User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Today’s Top News Highlights: COVID-19 -- Heart transplant patients face greater mortality, rheumatology drugs look safe
Here are the stories our MDedge editors across specialties think you need to know about today:
More fatalities in heart transplant patients with COVID-19
COVID-19 infection appears to be associated with a high risk for mortality in heart transplant recipients. The conclusion is based on a case series with 28 patients with a confirmed diagnosis of COVID-19 who received a heart transplant during March and April 2020. There was a case-fatality rate of 25%, according to the study published in JAMA Cardiology. “The high case fatality in our case series should alert physicians to the vulnerability of heart transplant recipients during the COVID-19 pandemic,” senior author Nir Uriel, MD, professor of medicine at Columbia University, New York, said in an interview. “These patients require extra precautions to prevent the development of infection.” Read more.
High costs for type 1 diabetes patients: It’s not just insulin
For privately insured individuals with type 1 diabetes in the United States, out-of-pocket costs for insulin are typically lower than for other diabetes-related supplies. But overall out-of-pocket costs – taking into account everything that is needed to manage diabetes – are still very high. Two separate research letters recently published in JAMA Internal Medicine examined some of the drivers behind these high costs. The first research letter examined all costs for privately insured patients with type 1 diabetes, finding a mean out-of-pocket spend of approximately $2,500 a year. “Policymakers should improve the affordability of all care for type 1 diabetes,” said the lead author of the first research letter, Kao-Ping Chua, MD, PhD, of the department of pediatrics, University of Michigan, Ann Arbor. Read more.
Most rheumatology drugs don’t up COVID-19 hospitalizations
The vast majority of patients with rheumatic and musculoskeletal diseases who contract COVID-19 recover from the virus, regardless of which medication they receive for their rheumatic condition, new international research suggests. Researchers looked at 600 COVID-19 patients from 40 countries, and found that those taking TNF inhibitors for their rheumatic disease were less likely to be hospitalized for COVID-19. Treatment with more than 10 mg of prednisone daily – considered a moderate to high dose – was associated with a higher probability of hospitalization, however. “These results provide, for the first time, information about the outcome of COVID-19 in patients with rheumatic and musculoskeletal diseases,” said study investigator Pedro Machado, MD, PhD, from University College London. “They should provide some reassurance to patients and healthcare providers.” Read more.
A bumpy virtual #ASCO20
Some prominent oncologists gave up on the virtual meeting of the American Society of Clinical Oncology after facing technical problems with online sessions. Despite those glitches, dozens of virtual meeting attendees praised the online effort, which was assembled in just a few months, and called out virtues such as the quick availability of video transcripts as well as the obvious benefits of low cost, zero travel, and overall convenience. But one sentiment was nearly universal: there’s nothing like the real thing. This year’s meeting, which involved 40,000-plus attendees, was shortened to 3 days and limited to scientific presentations because of the COVID-19 pandemic. Education sessions will be held online August 8-10. Read more.
Parenting special needs children: An unlikely model
As families adjust to daily life during a pandemic, the parents of special needs children may be able to offer them some lessons. The chronic struggles of many special needs parents – from staying home often to taking on roles in which they have not been trained – strongly resemble the challenges facing most families in the COVID-19 pandemic, according to Migdalia Miranda Sotir, MD, a psychiatrist in private practice in Wheaton, Ill. “Parents may take on active roles supplementing their developmentally delayed children with educational experiences or therapeutic modalities in their own homes given that the needs might be too great to just rely on the school or therapy time,” she writes on MDedge. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
More fatalities in heart transplant patients with COVID-19
COVID-19 infection appears to be associated with a high risk for mortality in heart transplant recipients. The conclusion is based on a case series with 28 patients with a confirmed diagnosis of COVID-19 who received a heart transplant during March and April 2020. There was a case-fatality rate of 25%, according to the study published in JAMA Cardiology. “The high case fatality in our case series should alert physicians to the vulnerability of heart transplant recipients during the COVID-19 pandemic,” senior author Nir Uriel, MD, professor of medicine at Columbia University, New York, said in an interview. “These patients require extra precautions to prevent the development of infection.” Read more.
High costs for type 1 diabetes patients: It’s not just insulin
For privately insured individuals with type 1 diabetes in the United States, out-of-pocket costs for insulin are typically lower than for other diabetes-related supplies. But overall out-of-pocket costs – taking into account everything that is needed to manage diabetes – are still very high. Two separate research letters recently published in JAMA Internal Medicine examined some of the drivers behind these high costs. The first research letter examined all costs for privately insured patients with type 1 diabetes, finding a mean out-of-pocket spend of approximately $2,500 a year. “Policymakers should improve the affordability of all care for type 1 diabetes,” said the lead author of the first research letter, Kao-Ping Chua, MD, PhD, of the department of pediatrics, University of Michigan, Ann Arbor. Read more.
Most rheumatology drugs don’t up COVID-19 hospitalizations
The vast majority of patients with rheumatic and musculoskeletal diseases who contract COVID-19 recover from the virus, regardless of which medication they receive for their rheumatic condition, new international research suggests. Researchers looked at 600 COVID-19 patients from 40 countries, and found that those taking TNF inhibitors for their rheumatic disease were less likely to be hospitalized for COVID-19. Treatment with more than 10 mg of prednisone daily – considered a moderate to high dose – was associated with a higher probability of hospitalization, however. “These results provide, for the first time, information about the outcome of COVID-19 in patients with rheumatic and musculoskeletal diseases,” said study investigator Pedro Machado, MD, PhD, from University College London. “They should provide some reassurance to patients and healthcare providers.” Read more.
A bumpy virtual #ASCO20
Some prominent oncologists gave up on the virtual meeting of the American Society of Clinical Oncology after facing technical problems with online sessions. Despite those glitches, dozens of virtual meeting attendees praised the online effort, which was assembled in just a few months, and called out virtues such as the quick availability of video transcripts as well as the obvious benefits of low cost, zero travel, and overall convenience. But one sentiment was nearly universal: there’s nothing like the real thing. This year’s meeting, which involved 40,000-plus attendees, was shortened to 3 days and limited to scientific presentations because of the COVID-19 pandemic. Education sessions will be held online August 8-10. Read more.
Parenting special needs children: An unlikely model
As families adjust to daily life during a pandemic, the parents of special needs children may be able to offer them some lessons. The chronic struggles of many special needs parents – from staying home often to taking on roles in which they have not been trained – strongly resemble the challenges facing most families in the COVID-19 pandemic, according to Migdalia Miranda Sotir, MD, a psychiatrist in private practice in Wheaton, Ill. “Parents may take on active roles supplementing their developmentally delayed children with educational experiences or therapeutic modalities in their own homes given that the needs might be too great to just rely on the school or therapy time,” she writes on MDedge. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
More fatalities in heart transplant patients with COVID-19
COVID-19 infection appears to be associated with a high risk for mortality in heart transplant recipients. The conclusion is based on a case series with 28 patients with a confirmed diagnosis of COVID-19 who received a heart transplant during March and April 2020. There was a case-fatality rate of 25%, according to the study published in JAMA Cardiology. “The high case fatality in our case series should alert physicians to the vulnerability of heart transplant recipients during the COVID-19 pandemic,” senior author Nir Uriel, MD, professor of medicine at Columbia University, New York, said in an interview. “These patients require extra precautions to prevent the development of infection.” Read more.
High costs for type 1 diabetes patients: It’s not just insulin
For privately insured individuals with type 1 diabetes in the United States, out-of-pocket costs for insulin are typically lower than for other diabetes-related supplies. But overall out-of-pocket costs – taking into account everything that is needed to manage diabetes – are still very high. Two separate research letters recently published in JAMA Internal Medicine examined some of the drivers behind these high costs. The first research letter examined all costs for privately insured patients with type 1 diabetes, finding a mean out-of-pocket spend of approximately $2,500 a year. “Policymakers should improve the affordability of all care for type 1 diabetes,” said the lead author of the first research letter, Kao-Ping Chua, MD, PhD, of the department of pediatrics, University of Michigan, Ann Arbor. Read more.
Most rheumatology drugs don’t up COVID-19 hospitalizations
The vast majority of patients with rheumatic and musculoskeletal diseases who contract COVID-19 recover from the virus, regardless of which medication they receive for their rheumatic condition, new international research suggests. Researchers looked at 600 COVID-19 patients from 40 countries, and found that those taking TNF inhibitors for their rheumatic disease were less likely to be hospitalized for COVID-19. Treatment with more than 10 mg of prednisone daily – considered a moderate to high dose – was associated with a higher probability of hospitalization, however. “These results provide, for the first time, information about the outcome of COVID-19 in patients with rheumatic and musculoskeletal diseases,” said study investigator Pedro Machado, MD, PhD, from University College London. “They should provide some reassurance to patients and healthcare providers.” Read more.
A bumpy virtual #ASCO20
Some prominent oncologists gave up on the virtual meeting of the American Society of Clinical Oncology after facing technical problems with online sessions. Despite those glitches, dozens of virtual meeting attendees praised the online effort, which was assembled in just a few months, and called out virtues such as the quick availability of video transcripts as well as the obvious benefits of low cost, zero travel, and overall convenience. But one sentiment was nearly universal: there’s nothing like the real thing. This year’s meeting, which involved 40,000-plus attendees, was shortened to 3 days and limited to scientific presentations because of the COVID-19 pandemic. Education sessions will be held online August 8-10. Read more.
Parenting special needs children: An unlikely model
As families adjust to daily life during a pandemic, the parents of special needs children may be able to offer them some lessons. The chronic struggles of many special needs parents – from staying home often to taking on roles in which they have not been trained – strongly resemble the challenges facing most families in the COVID-19 pandemic, according to Migdalia Miranda Sotir, MD, a psychiatrist in private practice in Wheaton, Ill. “Parents may take on active roles supplementing their developmentally delayed children with educational experiences or therapeutic modalities in their own homes given that the needs might be too great to just rely on the school or therapy time,” she writes on MDedge. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Most rheumatology drugs don’t increase COVID-19 hospitalization risk
The vast majority of patients with rheumatic and musculoskeletal diseases who contract COVID-19 recover from the virus, regardless of which medication they receive for their rheumatic condition, new international research suggests.
“These results provide, for the first time, information about the outcome of COVID-19 in patients with rheumatic and musculoskeletal diseases,” said study investigator Pedro Machado, MD, PhD, from University College London. “They should provide some reassurance to patients and healthcare providers.”
Machado and his colleagues looked at 600 COVID-19 patients from 40 countries, and found that those taking TNF inhibitors for their rheumatic disease were less likely to be hospitalized for COVID-19. However, treatment with more than 10 mg of prednisone daily — considered a moderate to high dose — was associated with a higher probability of hospitalization.
In addition, hospitalization was not associated with biologics; JAK inhibitors; conventional disease-modifying antirheumatic drugs (DMARDs), such as methotrexate; antimalarials, such as hydroxychloroquine; or nonsteroidal anti-inflammatory drugs (NSAIDs) — either alone or in combination with other biologics, such as TNF-alpha inhibitors.
The findings were presented at the virtual European League Against Rheumatism (EULAR) 2020 Congress and were published online in Annals of the Rheumatic Diseases.
“Initially, there was a huge concern that these drugs could affect the outcome of patients getting COVID-19, but what this is showing is that probably these drugs do not increase their risk of severe outcome,” Machado, who is chair of the EULAR standing committee on epidemiology and health services research, told Medscape Medical News.
As of June 1, 1061 patients from 28 participating countries had been entered into the EULAR COVID-19 database, which was launched as part of the international Global Rheumatology Alliance registry. Patient data are categorized by factors such as top rheumatology diagnosis, comorbidities, top-five COVID-19 symptoms, and DMARD therapy at the time of virus infection. Anonymized data will be shared with an international register based in the United States.
Machado’s team combined data from the EULAR and Global Rheumatology Alliance COVID-19 registries from March 24 to April 20. They looked at patient factors — such as age, sex, smoking status, rheumatic diagnosis, comorbidities, and rheumatic therapies — to examine the association of rheumatic therapies with hospitalization rates and COVID-19 disease course.
Of the 277 patients (46%) in the study cohort who required hospitalization, 55 (9%) died. But this finding shouldn’t be viewed as the true rate of hospitalization or death in patients with rheumatic disease and COVID-19, said Gerd Burmester, MD, from Charité–University Medicine Berlin.
“There’s tremendous bias in terms of more serious cases of COVID-19 being reported to the registries,” he explained, “because the mild cases won’t even show up at their rheumatologist’s office.”
“This can skew the idea that COVID-19 is much more dangerous to rheumatic patients than to the regular population,” Burmester told Medscape Medical News. “It scares the patients, obviously, but we believe this is not justified.”
It’s still unclear whether rituximab use raises the risk for severe COVID-19, he said. “It appears to be the only biologic for which the jury is still out,” he said.
“Anti-TNFs and anti-IL-6 drugs may even be beneficial, although we don’t have robust data,” he added.
The study can only highlight associations between rheumatic drugs and COVID-19 outcomes. “We cannot say there is a causal relationship between the findings,” Machado said.
Longer-term data, when available, should illuminate “more granular” aspects of COVID-19 outcomes in rheumatic patients, including their risks of requiring ventilation or developing a cytokine storm, he noted.
Burmester and Machado agree that research needs to continue as the pandemic rages on. But so far, “there are no data suggesting that, if you’re on a targeted, dedicated immunomodulator, your risk is higher to have a worse course of COVID-19 than the general population,” Burmester said.
“We simply didn’t know that when the pandemic started, and some patients even discontinued their drugs out of this fear,” he added. “It’s more reassuring than we originally thought.”
This article first appeared on Medscape.com.
The vast majority of patients with rheumatic and musculoskeletal diseases who contract COVID-19 recover from the virus, regardless of which medication they receive for their rheumatic condition, new international research suggests.
“These results provide, for the first time, information about the outcome of COVID-19 in patients with rheumatic and musculoskeletal diseases,” said study investigator Pedro Machado, MD, PhD, from University College London. “They should provide some reassurance to patients and healthcare providers.”
Machado and his colleagues looked at 600 COVID-19 patients from 40 countries, and found that those taking TNF inhibitors for their rheumatic disease were less likely to be hospitalized for COVID-19. However, treatment with more than 10 mg of prednisone daily — considered a moderate to high dose — was associated with a higher probability of hospitalization.
In addition, hospitalization was not associated with biologics; JAK inhibitors; conventional disease-modifying antirheumatic drugs (DMARDs), such as methotrexate; antimalarials, such as hydroxychloroquine; or nonsteroidal anti-inflammatory drugs (NSAIDs) — either alone or in combination with other biologics, such as TNF-alpha inhibitors.
The findings were presented at the virtual European League Against Rheumatism (EULAR) 2020 Congress and were published online in Annals of the Rheumatic Diseases.
“Initially, there was a huge concern that these drugs could affect the outcome of patients getting COVID-19, but what this is showing is that probably these drugs do not increase their risk of severe outcome,” Machado, who is chair of the EULAR standing committee on epidemiology and health services research, told Medscape Medical News.
As of June 1, 1061 patients from 28 participating countries had been entered into the EULAR COVID-19 database, which was launched as part of the international Global Rheumatology Alliance registry. Patient data are categorized by factors such as top rheumatology diagnosis, comorbidities, top-five COVID-19 symptoms, and DMARD therapy at the time of virus infection. Anonymized data will be shared with an international register based in the United States.
Machado’s team combined data from the EULAR and Global Rheumatology Alliance COVID-19 registries from March 24 to April 20. They looked at patient factors — such as age, sex, smoking status, rheumatic diagnosis, comorbidities, and rheumatic therapies — to examine the association of rheumatic therapies with hospitalization rates and COVID-19 disease course.
Of the 277 patients (46%) in the study cohort who required hospitalization, 55 (9%) died. But this finding shouldn’t be viewed as the true rate of hospitalization or death in patients with rheumatic disease and COVID-19, said Gerd Burmester, MD, from Charité–University Medicine Berlin.
“There’s tremendous bias in terms of more serious cases of COVID-19 being reported to the registries,” he explained, “because the mild cases won’t even show up at their rheumatologist’s office.”
“This can skew the idea that COVID-19 is much more dangerous to rheumatic patients than to the regular population,” Burmester told Medscape Medical News. “It scares the patients, obviously, but we believe this is not justified.”
It’s still unclear whether rituximab use raises the risk for severe COVID-19, he said. “It appears to be the only biologic for which the jury is still out,” he said.
“Anti-TNFs and anti-IL-6 drugs may even be beneficial, although we don’t have robust data,” he added.
The study can only highlight associations between rheumatic drugs and COVID-19 outcomes. “We cannot say there is a causal relationship between the findings,” Machado said.
