User login
Review protocols, follow reprocessing guidelines to cut device-related HAIs
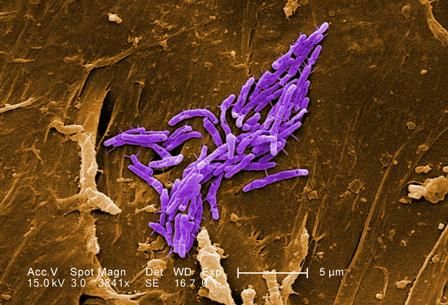
ATLANTA – Ongoing vigilance regarding the role of and transmission of antimicrobial-resistant pathogen is needed, according to Isaac Benowitz, MD, of the Centers for Disease Control and Prevention’s Division of Healthcare Quality Promotion (DHQP).
A review of records from the DHQP, which investigates and responds to infections and related adverse events in health care settings upon invitation, showed that in 2017 environmental pathogens were most often the triggers for these investigations, said Dr. Benowitz, a medical epidemiologist.
He reviewed internal records for consultations with state and local health departments involving medical devices and collected data on health care setting, pathogen, investigation findings including possible exposure or transmission, and public health actions.
Of 285 consultations, 48 involved a specific medical device or general medical device reprocessing, he said, noting that most of those 48 were in an acute care hospital (63%) or clinic (19%).
“The most frequent pathogens noted in these consultations were nontuberculous mycobacteria at 21%, Candida species ... at 10%, and Burkholderia species ... at 8%,” he said, noting that a wide variety of devices were implicated.
In the inpatient setting these devices included ventilators, dialysis machines, breast pumps, central lines, and respiratory therapy equipment. In the outpatient setting they included glucometers and opthalmic equipment.
“In many settings we saw issues with endoscopes, including duodenoscopes, but also bronchoscopes,” he added.
Actions taken as part of the investigations included medical device recalls, improved infection control and reprocessing procedures, and patient notification, education, guidance, testing, and treatment.
In some cases there was disciplinary action or oversight for health care professionals, he added.
Investigations identified medical devices contaminated in manufacturing, incorrect reprocessing of endoscopes or ventilators, and inappropriate medical device use or reuse, he said.
A number of lessons can be learned from these and other investigations, he added.
“First, devices can be reservoirs and transmission vectors for health care–associated infections. Second, health care facilities, health care facility staff, and public health partners should take opportunities to review protocols and the practices within those protocol,” he said. “These are opportunities to strengthen infection control practices even in the absence of documented transmission.”
In fact, in most of the investigations he discussed, transmission was rarely confirmed to be associated with a medical device. This was largely because of a lack of “epidemiological rigor,” but associations between health care–associated infections and medical devices “are still quite meaningful and often actionable,” he said.
Dr. Benowitz stressed the importance of engaging public health partners to discuss findings and actions, explaining that “what may look like a single-facility issue may have a very different perspective when you realize that there’s a similar issue at another facility elsewhere.”
“For all devices, it’s important to ensure adherence to the device reprocessing guidelines, “ he added, noting that these include a combination of facility protocols, manufacturer instructions for use, and guidance from organizations like the Food and Drug Administration and the CDC.
Dr. Benowitz reported having no disclosures.
[email protected]
SOURCE: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
ATLANTA – Ongoing vigilance regarding the role of and transmission of antimicrobial-resistant pathogen is needed, according to Isaac Benowitz, MD, of the Centers for Disease Control and Prevention’s Division of Healthcare Quality Promotion (DHQP).
A review of records from the DHQP, which investigates and responds to infections and related adverse events in health care settings upon invitation, showed that in 2017 environmental pathogens were most often the triggers for these investigations, said Dr. Benowitz, a medical epidemiologist.
He reviewed internal records for consultations with state and local health departments involving medical devices and collected data on health care setting, pathogen, investigation findings including possible exposure or transmission, and public health actions.
Of 285 consultations, 48 involved a specific medical device or general medical device reprocessing, he said, noting that most of those 48 were in an acute care hospital (63%) or clinic (19%).
“The most frequent pathogens noted in these consultations were nontuberculous mycobacteria at 21%, Candida species ... at 10%, and Burkholderia species ... at 8%,” he said, noting that a wide variety of devices were implicated.
In the inpatient setting these devices included ventilators, dialysis machines, breast pumps, central lines, and respiratory therapy equipment. In the outpatient setting they included glucometers and opthalmic equipment.
“In many settings we saw issues with endoscopes, including duodenoscopes, but also bronchoscopes,” he added.
Actions taken as part of the investigations included medical device recalls, improved infection control and reprocessing procedures, and patient notification, education, guidance, testing, and treatment.
In some cases there was disciplinary action or oversight for health care professionals, he added.
Investigations identified medical devices contaminated in manufacturing, incorrect reprocessing of endoscopes or ventilators, and inappropriate medical device use or reuse, he said.
A number of lessons can be learned from these and other investigations, he added.
“First, devices can be reservoirs and transmission vectors for health care–associated infections. Second, health care facilities, health care facility staff, and public health partners should take opportunities to review protocols and the practices within those protocol,” he said. “These are opportunities to strengthen infection control practices even in the absence of documented transmission.”
In fact, in most of the investigations he discussed, transmission was rarely confirmed to be associated with a medical device. This was largely because of a lack of “epidemiological rigor,” but associations between health care–associated infections and medical devices “are still quite meaningful and often actionable,” he said.
Dr. Benowitz stressed the importance of engaging public health partners to discuss findings and actions, explaining that “what may look like a single-facility issue may have a very different perspective when you realize that there’s a similar issue at another facility elsewhere.”
“For all devices, it’s important to ensure adherence to the device reprocessing guidelines, “ he added, noting that these include a combination of facility protocols, manufacturer instructions for use, and guidance from organizations like the Food and Drug Administration and the CDC.
Dr. Benowitz reported having no disclosures.
[email protected]
SOURCE: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
ATLANTA – Ongoing vigilance regarding the role of and transmission of antimicrobial-resistant pathogen is needed, according to Isaac Benowitz, MD, of the Centers for Disease Control and Prevention’s Division of Healthcare Quality Promotion (DHQP).
A review of records from the DHQP, which investigates and responds to infections and related adverse events in health care settings upon invitation, showed that in 2017 environmental pathogens were most often the triggers for these investigations, said Dr. Benowitz, a medical epidemiologist.
He reviewed internal records for consultations with state and local health departments involving medical devices and collected data on health care setting, pathogen, investigation findings including possible exposure or transmission, and public health actions.
Of 285 consultations, 48 involved a specific medical device or general medical device reprocessing, he said, noting that most of those 48 were in an acute care hospital (63%) or clinic (19%).
“The most frequent pathogens noted in these consultations were nontuberculous mycobacteria at 21%, Candida species ... at 10%, and Burkholderia species ... at 8%,” he said, noting that a wide variety of devices were implicated.
In the inpatient setting these devices included ventilators, dialysis machines, breast pumps, central lines, and respiratory therapy equipment. In the outpatient setting they included glucometers and opthalmic equipment.
“In many settings we saw issues with endoscopes, including duodenoscopes, but also bronchoscopes,” he added.
Actions taken as part of the investigations included medical device recalls, improved infection control and reprocessing procedures, and patient notification, education, guidance, testing, and treatment.
In some cases there was disciplinary action or oversight for health care professionals, he added.
Investigations identified medical devices contaminated in manufacturing, incorrect reprocessing of endoscopes or ventilators, and inappropriate medical device use or reuse, he said.
A number of lessons can be learned from these and other investigations, he added.
“First, devices can be reservoirs and transmission vectors for health care–associated infections. Second, health care facilities, health care facility staff, and public health partners should take opportunities to review protocols and the practices within those protocol,” he said. “These are opportunities to strengthen infection control practices even in the absence of documented transmission.”
In fact, in most of the investigations he discussed, transmission was rarely confirmed to be associated with a medical device. This was largely because of a lack of “epidemiological rigor,” but associations between health care–associated infections and medical devices “are still quite meaningful and often actionable,” he said.
Dr. Benowitz stressed the importance of engaging public health partners to discuss findings and actions, explaining that “what may look like a single-facility issue may have a very different perspective when you realize that there’s a similar issue at another facility elsewhere.”
“For all devices, it’s important to ensure adherence to the device reprocessing guidelines, “ he added, noting that these include a combination of facility protocols, manufacturer instructions for use, and guidance from organizations like the Food and Drug Administration and the CDC.
Dr. Benowitz reported having no disclosures.
[email protected]
SOURCE: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
REPORTING FROM ICEID 2018
Key clinical point: Medical devices can be reservoirs and transmission vectors for health care–associated infections.
Major finding: Of 285 consultations, 48 involved medical devices or device reprocessing.
Study details: A review of records from 285 consultations
Disclosures: Dr. Benowitz reported having no disclosures
Source: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
Coronary CT angiography radiation dose fell 78% from 2007-2017
MUNICH – The median radiation dosage received by patients worldwide undergoing coronary CT angiography fell by 78% from 2007 to 2017, according to a prospective study with more than 4,500 patients.
This substantial drop in radiation occurred with a steady rate of nondiagnostic CT scans, less than 2% in both 2007 and 2017.
“Given the high diagnostic accuracy and the low radiation dose, coronary CT angiography should be considered as a first-line diagnostic test,” Jörg Hausleiter, MD, said at the annual congress of the European Society of Cardiology.
The results also showed a huge disparity in the range of radiation doses used worldwide, with a 37-fold intersite variability in the median dose. This finding “underlines the need for further site-specific training and adaptation of contemporary cardiac scan protocols,” said Dr. Hausleiter, professor of medicine at the University of Munich Clinic. He suggested updated imaging guidelines on radiation levels, more educational sessions on how to perform coronary CT angiography, and actions by vendors to adjust their standard imaging protocols.
The Prospective Multicenter Registry on Radiation Dose Estimates of Cardiac CT Angiography in Daily Practice in 2017 (PROTECTION-VI) study included 4,502 patients from a total of 61 sites in 32 countries. At each participating site, investigators enrolled consecutive adults during a randomly selected month in 2017, with a median of 51 patients enrolled at each site undergoing diagnostic coronary CT angiography. Comparison data for 2007 came from a similar study run by Dr. Hausleiter and his associates at that time, with 1,965 patients undergoing coronary CT angiography (JAMA. 2009 Feb 4;301[5]:500-7). In 2007, the median dose-length product of radiation for each scan was 885 mGy x cm, which corresponds to a radiation dose of about 12.4 mSv. In 2017, the median dose-length product was 195 mGy x cm, corresponding to a dose of about 2.7 mSv. By both measures the median dose dropped by roughly 78%.
A multivariate analysis identified three changes in the way clinicians obtained most of the CT scans during the two studied time periods that seemed to explain the drop in radiation dose. First, more scan protocols in 2017 used low tube potential; second, more protocols in 2017 used prospectively ECG-triggered axial high-pitch scans; and third, 2017 had increased use of iterative image reconstruction, Dr. Hausleiter said. Patient variables that had modest but significant links with increased radiation doses were higher body weight, higher heart rate, and no sinus rhythm.
Concurrently with Dr. Hausleiter’s talk at the congress, the results appeared in an article online (Euro Heart J. 2018 Aug 25. doi: 10.1093/eurheartj/ehy546).
The results from the PROTECTION VI study show that the radiation doses used today for coronary CT angiography are very low. But the study is limited by looking only at the median doses used at 61 sites worldwide. I hope that the dose level seen in the study is what is now used at community hospitals across the United States, but for the time being we can’t be sure.
With today’s CT technology, as long as the dose-length product a patient receives is less than 200 mGy x cm, the facility is doing a good job of minimizing radiation exposure. As CT technology continues to improve, we can expect the median dose to fall even more in the future.
