User login
What’s the price of rude behavior in the hospital?
SAN DIEGO – Does rudeness from a colleague prevent physicians from noticing a diagnostic error and challenging it? A new study suggests it might not, at least in the context of hand-offs from dismissive and insulting fellow doctors.
Instead, a simulation found that experience seems to be the key factor in giving physicians the guts – or the awareness – to change course. Still, the findings hint that rudeness may still have a negative effect on one group – resident physicians.
“It appears that we are building resilience somewhere in training,” said study lead author Michael Avesar, MD, a pediatric critical care medicine fellow at Children’s Hospital Los Angeles.
Dr. Avesar spoke in an interview following the presentation of the study findings at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
The initial motivation of the study wasn’t to gain more understanding of rudeness in medicine. Instead, Dr. Avesar said, “We started off with trying to find ways to understand how physicians think during high-stakes decisions in stressful or time-limited situations. We wanted to see if people were able to challenge the momentum of diagnostic error. That’s when we learned more about the rudeness literature.”
Yes, it’s true: Researchers have devoted time to studying rudeness in medicine. After all, it’s quite common. A 2017 Israeli study in Pediatrics declared it’s “routinely experienced by medical teams.” That study, also based on simulations, determined that “rudeness has robust, deleterious effects on the performance of medical teams. Moreover, exposure to rudeness debilitated the very collaborative mechanisms recognized as essential for patient care and safety” (Pediatrics. 2017 Feb. doi: 10.1542/peds.2016-2305).
For the new study, Dr. Avesar and his colleagues ultimately decided to explore possible links between rudeness and diagnostic error. To explore the issue, they created a simulation of a hand-off of a pediatric patient from the operating team to the ICU.
In the simulation, the “physician” handing off the “patient” incorrectly noted a diagnosis of sepsis. In fact, the patient had cardiac tamponade.
The physician, played by an actor, was instructed to either act in a neutral fashion during the hand-off or be rude. But rudeness, it turns out, isn’t easy to define, even if we all think we know it when we see it.
“There’s a lot of debate as to what is ‘rude,’ ” Dr. Avesar said. The researchers settled on a level of rudeness that wasn’t “too mean” but was still inappropriate: It featured frequent interruptions during the hand-off, lack of eye contact, and abrupt departures. In some simulations, the actor insulted the colleagues of the recipient of the hand-off.
In other words, Dr. Avesar said, the actor was a jerk.
The researchers tested the “neutral” and “rude” hand-off scenarios in 41 simulations. The physicians who played the recipients of the hand-offs included 11 attendings, 14 fellows, and 16 residents.
Eighty-two percent of the attendings (9/11) challenged the diagnosis, as did 86% (12/14) of the fellows. Only 31% (5/16) of residents challenged the diagnosis; this difference from the other groups was statistically significant.
Half of the eight residents exposed to a “neutral” handoff challenged the correct diagnosis, while only 13% (1/8) of those who were treated rudely did. “While the P value was not significant, previous literature focused on residents supports this trend,” Dr. Avesar said.
It’s possible that certain residents gain the knowledge and experience to overcome rudeness over time, he said. That, he said, leads to an intriguing question: “Could we find out how resilience is learned and how to replicate it?”
Moving forward, he said, the team will try to figure out whether there’s a link between personality types and reactions to rudeness.
Eventually, he said, the team may test ways to reduce the effects of rudeness and boost critical thinking. “We see this as a long-term strategy to enhance medical education and patient safety,” he said.
No study funding is reported. Dr. Avesar reports no relevant disclosures.
SOURCE: Avesar M et al. Crit Care Med. 2019 Jan;47(1):682, Abstract 1412.
SAN DIEGO – Does rudeness from a colleague prevent physicians from noticing a diagnostic error and challenging it? A new study suggests it might not, at least in the context of hand-offs from dismissive and insulting fellow doctors.
Instead, a simulation found that experience seems to be the key factor in giving physicians the guts – or the awareness – to change course. Still, the findings hint that rudeness may still have a negative effect on one group – resident physicians.
“It appears that we are building resilience somewhere in training,” said study lead author Michael Avesar, MD, a pediatric critical care medicine fellow at Children’s Hospital Los Angeles.
Dr. Avesar spoke in an interview following the presentation of the study findings at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
The initial motivation of the study wasn’t to gain more understanding of rudeness in medicine. Instead, Dr. Avesar said, “We started off with trying to find ways to understand how physicians think during high-stakes decisions in stressful or time-limited situations. We wanted to see if people were able to challenge the momentum of diagnostic error. That’s when we learned more about the rudeness literature.”
Yes, it’s true: Researchers have devoted time to studying rudeness in medicine. After all, it’s quite common. A 2017 Israeli study in Pediatrics declared it’s “routinely experienced by medical teams.” That study, also based on simulations, determined that “rudeness has robust, deleterious effects on the performance of medical teams. Moreover, exposure to rudeness debilitated the very collaborative mechanisms recognized as essential for patient care and safety” (Pediatrics. 2017 Feb. doi: 10.1542/peds.2016-2305).
For the new study, Dr. Avesar and his colleagues ultimately decided to explore possible links between rudeness and diagnostic error. To explore the issue, they created a simulation of a hand-off of a pediatric patient from the operating team to the ICU.
In the simulation, the “physician” handing off the “patient” incorrectly noted a diagnosis of sepsis. In fact, the patient had cardiac tamponade.
The physician, played by an actor, was instructed to either act in a neutral fashion during the hand-off or be rude. But rudeness, it turns out, isn’t easy to define, even if we all think we know it when we see it.
“There’s a lot of debate as to what is ‘rude,’ ” Dr. Avesar said. The researchers settled on a level of rudeness that wasn’t “too mean” but was still inappropriate: It featured frequent interruptions during the hand-off, lack of eye contact, and abrupt departures. In some simulations, the actor insulted the colleagues of the recipient of the hand-off.
In other words, Dr. Avesar said, the actor was a jerk.
The researchers tested the “neutral” and “rude” hand-off scenarios in 41 simulations. The physicians who played the recipients of the hand-offs included 11 attendings, 14 fellows, and 16 residents.
Eighty-two percent of the attendings (9/11) challenged the diagnosis, as did 86% (12/14) of the fellows. Only 31% (5/16) of residents challenged the diagnosis; this difference from the other groups was statistically significant.
Half of the eight residents exposed to a “neutral” handoff challenged the correct diagnosis, while only 13% (1/8) of those who were treated rudely did. “While the P value was not significant, previous literature focused on residents supports this trend,” Dr. Avesar said.
It’s possible that certain residents gain the knowledge and experience to overcome rudeness over time, he said. That, he said, leads to an intriguing question: “Could we find out how resilience is learned and how to replicate it?”
Moving forward, he said, the team will try to figure out whether there’s a link between personality types and reactions to rudeness.
Eventually, he said, the team may test ways to reduce the effects of rudeness and boost critical thinking. “We see this as a long-term strategy to enhance medical education and patient safety,” he said.
No study funding is reported. Dr. Avesar reports no relevant disclosures.
SOURCE: Avesar M et al. Crit Care Med. 2019 Jan;47(1):682, Abstract 1412.
SAN DIEGO – Does rudeness from a colleague prevent physicians from noticing a diagnostic error and challenging it? A new study suggests it might not, at least in the context of hand-offs from dismissive and insulting fellow doctors.
Instead, a simulation found that experience seems to be the key factor in giving physicians the guts – or the awareness – to change course. Still, the findings hint that rudeness may still have a negative effect on one group – resident physicians.
“It appears that we are building resilience somewhere in training,” said study lead author Michael Avesar, MD, a pediatric critical care medicine fellow at Children’s Hospital Los Angeles.
Dr. Avesar spoke in an interview following the presentation of the study findings at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
The initial motivation of the study wasn’t to gain more understanding of rudeness in medicine. Instead, Dr. Avesar said, “We started off with trying to find ways to understand how physicians think during high-stakes decisions in stressful or time-limited situations. We wanted to see if people were able to challenge the momentum of diagnostic error. That’s when we learned more about the rudeness literature.”
Yes, it’s true: Researchers have devoted time to studying rudeness in medicine. After all, it’s quite common. A 2017 Israeli study in Pediatrics declared it’s “routinely experienced by medical teams.” That study, also based on simulations, determined that “rudeness has robust, deleterious effects on the performance of medical teams. Moreover, exposure to rudeness debilitated the very collaborative mechanisms recognized as essential for patient care and safety” (Pediatrics. 2017 Feb. doi: 10.1542/peds.2016-2305).
For the new study, Dr. Avesar and his colleagues ultimately decided to explore possible links between rudeness and diagnostic error. To explore the issue, they created a simulation of a hand-off of a pediatric patient from the operating team to the ICU.
In the simulation, the “physician” handing off the “patient” incorrectly noted a diagnosis of sepsis. In fact, the patient had cardiac tamponade.
The physician, played by an actor, was instructed to either act in a neutral fashion during the hand-off or be rude. But rudeness, it turns out, isn’t easy to define, even if we all think we know it when we see it.
“There’s a lot of debate as to what is ‘rude,’ ” Dr. Avesar said. The researchers settled on a level of rudeness that wasn’t “too mean” but was still inappropriate: It featured frequent interruptions during the hand-off, lack of eye contact, and abrupt departures. In some simulations, the actor insulted the colleagues of the recipient of the hand-off.
In other words, Dr. Avesar said, the actor was a jerk.
The researchers tested the “neutral” and “rude” hand-off scenarios in 41 simulations. The physicians who played the recipients of the hand-offs included 11 attendings, 14 fellows, and 16 residents.
Eighty-two percent of the attendings (9/11) challenged the diagnosis, as did 86% (12/14) of the fellows. Only 31% (5/16) of residents challenged the diagnosis; this difference from the other groups was statistically significant.
Half of the eight residents exposed to a “neutral” handoff challenged the correct diagnosis, while only 13% (1/8) of those who were treated rudely did. “While the P value was not significant, previous literature focused on residents supports this trend,” Dr. Avesar said.
It’s possible that certain residents gain the knowledge and experience to overcome rudeness over time, he said. That, he said, leads to an intriguing question: “Could we find out how resilience is learned and how to replicate it?”
Moving forward, he said, the team will try to figure out whether there’s a link between personality types and reactions to rudeness.
Eventually, he said, the team may test ways to reduce the effects of rudeness and boost critical thinking. “We see this as a long-term strategy to enhance medical education and patient safety,” he said.
No study funding is reported. Dr. Avesar reports no relevant disclosures.
SOURCE: Avesar M et al. Crit Care Med. 2019 Jan;47(1):682, Abstract 1412.
REPORTING FROM CCC48
Scott Gottlieb to step down as FDA commissioner
According to reports, he is stepping down to spend more time with his family, who live in Westport, Conn. He splits time between there and Washington. He was confirmed by the Senate in May 2017 with five Democrats and one independent joining Republicans in voting him in.
President Trump confirmed Dr. Gottlieb’s resignation, praising him in a tweet for the “terrific job” he has done in this role and commending his efforts to help “us to lower drug prices, get a record number of generic drugs approved and onto the market, and so many other things. ”
Dr. Gottlieb’s legacy may be his work on regulating e-cigarettes, although that work is unfinished. His passion for this subject can be found in a statement made in Nov. 2018, announcing an advanced notice of proposed rule making to regulate e-cigarettes.
“Today, I’m pursuing actions aimed at addressing the disturbing trend of youth nicotine use and continuing to advance the historic declines we’ve achieved in recent years in the rates of combustible cigarette use among kids,” Dr. Gottlieb said in the statement.
More recently, the agency announced March 4 enforcement actions aimed at both retailers and manufacturers, including requesting a meeting with Walgreens to discuss the nearly 1,800 violations the chain has amassed across the country for selling tobacco products to minors.
“Because tobacco use is almost always initiated and established during adolescence, early intervention ‒ including making sure tobacco products aren’t being marketed to, sold to, or used by kids ‒ is critical,” he said in announcing the enforcement actions. He added that the FDA will “continue vigorous enforcement activities, with a sustained campaign to monitor, penalize, and help prevent e-cigarette sales to minors in retail locations, including manufacturers’ Internet storefronts, as well as take additional steps to tackle other concerns related to the youth access and appeal of these products. The FDA is also exploring additional enforcement avenues to target violative sales and marketing practices by manufacturers and retailers.”
The American Heart Association praised Dr. Gottlieb’s work.
“Commissioner Gottlieb departs the FDA having established himself as a tireless champion of tobacco control,” the organization said in a statement. “He elevated the war on tobacco use – and particularly the epidemic of electronic cigarette use among youth – to unprecedented levels. Because of his efforts, millions more people nationwide are aware of the grave threats posed by e-cigarettes and other tobacco products that are addicting a new generation of youth. We urge the FDA in the strongest possible terms to move forward with effective regulation of an industry that continues to prioritize profits over the lives of consumers.”
Department of Health & Human Services Secretary Alex Azar acknowledged Dr. Gottlieb’s work in combating youth e-cigarette use among a number of areas that the outgoing official has had a positive impact on.
“Scott’s leadership inspired historic results from the FDA team, which delivered record approvals of both innovative treatments and affordable generic drugs, while advancing important policies to confront opioid addiction, tobacco and youth e-cigarette use, chronic disease, and more,” Secretary Azar said in a statement. “The public health of our country is better off for the work Scott and the entire FDA team have done over the last two years.”
Under his leadership, FDA has approved a record number of generic drugs, although many still are not on the market yet.
In the area of opioids, his tenure could be a mixed bag as the FDA on the one hand removed an opioid product from the market, but on the other, controversially approved a new, powerful one.
According to reports, he is stepping down to spend more time with his family, who live in Westport, Conn. He splits time between there and Washington. He was confirmed by the Senate in May 2017 with five Democrats and one independent joining Republicans in voting him in.
President Trump confirmed Dr. Gottlieb’s resignation, praising him in a tweet for the “terrific job” he has done in this role and commending his efforts to help “us to lower drug prices, get a record number of generic drugs approved and onto the market, and so many other things. ”
Dr. Gottlieb’s legacy may be his work on regulating e-cigarettes, although that work is unfinished. His passion for this subject can be found in a statement made in Nov. 2018, announcing an advanced notice of proposed rule making to regulate e-cigarettes.
“Today, I’m pursuing actions aimed at addressing the disturbing trend of youth nicotine use and continuing to advance the historic declines we’ve achieved in recent years in the rates of combustible cigarette use among kids,” Dr. Gottlieb said in the statement.
More recently, the agency announced March 4 enforcement actions aimed at both retailers and manufacturers, including requesting a meeting with Walgreens to discuss the nearly 1,800 violations the chain has amassed across the country for selling tobacco products to minors.
“Because tobacco use is almost always initiated and established during adolescence, early intervention ‒ including making sure tobacco products aren’t being marketed to, sold to, or used by kids ‒ is critical,” he said in announcing the enforcement actions. He added that the FDA will “continue vigorous enforcement activities, with a sustained campaign to monitor, penalize, and help prevent e-cigarette sales to minors in retail locations, including manufacturers’ Internet storefronts, as well as take additional steps to tackle other concerns related to the youth access and appeal of these products. The FDA is also exploring additional enforcement avenues to target violative sales and marketing practices by manufacturers and retailers.”
The American Heart Association praised Dr. Gottlieb’s work.
