User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Half of type 1 diabetes patients with COVID-19 manage at home
New preliminary data from the T1D Exchange suggest that, although hyperglycemia and diabetic ketoacidosis (DKA) are common in people with type 1 diabetes who develop COVID-19, many are still able to manage the illness at home and overall mortality is relatively low.
The new findings – the first US data on individuals with type 1 diabetes and COVID-19 – were published online June 5 in Diabetes Care by Osagie A. Ebekozien, MD, vice president, quality improvement and population health at the T1D Exchange, and colleagues.
Two UK studies are the only prior ones to previously examine the topic.
The newly published study includes data as of May 5 on 64 individuals from a total of 64 US sites, including 15 T1D Exchange member clinics and an additional 49 endocrinology clinics from around the country. Since the paper was submitted, there are now 220 patients from 68 sites. Another publication with a more detailed analysis of risk factors and adjustment for confounders is planned for later this year.
Some of the findings from the preliminary data have shifted, but many aspects remain consistent, Ebekozien told Medscape Medical News.
“One thing still very true, even with the unpublished findings, is the influence of A1c and glycemic management. ...With higher A1c levels, we’re seeing more COVID-19 hospitalizations and worse outcomes,” he said.
And as has been generally reported for COVID-19, high body mass index was a major risk factor in the preliminary dataset – and remains so.
There were two deaths in the preliminary report, both individuals with comorbidities in addition to type 1 diabetes, Ebekozien said. There have been a few more deaths in the larger dataset, but the mortality rate remains relatively low.
Interestingly, females predominate in both cohorts. That may be a reporting phenomenon, another factor that is being analyzed.
Hyperglycemia Remains a Major Risk Factor
The study is specifically being conducted by the T1D Exchange’s Quality Improvement Collaborative, which Ebekozien heads.
Data were obtained for 33 patients with type 1 diabetes who tested positive for COVID-19, and another 31 who were classified as “COVID-19–like” because they had symptoms consistent with COVID-19, as identified by the Centers for Disease Control and Prevention, but hadn’t been tested for the virus.
For all 64 patients, the mean age was 20.9 years and two thirds (65.6%) were aged 18 or younger. A higher proportion of the COVID-19–like patients were pediatric than the confirmed cases. The larger dataset includes more adult patients, Ebekozien told Medscape Medical News.
Overall, 60.9% of patients were female. Nearly half were white, a quarter Hispanic, and 18.8% black. More confirmed COVID-19 cases were black compared with suspected cases (30.3% vs 6.5%).
Median A1c for the overall group (including suspected COVID-19 cases) was 8.0%, but it was 8.5% among confirmed cases. Overall, six patients (9.8%) presented with new-onset type 1 diabetes after they developed COVID-19.
Hyperglycemia was present in half (32) of patients overall. DKA occurred in 19 people (30.2%): 15 of the confirmed COVID-19 cases (45.5%) versus just 4 (13.3%) of the COVID-19–like cases. Nausea was reported in 30.2% of patients overall.
Other symptoms were typical of COVID-19, including fever (41.3%), dry cough (38.1%), and shortness of breath (27.0%). Loss of taste and smell was less common, at just 9.5% overall.
Obesity was present in 39.7% of patients overall, with similar proportions in the confirmed and suspected COVID-19 groups. Hypertension and/or cardiovascular disease were present in 14.3% of patients overall, and the rate was similar between the two subgroups.
One of the two patients who died was a 79-year-old man who had hypertension and a prior stroke in addition to type 1 diabetes. The other was a 19-year-old woman with a history of asthma who developed a pulmonary embolism during the onset of COVID-19. Neither had DKA.
Even in Type 1 Diabetes, COVID-19 Can Be Managed at Home
Overall, 34.9% of patients were able to manage COVID-19 entirely at home, with 27.3% of the confirmed and 43.3% of the suspected cases able to do so.
At the other extreme, 22.2% of patients overall were admitted to the intensive care unit; 30.3% of the confirmed versus 13.3% of suspected cases.
Including the small proportion of patients sent home after being seen in emergency or urgent care, overall roughly half were not admitted to hospital.
“Interestingly, even in this preliminary study, half were managed at home via telemedicine with an endocrinologist and infectious disease specialist. ... I think it continues to be a case-by-case clinical decision between the patient and their provider,” Ebekozien said.
“But, we’re seeing a good number of patients who are managed at home and the symptoms resolve in a week or two, and the illness runs its course, and they don’t have to even be seen,” he added.
The research team is also collecting data on barriers to remote care, including challenges with telemedicine and how frontline providers are navigating them.
“Those are all things that our future paper will be able to shed more light on,” he explained.
Endocrinologists around the country are invited to report cases of COVID-19 in patients with type 1 diabetes to the T1D Exchange by emailing [email protected].
And in fact, Ebekozien also requested that clinicians with a large type 1 diabetes population also report if they’ve had no COVID-19 cases.
“Even if they haven’t had a case, that’s very useful information for us to know. One of the things we want to calculate down the line is the incidence ratio. Not all participating sites have had a case.”
Endocrinologists from all the participating sites have formed a dedicated community that meets regularly via webinars to share information, he noted. “It’s been a very selfless effort to work collaboratively as a community to quickly answer critical questions.”
The Helmsley Charitable Trust funds the T1D Exchange Quality Improvement Collaborative. The T1D Exchange received financial support for this study from Abbott Diabetes, Dexcom, JDRF, Insulet Corporation, Lilly, Medtronic, and Tandem Diabetes Care. No other relevant financial relationships were reported.
This article first appeared on Medscape.com.
New preliminary data from the T1D Exchange suggest that, although hyperglycemia and diabetic ketoacidosis (DKA) are common in people with type 1 diabetes who develop COVID-19, many are still able to manage the illness at home and overall mortality is relatively low.
The new findings – the first US data on individuals with type 1 diabetes and COVID-19 – were published online June 5 in Diabetes Care by Osagie A. Ebekozien, MD, vice president, quality improvement and population health at the T1D Exchange, and colleagues.
Two UK studies are the only prior ones to previously examine the topic.
The newly published study includes data as of May 5 on 64 individuals from a total of 64 US sites, including 15 T1D Exchange member clinics and an additional 49 endocrinology clinics from around the country. Since the paper was submitted, there are now 220 patients from 68 sites. Another publication with a more detailed analysis of risk factors and adjustment for confounders is planned for later this year.
Some of the findings from the preliminary data have shifted, but many aspects remain consistent, Ebekozien told Medscape Medical News.
“One thing still very true, even with the unpublished findings, is the influence of A1c and glycemic management. ...With higher A1c levels, we’re seeing more COVID-19 hospitalizations and worse outcomes,” he said.
And as has been generally reported for COVID-19, high body mass index was a major risk factor in the preliminary dataset – and remains so.
There were two deaths in the preliminary report, both individuals with comorbidities in addition to type 1 diabetes, Ebekozien said. There have been a few more deaths in the larger dataset, but the mortality rate remains relatively low.
Interestingly, females predominate in both cohorts. That may be a reporting phenomenon, another factor that is being analyzed.
Hyperglycemia Remains a Major Risk Factor
The study is specifically being conducted by the T1D Exchange’s Quality Improvement Collaborative, which Ebekozien heads.
Data were obtained for 33 patients with type 1 diabetes who tested positive for COVID-19, and another 31 who were classified as “COVID-19–like” because they had symptoms consistent with COVID-19, as identified by the Centers for Disease Control and Prevention, but hadn’t been tested for the virus.
For all 64 patients, the mean age was 20.9 years and two thirds (65.6%) were aged 18 or younger. A higher proportion of the COVID-19–like patients were pediatric than the confirmed cases. The larger dataset includes more adult patients, Ebekozien told Medscape Medical News.
Overall, 60.9% of patients were female. Nearly half were white, a quarter Hispanic, and 18.8% black. More confirmed COVID-19 cases were black compared with suspected cases (30.3% vs 6.5%).
Median A1c for the overall group (including suspected COVID-19 cases) was 8.0%, but it was 8.5% among confirmed cases. Overall, six patients (9.8%) presented with new-onset type 1 diabetes after they developed COVID-19.
Hyperglycemia was present in half (32) of patients overall. DKA occurred in 19 people (30.2%): 15 of the confirmed COVID-19 cases (45.5%) versus just 4 (13.3%) of the COVID-19–like cases. Nausea was reported in 30.2% of patients overall.
Other symptoms were typical of COVID-19, including fever (41.3%), dry cough (38.1%), and shortness of breath (27.0%). Loss of taste and smell was less common, at just 9.5% overall.
Obesity was present in 39.7% of patients overall, with similar proportions in the confirmed and suspected COVID-19 groups. Hypertension and/or cardiovascular disease were present in 14.3% of patients overall, and the rate was similar between the two subgroups.
One of the two patients who died was a 79-year-old man who had hypertension and a prior stroke in addition to type 1 diabetes. The other was a 19-year-old woman with a history of asthma who developed a pulmonary embolism during the onset of COVID-19. Neither had DKA.
Even in Type 1 Diabetes, COVID-19 Can Be Managed at Home
Overall, 34.9% of patients were able to manage COVID-19 entirely at home, with 27.3% of the confirmed and 43.3% of the suspected cases able to do so.
At the other extreme, 22.2% of patients overall were admitted to the intensive care unit; 30.3% of the confirmed versus 13.3% of suspected cases.
Including the small proportion of patients sent home after being seen in emergency or urgent care, overall roughly half were not admitted to hospital.
“Interestingly, even in this preliminary study, half were managed at home via telemedicine with an endocrinologist and infectious disease specialist. ... I think it continues to be a case-by-case clinical decision between the patient and their provider,” Ebekozien said.
“But, we’re seeing a good number of patients who are managed at home and the symptoms resolve in a week or two, and the illness runs its course, and they don’t have to even be seen,” he added.
The research team is also collecting data on barriers to remote care, including challenges with telemedicine and how frontline providers are navigating them.
“Those are all things that our future paper will be able to shed more light on,” he explained.
Endocrinologists around the country are invited to report cases of COVID-19 in patients with type 1 diabetes to the T1D Exchange by emailing [email protected].
And in fact, Ebekozien also requested that clinicians with a large type 1 diabetes population also report if they’ve had no COVID-19 cases.
“Even if they haven’t had a case, that’s very useful information for us to know. One of the things we want to calculate down the line is the incidence ratio. Not all participating sites have had a case.”
Endocrinologists from all the participating sites have formed a dedicated community that meets regularly via webinars to share information, he noted. “It’s been a very selfless effort to work collaboratively as a community to quickly answer critical questions.”
The Helmsley Charitable Trust funds the T1D Exchange Quality Improvement Collaborative. The T1D Exchange received financial support for this study from Abbott Diabetes, Dexcom, JDRF, Insulet Corporation, Lilly, Medtronic, and Tandem Diabetes Care. No other relevant financial relationships were reported.
This article first appeared on Medscape.com.
New preliminary data from the T1D Exchange suggest that, although hyperglycemia and diabetic ketoacidosis (DKA) are common in people with type 1 diabetes who develop COVID-19, many are still able to manage the illness at home and overall mortality is relatively low.
The new findings – the first US data on individuals with type 1 diabetes and COVID-19 – were published online June 5 in Diabetes Care by Osagie A. Ebekozien, MD, vice president, quality improvement and population health at the T1D Exchange, and colleagues.
Two UK studies are the only prior ones to previously examine the topic.
The newly published study includes data as of May 5 on 64 individuals from a total of 64 US sites, including 15 T1D Exchange member clinics and an additional 49 endocrinology clinics from around the country. Since the paper was submitted, there are now 220 patients from 68 sites. Another publication with a more detailed analysis of risk factors and adjustment for confounders is planned for later this year.
Some of the findings from the preliminary data have shifted, but many aspects remain consistent, Ebekozien told Medscape Medical News.
“One thing still very true, even with the unpublished findings, is the influence of A1c and glycemic management. ...With higher A1c levels, we’re seeing more COVID-19 hospitalizations and worse outcomes,” he said.
And as has been generally reported for COVID-19, high body mass index was a major risk factor in the preliminary dataset – and remains so.
There were two deaths in the preliminary report, both individuals with comorbidities in addition to type 1 diabetes, Ebekozien said. There have been a few more deaths in the larger dataset, but the mortality rate remains relatively low.
Interestingly, females predominate in both cohorts. That may be a reporting phenomenon, another factor that is being analyzed.
Hyperglycemia Remains a Major Risk Factor
The study is specifically being conducted by the T1D Exchange’s Quality Improvement Collaborative, which Ebekozien heads.
Data were obtained for 33 patients with type 1 diabetes who tested positive for COVID-19, and another 31 who were classified as “COVID-19–like” because they had symptoms consistent with COVID-19, as identified by the Centers for Disease Control and Prevention, but hadn’t been tested for the virus.
For all 64 patients, the mean age was 20.9 years and two thirds (65.6%) were aged 18 or younger. A higher proportion of the COVID-19–like patients were pediatric than the confirmed cases. The larger dataset includes more adult patients, Ebekozien told Medscape Medical News.
Overall, 60.9% of patients were female. Nearly half were white, a quarter Hispanic, and 18.8% black. More confirmed COVID-19 cases were black compared with suspected cases (30.3% vs 6.5%).
Median A1c for the overall group (including suspected COVID-19 cases) was 8.0%, but it was 8.5% among confirmed cases. Overall, six patients (9.8%) presented with new-onset type 1 diabetes after they developed COVID-19.
Hyperglycemia was present in half (32) of patients overall. DKA occurred in 19 people (30.2%): 15 of the confirmed COVID-19 cases (45.5%) versus just 4 (13.3%) of the COVID-19–like cases. Nausea was reported in 30.2% of patients overall.
Other symptoms were typical of COVID-19, including fever (41.3%), dry cough (38.1%), and shortness of breath (27.0%). Loss of taste and smell was less common, at just 9.5% overall.
Obesity was present in 39.7% of patients overall, with similar proportions in the confirmed and suspected COVID-19 groups. Hypertension and/or cardiovascular disease were present in 14.3% of patients overall, and the rate was similar between the two subgroups.
One of the two patients who died was a 79-year-old man who had hypertension and a prior stroke in addition to type 1 diabetes. The other was a 19-year-old woman with a history of asthma who developed a pulmonary embolism during the onset of COVID-19. Neither had DKA.
Even in Type 1 Diabetes, COVID-19 Can Be Managed at Home
Overall, 34.9% of patients were able to manage COVID-19 entirely at home, with 27.3% of the confirmed and 43.3% of the suspected cases able to do so.
At the other extreme, 22.2% of patients overall were admitted to the intensive care unit; 30.3% of the confirmed versus 13.3% of suspected cases.
Including the small proportion of patients sent home after being seen in emergency or urgent care, overall roughly half were not admitted to hospital.
“Interestingly, even in this preliminary study, half were managed at home via telemedicine with an endocrinologist and infectious disease specialist. ... I think it continues to be a case-by-case clinical decision between the patient and their provider,” Ebekozien said.
“But, we’re seeing a good number of patients who are managed at home and the symptoms resolve in a week or two, and the illness runs its course, and they don’t have to even be seen,” he added.
The research team is also collecting data on barriers to remote care, including challenges with telemedicine and how frontline providers are navigating them.
“Those are all things that our future paper will be able to shed more light on,” he explained.
Endocrinologists around the country are invited to report cases of COVID-19 in patients with type 1 diabetes to the T1D Exchange by emailing [email protected].
And in fact, Ebekozien also requested that clinicians with a large type 1 diabetes population also report if they’ve had no COVID-19 cases.
“Even if they haven’t had a case, that’s very useful information for us to know. One of the things we want to calculate down the line is the incidence ratio. Not all participating sites have had a case.”
Endocrinologists from all the participating sites have formed a dedicated community that meets regularly via webinars to share information, he noted. “It’s been a very selfless effort to work collaboratively as a community to quickly answer critical questions.”
The Helmsley Charitable Trust funds the T1D Exchange Quality Improvement Collaborative. The T1D Exchange received financial support for this study from Abbott Diabetes, Dexcom, JDRF, Insulet Corporation, Lilly, Medtronic, and Tandem Diabetes Care. No other relevant financial relationships were reported.
This article first appeared on Medscape.com.
Addressing suicide prevention among South Asian Americans
Multifaceted strategies are needed to address unique cultural factors
On first glance, the age-adjusted rate of suicide for Asian and Pacific Islander populations living in the United States looks comparatively low.
Over the past 2 decades in the United States, for example, the overall rate increased by 35%, from, 10.5 to 14.2 per 100,000 individuals. That compares with a rate of 7.0 per 100,000 among Asian and Pacific Islander communities.1
However, because of the aggregate nature (national suicide mortality data combine people of Asian, Native Hawaiian, and other Pacific Islander descent into a single group) in which these data are reported, a significant amount of salient information on subgroups of Asian Americans is lost.2 There is a growing body of research on the mental health of Asian Americans, but the dearth of information and research on suicide in South Asians is striking.3 In fact, a review of literature finds fewer than 10 articles on the topic that have been published in peer-reviewed journals in the last decade. to provide effective, culturally sensitive care.
Diverse group
There are 3.4 million individuals of South Asian descent in the United States. Geographically, South Asians may have familial and cultural/historical roots in Bangladesh, Bhutan, India, Maldives, Nepal, and Pakistan.4 They enjoy a rich diversity in terms of cultural and religious beliefs, language, socioeconomic status, modes of acculturation, and immigration patterns. Asian Indians are the largest group of South Asians in the United States. They are highly educated, with a larger proportion of them pursuing an undergraduate and/or graduate level education than the general population. The median household income of Asian Indians is also higher than the national average.5
In general, suicide, like all mental health issues, is a stigmatized and taboo topic in the South Asian community.6 Also, South Asian Americans are hesitant to seek mental health care because of a perceived inability of Western health care professionals to understand their cultural views. Extrapolation from data on South Asians in the United Kingdom, aggregate statistics for Asian Americans and Pacific Islanders, and studies on South Asians in the United States highlight two South Asian subgroups that are particularly vulnerable to suicide. These are young adults (aged 18-24 years) and women.7
Suicide is the second-leading cause of death for young Asian American men in the United States. Rates of lifetime suicidal ideation and attempts are higher among younger Asian Americans (aged 18-24 years) than among older Asian American adults. Young Asian American adults have been found to have higher levels of suicidal ideation than their white counterparts.8,9 Acculturation or assimilating into a different culture, familial violence as a child, hopelessness or a thought pattern with a pessimistic outlook, depression, and childhood sexual abuse have all been found to be positively correlated with suicidal ideation and attempted suicide in South Asian Americans. One study that conducted0 in-group analysis on undergraduate university students of South Asian descent living in New York found higher levels of hopelessness and depression in Asian Indians relative to Bangladeshi or Pakistani Americans.10
In addition, higher levels of suicidal ideation are reported in Asian Indians relative to Bangladeshi or Pakistani Americans. These results resemble findings from similar studies in the United Kingdom. A posited reason for these findings is a difference in religious beliefs. Pakistani and Bangladeshi Americans are predominantly Muslim, have stronger moral beliefs against suicide, and consider it a sin as defined by Islamic beliefs. Asian Indians, in contrast, are majority Hindu and believe in reincarnation – a context that might make suicide seem more permissible.11
South Asian women are particularly vulnerable to domestic violence, childhood sexual abuse, intimate partner violence, and/or familial violence. Cultural gender norms, traditional norms, and patriarchal ideology in the South Asian community make quantifying the level of childhood sexual abuse and familial violence a challenge. Furthermore, culturally, South Asian women are often considered subordinate relative to men, and discussion around family violence and childhood sexual abuse is avoided. Studies from the United Kingdom find a lack of knowledge around, disclosure of, and fear of reporting childhood sexual abuse in South Asian women. A study of a sample of representative South Asian American women found that 25.2% had experienced some form of childhood sexual abuse.12
Research also suggests that South Asians in the United States have some of the highest rates of intimate partner violence. Another study in the United States found that two out of five South Asian women have experienced physical and/or sexual intimate partner violence. This is much higher than the rate found in representative general U.S. population samples.
Literature suggests that exposure to these factors increases womens’ risk for suicidal ideation and attempted suicide. In the United Kingdom, research on South Asian women (aged 18-24 years) has found rates of attempted suicide to be three times higher than those of their white counterparts. Research from the United Kingdom and the United States suggests that younger married South Asian women are exposed to emotional and/or physical abuse from their spouse or in-laws, which is often a mediating factor in their increased risk for suicide.
Attempts to address suicide in the South Asian American community have to be multifaceted. An ideal approach would consist of educating, and connecting with, the community through ethnic media and trusted community sources, such as primary care doctors, caregivers, and social workers. In line with established American Psychological Association guidelines on caring for individuals of immigrant origin, health care professionals should document the patient’s number of generations in the country, number of years in the country, language fluency, family and community support, educational level, social status changes related to immigration, intimate relationships with people of different backgrounds, and stress related to acculturation. Special attention should be paid to South Asian women. Health care professionals should screen South Asian women for past and current intimate partner violence, provide culturally appropriate intimate partner violence resources, and be prepared to refer them to legal counseling services. Also, South Asian women should be screened for a history of exposure to familial violence and childhood sexual abuse.1
To adequately serve this population, there is a need to build capacity in the provision of culturally appropriate mental health services. Access to mental health care professionals through settings such as shelters for abused women, South Asian community–based organizations, youth centers, college counseling, and senior centers would encourage individuals to seek care without the threat of being stigmatized.
References
1. Hedegaard H et al. Suicide mortality in the United States, 1999–2017. NCHS Data Brief, No. 330. 2018 Nov.
2. Ahmad-Stout DJ and Nath SR. J College Stud Psychother. 2013 Jan 10;27(1):43-61.
3. Li H and Keshavan M. Asian J Psychiatry. 2011;4(1):1.
4. Nagaraj NC et al. J Immigr Minor Health. 2019 Oct;21(5):978-1003.
5. Nagaraj NC et al. J Comm Health. 2018;43(3):543-51.
6. Cao KO. Generations. 2014;30(4):82-5.
7. Hurwitz EJ et al. J Immigr Minor Health. 2006;8(3):251-61.
8. Polanco-Roman L et al. Cultur Divers Ethnic Minor Psychol. 2019 Dec 23. doi: 10.1037/cpd0000313.
9. Erausquin JT et al. J Youth Adolesc. 2019 Sep;48(9):1796-1805.
10. Lane R et al. Asian Am J Psychol. 2016;7(2):120-8.
11. Nath SR et al. Asian Am J Psychol. 2018;9(4):334-343.
12. Robertson HA et al. J Immigr Minor Health. 2016 Jul 31;18(4):921-7.
Mr. Kaleka is a medical student in the class of 2021 at Central Michigan University (CMU) College of Medicine, Mt. Pleasant. He has no disclosures. Mr. Kaleka would like to thank his mentor, Furhut Janssen, DO, for her continued guidance and support in research on mental health in immigrant populations.
Multifaceted strategies are needed to address unique cultural factors
Multifaceted strategies are needed to address unique cultural factors
On first glance, the age-adjusted rate of suicide for Asian and Pacific Islander populations living in the United States looks comparatively low.
Over the past 2 decades in the United States, for example, the overall rate increased by 35%, from, 10.5 to 14.2 per 100,000 individuals. That compares with a rate of 7.0 per 100,000 among Asian and Pacific Islander communities.1
However, because of the aggregate nature (national suicide mortality data combine people of Asian, Native Hawaiian, and other Pacific Islander descent into a single group) in which these data are reported, a significant amount of salient information on subgroups of Asian Americans is lost.2 There is a growing body of research on the mental health of Asian Americans, but the dearth of information and research on suicide in South Asians is striking.3 In fact, a review of literature finds fewer than 10 articles on the topic that have been published in peer-reviewed journals in the last decade. to provide effective, culturally sensitive care.
Diverse group
There are 3.4 million individuals of South Asian descent in the United States. Geographically, South Asians may have familial and cultural/historical roots in Bangladesh, Bhutan, India, Maldives, Nepal, and Pakistan.4 They enjoy a rich diversity in terms of cultural and religious beliefs, language, socioeconomic status, modes of acculturation, and immigration patterns. Asian Indians are the largest group of South Asians in the United States. They are highly educated, with a larger proportion of them pursuing an undergraduate and/or graduate level education than the general population. The median household income of Asian Indians is also higher than the national average.5
In general, suicide, like all mental health issues, is a stigmatized and taboo topic in the South Asian community.6 Also, South Asian Americans are hesitant to seek mental health care because of a perceived inability of Western health care professionals to understand their cultural views. Extrapolation from data on South Asians in the United Kingdom, aggregate statistics for Asian Americans and Pacific Islanders, and studies on South Asians in the United States highlight two South Asian subgroups that are particularly vulnerable to suicide. These are young adults (aged 18-24 years) and women.7
Suicide is the second-leading cause of death for young Asian American men in the United States. Rates of lifetime suicidal ideation and attempts are higher among younger Asian Americans (aged 18-24 years) than among older Asian American adults. Young Asian American adults have been found to have higher levels of suicidal ideation than their white counterparts.8,9 Acculturation or assimilating into a different culture, familial violence as a child, hopelessness or a thought pattern with a pessimistic outlook, depression, and childhood sexual abuse have all been found to be positively correlated with suicidal ideation and attempted suicide in South Asian Americans. One study that conducted0 in-group analysis on undergraduate university students of South Asian descent living in New York found higher levels of hopelessness and depression in Asian Indians relative to Bangladeshi or Pakistani Americans.10
In addition, higher levels of suicidal ideation are reported in Asian Indians relative to Bangladeshi or Pakistani Americans. These results resemble findings from similar studies in the United Kingdom. A posited reason for these findings is a difference in religious beliefs. Pakistani and Bangladeshi Americans are predominantly Muslim, have stronger moral beliefs against suicide, and consider it a sin as defined by Islamic beliefs. Asian Indians, in contrast, are majority Hindu and believe in reincarnation – a context that might make suicide seem more permissible.11
South Asian women are particularly vulnerable to domestic violence, childhood sexual abuse, intimate partner violence, and/or familial violence. Cultural gender norms, traditional norms, and patriarchal ideology in the South Asian community make quantifying the level of childhood sexual abuse and familial violence a challenge. Furthermore, culturally, South Asian women are often considered subordinate relative to men, and discussion around family violence and childhood sexual abuse is avoided. Studies from the United Kingdom find a lack of knowledge around, disclosure of, and fear of reporting childhood sexual abuse in South Asian women. A study of a sample of representative South Asian American women found that 25.2% had experienced some form of childhood sexual abuse.12
Research also suggests that South Asians in the United States have some of the highest rates of intimate partner violence. Another study in the United States found that two out of five South Asian women have experienced physical and/or sexual intimate partner violence. This is much higher than the rate found in representative general U.S. population samples.
Literature suggests that exposure to these factors increases womens’ risk for suicidal ideation and attempted suicide. In the United Kingdom, research on South Asian women (aged 18-24 years) has found rates of attempted suicide to be three times higher than those of their white counterparts. Research from the United Kingdom and the United States suggests that younger married South Asian women are exposed to emotional and/or physical abuse from their spouse or in-laws, which is often a mediating factor in their increased risk for suicide.