Todd C. Villines, MD , a cardiologist at Georgetown University in Washington and immediate past president of the Society of Cardiovascular CT, made these comments in an interview. He had no relevant disclosures.
The results from the PROTECTION VI study show that the radiation doses used today for coronary CT angiography are very low. But the study is limited by looking only at the median doses used at 61 sites worldwide. I hope that the dose level seen in the study is what is now used at community hospitals across the United States, but for the time being we can’t be sure.
With today’s CT technology, as long as the dose-length product a patient receives is less than 200 mGy x cm, the facility is doing a good job of minimizing radiation exposure. As CT technology continues to improve, we can expect the median dose to fall even more in the future.
Todd C. Villines, MD , a cardiologist at Georgetown University in Washington and immediate past president of the Society of Cardiovascular CT, made these comments in an interview. He had no relevant disclosures.
The results from the PROTECTION VI study show that the radiation doses used today for coronary CT angiography are very low. But the study is limited by looking only at the median doses used at 61 sites worldwide. I hope that the dose level seen in the study is what is now used at community hospitals across the United States, but for the time being we can’t be sure.
With today’s CT technology, as long as the dose-length product a patient receives is less than 200 mGy x cm, the facility is doing a good job of minimizing radiation exposure. As CT technology continues to improve, we can expect the median dose to fall even more in the future.
Todd C. Villines, MD , a cardiologist at Georgetown University in Washington and immediate past president of the Society of Cardiovascular CT, made these comments in an interview. He had no relevant disclosures.
MUNICH – The median radiation dosage received by patients worldwide undergoing coronary CT angiography fell by 78% from 2007 to 2017, according to a prospective study with more than 4,500 patients.
This substantial drop in radiation occurred with a steady rate of nondiagnostic CT scans, less than 2% in both 2007 and 2017.
“Given the high diagnostic accuracy and the low radiation dose, coronary CT angiography should be considered as a first-line diagnostic test,” Jörg Hausleiter, MD, said at the annual congress of the European Society of Cardiology.
The results also showed a huge disparity in the range of radiation doses used worldwide, with a 37-fold intersite variability in the median dose. This finding “underlines the need for further site-specific training and adaptation of contemporary cardiac scan protocols,” said Dr. Hausleiter, professor of medicine at the University of Munich Clinic. He suggested updated imaging guidelines on radiation levels, more educational sessions on how to perform coronary CT angiography, and actions by vendors to adjust their standard imaging protocols.
The Prospective Multicenter Registry on Radiation Dose Estimates of Cardiac CT Angiography in Daily Practice in 2017 (PROTECTION-VI) study included 4,502 patients from a total of 61 sites in 32 countries. At each participating site, investigators enrolled consecutive adults during a randomly selected month in 2017, with a median of 51 patients enrolled at each site undergoing diagnostic coronary CT angiography. Comparison data for 2007 came from a similar study run by Dr. Hausleiter and his associates at that time, with 1,965 patients undergoing coronary CT angiography (JAMA. 2009 Feb 4;301[5]:500-7). In 2007, the median dose-length product of radiation for each scan was 885 mGy x cm, which corresponds to a radiation dose of about 12.4 mSv. In 2017, the median dose-length product was 195 mGy x cm, corresponding to a dose of about 2.7 mSv. By both measures the median dose dropped by roughly 78%.
A multivariate analysis identified three changes in the way clinicians obtained most of the CT scans during the two studied time periods that seemed to explain the drop in radiation dose. First, more scan protocols in 2017 used low tube potential; second, more protocols in 2017 used prospectively ECG-triggered axial high-pitch scans; and third, 2017 had increased use of iterative image reconstruction, Dr. Hausleiter said. Patient variables that had modest but significant links with increased radiation doses were higher body weight, higher heart rate, and no sinus rhythm.
Concurrently with Dr. Hausleiter’s talk at the congress, the results appeared in an article online (Euro Heart J. 2018 Aug 25. doi: 10.1093/eurheartj/ehy546).
MUNICH – The median radiation dosage received by patients worldwide undergoing coronary CT angiography fell by 78% from 2007 to 2017, according to a prospective study with more than 4,500 patients.
This substantial drop in radiation occurred with a steady rate of nondiagnostic CT scans, less than 2% in both 2007 and 2017.
“Given the high diagnostic accuracy and the low radiation dose, coronary CT angiography should be considered as a first-line diagnostic test,” Jörg Hausleiter, MD, said at the annual congress of the European Society of Cardiology.
The results also showed a huge disparity in the range of radiation doses used worldwide, with a 37-fold intersite variability in the median dose. This finding “underlines the need for further site-specific training and adaptation of contemporary cardiac scan protocols,” said Dr. Hausleiter, professor of medicine at the University of Munich Clinic. He suggested updated imaging guidelines on radiation levels, more educational sessions on how to perform coronary CT angiography, and actions by vendors to adjust their standard imaging protocols.
The Prospective Multicenter Registry on Radiation Dose Estimates of Cardiac CT Angiography in Daily Practice in 2017 (PROTECTION-VI) study included 4,502 patients from a total of 61 sites in 32 countries. At each participating site, investigators enrolled consecutive adults during a randomly selected month in 2017, with a median of 51 patients enrolled at each site undergoing diagnostic coronary CT angiography. Comparison data for 2007 came from a similar study run by Dr. Hausleiter and his associates at that time, with 1,965 patients undergoing coronary CT angiography (JAMA. 2009 Feb 4;301[5]:500-7). In 2007, the median dose-length product of radiation for each scan was 885 mGy x cm, which corresponds to a radiation dose of about 12.4 mSv. In 2017, the median dose-length product was 195 mGy x cm, corresponding to a dose of about 2.7 mSv. By both measures the median dose dropped by roughly 78%.
A multivariate analysis identified three changes in the way clinicians obtained most of the CT scans during the two studied time periods that seemed to explain the drop in radiation dose. First, more scan protocols in 2017 used low tube potential; second, more protocols in 2017 used prospectively ECG-triggered axial high-pitch scans; and third, 2017 had increased use of iterative image reconstruction, Dr. Hausleiter said. Patient variables that had modest but significant links with increased radiation doses were higher body weight, higher heart rate, and no sinus rhythm.
Concurrently with Dr. Hausleiter’s talk at the congress, the results appeared in an article online (Euro Heart J. 2018 Aug 25. doi: 10.1093/eurheartj/ehy546).
REPORTING FROM THE ESC CONGRESS 2018
Key clinical point: The median radiation dose during coronary CT angiography fell from 2007 to 2017.
Major finding: The median dose-length product was 195 mGY x cm in 2017 and 885 mGy x cm in 2007.
Study details: PROTECTION VI, a prospective study run at 61 sites in 32 countries.
Disclosures: PROTECTION VI received no commercial funding. Dr. Hausleiter has received research funding from Abbott Vascular.
Cutaneous lesions? Consider C. diphtheriae in those with foreign travel
ATLANTA – Seven cases of imported Corynebacterium diphtheriae in Minnesota highlight the importance of maintaining suspicion that cutaneous lesions in individuals with recent travel to endemic countries might be associated with C. diphtheriae infection.
The cases also underscore the importance of referring C. diphtheriae isolates to state health departments for confirmatory testing, Jayne Griffith, of the Minnesota Department of Health, and her colleagues reported in a poster at the International Conference on Emerging Infectious Diseases.
“C. diphtheriae infections was not clinically suspected in any of these case-patients. All infections were initially identified solely by [matrix-assisted laser desorption/ionization time-of-flight spectrometry] testing performed at the clinical institutions,” the investigators wrote. “Confirmation and further toxigenicity testing allowed for prompt case investigation and public health response, preventing disease spread.”
Infections caused by toxigenic C. diphtheriae are rare in the United States because of widespread vaccination, but remain endemic in countries with suboptimal vaccine coverage. For this reason, infection is a concern for unvaccinated individuals traveling to diphtheria-endemic countries as well as for those who have contact with people from these areas. The investigators noted that “infections are primarily respiratory or cutaneous; respiratory infections can be life-threatening and cutaneous wounds may serve as a reservoir from which bacteria can be transmitted to susceptible contacts.”
The Minnesota cases involved patients who presented with cutaneous ulcers between 2014 and 2017. The Minnesota Department of Health confirmed C. diphtheriae status by culture after the initial identification at private institutions or providers using matrix-assisted laser desorption/ionization time-of-flight spectrometry. Isolates were sent to the Centers for Disease Control and Prevention Pertussis and Diphtheria Laboratory for biotyping and confirmation of toxigenicity.
The CDC confirmed that isolates from two patients were toxigenic C. diphtheriae biotype mitis. The remaining cases were nontoxigenic diphtheria, including C. diphtheriae mitis (three case-patients, including one who also had Staphylococcus aureus, and another who also had methicillin-resistant S. aureus) and two case-patients with C. diphtheriae belfanti.
The patients with toxigenic infection included a 35-year-old woman who developed an abdominal boil after spending months in Somalia, and a 48-year-old man who cut his leg while in Ethiopia.
The patients with nontoxigenic infection included four foreign-born individuals ranging in age from 7 to 66 years and one 24-year-old man from the United States. One of the foreign-born individuals had immigrated from a diphtheria-endemic country 3 months prior to his diagnosis, but none of the remaining four had traveled outside the United States in the 6 months prior to infection onset. One, however, lived in a home with family members who traveled frequently to eastern Africa. The vaccination status of these patients was unknown.
Contact tracing was conducted and prophylactic antibiotics were recommended as appropriate. Vaccination was recommended when a case-patient and/or contact was inadequately immunized.
Both patients with toxigenic infection experienced wound healing after appropriate antibiotic therapy.
Ms. Griffith reported having no disclosures.
ATLANTA – Seven cases of imported Corynebacterium diphtheriae in Minnesota highlight the importance of maintaining suspicion that cutaneous lesions in individuals with recent travel to endemic countries might be associated with C. diphtheriae infection.
The cases also underscore the importance of referring C. diphtheriae isolates to state health departments for confirmatory testing, Jayne Griffith, of the Minnesota Department of Health, and her colleagues reported in a poster at the International Conference on Emerging Infectious Diseases.
“C. diphtheriae infections was not clinically suspected in any of these case-patients. All infections were initially identified solely by [matrix-assisted laser desorption/ionization time-of-flight spectrometry] testing performed at the clinical institutions,” the investigators wrote. “Confirmation and further toxigenicity testing allowed for prompt case investigation and public health response, preventing disease spread.”
Infections caused by toxigenic C. diphtheriae are rare in the United States because of widespread vaccination, but remain endemic in countries with suboptimal vaccine coverage. For this reason, infection is a concern for unvaccinated individuals traveling to diphtheria-endemic countries as well as for those who have contact with people from these areas. The investigators noted that “infections are primarily respiratory or cutaneous; respiratory infections can be life-threatening and cutaneous wounds may serve as a reservoir from which bacteria can be transmitted to susceptible contacts.”
The Minnesota cases involved patients who presented with cutaneous ulcers between 2014 and 2017. The Minnesota Department of Health confirmed C. diphtheriae status by culture after the initial identification at private institutions or providers using matrix-assisted laser desorption/ionization time-of-flight spectrometry. Isolates were sent to the Centers for Disease Control and Prevention Pertussis and Diphtheria Laboratory for biotyping and confirmation of toxigenicity.
The CDC confirmed that isolates from two patients were toxigenic C. diphtheriae biotype mitis. The remaining cases were nontoxigenic diphtheria, including C. diphtheriae mitis (three case-patients, including one who also had Staphylococcus aureus, and another who also had methicillin-resistant S. aureus) and two case-patients with C. diphtheriae belfanti.
The patients with toxigenic infection included a 35-year-old woman who developed an abdominal boil after spending months in Somalia, and a 48-year-old man who cut his leg while in Ethiopia.