“Commissioner Gottlieb departs the FDA having established himself as a tireless champion of tobacco control,” the organization said in a statement. “He elevated the war on tobacco use – and particularly the epidemic of electronic cigarette use among youth – to unprecedented levels. Because of his efforts, millions more people nationwide are aware of the grave threats posed by e-cigarettes and other tobacco products that are addicting a new generation of youth. We urge the FDA in the strongest possible terms to move forward with effective regulation of an industry that continues to prioritize profits over the lives of consumers.”
Department of Health & Human Services Secretary Alex Azar acknowledged Dr. Gottlieb’s work in combating youth e-cigarette use among a number of areas that the outgoing official has had a positive impact on.
“Scott’s leadership inspired historic results from the FDA team, which delivered record approvals of both innovative treatments and affordable generic drugs, while advancing important policies to confront opioid addiction, tobacco and youth e-cigarette use, chronic disease, and more,” Secretary Azar said in a statement. “The public health of our country is better off for the work Scott and the entire FDA team have done over the last two years.”
Under his leadership, FDA has approved a record number of generic drugs, although many still are not on the market yet.
In the area of opioids, his tenure could be a mixed bag as the FDA on the one hand removed an opioid product from the market, but on the other, controversially approved a new, powerful one.
According to reports, he is stepping down to spend more time with his family, who live in Westport, Conn. He splits time between there and Washington. He was confirmed by the Senate in May 2017 with five Democrats and one independent joining Republicans in voting him in.
President Trump confirmed Dr. Gottlieb’s resignation, praising him in a tweet for the “terrific job” he has done in this role and commending his efforts to help “us to lower drug prices, get a record number of generic drugs approved and onto the market, and so many other things. ”
Dr. Gottlieb’s legacy may be his work on regulating e-cigarettes, although that work is unfinished. His passion for this subject can be found in a statement made in Nov. 2018, announcing an advanced notice of proposed rule making to regulate e-cigarettes.
“Today, I’m pursuing actions aimed at addressing the disturbing trend of youth nicotine use and continuing to advance the historic declines we’ve achieved in recent years in the rates of combustible cigarette use among kids,” Dr. Gottlieb said in the statement.
More recently, the agency announced March 4 enforcement actions aimed at both retailers and manufacturers, including requesting a meeting with Walgreens to discuss the nearly 1,800 violations the chain has amassed across the country for selling tobacco products to minors.
“Because tobacco use is almost always initiated and established during adolescence, early intervention ‒ including making sure tobacco products aren’t being marketed to, sold to, or used by kids ‒ is critical,” he said in announcing the enforcement actions. He added that the FDA will “continue vigorous enforcement activities, with a sustained campaign to monitor, penalize, and help prevent e-cigarette sales to minors in retail locations, including manufacturers’ Internet storefronts, as well as take additional steps to tackle other concerns related to the youth access and appeal of these products. The FDA is also exploring additional enforcement avenues to target violative sales and marketing practices by manufacturers and retailers.”
The American Heart Association praised Dr. Gottlieb’s work.
“Commissioner Gottlieb departs the FDA having established himself as a tireless champion of tobacco control,” the organization said in a statement. “He elevated the war on tobacco use – and particularly the epidemic of electronic cigarette use among youth – to unprecedented levels. Because of his efforts, millions more people nationwide are aware of the grave threats posed by e-cigarettes and other tobacco products that are addicting a new generation of youth. We urge the FDA in the strongest possible terms to move forward with effective regulation of an industry that continues to prioritize profits over the lives of consumers.”
Department of Health & Human Services Secretary Alex Azar acknowledged Dr. Gottlieb’s work in combating youth e-cigarette use among a number of areas that the outgoing official has had a positive impact on.
“Scott’s leadership inspired historic results from the FDA team, which delivered record approvals of both innovative treatments and affordable generic drugs, while advancing important policies to confront opioid addiction, tobacco and youth e-cigarette use, chronic disease, and more,” Secretary Azar said in a statement. “The public health of our country is better off for the work Scott and the entire FDA team have done over the last two years.”
Under his leadership, FDA has approved a record number of generic drugs, although many still are not on the market yet.
In the area of opioids, his tenure could be a mixed bag as the FDA on the one hand removed an opioid product from the market, but on the other, controversially approved a new, powerful one.
Take stronger steps to prevent staph infections and sepsis
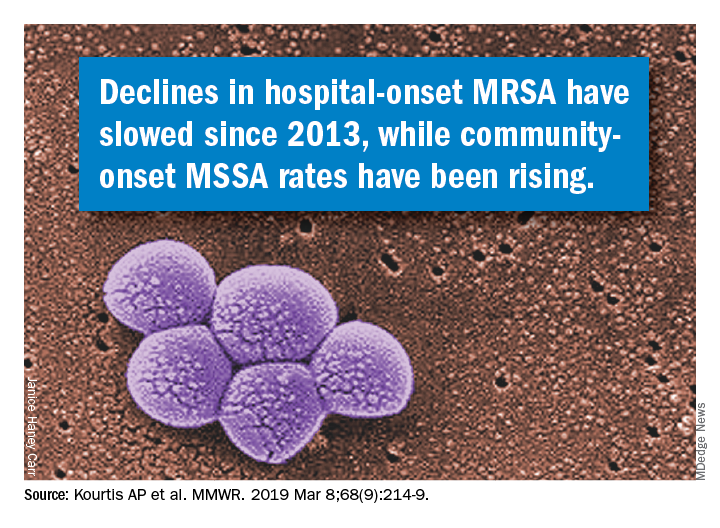
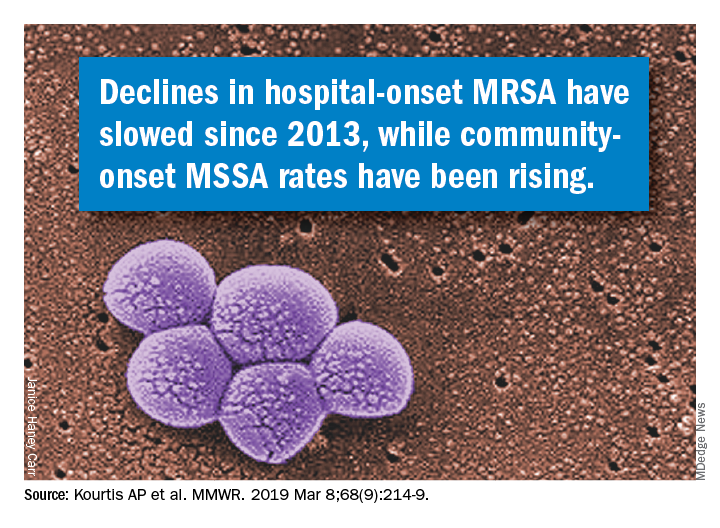
according to data from a Vital Signs report issued by the Centers for Disease Control and Prevention. The data include both methicillin-resistant S. aureus (MRSA) and methicillin-susceptible S. aureus (MSSA).
Although MRSA infections in health care settings declined by approximately 17% during 2005-2012, rates plateaued during 2012-2017, Anne Schuchat, MD, principal deputy director of the CDC, said in a teleconference March 5 to present the findings. The report emphasizes the potential for serious illness and death with any staph infection and the need for ongoing vigilance on the part of clinicians, she said.
In addition, community-onset MSSA infections increased by 3.9%/year during 2012-2017. Data from previous studies suggest that this increase may be connected to the opioid epidemic, said Dr. Schuchat.
“People who inject drugs are 16% more likely to develop a staph infection” than are those who don’t inject drugs, she said.
Community-onset MRSA declined by 6.9% during 2001-2016, attributed to declines in health care–associated infections, according to Vital Signs author Athena P. Kourtis, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, and her colleagues. Rates of hospital-associated MSSA infection remained essentially unchanged (P = .11). The overall unadjusted in-hospital mortality among patients with S. aureus bloodstream infections over the study period was 18%.
The data for the report were collected from electronic health records at more than 400 acute care hospitals, as well as population-based surveillance data from the CDC’s Emerging Infections Program.
Most people carry staph on their skin with no ill effects, but the bacteria become dangerous when they enter the bloodstream, Dr. Schuchat emphasized. “We hope the new data today will refocus the nation’s efforts to protect patients from staph infections,” she said.
Dr. Schuchat advised clinicians and hospital administrators to review their data and step up their safety protocols to prevent staph infections. Precautions include wearing gowns and gloves, following proper hand washing protocols, cautious use of antibiotics, and treating infections rapidly when they occur, she said. Dr. Schuchat noted that lack of adherence to these recommendations may have declined in recent years if clinicians and hospital administrators were wondering whether their protocols have an effect and have value. However, “this is a very serious infection, and we think it is very much worth preventing,” she emphasized.
Other strategies to prevent staph infections in health care settings include reviewing infection data regularly, exploring new approaches to prevent infections, and educating patients about when they may be at increased risk for infection, such as when invasive devices are in place or during surgical procedures. Also, clinicians should be aware of the increased risk for patients who inject drugs, Dr. Schuchat said.
Dr. Schuchat commended the Department of Veterans Affairs Medical Centers (VAMC), which overall reduced their rate of staph infections by 43% during the period from 2005 through 2017 in contrast to the national trend. These findings also appeared in the MMWR on March 5. The VAMC implemented additional interventions and increased their adherence to CDC recommendations during this period, she noted.
The Vital Signs data were published March 5 in the CDC’s Morbidity and Mortality Weekly Report; read the full report here.
The CDC researchers had no financial conflicts to disclose.
SOURCE: Kourtis AP et al. MMWR. 2019 Mar 5; 68:1-6.
according to data from a Vital Signs report issued by the Centers for Disease Control and Prevention. The data include both methicillin-resistant S. aureus (MRSA) and methicillin-susceptible S. aureus (MSSA).
Although MRSA infections in health care settings declined by approximately 17% during 2005-2012, rates plateaued during 2012-2017, Anne Schuchat, MD, principal deputy director of the CDC, said in a teleconference March 5 to present the findings. The report emphasizes the potential for serious illness and death with any staph infection and the need for ongoing vigilance on the part of clinicians, she said.
In addition, community-onset MSSA infections increased by 3.9%/year during 2012-2017. Data from previous studies suggest that this increase may be connected to the opioid epidemic, said Dr. Schuchat.
“People who inject drugs are 16% more likely to develop a staph infection” than are those who don’t inject drugs, she said.
Community-onset MRSA declined by 6.9% during 2001-2016, attributed to declines in health care–associated infections, according to Vital Signs author Athena P. Kourtis, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, and her colleagues. Rates of hospital-associated MSSA infection remained essentially unchanged (P = .11). The overall unadjusted in-hospital mortality among patients with S. aureus bloodstream infections over the study period was 18%.
The data for the report were collected from electronic health records at more than 400 acute care hospitals, as well as population-based surveillance data from the CDC’s Emerging Infections Program.
Most people carry staph on their skin with no ill effects, but the bacteria become dangerous when they enter the bloodstream, Dr. Schuchat emphasized. “We hope the new data today will refocus the nation’s efforts to protect patients from staph infections,” she said.
Dr. Schuchat advised clinicians and hospital administrators to review their data and step up their safety protocols to prevent staph infections. Precautions include wearing gowns and gloves, following proper hand washing protocols, cautious use of antibiotics, and treating infections rapidly when they occur, she said. Dr. Schuchat noted that lack of adherence to these recommendations may have declined in recent years if clinicians and hospital administrators were wondering whether their protocols have an effect and have value. However, “this is a very serious infection, and we think it is very much worth preventing,” she emphasized.
Other strategies to prevent staph infections in health care settings include reviewing infection data regularly, exploring new approaches to prevent infections, and educating patients about when they may be at increased risk for infection, such as when invasive devices are in place or during surgical procedures. Also, clinicians should be aware of the increased risk for patients who inject drugs, Dr. Schuchat said.
Dr. Schuchat commended the Department of Veterans Affairs Medical Centers (VAMC), which overall reduced their rate of staph infections by 43% during the period from 2005 through 2017 in contrast to the national trend. These findings also appeared in the MMWR on March 5. The VAMC implemented additional interventions and increased their adherence to CDC recommendations during this period, she noted.
The Vital Signs data were published March 5 in the CDC’s Morbidity and Mortality Weekly Report; read the full report here.
The CDC researchers had no financial conflicts to disclose.
SOURCE: Kourtis AP et al. MMWR. 2019 Mar 5; 68:1-6.
according to data from a Vital Signs report issued by the Centers for Disease Control and Prevention. The data include both methicillin-resistant S. aureus (MRSA) and methicillin-susceptible S. aureus (MSSA).
Although MRSA infections in health care settings declined by approximately 17% during 2005-2012, rates plateaued during 2012-2017, Anne Schuchat, MD, principal deputy director of the CDC, said in a teleconference March 5 to present the findings. The report emphasizes the potential for serious illness and death with any staph infection and the need for ongoing vigilance on the part of clinicians, she said.
In addition, community-onset MSSA infections increased by 3.9%/year during 2012-2017. Data from previous studies suggest that this increase may be connected to the opioid epidemic, said Dr. Schuchat.
“People who inject drugs are 16% more likely to develop a staph infection” than are those who don’t inject drugs, she said.
Community-onset MRSA declined by 6.9% during 2001-2016, attributed to declines in health care–associated infections, according to Vital Signs author Athena P. Kourtis, MD, of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, and her colleagues. Rates of hospital-associated MSSA infection remained essentially unchanged (P = .11). The overall unadjusted in-hospital mortality among patients with S. aureus bloodstream infections over the study period was 18%.
The data for the report were collected from electronic health records at more than 400 acute care hospitals, as well as population-based surveillance data from the CDC’s Emerging Infections Program.
Most people carry staph on their skin with no ill effects, but the bacteria become dangerous when they enter the bloodstream, Dr. Schuchat emphasized. “We hope the new data today will refocus the nation’s efforts to protect patients from staph infections,” she said.
Dr. Schuchat advised clinicians and hospital administrators to review their data and step up their safety protocols to prevent staph infections. Precautions include wearing gowns and gloves, following proper hand washing protocols, cautious use of antibiotics, and treating infections rapidly when they occur, she said. Dr. Schuchat noted that lack of adherence to these recommendations may have declined in recent years if clinicians and hospital administrators were wondering whether their protocols have an effect and have value. However, “this is a very serious infection, and we think it is very much worth preventing,” she emphasized.
Other strategies to prevent staph infections in health care settings include reviewing infection data regularly, exploring new approaches to prevent infections, and educating patients about when they may be at increased risk for infection, such as when invasive devices are in place or during surgical procedures. Also, clinicians should be aware of the increased risk for patients who inject drugs, Dr. Schuchat said.
Dr. Schuchat commended the Department of Veterans Affairs Medical Centers (VAMC), which overall reduced their rate of staph infections by 43% during the period from 2005 through 2017 in contrast to the national trend. These findings also appeared in the MMWR on March 5. The VAMC implemented additional interventions and increased their adherence to CDC recommendations during this period, she noted.
The Vital Signs data were published March 5 in the CDC’s Morbidity and Mortality Weekly Report; read the full report here.
The CDC researchers had no financial conflicts to disclose.
SOURCE: Kourtis AP et al. MMWR. 2019 Mar 5; 68:1-6.
FROM THE MORBIDITY AND MORTALITY WEEKLY REPORT
New SOFA version could streamline outcomes research
SAN DIEGO – The new method replaces some of SOFA’s more subjective criteria with objective measures.
eSOFA relies on electronic health records to reduce reliance on administrative records, which suffer from cross-hospital variability in diagnosis and coding practices, as well as changes in these practices over time. The diagnosis of sepsis itself is also highly subjective. Instead, eSOFA determines dysfunction in six organ systems, indicated by use of vasopressors and mechanical ventilation, and the presence of abnormal laboratory values.
