User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'medstat-accordion-set article-series')]
EHR Copy and Paste Can Get Physicians Into Trouble
Physicians who misuse the “copy-and-paste” feature in patients’ electronic health records (EHRs) can face serious consequences, including lost hospital privileges, fines, and malpractice lawsuits.
In California, a locum tenens physician lost her hospital privileges after repeatedly violating the copy-and-paste policy developed at Santa Rosa Memorial Hospital, Santa Rosa, California.
“Her use of copy and paste impaired continuity of care,” said Alvin Gore, MD, who was involved in the case as the hospital’s director of utilization management.
Dr. Gore said the hospital warned the doctor, but she did not change her behavior. He did not identify the physician, citing confidentiality. The case occurred more than 5 years ago. Since then, several physicians have been called onto the carpet for violations of the policy, but no one else has lost privileges, Dr. Gore said.
“EHRs are imperfect, time consuming, and somewhat rigid,” said Robert A. Dowling, MD, a practice management consultant for large medical groups. “If physicians can’t easily figure out a complex system, they’re likely to use a workaround like copy and paste.”
Copy-and-paste abuse has also led to fines. A six-member cardiology group in Somerville, New Jersey, paid a $422,000 fine to the federal government to settle copy-and-paste charges, following an investigation by the Office of the Inspector General of the Department of Health and Human Services, according to the Report on Medicare Compliance.
This big settlement, announced in 2016, is a rare case in which physicians were charged with copy-and-paste fraud — intentionally using it to enhance reimbursement.
More commonly, Medicare contractors identify physicians who unintentionally received overpayments through sloppy copy-and-paste practices, according to a coding and documentation auditor who worked for 10 years at a Medicare contractor in Pennsylvania.
Such cases are frequent and are handled confidentially, said the auditor, who asked not to be identified. Practices must return the overpayment, and the physicians involved are “contacted and educated,” she said.
Copy and paste can also show up in malpractice lawsuits. In a 2012 survey, 53% of professional liability carriers said they had handled an EHR-related malpractice claim, and 71% of those claims included copy-and-paste use.
One such case, described by CRICO, a malpractice carrier based in Massachusetts, took place in 2012-2013. “A patient developed amiodarone toxicity because the patient›s history and medications were copied from a previous note that did not document that the patient was already on the medication,» CRICO stated.
“If you do face a malpractice claim, copying and pasting the same note repeatedly makes you look clinically inattentive, even if the copy/pasted material is unrelated to the adverse event,” CRICO officials noted in a report.
The Push to Use Copy and Paste
Copy and paste is a great time-saver. One study linked its use to lower burnout rates. However, it can easily introduce errors into the medical record. “This can be a huge problem,” Dr. Dowling said. “If, for example, you copy forward a previous note that said the patient had blood in their urine ‘6 days ago,’ it is immediately inaccurate.”
Practices can control use of copy and paste through coding clerks who read the medical records and then educate doctors when problems crop up.
The Pennsylvania auditor, who now works for a large group practice, said the group has very few copy-and-paste problems because of her role. “Not charting responsibly rarely happens because I work very closely with the doctors,” she said.
Dr. Dowling, however, reports that many physicians continue to overuse copy and paste. He points to a 2022 study which found that, on average, half the clinical note at one health system had been copied and pasted.
One solution might be to sanction physicians for overusing copy and paste, just as they’re sometimes penalized for not completing their notes on time with a reduction in income or possible termination.
Practices could periodically audit medical records for excessive copy-paste use. EHR systems like Epic’s can indicate how much of a doctor’s note has been copied. But Dr. Dowling doesn’t know of any practices that do this.
“There is little appetite to introduce a new enforcement activity for physicians,” he said. “Physicians would see it just as a way to make their lives more difficult than they already are.”
Monitoring in Hospitals and Health Systems
Some hospitals and health systems have gone as far as disabling copy-and-paste function in their EHR systems. However, enterprising physicians have found ways around these blocks.
Some institutions have also introduced formal policies, directing doctors on how they can copy and paste, including Banner Health in Arizona, Northwell Health in New York, UConn Health in Connecticut, University of Maryland Medical System, and University of Toledo in Ohio.
Definitions of what is not acceptable vary, but most of these policies oppose copying someone else’s notes and direct physicians to indicate the origin of pasted material.
Santa Rosa Memorial’s policy is quite specific. It still allows some copy and paste but stipulates that it cannot be used for the chief complaint, the review of systems, the physical examination, and the assessment and plan in the medical record, except when the information can’t be obtained directly from the patient. Also, physicians must summarize test results and provide references to other providers’ notes.
Dr. Gore said he and a physician educator who works with physicians on clinical documentation proposed the policy about a decade ago. When physicians on staff were asked to comment, some said they would be opposed to a complete ban, but they generally agreed that copy and paste was a serious problem that needed to be addressed, he said.
The hospital could have simply adopted guidelines, as opposed to rules with consequences, but “we wanted our policy to have teeth,” Dr. Gore said.
When violators are identified, Dr. Gore says he meets with them confidentially and educates them on proper use of copy and paste. Sometimes, the department head is brought in. Some physicians go on to violate the policy again and have to attend another meeting, he said, but aside from the one case, no one else has been disciplined.
It’s unclear how many physicians have faced consequences for misusing copy-paste features — such data aren’t tracked, and sanctions are likely to be handled confidentially, as a personnel matter.
Geisinger Health in Pennsylvania regularly monitors copy-and-paste usage and makes it part of physicians’ professional evaluations, according to a 2022 presentation by a Geisinger official.
Meanwhile, even when systems don’t have specific policies, they may still discipline physicians when copy and paste leads to errors. Scott MacDonald, MD, chief medical information officer at UC Davis Health in Sacramento, California, told this news organization that copy-and-paste abuse has come up a few times over the years in investigations of clinical errors.
Holding Physicians Accountable
Physicians can be held accountable for copy and paste by Medicare contractors and in malpractice lawsuits, but the most obvious way is at their place of work: A practice, hospital, or health system.
One physician has lost staff privileges, but more typically, coding clerks or colleagues talk to offending physicians and try to educate them on proper use of copy and paste.
Educational outreach, however, is often ineffective, said Robert Hirschtick, MD, a retired teaching physician at Northwestern University Feinberg School of Medicine, Chicago, Illinois. “The physician may be directed to take an online course,” he said. “When they take the course, the goal is to get it done with, rather than to learn something new.”
Dr. Hirschtick’s articles on copy and paste, including one titled, “Sloppy and Paste,” have put him at the front lines of the debate. “This is an ethical issue,” he said in an interview. He agrees that some forms of copy and paste are permissible, but in many cases, “it is intellectually dishonest and potentially even plagiarism,” he said.
Dr. Hirschtick argues that copy-and-paste policies need more teeth. “Tying violations to compensation would be quite effective,” he said. “Even if physicians were rarely penalized, just knowing that it could happen to you might be enough. But I haven’t heard of anyone doing this.”
A version of this article appeared on Medscape.com.
Physicians who misuse the “copy-and-paste” feature in patients’ electronic health records (EHRs) can face serious consequences, including lost hospital privileges, fines, and malpractice lawsuits.
In California, a locum tenens physician lost her hospital privileges after repeatedly violating the copy-and-paste policy developed at Santa Rosa Memorial Hospital, Santa Rosa, California.
“Her use of copy and paste impaired continuity of care,” said Alvin Gore, MD, who was involved in the case as the hospital’s director of utilization management.
Dr. Gore said the hospital warned the doctor, but she did not change her behavior. He did not identify the physician, citing confidentiality. The case occurred more than 5 years ago. Since then, several physicians have been called onto the carpet for violations of the policy, but no one else has lost privileges, Dr. Gore said.
“EHRs are imperfect, time consuming, and somewhat rigid,” said Robert A. Dowling, MD, a practice management consultant for large medical groups. “If physicians can’t easily figure out a complex system, they’re likely to use a workaround like copy and paste.”
Copy-and-paste abuse has also led to fines. A six-member cardiology group in Somerville, New Jersey, paid a $422,000 fine to the federal government to settle copy-and-paste charges, following an investigation by the Office of the Inspector General of the Department of Health and Human Services, according to the Report on Medicare Compliance.
This big settlement, announced in 2016, is a rare case in which physicians were charged with copy-and-paste fraud — intentionally using it to enhance reimbursement.
More commonly, Medicare contractors identify physicians who unintentionally received overpayments through sloppy copy-and-paste practices, according to a coding and documentation auditor who worked for 10 years at a Medicare contractor in Pennsylvania.
Such cases are frequent and are handled confidentially, said the auditor, who asked not to be identified. Practices must return the overpayment, and the physicians involved are “contacted and educated,” she said.
Copy and paste can also show up in malpractice lawsuits. In a 2012 survey, 53% of professional liability carriers said they had handled an EHR-related malpractice claim, and 71% of those claims included copy-and-paste use.
One such case, described by CRICO, a malpractice carrier based in Massachusetts, took place in 2012-2013. “A patient developed amiodarone toxicity because the patient›s history and medications were copied from a previous note that did not document that the patient was already on the medication,» CRICO stated.
“If you do face a malpractice claim, copying and pasting the same note repeatedly makes you look clinically inattentive, even if the copy/pasted material is unrelated to the adverse event,” CRICO officials noted in a report.
The Push to Use Copy and Paste
Copy and paste is a great time-saver. One study linked its use to lower burnout rates. However, it can easily introduce errors into the medical record. “This can be a huge problem,” Dr. Dowling said. “If, for example, you copy forward a previous note that said the patient had blood in their urine ‘6 days ago,’ it is immediately inaccurate.”
Practices can control use of copy and paste through coding clerks who read the medical records and then educate doctors when problems crop up.
The Pennsylvania auditor, who now works for a large group practice, said the group has very few copy-and-paste problems because of her role. “Not charting responsibly rarely happens because I work very closely with the doctors,” she said.
Dr. Dowling, however, reports that many physicians continue to overuse copy and paste. He points to a 2022 study which found that, on average, half the clinical note at one health system had been copied and pasted.
One solution might be to sanction physicians for overusing copy and paste, just as they’re sometimes penalized for not completing their notes on time with a reduction in income or possible termination.
Practices could periodically audit medical records for excessive copy-paste use. EHR systems like Epic’s can indicate how much of a doctor’s note has been copied. But Dr. Dowling doesn’t know of any practices that do this.
“There is little appetite to introduce a new enforcement activity for physicians,” he said. “Physicians would see it just as a way to make their lives more difficult than they already are.”
Monitoring in Hospitals and Health Systems
Some hospitals and health systems have gone as far as disabling copy-and-paste function in their EHR systems. However, enterprising physicians have found ways around these blocks.
Some institutions have also introduced formal policies, directing doctors on how they can copy and paste, including Banner Health in Arizona, Northwell Health in New York, UConn Health in Connecticut, University of Maryland Medical System, and University of Toledo in Ohio.
Definitions of what is not acceptable vary, but most of these policies oppose copying someone else’s notes and direct physicians to indicate the origin of pasted material.
Santa Rosa Memorial’s policy is quite specific. It still allows some copy and paste but stipulates that it cannot be used for the chief complaint, the review of systems, the physical examination, and the assessment and plan in the medical record, except when the information can’t be obtained directly from the patient. Also, physicians must summarize test results and provide references to other providers’ notes.
Dr. Gore said he and a physician educator who works with physicians on clinical documentation proposed the policy about a decade ago. When physicians on staff were asked to comment, some said they would be opposed to a complete ban, but they generally agreed that copy and paste was a serious problem that needed to be addressed, he said.
The hospital could have simply adopted guidelines, as opposed to rules with consequences, but “we wanted our policy to have teeth,” Dr. Gore said.
When violators are identified, Dr. Gore says he meets with them confidentially and educates them on proper use of copy and paste. Sometimes, the department head is brought in. Some physicians go on to violate the policy again and have to attend another meeting, he said, but aside from the one case, no one else has been disciplined.
It’s unclear how many physicians have faced consequences for misusing copy-paste features — such data aren’t tracked, and sanctions are likely to be handled confidentially, as a personnel matter.
Geisinger Health in Pennsylvania regularly monitors copy-and-paste usage and makes it part of physicians’ professional evaluations, according to a 2022 presentation by a Geisinger official.
Meanwhile, even when systems don’t have specific policies, they may still discipline physicians when copy and paste leads to errors. Scott MacDonald, MD, chief medical information officer at UC Davis Health in Sacramento, California, told this news organization that copy-and-paste abuse has come up a few times over the years in investigations of clinical errors.
Holding Physicians Accountable
Physicians can be held accountable for copy and paste by Medicare contractors and in malpractice lawsuits, but the most obvious way is at their place of work: A practice, hospital, or health system.
One physician has lost staff privileges, but more typically, coding clerks or colleagues talk to offending physicians and try to educate them on proper use of copy and paste.
Educational outreach, however, is often ineffective, said Robert Hirschtick, MD, a retired teaching physician at Northwestern University Feinberg School of Medicine, Chicago, Illinois. “The physician may be directed to take an online course,” he said. “When they take the course, the goal is to get it done with, rather than to learn something new.”
Dr. Hirschtick’s articles on copy and paste, including one titled, “Sloppy and Paste,” have put him at the front lines of the debate. “This is an ethical issue,” he said in an interview. He agrees that some forms of copy and paste are permissible, but in many cases, “it is intellectually dishonest and potentially even plagiarism,” he said.
Dr. Hirschtick argues that copy-and-paste policies need more teeth. “Tying violations to compensation would be quite effective,” he said. “Even if physicians were rarely penalized, just knowing that it could happen to you might be enough. But I haven’t heard of anyone doing this.”
A version of this article appeared on Medscape.com.
Physicians who misuse the “copy-and-paste” feature in patients’ electronic health records (EHRs) can face serious consequences, including lost hospital privileges, fines, and malpractice lawsuits.
In California, a locum tenens physician lost her hospital privileges after repeatedly violating the copy-and-paste policy developed at Santa Rosa Memorial Hospital, Santa Rosa, California.
“Her use of copy and paste impaired continuity of care,” said Alvin Gore, MD, who was involved in the case as the hospital’s director of utilization management.
Dr. Gore said the hospital warned the doctor, but she did not change her behavior. He did not identify the physician, citing confidentiality. The case occurred more than 5 years ago. Since then, several physicians have been called onto the carpet for violations of the policy, but no one else has lost privileges, Dr. Gore said.
“EHRs are imperfect, time consuming, and somewhat rigid,” said Robert A. Dowling, MD, a practice management consultant for large medical groups. “If physicians can’t easily figure out a complex system, they’re likely to use a workaround like copy and paste.”
Copy-and-paste abuse has also led to fines. A six-member cardiology group in Somerville, New Jersey, paid a $422,000 fine to the federal government to settle copy-and-paste charges, following an investigation by the Office of the Inspector General of the Department of Health and Human Services, according to the Report on Medicare Compliance.
This big settlement, announced in 2016, is a rare case in which physicians were charged with copy-and-paste fraud — intentionally using it to enhance reimbursement.
More commonly, Medicare contractors identify physicians who unintentionally received overpayments through sloppy copy-and-paste practices, according to a coding and documentation auditor who worked for 10 years at a Medicare contractor in Pennsylvania.
Such cases are frequent and are handled confidentially, said the auditor, who asked not to be identified. Practices must return the overpayment, and the physicians involved are “contacted and educated,” she said.
Copy and paste can also show up in malpractice lawsuits. In a 2012 survey, 53% of professional liability carriers said they had handled an EHR-related malpractice claim, and 71% of those claims included copy-and-paste use.
One such case, described by CRICO, a malpractice carrier based in Massachusetts, took place in 2012-2013. “A patient developed amiodarone toxicity because the patient›s history and medications were copied from a previous note that did not document that the patient was already on the medication,» CRICO stated.
“If you do face a malpractice claim, copying and pasting the same note repeatedly makes you look clinically inattentive, even if the copy/pasted material is unrelated to the adverse event,” CRICO officials noted in a report.
The Push to Use Copy and Paste
Copy and paste is a great time-saver. One study linked its use to lower burnout rates. However, it can easily introduce errors into the medical record. “This can be a huge problem,” Dr. Dowling said. “If, for example, you copy forward a previous note that said the patient had blood in their urine ‘6 days ago,’ it is immediately inaccurate.”
Practices can control use of copy and paste through coding clerks who read the medical records and then educate doctors when problems crop up.
The Pennsylvania auditor, who now works for a large group practice, said the group has very few copy-and-paste problems because of her role. “Not charting responsibly rarely happens because I work very closely with the doctors,” she said.
Dr. Dowling, however, reports that many physicians continue to overuse copy and paste. He points to a 2022 study which found that, on average, half the clinical note at one health system had been copied and pasted.
One solution might be to sanction physicians for overusing copy and paste, just as they’re sometimes penalized for not completing their notes on time with a reduction in income or possible termination.
Practices could periodically audit medical records for excessive copy-paste use. EHR systems like Epic’s can indicate how much of a doctor’s note has been copied. But Dr. Dowling doesn’t know of any practices that do this.
“There is little appetite to introduce a new enforcement activity for physicians,” he said. “Physicians would see it just as a way to make their lives more difficult than they already are.”
