User login
‘COVID toes’ chilblain-like lesions not related to COVID-19
from Italy.
These lesions are “most likely are benign” and resolve on their own after 2-6 weeks, Valentina Discepolo, MD, PhD, University of Naples Federico II, told this news organization.
“They do not seem to be the manifestation of systemic inflammatory or autoimmune phenomena. According to our experience, they should not require a SARS-CoV-2–specific molecular or serological test since in all cases in our series they were negative,” said Dr. Discepolo.
The study was published online June 10, 2021, in JAMA Network Open.
‘COVID toes’ a fallacy?
The temporal association between the COVID-19 pandemic and the increasing number of chilblain-like lesions has led some in the media to call it “COVID toes,” the investigators wrote. However, data on the association with SARS-CoV-2 are controversial.
For this report, Dr. Discepolo and colleagues evaluated 17 adolescents who presented with chilblain-like lesions of the toes during the first wave of the pandemic in southern Italy.
None had evidence of current, past, or local SARS-CoV-2 infection.
“In our experience, chilblain-like lesions are not a manifestation of COVID-19, as shown by negative serological and molecular specific for SARS-CoV2,” Dr. Discepolo said in an interview.
The lesions were bilaterally distributed in 16 adolescents (94.1%) and heel skin was involved in 7 (41.2%). Ulceration complicated one patient during the active phase of the disease, and desquamation developed over time in three patients (17.6%). Only two patients (11.8%) had concurrent involvement of the fingers.
Self-administered therapies included topical antibiotics and/or corticosteroids, disinfectants, and antifungal agents; systemic antibiotics or corticosteroids were used rarely.
None of the therapies substantially changed the course of the lesions. Duration was “extremely variable,” ranging from 49 to 145 days; however, at follow-up, all patients had full resolution.
Almost invariably, the lesions were characterized by a triad of red dots, white rosettes, and white streaks on an erythematous background, the investigators reported.
In more than half the patients (56%), red dots often appeared as dotted and comma-shaped congested vessels that surrounded the rosettes in the early stage of the lesions. In later stages, red dots were still present, but the rosettes had disappeared.
Although found inconsistently in inflammatory cutaneous conditions, these three signs do not characterize the dermoscopic picture of perniosis, suggesting a distinct disease process, the investigators said.
Don’t blame it on ischemia, clots
Histologic analysis revealed “remodeling of the dermal blood vessels with a lobular arrangement, wall thickening, and a mild perivascular lymphocytic infiltrate,” they noted.
Punch biopsy of the involved skin mostly showed endothelial hyperplasia, mild lymphocytic infiltrate, and vessels’ architecture disruption with no papillary dermal edema or eosinophilic or neutrophilic infiltrate.
Pathology did not reveal any ischemic changes, which argues against systemic vasculopathy, Farzam Gorouhi, MD, from Kaiser Permanente, South Sacramento Medical Center, noted in a linked editorial. “Thus, this study provides further evidence against the thromboembolic nature of the presented pattern in adolescents during the COVID-19 pandemic.”
Results of capillaroscopy, used to investigate structural changes in peripheral microcirculation, were either completely normal or showed rare ectasias, supporting a lack of systemic inflammatory process.
“The lack of capillaroscopic features of a major vasculopathic event in the study by Discepolo et al. argues against the ischemic nature of this disease and, thus, indicates that this presentation is not associated with systemic ischemia or an embolic event,” Dr. Gorouhi noted.
Chilblain-like lesions have been one of the most commonly described cutaneous manifestations during the COVID-19 pandemic, but their etiopathogenesis, including the role of SARS-CoV-2, has remained elusive, the investigators wrote.
The findings in this case series do not support the association of the lesions with SARS-CoV-2 infection, they concluded.
The fact that only three new cases of chilblain-like lesions were reported during the highest peaks of the pandemic further supports a lack of association with SARS-CoV-2 infection, they noted.
In addition, none of these patients tested positive for SARS-CoV-2 and all three cases during the second wave occurred in the winter months, suggesting that exposure to the cold might, at least in some cases, trigger the skin lesions, the investigators said.
In line with this hypothesis, seven of the adolescents in this case series (41.2%) relapsed during the winter months while again testing negative for SARS-CoV-2.
“We believe that lifestyle modifications [reduced physical activity, microtraumatisms caused by walking barefoot at home] during the first strict lockdown played a role, likely promoting a local inflammatory process promoted by vascular stasis that led in genetically susceptible individuals to the onset of these lesions,” Dr. Discepolo said in an interview.
This research had no specific funding. The investigators and Dr. Gorouhi declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
from Italy.
These lesions are “most likely are benign” and resolve on their own after 2-6 weeks, Valentina Discepolo, MD, PhD, University of Naples Federico II, told this news organization.
“They do not seem to be the manifestation of systemic inflammatory or autoimmune phenomena. According to our experience, they should not require a SARS-CoV-2–specific molecular or serological test since in all cases in our series they were negative,” said Dr. Discepolo.
The study was published online June 10, 2021, in JAMA Network Open.
‘COVID toes’ a fallacy?
The temporal association between the COVID-19 pandemic and the increasing number of chilblain-like lesions has led some in the media to call it “COVID toes,” the investigators wrote. However, data on the association with SARS-CoV-2 are controversial.
For this report, Dr. Discepolo and colleagues evaluated 17 adolescents who presented with chilblain-like lesions of the toes during the first wave of the pandemic in southern Italy.
None had evidence of current, past, or local SARS-CoV-2 infection.
“In our experience, chilblain-like lesions are not a manifestation of COVID-19, as shown by negative serological and molecular specific for SARS-CoV2,” Dr. Discepolo said in an interview.
The lesions were bilaterally distributed in 16 adolescents (94.1%) and heel skin was involved in 7 (41.2%). Ulceration complicated one patient during the active phase of the disease, and desquamation developed over time in three patients (17.6%). Only two patients (11.8%) had concurrent involvement of the fingers.
Self-administered therapies included topical antibiotics and/or corticosteroids, disinfectants, and antifungal agents; systemic antibiotics or corticosteroids were used rarely.
None of the therapies substantially changed the course of the lesions. Duration was “extremely variable,” ranging from 49 to 145 days; however, at follow-up, all patients had full resolution.
Almost invariably, the lesions were characterized by a triad of red dots, white rosettes, and white streaks on an erythematous background, the investigators reported.
In more than half the patients (56%), red dots often appeared as dotted and comma-shaped congested vessels that surrounded the rosettes in the early stage of the lesions. In later stages, red dots were still present, but the rosettes had disappeared.
Although found inconsistently in inflammatory cutaneous conditions, these three signs do not characterize the dermoscopic picture of perniosis, suggesting a distinct disease process, the investigators said.
Don’t blame it on ischemia, clots
Histologic analysis revealed “remodeling of the dermal blood vessels with a lobular arrangement, wall thickening, and a mild perivascular lymphocytic infiltrate,” they noted.
Punch biopsy of the involved skin mostly showed endothelial hyperplasia, mild lymphocytic infiltrate, and vessels’ architecture disruption with no papillary dermal edema or eosinophilic or neutrophilic infiltrate.
Pathology did not reveal any ischemic changes, which argues against systemic vasculopathy, Farzam Gorouhi, MD, from Kaiser Permanente, South Sacramento Medical Center, noted in a linked editorial. “Thus, this study provides further evidence against the thromboembolic nature of the presented pattern in adolescents during the COVID-19 pandemic.”
Results of capillaroscopy, used to investigate structural changes in peripheral microcirculation, were either completely normal or showed rare ectasias, supporting a lack of systemic inflammatory process.
“The lack of capillaroscopic features of a major vasculopathic event in the study by Discepolo et al. argues against the ischemic nature of this disease and, thus, indicates that this presentation is not associated with systemic ischemia or an embolic event,” Dr. Gorouhi noted.
Chilblain-like lesions have been one of the most commonly described cutaneous manifestations during the COVID-19 pandemic, but their etiopathogenesis, including the role of SARS-CoV-2, has remained elusive, the investigators wrote.
The findings in this case series do not support the association of the lesions with SARS-CoV-2 infection, they concluded.
The fact that only three new cases of chilblain-like lesions were reported during the highest peaks of the pandemic further supports a lack of association with SARS-CoV-2 infection, they noted.
In addition, none of these patients tested positive for SARS-CoV-2 and all three cases during the second wave occurred in the winter months, suggesting that exposure to the cold might, at least in some cases, trigger the skin lesions, the investigators said.
In line with this hypothesis, seven of the adolescents in this case series (41.2%) relapsed during the winter months while again testing negative for SARS-CoV-2.
“We believe that lifestyle modifications [reduced physical activity, microtraumatisms caused by walking barefoot at home] during the first strict lockdown played a role, likely promoting a local inflammatory process promoted by vascular stasis that led in genetically susceptible individuals to the onset of these lesions,” Dr. Discepolo said in an interview.
This research had no specific funding. The investigators and Dr. Gorouhi declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
from Italy.
These lesions are “most likely are benign” and resolve on their own after 2-6 weeks, Valentina Discepolo, MD, PhD, University of Naples Federico II, told this news organization.
“They do not seem to be the manifestation of systemic inflammatory or autoimmune phenomena. According to our experience, they should not require a SARS-CoV-2–specific molecular or serological test since in all cases in our series they were negative,” said Dr. Discepolo.
The study was published online June 10, 2021, in JAMA Network Open.
‘COVID toes’ a fallacy?
The temporal association between the COVID-19 pandemic and the increasing number of chilblain-like lesions has led some in the media to call it “COVID toes,” the investigators wrote. However, data on the association with SARS-CoV-2 are controversial.
For this report, Dr. Discepolo and colleagues evaluated 17 adolescents who presented with chilblain-like lesions of the toes during the first wave of the pandemic in southern Italy.
None had evidence of current, past, or local SARS-CoV-2 infection.
“In our experience, chilblain-like lesions are not a manifestation of COVID-19, as shown by negative serological and molecular specific for SARS-CoV2,” Dr. Discepolo said in an interview.
The lesions were bilaterally distributed in 16 adolescents (94.1%) and heel skin was involved in 7 (41.2%). Ulceration complicated one patient during the active phase of the disease, and desquamation developed over time in three patients (17.6%). Only two patients (11.8%) had concurrent involvement of the fingers.
Self-administered therapies included topical antibiotics and/or corticosteroids, disinfectants, and antifungal agents; systemic antibiotics or corticosteroids were used rarely.
None of the therapies substantially changed the course of the lesions. Duration was “extremely variable,” ranging from 49 to 145 days; however, at follow-up, all patients had full resolution.
Almost invariably, the lesions were characterized by a triad of red dots, white rosettes, and white streaks on an erythematous background, the investigators reported.
In more than half the patients (56%), red dots often appeared as dotted and comma-shaped congested vessels that surrounded the rosettes in the early stage of the lesions. In later stages, red dots were still present, but the rosettes had disappeared.
Although found inconsistently in inflammatory cutaneous conditions, these three signs do not characterize the dermoscopic picture of perniosis, suggesting a distinct disease process, the investigators said.
Don’t blame it on ischemia, clots
Histologic analysis revealed “remodeling of the dermal blood vessels with a lobular arrangement, wall thickening, and a mild perivascular lymphocytic infiltrate,” they noted.
Punch biopsy of the involved skin mostly showed endothelial hyperplasia, mild lymphocytic infiltrate, and vessels’ architecture disruption with no papillary dermal edema or eosinophilic or neutrophilic infiltrate.
Pathology did not reveal any ischemic changes, which argues against systemic vasculopathy, Farzam Gorouhi, MD, from Kaiser Permanente, South Sacramento Medical Center, noted in a linked editorial. “Thus, this study provides further evidence against the thromboembolic nature of the presented pattern in adolescents during the COVID-19 pandemic.”
Results of capillaroscopy, used to investigate structural changes in peripheral microcirculation, were either completely normal or showed rare ectasias, supporting a lack of systemic inflammatory process.
“The lack of capillaroscopic features of a major vasculopathic event in the study by Discepolo et al. argues against the ischemic nature of this disease and, thus, indicates that this presentation is not associated with systemic ischemia or an embolic event,” Dr. Gorouhi noted.
Chilblain-like lesions have been one of the most commonly described cutaneous manifestations during the COVID-19 pandemic, but their etiopathogenesis, including the role of SARS-CoV-2, has remained elusive, the investigators wrote.
The findings in this case series do not support the association of the lesions with SARS-CoV-2 infection, they concluded.
The fact that only three new cases of chilblain-like lesions were reported during the highest peaks of the pandemic further supports a lack of association with SARS-CoV-2 infection, they noted.
In addition, none of these patients tested positive for SARS-CoV-2 and all three cases during the second wave occurred in the winter months, suggesting that exposure to the cold might, at least in some cases, trigger the skin lesions, the investigators said.
In line with this hypothesis, seven of the adolescents in this case series (41.2%) relapsed during the winter months while again testing negative for SARS-CoV-2.
“We believe that lifestyle modifications [reduced physical activity, microtraumatisms caused by walking barefoot at home] during the first strict lockdown played a role, likely promoting a local inflammatory process promoted by vascular stasis that led in genetically susceptible individuals to the onset of these lesions,” Dr. Discepolo said in an interview.
This research had no specific funding. The investigators and Dr. Gorouhi declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Converging to build for tomorrow
Last month we converged virtually for our annual conference, SHM Converge – the second time since the start of the coronavirus pandemic. We are thankful for innovations and advancements in technology that have allowed the world, including SHM, to continue connecting us all together. And yet, 18 months in, having forged new roads, experienced unique and life-changing events, we long for the in-person human connection that allows us to share a common experience. At a time of imperatives in our world – a global pandemic, systemic racism, and deep geopolitical divides – more than ever, we need to converge. Isolation only festers, deepening our divisions and conflicts.
In high school, I read Robert Frost’s poem “The Road Not Taken” and clung to the notion of diverging roads and choosing the road less traveled. Like most young people, my years since reading the poem were filled with attempts at forging new paths and experiencing great things – and yet, always feeling unaccomplished. Was Oscar Wilde right when he wrote: “Life imitates Art far more than Art imitates Life?” After all, these past 18 months, we have shared in the traumas of our times, and still, we remain isolated and alone. Our diverse experiences have been real, both tragic and heroic, from east to west, city to country, black to white, and red to blue.
At SHM, it’s time to converge and face the great challenges of our lifetime. A deadly pandemic continues to rage around the world, bringing unprecedented human suffering and loss of lives. In its wake, this pandemic also laid bare the ugly face of systemic racism, brought our deepest divisions to the surface – all threatening the very fabric of our society. This pandemic has been a stress test for health care systems, revealing our vulnerabilities and expanding the chasm of care between urban and rural communities, all in turn worsening our growing health disparities. This moment needs convergence to rekindle connection and solidarity.
Scholars do not interpret “The Road Not Taken” as a recommendation to take the road less traveled. Instead, it is a suggestion that the diverging roads lead to a common place having been “worn about the same” as they “equally lay.” It is true that our roads are unique and shape our lives, but so, too, does the destination and common place our roads lead us to. At that common place, during these taxing times, SHM enables hospitalists to tackle these great challenges.
For over 2 decades of dynamic changes in health care, SHM has been the workshop where hospitalists converged to sharpen clinical skills, improve quality and safety, develop acute care models inside and outside of hospitals, advocate for better health policy and blaze new trails. Though the issues evolved, and new ones emerge, today is no different.
Indeed, this is an historic time. This weighted moment meets us at the crossroads. A moment that demands synergy, cooperation, and creativity. A dynamic change to health care policy, advances in care innovation, renewed prioritization of public health, and rich national discourse on our social fabric; hospitalists are essential to every one of those conversations. SHM has evolved to meet our growing needs, equipping hospitalists with tools to engage at every level, and most importantly, enabled us to find our common place.
Where do we go now? I suggest we continue to take the roads not taken and at the destination, build the map of tomorrow, together.
Dr. Siy is division medical director, hospital specialties, in the departments of hospital medicine and community senior and palliative care at HealthPartners in Bloomington, Minn. He is the new president of SHM.
Last month we converged virtually for our annual conference, SHM Converge – the second time since the start of the coronavirus pandemic. We are thankful for innovations and advancements in technology that have allowed the world, including SHM, to continue connecting us all together. And yet, 18 months in, having forged new roads, experienced unique and life-changing events, we long for the in-person human connection that allows us to share a common experience. At a time of imperatives in our world – a global pandemic, systemic racism, and deep geopolitical divides – more than ever, we need to converge. Isolation only festers, deepening our divisions and conflicts.
In high school, I read Robert Frost’s poem “The Road Not Taken” and clung to the notion of diverging roads and choosing the road less traveled. Like most young people, my years since reading the poem were filled with attempts at forging new paths and experiencing great things – and yet, always feeling unaccomplished. Was Oscar Wilde right when he wrote: “Life imitates Art far more than Art imitates Life?” After all, these past 18 months, we have shared in the traumas of our times, and still, we remain isolated and alone. Our diverse experiences have been real, both tragic and heroic, from east to west, city to country, black to white, and red to blue.
At SHM, it’s time to converge and face the great challenges of our lifetime. A deadly pandemic continues to rage around the world, bringing unprecedented human suffering and loss of lives. In its wake, this pandemic also laid bare the ugly face of systemic racism, brought our deepest divisions to the surface – all threatening the very fabric of our society. This pandemic has been a stress test for health care systems, revealing our vulnerabilities and expanding the chasm of care between urban and rural communities, all in turn worsening our growing health disparities. This moment needs convergence to rekindle connection and solidarity.
Scholars do not interpret “The Road Not Taken” as a recommendation to take the road less traveled. Instead, it is a suggestion that the diverging roads lead to a common place having been “worn about the same” as they “equally lay.” It is true that our roads are unique and shape our lives, but so, too, does the destination and common place our roads lead us to. At that common place, during these taxing times, SHM enables hospitalists to tackle these great challenges.
For over 2 decades of dynamic changes in health care, SHM has been the workshop where hospitalists converged to sharpen clinical skills, improve quality and safety, develop acute care models inside and outside of hospitals, advocate for better health policy and blaze new trails. Though the issues evolved, and new ones emerge, today is no different.
Indeed, this is an historic time. This weighted moment meets us at the crossroads. A moment that demands synergy, cooperation, and creativity. A dynamic change to health care policy, advances in care innovation, renewed prioritization of public health, and rich national discourse on our social fabric; hospitalists are essential to every one of those conversations. SHM has evolved to meet our growing needs, equipping hospitalists with tools to engage at every level, and most importantly, enabled us to find our common place.
Where do we go now? I suggest we continue to take the roads not taken and at the destination, build the map of tomorrow, together.
Dr. Siy is division medical director, hospital specialties, in the departments of hospital medicine and community senior and palliative care at HealthPartners in Bloomington, Minn. He is the new president of SHM.