Longer-term data, when available, should illuminate “more granular” aspects of COVID-19 outcomes in rheumatic patients, including their risks of requiring ventilation or developing a cytokine storm, he noted.
Burmester and Machado agree that research needs to continue as the pandemic rages on. But so far, “there are no data suggesting that, if you’re on a targeted, dedicated immunomodulator, your risk is higher to have a worse course of COVID-19 than the general population,” Burmester said.
“We simply didn’t know that when the pandemic started, and some patients even discontinued their drugs out of this fear,” he added. “It’s more reassuring than we originally thought.”
This article first appeared on Medscape.com.
The vast majority of patients with rheumatic and musculoskeletal diseases who contract COVID-19 recover from the virus, regardless of which medication they receive for their rheumatic condition, new international research suggests.
“These results provide, for the first time, information about the outcome of COVID-19 in patients with rheumatic and musculoskeletal diseases,” said study investigator Pedro Machado, MD, PhD, from University College London. “They should provide some reassurance to patients and healthcare providers.”
Machado and his colleagues looked at 600 COVID-19 patients from 40 countries, and found that those taking TNF inhibitors for their rheumatic disease were less likely to be hospitalized for COVID-19. However, treatment with more than 10 mg of prednisone daily — considered a moderate to high dose — was associated with a higher probability of hospitalization.
In addition, hospitalization was not associated with biologics; JAK inhibitors; conventional disease-modifying antirheumatic drugs (DMARDs), such as methotrexate; antimalarials, such as hydroxychloroquine; or nonsteroidal anti-inflammatory drugs (NSAIDs) — either alone or in combination with other biologics, such as TNF-alpha inhibitors.
The findings were presented at the virtual European League Against Rheumatism (EULAR) 2020 Congress and were published online in Annals of the Rheumatic Diseases.
“Initially, there was a huge concern that these drugs could affect the outcome of patients getting COVID-19, but what this is showing is that probably these drugs do not increase their risk of severe outcome,” Machado, who is chair of the EULAR standing committee on epidemiology and health services research, told Medscape Medical News.
As of June 1, 1061 patients from 28 participating countries had been entered into the EULAR COVID-19 database, which was launched as part of the international Global Rheumatology Alliance registry. Patient data are categorized by factors such as top rheumatology diagnosis, comorbidities, top-five COVID-19 symptoms, and DMARD therapy at the time of virus infection. Anonymized data will be shared with an international register based in the United States.
Machado’s team combined data from the EULAR and Global Rheumatology Alliance COVID-19 registries from March 24 to April 20. They looked at patient factors — such as age, sex, smoking status, rheumatic diagnosis, comorbidities, and rheumatic therapies — to examine the association of rheumatic therapies with hospitalization rates and COVID-19 disease course.
Of the 277 patients (46%) in the study cohort who required hospitalization, 55 (9%) died. But this finding shouldn’t be viewed as the true rate of hospitalization or death in patients with rheumatic disease and COVID-19, said Gerd Burmester, MD, from Charité–University Medicine Berlin.
“There’s tremendous bias in terms of more serious cases of COVID-19 being reported to the registries,” he explained, “because the mild cases won’t even show up at their rheumatologist’s office.”
“This can skew the idea that COVID-19 is much more dangerous to rheumatic patients than to the regular population,” Burmester told Medscape Medical News. “It scares the patients, obviously, but we believe this is not justified.”
It’s still unclear whether rituximab use raises the risk for severe COVID-19, he said. “It appears to be the only biologic for which the jury is still out,” he said.
“Anti-TNFs and anti-IL-6 drugs may even be beneficial, although we don’t have robust data,” he added.
The study can only highlight associations between rheumatic drugs and COVID-19 outcomes. “We cannot say there is a causal relationship between the findings,” Machado said.
Longer-term data, when available, should illuminate “more granular” aspects of COVID-19 outcomes in rheumatic patients, including their risks of requiring ventilation or developing a cytokine storm, he noted.
Burmester and Machado agree that research needs to continue as the pandemic rages on. But so far, “there are no data suggesting that, if you’re on a targeted, dedicated immunomodulator, your risk is higher to have a worse course of COVID-19 than the general population,” Burmester said.
“We simply didn’t know that when the pandemic started, and some patients even discontinued their drugs out of this fear,” he added. “It’s more reassuring than we originally thought.”
This article first appeared on Medscape.com.
NIMH strategic plan returns balance to research priorities
Digital health, suicide prevention, innovation addressed
The National Institute of Mental Health’s 2020 Strategic Plan outlines priorities in basic science research and clinical trials for psychiatry over the next 5 years, emphasizing where advances are needed in suicide prevention, digital health technology, early diagnosis in psychosis, and much more.
Experts’ reaction to the strategic plan is mixed. Some applaud the NIMH for addressing many essential research priorities and for returning a balance to the focus on basic/translational research and clinical advances. Others would have liked to see a different emphasis on some components of the plan.
Focusing on diversity
A greater weight on research in diverse populations and a renewed focus on studies across the lifespan – including developmental origins of psychiatric illness – are among the novel aspects of the plan.
“The enhanced attention to recruiting diverse subjects and focusing on diversity in our research is new and very welcome,” Jonathan E. Alpert, MD, PhD, chair of the American Psychiatric Association’s Council on Research, said in an interview.
Addressing the entire lifespan is likewise important, added Dr. Alpert, who holds the Dorothy and Marty Silverman Chair of Psychiatry at the Albert Einstein College of Medicine in New York. “Many of the conditions we treat – whether they are mood disorders or even dementia– might have developmental origins that would be best studied early in life.”
Furthermore, the plan promotes more interdisciplinary collaboration. For example, there are new cross-cutting research themes, including prevention, environmental influences, global health, and more. These are areas where psychiatry needs strengthening, said Stevan M. Weine, MD, director of Global Medicine at the University of Illinois at Chicago, in an interview.
In the era of COVID-19, which will involve ongoing diseases and disasters such as those tied to climate changes and disparities, there will be a need to conduct research and train researchers who are more open to new research questions, said Dr. Weine, also director of the Center for Global Health and professor of psychiatry at the university. It also will be important to partner with researchers from multiple disciplines, he added.
The plan also recognizes novel applications of digital technology. In addition, the plan outlines the promise of “harnessing the power of data,” such as machine learning, to help identify suicide risk factors based on large data, for example. However, Igor Galynker, MD, PhD, predicted that this technology will likely identify factors that “we see again and again,” such as depression, other forms of mental illness, and previous attempt history.
“Machine learning is useful but should not be emphasized” even if it is “technologically sexy and almost seductive,” Dr. Galynker, director of the Suicide Research & Prevention Laboratory at the Icahn School of Medicine at Mount Sinai in New York, said in an interview.
Addressing suicide
The strategic plan places a renewed emphasis on suicide prevention. The report cites a “troubling rise in the national suicide rate.” The authors suggested expanding initial success with brief screening tools in emergency departments to other clinical settings. Furthermore, the report highlights evidence that pairing such screening with low-cost follow-up interventions, such as telephone calls, can reduce the number of suicide attempts the following year.
Widespread screening could help identify people at risk, but it relies on the honesty of self-reporting, Dr. Galynker said, adding that about 75% of people who end their own lives never disclose their plan to anyone. Furthermore, suicide intent can be very short-lived – a crisis lasting as little as 15 minutes for some – reducing the likelihood that routine screening will flag a person in crisis.
“What is missing is an individual approach,” Dr. Galynker said while also endorsing the systemic approach to suicide prevention in the plan. “One thing in the strategic plan I may not agree with is the emphasis on administrative prediction measures ... based on drop-down menus and risk factors, and not on patient stories.” Risk factors are useful for long-term or lifetime risk, but they are not going to predict who will switch to acute suicidal state in the next several days or hours.”
Instead, Dr. Galynker suggested screening people for suicide crisis syndrome, which is “a very defined, characteristic, reproducible, and importantly, treatable,” state.
Covering basic neuroscience
Suicide prevention is just one of seven challenges and opportunities highlighted in the strategic plan. The authors also address research priorities for early treatment of psychosis and for research into mental health equity, HIV/AIDS research, genetics, and neural circuits.
“My overall impression is it’s very positive,” said Dr. Alpert, who is also professor and chair of the psychiatry and behavioral sciences department at Albert Einstein. “It really spans basic and translational neuroscience all the way to health services research and health disparities research. And I think, for many of us, we welcome that. It feels very relevant to the broad span of meaningful psychiatric research.”
Dr. Weine agreed. The strategic plan is “very helpful,” he said. “It is comprehensive, broad, and multidisciplinary.”
Promoting four overall goals
The plan seeks to promote the four following goals:
- Define the brain mechanisms underlying complex behaviors.
- Examine mental illness trajectories across the lifespan.
- Strive for prevention and cures.
- Strengthen the public health effects of National Institutes of Health–supported research.
The first goal is “an effort to try to make sense of the underlying biology, and that has to be your foundation point,” Ken Duckworth, MD, chief medical officer at the National Alliance on Mental Illness in Arlington, Va., said in an interview. “The reason we don’t have a lot of new drug discovery is because the fundamentals of biology still need understanding. It’s a long-term goal, so it’s hard,” he added. “Everyone living with someone in their life with an illness wants better ideas now.”
The third goal is likewise challenging, Dr. Duckworth said. “That is optimistic and ... aspirational, but very important and valuable.”
Developing innovative models
Regarding the public health goal, Dr. Duckworth cited one of the objectives, to “Develop innovative service delivery models to dramatically improve the outcomes of mental health services received in diverse communities and populations.” Dr. Duckworth explained, “Trying to solve for the problem in the context of an inadequate workforce that is insufficiently diverse – it just gets to something that I’m not sure would have been a priority in the past.
“That speaks to the awakening we’re having as a society. To address some of these historic and systemic injustices and how research can play into that is really important,” Dr. Duckworth added.
Overall, he saluted the plan and its goals. Dr. Duckworth added, “We gave some feedback that we wanted more emphasis on co-occurring disorders, such as research into people with mental health and addiction [issues] and on premature mortality. I think they took some of that feedback.”
Facing ‘significant challenges’
Dr. Weine added. “It sets a path for scientific advances that are responsive to these problems.”
“The future is bright. Looking forward to the next 5 years and beyond, the new NIMH Strategic Plan for Research aims to build on these advances,” Joshua A. Gordon, MD, PhD, NIMH director, noted in his Director’s Messages blog.
“Nonetheless, we face significant challenges,” he adds. “Studies of the origins of mental illnesses suggest that a combination of causes – genetic, environmental, social, and psychological – act on the brain through a complex web of interactions, resulting in a set of heterogeneous and overlapping illnesses.”
“My hope is that the actual funding of research over the coming years reflects the comprehensive, broad, and multidisciplinary characteristics of this strategic plan,” Dr. Weine said.
The NIMH plans to its post progress for each goal on an ongoing basis on the Strategic Plan website.
Dr. Alpert, Dr. Galynker, Dr. Weine, and Dr. Duckworth had no relevant disclosures.
Digital health, suicide prevention, innovation addressed
Digital health, suicide prevention, innovation addressed
The National Institute of Mental Health’s 2020 Strategic Plan outlines priorities in basic science research and clinical trials for psychiatry over the next 5 years, emphasizing where advances are needed in suicide prevention, digital health technology, early diagnosis in psychosis, and much more.
Experts’ reaction to the strategic plan is mixed. Some applaud the NIMH for addressing many essential research priorities and for returning a balance to the focus on basic/translational research and clinical advances. Others would have liked to see a different emphasis on some components of the plan.
Focusing on diversity
A greater weight on research in diverse populations and a renewed focus on studies across the lifespan – including developmental origins of psychiatric illness – are among the novel aspects of the plan.
“The enhanced attention to recruiting diverse subjects and focusing on diversity in our research is new and very welcome,” Jonathan E. Alpert, MD, PhD, chair of the American Psychiatric Association’s Council on Research, said in an interview.
Addressing the entire lifespan is likewise important, added Dr. Alpert, who holds the Dorothy and Marty Silverman Chair of Psychiatry at the Albert Einstein College of Medicine in New York. “Many of the conditions we treat – whether they are mood disorders or even dementia– might have developmental origins that would be best studied early in life.”
Furthermore, the plan promotes more interdisciplinary collaboration. For example, there are new cross-cutting research themes, including prevention, environmental influences, global health, and more. These are areas where psychiatry needs strengthening, said Stevan M. Weine, MD, director of Global Medicine at the University of Illinois at Chicago, in an interview.
In the era of COVID-19, which will involve ongoing diseases and disasters such as those tied to climate changes and disparities, there will be a need to conduct research and train researchers who are more open to new research questions, said Dr. Weine, also director of the Center for Global Health and professor of psychiatry at the university. It also will be important to partner with researchers from multiple disciplines, he added.
The plan also recognizes novel applications of digital technology. In addition, the plan outlines the promise of “harnessing the power of data,” such as machine learning, to help identify suicide risk factors based on large data, for example. However, Igor Galynker, MD, PhD, predicted that this technology will likely identify factors that “we see again and again,” such as depression, other forms of mental illness, and previous attempt history.
“Machine learning is useful but should not be emphasized” even if it is “technologically sexy and almost seductive,” Dr. Galynker, director of the Suicide Research & Prevention Laboratory at the Icahn School of Medicine at Mount Sinai in New York, said in an interview.
Addressing suicide
The strategic plan places a renewed emphasis on suicide prevention. The report cites a “troubling rise in the national suicide rate.” The authors suggested expanding initial success with brief screening tools in emergency departments to other clinical settings. Furthermore, the report highlights evidence that pairing such screening with low-cost follow-up interventions, such as telephone calls, can reduce the number of suicide attempts the following year.
Widespread screening could help identify people at risk, but it relies on the honesty of self-reporting, Dr. Galynker said, adding that about 75% of people who end their own lives never disclose their plan to anyone. Furthermore, suicide intent can be very short-lived – a crisis lasting as little as 15 minutes for some – reducing the likelihood that routine screening will flag a person in crisis.
“What is missing is an individual approach,” Dr. Galynker said while also endorsing the systemic approach to suicide prevention in the plan. “One thing in the strategic plan I may not agree with is the emphasis on administrative prediction measures ... based on drop-down menus and risk factors, and not on patient stories.” Risk factors are useful for long-term or lifetime risk, but they are not going to predict who will switch to acute suicidal state in the next several days or hours.”
Instead, Dr. Galynker suggested screening people for suicide crisis syndrome, which is “a very defined, characteristic, reproducible, and importantly, treatable,” state.
Covering basic neuroscience
Suicide prevention is just one of seven challenges and opportunities highlighted in the strategic plan. The authors also address research priorities for early treatment of psychosis and for research into mental health equity, HIV/AIDS research, genetics, and neural circuits.
“My overall impression is it’s very positive,” said Dr. Alpert, who is also professor and chair of the psychiatry and behavioral sciences department at Albert Einstein. “It really spans basic and translational neuroscience all the way to health services research and health disparities research. And I think, for many of us, we welcome that. It feels very relevant to the broad span of meaningful psychiatric research.”
Dr. Weine agreed. The strategic plan is “very helpful,” he said. “It is comprehensive, broad, and multidisciplinary.”
Promoting four overall goals
The plan seeks to promote the four following goals:
- Define the brain mechanisms underlying complex behaviors.
- Examine mental illness trajectories across the lifespan.
- Strive for prevention and cures.
- Strengthen the public health effects of National Institutes of Health–supported research.
The first goal is “an effort to try to make sense of the underlying biology, and that has to be your foundation point,” Ken Duckworth, MD, chief medical officer at the National Alliance on Mental Illness in Arlington, Va., said in an interview. “The reason we don’t have a lot of new drug discovery is because the fundamentals of biology still need understanding. It’s a long-term goal, so it’s hard,” he added. “Everyone living with someone in their life with an illness wants better ideas now.”
The third goal is likewise challenging, Dr. Duckworth said. “That is optimistic and ... aspirational, but very important and valuable.”
Developing innovative models
Regarding the public health goal, Dr. Duckworth cited one of the objectives, to “Develop innovative service delivery models to dramatically improve the outcomes of mental health services received in diverse communities and populations.” Dr. Duckworth explained, “Trying to solve for the problem in the context of an inadequate workforce that is insufficiently diverse – it just gets to something that I’m not sure would have been a priority in the past.
“That speaks to the awakening we’re having as a society. To address some of these historic and systemic injustices and how research can play into that is really important,” Dr. Duckworth added.
Overall, he saluted the plan and its goals. Dr. Duckworth added, “We gave some feedback that we wanted more emphasis on co-occurring disorders, such as research into people with mental health and addiction [issues] and on premature mortality. I think they took some of that feedback.”