Monitoring in Hospitals and Health Systems
Some hospitals and health systems have gone as far as disabling copy-and-paste function in their EHR systems. However, enterprising physicians have found ways around these blocks.
Some institutions have also introduced formal policies, directing doctors on how they can copy and paste, including Banner Health in Arizona, Northwell Health in New York, UConn Health in Connecticut, University of Maryland Medical System, and University of Toledo in Ohio.
Definitions of what is not acceptable vary, but most of these policies oppose copying someone else’s notes and direct physicians to indicate the origin of pasted material.
Santa Rosa Memorial’s policy is quite specific. It still allows some copy and paste but stipulates that it cannot be used for the chief complaint, the review of systems, the physical examination, and the assessment and plan in the medical record, except when the information can’t be obtained directly from the patient. Also, physicians must summarize test results and provide references to other providers’ notes.
Dr. Gore said he and a physician educator who works with physicians on clinical documentation proposed the policy about a decade ago. When physicians on staff were asked to comment, some said they would be opposed to a complete ban, but they generally agreed that copy and paste was a serious problem that needed to be addressed, he said.
The hospital could have simply adopted guidelines, as opposed to rules with consequences, but “we wanted our policy to have teeth,” Dr. Gore said.
When violators are identified, Dr. Gore says he meets with them confidentially and educates them on proper use of copy and paste. Sometimes, the department head is brought in. Some physicians go on to violate the policy again and have to attend another meeting, he said, but aside from the one case, no one else has been disciplined.
It’s unclear how many physicians have faced consequences for misusing copy-paste features — such data aren’t tracked, and sanctions are likely to be handled confidentially, as a personnel matter.
Geisinger Health in Pennsylvania regularly monitors copy-and-paste usage and makes it part of physicians’ professional evaluations, according to a 2022 presentation by a Geisinger official.
Meanwhile, even when systems don’t have specific policies, they may still discipline physicians when copy and paste leads to errors. Scott MacDonald, MD, chief medical information officer at UC Davis Health in Sacramento, California, told this news organization that copy-and-paste abuse has come up a few times over the years in investigations of clinical errors.
Holding Physicians Accountable
Physicians can be held accountable for copy and paste by Medicare contractors and in malpractice lawsuits, but the most obvious way is at their place of work: A practice, hospital, or health system.
One physician has lost staff privileges, but more typically, coding clerks or colleagues talk to offending physicians and try to educate them on proper use of copy and paste.
Educational outreach, however, is often ineffective, said Robert Hirschtick, MD, a retired teaching physician at Northwestern University Feinberg School of Medicine, Chicago, Illinois. “The physician may be directed to take an online course,” he said. “When they take the course, the goal is to get it done with, rather than to learn something new.”
Dr. Hirschtick’s articles on copy and paste, including one titled, “Sloppy and Paste,” have put him at the front lines of the debate. “This is an ethical issue,” he said in an interview. He agrees that some forms of copy and paste are permissible, but in many cases, “it is intellectually dishonest and potentially even plagiarism,” he said.
Dr. Hirschtick argues that copy-and-paste policies need more teeth. “Tying violations to compensation would be quite effective,” he said. “Even if physicians were rarely penalized, just knowing that it could happen to you might be enough. But I haven’t heard of anyone doing this.”
A version of this article appeared on Medscape.com.
Metabolite in Red Meat Increases Kidney Disease Risk
TOPLINE:
Trimethylamine N-oxide (TMAO) is a gut microbiota-derived metabolite generated by metabolism of dietary L-carnitine, primarily from red meat, and choline, from a variety of animal source foods. TMAO has been shown to cause kidney injury and tubulointerstitial fibrosis in experimental models.
In this study, TMAO was independently associated with higher risks for incident chronic kidney disease (CKD) and faster kidney function decline in humans.
METHODOLOGY:
- Study population was 10,564 participants from two community-based, prospective cohorts without baseline CKD (estimated glomerular filtration rate [eGFR] ≥ 60 mL/min/1.73 m2).
- Incident CKD was defined as eGFR decline ≥ 30% from baseline, resulting in eGFR < 60 mL/min/1.73 m2.
TAKEAWAY:
- During a median 9.4 years, 979 incident CKD events occurred.
- Correlation between baseline TMAO and total meat intake was small but statistically significant (P = .08).
- After adjustments for sociodemographic, lifestyle, diet, and cardiovascular risk factors, higher plasma TMAO was associated with more than doubled CKD incidence (hazard ratio, 2.24 for top vs bottom quintile).
- Higher TMAO levels were also associated with greater annual eGFR decline (top vs bottom quintile eGFR change = −0.43 mL/min/1.73 m2 per year.
- Compared with other major CKD risk factors, the association for the top vs bottom TMAO quintile (−0.43 mL/min/1.73 m2 per year) was similar to that seen per 10 years of older age (−0.43) and presence of diabetes (−0.51), and larger than that seen comparing Black vs non-Black race (−0.28) and per 10 mm Hg systolic blood pressure (−0.16).
IN PRACTICE:
“TMAO levels are highly modifiable by both lifestyle-like diet and pharmacologic interventions. Besides using novel drugs to lower TMAO in patients, using dietary interventions to lower TMAO in the general population could be a cost-efficient and low-risk preventive strategy for chronic kidney disease development. ... These findings support future studies to investigate whether lifestyle and pharmacologic interventions to lower TMAO may prevent CKD development and progression.”
SOURCE:
The study was conducted by Meng Wang, PhD, of Tufts University, Boston, and colleagues and published online in the Journal of the American Society of Nephrology.
LIMITATIONS:
Observational design, can’t exclude residual confounding.
Inter-assay variability.
Use of International Classification of Diseases codes for hospitalization-based CKD, subject to reporting errors.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health and an American Heart Association Postdoctoral Fellowship. Dr. Wang had no disclosures but several coauthors have patents on various diagnostics and/or industry disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
Trimethylamine N-oxide (TMAO) is a gut microbiota-derived metabolite generated by metabolism of dietary L-carnitine, primarily from red meat, and choline, from a variety of animal source foods. TMAO has been shown to cause kidney injury and tubulointerstitial fibrosis in experimental models.
In this study, TMAO was independently associated with higher risks for incident chronic kidney disease (CKD) and faster kidney function decline in humans.
METHODOLOGY:
- Study population was 10,564 participants from two community-based, prospective cohorts without baseline CKD (estimated glomerular filtration rate [eGFR] ≥ 60 mL/min/1.73 m2).
- Incident CKD was defined as eGFR decline ≥ 30% from baseline, resulting in eGFR < 60 mL/min/1.73 m2.
TAKEAWAY:
- During a median 9.4 years, 979 incident CKD events occurred.
- Correlation between baseline TMAO and total meat intake was small but statistically significant (P = .08).
- After adjustments for sociodemographic, lifestyle, diet, and cardiovascular risk factors, higher plasma TMAO was associated with more than doubled CKD incidence (hazard ratio, 2.24 for top vs bottom quintile).
- Higher TMAO levels were also associated with greater annual eGFR decline (top vs bottom quintile eGFR change = −0.43 mL/min/1.73 m2 per year.
- Compared with other major CKD risk factors, the association for the top vs bottom TMAO quintile (−0.43 mL/min/1.73 m2 per year) was similar to that seen per 10 years of older age (−0.43) and presence of diabetes (−0.51), and larger than that seen comparing Black vs non-Black race (−0.28) and per 10 mm Hg systolic blood pressure (−0.16).
IN PRACTICE:
“TMAO levels are highly modifiable by both lifestyle-like diet and pharmacologic interventions. Besides using novel drugs to lower TMAO in patients, using dietary interventions to lower TMAO in the general population could be a cost-efficient and low-risk preventive strategy for chronic kidney disease development. ... These findings support future studies to investigate whether lifestyle and pharmacologic interventions to lower TMAO may prevent CKD development and progression.”
SOURCE:
The study was conducted by Meng Wang, PhD, of Tufts University, Boston, and colleagues and published online in the Journal of the American Society of Nephrology.
LIMITATIONS:
Observational design, can’t exclude residual confounding.
Inter-assay variability.
Use of International Classification of Diseases codes for hospitalization-based CKD, subject to reporting errors.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health and an American Heart Association Postdoctoral Fellowship. Dr. Wang had no disclosures but several coauthors have patents on various diagnostics and/or industry disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
Trimethylamine N-oxide (TMAO) is a gut microbiota-derived metabolite generated by metabolism of dietary L-carnitine, primarily from red meat, and choline, from a variety of animal source foods. TMAO has been shown to cause kidney injury and tubulointerstitial fibrosis in experimental models.
In this study, TMAO was independently associated with higher risks for incident chronic kidney disease (CKD) and faster kidney function decline in humans.
METHODOLOGY:
- Study population was 10,564 participants from two community-based, prospective cohorts without baseline CKD (estimated glomerular filtration rate [eGFR] ≥ 60 mL/min/1.73 m2).
- Incident CKD was defined as eGFR decline ≥ 30% from baseline, resulting in eGFR < 60 mL/min/1.73 m2.
TAKEAWAY:
- During a median 9.4 years, 979 incident CKD events occurred.
- Correlation between baseline TMAO and total meat intake was small but statistically significant (P = .08).
- After adjustments for sociodemographic, lifestyle, diet, and cardiovascular risk factors, higher plasma TMAO was associated with more than doubled CKD incidence (hazard ratio, 2.24 for top vs bottom quintile).
- Higher TMAO levels were also associated with greater annual eGFR decline (top vs bottom quintile eGFR change = −0.43 mL/min/1.73 m2 per year.
- Compared with other major CKD risk factors, the association for the top vs bottom TMAO quintile (−0.43 mL/min/1.73 m2 per year) was similar to that seen per 10 years of older age (−0.43) and presence of diabetes (−0.51), and larger than that seen comparing Black vs non-Black race (−0.28) and per 10 mm Hg systolic blood pressure (−0.16).
IN PRACTICE:
“TMAO levels are highly modifiable by both lifestyle-like diet and pharmacologic interventions. Besides using novel drugs to lower TMAO in patients, using dietary interventions to lower TMAO in the general population could be a cost-efficient and low-risk preventive strategy for chronic kidney disease development. ... These findings support future studies to investigate whether lifestyle and pharmacologic interventions to lower TMAO may prevent CKD development and progression.”
SOURCE:
The study was conducted by Meng Wang, PhD, of Tufts University, Boston, and colleagues and published online in the Journal of the American Society of Nephrology.
LIMITATIONS:
Observational design, can’t exclude residual confounding.
Inter-assay variability.
Use of International Classification of Diseases codes for hospitalization-based CKD, subject to reporting errors.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health and an American Heart Association Postdoctoral Fellowship. Dr. Wang had no disclosures but several coauthors have patents on various diagnostics and/or industry disclosures.
A version of this article appeared on Medscape.com.
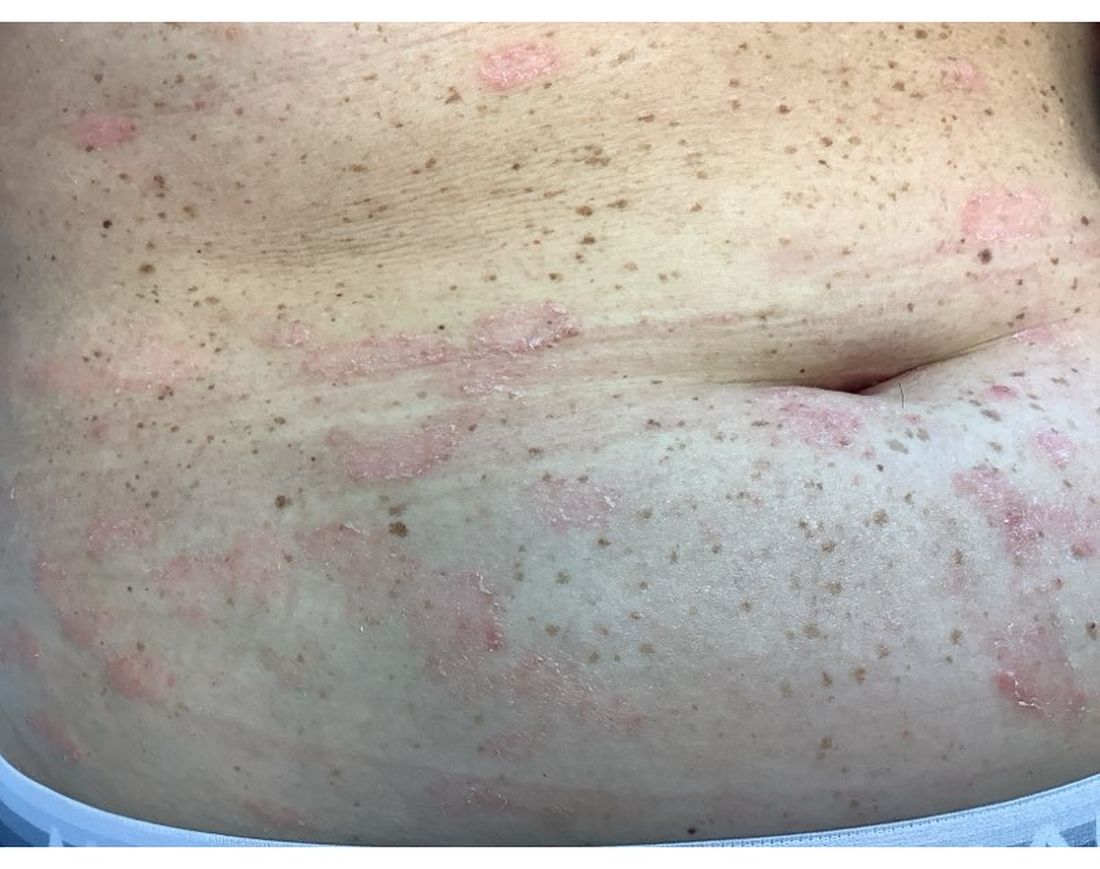
A 30-Year-Old White Female Presented With a 4-Month History of Scaly, Erythematous Patches and Plaques on Her Trunk and Extremities
Tumor necrosis factor (TNF)-alpha inhibitors are used to treat a variety of autoimmune conditions including psoriasis, psoriatic arthritis, rheumatoid arthritis (RA), spondyloarthritis, and inflammatory bowel disease (IBD). Interestingly, they have also been observed to cause paradoxical psoriasis with an incidence between 0.6%-5.3%, most commonly occurring in patients with underlying Crohn’s disease and rheumatoid arthritis (RA). Infliximab is the most common TNF inhibitor associated with this condition (52.6%-62.6% of cases) followed by etanercept (12%-29%). .
Psoriasis is traditionally divided into two types. Patients with type I psoriasis have a family history, develop symptoms before the age of 40 and are often positive for HLA-Cw6. Type II psoriasis is not related to HLA-Cw6, lacks a family history, and typically manifests after age 40. Psoriatic lesions are well-defined, erythematous plaques with silvery scales most commonly appearing on extensor surfaces and the scalp. Variants include nail psoriasis, pustular psoriasis, inverse psoriasis, and guttate psoriasis.
Although psoriasis is typically a clinical diagnosis, histologic examination may be used to differentiate from other dermatoses if necessary. The lesions of TNF inhibitor-induced psoriasis characteristically display patterns similar to primary psoriasis, including parakeratosis, microabscesses, and rete ridges. Eosinophilic hypersensitivity reactions and features overlapping with eczematous hypersensitivity (psoriasiform dermatitis) may also be present.
The pathogenesis of this condition is not well understood, but theories include a variety of immune processes including interferon overproduction, interleukin and T-cell activation, and the presence of an infectious nidus. Classical psoriasis is related to type 1 interferon release, so theoretically, immunosuppression caused by TNF inhibitor treatment may permit uncontrolled production of interferons, resulting in psoriatic lesions. Another theory is that interleukin (IL)-23, a pro-inflammatory cytokine, promotes activation of T-helper 17 (Th17) cells. Th17 cells are part of the pathogenesis of primary psoriasis and other inflammatory conditions, such as RA and inflammatory bowel disease. Of note, individuals with gastrointestinal inflammatory diseases are already known to be at a greater risk for developing psoriasis. Immunosuppression caused by a TNF inhibitor may leave patients more susceptible to other infections, which may induce psoriatic plaques.
There are multiple approaches to treatment depending on the severity of the disease. If the psoriatic eruption is mild, the medication may be continued. This “treat-through” method is often considered when stopping the current immunotherapy would cause the patient significant issues. Moderate to severe cases of TNF inhibitor-induced psoriasis may warrant switching TNF inhibitor therapy or completely changing the drug class used in the treatment of the underlying autoimmune condition. Additional treatments include topical and oral steroids, UV therapy, methotrexate, cyclosporine, and acitretin.
This case and the photo were submitted by Lucas Shapiro, BS, of Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Florida, and Leon S. Maratchi, MD, Gastro Health, Hollywood, Florida. The column was edited by Donna Bilu Martin, MD.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Li SJ et al. J Psoriasis Psoriatic Arthritis. 2019 Apr;4(2):70-80. doi: 10.1177/2475530318810851.