The patients with nontoxigenic infection included four foreign-born individuals ranging in age from 7 to 66 years and one 24-year-old man from the United States. One of the foreign-born individuals had immigrated from a diphtheria-endemic country 3 months prior to his diagnosis, but none of the remaining four had traveled outside the United States in the 6 months prior to infection onset. One, however, lived in a home with family members who traveled frequently to eastern Africa. The vaccination status of these patients was unknown.
Contact tracing was conducted and prophylactic antibiotics were recommended as appropriate. Vaccination was recommended when a case-patient and/or contact was inadequately immunized.
Both patients with toxigenic infection experienced wound healing after appropriate antibiotic therapy.
Ms. Griffith reported having no disclosures.
ATLANTA – Seven cases of imported Corynebacterium diphtheriae in Minnesota highlight the importance of maintaining suspicion that cutaneous lesions in individuals with recent travel to endemic countries might be associated with C. diphtheriae infection.
The cases also underscore the importance of referring C. diphtheriae isolates to state health departments for confirmatory testing, Jayne Griffith, of the Minnesota Department of Health, and her colleagues reported in a poster at the International Conference on Emerging Infectious Diseases.
“C. diphtheriae infections was not clinically suspected in any of these case-patients. All infections were initially identified solely by [matrix-assisted laser desorption/ionization time-of-flight spectrometry] testing performed at the clinical institutions,” the investigators wrote. “Confirmation and further toxigenicity testing allowed for prompt case investigation and public health response, preventing disease spread.”
Infections caused by toxigenic C. diphtheriae are rare in the United States because of widespread vaccination, but remain endemic in countries with suboptimal vaccine coverage. For this reason, infection is a concern for unvaccinated individuals traveling to diphtheria-endemic countries as well as for those who have contact with people from these areas. The investigators noted that “infections are primarily respiratory or cutaneous; respiratory infections can be life-threatening and cutaneous wounds may serve as a reservoir from which bacteria can be transmitted to susceptible contacts.”
The Minnesota cases involved patients who presented with cutaneous ulcers between 2014 and 2017. The Minnesota Department of Health confirmed C. diphtheriae status by culture after the initial identification at private institutions or providers using matrix-assisted laser desorption/ionization time-of-flight spectrometry. Isolates were sent to the Centers for Disease Control and Prevention Pertussis and Diphtheria Laboratory for biotyping and confirmation of toxigenicity.
The CDC confirmed that isolates from two patients were toxigenic C. diphtheriae biotype mitis. The remaining cases were nontoxigenic diphtheria, including C. diphtheriae mitis (three case-patients, including one who also had Staphylococcus aureus, and another who also had methicillin-resistant S. aureus) and two case-patients with C. diphtheriae belfanti.
The patients with toxigenic infection included a 35-year-old woman who developed an abdominal boil after spending months in Somalia, and a 48-year-old man who cut his leg while in Ethiopia.
The patients with nontoxigenic infection included four foreign-born individuals ranging in age from 7 to 66 years and one 24-year-old man from the United States. One of the foreign-born individuals had immigrated from a diphtheria-endemic country 3 months prior to his diagnosis, but none of the remaining four had traveled outside the United States in the 6 months prior to infection onset. One, however, lived in a home with family members who traveled frequently to eastern Africa. The vaccination status of these patients was unknown.
Contact tracing was conducted and prophylactic antibiotics were recommended as appropriate. Vaccination was recommended when a case-patient and/or contact was inadequately immunized.
Both patients with toxigenic infection experienced wound healing after appropriate antibiotic therapy.
Ms. Griffith reported having no disclosures.
REPORTING FROM ICEID 2018
Key clinical point: Corynebacterium diphtheriae should be considered in individuals who present with cutaneous lesions after traveling to diphtheria-endemic countries.
Major finding: Refer suspect C. diphtheriae isolates to state health departments.
Study details: A review of seven C. diphtheriae cases.
Disclosures: Ms. Griffith reported having no disclosures.
Danish endocarditis strategy halved hospital days
MUNICH – Patients with left-sided endocarditis who are clinically stable after a couple weeks of inpatient intravenous antibiotics may at that point become candidates for discharge on oral antibiotics for the remainder of their treatment course, according to the findings of the randomized, multicenter, Danish POET trial.
“Shifting to oral antibiotic treatment in stabilized patients with endocarditis was as effective and safe as continued intravenous antibiotic treatment and was given during half the antibiotic treatment period. These novel findings may have a significant impact on future clinical practice for the management of patients who are stable,” Henning Bundgård, MD, said at the annual congress of the European Society of Cardiology.
Both ESC and American Heart Association/American College of Cardiology guidelines now recommend treatment of infective endocarditis with intravenous antibiotics for up to 6 weeks. Safely cutting the duration of in-hospital intravenous antibiotics in half is likely to generate major cost savings while improving patient quality of life and avoiding prolonged exposure to the iatrogenic risks inherent to the hospital environment, noted Dr. Bundgård, a cardiologist at Copenhagen University Hospital.
The rationale for the POET (Partial Oral Treatment of Endocarditis) trial was the investigators’ recognition that, even though infectious endocarditis is a feared disease with an in-hospital mortality of 15% or more, the great majority of serious complications occur in the early critical phase of therapy; that is, during the first 10 days or so of inpatient intravenous antibiotic therapy.
“After stabilization, the main reason for staying in the hospital is just to receive IV antibiotics,” Dr. Bundgård noted.
POET included 400 patients with left-sided endocarditis hospitalized at multiple cardiac centers across Denmark, 35% of whom had at least one major comorbid condition. When this reporter observed that this was the smallest study he’d ever seen reported from Denmark, where researchers famously like to utilize interconnected national databases to conduct nationwide observational studies incorporating the country’s entire population, the cardiologist replied, “Denmark is a small country, but we like to make big trials. And this is actually the largest-ever clinical trial in endocarditis, so we are still going big.”
Important to the generalizability of the POET results was the requirement that all 400 participants had to be infected with streptococcus, Staphylococcus aureus, Enterococcus faecalis, or coagulase-negative staphylococci – the major pathogens responsible for three-quarters of all cases of infectious endocarditis.
Once participants were clinically stable after a median of 17 days of intravenous antibiotics, they were randomized to continued in-hospital intravenous antibiotic therapy for a median of another 19 days or to discharge on two oral antibiotics from different classes with different mechanisms of action administered for a median of 17 days, with selection of the oral agents being guided by the results of bacterial susceptibility testing.
The primary outcome was a composite of all-cause mortality, embolic events, unplanned cardiac surgery, and relapse of bacteremia from randomization through 6 months after completion of antibiotic therapy. This occurred in 9.0% of the orally treated group and 12.1% of patients on full-course intravenous therapy for a 28% relative risk reduction, which statistically established the noninferioritiy of the partial oral regimen. The results were similar in patients with native as compared with prosthetic valves, with or without major comorbidities, and in surgically as opposed to conservatively treated patients.
Rates of three of the four components of the composite endpoint were similar in both groups. However, all-cause mortality occurred in 3.5% of the oral therapy group, compared with 6.5% of those on intravenous therapy. Dr. Bundgård said he and his coinvestigators think the disparity in mortality was probably caused by play of chance, although he added that they were struck that four sudden deaths occurred in the intravenous group and none in patients who got oral antibiotics.
Side effects were similarly mild and low frequency in both study arms.
Audience members were eager for details on how the Danish investigators decided patients were clinically stable on intravenous antibiotics and thus ready for randomization, as well as the outpatient follow-up procedures employed in those discharged on oral therapy.
Dr. Bundgård explained that clinical stability required that a patient be afebrile, have C-reactive protein and leukocyte levels less than 35% of their peaks, and needed to have been on intravenous antibiotics for a minimum of 10 days. Moreover, patients who underwent valve surgery during their hospitalization, as did 38% of POET participants, had to wait a minimum of 7 days afterwards before they could be declared clinically stable. Lastly, just prior to randomization all participants underwent transesophageal echocardiography to rule out abscess formation or other valve abnormalities requiring surgery.
Outpatient follow-up required that patients drop in two or three times per week to be checked by a familiar physician or nurse at the hospital ward where they had stayed. Compliance was very good, although it should be noted that only five patients in the POET study were intravenous drug abusers.
Asked why investigators discharged patients on oral therapy rather than on home intravenous antibiotics, Dr. Bundgård explained that home intravenous antibiotic therapy isn’t utilized in Denmark because of the expense and logistic complexity.
Discussant Chris P. Gale, MD, urged care in generalizing the study findings.
“The ‘O’ in POET does not stand for ‘outpatient.’ Outpatients were only selected for oral therapy if they had no heart failure, no emboli, no arrhythmia, no complicating comorbidities, and they were strictly monitored – and frequently. Should we elect to adopt POET into practice, I would recommend strict adherence to the study’s patient selection and monitoring criteria,” said Dr. Gale, a cardiologist at the University of Leeds (England).
The POET results clearly swayed the full-house audience attending the late-breaking Hot Line session in the conference main arena. Immediately before Dr. Bundgård’s presentation, 66% of the audience indicated electronically that they would continue intravenous antibiotics for another 2-4 weeks in a patient with infectious endocarditis who had responded well to 2 weeks of such therapy. After seeing the study results, however, only 19% would still follow that course of action, while 59% of the audience would switch to oral antibiotics and discharge the patient.
Dr. Bundgård reported having no financial conflicts regarding the POET study, which was funded by the Danish Heart Foundation and other research foundations.
Simultaneous with Dr. Bundgård’s presentation in Munich, the POET results were published online by the New England Journal of Medicine (2018 Aug 28. doi: 10.1056/NEJMoa1808312).
MUNICH – Patients with left-sided endocarditis who are clinically stable after a couple weeks of inpatient intravenous antibiotics may at that point become candidates for discharge on oral antibiotics for the remainder of their treatment course, according to the findings of the randomized, multicenter, Danish POET trial.
“Shifting to oral antibiotic treatment in stabilized patients with endocarditis was as effective and safe as continued intravenous antibiotic treatment and was given during half the antibiotic treatment period. These novel findings may have a significant impact on future clinical practice for the management of patients who are stable,” Henning Bundgård, MD, said at the annual congress of the European Society of Cardiology.
Both ESC and American Heart Association/American College of Cardiology guidelines now recommend treatment of infective endocarditis with intravenous antibiotics for up to 6 weeks. Safely cutting the duration of in-hospital intravenous antibiotics in half is likely to generate major cost savings while improving patient quality of life and avoiding prolonged exposure to the iatrogenic risks inherent to the hospital environment, noted Dr. Bundgård, a cardiologist at Copenhagen University Hospital.
The rationale for the POET (Partial Oral Treatment of Endocarditis) trial was the investigators’ recognition that, even though infectious endocarditis is a feared disease with an in-hospital mortality of 15% or more, the great majority of serious complications occur in the early critical phase of therapy; that is, during the first 10 days or so of inpatient intravenous antibiotic therapy.
“After stabilization, the main reason for staying in the hospital is just to receive IV antibiotics,” Dr. Bundgård noted.
POET included 400 patients with left-sided endocarditis hospitalized at multiple cardiac centers across Denmark, 35% of whom had at least one major comorbid condition. When this reporter observed that this was the smallest study he’d ever seen reported from Denmark, where researchers famously like to utilize interconnected national databases to conduct nationwide observational studies incorporating the country’s entire population, the cardiologist replied, “Denmark is a small country, but we like to make big trials. And this is actually the largest-ever clinical trial in endocarditis, so we are still going big.”
Important to the generalizability of the POET results was the requirement that all 400 participants had to be infected with streptococcus, Staphylococcus aureus, Enterococcus faecalis, or coagulase-negative staphylococci – the major pathogens responsible for three-quarters of all cases of infectious endocarditis.