Last month we converged virtually for our annual conference, SHM Converge – the second time since the start of the coronavirus pandemic. We are thankful for innovations and advancements in technology that have allowed the world, including SHM, to continue connecting us all together. And yet, 18 months in, having forged new roads, experienced unique and life-changing events, we long for the in-person human connection that allows us to share a common experience. At a time of imperatives in our world – a global pandemic, systemic racism, and deep geopolitical divides – more than ever, we need to converge. Isolation only festers, deepening our divisions and conflicts.
In high school, I read Robert Frost’s poem “The Road Not Taken” and clung to the notion of diverging roads and choosing the road less traveled. Like most young people, my years since reading the poem were filled with attempts at forging new paths and experiencing great things – and yet, always feeling unaccomplished. Was Oscar Wilde right when he wrote: “Life imitates Art far more than Art imitates Life?” After all, these past 18 months, we have shared in the traumas of our times, and still, we remain isolated and alone. Our diverse experiences have been real, both tragic and heroic, from east to west, city to country, black to white, and red to blue.
At SHM, it’s time to converge and face the great challenges of our lifetime. A deadly pandemic continues to rage around the world, bringing unprecedented human suffering and loss of lives. In its wake, this pandemic also laid bare the ugly face of systemic racism, brought our deepest divisions to the surface – all threatening the very fabric of our society. This pandemic has been a stress test for health care systems, revealing our vulnerabilities and expanding the chasm of care between urban and rural communities, all in turn worsening our growing health disparities. This moment needs convergence to rekindle connection and solidarity.
Scholars do not interpret “The Road Not Taken” as a recommendation to take the road less traveled. Instead, it is a suggestion that the diverging roads lead to a common place having been “worn about the same” as they “equally lay.” It is true that our roads are unique and shape our lives, but so, too, does the destination and common place our roads lead us to. At that common place, during these taxing times, SHM enables hospitalists to tackle these great challenges.
For over 2 decades of dynamic changes in health care, SHM has been the workshop where hospitalists converged to sharpen clinical skills, improve quality and safety, develop acute care models inside and outside of hospitals, advocate for better health policy and blaze new trails. Though the issues evolved, and new ones emerge, today is no different.
Indeed, this is an historic time. This weighted moment meets us at the crossroads. A moment that demands synergy, cooperation, and creativity. A dynamic change to health care policy, advances in care innovation, renewed prioritization of public health, and rich national discourse on our social fabric; hospitalists are essential to every one of those conversations. SHM has evolved to meet our growing needs, equipping hospitalists with tools to engage at every level, and most importantly, enabled us to find our common place.
Where do we go now? I suggest we continue to take the roads not taken and at the destination, build the map of tomorrow, together.
Dr. Siy is division medical director, hospital specialties, in the departments of hospital medicine and community senior and palliative care at HealthPartners in Bloomington, Minn. He is the new president of SHM.
As new cases fall, U.S. passes 4 million children with COVID-19
Even as the number of new COVID-19 cases continues to drop, the United States reached the 4-million mark for infected children, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
. That weekly total, the lowest since June of 2020, comes from 49 states (excluding N.Y.), the District of Columbia, New York City, Puerto Rico, and Guam, the AAP and CHA said in their weekly COVID-19 report.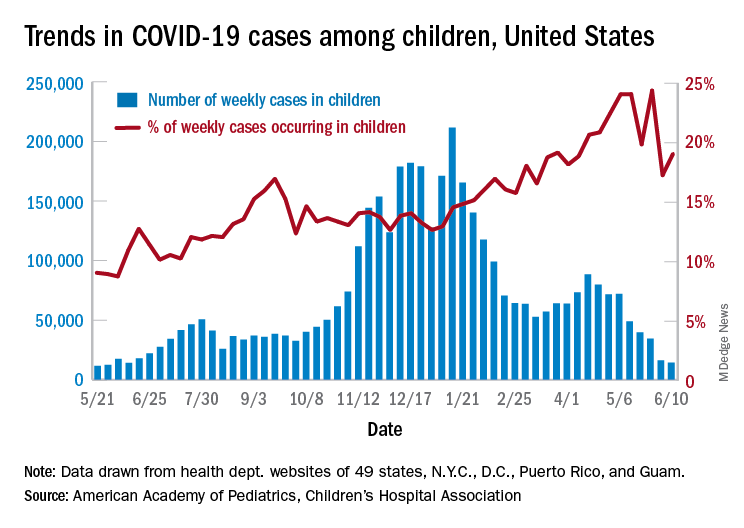
Children represent 14.1% of all COVID-19 cases since the beginning of the pandemic, while the corresponding figure for the week ending June 10 was 19.0%. That weekly proportion of cases among children had been rising pretty steadily through the winter and early spring, but the situation has become much more volatile over the last month, the AAP/CHA data show.
Use of the Pfizer-BioNTech vaccine in children aged 16-17 years, of course, didn’t begin until April, and the vaccine wasn’t authorized for children aged 12-15 years until mid-May. The Moderna and Johnson & Johnson vaccines have not received such authorization yet, but Moderna is in the process of seeking an emergency-use recommendation from the Food and Drug Administration.
In the younger group of children who are currently eligible, completion of the vaccine regimen took a big jump in the week ending June 14, according to the Centers for Disease Control and Prevention. The cumulative share of those aged 12-15 years who had received a second dose jumped from 4.1% on June 7 to 11.4% on June 14, with comparable numbers for 16- and 17-year-olds coming in at 26.4% and 29.1%.
Activity over just the last 14 days, however, shows a slight decrease in children aged 12-15 getting a first dose: For just the 2 weeks ending June 7, 17.9% of all children in the age group initiated a first dose, but for the 14 days ending June 14, only 17.1% of the age group did so, the CDC said on its COVID Data Tracker site.
For children aged 16-17 years – of whom less than 30% have reached full vaccination – activity seems to have stagnated: 4.8% of all 16- to 17-year-olds initiated a first vaccination during the 14 days ending June 7, compared with 4.7% who did so during the 14 days ending June 14, the CDC reported.
Older age groups with higher completion rates are still producing greater vaccine initiation. As of June 14, those aged 25-39 years had a completion rate of 41.9% and 24.0% of the age group had received a first dose in the previous 2 weeks, while 61.4% of those aged 50-64 were fully vaccinated, and 18.0% had gotten their first dose, the CDC data indicate.
Even as the number of new COVID-19 cases continues to drop, the United States reached the 4-million mark for infected children, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
. That weekly total, the lowest since June of 2020, comes from 49 states (excluding N.Y.), the District of Columbia, New York City, Puerto Rico, and Guam, the AAP and CHA said in their weekly COVID-19 report.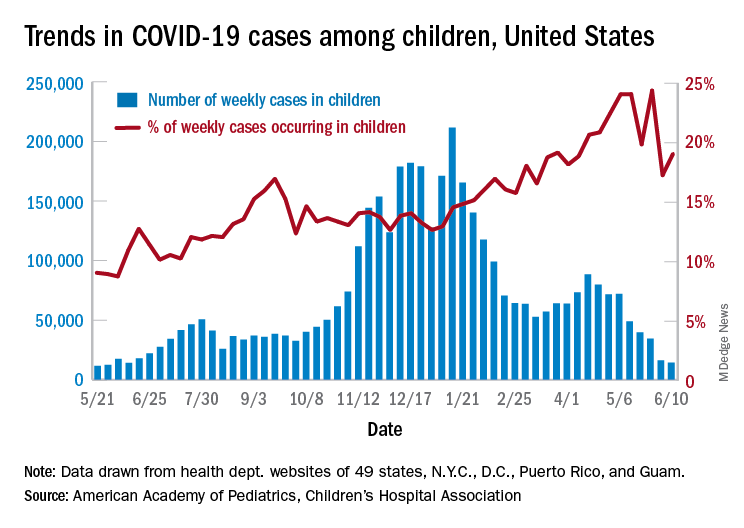
Children represent 14.1% of all COVID-19 cases since the beginning of the pandemic, while the corresponding figure for the week ending June 10 was 19.0%. That weekly proportion of cases among children had been rising pretty steadily through the winter and early spring, but the situation has become much more volatile over the last month, the AAP/CHA data show.
Use of the Pfizer-BioNTech vaccine in children aged 16-17 years, of course, didn’t begin until April, and the vaccine wasn’t authorized for children aged 12-15 years until mid-May. The Moderna and Johnson & Johnson vaccines have not received such authorization yet, but Moderna is in the process of seeking an emergency-use recommendation from the Food and Drug Administration.
In the younger group of children who are currently eligible, completion of the vaccine regimen took a big jump in the week ending June 14, according to the Centers for Disease Control and Prevention. The cumulative share of those aged 12-15 years who had received a second dose jumped from 4.1% on June 7 to 11.4% on June 14, with comparable numbers for 16- and 17-year-olds coming in at 26.4% and 29.1%.
Activity over just the last 14 days, however, shows a slight decrease in children aged 12-15 getting a first dose: For just the 2 weeks ending June 7, 17.9% of all children in the age group initiated a first dose, but for the 14 days ending June 14, only 17.1% of the age group did so, the CDC said on its COVID Data Tracker site.
For children aged 16-17 years – of whom less than 30% have reached full vaccination – activity seems to have stagnated: 4.8% of all 16- to 17-year-olds initiated a first vaccination during the 14 days ending June 7, compared with 4.7% who did so during the 14 days ending June 14, the CDC reported.
Older age groups with higher completion rates are still producing greater vaccine initiation. As of June 14, those aged 25-39 years had a completion rate of 41.9% and 24.0% of the age group had received a first dose in the previous 2 weeks, while 61.4% of those aged 50-64 were fully vaccinated, and 18.0% had gotten their first dose, the CDC data indicate.
Even as the number of new COVID-19 cases continues to drop, the United States reached the 4-million mark for infected children, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
. That weekly total, the lowest since June of 2020, comes from 49 states (excluding N.Y.), the District of Columbia, New York City, Puerto Rico, and Guam, the AAP and CHA said in their weekly COVID-19 report.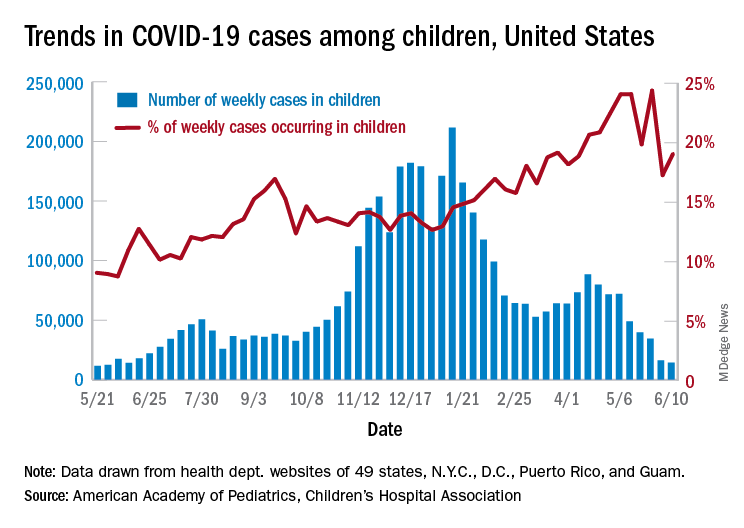
Children represent 14.1% of all COVID-19 cases since the beginning of the pandemic, while the corresponding figure for the week ending June 10 was 19.0%. That weekly proportion of cases among children had been rising pretty steadily through the winter and early spring, but the situation has become much more volatile over the last month, the AAP/CHA data show.
Use of the Pfizer-BioNTech vaccine in children aged 16-17 years, of course, didn’t begin until April, and the vaccine wasn’t authorized for children aged 12-15 years until mid-May. The Moderna and Johnson & Johnson vaccines have not received such authorization yet, but Moderna is in the process of seeking an emergency-use recommendation from the Food and Drug Administration.
In the younger group of children who are currently eligible, completion of the vaccine regimen took a big jump in the week ending June 14, according to the Centers for Disease Control and Prevention. The cumulative share of those aged 12-15 years who had received a second dose jumped from 4.1% on June 7 to 11.4% on June 14, with comparable numbers for 16- and 17-year-olds coming in at 26.4% and 29.1%.
Activity over just the last 14 days, however, shows a slight decrease in children aged 12-15 getting a first dose: For just the 2 weeks ending June 7, 17.9% of all children in the age group initiated a first dose, but for the 14 days ending June 14, only 17.1% of the age group did so, the CDC said on its COVID Data Tracker site.
For children aged 16-17 years – of whom less than 30% have reached full vaccination – activity seems to have stagnated: 4.8% of all 16- to 17-year-olds initiated a first vaccination during the 14 days ending June 7, compared with 4.7% who did so during the 14 days ending June 14, the CDC reported.
Older age groups with higher completion rates are still producing greater vaccine initiation. As of June 14, those aged 25-39 years had a completion rate of 41.9% and 24.0% of the age group had received a first dose in the previous 2 weeks, while 61.4% of those aged 50-64 were fully vaccinated, and 18.0% had gotten their first dose, the CDC data indicate.
U.S. News releases Best Children’s Hospitals list, with changes
Released June 15, the 2021-2022 rankings, which acknowledge 50 U.S. centers for delivering exceptional care in several specialties, also give the Massachusetts hospital the top spot in 4 of 10 pediatric specialties assessed: nephrology, neurology and neurosurgery, pulmonology and lung surgery, and urology.
Children’s Hospital of Philadelphia retains second spot in the annually updated list, and Texas Children’s Hospital, in Houston, moves up a rung to third place, bumping Cincinnati Children’s Hospital Medical Center from third to fourth place. Children’s Hospital Los Angeles comes in at no. 5.
The remaining top 10 placements, in descending order, are as follows:
Children’s Hospital Colorado in Aurora; Children’s National Hospital in Washington; Nationwide Children’s Hospital in Columbus, Ohio; UPMS Children’s Hospital of Pittsburgh; and Lucile Packard Children’s Hospital Stanford (Calif.).
New regional rankings
This year’s edition offers something new, adding rankings within states and multiple-state rankings within seven regions to facilitate choice. “The Best Children’s Hospitals rankings have always highlighted hospitals that excel in specialized care,” said Ben Harder, chief of health analysis and managing editor at U.S. News, in a press release. “Now, this year’s new state and regional rankings can help families identify conveniently located hospitals capable of meeting their child’s needs. As the pandemic continues to affect travel, finding high-quality care close to home has never been more important.”
Across the seven regions, the top-ranked institutions are as follows:
- Mid-Atlantic – Children’s Hospital of Philadelphia.
- Midwest – Cincinnati Children’s Hospital Medical Center.
- New England – Boston Children’s Hospital.
- Pacific – Children’s Hospital Los Angeles.
- Rocky Mountains – Children’s Hospital Colorado.
- Southeast – Children’s Healthcare of Atlanta and Monroe Carell Jr. Children’s Hospital of Vanderbilt, in Nashville, Tenn.
- Southwest – Texas Children’s Hospital.
Specialties
Boston Children’s not only topped the overall list but also led in four specialties. For the other six specialties that were ranked, the top hospitals on the honor roll are as follows:
- Cancer – Children’s Hospital of Philadelphia.
- Cardiology and heart surgery – Texas Children’s Hospital.
- Diabetes and endocrinology – Children’s Hospital of Philadelphia.
- Gastroenterology and gastrointestinal surgery – Children’s Hospital Colorado.
- Neonatology – Children’s National Hospital.
- Orthopedics – Children’s Hospital of Philadelphia.
For the past 15 years, the objective of the rankings has been to offer a starting point for parents in making decisions about the best place to take very sick children for high-quality care. The editors of the rankings acknowledge that considerations of travel costs and insurance coverage are other factors to consider.
Helpful for families
The rankings are helpful for families, according to Joe W. St. Geme, III, MD, Children’s Hospital of Philadelphia’s physician-in-chief and chair of its department of pediatrics. “Some parents, especially those coming from outside an area, find them useful when deciding on care away from home,” he told this news organization. “Most types of pediatric care are available in the community, but sometimes a child has an unusual disease or complex disease for which local care is not available.”
Dr. St. Geme said the new regional rankings may be useful in helping parents decide where to bring a child for care that is closer to where they live.
A top ranking from U.S. News is just one indication of a hospital›s overall performance, according to Angela Lorts, MD, MBA, director of the Ventricular Assist Device Program, at Cincinnati Children’s Hospital Medical Center.
“Parents seeking care for their child should use the data to ask questions and understand the limitations,” she told this news organization. “Rankings are only based on a small subset of the children we care for. Many of the metrics may not pertain to their child and may not reflect the care they will receive.”
In her view, ranking will not give parents all the information they need about medical care and outcomes for specific conditions.
Hospital reaction
Hospitals can use the rankings to target improvements, says Dr. St. Geme. “These rankings can provide an opportunity for some benchmarking, to see what other institutions are doing and how they’re able to deliver care. They can serve as a source of ideas and can influence planning,” he said.
He cautioned that the data are not as complete as they could be. “A number of services are not included, and we try to keep that in mind,” he said.
Rankings may also affect recruitment, Dr. St. Geme added, because higher-ranked institutions may find it easier to attract sought-after clinicians and investigators in needed areas.
Another sphere of influence is philanthropy and fund raising. “People are much more likely to consider making both small and large donations to a high-ranked institution,” said J. Howard Smart, MD, chair of pediatrics at Sharp Rees-Stealy Medical Group and chair-elect of the physician leadership council at Sharp Mary Birch Hospital for Women and Newborns in San Diego.
Dr. St. Geme agrees. “Philanthropists are interested in making investments where they feel they’re a sure bet, and rankings may indicate a sure bet. But their impact on government funding and grant support is probably less.”
Ultimately, however, some families may not have lot of choice in where to go when their children are sick, Dr. Smart said. “And people probably don’t choose a location to live in based on nearby children’s hospitals the way they do for schools,” he said.
What about hospitals that continue to rank much lower on the 50-institution list – excellent though they must be to make it onto the honor roll. “To be on the list but not to have risen in rank in recent years might be a disappointment,” said Dr. St. Geme. “But it might also motivate a hospital to think about making internal investments in order to strengthen a particular service. And it may motivate nonranked hospitals to improve care in order to break into the list.”
Dr. Lorts points out that the annual survey process requires hospitals to track the clinical outcomes of a subset of patients, which may lead to improvement in these areas. It also requires data collection on structure and process, which drives needs assessments of select hospital areas. “But ideally, all hospitals would be tracking important outcomes, benchmarking to peer hospitals, and improving where needed without the U.S. News incentive,” she said.
This year’s data, compiled by research and consulting firm RTI International, derive from feedback on more than 1,200 questions provided by 118 responding institutions. Details on each hospital on the list and the methodology used in the analysis are available on U.S. News & World Report’s website.