“The SOFA score includes measures like the Glasgow Coma Scale, which undoubtedly at the bedside is a very important clinical sign, but when trying to implement something that is objective for purposes of retrospective case counting and standardization, it can be problematic. The measures we chose [for eSOFA] are concrete, important maneuvers that were initiated by clinicians,” Chanu Rhee, MD, said in an interview.
Dr. Rhee is assistant professor of population medicine at Harvard Medical School and Brigham and Women’s Hospital, Boston. He presented the results of the study at the Critical Care Congress sponsored by the Society of Critical Care Medicine, and the work was simultaneously published online in Critical Care Medicine.
Key elements of SOFA that pose challenges for administrative data include: PaO2/FiO2, which are not routinely measured, and can be difficult to assign to arterial or venous samples; inconsistency in blood pressure and transient increases in vasopressor dose; the subjectivity of the Glasgow Coma Scale, which is also difficult to assess in sedated patients; and inconsistent urine output.
eSOFA introduced new measures for various organ functions, including cardiovascular (vasopressor initiation), pulmonary (mechanical ventilation initiation), renal (doubling of creatinine levels or a 50% or greater decrease in estimated glomerular filtration rate, compared with baseline), hepatic (bilirubin levels greater than or equal to 2.0 mg/dL and at least doubled from baseline), coagulation (platelet count less than 100 cells/mcL and at least a 50% decrease from a baseline of at least 100 cells/mcL), and neurological (lactate greater than or equal to 2.0 mmol/L).
“[eSOFA] opens a window into inter-facility comparisons that has not been possible to do. It’s really critical to ask, ‘How am I doing compared to my peer institutions?’ If you’re doing worse, you can look at the whole spectrum of things to try to drive improvements in care,” said Dr. Rhee.
The new tool isn’t just limited to quality improvement research. Shaeesta Khan, MD, assistant professor of critical care medicine at Geisinger Medical Center,Danville, Pa., has found eSOFA to be useful in her research into how genetic polymorphisms play a role in sepsis outcomes. Geisinger has a large population of patients with completed whole genome sequencing, and Dr. Khan began by trying to glean sepsis outcomes from administrative data.
“I explained SOFA scores to our data broker, and he pulled up 3,000 patients and gave everybody a SOFA score based on the algorithm he created, and it was all over the chart. Once I started doing chart review and phenotype verification, it was just a nightmare,” Dr. Khan said in an interview.
After struggling with the project, one of her mentors put her in touch with one of Dr. Rhee’s colleagues, and she asked the data broker to modify the eSOFA algorithm to fit her specific criteria. “It was a blessing,” she said.
Now, she has data from 5,000 patients with sepsis and sequenced DNA, and can begin comparing outcomes and genetic variants. About 20 candidate genes for sepsis outcomes have been identified to date, but she has a particular interest in PCSK9, which is an innate immune system regulator. She hopes to present results at CCC49 in 2020.
Validating mortality prediction
The researchers compared eSOFA and SOFA in a sample from 111 U.S. acute care hospitals to see if eSOFA had a comparable predictive validity for mortality. The analysis included 942,360 adults seen between 2013 and 2015. A total of 11.1% (104,903) had a presumed serious infection based on a blood culture order and at least 4 consecutive days of antibiotic use.
The analysis showed that 6.1% of those with infections had a sepsis event based on at least a 2-point increase in SOFA score from baseline (Sepsis-3 criteria), compared with 4.4% identified by at least a 1-point increase in eSOFA score. A total of 34,174 patients (3.6%) overlapped between SOFA and eSOFA, which represented good agreement (Cronbach’s alpha, 0.81). Compared with SOFA/Sepsis-3, eSOFA had a sensitivity of 60%, and a positive predictive value of 82%.
Patients identified by eSOFA were slightly more ill, with more requiring ICU admission (41% vs. 35%), and a greater frequency of in-hospital mortality (17% vs. 14%). Those patients who were identified by SOFA/Sepsis-3, but missed by eSOFA, had an overall lower mortality (6%).
There was a similar risk of mortality across deciles between SOFA- and eSOFA-identified sepsis patients. In an independent analysis of four hospitals from the Emory system, the area under the receiver operating characteristics was 0.77 for eSOFA and 0.76 for SOFA (P less than .001).
The Centers for Disease Control and Prevention and the Agency for Healthcare Research and Quality funded the study. Dr. Rhee and Dr. Khan have no relevant financial conflicts.
SOURCE: Rhee C et al. Crit Care Med. 2019;47(3):307-14.
SAN DIEGO – The new method replaces some of SOFA’s more subjective criteria with objective measures.
eSOFA relies on electronic health records to reduce reliance on administrative records, which suffer from cross-hospital variability in diagnosis and coding practices, as well as changes in these practices over time. The diagnosis of sepsis itself is also highly subjective. Instead, eSOFA determines dysfunction in six organ systems, indicated by use of vasopressors and mechanical ventilation, and the presence of abnormal laboratory values.
“The SOFA score includes measures like the Glasgow Coma Scale, which undoubtedly at the bedside is a very important clinical sign, but when trying to implement something that is objective for purposes of retrospective case counting and standardization, it can be problematic. The measures we chose [for eSOFA] are concrete, important maneuvers that were initiated by clinicians,” Chanu Rhee, MD, said in an interview.
Dr. Rhee is assistant professor of population medicine at Harvard Medical School and Brigham and Women’s Hospital, Boston. He presented the results of the study at the Critical Care Congress sponsored by the Society of Critical Care Medicine, and the work was simultaneously published online in Critical Care Medicine.
Key elements of SOFA that pose challenges for administrative data include: PaO2/FiO2, which are not routinely measured, and can be difficult to assign to arterial or venous samples; inconsistency in blood pressure and transient increases in vasopressor dose; the subjectivity of the Glasgow Coma Scale, which is also difficult to assess in sedated patients; and inconsistent urine output.
eSOFA introduced new measures for various organ functions, including cardiovascular (vasopressor initiation), pulmonary (mechanical ventilation initiation), renal (doubling of creatinine levels or a 50% or greater decrease in estimated glomerular filtration rate, compared with baseline), hepatic (bilirubin levels greater than or equal to 2.0 mg/dL and at least doubled from baseline), coagulation (platelet count less than 100 cells/mcL and at least a 50% decrease from a baseline of at least 100 cells/mcL), and neurological (lactate greater than or equal to 2.0 mmol/L).
“[eSOFA] opens a window into inter-facility comparisons that has not been possible to do. It’s really critical to ask, ‘How am I doing compared to my peer institutions?’ If you’re doing worse, you can look at the whole spectrum of things to try to drive improvements in care,” said Dr. Rhee.
The new tool isn’t just limited to quality improvement research. Shaeesta Khan, MD, assistant professor of critical care medicine at Geisinger Medical Center,Danville, Pa., has found eSOFA to be useful in her research into how genetic polymorphisms play a role in sepsis outcomes. Geisinger has a large population of patients with completed whole genome sequencing, and Dr. Khan began by trying to glean sepsis outcomes from administrative data.
“I explained SOFA scores to our data broker, and he pulled up 3,000 patients and gave everybody a SOFA score based on the algorithm he created, and it was all over the chart. Once I started doing chart review and phenotype verification, it was just a nightmare,” Dr. Khan said in an interview.
After struggling with the project, one of her mentors put her in touch with one of Dr. Rhee’s colleagues, and she asked the data broker to modify the eSOFA algorithm to fit her specific criteria. “It was a blessing,” she said.
Now, she has data from 5,000 patients with sepsis and sequenced DNA, and can begin comparing outcomes and genetic variants. About 20 candidate genes for sepsis outcomes have been identified to date, but she has a particular interest in PCSK9, which is an innate immune system regulator. She hopes to present results at CCC49 in 2020.
Validating mortality prediction
The researchers compared eSOFA and SOFA in a sample from 111 U.S. acute care hospitals to see if eSOFA had a comparable predictive validity for mortality. The analysis included 942,360 adults seen between 2013 and 2015. A total of 11.1% (104,903) had a presumed serious infection based on a blood culture order and at least 4 consecutive days of antibiotic use.
The analysis showed that 6.1% of those with infections had a sepsis event based on at least a 2-point increase in SOFA score from baseline (Sepsis-3 criteria), compared with 4.4% identified by at least a 1-point increase in eSOFA score. A total of 34,174 patients (3.6%) overlapped between SOFA and eSOFA, which represented good agreement (Cronbach’s alpha, 0.81). Compared with SOFA/Sepsis-3, eSOFA had a sensitivity of 60%, and a positive predictive value of 82%.
Patients identified by eSOFA were slightly more ill, with more requiring ICU admission (41% vs. 35%), and a greater frequency of in-hospital mortality (17% vs. 14%). Those patients who were identified by SOFA/Sepsis-3, but missed by eSOFA, had an overall lower mortality (6%).
There was a similar risk of mortality across deciles between SOFA- and eSOFA-identified sepsis patients. In an independent analysis of four hospitals from the Emory system, the area under the receiver operating characteristics was 0.77 for eSOFA and 0.76 for SOFA (P less than .001).
The Centers for Disease Control and Prevention and the Agency for Healthcare Research and Quality funded the study. Dr. Rhee and Dr. Khan have no relevant financial conflicts.
SOURCE: Rhee C et al. Crit Care Med. 2019;47(3):307-14.
SAN DIEGO – The new method replaces some of SOFA’s more subjective criteria with objective measures.
eSOFA relies on electronic health records to reduce reliance on administrative records, which suffer from cross-hospital variability in diagnosis and coding practices, as well as changes in these practices over time. The diagnosis of sepsis itself is also highly subjective. Instead, eSOFA determines dysfunction in six organ systems, indicated by use of vasopressors and mechanical ventilation, and the presence of abnormal laboratory values.
“The SOFA score includes measures like the Glasgow Coma Scale, which undoubtedly at the bedside is a very important clinical sign, but when trying to implement something that is objective for purposes of retrospective case counting and standardization, it can be problematic. The measures we chose [for eSOFA] are concrete, important maneuvers that were initiated by clinicians,” Chanu Rhee, MD, said in an interview.
Dr. Rhee is assistant professor of population medicine at Harvard Medical School and Brigham and Women’s Hospital, Boston. He presented the results of the study at the Critical Care Congress sponsored by the Society of Critical Care Medicine, and the work was simultaneously published online in Critical Care Medicine.
Key elements of SOFA that pose challenges for administrative data include: PaO2/FiO2, which are not routinely measured, and can be difficult to assign to arterial or venous samples; inconsistency in blood pressure and transient increases in vasopressor dose; the subjectivity of the Glasgow Coma Scale, which is also difficult to assess in sedated patients; and inconsistent urine output.
eSOFA introduced new measures for various organ functions, including cardiovascular (vasopressor initiation), pulmonary (mechanical ventilation initiation), renal (doubling of creatinine levels or a 50% or greater decrease in estimated glomerular filtration rate, compared with baseline), hepatic (bilirubin levels greater than or equal to 2.0 mg/dL and at least doubled from baseline), coagulation (platelet count less than 100 cells/mcL and at least a 50% decrease from a baseline of at least 100 cells/mcL), and neurological (lactate greater than or equal to 2.0 mmol/L).
“[eSOFA] opens a window into inter-facility comparisons that has not been possible to do. It’s really critical to ask, ‘How am I doing compared to my peer institutions?’ If you’re doing worse, you can look at the whole spectrum of things to try to drive improvements in care,” said Dr. Rhee.
The new tool isn’t just limited to quality improvement research. Shaeesta Khan, MD, assistant professor of critical care medicine at Geisinger Medical Center,Danville, Pa., has found eSOFA to be useful in her research into how genetic polymorphisms play a role in sepsis outcomes. Geisinger has a large population of patients with completed whole genome sequencing, and Dr. Khan began by trying to glean sepsis outcomes from administrative data.
“I explained SOFA scores to our data broker, and he pulled up 3,000 patients and gave everybody a SOFA score based on the algorithm he created, and it was all over the chart. Once I started doing chart review and phenotype verification, it was just a nightmare,” Dr. Khan said in an interview.
After struggling with the project, one of her mentors put her in touch with one of Dr. Rhee’s colleagues, and she asked the data broker to modify the eSOFA algorithm to fit her specific criteria. “It was a blessing,” she said.
Now, she has data from 5,000 patients with sepsis and sequenced DNA, and can begin comparing outcomes and genetic variants. About 20 candidate genes for sepsis outcomes have been identified to date, but she has a particular interest in PCSK9, which is an innate immune system regulator. She hopes to present results at CCC49 in 2020.
Validating mortality prediction
The researchers compared eSOFA and SOFA in a sample from 111 U.S. acute care hospitals to see if eSOFA had a comparable predictive validity for mortality. The analysis included 942,360 adults seen between 2013 and 2015. A total of 11.1% (104,903) had a presumed serious infection based on a blood culture order and at least 4 consecutive days of antibiotic use.
The analysis showed that 6.1% of those with infections had a sepsis event based on at least a 2-point increase in SOFA score from baseline (Sepsis-3 criteria), compared with 4.4% identified by at least a 1-point increase in eSOFA score. A total of 34,174 patients (3.6%) overlapped between SOFA and eSOFA, which represented good agreement (Cronbach’s alpha, 0.81). Compared with SOFA/Sepsis-3, eSOFA had a sensitivity of 60%, and a positive predictive value of 82%.
Patients identified by eSOFA were slightly more ill, with more requiring ICU admission (41% vs. 35%), and a greater frequency of in-hospital mortality (17% vs. 14%). Those patients who were identified by SOFA/Sepsis-3, but missed by eSOFA, had an overall lower mortality (6%).
There was a similar risk of mortality across deciles between SOFA- and eSOFA-identified sepsis patients. In an independent analysis of four hospitals from the Emory system, the area under the receiver operating characteristics was 0.77 for eSOFA and 0.76 for SOFA (P less than .001).
The Centers for Disease Control and Prevention and the Agency for Healthcare Research and Quality funded the study. Dr. Rhee and Dr. Khan have no relevant financial conflicts.
SOURCE: Rhee C et al. Crit Care Med. 2019;47(3):307-14.
REPORTING FROM CCC48
Hospitalists on the Hill
Advocating for HM in DC
Another Hill Day is coming – the all-day advocacy event on Capitol Hill is scheduled in conjunction with the Society of Hospital Medicine’s Annual Conference whenever it is held in Washington, DC. In 2019, Hill Day will take place on March 27, the final day of HM19.
This will be the fourth Hill Day, and the last for some time, said Ron Greeno, MD, FCCP, MHM, senior advisor for government affairs at SHM and the society’s immediate past president. For at least the next 5 years, SHM’s annual conferences won’t be held in Washington, so there will not be any opportunities to plan a Hill Day during that time. “Members may want to take advantage of this opportunity,” Dr. Greeno said. “The people who do this never forget it.”
How Hill Day works
Sign up for Hill Day and you’ll spend a day visiting legislators and their health care staffers to educate them on what hospital medicine is, what a hospitalist does, and some of the pressing issues that affect the profession, said Joshua Lenchus, DO, RPh, FACP, SFHM, chair of the SHM Public Policy Committee. “We try to leverage participants’ work and home addresses to pair them up with legislators from that area. Some hospitalists have personal or professional relationships with some of the legislators, and even if they’re not in their area, we’ll try to leverage that. And for people who have expertise in a particular topic, we try to arrange an audience with a member of Congress who may be promoting or sponsoring a bill related to that.”