Once participants were clinically stable after a median of 17 days of intravenous antibiotics, they were randomized to continued in-hospital intravenous antibiotic therapy for a median of another 19 days or to discharge on two oral antibiotics from different classes with different mechanisms of action administered for a median of 17 days, with selection of the oral agents being guided by the results of bacterial susceptibility testing.
The primary outcome was a composite of all-cause mortality, embolic events, unplanned cardiac surgery, and relapse of bacteremia from randomization through 6 months after completion of antibiotic therapy. This occurred in 9.0% of the orally treated group and 12.1% of patients on full-course intravenous therapy for a 28% relative risk reduction, which statistically established the noninferioritiy of the partial oral regimen. The results were similar in patients with native as compared with prosthetic valves, with or without major comorbidities, and in surgically as opposed to conservatively treated patients.
Rates of three of the four components of the composite endpoint were similar in both groups. However, all-cause mortality occurred in 3.5% of the oral therapy group, compared with 6.5% of those on intravenous therapy. Dr. Bundgård said he and his coinvestigators think the disparity in mortality was probably caused by play of chance, although he added that they were struck that four sudden deaths occurred in the intravenous group and none in patients who got oral antibiotics.
Side effects were similarly mild and low frequency in both study arms.
Audience members were eager for details on how the Danish investigators decided patients were clinically stable on intravenous antibiotics and thus ready for randomization, as well as the outpatient follow-up procedures employed in those discharged on oral therapy.
Dr. Bundgård explained that clinical stability required that a patient be afebrile, have C-reactive protein and leukocyte levels less than 35% of their peaks, and needed to have been on intravenous antibiotics for a minimum of 10 days. Moreover, patients who underwent valve surgery during their hospitalization, as did 38% of POET participants, had to wait a minimum of 7 days afterwards before they could be declared clinically stable. Lastly, just prior to randomization all participants underwent transesophageal echocardiography to rule out abscess formation or other valve abnormalities requiring surgery.
Outpatient follow-up required that patients drop in two or three times per week to be checked by a familiar physician or nurse at the hospital ward where they had stayed. Compliance was very good, although it should be noted that only five patients in the POET study were intravenous drug abusers.
Asked why investigators discharged patients on oral therapy rather than on home intravenous antibiotics, Dr. Bundgård explained that home intravenous antibiotic therapy isn’t utilized in Denmark because of the expense and logistic complexity.
Discussant Chris P. Gale, MD, urged care in generalizing the study findings.
“The ‘O’ in POET does not stand for ‘outpatient.’ Outpatients were only selected for oral therapy if they had no heart failure, no emboli, no arrhythmia, no complicating comorbidities, and they were strictly monitored – and frequently. Should we elect to adopt POET into practice, I would recommend strict adherence to the study’s patient selection and monitoring criteria,” said Dr. Gale, a cardiologist at the University of Leeds (England).
The POET results clearly swayed the full-house audience attending the late-breaking Hot Line session in the conference main arena. Immediately before Dr. Bundgård’s presentation, 66% of the audience indicated electronically that they would continue intravenous antibiotics for another 2-4 weeks in a patient with infectious endocarditis who had responded well to 2 weeks of such therapy. After seeing the study results, however, only 19% would still follow that course of action, while 59% of the audience would switch to oral antibiotics and discharge the patient.
Dr. Bundgård reported having no financial conflicts regarding the POET study, which was funded by the Danish Heart Foundation and other research foundations.
Simultaneous with Dr. Bundgård’s presentation in Munich, the POET results were published online by the New England Journal of Medicine (2018 Aug 28. doi: 10.1056/NEJMoa1808312).
MUNICH – Patients with left-sided endocarditis who are clinically stable after a couple weeks of inpatient intravenous antibiotics may at that point become candidates for discharge on oral antibiotics for the remainder of their treatment course, according to the findings of the randomized, multicenter, Danish POET trial.
“Shifting to oral antibiotic treatment in stabilized patients with endocarditis was as effective and safe as continued intravenous antibiotic treatment and was given during half the antibiotic treatment period. These novel findings may have a significant impact on future clinical practice for the management of patients who are stable,” Henning Bundgård, MD, said at the annual congress of the European Society of Cardiology.
Both ESC and American Heart Association/American College of Cardiology guidelines now recommend treatment of infective endocarditis with intravenous antibiotics for up to 6 weeks. Safely cutting the duration of in-hospital intravenous antibiotics in half is likely to generate major cost savings while improving patient quality of life and avoiding prolonged exposure to the iatrogenic risks inherent to the hospital environment, noted Dr. Bundgård, a cardiologist at Copenhagen University Hospital.
The rationale for the POET (Partial Oral Treatment of Endocarditis) trial was the investigators’ recognition that, even though infectious endocarditis is a feared disease with an in-hospital mortality of 15% or more, the great majority of serious complications occur in the early critical phase of therapy; that is, during the first 10 days or so of inpatient intravenous antibiotic therapy.
“After stabilization, the main reason for staying in the hospital is just to receive IV antibiotics,” Dr. Bundgård noted.
POET included 400 patients with left-sided endocarditis hospitalized at multiple cardiac centers across Denmark, 35% of whom had at least one major comorbid condition. When this reporter observed that this was the smallest study he’d ever seen reported from Denmark, where researchers famously like to utilize interconnected national databases to conduct nationwide observational studies incorporating the country’s entire population, the cardiologist replied, “Denmark is a small country, but we like to make big trials. And this is actually the largest-ever clinical trial in endocarditis, so we are still going big.”
Important to the generalizability of the POET results was the requirement that all 400 participants had to be infected with streptococcus, Staphylococcus aureus, Enterococcus faecalis, or coagulase-negative staphylococci – the major pathogens responsible for three-quarters of all cases of infectious endocarditis.
Once participants were clinically stable after a median of 17 days of intravenous antibiotics, they were randomized to continued in-hospital intravenous antibiotic therapy for a median of another 19 days or to discharge on two oral antibiotics from different classes with different mechanisms of action administered for a median of 17 days, with selection of the oral agents being guided by the results of bacterial susceptibility testing.
The primary outcome was a composite of all-cause mortality, embolic events, unplanned cardiac surgery, and relapse of bacteremia from randomization through 6 months after completion of antibiotic therapy. This occurred in 9.0% of the orally treated group and 12.1% of patients on full-course intravenous therapy for a 28% relative risk reduction, which statistically established the noninferioritiy of the partial oral regimen. The results were similar in patients with native as compared with prosthetic valves, with or without major comorbidities, and in surgically as opposed to conservatively treated patients.
Rates of three of the four components of the composite endpoint were similar in both groups. However, all-cause mortality occurred in 3.5% of the oral therapy group, compared with 6.5% of those on intravenous therapy. Dr. Bundgård said he and his coinvestigators think the disparity in mortality was probably caused by play of chance, although he added that they were struck that four sudden deaths occurred in the intravenous group and none in patients who got oral antibiotics.
Side effects were similarly mild and low frequency in both study arms.
Audience members were eager for details on how the Danish investigators decided patients were clinically stable on intravenous antibiotics and thus ready for randomization, as well as the outpatient follow-up procedures employed in those discharged on oral therapy.
Dr. Bundgård explained that clinical stability required that a patient be afebrile, have C-reactive protein and leukocyte levels less than 35% of their peaks, and needed to have been on intravenous antibiotics for a minimum of 10 days. Moreover, patients who underwent valve surgery during their hospitalization, as did 38% of POET participants, had to wait a minimum of 7 days afterwards before they could be declared clinically stable. Lastly, just prior to randomization all participants underwent transesophageal echocardiography to rule out abscess formation or other valve abnormalities requiring surgery.
Outpatient follow-up required that patients drop in two or three times per week to be checked by a familiar physician or nurse at the hospital ward where they had stayed. Compliance was very good, although it should be noted that only five patients in the POET study were intravenous drug abusers.
Asked why investigators discharged patients on oral therapy rather than on home intravenous antibiotics, Dr. Bundgård explained that home intravenous antibiotic therapy isn’t utilized in Denmark because of the expense and logistic complexity.
Discussant Chris P. Gale, MD, urged care in generalizing the study findings.
“The ‘O’ in POET does not stand for ‘outpatient.’ Outpatients were only selected for oral therapy if they had no heart failure, no emboli, no arrhythmia, no complicating comorbidities, and they were strictly monitored – and frequently. Should we elect to adopt POET into practice, I would recommend strict adherence to the study’s patient selection and monitoring criteria,” said Dr. Gale, a cardiologist at the University of Leeds (England).
The POET results clearly swayed the full-house audience attending the late-breaking Hot Line session in the conference main arena. Immediately before Dr. Bundgård’s presentation, 66% of the audience indicated electronically that they would continue intravenous antibiotics for another 2-4 weeks in a patient with infectious endocarditis who had responded well to 2 weeks of such therapy. After seeing the study results, however, only 19% would still follow that course of action, while 59% of the audience would switch to oral antibiotics and discharge the patient.
Dr. Bundgård reported having no financial conflicts regarding the POET study, which was funded by the Danish Heart Foundation and other research foundations.
Simultaneous with Dr. Bundgård’s presentation in Munich, the POET results were published online by the New England Journal of Medicine (2018 Aug 28. doi: 10.1056/NEJMoa1808312).
REPORTING FROM THE ESC CONGRESS 2018
Key clinical point: Clinically stable patients with left-sided infectious endocarditis can safely and effectively be discharged on oral antibiotics after completing half of a full course of intravenous antibiotics.
Major finding: Key 6-month outcomes were similar in patients with left-sided infectious endocarditis regardless of whether they were discharged early on carefully selected oral antibiotics or remained in hospital to complete a full course of intravenous antibiotics.
Study details: This prospective, multicenter, Danish randomized trial included 400 patients with left-sided infectious endocarditis.
Disclosures: The presenter reported having no financial conflicts regarding the POET study, which was funded by the Danish Heart Foundation and other research foundations.
Factor Xa inhibitors versus vitamin K antagonists for preventing embolism in AF patients
Clinical question: Do factor Xa inhibitors reduce the incidence of strokes and systemic embolic events, compared with warfarin, in people with atrial fibrillation?
Background: Factor Xa inhibitors, called DOACs or direct-acting anticoagulants, and vitamin K antagonists (VKAs) are part of treatment guidelines for preventing stroke and systemic embolic events in people with atrial fibrillation (AF). This study assessed the effectiveness and safety of treatment with factor Xa inhibitors versus VKAs for preventing cerebral or systemic embolic events in AF.
Study design: Cochrane Review update.
Setting: Data obtained from trial registers of the Cochrane Central Register of Controlled Trials (August 2017), the Cochrane Heart Group and the Cochrane Stroke Group (September 2016), Embase (1980 to April 2017), and MEDLINE (1950 to April 2017). Authors also screened reference lists and contacted pharmaceutical companies, authors, and sponsors of relevant published trials.
Synopsis: The study included 42,084 participants from 10 trials with a diagnosis of AF who were eligible for long-term anticoagulation with warfarin (target INR 2-3).
The trials directly compared dose-adjusted warfarin with factor Xa inhibitors. Median follow-up ranged from 12 weeks to 1.9 years, and composite primary endpoint was all strokes (both ischemic and hemorrhagic) and non–central nervous systemic embolic events. Factor Xa inhibitor significantly decreased the number of strokes and systemic embolic events, compared with dose-adjusted warfarin (odds ratio, 0.81; 95% confidence interval, 0.72-0.91), reduced the number of major bleeding events (OR, 0.92; 95% CI, 0.63-1.34), and significantly reduced the risk of intracranial hemorrhage (OR, 0.56; 95% CI, 0.45-0.70). They also significantly reduced the number of all-cause deaths (OR, 0.88; 95% CI, 0.81-0.97). One limitation of this study is the heterogeneity and hence lower quality of evidence. This study shows a small net clinical benefit of using factor Xa inhibitors in AF because of a reduction in strokes and systemic embolic events and also a lower risk of bleeding (including intracranial hemorrhages), compared with using warfarin.