A version of this article first appeared on Medscape.com.
Released June 15, the 2021-2022 rankings, which acknowledge 50 U.S. centers for delivering exceptional care in several specialties, also give the Massachusetts hospital the top spot in 4 of 10 pediatric specialties assessed: nephrology, neurology and neurosurgery, pulmonology and lung surgery, and urology.
Children’s Hospital of Philadelphia retains second spot in the annually updated list, and Texas Children’s Hospital, in Houston, moves up a rung to third place, bumping Cincinnati Children’s Hospital Medical Center from third to fourth place. Children’s Hospital Los Angeles comes in at no. 5.
The remaining top 10 placements, in descending order, are as follows:
Children’s Hospital Colorado in Aurora; Children’s National Hospital in Washington; Nationwide Children’s Hospital in Columbus, Ohio; UPMS Children’s Hospital of Pittsburgh; and Lucile Packard Children’s Hospital Stanford (Calif.).
New regional rankings
This year’s edition offers something new, adding rankings within states and multiple-state rankings within seven regions to facilitate choice. “The Best Children’s Hospitals rankings have always highlighted hospitals that excel in specialized care,” said Ben Harder, chief of health analysis and managing editor at U.S. News, in a press release. “Now, this year’s new state and regional rankings can help families identify conveniently located hospitals capable of meeting their child’s needs. As the pandemic continues to affect travel, finding high-quality care close to home has never been more important.”
Across the seven regions, the top-ranked institutions are as follows:
- Mid-Atlantic – Children’s Hospital of Philadelphia.
- Midwest – Cincinnati Children’s Hospital Medical Center.
- New England – Boston Children’s Hospital.
- Pacific – Children’s Hospital Los Angeles.
- Rocky Mountains – Children’s Hospital Colorado.
- Southeast – Children’s Healthcare of Atlanta and Monroe Carell Jr. Children’s Hospital of Vanderbilt, in Nashville, Tenn.
- Southwest – Texas Children’s Hospital.
Specialties
Boston Children’s not only topped the overall list but also led in four specialties. For the other six specialties that were ranked, the top hospitals on the honor roll are as follows:
- Cancer – Children’s Hospital of Philadelphia.
- Cardiology and heart surgery – Texas Children’s Hospital.
- Diabetes and endocrinology – Children’s Hospital of Philadelphia.
- Gastroenterology and gastrointestinal surgery – Children’s Hospital Colorado.
- Neonatology – Children’s National Hospital.
- Orthopedics – Children’s Hospital of Philadelphia.
For the past 15 years, the objective of the rankings has been to offer a starting point for parents in making decisions about the best place to take very sick children for high-quality care. The editors of the rankings acknowledge that considerations of travel costs and insurance coverage are other factors to consider.
Helpful for families
The rankings are helpful for families, according to Joe W. St. Geme, III, MD, Children’s Hospital of Philadelphia’s physician-in-chief and chair of its department of pediatrics. “Some parents, especially those coming from outside an area, find them useful when deciding on care away from home,” he told this news organization. “Most types of pediatric care are available in the community, but sometimes a child has an unusual disease or complex disease for which local care is not available.”
Dr. St. Geme said the new regional rankings may be useful in helping parents decide where to bring a child for care that is closer to where they live.
A top ranking from U.S. News is just one indication of a hospital›s overall performance, according to Angela Lorts, MD, MBA, director of the Ventricular Assist Device Program, at Cincinnati Children’s Hospital Medical Center.
“Parents seeking care for their child should use the data to ask questions and understand the limitations,” she told this news organization. “Rankings are only based on a small subset of the children we care for. Many of the metrics may not pertain to their child and may not reflect the care they will receive.”
In her view, ranking will not give parents all the information they need about medical care and outcomes for specific conditions.
Hospital reaction
Hospitals can use the rankings to target improvements, says Dr. St. Geme. “These rankings can provide an opportunity for some benchmarking, to see what other institutions are doing and how they’re able to deliver care. They can serve as a source of ideas and can influence planning,” he said.
He cautioned that the data are not as complete as they could be. “A number of services are not included, and we try to keep that in mind,” he said.
Rankings may also affect recruitment, Dr. St. Geme added, because higher-ranked institutions may find it easier to attract sought-after clinicians and investigators in needed areas.
Another sphere of influence is philanthropy and fund raising. “People are much more likely to consider making both small and large donations to a high-ranked institution,” said J. Howard Smart, MD, chair of pediatrics at Sharp Rees-Stealy Medical Group and chair-elect of the physician leadership council at Sharp Mary Birch Hospital for Women and Newborns in San Diego.
Dr. St. Geme agrees. “Philanthropists are interested in making investments where they feel they’re a sure bet, and rankings may indicate a sure bet. But their impact on government funding and grant support is probably less.”
Ultimately, however, some families may not have lot of choice in where to go when their children are sick, Dr. Smart said. “And people probably don’t choose a location to live in based on nearby children’s hospitals the way they do for schools,” he said.
What about hospitals that continue to rank much lower on the 50-institution list – excellent though they must be to make it onto the honor roll. “To be on the list but not to have risen in rank in recent years might be a disappointment,” said Dr. St. Geme. “But it might also motivate a hospital to think about making internal investments in order to strengthen a particular service. And it may motivate nonranked hospitals to improve care in order to break into the list.”
Dr. Lorts points out that the annual survey process requires hospitals to track the clinical outcomes of a subset of patients, which may lead to improvement in these areas. It also requires data collection on structure and process, which drives needs assessments of select hospital areas. “But ideally, all hospitals would be tracking important outcomes, benchmarking to peer hospitals, and improving where needed without the U.S. News incentive,” she said.
This year’s data, compiled by research and consulting firm RTI International, derive from feedback on more than 1,200 questions provided by 118 responding institutions. Details on each hospital on the list and the methodology used in the analysis are available on U.S. News & World Report’s website.
A version of this article first appeared on Medscape.com.
Released June 15, the 2021-2022 rankings, which acknowledge 50 U.S. centers for delivering exceptional care in several specialties, also give the Massachusetts hospital the top spot in 4 of 10 pediatric specialties assessed: nephrology, neurology and neurosurgery, pulmonology and lung surgery, and urology.
Children’s Hospital of Philadelphia retains second spot in the annually updated list, and Texas Children’s Hospital, in Houston, moves up a rung to third place, bumping Cincinnati Children’s Hospital Medical Center from third to fourth place. Children’s Hospital Los Angeles comes in at no. 5.
The remaining top 10 placements, in descending order, are as follows:
Children’s Hospital Colorado in Aurora; Children’s National Hospital in Washington; Nationwide Children’s Hospital in Columbus, Ohio; UPMS Children’s Hospital of Pittsburgh; and Lucile Packard Children’s Hospital Stanford (Calif.).
New regional rankings
This year’s edition offers something new, adding rankings within states and multiple-state rankings within seven regions to facilitate choice. “The Best Children’s Hospitals rankings have always highlighted hospitals that excel in specialized care,” said Ben Harder, chief of health analysis and managing editor at U.S. News, in a press release. “Now, this year’s new state and regional rankings can help families identify conveniently located hospitals capable of meeting their child’s needs. As the pandemic continues to affect travel, finding high-quality care close to home has never been more important.”
Across the seven regions, the top-ranked institutions are as follows:
- Mid-Atlantic – Children’s Hospital of Philadelphia.
- Midwest – Cincinnati Children’s Hospital Medical Center.
- New England – Boston Children’s Hospital.
- Pacific – Children’s Hospital Los Angeles.
- Rocky Mountains – Children’s Hospital Colorado.
- Southeast – Children’s Healthcare of Atlanta and Monroe Carell Jr. Children’s Hospital of Vanderbilt, in Nashville, Tenn.
- Southwest – Texas Children’s Hospital.
Specialties
Boston Children’s not only topped the overall list but also led in four specialties. For the other six specialties that were ranked, the top hospitals on the honor roll are as follows:
- Cancer – Children’s Hospital of Philadelphia.
- Cardiology and heart surgery – Texas Children’s Hospital.
- Diabetes and endocrinology – Children’s Hospital of Philadelphia.
- Gastroenterology and gastrointestinal surgery – Children’s Hospital Colorado.
- Neonatology – Children’s National Hospital.
- Orthopedics – Children’s Hospital of Philadelphia.
For the past 15 years, the objective of the rankings has been to offer a starting point for parents in making decisions about the best place to take very sick children for high-quality care. The editors of the rankings acknowledge that considerations of travel costs and insurance coverage are other factors to consider.
Helpful for families
The rankings are helpful for families, according to Joe W. St. Geme, III, MD, Children’s Hospital of Philadelphia’s physician-in-chief and chair of its department of pediatrics. “Some parents, especially those coming from outside an area, find them useful when deciding on care away from home,” he told this news organization. “Most types of pediatric care are available in the community, but sometimes a child has an unusual disease or complex disease for which local care is not available.”
Dr. St. Geme said the new regional rankings may be useful in helping parents decide where to bring a child for care that is closer to where they live.
A top ranking from U.S. News is just one indication of a hospital›s overall performance, according to Angela Lorts, MD, MBA, director of the Ventricular Assist Device Program, at Cincinnati Children’s Hospital Medical Center.
“Parents seeking care for their child should use the data to ask questions and understand the limitations,” she told this news organization. “Rankings are only based on a small subset of the children we care for. Many of the metrics may not pertain to their child and may not reflect the care they will receive.”
In her view, ranking will not give parents all the information they need about medical care and outcomes for specific conditions.
Hospital reaction
Hospitals can use the rankings to target improvements, says Dr. St. Geme. “These rankings can provide an opportunity for some benchmarking, to see what other institutions are doing and how they’re able to deliver care. They can serve as a source of ideas and can influence planning,” he said.
He cautioned that the data are not as complete as they could be. “A number of services are not included, and we try to keep that in mind,” he said.
Rankings may also affect recruitment, Dr. St. Geme added, because higher-ranked institutions may find it easier to attract sought-after clinicians and investigators in needed areas.
Another sphere of influence is philanthropy and fund raising. “People are much more likely to consider making both small and large donations to a high-ranked institution,” said J. Howard Smart, MD, chair of pediatrics at Sharp Rees-Stealy Medical Group and chair-elect of the physician leadership council at Sharp Mary Birch Hospital for Women and Newborns in San Diego.
Dr. St. Geme agrees. “Philanthropists are interested in making investments where they feel they’re a sure bet, and rankings may indicate a sure bet. But their impact on government funding and grant support is probably less.”
Ultimately, however, some families may not have lot of choice in where to go when their children are sick, Dr. Smart said. “And people probably don’t choose a location to live in based on nearby children’s hospitals the way they do for schools,” he said.
What about hospitals that continue to rank much lower on the 50-institution list – excellent though they must be to make it onto the honor roll. “To be on the list but not to have risen in rank in recent years might be a disappointment,” said Dr. St. Geme. “But it might also motivate a hospital to think about making internal investments in order to strengthen a particular service. And it may motivate nonranked hospitals to improve care in order to break into the list.”
Dr. Lorts points out that the annual survey process requires hospitals to track the clinical outcomes of a subset of patients, which may lead to improvement in these areas. It also requires data collection on structure and process, which drives needs assessments of select hospital areas. “But ideally, all hospitals would be tracking important outcomes, benchmarking to peer hospitals, and improving where needed without the U.S. News incentive,” she said.
This year’s data, compiled by research and consulting firm RTI International, derive from feedback on more than 1,200 questions provided by 118 responding institutions. Details on each hospital on the list and the methodology used in the analysis are available on U.S. News & World Report’s website.
A version of this article first appeared on Medscape.com.
Simple risk assessment predicts post-PCI ischemic events
A patient’s risk for ischemic events, but not bleeding, after percutaneous coronary intervention (PCI) can be predicted simply based on whether they have one or more guideline-based standardized risk criteria, a large-scale real-world analysis suggests.
Haoyu Wang, MD, and colleagues showed that having at least one high-risk feature, as outlined in the 2018 European Society of Cardiology and European Association for Cardiothoracic Surgery (ESC/EACTS) Guidelines on Myocardial Revascularization, was associated with an increased risk for target vessel failure by 48% and for a patient-oriented composite outcome by 44%.
Moreover, they showed that implantation of at least three stents and the presence of diabetes and diffuse multivessel disease were the only high-risk features from the guidelines that were independent predictors of the two outcomes.
The study of more than 10,000 PCI patients also showed that determining whether patients were at high bleeding risk (HBR) did not modify their ischemic risk.
This, said Dr. Wang, from the National Center for Cardiovascular Diseases, Fuwai Hospital, Beijing, underscores the importance of applying the high ischemic risk (HIR) criteria from the ESC/EACTS guidelines when tailoring dual antiplatelet therapy (DAPT).
The research was presented at the European Atherosclerosis Society 2021 Virtual Congress on June 2, and published online in the Journal of Atherosclerosis and Thrombosis.
Dr. Wang told theheart.org | Medscape Cardiology that they conducted the study to determine which – HIR or HBR – is “most important to balance when treating patients undergoing PCI and then having dual antiplatelet therapy.”
The results showed that when patients have both a HIR and HBR, it is the ESC/EACTS guideline HIR criteria that have “a higher impact” than the bleeding risk, and that this can be “used to guide our choice of the duration of dual anti-platelet therapy.”
“Maybe we can extend, or use more potent, P2Y12 inhibitors” in those situations, he said.
S. Lale Tokgözoglu, MD, PhD, professor of cardiology, Hacettepe University, Ankara, Turkey, who was not involved in the study, said the HIR assessment “performed well,” adding that the HBR score might have been expected to attenuate its “prognostic advantage.”
She told this news organization that the results “are interesting since previous observations have suggested that Asian patients may be more prone to medication side effects and bleeding.”
These findings emphasize the importance of assessing HIR in daily PCI practice and confirm that it “performs well in different populations in real life,” added Dr. Tokgözoglu, a former president of the EAS.
The ESC/EACTS guidelines aimed to standardize the definition of HIR, Dr. Wang said during the presentation.
They set out 10 high-risk features for ischemic events for patients undergoing revascularization, which included patient medical history, comorbid conditions, and the characteristics of the PCI procedure.
Although the goals of the criteria are to inform decision-making and stimulate research, Dr. Wang said that their “prevalence and prognostic association with clinical outcomes are yet to be established in real-world PCI practice.”
Alongside, the Predicting Bleeding Complication in Patients Undergoing Stent Implantation and Subsequent Dual Antiplatelet Therapy (PRECISE-DAPT) score was developed to predict out-of-hospital bleeding in patients receiving DAPT after stent implantation.
Although a PRECISE-DAPT score of at least 25 constitutes a patient at high bleeding risk, Dr. Wang pointed out that such patients are typically also at risk for ischemic events after PCI, and it is “unclear” whether being at HBR modifies this risk.
To investigate further, they used the prospective, real-world Fuwai PCI registry to collate an all-comer patient population with unselected use of drug-eluting stents at the National Center for Cardiovascular Diseases at Fuwai Hospital.
They excluded individuals who were treated with balloon angioplasty alone, bioresorbable scaffolds, or bare metal stents, leaving a total population of 10,167 patients who were treated in 2013.
In that cohort, 5,149 patients (50.6%) met at least one risk criterion from the ESC/EACTS guidelines (HIR patients) and 5,018 (49.4%) met none of the risk criteria (non-HIR patients).
The most common criteria were implantation of at least three stents (23.5%); total stent length greater than 60 mm (20.2%); diffuse multivessel disease, especially in diabetic patients (18.5%); and a history of ST-segment elevation myocardial infarction (13.9%).
HIR patients were significantly older than non-HIR patients (average age, 58.86 vs. 57.77 years; P < .001), were more likely to have diabetes mellitus (42.6% vs. 16.9%; P < .001); and were more likely to have already had a myocardial infarction (32.2% vs. 5.2%; P < .001).
HIR patients also had higher average PRECISE-ADAPT scores than those without HIR (11.22 vs. 9.94; P < .001), and were conversely less likely to have the left anterior descending artery as the target vessel than non-HIR patients (86.0% vs. 94.6%; P < .001).
Cox regression analysis taking into account a range of patient and clinical factors revealed that HIR patients were significantly more likely than their non-HIR counterparts to experience target vessel failure (hazard ratio, 1.48; 95% confidence interval, 1.25-1.74; P < .001).
They were also significantly more likely to have a patient-oriented composite outcome, defined as all-cause death, any myocardial infarction, or any revascularization (HR, 1.44; 95% CI, 1.28-1.63; P < .001).
There was also a significantly higher risk for cardiac death in HIR than in non-HIR patients (HR, 1.95; 95% CI, 1.16-3.29; P = .012).
However, there was no significant association between HIR status and clinically relevant bleeding (HR, 0.84; 95% CI, 0.66-1.06; P = .143).
When the researchers looked at individual ischemic risk features, they found that, on fully adjusted analyses, only two were independent predictors of target vessel failure and the patient-oriented composite outcome.
Having at least three stents implanted was significantly associated with target vessel failure (HR, 1.36; 95% CI, 1.02-1.80; P = .038), and borderline significantly associated with the patient oriented composite outcome (HR, 1.23; 95% CI, 1.00-1.53; P = .056).
Diffuse multivessel disease, especially in diabetic patients, was significantly associated with both target vessel failure (HR, 1.24; 95% CI, 1.02-1.51; P = .035) and with the patient-oriented composite outcome (HR, 1.20; 95% CI, 1.04-1.39; P = .012).
Neither risk feature was significantly associated with clinically relevant bleeding, Dr. Wang noted.
Stratifying the patients by HBR status, the team found that rates of target vessel failure, the patient-oriented composite outcome, cardiac death, myocardial infarction, and definite/probable stent thrombosis were higher in patients with both HIR and HBR than those with neither HIR nor HBR (P < .001).
Further stratifying patients by PRECISE-ADAPT scores – 10 or less indicating very low risk, 11-17 indicating low risk, 18-24 indicating moderate risk, and at least 25 indicating high risk – showed that HIR features had a consistent effect on ischemic and bleeding outcomes, regardless of bleeding risk.
No funding declared. No relevant financial relationships declared.
A version of this article first appeared on Medscape.com.
A patient’s risk for ischemic events, but not bleeding, after percutaneous coronary intervention (PCI) can be predicted simply based on whether they have one or more guideline-based standardized risk criteria, a large-scale real-world analysis suggests.
Haoyu Wang, MD, and colleagues showed that having at least one high-risk feature, as outlined in the 2018 European Society of Cardiology and European Association for Cardiothoracic Surgery (ESC/EACTS) Guidelines on Myocardial Revascularization, was associated with an increased risk for target vessel failure by 48% and for a patient-oriented composite outcome by 44%.
Moreover, they showed that implantation of at least three stents and the presence of diabetes and diffuse multivessel disease were the only high-risk features from the guidelines that were independent predictors of the two outcomes.