Facing ‘significant challenges’
Dr. Weine added. “It sets a path for scientific advances that are responsive to these problems.”
“The future is bright. Looking forward to the next 5 years and beyond, the new NIMH Strategic Plan for Research aims to build on these advances,” Joshua A. Gordon, MD, PhD, NIMH director, noted in his Director’s Messages blog.
“Nonetheless, we face significant challenges,” he adds. “Studies of the origins of mental illnesses suggest that a combination of causes – genetic, environmental, social, and psychological – act on the brain through a complex web of interactions, resulting in a set of heterogeneous and overlapping illnesses.”
“My hope is that the actual funding of research over the coming years reflects the comprehensive, broad, and multidisciplinary characteristics of this strategic plan,” Dr. Weine said.
The NIMH plans to its post progress for each goal on an ongoing basis on the Strategic Plan website.
Dr. Alpert, Dr. Galynker, Dr. Weine, and Dr. Duckworth had no relevant disclosures.
The National Institute of Mental Health’s 2020 Strategic Plan outlines priorities in basic science research and clinical trials for psychiatry over the next 5 years, emphasizing where advances are needed in suicide prevention, digital health technology, early diagnosis in psychosis, and much more.
Experts’ reaction to the strategic plan is mixed. Some applaud the NIMH for addressing many essential research priorities and for returning a balance to the focus on basic/translational research and clinical advances. Others would have liked to see a different emphasis on some components of the plan.
Focusing on diversity
A greater weight on research in diverse populations and a renewed focus on studies across the lifespan – including developmental origins of psychiatric illness – are among the novel aspects of the plan.
“The enhanced attention to recruiting diverse subjects and focusing on diversity in our research is new and very welcome,” Jonathan E. Alpert, MD, PhD, chair of the American Psychiatric Association’s Council on Research, said in an interview.
Addressing the entire lifespan is likewise important, added Dr. Alpert, who holds the Dorothy and Marty Silverman Chair of Psychiatry at the Albert Einstein College of Medicine in New York. “Many of the conditions we treat – whether they are mood disorders or even dementia– might have developmental origins that would be best studied early in life.”
Furthermore, the plan promotes more interdisciplinary collaboration. For example, there are new cross-cutting research themes, including prevention, environmental influences, global health, and more. These are areas where psychiatry needs strengthening, said Stevan M. Weine, MD, director of Global Medicine at the University of Illinois at Chicago, in an interview.
In the era of COVID-19, which will involve ongoing diseases and disasters such as those tied to climate changes and disparities, there will be a need to conduct research and train researchers who are more open to new research questions, said Dr. Weine, also director of the Center for Global Health and professor of psychiatry at the university. It also will be important to partner with researchers from multiple disciplines, he added.
The plan also recognizes novel applications of digital technology. In addition, the plan outlines the promise of “harnessing the power of data,” such as machine learning, to help identify suicide risk factors based on large data, for example. However, Igor Galynker, MD, PhD, predicted that this technology will likely identify factors that “we see again and again,” such as depression, other forms of mental illness, and previous attempt history.
“Machine learning is useful but should not be emphasized” even if it is “technologically sexy and almost seductive,” Dr. Galynker, director of the Suicide Research & Prevention Laboratory at the Icahn School of Medicine at Mount Sinai in New York, said in an interview.
Addressing suicide
The strategic plan places a renewed emphasis on suicide prevention. The report cites a “troubling rise in the national suicide rate.” The authors suggested expanding initial success with brief screening tools in emergency departments to other clinical settings. Furthermore, the report highlights evidence that pairing such screening with low-cost follow-up interventions, such as telephone calls, can reduce the number of suicide attempts the following year.
Widespread screening could help identify people at risk, but it relies on the honesty of self-reporting, Dr. Galynker said, adding that about 75% of people who end their own lives never disclose their plan to anyone. Furthermore, suicide intent can be very short-lived – a crisis lasting as little as 15 minutes for some – reducing the likelihood that routine screening will flag a person in crisis.
“What is missing is an individual approach,” Dr. Galynker said while also endorsing the systemic approach to suicide prevention in the plan. “One thing in the strategic plan I may not agree with is the emphasis on administrative prediction measures ... based on drop-down menus and risk factors, and not on patient stories.” Risk factors are useful for long-term or lifetime risk, but they are not going to predict who will switch to acute suicidal state in the next several days or hours.”
Instead, Dr. Galynker suggested screening people for suicide crisis syndrome, which is “a very defined, characteristic, reproducible, and importantly, treatable,” state.
Covering basic neuroscience
Suicide prevention is just one of seven challenges and opportunities highlighted in the strategic plan. The authors also address research priorities for early treatment of psychosis and for research into mental health equity, HIV/AIDS research, genetics, and neural circuits.
“My overall impression is it’s very positive,” said Dr. Alpert, who is also professor and chair of the psychiatry and behavioral sciences department at Albert Einstein. “It really spans basic and translational neuroscience all the way to health services research and health disparities research. And I think, for many of us, we welcome that. It feels very relevant to the broad span of meaningful psychiatric research.”
Dr. Weine agreed. The strategic plan is “very helpful,” he said. “It is comprehensive, broad, and multidisciplinary.”
Promoting four overall goals
The plan seeks to promote the four following goals:
- Define the brain mechanisms underlying complex behaviors.
- Examine mental illness trajectories across the lifespan.
- Strive for prevention and cures.
- Strengthen the public health effects of National Institutes of Health–supported research.
The first goal is “an effort to try to make sense of the underlying biology, and that has to be your foundation point,” Ken Duckworth, MD, chief medical officer at the National Alliance on Mental Illness in Arlington, Va., said in an interview. “The reason we don’t have a lot of new drug discovery is because the fundamentals of biology still need understanding. It’s a long-term goal, so it’s hard,” he added. “Everyone living with someone in their life with an illness wants better ideas now.”
The third goal is likewise challenging, Dr. Duckworth said. “That is optimistic and ... aspirational, but very important and valuable.”
Developing innovative models
Regarding the public health goal, Dr. Duckworth cited one of the objectives, to “Develop innovative service delivery models to dramatically improve the outcomes of mental health services received in diverse communities and populations.” Dr. Duckworth explained, “Trying to solve for the problem in the context of an inadequate workforce that is insufficiently diverse – it just gets to something that I’m not sure would have been a priority in the past.
“That speaks to the awakening we’re having as a society. To address some of these historic and systemic injustices and how research can play into that is really important,” Dr. Duckworth added.
Overall, he saluted the plan and its goals. Dr. Duckworth added, “We gave some feedback that we wanted more emphasis on co-occurring disorders, such as research into people with mental health and addiction [issues] and on premature mortality. I think they took some of that feedback.”
Facing ‘significant challenges’
Dr. Weine added. “It sets a path for scientific advances that are responsive to these problems.”
“The future is bright. Looking forward to the next 5 years and beyond, the new NIMH Strategic Plan for Research aims to build on these advances,” Joshua A. Gordon, MD, PhD, NIMH director, noted in his Director’s Messages blog.
“Nonetheless, we face significant challenges,” he adds. “Studies of the origins of mental illnesses suggest that a combination of causes – genetic, environmental, social, and psychological – act on the brain through a complex web of interactions, resulting in a set of heterogeneous and overlapping illnesses.”
“My hope is that the actual funding of research over the coming years reflects the comprehensive, broad, and multidisciplinary characteristics of this strategic plan,” Dr. Weine said.
The NIMH plans to its post progress for each goal on an ongoing basis on the Strategic Plan website.
Dr. Alpert, Dr. Galynker, Dr. Weine, and Dr. Duckworth had no relevant disclosures.
Parenting special needs children: An unlikely model
COVID-19 can give physicians a window into lives of families
The last few months have tested the stamina of most families. Many people are struggling to keep some semblance of normalcy amid a radical transformation of everyday life. It seems as if everything changed overnight.
In a similar way, when a child with many needs is born into a family, adjustments also have to take place to receive the new baby. Families are, in most cases, not prepared for what is to come. Their expectations usually are not in sync with how their lives end up. They are crunched for time. They need to adjust, and at the same time, they mourn the loss of their previous less demanding lifestyle. More importantly, these parents learn that this might be an adjustment that they might need to make for a long time – in some instances, for a lifetime.
Stress load over time can correlate with a sense of burnout, and mental health professionals need to be prepared to address these issues in our patients.
Here is a list of some chronic struggles with which many special needs parents must contend. These strongly resemble the challenges parents in the general population have been facing with their families during this pandemic:
- Bypassing breaks to unwind and having to be always “on” while at home: These parents take care of children who need to be chronically tube fed, can’t sleep well at night because they are often sick, have recurrent seizures or maladaptive behaviors that affect the caretakers and the rest of the family. For parents of children who are on the autism spectrum, these challenges can be a constant struggle. Almost 60% of children with autism spectrum disorder (ASD) experience bodily difficulties, such as trouble breathing. However, nearly 100% of children with ASD experienced difficulties with their abilities and activities, such as self-care tasks like eating and dressing, and emotional or behavioral health, according to a 2016 report on child and adolescent health by the Johns Hopkins Bloomberg School of Public Health.
- Taking on roles for which they are not trained: Parents may take on active roles supplementing their developmentally delayed children with educational experiences or therapeutic modalities in their own homes given that the needs might be too great to just rely on the school or therapy time. There are about 1.17 million children in the United States living with ASD and more than 12% of children with ASD have severe cases, the Hopkins report said. Parents frequently are forced to take on the role of “therapist” to meet the needs of their child.
- Staying home often: Some parents are unable to have a “regular sitter” to provide respite, because the needs of the child require a higher level of care, training, and consideration. Caring for a special child means parents often don’t have the option of leaving their older child alone. As a result, they may end up spending more time at home than their counterpart parents with children who are the same age.
- Struggling to meet everyone’s demands for attention while at home: The child might require full-time attention or prolonged hospitalizations, and the needs of other siblings are sometimes put on hold until time or energy are available for all.
- Not traveling unless absolutely necessary: Families have a hard time leaving home for vacations or for other reasons. They may have to travel with medical supplies and equipment. They need to make sure that their destination is ready to welcome their child with all needs taken into consideration (special diets, activities, and facilities). Will the vacation set them back because it might take more effort to go than to stay home?
- Avoiding unnecessary exposures: Trying to avoid infections (even the ones that may be innocuous to others) if their child is immunocompromised. These children may readily decompensate and end up hospitalized with a more serious medical complication.
- Being very aware of remaining physically distant from others: Parents must go to great lengths not to impinge on other people’s space if the child is being loud or moving in a disruptive way, or if other people negatively affect how the child responds. Some families are apprehensive because they have felt judged by others when they are in the community, restaurants, or other places of gathering.
- Feeling concerned about having the right food, medicines, and supplements in the house: Parents are constantly trying to fulfill special dietary requirements and have the reserve to make sure that all meals and treatments are accounted for in the near future. They might need oxygen or specialized formulas that are hard to find in local stores. Some treatments, when withdrawn or unavailable, can prove life threatening.
- Restricting social circles: Some families with children with severe autism may self-isolate when they feel it is hard to be around them and be friends with them, since they can’t readily participate in “usual family activities,” and the regular norms of socialization can’t apply to their family’s set of behaviors. Their child might seem to be disruptive, or loud, nonverbal, mute, or unable to easily relate to others.
- Experiencing a pervasive sense of uncertainty about the future: A child might continue to miss milestones, or might have a rare condition that hasn’t been diagnosed. When thinking of the future, parents can’t predict what level of care they need to plan and budget for.
- Being concerned about dying early and not being able to provide for their child: Parents worry about who would take care of their child for life. Who would take care of their aging adult “child” after parents are gone? They might have concerns about having a will in place early on.
- Facing financial stress secondary to losing a job or the cost of treatments: Absenteeism might be the end result of having to care for their child’s ongoing needs, appointments, and medical emergencies. Sometimes, they might depend on a caretaker who might be very difficult to replace. It might take extensive training once a candidate is found. Direct costs include medical care, hospitalizations, special education, special therapies (occupational, speech, and physical therapy), and paid caregivers. Indirect costs include lost productivity for family caregivers because of the inability to maintain employment while caring for affected individuals, as well as lost wages and benefits, the Hopkins report said.
- Struggling to coordinate daily schedules: Parents face this challenge not only with young children but with those who are chronically ill and might need ongoing 24/7 care. The schedule might include educational and therapeutic (physical, occupational, speech, language therapy, recreational) interventions regularly or daily. This schedule is to be superimposed on all the other necessary responsibilities parents already have to contend with. Forty-eight percent of school-aged children with ASD use three or more services. In addition, children with moderate or severe cases of ASD used three or more services at almost twice the rate of children with mild cases of ASD (60% vs. 35%).
- Longing for a cure or a medicine that will improve the outcome: Often, parents search for treatments so that their child could live a more comfortable or healthier life. For children who have a rare condition, there may not be sufficient research dedicated to their cause or diagnostic pursuits. Currently, it is estimated that 1 in 10 Americans has a rare disease – about 80% of which are genetically based. Of the nearly 7,000 rare diseases known to exist, less than 500 – roughly 5% – have a known treatment approved by the U.S. Food and Drug Administration, reports the National Center for Advancing Translational Diseases and the Genetic and Rare Diseases Information Center.
- Hoping for better times to come: It is difficult at times to appreciate the present when it happens to be so chronically challenging and exhausting for everyone.
Parents of children with significant special needs experience many hurdles that they learn to endure, overcome, and master. This pandemic can provide physicians with a window into the lives of these families.
Dr. Sotir is a psychiatrist in private practice in Wheaton, Ill. As a parent of three children, one with special needs, she has extensive experience helping parents challenged by having special needs children find balance, support, direction, and joy in all dimensions of individual and family life. This area is the focus of her practice and public speaking. In Part 2, she will explore how psychiatrists as a specialty can support these families. She has no disclosures.
COVID-19 can give physicians a window into lives of families
COVID-19 can give physicians a window into lives of families
The last few months have tested the stamina of most families. Many people are struggling to keep some semblance of normalcy amid a radical transformation of everyday life. It seems as if everything changed overnight.
In a similar way, when a child with many needs is born into a family, adjustments also have to take place to receive the new baby. Families are, in most cases, not prepared for what is to come. Their expectations usually are not in sync with how their lives end up. They are crunched for time. They need to adjust, and at the same time, they mourn the loss of their previous less demanding lifestyle. More importantly, these parents learn that this might be an adjustment that they might need to make for a long time – in some instances, for a lifetime.
Stress load over time can correlate with a sense of burnout, and mental health professionals need to be prepared to address these issues in our patients.
Here is a list of some chronic struggles with which many special needs parents must contend. These strongly resemble the challenges parents in the general population have been facing with their families during this pandemic:
- Bypassing breaks to unwind and having to be always “on” while at home: These parents take care of children who need to be chronically tube fed, can’t sleep well at night because they are often sick, have recurrent seizures or maladaptive behaviors that affect the caretakers and the rest of the family. For parents of children who are on the autism spectrum, these challenges can be a constant struggle. Almost 60% of children with autism spectrum disorder (ASD) experience bodily difficulties, such as trouble breathing. However, nearly 100% of children with ASD experienced difficulties with their abilities and activities, such as self-care tasks like eating and dressing, and emotional or behavioral health, according to a 2016 report on child and adolescent health by the Johns Hopkins Bloomberg School of Public Health.
- Taking on roles for which they are not trained: Parents may take on active roles supplementing their developmentally delayed children with educational experiences or therapeutic modalities in their own homes given that the needs might be too great to just rely on the school or therapy time. There are about 1.17 million children in the United States living with ASD and more than 12% of children with ASD have severe cases, the Hopkins report said. Parents frequently are forced to take on the role of “therapist” to meet the needs of their child.
- Staying home often: Some parents are unable to have a “regular sitter” to provide respite, because the needs of the child require a higher level of care, training, and consideration. Caring for a special child means parents often don’t have the option of leaving their older child alone. As a result, they may end up spending more time at home than their counterpart parents with children who are the same age.
- Struggling to meet everyone’s demands for attention while at home: The child might require full-time attention or prolonged hospitalizations, and the needs of other siblings are sometimes put on hold until time or energy are available for all.
- Not traveling unless absolutely necessary: Families have a hard time leaving home for vacations or for other reasons. They may have to travel with medical supplies and equipment. They need to make sure that their destination is ready to welcome their child with all needs taken into consideration (special diets, activities, and facilities). Will the vacation set them back because it might take more effort to go than to stay home?
- Avoiding unnecessary exposures: Trying to avoid infections (even the ones that may be innocuous to others) if their child is immunocompromised. These children may readily decompensate and end up hospitalized with a more serious medical complication.