Attempts to address suicide in the South Asian American community have to be multifaceted. An ideal approach would consist of educating, and connecting with, the community through ethnic media and trusted community sources, such as primary care doctors, caregivers, and social workers. In line with established American Psychological Association guidelines on caring for individuals of immigrant origin, health care professionals should document the patient’s number of generations in the country, number of years in the country, language fluency, family and community support, educational level, social status changes related to immigration, intimate relationships with people of different backgrounds, and stress related to acculturation. Special attention should be paid to South Asian women. Health care professionals should screen South Asian women for past and current intimate partner violence, provide culturally appropriate intimate partner violence resources, and be prepared to refer them to legal counseling services. Also, South Asian women should be screened for a history of exposure to familial violence and childhood sexual abuse.1
To adequately serve this population, there is a need to build capacity in the provision of culturally appropriate mental health services. Access to mental health care professionals through settings such as shelters for abused women, South Asian community–based organizations, youth centers, college counseling, and senior centers would encourage individuals to seek care without the threat of being stigmatized.
References
1. Hedegaard H et al. Suicide mortality in the United States, 1999–2017. NCHS Data Brief, No. 330. 2018 Nov.
2. Ahmad-Stout DJ and Nath SR. J College Stud Psychother. 2013 Jan 10;27(1):43-61.
3. Li H and Keshavan M. Asian J Psychiatry. 2011;4(1):1.
4. Nagaraj NC et al. J Immigr Minor Health. 2019 Oct;21(5):978-1003.
5. Nagaraj NC et al. J Comm Health. 2018;43(3):543-51.
6. Cao KO. Generations. 2014;30(4):82-5.
7. Hurwitz EJ et al. J Immigr Minor Health. 2006;8(3):251-61.
8. Polanco-Roman L et al. Cultur Divers Ethnic Minor Psychol. 2019 Dec 23. doi: 10.1037/cpd0000313.
9. Erausquin JT et al. J Youth Adolesc. 2019 Sep;48(9):1796-1805.
10. Lane R et al. Asian Am J Psychol. 2016;7(2):120-8.
11. Nath SR et al. Asian Am J Psychol. 2018;9(4):334-343.
12. Robertson HA et al. J Immigr Minor Health. 2016 Jul 31;18(4):921-7.
Mr. Kaleka is a medical student in the class of 2021 at Central Michigan University (CMU) College of Medicine, Mt. Pleasant. He has no disclosures. Mr. Kaleka would like to thank his mentor, Furhut Janssen, DO, for her continued guidance and support in research on mental health in immigrant populations.
On first glance, the age-adjusted rate of suicide for Asian and Pacific Islander populations living in the United States looks comparatively low.
Over the past 2 decades in the United States, for example, the overall rate increased by 35%, from, 10.5 to 14.2 per 100,000 individuals. That compares with a rate of 7.0 per 100,000 among Asian and Pacific Islander communities.1
However, because of the aggregate nature (national suicide mortality data combine people of Asian, Native Hawaiian, and other Pacific Islander descent into a single group) in which these data are reported, a significant amount of salient information on subgroups of Asian Americans is lost.2 There is a growing body of research on the mental health of Asian Americans, but the dearth of information and research on suicide in South Asians is striking.3 In fact, a review of literature finds fewer than 10 articles on the topic that have been published in peer-reviewed journals in the last decade. to provide effective, culturally sensitive care.
Diverse group
There are 3.4 million individuals of South Asian descent in the United States. Geographically, South Asians may have familial and cultural/historical roots in Bangladesh, Bhutan, India, Maldives, Nepal, and Pakistan.4 They enjoy a rich diversity in terms of cultural and religious beliefs, language, socioeconomic status, modes of acculturation, and immigration patterns. Asian Indians are the largest group of South Asians in the United States. They are highly educated, with a larger proportion of them pursuing an undergraduate and/or graduate level education than the general population. The median household income of Asian Indians is also higher than the national average.5
In general, suicide, like all mental health issues, is a stigmatized and taboo topic in the South Asian community.6 Also, South Asian Americans are hesitant to seek mental health care because of a perceived inability of Western health care professionals to understand their cultural views. Extrapolation from data on South Asians in the United Kingdom, aggregate statistics for Asian Americans and Pacific Islanders, and studies on South Asians in the United States highlight two South Asian subgroups that are particularly vulnerable to suicide. These are young adults (aged 18-24 years) and women.7
Suicide is the second-leading cause of death for young Asian American men in the United States. Rates of lifetime suicidal ideation and attempts are higher among younger Asian Americans (aged 18-24 years) than among older Asian American adults. Young Asian American adults have been found to have higher levels of suicidal ideation than their white counterparts.8,9 Acculturation or assimilating into a different culture, familial violence as a child, hopelessness or a thought pattern with a pessimistic outlook, depression, and childhood sexual abuse have all been found to be positively correlated with suicidal ideation and attempted suicide in South Asian Americans. One study that conducted0 in-group analysis on undergraduate university students of South Asian descent living in New York found higher levels of hopelessness and depression in Asian Indians relative to Bangladeshi or Pakistani Americans.10
In addition, higher levels of suicidal ideation are reported in Asian Indians relative to Bangladeshi or Pakistani Americans. These results resemble findings from similar studies in the United Kingdom. A posited reason for these findings is a difference in religious beliefs. Pakistani and Bangladeshi Americans are predominantly Muslim, have stronger moral beliefs against suicide, and consider it a sin as defined by Islamic beliefs. Asian Indians, in contrast, are majority Hindu and believe in reincarnation – a context that might make suicide seem more permissible.11
South Asian women are particularly vulnerable to domestic violence, childhood sexual abuse, intimate partner violence, and/or familial violence. Cultural gender norms, traditional norms, and patriarchal ideology in the South Asian community make quantifying the level of childhood sexual abuse and familial violence a challenge. Furthermore, culturally, South Asian women are often considered subordinate relative to men, and discussion around family violence and childhood sexual abuse is avoided. Studies from the United Kingdom find a lack of knowledge around, disclosure of, and fear of reporting childhood sexual abuse in South Asian women. A study of a sample of representative South Asian American women found that 25.2% had experienced some form of childhood sexual abuse.12
Research also suggests that South Asians in the United States have some of the highest rates of intimate partner violence. Another study in the United States found that two out of five South Asian women have experienced physical and/or sexual intimate partner violence. This is much higher than the rate found in representative general U.S. population samples.
Literature suggests that exposure to these factors increases womens’ risk for suicidal ideation and attempted suicide. In the United Kingdom, research on South Asian women (aged 18-24 years) has found rates of attempted suicide to be three times higher than those of their white counterparts. Research from the United Kingdom and the United States suggests that younger married South Asian women are exposed to emotional and/or physical abuse from their spouse or in-laws, which is often a mediating factor in their increased risk for suicide.
Attempts to address suicide in the South Asian American community have to be multifaceted. An ideal approach would consist of educating, and connecting with, the community through ethnic media and trusted community sources, such as primary care doctors, caregivers, and social workers. In line with established American Psychological Association guidelines on caring for individuals of immigrant origin, health care professionals should document the patient’s number of generations in the country, number of years in the country, language fluency, family and community support, educational level, social status changes related to immigration, intimate relationships with people of different backgrounds, and stress related to acculturation. Special attention should be paid to South Asian women. Health care professionals should screen South Asian women for past and current intimate partner violence, provide culturally appropriate intimate partner violence resources, and be prepared to refer them to legal counseling services. Also, South Asian women should be screened for a history of exposure to familial violence and childhood sexual abuse.1
To adequately serve this population, there is a need to build capacity in the provision of culturally appropriate mental health services. Access to mental health care professionals through settings such as shelters for abused women, South Asian community–based organizations, youth centers, college counseling, and senior centers would encourage individuals to seek care without the threat of being stigmatized.
References
1. Hedegaard H et al. Suicide mortality in the United States, 1999–2017. NCHS Data Brief, No. 330. 2018 Nov.
2. Ahmad-Stout DJ and Nath SR. J College Stud Psychother. 2013 Jan 10;27(1):43-61.
3. Li H and Keshavan M. Asian J Psychiatry. 2011;4(1):1.
4. Nagaraj NC et al. J Immigr Minor Health. 2019 Oct;21(5):978-1003.
5. Nagaraj NC et al. J Comm Health. 2018;43(3):543-51.
6. Cao KO. Generations. 2014;30(4):82-5.
7. Hurwitz EJ et al. J Immigr Minor Health. 2006;8(3):251-61.
8. Polanco-Roman L et al. Cultur Divers Ethnic Minor Psychol. 2019 Dec 23. doi: 10.1037/cpd0000313.
9. Erausquin JT et al. J Youth Adolesc. 2019 Sep;48(9):1796-1805.
10. Lane R et al. Asian Am J Psychol. 2016;7(2):120-8.
11. Nath SR et al. Asian Am J Psychol. 2018;9(4):334-343.
12. Robertson HA et al. J Immigr Minor Health. 2016 Jul 31;18(4):921-7.
Mr. Kaleka is a medical student in the class of 2021 at Central Michigan University (CMU) College of Medicine, Mt. Pleasant. He has no disclosures. Mr. Kaleka would like to thank his mentor, Furhut Janssen, DO, for her continued guidance and support in research on mental health in immigrant populations.
Fighting COVID and police brutality, medical teams take to streets to treat protesters
Amid clouds of choking tear gas, booming flash-bang grenades and other “riot control agents,” volunteer medics plunged into street protests over the past weeks to help the injured – sometimes rushing to the front lines as soon as their hospital shifts ended.
Known as “street medics,” these unorthodox teams of nursing students, veterinarians, doctors, trauma surgeons, security guards, ski patrollers, nurses, wilderness EMTs, and off-the-clock ambulance workers poured water – not milk – into the eyes of tear-gassed protesters. They stanched bleeding wounds and plucked disoriented teenagers from clouds of gas, entering dangerous corners where on-duty emergency health responders may fear to go.
So donning cloth masks to protect against the virus – plus helmets, makeshift shields and other gear to guard against rubber bullets, projectiles and tear gas – the volunteer medics organized themselves into a web of first responders to care for people on the streets. They showed up early, set up first-aid stations, established transportation networks and covered their arms, helmets and backpacks with crosses made of red duct tape, to signify that they were medics. Some stayed late into the night past curfews until every protester had left.
Iris Butler, a 21-year-old certified nursing assistant who works in a nursing home, decided to offer her skills after seeing a man injured by a rubber bullet on her first night at the Denver protests. She showed up as a medic every night thereafter. She didn’t see it as a choice.
“I am working full time and basically being at the protest after getting straight off of work,” said Butler, who is black. That’s tiring, she added, but so is being a black woman in America.
After going out as a medic on her own, she soon met other volunteers. Together they used text-message chains to organize their efforts. One night, she responded to a man who had been shot with a rubber bullet in the chest; she said his torso had turned blue and purple from the impact. She also provided aid after a shooting near the protest left someone in critical condition.
“It’s hard, but bills need to be paid and justice needs to be served,” she said.
The street medic movement traces its roots, in part, to the 1960s protests, as well as the American Indian Movement and the Black Panther Party. Denver Action Medic Network offers a 20-hour training course that prepares them to treat patients in conflicts with police and large crowds; a four-hour session is offered to medical professionals as “bridge” training.
Since the coronavirus pandemic began, the Denver Action Medic Network has added new training guidelines: Don’t go to protests if sick or in contact with those who are infected; wear a mask; give people lots of space and use hand sanitizer. Jordan Garcia, a 39-year-old medic for over 20 years who works with the network of veteran street medics, said they also warn medics about the increased risk of transmission because of protesters coughing from tear gas, and urge them to get tested for the virus after the protests.
The number of volunteer medics swelled after George Floyd’s May 25 killing in Minneapolis. In Denver alone, at least 40 people reached out to the Denver Action Medic Network for training.
On June 3, Dr. Rupa Marya, an associate professor of medicine at the University of California,San Francisco, and the co-founder of the Do No Harm Coalition, which runs street medic training in the Bay Area, hosted a national webinar attended by over 3,000 medical professionals to provide the bridge training to be a street medic. In her online bio, Marya describes the coalition as “an organization of over 450 health workers committed to structural change” in addressing health problems.
“When we see suffering, that’s where we go,” Marya said. “And right now that suffering is happening on the streets.”
In the recent Denver protests, street medics responded to major head, face and eye injuries among protesters from what are sometimes described as “kinetic impact projectiles” or “less-than-lethal” bullets shot at protesters, along with tear-gas and flash-bang stun grenade canisters that either hit them or exploded in their faces.
Garcia, who by day works for an immigrant rights nonprofit, said that these weapons are not designed to be shot directly at people.
“We’re seeing police use these less-lethal weapons in lethal ways, and that is pretty upsetting,” Garcia said about the recent protests.
Denver police Chief Paul Pazen promised to make changes, including banning chokeholds and requiring SWAT teams to turn on their body cameras. Last week, a federal judge also issued a temporary injunction to stop Denver police from using tear gas and other less-than-lethal weapons in response to a class action lawsuit, in which a medic stated he was shot multiple times by police with pepper balls while treating patients. (Last week in North Carolina police were recorded destroying medic stations.)
Denver street medic Kevin Connell, a 30-year-old emergency room nurse, said he was hit with pepper balls in the back of his medic vest – which was clearly marked by red crosses – while treating a patient. He showed up to the Denver protests every night he did not have to work, he said, wearing a Kevlar medic vest, protective goggles and a homemade gas mask fashioned from a water bottle. As a member of the Denver Action Medic Network, Connell also served at the Standing Rock protests in North Dakota in a dispute over the building of the Dakota Access Pipeline.
“I mean, as bad as it sounds, it was only tear gas, pepper balls and rubber bullets that were being fired on us,” Connell said of his recent experience in Denver. “When I was at Standing Rock, they were using high-powered water hoses even when it was, like, freezing cold. … So I think the police here had a little bit more restraint.”
Still, first-time street medic Aj Mossman, a 31-year-old Denver emergency medical technician studying for nursing school, was shocked to be tear-gassed and struck in the back of the leg with a flash grenade while treating a protester on May 30. Mossman still has a large leg bruise.
The following night, Mossman, who uses the pronoun they, brought more protective gear, but said they are still having difficulty processing what felt like a war zone.
“I thought I understood what my black friends went through. I thought I understood what the black community went through,” said Mossman, who is white. “But I had absolutely no idea how violent the police were and how little they cared about who they hurt.”
For Butler, serving as a medic with others from various walks of life was inspiring. “They’re also out there to protect black and brown bodies. And that’s amazing,” she said. “That’s just a beautiful sight.”
This article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Amid clouds of choking tear gas, booming flash-bang grenades and other “riot control agents,” volunteer medics plunged into street protests over the past weeks to help the injured – sometimes rushing to the front lines as soon as their hospital shifts ended.
Known as “street medics,” these unorthodox teams of nursing students, veterinarians, doctors, trauma surgeons, security guards, ski patrollers, nurses, wilderness EMTs, and off-the-clock ambulance workers poured water – not milk – into the eyes of tear-gassed protesters. They stanched bleeding wounds and plucked disoriented teenagers from clouds of gas, entering dangerous corners where on-duty emergency health responders may fear to go.
So donning cloth masks to protect against the virus – plus helmets, makeshift shields and other gear to guard against rubber bullets, projectiles and tear gas – the volunteer medics organized themselves into a web of first responders to care for people on the streets. They showed up early, set up first-aid stations, established transportation networks and covered their arms, helmets and backpacks with crosses made of red duct tape, to signify that they were medics. Some stayed late into the night past curfews until every protester had left.
Iris Butler, a 21-year-old certified nursing assistant who works in a nursing home, decided to offer her skills after seeing a man injured by a rubber bullet on her first night at the Denver protests. She showed up as a medic every night thereafter. She didn’t see it as a choice.
“I am working full time and basically being at the protest after getting straight off of work,” said Butler, who is black. That’s tiring, she added, but so is being a black woman in America.
After going out as a medic on her own, she soon met other volunteers. Together they used text-message chains to organize their efforts. One night, she responded to a man who had been shot with a rubber bullet in the chest; she said his torso had turned blue and purple from the impact. She also provided aid after a shooting near the protest left someone in critical condition.
“It’s hard, but bills need to be paid and justice needs to be served,” she said.
The street medic movement traces its roots, in part, to the 1960s protests, as well as the American Indian Movement and the Black Panther Party. Denver Action Medic Network offers a 20-hour training course that prepares them to treat patients in conflicts with police and large crowds; a four-hour session is offered to medical professionals as “bridge” training.
Since the coronavirus pandemic began, the Denver Action Medic Network has added new training guidelines: Don’t go to protests if sick or in contact with those who are infected; wear a mask; give people lots of space and use hand sanitizer. Jordan Garcia, a 39-year-old medic for over 20 years who works with the network of veteran street medics, said they also warn medics about the increased risk of transmission because of protesters coughing from tear gas, and urge them to get tested for the virus after the protests.
The number of volunteer medics swelled after George Floyd’s May 25 killing in Minneapolis. In Denver alone, at least 40 people reached out to the Denver Action Medic Network for training.
On June 3, Dr. Rupa Marya, an associate professor of medicine at the University of California,San Francisco, and the co-founder of the Do No Harm Coalition, which runs street medic training in the Bay Area, hosted a national webinar attended by over 3,000 medical professionals to provide the bridge training to be a street medic. In her online bio, Marya describes the coalition as “an organization of over 450 health workers committed to structural change” in addressing health problems.
“When we see suffering, that’s where we go,” Marya said. “And right now that suffering is happening on the streets.”
In the recent Denver protests, street medics responded to major head, face and eye injuries among protesters from what are sometimes described as “kinetic impact projectiles” or “less-than-lethal” bullets shot at protesters, along with tear-gas and flash-bang stun grenade canisters that either hit them or exploded in their faces.
Garcia, who by day works for an immigrant rights nonprofit, said that these weapons are not designed to be shot directly at people.
“We’re seeing police use these less-lethal weapons in lethal ways, and that is pretty upsetting,” Garcia said about the recent protests.
Denver police Chief Paul Pazen promised to make changes, including banning chokeholds and requiring SWAT teams to turn on their body cameras. Last week, a federal judge also issued a temporary injunction to stop Denver police from using tear gas and other less-than-lethal weapons in response to a class action lawsuit, in which a medic stated he was shot multiple times by police with pepper balls while treating patients. (Last week in North Carolina police were recorded destroying medic stations.)
Denver street medic Kevin Connell, a 30-year-old emergency room nurse, said he was hit with pepper balls in the back of his medic vest – which was clearly marked by red crosses – while treating a patient. He showed up to the Denver protests every night he did not have to work, he said, wearing a Kevlar medic vest, protective goggles and a homemade gas mask fashioned from a water bottle. As a member of the Denver Action Medic Network, Connell also served at the Standing Rock protests in North Dakota in a dispute over the building of the Dakota Access Pipeline.
“I mean, as bad as it sounds, it was only tear gas, pepper balls and rubber bullets that were being fired on us,” Connell said of his recent experience in Denver. “When I was at Standing Rock, they were using high-powered water hoses even when it was, like, freezing cold. … So I think the police here had a little bit more restraint.”
Still, first-time street medic Aj Mossman, a 31-year-old Denver emergency medical technician studying for nursing school, was shocked to be tear-gassed and struck in the back of the leg with a flash grenade while treating a protester on May 30. Mossman still has a large leg bruise.
The following night, Mossman, who uses the pronoun they, brought more protective gear, but said they are still having difficulty processing what felt like a war zone.
“I thought I understood what my black friends went through. I thought I understood what the black community went through,” said Mossman, who is white. “But I had absolutely no idea how violent the police were and how little they cared about who they hurt.”
For Butler, serving as a medic with others from various walks of life was inspiring. “They’re also out there to protect black and brown bodies. And that’s amazing,” she said. “That’s just a beautiful sight.”
This article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Amid clouds of choking tear gas, booming flash-bang grenades and other “riot control agents,” volunteer medics plunged into street protests over the past weeks to help the injured – sometimes rushing to the front lines as soon as their hospital shifts ended.
Known as “street medics,” these unorthodox teams of nursing students, veterinarians, doctors, trauma surgeons, security guards, ski patrollers, nurses, wilderness EMTs, and off-the-clock ambulance workers poured water – not milk – into the eyes of tear-gassed protesters. They stanched bleeding wounds and plucked disoriented teenagers from clouds of gas, entering dangerous corners where on-duty emergency health responders may fear to go.
So donning cloth masks to protect against the virus – plus helmets, makeshift shields and other gear to guard against rubber bullets, projectiles and tear gas – the volunteer medics organized themselves into a web of first responders to care for people on the streets. They showed up early, set up first-aid stations, established transportation networks and covered their arms, helmets and backpacks with crosses made of red duct tape, to signify that they were medics. Some stayed late into the night past curfews until every protester had left.
Iris Butler, a 21-year-old certified nursing assistant who works in a nursing home, decided to offer her skills after seeing a man injured by a rubber bullet on her first night at the Denver protests. She showed up as a medic every night thereafter. She didn’t see it as a choice.
“I am working full time and basically being at the protest after getting straight off of work,” said Butler, who is black. That’s tiring, she added, but so is being a black woman in America.
After going out as a medic on her own, she soon met other volunteers. Together they used text-message chains to organize their efforts. One night, she responded to a man who had been shot with a rubber bullet in the chest; she said his torso had turned blue and purple from the impact. She also provided aid after a shooting near the protest left someone in critical condition.
“It’s hard, but bills need to be paid and justice needs to be served,” she said.
The street medic movement traces its roots, in part, to the 1960s protests, as well as the American Indian Movement and the Black Panther Party. Denver Action Medic Network offers a 20-hour training course that prepares them to treat patients in conflicts with police and large crowds; a four-hour session is offered to medical professionals as “bridge” training.
Since the coronavirus pandemic began, the Denver Action Medic Network has added new training guidelines: Don’t go to protests if sick or in contact with those who are infected; wear a mask; give people lots of space and use hand sanitizer. Jordan Garcia, a 39-year-old medic for over 20 years who works with the network of veteran street medics, said they also warn medics about the increased risk of transmission because of protesters coughing from tear gas, and urge them to get tested for the virus after the protests.
The number of volunteer medics swelled after George Floyd’s May 25 killing in Minneapolis. In Denver alone, at least 40 people reached out to the Denver Action Medic Network for training.
On June 3, Dr. Rupa Marya, an associate professor of medicine at the University of California,San Francisco, and the co-founder of the Do No Harm Coalition, which runs street medic training in the Bay Area, hosted a national webinar attended by over 3,000 medical professionals to provide the bridge training to be a street medic. In her online bio, Marya describes the coalition as “an organization of over 450 health workers committed to structural change” in addressing health problems.
“When we see suffering, that’s where we go,” Marya said. “And right now that suffering is happening on the streets.”
In the recent Denver protests, street medics responded to major head, face and eye injuries among protesters from what are sometimes described as “kinetic impact projectiles” or “less-than-lethal” bullets shot at protesters, along with tear-gas and flash-bang stun grenade canisters that either hit them or exploded in their faces.
Garcia, who by day works for an immigrant rights nonprofit, said that these weapons are not designed to be shot directly at people.
“We’re seeing police use these less-lethal weapons in lethal ways, and that is pretty upsetting,” Garcia said about the recent protests.
Denver police Chief Paul Pazen promised to make changes, including banning chokeholds and requiring SWAT teams to turn on their body cameras. Last week, a federal judge also issued a temporary injunction to stop Denver police from using tear gas and other less-than-lethal weapons in response to a class action lawsuit, in which a medic stated he was shot multiple times by police with pepper balls while treating patients. (Last week in North Carolina police were recorded destroying medic stations.)
Denver street medic Kevin Connell, a 30-year-old emergency room nurse, said he was hit with pepper balls in the back of his medic vest – which was clearly marked by red crosses – while treating a patient. He showed up to the Denver protests every night he did not have to work, he said, wearing a Kevlar medic vest, protective goggles and a homemade gas mask fashioned from a water bottle. As a member of the Denver Action Medic Network, Connell also served at the Standing Rock protests in North Dakota in a dispute over the building of the Dakota Access Pipeline.
“I mean, as bad as it sounds, it was only tear gas, pepper balls and rubber bullets that were being fired on us,” Connell said of his recent experience in Denver. “When I was at Standing Rock, they were using high-powered water hoses even when it was, like, freezing cold. … So I think the police here had a little bit more restraint.”
Still, first-time street medic Aj Mossman, a 31-year-old Denver emergency medical technician studying for nursing school, was shocked to be tear-gassed and struck in the back of the leg with a flash grenade while treating a protester on May 30. Mossman still has a large leg bruise.
The following night, Mossman, who uses the pronoun they, brought more protective gear, but said they are still having difficulty processing what felt like a war zone.
“I thought I understood what my black friends went through. I thought I understood what the black community went through,” said Mossman, who is white. “But I had absolutely no idea how violent the police were and how little they cared about who they hurt.”
For Butler, serving as a medic with others from various walks of life was inspiring. “They’re also out there to protect black and brown bodies. And that’s amazing,” she said. “That’s just a beautiful sight.”
This article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
If you reopen it, will they come?
On April 16, the White House released federal guidelines for reopening American businesses – followed 3 days later by specific recommendations from the Centers for Medicare and Medicaid Services for .
Depending on where you live, you may have already reopened (or even never closed), or you may be awaiting the relaxation of restrictions in your state. (As I write this on June 10, the stay-at-home order in my state, New Jersey, is being rescinded.)
The big question, of course, is whether patients can be convinced that it is safe to leave their homes and come to your office. The answer may depend on how well you time your reopening and adhere to the appropriate federal, state, and independent guidelines.
The federal guidelines have three sections: criteria, which outline conditions each region or state should satisfy before reopening; preparedness, which lists how states should prepare for reopening; and phase guidelines, which detail responsibilities of individuals and employers during distinct reopening phases.
You should pay the most attention to the “criteria” section. The key question to ask: “Has my state or region satisfied the basic criteria for reopening?”
Those criteria are as follows:
- Symptoms reported within a 14-day period should be on a downward trajectory.
- Cases documented (or positive tests as a percentage of total tests) within a 14-day period should also be on a downward trajectory.
- Hospitals should be treating all patients without crisis care. They should also have a robust testing program in place for at-risk health care workers.
If your area meets these criteria, you can proceed to the CMS recommendations. They cover general advice related to personal protective equipment (PPE), workforce availability, facility considerations, sanitation protocols, supplies, and testing capacity.
The key takeaway: As long as your area has the resources to quickly respond to a surge of COVID-19 cases, you can start offering care to non-COVID patients. Keep seeing patients via telehealth as often as possible, and prioritize surgical/procedural care and high-complexity chronic disease management before moving on to preventive and cosmetic services.
The American Medical Association has issued its own checklist of criteria for reopening your practice to supplement the federal guidelines. Highlights include the following:
- Sit down with a calendar and pick an expected reopening day. Ideally, this should include a “soft reopening.” Make a plan to stock necessary PPE and write down plans for cleaning and staffing if an employee or patient is diagnosed with COVID-19 after visiting your office.
- Take a stepwise approach so you can identify challenges early and address them. It’s important to figure out which visits can continue via telehealth, and begin with just a few in-person visits each day. Plan out a schedule and clearly communicate it to patients, clinicians, and staff.
- Patient safety is your top concern. Encourage patients to visit without companions whenever possible, and of course, all individuals who visit the office should wear a cloth face covering.
- Screen employees for fevers and other symptoms of COVID-19; remember that those records are subject to HIPAA rules and must be kept confidential. Minimize contact between employees as much as possible.
- Do your best to screen patients before in-person visits, to verify they don’t have symptoms of COVID-19. Consider creating a script that office staff can use to contact patients 24 hours before they come in. Use this as a chance to ask about symptoms, and explain any reopening logistics they should know about.
- Contact your malpractice insurance carrier to discuss whether you need to make any changes to your coverage.