Hill Day volunteers will attend an orientation to learn more about what the day will look like and what they’ll be talking about in their meetings. “We’ll only have time to cover one or two issues, and we’re in the process now of choosing the issues we want to address. We orient participants on those subjects so everybody is kind of saying the same thing,” Dr. Greeno said. “People shouldn’t be afraid of not being conversant with the issues because we do sufficient orientation that everybody gets comfortable enough to do a good job.”
Registration for Hill Day is happening online now. HM19 attendees can register at https://s1.goeshow.com/shm/annual/2019/registration_form.cfm.
“We beg people: If you sign up, show up, because we have many more people trying to participate than we can accommodate,” Dr. Greeno said. “If you change your mind, that’s fine because we have a waiting list, but please let us know because somebody else wants to take your place.”
The purpose of Hill Day
Educating legislators and their health care staff is the goal of the day, and it’s an important job. “Hospital medicine is still a relatively new field,” Dr. Lenchus said. “There are a fair number of legislators who still don’t know what a hospitalist is or what hospital medicine is. Part of our visits is always to educate them about what we do and what our impact is on the health care landscape of the country.” He added that educating Hill staff about the most pressing issues is another primary goal.
“Finally, and this is what separates us from other organizations that do legislative advocacy, we try to leave them with the idea that we’re here to help,” Dr. Lenchus said. “If there’s an issue or a particular bill that we’re asking them to sponsor or cosponsor, that’s one part of a visit. But by and large, we are trying to leave them with the sense that SHM is a resource when it comes to health care–related issues. We want to be there for legislators so that they can understand our position accurately from the outset.”
In short, Hill Day offers a rare opportunity to have direct access to the people who are voting on new legislation affecting hospitalists and affecting the implementation of existing legislation. “This is where the rubber meets the road,” Dr. Lenchus said. Each time a Hill Day is held, he noted, attendance increases. “That’s a true testament to the level of involvement and the interest that hospitalists have across the country. If you’re at all interested, you should absolutely sign up. This will be an amazing experience.”
The lasting impact
Though it’s just one day, Hill Day’s effects are significant.
“Before I started doing this work, I often thought, ‘What impact could someone have going into a legislator’s office?’ ” Dr. Greeno said. “But the answer is ‘A lot.’ The members and staff really do listen – especially if an advocate is highly educated and represent what legislators consider an important constituency, like health care providers. Health care is a hot topic, and it’s probably going to be one of the hot topics in the next election. Hospitalists have good ideas, and as a result these meetings are extremely influential; we wouldn’t do it otherwise. It is fun, but we’re not doing it for fun. We’re doing it because we know we can make a difference.”
In fact, in terms of impact on Capitol Hill, SHM punches above its weight, he added.
“We’re a relatively new society; we’re not huge. There are lots of societies that are much bigger than us and have many more resources, but people on the Hill have told us they like talking with us because they know we’re not looking at things the same way,” Dr. Greeno revealed. “We’re trying to help, and the issues that we’re addressing are not necessarily self-serving. We’re not saying, ‘You need to do this because it will make more money for our doctors.’ Instead, we’re saying, ‘You need to do this because the way it’s being done now is hurting patients. It’s hurting the health care system, and we have ideas about how to make that better.’ ”
SHM’s impressive track record has earned the society a positive reputation that will underlie the Hill Day meetings. “When we first set up the policy shop at SHM, we wanted to be seen as providers who cared about the American health care system and our patients,” Dr. Greeno said. “We have established that reputation, and that has led members on Capitol Hill to recognize us as being well intentioned and knowledgeable. So we have an outsize influence in Congress for our age and our size. When 200 hospitalists go to Capitol Hill, it’s an important thing.”
For more information about Hill Day, including details about participation, visit shmannualconference.org/hill-day/.
Advocating for HM in DC
Advocating for HM in DC
Another Hill Day is coming – the all-day advocacy event on Capitol Hill is scheduled in conjunction with the Society of Hospital Medicine’s Annual Conference whenever it is held in Washington, DC. In 2019, Hill Day will take place on March 27, the final day of HM19.
This will be the fourth Hill Day, and the last for some time, said Ron Greeno, MD, FCCP, MHM, senior advisor for government affairs at SHM and the society’s immediate past president. For at least the next 5 years, SHM’s annual conferences won’t be held in Washington, so there will not be any opportunities to plan a Hill Day during that time. “Members may want to take advantage of this opportunity,” Dr. Greeno said. “The people who do this never forget it.”
How Hill Day works
Sign up for Hill Day and you’ll spend a day visiting legislators and their health care staffers to educate them on what hospital medicine is, what a hospitalist does, and some of the pressing issues that affect the profession, said Joshua Lenchus, DO, RPh, FACP, SFHM, chair of the SHM Public Policy Committee. “We try to leverage participants’ work and home addresses to pair them up with legislators from that area. Some hospitalists have personal or professional relationships with some of the legislators, and even if they’re not in their area, we’ll try to leverage that. And for people who have expertise in a particular topic, we try to arrange an audience with a member of Congress who may be promoting or sponsoring a bill related to that.”
Hill Day volunteers will attend an orientation to learn more about what the day will look like and what they’ll be talking about in their meetings. “We’ll only have time to cover one or two issues, and we’re in the process now of choosing the issues we want to address. We orient participants on those subjects so everybody is kind of saying the same thing,” Dr. Greeno said. “People shouldn’t be afraid of not being conversant with the issues because we do sufficient orientation that everybody gets comfortable enough to do a good job.”
Registration for Hill Day is happening online now. HM19 attendees can register at https://s1.goeshow.com/shm/annual/2019/registration_form.cfm.
“We beg people: If you sign up, show up, because we have many more people trying to participate than we can accommodate,” Dr. Greeno said. “If you change your mind, that’s fine because we have a waiting list, but please let us know because somebody else wants to take your place.”
The purpose of Hill Day
Educating legislators and their health care staff is the goal of the day, and it’s an important job. “Hospital medicine is still a relatively new field,” Dr. Lenchus said. “There are a fair number of legislators who still don’t know what a hospitalist is or what hospital medicine is. Part of our visits is always to educate them about what we do and what our impact is on the health care landscape of the country.” He added that educating Hill staff about the most pressing issues is another primary goal.
“Finally, and this is what separates us from other organizations that do legislative advocacy, we try to leave them with the idea that we’re here to help,” Dr. Lenchus said. “If there’s an issue or a particular bill that we’re asking them to sponsor or cosponsor, that’s one part of a visit. But by and large, we are trying to leave them with the sense that SHM is a resource when it comes to health care–related issues. We want to be there for legislators so that they can understand our position accurately from the outset.”
In short, Hill Day offers a rare opportunity to have direct access to the people who are voting on new legislation affecting hospitalists and affecting the implementation of existing legislation. “This is where the rubber meets the road,” Dr. Lenchus said. Each time a Hill Day is held, he noted, attendance increases. “That’s a true testament to the level of involvement and the interest that hospitalists have across the country. If you’re at all interested, you should absolutely sign up. This will be an amazing experience.”
The lasting impact
Though it’s just one day, Hill Day’s effects are significant.
“Before I started doing this work, I often thought, ‘What impact could someone have going into a legislator’s office?’ ” Dr. Greeno said. “But the answer is ‘A lot.’ The members and staff really do listen – especially if an advocate is highly educated and represent what legislators consider an important constituency, like health care providers. Health care is a hot topic, and it’s probably going to be one of the hot topics in the next election. Hospitalists have good ideas, and as a result these meetings are extremely influential; we wouldn’t do it otherwise. It is fun, but we’re not doing it for fun. We’re doing it because we know we can make a difference.”
In fact, in terms of impact on Capitol Hill, SHM punches above its weight, he added.
“We’re a relatively new society; we’re not huge. There are lots of societies that are much bigger than us and have many more resources, but people on the Hill have told us they like talking with us because they know we’re not looking at things the same way,” Dr. Greeno revealed. “We’re trying to help, and the issues that we’re addressing are not necessarily self-serving. We’re not saying, ‘You need to do this because it will make more money for our doctors.’ Instead, we’re saying, ‘You need to do this because the way it’s being done now is hurting patients. It’s hurting the health care system, and we have ideas about how to make that better.’ ”
SHM’s impressive track record has earned the society a positive reputation that will underlie the Hill Day meetings. “When we first set up the policy shop at SHM, we wanted to be seen as providers who cared about the American health care system and our patients,” Dr. Greeno said. “We have established that reputation, and that has led members on Capitol Hill to recognize us as being well intentioned and knowledgeable. So we have an outsize influence in Congress for our age and our size. When 200 hospitalists go to Capitol Hill, it’s an important thing.”
For more information about Hill Day, including details about participation, visit shmannualconference.org/hill-day/.
Another Hill Day is coming – the all-day advocacy event on Capitol Hill is scheduled in conjunction with the Society of Hospital Medicine’s Annual Conference whenever it is held in Washington, DC. In 2019, Hill Day will take place on March 27, the final day of HM19.
This will be the fourth Hill Day, and the last for some time, said Ron Greeno, MD, FCCP, MHM, senior advisor for government affairs at SHM and the society’s immediate past president. For at least the next 5 years, SHM’s annual conferences won’t be held in Washington, so there will not be any opportunities to plan a Hill Day during that time. “Members may want to take advantage of this opportunity,” Dr. Greeno said. “The people who do this never forget it.”
How Hill Day works
Sign up for Hill Day and you’ll spend a day visiting legislators and their health care staffers to educate them on what hospital medicine is, what a hospitalist does, and some of the pressing issues that affect the profession, said Joshua Lenchus, DO, RPh, FACP, SFHM, chair of the SHM Public Policy Committee. “We try to leverage participants’ work and home addresses to pair them up with legislators from that area. Some hospitalists have personal or professional relationships with some of the legislators, and even if they’re not in their area, we’ll try to leverage that. And for people who have expertise in a particular topic, we try to arrange an audience with a member of Congress who may be promoting or sponsoring a bill related to that.”
Hill Day volunteers will attend an orientation to learn more about what the day will look like and what they’ll be talking about in their meetings. “We’ll only have time to cover one or two issues, and we’re in the process now of choosing the issues we want to address. We orient participants on those subjects so everybody is kind of saying the same thing,” Dr. Greeno said. “People shouldn’t be afraid of not being conversant with the issues because we do sufficient orientation that everybody gets comfortable enough to do a good job.”
Registration for Hill Day is happening online now. HM19 attendees can register at https://s1.goeshow.com/shm/annual/2019/registration_form.cfm.
“We beg people: If you sign up, show up, because we have many more people trying to participate than we can accommodate,” Dr. Greeno said. “If you change your mind, that’s fine because we have a waiting list, but please let us know because somebody else wants to take your place.”
The purpose of Hill Day
Educating legislators and their health care staff is the goal of the day, and it’s an important job. “Hospital medicine is still a relatively new field,” Dr. Lenchus said. “There are a fair number of legislators who still don’t know what a hospitalist is or what hospital medicine is. Part of our visits is always to educate them about what we do and what our impact is on the health care landscape of the country.” He added that educating Hill staff about the most pressing issues is another primary goal.
“Finally, and this is what separates us from other organizations that do legislative advocacy, we try to leave them with the idea that we’re here to help,” Dr. Lenchus said. “If there’s an issue or a particular bill that we’re asking them to sponsor or cosponsor, that’s one part of a visit. But by and large, we are trying to leave them with the sense that SHM is a resource when it comes to health care–related issues. We want to be there for legislators so that they can understand our position accurately from the outset.”
In short, Hill Day offers a rare opportunity to have direct access to the people who are voting on new legislation affecting hospitalists and affecting the implementation of existing legislation. “This is where the rubber meets the road,” Dr. Lenchus said. Each time a Hill Day is held, he noted, attendance increases. “That’s a true testament to the level of involvement and the interest that hospitalists have across the country. If you’re at all interested, you should absolutely sign up. This will be an amazing experience.”
The lasting impact
Though it’s just one day, Hill Day’s effects are significant.
“Before I started doing this work, I often thought, ‘What impact could someone have going into a legislator’s office?’ ” Dr. Greeno said. “But the answer is ‘A lot.’ The members and staff really do listen – especially if an advocate is highly educated and represent what legislators consider an important constituency, like health care providers. Health care is a hot topic, and it’s probably going to be one of the hot topics in the next election. Hospitalists have good ideas, and as a result these meetings are extremely influential; we wouldn’t do it otherwise. It is fun, but we’re not doing it for fun. We’re doing it because we know we can make a difference.”
In fact, in terms of impact on Capitol Hill, SHM punches above its weight, he added.
“We’re a relatively new society; we’re not huge. There are lots of societies that are much bigger than us and have many more resources, but people on the Hill have told us they like talking with us because they know we’re not looking at things the same way,” Dr. Greeno revealed. “We’re trying to help, and the issues that we’re addressing are not necessarily self-serving. We’re not saying, ‘You need to do this because it will make more money for our doctors.’ Instead, we’re saying, ‘You need to do this because the way it’s being done now is hurting patients. It’s hurting the health care system, and we have ideas about how to make that better.’ ”
SHM’s impressive track record has earned the society a positive reputation that will underlie the Hill Day meetings. “When we first set up the policy shop at SHM, we wanted to be seen as providers who cared about the American health care system and our patients,” Dr. Greeno said. “We have established that reputation, and that has led members on Capitol Hill to recognize us as being well intentioned and knowledgeable. So we have an outsize influence in Congress for our age and our size. When 200 hospitalists go to Capitol Hill, it’s an important thing.”
For more information about Hill Day, including details about participation, visit shmannualconference.org/hill-day/.
AAP: Treating patients during disasters raises liability risks
In a 2019 technical report, the AAP outlines common claims that can arise when treating children during disasters and how certain circumstances can force you to deviate from routine medical practices. In an accompanying policy statement by the AAP committee on medical liability and risk management, recommendations are offered for how to prepare for and prevent such legal risks.
During disasters, liability dangers can increase when circumstances “devolve into an environment of limited choices for both patients and providers,” and you have fewer treatment options available to you, according to the guidance authored by New York pediatrician Dr. Robin L. Altman and her associates.
Common claims that stem from treating patients during disasters are negligence, abandonment, and lack of informed consent. The AAP technical report offers examples about how these accusations can occur, including:
- When during a disaster, you are forced to alter treatment because of scarce medical supplies or equipment, you may later be accused of negligence if the patient’s outcome is negatively affected by the modified treatment.
- When a disaster progresses to overwhelming conditions, and you must practice in an altered health care environment that demands atypical actions, such actions may later be questioned and be accused of providing suboptimal care. Documentation of medical decision making for instance, a primary defense for one’s actions, may be compromised because of an inoperable electronic medical record. Similarly, past medical history may be unavailable, which may impact the appropriateness of care provision.
- In chaotic conditions, you may have to stop treating some patients to focus their time and resources elsewhere, which may lead to an abandonment claim, defined as unilateral termination of a physician-patient relationship – without proper patient notice – when treatment is still required. An abandonment claim also may arise when you have to make decisions in extreme conditions about which patients to transfer or evacuate first and whom to leave behind.
- When providing medical care to children during disasters, a lack of informed consent claim can arise if adequate parental permission is unattainable. This may result from families that are separated or displaced children in need of medical care.
Other claims that can arise from providing care during disasters include HIPAA breaches, licensing violations, discrimination claims, and Emergency Medical Treatment and Labor Act (EMTALA) violations, among others.
To reduce liability risks, you should strive to understand liability risks and limitations during disasters and take steps to mitigate them by crafting a disaster readiness plan, according to the AAP policy statement. The plan should include provider and staff education on improving medical care during disasters and how best to document medical decisions made in disaster-affected health care environments. Proactively identifying obstacles to care during disasters also is key. You can use the AAP division of state government affairs as a resource; it can provide current information on disaster liability in the different states.