- Being very aware of remaining physically distant from others: Parents must go to great lengths not to impinge on other people’s space if the child is being loud or moving in a disruptive way, or if other people negatively affect how the child responds. Some families are apprehensive because they have felt judged by others when they are in the community, restaurants, or other places of gathering.
- Feeling concerned about having the right food, medicines, and supplements in the house: Parents are constantly trying to fulfill special dietary requirements and have the reserve to make sure that all meals and treatments are accounted for in the near future. They might need oxygen or specialized formulas that are hard to find in local stores. Some treatments, when withdrawn or unavailable, can prove life threatening.
- Restricting social circles: Some families with children with severe autism may self-isolate when they feel it is hard to be around them and be friends with them, since they can’t readily participate in “usual family activities,” and the regular norms of socialization can’t apply to their family’s set of behaviors. Their child might seem to be disruptive, or loud, nonverbal, mute, or unable to easily relate to others.
- Experiencing a pervasive sense of uncertainty about the future: A child might continue to miss milestones, or might have a rare condition that hasn’t been diagnosed. When thinking of the future, parents can’t predict what level of care they need to plan and budget for.
- Being concerned about dying early and not being able to provide for their child: Parents worry about who would take care of their child for life. Who would take care of their aging adult “child” after parents are gone? They might have concerns about having a will in place early on.
- Facing financial stress secondary to losing a job or the cost of treatments: Absenteeism might be the end result of having to care for their child’s ongoing needs, appointments, and medical emergencies. Sometimes, they might depend on a caretaker who might be very difficult to replace. It might take extensive training once a candidate is found. Direct costs include medical care, hospitalizations, special education, special therapies (occupational, speech, and physical therapy), and paid caregivers. Indirect costs include lost productivity for family caregivers because of the inability to maintain employment while caring for affected individuals, as well as lost wages and benefits, the Hopkins report said.
- Struggling to coordinate daily schedules: Parents face this challenge not only with young children but with those who are chronically ill and might need ongoing 24/7 care. The schedule might include educational and therapeutic (physical, occupational, speech, language therapy, recreational) interventions regularly or daily. This schedule is to be superimposed on all the other necessary responsibilities parents already have to contend with. Forty-eight percent of school-aged children with ASD use three or more services. In addition, children with moderate or severe cases of ASD used three or more services at almost twice the rate of children with mild cases of ASD (60% vs. 35%).
- Longing for a cure or a medicine that will improve the outcome: Often, parents search for treatments so that their child could live a more comfortable or healthier life. For children who have a rare condition, there may not be sufficient research dedicated to their cause or diagnostic pursuits. Currently, it is estimated that 1 in 10 Americans has a rare disease – about 80% of which are genetically based. Of the nearly 7,000 rare diseases known to exist, less than 500 – roughly 5% – have a known treatment approved by the U.S. Food and Drug Administration, reports the National Center for Advancing Translational Diseases and the Genetic and Rare Diseases Information Center.
- Hoping for better times to come: It is difficult at times to appreciate the present when it happens to be so chronically challenging and exhausting for everyone.
Parents of children with significant special needs experience many hurdles that they learn to endure, overcome, and master. This pandemic can provide physicians with a window into the lives of these families.
Dr. Sotir is a psychiatrist in private practice in Wheaton, Ill. As a parent of three children, one with special needs, she has extensive experience helping parents challenged by having special needs children find balance, support, direction, and joy in all dimensions of individual and family life. This area is the focus of her practice and public speaking. In Part 2, she will explore how psychiatrists as a specialty can support these families. She has no disclosures.
The last few months have tested the stamina of most families. Many people are struggling to keep some semblance of normalcy amid a radical transformation of everyday life. It seems as if everything changed overnight.
In a similar way, when a child with many needs is born into a family, adjustments also have to take place to receive the new baby. Families are, in most cases, not prepared for what is to come. Their expectations usually are not in sync with how their lives end up. They are crunched for time. They need to adjust, and at the same time, they mourn the loss of their previous less demanding lifestyle. More importantly, these parents learn that this might be an adjustment that they might need to make for a long time – in some instances, for a lifetime.
Stress load over time can correlate with a sense of burnout, and mental health professionals need to be prepared to address these issues in our patients.
Here is a list of some chronic struggles with which many special needs parents must contend. These strongly resemble the challenges parents in the general population have been facing with their families during this pandemic:
- Bypassing breaks to unwind and having to be always “on” while at home: These parents take care of children who need to be chronically tube fed, can’t sleep well at night because they are often sick, have recurrent seizures or maladaptive behaviors that affect the caretakers and the rest of the family. For parents of children who are on the autism spectrum, these challenges can be a constant struggle. Almost 60% of children with autism spectrum disorder (ASD) experience bodily difficulties, such as trouble breathing. However, nearly 100% of children with ASD experienced difficulties with their abilities and activities, such as self-care tasks like eating and dressing, and emotional or behavioral health, according to a 2016 report on child and adolescent health by the Johns Hopkins Bloomberg School of Public Health.
- Taking on roles for which they are not trained: Parents may take on active roles supplementing their developmentally delayed children with educational experiences or therapeutic modalities in their own homes given that the needs might be too great to just rely on the school or therapy time. There are about 1.17 million children in the United States living with ASD and more than 12% of children with ASD have severe cases, the Hopkins report said. Parents frequently are forced to take on the role of “therapist” to meet the needs of their child.
- Staying home often: Some parents are unable to have a “regular sitter” to provide respite, because the needs of the child require a higher level of care, training, and consideration. Caring for a special child means parents often don’t have the option of leaving their older child alone. As a result, they may end up spending more time at home than their counterpart parents with children who are the same age.
- Struggling to meet everyone’s demands for attention while at home: The child might require full-time attention or prolonged hospitalizations, and the needs of other siblings are sometimes put on hold until time or energy are available for all.
- Not traveling unless absolutely necessary: Families have a hard time leaving home for vacations or for other reasons. They may have to travel with medical supplies and equipment. They need to make sure that their destination is ready to welcome their child with all needs taken into consideration (special diets, activities, and facilities). Will the vacation set them back because it might take more effort to go than to stay home?
- Avoiding unnecessary exposures: Trying to avoid infections (even the ones that may be innocuous to others) if their child is immunocompromised. These children may readily decompensate and end up hospitalized with a more serious medical complication.
- Being very aware of remaining physically distant from others: Parents must go to great lengths not to impinge on other people’s space if the child is being loud or moving in a disruptive way, or if other people negatively affect how the child responds. Some families are apprehensive because they have felt judged by others when they are in the community, restaurants, or other places of gathering.
- Feeling concerned about having the right food, medicines, and supplements in the house: Parents are constantly trying to fulfill special dietary requirements and have the reserve to make sure that all meals and treatments are accounted for in the near future. They might need oxygen or specialized formulas that are hard to find in local stores. Some treatments, when withdrawn or unavailable, can prove life threatening.
- Restricting social circles: Some families with children with severe autism may self-isolate when they feel it is hard to be around them and be friends with them, since they can’t readily participate in “usual family activities,” and the regular norms of socialization can’t apply to their family’s set of behaviors. Their child might seem to be disruptive, or loud, nonverbal, mute, or unable to easily relate to others.
- Experiencing a pervasive sense of uncertainty about the future: A child might continue to miss milestones, or might have a rare condition that hasn’t been diagnosed. When thinking of the future, parents can’t predict what level of care they need to plan and budget for.
- Being concerned about dying early and not being able to provide for their child: Parents worry about who would take care of their child for life. Who would take care of their aging adult “child” after parents are gone? They might have concerns about having a will in place early on.
- Facing financial stress secondary to losing a job or the cost of treatments: Absenteeism might be the end result of having to care for their child’s ongoing needs, appointments, and medical emergencies. Sometimes, they might depend on a caretaker who might be very difficult to replace. It might take extensive training once a candidate is found. Direct costs include medical care, hospitalizations, special education, special therapies (occupational, speech, and physical therapy), and paid caregivers. Indirect costs include lost productivity for family caregivers because of the inability to maintain employment while caring for affected individuals, as well as lost wages and benefits, the Hopkins report said.
- Struggling to coordinate daily schedules: Parents face this challenge not only with young children but with those who are chronically ill and might need ongoing 24/7 care. The schedule might include educational and therapeutic (physical, occupational, speech, language therapy, recreational) interventions regularly or daily. This schedule is to be superimposed on all the other necessary responsibilities parents already have to contend with. Forty-eight percent of school-aged children with ASD use three or more services. In addition, children with moderate or severe cases of ASD used three or more services at almost twice the rate of children with mild cases of ASD (60% vs. 35%).
- Longing for a cure or a medicine that will improve the outcome: Often, parents search for treatments so that their child could live a more comfortable or healthier life. For children who have a rare condition, there may not be sufficient research dedicated to their cause or diagnostic pursuits. Currently, it is estimated that 1 in 10 Americans has a rare disease – about 80% of which are genetically based. Of the nearly 7,000 rare diseases known to exist, less than 500 – roughly 5% – have a known treatment approved by the U.S. Food and Drug Administration, reports the National Center for Advancing Translational Diseases and the Genetic and Rare Diseases Information Center.
- Hoping for better times to come: It is difficult at times to appreciate the present when it happens to be so chronically challenging and exhausting for everyone.
Parents of children with significant special needs experience many hurdles that they learn to endure, overcome, and master. This pandemic can provide physicians with a window into the lives of these families.
Dr. Sotir is a psychiatrist in private practice in Wheaton, Ill. As a parent of three children, one with special needs, she has extensive experience helping parents challenged by having special needs children find balance, support, direction, and joy in all dimensions of individual and family life. This area is the focus of her practice and public speaking. In Part 2, she will explore how psychiatrists as a specialty can support these families. She has no disclosures.
More fatalities in heart transplant patients with COVID-19
COVID-19 infection is associated with a high risk for mortality in heart transplant (HT) recipients, a new case series suggests.
Investigators looked at data on 28 patients with a confirmed diagnosis of COVID-19 who received a HT between March 1, 2020, and April 24, 2020 and found a case-fatality rate of 25%.
“The high case fatality in our case series should alert physicians to the vulnerability of heart transplant recipients during the COVID-19 pandemic,” senior author Nir Uriel, MD, MSc, professor of medicine at Columbia University, New York, said in an interview.
“These patients require extra precautions to prevent the development of infection,” said Dr. Uriel, who is also a cardiologist at New York Presbyterian/Columbia University Irving Medical Center.
The study was published online May 13 in JAMA Cardiology.
Similar presentation
HT recipients can have several comorbidities after the procedure, including hypertension, diabetes, cardiac allograft vasculopathy, and ongoing immunosuppression, all of which can place them at risk for infection and adverse outcomes with COVID-19 infection, the authors wrote.
The researchers therefore embarked on a case series looking at 28 HT recipients with COVID-19 infection (median age, 64.0 years; interquartile range, 53.5-70.5; 79% male) to “describe the outcomes of recipients of HT who are chronically immunosuppressed and develop COVID-19 and raise important questions about the role of the immune system in the process.”
The median time from HT to study period was 8.6 (IQR, 4.2-14.5) years. Most patients had numerous comorbidities.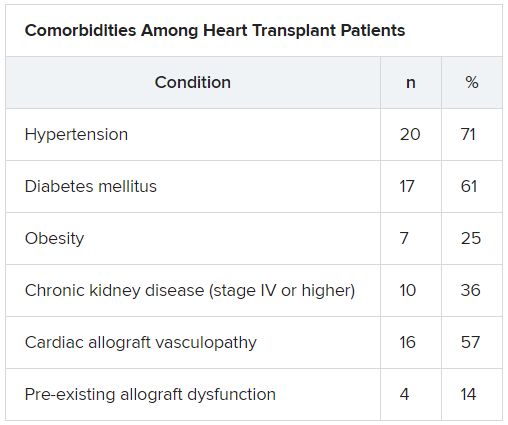
“The presentation of COVID-19 was similar to nontransplant patients with fever, dyspnea, cough, and GI symptoms,” Dr. Uriel reported.
No protective effect
Twenty-two patients (79%) required admission to the hospital, seven of whom (25%) required admission to the ICU and mechanical ventilation.
Despite the presence of immunosuppressive therapy, all patients had significant elevation of inflammatory biomarkers (median peak high-sensitivity C-reactive protein [hs-CRP], 11.83 mg/dL; IQR, 7.44-19.26; median peak interleukin [IL]-6, 105 pg/mL; IQR, 38-296).
Three-quarters had myocardial injury, with a median high-sensitivity troponin T of 0.055 (0.0205 - 0.1345) ng/mL.
Treatments of COVID-19 included hydroxychloroquine (18 patients; 78%), high-dose corticosteroids (eight patients; 47%), and IL-6 receptor antagonists (six patients; 26%).
Moreover, during hospitalization, mycophenolate mofetil was discontinued in most (70%) patients, and one-quarter had a reduction in their calcineurin inhibitor dose.
“Heart transplant recipients generally require more intense immunosuppressive therapy than most other solid organ transplant recipients, and this high baseline immunosuppression increases their propensity to develop infections and their likelihood of experiencing severe manifestations of infections,” Dr. Uriel commented.
“With COVID-19, in which the body’s inflammatory reaction appears to play a role in disease severity, there has been a question of whether immunosuppression may offer a protective effect,” he continued.
“This case series suggests that this is not the case, although this would need to be confirmed in larger studies,” he said.
Low threshold
Among the 22 patients who were admitted to the hospital, half were discharged home and four (18%) were still hospitalized at the end of the study.
Of the seven patients who died, two died at the study center, and five died in an outside institution.
“In the HT population, social distancing (or isolation), strict use of masks when in public, proper handwashing, and sanitization of surfaces are of paramount importance in the prevention of COVID-19 infection,” Dr. Uriel stated.
“In addition, we have restricted these patients’ contact with the hospital as much as possible during the pandemic,” he said.
However, “there should be a low threshold to hospitalize heart transplant patients who develop infection with COVID-19. Furthermore, in our series, outcomes were better for patients hospitalized at the transplant center; therefore, strong consideration should be given to transferring HT patients when hospitalized at another hospital,” he added.
The authors emphasized that COVID-19 patients “will require ongoing monitoring in the recovery phase, as an immunosuppression regimen is reintroduced and the consequences to the allograft itself become apparent.”
Vulnerable population
Commenting on the study, Mandeep R. Mehra, MD, MSc, William Harvey Distinguished Chair in Advanced Cardiovascular Medicine at Brigham and Women’s Hospital, Boston, suggested that “in epidemiological terms, [the findings] might not look as bad as the way they are reflected in the paper.”
Given that Columbia is “one of the larger heart transplant centers in the U.S., following probably 1,000 patients, having only 22 out of perhaps thousands whom they transplanted or are actively following would actually represent a low serious infection rate,” said Dr. Mehra, who is also the executive director of the Center for Advanced Heart Disease at Brigham and Women’s Hospital and a professor of medicine at Harvard Medical School, also in Boston.
“We must not forget to emphasize that, when assessing these case fatality rates, we must look at the entire population at risk, not only the handful that we were able to observe,” explained Dr. Mehra, who was not involved with the study.
Moreover, the patients were “older and had comorbidities, with poor underlying kidney function and other complications, and underlying coronary artery disease in the transplanted heart,” so “it would not surprise me that they had such a high fatality rate, since they had a high degree of vulnerability,” he said.
Dr. Mehra, who is also the editor-in-chief of the Journal of Heart and Lung Transplantation, said that the journal has received manuscripts still in the review process that suggest different fatality rates than those found in the current case series.
However, he acknowledged that, because these are patients with serious vulnerability due to underlying heart disease, “you can’t be lackadaisical and need to do everything to decrease this vulnerability.”
The authors noted that, although their study did not show a protective effect from immunosuppression against COVID-19, further studies are needed to assess each individual immunosuppressive agent and provide a definitive answer.
The study was supported by a grant to one of the investigators from the National Heart, Lung, and Blood Institute. Dr. Uriel reports no relevant financial relationships. The other authors’ disclosures are listed in the publication. Dr. Mehra reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19 infection is associated with a high risk for mortality in heart transplant (HT) recipients, a new case series suggests.
Investigators looked at data on 28 patients with a confirmed diagnosis of COVID-19 who received a HT between March 1, 2020, and April 24, 2020 and found a case-fatality rate of 25%.
“The high case fatality in our case series should alert physicians to the vulnerability of heart transplant recipients during the COVID-19 pandemic,” senior author Nir Uriel, MD, MSc, professor of medicine at Columbia University, New York, said in an interview.
“These patients require extra precautions to prevent the development of infection,” said Dr. Uriel, who is also a cardiologist at New York Presbyterian/Columbia University Irving Medical Center.
The study was published online May 13 in JAMA Cardiology.