This would also be a great time to review your confidentiality, privacy, and data security protocols. COVID-19 presents new challenges for data privacy – for example, if you must inform coworkers or patients that they have come into contact with someone who tested positive. Make a plan that follows HIPAA guidelines during COVID-19. Also, make sure you have a plan for handling issues like paid sick leave or reporting COVID-19 cases to your local health department.
Another useful resource is the Medical Group Management Association’s COVID-19 Medical Practice Reopening Checklist. You can use it to confirm that you are addressing all the important items, and that you haven’t missed anything.
As for me, I am advising patients who are reluctant to seek treatment that many medical problems pose more risk than COVID-19, faster treatment means better outcomes, and because we maintain strict disinfection protocols, they are far less likely to be infected with COVID-19 in my office than, say, at a grocery store.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
On April 16, the White House released federal guidelines for reopening American businesses – followed 3 days later by specific recommendations from the Centers for Medicare and Medicaid Services for .
Depending on where you live, you may have already reopened (or even never closed), or you may be awaiting the relaxation of restrictions in your state. (As I write this on June 10, the stay-at-home order in my state, New Jersey, is being rescinded.)
The big question, of course, is whether patients can be convinced that it is safe to leave their homes and come to your office. The answer may depend on how well you time your reopening and adhere to the appropriate federal, state, and independent guidelines.
The federal guidelines have three sections: criteria, which outline conditions each region or state should satisfy before reopening; preparedness, which lists how states should prepare for reopening; and phase guidelines, which detail responsibilities of individuals and employers during distinct reopening phases.
You should pay the most attention to the “criteria” section. The key question to ask: “Has my state or region satisfied the basic criteria for reopening?”
Those criteria are as follows:
- Symptoms reported within a 14-day period should be on a downward trajectory.
- Cases documented (or positive tests as a percentage of total tests) within a 14-day period should also be on a downward trajectory.
- Hospitals should be treating all patients without crisis care. They should also have a robust testing program in place for at-risk health care workers.
If your area meets these criteria, you can proceed to the CMS recommendations. They cover general advice related to personal protective equipment (PPE), workforce availability, facility considerations, sanitation protocols, supplies, and testing capacity.
The key takeaway: As long as your area has the resources to quickly respond to a surge of COVID-19 cases, you can start offering care to non-COVID patients. Keep seeing patients via telehealth as often as possible, and prioritize surgical/procedural care and high-complexity chronic disease management before moving on to preventive and cosmetic services.
The American Medical Association has issued its own checklist of criteria for reopening your practice to supplement the federal guidelines. Highlights include the following:
- Sit down with a calendar and pick an expected reopening day. Ideally, this should include a “soft reopening.” Make a plan to stock necessary PPE and write down plans for cleaning and staffing if an employee or patient is diagnosed with COVID-19 after visiting your office.
- Take a stepwise approach so you can identify challenges early and address them. It’s important to figure out which visits can continue via telehealth, and begin with just a few in-person visits each day. Plan out a schedule and clearly communicate it to patients, clinicians, and staff.
- Patient safety is your top concern. Encourage patients to visit without companions whenever possible, and of course, all individuals who visit the office should wear a cloth face covering.
- Screen employees for fevers and other symptoms of COVID-19; remember that those records are subject to HIPAA rules and must be kept confidential. Minimize contact between employees as much as possible.
- Do your best to screen patients before in-person visits, to verify they don’t have symptoms of COVID-19. Consider creating a script that office staff can use to contact patients 24 hours before they come in. Use this as a chance to ask about symptoms, and explain any reopening logistics they should know about.
- Contact your malpractice insurance carrier to discuss whether you need to make any changes to your coverage.
This would also be a great time to review your confidentiality, privacy, and data security protocols. COVID-19 presents new challenges for data privacy – for example, if you must inform coworkers or patients that they have come into contact with someone who tested positive. Make a plan that follows HIPAA guidelines during COVID-19. Also, make sure you have a plan for handling issues like paid sick leave or reporting COVID-19 cases to your local health department.
Another useful resource is the Medical Group Management Association’s COVID-19 Medical Practice Reopening Checklist. You can use it to confirm that you are addressing all the important items, and that you haven’t missed anything.
As for me, I am advising patients who are reluctant to seek treatment that many medical problems pose more risk than COVID-19, faster treatment means better outcomes, and because we maintain strict disinfection protocols, they are far less likely to be infected with COVID-19 in my office than, say, at a grocery store.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
On April 16, the White House released federal guidelines for reopening American businesses – followed 3 days later by specific recommendations from the Centers for Medicare and Medicaid Services for .
Depending on where you live, you may have already reopened (or even never closed), or you may be awaiting the relaxation of restrictions in your state. (As I write this on June 10, the stay-at-home order in my state, New Jersey, is being rescinded.)
The big question, of course, is whether patients can be convinced that it is safe to leave their homes and come to your office. The answer may depend on how well you time your reopening and adhere to the appropriate federal, state, and independent guidelines.
The federal guidelines have three sections: criteria, which outline conditions each region or state should satisfy before reopening; preparedness, which lists how states should prepare for reopening; and phase guidelines, which detail responsibilities of individuals and employers during distinct reopening phases.
You should pay the most attention to the “criteria” section. The key question to ask: “Has my state or region satisfied the basic criteria for reopening?”
Those criteria are as follows:
- Symptoms reported within a 14-day period should be on a downward trajectory.
- Cases documented (or positive tests as a percentage of total tests) within a 14-day period should also be on a downward trajectory.
- Hospitals should be treating all patients without crisis care. They should also have a robust testing program in place for at-risk health care workers.
If your area meets these criteria, you can proceed to the CMS recommendations. They cover general advice related to personal protective equipment (PPE), workforce availability, facility considerations, sanitation protocols, supplies, and testing capacity.
The key takeaway: As long as your area has the resources to quickly respond to a surge of COVID-19 cases, you can start offering care to non-COVID patients. Keep seeing patients via telehealth as often as possible, and prioritize surgical/procedural care and high-complexity chronic disease management before moving on to preventive and cosmetic services.
The American Medical Association has issued its own checklist of criteria for reopening your practice to supplement the federal guidelines. Highlights include the following:
- Sit down with a calendar and pick an expected reopening day. Ideally, this should include a “soft reopening.” Make a plan to stock necessary PPE and write down plans for cleaning and staffing if an employee or patient is diagnosed with COVID-19 after visiting your office.
- Take a stepwise approach so you can identify challenges early and address them. It’s important to figure out which visits can continue via telehealth, and begin with just a few in-person visits each day. Plan out a schedule and clearly communicate it to patients, clinicians, and staff.
- Patient safety is your top concern. Encourage patients to visit without companions whenever possible, and of course, all individuals who visit the office should wear a cloth face covering.
- Screen employees for fevers and other symptoms of COVID-19; remember that those records are subject to HIPAA rules and must be kept confidential. Minimize contact between employees as much as possible.
- Do your best to screen patients before in-person visits, to verify they don’t have symptoms of COVID-19. Consider creating a script that office staff can use to contact patients 24 hours before they come in. Use this as a chance to ask about symptoms, and explain any reopening logistics they should know about.
- Contact your malpractice insurance carrier to discuss whether you need to make any changes to your coverage.
This would also be a great time to review your confidentiality, privacy, and data security protocols. COVID-19 presents new challenges for data privacy – for example, if you must inform coworkers or patients that they have come into contact with someone who tested positive. Make a plan that follows HIPAA guidelines during COVID-19. Also, make sure you have a plan for handling issues like paid sick leave or reporting COVID-19 cases to your local health department.
Another useful resource is the Medical Group Management Association’s COVID-19 Medical Practice Reopening Checklist. You can use it to confirm that you are addressing all the important items, and that you haven’t missed anything.
As for me, I am advising patients who are reluctant to seek treatment that many medical problems pose more risk than COVID-19, faster treatment means better outcomes, and because we maintain strict disinfection protocols, they are far less likely to be infected with COVID-19 in my office than, say, at a grocery store.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
New long-term data for antipsychotic in pediatric bipolar depression
The antipsychotic lurasidone (Latuda, Sunovion Pharmaceuticals) has long-term efficacy in the treatment of bipolar depression (BD) in children and adolescents, new research suggests.
In an open-label extension study involving patients aged 10-17 years, up to 2 years of treatment with lurasidone was associated with continued improvement in depressive symptoms. There were progressively higher rates of remission, recovery, and sustained remission.
Coinvestigator Manpreet K. Singh, MD, director of the Stanford Pediatric Mood Disorders Program, Stanford (Calif.) University, noted that early onset of BD is common. Although in pediatric populations, prevalence has been fairly stable at around 1.8%, these patients have “a very limited number of treatment options available for the depressed phases of BD,” which is often predominant and can be difficult to identify.
“A lot of youths who are experiencing depressive symptoms in the context of having had a manic episode will often have a relapsing and remitting course, even after the acute phase of treatment, so because kids can be on medications for long periods of time, a better understanding of what works ... is very important,” Dr. Singh said in an interview.
The findings were presented at the virtual American Society of Clinical Psychopharmacology (ASCP) 2020 annual meeting.
Long-term Efficacy
The Food and Drug Administration approved lurasidone as monotherapy for BD in children and adolescents in 2018. The aim of the current study was to evaluate the drug’s long-term efficacy in achieving response or remission in this population.
A total of 305 children who completed an initial 6-week double-blind study of lurasidone versus placebo entered the 2-year, open-label extension study. In the extension, they either continued taking lurasidone or were switched from placebo to lurasidone 20-80 mg/day. Of this group, 195 children completed 52 weeks of treatment, and 93 completed 104 weeks of treatment.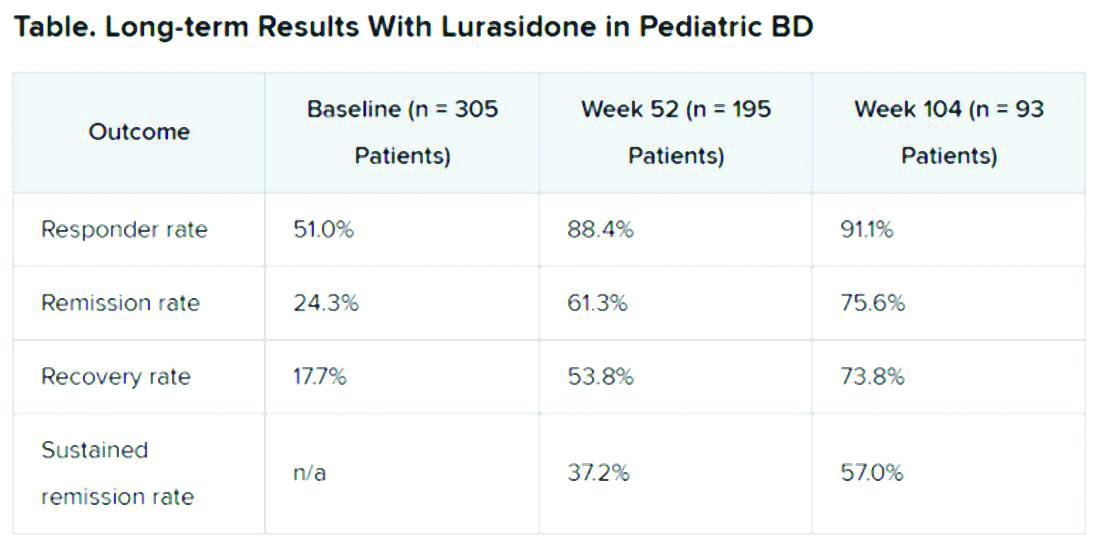
Efficacy was measured with the Children’s Depression Rating Scale, Revised (CDRS-R) and the Clinical Global Impression, Bipolar Depression Severity scale (CGI-BP-S). Functioning was evaluated with the clinician-rated Children’s Global Assessment Scale (CGAS); on that scale, a score of 70 or higher indicates no clinically meaningful functional impairment.
Remission criteria were met if a patient achieved a CDRS-R total score of 28 or less, a Young Mania Rating Scale (YMRS) total score of 8 or less, and a CGI-BP-S depression score of 3 or less.
Recovery criteria were met if a patient achieved remission and had a CGAS score of at least 70.
Sustained remission, a more stringent outcome, required that the patient meet remission criteria for at least 24 consecutive weeks.
In addition, there was a strong inverse correlation (r = –0.71) between depression severity, as measured by CDRS-R total score, and functioning, as measured by the CGAS.
“That’s the cool thing: As the depression symptoms and severity came down, the overall functioning in these kids improved,” Dr. Singh noted.
“This improvement in functioning ends up being much more clinically relevant and useful to clinicians than just showing an improvement in a set of symptoms because what brings a kid – or even an adult, for that matter – to see a clinician to get treatment is because something about their symptoms is causing significant functional impairment,” she said.
“So this is the take-home message: You can see that lurasidone ... demonstrates not just recovery from depressive symptoms but that this reduction in depressive symptoms corresponds to an improvement in functioning for these youths,” she added.
Potential Limitations
Commenting on the study, Christoph U. Correll, MD, professor of child and adolescent psychiatry, Charite Universitatsmedizin, Berlin, Germany, noted that BD is difficult to treat, especially for patients who are going through “a developmentally vulnerable phase of their lives.”
“Lurasidone is the only monotherapy approved for bipolar depression in youth and is fairly well tolerated,” said Dr. Correll, who was not part of the research. He added that the long-term effectiveness data on response and remission “add relevant information” to the field.
However, he noted that it is not clear whether the high and increasing rates of response and remission were based on the reporting of observed cases or on last-observation-carried-forward analyses. “Given the naturally high dropout rate in such a long-term study and the potential for a survival bias, this is a relevant methodological question that affects the interpretation of the data,” he said.
“Nevertheless, the very favorable results for cumulative response, remission, and sustained remission add to the evidence that lurasidone is an effective treatment for youth with bipolar depression. Since efficacy cannot be interpreted in isolation, data describing the tolerability, including long-term cardiometabolic effects, will be important complementary data to consider,” Dr. Correll said.
The study was funded by Sunovion Pharmaceuticals. Dr. Singh is on the advisory board for Sunovion, is a consultant for Google X and Limbix, and receives royalties from American Psychiatric Association Publishing. She has also received research support from Stanford’s Maternal Child Health Research Institute and Department of Psychiatry, the National Institute of Mental Health, the National Institute on Aging, Johnson and Johnson, Allergan, PCORI, and the Brain and Behavior Research Foundation. Dr. Correll has been a consultant or adviser to and has received honoraria from Sunovion, as well as Acadia, Alkermes, Allergan, Angelini, Axsome, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Janssen/J&J, LB Pharma, Lundbeck, MedAvante-ProPhase, Medscape, Neurocrine, Noven, Otsuka, Pfizer, Recordati, Rovi, Sumitomo Dainippon, Supernus, Takeda, and Teva.
A version of this article originally appeared on Medscape.com.
The antipsychotic lurasidone (Latuda, Sunovion Pharmaceuticals) has long-term efficacy in the treatment of bipolar depression (BD) in children and adolescents, new research suggests.
In an open-label extension study involving patients aged 10-17 years, up to 2 years of treatment with lurasidone was associated with continued improvement in depressive symptoms. There were progressively higher rates of remission, recovery, and sustained remission.
Coinvestigator Manpreet K. Singh, MD, director of the Stanford Pediatric Mood Disorders Program, Stanford (Calif.) University, noted that early onset of BD is common. Although in pediatric populations, prevalence has been fairly stable at around 1.8%, these patients have “a very limited number of treatment options available for the depressed phases of BD,” which is often predominant and can be difficult to identify.
“A lot of youths who are experiencing depressive symptoms in the context of having had a manic episode will often have a relapsing and remitting course, even after the acute phase of treatment, so because kids can be on medications for long periods of time, a better understanding of what works ... is very important,” Dr. Singh said in an interview.
The findings were presented at the virtual American Society of Clinical Psychopharmacology (ASCP) 2020 annual meeting.
Long-term Efficacy
The Food and Drug Administration approved lurasidone as monotherapy for BD in children and adolescents in 2018. The aim of the current study was to evaluate the drug’s long-term efficacy in achieving response or remission in this population.
A total of 305 children who completed an initial 6-week double-blind study of lurasidone versus placebo entered the 2-year, open-label extension study. In the extension, they either continued taking lurasidone or were switched from placebo to lurasidone 20-80 mg/day. Of this group, 195 children completed 52 weeks of treatment, and 93 completed 104 weeks of treatment.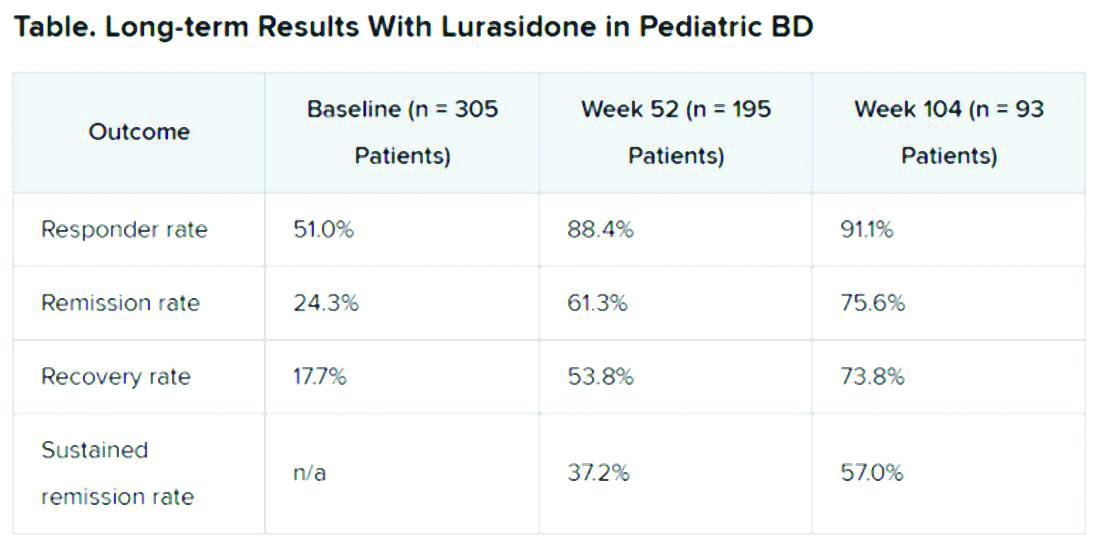
Efficacy was measured with the Children’s Depression Rating Scale, Revised (CDRS-R) and the Clinical Global Impression, Bipolar Depression Severity scale (CGI-BP-S). Functioning was evaluated with the clinician-rated Children’s Global Assessment Scale (CGAS); on that scale, a score of 70 or higher indicates no clinically meaningful functional impairment.
Remission criteria were met if a patient achieved a CDRS-R total score of 28 or less, a Young Mania Rating Scale (YMRS) total score of 8 or less, and a CGI-BP-S depression score of 3 or less.
Recovery criteria were met if a patient achieved remission and had a CGAS score of at least 70.
Sustained remission, a more stringent outcome, required that the patient meet remission criteria for at least 24 consecutive weeks.
In addition, there was a strong inverse correlation (r = –0.71) between depression severity, as measured by CDRS-R total score, and functioning, as measured by the CGAS.
“That’s the cool thing: As the depression symptoms and severity came down, the overall functioning in these kids improved,” Dr. Singh noted.
“This improvement in functioning ends up being much more clinically relevant and useful to clinicians than just showing an improvement in a set of symptoms because what brings a kid – or even an adult, for that matter – to see a clinician to get treatment is because something about their symptoms is causing significant functional impairment,” she said.
“So this is the take-home message: You can see that lurasidone ... demonstrates not just recovery from depressive symptoms but that this reduction in depressive symptoms corresponds to an improvement in functioning for these youths,” she added.
Potential Limitations
Commenting on the study, Christoph U. Correll, MD, professor of child and adolescent psychiatry, Charite Universitatsmedizin, Berlin, Germany, noted that BD is difficult to treat, especially for patients who are going through “a developmentally vulnerable phase of their lives.”
“Lurasidone is the only monotherapy approved for bipolar depression in youth and is fairly well tolerated,” said Dr. Correll, who was not part of the research. He added that the long-term effectiveness data on response and remission “add relevant information” to the field.
However, he noted that it is not clear whether the high and increasing rates of response and remission were based on the reporting of observed cases or on last-observation-carried-forward analyses. “Given the naturally high dropout rate in such a long-term study and the potential for a survival bias, this is a relevant methodological question that affects the interpretation of the data,” he said.
“Nevertheless, the very favorable results for cumulative response, remission, and sustained remission add to the evidence that lurasidone is an effective treatment for youth with bipolar depression. Since efficacy cannot be interpreted in isolation, data describing the tolerability, including long-term cardiometabolic effects, will be important complementary data to consider,” Dr. Correll said.
The study was funded by Sunovion Pharmaceuticals. Dr. Singh is on the advisory board for Sunovion, is a consultant for Google X and Limbix, and receives royalties from American Psychiatric Association Publishing. She has also received research support from Stanford’s Maternal Child Health Research Institute and Department of Psychiatry, the National Institute of Mental Health, the National Institute on Aging, Johnson and Johnson, Allergan, PCORI, and the Brain and Behavior Research Foundation. Dr. Correll has been a consultant or adviser to and has received honoraria from Sunovion, as well as Acadia, Alkermes, Allergan, Angelini, Axsome, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Janssen/J&J, LB Pharma, Lundbeck, MedAvante-ProPhase, Medscape, Neurocrine, Noven, Otsuka, Pfizer, Recordati, Rovi, Sumitomo Dainippon, Supernus, Takeda, and Teva.
A version of this article originally appeared on Medscape.com.
The antipsychotic lurasidone (Latuda, Sunovion Pharmaceuticals) has long-term efficacy in the treatment of bipolar depression (BD) in children and adolescents, new research suggests.
In an open-label extension study involving patients aged 10-17 years, up to 2 years of treatment with lurasidone was associated with continued improvement in depressive symptoms. There were progressively higher rates of remission, recovery, and sustained remission.
Coinvestigator Manpreet K. Singh, MD, director of the Stanford Pediatric Mood Disorders Program, Stanford (Calif.) University, noted that early onset of BD is common. Although in pediatric populations, prevalence has been fairly stable at around 1.8%, these patients have “a very limited number of treatment options available for the depressed phases of BD,” which is often predominant and can be difficult to identify.
“A lot of youths who are experiencing depressive symptoms in the context of having had a manic episode will often have a relapsing and remitting course, even after the acute phase of treatment, so because kids can be on medications for long periods of time, a better understanding of what works ... is very important,” Dr. Singh said in an interview.
The findings were presented at the virtual American Society of Clinical Psychopharmacology (ASCP) 2020 annual meeting.
Long-term Efficacy
The Food and Drug Administration approved lurasidone as monotherapy for BD in children and adolescents in 2018. The aim of the current study was to evaluate the drug’s long-term efficacy in achieving response or remission in this population.
A total of 305 children who completed an initial 6-week double-blind study of lurasidone versus placebo entered the 2-year, open-label extension study. In the extension, they either continued taking lurasidone or were switched from placebo to lurasidone 20-80 mg/day. Of this group, 195 children completed 52 weeks of treatment, and 93 completed 104 weeks of treatment.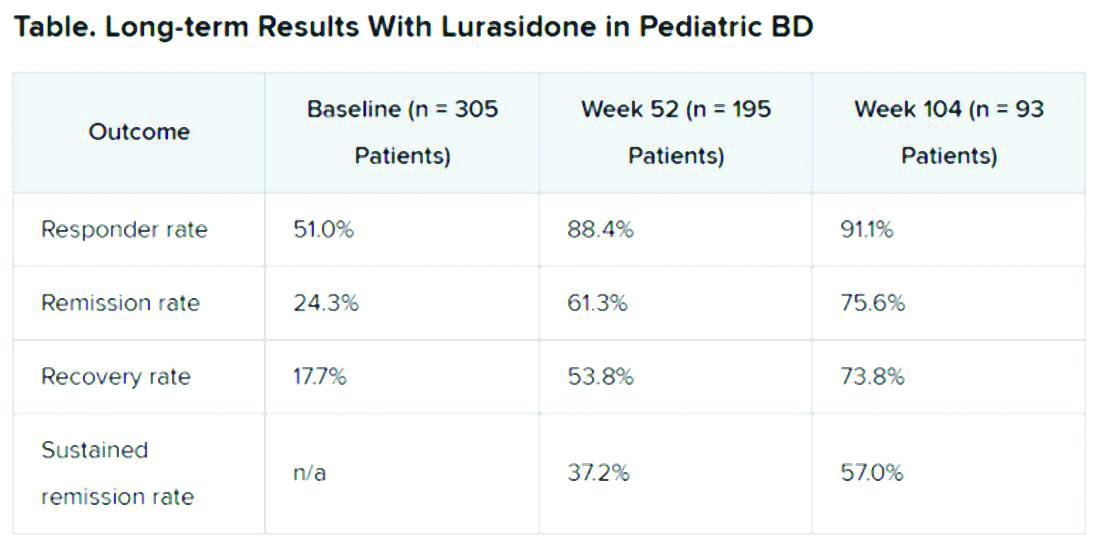
Efficacy was measured with the Children’s Depression Rating Scale, Revised (CDRS-R) and the Clinical Global Impression, Bipolar Depression Severity scale (CGI-BP-S). Functioning was evaluated with the clinician-rated Children’s Global Assessment Scale (CGAS); on that scale, a score of 70 or higher indicates no clinically meaningful functional impairment.
Remission criteria were met if a patient achieved a CDRS-R total score of 28 or less, a Young Mania Rating Scale (YMRS) total score of 8 or less, and a CGI-BP-S depression score of 3 or less.
Recovery criteria were met if a patient achieved remission and had a CGAS score of at least 70.
Sustained remission, a more stringent outcome, required that the patient meet remission criteria for at least 24 consecutive weeks.
In addition, there was a strong inverse correlation (r = –0.71) between depression severity, as measured by CDRS-R total score, and functioning, as measured by the CGAS.
“That’s the cool thing: As the depression symptoms and severity came down, the overall functioning in these kids improved,” Dr. Singh noted.
“This improvement in functioning ends up being much more clinically relevant and useful to clinicians than just showing an improvement in a set of symptoms because what brings a kid – or even an adult, for that matter – to see a clinician to get treatment is because something about their symptoms is causing significant functional impairment,” she said.
“So this is the take-home message: You can see that lurasidone ... demonstrates not just recovery from depressive symptoms but that this reduction in depressive symptoms corresponds to an improvement in functioning for these youths,” she added.
Potential Limitations
Commenting on the study, Christoph U. Correll, MD, professor of child and adolescent psychiatry, Charite Universitatsmedizin, Berlin, Germany, noted that BD is difficult to treat, especially for patients who are going through “a developmentally vulnerable phase of their lives.”
“Lurasidone is the only monotherapy approved for bipolar depression in youth and is fairly well tolerated,” said Dr. Correll, who was not part of the research. He added that the long-term effectiveness data on response and remission “add relevant information” to the field.
However, he noted that it is not clear whether the high and increasing rates of response and remission were based on the reporting of observed cases or on last-observation-carried-forward analyses. “Given the naturally high dropout rate in such a long-term study and the potential for a survival bias, this is a relevant methodological question that affects the interpretation of the data,” he said.
“Nevertheless, the very favorable results for cumulative response, remission, and sustained remission add to the evidence that lurasidone is an effective treatment for youth with bipolar depression. Since efficacy cannot be interpreted in isolation, data describing the tolerability, including long-term cardiometabolic effects, will be important complementary data to consider,” Dr. Correll said.