You also should understand potential limits to your medical malpractice insurance coverage during disasters and take steps to add coverage for identified gaps, according to the AAP guidelines.
AAP recommends that you advocate for your health center to have active disaster plans that cover children’s needs and for your hospital to conduct regular drills that test pediatric capabilities. Throughout the guidelines, the AAP calls on the U.S. Department of Health and Human Services to review current state and federal liability laws, and for the agency to recommend new laws that address disaster-response liability protections for doctors. HHS also should assess the liability coverage needs of physicians during crisis times and take action to reduce inconsistencies in state malpractice protections for volunteer physicians and nonvolunteer physicians, according to AAP.
The AAP policy statement is timely because of the number of recent disasters in the United States, said Dr. Altman, lead author of the two papers.
Citing the Federal Emergency Management Agency, Dr. Altman said there were 59 major disaster declarations and 16 emergency declarations in 2017, along with more than 300 mass shooting incidents and more than 110 other man-made disasters such as fires and industrial accidents.
“Disaster conditions can result in pediatric health care providers being faced with the need to address medical conditions outside of their scope of training and experience, without access to the usual fund of patient history and background information, without the usual input or consent from parents or guardians, without the usual assistance of data such as laboratory values or physiologic monitoring, and without knowledge of how long dire conditions will last,” Dr. Altman said in an AAP News statement. “In addition, this can occur within the backdrop of one’s own physical exhaustion, concerns for the safety of one’s own family members, and the risk of loss of valuable and expensive professional property and supplies.”
The AAP guidance can help pediatricians understand the unique professional liability risks that may occur when caring for pediatric patients and families during a disaster, she said.
“It is the hope that this will raise awareness, improve preparedness, and reduce potential deficiencies in professional liability protections for health care providers trying to do their best to care for patients during these infrequent, yet debilitating, events,” Dr. Altman said in the statement.
There was no external funding, and the authors indicated they had no relevant financial disclosures.
SOURCES: Pediatrics. 2019. doi: 10.1542/peds.2018-3892; Pediatrics. 2019. doi: 10.1542/peds.2018-3893.
In a 2019 technical report, the AAP outlines common claims that can arise when treating children during disasters and how certain circumstances can force you to deviate from routine medical practices. In an accompanying policy statement by the AAP committee on medical liability and risk management, recommendations are offered for how to prepare for and prevent such legal risks.
During disasters, liability dangers can increase when circumstances “devolve into an environment of limited choices for both patients and providers,” and you have fewer treatment options available to you, according to the guidance authored by New York pediatrician Dr. Robin L. Altman and her associates.
Common claims that stem from treating patients during disasters are negligence, abandonment, and lack of informed consent. The AAP technical report offers examples about how these accusations can occur, including:
- When during a disaster, you are forced to alter treatment because of scarce medical supplies or equipment, you may later be accused of negligence if the patient’s outcome is negatively affected by the modified treatment.
- When a disaster progresses to overwhelming conditions, and you must practice in an altered health care environment that demands atypical actions, such actions may later be questioned and be accused of providing suboptimal care. Documentation of medical decision making for instance, a primary defense for one’s actions, may be compromised because of an inoperable electronic medical record. Similarly, past medical history may be unavailable, which may impact the appropriateness of care provision.
- In chaotic conditions, you may have to stop treating some patients to focus their time and resources elsewhere, which may lead to an abandonment claim, defined as unilateral termination of a physician-patient relationship – without proper patient notice – when treatment is still required. An abandonment claim also may arise when you have to make decisions in extreme conditions about which patients to transfer or evacuate first and whom to leave behind.
- When providing medical care to children during disasters, a lack of informed consent claim can arise if adequate parental permission is unattainable. This may result from families that are separated or displaced children in need of medical care.
Other claims that can arise from providing care during disasters include HIPAA breaches, licensing violations, discrimination claims, and Emergency Medical Treatment and Labor Act (EMTALA) violations, among others.
To reduce liability risks, you should strive to understand liability risks and limitations during disasters and take steps to mitigate them by crafting a disaster readiness plan, according to the AAP policy statement. The plan should include provider and staff education on improving medical care during disasters and how best to document medical decisions made in disaster-affected health care environments. Proactively identifying obstacles to care during disasters also is key. You can use the AAP division of state government affairs as a resource; it can provide current information on disaster liability in the different states.
You also should understand potential limits to your medical malpractice insurance coverage during disasters and take steps to add coverage for identified gaps, according to the AAP guidelines.
AAP recommends that you advocate for your health center to have active disaster plans that cover children’s needs and for your hospital to conduct regular drills that test pediatric capabilities. Throughout the guidelines, the AAP calls on the U.S. Department of Health and Human Services to review current state and federal liability laws, and for the agency to recommend new laws that address disaster-response liability protections for doctors. HHS also should assess the liability coverage needs of physicians during crisis times and take action to reduce inconsistencies in state malpractice protections for volunteer physicians and nonvolunteer physicians, according to AAP.
The AAP policy statement is timely because of the number of recent disasters in the United States, said Dr. Altman, lead author of the two papers.
Citing the Federal Emergency Management Agency, Dr. Altman said there were 59 major disaster declarations and 16 emergency declarations in 2017, along with more than 300 mass shooting incidents and more than 110 other man-made disasters such as fires and industrial accidents.
“Disaster conditions can result in pediatric health care providers being faced with the need to address medical conditions outside of their scope of training and experience, without access to the usual fund of patient history and background information, without the usual input or consent from parents or guardians, without the usual assistance of data such as laboratory values or physiologic monitoring, and without knowledge of how long dire conditions will last,” Dr. Altman said in an AAP News statement. “In addition, this can occur within the backdrop of one’s own physical exhaustion, concerns for the safety of one’s own family members, and the risk of loss of valuable and expensive professional property and supplies.”
The AAP guidance can help pediatricians understand the unique professional liability risks that may occur when caring for pediatric patients and families during a disaster, she said.
“It is the hope that this will raise awareness, improve preparedness, and reduce potential deficiencies in professional liability protections for health care providers trying to do their best to care for patients during these infrequent, yet debilitating, events,” Dr. Altman said in the statement.
There was no external funding, and the authors indicated they had no relevant financial disclosures.
SOURCES: Pediatrics. 2019. doi: 10.1542/peds.2018-3892; Pediatrics. 2019. doi: 10.1542/peds.2018-3893.
In a 2019 technical report, the AAP outlines common claims that can arise when treating children during disasters and how certain circumstances can force you to deviate from routine medical practices. In an accompanying policy statement by the AAP committee on medical liability and risk management, recommendations are offered for how to prepare for and prevent such legal risks.
During disasters, liability dangers can increase when circumstances “devolve into an environment of limited choices for both patients and providers,” and you have fewer treatment options available to you, according to the guidance authored by New York pediatrician Dr. Robin L. Altman and her associates.
Common claims that stem from treating patients during disasters are negligence, abandonment, and lack of informed consent. The AAP technical report offers examples about how these accusations can occur, including:
- When during a disaster, you are forced to alter treatment because of scarce medical supplies or equipment, you may later be accused of negligence if the patient’s outcome is negatively affected by the modified treatment.
- When a disaster progresses to overwhelming conditions, and you must practice in an altered health care environment that demands atypical actions, such actions may later be questioned and be accused of providing suboptimal care. Documentation of medical decision making for instance, a primary defense for one’s actions, may be compromised because of an inoperable electronic medical record. Similarly, past medical history may be unavailable, which may impact the appropriateness of care provision.
- In chaotic conditions, you may have to stop treating some patients to focus their time and resources elsewhere, which may lead to an abandonment claim, defined as unilateral termination of a physician-patient relationship – without proper patient notice – when treatment is still required. An abandonment claim also may arise when you have to make decisions in extreme conditions about which patients to transfer or evacuate first and whom to leave behind.
- When providing medical care to children during disasters, a lack of informed consent claim can arise if adequate parental permission is unattainable. This may result from families that are separated or displaced children in need of medical care.
Other claims that can arise from providing care during disasters include HIPAA breaches, licensing violations, discrimination claims, and Emergency Medical Treatment and Labor Act (EMTALA) violations, among others.
To reduce liability risks, you should strive to understand liability risks and limitations during disasters and take steps to mitigate them by crafting a disaster readiness plan, according to the AAP policy statement. The plan should include provider and staff education on improving medical care during disasters and how best to document medical decisions made in disaster-affected health care environments. Proactively identifying obstacles to care during disasters also is key. You can use the AAP division of state government affairs as a resource; it can provide current information on disaster liability in the different states.
You also should understand potential limits to your medical malpractice insurance coverage during disasters and take steps to add coverage for identified gaps, according to the AAP guidelines.
AAP recommends that you advocate for your health center to have active disaster plans that cover children’s needs and for your hospital to conduct regular drills that test pediatric capabilities. Throughout the guidelines, the AAP calls on the U.S. Department of Health and Human Services to review current state and federal liability laws, and for the agency to recommend new laws that address disaster-response liability protections for doctors. HHS also should assess the liability coverage needs of physicians during crisis times and take action to reduce inconsistencies in state malpractice protections for volunteer physicians and nonvolunteer physicians, according to AAP.
The AAP policy statement is timely because of the number of recent disasters in the United States, said Dr. Altman, lead author of the two papers.
Citing the Federal Emergency Management Agency, Dr. Altman said there were 59 major disaster declarations and 16 emergency declarations in 2017, along with more than 300 mass shooting incidents and more than 110 other man-made disasters such as fires and industrial accidents.
“Disaster conditions can result in pediatric health care providers being faced with the need to address medical conditions outside of their scope of training and experience, without access to the usual fund of patient history and background information, without the usual input or consent from parents or guardians, without the usual assistance of data such as laboratory values or physiologic monitoring, and without knowledge of how long dire conditions will last,” Dr. Altman said in an AAP News statement. “In addition, this can occur within the backdrop of one’s own physical exhaustion, concerns for the safety of one’s own family members, and the risk of loss of valuable and expensive professional property and supplies.”
The AAP guidance can help pediatricians understand the unique professional liability risks that may occur when caring for pediatric patients and families during a disaster, she said.
“It is the hope that this will raise awareness, improve preparedness, and reduce potential deficiencies in professional liability protections for health care providers trying to do their best to care for patients during these infrequent, yet debilitating, events,” Dr. Altman said in the statement.
There was no external funding, and the authors indicated they had no relevant financial disclosures.
SOURCES: Pediatrics. 2019. doi: 10.1542/peds.2018-3892; Pediatrics. 2019. doi: 10.1542/peds.2018-3893.
Second extubation attempts should be judged on their own merits
SAN DIEGO – When attempting a second extubation, improvements in weaning parameters, compared with the first extubation attempt, do not predict success. Instead, the best predictors were the values of the parameters immediately before the second attempt.
“We hypothesized that the change in parameter values was more important than the actual values right before we tried to re-extubate, and that didn’t turn out to be the case. Because it was a smaller study, we can’t say [change in values] is not useful at all, but we didn’t find a strong association. We showed that the magnitude of the effect with the number measured right before the re-extubation is probably your best bet, but you should obviously evaluate the whole clinical scenario,” commented senior author Michael David Maile, MD, assistant professor of anesthesiology at the University of Michigan, Ann Arbor.
The study was presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine by Suraj Trivedi, MD, who is currently an anesthesiology fellow at Stanford (Calif.) Medicine.
Factors such as rapid shallow breathing index (RSBI), negative inspiratory force (NIF), vital capacity (VC), and partial pressure of arterial carbon dioxide (PaCO2) have been shown to predict success or failure of an initial extubation attempt.
There is currently little available guidance on how to proceed when a first extubation attempt fails. The researchers had anticipated that RSBI, NIF, VC, and PaCO2 levels matching the first attempt would be associated with success the second time around.
But their retrospective study of adult patients at the University of Michigan critical care units found that only the change in RSBI values predicted success on a univariate analysis, and that association became statistically insignificant once they corrected for baseline RSBI previous to the re-extubation attempt.
“I think the biggest take-home message is that we have to figure out each attempt to extubate on its own merits. If you’re trying to extubate a patient in the ICU who has potentially been intubated and extubated multiple times, the clinical gut feeling is always that [the patient has] to be better off than the previous attempt. What we are pointing out is that it really doesn’t matter. If the parameters are all within the overall guidelines, it’s still okay to extubate, even if the absolute change in the variables is not better [than the previous attempt],” Dr. Trivedi said in an interview.
“People put a lot of emphasis on the improvement from the first to the second attempt, and this should temper that enthusiasm to put a lot of weight on the change. But I don’t think our data support that the change means nothing,” added Dr. Maile.
The study included 525 patients (42% female). Comorbidities were common: 72% had cardiac arrhythmias, 58% had hypertension, 33% had renal failure, 39% had a pulmonary disorder, and 25% had liver disease.
Univariate analyses showed associations between values of parameters immediately before the second extubation attempt and success in the second extubation attempt, including RSBI (re-extubation success, mean 53.1 vs failure, mean 68.8; P =.0002) and NIF (success, mean –41.2 vs. failure, mean –38.4; P =.036), and VC (success, mean 1009.8 vs. failure, mean 906.8; P =.017).
When the researchers examined changes in parameters between the first and second attempt, only a change in RSBI predicted success (success, value change of 7.1 vs. failure, value change of 0.05; P less than .031). But when they corrected for the RSBI value immediately before the second attempt, the difference was not statistically significant (P = .892).
The study was not funded. Dr. Maile and Dr. Trivedi have no relevant financial disclosures.
SOURCE: Trivedi S et al. CCC48 2019, Abstract 27.
SAN DIEGO – When attempting a second extubation, improvements in weaning parameters, compared with the first extubation attempt, do not predict success. Instead, the best predictors were the values of the parameters immediately before the second attempt.
“We hypothesized that the change in parameter values was more important than the actual values right before we tried to re-extubate, and that didn’t turn out to be the case. Because it was a smaller study, we can’t say [change in values] is not useful at all, but we didn’t find a strong association. We showed that the magnitude of the effect with the number measured right before the re-extubation is probably your best bet, but you should obviously evaluate the whole clinical scenario,” commented senior author Michael David Maile, MD, assistant professor of anesthesiology at the University of Michigan, Ann Arbor.
The study was presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine by Suraj Trivedi, MD, who is currently an anesthesiology fellow at Stanford (Calif.) Medicine.
Factors such as rapid shallow breathing index (RSBI), negative inspiratory force (NIF), vital capacity (VC), and partial pressure of arterial carbon dioxide (PaCO2) have been shown to predict success or failure of an initial extubation attempt.
There is currently little available guidance on how to proceed when a first extubation attempt fails. The researchers had anticipated that RSBI, NIF, VC, and PaCO2 levels matching the first attempt would be associated with success the second time around.
But their retrospective study of adult patients at the University of Michigan critical care units found that only the change in RSBI values predicted success on a univariate analysis, and that association became statistically insignificant once they corrected for baseline RSBI previous to the re-extubation attempt.
“I think the biggest take-home message is that we have to figure out each attempt to extubate on its own merits. If you’re trying to extubate a patient in the ICU who has potentially been intubated and extubated multiple times, the clinical gut feeling is always that [the patient has] to be better off than the previous attempt. What we are pointing out is that it really doesn’t matter. If the parameters are all within the overall guidelines, it’s still okay to extubate, even if the absolute change in the variables is not better [than the previous attempt],” Dr. Trivedi said in an interview.