The study of more than 10,000 PCI patients also showed that determining whether patients were at high bleeding risk (HBR) did not modify their ischemic risk.
This, said Dr. Wang, from the National Center for Cardiovascular Diseases, Fuwai Hospital, Beijing, underscores the importance of applying the high ischemic risk (HIR) criteria from the ESC/EACTS guidelines when tailoring dual antiplatelet therapy (DAPT).
The research was presented at the European Atherosclerosis Society 2021 Virtual Congress on June 2, and published online in the Journal of Atherosclerosis and Thrombosis.
Dr. Wang told theheart.org | Medscape Cardiology that they conducted the study to determine which – HIR or HBR – is “most important to balance when treating patients undergoing PCI and then having dual antiplatelet therapy.”
The results showed that when patients have both a HIR and HBR, it is the ESC/EACTS guideline HIR criteria that have “a higher impact” than the bleeding risk, and that this can be “used to guide our choice of the duration of dual anti-platelet therapy.”
“Maybe we can extend, or use more potent, P2Y12 inhibitors” in those situations, he said.
S. Lale Tokgözoglu, MD, PhD, professor of cardiology, Hacettepe University, Ankara, Turkey, who was not involved in the study, said the HIR assessment “performed well,” adding that the HBR score might have been expected to attenuate its “prognostic advantage.”
She told this news organization that the results “are interesting since previous observations have suggested that Asian patients may be more prone to medication side effects and bleeding.”
These findings emphasize the importance of assessing HIR in daily PCI practice and confirm that it “performs well in different populations in real life,” added Dr. Tokgözoglu, a former president of the EAS.
The ESC/EACTS guidelines aimed to standardize the definition of HIR, Dr. Wang said during the presentation.
They set out 10 high-risk features for ischemic events for patients undergoing revascularization, which included patient medical history, comorbid conditions, and the characteristics of the PCI procedure.
Although the goals of the criteria are to inform decision-making and stimulate research, Dr. Wang said that their “prevalence and prognostic association with clinical outcomes are yet to be established in real-world PCI practice.”
Alongside, the Predicting Bleeding Complication in Patients Undergoing Stent Implantation and Subsequent Dual Antiplatelet Therapy (PRECISE-DAPT) score was developed to predict out-of-hospital bleeding in patients receiving DAPT after stent implantation.
Although a PRECISE-DAPT score of at least 25 constitutes a patient at high bleeding risk, Dr. Wang pointed out that such patients are typically also at risk for ischemic events after PCI, and it is “unclear” whether being at HBR modifies this risk.
To investigate further, they used the prospective, real-world Fuwai PCI registry to collate an all-comer patient population with unselected use of drug-eluting stents at the National Center for Cardiovascular Diseases at Fuwai Hospital.
They excluded individuals who were treated with balloon angioplasty alone, bioresorbable scaffolds, or bare metal stents, leaving a total population of 10,167 patients who were treated in 2013.
In that cohort, 5,149 patients (50.6%) met at least one risk criterion from the ESC/EACTS guidelines (HIR patients) and 5,018 (49.4%) met none of the risk criteria (non-HIR patients).
The most common criteria were implantation of at least three stents (23.5%); total stent length greater than 60 mm (20.2%); diffuse multivessel disease, especially in diabetic patients (18.5%); and a history of ST-segment elevation myocardial infarction (13.9%).
HIR patients were significantly older than non-HIR patients (average age, 58.86 vs. 57.77 years; P < .001), were more likely to have diabetes mellitus (42.6% vs. 16.9%; P < .001); and were more likely to have already had a myocardial infarction (32.2% vs. 5.2%; P < .001).
HIR patients also had higher average PRECISE-ADAPT scores than those without HIR (11.22 vs. 9.94; P < .001), and were conversely less likely to have the left anterior descending artery as the target vessel than non-HIR patients (86.0% vs. 94.6%; P < .001).
Cox regression analysis taking into account a range of patient and clinical factors revealed that HIR patients were significantly more likely than their non-HIR counterparts to experience target vessel failure (hazard ratio, 1.48; 95% confidence interval, 1.25-1.74; P < .001).
They were also significantly more likely to have a patient-oriented composite outcome, defined as all-cause death, any myocardial infarction, or any revascularization (HR, 1.44; 95% CI, 1.28-1.63; P < .001).
There was also a significantly higher risk for cardiac death in HIR than in non-HIR patients (HR, 1.95; 95% CI, 1.16-3.29; P = .012).
However, there was no significant association between HIR status and clinically relevant bleeding (HR, 0.84; 95% CI, 0.66-1.06; P = .143).
When the researchers looked at individual ischemic risk features, they found that, on fully adjusted analyses, only two were independent predictors of target vessel failure and the patient-oriented composite outcome.
Having at least three stents implanted was significantly associated with target vessel failure (HR, 1.36; 95% CI, 1.02-1.80; P = .038), and borderline significantly associated with the patient oriented composite outcome (HR, 1.23; 95% CI, 1.00-1.53; P = .056).
Diffuse multivessel disease, especially in diabetic patients, was significantly associated with both target vessel failure (HR, 1.24; 95% CI, 1.02-1.51; P = .035) and with the patient-oriented composite outcome (HR, 1.20; 95% CI, 1.04-1.39; P = .012).
Neither risk feature was significantly associated with clinically relevant bleeding, Dr. Wang noted.
Stratifying the patients by HBR status, the team found that rates of target vessel failure, the patient-oriented composite outcome, cardiac death, myocardial infarction, and definite/probable stent thrombosis were higher in patients with both HIR and HBR than those with neither HIR nor HBR (P < .001).
Further stratifying patients by PRECISE-ADAPT scores – 10 or less indicating very low risk, 11-17 indicating low risk, 18-24 indicating moderate risk, and at least 25 indicating high risk – showed that HIR features had a consistent effect on ischemic and bleeding outcomes, regardless of bleeding risk.
No funding declared. No relevant financial relationships declared.
A version of this article first appeared on Medscape.com.
A patient’s risk for ischemic events, but not bleeding, after percutaneous coronary intervention (PCI) can be predicted simply based on whether they have one or more guideline-based standardized risk criteria, a large-scale real-world analysis suggests.
Haoyu Wang, MD, and colleagues showed that having at least one high-risk feature, as outlined in the 2018 European Society of Cardiology and European Association for Cardiothoracic Surgery (ESC/EACTS) Guidelines on Myocardial Revascularization, was associated with an increased risk for target vessel failure by 48% and for a patient-oriented composite outcome by 44%.
Moreover, they showed that implantation of at least three stents and the presence of diabetes and diffuse multivessel disease were the only high-risk features from the guidelines that were independent predictors of the two outcomes.
The study of more than 10,000 PCI patients also showed that determining whether patients were at high bleeding risk (HBR) did not modify their ischemic risk.
This, said Dr. Wang, from the National Center for Cardiovascular Diseases, Fuwai Hospital, Beijing, underscores the importance of applying the high ischemic risk (HIR) criteria from the ESC/EACTS guidelines when tailoring dual antiplatelet therapy (DAPT).
The research was presented at the European Atherosclerosis Society 2021 Virtual Congress on June 2, and published online in the Journal of Atherosclerosis and Thrombosis.
Dr. Wang told theheart.org | Medscape Cardiology that they conducted the study to determine which – HIR or HBR – is “most important to balance when treating patients undergoing PCI and then having dual antiplatelet therapy.”
The results showed that when patients have both a HIR and HBR, it is the ESC/EACTS guideline HIR criteria that have “a higher impact” than the bleeding risk, and that this can be “used to guide our choice of the duration of dual anti-platelet therapy.”
“Maybe we can extend, or use more potent, P2Y12 inhibitors” in those situations, he said.
S. Lale Tokgözoglu, MD, PhD, professor of cardiology, Hacettepe University, Ankara, Turkey, who was not involved in the study, said the HIR assessment “performed well,” adding that the HBR score might have been expected to attenuate its “prognostic advantage.”
She told this news organization that the results “are interesting since previous observations have suggested that Asian patients may be more prone to medication side effects and bleeding.”
These findings emphasize the importance of assessing HIR in daily PCI practice and confirm that it “performs well in different populations in real life,” added Dr. Tokgözoglu, a former president of the EAS.
The ESC/EACTS guidelines aimed to standardize the definition of HIR, Dr. Wang said during the presentation.
They set out 10 high-risk features for ischemic events for patients undergoing revascularization, which included patient medical history, comorbid conditions, and the characteristics of the PCI procedure.
Although the goals of the criteria are to inform decision-making and stimulate research, Dr. Wang said that their “prevalence and prognostic association with clinical outcomes are yet to be established in real-world PCI practice.”
Alongside, the Predicting Bleeding Complication in Patients Undergoing Stent Implantation and Subsequent Dual Antiplatelet Therapy (PRECISE-DAPT) score was developed to predict out-of-hospital bleeding in patients receiving DAPT after stent implantation.
Although a PRECISE-DAPT score of at least 25 constitutes a patient at high bleeding risk, Dr. Wang pointed out that such patients are typically also at risk for ischemic events after PCI, and it is “unclear” whether being at HBR modifies this risk.
To investigate further, they used the prospective, real-world Fuwai PCI registry to collate an all-comer patient population with unselected use of drug-eluting stents at the National Center for Cardiovascular Diseases at Fuwai Hospital.
They excluded individuals who were treated with balloon angioplasty alone, bioresorbable scaffolds, or bare metal stents, leaving a total population of 10,167 patients who were treated in 2013.
In that cohort, 5,149 patients (50.6%) met at least one risk criterion from the ESC/EACTS guidelines (HIR patients) and 5,018 (49.4%) met none of the risk criteria (non-HIR patients).
The most common criteria were implantation of at least three stents (23.5%); total stent length greater than 60 mm (20.2%); diffuse multivessel disease, especially in diabetic patients (18.5%); and a history of ST-segment elevation myocardial infarction (13.9%).
HIR patients were significantly older than non-HIR patients (average age, 58.86 vs. 57.77 years; P < .001), were more likely to have diabetes mellitus (42.6% vs. 16.9%; P < .001); and were more likely to have already had a myocardial infarction (32.2% vs. 5.2%; P < .001).
HIR patients also had higher average PRECISE-ADAPT scores than those without HIR (11.22 vs. 9.94; P < .001), and were conversely less likely to have the left anterior descending artery as the target vessel than non-HIR patients (86.0% vs. 94.6%; P < .001).
Cox regression analysis taking into account a range of patient and clinical factors revealed that HIR patients were significantly more likely than their non-HIR counterparts to experience target vessel failure (hazard ratio, 1.48; 95% confidence interval, 1.25-1.74; P < .001).
They were also significantly more likely to have a patient-oriented composite outcome, defined as all-cause death, any myocardial infarction, or any revascularization (HR, 1.44; 95% CI, 1.28-1.63; P < .001).
There was also a significantly higher risk for cardiac death in HIR than in non-HIR patients (HR, 1.95; 95% CI, 1.16-3.29; P = .012).
However, there was no significant association between HIR status and clinically relevant bleeding (HR, 0.84; 95% CI, 0.66-1.06; P = .143).
When the researchers looked at individual ischemic risk features, they found that, on fully adjusted analyses, only two were independent predictors of target vessel failure and the patient-oriented composite outcome.
Having at least three stents implanted was significantly associated with target vessel failure (HR, 1.36; 95% CI, 1.02-1.80; P = .038), and borderline significantly associated with the patient oriented composite outcome (HR, 1.23; 95% CI, 1.00-1.53; P = .056).
Diffuse multivessel disease, especially in diabetic patients, was significantly associated with both target vessel failure (HR, 1.24; 95% CI, 1.02-1.51; P = .035) and with the patient-oriented composite outcome (HR, 1.20; 95% CI, 1.04-1.39; P = .012).
Neither risk feature was significantly associated with clinically relevant bleeding, Dr. Wang noted.
Stratifying the patients by HBR status, the team found that rates of target vessel failure, the patient-oriented composite outcome, cardiac death, myocardial infarction, and definite/probable stent thrombosis were higher in patients with both HIR and HBR than those with neither HIR nor HBR (P < .001).
Further stratifying patients by PRECISE-ADAPT scores – 10 or less indicating very low risk, 11-17 indicating low risk, 18-24 indicating moderate risk, and at least 25 indicating high risk – showed that HIR features had a consistent effect on ischemic and bleeding outcomes, regardless of bleeding risk.
No funding declared. No relevant financial relationships declared.
A version of this article first appeared on Medscape.com.
Professional versus facility billing: What hospitalists must know
Dramatic impact on hospital margins
Coding and billing for the professional services of physicians and other practitioners in the hospital and for the hospital’s facility costs are separate and distinct processes. But both reflect the totality of care given to patients in the complex, costly, heavily regulated setting of an acute care hospital. And both are essential to the financial well-being of the hospital and its providers, and to their mutual ability to survive current financial uncertainties imposed by the COVID pandemic.
“What hospitalists don’t realize is that your professional billing is a completely separate entity [from the facility’s billing],” said Aziz Ansari, DO, SFHM, hospitalist, professor of medicine, and associate chief medical officer for clinical optimization and revenue integrity at Loyola University Medical Center in Maywood, Ill. “Your E/M [Evaluation and Management] coding has a separate set of rules, which are not married at all to facility billing.”
Dr. Ansari presented a session at Converge – the annual conference of SHM – in May 2021, on the hospitalist’s role in “Piloting the Twin Engines of the Mid-Revenue Cycle Ship,” with a focus on how physician documentation can optimize both facility billing and quality of care. Hospitalists generally don’t realize how much impact they actually have on their hospital’s revenue cycle and quality, he said. Thorough documentation, accurately and specifically describing the patient’s severity of illness and complexity, affects both.
“When a utilization management nurse calls you about a case, you need to realize they are your partner in getting it right.” A simple documentation lapse that would change a case from observation to inpatient could cost the hospital $3,000 or more per case, and that can add up quickly, Dr. Ansari said. “We’ve seen what happened with COVID. We realized how fragile the system is, and how razor-thin hospital margins are.”
Distinction between professional and facility billing
Professional billing by hospitalist physicians and advanced practice providers is done for their individual encounters with patients and charged per visit for every day the patient is in the hospital based on the treatments, examinations, and medical decision-making required to care for that patient.
These are spelled out using E/M codes derived from Current Procedural Terminology, which is maintained by the American Medical Association for specifying what the provider did during the encounter. Other parameters of professional billing include complexity of decision-making versus amount of time spent, and a variety of modifiers.
By contrast, facility billing by hospitals is based on the complexity of the patient’s condition and is generally done whether the hospitalization is considered an inpatient hospitalization or an outpatient hospitalization such as an observation stay. Inpatient hospital stays are often paid using diagnosis-related groupings (DRGs), Medicare’s patient classification system for standardizing prospective payment to hospitals and encouraging cost-containment strategies.
DRGs, which represent about half of total hospital reimbursement, are a separate payment mechanism covering all facility charges associated with the inpatient stay from admission to discharge, incorporating the costs of providing hospital care, including but not limited to space, equipment, supplies, tests, and medications. Outpatient hospital stays, by contrast, are paid based on Ambulatory Payment Classifications.
A facility bill is submitted to the payer at the end of the hospital stay, describing the patient’s condition using ICD-10 diagnostic codes. All of the patient’s diagnoses and comorbidities contribute to the assignment of a DRG that best captures the total hospital stay. But to make the issue more complicated, the system is evolving toward models of bundled payment that will eventually phase out traditional DRGs in favor of new systems combining inpatient and outpatient reimbursement into a single bundled episode of care.
Professional and facility bills for a single hospitalization may be prepared by different personnel on separate teams following different rules, although they may both be housed in the hospital’s billing department. The differing rules for coding professional services versus facility services can be hard for hospitalists to appreciate, said Wendy Arafiles, MD, a pediatric hospitalist at Phoenix Children’s Hospital and medical director for its clinical documentation integrity (CDI) team. An example is for uncertain diagnoses. There may be a clinical suspicion of a diagnosis, and language such as “likely bacterial pneumonia” might be sufficient for facility coding but not for professional services coding.
Hospitalists, depending on their group’s size, structure, and relationship to the hospital, may be responsible for selecting the CPT codes or other parameters for the insurance claim and bill. Or these may be left to billing specialists. And those specialists could be employed by the hospital or by the hospitalist group or multispecialty medical group, or they could be contracted outside agencies that handle the billing for a fee.
The revenue cycle
The hospital revenue cycle has a lot of cogs in the machine, Dr. Arafiles said. “This is just one of the many nuances of our crazy system. I will go out on a limb and say it is not our job as clinicians to know all of those nuances.” The DRG assignment is dependent on how providers can describe the complexity of the patient and severity of the illness, even if it doesn’t impact professional billing, Dr. Arafiles added.
Hospitalists don’t want to think about money when providing patient care. “Our job is to provide the best care to our patients. We often utilize resources without thinking about how much they are going to cost, so that we can do what we think is necessary for our patients,” she explained. But accurate diagnosis codes can capture the complexity of the care. “Maybe we don’t take that part seriously enough. As long as I, as the provider, can accurately describe the complexity of my patient, I can justify why I spent all those resources and so many days caring for him or her.”
Charles Locke, MD, executive medical director of care management for LifeBridge Health and assistant professor of medicine at Johns Hopkins University, Baltimore, said hospitalists typically are paid set salaries directly by the hospital, in some cases with productivity bonuses based in part on their billing and posted RVUs (relative value units). RVUs are the cornerstone of Medicare’s reimbursement formula for physician services.
“Another thing to keep in mind, one might think in 2021 that the computer systems would be sophisticated enough to link up professional and facility billing to ensure that bills for each are concordant for services provided on a given day. But it turns out they are not yet well connected,” Dr. Locke said.
“These are issues that everybody struggles with. Hospitalists need to know and order the appropriate status, inpatient versus outpatient, and whether and when to order observation services, as this will affect hospital reimbursement and, potentially, patient liability,” he explained.1 If the hospital is denied its facility claim because of improper status, that denial doesn’t necessary extend to a denial for the doctor’s professional fee. “Hospitalists need to know these are often separated. Even though their professional fee is honored, the hospital’s service charges may not be.”
Dr. Locke said knowing the history of Medicare might help hospitalists to better appreciate the distinctions. When this federal entitlement was first proposed in the 1960s as a way to help older Americans in poverty obtain needed health care, organized medicine sought to be excluded from the program. “Nonhospital services and doctors’ service fees were not included in the original Medicare proposal,” he said. Medicare Part B was created to provide insurance for doctors’ professional fees, which are still handled separately under Medicare.
Many institutions use clinical documentation for multiple purposes. “There are so many masters for this one document,” Dr. Arafiles said. The information is also used for various quality and patient safety metrics and data gathering. “Every code we choose is used in many different ways by the institution. We don’t know where all it goes. But we need to know how to describe how complex the case was, and how much work it entailed. The more we know about how to describe that, the better for the institution.”
