perspired profusely, trembled, blew up her cheeks, and ... seemed to imitate a chicken, [making noises] like clucking, cackling, and crowing like a rooster,” they say.
“After about 10 minutes she seemed to tighten her muscles for a few seconds, her face turned red and for a short time she didn’t react. These symptoms repeated themselves at intervals of a few minutes [and her] consciousness was fluctuating,” with the patient “disoriented in time and space.”
Lead author Dr Athena Beckers of University Psychiatric Centre, KU Leuven, Belgium, said in an interview with MediQuality: “With only 56 case descriptions in the medical literature from 1850 to the present day, the condition is rare. It amounts to about one description every 3 years.
“We suspect, however, that the delusion is not always noticed: the patient shows bizarre behaviour or makes animal sounds, it is probably often catalogued under the general term ‘psychosis’.”
Dr Beckers adds that it is important that the symptoms are recognised, because of the possible underlying causes which can include epilepsy. So this might require a different or complementary treatment “with, for example, antiepileptic drugs”.
“I myself have only seen this type of delusion once, but I ... heard anecdotal stories from other patients whose family member, for example with schizophrenia, sometimes thought he was a cow [during] ... a psychosis.
“After the publication of my article I was also contacted by someone who told me they had experienced the same thing 30 years ago – he thought he was a chicken.
“I think it’s a good thing that we psychiatrists are aware of the fact that clinical zoanthropy exists and may require additional research,” she observed.
Fortunately, this woman’s experience ended well. After about one year of disability, the patient was able to return to work progressively. Her mood remained stable and there were no more psychotic symptoms or any indication of epileptic episodes.
Such Delusions Are Rare
Dr Georges Otte, a recently retired neuropsychiatrist who formerly worked at Ghent University, Belgium, gave his thoughts to Mediquality: “The interface between neurology and psychiatry ... is a fertile meadow on which many crops thrive. But it is in the darkest corners of psychosis that one finds the most bizarre and also rarest excesses.”
There are a number of delusions of identity, said Dr Otte.
These include Cotard’s syndrome, a rare condition marked by the false belief that the person or their body parts are dead, dying, or don’t exist, or Capgras delusion, where the affected person believes that a spouse or close family member has been replaced with an imposter. Delusions can also occur as a result of substance abuse, for example after using psilocybin (magic mushrooms), he added.
“Delusions in which patients are convinced of ‘shape shifting’ (man to animal) are quite rare,” Dr Otte observed.
“In the literature we know that lycanthropy [a person thinks he or she is turning into a werewolf],” has been reported, and has “apparently inspired many authors of horror stories,” he added.
“But it’s not every day that as a psychiatrist, you will encounter such an extreme psychotic depersonalization as someone turning into a chicken.”
This article first appeared on Medscape.com.
LEUVEN, Belgium — A 54-year-old woman has suffered the delusion of thinking she is a chicken for 24 hours. This very rare condition, known as zoanthropy, in which people think they are an animal is often not recognised, say researchers from the University of Leuven.
Zoanthropy can include people believing they are, or behaving like, any kind of animal: from a dog, to a lion or tiger, crocodile, snake, or bee.
It’s important to recognise this as a potential symptom of something serious, say the researchers in the July issue of the Belgian Journal of Psychiatry, Tijdschrift voor Psychiatrie.
“Additional investigations with brain imaging and electroencephalogram are therefore advised,” say the authors.
Psychiatrists Need to Be Aware That Clinical Zoanthropy Exists
In their paper, they describe the case of the woman who briefly thought she was a chicken, which was followed by her having a generalized epileptic seizure.
“Clinically, we saw a lady who perspired profusely, trembled, blew up her cheeks, and ... seemed to imitate a chicken, [making noises] like clucking, cackling, and crowing like a rooster,” they say.
“After about 10 minutes she seemed to tighten her muscles for a few seconds, her face turned red and for a short time she didn’t react. These symptoms repeated themselves at intervals of a few minutes [and her] consciousness was fluctuating,” with the patient “disoriented in time and space.”
Lead author Dr Athena Beckers of University Psychiatric Centre, KU Leuven, Belgium, said in an interview with MediQuality: “With only 56 case descriptions in the medical literature from 1850 to the present day, the condition is rare. It amounts to about one description every 3 years.
“We suspect, however, that the delusion is not always noticed: the patient shows bizarre behaviour or makes animal sounds, it is probably often catalogued under the general term ‘psychosis’.”
Dr Beckers adds that it is important that the symptoms are recognised, because of the possible underlying causes which can include epilepsy. So this might require a different or complementary treatment “with, for example, antiepileptic drugs”.
“I myself have only seen this type of delusion once, but I ... heard anecdotal stories from other patients whose family member, for example with schizophrenia, sometimes thought he was a cow [during] ... a psychosis.
“After the publication of my article I was also contacted by someone who told me they had experienced the same thing 30 years ago – he thought he was a chicken.
“I think it’s a good thing that we psychiatrists are aware of the fact that clinical zoanthropy exists and may require additional research,” she observed.
Fortunately, this woman’s experience ended well. After about one year of disability, the patient was able to return to work progressively. Her mood remained stable and there were no more psychotic symptoms or any indication of epileptic episodes.
Such Delusions Are Rare
Dr Georges Otte, a recently retired neuropsychiatrist who formerly worked at Ghent University, Belgium, gave his thoughts to Mediquality: “The interface between neurology and psychiatry ... is a fertile meadow on which many crops thrive. But it is in the darkest corners of psychosis that one finds the most bizarre and also rarest excesses.”
There are a number of delusions of identity, said Dr Otte.
These include Cotard’s syndrome, a rare condition marked by the false belief that the person or their body parts are dead, dying, or don’t exist, or Capgras delusion, where the affected person believes that a spouse or close family member has been replaced with an imposter. Delusions can also occur as a result of substance abuse, for example after using psilocybin (magic mushrooms), he added.
“Delusions in which patients are convinced of ‘shape shifting’ (man to animal) are quite rare,” Dr Otte observed.
“In the literature we know that lycanthropy [a person thinks he or she is turning into a werewolf],” has been reported, and has “apparently inspired many authors of horror stories,” he added.
“But it’s not every day that as a psychiatrist, you will encounter such an extreme psychotic depersonalization as someone turning into a chicken.”
This article first appeared on Medscape.com.
LEUVEN, Belgium — A 54-year-old woman has suffered the delusion of thinking she is a chicken for 24 hours. This very rare condition, known as zoanthropy, in which people think they are an animal is often not recognised, say researchers from the University of Leuven.
Zoanthropy can include people believing they are, or behaving like, any kind of animal: from a dog, to a lion or tiger, crocodile, snake, or bee.
It’s important to recognise this as a potential symptom of something serious, say the researchers in the July issue of the Belgian Journal of Psychiatry, Tijdschrift voor Psychiatrie.
“Additional investigations with brain imaging and electroencephalogram are therefore advised,” say the authors.
Psychiatrists Need to Be Aware That Clinical Zoanthropy Exists
In their paper, they describe the case of the woman who briefly thought she was a chicken, which was followed by her having a generalized epileptic seizure.
“Clinically, we saw a lady who perspired profusely, trembled, blew up her cheeks, and ... seemed to imitate a chicken, [making noises] like clucking, cackling, and crowing like a rooster,” they say.
“After about 10 minutes she seemed to tighten her muscles for a few seconds, her face turned red and for a short time she didn’t react. These symptoms repeated themselves at intervals of a few minutes [and her] consciousness was fluctuating,” with the patient “disoriented in time and space.”
Lead author Dr Athena Beckers of University Psychiatric Centre, KU Leuven, Belgium, said in an interview with MediQuality: “With only 56 case descriptions in the medical literature from 1850 to the present day, the condition is rare. It amounts to about one description every 3 years.
“We suspect, however, that the delusion is not always noticed: the patient shows bizarre behaviour or makes animal sounds, it is probably often catalogued under the general term ‘psychosis’.”
Dr Beckers adds that it is important that the symptoms are recognised, because of the possible underlying causes which can include epilepsy. So this might require a different or complementary treatment “with, for example, antiepileptic drugs”.
“I myself have only seen this type of delusion once, but I ... heard anecdotal stories from other patients whose family member, for example with schizophrenia, sometimes thought he was a cow [during] ... a psychosis.