The study was funded by Sunovion Pharmaceuticals. Dr. Singh is on the advisory board for Sunovion, is a consultant for Google X and Limbix, and receives royalties from American Psychiatric Association Publishing. She has also received research support from Stanford’s Maternal Child Health Research Institute and Department of Psychiatry, the National Institute of Mental Health, the National Institute on Aging, Johnson and Johnson, Allergan, PCORI, and the Brain and Behavior Research Foundation. Dr. Correll has been a consultant or adviser to and has received honoraria from Sunovion, as well as Acadia, Alkermes, Allergan, Angelini, Axsome, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Janssen/J&J, LB Pharma, Lundbeck, MedAvante-ProPhase, Medscape, Neurocrine, Noven, Otsuka, Pfizer, Recordati, Rovi, Sumitomo Dainippon, Supernus, Takeda, and Teva.
A version of this article originally appeared on Medscape.com.
FROM ASCP 2020
Daily Recap: Feds seek COVID-19 info through app, hospitalists take on new roles
Here are the stories our MDedge editors across specialties think you need to know about today:
FDA seeks COVID-19 info through CURE ID
Federal health officials are asking clinicians to use the free CURE ID mobile app and web platform as a tool to collect information on the treatment of patients with COVID-19. CURE ID is an Internet-based data repository first developed in 2013 as a collaboration between the Food and Drug Administration and the National Center for Advancing Translational Sciences, part of the National Institutes of Health. It provides licensed clinicians worldwide with an opportunity to report novel uses of existing drugs for patients with difficult-to-treat infectious diseases, including COVID-19, through a website, a smartphone, or other mobile device. “By utilizing the CURE ID platform now for COVID-19 case collection – in conjunction with data gathered from other registries, EHR systems, and clinical trials – data collected during an outbreak can be improved and coordinated,” said Heather A. Stone, MPH, a health science policy analyst in the office of medical policy at the FDA’s Center for Drug Evaluation and Research. “This may allow us to find possible treatments to help ease this pandemic, and prepare us better to fight the next one.” Read more.
Hospitalists take on new roles in COVID era
Whether it’s working shifts in the ICU, caring for ventilator patients, or reporting to postanesthesia care units and post-acute or step-down units, hospitalists are stepping into a variety of new roles as part of their frontline response to the COVID-19 pandemic. Valerie Vaughn, MD, a hospitalist with Michigan Medicine and assistant professor of medicine at the University of Michigan in Ann Arbor, was doing research on how to reduce overuse of antibiotics in hospitals when the COVID-19 crisis hit and dramatically redefined her job. “We were afraid that we might have 3,000 to 5,000 hospitalized COVID patients by now, based on predictive modeling done while the pandemic was still growing exponentially,” she explained. Although Michigan continues to have high COVID-19 infection rates, centered on nearby Detroit, “things are a lot better today than they were 4 weeks ago.” Dr. Vaughn helped to mobilize a team of 25 hospitalists, along with other health care professionals, who volunteered to manage COVID-19 patients in the ICU and other hospital units. Read more.
COVID-19 recommendations for rheumatic disease treatment
The European League Against Rheumatism (EULAR) issued provisional recommendations for the management of rheumatic and musculoskeletal diseases in the context of SARS-CoV-2. Contrary to earlier expectations, there is no indication that patients with rheumatic and musculoskeletal diseases have a higher risk of contracting the virus or have a worse course if they do, according to the task force that worked on the recommendations. The task force also pointed out that rheumatology drugs are being used to treat COVID-19 patients who don’t have rheumatic diseases, raising the possibility of a shortage of disease-modifying antirheumatic drugs. Read more.
Mental health visits are 19% of ED costs
Mental and substance use disorders represented 19% of all emergency department visits in 2017 and cost $14.6 billion, according to figures from the Agency for Healthcare Research and Quality. The most costly mental and substance use disorder diagnosis was anxiety and fear-related disorders, accounting for $5.6 billion worth of visits, following by depressive disorders and alcohol-related disorders. Read more.
Food deserts linked to health issues in pregnancy
Living in a neighborhood lacking adequate access to affordable, high-quality food is associated with a somewhat greater risk of developing pregnancy morbidity, according to an observational study. Researchers found that women who lived in a food desert had a 1.6 times greater odds of pregnancy comorbidity than if they did not. “An additional, albeit less obvious factor that may be unique to patients suffering disproportionately from obstetric morbidity is exposure to toxic elements,” the researchers reported in Obstetrics & Gynecology. “It has been shown in a previous study that low-income, predominantly black communities of pregnant women may suffer disproportionately from lead or arsenic exposure.” Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
FDA seeks COVID-19 info through CURE ID
Federal health officials are asking clinicians to use the free CURE ID mobile app and web platform as a tool to collect information on the treatment of patients with COVID-19. CURE ID is an Internet-based data repository first developed in 2013 as a collaboration between the Food and Drug Administration and the National Center for Advancing Translational Sciences, part of the National Institutes of Health. It provides licensed clinicians worldwide with an opportunity to report novel uses of existing drugs for patients with difficult-to-treat infectious diseases, including COVID-19, through a website, a smartphone, or other mobile device. “By utilizing the CURE ID platform now for COVID-19 case collection – in conjunction with data gathered from other registries, EHR systems, and clinical trials – data collected during an outbreak can be improved and coordinated,” said Heather A. Stone, MPH, a health science policy analyst in the office of medical policy at the FDA’s Center for Drug Evaluation and Research. “This may allow us to find possible treatments to help ease this pandemic, and prepare us better to fight the next one.” Read more.
Hospitalists take on new roles in COVID era
Whether it’s working shifts in the ICU, caring for ventilator patients, or reporting to postanesthesia care units and post-acute or step-down units, hospitalists are stepping into a variety of new roles as part of their frontline response to the COVID-19 pandemic. Valerie Vaughn, MD, a hospitalist with Michigan Medicine and assistant professor of medicine at the University of Michigan in Ann Arbor, was doing research on how to reduce overuse of antibiotics in hospitals when the COVID-19 crisis hit and dramatically redefined her job. “We were afraid that we might have 3,000 to 5,000 hospitalized COVID patients by now, based on predictive modeling done while the pandemic was still growing exponentially,” she explained. Although Michigan continues to have high COVID-19 infection rates, centered on nearby Detroit, “things are a lot better today than they were 4 weeks ago.” Dr. Vaughn helped to mobilize a team of 25 hospitalists, along with other health care professionals, who volunteered to manage COVID-19 patients in the ICU and other hospital units. Read more.
COVID-19 recommendations for rheumatic disease treatment
The European League Against Rheumatism (EULAR) issued provisional recommendations for the management of rheumatic and musculoskeletal diseases in the context of SARS-CoV-2. Contrary to earlier expectations, there is no indication that patients with rheumatic and musculoskeletal diseases have a higher risk of contracting the virus or have a worse course if they do, according to the task force that worked on the recommendations. The task force also pointed out that rheumatology drugs are being used to treat COVID-19 patients who don’t have rheumatic diseases, raising the possibility of a shortage of disease-modifying antirheumatic drugs. Read more.
Mental health visits are 19% of ED costs
Mental and substance use disorders represented 19% of all emergency department visits in 2017 and cost $14.6 billion, according to figures from the Agency for Healthcare Research and Quality. The most costly mental and substance use disorder diagnosis was anxiety and fear-related disorders, accounting for $5.6 billion worth of visits, following by depressive disorders and alcohol-related disorders. Read more.
Food deserts linked to health issues in pregnancy
Living in a neighborhood lacking adequate access to affordable, high-quality food is associated with a somewhat greater risk of developing pregnancy morbidity, according to an observational study. Researchers found that women who lived in a food desert had a 1.6 times greater odds of pregnancy comorbidity than if they did not. “An additional, albeit less obvious factor that may be unique to patients suffering disproportionately from obstetric morbidity is exposure to toxic elements,” the researchers reported in Obstetrics & Gynecology. “It has been shown in a previous study that low-income, predominantly black communities of pregnant women may suffer disproportionately from lead or arsenic exposure.” Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
FDA seeks COVID-19 info through CURE ID
Federal health officials are asking clinicians to use the free CURE ID mobile app and web platform as a tool to collect information on the treatment of patients with COVID-19. CURE ID is an Internet-based data repository first developed in 2013 as a collaboration between the Food and Drug Administration and the National Center for Advancing Translational Sciences, part of the National Institutes of Health. It provides licensed clinicians worldwide with an opportunity to report novel uses of existing drugs for patients with difficult-to-treat infectious diseases, including COVID-19, through a website, a smartphone, or other mobile device. “By utilizing the CURE ID platform now for COVID-19 case collection – in conjunction with data gathered from other registries, EHR systems, and clinical trials – data collected during an outbreak can be improved and coordinated,” said Heather A. Stone, MPH, a health science policy analyst in the office of medical policy at the FDA’s Center for Drug Evaluation and Research. “This may allow us to find possible treatments to help ease this pandemic, and prepare us better to fight the next one.” Read more.
Hospitalists take on new roles in COVID era
Whether it’s working shifts in the ICU, caring for ventilator patients, or reporting to postanesthesia care units and post-acute or step-down units, hospitalists are stepping into a variety of new roles as part of their frontline response to the COVID-19 pandemic. Valerie Vaughn, MD, a hospitalist with Michigan Medicine and assistant professor of medicine at the University of Michigan in Ann Arbor, was doing research on how to reduce overuse of antibiotics in hospitals when the COVID-19 crisis hit and dramatically redefined her job. “We were afraid that we might have 3,000 to 5,000 hospitalized COVID patients by now, based on predictive modeling done while the pandemic was still growing exponentially,” she explained. Although Michigan continues to have high COVID-19 infection rates, centered on nearby Detroit, “things are a lot better today than they were 4 weeks ago.” Dr. Vaughn helped to mobilize a team of 25 hospitalists, along with other health care professionals, who volunteered to manage COVID-19 patients in the ICU and other hospital units. Read more.
COVID-19 recommendations for rheumatic disease treatment
The European League Against Rheumatism (EULAR) issued provisional recommendations for the management of rheumatic and musculoskeletal diseases in the context of SARS-CoV-2. Contrary to earlier expectations, there is no indication that patients with rheumatic and musculoskeletal diseases have a higher risk of contracting the virus or have a worse course if they do, according to the task force that worked on the recommendations. The task force also pointed out that rheumatology drugs are being used to treat COVID-19 patients who don’t have rheumatic diseases, raising the possibility of a shortage of disease-modifying antirheumatic drugs. Read more.
Mental health visits are 19% of ED costs
Mental and substance use disorders represented 19% of all emergency department visits in 2017 and cost $14.6 billion, according to figures from the Agency for Healthcare Research and Quality. The most costly mental and substance use disorder diagnosis was anxiety and fear-related disorders, accounting for $5.6 billion worth of visits, following by depressive disorders and alcohol-related disorders. Read more.
Food deserts linked to health issues in pregnancy
Living in a neighborhood lacking adequate access to affordable, high-quality food is associated with a somewhat greater risk of developing pregnancy morbidity, according to an observational study. Researchers found that women who lived in a food desert had a 1.6 times greater odds of pregnancy comorbidity than if they did not. “An additional, albeit less obvious factor that may be unique to patients suffering disproportionately from obstetric morbidity is exposure to toxic elements,” the researchers reported in Obstetrics & Gynecology. “It has been shown in a previous study that low-income, predominantly black communities of pregnant women may suffer disproportionately from lead or arsenic exposure.” Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Hospitalists stretch into new roles on COVID-19 front lines
‘Every single day is different’
In the midst of the COVID-19 pandemic, health systems, hospitals, and hospitalists – especially in hot spots like New York, Detroit, or Boston – have been challenged to stretch limits, redefine roles, and redeploy critical staff in response to rapidly changing needs on the ground.
Many hospitalists are working above and beyond their normal duties, sometimes beyond their training, specialty, or comfort zone and are rising to the occasion in ways they never imagined. These include doing shifts in ICUs, working with ventilator patients, and reporting to other atypical sites of care like postanesthesia care units and post-acute or step-down units.
Valerie Vaughn, MD, MSc, a hospitalist with Michigan Medicine and assistant professor of medicine at the University of Michigan in Ann Arbor, was doing research on how to reduce overuse of antibiotics in hospitals when the COVID-19 crisis hit and dramatically redefined her job. “We were afraid that we might have 3,000 to 5,000 hospitalized COVID patients by now, based on predictive modeling done while the pandemic was still growing exponentially,” she explained. Although Michigan continues to have high COVID-19 infection rates, centered on nearby Detroit, “things are a lot better today than they were 4 weeks ago.”
Dr. Vaughn helped to mobilize a team of 25 hospitalists, along with other health care providers, who volunteered to manage COVID-19 patients in the ICU and other hospital units. She was asked to help develop an all-COVID unit called the Regional Infectious Containment Unit or RICU, which opened March 16. Then, when the RICU became full, it was supplemented by two COVID-19 Moderate Care Units staffed by hospitalists who had “learned the ropes” in the RICU.
Both of these new models were defined in relation to the ICUs at Michigan Medicine – which were doubling in capacity, up to 200 beds at last count – and to the provision of intensive-level and long-term ventilator care for the sickest patients. The moderate care units are for patients who are not on ventilators but still very sick, for example, those receiving massive high-flow oxygen, often with a medical do-not-resuscitate/do-not-intubate order. “We established these units to do everything (medically) short of vents,” Dr. Vaughn said.
“We are having in-depth conversations about goals of care with patients soon after they arrive at the hospital. We know outcomes from ventilators are worse for COVID-positive patients who have comorbidities, and we’re using that information to inform these conversations. We’ve given scripts to clinicians to help guide them in leading these conversations. We can do other things than `use ventilators to manage their symptoms. But these are still difficult conversations,” Dr. Vaughn said.

“We also engaged palliative care early on and asked them to round with us on every [COVID] patient – until demand got too high.” The bottleneck has been the number of ICU beds available, she explained. “If you want your patient to come in and take that bed, make sure you’ve talked to the family about it.”
The COVID-19 team developed guidelines printed on pocket cards addressing critical care issues such as a refresher on how to treat acute respiratory distress syndrome and how to use vasopressors. (See the COVID-19 Continuing Medical Education Portal for web-accessible educational resources developed by Michigan Health).
It’s amazing how quickly patients can become very sick with COVID-19, Dr. Vaughn said. “One of the good things to happen from the beginning with our RICU is that a group of doctors became COVID care experts very quickly. We joined four to five hospitalists and their teams with each intensivist, so one critical care expert is there to do teaching and answer clinicians’ questions. The hospitalists coordinate the COVID care and talk to the families.”
Working on the front lines of this crisis, Dr. Vaughn said, has generated a powerful sense of purpose and camaraderie, creating bonds like in war time. “All of us on our days off feel a twinge of guilt for not being there in the hospital. The sense of gratitude we get from patients and families has been enormous, even when we were telling them bad news. That just brings us to tears.”
One of the hardest things for the doctors practicing above their typical scope of practice is that, when something bad happens, they can’t know whether it was a mistake on their part or not, she noted. “But I’ve never been so proud of our group or to be a hospitalist. No one has complained or pushed back. Everyone has responded by saying: ‘What can I do to help?’ ”
Enough work in hospital medicine
Hospitalists had not been deployed to care for ICU patients at Beth Israel Deaconess Medical Center (BIDMC) in Boston, a major hot spot for COVID-19, said Joseph Ming Wah Li, MD, SFHM, director of the hospital medicine program at BIDMC, when he spoke to The Hospitalist in mid-May. That’s because there were plenty of hospital medicine assignments to keep them busy. Dr. Li leads a service of 120 hospitalists practicing at four hospitals.
“As we speak today, we have 300 patients with COVID, with 70 or 80 of them in our ICU. I’m taking care of 17 patients today, 15 of them COVID-positive, and the other two placed in a former radiology holding suite adapted for COVID-negative patients. Our postanesthesia care unit is now an ICU filled with COVID patients,” he said.
“Half of my day is seeing patients and the other half I’m on Zoom calls. I’m also one of the resource allocation officers for BIDMC,” Dr. Li said. He helped to create a standard of care for the hospital, addressing what to do if there weren’t enough ICU beds or ventilators. “We’ve never actualized it and probably won’t, but it was important to go through this exercise, with a lot of discussion up front.”
Haki Laho, MD, an orthopedic hospitalist at New England Baptist Hospital (NEBH), also in Boston, has been redeployed to care for a different population of patients as his system tries to bunch patients. “All of a sudden – within hours and days – at the beginning of the pandemic and based on the recommendations, our whole system decided to stop all elective procedures and devote the resources to COVID,” he said.
NEBH is Beth Israel Lahey Health’s 141-bed orthopedic and surgical hospital, and the system has tried to keep the specialty facility COVID-19–free as much as possible, with the COVID-19 patients grouped together at BIDMC. Dr. Laho’s orthopedic hospitalist group, just five doctors, has been managing the influx of medical patients with multiple comorbidities – not COVID-19–infected but still a different kind of patient than they are used to.
“So far, so good. We’re dealing with it,” he said. “But if one of us got sick, the others would have to step up and do more shifts. We are physicians, internal medicine trained, but since my residency I hadn’t had to deal with these kinds of issues on a daily basis, such as setting up IV lines. I feel like I am back in residency mode.”
Convention Center medicine
Another Boston hospitalist, Amy Baughman, MD, who practices at Massachusetts General Hospital, is using her skills in a new setting, serving as a co-medical director at Boston Hope Medical Center, a 1,000-bed field hospital for patients with COVID-19. Open since April 10 and housed in the Boston Convention and Exhibition Center, it is a four-way collaboration between the Commonwealth of Massachusetts, the City of Boston, Partners HealthCare, and the Boston Health Care for the Homeless Program.
Boston Hope is divided into a post-acute care section for recovering COVID-19 patients and a respite section for undomiciled patients with COVID-19 who need a place to safely quarantine. Built for a maximum of 1,000 beds, it is currently using fewer, with 83 patients on the post-acute side and 73 on the respite side as of May 12. A total of 370 and 315, respectively, had been admitted through May 12.
The team had 5 days to put the field hospital together with the help of the Army National Guard. “During that first week I was installing hand sanitizer dispensers and making [personal protective equipment] signs. Everyone here has had to do things like that,” Dr. Baughman said. “We’ve had to be incredibly creative in our staffing, using doctors from primary care and subspecialties including dermatology, radiology, and orthopedics. We had to fast-track trainings on how to use EPIC and to provide post-acute COVID care. How do you simultaneously build a medical facility and lead teams to provide high quality care?”
Dr. Baughman still works hospitalist shifts half-time at Massachusetts General. Her prior experience providing post-acute care in the VA system was helpful in creating the post-acute level of care at Boston Hope.
“My medical director role involves supervising, staffing, and scheduling. My co-medical director, Dr. Kerri Palamara, and I also supervise the clinical care,” she said. “There are a lot of systems issues, like ordering labs or prescriptions, with couriers going back and forth. And we developed clinical pathways, such as for [deep vein thrombosis] prophylaxis or for COVID retesting to determine when it is safe to end a quarantine. We’re just now rolling out virtual specialist consultations,” she noted.
“It has gone incredibly well. So much of it has been about our ability and willingness to work hard, and take feedback and go forward. We don’t have time to harp on things. We have to be very solution oriented. At the same time, honestly, it’s been fun. Every single day is different,” Dr. Baughman said.
“It’s been an opportunity to use my skills in a totally new setting, and at a level of responsibility I haven’t had before, although that’s probably a common theme with COVID-19. I was put on this team because I am a hospitalist,” she said. “I think hospitalists have been the backbone of the response to COVID in this country. It’s been an opportunity for our specialty to shine. We need to embrace the opportunity.”
Balancing expertise and supervision
Mount Sinai Hospital (MSH) in Manhattan is in the New York epicenter of the COVID-19 crisis and has mobilized large numbers of pulmonary critical care and anesthesia physicians to staff up multiple ICUs for COVID-19 patients, said Andrew Dunn, MD, chief of the division of hospital medicine at Mount Sinai School of Medicine.
“My hospitalist group is covering many step-down units, medical wards, and atypical locations, providing advanced oxygen therapies, [bilevel positive airway pressure], high-flow nasal cannulas, and managing some patients on ventilators,” he said.
MSH has teaching services with house staff and nonteaching services. “We combined them into a unified service with house staff dispersed across all of the teams. We drafted a lot of nonhospitalists from different specialties to be attendings, and that has given us a tiered model, with a hospitalist supervising three or four nonhospitalist-led teams. Although the supervising hospitalists carry no patient caseloads of their own, this is primarily a clinical rather than an administrative role.”
At the peak, there were 40 rounding teams at MSH, each with a typical census of 15 patients or more, which meant that 10 supervisory hospitalists were responsible for 300 to 400 patients. “What we learned first was the need to balance the level of expertise. For example, a team may include a postgraduate year 3 resident and a radiology intern,” Dr. Dunn said. As COVID-19 census has started coming down, supervisory hospitalists are returning to direct care attending roles, and some hospitalists have been shared across the Mount Sinai system’s hospitals.
Dr. Dunn’s advice for hospitalists filling a supervisory role like this in a tiered model: Make sure you talk to your team the night before the first day of a scheduling block and try to address as many of their questions as possible. “If you wait until the morning of the shift to connect with them, anxiety will be high. But after going through a couple of scheduling cycles, we find that things are getting better. I think we’ve paid a lot of attention to the risks of burnout by our physicians. We’re using a model of 4 days on/4 off.”
Another variation on these themes is Joshua Shatzkes, MD, assistant professor of medicine and cardiology at Mount Sinai, who practices outpatient cardiology at MSH and in several off-site offices in Brooklyn. He saw early on that COVID-19 would have a huge effect on his practice, so he volunteered to help out with inpatient care. “I made it known to my chief that I was available, and I was deployed in the first week, after a weekend of cramming webinars and lectures on critical care and pulling out critical concepts that I already knew.”
Dr. Shatzkes said his career path led him into outpatient cardiology 11 years ago, where he was quickly too busy to see his patients when they went into the hospital, even though he missed hospital medicine. Working as a temporary hospitalist with the arrival of COVID-19, he has been invigorated and mobilized by the experience and reminded of why he went to medical school in the first place. “Each day’s shift went quickly but felt long. At the end of the day, I was tired but not exhausted. When I walked out of a patient’s room, they could tell, ‘This is a doctor who cared for me,’ ” he said.
After Dr. Shatzkes volunteered, he got the call from his division chief. “I was officially deployed for a 4-day shift at Mount Sinai and then as a backup.” On his first morning as an inpatient doctor, he was still getting oriented when calls started coming from the nurses. “I had five patients struggling to breathe. Their degree of hypoxia was remarkable. I kept them out of the ICU, at least for that day.”
Since then, he has continued to follow some of those patients in the hospital, along with some from his outpatient practice who were hospitalized, and others referred by colleagues, while remaining available to his outpatients through telemedicine. When this is all over, Dr. Shatzkes said, he would love to find a way to incorporate a hospital practice in his job – depending on the realities of New York traffic.
“Joshua is not a hospitalist, but he went on service and felt so fulfilled and rewarded, he asked me if he could stay on service,” Dr. Dunn said. “I also got an email from the nurse manager on the unit. They want him back.”
‘Every single day is different’
‘Every single day is different’
In the midst of the COVID-19 pandemic, health systems, hospitals, and hospitalists – especially in hot spots like New York, Detroit, or Boston – have been challenged to stretch limits, redefine roles, and redeploy critical staff in response to rapidly changing needs on the ground.
Many hospitalists are working above and beyond their normal duties, sometimes beyond their training, specialty, or comfort zone and are rising to the occasion in ways they never imagined. These include doing shifts in ICUs, working with ventilator patients, and reporting to other atypical sites of care like postanesthesia care units and post-acute or step-down units.
Valerie Vaughn, MD, MSc, a hospitalist with Michigan Medicine and assistant professor of medicine at the University of Michigan in Ann Arbor, was doing research on how to reduce overuse of antibiotics in hospitals when the COVID-19 crisis hit and dramatically redefined her job. “We were afraid that we might have 3,000 to 5,000 hospitalized COVID patients by now, based on predictive modeling done while the pandemic was still growing exponentially,” she explained. Although Michigan continues to have high COVID-19 infection rates, centered on nearby Detroit, “things are a lot better today than they were 4 weeks ago.”
Dr. Vaughn helped to mobilize a team of 25 hospitalists, along with other health care providers, who volunteered to manage COVID-19 patients in the ICU and other hospital units. She was asked to help develop an all-COVID unit called the Regional Infectious Containment Unit or RICU, which opened March 16. Then, when the RICU became full, it was supplemented by two COVID-19 Moderate Care Units staffed by hospitalists who had “learned the ropes” in the RICU.
Both of these new models were defined in relation to the ICUs at Michigan Medicine – which were doubling in capacity, up to 200 beds at last count – and to the provision of intensive-level and long-term ventilator care for the sickest patients. The moderate care units are for patients who are not on ventilators but still very sick, for example, those receiving massive high-flow oxygen, often with a medical do-not-resuscitate/do-not-intubate order. “We established these units to do everything (medically) short of vents,” Dr. Vaughn said.
“We are having in-depth conversations about goals of care with patients soon after they arrive at the hospital. We know outcomes from ventilators are worse for COVID-positive patients who have comorbidities, and we’re using that information to inform these conversations. We’ve given scripts to clinicians to help guide them in leading these conversations. We can do other things than `use ventilators to manage their symptoms. But these are still difficult conversations,” Dr. Vaughn said.

“We also engaged palliative care early on and asked them to round with us on every [COVID] patient – until demand got too high.” The bottleneck has been the number of ICU beds available, she explained. “If you want your patient to come in and take that bed, make sure you’ve talked to the family about it.”
The COVID-19 team developed guidelines printed on pocket cards addressing critical care issues such as a refresher on how to treat acute respiratory distress syndrome and how to use vasopressors. (See the COVID-19 Continuing Medical Education Portal for web-accessible educational resources developed by Michigan Health).
It’s amazing how quickly patients can become very sick with COVID-19, Dr. Vaughn said. “One of the good things to happen from the beginning with our RICU is that a group of doctors became COVID care experts very quickly. We joined four to five hospitalists and their teams with each intensivist, so one critical care expert is there to do teaching and answer clinicians’ questions. The hospitalists coordinate the COVID care and talk to the families.”
Working on the front lines of this crisis, Dr. Vaughn said, has generated a powerful sense of purpose and camaraderie, creating bonds like in war time. “All of us on our days off feel a twinge of guilt for not being there in the hospital. The sense of gratitude we get from patients and families has been enormous, even when we were telling them bad news. That just brings us to tears.”
One of the hardest things for the doctors practicing above their typical scope of practice is that, when something bad happens, they can’t know whether it was a mistake on their part or not, she noted. “But I’ve never been so proud of our group or to be a hospitalist. No one has complained or pushed back. Everyone has responded by saying: ‘What can I do to help?’ ”
Enough work in hospital medicine
Hospitalists had not been deployed to care for ICU patients at Beth Israel Deaconess Medical Center (BIDMC) in Boston, a major hot spot for COVID-19, said Joseph Ming Wah Li, MD, SFHM, director of the hospital medicine program at BIDMC, when he spoke to The Hospitalist in mid-May. That’s because there were plenty of hospital medicine assignments to keep them busy. Dr. Li leads a service of 120 hospitalists practicing at four hospitals.
“As we speak today, we have 300 patients with COVID, with 70 or 80 of them in our ICU. I’m taking care of 17 patients today, 15 of them COVID-positive, and the other two placed in a former radiology holding suite adapted for COVID-negative patients. Our postanesthesia care unit is now an ICU filled with COVID patients,” he said.