“People put a lot of emphasis on the improvement from the first to the second attempt, and this should temper that enthusiasm to put a lot of weight on the change. But I don’t think our data support that the change means nothing,” added Dr. Maile.
The study included 525 patients (42% female). Comorbidities were common: 72% had cardiac arrhythmias, 58% had hypertension, 33% had renal failure, 39% had a pulmonary disorder, and 25% had liver disease.
Univariate analyses showed associations between values of parameters immediately before the second extubation attempt and success in the second extubation attempt, including RSBI (re-extubation success, mean 53.1 vs failure, mean 68.8; P =.0002) and NIF (success, mean –41.2 vs. failure, mean –38.4; P =.036), and VC (success, mean 1009.8 vs. failure, mean 906.8; P =.017).
When the researchers examined changes in parameters between the first and second attempt, only a change in RSBI predicted success (success, value change of 7.1 vs. failure, value change of 0.05; P less than .031). But when they corrected for the RSBI value immediately before the second attempt, the difference was not statistically significant (P = .892).
The study was not funded. Dr. Maile and Dr. Trivedi have no relevant financial disclosures.
SOURCE: Trivedi S et al. CCC48 2019, Abstract 27.
SAN DIEGO – When attempting a second extubation, improvements in weaning parameters, compared with the first extubation attempt, do not predict success. Instead, the best predictors were the values of the parameters immediately before the second attempt.
“We hypothesized that the change in parameter values was more important than the actual values right before we tried to re-extubate, and that didn’t turn out to be the case. Because it was a smaller study, we can’t say [change in values] is not useful at all, but we didn’t find a strong association. We showed that the magnitude of the effect with the number measured right before the re-extubation is probably your best bet, but you should obviously evaluate the whole clinical scenario,” commented senior author Michael David Maile, MD, assistant professor of anesthesiology at the University of Michigan, Ann Arbor.
The study was presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine by Suraj Trivedi, MD, who is currently an anesthesiology fellow at Stanford (Calif.) Medicine.
Factors such as rapid shallow breathing index (RSBI), negative inspiratory force (NIF), vital capacity (VC), and partial pressure of arterial carbon dioxide (PaCO2) have been shown to predict success or failure of an initial extubation attempt.
There is currently little available guidance on how to proceed when a first extubation attempt fails. The researchers had anticipated that RSBI, NIF, VC, and PaCO2 levels matching the first attempt would be associated with success the second time around.
But their retrospective study of adult patients at the University of Michigan critical care units found that only the change in RSBI values predicted success on a univariate analysis, and that association became statistically insignificant once they corrected for baseline RSBI previous to the re-extubation attempt.
“I think the biggest take-home message is that we have to figure out each attempt to extubate on its own merits. If you’re trying to extubate a patient in the ICU who has potentially been intubated and extubated multiple times, the clinical gut feeling is always that [the patient has] to be better off than the previous attempt. What we are pointing out is that it really doesn’t matter. If the parameters are all within the overall guidelines, it’s still okay to extubate, even if the absolute change in the variables is not better [than the previous attempt],” Dr. Trivedi said in an interview.
“People put a lot of emphasis on the improvement from the first to the second attempt, and this should temper that enthusiasm to put a lot of weight on the change. But I don’t think our data support that the change means nothing,” added Dr. Maile.
The study included 525 patients (42% female). Comorbidities were common: 72% had cardiac arrhythmias, 58% had hypertension, 33% had renal failure, 39% had a pulmonary disorder, and 25% had liver disease.
Univariate analyses showed associations between values of parameters immediately before the second extubation attempt and success in the second extubation attempt, including RSBI (re-extubation success, mean 53.1 vs failure, mean 68.8; P =.0002) and NIF (success, mean –41.2 vs. failure, mean –38.4; P =.036), and VC (success, mean 1009.8 vs. failure, mean 906.8; P =.017).
When the researchers examined changes in parameters between the first and second attempt, only a change in RSBI predicted success (success, value change of 7.1 vs. failure, value change of 0.05; P less than .031). But when they corrected for the RSBI value immediately before the second attempt, the difference was not statistically significant (P = .892).
The study was not funded. Dr. Maile and Dr. Trivedi have no relevant financial disclosures.
SOURCE: Trivedi S et al. CCC48 2019, Abstract 27.
REPORTING FROM CCC48
Key clinical point: Patient readiness for a second extubation should be judged by current parameters alone.
Major finding: The change in parameter values between first and second extubation attempts was not predictive of success.
Study details: A retrospective analysis of 525 patients.
Disclosures: The study was not funded. Dr. Maile and Dr. Trivedi have no relevant financial disclosures.
Source: Trivedi S et al. CCC48 2019, Abstract 27.
Malpractice suits are less frequent – but more costly
Lawsuits against physicians declined across virtually all specialties by more than a quarter over a 10-year span, but the cost to manage legal challenges went up, a recent analysis finds.
From 2007 to 2016, the rate of claims dropped by 27% per 100 doctors from 5.1 to 3.7, according to a review of 124,000 cases by CRICO Strategies, a division of CRICO, the medical liability insurance provider for the Harvard medical community. CRICO’s database of claims contains about 30% of legal cases filed against health providers across the U.S.
For internists, the rate of lawsuits decreased by 35% between 2007 and 2016, according to CRICO data provided to MDedge News. Ob.gyns. saw a 44% drop in claims over the 10-year period, and surgeons experienced a 23% rate decrease. The analysis did not break down the rate of claims by other single subspecialists. Claims decreased by a combined 29% for cardiologists, dermatologists, endocrinologists, family physicians, gastroenterologists, hematologists/oncologists, hospitalists, infectious disease specialists, internists, nephrologists, neurologists, pulmonologists, and rheumatologists/immunologists, according to the report published in February 2019 on CRICO’s website.
The findings are consistent with prior research on claim trends, said Seth Seabury, PhD, a medical liability researcher and director of the Keck-Schaeffer Initiative for Population Health Policy at the University of Southern California, Los Angeles.
“Malpractice claim frequency has been falling pretty steadily for a while now, reflecting a number of factors including the widespread adoption of tort reform and other measures to shield physicians from malpractice risk,” Dr. Seabury said in an interview. “Interestingly, the decline seems greatest in the claims with lower potential stakes, as you see average indemnity holding flat or rising. Some of this likely reflects the unwillingness of attorneys to take cases with lower potential payouts, because of the high cost of litigating a malpractice case.”
While frequency went down, the cost to manage a legal claim went up, according to CRICO data. The price of defending a malpractice lawsuit rose an average of 3.5% annually over the 10-year period from $36,000 to $46,000. For cases that ended with no payment (indemnity) to plaintiffs, the cost to manage a case rose an average of 5% annually.
The upward trends in case management expenses are striking, particularly since the time to resolve cases has decreased, said Michelle Mello, PhD, a health research and policy professor at Stanford (Calif.) University. From 2007 to 2016, the average time to resolve a case dropped from 29 to 27 months, the CRICO report found.
“CRICO nods to disclosure and apology approaches as perhaps underlying the more encouraging trend in time to resolution, but it was surprising to me that such approaches have not translated into lower defense costs,” Dr. Mello said in an interview. “In particular, a lot is still being spent to manage cases that never result in a payment to the patient. My hope was that, as hospitals got better at communicating with patients about adverse events, including the fact that about three-quarters of them are not due to substandard care, there would be fewer claims involving such events and also less money spent dealing with such claims when they do arise.”
For cases that do end in payment, high payouts are on the rise. Cases that ended in payments of $1 million or more increased 4% over the 10-year time frame, while payments of $3 million to $11 million increased 7% annually, according to the CRICO report. Cases that ended in payment lower than $1 million dropped over the 10-year span.
The reasons behind increasing plaintiff payouts is uncertain, Dr. Seabury said.
“It’s hard to say exactly why high payouts are on the rise, as payout levels reflect a number of factors – [such as] economic damages, clinical severity, pain and suffering – that can be difficult to disentangle,” he said. “But it is probably concerning for doctors in the sense that, while claims are becoming less likely, when they do happen, it could be more catastrophic in the sense of having large damages that exceed the policy limit.”
Lawsuits against physicians declined across virtually all specialties by more than a quarter over a 10-year span, but the cost to manage legal challenges went up, a recent analysis finds.
From 2007 to 2016, the rate of claims dropped by 27% per 100 doctors from 5.1 to 3.7, according to a review of 124,000 cases by CRICO Strategies, a division of CRICO, the medical liability insurance provider for the Harvard medical community. CRICO’s database of claims contains about 30% of legal cases filed against health providers across the U.S.
For internists, the rate of lawsuits decreased by 35% between 2007 and 2016, according to CRICO data provided to MDedge News. Ob.gyns. saw a 44% drop in claims over the 10-year period, and surgeons experienced a 23% rate decrease. The analysis did not break down the rate of claims by other single subspecialists. Claims decreased by a combined 29% for cardiologists, dermatologists, endocrinologists, family physicians, gastroenterologists, hematologists/oncologists, hospitalists, infectious disease specialists, internists, nephrologists, neurologists, pulmonologists, and rheumatologists/immunologists, according to the report published in February 2019 on CRICO’s website.
The findings are consistent with prior research on claim trends, said Seth Seabury, PhD, a medical liability researcher and director of the Keck-Schaeffer Initiative for Population Health Policy at the University of Southern California, Los Angeles.
“Malpractice claim frequency has been falling pretty steadily for a while now, reflecting a number of factors including the widespread adoption of tort reform and other measures to shield physicians from malpractice risk,” Dr. Seabury said in an interview. “Interestingly, the decline seems greatest in the claims with lower potential stakes, as you see average indemnity holding flat or rising. Some of this likely reflects the unwillingness of attorneys to take cases with lower potential payouts, because of the high cost of litigating a malpractice case.”
While frequency went down, the cost to manage a legal claim went up, according to CRICO data. The price of defending a malpractice lawsuit rose an average of 3.5% annually over the 10-year period from $36,000 to $46,000. For cases that ended with no payment (indemnity) to plaintiffs, the cost to manage a case rose an average of 5% annually.
The upward trends in case management expenses are striking, particularly since the time to resolve cases has decreased, said Michelle Mello, PhD, a health research and policy professor at Stanford (Calif.) University. From 2007 to 2016, the average time to resolve a case dropped from 29 to 27 months, the CRICO report found.
“CRICO nods to disclosure and apology approaches as perhaps underlying the more encouraging trend in time to resolution, but it was surprising to me that such approaches have not translated into lower defense costs,” Dr. Mello said in an interview. “In particular, a lot is still being spent to manage cases that never result in a payment to the patient. My hope was that, as hospitals got better at communicating with patients about adverse events, including the fact that about three-quarters of them are not due to substandard care, there would be fewer claims involving such events and also less money spent dealing with such claims when they do arise.”
For cases that do end in payment, high payouts are on the rise. Cases that ended in payments of $1 million or more increased 4% over the 10-year time frame, while payments of $3 million to $11 million increased 7% annually, according to the CRICO report. Cases that ended in payment lower than $1 million dropped over the 10-year span.
The reasons behind increasing plaintiff payouts is uncertain, Dr. Seabury said.
“It’s hard to say exactly why high payouts are on the rise, as payout levels reflect a number of factors – [such as] economic damages, clinical severity, pain and suffering – that can be difficult to disentangle,” he said. “But it is probably concerning for doctors in the sense that, while claims are becoming less likely, when they do happen, it could be more catastrophic in the sense of having large damages that exceed the policy limit.”
Lawsuits against physicians declined across virtually all specialties by more than a quarter over a 10-year span, but the cost to manage legal challenges went up, a recent analysis finds.
From 2007 to 2016, the rate of claims dropped by 27% per 100 doctors from 5.1 to 3.7, according to a review of 124,000 cases by CRICO Strategies, a division of CRICO, the medical liability insurance provider for the Harvard medical community. CRICO’s database of claims contains about 30% of legal cases filed against health providers across the U.S.
For internists, the rate of lawsuits decreased by 35% between 2007 and 2016, according to CRICO data provided to MDedge News. Ob.gyns. saw a 44% drop in claims over the 10-year period, and surgeons experienced a 23% rate decrease. The analysis did not break down the rate of claims by other single subspecialists. Claims decreased by a combined 29% for cardiologists, dermatologists, endocrinologists, family physicians, gastroenterologists, hematologists/oncologists, hospitalists, infectious disease specialists, internists, nephrologists, neurologists, pulmonologists, and rheumatologists/immunologists, according to the report published in February 2019 on CRICO’s website.
The findings are consistent with prior research on claim trends, said Seth Seabury, PhD, a medical liability researcher and director of the Keck-Schaeffer Initiative for Population Health Policy at the University of Southern California, Los Angeles.
“Malpractice claim frequency has been falling pretty steadily for a while now, reflecting a number of factors including the widespread adoption of tort reform and other measures to shield physicians from malpractice risk,” Dr. Seabury said in an interview. “Interestingly, the decline seems greatest in the claims with lower potential stakes, as you see average indemnity holding flat or rising. Some of this likely reflects the unwillingness of attorneys to take cases with lower potential payouts, because of the high cost of litigating a malpractice case.”
While frequency went down, the cost to manage a legal claim went up, according to CRICO data. The price of defending a malpractice lawsuit rose an average of 3.5% annually over the 10-year period from $36,000 to $46,000. For cases that ended with no payment (indemnity) to plaintiffs, the cost to manage a case rose an average of 5% annually.
The upward trends in case management expenses are striking, particularly since the time to resolve cases has decreased, said Michelle Mello, PhD, a health research and policy professor at Stanford (Calif.) University. From 2007 to 2016, the average time to resolve a case dropped from 29 to 27 months, the CRICO report found.
“CRICO nods to disclosure and apology approaches as perhaps underlying the more encouraging trend in time to resolution, but it was surprising to me that such approaches have not translated into lower defense costs,” Dr. Mello said in an interview. “In particular, a lot is still being spent to manage cases that never result in a payment to the patient. My hope was that, as hospitals got better at communicating with patients about adverse events, including the fact that about three-quarters of them are not due to substandard care, there would be fewer claims involving such events and also less money spent dealing with such claims when they do arise.”
For cases that do end in payment, high payouts are on the rise. Cases that ended in payments of $1 million or more increased 4% over the 10-year time frame, while payments of $3 million to $11 million increased 7% annually, according to the CRICO report. Cases that ended in payment lower than $1 million dropped over the 10-year span.
The reasons behind increasing plaintiff payouts is uncertain, Dr. Seabury said.
“It’s hard to say exactly why high payouts are on the rise, as payout levels reflect a number of factors – [such as] economic damages, clinical severity, pain and suffering – that can be difficult to disentangle,” he said. “But it is probably concerning for doctors in the sense that, while claims are becoming less likely, when they do happen, it could be more catastrophic in the sense of having large damages that exceed the policy limit.”
Advancing coherence: Your “meta-leadership” objective
Learn to balance organizational priorities
For the many people who expect you to lead, your role – among others – is to create coherence. That coherence characterizes the logic and consistency of what you do in your organization. It assembles the individual work of many different people into a whole that functions well. Coherence in your workplace helps people make sense of what they are doing and why it matters.
Our very rational brain craves coherence. We assemble facts, emotions, ambitions and our life stories into narratives that define who we are, what we are doing, and why it is important. An effective organizational “metaleader” encourages that process for followers. It helps people make sense of the work side of their life.