“After the publication of my article I was also contacted by someone who told me they had experienced the same thing 30 years ago – he thought he was a chicken.
“I think it’s a good thing that we psychiatrists are aware of the fact that clinical zoanthropy exists and may require additional research,” she observed.
Fortunately, this woman’s experience ended well. After about one year of disability, the patient was able to return to work progressively. Her mood remained stable and there were no more psychotic symptoms or any indication of epileptic episodes.
Such Delusions Are Rare
Dr Georges Otte, a recently retired neuropsychiatrist who formerly worked at Ghent University, Belgium, gave his thoughts to Mediquality: “The interface between neurology and psychiatry ... is a fertile meadow on which many crops thrive. But it is in the darkest corners of psychosis that one finds the most bizarre and also rarest excesses.”
There are a number of delusions of identity, said Dr Otte.
These include Cotard’s syndrome, a rare condition marked by the false belief that the person or their body parts are dead, dying, or don’t exist, or Capgras delusion, where the affected person believes that a spouse or close family member has been replaced with an imposter. Delusions can also occur as a result of substance abuse, for example after using psilocybin (magic mushrooms), he added.
“Delusions in which patients are convinced of ‘shape shifting’ (man to animal) are quite rare,” Dr Otte observed.
“In the literature we know that lycanthropy [a person thinks he or she is turning into a werewolf],” has been reported, and has “apparently inspired many authors of horror stories,” he added.
“But it’s not every day that as a psychiatrist, you will encounter such an extreme psychotic depersonalization as someone turning into a chicken.”
This article first appeared on Medscape.com.
Patients with COPD plus sleep problems should be screened for mood disorders
A study has shown a strong link between sleeping disturbances and depression in patients with chronic obstructive pulmonary disease.
Adults with clinically stable COPD who reported sleep problems were significantly more likely to report depression or anxiety, poor self-efficacy, and poor health-related quality of life, compared with those not reporting sleep problems, according to the findings from a study of 245 patients.
Sleep problems are common in patients with COPD and have been associated with poor COPD-related outcomes, wrote Sang Hee Lee, MD, of Wonkwang University Sanbon Hospital, Gunpo-si, South Korea, and colleagues.
“However, there is a lack of research on factors associated with sleep disturbance in patients with COPD,” they wrote.
In a prospective, multicenter, cross-sectional study published in the Clinical Respiratory Journal, the researchers enrolled 245 adults with COPD who completed the COPD and Asthma Impact Scale (CASIS) to determine sleep impairment. The CASIS was developed to measure sleep-related problems associated with respiratory disease, and scored on a scale of 1-100, with higher scores indicating greater sleep impairment. The average CASIS score was 40.9. The average age of the patients was 67 years, and 92% were men.
Patients’ health-related quality of life, anxiety/depression, and self-efficacy were assessed using the St. George’s Respiratory Questionnaire (SGRQ), the 36-item Short-Form Health Survey (SF-36), Hospital Anxiety and Depression Scale (HADS), and the COPD Self-Efficacy Scale (CSES). The average scores on these measures were 36.0 for the SGRQ; 48.1 and 50.6, respectively, for the physical and mental components of the SF-36; 3.8 and 6.4, respectively, for the HADS-A and HADS-D measures of anxiety and depression; and 3.3 on the CSES.
Worse sleep in these patients was associated with worse scores on measures of mood. In a multivariate analysis, higher scores on all four measures of health-related quality of life were significantly associated with higher CASIS scores (P = .006 for SGRQ; P = .037 for SF-36, P < .001 for HADS, and P = .010 for CSES).
Although the CASIS did not allow for measurement of symptom severity and did not include many items related to breathing problems, the test “shows good internal consistency, test-retest reproducibility, and construct validity according to previous studies,” the researchers wrote. “The CASIS may be a good tool for evaluating sleep disturbances in COPD patients, and further study is needed,” they added.
The study findings were limited by several factors including the cross-sectional study design, lack of data on obstructive sleep apnea, and lack of information on specific treatments such as at-home oxygen use or high-dose steroid use, the researchers noted. However, the results were strengthened by the use of a disease-specific sleep measure, and the study is the first known to include self-efficacy in relation to sleep quality in COPD patients, they reported.
The results highlight the association between depression, poor quality of life, and self-efficacy in relation to poor sleep, and suggest that “Sleep quality could be improved by enhancing HRQL and self-efficacy,” the researchers said. “Screening for mood disorder in patients with COPD is also needed,” they concluded.
The study was supported by the Basic Science Research Program of the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology. The researchers had no financial conflicts to disclose.
SOURCE: Lee SH et al. Clin Respir J. 2020 Jul 24. doi: 10.1111/crj.13235.
A study has shown a strong link between sleeping disturbances and depression in patients with chronic obstructive pulmonary disease.
Adults with clinically stable COPD who reported sleep problems were significantly more likely to report depression or anxiety, poor self-efficacy, and poor health-related quality of life, compared with those not reporting sleep problems, according to the findings from a study of 245 patients.
Sleep problems are common in patients with COPD and have been associated with poor COPD-related outcomes, wrote Sang Hee Lee, MD, of Wonkwang University Sanbon Hospital, Gunpo-si, South Korea, and colleagues.
“However, there is a lack of research on factors associated with sleep disturbance in patients with COPD,” they wrote.
In a prospective, multicenter, cross-sectional study published in the Clinical Respiratory Journal, the researchers enrolled 245 adults with COPD who completed the COPD and Asthma Impact Scale (CASIS) to determine sleep impairment. The CASIS was developed to measure sleep-related problems associated with respiratory disease, and scored on a scale of 1-100, with higher scores indicating greater sleep impairment. The average CASIS score was 40.9. The average age of the patients was 67 years, and 92% were men.
Patients’ health-related quality of life, anxiety/depression, and self-efficacy were assessed using the St. George’s Respiratory Questionnaire (SGRQ), the 36-item Short-Form Health Survey (SF-36), Hospital Anxiety and Depression Scale (HADS), and the COPD Self-Efficacy Scale (CSES). The average scores on these measures were 36.0 for the SGRQ; 48.1 and 50.6, respectively, for the physical and mental components of the SF-36; 3.8 and 6.4, respectively, for the HADS-A and HADS-D measures of anxiety and depression; and 3.3 on the CSES.
Worse sleep in these patients was associated with worse scores on measures of mood. In a multivariate analysis, higher scores on all four measures of health-related quality of life were significantly associated with higher CASIS scores (P = .006 for SGRQ; P = .037 for SF-36, P < .001 for HADS, and P = .010 for CSES).
Although the CASIS did not allow for measurement of symptom severity and did not include many items related to breathing problems, the test “shows good internal consistency, test-retest reproducibility, and construct validity according to previous studies,” the researchers wrote. “The CASIS may be a good tool for evaluating sleep disturbances in COPD patients, and further study is needed,” they added.
The study findings were limited by several factors including the cross-sectional study design, lack of data on obstructive sleep apnea, and lack of information on specific treatments such as at-home oxygen use or high-dose steroid use, the researchers noted. However, the results were strengthened by the use of a disease-specific sleep measure, and the study is the first known to include self-efficacy in relation to sleep quality in COPD patients, they reported.
The results highlight the association between depression, poor quality of life, and self-efficacy in relation to poor sleep, and suggest that “Sleep quality could be improved by enhancing HRQL and self-efficacy,” the researchers said. “Screening for mood disorder in patients with COPD is also needed,” they concluded.
The study was supported by the Basic Science Research Program of the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology. The researchers had no financial conflicts to disclose.
SOURCE: Lee SH et al. Clin Respir J. 2020 Jul 24. doi: 10.1111/crj.13235.
A study has shown a strong link between sleeping disturbances and depression in patients with chronic obstructive pulmonary disease.
Adults with clinically stable COPD who reported sleep problems were significantly more likely to report depression or anxiety, poor self-efficacy, and poor health-related quality of life, compared with those not reporting sleep problems, according to the findings from a study of 245 patients.
Sleep problems are common in patients with COPD and have been associated with poor COPD-related outcomes, wrote Sang Hee Lee, MD, of Wonkwang University Sanbon Hospital, Gunpo-si, South Korea, and colleagues.