“Half of my day is seeing patients and the other half I’m on Zoom calls. I’m also one of the resource allocation officers for BIDMC,” Dr. Li said. He helped to create a standard of care for the hospital, addressing what to do if there weren’t enough ICU beds or ventilators. “We’ve never actualized it and probably won’t, but it was important to go through this exercise, with a lot of discussion up front.”
Haki Laho, MD, an orthopedic hospitalist at New England Baptist Hospital (NEBH), also in Boston, has been redeployed to care for a different population of patients as his system tries to bunch patients. “All of a sudden – within hours and days – at the beginning of the pandemic and based on the recommendations, our whole system decided to stop all elective procedures and devote the resources to COVID,” he said.
NEBH is Beth Israel Lahey Health’s 141-bed orthopedic and surgical hospital, and the system has tried to keep the specialty facility COVID-19–free as much as possible, with the COVID-19 patients grouped together at BIDMC. Dr. Laho’s orthopedic hospitalist group, just five doctors, has been managing the influx of medical patients with multiple comorbidities – not COVID-19–infected but still a different kind of patient than they are used to.
“So far, so good. We’re dealing with it,” he said. “But if one of us got sick, the others would have to step up and do more shifts. We are physicians, internal medicine trained, but since my residency I hadn’t had to deal with these kinds of issues on a daily basis, such as setting up IV lines. I feel like I am back in residency mode.”
Convention Center medicine
Another Boston hospitalist, Amy Baughman, MD, who practices at Massachusetts General Hospital, is using her skills in a new setting, serving as a co-medical director at Boston Hope Medical Center, a 1,000-bed field hospital for patients with COVID-19. Open since April 10 and housed in the Boston Convention and Exhibition Center, it is a four-way collaboration between the Commonwealth of Massachusetts, the City of Boston, Partners HealthCare, and the Boston Health Care for the Homeless Program.
Boston Hope is divided into a post-acute care section for recovering COVID-19 patients and a respite section for undomiciled patients with COVID-19 who need a place to safely quarantine. Built for a maximum of 1,000 beds, it is currently using fewer, with 83 patients on the post-acute side and 73 on the respite side as of May 12. A total of 370 and 315, respectively, had been admitted through May 12.
The team had 5 days to put the field hospital together with the help of the Army National Guard. “During that first week I was installing hand sanitizer dispensers and making [personal protective equipment] signs. Everyone here has had to do things like that,” Dr. Baughman said. “We’ve had to be incredibly creative in our staffing, using doctors from primary care and subspecialties including dermatology, radiology, and orthopedics. We had to fast-track trainings on how to use EPIC and to provide post-acute COVID care. How do you simultaneously build a medical facility and lead teams to provide high quality care?”
Dr. Baughman still works hospitalist shifts half-time at Massachusetts General. Her prior experience providing post-acute care in the VA system was helpful in creating the post-acute level of care at Boston Hope.
“My medical director role involves supervising, staffing, and scheduling. My co-medical director, Dr. Kerri Palamara, and I also supervise the clinical care,” she said. “There are a lot of systems issues, like ordering labs or prescriptions, with couriers going back and forth. And we developed clinical pathways, such as for [deep vein thrombosis] prophylaxis or for COVID retesting to determine when it is safe to end a quarantine. We’re just now rolling out virtual specialist consultations,” she noted.
“It has gone incredibly well. So much of it has been about our ability and willingness to work hard, and take feedback and go forward. We don’t have time to harp on things. We have to be very solution oriented. At the same time, honestly, it’s been fun. Every single day is different,” Dr. Baughman said.
“It’s been an opportunity to use my skills in a totally new setting, and at a level of responsibility I haven’t had before, although that’s probably a common theme with COVID-19. I was put on this team because I am a hospitalist,” she said. “I think hospitalists have been the backbone of the response to COVID in this country. It’s been an opportunity for our specialty to shine. We need to embrace the opportunity.”
Balancing expertise and supervision
Mount Sinai Hospital (MSH) in Manhattan is in the New York epicenter of the COVID-19 crisis and has mobilized large numbers of pulmonary critical care and anesthesia physicians to staff up multiple ICUs for COVID-19 patients, said Andrew Dunn, MD, chief of the division of hospital medicine at Mount Sinai School of Medicine.
“My hospitalist group is covering many step-down units, medical wards, and atypical locations, providing advanced oxygen therapies, [bilevel positive airway pressure], high-flow nasal cannulas, and managing some patients on ventilators,” he said.
MSH has teaching services with house staff and nonteaching services. “We combined them into a unified service with house staff dispersed across all of the teams. We drafted a lot of nonhospitalists from different specialties to be attendings, and that has given us a tiered model, with a hospitalist supervising three or four nonhospitalist-led teams. Although the supervising hospitalists carry no patient caseloads of their own, this is primarily a clinical rather than an administrative role.”
At the peak, there were 40 rounding teams at MSH, each with a typical census of 15 patients or more, which meant that 10 supervisory hospitalists were responsible for 300 to 400 patients. “What we learned first was the need to balance the level of expertise. For example, a team may include a postgraduate year 3 resident and a radiology intern,” Dr. Dunn said. As COVID-19 census has started coming down, supervisory hospitalists are returning to direct care attending roles, and some hospitalists have been shared across the Mount Sinai system’s hospitals.
Dr. Dunn’s advice for hospitalists filling a supervisory role like this in a tiered model: Make sure you talk to your team the night before the first day of a scheduling block and try to address as many of their questions as possible. “If you wait until the morning of the shift to connect with them, anxiety will be high. But after going through a couple of scheduling cycles, we find that things are getting better. I think we’ve paid a lot of attention to the risks of burnout by our physicians. We’re using a model of 4 days on/4 off.”
Another variation on these themes is Joshua Shatzkes, MD, assistant professor of medicine and cardiology at Mount Sinai, who practices outpatient cardiology at MSH and in several off-site offices in Brooklyn. He saw early on that COVID-19 would have a huge effect on his practice, so he volunteered to help out with inpatient care. “I made it known to my chief that I was available, and I was deployed in the first week, after a weekend of cramming webinars and lectures on critical care and pulling out critical concepts that I already knew.”
Dr. Shatzkes said his career path led him into outpatient cardiology 11 years ago, where he was quickly too busy to see his patients when they went into the hospital, even though he missed hospital medicine. Working as a temporary hospitalist with the arrival of COVID-19, he has been invigorated and mobilized by the experience and reminded of why he went to medical school in the first place. “Each day’s shift went quickly but felt long. At the end of the day, I was tired but not exhausted. When I walked out of a patient’s room, they could tell, ‘This is a doctor who cared for me,’ ” he said.
After Dr. Shatzkes volunteered, he got the call from his division chief. “I was officially deployed for a 4-day shift at Mount Sinai and then as a backup.” On his first morning as an inpatient doctor, he was still getting oriented when calls started coming from the nurses. “I had five patients struggling to breathe. Their degree of hypoxia was remarkable. I kept them out of the ICU, at least for that day.”
Since then, he has continued to follow some of those patients in the hospital, along with some from his outpatient practice who were hospitalized, and others referred by colleagues, while remaining available to his outpatients through telemedicine. When this is all over, Dr. Shatzkes said, he would love to find a way to incorporate a hospital practice in his job – depending on the realities of New York traffic.
“Joshua is not a hospitalist, but he went on service and felt so fulfilled and rewarded, he asked me if he could stay on service,” Dr. Dunn said. “I also got an email from the nurse manager on the unit. They want him back.”
In the midst of the COVID-19 pandemic, health systems, hospitals, and hospitalists – especially in hot spots like New York, Detroit, or Boston – have been challenged to stretch limits, redefine roles, and redeploy critical staff in response to rapidly changing needs on the ground.
Many hospitalists are working above and beyond their normal duties, sometimes beyond their training, specialty, or comfort zone and are rising to the occasion in ways they never imagined. These include doing shifts in ICUs, working with ventilator patients, and reporting to other atypical sites of care like postanesthesia care units and post-acute or step-down units.
Valerie Vaughn, MD, MSc, a hospitalist with Michigan Medicine and assistant professor of medicine at the University of Michigan in Ann Arbor, was doing research on how to reduce overuse of antibiotics in hospitals when the COVID-19 crisis hit and dramatically redefined her job. “We were afraid that we might have 3,000 to 5,000 hospitalized COVID patients by now, based on predictive modeling done while the pandemic was still growing exponentially,” she explained. Although Michigan continues to have high COVID-19 infection rates, centered on nearby Detroit, “things are a lot better today than they were 4 weeks ago.”
Dr. Vaughn helped to mobilize a team of 25 hospitalists, along with other health care providers, who volunteered to manage COVID-19 patients in the ICU and other hospital units. She was asked to help develop an all-COVID unit called the Regional Infectious Containment Unit or RICU, which opened March 16. Then, when the RICU became full, it was supplemented by two COVID-19 Moderate Care Units staffed by hospitalists who had “learned the ropes” in the RICU.
Both of these new models were defined in relation to the ICUs at Michigan Medicine – which were doubling in capacity, up to 200 beds at last count – and to the provision of intensive-level and long-term ventilator care for the sickest patients. The moderate care units are for patients who are not on ventilators but still very sick, for example, those receiving massive high-flow oxygen, often with a medical do-not-resuscitate/do-not-intubate order. “We established these units to do everything (medically) short of vents,” Dr. Vaughn said.
“We are having in-depth conversations about goals of care with patients soon after they arrive at the hospital. We know outcomes from ventilators are worse for COVID-positive patients who have comorbidities, and we’re using that information to inform these conversations. We’ve given scripts to clinicians to help guide them in leading these conversations. We can do other things than `use ventilators to manage their symptoms. But these are still difficult conversations,” Dr. Vaughn said.

“We also engaged palliative care early on and asked them to round with us on every [COVID] patient – until demand got too high.” The bottleneck has been the number of ICU beds available, she explained. “If you want your patient to come in and take that bed, make sure you’ve talked to the family about it.”
The COVID-19 team developed guidelines printed on pocket cards addressing critical care issues such as a refresher on how to treat acute respiratory distress syndrome and how to use vasopressors. (See the COVID-19 Continuing Medical Education Portal for web-accessible educational resources developed by Michigan Health).
It’s amazing how quickly patients can become very sick with COVID-19, Dr. Vaughn said. “One of the good things to happen from the beginning with our RICU is that a group of doctors became COVID care experts very quickly. We joined four to five hospitalists and their teams with each intensivist, so one critical care expert is there to do teaching and answer clinicians’ questions. The hospitalists coordinate the COVID care and talk to the families.”
Working on the front lines of this crisis, Dr. Vaughn said, has generated a powerful sense of purpose and camaraderie, creating bonds like in war time. “All of us on our days off feel a twinge of guilt for not being there in the hospital. The sense of gratitude we get from patients and families has been enormous, even when we were telling them bad news. That just brings us to tears.”
One of the hardest things for the doctors practicing above their typical scope of practice is that, when something bad happens, they can’t know whether it was a mistake on their part or not, she noted. “But I’ve never been so proud of our group or to be a hospitalist. No one has complained or pushed back. Everyone has responded by saying: ‘What can I do to help?’ ”
Enough work in hospital medicine
Hospitalists had not been deployed to care for ICU patients at Beth Israel Deaconess Medical Center (BIDMC) in Boston, a major hot spot for COVID-19, said Joseph Ming Wah Li, MD, SFHM, director of the hospital medicine program at BIDMC, when he spoke to The Hospitalist in mid-May. That’s because there were plenty of hospital medicine assignments to keep them busy. Dr. Li leads a service of 120 hospitalists practicing at four hospitals.
“As we speak today, we have 300 patients with COVID, with 70 or 80 of them in our ICU. I’m taking care of 17 patients today, 15 of them COVID-positive, and the other two placed in a former radiology holding suite adapted for COVID-negative patients. Our postanesthesia care unit is now an ICU filled with COVID patients,” he said.
“Half of my day is seeing patients and the other half I’m on Zoom calls. I’m also one of the resource allocation officers for BIDMC,” Dr. Li said. He helped to create a standard of care for the hospital, addressing what to do if there weren’t enough ICU beds or ventilators. “We’ve never actualized it and probably won’t, but it was important to go through this exercise, with a lot of discussion up front.”
Haki Laho, MD, an orthopedic hospitalist at New England Baptist Hospital (NEBH), also in Boston, has been redeployed to care for a different population of patients as his system tries to bunch patients. “All of a sudden – within hours and days – at the beginning of the pandemic and based on the recommendations, our whole system decided to stop all elective procedures and devote the resources to COVID,” he said.
NEBH is Beth Israel Lahey Health’s 141-bed orthopedic and surgical hospital, and the system has tried to keep the specialty facility COVID-19–free as much as possible, with the COVID-19 patients grouped together at BIDMC. Dr. Laho’s orthopedic hospitalist group, just five doctors, has been managing the influx of medical patients with multiple comorbidities – not COVID-19–infected but still a different kind of patient than they are used to.
“So far, so good. We’re dealing with it,” he said. “But if one of us got sick, the others would have to step up and do more shifts. We are physicians, internal medicine trained, but since my residency I hadn’t had to deal with these kinds of issues on a daily basis, such as setting up IV lines. I feel like I am back in residency mode.”
Convention Center medicine
Another Boston hospitalist, Amy Baughman, MD, who practices at Massachusetts General Hospital, is using her skills in a new setting, serving as a co-medical director at Boston Hope Medical Center, a 1,000-bed field hospital for patients with COVID-19. Open since April 10 and housed in the Boston Convention and Exhibition Center, it is a four-way collaboration between the Commonwealth of Massachusetts, the City of Boston, Partners HealthCare, and the Boston Health Care for the Homeless Program.
Boston Hope is divided into a post-acute care section for recovering COVID-19 patients and a respite section for undomiciled patients with COVID-19 who need a place to safely quarantine. Built for a maximum of 1,000 beds, it is currently using fewer, with 83 patients on the post-acute side and 73 on the respite side as of May 12. A total of 370 and 315, respectively, had been admitted through May 12.
The team had 5 days to put the field hospital together with the help of the Army National Guard. “During that first week I was installing hand sanitizer dispensers and making [personal protective equipment] signs. Everyone here has had to do things like that,” Dr. Baughman said. “We’ve had to be incredibly creative in our staffing, using doctors from primary care and subspecialties including dermatology, radiology, and orthopedics. We had to fast-track trainings on how to use EPIC and to provide post-acute COVID care. How do you simultaneously build a medical facility and lead teams to provide high quality care?”
Dr. Baughman still works hospitalist shifts half-time at Massachusetts General. Her prior experience providing post-acute care in the VA system was helpful in creating the post-acute level of care at Boston Hope.
“My medical director role involves supervising, staffing, and scheduling. My co-medical director, Dr. Kerri Palamara, and I also supervise the clinical care,” she said. “There are a lot of systems issues, like ordering labs or prescriptions, with couriers going back and forth. And we developed clinical pathways, such as for [deep vein thrombosis] prophylaxis or for COVID retesting to determine when it is safe to end a quarantine. We’re just now rolling out virtual specialist consultations,” she noted.
“It has gone incredibly well. So much of it has been about our ability and willingness to work hard, and take feedback and go forward. We don’t have time to harp on things. We have to be very solution oriented. At the same time, honestly, it’s been fun. Every single day is different,” Dr. Baughman said.
“It’s been an opportunity to use my skills in a totally new setting, and at a level of responsibility I haven’t had before, although that’s probably a common theme with COVID-19. I was put on this team because I am a hospitalist,” she said. “I think hospitalists have been the backbone of the response to COVID in this country. It’s been an opportunity for our specialty to shine. We need to embrace the opportunity.”
Balancing expertise and supervision
Mount Sinai Hospital (MSH) in Manhattan is in the New York epicenter of the COVID-19 crisis and has mobilized large numbers of pulmonary critical care and anesthesia physicians to staff up multiple ICUs for COVID-19 patients, said Andrew Dunn, MD, chief of the division of hospital medicine at Mount Sinai School of Medicine.
“My hospitalist group is covering many step-down units, medical wards, and atypical locations, providing advanced oxygen therapies, [bilevel positive airway pressure], high-flow nasal cannulas, and managing some patients on ventilators,” he said.
MSH has teaching services with house staff and nonteaching services. “We combined them into a unified service with house staff dispersed across all of the teams. We drafted a lot of nonhospitalists from different specialties to be attendings, and that has given us a tiered model, with a hospitalist supervising three or four nonhospitalist-led teams. Although the supervising hospitalists carry no patient caseloads of their own, this is primarily a clinical rather than an administrative role.”
At the peak, there were 40 rounding teams at MSH, each with a typical census of 15 patients or more, which meant that 10 supervisory hospitalists were responsible for 300 to 400 patients. “What we learned first was the need to balance the level of expertise. For example, a team may include a postgraduate year 3 resident and a radiology intern,” Dr. Dunn said. As COVID-19 census has started coming down, supervisory hospitalists are returning to direct care attending roles, and some hospitalists have been shared across the Mount Sinai system’s hospitals.
Dr. Dunn’s advice for hospitalists filling a supervisory role like this in a tiered model: Make sure you talk to your team the night before the first day of a scheduling block and try to address as many of their questions as possible. “If you wait until the morning of the shift to connect with them, anxiety will be high. But after going through a couple of scheduling cycles, we find that things are getting better. I think we’ve paid a lot of attention to the risks of burnout by our physicians. We’re using a model of 4 days on/4 off.”
Another variation on these themes is Joshua Shatzkes, MD, assistant professor of medicine and cardiology at Mount Sinai, who practices outpatient cardiology at MSH and in several off-site offices in Brooklyn. He saw early on that COVID-19 would have a huge effect on his practice, so he volunteered to help out with inpatient care. “I made it known to my chief that I was available, and I was deployed in the first week, after a weekend of cramming webinars and lectures on critical care and pulling out critical concepts that I already knew.”
Dr. Shatzkes said his career path led him into outpatient cardiology 11 years ago, where he was quickly too busy to see his patients when they went into the hospital, even though he missed hospital medicine. Working as a temporary hospitalist with the arrival of COVID-19, he has been invigorated and mobilized by the experience and reminded of why he went to medical school in the first place. “Each day’s shift went quickly but felt long. At the end of the day, I was tired but not exhausted. When I walked out of a patient’s room, they could tell, ‘This is a doctor who cared for me,’ ” he said.
After Dr. Shatzkes volunteered, he got the call from his division chief. “I was officially deployed for a 4-day shift at Mount Sinai and then as a backup.” On his first morning as an inpatient doctor, he was still getting oriented when calls started coming from the nurses. “I had five patients struggling to breathe. Their degree of hypoxia was remarkable. I kept them out of the ICU, at least for that day.”
Since then, he has continued to follow some of those patients in the hospital, along with some from his outpatient practice who were hospitalized, and others referred by colleagues, while remaining available to his outpatients through telemedicine. When this is all over, Dr. Shatzkes said, he would love to find a way to incorporate a hospital practice in his job – depending on the realities of New York traffic.
“Joshua is not a hospitalist, but he went on service and felt so fulfilled and rewarded, he asked me if he could stay on service,” Dr. Dunn said. “I also got an email from the nurse manager on the unit. They want him back.”
The future of psychiatric diagnosis
Melissa R. Arbuckle, MD: Hi. I’m Dr. Melissa Arbuckle, vice chair for education and training in the Department of Psychiatry at Columbia University. I’m reporting on behalf of Medscape and our Columbia Psychiatry partnership. Today we’ll be discussing biomarkers with Dr. Jeffrey Lieberman. Welcome.
Jeffrey A. Lieberman, MD: Thanks, Melissa. Great to be here to talk about a subject that is near and dear to my heart.
Dr. Arbuckle: Dr. Lieberman is chair of the Department of Psychiatry at Columbia and is also director of the New York State Psychiatric Institute. Tell us about biomarkers and psychiatry, Dr Lieberman.
Dr. Lieberman: It would be nice if we had some! But first let me tell you what a biomarker is and what it would do for us. A biomarker is a biologic measure, a biologic feature, whether it’s blood pressure, pulse rate, an analyte in blood or cerebrospinal fluid, or a feature of an MRI or PET scan image of the brain that has diagnostic, prognostic, or theragnostic significance. A biomarker identifies an individual with symptoms of a specific disorder, indicates that they have this disorder, and can suggest a particular prognosis – less severe, more severe – or specify which treatment a person would likely respond to. For the entire history of our discipline, as long as physicians have studied mental illness, we have not had a diagnostic test for it. It’s a clinical diagnosis.
All illnesses in medicine began with clinical diagnosis: seizure disorder, epilepsy, was falling sickness; congestive heart failure was dropsy; for diabetes you tasted the urine to see if it was sweet or watery. But when we began to measure glucose and hemoglobin A1c, or when we developed the electrocardiogram to measure heart rhythms, and the electroencephalogram to measure brain activity, those were diagnostic tests based on biomarkers. We just don’t have them yet in psychiatry. The day we do have our first diagnostic tests, courtesy of a validated biomarker, will be a real milestone in the history of our profession.
Dr. Arbuckle: How far off might that be for psychiatry?
Dr. Lieberman: I’ve been in this profession for more than 30 years, and I’ve been saying for a while that it is coming soon. But we’re still waiting. Let me just add a cautionary note. Ever since psychiatry became scientifically minded and used scientific methodology and technology to understand the underpinnings of mental illness, there’s been an effort to identify biomarkers. It began in the 1960s with a series of false leads. There was something called the pink spot, as well as other metabolites, which were indicators on chromatographs linked to schizophrenia. This turned out to be wrong.
There was also the dexamethasone suppression test, to identify people who hypersecreted cortisol, which was believed to be diagnostic of depression. That turned out to be inadequate also.
There was the identification of genes beginning in the late 1980s. But the specific genes that indicated manic depressive illness and schizophrenia were not replicated. And now we know that the genetics of these disorders is polygenic and very complex.
So we cannot overpromise. I don’t want to say exactly when, but I will say that this is an area of intense research. There are a variety of different technologies that could yield this holy grail of diagnostic measures, including imaging measures such as MRI, PET, and nuclear medicine imaging, the use of genetics to create a polygenic risk score, and serologic analyses of blood to develop a panel of measures that may predict a specific condition or specific subtype of a condition.
It’s very likely, though, that we’ll not have a single pathognomonic test. I suspect that we’ll have several measures that, in combination, will be diagnostic or prognostic, in the same way that with cancer you have nomograms that give a prognosis. Or in the case of cardiovascular disease, where you have a lipid panel that takes into account a variety of lipid analytes to give you a risk score. I do believe that certainly within my professional lifetime, and hopefully sooner rather than later, we will see a diagnostic test.
Dr. Arbuckle: Given the different tests that did not pan out, what guidance can we offer clinicians as data come out and new potential biomarkers hit the media? How can we sift through what may or may not hold real promise?
Dr. Lieberman: I can tell practicing clinicians what not to do. Do not do what some of the charlatans in our field do. There are self-promoting psychiatrists out there who use SPECT scans to get a picture of the brain that is little more than pseudo color phrenology, and then they tell patients, “See this? This indicates that you have (this condition or that condition).” You can’t do that. Nothing we have now has that kind of validity or specificity.
However, even though a standard workup for an illness like schizophrenia does not require specific diagnostic tests, other than to rule out other conditions, imaging procedures can be useful additional information. For example, if you have an individual who presents with symptoms that meet criteria for schizophrenia and you obtain an MRI to rule out other possibilities, and the patient turns out to have dilated lateral ventricles or specific reductions in the size or distortions in the shape of certain temporal cortical structures, particularly in the hippocampus, that adds substance to your clinical diagnosis. So those kinds of things are useful. Similarly, with genetic testing, some institutions are now doing exome sequencing or whole genome sequencing that can provide a risk score. It adds something beyond a family history. These are not diagnostic, but they can add to your understanding.
Finally, with respect to schizophrenia and MRI in particular, if it does show structural abnormalities that are among the ones that have been reported for schizophrenia, this can be informative prognostically; such an individual may have a greater likelihood of having a chronic course with progression of the illness. And if that were my patient, I would be thinking that greater effort needs to be taken to ensure that the patient remains on treatment and does not suffer relapse.
Dr. Arbuckle: How do we prepare our trainees for a future of psychiatry with more biomarkers?
Dr. Lieberman: In medical school and postgraduate training, apart from understanding the method of diagnosis and the criteria for diagnoses, it’s important to understand the ancillary measures that are used in clinical medicine: blood testing, electrophysiologic measures, imaging procedures, neurocognitive testing, etc. This is a standard in terms of general medical training.
In terms of then applying it to mental illness and psychiatry, it’s a matter of knowing that these will be relevant at some point, staying apprised of the research literature that is generating data that pertain to the use of these measures for diagnostic, prognostic, or treatment-specific purposes, and then gauging how useful these will be. Right now, these measures are not required for diagnosis. They’re not validated sufficiently so that third-party payers will uniformly reimburse for them, but at some point they will be. Even before that time occurs, there are some measures that can be informative and enhance confidence in the diagnosis or add information about treatment response and outcome.
Dr. Arbuckle: We’re hearing about biotypes and how biotypes may not map to our current diagnostic systems. What are your thoughts about that?
Dr. Lieberman: You know, psychiatry has always been kind of the stepchild of medicine. And related to that, the Diagnostic and Statistical Manual of Mental Disorders (DSM) is the punching bag of the critics of psychiatry and the purported reason it hasn’t progressed faster. Sitting here at Columbia, the home of Robert Spitzer, who was the pioneer of the modern method of nosology that we still use in the DSM, it’s disappointing that we continue to lob tomatoes at this system, which is the best. It took psychiatry out of what was a dark age of clinical methodology and put it on solid scientific footing. That was in the late 1970s with [the development of] DSM-III.
And as much as we would like to have further progress, which would allow for not using a list of criteria in a menu-driven fashion to establish diagnoses, we’d like to have it be like a glucose tolerance test or an angiogram.
We’d like to do that, but we can’t yet. So there’s this aspirational desire to have something better, and this is permeating and motivating a lot of the research, which is good. But to claim that these don’t map to the current DSM and therefore invalidate the DSM-defined diagnoses is wrong and self-defeating. So if they don’t map to the current DSM diagnosis, is the diagnosis wrong or are the biotypes wrong? I believe it’s wishful thinking; individuals are trying to project their desires onto clinical practice, and it’s not desirable to do that. If there was anything that was an improvement on the DSM, it would have been incorporated into our practice.
The question about the limitations of DSM and the improved methods of neuroscientifically informed diagnostic systems was an issue that brought me into a confrontation with our former director of the National Institute of Mental Health (NIMH) in 2013.
After 5 years of the DSM task force laboring to revise the fifth edition of the DSM, as it was about to be launched, our former director, Tom Insel, disavowed it and proposed as a preferable alternative the research domains criteria (RDoC) system that was in development at the NIMH, which I believe epitomized this kind of sour grapes at what psychiatry didn’t have – an aspiration to have a more neuroscientifically informed diagnostic system. And as soon as he made the statement publicly, he had to walk it back because the RDoC system or any other system was not ready for prime time. It would have been a catastrophe if it would have been the one that informed clinical psychiatry. There was nothing that was superior to the DSM to be used at the time. This shows how frustration sometimes impels people to make rash statements.
We’re on the right track. Our field is progressing enormously, and one has to remember that everything that’s relevant in terms of being scientifically based and validated through empirical research in clinical psychiatry and mental illness has happened since the last half of the 20th century.
It is a very short period of time. We’ve made tremendous progress, and we’re continuing to make progress toward the milestone we’re all hoping for, where we have diagnostic tests. But we shouldn’t shortchange ourselves or underestimate the progress we have made in the meantime.
Dr. Arbuckle: This has been a great conversation. Signing off for Medscape and Columbia Psychiatry. Thank you.
