User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Case series suggests biologics, JAK inhibitors safe during pandemic
Use of biologics and Janus kinase (JAK) inhibitors was not associated with worse outcomes in 86 people with inflammatory diseases who contracted COVID-19, according to a case series from New York University Langone Health.
“We are not seeing worse outcomes with overall use of either. It’s reassuring” that the data support continued use during the pandemic, said rheumatologist and senior investigator Jose Scher, MD, an associate professor at New York University.
There have been concerns among rheumatologists, gastroenterologists, and dermatologists that underlying inflammatory diseases and the agents used to treat them would impact outcomes in COVID-19.
Dr. Scher and colleagues, including lead author and rheumatologist Rebecca Haberman, MD, wanted to address the issue, so they reviewed the experience in their own health system of patients with inflammatory diseases – most commonly psoriatic arthritis, RA, and Crohn’s disease – who were assessed for COVID-19 from March 3 to April 3.
Fever, cough, and shortness of breath were the most common symptoms. The infection was confirmed by polymerase chain reaction in 59 (69%) and highly suspected in 27.
A total of 62 patients (72%) were on JAK inhibitors or biologics at baseline, including 38 (44%) on tumor necrosis factor inhibitors.
Overall, 14 patients (16%) were hospitalized with COVID-19, which is consistent the 26% hospitalization rate among the general population in New York City.
Baseline biologic and JAK inhibitor use was actually lower among hospitalized patients than among those who weren’t hospitalized (50% vs. 76%), and the hospitalization rate was only 11% among 62 subjects who had been on the agents long term, more than a year among most.
Hospitalized patients tended to be slightly older (mean, 50 vs. 46 years) with a higher prevalence of hypertension, diabetes, and chronic obstructive pulmonary disease. They also had a higher prevalence of RA (43% vs. 19%), methotrexate use (43% vs. 15%), and use of hydroxychloroquine (21% vs. 7%) and oral glucocorticoids (29% vs. 6%).
It’s unknown what to make of those findings for now, Dr. Scher said. The study didn’t address differences in the severity of the underlying inflammatory illness, but a new and significantly larger case series is in the works that will analyze that and other potential confounders.
Dr. Scher noted that he’s particularly interested in drilling down further on the higher prevalence of RA and methotrexate in hospitalized patients. “We want to understand those signals better. All of this needs further validation,” he said.
Of the 14 hospitalized patients, 11 (79%) were discharged after a mean of 5.6 days. One died in the ED, and two remained hospitalized as of April 3, including one in the ICU.
The investigators are contributing to COVID-19 registries for inflammatory disease patients. The registries are tending to report higher hospitalization rates, but Dr. Scher noted they might be biased towards more severe cases, among other issues.
As for the current situation in New York City, he said that the “last week in March and first 3 in April were indescribable in terms of admissions, intubations, and deaths. Over the last week or so, it has calmed down significantly.”
There was no external funding. Dr. Haberman reported ties to Janssen, and Dr. Scher reported ties to Janssen, Novartis, Pfizer, and other companies.
SOURCE: Haberman R et al. N Engl J Med. 2020 Apr 29. doi: 10.1056/NEJMc2009567.
Use of biologics and Janus kinase (JAK) inhibitors was not associated with worse outcomes in 86 people with inflammatory diseases who contracted COVID-19, according to a case series from New York University Langone Health.
“We are not seeing worse outcomes with overall use of either. It’s reassuring” that the data support continued use during the pandemic, said rheumatologist and senior investigator Jose Scher, MD, an associate professor at New York University.
There have been concerns among rheumatologists, gastroenterologists, and dermatologists that underlying inflammatory diseases and the agents used to treat them would impact outcomes in COVID-19.
Dr. Scher and colleagues, including lead author and rheumatologist Rebecca Haberman, MD, wanted to address the issue, so they reviewed the experience in their own health system of patients with inflammatory diseases – most commonly psoriatic arthritis, RA, and Crohn’s disease – who were assessed for COVID-19 from March 3 to April 3.
Fever, cough, and shortness of breath were the most common symptoms. The infection was confirmed by polymerase chain reaction in 59 (69%) and highly suspected in 27.
A total of 62 patients (72%) were on JAK inhibitors or biologics at baseline, including 38 (44%) on tumor necrosis factor inhibitors.
Overall, 14 patients (16%) were hospitalized with COVID-19, which is consistent the 26% hospitalization rate among the general population in New York City.
Baseline biologic and JAK inhibitor use was actually lower among hospitalized patients than among those who weren’t hospitalized (50% vs. 76%), and the hospitalization rate was only 11% among 62 subjects who had been on the agents long term, more than a year among most.
Hospitalized patients tended to be slightly older (mean, 50 vs. 46 years) with a higher prevalence of hypertension, diabetes, and chronic obstructive pulmonary disease. They also had a higher prevalence of RA (43% vs. 19%), methotrexate use (43% vs. 15%), and use of hydroxychloroquine (21% vs. 7%) and oral glucocorticoids (29% vs. 6%).
It’s unknown what to make of those findings for now, Dr. Scher said. The study didn’t address differences in the severity of the underlying inflammatory illness, but a new and significantly larger case series is in the works that will analyze that and other potential confounders.
Dr. Scher noted that he’s particularly interested in drilling down further on the higher prevalence of RA and methotrexate in hospitalized patients. “We want to understand those signals better. All of this needs further validation,” he said.
Of the 14 hospitalized patients, 11 (79%) were discharged after a mean of 5.6 days. One died in the ED, and two remained hospitalized as of April 3, including one in the ICU.
The investigators are contributing to COVID-19 registries for inflammatory disease patients. The registries are tending to report higher hospitalization rates, but Dr. Scher noted they might be biased towards more severe cases, among other issues.
As for the current situation in New York City, he said that the “last week in March and first 3 in April were indescribable in terms of admissions, intubations, and deaths. Over the last week or so, it has calmed down significantly.”
There was no external funding. Dr. Haberman reported ties to Janssen, and Dr. Scher reported ties to Janssen, Novartis, Pfizer, and other companies.
SOURCE: Haberman R et al. N Engl J Med. 2020 Apr 29. doi: 10.1056/NEJMc2009567.
Use of biologics and Janus kinase (JAK) inhibitors was not associated with worse outcomes in 86 people with inflammatory diseases who contracted COVID-19, according to a case series from New York University Langone Health.
“We are not seeing worse outcomes with overall use of either. It’s reassuring” that the data support continued use during the pandemic, said rheumatologist and senior investigator Jose Scher, MD, an associate professor at New York University.
There have been concerns among rheumatologists, gastroenterologists, and dermatologists that underlying inflammatory diseases and the agents used to treat them would impact outcomes in COVID-19.
Dr. Scher and colleagues, including lead author and rheumatologist Rebecca Haberman, MD, wanted to address the issue, so they reviewed the experience in their own health system of patients with inflammatory diseases – most commonly psoriatic arthritis, RA, and Crohn’s disease – who were assessed for COVID-19 from March 3 to April 3.
Fever, cough, and shortness of breath were the most common symptoms. The infection was confirmed by polymerase chain reaction in 59 (69%) and highly suspected in 27.
A total of 62 patients (72%) were on JAK inhibitors or biologics at baseline, including 38 (44%) on tumor necrosis factor inhibitors.
Overall, 14 patients (16%) were hospitalized with COVID-19, which is consistent the 26% hospitalization rate among the general population in New York City.
Baseline biologic and JAK inhibitor use was actually lower among hospitalized patients than among those who weren’t hospitalized (50% vs. 76%), and the hospitalization rate was only 11% among 62 subjects who had been on the agents long term, more than a year among most.
Hospitalized patients tended to be slightly older (mean, 50 vs. 46 years) with a higher prevalence of hypertension, diabetes, and chronic obstructive pulmonary disease. They also had a higher prevalence of RA (43% vs. 19%), methotrexate use (43% vs. 15%), and use of hydroxychloroquine (21% vs. 7%) and oral glucocorticoids (29% vs. 6%).
It’s unknown what to make of those findings for now, Dr. Scher said. The study didn’t address differences in the severity of the underlying inflammatory illness, but a new and significantly larger case series is in the works that will analyze that and other potential confounders.
Dr. Scher noted that he’s particularly interested in drilling down further on the higher prevalence of RA and methotrexate in hospitalized patients. “We want to understand those signals better. All of this needs further validation,” he said.
Of the 14 hospitalized patients, 11 (79%) were discharged after a mean of 5.6 days. One died in the ED, and two remained hospitalized as of April 3, including one in the ICU.
The investigators are contributing to COVID-19 registries for inflammatory disease patients. The registries are tending to report higher hospitalization rates, but Dr. Scher noted they might be biased towards more severe cases, among other issues.
As for the current situation in New York City, he said that the “last week in March and first 3 in April were indescribable in terms of admissions, intubations, and deaths. Over the last week or so, it has calmed down significantly.”
There was no external funding. Dr. Haberman reported ties to Janssen, and Dr. Scher reported ties to Janssen, Novartis, Pfizer, and other companies.
SOURCE: Haberman R et al. N Engl J Med. 2020 Apr 29. doi: 10.1056/NEJMc2009567.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Antitumor treatment may increase risk of severe events in COVID-19 patients
Cancer patients who received antitumor treatment within 14 days of COVID-19 diagnosis had an increased risk of severe events, according to data from three hospitals in Wuhan.
Patients with patchy consolidation at hospital admission also had an increased risk of severe events, defined as ICU admission, mechanical ventilation, or death.
However, these findings are limited by the small number of patients studied and the retrospective nature of the analysis, according to researchers.
Li Zhang, MD, PhD, of Tongji Hospital in Wuhan, China, presented this research at the AACR virtual meeting I. Some of the data were previously published in Annals of Oncology.
The researchers studied 28 patients with cancer among 1,276 patients with COVID-19 treated at three hospitals in Wuhan. The most common cancer types were lung (n = 7), esophageal (n = 4), and breast (n = 3). Patients had other gastrointestinal, gynecologic, genitourinary, and head and neck cancers as well.
The patients’ median age was 65 years (range, 56-70 years), 60.9% were men, 35.7% had stage IV cancer, and 28.6% had hospital-acquired COVID-19. Antitumor treatments included chemotherapy (n = 22), surgery (n = 21), radiotherapy (n = 21), targeted therapy (n = 5), and immune checkpoint inhibitors (n = 2).
COVID-19 treatment
Most patients (n = 22) received oxygen as their only respiratory intervention, although 10 received mechanical ventilation.
For systemic therapy, patients received antibiotic treatment (n = 23), corticosteroids (n = 15), intravenous immunoglobulin (n = 10), and tocilizumab (n = 1).
Antiviral treatments included umifenovir (n = 14), lopinavir/ritonavir (n = 10), ganciclovir (n = 9), ribavirin (n = 1), or a combination of antiviral drugs (n = 9).
“No cancer patients were enrolled in clinical trials, so no one received hydroxychloroquine or remdesivir,” Dr. Zhang noted.
Outcomes
In all, 15 patients (53.6%) had severe events. The median time from COVID-19 diagnosis to severe events was 7 days (range, 5-15 days).
A total of eight patients (28.6%) died – three with lung cancer, two with prostate cancer, one with liver cancer, one with rectal cancer, and one with testicular cancer.
Causes of death were acute respiratory distress syndrome (n = 5), septic shock (n = 1), suspected pulmonary embolism (n = 1), and acute myocardial infarction (n = 1).
By April 4, 14 patients had been discharged from the hospital, and 6 were still hospitalized. The median duration of hospitalization was 18.4 days for discharged patients and 29.4 days for patients still in hospital.
Follow-up CT scans showed improvement in 13 patients, no changes in 5 patients, and deterioration in 6 patients.
Factors associated with severe events
In a multivariable analysis, receiving antitumor treatment within 14 days of COVID-19 diagnosis was associated with severe events (hazard ratio, 4.079; P = .037).
However, only seven patients received antitumor treatments within 14 days of COVID-19 diagnosis – three chemotherapy, two targeted therapy, one radiotherapy, and one immune checkpoint inhibitor. Five of these seven patients had severe events.
Another factor associated with severe events in multivariable analysis was patchy consolidation on CT scan at admission (HR, 5.438; P = .01). Age and gender were not significantly associated with severe events.
Immune checkpoint inhibitors
Dr. Zhang and colleagues also analyzed a second group of cancer patients and their family members to determine if patients on immune checkpoint inhibitors have an increased risk of COVID-19.
This group included 124 cancer patients treated with immune checkpoint inhibitors for at least 2 months. The patients had a median age of 59 years (range, 54-65 years), and 61.8% were men. Most patients (95.2%) had stage IV cancer, and the most common cancers were lung (54.0%), esophageal (18.6%), and head and neck (10.7%).
In this group, only one cancer patient developed COVID-19 (via nosocomial infection). In another case, a patient’s spouse developed COVID-19, but the patient did not.
Dr. Zhang said this “limited information did not suggest cancer patients treated with immune checkpoint inhibitors were more vulnerable to COVID infection.”
Dr. Zhang and colleagues reported no conflicts of interest. This research was funded by the National Natural Science Foundation of China and Huazhong University of Science and Technology COVID-19 Rapid Response Call China.
SOURCE: Zhang L et al. Ann Oncol. 2020 Mar 26. doi: 10.1016/j.annonc.2020.03.296.
Cancer patients who received antitumor treatment within 14 days of COVID-19 diagnosis had an increased risk of severe events, according to data from three hospitals in Wuhan.
Patients with patchy consolidation at hospital admission also had an increased risk of severe events, defined as ICU admission, mechanical ventilation, or death.
However, these findings are limited by the small number of patients studied and the retrospective nature of the analysis, according to researchers.
Li Zhang, MD, PhD, of Tongji Hospital in Wuhan, China, presented this research at the AACR virtual meeting I. Some of the data were previously published in Annals of Oncology.
The researchers studied 28 patients with cancer among 1,276 patients with COVID-19 treated at three hospitals in Wuhan. The most common cancer types were lung (n = 7), esophageal (n = 4), and breast (n = 3). Patients had other gastrointestinal, gynecologic, genitourinary, and head and neck cancers as well.
The patients’ median age was 65 years (range, 56-70 years), 60.9% were men, 35.7% had stage IV cancer, and 28.6% had hospital-acquired COVID-19. Antitumor treatments included chemotherapy (n = 22), surgery (n = 21), radiotherapy (n = 21), targeted therapy (n = 5), and immune checkpoint inhibitors (n = 2).
COVID-19 treatment
Most patients (n = 22) received oxygen as their only respiratory intervention, although 10 received mechanical ventilation.
For systemic therapy, patients received antibiotic treatment (n = 23), corticosteroids (n = 15), intravenous immunoglobulin (n = 10), and tocilizumab (n = 1).
Antiviral treatments included umifenovir (n = 14), lopinavir/ritonavir (n = 10), ganciclovir (n = 9), ribavirin (n = 1), or a combination of antiviral drugs (n = 9).
“No cancer patients were enrolled in clinical trials, so no one received hydroxychloroquine or remdesivir,” Dr. Zhang noted.
Outcomes
In all, 15 patients (53.6%) had severe events. The median time from COVID-19 diagnosis to severe events was 7 days (range, 5-15 days).
A total of eight patients (28.6%) died – three with lung cancer, two with prostate cancer, one with liver cancer, one with rectal cancer, and one with testicular cancer.
Causes of death were acute respiratory distress syndrome (n = 5), septic shock (n = 1), suspected pulmonary embolism (n = 1), and acute myocardial infarction (n = 1).
By April 4, 14 patients had been discharged from the hospital, and 6 were still hospitalized. The median duration of hospitalization was 18.4 days for discharged patients and 29.4 days for patients still in hospital.
Follow-up CT scans showed improvement in 13 patients, no changes in 5 patients, and deterioration in 6 patients.
Factors associated with severe events
In a multivariable analysis, receiving antitumor treatment within 14 days of COVID-19 diagnosis was associated with severe events (hazard ratio, 4.079; P = .037).
However, only seven patients received antitumor treatments within 14 days of COVID-19 diagnosis – three chemotherapy, two targeted therapy, one radiotherapy, and one immune checkpoint inhibitor. Five of these seven patients had severe events.
Another factor associated with severe events in multivariable analysis was patchy consolidation on CT scan at admission (HR, 5.438; P = .01). Age and gender were not significantly associated with severe events.
Immune checkpoint inhibitors
Dr. Zhang and colleagues also analyzed a second group of cancer patients and their family members to determine if patients on immune checkpoint inhibitors have an increased risk of COVID-19.
This group included 124 cancer patients treated with immune checkpoint inhibitors for at least 2 months. The patients had a median age of 59 years (range, 54-65 years), and 61.8% were men. Most patients (95.2%) had stage IV cancer, and the most common cancers were lung (54.0%), esophageal (18.6%), and head and neck (10.7%).
In this group, only one cancer patient developed COVID-19 (via nosocomial infection). In another case, a patient’s spouse developed COVID-19, but the patient did not.
Dr. Zhang said this “limited information did not suggest cancer patients treated with immune checkpoint inhibitors were more vulnerable to COVID infection.”
Dr. Zhang and colleagues reported no conflicts of interest. This research was funded by the National Natural Science Foundation of China and Huazhong University of Science and Technology COVID-19 Rapid Response Call China.
SOURCE: Zhang L et al. Ann Oncol. 2020 Mar 26. doi: 10.1016/j.annonc.2020.03.296.
Cancer patients who received antitumor treatment within 14 days of COVID-19 diagnosis had an increased risk of severe events, according to data from three hospitals in Wuhan.
Patients with patchy consolidation at hospital admission also had an increased risk of severe events, defined as ICU admission, mechanical ventilation, or death.
However, these findings are limited by the small number of patients studied and the retrospective nature of the analysis, according to researchers.
Li Zhang, MD, PhD, of Tongji Hospital in Wuhan, China, presented this research at the AACR virtual meeting I. Some of the data were previously published in Annals of Oncology.
The researchers studied 28 patients with cancer among 1,276 patients with COVID-19 treated at three hospitals in Wuhan. The most common cancer types were lung (n = 7), esophageal (n = 4), and breast (n = 3). Patients had other gastrointestinal, gynecologic, genitourinary, and head and neck cancers as well.
The patients’ median age was 65 years (range, 56-70 years), 60.9% were men, 35.7% had stage IV cancer, and 28.6% had hospital-acquired COVID-19. Antitumor treatments included chemotherapy (n = 22), surgery (n = 21), radiotherapy (n = 21), targeted therapy (n = 5), and immune checkpoint inhibitors (n = 2).
COVID-19 treatment
Most patients (n = 22) received oxygen as their only respiratory intervention, although 10 received mechanical ventilation.
For systemic therapy, patients received antibiotic treatment (n = 23), corticosteroids (n = 15), intravenous immunoglobulin (n = 10), and tocilizumab (n = 1).
Antiviral treatments included umifenovir (n = 14), lopinavir/ritonavir (n = 10), ganciclovir (n = 9), ribavirin (n = 1), or a combination of antiviral drugs (n = 9).
“No cancer patients were enrolled in clinical trials, so no one received hydroxychloroquine or remdesivir,” Dr. Zhang noted.
Outcomes
In all, 15 patients (53.6%) had severe events. The median time from COVID-19 diagnosis to severe events was 7 days (range, 5-15 days).
A total of eight patients (28.6%) died – three with lung cancer, two with prostate cancer, one with liver cancer, one with rectal cancer, and one with testicular cancer.
Causes of death were acute respiratory distress syndrome (n = 5), septic shock (n = 1), suspected pulmonary embolism (n = 1), and acute myocardial infarction (n = 1).
By April 4, 14 patients had been discharged from the hospital, and 6 were still hospitalized. The median duration of hospitalization was 18.4 days for discharged patients and 29.4 days for patients still in hospital.
Follow-up CT scans showed improvement in 13 patients, no changes in 5 patients, and deterioration in 6 patients.
Factors associated with severe events
In a multivariable analysis, receiving antitumor treatment within 14 days of COVID-19 diagnosis was associated with severe events (hazard ratio, 4.079; P = .037).
However, only seven patients received antitumor treatments within 14 days of COVID-19 diagnosis – three chemotherapy, two targeted therapy, one radiotherapy, and one immune checkpoint inhibitor. Five of these seven patients had severe events.
Another factor associated with severe events in multivariable analysis was patchy consolidation on CT scan at admission (HR, 5.438; P = .01). Age and gender were not significantly associated with severe events.
Immune checkpoint inhibitors
Dr. Zhang and colleagues also analyzed a second group of cancer patients and their family members to determine if patients on immune checkpoint inhibitors have an increased risk of COVID-19.
This group included 124 cancer patients treated with immune checkpoint inhibitors for at least 2 months. The patients had a median age of 59 years (range, 54-65 years), and 61.8% were men. Most patients (95.2%) had stage IV cancer, and the most common cancers were lung (54.0%), esophageal (18.6%), and head and neck (10.7%).
In this group, only one cancer patient developed COVID-19 (via nosocomial infection). In another case, a patient’s spouse developed COVID-19, but the patient did not.
Dr. Zhang said this “limited information did not suggest cancer patients treated with immune checkpoint inhibitors were more vulnerable to COVID infection.”
Dr. Zhang and colleagues reported no conflicts of interest. This research was funded by the National Natural Science Foundation of China and Huazhong University of Science and Technology COVID-19 Rapid Response Call China.
SOURCE: Zhang L et al. Ann Oncol. 2020 Mar 26. doi: 10.1016/j.annonc.2020.03.296.
FROM AACR 2020
Time to retire haloperidol?
For more than half a century, haloperidol has been used as a first-line medication for psychiatric agitation constituting a “behavioral emergency” when a patient cannot or will not take oral medication. Today, haloperidol is most commonly administered as an IM injection along with an anticholinergic medication to minimize extrapyramidal symptoms (EPS) and a benzodiazepine for additional sedation. The multiple-medication “cocktail” is often referred to by double-entendre nicknames, such as “B-52” or “5250” (ie, haloperidol, 5 mg; lorazepam, 2 mg; and
Earlier evidence of haloperidol’s efficacy
The initial “discovery” of antipsychotic medications was made in 1951 based on the inadvertent observation that chlorpromazine had the potential to calm surgical patients with autonomic activation. This calming effect, described as “désintéressment” (meaning a kind of “indifference to the world”),1 resulted in a new class of medications replacing barbiturates and bromides as go-to options to achieve “rapid tranquilization” of psychiatric agitation.2 Although the ability of antipsychotic medications to gradually reduce positive symptoms, such as delusions and hallucinations, has been attributed to dopamine (D2) antagonism, their more immediate sedating and anti-agitation effects are the result of broader effects as histamine (H1) and alpha-1 adrenergic antagonists.
In the 1970s, haloperidol emerged as a first-line option to manage agitation due to its IM and IV availability, as well as its relative lack of sedation and orthostasis compared with low-potency D2 antagonists such as chlorpromazine. However, haloperidol was observed to have a significant risk of acute EPS, including dystonic reactions.2 From the 1970s to the 1990s, numerous prospective clinical trials of haloperidol for the treatment of acute psychotic agitation, including several randomized controlled trials (RCTs) comparing haloperidol to lorazepam, were conducted.3 The design and outcomes of the haloperidol vs lorazepam RCTs were fairly consistent4-7:
- adult participants with acute agitation and a variety of psychiatric diagnoses, for whom informed consent often was waived due to agitation severity
- randomization to either IM haloperidol, 5 mg, or IM lorazepam, 2 mg, administered every 30 minutes until agitation resolved
- behavioral outcomes measured over several hours using various rating scales, without consistent assessment of EPS
- equivalent efficacy of haloperidol and lorazepam, with symptom resolution usually achieved after 1 to 2 doses (in 30 to 60 minutes), but sometimes longer
- anticholinergic “rescue” allowed for EPS, but not administered prophylactically
- EPS, including dystonia and akathisia, were significantly more frequent with haloperidol compared with lorazepam.8
In recognition of the greater risk of EPS with haloperidol compared with lorazepam, and the fact that most study participants were already taking standing doses of antipsychotic medications, some researchers have recommended using benzodiazepines alone as the optimal treatment for agitation.4,9 A 2012 Cochrane review concluded that the involuntary use of haloperidol alone “could be considered unethical.”10,11 However, other studies that examined the combination of haloperidol and lorazepam compared with either medication alone found that the combination of the 2 medications was associated with a more rapid resolution of symptoms, which suggests a superior synergistic effect.6,7,12 By the late 1990s, combined haloperidol and lorazepam, often mixed within a single injection, became the most common strategy to achieve rapid tranquilization in the psychiatric emergency setting.13 However, while the combination has been justified as a way to reduce the antipsychotic medication dose and EPS risk,2 few studies have compared combinations containing <5 mg of haloperidol. As a result, the apparent superiority of combined haloperidol and lorazepam compared with either medication alone may be a simple cumulative dose effect rather than true synergism. It is also important to note that adding lorazepam to haloperidol does not mitigate the risk of EPS such as dystonia in the absence of anticholinergic medication.8 To date, however, there have been no clinical trials investigating the efficacy of IM haloperidol, lorazepam, and
Newer RCTs tell a different story
With the availability of second-generation antipsychotics (SGAs) in IM formulations, clinical trials over the past 2 decades have focused on comparing SGAs with haloperidol alone as the “gold standard” control for acute agitation. Compared with previous trials of
- Study participants who signed informed consent (and were likely less agitated)
- IM haloperidol doses typically >5 mg (eg, 6.5 to 10 mg).
As with studies comparing lorazepam with haloperidol, the results of these RCTs revealed that IM
An updated 2017 Cochrane review of haloperidol for psychosis-induced aggression or agitation concluded that9:
- haloperidol is an effective intervention, although the evidence is “weak”
- significant treatment effects may take as long as 1 to 2 hours following multiple IM injections
- in contrast to SGAs, treatment with haloperidol carries a significant risk of EPS
- adding a benzodiazepine “does not have strong evidence of benefit and carries risk of additional harm.”
Continue to: Haloperidol's well-known toxicity
Haloperidol’s well-known toxicity
Haloperidol has been associated with numerous adverse effects:
Akathisia and other acute EPS. Treatment with even a single dose of IM haloperidol can result in acute EPS, including dystonia and akathisia. At best, such adverse effects are subjectively troubling and unpleasant; at worst, akathisia can exacerbate and be mistaken for agitation, leading to administration of more medication23 and the possible development of suicidal or violent behavior.24-25 In the studies reviewed above, the overall rate of EPS was as high as 21% after treatment with haloperidol,16 with parkinsonism occurring in up to 17% of patients,19 dystonia in up to 11%,7 and akathisia in up to 10%.15 However, because specific EPS were assessed inconsistently, and sometimes not at all, the rate of akathisia—arguably the most relevant and counter-therapeutic adverse effect related to agitation—remains unclear.
In another study that specifically assessed for akathisia in patients treated with haloperidol, up to 40% experienced akathisia 6 hours after a single oral dose of 5 mg.26 Even a single dose of IV
Although anticholinergic medications or benzodiazepinesare often administered as part of a haloperidol “cocktail,” these medications often do not adequately resolve emergent akathisia.26,28 No clinical trials of IM haloperidol combined with benztropine or diphenhydramine have been published, but several studies suggest that combining haloperidol with
Cardiotoxicity. Although low-potency antipsychotic medications such as
Continue to: Although there is no direct evidence...
Although there is no direct evidence that the cardiac risks associated with IV haloperidol apply to IM administration, epidemiologic studies indicate that oral haloperidol carries an elevated risk of ventricular arrhythmia and sudden cardiac death,35,36 with 1 study reporting greater risk compared with other SGAs.37 Haloperidol, whether administered orally or IM, may therefore be an especially poor choice for patients with agitation who are at risk for arrhythmia, including those with relevant medical comorbidities or delirium.34
Neuronal cell death. Several lines of research evidence have demonstrated that haloperidol can cause cellular injury or death in neuronal tissue in a dose-dependent fashion through a variety of mechanisms.38 By contrast, SGAs have been shown to have neuroprotective effects.39 While these findings have mostly come from studies conducted in animals or in vitro human tumor cell lines, some researchers have nonetheless called for haloperidol to be banned, noting that if its neurotoxic effects were more widely known, “we would realize what a travesty it is to use [such] a brain-unfriendly drug.”40
Several reasonable alternatives
Echoing the earlier Cochrane review of haloperidol for psychosis-induced aggression or agitation,10 a 2017 update concluded, “If no other alternative exists, sole use of intramuscular haloperidol could be life-saving. Where additional drugs are available, sole use of haloperidol for extreme emergency could be considered unethical.”9
What then are reasonable alternatives to replace IM haloperidol for agitation? Clinicians should consider the following nonpharmacologic and pharmacologic interventions:
Nonpharmacologic interventions. Several behavioral interventions have been demonstrated to be effective for managing acute agitation, including verbal de-escalation, enhanced “programming” on the inpatient units, and the judicious use of seclusion.41-43 While such interventions may demand additional staff or resources, they have the potential to lower long-term costs, reduce injuries to patients and staff, and improve the quality of care.43 The use of IM haloperidol as a form of “chemical restraint” does not represent standard-of-care treatment,3 and from an ethical perspective, should never be implemented punitively or to compensate for substandard care in the form of inadequate staffing or staff training.
Continue to: Benzodiazepines
Benzodiazepines. Lorazepam offers an attractive alternative to haloperidol without the risk of EPS.2,4,8 However, lorazepam alone may be perceived as less efficacious than a haloperidol “cocktail” because it represents less overall medication. Some evidence has suggested that lorazepam, 4 mg, might be the most appropriate dose, although it has only rarely been studied in clinical trials of acute agitation.3
Respiratory depression is frequently cited as an argument against using lorazepam for agitation, as if the therapeutic window is extremely narrow with ineffectiveness at 2 mg, but potential lethality beyond that dose. In fact, serious respiratory depression with lorazepam is unlikely in the absence of chronic obstructive pulmonary disease (COPD), obstructive sleep apnea, or concomitant alcohol or other sedative use.46 Case reports have documented therapeutic lorazepam dosing of 2 to 4 mg every 2 hours up to 20 to 30 mg/d in patients with manic agitation.47 Even in patients with COPD, significant respiratory depression tends not to occur at doses <8 mg.48 A more evidence-based concern about lorazepam dosing is that 2 mg might be ineffective in patients with established tolerance. For example, 1 report described a patient in acute alcohol withdrawal who required dosing lorazepam to 1,600 mg within 24 hours.49 Collectively, these reports suggest that lorazepam has a much wider therapeutic window than is typically perceived, and that dosing with 3 to 4 mg IM is a reasonable option for agitation when 2 mg is likely to be inadequate.
Paradoxical disinhibition is another concern that might prevent benzodiazepines from being used alone as a first-line intervention for emergency treatment of agitation. However, similar to respiratory depression, this adverse event is relatively rare and tends to occur in children and geriatric patients, individuals intoxicated with alcohol or other sedatives, and patients with brain injury, developmental delay, or dementia.23,46 Although exacerbation of aggression has not been demonstrated in the RCTs examining benzodiazepines for agitation reviewed above, based on other research, some clinicians have expressed concerns about the potential for benzodiazepines to exacerbate aggression in patients with impulse control disorders and a history of violent behavior.50
The 2005 Expert Consensus Panel for Behavioral Emergencies51 recommended the use of lorazepam alone over haloperidol for agitation for patients for whom the diagnosis is unknown or includes the following:
- stimulant intoxication
- personality disorder
- comorbid obesity
- comorbid cardiac arrhythmia
- a history of akathisia and other EPS
- a history of amenorrhea/galactorrhea
- a history of seizures.
In surveys, patients have ranked lorazepam as the preferred medication for emergency agitation, whereas haloperidol was ranked as one of the least-preferred options.51,52
Continue to: Second-generation antipsychotics
Second-generation antipsychotics. The SGAs available in IM formulations, such as aripiprazole, olanzapine, and ziprasidone, have been shown to be at least as effective as haloperidol for the treatment of acute agitation (in 2015, the short-acting injectable formulation of aripiprazole was discontinued in the United States independent of safety or efficacy issues53). A review of RCTs examining IM SGAs for the treatment of agitation concluded that the number needed to treat for response compared with placebo was 5 for aripiprazole, 3 for olanzapine, and 3 for ziprasidone.54 In terms of safety, a meta-analysis of studies examining IM medications for agitation confirmed that the risk of acute EPS, including dystonia, akathisia, and parkinsonism, is significantly lower with SGAs compared with haloperidol.55 An RCT comparing IM ziprasidone with haloperidol found equivalently modest effects on QTc prolongation.56 Therefore, SGAs are an obvious and evidence-based option for replacing haloperidol as a treatment for acute agitation.
Unfortunately, for clinicians hoping to replace haloperidol within a multiple-medication IM “cocktail,” there have been no published controlled trials of SGAs combined with benzodiazepines. Although a short report indicated that aripiprazole and lorazepam are chemically compatible to be combined within a single injection,57 the package insert for aripiprazole warns that “If parenteral benzodiazepine therapy is deemed necessary in addition to ABILIFY injection treatment, patients should be monitored for excessive sedation and for orthostatic hypotension.”58 The package insert for olanzapine likewise lists the combination of lorazepam and olanzapine as a drug interaction that can potentiate sedation, and the manufacturer issued specific warnings about parenteral combination.59,60 A single published case of significant hypotension with combined IM olanzapine and lorazepam,60 together with the fact that IM olanzapine can cause hypotension by itself,61 has discouraged the coadministration of these medications. Nonetheless, the combination is used in some emergency settings, with several retrospective studies failing to provide evidence of hypotension or respiratory depression as adverse effects.62-64
Droperidol.
Over the past decade, however, droperidol has returned to the US market68 and its IV and IM usage has been revitalized for managing patients with agitation within or en route to the ED. Studies have demonstrated droperidol efficacy comparable to midazolam, ziprasidone, or olanzapine, as well as effectiveness as an IV adjunct to midazolam.69-71 In contrast to the FDA black-box warning, retrospective studies and RCTs of both IV and IM droperidol suggest that QTc prolongation and torsades de pointes are rare events that do not occur any more frequently than they do with haloperidol, even at doses >10 mg.72,73 However, in studies involving patients with drug intoxication and treatment with multiple medications, oversedation to the point of needing rescue intervention was reported. In an emergency setting where these issues are relatively easily managed, such risks may be better tolerated than in psychiatric settings.
With earlier studies examining the use of droperidol in an acute psychiatric setting that reported a more rapid onset of action than haloperidol,65-67 a 2016 Cochrane review concluded that there was high-quality evidence to support droperidol’s use for psychosis-induced agitation.74 However, a 2015 RCT comparing IM droperidol, 10 mg, to haloperidol, 10 mg, found equivalent efficacy and response times (with maximal response occurring within 2 hours) and concluded that droperidol had no advantage over haloperidol.75 Because none of the clinical trials that evaluated droperidol have included assessments for EPS, its risk of akathisia remains uncertain.
Continue to: Ketamine
Ketamine. In recent years, ketamine has been used to treat acute agitation within or en route to the ED. Preliminary observational studies support ketamine’s efficacy when administered via IV or IM routes,76 with more rapid symptomatic improvement compared with haloperidol, lorazepam, or midazolam alone.77 Reported adverse effects of ketamine include dissociation, psychotic exacerbation, and respiratory depression,76 although 1 small naturalistic study found no evidence of exacerbation of psychotic or other psychiatric symptoms.78 An ongoing RCT is comparing IM ketamine, 5 mg/kg, to combined IM haloperidol, 5 mg, and midazolam, 5 mg.79 Although various ketamine formulations are increasingly being used in psychiatry, active psychosis is generally regarded as a contraindication. It is premature to recommend parenteral ketamine administration for agitation within most psychiatric settings until more research on safety has been completed.
Haloperidol, or something else? Practical considerations
Consider the following factors when deciding whether to use haloperidol or one of its alternatives:
Limitations of the evidence. Modern clinical trials requiring informed consent often do not include the kind of severe agitation that clinicians encounter in acute psychiatric, emergency, or forensic settings. In addition, standard interventions, such as 3-medication haloperidol “cocktails,” have not been evaluated in clinical trials. Clinicians are therefore often in the dark about optimal evidence-based practices.
Treatment goals. Psychiatric agitation has many causes, with a range of severity that warrants a commensurate range of responses. Protocols for managing acute agitation should include graded interventions that begin with nonpharmacologic interventions and voluntary oral medications, and move to involuntary IM medications when necessary.
While treatment guidelines clearly recommend against IM medications as “chemical restraint” with a goal of sedating a patient until he/she is unconscious,3,51 such outcomes are nonetheless often sought by staff who are concerned about the risk of injuries during a behavioral emergency. In such instances, the risks of violence towards patients and staff may outweigh concerns about adverse effects in a risk-benefit analysis. Consequently, clinicians may be prone to “skip over” graded interventions because they assume they “won’t work” in favor of administering involuntary multiple-medication haloperidol “cocktails” despite risks of excess sedation, EPS, and cardiotoxicity. Treatment settings should critically evaluate such biased preferences, with a goal of developing tailored, evidence-based strategies that maximize benefits while minimizing excess sedation and other untoward adverse effects, with an eye towards promoting better overall patient care and reducing length of stay.42,43,80
Continue to: Limitations of available medications
Limitations of available medications. There is no perfect medication for the management of acute agitation. Evidence indicates that pharmacologic options take 15 minutes to several hours to resolve acute agitation, even potentially more rapid-acting medications such as midazolam and droperidol. This is well beyond most clinicians’ desired window for response time in a behavioral emergency. Multiple-medication “cocktails” may be used with the hope of hastening response time, but may not achieve this goal at the expense of increasing the risk of adverse effects and the likelihood that a patient will remain sedated for a prolonged time. In the real world, this often means that by the time a psychiatrist comes to evaluate a patient who has been given emergency medications, the patient cannot be aroused for an interview. Ideally, medications would calm an agitated patient rapidly, without excess or prolonged sedation.80 Less-sedating SGAs, such as ziprasidone, might have this potential, but can sometimes be perceived as ineffective.
Avoiding akathisia. Akathisia’s potential to worsen and be mistaken for agitation makes it an especially concerning, if underappreciated, adverse effect of haloperidol that is often not adequately assessed in clinical trials or practice. In light of evidence that akathisia can occur in nearly half of patients receiving a single 5 mg-dose of haloperidol, it is difficult to justify the use of this medication for agitation when equally effective options exist with a lower risk of EPS.
While haloperidol-induced akathisia could in theory be mitigated by adding anticholinergic medications or benzodiazepines, previous studies have found that such strategies have limited effectiveness compared to “gold standard” treatment with propranolol.28,81,82 Furthermore, the half-lives of anticholinergic medications, such as benztropine or diphenhydramine, are significantly shorter than that of a single dose of haloperidol, which can be as long as 37 hours.83 Therefore, akathisia and other EPS could emerge or worsen several hours or even days after receiving an IM haloperidol “cocktail” as the shorter-acting medications wear off. Akathisia is best minimized by avoiding FGAs, such as haloperidol, when treating acute agitation.
Promoting adherence. Although haloperidol is often recommended for acute agitation in patients with schizophrenia or bipolar disorder on the basis that it would treat the underlying condition, many patients who receive IM medications for acute agitation are already prescribed standing doses of oral medication, which increases the risk of cumulative toxicity. In addition, receiving a medication likely to cause acute EPS that is ranked near the bottom of patient preferences may erode the potential for a therapeutic alliance and hamper longer-term antipsychotic medication adherence.

Time for a change
For nearly half a century, haloperidol has been a “gold standard” intervention for IM control in patients with agitation. However, given its potential to produce adverse effects, including a significant risk of akathisia that can worsen agitation, along with the availability of newer pharmacologic options that are at least as effective (Table 1, and Table 2), haloperidol should be retired as a first-line medication for the treatment of agitation. Clinicians would benefit from RCTs investigating the safety and efficacy of novel interventions including frequently-used, but untested medication combinations, as well as nonpharmacologic interventions.

Continue to: Bottom Line
Bottom Line
Although there is no perfect IM medication to treat acute agitation, haloperidol’s higher risk of adverse effects relative to newer alternatives suggest that it should no longer be considered a first-line intervention.
Related Resources
- Zun LS. Evidence-based review of pharmacotherapy for acute agitation. Part 1: onset of efficacy. J Emerg Med. 2018;54(3):364-374.