Bottom line: Patients with AF have a lower incidence of strokes and systemic embolic events when treated with factor Xa inhibitors, compared with those treated with warfarin.
Citation: Bruins Slot KM et al. Factor Xa inhibitors versus vitamin K antagonists for preventing cerebral or systemic embolism in patients with atrial fibrillation. Cochrane Database Syst Rev. 2018 Mar 6. doi: 10.1002/14651858.CD008980.pub3.
Dr. Veedu is a hospitalist and instructor in the division of hospital medicine at the University of Kentucky, Lexington.
Clinical question: Do factor Xa inhibitors reduce the incidence of strokes and systemic embolic events, compared with warfarin, in people with atrial fibrillation?
Background: Factor Xa inhibitors, called DOACs or direct-acting anticoagulants, and vitamin K antagonists (VKAs) are part of treatment guidelines for preventing stroke and systemic embolic events in people with atrial fibrillation (AF). This study assessed the effectiveness and safety of treatment with factor Xa inhibitors versus VKAs for preventing cerebral or systemic embolic events in AF.
Study design: Cochrane Review update.
Setting: Data obtained from trial registers of the Cochrane Central Register of Controlled Trials (August 2017), the Cochrane Heart Group and the Cochrane Stroke Group (September 2016), Embase (1980 to April 2017), and MEDLINE (1950 to April 2017). Authors also screened reference lists and contacted pharmaceutical companies, authors, and sponsors of relevant published trials.
Synopsis: The study included 42,084 participants from 10 trials with a diagnosis of AF who were eligible for long-term anticoagulation with warfarin (target INR 2-3).
The trials directly compared dose-adjusted warfarin with factor Xa inhibitors. Median follow-up ranged from 12 weeks to 1.9 years, and composite primary endpoint was all strokes (both ischemic and hemorrhagic) and non–central nervous systemic embolic events. Factor Xa inhibitor significantly decreased the number of strokes and systemic embolic events, compared with dose-adjusted warfarin (odds ratio, 0.81; 95% confidence interval, 0.72-0.91), reduced the number of major bleeding events (OR, 0.92; 95% CI, 0.63-1.34), and significantly reduced the risk of intracranial hemorrhage (OR, 0.56; 95% CI, 0.45-0.70). They also significantly reduced the number of all-cause deaths (OR, 0.88; 95% CI, 0.81-0.97). One limitation of this study is the heterogeneity and hence lower quality of evidence. This study shows a small net clinical benefit of using factor Xa inhibitors in AF because of a reduction in strokes and systemic embolic events and also a lower risk of bleeding (including intracranial hemorrhages), compared with using warfarin.
Bottom line: Patients with AF have a lower incidence of strokes and systemic embolic events when treated with factor Xa inhibitors, compared with those treated with warfarin.
Citation: Bruins Slot KM et al. Factor Xa inhibitors versus vitamin K antagonists for preventing cerebral or systemic embolism in patients with atrial fibrillation. Cochrane Database Syst Rev. 2018 Mar 6. doi: 10.1002/14651858.CD008980.pub3.
Dr. Veedu is a hospitalist and instructor in the division of hospital medicine at the University of Kentucky, Lexington.
Clinical question: Do factor Xa inhibitors reduce the incidence of strokes and systemic embolic events, compared with warfarin, in people with atrial fibrillation?
Background: Factor Xa inhibitors, called DOACs or direct-acting anticoagulants, and vitamin K antagonists (VKAs) are part of treatment guidelines for preventing stroke and systemic embolic events in people with atrial fibrillation (AF). This study assessed the effectiveness and safety of treatment with factor Xa inhibitors versus VKAs for preventing cerebral or systemic embolic events in AF.
Study design: Cochrane Review update.
Setting: Data obtained from trial registers of the Cochrane Central Register of Controlled Trials (August 2017), the Cochrane Heart Group and the Cochrane Stroke Group (September 2016), Embase (1980 to April 2017), and MEDLINE (1950 to April 2017). Authors also screened reference lists and contacted pharmaceutical companies, authors, and sponsors of relevant published trials.
Synopsis: The study included 42,084 participants from 10 trials with a diagnosis of AF who were eligible for long-term anticoagulation with warfarin (target INR 2-3).
The trials directly compared dose-adjusted warfarin with factor Xa inhibitors. Median follow-up ranged from 12 weeks to 1.9 years, and composite primary endpoint was all strokes (both ischemic and hemorrhagic) and non–central nervous systemic embolic events. Factor Xa inhibitor significantly decreased the number of strokes and systemic embolic events, compared with dose-adjusted warfarin (odds ratio, 0.81; 95% confidence interval, 0.72-0.91), reduced the number of major bleeding events (OR, 0.92; 95% CI, 0.63-1.34), and significantly reduced the risk of intracranial hemorrhage (OR, 0.56; 95% CI, 0.45-0.70). They also significantly reduced the number of all-cause deaths (OR, 0.88; 95% CI, 0.81-0.97). One limitation of this study is the heterogeneity and hence lower quality of evidence. This study shows a small net clinical benefit of using factor Xa inhibitors in AF because of a reduction in strokes and systemic embolic events and also a lower risk of bleeding (including intracranial hemorrhages), compared with using warfarin.
Bottom line: Patients with AF have a lower incidence of strokes and systemic embolic events when treated with factor Xa inhibitors, compared with those treated with warfarin.
Citation: Bruins Slot KM et al. Factor Xa inhibitors versus vitamin K antagonists for preventing cerebral or systemic embolism in patients with atrial fibrillation. Cochrane Database Syst Rev. 2018 Mar 6. doi: 10.1002/14651858.CD008980.pub3.
Dr. Veedu is a hospitalist and instructor in the division of hospital medicine at the University of Kentucky, Lexington.
How to handle anorexia in community hospitals
Food is nonnegotiable
ATLANTA – Everyone has to be on the same page when it comes to anorexia nervosa in a community hospital, according to pediatric hospitalists at Moses H. Cone Memorial Hospital in Greensboro, N.C.
Anorexia cases used to be rare there. When one came in, “everyone was anxious because we just didn’t know quite what to do,” said Suresh Nagappan, MD, a pediatrician and member of the teaching faculty at the hospital. Parents would hear one thing from one provider, something else from the next, and leave angry and confused. “Basically, it was a mess. We needed to standardize it,” he added.
So Dr. Nagappan and his colleagues created guidelines for treating patients with eating disorders about 3 years ago. “It was meeting after meeting for months, but well worth it,” he said at Pediatric Hospital Medicine.
Word of the hospital’s newfound expertise in anorexia has spread since then, and now it’s not unusual for Moses H. Cone to handle a few cases a week.
The pediatric hospitalist team has come to realize that, first and foremost, patients and families need to know why they are there; it’s about medical stabilization, not treating the eating disorder. That comes after discharge. Families need help sometimes to understand that it’s not a quick fix.
To make things clear, there’s strict criteria now for admission, based on American Academy of Pediatrics guidance. The main trigger is being under 75% of ideal body weight, but patients must also have systolic blood pressure below 90 mm Hg and other worrisome signs. “Sometimes, it feels like we’re splitting hairs” on who gets admitted, “but if we don’t have strict criteria on admission, we don’t have an end goal for discharge,” said pediatrician Maggie S. Hall, MD, also on the Moses H. Cone teaching faculty.
As for treatment, “food is medicine, and it’s not negotiable. We make that clear to everyone on day 1. If patients don’t eat their actual meal, they have 20 minutes to drink a supplement. If they can’t do that, they get a nasogastric tube,” Dr. Nagappan said. The tube is pulled after each meal, so that it remains an incentive to eat.
The team start patients with 1,600 calories a day and increase the intake by 200-250 calories a day. The goal is for a patient to gain 100-200 grams per day. Patients pick out what they want to eat with the help of a dietitian. When meals set off overwhelming anxiety, the Moses H. Cone team has learned that benzodiazepines can help.
Ironically, the initiation of regular meals is the most dangerous time for patients. As anorexic bodies switch from catabolic to anabolic metabolism, electrolytes can drop to dangerously low levels, causing arrhythmias, heart failure, and death. In general, “the reason these kids die is cardiac,” Dr. Nagappan said at the meeting, sponsored by the Society of Hospital Medicine, the AAP, and the Academic Pediatric Association.
Refeeding syndrome, as it’s known, is clinically significant in perhaps 6% of patients. The risk goes up if they are below 70% of their ideal body weight; have a prolonged QTc interval; or begin treatment with low phosphorous, magnesium, or potassium.
To counter the threat, electrolytes are measured twice a day at Moses H. Cone during the first week of treatment, and ECGs are taken daily for the first few days. “One thing to be really careful about is when you notice their heart rate beginning to creep up during rest. That can be a sign of developing cardiomyopathy; it’s an indication for us to get echocardiograms,” Dr. Hall said.
The Moses H. Cone team like to include families in meal times – it’s been shown to help – but family members need to be coached beforehand. They can’t be punitive. Mealtime talk has to be positive, and can’t focus on eating. Parents often need help handling their own anger and guilt before trying to eat with their child. Progress has to be monitored, but Dr. Nagappan cautioned that “you have to be really careful about how you get weights”; it should always be in the morning after the first void. Urine needs to be checked to make sure patients aren’t water loading.
Staff should be neutral about weight results, and keep them to themselves. Even something as benign as “good job” can be a problem. “You don’t want these patients focused on their weight. You want them focused on getting better and eating and taking it step by step,” he said.
The presenters had no disclosures to report.
Food is nonnegotiable
Food is nonnegotiable
ATLANTA – Everyone has to be on the same page when it comes to anorexia nervosa in a community hospital, according to pediatric hospitalists at Moses H. Cone Memorial Hospital in Greensboro, N.C.
Anorexia cases used to be rare there. When one came in, “everyone was anxious because we just didn’t know quite what to do,” said Suresh Nagappan, MD, a pediatrician and member of the teaching faculty at the hospital. Parents would hear one thing from one provider, something else from the next, and leave angry and confused. “Basically, it was a mess. We needed to standardize it,” he added.
So Dr. Nagappan and his colleagues created guidelines for treating patients with eating disorders about 3 years ago. “It was meeting after meeting for months, but well worth it,” he said at Pediatric Hospital Medicine.
Word of the hospital’s newfound expertise in anorexia has spread since then, and now it’s not unusual for Moses H. Cone to handle a few cases a week.
The pediatric hospitalist team has come to realize that, first and foremost, patients and families need to know why they are there; it’s about medical stabilization, not treating the eating disorder. That comes after discharge. Families need help sometimes to understand that it’s not a quick fix.
To make things clear, there’s strict criteria now for admission, based on American Academy of Pediatrics guidance. The main trigger is being under 75% of ideal body weight, but patients must also have systolic blood pressure below 90 mm Hg and other worrisome signs. “Sometimes, it feels like we’re splitting hairs” on who gets admitted, “but if we don’t have strict criteria on admission, we don’t have an end goal for discharge,” said pediatrician Maggie S. Hall, MD, also on the Moses H. Cone teaching faculty.
As for treatment, “food is medicine, and it’s not negotiable. We make that clear to everyone on day 1. If patients don’t eat their actual meal, they have 20 minutes to drink a supplement. If they can’t do that, they get a nasogastric tube,” Dr. Nagappan said. The tube is pulled after each meal, so that it remains an incentive to eat.