Dr. Lieberman is chairman of the Department of Psychiatry at Columbia University. He is a former president of the American Psychiatric Association. Dr. Arbuckle is vice chair for education and director of resident education in the Department of Psychiatry at Columbia University. She is particularly interested in the role of medical education in translating research into the practice of psychiatry.
This article first appeared on Medscape.com.
Melissa R. Arbuckle, MD: Hi. I’m Dr. Melissa Arbuckle, vice chair for education and training in the Department of Psychiatry at Columbia University. I’m reporting on behalf of Medscape and our Columbia Psychiatry partnership. Today we’ll be discussing biomarkers with Dr. Jeffrey Lieberman. Welcome.
Jeffrey A. Lieberman, MD: Thanks, Melissa. Great to be here to talk about a subject that is near and dear to my heart.
Dr. Arbuckle: Dr. Lieberman is chair of the Department of Psychiatry at Columbia and is also director of the New York State Psychiatric Institute. Tell us about biomarkers and psychiatry, Dr Lieberman.
Dr. Lieberman: It would be nice if we had some! But first let me tell you what a biomarker is and what it would do for us. A biomarker is a biologic measure, a biologic feature, whether it’s blood pressure, pulse rate, an analyte in blood or cerebrospinal fluid, or a feature of an MRI or PET scan image of the brain that has diagnostic, prognostic, or theragnostic significance. A biomarker identifies an individual with symptoms of a specific disorder, indicates that they have this disorder, and can suggest a particular prognosis – less severe, more severe – or specify which treatment a person would likely respond to. For the entire history of our discipline, as long as physicians have studied mental illness, we have not had a diagnostic test for it. It’s a clinical diagnosis.
All illnesses in medicine began with clinical diagnosis: seizure disorder, epilepsy, was falling sickness; congestive heart failure was dropsy; for diabetes you tasted the urine to see if it was sweet or watery. But when we began to measure glucose and hemoglobin A1c, or when we developed the electrocardiogram to measure heart rhythms, and the electroencephalogram to measure brain activity, those were diagnostic tests based on biomarkers. We just don’t have them yet in psychiatry. The day we do have our first diagnostic tests, courtesy of a validated biomarker, will be a real milestone in the history of our profession.
Dr. Arbuckle: How far off might that be for psychiatry?
Dr. Lieberman: I’ve been in this profession for more than 30 years, and I’ve been saying for a while that it is coming soon. But we’re still waiting. Let me just add a cautionary note. Ever since psychiatry became scientifically minded and used scientific methodology and technology to understand the underpinnings of mental illness, there’s been an effort to identify biomarkers. It began in the 1960s with a series of false leads. There was something called the pink spot, as well as other metabolites, which were indicators on chromatographs linked to schizophrenia. This turned out to be wrong.
There was also the dexamethasone suppression test, to identify people who hypersecreted cortisol, which was believed to be diagnostic of depression. That turned out to be inadequate also.
There was the identification of genes beginning in the late 1980s. But the specific genes that indicated manic depressive illness and schizophrenia were not replicated. And now we know that the genetics of these disorders is polygenic and very complex.
So we cannot overpromise. I don’t want to say exactly when, but I will say that this is an area of intense research. There are a variety of different technologies that could yield this holy grail of diagnostic measures, including imaging measures such as MRI, PET, and nuclear medicine imaging, the use of genetics to create a polygenic risk score, and serologic analyses of blood to develop a panel of measures that may predict a specific condition or specific subtype of a condition.
It’s very likely, though, that we’ll not have a single pathognomonic test. I suspect that we’ll have several measures that, in combination, will be diagnostic or prognostic, in the same way that with cancer you have nomograms that give a prognosis. Or in the case of cardiovascular disease, where you have a lipid panel that takes into account a variety of lipid analytes to give you a risk score. I do believe that certainly within my professional lifetime, and hopefully sooner rather than later, we will see a diagnostic test.
Dr. Arbuckle: Given the different tests that did not pan out, what guidance can we offer clinicians as data come out and new potential biomarkers hit the media? How can we sift through what may or may not hold real promise?
Dr. Lieberman: I can tell practicing clinicians what not to do. Do not do what some of the charlatans in our field do. There are self-promoting psychiatrists out there who use SPECT scans to get a picture of the brain that is little more than pseudo color phrenology, and then they tell patients, “See this? This indicates that you have (this condition or that condition).” You can’t do that. Nothing we have now has that kind of validity or specificity.
However, even though a standard workup for an illness like schizophrenia does not require specific diagnostic tests, other than to rule out other conditions, imaging procedures can be useful additional information. For example, if you have an individual who presents with symptoms that meet criteria for schizophrenia and you obtain an MRI to rule out other possibilities, and the patient turns out to have dilated lateral ventricles or specific reductions in the size or distortions in the shape of certain temporal cortical structures, particularly in the hippocampus, that adds substance to your clinical diagnosis. So those kinds of things are useful. Similarly, with genetic testing, some institutions are now doing exome sequencing or whole genome sequencing that can provide a risk score. It adds something beyond a family history. These are not diagnostic, but they can add to your understanding.
Finally, with respect to schizophrenia and MRI in particular, if it does show structural abnormalities that are among the ones that have been reported for schizophrenia, this can be informative prognostically; such an individual may have a greater likelihood of having a chronic course with progression of the illness. And if that were my patient, I would be thinking that greater effort needs to be taken to ensure that the patient remains on treatment and does not suffer relapse.
Dr. Arbuckle: How do we prepare our trainees for a future of psychiatry with more biomarkers?
Dr. Lieberman: In medical school and postgraduate training, apart from understanding the method of diagnosis and the criteria for diagnoses, it’s important to understand the ancillary measures that are used in clinical medicine: blood testing, electrophysiologic measures, imaging procedures, neurocognitive testing, etc. This is a standard in terms of general medical training.
In terms of then applying it to mental illness and psychiatry, it’s a matter of knowing that these will be relevant at some point, staying apprised of the research literature that is generating data that pertain to the use of these measures for diagnostic, prognostic, or treatment-specific purposes, and then gauging how useful these will be. Right now, these measures are not required for diagnosis. They’re not validated sufficiently so that third-party payers will uniformly reimburse for them, but at some point they will be. Even before that time occurs, there are some measures that can be informative and enhance confidence in the diagnosis or add information about treatment response and outcome.
Dr. Arbuckle: We’re hearing about biotypes and how biotypes may not map to our current diagnostic systems. What are your thoughts about that?
Dr. Lieberman: You know, psychiatry has always been kind of the stepchild of medicine. And related to that, the Diagnostic and Statistical Manual of Mental Disorders (DSM) is the punching bag of the critics of psychiatry and the purported reason it hasn’t progressed faster. Sitting here at Columbia, the home of Robert Spitzer, who was the pioneer of the modern method of nosology that we still use in the DSM, it’s disappointing that we continue to lob tomatoes at this system, which is the best. It took psychiatry out of what was a dark age of clinical methodology and put it on solid scientific footing. That was in the late 1970s with [the development of] DSM-III.
And as much as we would like to have further progress, which would allow for not using a list of criteria in a menu-driven fashion to establish diagnoses, we’d like to have it be like a glucose tolerance test or an angiogram.
We’d like to do that, but we can’t yet. So there’s this aspirational desire to have something better, and this is permeating and motivating a lot of the research, which is good. But to claim that these don’t map to the current DSM and therefore invalidate the DSM-defined diagnoses is wrong and self-defeating. So if they don’t map to the current DSM diagnosis, is the diagnosis wrong or are the biotypes wrong? I believe it’s wishful thinking; individuals are trying to project their desires onto clinical practice, and it’s not desirable to do that. If there was anything that was an improvement on the DSM, it would have been incorporated into our practice.
The question about the limitations of DSM and the improved methods of neuroscientifically informed diagnostic systems was an issue that brought me into a confrontation with our former director of the National Institute of Mental Health (NIMH) in 2013.
After 5 years of the DSM task force laboring to revise the fifth edition of the DSM, as it was about to be launched, our former director, Tom Insel, disavowed it and proposed as a preferable alternative the research domains criteria (RDoC) system that was in development at the NIMH, which I believe epitomized this kind of sour grapes at what psychiatry didn’t have – an aspiration to have a more neuroscientifically informed diagnostic system. And as soon as he made the statement publicly, he had to walk it back because the RDoC system or any other system was not ready for prime time. It would have been a catastrophe if it would have been the one that informed clinical psychiatry. There was nothing that was superior to the DSM to be used at the time. This shows how frustration sometimes impels people to make rash statements.
We’re on the right track. Our field is progressing enormously, and one has to remember that everything that’s relevant in terms of being scientifically based and validated through empirical research in clinical psychiatry and mental illness has happened since the last half of the 20th century.
It is a very short period of time. We’ve made tremendous progress, and we’re continuing to make progress toward the milestone we’re all hoping for, where we have diagnostic tests. But we shouldn’t shortchange ourselves or underestimate the progress we have made in the meantime.
Dr. Arbuckle: This has been a great conversation. Signing off for Medscape and Columbia Psychiatry. Thank you.
Dr. Lieberman is chairman of the Department of Psychiatry at Columbia University. He is a former president of the American Psychiatric Association. Dr. Arbuckle is vice chair for education and director of resident education in the Department of Psychiatry at Columbia University. She is particularly interested in the role of medical education in translating research into the practice of psychiatry.
This article first appeared on Medscape.com.
Melissa R. Arbuckle, MD: Hi. I’m Dr. Melissa Arbuckle, vice chair for education and training in the Department of Psychiatry at Columbia University. I’m reporting on behalf of Medscape and our Columbia Psychiatry partnership. Today we’ll be discussing biomarkers with Dr. Jeffrey Lieberman. Welcome.
Jeffrey A. Lieberman, MD: Thanks, Melissa. Great to be here to talk about a subject that is near and dear to my heart.
Dr. Arbuckle: Dr. Lieberman is chair of the Department of Psychiatry at Columbia and is also director of the New York State Psychiatric Institute. Tell us about biomarkers and psychiatry, Dr Lieberman.
Dr. Lieberman: It would be nice if we had some! But first let me tell you what a biomarker is and what it would do for us. A biomarker is a biologic measure, a biologic feature, whether it’s blood pressure, pulse rate, an analyte in blood or cerebrospinal fluid, or a feature of an MRI or PET scan image of the brain that has diagnostic, prognostic, or theragnostic significance. A biomarker identifies an individual with symptoms of a specific disorder, indicates that they have this disorder, and can suggest a particular prognosis – less severe, more severe – or specify which treatment a person would likely respond to. For the entire history of our discipline, as long as physicians have studied mental illness, we have not had a diagnostic test for it. It’s a clinical diagnosis.
All illnesses in medicine began with clinical diagnosis: seizure disorder, epilepsy, was falling sickness; congestive heart failure was dropsy; for diabetes you tasted the urine to see if it was sweet or watery. But when we began to measure glucose and hemoglobin A1c, or when we developed the electrocardiogram to measure heart rhythms, and the electroencephalogram to measure brain activity, those were diagnostic tests based on biomarkers. We just don’t have them yet in psychiatry. The day we do have our first diagnostic tests, courtesy of a validated biomarker, will be a real milestone in the history of our profession.
Dr. Arbuckle: How far off might that be for psychiatry?
Dr. Lieberman: I’ve been in this profession for more than 30 years, and I’ve been saying for a while that it is coming soon. But we’re still waiting. Let me just add a cautionary note. Ever since psychiatry became scientifically minded and used scientific methodology and technology to understand the underpinnings of mental illness, there’s been an effort to identify biomarkers. It began in the 1960s with a series of false leads. There was something called the pink spot, as well as other metabolites, which were indicators on chromatographs linked to schizophrenia. This turned out to be wrong.
There was also the dexamethasone suppression test, to identify people who hypersecreted cortisol, which was believed to be diagnostic of depression. That turned out to be inadequate also.
There was the identification of genes beginning in the late 1980s. But the specific genes that indicated manic depressive illness and schizophrenia were not replicated. And now we know that the genetics of these disorders is polygenic and very complex.
So we cannot overpromise. I don’t want to say exactly when, but I will say that this is an area of intense research. There are a variety of different technologies that could yield this holy grail of diagnostic measures, including imaging measures such as MRI, PET, and nuclear medicine imaging, the use of genetics to create a polygenic risk score, and serologic analyses of blood to develop a panel of measures that may predict a specific condition or specific subtype of a condition.
It’s very likely, though, that we’ll not have a single pathognomonic test. I suspect that we’ll have several measures that, in combination, will be diagnostic or prognostic, in the same way that with cancer you have nomograms that give a prognosis. Or in the case of cardiovascular disease, where you have a lipid panel that takes into account a variety of lipid analytes to give you a risk score. I do believe that certainly within my professional lifetime, and hopefully sooner rather than later, we will see a diagnostic test.
Dr. Arbuckle: Given the different tests that did not pan out, what guidance can we offer clinicians as data come out and new potential biomarkers hit the media? How can we sift through what may or may not hold real promise?
Dr. Lieberman: I can tell practicing clinicians what not to do. Do not do what some of the charlatans in our field do. There are self-promoting psychiatrists out there who use SPECT scans to get a picture of the brain that is little more than pseudo color phrenology, and then they tell patients, “See this? This indicates that you have (this condition or that condition).” You can’t do that. Nothing we have now has that kind of validity or specificity.
However, even though a standard workup for an illness like schizophrenia does not require specific diagnostic tests, other than to rule out other conditions, imaging procedures can be useful additional information. For example, if you have an individual who presents with symptoms that meet criteria for schizophrenia and you obtain an MRI to rule out other possibilities, and the patient turns out to have dilated lateral ventricles or specific reductions in the size or distortions in the shape of certain temporal cortical structures, particularly in the hippocampus, that adds substance to your clinical diagnosis. So those kinds of things are useful. Similarly, with genetic testing, some institutions are now doing exome sequencing or whole genome sequencing that can provide a risk score. It adds something beyond a family history. These are not diagnostic, but they can add to your understanding.
Finally, with respect to schizophrenia and MRI in particular, if it does show structural abnormalities that are among the ones that have been reported for schizophrenia, this can be informative prognostically; such an individual may have a greater likelihood of having a chronic course with progression of the illness. And if that were my patient, I would be thinking that greater effort needs to be taken to ensure that the patient remains on treatment and does not suffer relapse.
Dr. Arbuckle: How do we prepare our trainees for a future of psychiatry with more biomarkers?
Dr. Lieberman: In medical school and postgraduate training, apart from understanding the method of diagnosis and the criteria for diagnoses, it’s important to understand the ancillary measures that are used in clinical medicine: blood testing, electrophysiologic measures, imaging procedures, neurocognitive testing, etc. This is a standard in terms of general medical training.
In terms of then applying it to mental illness and psychiatry, it’s a matter of knowing that these will be relevant at some point, staying apprised of the research literature that is generating data that pertain to the use of these measures for diagnostic, prognostic, or treatment-specific purposes, and then gauging how useful these will be. Right now, these measures are not required for diagnosis. They’re not validated sufficiently so that third-party payers will uniformly reimburse for them, but at some point they will be. Even before that time occurs, there are some measures that can be informative and enhance confidence in the diagnosis or add information about treatment response and outcome.
Dr. Arbuckle: We’re hearing about biotypes and how biotypes may not map to our current diagnostic systems. What are your thoughts about that?
Dr. Lieberman: You know, psychiatry has always been kind of the stepchild of medicine. And related to that, the Diagnostic and Statistical Manual of Mental Disorders (DSM) is the punching bag of the critics of psychiatry and the purported reason it hasn’t progressed faster. Sitting here at Columbia, the home of Robert Spitzer, who was the pioneer of the modern method of nosology that we still use in the DSM, it’s disappointing that we continue to lob tomatoes at this system, which is the best. It took psychiatry out of what was a dark age of clinical methodology and put it on solid scientific footing. That was in the late 1970s with [the development of] DSM-III.
And as much as we would like to have further progress, which would allow for not using a list of criteria in a menu-driven fashion to establish diagnoses, we’d like to have it be like a glucose tolerance test or an angiogram.
We’d like to do that, but we can’t yet. So there’s this aspirational desire to have something better, and this is permeating and motivating a lot of the research, which is good. But to claim that these don’t map to the current DSM and therefore invalidate the DSM-defined diagnoses is wrong and self-defeating. So if they don’t map to the current DSM diagnosis, is the diagnosis wrong or are the biotypes wrong? I believe it’s wishful thinking; individuals are trying to project their desires onto clinical practice, and it’s not desirable to do that. If there was anything that was an improvement on the DSM, it would have been incorporated into our practice.
The question about the limitations of DSM and the improved methods of neuroscientifically informed diagnostic systems was an issue that brought me into a confrontation with our former director of the National Institute of Mental Health (NIMH) in 2013.
After 5 years of the DSM task force laboring to revise the fifth edition of the DSM, as it was about to be launched, our former director, Tom Insel, disavowed it and proposed as a preferable alternative the research domains criteria (RDoC) system that was in development at the NIMH, which I believe epitomized this kind of sour grapes at what psychiatry didn’t have – an aspiration to have a more neuroscientifically informed diagnostic system. And as soon as he made the statement publicly, he had to walk it back because the RDoC system or any other system was not ready for prime time. It would have been a catastrophe if it would have been the one that informed clinical psychiatry. There was nothing that was superior to the DSM to be used at the time. This shows how frustration sometimes impels people to make rash statements.
We’re on the right track. Our field is progressing enormously, and one has to remember that everything that’s relevant in terms of being scientifically based and validated through empirical research in clinical psychiatry and mental illness has happened since the last half of the 20th century.
It is a very short period of time. We’ve made tremendous progress, and we’re continuing to make progress toward the milestone we’re all hoping for, where we have diagnostic tests. But we shouldn’t shortchange ourselves or underestimate the progress we have made in the meantime.
Dr. Arbuckle: This has been a great conversation. Signing off for Medscape and Columbia Psychiatry. Thank you.
Dr. Lieberman is chairman of the Department of Psychiatry at Columbia University. He is a former president of the American Psychiatric Association. Dr. Arbuckle is vice chair for education and director of resident education in the Department of Psychiatry at Columbia University. She is particularly interested in the role of medical education in translating research into the practice of psychiatry.
This article first appeared on Medscape.com.
EULAR’s COVID-19 recommendations offer no surprises
As might be expected, the “EULAR [European League Against Rheumatism] provisional recommendations for the management of rheumatic and musculoskeletal diseases [RMDs] in the context of SARS-CoV-2” concur with much of the guidance already released on how best to manage patients during the current pandemic.
Highlights of the five overarching principles are that, contrary to earlier expectations, “there is no indication that patients with RMDs have an additional, or have a higher, risk of contracting the virus, or that they fare a worse course” than the general population, said the task force convener Robert Landewé, MD, PhD, professor of rheumatology at the University of Amsterdam.
“The second pertinent highlight is that, when it comes to managerial discussions, whether or not to stop or to start treatment for RMDs, rheumatologists should definitely be involved,” Dr. Landewé said during a live session at the annual European Congress of Rheumatology, held online this year due to COVID-19. “In practice, something that happens very often is that immunosuppressive drugs are stopped by medical specialists involved in the care of COVID but without any expertise in treating patients with rheumatic diseases. We should try to avoid that situation.”
The third highlight, something many rheumatologists may already be well aware of, is that rheumatology drugs are being used to treat COVID-19 patients without RMDs and a shortage of disease-modifying antirheumatic drugs (DMARDs) agents is a real possibility. As such, the fifth overarching highlight states that the availability of both synthetic and biologic DMARDs is “a delicate societal responsibility” and that “the off-label use of DMARDs in COVID-19 outside the context of clinical trials should be discouraged.”
The EULAR recommendation are now published online in Annals of the Rheumatic Diseases and they are “what you could call an unprecedented set of recommendations,” Dr. Landewé said. “We have never done this before,” he added, referring to the speed and way in which they had to be put together, remotely, and with little scientific evidence currently available. “Three months ago we hadn’t even heard about the virus.”
From the first patient being identified in the Hubei province of China in November 2019, to the first U.S. patient in the state of Washington on Jan. 20, 2020, and to the first European patient identified a little over 10 days later, the COVID-19 pandemic has taken the world by storm. It was only declared a pandemic on March 11, 2020, however, and Dr. Landewé noted that the response to the pandemic had been very variable – some countries locking down their borders early, while others took their time to make an appropriate response, if at all.
The rheumatology community was particularly concerned, Dr. Landewé said, because people with autoimmune diseases who were taking immunosuppressant drugs might be at higher risk for becoming infected with SARS-CoV-2, and may be at higher risk than others for a worse disease course. Thankfully, that seems not to be the case according to data that are emerging from new registries that have been set up, including EULAR’s own COVID-19 registry.
There are 13 recommendations that cover 4 themes: general measures and prevention of SARS-CoV-2 infection; the management of RMD patients during the pandemic; the management of RMD patients who have COVID-19; and the prevention of other pulmonary infections in RMD patients.
Highlighting the first three general recommendations, Dr. Landewé said: “Follow the regular guidelines in your country; if a patient with RMD does not have symptoms of COVID-19, simply continue RMD treatments,” albeit with a couple of exceptions.
The next four recommendation highlights are to avoid visits to the hospital or to the office; use remote monitoring via the telephone, for example; and if visits cannot be avoided, then take appropriate precautions. Finally, if you suspect a patient has COVID-19, do a test.
If patients test positive, then the next four recommendations cover what to do, such as continuing use of RMD treatments, but in the case of glucocorticoids this should be the lowest possible dose necessary. There is no consensus on what to do in cases of mild symptoms; the recommendation is to “decide on a case-by-case basis,” said Dr. Landewé. If a patient’s symptoms worsen, then “seek expert advice immediately and follow local treatment recommendations. The rheumatologist is not the expert to treat COVID-19,” he added. That responsibility lies with the pulmonologist, infectious disease specialist, or maybe the intensive care specialist, depending on local situations.
On the whole, the EULAR recommendations are pretty similar to those already released by the American College of Rheumatology, said Ted Mikuls, MD, of the University of Nebraska Medical Center, Omaha. The ACR recommendations are “slightly more prescriptive”, he suggested, with 25 final guidance statements. For example, general statements focused not only on the use of glucocorticoids, but also other medicines, such as antihypertensives.
“There’s really not a [lot of], I would say, major differences in the two efforts and that’s ... somewhat reassuring that we’re approaching the unknown from very different parts of the world, and driving in a very similar place,” commented Dr. Mikuls, who is a member of the ACR COVID-19 recommendations task force.
“I think one of the very important similarities that I would highlight is that, in the absence of known exposure, in the absence of COVID-19 infection, our panel felt very strongly about the importance of continuing rheumatic disease treatments,” Dr. Mikuls observed. The ACR guidelines also touch upon societal perspectives, including “some statements that were made very specific to lupus, and the use of antimalarials, given supply chain issues that we have encountered.”
Dr. Mikuls also said that the American recommendations emphasized that “you really have to manage active inflammatory rheumatic disease. Even in the context of the COVID-19 pandemic, given what we saw as the potential risk of unchecked inflammation and unchecked rheumatic disease.”
One notable difference, however, is that the European recommendations advise on immunizations and pneumonia prophylaxis, saying that all patients without COVID-19 symptoms should make sure they are up to date with any recommended vaccinations, “with a particular focus on pneumococcal and influenza vaccinations,” Dr. Landewé said.
Another difference is that the ACR recommendations are a living document and could potentially be updated monthly if the evidence arrives to allow that. In that sense, the American guidance is more agile, with EULAR expecting to update its recommendations every 3 months.
“The current evidence is extremely sparse and fragmented,” Dr. Landewé said. “We, as a task force are essentially flying blindly. We also have to cover many jurisdictions within Europe, with many conflicting opinions. So the last word to say is that updates are truly necessary, but we have to wait a while.”
SOURCE: Landewé RB et al. Ann Rheum Dis. 2020 Jun 5. doi: 10.1136/annrheumdis-2020-217877.
As might be expected, the “EULAR [European League Against Rheumatism] provisional recommendations for the management of rheumatic and musculoskeletal diseases [RMDs] in the context of SARS-CoV-2” concur with much of the guidance already released on how best to manage patients during the current pandemic.
Highlights of the five overarching principles are that, contrary to earlier expectations, “there is no indication that patients with RMDs have an additional, or have a higher, risk of contracting the virus, or that they fare a worse course” than the general population, said the task force convener Robert Landewé, MD, PhD, professor of rheumatology at the University of Amsterdam.
“The second pertinent highlight is that, when it comes to managerial discussions, whether or not to stop or to start treatment for RMDs, rheumatologists should definitely be involved,” Dr. Landewé said during a live session at the annual European Congress of Rheumatology, held online this year due to COVID-19. “In practice, something that happens very often is that immunosuppressive drugs are stopped by medical specialists involved in the care of COVID but without any expertise in treating patients with rheumatic diseases. We should try to avoid that situation.”
The third highlight, something many rheumatologists may already be well aware of, is that rheumatology drugs are being used to treat COVID-19 patients without RMDs and a shortage of disease-modifying antirheumatic drugs (DMARDs) agents is a real possibility. As such, the fifth overarching highlight states that the availability of both synthetic and biologic DMARDs is “a delicate societal responsibility” and that “the off-label use of DMARDs in COVID-19 outside the context of clinical trials should be discouraged.”
The EULAR recommendation are now published online in Annals of the Rheumatic Diseases and they are “what you could call an unprecedented set of recommendations,” Dr. Landewé said. “We have never done this before,” he added, referring to the speed and way in which they had to be put together, remotely, and with little scientific evidence currently available. “Three months ago we hadn’t even heard about the virus.”
From the first patient being identified in the Hubei province of China in November 2019, to the first U.S. patient in the state of Washington on Jan. 20, 2020, and to the first European patient identified a little over 10 days later, the COVID-19 pandemic has taken the world by storm. It was only declared a pandemic on March 11, 2020, however, and Dr. Landewé noted that the response to the pandemic had been very variable – some countries locking down their borders early, while others took their time to make an appropriate response, if at all.
The rheumatology community was particularly concerned, Dr. Landewé said, because people with autoimmune diseases who were taking immunosuppressant drugs might be at higher risk for becoming infected with SARS-CoV-2, and may be at higher risk than others for a worse disease course. Thankfully, that seems not to be the case according to data that are emerging from new registries that have been set up, including EULAR’s own COVID-19 registry.
There are 13 recommendations that cover 4 themes: general measures and prevention of SARS-CoV-2 infection; the management of RMD patients during the pandemic; the management of RMD patients who have COVID-19; and the prevention of other pulmonary infections in RMD patients.
Highlighting the first three general recommendations, Dr. Landewé said: “Follow the regular guidelines in your country; if a patient with RMD does not have symptoms of COVID-19, simply continue RMD treatments,” albeit with a couple of exceptions.
The next four recommendation highlights are to avoid visits to the hospital or to the office; use remote monitoring via the telephone, for example; and if visits cannot be avoided, then take appropriate precautions. Finally, if you suspect a patient has COVID-19, do a test.
If patients test positive, then the next four recommendations cover what to do, such as continuing use of RMD treatments, but in the case of glucocorticoids this should be the lowest possible dose necessary. There is no consensus on what to do in cases of mild symptoms; the recommendation is to “decide on a case-by-case basis,” said Dr. Landewé. If a patient’s symptoms worsen, then “seek expert advice immediately and follow local treatment recommendations. The rheumatologist is not the expert to treat COVID-19,” he added. That responsibility lies with the pulmonologist, infectious disease specialist, or maybe the intensive care specialist, depending on local situations.