Similar presentation
HT recipients can have several comorbidities after the procedure, including hypertension, diabetes, cardiac allograft vasculopathy, and ongoing immunosuppression, all of which can place them at risk for infection and adverse outcomes with COVID-19 infection, the authors wrote.
The researchers therefore embarked on a case series looking at 28 HT recipients with COVID-19 infection (median age, 64.0 years; interquartile range, 53.5-70.5; 79% male) to “describe the outcomes of recipients of HT who are chronically immunosuppressed and develop COVID-19 and raise important questions about the role of the immune system in the process.”
The median time from HT to study period was 8.6 (IQR, 4.2-14.5) years. Most patients had numerous comorbidities.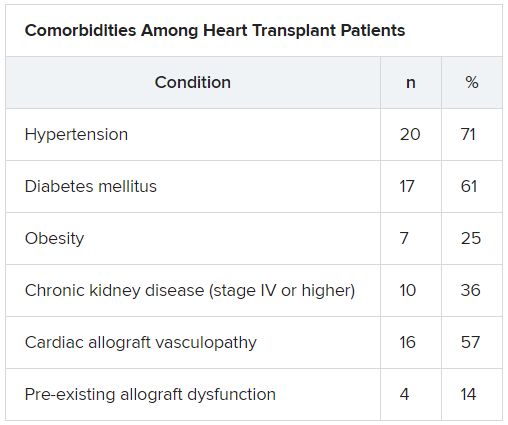
“The presentation of COVID-19 was similar to nontransplant patients with fever, dyspnea, cough, and GI symptoms,” Dr. Uriel reported.
No protective effect
Twenty-two patients (79%) required admission to the hospital, seven of whom (25%) required admission to the ICU and mechanical ventilation.
Despite the presence of immunosuppressive therapy, all patients had significant elevation of inflammatory biomarkers (median peak high-sensitivity C-reactive protein [hs-CRP], 11.83 mg/dL; IQR, 7.44-19.26; median peak interleukin [IL]-6, 105 pg/mL; IQR, 38-296).
Three-quarters had myocardial injury, with a median high-sensitivity troponin T of 0.055 (0.0205 - 0.1345) ng/mL.
Treatments of COVID-19 included hydroxychloroquine (18 patients; 78%), high-dose corticosteroids (eight patients; 47%), and IL-6 receptor antagonists (six patients; 26%).
Moreover, during hospitalization, mycophenolate mofetil was discontinued in most (70%) patients, and one-quarter had a reduction in their calcineurin inhibitor dose.
“Heart transplant recipients generally require more intense immunosuppressive therapy than most other solid organ transplant recipients, and this high baseline immunosuppression increases their propensity to develop infections and their likelihood of experiencing severe manifestations of infections,” Dr. Uriel commented.
“With COVID-19, in which the body’s inflammatory reaction appears to play a role in disease severity, there has been a question of whether immunosuppression may offer a protective effect,” he continued.
“This case series suggests that this is not the case, although this would need to be confirmed in larger studies,” he said.
Low threshold
Among the 22 patients who were admitted to the hospital, half were discharged home and four (18%) were still hospitalized at the end of the study.
Of the seven patients who died, two died at the study center, and five died in an outside institution.
“In the HT population, social distancing (or isolation), strict use of masks when in public, proper handwashing, and sanitization of surfaces are of paramount importance in the prevention of COVID-19 infection,” Dr. Uriel stated.
“In addition, we have restricted these patients’ contact with the hospital as much as possible during the pandemic,” he said.
However, “there should be a low threshold to hospitalize heart transplant patients who develop infection with COVID-19. Furthermore, in our series, outcomes were better for patients hospitalized at the transplant center; therefore, strong consideration should be given to transferring HT patients when hospitalized at another hospital,” he added.
The authors emphasized that COVID-19 patients “will require ongoing monitoring in the recovery phase, as an immunosuppression regimen is reintroduced and the consequences to the allograft itself become apparent.”
Vulnerable population
Commenting on the study, Mandeep R. Mehra, MD, MSc, William Harvey Distinguished Chair in Advanced Cardiovascular Medicine at Brigham and Women’s Hospital, Boston, suggested that “in epidemiological terms, [the findings] might not look as bad as the way they are reflected in the paper.”
Given that Columbia is “one of the larger heart transplant centers in the U.S., following probably 1,000 patients, having only 22 out of perhaps thousands whom they transplanted or are actively following would actually represent a low serious infection rate,” said Dr. Mehra, who is also the executive director of the Center for Advanced Heart Disease at Brigham and Women’s Hospital and a professor of medicine at Harvard Medical School, also in Boston.
“We must not forget to emphasize that, when assessing these case fatality rates, we must look at the entire population at risk, not only the handful that we were able to observe,” explained Dr. Mehra, who was not involved with the study.
Moreover, the patients were “older and had comorbidities, with poor underlying kidney function and other complications, and underlying coronary artery disease in the transplanted heart,” so “it would not surprise me that they had such a high fatality rate, since they had a high degree of vulnerability,” he said.
Dr. Mehra, who is also the editor-in-chief of the Journal of Heart and Lung Transplantation, said that the journal has received manuscripts still in the review process that suggest different fatality rates than those found in the current case series.
However, he acknowledged that, because these are patients with serious vulnerability due to underlying heart disease, “you can’t be lackadaisical and need to do everything to decrease this vulnerability.”
The authors noted that, although their study did not show a protective effect from immunosuppression against COVID-19, further studies are needed to assess each individual immunosuppressive agent and provide a definitive answer.
The study was supported by a grant to one of the investigators from the National Heart, Lung, and Blood Institute. Dr. Uriel reports no relevant financial relationships. The other authors’ disclosures are listed in the publication. Dr. Mehra reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19 infection is associated with a high risk for mortality in heart transplant (HT) recipients, a new case series suggests.
Investigators looked at data on 28 patients with a confirmed diagnosis of COVID-19 who received a HT between March 1, 2020, and April 24, 2020 and found a case-fatality rate of 25%.
“The high case fatality in our case series should alert physicians to the vulnerability of heart transplant recipients during the COVID-19 pandemic,” senior author Nir Uriel, MD, MSc, professor of medicine at Columbia University, New York, said in an interview.
“These patients require extra precautions to prevent the development of infection,” said Dr. Uriel, who is also a cardiologist at New York Presbyterian/Columbia University Irving Medical Center.
The study was published online May 13 in JAMA Cardiology.
Similar presentation
HT recipients can have several comorbidities after the procedure, including hypertension, diabetes, cardiac allograft vasculopathy, and ongoing immunosuppression, all of which can place them at risk for infection and adverse outcomes with COVID-19 infection, the authors wrote.
The researchers therefore embarked on a case series looking at 28 HT recipients with COVID-19 infection (median age, 64.0 years; interquartile range, 53.5-70.5; 79% male) to “describe the outcomes of recipients of HT who are chronically immunosuppressed and develop COVID-19 and raise important questions about the role of the immune system in the process.”
The median time from HT to study period was 8.6 (IQR, 4.2-14.5) years. Most patients had numerous comorbidities.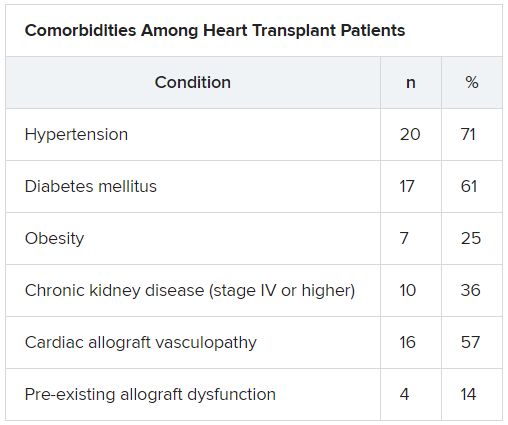
“The presentation of COVID-19 was similar to nontransplant patients with fever, dyspnea, cough, and GI symptoms,” Dr. Uriel reported.
No protective effect
Twenty-two patients (79%) required admission to the hospital, seven of whom (25%) required admission to the ICU and mechanical ventilation.
Despite the presence of immunosuppressive therapy, all patients had significant elevation of inflammatory biomarkers (median peak high-sensitivity C-reactive protein [hs-CRP], 11.83 mg/dL; IQR, 7.44-19.26; median peak interleukin [IL]-6, 105 pg/mL; IQR, 38-296).
Three-quarters had myocardial injury, with a median high-sensitivity troponin T of 0.055 (0.0205 - 0.1345) ng/mL.
Treatments of COVID-19 included hydroxychloroquine (18 patients; 78%), high-dose corticosteroids (eight patients; 47%), and IL-6 receptor antagonists (six patients; 26%).
Moreover, during hospitalization, mycophenolate mofetil was discontinued in most (70%) patients, and one-quarter had a reduction in their calcineurin inhibitor dose.
“Heart transplant recipients generally require more intense immunosuppressive therapy than most other solid organ transplant recipients, and this high baseline immunosuppression increases their propensity to develop infections and their likelihood of experiencing severe manifestations of infections,” Dr. Uriel commented.
“With COVID-19, in which the body’s inflammatory reaction appears to play a role in disease severity, there has been a question of whether immunosuppression may offer a protective effect,” he continued.
“This case series suggests that this is not the case, although this would need to be confirmed in larger studies,” he said.
Low threshold
Among the 22 patients who were admitted to the hospital, half were discharged home and four (18%) were still hospitalized at the end of the study.
Of the seven patients who died, two died at the study center, and five died in an outside institution.
“In the HT population, social distancing (or isolation), strict use of masks when in public, proper handwashing, and sanitization of surfaces are of paramount importance in the prevention of COVID-19 infection,” Dr. Uriel stated.
“In addition, we have restricted these patients’ contact with the hospital as much as possible during the pandemic,” he said.
However, “there should be a low threshold to hospitalize heart transplant patients who develop infection with COVID-19. Furthermore, in our series, outcomes were better for patients hospitalized at the transplant center; therefore, strong consideration should be given to transferring HT patients when hospitalized at another hospital,” he added.
The authors emphasized that COVID-19 patients “will require ongoing monitoring in the recovery phase, as an immunosuppression regimen is reintroduced and the consequences to the allograft itself become apparent.”
Vulnerable population
Commenting on the study, Mandeep R. Mehra, MD, MSc, William Harvey Distinguished Chair in Advanced Cardiovascular Medicine at Brigham and Women’s Hospital, Boston, suggested that “in epidemiological terms, [the findings] might not look as bad as the way they are reflected in the paper.”
Given that Columbia is “one of the larger heart transplant centers in the U.S., following probably 1,000 patients, having only 22 out of perhaps thousands whom they transplanted or are actively following would actually represent a low serious infection rate,” said Dr. Mehra, who is also the executive director of the Center for Advanced Heart Disease at Brigham and Women’s Hospital and a professor of medicine at Harvard Medical School, also in Boston.
“We must not forget to emphasize that, when assessing these case fatality rates, we must look at the entire population at risk, not only the handful that we were able to observe,” explained Dr. Mehra, who was not involved with the study.
Moreover, the patients were “older and had comorbidities, with poor underlying kidney function and other complications, and underlying coronary artery disease in the transplanted heart,” so “it would not surprise me that they had such a high fatality rate, since they had a high degree of vulnerability,” he said.
Dr. Mehra, who is also the editor-in-chief of the Journal of Heart and Lung Transplantation, said that the journal has received manuscripts still in the review process that suggest different fatality rates than those found in the current case series.
However, he acknowledged that, because these are patients with serious vulnerability due to underlying heart disease, “you can’t be lackadaisical and need to do everything to decrease this vulnerability.”
The authors noted that, although their study did not show a protective effect from immunosuppression against COVID-19, further studies are needed to assess each individual immunosuppressive agent and provide a definitive answer.
The study was supported by a grant to one of the investigators from the National Heart, Lung, and Blood Institute. Dr. Uriel reports no relevant financial relationships. The other authors’ disclosures are listed in the publication. Dr. Mehra reports no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Fracture risk higher for children with anxiety on benzodiazepines
a new study found, which offers further argument for caution with this class of drugs in young patients.
In research published in Pediatrics, Greta A. Bushnell, PhD, of Columbia University in New York and colleagues, looked at private insurance claims data including prescription records from 120,715 children aged 6-17 years diagnosed with an anxiety disorder and from 179,768 young adults aged 18-24 years also diagnosed with anxiety.
The investigators compared fracture incidence within 3 months of treatment initiation between the group prescribed benzodiazepines for anxiety and the group prescribed SSRIs. Subjects prescribed both classes of drugs were excluded from the analysis.
Of patients aged 6-17 years, 11% were prescribed benzodiazepines, with the remainder receiving SSRIs. Children on benzodiazepines saw 33 fractures per 1,000 person-years, compared with 25 of those on SSRIs, with an adjusted incidence rate ratio of 1.53. These were fractures in the upper and lower limbs.
Similar differences in fracture risk were not seen among the young adults in the study, of whom 32% were prescribed benzodiazepines and among whom fracture rates were low overall, 9 per 1,000 person-years in both medication groups.
Several SSRIs have been approved by the Food and Drug Administration to treat anxiety disorders in children, but benzodiazepines are used off label in youth. The drugs most commonly prescribed in the study were alprazolam and lorazepam, and 82% of the group in this study aged 6-17 years did not fill their prescriptions beyond 1 month.
In adults, benzodiazepine treatment has been shown to cause drowsiness, dizziness, and weakness, which can result in injury, and it also is associated with increased risk of car accidents, falls, and fractures. The higher fracture rate among children on benzodiazepine treatment seen in this study is similar to rates reported in studies of older adults, Dr. Bushnell and colleagues noted.
The researchers could not explain why the young adults in the study did not see a higher risk of fractures on benzodiazepines, compared with that among those taking SSRIs. They hypothesized that young adults are less active than children, with fewer opportunities for falls, and there were few fractures among the 18- to 24-year-old cohort in general.
David C. Rettew, MD, from the University of Vermont in Burlington, commented in an interview that, while there are plenty of reasons to be cautious about using benzodiazepines in youth, “fracture risk isn’t usually very prominent among them, so it is a nice reminder to have this on the radar screen.” Most clinicians, he said, already are quite wary of using benzodiazepines in children, which is suggested by the small proportion of children treated with them in this study.
“It seems quite possible that children and adolescents prescribed benzodiazepines are quite different clinically than the group prescribed SSRIs, despite the strong measures the study authors took to control for other variables between the two groups,” Dr. Rettew added. “I’d have to wonder if those clinical differences may be behind some of the fracture rate differences” seen in the study.
Dr. Bushnell and her colleagues acknowledged this among the study’s several limitations. “It is unclear how much unmeasured differences in psychiatric condition severity exist between youth initiating a benzodiazepine versus SSRI and how anxiety severity impacts fracture risk.” The researchers also noted that they could not measure use of the drugs beyond whether and when prescriptions were filled.
Dr. Bushnell and colleagues’ study was funded by the National Institute of Mental Health and by grants from the Agency for Healthcare Research and Quality, the Patient-Centered Outcomes Research Institute, and the National Institutes of Health. One of its coauthors disclosed financial relationships with several pharmaceutical manufacturers. Dr. Rettew said he had no relevant financial disclosures
SOURCE: Bushnell GA et al. Pediatrics. 2020 Jun. doi: 10.1542/peds.2019-3478.
a new study found, which offers further argument for caution with this class of drugs in young patients.
In research published in Pediatrics, Greta A. Bushnell, PhD, of Columbia University in New York and colleagues, looked at private insurance claims data including prescription records from 120,715 children aged 6-17 years diagnosed with an anxiety disorder and from 179,768 young adults aged 18-24 years also diagnosed with anxiety.
The investigators compared fracture incidence within 3 months of treatment initiation between the group prescribed benzodiazepines for anxiety and the group prescribed SSRIs. Subjects prescribed both classes of drugs were excluded from the analysis.
Of patients aged 6-17 years, 11% were prescribed benzodiazepines, with the remainder receiving SSRIs. Children on benzodiazepines saw 33 fractures per 1,000 person-years, compared with 25 of those on SSRIs, with an adjusted incidence rate ratio of 1.53. These were fractures in the upper and lower limbs.
Similar differences in fracture risk were not seen among the young adults in the study, of whom 32% were prescribed benzodiazepines and among whom fracture rates were low overall, 9 per 1,000 person-years in both medication groups.
Several SSRIs have been approved by the Food and Drug Administration to treat anxiety disorders in children, but benzodiazepines are used off label in youth. The drugs most commonly prescribed in the study were alprazolam and lorazepam, and 82% of the group in this study aged 6-17 years did not fill their prescriptions beyond 1 month.
In adults, benzodiazepine treatment has been shown to cause drowsiness, dizziness, and weakness, which can result in injury, and it also is associated with increased risk of car accidents, falls, and fractures. The higher fracture rate among children on benzodiazepine treatment seen in this study is similar to rates reported in studies of older adults, Dr. Bushnell and colleagues noted.