The team start patients with 1,600 calories a day and increase the intake by 200-250 calories a day. The goal is for a patient to gain 100-200 grams per day. Patients pick out what they want to eat with the help of a dietitian. When meals set off overwhelming anxiety, the Moses H. Cone team has learned that benzodiazepines can help.
Ironically, the initiation of regular meals is the most dangerous time for patients. As anorexic bodies switch from catabolic to anabolic metabolism, electrolytes can drop to dangerously low levels, causing arrhythmias, heart failure, and death. In general, “the reason these kids die is cardiac,” Dr. Nagappan said at the meeting, sponsored by the Society of Hospital Medicine, the AAP, and the Academic Pediatric Association.
Refeeding syndrome, as it’s known, is clinically significant in perhaps 6% of patients. The risk goes up if they are below 70% of their ideal body weight; have a prolonged QTc interval; or begin treatment with low phosphorous, magnesium, or potassium.
To counter the threat, electrolytes are measured twice a day at Moses H. Cone during the first week of treatment, and ECGs are taken daily for the first few days. “One thing to be really careful about is when you notice their heart rate beginning to creep up during rest. That can be a sign of developing cardiomyopathy; it’s an indication for us to get echocardiograms,” Dr. Hall said.
The Moses H. Cone team like to include families in meal times – it’s been shown to help – but family members need to be coached beforehand. They can’t be punitive. Mealtime talk has to be positive, and can’t focus on eating. Parents often need help handling their own anger and guilt before trying to eat with their child. Progress has to be monitored, but Dr. Nagappan cautioned that “you have to be really careful about how you get weights”; it should always be in the morning after the first void. Urine needs to be checked to make sure patients aren’t water loading.
Staff should be neutral about weight results, and keep them to themselves. Even something as benign as “good job” can be a problem. “You don’t want these patients focused on their weight. You want them focused on getting better and eating and taking it step by step,” he said.
The presenters had no disclosures to report.
ATLANTA – Everyone has to be on the same page when it comes to anorexia nervosa in a community hospital, according to pediatric hospitalists at Moses H. Cone Memorial Hospital in Greensboro, N.C.
Anorexia cases used to be rare there. When one came in, “everyone was anxious because we just didn’t know quite what to do,” said Suresh Nagappan, MD, a pediatrician and member of the teaching faculty at the hospital. Parents would hear one thing from one provider, something else from the next, and leave angry and confused. “Basically, it was a mess. We needed to standardize it,” he added.
So Dr. Nagappan and his colleagues created guidelines for treating patients with eating disorders about 3 years ago. “It was meeting after meeting for months, but well worth it,” he said at Pediatric Hospital Medicine.
Word of the hospital’s newfound expertise in anorexia has spread since then, and now it’s not unusual for Moses H. Cone to handle a few cases a week.
The pediatric hospitalist team has come to realize that, first and foremost, patients and families need to know why they are there; it’s about medical stabilization, not treating the eating disorder. That comes after discharge. Families need help sometimes to understand that it’s not a quick fix.
To make things clear, there’s strict criteria now for admission, based on American Academy of Pediatrics guidance. The main trigger is being under 75% of ideal body weight, but patients must also have systolic blood pressure below 90 mm Hg and other worrisome signs. “Sometimes, it feels like we’re splitting hairs” on who gets admitted, “but if we don’t have strict criteria on admission, we don’t have an end goal for discharge,” said pediatrician Maggie S. Hall, MD, also on the Moses H. Cone teaching faculty.
As for treatment, “food is medicine, and it’s not negotiable. We make that clear to everyone on day 1. If patients don’t eat their actual meal, they have 20 minutes to drink a supplement. If they can’t do that, they get a nasogastric tube,” Dr. Nagappan said. The tube is pulled after each meal, so that it remains an incentive to eat.
The team start patients with 1,600 calories a day and increase the intake by 200-250 calories a day. The goal is for a patient to gain 100-200 grams per day. Patients pick out what they want to eat with the help of a dietitian. When meals set off overwhelming anxiety, the Moses H. Cone team has learned that benzodiazepines can help.
Ironically, the initiation of regular meals is the most dangerous time for patients. As anorexic bodies switch from catabolic to anabolic metabolism, electrolytes can drop to dangerously low levels, causing arrhythmias, heart failure, and death. In general, “the reason these kids die is cardiac,” Dr. Nagappan said at the meeting, sponsored by the Society of Hospital Medicine, the AAP, and the Academic Pediatric Association.
Refeeding syndrome, as it’s known, is clinically significant in perhaps 6% of patients. The risk goes up if they are below 70% of their ideal body weight; have a prolonged QTc interval; or begin treatment with low phosphorous, magnesium, or potassium.
To counter the threat, electrolytes are measured twice a day at Moses H. Cone during the first week of treatment, and ECGs are taken daily for the first few days. “One thing to be really careful about is when you notice their heart rate beginning to creep up during rest. That can be a sign of developing cardiomyopathy; it’s an indication for us to get echocardiograms,” Dr. Hall said.
The Moses H. Cone team like to include families in meal times – it’s been shown to help – but family members need to be coached beforehand. They can’t be punitive. Mealtime talk has to be positive, and can’t focus on eating. Parents often need help handling their own anger and guilt before trying to eat with their child. Progress has to be monitored, but Dr. Nagappan cautioned that “you have to be really careful about how you get weights”; it should always be in the morning after the first void. Urine needs to be checked to make sure patients aren’t water loading.
Staff should be neutral about weight results, and keep them to themselves. Even something as benign as “good job” can be a problem. “You don’t want these patients focused on their weight. You want them focused on getting better and eating and taking it step by step,” he said.
The presenters had no disclosures to report.
EXPERT ANALYSIS FROM PHM 2018
Short Takes
Digoxin and mortality in atrial fibrillation
Using propensity score-matched controls, post hoc subgroup analysis of the ARISTOTLE trial showed an independent dose-dependent association between serum digoxin levels and mortality in those receiving digoxin, with a 19% higher adjusted hazard of death for each increase of 0.5 ng/mL (P = .001). For those initiating digoxin there was an independent association with higher mortality, regardless of heart failure (adjusted hazard ratio, 1.78; 95% confidence interval, 1.37-2.31; P less than .0001).
Citation: Lopes RD et al. Digoxin and mortality in patients with atrial fibrillation. J Am Coll Cardiol. 2018 Mar 13;71(10):1063-74.
ED opioid overdoses
Prior studies have shown a recent increase in opioid overdose-related deaths, and this analysis of 136 million ED visits in 45 states showed a continued upward trend from July 2016 to September 2017 with average increases of 5.6% per quarter in all regions and across all demographic groups, but this increase was especially pronounced in urban areas. The authors of this analysis called for the medical community to use these data to educate providers and organize resources for the rapidly evolving opioid epidemic.
Citation: Vivolo-Kantor AM et al. Vital signs: Trends in emergency department visits for suspected opioid overdoses - United States, July 2016-September 2017. MMWR Morb Mortal Wkly Rep. 2018;67:279-85.
Routine oxygen therapy in patients with acute MI with normal oxygen saturation levels has no benefit
A large meta-analysis showed no decrease in all-cause mortality, recurrent ischemia, or myocardial infarction, heart failure, and arrhythmia from using routine oxygen therapy in patients with acute myocardial infarction with normal oxygen saturation levels. This meta-analysis confirmed prior studies and supported the changing trend in recommendations to avoid supplemental oxygen in patients with peripheral oxygen saturations greater than 90%.
Citation: Abuzaid A et al. Oxygen therapy in patients with acute myocardial infarction: A systemic review and meta-analysis. Am J Med. 2018 Jun;131(6):693-701.
Predicting hospitalization for acute kidney injury
Data from the 2000-2014 National Inpatient Sample and National Health Interview Surveys indicated that people with diabetes are nearly four times more likely to have acute kidney injury-related hospitalization than are people without. The analysis may have limitations for multiple admissions being counted several times, underestimation of prevalence of acute kidney injury, increased awareness regarding acute kidney injury, and unknown effects of type and duration of diabetes.
Citation: Pavkov ME et al. Trends in hospitalization of acute kidney injury - United States, 2000-2014. MMWR. 2018 Mar 16;67(10):289-93.
Digoxin and mortality in atrial fibrillation
Using propensity score-matched controls, post hoc subgroup analysis of the ARISTOTLE trial showed an independent dose-dependent association between serum digoxin levels and mortality in those receiving digoxin, with a 19% higher adjusted hazard of death for each increase of 0.5 ng/mL (P = .001). For those initiating digoxin there was an independent association with higher mortality, regardless of heart failure (adjusted hazard ratio, 1.78; 95% confidence interval, 1.37-2.31; P less than .0001).
Citation: Lopes RD et al. Digoxin and mortality in patients with atrial fibrillation. J Am Coll Cardiol. 2018 Mar 13;71(10):1063-74.
ED opioid overdoses
Prior studies have shown a recent increase in opioid overdose-related deaths, and this analysis of 136 million ED visits in 45 states showed a continued upward trend from July 2016 to September 2017 with average increases of 5.6% per quarter in all regions and across all demographic groups, but this increase was especially pronounced in urban areas. The authors of this analysis called for the medical community to use these data to educate providers and organize resources for the rapidly evolving opioid epidemic.
Citation: Vivolo-Kantor AM et al. Vital signs: Trends in emergency department visits for suspected opioid overdoses - United States, July 2016-September 2017. MMWR Morb Mortal Wkly Rep. 2018;67:279-85.
Routine oxygen therapy in patients with acute MI with normal oxygen saturation levels has no benefit
A large meta-analysis showed no decrease in all-cause mortality, recurrent ischemia, or myocardial infarction, heart failure, and arrhythmia from using routine oxygen therapy in patients with acute myocardial infarction with normal oxygen saturation levels. This meta-analysis confirmed prior studies and supported the changing trend in recommendations to avoid supplemental oxygen in patients with peripheral oxygen saturations greater than 90%.
Citation: Abuzaid A et al. Oxygen therapy in patients with acute myocardial infarction: A systemic review and meta-analysis. Am J Med. 2018 Jun;131(6):693-701.
Predicting hospitalization for acute kidney injury
Data from the 2000-2014 National Inpatient Sample and National Health Interview Surveys indicated that people with diabetes are nearly four times more likely to have acute kidney injury-related hospitalization than are people without. The analysis may have limitations for multiple admissions being counted several times, underestimation of prevalence of acute kidney injury, increased awareness regarding acute kidney injury, and unknown effects of type and duration of diabetes.
Citation: Pavkov ME et al. Trends in hospitalization of acute kidney injury - United States, 2000-2014. MMWR. 2018 Mar 16;67(10):289-93.
Digoxin and mortality in atrial fibrillation
Using propensity score-matched controls, post hoc subgroup analysis of the ARISTOTLE trial showed an independent dose-dependent association between serum digoxin levels and mortality in those receiving digoxin, with a 19% higher adjusted hazard of death for each increase of 0.5 ng/mL (P = .001). For those initiating digoxin there was an independent association with higher mortality, regardless of heart failure (adjusted hazard ratio, 1.78; 95% confidence interval, 1.37-2.31; P less than .0001).
Citation: Lopes RD et al. Digoxin and mortality in patients with atrial fibrillation. J Am Coll Cardiol. 2018 Mar 13;71(10):1063-74.
ED opioid overdoses
Prior studies have shown a recent increase in opioid overdose-related deaths, and this analysis of 136 million ED visits in 45 states showed a continued upward trend from July 2016 to September 2017 with average increases of 5.6% per quarter in all regions and across all demographic groups, but this increase was especially pronounced in urban areas. The authors of this analysis called for the medical community to use these data to educate providers and organize resources for the rapidly evolving opioid epidemic.