2. Lu J and Lu Y. J Transl Autoimmun. 2023 Sep 6:7:100211. doi: 10.1016/j.jtauto.2023.100211.
3. Nair PA and Badri T. Psoriasis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK448194/
Tumor necrosis factor (TNF)-alpha inhibitors are used to treat a variety of autoimmune conditions including psoriasis, psoriatic arthritis, rheumatoid arthritis (RA), spondyloarthritis, and inflammatory bowel disease (IBD). Interestingly, they have also been observed to cause paradoxical psoriasis with an incidence between 0.6%-5.3%, most commonly occurring in patients with underlying Crohn’s disease and rheumatoid arthritis (RA). Infliximab is the most common TNF inhibitor associated with this condition (52.6%-62.6% of cases) followed by etanercept (12%-29%). .
Psoriasis is traditionally divided into two types. Patients with type I psoriasis have a family history, develop symptoms before the age of 40 and are often positive for HLA-Cw6. Type II psoriasis is not related to HLA-Cw6, lacks a family history, and typically manifests after age 40. Psoriatic lesions are well-defined, erythematous plaques with silvery scales most commonly appearing on extensor surfaces and the scalp. Variants include nail psoriasis, pustular psoriasis, inverse psoriasis, and guttate psoriasis.
Although psoriasis is typically a clinical diagnosis, histologic examination may be used to differentiate from other dermatoses if necessary. The lesions of TNF inhibitor-induced psoriasis characteristically display patterns similar to primary psoriasis, including parakeratosis, microabscesses, and rete ridges. Eosinophilic hypersensitivity reactions and features overlapping with eczematous hypersensitivity (psoriasiform dermatitis) may also be present.
The pathogenesis of this condition is not well understood, but theories include a variety of immune processes including interferon overproduction, interleukin and T-cell activation, and the presence of an infectious nidus. Classical psoriasis is related to type 1 interferon release, so theoretically, immunosuppression caused by TNF inhibitor treatment may permit uncontrolled production of interferons, resulting in psoriatic lesions. Another theory is that interleukin (IL)-23, a pro-inflammatory cytokine, promotes activation of T-helper 17 (Th17) cells. Th17 cells are part of the pathogenesis of primary psoriasis and other inflammatory conditions, such as RA and inflammatory bowel disease. Of note, individuals with gastrointestinal inflammatory diseases are already known to be at a greater risk for developing psoriasis. Immunosuppression caused by a TNF inhibitor may leave patients more susceptible to other infections, which may induce psoriatic plaques.
There are multiple approaches to treatment depending on the severity of the disease. If the psoriatic eruption is mild, the medication may be continued. This “treat-through” method is often considered when stopping the current immunotherapy would cause the patient significant issues. Moderate to severe cases of TNF inhibitor-induced psoriasis may warrant switching TNF inhibitor therapy or completely changing the drug class used in the treatment of the underlying autoimmune condition. Additional treatments include topical and oral steroids, UV therapy, methotrexate, cyclosporine, and acitretin.
This case and the photo were submitted by Lucas Shapiro, BS, of Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Florida, and Leon S. Maratchi, MD, Gastro Health, Hollywood, Florida. The column was edited by Donna Bilu Martin, MD.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Li SJ et al. J Psoriasis Psoriatic Arthritis. 2019 Apr;4(2):70-80. doi: 10.1177/2475530318810851.
2. Lu J and Lu Y. J Transl Autoimmun. 2023 Sep 6:7:100211. doi: 10.1016/j.jtauto.2023.100211.
3. Nair PA and Badri T. Psoriasis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK448194/
Tumor necrosis factor (TNF)-alpha inhibitors are used to treat a variety of autoimmune conditions including psoriasis, psoriatic arthritis, rheumatoid arthritis (RA), spondyloarthritis, and inflammatory bowel disease (IBD). Interestingly, they have also been observed to cause paradoxical psoriasis with an incidence between 0.6%-5.3%, most commonly occurring in patients with underlying Crohn’s disease and rheumatoid arthritis (RA). Infliximab is the most common TNF inhibitor associated with this condition (52.6%-62.6% of cases) followed by etanercept (12%-29%). .
Psoriasis is traditionally divided into two types. Patients with type I psoriasis have a family history, develop symptoms before the age of 40 and are often positive for HLA-Cw6. Type II psoriasis is not related to HLA-Cw6, lacks a family history, and typically manifests after age 40. Psoriatic lesions are well-defined, erythematous plaques with silvery scales most commonly appearing on extensor surfaces and the scalp. Variants include nail psoriasis, pustular psoriasis, inverse psoriasis, and guttate psoriasis.
Although psoriasis is typically a clinical diagnosis, histologic examination may be used to differentiate from other dermatoses if necessary. The lesions of TNF inhibitor-induced psoriasis characteristically display patterns similar to primary psoriasis, including parakeratosis, microabscesses, and rete ridges. Eosinophilic hypersensitivity reactions and features overlapping with eczematous hypersensitivity (psoriasiform dermatitis) may also be present.
The pathogenesis of this condition is not well understood, but theories include a variety of immune processes including interferon overproduction, interleukin and T-cell activation, and the presence of an infectious nidus. Classical psoriasis is related to type 1 interferon release, so theoretically, immunosuppression caused by TNF inhibitor treatment may permit uncontrolled production of interferons, resulting in psoriatic lesions. Another theory is that interleukin (IL)-23, a pro-inflammatory cytokine, promotes activation of T-helper 17 (Th17) cells. Th17 cells are part of the pathogenesis of primary psoriasis and other inflammatory conditions, such as RA and inflammatory bowel disease. Of note, individuals with gastrointestinal inflammatory diseases are already known to be at a greater risk for developing psoriasis. Immunosuppression caused by a TNF inhibitor may leave patients more susceptible to other infections, which may induce psoriatic plaques.
There are multiple approaches to treatment depending on the severity of the disease. If the psoriatic eruption is mild, the medication may be continued. This “treat-through” method is often considered when stopping the current immunotherapy would cause the patient significant issues. Moderate to severe cases of TNF inhibitor-induced psoriasis may warrant switching TNF inhibitor therapy or completely changing the drug class used in the treatment of the underlying autoimmune condition. Additional treatments include topical and oral steroids, UV therapy, methotrexate, cyclosporine, and acitretin.
This case and the photo were submitted by Lucas Shapiro, BS, of Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Florida, and Leon S. Maratchi, MD, Gastro Health, Hollywood, Florida. The column was edited by Donna Bilu Martin, MD.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Li SJ et al. J Psoriasis Psoriatic Arthritis. 2019 Apr;4(2):70-80. doi: 10.1177/2475530318810851.
2. Lu J and Lu Y. J Transl Autoimmun. 2023 Sep 6:7:100211. doi: 10.1016/j.jtauto.2023.100211.
3. Nair PA and Badri T. Psoriasis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK448194/
Chronic Pain Linked to Accelerated Brain Aging
, new research showed.
Using structural MRI data from more than 9000 adults with knee osteoarthritis (KOA) from the UK Biobank, investigators developed a brain age model to compare an individual’s brain age with their chronological age. Those with KOA showed a much faster rate of brain aging than healthy individuals.
The acceleration in brain aging was largely driven by the hippocampus and predicted memory decline and incident dementia during follow-up. Researchers identified a gene highly expressed in glial cells as a possible genetic factor for accelerated brain aging.
“We demonstrate the accelerated brain aging and cognitive decline in chronic musculoskeletal pain, in particular knee osteoarthritis, and provide a neural marker for early detection and intervention,” said co-first author Jiao Liu, PhD candidate, Chinese Academy of Sciences, Beijing.
“We are interested to know how to slow down the aging brain in chronic musculoskeletal pain patients. Proper exercise and lifestyle may reduce the risk,” Dr. Liu said.
The study was published online in Nature Mental Health.
Common Condition
CMP affects more than 40% of the world’s population and has been shown to have a harmful impact on cognitive function, although the exact mechanisms remain unclear. Prior research suggests that inflammatory markers associated with brain aging are higher in patients with CMP, suggesting a link between brain aging and CMP.
To investigate further, researchers explored patterns of brain aging in healthy cohorts and cohorts with four common types of CMP — chronic knee pain, chronic back pain, chronic neck pain, and chronic hip pain.
Using their brain age model, investigators observed significantly increased brain aging, or “predicted age difference,” only in individuals with KOA (P < .001). The observation was validated in an independent dataset (P = .020), suggesting a pattern of brain aging acceleration specific to KOA.
This acceleration was primarily driven by key brain regions involved in cognitive processing, including hippocampus and orbitofrontal cortex, and was correlated with longitudinal memory decline and dementia risk.
These data also suggest that the SLC39A8 gene, which is highly expressed in glial cells, might be a key genetic factor underpinning this acceleration.
“We not only revealed the specificity of accelerated brain aging in knee osteoarthritis patients, but importantly, we also provided longitudinal evidence suggesting the ability of our brain aging marker to predict future memory decline and increased dementia risk,” corresponding author Yiheng Tu, PhD, also with Chinese Academy of Sciences, Beijing, said in a news release.
A Future Treatment Target?
Commenting on this research, Shaheen Lakhan, MD, PhD, a neurologist and researcher based in Miami, noted that in this study, people with KOA showed signs of “faster brain aging on scans. Think of it as your brain wearing a disguise, appearing older than its actual years,” Dr. Lakhan said.
“Inflammation, a key player in osteoarthritis, might be playing a double agent, wreaking havoc not just on your joints but potentially on your memory too. Researchers even identified a specific gene linked to both knee pain and faster brain aging, hinting at a potential target for future treatments,” he added.
“Importantly, the increased risk of cognitive decline and dementia associated with chronic pain is likely one of many factors, and probably not a very high one on its own,” Dr. Lakhan noted.
The “good news,” he said, is that there are many “well-established ways to keep your brain sharp. Regular exercise, a healthy diet, and staying mentally stimulated are all proven strategies to reduce dementia risk. Think of chronic pain management as another tool you can add to your brain health toolbox.”
Support for the study was provided by the STI-2030 Major Project, the National Natural Science Foundation of China, the Scientific Foundation of the Institute of Psychology, Chinese Academy of Sciences, and the Young Elite Scientist Sponsorship Program by the China Association for Science and Technology. Dr. Liu and Dr. Lakhan had no relevant disclosures.
A version of this article appeared on Medscape.com.
, new research showed.
Using structural MRI data from more than 9000 adults with knee osteoarthritis (KOA) from the UK Biobank, investigators developed a brain age model to compare an individual’s brain age with their chronological age. Those with KOA showed a much faster rate of brain aging than healthy individuals.
The acceleration in brain aging was largely driven by the hippocampus and predicted memory decline and incident dementia during follow-up. Researchers identified a gene highly expressed in glial cells as a possible genetic factor for accelerated brain aging.
“We demonstrate the accelerated brain aging and cognitive decline in chronic musculoskeletal pain, in particular knee osteoarthritis, and provide a neural marker for early detection and intervention,” said co-first author Jiao Liu, PhD candidate, Chinese Academy of Sciences, Beijing.
“We are interested to know how to slow down the aging brain in chronic musculoskeletal pain patients. Proper exercise and lifestyle may reduce the risk,” Dr. Liu said.
The study was published online in Nature Mental Health.
Common Condition
CMP affects more than 40% of the world’s population and has been shown to have a harmful impact on cognitive function, although the exact mechanisms remain unclear. Prior research suggests that inflammatory markers associated with brain aging are higher in patients with CMP, suggesting a link between brain aging and CMP.
To investigate further, researchers explored patterns of brain aging in healthy cohorts and cohorts with four common types of CMP — chronic knee pain, chronic back pain, chronic neck pain, and chronic hip pain.
Using their brain age model, investigators observed significantly increased brain aging, or “predicted age difference,” only in individuals with KOA (P < .001). The observation was validated in an independent dataset (P = .020), suggesting a pattern of brain aging acceleration specific to KOA.
This acceleration was primarily driven by key brain regions involved in cognitive processing, including hippocampus and orbitofrontal cortex, and was correlated with longitudinal memory decline and dementia risk.
These data also suggest that the SLC39A8 gene, which is highly expressed in glial cells, might be a key genetic factor underpinning this acceleration.
“We not only revealed the specificity of accelerated brain aging in knee osteoarthritis patients, but importantly, we also provided longitudinal evidence suggesting the ability of our brain aging marker to predict future memory decline and increased dementia risk,” corresponding author Yiheng Tu, PhD, also with Chinese Academy of Sciences, Beijing, said in a news release.
A Future Treatment Target?
Commenting on this research, Shaheen Lakhan, MD, PhD, a neurologist and researcher based in Miami, noted that in this study, people with KOA showed signs of “faster brain aging on scans. Think of it as your brain wearing a disguise, appearing older than its actual years,” Dr. Lakhan said.
“Inflammation, a key player in osteoarthritis, might be playing a double agent, wreaking havoc not just on your joints but potentially on your memory too. Researchers even identified a specific gene linked to both knee pain and faster brain aging, hinting at a potential target for future treatments,” he added.
“Importantly, the increased risk of cognitive decline and dementia associated with chronic pain is likely one of many factors, and probably not a very high one on its own,” Dr. Lakhan noted.
The “good news,” he said, is that there are many “well-established ways to keep your brain sharp. Regular exercise, a healthy diet, and staying mentally stimulated are all proven strategies to reduce dementia risk. Think of chronic pain management as another tool you can add to your brain health toolbox.”
Support for the study was provided by the STI-2030 Major Project, the National Natural Science Foundation of China, the Scientific Foundation of the Institute of Psychology, Chinese Academy of Sciences, and the Young Elite Scientist Sponsorship Program by the China Association for Science and Technology. Dr. Liu and Dr. Lakhan had no relevant disclosures.
A version of this article appeared on Medscape.com.
, new research showed.
Using structural MRI data from more than 9000 adults with knee osteoarthritis (KOA) from the UK Biobank, investigators developed a brain age model to compare an individual’s brain age with their chronological age. Those with KOA showed a much faster rate of brain aging than healthy individuals.
The acceleration in brain aging was largely driven by the hippocampus and predicted memory decline and incident dementia during follow-up. Researchers identified a gene highly expressed in glial cells as a possible genetic factor for accelerated brain aging.
“We demonstrate the accelerated brain aging and cognitive decline in chronic musculoskeletal pain, in particular knee osteoarthritis, and provide a neural marker for early detection and intervention,” said co-first author Jiao Liu, PhD candidate, Chinese Academy of Sciences, Beijing.
“We are interested to know how to slow down the aging brain in chronic musculoskeletal pain patients. Proper exercise and lifestyle may reduce the risk,” Dr. Liu said.
The study was published online in Nature Mental Health.
Common Condition
CMP affects more than 40% of the world’s population and has been shown to have a harmful impact on cognitive function, although the exact mechanisms remain unclear. Prior research suggests that inflammatory markers associated with brain aging are higher in patients with CMP, suggesting a link between brain aging and CMP.
To investigate further, researchers explored patterns of brain aging in healthy cohorts and cohorts with four common types of CMP — chronic knee pain, chronic back pain, chronic neck pain, and chronic hip pain.
Using their brain age model, investigators observed significantly increased brain aging, or “predicted age difference,” only in individuals with KOA (P < .001). The observation was validated in an independent dataset (P = .020), suggesting a pattern of brain aging acceleration specific to KOA.
This acceleration was primarily driven by key brain regions involved in cognitive processing, including hippocampus and orbitofrontal cortex, and was correlated with longitudinal memory decline and dementia risk.
These data also suggest that the SLC39A8 gene, which is highly expressed in glial cells, might be a key genetic factor underpinning this acceleration.
“We not only revealed the specificity of accelerated brain aging in knee osteoarthritis patients, but importantly, we also provided longitudinal evidence suggesting the ability of our brain aging marker to predict future memory decline and increased dementia risk,” corresponding author Yiheng Tu, PhD, also with Chinese Academy of Sciences, Beijing, said in a news release.
A Future Treatment Target?
Commenting on this research, Shaheen Lakhan, MD, PhD, a neurologist and researcher based in Miami, noted that in this study, people with KOA showed signs of “faster brain aging on scans. Think of it as your brain wearing a disguise, appearing older than its actual years,” Dr. Lakhan said.
“Inflammation, a key player in osteoarthritis, might be playing a double agent, wreaking havoc not just on your joints but potentially on your memory too. Researchers even identified a specific gene linked to both knee pain and faster brain aging, hinting at a potential target for future treatments,” he added.
“Importantly, the increased risk of cognitive decline and dementia associated with chronic pain is likely one of many factors, and probably not a very high one on its own,” Dr. Lakhan noted.
The “good news,” he said, is that there are many “well-established ways to keep your brain sharp. Regular exercise, a healthy diet, and staying mentally stimulated are all proven strategies to reduce dementia risk. Think of chronic pain management as another tool you can add to your brain health toolbox.”