The researchers could not explain why the young adults in the study did not see a higher risk of fractures on benzodiazepines, compared with that among those taking SSRIs. They hypothesized that young adults are less active than children, with fewer opportunities for falls, and there were few fractures among the 18- to 24-year-old cohort in general.
David C. Rettew, MD, from the University of Vermont in Burlington, commented in an interview that, while there are plenty of reasons to be cautious about using benzodiazepines in youth, “fracture risk isn’t usually very prominent among them, so it is a nice reminder to have this on the radar screen.” Most clinicians, he said, already are quite wary of using benzodiazepines in children, which is suggested by the small proportion of children treated with them in this study.
“It seems quite possible that children and adolescents prescribed benzodiazepines are quite different clinically than the group prescribed SSRIs, despite the strong measures the study authors took to control for other variables between the two groups,” Dr. Rettew added. “I’d have to wonder if those clinical differences may be behind some of the fracture rate differences” seen in the study.
Dr. Bushnell and her colleagues acknowledged this among the study’s several limitations. “It is unclear how much unmeasured differences in psychiatric condition severity exist between youth initiating a benzodiazepine versus SSRI and how anxiety severity impacts fracture risk.” The researchers also noted that they could not measure use of the drugs beyond whether and when prescriptions were filled.
Dr. Bushnell and colleagues’ study was funded by the National Institute of Mental Health and by grants from the Agency for Healthcare Research and Quality, the Patient-Centered Outcomes Research Institute, and the National Institutes of Health. One of its coauthors disclosed financial relationships with several pharmaceutical manufacturers. Dr. Rettew said he had no relevant financial disclosures
SOURCE: Bushnell GA et al. Pediatrics. 2020 Jun. doi: 10.1542/peds.2019-3478.
a new study found, which offers further argument for caution with this class of drugs in young patients.
In research published in Pediatrics, Greta A. Bushnell, PhD, of Columbia University in New York and colleagues, looked at private insurance claims data including prescription records from 120,715 children aged 6-17 years diagnosed with an anxiety disorder and from 179,768 young adults aged 18-24 years also diagnosed with anxiety.
The investigators compared fracture incidence within 3 months of treatment initiation between the group prescribed benzodiazepines for anxiety and the group prescribed SSRIs. Subjects prescribed both classes of drugs were excluded from the analysis.
Of patients aged 6-17 years, 11% were prescribed benzodiazepines, with the remainder receiving SSRIs. Children on benzodiazepines saw 33 fractures per 1,000 person-years, compared with 25 of those on SSRIs, with an adjusted incidence rate ratio of 1.53. These were fractures in the upper and lower limbs.
Similar differences in fracture risk were not seen among the young adults in the study, of whom 32% were prescribed benzodiazepines and among whom fracture rates were low overall, 9 per 1,000 person-years in both medication groups.
Several SSRIs have been approved by the Food and Drug Administration to treat anxiety disorders in children, but benzodiazepines are used off label in youth. The drugs most commonly prescribed in the study were alprazolam and lorazepam, and 82% of the group in this study aged 6-17 years did not fill their prescriptions beyond 1 month.
In adults, benzodiazepine treatment has been shown to cause drowsiness, dizziness, and weakness, which can result in injury, and it also is associated with increased risk of car accidents, falls, and fractures. The higher fracture rate among children on benzodiazepine treatment seen in this study is similar to rates reported in studies of older adults, Dr. Bushnell and colleagues noted.
The researchers could not explain why the young adults in the study did not see a higher risk of fractures on benzodiazepines, compared with that among those taking SSRIs. They hypothesized that young adults are less active than children, with fewer opportunities for falls, and there were few fractures among the 18- to 24-year-old cohort in general.
David C. Rettew, MD, from the University of Vermont in Burlington, commented in an interview that, while there are plenty of reasons to be cautious about using benzodiazepines in youth, “fracture risk isn’t usually very prominent among them, so it is a nice reminder to have this on the radar screen.” Most clinicians, he said, already are quite wary of using benzodiazepines in children, which is suggested by the small proportion of children treated with them in this study.
“It seems quite possible that children and adolescents prescribed benzodiazepines are quite different clinically than the group prescribed SSRIs, despite the strong measures the study authors took to control for other variables between the two groups,” Dr. Rettew added. “I’d have to wonder if those clinical differences may be behind some of the fracture rate differences” seen in the study.
Dr. Bushnell and her colleagues acknowledged this among the study’s several limitations. “It is unclear how much unmeasured differences in psychiatric condition severity exist between youth initiating a benzodiazepine versus SSRI and how anxiety severity impacts fracture risk.” The researchers also noted that they could not measure use of the drugs beyond whether and when prescriptions were filled.
Dr. Bushnell and colleagues’ study was funded by the National Institute of Mental Health and by grants from the Agency for Healthcare Research and Quality, the Patient-Centered Outcomes Research Institute, and the National Institutes of Health. One of its coauthors disclosed financial relationships with several pharmaceutical manufacturers. Dr. Rettew said he had no relevant financial disclosures
SOURCE: Bushnell GA et al. Pediatrics. 2020 Jun. doi: 10.1542/peds.2019-3478.
FROM PEDIATRICS
Key clinical point: Children aged 6-17 years prescribed sedatives for anxiety saw a higher risk of fractures, compared with those on SSRIs.
Major finding: Children prescribed benzodiazepines for anxiety had 33 fractures per 1,000 person-years versus 25 among children prescribed SSRIs (adjusted incidence rate ratio, 1.53).
Study details: A retrospective cohort study using commercial insurance claims data from 120,715 children aged 6-17 years and 179,768 young adults ages 18-24 years from 2007 through 2016, all with anxiety diagnoses and prescribed either benzodiazepines or SSRIs.
Disclosures: Dr. Bushnell and colleagues’ study was funded by the National Institute of Mental Health, and grants from the Agency for Healthcare Research and Quality, the Patient-Centered Outcomes Research Institute, and the National Institutes of Health. One of its coauthors disclosed financial relationships with several pharmaceutical manufacturers.
Source: Bushnell GA et al. Pediatrics. 2020 Jun. doi: 10.1542/peds.2019-3478.
Today’s top news highlights: COVID-19 could worsen gambling problems, food allergies less common than thought
Here are the stories our MDedge editors across specialties think you need to know about today:
Could COVID-19 worsen gambling problems?
Take isolation, add excess available time and anxiety about illness or finances and you get the potential to increase problem gambling behaviors during the COVID-19 pandemic. A call to action, recently published in the Journal of Addiction Medicine, says it’s essential to gather data and supply guidance on this issue. “People are likely to be experiencing stress at levels they haven’t experienced previously,” said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said. Read more.
Food allergies in children are less frequent than expected
Food allergies appear to be less common than previously reported among 6- to 10-year-olds in Europe, according to a recent study. Prevalance ranged from a low of 1.4% to a high of 3.8%, both of which are “considerably lower” than the 16% rate based on parental reports of symptoms such as rash, itching, or diarrhea, Linus Grabenhenrich, MD, MPH, and colleagues reported in Allergy. The most commonly reported allergies were to peanuts and hazelnuts, with a prevalence of just over 5% for both. Previous research on pediatric food allergy prevalence has largely consisted of single-center studies with heterogeneous designs, the researchers noted. Read more.
The grocery store hug
William G. Wilkoff, MD, grew up in a family that didn’t embrace hugging, but as a small-town pediatrician he warmed up to the concept so much that he would frequently hug a passing acquaintance at the grocery store. That’s something he misses in the current environment and that he doesn’t expect will return. “[N]early every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship,” Dr. Wilkoff wrote in a column on MDedge. “Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child. I’m sure you have your own list of people who send off that we-need-to-hug spark.” Read more.
Identifying structural lesions of axial spondyloarthritis
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that show a high degree of specificity in identifying such lesions in the disease. “Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19. “The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort.” Read more.
Making the world’s skin crawl
Clinicians should be aware of the skin manifestations of COVID-19, especially when triaging patients. In a commentary published on MDedge, Kathleen M. Coerdt and Amor Khachemoune, MD, describe the dermatologic implications of COVID-19, including the clinical manifestations of the disease, risk reduction techniques for patients and providers, personal protective equipment-associated adverse reactions, and the financial impact on dermatologists. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Could COVID-19 worsen gambling problems?
Take isolation, add excess available time and anxiety about illness or finances and you get the potential to increase problem gambling behaviors during the COVID-19 pandemic. A call to action, recently published in the Journal of Addiction Medicine, says it’s essential to gather data and supply guidance on this issue. “People are likely to be experiencing stress at levels they haven’t experienced previously,” said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said. Read more.
Food allergies in children are less frequent than expected
Food allergies appear to be less common than previously reported among 6- to 10-year-olds in Europe, according to a recent study. Prevalance ranged from a low of 1.4% to a high of 3.8%, both of which are “considerably lower” than the 16% rate based on parental reports of symptoms such as rash, itching, or diarrhea, Linus Grabenhenrich, MD, MPH, and colleagues reported in Allergy. The most commonly reported allergies were to peanuts and hazelnuts, with a prevalence of just over 5% for both. Previous research on pediatric food allergy prevalence has largely consisted of single-center studies with heterogeneous designs, the researchers noted. Read more.
The grocery store hug
William G. Wilkoff, MD, grew up in a family that didn’t embrace hugging, but as a small-town pediatrician he warmed up to the concept so much that he would frequently hug a passing acquaintance at the grocery store. That’s something he misses in the current environment and that he doesn’t expect will return. “[N]early every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship,” Dr. Wilkoff wrote in a column on MDedge. “Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child. I’m sure you have your own list of people who send off that we-need-to-hug spark.” Read more.
Identifying structural lesions of axial spondyloarthritis
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that show a high degree of specificity in identifying such lesions in the disease. “Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19. “The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort.” Read more.
Making the world’s skin crawl
Clinicians should be aware of the skin manifestations of COVID-19, especially when triaging patients. In a commentary published on MDedge, Kathleen M. Coerdt and Amor Khachemoune, MD, describe the dermatologic implications of COVID-19, including the clinical manifestations of the disease, risk reduction techniques for patients and providers, personal protective equipment-associated adverse reactions, and the financial impact on dermatologists. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Could COVID-19 worsen gambling problems?
Take isolation, add excess available time and anxiety about illness or finances and you get the potential to increase problem gambling behaviors during the COVID-19 pandemic. A call to action, recently published in the Journal of Addiction Medicine, says it’s essential to gather data and supply guidance on this issue. “People are likely to be experiencing stress at levels they haven’t experienced previously,” said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said. Read more.
Food allergies in children are less frequent than expected
Food allergies appear to be less common than previously reported among 6- to 10-year-olds in Europe, according to a recent study. Prevalance ranged from a low of 1.4% to a high of 3.8%, both of which are “considerably lower” than the 16% rate based on parental reports of symptoms such as rash, itching, or diarrhea, Linus Grabenhenrich, MD, MPH, and colleagues reported in Allergy. The most commonly reported allergies were to peanuts and hazelnuts, with a prevalence of just over 5% for both. Previous research on pediatric food allergy prevalence has largely consisted of single-center studies with heterogeneous designs, the researchers noted. Read more.
The grocery store hug
William G. Wilkoff, MD, grew up in a family that didn’t embrace hugging, but as a small-town pediatrician he warmed up to the concept so much that he would frequently hug a passing acquaintance at the grocery store. That’s something he misses in the current environment and that he doesn’t expect will return. “[N]early every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship,” Dr. Wilkoff wrote in a column on MDedge. “Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child. I’m sure you have your own list of people who send off that we-need-to-hug spark.” Read more.
Identifying structural lesions of axial spondyloarthritis
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that show a high degree of specificity in identifying such lesions in the disease. “Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19. “The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort.” Read more.
Making the world’s skin crawl
Clinicians should be aware of the skin manifestations of COVID-19, especially when triaging patients. In a commentary published on MDedge, Kathleen M. Coerdt and Amor Khachemoune, MD, describe the dermatologic implications of COVID-19, including the clinical manifestations of the disease, risk reduction techniques for patients and providers, personal protective equipment-associated adverse reactions, and the financial impact on dermatologists. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Americans avoided emergency departments early in the pandemic
compared with the corresponding period in 2019, according to a report from the Centers for Disease Control and Prevention.
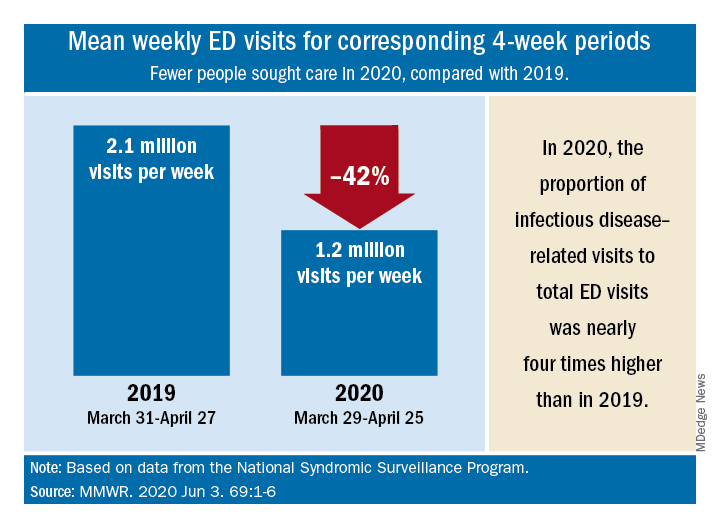
“The striking decline in ED visits nationwide … suggests that the pandemic has altered the use of the ED by the public,” Kathleen P. Hartnett, PhD, and associates at the CDC said June 3 in the Mortality and Morbidity Weekly Report.
The weekly mean was just over 1.2 million ED visits for the 4 weeks from March 29 to April 25, 2020, compared with the nearly 2.2 million visits per week recorded from March 31 to April 27, 2019 – a drop of 42%, based on an analysis of data from the National Syndromic Surveillance Program.
Despite that drop, ED visits for infectious disease–related reasons, taken as a proportion of all 1.2 ED visits during the early pandemic period, were 3.8 times higher than the comparison period in 2019, the investigators reported.
ED visits also were higher in 2020 for specified and unspecified lower respiratory disease not including influenza, pneumonia, asthma, or bronchitis (prevalence ratio of 1.99, compared with 2019), cardiac arrest and ventricular fibrillation (PR, 1.98), and pneumonia not caused by tuberculosis (PR, 1.91), Dr. Hartnett and associates said.
Prevalence ratios for the early pandemic period were down for most other conditions, with some of the largest decreases seen for influenza (PR, 0.16), otitis media (PR, 0.35), and neoplasm-related encounters (PR, 0.40), they said.
Visits have increased each week since reaching their lowest point during April 12-18, but the number for the most recent full week, May 24-30, which was not included in the analysis, was still 26% lower than the corresponding week in 2019, the CDC team pointed out.
“Some persons could be delaying care for conditions that might result in additional mortality if left untreated,” the investigators noted, and those “who use the ED as a safety net because they lack access to primary care and telemedicine might be disproportionately affected if they avoid seeking care because of concerns about the infection risk in the ED.”
SOURCE: Hartnett KP et al. MMWR. 2020 Jun 3. 69:1-6.
compared with the corresponding period in 2019, according to a report from the Centers for Disease Control and Prevention.
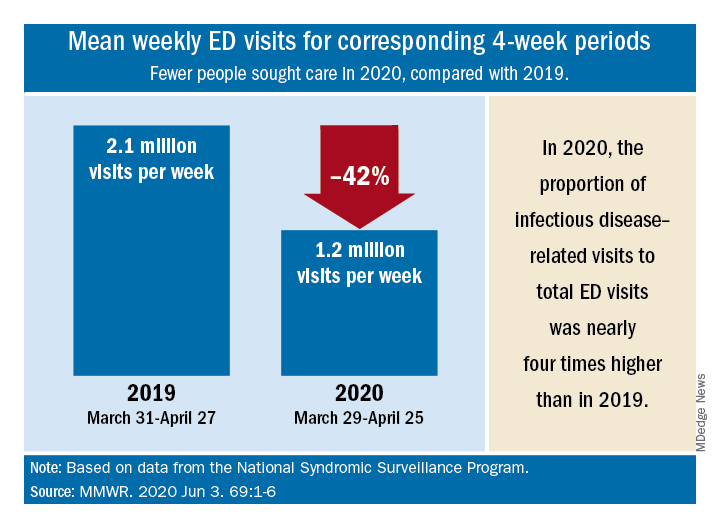
“The striking decline in ED visits nationwide … suggests that the pandemic has altered the use of the ED by the public,” Kathleen P. Hartnett, PhD, and associates at the CDC said June 3 in the Mortality and Morbidity Weekly Report.