When coherence is absent, the workplace is riddled with contradictions, unpredictability, and dissonance. People are expected to accomplish tasks for which the time, tools, and talent are missing. There is a perplexed swirl of high activity and low productivity. Expectations for high quality of care and patient satisfaction are contradicted by an overbearing workload, reams of paper work, and the low morale that leaves the work force lethargic. “What we are doing here and how we are doing it doesn’t make sense,” exemplifies the exasperation of working amid incoherence. The department does not drive together toward success-oriented performance. Instead, different people, priorities, and opportunities will be positioned in conflict with one another. For people in your group and those surrounding it, morale and motivation suffer. There is the risk that people will descend into malaise.
Creating coherence is a complex metaleadership process. A large health care center is a cacophony of priorities, of which advancing quality of care is but one. There are other objectives, some contradictory, that also absorb time and attention: achievement of financial benchmarks, promotion of professional careers, and the individual hopes and desires of patients. Systematically aligning those many priorities and objectives is a process of both design and leadership.
The metaleadership model is a strategy for building coherence amid the complexity of health care operations. For those unfamiliar with metaleadership: The prefix “meta-” refers to a wider perspective on what is happening, the people involved, and the overall combination of objectives. The three dimensions of practice are: 1) the Person of the metaleader – your own priorities, values and emotional intelligence; 2) the Situation – what is happening and what ought to be done about it; and 3) Connectivity of Effort, which leads down to subordinates, up to bosses, across to other internal departments, and beyond to external organizations and professionals.
In building connectivity of effort, the metaleader links the many sides of the work being accomplished. The intent is to balance – purposefully – different organizational objectives into a combined whole that gets the jobs done. Furthermore, that coherence links and adapts what people are doing to the situation at hand. And in essence, the person of the leader cannot lead broader coherence if not coherent in her or his own thinking, attitudes, and behaviors, so achievement of personal and professional clarity of purpose is important.
The question for you: How do you as a hospitalist leader create coherence in what you are leading given the changing priorities, actions, and turbulence of current health policy and the market?
The answers lie in the communication you foster and clarify. That communication demands clarity and diplomacy. It is multidirectional such that messages and information in your leading down, up, across, and beyond complement and inform one another.
An illustration of one pathway: You learn from senior management about cuts in the budget. You reflect with them on the choices implicit in those cuts. Perhaps there are better ways to reduce expenditures and increase revenues that offer an alternative pathway to a balanced budget? When communicating with your subordinates, you open conversation on ways to enhance efficiencies and assure quality. You explore avenues to partner with other departments within your institution on how you can link and leverage services and capabilities. And you consider your marketplace and the actions you can take to reinforce your department and assure the volume necessary to achieve budget and quality objectives. And through it all, you monitor the situation. What are the effects of the budget adjustments, and what can be done to sustain the coherence of the work and output of the department? It is a leadership process of constant situational awareness, personal commitment, and connectivity of effort.
An illustration of another pathway: Resist the change and argue forcefully for holding onto the current budget and workforce. Though you do not possess the authority to control larger budgetary decisions, you employ influence well beyond your authority. You recruit allies to your cause, advocates who believe in the purpose you are promoting. You build an alternative coherence, mindful of fostering friendship and minimizing alienation. You are recognized for the passion of your professional commitment and your capacity to uphold quality care and organizational balance.
Two very different pathways to crafting coherence. Leaders of each perceive their actions to advance priority coherence objectives. Apply this question to your own complex problem solving.
Metaleaders forge coherence through the narratives they build and the consistency with those themes and priorities. When everyone on your staff, from physicians to housekeeping personnel, can say “I am here to help save lives,” you know that your followers are on board with a shared mission. They recognize that their efforts contribute to that overall mission. Each person has a role to play, and her or his work fits with the efforts of others, and the bottom line accomplishments of the department.
The coherence you forge assists your followers to make sense of what they are doing and how it fits what others are doing. Work is fulfilling. Beyond that, in a turbulent health care system, you anticipate both problems and opportunities with strategies to meet them. You stay ahead of the game to ensure that people within and outside the department are aligned to maximize opportunities for success.
This is particularly important for the hospitalist. Your job is to fashion coherence on many levels. First, coherent patient care for the patient. Second, coherent interactions among professionals. Finally, organizational coherence, so one piece of the puzzle fits with others. And, when there is a need to recalculate, you adapt and develop solutions that fit the people and situation at hand.
Dr. Marcus is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is Director of the Program for Health Care Negotiation and Conflict Resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
Learn to balance organizational priorities
Learn to balance organizational priorities
For the many people who expect you to lead, your role – among others – is to create coherence. That coherence characterizes the logic and consistency of what you do in your organization. It assembles the individual work of many different people into a whole that functions well. Coherence in your workplace helps people make sense of what they are doing and why it matters.
Our very rational brain craves coherence. We assemble facts, emotions, ambitions and our life stories into narratives that define who we are, what we are doing, and why it is important. An effective organizational “metaleader” encourages that process for followers. It helps people make sense of the work side of their life.
When coherence is absent, the workplace is riddled with contradictions, unpredictability, and dissonance. People are expected to accomplish tasks for which the time, tools, and talent are missing. There is a perplexed swirl of high activity and low productivity. Expectations for high quality of care and patient satisfaction are contradicted by an overbearing workload, reams of paper work, and the low morale that leaves the work force lethargic. “What we are doing here and how we are doing it doesn’t make sense,” exemplifies the exasperation of working amid incoherence. The department does not drive together toward success-oriented performance. Instead, different people, priorities, and opportunities will be positioned in conflict with one another. For people in your group and those surrounding it, morale and motivation suffer. There is the risk that people will descend into malaise.
Creating coherence is a complex metaleadership process. A large health care center is a cacophony of priorities, of which advancing quality of care is but one. There are other objectives, some contradictory, that also absorb time and attention: achievement of financial benchmarks, promotion of professional careers, and the individual hopes and desires of patients. Systematically aligning those many priorities and objectives is a process of both design and leadership.
The metaleadership model is a strategy for building coherence amid the complexity of health care operations. For those unfamiliar with metaleadership: The prefix “meta-” refers to a wider perspective on what is happening, the people involved, and the overall combination of objectives. The three dimensions of practice are: 1) the Person of the metaleader – your own priorities, values and emotional intelligence; 2) the Situation – what is happening and what ought to be done about it; and 3) Connectivity of Effort, which leads down to subordinates, up to bosses, across to other internal departments, and beyond to external organizations and professionals.
In building connectivity of effort, the metaleader links the many sides of the work being accomplished. The intent is to balance – purposefully – different organizational objectives into a combined whole that gets the jobs done. Furthermore, that coherence links and adapts what people are doing to the situation at hand. And in essence, the person of the leader cannot lead broader coherence if not coherent in her or his own thinking, attitudes, and behaviors, so achievement of personal and professional clarity of purpose is important.
The question for you: How do you as a hospitalist leader create coherence in what you are leading given the changing priorities, actions, and turbulence of current health policy and the market?
The answers lie in the communication you foster and clarify. That communication demands clarity and diplomacy. It is multidirectional such that messages and information in your leading down, up, across, and beyond complement and inform one another.
An illustration of one pathway: You learn from senior management about cuts in the budget. You reflect with them on the choices implicit in those cuts. Perhaps there are better ways to reduce expenditures and increase revenues that offer an alternative pathway to a balanced budget? When communicating with your subordinates, you open conversation on ways to enhance efficiencies and assure quality. You explore avenues to partner with other departments within your institution on how you can link and leverage services and capabilities. And you consider your marketplace and the actions you can take to reinforce your department and assure the volume necessary to achieve budget and quality objectives. And through it all, you monitor the situation. What are the effects of the budget adjustments, and what can be done to sustain the coherence of the work and output of the department? It is a leadership process of constant situational awareness, personal commitment, and connectivity of effort.
An illustration of another pathway: Resist the change and argue forcefully for holding onto the current budget and workforce. Though you do not possess the authority to control larger budgetary decisions, you employ influence well beyond your authority. You recruit allies to your cause, advocates who believe in the purpose you are promoting. You build an alternative coherence, mindful of fostering friendship and minimizing alienation. You are recognized for the passion of your professional commitment and your capacity to uphold quality care and organizational balance.
Two very different pathways to crafting coherence. Leaders of each perceive their actions to advance priority coherence objectives. Apply this question to your own complex problem solving.
Metaleaders forge coherence through the narratives they build and the consistency with those themes and priorities. When everyone on your staff, from physicians to housekeeping personnel, can say “I am here to help save lives,” you know that your followers are on board with a shared mission. They recognize that their efforts contribute to that overall mission. Each person has a role to play, and her or his work fits with the efforts of others, and the bottom line accomplishments of the department.
The coherence you forge assists your followers to make sense of what they are doing and how it fits what others are doing. Work is fulfilling. Beyond that, in a turbulent health care system, you anticipate both problems and opportunities with strategies to meet them. You stay ahead of the game to ensure that people within and outside the department are aligned to maximize opportunities for success.
This is particularly important for the hospitalist. Your job is to fashion coherence on many levels. First, coherent patient care for the patient. Second, coherent interactions among professionals. Finally, organizational coherence, so one piece of the puzzle fits with others. And, when there is a need to recalculate, you adapt and develop solutions that fit the people and situation at hand.
Dr. Marcus is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is Director of the Program for Health Care Negotiation and Conflict Resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
For the many people who expect you to lead, your role – among others – is to create coherence. That coherence characterizes the logic and consistency of what you do in your organization. It assembles the individual work of many different people into a whole that functions well. Coherence in your workplace helps people make sense of what they are doing and why it matters.
Our very rational brain craves coherence. We assemble facts, emotions, ambitions and our life stories into narratives that define who we are, what we are doing, and why it is important. An effective organizational “metaleader” encourages that process for followers. It helps people make sense of the work side of their life.
When coherence is absent, the workplace is riddled with contradictions, unpredictability, and dissonance. People are expected to accomplish tasks for which the time, tools, and talent are missing. There is a perplexed swirl of high activity and low productivity. Expectations for high quality of care and patient satisfaction are contradicted by an overbearing workload, reams of paper work, and the low morale that leaves the work force lethargic. “What we are doing here and how we are doing it doesn’t make sense,” exemplifies the exasperation of working amid incoherence. The department does not drive together toward success-oriented performance. Instead, different people, priorities, and opportunities will be positioned in conflict with one another. For people in your group and those surrounding it, morale and motivation suffer. There is the risk that people will descend into malaise.
Creating coherence is a complex metaleadership process. A large health care center is a cacophony of priorities, of which advancing quality of care is but one. There are other objectives, some contradictory, that also absorb time and attention: achievement of financial benchmarks, promotion of professional careers, and the individual hopes and desires of patients. Systematically aligning those many priorities and objectives is a process of both design and leadership.
The metaleadership model is a strategy for building coherence amid the complexity of health care operations. For those unfamiliar with metaleadership: The prefix “meta-” refers to a wider perspective on what is happening, the people involved, and the overall combination of objectives. The three dimensions of practice are: 1) the Person of the metaleader – your own priorities, values and emotional intelligence; 2) the Situation – what is happening and what ought to be done about it; and 3) Connectivity of Effort, which leads down to subordinates, up to bosses, across to other internal departments, and beyond to external organizations and professionals.
In building connectivity of effort, the metaleader links the many sides of the work being accomplished. The intent is to balance – purposefully – different organizational objectives into a combined whole that gets the jobs done. Furthermore, that coherence links and adapts what people are doing to the situation at hand. And in essence, the person of the leader cannot lead broader coherence if not coherent in her or his own thinking, attitudes, and behaviors, so achievement of personal and professional clarity of purpose is important.
The question for you: How do you as a hospitalist leader create coherence in what you are leading given the changing priorities, actions, and turbulence of current health policy and the market?
The answers lie in the communication you foster and clarify. That communication demands clarity and diplomacy. It is multidirectional such that messages and information in your leading down, up, across, and beyond complement and inform one another.
An illustration of one pathway: You learn from senior management about cuts in the budget. You reflect with them on the choices implicit in those cuts. Perhaps there are better ways to reduce expenditures and increase revenues that offer an alternative pathway to a balanced budget? When communicating with your subordinates, you open conversation on ways to enhance efficiencies and assure quality. You explore avenues to partner with other departments within your institution on how you can link and leverage services and capabilities. And you consider your marketplace and the actions you can take to reinforce your department and assure the volume necessary to achieve budget and quality objectives. And through it all, you monitor the situation. What are the effects of the budget adjustments, and what can be done to sustain the coherence of the work and output of the department? It is a leadership process of constant situational awareness, personal commitment, and connectivity of effort.
An illustration of another pathway: Resist the change and argue forcefully for holding onto the current budget and workforce. Though you do not possess the authority to control larger budgetary decisions, you employ influence well beyond your authority. You recruit allies to your cause, advocates who believe in the purpose you are promoting. You build an alternative coherence, mindful of fostering friendship and minimizing alienation. You are recognized for the passion of your professional commitment and your capacity to uphold quality care and organizational balance.
Two very different pathways to crafting coherence. Leaders of each perceive their actions to advance priority coherence objectives. Apply this question to your own complex problem solving.
Metaleaders forge coherence through the narratives they build and the consistency with those themes and priorities. When everyone on your staff, from physicians to housekeeping personnel, can say “I am here to help save lives,” you know that your followers are on board with a shared mission. They recognize that their efforts contribute to that overall mission. Each person has a role to play, and her or his work fits with the efforts of others, and the bottom line accomplishments of the department.
The coherence you forge assists your followers to make sense of what they are doing and how it fits what others are doing. Work is fulfilling. Beyond that, in a turbulent health care system, you anticipate both problems and opportunities with strategies to meet them. You stay ahead of the game to ensure that people within and outside the department are aligned to maximize opportunities for success.
This is particularly important for the hospitalist. Your job is to fashion coherence on many levels. First, coherent patient care for the patient. Second, coherent interactions among professionals. Finally, organizational coherence, so one piece of the puzzle fits with others. And, when there is a need to recalculate, you adapt and develop solutions that fit the people and situation at hand.
Dr. Marcus is coauthor of Renegotiating Health Care: Resolving Conflict to Build Collaboration, Second Edition (San Francisco: Jossey-Bass Publishers, 2011) and is Director of the Program for Health Care Negotiation and Conflict Resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
Delaying antibiotics in elderly with UTI linked to higher sepsis, death rates
results of a large, population-based study suggest.
The risk of bloodstream infection was more than seven times greater in patients who did not receive antibiotics immediately after seeing a general practitioner for a UTI versus those who did, according to results of the study based on primary care records and other data for nearly 160,000 U.K. patients aged 65 years or older. Death rates and hospital admissions were significantly higher for these patients, according to the study published in The BMJ by Myriam Gharbi, PharmD, Phd, Imperial College London, and her colleagues.
The publication of these findings coincides with an increase in Escherichia coli bloodstream infections in England.
“Our study suggests the early initiation of antibiotics for UTI in older high risk adult populations (especially men aged [older than] 85 years) should be recommended to prevent serious complications,” Dr. Gharbi and her coauthors said in their report.
The population-based cohort study comprised 157,264 adult primary care patients at least 65 years of age who had one or more suspected or confirmed lower UTIs from November 2007 to May 2015. The researchers found that health care providers had diagnosed a total of 312,896 UTI episodes in these patients during the period they studied. In 7.2% (22,534) of the UTI episodes, the researchers were unable to find records of the patients having been prescribed antibiotics by a general practitioner within 7 days of the UTI diagnosis. These 22,534 episodes included those that occurred in patients who had a complication before an antibiotic was prescribed. An additional 6.2% (19,292) of the episodes occurred in patients who were prescribed antibiotics, but not during their first UTI-related visit to a general practitioner or on the same day of such a visit. The researchers classified this group of patients as having been prescribed antibiotics on a deferred or delayed basis, as they were not prescribed such drugs within 7 days of their visit.