Support for the study was provided by the STI-2030 Major Project, the National Natural Science Foundation of China, the Scientific Foundation of the Institute of Psychology, Chinese Academy of Sciences, and the Young Elite Scientist Sponsorship Program by the China Association for Science and Technology. Dr. Liu and Dr. Lakhan had no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM NATURE MENTAL HEALTH
Medicine or Politics? Doctors Defend Their Social Activism
It should come as no surprise that when physicians speak out on social and political issues, there is sometimes a backlash. This can range from the typical trolling that occurs online to rarer cases of professional penalties. Two doctors were fired by NYU Langone Health late last year after they posted social media messages about the Israel-Hamas war. Still, many physicians are not only willing to stand up for what they believe in, but they see it as an essential part of their profession.
"We're now at a place where doctors need to engage in public advocacy as an urgent part of our job," wrote Rob Davidson, MD, an emergency department physician, at the onslaught of the COVID-19 pandemic. In an Op-Ed piece for The Guardian, Dr. Davidson noted how the virus forced many physicians into becoming "activist doctors," calling for adequate personal protective equipment and correcting misinformation. "What we want above all is for the administration to listen to doctors, nurses, and frontline health workers - and stop playing politics," he wrote.
'It's Not About Being Political'
The intersection of medicine and politics is hardly new. Doctors frequently testify before Congress, sharing their expertise on issues concerning public health. This, however, isn't the same as "playing politics."
"I'm not taking political stances," said Megan Ranney, MD, Dean of the Yale School of Public Health. "Rather, I'm using science to inform best practices, and I'm vocal around the area where I have expertise where we could do collectively better."
Dr. Ranney's work to end firearm injury and death garnered particular attention when she co-authored an open letter to the National Rifle Association (NRA) in 2018. She wrote the letter in response to a tweet by the organization, admonishing physicians to "stay in their lane" when it comes to gun control.
Dr. Ranney's letter discussed gun violence as a public health crisis and urged the NRA to "be part of the solution" by joining the collective effort to reduce firearm injury and death through research, education, and advocacy. "We are not anti-gun," she stated. "We are anti-bullet hole," adding that "almost half of doctors own guns."
The NRA disagreed. When Dr. Ranney testified before Congress during a hearing on gun violence in 2023, NRA spokesperson Billy McLaughlin condemned her testimony as an effort to "dismantle the Second Amendment," calling Dr. Ranney "a known gun control extremist."
"If you actually read what I write, or if you actually listen to what I say, I'm not saying things on behalf of one political party or another," said Dr. Ranney. "It's not about being political. It's about recognizing our role in describing what's happening and making it clear for the world to see. Showing where, based off of data, there may be a better path to improve health and wellbeing."
In spite of the backlash, Dr. Ranney has no regrets about being an activist. "In the current media landscape, folks love to slap labels on people that may or may not be accurate. To me, what matters isn't where I land with a particular politician or political party, but how the work that I do improves health for populations."
When the Need to Act Outweighs the Fear
Laura Andreson, DO, an ob.gyn, took activism a step further when she joined a group of women in Tennessee to file a suit against the state, the attorney general, and the state board of medical examiners. The issue was the Tennessee's abortion ban, which the suit claimed prevented women from getting "necessary and potentially life-saving medical care."
Dr. Andreson, who says she was "not at all" politically active in the past, began to realize how the abortion ban could drastically affect her profession and her patients. "I don't know what flipped in me, but I just felt like I could do this," she said.
Like Dr. Ranney, Dr. Andreson has been as visible as she has been vocal, giving press conferences and interviews, but she acknowledges she has some fears about safety. In fact, after filing the lawsuit, the Center for Reproductive Rights recommended that she go to a website, DeleteMe, that removes personal data from the internet, making it more difficult for people to find her information. "But my need to do this and my desire to do this is stronger than my fears," she added.
Dr. Andreson, who is part of a small practice, did check with both her coworkers and the hospital administration before moving forward with the lawsuit. She was relieved to find that she had the support of her practice and that there wasn't anything in the hospital bylaws to prevent her from filing the lawsuit. "But the people in the bigger institutions who probably have an even better expert base than I do, they are handcuffed," she said.
It has been, in Dr. Andreson's words, "a little uncomfortable" being on the board of the Tennessee Medical Association when the Tennessee Board of Medical Examiners is part of the lawsuit. "We're all members of the same group," she said. "But I'm not suing them as individuals; I'm suing them as an entity that is under our government."
Dr. Andreson said most people have been supportive of her activist work, though she admitted to feeling frustrated when she encounters apathy from fellow ob.gyns. She got little response when she circulated information explaining the abortion laws and trying to get others involved. But she still sees education as being a key part of making change happen.
"I think advocacy, as someone who is considered a responsible, trustworthy person by your community, is important, because you can sway some people just by educating them," she said.
Fighting Inequities in Medicine and Beyond
Christina Chen, MD, says she felt very supported by her medical community at the Mayo Clinic in Rochester, Minnesota, when she and 16 other Asian American physicians posted a video on Instagram in 2020 highlighting increased violence and harassment of Asian Americans during COVID-19. It soon went viral, and the Mayo Clinic distributed it across their social media channels. The only negative repercussions Mayo faced were a few posts on social media saying that politics should not be brought into the healthcare space. Dr. Chen disagrees.
"Social issues and political decisions have direct impact on the health of our communities," Dr. Chen said. "We know that we still have a long way to go to solve health inequities, which is a public health problem, and we all play a huge role in voicing our concerns."
Activism, however, seems to be more complicated when it involves physicians being critical of inequities within the medical field. Nephrologist, Vanessa Grubbs, MD, MPH, founded the nonprofit Black Doc Village in 2022 to raise awareness about the wrongful dismissal of Black residents and expand the Black physician workforce.
Dr. Grubbs said that the medical community has not been supportive of her activism. "The reason why I'm no longer in academia is in part because they got very upset with me tweeting about how some trainees are biased in their treatment of attendings," she said. "Senior White men attendings are often treated very differently than junior women of color faculty."
Dr. Grubbs also expressed her views in 2020 essay in the New England Journal of Medicine where she criticized academic medical institutions for ignoring systemic racism, paying lip service to diversity, equity, and inclusion, and staying "deafeningly silent" when issues of racism are raised.
Today, Black Doc Village is focused on conducting research that can be used to change policy. And Dr. Grubbs now has the full support of her colleagues at West Oakland Health, in Oakland, California, which aspires to advance the Bay Area Black community's health and dignity. "So, no one here has a problem with me speaking out," she added.
The emphasis on data-driven activism as opposed to "playing politics," is a recurring theme for many physicians who publicly engage with social issues.
"It's not partisan," Dr. Ranney said. "Rather, it's a commitment to translating science into actionable steps that can be used regardless of what political party you are in. My job is not to be on one side or the other, but to advance human health." These doctors challenge their critics to explain how such a goal is outside their purview.
A version of this article first appeared on Medscape.com.
It should come as no surprise that when physicians speak out on social and political issues, there is sometimes a backlash. This can range from the typical trolling that occurs online to rarer cases of professional penalties. Two doctors were fired by NYU Langone Health late last year after they posted social media messages about the Israel-Hamas war. Still, many physicians are not only willing to stand up for what they believe in, but they see it as an essential part of their profession.
"We're now at a place where doctors need to engage in public advocacy as an urgent part of our job," wrote Rob Davidson, MD, an emergency department physician, at the onslaught of the COVID-19 pandemic. In an Op-Ed piece for The Guardian, Dr. Davidson noted how the virus forced many physicians into becoming "activist doctors," calling for adequate personal protective equipment and correcting misinformation. "What we want above all is for the administration to listen to doctors, nurses, and frontline health workers - and stop playing politics," he wrote.
'It's Not About Being Political'
The intersection of medicine and politics is hardly new. Doctors frequently testify before Congress, sharing their expertise on issues concerning public health. This, however, isn't the same as "playing politics."
"I'm not taking political stances," said Megan Ranney, MD, Dean of the Yale School of Public Health. "Rather, I'm using science to inform best practices, and I'm vocal around the area where I have expertise where we could do collectively better."
Dr. Ranney's work to end firearm injury and death garnered particular attention when she co-authored an open letter to the National Rifle Association (NRA) in 2018. She wrote the letter in response to a tweet by the organization, admonishing physicians to "stay in their lane" when it comes to gun control.
Dr. Ranney's letter discussed gun violence as a public health crisis and urged the NRA to "be part of the solution" by joining the collective effort to reduce firearm injury and death through research, education, and advocacy. "We are not anti-gun," she stated. "We are anti-bullet hole," adding that "almost half of doctors own guns."
The NRA disagreed. When Dr. Ranney testified before Congress during a hearing on gun violence in 2023, NRA spokesperson Billy McLaughlin condemned her testimony as an effort to "dismantle the Second Amendment," calling Dr. Ranney "a known gun control extremist."
"If you actually read what I write, or if you actually listen to what I say, I'm not saying things on behalf of one political party or another," said Dr. Ranney. "It's not about being political. It's about recognizing our role in describing what's happening and making it clear for the world to see. Showing where, based off of data, there may be a better path to improve health and wellbeing."
In spite of the backlash, Dr. Ranney has no regrets about being an activist. "In the current media landscape, folks love to slap labels on people that may or may not be accurate. To me, what matters isn't where I land with a particular politician or political party, but how the work that I do improves health for populations."
When the Need to Act Outweighs the Fear
Laura Andreson, DO, an ob.gyn, took activism a step further when she joined a group of women in Tennessee to file a suit against the state, the attorney general, and the state board of medical examiners. The issue was the Tennessee's abortion ban, which the suit claimed prevented women from getting "necessary and potentially life-saving medical care."
Dr. Andreson, who says she was "not at all" politically active in the past, began to realize how the abortion ban could drastically affect her profession and her patients. "I don't know what flipped in me, but I just felt like I could do this," she said.
Like Dr. Ranney, Dr. Andreson has been as visible as she has been vocal, giving press conferences and interviews, but she acknowledges she has some fears about safety. In fact, after filing the lawsuit, the Center for Reproductive Rights recommended that she go to a website, DeleteMe, that removes personal data from the internet, making it more difficult for people to find her information. "But my need to do this and my desire to do this is stronger than my fears," she added.
Dr. Andreson, who is part of a small practice, did check with both her coworkers and the hospital administration before moving forward with the lawsuit. She was relieved to find that she had the support of her practice and that there wasn't anything in the hospital bylaws to prevent her from filing the lawsuit. "But the people in the bigger institutions who probably have an even better expert base than I do, they are handcuffed," she said.
It has been, in Dr. Andreson's words, "a little uncomfortable" being on the board of the Tennessee Medical Association when the Tennessee Board of Medical Examiners is part of the lawsuit. "We're all members of the same group," she said. "But I'm not suing them as individuals; I'm suing them as an entity that is under our government."
Dr. Andreson said most people have been supportive of her activist work, though she admitted to feeling frustrated when she encounters apathy from fellow ob.gyns. She got little response when she circulated information explaining the abortion laws and trying to get others involved. But she still sees education as being a key part of making change happen.
"I think advocacy, as someone who is considered a responsible, trustworthy person by your community, is important, because you can sway some people just by educating them," she said.
Fighting Inequities in Medicine and Beyond
Christina Chen, MD, says she felt very supported by her medical community at the Mayo Clinic in Rochester, Minnesota, when she and 16 other Asian American physicians posted a video on Instagram in 2020 highlighting increased violence and harassment of Asian Americans during COVID-19. It soon went viral, and the Mayo Clinic distributed it across their social media channels. The only negative repercussions Mayo faced were a few posts on social media saying that politics should not be brought into the healthcare space. Dr. Chen disagrees.
"Social issues and political decisions have direct impact on the health of our communities," Dr. Chen said. "We know that we still have a long way to go to solve health inequities, which is a public health problem, and we all play a huge role in voicing our concerns."
Activism, however, seems to be more complicated when it involves physicians being critical of inequities within the medical field. Nephrologist, Vanessa Grubbs, MD, MPH, founded the nonprofit Black Doc Village in 2022 to raise awareness about the wrongful dismissal of Black residents and expand the Black physician workforce.
Dr. Grubbs said that the medical community has not been supportive of her activism. "The reason why I'm no longer in academia is in part because they got very upset with me tweeting about how some trainees are biased in their treatment of attendings," she said. "Senior White men attendings are often treated very differently than junior women of color faculty."
Dr. Grubbs also expressed her views in 2020 essay in the New England Journal of Medicine where she criticized academic medical institutions for ignoring systemic racism, paying lip service to diversity, equity, and inclusion, and staying "deafeningly silent" when issues of racism are raised.
Today, Black Doc Village is focused on conducting research that can be used to change policy. And Dr. Grubbs now has the full support of her colleagues at West Oakland Health, in Oakland, California, which aspires to advance the Bay Area Black community's health and dignity. "So, no one here has a problem with me speaking out," she added.
The emphasis on data-driven activism as opposed to "playing politics," is a recurring theme for many physicians who publicly engage with social issues.
"It's not partisan," Dr. Ranney said. "Rather, it's a commitment to translating science into actionable steps that can be used regardless of what political party you are in. My job is not to be on one side or the other, but to advance human health." These doctors challenge their critics to explain how such a goal is outside their purview.
A version of this article first appeared on Medscape.com.
It should come as no surprise that when physicians speak out on social and political issues, there is sometimes a backlash. This can range from the typical trolling that occurs online to rarer cases of professional penalties. Two doctors were fired by NYU Langone Health late last year after they posted social media messages about the Israel-Hamas war. Still, many physicians are not only willing to stand up for what they believe in, but they see it as an essential part of their profession.
"We're now at a place where doctors need to engage in public advocacy as an urgent part of our job," wrote Rob Davidson, MD, an emergency department physician, at the onslaught of the COVID-19 pandemic. In an Op-Ed piece for The Guardian, Dr. Davidson noted how the virus forced many physicians into becoming "activist doctors," calling for adequate personal protective equipment and correcting misinformation. "What we want above all is for the administration to listen to doctors, nurses, and frontline health workers - and stop playing politics," he wrote.
'It's Not About Being Political'
The intersection of medicine and politics is hardly new. Doctors frequently testify before Congress, sharing their expertise on issues concerning public health. This, however, isn't the same as "playing politics."
"I'm not taking political stances," said Megan Ranney, MD, Dean of the Yale School of Public Health. "Rather, I'm using science to inform best practices, and I'm vocal around the area where I have expertise where we could do collectively better."
Dr. Ranney's work to end firearm injury and death garnered particular attention when she co-authored an open letter to the National Rifle Association (NRA) in 2018. She wrote the letter in response to a tweet by the organization, admonishing physicians to "stay in their lane" when it comes to gun control.
Dr. Ranney's letter discussed gun violence as a public health crisis and urged the NRA to "be part of the solution" by joining the collective effort to reduce firearm injury and death through research, education, and advocacy. "We are not anti-gun," she stated. "We are anti-bullet hole," adding that "almost half of doctors own guns."
The NRA disagreed. When Dr. Ranney testified before Congress during a hearing on gun violence in 2023, NRA spokesperson Billy McLaughlin condemned her testimony as an effort to "dismantle the Second Amendment," calling Dr. Ranney "a known gun control extremist."
"If you actually read what I write, or if you actually listen to what I say, I'm not saying things on behalf of one political party or another," said Dr. Ranney. "It's not about being political. It's about recognizing our role in describing what's happening and making it clear for the world to see. Showing where, based off of data, there may be a better path to improve health and wellbeing."
In spite of the backlash, Dr. Ranney has no regrets about being an activist. "In the current media landscape, folks love to slap labels on people that may or may not be accurate. To me, what matters isn't where I land with a particular politician or political party, but how the work that I do improves health for populations."
When the Need to Act Outweighs the Fear
Laura Andreson, DO, an ob.gyn, took activism a step further when she joined a group of women in Tennessee to file a suit against the state, the attorney general, and the state board of medical examiners. The issue was the Tennessee's abortion ban, which the suit claimed prevented women from getting "necessary and potentially life-saving medical care."
Dr. Andreson, who says she was "not at all" politically active in the past, began to realize how the abortion ban could drastically affect her profession and her patients. "I don't know what flipped in me, but I just felt like I could do this," she said.
Like Dr. Ranney, Dr. Andreson has been as visible as she has been vocal, giving press conferences and interviews, but she acknowledges she has some fears about safety. In fact, after filing the lawsuit, the Center for Reproductive Rights recommended that she go to a website, DeleteMe, that removes personal data from the internet, making it more difficult for people to find her information. "But my need to do this and my desire to do this is stronger than my fears," she added.
Dr. Andreson, who is part of a small practice, did check with both her coworkers and the hospital administration before moving forward with the lawsuit. She was relieved to find that she had the support of her practice and that there wasn't anything in the hospital bylaws to prevent her from filing the lawsuit. "But the people in the bigger institutions who probably have an even better expert base than I do, they are handcuffed," she said.
It has been, in Dr. Andreson's words, "a little uncomfortable" being on the board of the Tennessee Medical Association when the Tennessee Board of Medical Examiners is part of the lawsuit. "We're all members of the same group," she said. "But I'm not suing them as individuals; I'm suing them as an entity that is under our government."
Dr. Andreson said most people have been supportive of her activist work, though she admitted to feeling frustrated when she encounters apathy from fellow ob.gyns. She got little response when she circulated information explaining the abortion laws and trying to get others involved. But she still sees education as being a key part of making change happen.