The weekly mean was just over 1.2 million ED visits for the 4 weeks from March 29 to April 25, 2020, compared with the nearly 2.2 million visits per week recorded from March 31 to April 27, 2019 – a drop of 42%, based on an analysis of data from the National Syndromic Surveillance Program.
Despite that drop, ED visits for infectious disease–related reasons, taken as a proportion of all 1.2 ED visits during the early pandemic period, were 3.8 times higher than the comparison period in 2019, the investigators reported.
ED visits also were higher in 2020 for specified and unspecified lower respiratory disease not including influenza, pneumonia, asthma, or bronchitis (prevalence ratio of 1.99, compared with 2019), cardiac arrest and ventricular fibrillation (PR, 1.98), and pneumonia not caused by tuberculosis (PR, 1.91), Dr. Hartnett and associates said.
Prevalence ratios for the early pandemic period were down for most other conditions, with some of the largest decreases seen for influenza (PR, 0.16), otitis media (PR, 0.35), and neoplasm-related encounters (PR, 0.40), they said.
Visits have increased each week since reaching their lowest point during April 12-18, but the number for the most recent full week, May 24-30, which was not included in the analysis, was still 26% lower than the corresponding week in 2019, the CDC team pointed out.
“Some persons could be delaying care for conditions that might result in additional mortality if left untreated,” the investigators noted, and those “who use the ED as a safety net because they lack access to primary care and telemedicine might be disproportionately affected if they avoid seeking care because of concerns about the infection risk in the ED.”
SOURCE: Hartnett KP et al. MMWR. 2020 Jun 3. 69:1-6.
compared with the corresponding period in 2019, according to a report from the Centers for Disease Control and Prevention.
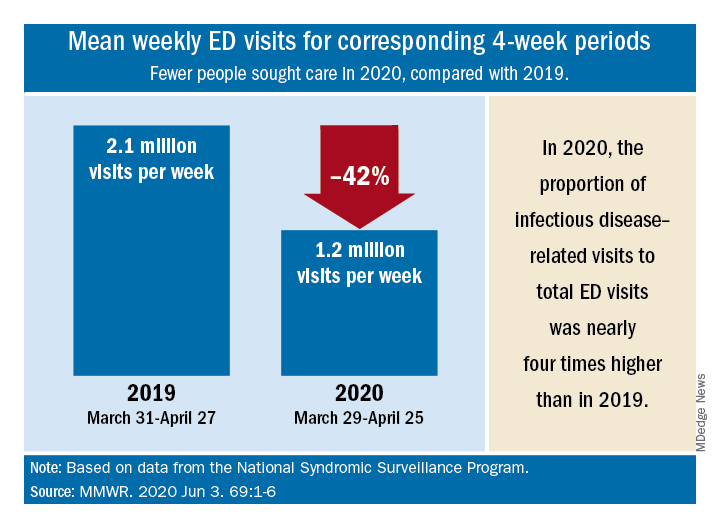
“The striking decline in ED visits nationwide … suggests that the pandemic has altered the use of the ED by the public,” Kathleen P. Hartnett, PhD, and associates at the CDC said June 3 in the Mortality and Morbidity Weekly Report.
The weekly mean was just over 1.2 million ED visits for the 4 weeks from March 29 to April 25, 2020, compared with the nearly 2.2 million visits per week recorded from March 31 to April 27, 2019 – a drop of 42%, based on an analysis of data from the National Syndromic Surveillance Program.
Despite that drop, ED visits for infectious disease–related reasons, taken as a proportion of all 1.2 ED visits during the early pandemic period, were 3.8 times higher than the comparison period in 2019, the investigators reported.
ED visits also were higher in 2020 for specified and unspecified lower respiratory disease not including influenza, pneumonia, asthma, or bronchitis (prevalence ratio of 1.99, compared with 2019), cardiac arrest and ventricular fibrillation (PR, 1.98), and pneumonia not caused by tuberculosis (PR, 1.91), Dr. Hartnett and associates said.
Prevalence ratios for the early pandemic period were down for most other conditions, with some of the largest decreases seen for influenza (PR, 0.16), otitis media (PR, 0.35), and neoplasm-related encounters (PR, 0.40), they said.
Visits have increased each week since reaching their lowest point during April 12-18, but the number for the most recent full week, May 24-30, which was not included in the analysis, was still 26% lower than the corresponding week in 2019, the CDC team pointed out.
“Some persons could be delaying care for conditions that might result in additional mortality if left untreated,” the investigators noted, and those “who use the ED as a safety net because they lack access to primary care and telemedicine might be disproportionately affected if they avoid seeking care because of concerns about the infection risk in the ED.”
SOURCE: Hartnett KP et al. MMWR. 2020 Jun 3. 69:1-6.
FROM MMWR
Is cannabis gaining acceptance as a treatment for neuropathic pain?
, a recent debate on the topic suggests. During the debate, one expert argued for, and another against, there being sufficient evidence for the use of cannabis to treat neuropathic pain, but in the end, they agreed that some patients do benefit.
The discussion took place at the Congress of the European Academy of Neurology (EAN) 2020, which transitioned to a virtual online meeting because of the COVID-19 pandemic.
The cannabis plant has 460 constituents. The two main components are tetrahydrocannabinol (THC) and cannabidiol (CBD). It can be consumed by swallowing oil extracts, by the sublingual route, or by smoking or eating the plant. Cannabis medications already in use include oral THC (nabilone, dronabinol) and an oral mucosal spray, nabiximols (Sativex).
Arguing that therapeutic cannabis is helpful for neuropathic pain, Elon Eisenberg, MD, professor of neurology and pain medicine, Israel Institute of Technology, Haifa, cited a number of encouraging randomized, controlled trials and meta-analyses of studies on the subject.
Opioid substitute
Dr. Eisenberg discussed three relevant articles. One was a 2016 viewpoint article published in JAMA that concluded that “cannabis seems to be a substitute, a rather good one, for opioids,” said Dr. Eisenberg.
A “comprehensive” 440-page review, published by the National Academies Press in 2017, evaluated the evidence to that point and “came to the conclusion there is substantial evidence that cannabis is an effective treatment for chronic pain in adults,” said Dr. Eisenberg.
And a 2018 position paper from the European Pain Federation determined that “the quantity and quality of evidence is such that cannabis-based medicines may be reasonably considered for chronic neuropathic pain,” he said.
He noted that the most recent results from an Israeli prospective cohort registry study that is following more than 851 patients who are taking cannabis over 1 year are positive. Analyses show a steady reduction in pain intensity and improvements in catastrophizing and disability. Importantly, he said, participants are using fewer opioids. However, about 40% of patients in that registry study experienced some adverse event, although most were not serious, said Dr. Eisenberg.
Not convinced
Arguing on the other side – that therapeutic cannabis is not helpful for neuropathic pain – was Nadine Attal, MD, PhD, professor of therapeutics and pain at the University Versailles Saint Quentin, France. She questioned the quality of some of the research to date and stressed that studies should consider neuropathic pain as a primary outcome – not spasticity or pain in general. They should also be double-blind, randomized, and placebo controlled, she said.
In addition, she said these studies should enroll at least 10 patients per group and should continue for 3 weeks or longer.
Dr. Attal wondered which of the many plant derivatives (phytocannabinoids) are used in cannabis studies.
She discussed four meta-analyses or reviews on the topic, some of which she said are “heterogeneous” and don’t provide convincing evidence for cannabis use in neuropathic pain.
For example, one review examined only marijuana, and all studies in it were short term. One of the studies in this review was of spasticity. Another review included two studies of cancer pain, and the most positive study in NP used short-term inhaled THC.
“There is no evidence to date that cannabinoids, including nabiximols or oral THC, administered for at least 3 weeks are more effective than placebo in neuropathic pain,” she concluded.
Some responders
However, Dr. Attal acknowledged that cannabis might be effective for some patients. In her experience, which has been borne out by some observational studies, patients with paroxysmal pain, or sudden stabbing pain, seem to get more relief from cannabis. “It’s absolutely possible that there’s a subgroup of symptoms or a subgroup of patients with specific symptoms who are much better responders to cannabis than others,” she said.
Asked if patients experience increased pain after withdrawing from cannabis, Dr. Eisenberg said he has observed that many patients stop taking cannabis when they start feeling better, but he hasn’t seen severe withdrawal symptoms.
However, there are other concerns related to cannabis use, said Dr. Eisenberg. A major concern regards driving a vehicle. In Israel, getting behind the wheel is prohibited within 6 hours of using cannabis.
But Dr. Eisenberg pointed out that published data on the safety of cannabis and driving were based on recreational users. “We need to keep in mind that recreational users typically use other substances, so we’re not sure the data is accurate,” he said.
There are increasing reports of stroke, transient ischemic attack, and MI among cannabis users. This is especially concerning because many of these cases involve young male adults who have no risk factors, said Dr. Eisenberg.
One conference delegate asked whether legal issues make it difficult to properly investigate cannabis in large studies. Dr. Eisenberg noted that legal concerns may help explain why there have not been any new randomized, controlled trials for about 2 years. “In the U.S., you can’t do clinical trials; cannabis is still regarded as schedule I substance,” he said.
Some physicians “are reluctant to deal with cannabis unless they get better data,” he said. “Doing research on cannabis seems to be somehow out of the mainstream.” Moreover, the research is difficult to carry out, owing to the complexity of the cannabis plant, which has many constituents. Perhaps it’s a matter of identifying and adding particular components to better demonstrate reduced pain, said Dr. Eisenberg.
Another complicating factor is that bioavailability differs considerably from one patient to another, “sometimes even by 10-fold,” he said.
Dr. Attal’s group will be starting a study next January that will enroll a large sample of patients with neuropathic pain or spasticity. In that study, cannabis will be dispensed through pharmacies and primary care. The aim of the study is “to see how it works in a real-life setting,” she said
Those participating in the virtual session were asked to vote on which side they agreed with. About 57% voted in favor of cannabis use, 14% voted against, and 28% had no opinion.
Dr. Eisenberg has received research grants from Rafa Laboratories, Saga Medical Ltd., Israel Pain Association, and Teva Israel. Dr. Attal has received support from Merck Sharp & Dohme, Sanofi, Ipsen, Novartis, Aptinyx, Air Liquide, Lilly, and Grunenthal.
A version of this article originally appeared on Medscape.com.
, a recent debate on the topic suggests. During the debate, one expert argued for, and another against, there being sufficient evidence for the use of cannabis to treat neuropathic pain, but in the end, they agreed that some patients do benefit.
The discussion took place at the Congress of the European Academy of Neurology (EAN) 2020, which transitioned to a virtual online meeting because of the COVID-19 pandemic.
The cannabis plant has 460 constituents. The two main components are tetrahydrocannabinol (THC) and cannabidiol (CBD). It can be consumed by swallowing oil extracts, by the sublingual route, or by smoking or eating the plant. Cannabis medications already in use include oral THC (nabilone, dronabinol) and an oral mucosal spray, nabiximols (Sativex).
Arguing that therapeutic cannabis is helpful for neuropathic pain, Elon Eisenberg, MD, professor of neurology and pain medicine, Israel Institute of Technology, Haifa, cited a number of encouraging randomized, controlled trials and meta-analyses of studies on the subject.
Opioid substitute
Dr. Eisenberg discussed three relevant articles. One was a 2016 viewpoint article published in JAMA that concluded that “cannabis seems to be a substitute, a rather good one, for opioids,” said Dr. Eisenberg.
A “comprehensive” 440-page review, published by the National Academies Press in 2017, evaluated the evidence to that point and “came to the conclusion there is substantial evidence that cannabis is an effective treatment for chronic pain in adults,” said Dr. Eisenberg.
And a 2018 position paper from the European Pain Federation determined that “the quantity and quality of evidence is such that cannabis-based medicines may be reasonably considered for chronic neuropathic pain,” he said.
He noted that the most recent results from an Israeli prospective cohort registry study that is following more than 851 patients who are taking cannabis over 1 year are positive. Analyses show a steady reduction in pain intensity and improvements in catastrophizing and disability. Importantly, he said, participants are using fewer opioids. However, about 40% of patients in that registry study experienced some adverse event, although most were not serious, said Dr. Eisenberg.
Not convinced
Arguing on the other side – that therapeutic cannabis is not helpful for neuropathic pain – was Nadine Attal, MD, PhD, professor of therapeutics and pain at the University Versailles Saint Quentin, France. She questioned the quality of some of the research to date and stressed that studies should consider neuropathic pain as a primary outcome – not spasticity or pain in general. They should also be double-blind, randomized, and placebo controlled, she said.
In addition, she said these studies should enroll at least 10 patients per group and should continue for 3 weeks or longer.
Dr. Attal wondered which of the many plant derivatives (phytocannabinoids) are used in cannabis studies.
She discussed four meta-analyses or reviews on the topic, some of which she said are “heterogeneous” and don’t provide convincing evidence for cannabis use in neuropathic pain.
For example, one review examined only marijuana, and all studies in it were short term. One of the studies in this review was of spasticity. Another review included two studies of cancer pain, and the most positive study in NP used short-term inhaled THC.
“There is no evidence to date that cannabinoids, including nabiximols or oral THC, administered for at least 3 weeks are more effective than placebo in neuropathic pain,” she concluded.
Some responders
However, Dr. Attal acknowledged that cannabis might be effective for some patients. In her experience, which has been borne out by some observational studies, patients with paroxysmal pain, or sudden stabbing pain, seem to get more relief from cannabis. “It’s absolutely possible that there’s a subgroup of symptoms or a subgroup of patients with specific symptoms who are much better responders to cannabis than others,” she said.
Asked if patients experience increased pain after withdrawing from cannabis, Dr. Eisenberg said he has observed that many patients stop taking cannabis when they start feeling better, but he hasn’t seen severe withdrawal symptoms.
However, there are other concerns related to cannabis use, said Dr. Eisenberg. A major concern regards driving a vehicle. In Israel, getting behind the wheel is prohibited within 6 hours of using cannabis.
But Dr. Eisenberg pointed out that published data on the safety of cannabis and driving were based on recreational users. “We need to keep in mind that recreational users typically use other substances, so we’re not sure the data is accurate,” he said.
There are increasing reports of stroke, transient ischemic attack, and MI among cannabis users. This is especially concerning because many of these cases involve young male adults who have no risk factors, said Dr. Eisenberg.
One conference delegate asked whether legal issues make it difficult to properly investigate cannabis in large studies. Dr. Eisenberg noted that legal concerns may help explain why there have not been any new randomized, controlled trials for about 2 years. “In the U.S., you can’t do clinical trials; cannabis is still regarded as schedule I substance,” he said.
Some physicians “are reluctant to deal with cannabis unless they get better data,” he said. “Doing research on cannabis seems to be somehow out of the mainstream.” Moreover, the research is difficult to carry out, owing to the complexity of the cannabis plant, which has many constituents. Perhaps it’s a matter of identifying and adding particular components to better demonstrate reduced pain, said Dr. Eisenberg.
Another complicating factor is that bioavailability differs considerably from one patient to another, “sometimes even by 10-fold,” he said.
Dr. Attal’s group will be starting a study next January that will enroll a large sample of patients with neuropathic pain or spasticity. In that study, cannabis will be dispensed through pharmacies and primary care. The aim of the study is “to see how it works in a real-life setting,” she said
Those participating in the virtual session were asked to vote on which side they agreed with. About 57% voted in favor of cannabis use, 14% voted against, and 28% had no opinion.
Dr. Eisenberg has received research grants from Rafa Laboratories, Saga Medical Ltd., Israel Pain Association, and Teva Israel. Dr. Attal has received support from Merck Sharp & Dohme, Sanofi, Ipsen, Novartis, Aptinyx, Air Liquide, Lilly, and Grunenthal.
A version of this article originally appeared on Medscape.com.
, a recent debate on the topic suggests. During the debate, one expert argued for, and another against, there being sufficient evidence for the use of cannabis to treat neuropathic pain, but in the end, they agreed that some patients do benefit.
The discussion took place at the Congress of the European Academy of Neurology (EAN) 2020, which transitioned to a virtual online meeting because of the COVID-19 pandemic.
The cannabis plant has 460 constituents. The two main components are tetrahydrocannabinol (THC) and cannabidiol (CBD). It can be consumed by swallowing oil extracts, by the sublingual route, or by smoking or eating the plant. Cannabis medications already in use include oral THC (nabilone, dronabinol) and an oral mucosal spray, nabiximols (Sativex).
Arguing that therapeutic cannabis is helpful for neuropathic pain, Elon Eisenberg, MD, professor of neurology and pain medicine, Israel Institute of Technology, Haifa, cited a number of encouraging randomized, controlled trials and meta-analyses of studies on the subject.