“However, there is a lack of research on factors associated with sleep disturbance in patients with COPD,” they wrote.
In a prospective, multicenter, cross-sectional study published in the Clinical Respiratory Journal, the researchers enrolled 245 adults with COPD who completed the COPD and Asthma Impact Scale (CASIS) to determine sleep impairment. The CASIS was developed to measure sleep-related problems associated with respiratory disease, and scored on a scale of 1-100, with higher scores indicating greater sleep impairment. The average CASIS score was 40.9. The average age of the patients was 67 years, and 92% were men.
Patients’ health-related quality of life, anxiety/depression, and self-efficacy were assessed using the St. George’s Respiratory Questionnaire (SGRQ), the 36-item Short-Form Health Survey (SF-36), Hospital Anxiety and Depression Scale (HADS), and the COPD Self-Efficacy Scale (CSES). The average scores on these measures were 36.0 for the SGRQ; 48.1 and 50.6, respectively, for the physical and mental components of the SF-36; 3.8 and 6.4, respectively, for the HADS-A and HADS-D measures of anxiety and depression; and 3.3 on the CSES.
Worse sleep in these patients was associated with worse scores on measures of mood. In a multivariate analysis, higher scores on all four measures of health-related quality of life were significantly associated with higher CASIS scores (P = .006 for SGRQ; P = .037 for SF-36, P < .001 for HADS, and P = .010 for CSES).
Although the CASIS did not allow for measurement of symptom severity and did not include many items related to breathing problems, the test “shows good internal consistency, test-retest reproducibility, and construct validity according to previous studies,” the researchers wrote. “The CASIS may be a good tool for evaluating sleep disturbances in COPD patients, and further study is needed,” they added.
The study findings were limited by several factors including the cross-sectional study design, lack of data on obstructive sleep apnea, and lack of information on specific treatments such as at-home oxygen use or high-dose steroid use, the researchers noted. However, the results were strengthened by the use of a disease-specific sleep measure, and the study is the first known to include self-efficacy in relation to sleep quality in COPD patients, they reported.
The results highlight the association between depression, poor quality of life, and self-efficacy in relation to poor sleep, and suggest that “Sleep quality could be improved by enhancing HRQL and self-efficacy,” the researchers said. “Screening for mood disorder in patients with COPD is also needed,” they concluded.
The study was supported by the Basic Science Research Program of the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology. The researchers had no financial conflicts to disclose.
SOURCE: Lee SH et al. Clin Respir J. 2020 Jul 24. doi: 10.1111/crj.13235.
FROM THE CLINICAL RESPIRATORY JOURNAL
More data needed to better understand COVID-19 skin manifestations
Qing Zhao, MD, Xiaokai Fang, MD, and their colleagues at the Shandong Provincial Hospital for Skin Diseases & Shandong Provincial Institute of Dermatology and Venereology, in Jinan, China, reported the results of a literature review of 44 articles published through May 2020 that included 507 patients with cutaneous manifestations of COVID-19. The review was published in the Journal of The European Academy of Dermatology and Venereology.
Nearly all of the patients (96%) were from Europe, and more than half were women (60%), with an average age of 49 years. Most patients had multiple skin symptoms, with the most common being erythema (44%), chilblain-like lesions (20%), urticaria-like lesions (16%), vesicular manifestations (13%), livedo/necrosis (6%), and petechiae (almost 2%). The authors described erythema as being present in specific sites, such as the trunk, extremities, flexural regions, face, and mucous membranes. Slightly less than half of all patients had significant pruritus.
Data on systemic COVID-19 symptoms were available for 431 patients and included fever in about two-thirds of patients and cough in almost 70%, with dyspnea in almost half of patients. Almost 60% had fatigue, and almost 60% had asthenia. Information about the onset of skin symptoms was available in 88 patients; of these patients, lesions were seen an average of almost 10 days after systemic symptoms appeared and, in almost 15%, were the first symptoms noted.
Histopathologic exams were done for only 23 patients and, in all cases, showed “inflammatory features without specific pathological changes, such as lymphocyte infiltration.” In one study, reverse transcription polymerase chain reaction testing of skin biopsy specimens tested negative for SARS-CoV-2.
Expression of ACE2, the receptor of SARS-CoV-2, in the skin was evaluated in six of the studies. “Higher ACE2 expression was identified in keratinocytes, mainly in differentiating keratinocytes and basal cells compared to the other cells of skin tissues,” the authors wrote. These results were confirmed with immunohistochemistry, which, they said, found “ACE2-positive keratinocytes in the stratum basal, the stratum spinosum, and the stratum granulosum of epiderma.” They added that this provides evidence “for percutaneous infection or the entry of virus into patients through skin tissues,” but cautioned that more research is needed.
The authors acknowledged that there are still many unanswered questions about COVID-19, and that more clinical data and research are needed, to improve the understanding of the cutaneous manifestations associated with COVID-19.
In an interview, Alisa N. Femia, MD, director of inpatient dermatology in the department of dermatology at New York University, said that the cutaneous signs described in the review align well with what she has seen in patients with COVID-19.
At this point, it is unclear whether cutaneous manifestations of COVID-19 are a result of SARS-CoV-2 invading the skin or an immune response related to SARS-CoV-2, noted Dr. Femia, who was not involved in the research. One method of entry could be through transmitting virus present on the skin to another part of the body where infection is more likely.
While it is possible COVID-19 could be contracted through the skin, she noted, it is much more likely an individual would be infected by SARS-CoV-2 through more traditionally understood means of transmission, such as through respiratory droplets in person-to-person contact. “I think we are far away from drawing that conclusion, that one could touch a surface or a person who has COVID and contract it through their skin,” Dr. Femia said. “The skin has a lot of other ways to protect against that from occurring,” she added.
“SAR-CoV-2 obviously enters through the ACE2 receptor, which is fairly ubiquitous, and it has been seen in keratinocytes,” she said. “But the skin is one of our biggest barriers ... and further, studies to date have shown that that receptor is expressed in relatively low levels of the keratinocytes.”
Pathogenesis of different cutaneous manifestations may be different, Dr. Femia said. For example, urticaria and morbilliform eruption were described by the authors of the review as more benign eruptions, but pathogenesis may differ from that of so-called COVID toes and from the pathogenesis of purpura and ulcerations seen in patients with more severe disease, she noted. It is plausible, she added, that purpura and ulcerations may be a “direct invasion of SARS-CoV-2 into endothelial cells,” which creates secondary processes “that ultimately destroy the skin.”
Urticaria and morbilliform eruptions, on the other hand, “are more simply that the immune system is recognizing COVID, and in doing so, is also recognizing some antigens in the skin and creating a hypersensitive response to the skin” and has “nothing to do with the SARS-CoV-2 virus actually being in that location,” she said.
It is important to differentiate between patients who have skin manifestations attributed to COVID-19 and those with manifestations independent of COVID-19, which is difficult, Dr. Femia noted. A patient with COVID-19 and a cutaneous manifestation may be having a reaction to a medication. “It’s important to have a critical eye and to remember that, when we see these manifestations, we should always be investigating whether there was an alternative cause so that we can better learn what exactly we should be attributing to this infection,” she said
Adam Friedman, MD, professor and interim chair of dermatology at George Washington University, Washington, said the authors of the review had presented interesting work, but made some “assumptions that need to be proven.” Dr. Friedman also was not involved in the research, but agreed in an interview with the assessment that it is unlikely SARS-CoV-2 would penetrate the skin. While some viruses – such as the poxvirus that causes molluscum contagiosum and the herpes simplex virus – invade keratinocytes specifically, there is a particular clinical phenotype that results that is associated with changes in the epidermis. However, “the skin manifestations of COVID-19 do not fit with direct skin invasion, [but] rather the immune response to systemic disease,” he said.
“[I]n terms of systemic invasion through the skin, it is possible, but this study certainly doesn’t show that. The presence/expression of ACE2 in the epidermis doesn’t translate to route of infection,” Dr. Friedman said..
The study received financial support from Shandong First Medical University, the Innovation Project of Shandong Academy of Medical Sciences and the Shandong Province Taishan Scholar Project. The authors report no relevant financial disclosures. Dr. Femia and Dr. Friedman had no relevant financial disclosures.