- Zun LS. Evidence-based review of pharmacotherapy for acute agitation. Part 2: safety. J Emerg Med. 2018;54(4): 522-532.
Drug Brand Names
Aripiprazole • Abilify
Benztropine • Cogentin
Chlorpromazine • Thorazine
Diphenhydramine • Benadryl
Droperidol • Inapsine
Haloperidol • Haldol
Ketamine • Ketalar
Lorazepam • Ativan
Midazolam • Versed
Olanzapine • Zyprexa
Prochlorperazine • Compazine
Promethazine • Phenergan
Propranolol • Inderal, Pronol
Ziprasidone • Geodon
1. Shorter E. A history of psychiatry. New York, NY: John Wiley & Sons, Inc.; 1997:249.
2. Salzman C, Green AI, Rodriguez-Villa F, et al. Benzodiazepines combined with neuroleptics for management of severe disruptive behavior. Psychosomatics. 1986;27(suppl 1):17-22.
3. Allen MH. Managing the agitated psychotic patient: a reappraisal of the evidence. J Clin Psychiatr. 2000;61(suppl 14):11-20.
4. Salzman C, Solomon D, Miyawaki E, et al. Parenteral lorazepam versus parenteral haloperidol for the control of psychotic disruptive behavior. J Clin Psychiatr. 1991:52(4):177-180.
5. Allen MH, Currier GW, Hughes DH, et al. The expert consensus guideline series: treatment of behavioral emergencies. Postgrad Med. 2001;(Spec No):1-88; quiz 89-90.
6. Foster S, Kessel J, Berman ME, et al. Efficacy of lorazepam and haloperidol for rapid tranquilization in a psychiatric emergency room setting. Int Clin Psychopharmacol. 1997;12(3):175-179.
7. Garza-Trevino WS, Hollister LE, Overall JE, et al. Efficacy of combinations of intramuscular antipsychotics and sedative-hypnotics for control of psychotic agitation. Am J Psychiatr. 1989:146(12):1598-1601.
8. Battaglia J, Moss S, Rush J, et al. Haloperidol, lorazepam, or both for psychotic agitation? A multicenter, prospective double-blind, emergency study. Am J Emerg Med 1997;15(4):335-340.
9. Ostinelli EG, Brooke-Powney MJ, Li X, et al. Haloperidol for psychosis-induced aggression or agitation (rapid tranquillisation). Cochrane Database Syst Rev. 2017; 7:CD009377. doi: 10.1002/14651858.CD009377.pub3.
10. Powney MJ, Adams CE, Jones H. Haloperidol for psychosis-induced aggression or agitation (rapid tranquillisation). Cochrane Database Syst Rev. 2012;11:CD009377. doi: 10.1002/14651858.CD009377.pub2.
11. Citrome L. Review: limited evidence on effects of haloperidol alone for rapid tranquillisation in psychosis-induced aggression. Evid Based Ment Health. 2013;16(2):47.
12. Bienek SA, Ownby R, Penalver A, et al. A double-blind study of lorazepam versus the combination of haloperidol and lorazepam in managing agitation. Pharmacother. 1998;18(1):57-62.
13. Binder RL, McNiel DE. Contemporary practices in managing acutely violent patients in 20 psychiatric emergency rooms. Psychiatric Serv. 1999;50(2):1553-1554.
14. Andrezina R, Josiassen RC, Marcus RN, et al. Intramuscular aripiprazole for the treatment of acute agitation in patients with schizophrenia or schizoaffective disorder: a double-blind, placebo-controlled comparison with intramuscular haloperidol. Psychopharmacology (Berl). 2006;188(3):281-292.
15. Tran-Johnson TK, Sack DA, Marcus RN, et al. Efficacy and safety of intramuscular aripiprazole in patients with acute agitation: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatr. 2007;68(1):111-119.
16. Brook S, Lucey JV, Gunn KP. Intramuscular ziprasidone compared with intramuscular haloperidol in the treatment of acute psychosis. J Clin Psychiatr. 2000;61(12):933-941.
17. Brook S, Walden J, Benattia I, et al. Ziprasidone and haloperidol in the treatment of acute exacerbation of schizophrenia and schizoaffective disorder: comparison of intramuscular and oral formulations in a 6-week, randomized, blinded-assessment study. Psychopharmacology (Berl). 2005;178(4):514-523.
18. Wright P, Birkett M, David SR, et al. Double-blind, placebo-controlled comparison of intramuscular olanzapine and intramuscular haloperidol in the treatment of acute agitation in schizophrenia. Am J Psychiatr. 2001;158(7):1149-1151.
19. Breier A, Meehan K, Birkett M, et al. A double-blind, placebo-controlled dose-response comparison of intramuscular olanzapine and haloperidol in the treatment of acute agitation in schizophrenia. Arch Gen Psych. 2002;59(5):441-448.
20. Hsu W, Huang S, Lee B, et al. Comparison of intramuscular olanzapine, orally disintegrating olanzapine tablets, oral risperidone solution, and intramuscular haloperidol in the management of acute agitation in an acute care psychiatric ward in Taiwan. J Clin Psychopharmacol. 2010;30(3):230-234.
21. Chan H, Ree S, Su L, et al. A double-blind, randomized comparison study of efficacy and safety of intramuscular olanzapine and intramuscular haloperidol in patients with schizophrenia and acute agitated behavior. J Clin Psychopharmacol. 2014;34(3):355-358.
22. Baldaçara L, Sanches M, Cordeiro DC, et al. Rapid tranquilization for agitated patients in emergency psychiatric rooms: a randomized trial of olanzapine, ziprasidone, haloperidol plus promethazine, haloperidol plus midazolam and haloperidol alone. Braz J Psychiatry. 2011;33(1):30-39.
23. Hillard JR. Defusing patient violence. Current Psychiatry. 2002;1(4):22-29.
24. Seemüller F, Schennach R, Mayr A, et al. Akathisia and suicidal ideation in first-episode schizophrenia. J Clin Psychopharmacol. 2012;32(5):694-698.
25. Eikelenboom-Schieveld SJM, Lucire Y, Fogleman JC. The relevance of cytochrome P450 polymorphism in forensic medicine and akathisia-related violence and suicide. J Forens Leg Med. 2016;41:65-71.
26. Van Putten T, May PRA, Marder SR. Akathisia with haloperidol and thiothixene. Arch Gen Psych. 1984;41:1036-1039.
27. Drotts DL, Vinson DR. Prochlorperazine induced akathisia in emergency patients. Ann Emerg Med. 1999;34(4):469-475.
28. Salem H, Negpal C, Pigott T. Revisiting antipsychotic-induced akathisia: current issues and prospective challenges. Curr Neuropharmacol. 2017;15(5):789-798.
29. Huf G, Coutinho ESF, Adams CE. Rapid tranquilization in psychiatric emergency settings in Brazil: pragmatic randomized controlled trial of intramuscular haloperidol versus intramuscular haloperidol plus promethazine. BMJ. 2007;335(7625):869.
30. Mantovani C, Labate CM, Sponholz A, et al. Are low doses of antipsychotics effective in the management of psychomotor agitation? A randomized, rated-blind trial of 4 intramuscular interventions. J Clin Psychopharmacol. 2013;33(3):306-312.
31. Darwish H, Grant R, Haslam R, et al. Promethazine-induced acute dystonic reactions. Am J Dis Child. 1980;134(10):990-991.
32. Jyothi CH, Rudraiah HGM, Vidya HK, et al. Promethazine induced acute dystonia: a case report. Manipal J Med Sci. 2016;1(2):63-64.
33. Ames D, Carr-Lopez SM, Gutierrez MA, et al. Detecting and managing adverse effects of antipsychotic medications: current state of play. Psychiatr Clin North Am. 2016;39(2):275-311.
34. Meyer-Massetti C, Cheng CM, Sharpe MA, et al. The FDA extended warning for intravenous haloperidol and torsades de pointes: how should institutions respond? J Hosp Med. 2010;5(4):E8-E16. doi: 10.1002/jhm.691.
35. Wu C, Tsai Y, Tsai H. Antipsychotic drugs and the risk of ventricular arrhythmia and/or sudden cardiac death: a nation-wide case-crossover study. J Am Heart Dis. 2015;4(2):e001568. doi: 10.1161/JAHA.114.001568.
36. Beach SR, Celano CM, Sugrue AM, et al. QT prolongation, torsades de pointe, and psychotropic medications: a 5-year update. Psychosomatics. 2018;59(1):105-122.
37. Leonard CE, Freeman CP, Newcomb CW, et al. Antipsychotics and the risks of sudden cardiac death and all-cause death: cohort studies in Medicaid and dually-eligible Medicaid-Medicare beneficiaries of five states. J Clin Exp Cardiol. 2013;suppl 10(6):1-9.
38. Nasrallah H, Chen AT. Multiple neurotoxic effects of haloperidol resulting in neuronal death. Ann Clin Psychiatr. 2017;29(3):195-202.
39. Chen AT, Nasrallah HA. Neuroprotective effects of the second generation antipsychotics. Schizophr Res. 2019;208:1-7.
40. Nasrallah HA. Haloperidol clearly is neurotoxic. Should it be banned? Current Psychiatry. 2013;12(7):7-8.
41. Corrigan PW, Yudofsky SC, Silver JM. Pharmacological and behavioral treatments for aggressive psychiatric inpatients. Hosp Comm Psychiatr. 1993;44(2):125-133.
42. Zeller SL, Citrome L. Managing agitation associated with schizophrenia and bipolar disorder in the emergency setting. West J Emerg Med. 2016;17(2):165-172.
43. Vieta E, Garriga M, Cardete L, et al. Protocol for the management of psychiatric patients with psychomotor agitation. BMC Psychiatr. 2017;17:328.
44. Nobay F, Simon BC, Levitt A, et al. A prospective, double-blind, randomized trial of midazolam versus haloperidol versus lorazepam in the chemical restraint of violent and severely agitated patients. Acad Emerg Med. 2004;11(7):744-749.
45. Klein LR, Driver BE, Miner JR, et al. Intramuscular midazolam, olanzapine, ziprasidone, or haloperidol for treating acute agitation in the emergency department. Ann Emerg Med. 2018;72(4):374-385.
46. Hillard JR. Emergency treatment of acute psychosis. J Clin Psychiatr. 1998;59(suppl 1):57-60.
47. Modell JG, Lenox RH, Weiner S. Inpatient clinical trial of lorazepam for the management of manic agitation. J Clin Psychopharmacol. 1985;5(2):109-110.
48. Denaut M, Yernault JC, De Coster A. Double-blind comparison of the respiratory effects of parenteral lorazepam and diazepam in patients with chronic obstructive lung disease. Curr Med Res Opin. 1975;2(10):611-615.
49. Kahn DR, Barnhorst AV, Bourgeois JA. A case of alcohol withdrawal requiring 1,600 mg of lorazepam in 24 hours. CNS Spectr. 2009;14(7):385-389.
50. Jones KA. Benzodiazepines: their role in aggression and why GPs should prescribe with caution. Austral Fam Physician. 2011;40(11):862-865.
51. Allen MH, Currier GW, Carpenter D, et al. The expert consensus guideline series. Treatment of behavioral emergencies 2005. J Psychiatr Pract. 2005;11(suppl 1):5-108.
52. Allen MH, Carpenter D, Sheets JL, et al. What do consumers say they want and need during a psychiatric emergency? J Psychiatr Pract. 2003;9(1):39-58.
53. Han DH. Some Abilify formulations to discontinue in 2015. MPR. https://www.empr.com/home/news/some-abilify-formulations-to-discontinue-in-2015/. Published January 13, 2015. Accessed April 17, 2020.
54. Citrome L. Comparison of intramuscular ziprasidone, olanzapine, or aripiprazole for agitation: a quantitative review of efficacy and safety. J Clin Psychiatry. 2007;68(12):1876-1885.
55. Satterthwaite TD, Wolf DH, Rosenheck RA, et al. A meta-analysis of the risk of acute extrapyramidal symptoms with intramuscular antipsychotics for the treatment for agitation. J Clin Psychiatr. 2008;69(12):1869-1879.
56. Miceli JJ, Tensfeldt TG, Shiovitz T, et al. Effects of high-dose ziprasidone and haloperidol on the QTc interval after intramuscular administration: a randomized, single-blind, parallel-group study in patients with schizophrenia or schizoaffective disorder. Clin Ther. 2010;32(3):472-491.
57. Kovalick LJ, Pikalov AA, Ni N, et al. Short-term physical compatibility of intramuscular aripiprazole with intramuscular lorazepam. Am J Health-Syst Pharm. 2008;65(21):2007-2008.
58. Abilify [package insert]. Princeton, NJ: Bristol-Myers Squibb Company; 2014.
59. Zyprexa [package insert]. Indianapolis, IN: Lilly Research Laboratories; 2005.
60. Zacher JL, Roche-Desilets J. Hypotension secondary to the combination of intramuscular olanzapine and intramuscular lorazepam. J Clin Psychiatr. 2005;66(12):1614-1615.
61. Marder SR, Sorsaburu S, Dunayevich E, et al. Case reports of postmarketing adverse event experiences with olanzapine intramuscular treatment in patients with agitation. J Clin Psychiatr 2010;71(4):433-441.
62. Wilson MP, MacDonald K, Vilke GM, et al. A comparison of the safety of olanzapine and haloperidol in combination with benzodiazepines in emergency department patients with acute agitation. J Emerg Med. 2012;43(5):790-797.
63. Wilson MP, MacDonald K, Vilke GM, et al. Potential complications of combining intramuscular olanzapine with benzodiazepines in emergency department patients. J Emerg Med. 2012;43(5):889-896.
64. Williams AM. Coadministration of intramuscular olanzapine and benzodiazepines in agitated patients with mental illness. Ment Health Clin [Internet]. 2018;8(5):208-213.
65. Resnick M, Burton BT. Droperidol vs. haloperidol in the initial management of acutely agitated patients. J Clin Psychiatry. 1984;45(7):298-299.
66. Thomas H, Schwartz E, Petrilli R. Droperidol versus haloperidol for chemical restraint of agitated and combative patients. Ann Emerg Med. 1992;21(4):407-413.
67. Richards JR, Derlet RW, Duncan DR. Chemical restraint for the agitated patient in the emergency department: lorazepam versus droperidol. J Emerg Med. 1998;16(4):567-573.
68. Boyer EW. Droperidol is back (and here’s what you need to know). ACEP Now. https://www.acepnow.com/article/droperidol-is-back-and-heres-what-you-need-to-know/. Published September 16, 2019. Accessed April 17, 2020.
69. Martel M, Sterzinger A, Miner J, et al. Management of acute undifferentiated agitation in the emergency department: a randomized double-blind trial of droperidol, ziprasidone, and midazolam. Acad Emerg Med. 2005;12(12):1167-1172.
70. Chan EW, Taylor DM, Knott JC, et al. Intravenous droperidol or olanzapine as an adjunct to midazolam for the acutely agitated patient: a multicenter, randomized, double-blind, placebo-controlled clinical trial. Ann Emerg Med. 2013;61(1):72-81.
71. Isbister GK, Calver LA, Page CB, et al. Randomized controlled trial of intramuscular droperidol versus midazolam for violence and acute behavioral disturbance: the DORM study. Ann Emerg Med. 2010;56(4):392-401.
72. Macht M, Mull AC, McVaney KE, et al. Comparison of droperidol and haloperidol for use by paramedics assessment of safety and effectiveness. Prehosp Emerg Care. 2014;18(3):375-380.
73. Calver L, Page CB, Downes MA, et al. The safety and effectiveness of droperidol for sedation of acute behavioral disturbance in the emergency department. Ann Emerg Med. 2015;66(3):230-238.
74. Kohokar MA, Rathbone J. Droperidol for psychosis-induced aggression or agitation. Cochrane Database Syst Rev. 2016;12:CD002830.
75. Calver L, Drinkwater V, Gupta R, et al. Droperidol v. haloperidol for sedation of aggressive behavior in acute mental health: randomized controlled trial. Brit J Psychiatr. 2015;206(3):223-228.
76. Hopper AB, Vilke GM, Castillo EM, et al. Ketamine use for acute agitation in the emergency department. J Emerg Med. 2015;48(6):712-719.
77. Riddell J, Tran A, Bengiamin R, et al. Ketamine as a first-line treatment for severely agitated emergency department patients. Am J Emerg Med. 2017;35:1000-1004.
78. Lebin JA, Akhavan AR, Hippe DS, et al. Psychiatric outcomes of patients with severe agitation following administration of prehospital ketamine. Acad Emerg Med. 2019;26(8):889-896.
79. Barbic D, Andolfatto G, Grunau B, et al. Rapid agitation control with ketamine in the emergency department (RACKED): a randomized controlled trial protocol. Trials. 2018;19(1):651.
80. Garriga M, Pacchiarotti I, Kasper S, et al. Assessment and management of agitation in psychiatry: expert consensus. World J Biol Psychiatr. 2016;17(2):86-128.
81. Adler L, Angrist B, Peselow E, et al. Efficacy of propranolol in neuroleptic-induced akathesia. J Clin Psychopharmacol. 1985;5(3):164-166.
82. Adler LA, Reiter S, Corwin J, et al. Neuroleptic-induced akathisia: propranolol versus benztropine. Biol Psychiatry. 1988;23(2):211-213.
83. de Leon J, Diaz FJ, Wedlund P, et al. Haloperidol half-life after chronic dosing. J Clin Psychopharmacol. 2004;24(6):656-660.
For more than half a century, haloperidol has been used as a first-line medication for psychiatric agitation constituting a “behavioral emergency” when a patient cannot or will not take oral medication. Today, haloperidol is most commonly administered as an IM injection along with an anticholinergic medication to minimize extrapyramidal symptoms (EPS) and a benzodiazepine for additional sedation. The multiple-medication “cocktail” is often referred to by double-entendre nicknames, such as “B-52” or “5250” (ie, haloperidol, 5 mg; lorazepam, 2 mg; and
Earlier evidence of haloperidol’s efficacy
The initial “discovery” of antipsychotic medications was made in 1951 based on the inadvertent observation that chlorpromazine had the potential to calm surgical patients with autonomic activation. This calming effect, described as “désintéressment” (meaning a kind of “indifference to the world”),1 resulted in a new class of medications replacing barbiturates and bromides as go-to options to achieve “rapid tranquilization” of psychiatric agitation.2 Although the ability of antipsychotic medications to gradually reduce positive symptoms, such as delusions and hallucinations, has been attributed to dopamine (D2) antagonism, their more immediate sedating and anti-agitation effects are the result of broader effects as histamine (H1) and alpha-1 adrenergic antagonists.
In the 1970s, haloperidol emerged as a first-line option to manage agitation due to its IM and IV availability, as well as its relative lack of sedation and orthostasis compared with low-potency D2 antagonists such as chlorpromazine. However, haloperidol was observed to have a significant risk of acute EPS, including dystonic reactions.2 From the 1970s to the 1990s, numerous prospective clinical trials of haloperidol for the treatment of acute psychotic agitation, including several randomized controlled trials (RCTs) comparing haloperidol to lorazepam, were conducted.3 The design and outcomes of the haloperidol vs lorazepam RCTs were fairly consistent4-7:
- adult participants with acute agitation and a variety of psychiatric diagnoses, for whom informed consent often was waived due to agitation severity
- randomization to either IM haloperidol, 5 mg, or IM lorazepam, 2 mg, administered every 30 minutes until agitation resolved
- behavioral outcomes measured over several hours using various rating scales, without consistent assessment of EPS
- equivalent efficacy of haloperidol and lorazepam, with symptom resolution usually achieved after 1 to 2 doses (in 30 to 60 minutes), but sometimes longer
- anticholinergic “rescue” allowed for EPS, but not administered prophylactically
- EPS, including dystonia and akathisia, were significantly more frequent with haloperidol compared with lorazepam.8
In recognition of the greater risk of EPS with haloperidol compared with lorazepam, and the fact that most study participants were already taking standing doses of antipsychotic medications, some researchers have recommended using benzodiazepines alone as the optimal treatment for agitation.4,9 A 2012 Cochrane review concluded that the involuntary use of haloperidol alone “could be considered unethical.”10,11 However, other studies that examined the combination of haloperidol and lorazepam compared with either medication alone found that the combination of the 2 medications was associated with a more rapid resolution of symptoms, which suggests a superior synergistic effect.6,7,12 By the late 1990s, combined haloperidol and lorazepam, often mixed within a single injection, became the most common strategy to achieve rapid tranquilization in the psychiatric emergency setting.13 However, while the combination has been justified as a way to reduce the antipsychotic medication dose and EPS risk,2 few studies have compared combinations containing <5 mg of haloperidol. As a result, the apparent superiority of combined haloperidol and lorazepam compared with either medication alone may be a simple cumulative dose effect rather than true synergism. It is also important to note that adding lorazepam to haloperidol does not mitigate the risk of EPS such as dystonia in the absence of anticholinergic medication.8 To date, however, there have been no clinical trials investigating the efficacy of IM haloperidol, lorazepam, and
Newer RCTs tell a different story
With the availability of second-generation antipsychotics (SGAs) in IM formulations, clinical trials over the past 2 decades have focused on comparing SGAs with haloperidol alone as the “gold standard” control for acute agitation. Compared with previous trials of
- Study participants who signed informed consent (and were likely less agitated)
- IM haloperidol doses typically >5 mg (eg, 6.5 to 10 mg).
As with studies comparing lorazepam with haloperidol, the results of these RCTs revealed that IM
An updated 2017 Cochrane review of haloperidol for psychosis-induced aggression or agitation concluded that9:
- haloperidol is an effective intervention, although the evidence is “weak”
- significant treatment effects may take as long as 1 to 2 hours following multiple IM injections
- in contrast to SGAs, treatment with haloperidol carries a significant risk of EPS
- adding a benzodiazepine “does not have strong evidence of benefit and carries risk of additional harm.”
Continue to: Haloperidol's well-known toxicity
Haloperidol’s well-known toxicity
Haloperidol has been associated with numerous adverse effects:
Akathisia and other acute EPS. Treatment with even a single dose of IM haloperidol can result in acute EPS, including dystonia and akathisia. At best, such adverse effects are subjectively troubling and unpleasant; at worst, akathisia can exacerbate and be mistaken for agitation, leading to administration of more medication23 and the possible development of suicidal or violent behavior.24-25 In the studies reviewed above, the overall rate of EPS was as high as 21% after treatment with haloperidol,16 with parkinsonism occurring in up to 17% of patients,19 dystonia in up to 11%,7 and akathisia in up to 10%.15 However, because specific EPS were assessed inconsistently, and sometimes not at all, the rate of akathisia—arguably the most relevant and counter-therapeutic adverse effect related to agitation—remains unclear.
In another study that specifically assessed for akathisia in patients treated with haloperidol, up to 40% experienced akathisia 6 hours after a single oral dose of 5 mg.26 Even a single dose of IV
Although anticholinergic medications or benzodiazepinesare often administered as part of a haloperidol “cocktail,” these medications often do not adequately resolve emergent akathisia.26,28 No clinical trials of IM haloperidol combined with benztropine or diphenhydramine have been published, but several studies suggest that combining haloperidol with
Cardiotoxicity. Although low-potency antipsychotic medications such as
Continue to: Although there is no direct evidence...
Although there is no direct evidence that the cardiac risks associated with IV haloperidol apply to IM administration, epidemiologic studies indicate that oral haloperidol carries an elevated risk of ventricular arrhythmia and sudden cardiac death,35,36 with 1 study reporting greater risk compared with other SGAs.37 Haloperidol, whether administered orally or IM, may therefore be an especially poor choice for patients with agitation who are at risk for arrhythmia, including those with relevant medical comorbidities or delirium.34
Neuronal cell death. Several lines of research evidence have demonstrated that haloperidol can cause cellular injury or death in neuronal tissue in a dose-dependent fashion through a variety of mechanisms.38 By contrast, SGAs have been shown to have neuroprotective effects.39 While these findings have mostly come from studies conducted in animals or in vitro human tumor cell lines, some researchers have nonetheless called for haloperidol to be banned, noting that if its neurotoxic effects were more widely known, “we would realize what a travesty it is to use [such] a brain-unfriendly drug.”40
Several reasonable alternatives
Echoing the earlier Cochrane review of haloperidol for psychosis-induced aggression or agitation,10 a 2017 update concluded, “If no other alternative exists, sole use of intramuscular haloperidol could be life-saving. Where additional drugs are available, sole use of haloperidol for extreme emergency could be considered unethical.”9
What then are reasonable alternatives to replace IM haloperidol for agitation? Clinicians should consider the following nonpharmacologic and pharmacologic interventions:
Nonpharmacologic interventions. Several behavioral interventions have been demonstrated to be effective for managing acute agitation, including verbal de-escalation, enhanced “programming” on the inpatient units, and the judicious use of seclusion.41-43 While such interventions may demand additional staff or resources, they have the potential to lower long-term costs, reduce injuries to patients and staff, and improve the quality of care.43 The use of IM haloperidol as a form of “chemical restraint” does not represent standard-of-care treatment,3 and from an ethical perspective, should never be implemented punitively or to compensate for substandard care in the form of inadequate staffing or staff training.
Continue to: Benzodiazepines
Benzodiazepines. Lorazepam offers an attractive alternative to haloperidol without the risk of EPS.2,4,8 However, lorazepam alone may be perceived as less efficacious than a haloperidol “cocktail” because it represents less overall medication. Some evidence has suggested that lorazepam, 4 mg, might be the most appropriate dose, although it has only rarely been studied in clinical trials of acute agitation.3
Respiratory depression is frequently cited as an argument against using lorazepam for agitation, as if the therapeutic window is extremely narrow with ineffectiveness at 2 mg, but potential lethality beyond that dose. In fact, serious respiratory depression with lorazepam is unlikely in the absence of chronic obstructive pulmonary disease (COPD), obstructive sleep apnea, or concomitant alcohol or other sedative use.46 Case reports have documented therapeutic lorazepam dosing of 2 to 4 mg every 2 hours up to 20 to 30 mg/d in patients with manic agitation.47 Even in patients with COPD, significant respiratory depression tends not to occur at doses <8 mg.48 A more evidence-based concern about lorazepam dosing is that 2 mg might be ineffective in patients with established tolerance. For example, 1 report described a patient in acute alcohol withdrawal who required dosing lorazepam to 1,600 mg within 24 hours.49 Collectively, these reports suggest that lorazepam has a much wider therapeutic window than is typically perceived, and that dosing with 3 to 4 mg IM is a reasonable option for agitation when 2 mg is likely to be inadequate.
Paradoxical disinhibition is another concern that might prevent benzodiazepines from being used alone as a first-line intervention for emergency treatment of agitation. However, similar to respiratory depression, this adverse event is relatively rare and tends to occur in children and geriatric patients, individuals intoxicated with alcohol or other sedatives, and patients with brain injury, developmental delay, or dementia.23,46 Although exacerbation of aggression has not been demonstrated in the RCTs examining benzodiazepines for agitation reviewed above, based on other research, some clinicians have expressed concerns about the potential for benzodiazepines to exacerbate aggression in patients with impulse control disorders and a history of violent behavior.50
The 2005 Expert Consensus Panel for Behavioral Emergencies51 recommended the use of lorazepam alone over haloperidol for agitation for patients for whom the diagnosis is unknown or includes the following:
- stimulant intoxication
- personality disorder
- comorbid obesity
- comorbid cardiac arrhythmia
- a history of akathisia and other EPS
- a history of amenorrhea/galactorrhea
- a history of seizures.
In surveys, patients have ranked lorazepam as the preferred medication for emergency agitation, whereas haloperidol was ranked as one of the least-preferred options.51,52
Continue to: Second-generation antipsychotics
Second-generation antipsychotics. The SGAs available in IM formulations, such as aripiprazole, olanzapine, and ziprasidone, have been shown to be at least as effective as haloperidol for the treatment of acute agitation (in 2015, the short-acting injectable formulation of aripiprazole was discontinued in the United States independent of safety or efficacy issues53). A review of RCTs examining IM SGAs for the treatment of agitation concluded that the number needed to treat for response compared with placebo was 5 for aripiprazole, 3 for olanzapine, and 3 for ziprasidone.54 In terms of safety, a meta-analysis of studies examining IM medications for agitation confirmed that the risk of acute EPS, including dystonia, akathisia, and parkinsonism, is significantly lower with SGAs compared with haloperidol.55 An RCT comparing IM ziprasidone with haloperidol found equivalently modest effects on QTc prolongation.56 Therefore, SGAs are an obvious and evidence-based option for replacing haloperidol as a treatment for acute agitation.
Unfortunately, for clinicians hoping to replace haloperidol within a multiple-medication IM “cocktail,” there have been no published controlled trials of SGAs combined with benzodiazepines. Although a short report indicated that aripiprazole and lorazepam are chemically compatible to be combined within a single injection,57 the package insert for aripiprazole warns that “If parenteral benzodiazepine therapy is deemed necessary in addition to ABILIFY injection treatment, patients should be monitored for excessive sedation and for orthostatic hypotension.”58 The package insert for olanzapine likewise lists the combination of lorazepam and olanzapine as a drug interaction that can potentiate sedation, and the manufacturer issued specific warnings about parenteral combination.59,60 A single published case of significant hypotension with combined IM olanzapine and lorazepam,60 together with the fact that IM olanzapine can cause hypotension by itself,61 has discouraged the coadministration of these medications. Nonetheless, the combination is used in some emergency settings, with several retrospective studies failing to provide evidence of hypotension or respiratory depression as adverse effects.62-64
Droperidol.
Over the past decade, however, droperidol has returned to the US market68 and its IV and IM usage has been revitalized for managing patients with agitation within or en route to the ED. Studies have demonstrated droperidol efficacy comparable to midazolam, ziprasidone, or olanzapine, as well as effectiveness as an IV adjunct to midazolam.69-71 In contrast to the FDA black-box warning, retrospective studies and RCTs of both IV and IM droperidol suggest that QTc prolongation and torsades de pointes are rare events that do not occur any more frequently than they do with haloperidol, even at doses >10 mg.72,73 However, in studies involving patients with drug intoxication and treatment with multiple medications, oversedation to the point of needing rescue intervention was reported. In an emergency setting where these issues are relatively easily managed, such risks may be better tolerated than in psychiatric settings.
With earlier studies examining the use of droperidol in an acute psychiatric setting that reported a more rapid onset of action than haloperidol,65-67 a 2016 Cochrane review concluded that there was high-quality evidence to support droperidol’s use for psychosis-induced agitation.74 However, a 2015 RCT comparing IM droperidol, 10 mg, to haloperidol, 10 mg, found equivalent efficacy and response times (with maximal response occurring within 2 hours) and concluded that droperidol had no advantage over haloperidol.75 Because none of the clinical trials that evaluated droperidol have included assessments for EPS, its risk of akathisia remains uncertain.
Continue to: Ketamine
Ketamine. In recent years, ketamine has been used to treat acute agitation within or en route to the ED. Preliminary observational studies support ketamine’s efficacy when administered via IV or IM routes,76 with more rapid symptomatic improvement compared with haloperidol, lorazepam, or midazolam alone.77 Reported adverse effects of ketamine include dissociation, psychotic exacerbation, and respiratory depression,76 although 1 small naturalistic study found no evidence of exacerbation of psychotic or other psychiatric symptoms.78 An ongoing RCT is comparing IM ketamine, 5 mg/kg, to combined IM haloperidol, 5 mg, and midazolam, 5 mg.79 Although various ketamine formulations are increasingly being used in psychiatry, active psychosis is generally regarded as a contraindication. It is premature to recommend parenteral ketamine administration for agitation within most psychiatric settings until more research on safety has been completed.
Haloperidol, or something else? Practical considerations
Consider the following factors when deciding whether to use haloperidol or one of its alternatives:
Limitations of the evidence. Modern clinical trials requiring informed consent often do not include the kind of severe agitation that clinicians encounter in acute psychiatric, emergency, or forensic settings. In addition, standard interventions, such as 3-medication haloperidol “cocktails,” have not been evaluated in clinical trials. Clinicians are therefore often in the dark about optimal evidence-based practices.
Treatment goals. Psychiatric agitation has many causes, with a range of severity that warrants a commensurate range of responses. Protocols for managing acute agitation should include graded interventions that begin with nonpharmacologic interventions and voluntary oral medications, and move to involuntary IM medications when necessary.
While treatment guidelines clearly recommend against IM medications as “chemical restraint” with a goal of sedating a patient until he/she is unconscious,3,51 such outcomes are nonetheless often sought by staff who are concerned about the risk of injuries during a behavioral emergency. In such instances, the risks of violence towards patients and staff may outweigh concerns about adverse effects in a risk-benefit analysis. Consequently, clinicians may be prone to “skip over” graded interventions because they assume they “won’t work” in favor of administering involuntary multiple-medication haloperidol “cocktails” despite risks of excess sedation, EPS, and cardiotoxicity. Treatment settings should critically evaluate such biased preferences, with a goal of developing tailored, evidence-based strategies that maximize benefits while minimizing excess sedation and other untoward adverse effects, with an eye towards promoting better overall patient care and reducing length of stay.42,43,80
Continue to: Limitations of available medications
Limitations of available medications. There is no perfect medication for the management of acute agitation. Evidence indicates that pharmacologic options take 15 minutes to several hours to resolve acute agitation, even potentially more rapid-acting medications such as midazolam and droperidol. This is well beyond most clinicians’ desired window for response time in a behavioral emergency. Multiple-medication “cocktails” may be used with the hope of hastening response time, but may not achieve this goal at the expense of increasing the risk of adverse effects and the likelihood that a patient will remain sedated for a prolonged time. In the real world, this often means that by the time a psychiatrist comes to evaluate a patient who has been given emergency medications, the patient cannot be aroused for an interview. Ideally, medications would calm an agitated patient rapidly, without excess or prolonged sedation.80 Less-sedating SGAs, such as ziprasidone, might have this potential, but can sometimes be perceived as ineffective.
Avoiding akathisia. Akathisia’s potential to worsen and be mistaken for agitation makes it an especially concerning, if underappreciated, adverse effect of haloperidol that is often not adequately assessed in clinical trials or practice. In light of evidence that akathisia can occur in nearly half of patients receiving a single 5 mg-dose of haloperidol, it is difficult to justify the use of this medication for agitation when equally effective options exist with a lower risk of EPS.
While haloperidol-induced akathisia could in theory be mitigated by adding anticholinergic medications or benzodiazepines, previous studies have found that such strategies have limited effectiveness compared to “gold standard” treatment with propranolol.28,81,82 Furthermore, the half-lives of anticholinergic medications, such as benztropine or diphenhydramine, are significantly shorter than that of a single dose of haloperidol, which can be as long as 37 hours.83 Therefore, akathisia and other EPS could emerge or worsen several hours or even days after receiving an IM haloperidol “cocktail” as the shorter-acting medications wear off. Akathisia is best minimized by avoiding FGAs, such as haloperidol, when treating acute agitation.
Promoting adherence. Although haloperidol is often recommended for acute agitation in patients with schizophrenia or bipolar disorder on the basis that it would treat the underlying condition, many patients who receive IM medications for acute agitation are already prescribed standing doses of oral medication, which increases the risk of cumulative toxicity. In addition, receiving a medication likely to cause acute EPS that is ranked near the bottom of patient preferences may erode the potential for a therapeutic alliance and hamper longer-term antipsychotic medication adherence.

Time for a change
For nearly half a century, haloperidol has been a “gold standard” intervention for IM control in patients with agitation. However, given its potential to produce adverse effects, including a significant risk of akathisia that can worsen agitation, along with the availability of newer pharmacologic options that are at least as effective (Table 1, and Table 2), haloperidol should be retired as a first-line medication for the treatment of agitation. Clinicians would benefit from RCTs investigating the safety and efficacy of novel interventions including frequently-used, but untested medication combinations, as well as nonpharmacologic interventions.

Continue to: Bottom Line
Bottom Line
Although there is no perfect IM medication to treat acute agitation, haloperidol’s higher risk of adverse effects relative to newer alternatives suggest that it should no longer be considered a first-line intervention.
Related Resources
- Zun LS. Evidence-based review of pharmacotherapy for acute agitation. Part 1: onset of efficacy. J Emerg Med. 2018;54(3):364-374.
- Zun LS. Evidence-based review of pharmacotherapy for acute agitation. Part 2: safety. J Emerg Med. 2018;54(4): 522-532.
Drug Brand Names
Aripiprazole • Abilify
Benztropine • Cogentin
Chlorpromazine • Thorazine
Diphenhydramine • Benadryl
Droperidol • Inapsine
Haloperidol • Haldol
Ketamine • Ketalar
Lorazepam • Ativan
Midazolam • Versed
Olanzapine • Zyprexa
Prochlorperazine • Compazine
Promethazine • Phenergan
Propranolol • Inderal, Pronol
Ziprasidone • Geodon
For more than half a century, haloperidol has been used as a first-line medication for psychiatric agitation constituting a “behavioral emergency” when a patient cannot or will not take oral medication. Today, haloperidol is most commonly administered as an IM injection along with an anticholinergic medication to minimize extrapyramidal symptoms (EPS) and a benzodiazepine for additional sedation. The multiple-medication “cocktail” is often referred to by double-entendre nicknames, such as “B-52” or “5250” (ie, haloperidol, 5 mg; lorazepam, 2 mg; and
Earlier evidence of haloperidol’s efficacy
The initial “discovery” of antipsychotic medications was made in 1951 based on the inadvertent observation that chlorpromazine had the potential to calm surgical patients with autonomic activation. This calming effect, described as “désintéressment” (meaning a kind of “indifference to the world”),1 resulted in a new class of medications replacing barbiturates and bromides as go-to options to achieve “rapid tranquilization” of psychiatric agitation.2 Although the ability of antipsychotic medications to gradually reduce positive symptoms, such as delusions and hallucinations, has been attributed to dopamine (D2) antagonism, their more immediate sedating and anti-agitation effects are the result of broader effects as histamine (H1) and alpha-1 adrenergic antagonists.
In the 1970s, haloperidol emerged as a first-line option to manage agitation due to its IM and IV availability, as well as its relative lack of sedation and orthostasis compared with low-potency D2 antagonists such as chlorpromazine. However, haloperidol was observed to have a significant risk of acute EPS, including dystonic reactions.2 From the 1970s to the 1990s, numerous prospective clinical trials of haloperidol for the treatment of acute psychotic agitation, including several randomized controlled trials (RCTs) comparing haloperidol to lorazepam, were conducted.3 The design and outcomes of the haloperidol vs lorazepam RCTs were fairly consistent4-7:
- adult participants with acute agitation and a variety of psychiatric diagnoses, for whom informed consent often was waived due to agitation severity
- randomization to either IM haloperidol, 5 mg, or IM lorazepam, 2 mg, administered every 30 minutes until agitation resolved
- behavioral outcomes measured over several hours using various rating scales, without consistent assessment of EPS
- equivalent efficacy of haloperidol and lorazepam, with symptom resolution usually achieved after 1 to 2 doses (in 30 to 60 minutes), but sometimes longer
- anticholinergic “rescue” allowed for EPS, but not administered prophylactically
- EPS, including dystonia and akathisia, were significantly more frequent with haloperidol compared with lorazepam.8
In recognition of the greater risk of EPS with haloperidol compared with lorazepam, and the fact that most study participants were already taking standing doses of antipsychotic medications, some researchers have recommended using benzodiazepines alone as the optimal treatment for agitation.4,9 A 2012 Cochrane review concluded that the involuntary use of haloperidol alone “could be considered unethical.”10,11 However, other studies that examined the combination of haloperidol and lorazepam compared with either medication alone found that the combination of the 2 medications was associated with a more rapid resolution of symptoms, which suggests a superior synergistic effect.6,7,12 By the late 1990s, combined haloperidol and lorazepam, often mixed within a single injection, became the most common strategy to achieve rapid tranquilization in the psychiatric emergency setting.13 However, while the combination has been justified as a way to reduce the antipsychotic medication dose and EPS risk,2 few studies have compared combinations containing <5 mg of haloperidol. As a result, the apparent superiority of combined haloperidol and lorazepam compared with either medication alone may be a simple cumulative dose effect rather than true synergism. It is also important to note that adding lorazepam to haloperidol does not mitigate the risk of EPS such as dystonia in the absence of anticholinergic medication.8 To date, however, there have been no clinical trials investigating the efficacy of IM haloperidol, lorazepam, and
Newer RCTs tell a different story
With the availability of second-generation antipsychotics (SGAs) in IM formulations, clinical trials over the past 2 decades have focused on comparing SGAs with haloperidol alone as the “gold standard” control for acute agitation. Compared with previous trials of
- Study participants who signed informed consent (and were likely less agitated)
- IM haloperidol doses typically >5 mg (eg, 6.5 to 10 mg).
As with studies comparing lorazepam with haloperidol, the results of these RCTs revealed that IM
An updated 2017 Cochrane review of haloperidol for psychosis-induced aggression or agitation concluded that9:
- haloperidol is an effective intervention, although the evidence is “weak”
- significant treatment effects may take as long as 1 to 2 hours following multiple IM injections
- in contrast to SGAs, treatment with haloperidol carries a significant risk of EPS
- adding a benzodiazepine “does not have strong evidence of benefit and carries risk of additional harm.”
Continue to: Haloperidol's well-known toxicity
Haloperidol’s well-known toxicity
Haloperidol has been associated with numerous adverse effects:
Akathisia and other acute EPS. Treatment with even a single dose of IM haloperidol can result in acute EPS, including dystonia and akathisia. At best, such adverse effects are subjectively troubling and unpleasant; at worst, akathisia can exacerbate and be mistaken for agitation, leading to administration of more medication23 and the possible development of suicidal or violent behavior.24-25 In the studies reviewed above, the overall rate of EPS was as high as 21% after treatment with haloperidol,16 with parkinsonism occurring in up to 17% of patients,19 dystonia in up to 11%,7 and akathisia in up to 10%.15 However, because specific EPS were assessed inconsistently, and sometimes not at all, the rate of akathisia—arguably the most relevant and counter-therapeutic adverse effect related to agitation—remains unclear.
In another study that specifically assessed for akathisia in patients treated with haloperidol, up to 40% experienced akathisia 6 hours after a single oral dose of 5 mg.26 Even a single dose of IV
Although anticholinergic medications or benzodiazepinesare often administered as part of a haloperidol “cocktail,” these medications often do not adequately resolve emergent akathisia.26,28 No clinical trials of IM haloperidol combined with benztropine or diphenhydramine have been published, but several studies suggest that combining haloperidol with
Cardiotoxicity. Although low-potency antipsychotic medications such as
Continue to: Although there is no direct evidence...
Although there is no direct evidence that the cardiac risks associated with IV haloperidol apply to IM administration, epidemiologic studies indicate that oral haloperidol carries an elevated risk of ventricular arrhythmia and sudden cardiac death,35,36 with 1 study reporting greater risk compared with other SGAs.37 Haloperidol, whether administered orally or IM, may therefore be an especially poor choice for patients with agitation who are at risk for arrhythmia, including those with relevant medical comorbidities or delirium.34
Neuronal cell death. Several lines of research evidence have demonstrated that haloperidol can cause cellular injury or death in neuronal tissue in a dose-dependent fashion through a variety of mechanisms.38 By contrast, SGAs have been shown to have neuroprotective effects.39 While these findings have mostly come from studies conducted in animals or in vitro human tumor cell lines, some researchers have nonetheless called for haloperidol to be banned, noting that if its neurotoxic effects were more widely known, “we would realize what a travesty it is to use [such] a brain-unfriendly drug.”40
Several reasonable alternatives
Echoing the earlier Cochrane review of haloperidol for psychosis-induced aggression or agitation,10 a 2017 update concluded, “If no other alternative exists, sole use of intramuscular haloperidol could be life-saving. Where additional drugs are available, sole use of haloperidol for extreme emergency could be considered unethical.”9
What then are reasonable alternatives to replace IM haloperidol for agitation? Clinicians should consider the following nonpharmacologic and pharmacologic interventions:
Nonpharmacologic interventions. Several behavioral interventions have been demonstrated to be effective for managing acute agitation, including verbal de-escalation, enhanced “programming” on the inpatient units, and the judicious use of seclusion.41-43 While such interventions may demand additional staff or resources, they have the potential to lower long-term costs, reduce injuries to patients and staff, and improve the quality of care.43 The use of IM haloperidol as a form of “chemical restraint” does not represent standard-of-care treatment,3 and from an ethical perspective, should never be implemented punitively or to compensate for substandard care in the form of inadequate staffing or staff training.
Continue to: Benzodiazepines
Benzodiazepines. Lorazepam offers an attractive alternative to haloperidol without the risk of EPS.2,4,8 However, lorazepam alone may be perceived as less efficacious than a haloperidol “cocktail” because it represents less overall medication. Some evidence has suggested that lorazepam, 4 mg, might be the most appropriate dose, although it has only rarely been studied in clinical trials of acute agitation.3
Respiratory depression is frequently cited as an argument against using lorazepam for agitation, as if the therapeutic window is extremely narrow with ineffectiveness at 2 mg, but potential lethality beyond that dose. In fact, serious respiratory depression with lorazepam is unlikely in the absence of chronic obstructive pulmonary disease (COPD), obstructive sleep apnea, or concomitant alcohol or other sedative use.46 Case reports have documented therapeutic lorazepam dosing of 2 to 4 mg every 2 hours up to 20 to 30 mg/d in patients with manic agitation.47 Even in patients with COPD, significant respiratory depression tends not to occur at doses <8 mg.48 A more evidence-based concern about lorazepam dosing is that 2 mg might be ineffective in patients with established tolerance. For example, 1 report described a patient in acute alcohol withdrawal who required dosing lorazepam to 1,600 mg within 24 hours.49 Collectively, these reports suggest that lorazepam has a much wider therapeutic window than is typically perceived, and that dosing with 3 to 4 mg IM is a reasonable option for agitation when 2 mg is likely to be inadequate.
Paradoxical disinhibition is another concern that might prevent benzodiazepines from being used alone as a first-line intervention for emergency treatment of agitation. However, similar to respiratory depression, this adverse event is relatively rare and tends to occur in children and geriatric patients, individuals intoxicated with alcohol or other sedatives, and patients with brain injury, developmental delay, or dementia.23,46 Although exacerbation of aggression has not been demonstrated in the RCTs examining benzodiazepines for agitation reviewed above, based on other research, some clinicians have expressed concerns about the potential for benzodiazepines to exacerbate aggression in patients with impulse control disorders and a history of violent behavior.50
The 2005 Expert Consensus Panel for Behavioral Emergencies51 recommended the use of lorazepam alone over haloperidol for agitation for patients for whom the diagnosis is unknown or includes the following:
- stimulant intoxication
- personality disorder
- comorbid obesity
- comorbid cardiac arrhythmia
- a history of akathisia and other EPS
- a history of amenorrhea/galactorrhea
- a history of seizures.
In surveys, patients have ranked lorazepam as the preferred medication for emergency agitation, whereas haloperidol was ranked as one of the least-preferred options.51,52
Continue to: Second-generation antipsychotics
Second-generation antipsychotics. The SGAs available in IM formulations, such as aripiprazole, olanzapine, and ziprasidone, have been shown to be at least as effective as haloperidol for the treatment of acute agitation (in 2015, the short-acting injectable formulation of aripiprazole was discontinued in the United States independent of safety or efficacy issues53). A review of RCTs examining IM SGAs for the treatment of agitation concluded that the number needed to treat for response compared with placebo was 5 for aripiprazole, 3 for olanzapine, and 3 for ziprasidone.54 In terms of safety, a meta-analysis of studies examining IM medications for agitation confirmed that the risk of acute EPS, including dystonia, akathisia, and parkinsonism, is significantly lower with SGAs compared with haloperidol.55 An RCT comparing IM ziprasidone with haloperidol found equivalently modest effects on QTc prolongation.56 Therefore, SGAs are an obvious and evidence-based option for replacing haloperidol as a treatment for acute agitation.
Unfortunately, for clinicians hoping to replace haloperidol within a multiple-medication IM “cocktail,” there have been no published controlled trials of SGAs combined with benzodiazepines. Although a short report indicated that aripiprazole and lorazepam are chemically compatible to be combined within a single injection,57 the package insert for aripiprazole warns that “If parenteral benzodiazepine therapy is deemed necessary in addition to ABILIFY injection treatment, patients should be monitored for excessive sedation and for orthostatic hypotension.”58 The package insert for olanzapine likewise lists the combination of lorazepam and olanzapine as a drug interaction that can potentiate sedation, and the manufacturer issued specific warnings about parenteral combination.59,60 A single published case of significant hypotension with combined IM olanzapine and lorazepam,60 together with the fact that IM olanzapine can cause hypotension by itself,61 has discouraged the coadministration of these medications. Nonetheless, the combination is used in some emergency settings, with several retrospective studies failing to provide evidence of hypotension or respiratory depression as adverse effects.62-64
Droperidol.
Over the past decade, however, droperidol has returned to the US market68 and its IV and IM usage has been revitalized for managing patients with agitation within or en route to the ED. Studies have demonstrated droperidol efficacy comparable to midazolam, ziprasidone, or olanzapine, as well as effectiveness as an IV adjunct to midazolam.69-71 In contrast to the FDA black-box warning, retrospective studies and RCTs of both IV and IM droperidol suggest that QTc prolongation and torsades de pointes are rare events that do not occur any more frequently than they do with haloperidol, even at doses >10 mg.72,73 However, in studies involving patients with drug intoxication and treatment with multiple medications, oversedation to the point of needing rescue intervention was reported. In an emergency setting where these issues are relatively easily managed, such risks may be better tolerated than in psychiatric settings.
With earlier studies examining the use of droperidol in an acute psychiatric setting that reported a more rapid onset of action than haloperidol,65-67 a 2016 Cochrane review concluded that there was high-quality evidence to support droperidol’s use for psychosis-induced agitation.74 However, a 2015 RCT comparing IM droperidol, 10 mg, to haloperidol, 10 mg, found equivalent efficacy and response times (with maximal response occurring within 2 hours) and concluded that droperidol had no advantage over haloperidol.75 Because none of the clinical trials that evaluated droperidol have included assessments for EPS, its risk of akathisia remains uncertain.
Continue to: Ketamine
Ketamine. In recent years, ketamine has been used to treat acute agitation within or en route to the ED. Preliminary observational studies support ketamine’s efficacy when administered via IV or IM routes,76 with more rapid symptomatic improvement compared with haloperidol, lorazepam, or midazolam alone.77 Reported adverse effects of ketamine include dissociation, psychotic exacerbation, and respiratory depression,76 although 1 small naturalistic study found no evidence of exacerbation of psychotic or other psychiatric symptoms.78 An ongoing RCT is comparing IM ketamine, 5 mg/kg, to combined IM haloperidol, 5 mg, and midazolam, 5 mg.79 Although various ketamine formulations are increasingly being used in psychiatry, active psychosis is generally regarded as a contraindication. It is premature to recommend parenteral ketamine administration for agitation within most psychiatric settings until more research on safety has been completed.
Haloperidol, or something else? Practical considerations
Consider the following factors when deciding whether to use haloperidol or one of its alternatives:
Limitations of the evidence. Modern clinical trials requiring informed consent often do not include the kind of severe agitation that clinicians encounter in acute psychiatric, emergency, or forensic settings. In addition, standard interventions, such as 3-medication haloperidol “cocktails,” have not been evaluated in clinical trials. Clinicians are therefore often in the dark about optimal evidence-based practices.
Treatment goals. Psychiatric agitation has many causes, with a range of severity that warrants a commensurate range of responses. Protocols for managing acute agitation should include graded interventions that begin with nonpharmacologic interventions and voluntary oral medications, and move to involuntary IM medications when necessary.
While treatment guidelines clearly recommend against IM medications as “chemical restraint” with a goal of sedating a patient until he/she is unconscious,3,51 such outcomes are nonetheless often sought by staff who are concerned about the risk of injuries during a behavioral emergency. In such instances, the risks of violence towards patients and staff may outweigh concerns about adverse effects in a risk-benefit analysis. Consequently, clinicians may be prone to “skip over” graded interventions because they assume they “won’t work” in favor of administering involuntary multiple-medication haloperidol “cocktails” despite risks of excess sedation, EPS, and cardiotoxicity. Treatment settings should critically evaluate such biased preferences, with a goal of developing tailored, evidence-based strategies that maximize benefits while minimizing excess sedation and other untoward adverse effects, with an eye towards promoting better overall patient care and reducing length of stay.42,43,80
Continue to: Limitations of available medications
Limitations of available medications. There is no perfect medication for the management of acute agitation. Evidence indicates that pharmacologic options take 15 minutes to several hours to resolve acute agitation, even potentially more rapid-acting medications such as midazolam and droperidol. This is well beyond most clinicians’ desired window for response time in a behavioral emergency. Multiple-medication “cocktails” may be used with the hope of hastening response time, but may not achieve this goal at the expense of increasing the risk of adverse effects and the likelihood that a patient will remain sedated for a prolonged time. In the real world, this often means that by the time a psychiatrist comes to evaluate a patient who has been given emergency medications, the patient cannot be aroused for an interview. Ideally, medications would calm an agitated patient rapidly, without excess or prolonged sedation.80 Less-sedating SGAs, such as ziprasidone, might have this potential, but can sometimes be perceived as ineffective.
Avoiding akathisia. Akathisia’s potential to worsen and be mistaken for agitation makes it an especially concerning, if underappreciated, adverse effect of haloperidol that is often not adequately assessed in clinical trials or practice. In light of evidence that akathisia can occur in nearly half of patients receiving a single 5 mg-dose of haloperidol, it is difficult to justify the use of this medication for agitation when equally effective options exist with a lower risk of EPS.
While haloperidol-induced akathisia could in theory be mitigated by adding anticholinergic medications or benzodiazepines, previous studies have found that such strategies have limited effectiveness compared to “gold standard” treatment with propranolol.28,81,82 Furthermore, the half-lives of anticholinergic medications, such as benztropine or diphenhydramine, are significantly shorter than that of a single dose of haloperidol, which can be as long as 37 hours.83 Therefore, akathisia and other EPS could emerge or worsen several hours or even days after receiving an IM haloperidol “cocktail” as the shorter-acting medications wear off. Akathisia is best minimized by avoiding FGAs, such as haloperidol, when treating acute agitation.
Promoting adherence. Although haloperidol is often recommended for acute agitation in patients with schizophrenia or bipolar disorder on the basis that it would treat the underlying condition, many patients who receive IM medications for acute agitation are already prescribed standing doses of oral medication, which increases the risk of cumulative toxicity. In addition, receiving a medication likely to cause acute EPS that is ranked near the bottom of patient preferences may erode the potential for a therapeutic alliance and hamper longer-term antipsychotic medication adherence.

Time for a change
For nearly half a century, haloperidol has been a “gold standard” intervention for IM control in patients with agitation. However, given its potential to produce adverse effects, including a significant risk of akathisia that can worsen agitation, along with the availability of newer pharmacologic options that are at least as effective (Table 1, and Table 2), haloperidol should be retired as a first-line medication for the treatment of agitation. Clinicians would benefit from RCTs investigating the safety and efficacy of novel interventions including frequently-used, but untested medication combinations, as well as nonpharmacologic interventions.

Continue to: Bottom Line
Bottom Line
Although there is no perfect IM medication to treat acute agitation, haloperidol’s higher risk of adverse effects relative to newer alternatives suggest that it should no longer be considered a first-line intervention.
Related Resources
- Zun LS. Evidence-based review of pharmacotherapy for acute agitation. Part 1: onset of efficacy. J Emerg Med. 2018;54(3):364-374.
- Zun LS. Evidence-based review of pharmacotherapy for acute agitation. Part 2: safety. J Emerg Med. 2018;54(4): 522-532.
Drug Brand Names
Aripiprazole • Abilify
Benztropine • Cogentin
Chlorpromazine • Thorazine
Diphenhydramine • Benadryl
Droperidol • Inapsine
Haloperidol • Haldol
Ketamine • Ketalar
Lorazepam • Ativan
Midazolam • Versed
Olanzapine • Zyprexa
Prochlorperazine • Compazine
Promethazine • Phenergan
Propranolol • Inderal, Pronol
Ziprasidone • Geodon
1. Shorter E. A history of psychiatry. New York, NY: John Wiley & Sons, Inc.; 1997:249.
2. Salzman C, Green AI, Rodriguez-Villa F, et al. Benzodiazepines combined with neuroleptics for management of severe disruptive behavior. Psychosomatics. 1986;27(suppl 1):17-22.
3. Allen MH. Managing the agitated psychotic patient: a reappraisal of the evidence. J Clin Psychiatr. 2000;61(suppl 14):11-20.
4. Salzman C, Solomon D, Miyawaki E, et al. Parenteral lorazepam versus parenteral haloperidol for the control of psychotic disruptive behavior. J Clin Psychiatr. 1991:52(4):177-180.
5. Allen MH, Currier GW, Hughes DH, et al. The expert consensus guideline series: treatment of behavioral emergencies. Postgrad Med. 2001;(Spec No):1-88; quiz 89-90.
6. Foster S, Kessel J, Berman ME, et al. Efficacy of lorazepam and haloperidol for rapid tranquilization in a psychiatric emergency room setting. Int Clin Psychopharmacol. 1997;12(3):175-179.
7. Garza-Trevino WS, Hollister LE, Overall JE, et al. Efficacy of combinations of intramuscular antipsychotics and sedative-hypnotics for control of psychotic agitation. Am J Psychiatr. 1989:146(12):1598-1601.
8. Battaglia J, Moss S, Rush J, et al. Haloperidol, lorazepam, or both for psychotic agitation? A multicenter, prospective double-blind, emergency study. Am J Emerg Med 1997;15(4):335-340.
9. Ostinelli EG, Brooke-Powney MJ, Li X, et al. Haloperidol for psychosis-induced aggression or agitation (rapid tranquillisation). Cochrane Database Syst Rev. 2017; 7:CD009377. doi: 10.1002/14651858.CD009377.pub3.
10. Powney MJ, Adams CE, Jones H. Haloperidol for psychosis-induced aggression or agitation (rapid tranquillisation). Cochrane Database Syst Rev. 2012;11:CD009377. doi: 10.1002/14651858.CD009377.pub2.
11. Citrome L. Review: limited evidence on effects of haloperidol alone for rapid tranquillisation in psychosis-induced aggression. Evid Based Ment Health. 2013;16(2):47.
12. Bienek SA, Ownby R, Penalver A, et al. A double-blind study of lorazepam versus the combination of haloperidol and lorazepam in managing agitation. Pharmacother. 1998;18(1):57-62.
13. Binder RL, McNiel DE. Contemporary practices in managing acutely violent patients in 20 psychiatric emergency rooms. Psychiatric Serv. 1999;50(2):1553-1554.
14. Andrezina R, Josiassen RC, Marcus RN, et al. Intramuscular aripiprazole for the treatment of acute agitation in patients with schizophrenia or schizoaffective disorder: a double-blind, placebo-controlled comparison with intramuscular haloperidol. Psychopharmacology (Berl). 2006;188(3):281-292.
15. Tran-Johnson TK, Sack DA, Marcus RN, et al. Efficacy and safety of intramuscular aripiprazole in patients with acute agitation: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatr. 2007;68(1):111-119.
16. Brook S, Lucey JV, Gunn KP. Intramuscular ziprasidone compared with intramuscular haloperidol in the treatment of acute psychosis. J Clin Psychiatr. 2000;61(12):933-941.
17. Brook S, Walden J, Benattia I, et al. Ziprasidone and haloperidol in the treatment of acute exacerbation of schizophrenia and schizoaffective disorder: comparison of intramuscular and oral formulations in a 6-week, randomized, blinded-assessment study. Psychopharmacology (Berl). 2005;178(4):514-523.
18. Wright P, Birkett M, David SR, et al. Double-blind, placebo-controlled comparison of intramuscular olanzapine and intramuscular haloperidol in the treatment of acute agitation in schizophrenia. Am J Psychiatr. 2001;158(7):1149-1151.
19. Breier A, Meehan K, Birkett M, et al. A double-blind, placebo-controlled dose-response comparison of intramuscular olanzapine and haloperidol in the treatment of acute agitation in schizophrenia. Arch Gen Psych. 2002;59(5):441-448.
20. Hsu W, Huang S, Lee B, et al. Comparison of intramuscular olanzapine, orally disintegrating olanzapine tablets, oral risperidone solution, and intramuscular haloperidol in the management of acute agitation in an acute care psychiatric ward in Taiwan. J Clin Psychopharmacol. 2010;30(3):230-234.
21. Chan H, Ree S, Su L, et al. A double-blind, randomized comparison study of efficacy and safety of intramuscular olanzapine and intramuscular haloperidol in patients with schizophrenia and acute agitated behavior. J Clin Psychopharmacol. 2014;34(3):355-358.
22. Baldaçara L, Sanches M, Cordeiro DC, et al. Rapid tranquilization for agitated patients in emergency psychiatric rooms: a randomized trial of olanzapine, ziprasidone, haloperidol plus promethazine, haloperidol plus midazolam and haloperidol alone. Braz J Psychiatry. 2011;33(1):30-39.
23. Hillard JR. Defusing patient violence. Current Psychiatry. 2002;1(4):22-29.
24. Seemüller F, Schennach R, Mayr A, et al. Akathisia and suicidal ideation in first-episode schizophrenia. J Clin Psychopharmacol. 2012;32(5):694-698.
25. Eikelenboom-Schieveld SJM, Lucire Y, Fogleman JC. The relevance of cytochrome P450 polymorphism in forensic medicine and akathisia-related violence and suicide. J Forens Leg Med. 2016;41:65-71.
26. Van Putten T, May PRA, Marder SR. Akathisia with haloperidol and thiothixene. Arch Gen Psych. 1984;41:1036-1039.
27. Drotts DL, Vinson DR. Prochlorperazine induced akathisia in emergency patients. Ann Emerg Med. 1999;34(4):469-475.
28. Salem H, Negpal C, Pigott T. Revisiting antipsychotic-induced akathisia: current issues and prospective challenges. Curr Neuropharmacol. 2017;15(5):789-798.
29. Huf G, Coutinho ESF, Adams CE. Rapid tranquilization in psychiatric emergency settings in Brazil: pragmatic randomized controlled trial of intramuscular haloperidol versus intramuscular haloperidol plus promethazine. BMJ. 2007;335(7625):869.
30. Mantovani C, Labate CM, Sponholz A, et al. Are low doses of antipsychotics effective in the management of psychomotor agitation? A randomized, rated-blind trial of 4 intramuscular interventions. J Clin Psychopharmacol. 2013;33(3):306-312.
31. Darwish H, Grant R, Haslam R, et al. Promethazine-induced acute dystonic reactions. Am J Dis Child. 1980;134(10):990-991.
32. Jyothi CH, Rudraiah HGM, Vidya HK, et al. Promethazine induced acute dystonia: a case report. Manipal J Med Sci. 2016;1(2):63-64.
33. Ames D, Carr-Lopez SM, Gutierrez MA, et al. Detecting and managing adverse effects of antipsychotic medications: current state of play. Psychiatr Clin North Am. 2016;39(2):275-311.
34. Meyer-Massetti C, Cheng CM, Sharpe MA, et al. The FDA extended warning for intravenous haloperidol and torsades de pointes: how should institutions respond? J Hosp Med. 2010;5(4):E8-E16. doi: 10.1002/jhm.691.
35. Wu C, Tsai Y, Tsai H. Antipsychotic drugs and the risk of ventricular arrhythmia and/or sudden cardiac death: a nation-wide case-crossover study. J Am Heart Dis. 2015;4(2):e001568. doi: 10.1161/JAHA.114.001568.
36. Beach SR, Celano CM, Sugrue AM, et al. QT prolongation, torsades de pointe, and psychotropic medications: a 5-year update. Psychosomatics. 2018;59(1):105-122.
37. Leonard CE, Freeman CP, Newcomb CW, et al. Antipsychotics and the risks of sudden cardiac death and all-cause death: cohort studies in Medicaid and dually-eligible Medicaid-Medicare beneficiaries of five states. J Clin Exp Cardiol. 2013;suppl 10(6):1-9.
38. Nasrallah H, Chen AT. Multiple neurotoxic effects of haloperidol resulting in neuronal death. Ann Clin Psychiatr. 2017;29(3):195-202.
39. Chen AT, Nasrallah HA. Neuroprotective effects of the second generation antipsychotics. Schizophr Res. 2019;208:1-7.
40. Nasrallah HA. Haloperidol clearly is neurotoxic. Should it be banned? Current Psychiatry. 2013;12(7):7-8.
41. Corrigan PW, Yudofsky SC, Silver JM. Pharmacological and behavioral treatments for aggressive psychiatric inpatients. Hosp Comm Psychiatr. 1993;44(2):125-133.
42. Zeller SL, Citrome L. Managing agitation associated with schizophrenia and bipolar disorder in the emergency setting. West J Emerg Med. 2016;17(2):165-172.
43. Vieta E, Garriga M, Cardete L, et al. Protocol for the management of psychiatric patients with psychomotor agitation. BMC Psychiatr. 2017;17:328.
44. Nobay F, Simon BC, Levitt A, et al. A prospective, double-blind, randomized trial of midazolam versus haloperidol versus lorazepam in the chemical restraint of violent and severely agitated patients. Acad Emerg Med. 2004;11(7):744-749.
45. Klein LR, Driver BE, Miner JR, et al. Intramuscular midazolam, olanzapine, ziprasidone, or haloperidol for treating acute agitation in the emergency department. Ann Emerg Med. 2018;72(4):374-385.
46. Hillard JR. Emergency treatment of acute psychosis. J Clin Psychiatr. 1998;59(suppl 1):57-60.
47. Modell JG, Lenox RH, Weiner S. Inpatient clinical trial of lorazepam for the management of manic agitation. J Clin Psychopharmacol. 1985;5(2):109-110.
48. Denaut M, Yernault JC, De Coster A. Double-blind comparison of the respiratory effects of parenteral lorazepam and diazepam in patients with chronic obstructive lung disease. Curr Med Res Opin. 1975;2(10):611-615.
49. Kahn DR, Barnhorst AV, Bourgeois JA. A case of alcohol withdrawal requiring 1,600 mg of lorazepam in 24 hours. CNS Spectr. 2009;14(7):385-389.
50. Jones KA. Benzodiazepines: their role in aggression and why GPs should prescribe with caution. Austral Fam Physician. 2011;40(11):862-865.
51. Allen MH, Currier GW, Carpenter D, et al. The expert consensus guideline series. Treatment of behavioral emergencies 2005. J Psychiatr Pract. 2005;11(suppl 1):5-108.
52. Allen MH, Carpenter D, Sheets JL, et al. What do consumers say they want and need during a psychiatric emergency? J Psychiatr Pract. 2003;9(1):39-58.
53. Han DH. Some Abilify formulations to discontinue in 2015. MPR. https://www.empr.com/home/news/some-abilify-formulations-to-discontinue-in-2015/. Published January 13, 2015. Accessed April 17, 2020.
54. Citrome L. Comparison of intramuscular ziprasidone, olanzapine, or aripiprazole for agitation: a quantitative review of efficacy and safety. J Clin Psychiatry. 2007;68(12):1876-1885.
55. Satterthwaite TD, Wolf DH, Rosenheck RA, et al. A meta-analysis of the risk of acute extrapyramidal symptoms with intramuscular antipsychotics for the treatment for agitation. J Clin Psychiatr. 2008;69(12):1869-1879.
56. Miceli JJ, Tensfeldt TG, Shiovitz T, et al. Effects of high-dose ziprasidone and haloperidol on the QTc interval after intramuscular administration: a randomized, single-blind, parallel-group study in patients with schizophrenia or schizoaffective disorder. Clin Ther. 2010;32(3):472-491.
57. Kovalick LJ, Pikalov AA, Ni N, et al. Short-term physical compatibility of intramuscular aripiprazole with intramuscular lorazepam. Am J Health-Syst Pharm. 2008;65(21):2007-2008.
58. Abilify [package insert]. Princeton, NJ: Bristol-Myers Squibb Company; 2014.
59. Zyprexa [package insert]. Indianapolis, IN: Lilly Research Laboratories; 2005.
60. Zacher JL, Roche-Desilets J. Hypotension secondary to the combination of intramuscular olanzapine and intramuscular lorazepam. J Clin Psychiatr. 2005;66(12):1614-1615.
61. Marder SR, Sorsaburu S, Dunayevich E, et al. Case reports of postmarketing adverse event experiences with olanzapine intramuscular treatment in patients with agitation. J Clin Psychiatr 2010;71(4):433-441.
62. Wilson MP, MacDonald K, Vilke GM, et al. A comparison of the safety of olanzapine and haloperidol in combination with benzodiazepines in emergency department patients with acute agitation. J Emerg Med. 2012;43(5):790-797.
63. Wilson MP, MacDonald K, Vilke GM, et al. Potential complications of combining intramuscular olanzapine with benzodiazepines in emergency department patients. J Emerg Med. 2012;43(5):889-896.
64. Williams AM. Coadministration of intramuscular olanzapine and benzodiazepines in agitated patients with mental illness. Ment Health Clin [Internet]. 2018;8(5):208-213.
65. Resnick M, Burton BT. Droperidol vs. haloperidol in the initial management of acutely agitated patients. J Clin Psychiatry. 1984;45(7):298-299.
66. Thomas H, Schwartz E, Petrilli R. Droperidol versus haloperidol for chemical restraint of agitated and combative patients. Ann Emerg Med. 1992;21(4):407-413.
67. Richards JR, Derlet RW, Duncan DR. Chemical restraint for the agitated patient in the emergency department: lorazepam versus droperidol. J Emerg Med. 1998;16(4):567-573.
68. Boyer EW. Droperidol is back (and here’s what you need to know). ACEP Now. https://www.acepnow.com/article/droperidol-is-back-and-heres-what-you-need-to-know/. Published September 16, 2019. Accessed April 17, 2020.
69. Martel M, Sterzinger A, Miner J, et al. Management of acute undifferentiated agitation in the emergency department: a randomized double-blind trial of droperidol, ziprasidone, and midazolam. Acad Emerg Med. 2005;12(12):1167-1172.
70. Chan EW, Taylor DM, Knott JC, et al. Intravenous droperidol or olanzapine as an adjunct to midazolam for the acutely agitated patient: a multicenter, randomized, double-blind, placebo-controlled clinical trial. Ann Emerg Med. 2013;61(1):72-81.
71. Isbister GK, Calver LA, Page CB, et al. Randomized controlled trial of intramuscular droperidol versus midazolam for violence and acute behavioral disturbance: the DORM study. Ann Emerg Med. 2010;56(4):392-401.
72. Macht M, Mull AC, McVaney KE, et al. Comparison of droperidol and haloperidol for use by paramedics assessment of safety and effectiveness. Prehosp Emerg Care. 2014;18(3):375-380.
73. Calver L, Page CB, Downes MA, et al. The safety and effectiveness of droperidol for sedation of acute behavioral disturbance in the emergency department. Ann Emerg Med. 2015;66(3):230-238.
74. Kohokar MA, Rathbone J. Droperidol for psychosis-induced aggression or agitation. Cochrane Database Syst Rev. 2016;12:CD002830.
75. Calver L, Drinkwater V, Gupta R, et al. Droperidol v. haloperidol for sedation of aggressive behavior in acute mental health: randomized controlled trial. Brit J Psychiatr. 2015;206(3):223-228.
76. Hopper AB, Vilke GM, Castillo EM, et al. Ketamine use for acute agitation in the emergency department. J Emerg Med. 2015;48(6):712-719.
77. Riddell J, Tran A, Bengiamin R, et al. Ketamine as a first-line treatment for severely agitated emergency department patients. Am J Emerg Med. 2017;35:1000-1004.
78. Lebin JA, Akhavan AR, Hippe DS, et al. Psychiatric outcomes of patients with severe agitation following administration of prehospital ketamine. Acad Emerg Med. 2019;26(8):889-896.
79. Barbic D, Andolfatto G, Grunau B, et al. Rapid agitation control with ketamine in the emergency department (RACKED): a randomized controlled trial protocol. Trials. 2018;19(1):651.
80. Garriga M, Pacchiarotti I, Kasper S, et al. Assessment and management of agitation in psychiatry: expert consensus. World J Biol Psychiatr. 2016;17(2):86-128.
81. Adler L, Angrist B, Peselow E, et al. Efficacy of propranolol in neuroleptic-induced akathesia. J Clin Psychopharmacol. 1985;5(3):164-166.
82. Adler LA, Reiter S, Corwin J, et al. Neuroleptic-induced akathisia: propranolol versus benztropine. Biol Psychiatry. 1988;23(2):211-213.
83. de Leon J, Diaz FJ, Wedlund P, et al. Haloperidol half-life after chronic dosing. J Clin Psychopharmacol. 2004;24(6):656-660.
1. Shorter E. A history of psychiatry. New York, NY: John Wiley & Sons, Inc.; 1997:249.
2. Salzman C, Green AI, Rodriguez-Villa F, et al. Benzodiazepines combined with neuroleptics for management of severe disruptive behavior. Psychosomatics. 1986;27(suppl 1):17-22.
3. Allen MH. Managing the agitated psychotic patient: a reappraisal of the evidence. J Clin Psychiatr. 2000;61(suppl 14):11-20.
4. Salzman C, Solomon D, Miyawaki E, et al. Parenteral lorazepam versus parenteral haloperidol for the control of psychotic disruptive behavior. J Clin Psychiatr. 1991:52(4):177-180.
5. Allen MH, Currier GW, Hughes DH, et al. The expert consensus guideline series: treatment of behavioral emergencies. Postgrad Med. 2001;(Spec No):1-88; quiz 89-90.
6. Foster S, Kessel J, Berman ME, et al. Efficacy of lorazepam and haloperidol for rapid tranquilization in a psychiatric emergency room setting. Int Clin Psychopharmacol. 1997;12(3):175-179.
7. Garza-Trevino WS, Hollister LE, Overall JE, et al. Efficacy of combinations of intramuscular antipsychotics and sedative-hypnotics for control of psychotic agitation. Am J Psychiatr. 1989:146(12):1598-1601.
8. Battaglia J, Moss S, Rush J, et al. Haloperidol, lorazepam, or both for psychotic agitation? A multicenter, prospective double-blind, emergency study. Am J Emerg Med 1997;15(4):335-340.
9. Ostinelli EG, Brooke-Powney MJ, Li X, et al. Haloperidol for psychosis-induced aggression or agitation (rapid tranquillisation). Cochrane Database Syst Rev. 2017; 7:CD009377. doi: 10.1002/14651858.CD009377.pub3.
10. Powney MJ, Adams CE, Jones H. Haloperidol for psychosis-induced aggression or agitation (rapid tranquillisation). Cochrane Database Syst Rev. 2012;11:CD009377. doi: 10.1002/14651858.CD009377.pub2.
11. Citrome L. Review: limited evidence on effects of haloperidol alone for rapid tranquillisation in psychosis-induced aggression. Evid Based Ment Health. 2013;16(2):47.
12. Bienek SA, Ownby R, Penalver A, et al. A double-blind study of lorazepam versus the combination of haloperidol and lorazepam in managing agitation. Pharmacother. 1998;18(1):57-62.
13. Binder RL, McNiel DE. Contemporary practices in managing acutely violent patients in 20 psychiatric emergency rooms. Psychiatric Serv. 1999;50(2):1553-1554.
14. Andrezina R, Josiassen RC, Marcus RN, et al. Intramuscular aripiprazole for the treatment of acute agitation in patients with schizophrenia or schizoaffective disorder: a double-blind, placebo-controlled comparison with intramuscular haloperidol. Psychopharmacology (Berl). 2006;188(3):281-292.
15. Tran-Johnson TK, Sack DA, Marcus RN, et al. Efficacy and safety of intramuscular aripiprazole in patients with acute agitation: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatr. 2007;68(1):111-119.
16. Brook S, Lucey JV, Gunn KP. Intramuscular ziprasidone compared with intramuscular haloperidol in the treatment of acute psychosis. J Clin Psychiatr. 2000;61(12):933-941.
17. Brook S, Walden J, Benattia I, et al. Ziprasidone and haloperidol in the treatment of acute exacerbation of schizophrenia and schizoaffective disorder: comparison of intramuscular and oral formulations in a 6-week, randomized, blinded-assessment study. Psychopharmacology (Berl). 2005;178(4):514-523.
18. Wright P, Birkett M, David SR, et al. Double-blind, placebo-controlled comparison of intramuscular olanzapine and intramuscular haloperidol in the treatment of acute agitation in schizophrenia. Am J Psychiatr. 2001;158(7):1149-1151.
19. Breier A, Meehan K, Birkett M, et al. A double-blind, placebo-controlled dose-response comparison of intramuscular olanzapine and haloperidol in the treatment of acute agitation in schizophrenia. Arch Gen Psych. 2002;59(5):441-448.
20. Hsu W, Huang S, Lee B, et al. Comparison of intramuscular olanzapine, orally disintegrating olanzapine tablets, oral risperidone solution, and intramuscular haloperidol in the management of acute agitation in an acute care psychiatric ward in Taiwan. J Clin Psychopharmacol. 2010;30(3):230-234.
21. Chan H, Ree S, Su L, et al. A double-blind, randomized comparison study of efficacy and safety of intramuscular olanzapine and intramuscular haloperidol in patients with schizophrenia and acute agitated behavior. J Clin Psychopharmacol. 2014;34(3):355-358.
22. Baldaçara L, Sanches M, Cordeiro DC, et al. Rapid tranquilization for agitated patients in emergency psychiatric rooms: a randomized trial of olanzapine, ziprasidone, haloperidol plus promethazine, haloperidol plus midazolam and haloperidol alone. Braz J Psychiatry. 2011;33(1):30-39.
23. Hillard JR. Defusing patient violence. Current Psychiatry. 2002;1(4):22-29.
24. Seemüller F, Schennach R, Mayr A, et al. Akathisia and suicidal ideation in first-episode schizophrenia. J Clin Psychopharmacol. 2012;32(5):694-698.
25. Eikelenboom-Schieveld SJM, Lucire Y, Fogleman JC. The relevance of cytochrome P450 polymorphism in forensic medicine and akathisia-related violence and suicide. J Forens Leg Med. 2016;41:65-71.
26. Van Putten T, May PRA, Marder SR. Akathisia with haloperidol and thiothixene. Arch Gen Psych. 1984;41:1036-1039.
27. Drotts DL, Vinson DR. Prochlorperazine induced akathisia in emergency patients. Ann Emerg Med. 1999;34(4):469-475.
28. Salem H, Negpal C, Pigott T. Revisiting antipsychotic-induced akathisia: current issues and prospective challenges. Curr Neuropharmacol. 2017;15(5):789-798.
29. Huf G, Coutinho ESF, Adams CE. Rapid tranquilization in psychiatric emergency settings in Brazil: pragmatic randomized controlled trial of intramuscular haloperidol versus intramuscular haloperidol plus promethazine. BMJ. 2007;335(7625):869.
30. Mantovani C, Labate CM, Sponholz A, et al. Are low doses of antipsychotics effective in the management of psychomotor agitation? A randomized, rated-blind trial of 4 intramuscular interventions. J Clin Psychopharmacol. 2013;33(3):306-312.
31. Darwish H, Grant R, Haslam R, et al. Promethazine-induced acute dystonic reactions. Am J Dis Child. 1980;134(10):990-991.
32. Jyothi CH, Rudraiah HGM, Vidya HK, et al. Promethazine induced acute dystonia: a case report. Manipal J Med Sci. 2016;1(2):63-64.
33. Ames D, Carr-Lopez SM, Gutierrez MA, et al. Detecting and managing adverse effects of antipsychotic medications: current state of play. Psychiatr Clin North Am. 2016;39(2):275-311.
34. Meyer-Massetti C, Cheng CM, Sharpe MA, et al. The FDA extended warning for intravenous haloperidol and torsades de pointes: how should institutions respond? J Hosp Med. 2010;5(4):E8-E16. doi: 10.1002/jhm.691.
35. Wu C, Tsai Y, Tsai H. Antipsychotic drugs and the risk of ventricular arrhythmia and/or sudden cardiac death: a nation-wide case-crossover study. J Am Heart Dis. 2015;4(2):e001568. doi: 10.1161/JAHA.114.001568.
36. Beach SR, Celano CM, Sugrue AM, et al. QT prolongation, torsades de pointe, and psychotropic medications: a 5-year update. Psychosomatics. 2018;59(1):105-122.
37. Leonard CE, Freeman CP, Newcomb CW, et al. Antipsychotics and the risks of sudden cardiac death and all-cause death: cohort studies in Medicaid and dually-eligible Medicaid-Medicare beneficiaries of five states. J Clin Exp Cardiol. 2013;suppl 10(6):1-9.
38. Nasrallah H, Chen AT. Multiple neurotoxic effects of haloperidol resulting in neuronal death. Ann Clin Psychiatr. 2017;29(3):195-202.
39. Chen AT, Nasrallah HA. Neuroprotective effects of the second generation antipsychotics. Schizophr Res. 2019;208:1-7.
40. Nasrallah HA. Haloperidol clearly is neurotoxic. Should it be banned? Current Psychiatry. 2013;12(7):7-8.
41. Corrigan PW, Yudofsky SC, Silver JM. Pharmacological and behavioral treatments for aggressive psychiatric inpatients. Hosp Comm Psychiatr. 1993;44(2):125-133.
42. Zeller SL, Citrome L. Managing agitation associated with schizophrenia and bipolar disorder in the emergency setting. West J Emerg Med. 2016;17(2):165-172.
43. Vieta E, Garriga M, Cardete L, et al. Protocol for the management of psychiatric patients with psychomotor agitation. BMC Psychiatr. 2017;17:328.
44. Nobay F, Simon BC, Levitt A, et al. A prospective, double-blind, randomized trial of midazolam versus haloperidol versus lorazepam in the chemical restraint of violent and severely agitated patients. Acad Emerg Med. 2004;11(7):744-749.
45. Klein LR, Driver BE, Miner JR, et al. Intramuscular midazolam, olanzapine, ziprasidone, or haloperidol for treating acute agitation in the emergency department. Ann Emerg Med. 2018;72(4):374-385.
46. Hillard JR. Emergency treatment of acute psychosis. J Clin Psychiatr. 1998;59(suppl 1):57-60.
47. Modell JG, Lenox RH, Weiner S. Inpatient clinical trial of lorazepam for the management of manic agitation. J Clin Psychopharmacol. 1985;5(2):109-110.
48. Denaut M, Yernault JC, De Coster A. Double-blind comparison of the respiratory effects of parenteral lorazepam and diazepam in patients with chronic obstructive lung disease. Curr Med Res Opin. 1975;2(10):611-615.
49. Kahn DR, Barnhorst AV, Bourgeois JA. A case of alcohol withdrawal requiring 1,600 mg of lorazepam in 24 hours. CNS Spectr. 2009;14(7):385-389.
50. Jones KA. Benzodiazepines: their role in aggression and why GPs should prescribe with caution. Austral Fam Physician. 2011;40(11):862-865.
51. Allen MH, Currier GW, Carpenter D, et al. The expert consensus guideline series. Treatment of behavioral emergencies 2005. J Psychiatr Pract. 2005;11(suppl 1):5-108.
52. Allen MH, Carpenter D, Sheets JL, et al. What do consumers say they want and need during a psychiatric emergency? J Psychiatr Pract. 2003;9(1):39-58.
53. Han DH. Some Abilify formulations to discontinue in 2015. MPR. https://www.empr.com/home/news/some-abilify-formulations-to-discontinue-in-2015/. Published January 13, 2015. Accessed April 17, 2020.
54. Citrome L. Comparison of intramuscular ziprasidone, olanzapine, or aripiprazole for agitation: a quantitative review of efficacy and safety. J Clin Psychiatry. 2007;68(12):1876-1885.
55. Satterthwaite TD, Wolf DH, Rosenheck RA, et al. A meta-analysis of the risk of acute extrapyramidal symptoms with intramuscular antipsychotics for the treatment for agitation. J Clin Psychiatr. 2008;69(12):1869-1879.
56. Miceli JJ, Tensfeldt TG, Shiovitz T, et al. Effects of high-dose ziprasidone and haloperidol on the QTc interval after intramuscular administration: a randomized, single-blind, parallel-group study in patients with schizophrenia or schizoaffective disorder. Clin Ther. 2010;32(3):472-491.
57. Kovalick LJ, Pikalov AA, Ni N, et al. Short-term physical compatibility of intramuscular aripiprazole with intramuscular lorazepam. Am J Health-Syst Pharm. 2008;65(21):2007-2008.
58. Abilify [package insert]. Princeton, NJ: Bristol-Myers Squibb Company; 2014.
59. Zyprexa [package insert]. Indianapolis, IN: Lilly Research Laboratories; 2005.
60. Zacher JL, Roche-Desilets J. Hypotension secondary to the combination of intramuscular olanzapine and intramuscular lorazepam. J Clin Psychiatr. 2005;66(12):1614-1615.
61. Marder SR, Sorsaburu S, Dunayevich E, et al. Case reports of postmarketing adverse event experiences with olanzapine intramuscular treatment in patients with agitation. J Clin Psychiatr 2010;71(4):433-441.
62. Wilson MP, MacDonald K, Vilke GM, et al. A comparison of the safety of olanzapine and haloperidol in combination with benzodiazepines in emergency department patients with acute agitation. J Emerg Med. 2012;43(5):790-797.
63. Wilson MP, MacDonald K, Vilke GM, et al. Potential complications of combining intramuscular olanzapine with benzodiazepines in emergency department patients. J Emerg Med. 2012;43(5):889-896.
64. Williams AM. Coadministration of intramuscular olanzapine and benzodiazepines in agitated patients with mental illness. Ment Health Clin [Internet]. 2018;8(5):208-213.
65. Resnick M, Burton BT. Droperidol vs. haloperidol in the initial management of acutely agitated patients. J Clin Psychiatry. 1984;45(7):298-299.
66. Thomas H, Schwartz E, Petrilli R. Droperidol versus haloperidol for chemical restraint of agitated and combative patients. Ann Emerg Med. 1992;21(4):407-413.
67. Richards JR, Derlet RW, Duncan DR. Chemical restraint for the agitated patient in the emergency department: lorazepam versus droperidol. J Emerg Med. 1998;16(4):567-573.
68. Boyer EW. Droperidol is back (and here’s what you need to know). ACEP Now. https://www.acepnow.com/article/droperidol-is-back-and-heres-what-you-need-to-know/. Published September 16, 2019. Accessed April 17, 2020.
69. Martel M, Sterzinger A, Miner J, et al. Management of acute undifferentiated agitation in the emergency department: a randomized double-blind trial of droperidol, ziprasidone, and midazolam. Acad Emerg Med. 2005;12(12):1167-1172.
70. Chan EW, Taylor DM, Knott JC, et al. Intravenous droperidol or olanzapine as an adjunct to midazolam for the acutely agitated patient: a multicenter, randomized, double-blind, placebo-controlled clinical trial. Ann Emerg Med. 2013;61(1):72-81.
71. Isbister GK, Calver LA, Page CB, et al. Randomized controlled trial of intramuscular droperidol versus midazolam for violence and acute behavioral disturbance: the DORM study. Ann Emerg Med. 2010;56(4):392-401.
72. Macht M, Mull AC, McVaney KE, et al. Comparison of droperidol and haloperidol for use by paramedics assessment of safety and effectiveness. Prehosp Emerg Care. 2014;18(3):375-380.
73. Calver L, Page CB, Downes MA, et al. The safety and effectiveness of droperidol for sedation of acute behavioral disturbance in the emergency department. Ann Emerg Med. 2015;66(3):230-238.
74. Kohokar MA, Rathbone J. Droperidol for psychosis-induced aggression or agitation. Cochrane Database Syst Rev. 2016;12:CD002830.
75. Calver L, Drinkwater V, Gupta R, et al. Droperidol v. haloperidol for sedation of aggressive behavior in acute mental health: randomized controlled trial. Brit J Psychiatr. 2015;206(3):223-228.
76. Hopper AB, Vilke GM, Castillo EM, et al. Ketamine use for acute agitation in the emergency department. J Emerg Med. 2015;48(6):712-719.
77. Riddell J, Tran A, Bengiamin R, et al. Ketamine as a first-line treatment for severely agitated emergency department patients. Am J Emerg Med. 2017;35:1000-1004.
78. Lebin JA, Akhavan AR, Hippe DS, et al. Psychiatric outcomes of patients with severe agitation following administration of prehospital ketamine. Acad Emerg Med. 2019;26(8):889-896.
79. Barbic D, Andolfatto G, Grunau B, et al. Rapid agitation control with ketamine in the emergency department (RACKED): a randomized controlled trial protocol. Trials. 2018;19(1):651.
80. Garriga M, Pacchiarotti I, Kasper S, et al. Assessment and management of agitation in psychiatry: expert consensus. World J Biol Psychiatr. 2016;17(2):86-128.
81. Adler L, Angrist B, Peselow E, et al. Efficacy of propranolol in neuroleptic-induced akathesia. J Clin Psychopharmacol. 1985;5(3):164-166.
82. Adler LA, Reiter S, Corwin J, et al. Neuroleptic-induced akathisia: propranolol versus benztropine. Biol Psychiatry. 1988;23(2):211-213.
83. de Leon J, Diaz FJ, Wedlund P, et al. Haloperidol half-life after chronic dosing. J Clin Psychopharmacol. 2004;24(6):656-660.
COVID-19 in the era of loneliness
The natural state of human beings is to live together and function as organized groups. The beginnings of communities have primeval origins; evolutionarily, societies that worked together were more productive, efficient and—probably most important—safer. Thousands of years of evolution have ingrained these behaviors as part of our genetic constitution and developmental process. Social integration and acceptance thus are an integral part of basic human behavior and provide a sense of protection, pleasure, and purpose in life.
Unfortunately, the social isolation necessary to address the coronavirus disease 2019 (COVID-19) pandemic is preventing this integration, and is likely to worsen what some have called an epidemic of loneliness. As mental health clinicians, we need to use technology to strengthen our patients’ social support systems.
Loneliness: A growing problem
Changes in society over the last few decades have led to increased isolation. In the last 50 years, there has been a rise in single-person households in the United States. This is most common in large cities, where the prevalence is approximately 40%.1 The average number of confidants or the size of an American’s social network reduced by more than one-third from 1985 to 2009.2 In a study published in 2018, the health service company Cigna used the UCLA Loneliness Scale to survey >20,000 American adults.3 Nearly half of respondents reported always feeling alone (46%) or left out (47%), and individuals age 18 to 22 were the loneliest age group and claimed to be in worse health than older age groups. Furthermore, the results suggested that people who felt lonelier were more likely to have poor sleep and be less physically active. Americans who lived with others were less likely to report feeling lonely, except for single parents living only with their children. The results also showed that people who engage in meaningful interactions with others had lower loneliness scores and perceived that they were in better overall health.3
Studies have consistently demonstrated a link between loneliness and health problems such as cardiovascular disease, substance use disorders (SUDs), and mood disorders. A 2010 meta-analysis of 148 prospective studies with 308,849 participants found that the influence of social relationships on the risk of mortality is comparable to well-established risk factors for mortality such as smoking and alcohol consumption.4 These findings were confirmed in a 2015 meta-analysis that included 70 studies with 3.4 million participants followed for an average of 7 years. 5
Loneliness has been identified as a social determinant of health and is considered by many to be epidemic in proportion in developed countries. According to a 2019 Business Insider survey, almost 20% of US health care leaders planned to address social isolation in the next 12 months.6
Increased vulnerability during COVID-19 isolation
The forced quarantines and social distancing imposed by the COVID-19 crisis are likely to further exacerbate the loneliness epidemic. Hopefully, this increased isolation will not last more than several months, and its effect on chronic medical illnesses will be minor. However, for patients with mental illness, this further isolation, in conjunction with rising societal anxiety and fear of the potentially devastating financial consequences, could worsen their illness, and might even lead to suicidal ideation or behavior.
Individuals with SUDs are particularly vulnerable to the social limitations required by COVID-19. While social isolation is essential to limit the spread of COVID-19, this restriction poses unique challenges for these patients because connection and social support are important aspects of achieving and maintaining sobriety.7
Continue to: A call to action
A call to action
As mental health clinicians, we need to proactively engage with our patients to develop a plan to strengthen their social support systems. This may mean suggesting that they stay in contact with their network of people via video conferencing or by using the phone. We need to identify high-risk patients and continue to provide treatment via telepsychiatry. This is especially necessary to prevent relapse among patients with SUDs or mood disorders, and to minimize the risk of suicide.
We are ethically required to provide an atmosphere of trust, safety, and social inclusion by using resources, such as telehealth, video conferencing, and other online tools, to ameliorate the short- and long-term impact of COVID-19 isolation. Providing avenues that are easily accessible, are supportive, and maintain standards of care are essential. These resources should be implemented as early as possible to avoid negative outcomes regarding both COVID-19 and mental health.
There is also a significant risk that once circumstances improve, there will be a surge in the number of patients seeking a higher level of mental health care. Our actions and preparedness today will define the trajectory of our patients’ mental health in the future, potentially for years to come. While presently we are forced to be reactive, hopefully what is borne out of this crisis will translate into proactive measures for future crises.
Let this brief commentary serve as a call to action. As society finds ways to work from home, mental health clinicians need to lead the charge to use these same technologies to increase our patients’ social interactions. If we do not find ways to address the mental health burden of the COVID-19 pandemic, who will? We are all part of the mental health community, and we need to continue to function as an organized group, as has been the natural state of human beings for thousands of years.
Bottom Line
The social isolation required to limit the spread of the coronavirus disease 2019 pandemic is likely to increase loneliness, particularly among vulnerable patients with mood disorders and/or substance use disorders. As mental health clinicians, we need to work to strengthen our patients’ social support systems using resources such as video conferencing and other technologies.
Related Resources
- Cacioppo S, Grippo AJ, London S, et al. Loneliness: clinical import and interventions. Perspect Psychol Sci. 2015;10(2):238-249.
- Geriatric loneliness with Dr. Steven Wengel. Psychcast (podcast). https://www.mdedge.com/podcasts/psychcast/geriatricloneliness-dr-steven-wengel. Published April 1, 2020.
1. Howe N. Millennials and the loneliness epidemic. Forbes. https://www.forbes.com/sites/neilhowe/2019/05/03/millennials-and-the-loneliness-epidemic/. Published May 3, 2019. Accessed April 10, 2020.
2. The Economist. All the lonely people: loneliness is a serious public-health problem. https://www.economist.com/international/2018/09/01/loneliness-is-a-serious-public-health-problem. Published September 1, 2018. Accessed April 10, 2020.
3. Cigna. New Cigna study reveals loneliness at epidemic levels in America. https://www.cigna.com/newsroom/news-releases/2018/new-cigna-study-reveals-loneliness-at-epidemic-levels-in-america. Published May 1, 2018. Accessed April 10, 2020.
4. Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316.
5. Holt-Lunstad J, Smith TB, Baker M, et al. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10(2):227-237.
6. Finley D. How increased social distancing for the coronavirus could spur a loneliness epidemic. Business Insider. https://www.businessinsider.com/coronavirus-could-spur-loneliness-epidemic-2020-3. Published March 16, 2020. Accessed April 10, 2020.
7. Roy L. Addiction treatment facilities: are they prepared for the COVID-19 coronavirus outbreak? Forbes. https://www.forbes.com/sites/lipiroy/2020/03/16/addiction-treatment-facilities-are-they-prepared-for-covid-19/#555149b544ea. Published March 16, 2020. Accessed April 10, 2020.
The natural state of human beings is to live together and function as organized groups. The beginnings of communities have primeval origins; evolutionarily, societies that worked together were more productive, efficient and—probably most important—safer. Thousands of years of evolution have ingrained these behaviors as part of our genetic constitution and developmental process. Social integration and acceptance thus are an integral part of basic human behavior and provide a sense of protection, pleasure, and purpose in life.
Unfortunately, the social isolation necessary to address the coronavirus disease 2019 (COVID-19) pandemic is preventing this integration, and is likely to worsen what some have called an epidemic of loneliness. As mental health clinicians, we need to use technology to strengthen our patients’ social support systems.
Loneliness: A growing problem
Changes in society over the last few decades have led to increased isolation. In the last 50 years, there has been a rise in single-person households in the United States. This is most common in large cities, where the prevalence is approximately 40%.1 The average number of confidants or the size of an American’s social network reduced by more than one-third from 1985 to 2009.2 In a study published in 2018, the health service company Cigna used the UCLA Loneliness Scale to survey >20,000 American adults.3 Nearly half of respondents reported always feeling alone (46%) or left out (47%), and individuals age 18 to 22 were the loneliest age group and claimed to be in worse health than older age groups. Furthermore, the results suggested that people who felt lonelier were more likely to have poor sleep and be less physically active. Americans who lived with others were less likely to report feeling lonely, except for single parents living only with their children. The results also showed that people who engage in meaningful interactions with others had lower loneliness scores and perceived that they were in better overall health.3
Studies have consistently demonstrated a link between loneliness and health problems such as cardiovascular disease, substance use disorders (SUDs), and mood disorders. A 2010 meta-analysis of 148 prospective studies with 308,849 participants found that the influence of social relationships on the risk of mortality is comparable to well-established risk factors for mortality such as smoking and alcohol consumption.4 These findings were confirmed in a 2015 meta-analysis that included 70 studies with 3.4 million participants followed for an average of 7 years. 5
Loneliness has been identified as a social determinant of health and is considered by many to be epidemic in proportion in developed countries. According to a 2019 Business Insider survey, almost 20% of US health care leaders planned to address social isolation in the next 12 months.6
Increased vulnerability during COVID-19 isolation
The forced quarantines and social distancing imposed by the COVID-19 crisis are likely to further exacerbate the loneliness epidemic. Hopefully, this increased isolation will not last more than several months, and its effect on chronic medical illnesses will be minor. However, for patients with mental illness, this further isolation, in conjunction with rising societal anxiety and fear of the potentially devastating financial consequences, could worsen their illness, and might even lead to suicidal ideation or behavior.
Individuals with SUDs are particularly vulnerable to the social limitations required by COVID-19. While social isolation is essential to limit the spread of COVID-19, this restriction poses unique challenges for these patients because connection and social support are important aspects of achieving and maintaining sobriety.7
Continue to: A call to action
A call to action
As mental health clinicians, we need to proactively engage with our patients to develop a plan to strengthen their social support systems. This may mean suggesting that they stay in contact with their network of people via video conferencing or by using the phone. We need to identify high-risk patients and continue to provide treatment via telepsychiatry. This is especially necessary to prevent relapse among patients with SUDs or mood disorders, and to minimize the risk of suicide.
We are ethically required to provide an atmosphere of trust, safety, and social inclusion by using resources, such as telehealth, video conferencing, and other online tools, to ameliorate the short- and long-term impact of COVID-19 isolation. Providing avenues that are easily accessible, are supportive, and maintain standards of care are essential. These resources should be implemented as early as possible to avoid negative outcomes regarding both COVID-19 and mental health.
There is also a significant risk that once circumstances improve, there will be a surge in the number of patients seeking a higher level of mental health care. Our actions and preparedness today will define the trajectory of our patients’ mental health in the future, potentially for years to come. While presently we are forced to be reactive, hopefully what is borne out of this crisis will translate into proactive measures for future crises.
Let this brief commentary serve as a call to action. As society finds ways to work from home, mental health clinicians need to lead the charge to use these same technologies to increase our patients’ social interactions. If we do not find ways to address the mental health burden of the COVID-19 pandemic, who will? We are all part of the mental health community, and we need to continue to function as an organized group, as has been the natural state of human beings for thousands of years.
Bottom Line
The social isolation required to limit the spread of the coronavirus disease 2019 pandemic is likely to increase loneliness, particularly among vulnerable patients with mood disorders and/or substance use disorders. As mental health clinicians, we need to work to strengthen our patients’ social support systems using resources such as video conferencing and other technologies.
Related Resources
- Cacioppo S, Grippo AJ, London S, et al. Loneliness: clinical import and interventions. Perspect Psychol Sci. 2015;10(2):238-249.
- Geriatric loneliness with Dr. Steven Wengel. Psychcast (podcast). https://www.mdedge.com/podcasts/psychcast/geriatricloneliness-dr-steven-wengel. Published April 1, 2020.
The natural state of human beings is to live together and function as organized groups. The beginnings of communities have primeval origins; evolutionarily, societies that worked together were more productive, efficient and—probably most important—safer. Thousands of years of evolution have ingrained these behaviors as part of our genetic constitution and developmental process. Social integration and acceptance thus are an integral part of basic human behavior and provide a sense of protection, pleasure, and purpose in life.
Unfortunately, the social isolation necessary to address the coronavirus disease 2019 (COVID-19) pandemic is preventing this integration, and is likely to worsen what some have called an epidemic of loneliness. As mental health clinicians, we need to use technology to strengthen our patients’ social support systems.
Loneliness: A growing problem
Changes in society over the last few decades have led to increased isolation. In the last 50 years, there has been a rise in single-person households in the United States. This is most common in large cities, where the prevalence is approximately 40%.1 The average number of confidants or the size of an American’s social network reduced by more than one-third from 1985 to 2009.2 In a study published in 2018, the health service company Cigna used the UCLA Loneliness Scale to survey >20,000 American adults.3 Nearly half of respondents reported always feeling alone (46%) or left out (47%), and individuals age 18 to 22 were the loneliest age group and claimed to be in worse health than older age groups. Furthermore, the results suggested that people who felt lonelier were more likely to have poor sleep and be less physically active. Americans who lived with others were less likely to report feeling lonely, except for single parents living only with their children. The results also showed that people who engage in meaningful interactions with others had lower loneliness scores and perceived that they were in better overall health.3
Studies have consistently demonstrated a link between loneliness and health problems such as cardiovascular disease, substance use disorders (SUDs), and mood disorders. A 2010 meta-analysis of 148 prospective studies with 308,849 participants found that the influence of social relationships on the risk of mortality is comparable to well-established risk factors for mortality such as smoking and alcohol consumption.4 These findings were confirmed in a 2015 meta-analysis that included 70 studies with 3.4 million participants followed for an average of 7 years. 5
Loneliness has been identified as a social determinant of health and is considered by many to be epidemic in proportion in developed countries. According to a 2019 Business Insider survey, almost 20% of US health care leaders planned to address social isolation in the next 12 months.6
Increased vulnerability during COVID-19 isolation
The forced quarantines and social distancing imposed by the COVID-19 crisis are likely to further exacerbate the loneliness epidemic. Hopefully, this increased isolation will not last more than several months, and its effect on chronic medical illnesses will be minor. However, for patients with mental illness, this further isolation, in conjunction with rising societal anxiety and fear of the potentially devastating financial consequences, could worsen their illness, and might even lead to suicidal ideation or behavior.
Individuals with SUDs are particularly vulnerable to the social limitations required by COVID-19. While social isolation is essential to limit the spread of COVID-19, this restriction poses unique challenges for these patients because connection and social support are important aspects of achieving and maintaining sobriety.7
Continue to: A call to action
A call to action
As mental health clinicians, we need to proactively engage with our patients to develop a plan to strengthen their social support systems. This may mean suggesting that they stay in contact with their network of people via video conferencing or by using the phone. We need to identify high-risk patients and continue to provide treatment via telepsychiatry. This is especially necessary to prevent relapse among patients with SUDs or mood disorders, and to minimize the risk of suicide.
We are ethically required to provide an atmosphere of trust, safety, and social inclusion by using resources, such as telehealth, video conferencing, and other online tools, to ameliorate the short- and long-term impact of COVID-19 isolation. Providing avenues that are easily accessible, are supportive, and maintain standards of care are essential. These resources should be implemented as early as possible to avoid negative outcomes regarding both COVID-19 and mental health.
There is also a significant risk that once circumstances improve, there will be a surge in the number of patients seeking a higher level of mental health care. Our actions and preparedness today will define the trajectory of our patients’ mental health in the future, potentially for years to come. While presently we are forced to be reactive, hopefully what is borne out of this crisis will translate into proactive measures for future crises.
Let this brief commentary serve as a call to action. As society finds ways to work from home, mental health clinicians need to lead the charge to use these same technologies to increase our patients’ social interactions. If we do not find ways to address the mental health burden of the COVID-19 pandemic, who will? We are all part of the mental health community, and we need to continue to function as an organized group, as has been the natural state of human beings for thousands of years.
Bottom Line
The social isolation required to limit the spread of the coronavirus disease 2019 pandemic is likely to increase loneliness, particularly among vulnerable patients with mood disorders and/or substance use disorders. As mental health clinicians, we need to work to strengthen our patients’ social support systems using resources such as video conferencing and other technologies.
Related Resources
- Cacioppo S, Grippo AJ, London S, et al. Loneliness: clinical import and interventions. Perspect Psychol Sci. 2015;10(2):238-249.
- Geriatric loneliness with Dr. Steven Wengel. Psychcast (podcast). https://www.mdedge.com/podcasts/psychcast/geriatricloneliness-dr-steven-wengel. Published April 1, 2020.
1. Howe N. Millennials and the loneliness epidemic. Forbes. https://www.forbes.com/sites/neilhowe/2019/05/03/millennials-and-the-loneliness-epidemic/. Published May 3, 2019. Accessed April 10, 2020.
2. The Economist. All the lonely people: loneliness is a serious public-health problem. https://www.economist.com/international/2018/09/01/loneliness-is-a-serious-public-health-problem. Published September 1, 2018. Accessed April 10, 2020.
3. Cigna. New Cigna study reveals loneliness at epidemic levels in America. https://www.cigna.com/newsroom/news-releases/2018/new-cigna-study-reveals-loneliness-at-epidemic-levels-in-america. Published May 1, 2018. Accessed April 10, 2020.
4. Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316.
5. Holt-Lunstad J, Smith TB, Baker M, et al. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10(2):227-237.
6. Finley D. How increased social distancing for the coronavirus could spur a loneliness epidemic. Business Insider. https://www.businessinsider.com/coronavirus-could-spur-loneliness-epidemic-2020-3. Published March 16, 2020. Accessed April 10, 2020.
7. Roy L. Addiction treatment facilities: are they prepared for the COVID-19 coronavirus outbreak? Forbes. https://www.forbes.com/sites/lipiroy/2020/03/16/addiction-treatment-facilities-are-they-prepared-for-covid-19/#555149b544ea. Published March 16, 2020. Accessed April 10, 2020.
1. Howe N. Millennials and the loneliness epidemic. Forbes. https://www.forbes.com/sites/neilhowe/2019/05/03/millennials-and-the-loneliness-epidemic/. Published May 3, 2019. Accessed April 10, 2020.
2. The Economist. All the lonely people: loneliness is a serious public-health problem. https://www.economist.com/international/2018/09/01/loneliness-is-a-serious-public-health-problem. Published September 1, 2018. Accessed April 10, 2020.
3. Cigna. New Cigna study reveals loneliness at epidemic levels in America. https://www.cigna.com/newsroom/news-releases/2018/new-cigna-study-reveals-loneliness-at-epidemic-levels-in-america. Published May 1, 2018. Accessed April 10, 2020.
4. Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316.
5. Holt-Lunstad J, Smith TB, Baker M, et al. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10(2):227-237.
6. Finley D. How increased social distancing for the coronavirus could spur a loneliness epidemic. Business Insider. https://www.businessinsider.com/coronavirus-could-spur-loneliness-epidemic-2020-3. Published March 16, 2020. Accessed April 10, 2020.
7. Roy L. Addiction treatment facilities: are they prepared for the COVID-19 coronavirus outbreak? Forbes. https://www.forbes.com/sites/lipiroy/2020/03/16/addiction-treatment-facilities-are-they-prepared-for-covid-19/#555149b544ea. Published March 16, 2020. Accessed April 10, 2020.
COVID-19: A psychiatry resident’s perspective
During these unprecedented times, venturing into the unknown of the coronavirus disease 2019 (COVID-19) pandemic, a feeling of impending doom prevails. Almost all of us have been restricted to our homes. Although the physical dimensions of what we call home may vary, the meaning of this restriction is fairly universal. No matter how our sociodemographics differ, with no guidance for this situation from anything even remotely comparable in the past, our lives have been transformed into a work in progress.
During this pandemic, I have observed a wide range of human emotions and behavior—many of them familiar and predictable, some abysmal, and some inspiring.
’Why should I care?’
On December 31, 2019, health officials in China informed the World Health Organization about a pneumonia-like presentation in a group of people in Wuhan. On January 7, 2020, a novel coronavirus was identified as the cause, and the first death was reported a few days later. In the following days and weeks the disease rapidly spread, as did the growing sense that this was not a typical virus.
While these events occurred, the rest of the world was in what I call a ”Why should I care?” mode. Most humans tend to suffer from this indifference. This has been observed repeatedly through the years, such as when the Ebola outbreak occurred in Africa in 2014-2016. It was only when cases started to develop in Europe and the United States that other countries started to pay attention. A similar phenomenon has been observed every time we’ve faced a global outbreak (avian influenza, Middle East respiratory syndrome, etc.).
When are we going to learn? It is time to realize that global borders are more porous than we think, and human interactions cannot be blocked by any wall. When a catastrophic event, outbreak, or disaster starts in any part of the world, it is naive to assume that we will not be affected. We will eventually be affected—the only question is how, when, and to what extent? We are always all in this together.
An abundance of ignorance and stupidity
Within a few weeks of the first reports from China, cases of COVID-19 were reported in South Korea, Italy, Spain, Germany, and many other countries. Slowly, COVID-19 reached the United States, which as of mid-April had the highest number of cases worldwide. When COVID-19 hit the United States, the response was that of shock and anger. How could this happen to us? Why is the government not doing anything?
Amidst this pandemonium, ignorance and stupidity of the highest degree were commonplace. This was not restricted to any particular country or region. Almost 2 months into the pandemic, the Ministry of Tourism in my home country of Nepal declared Nepal a ”coronavirus-free zone” and took measures to bring in tourists, focusing specifically on China, where COVID-19 had already killed hundreds. In India, some people were drinking cow urine in hopes of warding off the virus. In the United Sates, thousands of young people flocked to beaches for Spring Break, disregarding measures for social distancing. ”If I get corona, I get corona,” one young man said in an interview that went viral. Personally, I have encountered people who responded to this pandemic by saying the disease was ”cooties” or ”just a flu,” and dismissing it with ”If I die from this, I die.”
Continue to: Rising panic and fear
Rising panic and fear
For most people, seeing COVID-19 at their doorstep triggered a panic, and sent many into a frenzy of buying and hoarding. Once again, we proved that people everywhere are equally stupid, as toilet paper began to vanish from stores across the globe. And yet, this again was a moment when some people began to experience a false sense of immunity: ”I have enough food, money, and toilet paper to last me for 2 years. Why should I be worried?”
When the numbers of COVID-19 deaths in Europe were first reported, the fear became palpable. In Italy and Spain, towns were locked down, and tens of thousands of people (mostly older adults) have died. It was truly heartbreaking to see people alone and at their weakest with no family members allowed to be by their side.
A glimmer of hope
Despite all of this, there were superheroes—the nurses, physicians, allied health professionals, first responders, store workers, restaurant workers, delivery personnel, and others who didn’t have the option of staying home, or who volunteered to help people in need. In moments like this, the actions of these individuals give us hope, reminding us that the human spirit is resilient, and that we will get through this.
A rotation in the emergency department during COVID-19
As a psychiatry resident, it is unlikely that my peers and I face the same risks as our colleagues in other medical specialities. But those of us who happened to be in medical rotations during this time have had the chance to experience this very closely. My personal experience, albeit a brief one, of working in an emergency department with suspected COVID-19 patients has been sobering. Watching nurses and physicians walk into a room wearing personal protective equipment, fearful inside but with a reassuring smile for a scared patient, definitely was one of the most compelling moments of my life. Living in a distant land, with my daughter, wife, parents, and extended family back home in Nepal, has made this even more challenging.
We will overcome this as we have overcome previous challenges in the past. There will be death and chaos, but we will prevail. The only thing is to ask ourselves: How do we want to continue living when this is over?
During these unprecedented times, venturing into the unknown of the coronavirus disease 2019 (COVID-19) pandemic, a feeling of impending doom prevails. Almost all of us have been restricted to our homes. Although the physical dimensions of what we call home may vary, the meaning of this restriction is fairly universal. No matter how our sociodemographics differ, with no guidance for this situation from anything even remotely comparable in the past, our lives have been transformed into a work in progress.
During this pandemic, I have observed a wide range of human emotions and behavior—many of them familiar and predictable, some abysmal, and some inspiring.
’Why should I care?’
On December 31, 2019, health officials in China informed the World Health Organization about a pneumonia-like presentation in a group of people in Wuhan. On January 7, 2020, a novel coronavirus was identified as the cause, and the first death was reported a few days later. In the following days and weeks the disease rapidly spread, as did the growing sense that this was not a typical virus.
While these events occurred, the rest of the world was in what I call a ”Why should I care?” mode. Most humans tend to suffer from this indifference. This has been observed repeatedly through the years, such as when the Ebola outbreak occurred in Africa in 2014-2016. It was only when cases started to develop in Europe and the United States that other countries started to pay attention. A similar phenomenon has been observed every time we’ve faced a global outbreak (avian influenza, Middle East respiratory syndrome, etc.).
When are we going to learn? It is time to realize that global borders are more porous than we think, and human interactions cannot be blocked by any wall. When a catastrophic event, outbreak, or disaster starts in any part of the world, it is naive to assume that we will not be affected. We will eventually be affected—the only question is how, when, and to what extent? We are always all in this together.
An abundance of ignorance and stupidity
Within a few weeks of the first reports from China, cases of COVID-19 were reported in South Korea, Italy, Spain, Germany, and many other countries. Slowly, COVID-19 reached the United States, which as of mid-April had the highest number of cases worldwide. When COVID-19 hit the United States, the response was that of shock and anger. How could this happen to us? Why is the government not doing anything?
Amidst this pandemonium, ignorance and stupidity of the highest degree were commonplace. This was not restricted to any particular country or region. Almost 2 months into the pandemic, the Ministry of Tourism in my home country of Nepal declared Nepal a ”coronavirus-free zone” and took measures to bring in tourists, focusing specifically on China, where COVID-19 had already killed hundreds. In India, some people were drinking cow urine in hopes of warding off the virus. In the United Sates, thousands of young people flocked to beaches for Spring Break, disregarding measures for social distancing. ”If I get corona, I get corona,” one young man said in an interview that went viral. Personally, I have encountered people who responded to this pandemic by saying the disease was ”cooties” or ”just a flu,” and dismissing it with ”If I die from this, I die.”
Continue to: Rising panic and fear
Rising panic and fear
For most people, seeing COVID-19 at their doorstep triggered a panic, and sent many into a frenzy of buying and hoarding. Once again, we proved that people everywhere are equally stupid, as toilet paper began to vanish from stores across the globe. And yet, this again was a moment when some people began to experience a false sense of immunity: ”I have enough food, money, and toilet paper to last me for 2 years. Why should I be worried?”
When the numbers of COVID-19 deaths in Europe were first reported, the fear became palpable. In Italy and Spain, towns were locked down, and tens of thousands of people (mostly older adults) have died. It was truly heartbreaking to see people alone and at their weakest with no family members allowed to be by their side.
A glimmer of hope
Despite all of this, there were superheroes—the nurses, physicians, allied health professionals, first responders, store workers, restaurant workers, delivery personnel, and others who didn’t have the option of staying home, or who volunteered to help people in need. In moments like this, the actions of these individuals give us hope, reminding us that the human spirit is resilient, and that we will get through this.
A rotation in the emergency department during COVID-19
As a psychiatry resident, it is unlikely that my peers and I face the same risks as our colleagues in other medical specialities. But those of us who happened to be in medical rotations during this time have had the chance to experience this very closely. My personal experience, albeit a brief one, of working in an emergency department with suspected COVID-19 patients has been sobering. Watching nurses and physicians walk into a room wearing personal protective equipment, fearful inside but with a reassuring smile for a scared patient, definitely was one of the most compelling moments of my life. Living in a distant land, with my daughter, wife, parents, and extended family back home in Nepal, has made this even more challenging.
We will overcome this as we have overcome previous challenges in the past. There will be death and chaos, but we will prevail. The only thing is to ask ourselves: How do we want to continue living when this is over?
During these unprecedented times, venturing into the unknown of the coronavirus disease 2019 (COVID-19) pandemic, a feeling of impending doom prevails. Almost all of us have been restricted to our homes. Although the physical dimensions of what we call home may vary, the meaning of this restriction is fairly universal. No matter how our sociodemographics differ, with no guidance for this situation from anything even remotely comparable in the past, our lives have been transformed into a work in progress.
During this pandemic, I have observed a wide range of human emotions and behavior—many of them familiar and predictable, some abysmal, and some inspiring.
’Why should I care?’
On December 31, 2019, health officials in China informed the World Health Organization about a pneumonia-like presentation in a group of people in Wuhan. On January 7, 2020, a novel coronavirus was identified as the cause, and the first death was reported a few days later. In the following days and weeks the disease rapidly spread, as did the growing sense that this was not a typical virus.
While these events occurred, the rest of the world was in what I call a ”Why should I care?” mode. Most humans tend to suffer from this indifference. This has been observed repeatedly through the years, such as when the Ebola outbreak occurred in Africa in 2014-2016. It was only when cases started to develop in Europe and the United States that other countries started to pay attention. A similar phenomenon has been observed every time we’ve faced a global outbreak (avian influenza, Middle East respiratory syndrome, etc.).
When are we going to learn? It is time to realize that global borders are more porous than we think, and human interactions cannot be blocked by any wall. When a catastrophic event, outbreak, or disaster starts in any part of the world, it is naive to assume that we will not be affected. We will eventually be affected—the only question is how, when, and to what extent? We are always all in this together.
An abundance of ignorance and stupidity
Within a few weeks of the first reports from China, cases of COVID-19 were reported in South Korea, Italy, Spain, Germany, and many other countries. Slowly, COVID-19 reached the United States, which as of mid-April had the highest number of cases worldwide. When COVID-19 hit the United States, the response was that of shock and anger. How could this happen to us? Why is the government not doing anything?
Amidst this pandemonium, ignorance and stupidity of the highest degree were commonplace. This was not restricted to any particular country or region. Almost 2 months into the pandemic, the Ministry of Tourism in my home country of Nepal declared Nepal a ”coronavirus-free zone” and took measures to bring in tourists, focusing specifically on China, where COVID-19 had already killed hundreds. In India, some people were drinking cow urine in hopes of warding off the virus. In the United Sates, thousands of young people flocked to beaches for Spring Break, disregarding measures for social distancing. ”If I get corona, I get corona,” one young man said in an interview that went viral. Personally, I have encountered people who responded to this pandemic by saying the disease was ”cooties” or ”just a flu,” and dismissing it with ”If I die from this, I die.”
Continue to: Rising panic and fear
Rising panic and fear
For most people, seeing COVID-19 at their doorstep triggered a panic, and sent many into a frenzy of buying and hoarding. Once again, we proved that people everywhere are equally stupid, as toilet paper began to vanish from stores across the globe. And yet, this again was a moment when some people began to experience a false sense of immunity: ”I have enough food, money, and toilet paper to last me for 2 years. Why should I be worried?”
When the numbers of COVID-19 deaths in Europe were first reported, the fear became palpable. In Italy and Spain, towns were locked down, and tens of thousands of people (mostly older adults) have died. It was truly heartbreaking to see people alone and at their weakest with no family members allowed to be by their side.
A glimmer of hope
Despite all of this, there were superheroes—the nurses, physicians, allied health professionals, first responders, store workers, restaurant workers, delivery personnel, and others who didn’t have the option of staying home, or who volunteered to help people in need. In moments like this, the actions of these individuals give us hope, reminding us that the human spirit is resilient, and that we will get through this.
A rotation in the emergency department during COVID-19
As a psychiatry resident, it is unlikely that my peers and I face the same risks as our colleagues in other medical specialities. But those of us who happened to be in medical rotations during this time have had the chance to experience this very closely. My personal experience, albeit a brief one, of working in an emergency department with suspected COVID-19 patients has been sobering. Watching nurses and physicians walk into a room wearing personal protective equipment, fearful inside but with a reassuring smile for a scared patient, definitely was one of the most compelling moments of my life. Living in a distant land, with my daughter, wife, parents, and extended family back home in Nepal, has made this even more challenging.
We will overcome this as we have overcome previous challenges in the past. There will be death and chaos, but we will prevail. The only thing is to ask ourselves: How do we want to continue living when this is over?
Screening for adolescent substance use; Changing routines during COVID-19
Screening for adolescent substance use
I want to congratulate Dr. Verma on her article “Opioid use disorder in adolescents: An overview” (Evidence-Based Reviews,
Because evidence suggests there are continued barriers, such as time constraints, in evaluating for adolescent SUD,1,2 I believe the Screen to Brief Intervention (S2BI) and Brief Screener for Tobacco, Alcohol and Drug (BSTAD) should be included.3,4 The S2BI and BSTAD are brief screeners that assess substance use, are validated for adolescent patients, can be completed online, and can assist in identifying DSM-5 criteria for SUD.
The S2BI has demonstrated high sensitivity and specificity for identifying SUD.3 The single screening assessment for “past-year use” is quick and can be administered in a variety of clinical settings. The S2BI begins by asking a patient about his/her frequency of tobacco, alcohol, and/or marijuana use in the past year. If the patient endorses past-year use of any of these substances, the S2BI prompts follow-up questions about the use of prescription medications, illicit drugs, inhalants, and herbal products. A patient’s frequency of use is strongly correlated with the likelihood of having a SUD. Adolescents who report using a substance “once or twice” in the past year are very unlikely to have a SUD. Patients who endorse “monthly” use are more likely to meet the criteria for a mild or moderate SUD, and those reporting “weekly or more” use are more likely to have a severe SUD.
The BSTAD is an electronic, validated, high-sensitivity, high-specificity instrument for identifying SUD.1 It asks a single frequency question about past-year use of tobacco, alcohol, and marijuana, which are the most commonly used substances among adolescents. Patients who report using any of these substances are then asked about additional substance use. Based on the patient’s self-report of past year use, the screen places him/her into 1 of 3 risk categories for SUD: no reported use, lower risk, and higher risk. Each risk level maps to suggested clinical actions that are summarized in the results section.
Kevin M. Simon, MD
Child & Adolescent Psychiatry Fellow
Boston Children’s Hospital
Clinical Fellow in Psychiatry
Harvard Medical School
Boston, Massachusetts
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
References
1. Palmer A, Karakus M, Mark T. Barriers faced by physicians in screening for substance use disorders among adolescents. Psychiatr Serv. 2019;70(5):409-412.
2. D’Souza-Li L, Harris SK. The future of screening, brief intervention and referral to treatment in adolescent primary care: research directions and dissemination challenges. Curr Opin Pediatr. 2016;28(4):434-440.
3. Levy S, Weiss R, Sherritt L, et al. An electronic screen for triaging adolescent substance use by risk levels. JAMA Pediatr. 2014;168(9):822-828.
4. Kelly SM, Gryczynski J, Mitchell SG, et al. Validity of brief screening instrument for adolescent tobacco, alcohol, and drug use. Pediatrics. 2014;133(5):819-826.
Continue to: The author responds
The author responds
I thank Dr. Simon for his words of encouragement. I agree that both the S2BI and BSTAD have high sensitivity and specificity and are easy to use for screening for the use of multiple substances. Once substance use is established, both tools recommend administering high-risk assessment with additional scales such as the CRAFFT. During the initial evaluation, many psychiatrists take their patient’s history of substance use in detail, including age of onset, frequency, amount used, severity, and the time of his/her last use, without using a screening instrument. My article focused on instruments that can determine whether there is need for a further detailed evaluation. I agree that the S2BI and BSTAD would assist psychiatrists or physicians in other specialties (eg, pediatrics, family medicine) who might not take a complete substance use history during their initial evaluations.
Shikha Verma, MD
Rogers Behavioral Health
Kenosha, Wisconsin
Assistant Professor
Department of Psychiatry and Behavioral Health
Rosalind Franklin University of Medicine and Science
North Chicago, Illinois
Continue to: Changes as a result of COVID-19
Changes as a result of COVID-19
I thank Dr. Nasrallah for his editorial “During a viral pandemic, anxiety is endemic: The psychiatric aspects of COVID-19” (From the Editor,
I appreciated the editorial because it got me thinking about how the pandemic has changed me and my family:
1. We are engaging more in social media.
2. I feel uncomfortable when I go to the grocery store.
3. I feel better when I don’t access the news about COVID-19.
4. My children need physical socialization with their friends (sports, games, other activities, etc.).
5. My children function better with a schedule, but we find it difficult to keep them on a good schedule. Our teenagers stay up late at night (because all of their friends do), and they sleep in late the next morning.
Here are some positive changes:
1. Creating a weekly family calendar on a dry-erase board, so the family can see what is going on during the week.
2. Creating responsibility for our older children (eg, washing their own clothes, cleaning their bathroom).
3. Eating most meals as a family and organizing meals better, too.
4. Playing games together.
5. Cleaning the house together.
6. Getting outside to walk the dog and appreciate nature more.
7. Exercising.
8. Utilizing positive social media.
9. Getting caught up on life.
Again, I thank Dr. Nasrallah for writing this editorial because it led me to self-reflect on this situation, and helped me feel normal.
Doug Dolenc
Westfield, Indiana
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
Screening for adolescent substance use
I want to congratulate Dr. Verma on her article “Opioid use disorder in adolescents: An overview” (Evidence-Based Reviews,
Because evidence suggests there are continued barriers, such as time constraints, in evaluating for adolescent SUD,1,2 I believe the Screen to Brief Intervention (S2BI) and Brief Screener for Tobacco, Alcohol and Drug (BSTAD) should be included.3,4 The S2BI and BSTAD are brief screeners that assess substance use, are validated for adolescent patients, can be completed online, and can assist in identifying DSM-5 criteria for SUD.
The S2BI has demonstrated high sensitivity and specificity for identifying SUD.3 The single screening assessment for “past-year use” is quick and can be administered in a variety of clinical settings. The S2BI begins by asking a patient about his/her frequency of tobacco, alcohol, and/or marijuana use in the past year. If the patient endorses past-year use of any of these substances, the S2BI prompts follow-up questions about the use of prescription medications, illicit drugs, inhalants, and herbal products. A patient’s frequency of use is strongly correlated with the likelihood of having a SUD. Adolescents who report using a substance “once or twice” in the past year are very unlikely to have a SUD. Patients who endorse “monthly” use are more likely to meet the criteria for a mild or moderate SUD, and those reporting “weekly or more” use are more likely to have a severe SUD.
The BSTAD is an electronic, validated, high-sensitivity, high-specificity instrument for identifying SUD.1 It asks a single frequency question about past-year use of tobacco, alcohol, and marijuana, which are the most commonly used substances among adolescents. Patients who report using any of these substances are then asked about additional substance use. Based on the patient’s self-report of past year use, the screen places him/her into 1 of 3 risk categories for SUD: no reported use, lower risk, and higher risk. Each risk level maps to suggested clinical actions that are summarized in the results section.
Kevin M. Simon, MD
Child & Adolescent Psychiatry Fellow
Boston Children’s Hospital
Clinical Fellow in Psychiatry
Harvard Medical School
Boston, Massachusetts
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
References
1. Palmer A, Karakus M, Mark T. Barriers faced by physicians in screening for substance use disorders among adolescents. Psychiatr Serv. 2019;70(5):409-412.
2. D’Souza-Li L, Harris SK. The future of screening, brief intervention and referral to treatment in adolescent primary care: research directions and dissemination challenges. Curr Opin Pediatr. 2016;28(4):434-440.
3. Levy S, Weiss R, Sherritt L, et al. An electronic screen for triaging adolescent substance use by risk levels. JAMA Pediatr. 2014;168(9):822-828.
4. Kelly SM, Gryczynski J, Mitchell SG, et al. Validity of brief screening instrument for adolescent tobacco, alcohol, and drug use. Pediatrics. 2014;133(5):819-826.
Continue to: The author responds
The author responds
I thank Dr. Simon for his words of encouragement. I agree that both the S2BI and BSTAD have high sensitivity and specificity and are easy to use for screening for the use of multiple substances. Once substance use is established, both tools recommend administering high-risk assessment with additional scales such as the CRAFFT. During the initial evaluation, many psychiatrists take their patient’s history of substance use in detail, including age of onset, frequency, amount used, severity, and the time of his/her last use, without using a screening instrument. My article focused on instruments that can determine whether there is need for a further detailed evaluation. I agree that the S2BI and BSTAD would assist psychiatrists or physicians in other specialties (eg, pediatrics, family medicine) who might not take a complete substance use history during their initial evaluations.
Shikha Verma, MD
Rogers Behavioral Health
Kenosha, Wisconsin
Assistant Professor
Department of Psychiatry and Behavioral Health
Rosalind Franklin University of Medicine and Science
North Chicago, Illinois
Continue to: Changes as a result of COVID-19
Changes as a result of COVID-19
I thank Dr. Nasrallah for his editorial “During a viral pandemic, anxiety is endemic: The psychiatric aspects of COVID-19” (From the Editor,
I appreciated the editorial because it got me thinking about how the pandemic has changed me and my family:
1. We are engaging more in social media.
2. I feel uncomfortable when I go to the grocery store.
3. I feel better when I don’t access the news about COVID-19.
4. My children need physical socialization with their friends (sports, games, other activities, etc.).
5. My children function better with a schedule, but we find it difficult to keep them on a good schedule. Our teenagers stay up late at night (because all of their friends do), and they sleep in late the next morning.
Here are some positive changes:
1. Creating a weekly family calendar on a dry-erase board, so the family can see what is going on during the week.
2. Creating responsibility for our older children (eg, washing their own clothes, cleaning their bathroom).
3. Eating most meals as a family and organizing meals better, too.
4. Playing games together.
5. Cleaning the house together.
6. Getting outside to walk the dog and appreciate nature more.
7. Exercising.
8. Utilizing positive social media.
9. Getting caught up on life.
Again, I thank Dr. Nasrallah for writing this editorial because it led me to self-reflect on this situation, and helped me feel normal.
Doug Dolenc
Westfield, Indiana
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
Screening for adolescent substance use
I want to congratulate Dr. Verma on her article “Opioid use disorder in adolescents: An overview” (Evidence-Based Reviews,
Because evidence suggests there are continued barriers, such as time constraints, in evaluating for adolescent SUD,1,2 I believe the Screen to Brief Intervention (S2BI) and Brief Screener for Tobacco, Alcohol and Drug (BSTAD) should be included.3,4 The S2BI and BSTAD are brief screeners that assess substance use, are validated for adolescent patients, can be completed online, and can assist in identifying DSM-5 criteria for SUD.
The S2BI has demonstrated high sensitivity and specificity for identifying SUD.3 The single screening assessment for “past-year use” is quick and can be administered in a variety of clinical settings. The S2BI begins by asking a patient about his/her frequency of tobacco, alcohol, and/or marijuana use in the past year. If the patient endorses past-year use of any of these substances, the S2BI prompts follow-up questions about the use of prescription medications, illicit drugs, inhalants, and herbal products. A patient’s frequency of use is strongly correlated with the likelihood of having a SUD. Adolescents who report using a substance “once or twice” in the past year are very unlikely to have a SUD. Patients who endorse “monthly” use are more likely to meet the criteria for a mild or moderate SUD, and those reporting “weekly or more” use are more likely to have a severe SUD.
The BSTAD is an electronic, validated, high-sensitivity, high-specificity instrument for identifying SUD.1 It asks a single frequency question about past-year use of tobacco, alcohol, and marijuana, which are the most commonly used substances among adolescents. Patients who report using any of these substances are then asked about additional substance use. Based on the patient’s self-report of past year use, the screen places him/her into 1 of 3 risk categories for SUD: no reported use, lower risk, and higher risk. Each risk level maps to suggested clinical actions that are summarized in the results section.
Kevin M. Simon, MD
Child & Adolescent Psychiatry Fellow
Boston Children’s Hospital
Clinical Fellow in Psychiatry
Harvard Medical School
Boston, Massachusetts
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
References
1. Palmer A, Karakus M, Mark T. Barriers faced by physicians in screening for substance use disorders among adolescents. Psychiatr Serv. 2019;70(5):409-412.
2. D’Souza-Li L, Harris SK. The future of screening, brief intervention and referral to treatment in adolescent primary care: research directions and dissemination challenges. Curr Opin Pediatr. 2016;28(4):434-440.
3. Levy S, Weiss R, Sherritt L, et al. An electronic screen for triaging adolescent substance use by risk levels. JAMA Pediatr. 2014;168(9):822-828.
4. Kelly SM, Gryczynski J, Mitchell SG, et al. Validity of brief screening instrument for adolescent tobacco, alcohol, and drug use. Pediatrics. 2014;133(5):819-826.
Continue to: The author responds
The author responds
I thank Dr. Simon for his words of encouragement. I agree that both the S2BI and BSTAD have high sensitivity and specificity and are easy to use for screening for the use of multiple substances. Once substance use is established, both tools recommend administering high-risk assessment with additional scales such as the CRAFFT. During the initial evaluation, many psychiatrists take their patient’s history of substance use in detail, including age of onset, frequency, amount used, severity, and the time of his/her last use, without using a screening instrument. My article focused on instruments that can determine whether there is need for a further detailed evaluation. I agree that the S2BI and BSTAD would assist psychiatrists or physicians in other specialties (eg, pediatrics, family medicine) who might not take a complete substance use history during their initial evaluations.
Shikha Verma, MD
Rogers Behavioral Health
Kenosha, Wisconsin
Assistant Professor
Department of Psychiatry and Behavioral Health
Rosalind Franklin University of Medicine and Science
North Chicago, Illinois
Continue to: Changes as a result of COVID-19
Changes as a result of COVID-19
I thank Dr. Nasrallah for his editorial “During a viral pandemic, anxiety is endemic: The psychiatric aspects of COVID-19” (From the Editor,
I appreciated the editorial because it got me thinking about how the pandemic has changed me and my family:
1. We are engaging more in social media.
2. I feel uncomfortable when I go to the grocery store.
3. I feel better when I don’t access the news about COVID-19.
4. My children need physical socialization with their friends (sports, games, other activities, etc.).
5. My children function better with a schedule, but we find it difficult to keep them on a good schedule. Our teenagers stay up late at night (because all of their friends do), and they sleep in late the next morning.
Here are some positive changes:
1. Creating a weekly family calendar on a dry-erase board, so the family can see what is going on during the week.
2. Creating responsibility for our older children (eg, washing their own clothes, cleaning their bathroom).
3. Eating most meals as a family and organizing meals better, too.
4. Playing games together.
5. Cleaning the house together.
6. Getting outside to walk the dog and appreciate nature more.
7. Exercising.
8. Utilizing positive social media.
9. Getting caught up on life.
Again, I thank Dr. Nasrallah for writing this editorial because it led me to self-reflect on this situation, and helped me feel normal.
Doug Dolenc
Westfield, Indiana
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
Love in the time of coronavirus
Several months ago, I sat with a woman just a few days after the emergent Cesarean section delivery of her first child. She cried as she told me about her entire life—childhood trauma, a pattern of difficult relationships, several miscarriages, and now, finally, a baby—delivered under circumstances so scary, all she remembered was overwhelming fear. Now, she had returned to the hospital with severe postpartum depression, layered with struggles that are common during the first days with a newborn—little sleep, loss of autonomy, guilt, and loneliness. It was hard to listen to it all, but I encouraged her to express her pain, believing that burdens are lighter when shared.
Words often fail us in times of desperation. Much of my education has involved borrowing words, phrases, or ideas from my experienced attendings and mentors, applying them like a salve when I don’t know what else to say. Sitting with another person in silence is often powerful enough, but when something needs to be said, I fall back on these inherited ideas. One of the mantras I often use, and what I said to my patient that day, is about hope: “When you’re down in this depression, you feel hopeless, and you can’t see the hope. It doesn’t mean there isn’t hope; just that you can’t see it.” I’ve watched that idea take root in patients who—despite their own beliefs in the moment—do get better, thus proving the point. Another favorite phrase: “With any luck at all, tomorrow will be better than today.” When you talk to someone on the worst day of their life, what else is there to say?
Today, my conversation with that woman seems like an eternity ago. Public discourse has been overtaken by coronavirus disease 2019 (COVID-19)—the journalism, reflections on the journalism, medical advice, debate about the medical advice, and the innumerable ways in which this worldwide strife has created pain: celebrations and long-awaited plans cancelled, weddings and funerals put on hold, isolation, loneliness, death, and, of course, the fear of death. Those feelings and any other permutations are valid; another phrase, “It’s OK to feel what you are feeling,” carries weight for me these days. I work in a hospital, so I add to the list the breathless fears about what’s going to happen in our local environment. The chronic uncertainty was wearing us thin even before we had begun to do here in Ohio what was already being done elsewhere: working extra shifts, intubating new patients, praying we don’t get sick ourselves.
Our work during COVID-19
Amidst this, my colleagues and I continue our work as psychiatrists, sitting with humans experiencing complex grief (a man whose wife died alone in a nursing home, because of visitor restrictions), confusion (delirium resulting from respiratory failure), and even psychosis (inability to access stabilizing medications coupled with crippling paranoia). These remain just as real and debilitating in a pandemic as they do in other times. In addition to pre-existing mental illnesses, for some individuals, the shared anxiety will progress to clinically significant disorders that may last even longer than the effects of the virus. The resulting complex symptoms could affect everything from home lives to interpersonal relationships to our local and global economies. These are not minor issues. Although often triaged aside in a disaster, our collective mental health remains in some ways more central than ever.
Modern psychiatry would not often use the word “love,” but that’s what I am trying to do—show love to the people who need it the most right now (which is all of us, really). This love takes strange shapes, and sometimes new forms, but it’s just about all I have to give. Like everyone else, I don’t have concrete answers for the grief and fear and panic. But I’m content to share the burden of pain, believing that burdens are lighter when shared. And I have a few words that, however little comfort they offer in the moment, are eventually proven true: Just because you can’t see the hope doesn’t mean it isn’t there. It’s OK to feel what you are feeling. With any luck at all, tomorrow will be better than today.
Several months ago, I sat with a woman just a few days after the emergent Cesarean section delivery of her first child. She cried as she told me about her entire life—childhood trauma, a pattern of difficult relationships, several miscarriages, and now, finally, a baby—delivered under circumstances so scary, all she remembered was overwhelming fear. Now, she had returned to the hospital with severe postpartum depression, layered with struggles that are common during the first days with a newborn—little sleep, loss of autonomy, guilt, and loneliness. It was hard to listen to it all, but I encouraged her to express her pain, believing that burdens are lighter when shared.
Words often fail us in times of desperation. Much of my education has involved borrowing words, phrases, or ideas from my experienced attendings and mentors, applying them like a salve when I don’t know what else to say. Sitting with another person in silence is often powerful enough, but when something needs to be said, I fall back on these inherited ideas. One of the mantras I often use, and what I said to my patient that day, is about hope: “When you’re down in this depression, you feel hopeless, and you can’t see the hope. It doesn’t mean there isn’t hope; just that you can’t see it.” I’ve watched that idea take root in patients who—despite their own beliefs in the moment—do get better, thus proving the point. Another favorite phrase: “With any luck at all, tomorrow will be better than today.” When you talk to someone on the worst day of their life, what else is there to say?
Today, my conversation with that woman seems like an eternity ago. Public discourse has been overtaken by coronavirus disease 2019 (COVID-19)—the journalism, reflections on the journalism, medical advice, debate about the medical advice, and the innumerable ways in which this worldwide strife has created pain: celebrations and long-awaited plans cancelled, weddings and funerals put on hold, isolation, loneliness, death, and, of course, the fear of death. Those feelings and any other permutations are valid; another phrase, “It’s OK to feel what you are feeling,” carries weight for me these days. I work in a hospital, so I add to the list the breathless fears about what’s going to happen in our local environment. The chronic uncertainty was wearing us thin even before we had begun to do here in Ohio what was already being done elsewhere: working extra shifts, intubating new patients, praying we don’t get sick ourselves.
Our work during COVID-19
Amidst this, my colleagues and I continue our work as psychiatrists, sitting with humans experiencing complex grief (a man whose wife died alone in a nursing home, because of visitor restrictions), confusion (delirium resulting from respiratory failure), and even psychosis (inability to access stabilizing medications coupled with crippling paranoia). These remain just as real and debilitating in a pandemic as they do in other times. In addition to pre-existing mental illnesses, for some individuals, the shared anxiety will progress to clinically significant disorders that may last even longer than the effects of the virus. The resulting complex symptoms could affect everything from home lives to interpersonal relationships to our local and global economies. These are not minor issues. Although often triaged aside in a disaster, our collective mental health remains in some ways more central than ever.
Modern psychiatry would not often use the word “love,” but that’s what I am trying to do—show love to the people who need it the most right now (which is all of us, really). This love takes strange shapes, and sometimes new forms, but it’s just about all I have to give. Like everyone else, I don’t have concrete answers for the grief and fear and panic. But I’m content to share the burden of pain, believing that burdens are lighter when shared. And I have a few words that, however little comfort they offer in the moment, are eventually proven true: Just because you can’t see the hope doesn’t mean it isn’t there. It’s OK to feel what you are feeling. With any luck at all, tomorrow will be better than today.
Several months ago, I sat with a woman just a few days after the emergent Cesarean section delivery of her first child. She cried as she told me about her entire life—childhood trauma, a pattern of difficult relationships, several miscarriages, and now, finally, a baby—delivered under circumstances so scary, all she remembered was overwhelming fear. Now, she had returned to the hospital with severe postpartum depression, layered with struggles that are common during the first days with a newborn—little sleep, loss of autonomy, guilt, and loneliness. It was hard to listen to it all, but I encouraged her to express her pain, believing that burdens are lighter when shared.
Words often fail us in times of desperation. Much of my education has involved borrowing words, phrases, or ideas from my experienced attendings and mentors, applying them like a salve when I don’t know what else to say. Sitting with another person in silence is often powerful enough, but when something needs to be said, I fall back on these inherited ideas. One of the mantras I often use, and what I said to my patient that day, is about hope: “When you’re down in this depression, you feel hopeless, and you can’t see the hope. It doesn’t mean there isn’t hope; just that you can’t see it.” I’ve watched that idea take root in patients who—despite their own beliefs in the moment—do get better, thus proving the point. Another favorite phrase: “With any luck at all, tomorrow will be better than today.” When you talk to someone on the worst day of their life, what else is there to say?
Today, my conversation with that woman seems like an eternity ago. Public discourse has been overtaken by coronavirus disease 2019 (COVID-19)—the journalism, reflections on the journalism, medical advice, debate about the medical advice, and the innumerable ways in which this worldwide strife has created pain: celebrations and long-awaited plans cancelled, weddings and funerals put on hold, isolation, loneliness, death, and, of course, the fear of death. Those feelings and any other permutations are valid; another phrase, “It’s OK to feel what you are feeling,” carries weight for me these days. I work in a hospital, so I add to the list the breathless fears about what’s going to happen in our local environment. The chronic uncertainty was wearing us thin even before we had begun to do here in Ohio what was already being done elsewhere: working extra shifts, intubating new patients, praying we don’t get sick ourselves.
Our work during COVID-19
Amidst this, my colleagues and I continue our work as psychiatrists, sitting with humans experiencing complex grief (a man whose wife died alone in a nursing home, because of visitor restrictions), confusion (delirium resulting from respiratory failure), and even psychosis (inability to access stabilizing medications coupled with crippling paranoia). These remain just as real and debilitating in a pandemic as they do in other times. In addition to pre-existing mental illnesses, for some individuals, the shared anxiety will progress to clinically significant disorders that may last even longer than the effects of the virus. The resulting complex symptoms could affect everything from home lives to interpersonal relationships to our local and global economies. These are not minor issues. Although often triaged aside in a disaster, our collective mental health remains in some ways more central than ever.
Modern psychiatry would not often use the word “love,” but that’s what I am trying to do—show love to the people who need it the most right now (which is all of us, really). This love takes strange shapes, and sometimes new forms, but it’s just about all I have to give. Like everyone else, I don’t have concrete answers for the grief and fear and panic. But I’m content to share the burden of pain, believing that burdens are lighter when shared. And I have a few words that, however little comfort they offer in the moment, are eventually proven true: Just because you can’t see the hope doesn’t mean it isn’t there. It’s OK to feel what you are feeling. With any luck at all, tomorrow will be better than today.
Posttraumatic stress disorder: From pathophysiology to pharmacology
Posttraumatic stress disorder (PTSD) occurs acutely and chronically in the aftermath of severe and potentially life-threatening trauma.1 The prevalence of PTSD varies significantly across countries and by type of trauma (Box1-7).
Box
In the general population, the prevalence of posttraumatic stress disorder (PTSD) varies from as low as 0.3% in China to as high as 6.1% in New Zealand1 and 6.8% in the United States.2 These rates are actually much lower than expected when one considers that severe trauma is experienced by 60.7% of men and 51.2% of women.3,4 Although the majority of individuals exposed to trauma experience emotional distress immediately following a traumatic event, most of them do not develop PTSD.5
It appears that the context of trauma is important: 12% to 15% of veterans experience PTSD, compared with 19% to 75% of crime victims and 80% of rape victims.1 The lifetime risk for PTSD is twice as high in women as it is in men,6 and genetic vulnerability may play a role. For example, twin studies showed that approximately 30% of the risk for PTSD may be mediated by genetic predisposition.7
Individuals who develop PTSD experience a wide range of symptoms.8 These can be categorized as PTSD-specific symptoms, or nonspecific symptoms. PTSD-specific symptoms include nightmares, flashbacks, dissociative reactions, hyperreactivity or hyperarousal, distress with reminders of trauma, and avoidance of trauma-related physical reminders and thoughts/feelings (Table8). Nonspecific symptoms include depressive and anxiety symptoms and significant problems in social, relationship, or work situations.8
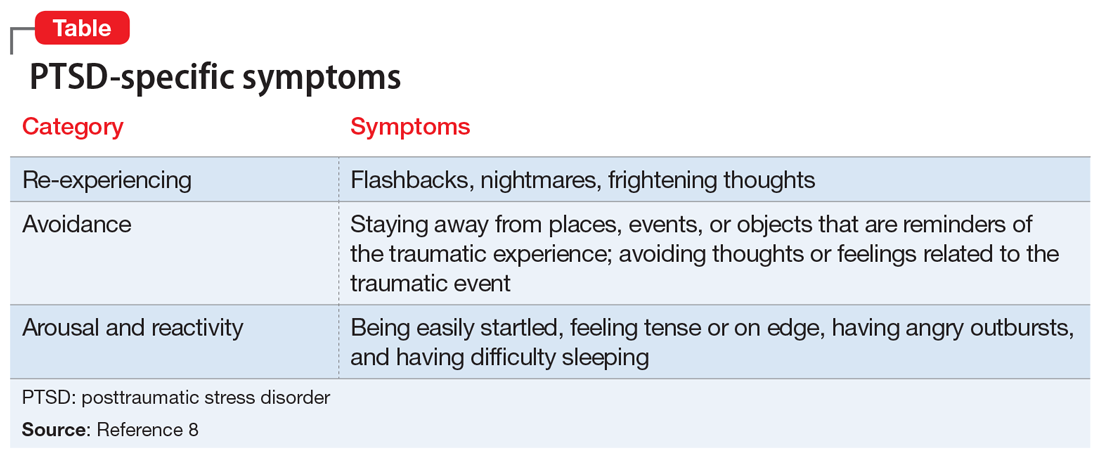
While successful treatment necessitates taking all of these symptoms into account, understanding the pathophysiology of PTSD can inform a more focused and rational treatment approach. In this article, we describe some key pathophysiologic PTSD studies, and focus on PTSD-specific psychopathology to inform treatment.
Brain systems implicated in PTSD
Neuropeptide Y (NPY) is an anxiolytic endogenous peptide that has connections to the hypothalamic-pituitary-adrenal (HPA) axis. Its levels can be modulated by stress.9 Preclinical and clinical studies strongly support a potential role of NPY dysfunction in the pathophysiology of PTSD. Lower concentrations of NPY increase susceptibility to PTSD in combat veterans10 and in animal models.11 Three single-nucleotide polymorphisms (SNPs) appear to mediate this effect.12 These findings strongly support pharmaceutical targeting this system as a useful therapeutic approach.13,14 Indeed, intranasal NPY administered as a single dose reduces anxiety in animal models15 and in humans,16 but this work has not yet translated into clinical tools.
Corticotropin-releasing hormone receptor (CRHR1) gene. Corticotropin-releasing hormone has been implicated in PTSD.17 Corticotropin-releasing hormone receptors (CRHR) are important mediators in response to stress.18,19 They bind corticotropin-releasing hormone and contribute to the integration of autonomic, behavioral, and immune responses to stress.20 Single-nucleotide polymorphisms in the regulatory portion of the CRHR1 gene are associated with an increased risk for depression in adults who have a history of child abuse.21
The CRHR1 receptor antagonist GSK561679 is an investigational agent for the treatment of mood and anxiety disorders.22 In exploratory studies,23,24 GSK561679 was found to inhibit fear-potentiated startle in patients with PTSD, but not overall PTSD symptoms, although a subset of women with a specific genetic variant of the CRHR1 gene (rs110402) experienced significant benefit.25,26 This suggests that we must learn more about this system before we proceed.27
Brain-derived neurotrophic factor (BDNF). The synthesis of BDNF is influenced by neuronal activity in the brain and plays a role in synaptic transmission and plasticity.28 Brain-derived neurotrophic factor is encoded by the BDNF gene, which has been implicated in stress vulnerability.29 A common SNP in the pro-region of the human BDNF gene results in a valine-to-methionine substitution at the 66th amino acid (Val66Met). The functional Val66Met polymorphism may have a role in the risk of developing PTSD. However, not all studies support this finding. One study found that an SNP with a resulting Val66Met polymorphism is associated with adult PTSD symptoms after childhood abuse, while a meta-analysis of 7 studies did not confirm this.30,31 We need to learn more about BDNF before we proceed.32
Continue to: Serotonin transporter (5-HTT) gene
Serotonin transporter (5-HTT) gene. Serotonin transporter is a monoamine transporter protein that terminates the neurotransmitter signal by transporting serotonin from the synaptic cleft back into the presynaptic neuron. It is encoded by the SLC6A4 gene, which resides on the long arm of chromosome 17(17q11.1-q12). It is a large gene with 31 kilo bases and 14 separate exons (transcribed regions).33,34
This gene has several variants. The best-studied is a variation in the promoter region. A 44-bp insertion or deletion yields the “long” and “short” alleles, respectively. The proteins produced by the 2 alleles are identical, but the amount of expressed protein is different. The short allele (“S”) is associated with a nearly 50% reduction in 5-HTT expression in both homozygotes and heterozygotes.35 A greater incidence of serotonin transporter promoter region (5-HTTLPR) S has been found in individuals with PTSD compared with those without PTSD,36-38 and 5-HTTLPR S increases the risk of PTSD in individuals with low social support39 or after very few traumatic events.40 The short allele variant is also associated with depression in individuals who face adversity.35,41
The overrepresentation of the short form of 5-HTTLPR in individuals who develop PTSD may represent a potential problem with current treatment paradigms, in which an antidepressant is the first-line treatment, because this allele is associated with reduced response to antidepressants.42,43 More distressing is the possible association of this allele with increased suicide risk, particularly violent suicide44 or repeated suicide attempts.45
Furthermore, a functional MRI study of patients who were anxious revealed that in individuals with the short allele, administration of
Catechol-o-methyltransferase (COMT) is one of the enzymes that degrades catecholamines such as dopamine, epinephrine, and norepinephrine (NE).47 In humans, COMT protein is encoded by the COMT gene. This gene is associated with allelic variants; the best-studied of these is Val158Met. COMT Val158Met polymorphism (rs4860) has been linked to deficits in stress response and emotional resilience.48,49 Val158Met is associated with a 40% reduction in enzyme activity and slower catalysis of catecholamines, resulting in increases in catecholamines levels in the brain, which may increase the risk of developing PTSD.50 Individuals homozygous for this SNP (Met/Met) are highly susceptible to develop PTSD independently of the severity of the trauma they experienced.51 The Val158Met polymorphism may be associated with other abnormalities, such as cognitive problems with specific frontal cortical activity, and also with improved antidepressant response (valine homozygotes less responsive than methionine homozygotes).52 This gene is available on gene testing profiles.
Continue to: The role of norepinephrine in PTSD
The role of norepinephrine in PTSD
Perhaps the greatest advance in the understanding of the pathophysiology of PTSD relates to changes in brain NE. The HPA axis is responsible for coordinating the hormonal response to stress. Dysregulation of this axis and increased activity of the central and peripheral noradrenergic systems are usually observed in patients with PTSD.53 Several monoamine neurotransmitters are important in the regulation and function of the HPA axis. Norepinephrine plays a major role in stress.
The clinical PTSD-specific criteria are all descriptions of excessive noradrenergic tone.54 For example, hypervigilance and hyperstartle are clearly anticipated as evidence of NE stimulation. Flashbacks, particularly those that might be precipitated by environmental cues, also can be a manifestation of the vigilance induced by NE. Sleep disturbances (insomnia and nightmares) are present; insomnia is reported more often than nightmares.55 Increased catecholamine levels, particularly NE, are a feature of sleep disturbances associated with middle insomnia. Dreams can be remembered only if you wake up during dreaming. Catecholamines do not change the content of dreams, just recall.56
In a study of central noradrenergic tone in patients with PTSD, 6 hourly CSF samples were collected from 11 male combat veterans with PTSD and 8 healthy controls.57 Participants with PTSD had significantly higher CSF NE concentrations (0.55 ± 0.17 pmol/ml vs 0.39 ± 0.16 pmol/mL in the PTSD and control groups, respectively; F = 4.49, P < .05).57 Overall PTSD symptoms correlated significantly with CSF NE levels (r = 0.82, P <.005), and PTSD-specific symptoms such as avoidance (r = 0.79, P = .004). Intrusive thoughts (r = 0.57, P = .07) and hyperarousal (r = 0.54, P = .09) were also related.57 This relationship is unique; patients with PTSD with predominant depressive symptoms do not have elevated plasma NE levels.58
In the human brain, there are 3 main groups of NE receptors: alpha-1 receptors, alpha-2 receptors, and beta receptors.59 Alpha-1 receptors (alpha-1A, alpha-1B, and alpha-1D) are postsynaptic and mediate increase in inositol trisphosphate (IP3) and intracellular calcium (Ca2+). Alpha-2 receptors (alpha-2A, alpha-2B, alpha-2C) in the CNS are presynaptic autoreceptors and serve to reduce NE release. Beta receptors (beta-1, beta-2, beta-3) inhibit cyclic adenosine monophosphate (cAMP) production.59 The effects of inhibition of alpha or beta receptors are different. Inhibition of beta receptors is associated with depressive symptoms and depressive syndrome, inhibition of peripheral beta receptors is associated with reductions in anxiety (generally reduction of pulse, sweating, tremor),60 and inhibition of central alpha-1 receptors is associated with reduced PTSD symptoms.61
Choice of agents for PTSD-specific symptoms
As outlined in the Table,8 PTSD is characterized by 3 types of symptoms that are specific for PTSD. Trauma-focused psychotherapy62,63 and selective serotonin reuptake inhibitors (SSRIs)64 are considered first-line therapy for PTSD. Only
Continue to: Serotonin transporter promoter...
Serotonin transporter promoter region gene short-type variants, which possibly increase an individual’s predisposition to developing PTSD, may explain the abundance of depressive symptoms in this condition and the subdued response to antidepressants. Specifically, an anticipated preponderance of these alleles may be associated with poorer outcomes. Non-SSRI treatments, such as low-dose
On the other hand, animal models support antagonism of the postsynaptic alpha-1 adrenergic receptor of the CNS as a target for PTSD treatment.71 Although
Quetiapine might be another non-SSRI option for treating patients with PTSD. It is an antagonist with high affinity tothehistamine-1 receptor at low doses. Norquetiapine is an alpha-2 antagonist that increases brain NE levels. Both quetiapine and norquetiapine are alpha-1 antagonists. There is no beta blockade and no SSRI effect, but some 5HT2A blockade, which may be anxiolytic. Compared with placebo, an average quetiapine dose of 258 mg/d resulted in significantly greater reductions in Clinician-Administered PTSD Scale total score, re-experiencing score, and hyperarousal score.73
Unfortunately, none of the non-SSRI options have been adequately evaluated. For now, clinicians need to continue to use SSRIs, and researchers need to continue to explore mechanism-guided alternatives.
Bottom Line
Understanding the mechanisms of the pathophysiology of posttraumatic stress disorder (PTSD) may allow clinicians to “jump ahead” of clinical studies and FDA indications. Clinicians may reasonably use alpha-1 antagonists (eg, prazosin, quetiapine) for general clinical improvement of patients with PTSD, particularly for PTSD-specific symptoms. Using antihistamines to reduce anxiety (especially in patients who have the COMT Val158Met polymorphism) may also be reasonable.
Related Resources
- North CS, Hong BA, Downs DL. PTSD: a systematic approach to diagnosis and treatment. Current Psychiatry. 2018;17(4):35-43.
- Zhang Y, Ren R, Sanford LD, et al. The effects of prazosin on sleep disturbances in post-traumatic stress disorder: a systematic review and meta-analysis. Sleep Med. 2019; 67:225-231.
Drug Brand Names
Aripiprazole • Abilify
Citalopram • Celexa
Paroxetine • Paxil
Prazosin • Minipress
Quetiapine • Seroquel
Sertraline • Zoloft
1. Javidi H, Yadollahie M. Post-traumatic stress disorder. Int J Occup Environ Med. 2012;3(1):2-9.
2. Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627.
3. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048-1060.
4. Breslau N, Kessler RC, Chilcoat HD, et al. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55(7):626-632.
5. Cerda M, Sagdeo A, Johnson J, et al. Genetic and environmental influences on psychiatric comorbidity: a systematic review. J Affect Disord. 2010;126(1-2):14-38.
6. Yehuda R, Hoge CW, McFarlane AC, et al. Post-traumatic stress disorder. Nat Rev Dis Primers. 2015;1:15057. doi: 10.1038/nrdp.2015.57.
7. True WR, Rice J, Eisen SA, et al. A twin study of genetic and environmental contributions to liability for posttraumatic stress symptoms. Arch Gen Psychiatry. 1993;50(4):257-264.
8. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013:271-280.
9. Reichmann F, Holzer P. Neuropeptide Y: a stressful review. Neuropeptides. 2016;55:99-109.
10. Yehuda R, Brand S, Yang RK. Plasma neuropeptide Y concentrations in combat exposed veterans: relationship to trauma exposure, recovery from PTSD, and coping. Biol Psychiatry. 2006;59(7):660-663.
11. Cohen H, Liu T, Kozlovsky N, et al. The neuropeptide Y (NPY)-ergic system is associated with behavioral resilience to stress exposure in an animal model of post-traumatic stress disorder. Neuropsychopharmacology. 2012;37(2):350-363.
12. Donner J, Sipilä T, Ripatti S, et al. Support for involvement of glutamate decarboxylase 1 and neuropeptide Y in anxiety susceptibility. Am J Med Genet B Neuropsychiatr Genet. 2012;159B(3):316-327.
13. Schmeltzer SN, Herman JP, Sah R. Neuropeptide Y (NPY) and posttraumatic stress disorder (PTSD): a translational update. Exp Neurol. 2016;284(pt B):196-210.
14. Kautz M, Charney DS, Murrough JW. Neuropeptide Y, resilience, and PTSD therapeutics. Neurosci Lett. 2017;649:164-169.
15. Serova LI, Laukova M, Alaluf LG, et al. Intranasal neuropeptide Y reverses anxiety and depressive-like behavior impaired by single prolonged stress PTSD model. Eur Neuropsychopharmacol. 2014;24(1):142-147.
16. Sayed S, Van Dam NT, Horn SR, et al. A randomized dose-ranging study of neuropeptide Y in patients with posttraumatic stress disorder. Int J Neuropsychopharmacol. 2018;21(1):3-11.
17. Toth M, Flandreau EI, Deslauriers J, et al. Overexpression of forebrain CRH during early life increases trauma susceptibility in adulthood. Neuropsychopharmacology. 2016;41(6):1681-1690.
18. White S, Acierno R, Ruggiero KJ, et al. Association of CRHR1 variants and posttraumatic stress symptoms in hurricane exposed adults. J Anxiety Disord. 2013;27(7):678-683.
19. Wolf EJ, Mitchell KS, Logue MW, et al. Corticotropin releasing hormone receptor 2 (CRHR-2) gene is associated with decreased risk and severity of posttraumatic stress disorder in women. Depress Anxiety. 2013;30(12):1161-1169.
20. Whitnall MH. Regulation of the hypothalamic corticotropin-releasing hormone neurosecretory system. Prog Neurobiol. 1993;40(5):573-629.
21. Bradley RG, Binder EB, Epstein MP, et al. Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Arch Gen Psychiatry. 2008;65(2):190-200.
22. Tellew JE, Lanier M, Moorjani M, et al. Discovery of NBI-77860/GSK561679, a potent corticotropin-releasing factor (CRF1) receptor antagonist with improved pharmacokinetic properties. Bioorg Med Chem Lett. 2010;20(24):7259-7264.
23. Dunlop BW, Rothbaum BO, Binder EB, et al. Evaluation of a corticotropin releasing hormone type 1 receptor antagonist in women with posttraumatic stress disorder: study protocol for a randomized controlled trial. Trials. 2014;15:240. doi: 10.1186/1745-6215-15-240.
24. Jovanovic T, Duncan EJ, Kaye J, et al. Psychophysiological treatment outcomes: Corticotropin-releasing factor type 1 receptor antagonist increases inhibition of fear-potentiated startle in PTSD patients. Psychophysiology. 2019:e13356. doi: 10.1111/psyp.13356.
25. Dunlop BW, Binder EB, Iosifescu D, et al. Corticotropin-releasing factor receptor 1 antagonism is ineffective for women with posttraumatic stress disorder. Biol Psychiatry. 2017;82(12):866-874.
26. Pape JC, Carrillo-Roa T, Rothbaum BO, et al. DNA methylation levels are associated with CRF1 receptor antagonist treatment outcome in women with post-traumatic stress disorder. Clin Epigenetics. 2018;10(1):136. doi: 10.1186/s13148-018-0569-x.
27. Murrough JW, Charney DS. Corticotropin-releasing factor type 1 receptor antagonists for stress-related disorders: time to call it quits? Biol Psychiatry. 2017;82(12):858-860.
28. Leal G, Bramham CR, Duarte CB. BDNF and hippocampal synaptic plasticity. Vitam Horm. 2017;104:153-195.
29. Groves JO. Is it time to reassess the BDNF hypothesis of depression? Mol Psychiatry. 2007;12:1079-1088.
30. Frustaci A, Pozzi G, Gianfagna F, et al. Meta-analysis of the brain-derived neurotrophic factor gene (BDNF) Val66Met polymorphism in anxiety disorders and anxiety-related personality traits. Neuropsychobiology. 2008;58(3-4):163-170.
31. Gatt JM, Nemeroff CB, Dobson-Stone C, et al. Interactions between BDNF Val66Met polymorphism and early life stress predict brain and arousal pathways to syndromal depression and anxiety. Mol Psychiatry. 2009;14(7):681-695.
32. Ragen BJ, Seidel J, Chollak C, et al. Investigational drugs under development for the treatment of PTSD. Expert Opin Investig Drugs. 2015;24(5):659-672.
33. Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301(5631):386-389.
34. Murphy DL, Fox MA, Timpano KR, et al. How the serotonin story is being rewritten by new gene-based discoveries principally related to SLC6A4, the serotonin transporter gene, which functions to influence all cellular serotonin systems. Neuropharmacology. 2008;55(6):932-960.
35. Luddington NS, Mandadapu A, Husk M, et al. Clinical implications of genetic variation in the serotonin transporter promoter region: a review. Prim Care Compan J Clin Psychiatry. 2009;11:(3):93-102.
36. Lee HJ, Lee MS, Kang RH, et al. Influence of the serotonin transporter promoter gene polymorphism on susceptibility to posttraumatic stress disorder. Depress Anxiety. 2005;21(3):135-139.
37. Liu Y, Garrett ME, Dennis MF, et al. An examination of the association between 5-HTTLPR, combat exposure, and PTSD diagnosis among U.S. veterans. PLoS One. 2015;10(3):e0119998. doi: 10.1371/journal.pone.0119998.
38. Mehta D, Voisey J, Bruenig D, et al. Transcriptome analysis reveals novel genes and immune networks dysregulated in veterans with PTSD. Brain Behav Immun. 2018;74:133-142. doi: 10.1016/j.bbi.2018.08.014.
39. Kilpatrick DG, Koenen KC, Ruggiero KJ, et al. The serotonin transporter genotype and social support and moderation of posttraumatic stress disorder and depression in hurricane-exposed adults. Am J Psychiatry. 2007;164(11):1693-1699.
40. Kolassa IT, Ertl V, Eckart C, et al. Association study of trauma load and SLC6A4 promoter polymorphism in posttraumatic stress disorder: evidence from survivors of the Rwandan genocide. J Clin Psychiatry. 2010;71(5):543-547.
41. Bryant RA, Felmingham KL, Falconer EM, et al. Preliminary evidence of the short allele of the serotonin transporter gene predicting poor response to cognitive behavior therapy in posttraumatic stress disorder. Biol Psychiatry. 2010;67(12):1217-1219.
42. Mrazek DA, Rush AJ, Biernacka JM, et al. SLC6A4 variation and citalopram response. Am J Med Genet B Neuropsychiatr Genet. 2009;150B(3):341-351.
43. Shiroma PR, Drews MS, Geske JR, et al. SLC6A4 polymorphisms and age of onset in late-life depression on treatment outcomes with citalopram: a Sequenced Treatment Alternatives to Relieve Depression (STAR*D) report. Am J Geriatr Psychiatry. 2014;22(11):1140-1148.
44. Fanelli G, Serretti A. The influence of the serotonin transporter gene 5-HTTLPR polymorphism on suicidal behaviors: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2019;88:375-387.
45. Courtet P, Picot MC, Bellivier F, et al. Serotonin transporter gene may be involved in short-term risk of subsequent suicide attempts. Biol Psychiatry. 2003;55(1):46-51.
46. Outhred T, Das P, Dobson-Stone C, et al. The impact of 5-HTTLPR on acute serotonin transporter blockade by escitalopram on emotion processing: Preliminary findings from a randomised, crossover fMRI study. Aust NZ J Psychiatry. 2014;48(12):1115-1125.
47. Lachman HM, Papolos DF, Saito T, et al. Human catechol-O-methyltransferase pharmacogenetics: description of a functional polymorphism and its potential application to neuropsychiatric disorders. Pharmacogenetics. 1996;6(3):243-250.
48. Valente NL, Vallada H, Cordeiro Q, et al. Catechol-O-methyltransferase (COMT) val158met polymorphism as a risk factor for PTSD after urban violence. J Mol Neurosci. 2011;43(3):516-523.
49. van Rooij SJ, Stevens JS, Ely TD, et al. Childhood trauma and COMT genotype interact to increase hippocampal activation in resilient individuals. Front Psychiatry. 2016;7:156. doi: 10.3389/fpsyt.2016.00156.
50. Wu G, Feder A, Cohen H, et al. Understanding resilience. Front Behav Neuroscience. 2013;7:10. doi: 10.3389/fnbeh.2013.00010.
51. Kolassa I, Kolassa S, Ertl V, et al. The risk of posttraumatic stress disorder after trauma depends on traumatic load and the catechol-O-methyltransferase Val(158)Met polymorphism. Biol Psychiatry. 2010;67(4):304-308.
52. Bruder GE, Keilp JG, Xu H, et al. Catechol-O-methyltransferase (COMT) genotypes and working memory: associations with differing cognitive operations. Biol Psychiatry. 2005;58(11):901-907.
53. Strawn JR, Geracioti TD Jr. Noradrenergic dysfunction and the psychopharmacology of posttraumatic stress disorder. Depress Anxiety. 2008;25(3):260-271.
54. Hendrickson RC, Raskind MA. Noradrenergic dysregulation in the pathophysiology of PTSD. Exp Neurol. 2016;284(pt B):181-195.
55. Neylan TC, Marmar CR, Metzler TJ, et al. Sleep disturbances in the Vietnam generation: findings from a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1998;155(7):929-933.
56. Roehrs TA, Roth T. Hyperarousal in insomnia and hypnotic dose escalation. Sleep Med. 2016;23:16-20.
57. Geracioti TD Jr, Baker DG, Ekhator NN, et al. CSF Norepinephrine concentrations in posttraumatic stress disorder. Am J Psychiatry. 2001;158(8):1227-1230.
58. Yehuda R, Siever LJ, Teicher MH, et al. Plasma norepinephrine and 3-methoxy-4-hydroxyphenylglycol concentrations and severity of depression in combat posttraumatic stress disorder and major depressive disorder. Biol Psychiatry. 1998;44(1):56-63.
59. Molinoff PB. Alpha- and beta-adrenergic receptor subtypes properties, distribution and regulation. Drugs. 1984;28(suppl 2):1-15.
60. El-Mallakh RS. The use of beta-blockers in psychiatry. Res Staff Phys. 1989;35:49-52,59,62.
61. Raskind MA, Peterson K, Williams T, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. 2013;170(9):1003-1010.
62. Bisson JI, Roberts NP, Andrew M, et al. Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev. 2013;(12):CD003388.
63. Steenkamp MM, Litz BT, Hoge CW, et al. Psychotherapy for military-related PTSD: a review of randomized clinical trials. JAMA. 2015;314(5):489-500.
64. Hoskins M, Pearce J, Bethell A, et al. Pharmacotherapy for post-traumatic stress disorder: systematic review and meta-analysis. Br J Psychiatry. 2015;206(2):93-100.
65. Belkin MR, Schwartz TL. Alpha-2 receptor agonists for the treatment of posttraumatic stress disorder. Drugs Context. 2015;4:212286. doi: 10.7573/dic.212286.
66. Brady K, Pearlstein T, Asnis GM, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA. 2000;283(14):1837-1844.
67. Davidson JRT, Landerman LR, Farfel GM, et al. Characterizing the effects of sertraline in post-traumatic stress disorder. Psychol Med. 2002;32(4):661-670.
68. Hertzberg MA, Feldman ME, Beckham JC, et al. Lack of efficacy for fluoxetine in PTSD: a placebo controlled trial in combat veterans. Ann Clin Psychiatry. 2000;12(2):101-105.
69. Friedman MJ, Marmar CR, Baker DG, et al. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. J Clin Psychiatry. 2007;68(5):711-720.
70. Mello MF, Costa MCP, Schoedl AF, et al. Aripiprazole in the treatment of posttraumatic stress disorder: an open-label trial. Rev Bras Psiquiatr. 2008;30(4):358-361.
71. Birnbaum S, Gobeske KT, Auerbach J, et al. A role for norepinephrine in stress-induced cognitive deficits: alpha-1-adrenoceptor mediation in the prefrontal cortex. Biol Psychiatry. 1999;46(9):1266-1274.
72. Ahmadpanah M, Sabzeiee P, Hosseini SM, et al. Comparing the effect of prazosin and hydroxyzine on sleep quality in patients suffering from posttraumatic stress disorder. Neuropsychobiology. 2014;69(4):235-242.
73. Villarreal G, Hamner MB, Cañive JM, et al. Efficacy of quetiapine monotherapy in posttraumatic stress disorder: a randomized, placebo-controlled trial. Am J Psychiatry. 2016;173(12):1205-1212.
Posttraumatic stress disorder (PTSD) occurs acutely and chronically in the aftermath of severe and potentially life-threatening trauma.1 The prevalence of PTSD varies significantly across countries and by type of trauma (Box1-7).
Box
In the general population, the prevalence of posttraumatic stress disorder (PTSD) varies from as low as 0.3% in China to as high as 6.1% in New Zealand1 and 6.8% in the United States.2 These rates are actually much lower than expected when one considers that severe trauma is experienced by 60.7% of men and 51.2% of women.3,4 Although the majority of individuals exposed to trauma experience emotional distress immediately following a traumatic event, most of them do not develop PTSD.5
It appears that the context of trauma is important: 12% to 15% of veterans experience PTSD, compared with 19% to 75% of crime victims and 80% of rape victims.1 The lifetime risk for PTSD is twice as high in women as it is in men,6 and genetic vulnerability may play a role. For example, twin studies showed that approximately 30% of the risk for PTSD may be mediated by genetic predisposition.7
Individuals who develop PTSD experience a wide range of symptoms.8 These can be categorized as PTSD-specific symptoms, or nonspecific symptoms. PTSD-specific symptoms include nightmares, flashbacks, dissociative reactions, hyperreactivity or hyperarousal, distress with reminders of trauma, and avoidance of trauma-related physical reminders and thoughts/feelings (Table8). Nonspecific symptoms include depressive and anxiety symptoms and significant problems in social, relationship, or work situations.8
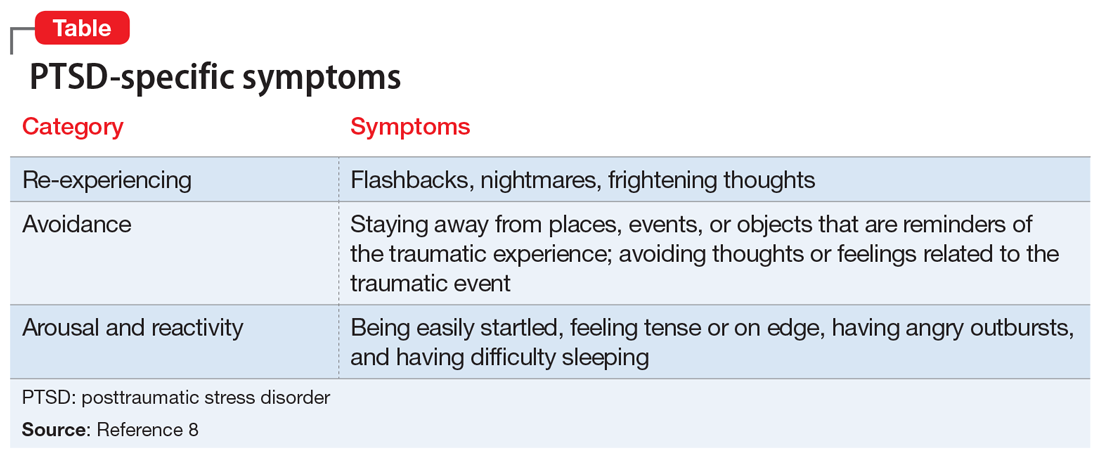
While successful treatment necessitates taking all of these symptoms into account, understanding the pathophysiology of PTSD can inform a more focused and rational treatment approach. In this article, we describe some key pathophysiologic PTSD studies, and focus on PTSD-specific psychopathology to inform treatment.
Brain systems implicated in PTSD
Neuropeptide Y (NPY) is an anxiolytic endogenous peptide that has connections to the hypothalamic-pituitary-adrenal (HPA) axis. Its levels can be modulated by stress.9 Preclinical and clinical studies strongly support a potential role of NPY dysfunction in the pathophysiology of PTSD. Lower concentrations of NPY increase susceptibility to PTSD in combat veterans10 and in animal models.11 Three single-nucleotide polymorphisms (SNPs) appear to mediate this effect.12 These findings strongly support pharmaceutical targeting this system as a useful therapeutic approach.13,14 Indeed, intranasal NPY administered as a single dose reduces anxiety in animal models15 and in humans,16 but this work has not yet translated into clinical tools.
Corticotropin-releasing hormone receptor (CRHR1) gene. Corticotropin-releasing hormone has been implicated in PTSD.17 Corticotropin-releasing hormone receptors (CRHR) are important mediators in response to stress.18,19 They bind corticotropin-releasing hormone and contribute to the integration of autonomic, behavioral, and immune responses to stress.20 Single-nucleotide polymorphisms in the regulatory portion of the CRHR1 gene are associated with an increased risk for depression in adults who have a history of child abuse.21
The CRHR1 receptor antagonist GSK561679 is an investigational agent for the treatment of mood and anxiety disorders.22 In exploratory studies,23,24 GSK561679 was found to inhibit fear-potentiated startle in patients with PTSD, but not overall PTSD symptoms, although a subset of women with a specific genetic variant of the CRHR1 gene (rs110402) experienced significant benefit.25,26 This suggests that we must learn more about this system before we proceed.27
Brain-derived neurotrophic factor (BDNF). The synthesis of BDNF is influenced by neuronal activity in the brain and plays a role in synaptic transmission and plasticity.28 Brain-derived neurotrophic factor is encoded by the BDNF gene, which has been implicated in stress vulnerability.29 A common SNP in the pro-region of the human BDNF gene results in a valine-to-methionine substitution at the 66th amino acid (Val66Met). The functional Val66Met polymorphism may have a role in the risk of developing PTSD. However, not all studies support this finding. One study found that an SNP with a resulting Val66Met polymorphism is associated with adult PTSD symptoms after childhood abuse, while a meta-analysis of 7 studies did not confirm this.30,31 We need to learn more about BDNF before we proceed.32
Continue to: Serotonin transporter (5-HTT) gene
Serotonin transporter (5-HTT) gene. Serotonin transporter is a monoamine transporter protein that terminates the neurotransmitter signal by transporting serotonin from the synaptic cleft back into the presynaptic neuron. It is encoded by the SLC6A4 gene, which resides on the long arm of chromosome 17(17q11.1-q12). It is a large gene with 31 kilo bases and 14 separate exons (transcribed regions).33,34
This gene has several variants. The best-studied is a variation in the promoter region. A 44-bp insertion or deletion yields the “long” and “short” alleles, respectively. The proteins produced by the 2 alleles are identical, but the amount of expressed protein is different. The short allele (“S”) is associated with a nearly 50% reduction in 5-HTT expression in both homozygotes and heterozygotes.35 A greater incidence of serotonin transporter promoter region (5-HTTLPR) S has been found in individuals with PTSD compared with those without PTSD,36-38 and 5-HTTLPR S increases the risk of PTSD in individuals with low social support39 or after very few traumatic events.40 The short allele variant is also associated with depression in individuals who face adversity.35,41
The overrepresentation of the short form of 5-HTTLPR in individuals who develop PTSD may represent a potential problem with current treatment paradigms, in which an antidepressant is the first-line treatment, because this allele is associated with reduced response to antidepressants.42,43 More distressing is the possible association of this allele with increased suicide risk, particularly violent suicide44 or repeated suicide attempts.45
Furthermore, a functional MRI study of patients who were anxious revealed that in individuals with the short allele, administration of
Catechol-o-methyltransferase (COMT) is one of the enzymes that degrades catecholamines such as dopamine, epinephrine, and norepinephrine (NE).47 In humans, COMT protein is encoded by the COMT gene. This gene is associated with allelic variants; the best-studied of these is Val158Met. COMT Val158Met polymorphism (rs4860) has been linked to deficits in stress response and emotional resilience.48,49 Val158Met is associated with a 40% reduction in enzyme activity and slower catalysis of catecholamines, resulting in increases in catecholamines levels in the brain, which may increase the risk of developing PTSD.50 Individuals homozygous for this SNP (Met/Met) are highly susceptible to develop PTSD independently of the severity of the trauma they experienced.51 The Val158Met polymorphism may be associated with other abnormalities, such as cognitive problems with specific frontal cortical activity, and also with improved antidepressant response (valine homozygotes less responsive than methionine homozygotes).52 This gene is available on gene testing profiles.
Continue to: The role of norepinephrine in PTSD
The role of norepinephrine in PTSD
Perhaps the greatest advance in the understanding of the pathophysiology of PTSD relates to changes in brain NE. The HPA axis is responsible for coordinating the hormonal response to stress. Dysregulation of this axis and increased activity of the central and peripheral noradrenergic systems are usually observed in patients with PTSD.53 Several monoamine neurotransmitters are important in the regulation and function of the HPA axis. Norepinephrine plays a major role in stress.
The clinical PTSD-specific criteria are all descriptions of excessive noradrenergic tone.54 For example, hypervigilance and hyperstartle are clearly anticipated as evidence of NE stimulation. Flashbacks, particularly those that might be precipitated by environmental cues, also can be a manifestation of the vigilance induced by NE. Sleep disturbances (insomnia and nightmares) are present; insomnia is reported more often than nightmares.55 Increased catecholamine levels, particularly NE, are a feature of sleep disturbances associated with middle insomnia. Dreams can be remembered only if you wake up during dreaming. Catecholamines do not change the content of dreams, just recall.56
In a study of central noradrenergic tone in patients with PTSD, 6 hourly CSF samples were collected from 11 male combat veterans with PTSD and 8 healthy controls.57 Participants with PTSD had significantly higher CSF NE concentrations (0.55 ± 0.17 pmol/ml vs 0.39 ± 0.16 pmol/mL in the PTSD and control groups, respectively; F = 4.49, P < .05).57 Overall PTSD symptoms correlated significantly with CSF NE levels (r = 0.82, P <.005), and PTSD-specific symptoms such as avoidance (r = 0.79, P = .004). Intrusive thoughts (r = 0.57, P = .07) and hyperarousal (r = 0.54, P = .09) were also related.57 This relationship is unique; patients with PTSD with predominant depressive symptoms do not have elevated plasma NE levels.58
In the human brain, there are 3 main groups of NE receptors: alpha-1 receptors, alpha-2 receptors, and beta receptors.59 Alpha-1 receptors (alpha-1A, alpha-1B, and alpha-1D) are postsynaptic and mediate increase in inositol trisphosphate (IP3) and intracellular calcium (Ca2+). Alpha-2 receptors (alpha-2A, alpha-2B, alpha-2C) in the CNS are presynaptic autoreceptors and serve to reduce NE release. Beta receptors (beta-1, beta-2, beta-3) inhibit cyclic adenosine monophosphate (cAMP) production.59 The effects of inhibition of alpha or beta receptors are different. Inhibition of beta receptors is associated with depressive symptoms and depressive syndrome, inhibition of peripheral beta receptors is associated with reductions in anxiety (generally reduction of pulse, sweating, tremor),60 and inhibition of central alpha-1 receptors is associated with reduced PTSD symptoms.61
Choice of agents for PTSD-specific symptoms
As outlined in the Table,8 PTSD is characterized by 3 types of symptoms that are specific for PTSD. Trauma-focused psychotherapy62,63 and selective serotonin reuptake inhibitors (SSRIs)64 are considered first-line therapy for PTSD. Only
Continue to: Serotonin transporter promoter...
Serotonin transporter promoter region gene short-type variants, which possibly increase an individual’s predisposition to developing PTSD, may explain the abundance of depressive symptoms in this condition and the subdued response to antidepressants. Specifically, an anticipated preponderance of these alleles may be associated with poorer outcomes. Non-SSRI treatments, such as low-dose
On the other hand, animal models support antagonism of the postsynaptic alpha-1 adrenergic receptor of the CNS as a target for PTSD treatment.71 Although
Quetiapine might be another non-SSRI option for treating patients with PTSD. It is an antagonist with high affinity tothehistamine-1 receptor at low doses. Norquetiapine is an alpha-2 antagonist that increases brain NE levels. Both quetiapine and norquetiapine are alpha-1 antagonists. There is no beta blockade and no SSRI effect, but some 5HT2A blockade, which may be anxiolytic. Compared with placebo, an average quetiapine dose of 258 mg/d resulted in significantly greater reductions in Clinician-Administered PTSD Scale total score, re-experiencing score, and hyperarousal score.73
Unfortunately, none of the non-SSRI options have been adequately evaluated. For now, clinicians need to continue to use SSRIs, and researchers need to continue to explore mechanism-guided alternatives.
Bottom Line
Understanding the mechanisms of the pathophysiology of posttraumatic stress disorder (PTSD) may allow clinicians to “jump ahead” of clinical studies and FDA indications. Clinicians may reasonably use alpha-1 antagonists (eg, prazosin, quetiapine) for general clinical improvement of patients with PTSD, particularly for PTSD-specific symptoms. Using antihistamines to reduce anxiety (especially in patients who have the COMT Val158Met polymorphism) may also be reasonable.
Related Resources
- North CS, Hong BA, Downs DL. PTSD: a systematic approach to diagnosis and treatment. Current Psychiatry. 2018;17(4):35-43.
- Zhang Y, Ren R, Sanford LD, et al. The effects of prazosin on sleep disturbances in post-traumatic stress disorder: a systematic review and meta-analysis. Sleep Med. 2019; 67:225-231.
Drug Brand Names
Aripiprazole • Abilify
Citalopram • Celexa
Paroxetine • Paxil
Prazosin • Minipress
Quetiapine • Seroquel
Sertraline • Zoloft
Posttraumatic stress disorder (PTSD) occurs acutely and chronically in the aftermath of severe and potentially life-threatening trauma.1 The prevalence of PTSD varies significantly across countries and by type of trauma (Box1-7).
Box
In the general population, the prevalence of posttraumatic stress disorder (PTSD) varies from as low as 0.3% in China to as high as 6.1% in New Zealand1 and 6.8% in the United States.2 These rates are actually much lower than expected when one considers that severe trauma is experienced by 60.7% of men and 51.2% of women.3,4 Although the majority of individuals exposed to trauma experience emotional distress immediately following a traumatic event, most of them do not develop PTSD.5
It appears that the context of trauma is important: 12% to 15% of veterans experience PTSD, compared with 19% to 75% of crime victims and 80% of rape victims.1 The lifetime risk for PTSD is twice as high in women as it is in men,6 and genetic vulnerability may play a role. For example, twin studies showed that approximately 30% of the risk for PTSD may be mediated by genetic predisposition.7
Individuals who develop PTSD experience a wide range of symptoms.8 These can be categorized as PTSD-specific symptoms, or nonspecific symptoms. PTSD-specific symptoms include nightmares, flashbacks, dissociative reactions, hyperreactivity or hyperarousal, distress with reminders of trauma, and avoidance of trauma-related physical reminders and thoughts/feelings (Table8). Nonspecific symptoms include depressive and anxiety symptoms and significant problems in social, relationship, or work situations.8
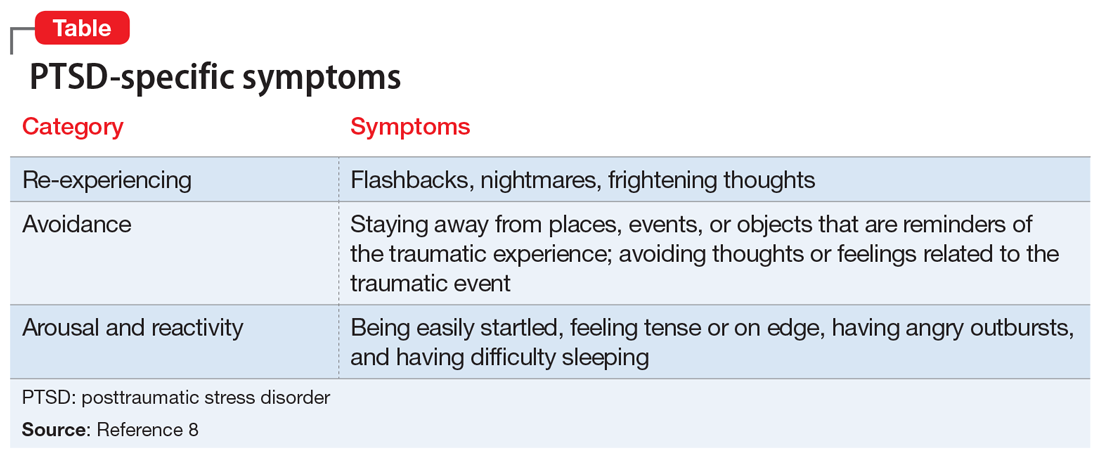
While successful treatment necessitates taking all of these symptoms into account, understanding the pathophysiology of PTSD can inform a more focused and rational treatment approach. In this article, we describe some key pathophysiologic PTSD studies, and focus on PTSD-specific psychopathology to inform treatment.
Brain systems implicated in PTSD
Neuropeptide Y (NPY) is an anxiolytic endogenous peptide that has connections to the hypothalamic-pituitary-adrenal (HPA) axis. Its levels can be modulated by stress.9 Preclinical and clinical studies strongly support a potential role of NPY dysfunction in the pathophysiology of PTSD. Lower concentrations of NPY increase susceptibility to PTSD in combat veterans10 and in animal models.11 Three single-nucleotide polymorphisms (SNPs) appear to mediate this effect.12 These findings strongly support pharmaceutical targeting this system as a useful therapeutic approach.13,14 Indeed, intranasal NPY administered as a single dose reduces anxiety in animal models15 and in humans,16 but this work has not yet translated into clinical tools.
Corticotropin-releasing hormone receptor (CRHR1) gene. Corticotropin-releasing hormone has been implicated in PTSD.17 Corticotropin-releasing hormone receptors (CRHR) are important mediators in response to stress.18,19 They bind corticotropin-releasing hormone and contribute to the integration of autonomic, behavioral, and immune responses to stress.20 Single-nucleotide polymorphisms in the regulatory portion of the CRHR1 gene are associated with an increased risk for depression in adults who have a history of child abuse.21
The CRHR1 receptor antagonist GSK561679 is an investigational agent for the treatment of mood and anxiety disorders.22 In exploratory studies,23,24 GSK561679 was found to inhibit fear-potentiated startle in patients with PTSD, but not overall PTSD symptoms, although a subset of women with a specific genetic variant of the CRHR1 gene (rs110402) experienced significant benefit.25,26 This suggests that we must learn more about this system before we proceed.27
Brain-derived neurotrophic factor (BDNF). The synthesis of BDNF is influenced by neuronal activity in the brain and plays a role in synaptic transmission and plasticity.28 Brain-derived neurotrophic factor is encoded by the BDNF gene, which has been implicated in stress vulnerability.29 A common SNP in the pro-region of the human BDNF gene results in a valine-to-methionine substitution at the 66th amino acid (Val66Met). The functional Val66Met polymorphism may have a role in the risk of developing PTSD. However, not all studies support this finding. One study found that an SNP with a resulting Val66Met polymorphism is associated with adult PTSD symptoms after childhood abuse, while a meta-analysis of 7 studies did not confirm this.30,31 We need to learn more about BDNF before we proceed.32
Continue to: Serotonin transporter (5-HTT) gene
Serotonin transporter (5-HTT) gene. Serotonin transporter is a monoamine transporter protein that terminates the neurotransmitter signal by transporting serotonin from the synaptic cleft back into the presynaptic neuron. It is encoded by the SLC6A4 gene, which resides on the long arm of chromosome 17(17q11.1-q12). It is a large gene with 31 kilo bases and 14 separate exons (transcribed regions).33,34
This gene has several variants. The best-studied is a variation in the promoter region. A 44-bp insertion or deletion yields the “long” and “short” alleles, respectively. The proteins produced by the 2 alleles are identical, but the amount of expressed protein is different. The short allele (“S”) is associated with a nearly 50% reduction in 5-HTT expression in both homozygotes and heterozygotes.35 A greater incidence of serotonin transporter promoter region (5-HTTLPR) S has been found in individuals with PTSD compared with those without PTSD,36-38 and 5-HTTLPR S increases the risk of PTSD in individuals with low social support39 or after very few traumatic events.40 The short allele variant is also associated with depression in individuals who face adversity.35,41
The overrepresentation of the short form of 5-HTTLPR in individuals who develop PTSD may represent a potential problem with current treatment paradigms, in which an antidepressant is the first-line treatment, because this allele is associated with reduced response to antidepressants.42,43 More distressing is the possible association of this allele with increased suicide risk, particularly violent suicide44 or repeated suicide attempts.45
Furthermore, a functional MRI study of patients who were anxious revealed that in individuals with the short allele, administration of
Catechol-o-methyltransferase (COMT) is one of the enzymes that degrades catecholamines such as dopamine, epinephrine, and norepinephrine (NE).47 In humans, COMT protein is encoded by the COMT gene. This gene is associated with allelic variants; the best-studied of these is Val158Met. COMT Val158Met polymorphism (rs4860) has been linked to deficits in stress response and emotional resilience.48,49 Val158Met is associated with a 40% reduction in enzyme activity and slower catalysis of catecholamines, resulting in increases in catecholamines levels in the brain, which may increase the risk of developing PTSD.50 Individuals homozygous for this SNP (Met/Met) are highly susceptible to develop PTSD independently of the severity of the trauma they experienced.51 The Val158Met polymorphism may be associated with other abnormalities, such as cognitive problems with specific frontal cortical activity, and also with improved antidepressant response (valine homozygotes less responsive than methionine homozygotes).52 This gene is available on gene testing profiles.
Continue to: The role of norepinephrine in PTSD
The role of norepinephrine in PTSD
Perhaps the greatest advance in the understanding of the pathophysiology of PTSD relates to changes in brain NE. The HPA axis is responsible for coordinating the hormonal response to stress. Dysregulation of this axis and increased activity of the central and peripheral noradrenergic systems are usually observed in patients with PTSD.53 Several monoamine neurotransmitters are important in the regulation and function of the HPA axis. Norepinephrine plays a major role in stress.
The clinical PTSD-specific criteria are all descriptions of excessive noradrenergic tone.54 For example, hypervigilance and hyperstartle are clearly anticipated as evidence of NE stimulation. Flashbacks, particularly those that might be precipitated by environmental cues, also can be a manifestation of the vigilance induced by NE. Sleep disturbances (insomnia and nightmares) are present; insomnia is reported more often than nightmares.55 Increased catecholamine levels, particularly NE, are a feature of sleep disturbances associated with middle insomnia. Dreams can be remembered only if you wake up during dreaming. Catecholamines do not change the content of dreams, just recall.56
In a study of central noradrenergic tone in patients with PTSD, 6 hourly CSF samples were collected from 11 male combat veterans with PTSD and 8 healthy controls.57 Participants with PTSD had significantly higher CSF NE concentrations (0.55 ± 0.17 pmol/ml vs 0.39 ± 0.16 pmol/mL in the PTSD and control groups, respectively; F = 4.49, P < .05).57 Overall PTSD symptoms correlated significantly with CSF NE levels (r = 0.82, P <.005), and PTSD-specific symptoms such as avoidance (r = 0.79, P = .004). Intrusive thoughts (r = 0.57, P = .07) and hyperarousal (r = 0.54, P = .09) were also related.57 This relationship is unique; patients with PTSD with predominant depressive symptoms do not have elevated plasma NE levels.58
In the human brain, there are 3 main groups of NE receptors: alpha-1 receptors, alpha-2 receptors, and beta receptors.59 Alpha-1 receptors (alpha-1A, alpha-1B, and alpha-1D) are postsynaptic and mediate increase in inositol trisphosphate (IP3) and intracellular calcium (Ca2+). Alpha-2 receptors (alpha-2A, alpha-2B, alpha-2C) in the CNS are presynaptic autoreceptors and serve to reduce NE release. Beta receptors (beta-1, beta-2, beta-3) inhibit cyclic adenosine monophosphate (cAMP) production.59 The effects of inhibition of alpha or beta receptors are different. Inhibition of beta receptors is associated with depressive symptoms and depressive syndrome, inhibition of peripheral beta receptors is associated with reductions in anxiety (generally reduction of pulse, sweating, tremor),60 and inhibition of central alpha-1 receptors is associated with reduced PTSD symptoms.61
Choice of agents for PTSD-specific symptoms
As outlined in the Table,8 PTSD is characterized by 3 types of symptoms that are specific for PTSD. Trauma-focused psychotherapy62,63 and selective serotonin reuptake inhibitors (SSRIs)64 are considered first-line therapy for PTSD. Only
Continue to: Serotonin transporter promoter...
Serotonin transporter promoter region gene short-type variants, which possibly increase an individual’s predisposition to developing PTSD, may explain the abundance of depressive symptoms in this condition and the subdued response to antidepressants. Specifically, an anticipated preponderance of these alleles may be associated with poorer outcomes. Non-SSRI treatments, such as low-dose
On the other hand, animal models support antagonism of the postsynaptic alpha-1 adrenergic receptor of the CNS as a target for PTSD treatment.71 Although
Quetiapine might be another non-SSRI option for treating patients with PTSD. It is an antagonist with high affinity tothehistamine-1 receptor at low doses. Norquetiapine is an alpha-2 antagonist that increases brain NE levels. Both quetiapine and norquetiapine are alpha-1 antagonists. There is no beta blockade and no SSRI effect, but some 5HT2A blockade, which may be anxiolytic. Compared with placebo, an average quetiapine dose of 258 mg/d resulted in significantly greater reductions in Clinician-Administered PTSD Scale total score, re-experiencing score, and hyperarousal score.73
Unfortunately, none of the non-SSRI options have been adequately evaluated. For now, clinicians need to continue to use SSRIs, and researchers need to continue to explore mechanism-guided alternatives.
Bottom Line
Understanding the mechanisms of the pathophysiology of posttraumatic stress disorder (PTSD) may allow clinicians to “jump ahead” of clinical studies and FDA indications. Clinicians may reasonably use alpha-1 antagonists (eg, prazosin, quetiapine) for general clinical improvement of patients with PTSD, particularly for PTSD-specific symptoms. Using antihistamines to reduce anxiety (especially in patients who have the COMT Val158Met polymorphism) may also be reasonable.
Related Resources
- North CS, Hong BA, Downs DL. PTSD: a systematic approach to diagnosis and treatment. Current Psychiatry. 2018;17(4):35-43.
- Zhang Y, Ren R, Sanford LD, et al. The effects of prazosin on sleep disturbances in post-traumatic stress disorder: a systematic review and meta-analysis. Sleep Med. 2019; 67:225-231.
Drug Brand Names
Aripiprazole • Abilify
Citalopram • Celexa
Paroxetine • Paxil
Prazosin • Minipress
Quetiapine • Seroquel
Sertraline • Zoloft
1. Javidi H, Yadollahie M. Post-traumatic stress disorder. Int J Occup Environ Med. 2012;3(1):2-9.
2. Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627.
3. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048-1060.
4. Breslau N, Kessler RC, Chilcoat HD, et al. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55(7):626-632.
5. Cerda M, Sagdeo A, Johnson J, et al. Genetic and environmental influences on psychiatric comorbidity: a systematic review. J Affect Disord. 2010;126(1-2):14-38.
6. Yehuda R, Hoge CW, McFarlane AC, et al. Post-traumatic stress disorder. Nat Rev Dis Primers. 2015;1:15057. doi: 10.1038/nrdp.2015.57.
7. True WR, Rice J, Eisen SA, et al. A twin study of genetic and environmental contributions to liability for posttraumatic stress symptoms. Arch Gen Psychiatry. 1993;50(4):257-264.
8. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013:271-280.
9. Reichmann F, Holzer P. Neuropeptide Y: a stressful review. Neuropeptides. 2016;55:99-109.
10. Yehuda R, Brand S, Yang RK. Plasma neuropeptide Y concentrations in combat exposed veterans: relationship to trauma exposure, recovery from PTSD, and coping. Biol Psychiatry. 2006;59(7):660-663.
11. Cohen H, Liu T, Kozlovsky N, et al. The neuropeptide Y (NPY)-ergic system is associated with behavioral resilience to stress exposure in an animal model of post-traumatic stress disorder. Neuropsychopharmacology. 2012;37(2):350-363.
12. Donner J, Sipilä T, Ripatti S, et al. Support for involvement of glutamate decarboxylase 1 and neuropeptide Y in anxiety susceptibility. Am J Med Genet B Neuropsychiatr Genet. 2012;159B(3):316-327.
13. Schmeltzer SN, Herman JP, Sah R. Neuropeptide Y (NPY) and posttraumatic stress disorder (PTSD): a translational update. Exp Neurol. 2016;284(pt B):196-210.
14. Kautz M, Charney DS, Murrough JW. Neuropeptide Y, resilience, and PTSD therapeutics. Neurosci Lett. 2017;649:164-169.
15. Serova LI, Laukova M, Alaluf LG, et al. Intranasal neuropeptide Y reverses anxiety and depressive-like behavior impaired by single prolonged stress PTSD model. Eur Neuropsychopharmacol. 2014;24(1):142-147.
16. Sayed S, Van Dam NT, Horn SR, et al. A randomized dose-ranging study of neuropeptide Y in patients with posttraumatic stress disorder. Int J Neuropsychopharmacol. 2018;21(1):3-11.
17. Toth M, Flandreau EI, Deslauriers J, et al. Overexpression of forebrain CRH during early life increases trauma susceptibility in adulthood. Neuropsychopharmacology. 2016;41(6):1681-1690.
18. White S, Acierno R, Ruggiero KJ, et al. Association of CRHR1 variants and posttraumatic stress symptoms in hurricane exposed adults. J Anxiety Disord. 2013;27(7):678-683.
19. Wolf EJ, Mitchell KS, Logue MW, et al. Corticotropin releasing hormone receptor 2 (CRHR-2) gene is associated with decreased risk and severity of posttraumatic stress disorder in women. Depress Anxiety. 2013;30(12):1161-1169.
20. Whitnall MH. Regulation of the hypothalamic corticotropin-releasing hormone neurosecretory system. Prog Neurobiol. 1993;40(5):573-629.
21. Bradley RG, Binder EB, Epstein MP, et al. Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Arch Gen Psychiatry. 2008;65(2):190-200.
22. Tellew JE, Lanier M, Moorjani M, et al. Discovery of NBI-77860/GSK561679, a potent corticotropin-releasing factor (CRF1) receptor antagonist with improved pharmacokinetic properties. Bioorg Med Chem Lett. 2010;20(24):7259-7264.
23. Dunlop BW, Rothbaum BO, Binder EB, et al. Evaluation of a corticotropin releasing hormone type 1 receptor antagonist in women with posttraumatic stress disorder: study protocol for a randomized controlled trial. Trials. 2014;15:240. doi: 10.1186/1745-6215-15-240.
24. Jovanovic T, Duncan EJ, Kaye J, et al. Psychophysiological treatment outcomes: Corticotropin-releasing factor type 1 receptor antagonist increases inhibition of fear-potentiated startle in PTSD patients. Psychophysiology. 2019:e13356. doi: 10.1111/psyp.13356.
25. Dunlop BW, Binder EB, Iosifescu D, et al. Corticotropin-releasing factor receptor 1 antagonism is ineffective for women with posttraumatic stress disorder. Biol Psychiatry. 2017;82(12):866-874.
26. Pape JC, Carrillo-Roa T, Rothbaum BO, et al. DNA methylation levels are associated with CRF1 receptor antagonist treatment outcome in women with post-traumatic stress disorder. Clin Epigenetics. 2018;10(1):136. doi: 10.1186/s13148-018-0569-x.
27. Murrough JW, Charney DS. Corticotropin-releasing factor type 1 receptor antagonists for stress-related disorders: time to call it quits? Biol Psychiatry. 2017;82(12):858-860.
28. Leal G, Bramham CR, Duarte CB. BDNF and hippocampal synaptic plasticity. Vitam Horm. 2017;104:153-195.
29. Groves JO. Is it time to reassess the BDNF hypothesis of depression? Mol Psychiatry. 2007;12:1079-1088.
30. Frustaci A, Pozzi G, Gianfagna F, et al. Meta-analysis of the brain-derived neurotrophic factor gene (BDNF) Val66Met polymorphism in anxiety disorders and anxiety-related personality traits. Neuropsychobiology. 2008;58(3-4):163-170.
31. Gatt JM, Nemeroff CB, Dobson-Stone C, et al. Interactions between BDNF Val66Met polymorphism and early life stress predict brain and arousal pathways to syndromal depression and anxiety. Mol Psychiatry. 2009;14(7):681-695.
32. Ragen BJ, Seidel J, Chollak C, et al. Investigational drugs under development for the treatment of PTSD. Expert Opin Investig Drugs. 2015;24(5):659-672.
33. Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301(5631):386-389.
34. Murphy DL, Fox MA, Timpano KR, et al. How the serotonin story is being rewritten by new gene-based discoveries principally related to SLC6A4, the serotonin transporter gene, which functions to influence all cellular serotonin systems. Neuropharmacology. 2008;55(6):932-960.
35. Luddington NS, Mandadapu A, Husk M, et al. Clinical implications of genetic variation in the serotonin transporter promoter region: a review. Prim Care Compan J Clin Psychiatry. 2009;11:(3):93-102.
36. Lee HJ, Lee MS, Kang RH, et al. Influence of the serotonin transporter promoter gene polymorphism on susceptibility to posttraumatic stress disorder. Depress Anxiety. 2005;21(3):135-139.
37. Liu Y, Garrett ME, Dennis MF, et al. An examination of the association between 5-HTTLPR, combat exposure, and PTSD diagnosis among U.S. veterans. PLoS One. 2015;10(3):e0119998. doi: 10.1371/journal.pone.0119998.
38. Mehta D, Voisey J, Bruenig D, et al. Transcriptome analysis reveals novel genes and immune networks dysregulated in veterans with PTSD. Brain Behav Immun. 2018;74:133-142. doi: 10.1016/j.bbi.2018.08.014.
39. Kilpatrick DG, Koenen KC, Ruggiero KJ, et al. The serotonin transporter genotype and social support and moderation of posttraumatic stress disorder and depression in hurricane-exposed adults. Am J Psychiatry. 2007;164(11):1693-1699.
40. Kolassa IT, Ertl V, Eckart C, et al. Association study of trauma load and SLC6A4 promoter polymorphism in posttraumatic stress disorder: evidence from survivors of the Rwandan genocide. J Clin Psychiatry. 2010;71(5):543-547.
41. Bryant RA, Felmingham KL, Falconer EM, et al. Preliminary evidence of the short allele of the serotonin transporter gene predicting poor response to cognitive behavior therapy in posttraumatic stress disorder. Biol Psychiatry. 2010;67(12):1217-1219.
42. Mrazek DA, Rush AJ, Biernacka JM, et al. SLC6A4 variation and citalopram response. Am J Med Genet B Neuropsychiatr Genet. 2009;150B(3):341-351.
43. Shiroma PR, Drews MS, Geske JR, et al. SLC6A4 polymorphisms and age of onset in late-life depression on treatment outcomes with citalopram: a Sequenced Treatment Alternatives to Relieve Depression (STAR*D) report. Am J Geriatr Psychiatry. 2014;22(11):1140-1148.
44. Fanelli G, Serretti A. The influence of the serotonin transporter gene 5-HTTLPR polymorphism on suicidal behaviors: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2019;88:375-387.
45. Courtet P, Picot MC, Bellivier F, et al. Serotonin transporter gene may be involved in short-term risk of subsequent suicide attempts. Biol Psychiatry. 2003;55(1):46-51.
46. Outhred T, Das P, Dobson-Stone C, et al. The impact of 5-HTTLPR on acute serotonin transporter blockade by escitalopram on emotion processing: Preliminary findings from a randomised, crossover fMRI study. Aust NZ J Psychiatry. 2014;48(12):1115-1125.
47. Lachman HM, Papolos DF, Saito T, et al. Human catechol-O-methyltransferase pharmacogenetics: description of a functional polymorphism and its potential application to neuropsychiatric disorders. Pharmacogenetics. 1996;6(3):243-250.
48. Valente NL, Vallada H, Cordeiro Q, et al. Catechol-O-methyltransferase (COMT) val158met polymorphism as a risk factor for PTSD after urban violence. J Mol Neurosci. 2011;43(3):516-523.
49. van Rooij SJ, Stevens JS, Ely TD, et al. Childhood trauma and COMT genotype interact to increase hippocampal activation in resilient individuals. Front Psychiatry. 2016;7:156. doi: 10.3389/fpsyt.2016.00156.
50. Wu G, Feder A, Cohen H, et al. Understanding resilience. Front Behav Neuroscience. 2013;7:10. doi: 10.3389/fnbeh.2013.00010.
51. Kolassa I, Kolassa S, Ertl V, et al. The risk of posttraumatic stress disorder after trauma depends on traumatic load and the catechol-O-methyltransferase Val(158)Met polymorphism. Biol Psychiatry. 2010;67(4):304-308.
52. Bruder GE, Keilp JG, Xu H, et al. Catechol-O-methyltransferase (COMT) genotypes and working memory: associations with differing cognitive operations. Biol Psychiatry. 2005;58(11):901-907.
53. Strawn JR, Geracioti TD Jr. Noradrenergic dysfunction and the psychopharmacology of posttraumatic stress disorder. Depress Anxiety. 2008;25(3):260-271.
54. Hendrickson RC, Raskind MA. Noradrenergic dysregulation in the pathophysiology of PTSD. Exp Neurol. 2016;284(pt B):181-195.
55. Neylan TC, Marmar CR, Metzler TJ, et al. Sleep disturbances in the Vietnam generation: findings from a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1998;155(7):929-933.
56. Roehrs TA, Roth T. Hyperarousal in insomnia and hypnotic dose escalation. Sleep Med. 2016;23:16-20.
57. Geracioti TD Jr, Baker DG, Ekhator NN, et al. CSF Norepinephrine concentrations in posttraumatic stress disorder. Am J Psychiatry. 2001;158(8):1227-1230.
58. Yehuda R, Siever LJ, Teicher MH, et al. Plasma norepinephrine and 3-methoxy-4-hydroxyphenylglycol concentrations and severity of depression in combat posttraumatic stress disorder and major depressive disorder. Biol Psychiatry. 1998;44(1):56-63.
59. Molinoff PB. Alpha- and beta-adrenergic receptor subtypes properties, distribution and regulation. Drugs. 1984;28(suppl 2):1-15.
60. El-Mallakh RS. The use of beta-blockers in psychiatry. Res Staff Phys. 1989;35:49-52,59,62.
61. Raskind MA, Peterson K, Williams T, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. 2013;170(9):1003-1010.
62. Bisson JI, Roberts NP, Andrew M, et al. Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev. 2013;(12):CD003388.
63. Steenkamp MM, Litz BT, Hoge CW, et al. Psychotherapy for military-related PTSD: a review of randomized clinical trials. JAMA. 2015;314(5):489-500.
64. Hoskins M, Pearce J, Bethell A, et al. Pharmacotherapy for post-traumatic stress disorder: systematic review and meta-analysis. Br J Psychiatry. 2015;206(2):93-100.
65. Belkin MR, Schwartz TL. Alpha-2 receptor agonists for the treatment of posttraumatic stress disorder. Drugs Context. 2015;4:212286. doi: 10.7573/dic.212286.
66. Brady K, Pearlstein T, Asnis GM, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA. 2000;283(14):1837-1844.
67. Davidson JRT, Landerman LR, Farfel GM, et al. Characterizing the effects of sertraline in post-traumatic stress disorder. Psychol Med. 2002;32(4):661-670.
68. Hertzberg MA, Feldman ME, Beckham JC, et al. Lack of efficacy for fluoxetine in PTSD: a placebo controlled trial in combat veterans. Ann Clin Psychiatry. 2000;12(2):101-105.
69. Friedman MJ, Marmar CR, Baker DG, et al. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. J Clin Psychiatry. 2007;68(5):711-720.
70. Mello MF, Costa MCP, Schoedl AF, et al. Aripiprazole in the treatment of posttraumatic stress disorder: an open-label trial. Rev Bras Psiquiatr. 2008;30(4):358-361.
71. Birnbaum S, Gobeske KT, Auerbach J, et al. A role for norepinephrine in stress-induced cognitive deficits: alpha-1-adrenoceptor mediation in the prefrontal cortex. Biol Psychiatry. 1999;46(9):1266-1274.
72. Ahmadpanah M, Sabzeiee P, Hosseini SM, et al. Comparing the effect of prazosin and hydroxyzine on sleep quality in patients suffering from posttraumatic stress disorder. Neuropsychobiology. 2014;69(4):235-242.
73. Villarreal G, Hamner MB, Cañive JM, et al. Efficacy of quetiapine monotherapy in posttraumatic stress disorder: a randomized, placebo-controlled trial. Am J Psychiatry. 2016;173(12):1205-1212.
1. Javidi H, Yadollahie M. Post-traumatic stress disorder. Int J Occup Environ Med. 2012;3(1):2-9.
2. Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-627.
3. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048-1060.
4. Breslau N, Kessler RC, Chilcoat HD, et al. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55(7):626-632.
5. Cerda M, Sagdeo A, Johnson J, et al. Genetic and environmental influences on psychiatric comorbidity: a systematic review. J Affect Disord. 2010;126(1-2):14-38.
6. Yehuda R, Hoge CW, McFarlane AC, et al. Post-traumatic stress disorder. Nat Rev Dis Primers. 2015;1:15057. doi: 10.1038/nrdp.2015.57.
7. True WR, Rice J, Eisen SA, et al. A twin study of genetic and environmental contributions to liability for posttraumatic stress symptoms. Arch Gen Psychiatry. 1993;50(4):257-264.
8. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013:271-280.
9. Reichmann F, Holzer P. Neuropeptide Y: a stressful review. Neuropeptides. 2016;55:99-109.
10. Yehuda R, Brand S, Yang RK. Plasma neuropeptide Y concentrations in combat exposed veterans: relationship to trauma exposure, recovery from PTSD, and coping. Biol Psychiatry. 2006;59(7):660-663.
11. Cohen H, Liu T, Kozlovsky N, et al. The neuropeptide Y (NPY)-ergic system is associated with behavioral resilience to stress exposure in an animal model of post-traumatic stress disorder. Neuropsychopharmacology. 2012;37(2):350-363.
12. Donner J, Sipilä T, Ripatti S, et al. Support for involvement of glutamate decarboxylase 1 and neuropeptide Y in anxiety susceptibility. Am J Med Genet B Neuropsychiatr Genet. 2012;159B(3):316-327.
13. Schmeltzer SN, Herman JP, Sah R. Neuropeptide Y (NPY) and posttraumatic stress disorder (PTSD): a translational update. Exp Neurol. 2016;284(pt B):196-210.
14. Kautz M, Charney DS, Murrough JW. Neuropeptide Y, resilience, and PTSD therapeutics. Neurosci Lett. 2017;649:164-169.
15. Serova LI, Laukova M, Alaluf LG, et al. Intranasal neuropeptide Y reverses anxiety and depressive-like behavior impaired by single prolonged stress PTSD model. Eur Neuropsychopharmacol. 2014;24(1):142-147.
16. Sayed S, Van Dam NT, Horn SR, et al. A randomized dose-ranging study of neuropeptide Y in patients with posttraumatic stress disorder. Int J Neuropsychopharmacol. 2018;21(1):3-11.
17. Toth M, Flandreau EI, Deslauriers J, et al. Overexpression of forebrain CRH during early life increases trauma susceptibility in adulthood. Neuropsychopharmacology. 2016;41(6):1681-1690.
18. White S, Acierno R, Ruggiero KJ, et al. Association of CRHR1 variants and posttraumatic stress symptoms in hurricane exposed adults. J Anxiety Disord. 2013;27(7):678-683.
19. Wolf EJ, Mitchell KS, Logue MW, et al. Corticotropin releasing hormone receptor 2 (CRHR-2) gene is associated with decreased risk and severity of posttraumatic stress disorder in women. Depress Anxiety. 2013;30(12):1161-1169.
20. Whitnall MH. Regulation of the hypothalamic corticotropin-releasing hormone neurosecretory system. Prog Neurobiol. 1993;40(5):573-629.
21. Bradley RG, Binder EB, Epstein MP, et al. Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Arch Gen Psychiatry. 2008;65(2):190-200.
22. Tellew JE, Lanier M, Moorjani M, et al. Discovery of NBI-77860/GSK561679, a potent corticotropin-releasing factor (CRF1) receptor antagonist with improved pharmacokinetic properties. Bioorg Med Chem Lett. 2010;20(24):7259-7264.
23. Dunlop BW, Rothbaum BO, Binder EB, et al. Evaluation of a corticotropin releasing hormone type 1 receptor antagonist in women with posttraumatic stress disorder: study protocol for a randomized controlled trial. Trials. 2014;15:240. doi: 10.1186/1745-6215-15-240.
24. Jovanovic T, Duncan EJ, Kaye J, et al. Psychophysiological treatment outcomes: Corticotropin-releasing factor type 1 receptor antagonist increases inhibition of fear-potentiated startle in PTSD patients. Psychophysiology. 2019:e13356. doi: 10.1111/psyp.13356.
25. Dunlop BW, Binder EB, Iosifescu D, et al. Corticotropin-releasing factor receptor 1 antagonism is ineffective for women with posttraumatic stress disorder. Biol Psychiatry. 2017;82(12):866-874.
26. Pape JC, Carrillo-Roa T, Rothbaum BO, et al. DNA methylation levels are associated with CRF1 receptor antagonist treatment outcome in women with post-traumatic stress disorder. Clin Epigenetics. 2018;10(1):136. doi: 10.1186/s13148-018-0569-x.
27. Murrough JW, Charney DS. Corticotropin-releasing factor type 1 receptor antagonists for stress-related disorders: time to call it quits? Biol Psychiatry. 2017;82(12):858-860.
28. Leal G, Bramham CR, Duarte CB. BDNF and hippocampal synaptic plasticity. Vitam Horm. 2017;104:153-195.
29. Groves JO. Is it time to reassess the BDNF hypothesis of depression? Mol Psychiatry. 2007;12:1079-1088.
30. Frustaci A, Pozzi G, Gianfagna F, et al. Meta-analysis of the brain-derived neurotrophic factor gene (BDNF) Val66Met polymorphism in anxiety disorders and anxiety-related personality traits. Neuropsychobiology. 2008;58(3-4):163-170.
31. Gatt JM, Nemeroff CB, Dobson-Stone C, et al. Interactions between BDNF Val66Met polymorphism and early life stress predict brain and arousal pathways to syndromal depression and anxiety. Mol Psychiatry. 2009;14(7):681-695.
32. Ragen BJ, Seidel J, Chollak C, et al. Investigational drugs under development for the treatment of PTSD. Expert Opin Investig Drugs. 2015;24(5):659-672.
33. Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301(5631):386-389.
34. Murphy DL, Fox MA, Timpano KR, et al. How the serotonin story is being rewritten by new gene-based discoveries principally related to SLC6A4, the serotonin transporter gene, which functions to influence all cellular serotonin systems. Neuropharmacology. 2008;55(6):932-960.
35. Luddington NS, Mandadapu A, Husk M, et al. Clinical implications of genetic variation in the serotonin transporter promoter region: a review. Prim Care Compan J Clin Psychiatry. 2009;11:(3):93-102.
36. Lee HJ, Lee MS, Kang RH, et al. Influence of the serotonin transporter promoter gene polymorphism on susceptibility to posttraumatic stress disorder. Depress Anxiety. 2005;21(3):135-139.
37. Liu Y, Garrett ME, Dennis MF, et al. An examination of the association between 5-HTTLPR, combat exposure, and PTSD diagnosis among U.S. veterans. PLoS One. 2015;10(3):e0119998. doi: 10.1371/journal.pone.0119998.
38. Mehta D, Voisey J, Bruenig D, et al. Transcriptome analysis reveals novel genes and immune networks dysregulated in veterans with PTSD. Brain Behav Immun. 2018;74:133-142. doi: 10.1016/j.bbi.2018.08.014.
39. Kilpatrick DG, Koenen KC, Ruggiero KJ, et al. The serotonin transporter genotype and social support and moderation of posttraumatic stress disorder and depression in hurricane-exposed adults. Am J Psychiatry. 2007;164(11):1693-1699.
40. Kolassa IT, Ertl V, Eckart C, et al. Association study of trauma load and SLC6A4 promoter polymorphism in posttraumatic stress disorder: evidence from survivors of the Rwandan genocide. J Clin Psychiatry. 2010;71(5):543-547.
41. Bryant RA, Felmingham KL, Falconer EM, et al. Preliminary evidence of the short allele of the serotonin transporter gene predicting poor response to cognitive behavior therapy in posttraumatic stress disorder. Biol Psychiatry. 2010;67(12):1217-1219.
42. Mrazek DA, Rush AJ, Biernacka JM, et al. SLC6A4 variation and citalopram response. Am J Med Genet B Neuropsychiatr Genet. 2009;150B(3):341-351.
43. Shiroma PR, Drews MS, Geske JR, et al. SLC6A4 polymorphisms and age of onset in late-life depression on treatment outcomes with citalopram: a Sequenced Treatment Alternatives to Relieve Depression (STAR*D) report. Am J Geriatr Psychiatry. 2014;22(11):1140-1148.
44. Fanelli G, Serretti A. The influence of the serotonin transporter gene 5-HTTLPR polymorphism on suicidal behaviors: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2019;88:375-387.
45. Courtet P, Picot MC, Bellivier F, et al. Serotonin transporter gene may be involved in short-term risk of subsequent suicide attempts. Biol Psychiatry. 2003;55(1):46-51.
46. Outhred T, Das P, Dobson-Stone C, et al. The impact of 5-HTTLPR on acute serotonin transporter blockade by escitalopram on emotion processing: Preliminary findings from a randomised, crossover fMRI study. Aust NZ J Psychiatry. 2014;48(12):1115-1125.
47. Lachman HM, Papolos DF, Saito T, et al. Human catechol-O-methyltransferase pharmacogenetics: description of a functional polymorphism and its potential application to neuropsychiatric disorders. Pharmacogenetics. 1996;6(3):243-250.
48. Valente NL, Vallada H, Cordeiro Q, et al. Catechol-O-methyltransferase (COMT) val158met polymorphism as a risk factor for PTSD after urban violence. J Mol Neurosci. 2011;43(3):516-523.
49. van Rooij SJ, Stevens JS, Ely TD, et al. Childhood trauma and COMT genotype interact to increase hippocampal activation in resilient individuals. Front Psychiatry. 2016;7:156. doi: 10.3389/fpsyt.2016.00156.
50. Wu G, Feder A, Cohen H, et al. Understanding resilience. Front Behav Neuroscience. 2013;7:10. doi: 10.3389/fnbeh.2013.00010.
51. Kolassa I, Kolassa S, Ertl V, et al. The risk of posttraumatic stress disorder after trauma depends on traumatic load and the catechol-O-methyltransferase Val(158)Met polymorphism. Biol Psychiatry. 2010;67(4):304-308.
52. Bruder GE, Keilp JG, Xu H, et al. Catechol-O-methyltransferase (COMT) genotypes and working memory: associations with differing cognitive operations. Biol Psychiatry. 2005;58(11):901-907.
53. Strawn JR, Geracioti TD Jr. Noradrenergic dysfunction and the psychopharmacology of posttraumatic stress disorder. Depress Anxiety. 2008;25(3):260-271.
54. Hendrickson RC, Raskind MA. Noradrenergic dysregulation in the pathophysiology of PTSD. Exp Neurol. 2016;284(pt B):181-195.
55. Neylan TC, Marmar CR, Metzler TJ, et al. Sleep disturbances in the Vietnam generation: findings from a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1998;155(7):929-933.
56. Roehrs TA, Roth T. Hyperarousal in insomnia and hypnotic dose escalation. Sleep Med. 2016;23:16-20.
57. Geracioti TD Jr, Baker DG, Ekhator NN, et al. CSF Norepinephrine concentrations in posttraumatic stress disorder. Am J Psychiatry. 2001;158(8):1227-1230.
58. Yehuda R, Siever LJ, Teicher MH, et al. Plasma norepinephrine and 3-methoxy-4-hydroxyphenylglycol concentrations and severity of depression in combat posttraumatic stress disorder and major depressive disorder. Biol Psychiatry. 1998;44(1):56-63.
59. Molinoff PB. Alpha- and beta-adrenergic receptor subtypes properties, distribution and regulation. Drugs. 1984;28(suppl 2):1-15.
60. El-Mallakh RS. The use of beta-blockers in psychiatry. Res Staff Phys. 1989;35:49-52,59,62.
61. Raskind MA, Peterson K, Williams T, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. 2013;170(9):1003-1010.
62. Bisson JI, Roberts NP, Andrew M, et al. Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev. 2013;(12):CD003388.
63. Steenkamp MM, Litz BT, Hoge CW, et al. Psychotherapy for military-related PTSD: a review of randomized clinical trials. JAMA. 2015;314(5):489-500.
64. Hoskins M, Pearce J, Bethell A, et al. Pharmacotherapy for post-traumatic stress disorder: systematic review and meta-analysis. Br J Psychiatry. 2015;206(2):93-100.
65. Belkin MR, Schwartz TL. Alpha-2 receptor agonists for the treatment of posttraumatic stress disorder. Drugs Context. 2015;4:212286. doi: 10.7573/dic.212286.
66. Brady K, Pearlstein T, Asnis GM, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA. 2000;283(14):1837-1844.
67. Davidson JRT, Landerman LR, Farfel GM, et al. Characterizing the effects of sertraline in post-traumatic stress disorder. Psychol Med. 2002;32(4):661-670.
68. Hertzberg MA, Feldman ME, Beckham JC, et al. Lack of efficacy for fluoxetine in PTSD: a placebo controlled trial in combat veterans. Ann Clin Psychiatry. 2000;12(2):101-105.
69. Friedman MJ, Marmar CR, Baker DG, et al. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. J Clin Psychiatry. 2007;68(5):711-720.
70. Mello MF, Costa MCP, Schoedl AF, et al. Aripiprazole in the treatment of posttraumatic stress disorder: an open-label trial. Rev Bras Psiquiatr. 2008;30(4):358-361.
71. Birnbaum S, Gobeske KT, Auerbach J, et al. A role for norepinephrine in stress-induced cognitive deficits: alpha-1-adrenoceptor mediation in the prefrontal cortex. Biol Psychiatry. 1999;46(9):1266-1274.
72. Ahmadpanah M, Sabzeiee P, Hosseini SM, et al. Comparing the effect of prazosin and hydroxyzine on sleep quality in patients suffering from posttraumatic stress disorder. Neuropsychobiology. 2014;69(4):235-242.
73. Villarreal G, Hamner MB, Cañive JM, et al. Efficacy of quetiapine monotherapy in posttraumatic stress disorder: a randomized, placebo-controlled trial. Am J Psychiatry. 2016;173(12):1205-1212.
When mania isn’t what it seems
CASE Aggressive, impulsive, and not sleeping
Mr. S, age 22, is brought by his family to his outpatient psychiatrist because he has begun to
Mr. S has significant language impairment and is unreliable as a narrator. His family reports that Mr. S’s behavior has resulted in declining academic performance, and they have curtailed his social activities due to behavioral issues. Both his family and teachers report that it is increasingly difficult to redirect Mr. S’s behavior. Although not physically aggressive, Mr. S becomes verbally agitated when rituals are incomplete. He has gone from sleeping 8 hours each night to only 3 to 4 hours, but he does not appear tired during the day.
HISTORY Multiple hospitalizations
As a child, Mr. S had been diagnosed with autism and intellectual disability. When he was 13, he began exhibiting marked stereotypy, restlessness, impulsivity, frenzy, agitation, combativeness, and purposeless motor activity. At that time, he was not receiving any medications. Mr. S had not slept for 2 days and had been walking in circles nonstop. He became aggressive whenever anyone attempted to redirect his behavior. The family took Mr. S to the emergency department (ED), where clinicians ruled out organic causes for his behavioral disturbances, including infections, drug intoxication, and use of illicit substances. Mr. S was transferred from the ED to a child and adolescent psychiatry ward at a nearby university hospital for inpatient treatment.
On the inpatient unit, the treatment team diagnosed Mr. S with bipolar disorder and believed that he was experiencing a manic episode. He was prescribed quetiapine, 25 mg by mouth during the day and 75 mg by mouth at night, to stabilize his agitation, and was discharged with a plan to follow up with his outpatient psychiatrist. However, within 1 week, his symptoms returned, with markedly increased aggression and agitation, so he was readmitted, tapered off quetiapine, and prescribed valproic acid, 125 mg by mouth during the day and 375 mg by mouth at bedtime. With this regimen, Mr. S became calmer, but when he was discharged home, he was subdued and withdrawn, overly adherent to rules and routines, constantly irritable, and often unable to focus.
Two years later, Mr. S developed hyperammonemia. Valproic acid was discontinued, and many of his behavioral issues resolved. He flourished both academically and socially. He experienced no exacerbation of symptoms until his current presentation.
[polldaddy:10544547]
EVALUATION Pinpointing the cause
Mr. S’s physical examination reveals that his vital signs are within normal limits. Mr. S is mildly tachycardic (heart rate, 105 bpm), with regular rate and rhythm. No murmurs, gallops, or rubs are auscultated. The remainder of the physical exam, including a detailed neurologic exam, is normal.
On mental status examination, Mr. S makes limited eye contact. He has difficulty sitting in the chair, with increased rocking, finger flicking, and hand flapping from baseline. Some compulsive behaviors are noted, such as tapping his neck. He has increased tics (eye blinking and mouth opening) and increased verbigeration and repetitive verbal statements. He loudly and repeatedly demands to go home, and uses short sentences with incorrect pronouns. His affect is difficult to assess, but he is agitated. His thought process is concrete. There is no evidence of suicidal ideation, homicidal ideation, or psychosis. Mr. S denies auditory hallucinations. His insight and judgment are limited.
Continue to: The psychiatrist rules out...
The psychiatrist rules out a behavioral exacerbation of autism based on an interview with Mr. S’s family and established rapport from treating him for several years. Mr. S’s family reports that many of his behaviors are not new but that the increased drive and intensity is worrisome. Further, his family cannot identify any stressors or precipitants for the behaviors and reports that offering preferred reinforcers did not help. An anxiety disorder is ruled out because according to the family, Mr. S’s drive to constantly move and complete rituals is fueling his anxiety. Schizoaffective disorder is ruled out because Mr. S denies auditory hallucinations and has not been observed responding to internal stimuli.
His Bush-Francis Catatonia Rating Scale (BFCRS) score is 26, which suggests a high likelihood of catatonia. Based on the BFCRS score, Mr. S’s psychiatrist makes the diagnosis of hyperkinetic catatonia.
The authors’ observations
The psychiatrist determined that Mr. S had been misdiagnosed with bipolar disorder at age 13. At that time, he had experienced his first episode of hyperkinetic catatonia and his symptoms decreased after he received lorazepam in the ED. However, the treatment team did not correctly identify this, most likely due to limited knowledge of catatonia among emergency medicine clinicians.
This case exemplifies a cognitive error of premature closure. Rather than considering catatonia as a complication of autism when Mr. S was 13, the clinicians added a second psychiatric diagnosis of bipolar disorder.Although premature closure errors generally occur when the physician assumes the patient is having a common complication of a known illness,1 in Mr. S’s case, the opposite occurred.
Conceptualizing catatonia
One helpful model for conceptualizing catatonia is to think of it as a basal ganglia disorder, with lesions in the basal ganglia thalamocortical tracts and the anterior cingulate/medial orbitofrontal circuit. Disrupting these pathways can result in symptoms such as mutism or repetitive and imitative behaviors. This is likely due to decreased disinhibition by gamma-aminobutyric acid (GABA), resulting in a hypodopaminergic state. This explains why benzodiazepines, which act to increase GABA, are effective for treating catatonia, and antipsychotics that act to decrease dopamine can exacerbate symptoms. Fricchione et al2 developed a model to visually represent the neurobiologic pathophysiology of catatonia (Figure2).
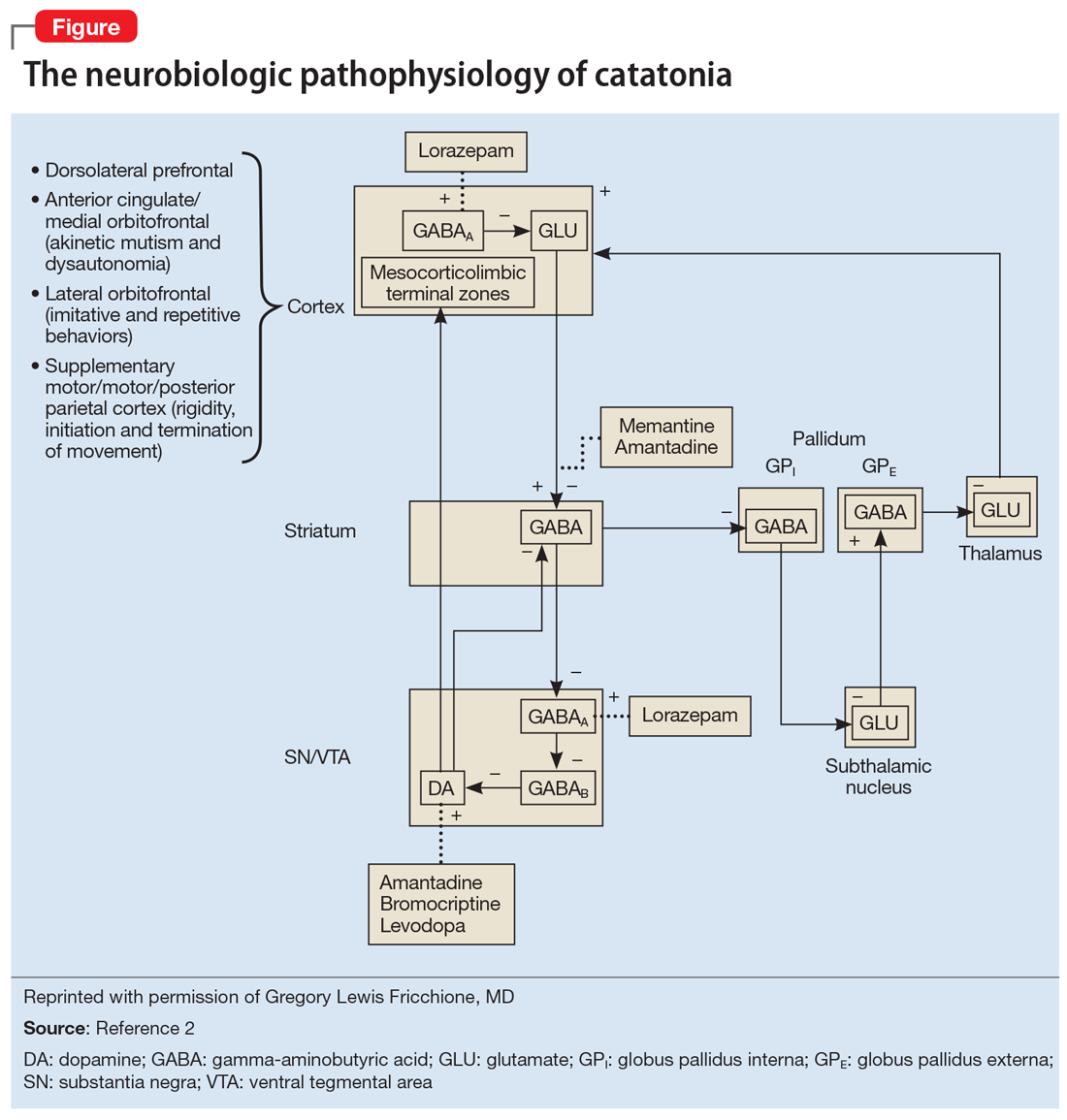
Continue to: Underlying causes of catatonia
Underlying causes of catatonia
Catatonia is most often seen in individuals with an underlying psychiatric condition such as schizophrenia, mood disorders, or autism. However, catatonia also occurs in the context of general neurologic and medical disorders, including (but not limited to) infections, metabolic disorders, endocrinopathies, epilepsy, neurodegenerative diseases, delirium, hypertensive encephalopathy, autoimmune encephalitis, and liver and kidney transplantation.3
Subtypes of catatonia include4:
- hypokinetic catatonia, which presents as stupor, mutism, and negativism
- hyperkinetic catatonia, which presents as hyperactivity, agitation, and stereotypy (as observed in Mr. S)
- malignant catatonia, which is a potentially lethal form of catatonia that occurs when hypo- or hyperkinetic catatonia is accompanied by autonomic instability such as tachycardia, tachypnea, hypertension, fever, and muscle rigidity
- periodic catatonia, which is characterized by brief episodes of stupor or excitatory catatonia lasting 4 to 10 days. These episodes recur over weeks to years, with patients remaining asymptomatic between episodes, or showing mild symptoms, such as facial grimacing or negativisms. Periodic catatonia often is autosomal dominant, involves linkage for the long arm of chromosome 15, and has a better prognosis than the other forms.
Autism and catatonia
Most individuals with autism who experience a catatonic episode first do so between age 10 and 19, and many episodes are precipitated by sudden changes in routine resulting in stress.5 An estimated 12% to 18% of patients with autism are diagnosed with catatonia in their lifetime, but the actual prevalence is likely higher.4
One of the reasons for this might be that although catatonia is well known in the psychiatric community, it is relatively unknown in the general medical community. Children and adolescents with psychiatric illness are likely to have symptoms of catatonia overlooked because catatonia often is not included in the differential diagnosis.6
In Mr. S’s case, it became clear that he did not have a mood disorder, but was prone to episodes of hyperkinetic catatonia due to his autism.
Continue to: Better recognition of catatonia
Better recognition of catatonia
As catatonia becomes better elucidated and more clearly described in the literature, there is increasing awareness that symptoms do not always involve stupor, mutism, and slowed motor activity, but can include increased motor activity, agitation, and stereotypies. The BFCRS is extremely useful for quantifying symptoms of catatonia. The best way to confirm the diagnosis is to use a lorazepam challenge in an inpatient setting, or a trial of lorazepam in an outpatient setting.5
[polldaddy:10544548]
The authors’ observations
Lorazepam is often considered the first-line treatment for catatonia because it is one of the most widely studied medications. Other benzodiazepines, such as oxazepam and clonazepam, and the sedative/hypnotic zolpidem have also been shown to be effective. Antipsychotics with dopamine-blocking mechanisms can exacerbate symptoms of catatonia and should be avoided in these patients. Furthermore, in cases of refractory catatonia, bilateral electroconvulsive therapy is an important and necessary treatment.7
TREATMENT Pharmacologic agents decrease BFCRS score
Mr. S is prescribed a regimen of lorazepam, 2 mg by mouth daily, and the supplement N-acetylcysteine, 600 mg by mouth daily. Within 2 weeks of starting this regimen, Mr. S’s BFCRS score decreases from 26 to 14. After 6 months of treatment with lorazepam, Mr. S shows considerable improvement. The stereotypic behaviors and impulsivity decrease significantly, leading to improved sleep and performance in school. After 6 months Mr. S is successfully tapered off the lorazepam, with a complete return to baseline.
Bottom Line
Hyperkinetic catatonia is easily overlooked, especially in the emergency setting. Catatonia should always be ruled out, particularly in patients with underlying conditions associated with it. Hyperkinetic catatonia is an underrecognized comorbidity in patients with autism.
Related Resources
- Dhossche DM, Wing L, Ohta M, et al. International Review of Neurobiology: Catatonia in autism spectrum disorders, vol 72. New York, NY: Academic Press/Elsevier; 2006.
- Taylor MA, Fink M. Catatonia in psychiatric classification: a home of its own. Am J Psychiatry. 2003;160(7):1233-1241.
Drug Brand Names
Amantadine • Symmetrel
Bromocriptine • Parlodel
Clonazepam • Klonopin
Lorazepam • Ativan
Memantine • Namenda
Oxazepam • Serax
Quetiapine • Seroquel
Valproic acid • Depakene, Depakote
Zolpidem • Ambien
1. McGee DL. Cognitive errors in clinical decision making. Merck Manual. https://www.merckmanuals.com/professional/special-subjects/clinical-decision-making/cognitive-errors-in-clinical-decision-making. Published November 2018. Accessed February 10, 2020.
2. Fricchione GL, Gross AF, Stern TA. Catatonia, neuroleptic malignant syndrome, and serotonin syndrome. Fricchione GL, Huffman JC, Stern TA, Bush G, eds. Massachusetts General Hospital Handbook of General Hospital Psychiatry. 6th ed. Philadelphia, PA: Saunders Elsevier; 2004:513-530.
3. Oldham MA, Lee HB. Catatonia vis-à-vis delirium: the significance of recognizing catatonia in altered mental status. Gen Hosp Psychiatry. 2015;37(6):554-559.
4. Wijemanne S, Jankovic J. Movement disorders in catatonia. J Neurol Neurosurg Psychiatry. 2014;86(8):825-832.
5. Dhossche DM, Shah A, Wing L. Blueprints for the assessment, treatment, and future study of catatonia in autism spectrum disorders. Int Rev Neurobiol. 2006:72;267-284.
6. Wing L, Shah A. Catatonia in autistic spectrum disorders. Br J Psychiatry. 2000:176(4):357-362.
7. Seinaert P, Dhossche DM, Vancampfort D, et al. A clinical review of the treatment of catatonia. Front Psychiatry. 2014;5:181.
CASE Aggressive, impulsive, and not sleeping
Mr. S, age 22, is brought by his family to his outpatient psychiatrist because he has begun to
Mr. S has significant language impairment and is unreliable as a narrator. His family reports that Mr. S’s behavior has resulted in declining academic performance, and they have curtailed his social activities due to behavioral issues. Both his family and teachers report that it is increasingly difficult to redirect Mr. S’s behavior. Although not physically aggressive, Mr. S becomes verbally agitated when rituals are incomplete. He has gone from sleeping 8 hours each night to only 3 to 4 hours, but he does not appear tired during the day.