Dr. Arafiles views the clinical note, first and foremost, as clinical communication, so that one provider can seamlessly pick up where the previous left off. “If I use language in my note that is accurate and specific, it will be useful to all who later need it.” Building on metrics such as expected versus actual 30-day readmission rates, risk-adjusted mortality, and all the ways government agencies report hospital quality, she said, “what we document has lasting impact. That’s where the facility side of billing and coding is ever more important. You can’t just think about your professional billing and RVUs.”
Support from the hospital
Some hospitalists may think facility billing is not their concern. But consider this: The average support or subsidy paid by U.S. hospitals for a full-time equivalent hospitalist is estimated at $198,750, according to SHM’s 2020 State of Hospital Medicine.2 That support reflects the difference between the cost of employing a hospitalist in a competitive labor environment and what that provider is actually able to generate in billing income, said Hardik Vora, MD, MPH, SFHM, chair of SHM’s practice management committee.
With a lot of medical specialties, the physician’s salary is only or largely supported by professional billing, said Dr. Vora, who is medical director for Hospital Medicine and physician advisor for utilization management and CDI at Riverside Health System, Yorktown, Va.
“Hospital medicine is different in that aspect, regardless of employment model. And that’s where the concept of value comes in – how else do you bring value to the hospital that supports you,” said Dr. Vora.
Hospitalists often emphasize their contributions to quality improvement, patient safety, and hospital governance committees – all the ways they contribute to the health of the institution – as justification for their support from the hospital. But beneath all of that is the income the hospital generates from facility billing and from the hospitalist’s contributions to complete, accurate, and timely documentation that can support the hospital’s bills.
Typically, this hospital support to supplement hospitalist billing income is not directly tied to the income generated by facility billing or to the hospitalist’s contribution to its completeness. But between growing technological sophistication and greater belt-tightening, that link may get closer over time.
Other players
Because of the importance of complete and accurate billing to the hospital’s financial well-being, specialized supportive services have evolved, from traditional utilization review or utilization management to CDI services and the role of physician advisors – experienced doctors who know well how these processes work and are able to teach providers about regulatory compliance and medical necessity.
“One of my jobs as the medical director for our hospital’s CDI program is to educate residents, fellows, and newly onboarded providers to be descriptive enough in their charting to capture the complexity of the patient’s condition,” Dr. Arafiles said. Physician advisors and CDI programs can involve clinical providers in bringing value to the institution through their documentation. They serve as the intermediaries between the coders and the clinicians.
The CDI specialist’s job description focuses on diagnosis capture and associated reimbursement. But integrity broadly defined goes to the integrity of the medical record and its contribution to quality and patient safety as well as providing a medical record that is defensible to audits, physician revenue cycle expert Glenn Krauss noted in a recent post at ICD10 Monitor.3
Dr. Vora sees his role as physician advisor to be the link between the hospital’s executive team and the hospital’s medical providers. “Providers need help in understanding a complex set of ever-changing rules of facility billing and the frequently competing priorities between facility and professional billing. I tell my providers: The longer the patient stays in the hospital, you may be generating more RVUs, but our facility may be losing money.”
Hospital administrators are acutely aware of facility billing, but they don’t necessarily understand the nuances of professional billing, said Jay Weatherly, MS, the cofounder of Hospitalist Billing, a company that specializes in comprehensive billing and collection solutions for hospitalist groups that are employed directly by their hospitals. But he sees an essential symbiotic relationship between hospital administrators and clinicians.
“We rely on hospitalists’ record keeping to do our job. We rely on them to get it right,” he said. “We want to encourage doctors to cooperate with the process. Billing should never be a physician’s top priority, but it is important, nonetheless.”
HBI is relentless in pursuit of the information needed for its coding and billing, but does so gently, in a way not to put off doctors, Mr. Weatherly said. “There is an art and a science associated with securing the needed information. We have great respect for the doctors we work with, yet we’re all spokes in a bigger wheel, and we need to bill effectively in order to keep the wheel moving.”
What can hospitalists do?
Sources for this article say one of the best places for hospitalists to start improving their understanding of these distinctions is to ask the coders in their institution for advice on how to make the process run more smoothly.
“If you have a CDI team, they are there to help. Reach out to them,” Dr. Arafiles said. Generally, medical schools and residency programs fail to convey the complexities of contemporary hospital economics to future doctors.
Hospitalists have become indispensable, Dr. Vora said. But salaries for hospitalists are going up while hospital reimbursement is going down, and hospitalists are not seeing more patients. “At some point we will no longer be able to say financial support for hospital medicine groups is just a cost of doing business for the hospital. COVID tested us – and demonstrated how much hospital executives value us as part of the team. Our organization absolutely stood behind its physicians despite financially challenging times. Now we need to do what we can to support the organization,” he added.
Hospitalists can also continue to educate themselves on good documentation and coding practices, by finding programs like SHM’s Utilization Management and Clinical Documentation for Hospitalists.
“As we see a significant shift to value-based payment, with its focus on value, efficiency, quality – the best care at the lowest possible price – hospital medicine as a specialty will be best positioned to help with that. If the hospital does well, we do well. We should be building relationships with the hospital’s leadership team,” Dr. Vora said. “You always want to contribute to that partnership to the highest level possible. When they look at us, they should see their most reliable partner.”
References
1. Locke C, Hu E. Medicare’s two-midnight rule: What hospitalists must know. The Hospitalist. 2019 Feb 22.
2. Beresford L. Hospital medicine in a worldwide pandemic: State of Hospital Medicine 2020. The Hospitalist. 2020 Sep 20.
3. Krauss G. Clinical documentation integrity: rebranding and repurposing. ICD10 Monitor. March 16, 2020 Mar 16. https://www.icd10monitor.com/clinical-documentation-integrity-rebranding-and-repurposing.
Dramatic impact on hospital margins
Dramatic impact on hospital margins
Coding and billing for the professional services of physicians and other practitioners in the hospital and for the hospital’s facility costs are separate and distinct processes. But both reflect the totality of care given to patients in the complex, costly, heavily regulated setting of an acute care hospital. And both are essential to the financial well-being of the hospital and its providers, and to their mutual ability to survive current financial uncertainties imposed by the COVID pandemic.
“What hospitalists don’t realize is that your professional billing is a completely separate entity [from the facility’s billing],” said Aziz Ansari, DO, SFHM, hospitalist, professor of medicine, and associate chief medical officer for clinical optimization and revenue integrity at Loyola University Medical Center in Maywood, Ill. “Your E/M [Evaluation and Management] coding has a separate set of rules, which are not married at all to facility billing.”
Dr. Ansari presented a session at Converge – the annual conference of SHM – in May 2021, on the hospitalist’s role in “Piloting the Twin Engines of the Mid-Revenue Cycle Ship,” with a focus on how physician documentation can optimize both facility billing and quality of care. Hospitalists generally don’t realize how much impact they actually have on their hospital’s revenue cycle and quality, he said. Thorough documentation, accurately and specifically describing the patient’s severity of illness and complexity, affects both.
“When a utilization management nurse calls you about a case, you need to realize they are your partner in getting it right.” A simple documentation lapse that would change a case from observation to inpatient could cost the hospital $3,000 or more per case, and that can add up quickly, Dr. Ansari said. “We’ve seen what happened with COVID. We realized how fragile the system is, and how razor-thin hospital margins are.”
Distinction between professional and facility billing
Professional billing by hospitalist physicians and advanced practice providers is done for their individual encounters with patients and charged per visit for every day the patient is in the hospital based on the treatments, examinations, and medical decision-making required to care for that patient.
These are spelled out using E/M codes derived from Current Procedural Terminology, which is maintained by the American Medical Association for specifying what the provider did during the encounter. Other parameters of professional billing include complexity of decision-making versus amount of time spent, and a variety of modifiers.
By contrast, facility billing by hospitals is based on the complexity of the patient’s condition and is generally done whether the hospitalization is considered an inpatient hospitalization or an outpatient hospitalization such as an observation stay. Inpatient hospital stays are often paid using diagnosis-related groupings (DRGs), Medicare’s patient classification system for standardizing prospective payment to hospitals and encouraging cost-containment strategies.
DRGs, which represent about half of total hospital reimbursement, are a separate payment mechanism covering all facility charges associated with the inpatient stay from admission to discharge, incorporating the costs of providing hospital care, including but not limited to space, equipment, supplies, tests, and medications. Outpatient hospital stays, by contrast, are paid based on Ambulatory Payment Classifications.
A facility bill is submitted to the payer at the end of the hospital stay, describing the patient’s condition using ICD-10 diagnostic codes. All of the patient’s diagnoses and comorbidities contribute to the assignment of a DRG that best captures the total hospital stay. But to make the issue more complicated, the system is evolving toward models of bundled payment that will eventually phase out traditional DRGs in favor of new systems combining inpatient and outpatient reimbursement into a single bundled episode of care.
Professional and facility bills for a single hospitalization may be prepared by different personnel on separate teams following different rules, although they may both be housed in the hospital’s billing department. The differing rules for coding professional services versus facility services can be hard for hospitalists to appreciate, said Wendy Arafiles, MD, a pediatric hospitalist at Phoenix Children’s Hospital and medical director for its clinical documentation integrity (CDI) team. An example is for uncertain diagnoses. There may be a clinical suspicion of a diagnosis, and language such as “likely bacterial pneumonia” might be sufficient for facility coding but not for professional services coding.
Hospitalists, depending on their group’s size, structure, and relationship to the hospital, may be responsible for selecting the CPT codes or other parameters for the insurance claim and bill. Or these may be left to billing specialists. And those specialists could be employed by the hospital or by the hospitalist group or multispecialty medical group, or they could be contracted outside agencies that handle the billing for a fee.
The revenue cycle
The hospital revenue cycle has a lot of cogs in the machine, Dr. Arafiles said. “This is just one of the many nuances of our crazy system. I will go out on a limb and say it is not our job as clinicians to know all of those nuances.” The DRG assignment is dependent on how providers can describe the complexity of the patient and severity of the illness, even if it doesn’t impact professional billing, Dr. Arafiles added.
Hospitalists don’t want to think about money when providing patient care. “Our job is to provide the best care to our patients. We often utilize resources without thinking about how much they are going to cost, so that we can do what we think is necessary for our patients,” she explained. But accurate diagnosis codes can capture the complexity of the care. “Maybe we don’t take that part seriously enough. As long as I, as the provider, can accurately describe the complexity of my patient, I can justify why I spent all those resources and so many days caring for him or her.”
Charles Locke, MD, executive medical director of care management for LifeBridge Health and assistant professor of medicine at Johns Hopkins University, Baltimore, said hospitalists typically are paid set salaries directly by the hospital, in some cases with productivity bonuses based in part on their billing and posted RVUs (relative value units). RVUs are the cornerstone of Medicare’s reimbursement formula for physician services.
“Another thing to keep in mind, one might think in 2021 that the computer systems would be sophisticated enough to link up professional and facility billing to ensure that bills for each are concordant for services provided on a given day. But it turns out they are not yet well connected,” Dr. Locke said.
“These are issues that everybody struggles with. Hospitalists need to know and order the appropriate status, inpatient versus outpatient, and whether and when to order observation services, as this will affect hospital reimbursement and, potentially, patient liability,” he explained.1 If the hospital is denied its facility claim because of improper status, that denial doesn’t necessary extend to a denial for the doctor’s professional fee. “Hospitalists need to know these are often separated. Even though their professional fee is honored, the hospital’s service charges may not be.”
Dr. Locke said knowing the history of Medicare might help hospitalists to better appreciate the distinctions. When this federal entitlement was first proposed in the 1960s as a way to help older Americans in poverty obtain needed health care, organized medicine sought to be excluded from the program. “Nonhospital services and doctors’ service fees were not included in the original Medicare proposal,” he said. Medicare Part B was created to provide insurance for doctors’ professional fees, which are still handled separately under Medicare.
Many institutions use clinical documentation for multiple purposes. “There are so many masters for this one document,” Dr. Arafiles said. The information is also used for various quality and patient safety metrics and data gathering. “Every code we choose is used in many different ways by the institution. We don’t know where all it goes. But we need to know how to describe how complex the case was, and how much work it entailed. The more we know about how to describe that, the better for the institution.”
Dr. Arafiles views the clinical note, first and foremost, as clinical communication, so that one provider can seamlessly pick up where the previous left off. “If I use language in my note that is accurate and specific, it will be useful to all who later need it.” Building on metrics such as expected versus actual 30-day readmission rates, risk-adjusted mortality, and all the ways government agencies report hospital quality, she said, “what we document has lasting impact. That’s where the facility side of billing and coding is ever more important. You can’t just think about your professional billing and RVUs.”
Support from the hospital
Some hospitalists may think facility billing is not their concern. But consider this: The average support or subsidy paid by U.S. hospitals for a full-time equivalent hospitalist is estimated at $198,750, according to SHM’s 2020 State of Hospital Medicine.2 That support reflects the difference between the cost of employing a hospitalist in a competitive labor environment and what that provider is actually able to generate in billing income, said Hardik Vora, MD, MPH, SFHM, chair of SHM’s practice management committee.
With a lot of medical specialties, the physician’s salary is only or largely supported by professional billing, said Dr. Vora, who is medical director for Hospital Medicine and physician advisor for utilization management and CDI at Riverside Health System, Yorktown, Va.
“Hospital medicine is different in that aspect, regardless of employment model. And that’s where the concept of value comes in – how else do you bring value to the hospital that supports you,” said Dr. Vora.
Hospitalists often emphasize their contributions to quality improvement, patient safety, and hospital governance committees – all the ways they contribute to the health of the institution – as justification for their support from the hospital. But beneath all of that is the income the hospital generates from facility billing and from the hospitalist’s contributions to complete, accurate, and timely documentation that can support the hospital’s bills.
Typically, this hospital support to supplement hospitalist billing income is not directly tied to the income generated by facility billing or to the hospitalist’s contribution to its completeness. But between growing technological sophistication and greater belt-tightening, that link may get closer over time.
Other players
Because of the importance of complete and accurate billing to the hospital’s financial well-being, specialized supportive services have evolved, from traditional utilization review or utilization management to CDI services and the role of physician advisors – experienced doctors who know well how these processes work and are able to teach providers about regulatory compliance and medical necessity.
“One of my jobs as the medical director for our hospital’s CDI program is to educate residents, fellows, and newly onboarded providers to be descriptive enough in their charting to capture the complexity of the patient’s condition,” Dr. Arafiles said. Physician advisors and CDI programs can involve clinical providers in bringing value to the institution through their documentation. They serve as the intermediaries between the coders and the clinicians.
The CDI specialist’s job description focuses on diagnosis capture and associated reimbursement. But integrity broadly defined goes to the integrity of the medical record and its contribution to quality and patient safety as well as providing a medical record that is defensible to audits, physician revenue cycle expert Glenn Krauss noted in a recent post at ICD10 Monitor.3
Dr. Vora sees his role as physician advisor to be the link between the hospital’s executive team and the hospital’s medical providers. “Providers need help in understanding a complex set of ever-changing rules of facility billing and the frequently competing priorities between facility and professional billing. I tell my providers: The longer the patient stays in the hospital, you may be generating more RVUs, but our facility may be losing money.”
Hospital administrators are acutely aware of facility billing, but they don’t necessarily understand the nuances of professional billing, said Jay Weatherly, MS, the cofounder of Hospitalist Billing, a company that specializes in comprehensive billing and collection solutions for hospitalist groups that are employed directly by their hospitals. But he sees an essential symbiotic relationship between hospital administrators and clinicians.
“We rely on hospitalists’ record keeping to do our job. We rely on them to get it right,” he said. “We want to encourage doctors to cooperate with the process. Billing should never be a physician’s top priority, but it is important, nonetheless.”
HBI is relentless in pursuit of the information needed for its coding and billing, but does so gently, in a way not to put off doctors, Mr. Weatherly said. “There is an art and a science associated with securing the needed information. We have great respect for the doctors we work with, yet we’re all spokes in a bigger wheel, and we need to bill effectively in order to keep the wheel moving.”
What can hospitalists do?
Sources for this article say one of the best places for hospitalists to start improving their understanding of these distinctions is to ask the coders in their institution for advice on how to make the process run more smoothly.
“If you have a CDI team, they are there to help. Reach out to them,” Dr. Arafiles said. Generally, medical schools and residency programs fail to convey the complexities of contemporary hospital economics to future doctors.
Hospitalists have become indispensable, Dr. Vora said. But salaries for hospitalists are going up while hospital reimbursement is going down, and hospitalists are not seeing more patients. “At some point we will no longer be able to say financial support for hospital medicine groups is just a cost of doing business for the hospital. COVID tested us – and demonstrated how much hospital executives value us as part of the team. Our organization absolutely stood behind its physicians despite financially challenging times. Now we need to do what we can to support the organization,” he added.
Hospitalists can also continue to educate themselves on good documentation and coding practices, by finding programs like SHM’s Utilization Management and Clinical Documentation for Hospitalists.
“As we see a significant shift to value-based payment, with its focus on value, efficiency, quality – the best care at the lowest possible price – hospital medicine as a specialty will be best positioned to help with that. If the hospital does well, we do well. We should be building relationships with the hospital’s leadership team,” Dr. Vora said. “You always want to contribute to that partnership to the highest level possible. When they look at us, they should see their most reliable partner.”
References
1. Locke C, Hu E. Medicare’s two-midnight rule: What hospitalists must know. The Hospitalist. 2019 Feb 22.
2. Beresford L. Hospital medicine in a worldwide pandemic: State of Hospital Medicine 2020. The Hospitalist. 2020 Sep 20.
3. Krauss G. Clinical documentation integrity: rebranding and repurposing. ICD10 Monitor. March 16, 2020 Mar 16. https://www.icd10monitor.com/clinical-documentation-integrity-rebranding-and-repurposing.
Coding and billing for the professional services of physicians and other practitioners in the hospital and for the hospital’s facility costs are separate and distinct processes. But both reflect the totality of care given to patients in the complex, costly, heavily regulated setting of an acute care hospital. And both are essential to the financial well-being of the hospital and its providers, and to their mutual ability to survive current financial uncertainties imposed by the COVID pandemic.
“What hospitalists don’t realize is that your professional billing is a completely separate entity [from the facility’s billing],” said Aziz Ansari, DO, SFHM, hospitalist, professor of medicine, and associate chief medical officer for clinical optimization and revenue integrity at Loyola University Medical Center in Maywood, Ill. “Your E/M [Evaluation and Management] coding has a separate set of rules, which are not married at all to facility billing.”
