User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Anorexia nervosa and COVID-19
Recent concerns surrounding coronavirus disease 2019 (COVID-19) make it timely to reexamine the complex findings related to eating disorders and the immune system, and the risks for and detection of infection in patients with anorexia nervosa (AN) and similar disorders. To date, there are no published studies evaluating patients with eating disorders and COVID-19. However, it may be helpful to review the data on the infectious process in this patient population to improve patient communication, enhance surveillance and detection, and possibly reduce morbidity and mortality.
The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) issued warnings that individuals who are older, have underlying medical conditions, and/or are immunocompromised face the greatest risk of serious complications and death as a result of COVID-19, the disease process caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Due to malnutrition, patients with eating disorders, especially AN, may be perceived to have an increased risk of medical conditions and infection. Despite many studies on specific changes and differences in the immune system of patients with eating disorders, the consequences of these changes remain controversial and inconclusive.
This article reviews research on eating disorders, focusing on published data regarding the effects of AN on the immune system, susceptibility to infections, infectious detection, and morbidity. We also discuss clinical considerations related to COVID-19 and patients with AN.
Infection risks: Conflicting data
In a 1981 study that included 9 participants, Golla et al1 concluded that patients with AN may have “resistance” to infections based on a suggested protective factor within the immune system of these patients. Because this study has been cited repeatedly in multiple articles about AN and cell-mediated immunity,2-7 some clinicians have accepted this evidence of resistance to infection in patients with AN, which may lower their suspicion for and detection of infections in patients with AN.
However, studies published both before and after Golla et al1 have shown statistically significant results that contradict those researchers’ conclusion. A study that compared the medical records of 68 patients with AN with those who did not have AN found no significant difference, and concluded that the rate of infection among patients with AN is the same as among controls.8 These researchers noted that infection rates may be higher among patients with later-stage, more severe AN. In a 1986 study of 12 patients with AN, Cason et al9 concluded that while cellular immunity function is abnormal in patients with AN, their results were not compatible with prior studies that suggested AN patients were more resistant to infection.1,2,8
More recently, researchers compared 1,592 patients with eating disorders with 6,368 matched controls; they reviewed prescriptions of antibacterial, antifungal, and antiviral medications as a measure of infection rates.10 Compared with controls, patients with binge eating disorder (BED), patients with bulimia nervosa (BN), and males with AN more often received prescriptions for antimicrobial medications. There was no statistically significant difference between controls and females with AN, which is consistent with other reports of no increased or decreased risk of infection among females with AN. In terms of antiviral use, this study showed an increased prescription of antivirals only in the BN group.
Several other studies examining the rate of infection in patients with AN concluded that there is neither an increased nor decreased rate of infection in patients with AN, and that the rate of infection in this population is similar to that of the general population.8,10-12 Because studies that have included patients with AN have evaluated only symptomatic viral infections, some researchers have proposed that patients with AN may show lower rates of symptomatic viral infection but higher rates of asymptomatic infection, as evidenced by higher viral titers.6 Further research is required. Despite controversy regarding infection rates, studies have found that patients with AN have increased rates of morbidity and mortality from infections.6,12-16
Continue to: Obstacles to detecting infections
Obstacles to detecting infections
Several factors can complicate the surveillance and detection of infections in patients with eating disorders, especially those with AN. These include:
- an accepted predisposition to infection secondary to malnutrition
- a lack of visual or reported infectious symptoms
- misrepresentation and assumptions from published research.
Clinicians who report fewer observed cases of infections among patients with AN may be overlooking comorbid disease processes due to a bias from the literature and/or a lack of awareness of symptom parameters in patients with AN.
Features of AN include a loss of adipose tissue responsible for pro-inflammatory cytokines, and excessive exercise, which stimulates anti-inflammatory myokines. This can modulate the experience of illness that impacts the core features of disease,17 possibly reducing symptomatic presentation of infections.
Fever. The presence and intensity of fever may be altered in patients with eating disorders, especially those with AN. In a study of 311 inpatients with AN, researchers found that patients with AN had a significant delay in fever response in AN.12 Of 23 patients with an active bacterial infection, all but 5 had a fever <37°C, with some as low as 35.5°C. A detectable fever response and unexplained fevers were found in 2 of the 6 patients with a viral infection. A series of case studies found that patients with AN with bacterial infections also had a delayed fever response.18
For patients with infections that commonly present with fever, such as COVID-19, a delayed fever response can delay or evade the detection of infection, thus increasing potential complications as well viral exposure to others. Thus, clinicians should use caution when ruling out COVID-19 or other infections because of a lack of significant fever.
Continue to: Overlapping symptoms
Overlapping symptoms. The symptoms of viral infection can mimic the symptoms of AN, which further complicates screening and diagnosis of infection in these patients. Although up to 80% of individuals infected with COVID-19 may be asymptomatic or have a mild presentation, the most common reported symptoms are fever (92.6%), shortness of breath (50.8%), expectoration (41.4%), fatigue (46.4%), dry cough (33.3%), and myalgia (21.4%).19-21 Gastrointestinal (GI) symptoms have been reported in patients with COVID-19, as well as a loss of taste and smell.
Commonly reported physical symptoms of AN include an intolerance to cold, general fatigue, muscle aches and pains, restlessness, emesis, and a multitude of GI complaints. Patients with AN also have been reported to experience shortness of breath due to conditions such as respiratory muscle weakness,22 nutritional emphysema,23 and anxiety and panic attack.24 These conditions could lead to an increased susceptibility to COVID-19 and increased complications during treatment. Cardiac abnormalities, which are common in patients with AN and BN, may increase the risk of adverse events. While these symptoms may be an important part of screening for diseases such as COVID-19, suspicion of infection also may be lower because of the overlap of AN symptomology, underlying conditions, and a delayed fever response.
Laboratory findings. Laboratory testing results for patients with COVID-19 include lower lymphocyte counts, higher leukocyte counts, elevated levels of infection-related biomarkers and inflammatory cytokines, and significantly decreased T-cell counts.19 Similar values are also found in patients with AN.
The similar clinical presentations and laboratory values of AN and COVID-19 could lead to delayed diagnosis, increased disease transmission, cross-contamination of facilities, and higher incidences of medical complications and mortality.
The immunology of AN and correlations with COVID-19
Many studies examining the immune system of patients with eating disorders, especially those with AN, have discovered changes and differences in both cell-mediated and humoral response to infections.1,3,5,7,9,11,16,21,25-27 Whether these differences represent a dysfunctional immune system, an immunocompromised state, or even a protective factor remains unclear.
Continue to: While some studies have reported...
While some studies have reported that AN represents an immunocompromised state, others describe the immune system of patients with AN as dysfunctional or simply altered.9,11,22,28 Some studies have found that patients with AN had delayed reactions to pathogen skin exposures compared with healthy controls, which provides evidence of an impaired cell-mediated immune system.9,27,29
Some studies have considered the consequences of infection and immunologic findings as markers of or contributing to the onset of AN.2,30,31 Numerous studies have noted abnormalities in AN with regards to cell-mediated immunity, the humoral system, the lymphoreticular system, and the innate immune system, and potential contributions from increased oxidative stress, a chronically activated sympathetic nervous system and hypothalamic-pituitary-adrenal axis, altered intestinal microbiota, and an abnormal bone marrow microenvironment.2
Box 1
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a new beta-coronavirus that is still being studied for its effects on the immune system. It may take years to fully understand the nature of the pathogen and the response of the human immune system. To better understand COVID19, researchers have been turning to what they learned from the past outbreaks of severe acute respiratory syndrome (SARS) in 2003- 2004 and Middle East respiratory syndrome (MERS) in 2011, both caused by betacoronaviruses with a zoonotic origin.25,32
The proposed pathogenesis for infection of SARS-CoV-2 is similar to SARS and occurs when aerosolized droplets containing the virus enter the host.32 While currently there is only initial data on the host innate immune status of patients infected with SARS-CoV-2, initial findings of a report on 99 cases in Wuhan, China included increased total neutrophils (38%), reduced total lymphocytes (35%), increased serum interleukin-6 (52%), and increased C-reactive protein (84%).33 Additional findings were decreased percentages of monocytes, eosinophils, and basophils, as well as significantly decreased levels of cytokines and T-cells in more severe cases.19 Past research with SARS reported similar T-cell findings, with a more frequent CD8+ response and a greater magnitude of CD4+.34
Box 119,25,32-34 describes some of the initial immunologic findings reported in patients with COVID-19. In Box 2,5,8,11,13,14,19,26,28,35-40 we discuss reports that describe the immunologic overlay of COVID-19 and AN.
Box 2
Leukopenia (low leukocyte levels) is a common finding in patients with anorexia nervosa (AN),8 and often leads clinicians to lower their suspicion for infection. A 2008 Hungarian study that evaluated lymphocyte activation parameters and clinical status in 11 adolescents (10 girls and 1 boy) with AN, 12 obese adolescents, and 10 healthy controls did not find any association between the variables.35 While many studies have focused on adults, it is important to note that leukopenia is a common finding in adolescents (age 12 to 17) with AN.36
Leukocyte counts are elevated in coronavirus disease 2019 (COVID-19), possibly offsetting AN’s leukopenia. In addition, neutrophil counts are elevated and monocyte, eosinophil, basophil, and especially lymphocyte counts are significantly decreased. A meta-analysis that included 22 studies and 924 participants (512 with AN and 412 controls) examined common inflammatory cytokine findings in patients with AN.11 Compared with healthy controls, patients with AN had significantly elevated levels of tumor necrosis factor alpha (TNF-alpha), interleukin (IL)-1, IL-6, and TNF-receptor II, and significantly decreased levels of C-reactive protein and IL-6 receptor. Elevated levels of TNF-alpha and IL-6 also have been reported in patients with COVID-19.19 These findings may mask suspicion for infection in patients with AN.19
In patients with AN and those with bulimia nervosa, CD4+-to-CD8+ ratios also have been found to be low as a result of normal-tohigher levels of CD4+ cells and lower levels of CD8+ cells.36-39 Researchers have also proposed that the lymphocytosis observed in AN is a result of increased naïve CD4+.36 In AN, total lymphocyte counts have been found to correlate positively with a patient’s body mass index (BMI), while the CD4+ T-lymphocyte correlated negatively with BMI and were critically low in patients with severe malnutrition.26,40 In patients with COVID-19, CD4+ levels have reported to be within normal range, naïve CD4+ cells were elevated, and CD8+ cells were slightly decreased,19 which is similar to the findings in AN.
Fewer studies have evaluated humoral immune response in AN, and results have varied. One study (N = 46) found elevated B-cell counts in adolescents with AN-restricting type,36 while another (N = 40) reported normal levels of B-cells.5 Specific decreases in immunoglobulin (Ig) G and IgM have also been reported in AN, while IgA, IgG, and IgM usually are normal in COVID-19.19
Despite differences in immune system function, cellular immunity appears to remain relatively intact in patients with AN, but can become compromised with severe malnutrition or with advanced weight loss.28,40 This compromised immunity related to severe AN with a very low BMI likely leads to the increased morbidity and mortality.8,13,14
Malnutrition and the immune system
Differences in the type of malnutrition observed in low-weight patients with AN may help explain why patients with AN can maintain a relatively intact cell-mediated immune system.1 Protein-energy malnutrition (PEM), which is found in typical states of starvation, consists of deficiencies in multiple vitamins, protein, and energy (caloric content), whereas the dietary habits of patients with AN usually result in a deficiency of carbohydrates and fats.41 Studies that examined the impact of PEM on immunity to influenza infection have suggested that balanced protein energy replenishment may be a strategy for boosting immunity against influenza viral infections.42 However, carbohydrates are the primary nutrients for human bone marrow fat cells, which play a crucial role in the maturation of white blood cells. This may account for the leukopenia that is common in patients with AN.6,43 The protein-sparing aspect of the typical AN diet may account for the immune system changes observed in patients with AN.44
Although some studies have proposed that immune deficiencies observed in patients with AN are secondary to malnutrition and return to normal with refeeding,5,40,45 others have concluded that immune function is not compromised by factors such as nutritional status or body weight in AN.26,43,46
Continue to: Clinical considerations
Clinical considerations
Neither the CDC nor the WHO have issued a specific protocol for monitoring for and treating COVID-19 in patients with eating disorders; however, the guidelines offered by these organizations for the general population should be followed for patients with eating disorders.
When screening a patient with an eating disorder, keep in mind that the symptoms of eating disorders, such as AN, may mimic an infectious process. Mood symptoms, such as depression or anxiety, could represent physiological responses to infection. Patients with GI symptoms that typically are considered part of the pathology of an eating disorder should be more carefully considered for COVID-19. Monitor a patient’s basal body temperature, and be mindful that a patient with AN may exhibit a delayed fever response. Be vigilant for a recent loss of taste or smell, which should raise suspicion for COVID-19. When monitoring vital signs, pay careful attention for any decompensation in a patient’s pulse oximetry. Whenever possible, order COVID-19 testing for any patient you suspect may be infected.
Outpatient clinicians should work closely in a collaborative manner with a patient’s eating disorder treatment team. Psychiatrists, primary care physicians, psychotherapists, nutritionists, and other clinicians should all follow CDC/WHO guidelines regarding COVID-19, provide surveillance, and communicate any suspicions to the medical team. Eating disorder treatment programs, including residential centers, partial hospital programs (PHP), and intensive outpatient programs (IOP), must enhance monitoring for COVID-19, and exercise caution by practicing social distancing and providing adequate personal protective equipment for patients and staff. To reduce the spread of COVID-19, many IOPs and PHPs have transitioned to virtual treatment. Residential centers must carefully screen patients before admission to weigh the risks and benefits of inpatient vs outpatient care.
Bottom Line
Differences in the immune system of patients with an eating disorder do not necessarily confer a higher or lower risk of infection. Symptoms of some infections can mimic the symptoms of anorexia nervosa. Recognizing infections in patients with eating disorders is critical because compared with the general population, they have higher rates of infection-related morbidity and mortality.
Related Resources
- Congress J, Madaan V. 6 ‘M’s to keep in mind when you next see a patient with anorexia nervosa. Current Psychiatry. 2014;13(5):58-59.
- Westmoreland P. Eating disorders: Masterclass lecture part I. Psychcast (podcast). https://www.mdedge.com/podcasts/psychcast/eating-disorders-masterclass-lecture-part-i.
1. Golla JA, Larson LA, Anderson CF, et al. An immunological assessment of patients with anorexia nervosa. Am J Clin Nutr. 1981;34(12):2756-2762.
2. Gibson D, Mehler PS. Anorexia nervosa and the immune system—a narrative review. J Clin Med. 2019;8(11):1915. doi: 10.3390/jcm8111915.
3. Słotwin
4. Nova E, Samartín S, Gómez S, et al. The adaptive response of the immune system to the particular malnutrition of eating disorders. Eur J Clin Nutr. 2002;56(suppl 3):S34-S37.
5. Allende LM, Corell A, Manzanares J, et al. Immunodeficiency associated with anorexia nervosa is secondary and improves after refeeding. Immunology. 1998;94(4):543-551.
6. Brown RF, Bartrop R, Birmingham CL. Immunological disturbance and infectious disease in anorexia nervosa: a review. Acta Neuropsychiatr. 2008;20(3):117-128.
7. Polack E, Nahmod VE, Emeric-Sauval E, et al. Low lymphocyte interferon-gamma production and variable proliferative response in anorexia nervosa patients. J Clin Immunol. 1993;13(6):445-451.
8. Bowers TK, Eckert E. Leukopenia in anorexia nervosa. Lack of increased risk of infection. Arch Intern Med. 1978;138(10):1520-1523.
9. Cason J, Ainley CC, Wolstencroft RA, et al. Cell-mediated immunity in anorexia nervosa. Clin Exp Immunol. 1986;64(2):370-375.
10. Raevuori A, Lukkariniemi L, Suokas JT, et al. Increased use of antimicrobial medication in bulimia nervosa and binge-eating disorder prior to the eating disorder treatment. Int J Eat Disord. 2016;49(6):542-552.
11. Solmi M, Veronese N, Favaro A, et al. Inflammatory cytokines and anorexia nervosa: a meta-analysis of cross-sectional and longitudinal studies. Psychoneuroendocrinology. 2015;51:237-252.
12. Brown RF, Bartrop R, Beumont P, et al. Bacterial infections in anorexia nervosa: delayed recognition increases complications. Int J Eat Disord. 2005;37(3):261-265.
13. Theander S. Anorexia nervosa. A psychiatric investigation of 94 female patients. Acta Psychiatr Scand Suppl. 1970;214:1-194.
14. Warren MP, Vande Wiele RL. Clinical and metabolic features of anorexia nervosa. Am J Obstet Gynecol. 1973;117(3):435-449.
15. Copeland PM, Herzog DB. Hypoglycemia and death in anorexia nervosa. Psychother Psychosom. 1987;48(1-4):146-150.
16. Devuyst O, Lambert M, Rodhain J, et al. Haematological changes and infectious complications in anorexia nervosa: a case-control study. Q J Med. 1993;86(12):791-799.
17. Pisetsky DS, Trace SE, Brownley KA, et al. The expression of cytokines and chemokines in the blood of patients with severe weight loss from anorexia nervosa: an exploratory study. Cytokine. 2014;69(1):110-115.
18. Birmingham CL, Hodgson DM, Fung J, et al. Reduced febrile response to bacterial infection in anorexia nervosa patients. Int J Eat Disord. 2003;34(2):269-272.
19. Qin C, Zhou L, Hu Z, et al. Dysregulation of immune response in patients with COVID-19 in Wuhan, China [published online March 12, 2020]. Clin Infect Dis. doi: 10.1093/cid/ciaa248.
20. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506.
21. Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514-523.
22. Birmingham CL, Tan AO. Respiratory muscle weakness and anorexia nervosa. Int J Eat Disord. 2003;33(2):230-233.
23. Cook VJ, Coxson HO, Mason AG, et al. Bullae, bronchiectasis and nutritional emphysema in severe anorexia nervosa. Can Respir J. 2001;8(5):361-365.
24. Khalsa SS, Hassanpour MS, Strober M, et al. Interoceptive anxiety and body representation in anorexia nervosa [published online September 21, 2018]. Front Psychiatry. 2018;9:444. doi: 10.3389/fpsyt.2018.00444.
25. van West D, Maes M. Cytokines in de obsessief compulsieve stoornis en in anorexia nervosa: een overzicht. Acta Neuropsychiatr. 1999;11(4):125-129.
26. Komorowska-Pietrzykowska R, Rajewski A, Wiktorowicz K, et al. Czynnos
27. Marcos A, Varela P, Toro O, et al. Interactions between nutrition and immunity in anorexia nervosa: a 1-y follow-up study. Am J Clin Nutr. 1997;66(2):485S-490S.
28. Pertschuk MJ, Crosby LO, Barot L, et al. Immunocompetency in anorexia nervosa. Am J Clin Nutr. 1982;35(5):968-972.
29. Varela P, Marcos A, Navarro MP. Zinc status in anorexia nervosa. Ann Nutr Metab. 1992;36(4):197-202.
30. Breithaupt L, Köhler-Forsberg O, Larsen JT, et al. Association of exposure to infections in childhood with risk of eating disorders in adolescent girls. JAMA Psychiatry. 2019;76(8):800-809.
31. Brambilla F, Monti D, Franceschi C. Plasma concentrations of interleukin-1-beta, interleukin-6 and tumor necrosis factor-alpha, and of their soluble receptors and receptor antagonist in anorexia nervosa. Psychiatry Res. 2001;103(2-3):107-114.
32. Prompetchara E, Ketloy C, Palaga T. Immune responses in COVID-19 and potential vaccines: lessons learned from SARS and MERS epidemic [published online February 27, 2020]. Asian Pac J Allergy Immunol. doi: 10.12932/AP-200220-0772.
33. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270-273.
34. Li CK, Wu H, Yan H, et al. T cell responses to whole SARS coronavirus in humans. J Immunol. 2008;181(8):5490-5500.
35. Páli AA, Pászthy B. Az immunrendszer muködésének megváltozása a táplálkozási magatartás zavarai esetén [Changes of the immune functions in patients with eating disorders]. Ideggyogy Sz. 2008;61(11-12):381‐384.
36. Elegido A, Graell M, Andrés P, et al. Increased naive CD4+ and B lymphocyte subsets are associated with body mass loss and drive relative lymphocytosis in anorexia nervosa patients. Nutr Res. 2017;39:43-50.
37. Marcos A, Varela P, Santacruz I, et al. Nutritional status and immunocompetence in eating disorders. A comparative study. Eur J Clin Nutr. 1993;47(11):787-793.
38. Mustafa A, Ward A, Treasure J, et al. T lymphocyte subpopulations in anorexia nervosa and refeeding. Clin Immunol Immunopathol. 1997;82(3):282-289.
39. Nagata T, Kiriike N, Tobitani W, et al. Lymphocyte subset, lymphocyte proliferative response, and soluble interleukin-2 receptor in anorexic patients. Biol Psychiatry. 1999;45(4):471-474.
40. Saito H, Nomura K, Hotta M, et al. Malnutrition induces dissociated changes in lymphocyte count and subset proportion in patients with anorexia nervosa. Int J Eat Disord. 2007;40(6):575-579.
41. Nova E, Varela P, López-Vidriero I, et al. A one-year follow-up study in anorexia nervosa. Dietary pattern and anthropometrical evolution. Eur J Clin Nutr. 2001;55(7):547-554.
42. Taylor AK, Cao W, Vora KP, et al. Protein energy malnutrition decreases immunity and increases susceptibility to influenza infection in mice. J Infect Dis. 2013;207(3):501-510.
43. Mant MJ, Faragher BS. The hematology of anorexia nervosa. Br J Haematol. 1972;23(6):737-749.
44. Marcos A. The immune system in eating disorders: an overview. Nutrition. 1997;13(10):853-862.
45. Schattner A, Tepper R, Steinbock M, et al. TNF, interferon-gamma and cell-mediated cytotoxicity in anorexia nervosa; effect of refeeding. J Clin Lab Immunol. 1990;32(4):183-184.
46. Nagata T, Tobitani W, Kiriike N, et al. Capacity to produce cytokines during weight restoration in patients with anorexia nervosa. Psychosom Med. 1999;61(3):371-377.
Recent concerns surrounding coronavirus disease 2019 (COVID-19) make it timely to reexamine the complex findings related to eating disorders and the immune system, and the risks for and detection of infection in patients with anorexia nervosa (AN) and similar disorders. To date, there are no published studies evaluating patients with eating disorders and COVID-19. However, it may be helpful to review the data on the infectious process in this patient population to improve patient communication, enhance surveillance and detection, and possibly reduce morbidity and mortality.
The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) issued warnings that individuals who are older, have underlying medical conditions, and/or are immunocompromised face the greatest risk of serious complications and death as a result of COVID-19, the disease process caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Due to malnutrition, patients with eating disorders, especially AN, may be perceived to have an increased risk of medical conditions and infection. Despite many studies on specific changes and differences in the immune system of patients with eating disorders, the consequences of these changes remain controversial and inconclusive.
This article reviews research on eating disorders, focusing on published data regarding the effects of AN on the immune system, susceptibility to infections, infectious detection, and morbidity. We also discuss clinical considerations related to COVID-19 and patients with AN.
Infection risks: Conflicting data
In a 1981 study that included 9 participants, Golla et al1 concluded that patients with AN may have “resistance” to infections based on a suggested protective factor within the immune system of these patients. Because this study has been cited repeatedly in multiple articles about AN and cell-mediated immunity,2-7 some clinicians have accepted this evidence of resistance to infection in patients with AN, which may lower their suspicion for and detection of infections in patients with AN.