SOURCE: Zhao Q et al. J Eur Acad Dermatol Venereol. 2020 Jun 28. doi: 10.1111/jdv.16778.
Qing Zhao, MD, Xiaokai Fang, MD, and their colleagues at the Shandong Provincial Hospital for Skin Diseases & Shandong Provincial Institute of Dermatology and Venereology, in Jinan, China, reported the results of a literature review of 44 articles published through May 2020 that included 507 patients with cutaneous manifestations of COVID-19. The review was published in the Journal of The European Academy of Dermatology and Venereology.
Nearly all of the patients (96%) were from Europe, and more than half were women (60%), with an average age of 49 years. Most patients had multiple skin symptoms, with the most common being erythema (44%), chilblain-like lesions (20%), urticaria-like lesions (16%), vesicular manifestations (13%), livedo/necrosis (6%), and petechiae (almost 2%). The authors described erythema as being present in specific sites, such as the trunk, extremities, flexural regions, face, and mucous membranes. Slightly less than half of all patients had significant pruritus.
Data on systemic COVID-19 symptoms were available for 431 patients and included fever in about two-thirds of patients and cough in almost 70%, with dyspnea in almost half of patients. Almost 60% had fatigue, and almost 60% had asthenia. Information about the onset of skin symptoms was available in 88 patients; of these patients, lesions were seen an average of almost 10 days after systemic symptoms appeared and, in almost 15%, were the first symptoms noted.
Histopathologic exams were done for only 23 patients and, in all cases, showed “inflammatory features without specific pathological changes, such as lymphocyte infiltration.” In one study, reverse transcription polymerase chain reaction testing of skin biopsy specimens tested negative for SARS-CoV-2.
Expression of ACE2, the receptor of SARS-CoV-2, in the skin was evaluated in six of the studies. “Higher ACE2 expression was identified in keratinocytes, mainly in differentiating keratinocytes and basal cells compared to the other cells of skin tissues,” the authors wrote. These results were confirmed with immunohistochemistry, which, they said, found “ACE2-positive keratinocytes in the stratum basal, the stratum spinosum, and the stratum granulosum of epiderma.” They added that this provides evidence “for percutaneous infection or the entry of virus into patients through skin tissues,” but cautioned that more research is needed.
The authors acknowledged that there are still many unanswered questions about COVID-19, and that more clinical data and research are needed, to improve the understanding of the cutaneous manifestations associated with COVID-19.
In an interview, Alisa N. Femia, MD, director of inpatient dermatology in the department of dermatology at New York University, said that the cutaneous signs described in the review align well with what she has seen in patients with COVID-19.
At this point, it is unclear whether cutaneous manifestations of COVID-19 are a result of SARS-CoV-2 invading the skin or an immune response related to SARS-CoV-2, noted Dr. Femia, who was not involved in the research. One method of entry could be through transmitting virus present on the skin to another part of the body where infection is more likely.
While it is possible COVID-19 could be contracted through the skin, she noted, it is much more likely an individual would be infected by SARS-CoV-2 through more traditionally understood means of transmission, such as through respiratory droplets in person-to-person contact. “I think we are far away from drawing that conclusion, that one could touch a surface or a person who has COVID and contract it through their skin,” Dr. Femia said. “The skin has a lot of other ways to protect against that from occurring,” she added.
“SAR-CoV-2 obviously enters through the ACE2 receptor, which is fairly ubiquitous, and it has been seen in keratinocytes,” she said. “But the skin is one of our biggest barriers ... and further, studies to date have shown that that receptor is expressed in relatively low levels of the keratinocytes.”
Pathogenesis of different cutaneous manifestations may be different, Dr. Femia said. For example, urticaria and morbilliform eruption were described by the authors of the review as more benign eruptions, but pathogenesis may differ from that of so-called COVID toes and from the pathogenesis of purpura and ulcerations seen in patients with more severe disease, she noted. It is plausible, she added, that purpura and ulcerations may be a “direct invasion of SARS-CoV-2 into endothelial cells,” which creates secondary processes “that ultimately destroy the skin.”
Urticaria and morbilliform eruptions, on the other hand, “are more simply that the immune system is recognizing COVID, and in doing so, is also recognizing some antigens in the skin and creating a hypersensitive response to the skin” and has “nothing to do with the SARS-CoV-2 virus actually being in that location,” she said.
It is important to differentiate between patients who have skin manifestations attributed to COVID-19 and those with manifestations independent of COVID-19, which is difficult, Dr. Femia noted. A patient with COVID-19 and a cutaneous manifestation may be having a reaction to a medication. “It’s important to have a critical eye and to remember that, when we see these manifestations, we should always be investigating whether there was an alternative cause so that we can better learn what exactly we should be attributing to this infection,” she said
Adam Friedman, MD, professor and interim chair of dermatology at George Washington University, Washington, said the authors of the review had presented interesting work, but made some “assumptions that need to be proven.” Dr. Friedman also was not involved in the research, but agreed in an interview with the assessment that it is unlikely SARS-CoV-2 would penetrate the skin. While some viruses – such as the poxvirus that causes molluscum contagiosum and the herpes simplex virus – invade keratinocytes specifically, there is a particular clinical phenotype that results that is associated with changes in the epidermis. However, “the skin manifestations of COVID-19 do not fit with direct skin invasion, [but] rather the immune response to systemic disease,” he said.
“[I]n terms of systemic invasion through the skin, it is possible, but this study certainly doesn’t show that. The presence/expression of ACE2 in the epidermis doesn’t translate to route of infection,” Dr. Friedman said..
The study received financial support from Shandong First Medical University, the Innovation Project of Shandong Academy of Medical Sciences and the Shandong Province Taishan Scholar Project. The authors report no relevant financial disclosures. Dr. Femia and Dr. Friedman had no relevant financial disclosures.
SOURCE: Zhao Q et al. J Eur Acad Dermatol Venereol. 2020 Jun 28. doi: 10.1111/jdv.16778.
Qing Zhao, MD, Xiaokai Fang, MD, and their colleagues at the Shandong Provincial Hospital for Skin Diseases & Shandong Provincial Institute of Dermatology and Venereology, in Jinan, China, reported the results of a literature review of 44 articles published through May 2020 that included 507 patients with cutaneous manifestations of COVID-19. The review was published in the Journal of The European Academy of Dermatology and Venereology.
Nearly all of the patients (96%) were from Europe, and more than half were women (60%), with an average age of 49 years. Most patients had multiple skin symptoms, with the most common being erythema (44%), chilblain-like lesions (20%), urticaria-like lesions (16%), vesicular manifestations (13%), livedo/necrosis (6%), and petechiae (almost 2%). The authors described erythema as being present in specific sites, such as the trunk, extremities, flexural regions, face, and mucous membranes. Slightly less than half of all patients had significant pruritus.
Data on systemic COVID-19 symptoms were available for 431 patients and included fever in about two-thirds of patients and cough in almost 70%, with dyspnea in almost half of patients. Almost 60% had fatigue, and almost 60% had asthenia. Information about the onset of skin symptoms was available in 88 patients; of these patients, lesions were seen an average of almost 10 days after systemic symptoms appeared and, in almost 15%, were the first symptoms noted.
Histopathologic exams were done for only 23 patients and, in all cases, showed “inflammatory features without specific pathological changes, such as lymphocyte infiltration.” In one study, reverse transcription polymerase chain reaction testing of skin biopsy specimens tested negative for SARS-CoV-2.
Expression of ACE2, the receptor of SARS-CoV-2, in the skin was evaluated in six of the studies. “Higher ACE2 expression was identified in keratinocytes, mainly in differentiating keratinocytes and basal cells compared to the other cells of skin tissues,” the authors wrote. These results were confirmed with immunohistochemistry, which, they said, found “ACE2-positive keratinocytes in the stratum basal, the stratum spinosum, and the stratum granulosum of epiderma.” They added that this provides evidence “for percutaneous infection or the entry of virus into patients through skin tissues,” but cautioned that more research is needed.
The authors acknowledged that there are still many unanswered questions about COVID-19, and that more clinical data and research are needed, to improve the understanding of the cutaneous manifestations associated with COVID-19.
In an interview, Alisa N. Femia, MD, director of inpatient dermatology in the department of dermatology at New York University, said that the cutaneous signs described in the review align well with what she has seen in patients with COVID-19.