Dr. Ansari presented a session at Converge – the annual conference of SHM – in May 2021, on the hospitalist’s role in “Piloting the Twin Engines of the Mid-Revenue Cycle Ship,” with a focus on how physician documentation can optimize both facility billing and quality of care. Hospitalists generally don’t realize how much impact they actually have on their hospital’s revenue cycle and quality, he said. Thorough documentation, accurately and specifically describing the patient’s severity of illness and complexity, affects both.
“When a utilization management nurse calls you about a case, you need to realize they are your partner in getting it right.” A simple documentation lapse that would change a case from observation to inpatient could cost the hospital $3,000 or more per case, and that can add up quickly, Dr. Ansari said. “We’ve seen what happened with COVID. We realized how fragile the system is, and how razor-thin hospital margins are.”
Distinction between professional and facility billing
Professional billing by hospitalist physicians and advanced practice providers is done for their individual encounters with patients and charged per visit for every day the patient is in the hospital based on the treatments, examinations, and medical decision-making required to care for that patient.
These are spelled out using E/M codes derived from Current Procedural Terminology, which is maintained by the American Medical Association for specifying what the provider did during the encounter. Other parameters of professional billing include complexity of decision-making versus amount of time spent, and a variety of modifiers.
By contrast, facility billing by hospitals is based on the complexity of the patient’s condition and is generally done whether the hospitalization is considered an inpatient hospitalization or an outpatient hospitalization such as an observation stay. Inpatient hospital stays are often paid using diagnosis-related groupings (DRGs), Medicare’s patient classification system for standardizing prospective payment to hospitals and encouraging cost-containment strategies.
DRGs, which represent about half of total hospital reimbursement, are a separate payment mechanism covering all facility charges associated with the inpatient stay from admission to discharge, incorporating the costs of providing hospital care, including but not limited to space, equipment, supplies, tests, and medications. Outpatient hospital stays, by contrast, are paid based on Ambulatory Payment Classifications.
A facility bill is submitted to the payer at the end of the hospital stay, describing the patient’s condition using ICD-10 diagnostic codes. All of the patient’s diagnoses and comorbidities contribute to the assignment of a DRG that best captures the total hospital stay. But to make the issue more complicated, the system is evolving toward models of bundled payment that will eventually phase out traditional DRGs in favor of new systems combining inpatient and outpatient reimbursement into a single bundled episode of care.
Professional and facility bills for a single hospitalization may be prepared by different personnel on separate teams following different rules, although they may both be housed in the hospital’s billing department. The differing rules for coding professional services versus facility services can be hard for hospitalists to appreciate, said Wendy Arafiles, MD, a pediatric hospitalist at Phoenix Children’s Hospital and medical director for its clinical documentation integrity (CDI) team. An example is for uncertain diagnoses. There may be a clinical suspicion of a diagnosis, and language such as “likely bacterial pneumonia” might be sufficient for facility coding but not for professional services coding.
Hospitalists, depending on their group’s size, structure, and relationship to the hospital, may be responsible for selecting the CPT codes or other parameters for the insurance claim and bill. Or these may be left to billing specialists. And those specialists could be employed by the hospital or by the hospitalist group or multispecialty medical group, or they could be contracted outside agencies that handle the billing for a fee.
The revenue cycle
The hospital revenue cycle has a lot of cogs in the machine, Dr. Arafiles said. “This is just one of the many nuances of our crazy system. I will go out on a limb and say it is not our job as clinicians to know all of those nuances.” The DRG assignment is dependent on how providers can describe the complexity of the patient and severity of the illness, even if it doesn’t impact professional billing, Dr. Arafiles added.
Hospitalists don’t want to think about money when providing patient care. “Our job is to provide the best care to our patients. We often utilize resources without thinking about how much they are going to cost, so that we can do what we think is necessary for our patients,” she explained. But accurate diagnosis codes can capture the complexity of the care. “Maybe we don’t take that part seriously enough. As long as I, as the provider, can accurately describe the complexity of my patient, I can justify why I spent all those resources and so many days caring for him or her.”
Charles Locke, MD, executive medical director of care management for LifeBridge Health and assistant professor of medicine at Johns Hopkins University, Baltimore, said hospitalists typically are paid set salaries directly by the hospital, in some cases with productivity bonuses based in part on their billing and posted RVUs (relative value units). RVUs are the cornerstone of Medicare’s reimbursement formula for physician services.
“Another thing to keep in mind, one might think in 2021 that the computer systems would be sophisticated enough to link up professional and facility billing to ensure that bills for each are concordant for services provided on a given day. But it turns out they are not yet well connected,” Dr. Locke said.
“These are issues that everybody struggles with. Hospitalists need to know and order the appropriate status, inpatient versus outpatient, and whether and when to order observation services, as this will affect hospital reimbursement and, potentially, patient liability,” he explained.1 If the hospital is denied its facility claim because of improper status, that denial doesn’t necessary extend to a denial for the doctor’s professional fee. “Hospitalists need to know these are often separated. Even though their professional fee is honored, the hospital’s service charges may not be.”
Dr. Locke said knowing the history of Medicare might help hospitalists to better appreciate the distinctions. When this federal entitlement was first proposed in the 1960s as a way to help older Americans in poverty obtain needed health care, organized medicine sought to be excluded from the program. “Nonhospital services and doctors’ service fees were not included in the original Medicare proposal,” he said. Medicare Part B was created to provide insurance for doctors’ professional fees, which are still handled separately under Medicare.
Many institutions use clinical documentation for multiple purposes. “There are so many masters for this one document,” Dr. Arafiles said. The information is also used for various quality and patient safety metrics and data gathering. “Every code we choose is used in many different ways by the institution. We don’t know where all it goes. But we need to know how to describe how complex the case was, and how much work it entailed. The more we know about how to describe that, the better for the institution.”
Dr. Arafiles views the clinical note, first and foremost, as clinical communication, so that one provider can seamlessly pick up where the previous left off. “If I use language in my note that is accurate and specific, it will be useful to all who later need it.” Building on metrics such as expected versus actual 30-day readmission rates, risk-adjusted mortality, and all the ways government agencies report hospital quality, she said, “what we document has lasting impact. That’s where the facility side of billing and coding is ever more important. You can’t just think about your professional billing and RVUs.”
Support from the hospital
Some hospitalists may think facility billing is not their concern. But consider this: The average support or subsidy paid by U.S. hospitals for a full-time equivalent hospitalist is estimated at $198,750, according to SHM’s 2020 State of Hospital Medicine.2 That support reflects the difference between the cost of employing a hospitalist in a competitive labor environment and what that provider is actually able to generate in billing income, said Hardik Vora, MD, MPH, SFHM, chair of SHM’s practice management committee.
With a lot of medical specialties, the physician’s salary is only or largely supported by professional billing, said Dr. Vora, who is medical director for Hospital Medicine and physician advisor for utilization management and CDI at Riverside Health System, Yorktown, Va.
“Hospital medicine is different in that aspect, regardless of employment model. And that’s where the concept of value comes in – how else do you bring value to the hospital that supports you,” said Dr. Vora.
Hospitalists often emphasize their contributions to quality improvement, patient safety, and hospital governance committees – all the ways they contribute to the health of the institution – as justification for their support from the hospital. But beneath all of that is the income the hospital generates from facility billing and from the hospitalist’s contributions to complete, accurate, and timely documentation that can support the hospital’s bills.
Typically, this hospital support to supplement hospitalist billing income is not directly tied to the income generated by facility billing or to the hospitalist’s contribution to its completeness. But between growing technological sophistication and greater belt-tightening, that link may get closer over time.
Other players
Because of the importance of complete and accurate billing to the hospital’s financial well-being, specialized supportive services have evolved, from traditional utilization review or utilization management to CDI services and the role of physician advisors – experienced doctors who know well how these processes work and are able to teach providers about regulatory compliance and medical necessity.
“One of my jobs as the medical director for our hospital’s CDI program is to educate residents, fellows, and newly onboarded providers to be descriptive enough in their charting to capture the complexity of the patient’s condition,” Dr. Arafiles said. Physician advisors and CDI programs can involve clinical providers in bringing value to the institution through their documentation. They serve as the intermediaries between the coders and the clinicians.
The CDI specialist’s job description focuses on diagnosis capture and associated reimbursement. But integrity broadly defined goes to the integrity of the medical record and its contribution to quality and patient safety as well as providing a medical record that is defensible to audits, physician revenue cycle expert Glenn Krauss noted in a recent post at ICD10 Monitor.3
Dr. Vora sees his role as physician advisor to be the link between the hospital’s executive team and the hospital’s medical providers. “Providers need help in understanding a complex set of ever-changing rules of facility billing and the frequently competing priorities between facility and professional billing. I tell my providers: The longer the patient stays in the hospital, you may be generating more RVUs, but our facility may be losing money.”
Hospital administrators are acutely aware of facility billing, but they don’t necessarily understand the nuances of professional billing, said Jay Weatherly, MS, the cofounder of Hospitalist Billing, a company that specializes in comprehensive billing and collection solutions for hospitalist groups that are employed directly by their hospitals. But he sees an essential symbiotic relationship between hospital administrators and clinicians.
“We rely on hospitalists’ record keeping to do our job. We rely on them to get it right,” he said. “We want to encourage doctors to cooperate with the process. Billing should never be a physician’s top priority, but it is important, nonetheless.”
HBI is relentless in pursuit of the information needed for its coding and billing, but does so gently, in a way not to put off doctors, Mr. Weatherly said. “There is an art and a science associated with securing the needed information. We have great respect for the doctors we work with, yet we’re all spokes in a bigger wheel, and we need to bill effectively in order to keep the wheel moving.”
What can hospitalists do?
Sources for this article say one of the best places for hospitalists to start improving their understanding of these distinctions is to ask the coders in their institution for advice on how to make the process run more smoothly.
“If you have a CDI team, they are there to help. Reach out to them,” Dr. Arafiles said. Generally, medical schools and residency programs fail to convey the complexities of contemporary hospital economics to future doctors.
Hospitalists have become indispensable, Dr. Vora said. But salaries for hospitalists are going up while hospital reimbursement is going down, and hospitalists are not seeing more patients. “At some point we will no longer be able to say financial support for hospital medicine groups is just a cost of doing business for the hospital. COVID tested us – and demonstrated how much hospital executives value us as part of the team. Our organization absolutely stood behind its physicians despite financially challenging times. Now we need to do what we can to support the organization,” he added.
Hospitalists can also continue to educate themselves on good documentation and coding practices, by finding programs like SHM’s Utilization Management and Clinical Documentation for Hospitalists.
“As we see a significant shift to value-based payment, with its focus on value, efficiency, quality – the best care at the lowest possible price – hospital medicine as a specialty will be best positioned to help with that. If the hospital does well, we do well. We should be building relationships with the hospital’s leadership team,” Dr. Vora said. “You always want to contribute to that partnership to the highest level possible. When they look at us, they should see their most reliable partner.”
References
1. Locke C, Hu E. Medicare’s two-midnight rule: What hospitalists must know. The Hospitalist. 2019 Feb 22.
2. Beresford L. Hospital medicine in a worldwide pandemic: State of Hospital Medicine 2020. The Hospitalist. 2020 Sep 20.
3. Krauss G. Clinical documentation integrity: rebranding and repurposing. ICD10 Monitor. March 16, 2020 Mar 16. https://www.icd10monitor.com/clinical-documentation-integrity-rebranding-and-repurposing.
Judge tosses hospital staff suit over vaccine mandate
A federal judge in Texas has dismissed a lawsuit from 117 Houston Methodist Hospital workers who refused to get a COVID-19 vaccine and said it was illegal to require them to do so.
In the ruling issued June 12, U.S. District Judge Lynn Hughes upheld the hospital’s policy and said the vaccination requirement didn’t break any federal laws.
“This is not coercion,” Judge Hughes wrote in the ruling.
“Methodist is trying to do their business of saving lives without giving them the COVID-19 virus,” he wrote. “It is a choice made to keep staff, patients, and their families safer.”
In April, the Houston Methodist Hospital system announced a policy that required employees to be vaccinated by June 7 or request an exemption. After the deadline, 178 of 26,000 employees refused to get inoculated and were placed on suspension without pay. The employees said the vaccine was unsafe and “experimental.” In his ruling, Judge Hughes said their claim was false and irrelevant.
“Texas law only protects employees from being terminated for refusing to commit an act carrying criminal penalties to the worker,” he wrote. “Receiving a COVID-19 vaccination is not an illegal act, and it carries no criminal penalties.”
He denounced the “press-release style of the complaint” and the comparison of the hospital’s vaccine policy to forced experimentation by the Nazis against Jewish people during the Holocaust.
“Equating the injection requirement to medical experimentation in concentration camps is reprehensible,” he wrote. “Nazi doctors conducted medical experiments on victims that caused pain, mutilation, permanent disability, and in many cases, death.”
Judge Hughes also said that employees can “freely choose” to accept or refuse a COVID-19 vaccine. If they refuse, they “simply need to work somewhere else,” he wrote.
“If a worker refuses an assignment, changed office, earlier start time, or other directive, he may be properly fired,” Judge Hughes said. “Every employment includes limits on the worker’s behavior in exchange for his remuneration. This is all part of the bargain.”
The ruling could set a precedent for similar COVID-19 vaccine lawsuits across the country, NPR reported. Houston Methodist was one of the first hospitals to require staff to be vaccinated. After the ruling on June 12, the hospital system wrote in a statement that it was “pleased and reassured” that Judge Hughes dismissed a “frivolous lawsuit.”
The hospital system will begin to terminate the 178 employees who were suspended if they don’t get a vaccine by June 21.
Jennifer Bridges, a nurse who has led the campaign against the vaccine policy, said she and the other plaintiffs will appeal the decision, according to KHOU.
“We’re OK with this decision. We are appealing. This will be taken all the way to the Supreme Court,” she told the news station. “This is far from over. This is literally only the beginning.”
A version of this article first appeared on WebMD.com.
A federal judge in Texas has dismissed a lawsuit from 117 Houston Methodist Hospital workers who refused to get a COVID-19 vaccine and said it was illegal to require them to do so.
In the ruling issued June 12, U.S. District Judge Lynn Hughes upheld the hospital’s policy and said the vaccination requirement didn’t break any federal laws.
“This is not coercion,” Judge Hughes wrote in the ruling.
“Methodist is trying to do their business of saving lives without giving them the COVID-19 virus,” he wrote. “It is a choice made to keep staff, patients, and their families safer.”
In April, the Houston Methodist Hospital system announced a policy that required employees to be vaccinated by June 7 or request an exemption. After the deadline, 178 of 26,000 employees refused to get inoculated and were placed on suspension without pay. The employees said the vaccine was unsafe and “experimental.” In his ruling, Judge Hughes said their claim was false and irrelevant.
“Texas law only protects employees from being terminated for refusing to commit an act carrying criminal penalties to the worker,” he wrote. “Receiving a COVID-19 vaccination is not an illegal act, and it carries no criminal penalties.”
He denounced the “press-release style of the complaint” and the comparison of the hospital’s vaccine policy to forced experimentation by the Nazis against Jewish people during the Holocaust.
“Equating the injection requirement to medical experimentation in concentration camps is reprehensible,” he wrote. “Nazi doctors conducted medical experiments on victims that caused pain, mutilation, permanent disability, and in many cases, death.”
Judge Hughes also said that employees can “freely choose” to accept or refuse a COVID-19 vaccine. If they refuse, they “simply need to work somewhere else,” he wrote.
“If a worker refuses an assignment, changed office, earlier start time, or other directive, he may be properly fired,” Judge Hughes said. “Every employment includes limits on the worker’s behavior in exchange for his remuneration. This is all part of the bargain.”
The ruling could set a precedent for similar COVID-19 vaccine lawsuits across the country, NPR reported. Houston Methodist was one of the first hospitals to require staff to be vaccinated. After the ruling on June 12, the hospital system wrote in a statement that it was “pleased and reassured” that Judge Hughes dismissed a “frivolous lawsuit.”
The hospital system will begin to terminate the 178 employees who were suspended if they don’t get a vaccine by June 21.
Jennifer Bridges, a nurse who has led the campaign against the vaccine policy, said she and the other plaintiffs will appeal the decision, according to KHOU.
“We’re OK with this decision. We are appealing. This will be taken all the way to the Supreme Court,” she told the news station. “This is far from over. This is literally only the beginning.”
A version of this article first appeared on WebMD.com.
A federal judge in Texas has dismissed a lawsuit from 117 Houston Methodist Hospital workers who refused to get a COVID-19 vaccine and said it was illegal to require them to do so.
In the ruling issued June 12, U.S. District Judge Lynn Hughes upheld the hospital’s policy and said the vaccination requirement didn’t break any federal laws.
“This is not coercion,” Judge Hughes wrote in the ruling.
“Methodist is trying to do their business of saving lives without giving them the COVID-19 virus,” he wrote. “It is a choice made to keep staff, patients, and their families safer.”
In April, the Houston Methodist Hospital system announced a policy that required employees to be vaccinated by June 7 or request an exemption. After the deadline, 178 of 26,000 employees refused to get inoculated and were placed on suspension without pay. The employees said the vaccine was unsafe and “experimental.” In his ruling, Judge Hughes said their claim was false and irrelevant.
“Texas law only protects employees from being terminated for refusing to commit an act carrying criminal penalties to the worker,” he wrote. “Receiving a COVID-19 vaccination is not an illegal act, and it carries no criminal penalties.”
He denounced the “press-release style of the complaint” and the comparison of the hospital’s vaccine policy to forced experimentation by the Nazis against Jewish people during the Holocaust.
“Equating the injection requirement to medical experimentation in concentration camps is reprehensible,” he wrote. “Nazi doctors conducted medical experiments on victims that caused pain, mutilation, permanent disability, and in many cases, death.”
Judge Hughes also said that employees can “freely choose” to accept or refuse a COVID-19 vaccine. If they refuse, they “simply need to work somewhere else,” he wrote.
“If a worker refuses an assignment, changed office, earlier start time, or other directive, he may be properly fired,” Judge Hughes said. “Every employment includes limits on the worker’s behavior in exchange for his remuneration. This is all part of the bargain.”
The ruling could set a precedent for similar COVID-19 vaccine lawsuits across the country, NPR reported. Houston Methodist was one of the first hospitals to require staff to be vaccinated. After the ruling on June 12, the hospital system wrote in a statement that it was “pleased and reassured” that Judge Hughes dismissed a “frivolous lawsuit.”
The hospital system will begin to terminate the 178 employees who were suspended if they don’t get a vaccine by June 21.
Jennifer Bridges, a nurse who has led the campaign against the vaccine policy, said she and the other plaintiffs will appeal the decision, according to KHOU.
“We’re OK with this decision. We are appealing. This will be taken all the way to the Supreme Court,” she told the news station. “This is far from over. This is literally only the beginning.”
A version of this article first appeared on WebMD.com.