However, studies published both before and after Golla et al1 have shown statistically significant results that contradict those researchers’ conclusion. A study that compared the medical records of 68 patients with AN with those who did not have AN found no significant difference, and concluded that the rate of infection among patients with AN is the same as among controls.8 These researchers noted that infection rates may be higher among patients with later-stage, more severe AN. In a 1986 study of 12 patients with AN, Cason et al9 concluded that while cellular immunity function is abnormal in patients with AN, their results were not compatible with prior studies that suggested AN patients were more resistant to infection.1,2,8
More recently, researchers compared 1,592 patients with eating disorders with 6,368 matched controls; they reviewed prescriptions of antibacterial, antifungal, and antiviral medications as a measure of infection rates.10 Compared with controls, patients with binge eating disorder (BED), patients with bulimia nervosa (BN), and males with AN more often received prescriptions for antimicrobial medications. There was no statistically significant difference between controls and females with AN, which is consistent with other reports of no increased or decreased risk of infection among females with AN. In terms of antiviral use, this study showed an increased prescription of antivirals only in the BN group.
Several other studies examining the rate of infection in patients with AN concluded that there is neither an increased nor decreased rate of infection in patients with AN, and that the rate of infection in this population is similar to that of the general population.8,10-12 Because studies that have included patients with AN have evaluated only symptomatic viral infections, some researchers have proposed that patients with AN may show lower rates of symptomatic viral infection but higher rates of asymptomatic infection, as evidenced by higher viral titers.6 Further research is required. Despite controversy regarding infection rates, studies have found that patients with AN have increased rates of morbidity and mortality from infections.6,12-16
Continue to: Obstacles to detecting infections
Obstacles to detecting infections
Several factors can complicate the surveillance and detection of infections in patients with eating disorders, especially those with AN. These include:
- an accepted predisposition to infection secondary to malnutrition
- a lack of visual or reported infectious symptoms
- misrepresentation and assumptions from published research.
Clinicians who report fewer observed cases of infections among patients with AN may be overlooking comorbid disease processes due to a bias from the literature and/or a lack of awareness of symptom parameters in patients with AN.
Features of AN include a loss of adipose tissue responsible for pro-inflammatory cytokines, and excessive exercise, which stimulates anti-inflammatory myokines. This can modulate the experience of illness that impacts the core features of disease,17 possibly reducing symptomatic presentation of infections.
Fever. The presence and intensity of fever may be altered in patients with eating disorders, especially those with AN. In a study of 311 inpatients with AN, researchers found that patients with AN had a significant delay in fever response in AN.12 Of 23 patients with an active bacterial infection, all but 5 had a fever <37°C, with some as low as 35.5°C. A detectable fever response and unexplained fevers were found in 2 of the 6 patients with a viral infection. A series of case studies found that patients with AN with bacterial infections also had a delayed fever response.18
For patients with infections that commonly present with fever, such as COVID-19, a delayed fever response can delay or evade the detection of infection, thus increasing potential complications as well viral exposure to others. Thus, clinicians should use caution when ruling out COVID-19 or other infections because of a lack of significant fever.
Continue to: Overlapping symptoms
Overlapping symptoms. The symptoms of viral infection can mimic the symptoms of AN, which further complicates screening and diagnosis of infection in these patients. Although up to 80% of individuals infected with COVID-19 may be asymptomatic or have a mild presentation, the most common reported symptoms are fever (92.6%), shortness of breath (50.8%), expectoration (41.4%), fatigue (46.4%), dry cough (33.3%), and myalgia (21.4%).19-21 Gastrointestinal (GI) symptoms have been reported in patients with COVID-19, as well as a loss of taste and smell.
Commonly reported physical symptoms of AN include an intolerance to cold, general fatigue, muscle aches and pains, restlessness, emesis, and a multitude of GI complaints. Patients with AN also have been reported to experience shortness of breath due to conditions such as respiratory muscle weakness,22 nutritional emphysema,23 and anxiety and panic attack.24 These conditions could lead to an increased susceptibility to COVID-19 and increased complications during treatment. Cardiac abnormalities, which are common in patients with AN and BN, may increase the risk of adverse events. While these symptoms may be an important part of screening for diseases such as COVID-19, suspicion of infection also may be lower because of the overlap of AN symptomology, underlying conditions, and a delayed fever response.
Laboratory findings. Laboratory testing results for patients with COVID-19 include lower lymphocyte counts, higher leukocyte counts, elevated levels of infection-related biomarkers and inflammatory cytokines, and significantly decreased T-cell counts.19 Similar values are also found in patients with AN.
The similar clinical presentations and laboratory values of AN and COVID-19 could lead to delayed diagnosis, increased disease transmission, cross-contamination of facilities, and higher incidences of medical complications and mortality.
The immunology of AN and correlations with COVID-19
Many studies examining the immune system of patients with eating disorders, especially those with AN, have discovered changes and differences in both cell-mediated and humoral response to infections.1,3,5,7,9,11,16,21,25-27 Whether these differences represent a dysfunctional immune system, an immunocompromised state, or even a protective factor remains unclear.
Continue to: While some studies have reported...
While some studies have reported that AN represents an immunocompromised state, others describe the immune system of patients with AN as dysfunctional or simply altered.9,11,22,28 Some studies have found that patients with AN had delayed reactions to pathogen skin exposures compared with healthy controls, which provides evidence of an impaired cell-mediated immune system.9,27,29
Some studies have considered the consequences of infection and immunologic findings as markers of or contributing to the onset of AN.2,30,31 Numerous studies have noted abnormalities in AN with regards to cell-mediated immunity, the humoral system, the lymphoreticular system, and the innate immune system, and potential contributions from increased oxidative stress, a chronically activated sympathetic nervous system and hypothalamic-pituitary-adrenal axis, altered intestinal microbiota, and an abnormal bone marrow microenvironment.2
Box 1
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a new beta-coronavirus that is still being studied for its effects on the immune system. It may take years to fully understand the nature of the pathogen and the response of the human immune system. To better understand COVID19, researchers have been turning to what they learned from the past outbreaks of severe acute respiratory syndrome (SARS) in 2003- 2004 and Middle East respiratory syndrome (MERS) in 2011, both caused by betacoronaviruses with a zoonotic origin.25,32
The proposed pathogenesis for infection of SARS-CoV-2 is similar to SARS and occurs when aerosolized droplets containing the virus enter the host.32 While currently there is only initial data on the host innate immune status of patients infected with SARS-CoV-2, initial findings of a report on 99 cases in Wuhan, China included increased total neutrophils (38%), reduced total lymphocytes (35%), increased serum interleukin-6 (52%), and increased C-reactive protein (84%).33 Additional findings were decreased percentages of monocytes, eosinophils, and basophils, as well as significantly decreased levels of cytokines and T-cells in more severe cases.19 Past research with SARS reported similar T-cell findings, with a more frequent CD8+ response and a greater magnitude of CD4+.34
Box 119,25,32-34 describes some of the initial immunologic findings reported in patients with COVID-19. In Box 2,5,8,11,13,14,19,26,28,35-40 we discuss reports that describe the immunologic overlay of COVID-19 and AN.
Box 2
Leukopenia (low leukocyte levels) is a common finding in patients with anorexia nervosa (AN),8 and often leads clinicians to lower their suspicion for infection. A 2008 Hungarian study that evaluated lymphocyte activation parameters and clinical status in 11 adolescents (10 girls and 1 boy) with AN, 12 obese adolescents, and 10 healthy controls did not find any association between the variables.35 While many studies have focused on adults, it is important to note that leukopenia is a common finding in adolescents (age 12 to 17) with AN.36
Leukocyte counts are elevated in coronavirus disease 2019 (COVID-19), possibly offsetting AN’s leukopenia. In addition, neutrophil counts are elevated and monocyte, eosinophil, basophil, and especially lymphocyte counts are significantly decreased. A meta-analysis that included 22 studies and 924 participants (512 with AN and 412 controls) examined common inflammatory cytokine findings in patients with AN.11 Compared with healthy controls, patients with AN had significantly elevated levels of tumor necrosis factor alpha (TNF-alpha), interleukin (IL)-1, IL-6, and TNF-receptor II, and significantly decreased levels of C-reactive protein and IL-6 receptor. Elevated levels of TNF-alpha and IL-6 also have been reported in patients with COVID-19.19 These findings may mask suspicion for infection in patients with AN.19
In patients with AN and those with bulimia nervosa, CD4+-to-CD8+ ratios also have been found to be low as a result of normal-tohigher levels of CD4+ cells and lower levels of CD8+ cells.36-39 Researchers have also proposed that the lymphocytosis observed in AN is a result of increased naïve CD4+.36 In AN, total lymphocyte counts have been found to correlate positively with a patient’s body mass index (BMI), while the CD4+ T-lymphocyte correlated negatively with BMI and were critically low in patients with severe malnutrition.26,40 In patients with COVID-19, CD4+ levels have reported to be within normal range, naïve CD4+ cells were elevated, and CD8+ cells were slightly decreased,19 which is similar to the findings in AN.
Fewer studies have evaluated humoral immune response in AN, and results have varied. One study (N = 46) found elevated B-cell counts in adolescents with AN-restricting type,36 while another (N = 40) reported normal levels of B-cells.5 Specific decreases in immunoglobulin (Ig) G and IgM have also been reported in AN, while IgA, IgG, and IgM usually are normal in COVID-19.19
Despite differences in immune system function, cellular immunity appears to remain relatively intact in patients with AN, but can become compromised with severe malnutrition or with advanced weight loss.28,40 This compromised immunity related to severe AN with a very low BMI likely leads to the increased morbidity and mortality.8,13,14
Malnutrition and the immune system
Differences in the type of malnutrition observed in low-weight patients with AN may help explain why patients with AN can maintain a relatively intact cell-mediated immune system.1 Protein-energy malnutrition (PEM), which is found in typical states of starvation, consists of deficiencies in multiple vitamins, protein, and energy (caloric content), whereas the dietary habits of patients with AN usually result in a deficiency of carbohydrates and fats.41 Studies that examined the impact of PEM on immunity to influenza infection have suggested that balanced protein energy replenishment may be a strategy for boosting immunity against influenza viral infections.42 However, carbohydrates are the primary nutrients for human bone marrow fat cells, which play a crucial role in the maturation of white blood cells. This may account for the leukopenia that is common in patients with AN.6,43 The protein-sparing aspect of the typical AN diet may account for the immune system changes observed in patients with AN.44
Although some studies have proposed that immune deficiencies observed in patients with AN are secondary to malnutrition and return to normal with refeeding,5,40,45 others have concluded that immune function is not compromised by factors such as nutritional status or body weight in AN.26,43,46
Continue to: Clinical considerations
Clinical considerations
Neither the CDC nor the WHO have issued a specific protocol for monitoring for and treating COVID-19 in patients with eating disorders; however, the guidelines offered by these organizations for the general population should be followed for patients with eating disorders.
When screening a patient with an eating disorder, keep in mind that the symptoms of eating disorders, such as AN, may mimic an infectious process. Mood symptoms, such as depression or anxiety, could represent physiological responses to infection. Patients with GI symptoms that typically are considered part of the pathology of an eating disorder should be more carefully considered for COVID-19. Monitor a patient’s basal body temperature, and be mindful that a patient with AN may exhibit a delayed fever response. Be vigilant for a recent loss of taste or smell, which should raise suspicion for COVID-19. When monitoring vital signs, pay careful attention for any decompensation in a patient’s pulse oximetry. Whenever possible, order COVID-19 testing for any patient you suspect may be infected.
Outpatient clinicians should work closely in a collaborative manner with a patient’s eating disorder treatment team. Psychiatrists, primary care physicians, psychotherapists, nutritionists, and other clinicians should all follow CDC/WHO guidelines regarding COVID-19, provide surveillance, and communicate any suspicions to the medical team. Eating disorder treatment programs, including residential centers, partial hospital programs (PHP), and intensive outpatient programs (IOP), must enhance monitoring for COVID-19, and exercise caution by practicing social distancing and providing adequate personal protective equipment for patients and staff. To reduce the spread of COVID-19, many IOPs and PHPs have transitioned to virtual treatment. Residential centers must carefully screen patients before admission to weigh the risks and benefits of inpatient vs outpatient care.
Bottom Line
Differences in the immune system of patients with an eating disorder do not necessarily confer a higher or lower risk of infection. Symptoms of some infections can mimic the symptoms of anorexia nervosa. Recognizing infections in patients with eating disorders is critical because compared with the general population, they have higher rates of infection-related morbidity and mortality.
Related Resources
- Congress J, Madaan V. 6 ‘M’s to keep in mind when you next see a patient with anorexia nervosa. Current Psychiatry. 2014;13(5):58-59.
- Westmoreland P. Eating disorders: Masterclass lecture part I. Psychcast (podcast). https://www.mdedge.com/podcasts/psychcast/eating-disorders-masterclass-lecture-part-i.
Recent concerns surrounding coronavirus disease 2019 (COVID-19) make it timely to reexamine the complex findings related to eating disorders and the immune system, and the risks for and detection of infection in patients with anorexia nervosa (AN) and similar disorders. To date, there are no published studies evaluating patients with eating disorders and COVID-19. However, it may be helpful to review the data on the infectious process in this patient population to improve patient communication, enhance surveillance and detection, and possibly reduce morbidity and mortality.
The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) issued warnings that individuals who are older, have underlying medical conditions, and/or are immunocompromised face the greatest risk of serious complications and death as a result of COVID-19, the disease process caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Due to malnutrition, patients with eating disorders, especially AN, may be perceived to have an increased risk of medical conditions and infection. Despite many studies on specific changes and differences in the immune system of patients with eating disorders, the consequences of these changes remain controversial and inconclusive.
This article reviews research on eating disorders, focusing on published data regarding the effects of AN on the immune system, susceptibility to infections, infectious detection, and morbidity. We also discuss clinical considerations related to COVID-19 and patients with AN.
Infection risks: Conflicting data
In a 1981 study that included 9 participants, Golla et al1 concluded that patients with AN may have “resistance” to infections based on a suggested protective factor within the immune system of these patients. Because this study has been cited repeatedly in multiple articles about AN and cell-mediated immunity,2-7 some clinicians have accepted this evidence of resistance to infection in patients with AN, which may lower their suspicion for and detection of infections in patients with AN.
However, studies published both before and after Golla et al1 have shown statistically significant results that contradict those researchers’ conclusion. A study that compared the medical records of 68 patients with AN with those who did not have AN found no significant difference, and concluded that the rate of infection among patients with AN is the same as among controls.8 These researchers noted that infection rates may be higher among patients with later-stage, more severe AN. In a 1986 study of 12 patients with AN, Cason et al9 concluded that while cellular immunity function is abnormal in patients with AN, their results were not compatible with prior studies that suggested AN patients were more resistant to infection.1,2,8
More recently, researchers compared 1,592 patients with eating disorders with 6,368 matched controls; they reviewed prescriptions of antibacterial, antifungal, and antiviral medications as a measure of infection rates.10 Compared with controls, patients with binge eating disorder (BED), patients with bulimia nervosa (BN), and males with AN more often received prescriptions for antimicrobial medications. There was no statistically significant difference between controls and females with AN, which is consistent with other reports of no increased or decreased risk of infection among females with AN. In terms of antiviral use, this study showed an increased prescription of antivirals only in the BN group.
Several other studies examining the rate of infection in patients with AN concluded that there is neither an increased nor decreased rate of infection in patients with AN, and that the rate of infection in this population is similar to that of the general population.8,10-12 Because studies that have included patients with AN have evaluated only symptomatic viral infections, some researchers have proposed that patients with AN may show lower rates of symptomatic viral infection but higher rates of asymptomatic infection, as evidenced by higher viral titers.6 Further research is required. Despite controversy regarding infection rates, studies have found that patients with AN have increased rates of morbidity and mortality from infections.6,12-16
Continue to: Obstacles to detecting infections
Obstacles to detecting infections
Several factors can complicate the surveillance and detection of infections in patients with eating disorders, especially those with AN. These include:
- an accepted predisposition to infection secondary to malnutrition
- a lack of visual or reported infectious symptoms
- misrepresentation and assumptions from published research.
Clinicians who report fewer observed cases of infections among patients with AN may be overlooking comorbid disease processes due to a bias from the literature and/or a lack of awareness of symptom parameters in patients with AN.
Features of AN include a loss of adipose tissue responsible for pro-inflammatory cytokines, and excessive exercise, which stimulates anti-inflammatory myokines. This can modulate the experience of illness that impacts the core features of disease,17 possibly reducing symptomatic presentation of infections.
Fever. The presence and intensity of fever may be altered in patients with eating disorders, especially those with AN. In a study of 311 inpatients with AN, researchers found that patients with AN had a significant delay in fever response in AN.12 Of 23 patients with an active bacterial infection, all but 5 had a fever <37°C, with some as low as 35.5°C. A detectable fever response and unexplained fevers were found in 2 of the 6 patients with a viral infection. A series of case studies found that patients with AN with bacterial infections also had a delayed fever response.18
For patients with infections that commonly present with fever, such as COVID-19, a delayed fever response can delay or evade the detection of infection, thus increasing potential complications as well viral exposure to others. Thus, clinicians should use caution when ruling out COVID-19 or other infections because of a lack of significant fever.
Continue to: Overlapping symptoms
Overlapping symptoms. The symptoms of viral infection can mimic the symptoms of AN, which further complicates screening and diagnosis of infection in these patients. Although up to 80% of individuals infected with COVID-19 may be asymptomatic or have a mild presentation, the most common reported symptoms are fever (92.6%), shortness of breath (50.8%), expectoration (41.4%), fatigue (46.4%), dry cough (33.3%), and myalgia (21.4%).19-21 Gastrointestinal (GI) symptoms have been reported in patients with COVID-19, as well as a loss of taste and smell.
Commonly reported physical symptoms of AN include an intolerance to cold, general fatigue, muscle aches and pains, restlessness, emesis, and a multitude of GI complaints. Patients with AN also have been reported to experience shortness of breath due to conditions such as respiratory muscle weakness,22 nutritional emphysema,23 and anxiety and panic attack.24 These conditions could lead to an increased susceptibility to COVID-19 and increased complications during treatment. Cardiac abnormalities, which are common in patients with AN and BN, may increase the risk of adverse events. While these symptoms may be an important part of screening for diseases such as COVID-19, suspicion of infection also may be lower because of the overlap of AN symptomology, underlying conditions, and a delayed fever response.
Laboratory findings. Laboratory testing results for patients with COVID-19 include lower lymphocyte counts, higher leukocyte counts, elevated levels of infection-related biomarkers and inflammatory cytokines, and significantly decreased T-cell counts.19 Similar values are also found in patients with AN.
The similar clinical presentations and laboratory values of AN and COVID-19 could lead to delayed diagnosis, increased disease transmission, cross-contamination of facilities, and higher incidences of medical complications and mortality.
The immunology of AN and correlations with COVID-19
Many studies examining the immune system of patients with eating disorders, especially those with AN, have discovered changes and differences in both cell-mediated and humoral response to infections.1,3,5,7,9,11,16,21,25-27 Whether these differences represent a dysfunctional immune system, an immunocompromised state, or even a protective factor remains unclear.
Continue to: While some studies have reported...
While some studies have reported that AN represents an immunocompromised state, others describe the immune system of patients with AN as dysfunctional or simply altered.9,11,22,28 Some studies have found that patients with AN had delayed reactions to pathogen skin exposures compared with healthy controls, which provides evidence of an impaired cell-mediated immune system.9,27,29
Some studies have considered the consequences of infection and immunologic findings as markers of or contributing to the onset of AN.2,30,31 Numerous studies have noted abnormalities in AN with regards to cell-mediated immunity, the humoral system, the lymphoreticular system, and the innate immune system, and potential contributions from increased oxidative stress, a chronically activated sympathetic nervous system and hypothalamic-pituitary-adrenal axis, altered intestinal microbiota, and an abnormal bone marrow microenvironment.2
Box 1
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a new beta-coronavirus that is still being studied for its effects on the immune system. It may take years to fully understand the nature of the pathogen and the response of the human immune system. To better understand COVID19, researchers have been turning to what they learned from the past outbreaks of severe acute respiratory syndrome (SARS) in 2003- 2004 and Middle East respiratory syndrome (MERS) in 2011, both caused by betacoronaviruses with a zoonotic origin.25,32
The proposed pathogenesis for infection of SARS-CoV-2 is similar to SARS and occurs when aerosolized droplets containing the virus enter the host.32 While currently there is only initial data on the host innate immune status of patients infected with SARS-CoV-2, initial findings of a report on 99 cases in Wuhan, China included increased total neutrophils (38%), reduced total lymphocytes (35%), increased serum interleukin-6 (52%), and increased C-reactive protein (84%).33 Additional findings were decreased percentages of monocytes, eosinophils, and basophils, as well as significantly decreased levels of cytokines and T-cells in more severe cases.19 Past research with SARS reported similar T-cell findings, with a more frequent CD8+ response and a greater magnitude of CD4+.34
Box 119,25,32-34 describes some of the initial immunologic findings reported in patients with COVID-19. In Box 2,5,8,11,13,14,19,26,28,35-40 we discuss reports that describe the immunologic overlay of COVID-19 and AN.
Box 2
Leukopenia (low leukocyte levels) is a common finding in patients with anorexia nervosa (AN),8 and often leads clinicians to lower their suspicion for infection. A 2008 Hungarian study that evaluated lymphocyte activation parameters and clinical status in 11 adolescents (10 girls and 1 boy) with AN, 12 obese adolescents, and 10 healthy controls did not find any association between the variables.35 While many studies have focused on adults, it is important to note that leukopenia is a common finding in adolescents (age 12 to 17) with AN.36
Leukocyte counts are elevated in coronavirus disease 2019 (COVID-19), possibly offsetting AN’s leukopenia. In addition, neutrophil counts are elevated and monocyte, eosinophil, basophil, and especially lymphocyte counts are significantly decreased. A meta-analysis that included 22 studies and 924 participants (512 with AN and 412 controls) examined common inflammatory cytokine findings in patients with AN.11 Compared with healthy controls, patients with AN had significantly elevated levels of tumor necrosis factor alpha (TNF-alpha), interleukin (IL)-1, IL-6, and TNF-receptor II, and significantly decreased levels of C-reactive protein and IL-6 receptor. Elevated levels of TNF-alpha and IL-6 also have been reported in patients with COVID-19.19 These findings may mask suspicion for infection in patients with AN.19
In patients with AN and those with bulimia nervosa, CD4+-to-CD8+ ratios also have been found to be low as a result of normal-tohigher levels of CD4+ cells and lower levels of CD8+ cells.36-39 Researchers have also proposed that the lymphocytosis observed in AN is a result of increased naïve CD4+.36 In AN, total lymphocyte counts have been found to correlate positively with a patient’s body mass index (BMI), while the CD4+ T-lymphocyte correlated negatively with BMI and were critically low in patients with severe malnutrition.26,40 In patients with COVID-19, CD4+ levels have reported to be within normal range, naïve CD4+ cells were elevated, and CD8+ cells were slightly decreased,19 which is similar to the findings in AN.