At this point, it is unclear whether cutaneous manifestations of COVID-19 are a result of SARS-CoV-2 invading the skin or an immune response related to SARS-CoV-2, noted Dr. Femia, who was not involved in the research. One method of entry could be through transmitting virus present on the skin to another part of the body where infection is more likely.
While it is possible COVID-19 could be contracted through the skin, she noted, it is much more likely an individual would be infected by SARS-CoV-2 through more traditionally understood means of transmission, such as through respiratory droplets in person-to-person contact. “I think we are far away from drawing that conclusion, that one could touch a surface or a person who has COVID and contract it through their skin,” Dr. Femia said. “The skin has a lot of other ways to protect against that from occurring,” she added.
“SAR-CoV-2 obviously enters through the ACE2 receptor, which is fairly ubiquitous, and it has been seen in keratinocytes,” she said. “But the skin is one of our biggest barriers ... and further, studies to date have shown that that receptor is expressed in relatively low levels of the keratinocytes.”
Pathogenesis of different cutaneous manifestations may be different, Dr. Femia said. For example, urticaria and morbilliform eruption were described by the authors of the review as more benign eruptions, but pathogenesis may differ from that of so-called COVID toes and from the pathogenesis of purpura and ulcerations seen in patients with more severe disease, she noted. It is plausible, she added, that purpura and ulcerations may be a “direct invasion of SARS-CoV-2 into endothelial cells,” which creates secondary processes “that ultimately destroy the skin.”
Urticaria and morbilliform eruptions, on the other hand, “are more simply that the immune system is recognizing COVID, and in doing so, is also recognizing some antigens in the skin and creating a hypersensitive response to the skin” and has “nothing to do with the SARS-CoV-2 virus actually being in that location,” she said.
It is important to differentiate between patients who have skin manifestations attributed to COVID-19 and those with manifestations independent of COVID-19, which is difficult, Dr. Femia noted. A patient with COVID-19 and a cutaneous manifestation may be having a reaction to a medication. “It’s important to have a critical eye and to remember that, when we see these manifestations, we should always be investigating whether there was an alternative cause so that we can better learn what exactly we should be attributing to this infection,” she said
Adam Friedman, MD, professor and interim chair of dermatology at George Washington University, Washington, said the authors of the review had presented interesting work, but made some “assumptions that need to be proven.” Dr. Friedman also was not involved in the research, but agreed in an interview with the assessment that it is unlikely SARS-CoV-2 would penetrate the skin. While some viruses – such as the poxvirus that causes molluscum contagiosum and the herpes simplex virus – invade keratinocytes specifically, there is a particular clinical phenotype that results that is associated with changes in the epidermis. However, “the skin manifestations of COVID-19 do not fit with direct skin invasion, [but] rather the immune response to systemic disease,” he said.
“[I]n terms of systemic invasion through the skin, it is possible, but this study certainly doesn’t show that. The presence/expression of ACE2 in the epidermis doesn’t translate to route of infection,” Dr. Friedman said..
The study received financial support from Shandong First Medical University, the Innovation Project of Shandong Academy of Medical Sciences and the Shandong Province Taishan Scholar Project. The authors report no relevant financial disclosures. Dr. Femia and Dr. Friedman had no relevant financial disclosures.
SOURCE: Zhao Q et al. J Eur Acad Dermatol Venereol. 2020 Jun 28. doi: 10.1111/jdv.16778.
FROM THE JOURNAL OF THE EUROPEAN ACADEMY OF DERMATOLOGY AND VENEREOLOGY
Are you SARS-CoV-2 vaccine hesitant?
When the pandemic was just emerging from its infancy and we were just beginning to think about social distancing, I was sitting around enjoying an adult beverage and some gluten free (not my choice) snacks with some friends. A retired nurse who had just celebrated her 80th birthday said, “I can’t wait until they’ve developed a vaccine.” A former electrical engineer sitting just short of 2 meters to her left responded, “Don’t save me a place near the front of the line for something that is being developed in a program called Warp Speed.”
How do you feel about the potential SARS-CoV-2 vaccine? Are you going to roll up your sleeve as soon as the vaccine becomes available in your community? What are you going to suggest to your patients, your children? I suspect many of you will answer, “It depends.”
Will it make any difference to you which biochemical-immune-bending strategy is being used to make the vaccine? All of them will probably be the result of a clever sounding but novel technique, all of them with a track record that is measured in months and not years. Will you be swayed by how large the trials were? Or how long the follow-up lasted? How effective must the vaccine be to convince you that it is worth receiving or recommending? Do you have the tools and experience to make a decision like that? I know I don’t. And should you and I even be put in a position to make that decision?
In the past, you and I may have relied on the Centers for Disease Control and Prevention for advice. But given the somewhat murky and stormy relationship between the CDC and the president, the vaccine recommendation may be issued by the White House and not the CDC.
For those of us who were practicing medicine during the Swine Flu fiasco of 1976, the pace and the politics surrounding the development of a SARS-CoV-2 vaccine has a discomforting déjà vu quality about it. The fact that like this year 1976 was an election year that infused the development process with a sense of urgency above and beyond any of the concerns about the pandemic that never happened. Although causality was never proven, there was a surge in Guillain-Barré syndrome cases that had been linked temporally to the vaccine.
Of course, our pandemic is real, and it would be imprudent to wait a year or more to watch for long-term vaccine sequelae. However, I am more than a little concerned that fast tracking the development process may result in unfortunate consequences in the short term that could have been avoided with a more measured approach to trialing the vaccines.
The sad reality is that as a nation we tend to be impatient. We are drawn to quick fixes that come in a vial or a capsule. We are learning that simple measures like mask wearing and social distancing can make a difference in slowing the spread of the virus. It would be tragic to rush a vaccine into production that at best turns out to simply be an expensive alternative to the measures that we know work or at worst injures more of us than it saves.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
When the pandemic was just emerging from its infancy and we were just beginning to think about social distancing, I was sitting around enjoying an adult beverage and some gluten free (not my choice) snacks with some friends. A retired nurse who had just celebrated her 80th birthday said, “I can’t wait until they’ve developed a vaccine.” A former electrical engineer sitting just short of 2 meters to her left responded, “Don’t save me a place near the front of the line for something that is being developed in a program called Warp Speed.”
How do you feel about the potential SARS-CoV-2 vaccine? Are you going to roll up your sleeve as soon as the vaccine becomes available in your community? What are you going to suggest to your patients, your children? I suspect many of you will answer, “It depends.”
Will it make any difference to you which biochemical-immune-bending strategy is being used to make the vaccine? All of them will probably be the result of a clever sounding but novel technique, all of them with a track record that is measured in months and not years. Will you be swayed by how large the trials were? Or how long the follow-up lasted? How effective must the vaccine be to convince you that it is worth receiving or recommending? Do you have the tools and experience to make a decision like that? I know I don’t. And should you and I even be put in a position to make that decision?
In the past, you and I may have relied on the Centers for Disease Control and Prevention for advice. But given the somewhat murky and stormy relationship between the CDC and the president, the vaccine recommendation may be issued by the White House and not the CDC.
For those of us who were practicing medicine during the Swine Flu fiasco of 1976, the pace and the politics surrounding the development of a SARS-CoV-2 vaccine has a discomforting déjà vu quality about it. The fact that like this year 1976 was an election year that infused the development process with a sense of urgency above and beyond any of the concerns about the pandemic that never happened. Although causality was never proven, there was a surge in Guillain-Barré syndrome cases that had been linked temporally to the vaccine.
Of course, our pandemic is real, and it would be imprudent to wait a year or more to watch for long-term vaccine sequelae. However, I am more than a little concerned that fast tracking the development process may result in unfortunate consequences in the short term that could have been avoided with a more measured approach to trialing the vaccines.
The sad reality is that as a nation we tend to be impatient. We are drawn to quick fixes that come in a vial or a capsule. We are learning that simple measures like mask wearing and social distancing can make a difference in slowing the spread of the virus. It would be tragic to rush a vaccine into production that at best turns out to simply be an expensive alternative to the measures that we know work or at worst injures more of us than it saves.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
When the pandemic was just emerging from its infancy and we were just beginning to think about social distancing, I was sitting around enjoying an adult beverage and some gluten free (not my choice) snacks with some friends. A retired nurse who had just celebrated her 80th birthday said, “I can’t wait until they’ve developed a vaccine.” A former electrical engineer sitting just short of 2 meters to her left responded, “Don’t save me a place near the front of the line for something that is being developed in a program called Warp Speed.”