"I think advocacy, as someone who is considered a responsible, trustworthy person by your community, is important, because you can sway some people just by educating them," she said.
Fighting Inequities in Medicine and Beyond
Christina Chen, MD, says she felt very supported by her medical community at the Mayo Clinic in Rochester, Minnesota, when she and 16 other Asian American physicians posted a video on Instagram in 2020 highlighting increased violence and harassment of Asian Americans during COVID-19. It soon went viral, and the Mayo Clinic distributed it across their social media channels. The only negative repercussions Mayo faced were a few posts on social media saying that politics should not be brought into the healthcare space. Dr. Chen disagrees.
"Social issues and political decisions have direct impact on the health of our communities," Dr. Chen said. "We know that we still have a long way to go to solve health inequities, which is a public health problem, and we all play a huge role in voicing our concerns."
Activism, however, seems to be more complicated when it involves physicians being critical of inequities within the medical field. Nephrologist, Vanessa Grubbs, MD, MPH, founded the nonprofit Black Doc Village in 2022 to raise awareness about the wrongful dismissal of Black residents and expand the Black physician workforce.
Dr. Grubbs said that the medical community has not been supportive of her activism. "The reason why I'm no longer in academia is in part because they got very upset with me tweeting about how some trainees are biased in their treatment of attendings," she said. "Senior White men attendings are often treated very differently than junior women of color faculty."
Dr. Grubbs also expressed her views in 2020 essay in the New England Journal of Medicine where she criticized academic medical institutions for ignoring systemic racism, paying lip service to diversity, equity, and inclusion, and staying "deafeningly silent" when issues of racism are raised.
Today, Black Doc Village is focused on conducting research that can be used to change policy. And Dr. Grubbs now has the full support of her colleagues at West Oakland Health, in Oakland, California, which aspires to advance the Bay Area Black community's health and dignity. "So, no one here has a problem with me speaking out," she added.
The emphasis on data-driven activism as opposed to "playing politics," is a recurring theme for many physicians who publicly engage with social issues.
"It's not partisan," Dr. Ranney said. "Rather, it's a commitment to translating science into actionable steps that can be used regardless of what political party you are in. My job is not to be on one side or the other, but to advance human health." These doctors challenge their critics to explain how such a goal is outside their purview.
A version of this article first appeared on Medscape.com.
Congress Directly Provides $10 Million for Arthritis Research for First Time
Congress provided $10 million to fund arthritis research in the recently passed federal fiscal year 2024 budget.
The new arthritis program is part of the Department of Defense’s (DOD’s) Congressionally Directed Medical Research Programs (CDMRP), which provides dedicated funding to study certain diseases and health conditions.
This is the first stand-alone research program for arthritis of the CDMRP, though the organization had previously funded arthritis-related research through their other programs, including chronic pain management, joint warfighter medical, peer-reviewed orthopedic, peer-reviewed medical, and tick-borne disease programs.
It is not yet known what specific aspects of arthritis this funding will go toward. The standard process for new programs involves speaking with researchers, clinicians, and individuals with these targeted health conditions to better understand research gaps and narrow focus, Akua Roach, PhD, the program manager for this new CDMRP arthritis research program, told this news organization.
“We’re not going to be able to solve every question,” she said, though the allocated $10 million is “a great number to do a lot of great work.”
While the CDMRP is under the DOD, research funding can go to studying patient populations outside of military personnel or veterans, she added.
“I think that is perhaps a common misconception that if you are getting funding from the DOD, that you have to have a DOD population, and that is not true,” she said.
Another misconception is that CDMRP funding only goes to military treatment facilities. In fact, on average, 92% of CDMRP funding goes to academia, industry, and other nonmilitary recipients, noted CDMRP Director Colonel Sarah Goldman.
“Anyone around the world can apply for funding,” she told this news organization. “We want to fund the best research.”
Because the funding is provided under the defense bill, there will be discussions around the military relevance of research, she added, which not only includes service members but also their families.
CDMRP anticipates that funding opportunities through this new arthritis research program will be available by July or August 2024.
A version of this article appeared on Medscape.com.
Congress provided $10 million to fund arthritis research in the recently passed federal fiscal year 2024 budget.
The new arthritis program is part of the Department of Defense’s (DOD’s) Congressionally Directed Medical Research Programs (CDMRP), which provides dedicated funding to study certain diseases and health conditions.
This is the first stand-alone research program for arthritis of the CDMRP, though the organization had previously funded arthritis-related research through their other programs, including chronic pain management, joint warfighter medical, peer-reviewed orthopedic, peer-reviewed medical, and tick-borne disease programs.
It is not yet known what specific aspects of arthritis this funding will go toward. The standard process for new programs involves speaking with researchers, clinicians, and individuals with these targeted health conditions to better understand research gaps and narrow focus, Akua Roach, PhD, the program manager for this new CDMRP arthritis research program, told this news organization.
“We’re not going to be able to solve every question,” she said, though the allocated $10 million is “a great number to do a lot of great work.”
While the CDMRP is under the DOD, research funding can go to studying patient populations outside of military personnel or veterans, she added.
“I think that is perhaps a common misconception that if you are getting funding from the DOD, that you have to have a DOD population, and that is not true,” she said.
Another misconception is that CDMRP funding only goes to military treatment facilities. In fact, on average, 92% of CDMRP funding goes to academia, industry, and other nonmilitary recipients, noted CDMRP Director Colonel Sarah Goldman.
“Anyone around the world can apply for funding,” she told this news organization. “We want to fund the best research.”
Because the funding is provided under the defense bill, there will be discussions around the military relevance of research, she added, which not only includes service members but also their families.
CDMRP anticipates that funding opportunities through this new arthritis research program will be available by July or August 2024.
A version of this article appeared on Medscape.com.
Congress provided $10 million to fund arthritis research in the recently passed federal fiscal year 2024 budget.
The new arthritis program is part of the Department of Defense’s (DOD’s) Congressionally Directed Medical Research Programs (CDMRP), which provides dedicated funding to study certain diseases and health conditions.
This is the first stand-alone research program for arthritis of the CDMRP, though the organization had previously funded arthritis-related research through their other programs, including chronic pain management, joint warfighter medical, peer-reviewed orthopedic, peer-reviewed medical, and tick-borne disease programs.
It is not yet known what specific aspects of arthritis this funding will go toward. The standard process for new programs involves speaking with researchers, clinicians, and individuals with these targeted health conditions to better understand research gaps and narrow focus, Akua Roach, PhD, the program manager for this new CDMRP arthritis research program, told this news organization.
“We’re not going to be able to solve every question,” she said, though the allocated $10 million is “a great number to do a lot of great work.”
While the CDMRP is under the DOD, research funding can go to studying patient populations outside of military personnel or veterans, she added.
“I think that is perhaps a common misconception that if you are getting funding from the DOD, that you have to have a DOD population, and that is not true,” she said.
Another misconception is that CDMRP funding only goes to military treatment facilities. In fact, on average, 92% of CDMRP funding goes to academia, industry, and other nonmilitary recipients, noted CDMRP Director Colonel Sarah Goldman.
“Anyone around the world can apply for funding,” she told this news organization. “We want to fund the best research.”
Because the funding is provided under the defense bill, there will be discussions around the military relevance of research, she added, which not only includes service members but also their families.
CDMRP anticipates that funding opportunities through this new arthritis research program will be available by July or August 2024.
A version of this article appeared on Medscape.com.
Bone Infections Increase After S. aureus Bacteremia in Patients With Rheumatoid Arthritis
TOPLINE:
After Staphylococcus aureus bacteremia, patients with rheumatoid arthritis (RA) face nearly double the risk for osteoarticular infections compared with those without RA, with similar mortality risks in both groups.
METHODOLOGY:
- The contraction of S aureus bacteremia is linked to poor clinical outcomes in patients with RA; however, no well-sized studies have evaluated the risk for osteoarticular infections and mortality outcomes in patients with RA following S aureus bacteremia.
- This Danish nationwide cohort study aimed to explore whether the cumulative incidence of osteoarticular infections and death would be higher in patients with RA than in those without RA after contracting S aureus bacteremia.
- The study cohort included 18,274 patients with a first episode of S aureus bacteremia between 2006 and 2018, of whom 367 had been diagnosed with RA before contracting S aureus bacteremia.
- The RA cohort had more women (62%) and a higher median age of participants (73 years) than the non-RA cohort (37% women; median age of participants, 70 years).
TAKEAWAY:
- The 90-day cumulative incidence of osteoarticular infections (septic arthritis, spondylitis, osteomyelitis, psoas muscle abscess, or prosthetic joint infection) was nearly double in patients with RA compared with in those without RA (23.1% vs 12.5%; hazard ratio [HR], 1.93; 95% CI, 1.54-2.41).
- In patients with RA, the risk for osteoarticular infections increased with tumor necrosis factor inhibitor use (HR, 2.27; 95% CI, 1.29-3.98) and orthopedic implants (HR, 1.75; 95% CI, 1.08-2.85).
- Moreover, 90-day all-cause mortality was comparable in the RA (35.4%) and non-RA cohorts (33.9%).
IN PRACTICE:
“Our findings stress the need for vigilance in patients with RA who present with S aureus bacteremia to ensure timely identification and treatment of osteoarticular infections, especially in current TNFi [tumor necrosis factor inhibitor] users and patients with orthopedic implants,” the authors wrote.
SOURCE:
This study, led by Sabine S. Dieperink, MD, of the Centre of Head and Orthopaedics, Copenhagen University Rigshospitalet Glostrup, Denmark, was published online March 9 in Rheumatology (Oxford).
LIMITATIONS:
There might have been chances of misclassification of metastatic S aureus infections owing to the lack of specificity in diagnoses or procedure codes. This study relied on administrative data to record osteoarticular infections, which might have led investigators to underestimate the true cumulative incidence of osteoarticular infections. Also, some patients might have passed away before being diagnosed with osteoarticular infection owing to the high mortality.
DISCLOSURES:
This work was supported by grants from The Danish Rheumatism Association and Beckett Fonden. Some of the authors, including the lead author, declared receiving grants from various funding agencies and other sources, including pharmaceutical companies.
A version of this article appeared on Medscape.com.
TOPLINE:
After Staphylococcus aureus bacteremia, patients with rheumatoid arthritis (RA) face nearly double the risk for osteoarticular infections compared with those without RA, with similar mortality risks in both groups.
METHODOLOGY:
- The contraction of S aureus bacteremia is linked to poor clinical outcomes in patients with RA; however, no well-sized studies have evaluated the risk for osteoarticular infections and mortality outcomes in patients with RA following S aureus bacteremia.
- This Danish nationwide cohort study aimed to explore whether the cumulative incidence of osteoarticular infections and death would be higher in patients with RA than in those without RA after contracting S aureus bacteremia.
- The study cohort included 18,274 patients with a first episode of S aureus bacteremia between 2006 and 2018, of whom 367 had been diagnosed with RA before contracting S aureus bacteremia.
- The RA cohort had more women (62%) and a higher median age of participants (73 years) than the non-RA cohort (37% women; median age of participants, 70 years).
TAKEAWAY:
- The 90-day cumulative incidence of osteoarticular infections (septic arthritis, spondylitis, osteomyelitis, psoas muscle abscess, or prosthetic joint infection) was nearly double in patients with RA compared with in those without RA (23.1% vs 12.5%; hazard ratio [HR], 1.93; 95% CI, 1.54-2.41).
- In patients with RA, the risk for osteoarticular infections increased with tumor necrosis factor inhibitor use (HR, 2.27; 95% CI, 1.29-3.98) and orthopedic implants (HR, 1.75; 95% CI, 1.08-2.85).
- Moreover, 90-day all-cause mortality was comparable in the RA (35.4%) and non-RA cohorts (33.9%).
IN PRACTICE:
“Our findings stress the need for vigilance in patients with RA who present with S aureus bacteremia to ensure timely identification and treatment of osteoarticular infections, especially in current TNFi [tumor necrosis factor inhibitor] users and patients with orthopedic implants,” the authors wrote.
SOURCE:
This study, led by Sabine S. Dieperink, MD, of the Centre of Head and Orthopaedics, Copenhagen University Rigshospitalet Glostrup, Denmark, was published online March 9 in Rheumatology (Oxford).
LIMITATIONS:
There might have been chances of misclassification of metastatic S aureus infections owing to the lack of specificity in diagnoses or procedure codes. This study relied on administrative data to record osteoarticular infections, which might have led investigators to underestimate the true cumulative incidence of osteoarticular infections. Also, some patients might have passed away before being diagnosed with osteoarticular infection owing to the high mortality.
DISCLOSURES:
This work was supported by grants from The Danish Rheumatism Association and Beckett Fonden. Some of the authors, including the lead author, declared receiving grants from various funding agencies and other sources, including pharmaceutical companies.
A version of this article appeared on Medscape.com.
TOPLINE:
After Staphylococcus aureus bacteremia, patients with rheumatoid arthritis (RA) face nearly double the risk for osteoarticular infections compared with those without RA, with similar mortality risks in both groups.
METHODOLOGY:
- The contraction of S aureus bacteremia is linked to poor clinical outcomes in patients with RA; however, no well-sized studies have evaluated the risk for osteoarticular infections and mortality outcomes in patients with RA following S aureus bacteremia.
- This Danish nationwide cohort study aimed to explore whether the cumulative incidence of osteoarticular infections and death would be higher in patients with RA than in those without RA after contracting S aureus bacteremia.
- The study cohort included 18,274 patients with a first episode of S aureus bacteremia between 2006 and 2018, of whom 367 had been diagnosed with RA before contracting S aureus bacteremia.
- The RA cohort had more women (62%) and a higher median age of participants (73 years) than the non-RA cohort (37% women; median age of participants, 70 years).
TAKEAWAY:
- The 90-day cumulative incidence of osteoarticular infections (septic arthritis, spondylitis, osteomyelitis, psoas muscle abscess, or prosthetic joint infection) was nearly double in patients with RA compared with in those without RA (23.1% vs 12.5%; hazard ratio [HR], 1.93; 95% CI, 1.54-2.41).
- In patients with RA, the risk for osteoarticular infections increased with tumor necrosis factor inhibitor use (HR, 2.27; 95% CI, 1.29-3.98) and orthopedic implants (HR, 1.75; 95% CI, 1.08-2.85).
- Moreover, 90-day all-cause mortality was comparable in the RA (35.4%) and non-RA cohorts (33.9%).
IN PRACTICE:
“Our findings stress the need for vigilance in patients with RA who present with S aureus bacteremia to ensure timely identification and treatment of osteoarticular infections, especially in current TNFi [tumor necrosis factor inhibitor] users and patients with orthopedic implants,” the authors wrote.
SOURCE:
This study, led by Sabine S. Dieperink, MD, of the Centre of Head and Orthopaedics, Copenhagen University Rigshospitalet Glostrup, Denmark, was published online March 9 in Rheumatology (Oxford).
LIMITATIONS:
There might have been chances of misclassification of metastatic S aureus infections owing to the lack of specificity in diagnoses or procedure codes. This study relied on administrative data to record osteoarticular infections, which might have led investigators to underestimate the true cumulative incidence of osteoarticular infections. Also, some patients might have passed away before being diagnosed with osteoarticular infection owing to the high mortality.
DISCLOSURES:
This work was supported by grants from The Danish Rheumatism Association and Beckett Fonden. Some of the authors, including the lead author, declared receiving grants from various funding agencies and other sources, including pharmaceutical companies.
A version of this article appeared on Medscape.com.
Study Shows Nirmatrelvir–Ritonavir No More Effective Than Placebo for COVID-19 Symptom Relief
Paxlovid does not significantly alleviate symptoms of COVID-19 compared with placebo among nonhospitalized adults, a new study published April 3 in The New England Journal of Medicine found.
The results suggest that the drug, a combination of nirmatrelvir and ritonavir, may not be particularly helpful for patients who are not at high risk for severe COVID-19. However, although the rate of hospitalization and death from any cause was low overall, the group that received Paxlovid had a reduced rate compared with people in the placebo group, according to the researchers.
“Clearly, the benefit observed among unvaccinated high-risk persons does not extend to those at lower risk for severe COVID-19,” Rajesh T. Gandhi, MD, and Martin Hirsch, MD, of Massachusetts General Hospital in Boston, wrote in an editorial accompanying the journal article. “This result supports guidelines that recommend nirmatrelvir–ritonavir only for persons who are at high risk for disease progression.”
The time from onset to relief of COVID-19 symptoms — including cough, shortness of breath, body aches, and chills — did not differ significantly between the two study groups, the researchers reported. The median time to sustained alleviation of symptoms was 12 days for the Paxlovid group compared with 13 days in the placebo group (P = .60).
However, the phase 2/3 trial found a 57.6% relative reduction in the risk for hospitalizations or death among people who took Paxlovid and were vaccinated but were at high risk for poor outcomes, according to Jennifer Hammond, PhD, head of antiviral development for Pfizer, which makes the drug, and the corresponding author on the study.
Paxlovid has “an increasing body of evidence supporting the strong clinical value of the treatment in preventing hospitalization and death among eligible patients across age groups, vaccination status, and predominant variants,” Dr. Hammond said.