Citation: Vivolo-Kantor AM et al. Vital signs: Trends in emergency department visits for suspected opioid overdoses - United States, July 2016-September 2017. MMWR Morb Mortal Wkly Rep. 2018;67:279-85.
Routine oxygen therapy in patients with acute MI with normal oxygen saturation levels has no benefit
A large meta-analysis showed no decrease in all-cause mortality, recurrent ischemia, or myocardial infarction, heart failure, and arrhythmia from using routine oxygen therapy in patients with acute myocardial infarction with normal oxygen saturation levels. This meta-analysis confirmed prior studies and supported the changing trend in recommendations to avoid supplemental oxygen in patients with peripheral oxygen saturations greater than 90%.
Citation: Abuzaid A et al. Oxygen therapy in patients with acute myocardial infarction: A systemic review and meta-analysis. Am J Med. 2018 Jun;131(6):693-701.
Predicting hospitalization for acute kidney injury
Data from the 2000-2014 National Inpatient Sample and National Health Interview Surveys indicated that people with diabetes are nearly four times more likely to have acute kidney injury-related hospitalization than are people without. The analysis may have limitations for multiple admissions being counted several times, underestimation of prevalence of acute kidney injury, increased awareness regarding acute kidney injury, and unknown effects of type and duration of diabetes.
Citation: Pavkov ME et al. Trends in hospitalization of acute kidney injury - United States, 2000-2014. MMWR. 2018 Mar 16;67(10):289-93.
A new antiemetic
Clinical question: Can aromatherapy with isopropyl alcohol confer an adjunctive and lasting benefit as an antiemetic in ED patients who do not otherwise need IV access?
Background: Prior studies have shown a benefit of aromatherapy with isopropyl alcohol for postoperative nausea and vomiting, and it is both widely available and safe. Only one randomized, controlled study exists documenting use of aromatherapy with isopropyl alcohol in the ED, but this monitored for effects for only 10 minutes and did not compare it with other antiemetic therapies used in the emergency department.
Study design: Randomized, double-blinded, placebo-controlled trial.
Setting: Single urban tertiary care center emergency department.
Synopsis: The study separated 120 patients with nausea who did not otherwise need intravenous access into three treatment groups. They were assessed for improvement in nausea using a visual analog scale 30 minutes after administration of either oral ondansetron 4 mg and inhaled isopropyl alcohol, oral placebo and inhaled isopropyl alcohol, or oral ondansetron and inhaled saline. The mean decrease in nausea visual analog scale score was 30 mm (95% confidence interval, 22-37 mm), 32 mm (95% CI, 25-39 mm), and 9 mm (95% CI, 5-14 mm), respectively. The need for rescue antiemetics was 27.5%, 25%, and 45%, respectively. This study is limited by its small size, its relatively healthy population with a predominant diagnosis of gastroenteritis, and that patients who required IV catheters were excluded; therefore, it may not be generalizable to sicker patients with alternative etiologies for nausea. Furthermore, many patients were able to distinguish isopropyl alcohol from placebo inhalant by smell so the blinding was possibly ineffective. However, since isopropyl alcohol is low risk, inexpensive, and readily available, it may be reasonable to consider this as a therapeutic option for some patients.
Bottom line: In ED patients who did not otherwise need intravenous access, aromatherapy with inhaled isopropyl alcohol alone or with ondansetron was superior for nausea relief when compared with ondansetron alone.
Citation: April MD et al. Aromatherapy versus oral ondansetron for antiemetic therapy among adult emergency department patients: A randomized controlled trial. Ann Emerg Med. 2018 Feb 17. doi: 10.1016/j.annemergmed.2018.01.016.
Dr. Sayers is an assistant professor in the division of hospital medicine at the University of Kentucky, Lexington.
Clinical question: Can aromatherapy with isopropyl alcohol confer an adjunctive and lasting benefit as an antiemetic in ED patients who do not otherwise need IV access?
Background: Prior studies have shown a benefit of aromatherapy with isopropyl alcohol for postoperative nausea and vomiting, and it is both widely available and safe. Only one randomized, controlled study exists documenting use of aromatherapy with isopropyl alcohol in the ED, but this monitored for effects for only 10 minutes and did not compare it with other antiemetic therapies used in the emergency department.
Study design: Randomized, double-blinded, placebo-controlled trial.
Setting: Single urban tertiary care center emergency department.
Synopsis: The study separated 120 patients with nausea who did not otherwise need intravenous access into three treatment groups. They were assessed for improvement in nausea using a visual analog scale 30 minutes after administration of either oral ondansetron 4 mg and inhaled isopropyl alcohol, oral placebo and inhaled isopropyl alcohol, or oral ondansetron and inhaled saline. The mean decrease in nausea visual analog scale score was 30 mm (95% confidence interval, 22-37 mm), 32 mm (95% CI, 25-39 mm), and 9 mm (95% CI, 5-14 mm), respectively. The need for rescue antiemetics was 27.5%, 25%, and 45%, respectively. This study is limited by its small size, its relatively healthy population with a predominant diagnosis of gastroenteritis, and that patients who required IV catheters were excluded; therefore, it may not be generalizable to sicker patients with alternative etiologies for nausea. Furthermore, many patients were able to distinguish isopropyl alcohol from placebo inhalant by smell so the blinding was possibly ineffective. However, since isopropyl alcohol is low risk, inexpensive, and readily available, it may be reasonable to consider this as a therapeutic option for some patients.
Bottom line: In ED patients who did not otherwise need intravenous access, aromatherapy with inhaled isopropyl alcohol alone or with ondansetron was superior for nausea relief when compared with ondansetron alone.
Citation: April MD et al. Aromatherapy versus oral ondansetron for antiemetic therapy among adult emergency department patients: A randomized controlled trial. Ann Emerg Med. 2018 Feb 17. doi: 10.1016/j.annemergmed.2018.01.016.
Dr. Sayers is an assistant professor in the division of hospital medicine at the University of Kentucky, Lexington.
Clinical question: Can aromatherapy with isopropyl alcohol confer an adjunctive and lasting benefit as an antiemetic in ED patients who do not otherwise need IV access?
Background: Prior studies have shown a benefit of aromatherapy with isopropyl alcohol for postoperative nausea and vomiting, and it is both widely available and safe. Only one randomized, controlled study exists documenting use of aromatherapy with isopropyl alcohol in the ED, but this monitored for effects for only 10 minutes and did not compare it with other antiemetic therapies used in the emergency department.
Study design: Randomized, double-blinded, placebo-controlled trial.
Setting: Single urban tertiary care center emergency department.
Synopsis: The study separated 120 patients with nausea who did not otherwise need intravenous access into three treatment groups. They were assessed for improvement in nausea using a visual analog scale 30 minutes after administration of either oral ondansetron 4 mg and inhaled isopropyl alcohol, oral placebo and inhaled isopropyl alcohol, or oral ondansetron and inhaled saline. The mean decrease in nausea visual analog scale score was 30 mm (95% confidence interval, 22-37 mm), 32 mm (95% CI, 25-39 mm), and 9 mm (95% CI, 5-14 mm), respectively. The need for rescue antiemetics was 27.5%, 25%, and 45%, respectively. This study is limited by its small size, its relatively healthy population with a predominant diagnosis of gastroenteritis, and that patients who required IV catheters were excluded; therefore, it may not be generalizable to sicker patients with alternative etiologies for nausea. Furthermore, many patients were able to distinguish isopropyl alcohol from placebo inhalant by smell so the blinding was possibly ineffective. However, since isopropyl alcohol is low risk, inexpensive, and readily available, it may be reasonable to consider this as a therapeutic option for some patients.
Bottom line: In ED patients who did not otherwise need intravenous access, aromatherapy with inhaled isopropyl alcohol alone or with ondansetron was superior for nausea relief when compared with ondansetron alone.
Citation: April MD et al. Aromatherapy versus oral ondansetron for antiemetic therapy among adult emergency department patients: A randomized controlled trial. Ann Emerg Med. 2018 Feb 17. doi: 10.1016/j.annemergmed.2018.01.016.
Dr. Sayers is an assistant professor in the division of hospital medicine at the University of Kentucky, Lexington.
Acute biliary pancreatitis linked to poor outcomes in elderly
Mortality was almost three times as high in elderly patients after stringent matching for confounding variables, wrote researcher Kishan Patel, MD, of the Ohio State University, Columbus, and coauthors.
These findings represent a “current health care concern,” since the elderly population in the United States is expected to double within the next several decades and the prevalence of acute pancreatitis is on the rise, Dr. Patel and colleagues wrote in a report on the analysis in the Journal of Clinical Gastroenterology.
The analysis is the first, to the investigators’ knowledge, that addresses national-level outcomes associated with acute biliary pancreatitis in elderly patients.
To evaluate clinical outcomes of elderly patients with acute biliary pancreatitis, Dr. Patel and colleagues queried the Nationwide Readmissions Database, which is the largest inpatient readmission database in the United States.
The investigators looked at outcomes associated with index hospitalizations, defined as a patient’s first hospitalization in a calendar year, and found 184,763 adult patients who received a diagnosis of acute biliary pancreatitis between 2011 and 2014. Of those, 41% were elderly.
The mortality rate associated with the index admission was 1.96% (n = 356) for the elderly patients, compared with just 0.32% (n = 1,473) for nonelderly patients (P less than .001), according to the report.
Mortality was increased in the elderly versus nonelderly patients, with an odds ratio of 2.8 (95% CI, 2.2-3.5), according to results of a propensity score matched analysis. Likewise, severe acute pancreatitis was increased in the elderly, with an OR of 1.2 (95% CI: 1.1-1.3) in that analysis.
By contrast, patient age did not impact 30-day readmission rates, according to results of a multivariate analysis that adjusted for confounding factors.
Mortality and severe acute pancreatitis both increased with age within the elderly cohort, further multivariate analysis showed. For example, the ORs for mortality were 1.39 for patients aged 75-84 years and 2.21 for patients aged 85 years and older, the results show.
The elderly population in the United States is expected to almost double by 2050, rising from 48 to 88 million, Dr. Patel and colleagues said. The number of those aged 85 years or older is expected to increase from 5.9 to 18 million by 2050, at which time they will make up nearly 5% of the total U.S. population.
“This specific demographic is more susceptible to common medical ailments, more troubling is acute pancreatitis is one of the most frequent causes of hospitalization in gastroenterology,” Dr. Patel and colleagues wrote.
Dr. Patel and coauthors reported no conflicts of interest related to the analysis.
SOURCE: Patel K et al. J Clin Gastroenterol. 2018 Aug 28. doi: 10.1097/MCG.0000000000001108.
Mortality was almost three times as high in elderly patients after stringent matching for confounding variables, wrote researcher Kishan Patel, MD, of the Ohio State University, Columbus, and coauthors.
These findings represent a “current health care concern,” since the elderly population in the United States is expected to double within the next several decades and the prevalence of acute pancreatitis is on the rise, Dr. Patel and colleagues wrote in a report on the analysis in the Journal of Clinical Gastroenterology.
The analysis is the first, to the investigators’ knowledge, that addresses national-level outcomes associated with acute biliary pancreatitis in elderly patients.
To evaluate clinical outcomes of elderly patients with acute biliary pancreatitis, Dr. Patel and colleagues queried the Nationwide Readmissions Database, which is the largest inpatient readmission database in the United States.
The investigators looked at outcomes associated with index hospitalizations, defined as a patient’s first hospitalization in a calendar year, and found 184,763 adult patients who received a diagnosis of acute biliary pancreatitis between 2011 and 2014. Of those, 41% were elderly.
The mortality rate associated with the index admission was 1.96% (n = 356) for the elderly patients, compared with just 0.32% (n = 1,473) for nonelderly patients (P less than .001), according to the report.