Fewer studies have evaluated humoral immune response in AN, and results have varied. One study (N = 46) found elevated B-cell counts in adolescents with AN-restricting type,36 while another (N = 40) reported normal levels of B-cells.5 Specific decreases in immunoglobulin (Ig) G and IgM have also been reported in AN, while IgA, IgG, and IgM usually are normal in COVID-19.19
Despite differences in immune system function, cellular immunity appears to remain relatively intact in patients with AN, but can become compromised with severe malnutrition or with advanced weight loss.28,40 This compromised immunity related to severe AN with a very low BMI likely leads to the increased morbidity and mortality.8,13,14
Malnutrition and the immune system
Differences in the type of malnutrition observed in low-weight patients with AN may help explain why patients with AN can maintain a relatively intact cell-mediated immune system.1 Protein-energy malnutrition (PEM), which is found in typical states of starvation, consists of deficiencies in multiple vitamins, protein, and energy (caloric content), whereas the dietary habits of patients with AN usually result in a deficiency of carbohydrates and fats.41 Studies that examined the impact of PEM on immunity to influenza infection have suggested that balanced protein energy replenishment may be a strategy for boosting immunity against influenza viral infections.42 However, carbohydrates are the primary nutrients for human bone marrow fat cells, which play a crucial role in the maturation of white blood cells. This may account for the leukopenia that is common in patients with AN.6,43 The protein-sparing aspect of the typical AN diet may account for the immune system changes observed in patients with AN.44
Although some studies have proposed that immune deficiencies observed in patients with AN are secondary to malnutrition and return to normal with refeeding,5,40,45 others have concluded that immune function is not compromised by factors such as nutritional status or body weight in AN.26,43,46
Continue to: Clinical considerations
Clinical considerations
Neither the CDC nor the WHO have issued a specific protocol for monitoring for and treating COVID-19 in patients with eating disorders; however, the guidelines offered by these organizations for the general population should be followed for patients with eating disorders.
When screening a patient with an eating disorder, keep in mind that the symptoms of eating disorders, such as AN, may mimic an infectious process. Mood symptoms, such as depression or anxiety, could represent physiological responses to infection. Patients with GI symptoms that typically are considered part of the pathology of an eating disorder should be more carefully considered for COVID-19. Monitor a patient’s basal body temperature, and be mindful that a patient with AN may exhibit a delayed fever response. Be vigilant for a recent loss of taste or smell, which should raise suspicion for COVID-19. When monitoring vital signs, pay careful attention for any decompensation in a patient’s pulse oximetry. Whenever possible, order COVID-19 testing for any patient you suspect may be infected.
Outpatient clinicians should work closely in a collaborative manner with a patient’s eating disorder treatment team. Psychiatrists, primary care physicians, psychotherapists, nutritionists, and other clinicians should all follow CDC/WHO guidelines regarding COVID-19, provide surveillance, and communicate any suspicions to the medical team. Eating disorder treatment programs, including residential centers, partial hospital programs (PHP), and intensive outpatient programs (IOP), must enhance monitoring for COVID-19, and exercise caution by practicing social distancing and providing adequate personal protective equipment for patients and staff. To reduce the spread of COVID-19, many IOPs and PHPs have transitioned to virtual treatment. Residential centers must carefully screen patients before admission to weigh the risks and benefits of inpatient vs outpatient care.
Bottom Line
Differences in the immune system of patients with an eating disorder do not necessarily confer a higher or lower risk of infection. Symptoms of some infections can mimic the symptoms of anorexia nervosa. Recognizing infections in patients with eating disorders is critical because compared with the general population, they have higher rates of infection-related morbidity and mortality.
Related Resources
- Congress J, Madaan V. 6 ‘M’s to keep in mind when you next see a patient with anorexia nervosa. Current Psychiatry. 2014;13(5):58-59.
- Westmoreland P. Eating disorders: Masterclass lecture part I. Psychcast (podcast). https://www.mdedge.com/podcasts/psychcast/eating-disorders-masterclass-lecture-part-i.
1. Golla JA, Larson LA, Anderson CF, et al. An immunological assessment of patients with anorexia nervosa. Am J Clin Nutr. 1981;34(12):2756-2762.
2. Gibson D, Mehler PS. Anorexia nervosa and the immune system—a narrative review. J Clin Med. 2019;8(11):1915. doi: 10.3390/jcm8111915.
3. Słotwin
4. Nova E, Samartín S, Gómez S, et al. The adaptive response of the immune system to the particular malnutrition of eating disorders. Eur J Clin Nutr. 2002;56(suppl 3):S34-S37.
5. Allende LM, Corell A, Manzanares J, et al. Immunodeficiency associated with anorexia nervosa is secondary and improves after refeeding. Immunology. 1998;94(4):543-551.
6. Brown RF, Bartrop R, Birmingham CL. Immunological disturbance and infectious disease in anorexia nervosa: a review. Acta Neuropsychiatr. 2008;20(3):117-128.
7. Polack E, Nahmod VE, Emeric-Sauval E, et al. Low lymphocyte interferon-gamma production and variable proliferative response in anorexia nervosa patients. J Clin Immunol. 1993;13(6):445-451.
8. Bowers TK, Eckert E. Leukopenia in anorexia nervosa. Lack of increased risk of infection. Arch Intern Med. 1978;138(10):1520-1523.
9. Cason J, Ainley CC, Wolstencroft RA, et al. Cell-mediated immunity in anorexia nervosa. Clin Exp Immunol. 1986;64(2):370-375.
10. Raevuori A, Lukkariniemi L, Suokas JT, et al. Increased use of antimicrobial medication in bulimia nervosa and binge-eating disorder prior to the eating disorder treatment. Int J Eat Disord. 2016;49(6):542-552.
11. Solmi M, Veronese N, Favaro A, et al. Inflammatory cytokines and anorexia nervosa: a meta-analysis of cross-sectional and longitudinal studies. Psychoneuroendocrinology. 2015;51:237-252.
12. Brown RF, Bartrop R, Beumont P, et al. Bacterial infections in anorexia nervosa: delayed recognition increases complications. Int J Eat Disord. 2005;37(3):261-265.
13. Theander S. Anorexia nervosa. A psychiatric investigation of 94 female patients. Acta Psychiatr Scand Suppl. 1970;214:1-194.
14. Warren MP, Vande Wiele RL. Clinical and metabolic features of anorexia nervosa. Am J Obstet Gynecol. 1973;117(3):435-449.
15. Copeland PM, Herzog DB. Hypoglycemia and death in anorexia nervosa. Psychother Psychosom. 1987;48(1-4):146-150.
16. Devuyst O, Lambert M, Rodhain J, et al. Haematological changes and infectious complications in anorexia nervosa: a case-control study. Q J Med. 1993;86(12):791-799.
17. Pisetsky DS, Trace SE, Brownley KA, et al. The expression of cytokines and chemokines in the blood of patients with severe weight loss from anorexia nervosa: an exploratory study. Cytokine. 2014;69(1):110-115.
18. Birmingham CL, Hodgson DM, Fung J, et al. Reduced febrile response to bacterial infection in anorexia nervosa patients. Int J Eat Disord. 2003;34(2):269-272.
19. Qin C, Zhou L, Hu Z, et al. Dysregulation of immune response in patients with COVID-19 in Wuhan, China [published online March 12, 2020]. Clin Infect Dis. doi: 10.1093/cid/ciaa248.
20. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506.
21. Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514-523.
22. Birmingham CL, Tan AO. Respiratory muscle weakness and anorexia nervosa. Int J Eat Disord. 2003;33(2):230-233.
23. Cook VJ, Coxson HO, Mason AG, et al. Bullae, bronchiectasis and nutritional emphysema in severe anorexia nervosa. Can Respir J. 2001;8(5):361-365.
24. Khalsa SS, Hassanpour MS, Strober M, et al. Interoceptive anxiety and body representation in anorexia nervosa [published online September 21, 2018]. Front Psychiatry. 2018;9:444. doi: 10.3389/fpsyt.2018.00444.
25. van West D, Maes M. Cytokines in de obsessief compulsieve stoornis en in anorexia nervosa: een overzicht. Acta Neuropsychiatr. 1999;11(4):125-129.
26. Komorowska-Pietrzykowska R, Rajewski A, Wiktorowicz K, et al. Czynnos
27. Marcos A, Varela P, Toro O, et al. Interactions between nutrition and immunity in anorexia nervosa: a 1-y follow-up study. Am J Clin Nutr. 1997;66(2):485S-490S.
28. Pertschuk MJ, Crosby LO, Barot L, et al. Immunocompetency in anorexia nervosa. Am J Clin Nutr. 1982;35(5):968-972.
29. Varela P, Marcos A, Navarro MP. Zinc status in anorexia nervosa. Ann Nutr Metab. 1992;36(4):197-202.
30. Breithaupt L, Köhler-Forsberg O, Larsen JT, et al. Association of exposure to infections in childhood with risk of eating disorders in adolescent girls. JAMA Psychiatry. 2019;76(8):800-809.
31. Brambilla F, Monti D, Franceschi C. Plasma concentrations of interleukin-1-beta, interleukin-6 and tumor necrosis factor-alpha, and of their soluble receptors and receptor antagonist in anorexia nervosa. Psychiatry Res. 2001;103(2-3):107-114.
32. Prompetchara E, Ketloy C, Palaga T. Immune responses in COVID-19 and potential vaccines: lessons learned from SARS and MERS epidemic [published online February 27, 2020]. Asian Pac J Allergy Immunol. doi: 10.12932/AP-200220-0772.
33. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270-273.
34. Li CK, Wu H, Yan H, et al. T cell responses to whole SARS coronavirus in humans. J Immunol. 2008;181(8):5490-5500.
35. Páli AA, Pászthy B. Az immunrendszer muködésének megváltozása a táplálkozási magatartás zavarai esetén [Changes of the immune functions in patients with eating disorders]. Ideggyogy Sz. 2008;61(11-12):381‐384.
36. Elegido A, Graell M, Andrés P, et al. Increased naive CD4+ and B lymphocyte subsets are associated with body mass loss and drive relative lymphocytosis in anorexia nervosa patients. Nutr Res. 2017;39:43-50.
37. Marcos A, Varela P, Santacruz I, et al. Nutritional status and immunocompetence in eating disorders. A comparative study. Eur J Clin Nutr. 1993;47(11):787-793.
38. Mustafa A, Ward A, Treasure J, et al. T lymphocyte subpopulations in anorexia nervosa and refeeding. Clin Immunol Immunopathol. 1997;82(3):282-289.
39. Nagata T, Kiriike N, Tobitani W, et al. Lymphocyte subset, lymphocyte proliferative response, and soluble interleukin-2 receptor in anorexic patients. Biol Psychiatry. 1999;45(4):471-474.
40. Saito H, Nomura K, Hotta M, et al. Malnutrition induces dissociated changes in lymphocyte count and subset proportion in patients with anorexia nervosa. Int J Eat Disord. 2007;40(6):575-579.
41. Nova E, Varela P, López-Vidriero I, et al. A one-year follow-up study in anorexia nervosa. Dietary pattern and anthropometrical evolution. Eur J Clin Nutr. 2001;55(7):547-554.
42. Taylor AK, Cao W, Vora KP, et al. Protein energy malnutrition decreases immunity and increases susceptibility to influenza infection in mice. J Infect Dis. 2013;207(3):501-510.
43. Mant MJ, Faragher BS. The hematology of anorexia nervosa. Br J Haematol. 1972;23(6):737-749.
44. Marcos A. The immune system in eating disorders: an overview. Nutrition. 1997;13(10):853-862.
45. Schattner A, Tepper R, Steinbock M, et al. TNF, interferon-gamma and cell-mediated cytotoxicity in anorexia nervosa; effect of refeeding. J Clin Lab Immunol. 1990;32(4):183-184.
46. Nagata T, Tobitani W, Kiriike N, et al. Capacity to produce cytokines during weight restoration in patients with anorexia nervosa. Psychosom Med. 1999;61(3):371-377.
1. Golla JA, Larson LA, Anderson CF, et al. An immunological assessment of patients with anorexia nervosa. Am J Clin Nutr. 1981;34(12):2756-2762.
2. Gibson D, Mehler PS. Anorexia nervosa and the immune system—a narrative review. J Clin Med. 2019;8(11):1915. doi: 10.3390/jcm8111915.
3. Słotwin
4. Nova E, Samartín S, Gómez S, et al. The adaptive response of the immune system to the particular malnutrition of eating disorders. Eur J Clin Nutr. 2002;56(suppl 3):S34-S37.
5. Allende LM, Corell A, Manzanares J, et al. Immunodeficiency associated with anorexia nervosa is secondary and improves after refeeding. Immunology. 1998;94(4):543-551.
6. Brown RF, Bartrop R, Birmingham CL. Immunological disturbance and infectious disease in anorexia nervosa: a review. Acta Neuropsychiatr. 2008;20(3):117-128.
7. Polack E, Nahmod VE, Emeric-Sauval E, et al. Low lymphocyte interferon-gamma production and variable proliferative response in anorexia nervosa patients. J Clin Immunol. 1993;13(6):445-451.
8. Bowers TK, Eckert E. Leukopenia in anorexia nervosa. Lack of increased risk of infection. Arch Intern Med. 1978;138(10):1520-1523.
9. Cason J, Ainley CC, Wolstencroft RA, et al. Cell-mediated immunity in anorexia nervosa. Clin Exp Immunol. 1986;64(2):370-375.
10. Raevuori A, Lukkariniemi L, Suokas JT, et al. Increased use of antimicrobial medication in bulimia nervosa and binge-eating disorder prior to the eating disorder treatment. Int J Eat Disord. 2016;49(6):542-552.
11. Solmi M, Veronese N, Favaro A, et al. Inflammatory cytokines and anorexia nervosa: a meta-analysis of cross-sectional and longitudinal studies. Psychoneuroendocrinology. 2015;51:237-252.
12. Brown RF, Bartrop R, Beumont P, et al. Bacterial infections in anorexia nervosa: delayed recognition increases complications. Int J Eat Disord. 2005;37(3):261-265.
13. Theander S. Anorexia nervosa. A psychiatric investigation of 94 female patients. Acta Psychiatr Scand Suppl. 1970;214:1-194.
14. Warren MP, Vande Wiele RL. Clinical and metabolic features of anorexia nervosa. Am J Obstet Gynecol. 1973;117(3):435-449.
15. Copeland PM, Herzog DB. Hypoglycemia and death in anorexia nervosa. Psychother Psychosom. 1987;48(1-4):146-150.
16. Devuyst O, Lambert M, Rodhain J, et al. Haematological changes and infectious complications in anorexia nervosa: a case-control study. Q J Med. 1993;86(12):791-799.
17. Pisetsky DS, Trace SE, Brownley KA, et al. The expression of cytokines and chemokines in the blood of patients with severe weight loss from anorexia nervosa: an exploratory study. Cytokine. 2014;69(1):110-115.
18. Birmingham CL, Hodgson DM, Fung J, et al. Reduced febrile response to bacterial infection in anorexia nervosa patients. Int J Eat Disord. 2003;34(2):269-272.
19. Qin C, Zhou L, Hu Z, et al. Dysregulation of immune response in patients with COVID-19 in Wuhan, China [published online March 12, 2020]. Clin Infect Dis. doi: 10.1093/cid/ciaa248.
20. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506.
21. Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514-523.
22. Birmingham CL, Tan AO. Respiratory muscle weakness and anorexia nervosa. Int J Eat Disord. 2003;33(2):230-233.
23. Cook VJ, Coxson HO, Mason AG, et al. Bullae, bronchiectasis and nutritional emphysema in severe anorexia nervosa. Can Respir J. 2001;8(5):361-365.
24. Khalsa SS, Hassanpour MS, Strober M, et al. Interoceptive anxiety and body representation in anorexia nervosa [published online September 21, 2018]. Front Psychiatry. 2018;9:444. doi: 10.3389/fpsyt.2018.00444.
25. van West D, Maes M. Cytokines in de obsessief compulsieve stoornis en in anorexia nervosa: een overzicht. Acta Neuropsychiatr. 1999;11(4):125-129.
26. Komorowska-Pietrzykowska R, Rajewski A, Wiktorowicz K, et al. Czynnos
27. Marcos A, Varela P, Toro O, et al. Interactions between nutrition and immunity in anorexia nervosa: a 1-y follow-up study. Am J Clin Nutr. 1997;66(2):485S-490S.
28. Pertschuk MJ, Crosby LO, Barot L, et al. Immunocompetency in anorexia nervosa. Am J Clin Nutr. 1982;35(5):968-972.
29. Varela P, Marcos A, Navarro MP. Zinc status in anorexia nervosa. Ann Nutr Metab. 1992;36(4):197-202.
30. Breithaupt L, Köhler-Forsberg O, Larsen JT, et al. Association of exposure to infections in childhood with risk of eating disorders in adolescent girls. JAMA Psychiatry. 2019;76(8):800-809.
31. Brambilla F, Monti D, Franceschi C. Plasma concentrations of interleukin-1-beta, interleukin-6 and tumor necrosis factor-alpha, and of their soluble receptors and receptor antagonist in anorexia nervosa. Psychiatry Res. 2001;103(2-3):107-114.
32. Prompetchara E, Ketloy C, Palaga T. Immune responses in COVID-19 and potential vaccines: lessons learned from SARS and MERS epidemic [published online February 27, 2020]. Asian Pac J Allergy Immunol. doi: 10.12932/AP-200220-0772.
33. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270-273.
34. Li CK, Wu H, Yan H, et al. T cell responses to whole SARS coronavirus in humans. J Immunol. 2008;181(8):5490-5500.
35. Páli AA, Pászthy B. Az immunrendszer muködésének megváltozása a táplálkozási magatartás zavarai esetén [Changes of the immune functions in patients with eating disorders]. Ideggyogy Sz. 2008;61(11-12):381‐384.
36. Elegido A, Graell M, Andrés P, et al. Increased naive CD4+ and B lymphocyte subsets are associated with body mass loss and drive relative lymphocytosis in anorexia nervosa patients. Nutr Res. 2017;39:43-50.
37. Marcos A, Varela P, Santacruz I, et al. Nutritional status and immunocompetence in eating disorders. A comparative study. Eur J Clin Nutr. 1993;47(11):787-793.
38. Mustafa A, Ward A, Treasure J, et al. T lymphocyte subpopulations in anorexia nervosa and refeeding. Clin Immunol Immunopathol. 1997;82(3):282-289.
39. Nagata T, Kiriike N, Tobitani W, et al. Lymphocyte subset, lymphocyte proliferative response, and soluble interleukin-2 receptor in anorexic patients. Biol Psychiatry. 1999;45(4):471-474.
40. Saito H, Nomura K, Hotta M, et al. Malnutrition induces dissociated changes in lymphocyte count and subset proportion in patients with anorexia nervosa. Int J Eat Disord. 2007;40(6):575-579.
41. Nova E, Varela P, López-Vidriero I, et al. A one-year follow-up study in anorexia nervosa. Dietary pattern and anthropometrical evolution. Eur J Clin Nutr. 2001;55(7):547-554.
42. Taylor AK, Cao W, Vora KP, et al. Protein energy malnutrition decreases immunity and increases susceptibility to influenza infection in mice. J Infect Dis. 2013;207(3):501-510.
43. Mant MJ, Faragher BS. The hematology of anorexia nervosa. Br J Haematol. 1972;23(6):737-749.
44. Marcos A. The immune system in eating disorders: an overview. Nutrition. 1997;13(10):853-862.
45. Schattner A, Tepper R, Steinbock M, et al. TNF, interferon-gamma and cell-mediated cytotoxicity in anorexia nervosa; effect of refeeding. J Clin Lab Immunol. 1990;32(4):183-184.
46. Nagata T, Tobitani W, Kiriike N, et al. Capacity to produce cytokines during weight restoration in patients with anorexia nervosa. Psychosom Med. 1999;61(3):371-377.
Huntington’s disease biomarkers appear 24 years before clinical symptoms
, according to a study published in the June Lancet Neurology. The data come from the Huntington’s disease Young Adult Study (HD-YAS) conducted in the United Kingdom.
The genetic cause of Huntington’s disease provides a potential target for biomarker treatment, wrote joint first authors Rachael I. Scahill, PhD, and Paul Zeun, BMBS, of University College London and colleagues.
“A detailed characterization of the premanifest period in Huntington’s disease is crucial for disease staging, informing the optimum time to initiate treatments, and identifying biomarkers for future trials in people with premanifest Huntington’s disease (preHD),” they said.
Identifying biomarkers of pre-Huntington’s disease
For their study, the researchers recruited 64 young adults with presymptomatic Huntington’s disease (preHD) and 67 controls, with an average age of 29 years. Brain imaging was conducted between Aug. 2, 2017, and April 25, 2019. Individuals with preexisting measurable cognitive and psychiatric disorders were excluded.
The researchers found no significant evidence of cognitive or psychiatric impairment in the preHD group at 23.6 years from the predicted onset of symptoms. The preHD group showed smaller putamen volumes, compared with controls, but this difference had no apparent relation to the timing of symptom onset, the researchers said.
Brain imaging revealed elevations in the CSF mutant huntingtin, neurofilament light protein (NfL), YKL-40, and plasma NfL among individuals with preHD, compared with controls. Of these, CSF NfL showed the highest effect size of measures in the study and showed a significant increasing association with estimated years to the onset of clinical symptoms of HD carriers. Overall, 53% of individuals with preHD had CSF NfL values in the normal range, and 47% had elevated values, compared with controls.
“NfL is therefore a potential candidate to provide a measure of disease progression in early preHD and might eventually be used as a marker of response to treatment in future preventive trials,” the researchers said.
The study findings were limited by several factors including potential underpowering to detect associations with age and CAG gene segment repeats, the researchers noted.
However, “By identifying a cohort of individuals with preHD and no detectable functional impairment but who begin to exhibit subtle elevations in select biological measures of neurodegeneration, we have highlighted a crucial point early in the disease process,” they concluded.
“Intervening at this stage might offer the prospect of delaying or preventing further neurodegeneration while function is intact, giving gene carriers many more years of life without impairment,” they added.
What is the best window for treatment?
The study is “particularly important since the absence of any subclinical symptoms in preHD individuals far from onset shows that the abnormal developmental aspect of Huntington’s disease has no substantial effect on adults’ clinical pattern,” wrote Anne-Catherine Bachoud-Lévi, MD, of Université Paris Est, Créteil, France, in an accompanying comment.
“The most robust findings of [the study] are the sensitiveness of NfL, compared with mutant huntingtin in CSF of individuals with preHD, and that degenerative rather than developmental disorders are clinically relevant,” she said. However, potential limitations to the study include the exclusion absence of language and calculation as part of the cognitive assessments, she noted. “Ideally, more sensitive cognitive tasks including these domains should be designed for preHD participants.”
In addition, the risks versus benefits of any long-term treatment must be considered, Dr. Bachoud-Lévi noted.
“The best window for treatment should instead target the time when a detectable subclinical slope of cognitive performance allows for predicting disease onset within a few years,” she said. “Turning to machine learning methodology, such as that in oncology, might also permit combining the best window and the best disease-modifying therapy for individuals with preHD,” she added.
The study was supported by the Wellcome Trust, CHDI Foundation. The researchers had no financial conflicts to disclose. Dr. Bachoud-Lévi disclosed grants and personal fees from Roche, and grants from the French Ministry of Health and Direction de la Recherche Clinique.
SOURCES: Scahill RI et al. Lancet Neurol. 2020 June;19:502-12; Bachoud-Lévi A-C. Lancet Neurol. 2020 June;19:473-5.
, according to a study published in the June Lancet Neurology. The data come from the Huntington’s disease Young Adult Study (HD-YAS) conducted in the United Kingdom.
The genetic cause of Huntington’s disease provides a potential target for biomarker treatment, wrote joint first authors Rachael I. Scahill, PhD, and Paul Zeun, BMBS, of University College London and colleagues.
“A detailed characterization of the premanifest period in Huntington’s disease is crucial for disease staging, informing the optimum time to initiate treatments, and identifying biomarkers for future trials in people with premanifest Huntington’s disease (preHD),” they said.
Identifying biomarkers of pre-Huntington’s disease
For their study, the researchers recruited 64 young adults with presymptomatic Huntington’s disease (preHD) and 67 controls, with an average age of 29 years. Brain imaging was conducted between Aug. 2, 2017, and April 25, 2019. Individuals with preexisting measurable cognitive and psychiatric disorders were excluded.
The researchers found no significant evidence of cognitive or psychiatric impairment in the preHD group at 23.6 years from the predicted onset of symptoms. The preHD group showed smaller putamen volumes, compared with controls, but this difference had no apparent relation to the timing of symptom onset, the researchers said.