On the whole, the EULAR recommendations are pretty similar to those already released by the American College of Rheumatology, said Ted Mikuls, MD, of the University of Nebraska Medical Center, Omaha. The ACR recommendations are “slightly more prescriptive”, he suggested, with 25 final guidance statements. For example, general statements focused not only on the use of glucocorticoids, but also other medicines, such as antihypertensives.
“There’s really not a [lot of], I would say, major differences in the two efforts and that’s ... somewhat reassuring that we’re approaching the unknown from very different parts of the world, and driving in a very similar place,” commented Dr. Mikuls, who is a member of the ACR COVID-19 recommendations task force.
“I think one of the very important similarities that I would highlight is that, in the absence of known exposure, in the absence of COVID-19 infection, our panel felt very strongly about the importance of continuing rheumatic disease treatments,” Dr. Mikuls observed. The ACR guidelines also touch upon societal perspectives, including “some statements that were made very specific to lupus, and the use of antimalarials, given supply chain issues that we have encountered.”
Dr. Mikuls also said that the American recommendations emphasized that “you really have to manage active inflammatory rheumatic disease. Even in the context of the COVID-19 pandemic, given what we saw as the potential risk of unchecked inflammation and unchecked rheumatic disease.”
One notable difference, however, is that the European recommendations advise on immunizations and pneumonia prophylaxis, saying that all patients without COVID-19 symptoms should make sure they are up to date with any recommended vaccinations, “with a particular focus on pneumococcal and influenza vaccinations,” Dr. Landewé said.
Another difference is that the ACR recommendations are a living document and could potentially be updated monthly if the evidence arrives to allow that. In that sense, the American guidance is more agile, with EULAR expecting to update its recommendations every 3 months.
“The current evidence is extremely sparse and fragmented,” Dr. Landewé said. “We, as a task force are essentially flying blindly. We also have to cover many jurisdictions within Europe, with many conflicting opinions. So the last word to say is that updates are truly necessary, but we have to wait a while.”
SOURCE: Landewé RB et al. Ann Rheum Dis. 2020 Jun 5. doi: 10.1136/annrheumdis-2020-217877.
As might be expected, the “EULAR [European League Against Rheumatism] provisional recommendations for the management of rheumatic and musculoskeletal diseases [RMDs] in the context of SARS-CoV-2” concur with much of the guidance already released on how best to manage patients during the current pandemic.
Highlights of the five overarching principles are that, contrary to earlier expectations, “there is no indication that patients with RMDs have an additional, or have a higher, risk of contracting the virus, or that they fare a worse course” than the general population, said the task force convener Robert Landewé, MD, PhD, professor of rheumatology at the University of Amsterdam.
“The second pertinent highlight is that, when it comes to managerial discussions, whether or not to stop or to start treatment for RMDs, rheumatologists should definitely be involved,” Dr. Landewé said during a live session at the annual European Congress of Rheumatology, held online this year due to COVID-19. “In practice, something that happens very often is that immunosuppressive drugs are stopped by medical specialists involved in the care of COVID but without any expertise in treating patients with rheumatic diseases. We should try to avoid that situation.”
The third highlight, something many rheumatologists may already be well aware of, is that rheumatology drugs are being used to treat COVID-19 patients without RMDs and a shortage of disease-modifying antirheumatic drugs (DMARDs) agents is a real possibility. As such, the fifth overarching highlight states that the availability of both synthetic and biologic DMARDs is “a delicate societal responsibility” and that “the off-label use of DMARDs in COVID-19 outside the context of clinical trials should be discouraged.”
The EULAR recommendation are now published online in Annals of the Rheumatic Diseases and they are “what you could call an unprecedented set of recommendations,” Dr. Landewé said. “We have never done this before,” he added, referring to the speed and way in which they had to be put together, remotely, and with little scientific evidence currently available. “Three months ago we hadn’t even heard about the virus.”
From the first patient being identified in the Hubei province of China in November 2019, to the first U.S. patient in the state of Washington on Jan. 20, 2020, and to the first European patient identified a little over 10 days later, the COVID-19 pandemic has taken the world by storm. It was only declared a pandemic on March 11, 2020, however, and Dr. Landewé noted that the response to the pandemic had been very variable – some countries locking down their borders early, while others took their time to make an appropriate response, if at all.
The rheumatology community was particularly concerned, Dr. Landewé said, because people with autoimmune diseases who were taking immunosuppressant drugs might be at higher risk for becoming infected with SARS-CoV-2, and may be at higher risk than others for a worse disease course. Thankfully, that seems not to be the case according to data that are emerging from new registries that have been set up, including EULAR’s own COVID-19 registry.
There are 13 recommendations that cover 4 themes: general measures and prevention of SARS-CoV-2 infection; the management of RMD patients during the pandemic; the management of RMD patients who have COVID-19; and the prevention of other pulmonary infections in RMD patients.
Highlighting the first three general recommendations, Dr. Landewé said: “Follow the regular guidelines in your country; if a patient with RMD does not have symptoms of COVID-19, simply continue RMD treatments,” albeit with a couple of exceptions.
The next four recommendation highlights are to avoid visits to the hospital or to the office; use remote monitoring via the telephone, for example; and if visits cannot be avoided, then take appropriate precautions. Finally, if you suspect a patient has COVID-19, do a test.
If patients test positive, then the next four recommendations cover what to do, such as continuing use of RMD treatments, but in the case of glucocorticoids this should be the lowest possible dose necessary. There is no consensus on what to do in cases of mild symptoms; the recommendation is to “decide on a case-by-case basis,” said Dr. Landewé. If a patient’s symptoms worsen, then “seek expert advice immediately and follow local treatment recommendations. The rheumatologist is not the expert to treat COVID-19,” he added. That responsibility lies with the pulmonologist, infectious disease specialist, or maybe the intensive care specialist, depending on local situations.
On the whole, the EULAR recommendations are pretty similar to those already released by the American College of Rheumatology, said Ted Mikuls, MD, of the University of Nebraska Medical Center, Omaha. The ACR recommendations are “slightly more prescriptive”, he suggested, with 25 final guidance statements. For example, general statements focused not only on the use of glucocorticoids, but also other medicines, such as antihypertensives.
“There’s really not a [lot of], I would say, major differences in the two efforts and that’s ... somewhat reassuring that we’re approaching the unknown from very different parts of the world, and driving in a very similar place,” commented Dr. Mikuls, who is a member of the ACR COVID-19 recommendations task force.
“I think one of the very important similarities that I would highlight is that, in the absence of known exposure, in the absence of COVID-19 infection, our panel felt very strongly about the importance of continuing rheumatic disease treatments,” Dr. Mikuls observed. The ACR guidelines also touch upon societal perspectives, including “some statements that were made very specific to lupus, and the use of antimalarials, given supply chain issues that we have encountered.”
Dr. Mikuls also said that the American recommendations emphasized that “you really have to manage active inflammatory rheumatic disease. Even in the context of the COVID-19 pandemic, given what we saw as the potential risk of unchecked inflammation and unchecked rheumatic disease.”
One notable difference, however, is that the European recommendations advise on immunizations and pneumonia prophylaxis, saying that all patients without COVID-19 symptoms should make sure they are up to date with any recommended vaccinations, “with a particular focus on pneumococcal and influenza vaccinations,” Dr. Landewé said.
Another difference is that the ACR recommendations are a living document and could potentially be updated monthly if the evidence arrives to allow that. In that sense, the American guidance is more agile, with EULAR expecting to update its recommendations every 3 months.
“The current evidence is extremely sparse and fragmented,” Dr. Landewé said. “We, as a task force are essentially flying blindly. We also have to cover many jurisdictions within Europe, with many conflicting opinions. So the last word to say is that updates are truly necessary, but we have to wait a while.”
SOURCE: Landewé RB et al. Ann Rheum Dis. 2020 Jun 5. doi: 10.1136/annrheumdis-2020-217877.
FROM THE EULAR 2020 E-CONGRESS
Medical ethics in the time of COVID-19
It is clear that the coronavirus 2019 disease (COVID-19) pandemic is one of the most extraordinary epochs of our professional and personal lives. Besides the challenges to the techniques and technologies of care for this illness, we are seeing challenges to the fundamentals of health care, both to the systems whereby it is delivered, and to the ethical principles that guide that delivery. There is unprecedented relevance of certain ethical issues in the practice of medicine, many of which have previously been discussed in classrooms and textbooks, but now are at play in daily practice, particularly at the frontlines of the war against COVID-19.1 In this article, I highlight several ethical dilemmas that are salient to these unique times. Some of the most compelling issues can be sorted into 2 clearly overlapping domains: triage ethics and equity ethics.
Triage ethics
In the areas most greatly affected by the COVID-19 pandemic, scarcity of treatment resources, such as ventilators, is a legitimate concern. French surgeon Dominique Jean Larry was the first to establish medical sorting protocols in the context of the battles of the Napoleonic wars, for which he used the French word triage, meaning “sorting.”2 He articulated 3 prognostic categories: 1) those who would die even with treatment, 2) those who would live without treatment, and 3) those who would die unless treated. Triage decisions arise in the context of insufficient resources, particularly space, staff, and supplies. Although usually identified with disasters, these decisions can arise in other contexts where personnel or technological resources are inadequate. Indeed, one of the first modern incarnations of triage ethics in American civilian life was in the early days of hemodialysis, when so-called “God committees” made complex decisions about which patients would be able to use this new, rare technology.3
Two fundamental moral constructs undergird medical ethics: deontological and utilitarian. The former, in which most clinicians traffic in ordinary practice, is driven by principles or moral rules such as the sanctity of life, the rule of fairness, and the principle of autonomy.4 They apply primarily in the context of treating an individual patient. The utilitarian way of reasoning is not as familiar to clinicians. It is focused on the broader context, the common good, the health of the group. It asks to calculate “the greatest good for the greatest number” as a means of navigating ethical dilemmas.5 The utilitarian perspective is far more familiar to policymakers, health care administrators, and public health professionals. It tends to be anathema to clinicians. However, disasters such as the COVID-19 pandemic ask some clinicians, particularly inpatient physicians, to shift from their usual deontological perspective to a utilitarian one, because triage ethics fundamentally draw on utilitarian reasoning. This can be quite anguishing to clinicians who typically work with individual patients in settings of more adequate, if not abundant, resources. What may feel wrong in a deontological mode can be seen as ethically right in a utilitarian framework.
The Table compares and contrasts these 2 paradigms and how they manifest in the clinical trenches, in a protracted health care crisis with limited resources.
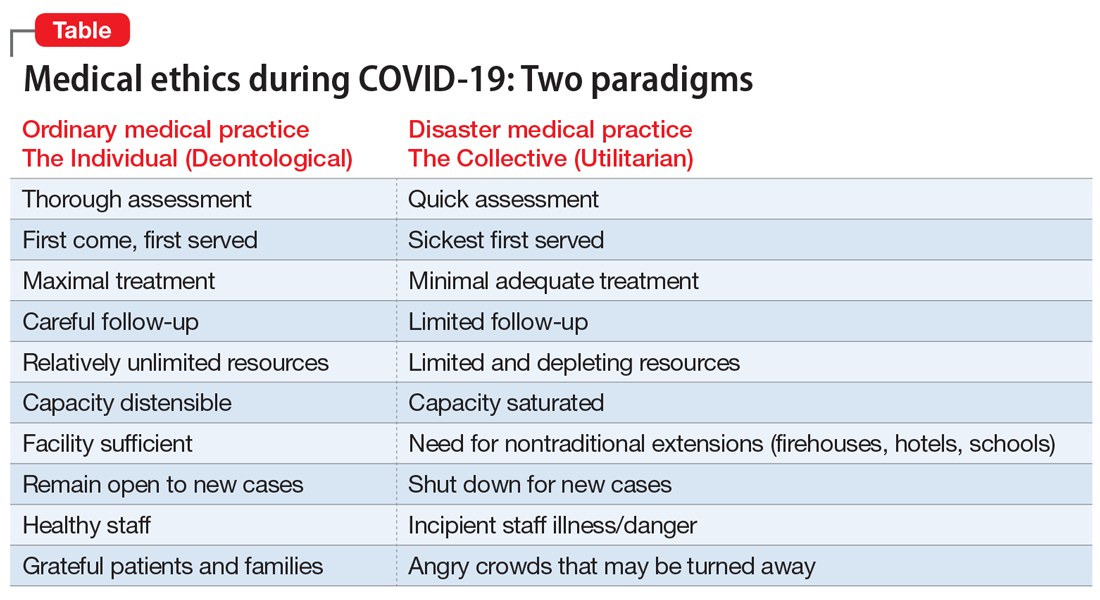
The COVID-19 crisis has produced an unprecedented and extended exposure of clinicians to triage situations in the face of limited resources such as ventilators, personnel, personal protective equipment, etc.6 Numerous possible approaches to deploying limited supplies are being considered. On what basis should such decisions be made? How can fairness be optimally manifest? Some possibilities include:
- first come, first served
- youngest first
- lottery
- short-term survivability
- long-term prognosis for quality of life
- value of a patient to the lives of others (eg, parents, health care workers, vaccine researchers).
One particularly interesting exploration of these questions was done in Maryland and reported in the “Maryland Framework for the Allocation of Scarce Life-sustaining Medical Resources in a Catastrophic Public Health Emergency.”7 This was the product of a multi-year consultation, ending in 2017, with several constituencies, including clinicians, politicians, hospital administrators, and members of the public brainstorming about approaches to allocating a hypothetical scarcity of ventilators. Interestingly, there was one broad consensus among these groups: a ventilator should not be withdrawn from a patient already using it to give to a “better” candidate who comes along later.
Some institutions have developed a method of making triage decisions that takes such decisions out of the hands of individual clinicians and instead assigns them to specialized “triage teams” made up of ethicists and clinicians experienced in critical care, to develop more distance from the emotions at the bedside. To minimize bias, such teams are often insulated from getting personal information about the patient, and receive only acute clinical information.8
Continue to: The pros and cons of these approaches...
The pros and cons of these approaches and the underlying ethical reasoning is beyond the scope of this overview. Policy documents from different states, regions, nations, and institutions have various approaches to making these choices. Presently, there is no coherent national or international agreement on triage ethics.9 It is important, however, that there be transparency in whatever approach an institution adopts for triage decisions.
Equity ethics
Though the equitable distribution of health care delivery has long been a concern, this problem has become magnified by the COVID-19 crisis. Race, sex, age, socioeconomic class, and type of illness have all been perennial sources of division between those who have better or worse access to health care and its outcomes. All of these distinctions have created differentials in rates of cases, hospitalizations, and deaths in the COVID-19 pandemic.10
The shifting of acute health care facilities to mostly COVID-19–related treatment, and postponing less critical and more “elective” care, creates a divide based on illness type. Many facilities have stopped taking admissions for other kinds of cases. This is particularly relevant to psychiatric units, many of which have had to decrease their bed capacities to make all rooms private, and limit their usual treatments offered to inpatients.11 Many long-term units, such as at state hospitals, are closing to new admissions. Many day hospitals and intensive outpatient programs remain closed, not even shifting to telehealth. In areas most affected by COVID-19, some institutions have closed psychiatric wards and reallocated psychiatrists to cover some of the medical units. So the availability of the more intensive, institutionally-based levels of care is significantly reduced, particularly for psychiatric patients.12 These patients already are a disadvantaged population in the distribution of health care resources, and the care of individuals with serious mental illness is more likely to be seen as “nonessential” in this time of suddenly scarcer institutional resources.
One of the cherished ethical values in health care is autonomy, and in a deontological triage environment, honoring patient autonomy is carefully and tenderly administered. However, in a utilitarian-driven triage environment, considerations of the common good can trump autonomy, even in subtle ways that create inequities. Clinicians have been advised to have more frank conversations with patients, particularly those with chronic illnesses, stepping up initiatives to make advanced directives during this crisis, explicitly reminding patients that there may not be enough ventilators for all who need one.13 Some have argued that such physician-initiated conversations can be inherently coercive, making these decisions not as autonomous as it may appear, similar to physicians suggesting medical euthanasia as an option.14 Interestingly, some jurisdictions that offer euthanasia have been suspending such services during the COVID-19 crisis.15 Some hospitals have even wrestled with the possibility that all COVID-19 admissions should be considered “do not resuscitate,” especially because cardiopulmonary resuscitation significantly elevates the risks of viral exposure for the treatment team.16,17 A more explicit example of how current standards protecting patient autonomy may be challenged is patients who are admitted involuntarily to a psychiatric unit. These are patients whose presumptively impaired autonomy is already being overridden by the involuntary nature of the admission. If a psychiatric unit requires admissions to be COVID-19–negative, and if patients refuse COVID-19 testing, should the testing be forced upon them to protect the entire milieu?
Many ethicists are highlighting the embedded equity bias known as “ableism” inherent in triage decisions—implicitly disfavoring resources for patients with COVID-19 who are already physically or intellectually disabled, chronically ill, aged, homeless, psychosocially low functioning, etc.18 Without explicit protections for individuals who are chronically disabled, triage decisions unguided by policy safeguards may reflexively favor the more “abled.” This bias towards the more abled is often inherent in how difficult it is to access health care. It can also be manifested in bedside triage decisions made in the moment by individual clinicians. Many disability rights advocates have been sounding this alarm during the COVID-19 crisis.19
Continue to: A special circumstance of equity...
A special circumstance of equity is arising during this ongoing pandemic—the possibility of treating health care workers as a privileged class. Unlike typical disasters, where health care workers come in afterwards, and therefore are in relatively less danger, pandemics create particularly high risks of danger for such individuals, with repeated exposure to the virus. They are both responders and potential victims. Should they have higher priority for ventilators, vaccines, funding, etc?6 This is a more robust degree of compensatory justice than merely giving appreciation. Giving health care workers such advantages may seem intuitively appealing, but perhaps professionalism and the self-obligation of duty mitigates such claims.20
A unique opportunity
The magnitude and pervasiveness of this pandemic crisis is unique in our lifetimes, as both professionals and as citizens. In the crucible of this extraordinary time, these and other medical ethics dilemmas burn hotter than ever before. Different societies and institutions may come up with different answers, based on their cultures and values. It is important, however, that the venerable ethos of medical ethics, which has evolved through the millennia, codified in oaths, codes, and scholarship, can be a compass at the bedside and in the meetings of legislatures, leaders, and policymakers. Perhaps we can emerge from this time with more clarity about how to balance the preciousness of individual rights with the needs of the common good.
Bottom Line
The coronavirus disease 2019 (COVID-19) pandemic has brought increased attention to triage ethics and equity ethics. There is no coherent national or international agreement on how to best deploy limited supplies such as ventilators and personal protective equipment. Although the equitable distribution of health care delivery has long been a concern, this problem has become magnified by COVID-19. Clinicians may be asked to view health care through the less familiar lens of the common good, as opposed to focusing strictly on an individual patient.
Related Resources
- Johns Hopkins Berman Institute of Bioethics. Coronavirus ethics and policy insights and resources. https://bioethics.jhu.edu/research-and-outreach/covid-19-bioethics-expert-insights/.
- Daugherty-Biddison L, Gwon H, Regenberg A, et al. Maryland framework for the allocation of scarce lifesustaining medical resources in a catastrophic public health emergency. www.law.umaryland.edu/media/SOL/pdfs/Programs/Health-Law/MHECN/ASR%20Framework_Final.pdf.
1. AMA Journal of Ethics. COVID-19 ethics resource center. https://journalofethics.ama-assn.org/COVID-19-ethics-resource-center. Updated May 2020. Accessed May 26, 2020.
2. Skandakalis PN, Lainas P, Zoras O, et al. “To afford the wounded speedy assistance”: Dominique Jean Larrey and Napoleon. World J Surg. 2006;30(8):1392-1399.
3. Ross W. God panels and the history of hemodialysis in America: a cautionary tale. Virtual Mentor. 2012;14(11):890-896.
4. Alexander L, Moore M. Deontological ethics. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/ethics-deontological/. Revised October 17, 2016. Accessed May 26, 2020.
5. Driver J. The history of utilitarianism. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/utilitarianism-history/. Revised September 22, 2014. Accessed May 26, 2020.
6. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. 2020;382(21):2049-2055.
7. Daugherty-Biddison EL, Faden R, Gwon HW, et al. Too many patients…a framework to guide statewide allocation of scarce mechanical ventilation during disasters. Chest. 2019;155(4):848-854.
8. Dudzinski D, Campelia G, Brazg T. Pandemic resources including COVID-19 materials. Department of Bioethics and Humanities, University of Washington Medicine. http://depts.washington.edu/bhdept/ethics-medicine/bioethics-topics/detail/245. Published April 6, 2020. Accessed May 26, 2020.
9. Antommaria AHM, Gibb TS, McGuire AL, et al; Task Force of the Association of Bioethics Program Directors. Ventilator triage policies during the COVID-19 pandemic at U.S. hospitals associated with members of the Association of Bioethics Program Directors [published online April 24, 2020]. Ann Intern Med. 2020;M20-1738. doi: 10.7326/M20-1738.
10. Cooney E. Who gets hospitalized for COVID-19? Report shows differences by race and sex. STAT. https://www.statnews.com/2020/04/09/hospitalized-COVID-19-patients-differences-by-race-and-sex/. Published April 9, 2020. Accessed May 26, 2020.
11. Gessen M. Why psychiatric wards are uniquely vulnerable to the coronavirus. The New Yorker. https://www.newyorker.com/news/news-desk/why-psychiatric-wards-are-uniquely-vulnerable-to-the-coronavirus. Published April 21, 2020. Accessed May 26, 2020.
12. American Psychiatric Association Ethics Committee. COVID-19 related opinions of the APA Ethics Committee. American Psychiatric Association. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Ethics/APA-COVID-19-Ethics-Opinions.pdf. Published May 5, 2020. Accessed May 26, 2020.
13. Wee M. Coronavirus and the misuse of ‘do not resuscitate’ orders. The Spectator. https://www.spectator.co.uk/article/coronavirus-and-the-misuse-of-do-not-resuscitate-orders. Published May 6, 2020. Accessed May 26, 2020.
14. Prokopetz JZ, Lehmann LS. Redefining physicians’ role in assisted dying. N Engl J Med. 2012;367(20):97-99.
15. Yuill K, Boer T. What COVID-19 has revealed about euthanasia. spiked. https://www.spiked-online.com/2020/04/14/COVID-19-has-revealed-the-ugliness-of-euthanasia/. Published April 14, 2020. Accessed May 26, 2020.
16. Plunkett AJ. COVID-19: hospitals should consider CoP carefully before deciding on DNR policy. PSQH. https://www.psqh.com/news/COVID-19-hospitals-should-consider-cop-carefully-before-deciding-on-dnr-policy/. Published March 26, 2020. Accessed May 26, 2020.
17. Kramer DB, Lo B, Dickert NW. CPR in the COVID-19 era: an ethical framework [published online May 6, 2020]. N Engl J Med. doi: 10.1056/NEJMp2010758.
18. Mykitiuk R, Lemmens T. Assessing the value of a life: COVID-19 triage orders mustn’t work against those with disabilities. CBC News. https://www.cbc.ca/news/opinion/opinion-disabled-COVID-19-triage-orders-1.5532137. Published April 19, 2020. Accessed May 26, 2020.
19. Solomon MZ, Wynia MK, Gostin LO. COVID-19 crisis triage—optimizing health outcomes and disability rights [published online May 19, 2020]. N Engl J Med. doi: 10.1056/NEJMp2008300.
20. Appel JM. Ethics consult: who’s first to get COVID-19 Vax? MD/JD bangs gavel. MedPage Today. https://www.medpagetoday.com/infectiousdisease/COVID19/86260. Published May 1, 2020. Accessed May 26, 2020.
It is clear that the coronavirus 2019 disease (COVID-19) pandemic is one of the most extraordinary epochs of our professional and personal lives. Besides the challenges to the techniques and technologies of care for this illness, we are seeing challenges to the fundamentals of health care, both to the systems whereby it is delivered, and to the ethical principles that guide that delivery. There is unprecedented relevance of certain ethical issues in the practice of medicine, many of which have previously been discussed in classrooms and textbooks, but now are at play in daily practice, particularly at the frontlines of the war against COVID-19.1 In this article, I highlight several ethical dilemmas that are salient to these unique times. Some of the most compelling issues can be sorted into 2 clearly overlapping domains: triage ethics and equity ethics.
Triage ethics
In the areas most greatly affected by the COVID-19 pandemic, scarcity of treatment resources, such as ventilators, is a legitimate concern. French surgeon Dominique Jean Larry was the first to establish medical sorting protocols in the context of the battles of the Napoleonic wars, for which he used the French word triage, meaning “sorting.”2 He articulated 3 prognostic categories: 1) those who would die even with treatment, 2) those who would live without treatment, and 3) those who would die unless treated. Triage decisions arise in the context of insufficient resources, particularly space, staff, and supplies. Although usually identified with disasters, these decisions can arise in other contexts where personnel or technological resources are inadequate. Indeed, one of the first modern incarnations of triage ethics in American civilian life was in the early days of hemodialysis, when so-called “God committees” made complex decisions about which patients would be able to use this new, rare technology.3
Two fundamental moral constructs undergird medical ethics: deontological and utilitarian. The former, in which most clinicians traffic in ordinary practice, is driven by principles or moral rules such as the sanctity of life, the rule of fairness, and the principle of autonomy.4 They apply primarily in the context of treating an individual patient. The utilitarian way of reasoning is not as familiar to clinicians. It is focused on the broader context, the common good, the health of the group. It asks to calculate “the greatest good for the greatest number” as a means of navigating ethical dilemmas.5 The utilitarian perspective is far more familiar to policymakers, health care administrators, and public health professionals. It tends to be anathema to clinicians. However, disasters such as the COVID-19 pandemic ask some clinicians, particularly inpatient physicians, to shift from their usual deontological perspective to a utilitarian one, because triage ethics fundamentally draw on utilitarian reasoning. This can be quite anguishing to clinicians who typically work with individual patients in settings of more adequate, if not abundant, resources. What may feel wrong in a deontological mode can be seen as ethically right in a utilitarian framework.
The Table compares and contrasts these 2 paradigms and how they manifest in the clinical trenches, in a protracted health care crisis with limited resources.
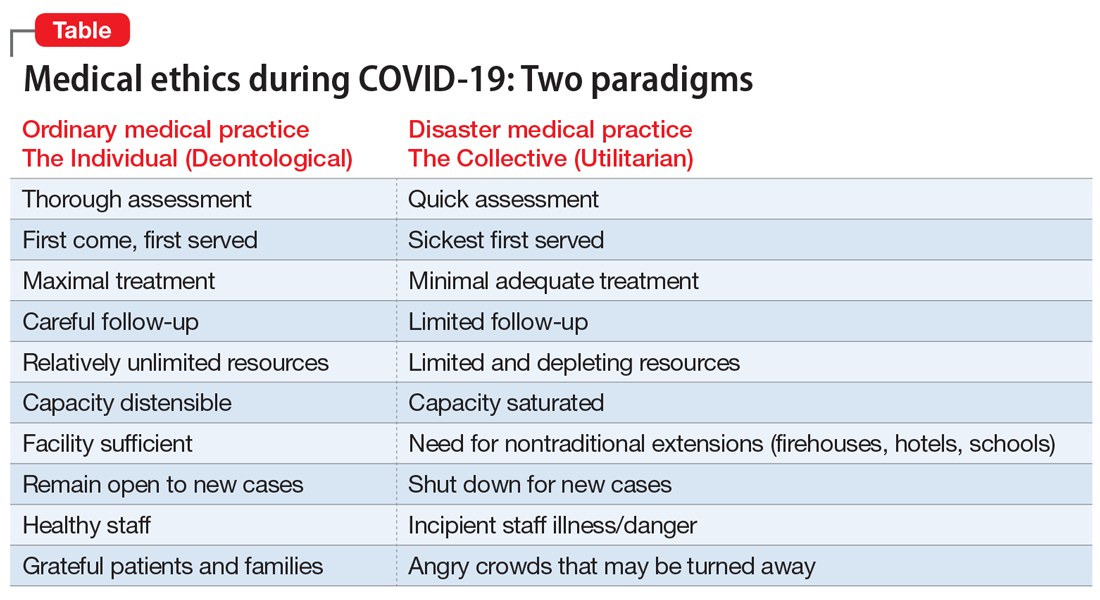
The COVID-19 crisis has produced an unprecedented and extended exposure of clinicians to triage situations in the face of limited resources such as ventilators, personnel, personal protective equipment, etc.6 Numerous possible approaches to deploying limited supplies are being considered. On what basis should such decisions be made? How can fairness be optimally manifest? Some possibilities include:
- first come, first served
- youngest first
- lottery
- short-term survivability
- long-term prognosis for quality of life
- value of a patient to the lives of others (eg, parents, health care workers, vaccine researchers).