OSHA issues new rules on COVID-19 safety for health care workers
The U.S. Occupational Safety and Health Administration issued its long-awaited Emergency Temporary Standard (ETS) for COVID-19 June 10, surprising many by including only health care workers in the new emergency workplace safety rules.
“The ETS is an overdue step toward protecting health care workers, especially those working in long-term care facilities and home health care who are at greatly increased risk of infection,” said George Washington University, Washington, professor and former Obama administration Assistant Secretary of Labor David Michaels, PhD, MPH. “OSHA’s failure to issue a COVID-specific standard in other high-risk industries, like meat and poultry processing, corrections, homeless shelters, and retail establishments is disappointing. If exposure is not controlled in these workplaces, they will continue to be important drivers of infections.”
With the new regulations in place, about 10.3 million health care workers at hospitals, nursing homes, and assisted living facilities, as well as emergency responders and home health care workers, should be guaranteed protection standards that replace former guidance.
The new protections include supplying personal protective equipment and ensuring proper usage (for example, mandatory seal checks on respirators); screening everyone who enters the facility for COVID-19; ensuring proper ventilation; and establishing physical distancing requirements (6 feet) for unvaccinated workers. It also requires employers to give workers time off for vaccination. An antiretaliation clause could shield workers who complain about unsafe conditions.
“The science tells us that health care workers, particularly those who come into regular contact with the virus, are most at risk at this point in the pandemic,” Labor Secretary Marty Walsh said on a press call. “So following an extensive review of the science and data, OSHA determined that a health care–specific safety requirement will make the biggest impact.”
But questions remain, said James Brudney, JD, a professor at Fordham Law School in New York and former chief counsel of the U.S. Senate Subcommittee on Labor. The standard doesn’t amplify or address existing rules regarding a right to refuse unsafe work, for example, so employees may still feel they are risking their jobs to complain, despite the antiretaliation clause.
And although vaccinated employees don’t have to adhere to the same distancing and masking standards in many instances, the standard doesn’t spell out how employers should determine their workers’ vaccination status – instead leaving that determination to employers through their own policies and procedures. (California’s state OSHA office rules specify the mechanism for documentation of vaccination.)
The Trump administration did not issue an ETS, saying OSHA’s general duty clause sufficed. President Joe Biden took the opposite approach, calling for an investigation into an ETS on his first day in office. But the process took months longer than promised.
“I know it’s been a long time coming,” Mr. Walsh acknowledged. “Our health care workers from the very beginning have been put at risk.
While health care unions had asked for mandated safety standards sooner, National Nurses United, the country’s largest labor union for registered nurses, still welcomed the rules.
“An ETS is a major step toward requiring accountability for hospitals who consistently put their budget goals and profits over our health and safety,” Zenei Triunfo-Cortez, RN, one of NNU’s three presidents, said in a statement June 9 anticipating the publication of the rules.
The rules do not apply to retail pharmacies, ambulatory care settings that screen nonemployees for COVID-19, or certain other settings in which all employees are vaccinated and people with suspected or confirmed COVID-19 cannot enter.
The agency said it will work with states that have already issued local regulations, including two states that issued temporary standards of their own, Virginia and California.
Employers will have 2 weeks to comply with most of the regulations after they’re published in the Federal Register. The standards will expire in 6 months but could then become permanent, as Virginia’s did in January.
A version of this article first appeared on Medscape.com.
The U.S. Occupational Safety and Health Administration issued its long-awaited Emergency Temporary Standard (ETS) for COVID-19 June 10, surprising many by including only health care workers in the new emergency workplace safety rules.
“The ETS is an overdue step toward protecting health care workers, especially those working in long-term care facilities and home health care who are at greatly increased risk of infection,” said George Washington University, Washington, professor and former Obama administration Assistant Secretary of Labor David Michaels, PhD, MPH. “OSHA’s failure to issue a COVID-specific standard in other high-risk industries, like meat and poultry processing, corrections, homeless shelters, and retail establishments is disappointing. If exposure is not controlled in these workplaces, they will continue to be important drivers of infections.”
With the new regulations in place, about 10.3 million health care workers at hospitals, nursing homes, and assisted living facilities, as well as emergency responders and home health care workers, should be guaranteed protection standards that replace former guidance.
The new protections include supplying personal protective equipment and ensuring proper usage (for example, mandatory seal checks on respirators); screening everyone who enters the facility for COVID-19; ensuring proper ventilation; and establishing physical distancing requirements (6 feet) for unvaccinated workers. It also requires employers to give workers time off for vaccination. An antiretaliation clause could shield workers who complain about unsafe conditions.
“The science tells us that health care workers, particularly those who come into regular contact with the virus, are most at risk at this point in the pandemic,” Labor Secretary Marty Walsh said on a press call. “So following an extensive review of the science and data, OSHA determined that a health care–specific safety requirement will make the biggest impact.”
But questions remain, said James Brudney, JD, a professor at Fordham Law School in New York and former chief counsel of the U.S. Senate Subcommittee on Labor. The standard doesn’t amplify or address existing rules regarding a right to refuse unsafe work, for example, so employees may still feel they are risking their jobs to complain, despite the antiretaliation clause.
And although vaccinated employees don’t have to adhere to the same distancing and masking standards in many instances, the standard doesn’t spell out how employers should determine their workers’ vaccination status – instead leaving that determination to employers through their own policies and procedures. (California’s state OSHA office rules specify the mechanism for documentation of vaccination.)
The Trump administration did not issue an ETS, saying OSHA’s general duty clause sufficed. President Joe Biden took the opposite approach, calling for an investigation into an ETS on his first day in office. But the process took months longer than promised.
“I know it’s been a long time coming,” Mr. Walsh acknowledged. “Our health care workers from the very beginning have been put at risk.
While health care unions had asked for mandated safety standards sooner, National Nurses United, the country’s largest labor union for registered nurses, still welcomed the rules.
“An ETS is a major step toward requiring accountability for hospitals who consistently put their budget goals and profits over our health and safety,” Zenei Triunfo-Cortez, RN, one of NNU’s three presidents, said in a statement June 9 anticipating the publication of the rules.
The rules do not apply to retail pharmacies, ambulatory care settings that screen nonemployees for COVID-19, or certain other settings in which all employees are vaccinated and people with suspected or confirmed COVID-19 cannot enter.
The agency said it will work with states that have already issued local regulations, including two states that issued temporary standards of their own, Virginia and California.
Employers will have 2 weeks to comply with most of the regulations after they’re published in the Federal Register. The standards will expire in 6 months but could then become permanent, as Virginia’s did in January.
A version of this article first appeared on Medscape.com.
The U.S. Occupational Safety and Health Administration issued its long-awaited Emergency Temporary Standard (ETS) for COVID-19 June 10, surprising many by including only health care workers in the new emergency workplace safety rules.
“The ETS is an overdue step toward protecting health care workers, especially those working in long-term care facilities and home health care who are at greatly increased risk of infection,” said George Washington University, Washington, professor and former Obama administration Assistant Secretary of Labor David Michaels, PhD, MPH. “OSHA’s failure to issue a COVID-specific standard in other high-risk industries, like meat and poultry processing, corrections, homeless shelters, and retail establishments is disappointing. If exposure is not controlled in these workplaces, they will continue to be important drivers of infections.”
With the new regulations in place, about 10.3 million health care workers at hospitals, nursing homes, and assisted living facilities, as well as emergency responders and home health care workers, should be guaranteed protection standards that replace former guidance.
The new protections include supplying personal protective equipment and ensuring proper usage (for example, mandatory seal checks on respirators); screening everyone who enters the facility for COVID-19; ensuring proper ventilation; and establishing physical distancing requirements (6 feet) for unvaccinated workers. It also requires employers to give workers time off for vaccination. An antiretaliation clause could shield workers who complain about unsafe conditions.
“The science tells us that health care workers, particularly those who come into regular contact with the virus, are most at risk at this point in the pandemic,” Labor Secretary Marty Walsh said on a press call. “So following an extensive review of the science and data, OSHA determined that a health care–specific safety requirement will make the biggest impact.”
But questions remain, said James Brudney, JD, a professor at Fordham Law School in New York and former chief counsel of the U.S. Senate Subcommittee on Labor. The standard doesn’t amplify or address existing rules regarding a right to refuse unsafe work, for example, so employees may still feel they are risking their jobs to complain, despite the antiretaliation clause.
And although vaccinated employees don’t have to adhere to the same distancing and masking standards in many instances, the standard doesn’t spell out how employers should determine their workers’ vaccination status – instead leaving that determination to employers through their own policies and procedures. (California’s state OSHA office rules specify the mechanism for documentation of vaccination.)
The Trump administration did not issue an ETS, saying OSHA’s general duty clause sufficed. President Joe Biden took the opposite approach, calling for an investigation into an ETS on his first day in office. But the process took months longer than promised.
“I know it’s been a long time coming,” Mr. Walsh acknowledged. “Our health care workers from the very beginning have been put at risk.
While health care unions had asked for mandated safety standards sooner, National Nurses United, the country’s largest labor union for registered nurses, still welcomed the rules.
“An ETS is a major step toward requiring accountability for hospitals who consistently put their budget goals and profits over our health and safety,” Zenei Triunfo-Cortez, RN, one of NNU’s three presidents, said in a statement June 9 anticipating the publication of the rules.
The rules do not apply to retail pharmacies, ambulatory care settings that screen nonemployees for COVID-19, or certain other settings in which all employees are vaccinated and people with suspected or confirmed COVID-19 cannot enter.
The agency said it will work with states that have already issued local regulations, including two states that issued temporary standards of their own, Virginia and California.
Employers will have 2 weeks to comply with most of the regulations after they’re published in the Federal Register. The standards will expire in 6 months but could then become permanent, as Virginia’s did in January.
A version of this article first appeared on Medscape.com.
Infections in infants: An update
Converge 2021 session
Febrile Infant Update
Presenter
Russell J. McCulloh, MD
Session summary
Infections in infants aged younger than 90 days have been the subject of intense study in pediatric hospital medicine for many years. With the guidance of our talented presenter Dr. Russell McCulloh of Children’s Hospital & Medical Center in Omaha, Neb., the audience explored the historical perspective and evolution of this scientific question, including successes, special situations, newer screening tests, and description of cutting-edge scoring tools and platforms.
The challenge – Tens of thousands of infants present for care in the setting of fever each year. We know that our physical exam and history-taking skills are unlikely to be helpful in risk stratification. We have been guided by the desire to separate serious bacterial infection (SBI: bone infection, meningitis, pneumonia, urinary tract infection, bacteremia, enteritis) from invasive bacterial infection (IBI: meningitis and bacteremia). Data has shown that no test is 100% sensitive or specific, therefore we have to balance risk of disease to cost and invasiveness of tests. Important questions include whether to test and how to stratify by age, who to admit, and who to provide antibiotics.
The wins and exceptions – Fortunately, the early Boston, Philadelphia, and Rochester criteria set the stage for safely reducing testing. The current American College of Emergency Physicians guidelines for infants aged 29-90 days allows for lumbar puncture to be optional knowing that a look back using prior criteria identified no cases of meningitis in the low risk group. Similarly, in low-risk infants aged less that 29 days in nearly 4,000 cases there were just 2 infants with meningitis. Universal screening of moms for Group B Streptococcus with delivery of antibiotics in appropriate cases has dramatically decreased incidence of SBI. The Hib and pneumovax vaccines have likewise decreased incidence of SBI. Exceptions persist, including knowledge that infants with herpes simplex virus disease will not have fever in 50% of cases and that risk of HSV transmission is highest (25%-60% transmission) in mothers with primary disease. Given risk of HSV CNS disease after 1 week of age, in any high-risk infant less than 21 days, the mantra remains to test and treat.
The cutting edge – Thanks to ongoing research, we now have the PECARN and REVISE study groups to further aid decision-making. With PECARN we know that SBI in infants is extremely unlikely (negative predictive value, 99.7%) with a negative urinalysis , absolute neutrophil count less than 4,090, and procalcitonin less than 1.71. REVISE has revealed that infants with positive viral testing are unlikely to have SBI (7%-12%), particularly with influenza and RSV disease. Procalcitonin has also recently been shown to be an effective tool to rule out disease with the highest negative predictive value among available inflammatory markers. The just-published Aronson rule identifies a scoring system for IBI (using age less than 21 days/1pt; temp 38-38.4° C/2pt; >38.5° C/4pt; abnormal urinalysis/3pt; and absolute neutrophil count >5185/2pt) where any score greater than2 provides a sensitivity of 98.8% and NPV in validation studies of 99.4%. Likewise, multiplex polymerase chain reaction testing of spinal fluid has allowed for additional insight in pretreated cases and has helped us to remove antibiotic treatment from cases where parechovirus and enterovirus are positive because of the low risk for concomitant bacterial meningitis. As we await the release of revised national American Academy of Pediatrics guidelines, it is safe to say great progress has been made in the care of young febrile infants with shorter length of stay and fewer tests for all.
Key takeaways
- Numerous screening tests, rules, and scoring tools have been created to improve identification of infants with IBI, a low-frequency, high-morbidity event. The most recent with negative predictive values of 99.7% and 99.4% are the PECARN and Aronson scoring tools.
- Recent studies of the febrile infant population indicate that the odds of UTI or bacteremia in infants with respiratory symptoms is low, particularly for RSV and influenza.
- Among newer tests developed, a negative procalcitonin has the highest negative predictive value.
- Viral pathogens identified on cerebrospinal fluid molecular testing can be helpful in pretreated cases and indicative of low likelihood of bacterial meningitis allowing for observation off of antibiotics.
Dr. King is a hospitalist, associate director for medical education and associate program director for the pediatrics residency program at Children’s Minnesota in Minneapolis. She has shared some of her resident teaching, presentation skills, and peer-coaching work on a national level.
Converge 2021 session
Febrile Infant Update
Presenter
Russell J. McCulloh, MD
Session summary
Infections in infants aged younger than 90 days have been the subject of intense study in pediatric hospital medicine for many years. With the guidance of our talented presenter Dr. Russell McCulloh of Children’s Hospital & Medical Center in Omaha, Neb., the audience explored the historical perspective and evolution of this scientific question, including successes, special situations, newer screening tests, and description of cutting-edge scoring tools and platforms.
The challenge – Tens of thousands of infants present for care in the setting of fever each year. We know that our physical exam and history-taking skills are unlikely to be helpful in risk stratification. We have been guided by the desire to separate serious bacterial infection (SBI: bone infection, meningitis, pneumonia, urinary tract infection, bacteremia, enteritis) from invasive bacterial infection (IBI: meningitis and bacteremia). Data has shown that no test is 100% sensitive or specific, therefore we have to balance risk of disease to cost and invasiveness of tests. Important questions include whether to test and how to stratify by age, who to admit, and who to provide antibiotics.
The wins and exceptions – Fortunately, the early Boston, Philadelphia, and Rochester criteria set the stage for safely reducing testing. The current American College of Emergency Physicians guidelines for infants aged 29-90 days allows for lumbar puncture to be optional knowing that a look back using prior criteria identified no cases of meningitis in the low risk group. Similarly, in low-risk infants aged less that 29 days in nearly 4,000 cases there were just 2 infants with meningitis. Universal screening of moms for Group B Streptococcus with delivery of antibiotics in appropriate cases has dramatically decreased incidence of SBI. The Hib and pneumovax vaccines have likewise decreased incidence of SBI. Exceptions persist, including knowledge that infants with herpes simplex virus disease will not have fever in 50% of cases and that risk of HSV transmission is highest (25%-60% transmission) in mothers with primary disease. Given risk of HSV CNS disease after 1 week of age, in any high-risk infant less than 21 days, the mantra remains to test and treat.
The cutting edge – Thanks to ongoing research, we now have the PECARN and REVISE study groups to further aid decision-making. With PECARN we know that SBI in infants is extremely unlikely (negative predictive value, 99.7%) with a negative urinalysis , absolute neutrophil count less than 4,090, and procalcitonin less than 1.71. REVISE has revealed that infants with positive viral testing are unlikely to have SBI (7%-12%), particularly with influenza and RSV disease. Procalcitonin has also recently been shown to be an effective tool to rule out disease with the highest negative predictive value among available inflammatory markers. The just-published Aronson rule identifies a scoring system for IBI (using age less than 21 days/1pt; temp 38-38.4° C/2pt; >38.5° C/4pt; abnormal urinalysis/3pt; and absolute neutrophil count >5185/2pt) where any score greater than2 provides a sensitivity of 98.8% and NPV in validation studies of 99.4%. Likewise, multiplex polymerase chain reaction testing of spinal fluid has allowed for additional insight in pretreated cases and has helped us to remove antibiotic treatment from cases where parechovirus and enterovirus are positive because of the low risk for concomitant bacterial meningitis. As we await the release of revised national American Academy of Pediatrics guidelines, it is safe to say great progress has been made in the care of young febrile infants with shorter length of stay and fewer tests for all.
Key takeaways
- Numerous screening tests, rules, and scoring tools have been created to improve identification of infants with IBI, a low-frequency, high-morbidity event. The most recent with negative predictive values of 99.7% and 99.4% are the PECARN and Aronson scoring tools.
- Recent studies of the febrile infant population indicate that the odds of UTI or bacteremia in infants with respiratory symptoms is low, particularly for RSV and influenza.
- Among newer tests developed, a negative procalcitonin has the highest negative predictive value.
- Viral pathogens identified on cerebrospinal fluid molecular testing can be helpful in pretreated cases and indicative of low likelihood of bacterial meningitis allowing for observation off of antibiotics.
Dr. King is a hospitalist, associate director for medical education and associate program director for the pediatrics residency program at Children’s Minnesota in Minneapolis. She has shared some of her resident teaching, presentation skills, and peer-coaching work on a national level.
Converge 2021 session
Febrile Infant Update
Presenter
Russell J. McCulloh, MD
Session summary
Infections in infants aged younger than 90 days have been the subject of intense study in pediatric hospital medicine for many years. With the guidance of our talented presenter Dr. Russell McCulloh of Children’s Hospital & Medical Center in Omaha, Neb., the audience explored the historical perspective and evolution of this scientific question, including successes, special situations, newer screening tests, and description of cutting-edge scoring tools and platforms.
The challenge – Tens of thousands of infants present for care in the setting of fever each year. We know that our physical exam and history-taking skills are unlikely to be helpful in risk stratification. We have been guided by the desire to separate serious bacterial infection (SBI: bone infection, meningitis, pneumonia, urinary tract infection, bacteremia, enteritis) from invasive bacterial infection (IBI: meningitis and bacteremia). Data has shown that no test is 100% sensitive or specific, therefore we have to balance risk of disease to cost and invasiveness of tests. Important questions include whether to test and how to stratify by age, who to admit, and who to provide antibiotics.