HISTORY Multiple hospitalizations
As a child, Mr. S had been diagnosed with autism and intellectual disability. When he was 13, he began exhibiting marked stereotypy, restlessness, impulsivity, frenzy, agitation, combativeness, and purposeless motor activity. At that time, he was not receiving any medications. Mr. S had not slept for 2 days and had been walking in circles nonstop. He became aggressive whenever anyone attempted to redirect his behavior. The family took Mr. S to the emergency department (ED), where clinicians ruled out organic causes for his behavioral disturbances, including infections, drug intoxication, and use of illicit substances. Mr. S was transferred from the ED to a child and adolescent psychiatry ward at a nearby university hospital for inpatient treatment.
On the inpatient unit, the treatment team diagnosed Mr. S with bipolar disorder and believed that he was experiencing a manic episode. He was prescribed quetiapine, 25 mg by mouth during the day and 75 mg by mouth at night, to stabilize his agitation, and was discharged with a plan to follow up with his outpatient psychiatrist. However, within 1 week, his symptoms returned, with markedly increased aggression and agitation, so he was readmitted, tapered off quetiapine, and prescribed valproic acid, 125 mg by mouth during the day and 375 mg by mouth at bedtime. With this regimen, Mr. S became calmer, but when he was discharged home, he was subdued and withdrawn, overly adherent to rules and routines, constantly irritable, and often unable to focus.
Two years later, Mr. S developed hyperammonemia. Valproic acid was discontinued, and many of his behavioral issues resolved. He flourished both academically and socially. He experienced no exacerbation of symptoms until his current presentation.
[polldaddy:10544547]
EVALUATION Pinpointing the cause
Mr. S’s physical examination reveals that his vital signs are within normal limits. Mr. S is mildly tachycardic (heart rate, 105 bpm), with regular rate and rhythm. No murmurs, gallops, or rubs are auscultated. The remainder of the physical exam, including a detailed neurologic exam, is normal.
On mental status examination, Mr. S makes limited eye contact. He has difficulty sitting in the chair, with increased rocking, finger flicking, and hand flapping from baseline. Some compulsive behaviors are noted, such as tapping his neck. He has increased tics (eye blinking and mouth opening) and increased verbigeration and repetitive verbal statements. He loudly and repeatedly demands to go home, and uses short sentences with incorrect pronouns. His affect is difficult to assess, but he is agitated. His thought process is concrete. There is no evidence of suicidal ideation, homicidal ideation, or psychosis. Mr. S denies auditory hallucinations. His insight and judgment are limited.
Continue to: The psychiatrist rules out...
The psychiatrist rules out a behavioral exacerbation of autism based on an interview with Mr. S’s family and established rapport from treating him for several years. Mr. S’s family reports that many of his behaviors are not new but that the increased drive and intensity is worrisome. Further, his family cannot identify any stressors or precipitants for the behaviors and reports that offering preferred reinforcers did not help. An anxiety disorder is ruled out because according to the family, Mr. S’s drive to constantly move and complete rituals is fueling his anxiety. Schizoaffective disorder is ruled out because Mr. S denies auditory hallucinations and has not been observed responding to internal stimuli.
His Bush-Francis Catatonia Rating Scale (BFCRS) score is 26, which suggests a high likelihood of catatonia. Based on the BFCRS score, Mr. S’s psychiatrist makes the diagnosis of hyperkinetic catatonia.
The authors’ observations
The psychiatrist determined that Mr. S had been misdiagnosed with bipolar disorder at age 13. At that time, he had experienced his first episode of hyperkinetic catatonia and his symptoms decreased after he received lorazepam in the ED. However, the treatment team did not correctly identify this, most likely due to limited knowledge of catatonia among emergency medicine clinicians.
This case exemplifies a cognitive error of premature closure. Rather than considering catatonia as a complication of autism when Mr. S was 13, the clinicians added a second psychiatric diagnosis of bipolar disorder.Although premature closure errors generally occur when the physician assumes the patient is having a common complication of a known illness,1 in Mr. S’s case, the opposite occurred.
Conceptualizing catatonia
One helpful model for conceptualizing catatonia is to think of it as a basal ganglia disorder, with lesions in the basal ganglia thalamocortical tracts and the anterior cingulate/medial orbitofrontal circuit. Disrupting these pathways can result in symptoms such as mutism or repetitive and imitative behaviors. This is likely due to decreased disinhibition by gamma-aminobutyric acid (GABA), resulting in a hypodopaminergic state. This explains why benzodiazepines, which act to increase GABA, are effective for treating catatonia, and antipsychotics that act to decrease dopamine can exacerbate symptoms. Fricchione et al2 developed a model to visually represent the neurobiologic pathophysiology of catatonia (Figure2).
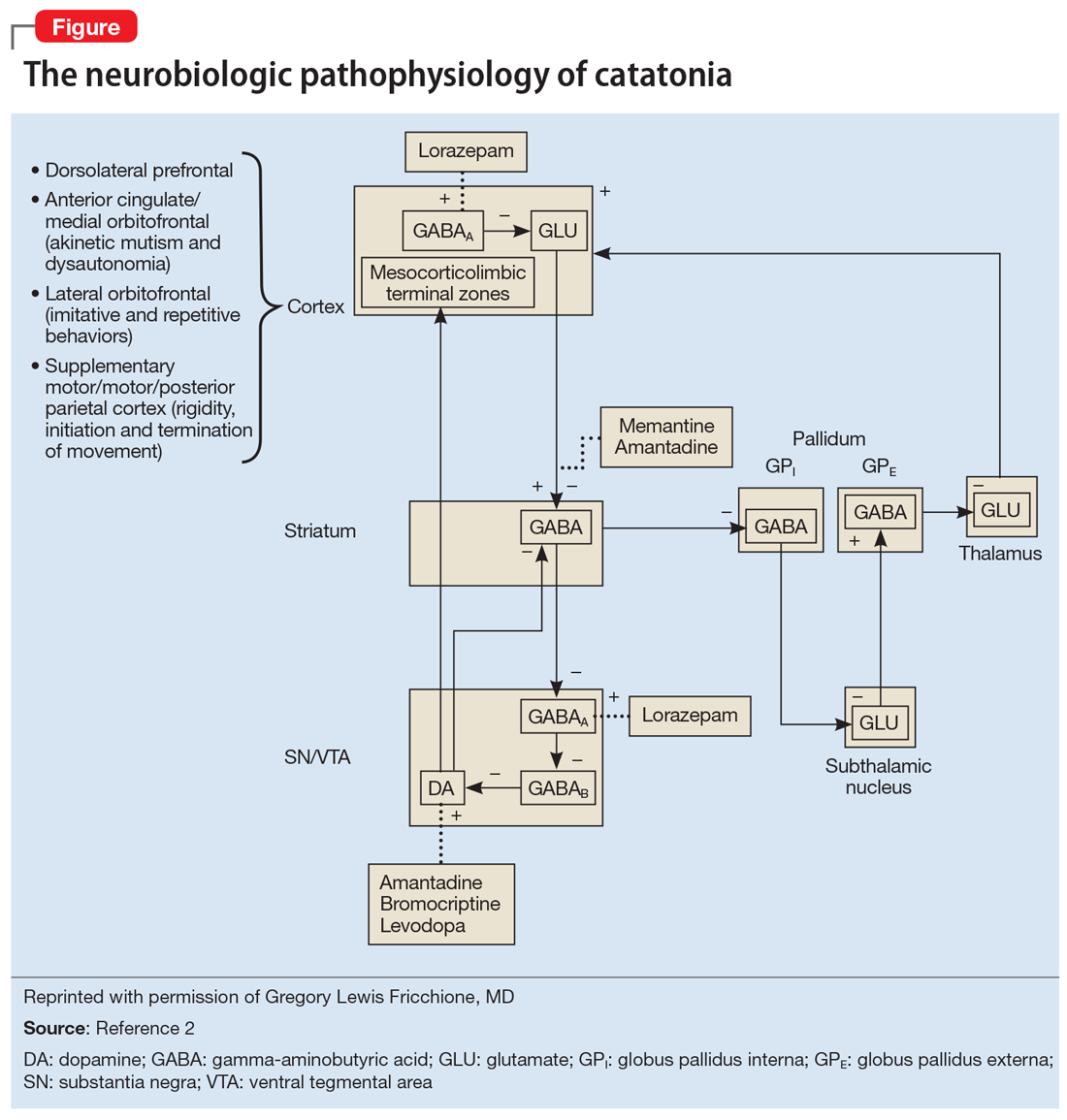
Continue to: Underlying causes of catatonia
Underlying causes of catatonia
Catatonia is most often seen in individuals with an underlying psychiatric condition such as schizophrenia, mood disorders, or autism. However, catatonia also occurs in the context of general neurologic and medical disorders, including (but not limited to) infections, metabolic disorders, endocrinopathies, epilepsy, neurodegenerative diseases, delirium, hypertensive encephalopathy, autoimmune encephalitis, and liver and kidney transplantation.3
Subtypes of catatonia include4:
- hypokinetic catatonia, which presents as stupor, mutism, and negativism
- hyperkinetic catatonia, which presents as hyperactivity, agitation, and stereotypy (as observed in Mr. S)
- malignant catatonia, which is a potentially lethal form of catatonia that occurs when hypo- or hyperkinetic catatonia is accompanied by autonomic instability such as tachycardia, tachypnea, hypertension, fever, and muscle rigidity
- periodic catatonia, which is characterized by brief episodes of stupor or excitatory catatonia lasting 4 to 10 days. These episodes recur over weeks to years, with patients remaining asymptomatic between episodes, or showing mild symptoms, such as facial grimacing or negativisms. Periodic catatonia often is autosomal dominant, involves linkage for the long arm of chromosome 15, and has a better prognosis than the other forms.
Autism and catatonia
Most individuals with autism who experience a catatonic episode first do so between age 10 and 19, and many episodes are precipitated by sudden changes in routine resulting in stress.5 An estimated 12% to 18% of patients with autism are diagnosed with catatonia in their lifetime, but the actual prevalence is likely higher.4
One of the reasons for this might be that although catatonia is well known in the psychiatric community, it is relatively unknown in the general medical community. Children and adolescents with psychiatric illness are likely to have symptoms of catatonia overlooked because catatonia often is not included in the differential diagnosis.6
In Mr. S’s case, it became clear that he did not have a mood disorder, but was prone to episodes of hyperkinetic catatonia due to his autism.
Continue to: Better recognition of catatonia
Better recognition of catatonia
As catatonia becomes better elucidated and more clearly described in the literature, there is increasing awareness that symptoms do not always involve stupor, mutism, and slowed motor activity, but can include increased motor activity, agitation, and stereotypies. The BFCRS is extremely useful for quantifying symptoms of catatonia. The best way to confirm the diagnosis is to use a lorazepam challenge in an inpatient setting, or a trial of lorazepam in an outpatient setting.5
[polldaddy:10544548]
The authors’ observations
Lorazepam is often considered the first-line treatment for catatonia because it is one of the most widely studied medications. Other benzodiazepines, such as oxazepam and clonazepam, and the sedative/hypnotic zolpidem have also been shown to be effective. Antipsychotics with dopamine-blocking mechanisms can exacerbate symptoms of catatonia and should be avoided in these patients. Furthermore, in cases of refractory catatonia, bilateral electroconvulsive therapy is an important and necessary treatment.7
TREATMENT Pharmacologic agents decrease BFCRS score
Mr. S is prescribed a regimen of lorazepam, 2 mg by mouth daily, and the supplement N-acetylcysteine, 600 mg by mouth daily. Within 2 weeks of starting this regimen, Mr. S’s BFCRS score decreases from 26 to 14. After 6 months of treatment with lorazepam, Mr. S shows considerable improvement. The stereotypic behaviors and impulsivity decrease significantly, leading to improved sleep and performance in school. After 6 months Mr. S is successfully tapered off the lorazepam, with a complete return to baseline.
Bottom Line
Hyperkinetic catatonia is easily overlooked, especially in the emergency setting. Catatonia should always be ruled out, particularly in patients with underlying conditions associated with it. Hyperkinetic catatonia is an underrecognized comorbidity in patients with autism.
Related Resources
- Dhossche DM, Wing L, Ohta M, et al. International Review of Neurobiology: Catatonia in autism spectrum disorders, vol 72. New York, NY: Academic Press/Elsevier; 2006.
- Taylor MA, Fink M. Catatonia in psychiatric classification: a home of its own. Am J Psychiatry. 2003;160(7):1233-1241.
Drug Brand Names
Amantadine • Symmetrel
Bromocriptine • Parlodel
Clonazepam • Klonopin
Lorazepam • Ativan
Memantine • Namenda
Oxazepam • Serax
Quetiapine • Seroquel
Valproic acid • Depakene, Depakote
Zolpidem • Ambien
CASE Aggressive, impulsive, and not sleeping
Mr. S, age 22, is brought by his family to his outpatient psychiatrist because he has begun to
Mr. S has significant language impairment and is unreliable as a narrator. His family reports that Mr. S’s behavior has resulted in declining academic performance, and they have curtailed his social activities due to behavioral issues. Both his family and teachers report that it is increasingly difficult to redirect Mr. S’s behavior. Although not physically aggressive, Mr. S becomes verbally agitated when rituals are incomplete. He has gone from sleeping 8 hours each night to only 3 to 4 hours, but he does not appear tired during the day.
HISTORY Multiple hospitalizations
As a child, Mr. S had been diagnosed with autism and intellectual disability. When he was 13, he began exhibiting marked stereotypy, restlessness, impulsivity, frenzy, agitation, combativeness, and purposeless motor activity. At that time, he was not receiving any medications. Mr. S had not slept for 2 days and had been walking in circles nonstop. He became aggressive whenever anyone attempted to redirect his behavior. The family took Mr. S to the emergency department (ED), where clinicians ruled out organic causes for his behavioral disturbances, including infections, drug intoxication, and use of illicit substances. Mr. S was transferred from the ED to a child and adolescent psychiatry ward at a nearby university hospital for inpatient treatment.
On the inpatient unit, the treatment team diagnosed Mr. S with bipolar disorder and believed that he was experiencing a manic episode. He was prescribed quetiapine, 25 mg by mouth during the day and 75 mg by mouth at night, to stabilize his agitation, and was discharged with a plan to follow up with his outpatient psychiatrist. However, within 1 week, his symptoms returned, with markedly increased aggression and agitation, so he was readmitted, tapered off quetiapine, and prescribed valproic acid, 125 mg by mouth during the day and 375 mg by mouth at bedtime. With this regimen, Mr. S became calmer, but when he was discharged home, he was subdued and withdrawn, overly adherent to rules and routines, constantly irritable, and often unable to focus.
Two years later, Mr. S developed hyperammonemia. Valproic acid was discontinued, and many of his behavioral issues resolved. He flourished both academically and socially. He experienced no exacerbation of symptoms until his current presentation.
[polldaddy:10544547]
EVALUATION Pinpointing the cause
Mr. S’s physical examination reveals that his vital signs are within normal limits. Mr. S is mildly tachycardic (heart rate, 105 bpm), with regular rate and rhythm. No murmurs, gallops, or rubs are auscultated. The remainder of the physical exam, including a detailed neurologic exam, is normal.
On mental status examination, Mr. S makes limited eye contact. He has difficulty sitting in the chair, with increased rocking, finger flicking, and hand flapping from baseline. Some compulsive behaviors are noted, such as tapping his neck. He has increased tics (eye blinking and mouth opening) and increased verbigeration and repetitive verbal statements. He loudly and repeatedly demands to go home, and uses short sentences with incorrect pronouns. His affect is difficult to assess, but he is agitated. His thought process is concrete. There is no evidence of suicidal ideation, homicidal ideation, or psychosis. Mr. S denies auditory hallucinations. His insight and judgment are limited.
Continue to: The psychiatrist rules out...
The psychiatrist rules out a behavioral exacerbation of autism based on an interview with Mr. S’s family and established rapport from treating him for several years. Mr. S’s family reports that many of his behaviors are not new but that the increased drive and intensity is worrisome. Further, his family cannot identify any stressors or precipitants for the behaviors and reports that offering preferred reinforcers did not help. An anxiety disorder is ruled out because according to the family, Mr. S’s drive to constantly move and complete rituals is fueling his anxiety. Schizoaffective disorder is ruled out because Mr. S denies auditory hallucinations and has not been observed responding to internal stimuli.
His Bush-Francis Catatonia Rating Scale (BFCRS) score is 26, which suggests a high likelihood of catatonia. Based on the BFCRS score, Mr. S’s psychiatrist makes the diagnosis of hyperkinetic catatonia.
The authors’ observations
The psychiatrist determined that Mr. S had been misdiagnosed with bipolar disorder at age 13. At that time, he had experienced his first episode of hyperkinetic catatonia and his symptoms decreased after he received lorazepam in the ED. However, the treatment team did not correctly identify this, most likely due to limited knowledge of catatonia among emergency medicine clinicians.
This case exemplifies a cognitive error of premature closure. Rather than considering catatonia as a complication of autism when Mr. S was 13, the clinicians added a second psychiatric diagnosis of bipolar disorder.Although premature closure errors generally occur when the physician assumes the patient is having a common complication of a known illness,1 in Mr. S’s case, the opposite occurred.
Conceptualizing catatonia
One helpful model for conceptualizing catatonia is to think of it as a basal ganglia disorder, with lesions in the basal ganglia thalamocortical tracts and the anterior cingulate/medial orbitofrontal circuit. Disrupting these pathways can result in symptoms such as mutism or repetitive and imitative behaviors. This is likely due to decreased disinhibition by gamma-aminobutyric acid (GABA), resulting in a hypodopaminergic state. This explains why benzodiazepines, which act to increase GABA, are effective for treating catatonia, and antipsychotics that act to decrease dopamine can exacerbate symptoms. Fricchione et al2 developed a model to visually represent the neurobiologic pathophysiology of catatonia (Figure2).
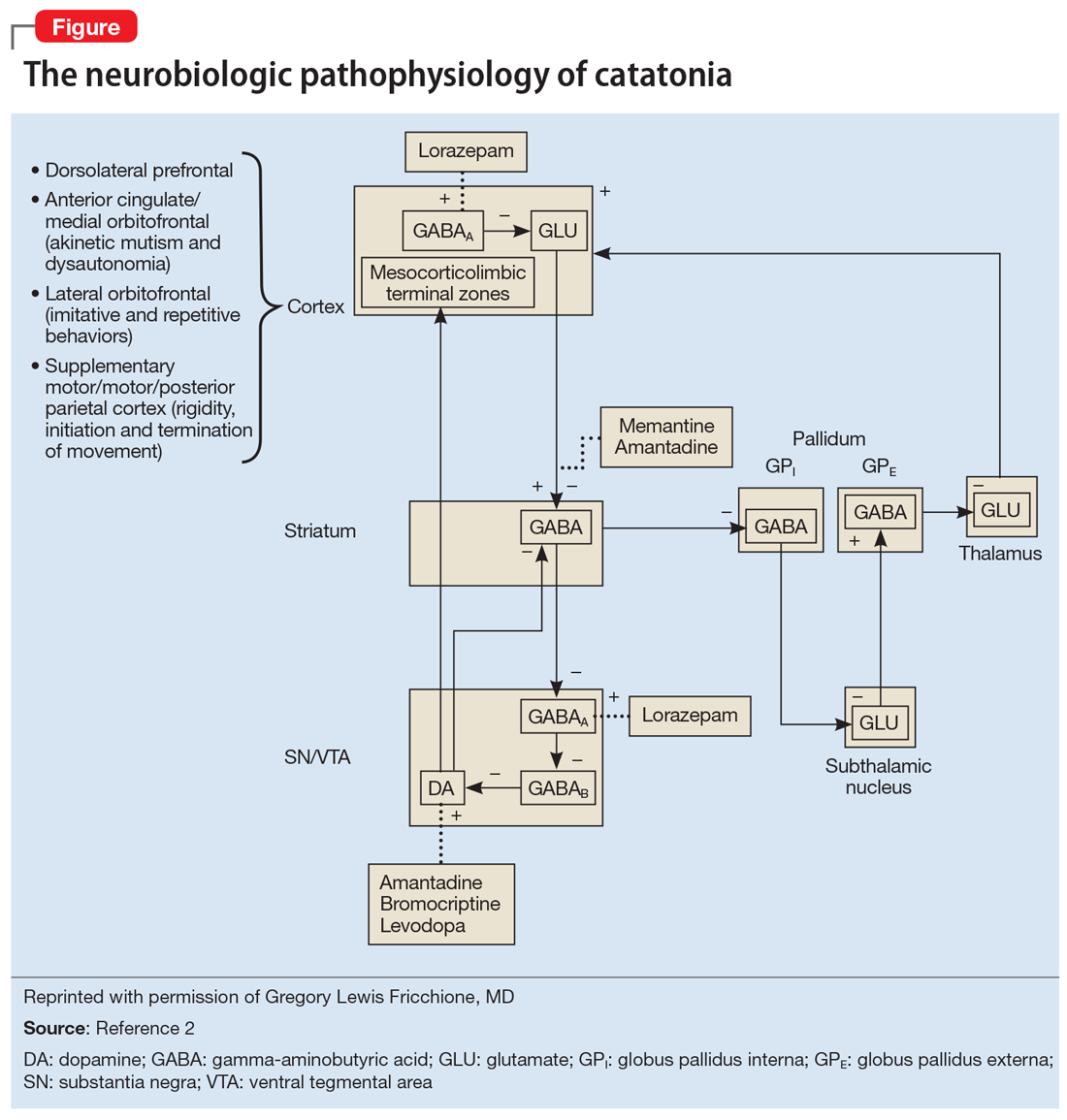
Continue to: Underlying causes of catatonia
Underlying causes of catatonia
Catatonia is most often seen in individuals with an underlying psychiatric condition such as schizophrenia, mood disorders, or autism. However, catatonia also occurs in the context of general neurologic and medical disorders, including (but not limited to) infections, metabolic disorders, endocrinopathies, epilepsy, neurodegenerative diseases, delirium, hypertensive encephalopathy, autoimmune encephalitis, and liver and kidney transplantation.3
Subtypes of catatonia include4:
- hypokinetic catatonia, which presents as stupor, mutism, and negativism
- hyperkinetic catatonia, which presents as hyperactivity, agitation, and stereotypy (as observed in Mr. S)
- malignant catatonia, which is a potentially lethal form of catatonia that occurs when hypo- or hyperkinetic catatonia is accompanied by autonomic instability such as tachycardia, tachypnea, hypertension, fever, and muscle rigidity
- periodic catatonia, which is characterized by brief episodes of stupor or excitatory catatonia lasting 4 to 10 days. These episodes recur over weeks to years, with patients remaining asymptomatic between episodes, or showing mild symptoms, such as facial grimacing or negativisms. Periodic catatonia often is autosomal dominant, involves linkage for the long arm of chromosome 15, and has a better prognosis than the other forms.
Autism and catatonia
Most individuals with autism who experience a catatonic episode first do so between age 10 and 19, and many episodes are precipitated by sudden changes in routine resulting in stress.5 An estimated 12% to 18% of patients with autism are diagnosed with catatonia in their lifetime, but the actual prevalence is likely higher.4
One of the reasons for this might be that although catatonia is well known in the psychiatric community, it is relatively unknown in the general medical community. Children and adolescents with psychiatric illness are likely to have symptoms of catatonia overlooked because catatonia often is not included in the differential diagnosis.6
In Mr. S’s case, it became clear that he did not have a mood disorder, but was prone to episodes of hyperkinetic catatonia due to his autism.
Continue to: Better recognition of catatonia
Better recognition of catatonia
As catatonia becomes better elucidated and more clearly described in the literature, there is increasing awareness that symptoms do not always involve stupor, mutism, and slowed motor activity, but can include increased motor activity, agitation, and stereotypies. The BFCRS is extremely useful for quantifying symptoms of catatonia. The best way to confirm the diagnosis is to use a lorazepam challenge in an inpatient setting, or a trial of lorazepam in an outpatient setting.5
[polldaddy:10544548]
The authors’ observations
Lorazepam is often considered the first-line treatment for catatonia because it is one of the most widely studied medications. Other benzodiazepines, such as oxazepam and clonazepam, and the sedative/hypnotic zolpidem have also been shown to be effective. Antipsychotics with dopamine-blocking mechanisms can exacerbate symptoms of catatonia and should be avoided in these patients. Furthermore, in cases of refractory catatonia, bilateral electroconvulsive therapy is an important and necessary treatment.7
TREATMENT Pharmacologic agents decrease BFCRS score
Mr. S is prescribed a regimen of lorazepam, 2 mg by mouth daily, and the supplement N-acetylcysteine, 600 mg by mouth daily. Within 2 weeks of starting this regimen, Mr. S’s BFCRS score decreases from 26 to 14. After 6 months of treatment with lorazepam, Mr. S shows considerable improvement. The stereotypic behaviors and impulsivity decrease significantly, leading to improved sleep and performance in school. After 6 months Mr. S is successfully tapered off the lorazepam, with a complete return to baseline.
Bottom Line
Hyperkinetic catatonia is easily overlooked, especially in the emergency setting. Catatonia should always be ruled out, particularly in patients with underlying conditions associated with it. Hyperkinetic catatonia is an underrecognized comorbidity in patients with autism.
Related Resources
- Dhossche DM, Wing L, Ohta M, et al. International Review of Neurobiology: Catatonia in autism spectrum disorders, vol 72. New York, NY: Academic Press/Elsevier; 2006.
- Taylor MA, Fink M. Catatonia in psychiatric classification: a home of its own. Am J Psychiatry. 2003;160(7):1233-1241.
Drug Brand Names
Amantadine • Symmetrel
Bromocriptine • Parlodel
Clonazepam • Klonopin
Lorazepam • Ativan
Memantine • Namenda
Oxazepam • Serax
Quetiapine • Seroquel
Valproic acid • Depakene, Depakote
Zolpidem • Ambien
1. McGee DL. Cognitive errors in clinical decision making. Merck Manual. https://www.merckmanuals.com/professional/special-subjects/clinical-decision-making/cognitive-errors-in-clinical-decision-making. Published November 2018. Accessed February 10, 2020.
2. Fricchione GL, Gross AF, Stern TA. Catatonia, neuroleptic malignant syndrome, and serotonin syndrome. Fricchione GL, Huffman JC, Stern TA, Bush G, eds. Massachusetts General Hospital Handbook of General Hospital Psychiatry. 6th ed. Philadelphia, PA: Saunders Elsevier; 2004:513-530.
3. Oldham MA, Lee HB. Catatonia vis-à-vis delirium: the significance of recognizing catatonia in altered mental status. Gen Hosp Psychiatry. 2015;37(6):554-559.
4. Wijemanne S, Jankovic J. Movement disorders in catatonia. J Neurol Neurosurg Psychiatry. 2014;86(8):825-832.
5. Dhossche DM, Shah A, Wing L. Blueprints for the assessment, treatment, and future study of catatonia in autism spectrum disorders. Int Rev Neurobiol. 2006:72;267-284.
6. Wing L, Shah A. Catatonia in autistic spectrum disorders. Br J Psychiatry. 2000:176(4):357-362.
7. Seinaert P, Dhossche DM, Vancampfort D, et al. A clinical review of the treatment of catatonia. Front Psychiatry. 2014;5:181.
1. McGee DL. Cognitive errors in clinical decision making. Merck Manual. https://www.merckmanuals.com/professional/special-subjects/clinical-decision-making/cognitive-errors-in-clinical-decision-making. Published November 2018. Accessed February 10, 2020.
2. Fricchione GL, Gross AF, Stern TA. Catatonia, neuroleptic malignant syndrome, and serotonin syndrome. Fricchione GL, Huffman JC, Stern TA, Bush G, eds. Massachusetts General Hospital Handbook of General Hospital Psychiatry. 6th ed. Philadelphia, PA: Saunders Elsevier; 2004:513-530.
3. Oldham MA, Lee HB. Catatonia vis-à-vis delirium: the significance of recognizing catatonia in altered mental status. Gen Hosp Psychiatry. 2015;37(6):554-559.
4. Wijemanne S, Jankovic J. Movement disorders in catatonia. J Neurol Neurosurg Psychiatry. 2014;86(8):825-832.
5. Dhossche DM, Shah A, Wing L. Blueprints for the assessment, treatment, and future study of catatonia in autism spectrum disorders. Int Rev Neurobiol. 2006:72;267-284.
6. Wing L, Shah A. Catatonia in autistic spectrum disorders. Br J Psychiatry. 2000:176(4):357-362.
7. Seinaert P, Dhossche DM, Vancampfort D, et al. A clinical review of the treatment of catatonia. Front Psychiatry. 2014;5:181.
Yale’s COVID-19 inpatient protocol: Hydroxychloroquine plus/minus tocilizumab
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
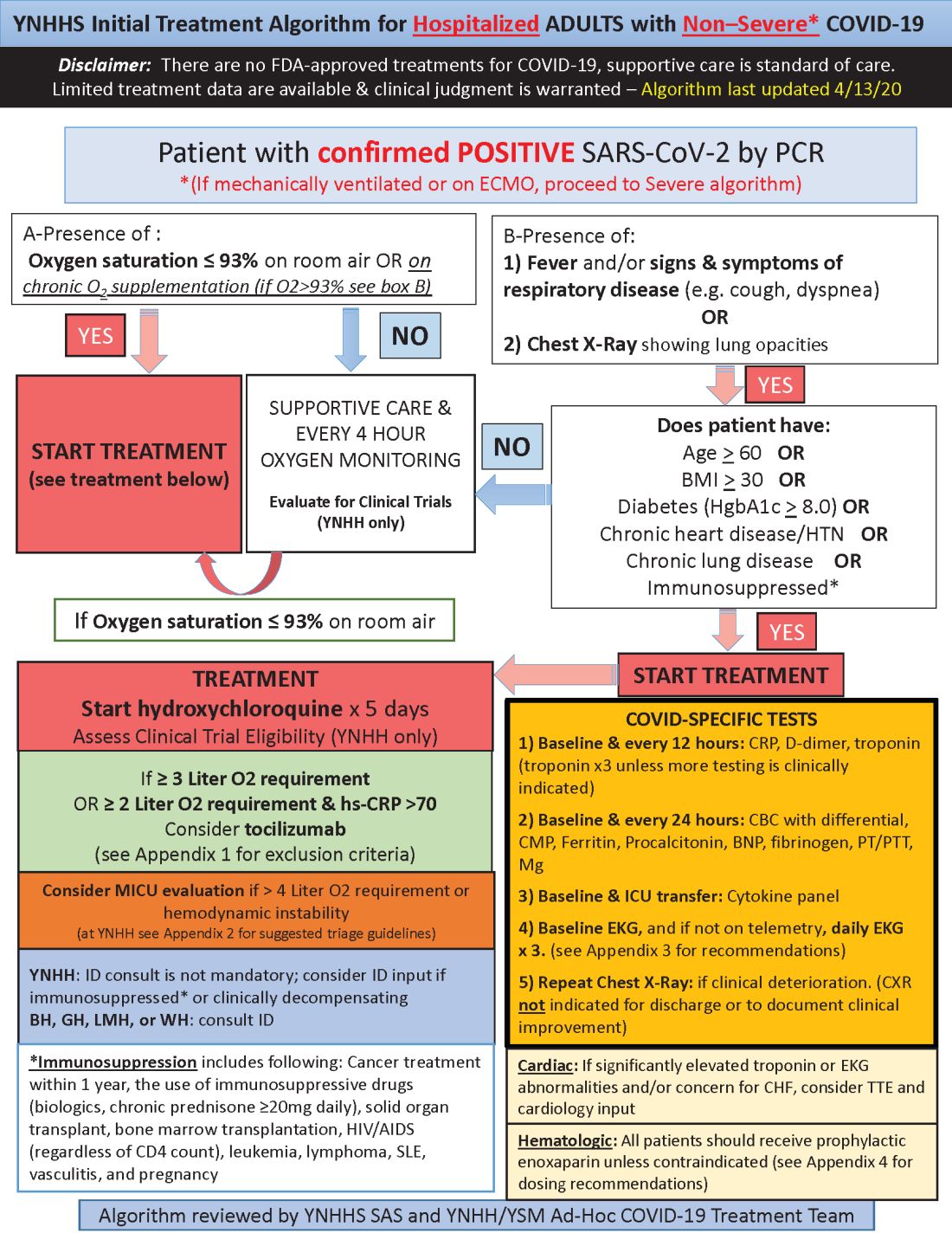
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
[email protected]
This article was updated with the latest treatment algorithm on 5/6/2020.
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
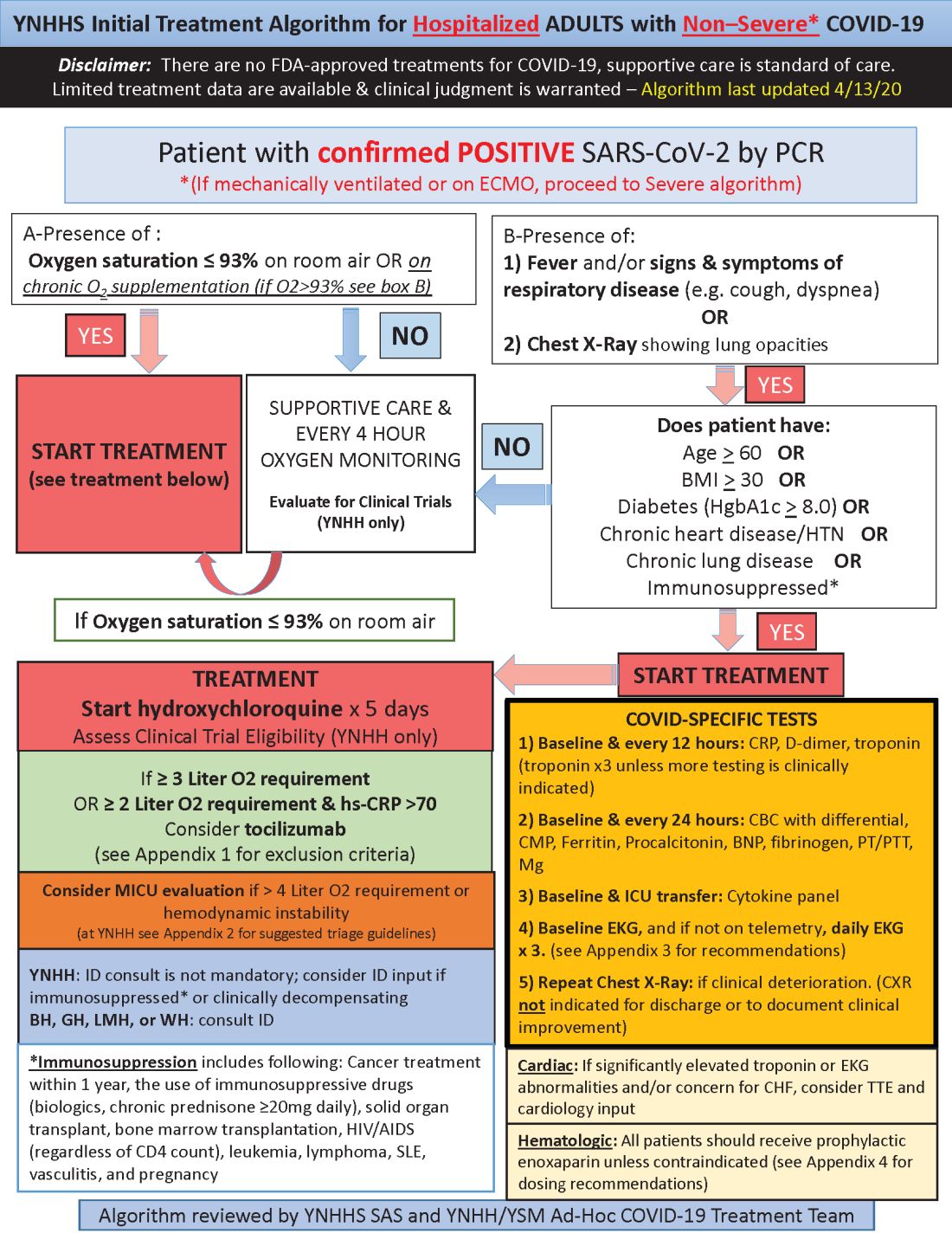
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
[email protected]
This article was updated with the latest treatment algorithm on 5/6/2020.
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
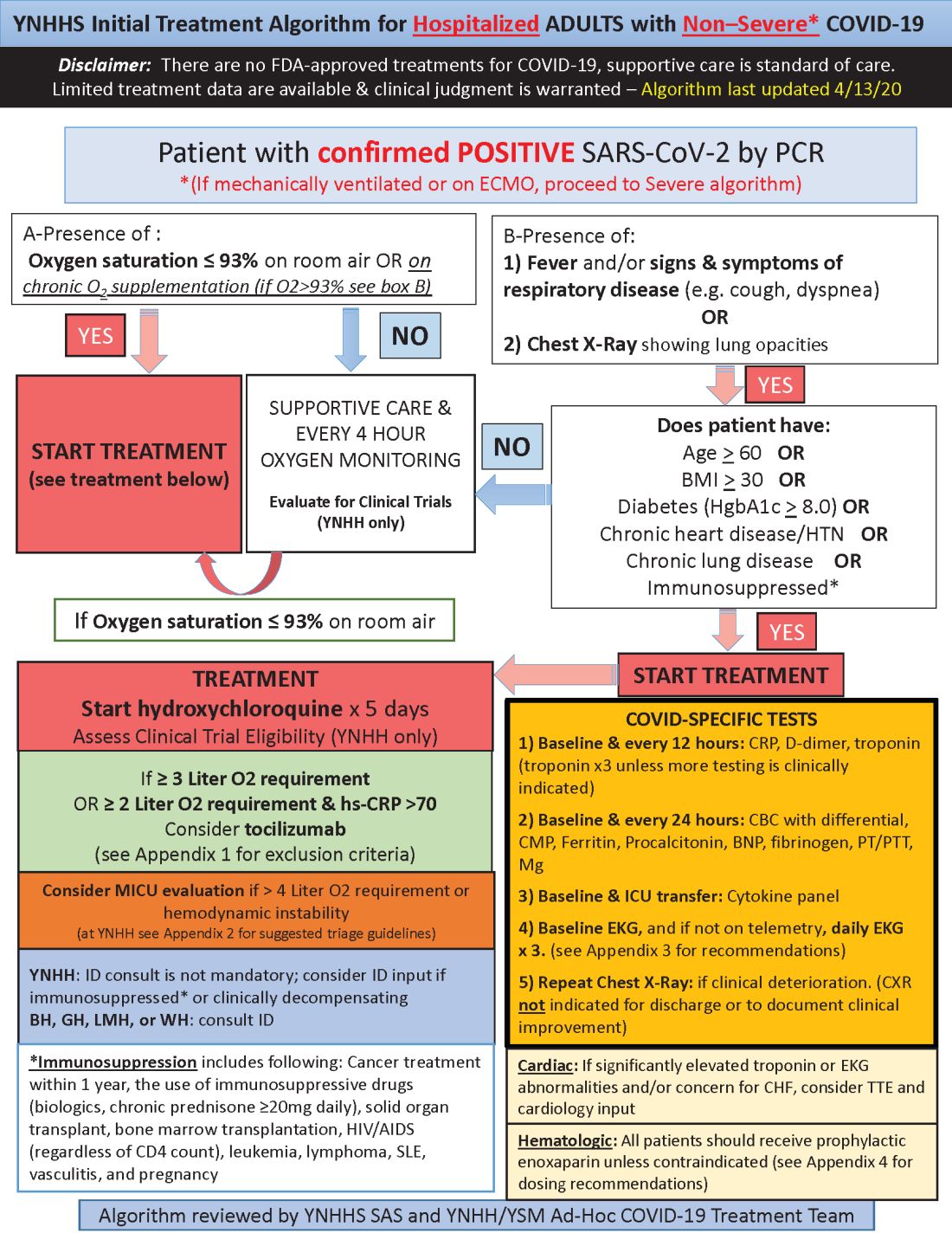
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
[email protected]
This article was updated with the latest treatment algorithm on 5/6/2020.