Brain imaging revealed elevations in the CSF mutant huntingtin, neurofilament light protein (NfL), YKL-40, and plasma NfL among individuals with preHD, compared with controls. Of these, CSF NfL showed the highest effect size of measures in the study and showed a significant increasing association with estimated years to the onset of clinical symptoms of HD carriers. Overall, 53% of individuals with preHD had CSF NfL values in the normal range, and 47% had elevated values, compared with controls.
“NfL is therefore a potential candidate to provide a measure of disease progression in early preHD and might eventually be used as a marker of response to treatment in future preventive trials,” the researchers said.
The study findings were limited by several factors including potential underpowering to detect associations with age and CAG gene segment repeats, the researchers noted.
However, “By identifying a cohort of individuals with preHD and no detectable functional impairment but who begin to exhibit subtle elevations in select biological measures of neurodegeneration, we have highlighted a crucial point early in the disease process,” they concluded.
“Intervening at this stage might offer the prospect of delaying or preventing further neurodegeneration while function is intact, giving gene carriers many more years of life without impairment,” they added.
What is the best window for treatment?
The study is “particularly important since the absence of any subclinical symptoms in preHD individuals far from onset shows that the abnormal developmental aspect of Huntington’s disease has no substantial effect on adults’ clinical pattern,” wrote Anne-Catherine Bachoud-Lévi, MD, of Université Paris Est, Créteil, France, in an accompanying comment.
“The most robust findings of [the study] are the sensitiveness of NfL, compared with mutant huntingtin in CSF of individuals with preHD, and that degenerative rather than developmental disorders are clinically relevant,” she said. However, potential limitations to the study include the exclusion absence of language and calculation as part of the cognitive assessments, she noted. “Ideally, more sensitive cognitive tasks including these domains should be designed for preHD participants.”
In addition, the risks versus benefits of any long-term treatment must be considered, Dr. Bachoud-Lévi noted.
“The best window for treatment should instead target the time when a detectable subclinical slope of cognitive performance allows for predicting disease onset within a few years,” she said. “Turning to machine learning methodology, such as that in oncology, might also permit combining the best window and the best disease-modifying therapy for individuals with preHD,” she added.
The study was supported by the Wellcome Trust, CHDI Foundation. The researchers had no financial conflicts to disclose. Dr. Bachoud-Lévi disclosed grants and personal fees from Roche, and grants from the French Ministry of Health and Direction de la Recherche Clinique.
SOURCES: Scahill RI et al. Lancet Neurol. 2020 June;19:502-12; Bachoud-Lévi A-C. Lancet Neurol. 2020 June;19:473-5.
, according to a study published in the June Lancet Neurology. The data come from the Huntington’s disease Young Adult Study (HD-YAS) conducted in the United Kingdom.
The genetic cause of Huntington’s disease provides a potential target for biomarker treatment, wrote joint first authors Rachael I. Scahill, PhD, and Paul Zeun, BMBS, of University College London and colleagues.
“A detailed characterization of the premanifest period in Huntington’s disease is crucial for disease staging, informing the optimum time to initiate treatments, and identifying biomarkers for future trials in people with premanifest Huntington’s disease (preHD),” they said.
Identifying biomarkers of pre-Huntington’s disease
For their study, the researchers recruited 64 young adults with presymptomatic Huntington’s disease (preHD) and 67 controls, with an average age of 29 years. Brain imaging was conducted between Aug. 2, 2017, and April 25, 2019. Individuals with preexisting measurable cognitive and psychiatric disorders were excluded.
The researchers found no significant evidence of cognitive or psychiatric impairment in the preHD group at 23.6 years from the predicted onset of symptoms. The preHD group showed smaller putamen volumes, compared with controls, but this difference had no apparent relation to the timing of symptom onset, the researchers said.
Brain imaging revealed elevations in the CSF mutant huntingtin, neurofilament light protein (NfL), YKL-40, and plasma NfL among individuals with preHD, compared with controls. Of these, CSF NfL showed the highest effect size of measures in the study and showed a significant increasing association with estimated years to the onset of clinical symptoms of HD carriers. Overall, 53% of individuals with preHD had CSF NfL values in the normal range, and 47% had elevated values, compared with controls.
“NfL is therefore a potential candidate to provide a measure of disease progression in early preHD and might eventually be used as a marker of response to treatment in future preventive trials,” the researchers said.
The study findings were limited by several factors including potential underpowering to detect associations with age and CAG gene segment repeats, the researchers noted.
However, “By identifying a cohort of individuals with preHD and no detectable functional impairment but who begin to exhibit subtle elevations in select biological measures of neurodegeneration, we have highlighted a crucial point early in the disease process,” they concluded.
“Intervening at this stage might offer the prospect of delaying or preventing further neurodegeneration while function is intact, giving gene carriers many more years of life without impairment,” they added.
What is the best window for treatment?
The study is “particularly important since the absence of any subclinical symptoms in preHD individuals far from onset shows that the abnormal developmental aspect of Huntington’s disease has no substantial effect on adults’ clinical pattern,” wrote Anne-Catherine Bachoud-Lévi, MD, of Université Paris Est, Créteil, France, in an accompanying comment.
“The most robust findings of [the study] are the sensitiveness of NfL, compared with mutant huntingtin in CSF of individuals with preHD, and that degenerative rather than developmental disorders are clinically relevant,” she said. However, potential limitations to the study include the exclusion absence of language and calculation as part of the cognitive assessments, she noted. “Ideally, more sensitive cognitive tasks including these domains should be designed for preHD participants.”
In addition, the risks versus benefits of any long-term treatment must be considered, Dr. Bachoud-Lévi noted.
“The best window for treatment should instead target the time when a detectable subclinical slope of cognitive performance allows for predicting disease onset within a few years,” she said. “Turning to machine learning methodology, such as that in oncology, might also permit combining the best window and the best disease-modifying therapy for individuals with preHD,” she added.
The study was supported by the Wellcome Trust, CHDI Foundation. The researchers had no financial conflicts to disclose. Dr. Bachoud-Lévi disclosed grants and personal fees from Roche, and grants from the French Ministry of Health and Direction de la Recherche Clinique.
SOURCES: Scahill RI et al. Lancet Neurol. 2020 June;19:502-12; Bachoud-Lévi A-C. Lancet Neurol. 2020 June;19:473-5.
FROM LANCET NEUROLOGY
Today’s Top News Highlights: Doctors protest racism, controversial studies retracted
Here are the stories our MDedge editors across specialties think you need to know about today:
#WhiteCoats4BlackLives stands up to racism
Participants in the growing #WhiteCoats4BlackLives protest against racism say it is a chance to use their status as trusted messengers, show themselves as allies of people of color, and demonstrate that they are familiar with how racism has contributed to health disparities.
The medical student-run group WhiteCoats4BlackLives has helped organize ongoing, large-scale events at hospitals, medical campuses, and city centers nationwide.“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in late last month in a city park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Read more.
A conversation on race
In this special episode of the Psychcast podast, host Lorenzo Norris, MD, and fourth-year psychiatry resident Brandon C. Newsome, MD, discuss race relations as physicians in the wake of the death of George Floyd. The pair discuss what their patients are experiencing and what they’re experiencing as black physicians.
“Racism – whether or not you witness it, whether or not you utilize it, whether or not you are the subject of it – affects and hurts us all,” Dr. Norris says. “We all have to start to own that. You can’t just stay siloed, because it is going to affect you.” Listen here.
Two journals retract studies on HCQ
The Lancet has retracted a highly cited study that suggested hydroxychloroquine (HCQ) may cause more harm than benefit in patients with COVID-19. Hours later, the New England Journal of Medicine announced that it had retracted a second article by some of the same authors, also on heart disease and COVID-19.
Three authors of the Lancet article wrote in a letter that the action came after concerns were raised about the integrity of the data, and about how the analysis was conducted by Chicago-based Surgisphere Corp and study coauthor Sapan Desai, MD, Surgisphere’s founder and CEO. The authors asked for an independent third-party review of Surgisphere to evaluate the integrity of the trial elements and to replicate the analyses in the article.
“Our independent peer reviewers informed us that Surgisphere would not transfer the full dataset, client contracts, and the full ISO audit report to their servers for analysis, as such transfer would violate client agreements and confidentiality requirements,” the authors wrote, leading them to request a retraction of the paper.
In a similar note, the authors requested that the New England Journal of Medicine retract the earlier article as well.
Both journals had already published “Expression of Concern” notices about the articles. The expression of concern followed an open letter, endorsed by more than 200 scientists, ethicists, and clinicians and posted on May 28, questioning the data and ethics of the study.
Read more.
FDA approves antibiotic to treat pneumonia
The Food and Drug Administration has approved Recarbrio (imipenem-cilastatin and relebactam) for the treatment of hospital-acquired and ventilator-associated bacterial pneumonia in people aged 18 years and older.
Approval for Recarbrio was based on results of a randomized, controlled clinical trial of 535 hospitalized adults with hospital-acquired and ventilator-associated bacterial pneumonia who received either Recarbrio or piperacillin-tazobactam. After 28 days, 16% of patients who received Recarbrio and 21% of patients who received piperacillin-tazobactam had died.
“As a public health agency, the FDA addresses the threat of antimicrobial-resistant infections by facilitating the development of safe and effective new treatments. These efforts provide more options to fight serious bacterial infections and get new, safe and effective therapies to patients as soon as possible,” said Sumathi Nambiar, MD, MPH, of the agency’s Center for Drug Evaluation and Research.
Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
#WhiteCoats4BlackLives stands up to racism
Participants in the growing #WhiteCoats4BlackLives protest against racism say it is a chance to use their status as trusted messengers, show themselves as allies of people of color, and demonstrate that they are familiar with how racism has contributed to health disparities.
The medical student-run group WhiteCoats4BlackLives has helped organize ongoing, large-scale events at hospitals, medical campuses, and city centers nationwide.“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in late last month in a city park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Read more.
A conversation on race
In this special episode of the Psychcast podast, host Lorenzo Norris, MD, and fourth-year psychiatry resident Brandon C. Newsome, MD, discuss race relations as physicians in the wake of the death of George Floyd. The pair discuss what their patients are experiencing and what they’re experiencing as black physicians.
“Racism – whether or not you witness it, whether or not you utilize it, whether or not you are the subject of it – affects and hurts us all,” Dr. Norris says. “We all have to start to own that. You can’t just stay siloed, because it is going to affect you.” Listen here.
Two journals retract studies on HCQ
The Lancet has retracted a highly cited study that suggested hydroxychloroquine (HCQ) may cause more harm than benefit in patients with COVID-19. Hours later, the New England Journal of Medicine announced that it had retracted a second article by some of the same authors, also on heart disease and COVID-19.
Three authors of the Lancet article wrote in a letter that the action came after concerns were raised about the integrity of the data, and about how the analysis was conducted by Chicago-based Surgisphere Corp and study coauthor Sapan Desai, MD, Surgisphere’s founder and CEO. The authors asked for an independent third-party review of Surgisphere to evaluate the integrity of the trial elements and to replicate the analyses in the article.
“Our independent peer reviewers informed us that Surgisphere would not transfer the full dataset, client contracts, and the full ISO audit report to their servers for analysis, as such transfer would violate client agreements and confidentiality requirements,” the authors wrote, leading them to request a retraction of the paper.
In a similar note, the authors requested that the New England Journal of Medicine retract the earlier article as well.
Both journals had already published “Expression of Concern” notices about the articles. The expression of concern followed an open letter, endorsed by more than 200 scientists, ethicists, and clinicians and posted on May 28, questioning the data and ethics of the study.
Read more.
FDA approves antibiotic to treat pneumonia
The Food and Drug Administration has approved Recarbrio (imipenem-cilastatin and relebactam) for the treatment of hospital-acquired and ventilator-associated bacterial pneumonia in people aged 18 years and older.
Approval for Recarbrio was based on results of a randomized, controlled clinical trial of 535 hospitalized adults with hospital-acquired and ventilator-associated bacterial pneumonia who received either Recarbrio or piperacillin-tazobactam. After 28 days, 16% of patients who received Recarbrio and 21% of patients who received piperacillin-tazobactam had died.
“As a public health agency, the FDA addresses the threat of antimicrobial-resistant infections by facilitating the development of safe and effective new treatments. These efforts provide more options to fight serious bacterial infections and get new, safe and effective therapies to patients as soon as possible,” said Sumathi Nambiar, MD, MPH, of the agency’s Center for Drug Evaluation and Research.
Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
#WhiteCoats4BlackLives stands up to racism
Participants in the growing #WhiteCoats4BlackLives protest against racism say it is a chance to use their status as trusted messengers, show themselves as allies of people of color, and demonstrate that they are familiar with how racism has contributed to health disparities.
The medical student-run group WhiteCoats4BlackLives has helped organize ongoing, large-scale events at hospitals, medical campuses, and city centers nationwide.“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in late last month in a city park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Read more.
A conversation on race
In this special episode of the Psychcast podast, host Lorenzo Norris, MD, and fourth-year psychiatry resident Brandon C. Newsome, MD, discuss race relations as physicians in the wake of the death of George Floyd. The pair discuss what their patients are experiencing and what they’re experiencing as black physicians.
“Racism – whether or not you witness it, whether or not you utilize it, whether or not you are the subject of it – affects and hurts us all,” Dr. Norris says. “We all have to start to own that. You can’t just stay siloed, because it is going to affect you.” Listen here.
Two journals retract studies on HCQ
The Lancet has retracted a highly cited study that suggested hydroxychloroquine (HCQ) may cause more harm than benefit in patients with COVID-19. Hours later, the New England Journal of Medicine announced that it had retracted a second article by some of the same authors, also on heart disease and COVID-19.
Three authors of the Lancet article wrote in a letter that the action came after concerns were raised about the integrity of the data, and about how the analysis was conducted by Chicago-based Surgisphere Corp and study coauthor Sapan Desai, MD, Surgisphere’s founder and CEO. The authors asked for an independent third-party review of Surgisphere to evaluate the integrity of the trial elements and to replicate the analyses in the article.
“Our independent peer reviewers informed us that Surgisphere would not transfer the full dataset, client contracts, and the full ISO audit report to their servers for analysis, as such transfer would violate client agreements and confidentiality requirements,” the authors wrote, leading them to request a retraction of the paper.
In a similar note, the authors requested that the New England Journal of Medicine retract the earlier article as well.
Both journals had already published “Expression of Concern” notices about the articles. The expression of concern followed an open letter, endorsed by more than 200 scientists, ethicists, and clinicians and posted on May 28, questioning the data and ethics of the study.
Read more.
FDA approves antibiotic to treat pneumonia
The Food and Drug Administration has approved Recarbrio (imipenem-cilastatin and relebactam) for the treatment of hospital-acquired and ventilator-associated bacterial pneumonia in people aged 18 years and older.
Approval for Recarbrio was based on results of a randomized, controlled clinical trial of 535 hospitalized adults with hospital-acquired and ventilator-associated bacterial pneumonia who received either Recarbrio or piperacillin-tazobactam. After 28 days, 16% of patients who received Recarbrio and 21% of patients who received piperacillin-tazobactam had died.
“As a public health agency, the FDA addresses the threat of antimicrobial-resistant infections by facilitating the development of safe and effective new treatments. These efforts provide more options to fight serious bacterial infections and get new, safe and effective therapies to patients as soon as possible,” said Sumathi Nambiar, MD, MPH, of the agency’s Center for Drug Evaluation and Research.
Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
#WhiteCoats4BlackLives: A ‘platform for good’
like those on vivid display during the COVID-19 pandemic.
Sporadic protests – with participants in scrubs or white coats kneeling for 8 minutes and 46 seconds in memory of George Floyd – have quickly grown into organized, ongoing, large-scale events at hospitals, medical campuses, and city centers in New York, Indianapolis, Atlanta, Austin, Houston, Boston, Miami, Portland, Sacramento, Los Angeles, Philadelphia, and Albuquerque, among others.
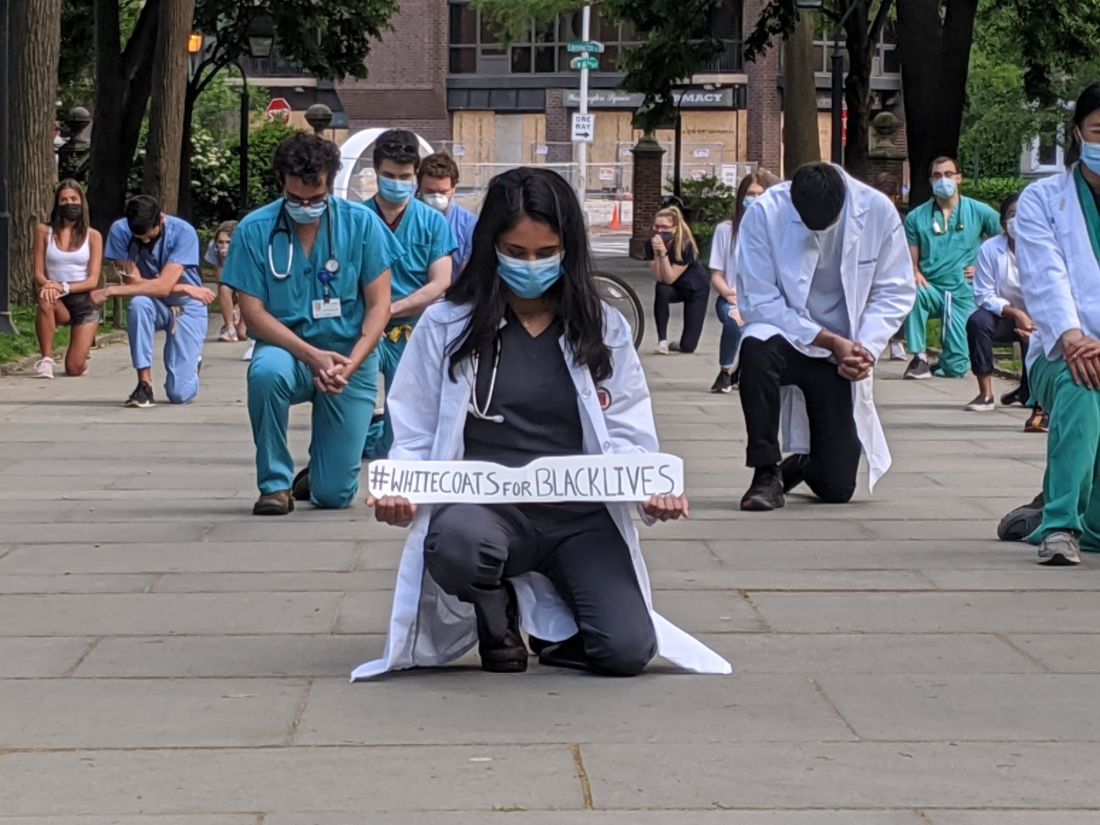
The group WhiteCoats4BlackLives began with a “die-in” protest in 2014, and the medical student–run organization continues to organize, with a large number of protests scheduled to occur simultaneously on June 5 at 1:00 p.m. Eastern Time.
“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in on May 31 in the city’s Washington Square Park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Crystal Nnenne Azu, MD, a third-year internal medicine resident at Indiana University, who has long worked on increasing diversity in medicine, said she helped organize a march and kneel-in at the school’s Eskenazi Hospital campus on June 3 to educate and show support.
Some 500-1,000 health care providers in scrubs and white coats turned out, tweeted one observer.
“Racism is a public health crisis,” Dr. Azu said. “This COVID epidemic has definitely raised that awareness even more for many of our colleagues.”
Disproportionate death rates in blacks and Latinos are “not just related to individual choices but also systemic racism,” she said.
The march also called out police brutality and the “angst” that many people feel about it, said Dr. Azu. “People want an avenue to express their discomfort, to raise awareness, and also show their solidarity and support for peaceful protests,” she said.
A June 4 protest and “die-in” – held to honor black and indigenous lives at the University of New Mexico Health Sciences campus in Albuquerque – was personal for Jaron Kee, MD, a first-year family medicine resident. He was raised on the Navajo reservation in Crystal, New Mexico, and has watched COVID-19 devastate the tribe, adding insult to years of health disparities, police brutality, and neglect of thousands of missing and murdered indigenous women, he said.
Participating is a means of reassuring the community that “we’re allies and that their suffering and their livelihood is something that we don’t underrecognize,” Dr. Kee said. These values spurred him to enter medicine, he said.
Eileen Barrett, MD, MPH, a hospitalist and assistant professor of internal medicine at the University of New Mexico School of Medicine, who also attended the “die-in,” said she hopes that peers, in particular people of color, see that they have allies at work “who are committed to being anti-racist.”
It’s also “a statement to the community at large that physicians and other healthcare workers strive to be anti-racist and do our best to support our African American and indigenous peers, students, patients, and community members,” she said.
Now is different
Some residents said they felt particularly moved to act now – as the country entered a second week of protests in response to George Floyd’s death and as the COVID-19 pandemic highlighted the devastating toll of health disparities.
“This protest feels different to me,” said Ian Fields, MD, a urogynecology fellow at Oregon Health Sciences University (OHSU) School of Medicine. “The events over the last couple of weeks were just a big catalyst for this to explode,” he said.
“I was very intent, as a white male physician, just coming to acknowledge the privilege that I have, and to do something,” Dr. Fields said, adding that as an obstetrician-gynecologist, he sees the results of health disparities daily. He took part in a kneel-in and demonstration with OHSU colleagues on June 2 at Portland’s Pioneer Courthouse Square.
It’s okay to be sad and mourn, Dr. Fields said, but, he added, “nobody needs our tears necessarily right now. They need us to show up and to speak up about what we see going on.”
“It feels like it’s a national conversation,” said Dr. Verghese. The White Coats movement is “not an issue that’s confined to the black community – this is not an issue that’s a ‘black thing’ – this is a humanitarian thing,” she said.
Dr. Verghese, an Indian American who said that no one would mistake her for being white, said she still wants to acknowledge that she has privilege, as well as biases. All the patients in the COVID-19 unit where she works are African American, but she said she hadn’t initially noticed.
“What’s shocking is that I didn’t think about it,” she said. “I do have to recognize my own biases.”
Protesting During a Pandemic
Despite the demands of treating COVID-19 patients, healthcare professionals have made the White Coat protests a priority, they said. Most – but not all – of the White Coats protests have been on medical campuses, allowing health care professionals to quickly assemble and get back to work. Plus, all of the protests have called on attendees to march and gather safely – with masks and distancing.
“Seeing that we are working in the hospital, it’s important for us to be wearing our masks, to be social distancing,” Dr. Azu said. Organizers asked attendees to ensure that they protested in a way that kept them “from worsening the COVID epidemic,” said Dr. Azu.
Unlike many others, the first protest in Portland was in conjunction with a larger group that assembles every evening in the square, said Dr. Fields. The physician protesters were wearing masks and maintaining distance from each other, especially when they kneeled, he said.
The protests have provided an escape from the futility of not being able to do anything for COVID-19 patients except to provide support, said Dr. Verghese. “In so many ways, we find ourselves powerless,” she said.
Protesting, Dr. Verghese added, was “one tiny moment where I got to regain my sense of agency, that I could actually do something about this.”
This article first appeared on Medscape.com.
like those on vivid display during the COVID-19 pandemic.
Sporadic protests – with participants in scrubs or white coats kneeling for 8 minutes and 46 seconds in memory of George Floyd – have quickly grown into organized, ongoing, large-scale events at hospitals, medical campuses, and city centers in New York, Indianapolis, Atlanta, Austin, Houston, Boston, Miami, Portland, Sacramento, Los Angeles, Philadelphia, and Albuquerque, among others.