The wins and exceptions – Fortunately, the early Boston, Philadelphia, and Rochester criteria set the stage for safely reducing testing. The current American College of Emergency Physicians guidelines for infants aged 29-90 days allows for lumbar puncture to be optional knowing that a look back using prior criteria identified no cases of meningitis in the low risk group. Similarly, in low-risk infants aged less that 29 days in nearly 4,000 cases there were just 2 infants with meningitis. Universal screening of moms for Group B Streptococcus with delivery of antibiotics in appropriate cases has dramatically decreased incidence of SBI. The Hib and pneumovax vaccines have likewise decreased incidence of SBI. Exceptions persist, including knowledge that infants with herpes simplex virus disease will not have fever in 50% of cases and that risk of HSV transmission is highest (25%-60% transmission) in mothers with primary disease. Given risk of HSV CNS disease after 1 week of age, in any high-risk infant less than 21 days, the mantra remains to test and treat.
The cutting edge – Thanks to ongoing research, we now have the PECARN and REVISE study groups to further aid decision-making. With PECARN we know that SBI in infants is extremely unlikely (negative predictive value, 99.7%) with a negative urinalysis , absolute neutrophil count less than 4,090, and procalcitonin less than 1.71. REVISE has revealed that infants with positive viral testing are unlikely to have SBI (7%-12%), particularly with influenza and RSV disease. Procalcitonin has also recently been shown to be an effective tool to rule out disease with the highest negative predictive value among available inflammatory markers. The just-published Aronson rule identifies a scoring system for IBI (using age less than 21 days/1pt; temp 38-38.4° C/2pt; >38.5° C/4pt; abnormal urinalysis/3pt; and absolute neutrophil count >5185/2pt) where any score greater than2 provides a sensitivity of 98.8% and NPV in validation studies of 99.4%. Likewise, multiplex polymerase chain reaction testing of spinal fluid has allowed for additional insight in pretreated cases and has helped us to remove antibiotic treatment from cases where parechovirus and enterovirus are positive because of the low risk for concomitant bacterial meningitis. As we await the release of revised national American Academy of Pediatrics guidelines, it is safe to say great progress has been made in the care of young febrile infants with shorter length of stay and fewer tests for all.
Key takeaways
- Numerous screening tests, rules, and scoring tools have been created to improve identification of infants with IBI, a low-frequency, high-morbidity event. The most recent with negative predictive values of 99.7% and 99.4% are the PECARN and Aronson scoring tools.
- Recent studies of the febrile infant population indicate that the odds of UTI or bacteremia in infants with respiratory symptoms is low, particularly for RSV and influenza.
- Among newer tests developed, a negative procalcitonin has the highest negative predictive value.
- Viral pathogens identified on cerebrospinal fluid molecular testing can be helpful in pretreated cases and indicative of low likelihood of bacterial meningitis allowing for observation off of antibiotics.
Dr. King is a hospitalist, associate director for medical education and associate program director for the pediatrics residency program at Children’s Minnesota in Minneapolis. She has shared some of her resident teaching, presentation skills, and peer-coaching work on a national level.
FROM SHM CONVERGE 2021
Are left atrial thrombi that defy preprocedure anticoagulation predictable?
Three or more weeks of oral anticoagulation (OAC) sometimes isn’t up to the job of clearing any potentially embolic left atrial (LA) thrombi before procedures like cardioversion or catheter ablation in patients with atrial fibrillation (AF). Such OAC-defiant LA thrombi aren’t common, nor are they rare enough to ignore, suggests a new meta-analysis that might also have identified features that predispose to them.
Such predictors of LA clots that persist despite OAC could potentially guide selective use of transesophageal echocardiography (TEE) instead of more routine policies to either use or not use TEE for thrombus rule-out before rhythm-control procedures, researchers propose.
Their prevalence was about 2.7% among the study’s more than 14,000 patients who received at least 3 weeks of OAC with either vitamin K antagonists (VKA) or direct oral anticoagulants (DOAC) before undergoing TEE.
But OAC-resistant LA thrombi were two- to four-times as common in patients with than without certain features, including AF other than paroxysmal and higher CHADS2 and CHA2DS2-VASc stroke risk-stratification scores.
“TEE imaging in select patients at an elevated risk of LA thrombus, despite anticoagulation status, may be a reasonable approach to minimize the risk of thromboembolic complications following cardioversion or catheter ablation,” propose the study’s authors, led by Antony Lurie, BMSC, Population Health Research Institute, Hamilton, Ont. Their report was published in the June 15 issue of the Journal of the American College of Cardiology.
Guidelines don’t encourage TEE before cardioversion in patients who have been on OAC for at least 3 weeks, the group notes, and policies on TEE use before AF ablation vary widely regardless of anticoagulation status.
The current study suggests that 3 weeks of OAC isn’t enough for a substantial number of patients, who might be put at thromboembolic risk if TEE were to be skipped before rhythm-control procedures.
Conversely, many patients unlikely to have LA thrombi get preprocedure TEE anyway. That can happen “irrespective of how long they’ve been anticoagulated, their pattern of atrial fibrillation, or their stroke risk,” senior author Jorge A. Wong, MD, MPH, Population Health Research Institute and McMaster University, Hamilton, Ont., told this news organization.
But “TEE is an invasive imaging modality, so it is associated with small element of risk.” The current study, Dr. Wong said, points to potential risk-stratification tools clinicians might use to guide more selective TEE screening.
“At sites where TEEs are done all the time for patients undergoing ablation, one could use several of these risk markers to perhaps tailor use of TEE in individuals,” Dr. Wong said. “For example, in people with paroxysmal atrial fibrillation, we found that the risk of left atrial appendage clot was approximately 1% or less.” Screening by TEE might reasonably be avoided in such patients.
“Fortunately, continued oral anticoagulation already yields low peri-procedural stroke rates,” observes an accompanying editorial from Paulus Kirchhof, MD, and Christoph Sinning, MD, from the University Heart & Vascular Center and German Centre of Cardiovascular Research, Hamburg.
“Based on this new analysis of existing data, a risk-based use of TEE imaging in anticoagulated patients could enable further improvement in the safe delivery of rhythm control interventions in patients with AF,” the editorialists agree.
The meta-analysis covered 10 prospective and 25 retrospective studies with a total of 14,653 patients that reported whether LA thrombus was present in patients with AF or atrial flutter (AFL) who underwent TEE after at least 3 weeks of VKA or DOAC therapy. Reports for 30 of the studies identified patients by rhythm-control procedure, and the remaining five didn’t specify TEE indications.
The weighted mean prevalence of LA thrombus at TEE was 2.73% (95% confidence interval, 1.95%-3.80%). The finding was not significantly changed in separate sensitivity analyses, the report says, including one limited to studies with low risk of bias and others excluding patients with valvular AF, interrupted OAC, heparin bridging, or subtherapeutic anticoagulation, respectively.
Patients treated with VKA and DOACs showed similar prevalences of LA thrombi, with means of 2.80% and 3.12%, respectively (P = .674). The prevalence was significantly higher in patients:
- with nonparoxysmal than with paroxysmal AF/AFL (4.81% vs. 1.03%; P < .001)
- undergoing cardioversion than ablation (5.55% vs. 1.65; P < .001)
- with CHA2DS2-VASc scores of at least 3 than with scores of 2 or less (6.31% vs. 1.06%; P < .001).
A limitation of the study, observe Dr. Kirchhof and Dr. Sinning, “is that all patients had a clinical indication for a TEE, which might be a selection bias. When a thrombus was found on TEE, clinical judgment led to postponing of the procedure,” thereby avoiding potential thromboembolism.
“Thus, the paper cannot demonstrate that presence of a thrombus on TEE is related to peri-procedural ischemic stroke,” they write.
The literature puts the risk for stroke or systemic embolism at well under 1% for patients anticoagulated with either VKA or DOACs for at least 3 weeks prior to cardioversion, in contrast to the nearly 3% prevalence of LA appendage thrombus by TEE in the current analysis, Dr. Wong observed.
“So we’re seeing a lot more left atrial appendage thrombus than we would see stroke,” but there wasn’t a way to determine whether that increases the stroke risk, he agreed.Dr. Wong, Dr. Lurie, and the other authors report no relevant conflicts. Dr. Kirchhof discloses receiving partial support “from several drug and device companies active in atrial fibrillation” and to being listed as inventor on two AF-related patents held by the University of Birmingham. Dr. Sinning reports no relevant relationships.
A version of this article first appeared on Medscape.com.
Three or more weeks of oral anticoagulation (OAC) sometimes isn’t up to the job of clearing any potentially embolic left atrial (LA) thrombi before procedures like cardioversion or catheter ablation in patients with atrial fibrillation (AF). Such OAC-defiant LA thrombi aren’t common, nor are they rare enough to ignore, suggests a new meta-analysis that might also have identified features that predispose to them.
Such predictors of LA clots that persist despite OAC could potentially guide selective use of transesophageal echocardiography (TEE) instead of more routine policies to either use or not use TEE for thrombus rule-out before rhythm-control procedures, researchers propose.
Their prevalence was about 2.7% among the study’s more than 14,000 patients who received at least 3 weeks of OAC with either vitamin K antagonists (VKA) or direct oral anticoagulants (DOAC) before undergoing TEE.
But OAC-resistant LA thrombi were two- to four-times as common in patients with than without certain features, including AF other than paroxysmal and higher CHADS2 and CHA2DS2-VASc stroke risk-stratification scores.
“TEE imaging in select patients at an elevated risk of LA thrombus, despite anticoagulation status, may be a reasonable approach to minimize the risk of thromboembolic complications following cardioversion or catheter ablation,” propose the study’s authors, led by Antony Lurie, BMSC, Population Health Research Institute, Hamilton, Ont. Their report was published in the June 15 issue of the Journal of the American College of Cardiology.
Guidelines don’t encourage TEE before cardioversion in patients who have been on OAC for at least 3 weeks, the group notes, and policies on TEE use before AF ablation vary widely regardless of anticoagulation status.
The current study suggests that 3 weeks of OAC isn’t enough for a substantial number of patients, who might be put at thromboembolic risk if TEE were to be skipped before rhythm-control procedures.
Conversely, many patients unlikely to have LA thrombi get preprocedure TEE anyway. That can happen “irrespective of how long they’ve been anticoagulated, their pattern of atrial fibrillation, or their stroke risk,” senior author Jorge A. Wong, MD, MPH, Population Health Research Institute and McMaster University, Hamilton, Ont., told this news organization.
But “TEE is an invasive imaging modality, so it is associated with small element of risk.” The current study, Dr. Wong said, points to potential risk-stratification tools clinicians might use to guide more selective TEE screening.
“At sites where TEEs are done all the time for patients undergoing ablation, one could use several of these risk markers to perhaps tailor use of TEE in individuals,” Dr. Wong said. “For example, in people with paroxysmal atrial fibrillation, we found that the risk of left atrial appendage clot was approximately 1% or less.” Screening by TEE might reasonably be avoided in such patients.
“Fortunately, continued oral anticoagulation already yields low peri-procedural stroke rates,” observes an accompanying editorial from Paulus Kirchhof, MD, and Christoph Sinning, MD, from the University Heart & Vascular Center and German Centre of Cardiovascular Research, Hamburg.
“Based on this new analysis of existing data, a risk-based use of TEE imaging in anticoagulated patients could enable further improvement in the safe delivery of rhythm control interventions in patients with AF,” the editorialists agree.
The meta-analysis covered 10 prospective and 25 retrospective studies with a total of 14,653 patients that reported whether LA thrombus was present in patients with AF or atrial flutter (AFL) who underwent TEE after at least 3 weeks of VKA or DOAC therapy. Reports for 30 of the studies identified patients by rhythm-control procedure, and the remaining five didn’t specify TEE indications.
The weighted mean prevalence of LA thrombus at TEE was 2.73% (95% confidence interval, 1.95%-3.80%). The finding was not significantly changed in separate sensitivity analyses, the report says, including one limited to studies with low risk of bias and others excluding patients with valvular AF, interrupted OAC, heparin bridging, or subtherapeutic anticoagulation, respectively.
Patients treated with VKA and DOACs showed similar prevalences of LA thrombi, with means of 2.80% and 3.12%, respectively (P = .674). The prevalence was significantly higher in patients:
- with nonparoxysmal than with paroxysmal AF/AFL (4.81% vs. 1.03%; P < .001)
- undergoing cardioversion than ablation (5.55% vs. 1.65; P < .001)
- with CHA2DS2-VASc scores of at least 3 than with scores of 2 or less (6.31% vs. 1.06%; P < .001).
A limitation of the study, observe Dr. Kirchhof and Dr. Sinning, “is that all patients had a clinical indication for a TEE, which might be a selection bias. When a thrombus was found on TEE, clinical judgment led to postponing of the procedure,” thereby avoiding potential thromboembolism.
“Thus, the paper cannot demonstrate that presence of a thrombus on TEE is related to peri-procedural ischemic stroke,” they write.
The literature puts the risk for stroke or systemic embolism at well under 1% for patients anticoagulated with either VKA or DOACs for at least 3 weeks prior to cardioversion, in contrast to the nearly 3% prevalence of LA appendage thrombus by TEE in the current analysis, Dr. Wong observed.
“So we’re seeing a lot more left atrial appendage thrombus than we would see stroke,” but there wasn’t a way to determine whether that increases the stroke risk, he agreed.Dr. Wong, Dr. Lurie, and the other authors report no relevant conflicts. Dr. Kirchhof discloses receiving partial support “from several drug and device companies active in atrial fibrillation” and to being listed as inventor on two AF-related patents held by the University of Birmingham. Dr. Sinning reports no relevant relationships.
A version of this article first appeared on Medscape.com.
Three or more weeks of oral anticoagulation (OAC) sometimes isn’t up to the job of clearing any potentially embolic left atrial (LA) thrombi before procedures like cardioversion or catheter ablation in patients with atrial fibrillation (AF). Such OAC-defiant LA thrombi aren’t common, nor are they rare enough to ignore, suggests a new meta-analysis that might also have identified features that predispose to them.
Such predictors of LA clots that persist despite OAC could potentially guide selective use of transesophageal echocardiography (TEE) instead of more routine policies to either use or not use TEE for thrombus rule-out before rhythm-control procedures, researchers propose.
Their prevalence was about 2.7% among the study’s more than 14,000 patients who received at least 3 weeks of OAC with either vitamin K antagonists (VKA) or direct oral anticoagulants (DOAC) before undergoing TEE.
But OAC-resistant LA thrombi were two- to four-times as common in patients with than without certain features, including AF other than paroxysmal and higher CHADS2 and CHA2DS2-VASc stroke risk-stratification scores.
“TEE imaging in select patients at an elevated risk of LA thrombus, despite anticoagulation status, may be a reasonable approach to minimize the risk of thromboembolic complications following cardioversion or catheter ablation,” propose the study’s authors, led by Antony Lurie, BMSC, Population Health Research Institute, Hamilton, Ont. Their report was published in the June 15 issue of the Journal of the American College of Cardiology.
Guidelines don’t encourage TEE before cardioversion in patients who have been on OAC for at least 3 weeks, the group notes, and policies on TEE use before AF ablation vary widely regardless of anticoagulation status.
The current study suggests that 3 weeks of OAC isn’t enough for a substantial number of patients, who might be put at thromboembolic risk if TEE were to be skipped before rhythm-control procedures.
Conversely, many patients unlikely to have LA thrombi get preprocedure TEE anyway. That can happen “irrespective of how long they’ve been anticoagulated, their pattern of atrial fibrillation, or their stroke risk,” senior author Jorge A. Wong, MD, MPH, Population Health Research Institute and McMaster University, Hamilton, Ont., told this news organization.
But “TEE is an invasive imaging modality, so it is associated with small element of risk.” The current study, Dr. Wong said, points to potential risk-stratification tools clinicians might use to guide more selective TEE screening.
“At sites where TEEs are done all the time for patients undergoing ablation, one could use several of these risk markers to perhaps tailor use of TEE in individuals,” Dr. Wong said. “For example, in people with paroxysmal atrial fibrillation, we found that the risk of left atrial appendage clot was approximately 1% or less.” Screening by TEE might reasonably be avoided in such patients.
“Fortunately, continued oral anticoagulation already yields low peri-procedural stroke rates,” observes an accompanying editorial from Paulus Kirchhof, MD, and Christoph Sinning, MD, from the University Heart & Vascular Center and German Centre of Cardiovascular Research, Hamburg.
“Based on this new analysis of existing data, a risk-based use of TEE imaging in anticoagulated patients could enable further improvement in the safe delivery of rhythm control interventions in patients with AF,” the editorialists agree.
The meta-analysis covered 10 prospective and 25 retrospective studies with a total of 14,653 patients that reported whether LA thrombus was present in patients with AF or atrial flutter (AFL) who underwent TEE after at least 3 weeks of VKA or DOAC therapy. Reports for 30 of the studies identified patients by rhythm-control procedure, and the remaining five didn’t specify TEE indications.
The weighted mean prevalence of LA thrombus at TEE was 2.73% (95% confidence interval, 1.95%-3.80%). The finding was not significantly changed in separate sensitivity analyses, the report says, including one limited to studies with low risk of bias and others excluding patients with valvular AF, interrupted OAC, heparin bridging, or subtherapeutic anticoagulation, respectively.
Patients treated with VKA and DOACs showed similar prevalences of LA thrombi, with means of 2.80% and 3.12%, respectively (P = .674). The prevalence was significantly higher in patients:
- with nonparoxysmal than with paroxysmal AF/AFL (4.81% vs. 1.03%; P < .001)
- undergoing cardioversion than ablation (5.55% vs. 1.65; P < .001)
- with CHA2DS2-VASc scores of at least 3 than with scores of 2 or less (6.31% vs. 1.06%; P < .001).
A limitation of the study, observe Dr. Kirchhof and Dr. Sinning, “is that all patients had a clinical indication for a TEE, which might be a selection bias. When a thrombus was found on TEE, clinical judgment led to postponing of the procedure,” thereby avoiding potential thromboembolism.
“Thus, the paper cannot demonstrate that presence of a thrombus on TEE is related to peri-procedural ischemic stroke,” they write.
The literature puts the risk for stroke or systemic embolism at well under 1% for patients anticoagulated with either VKA or DOACs for at least 3 weeks prior to cardioversion, in contrast to the nearly 3% prevalence of LA appendage thrombus by TEE in the current analysis, Dr. Wong observed.
“So we’re seeing a lot more left atrial appendage thrombus than we would see stroke,” but there wasn’t a way to determine whether that increases the stroke risk, he agreed.Dr. Wong, Dr. Lurie, and the other authors report no relevant conflicts. Dr. Kirchhof discloses receiving partial support “from several drug and device companies active in atrial fibrillation” and to being listed as inventor on two AF-related patents held by the University of Birmingham. Dr. Sinning reports no relevant relationships.
A version of this article first appeared on Medscape.com.