Overall, there were 1,539 cases (0.5% of the total number of UTIs) of bloodstream infection within 60 days of the initial urinary tract infection diagnosis, the researchers reported.
The bloodstream infection rate was 2.9% for patients who were not prescribed antibiotics ever or prior to an infection occurring, 2.2% in those who were prescribed antibiotics on a deferred basis, and 0.2% in those who were prescribed antibiotics immediately, meaning during their first visit to a general practitioner for a UTI or on the same day of such a visit (P less than .001). After adjustment for potential confounding variables such as age, sex, and region, the patients classified as having not been prescribed antibiotics or having been prescribed antibiotics on a deferred basis were significantly more likely to have a bloodstream infection within 60 days of their visit to a health care provider, compared with those who received antibiotics immediately, with odds ratios of 8.08 (95% confidence interval, 7.12-9.16) and 7.12 (95% CI, 6.22-8.14), respectively.
Hospital admissions after a UTI episode were nearly twice as high in the no- or deferred-antibiotics groups (27.0% and 26.8%, respectively), compared with the group that received antibiotics right away (14.8%), the investigators reported. The lengths of hospital stays were 12.1 days for the group classified as having not been prescribed antibiotics, 7.7 days for the group subject to delayed antibiotic prescribing, and 6.3 days for the group who received antibiotics immediately.
Deaths within 60 days of experiencing a urinary tract infection occurred in 5.4% of patients in the no-antibiotics group, 2.8% of the deferred-antibiotics group, and 1.6% of the immediate-antibiotics group. After adjustment for covariates, a regression analysis showed the risks for all-cause mortality were 1.16 and 2.18 times higher in the deferred-antibiotics group and the no-antibiotics group, respectively, according to the paper.
In the immediate-antibiotics group, those patients who received nitrofurantoin had a “small but significant increase” in 60-day survival versus those who received trimethoprim, the investigators noted in the discussion section of their report.
“This increase could reflect either higher levels of resistance to trimethoprim or a healthier population treated with nitrofurantoin, the latest being not recommended for patients with poor kidney function,” the researchers wrote.
This study was supported by the National Institute for Health Research and other U.K. sources. One study coauthor reported working as an epidemiologist with GSK in areas not related to the study.
SOURCE: Gharbi M et al. BMJ. 2019 Feb 27. doi: 10.1136/bmj.l525.
This study linking primary care prescribing to serious infections in elderly patients with urinary tract infections is timely, as rates of bloodstream infection and mortality are increasing in this age group, according to Alastair D. Hay, MB.ChB, a professor at University of Bristol, England.
“Prompt treatment should be offered to older patients, men (who are at higher risk than women), and those living in areas of greater socioeconomic deprivation who are at the highest risk of bloodstream infections,” Dr. Hay said in an editorial accompanying the report by Gharbi et al.
That said, the link between prescribing and infection in this particular study may not be causal: “The implications are likely to be more nuanced than primary care doctors risking the health of older adults to meet targets for antimicrobial stewardship,” Dr. Hay noted.
Doctors are cautious when managing infections in vulnerable groups, evidence shows, and the deferred prescribing reported in this study is likely not the same as the delayed prescribing seen in primary care, he explained.
“Most clinicians issue a prescription on the day of presentation, with verbal advice to delay treatment, rather than waiting for a patient to return or issuing a postdated prescription,” he said. “The group given immediate antibiotics in the study by Gharbi and colleagues likely contained some patients managed in this way.”
Patients who apparently had no prescription in this retrospective analysis may have had a same-day admission with a bloodstream infection; moreover, a number of bloodstream infections in older people are due to urinary tract bacteria, and so would not be prevented by treatment for urinary tract infection, Dr. Hay said.
“Further research is needed to establish whether treatment should be initiated with a broad or a narrow spectrum antibiotic and to identify those in whom delaying treatment (while awaiting investigation) is safe,” he concluded.
Dr. Hay is a professor in the Centre for Academic Primary Care, University of Bristol, England. His editorial appears in The BMJ (2019 Feb 27. doi: 10.1136/bmj.l780). Dr. Hay declared that he is a member of the managing common infections guideline committee for the National Institute for Health and Care Excellence (NICE).
This study linking primary care prescribing to serious infections in elderly patients with urinary tract infections is timely, as rates of bloodstream infection and mortality are increasing in this age group, according to Alastair D. Hay, MB.ChB, a professor at University of Bristol, England.
“Prompt treatment should be offered to older patients, men (who are at higher risk than women), and those living in areas of greater socioeconomic deprivation who are at the highest risk of bloodstream infections,” Dr. Hay said in an editorial accompanying the report by Gharbi et al.
That said, the link between prescribing and infection in this particular study may not be causal: “The implications are likely to be more nuanced than primary care doctors risking the health of older adults to meet targets for antimicrobial stewardship,” Dr. Hay noted.
Doctors are cautious when managing infections in vulnerable groups, evidence shows, and the deferred prescribing reported in this study is likely not the same as the delayed prescribing seen in primary care, he explained.
“Most clinicians issue a prescription on the day of presentation, with verbal advice to delay treatment, rather than waiting for a patient to return or issuing a postdated prescription,” he said. “The group given immediate antibiotics in the study by Gharbi and colleagues likely contained some patients managed in this way.”
Patients who apparently had no prescription in this retrospective analysis may have had a same-day admission with a bloodstream infection; moreover, a number of bloodstream infections in older people are due to urinary tract bacteria, and so would not be prevented by treatment for urinary tract infection, Dr. Hay said.
“Further research is needed to establish whether treatment should be initiated with a broad or a narrow spectrum antibiotic and to identify those in whom delaying treatment (while awaiting investigation) is safe,” he concluded.
Dr. Hay is a professor in the Centre for Academic Primary Care, University of Bristol, England. His editorial appears in The BMJ (2019 Feb 27. doi: 10.1136/bmj.l780). Dr. Hay declared that he is a member of the managing common infections guideline committee for the National Institute for Health and Care Excellence (NICE).
This study linking primary care prescribing to serious infections in elderly patients with urinary tract infections is timely, as rates of bloodstream infection and mortality are increasing in this age group, according to Alastair D. Hay, MB.ChB, a professor at University of Bristol, England.
“Prompt treatment should be offered to older patients, men (who are at higher risk than women), and those living in areas of greater socioeconomic deprivation who are at the highest risk of bloodstream infections,” Dr. Hay said in an editorial accompanying the report by Gharbi et al.
That said, the link between prescribing and infection in this particular study may not be causal: “The implications are likely to be more nuanced than primary care doctors risking the health of older adults to meet targets for antimicrobial stewardship,” Dr. Hay noted.
Doctors are cautious when managing infections in vulnerable groups, evidence shows, and the deferred prescribing reported in this study is likely not the same as the delayed prescribing seen in primary care, he explained.
“Most clinicians issue a prescription on the day of presentation, with verbal advice to delay treatment, rather than waiting for a patient to return or issuing a postdated prescription,” he said. “The group given immediate antibiotics in the study by Gharbi and colleagues likely contained some patients managed in this way.”
Patients who apparently had no prescription in this retrospective analysis may have had a same-day admission with a bloodstream infection; moreover, a number of bloodstream infections in older people are due to urinary tract bacteria, and so would not be prevented by treatment for urinary tract infection, Dr. Hay said.
“Further research is needed to establish whether treatment should be initiated with a broad or a narrow spectrum antibiotic and to identify those in whom delaying treatment (while awaiting investigation) is safe,” he concluded.
Dr. Hay is a professor in the Centre for Academic Primary Care, University of Bristol, England. His editorial appears in The BMJ (2019 Feb 27. doi: 10.1136/bmj.l780). Dr. Hay declared that he is a member of the managing common infections guideline committee for the National Institute for Health and Care Excellence (NICE).
results of a large, population-based study suggest.
The risk of bloodstream infection was more than seven times greater in patients who did not receive antibiotics immediately after seeing a general practitioner for a UTI versus those who did, according to results of the study based on primary care records and other data for nearly 160,000 U.K. patients aged 65 years or older. Death rates and hospital admissions were significantly higher for these patients, according to the study published in The BMJ by Myriam Gharbi, PharmD, Phd, Imperial College London, and her colleagues.
The publication of these findings coincides with an increase in Escherichia coli bloodstream infections in England.
“Our study suggests the early initiation of antibiotics for UTI in older high risk adult populations (especially men aged [older than] 85 years) should be recommended to prevent serious complications,” Dr. Gharbi and her coauthors said in their report.
The population-based cohort study comprised 157,264 adult primary care patients at least 65 years of age who had one or more suspected or confirmed lower UTIs from November 2007 to May 2015. The researchers found that health care providers had diagnosed a total of 312,896 UTI episodes in these patients during the period they studied. In 7.2% (22,534) of the UTI episodes, the researchers were unable to find records of the patients having been prescribed antibiotics by a general practitioner within 7 days of the UTI diagnosis. These 22,534 episodes included those that occurred in patients who had a complication before an antibiotic was prescribed. An additional 6.2% (19,292) of the episodes occurred in patients who were prescribed antibiotics, but not during their first UTI-related visit to a general practitioner or on the same day of such a visit. The researchers classified this group of patients as having been prescribed antibiotics on a deferred or delayed basis, as they were not prescribed such drugs within 7 days of their visit.
Overall, there were 1,539 cases (0.5% of the total number of UTIs) of bloodstream infection within 60 days of the initial urinary tract infection diagnosis, the researchers reported.
The bloodstream infection rate was 2.9% for patients who were not prescribed antibiotics ever or prior to an infection occurring, 2.2% in those who were prescribed antibiotics on a deferred basis, and 0.2% in those who were prescribed antibiotics immediately, meaning during their first visit to a general practitioner for a UTI or on the same day of such a visit (P less than .001). After adjustment for potential confounding variables such as age, sex, and region, the patients classified as having not been prescribed antibiotics or having been prescribed antibiotics on a deferred basis were significantly more likely to have a bloodstream infection within 60 days of their visit to a health care provider, compared with those who received antibiotics immediately, with odds ratios of 8.08 (95% confidence interval, 7.12-9.16) and 7.12 (95% CI, 6.22-8.14), respectively.
Hospital admissions after a UTI episode were nearly twice as high in the no- or deferred-antibiotics groups (27.0% and 26.8%, respectively), compared with the group that received antibiotics right away (14.8%), the investigators reported. The lengths of hospital stays were 12.1 days for the group classified as having not been prescribed antibiotics, 7.7 days for the group subject to delayed antibiotic prescribing, and 6.3 days for the group who received antibiotics immediately.
Deaths within 60 days of experiencing a urinary tract infection occurred in 5.4% of patients in the no-antibiotics group, 2.8% of the deferred-antibiotics group, and 1.6% of the immediate-antibiotics group. After adjustment for covariates, a regression analysis showed the risks for all-cause mortality were 1.16 and 2.18 times higher in the deferred-antibiotics group and the no-antibiotics group, respectively, according to the paper.
In the immediate-antibiotics group, those patients who received nitrofurantoin had a “small but significant increase” in 60-day survival versus those who received trimethoprim, the investigators noted in the discussion section of their report.
“This increase could reflect either higher levels of resistance to trimethoprim or a healthier population treated with nitrofurantoin, the latest being not recommended for patients with poor kidney function,” the researchers wrote.
This study was supported by the National Institute for Health Research and other U.K. sources. One study coauthor reported working as an epidemiologist with GSK in areas not related to the study.
SOURCE: Gharbi M et al. BMJ. 2019 Feb 27. doi: 10.1136/bmj.l525.
results of a large, population-based study suggest.
The risk of bloodstream infection was more than seven times greater in patients who did not receive antibiotics immediately after seeing a general practitioner for a UTI versus those who did, according to results of the study based on primary care records and other data for nearly 160,000 U.K. patients aged 65 years or older. Death rates and hospital admissions were significantly higher for these patients, according to the study published in The BMJ by Myriam Gharbi, PharmD, Phd, Imperial College London, and her colleagues.
The publication of these findings coincides with an increase in Escherichia coli bloodstream infections in England.
“Our study suggests the early initiation of antibiotics for UTI in older high risk adult populations (especially men aged [older than] 85 years) should be recommended to prevent serious complications,” Dr. Gharbi and her coauthors said in their report.
The population-based cohort study comprised 157,264 adult primary care patients at least 65 years of age who had one or more suspected or confirmed lower UTIs from November 2007 to May 2015. The researchers found that health care providers had diagnosed a total of 312,896 UTI episodes in these patients during the period they studied. In 7.2% (22,534) of the UTI episodes, the researchers were unable to find records of the patients having been prescribed antibiotics by a general practitioner within 7 days of the UTI diagnosis. These 22,534 episodes included those that occurred in patients who had a complication before an antibiotic was prescribed. An additional 6.2% (19,292) of the episodes occurred in patients who were prescribed antibiotics, but not during their first UTI-related visit to a general practitioner or on the same day of such a visit. The researchers classified this group of patients as having been prescribed antibiotics on a deferred or delayed basis, as they were not prescribed such drugs within 7 days of their visit.
Overall, there were 1,539 cases (0.5% of the total number of UTIs) of bloodstream infection within 60 days of the initial urinary tract infection diagnosis, the researchers reported.
The bloodstream infection rate was 2.9% for patients who were not prescribed antibiotics ever or prior to an infection occurring, 2.2% in those who were prescribed antibiotics on a deferred basis, and 0.2% in those who were prescribed antibiotics immediately, meaning during their first visit to a general practitioner for a UTI or on the same day of such a visit (P less than .001). After adjustment for potential confounding variables such as age, sex, and region, the patients classified as having not been prescribed antibiotics or having been prescribed antibiotics on a deferred basis were significantly more likely to have a bloodstream infection within 60 days of their visit to a health care provider, compared with those who received antibiotics immediately, with odds ratios of 8.08 (95% confidence interval, 7.12-9.16) and 7.12 (95% CI, 6.22-8.14), respectively.
Hospital admissions after a UTI episode were nearly twice as high in the no- or deferred-antibiotics groups (27.0% and 26.8%, respectively), compared with the group that received antibiotics right away (14.8%), the investigators reported. The lengths of hospital stays were 12.1 days for the group classified as having not been prescribed antibiotics, 7.7 days for the group subject to delayed antibiotic prescribing, and 6.3 days for the group who received antibiotics immediately.
Deaths within 60 days of experiencing a urinary tract infection occurred in 5.4% of patients in the no-antibiotics group, 2.8% of the deferred-antibiotics group, and 1.6% of the immediate-antibiotics group. After adjustment for covariates, a regression analysis showed the risks for all-cause mortality were 1.16 and 2.18 times higher in the deferred-antibiotics group and the no-antibiotics group, respectively, according to the paper.
In the immediate-antibiotics group, those patients who received nitrofurantoin had a “small but significant increase” in 60-day survival versus those who received trimethoprim, the investigators noted in the discussion section of their report.
“This increase could reflect either higher levels of resistance to trimethoprim or a healthier population treated with nitrofurantoin, the latest being not recommended for patients with poor kidney function,” the researchers wrote.
This study was supported by the National Institute for Health Research and other U.K. sources. One study coauthor reported working as an epidemiologist with GSK in areas not related to the study.
SOURCE: Gharbi M et al. BMJ. 2019 Feb 27. doi: 10.1136/bmj.l525.
FROM THE BMJ