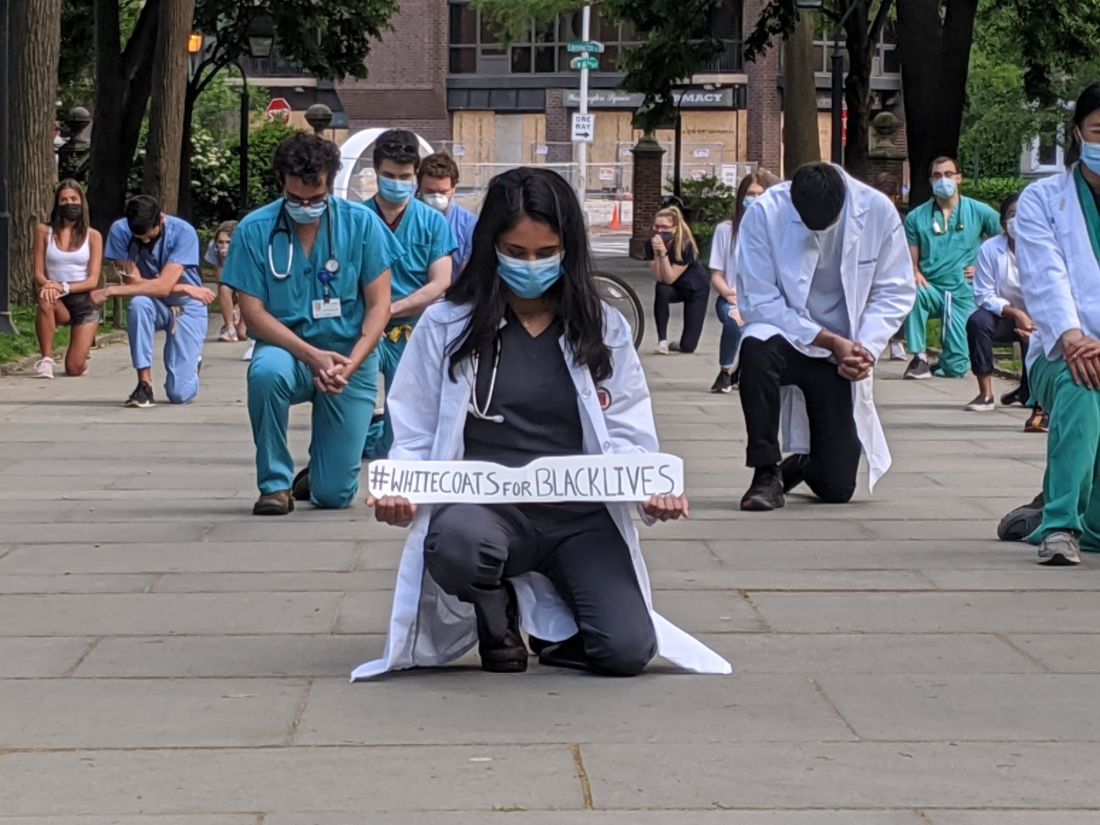
The group WhiteCoats4BlackLives began with a “die-in” protest in 2014, and the medical student–run organization continues to organize, with a large number of protests scheduled to occur simultaneously on June 5 at 1:00 p.m. Eastern Time.
“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in on May 31 in the city’s Washington Square Park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Crystal Nnenne Azu, MD, a third-year internal medicine resident at Indiana University, who has long worked on increasing diversity in medicine, said she helped organize a march and kneel-in at the school’s Eskenazi Hospital campus on June 3 to educate and show support.
Some 500-1,000 health care providers in scrubs and white coats turned out, tweeted one observer.
“Racism is a public health crisis,” Dr. Azu said. “This COVID epidemic has definitely raised that awareness even more for many of our colleagues.”
Disproportionate death rates in blacks and Latinos are “not just related to individual choices but also systemic racism,” she said.
The march also called out police brutality and the “angst” that many people feel about it, said Dr. Azu. “People want an avenue to express their discomfort, to raise awareness, and also show their solidarity and support for peaceful protests,” she said.
A June 4 protest and “die-in” – held to honor black and indigenous lives at the University of New Mexico Health Sciences campus in Albuquerque – was personal for Jaron Kee, MD, a first-year family medicine resident. He was raised on the Navajo reservation in Crystal, New Mexico, and has watched COVID-19 devastate the tribe, adding insult to years of health disparities, police brutality, and neglect of thousands of missing and murdered indigenous women, he said.
Participating is a means of reassuring the community that “we’re allies and that their suffering and their livelihood is something that we don’t underrecognize,” Dr. Kee said. These values spurred him to enter medicine, he said.
Eileen Barrett, MD, MPH, a hospitalist and assistant professor of internal medicine at the University of New Mexico School of Medicine, who also attended the “die-in,” said she hopes that peers, in particular people of color, see that they have allies at work “who are committed to being anti-racist.”
It’s also “a statement to the community at large that physicians and other healthcare workers strive to be anti-racist and do our best to support our African American and indigenous peers, students, patients, and community members,” she said.
Now is different
Some residents said they felt particularly moved to act now – as the country entered a second week of protests in response to George Floyd’s death and as the COVID-19 pandemic highlighted the devastating toll of health disparities.
“This protest feels different to me,” said Ian Fields, MD, a urogynecology fellow at Oregon Health Sciences University (OHSU) School of Medicine. “The events over the last couple of weeks were just a big catalyst for this to explode,” he said.
“I was very intent, as a white male physician, just coming to acknowledge the privilege that I have, and to do something,” Dr. Fields said, adding that as an obstetrician-gynecologist, he sees the results of health disparities daily. He took part in a kneel-in and demonstration with OHSU colleagues on June 2 at Portland’s Pioneer Courthouse Square.
It’s okay to be sad and mourn, Dr. Fields said, but, he added, “nobody needs our tears necessarily right now. They need us to show up and to speak up about what we see going on.”
“It feels like it’s a national conversation,” said Dr. Verghese. The White Coats movement is “not an issue that’s confined to the black community – this is not an issue that’s a ‘black thing’ – this is a humanitarian thing,” she said.
Dr. Verghese, an Indian American who said that no one would mistake her for being white, said she still wants to acknowledge that she has privilege, as well as biases. All the patients in the COVID-19 unit where she works are African American, but she said she hadn’t initially noticed.
“What’s shocking is that I didn’t think about it,” she said. “I do have to recognize my own biases.”
Protesting During a Pandemic
Despite the demands of treating COVID-19 patients, healthcare professionals have made the White Coat protests a priority, they said. Most – but not all – of the White Coats protests have been on medical campuses, allowing health care professionals to quickly assemble and get back to work. Plus, all of the protests have called on attendees to march and gather safely – with masks and distancing.
“Seeing that we are working in the hospital, it’s important for us to be wearing our masks, to be social distancing,” Dr. Azu said. Organizers asked attendees to ensure that they protested in a way that kept them “from worsening the COVID epidemic,” said Dr. Azu.
Unlike many others, the first protest in Portland was in conjunction with a larger group that assembles every evening in the square, said Dr. Fields. The physician protesters were wearing masks and maintaining distance from each other, especially when they kneeled, he said.
The protests have provided an escape from the futility of not being able to do anything for COVID-19 patients except to provide support, said Dr. Verghese. “In so many ways, we find ourselves powerless,” she said.
Protesting, Dr. Verghese added, was “one tiny moment where I got to regain my sense of agency, that I could actually do something about this.”
This article first appeared on Medscape.com.
like those on vivid display during the COVID-19 pandemic.
Sporadic protests – with participants in scrubs or white coats kneeling for 8 minutes and 46 seconds in memory of George Floyd – have quickly grown into organized, ongoing, large-scale events at hospitals, medical campuses, and city centers in New York, Indianapolis, Atlanta, Austin, Houston, Boston, Miami, Portland, Sacramento, Los Angeles, Philadelphia, and Albuquerque, among others.
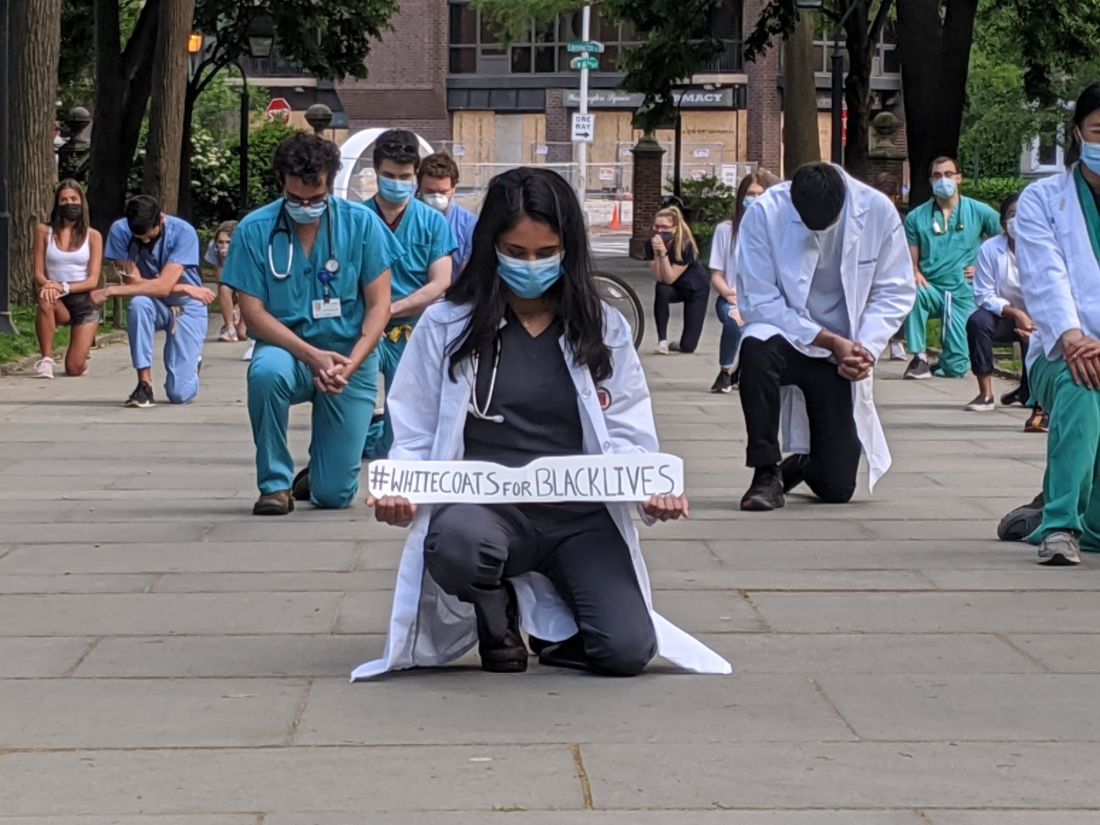
The group WhiteCoats4BlackLives began with a “die-in” protest in 2014, and the medical student–run organization continues to organize, with a large number of protests scheduled to occur simultaneously on June 5 at 1:00 p.m. Eastern Time.
“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in on May 31 in the city’s Washington Square Park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Crystal Nnenne Azu, MD, a third-year internal medicine resident at Indiana University, who has long worked on increasing diversity in medicine, said she helped organize a march and kneel-in at the school’s Eskenazi Hospital campus on June 3 to educate and show support.
Some 500-1,000 health care providers in scrubs and white coats turned out, tweeted one observer.
“Racism is a public health crisis,” Dr. Azu said. “This COVID epidemic has definitely raised that awareness even more for many of our colleagues.”
Disproportionate death rates in blacks and Latinos are “not just related to individual choices but also systemic racism,” she said.
The march also called out police brutality and the “angst” that many people feel about it, said Dr. Azu. “People want an avenue to express their discomfort, to raise awareness, and also show their solidarity and support for peaceful protests,” she said.
A June 4 protest and “die-in” – held to honor black and indigenous lives at the University of New Mexico Health Sciences campus in Albuquerque – was personal for Jaron Kee, MD, a first-year family medicine resident. He was raised on the Navajo reservation in Crystal, New Mexico, and has watched COVID-19 devastate the tribe, adding insult to years of health disparities, police brutality, and neglect of thousands of missing and murdered indigenous women, he said.
Participating is a means of reassuring the community that “we’re allies and that their suffering and their livelihood is something that we don’t underrecognize,” Dr. Kee said. These values spurred him to enter medicine, he said.
Eileen Barrett, MD, MPH, a hospitalist and assistant professor of internal medicine at the University of New Mexico School of Medicine, who also attended the “die-in,” said she hopes that peers, in particular people of color, see that they have allies at work “who are committed to being anti-racist.”
It’s also “a statement to the community at large that physicians and other healthcare workers strive to be anti-racist and do our best to support our African American and indigenous peers, students, patients, and community members,” she said.
Now is different
Some residents said they felt particularly moved to act now – as the country entered a second week of protests in response to George Floyd’s death and as the COVID-19 pandemic highlighted the devastating toll of health disparities.
“This protest feels different to me,” said Ian Fields, MD, a urogynecology fellow at Oregon Health Sciences University (OHSU) School of Medicine. “The events over the last couple of weeks were just a big catalyst for this to explode,” he said.
“I was very intent, as a white male physician, just coming to acknowledge the privilege that I have, and to do something,” Dr. Fields said, adding that as an obstetrician-gynecologist, he sees the results of health disparities daily. He took part in a kneel-in and demonstration with OHSU colleagues on June 2 at Portland’s Pioneer Courthouse Square.
It’s okay to be sad and mourn, Dr. Fields said, but, he added, “nobody needs our tears necessarily right now. They need us to show up and to speak up about what we see going on.”
“It feels like it’s a national conversation,” said Dr. Verghese. The White Coats movement is “not an issue that’s confined to the black community – this is not an issue that’s a ‘black thing’ – this is a humanitarian thing,” she said.
Dr. Verghese, an Indian American who said that no one would mistake her for being white, said she still wants to acknowledge that she has privilege, as well as biases. All the patients in the COVID-19 unit where she works are African American, but she said she hadn’t initially noticed.
“What’s shocking is that I didn’t think about it,” she said. “I do have to recognize my own biases.”
Protesting During a Pandemic
Despite the demands of treating COVID-19 patients, healthcare professionals have made the White Coat protests a priority, they said. Most – but not all – of the White Coats protests have been on medical campuses, allowing health care professionals to quickly assemble and get back to work. Plus, all of the protests have called on attendees to march and gather safely – with masks and distancing.
“Seeing that we are working in the hospital, it’s important for us to be wearing our masks, to be social distancing,” Dr. Azu said. Organizers asked attendees to ensure that they protested in a way that kept them “from worsening the COVID epidemic,” said Dr. Azu.
Unlike many others, the first protest in Portland was in conjunction with a larger group that assembles every evening in the square, said Dr. Fields. The physician protesters were wearing masks and maintaining distance from each other, especially when they kneeled, he said.
The protests have provided an escape from the futility of not being able to do anything for COVID-19 patients except to provide support, said Dr. Verghese. “In so many ways, we find ourselves powerless,” she said.
Protesting, Dr. Verghese added, was “one tiny moment where I got to regain my sense of agency, that I could actually do something about this.”
This article first appeared on Medscape.com.
COVID-19-related inflammatory condition more common in black children in small study
More evidence has linked the Kawasaki-like multisystem inflammatory syndrome in children to COVID-19 and suggests that black children have a greater risk of the condition, according to a study published in the BMJ.
A small observational study in Paris found more than half of the 21 children who were admitted for the condition at the city’s pediatric hospital for COVID-19 patients were of African ancestry.
“The observation of a higher proportion of patients of African ancestry is consistent with recent findings, suggesting an effect of either social and living conditions or genetic susceptibility,” wrote Julie Toubiana, MD, PhD, of the University of Paris and the Pasteur Institute, and colleagues.
The findings did not surprise Edward M. Behrens, MD, chief of the division of rheumatology at Children’s Hospital of Philadelphia, whose institution has seen similar disparities that he attributes to social disadvantages.
“Infection rate will be higher in vulnerable populations that are less able to socially distance, have disproportionate numbers of essential workers, and have less access to health care and other resources,” Dr. Behrens said in an interview. “While there may be a role for genetics, environment – including social disparities – is almost certainly playing a role.”
Although the study’s small size is a limitation, he said, “the features described seem to mirror the experience of our center and what has been discussed more broadly amongst U.S. physicians.”
Byron Whyte, MD, a pediatrician in private practice in southeast Washington, found the differences in race interesting, but said the study was too small to draw any conclusions or generalize to the United States. But social disparities related to race are likely similar in France as they are in the United States, he said.
The prospective observational study assessed the clinical and demographic characteristics of all patients under age 18 who met the criteria for Kawasaki disease and were admitted between April 27 and May 20 to the Necker Hospital for Sick Children in Paris.
The 21 children had an average age of 8 years (ranging from 3 to 16), and 57% had at least one parent from sub-Saharan Africa or a Caribbean island; 14% had parents from Asia (two from China and one from Sri Lanka). The authors noted in their discussion that past U.S. and U.K. studies of Kawasaki disease have found a 2.5 times greater risk in Asian-American children and 1.5 times greater risk in African-American children compared with children with European ancestry.
Most of the patients (81%) needed intensive care, with 57% presenting with Kawasaki disease shock syndrome and 67% with myocarditis. Dr. Toubiana and associates also noted that “gastrointestinal symptoms were also unusually common, affecting all of our 21 patients.”
Only nine of the children reported having symptoms of a viral-like illness when they were admitted, primarily headache, cough, coryza, and fever, plus anosmia in one child. Among those children, the Kawasaki symptoms began a median 45 days after onset of the viral symptoms (range 18-79 days).
Only two children showed no positive test result for current COVID-19 infection or antibodies. Eight (38%) of the children had positive PCR tests for SARS-CoV2, and 19 (90%) had positive tests for IgG antibodies. The two patients with both negative tests did not require intensive care and did not have myocarditis.
About half the patients (52%) met all the criteria of Kawasaki disease, and the other 10 had “incomplete Kawasaki disease.” The most common Kawasaki symptoms were the polymorphous skin rash, occurring in 76% of the patients, changes to the lips and oral cavity (76%), and bilateral bulbar conjunctival injection (81%). Three patients (14%) had pleural effusion, and 10 of them (48%) had pericardial effusion, Dr. Toubiana and associates reported.
But Dr. Behrens said he disagrees with the assertion that the illness described in the paper and what he is seeing at Children’s Hospital of Philadelphia is related to Kawasaki disease.
“Most experts here in the U.S. seem to agree this is not Kawasaki disease, but a distinct clinical syndrome called multisystem inflammatory syndrome in children, or MIS-C, that seems to have some overlap with the most nonspecific features of Kawasaki disease,” said Dr. Behrens, who is the Joseph Lee Hollander Chair in Pediatric Rheumatology at Children’s Hospital of Philadelphia. He has coauthored a study currently under review and available as a preprint soon that examines the biologic mechanisms underlying MIS-C.
Neither Dr. Behrens nor Dr. Whyte believed the findings had clinical implications that might change practice, but Dr. Whyte said he will be paying closer attention to the black children he treats – 99% of his practice – who are recovering from COVID-19.
“And, because we know that the concerns of African Americans are often overlooked in health care,” Dr. Whyte said, physicians should “pay a little more attention to symptom reporting on those kids, since there is a possibility that those kids would need hospitalization.”
All the patients in the study were treated with intravenous immunoglobulin, and corticosteroids were administered to 10 of them (48%). Their median hospital stay was 8 days (5 days in intensive care), and all were discharged without any deaths.
“Only one patient had symptoms suggestive of acute covid-19 and most had positive serum test results for IgG antibodies, suggesting that the development of Kawasaki disease in these patients is more likely to be the result of a postviral immunological reaction,” Dr. Toubiana and associates said.
The research received no external funding, and neither the authors nor other quoted physicians had any relevant financial disclosures.
SOURCE: Toubiana J et al. BMJ. 2020 Jun 3, doi: 10.1136 bmj.m2094.
More evidence has linked the Kawasaki-like multisystem inflammatory syndrome in children to COVID-19 and suggests that black children have a greater risk of the condition, according to a study published in the BMJ.
A small observational study in Paris found more than half of the 21 children who were admitted for the condition at the city’s pediatric hospital for COVID-19 patients were of African ancestry.
“The observation of a higher proportion of patients of African ancestry is consistent with recent findings, suggesting an effect of either social and living conditions or genetic susceptibility,” wrote Julie Toubiana, MD, PhD, of the University of Paris and the Pasteur Institute, and colleagues.
The findings did not surprise Edward M. Behrens, MD, chief of the division of rheumatology at Children’s Hospital of Philadelphia, whose institution has seen similar disparities that he attributes to social disadvantages.
“Infection rate will be higher in vulnerable populations that are less able to socially distance, have disproportionate numbers of essential workers, and have less access to health care and other resources,” Dr. Behrens said in an interview. “While there may be a role for genetics, environment – including social disparities – is almost certainly playing a role.”
Although the study’s small size is a limitation, he said, “the features described seem to mirror the experience of our center and what has been discussed more broadly amongst U.S. physicians.”
Byron Whyte, MD, a pediatrician in private practice in southeast Washington, found the differences in race interesting, but said the study was too small to draw any conclusions or generalize to the United States. But social disparities related to race are likely similar in France as they are in the United States, he said.
The prospective observational study assessed the clinical and demographic characteristics of all patients under age 18 who met the criteria for Kawasaki disease and were admitted between April 27 and May 20 to the Necker Hospital for Sick Children in Paris.
The 21 children had an average age of 8 years (ranging from 3 to 16), and 57% had at least one parent from sub-Saharan Africa or a Caribbean island; 14% had parents from Asia (two from China and one from Sri Lanka). The authors noted in their discussion that past U.S. and U.K. studies of Kawasaki disease have found a 2.5 times greater risk in Asian-American children and 1.5 times greater risk in African-American children compared with children with European ancestry.
Most of the patients (81%) needed intensive care, with 57% presenting with Kawasaki disease shock syndrome and 67% with myocarditis. Dr. Toubiana and associates also noted that “gastrointestinal symptoms were also unusually common, affecting all of our 21 patients.”
Only nine of the children reported having symptoms of a viral-like illness when they were admitted, primarily headache, cough, coryza, and fever, plus anosmia in one child. Among those children, the Kawasaki symptoms began a median 45 days after onset of the viral symptoms (range 18-79 days).
Only two children showed no positive test result for current COVID-19 infection or antibodies. Eight (38%) of the children had positive PCR tests for SARS-CoV2, and 19 (90%) had positive tests for IgG antibodies. The two patients with both negative tests did not require intensive care and did not have myocarditis.
About half the patients (52%) met all the criteria of Kawasaki disease, and the other 10 had “incomplete Kawasaki disease.” The most common Kawasaki symptoms were the polymorphous skin rash, occurring in 76% of the patients, changes to the lips and oral cavity (76%), and bilateral bulbar conjunctival injection (81%). Three patients (14%) had pleural effusion, and 10 of them (48%) had pericardial effusion, Dr. Toubiana and associates reported.
But Dr. Behrens said he disagrees with the assertion that the illness described in the paper and what he is seeing at Children’s Hospital of Philadelphia is related to Kawasaki disease.
“Most experts here in the U.S. seem to agree this is not Kawasaki disease, but a distinct clinical syndrome called multisystem inflammatory syndrome in children, or MIS-C, that seems to have some overlap with the most nonspecific features of Kawasaki disease,” said Dr. Behrens, who is the Joseph Lee Hollander Chair in Pediatric Rheumatology at Children’s Hospital of Philadelphia. He has coauthored a study currently under review and available as a preprint soon that examines the biologic mechanisms underlying MIS-C.
Neither Dr. Behrens nor Dr. Whyte believed the findings had clinical implications that might change practice, but Dr. Whyte said he will be paying closer attention to the black children he treats – 99% of his practice – who are recovering from COVID-19.
“And, because we know that the concerns of African Americans are often overlooked in health care,” Dr. Whyte said, physicians should “pay a little more attention to symptom reporting on those kids, since there is a possibility that those kids would need hospitalization.”