She and her colleagues analyzed data from 1250 adults with symptomatic COVID-19. Participants were fully vaccinated and had a high risk for progression to severe disease or were never vaccinated or had not been in the previous year and had no risk factors for progression to severe disease.
More than half of participants were women, 78.5% were White and 41.4% identified as Hispanic or Latinx. Almost three quarters underwent randomization within 3 days of the start of symptoms, and a little over half had previously received a COVID-19 vaccination. Almost half had one risk factor for severe illness, the most common of these being hypertension (12.3%).
In a subgroup analysis of high-risk participants, hospitalization or death occurred in 0.9% of patients in the Paxlovid group and 2.2% in the placebo group (95% CI, -3.3 to 0.7).
The study’s limitations include that the statistical analysis of COVID-19–related hospitalizations or death from any cause was only descriptive, “because the results for the primary efficacy end point were not significant,” the authors wrote.
Participants who were vaccinated and at high risk were also enrolled regardless of when they had last had a vaccine dose. Furthermore, Paxlovid has a telltale taste, which may have affected the blinding. Finally, the trial was started when the B.1.617.2 (Delta) variant was predominant.
Dr. Gandhi and Dr. Hirsch pointed out that only 5% of participants in the trial were older than 65 years and that other than risk factors such as obesity and smoking, just 2% of people had heart or lung disease.
“As with many medical interventions, there is likely to be a gradient of benefit for nirmatrelvir–ritonavir, with the patients at highest risk for progression most likely to derive the greatest benefit,” Dr. Gandhi and Dr. Hirsch wrote in the editorial. “Thus, it appears reasonable to recommend nirmatrelvir–ritonavir primarily for the treatment of COVID-19 in older patients (particularly those ≥ 65 years of age), those who are immunocompromised, and those who have conditions that substantially increase the risk of severe COVID-19, regardless of previous vaccination or infection status.”
The study was supported by Pfizer.
A version of this article appeared on Medscape.com .
Paxlovid does not significantly alleviate symptoms of COVID-19 compared with placebo among nonhospitalized adults, a new study published April 3 in The New England Journal of Medicine found.
The results suggest that the drug, a combination of nirmatrelvir and ritonavir, may not be particularly helpful for patients who are not at high risk for severe COVID-19. However, although the rate of hospitalization and death from any cause was low overall, the group that received Paxlovid had a reduced rate compared with people in the placebo group, according to the researchers.
“Clearly, the benefit observed among unvaccinated high-risk persons does not extend to those at lower risk for severe COVID-19,” Rajesh T. Gandhi, MD, and Martin Hirsch, MD, of Massachusetts General Hospital in Boston, wrote in an editorial accompanying the journal article. “This result supports guidelines that recommend nirmatrelvir–ritonavir only for persons who are at high risk for disease progression.”
The time from onset to relief of COVID-19 symptoms — including cough, shortness of breath, body aches, and chills — did not differ significantly between the two study groups, the researchers reported. The median time to sustained alleviation of symptoms was 12 days for the Paxlovid group compared with 13 days in the placebo group (P = .60).
However, the phase 2/3 trial found a 57.6% relative reduction in the risk for hospitalizations or death among people who took Paxlovid and were vaccinated but were at high risk for poor outcomes, according to Jennifer Hammond, PhD, head of antiviral development for Pfizer, which makes the drug, and the corresponding author on the study.
Paxlovid has “an increasing body of evidence supporting the strong clinical value of the treatment in preventing hospitalization and death among eligible patients across age groups, vaccination status, and predominant variants,” Dr. Hammond said.
She and her colleagues analyzed data from 1250 adults with symptomatic COVID-19. Participants were fully vaccinated and had a high risk for progression to severe disease or were never vaccinated or had not been in the previous year and had no risk factors for progression to severe disease.
More than half of participants were women, 78.5% were White and 41.4% identified as Hispanic or Latinx. Almost three quarters underwent randomization within 3 days of the start of symptoms, and a little over half had previously received a COVID-19 vaccination. Almost half had one risk factor for severe illness, the most common of these being hypertension (12.3%).
In a subgroup analysis of high-risk participants, hospitalization or death occurred in 0.9% of patients in the Paxlovid group and 2.2% in the placebo group (95% CI, -3.3 to 0.7).
The study’s limitations include that the statistical analysis of COVID-19–related hospitalizations or death from any cause was only descriptive, “because the results for the primary efficacy end point were not significant,” the authors wrote.
Participants who were vaccinated and at high risk were also enrolled regardless of when they had last had a vaccine dose. Furthermore, Paxlovid has a telltale taste, which may have affected the blinding. Finally, the trial was started when the B.1.617.2 (Delta) variant was predominant.
Dr. Gandhi and Dr. Hirsch pointed out that only 5% of participants in the trial were older than 65 years and that other than risk factors such as obesity and smoking, just 2% of people had heart or lung disease.
“As with many medical interventions, there is likely to be a gradient of benefit for nirmatrelvir–ritonavir, with the patients at highest risk for progression most likely to derive the greatest benefit,” Dr. Gandhi and Dr. Hirsch wrote in the editorial. “Thus, it appears reasonable to recommend nirmatrelvir–ritonavir primarily for the treatment of COVID-19 in older patients (particularly those ≥ 65 years of age), those who are immunocompromised, and those who have conditions that substantially increase the risk of severe COVID-19, regardless of previous vaccination or infection status.”
The study was supported by Pfizer.
A version of this article appeared on Medscape.com .
Paxlovid does not significantly alleviate symptoms of COVID-19 compared with placebo among nonhospitalized adults, a new study published April 3 in The New England Journal of Medicine found.
The results suggest that the drug, a combination of nirmatrelvir and ritonavir, may not be particularly helpful for patients who are not at high risk for severe COVID-19. However, although the rate of hospitalization and death from any cause was low overall, the group that received Paxlovid had a reduced rate compared with people in the placebo group, according to the researchers.
“Clearly, the benefit observed among unvaccinated high-risk persons does not extend to those at lower risk for severe COVID-19,” Rajesh T. Gandhi, MD, and Martin Hirsch, MD, of Massachusetts General Hospital in Boston, wrote in an editorial accompanying the journal article. “This result supports guidelines that recommend nirmatrelvir–ritonavir only for persons who are at high risk for disease progression.”
The time from onset to relief of COVID-19 symptoms — including cough, shortness of breath, body aches, and chills — did not differ significantly between the two study groups, the researchers reported. The median time to sustained alleviation of symptoms was 12 days for the Paxlovid group compared with 13 days in the placebo group (P = .60).
However, the phase 2/3 trial found a 57.6% relative reduction in the risk for hospitalizations or death among people who took Paxlovid and were vaccinated but were at high risk for poor outcomes, according to Jennifer Hammond, PhD, head of antiviral development for Pfizer, which makes the drug, and the corresponding author on the study.
Paxlovid has “an increasing body of evidence supporting the strong clinical value of the treatment in preventing hospitalization and death among eligible patients across age groups, vaccination status, and predominant variants,” Dr. Hammond said.
She and her colleagues analyzed data from 1250 adults with symptomatic COVID-19. Participants were fully vaccinated and had a high risk for progression to severe disease or were never vaccinated or had not been in the previous year and had no risk factors for progression to severe disease.
More than half of participants were women, 78.5% were White and 41.4% identified as Hispanic or Latinx. Almost three quarters underwent randomization within 3 days of the start of symptoms, and a little over half had previously received a COVID-19 vaccination. Almost half had one risk factor for severe illness, the most common of these being hypertension (12.3%).
In a subgroup analysis of high-risk participants, hospitalization or death occurred in 0.9% of patients in the Paxlovid group and 2.2% in the placebo group (95% CI, -3.3 to 0.7).
The study’s limitations include that the statistical analysis of COVID-19–related hospitalizations or death from any cause was only descriptive, “because the results for the primary efficacy end point were not significant,” the authors wrote.
Participants who were vaccinated and at high risk were also enrolled regardless of when they had last had a vaccine dose. Furthermore, Paxlovid has a telltale taste, which may have affected the blinding. Finally, the trial was started when the B.1.617.2 (Delta) variant was predominant.
Dr. Gandhi and Dr. Hirsch pointed out that only 5% of participants in the trial were older than 65 years and that other than risk factors such as obesity and smoking, just 2% of people had heart or lung disease.
“As with many medical interventions, there is likely to be a gradient of benefit for nirmatrelvir–ritonavir, with the patients at highest risk for progression most likely to derive the greatest benefit,” Dr. Gandhi and Dr. Hirsch wrote in the editorial. “Thus, it appears reasonable to recommend nirmatrelvir–ritonavir primarily for the treatment of COVID-19 in older patients (particularly those ≥ 65 years of age), those who are immunocompromised, and those who have conditions that substantially increase the risk of severe COVID-19, regardless of previous vaccination or infection status.”
The study was supported by Pfizer.
A version of this article appeared on Medscape.com .
Why Do So Many Doctors Embrace Superstitions and Rituals?
The second-floor operating rooms at Lehigh Valley Hospital in Allentown, Pennsylvania, are numbered sequentially — except when you get to what should be operation room (OR) 13. It’s OR M. The M doesn’t stand for Maternity or any other specialty. Rather in this high-tech, state-of-the art healthcare center, it’s there to ward off bad juju and evil spirits.
“Just as taller buildings usually don’t have a 13th floor or hotels don’t have a room 13, it revolves around the common superstition of the unlucky nature of number 13,” said a hospital spokesperson.
During the pandemic, the public was told repeatedly that modern medicine is science-based. But when I started talking to surgeons and other physicians for this article, I uncovered something decidedly unscientific.
In ORs and emergency rooms (ERs), small-town doctor’s offices, and mega hospitals, there’s a measure of dread before full moons and Friday the 13th, and no one dares utter the Q word (as in, “It sure is quiet today.”) That would risk bringing the wrath of the medical gods, and you’d earn the reputation of being a jinx or “black cloud.” Likewise, the songs “Stairway to Heaven” or “Another One Bites the Dust” will never be heard in any waiting room, elevator, or OR.
Indeed, when it comes to superstitions and rituals in medicine, it seems everyone has a story or a belief. …
A 2-Hour Ritual
Carmen Fong, MD, a colorectal surgeon in New York City, had a presurgical ritual that took her nearly 2 hours to complete. “I’d wake up at the same time every day, pack two hard-boiled eggs and a thermos of coffee in my small leather bag, walk to work via the same route, and swipe into the preop area while waving hi to the front desk,” she recounted. “I’d talk to the patient, sign the consent with the same ballpoint pen, go upstairs to my office, change into my scrubs [same cap and Danskos], then turn on my computer, and take a sip of coffee before heading back down to the OR. I’d always remove my badge and place it near the nurses’ workstation, then put on the patient’s SCDs [sequential compression devices] myself. I’d hold the oxygen mask while telling the patient, ‘See you later.’ Never ‘It will be okay’ or ‘Have a good sleep.’ Always ‘See you later.’ ”
Dr. Fong did this for 5 years prior to more than a thousand surgeries. She did it because it made her feel calm and in control, which translated to more successful operations. “It never failed me.”
Wonder Woman Clogs
Anureet Bajaj, MD, a plastic surgeon in Oklahoma City, wore Wonder Woman clogs in the OR for years because “they made me feel stronger, and my surgeries went better.” She’s also very specific about her OR playlist; “it must be ‘80s music.” And for a time, she wore a friendship bracelet that one of her employees made to commemorate getting through a particularly hard day. “If I forgot it, my heart sank, and my anxiety rose,” she said. “Wearing it gave me security and confidence that the day would go well.”
A Moment of Silence
Juliet Emamaullee, MD, PhD, is a liver and kidney transplant surgeon at Keck Hospital and Children’s Hospital Los Angeles. Because of the complexity of her operations, she must know every aspect of her patients’ medical history. This leads to a level of intimacy that most people never have with their doctors. “Transplant surgeons are playing god in many ways,” she said. “During procurement, after we prep and drape the donor and right before I make the incision, everyone in the OR has a moment of silence to acknowledge the donation. If the organ has been transported, then I’ll say a prayer to myself that I do good work with this generous gift of life.”
Magical Thinking
Before we go any further, I should clarify that there’s a difference between rituals and superstitions like the ones just shared and routines and practices such as handwashing or doublechecking that it’s the right hip and not the left. All pilots have a preflight checklist that’s necessary for safety, but some might also make the sign of the cross.
Lester Gottesman, MD, has been a surgeon at the Icahn School of Medicine at Mount Sinai Hospital in New York City for nearly 50 years. He believes rituals and superstitions are more prevalent in medicine than in any other profession, despite there being no definitive research confirming their effectiveness.
In fact, it’s the opposite.
One of the few studies to examine superstitions among physicians was published in the Annals of Surgery in 2021. Researchers analyzed the operational records of 27,914 consecutive patients who underwent general, visceral, or vascular surgery. They found no association of moon phases, zodiac signs, or Friday the 13th with poor outcomes. Having acute coronary syndrome on Friday the 13th also did not influence the 13-year mortality rate compared to other dates in the year. And although 70% of physicians believe that some colleagues are “black clouds,” an analysis of 96 physicians and 6149 admissions found no such pattern.
Granted, this is just one analysis, but the results aren’t surprising. No one really believes in this stuff. So, why does it persist?
Dr. Gottesman cited an episode from the popular medical TV show Grey’s Anatomy, in which chief surgeon Meredith Grey puts it this way: “Superstition lies in the space between what we can control and what we can’t. …We rely on superstitions because we are smart enough to know we don’t have all the answers and that life works in mysterious ways. Don’t diss the juju from wherever it comes.”
“Superstition and science both start at the same place — to explain an unexplainable event,” said Dr. Gottesman, who always checks his suture lines at the end of a surgery in the order in which he did them. “If science provides a coherent answer, so be it. If not, the human’s need for order will assign causality to otherwise inanimate objects, noncausal events, or divine influence.”
In other words, the more unknowns and trepidation, the greater the tendency toward what Dr. Gottesman called “magical thinking.” And when you consider healing’s long history, you realize that ritual and superstition defined medicine for centuries. Gottesman pointed out that it wasn’t until Hippocrates separated religion and superstition from disease around 430 BC that modern medicine was born. But because doctors still don’t know everything, an element of magic endures.
The question is, in this high-tech age, do these stubborn beliefs still have a place? Do they help or hinder doctors, and, most important, do they have any effect on patient outcomes?
Five Benefits
To reiterate, there are no studies showing that Wonder Woman clogs convey surgical superpowers or that eating two hard-boiled eggs boosts OR performance. But anecdotally, many doctors admit to experiencing noticeable perks from their quirks. Let’s start with the supposed benefits:
- Less stress: A quarter of US clinicians are considering switching careers, primarily due to burnout, according to a 2022 Bain survey. “The fact that [rituals and superstitions] are so prevalent in such a high-stress field can’t be coincidence,” said Dr. Fong. “Offloading some of the responsibility to whatever gods there may be is a way of taming our anxieties so we can function better.”
- Hyperfocus: Dr. Emamaullee played volleyball in high school and college. She suggested that her presurgical routine isn’t all that different from her warmup before a championship match. It’s habitual behavior that helps induce a state of heightened concentration, confidence, and immersion. Athletes call it being “in the zone” or in a “state of flow,” and Dr. Emamaullee said she experiences the same thing in the OR.
- More control: Remember those horrific images of patients with COVID-19 overwhelming ERs in Brooklyn and Queens during the pandemic? Dr. Fong was in the middle of that. “In crisis situations where there are more unknowns, rituals and superstitions become even more important,” she said. “I may not be able to control what’s happening, but I can control myself. Rituals help restore some normalcy and organization, and they give me a sense of calm.”
- Better performance: A series of general-population experiments published in the journal Psychological Science in 2010 concluded that “good-luck–related superstitions” boosted self-confidence in mastering upcoming tasks and improved motor dexterity, memory, and overall performance.
- Placebo effect: This phenomenon is well-established in medicine. Give someone a special pill or treatment, and a significant portion will claim benefit. “Placebo is magical thinking,” said Dr. Gottesman. “It has identifiable and quantifiable effects on human disease.” And perhaps on medical practitioners, too. If a doctor believes her friendship bracelet has special powers and helps her be a better physician, then it just might.
Four Drawbacks
- Compulsive behavior: When superstitious beliefs or repetitive behaviors begin causing personal distress, interfering with daily duties, or negatively affecting patient outcomes, then there’s a problem. There’s a story on Quora about a neurosurgeon who always ate two Hostess Ho Hos chocolate cakes before operations. When he forgot to do so one day, he supposedly left his patient on the table and ran off to eat them. Even if it’s urban legend, it’s a useful illustration of quirk disrupting work.
- Less flexibility: Every human body and every surgery is different. “When ritualistic behaviors or habits become so rigid that you lose the ability to adapt, then that becomes dangerous for the patient,” said Dr. Fong. “The art of medicine, not unlike jazz, often comes from the improvisation.”
- Self-fulfilling: Just as rituals and superstitions can empower and provide a sense of control, they can quickly turn on physicians who forget a part of their routine or leave their talisman on the bureau. Instead of confidence, they supply doubt. The karma becomes kryptonite.