How do you feel about the potential SARS-CoV-2 vaccine? Are you going to roll up your sleeve as soon as the vaccine becomes available in your community? What are you going to suggest to your patients, your children? I suspect many of you will answer, “It depends.”
Will it make any difference to you which biochemical-immune-bending strategy is being used to make the vaccine? All of them will probably be the result of a clever sounding but novel technique, all of them with a track record that is measured in months and not years. Will you be swayed by how large the trials were? Or how long the follow-up lasted? How effective must the vaccine be to convince you that it is worth receiving or recommending? Do you have the tools and experience to make a decision like that? I know I don’t. And should you and I even be put in a position to make that decision?
In the past, you and I may have relied on the Centers for Disease Control and Prevention for advice. But given the somewhat murky and stormy relationship between the CDC and the president, the vaccine recommendation may be issued by the White House and not the CDC.
For those of us who were practicing medicine during the Swine Flu fiasco of 1976, the pace and the politics surrounding the development of a SARS-CoV-2 vaccine has a discomforting déjà vu quality about it. The fact that like this year 1976 was an election year that infused the development process with a sense of urgency above and beyond any of the concerns about the pandemic that never happened. Although causality was never proven, there was a surge in Guillain-Barré syndrome cases that had been linked temporally to the vaccine.
Of course, our pandemic is real, and it would be imprudent to wait a year or more to watch for long-term vaccine sequelae. However, I am more than a little concerned that fast tracking the development process may result in unfortunate consequences in the short term that could have been avoided with a more measured approach to trialing the vaccines.
The sad reality is that as a nation we tend to be impatient. We are drawn to quick fixes that come in a vial or a capsule. We are learning that simple measures like mask wearing and social distancing can make a difference in slowing the spread of the virus. It would be tragic to rush a vaccine into production that at best turns out to simply be an expensive alternative to the measures that we know work or at worst injures more of us than it saves.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
COVID-19 bits and pieces
It turns out that a pandemic, at least this COVID-19 version, can be a challenge for folks like me who are seldom at a loss for words. The pandemic has so overwhelmed every corner of our lives that it is hard to think of another topic on which to pontificate and still not tromp on someone’s political toes. One can always write about the pandemic itself, and I’ve tried that, but as the curtain is gradually being pulled back on this crafty little germ one runs the risk of making an observation today that will be disproved in a week or 2. However, I can’t suppress my urge to write, and so I have decided to share a few brief random observations. Of course they are related to the pandemic. And of course I realize that there is a better than fifty percent chance that they will be proved wrong by the time you read my next Letters from Maine.
Under the radar
Two of the many mysteries about SARS-CoV-2 involve young children who as a group appear to be less easily infected than adults and even when infected seem to be less likely to spread the disease to other people, particularly adults. One explanation posited by some researchers in France is that young children are less likely to have symptoms such as cough and are less powerful speakers and so might be less likely to spew out a significant number of infected aerosolized droplets (“How to Reopen Schools: What Science and Other Countries Teach Us.” By Pam Belluck, Apoorva Mandavill, and Benedict Carey. New York Times, July 11, 2020). While there are probably several factors to explain this observation, one may be that young children are short, seldom taller than an adult waistline. I suspect the majority of aerosols they emit fall and inactivate harmlessly to the floor several feet below an adult’s nose and mouth. Regardless of the explanation, it appears to be good news for the opening of schools, at least for the early grades.
Forget the deep cleaning
There has been a glut of news stories about reopening schools, and many of these stories are accompanied by images of school custodians with buckets, mops, spray bottles, and sponges scouring desks and walls. The most recent image in our local newspaper was of someone scrubbing the underside of a desk. I know it’s taking the World Health Organization an unconscionable period of time to acknowledge that SARS-CoV-2 is airborne, but the rest of us should have gotten the message long ago and been directing our attention to air handling and ventilation. The urge to scrub and deep clean is a hard habit to break, but this nasty bug is not like influenza or a flesh eating bacteria in which deep cleaning might help. A better image to attach to a story on school reopening would be one of a custodian with a screwdriver struggling to pry open a classroom window that had been painted shut a decade ago.
Managing the inevitable
Middlebury College in Vermont and Bowdoin College here in Brunswick, Maine, are similar in many respects because they are small and situated in relatively isolated small New England towns with good track records for pandemic management. Middlebury has elected to invite all its 2,750 students back to campus, whereas Bowdoin has decided to allow only incoming first years and transfer students (for a total of about 600) to return. Both schools will institute similar testing and social distancing protocols and restrict students from access to their respective towns (“A Tale of 2 Colleges.” By Bill Burger. Inside Higher Ed, June 29,2020). It will be an interesting experiment. I’m voting for Middlebury and not because my son and daughter-in-law are alums, but because I think Middlebury seems to have acknowledged that no matter how diligent one is in creating a SARS-CoV-2–free environment at the outset, these are college kids and there will be some cases on both campuses. It is on how those inevitable realities are managed and contained that an institution should be judged.
Patience
Unfortunately, We always have been a restless and impatient population eager to get moving and it has driven us to greatness. Hopefully, patience will be a lesson that we will learn, along with many others.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
It turns out that a pandemic, at least this COVID-19 version, can be a challenge for folks like me who are seldom at a loss for words. The pandemic has so overwhelmed every corner of our lives that it is hard to think of another topic on which to pontificate and still not tromp on someone’s political toes. One can always write about the pandemic itself, and I’ve tried that, but as the curtain is gradually being pulled back on this crafty little germ one runs the risk of making an observation today that will be disproved in a week or 2. However, I can’t suppress my urge to write, and so I have decided to share a few brief random observations. Of course they are related to the pandemic. And of course I realize that there is a better than fifty percent chance that they will be proved wrong by the time you read my next Letters from Maine.
Under the radar
Two of the many mysteries about SARS-CoV-2 involve young children who as a group appear to be less easily infected than adults and even when infected seem to be less likely to spread the disease to other people, particularly adults. One explanation posited by some researchers in France is that young children are less likely to have symptoms such as cough and are less powerful speakers and so might be less likely to spew out a significant number of infected aerosolized droplets (“How to Reopen Schools: What Science and Other Countries Teach Us.” By Pam Belluck, Apoorva Mandavill, and Benedict Carey. New York Times, July 11, 2020). While there are probably several factors to explain this observation, one may be that young children are short, seldom taller than an adult waistline. I suspect the majority of aerosols they emit fall and inactivate harmlessly to the floor several feet below an adult’s nose and mouth. Regardless of the explanation, it appears to be good news for the opening of schools, at least for the early grades.
Forget the deep cleaning
There has been a glut of news stories about reopening schools, and many of these stories are accompanied by images of school custodians with buckets, mops, spray bottles, and sponges scouring desks and walls. The most recent image in our local newspaper was of someone scrubbing the underside of a desk. I know it’s taking the World Health Organization an unconscionable period of time to acknowledge that SARS-CoV-2 is airborne, but the rest of us should have gotten the message long ago and been directing our attention to air handling and ventilation. The urge to scrub and deep clean is a hard habit to break, but this nasty bug is not like influenza or a flesh eating bacteria in which deep cleaning might help. A better image to attach to a story on school reopening would be one of a custodian with a screwdriver struggling to pry open a classroom window that had been painted shut a decade ago.
Managing the inevitable
Middlebury College in Vermont and Bowdoin College here in Brunswick, Maine, are similar in many respects because they are small and situated in relatively isolated small New England towns with good track records for pandemic management. Middlebury has elected to invite all its 2,750 students back to campus, whereas Bowdoin has decided to allow only incoming first years and transfer students (for a total of about 600) to return. Both schools will institute similar testing and social distancing protocols and restrict students from access to their respective towns (“A Tale of 2 Colleges.” By Bill Burger. Inside Higher Ed, June 29,2020). It will be an interesting experiment. I’m voting for Middlebury and not because my son and daughter-in-law are alums, but because I think Middlebury seems to have acknowledged that no matter how diligent one is in creating a SARS-CoV-2–free environment at the outset, these are college kids and there will be some cases on both campuses. It is on how those inevitable realities are managed and contained that an institution should be judged.
Patience
Unfortunately, We always have been a restless and impatient population eager to get moving and it has driven us to greatness. Hopefully, patience will be a lesson that we will learn, along with many others.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
It turns out that a pandemic, at least this COVID-19 version, can be a challenge for folks like me who are seldom at a loss for words. The pandemic has so overwhelmed every corner of our lives that it is hard to think of another topic on which to pontificate and still not tromp on someone’s political toes. One can always write about the pandemic itself, and I’ve tried that, but as the curtain is gradually being pulled back on this crafty little germ one runs the risk of making an observation today that will be disproved in a week or 2. However, I can’t suppress my urge to write, and so I have decided to share a few brief random observations. Of course they are related to the pandemic. And of course I realize that there is a better than fifty percent chance that they will be proved wrong by the time you read my next Letters from Maine.
Under the radar
Two of the many mysteries about SARS-CoV-2 involve young children who as a group appear to be less easily infected than adults and even when infected seem to be less likely to spread the disease to other people, particularly adults. One explanation posited by some researchers in France is that young children are less likely to have symptoms such as cough and are less powerful speakers and so might be less likely to spew out a significant number of infected aerosolized droplets (“How to Reopen Schools: What Science and Other Countries Teach Us.” By Pam Belluck, Apoorva Mandavill, and Benedict Carey. New York Times, July 11, 2020). While there are probably several factors to explain this observation, one may be that young children are short, seldom taller than an adult waistline. I suspect the majority of aerosols they emit fall and inactivate harmlessly to the floor several feet below an adult’s nose and mouth. Regardless of the explanation, it appears to be good news for the opening of schools, at least for the early grades.
Forget the deep cleaning
There has been a glut of news stories about reopening schools, and many of these stories are accompanied by images of school custodians with buckets, mops, spray bottles, and sponges scouring desks and walls. The most recent image in our local newspaper was of someone scrubbing the underside of a desk. I know it’s taking the World Health Organization an unconscionable period of time to acknowledge that SARS-CoV-2 is airborne, but the rest of us should have gotten the message long ago and been directing our attention to air handling and ventilation. The urge to scrub and deep clean is a hard habit to break, but this nasty bug is not like influenza or a flesh eating bacteria in which deep cleaning might help. A better image to attach to a story on school reopening would be one of a custodian with a screwdriver struggling to pry open a classroom window that had been painted shut a decade ago.
Managing the inevitable
Middlebury College in Vermont and Bowdoin College here in Brunswick, Maine, are similar in many respects because they are small and situated in relatively isolated small New England towns with good track records for pandemic management. Middlebury has elected to invite all its 2,750 students back to campus, whereas Bowdoin has decided to allow only incoming first years and transfer students (for a total of about 600) to return. Both schools will institute similar testing and social distancing protocols and restrict students from access to their respective towns (“A Tale of 2 Colleges.” By Bill Burger. Inside Higher Ed, June 29,2020). It will be an interesting experiment. I’m voting for Middlebury and not because my son and daughter-in-law are alums, but because I think Middlebury seems to have acknowledged that no matter how diligent one is in creating a SARS-CoV-2–free environment at the outset, these are college kids and there will be some cases on both campuses. It is on how those inevitable realities are managed and contained that an institution should be judged.
Patience
Unfortunately, We always have been a restless and impatient population eager to get moving and it has driven us to greatness. Hopefully, patience will be a lesson that we will learn, along with many others.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Higher death rate seen in cancer patients with nosocomial COVID-19
, according to researchers.
In an observational study of patients with COVID-19 and cancer, 19% of patients had COVID-19 acquired during a non-COVID-related hospital stay, and 81% had community-acquired COVID-19.
At a median follow-up of 23 days, the overall mortality rate was 28%. However, the all-cause mortality rate in patients with nosocomial COVID-19 was more than double that of patients with community-acquired COVID-19, at 47% and 23%, respectively.
Arielle Elkrief, MD, of the University of Montreal, reported these results during the AACR virtual meeting: COVID-19 and Cancer.
“This is the first report that describes a high rate of hospital-acquired COVID-19 in patients with cancer, at a rate of 19%,” Dr. Elkrief said. “This was associated with high mortality in both univariate and multivariate analyses.”
The study included 250 adults and 3 children with COVID-19 and cancer who were identified between March 3 and May 23, 2020. They ranged in age from 4 to 95 years, but the median age was 73 years.
All patients had either laboratory-confirmed (95%) or presumed COVID-19 (5%) and invasive cancer. The most common cancer types were similar to those seen in the general population. Lung and breast cancer were the most common, followed by lymphoma, prostate cancer, and colorectal cancer. Most patients were on active anticancer therapy, most often chemotherapy.
Most patients (n = 236) were residents of Quebec, but 17 patients were residents of British Columbia.
“It is important to note that Quebec was one of the most heavily affected areas in North America at the time of the study,” Dr. Elkrief said.
Outcomes by group
There were 206 patients (81%) who had community-acquired COVID-19 and 47 (19%) who had nosocomial COVID-19. The two groups were similar with respect to sex, performance status, and cancer stage. A small trend toward more patients on active therapy was seen in the nosocomial group, but the difference did not reach statistical significance.
The median overall survival was 27 days in the nosocomial group and 71 days in the community-acquired group (hazard ratio, 2.2; P = .002).
A multivariate analysis showed that nosocomial infection was “strongly and independently associated with death,” Dr. Elkrief said. “Other risk factors for poor prognosis included age, poor [performance] status, and advanced stage of cancer.”
There were no significant differences between the hospital-acquired and community-acquired groups for other outcomes, including oxygen requirements (43% and 47%, respectively), ICU admission (13% and 11%), need for mechanical ventilation (6% and 5%), or length of stay (median, 9.5 days and 8.5 days).
The low rate of ICU admission, considering the mortality rate of 28%, “could reflect that patients with cancer are less likely to be admitted to the ICU,” Dr. Elkrief noted.
Applying the findings to practice
The findings reinforce the importance of adherence to stringent infection control guidelines to protect vulnerable patients, such as those with cancer, Dr. Elkrief said.
In ambulatory settings, this means decreasing in-person visits through increased use of teleconsultations, and for those who need to be seen in person, screening for symptoms or use of polymerase chain reaction testing should be used when resources are available, she said.
“Similar principles apply to chemotherapy treatment units,” Dr. Elkrief said. She added that staff must avoid cross-contamination between COVID and COVID-free zones, and that “dedicated personnel and equipment should be maintained and separate between these two zones.
“Adequate protective personal equipment and strict hand hygiene protocols are also of utmost importance,” Dr. Elkrief said. “The threat of COVID-19 is not behind us, and so we continue to enforce these strategies to protect our patients.”
Session moderator Gypsyamber D’Souza, PhD, an infectious disease epidemiologist at Johns Hopkins University in Baltimore, raised the question of whether the high nosocomial infection and death rate in this study was related to patients having more severe disease because of underlying comorbidities.
Dr. Elkrief explained that the overall mortality rate was indeed higher than the 13% reported in other studies, and it may reflect an overrepresentation of hospitalized or more severely ill patients in the cohort.
However, the investigators made every effort to include all patients with both cancer and COVID-19 by using systematic screening of inpatient and outpatients lists and registries.
Further, the multivariate analysis included both inpatients and outpatients and adjusted for known negative prognostic factors for COVID-19 outcomes. These included increasing age, poor performance status, and different comorbidities.
The finding that nosocomial infection was an independent predictor of death “pushed us to look at nosocomial infection as a new independent risk factor,” Dr. Elkrief said.
Dr. Elkrief reported grant support from AstraZeneca. Dr. D’Souza did not report any disclosures.
SOURCE: Elkrief A et al. AACR: COVID and Cancer, Abstract S12-01.
, according to researchers.
In an observational study of patients with COVID-19 and cancer, 19% of patients had COVID-19 acquired during a non-COVID-related hospital stay, and 81% had community-acquired COVID-19.
At a median follow-up of 23 days, the overall mortality rate was 28%. However, the all-cause mortality rate in patients with nosocomial COVID-19 was more than double that of patients with community-acquired COVID-19, at 47% and 23%, respectively.