All the patients in the study were treated with intravenous immunoglobulin, and corticosteroids were administered to 10 of them (48%). Their median hospital stay was 8 days (5 days in intensive care), and all were discharged without any deaths.
“Only one patient had symptoms suggestive of acute covid-19 and most had positive serum test results for IgG antibodies, suggesting that the development of Kawasaki disease in these patients is more likely to be the result of a postviral immunological reaction,” Dr. Toubiana and associates said.
The research received no external funding, and neither the authors nor other quoted physicians had any relevant financial disclosures.
SOURCE: Toubiana J et al. BMJ. 2020 Jun 3, doi: 10.1136 bmj.m2094.
More evidence has linked the Kawasaki-like multisystem inflammatory syndrome in children to COVID-19 and suggests that black children have a greater risk of the condition, according to a study published in the BMJ.
A small observational study in Paris found more than half of the 21 children who were admitted for the condition at the city’s pediatric hospital for COVID-19 patients were of African ancestry.
“The observation of a higher proportion of patients of African ancestry is consistent with recent findings, suggesting an effect of either social and living conditions or genetic susceptibility,” wrote Julie Toubiana, MD, PhD, of the University of Paris and the Pasteur Institute, and colleagues.
The findings did not surprise Edward M. Behrens, MD, chief of the division of rheumatology at Children’s Hospital of Philadelphia, whose institution has seen similar disparities that he attributes to social disadvantages.
“Infection rate will be higher in vulnerable populations that are less able to socially distance, have disproportionate numbers of essential workers, and have less access to health care and other resources,” Dr. Behrens said in an interview. “While there may be a role for genetics, environment – including social disparities – is almost certainly playing a role.”
Although the study’s small size is a limitation, he said, “the features described seem to mirror the experience of our center and what has been discussed more broadly amongst U.S. physicians.”
Byron Whyte, MD, a pediatrician in private practice in southeast Washington, found the differences in race interesting, but said the study was too small to draw any conclusions or generalize to the United States. But social disparities related to race are likely similar in France as they are in the United States, he said.
The prospective observational study assessed the clinical and demographic characteristics of all patients under age 18 who met the criteria for Kawasaki disease and were admitted between April 27 and May 20 to the Necker Hospital for Sick Children in Paris.
The 21 children had an average age of 8 years (ranging from 3 to 16), and 57% had at least one parent from sub-Saharan Africa or a Caribbean island; 14% had parents from Asia (two from China and one from Sri Lanka). The authors noted in their discussion that past U.S. and U.K. studies of Kawasaki disease have found a 2.5 times greater risk in Asian-American children and 1.5 times greater risk in African-American children compared with children with European ancestry.
Most of the patients (81%) needed intensive care, with 57% presenting with Kawasaki disease shock syndrome and 67% with myocarditis. Dr. Toubiana and associates also noted that “gastrointestinal symptoms were also unusually common, affecting all of our 21 patients.”
Only nine of the children reported having symptoms of a viral-like illness when they were admitted, primarily headache, cough, coryza, and fever, plus anosmia in one child. Among those children, the Kawasaki symptoms began a median 45 days after onset of the viral symptoms (range 18-79 days).
Only two children showed no positive test result for current COVID-19 infection or antibodies. Eight (38%) of the children had positive PCR tests for SARS-CoV2, and 19 (90%) had positive tests for IgG antibodies. The two patients with both negative tests did not require intensive care and did not have myocarditis.
About half the patients (52%) met all the criteria of Kawasaki disease, and the other 10 had “incomplete Kawasaki disease.” The most common Kawasaki symptoms were the polymorphous skin rash, occurring in 76% of the patients, changes to the lips and oral cavity (76%), and bilateral bulbar conjunctival injection (81%). Three patients (14%) had pleural effusion, and 10 of them (48%) had pericardial effusion, Dr. Toubiana and associates reported.
But Dr. Behrens said he disagrees with the assertion that the illness described in the paper and what he is seeing at Children’s Hospital of Philadelphia is related to Kawasaki disease.
“Most experts here in the U.S. seem to agree this is not Kawasaki disease, but a distinct clinical syndrome called multisystem inflammatory syndrome in children, or MIS-C, that seems to have some overlap with the most nonspecific features of Kawasaki disease,” said Dr. Behrens, who is the Joseph Lee Hollander Chair in Pediatric Rheumatology at Children’s Hospital of Philadelphia. He has coauthored a study currently under review and available as a preprint soon that examines the biologic mechanisms underlying MIS-C.
Neither Dr. Behrens nor Dr. Whyte believed the findings had clinical implications that might change practice, but Dr. Whyte said he will be paying closer attention to the black children he treats – 99% of his practice – who are recovering from COVID-19.
“And, because we know that the concerns of African Americans are often overlooked in health care,” Dr. Whyte said, physicians should “pay a little more attention to symptom reporting on those kids, since there is a possibility that those kids would need hospitalization.”
All the patients in the study were treated with intravenous immunoglobulin, and corticosteroids were administered to 10 of them (48%). Their median hospital stay was 8 days (5 days in intensive care), and all were discharged without any deaths.
“Only one patient had symptoms suggestive of acute covid-19 and most had positive serum test results for IgG antibodies, suggesting that the development of Kawasaki disease in these patients is more likely to be the result of a postviral immunological reaction,” Dr. Toubiana and associates said.
The research received no external funding, and neither the authors nor other quoted physicians had any relevant financial disclosures.
SOURCE: Toubiana J et al. BMJ. 2020 Jun 3, doi: 10.1136 bmj.m2094.
FROM BMJ
COVID-19 neurologic effects: Does the virus directly attack the brain?
A new review article summarizes what is known so far, and what clinicians need to look out for.
“We frequently see neurological conditions in people with COVID-19, but we understand very little about these effects. Is it the virus entering the brain/nerves or are they a result of a general inflammation or immune response – a bystander effect of people being severely ill. It is probably a combination of both,” said senior author Serena Spudich, MD, Gilbert H. Glaser Professor of Neurology; division chief of neurological infections & global neurology; and codirector of the Center for Neuroepidemiology and Clinical Neurological Research at Yale University, New Haven, Conn.
“Our message is that there are fairly frequent neurological sequelae of COVID-19 and we need to be alert to these, and to try to understand the potential long-term consequences,” she said.
The review was published online May 29 in JAMA Neurology.
Brain changes linked to loss of smell
In a separate article also published online in JAMA Neurology the same day, an Italian group describes a COVID-19 patient with anosmia (loss of sense of smell) who showed brain abnormalities on MRI in the areas associated with smell – the right gyrus rectus and the olfactory bulbs. These changes were resolved on later scan and the patient recovered her sense of smell.
“Based on the MRI findings, we can speculate that SARS-CoV-2 might invade the brain through the olfactory pathway,” conclude the researchers, led by first author Letterio S. Politi, MD, of the department of neuroradiology at IRCCS Istituto Clinico Humanitas and Humanitas University, Milan, Italy.
Can coronaviruses enter the CNS?
Dr. Spudich described this case report as “compelling evidence suggesting that loss of smell is a neurologic effect.”
“Loss of smell and/or taste is a common symptom in COVID-19, so this may suggest that an awful lot of people have some neurological involvement,” Dr. Spudich commented. “While a transient loss of smell or taste is not serious, if the virus has infected brain tissue the question is could this then spread to other parts of the brain and cause other more serious neurological effects,” she added.
In their review article, Dr. Spudich and colleagues present evidence showing that coronaviruses can enter the CNS.
“We know that SARS-1 and MERS have been shown to enter the nervous system and several coronaviruses have been shown to cause direct brain effects,” she said. “There is also some evidence that SARS-CoV-2 can do this too. As well as these latest MRI findings linked to loss of smell, there is a report of the virus being found in endothelial cells in the brain and a French autopsy study has also detected virus in the brain.”
Complications of other systemic effects?
Dr. Spudich is a neurologist specializing in neurologic consequences of infectious disease. “We don’t normally have such vast numbers of patients but in the last 3 months there has been an avalanche,” she says. From her personal experience, she believes the majority of neurologic symptoms in COVID-19 patients are most probably complications of other systemic effects, such as kidney, heart, or liver problems. But there is likely also a direct viral effect on the CNS in some patients.
“Reports from China suggested that serious neurologic effects were present in about one-third of hospitalized COVID-19 patients. I would say in our experience the figure would be less than that – maybe around 10%,” she noted.
Some COVID-19 patients are presenting with primary neurologic symptoms. For example, an elderly person may first develop confusion rather than a cough or shortness of breath; others have had severe headache as an initial COVID-19 symptom, Dr. Spudich reported. “Medical staff need to be aware of this – a severe headache in a patient who doesn’t normally get headaches could be a sign of the virus.”
Some of the neurologic symptoms could be caused by autoimmunity. Dr. Spudich explained that, in acute HIV infection a small proportion of patients can first present with autoimmune neurologic effects such as Guillain-Barré syndrome, an autoimmune condition of the nerves which causes a tingling sensation in the hands and feet. “This is well described in HIV, but we are also now seeing this in COVID-19 patients too,” she said. “A panoply of conditions can be caused by autoimmunity.”
On the increase in strokes that has been reported in COVID-19 patients, Dr. Spudich said, “this could be due to direct effects of the virus (e.g., causing an increase in coagulation or infecting the endothelial cells in the brain) or it could just be the final trigger for patients who were at risk of stroke anyway.”
There have been some very high-profile reports of younger patients with major strokes, she said, “but we haven’t seen that in our hospital. For the most part in my experience, strokes are happening in older COVID-19 patients with stroke risk factors such as AF [atrial fibrillation], hypertension, and diabetes. We haven’t seen a preponderance of strokes in young, otherwise healthy people.”
Even in patients who have neurologic effects as the first sign of COVID-19 infection, it is not known whether these symptoms are caused directly by the virus.
“We know that flu can cause people to have headaches, but that is because of an increase in inflammatory cytokines. On the other hand, patients with acute HIV infection often have headaches as a result of the virus getting into the brain. We don’t know where in this [cluster] COVID-19 virus falls,” Dr. Spudich said.
Much is still unknown
“The information we have is very sparse at this point. We need far more systematic information on this from CSF samples and imaging.” Dr. Spudich urged clinicians to try to collect such information in patients with neurologic symptoms.
Acknowledging that fewer such tests are being done at present because of concerns over infection risk, Dr. Spudich suggested that some changes in procedure may help. “In our hospital we have a portable MRI scanner which can be brought to the patient. This means the patient does not have to move across the hospital for a scan. This helps us to decide whether the patient has had a stroke, which can be missed when patients are on a ventilator.”
It is also unclear whether the neurologic effects seen during COVID-19 infection will last long term.
Dr. Spudich noted that there have been reports of COVID-19 patients discharged from intensive care having difficulty with higher cognitive function for some time thereafter. “This can happen after being in ICU but is it more pronounced in COVID-19 patients? An ongoing study is underway to look at this,” she said.
This article first appeared on Medscape.com.
A new review article summarizes what is known so far, and what clinicians need to look out for.
“We frequently see neurological conditions in people with COVID-19, but we understand very little about these effects. Is it the virus entering the brain/nerves or are they a result of a general inflammation or immune response – a bystander effect of people being severely ill. It is probably a combination of both,” said senior author Serena Spudich, MD, Gilbert H. Glaser Professor of Neurology; division chief of neurological infections & global neurology; and codirector of the Center for Neuroepidemiology and Clinical Neurological Research at Yale University, New Haven, Conn.
“Our message is that there are fairly frequent neurological sequelae of COVID-19 and we need to be alert to these, and to try to understand the potential long-term consequences,” she said.
The review was published online May 29 in JAMA Neurology.
Brain changes linked to loss of smell
In a separate article also published online in JAMA Neurology the same day, an Italian group describes a COVID-19 patient with anosmia (loss of sense of smell) who showed brain abnormalities on MRI in the areas associated with smell – the right gyrus rectus and the olfactory bulbs. These changes were resolved on later scan and the patient recovered her sense of smell.
“Based on the MRI findings, we can speculate that SARS-CoV-2 might invade the brain through the olfactory pathway,” conclude the researchers, led by first author Letterio S. Politi, MD, of the department of neuroradiology at IRCCS Istituto Clinico Humanitas and Humanitas University, Milan, Italy.
Can coronaviruses enter the CNS?
Dr. Spudich described this case report as “compelling evidence suggesting that loss of smell is a neurologic effect.”
“Loss of smell and/or taste is a common symptom in COVID-19, so this may suggest that an awful lot of people have some neurological involvement,” Dr. Spudich commented. “While a transient loss of smell or taste is not serious, if the virus has infected brain tissue the question is could this then spread to other parts of the brain and cause other more serious neurological effects,” she added.
In their review article, Dr. Spudich and colleagues present evidence showing that coronaviruses can enter the CNS.
“We know that SARS-1 and MERS have been shown to enter the nervous system and several coronaviruses have been shown to cause direct brain effects,” she said. “There is also some evidence that SARS-CoV-2 can do this too. As well as these latest MRI findings linked to loss of smell, there is a report of the virus being found in endothelial cells in the brain and a French autopsy study has also detected virus in the brain.”
Complications of other systemic effects?
Dr. Spudich is a neurologist specializing in neurologic consequences of infectious disease. “We don’t normally have such vast numbers of patients but in the last 3 months there has been an avalanche,” she says. From her personal experience, she believes the majority of neurologic symptoms in COVID-19 patients are most probably complications of other systemic effects, such as kidney, heart, or liver problems. But there is likely also a direct viral effect on the CNS in some patients.
“Reports from China suggested that serious neurologic effects were present in about one-third of hospitalized COVID-19 patients. I would say in our experience the figure would be less than that – maybe around 10%,” she noted.
Some COVID-19 patients are presenting with primary neurologic symptoms. For example, an elderly person may first develop confusion rather than a cough or shortness of breath; others have had severe headache as an initial COVID-19 symptom, Dr. Spudich reported. “Medical staff need to be aware of this – a severe headache in a patient who doesn’t normally get headaches could be a sign of the virus.”
Some of the neurologic symptoms could be caused by autoimmunity. Dr. Spudich explained that, in acute HIV infection a small proportion of patients can first present with autoimmune neurologic effects such as Guillain-Barré syndrome, an autoimmune condition of the nerves which causes a tingling sensation in the hands and feet. “This is well described in HIV, but we are also now seeing this in COVID-19 patients too,” she said. “A panoply of conditions can be caused by autoimmunity.”
On the increase in strokes that has been reported in COVID-19 patients, Dr. Spudich said, “this could be due to direct effects of the virus (e.g., causing an increase in coagulation or infecting the endothelial cells in the brain) or it could just be the final trigger for patients who were at risk of stroke anyway.”
There have been some very high-profile reports of younger patients with major strokes, she said, “but we haven’t seen that in our hospital. For the most part in my experience, strokes are happening in older COVID-19 patients with stroke risk factors such as AF [atrial fibrillation], hypertension, and diabetes. We haven’t seen a preponderance of strokes in young, otherwise healthy people.”
Even in patients who have neurologic effects as the first sign of COVID-19 infection, it is not known whether these symptoms are caused directly by the virus.
“We know that flu can cause people to have headaches, but that is because of an increase in inflammatory cytokines. On the other hand, patients with acute HIV infection often have headaches as a result of the virus getting into the brain. We don’t know where in this [cluster] COVID-19 virus falls,” Dr. Spudich said.
Much is still unknown
“The information we have is very sparse at this point. We need far more systematic information on this from CSF samples and imaging.” Dr. Spudich urged clinicians to try to collect such information in patients with neurologic symptoms.
Acknowledging that fewer such tests are being done at present because of concerns over infection risk, Dr. Spudich suggested that some changes in procedure may help. “In our hospital we have a portable MRI scanner which can be brought to the patient. This means the patient does not have to move across the hospital for a scan. This helps us to decide whether the patient has had a stroke, which can be missed when patients are on a ventilator.”
It is also unclear whether the neurologic effects seen during COVID-19 infection will last long term.
Dr. Spudich noted that there have been reports of COVID-19 patients discharged from intensive care having difficulty with higher cognitive function for some time thereafter. “This can happen after being in ICU but is it more pronounced in COVID-19 patients? An ongoing study is underway to look at this,” she said.
This article first appeared on Medscape.com.
A new review article summarizes what is known so far, and what clinicians need to look out for.
“We frequently see neurological conditions in people with COVID-19, but we understand very little about these effects. Is it the virus entering the brain/nerves or are they a result of a general inflammation or immune response – a bystander effect of people being severely ill. It is probably a combination of both,” said senior author Serena Spudich, MD, Gilbert H. Glaser Professor of Neurology; division chief of neurological infections & global neurology; and codirector of the Center for Neuroepidemiology and Clinical Neurological Research at Yale University, New Haven, Conn.
“Our message is that there are fairly frequent neurological sequelae of COVID-19 and we need to be alert to these, and to try to understand the potential long-term consequences,” she said.
The review was published online May 29 in JAMA Neurology.
Brain changes linked to loss of smell
In a separate article also published online in JAMA Neurology the same day, an Italian group describes a COVID-19 patient with anosmia (loss of sense of smell) who showed brain abnormalities on MRI in the areas associated with smell – the right gyrus rectus and the olfactory bulbs. These changes were resolved on later scan and the patient recovered her sense of smell.
“Based on the MRI findings, we can speculate that SARS-CoV-2 might invade the brain through the olfactory pathway,” conclude the researchers, led by first author Letterio S. Politi, MD, of the department of neuroradiology at IRCCS Istituto Clinico Humanitas and Humanitas University, Milan, Italy.
Can coronaviruses enter the CNS?
Dr. Spudich described this case report as “compelling evidence suggesting that loss of smell is a neurologic effect.”
“Loss of smell and/or taste is a common symptom in COVID-19, so this may suggest that an awful lot of people have some neurological involvement,” Dr. Spudich commented. “While a transient loss of smell or taste is not serious, if the virus has infected brain tissue the question is could this then spread to other parts of the brain and cause other more serious neurological effects,” she added.
In their review article, Dr. Spudich and colleagues present evidence showing that coronaviruses can enter the CNS.
“We know that SARS-1 and MERS have been shown to enter the nervous system and several coronaviruses have been shown to cause direct brain effects,” she said. “There is also some evidence that SARS-CoV-2 can do this too. As well as these latest MRI findings linked to loss of smell, there is a report of the virus being found in endothelial cells in the brain and a French autopsy study has also detected virus in the brain.”
Complications of other systemic effects?
Dr. Spudich is a neurologist specializing in neurologic consequences of infectious disease. “We don’t normally have such vast numbers of patients but in the last 3 months there has been an avalanche,” she says. From her personal experience, she believes the majority of neurologic symptoms in COVID-19 patients are most probably complications of other systemic effects, such as kidney, heart, or liver problems. But there is likely also a direct viral effect on the CNS in some patients.
“Reports from China suggested that serious neurologic effects were present in about one-third of hospitalized COVID-19 patients. I would say in our experience the figure would be less than that – maybe around 10%,” she noted.
Some COVID-19 patients are presenting with primary neurologic symptoms. For example, an elderly person may first develop confusion rather than a cough or shortness of breath; others have had severe headache as an initial COVID-19 symptom, Dr. Spudich reported. “Medical staff need to be aware of this – a severe headache in a patient who doesn’t normally get headaches could be a sign of the virus.”
Some of the neurologic symptoms could be caused by autoimmunity. Dr. Spudich explained that, in acute HIV infection a small proportion of patients can first present with autoimmune neurologic effects such as Guillain-Barré syndrome, an autoimmune condition of the nerves which causes a tingling sensation in the hands and feet. “This is well described in HIV, but we are also now seeing this in COVID-19 patients too,” she said. “A panoply of conditions can be caused by autoimmunity.”
On the increase in strokes that has been reported in COVID-19 patients, Dr. Spudich said, “this could be due to direct effects of the virus (e.g., causing an increase in coagulation or infecting the endothelial cells in the brain) or it could just be the final trigger for patients who were at risk of stroke anyway.”
There have been some very high-profile reports of younger patients with major strokes, she said, “but we haven’t seen that in our hospital. For the most part in my experience, strokes are happening in older COVID-19 patients with stroke risk factors such as AF [atrial fibrillation], hypertension, and diabetes. We haven’t seen a preponderance of strokes in young, otherwise healthy people.”
Even in patients who have neurologic effects as the first sign of COVID-19 infection, it is not known whether these symptoms are caused directly by the virus.
“We know that flu can cause people to have headaches, but that is because of an increase in inflammatory cytokines. On the other hand, patients with acute HIV infection often have headaches as a result of the virus getting into the brain. We don’t know where in this [cluster] COVID-19 virus falls,” Dr. Spudich said.
Much is still unknown
“The information we have is very sparse at this point. We need far more systematic information on this from CSF samples and imaging.” Dr. Spudich urged clinicians to try to collect such information in patients with neurologic symptoms.
Acknowledging that fewer such tests are being done at present because of concerns over infection risk, Dr. Spudich suggested that some changes in procedure may help. “In our hospital we have a portable MRI scanner which can be brought to the patient. This means the patient does not have to move across the hospital for a scan. This helps us to decide whether the patient has had a stroke, which can be missed when patients are on a ventilator.”
It is also unclear whether the neurologic effects seen during COVID-19 infection will last long term.
Dr. Spudich noted that there have been reports of COVID-19 patients discharged from intensive care having difficulty with higher cognitive function for some time thereafter. “This can happen after being in ICU but is it more pronounced in COVID-19 patients? An ongoing study is underway to look at this,” she said.
This article first appeared on Medscape.com.
COVID-19: Use these strategies to help parents with and without special needs children
Most people can cope, to some degree, with the multiple weeks of social distancing and stressors related to the pandemic. But what if those stressors became a way of life for a year – or longer? What sorts of skills would be essential not only to survive but to have a renewed sense of resilience?
I know of one group that has had experiences that mirror the challenges faced by the parents of children: the parents of special needs children. As I argued previously, those parents have faced many of the challenges presented by COVID-19. Among those challenges are social distancing and difficulty accessing everyday common experiences. These parents know that they have to manage more areas of their children’s rearing than do their counterparts.
In addition to having to plan for how to deal with acute urgent or emergent medical situations involving their special needs children, these parents also must prepare for the long-term effects of managing children who require ongoing daily care, attention, and dedication.
These strategies can help the parents of special needs kids find a sense of mastery and comfort. The hope is that, after practicing them for long periods of time, the strategies become second nature.
Here are several strategies that might help patients with children during this pandemic:
- Take time to reset: Sometimes it is helpful for parents to take a minute away from a difficult impasse with their kids to reset and take their own “time out.” A few seconds of mental time away from the “scene” provides space and a mental reminder that the minute that just happened is finite, and that a whole new one is coming up next. The break provides a sense of hope. This cognitive reframing could be practiced often.
- Re-enter the challenging scene with a warm voice: Parents model for their children, but they also are telling their own brains that they, too, can calm down. This approach also de-escalates the situation and allows children to get used to hearing directions from someone who is in control – without hostility or irritability.
- Keep a sense of humor; it might come in handy: This is especially the case when tension is in the home, or when facing a set of challenging bad news. As an example, consider how some situations are so repetitive that they border on the ridiculous – such as a grown child having a tantrum at a store. Encourage the children to give themselves permission to cry first so they can laugh second, and then move on.
- Establish a routine for children that is self-reinforcing, and allows for together and separate times: They can, as an example: A) Get ready for the day all by themselves, or as much as they can do independently, before they come down and then B) have breakfast. Then, the child can C) do homework, and then D) go play outside. The routine would then continue on its own without outside reinforcers.
- Tell the children that they can get to the reinforcing activity only after completing the previous one. Over time, they learn to take pride in completing the first activity and doing so more independently. Not having to wait to be told what to do all the time fosters a sense of independence.
- Plan for meals and fun tasks together, and separate for individual work. This creates a sense of change and gives the day a certain flow. Establish routines that are predictable for the children that can be easily documented for the whole family on a calendar. Establish a beginning and an end time to the work day. Mark the end of the day with a chalk line establishing when the family can engage in a certain activity, for example, going for a family bike ride. Let the routine honor healthy circadian rhythms for sleep/wakeful times, and be consistent.
- Feed the brain and body the “good stuff”: Limit negative news, and surround the children with people who bring them joy or provide hope. Listen to inspirational messages and uplifting music. Give the children food that nourishes and energizes their bodies. Take in the view outside, the greenery, or the sky if there is no green around. Connect with family/friends who are far away.
- Make time to replenish with something that is meaningful/productive/helpful: Parents have very little time for themselves when they are “on,” so when they can actually take a little time to recharge, the activity should check many boxes. For example, encourage them to go for a walk (exercise) while listening to music (relax), make a phone call to someone who can relate to their situation (socialize), pray with someone (be spiritual), or sit in their rooms to get some alone quiet time (meditate). Reach out to those who are lonely. Network. Mentor. Volunteer.
- Develop an eye for noticing the positive: Instead of hoping for things to go back to the way they were, tell your patients to practice embracing without judgment the new norm. Get them to notice the time they spend with their families. Break all tasks into many smaller tasks, so there is more possibility of observing progress, and it is evident for everyone to see. Learn to notice the small changes that they want to see in their children. Celebrate all that can be celebrated by stating the obvious: “You wiped your face after eating. You are observant; you are noticing when you have something on your face.”
- State when a child is forgiving, helpful, or puts forward some effort. Label the growth witnessed. The child will learn that that is who they are over time (“observant”). Verbalizing these behaviors also will provide patients with a sense of mastery over parenting, because they are driving the emotional and behavioral development of their children in a way that also complements their family values.
- Make everyone in the family a contributor and foster a sense of gratitude: Give everyone a reason to claim that their collaboration and effort are a big part of the plan’s success. Take turns to lessen everyone’s burden and to thank them for their contributions. Older children can take on leadership roles, even in small ways. Younger children can practice being good listeners, following directions, and helping. Reverse the roles when possible.
Special needs families sometimes have to work harder than others to overcome obstacles, grow, and learn to support one another. Since the pandemic, many parents have been just as challenged. Mastering the above skills might provide a sense of fulfillment and agency, as well as an appreciation for the unexpected gifts that special children – and all children – have to offer.
Dr. Sotir is a psychiatrist with a private practice in Wheaton, Ill. As a parent of three children, one with special needs, she has extensive experience helping parents challenged by having special needs children find balance, support, direction, and joy in all dimensions of individual and family life. This area is the focus of her practice and public speaking. She has no disclosures.
Most people can cope, to some degree, with the multiple weeks of social distancing and stressors related to the pandemic. But what if those stressors became a way of life for a year – or longer? What sorts of skills would be essential not only to survive but to have a renewed sense of resilience?
I know of one group that has had experiences that mirror the challenges faced by the parents of children: the parents of special needs children. As I argued previously, those parents have faced many of the challenges presented by COVID-19. Among those challenges are social distancing and difficulty accessing everyday common experiences. These parents know that they have to manage more areas of their children’s rearing than do their counterparts.
In addition to having to plan for how to deal with acute urgent or emergent medical situations involving their special needs children, these parents also must prepare for the long-term effects of managing children who require ongoing daily care, attention, and dedication.
These strategies can help the parents of special needs kids find a sense of mastery and comfort. The hope is that, after practicing them for long periods of time, the strategies become second nature.
Here are several strategies that might help patients with children during this pandemic:
- Take time to reset: Sometimes it is helpful for parents to take a minute away from a difficult impasse with their kids to reset and take their own “time out.” A few seconds of mental time away from the “scene” provides space and a mental reminder that the minute that just happened is finite, and that a whole new one is coming up next. The break provides a sense of hope. This cognitive reframing could be practiced often.
- Re-enter the challenging scene with a warm voice: Parents model for their children, but they also are telling their own brains that they, too, can calm down. This approach also de-escalates the situation and allows children to get used to hearing directions from someone who is in control – without hostility or irritability.
- Keep a sense of humor; it might come in handy: This is especially the case when tension is in the home, or when facing a set of challenging bad news. As an example, consider how some situations are so repetitive that they border on the ridiculous – such as a grown child having a tantrum at a store. Encourage the children to give themselves permission to cry first so they can laugh second, and then move on.
- Establish a routine for children that is self-reinforcing, and allows for together and separate times: They can, as an example: A) Get ready for the day all by themselves, or as much as they can do independently, before they come down and then B) have breakfast. Then, the child can C) do homework, and then D) go play outside. The routine would then continue on its own without outside reinforcers.
- Tell the children that they can get to the reinforcing activity only after completing the previous one. Over time, they learn to take pride in completing the first activity and doing so more independently. Not having to wait to be told what to do all the time fosters a sense of independence.
- Plan for meals and fun tasks together, and separate for individual work. This creates a sense of change and gives the day a certain flow. Establish routines that are predictable for the children that can be easily documented for the whole family on a calendar. Establish a beginning and an end time to the work day. Mark the end of the day with a chalk line establishing when the family can engage in a certain activity, for example, going for a family bike ride. Let the routine honor healthy circadian rhythms for sleep/wakeful times, and be consistent.
- Feed the brain and body the “good stuff”: Limit negative news, and surround the children with people who bring them joy or provide hope. Listen to inspirational messages and uplifting music. Give the children food that nourishes and energizes their bodies. Take in the view outside, the greenery, or the sky if there is no green around. Connect with family/friends who are far away.
- Make time to replenish with something that is meaningful/productive/helpful: Parents have very little time for themselves when they are “on,” so when they can actually take a little time to recharge, the activity should check many boxes. For example, encourage them to go for a walk (exercise) while listening to music (relax), make a phone call to someone who can relate to their situation (socialize), pray with someone (be spiritual), or sit in their rooms to get some alone quiet time (meditate). Reach out to those who are lonely. Network. Mentor. Volunteer.
- Develop an eye for noticing the positive: Instead of hoping for things to go back to the way they were, tell your patients to practice embracing without judgment the new norm. Get them to notice the time they spend with their families. Break all tasks into many smaller tasks, so there is more possibility of observing progress, and it is evident for everyone to see. Learn to notice the small changes that they want to see in their children. Celebrate all that can be celebrated by stating the obvious: “You wiped your face after eating. You are observant; you are noticing when you have something on your face.”
- State when a child is forgiving, helpful, or puts forward some effort. Label the growth witnessed. The child will learn that that is who they are over time (“observant”). Verbalizing these behaviors also will provide patients with a sense of mastery over parenting, because they are driving the emotional and behavioral development of their children in a way that also complements their family values.
- Make everyone in the family a contributor and foster a sense of gratitude: Give everyone a reason to claim that their collaboration and effort are a big part of the plan’s success. Take turns to lessen everyone’s burden and to thank them for their contributions. Older children can take on leadership roles, even in small ways. Younger children can practice being good listeners, following directions, and helping. Reverse the roles when possible.
Special needs families sometimes have to work harder than others to overcome obstacles, grow, and learn to support one another. Since the pandemic, many parents have been just as challenged. Mastering the above skills might provide a sense of fulfillment and agency, as well as an appreciation for the unexpected gifts that special children – and all children – have to offer.
Dr. Sotir is a psychiatrist with a private practice in Wheaton, Ill. As a parent of three children, one with special needs, she has extensive experience helping parents challenged by having special needs children find balance, support, direction, and joy in all dimensions of individual and family life. This area is the focus of her practice and public speaking. She has no disclosures.
Most people can cope, to some degree, with the multiple weeks of social distancing and stressors related to the pandemic. But what if those stressors became a way of life for a year – or longer? What sorts of skills would be essential not only to survive but to have a renewed sense of resilience?
I know of one group that has had experiences that mirror the challenges faced by the parents of children: the parents of special needs children. As I argued previously, those parents have faced many of the challenges presented by COVID-19. Among those challenges are social distancing and difficulty accessing everyday common experiences. These parents know that they have to manage more areas of their children’s rearing than do their counterparts.
In addition to having to plan for how to deal with acute urgent or emergent medical situations involving their special needs children, these parents also must prepare for the long-term effects of managing children who require ongoing daily care, attention, and dedication.
These strategies can help the parents of special needs kids find a sense of mastery and comfort. The hope is that, after practicing them for long periods of time, the strategies become second nature.
Here are several strategies that might help patients with children during this pandemic:
- Take time to reset: Sometimes it is helpful for parents to take a minute away from a difficult impasse with their kids to reset and take their own “time out.” A few seconds of mental time away from the “scene” provides space and a mental reminder that the minute that just happened is finite, and that a whole new one is coming up next. The break provides a sense of hope. This cognitive reframing could be practiced often.
- Re-enter the challenging scene with a warm voice: Parents model for their children, but they also are telling their own brains that they, too, can calm down. This approach also de-escalates the situation and allows children to get used to hearing directions from someone who is in control – without hostility or irritability.
- Keep a sense of humor; it might come in handy: This is especially the case when tension is in the home, or when facing a set of challenging bad news. As an example, consider how some situations are so repetitive that they border on the ridiculous – such as a grown child having a tantrum at a store. Encourage the children to give themselves permission to cry first so they can laugh second, and then move on.
- Establish a routine for children that is self-reinforcing, and allows for together and separate times: They can, as an example: A) Get ready for the day all by themselves, or as much as they can do independently, before they come down and then B) have breakfast. Then, the child can C) do homework, and then D) go play outside. The routine would then continue on its own without outside reinforcers.
- Tell the children that they can get to the reinforcing activity only after completing the previous one. Over time, they learn to take pride in completing the first activity and doing so more independently. Not having to wait to be told what to do all the time fosters a sense of independence.
- Plan for meals and fun tasks together, and separate for individual work. This creates a sense of change and gives the day a certain flow. Establish routines that are predictable for the children that can be easily documented for the whole family on a calendar. Establish a beginning and an end time to the work day. Mark the end of the day with a chalk line establishing when the family can engage in a certain activity, for example, going for a family bike ride. Let the routine honor healthy circadian rhythms for sleep/wakeful times, and be consistent.
- Feed the brain and body the “good stuff”: Limit negative news, and surround the children with people who bring them joy or provide hope. Listen to inspirational messages and uplifting music. Give the children food that nourishes and energizes their bodies. Take in the view outside, the greenery, or the sky if there is no green around. Connect with family/friends who are far away.
- Make time to replenish with something that is meaningful/productive/helpful: Parents have very little time for themselves when they are “on,” so when they can actually take a little time to recharge, the activity should check many boxes. For example, encourage them to go for a walk (exercise) while listening to music (relax), make a phone call to someone who can relate to their situation (socialize), pray with someone (be spiritual), or sit in their rooms to get some alone quiet time (meditate). Reach out to those who are lonely. Network. Mentor. Volunteer.
- Develop an eye for noticing the positive: Instead of hoping for things to go back to the way they were, tell your patients to practice embracing without judgment the new norm. Get them to notice the time they spend with their families. Break all tasks into many smaller tasks, so there is more possibility of observing progress, and it is evident for everyone to see. Learn to notice the small changes that they want to see in their children. Celebrate all that can be celebrated by stating the obvious: “You wiped your face after eating. You are observant; you are noticing when you have something on your face.”
- State when a child is forgiving, helpful, or puts forward some effort. Label the growth witnessed. The child will learn that that is who they are over time (“observant”). Verbalizing these behaviors also will provide patients with a sense of mastery over parenting, because they are driving the emotional and behavioral development of their children in a way that also complements their family values.
- Make everyone in the family a contributor and foster a sense of gratitude: Give everyone a reason to claim that their collaboration and effort are a big part of the plan’s success. Take turns to lessen everyone’s burden and to thank them for their contributions. Older children can take on leadership roles, even in small ways. Younger children can practice being good listeners, following directions, and helping. Reverse the roles when possible.
Special needs families sometimes have to work harder than others to overcome obstacles, grow, and learn to support one another. Since the pandemic, many parents have been just as challenged. Mastering the above skills might provide a sense of fulfillment and agency, as well as an appreciation for the unexpected gifts that special children – and all children – have to offer.
Dr. Sotir is a psychiatrist with a private practice in Wheaton, Ill. As a parent of three children, one with special needs, she has extensive experience helping parents challenged by having special needs children find balance, support, direction, and joy in all dimensions of individual and family life. This area is the focus of her practice and public speaking. She has no disclosures.
First-in-class antipsychotic linked to lower cardiometabolic risk
A recently approved first-in-class antipsychotic appears to have fewer adverse cardiometabolic effects than standard care with risperidone, new research suggests.
In post hoc analyses of two short-term randomized controlled trials plus an open-label long-term study, patients with schizophrenia on lumateperone (Caplyta, Intra-Cellular Therapies) had reduced rates of metabolic syndrome, compared with their counterparts taking placebo or the antipsychotic risperidone.
In the short-term studies, rates of metabolic syndrome were similar between groups at baseline, but by the end of 4 and 6 weeks of treatment, 25% of patients taking lumateperone no longer met criteria for metabolic syndrome. A similar finding occurred in 36% of patients in the 1-year open label study.
“One of the major advantages that we found during the drug’s development was that it has a very favorable profile with regard to changes in weight, and other [parameters] associated with cardiovascular disease risk, such as elevated glucose and lipids,” study investigator Andrew Satlin, MD, chief medical officer at Intra-Cellular Therapies, New York, told this news organization.
“So we went back to our data and looked to see whether the changes that we saw had an impact on either the development or the resolution of metabolic syndrome in the patients who came into our studies,” he said.
The findings were presented at the American Society of Clinical Psychopharmacology 2020 Virtual Conference.
Reduced cholesterol
Lumateperone was approved in December by the Food and Drug Administration. The drug acts synergistically through the serotonergic, dopaminergic, and glutamatergic systems.
The short-term studies included 511 patients randomly assigned to receive lumateperone 42 mg (n = 256 patients) or risperidone 4 mg (n = 255 patients).
At baseline, rates of metabolic syndrome were 16% in the lumateperone group and 19% in the risperidone group. At the end of treatment, metabolic syndrome was less common in the lumateperone group (13%) vs. those receiving risperidone (25%).
In addition, 46% of lumateperone patients with metabolic syndrome at baseline no longer had it at the end of the study period. This compared with 25% of patients on risperidone.
The differences in metabolic syndrome conversion rates appeared to be driven by greater reductions in total cholesterol with lumateperone, compared with risperidone (–2.8 mg/dL with lumateperone vs. 4.8 mg/dL with risperidone) and triglycerides (–0.7 mg/dL with lumateperone vs. 20.4 mg/dL with risperidone).
Greater increases in blood glucose were also seen with risperidone (7.7 mg/dL) than with lumateperone (0.9 mg/dL).
The long-term study included 602 patients with stable schizophrenia. All received lumateperone 42 mg, and 197 patients (33%) had metabolic syndrome at baseline.
At the end of the 1-year study, 72 of these patients (36%) no longer met criteria for metabolic syndrome.
“Safest antipsychotic so far”
“Lumateperone seems to be the safest antipsychotic we have seen so far,” Christoph U. Correll, MD, professor of child and adolescent psychiatry, Charité Universitatsmedizin, Berlin, who was also involved in clinical trials of lumateperone, told this news organization.
“It seems to be very safe when it comes to cardiometabolic parameters, and it shows similar reduction in symptoms as risperidone. It is certainly an agent one should consider, particularly when a patient cannot tolerate other medications or may not be in full adherence,” said Dr. Correll, who has a joint appointment as professor of psychiatry and molecular medicine at the Zucker School of Medicine at Hofstra University in Hempstead, New York.
The drug’s safety and efficacy profile would make it a good candidate in patients initiating antipsychotic treatment, but reimbursement issues may be a barrier, at least for now, he added.
He said that the drug may prevent the onset of metabolic side effects and added that once payers are willing to reimburse the drug it should become the “first-line standard of care.”
It is well known that atypical antipsychotics are associated with adverse and rapid metabolic changes. Dr. Correll noted that particularly early-phase and first-episode patients can be “very sensitive” to the side effects of these drugs and often experience rapid weight gain and other adverse metabolic changes. Lumateperone, he added, may help avoid some of this cardiometabolic risk.
Time will tell
Jessica M. Gannon, MD, a psychiatrist at the University of Pittsburgh said in commenting on the findings that the drug’s favorable metabolic profile has previously been reported.
She also noted that there has been some interest in lumateperone because of possible “downstream effects on NMDA-type glutamate receptor activity, a larger binding ratio at dopamine-2:5HT1A receptors than other atypical antipsychotics, and presynaptic D2 partial agonism and a postsynaptic D2 antagonism.”
“This latter feature may explain the reported low extrapyramidal symptom incidence in the clinical trials,” she said .
“While I think future studies and clinical use can help determine how clinically efficacious this medication will be for our patients when compared to others on the market, its favorable metabolic and EPS profile do make it of interest,” added Gannon, who was not involved in researching the drug.
The study was funded by Intra-Cellular Therapies. Dr. Satlin is chief medical officer of Intracellular Therapies. Dr. Correll has been a consultant or advisor to and has received honoraria from Acadia, Alkermes, Allergan, Angelini, Axsome, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Janssen/J&J, LB Pharma, Lundbeck, MedAvante-ProPhase, Medscape, Neurocrine, Noven, Otsuka, Pfizer, Recordati, Rovi, Sumitomo Dainippon, Sunovion, Supernus, Takeda, and Teva.
A version of this article originally appeared on Medscape.com.
A recently approved first-in-class antipsychotic appears to have fewer adverse cardiometabolic effects than standard care with risperidone, new research suggests.
In post hoc analyses of two short-term randomized controlled trials plus an open-label long-term study, patients with schizophrenia on lumateperone (Caplyta, Intra-Cellular Therapies) had reduced rates of metabolic syndrome, compared with their counterparts taking placebo or the antipsychotic risperidone.
In the short-term studies, rates of metabolic syndrome were similar between groups at baseline, but by the end of 4 and 6 weeks of treatment, 25% of patients taking lumateperone no longer met criteria for metabolic syndrome. A similar finding occurred in 36% of patients in the 1-year open label study.
“One of the major advantages that we found during the drug’s development was that it has a very favorable profile with regard to changes in weight, and other [parameters] associated with cardiovascular disease risk, such as elevated glucose and lipids,” study investigator Andrew Satlin, MD, chief medical officer at Intra-Cellular Therapies, New York, told this news organization.
“So we went back to our data and looked to see whether the changes that we saw had an impact on either the development or the resolution of metabolic syndrome in the patients who came into our studies,” he said.
The findings were presented at the American Society of Clinical Psychopharmacology 2020 Virtual Conference.
Reduced cholesterol
Lumateperone was approved in December by the Food and Drug Administration. The drug acts synergistically through the serotonergic, dopaminergic, and glutamatergic systems.
The short-term studies included 511 patients randomly assigned to receive lumateperone 42 mg (n = 256 patients) or risperidone 4 mg (n = 255 patients).
At baseline, rates of metabolic syndrome were 16% in the lumateperone group and 19% in the risperidone group. At the end of treatment, metabolic syndrome was less common in the lumateperone group (13%) vs. those receiving risperidone (25%).
In addition, 46% of lumateperone patients with metabolic syndrome at baseline no longer had it at the end of the study period. This compared with 25% of patients on risperidone.
The differences in metabolic syndrome conversion rates appeared to be driven by greater reductions in total cholesterol with lumateperone, compared with risperidone (–2.8 mg/dL with lumateperone vs. 4.8 mg/dL with risperidone) and triglycerides (–0.7 mg/dL with lumateperone vs. 20.4 mg/dL with risperidone).
Greater increases in blood glucose were also seen with risperidone (7.7 mg/dL) than with lumateperone (0.9 mg/dL).
The long-term study included 602 patients with stable schizophrenia. All received lumateperone 42 mg, and 197 patients (33%) had metabolic syndrome at baseline.
At the end of the 1-year study, 72 of these patients (36%) no longer met criteria for metabolic syndrome.
“Safest antipsychotic so far”
“Lumateperone seems to be the safest antipsychotic we have seen so far,” Christoph U. Correll, MD, professor of child and adolescent psychiatry, Charité Universitatsmedizin, Berlin, who was also involved in clinical trials of lumateperone, told this news organization.
“It seems to be very safe when it comes to cardiometabolic parameters, and it shows similar reduction in symptoms as risperidone. It is certainly an agent one should consider, particularly when a patient cannot tolerate other medications or may not be in full adherence,” said Dr. Correll, who has a joint appointment as professor of psychiatry and molecular medicine at the Zucker School of Medicine at Hofstra University in Hempstead, New York.
The drug’s safety and efficacy profile would make it a good candidate in patients initiating antipsychotic treatment, but reimbursement issues may be a barrier, at least for now, he added.
He said that the drug may prevent the onset of metabolic side effects and added that once payers are willing to reimburse the drug it should become the “first-line standard of care.”
It is well known that atypical antipsychotics are associated with adverse and rapid metabolic changes. Dr. Correll noted that particularly early-phase and first-episode patients can be “very sensitive” to the side effects of these drugs and often experience rapid weight gain and other adverse metabolic changes. Lumateperone, he added, may help avoid some of this cardiometabolic risk.
Time will tell
Jessica M. Gannon, MD, a psychiatrist at the University of Pittsburgh said in commenting on the findings that the drug’s favorable metabolic profile has previously been reported.
She also noted that there has been some interest in lumateperone because of possible “downstream effects on NMDA-type glutamate receptor activity, a larger binding ratio at dopamine-2:5HT1A receptors than other atypical antipsychotics, and presynaptic D2 partial agonism and a postsynaptic D2 antagonism.”
“This latter feature may explain the reported low extrapyramidal symptom incidence in the clinical trials,” she said .
“While I think future studies and clinical use can help determine how clinically efficacious this medication will be for our patients when compared to others on the market, its favorable metabolic and EPS profile do make it of interest,” added Gannon, who was not involved in researching the drug.
The study was funded by Intra-Cellular Therapies. Dr. Satlin is chief medical officer of Intracellular Therapies. Dr. Correll has been a consultant or advisor to and has received honoraria from Acadia, Alkermes, Allergan, Angelini, Axsome, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Janssen/J&J, LB Pharma, Lundbeck, MedAvante-ProPhase, Medscape, Neurocrine, Noven, Otsuka, Pfizer, Recordati, Rovi, Sumitomo Dainippon, Sunovion, Supernus, Takeda, and Teva.
A version of this article originally appeared on Medscape.com.
A recently approved first-in-class antipsychotic appears to have fewer adverse cardiometabolic effects than standard care with risperidone, new research suggests.
In post hoc analyses of two short-term randomized controlled trials plus an open-label long-term study, patients with schizophrenia on lumateperone (Caplyta, Intra-Cellular Therapies) had reduced rates of metabolic syndrome, compared with their counterparts taking placebo or the antipsychotic risperidone.
In the short-term studies, rates of metabolic syndrome were similar between groups at baseline, but by the end of 4 and 6 weeks of treatment, 25% of patients taking lumateperone no longer met criteria for metabolic syndrome. A similar finding occurred in 36% of patients in the 1-year open label study.
“One of the major advantages that we found during the drug’s development was that it has a very favorable profile with regard to changes in weight, and other [parameters] associated with cardiovascular disease risk, such as elevated glucose and lipids,” study investigator Andrew Satlin, MD, chief medical officer at Intra-Cellular Therapies, New York, told this news organization.
“So we went back to our data and looked to see whether the changes that we saw had an impact on either the development or the resolution of metabolic syndrome in the patients who came into our studies,” he said.
The findings were presented at the American Society of Clinical Psychopharmacology 2020 Virtual Conference.
Reduced cholesterol
Lumateperone was approved in December by the Food and Drug Administration. The drug acts synergistically through the serotonergic, dopaminergic, and glutamatergic systems.