- Avoiding responsibility: After years of friendship bracelets and Wonder Woman clogs, Dr. Bajaj is making a deliberate effort to excise magical thinking from her practice. “It can hold you back if you’re not careful,” she said. “If you start using it as a crutch when something goes wrong — like ‘Oh, I wasn’t wearing my clogs today and that’s why my flap failed’ — then you’re not doing your due diligence and figuring out what really happened.” Rather than placing the responsibility for her day going well on superstition, she’s trying to own it herself by living with more intent.
The Diagnosis
Most of the medical experts I spoke with didn’t think there was anything wrong with rituals or superstitions as long as they didn’t become compulsive or a convenient repository of blame.
“Rituals and superstitions are an acknowledgment that forces external to ourselves exist,” concluded Dr. Fong. “They’re like tiny offerings to whatever gods are out there to please be on our side. And we keep doing them because there’s a reward — better patient outcomes, which is all we want to achieve in the end. I say embrace them.”
A version of this article first appeared on Medscape.com.
The second-floor operating rooms at Lehigh Valley Hospital in Allentown, Pennsylvania, are numbered sequentially — except when you get to what should be operation room (OR) 13. It’s OR M. The M doesn’t stand for Maternity or any other specialty. Rather in this high-tech, state-of-the art healthcare center, it’s there to ward off bad juju and evil spirits.
“Just as taller buildings usually don’t have a 13th floor or hotels don’t have a room 13, it revolves around the common superstition of the unlucky nature of number 13,” said a hospital spokesperson.
During the pandemic, the public was told repeatedly that modern medicine is science-based. But when I started talking to surgeons and other physicians for this article, I uncovered something decidedly unscientific.
In ORs and emergency rooms (ERs), small-town doctor’s offices, and mega hospitals, there’s a measure of dread before full moons and Friday the 13th, and no one dares utter the Q word (as in, “It sure is quiet today.”) That would risk bringing the wrath of the medical gods, and you’d earn the reputation of being a jinx or “black cloud.” Likewise, the songs “Stairway to Heaven” or “Another One Bites the Dust” will never be heard in any waiting room, elevator, or OR.
Indeed, when it comes to superstitions and rituals in medicine, it seems everyone has a story or a belief. …
A 2-Hour Ritual
Carmen Fong, MD, a colorectal surgeon in New York City, had a presurgical ritual that took her nearly 2 hours to complete. “I’d wake up at the same time every day, pack two hard-boiled eggs and a thermos of coffee in my small leather bag, walk to work via the same route, and swipe into the preop area while waving hi to the front desk,” she recounted. “I’d talk to the patient, sign the consent with the same ballpoint pen, go upstairs to my office, change into my scrubs [same cap and Danskos], then turn on my computer, and take a sip of coffee before heading back down to the OR. I’d always remove my badge and place it near the nurses’ workstation, then put on the patient’s SCDs [sequential compression devices] myself. I’d hold the oxygen mask while telling the patient, ‘See you later.’ Never ‘It will be okay’ or ‘Have a good sleep.’ Always ‘See you later.’ ”
Dr. Fong did this for 5 years prior to more than a thousand surgeries. She did it because it made her feel calm and in control, which translated to more successful operations. “It never failed me.”
Wonder Woman Clogs
Anureet Bajaj, MD, a plastic surgeon in Oklahoma City, wore Wonder Woman clogs in the OR for years because “they made me feel stronger, and my surgeries went better.” She’s also very specific about her OR playlist; “it must be ‘80s music.” And for a time, she wore a friendship bracelet that one of her employees made to commemorate getting through a particularly hard day. “If I forgot it, my heart sank, and my anxiety rose,” she said. “Wearing it gave me security and confidence that the day would go well.”
A Moment of Silence
Juliet Emamaullee, MD, PhD, is a liver and kidney transplant surgeon at Keck Hospital and Children’s Hospital Los Angeles. Because of the complexity of her operations, she must know every aspect of her patients’ medical history. This leads to a level of intimacy that most people never have with their doctors. “Transplant surgeons are playing god in many ways,” she said. “During procurement, after we prep and drape the donor and right before I make the incision, everyone in the OR has a moment of silence to acknowledge the donation. If the organ has been transported, then I’ll say a prayer to myself that I do good work with this generous gift of life.”
Magical Thinking
Before we go any further, I should clarify that there’s a difference between rituals and superstitions like the ones just shared and routines and practices such as handwashing or doublechecking that it’s the right hip and not the left. All pilots have a preflight checklist that’s necessary for safety, but some might also make the sign of the cross.
Lester Gottesman, MD, has been a surgeon at the Icahn School of Medicine at Mount Sinai Hospital in New York City for nearly 50 years. He believes rituals and superstitions are more prevalent in medicine than in any other profession, despite there being no definitive research confirming their effectiveness.
In fact, it’s the opposite.
One of the few studies to examine superstitions among physicians was published in the Annals of Surgery in 2021. Researchers analyzed the operational records of 27,914 consecutive patients who underwent general, visceral, or vascular surgery. They found no association of moon phases, zodiac signs, or Friday the 13th with poor outcomes. Having acute coronary syndrome on Friday the 13th also did not influence the 13-year mortality rate compared to other dates in the year. And although 70% of physicians believe that some colleagues are “black clouds,” an analysis of 96 physicians and 6149 admissions found no such pattern.
Granted, this is just one analysis, but the results aren’t surprising. No one really believes in this stuff. So, why does it persist?
Dr. Gottesman cited an episode from the popular medical TV show Grey’s Anatomy, in which chief surgeon Meredith Grey puts it this way: “Superstition lies in the space between what we can control and what we can’t. …We rely on superstitions because we are smart enough to know we don’t have all the answers and that life works in mysterious ways. Don’t diss the juju from wherever it comes.”
“Superstition and science both start at the same place — to explain an unexplainable event,” said Dr. Gottesman, who always checks his suture lines at the end of a surgery in the order in which he did them. “If science provides a coherent answer, so be it. If not, the human’s need for order will assign causality to otherwise inanimate objects, noncausal events, or divine influence.”
In other words, the more unknowns and trepidation, the greater the tendency toward what Dr. Gottesman called “magical thinking.” And when you consider healing’s long history, you realize that ritual and superstition defined medicine for centuries. Gottesman pointed out that it wasn’t until Hippocrates separated religion and superstition from disease around 430 BC that modern medicine was born. But because doctors still don’t know everything, an element of magic endures.
The question is, in this high-tech age, do these stubborn beliefs still have a place? Do they help or hinder doctors, and, most important, do they have any effect on patient outcomes?
Five Benefits
To reiterate, there are no studies showing that Wonder Woman clogs convey surgical superpowers or that eating two hard-boiled eggs boosts OR performance. But anecdotally, many doctors admit to experiencing noticeable perks from their quirks. Let’s start with the supposed benefits:
- Less stress: A quarter of US clinicians are considering switching careers, primarily due to burnout, according to a 2022 Bain survey. “The fact that [rituals and superstitions] are so prevalent in such a high-stress field can’t be coincidence,” said Dr. Fong. “Offloading some of the responsibility to whatever gods there may be is a way of taming our anxieties so we can function better.”
- Hyperfocus: Dr. Emamaullee played volleyball in high school and college. She suggested that her presurgical routine isn’t all that different from her warmup before a championship match. It’s habitual behavior that helps induce a state of heightened concentration, confidence, and immersion. Athletes call it being “in the zone” or in a “state of flow,” and Dr. Emamaullee said she experiences the same thing in the OR.
- More control: Remember those horrific images of patients with COVID-19 overwhelming ERs in Brooklyn and Queens during the pandemic? Dr. Fong was in the middle of that. “In crisis situations where there are more unknowns, rituals and superstitions become even more important,” she said. “I may not be able to control what’s happening, but I can control myself. Rituals help restore some normalcy and organization, and they give me a sense of calm.”
- Better performance: A series of general-population experiments published in the journal Psychological Science in 2010 concluded that “good-luck–related superstitions” boosted self-confidence in mastering upcoming tasks and improved motor dexterity, memory, and overall performance.
- Placebo effect: This phenomenon is well-established in medicine. Give someone a special pill or treatment, and a significant portion will claim benefit. “Placebo is magical thinking,” said Dr. Gottesman. “It has identifiable and quantifiable effects on human disease.” And perhaps on medical practitioners, too. If a doctor believes her friendship bracelet has special powers and helps her be a better physician, then it just might.
Four Drawbacks
- Compulsive behavior: When superstitious beliefs or repetitive behaviors begin causing personal distress, interfering with daily duties, or negatively affecting patient outcomes, then there’s a problem. There’s a story on Quora about a neurosurgeon who always ate two Hostess Ho Hos chocolate cakes before operations. When he forgot to do so one day, he supposedly left his patient on the table and ran off to eat them. Even if it’s urban legend, it’s a useful illustration of quirk disrupting work.
- Less flexibility: Every human body and every surgery is different. “When ritualistic behaviors or habits become so rigid that you lose the ability to adapt, then that becomes dangerous for the patient,” said Dr. Fong. “The art of medicine, not unlike jazz, often comes from the improvisation.”
- Self-fulfilling: Just as rituals and superstitions can empower and provide a sense of control, they can quickly turn on physicians who forget a part of their routine or leave their talisman on the bureau. Instead of confidence, they supply doubt. The karma becomes kryptonite.
- Avoiding responsibility: After years of friendship bracelets and Wonder Woman clogs, Dr. Bajaj is making a deliberate effort to excise magical thinking from her practice. “It can hold you back if you’re not careful,” she said. “If you start using it as a crutch when something goes wrong — like ‘Oh, I wasn’t wearing my clogs today and that’s why my flap failed’ — then you’re not doing your due diligence and figuring out what really happened.” Rather than placing the responsibility for her day going well on superstition, she’s trying to own it herself by living with more intent.
The Diagnosis
Most of the medical experts I spoke with didn’t think there was anything wrong with rituals or superstitions as long as they didn’t become compulsive or a convenient repository of blame.
“Rituals and superstitions are an acknowledgment that forces external to ourselves exist,” concluded Dr. Fong. “They’re like tiny offerings to whatever gods are out there to please be on our side. And we keep doing them because there’s a reward — better patient outcomes, which is all we want to achieve in the end. I say embrace them.”
A version of this article first appeared on Medscape.com.
The second-floor operating rooms at Lehigh Valley Hospital in Allentown, Pennsylvania, are numbered sequentially — except when you get to what should be operation room (OR) 13. It’s OR M. The M doesn’t stand for Maternity or any other specialty. Rather in this high-tech, state-of-the art healthcare center, it’s there to ward off bad juju and evil spirits.
“Just as taller buildings usually don’t have a 13th floor or hotels don’t have a room 13, it revolves around the common superstition of the unlucky nature of number 13,” said a hospital spokesperson.
During the pandemic, the public was told repeatedly that modern medicine is science-based. But when I started talking to surgeons and other physicians for this article, I uncovered something decidedly unscientific.
In ORs and emergency rooms (ERs), small-town doctor’s offices, and mega hospitals, there’s a measure of dread before full moons and Friday the 13th, and no one dares utter the Q word (as in, “It sure is quiet today.”) That would risk bringing the wrath of the medical gods, and you’d earn the reputation of being a jinx or “black cloud.” Likewise, the songs “Stairway to Heaven” or “Another One Bites the Dust” will never be heard in any waiting room, elevator, or OR.
Indeed, when it comes to superstitions and rituals in medicine, it seems everyone has a story or a belief. …
A 2-Hour Ritual
Carmen Fong, MD, a colorectal surgeon in New York City, had a presurgical ritual that took her nearly 2 hours to complete. “I’d wake up at the same time every day, pack two hard-boiled eggs and a thermos of coffee in my small leather bag, walk to work via the same route, and swipe into the preop area while waving hi to the front desk,” she recounted. “I’d talk to the patient, sign the consent with the same ballpoint pen, go upstairs to my office, change into my scrubs [same cap and Danskos], then turn on my computer, and take a sip of coffee before heading back down to the OR. I’d always remove my badge and place it near the nurses’ workstation, then put on the patient’s SCDs [sequential compression devices] myself. I’d hold the oxygen mask while telling the patient, ‘See you later.’ Never ‘It will be okay’ or ‘Have a good sleep.’ Always ‘See you later.’ ”
Dr. Fong did this for 5 years prior to more than a thousand surgeries. She did it because it made her feel calm and in control, which translated to more successful operations. “It never failed me.”
Wonder Woman Clogs
Anureet Bajaj, MD, a plastic surgeon in Oklahoma City, wore Wonder Woman clogs in the OR for years because “they made me feel stronger, and my surgeries went better.” She’s also very specific about her OR playlist; “it must be ‘80s music.” And for a time, she wore a friendship bracelet that one of her employees made to commemorate getting through a particularly hard day. “If I forgot it, my heart sank, and my anxiety rose,” she said. “Wearing it gave me security and confidence that the day would go well.”
A Moment of Silence
Juliet Emamaullee, MD, PhD, is a liver and kidney transplant surgeon at Keck Hospital and Children’s Hospital Los Angeles. Because of the complexity of her operations, she must know every aspect of her patients’ medical history. This leads to a level of intimacy that most people never have with their doctors. “Transplant surgeons are playing god in many ways,” she said. “During procurement, after we prep and drape the donor and right before I make the incision, everyone in the OR has a moment of silence to acknowledge the donation. If the organ has been transported, then I’ll say a prayer to myself that I do good work with this generous gift of life.”
Magical Thinking
Before we go any further, I should clarify that there’s a difference between rituals and superstitions like the ones just shared and routines and practices such as handwashing or doublechecking that it’s the right hip and not the left. All pilots have a preflight checklist that’s necessary for safety, but some might also make the sign of the cross.
Lester Gottesman, MD, has been a surgeon at the Icahn School of Medicine at Mount Sinai Hospital in New York City for nearly 50 years. He believes rituals and superstitions are more prevalent in medicine than in any other profession, despite there being no definitive research confirming their effectiveness.
In fact, it’s the opposite.
One of the few studies to examine superstitions among physicians was published in the Annals of Surgery in 2021. Researchers analyzed the operational records of 27,914 consecutive patients who underwent general, visceral, or vascular surgery. They found no association of moon phases, zodiac signs, or Friday the 13th with poor outcomes. Having acute coronary syndrome on Friday the 13th also did not influence the 13-year mortality rate compared to other dates in the year. And although 70% of physicians believe that some colleagues are “black clouds,” an analysis of 96 physicians and 6149 admissions found no such pattern.
Granted, this is just one analysis, but the results aren’t surprising. No one really believes in this stuff. So, why does it persist?
Dr. Gottesman cited an episode from the popular medical TV show Grey’s Anatomy, in which chief surgeon Meredith Grey puts it this way: “Superstition lies in the space between what we can control and what we can’t. …We rely on superstitions because we are smart enough to know we don’t have all the answers and that life works in mysterious ways. Don’t diss the juju from wherever it comes.”
“Superstition and science both start at the same place — to explain an unexplainable event,” said Dr. Gottesman, who always checks his suture lines at the end of a surgery in the order in which he did them. “If science provides a coherent answer, so be it. If not, the human’s need for order will assign causality to otherwise inanimate objects, noncausal events, or divine influence.”
In other words, the more unknowns and trepidation, the greater the tendency toward what Dr. Gottesman called “magical thinking.” And when you consider healing’s long history, you realize that ritual and superstition defined medicine for centuries. Gottesman pointed out that it wasn’t until Hippocrates separated religion and superstition from disease around 430 BC that modern medicine was born. But because doctors still don’t know everything, an element of magic endures.
The question is, in this high-tech age, do these stubborn beliefs still have a place? Do they help or hinder doctors, and, most important, do they have any effect on patient outcomes?
Five Benefits
To reiterate, there are no studies showing that Wonder Woman clogs convey surgical superpowers or that eating two hard-boiled eggs boosts OR performance. But anecdotally, many doctors admit to experiencing noticeable perks from their quirks. Let’s start with the supposed benefits:
- Less stress: A quarter of US clinicians are considering switching careers, primarily due to burnout, according to a 2022 Bain survey. “The fact that [rituals and superstitions] are so prevalent in such a high-stress field can’t be coincidence,” said Dr. Fong. “Offloading some of the responsibility to whatever gods there may be is a way of taming our anxieties so we can function better.”
- Hyperfocus: Dr. Emamaullee played volleyball in high school and college. She suggested that her presurgical routine isn’t all that different from her warmup before a championship match. It’s habitual behavior that helps induce a state of heightened concentration, confidence, and immersion. Athletes call it being “in the zone” or in a “state of flow,” and Dr. Emamaullee said she experiences the same thing in the OR.
- More control: Remember those horrific images of patients with COVID-19 overwhelming ERs in Brooklyn and Queens during the pandemic? Dr. Fong was in the middle of that. “In crisis situations where there are more unknowns, rituals and superstitions become even more important,” she said. “I may not be able to control what’s happening, but I can control myself. Rituals help restore some normalcy and organization, and they give me a sense of calm.”