Opioid substitute
Dr. Eisenberg discussed three relevant articles. One was a 2016 viewpoint article published in JAMA that concluded that “cannabis seems to be a substitute, a rather good one, for opioids,” said Dr. Eisenberg.
A “comprehensive” 440-page review, published by the National Academies Press in 2017, evaluated the evidence to that point and “came to the conclusion there is substantial evidence that cannabis is an effective treatment for chronic pain in adults,” said Dr. Eisenberg.
And a 2018 position paper from the European Pain Federation determined that “the quantity and quality of evidence is such that cannabis-based medicines may be reasonably considered for chronic neuropathic pain,” he said.
He noted that the most recent results from an Israeli prospective cohort registry study that is following more than 851 patients who are taking cannabis over 1 year are positive. Analyses show a steady reduction in pain intensity and improvements in catastrophizing and disability. Importantly, he said, participants are using fewer opioids. However, about 40% of patients in that registry study experienced some adverse event, although most were not serious, said Dr. Eisenberg.
Not convinced
Arguing on the other side – that therapeutic cannabis is not helpful for neuropathic pain – was Nadine Attal, MD, PhD, professor of therapeutics and pain at the University Versailles Saint Quentin, France. She questioned the quality of some of the research to date and stressed that studies should consider neuropathic pain as a primary outcome – not spasticity or pain in general. They should also be double-blind, randomized, and placebo controlled, she said.
In addition, she said these studies should enroll at least 10 patients per group and should continue for 3 weeks or longer.
Dr. Attal wondered which of the many plant derivatives (phytocannabinoids) are used in cannabis studies.
She discussed four meta-analyses or reviews on the topic, some of which she said are “heterogeneous” and don’t provide convincing evidence for cannabis use in neuropathic pain.
For example, one review examined only marijuana, and all studies in it were short term. One of the studies in this review was of spasticity. Another review included two studies of cancer pain, and the most positive study in NP used short-term inhaled THC.
“There is no evidence to date that cannabinoids, including nabiximols or oral THC, administered for at least 3 weeks are more effective than placebo in neuropathic pain,” she concluded.
Some responders
However, Dr. Attal acknowledged that cannabis might be effective for some patients. In her experience, which has been borne out by some observational studies, patients with paroxysmal pain, or sudden stabbing pain, seem to get more relief from cannabis. “It’s absolutely possible that there’s a subgroup of symptoms or a subgroup of patients with specific symptoms who are much better responders to cannabis than others,” she said.
Asked if patients experience increased pain after withdrawing from cannabis, Dr. Eisenberg said he has observed that many patients stop taking cannabis when they start feeling better, but he hasn’t seen severe withdrawal symptoms.
However, there are other concerns related to cannabis use, said Dr. Eisenberg. A major concern regards driving a vehicle. In Israel, getting behind the wheel is prohibited within 6 hours of using cannabis.
But Dr. Eisenberg pointed out that published data on the safety of cannabis and driving were based on recreational users. “We need to keep in mind that recreational users typically use other substances, so we’re not sure the data is accurate,” he said.
There are increasing reports of stroke, transient ischemic attack, and MI among cannabis users. This is especially concerning because many of these cases involve young male adults who have no risk factors, said Dr. Eisenberg.
One conference delegate asked whether legal issues make it difficult to properly investigate cannabis in large studies. Dr. Eisenberg noted that legal concerns may help explain why there have not been any new randomized, controlled trials for about 2 years. “In the U.S., you can’t do clinical trials; cannabis is still regarded as schedule I substance,” he said.
Some physicians “are reluctant to deal with cannabis unless they get better data,” he said. “Doing research on cannabis seems to be somehow out of the mainstream.” Moreover, the research is difficult to carry out, owing to the complexity of the cannabis plant, which has many constituents. Perhaps it’s a matter of identifying and adding particular components to better demonstrate reduced pain, said Dr. Eisenberg.
Another complicating factor is that bioavailability differs considerably from one patient to another, “sometimes even by 10-fold,” he said.
Dr. Attal’s group will be starting a study next January that will enroll a large sample of patients with neuropathic pain or spasticity. In that study, cannabis will be dispensed through pharmacies and primary care. The aim of the study is “to see how it works in a real-life setting,” she said
Those participating in the virtual session were asked to vote on which side they agreed with. About 57% voted in favor of cannabis use, 14% voted against, and 28% had no opinion.
Dr. Eisenberg has received research grants from Rafa Laboratories, Saga Medical Ltd., Israel Pain Association, and Teva Israel. Dr. Attal has received support from Merck Sharp & Dohme, Sanofi, Ipsen, Novartis, Aptinyx, Air Liquide, Lilly, and Grunenthal.
A version of this article originally appeared on Medscape.com.
FROM EAN 2020
Atopic dermatitis in adults, children linked to neuropsychiatric disorders
according to a study presented at the annual meeting of the Society for Investigative Dermatology, held virtually.
“The risk increase ranges from as low as 5% up to 59%, depending on the outcome, with generally greater effects observed among the adults,” Joy Wan, MD, a postdoctoral dermatology fellow at the University of Pennsylvania, Philadelphia, said in her presentation. The risk was independent of other atopic disease, gender, age, and socioeconomic status.
Dr. Wan and colleagues conducted a cohort study of patients with AD in the United Kingdom using data from the Health Improvement Network (THIN) electronic records database, matching AD patients in THIN with up to five patients without AD, similar in age and also registered to general practices. The researchers validated AD disease status using an algorithm that identified patients with a diagnostic code and two therapy codes related to AD. Outcomes of interest included anxiety, depression, bipolar disorder, obsessive-compulsive disorder, ADHD, schizophrenia, and autism. Patients entered into the cohort when they were diagnosed with AD, registered by a practice, or when data from a practice was reported to THIN. The researchers stopped following patients when they developed a neuropsychiatric outcome of interest, left a practice, died, or when the study ended.
“Previous studies have found associations between atopic dermatitis and anxiety, depression, and attention-deficit/hyperactivity disorder. However, many previous studies had been cross-sectional and they were unable to evaluate the directionality of association between atopic dermatitis and neuropsychiatric outcomes, while other previous studies have relied on the self-report of atopic dermatitis and outcomes as well,” Dr. Wan said. “Thus, longitudinal studies, using validated measures of atopic dermatitis, and those that include the entire age span, are really needed.”
Overall, 434,859 children and adolescents under aged 18 with AD in the THIN database were matched to 1,983,589 controls, and 644,802 adults with AD were matched to almost 2,900,000 adults without AD. In the pediatric group, demographics were mostly balanced between children with and without AD: the average age ranged between about 5 and almost 6 years. In pediatric patients with AD, there was a higher rate of allergic rhinitis (6.2% vs. 4%) and asthma (13.5% vs. 9.3%) than in the control group.
For adults, the average age was about 48 years in both groups. Compared with patients who did not have AD, adults with AD also had higher rates of allergic rhinitis (15.2% vs. 9.6%) and asthma (19.9% vs. 12.6%).
After adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis, Dr. Wan and colleagues found greater rates of bipolar disorder (hazard ratio, 1.34; 95% confidence interval, 1.09-1.65), obsessive-compulsive disorder (HR, 1.30; 95% CI, 1.21-1.41), anxiety (HR, 1.09; 95% CI, 1.07-1.11), and depression (HR, 1.06; 95% CI, 1.04-1.08) among children and adolescents with AD, compared with controls.
In the adult cohort, a diagnosis of AD was associated with an increased risk of autism (HR, 1.53; 95% CI, 1.30-1.80), obsessive-compulsive disorder (HR, 1.49; 95% CI, 1.40-1.59), ADHD (HR, 1.31; 95% CI, 1.13-1.53), anxiety (HR, 1.17; 95% CI, 1.15-1.18), depression (HR, 1.15; 95% CI, 1.14-1.16), and bipolar disorder (HR, 1.12; 95% CI, 1.04-1.21), after adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis.
One reason for the increased associations among the adults, even for ADHD and autism, which are more characteristically diagnosed in childhood, Dr. Wan said, is that, since they looked at incident outcomes, “many children may already have had these prevalent comorbidities at the time of the entry in the cohort.”
She noted that the study may have observation bias or unknown confounders, but she hopes these results raise awareness of the association between AD and neuropsychiatric disorders, although more research is needed to determine how AD severity affects neuropsychiatric outcomes. “Additional work is needed to really understand the mechanisms that drive these associations, whether it’s mediated through symptoms of atopic dermatitis such as itch and poor sleep, or potentially the stigma of having a chronic skin disease, or perhaps shared pathophysiology between atopic dermatitis and these neuropsychiatric diseases,” she said.
The study was funded by a grant from Pfizer. Dr. Wan reports receiving research funding from Pfizer paid to the University of Pennsylvania.
according to a study presented at the annual meeting of the Society for Investigative Dermatology, held virtually.
“The risk increase ranges from as low as 5% up to 59%, depending on the outcome, with generally greater effects observed among the adults,” Joy Wan, MD, a postdoctoral dermatology fellow at the University of Pennsylvania, Philadelphia, said in her presentation. The risk was independent of other atopic disease, gender, age, and socioeconomic status.
Dr. Wan and colleagues conducted a cohort study of patients with AD in the United Kingdom using data from the Health Improvement Network (THIN) electronic records database, matching AD patients in THIN with up to five patients without AD, similar in age and also registered to general practices. The researchers validated AD disease status using an algorithm that identified patients with a diagnostic code and two therapy codes related to AD. Outcomes of interest included anxiety, depression, bipolar disorder, obsessive-compulsive disorder, ADHD, schizophrenia, and autism. Patients entered into the cohort when they were diagnosed with AD, registered by a practice, or when data from a practice was reported to THIN. The researchers stopped following patients when they developed a neuropsychiatric outcome of interest, left a practice, died, or when the study ended.
“Previous studies have found associations between atopic dermatitis and anxiety, depression, and attention-deficit/hyperactivity disorder. However, many previous studies had been cross-sectional and they were unable to evaluate the directionality of association between atopic dermatitis and neuropsychiatric outcomes, while other previous studies have relied on the self-report of atopic dermatitis and outcomes as well,” Dr. Wan said. “Thus, longitudinal studies, using validated measures of atopic dermatitis, and those that include the entire age span, are really needed.”
Overall, 434,859 children and adolescents under aged 18 with AD in the THIN database were matched to 1,983,589 controls, and 644,802 adults with AD were matched to almost 2,900,000 adults without AD. In the pediatric group, demographics were mostly balanced between children with and without AD: the average age ranged between about 5 and almost 6 years. In pediatric patients with AD, there was a higher rate of allergic rhinitis (6.2% vs. 4%) and asthma (13.5% vs. 9.3%) than in the control group.
For adults, the average age was about 48 years in both groups. Compared with patients who did not have AD, adults with AD also had higher rates of allergic rhinitis (15.2% vs. 9.6%) and asthma (19.9% vs. 12.6%).
After adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis, Dr. Wan and colleagues found greater rates of bipolar disorder (hazard ratio, 1.34; 95% confidence interval, 1.09-1.65), obsessive-compulsive disorder (HR, 1.30; 95% CI, 1.21-1.41), anxiety (HR, 1.09; 95% CI, 1.07-1.11), and depression (HR, 1.06; 95% CI, 1.04-1.08) among children and adolescents with AD, compared with controls.
In the adult cohort, a diagnosis of AD was associated with an increased risk of autism (HR, 1.53; 95% CI, 1.30-1.80), obsessive-compulsive disorder (HR, 1.49; 95% CI, 1.40-1.59), ADHD (HR, 1.31; 95% CI, 1.13-1.53), anxiety (HR, 1.17; 95% CI, 1.15-1.18), depression (HR, 1.15; 95% CI, 1.14-1.16), and bipolar disorder (HR, 1.12; 95% CI, 1.04-1.21), after adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis.
One reason for the increased associations among the adults, even for ADHD and autism, which are more characteristically diagnosed in childhood, Dr. Wan said, is that, since they looked at incident outcomes, “many children may already have had these prevalent comorbidities at the time of the entry in the cohort.”
She noted that the study may have observation bias or unknown confounders, but she hopes these results raise awareness of the association between AD and neuropsychiatric disorders, although more research is needed to determine how AD severity affects neuropsychiatric outcomes. “Additional work is needed to really understand the mechanisms that drive these associations, whether it’s mediated through symptoms of atopic dermatitis such as itch and poor sleep, or potentially the stigma of having a chronic skin disease, or perhaps shared pathophysiology between atopic dermatitis and these neuropsychiatric diseases,” she said.
The study was funded by a grant from Pfizer. Dr. Wan reports receiving research funding from Pfizer paid to the University of Pennsylvania.
according to a study presented at the annual meeting of the Society for Investigative Dermatology, held virtually.
“The risk increase ranges from as low as 5% up to 59%, depending on the outcome, with generally greater effects observed among the adults,” Joy Wan, MD, a postdoctoral dermatology fellow at the University of Pennsylvania, Philadelphia, said in her presentation. The risk was independent of other atopic disease, gender, age, and socioeconomic status.
Dr. Wan and colleagues conducted a cohort study of patients with AD in the United Kingdom using data from the Health Improvement Network (THIN) electronic records database, matching AD patients in THIN with up to five patients without AD, similar in age and also registered to general practices. The researchers validated AD disease status using an algorithm that identified patients with a diagnostic code and two therapy codes related to AD. Outcomes of interest included anxiety, depression, bipolar disorder, obsessive-compulsive disorder, ADHD, schizophrenia, and autism. Patients entered into the cohort when they were diagnosed with AD, registered by a practice, or when data from a practice was reported to THIN. The researchers stopped following patients when they developed a neuropsychiatric outcome of interest, left a practice, died, or when the study ended.
“Previous studies have found associations between atopic dermatitis and anxiety, depression, and attention-deficit/hyperactivity disorder. However, many previous studies had been cross-sectional and they were unable to evaluate the directionality of association between atopic dermatitis and neuropsychiatric outcomes, while other previous studies have relied on the self-report of atopic dermatitis and outcomes as well,” Dr. Wan said. “Thus, longitudinal studies, using validated measures of atopic dermatitis, and those that include the entire age span, are really needed.”
Overall, 434,859 children and adolescents under aged 18 with AD in the THIN database were matched to 1,983,589 controls, and 644,802 adults with AD were matched to almost 2,900,000 adults without AD. In the pediatric group, demographics were mostly balanced between children with and without AD: the average age ranged between about 5 and almost 6 years. In pediatric patients with AD, there was a higher rate of allergic rhinitis (6.2% vs. 4%) and asthma (13.5% vs. 9.3%) than in the control group.
For adults, the average age was about 48 years in both groups. Compared with patients who did not have AD, adults with AD also had higher rates of allergic rhinitis (15.2% vs. 9.6%) and asthma (19.9% vs. 12.6%).
After adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis, Dr. Wan and colleagues found greater rates of bipolar disorder (hazard ratio, 1.34; 95% confidence interval, 1.09-1.65), obsessive-compulsive disorder (HR, 1.30; 95% CI, 1.21-1.41), anxiety (HR, 1.09; 95% CI, 1.07-1.11), and depression (HR, 1.06; 95% CI, 1.04-1.08) among children and adolescents with AD, compared with controls.
In the adult cohort, a diagnosis of AD was associated with an increased risk of autism (HR, 1.53; 95% CI, 1.30-1.80), obsessive-compulsive disorder (HR, 1.49; 95% CI, 1.40-1.59), ADHD (HR, 1.31; 95% CI, 1.13-1.53), anxiety (HR, 1.17; 95% CI, 1.15-1.18), depression (HR, 1.15; 95% CI, 1.14-1.16), and bipolar disorder (HR, 1.12; 95% CI, 1.04-1.21), after adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis.
One reason for the increased associations among the adults, even for ADHD and autism, which are more characteristically diagnosed in childhood, Dr. Wan said, is that, since they looked at incident outcomes, “many children may already have had these prevalent comorbidities at the time of the entry in the cohort.”
She noted that the study may have observation bias or unknown confounders, but she hopes these results raise awareness of the association between AD and neuropsychiatric disorders, although more research is needed to determine how AD severity affects neuropsychiatric outcomes. “Additional work is needed to really understand the mechanisms that drive these associations, whether it’s mediated through symptoms of atopic dermatitis such as itch and poor sleep, or potentially the stigma of having a chronic skin disease, or perhaps shared pathophysiology between atopic dermatitis and these neuropsychiatric diseases,” she said.
The study was funded by a grant from Pfizer. Dr. Wan reports receiving research funding from Pfizer paid to the University of Pennsylvania.
FROM SID 2020