One particularly interesting exploration of these questions was done in Maryland and reported in the “Maryland Framework for the Allocation of Scarce Life-sustaining Medical Resources in a Catastrophic Public Health Emergency.”7 This was the product of a multi-year consultation, ending in 2017, with several constituencies, including clinicians, politicians, hospital administrators, and members of the public brainstorming about approaches to allocating a hypothetical scarcity of ventilators. Interestingly, there was one broad consensus among these groups: a ventilator should not be withdrawn from a patient already using it to give to a “better” candidate who comes along later.
Some institutions have developed a method of making triage decisions that takes such decisions out of the hands of individual clinicians and instead assigns them to specialized “triage teams” made up of ethicists and clinicians experienced in critical care, to develop more distance from the emotions at the bedside. To minimize bias, such teams are often insulated from getting personal information about the patient, and receive only acute clinical information.8
Continue to: The pros and cons of these approaches...
The pros and cons of these approaches and the underlying ethical reasoning is beyond the scope of this overview. Policy documents from different states, regions, nations, and institutions have various approaches to making these choices. Presently, there is no coherent national or international agreement on triage ethics.9 It is important, however, that there be transparency in whatever approach an institution adopts for triage decisions.
Equity ethics
Though the equitable distribution of health care delivery has long been a concern, this problem has become magnified by the COVID-19 crisis. Race, sex, age, socioeconomic class, and type of illness have all been perennial sources of division between those who have better or worse access to health care and its outcomes. All of these distinctions have created differentials in rates of cases, hospitalizations, and deaths in the COVID-19 pandemic.10
The shifting of acute health care facilities to mostly COVID-19–related treatment, and postponing less critical and more “elective” care, creates a divide based on illness type. Many facilities have stopped taking admissions for other kinds of cases. This is particularly relevant to psychiatric units, many of which have had to decrease their bed capacities to make all rooms private, and limit their usual treatments offered to inpatients.11 Many long-term units, such as at state hospitals, are closing to new admissions. Many day hospitals and intensive outpatient programs remain closed, not even shifting to telehealth. In areas most affected by COVID-19, some institutions have closed psychiatric wards and reallocated psychiatrists to cover some of the medical units. So the availability of the more intensive, institutionally-based levels of care is significantly reduced, particularly for psychiatric patients.12 These patients already are a disadvantaged population in the distribution of health care resources, and the care of individuals with serious mental illness is more likely to be seen as “nonessential” in this time of suddenly scarcer institutional resources.
One of the cherished ethical values in health care is autonomy, and in a deontological triage environment, honoring patient autonomy is carefully and tenderly administered. However, in a utilitarian-driven triage environment, considerations of the common good can trump autonomy, even in subtle ways that create inequities. Clinicians have been advised to have more frank conversations with patients, particularly those with chronic illnesses, stepping up initiatives to make advanced directives during this crisis, explicitly reminding patients that there may not be enough ventilators for all who need one.13 Some have argued that such physician-initiated conversations can be inherently coercive, making these decisions not as autonomous as it may appear, similar to physicians suggesting medical euthanasia as an option.14 Interestingly, some jurisdictions that offer euthanasia have been suspending such services during the COVID-19 crisis.15 Some hospitals have even wrestled with the possibility that all COVID-19 admissions should be considered “do not resuscitate,” especially because cardiopulmonary resuscitation significantly elevates the risks of viral exposure for the treatment team.16,17 A more explicit example of how current standards protecting patient autonomy may be challenged is patients who are admitted involuntarily to a psychiatric unit. These are patients whose presumptively impaired autonomy is already being overridden by the involuntary nature of the admission. If a psychiatric unit requires admissions to be COVID-19–negative, and if patients refuse COVID-19 testing, should the testing be forced upon them to protect the entire milieu?
Many ethicists are highlighting the embedded equity bias known as “ableism” inherent in triage decisions—implicitly disfavoring resources for patients with COVID-19 who are already physically or intellectually disabled, chronically ill, aged, homeless, psychosocially low functioning, etc.18 Without explicit protections for individuals who are chronically disabled, triage decisions unguided by policy safeguards may reflexively favor the more “abled.” This bias towards the more abled is often inherent in how difficult it is to access health care. It can also be manifested in bedside triage decisions made in the moment by individual clinicians. Many disability rights advocates have been sounding this alarm during the COVID-19 crisis.19
Continue to: A special circumstance of equity...
A special circumstance of equity is arising during this ongoing pandemic—the possibility of treating health care workers as a privileged class. Unlike typical disasters, where health care workers come in afterwards, and therefore are in relatively less danger, pandemics create particularly high risks of danger for such individuals, with repeated exposure to the virus. They are both responders and potential victims. Should they have higher priority for ventilators, vaccines, funding, etc?6 This is a more robust degree of compensatory justice than merely giving appreciation. Giving health care workers such advantages may seem intuitively appealing, but perhaps professionalism and the self-obligation of duty mitigates such claims.20
A unique opportunity
The magnitude and pervasiveness of this pandemic crisis is unique in our lifetimes, as both professionals and as citizens. In the crucible of this extraordinary time, these and other medical ethics dilemmas burn hotter than ever before. Different societies and institutions may come up with different answers, based on their cultures and values. It is important, however, that the venerable ethos of medical ethics, which has evolved through the millennia, codified in oaths, codes, and scholarship, can be a compass at the bedside and in the meetings of legislatures, leaders, and policymakers. Perhaps we can emerge from this time with more clarity about how to balance the preciousness of individual rights with the needs of the common good.
Bottom Line
The coronavirus disease 2019 (COVID-19) pandemic has brought increased attention to triage ethics and equity ethics. There is no coherent national or international agreement on how to best deploy limited supplies such as ventilators and personal protective equipment. Although the equitable distribution of health care delivery has long been a concern, this problem has become magnified by COVID-19. Clinicians may be asked to view health care through the less familiar lens of the common good, as opposed to focusing strictly on an individual patient.
Related Resources
- Johns Hopkins Berman Institute of Bioethics. Coronavirus ethics and policy insights and resources. https://bioethics.jhu.edu/research-and-outreach/covid-19-bioethics-expert-insights/.
- Daugherty-Biddison L, Gwon H, Regenberg A, et al. Maryland framework for the allocation of scarce lifesustaining medical resources in a catastrophic public health emergency. www.law.umaryland.edu/media/SOL/pdfs/Programs/Health-Law/MHECN/ASR%20Framework_Final.pdf.
It is clear that the coronavirus 2019 disease (COVID-19) pandemic is one of the most extraordinary epochs of our professional and personal lives. Besides the challenges to the techniques and technologies of care for this illness, we are seeing challenges to the fundamentals of health care, both to the systems whereby it is delivered, and to the ethical principles that guide that delivery. There is unprecedented relevance of certain ethical issues in the practice of medicine, many of which have previously been discussed in classrooms and textbooks, but now are at play in daily practice, particularly at the frontlines of the war against COVID-19.1 In this article, I highlight several ethical dilemmas that are salient to these unique times. Some of the most compelling issues can be sorted into 2 clearly overlapping domains: triage ethics and equity ethics.
Triage ethics
In the areas most greatly affected by the COVID-19 pandemic, scarcity of treatment resources, such as ventilators, is a legitimate concern. French surgeon Dominique Jean Larry was the first to establish medical sorting protocols in the context of the battles of the Napoleonic wars, for which he used the French word triage, meaning “sorting.”2 He articulated 3 prognostic categories: 1) those who would die even with treatment, 2) those who would live without treatment, and 3) those who would die unless treated. Triage decisions arise in the context of insufficient resources, particularly space, staff, and supplies. Although usually identified with disasters, these decisions can arise in other contexts where personnel or technological resources are inadequate. Indeed, one of the first modern incarnations of triage ethics in American civilian life was in the early days of hemodialysis, when so-called “God committees” made complex decisions about which patients would be able to use this new, rare technology.3
Two fundamental moral constructs undergird medical ethics: deontological and utilitarian. The former, in which most clinicians traffic in ordinary practice, is driven by principles or moral rules such as the sanctity of life, the rule of fairness, and the principle of autonomy.4 They apply primarily in the context of treating an individual patient. The utilitarian way of reasoning is not as familiar to clinicians. It is focused on the broader context, the common good, the health of the group. It asks to calculate “the greatest good for the greatest number” as a means of navigating ethical dilemmas.5 The utilitarian perspective is far more familiar to policymakers, health care administrators, and public health professionals. It tends to be anathema to clinicians. However, disasters such as the COVID-19 pandemic ask some clinicians, particularly inpatient physicians, to shift from their usual deontological perspective to a utilitarian one, because triage ethics fundamentally draw on utilitarian reasoning. This can be quite anguishing to clinicians who typically work with individual patients in settings of more adequate, if not abundant, resources. What may feel wrong in a deontological mode can be seen as ethically right in a utilitarian framework.
The Table compares and contrasts these 2 paradigms and how they manifest in the clinical trenches, in a protracted health care crisis with limited resources.
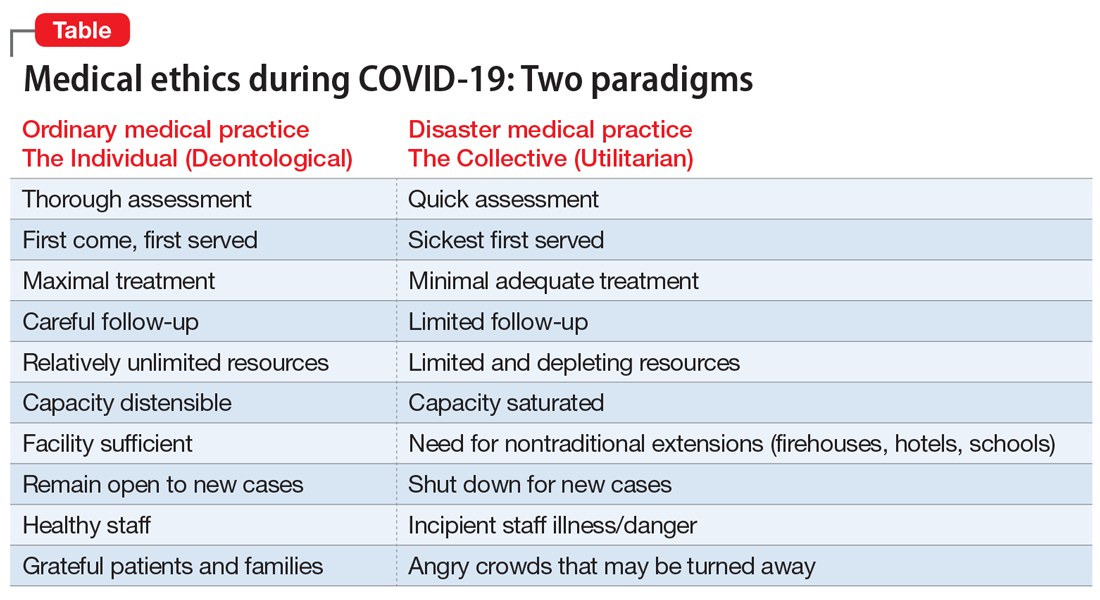
The COVID-19 crisis has produced an unprecedented and extended exposure of clinicians to triage situations in the face of limited resources such as ventilators, personnel, personal protective equipment, etc.6 Numerous possible approaches to deploying limited supplies are being considered. On what basis should such decisions be made? How can fairness be optimally manifest? Some possibilities include:
- first come, first served
- youngest first
- lottery
- short-term survivability
- long-term prognosis for quality of life
- value of a patient to the lives of others (eg, parents, health care workers, vaccine researchers).
One particularly interesting exploration of these questions was done in Maryland and reported in the “Maryland Framework for the Allocation of Scarce Life-sustaining Medical Resources in a Catastrophic Public Health Emergency.”7 This was the product of a multi-year consultation, ending in 2017, with several constituencies, including clinicians, politicians, hospital administrators, and members of the public brainstorming about approaches to allocating a hypothetical scarcity of ventilators. Interestingly, there was one broad consensus among these groups: a ventilator should not be withdrawn from a patient already using it to give to a “better” candidate who comes along later.
Some institutions have developed a method of making triage decisions that takes such decisions out of the hands of individual clinicians and instead assigns them to specialized “triage teams” made up of ethicists and clinicians experienced in critical care, to develop more distance from the emotions at the bedside. To minimize bias, such teams are often insulated from getting personal information about the patient, and receive only acute clinical information.8
Continue to: The pros and cons of these approaches...
The pros and cons of these approaches and the underlying ethical reasoning is beyond the scope of this overview. Policy documents from different states, regions, nations, and institutions have various approaches to making these choices. Presently, there is no coherent national or international agreement on triage ethics.9 It is important, however, that there be transparency in whatever approach an institution adopts for triage decisions.
Equity ethics
Though the equitable distribution of health care delivery has long been a concern, this problem has become magnified by the COVID-19 crisis. Race, sex, age, socioeconomic class, and type of illness have all been perennial sources of division between those who have better or worse access to health care and its outcomes. All of these distinctions have created differentials in rates of cases, hospitalizations, and deaths in the COVID-19 pandemic.10
The shifting of acute health care facilities to mostly COVID-19–related treatment, and postponing less critical and more “elective” care, creates a divide based on illness type. Many facilities have stopped taking admissions for other kinds of cases. This is particularly relevant to psychiatric units, many of which have had to decrease their bed capacities to make all rooms private, and limit their usual treatments offered to inpatients.11 Many long-term units, such as at state hospitals, are closing to new admissions. Many day hospitals and intensive outpatient programs remain closed, not even shifting to telehealth. In areas most affected by COVID-19, some institutions have closed psychiatric wards and reallocated psychiatrists to cover some of the medical units. So the availability of the more intensive, institutionally-based levels of care is significantly reduced, particularly for psychiatric patients.12 These patients already are a disadvantaged population in the distribution of health care resources, and the care of individuals with serious mental illness is more likely to be seen as “nonessential” in this time of suddenly scarcer institutional resources.
One of the cherished ethical values in health care is autonomy, and in a deontological triage environment, honoring patient autonomy is carefully and tenderly administered. However, in a utilitarian-driven triage environment, considerations of the common good can trump autonomy, even in subtle ways that create inequities. Clinicians have been advised to have more frank conversations with patients, particularly those with chronic illnesses, stepping up initiatives to make advanced directives during this crisis, explicitly reminding patients that there may not be enough ventilators for all who need one.13 Some have argued that such physician-initiated conversations can be inherently coercive, making these decisions not as autonomous as it may appear, similar to physicians suggesting medical euthanasia as an option.14 Interestingly, some jurisdictions that offer euthanasia have been suspending such services during the COVID-19 crisis.15 Some hospitals have even wrestled with the possibility that all COVID-19 admissions should be considered “do not resuscitate,” especially because cardiopulmonary resuscitation significantly elevates the risks of viral exposure for the treatment team.16,17 A more explicit example of how current standards protecting patient autonomy may be challenged is patients who are admitted involuntarily to a psychiatric unit. These are patients whose presumptively impaired autonomy is already being overridden by the involuntary nature of the admission. If a psychiatric unit requires admissions to be COVID-19–negative, and if patients refuse COVID-19 testing, should the testing be forced upon them to protect the entire milieu?
Many ethicists are highlighting the embedded equity bias known as “ableism” inherent in triage decisions—implicitly disfavoring resources for patients with COVID-19 who are already physically or intellectually disabled, chronically ill, aged, homeless, psychosocially low functioning, etc.18 Without explicit protections for individuals who are chronically disabled, triage decisions unguided by policy safeguards may reflexively favor the more “abled.” This bias towards the more abled is often inherent in how difficult it is to access health care. It can also be manifested in bedside triage decisions made in the moment by individual clinicians. Many disability rights advocates have been sounding this alarm during the COVID-19 crisis.19
Continue to: A special circumstance of equity...
A special circumstance of equity is arising during this ongoing pandemic—the possibility of treating health care workers as a privileged class. Unlike typical disasters, where health care workers come in afterwards, and therefore are in relatively less danger, pandemics create particularly high risks of danger for such individuals, with repeated exposure to the virus. They are both responders and potential victims. Should they have higher priority for ventilators, vaccines, funding, etc?6 This is a more robust degree of compensatory justice than merely giving appreciation. Giving health care workers such advantages may seem intuitively appealing, but perhaps professionalism and the self-obligation of duty mitigates such claims.20
A unique opportunity
The magnitude and pervasiveness of this pandemic crisis is unique in our lifetimes, as both professionals and as citizens. In the crucible of this extraordinary time, these and other medical ethics dilemmas burn hotter than ever before. Different societies and institutions may come up with different answers, based on their cultures and values. It is important, however, that the venerable ethos of medical ethics, which has evolved through the millennia, codified in oaths, codes, and scholarship, can be a compass at the bedside and in the meetings of legislatures, leaders, and policymakers. Perhaps we can emerge from this time with more clarity about how to balance the preciousness of individual rights with the needs of the common good.
Bottom Line
The coronavirus disease 2019 (COVID-19) pandemic has brought increased attention to triage ethics and equity ethics. There is no coherent national or international agreement on how to best deploy limited supplies such as ventilators and personal protective equipment. Although the equitable distribution of health care delivery has long been a concern, this problem has become magnified by COVID-19. Clinicians may be asked to view health care through the less familiar lens of the common good, as opposed to focusing strictly on an individual patient.
Related Resources
- Johns Hopkins Berman Institute of Bioethics. Coronavirus ethics and policy insights and resources. https://bioethics.jhu.edu/research-and-outreach/covid-19-bioethics-expert-insights/.
- Daugherty-Biddison L, Gwon H, Regenberg A, et al. Maryland framework for the allocation of scarce lifesustaining medical resources in a catastrophic public health emergency. www.law.umaryland.edu/media/SOL/pdfs/Programs/Health-Law/MHECN/ASR%20Framework_Final.pdf.
1. AMA Journal of Ethics. COVID-19 ethics resource center. https://journalofethics.ama-assn.org/COVID-19-ethics-resource-center. Updated May 2020. Accessed May 26, 2020.
2. Skandakalis PN, Lainas P, Zoras O, et al. “To afford the wounded speedy assistance”: Dominique Jean Larrey and Napoleon. World J Surg. 2006;30(8):1392-1399.
3. Ross W. God panels and the history of hemodialysis in America: a cautionary tale. Virtual Mentor. 2012;14(11):890-896.
4. Alexander L, Moore M. Deontological ethics. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/ethics-deontological/. Revised October 17, 2016. Accessed May 26, 2020.
5. Driver J. The history of utilitarianism. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/utilitarianism-history/. Revised September 22, 2014. Accessed May 26, 2020.
6. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. 2020;382(21):2049-2055.
7. Daugherty-Biddison EL, Faden R, Gwon HW, et al. Too many patients…a framework to guide statewide allocation of scarce mechanical ventilation during disasters. Chest. 2019;155(4):848-854.
8. Dudzinski D, Campelia G, Brazg T. Pandemic resources including COVID-19 materials. Department of Bioethics and Humanities, University of Washington Medicine. http://depts.washington.edu/bhdept/ethics-medicine/bioethics-topics/detail/245. Published April 6, 2020. Accessed May 26, 2020.
9. Antommaria AHM, Gibb TS, McGuire AL, et al; Task Force of the Association of Bioethics Program Directors. Ventilator triage policies during the COVID-19 pandemic at U.S. hospitals associated with members of the Association of Bioethics Program Directors [published online April 24, 2020]. Ann Intern Med. 2020;M20-1738. doi: 10.7326/M20-1738.
10. Cooney E. Who gets hospitalized for COVID-19? Report shows differences by race and sex. STAT. https://www.statnews.com/2020/04/09/hospitalized-COVID-19-patients-differences-by-race-and-sex/. Published April 9, 2020. Accessed May 26, 2020.
11. Gessen M. Why psychiatric wards are uniquely vulnerable to the coronavirus. The New Yorker. https://www.newyorker.com/news/news-desk/why-psychiatric-wards-are-uniquely-vulnerable-to-the-coronavirus. Published April 21, 2020. Accessed May 26, 2020.
12. American Psychiatric Association Ethics Committee. COVID-19 related opinions of the APA Ethics Committee. American Psychiatric Association. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Ethics/APA-COVID-19-Ethics-Opinions.pdf. Published May 5, 2020. Accessed May 26, 2020.
13. Wee M. Coronavirus and the misuse of ‘do not resuscitate’ orders. The Spectator. https://www.spectator.co.uk/article/coronavirus-and-the-misuse-of-do-not-resuscitate-orders. Published May 6, 2020. Accessed May 26, 2020.
14. Prokopetz JZ, Lehmann LS. Redefining physicians’ role in assisted dying. N Engl J Med. 2012;367(20):97-99.
15. Yuill K, Boer T. What COVID-19 has revealed about euthanasia. spiked. https://www.spiked-online.com/2020/04/14/COVID-19-has-revealed-the-ugliness-of-euthanasia/. Published April 14, 2020. Accessed May 26, 2020.
16. Plunkett AJ. COVID-19: hospitals should consider CoP carefully before deciding on DNR policy. PSQH. https://www.psqh.com/news/COVID-19-hospitals-should-consider-cop-carefully-before-deciding-on-dnr-policy/. Published March 26, 2020. Accessed May 26, 2020.
17. Kramer DB, Lo B, Dickert NW. CPR in the COVID-19 era: an ethical framework [published online May 6, 2020]. N Engl J Med. doi: 10.1056/NEJMp2010758.
18. Mykitiuk R, Lemmens T. Assessing the value of a life: COVID-19 triage orders mustn’t work against those with disabilities. CBC News. https://www.cbc.ca/news/opinion/opinion-disabled-COVID-19-triage-orders-1.5532137. Published April 19, 2020. Accessed May 26, 2020.
19. Solomon MZ, Wynia MK, Gostin LO. COVID-19 crisis triage—optimizing health outcomes and disability rights [published online May 19, 2020]. N Engl J Med. doi: 10.1056/NEJMp2008300.
20. Appel JM. Ethics consult: who’s first to get COVID-19 Vax? MD/JD bangs gavel. MedPage Today. https://www.medpagetoday.com/infectiousdisease/COVID19/86260. Published May 1, 2020. Accessed May 26, 2020.
1. AMA Journal of Ethics. COVID-19 ethics resource center. https://journalofethics.ama-assn.org/COVID-19-ethics-resource-center. Updated May 2020. Accessed May 26, 2020.
2. Skandakalis PN, Lainas P, Zoras O, et al. “To afford the wounded speedy assistance”: Dominique Jean Larrey and Napoleon. World J Surg. 2006;30(8):1392-1399.
3. Ross W. God panels and the history of hemodialysis in America: a cautionary tale. Virtual Mentor. 2012;14(11):890-896.
4. Alexander L, Moore M. Deontological ethics. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/ethics-deontological/. Revised October 17, 2016. Accessed May 26, 2020.
5. Driver J. The history of utilitarianism. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/utilitarianism-history/. Revised September 22, 2014. Accessed May 26, 2020.
6. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. 2020;382(21):2049-2055.
7. Daugherty-Biddison EL, Faden R, Gwon HW, et al. Too many patients…a framework to guide statewide allocation of scarce mechanical ventilation during disasters. Chest. 2019;155(4):848-854.
8. Dudzinski D, Campelia G, Brazg T. Pandemic resources including COVID-19 materials. Department of Bioethics and Humanities, University of Washington Medicine. http://depts.washington.edu/bhdept/ethics-medicine/bioethics-topics/detail/245. Published April 6, 2020. Accessed May 26, 2020.
9. Antommaria AHM, Gibb TS, McGuire AL, et al; Task Force of the Association of Bioethics Program Directors. Ventilator triage policies during the COVID-19 pandemic at U.S. hospitals associated with members of the Association of Bioethics Program Directors [published online April 24, 2020]. Ann Intern Med. 2020;M20-1738. doi: 10.7326/M20-1738.
10. Cooney E. Who gets hospitalized for COVID-19? Report shows differences by race and sex. STAT. https://www.statnews.com/2020/04/09/hospitalized-COVID-19-patients-differences-by-race-and-sex/. Published April 9, 2020. Accessed May 26, 2020.
11. Gessen M. Why psychiatric wards are uniquely vulnerable to the coronavirus. The New Yorker. https://www.newyorker.com/news/news-desk/why-psychiatric-wards-are-uniquely-vulnerable-to-the-coronavirus. Published April 21, 2020. Accessed May 26, 2020.
12. American Psychiatric Association Ethics Committee. COVID-19 related opinions of the APA Ethics Committee. American Psychiatric Association. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Ethics/APA-COVID-19-Ethics-Opinions.pdf. Published May 5, 2020. Accessed May 26, 2020.
13. Wee M. Coronavirus and the misuse of ‘do not resuscitate’ orders. The Spectator. https://www.spectator.co.uk/article/coronavirus-and-the-misuse-of-do-not-resuscitate-orders. Published May 6, 2020. Accessed May 26, 2020.
14. Prokopetz JZ, Lehmann LS. Redefining physicians’ role in assisted dying. N Engl J Med. 2012;367(20):97-99.
15. Yuill K, Boer T. What COVID-19 has revealed about euthanasia. spiked. https://www.spiked-online.com/2020/04/14/COVID-19-has-revealed-the-ugliness-of-euthanasia/. Published April 14, 2020. Accessed May 26, 2020.
16. Plunkett AJ. COVID-19: hospitals should consider CoP carefully before deciding on DNR policy. PSQH. https://www.psqh.com/news/COVID-19-hospitals-should-consider-cop-carefully-before-deciding-on-dnr-policy/. Published March 26, 2020. Accessed May 26, 2020.
17. Kramer DB, Lo B, Dickert NW. CPR in the COVID-19 era: an ethical framework [published online May 6, 2020]. N Engl J Med. doi: 10.1056/NEJMp2010758.
18. Mykitiuk R, Lemmens T. Assessing the value of a life: COVID-19 triage orders mustn’t work against those with disabilities. CBC News. https://www.cbc.ca/news/opinion/opinion-disabled-COVID-19-triage-orders-1.5532137. Published April 19, 2020. Accessed May 26, 2020.
19. Solomon MZ, Wynia MK, Gostin LO. COVID-19 crisis triage—optimizing health outcomes and disability rights [published online May 19, 2020]. N Engl J Med. doi: 10.1056/NEJMp2008300.
20. Appel JM. Ethics consult: who’s first to get COVID-19 Vax? MD/JD bangs gavel. MedPage Today. https://www.medpagetoday.com/infectiousdisease/COVID19/86260. Published May 1, 2020. Accessed May 26, 2020.