Arielle Elkrief, MD, of the University of Montreal, reported these results during the AACR virtual meeting: COVID-19 and Cancer.
“This is the first report that describes a high rate of hospital-acquired COVID-19 in patients with cancer, at a rate of 19%,” Dr. Elkrief said. “This was associated with high mortality in both univariate and multivariate analyses.”
The study included 250 adults and 3 children with COVID-19 and cancer who were identified between March 3 and May 23, 2020. They ranged in age from 4 to 95 years, but the median age was 73 years.
All patients had either laboratory-confirmed (95%) or presumed COVID-19 (5%) and invasive cancer. The most common cancer types were similar to those seen in the general population. Lung and breast cancer were the most common, followed by lymphoma, prostate cancer, and colorectal cancer. Most patients were on active anticancer therapy, most often chemotherapy.
Most patients (n = 236) were residents of Quebec, but 17 patients were residents of British Columbia.
“It is important to note that Quebec was one of the most heavily affected areas in North America at the time of the study,” Dr. Elkrief said.
Outcomes by group
There were 206 patients (81%) who had community-acquired COVID-19 and 47 (19%) who had nosocomial COVID-19. The two groups were similar with respect to sex, performance status, and cancer stage. A small trend toward more patients on active therapy was seen in the nosocomial group, but the difference did not reach statistical significance.
The median overall survival was 27 days in the nosocomial group and 71 days in the community-acquired group (hazard ratio, 2.2; P = .002).
A multivariate analysis showed that nosocomial infection was “strongly and independently associated with death,” Dr. Elkrief said. “Other risk factors for poor prognosis included age, poor [performance] status, and advanced stage of cancer.”
There were no significant differences between the hospital-acquired and community-acquired groups for other outcomes, including oxygen requirements (43% and 47%, respectively), ICU admission (13% and 11%), need for mechanical ventilation (6% and 5%), or length of stay (median, 9.5 days and 8.5 days).
The low rate of ICU admission, considering the mortality rate of 28%, “could reflect that patients with cancer are less likely to be admitted to the ICU,” Dr. Elkrief noted.
Applying the findings to practice
The findings reinforce the importance of adherence to stringent infection control guidelines to protect vulnerable patients, such as those with cancer, Dr. Elkrief said.
In ambulatory settings, this means decreasing in-person visits through increased use of teleconsultations, and for those who need to be seen in person, screening for symptoms or use of polymerase chain reaction testing should be used when resources are available, she said.
“Similar principles apply to chemotherapy treatment units,” Dr. Elkrief said. She added that staff must avoid cross-contamination between COVID and COVID-free zones, and that “dedicated personnel and equipment should be maintained and separate between these two zones.
“Adequate protective personal equipment and strict hand hygiene protocols are also of utmost importance,” Dr. Elkrief said. “The threat of COVID-19 is not behind us, and so we continue to enforce these strategies to protect our patients.”
Session moderator Gypsyamber D’Souza, PhD, an infectious disease epidemiologist at Johns Hopkins University in Baltimore, raised the question of whether the high nosocomial infection and death rate in this study was related to patients having more severe disease because of underlying comorbidities.
Dr. Elkrief explained that the overall mortality rate was indeed higher than the 13% reported in other studies, and it may reflect an overrepresentation of hospitalized or more severely ill patients in the cohort.
However, the investigators made every effort to include all patients with both cancer and COVID-19 by using systematic screening of inpatient and outpatients lists and registries.
Further, the multivariate analysis included both inpatients and outpatients and adjusted for known negative prognostic factors for COVID-19 outcomes. These included increasing age, poor performance status, and different comorbidities.
The finding that nosocomial infection was an independent predictor of death “pushed us to look at nosocomial infection as a new independent risk factor,” Dr. Elkrief said.
Dr. Elkrief reported grant support from AstraZeneca. Dr. D’Souza did not report any disclosures.
SOURCE: Elkrief A et al. AACR: COVID and Cancer, Abstract S12-01.
, according to researchers.
In an observational study of patients with COVID-19 and cancer, 19% of patients had COVID-19 acquired during a non-COVID-related hospital stay, and 81% had community-acquired COVID-19.
At a median follow-up of 23 days, the overall mortality rate was 28%. However, the all-cause mortality rate in patients with nosocomial COVID-19 was more than double that of patients with community-acquired COVID-19, at 47% and 23%, respectively.
Arielle Elkrief, MD, of the University of Montreal, reported these results during the AACR virtual meeting: COVID-19 and Cancer.
“This is the first report that describes a high rate of hospital-acquired COVID-19 in patients with cancer, at a rate of 19%,” Dr. Elkrief said. “This was associated with high mortality in both univariate and multivariate analyses.”
The study included 250 adults and 3 children with COVID-19 and cancer who were identified between March 3 and May 23, 2020. They ranged in age from 4 to 95 years, but the median age was 73 years.
All patients had either laboratory-confirmed (95%) or presumed COVID-19 (5%) and invasive cancer. The most common cancer types were similar to those seen in the general population. Lung and breast cancer were the most common, followed by lymphoma, prostate cancer, and colorectal cancer. Most patients were on active anticancer therapy, most often chemotherapy.
Most patients (n = 236) were residents of Quebec, but 17 patients were residents of British Columbia.
“It is important to note that Quebec was one of the most heavily affected areas in North America at the time of the study,” Dr. Elkrief said.
Outcomes by group
There were 206 patients (81%) who had community-acquired COVID-19 and 47 (19%) who had nosocomial COVID-19. The two groups were similar with respect to sex, performance status, and cancer stage. A small trend toward more patients on active therapy was seen in the nosocomial group, but the difference did not reach statistical significance.
The median overall survival was 27 days in the nosocomial group and 71 days in the community-acquired group (hazard ratio, 2.2; P = .002).
A multivariate analysis showed that nosocomial infection was “strongly and independently associated with death,” Dr. Elkrief said. “Other risk factors for poor prognosis included age, poor [performance] status, and advanced stage of cancer.”
There were no significant differences between the hospital-acquired and community-acquired groups for other outcomes, including oxygen requirements (43% and 47%, respectively), ICU admission (13% and 11%), need for mechanical ventilation (6% and 5%), or length of stay (median, 9.5 days and 8.5 days).
The low rate of ICU admission, considering the mortality rate of 28%, “could reflect that patients with cancer are less likely to be admitted to the ICU,” Dr. Elkrief noted.
Applying the findings to practice
The findings reinforce the importance of adherence to stringent infection control guidelines to protect vulnerable patients, such as those with cancer, Dr. Elkrief said.
In ambulatory settings, this means decreasing in-person visits through increased use of teleconsultations, and for those who need to be seen in person, screening for symptoms or use of polymerase chain reaction testing should be used when resources are available, she said.
“Similar principles apply to chemotherapy treatment units,” Dr. Elkrief said. She added that staff must avoid cross-contamination between COVID and COVID-free zones, and that “dedicated personnel and equipment should be maintained and separate between these two zones.
“Adequate protective personal equipment and strict hand hygiene protocols are also of utmost importance,” Dr. Elkrief said. “The threat of COVID-19 is not behind us, and so we continue to enforce these strategies to protect our patients.”
Session moderator Gypsyamber D’Souza, PhD, an infectious disease epidemiologist at Johns Hopkins University in Baltimore, raised the question of whether the high nosocomial infection and death rate in this study was related to patients having more severe disease because of underlying comorbidities.
Dr. Elkrief explained that the overall mortality rate was indeed higher than the 13% reported in other studies, and it may reflect an overrepresentation of hospitalized or more severely ill patients in the cohort.
However, the investigators made every effort to include all patients with both cancer and COVID-19 by using systematic screening of inpatient and outpatients lists and registries.
Further, the multivariate analysis included both inpatients and outpatients and adjusted for known negative prognostic factors for COVID-19 outcomes. These included increasing age, poor performance status, and different comorbidities.
The finding that nosocomial infection was an independent predictor of death “pushed us to look at nosocomial infection as a new independent risk factor,” Dr. Elkrief said.
Dr. Elkrief reported grant support from AstraZeneca. Dr. D’Souza did not report any disclosures.
SOURCE: Elkrief A et al. AACR: COVID and Cancer, Abstract S12-01.
FROM AACR: COVID-19 AND CANCER