The short-term studies included 511 patients randomly assigned to receive lumateperone 42 mg (n = 256 patients) or risperidone 4 mg (n = 255 patients).
At baseline, rates of metabolic syndrome were 16% in the lumateperone group and 19% in the risperidone group. At the end of treatment, metabolic syndrome was less common in the lumateperone group (13%) vs. those receiving risperidone (25%).
In addition, 46% of lumateperone patients with metabolic syndrome at baseline no longer had it at the end of the study period. This compared with 25% of patients on risperidone.
The differences in metabolic syndrome conversion rates appeared to be driven by greater reductions in total cholesterol with lumateperone, compared with risperidone (–2.8 mg/dL with lumateperone vs. 4.8 mg/dL with risperidone) and triglycerides (–0.7 mg/dL with lumateperone vs. 20.4 mg/dL with risperidone).
Greater increases in blood glucose were also seen with risperidone (7.7 mg/dL) than with lumateperone (0.9 mg/dL).
The long-term study included 602 patients with stable schizophrenia. All received lumateperone 42 mg, and 197 patients (33%) had metabolic syndrome at baseline.
At the end of the 1-year study, 72 of these patients (36%) no longer met criteria for metabolic syndrome.
“Safest antipsychotic so far”
“Lumateperone seems to be the safest antipsychotic we have seen so far,” Christoph U. Correll, MD, professor of child and adolescent psychiatry, Charité Universitatsmedizin, Berlin, who was also involved in clinical trials of lumateperone, told this news organization.
“It seems to be very safe when it comes to cardiometabolic parameters, and it shows similar reduction in symptoms as risperidone. It is certainly an agent one should consider, particularly when a patient cannot tolerate other medications or may not be in full adherence,” said Dr. Correll, who has a joint appointment as professor of psychiatry and molecular medicine at the Zucker School of Medicine at Hofstra University in Hempstead, New York.
The drug’s safety and efficacy profile would make it a good candidate in patients initiating antipsychotic treatment, but reimbursement issues may be a barrier, at least for now, he added.
He said that the drug may prevent the onset of metabolic side effects and added that once payers are willing to reimburse the drug it should become the “first-line standard of care.”
It is well known that atypical antipsychotics are associated with adverse and rapid metabolic changes. Dr. Correll noted that particularly early-phase and first-episode patients can be “very sensitive” to the side effects of these drugs and often experience rapid weight gain and other adverse metabolic changes. Lumateperone, he added, may help avoid some of this cardiometabolic risk.
Time will tell
Jessica M. Gannon, MD, a psychiatrist at the University of Pittsburgh said in commenting on the findings that the drug’s favorable metabolic profile has previously been reported.
She also noted that there has been some interest in lumateperone because of possible “downstream effects on NMDA-type glutamate receptor activity, a larger binding ratio at dopamine-2:5HT1A receptors than other atypical antipsychotics, and presynaptic D2 partial agonism and a postsynaptic D2 antagonism.”
“This latter feature may explain the reported low extrapyramidal symptom incidence in the clinical trials,” she said .
“While I think future studies and clinical use can help determine how clinically efficacious this medication will be for our patients when compared to others on the market, its favorable metabolic and EPS profile do make it of interest,” added Gannon, who was not involved in researching the drug.
The study was funded by Intra-Cellular Therapies. Dr. Satlin is chief medical officer of Intracellular Therapies. Dr. Correll has been a consultant or advisor to and has received honoraria from Acadia, Alkermes, Allergan, Angelini, Axsome, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Janssen/J&J, LB Pharma, Lundbeck, MedAvante-ProPhase, Medscape, Neurocrine, Noven, Otsuka, Pfizer, Recordati, Rovi, Sumitomo Dainippon, Sunovion, Supernus, Takeda, and Teva.
A version of this article originally appeared on Medscape.com.
Lancet, NEJM retract studies on hydroxychloroquine for COVID-19
The Lancet announced today that it has retracted a highly cited study that suggested hydroxychloroquine may cause more harm than benefit in patients with COVID-19. Hours later, the New England Journal of Medicine announced that it had retracted a second article by some of the same authors, also on heart disease and COVID-19.
The Lancet article, titled “Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: A multinational registry analysis” was originally published online May 22. The NEJM article, “Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19” was initially published May 1.
Three authors of the Lancet article, Mandeep R. Mehra, MD, Frank Ruschitzka, MD, and Amit N. Patel, MD, wrote in a letter that the action came after concerns were raised about the integrity of the data, and about how the analysis was conducted by Chicago-based Surgisphere Corp and study coauthor Sapan Desai, MD, Surgisphere’s founder and CEO.
The authors asked for an independent third-party review of Surgisphere to evaluate the integrity of the trial elements and to replicate the analyses in the article.
“Our independent peer reviewers informed us that Surgisphere would not transfer the full dataset, client contracts, and the full ISO audit report to their servers for analysis, as such transfer would violate client agreements and confidentiality requirements,” the authors wrote.
Therefore, reviewers were not able to conduct the review and notified the authors they would withdraw from the peer-review process.
The Lancet said in a statement: “The Lancet takes issues of scientific integrity extremely seriously, and there are many outstanding questions about Surgisphere and the data that were allegedly included in this study. Following guidelines from the Committee on Publication Ethics and International Committee of Medical Journal Editors, institutional reviews of Surgisphere’s research collaborations are urgently needed.”
The authors wrote, “We can never forget the responsibility we have as researchers to scrupulously ensure that we rely on data sources that adhere to our high standards. Based on this development, we can no longer vouch for the veracity of the primary data sources. Due to this unfortunate development, the authors request that the paper be retracted.
“We all entered this collaboration to contribute in good faith and at a time of great need during the COVID-19 pandemic. We deeply apologize to you, the editors, and the journal readership for any embarrassment or inconvenience that this may have caused.”
In a similar, if briefer, note, the authors requested that the New England Journal of Medicine retract the earlier article as well. The retraction notice on the website reads: “Because all the authors were not granted access to the raw data and the raw data could not be made available to a third-party auditor, we are unable to validate the primary data sources underlying our article, ‘Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19.’ We therefore request that the article be retracted. We apologize to the editors and to readers of the Journal for the difficulties that this has caused.”
Both journals had already published “Expression of Concern” notices about the articles. The expression of concern followed an open letter, endorsed by more than 200 scientists, ethicists, and clinicians and posted on May 28, questioning the data and ethics of the study.
A version of this article originally appeared on Medscape.com.
The Lancet announced today that it has retracted a highly cited study that suggested hydroxychloroquine may cause more harm than benefit in patients with COVID-19. Hours later, the New England Journal of Medicine announced that it had retracted a second article by some of the same authors, also on heart disease and COVID-19.
The Lancet article, titled “Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: A multinational registry analysis” was originally published online May 22. The NEJM article, “Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19” was initially published May 1.
Three authors of the Lancet article, Mandeep R. Mehra, MD, Frank Ruschitzka, MD, and Amit N. Patel, MD, wrote in a letter that the action came after concerns were raised about the integrity of the data, and about how the analysis was conducted by Chicago-based Surgisphere Corp and study coauthor Sapan Desai, MD, Surgisphere’s founder and CEO.
The authors asked for an independent third-party review of Surgisphere to evaluate the integrity of the trial elements and to replicate the analyses in the article.
“Our independent peer reviewers informed us that Surgisphere would not transfer the full dataset, client contracts, and the full ISO audit report to their servers for analysis, as such transfer would violate client agreements and confidentiality requirements,” the authors wrote.
Therefore, reviewers were not able to conduct the review and notified the authors they would withdraw from the peer-review process.
The Lancet said in a statement: “The Lancet takes issues of scientific integrity extremely seriously, and there are many outstanding questions about Surgisphere and the data that were allegedly included in this study. Following guidelines from the Committee on Publication Ethics and International Committee of Medical Journal Editors, institutional reviews of Surgisphere’s research collaborations are urgently needed.”
The authors wrote, “We can never forget the responsibility we have as researchers to scrupulously ensure that we rely on data sources that adhere to our high standards. Based on this development, we can no longer vouch for the veracity of the primary data sources. Due to this unfortunate development, the authors request that the paper be retracted.
“We all entered this collaboration to contribute in good faith and at a time of great need during the COVID-19 pandemic. We deeply apologize to you, the editors, and the journal readership for any embarrassment or inconvenience that this may have caused.”
In a similar, if briefer, note, the authors requested that the New England Journal of Medicine retract the earlier article as well. The retraction notice on the website reads: “Because all the authors were not granted access to the raw data and the raw data could not be made available to a third-party auditor, we are unable to validate the primary data sources underlying our article, ‘Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19.’ We therefore request that the article be retracted. We apologize to the editors and to readers of the Journal for the difficulties that this has caused.”
Both journals had already published “Expression of Concern” notices about the articles. The expression of concern followed an open letter, endorsed by more than 200 scientists, ethicists, and clinicians and posted on May 28, questioning the data and ethics of the study.
A version of this article originally appeared on Medscape.com.
The Lancet announced today that it has retracted a highly cited study that suggested hydroxychloroquine may cause more harm than benefit in patients with COVID-19. Hours later, the New England Journal of Medicine announced that it had retracted a second article by some of the same authors, also on heart disease and COVID-19.
The Lancet article, titled “Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: A multinational registry analysis” was originally published online May 22. The NEJM article, “Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19” was initially published May 1.
Three authors of the Lancet article, Mandeep R. Mehra, MD, Frank Ruschitzka, MD, and Amit N. Patel, MD, wrote in a letter that the action came after concerns were raised about the integrity of the data, and about how the analysis was conducted by Chicago-based Surgisphere Corp and study coauthor Sapan Desai, MD, Surgisphere’s founder and CEO.
The authors asked for an independent third-party review of Surgisphere to evaluate the integrity of the trial elements and to replicate the analyses in the article.
“Our independent peer reviewers informed us that Surgisphere would not transfer the full dataset, client contracts, and the full ISO audit report to their servers for analysis, as such transfer would violate client agreements and confidentiality requirements,” the authors wrote.
Therefore, reviewers were not able to conduct the review and notified the authors they would withdraw from the peer-review process.
The Lancet said in a statement: “The Lancet takes issues of scientific integrity extremely seriously, and there are many outstanding questions about Surgisphere and the data that were allegedly included in this study. Following guidelines from the Committee on Publication Ethics and International Committee of Medical Journal Editors, institutional reviews of Surgisphere’s research collaborations are urgently needed.”
The authors wrote, “We can never forget the responsibility we have as researchers to scrupulously ensure that we rely on data sources that adhere to our high standards. Based on this development, we can no longer vouch for the veracity of the primary data sources. Due to this unfortunate development, the authors request that the paper be retracted.
“We all entered this collaboration to contribute in good faith and at a time of great need during the COVID-19 pandemic. We deeply apologize to you, the editors, and the journal readership for any embarrassment or inconvenience that this may have caused.”
In a similar, if briefer, note, the authors requested that the New England Journal of Medicine retract the earlier article as well. The retraction notice on the website reads: “Because all the authors were not granted access to the raw data and the raw data could not be made available to a third-party auditor, we are unable to validate the primary data sources underlying our article, ‘Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19.’ We therefore request that the article be retracted. We apologize to the editors and to readers of the Journal for the difficulties that this has caused.”
Both journals had already published “Expression of Concern” notices about the articles. The expression of concern followed an open letter, endorsed by more than 200 scientists, ethicists, and clinicians and posted on May 28, questioning the data and ethics of the study.
A version of this article originally appeared on Medscape.com.
Should healthcare workers wear masks at home?
Wearing a mask at home, even when everyone is feeling fine, might reduce the risk of frontline healthcare workers transmitting SARS-CoV-2 infection to their families, a recent study from China suggests. But the benefits might not outweigh the costs, according to several physicians interviewed.
“My gut reaction is that home mask use for healthcare workers would place an inordinately high burden on those healthcare workers and their families,” said Jeanne Noble, MD, an emergency care physician at the University of California, San Francisco. “Wearing a mask for a 10-hour shift already represents significant physical discomfort, causing sores across the nose and behind the ears. The emotional toll of the physical distance that comes with mask use, with limited facial expression, is also quite real.”
The suggested benefit of home mask use comes from research published online May 28 in BMJ Global Health. To assess predictors of household transmission of SARS-CoV-2 infection, Yu Wang, MD, of the Beijing Center for Disease Prevention and Control and colleagues conducted a retrospective study of 124 families in Beijing in which there was a confirmed case of COVID-19 as of February 21. The researchers surveyed family members by telephone about household hygiene and behaviors during the pandemic to examine risk factors for transmission.
During the 2 weeks following onset of the primary case, secondary transmission occurred in 41 families. Overall, 77 of 335 family members developed COVID-19.
A multivariable logistic regression analysis found that in households in which family members wore masks at home before the first person became ill, there was less likelihood of transmission of disease to a family member, compared with families in which no one wore a mask prior to illness onset.
“Facemasks were 79% effective and disinfection was 77% effective in preventing transmission,” the researchers report, “whilst close frequent contact in the household increased the risk of transmission 18 times, and diarrhea in the index patient increased the risk by four times.
However, wearing masks after symptom onset was not protective, according to the analysis. The findings support “universal face mask use, and also provides guidance on risk reduction for families living with someone in quarantine or isolation, and families of health workers, who may face ongoing risk,” the authors write.
Still, other precautions may be more important, experts say.
“I think by far the best way for healthcare professionals to protect their families is to carefully employ appropriate infection prevention measures at work,” said Mark E. Rupp, MD, chief of the Division of Infectious Diseases at Nebraska Medical Center in Omaha. “The combination of administrative interventions, engineering improvements, and personal protective equipment is very effective in preventing SARS-CoV-2 acquisition in the workplace.”
Many physicians already wear masks at home, and this study “only reemphasized the importance of doing so,” said Raghavendra Tirupathi, MD, medical director of Keystone Infectious Diseases in Chambersburg, Pennsylvania, who recently reviewed studies about masks and COVID-19.
Home mask use provides “one more layer of protection that might help mitigate the risk of transmission to family members,” Tirupathi said. But it does not obviate the need to follow other preventive measures, such as social distancing and proper hygiene.
But Rupp, whose advice on how healthcare workers can protect their families was recently highlighted by the American Medical Association, isn’t convinced. He said he won’t be adding home mask use to his list of recommendations. “It would be intrusive, cumbersome, and impractical to wear a mask in the home setting,” Rupp said in an interview.
However, when out in the community, all family members must protect one another by practicing social distancing, wearing masks, and practicing proper hand hygiene. “I also think that it is a good idea to have some masks on hand in case anyone does develop symptoms in the household and to wear them if a family member falls ill ― at least until testing can confirm COVID-19,” Rupp said. “If a family member does fall ill, masks for the ill person as well as the well persons would be indicated along with other home quarantine measures.”
For her part, Noble, who has provided guidance about proper mask use, said that targeted use of masks at home, such as around older visiting relatives or other more vulnerable family members, may be more realistic than continuous in-home use.
When a household member becomes ill, recommendations for preventing disease spread include having a sick family member sleep in a separate bedroom, using a separate bathroom, and wearing a mask when within 6 feet of other household members. They also should avoid sharing meals. “For a household member who is a medical provider, to follow these self-isolation precautions while at home for months on end would have a significant emotional toll,” Noble said in an email. “With no end in sight for the pandemic, perpetual mask use in both the private and public sphere strikes me as overwhelming ― I write this near the end of my 10-hour shift wearing both an N95 and surgical mask and counting the minutes before I can take them off!”
A limitation of the study was its reliance on telephone interviews, which are subject to recall bias, the authors note.
The study was funded by the Beijing Science and Technology Planning Project. The researchers have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Wearing a mask at home, even when everyone is feeling fine, might reduce the risk of frontline healthcare workers transmitting SARS-CoV-2 infection to their families, a recent study from China suggests. But the benefits might not outweigh the costs, according to several physicians interviewed.
“My gut reaction is that home mask use for healthcare workers would place an inordinately high burden on those healthcare workers and their families,” said Jeanne Noble, MD, an emergency care physician at the University of California, San Francisco. “Wearing a mask for a 10-hour shift already represents significant physical discomfort, causing sores across the nose and behind the ears. The emotional toll of the physical distance that comes with mask use, with limited facial expression, is also quite real.”
The suggested benefit of home mask use comes from research published online May 28 in BMJ Global Health. To assess predictors of household transmission of SARS-CoV-2 infection, Yu Wang, MD, of the Beijing Center for Disease Prevention and Control and colleagues conducted a retrospective study of 124 families in Beijing in which there was a confirmed case of COVID-19 as of February 21. The researchers surveyed family members by telephone about household hygiene and behaviors during the pandemic to examine risk factors for transmission.
During the 2 weeks following onset of the primary case, secondary transmission occurred in 41 families. Overall, 77 of 335 family members developed COVID-19.
A multivariable logistic regression analysis found that in households in which family members wore masks at home before the first person became ill, there was less likelihood of transmission of disease to a family member, compared with families in which no one wore a mask prior to illness onset.
“Facemasks were 79% effective and disinfection was 77% effective in preventing transmission,” the researchers report, “whilst close frequent contact in the household increased the risk of transmission 18 times, and diarrhea in the index patient increased the risk by four times.
However, wearing masks after symptom onset was not protective, according to the analysis. The findings support “universal face mask use, and also provides guidance on risk reduction for families living with someone in quarantine or isolation, and families of health workers, who may face ongoing risk,” the authors write.
Still, other precautions may be more important, experts say.
“I think by far the best way for healthcare professionals to protect their families is to carefully employ appropriate infection prevention measures at work,” said Mark E. Rupp, MD, chief of the Division of Infectious Diseases at Nebraska Medical Center in Omaha. “The combination of administrative interventions, engineering improvements, and personal protective equipment is very effective in preventing SARS-CoV-2 acquisition in the workplace.”
Many physicians already wear masks at home, and this study “only reemphasized the importance of doing so,” said Raghavendra Tirupathi, MD, medical director of Keystone Infectious Diseases in Chambersburg, Pennsylvania, who recently reviewed studies about masks and COVID-19.
Home mask use provides “one more layer of protection that might help mitigate the risk of transmission to family members,” Tirupathi said. But it does not obviate the need to follow other preventive measures, such as social distancing and proper hygiene.
But Rupp, whose advice on how healthcare workers can protect their families was recently highlighted by the American Medical Association, isn’t convinced. He said he won’t be adding home mask use to his list of recommendations. “It would be intrusive, cumbersome, and impractical to wear a mask in the home setting,” Rupp said in an interview.
However, when out in the community, all family members must protect one another by practicing social distancing, wearing masks, and practicing proper hand hygiene. “I also think that it is a good idea to have some masks on hand in case anyone does develop symptoms in the household and to wear them if a family member falls ill ― at least until testing can confirm COVID-19,” Rupp said. “If a family member does fall ill, masks for the ill person as well as the well persons would be indicated along with other home quarantine measures.”
For her part, Noble, who has provided guidance about proper mask use, said that targeted use of masks at home, such as around older visiting relatives or other more vulnerable family members, may be more realistic than continuous in-home use.
When a household member becomes ill, recommendations for preventing disease spread include having a sick family member sleep in a separate bedroom, using a separate bathroom, and wearing a mask when within 6 feet of other household members. They also should avoid sharing meals. “For a household member who is a medical provider, to follow these self-isolation precautions while at home for months on end would have a significant emotional toll,” Noble said in an email. “With no end in sight for the pandemic, perpetual mask use in both the private and public sphere strikes me as overwhelming ― I write this near the end of my 10-hour shift wearing both an N95 and surgical mask and counting the minutes before I can take them off!”
A limitation of the study was its reliance on telephone interviews, which are subject to recall bias, the authors note.
The study was funded by the Beijing Science and Technology Planning Project. The researchers have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Wearing a mask at home, even when everyone is feeling fine, might reduce the risk of frontline healthcare workers transmitting SARS-CoV-2 infection to their families, a recent study from China suggests. But the benefits might not outweigh the costs, according to several physicians interviewed.
“My gut reaction is that home mask use for healthcare workers would place an inordinately high burden on those healthcare workers and their families,” said Jeanne Noble, MD, an emergency care physician at the University of California, San Francisco. “Wearing a mask for a 10-hour shift already represents significant physical discomfort, causing sores across the nose and behind the ears. The emotional toll of the physical distance that comes with mask use, with limited facial expression, is also quite real.”
The suggested benefit of home mask use comes from research published online May 28 in BMJ Global Health. To assess predictors of household transmission of SARS-CoV-2 infection, Yu Wang, MD, of the Beijing Center for Disease Prevention and Control and colleagues conducted a retrospective study of 124 families in Beijing in which there was a confirmed case of COVID-19 as of February 21. The researchers surveyed family members by telephone about household hygiene and behaviors during the pandemic to examine risk factors for transmission.
During the 2 weeks following onset of the primary case, secondary transmission occurred in 41 families. Overall, 77 of 335 family members developed COVID-19.
A multivariable logistic regression analysis found that in households in which family members wore masks at home before the first person became ill, there was less likelihood of transmission of disease to a family member, compared with families in which no one wore a mask prior to illness onset.
“Facemasks were 79% effective and disinfection was 77% effective in preventing transmission,” the researchers report, “whilst close frequent contact in the household increased the risk of transmission 18 times, and diarrhea in the index patient increased the risk by four times.
However, wearing masks after symptom onset was not protective, according to the analysis. The findings support “universal face mask use, and also provides guidance on risk reduction for families living with someone in quarantine or isolation, and families of health workers, who may face ongoing risk,” the authors write.
Still, other precautions may be more important, experts say.
“I think by far the best way for healthcare professionals to protect their families is to carefully employ appropriate infection prevention measures at work,” said Mark E. Rupp, MD, chief of the Division of Infectious Diseases at Nebraska Medical Center in Omaha. “The combination of administrative interventions, engineering improvements, and personal protective equipment is very effective in preventing SARS-CoV-2 acquisition in the workplace.”
Many physicians already wear masks at home, and this study “only reemphasized the importance of doing so,” said Raghavendra Tirupathi, MD, medical director of Keystone Infectious Diseases in Chambersburg, Pennsylvania, who recently reviewed studies about masks and COVID-19.
Home mask use provides “one more layer of protection that might help mitigate the risk of transmission to family members,” Tirupathi said. But it does not obviate the need to follow other preventive measures, such as social distancing and proper hygiene.
But Rupp, whose advice on how healthcare workers can protect their families was recently highlighted by the American Medical Association, isn’t convinced. He said he won’t be adding home mask use to his list of recommendations. “It would be intrusive, cumbersome, and impractical to wear a mask in the home setting,” Rupp said in an interview.
However, when out in the community, all family members must protect one another by practicing social distancing, wearing masks, and practicing proper hand hygiene. “I also think that it is a good idea to have some masks on hand in case anyone does develop symptoms in the household and to wear them if a family member falls ill ― at least until testing can confirm COVID-19,” Rupp said. “If a family member does fall ill, masks for the ill person as well as the well persons would be indicated along with other home quarantine measures.”
For her part, Noble, who has provided guidance about proper mask use, said that targeted use of masks at home, such as around older visiting relatives or other more vulnerable family members, may be more realistic than continuous in-home use.
When a household member becomes ill, recommendations for preventing disease spread include having a sick family member sleep in a separate bedroom, using a separate bathroom, and wearing a mask when within 6 feet of other household members. They also should avoid sharing meals. “For a household member who is a medical provider, to follow these self-isolation precautions while at home for months on end would have a significant emotional toll,” Noble said in an email. “With no end in sight for the pandemic, perpetual mask use in both the private and public sphere strikes me as overwhelming ― I write this near the end of my 10-hour shift wearing both an N95 and surgical mask and counting the minutes before I can take them off!”
A limitation of the study was its reliance on telephone interviews, which are subject to recall bias, the authors note.
The study was funded by the Beijing Science and Technology Planning Project. The researchers have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.