Mortality was increased in the elderly versus nonelderly patients, with an odds ratio of 2.8 (95% CI, 2.2-3.5), according to results of a propensity score matched analysis. Likewise, severe acute pancreatitis was increased in the elderly, with an OR of 1.2 (95% CI: 1.1-1.3) in that analysis.
By contrast, patient age did not impact 30-day readmission rates, according to results of a multivariate analysis that adjusted for confounding factors.
Mortality and severe acute pancreatitis both increased with age within the elderly cohort, further multivariate analysis showed. For example, the ORs for mortality were 1.39 for patients aged 75-84 years and 2.21 for patients aged 85 years and older, the results show.
The elderly population in the United States is expected to almost double by 2050, rising from 48 to 88 million, Dr. Patel and colleagues said. The number of those aged 85 years or older is expected to increase from 5.9 to 18 million by 2050, at which time they will make up nearly 5% of the total U.S. population.
“This specific demographic is more susceptible to common medical ailments, more troubling is acute pancreatitis is one of the most frequent causes of hospitalization in gastroenterology,” Dr. Patel and colleagues wrote.
Dr. Patel and coauthors reported no conflicts of interest related to the analysis.
SOURCE: Patel K et al. J Clin Gastroenterol. 2018 Aug 28. doi: 10.1097/MCG.0000000000001108.
Mortality was almost three times as high in elderly patients after stringent matching for confounding variables, wrote researcher Kishan Patel, MD, of the Ohio State University, Columbus, and coauthors.
These findings represent a “current health care concern,” since the elderly population in the United States is expected to double within the next several decades and the prevalence of acute pancreatitis is on the rise, Dr. Patel and colleagues wrote in a report on the analysis in the Journal of Clinical Gastroenterology.
The analysis is the first, to the investigators’ knowledge, that addresses national-level outcomes associated with acute biliary pancreatitis in elderly patients.
To evaluate clinical outcomes of elderly patients with acute biliary pancreatitis, Dr. Patel and colleagues queried the Nationwide Readmissions Database, which is the largest inpatient readmission database in the United States.
The investigators looked at outcomes associated with index hospitalizations, defined as a patient’s first hospitalization in a calendar year, and found 184,763 adult patients who received a diagnosis of acute biliary pancreatitis between 2011 and 2014. Of those, 41% were elderly.
The mortality rate associated with the index admission was 1.96% (n = 356) for the elderly patients, compared with just 0.32% (n = 1,473) for nonelderly patients (P less than .001), according to the report.
Mortality was increased in the elderly versus nonelderly patients, with an odds ratio of 2.8 (95% CI, 2.2-3.5), according to results of a propensity score matched analysis. Likewise, severe acute pancreatitis was increased in the elderly, with an OR of 1.2 (95% CI: 1.1-1.3) in that analysis.
By contrast, patient age did not impact 30-day readmission rates, according to results of a multivariate analysis that adjusted for confounding factors.
Mortality and severe acute pancreatitis both increased with age within the elderly cohort, further multivariate analysis showed. For example, the ORs for mortality were 1.39 for patients aged 75-84 years and 2.21 for patients aged 85 years and older, the results show.
The elderly population in the United States is expected to almost double by 2050, rising from 48 to 88 million, Dr. Patel and colleagues said. The number of those aged 85 years or older is expected to increase from 5.9 to 18 million by 2050, at which time they will make up nearly 5% of the total U.S. population.
“This specific demographic is more susceptible to common medical ailments, more troubling is acute pancreatitis is one of the most frequent causes of hospitalization in gastroenterology,” Dr. Patel and colleagues wrote.
Dr. Patel and coauthors reported no conflicts of interest related to the analysis.
SOURCE: Patel K et al. J Clin Gastroenterol. 2018 Aug 28. doi: 10.1097/MCG.0000000000001108.
FROM THE JOURNAL OF CLINICAL GASTROENTEROLOGY
Key clinical point: Compared with younger patients, elderly patients admitted for acute biliary pancreatitis have increased rates of adverse outcomes.
Major finding: Elderly patients had increased mortality (odds ratio, 2.8; 95% confidence interval, 2.2-3.5) and severe acute pancreatitis (OR, 1.2; 95% CI: 1.1-1.3).
Study details: A propensity score matched analysis of a large, nationally representative database including nearly 185,000 adults with acute biliary pancreatitis.
Disclosures: The study authors reported no conflicts of interest related to the study.
Source: Patel K et al. J Clin Gastroenterol. 2018 Aug 28. doi: 10.1097/MCG.0000000000001108.
Penalties not necessary to save money in some Medicare ACOs
The Centers for Medicare & Medicaid Services may be able to reduce spending through the Medicare Shared Savings Program (MSSP) without asking for health care professionals and organizations to take on penalties or so-called downside risk, according to a study published in Sept. 5 in the New England Journal of Medicine.
Researchers, using fee-for-service claims from 2009 through 2015 and performing difference-in-difference analyses to compare changes in Medicare spending, found that Accountable Care Organizations (ACOs) formed from physician practices were able to save money while hospital-based ACOs were not.
“Our results also suggest that shared-savings contracts that do not impose a downside risk of financial losses for spending above benchmarks – which may appeal to smaller organizations without sufficient reserves to withstand potential losses – may be effective in lowering Medicare spending,” J. Michael McWilliams, MD, PhD, of Harvard Medical School, Boston, and his colleagues wrote.
Researchers found that by 2015, groups participating in MSSP, as compared with those who did not participate, were “associated with a mean differential reduction of $302 in total Medicare spending per beneficiary in the 2012 entry of cohorts of ACOs,” without accounting for bonus payments.
“Accounting for shared-savings bonus payments, we determined that the differential spending reductions in the entry cohorts of physician-group ACOs from 2012 through 2014 constituted a net savings to Medicare of $256.4 million in 2015,” Dr. McWilliams and his colleagues wrote. “For hospital-integrated ACOs, bonus payments more than offset annual spending reductions.”
Dr. McWilliams and his colleagues noted that their findings were limited by a narrow focus on organizational structure (financial independence from hospitals), so other factors could have held to differences in savings; changes in coding practices for ACOs coming in as of 2013; lack of data on costs to ACOs or efforts to lower spending or improve quality; and the inability to assess the effects of the MSSP on many aspects of quality of care because of the nature of using claims-based measures.
“Our results probably underestimate savings to Medicare because they do not account for spillover effects of ACO efforts on nonattributed patients or effects of lower fee-for-service Medicare spending on payments to Medicare Advantage plans,” the researchers added.
The study was funded by a grant from the National Institute on Aging. Dr. McWilliams and Michael Chernew, PhD, also of Harvard Medical School, both have received consulting fees related to ACO research.
SOURCE: McWilliams JM et al. N Engl J Med. 2018 Sep 5. doi: 10.1056/NEJMsa1803388.
The Centers for Medicare & Medicaid Services may be able to reduce spending through the Medicare Shared Savings Program (MSSP) without asking for health care professionals and organizations to take on penalties or so-called downside risk, according to a study published in Sept. 5 in the New England Journal of Medicine.
Researchers, using fee-for-service claims from 2009 through 2015 and performing difference-in-difference analyses to compare changes in Medicare spending, found that Accountable Care Organizations (ACOs) formed from physician practices were able to save money while hospital-based ACOs were not.
“Our results also suggest that shared-savings contracts that do not impose a downside risk of financial losses for spending above benchmarks – which may appeal to smaller organizations without sufficient reserves to withstand potential losses – may be effective in lowering Medicare spending,” J. Michael McWilliams, MD, PhD, of Harvard Medical School, Boston, and his colleagues wrote.
Researchers found that by 2015, groups participating in MSSP, as compared with those who did not participate, were “associated with a mean differential reduction of $302 in total Medicare spending per beneficiary in the 2012 entry of cohorts of ACOs,” without accounting for bonus payments.
“Accounting for shared-savings bonus payments, we determined that the differential spending reductions in the entry cohorts of physician-group ACOs from 2012 through 2014 constituted a net savings to Medicare of $256.4 million in 2015,” Dr. McWilliams and his colleagues wrote. “For hospital-integrated ACOs, bonus payments more than offset annual spending reductions.”
Dr. McWilliams and his colleagues noted that their findings were limited by a narrow focus on organizational structure (financial independence from hospitals), so other factors could have held to differences in savings; changes in coding practices for ACOs coming in as of 2013; lack of data on costs to ACOs or efforts to lower spending or improve quality; and the inability to assess the effects of the MSSP on many aspects of quality of care because of the nature of using claims-based measures.
“Our results probably underestimate savings to Medicare because they do not account for spillover effects of ACO efforts on nonattributed patients or effects of lower fee-for-service Medicare spending on payments to Medicare Advantage plans,” the researchers added.
The study was funded by a grant from the National Institute on Aging. Dr. McWilliams and Michael Chernew, PhD, also of Harvard Medical School, both have received consulting fees related to ACO research.
SOURCE: McWilliams JM et al. N Engl J Med. 2018 Sep 5. doi: 10.1056/NEJMsa1803388.
The Centers for Medicare & Medicaid Services may be able to reduce spending through the Medicare Shared Savings Program (MSSP) without asking for health care professionals and organizations to take on penalties or so-called downside risk, according to a study published in Sept. 5 in the New England Journal of Medicine.
Researchers, using fee-for-service claims from 2009 through 2015 and performing difference-in-difference analyses to compare changes in Medicare spending, found that Accountable Care Organizations (ACOs) formed from physician practices were able to save money while hospital-based ACOs were not.
“Our results also suggest that shared-savings contracts that do not impose a downside risk of financial losses for spending above benchmarks – which may appeal to smaller organizations without sufficient reserves to withstand potential losses – may be effective in lowering Medicare spending,” J. Michael McWilliams, MD, PhD, of Harvard Medical School, Boston, and his colleagues wrote.
Researchers found that by 2015, groups participating in MSSP, as compared with those who did not participate, were “associated with a mean differential reduction of $302 in total Medicare spending per beneficiary in the 2012 entry of cohorts of ACOs,” without accounting for bonus payments.
“Accounting for shared-savings bonus payments, we determined that the differential spending reductions in the entry cohorts of physician-group ACOs from 2012 through 2014 constituted a net savings to Medicare of $256.4 million in 2015,” Dr. McWilliams and his colleagues wrote. “For hospital-integrated ACOs, bonus payments more than offset annual spending reductions.”
Dr. McWilliams and his colleagues noted that their findings were limited by a narrow focus on organizational structure (financial independence from hospitals), so other factors could have held to differences in savings; changes in coding practices for ACOs coming in as of 2013; lack of data on costs to ACOs or efforts to lower spending or improve quality; and the inability to assess the effects of the MSSP on many aspects of quality of care because of the nature of using claims-based measures.
“Our results probably underestimate savings to Medicare because they do not account for spillover effects of ACO efforts on nonattributed patients or effects of lower fee-for-service Medicare spending on payments to Medicare Advantage plans,” the researchers added.
The study was funded by a grant from the National Institute on Aging. Dr. McWilliams and Michael Chernew, PhD, also of Harvard Medical School, both have received consulting fees related to ACO research.
SOURCE: McWilliams JM et al. N Engl J Med. 2018 Sep 5. doi: 10.1056/NEJMsa1803388.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Physician group ACOs in the Medicare Shared Savings Program (MSSP) generated more savings than did hospital-led ACO groups.
Major finding: Physician group ACOs joining the MSSP in 2012-2014 generated $256.4 million in Medicare savings in 2015.
Study details: Analysis of fee-for-service Medicare claims during 2009-2015.
Disclosures: The study was funded by the National Institute on Aging. Dr. McWilliams and Dr. Chernew disclosed consulting fees related to ACO research.
Source: McWilliams JM et al. N Engl J Med. doi: 10.1056/NEJMsa1803388.