- Better performance: A series of general-population experiments published in the journal Psychological Science in 2010 concluded that “good-luck–related superstitions” boosted self-confidence in mastering upcoming tasks and improved motor dexterity, memory, and overall performance.
- Placebo effect: This phenomenon is well-established in medicine. Give someone a special pill or treatment, and a significant portion will claim benefit. “Placebo is magical thinking,” said Dr. Gottesman. “It has identifiable and quantifiable effects on human disease.” And perhaps on medical practitioners, too. If a doctor believes her friendship bracelet has special powers and helps her be a better physician, then it just might.
Four Drawbacks
- Compulsive behavior: When superstitious beliefs or repetitive behaviors begin causing personal distress, interfering with daily duties, or negatively affecting patient outcomes, then there’s a problem. There’s a story on Quora about a neurosurgeon who always ate two Hostess Ho Hos chocolate cakes before operations. When he forgot to do so one day, he supposedly left his patient on the table and ran off to eat them. Even if it’s urban legend, it’s a useful illustration of quirk disrupting work.
- Less flexibility: Every human body and every surgery is different. “When ritualistic behaviors or habits become so rigid that you lose the ability to adapt, then that becomes dangerous for the patient,” said Dr. Fong. “The art of medicine, not unlike jazz, often comes from the improvisation.”
- Self-fulfilling: Just as rituals and superstitions can empower and provide a sense of control, they can quickly turn on physicians who forget a part of their routine or leave their talisman on the bureau. Instead of confidence, they supply doubt. The karma becomes kryptonite.
- Avoiding responsibility: After years of friendship bracelets and Wonder Woman clogs, Dr. Bajaj is making a deliberate effort to excise magical thinking from her practice. “It can hold you back if you’re not careful,” she said. “If you start using it as a crutch when something goes wrong — like ‘Oh, I wasn’t wearing my clogs today and that’s why my flap failed’ — then you’re not doing your due diligence and figuring out what really happened.” Rather than placing the responsibility for her day going well on superstition, she’s trying to own it herself by living with more intent.
The Diagnosis
Most of the medical experts I spoke with didn’t think there was anything wrong with rituals or superstitions as long as they didn’t become compulsive or a convenient repository of blame.
“Rituals and superstitions are an acknowledgment that forces external to ourselves exist,” concluded Dr. Fong. “They’re like tiny offerings to whatever gods are out there to please be on our side. And we keep doing them because there’s a reward — better patient outcomes, which is all we want to achieve in the end. I say embrace them.”
A version of this article first appeared on Medscape.com.
Hospitals Cash In on a Private Equity-Backed Trend: Concierge Physician Care
Nonprofit hospitals created largely to serve the poor are adding concierge physician practices, charging patients annual membership fees of $2,000 or more for easier access to their doctors.
It’s a trend that began decades ago with physician practices. Thousands of doctors have shifted to the concierge model, in which they can increase their income while decreasing their patient load.
Northwestern Medicine in Chicago, Penn Medicine in Philadelphia, University Hospitals in the Cleveland area, and Baptist Health in Miami are among the large hospital systems offering concierge physician services. The fees, which can exceed $4,000 a year, are in addition to copayments, deductibles, and other charges not paid by patients’ insurance plans.
Critics of concierge medicine say the practice exacerbates primary care shortages, ensuring access only for the affluent, while driving up health care costs. But for tax-exempt hospitals, the financial benefits can be twofold.
“Hospitals are attracted to physicians that offer concierge services because their patients do not come with bad debts or a need for charity care, and most of them have private insurance which pays the hospital very well,” said Gerard Anderson, a hospital finance expert at Johns Hopkins University.
“They are the ideal patient, from the hospitals’ perspective.”
Concierge physicians typically limit their practices to a few hundred patients, compared with a couple of thousand for a traditional primary care doctor, so they can promise immediate access and longer visits.
“Every time we see these models expand, we are contracting the availability of primary care doctors for the general population,” said Jewel Mullen, associate dean for health equity at the University of Texas-Austin’s Dell Medical School. The former Connecticut health commissioner said concierge doctors join large hospital systems because of the institutions’ reputations, while hospitals sign up concierge physicians to ensure referrals to specialists and inpatient care. “It helps hospitals secure a bigger piece of their market,” she said.
Concierge physicians typically promise same-day or next-day appointments. Many provide patients their mobile phone number.
Aaron Klein, who oversees the concierge physician practices at Baptist Health, said the program was initially intended to serve donors.
“High-end donors wanted to make sure they have doctors to care for them,” he said.
Baptist opened its concierge program in 2019 and now has three practices across South Florida, where patients pay $2,500 a year.
“My philosophy is: It’s better to give world-class care to a few hundred patients rather than provide inadequate care to a few thousand patients,” Klein said.
Concierge physician practices started more than 20 years ago, mainly in upscale areas such as Boca Raton, Florida, and La Jolla, California. They catered mostly to wealthy retirees willing to pay extra for better physician access. Some of the first physician practices to enter the business were backed by private equity firms.
One of the largest, Boca Raton-based MDVIP, has more than 1,100 physicians and more than 390,000 patients. It was started in 2000, and since 2014 private equity firms have owned a majority stake in the company.
Some concierge physicians say their more attentive care means healthier patients. A study published last year by researchers at the University of California-Berkeley and University of Pennsylvania found no impact on mortality rates. What the study did find: higher costs.
Using Medicare claims data, the researchers found that concierge medicine enrollment corresponded with a 30%-50% increase in total health care spending by patients.
For hospitals, “this is an extension of them consolidating the market,” said Adam Leive, a study co-author and an assistant professor of public policy at UC Berkeley. Inova Health Care Services in Fairfax, Virginia, one of the state’s largest tax-exempt hospital chains, employs 18 concierge doctors, who each handle no more than 400 patients. Those patients pay $2,200 a year for the privilege.
George Salem, 70, of McLean, Virginia, has been a patient in Inova’s concierge practice for several years along with his wife. Earlier this year he slammed his finger in a hotel door, he said. As soon as he got home, he called his physician, who saw him immediately and stitched up the wound. He said he sees his doctor about 10 to 12 times a year.
“I loved my internist before, but it was impossible to get to see him,” Salem said. Immediate access to his doctor “very much gives me peace of mind,” he said.
Craig Cheifetz, a vice president at Inova who oversees the concierge program, said the hospital system took interest in the model after MDVIP began moving aggressively into the Washington, D.C., suburbs about a decade ago. Today, Inova’s program has 6,000 patients.
Cheifetz disputes the charge that concierge physician programs exacerbate primary care shortages. The model keeps doctors who were considering retiring early in the business with a lighter caseload, he said. And the fees amount to no more than a few dollars a day — about what some people spend on coffee, he said.
“Inova has an incredible primary care network for those who can’t afford the concierge care,” he said. “We are still providing all that is necessary in primary care for those who need it.”
Some hospitals are starting concierge physician practices far from their home locations. For example, Tampa General Hospital in Florida last year opened a concierge practice in upper-middle-class Palm Beach Gardens, a roughly three-hour drive from Tampa. Mount Sinai Health System in New York runs a concierge physician practice in West Palm Beach.
NCH Healthcare System in Naples, Florida, employs 12 concierge physicians who treat about 3,000 patients total. “We found a need in this community for those who wanted a more personalized health care experience,” said James Brinkert, regional administrator for the system. Members pay an annual fee of at least $3,500.
NCH patients whose doctors convert to concierge and who don’t want to pay the membership fee are referred to other primary care practices or to urgent care, Brinkert said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF .
Nonprofit hospitals created largely to serve the poor are adding concierge physician practices, charging patients annual membership fees of $2,000 or more for easier access to their doctors.
It’s a trend that began decades ago with physician practices. Thousands of doctors have shifted to the concierge model, in which they can increase their income while decreasing their patient load.
Northwestern Medicine in Chicago, Penn Medicine in Philadelphia, University Hospitals in the Cleveland area, and Baptist Health in Miami are among the large hospital systems offering concierge physician services. The fees, which can exceed $4,000 a year, are in addition to copayments, deductibles, and other charges not paid by patients’ insurance plans.
Critics of concierge medicine say the practice exacerbates primary care shortages, ensuring access only for the affluent, while driving up health care costs. But for tax-exempt hospitals, the financial benefits can be twofold.
“Hospitals are attracted to physicians that offer concierge services because their patients do not come with bad debts or a need for charity care, and most of them have private insurance which pays the hospital very well,” said Gerard Anderson, a hospital finance expert at Johns Hopkins University.
“They are the ideal patient, from the hospitals’ perspective.”
Concierge physicians typically limit their practices to a few hundred patients, compared with a couple of thousand for a traditional primary care doctor, so they can promise immediate access and longer visits.
“Every time we see these models expand, we are contracting the availability of primary care doctors for the general population,” said Jewel Mullen, associate dean for health equity at the University of Texas-Austin’s Dell Medical School. The former Connecticut health commissioner said concierge doctors join large hospital systems because of the institutions’ reputations, while hospitals sign up concierge physicians to ensure referrals to specialists and inpatient care. “It helps hospitals secure a bigger piece of their market,” she said.
Concierge physicians typically promise same-day or next-day appointments. Many provide patients their mobile phone number.
Aaron Klein, who oversees the concierge physician practices at Baptist Health, said the program was initially intended to serve donors.
“High-end donors wanted to make sure they have doctors to care for them,” he said.
Baptist opened its concierge program in 2019 and now has three practices across South Florida, where patients pay $2,500 a year.
“My philosophy is: It’s better to give world-class care to a few hundred patients rather than provide inadequate care to a few thousand patients,” Klein said.
Concierge physician practices started more than 20 years ago, mainly in upscale areas such as Boca Raton, Florida, and La Jolla, California. They catered mostly to wealthy retirees willing to pay extra for better physician access. Some of the first physician practices to enter the business were backed by private equity firms.
One of the largest, Boca Raton-based MDVIP, has more than 1,100 physicians and more than 390,000 patients. It was started in 2000, and since 2014 private equity firms have owned a majority stake in the company.
Some concierge physicians say their more attentive care means healthier patients. A study published last year by researchers at the University of California-Berkeley and University of Pennsylvania found no impact on mortality rates. What the study did find: higher costs.
Using Medicare claims data, the researchers found that concierge medicine enrollment corresponded with a 30%-50% increase in total health care spending by patients.
For hospitals, “this is an extension of them consolidating the market,” said Adam Leive, a study co-author and an assistant professor of public policy at UC Berkeley. Inova Health Care Services in Fairfax, Virginia, one of the state’s largest tax-exempt hospital chains, employs 18 concierge doctors, who each handle no more than 400 patients. Those patients pay $2,200 a year for the privilege.
George Salem, 70, of McLean, Virginia, has been a patient in Inova’s concierge practice for several years along with his wife. Earlier this year he slammed his finger in a hotel door, he said. As soon as he got home, he called his physician, who saw him immediately and stitched up the wound. He said he sees his doctor about 10 to 12 times a year.
“I loved my internist before, but it was impossible to get to see him,” Salem said. Immediate access to his doctor “very much gives me peace of mind,” he said.
Craig Cheifetz, a vice president at Inova who oversees the concierge program, said the hospital system took interest in the model after MDVIP began moving aggressively into the Washington, D.C., suburbs about a decade ago. Today, Inova’s program has 6,000 patients.
Cheifetz disputes the charge that concierge physician programs exacerbate primary care shortages. The model keeps doctors who were considering retiring early in the business with a lighter caseload, he said. And the fees amount to no more than a few dollars a day — about what some people spend on coffee, he said.
“Inova has an incredible primary care network for those who can’t afford the concierge care,” he said. “We are still providing all that is necessary in primary care for those who need it.”
Some hospitals are starting concierge physician practices far from their home locations. For example, Tampa General Hospital in Florida last year opened a concierge practice in upper-middle-class Palm Beach Gardens, a roughly three-hour drive from Tampa. Mount Sinai Health System in New York runs a concierge physician practice in West Palm Beach.
NCH Healthcare System in Naples, Florida, employs 12 concierge physicians who treat about 3,000 patients total. “We found a need in this community for those who wanted a more personalized health care experience,” said James Brinkert, regional administrator for the system. Members pay an annual fee of at least $3,500.
NCH patients whose doctors convert to concierge and who don’t want to pay the membership fee are referred to other primary care practices or to urgent care, Brinkert said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF .
Nonprofit hospitals created largely to serve the poor are adding concierge physician practices, charging patients annual membership fees of $2,000 or more for easier access to their doctors.
It’s a trend that began decades ago with physician practices. Thousands of doctors have shifted to the concierge model, in which they can increase their income while decreasing their patient load.
Northwestern Medicine in Chicago, Penn Medicine in Philadelphia, University Hospitals in the Cleveland area, and Baptist Health in Miami are among the large hospital systems offering concierge physician services. The fees, which can exceed $4,000 a year, are in addition to copayments, deductibles, and other charges not paid by patients’ insurance plans.
Critics of concierge medicine say the practice exacerbates primary care shortages, ensuring access only for the affluent, while driving up health care costs. But for tax-exempt hospitals, the financial benefits can be twofold.
“Hospitals are attracted to physicians that offer concierge services because their patients do not come with bad debts or a need for charity care, and most of them have private insurance which pays the hospital very well,” said Gerard Anderson, a hospital finance expert at Johns Hopkins University.
“They are the ideal patient, from the hospitals’ perspective.”
Concierge physicians typically limit their practices to a few hundred patients, compared with a couple of thousand for a traditional primary care doctor, so they can promise immediate access and longer visits.
“Every time we see these models expand, we are contracting the availability of primary care doctors for the general population,” said Jewel Mullen, associate dean for health equity at the University of Texas-Austin’s Dell Medical School. The former Connecticut health commissioner said concierge doctors join large hospital systems because of the institutions’ reputations, while hospitals sign up concierge physicians to ensure referrals to specialists and inpatient care. “It helps hospitals secure a bigger piece of their market,” she said.
Concierge physicians typically promise same-day or next-day appointments. Many provide patients their mobile phone number.
Aaron Klein, who oversees the concierge physician practices at Baptist Health, said the program was initially intended to serve donors.
“High-end donors wanted to make sure they have doctors to care for them,” he said.
Baptist opened its concierge program in 2019 and now has three practices across South Florida, where patients pay $2,500 a year.
“My philosophy is: It’s better to give world-class care to a few hundred patients rather than provide inadequate care to a few thousand patients,” Klein said.
Concierge physician practices started more than 20 years ago, mainly in upscale areas such as Boca Raton, Florida, and La Jolla, California. They catered mostly to wealthy retirees willing to pay extra for better physician access. Some of the first physician practices to enter the business were backed by private equity firms.
One of the largest, Boca Raton-based MDVIP, has more than 1,100 physicians and more than 390,000 patients. It was started in 2000, and since 2014 private equity firms have owned a majority stake in the company.
Some concierge physicians say their more attentive care means healthier patients. A study published last year by researchers at the University of California-Berkeley and University of Pennsylvania found no impact on mortality rates. What the study did find: higher costs.
Using Medicare claims data, the researchers found that concierge medicine enrollment corresponded with a 30%-50% increase in total health care spending by patients.
For hospitals, “this is an extension of them consolidating the market,” said Adam Leive, a study co-author and an assistant professor of public policy at UC Berkeley. Inova Health Care Services in Fairfax, Virginia, one of the state’s largest tax-exempt hospital chains, employs 18 concierge doctors, who each handle no more than 400 patients. Those patients pay $2,200 a year for the privilege.
George Salem, 70, of McLean, Virginia, has been a patient in Inova’s concierge practice for several years along with his wife. Earlier this year he slammed his finger in a hotel door, he said. As soon as he got home, he called his physician, who saw him immediately and stitched up the wound. He said he sees his doctor about 10 to 12 times a year.
“I loved my internist before, but it was impossible to get to see him,” Salem said. Immediate access to his doctor “very much gives me peace of mind,” he said.
Craig Cheifetz, a vice president at Inova who oversees the concierge program, said the hospital system took interest in the model after MDVIP began moving aggressively into the Washington, D.C., suburbs about a decade ago. Today, Inova’s program has 6,000 patients.
Cheifetz disputes the charge that concierge physician programs exacerbate primary care shortages. The model keeps doctors who were considering retiring early in the business with a lighter caseload, he said. And the fees amount to no more than a few dollars a day — about what some people spend on coffee, he said.
“Inova has an incredible primary care network for those who can’t afford the concierge care,” he said. “We are still providing all that is necessary in primary care for those who need it.”
Some hospitals are starting concierge physician practices far from their home locations. For example, Tampa General Hospital in Florida last year opened a concierge practice in upper-middle-class Palm Beach Gardens, a roughly three-hour drive from Tampa. Mount Sinai Health System in New York runs a concierge physician practice in West Palm Beach.
NCH Healthcare System in Naples, Florida, employs 12 concierge physicians who treat about 3,000 patients total. “We found a need in this community for those who wanted a more personalized health care experience,” said James Brinkert, regional administrator for the system. Members pay an annual fee of at least $3,500.
NCH patients whose doctors convert to concierge and who don’t want to pay the membership fee are referred to other primary care practices or to urgent care, Brinkert said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF .