User login
A better future for baby: Stemming the tide of fetal alcohol syndrome
Screen all females of childbearing age for alcohol use with standardized screening instruments such as TWEAK, T-ACE, or AUDIT. A
Use brief, in-office interventions to decrease alcohol consumption and increase effective contraception in sexually active women. Involve a supportive adult of the patient’s choosing where possible. A
Advise pregnant patients that complete abstinence from alcohol is safest. B
Refer a child who meets FAS referral criteria for multi-disciplinary evaluations as early as possible. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Family physicians who care for infants and young children are often asked to diagnose growth lags and failure to meet parents’ expectations for reaching developmental milestones: Why isn’t my child gaining weight? Why isn’t he talking? The other kids in the day-care center ride tricycles—why can’t he? Will he catch up? My mother thinks he’s funny looking. Do you?
Simple reassurance is all that most of these worried families need. But for families with children whose growth or developmental milestones are sufficiently outside the usual parameters, more than reassurance is called for. As you consider whether the lags that worry parents are signs of a serious disability, it’s important to make a place for fetal alcohol syndrome (FAS) in your differential.
FAS, a congenital disorder caused by alcohol exposure during pregnancy, is characterized by growth deficiency before and after birth, distinctive facial features, and central nervous system (CNS) dysfunctions. The cognitive and developmental effects of FAS persist throughout life and are severe enough to limit employment and independent living.1,2
A spectrum of severity. FAS is the most severe expression of prenatal alcohol exposure. The term fetal alcohol spectrum disorders (FASD) is a nondiagnostic umbrella term that includes FAS as well as ARND (alcohol-related neurobehavioral disorder) and ARBD (alcohol-related birth defects). Children with ARND and ARBD fail to meet the full FAS diagnostic criteria but still exhibit the negative effects of gestational alcohol exposure. Centers for Disease Control and Prevention (CDC) diagnostic criteria for FAS are summarized in TABLE 1. Studies by the CDC have reported FAS prevalence rates from 0.2 to 1.5 cases per 1000 live births, with a higher prevalence among minority (Native American and African American) and impoverished groups.1
An opportunity—and a challenge. As a family physician, you have a unique opportunity to modify the impact of FAS by recognizing the disorder in infancy or early childhood, actively engineering appropriate referrals, and supporting families in the difficult task of parenting a child with disabilities. Correctly diagnosing a child with FAS before age 6 can have a protective influence, decreasing the odds that he or she will suffer severe secondary disabilities in adolescence and adulthood. You can also help prevent FAS by screening for potentially harmful drinking patterns and helping sexually active female patients decrease alcohol consumption and use contraception successfully.
Providing these supportive and preventive services can be challenging. A recent survey of pediatricians revealed that only 34% felt prepared to manage and coordinate the treatment of children with FASD, and only 13% routinely counseled adolescent patients about the risks of drinking and pregnancy.3 Th is article will help you surmount the difficulties these tasks present and perform vital functions for alcohol-affected families you may encounter in your practice.
TABLE 1
Diagnostic criteria for fetal alcohol syndrome
Facial dysmorphia
| ≤10th percentile for age and racial norms Score of 4 or 5 on lip-philtrum guide* Score of 4 or 5 on lip-philtrum guide* |
| Growth problems | <10th percentile for age, sex, gestational age, racial norms in height or weight, prenatally or postnatally |
| CNS abnormalities | Any structural abnormality (head circumference <10% of age norm or clinically significant brain abnormalities observable through imaging); neurological abnormality not due to postnatal insult or fever; or functional abnormality demonstrated by cognitive performance less than expected for age, schooling, or family circumstances. An individual could meet the CNS abnormality criteria for a FAS diagnosis through a structural abnormality, yet not demonstrate detectable functional deficits. |
| CNS, central nervous system. | |
| *The lip-philtrum guide is available at http://depts.washington.edu/fasdpn/htmls/lip-philtrum-guides.htm. | |
| Source: Centers for Disease Control and Prevention. Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis. 2005. Available at www.cdc.gov/ncbddd/fasd/documents/FAS_guidelines_accessible.pdf. Accessed April 10, 2010. | |
The place to start: Spotting mothers at risk
Recognizing an infant with FAS starts by asking the baby’s mother about her pattern of drinking while she was pregnant. Most studies on the effects of gestational exposure to alcohol have emphasized moderate to high levels of exposure. In 1 study, children who were exposed to binge drinking were 1.7 times as likely to have IQ scores in the mentally retarded range and 2.5 times more likely to have clinically significant levels of delinquent behavior.4 Binge drinking is defined by the National Institute of Alcohol Abuse and Alcoholism as a pattern of drinking that brings blood alcohol concentration to 0.8% or above, which typically happens in women who consume 4 or more drinks in a period of about 2 hours.5
But a pregnant woman doesn’t have to be a binge drinker to put her fetus at risk. Even low levels of prenatal alcohol use—as low as 1 drink per week—have been associated with adverse behavioral changes in children, including increased aggressive behaviors documented at school age.6,7 The research documenting effects at these low levels has led the American Academy of Pediatrics (AAP) and the American Congress of Obstetricians and Gynecologists (ACOG) to recommend total abstinence from alcohol throughout pregnancy.8,9 Patterns of “at risk” drinking for women include binge drinking or persistent regular use (>7 drinks in 1 week). If a mother provides a history of that level of prenatal exposure, her child should be referred for multidisciplinary evaluation at an FAS center, even in the absence of the characteristic facial features.1
The face of FAS
Without a history of prenatal alcohol exposure, the cardinal features of facial dysmorphia (short palpebral fissures, smooth philtrum, and thin vermillion border) plus deficits in height and weight are the main physical findings of FAS. Evaluating height and weight percentiles is a routine part of well-child care, requiring minimal training. Height or weight or both at or below the 10th percentile, adjusted for age, sex, gestational age, and race or ethnicity, meet part of the CDC diagnostic criteria for FAS, but must be accompanied by at least 1 of the typical facial features associated with FAS to meet referral guidelines.1 The diagnostic guidelines are more restrictive, requiring all 3 facial features to meet the threshold for an FAS diagnosis, vs another diagnosis, such as alcohol-related neurodevelopmental disorders (TABLE 1).
Learning to measure faces. Examining a child for the facial characteristics of FAS requires a set of skills that can be learned in a relatively short time, with moderate interrater reliability when compared with dysmorphologists, according to 1 study.10
Tools for measuring. Palpebral fissure length (PFL) can be measured with a clear plastic ruler pressed onto the child’s cheek to determine the distance from the endocanthion to the exocanthion while the child is gazing upward.11 To meet the CDC criteria for FAS, this distance should be at or below the 10th percentile compared to norms. The shape of the lips and the nature of the philtrum are then compared to preestablished comparison photographs available on the University of Washington Lip-Philtrum Guides (see URL that follows).12 The vermillion border and the philtrum must both receive a rank of 4 or 5 to meet FAS criteria.11
Changes in the clinical presentation of fetal alcohol syndrome (FAS) occur across the lifespan. Clinicians searching for an explanation of an older child’s difficulties may need to reconsider a possible diagnosis of FAS, even if the facial features are less recognizable.
Preschool children with FAS may display a delay in early language acquisition and the beginnings of attention problems and hyperactivity. School-age children may have difficulty remembering material even when they have gone over it many times. They may lack social perception skills, be hyperactive, and show cognitive delays. Mathematics is often an area of severe delay, and sleep problems can persist.1
Teens and adults with FAS often have a wide range of secondary disabilities: disrupted schooling, inappropriate sexual behavior, mental health problems, aggression, trouble with the law, confinement in jail or as inpatients in psychiatric or substance abuse treatment facilities, alcohol and drug problems, and failure or inability to live independently at an appropriate age. They may have trouble finding a job and keeping one. More than 90% of patients with FAS exhibit mental health problems, with attention problems appearing in early childhood and persisting, and depression appearing in adolescence and adulthod.15
Tools available online for physicians include Lip-Philtrum Guides (www.depts.washington.edu/fasdpn/htmls/lip-philtrum-guides.htm) and an instructional video depicting PFL measurement techniques (www.depts.washington.edu/fasdpn/htmls/photo-face.htm), both from the University of Washington FAS Diagnostic and Prevention Network. In addition, a physical evaluation summary form, with reference data for PFL in Caucasian, black, and Hispanic children, is available at http://www.fas.academicedge.com/documents/phyevaln.pdf.
The Astley-Clarren criteria. The 4-digit diagnostic code developed by Astley and Clarren for diagnosis of FAS and employed at some FAS referral centers uses very strict criteria.13 Centers using these criteria define “abnormal” as ≥2 standard deviations below the mean or its equivalent, ≤2.5th percentile.13 Th is applies to the 3 facial features and CNS dysfunction (low IQ, eg). If all 3 facial features are identified in the Astley-Clarren system as abnormal (PFL ≤2.5th percentile, lip philtrum 5, vermillion 5), the sensitivity of the facial features is 100% and specificity is 99.8% for a diagnosis of FAS.13
The CDC criteria, developed with increased surveillance by providers as a goal, uses relaxed criteria of ≤10th percentile of PFL and 4 or 5 on the philtrum/vermillion border guide to identify abnormal facial features and <10th percentile in CNS dysfunctions. Sensitivity and specificity data for those CDC criteria are not available.1
CNS abnormalities may be noted early enough to trigger a referral for complete evaluation, but must be present in some degree to confirm a diagnosis of FAS. Abnormalities may include microcephaly with head circumference below the 10th percentile; clinically significant brain abnormalities observable through imaging, especially a small or absent corpus callosum; and functional deficits in any of a multitude of domains. In an infant, these deficits may be expressed in global developmental delays, sleep cycle problems, poor muscle tone, and feeding problems with poor suck and texture aversion.1
Evaluation may not confirm the diagnosis. Children referred for more extensive evaluation may or may not be confirmed to have FAS. In 2 demographically similar counties in New York state, only 5% of children initially identified in 1 county (10 of 208) and 13% (53 of 420) of children in the other county were confirmed to have FAS.12 The FAS diagnosis is complicated and the CNS and growth deficiencies may not be expressed until a later age.14 (See “Fetal alcohol syndrome across the lifespan”1,15)
Providers may feel reluctant to alarm or stigmatize families when they are unsure of the diagnosis, but the long-term benefit of confirming the diagnosis early on may be significant for the child and family. The case on page 341 (Tanya) illustrates the complexity of diagnosing FASD.
The encouraging news for family physicians is that the odds of escaping adverse life outcomes are increased 2- to 4-fold by receiving a diagnosis of FAS before age 6 and by being raised in a stable environment.16 Early diagnosis can be protective by helping with eligibility requirements for support services and by opening the door to medical management of FAS-associated conditions such as ADHD and depression. In addition, the diagnosis can alert family physicians to the family’s need for help with ongoing problems with alcohol use. The case on page 341 (Brianna) illustrates the complex secondary problems a teen with FAS may face.
Putting families in touch with resources
Multidisciplinary FAS teams may include physicians (a geneticist or developmental pediatrician), psychologists, speech pathologists, educational specialists, social workers, and occupational therapists. These groups typically have in-depth intake and evaluation processes, including neurodiagnostic studies that help clarify the cognitive and functional domains that are affected.
You can locate the nearest FAS evaluation team and other resources for providers and families on the National and State Resource Directory for the National Organization on Fetal Alcohol Syndrome. Go to www.nofas.org, click on Resources, then on National and State Resources Directory in the box on the left side of the page. There may be a waiting list for evaluation, but under Part C of the Individuals with Disabilities Education Act (IDEA), FAS is considered a “presumptive eligibility” diagnosis. Presumptive diagnoses allow children under age 3 at risk of later developmental delay to be served without meeting particular eligibility criteria.1 Physicians may refer these children for developmental assessment services and early intervention services while waiting for the more complete FAS evaluation.
After the age of 3, children and families are referred to preschool programs for children with disabilities that are administered through IDEA Part B, with no “presumptive eligibility” diagnoses. Eligibility for educational services under this program is entirely based on functional criteria.
Your best bet: Prevention
The key to preventing FAS is to find out whether your patient’s drinking patterns and contraceptive habits put her at risk for an alcohol-exposed pregnancy. Make it routine practice to ask women, in a way that encourages honest reporting, about both of these aspects of their lives. The US Preventive Services Task Force recommends screening and counseling intervention in primary care settings to reduce alcohol misuse in adults, including pregnant women.17 The case on page 341 (Clarice) illustrates how screening and brief intervention can be used to prevent alcohol-exposed pregnancy.
TANYA
Possible, though unconfirmed, FAS
This 1-month-old African American girl was admitted to the hospital with stridor, possible cardiorespiratory issues, and failure to thrive. She exhibited microcephaly, poor suck, floppy overall muscle tone, and small palpebral fissure lengths. The respiratory noise was attributed to tracheomalacia, secondary to her poor muscle tone.
An initial magnetic resonance imaging of the brain showed an almost complete absence of the corpus callosum. Obviously at risk for future delays, Tanya was referred for early childhood development intervention. By the age of 5½, she was within her peer group’s normal range in fine motor, gross motor, and speech skills. She was removed from her mother’s care for neglect and later placed in an extended family adoption.
Her initial evaluation took place before the widespread publication of fetal alcohol syndrome (FAS) criteria, and she was not referred for more specific FAS evaluation, as she would have been had she been seen more recently. Tanya has been lost to long-term follow-up from her initial medical home, but her mother returned to the same practice for a subsequent pregnancy and was screened as a problem drinker.
BRIANNA
Facing severe secondary disabilities
This 16-year-old Caucasian girl entered foster care for the second time because her first placement could not deal with her complex behavioral issues. Her mother committed suicide last year, and her father is in an alcohol rehabilitation program. No pregnancy history is available.
The social service agency supervising Brianna’s care decided not to return her to her father’s home. She made a suicidal gesture, her behavior is sometimes violent, and she has been diagnosed with attention deficit hyperactivity disorder (ADHD). She is being treated for depression, requiring multiple medications.
Brianna’s life has been difficult. Before she was 2 years old, she underwent surgery for a ventricular septal defect. Although her cardiac repair was successful, she remains significantly underweight, <3rd percentile on the growth curve. Because she is an adolescent, her facial features are less distinctive for FAS, but she appears to have a smooth philtrum and thin vermillion. Her learning disabilities are significant enough that she has been held back a grade and requires an individualized education plan.
It may be too late to help provide any assistance to Brianna, who is already experiencing severe secondary disabilities. But if a diagnosis of FAS (or alcohol-related neurobehavioral disorder) can be made, even at this point in her life, provisions may be made within the foster care system for transitional housing and emphasis on life skills training, rather than simply allowing her to “age out” of the system when she turns 18.
CLARICE
Preventing an alcohol-exposed pregnancy
Clarice is an 18-year-old, college-bound woman who came in for a pre-college health maintenance examination. She reported being sexually active and was using effective contraception only intermittently. On the TWEAK questionnaire, she said the most she has had to drink on a single occasion was 6 drinks, noted that she had never passed out and had not had any problems associated with drinking. The only worry she connected with drinking was a fear of gaining weight.
Clarice met the criteria for “at risk” drinking (TABLE 3). She was a candidate for a brief intervention, including information on the hazards of alcohol-exposed pregnancy and on effective contraceptive practices. We scheduled a telephone follow-up and checkup in 6 months.
* Drawn from the author’s case files. Names have been changed to protect patient privacy.
Screening should include simple quantity and frequency questions developed by the National Institute on Alcohol Abuse to clarify a patient’s current drinking patterns. The questions include the numbers of days per week of any drinking, the average number of drinks per day, and the maximum number of drinks consumed in 1 day during the past month. Determining that a woman drinks more than 7 drinks per week has a 29% sensitivity, but a 90% specificity for identifying lifetime risk of alcohol abuse or dependence.18
Other tools include TWEAK (Tolerance, Worry, Eye-opener, Amnesia, (K)Cut down), T-ACE (Tolerance, Annoyed, Cut down, Eye opener), and AUDIT (Alcohol Use Disorder Identification Test). They are detailed below and available online at Project Cork. Go to www.projectcork.org, and click on “clinical tools.”
The 5-item TWEAK tool (TABLE 2) appears to be the optimal screening questionnaire for identifying women in racially mixed populations with heavy drinking or alcohol abuse and dependence, but a score of 2 points should be the threshold for identifying female problem drinkers.19,20 Using the lower cutoff of 2, the sensitivity of TWEAK is in the 87% to 91% range for women, with a specificity of 77% to 90%.18
The T-ACE tool is a set of 4 questions, with the question addressing tolerance weighted more heavily than the others. With a score of 2 or more, the sensitivity of T-ACE is 70% to 88%; the specificity is 79% to 85%.18
The AUDIT tool is a self-administered screen that consists of a series of 10 questions that are each scored on a scale of 0 to 4. The maximum score is 40. A score of 2 indicates some harmful use of alcohol, but a score of 8 or more has a sensitivity of 59% to 66%, with a specificity of 93% to 97% in women.18
TABLE 2
TWEAK your patients for alcohol use
| Tolerance: How many drinks does it take for you to: | Score |
| 2 points for ≥3 drinks 2 points for ≥5 drinks |
| Worry about drinking | |
| Have your friends or relatives worried about your drinking in the past year? | 1 point for Yes |
| Eye-opener | |
| Do you sometimes take a drink in the morning when you first get up? | 1 point for Yes |
| Amnesia | |
| Are there times when you drink and afterwards can’t remember what you said or did? | 1 point for Yes |
| (K)Cut down | |
| Do you sometimes feel the need to cut down on your drinking? | 1 point for Yes |
| Scoring: ≥3 points is considered positive for alcoholism/heavy drinking. Thresholds differ for screening different populations, and a score of ≥2 points should be used as the threshold for identifying female problem drinkers. | |
| Source: Chan AW, et al. Alcohol Clin Exp Res. 1993.19 | |
When your patient is at risk
Brief interventions are recommended for nonpregnant and pregnant women who have exhibited a pattern of at-risk or problem drinking.21TABLE 3 summarizes patterns of drinking in women, from not drinking at all through various degrees of risk to alcohol dependency. Referral to an addiction specialist is recommended for women with alcohol dependence.
Brief interventions for alcohol abuse can be single-session encounters from 5 to 15 minutes’ duration, or multi-contact brief sessions, including possible phone follow-up contacts. Project TrEAT (Trial for Early Alcohol Treatment) provided two 15-minute sessions with the primary care physician (either a family physician or internist in community-based practice) scheduled 1 month apart, with nurse follow-up phone calls 2 weeks after each appointment.22
TABLE 3
Drinking patterns in women
Abstainer
|
Low-risk drinking
|
At-risk drinking
|
Problem drinking
|
Alcohol-dependent drinking: Maladaptive patterns of alcohol use leading to clinically significant impairment manifested by 3 or more of the following, occurring at any time during the same 12-month period:
|
| Source: Training program for medical students and other health professionals on fetal alcohol syndrome. Presented by the Midwest Regional Fetal Alcohol Syndrome Training Center; March 18, 2005; St. Louis, Mo. |
Patients received general information regarding adverse effects of alcohol and the prevalence of problem drinking, in addition to tools to help them identify drinking triggers and track their consumption. The patient and physician developed a “drinking agreement” in the form of a rescription. Men and non pregnant women were included in this study.
Women reduced their alcohol use by 47% and their frequency of binge drinking by 56%, as noted at a 6-month follow-up, with changes well maintained at 12 months. The reductions for female patients were actually slightly higher than for male participants.22
Chang and colleagues provided a 25-minute single session brief intervention to pregnant women who had screened positive on the T-ACE questionnaire with a score of 2 or more, and were identified as being at risk for prenatal alcohol use.23 Participants were randomly assigned to the intervention group or a control group. Both the control group and the brief intervention group decreased their use of alcohol after enrolling in the study and undergoing the initial detailed assessment.
For women who were heavier drinkers, the brief interventions for prenatal alcohol use were statistically more effective in reducing their frequency of alcohol consumption, vs the initial assessment alone. In addition, the effects of the brief intervention were significantly enhanced when a support partner of the woman’s choice also participated.23
The Project Choices Intervention Research Group studied an intervention that included 4 sessions of motivational interviewing regarding alcohol habits, and a contraception counseling session.24 Study participants were recruited from 6 community-based settings with high proportions of women at risk for an alcohol-exposed pregnancy, including a jail and 2 drug and alcohol treatment centers. Among the 143 women who completed the 6-month follow-up, 68.5% were no longer at risk of having an alcohol-exposed pregnancy.
These participants successfully lowered their risk by reducing alcohol use only (12.9%), adopting appropriate contraception use only (23.1%), or by changing both risk factors (32.9%). Even if all the study participants who were lost to follow-up were assumed to have been unsuccessful at eliminating their risk of alcohol-exposed pregnancy, more than half of the women (51.6%) successfully changed.24
Take advantage of opportunities
FAS is the most severe consequence of alcohol-exposed pregnancy, leaving the affected child with a lifelong disability. As a family physician, you have access to easy-touse, cost-effective clinical tools to screen for at-risk drinking behaviors and have sufficient rapport with your patients to encourage effective contraceptive practices. You also have effective tools for helping patients reduce their alcohol consumption.
Within the context of your long-term relationships with patients, you can provide brief interventions that include factual information and opportunities for goal setting. You can assist families with an FAS child to access services, manage medically related complications, and plan for special education and vocational skills training.
Recognition that 1 child in a family is affected by prenatal alcohol exposure gives you another window of opportunity to address the underlying substance use issues in the mother and the family, increasing the odds that future pregnancies will not be alcohol exposed.
CORRESPONDENCE Mary C. Boyce, MD, Wesley Family Medicine Residency, 850 N. Hillside, Wichita, KS 67214; [email protected]
1. Centers for Disease Control and Prevention. Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis. 2005. Available at: www.cdc.gov/ncbddd/fasd/documents/FAS_guidelines_accessible.pdf. Accessed April 10, 2010.
2. Spohr HL, Williams J, Steinhausen HC. Fetal alcohol spectrum disorders in young adulthood. J Pediatr. 2007;150:175-179.
3. Gahagan S, Sharpe TT, Brimacombe M, et al. Pediatricians’ knowledge, training, and experience in the care of children with fetal alcohol syndrome. Pediatrics. 2006;118:e657-e668.
4. Bailey BN, Delaney-Black V, Covington CY, et al. Prenatal exposure to binge drinking and cognitive and behavioral outcomes at age 7 years. Am J Obstet Gynecol. 2004;191:1037-1043.
5. CDC. Alcohol and public health/binge drinking. Quick stats. Available at: www.cdc.gov/alcohol/quickstats/binge_drinking.htm. Accessed April 21, 2010.
6. Sood B, Delaney-Black V, Covington C, et al. Prenatal alcohol exposure and childhood behavior at age 6 to 7 years: I. Doseresponse effect. Pediatrics. 2001;108:E34.-
7. Sokol RJ, Delaney-Black V, Nordstrom B. Fetal alcohol spectrum disorder. JAMA. 2003;290:2996-2999.
8. American Congress of Obstetricians and Gynecologists. ACOG Education Pamphlet AP170: Tobacco, alcohol, drugs, and pregnancy. Available at www.acog.org/publications/patient_education/bp170.cfm. Accessed May 3, 2010.
9. Committee on Substance Abuse and Committee on Children With Disabilities. Fetal alcohol syndrome and alcohol-related neurodevelopmental disorders. Pediatrics. 2000;106:358-361.
10. Jones KL, Robinson LK, Bakhireva LN, et al. Accuracy of the diagnosis of physical features of fetal alcohol syndrome by pediatricians after specialized training. Pediatrics. 2006;118:e1734-e1738.
11. University of Washington Fetal Alcohol Syndrome Diagnostic and Prevention Network. FAS facial photography and measurement instruction. Available at: www.depts.washington.edu/fasdpn/htmls/photo-face.htm. Accessed April 21,2010.
12. University of Washington Fetal Alcohol Syndrome Diagnostic and Prevention Network. Lip philtrum guides. Available at: www.depts.washington.edu/fasdpn/htmls/lip-philtrum-guides.htm. Accessed April 21, 2010.
13. Astley S. Comparison of the 4-digit diagnostic code and the Hoyme diagnostic guidelines for fetal alcohol spectrum disorder. Pediatrics. 2006;188:1532-1545.
14. Druschel CM, Fox DJ. Issues in estimating the prevalence of fetal alcohol syndrome: examination of 2 counties in New York State. Pediatrics. 2007;119:e384-e390.
15. Streissguth AP, Barr HM, Kogan J, et al. Understanding the occurrence of secondary disabilities in clients with fetal alcohol syndrome (FAS) and fetal alcohol effects (FAE). Final Report to the Centers for Disease Control and Prevention. Technical report no. 96-06. Seattle, WA: University of Washington, Fetal Alcohol and Drug Unit; 1996.
16. Streissguth AP, Bookstein FL, Barr H, et al. Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. J Dev Behav Pediatr. 2004;25:228-238.
17. US Preventive Services Task Force. Screening and behavioral interventions in primary care to reduce alcohol misuse: recommendation statement, April 2004. Available at: www.ahrq.gov/clinic/3rduspstf/alcohol/alcomisrs.htm. Accessed April 10, 2010.
18. Bradley KA, Boyd-Wickizer J, Powell SH, et al. Alcohol screening questionnaires in women: a critical review. JAMA. 1998;20:166-171.
19. Chan AW, Pristach EA, Welte JW, et al. Use of the TWEAK test in screening for alcoholism/heavy drinking in three populations. Alcohol Clin Exp Res. 1993;17:1188-1192.
20. Russell M, Bigler L. Screening for alcohol-related problems in an outpatient obstetric-gynecologic clinic. Am J Obstet Gynecol. 1979;134:4-12.
21. National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: a clinician’s guide. Updated January 2007. Available at: http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/clinicians_guide.htm. Accessed April 21, 2010.
22. Fleming MF, Barry KL, Manwell LB, et al. Brief physician advice for problem alcohol drinkers. JAMA. 1997;277:1039-1045.
23. Chang G, McNamara TK, Orav J, et al. Brief interventions for prenatal alcohol use: a randomized trial. Obstet Gynecol. 2005;105:991-998.
24. The Project Choices Intervention Research Group. Reducing the risk of alcohol-exposed pregnancies: a study of motivational intervention in community settings. Pediatrics. 2003;111:1131-1135.
Screen all females of childbearing age for alcohol use with standardized screening instruments such as TWEAK, T-ACE, or AUDIT. A
Use brief, in-office interventions to decrease alcohol consumption and increase effective contraception in sexually active women. Involve a supportive adult of the patient’s choosing where possible. A
Advise pregnant patients that complete abstinence from alcohol is safest. B
Refer a child who meets FAS referral criteria for multi-disciplinary evaluations as early as possible. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Family physicians who care for infants and young children are often asked to diagnose growth lags and failure to meet parents’ expectations for reaching developmental milestones: Why isn’t my child gaining weight? Why isn’t he talking? The other kids in the day-care center ride tricycles—why can’t he? Will he catch up? My mother thinks he’s funny looking. Do you?
Simple reassurance is all that most of these worried families need. But for families with children whose growth or developmental milestones are sufficiently outside the usual parameters, more than reassurance is called for. As you consider whether the lags that worry parents are signs of a serious disability, it’s important to make a place for fetal alcohol syndrome (FAS) in your differential.
FAS, a congenital disorder caused by alcohol exposure during pregnancy, is characterized by growth deficiency before and after birth, distinctive facial features, and central nervous system (CNS) dysfunctions. The cognitive and developmental effects of FAS persist throughout life and are severe enough to limit employment and independent living.1,2
A spectrum of severity. FAS is the most severe expression of prenatal alcohol exposure. The term fetal alcohol spectrum disorders (FASD) is a nondiagnostic umbrella term that includes FAS as well as ARND (alcohol-related neurobehavioral disorder) and ARBD (alcohol-related birth defects). Children with ARND and ARBD fail to meet the full FAS diagnostic criteria but still exhibit the negative effects of gestational alcohol exposure. Centers for Disease Control and Prevention (CDC) diagnostic criteria for FAS are summarized in TABLE 1. Studies by the CDC have reported FAS prevalence rates from 0.2 to 1.5 cases per 1000 live births, with a higher prevalence among minority (Native American and African American) and impoverished groups.1
An opportunity—and a challenge. As a family physician, you have a unique opportunity to modify the impact of FAS by recognizing the disorder in infancy or early childhood, actively engineering appropriate referrals, and supporting families in the difficult task of parenting a child with disabilities. Correctly diagnosing a child with FAS before age 6 can have a protective influence, decreasing the odds that he or she will suffer severe secondary disabilities in adolescence and adulthood. You can also help prevent FAS by screening for potentially harmful drinking patterns and helping sexually active female patients decrease alcohol consumption and use contraception successfully.
Providing these supportive and preventive services can be challenging. A recent survey of pediatricians revealed that only 34% felt prepared to manage and coordinate the treatment of children with FASD, and only 13% routinely counseled adolescent patients about the risks of drinking and pregnancy.3 Th is article will help you surmount the difficulties these tasks present and perform vital functions for alcohol-affected families you may encounter in your practice.
TABLE 1
Diagnostic criteria for fetal alcohol syndrome
Facial dysmorphia
| ≤10th percentile for age and racial norms Score of 4 or 5 on lip-philtrum guide* Score of 4 or 5 on lip-philtrum guide* |
| Growth problems | <10th percentile for age, sex, gestational age, racial norms in height or weight, prenatally or postnatally |
| CNS abnormalities | Any structural abnormality (head circumference <10% of age norm or clinically significant brain abnormalities observable through imaging); neurological abnormality not due to postnatal insult or fever; or functional abnormality demonstrated by cognitive performance less than expected for age, schooling, or family circumstances. An individual could meet the CNS abnormality criteria for a FAS diagnosis through a structural abnormality, yet not demonstrate detectable functional deficits. |
| CNS, central nervous system. | |
| *The lip-philtrum guide is available at http://depts.washington.edu/fasdpn/htmls/lip-philtrum-guides.htm. | |
| Source: Centers for Disease Control and Prevention. Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis. 2005. Available at www.cdc.gov/ncbddd/fasd/documents/FAS_guidelines_accessible.pdf. Accessed April 10, 2010. | |
The place to start: Spotting mothers at risk
Recognizing an infant with FAS starts by asking the baby’s mother about her pattern of drinking while she was pregnant. Most studies on the effects of gestational exposure to alcohol have emphasized moderate to high levels of exposure. In 1 study, children who were exposed to binge drinking were 1.7 times as likely to have IQ scores in the mentally retarded range and 2.5 times more likely to have clinically significant levels of delinquent behavior.4 Binge drinking is defined by the National Institute of Alcohol Abuse and Alcoholism as a pattern of drinking that brings blood alcohol concentration to 0.8% or above, which typically happens in women who consume 4 or more drinks in a period of about 2 hours.5
But a pregnant woman doesn’t have to be a binge drinker to put her fetus at risk. Even low levels of prenatal alcohol use—as low as 1 drink per week—have been associated with adverse behavioral changes in children, including increased aggressive behaviors documented at school age.6,7 The research documenting effects at these low levels has led the American Academy of Pediatrics (AAP) and the American Congress of Obstetricians and Gynecologists (ACOG) to recommend total abstinence from alcohol throughout pregnancy.8,9 Patterns of “at risk” drinking for women include binge drinking or persistent regular use (>7 drinks in 1 week). If a mother provides a history of that level of prenatal exposure, her child should be referred for multidisciplinary evaluation at an FAS center, even in the absence of the characteristic facial features.1
The face of FAS
Without a history of prenatal alcohol exposure, the cardinal features of facial dysmorphia (short palpebral fissures, smooth philtrum, and thin vermillion border) plus deficits in height and weight are the main physical findings of FAS. Evaluating height and weight percentiles is a routine part of well-child care, requiring minimal training. Height or weight or both at or below the 10th percentile, adjusted for age, sex, gestational age, and race or ethnicity, meet part of the CDC diagnostic criteria for FAS, but must be accompanied by at least 1 of the typical facial features associated with FAS to meet referral guidelines.1 The diagnostic guidelines are more restrictive, requiring all 3 facial features to meet the threshold for an FAS diagnosis, vs another diagnosis, such as alcohol-related neurodevelopmental disorders (TABLE 1).
Learning to measure faces. Examining a child for the facial characteristics of FAS requires a set of skills that can be learned in a relatively short time, with moderate interrater reliability when compared with dysmorphologists, according to 1 study.10
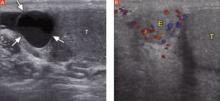
Tools for measuring. Palpebral fissure length (PFL) can be measured with a clear plastic ruler pressed onto the child’s cheek to determine the distance from the endocanthion to the exocanthion while the child is gazing upward.11 To meet the CDC criteria for FAS, this distance should be at or below the 10th percentile compared to norms. The shape of the lips and the nature of the philtrum are then compared to preestablished comparison photographs available on the University of Washington Lip-Philtrum Guides (see URL that follows).12 The vermillion border and the philtrum must both receive a rank of 4 or 5 to meet FAS criteria.11
Changes in the clinical presentation of fetal alcohol syndrome (FAS) occur across the lifespan. Clinicians searching for an explanation of an older child’s difficulties may need to reconsider a possible diagnosis of FAS, even if the facial features are less recognizable.
Preschool children with FAS may display a delay in early language acquisition and the beginnings of attention problems and hyperactivity. School-age children may have difficulty remembering material even when they have gone over it many times. They may lack social perception skills, be hyperactive, and show cognitive delays. Mathematics is often an area of severe delay, and sleep problems can persist.1
Teens and adults with FAS often have a wide range of secondary disabilities: disrupted schooling, inappropriate sexual behavior, mental health problems, aggression, trouble with the law, confinement in jail or as inpatients in psychiatric or substance abuse treatment facilities, alcohol and drug problems, and failure or inability to live independently at an appropriate age. They may have trouble finding a job and keeping one. More than 90% of patients with FAS exhibit mental health problems, with attention problems appearing in early childhood and persisting, and depression appearing in adolescence and adulthod.15
Tools available online for physicians include Lip-Philtrum Guides (www.depts.washington.edu/fasdpn/htmls/lip-philtrum-guides.htm) and an instructional video depicting PFL measurement techniques (www.depts.washington.edu/fasdpn/htmls/photo-face.htm), both from the University of Washington FAS Diagnostic and Prevention Network. In addition, a physical evaluation summary form, with reference data for PFL in Caucasian, black, and Hispanic children, is available at http://www.fas.academicedge.com/documents/phyevaln.pdf.
The Astley-Clarren criteria. The 4-digit diagnostic code developed by Astley and Clarren for diagnosis of FAS and employed at some FAS referral centers uses very strict criteria.13 Centers using these criteria define “abnormal” as ≥2 standard deviations below the mean or its equivalent, ≤2.5th percentile.13 Th is applies to the 3 facial features and CNS dysfunction (low IQ, eg). If all 3 facial features are identified in the Astley-Clarren system as abnormal (PFL ≤2.5th percentile, lip philtrum 5, vermillion 5), the sensitivity of the facial features is 100% and specificity is 99.8% for a diagnosis of FAS.13
The CDC criteria, developed with increased surveillance by providers as a goal, uses relaxed criteria of ≤10th percentile of PFL and 4 or 5 on the philtrum/vermillion border guide to identify abnormal facial features and <10th percentile in CNS dysfunctions. Sensitivity and specificity data for those CDC criteria are not available.1
CNS abnormalities may be noted early enough to trigger a referral for complete evaluation, but must be present in some degree to confirm a diagnosis of FAS. Abnormalities may include microcephaly with head circumference below the 10th percentile; clinically significant brain abnormalities observable through imaging, especially a small or absent corpus callosum; and functional deficits in any of a multitude of domains. In an infant, these deficits may be expressed in global developmental delays, sleep cycle problems, poor muscle tone, and feeding problems with poor suck and texture aversion.1
Evaluation may not confirm the diagnosis. Children referred for more extensive evaluation may or may not be confirmed to have FAS. In 2 demographically similar counties in New York state, only 5% of children initially identified in 1 county (10 of 208) and 13% (53 of 420) of children in the other county were confirmed to have FAS.12 The FAS diagnosis is complicated and the CNS and growth deficiencies may not be expressed until a later age.14 (See “Fetal alcohol syndrome across the lifespan”1,15)
Providers may feel reluctant to alarm or stigmatize families when they are unsure of the diagnosis, but the long-term benefit of confirming the diagnosis early on may be significant for the child and family. The case on page 341 (Tanya) illustrates the complexity of diagnosing FASD.
The encouraging news for family physicians is that the odds of escaping adverse life outcomes are increased 2- to 4-fold by receiving a diagnosis of FAS before age 6 and by being raised in a stable environment.16 Early diagnosis can be protective by helping with eligibility requirements for support services and by opening the door to medical management of FAS-associated conditions such as ADHD and depression. In addition, the diagnosis can alert family physicians to the family’s need for help with ongoing problems with alcohol use. The case on page 341 (Brianna) illustrates the complex secondary problems a teen with FAS may face.
Putting families in touch with resources
Multidisciplinary FAS teams may include physicians (a geneticist or developmental pediatrician), psychologists, speech pathologists, educational specialists, social workers, and occupational therapists. These groups typically have in-depth intake and evaluation processes, including neurodiagnostic studies that help clarify the cognitive and functional domains that are affected.
You can locate the nearest FAS evaluation team and other resources for providers and families on the National and State Resource Directory for the National Organization on Fetal Alcohol Syndrome. Go to www.nofas.org, click on Resources, then on National and State Resources Directory in the box on the left side of the page. There may be a waiting list for evaluation, but under Part C of the Individuals with Disabilities Education Act (IDEA), FAS is considered a “presumptive eligibility” diagnosis. Presumptive diagnoses allow children under age 3 at risk of later developmental delay to be served without meeting particular eligibility criteria.1 Physicians may refer these children for developmental assessment services and early intervention services while waiting for the more complete FAS evaluation.
After the age of 3, children and families are referred to preschool programs for children with disabilities that are administered through IDEA Part B, with no “presumptive eligibility” diagnoses. Eligibility for educational services under this program is entirely based on functional criteria.
Your best bet: Prevention
The key to preventing FAS is to find out whether your patient’s drinking patterns and contraceptive habits put her at risk for an alcohol-exposed pregnancy. Make it routine practice to ask women, in a way that encourages honest reporting, about both of these aspects of their lives. The US Preventive Services Task Force recommends screening and counseling intervention in primary care settings to reduce alcohol misuse in adults, including pregnant women.17 The case on page 341 (Clarice) illustrates how screening and brief intervention can be used to prevent alcohol-exposed pregnancy.
TANYA
Possible, though unconfirmed, FAS
This 1-month-old African American girl was admitted to the hospital with stridor, possible cardiorespiratory issues, and failure to thrive. She exhibited microcephaly, poor suck, floppy overall muscle tone, and small palpebral fissure lengths. The respiratory noise was attributed to tracheomalacia, secondary to her poor muscle tone.
An initial magnetic resonance imaging of the brain showed an almost complete absence of the corpus callosum. Obviously at risk for future delays, Tanya was referred for early childhood development intervention. By the age of 5½, she was within her peer group’s normal range in fine motor, gross motor, and speech skills. She was removed from her mother’s care for neglect and later placed in an extended family adoption.
Her initial evaluation took place before the widespread publication of fetal alcohol syndrome (FAS) criteria, and she was not referred for more specific FAS evaluation, as she would have been had she been seen more recently. Tanya has been lost to long-term follow-up from her initial medical home, but her mother returned to the same practice for a subsequent pregnancy and was screened as a problem drinker.
BRIANNA
Facing severe secondary disabilities
This 16-year-old Caucasian girl entered foster care for the second time because her first placement could not deal with her complex behavioral issues. Her mother committed suicide last year, and her father is in an alcohol rehabilitation program. No pregnancy history is available.
The social service agency supervising Brianna’s care decided not to return her to her father’s home. She made a suicidal gesture, her behavior is sometimes violent, and she has been diagnosed with attention deficit hyperactivity disorder (ADHD). She is being treated for depression, requiring multiple medications.
Brianna’s life has been difficult. Before she was 2 years old, she underwent surgery for a ventricular septal defect. Although her cardiac repair was successful, she remains significantly underweight, <3rd percentile on the growth curve. Because she is an adolescent, her facial features are less distinctive for FAS, but she appears to have a smooth philtrum and thin vermillion. Her learning disabilities are significant enough that she has been held back a grade and requires an individualized education plan.
It may be too late to help provide any assistance to Brianna, who is already experiencing severe secondary disabilities. But if a diagnosis of FAS (or alcohol-related neurobehavioral disorder) can be made, even at this point in her life, provisions may be made within the foster care system for transitional housing and emphasis on life skills training, rather than simply allowing her to “age out” of the system when she turns 18.
CLARICE
Preventing an alcohol-exposed pregnancy
Clarice is an 18-year-old, college-bound woman who came in for a pre-college health maintenance examination. She reported being sexually active and was using effective contraception only intermittently. On the TWEAK questionnaire, she said the most she has had to drink on a single occasion was 6 drinks, noted that she had never passed out and had not had any problems associated with drinking. The only worry she connected with drinking was a fear of gaining weight.
Clarice met the criteria for “at risk” drinking (TABLE 3). She was a candidate for a brief intervention, including information on the hazards of alcohol-exposed pregnancy and on effective contraceptive practices. We scheduled a telephone follow-up and checkup in 6 months.
* Drawn from the author’s case files. Names have been changed to protect patient privacy.
Screening should include simple quantity and frequency questions developed by the National Institute on Alcohol Abuse to clarify a patient’s current drinking patterns. The questions include the numbers of days per week of any drinking, the average number of drinks per day, and the maximum number of drinks consumed in 1 day during the past month. Determining that a woman drinks more than 7 drinks per week has a 29% sensitivity, but a 90% specificity for identifying lifetime risk of alcohol abuse or dependence.18
Other tools include TWEAK (Tolerance, Worry, Eye-opener, Amnesia, (K)Cut down), T-ACE (Tolerance, Annoyed, Cut down, Eye opener), and AUDIT (Alcohol Use Disorder Identification Test). They are detailed below and available online at Project Cork. Go to www.projectcork.org, and click on “clinical tools.”
The 5-item TWEAK tool (TABLE 2) appears to be the optimal screening questionnaire for identifying women in racially mixed populations with heavy drinking or alcohol abuse and dependence, but a score of 2 points should be the threshold for identifying female problem drinkers.19,20 Using the lower cutoff of 2, the sensitivity of TWEAK is in the 87% to 91% range for women, with a specificity of 77% to 90%.18
The T-ACE tool is a set of 4 questions, with the question addressing tolerance weighted more heavily than the others. With a score of 2 or more, the sensitivity of T-ACE is 70% to 88%; the specificity is 79% to 85%.18
The AUDIT tool is a self-administered screen that consists of a series of 10 questions that are each scored on a scale of 0 to 4. The maximum score is 40. A score of 2 indicates some harmful use of alcohol, but a score of 8 or more has a sensitivity of 59% to 66%, with a specificity of 93% to 97% in women.18
TABLE 2
TWEAK your patients for alcohol use
| Tolerance: How many drinks does it take for you to: | Score |
| 2 points for ≥3 drinks 2 points for ≥5 drinks |
| Worry about drinking | |
| Have your friends or relatives worried about your drinking in the past year? | 1 point for Yes |
| Eye-opener | |
| Do you sometimes take a drink in the morning when you first get up? | 1 point for Yes |
| Amnesia | |
| Are there times when you drink and afterwards can’t remember what you said or did? | 1 point for Yes |
| (K)Cut down | |
| Do you sometimes feel the need to cut down on your drinking? | 1 point for Yes |
| Scoring: ≥3 points is considered positive for alcoholism/heavy drinking. Thresholds differ for screening different populations, and a score of ≥2 points should be used as the threshold for identifying female problem drinkers. | |
| Source: Chan AW, et al. Alcohol Clin Exp Res. 1993.19 | |
When your patient is at risk
Brief interventions are recommended for nonpregnant and pregnant women who have exhibited a pattern of at-risk or problem drinking.21TABLE 3 summarizes patterns of drinking in women, from not drinking at all through various degrees of risk to alcohol dependency. Referral to an addiction specialist is recommended for women with alcohol dependence.
Brief interventions for alcohol abuse can be single-session encounters from 5 to 15 minutes’ duration, or multi-contact brief sessions, including possible phone follow-up contacts. Project TrEAT (Trial for Early Alcohol Treatment) provided two 15-minute sessions with the primary care physician (either a family physician or internist in community-based practice) scheduled 1 month apart, with nurse follow-up phone calls 2 weeks after each appointment.22
TABLE 3
Drinking patterns in women
Abstainer
|
Low-risk drinking
|
At-risk drinking
|
Problem drinking
|
Alcohol-dependent drinking: Maladaptive patterns of alcohol use leading to clinically significant impairment manifested by 3 or more of the following, occurring at any time during the same 12-month period:
|
| Source: Training program for medical students and other health professionals on fetal alcohol syndrome. Presented by the Midwest Regional Fetal Alcohol Syndrome Training Center; March 18, 2005; St. Louis, Mo. |
Patients received general information regarding adverse effects of alcohol and the prevalence of problem drinking, in addition to tools to help them identify drinking triggers and track their consumption. The patient and physician developed a “drinking agreement” in the form of a rescription. Men and non pregnant women were included in this study.
Women reduced their alcohol use by 47% and their frequency of binge drinking by 56%, as noted at a 6-month follow-up, with changes well maintained at 12 months. The reductions for female patients were actually slightly higher than for male participants.22
Chang and colleagues provided a 25-minute single session brief intervention to pregnant women who had screened positive on the T-ACE questionnaire with a score of 2 or more, and were identified as being at risk for prenatal alcohol use.23 Participants were randomly assigned to the intervention group or a control group. Both the control group and the brief intervention group decreased their use of alcohol after enrolling in the study and undergoing the initial detailed assessment.
For women who were heavier drinkers, the brief interventions for prenatal alcohol use were statistically more effective in reducing their frequency of alcohol consumption, vs the initial assessment alone. In addition, the effects of the brief intervention were significantly enhanced when a support partner of the woman’s choice also participated.23
The Project Choices Intervention Research Group studied an intervention that included 4 sessions of motivational interviewing regarding alcohol habits, and a contraception counseling session.24 Study participants were recruited from 6 community-based settings with high proportions of women at risk for an alcohol-exposed pregnancy, including a jail and 2 drug and alcohol treatment centers. Among the 143 women who completed the 6-month follow-up, 68.5% were no longer at risk of having an alcohol-exposed pregnancy.
These participants successfully lowered their risk by reducing alcohol use only (12.9%), adopting appropriate contraception use only (23.1%), or by changing both risk factors (32.9%). Even if all the study participants who were lost to follow-up were assumed to have been unsuccessful at eliminating their risk of alcohol-exposed pregnancy, more than half of the women (51.6%) successfully changed.24
Take advantage of opportunities
FAS is the most severe consequence of alcohol-exposed pregnancy, leaving the affected child with a lifelong disability. As a family physician, you have access to easy-touse, cost-effective clinical tools to screen for at-risk drinking behaviors and have sufficient rapport with your patients to encourage effective contraceptive practices. You also have effective tools for helping patients reduce their alcohol consumption.
Within the context of your long-term relationships with patients, you can provide brief interventions that include factual information and opportunities for goal setting. You can assist families with an FAS child to access services, manage medically related complications, and plan for special education and vocational skills training.
Recognition that 1 child in a family is affected by prenatal alcohol exposure gives you another window of opportunity to address the underlying substance use issues in the mother and the family, increasing the odds that future pregnancies will not be alcohol exposed.
CORRESPONDENCE Mary C. Boyce, MD, Wesley Family Medicine Residency, 850 N. Hillside, Wichita, KS 67214; [email protected]
Screen all females of childbearing age for alcohol use with standardized screening instruments such as TWEAK, T-ACE, or AUDIT. A
Use brief, in-office interventions to decrease alcohol consumption and increase effective contraception in sexually active women. Involve a supportive adult of the patient’s choosing where possible. A
Advise pregnant patients that complete abstinence from alcohol is safest. B
Refer a child who meets FAS referral criteria for multi-disciplinary evaluations as early as possible. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Family physicians who care for infants and young children are often asked to diagnose growth lags and failure to meet parents’ expectations for reaching developmental milestones: Why isn’t my child gaining weight? Why isn’t he talking? The other kids in the day-care center ride tricycles—why can’t he? Will he catch up? My mother thinks he’s funny looking. Do you?
Simple reassurance is all that most of these worried families need. But for families with children whose growth or developmental milestones are sufficiently outside the usual parameters, more than reassurance is called for. As you consider whether the lags that worry parents are signs of a serious disability, it’s important to make a place for fetal alcohol syndrome (FAS) in your differential.
FAS, a congenital disorder caused by alcohol exposure during pregnancy, is characterized by growth deficiency before and after birth, distinctive facial features, and central nervous system (CNS) dysfunctions. The cognitive and developmental effects of FAS persist throughout life and are severe enough to limit employment and independent living.1,2
A spectrum of severity. FAS is the most severe expression of prenatal alcohol exposure. The term fetal alcohol spectrum disorders (FASD) is a nondiagnostic umbrella term that includes FAS as well as ARND (alcohol-related neurobehavioral disorder) and ARBD (alcohol-related birth defects). Children with ARND and ARBD fail to meet the full FAS diagnostic criteria but still exhibit the negative effects of gestational alcohol exposure. Centers for Disease Control and Prevention (CDC) diagnostic criteria for FAS are summarized in TABLE 1. Studies by the CDC have reported FAS prevalence rates from 0.2 to 1.5 cases per 1000 live births, with a higher prevalence among minority (Native American and African American) and impoverished groups.1
An opportunity—and a challenge. As a family physician, you have a unique opportunity to modify the impact of FAS by recognizing the disorder in infancy or early childhood, actively engineering appropriate referrals, and supporting families in the difficult task of parenting a child with disabilities. Correctly diagnosing a child with FAS before age 6 can have a protective influence, decreasing the odds that he or she will suffer severe secondary disabilities in adolescence and adulthood. You can also help prevent FAS by screening for potentially harmful drinking patterns and helping sexually active female patients decrease alcohol consumption and use contraception successfully.
Providing these supportive and preventive services can be challenging. A recent survey of pediatricians revealed that only 34% felt prepared to manage and coordinate the treatment of children with FASD, and only 13% routinely counseled adolescent patients about the risks of drinking and pregnancy.3 Th is article will help you surmount the difficulties these tasks present and perform vital functions for alcohol-affected families you may encounter in your practice.
TABLE 1
Diagnostic criteria for fetal alcohol syndrome
Facial dysmorphia
| ≤10th percentile for age and racial norms Score of 4 or 5 on lip-philtrum guide* Score of 4 or 5 on lip-philtrum guide* |
| Growth problems | <10th percentile for age, sex, gestational age, racial norms in height or weight, prenatally or postnatally |
| CNS abnormalities | Any structural abnormality (head circumference <10% of age norm or clinically significant brain abnormalities observable through imaging); neurological abnormality not due to postnatal insult or fever; or functional abnormality demonstrated by cognitive performance less than expected for age, schooling, or family circumstances. An individual could meet the CNS abnormality criteria for a FAS diagnosis through a structural abnormality, yet not demonstrate detectable functional deficits. |
| CNS, central nervous system. | |
| *The lip-philtrum guide is available at http://depts.washington.edu/fasdpn/htmls/lip-philtrum-guides.htm. | |
| Source: Centers for Disease Control and Prevention. Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis. 2005. Available at www.cdc.gov/ncbddd/fasd/documents/FAS_guidelines_accessible.pdf. Accessed April 10, 2010. | |
The place to start: Spotting mothers at risk
Recognizing an infant with FAS starts by asking the baby’s mother about her pattern of drinking while she was pregnant. Most studies on the effects of gestational exposure to alcohol have emphasized moderate to high levels of exposure. In 1 study, children who were exposed to binge drinking were 1.7 times as likely to have IQ scores in the mentally retarded range and 2.5 times more likely to have clinically significant levels of delinquent behavior.4 Binge drinking is defined by the National Institute of Alcohol Abuse and Alcoholism as a pattern of drinking that brings blood alcohol concentration to 0.8% or above, which typically happens in women who consume 4 or more drinks in a period of about 2 hours.5
But a pregnant woman doesn’t have to be a binge drinker to put her fetus at risk. Even low levels of prenatal alcohol use—as low as 1 drink per week—have been associated with adverse behavioral changes in children, including increased aggressive behaviors documented at school age.6,7 The research documenting effects at these low levels has led the American Academy of Pediatrics (AAP) and the American Congress of Obstetricians and Gynecologists (ACOG) to recommend total abstinence from alcohol throughout pregnancy.8,9 Patterns of “at risk” drinking for women include binge drinking or persistent regular use (>7 drinks in 1 week). If a mother provides a history of that level of prenatal exposure, her child should be referred for multidisciplinary evaluation at an FAS center, even in the absence of the characteristic facial features.1
The face of FAS
Without a history of prenatal alcohol exposure, the cardinal features of facial dysmorphia (short palpebral fissures, smooth philtrum, and thin vermillion border) plus deficits in height and weight are the main physical findings of FAS. Evaluating height and weight percentiles is a routine part of well-child care, requiring minimal training. Height or weight or both at or below the 10th percentile, adjusted for age, sex, gestational age, and race or ethnicity, meet part of the CDC diagnostic criteria for FAS, but must be accompanied by at least 1 of the typical facial features associated with FAS to meet referral guidelines.1 The diagnostic guidelines are more restrictive, requiring all 3 facial features to meet the threshold for an FAS diagnosis, vs another diagnosis, such as alcohol-related neurodevelopmental disorders (TABLE 1).
Learning to measure faces. Examining a child for the facial characteristics of FAS requires a set of skills that can be learned in a relatively short time, with moderate interrater reliability when compared with dysmorphologists, according to 1 study.10
Tools for measuring. Palpebral fissure length (PFL) can be measured with a clear plastic ruler pressed onto the child’s cheek to determine the distance from the endocanthion to the exocanthion while the child is gazing upward.11 To meet the CDC criteria for FAS, this distance should be at or below the 10th percentile compared to norms. The shape of the lips and the nature of the philtrum are then compared to preestablished comparison photographs available on the University of Washington Lip-Philtrum Guides (see URL that follows).12 The vermillion border and the philtrum must both receive a rank of 4 or 5 to meet FAS criteria.11
Changes in the clinical presentation of fetal alcohol syndrome (FAS) occur across the lifespan. Clinicians searching for an explanation of an older child’s difficulties may need to reconsider a possible diagnosis of FAS, even if the facial features are less recognizable.
Preschool children with FAS may display a delay in early language acquisition and the beginnings of attention problems and hyperactivity. School-age children may have difficulty remembering material even when they have gone over it many times. They may lack social perception skills, be hyperactive, and show cognitive delays. Mathematics is often an area of severe delay, and sleep problems can persist.1
Teens and adults with FAS often have a wide range of secondary disabilities: disrupted schooling, inappropriate sexual behavior, mental health problems, aggression, trouble with the law, confinement in jail or as inpatients in psychiatric or substance abuse treatment facilities, alcohol and drug problems, and failure or inability to live independently at an appropriate age. They may have trouble finding a job and keeping one. More than 90% of patients with FAS exhibit mental health problems, with attention problems appearing in early childhood and persisting, and depression appearing in adolescence and adulthod.15
Tools available online for physicians include Lip-Philtrum Guides (www.depts.washington.edu/fasdpn/htmls/lip-philtrum-guides.htm) and an instructional video depicting PFL measurement techniques (www.depts.washington.edu/fasdpn/htmls/photo-face.htm), both from the University of Washington FAS Diagnostic and Prevention Network. In addition, a physical evaluation summary form, with reference data for PFL in Caucasian, black, and Hispanic children, is available at http://www.fas.academicedge.com/documents/phyevaln.pdf.
The Astley-Clarren criteria. The 4-digit diagnostic code developed by Astley and Clarren for diagnosis of FAS and employed at some FAS referral centers uses very strict criteria.13 Centers using these criteria define “abnormal” as ≥2 standard deviations below the mean or its equivalent, ≤2.5th percentile.13 Th is applies to the 3 facial features and CNS dysfunction (low IQ, eg). If all 3 facial features are identified in the Astley-Clarren system as abnormal (PFL ≤2.5th percentile, lip philtrum 5, vermillion 5), the sensitivity of the facial features is 100% and specificity is 99.8% for a diagnosis of FAS.13
The CDC criteria, developed with increased surveillance by providers as a goal, uses relaxed criteria of ≤10th percentile of PFL and 4 or 5 on the philtrum/vermillion border guide to identify abnormal facial features and <10th percentile in CNS dysfunctions. Sensitivity and specificity data for those CDC criteria are not available.1
CNS abnormalities may be noted early enough to trigger a referral for complete evaluation, but must be present in some degree to confirm a diagnosis of FAS. Abnormalities may include microcephaly with head circumference below the 10th percentile; clinically significant brain abnormalities observable through imaging, especially a small or absent corpus callosum; and functional deficits in any of a multitude of domains. In an infant, these deficits may be expressed in global developmental delays, sleep cycle problems, poor muscle tone, and feeding problems with poor suck and texture aversion.1
Evaluation may not confirm the diagnosis. Children referred for more extensive evaluation may or may not be confirmed to have FAS. In 2 demographically similar counties in New York state, only 5% of children initially identified in 1 county (10 of 208) and 13% (53 of 420) of children in the other county were confirmed to have FAS.12 The FAS diagnosis is complicated and the CNS and growth deficiencies may not be expressed until a later age.14 (See “Fetal alcohol syndrome across the lifespan”1,15)
Providers may feel reluctant to alarm or stigmatize families when they are unsure of the diagnosis, but the long-term benefit of confirming the diagnosis early on may be significant for the child and family. The case on page 341 (Tanya) illustrates the complexity of diagnosing FASD.
The encouraging news for family physicians is that the odds of escaping adverse life outcomes are increased 2- to 4-fold by receiving a diagnosis of FAS before age 6 and by being raised in a stable environment.16 Early diagnosis can be protective by helping with eligibility requirements for support services and by opening the door to medical management of FAS-associated conditions such as ADHD and depression. In addition, the diagnosis can alert family physicians to the family’s need for help with ongoing problems with alcohol use. The case on page 341 (Brianna) illustrates the complex secondary problems a teen with FAS may face.
Putting families in touch with resources
Multidisciplinary FAS teams may include physicians (a geneticist or developmental pediatrician), psychologists, speech pathologists, educational specialists, social workers, and occupational therapists. These groups typically have in-depth intake and evaluation processes, including neurodiagnostic studies that help clarify the cognitive and functional domains that are affected.
You can locate the nearest FAS evaluation team and other resources for providers and families on the National and State Resource Directory for the National Organization on Fetal Alcohol Syndrome. Go to www.nofas.org, click on Resources, then on National and State Resources Directory in the box on the left side of the page. There may be a waiting list for evaluation, but under Part C of the Individuals with Disabilities Education Act (IDEA), FAS is considered a “presumptive eligibility” diagnosis. Presumptive diagnoses allow children under age 3 at risk of later developmental delay to be served without meeting particular eligibility criteria.1 Physicians may refer these children for developmental assessment services and early intervention services while waiting for the more complete FAS evaluation.
After the age of 3, children and families are referred to preschool programs for children with disabilities that are administered through IDEA Part B, with no “presumptive eligibility” diagnoses. Eligibility for educational services under this program is entirely based on functional criteria.
Your best bet: Prevention
The key to preventing FAS is to find out whether your patient’s drinking patterns and contraceptive habits put her at risk for an alcohol-exposed pregnancy. Make it routine practice to ask women, in a way that encourages honest reporting, about both of these aspects of their lives. The US Preventive Services Task Force recommends screening and counseling intervention in primary care settings to reduce alcohol misuse in adults, including pregnant women.17 The case on page 341 (Clarice) illustrates how screening and brief intervention can be used to prevent alcohol-exposed pregnancy.
TANYA
Possible, though unconfirmed, FAS
This 1-month-old African American girl was admitted to the hospital with stridor, possible cardiorespiratory issues, and failure to thrive. She exhibited microcephaly, poor suck, floppy overall muscle tone, and small palpebral fissure lengths. The respiratory noise was attributed to tracheomalacia, secondary to her poor muscle tone.
An initial magnetic resonance imaging of the brain showed an almost complete absence of the corpus callosum. Obviously at risk for future delays, Tanya was referred for early childhood development intervention. By the age of 5½, she was within her peer group’s normal range in fine motor, gross motor, and speech skills. She was removed from her mother’s care for neglect and later placed in an extended family adoption.
Her initial evaluation took place before the widespread publication of fetal alcohol syndrome (FAS) criteria, and she was not referred for more specific FAS evaluation, as she would have been had she been seen more recently. Tanya has been lost to long-term follow-up from her initial medical home, but her mother returned to the same practice for a subsequent pregnancy and was screened as a problem drinker.
BRIANNA
Facing severe secondary disabilities
This 16-year-old Caucasian girl entered foster care for the second time because her first placement could not deal with her complex behavioral issues. Her mother committed suicide last year, and her father is in an alcohol rehabilitation program. No pregnancy history is available.
The social service agency supervising Brianna’s care decided not to return her to her father’s home. She made a suicidal gesture, her behavior is sometimes violent, and she has been diagnosed with attention deficit hyperactivity disorder (ADHD). She is being treated for depression, requiring multiple medications.
Brianna’s life has been difficult. Before she was 2 years old, she underwent surgery for a ventricular septal defect. Although her cardiac repair was successful, she remains significantly underweight, <3rd percentile on the growth curve. Because she is an adolescent, her facial features are less distinctive for FAS, but she appears to have a smooth philtrum and thin vermillion. Her learning disabilities are significant enough that she has been held back a grade and requires an individualized education plan.
It may be too late to help provide any assistance to Brianna, who is already experiencing severe secondary disabilities. But if a diagnosis of FAS (or alcohol-related neurobehavioral disorder) can be made, even at this point in her life, provisions may be made within the foster care system for transitional housing and emphasis on life skills training, rather than simply allowing her to “age out” of the system when she turns 18.
CLARICE
Preventing an alcohol-exposed pregnancy
Clarice is an 18-year-old, college-bound woman who came in for a pre-college health maintenance examination. She reported being sexually active and was using effective contraception only intermittently. On the TWEAK questionnaire, she said the most she has had to drink on a single occasion was 6 drinks, noted that she had never passed out and had not had any problems associated with drinking. The only worry she connected with drinking was a fear of gaining weight.
Clarice met the criteria for “at risk” drinking (TABLE 3). She was a candidate for a brief intervention, including information on the hazards of alcohol-exposed pregnancy and on effective contraceptive practices. We scheduled a telephone follow-up and checkup in 6 months.
* Drawn from the author’s case files. Names have been changed to protect patient privacy.
Screening should include simple quantity and frequency questions developed by the National Institute on Alcohol Abuse to clarify a patient’s current drinking patterns. The questions include the numbers of days per week of any drinking, the average number of drinks per day, and the maximum number of drinks consumed in 1 day during the past month. Determining that a woman drinks more than 7 drinks per week has a 29% sensitivity, but a 90% specificity for identifying lifetime risk of alcohol abuse or dependence.18
Other tools include TWEAK (Tolerance, Worry, Eye-opener, Amnesia, (K)Cut down), T-ACE (Tolerance, Annoyed, Cut down, Eye opener), and AUDIT (Alcohol Use Disorder Identification Test). They are detailed below and available online at Project Cork. Go to www.projectcork.org, and click on “clinical tools.”
The 5-item TWEAK tool (TABLE 2) appears to be the optimal screening questionnaire for identifying women in racially mixed populations with heavy drinking or alcohol abuse and dependence, but a score of 2 points should be the threshold for identifying female problem drinkers.19,20 Using the lower cutoff of 2, the sensitivity of TWEAK is in the 87% to 91% range for women, with a specificity of 77% to 90%.18
The T-ACE tool is a set of 4 questions, with the question addressing tolerance weighted more heavily than the others. With a score of 2 or more, the sensitivity of T-ACE is 70% to 88%; the specificity is 79% to 85%.18
The AUDIT tool is a self-administered screen that consists of a series of 10 questions that are each scored on a scale of 0 to 4. The maximum score is 40. A score of 2 indicates some harmful use of alcohol, but a score of 8 or more has a sensitivity of 59% to 66%, with a specificity of 93% to 97% in women.18
TABLE 2
TWEAK your patients for alcohol use
| Tolerance: How many drinks does it take for you to: | Score |
| 2 points for ≥3 drinks 2 points for ≥5 drinks |
| Worry about drinking | |
| Have your friends or relatives worried about your drinking in the past year? | 1 point for Yes |
| Eye-opener | |
| Do you sometimes take a drink in the morning when you first get up? | 1 point for Yes |
| Amnesia | |
| Are there times when you drink and afterwards can’t remember what you said or did? | 1 point for Yes |
| (K)Cut down | |
| Do you sometimes feel the need to cut down on your drinking? | 1 point for Yes |
| Scoring: ≥3 points is considered positive for alcoholism/heavy drinking. Thresholds differ for screening different populations, and a score of ≥2 points should be used as the threshold for identifying female problem drinkers. | |
| Source: Chan AW, et al. Alcohol Clin Exp Res. 1993.19 | |
When your patient is at risk
Brief interventions are recommended for nonpregnant and pregnant women who have exhibited a pattern of at-risk or problem drinking.21TABLE 3 summarizes patterns of drinking in women, from not drinking at all through various degrees of risk to alcohol dependency. Referral to an addiction specialist is recommended for women with alcohol dependence.
Brief interventions for alcohol abuse can be single-session encounters from 5 to 15 minutes’ duration, or multi-contact brief sessions, including possible phone follow-up contacts. Project TrEAT (Trial for Early Alcohol Treatment) provided two 15-minute sessions with the primary care physician (either a family physician or internist in community-based practice) scheduled 1 month apart, with nurse follow-up phone calls 2 weeks after each appointment.22
TABLE 3
Drinking patterns in women
Abstainer
|
Low-risk drinking
|
At-risk drinking
|
Problem drinking
|
Alcohol-dependent drinking: Maladaptive patterns of alcohol use leading to clinically significant impairment manifested by 3 or more of the following, occurring at any time during the same 12-month period:
|
| Source: Training program for medical students and other health professionals on fetal alcohol syndrome. Presented by the Midwest Regional Fetal Alcohol Syndrome Training Center; March 18, 2005; St. Louis, Mo. |
Patients received general information regarding adverse effects of alcohol and the prevalence of problem drinking, in addition to tools to help them identify drinking triggers and track their consumption. The patient and physician developed a “drinking agreement” in the form of a rescription. Men and non pregnant women were included in this study.
Women reduced their alcohol use by 47% and their frequency of binge drinking by 56%, as noted at a 6-month follow-up, with changes well maintained at 12 months. The reductions for female patients were actually slightly higher than for male participants.22
Chang and colleagues provided a 25-minute single session brief intervention to pregnant women who had screened positive on the T-ACE questionnaire with a score of 2 or more, and were identified as being at risk for prenatal alcohol use.23 Participants were randomly assigned to the intervention group or a control group. Both the control group and the brief intervention group decreased their use of alcohol after enrolling in the study and undergoing the initial detailed assessment.
For women who were heavier drinkers, the brief interventions for prenatal alcohol use were statistically more effective in reducing their frequency of alcohol consumption, vs the initial assessment alone. In addition, the effects of the brief intervention were significantly enhanced when a support partner of the woman’s choice also participated.23
The Project Choices Intervention Research Group studied an intervention that included 4 sessions of motivational interviewing regarding alcohol habits, and a contraception counseling session.24 Study participants were recruited from 6 community-based settings with high proportions of women at risk for an alcohol-exposed pregnancy, including a jail and 2 drug and alcohol treatment centers. Among the 143 women who completed the 6-month follow-up, 68.5% were no longer at risk of having an alcohol-exposed pregnancy.
These participants successfully lowered their risk by reducing alcohol use only (12.9%), adopting appropriate contraception use only (23.1%), or by changing both risk factors (32.9%). Even if all the study participants who were lost to follow-up were assumed to have been unsuccessful at eliminating their risk of alcohol-exposed pregnancy, more than half of the women (51.6%) successfully changed.24
Take advantage of opportunities
FAS is the most severe consequence of alcohol-exposed pregnancy, leaving the affected child with a lifelong disability. As a family physician, you have access to easy-touse, cost-effective clinical tools to screen for at-risk drinking behaviors and have sufficient rapport with your patients to encourage effective contraceptive practices. You also have effective tools for helping patients reduce their alcohol consumption.
Within the context of your long-term relationships with patients, you can provide brief interventions that include factual information and opportunities for goal setting. You can assist families with an FAS child to access services, manage medically related complications, and plan for special education and vocational skills training.
Recognition that 1 child in a family is affected by prenatal alcohol exposure gives you another window of opportunity to address the underlying substance use issues in the mother and the family, increasing the odds that future pregnancies will not be alcohol exposed.
CORRESPONDENCE Mary C. Boyce, MD, Wesley Family Medicine Residency, 850 N. Hillside, Wichita, KS 67214; [email protected]
1. Centers for Disease Control and Prevention. Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis. 2005. Available at: www.cdc.gov/ncbddd/fasd/documents/FAS_guidelines_accessible.pdf. Accessed April 10, 2010.
2. Spohr HL, Williams J, Steinhausen HC. Fetal alcohol spectrum disorders in young adulthood. J Pediatr. 2007;150:175-179.
3. Gahagan S, Sharpe TT, Brimacombe M, et al. Pediatricians’ knowledge, training, and experience in the care of children with fetal alcohol syndrome. Pediatrics. 2006;118:e657-e668.
4. Bailey BN, Delaney-Black V, Covington CY, et al. Prenatal exposure to binge drinking and cognitive and behavioral outcomes at age 7 years. Am J Obstet Gynecol. 2004;191:1037-1043.
5. CDC. Alcohol and public health/binge drinking. Quick stats. Available at: www.cdc.gov/alcohol/quickstats/binge_drinking.htm. Accessed April 21, 2010.
6. Sood B, Delaney-Black V, Covington C, et al. Prenatal alcohol exposure and childhood behavior at age 6 to 7 years: I. Doseresponse effect. Pediatrics. 2001;108:E34.-
7. Sokol RJ, Delaney-Black V, Nordstrom B. Fetal alcohol spectrum disorder. JAMA. 2003;290:2996-2999.
8. American Congress of Obstetricians and Gynecologists. ACOG Education Pamphlet AP170: Tobacco, alcohol, drugs, and pregnancy. Available at www.acog.org/publications/patient_education/bp170.cfm. Accessed May 3, 2010.
9. Committee on Substance Abuse and Committee on Children With Disabilities. Fetal alcohol syndrome and alcohol-related neurodevelopmental disorders. Pediatrics. 2000;106:358-361.
10. Jones KL, Robinson LK, Bakhireva LN, et al. Accuracy of the diagnosis of physical features of fetal alcohol syndrome by pediatricians after specialized training. Pediatrics. 2006;118:e1734-e1738.
11. University of Washington Fetal Alcohol Syndrome Diagnostic and Prevention Network. FAS facial photography and measurement instruction. Available at: www.depts.washington.edu/fasdpn/htmls/photo-face.htm. Accessed April 21,2010.
12. University of Washington Fetal Alcohol Syndrome Diagnostic and Prevention Network. Lip philtrum guides. Available at: www.depts.washington.edu/fasdpn/htmls/lip-philtrum-guides.htm. Accessed April 21, 2010.
13. Astley S. Comparison of the 4-digit diagnostic code and the Hoyme diagnostic guidelines for fetal alcohol spectrum disorder. Pediatrics. 2006;188:1532-1545.
14. Druschel CM, Fox DJ. Issues in estimating the prevalence of fetal alcohol syndrome: examination of 2 counties in New York State. Pediatrics. 2007;119:e384-e390.
15. Streissguth AP, Barr HM, Kogan J, et al. Understanding the occurrence of secondary disabilities in clients with fetal alcohol syndrome (FAS) and fetal alcohol effects (FAE). Final Report to the Centers for Disease Control and Prevention. Technical report no. 96-06. Seattle, WA: University of Washington, Fetal Alcohol and Drug Unit; 1996.
16. Streissguth AP, Bookstein FL, Barr H, et al. Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. J Dev Behav Pediatr. 2004;25:228-238.
17. US Preventive Services Task Force. Screening and behavioral interventions in primary care to reduce alcohol misuse: recommendation statement, April 2004. Available at: www.ahrq.gov/clinic/3rduspstf/alcohol/alcomisrs.htm. Accessed April 10, 2010.
18. Bradley KA, Boyd-Wickizer J, Powell SH, et al. Alcohol screening questionnaires in women: a critical review. JAMA. 1998;20:166-171.
19. Chan AW, Pristach EA, Welte JW, et al. Use of the TWEAK test in screening for alcoholism/heavy drinking in three populations. Alcohol Clin Exp Res. 1993;17:1188-1192.
20. Russell M, Bigler L. Screening for alcohol-related problems in an outpatient obstetric-gynecologic clinic. Am J Obstet Gynecol. 1979;134:4-12.
21. National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: a clinician’s guide. Updated January 2007. Available at: http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/clinicians_guide.htm. Accessed April 21, 2010.
22. Fleming MF, Barry KL, Manwell LB, et al. Brief physician advice for problem alcohol drinkers. JAMA. 1997;277:1039-1045.
23. Chang G, McNamara TK, Orav J, et al. Brief interventions for prenatal alcohol use: a randomized trial. Obstet Gynecol. 2005;105:991-998.
24. The Project Choices Intervention Research Group. Reducing the risk of alcohol-exposed pregnancies: a study of motivational intervention in community settings. Pediatrics. 2003;111:1131-1135.
1. Centers for Disease Control and Prevention. Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis. 2005. Available at: www.cdc.gov/ncbddd/fasd/documents/FAS_guidelines_accessible.pdf. Accessed April 10, 2010.
2. Spohr HL, Williams J, Steinhausen HC. Fetal alcohol spectrum disorders in young adulthood. J Pediatr. 2007;150:175-179.
3. Gahagan S, Sharpe TT, Brimacombe M, et al. Pediatricians’ knowledge, training, and experience in the care of children with fetal alcohol syndrome. Pediatrics. 2006;118:e657-e668.
4. Bailey BN, Delaney-Black V, Covington CY, et al. Prenatal exposure to binge drinking and cognitive and behavioral outcomes at age 7 years. Am J Obstet Gynecol. 2004;191:1037-1043.
5. CDC. Alcohol and public health/binge drinking. Quick stats. Available at: www.cdc.gov/alcohol/quickstats/binge_drinking.htm. Accessed April 21, 2010.
6. Sood B, Delaney-Black V, Covington C, et al. Prenatal alcohol exposure and childhood behavior at age 6 to 7 years: I. Doseresponse effect. Pediatrics. 2001;108:E34.-
7. Sokol RJ, Delaney-Black V, Nordstrom B. Fetal alcohol spectrum disorder. JAMA. 2003;290:2996-2999.
8. American Congress of Obstetricians and Gynecologists. ACOG Education Pamphlet AP170: Tobacco, alcohol, drugs, and pregnancy. Available at www.acog.org/publications/patient_education/bp170.cfm. Accessed May 3, 2010.
9. Committee on Substance Abuse and Committee on Children With Disabilities. Fetal alcohol syndrome and alcohol-related neurodevelopmental disorders. Pediatrics. 2000;106:358-361.
10. Jones KL, Robinson LK, Bakhireva LN, et al. Accuracy of the diagnosis of physical features of fetal alcohol syndrome by pediatricians after specialized training. Pediatrics. 2006;118:e1734-e1738.
11. University of Washington Fetal Alcohol Syndrome Diagnostic and Prevention Network. FAS facial photography and measurement instruction. Available at: www.depts.washington.edu/fasdpn/htmls/photo-face.htm. Accessed April 21,2010.
12. University of Washington Fetal Alcohol Syndrome Diagnostic and Prevention Network. Lip philtrum guides. Available at: www.depts.washington.edu/fasdpn/htmls/lip-philtrum-guides.htm. Accessed April 21, 2010.
13. Astley S. Comparison of the 4-digit diagnostic code and the Hoyme diagnostic guidelines for fetal alcohol spectrum disorder. Pediatrics. 2006;188:1532-1545.
14. Druschel CM, Fox DJ. Issues in estimating the prevalence of fetal alcohol syndrome: examination of 2 counties in New York State. Pediatrics. 2007;119:e384-e390.
15. Streissguth AP, Barr HM, Kogan J, et al. Understanding the occurrence of secondary disabilities in clients with fetal alcohol syndrome (FAS) and fetal alcohol effects (FAE). Final Report to the Centers for Disease Control and Prevention. Technical report no. 96-06. Seattle, WA: University of Washington, Fetal Alcohol and Drug Unit; 1996.
16. Streissguth AP, Bookstein FL, Barr H, et al. Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. J Dev Behav Pediatr. 2004;25:228-238.
17. US Preventive Services Task Force. Screening and behavioral interventions in primary care to reduce alcohol misuse: recommendation statement, April 2004. Available at: www.ahrq.gov/clinic/3rduspstf/alcohol/alcomisrs.htm. Accessed April 10, 2010.
18. Bradley KA, Boyd-Wickizer J, Powell SH, et al. Alcohol screening questionnaires in women: a critical review. JAMA. 1998;20:166-171.
19. Chan AW, Pristach EA, Welte JW, et al. Use of the TWEAK test in screening for alcoholism/heavy drinking in three populations. Alcohol Clin Exp Res. 1993;17:1188-1192.
20. Russell M, Bigler L. Screening for alcohol-related problems in an outpatient obstetric-gynecologic clinic. Am J Obstet Gynecol. 1979;134:4-12.
21. National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: a clinician’s guide. Updated January 2007. Available at: http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/clinicians_guide.htm. Accessed April 21, 2010.
22. Fleming MF, Barry KL, Manwell LB, et al. Brief physician advice for problem alcohol drinkers. JAMA. 1997;277:1039-1045.
23. Chang G, McNamara TK, Orav J, et al. Brief interventions for prenatal alcohol use: a randomized trial. Obstet Gynecol. 2005;105:991-998.
24. The Project Choices Intervention Research Group. Reducing the risk of alcohol-exposed pregnancies: a study of motivational intervention in community settings. Pediatrics. 2003;111:1131-1135.
An algorithm for the treatment of chronic testicular pain
Order ultrasound of the scrotum and testes to evaluate chronic testicular pain, with color Doppler to identify areas of hypervascularity. C
Treat suspected epididymitis with empiric coverage for chlamydia with either a 10-day regimen of doxycycline (100 mg twice daily) or a single dose (1 g) of azithromycin; treat suspected gonorrhea with a single intramuscular injection (125 mg) of ceftriaxone. A
Do not treat small epididymal cysts that do not correlate with testicular pain; larger, painful cysts can be aspirated, injected with a sclerosing agent, or surgically excised. C
Consider surgical options only after medical and conservative therapies have failed to alleviate chronic testicular pain. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE 1 Vincent B, a 33-year-old executive, visits his family physician for an evaluation of chronic orchialgia. Although his testicular pain has waxed and waned for several years, it has recently worsened, making it increasingly difficult for him to exercise or to sit for extended periods of time. In fact, this visit was prompted by a lengthy meeting during which he developed a “dull ache” that did not let up until he left the meeting and walked around.
CASE 2 Jason H, a 42-year-old married father of 3 who had a vasectomy 2 years ago, has had progressively worsening testicular pain ever since. He also has occasional pain after ejaculation, but no known hematospermia. Recently, the pain has become so bad that it limits both his physical and sexual activities and is having a negative effect on his relationship with his wife. Jason is sexually monogamous, has no significant medical history, and takes no prescription medications.
These 2 cases are based on actual patients we have seen in our practices. If Vincent and Jason (not their real names) were your patients, how would you initiate a work-up for testicular pain? What treatments would you offer? And at what point would you consider a referral to a urologist?
Chronic orchialgia is a complex urogenital focal pain syndrome in which neurogenic inflammation is the principal mediator. This debilitating condition is associated with substantial anxiety and frustration, and is characterized by intermittent or constant unilateral or bilateral testicular pain, occurring for at least 3 months, that has a significant negative impact on activities of daily living and physical activity.1
A variety of procedural and surgical options may help to minimize or alleviate chronic orchialgia. But which approach is best? There are no evidence-based guidelines for the treatment of this condition, and no randomized controlled trials to demonstrate the superiority of 1 modality over another. All diagnostic and treatment recommendations are based on expert opinion derived from small cohort studies.
With that in mind, we conducted a systematic review of the literature evaluating medical and surgical therapies for chronic testicular pain—and developed an algorithm (FIGURE 1), along with the text and TABLE that follow, for family physicians (FPs) to use as a guide.
FIGURE 1
Chronic orchialgia: A diagnosis and treatment algorithm1,3,4,6,10
NSAID, nonsteroidal anti-inflammatory drug; STIs, sexually transmitted infections.
CASE 1 Vincent B
Over the last few years, Vincent has had similar episodes of bilateral testicular pain. He denies any history of direct trauma to the testicles, and he works out regularly by lifting weights and running. When the pain becomes unbearable, he takes acetaminophen or ibuprofen and takes a few days off from exercising, which provides modest—but temporary—relief.
Vincent reports that he has had about a dozen lifetime sexual partners and had chlamydia over a decade ago as a college student. He is currently engaged and sexually monogamous, and tested negative for Chlamydia trachomatis, Neisseria gonorrhoeae, hepatitis, syphilis, and human immunodeficiency virus (HIV) at his annual health maintenance examination last month. Shortly before that, Vincent was treated empirically for epididymitis with a 4-week course of ciprofloxacin, with no significant improvement in symptoms. He has no significant past medical history, denies depression, and takes no prescription medications.
Physical examination reveals mild to moderate diffuse tenderness to palpation throughout the scrotum, including both testicles and spermatic cords. There is no erythema of the scrotum. Nor are there any palpable scrotal masses, varicoceles, or hydroceles; testicular, scrotal, or penile lesions; inguinal masses; or lymph nodes. His urethral meatus is patent. The prostate is smooth, nonnodular, and non-tender. The remainder of the physical exam is unremarkable.
Determining a cause can be a challenge
There are numerous possible causes of testicular pain (TABLE), including an inguinal hernia, torsion of the testicle, trauma, and a history of chlamydia or gonorrhea, to name a few.
TABLE
Causes of acute and chronic orchialgia1,3,4
Acute
|
Chronic
|
Chronic testicular pain can also be psychogenic, often relating to a history of sexual abuse or relationship stress. One study examining comorbid psychological conditions in men with chronic orchialgia identified a somatization disorder in 56% of the patients, nongenital chronic pain syndromes in 50%, and major depression or chemical dependency in 27%.2 Overall, however, estimates suggest that in about 25% of patients with chronic orchialgia, no identifiable etiology is found. 1
Establish a baseline with a physical exam
Conduct a physical examination of the scrotum, testes, spermatic cords, penis, inguinal region, and prostate as a baseline measurement in a patient who presents with chronic orchialgia.3,4 An initial urinalysis should be performed to rule out infection or identify microscopic hematuria, which may prompt a more targeted work-up and therapeutic plan. Take a thorough medical and psychosocial/ sexual history, as well.
Order an ultrasound of the scrotum and testes, the accepted gold standard to highlight structural abnormalities of the testicles. The addition of color Doppler makes it possible to find areas of hypervascularity, an indication of inflammation in the testicle and epididymis (FIGURES 2A AND B).
FIGURE 2
Well-circumscribed extratesticular mass
In the image at left, ultrasound reveals an anechoic mass (arrows), representing either an epididymal cyst or spermatocele, superior to the testicle (T). A color Doppler image (right) reveals increased vascularity to the epididymis (E), as compared with the testicle.
Epididymal cysts are common findings on scrotal ultrasound; they are frequently incidental, but may relate to the patient’s pain, depending on the size of the cyst. Smaller cysts that do not correlate with pain do not require treatment. Larger, painful cysts can be treated with aspiration or injection with a sclerosing agent—or with surgical excision, which offers the highest potential cure rate.3,4 A computed tomography (CT) scan without contrast is the best way to find genitourinary system calculi, which could be the source of referred renal pain to the groin and scrotum. A contrast-enhanced CT is best to evaluate for solid renal masses.
Start with the most conservative treatment
In the absence of any findings that require surgical intervention, start conservatively.
Initiate a trial of nonsteroidal anti-inflammatory drugs (NSAIDs) for at least 1 month. Although this is the standard first-line treatment, NSAIDs have been shown to help only a small percentage of patients with chronic orchialgia, and only on a short-term basis.1,3,4
Recommend scrotal elevation with supportive undergarments to decrease venous congestion. Tell the patient, too, that modifying his seated posture to avoid scrotal pressure may alleviate pain and poses no discernible risk of worsening orchialgia.5
Treat suspected STIs. The Centers for Disease Control and Prevention report that in men 14 to 35 years of age, epididymitis is most commonly caused by chlamydia or gonorrhea.6 In males younger than 14 or older than 35, epididymitis is most commonly caused by urinary coliform pathogens, including Eschericia coli.
If epididymitis is suspected to be due to chlamydia or gonorrhea, treatment should include either doxycycline 100 mg orally twice daily for 10 days or a single dose of azithromycin 1 g orally (for chlamydia eradication) and a single dose of ceftriaxone 125 mg intramuscularly (for gonorrhea eradication).6,7 If coliform bacteria is suspected, order a standard dose of a quinolone (eg, ciprofloxacin or levofloxacin 500 mg/d) for 10 days.6 For refractory cases, treatment with a standard dose of a quinolone for 4 weeks is recommended.6
It is generally reasonable to treat most patients empirically for suspected epididymitis with antibiotics if no other identifiable etiology can be determined. Multiple antibiotic treatments should be avoided, however, in the absence of either an identifiable urogenital infection or ultrasound findings consistent with epididymitis (eg, congestion and enlargement). Antibiotics have not been shown to decrease the severity of chronic orchialgia and their use, unless clearly indicated, may lead to drug resistance.3
Consider a tricyclic antidepressant or gabapentin
Both tricyclic antidepressants (TCAs) and gabapentin have demonstrated benefit in the treatment of chronic pelvic and neuropathic pain.8,9 Doses should be titrated to achieve a maximal therapeutic benefit while avoiding anticholinergic and neurologic side effects.
A cohort study using a multidisciplinary team consisting of a psychologist, an anesthetist, a physiotherapist, and an occupational therapist found >50% symptomatic improvement in 62% of men with chronic orchialgia treated with gabapentin up to 1800 mg per day, and 67% of men treated with nortriptyline up to 150 mg per day.10
However, a subgroup of patients who reported postvasectomy testicular pain did not achieve a 50% symptomatic improvement rate with either TCA or gabapentin therapy.
CASE 1 Vincent B
The FP reassured Vincent that his physical examination was normal and recommended a 1-month trial of ibuprofen (600 mg every 6 hours), and regular use of supportive briefs. Since the patient had been treated with antibiotics in the past with no change in symptoms—and because he was thought to be at low risk for an STI—the physician did not prescribe another empiric trial of antibiotics. He did send the patient for an ultrasound evaluation of the scrotum and testes, which revealed only a 0.5 × 0.4 × 0.6-cm right epididymal cyst that was not palpable on examination.
The patient returned after 1 month, noting that his symptoms had neither improved nor worsened. The FP suggested that he stop taking the ibuprofen and begin a trial of gabapentin 100 mg daily, titrating up to 3 times daily for the first month, then to 300 mg 3 times daily in the second month.
When he returned 3 months later, Vincent reported that his symptoms had improved by about 50%. He has since been able to increase both the intensity and frequency of physical activity. Vincent is not interested in further increasing the dose of gabapentin and declined a referral to a urologist for consideration of procedural and surgical therapeutic options, but agreed to follow up as needed if his testicular pain worsened.
Postvasectomy pain is not unusual
Several years after a vasectomy, the diameter of a man’s ejaculatory ducts often doubles in size to counteract the increase in fluid pressure.11 The specific cause of long-term post-vasectomy pain syndrome, or congestive epididymitis, is unknown, but has been reported in 5% to 43% of men who have undergone this procedure.12-14 Sperm granulomas or spermatoceles represent the body’s effort to spare the testicle from damage secondary to increasing fluid pressure. While these granulomas are benign lesions, their presence may predispose a man to postvasectomy pain syndrome.15-17
CASE 2 Jason H
Two months before Jason’s visit to the FP, his testicular pain had become so excrutiating that he went to the ED seeking treatment. He was given an ultrasound with color Doppler and found to have postvasectomy surgical changes consistent with bilateral spermatoceles, but no evidence of epididymitis or a mass. Before leaving the ED, Jason received ceftriaxone (125 mg IM) as gonorrhea prophylaxis. He was discharged home with prophylactic antibiotics for chlamydia, as well as ibuprofen. He was advised to avoid strenuous physical activity and told to follow-up with his FP if his symptoms did not improve.
During several months of conservative medical therapy, including trials of NSAIDs, quinolone antibiotics, TCAs, and gabapentin, Jason did not experience any significant pain relief. He was frustrated by the dull, aching pain in his scrotum that continued to limit his physical and sexual activities.
Finally, the FP recommended a urologic consultation.
Consider these minimally invasive procedures
When conservative medical management fails, minimally invasive techniques are the next step. There are 2 commonly used procedures, both of which can be performed by a urologist in an outpatient setting.
Spermatic cord blocks with lidocaine and methylprednisolone have been shown to provide relief for weeks up to several months in small case studies, and may be repeated at intervals of several months if modest relief is achieved.18,19
Transrectal ultrasound-guided periprostatic anesthetic injections, another microinvasive option, offers minimal risk and may provide some short-term relief. However, data on long-term benefit and resolution of pain and disability are lacking.20
Consider surgery only after all else fails
If all medical and conservative therapies have been tried and the patient continues to have debilitating pain, surgical options should be considered. Because current surgical therapies are not always effective and are not reversible (and research on the various options is limited), it is important to initiate a detailed discussion with the patient. Such conversations should be held in consultation with a urologist.
Highlight risks and benefits and provide realistic expectations of short- and long-term postsurgical outcomes. It is also important to address psychological factors and social stressors that often contribute to chronic pelvic pain syndromes, which can improve long-term outcomes regardless of the chosen treatment. For this reason, a referral to a psychiatrist may be indicated.
Microsurgical denervation of the spermatic cord. Removal of the afferent nerve stimulus to the testicle is believed to result in the downregulation of the peripheral and central nervous systems, so the patient no longer has the perception of testicular pain. Several small trials have yielded favorable symptomatic pain relief scores in up to 71% of patients, with reported adverse outcomes including rare testicular atrophy—but no complaints of hypoesthesia or hyperesthesia of the scrotum, penile shaft, inguinal, or medial thigh skin.21,22 This treatment should be considered only in patients who have experienced a significant degree of temporary relief from spermatic cord injection.
Epididymectomy is recommended only when pain is localized to the epididymis, as this is a testicle-sparing procedure. Unilateral or bilateral epididymectomy is a viable option for the treatment of chronic orchialgia related to postvasectomy pain syndrome or chronic epididymitis. Reports highlighting symptomatic improvement based on small case series range from 43% to 74%, with the highest success rate found during a 5½-year follow-up.23-25 In 1 study, 90% of patients reported that they were satisfied with their choice to undergo the procedure.25
Vasectomy reversal (vasovasostomy) and inguinal or scrotal orchiectomy should be considered only after all other treatment modalities have failed. Vasovasostomy has the potential to restore fertility in up to 98% of cases,26 which may or may not be desirable. One study of men who experienced post-vasectomy pain syndrome and underwent microsurgical vasovasostomy found that after nearly 2½ years, 84% experienced complete pain resolution.27
The goal of orchiectomy is to relieve orchialgia by releasing the entrapped ipsilateral genitofemoral and/or ilioinguinal nerves. One study determined that 90% of men who underwent unilateral epididymectomy for chronic orchialgia required an orchiectomy to resolve pain.1 Another study found that 80% of patients continued to suffer both short- and long-term debilitating orchialgia postorchiectomy.28
CASE 2 Jason H
Jason saw a urologist, who initially offered him bilateral spermatic cord blocks. They provided Jason with moderate symptom relief on most days of the week and allowed him to increase his physical and sexual activities. Three months later, Jason went back to the urologist for evaluation because he felt that the effects of the spermatic cord blocks had worn off. In the next 6 months, he had 2 additional bilateral blocks.
Nearly a year after a series of spermatic cord blocks, most of it spent in persistent discomfort, Jason returned to his FP with a request for narcotic pain medication. The FP tried to be supportive, but told Jason that chronic narcotic therapy was not an ideal choice—and referred him back to the urologist to discuss surgical options.
The urologist recommended a bilateral epididymectomy and the patient, who was desperate to obtain some pain relief and now regretted undergoing a vasectomy, agreed. Within the first few weeks after his surgery, he noticed a reduction in pain, and he slowly increased his physical activity. A year later, Jason reported only minimal testicular and scrotal discomfort that did not limit his physical or sexual activities—and he continues to be pleased with the outcome of his treatment.
CORRESPONDENCE Joel J. Heidelbaugh, MD, FAAFP, Ypsilanti Health Center, 200 Arnet, Suite 200, Ypsilanti, MI 48198; [email protected]
1. Davis B, Noble MJ, Weigel JD, et al. Analysis and management of chronic testicular pain. J Urol. 1990;143:936-939.
2. Schover LR. Psychological factors in men with genital pain. Cleve Clin J Med. 1990;57:697-700.
3. Masarani M, Cox R. Th e aetiology, pathophysiology and management of chronic orchialgia. Br J Urol Int. 2003;91:435-437.
4. Granitsiotis P, Kirk D. Chronic testicular pain: an overview. Eur Urol. 2004;45:430-436.
5. Coogan CL. Painful scrotum. In: Myers JA, Millikan KW, Sacla-rides TJ, eds. Common Surgical Diseases. New York: Springer; 2008:293-295.
6. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2006. MMWR Morb Mortal Wkly Rep. 2006;55(RR-11):1-94.
7. Newman LM, Moran JS, Workowski KA. Update on the management of gonorrhea in adults in the United States. Clin Infect Dis. 2007;44(suppl 3):S84-S101.
8. Wiffen PJ, McQuay HJ, Rees J, et al. Gabapentin for acute and chronic pain. Cochrane Database Syst Rev. 2005;(3):CD005452.-
9. American College of Obstetricians and Gynecologists. Chronic pelvic pain. ACOG Practice Bulletin No. 51. Obstet Gynecol. 2004;103:589-605.
10. Sinclair AM, Miller B, Lee LK. Chronic orchialgia: consider gabapentin or nortriptyline before considering surgery. Int J Urol. 2007;14:622-625.
11. Jarow JP, Budin RE, Dym M, et al. Quantitative pathologic changes in the human testis after vasectomy. N Engl J Med. 1985;313:1252-1256.
12. Choe J, Kirkemo A. Questionnaire-based outcomes study of nononcological post-vasectomy complications. J Urol. 1996;155:1284-1286.
13. McMahon A, Buckley J, Taylor A, et al. Chronic testicular pain following vasectomy. Br J Urol. 1992;69:188-191.
14. Ahmed I, Rasheed S, White C, et al. Th e incidence of post-vasectomy chronic testicular pain and the role of nerve stripping (denervation) of the spermatic cord in its management. Br J Urol. 1997;79:269-270.
15. Christiansen CG, Sandlow JI. Testicular pain following vasectomy: a review of postvasectomy pain syndrome. J Androl. 2003;24:293-298.
16. Shapiro EI, Silber SJ. Open-ended vasectomy, sperm granuloma, and postvasectomy orchialgia. Fertil Steril. 1979;32:546-550.
17. Taxy JB, Marshall FF, Erlickman RJ. Vasectomy: subclinical pathologic changes. Am J Surg Pathol. 1981;5:767-772.
18. Fuchs E. Cord block anesthesia for scrotal surgery. J Urol. 1982;128:718-719.
19. Issa M, Hsiao K, Bassel Y, et al. Spermatic cord anesthesia block for scrotal procedures in the outpatient clinic setting. J Urol. 2004;172:2358-2361.
20. Zorn B, Rauchenwald M, Steers WD. Periprostatic injection of local anesthesia for relief of chronic orchialgia. J Urol. 1994;151:411,A735.-
21. Levine LA, Matkov TG, Lubenow TR. Microsurgical denervation of the spermatic cord: a surgical alternative in the treatment of chronic orchialgia. J Urol. 1996;155:1005-1007.
22. Strom KH, Levine LA. Microsurgical denervation of the spermatic cord for chronic orchialgia: long-term results from a single center. J Urol. 2008;180:949-953.
23. Padmore DE, Norman RW, Millard OH. Analyses of indications for and outcomes of epdidymectomy. J Urol. 1996;156:95-96.
24. West AF, Leung HY, Powell PH. Epididymectomy is an effective treatment for scrotal pain after vasectomy. Br J Urol Int. 2000;85:1097-1099.
25. Siu W, Ohl DA, Schuster TG. Long-term follow-up after epididymectomy for chronic epidiymal pain. Urology. 2007;70:333-336.
26. Patel SR, Sigman M. Comparison of outcomes of vasovasostomy performed in the convoluted and straight vas deferens. J Urol. 2008;179:256-259.
27. Myers SA, Mershon CE, Fuchs EF. Vasectomy reversal for treatment of the post-vasectomy pain syndrome. J Urol. 1997;157:518-520.
28. Costabile RA, Hahn M, McLeod DG. Chronic orchialgia in the pain prone patient: the clinical perspective. J Urol. 1991;146:1571-1574.
Order ultrasound of the scrotum and testes to evaluate chronic testicular pain, with color Doppler to identify areas of hypervascularity. C
Treat suspected epididymitis with empiric coverage for chlamydia with either a 10-day regimen of doxycycline (100 mg twice daily) or a single dose (1 g) of azithromycin; treat suspected gonorrhea with a single intramuscular injection (125 mg) of ceftriaxone. A
Do not treat small epididymal cysts that do not correlate with testicular pain; larger, painful cysts can be aspirated, injected with a sclerosing agent, or surgically excised. C
Consider surgical options only after medical and conservative therapies have failed to alleviate chronic testicular pain. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE 1 Vincent B, a 33-year-old executive, visits his family physician for an evaluation of chronic orchialgia. Although his testicular pain has waxed and waned for several years, it has recently worsened, making it increasingly difficult for him to exercise or to sit for extended periods of time. In fact, this visit was prompted by a lengthy meeting during which he developed a “dull ache” that did not let up until he left the meeting and walked around.
CASE 2 Jason H, a 42-year-old married father of 3 who had a vasectomy 2 years ago, has had progressively worsening testicular pain ever since. He also has occasional pain after ejaculation, but no known hematospermia. Recently, the pain has become so bad that it limits both his physical and sexual activities and is having a negative effect on his relationship with his wife. Jason is sexually monogamous, has no significant medical history, and takes no prescription medications.
These 2 cases are based on actual patients we have seen in our practices. If Vincent and Jason (not their real names) were your patients, how would you initiate a work-up for testicular pain? What treatments would you offer? And at what point would you consider a referral to a urologist?
Chronic orchialgia is a complex urogenital focal pain syndrome in which neurogenic inflammation is the principal mediator. This debilitating condition is associated with substantial anxiety and frustration, and is characterized by intermittent or constant unilateral or bilateral testicular pain, occurring for at least 3 months, that has a significant negative impact on activities of daily living and physical activity.1
A variety of procedural and surgical options may help to minimize or alleviate chronic orchialgia. But which approach is best? There are no evidence-based guidelines for the treatment of this condition, and no randomized controlled trials to demonstrate the superiority of 1 modality over another. All diagnostic and treatment recommendations are based on expert opinion derived from small cohort studies.
With that in mind, we conducted a systematic review of the literature evaluating medical and surgical therapies for chronic testicular pain—and developed an algorithm (FIGURE 1), along with the text and TABLE that follow, for family physicians (FPs) to use as a guide.
FIGURE 1
Chronic orchialgia: A diagnosis and treatment algorithm1,3,4,6,10
NSAID, nonsteroidal anti-inflammatory drug; STIs, sexually transmitted infections.
CASE 1 Vincent B
Over the last few years, Vincent has had similar episodes of bilateral testicular pain. He denies any history of direct trauma to the testicles, and he works out regularly by lifting weights and running. When the pain becomes unbearable, he takes acetaminophen or ibuprofen and takes a few days off from exercising, which provides modest—but temporary—relief.
Vincent reports that he has had about a dozen lifetime sexual partners and had chlamydia over a decade ago as a college student. He is currently engaged and sexually monogamous, and tested negative for Chlamydia trachomatis, Neisseria gonorrhoeae, hepatitis, syphilis, and human immunodeficiency virus (HIV) at his annual health maintenance examination last month. Shortly before that, Vincent was treated empirically for epididymitis with a 4-week course of ciprofloxacin, with no significant improvement in symptoms. He has no significant past medical history, denies depression, and takes no prescription medications.
Physical examination reveals mild to moderate diffuse tenderness to palpation throughout the scrotum, including both testicles and spermatic cords. There is no erythema of the scrotum. Nor are there any palpable scrotal masses, varicoceles, or hydroceles; testicular, scrotal, or penile lesions; inguinal masses; or lymph nodes. His urethral meatus is patent. The prostate is smooth, nonnodular, and non-tender. The remainder of the physical exam is unremarkable.
Determining a cause can be a challenge
There are numerous possible causes of testicular pain (TABLE), including an inguinal hernia, torsion of the testicle, trauma, and a history of chlamydia or gonorrhea, to name a few.
TABLE
Causes of acute and chronic orchialgia1,3,4
Acute
|
Chronic
|
Chronic testicular pain can also be psychogenic, often relating to a history of sexual abuse or relationship stress. One study examining comorbid psychological conditions in men with chronic orchialgia identified a somatization disorder in 56% of the patients, nongenital chronic pain syndromes in 50%, and major depression or chemical dependency in 27%.2 Overall, however, estimates suggest that in about 25% of patients with chronic orchialgia, no identifiable etiology is found. 1
Establish a baseline with a physical exam
Conduct a physical examination of the scrotum, testes, spermatic cords, penis, inguinal region, and prostate as a baseline measurement in a patient who presents with chronic orchialgia.3,4 An initial urinalysis should be performed to rule out infection or identify microscopic hematuria, which may prompt a more targeted work-up and therapeutic plan. Take a thorough medical and psychosocial/ sexual history, as well.
Order an ultrasound of the scrotum and testes, the accepted gold standard to highlight structural abnormalities of the testicles. The addition of color Doppler makes it possible to find areas of hypervascularity, an indication of inflammation in the testicle and epididymis (FIGURES 2A AND B).
FIGURE 2
Well-circumscribed extratesticular mass
In the image at left, ultrasound reveals an anechoic mass (arrows), representing either an epididymal cyst or spermatocele, superior to the testicle (T). A color Doppler image (right) reveals increased vascularity to the epididymis (E), as compared with the testicle.
Epididymal cysts are common findings on scrotal ultrasound; they are frequently incidental, but may relate to the patient’s pain, depending on the size of the cyst. Smaller cysts that do not correlate with pain do not require treatment. Larger, painful cysts can be treated with aspiration or injection with a sclerosing agent—or with surgical excision, which offers the highest potential cure rate.3,4 A computed tomography (CT) scan without contrast is the best way to find genitourinary system calculi, which could be the source of referred renal pain to the groin and scrotum. A contrast-enhanced CT is best to evaluate for solid renal masses.
Start with the most conservative treatment
In the absence of any findings that require surgical intervention, start conservatively.
Initiate a trial of nonsteroidal anti-inflammatory drugs (NSAIDs) for at least 1 month. Although this is the standard first-line treatment, NSAIDs have been shown to help only a small percentage of patients with chronic orchialgia, and only on a short-term basis.1,3,4
Recommend scrotal elevation with supportive undergarments to decrease venous congestion. Tell the patient, too, that modifying his seated posture to avoid scrotal pressure may alleviate pain and poses no discernible risk of worsening orchialgia.5
Treat suspected STIs. The Centers for Disease Control and Prevention report that in men 14 to 35 years of age, epididymitis is most commonly caused by chlamydia or gonorrhea.6 In males younger than 14 or older than 35, epididymitis is most commonly caused by urinary coliform pathogens, including Eschericia coli.
If epididymitis is suspected to be due to chlamydia or gonorrhea, treatment should include either doxycycline 100 mg orally twice daily for 10 days or a single dose of azithromycin 1 g orally (for chlamydia eradication) and a single dose of ceftriaxone 125 mg intramuscularly (for gonorrhea eradication).6,7 If coliform bacteria is suspected, order a standard dose of a quinolone (eg, ciprofloxacin or levofloxacin 500 mg/d) for 10 days.6 For refractory cases, treatment with a standard dose of a quinolone for 4 weeks is recommended.6
It is generally reasonable to treat most patients empirically for suspected epididymitis with antibiotics if no other identifiable etiology can be determined. Multiple antibiotic treatments should be avoided, however, in the absence of either an identifiable urogenital infection or ultrasound findings consistent with epididymitis (eg, congestion and enlargement). Antibiotics have not been shown to decrease the severity of chronic orchialgia and their use, unless clearly indicated, may lead to drug resistance.3
Consider a tricyclic antidepressant or gabapentin
Both tricyclic antidepressants (TCAs) and gabapentin have demonstrated benefit in the treatment of chronic pelvic and neuropathic pain.8,9 Doses should be titrated to achieve a maximal therapeutic benefit while avoiding anticholinergic and neurologic side effects.
A cohort study using a multidisciplinary team consisting of a psychologist, an anesthetist, a physiotherapist, and an occupational therapist found >50% symptomatic improvement in 62% of men with chronic orchialgia treated with gabapentin up to 1800 mg per day, and 67% of men treated with nortriptyline up to 150 mg per day.10
However, a subgroup of patients who reported postvasectomy testicular pain did not achieve a 50% symptomatic improvement rate with either TCA or gabapentin therapy.
CASE 1 Vincent B
The FP reassured Vincent that his physical examination was normal and recommended a 1-month trial of ibuprofen (600 mg every 6 hours), and regular use of supportive briefs. Since the patient had been treated with antibiotics in the past with no change in symptoms—and because he was thought to be at low risk for an STI—the physician did not prescribe another empiric trial of antibiotics. He did send the patient for an ultrasound evaluation of the scrotum and testes, which revealed only a 0.5 × 0.4 × 0.6-cm right epididymal cyst that was not palpable on examination.
The patient returned after 1 month, noting that his symptoms had neither improved nor worsened. The FP suggested that he stop taking the ibuprofen and begin a trial of gabapentin 100 mg daily, titrating up to 3 times daily for the first month, then to 300 mg 3 times daily in the second month.
When he returned 3 months later, Vincent reported that his symptoms had improved by about 50%. He has since been able to increase both the intensity and frequency of physical activity. Vincent is not interested in further increasing the dose of gabapentin and declined a referral to a urologist for consideration of procedural and surgical therapeutic options, but agreed to follow up as needed if his testicular pain worsened.
Postvasectomy pain is not unusual
Several years after a vasectomy, the diameter of a man’s ejaculatory ducts often doubles in size to counteract the increase in fluid pressure.11 The specific cause of long-term post-vasectomy pain syndrome, or congestive epididymitis, is unknown, but has been reported in 5% to 43% of men who have undergone this procedure.12-14 Sperm granulomas or spermatoceles represent the body’s effort to spare the testicle from damage secondary to increasing fluid pressure. While these granulomas are benign lesions, their presence may predispose a man to postvasectomy pain syndrome.15-17
CASE 2 Jason H
Two months before Jason’s visit to the FP, his testicular pain had become so excrutiating that he went to the ED seeking treatment. He was given an ultrasound with color Doppler and found to have postvasectomy surgical changes consistent with bilateral spermatoceles, but no evidence of epididymitis or a mass. Before leaving the ED, Jason received ceftriaxone (125 mg IM) as gonorrhea prophylaxis. He was discharged home with prophylactic antibiotics for chlamydia, as well as ibuprofen. He was advised to avoid strenuous physical activity and told to follow-up with his FP if his symptoms did not improve.
During several months of conservative medical therapy, including trials of NSAIDs, quinolone antibiotics, TCAs, and gabapentin, Jason did not experience any significant pain relief. He was frustrated by the dull, aching pain in his scrotum that continued to limit his physical and sexual activities.
Finally, the FP recommended a urologic consultation.
Consider these minimally invasive procedures
When conservative medical management fails, minimally invasive techniques are the next step. There are 2 commonly used procedures, both of which can be performed by a urologist in an outpatient setting.
Spermatic cord blocks with lidocaine and methylprednisolone have been shown to provide relief for weeks up to several months in small case studies, and may be repeated at intervals of several months if modest relief is achieved.18,19
Transrectal ultrasound-guided periprostatic anesthetic injections, another microinvasive option, offers minimal risk and may provide some short-term relief. However, data on long-term benefit and resolution of pain and disability are lacking.20
Consider surgery only after all else fails
If all medical and conservative therapies have been tried and the patient continues to have debilitating pain, surgical options should be considered. Because current surgical therapies are not always effective and are not reversible (and research on the various options is limited), it is important to initiate a detailed discussion with the patient. Such conversations should be held in consultation with a urologist.
Highlight risks and benefits and provide realistic expectations of short- and long-term postsurgical outcomes. It is also important to address psychological factors and social stressors that often contribute to chronic pelvic pain syndromes, which can improve long-term outcomes regardless of the chosen treatment. For this reason, a referral to a psychiatrist may be indicated.
Microsurgical denervation of the spermatic cord. Removal of the afferent nerve stimulus to the testicle is believed to result in the downregulation of the peripheral and central nervous systems, so the patient no longer has the perception of testicular pain. Several small trials have yielded favorable symptomatic pain relief scores in up to 71% of patients, with reported adverse outcomes including rare testicular atrophy—but no complaints of hypoesthesia or hyperesthesia of the scrotum, penile shaft, inguinal, or medial thigh skin.21,22 This treatment should be considered only in patients who have experienced a significant degree of temporary relief from spermatic cord injection.
Epididymectomy is recommended only when pain is localized to the epididymis, as this is a testicle-sparing procedure. Unilateral or bilateral epididymectomy is a viable option for the treatment of chronic orchialgia related to postvasectomy pain syndrome or chronic epididymitis. Reports highlighting symptomatic improvement based on small case series range from 43% to 74%, with the highest success rate found during a 5½-year follow-up.23-25 In 1 study, 90% of patients reported that they were satisfied with their choice to undergo the procedure.25
Vasectomy reversal (vasovasostomy) and inguinal or scrotal orchiectomy should be considered only after all other treatment modalities have failed. Vasovasostomy has the potential to restore fertility in up to 98% of cases,26 which may or may not be desirable. One study of men who experienced post-vasectomy pain syndrome and underwent microsurgical vasovasostomy found that after nearly 2½ years, 84% experienced complete pain resolution.27
The goal of orchiectomy is to relieve orchialgia by releasing the entrapped ipsilateral genitofemoral and/or ilioinguinal nerves. One study determined that 90% of men who underwent unilateral epididymectomy for chronic orchialgia required an orchiectomy to resolve pain.1 Another study found that 80% of patients continued to suffer both short- and long-term debilitating orchialgia postorchiectomy.28
CASE 2 Jason H
Jason saw a urologist, who initially offered him bilateral spermatic cord blocks. They provided Jason with moderate symptom relief on most days of the week and allowed him to increase his physical and sexual activities. Three months later, Jason went back to the urologist for evaluation because he felt that the effects of the spermatic cord blocks had worn off. In the next 6 months, he had 2 additional bilateral blocks.
Nearly a year after a series of spermatic cord blocks, most of it spent in persistent discomfort, Jason returned to his FP with a request for narcotic pain medication. The FP tried to be supportive, but told Jason that chronic narcotic therapy was not an ideal choice—and referred him back to the urologist to discuss surgical options.
The urologist recommended a bilateral epididymectomy and the patient, who was desperate to obtain some pain relief and now regretted undergoing a vasectomy, agreed. Within the first few weeks after his surgery, he noticed a reduction in pain, and he slowly increased his physical activity. A year later, Jason reported only minimal testicular and scrotal discomfort that did not limit his physical or sexual activities—and he continues to be pleased with the outcome of his treatment.
CORRESPONDENCE Joel J. Heidelbaugh, MD, FAAFP, Ypsilanti Health Center, 200 Arnet, Suite 200, Ypsilanti, MI 48198; [email protected]
Order ultrasound of the scrotum and testes to evaluate chronic testicular pain, with color Doppler to identify areas of hypervascularity. C
Treat suspected epididymitis with empiric coverage for chlamydia with either a 10-day regimen of doxycycline (100 mg twice daily) or a single dose (1 g) of azithromycin; treat suspected gonorrhea with a single intramuscular injection (125 mg) of ceftriaxone. A
Do not treat small epididymal cysts that do not correlate with testicular pain; larger, painful cysts can be aspirated, injected with a sclerosing agent, or surgically excised. C
Consider surgical options only after medical and conservative therapies have failed to alleviate chronic testicular pain. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE 1 Vincent B, a 33-year-old executive, visits his family physician for an evaluation of chronic orchialgia. Although his testicular pain has waxed and waned for several years, it has recently worsened, making it increasingly difficult for him to exercise or to sit for extended periods of time. In fact, this visit was prompted by a lengthy meeting during which he developed a “dull ache” that did not let up until he left the meeting and walked around.
CASE 2 Jason H, a 42-year-old married father of 3 who had a vasectomy 2 years ago, has had progressively worsening testicular pain ever since. He also has occasional pain after ejaculation, but no known hematospermia. Recently, the pain has become so bad that it limits both his physical and sexual activities and is having a negative effect on his relationship with his wife. Jason is sexually monogamous, has no significant medical history, and takes no prescription medications.
These 2 cases are based on actual patients we have seen in our practices. If Vincent and Jason (not their real names) were your patients, how would you initiate a work-up for testicular pain? What treatments would you offer? And at what point would you consider a referral to a urologist?
Chronic orchialgia is a complex urogenital focal pain syndrome in which neurogenic inflammation is the principal mediator. This debilitating condition is associated with substantial anxiety and frustration, and is characterized by intermittent or constant unilateral or bilateral testicular pain, occurring for at least 3 months, that has a significant negative impact on activities of daily living and physical activity.1
A variety of procedural and surgical options may help to minimize or alleviate chronic orchialgia. But which approach is best? There are no evidence-based guidelines for the treatment of this condition, and no randomized controlled trials to demonstrate the superiority of 1 modality over another. All diagnostic and treatment recommendations are based on expert opinion derived from small cohort studies.
With that in mind, we conducted a systematic review of the literature evaluating medical and surgical therapies for chronic testicular pain—and developed an algorithm (FIGURE 1), along with the text and TABLE that follow, for family physicians (FPs) to use as a guide.
FIGURE 1
Chronic orchialgia: A diagnosis and treatment algorithm1,3,4,6,10
NSAID, nonsteroidal anti-inflammatory drug; STIs, sexually transmitted infections.
CASE 1 Vincent B
Over the last few years, Vincent has had similar episodes of bilateral testicular pain. He denies any history of direct trauma to the testicles, and he works out regularly by lifting weights and running. When the pain becomes unbearable, he takes acetaminophen or ibuprofen and takes a few days off from exercising, which provides modest—but temporary—relief.
Vincent reports that he has had about a dozen lifetime sexual partners and had chlamydia over a decade ago as a college student. He is currently engaged and sexually monogamous, and tested negative for Chlamydia trachomatis, Neisseria gonorrhoeae, hepatitis, syphilis, and human immunodeficiency virus (HIV) at his annual health maintenance examination last month. Shortly before that, Vincent was treated empirically for epididymitis with a 4-week course of ciprofloxacin, with no significant improvement in symptoms. He has no significant past medical history, denies depression, and takes no prescription medications.
Physical examination reveals mild to moderate diffuse tenderness to palpation throughout the scrotum, including both testicles and spermatic cords. There is no erythema of the scrotum. Nor are there any palpable scrotal masses, varicoceles, or hydroceles; testicular, scrotal, or penile lesions; inguinal masses; or lymph nodes. His urethral meatus is patent. The prostate is smooth, nonnodular, and non-tender. The remainder of the physical exam is unremarkable.
Determining a cause can be a challenge
There are numerous possible causes of testicular pain (TABLE), including an inguinal hernia, torsion of the testicle, trauma, and a history of chlamydia or gonorrhea, to name a few.
TABLE
Causes of acute and chronic orchialgia1,3,4
Acute
|
Chronic
|
Chronic testicular pain can also be psychogenic, often relating to a history of sexual abuse or relationship stress. One study examining comorbid psychological conditions in men with chronic orchialgia identified a somatization disorder in 56% of the patients, nongenital chronic pain syndromes in 50%, and major depression or chemical dependency in 27%.2 Overall, however, estimates suggest that in about 25% of patients with chronic orchialgia, no identifiable etiology is found. 1
Establish a baseline with a physical exam
Conduct a physical examination of the scrotum, testes, spermatic cords, penis, inguinal region, and prostate as a baseline measurement in a patient who presents with chronic orchialgia.3,4 An initial urinalysis should be performed to rule out infection or identify microscopic hematuria, which may prompt a more targeted work-up and therapeutic plan. Take a thorough medical and psychosocial/ sexual history, as well.
Order an ultrasound of the scrotum and testes, the accepted gold standard to highlight structural abnormalities of the testicles. The addition of color Doppler makes it possible to find areas of hypervascularity, an indication of inflammation in the testicle and epididymis (FIGURES 2A AND B).
FIGURE 2
Well-circumscribed extratesticular mass
In the image at left, ultrasound reveals an anechoic mass (arrows), representing either an epididymal cyst or spermatocele, superior to the testicle (T). A color Doppler image (right) reveals increased vascularity to the epididymis (E), as compared with the testicle.
Epididymal cysts are common findings on scrotal ultrasound; they are frequently incidental, but may relate to the patient’s pain, depending on the size of the cyst. Smaller cysts that do not correlate with pain do not require treatment. Larger, painful cysts can be treated with aspiration or injection with a sclerosing agent—or with surgical excision, which offers the highest potential cure rate.3,4 A computed tomography (CT) scan without contrast is the best way to find genitourinary system calculi, which could be the source of referred renal pain to the groin and scrotum. A contrast-enhanced CT is best to evaluate for solid renal masses.
Start with the most conservative treatment
In the absence of any findings that require surgical intervention, start conservatively.
Initiate a trial of nonsteroidal anti-inflammatory drugs (NSAIDs) for at least 1 month. Although this is the standard first-line treatment, NSAIDs have been shown to help only a small percentage of patients with chronic orchialgia, and only on a short-term basis.1,3,4
Recommend scrotal elevation with supportive undergarments to decrease venous congestion. Tell the patient, too, that modifying his seated posture to avoid scrotal pressure may alleviate pain and poses no discernible risk of worsening orchialgia.5
Treat suspected STIs. The Centers for Disease Control and Prevention report that in men 14 to 35 years of age, epididymitis is most commonly caused by chlamydia or gonorrhea.6 In males younger than 14 or older than 35, epididymitis is most commonly caused by urinary coliform pathogens, including Eschericia coli.
If epididymitis is suspected to be due to chlamydia or gonorrhea, treatment should include either doxycycline 100 mg orally twice daily for 10 days or a single dose of azithromycin 1 g orally (for chlamydia eradication) and a single dose of ceftriaxone 125 mg intramuscularly (for gonorrhea eradication).6,7 If coliform bacteria is suspected, order a standard dose of a quinolone (eg, ciprofloxacin or levofloxacin 500 mg/d) for 10 days.6 For refractory cases, treatment with a standard dose of a quinolone for 4 weeks is recommended.6
It is generally reasonable to treat most patients empirically for suspected epididymitis with antibiotics if no other identifiable etiology can be determined. Multiple antibiotic treatments should be avoided, however, in the absence of either an identifiable urogenital infection or ultrasound findings consistent with epididymitis (eg, congestion and enlargement). Antibiotics have not been shown to decrease the severity of chronic orchialgia and their use, unless clearly indicated, may lead to drug resistance.3
Consider a tricyclic antidepressant or gabapentin
Both tricyclic antidepressants (TCAs) and gabapentin have demonstrated benefit in the treatment of chronic pelvic and neuropathic pain.8,9 Doses should be titrated to achieve a maximal therapeutic benefit while avoiding anticholinergic and neurologic side effects.
A cohort study using a multidisciplinary team consisting of a psychologist, an anesthetist, a physiotherapist, and an occupational therapist found >50% symptomatic improvement in 62% of men with chronic orchialgia treated with gabapentin up to 1800 mg per day, and 67% of men treated with nortriptyline up to 150 mg per day.10
However, a subgroup of patients who reported postvasectomy testicular pain did not achieve a 50% symptomatic improvement rate with either TCA or gabapentin therapy.
CASE 1 Vincent B
The FP reassured Vincent that his physical examination was normal and recommended a 1-month trial of ibuprofen (600 mg every 6 hours), and regular use of supportive briefs. Since the patient had been treated with antibiotics in the past with no change in symptoms—and because he was thought to be at low risk for an STI—the physician did not prescribe another empiric trial of antibiotics. He did send the patient for an ultrasound evaluation of the scrotum and testes, which revealed only a 0.5 × 0.4 × 0.6-cm right epididymal cyst that was not palpable on examination.
The patient returned after 1 month, noting that his symptoms had neither improved nor worsened. The FP suggested that he stop taking the ibuprofen and begin a trial of gabapentin 100 mg daily, titrating up to 3 times daily for the first month, then to 300 mg 3 times daily in the second month.
When he returned 3 months later, Vincent reported that his symptoms had improved by about 50%. He has since been able to increase both the intensity and frequency of physical activity. Vincent is not interested in further increasing the dose of gabapentin and declined a referral to a urologist for consideration of procedural and surgical therapeutic options, but agreed to follow up as needed if his testicular pain worsened.
Postvasectomy pain is not unusual
Several years after a vasectomy, the diameter of a man’s ejaculatory ducts often doubles in size to counteract the increase in fluid pressure.11 The specific cause of long-term post-vasectomy pain syndrome, or congestive epididymitis, is unknown, but has been reported in 5% to 43% of men who have undergone this procedure.12-14 Sperm granulomas or spermatoceles represent the body’s effort to spare the testicle from damage secondary to increasing fluid pressure. While these granulomas are benign lesions, their presence may predispose a man to postvasectomy pain syndrome.15-17
CASE 2 Jason H
Two months before Jason’s visit to the FP, his testicular pain had become so excrutiating that he went to the ED seeking treatment. He was given an ultrasound with color Doppler and found to have postvasectomy surgical changes consistent with bilateral spermatoceles, but no evidence of epididymitis or a mass. Before leaving the ED, Jason received ceftriaxone (125 mg IM) as gonorrhea prophylaxis. He was discharged home with prophylactic antibiotics for chlamydia, as well as ibuprofen. He was advised to avoid strenuous physical activity and told to follow-up with his FP if his symptoms did not improve.
During several months of conservative medical therapy, including trials of NSAIDs, quinolone antibiotics, TCAs, and gabapentin, Jason did not experience any significant pain relief. He was frustrated by the dull, aching pain in his scrotum that continued to limit his physical and sexual activities.
Finally, the FP recommended a urologic consultation.
Consider these minimally invasive procedures
When conservative medical management fails, minimally invasive techniques are the next step. There are 2 commonly used procedures, both of which can be performed by a urologist in an outpatient setting.
Spermatic cord blocks with lidocaine and methylprednisolone have been shown to provide relief for weeks up to several months in small case studies, and may be repeated at intervals of several months if modest relief is achieved.18,19
Transrectal ultrasound-guided periprostatic anesthetic injections, another microinvasive option, offers minimal risk and may provide some short-term relief. However, data on long-term benefit and resolution of pain and disability are lacking.20
Consider surgery only after all else fails
If all medical and conservative therapies have been tried and the patient continues to have debilitating pain, surgical options should be considered. Because current surgical therapies are not always effective and are not reversible (and research on the various options is limited), it is important to initiate a detailed discussion with the patient. Such conversations should be held in consultation with a urologist.
Highlight risks and benefits and provide realistic expectations of short- and long-term postsurgical outcomes. It is also important to address psychological factors and social stressors that often contribute to chronic pelvic pain syndromes, which can improve long-term outcomes regardless of the chosen treatment. For this reason, a referral to a psychiatrist may be indicated.
Microsurgical denervation of the spermatic cord. Removal of the afferent nerve stimulus to the testicle is believed to result in the downregulation of the peripheral and central nervous systems, so the patient no longer has the perception of testicular pain. Several small trials have yielded favorable symptomatic pain relief scores in up to 71% of patients, with reported adverse outcomes including rare testicular atrophy—but no complaints of hypoesthesia or hyperesthesia of the scrotum, penile shaft, inguinal, or medial thigh skin.21,22 This treatment should be considered only in patients who have experienced a significant degree of temporary relief from spermatic cord injection.
Epididymectomy is recommended only when pain is localized to the epididymis, as this is a testicle-sparing procedure. Unilateral or bilateral epididymectomy is a viable option for the treatment of chronic orchialgia related to postvasectomy pain syndrome or chronic epididymitis. Reports highlighting symptomatic improvement based on small case series range from 43% to 74%, with the highest success rate found during a 5½-year follow-up.23-25 In 1 study, 90% of patients reported that they were satisfied with their choice to undergo the procedure.25
Vasectomy reversal (vasovasostomy) and inguinal or scrotal orchiectomy should be considered only after all other treatment modalities have failed. Vasovasostomy has the potential to restore fertility in up to 98% of cases,26 which may or may not be desirable. One study of men who experienced post-vasectomy pain syndrome and underwent microsurgical vasovasostomy found that after nearly 2½ years, 84% experienced complete pain resolution.27
The goal of orchiectomy is to relieve orchialgia by releasing the entrapped ipsilateral genitofemoral and/or ilioinguinal nerves. One study determined that 90% of men who underwent unilateral epididymectomy for chronic orchialgia required an orchiectomy to resolve pain.1 Another study found that 80% of patients continued to suffer both short- and long-term debilitating orchialgia postorchiectomy.28
CASE 2 Jason H
Jason saw a urologist, who initially offered him bilateral spermatic cord blocks. They provided Jason with moderate symptom relief on most days of the week and allowed him to increase his physical and sexual activities. Three months later, Jason went back to the urologist for evaluation because he felt that the effects of the spermatic cord blocks had worn off. In the next 6 months, he had 2 additional bilateral blocks.
Nearly a year after a series of spermatic cord blocks, most of it spent in persistent discomfort, Jason returned to his FP with a request for narcotic pain medication. The FP tried to be supportive, but told Jason that chronic narcotic therapy was not an ideal choice—and referred him back to the urologist to discuss surgical options.
The urologist recommended a bilateral epididymectomy and the patient, who was desperate to obtain some pain relief and now regretted undergoing a vasectomy, agreed. Within the first few weeks after his surgery, he noticed a reduction in pain, and he slowly increased his physical activity. A year later, Jason reported only minimal testicular and scrotal discomfort that did not limit his physical or sexual activities—and he continues to be pleased with the outcome of his treatment.
CORRESPONDENCE Joel J. Heidelbaugh, MD, FAAFP, Ypsilanti Health Center, 200 Arnet, Suite 200, Ypsilanti, MI 48198; [email protected]
1. Davis B, Noble MJ, Weigel JD, et al. Analysis and management of chronic testicular pain. J Urol. 1990;143:936-939.
2. Schover LR. Psychological factors in men with genital pain. Cleve Clin J Med. 1990;57:697-700.
3. Masarani M, Cox R. Th e aetiology, pathophysiology and management of chronic orchialgia. Br J Urol Int. 2003;91:435-437.
4. Granitsiotis P, Kirk D. Chronic testicular pain: an overview. Eur Urol. 2004;45:430-436.
5. Coogan CL. Painful scrotum. In: Myers JA, Millikan KW, Sacla-rides TJ, eds. Common Surgical Diseases. New York: Springer; 2008:293-295.
6. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2006. MMWR Morb Mortal Wkly Rep. 2006;55(RR-11):1-94.
7. Newman LM, Moran JS, Workowski KA. Update on the management of gonorrhea in adults in the United States. Clin Infect Dis. 2007;44(suppl 3):S84-S101.
8. Wiffen PJ, McQuay HJ, Rees J, et al. Gabapentin for acute and chronic pain. Cochrane Database Syst Rev. 2005;(3):CD005452.-
9. American College of Obstetricians and Gynecologists. Chronic pelvic pain. ACOG Practice Bulletin No. 51. Obstet Gynecol. 2004;103:589-605.
10. Sinclair AM, Miller B, Lee LK. Chronic orchialgia: consider gabapentin or nortriptyline before considering surgery. Int J Urol. 2007;14:622-625.
11. Jarow JP, Budin RE, Dym M, et al. Quantitative pathologic changes in the human testis after vasectomy. N Engl J Med. 1985;313:1252-1256.
12. Choe J, Kirkemo A. Questionnaire-based outcomes study of nononcological post-vasectomy complications. J Urol. 1996;155:1284-1286.
13. McMahon A, Buckley J, Taylor A, et al. Chronic testicular pain following vasectomy. Br J Urol. 1992;69:188-191.
14. Ahmed I, Rasheed S, White C, et al. Th e incidence of post-vasectomy chronic testicular pain and the role of nerve stripping (denervation) of the spermatic cord in its management. Br J Urol. 1997;79:269-270.
15. Christiansen CG, Sandlow JI. Testicular pain following vasectomy: a review of postvasectomy pain syndrome. J Androl. 2003;24:293-298.
16. Shapiro EI, Silber SJ. Open-ended vasectomy, sperm granuloma, and postvasectomy orchialgia. Fertil Steril. 1979;32:546-550.
17. Taxy JB, Marshall FF, Erlickman RJ. Vasectomy: subclinical pathologic changes. Am J Surg Pathol. 1981;5:767-772.
18. Fuchs E. Cord block anesthesia for scrotal surgery. J Urol. 1982;128:718-719.
19. Issa M, Hsiao K, Bassel Y, et al. Spermatic cord anesthesia block for scrotal procedures in the outpatient clinic setting. J Urol. 2004;172:2358-2361.
20. Zorn B, Rauchenwald M, Steers WD. Periprostatic injection of local anesthesia for relief of chronic orchialgia. J Urol. 1994;151:411,A735.-
21. Levine LA, Matkov TG, Lubenow TR. Microsurgical denervation of the spermatic cord: a surgical alternative in the treatment of chronic orchialgia. J Urol. 1996;155:1005-1007.
22. Strom KH, Levine LA. Microsurgical denervation of the spermatic cord for chronic orchialgia: long-term results from a single center. J Urol. 2008;180:949-953.
23. Padmore DE, Norman RW, Millard OH. Analyses of indications for and outcomes of epdidymectomy. J Urol. 1996;156:95-96.
24. West AF, Leung HY, Powell PH. Epididymectomy is an effective treatment for scrotal pain after vasectomy. Br J Urol Int. 2000;85:1097-1099.
25. Siu W, Ohl DA, Schuster TG. Long-term follow-up after epididymectomy for chronic epidiymal pain. Urology. 2007;70:333-336.
26. Patel SR, Sigman M. Comparison of outcomes of vasovasostomy performed in the convoluted and straight vas deferens. J Urol. 2008;179:256-259.
27. Myers SA, Mershon CE, Fuchs EF. Vasectomy reversal for treatment of the post-vasectomy pain syndrome. J Urol. 1997;157:518-520.
28. Costabile RA, Hahn M, McLeod DG. Chronic orchialgia in the pain prone patient: the clinical perspective. J Urol. 1991;146:1571-1574.
1. Davis B, Noble MJ, Weigel JD, et al. Analysis and management of chronic testicular pain. J Urol. 1990;143:936-939.
2. Schover LR. Psychological factors in men with genital pain. Cleve Clin J Med. 1990;57:697-700.
3. Masarani M, Cox R. Th e aetiology, pathophysiology and management of chronic orchialgia. Br J Urol Int. 2003;91:435-437.
4. Granitsiotis P, Kirk D. Chronic testicular pain: an overview. Eur Urol. 2004;45:430-436.
5. Coogan CL. Painful scrotum. In: Myers JA, Millikan KW, Sacla-rides TJ, eds. Common Surgical Diseases. New York: Springer; 2008:293-295.
6. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2006. MMWR Morb Mortal Wkly Rep. 2006;55(RR-11):1-94.
7. Newman LM, Moran JS, Workowski KA. Update on the management of gonorrhea in adults in the United States. Clin Infect Dis. 2007;44(suppl 3):S84-S101.
8. Wiffen PJ, McQuay HJ, Rees J, et al. Gabapentin for acute and chronic pain. Cochrane Database Syst Rev. 2005;(3):CD005452.-
9. American College of Obstetricians and Gynecologists. Chronic pelvic pain. ACOG Practice Bulletin No. 51. Obstet Gynecol. 2004;103:589-605.
10. Sinclair AM, Miller B, Lee LK. Chronic orchialgia: consider gabapentin or nortriptyline before considering surgery. Int J Urol. 2007;14:622-625.
11. Jarow JP, Budin RE, Dym M, et al. Quantitative pathologic changes in the human testis after vasectomy. N Engl J Med. 1985;313:1252-1256.
12. Choe J, Kirkemo A. Questionnaire-based outcomes study of nononcological post-vasectomy complications. J Urol. 1996;155:1284-1286.
13. McMahon A, Buckley J, Taylor A, et al. Chronic testicular pain following vasectomy. Br J Urol. 1992;69:188-191.
14. Ahmed I, Rasheed S, White C, et al. Th e incidence of post-vasectomy chronic testicular pain and the role of nerve stripping (denervation) of the spermatic cord in its management. Br J Urol. 1997;79:269-270.
15. Christiansen CG, Sandlow JI. Testicular pain following vasectomy: a review of postvasectomy pain syndrome. J Androl. 2003;24:293-298.
16. Shapiro EI, Silber SJ. Open-ended vasectomy, sperm granuloma, and postvasectomy orchialgia. Fertil Steril. 1979;32:546-550.
17. Taxy JB, Marshall FF, Erlickman RJ. Vasectomy: subclinical pathologic changes. Am J Surg Pathol. 1981;5:767-772.
18. Fuchs E. Cord block anesthesia for scrotal surgery. J Urol. 1982;128:718-719.
19. Issa M, Hsiao K, Bassel Y, et al. Spermatic cord anesthesia block for scrotal procedures in the outpatient clinic setting. J Urol. 2004;172:2358-2361.
20. Zorn B, Rauchenwald M, Steers WD. Periprostatic injection of local anesthesia for relief of chronic orchialgia. J Urol. 1994;151:411,A735.-
21. Levine LA, Matkov TG, Lubenow TR. Microsurgical denervation of the spermatic cord: a surgical alternative in the treatment of chronic orchialgia. J Urol. 1996;155:1005-1007.
22. Strom KH, Levine LA. Microsurgical denervation of the spermatic cord for chronic orchialgia: long-term results from a single center. J Urol. 2008;180:949-953.
23. Padmore DE, Norman RW, Millard OH. Analyses of indications for and outcomes of epdidymectomy. J Urol. 1996;156:95-96.
24. West AF, Leung HY, Powell PH. Epididymectomy is an effective treatment for scrotal pain after vasectomy. Br J Urol Int. 2000;85:1097-1099.
25. Siu W, Ohl DA, Schuster TG. Long-term follow-up after epididymectomy for chronic epidiymal pain. Urology. 2007;70:333-336.
26. Patel SR, Sigman M. Comparison of outcomes of vasovasostomy performed in the convoluted and straight vas deferens. J Urol. 2008;179:256-259.
27. Myers SA, Mershon CE, Fuchs EF. Vasectomy reversal for treatment of the post-vasectomy pain syndrome. J Urol. 1997;157:518-520.
28. Costabile RA, Hahn M, McLeod DG. Chronic orchialgia in the pain prone patient: the clinical perspective. J Urol. 1991;146:1571-1574.
Avoiding drug interactions: Here’s help
Be sure to inquire about over-the-counter drugs, herbal remedies, vitamins, and supplements when taking a medication history. A
Use an electronic prescribing software system that flags potential drug-drug interactions. A
Consider adjusting a dosing regimen or temporarily discontinuing a maintenance medication if the drug you are about to prescribe is likely to interact with another agent the patient is taking (and there are no alternatives you can prescribe). B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE John L, a 63-year-old man taking lovastatin (40 mg/d) and ramipril (5 mg/d) for hypercholesterolemia and arterial hypertension was hospitalized with atrial fibrillation. Three days later, he was discharged, with a prescription for amiodarone (200 mg/d). After a month, he was readmitted to the hospital with dark urine and intensifying thigh weakness and achiness. Laboratory testing revealed aspartate aminotransferase and alanine aminotransferase levels 10 times the upper limit of normal, and elevated urine and serum myoglobin.
Drug-drug interactions (DDIs) like the one John experienced between lovastatin and amiodarone are a common cause of readmissions, as well as emergency department visits and hospitalizations, for everything from myopathy to electrolyte imbalance, gastrointestinal (GI) bleeding, hepatotoxicity, renal dysfunction, and changes in blood pressure and heart rate.1-3
Yet many, if not most, DDIs can be avoided. With diligence and the right tools, you can do much to reduce the incidence of such interactions and adverse outcomes.
Polypharmacy and age pose the highest risks
The more medications a patient is taking, of course, the greater the likelihood of a clinically significant DDI. According to 1 study, 13% of patients taking 2 drugs develop a DDI; the incidence approaches 40% for patients taking 5 drugs, and exceeds 80% for patients taking 7 or more medications.4
In addition to polypharmacy, age alone is a key risk factor for DDIs.5 Pharmacokinetics and pharmacodynamics are frequently altered in older people, who may have slower intestinal transit time; diminished absorption capacity; decreased liver metabolism, mitochondrial function, and renal excretion; and alterations in volemia and body fat distribution.6 Although the speed at which these changes occur varies, aging is associated with a progressive deficiency in the regulation of most homeo-static mechanisms and an altered response to receptor stimulation.7
Whether age, multiple medications, or both are to blame, the impact on the elderly is striking. One recent retrospective study found 25% of elderly outpatients to be at risk for DDIs.8
Very young patients (<5 years) are also at risk for DDIs because of the immaturity of their enzymatic metabolic system.5,9,10 Additional risk factors, detailed in TABLE 1, include the presence of an infection or other acute medical condition, a metabolic or endocrine disorder, and taking 1 or more drugs with a narrow therapeutic range. Women are also at higher risk for DDIs than their male counterparts, the result of a slower metabolic capacity and interference with sex hormones.3-5,8,9 Pharmacogenetics may also play a big part in DDIs, and more and more studies are focusing on identifying patients at greatest risk.
TABLE 1
Risk factors for drug-drug interactions3-5,8,9
| Risk factor | Potential result |
|---|---|
| Acute medical condition (eg, dehydration, infection, alcoholism) | Augmented risk of elevated plasma drug concentration, increased catabolism, inhibition of hepatic drug metabolism |
| Age (very young [<5 years] and elderly) | Reduced metabolic capacity (greater accumulation of drugs) |
| Decreased renal and/or hepatic function | Decreased drug clearance/elimination; greater accumulation of drugs or their metabolites |
| Drug(s) with narrow therapeutic range | Increased risk for dose-related side effects |
| Female sex | Reduced metabolic capacity, interference with sex hormones |
| Metabolic or endocrine conditions (eg, fatty liver, obesity, hypothyroidism) | Altered hepatic metabolism, increased body distribution volumes, augmented risk of accumulation for hydrophobic molecules |
| Polypharmacy (≥3 medications) | Increased risk of metabolic and/or pharmacodynamic interference |
| Pharmacogenetics | Altered metabolic capacity (greater accumulation of drugs or their metabolites) |
Lack of coordinated care also increases risk
Another risk factor involves the use of multiple providers.9 A woman may be treated by—and receive prescriptions from—an endocrinolo-gist, a gynecologist, and a family physician (FP), for instance, and get medications from a local pharmacy, a nationwide discount chain, and a mail order pharmacy. As with the number of medications being taken, the greater the number of health care professionals a patient sees, the higher the risk.
To mitigate the risk, encourage your patients to fill all their prescriptions at the same pharmacy—and for your part, take a complete medication history before writing a new prescription.
Medication history in doubt? Schedule a “brown bag review”
Ask patients to provide the name and dose of every medication they’re taking. Inquire specifically about over-the-counter (OTC) cough and cold remedies and complementary and alternative medicines, including herbal remedies, vitamins, and supplements. Patients often neglect to mention nonprescription remedies and may not even think of them as medicine, but OTC products with the potential to interact adversely with prescription drugs may otherwise remain undetected.11-13
Consider a “brown bag review” for patients who don’t know what dosage they’re taking or have difficulty identifying the drugs other physicians have prescribed. Ask them to put all their medications in a brown bag and bring them in on their next visit.14,15
Steps to take to reduce risk
Software systems. A number of free and low-cost software systems identify potential DDIs (See “Check for drug interactions: Software programs to consider”). While such electronic programs can indeed lower the risk,16-18 they cannot be counted on to detect or avert every possible adverse interaction.
The downside. One problem is that some software programs fail to distinguish between clinically significant and nonsignificant interactions, causing some prescribers to override system alerts—and possibly miss an important warning.19 Another problem: While most systems do an excellent job of checking to see whether 2 drugs can be safely taken together, few are capable of checking for all potential interactions among multiple medications. What’s more, many drugs have not been evaluated for their potential to interact with other agents, so the absence of reported interactions is no guarantee of a lack of DDIs.
Other strategies to consider:
Minimize the number of prescriptions. While it may not be possible to avoid prescribing a new agent for a patient who is already taking multiple medications, limiting the number of new drugs to those that are absolutely essential will help to minimize DDIs. Whenever possible, select a compound with the desired effects. Prescribe a single agent with antihypertensive as well as uricosuric effects for a patient with elevated blood pressure and uric acid levels rather than 2 different drugs (eg, losartan instead of an anti-hypertensive agent plus allopurinol).
Alter the dosing regimen. Several active molecules may cause DDIs by interfering with intestinal absorption or GI transit time if they’re taken closely together. For example, a quinolone should not be administered at the same time as a cation because of possible chelation in the GI tract. If a patient needs both, however, you may be able to avert a DDI by advising the patient to take them at least 2 hours apart.20 Another possibility is to temporarily discontinue a maintenance medication if it has the potential to interact adversely with a drug that is needed for only a short duration.
Choose a different drug (or drug class). Some drug classes should never be mixed—nitrates and phosphodiesterase type-5 inhibitors, taken together, greatly increase the risk of vasodilation and may result in severe hypotension, for example. There are also drug classes with a low potential for DDIs, including cholinesterase inhibitors and anti-hypertensives (angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, beta-blockers, and thiazides).21
Frequently, though, medications within the same drug class do not share the same potential for DDIs. In such cases, an adverse outcome can often be averted by being aware of combinations likely to result in clinically significant DDIs (TABLE 2) and, whenever possible, prescribing another agent. If a patient taking carbamazepine needs a macro-lide antibiotic, for instance, azithromycin is a better choice than erythromycin. That’s because erythromycin inhibits the hepatic metabolism of the anticonvulsant, increasing the serum level of carbamazepine, while azithromycin does not interfere with carbamazepine metabolism.22
TABLE 2
Clinically significant drug-drug interactions21,22
| Combination (effect) |
|---|
| Allopurinol and captopril (augments allopurinol’s effect) |
| Antidepressants (SSRIs, MAOIs) and antiepileptics (augments antidepressant effect) |
| Clopidogrel and omeprazole or esomeprazole (reduces clopidogrel’s effect) |
| Erythromycin and carbamazepine (augments carbamazepine’s effect) |
| Erythromycin and terfenadine (augments terfenadine’s effect) |
| Ketoconazole and PPIs (reduces ketoconazole’s absorption) |
| Levodopa and metoclopramide (augments levodopa’s effect) |
| MAOIs and narcotic analgesics (augments effects of both drugs) |
| Nitrates and phosphodiesterase type-5 inhibitors (augments effects of both drugs) |
| OCs and penicillins, phenobarbital, or tetracycline (reduces OCs’ effect) |
| Phenobarbital and simvastatin* (reduces simvastatin’s effect) |
| Quinolone and cation (reduces quinolone’s absorption and effect) |
| Repaglinide and diltiazem (augments repaglinide’s effect) |
| Simvastatin* or lovastatin and amiodarone or itraconazole (augments statin’s effect) |
| Theophylline and cimetidine or ciprofloxacin (augments theophylline’s effect) |
| MAOIs, monoamine oxidase inhibitors; OCs, oral contraceptives; PPIs, proton pump inhibitors; SSRIs, selective serotonin reuptake inhibitors. |
| *For a complete list of drugs that may interact with simvastatin, see US Food and Drug Administration.28 |
FREE
- Epocrates Rx
http://www.epocrates.com/products/rx/ - eRx (National ePrescribing Patient Safety Initiative)
http://www.nationalerx.com/
FEE-BASED
- GeneMedRx (Drug-drug and drug-gene interactions)
http://www.genemedrx.com/provider-info.php
$199/year - iFacts (Drug Interaction Facts)
http://www.skyscape.com/EStore/ProductDetail.aspx?ProductID=217
$59.95/year - PEPID Portable Drug Companion
http://www.pepid.com/products/pdc/
$89.95/year
How is the drug metabolized?
DDIs may occur as a result of pharmaco-dynamic interaction (when 2 drugs act on the same receptor, site of action, or physiologic system) or pharmacokinetic changes (interference with absorption, albumin binding, distribution, metabolism, or elimination).23 As already noted, age-related changes in pharmacokinetics and pharmacodynamics contribute to the high prevalence of DDIs in elderly patients.
In the liver, drug metabolism, particularly via the cytochrome P450 (CYP450) system, is the cornerstone of drug transformation.23 Al-though the CYP system consists of “superfami-lies” with more than 100 types of enzymes, only a few are responsible for the majority of biotransformation.23 The CYP system is also subject to genetic polymorphism, making some patients especially prone to DDIs.
P-glycoproteins (PGPs), which regulate drug absorption by transporting the drugs across cell membranes, also play a key role. PGP inhibitors or inducers help determine whether the accumulation of the molecule or the increased delivery of toxic metabolites leads to adverse effects.10
Reviewing the mechanism of action of any drug you prescribe for a patient taking other medications may alert you to a potential DDI—and the need to either switch the newly prescribed agent or alter the individual’s drug regimen in some other way.
CASE When John was readmitted to the hospital, he was taken off both the lovastatin and amiodarone and hydrated with forced alkaline diuresis. After a week, his symptoms resolved, and he was discharged soon after. His blood tests normalized 1 month later. The severe DDI he experienced occurred because lovastatin (which is metabolized primarily by CYP3A4) and amiodarone (a CYP3A4 inhibitor) were taken together. (Statins that are substrates of CYP3A4 have the greatest potential for interacting with drugs known to inhibit the CYP450 system [eg, cyclosporine, morphine derivatives, ketoconazole, and amiodarone].)
This adverse interaction could have been avoided if the physician who started John on amiodarone had been aware of the potential DDI—and switched him to an HMG-CoA inhibitor other than lovastatin. Pravastatin, which is not metabolized via CYP450, would have been an excellent choice.
Warfarin warrants special attention
Medications that have a particularly high potential for adverse interactions require special attention and patient monitoring, warfarin foremost among them. Warfarin metabolism and its anticoagulant effects can be dramatically changed if it is administered with a drug with a higher affinity for PGPs or an agent that competes with it within the CYP450 system.24 Because of warfarin’s narrow therapeutic range, there are many drugs and drug classes that patients on warfarin should avoid (TABLE 3)—a fact that patients as well as their physicians need to be aware of.24 Indeed, warfarin is often involved in drug-related hospital admissions for DDIs, especially in elderly patients and in those who are also taking nonsteroidal anti-inflamma-tory drugs (NSAIDs) or macrolides—2 of the many drug classes that patients taking warfarin should avoid.24
TABLE 3
Patient on warfarin? Steer clear of these drugs10,20,23
| Drug class: agent(s) |
|---|
| Antiarrhythmics: amiodarone, propafenone |
| Antibiotics: ciprofloxacin, metronidazole, rifampin, trimethoprim/sulfamethoxazole |
| Anticonvulsants: carbamazepine, valproate |
| Antidepressants: fluoxetine, fluvoxamine, paroxetine, sertraline, trazodone |
| Antidiabetics: chlorpropamide |
| Antifungals: danazol, fluconazole, itraconazole, miconazole |
| Antimalarial agents: quinidine |
| Antineoplastics: azathioprine, fluorouracil, flutamide, ifosfamide, tamoxifen |
| Antiplatelet agents: ticlopidine |
| Antipsychotics: clozapine |
| Diuretics: spironolactone |
| GI drugs: cimetidine, esomeprazole, lansoprazole, omeprazole, pantoprazole, rabeprazole, ranitidine |
| Gout treatment: allopurinol |
| Hypolipidemics: atorvastatin, cholestyramine, ezetimibe, fenofibrate, fluvastatin, gemfibrozil, lovastatin, pravastatin, simvastatin |
| NSAIDs: aspirin, celecoxib, diclofenac, ibuprofen, indomethacin, ketoprofen, ketorolac, naproxen, piroxicam, sulindac |
| Thrombolytics: heparin, tissue plasminogen activator |
| Thyroid drugs: methimazole, propylthiouracil |
| Uricosuric agents: sulfinpyrazone |
| GI, gastrointestinal; NSAIDs, nonsteroidal anti-inflammatory drugs. |
Keep an eye on these drug combinations, as well
Among the many combinations likely to result in clinically significant DDIs (TABLE 2), the following are worth mentioning:
Clopidogrel + certain proton pump inhibitors. The addition of a PPI to clopidogrel has been associated with a significant increase of recurrent infarction.25 This may occur because clopidogrel is a prodrug and is converted in the liver to its active form by CYP2C19, an enzyme specifically inhibited by various PPIs—thereby altering the effectiveness of the antiplatelet agent. However, a recent analysis suggests that there is no need to avoid the concomitant use of a PPI and clopidogrel—and that the interference appears to be limited to omeprazole and esomeprazole.26
Oral contraceptives (OCs) + penicillins, phenobarbital, or tetracycline. Each of these drugs reduces the effect of OCs, and women who are taking them concomitantly need to be advised to use another means of contraception.
Phenobarbital + simvastatin. Pheno-barbital (a CYP3A4 inducer) may reduce the efficacy of simvastatin.
Repaglinide + diltiazem. Diltiazem inhibits the metabolism of repaglinide (a CYP3A4 substrate), thus increasing the risk of hypoglycemia.
Simvastatin + amiodarone or itraconazole. Either of these antiarrhythmic agents decreases simvastatin metabolism, raising the risk of myopathy; with amiodarone, however, the likelihood of an adverse outcome is especially high. In 2008, the US Food and Drug Administration (FDA) issued a warning to healthcare professionals of the increased risk for rhabdomyolysis when simvastatin doses greater than 20 mg are administered together with amiodarone.27 The agency issued a safety review of simvastatin, warning of its potential for DDIs with amiodarone and numerous other medications, earlier this year.28
As John’s case illustrates, use of lovastatin with amiodarone should be avoided, as well.
Keep others safe: Report adverse events
When a DDI occurs despite your best efforts, you can help ensure that other patients do not experience the same adverse outcome by reporting it to MedWatch, the FDA’s voluntary safety information and adverse event reporting program. Go to https://www.accessdata.fda.gov/scripts/medwatch/medwatch-online.htm to file a report online.
CORRESPONDENCE Ignazio Grattagliano, MD, General Medicine, Department of Internal and Public Medicine, University of Bari, P.zza G. Cesare, 11 – 70124, Bari, Italy; [email protected]
1. Becker ML, Kallewaard M, Caspers PW, et al. Hospitalisations and emergency department visits due to drug-drug interactions: a literature review. Pharmacoepidemiol Drug Saf. 2007;16:641-651.
2. Juurlink DN, Mamdani M, Kopp A, et al. Drug-drug interactions among elderly patients hospitalized for drug toxicity. JAMA. 2003;289:1652-1658.
3. Tulner LR, Frankfort SV, Gijsen GJ, et al. Drug-drug interactions in a geriatric outpatient cohort: prevalence and relevance. Drugs Aging. 2008;25:343-355.
4. Cadieux RJ. Drug interactions in the elderly. How multiple drug use increases risk exponentially. Postgrad Med. 1989;86:179-186.
5. Shapiro LE, Shear NH. Drug interactions: proteins, pumps, and P-450s. J Am Acad Dermatol. 2002;47:467-484.
6. Sitar DS. Aging issues in drug disposition and efficacy. Proc West Pharmacol Soc. 2007;50:16-20.
7. El Desoky ES, Derendorf H, Klotz U. Variability in response to cardiovascular drugs. Curr Clin Pharmacol. 2006;1:35-46.
8. Aparasu R, Baer R, Aparasu A. Clinically important potential drug-drug interactions in outpatient settings. Res Social Adm Pharm. 2007;3:426-437.
9. Becker ML, Kallewaard M, Caspers PW, et al. Potential determinants of drug-drug interaction associated dispensing in community pharmacies. Drug Saf. 2005;28:371-378.
10. Johnson TN, Thomson M. Intestinal metabolism and transport of drugs in children: the effects of age and disease. J Pediatr Gastroenterol Nutr. 2008;47:3-10.
11. Buurma H, Bouvy ML, De Smet PA, et al. Prevalence and determinants of pharmacy shopping behaviour. J Clin Pharm Ther. 2008;33:17-23.
12. Russmann S, Barguil Y, Cabalion P, et al. Hepatic injury due to traditional aqueous extracts of kava root in New Caledonia. Eur J Gastroenterol Hepatol. 2003;5:1033-1036.
13. Stickel F, Patsenker E, Schuppan D. Herbal hepatotoxicity. J Hepatol. 2005;43:901-910.
14. Institute for Safe Medication Practices. ISMP medication safety alert! Available at: http://www.ismp.org/Newsletters/consumer/alerts/BrownBag.asp. Accessed May 5, 2010.
15. National Institute on Aging. Obtaining the medical history. Available at: http://www.nia.nih.gov/Healthinformation/Publications/ClinicianHB/03_history.htm. Accessed May 5, 2010.
16. Glassman PA, Simon B, Belperio P, et al. Improving recognition of drug interactions: benefits and barriers to using automated drug alerts. Med Care. 2002;40:1161-1171.
17. Goldberg RM, Mabee J, Chan L, et al. Drug-drug and drug-disease interactions in the ED: analysis of a high-risk population. Am J Emerg Med. 1996;14:447-450.
18. Lapane KL, Waring ME, Schneider KL, et al. A mixed method study of the merits of e-prescribing drug alerts in primary care. J Gen Intern Med. 2008;23:442-446.
19. Magnus D, Rodgers S, Avery AJ. GPs’ views on computerized drug interaction alerts: questionnaire survey. J Clin Pharm Ther. 2002;27:377-382.
20. Shukla UA, Pittman KA, Barbhaiya RH. Pharmacokinetic interactions of cefprozil with food, propantheline, metoclopramide, and probenecid in healthy volunteers. J Clin Pharmacol. 1992;32:725-731.
21. Levy RH, Collins C. Risk and predictability of drug interactions in the elderly. Int Rev Neurobiol. 2007;81:235-251.
22. Pauwels O. Factors contributing to carbamazepine-macrolide interactions. Pharmacol Res. 2002;45:291-298.
23. Beaird SL. HMG-CoA reductase inhibitors: assessing differences in drug interactions and safety profiles. J Am Pharm Assoc (Wash). 2000;40:637-644.
24. Snaith A, Pugh L, Simpson CR, et al. The potential for interaction between warfarin and coprescribed medication: a retrospective study in primary care. Am J Cardiovasc Drugs. 2008;8:207-212.
25. Juurlink DN, Gomes T, Ko DT, et al. A population-based study of the drug interaction between proton pump inhibitors and clopidogrel. CMAJ. 2009;180:713-718.
26. O’Donoghue ML, Braunwald E, Antman EM, et al. Pharmaco-dynamic effect and clinical efficacy of clopidogrel and prasugrel with or without a proton-pump inhibitor: an analysis of two randomised trials. Lancet. 2009;374:989-997.
27. US Food and Drug Administration. Serious muscle injury with simvastatin/amiodarone combination. November 2008. Available at: http://www.accessdata.fda.gov/psn/printer.cfm?id=886. Accessed May 5, 2010.
28. US Food and Drug Administration. FDA drug safety communication: ongoing safety review of high-dose Zocor (simvastatin) and increased risk of muscle injury. March 19, 2010. Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/
ucm204882.htm. Accessed May 5, 2010.
Be sure to inquire about over-the-counter drugs, herbal remedies, vitamins, and supplements when taking a medication history. A
Use an electronic prescribing software system that flags potential drug-drug interactions. A
Consider adjusting a dosing regimen or temporarily discontinuing a maintenance medication if the drug you are about to prescribe is likely to interact with another agent the patient is taking (and there are no alternatives you can prescribe). B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE John L, a 63-year-old man taking lovastatin (40 mg/d) and ramipril (5 mg/d) for hypercholesterolemia and arterial hypertension was hospitalized with atrial fibrillation. Three days later, he was discharged, with a prescription for amiodarone (200 mg/d). After a month, he was readmitted to the hospital with dark urine and intensifying thigh weakness and achiness. Laboratory testing revealed aspartate aminotransferase and alanine aminotransferase levels 10 times the upper limit of normal, and elevated urine and serum myoglobin.
Drug-drug interactions (DDIs) like the one John experienced between lovastatin and amiodarone are a common cause of readmissions, as well as emergency department visits and hospitalizations, for everything from myopathy to electrolyte imbalance, gastrointestinal (GI) bleeding, hepatotoxicity, renal dysfunction, and changes in blood pressure and heart rate.1-3
Yet many, if not most, DDIs can be avoided. With diligence and the right tools, you can do much to reduce the incidence of such interactions and adverse outcomes.
Polypharmacy and age pose the highest risks
The more medications a patient is taking, of course, the greater the likelihood of a clinically significant DDI. According to 1 study, 13% of patients taking 2 drugs develop a DDI; the incidence approaches 40% for patients taking 5 drugs, and exceeds 80% for patients taking 7 or more medications.4
In addition to polypharmacy, age alone is a key risk factor for DDIs.5 Pharmacokinetics and pharmacodynamics are frequently altered in older people, who may have slower intestinal transit time; diminished absorption capacity; decreased liver metabolism, mitochondrial function, and renal excretion; and alterations in volemia and body fat distribution.6 Although the speed at which these changes occur varies, aging is associated with a progressive deficiency in the regulation of most homeo-static mechanisms and an altered response to receptor stimulation.7
Whether age, multiple medications, or both are to blame, the impact on the elderly is striking. One recent retrospective study found 25% of elderly outpatients to be at risk for DDIs.8
Very young patients (<5 years) are also at risk for DDIs because of the immaturity of their enzymatic metabolic system.5,9,10 Additional risk factors, detailed in TABLE 1, include the presence of an infection or other acute medical condition, a metabolic or endocrine disorder, and taking 1 or more drugs with a narrow therapeutic range. Women are also at higher risk for DDIs than their male counterparts, the result of a slower metabolic capacity and interference with sex hormones.3-5,8,9 Pharmacogenetics may also play a big part in DDIs, and more and more studies are focusing on identifying patients at greatest risk.
TABLE 1
Risk factors for drug-drug interactions3-5,8,9
| Risk factor | Potential result |
|---|---|
| Acute medical condition (eg, dehydration, infection, alcoholism) | Augmented risk of elevated plasma drug concentration, increased catabolism, inhibition of hepatic drug metabolism |
| Age (very young [<5 years] and elderly) | Reduced metabolic capacity (greater accumulation of drugs) |
| Decreased renal and/or hepatic function | Decreased drug clearance/elimination; greater accumulation of drugs or their metabolites |
| Drug(s) with narrow therapeutic range | Increased risk for dose-related side effects |
| Female sex | Reduced metabolic capacity, interference with sex hormones |
| Metabolic or endocrine conditions (eg, fatty liver, obesity, hypothyroidism) | Altered hepatic metabolism, increased body distribution volumes, augmented risk of accumulation for hydrophobic molecules |
| Polypharmacy (≥3 medications) | Increased risk of metabolic and/or pharmacodynamic interference |
| Pharmacogenetics | Altered metabolic capacity (greater accumulation of drugs or their metabolites) |
Lack of coordinated care also increases risk
Another risk factor involves the use of multiple providers.9 A woman may be treated by—and receive prescriptions from—an endocrinolo-gist, a gynecologist, and a family physician (FP), for instance, and get medications from a local pharmacy, a nationwide discount chain, and a mail order pharmacy. As with the number of medications being taken, the greater the number of health care professionals a patient sees, the higher the risk.
To mitigate the risk, encourage your patients to fill all their prescriptions at the same pharmacy—and for your part, take a complete medication history before writing a new prescription.
Medication history in doubt? Schedule a “brown bag review”
Ask patients to provide the name and dose of every medication they’re taking. Inquire specifically about over-the-counter (OTC) cough and cold remedies and complementary and alternative medicines, including herbal remedies, vitamins, and supplements. Patients often neglect to mention nonprescription remedies and may not even think of them as medicine, but OTC products with the potential to interact adversely with prescription drugs may otherwise remain undetected.11-13
Consider a “brown bag review” for patients who don’t know what dosage they’re taking or have difficulty identifying the drugs other physicians have prescribed. Ask them to put all their medications in a brown bag and bring them in on their next visit.14,15
Steps to take to reduce risk
Software systems. A number of free and low-cost software systems identify potential DDIs (See “Check for drug interactions: Software programs to consider”). While such electronic programs can indeed lower the risk,16-18 they cannot be counted on to detect or avert every possible adverse interaction.
The downside. One problem is that some software programs fail to distinguish between clinically significant and nonsignificant interactions, causing some prescribers to override system alerts—and possibly miss an important warning.19 Another problem: While most systems do an excellent job of checking to see whether 2 drugs can be safely taken together, few are capable of checking for all potential interactions among multiple medications. What’s more, many drugs have not been evaluated for their potential to interact with other agents, so the absence of reported interactions is no guarantee of a lack of DDIs.
Other strategies to consider:
Minimize the number of prescriptions. While it may not be possible to avoid prescribing a new agent for a patient who is already taking multiple medications, limiting the number of new drugs to those that are absolutely essential will help to minimize DDIs. Whenever possible, select a compound with the desired effects. Prescribe a single agent with antihypertensive as well as uricosuric effects for a patient with elevated blood pressure and uric acid levels rather than 2 different drugs (eg, losartan instead of an anti-hypertensive agent plus allopurinol).
Alter the dosing regimen. Several active molecules may cause DDIs by interfering with intestinal absorption or GI transit time if they’re taken closely together. For example, a quinolone should not be administered at the same time as a cation because of possible chelation in the GI tract. If a patient needs both, however, you may be able to avert a DDI by advising the patient to take them at least 2 hours apart.20 Another possibility is to temporarily discontinue a maintenance medication if it has the potential to interact adversely with a drug that is needed for only a short duration.
Choose a different drug (or drug class). Some drug classes should never be mixed—nitrates and phosphodiesterase type-5 inhibitors, taken together, greatly increase the risk of vasodilation and may result in severe hypotension, for example. There are also drug classes with a low potential for DDIs, including cholinesterase inhibitors and anti-hypertensives (angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, beta-blockers, and thiazides).21
Frequently, though, medications within the same drug class do not share the same potential for DDIs. In such cases, an adverse outcome can often be averted by being aware of combinations likely to result in clinically significant DDIs (TABLE 2) and, whenever possible, prescribing another agent. If a patient taking carbamazepine needs a macro-lide antibiotic, for instance, azithromycin is a better choice than erythromycin. That’s because erythromycin inhibits the hepatic metabolism of the anticonvulsant, increasing the serum level of carbamazepine, while azithromycin does not interfere with carbamazepine metabolism.22
TABLE 2
Clinically significant drug-drug interactions21,22
| Combination (effect) |
|---|
| Allopurinol and captopril (augments allopurinol’s effect) |
| Antidepressants (SSRIs, MAOIs) and antiepileptics (augments antidepressant effect) |
| Clopidogrel and omeprazole or esomeprazole (reduces clopidogrel’s effect) |
| Erythromycin and carbamazepine (augments carbamazepine’s effect) |
| Erythromycin and terfenadine (augments terfenadine’s effect) |
| Ketoconazole and PPIs (reduces ketoconazole’s absorption) |
| Levodopa and metoclopramide (augments levodopa’s effect) |
| MAOIs and narcotic analgesics (augments effects of both drugs) |
| Nitrates and phosphodiesterase type-5 inhibitors (augments effects of both drugs) |
| OCs and penicillins, phenobarbital, or tetracycline (reduces OCs’ effect) |
| Phenobarbital and simvastatin* (reduces simvastatin’s effect) |
| Quinolone and cation (reduces quinolone’s absorption and effect) |
| Repaglinide and diltiazem (augments repaglinide’s effect) |
| Simvastatin* or lovastatin and amiodarone or itraconazole (augments statin’s effect) |
| Theophylline and cimetidine or ciprofloxacin (augments theophylline’s effect) |
| MAOIs, monoamine oxidase inhibitors; OCs, oral contraceptives; PPIs, proton pump inhibitors; SSRIs, selective serotonin reuptake inhibitors. |
| *For a complete list of drugs that may interact with simvastatin, see US Food and Drug Administration.28 |
FREE
- Epocrates Rx
http://www.epocrates.com/products/rx/ - eRx (National ePrescribing Patient Safety Initiative)
http://www.nationalerx.com/
FEE-BASED
- GeneMedRx (Drug-drug and drug-gene interactions)
http://www.genemedrx.com/provider-info.php
$199/year - iFacts (Drug Interaction Facts)
http://www.skyscape.com/EStore/ProductDetail.aspx?ProductID=217
$59.95/year - PEPID Portable Drug Companion
http://www.pepid.com/products/pdc/
$89.95/year
How is the drug metabolized?
DDIs may occur as a result of pharmaco-dynamic interaction (when 2 drugs act on the same receptor, site of action, or physiologic system) or pharmacokinetic changes (interference with absorption, albumin binding, distribution, metabolism, or elimination).23 As already noted, age-related changes in pharmacokinetics and pharmacodynamics contribute to the high prevalence of DDIs in elderly patients.
In the liver, drug metabolism, particularly via the cytochrome P450 (CYP450) system, is the cornerstone of drug transformation.23 Al-though the CYP system consists of “superfami-lies” with more than 100 types of enzymes, only a few are responsible for the majority of biotransformation.23 The CYP system is also subject to genetic polymorphism, making some patients especially prone to DDIs.
P-glycoproteins (PGPs), which regulate drug absorption by transporting the drugs across cell membranes, also play a key role. PGP inhibitors or inducers help determine whether the accumulation of the molecule or the increased delivery of toxic metabolites leads to adverse effects.10
Reviewing the mechanism of action of any drug you prescribe for a patient taking other medications may alert you to a potential DDI—and the need to either switch the newly prescribed agent or alter the individual’s drug regimen in some other way.
CASE When John was readmitted to the hospital, he was taken off both the lovastatin and amiodarone and hydrated with forced alkaline diuresis. After a week, his symptoms resolved, and he was discharged soon after. His blood tests normalized 1 month later. The severe DDI he experienced occurred because lovastatin (which is metabolized primarily by CYP3A4) and amiodarone (a CYP3A4 inhibitor) were taken together. (Statins that are substrates of CYP3A4 have the greatest potential for interacting with drugs known to inhibit the CYP450 system [eg, cyclosporine, morphine derivatives, ketoconazole, and amiodarone].)
This adverse interaction could have been avoided if the physician who started John on amiodarone had been aware of the potential DDI—and switched him to an HMG-CoA inhibitor other than lovastatin. Pravastatin, which is not metabolized via CYP450, would have been an excellent choice.
Warfarin warrants special attention
Medications that have a particularly high potential for adverse interactions require special attention and patient monitoring, warfarin foremost among them. Warfarin metabolism and its anticoagulant effects can be dramatically changed if it is administered with a drug with a higher affinity for PGPs or an agent that competes with it within the CYP450 system.24 Because of warfarin’s narrow therapeutic range, there are many drugs and drug classes that patients on warfarin should avoid (TABLE 3)—a fact that patients as well as their physicians need to be aware of.24 Indeed, warfarin is often involved in drug-related hospital admissions for DDIs, especially in elderly patients and in those who are also taking nonsteroidal anti-inflamma-tory drugs (NSAIDs) or macrolides—2 of the many drug classes that patients taking warfarin should avoid.24
TABLE 3
Patient on warfarin? Steer clear of these drugs10,20,23
| Drug class: agent(s) |
|---|
| Antiarrhythmics: amiodarone, propafenone |
| Antibiotics: ciprofloxacin, metronidazole, rifampin, trimethoprim/sulfamethoxazole |
| Anticonvulsants: carbamazepine, valproate |
| Antidepressants: fluoxetine, fluvoxamine, paroxetine, sertraline, trazodone |
| Antidiabetics: chlorpropamide |
| Antifungals: danazol, fluconazole, itraconazole, miconazole |
| Antimalarial agents: quinidine |
| Antineoplastics: azathioprine, fluorouracil, flutamide, ifosfamide, tamoxifen |
| Antiplatelet agents: ticlopidine |
| Antipsychotics: clozapine |
| Diuretics: spironolactone |
| GI drugs: cimetidine, esomeprazole, lansoprazole, omeprazole, pantoprazole, rabeprazole, ranitidine |
| Gout treatment: allopurinol |
| Hypolipidemics: atorvastatin, cholestyramine, ezetimibe, fenofibrate, fluvastatin, gemfibrozil, lovastatin, pravastatin, simvastatin |
| NSAIDs: aspirin, celecoxib, diclofenac, ibuprofen, indomethacin, ketoprofen, ketorolac, naproxen, piroxicam, sulindac |
| Thrombolytics: heparin, tissue plasminogen activator |
| Thyroid drugs: methimazole, propylthiouracil |
| Uricosuric agents: sulfinpyrazone |
| GI, gastrointestinal; NSAIDs, nonsteroidal anti-inflammatory drugs. |
Keep an eye on these drug combinations, as well
Among the many combinations likely to result in clinically significant DDIs (TABLE 2), the following are worth mentioning:
Clopidogrel + certain proton pump inhibitors. The addition of a PPI to clopidogrel has been associated with a significant increase of recurrent infarction.25 This may occur because clopidogrel is a prodrug and is converted in the liver to its active form by CYP2C19, an enzyme specifically inhibited by various PPIs—thereby altering the effectiveness of the antiplatelet agent. However, a recent analysis suggests that there is no need to avoid the concomitant use of a PPI and clopidogrel—and that the interference appears to be limited to omeprazole and esomeprazole.26
Oral contraceptives (OCs) + penicillins, phenobarbital, or tetracycline. Each of these drugs reduces the effect of OCs, and women who are taking them concomitantly need to be advised to use another means of contraception.
Phenobarbital + simvastatin. Pheno-barbital (a CYP3A4 inducer) may reduce the efficacy of simvastatin.
Repaglinide + diltiazem. Diltiazem inhibits the metabolism of repaglinide (a CYP3A4 substrate), thus increasing the risk of hypoglycemia.
Simvastatin + amiodarone or itraconazole. Either of these antiarrhythmic agents decreases simvastatin metabolism, raising the risk of myopathy; with amiodarone, however, the likelihood of an adverse outcome is especially high. In 2008, the US Food and Drug Administration (FDA) issued a warning to healthcare professionals of the increased risk for rhabdomyolysis when simvastatin doses greater than 20 mg are administered together with amiodarone.27 The agency issued a safety review of simvastatin, warning of its potential for DDIs with amiodarone and numerous other medications, earlier this year.28
As John’s case illustrates, use of lovastatin with amiodarone should be avoided, as well.
Keep others safe: Report adverse events
When a DDI occurs despite your best efforts, you can help ensure that other patients do not experience the same adverse outcome by reporting it to MedWatch, the FDA’s voluntary safety information and adverse event reporting program. Go to https://www.accessdata.fda.gov/scripts/medwatch/medwatch-online.htm to file a report online.
CORRESPONDENCE Ignazio Grattagliano, MD, General Medicine, Department of Internal and Public Medicine, University of Bari, P.zza G. Cesare, 11 – 70124, Bari, Italy; [email protected]
Be sure to inquire about over-the-counter drugs, herbal remedies, vitamins, and supplements when taking a medication history. A
Use an electronic prescribing software system that flags potential drug-drug interactions. A
Consider adjusting a dosing regimen or temporarily discontinuing a maintenance medication if the drug you are about to prescribe is likely to interact with another agent the patient is taking (and there are no alternatives you can prescribe). B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE John L, a 63-year-old man taking lovastatin (40 mg/d) and ramipril (5 mg/d) for hypercholesterolemia and arterial hypertension was hospitalized with atrial fibrillation. Three days later, he was discharged, with a prescription for amiodarone (200 mg/d). After a month, he was readmitted to the hospital with dark urine and intensifying thigh weakness and achiness. Laboratory testing revealed aspartate aminotransferase and alanine aminotransferase levels 10 times the upper limit of normal, and elevated urine and serum myoglobin.
Drug-drug interactions (DDIs) like the one John experienced between lovastatin and amiodarone are a common cause of readmissions, as well as emergency department visits and hospitalizations, for everything from myopathy to electrolyte imbalance, gastrointestinal (GI) bleeding, hepatotoxicity, renal dysfunction, and changes in blood pressure and heart rate.1-3
Yet many, if not most, DDIs can be avoided. With diligence and the right tools, you can do much to reduce the incidence of such interactions and adverse outcomes.
Polypharmacy and age pose the highest risks
The more medications a patient is taking, of course, the greater the likelihood of a clinically significant DDI. According to 1 study, 13% of patients taking 2 drugs develop a DDI; the incidence approaches 40% for patients taking 5 drugs, and exceeds 80% for patients taking 7 or more medications.4
In addition to polypharmacy, age alone is a key risk factor for DDIs.5 Pharmacokinetics and pharmacodynamics are frequently altered in older people, who may have slower intestinal transit time; diminished absorption capacity; decreased liver metabolism, mitochondrial function, and renal excretion; and alterations in volemia and body fat distribution.6 Although the speed at which these changes occur varies, aging is associated with a progressive deficiency in the regulation of most homeo-static mechanisms and an altered response to receptor stimulation.7
Whether age, multiple medications, or both are to blame, the impact on the elderly is striking. One recent retrospective study found 25% of elderly outpatients to be at risk for DDIs.8
Very young patients (<5 years) are also at risk for DDIs because of the immaturity of their enzymatic metabolic system.5,9,10 Additional risk factors, detailed in TABLE 1, include the presence of an infection or other acute medical condition, a metabolic or endocrine disorder, and taking 1 or more drugs with a narrow therapeutic range. Women are also at higher risk for DDIs than their male counterparts, the result of a slower metabolic capacity and interference with sex hormones.3-5,8,9 Pharmacogenetics may also play a big part in DDIs, and more and more studies are focusing on identifying patients at greatest risk.
TABLE 1
Risk factors for drug-drug interactions3-5,8,9
| Risk factor | Potential result |
|---|---|
| Acute medical condition (eg, dehydration, infection, alcoholism) | Augmented risk of elevated plasma drug concentration, increased catabolism, inhibition of hepatic drug metabolism |
| Age (very young [<5 years] and elderly) | Reduced metabolic capacity (greater accumulation of drugs) |
| Decreased renal and/or hepatic function | Decreased drug clearance/elimination; greater accumulation of drugs or their metabolites |
| Drug(s) with narrow therapeutic range | Increased risk for dose-related side effects |
| Female sex | Reduced metabolic capacity, interference with sex hormones |
| Metabolic or endocrine conditions (eg, fatty liver, obesity, hypothyroidism) | Altered hepatic metabolism, increased body distribution volumes, augmented risk of accumulation for hydrophobic molecules |
| Polypharmacy (≥3 medications) | Increased risk of metabolic and/or pharmacodynamic interference |
| Pharmacogenetics | Altered metabolic capacity (greater accumulation of drugs or their metabolites) |
Lack of coordinated care also increases risk
Another risk factor involves the use of multiple providers.9 A woman may be treated by—and receive prescriptions from—an endocrinolo-gist, a gynecologist, and a family physician (FP), for instance, and get medications from a local pharmacy, a nationwide discount chain, and a mail order pharmacy. As with the number of medications being taken, the greater the number of health care professionals a patient sees, the higher the risk.
To mitigate the risk, encourage your patients to fill all their prescriptions at the same pharmacy—and for your part, take a complete medication history before writing a new prescription.
Medication history in doubt? Schedule a “brown bag review”
Ask patients to provide the name and dose of every medication they’re taking. Inquire specifically about over-the-counter (OTC) cough and cold remedies and complementary and alternative medicines, including herbal remedies, vitamins, and supplements. Patients often neglect to mention nonprescription remedies and may not even think of them as medicine, but OTC products with the potential to interact adversely with prescription drugs may otherwise remain undetected.11-13
Consider a “brown bag review” for patients who don’t know what dosage they’re taking or have difficulty identifying the drugs other physicians have prescribed. Ask them to put all their medications in a brown bag and bring them in on their next visit.14,15
Steps to take to reduce risk
Software systems. A number of free and low-cost software systems identify potential DDIs (See “Check for drug interactions: Software programs to consider”). While such electronic programs can indeed lower the risk,16-18 they cannot be counted on to detect or avert every possible adverse interaction.
The downside. One problem is that some software programs fail to distinguish between clinically significant and nonsignificant interactions, causing some prescribers to override system alerts—and possibly miss an important warning.19 Another problem: While most systems do an excellent job of checking to see whether 2 drugs can be safely taken together, few are capable of checking for all potential interactions among multiple medications. What’s more, many drugs have not been evaluated for their potential to interact with other agents, so the absence of reported interactions is no guarantee of a lack of DDIs.
Other strategies to consider:
Minimize the number of prescriptions. While it may not be possible to avoid prescribing a new agent for a patient who is already taking multiple medications, limiting the number of new drugs to those that are absolutely essential will help to minimize DDIs. Whenever possible, select a compound with the desired effects. Prescribe a single agent with antihypertensive as well as uricosuric effects for a patient with elevated blood pressure and uric acid levels rather than 2 different drugs (eg, losartan instead of an anti-hypertensive agent plus allopurinol).
Alter the dosing regimen. Several active molecules may cause DDIs by interfering with intestinal absorption or GI transit time if they’re taken closely together. For example, a quinolone should not be administered at the same time as a cation because of possible chelation in the GI tract. If a patient needs both, however, you may be able to avert a DDI by advising the patient to take them at least 2 hours apart.20 Another possibility is to temporarily discontinue a maintenance medication if it has the potential to interact adversely with a drug that is needed for only a short duration.
Choose a different drug (or drug class). Some drug classes should never be mixed—nitrates and phosphodiesterase type-5 inhibitors, taken together, greatly increase the risk of vasodilation and may result in severe hypotension, for example. There are also drug classes with a low potential for DDIs, including cholinesterase inhibitors and anti-hypertensives (angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, beta-blockers, and thiazides).21
Frequently, though, medications within the same drug class do not share the same potential for DDIs. In such cases, an adverse outcome can often be averted by being aware of combinations likely to result in clinically significant DDIs (TABLE 2) and, whenever possible, prescribing another agent. If a patient taking carbamazepine needs a macro-lide antibiotic, for instance, azithromycin is a better choice than erythromycin. That’s because erythromycin inhibits the hepatic metabolism of the anticonvulsant, increasing the serum level of carbamazepine, while azithromycin does not interfere with carbamazepine metabolism.22
TABLE 2
Clinically significant drug-drug interactions21,22
| Combination (effect) |
|---|
| Allopurinol and captopril (augments allopurinol’s effect) |
| Antidepressants (SSRIs, MAOIs) and antiepileptics (augments antidepressant effect) |
| Clopidogrel and omeprazole or esomeprazole (reduces clopidogrel’s effect) |
| Erythromycin and carbamazepine (augments carbamazepine’s effect) |
| Erythromycin and terfenadine (augments terfenadine’s effect) |
| Ketoconazole and PPIs (reduces ketoconazole’s absorption) |
| Levodopa and metoclopramide (augments levodopa’s effect) |
| MAOIs and narcotic analgesics (augments effects of both drugs) |
| Nitrates and phosphodiesterase type-5 inhibitors (augments effects of both drugs) |
| OCs and penicillins, phenobarbital, or tetracycline (reduces OCs’ effect) |
| Phenobarbital and simvastatin* (reduces simvastatin’s effect) |
| Quinolone and cation (reduces quinolone’s absorption and effect) |
| Repaglinide and diltiazem (augments repaglinide’s effect) |
| Simvastatin* or lovastatin and amiodarone or itraconazole (augments statin’s effect) |
| Theophylline and cimetidine or ciprofloxacin (augments theophylline’s effect) |
| MAOIs, monoamine oxidase inhibitors; OCs, oral contraceptives; PPIs, proton pump inhibitors; SSRIs, selective serotonin reuptake inhibitors. |
| *For a complete list of drugs that may interact with simvastatin, see US Food and Drug Administration.28 |
FREE
- Epocrates Rx
http://www.epocrates.com/products/rx/ - eRx (National ePrescribing Patient Safety Initiative)
http://www.nationalerx.com/
FEE-BASED
- GeneMedRx (Drug-drug and drug-gene interactions)
http://www.genemedrx.com/provider-info.php
$199/year - iFacts (Drug Interaction Facts)
http://www.skyscape.com/EStore/ProductDetail.aspx?ProductID=217
$59.95/year - PEPID Portable Drug Companion
http://www.pepid.com/products/pdc/
$89.95/year
How is the drug metabolized?
DDIs may occur as a result of pharmaco-dynamic interaction (when 2 drugs act on the same receptor, site of action, or physiologic system) or pharmacokinetic changes (interference with absorption, albumin binding, distribution, metabolism, or elimination).23 As already noted, age-related changes in pharmacokinetics and pharmacodynamics contribute to the high prevalence of DDIs in elderly patients.
In the liver, drug metabolism, particularly via the cytochrome P450 (CYP450) system, is the cornerstone of drug transformation.23 Al-though the CYP system consists of “superfami-lies” with more than 100 types of enzymes, only a few are responsible for the majority of biotransformation.23 The CYP system is also subject to genetic polymorphism, making some patients especially prone to DDIs.
P-glycoproteins (PGPs), which regulate drug absorption by transporting the drugs across cell membranes, also play a key role. PGP inhibitors or inducers help determine whether the accumulation of the molecule or the increased delivery of toxic metabolites leads to adverse effects.10
Reviewing the mechanism of action of any drug you prescribe for a patient taking other medications may alert you to a potential DDI—and the need to either switch the newly prescribed agent or alter the individual’s drug regimen in some other way.
CASE When John was readmitted to the hospital, he was taken off both the lovastatin and amiodarone and hydrated with forced alkaline diuresis. After a week, his symptoms resolved, and he was discharged soon after. His blood tests normalized 1 month later. The severe DDI he experienced occurred because lovastatin (which is metabolized primarily by CYP3A4) and amiodarone (a CYP3A4 inhibitor) were taken together. (Statins that are substrates of CYP3A4 have the greatest potential for interacting with drugs known to inhibit the CYP450 system [eg, cyclosporine, morphine derivatives, ketoconazole, and amiodarone].)
This adverse interaction could have been avoided if the physician who started John on amiodarone had been aware of the potential DDI—and switched him to an HMG-CoA inhibitor other than lovastatin. Pravastatin, which is not metabolized via CYP450, would have been an excellent choice.
Warfarin warrants special attention
Medications that have a particularly high potential for adverse interactions require special attention and patient monitoring, warfarin foremost among them. Warfarin metabolism and its anticoagulant effects can be dramatically changed if it is administered with a drug with a higher affinity for PGPs or an agent that competes with it within the CYP450 system.24 Because of warfarin’s narrow therapeutic range, there are many drugs and drug classes that patients on warfarin should avoid (TABLE 3)—a fact that patients as well as their physicians need to be aware of.24 Indeed, warfarin is often involved in drug-related hospital admissions for DDIs, especially in elderly patients and in those who are also taking nonsteroidal anti-inflamma-tory drugs (NSAIDs) or macrolides—2 of the many drug classes that patients taking warfarin should avoid.24
TABLE 3
Patient on warfarin? Steer clear of these drugs10,20,23
| Drug class: agent(s) |
|---|
| Antiarrhythmics: amiodarone, propafenone |
| Antibiotics: ciprofloxacin, metronidazole, rifampin, trimethoprim/sulfamethoxazole |
| Anticonvulsants: carbamazepine, valproate |
| Antidepressants: fluoxetine, fluvoxamine, paroxetine, sertraline, trazodone |
| Antidiabetics: chlorpropamide |
| Antifungals: danazol, fluconazole, itraconazole, miconazole |
| Antimalarial agents: quinidine |
| Antineoplastics: azathioprine, fluorouracil, flutamide, ifosfamide, tamoxifen |
| Antiplatelet agents: ticlopidine |
| Antipsychotics: clozapine |
| Diuretics: spironolactone |
| GI drugs: cimetidine, esomeprazole, lansoprazole, omeprazole, pantoprazole, rabeprazole, ranitidine |
| Gout treatment: allopurinol |
| Hypolipidemics: atorvastatin, cholestyramine, ezetimibe, fenofibrate, fluvastatin, gemfibrozil, lovastatin, pravastatin, simvastatin |
| NSAIDs: aspirin, celecoxib, diclofenac, ibuprofen, indomethacin, ketoprofen, ketorolac, naproxen, piroxicam, sulindac |
| Thrombolytics: heparin, tissue plasminogen activator |
| Thyroid drugs: methimazole, propylthiouracil |
| Uricosuric agents: sulfinpyrazone |
| GI, gastrointestinal; NSAIDs, nonsteroidal anti-inflammatory drugs. |
Keep an eye on these drug combinations, as well
Among the many combinations likely to result in clinically significant DDIs (TABLE 2), the following are worth mentioning:
Clopidogrel + certain proton pump inhibitors. The addition of a PPI to clopidogrel has been associated with a significant increase of recurrent infarction.25 This may occur because clopidogrel is a prodrug and is converted in the liver to its active form by CYP2C19, an enzyme specifically inhibited by various PPIs—thereby altering the effectiveness of the antiplatelet agent. However, a recent analysis suggests that there is no need to avoid the concomitant use of a PPI and clopidogrel—and that the interference appears to be limited to omeprazole and esomeprazole.26
Oral contraceptives (OCs) + penicillins, phenobarbital, or tetracycline. Each of these drugs reduces the effect of OCs, and women who are taking them concomitantly need to be advised to use another means of contraception.
Phenobarbital + simvastatin. Pheno-barbital (a CYP3A4 inducer) may reduce the efficacy of simvastatin.
Repaglinide + diltiazem. Diltiazem inhibits the metabolism of repaglinide (a CYP3A4 substrate), thus increasing the risk of hypoglycemia.
Simvastatin + amiodarone or itraconazole. Either of these antiarrhythmic agents decreases simvastatin metabolism, raising the risk of myopathy; with amiodarone, however, the likelihood of an adverse outcome is especially high. In 2008, the US Food and Drug Administration (FDA) issued a warning to healthcare professionals of the increased risk for rhabdomyolysis when simvastatin doses greater than 20 mg are administered together with amiodarone.27 The agency issued a safety review of simvastatin, warning of its potential for DDIs with amiodarone and numerous other medications, earlier this year.28
As John’s case illustrates, use of lovastatin with amiodarone should be avoided, as well.
Keep others safe: Report adverse events
When a DDI occurs despite your best efforts, you can help ensure that other patients do not experience the same adverse outcome by reporting it to MedWatch, the FDA’s voluntary safety information and adverse event reporting program. Go to https://www.accessdata.fda.gov/scripts/medwatch/medwatch-online.htm to file a report online.
CORRESPONDENCE Ignazio Grattagliano, MD, General Medicine, Department of Internal and Public Medicine, University of Bari, P.zza G. Cesare, 11 – 70124, Bari, Italy; [email protected]
1. Becker ML, Kallewaard M, Caspers PW, et al. Hospitalisations and emergency department visits due to drug-drug interactions: a literature review. Pharmacoepidemiol Drug Saf. 2007;16:641-651.
2. Juurlink DN, Mamdani M, Kopp A, et al. Drug-drug interactions among elderly patients hospitalized for drug toxicity. JAMA. 2003;289:1652-1658.
3. Tulner LR, Frankfort SV, Gijsen GJ, et al. Drug-drug interactions in a geriatric outpatient cohort: prevalence and relevance. Drugs Aging. 2008;25:343-355.
4. Cadieux RJ. Drug interactions in the elderly. How multiple drug use increases risk exponentially. Postgrad Med. 1989;86:179-186.
5. Shapiro LE, Shear NH. Drug interactions: proteins, pumps, and P-450s. J Am Acad Dermatol. 2002;47:467-484.
6. Sitar DS. Aging issues in drug disposition and efficacy. Proc West Pharmacol Soc. 2007;50:16-20.
7. El Desoky ES, Derendorf H, Klotz U. Variability in response to cardiovascular drugs. Curr Clin Pharmacol. 2006;1:35-46.
8. Aparasu R, Baer R, Aparasu A. Clinically important potential drug-drug interactions in outpatient settings. Res Social Adm Pharm. 2007;3:426-437.
9. Becker ML, Kallewaard M, Caspers PW, et al. Potential determinants of drug-drug interaction associated dispensing in community pharmacies. Drug Saf. 2005;28:371-378.
10. Johnson TN, Thomson M. Intestinal metabolism and transport of drugs in children: the effects of age and disease. J Pediatr Gastroenterol Nutr. 2008;47:3-10.
11. Buurma H, Bouvy ML, De Smet PA, et al. Prevalence and determinants of pharmacy shopping behaviour. J Clin Pharm Ther. 2008;33:17-23.
12. Russmann S, Barguil Y, Cabalion P, et al. Hepatic injury due to traditional aqueous extracts of kava root in New Caledonia. Eur J Gastroenterol Hepatol. 2003;5:1033-1036.
13. Stickel F, Patsenker E, Schuppan D. Herbal hepatotoxicity. J Hepatol. 2005;43:901-910.
14. Institute for Safe Medication Practices. ISMP medication safety alert! Available at: http://www.ismp.org/Newsletters/consumer/alerts/BrownBag.asp. Accessed May 5, 2010.
15. National Institute on Aging. Obtaining the medical history. Available at: http://www.nia.nih.gov/Healthinformation/Publications/ClinicianHB/03_history.htm. Accessed May 5, 2010.
16. Glassman PA, Simon B, Belperio P, et al. Improving recognition of drug interactions: benefits and barriers to using automated drug alerts. Med Care. 2002;40:1161-1171.
17. Goldberg RM, Mabee J, Chan L, et al. Drug-drug and drug-disease interactions in the ED: analysis of a high-risk population. Am J Emerg Med. 1996;14:447-450.
18. Lapane KL, Waring ME, Schneider KL, et al. A mixed method study of the merits of e-prescribing drug alerts in primary care. J Gen Intern Med. 2008;23:442-446.
19. Magnus D, Rodgers S, Avery AJ. GPs’ views on computerized drug interaction alerts: questionnaire survey. J Clin Pharm Ther. 2002;27:377-382.
20. Shukla UA, Pittman KA, Barbhaiya RH. Pharmacokinetic interactions of cefprozil with food, propantheline, metoclopramide, and probenecid in healthy volunteers. J Clin Pharmacol. 1992;32:725-731.
21. Levy RH, Collins C. Risk and predictability of drug interactions in the elderly. Int Rev Neurobiol. 2007;81:235-251.
22. Pauwels O. Factors contributing to carbamazepine-macrolide interactions. Pharmacol Res. 2002;45:291-298.
23. Beaird SL. HMG-CoA reductase inhibitors: assessing differences in drug interactions and safety profiles. J Am Pharm Assoc (Wash). 2000;40:637-644.
24. Snaith A, Pugh L, Simpson CR, et al. The potential for interaction between warfarin and coprescribed medication: a retrospective study in primary care. Am J Cardiovasc Drugs. 2008;8:207-212.
25. Juurlink DN, Gomes T, Ko DT, et al. A population-based study of the drug interaction between proton pump inhibitors and clopidogrel. CMAJ. 2009;180:713-718.
26. O’Donoghue ML, Braunwald E, Antman EM, et al. Pharmaco-dynamic effect and clinical efficacy of clopidogrel and prasugrel with or without a proton-pump inhibitor: an analysis of two randomised trials. Lancet. 2009;374:989-997.
27. US Food and Drug Administration. Serious muscle injury with simvastatin/amiodarone combination. November 2008. Available at: http://www.accessdata.fda.gov/psn/printer.cfm?id=886. Accessed May 5, 2010.
28. US Food and Drug Administration. FDA drug safety communication: ongoing safety review of high-dose Zocor (simvastatin) and increased risk of muscle injury. March 19, 2010. Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/
ucm204882.htm. Accessed May 5, 2010.
1. Becker ML, Kallewaard M, Caspers PW, et al. Hospitalisations and emergency department visits due to drug-drug interactions: a literature review. Pharmacoepidemiol Drug Saf. 2007;16:641-651.
2. Juurlink DN, Mamdani M, Kopp A, et al. Drug-drug interactions among elderly patients hospitalized for drug toxicity. JAMA. 2003;289:1652-1658.
3. Tulner LR, Frankfort SV, Gijsen GJ, et al. Drug-drug interactions in a geriatric outpatient cohort: prevalence and relevance. Drugs Aging. 2008;25:343-355.
4. Cadieux RJ. Drug interactions in the elderly. How multiple drug use increases risk exponentially. Postgrad Med. 1989;86:179-186.
5. Shapiro LE, Shear NH. Drug interactions: proteins, pumps, and P-450s. J Am Acad Dermatol. 2002;47:467-484.
6. Sitar DS. Aging issues in drug disposition and efficacy. Proc West Pharmacol Soc. 2007;50:16-20.
7. El Desoky ES, Derendorf H, Klotz U. Variability in response to cardiovascular drugs. Curr Clin Pharmacol. 2006;1:35-46.
8. Aparasu R, Baer R, Aparasu A. Clinically important potential drug-drug interactions in outpatient settings. Res Social Adm Pharm. 2007;3:426-437.
9. Becker ML, Kallewaard M, Caspers PW, et al. Potential determinants of drug-drug interaction associated dispensing in community pharmacies. Drug Saf. 2005;28:371-378.
10. Johnson TN, Thomson M. Intestinal metabolism and transport of drugs in children: the effects of age and disease. J Pediatr Gastroenterol Nutr. 2008;47:3-10.
11. Buurma H, Bouvy ML, De Smet PA, et al. Prevalence and determinants of pharmacy shopping behaviour. J Clin Pharm Ther. 2008;33:17-23.
12. Russmann S, Barguil Y, Cabalion P, et al. Hepatic injury due to traditional aqueous extracts of kava root in New Caledonia. Eur J Gastroenterol Hepatol. 2003;5:1033-1036.
13. Stickel F, Patsenker E, Schuppan D. Herbal hepatotoxicity. J Hepatol. 2005;43:901-910.
14. Institute for Safe Medication Practices. ISMP medication safety alert! Available at: http://www.ismp.org/Newsletters/consumer/alerts/BrownBag.asp. Accessed May 5, 2010.
15. National Institute on Aging. Obtaining the medical history. Available at: http://www.nia.nih.gov/Healthinformation/Publications/ClinicianHB/03_history.htm. Accessed May 5, 2010.
16. Glassman PA, Simon B, Belperio P, et al. Improving recognition of drug interactions: benefits and barriers to using automated drug alerts. Med Care. 2002;40:1161-1171.
17. Goldberg RM, Mabee J, Chan L, et al. Drug-drug and drug-disease interactions in the ED: analysis of a high-risk population. Am J Emerg Med. 1996;14:447-450.
18. Lapane KL, Waring ME, Schneider KL, et al. A mixed method study of the merits of e-prescribing drug alerts in primary care. J Gen Intern Med. 2008;23:442-446.
19. Magnus D, Rodgers S, Avery AJ. GPs’ views on computerized drug interaction alerts: questionnaire survey. J Clin Pharm Ther. 2002;27:377-382.
20. Shukla UA, Pittman KA, Barbhaiya RH. Pharmacokinetic interactions of cefprozil with food, propantheline, metoclopramide, and probenecid in healthy volunteers. J Clin Pharmacol. 1992;32:725-731.
21. Levy RH, Collins C. Risk and predictability of drug interactions in the elderly. Int Rev Neurobiol. 2007;81:235-251.
22. Pauwels O. Factors contributing to carbamazepine-macrolide interactions. Pharmacol Res. 2002;45:291-298.
23. Beaird SL. HMG-CoA reductase inhibitors: assessing differences in drug interactions and safety profiles. J Am Pharm Assoc (Wash). 2000;40:637-644.
24. Snaith A, Pugh L, Simpson CR, et al. The potential for interaction between warfarin and coprescribed medication: a retrospective study in primary care. Am J Cardiovasc Drugs. 2008;8:207-212.
25. Juurlink DN, Gomes T, Ko DT, et al. A population-based study of the drug interaction between proton pump inhibitors and clopidogrel. CMAJ. 2009;180:713-718.
26. O’Donoghue ML, Braunwald E, Antman EM, et al. Pharmaco-dynamic effect and clinical efficacy of clopidogrel and prasugrel with or without a proton-pump inhibitor: an analysis of two randomised trials. Lancet. 2009;374:989-997.
27. US Food and Drug Administration. Serious muscle injury with simvastatin/amiodarone combination. November 2008. Available at: http://www.accessdata.fda.gov/psn/printer.cfm?id=886. Accessed May 5, 2010.
28. US Food and Drug Administration. FDA drug safety communication: ongoing safety review of high-dose Zocor (simvastatin) and increased risk of muscle injury. March 19, 2010. Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/
ucm204882.htm. Accessed May 5, 2010.
Venous thrombosis: Preventing clots in patients at risk
• Testing for inherited hypercoagulable disorders should focus on the identification of individuals most likely to benefit from it. C
• Avoid testing asymptomatic individuals for the sole purpose of initiating long-term prophylactic therapy. C
• Long-term anticoagulant therapy may be warranted for patients with antithrombin III, protein C, or protein S deficiency, who may be at increased risk of recurrent thrombosis. C
• A definitive diagnosis of antiphospholipid antibody syndrome requires a history of either vascular thrombosis or pregnancy morbidity. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Each year, venous thrombosis develops in approximately 1 in 1000 people.1 The cause: An alteration in blood composition, venous stasis, or vascular damage—commonly known as Virchow’s triad. Changes in blood composition are associated with hereditary thrombophilias, such as factor V Leiden mutation or a deficiency in protein C or S or antithrombin III (AT). Changes in blood flow (stasis) and vessel damage stem from acquired conditions that commonly lead to hypercoagulability—pregnancy, malignancy, and estrogen use among them.
Regardless of the reason a patient is at elevated risk, however, the goal is the same: to prevent the development of thrombi, thereby reducing the increased morbidity and mortality associated with thromboembolism. Achieving that goal requires an understanding of both inherited and acquired risk factors, familiarity with diagnostic tools, and knowledge of appropriate treatment. This review, which begins with hereditary hypercoagulable states before turning to acquired conditions associated with hypercoagulability, will help toward that end.
Keep these thrombophilias on your radar screen
Factor V Leiden mutation is the most common inherited hypercoagulable disorder, and the most common form of activated protein C resistance. The mutation is found in an estimated 5% to 10% of the general population.2 Among patients with thromboembolic disorders, however, the incidence is considerably higher, with estimates ranging from 21% to 60%.3,4 Factor V Leiden mutation is more prevalent among Caucasian populations, and rarely found in people of Asian or African descent.2
Prothrombin G20210A mutation, an autosomal-dominant disorder, is the second most common inherited hypercoagulable state.4 This mutation is associated with an increase in prothrombin levels, causing an elevation in thrombin and, in turn, a heightened risk of thrombosis.
Although prothrombin G20210A mutation is found in only 1% to 2% of the general population, its prevalence among those with a history of thromboembolic events is estimated at 5% to 19%.4 This disorder, too, varies significantly by ethnicity: People from southern Europe are twice as likely to be affected as northern Europeans, and the mutation is rarely found in people of Asian or African descent.2,5
Protein C deficiency. Protein C, a vitamin K-dependent anticoagulant produced in the liver, is activated when thrombomodulin binds with thrombin in the presence of protein S, which serves as the cofactor. Protein C is required to inactivate clotting factors V and VIII.2 The deficiency is an autosomal-dominant disorder, and is more likely to result in venous than arterial thrombosis.2
Protein C deficiency affects 1 in every 200 to 500 people in the general population; among patients with a history of venous thrombosis, its prevalence is 2% to 9%.2,3 Generally, people with a protein C deficiency begin developing thrombi in their late teens, and about 75% suffer from 1 or more thrombotic events during the course of their lives.2
There are 2 types of protein C deficiency: Patients with type I have a decreased production of protein C, while those with type II have normal levels of the protein, but in a form that is dysfunctional.6
AT deficiency. AT, a natural anticoagulant synthesized by the liver and endothelial cells, is responsible for inactivating several clotting factors, including thrombin and factors IXa, Xa, XIa, and XIIa. Like protein C deficiency, AT deficiency is an autosomal-dominant disorder with 2 subtypes. Individuals with type I deficiency have normal plasma levels of AT, but the anticoagulant has reduced biological activity or is dysfunctional; those with type II deficiency have decreased plasma levels of fully functional AT.2 Both types are more likely to lead to venous than arterial thrombosis.
AT deficiency affects approximately 1 in 2000 to 5000 people, including 2.8% of patients who develop venous thrombosis.7 Nearly two-thirds of those with AT deficiency develop thrombi before the age of 35.2
Protein S deficiency. Endothelial cells are responsible for the synthesis of protein S, which, like protein C (for which it serves as a cofactor), is vitamin K-dependent. Protein S deficiency, also an autosomal-dominant disorder, has 3 subtypes: Type I, also known as classical deficiency, is characterized by reduced free and total levels of functional protein S; type II patients have a normal total level of protein S, but a decreased amount of free protein; and type III patients have normal levels of both free and total protein S, but the available proteins are dysfunctional.2,6
The prevalence of this hypercoagulable state in the general population is unknown, and protein S deficiencies have been found in only 1% of patients with a history of deep vein thrombosis (DVT).3,8 Although this hypercoagulable state is less common than other hereditary thrombophilias, 74% of people with this disorder develop DVT—half of them before the age of 25.2
Hyperhomocysteinemia. Elevations in homocysteine may occur as a result of a hereditary disorder (deficiencies in cystathionine beta-synthase or methylene-tetrahydrofolate reductase). Hyperhomocysteinemia may also be an acquired condition, associated with deficiencies in vitamins B6, B12, or folic acid; chronic kidney disease; hypothyroidism; and certain malignancies.
The prevalence of hyperhomocysteinemia varies, based on the underlying disorder. Only about 0.3% of the general population has a cystathionine beta-synthase deficiency. Methylene-tetrahydrofolate reductase deficiency, however, is common among Italian and Hispanic populations (occurring in about 20%), but rare (<1%) among African American people.3
When to test for thrombophilias
Idiopathic venous thrombosis is probably the most common reason for ordering testing for inherited hypercoagulable states, and an underlying thrombophilia is found in about 50% of cases.9 Other indications for testing include thrombus development in an unusual site (eg, splanchic, renal, retinal, or ovarian veins; cerebral venous sinuses; or upper limbs), recurrent venous thromboembolism (VTE), venous thrombosis at an early age (<45 years) or in a patient with a strong family history of VTE, and unexplained recurrent pregnancy loss.
Testing may also be considered for relatives of patients with known inherited hypercoagulability disorders, but this should be done only if the results could affect a treatment decision: Can a man safely undergo surgery with a high postoperative risk for thrombosis, for example? Should a woman take oral contraceptives (OCs), start hormone replacement therapy (HRT), or attempt another pregnancy?
Overall, testing for inherited hypercoagulable states should focus on the identification of individuals most likely to benefit from it; only tests yielding useful data should be performed. Testing of asymptomatic individuals for the sole purpose of initiating long-term prophylactic therapy is not recommended.
Which tests for which patients?
In some cases, selective assays may be more useful than test panels, for reasons associated with patient presentation as well as cost. Proper selection of specific tests should be individualized based on the patient’s age, thrombotic presentation, and family history, and on potential effects on patient management.
For patients with heparin resistance, cerebral vein thrombosis, intra-abdominal vein thrombosis, or recurrent superficial thrombophlebitis, AT testing may be in order. Patients with recurrent superficial thrombophlebitis may also benefit from testing for factor V Leiden mutation, and protein C and protein S testing may be beneficial for patients with warfarin skin necrosis, recurrent superficial thrombophlebitis, or neonatal purpura fulminans. Cerebral vein thrombosis in the general population and in women using OCs, in particular, is suggestive of a G20210A mutation,9 and is a possible indication for testing. Hyperhomocysteinemia testing may be considered for patients with premature arterial and venous thrombosis, as well as mental retardation, skeletal abnormalities, and vitamin B6 or B12 deficiency.
Many physicians prefer to order testing in stages, starting with tests for the most common thrombophilias. When ordering tests for the conditions detailed above and in the TABLE, be aware that test panels vary among facilities, so it may be necessary to check with the testing laboratory to ensure that it offers the tests that are indicated for a particular patient.
TABLE
Suspect a hereditary hypercoagulable disorder? Testing considerations to keep in mind2,3,8,9,11,12
| Disorder | Potential indication(s) for testing | Timing of test | Interaction with warfarin | Interaction with LMWH and UFH |
|---|---|---|---|---|
| Factor V Leiden mutation | Recurrent superficial thrombophlebitis | Not during an acute event | Modified aPTT test does not interact | Modified aPTT test does not interact |
| Prothrombin G20210A mutation | Cerebral vein thrombosis | Not during an acute event | No | No |
| Protein C deficiency |
| 7-10 days after cessation of warfarin therapy | Yes | No |
| Antithrombin III deficiency |
| 7-10 days after cessation of warfarin therapy | Yes | Yes |
| Protein S deficiency |
| 7-10 days after cessation of warfarin therapy | Yes | No |
| Hyperhomocysteinemia |
| Not during an acute event | No | No |
| aPTT, activated partial thromboplastin time; LMWH, low-molecular-weight heparin; UFH, unfractionated heparin. | ||||
Timing of tests, and other specifics
Acute thrombosis, anticoagulation therapy, and some disease states—eg, liver disease, nephritic syndrome, disseminated intravascular coagulation, and acute illness—can affect levels of AT, protein C, and protein S. Within the first 48 hours of warfarin therapy, for example, a patient’s protein C and protein S levels decline about 50%; after 2 weeks, the levels rise to about 70% of their normal range. Because of warfarin’s effect on these proteins, evaluation for these deficiencies should be performed at least 1 week to 10 days after cessation of a 3- to 6-month course of anticoagulation therapy. Abnormal findings should be confirmed with a second test approximately 3 weeks later.2,3,9
Several tests are used to detect factor V Leiden mutation, including the polymerase chain reaction-based test and the modified activated partial thromboplastin time (aPTT)-based test. The latter can be given to patients who are receiving anticoagulants. The results indicate the ratio of activated protein C (APC), and a finding of <2.0 is considered abnormal.8 The presence of lupus anticoagulant—autoantibodies that bind to phospholipids and proteins associated with the cell membrane—may yield a false-positive result on the modified aPTT test.
While the prothrombin G20210A mutation is linked to elevations in prothrombin, measuring prothrombin levels is not an accurate way to test for this hypercoagulable state. The prothrombin G20210A mutation generally is detected through DNA analysis instead.2,8
Hyperhomocysteinemia is diagnosed by measuring fasting plasma levels of homocysteine. Although the results are not standardized, they generally correlate with the severity of disease (mild, 15-30 μmol/L; moderate, >30-100 μmol/L; severe, >100 μmol/L). However, plasma levels may be falsely elevated during an acute thrombotic episode and decreased by supplementation with folic acid, B6, and B12. The decrease, however, does not indicate a reduction in the risk of thrombosis.
Treatment, yes, but for how long?
Most thrombotic events are initially treated with a combination of a heparin product (low-molecular-weight heparin [LMWH] or unfractionated heparin [UFH]) and warfarin—commonly known as bridging therapy. The heparin is discontinued once the patient’s international normalized ratio (INR) has been maintained at a therapeutic level for more than 24 hours, which usually takes about 5 days. Warfarin therapy, however, should continue for at least 3 to 6 months, depending on the severity and cause of the thrombosis.
Individuals with an AT, protein C, or protein S deficiency may be at increased risk of recurrence, and long-term anticoagulant therapy may be warranted.5 Under current guidelines from the American College of Chest Physicians (ACCP), however, hereditary thrombophilias are not considered to be major determinants of recurrence or a major factor guiding the duration of anticoagulation therapy.10 Practitioners must use their judgment to determine the need for treatment; if anticoagulation therapy is initiated, the duration should be based on an individual assessment of benefit and risk.
Recognizing and responding to acquired risks
Several conditions associated with vessel wall changes and venous stasis—the hallmarks of acquired hypercoagulable states—put patients at increased risk of venous thrombosis. Following is a review of the most likely risk factors, including antiphospholipid antibody syndrome (APS), previously known as lupus anticoagulant syndrome; heparin-induced thrombocytopenia (HIT); pregnancy; trauma; estrogen; and malignancy.
When to test for—and treat—APS
APS, a systemic autoimmune disorder that can result in arterial or venous thrombosis or pregnancy loss and morbidity, is characterized by the presence of autoantibodies. Patients of all ages may be affected by APS, one of the most common acquired hypercoagulability disorders. APS affects an estimated 28% of the general population.2 About 15% of recurrent pregnancy losses and 20% of recurrent thromboses in young adults are attributed to this autoimmune disorder.11
A definitive diagnosis of APS requires a history of either vascular thrombosis or pregnancy morbidity—defined as miscarriage after the 10th gestational week, consecutive fetal losses before the 10th gestational week, or placental insufficiency and premature birth before 34 weeks.11,12 APS testing may be useful in patients with cerebral vein thrombosis, intra-abdominal vein thrombosis, or unexplained recurrent fetal loss.9
In addition to clinical criteria, a diagnosis of APS is based on the presence of plasma antibodies on 2 or more occasions at least 12 weeks apart. APS encompasses 3 types of antiphospholipid antibodies—lupus anticoagulant antibodies, anticardiolipin antibodies, and anti-beta 2-glycoprotein I antibodies—which can be detected with 2 different tests. Coagulation assays are used to identify lupus anticoagulant antibodies because they prolong clotting time; however, immunoassays are used to measure immunologic reactivity to phospholipids to determine the presence of anticardiolipin antibodies and anti-beta 2-glycoprotein I antibodies.11,12
Treatment for APS generally involves anticoagulant therapy for the prevention and treatment of acute thrombotic events, or as prophylaxis during pregnancy. ACCP guidelines call for initiating warfarin therapy with a target INR of 2.5 (range 2.0-3.0) in patients with no other risk factors. In patients who have had recurrent thromboembolic events or have additional risk factors, a target INR of 3.0 (range 2.5-3.5) is suggested.10 LMWH and UFH are also options for use in the event of recurrence or for prophylaxis during pregnancy.11,13,14
HIT can be benign, or life threatening
HIT—defined by a decrease in platelet count to less than 150,000 (or a 50% drop from baseline) after initiation of heparin therapy—may or may not be benign. HIT type I (previously called heparin-associated thrombocytopenia), which affects approximately 10% of patients treated with heparin, is transient, asymptomatic, and not associated with an increased risk of thrombosis. Type I typically occurs within the first 2 days of heparin therapy.15
HIT type II is an immune-mediated response that does increase the risk of thrombosis. Patients usually develop type II 5 to 12 days after initiation of heparin, but in rare instances onset is delayed, occurring up to 40 days after heparin therapy. Approximately 5% of patients on heparin develop HIT type II, and the risk increases with frequent heparin use. Unlike other states of thrombocytopenia, HIT rarely causes bleeding. However, patients with HIT type II are at risk for a paradoxical thrombotic syndrome that may become life threatening.13,15
To diagnose HIT, an enzyme-linked immunosorbent assay or other specific blood tests must be used to confirm the presence of circulating antibodies.13 The diagnosis is based on the following criteria: (1) thrombocytopenia, (2) exclusion of other possible causes of thrombocytopenia, and (3) resolution of thrombocytopenia after discontinuation of heparin.13,15
When HIT is suspected, all heparin-containing products must be discontinued immediately and alternative anticoagulant therapy (typically, with danaparoid, lepirudin, or argatroban) should be initiated to reduce the risk of thrombosis. Warfarin alone should not be used for the treatment of HIT because of its association with worsening thrombosis and venous limb gangrene.13 However, warfarin should be initiated while the patient is receiving danaparoid or a thrombin-specific inhibitor—with at least 5 days of overlapping therapy recommended. Duration of therapy has not been well defined, but an overall course of at least 2 to 3 months is recommended to reduce the risk of recurrent thrombosis.13,15
Pregnancy raises risk, but limits Tx options
By altering the body’s normal physiologic state in a way that may lead to hypercoagulability, pregnancy increases the risk of VTE 6-fold.16 The risk continues throughout pregnancy and peaks during puerperium, the 6-week period after delivery. Cesarean delivery, prolonged immobility, and obesity elevate the risk.13,16
Treatment options for acute thrombotic events during pregnancy are limited because warfarin is contraindicated. Current ACCP guidelines recommend substituting UFH or LMWH for oral anticoagulant therapy when treatment for an acute thrombotic event is required.10 While no pharmacologic prophylaxis is currently recommended for pregnant patients with thrombophilias but no history of thrombotic events,10,17 there are cases when it may be necessary. Patients with an AT deficiency, for example, may require prenatal and postpartum prophylaxis,10 and patients who deliver by cesarean and have 1 or more additional risk factors should receive prophylaxis for the duration of their hospitalization. Women with multiple risk factors, in addition to pregnancy and cesarean section, should receive pharmacologic prophylaxis for up to 4 to 6 weeks postpartum.
Choices for postpartum anticoagulation for the treatment of an acute thrombotic event should be based on guidelines developed for nonpregnant patients, with this caveat: For women who are breastfeeding, safety during lactation must be considered. Neither UFH nor warfarin enters breast milk, so both are safe for such patients.18 LMWH, although smaller in molecular weight than UFH, is considered moderately safe during breastfeeding, as well.18
Prophylaxis is vital for trauma patients
Trauma and major injuries increase the risk of thrombosis by approximately 50%. Patients who are hospitalized after a major trauma are at high risk for the development of a VTE. At the greatest risk are those with spinal cord injuries (62%), pelvic fractures (61%), and leg fractures (80%).16 Current ACCP guidelines recommend the use of LMWH as soon as it is safe for trauma patients, and continuing it until discharge in patients with no apparent contraindication. If a patient has an active bleed or other contraindication, mechanical thromboprophylaxis is indicated until the bleeding risk decreases.15
Estrogens increase platelet aggregation
Estrogens are considered a risk factor because of their effect on both natural anticoagulants and clotting factors. A reduction in AT activity and increasing concentrations of clotting factors VII, X, and XII result from the use of estrogens. Estrogen is also thought to be responsible for the increase in platelet count and aggregation associated with the use of combination OCs.19 In fact, OC use is associated with about a 3-fold overall risk of thrombosis, a risk reported to be highest during the first year of use.16 Among hormonal contraceptives, the transdermal formulation has the highest risk.20-22 Hormone replacement therapy taken during menopause confers approximately a 2- to 4-fold increase in risk for VTE, and selective estrogen receptor modulators are associated with a 2-fold risk.16 Physicians should educate patients about the risks associated with these agents and signs and symptoms of thrombosis.
Cancer and hypercoagulability: Which patients need treatment?
Although the pathophysiologic process is not fully understood, a link between cancer and hypercoagulability has long been recognized. In fact, malignancy—the second most common cause of acquired hypercoagulability—is associated with 10% to 20% of spontaneous DVTs.2
One possible mechanism is the interaction of tumor cells with thrombin and plasmin-generating systems, directly influencing thrombus formation.7
Cancer patients also have an elevated risk for thrombosis related to immobilization, infection, treatment with antineoplastic agents, surgery, and the insertion of central venous catheters. Approximately 30% of patients with central venous catheters develop a DVT of the arm.16
Anticoagulant therapy in cancer patients varies, depending on the severity and circumstances of the patient. According to American Society of Clinical Oncology, National Comprehensive Cancer Center Network, and ACCP guidelines, LMWH is the preferred initial treatment for thromboses in patients with cancer— that is, in the first 3 to 6 months of therapy after a thrombotic event.17,23,24 The guidelines also mention warfarin as an alternative for long-term (>6 months) anticoagulant therapy, if no contraindications exist.
Because cancer is usually a long-term illness, anticoagulant therapy should be continued indefinitely, or until the cancer has resolved.10,23,24 Prophylaxis is recommended for cancer patients who are bedridden with an acute medical illness, but should not be routinely used in patients with indwelling venous catheters or those receiving chemotherapy or hormonal therapy.13,15
CORRESPONDENCE Haley M. Phillippe, PharmD, BCPS, University of Alabama Birmingham School of Medicine-Huntsville Campus, Department of Family Medicine, 301 Governors Drive, Huntsville, AL 35801; [email protected]
1. Beckman MG, Critchley SE, Hooper WC, et al. Venous thromboembolism: mechanisms, treatment and public awareness. Arteriosclerosis, Thrombosis, Vasc Biol. 2008;28:394-395.
2. Thomas RH. Hypercoagulability syndromes. Arch Intern Med. 2001;161:2433-2439.
3. Zwicker JI, Bauer KA. Thrombogenesis and hypercoagulable states. In: Ansell J, Oertel L, Wittkowsky A, eds. Managing Oral Anticoagulation Therapy. 2nd ed. St. Louis: Wolters Kluwer; 2005, p. 17:1-17:7.
4. Jebeleanu G, Procopciuc L. G20210A prothrombin gene mutation identified in patients with venous leg ulcers. J Cell Mol Med. 2001;5:397-401.
5. Dahlback B. Advances in understanding pathogenic mechanisms of thrombophilic disorders. Blood. 2008;112:19-27.
6. Beutler E, Lichtman MA, Coller BS, et al. Williams Hematology. 5th ed. New York: McGraw-Hill; 1995:1531–1542.
7. Nachman RL, Silverstein R. Hypercoagulable states. Ann Intern Med. 1993;119:819-827.
8. Federman DG, Kirsner RS. An update on hypercoagulable disorders. Arch Intern Med. 2001;161:1051-1056.
9. Deitcher S, Gomes M. Hypercoagulable state testing and malignancy screening following venous thromboembolic events. Vasc Med. 2003;8:33-46.
10. Hirsh J, Guyatt G, Albers W, et al. Executive summary: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th ed.) Chest. 2008;133(6 suppl):71S-109S.
11. Muscal E, Brey RL. Neurological manifestations of the antiphospholipid syndrome: risk assessment and evidence-based medicine. Int J Clin Pract. 2007;61:1561-1568.
12. Levine J, Branch D, Rauch J. The antiphospholipid syndrome. N Engl J Med. 2002;346:752-763.
13. Kuntz JG, Cheesman JD, Powers RD. Acute thrombotic disorders. Am J Emerg Med. 2006;24:460-467.
14. Sammaritano LR. Antiphospholipid syndrome: review. South Med J. 2005;98:617-625.
15. Franchini M. Heparin-induced thrombocytopenia: an update. Thrombosis J. 2005;3:14.-
16. Kyrle PA, Eichinger S. Deep vein thrombosis. Lancet. 2005;365:1163-1174.
17. Kearon C, Kahn SR, Agnelli G, et al. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th ed). Chest. 2008;133(6 suppl):454S-545S.
18. Hale MC. Medications and Mothers’ Milk. 11th ed. Amarillo, TX: Pharmasoft Publishing; 2004:282–283.
19. Ward MC, King DA, Link M, et al. Thrombosis secondary to medroxyprogesterone in patient at risk for thromboembolism. J Pharm Technol. 2005;21:276-280.
20. Vlijmen E, Brouwer J, Veeger N, et al. Oral contraceptives and the absolute risk of venous thromboembolism in women with single or multiple thrombophilic defects. Arch Intern Med. 2007;167:282-288.
21. Petitti D. Combination estrogen-progestin oral contraceptives. N Engl J Med. 2003;349:1443-1450.
22. Vandenbroucke J, Rosing J, Bloemenkamp K, et al. Oral contraceptives and the risk of venous thrombosis. N Engl J Med. 2001;344:1527-1535.
23. Lyman GH, Khorana A, Falanga A, et al. American Society of Clinical Oncology Guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol. 2007;25:1-16.
24. National Comprehensive Cancer Network. NCCN guidelines Available at: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp. Accessed May 14, 2010.
• Testing for inherited hypercoagulable disorders should focus on the identification of individuals most likely to benefit from it. C
• Avoid testing asymptomatic individuals for the sole purpose of initiating long-term prophylactic therapy. C
• Long-term anticoagulant therapy may be warranted for patients with antithrombin III, protein C, or protein S deficiency, who may be at increased risk of recurrent thrombosis. C
• A definitive diagnosis of antiphospholipid antibody syndrome requires a history of either vascular thrombosis or pregnancy morbidity. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Each year, venous thrombosis develops in approximately 1 in 1000 people.1 The cause: An alteration in blood composition, venous stasis, or vascular damage—commonly known as Virchow’s triad. Changes in blood composition are associated with hereditary thrombophilias, such as factor V Leiden mutation or a deficiency in protein C or S or antithrombin III (AT). Changes in blood flow (stasis) and vessel damage stem from acquired conditions that commonly lead to hypercoagulability—pregnancy, malignancy, and estrogen use among them.
Regardless of the reason a patient is at elevated risk, however, the goal is the same: to prevent the development of thrombi, thereby reducing the increased morbidity and mortality associated with thromboembolism. Achieving that goal requires an understanding of both inherited and acquired risk factors, familiarity with diagnostic tools, and knowledge of appropriate treatment. This review, which begins with hereditary hypercoagulable states before turning to acquired conditions associated with hypercoagulability, will help toward that end.
Keep these thrombophilias on your radar screen
Factor V Leiden mutation is the most common inherited hypercoagulable disorder, and the most common form of activated protein C resistance. The mutation is found in an estimated 5% to 10% of the general population.2 Among patients with thromboembolic disorders, however, the incidence is considerably higher, with estimates ranging from 21% to 60%.3,4 Factor V Leiden mutation is more prevalent among Caucasian populations, and rarely found in people of Asian or African descent.2
Prothrombin G20210A mutation, an autosomal-dominant disorder, is the second most common inherited hypercoagulable state.4 This mutation is associated with an increase in prothrombin levels, causing an elevation in thrombin and, in turn, a heightened risk of thrombosis.
Although prothrombin G20210A mutation is found in only 1% to 2% of the general population, its prevalence among those with a history of thromboembolic events is estimated at 5% to 19%.4 This disorder, too, varies significantly by ethnicity: People from southern Europe are twice as likely to be affected as northern Europeans, and the mutation is rarely found in people of Asian or African descent.2,5
Protein C deficiency. Protein C, a vitamin K-dependent anticoagulant produced in the liver, is activated when thrombomodulin binds with thrombin in the presence of protein S, which serves as the cofactor. Protein C is required to inactivate clotting factors V and VIII.2 The deficiency is an autosomal-dominant disorder, and is more likely to result in venous than arterial thrombosis.2
Protein C deficiency affects 1 in every 200 to 500 people in the general population; among patients with a history of venous thrombosis, its prevalence is 2% to 9%.2,3 Generally, people with a protein C deficiency begin developing thrombi in their late teens, and about 75% suffer from 1 or more thrombotic events during the course of their lives.2
There are 2 types of protein C deficiency: Patients with type I have a decreased production of protein C, while those with type II have normal levels of the protein, but in a form that is dysfunctional.6
AT deficiency. AT, a natural anticoagulant synthesized by the liver and endothelial cells, is responsible for inactivating several clotting factors, including thrombin and factors IXa, Xa, XIa, and XIIa. Like protein C deficiency, AT deficiency is an autosomal-dominant disorder with 2 subtypes. Individuals with type I deficiency have normal plasma levels of AT, but the anticoagulant has reduced biological activity or is dysfunctional; those with type II deficiency have decreased plasma levels of fully functional AT.2 Both types are more likely to lead to venous than arterial thrombosis.
AT deficiency affects approximately 1 in 2000 to 5000 people, including 2.8% of patients who develop venous thrombosis.7 Nearly two-thirds of those with AT deficiency develop thrombi before the age of 35.2
Protein S deficiency. Endothelial cells are responsible for the synthesis of protein S, which, like protein C (for which it serves as a cofactor), is vitamin K-dependent. Protein S deficiency, also an autosomal-dominant disorder, has 3 subtypes: Type I, also known as classical deficiency, is characterized by reduced free and total levels of functional protein S; type II patients have a normal total level of protein S, but a decreased amount of free protein; and type III patients have normal levels of both free and total protein S, but the available proteins are dysfunctional.2,6
The prevalence of this hypercoagulable state in the general population is unknown, and protein S deficiencies have been found in only 1% of patients with a history of deep vein thrombosis (DVT).3,8 Although this hypercoagulable state is less common than other hereditary thrombophilias, 74% of people with this disorder develop DVT—half of them before the age of 25.2
Hyperhomocysteinemia. Elevations in homocysteine may occur as a result of a hereditary disorder (deficiencies in cystathionine beta-synthase or methylene-tetrahydrofolate reductase). Hyperhomocysteinemia may also be an acquired condition, associated with deficiencies in vitamins B6, B12, or folic acid; chronic kidney disease; hypothyroidism; and certain malignancies.
The prevalence of hyperhomocysteinemia varies, based on the underlying disorder. Only about 0.3% of the general population has a cystathionine beta-synthase deficiency. Methylene-tetrahydrofolate reductase deficiency, however, is common among Italian and Hispanic populations (occurring in about 20%), but rare (<1%) among African American people.3
When to test for thrombophilias
Idiopathic venous thrombosis is probably the most common reason for ordering testing for inherited hypercoagulable states, and an underlying thrombophilia is found in about 50% of cases.9 Other indications for testing include thrombus development in an unusual site (eg, splanchic, renal, retinal, or ovarian veins; cerebral venous sinuses; or upper limbs), recurrent venous thromboembolism (VTE), venous thrombosis at an early age (<45 years) or in a patient with a strong family history of VTE, and unexplained recurrent pregnancy loss.
Testing may also be considered for relatives of patients with known inherited hypercoagulability disorders, but this should be done only if the results could affect a treatment decision: Can a man safely undergo surgery with a high postoperative risk for thrombosis, for example? Should a woman take oral contraceptives (OCs), start hormone replacement therapy (HRT), or attempt another pregnancy?
Overall, testing for inherited hypercoagulable states should focus on the identification of individuals most likely to benefit from it; only tests yielding useful data should be performed. Testing of asymptomatic individuals for the sole purpose of initiating long-term prophylactic therapy is not recommended.
Which tests for which patients?
In some cases, selective assays may be more useful than test panels, for reasons associated with patient presentation as well as cost. Proper selection of specific tests should be individualized based on the patient’s age, thrombotic presentation, and family history, and on potential effects on patient management.
For patients with heparin resistance, cerebral vein thrombosis, intra-abdominal vein thrombosis, or recurrent superficial thrombophlebitis, AT testing may be in order. Patients with recurrent superficial thrombophlebitis may also benefit from testing for factor V Leiden mutation, and protein C and protein S testing may be beneficial for patients with warfarin skin necrosis, recurrent superficial thrombophlebitis, or neonatal purpura fulminans. Cerebral vein thrombosis in the general population and in women using OCs, in particular, is suggestive of a G20210A mutation,9 and is a possible indication for testing. Hyperhomocysteinemia testing may be considered for patients with premature arterial and venous thrombosis, as well as mental retardation, skeletal abnormalities, and vitamin B6 or B12 deficiency.
Many physicians prefer to order testing in stages, starting with tests for the most common thrombophilias. When ordering tests for the conditions detailed above and in the TABLE, be aware that test panels vary among facilities, so it may be necessary to check with the testing laboratory to ensure that it offers the tests that are indicated for a particular patient.
TABLE
Suspect a hereditary hypercoagulable disorder? Testing considerations to keep in mind2,3,8,9,11,12
| Disorder | Potential indication(s) for testing | Timing of test | Interaction with warfarin | Interaction with LMWH and UFH |
|---|---|---|---|---|
| Factor V Leiden mutation | Recurrent superficial thrombophlebitis | Not during an acute event | Modified aPTT test does not interact | Modified aPTT test does not interact |
| Prothrombin G20210A mutation | Cerebral vein thrombosis | Not during an acute event | No | No |
| Protein C deficiency |
| 7-10 days after cessation of warfarin therapy | Yes | No |
| Antithrombin III deficiency |
| 7-10 days after cessation of warfarin therapy | Yes | Yes |
| Protein S deficiency |
| 7-10 days after cessation of warfarin therapy | Yes | No |
| Hyperhomocysteinemia |
| Not during an acute event | No | No |
| aPTT, activated partial thromboplastin time; LMWH, low-molecular-weight heparin; UFH, unfractionated heparin. | ||||
Timing of tests, and other specifics
Acute thrombosis, anticoagulation therapy, and some disease states—eg, liver disease, nephritic syndrome, disseminated intravascular coagulation, and acute illness—can affect levels of AT, protein C, and protein S. Within the first 48 hours of warfarin therapy, for example, a patient’s protein C and protein S levels decline about 50%; after 2 weeks, the levels rise to about 70% of their normal range. Because of warfarin’s effect on these proteins, evaluation for these deficiencies should be performed at least 1 week to 10 days after cessation of a 3- to 6-month course of anticoagulation therapy. Abnormal findings should be confirmed with a second test approximately 3 weeks later.2,3,9
Several tests are used to detect factor V Leiden mutation, including the polymerase chain reaction-based test and the modified activated partial thromboplastin time (aPTT)-based test. The latter can be given to patients who are receiving anticoagulants. The results indicate the ratio of activated protein C (APC), and a finding of <2.0 is considered abnormal.8 The presence of lupus anticoagulant—autoantibodies that bind to phospholipids and proteins associated with the cell membrane—may yield a false-positive result on the modified aPTT test.
While the prothrombin G20210A mutation is linked to elevations in prothrombin, measuring prothrombin levels is not an accurate way to test for this hypercoagulable state. The prothrombin G20210A mutation generally is detected through DNA analysis instead.2,8
Hyperhomocysteinemia is diagnosed by measuring fasting plasma levels of homocysteine. Although the results are not standardized, they generally correlate with the severity of disease (mild, 15-30 μmol/L; moderate, >30-100 μmol/L; severe, >100 μmol/L). However, plasma levels may be falsely elevated during an acute thrombotic episode and decreased by supplementation with folic acid, B6, and B12. The decrease, however, does not indicate a reduction in the risk of thrombosis.
Treatment, yes, but for how long?
Most thrombotic events are initially treated with a combination of a heparin product (low-molecular-weight heparin [LMWH] or unfractionated heparin [UFH]) and warfarin—commonly known as bridging therapy. The heparin is discontinued once the patient’s international normalized ratio (INR) has been maintained at a therapeutic level for more than 24 hours, which usually takes about 5 days. Warfarin therapy, however, should continue for at least 3 to 6 months, depending on the severity and cause of the thrombosis.
Individuals with an AT, protein C, or protein S deficiency may be at increased risk of recurrence, and long-term anticoagulant therapy may be warranted.5 Under current guidelines from the American College of Chest Physicians (ACCP), however, hereditary thrombophilias are not considered to be major determinants of recurrence or a major factor guiding the duration of anticoagulation therapy.10 Practitioners must use their judgment to determine the need for treatment; if anticoagulation therapy is initiated, the duration should be based on an individual assessment of benefit and risk.
Recognizing and responding to acquired risks
Several conditions associated with vessel wall changes and venous stasis—the hallmarks of acquired hypercoagulable states—put patients at increased risk of venous thrombosis. Following is a review of the most likely risk factors, including antiphospholipid antibody syndrome (APS), previously known as lupus anticoagulant syndrome; heparin-induced thrombocytopenia (HIT); pregnancy; trauma; estrogen; and malignancy.
When to test for—and treat—APS
APS, a systemic autoimmune disorder that can result in arterial or venous thrombosis or pregnancy loss and morbidity, is characterized by the presence of autoantibodies. Patients of all ages may be affected by APS, one of the most common acquired hypercoagulability disorders. APS affects an estimated 28% of the general population.2 About 15% of recurrent pregnancy losses and 20% of recurrent thromboses in young adults are attributed to this autoimmune disorder.11
A definitive diagnosis of APS requires a history of either vascular thrombosis or pregnancy morbidity—defined as miscarriage after the 10th gestational week, consecutive fetal losses before the 10th gestational week, or placental insufficiency and premature birth before 34 weeks.11,12 APS testing may be useful in patients with cerebral vein thrombosis, intra-abdominal vein thrombosis, or unexplained recurrent fetal loss.9
In addition to clinical criteria, a diagnosis of APS is based on the presence of plasma antibodies on 2 or more occasions at least 12 weeks apart. APS encompasses 3 types of antiphospholipid antibodies—lupus anticoagulant antibodies, anticardiolipin antibodies, and anti-beta 2-glycoprotein I antibodies—which can be detected with 2 different tests. Coagulation assays are used to identify lupus anticoagulant antibodies because they prolong clotting time; however, immunoassays are used to measure immunologic reactivity to phospholipids to determine the presence of anticardiolipin antibodies and anti-beta 2-glycoprotein I antibodies.11,12
Treatment for APS generally involves anticoagulant therapy for the prevention and treatment of acute thrombotic events, or as prophylaxis during pregnancy. ACCP guidelines call for initiating warfarin therapy with a target INR of 2.5 (range 2.0-3.0) in patients with no other risk factors. In patients who have had recurrent thromboembolic events or have additional risk factors, a target INR of 3.0 (range 2.5-3.5) is suggested.10 LMWH and UFH are also options for use in the event of recurrence or for prophylaxis during pregnancy.11,13,14
HIT can be benign, or life threatening
HIT—defined by a decrease in platelet count to less than 150,000 (or a 50% drop from baseline) after initiation of heparin therapy—may or may not be benign. HIT type I (previously called heparin-associated thrombocytopenia), which affects approximately 10% of patients treated with heparin, is transient, asymptomatic, and not associated with an increased risk of thrombosis. Type I typically occurs within the first 2 days of heparin therapy.15
HIT type II is an immune-mediated response that does increase the risk of thrombosis. Patients usually develop type II 5 to 12 days after initiation of heparin, but in rare instances onset is delayed, occurring up to 40 days after heparin therapy. Approximately 5% of patients on heparin develop HIT type II, and the risk increases with frequent heparin use. Unlike other states of thrombocytopenia, HIT rarely causes bleeding. However, patients with HIT type II are at risk for a paradoxical thrombotic syndrome that may become life threatening.13,15
To diagnose HIT, an enzyme-linked immunosorbent assay or other specific blood tests must be used to confirm the presence of circulating antibodies.13 The diagnosis is based on the following criteria: (1) thrombocytopenia, (2) exclusion of other possible causes of thrombocytopenia, and (3) resolution of thrombocytopenia after discontinuation of heparin.13,15
When HIT is suspected, all heparin-containing products must be discontinued immediately and alternative anticoagulant therapy (typically, with danaparoid, lepirudin, or argatroban) should be initiated to reduce the risk of thrombosis. Warfarin alone should not be used for the treatment of HIT because of its association with worsening thrombosis and venous limb gangrene.13 However, warfarin should be initiated while the patient is receiving danaparoid or a thrombin-specific inhibitor—with at least 5 days of overlapping therapy recommended. Duration of therapy has not been well defined, but an overall course of at least 2 to 3 months is recommended to reduce the risk of recurrent thrombosis.13,15
Pregnancy raises risk, but limits Tx options
By altering the body’s normal physiologic state in a way that may lead to hypercoagulability, pregnancy increases the risk of VTE 6-fold.16 The risk continues throughout pregnancy and peaks during puerperium, the 6-week period after delivery. Cesarean delivery, prolonged immobility, and obesity elevate the risk.13,16
Treatment options for acute thrombotic events during pregnancy are limited because warfarin is contraindicated. Current ACCP guidelines recommend substituting UFH or LMWH for oral anticoagulant therapy when treatment for an acute thrombotic event is required.10 While no pharmacologic prophylaxis is currently recommended for pregnant patients with thrombophilias but no history of thrombotic events,10,17 there are cases when it may be necessary. Patients with an AT deficiency, for example, may require prenatal and postpartum prophylaxis,10 and patients who deliver by cesarean and have 1 or more additional risk factors should receive prophylaxis for the duration of their hospitalization. Women with multiple risk factors, in addition to pregnancy and cesarean section, should receive pharmacologic prophylaxis for up to 4 to 6 weeks postpartum.
Choices for postpartum anticoagulation for the treatment of an acute thrombotic event should be based on guidelines developed for nonpregnant patients, with this caveat: For women who are breastfeeding, safety during lactation must be considered. Neither UFH nor warfarin enters breast milk, so both are safe for such patients.18 LMWH, although smaller in molecular weight than UFH, is considered moderately safe during breastfeeding, as well.18
Prophylaxis is vital for trauma patients
Trauma and major injuries increase the risk of thrombosis by approximately 50%. Patients who are hospitalized after a major trauma are at high risk for the development of a VTE. At the greatest risk are those with spinal cord injuries (62%), pelvic fractures (61%), and leg fractures (80%).16 Current ACCP guidelines recommend the use of LMWH as soon as it is safe for trauma patients, and continuing it until discharge in patients with no apparent contraindication. If a patient has an active bleed or other contraindication, mechanical thromboprophylaxis is indicated until the bleeding risk decreases.15
Estrogens increase platelet aggregation
Estrogens are considered a risk factor because of their effect on both natural anticoagulants and clotting factors. A reduction in AT activity and increasing concentrations of clotting factors VII, X, and XII result from the use of estrogens. Estrogen is also thought to be responsible for the increase in platelet count and aggregation associated with the use of combination OCs.19 In fact, OC use is associated with about a 3-fold overall risk of thrombosis, a risk reported to be highest during the first year of use.16 Among hormonal contraceptives, the transdermal formulation has the highest risk.20-22 Hormone replacement therapy taken during menopause confers approximately a 2- to 4-fold increase in risk for VTE, and selective estrogen receptor modulators are associated with a 2-fold risk.16 Physicians should educate patients about the risks associated with these agents and signs and symptoms of thrombosis.
Cancer and hypercoagulability: Which patients need treatment?
Although the pathophysiologic process is not fully understood, a link between cancer and hypercoagulability has long been recognized. In fact, malignancy—the second most common cause of acquired hypercoagulability—is associated with 10% to 20% of spontaneous DVTs.2
One possible mechanism is the interaction of tumor cells with thrombin and plasmin-generating systems, directly influencing thrombus formation.7
Cancer patients also have an elevated risk for thrombosis related to immobilization, infection, treatment with antineoplastic agents, surgery, and the insertion of central venous catheters. Approximately 30% of patients with central venous catheters develop a DVT of the arm.16
Anticoagulant therapy in cancer patients varies, depending on the severity and circumstances of the patient. According to American Society of Clinical Oncology, National Comprehensive Cancer Center Network, and ACCP guidelines, LMWH is the preferred initial treatment for thromboses in patients with cancer— that is, in the first 3 to 6 months of therapy after a thrombotic event.17,23,24 The guidelines also mention warfarin as an alternative for long-term (>6 months) anticoagulant therapy, if no contraindications exist.
Because cancer is usually a long-term illness, anticoagulant therapy should be continued indefinitely, or until the cancer has resolved.10,23,24 Prophylaxis is recommended for cancer patients who are bedridden with an acute medical illness, but should not be routinely used in patients with indwelling venous catheters or those receiving chemotherapy or hormonal therapy.13,15
CORRESPONDENCE Haley M. Phillippe, PharmD, BCPS, University of Alabama Birmingham School of Medicine-Huntsville Campus, Department of Family Medicine, 301 Governors Drive, Huntsville, AL 35801; [email protected]
• Testing for inherited hypercoagulable disorders should focus on the identification of individuals most likely to benefit from it. C
• Avoid testing asymptomatic individuals for the sole purpose of initiating long-term prophylactic therapy. C
• Long-term anticoagulant therapy may be warranted for patients with antithrombin III, protein C, or protein S deficiency, who may be at increased risk of recurrent thrombosis. C
• A definitive diagnosis of antiphospholipid antibody syndrome requires a history of either vascular thrombosis or pregnancy morbidity. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Each year, venous thrombosis develops in approximately 1 in 1000 people.1 The cause: An alteration in blood composition, venous stasis, or vascular damage—commonly known as Virchow’s triad. Changes in blood composition are associated with hereditary thrombophilias, such as factor V Leiden mutation or a deficiency in protein C or S or antithrombin III (AT). Changes in blood flow (stasis) and vessel damage stem from acquired conditions that commonly lead to hypercoagulability—pregnancy, malignancy, and estrogen use among them.
Regardless of the reason a patient is at elevated risk, however, the goal is the same: to prevent the development of thrombi, thereby reducing the increased morbidity and mortality associated with thromboembolism. Achieving that goal requires an understanding of both inherited and acquired risk factors, familiarity with diagnostic tools, and knowledge of appropriate treatment. This review, which begins with hereditary hypercoagulable states before turning to acquired conditions associated with hypercoagulability, will help toward that end.
Keep these thrombophilias on your radar screen
Factor V Leiden mutation is the most common inherited hypercoagulable disorder, and the most common form of activated protein C resistance. The mutation is found in an estimated 5% to 10% of the general population.2 Among patients with thromboembolic disorders, however, the incidence is considerably higher, with estimates ranging from 21% to 60%.3,4 Factor V Leiden mutation is more prevalent among Caucasian populations, and rarely found in people of Asian or African descent.2
Prothrombin G20210A mutation, an autosomal-dominant disorder, is the second most common inherited hypercoagulable state.4 This mutation is associated with an increase in prothrombin levels, causing an elevation in thrombin and, in turn, a heightened risk of thrombosis.
Although prothrombin G20210A mutation is found in only 1% to 2% of the general population, its prevalence among those with a history of thromboembolic events is estimated at 5% to 19%.4 This disorder, too, varies significantly by ethnicity: People from southern Europe are twice as likely to be affected as northern Europeans, and the mutation is rarely found in people of Asian or African descent.2,5
Protein C deficiency. Protein C, a vitamin K-dependent anticoagulant produced in the liver, is activated when thrombomodulin binds with thrombin in the presence of protein S, which serves as the cofactor. Protein C is required to inactivate clotting factors V and VIII.2 The deficiency is an autosomal-dominant disorder, and is more likely to result in venous than arterial thrombosis.2
Protein C deficiency affects 1 in every 200 to 500 people in the general population; among patients with a history of venous thrombosis, its prevalence is 2% to 9%.2,3 Generally, people with a protein C deficiency begin developing thrombi in their late teens, and about 75% suffer from 1 or more thrombotic events during the course of their lives.2
There are 2 types of protein C deficiency: Patients with type I have a decreased production of protein C, while those with type II have normal levels of the protein, but in a form that is dysfunctional.6
AT deficiency. AT, a natural anticoagulant synthesized by the liver and endothelial cells, is responsible for inactivating several clotting factors, including thrombin and factors IXa, Xa, XIa, and XIIa. Like protein C deficiency, AT deficiency is an autosomal-dominant disorder with 2 subtypes. Individuals with type I deficiency have normal plasma levels of AT, but the anticoagulant has reduced biological activity or is dysfunctional; those with type II deficiency have decreased plasma levels of fully functional AT.2 Both types are more likely to lead to venous than arterial thrombosis.
AT deficiency affects approximately 1 in 2000 to 5000 people, including 2.8% of patients who develop venous thrombosis.7 Nearly two-thirds of those with AT deficiency develop thrombi before the age of 35.2
Protein S deficiency. Endothelial cells are responsible for the synthesis of protein S, which, like protein C (for which it serves as a cofactor), is vitamin K-dependent. Protein S deficiency, also an autosomal-dominant disorder, has 3 subtypes: Type I, also known as classical deficiency, is characterized by reduced free and total levels of functional protein S; type II patients have a normal total level of protein S, but a decreased amount of free protein; and type III patients have normal levels of both free and total protein S, but the available proteins are dysfunctional.2,6
The prevalence of this hypercoagulable state in the general population is unknown, and protein S deficiencies have been found in only 1% of patients with a history of deep vein thrombosis (DVT).3,8 Although this hypercoagulable state is less common than other hereditary thrombophilias, 74% of people with this disorder develop DVT—half of them before the age of 25.2
Hyperhomocysteinemia. Elevations in homocysteine may occur as a result of a hereditary disorder (deficiencies in cystathionine beta-synthase or methylene-tetrahydrofolate reductase). Hyperhomocysteinemia may also be an acquired condition, associated with deficiencies in vitamins B6, B12, or folic acid; chronic kidney disease; hypothyroidism; and certain malignancies.
The prevalence of hyperhomocysteinemia varies, based on the underlying disorder. Only about 0.3% of the general population has a cystathionine beta-synthase deficiency. Methylene-tetrahydrofolate reductase deficiency, however, is common among Italian and Hispanic populations (occurring in about 20%), but rare (<1%) among African American people.3
When to test for thrombophilias
Idiopathic venous thrombosis is probably the most common reason for ordering testing for inherited hypercoagulable states, and an underlying thrombophilia is found in about 50% of cases.9 Other indications for testing include thrombus development in an unusual site (eg, splanchic, renal, retinal, or ovarian veins; cerebral venous sinuses; or upper limbs), recurrent venous thromboembolism (VTE), venous thrombosis at an early age (<45 years) or in a patient with a strong family history of VTE, and unexplained recurrent pregnancy loss.
Testing may also be considered for relatives of patients with known inherited hypercoagulability disorders, but this should be done only if the results could affect a treatment decision: Can a man safely undergo surgery with a high postoperative risk for thrombosis, for example? Should a woman take oral contraceptives (OCs), start hormone replacement therapy (HRT), or attempt another pregnancy?
Overall, testing for inherited hypercoagulable states should focus on the identification of individuals most likely to benefit from it; only tests yielding useful data should be performed. Testing of asymptomatic individuals for the sole purpose of initiating long-term prophylactic therapy is not recommended.
Which tests for which patients?
In some cases, selective assays may be more useful than test panels, for reasons associated with patient presentation as well as cost. Proper selection of specific tests should be individualized based on the patient’s age, thrombotic presentation, and family history, and on potential effects on patient management.
For patients with heparin resistance, cerebral vein thrombosis, intra-abdominal vein thrombosis, or recurrent superficial thrombophlebitis, AT testing may be in order. Patients with recurrent superficial thrombophlebitis may also benefit from testing for factor V Leiden mutation, and protein C and protein S testing may be beneficial for patients with warfarin skin necrosis, recurrent superficial thrombophlebitis, or neonatal purpura fulminans. Cerebral vein thrombosis in the general population and in women using OCs, in particular, is suggestive of a G20210A mutation,9 and is a possible indication for testing. Hyperhomocysteinemia testing may be considered for patients with premature arterial and venous thrombosis, as well as mental retardation, skeletal abnormalities, and vitamin B6 or B12 deficiency.
Many physicians prefer to order testing in stages, starting with tests for the most common thrombophilias. When ordering tests for the conditions detailed above and in the TABLE, be aware that test panels vary among facilities, so it may be necessary to check with the testing laboratory to ensure that it offers the tests that are indicated for a particular patient.
TABLE
Suspect a hereditary hypercoagulable disorder? Testing considerations to keep in mind2,3,8,9,11,12
| Disorder | Potential indication(s) for testing | Timing of test | Interaction with warfarin | Interaction with LMWH and UFH |
|---|---|---|---|---|
| Factor V Leiden mutation | Recurrent superficial thrombophlebitis | Not during an acute event | Modified aPTT test does not interact | Modified aPTT test does not interact |
| Prothrombin G20210A mutation | Cerebral vein thrombosis | Not during an acute event | No | No |
| Protein C deficiency |
| 7-10 days after cessation of warfarin therapy | Yes | No |
| Antithrombin III deficiency |
| 7-10 days after cessation of warfarin therapy | Yes | Yes |
| Protein S deficiency |
| 7-10 days after cessation of warfarin therapy | Yes | No |
| Hyperhomocysteinemia |
| Not during an acute event | No | No |
| aPTT, activated partial thromboplastin time; LMWH, low-molecular-weight heparin; UFH, unfractionated heparin. | ||||
Timing of tests, and other specifics
Acute thrombosis, anticoagulation therapy, and some disease states—eg, liver disease, nephritic syndrome, disseminated intravascular coagulation, and acute illness—can affect levels of AT, protein C, and protein S. Within the first 48 hours of warfarin therapy, for example, a patient’s protein C and protein S levels decline about 50%; after 2 weeks, the levels rise to about 70% of their normal range. Because of warfarin’s effect on these proteins, evaluation for these deficiencies should be performed at least 1 week to 10 days after cessation of a 3- to 6-month course of anticoagulation therapy. Abnormal findings should be confirmed with a second test approximately 3 weeks later.2,3,9
Several tests are used to detect factor V Leiden mutation, including the polymerase chain reaction-based test and the modified activated partial thromboplastin time (aPTT)-based test. The latter can be given to patients who are receiving anticoagulants. The results indicate the ratio of activated protein C (APC), and a finding of <2.0 is considered abnormal.8 The presence of lupus anticoagulant—autoantibodies that bind to phospholipids and proteins associated with the cell membrane—may yield a false-positive result on the modified aPTT test.
While the prothrombin G20210A mutation is linked to elevations in prothrombin, measuring prothrombin levels is not an accurate way to test for this hypercoagulable state. The prothrombin G20210A mutation generally is detected through DNA analysis instead.2,8
Hyperhomocysteinemia is diagnosed by measuring fasting plasma levels of homocysteine. Although the results are not standardized, they generally correlate with the severity of disease (mild, 15-30 μmol/L; moderate, >30-100 μmol/L; severe, >100 μmol/L). However, plasma levels may be falsely elevated during an acute thrombotic episode and decreased by supplementation with folic acid, B6, and B12. The decrease, however, does not indicate a reduction in the risk of thrombosis.
Treatment, yes, but for how long?
Most thrombotic events are initially treated with a combination of a heparin product (low-molecular-weight heparin [LMWH] or unfractionated heparin [UFH]) and warfarin—commonly known as bridging therapy. The heparin is discontinued once the patient’s international normalized ratio (INR) has been maintained at a therapeutic level for more than 24 hours, which usually takes about 5 days. Warfarin therapy, however, should continue for at least 3 to 6 months, depending on the severity and cause of the thrombosis.
Individuals with an AT, protein C, or protein S deficiency may be at increased risk of recurrence, and long-term anticoagulant therapy may be warranted.5 Under current guidelines from the American College of Chest Physicians (ACCP), however, hereditary thrombophilias are not considered to be major determinants of recurrence or a major factor guiding the duration of anticoagulation therapy.10 Practitioners must use their judgment to determine the need for treatment; if anticoagulation therapy is initiated, the duration should be based on an individual assessment of benefit and risk.
Recognizing and responding to acquired risks
Several conditions associated with vessel wall changes and venous stasis—the hallmarks of acquired hypercoagulable states—put patients at increased risk of venous thrombosis. Following is a review of the most likely risk factors, including antiphospholipid antibody syndrome (APS), previously known as lupus anticoagulant syndrome; heparin-induced thrombocytopenia (HIT); pregnancy; trauma; estrogen; and malignancy.
When to test for—and treat—APS
APS, a systemic autoimmune disorder that can result in arterial or venous thrombosis or pregnancy loss and morbidity, is characterized by the presence of autoantibodies. Patients of all ages may be affected by APS, one of the most common acquired hypercoagulability disorders. APS affects an estimated 28% of the general population.2 About 15% of recurrent pregnancy losses and 20% of recurrent thromboses in young adults are attributed to this autoimmune disorder.11
A definitive diagnosis of APS requires a history of either vascular thrombosis or pregnancy morbidity—defined as miscarriage after the 10th gestational week, consecutive fetal losses before the 10th gestational week, or placental insufficiency and premature birth before 34 weeks.11,12 APS testing may be useful in patients with cerebral vein thrombosis, intra-abdominal vein thrombosis, or unexplained recurrent fetal loss.9
In addition to clinical criteria, a diagnosis of APS is based on the presence of plasma antibodies on 2 or more occasions at least 12 weeks apart. APS encompasses 3 types of antiphospholipid antibodies—lupus anticoagulant antibodies, anticardiolipin antibodies, and anti-beta 2-glycoprotein I antibodies—which can be detected with 2 different tests. Coagulation assays are used to identify lupus anticoagulant antibodies because they prolong clotting time; however, immunoassays are used to measure immunologic reactivity to phospholipids to determine the presence of anticardiolipin antibodies and anti-beta 2-glycoprotein I antibodies.11,12
Treatment for APS generally involves anticoagulant therapy for the prevention and treatment of acute thrombotic events, or as prophylaxis during pregnancy. ACCP guidelines call for initiating warfarin therapy with a target INR of 2.5 (range 2.0-3.0) in patients with no other risk factors. In patients who have had recurrent thromboembolic events or have additional risk factors, a target INR of 3.0 (range 2.5-3.5) is suggested.10 LMWH and UFH are also options for use in the event of recurrence or for prophylaxis during pregnancy.11,13,14
HIT can be benign, or life threatening
HIT—defined by a decrease in platelet count to less than 150,000 (or a 50% drop from baseline) after initiation of heparin therapy—may or may not be benign. HIT type I (previously called heparin-associated thrombocytopenia), which affects approximately 10% of patients treated with heparin, is transient, asymptomatic, and not associated with an increased risk of thrombosis. Type I typically occurs within the first 2 days of heparin therapy.15
HIT type II is an immune-mediated response that does increase the risk of thrombosis. Patients usually develop type II 5 to 12 days after initiation of heparin, but in rare instances onset is delayed, occurring up to 40 days after heparin therapy. Approximately 5% of patients on heparin develop HIT type II, and the risk increases with frequent heparin use. Unlike other states of thrombocytopenia, HIT rarely causes bleeding. However, patients with HIT type II are at risk for a paradoxical thrombotic syndrome that may become life threatening.13,15
To diagnose HIT, an enzyme-linked immunosorbent assay or other specific blood tests must be used to confirm the presence of circulating antibodies.13 The diagnosis is based on the following criteria: (1) thrombocytopenia, (2) exclusion of other possible causes of thrombocytopenia, and (3) resolution of thrombocytopenia after discontinuation of heparin.13,15
When HIT is suspected, all heparin-containing products must be discontinued immediately and alternative anticoagulant therapy (typically, with danaparoid, lepirudin, or argatroban) should be initiated to reduce the risk of thrombosis. Warfarin alone should not be used for the treatment of HIT because of its association with worsening thrombosis and venous limb gangrene.13 However, warfarin should be initiated while the patient is receiving danaparoid or a thrombin-specific inhibitor—with at least 5 days of overlapping therapy recommended. Duration of therapy has not been well defined, but an overall course of at least 2 to 3 months is recommended to reduce the risk of recurrent thrombosis.13,15
Pregnancy raises risk, but limits Tx options
By altering the body’s normal physiologic state in a way that may lead to hypercoagulability, pregnancy increases the risk of VTE 6-fold.16 The risk continues throughout pregnancy and peaks during puerperium, the 6-week period after delivery. Cesarean delivery, prolonged immobility, and obesity elevate the risk.13,16
Treatment options for acute thrombotic events during pregnancy are limited because warfarin is contraindicated. Current ACCP guidelines recommend substituting UFH or LMWH for oral anticoagulant therapy when treatment for an acute thrombotic event is required.10 While no pharmacologic prophylaxis is currently recommended for pregnant patients with thrombophilias but no history of thrombotic events,10,17 there are cases when it may be necessary. Patients with an AT deficiency, for example, may require prenatal and postpartum prophylaxis,10 and patients who deliver by cesarean and have 1 or more additional risk factors should receive prophylaxis for the duration of their hospitalization. Women with multiple risk factors, in addition to pregnancy and cesarean section, should receive pharmacologic prophylaxis for up to 4 to 6 weeks postpartum.
Choices for postpartum anticoagulation for the treatment of an acute thrombotic event should be based on guidelines developed for nonpregnant patients, with this caveat: For women who are breastfeeding, safety during lactation must be considered. Neither UFH nor warfarin enters breast milk, so both are safe for such patients.18 LMWH, although smaller in molecular weight than UFH, is considered moderately safe during breastfeeding, as well.18
Prophylaxis is vital for trauma patients
Trauma and major injuries increase the risk of thrombosis by approximately 50%. Patients who are hospitalized after a major trauma are at high risk for the development of a VTE. At the greatest risk are those with spinal cord injuries (62%), pelvic fractures (61%), and leg fractures (80%).16 Current ACCP guidelines recommend the use of LMWH as soon as it is safe for trauma patients, and continuing it until discharge in patients with no apparent contraindication. If a patient has an active bleed or other contraindication, mechanical thromboprophylaxis is indicated until the bleeding risk decreases.15
Estrogens increase platelet aggregation
Estrogens are considered a risk factor because of their effect on both natural anticoagulants and clotting factors. A reduction in AT activity and increasing concentrations of clotting factors VII, X, and XII result from the use of estrogens. Estrogen is also thought to be responsible for the increase in platelet count and aggregation associated with the use of combination OCs.19 In fact, OC use is associated with about a 3-fold overall risk of thrombosis, a risk reported to be highest during the first year of use.16 Among hormonal contraceptives, the transdermal formulation has the highest risk.20-22 Hormone replacement therapy taken during menopause confers approximately a 2- to 4-fold increase in risk for VTE, and selective estrogen receptor modulators are associated with a 2-fold risk.16 Physicians should educate patients about the risks associated with these agents and signs and symptoms of thrombosis.
Cancer and hypercoagulability: Which patients need treatment?
Although the pathophysiologic process is not fully understood, a link between cancer and hypercoagulability has long been recognized. In fact, malignancy—the second most common cause of acquired hypercoagulability—is associated with 10% to 20% of spontaneous DVTs.2
One possible mechanism is the interaction of tumor cells with thrombin and plasmin-generating systems, directly influencing thrombus formation.7
Cancer patients also have an elevated risk for thrombosis related to immobilization, infection, treatment with antineoplastic agents, surgery, and the insertion of central venous catheters. Approximately 30% of patients with central venous catheters develop a DVT of the arm.16
Anticoagulant therapy in cancer patients varies, depending on the severity and circumstances of the patient. According to American Society of Clinical Oncology, National Comprehensive Cancer Center Network, and ACCP guidelines, LMWH is the preferred initial treatment for thromboses in patients with cancer— that is, in the first 3 to 6 months of therapy after a thrombotic event.17,23,24 The guidelines also mention warfarin as an alternative for long-term (>6 months) anticoagulant therapy, if no contraindications exist.
Because cancer is usually a long-term illness, anticoagulant therapy should be continued indefinitely, or until the cancer has resolved.10,23,24 Prophylaxis is recommended for cancer patients who are bedridden with an acute medical illness, but should not be routinely used in patients with indwelling venous catheters or those receiving chemotherapy or hormonal therapy.13,15
CORRESPONDENCE Haley M. Phillippe, PharmD, BCPS, University of Alabama Birmingham School of Medicine-Huntsville Campus, Department of Family Medicine, 301 Governors Drive, Huntsville, AL 35801; [email protected]
1. Beckman MG, Critchley SE, Hooper WC, et al. Venous thromboembolism: mechanisms, treatment and public awareness. Arteriosclerosis, Thrombosis, Vasc Biol. 2008;28:394-395.
2. Thomas RH. Hypercoagulability syndromes. Arch Intern Med. 2001;161:2433-2439.
3. Zwicker JI, Bauer KA. Thrombogenesis and hypercoagulable states. In: Ansell J, Oertel L, Wittkowsky A, eds. Managing Oral Anticoagulation Therapy. 2nd ed. St. Louis: Wolters Kluwer; 2005, p. 17:1-17:7.
4. Jebeleanu G, Procopciuc L. G20210A prothrombin gene mutation identified in patients with venous leg ulcers. J Cell Mol Med. 2001;5:397-401.
5. Dahlback B. Advances in understanding pathogenic mechanisms of thrombophilic disorders. Blood. 2008;112:19-27.
6. Beutler E, Lichtman MA, Coller BS, et al. Williams Hematology. 5th ed. New York: McGraw-Hill; 1995:1531–1542.
7. Nachman RL, Silverstein R. Hypercoagulable states. Ann Intern Med. 1993;119:819-827.
8. Federman DG, Kirsner RS. An update on hypercoagulable disorders. Arch Intern Med. 2001;161:1051-1056.
9. Deitcher S, Gomes M. Hypercoagulable state testing and malignancy screening following venous thromboembolic events. Vasc Med. 2003;8:33-46.
10. Hirsh J, Guyatt G, Albers W, et al. Executive summary: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th ed.) Chest. 2008;133(6 suppl):71S-109S.
11. Muscal E, Brey RL. Neurological manifestations of the antiphospholipid syndrome: risk assessment and evidence-based medicine. Int J Clin Pract. 2007;61:1561-1568.
12. Levine J, Branch D, Rauch J. The antiphospholipid syndrome. N Engl J Med. 2002;346:752-763.
13. Kuntz JG, Cheesman JD, Powers RD. Acute thrombotic disorders. Am J Emerg Med. 2006;24:460-467.
14. Sammaritano LR. Antiphospholipid syndrome: review. South Med J. 2005;98:617-625.
15. Franchini M. Heparin-induced thrombocytopenia: an update. Thrombosis J. 2005;3:14.-
16. Kyrle PA, Eichinger S. Deep vein thrombosis. Lancet. 2005;365:1163-1174.
17. Kearon C, Kahn SR, Agnelli G, et al. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th ed). Chest. 2008;133(6 suppl):454S-545S.
18. Hale MC. Medications and Mothers’ Milk. 11th ed. Amarillo, TX: Pharmasoft Publishing; 2004:282–283.
19. Ward MC, King DA, Link M, et al. Thrombosis secondary to medroxyprogesterone in patient at risk for thromboembolism. J Pharm Technol. 2005;21:276-280.
20. Vlijmen E, Brouwer J, Veeger N, et al. Oral contraceptives and the absolute risk of venous thromboembolism in women with single or multiple thrombophilic defects. Arch Intern Med. 2007;167:282-288.
21. Petitti D. Combination estrogen-progestin oral contraceptives. N Engl J Med. 2003;349:1443-1450.
22. Vandenbroucke J, Rosing J, Bloemenkamp K, et al. Oral contraceptives and the risk of venous thrombosis. N Engl J Med. 2001;344:1527-1535.
23. Lyman GH, Khorana A, Falanga A, et al. American Society of Clinical Oncology Guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol. 2007;25:1-16.
24. National Comprehensive Cancer Network. NCCN guidelines Available at: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp. Accessed May 14, 2010.
1. Beckman MG, Critchley SE, Hooper WC, et al. Venous thromboembolism: mechanisms, treatment and public awareness. Arteriosclerosis, Thrombosis, Vasc Biol. 2008;28:394-395.
2. Thomas RH. Hypercoagulability syndromes. Arch Intern Med. 2001;161:2433-2439.
3. Zwicker JI, Bauer KA. Thrombogenesis and hypercoagulable states. In: Ansell J, Oertel L, Wittkowsky A, eds. Managing Oral Anticoagulation Therapy. 2nd ed. St. Louis: Wolters Kluwer; 2005, p. 17:1-17:7.
4. Jebeleanu G, Procopciuc L. G20210A prothrombin gene mutation identified in patients with venous leg ulcers. J Cell Mol Med. 2001;5:397-401.
5. Dahlback B. Advances in understanding pathogenic mechanisms of thrombophilic disorders. Blood. 2008;112:19-27.
6. Beutler E, Lichtman MA, Coller BS, et al. Williams Hematology. 5th ed. New York: McGraw-Hill; 1995:1531–1542.
7. Nachman RL, Silverstein R. Hypercoagulable states. Ann Intern Med. 1993;119:819-827.
8. Federman DG, Kirsner RS. An update on hypercoagulable disorders. Arch Intern Med. 2001;161:1051-1056.
9. Deitcher S, Gomes M. Hypercoagulable state testing and malignancy screening following venous thromboembolic events. Vasc Med. 2003;8:33-46.
10. Hirsh J, Guyatt G, Albers W, et al. Executive summary: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th ed.) Chest. 2008;133(6 suppl):71S-109S.
11. Muscal E, Brey RL. Neurological manifestations of the antiphospholipid syndrome: risk assessment and evidence-based medicine. Int J Clin Pract. 2007;61:1561-1568.
12. Levine J, Branch D, Rauch J. The antiphospholipid syndrome. N Engl J Med. 2002;346:752-763.
13. Kuntz JG, Cheesman JD, Powers RD. Acute thrombotic disorders. Am J Emerg Med. 2006;24:460-467.
14. Sammaritano LR. Antiphospholipid syndrome: review. South Med J. 2005;98:617-625.
15. Franchini M. Heparin-induced thrombocytopenia: an update. Thrombosis J. 2005;3:14.-
16. Kyrle PA, Eichinger S. Deep vein thrombosis. Lancet. 2005;365:1163-1174.
17. Kearon C, Kahn SR, Agnelli G, et al. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th ed). Chest. 2008;133(6 suppl):454S-545S.
18. Hale MC. Medications and Mothers’ Milk. 11th ed. Amarillo, TX: Pharmasoft Publishing; 2004:282–283.
19. Ward MC, King DA, Link M, et al. Thrombosis secondary to medroxyprogesterone in patient at risk for thromboembolism. J Pharm Technol. 2005;21:276-280.
20. Vlijmen E, Brouwer J, Veeger N, et al. Oral contraceptives and the absolute risk of venous thromboembolism in women with single or multiple thrombophilic defects. Arch Intern Med. 2007;167:282-288.
21. Petitti D. Combination estrogen-progestin oral contraceptives. N Engl J Med. 2003;349:1443-1450.
22. Vandenbroucke J, Rosing J, Bloemenkamp K, et al. Oral contraceptives and the risk of venous thrombosis. N Engl J Med. 2001;344:1527-1535.
23. Lyman GH, Khorana A, Falanga A, et al. American Society of Clinical Oncology Guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol. 2007;25:1-16.
24. National Comprehensive Cancer Network. NCCN guidelines Available at: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp. Accessed May 14, 2010.
When to consider osteopathic manipulation
• Consider osteopathic manipulation for low back pain that has not responded to customary care, and other musculoskeletal pain such as headache or neck pain. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A patient of yours has nonspecific back pain that fails to improve with the usual self-care measures. He asks you whether osteopathic manipulation might help. Would you be prepared to discuss the relevant clinical evidence?
For a patient such as this, expert guidelines do recommend referral for osteopathic spinal manipulation, which, if performed by a qualified physician, may be efficacious and cost effective. Limited data show that osteopathic manipulation may also be effective for nonspinal disorders.
We conducted a systematic review of the evidence for osteopathic manipulative treatment (OMT) as applied to several conditions. Specifically, we searched PubMed for English language articles published between 1970 and December 2007, using the keywords osteopathy, osteopathic medicine, osteopathic manipulation, spinal manipulation, and somatic dysfunction. Our findings follow.
How OMT contributes to wellness
Osteopathic manipulative procedures are based on the premise that the neuromuscular system is vital to maintaining homeostasis. Changes in the musculoskeletal system can affect other organs (somatovisceral reflex), and visceral pathology can manifest as abnormalities in musculoskeletal tissue texture and articular motion (viscerosomatic reflex).1 These musculoskeletal changes are diagnosed as somatic dysfunction and are assigned International Statistical Classification of Diseases and Related Health Problems (ICD-9) codes corresponding to the area of the body in which these changes are palpated.2 Similarly, OMT therapeutic procedures are assigned Evaluation and Management (E&M) codes corresponding to the number of body areas treated.
OMT comprises more than 100 different techniques used to treat somatic dysfunction. Some techniques are similar to those used by chiropractors and physical or massage therapists; others are unique to osteopathically trained physicians.
OMT has multiple physiologic effects. Mechanically, OMT causes articular release, freeing joint motion. Neuromuscularly, OMT generates afferent input into the dorsal root ganglion, diminishing motor neuron discharge and relaxing muscle fibers.3 Vascularly, OMT may increase nitric oxide concentration in the blood, promoting vasodilatation and increasing blood flow to peripheral vascular tissue.4 Neurochemically, OMT can transiently increase serum levels of anandamide, stimulating cannabinoid receptors in the brain.5
What the evidence says about OMT for back pain
Joint clinical practice guidelines issued in 2007 by the American College of Physicians and the American Pain Society give a weak recommendation based on moderate-quality evidence that manipulation is an appropriate nonpharmacologic modality for treating nonspecific acute and chronic low back pain that fails to improve with self-care.6
The Institute for Clinical Systems Improvement guidelines for back pain, updated in 2008, recommend referral to a spine therapy professional for manipulative treatment of nonspecific low back pain that has failed to improve with self-care after 2 weeks, or for a patient experiencing incapacitating pain. The guidelines suggest that referred patients usually demonstrate improvement within 3 to 4 visits and typically require no more than 6 visits.7
DO family practitioners appear to use OMT more often for pain in the back than for pain in other areas of the body.8 Although a large number of randomized controlled trials (RCTs) have examined the role of spinal manipulation for adults with back pain, regardless of the type of practitioner, fewer trials have focused on manipulation specifically performed by osteopathically trained physicians.
Pain reduction is significant. A meta-analysis was conducted on 8 RCTs involving patients with back pain of at least 3 weeks’ duration, with 318 patients assigned to receive OMT vs 231 controls. Subjects in the OMT group received a variable number of OMT sessions over a given time frame per study protocol, while subjects in the control group were allowed to pursue standard care for back pain, including nonsteroidal anti-inflammatory agents (NSAIDs), muscle relaxants, narcotics, physical therapy, and home exercises. The authors found a significant (30%) overall reduction in pain rating in the OMT group compared with various control therapies at 4 and 12 weeks’ follow-up (95% confidence interval [CI], -0.47 to -0.13; P=.001).9
Another study randomized 155 patients with subacute low back pain to receive standard care or standard care plus 8 sessions of OMT over 2 months. At follow-up, both groups had similar pain ratings on a visual analog scale, but participants in the OMT group required significantly less NSAIDs, muscle relaxants, and physical therapy.10
A few RCTs have investigated the role of OMT in adults with chronic low back pain. One study randomized 91 patients with non-specific back pain of more than 3 months’ duration to receive 7 sessions of OMT, 7 sessions of sham manipulative therapy, or usual care. (Sham manipulation consisted of range of motion and light touch without therapeutic intention.) Both OMT and sham therapy significantly decreased back pain at 1 month (P=.01 and P=.003, respectively), 3 months (P=.001, P=.01), and 6 months (P=.02, P=.02) compared with usual care.11
A study conducted in the United Kingdom randomized 201 patients with spinal pain of 2 to 12 weeks’ duration to receive usual care or usual care plus 3 OMT sessions. At 2 months’ follow-up, the OMT group, compared with the usual care group, exhibited a significant reduction in spinal pain levels (95% CI, 0.7-9.8; P=.02) and in psychological distress secondary to spinal pain (95% CI, 2.7-10.7; P=.001). Both measures were rated on a scale of 0 to 100.12
A follow-up cost analysis between the usual care and usual care/OMT group found a nonsignificant difference in mean health care costs due to spinal pain for the duration of the study, estimated to be 58 £ ($88.13 US) in the usual care group and 47 £ ($71.42 US) in the OMT group.13 Authors of other studies have inferred potential health care cost savings associated with OMT for back pain based on workers’ compensation claims, lost work time, provider services, medication use, or length of hospital stay.14
Evidence basis for OMT in other disorders
Headache
One study randomized 22 subjects with tension-type headaches lasting longer than 6 months to 10-minute sessions of OMT, sham therapy, or supine rest. Participants rated their discomfort on a scale of 0 (absence of headache) to 7 (debilitating headache) before and after study intervention. Only the OMT group showed a significant immediate post-treatment reduction in patient-rated headache severity (P<.003).15
A more recent study examined 26 patients with tension headaches of similar severity and frequency at baseline. All 26 subjects received training in progressive muscular relaxation home exercises, while 14 subjects also received 3 OMT sessions over 3 weeks. At 6 weeks’ follow-up, the OMT group noted 1.79 headache-free days per week, compared with 0.21 headache-free days per week in the control group (P=.016).16
Neck pain
Fifty-eight patients with neck pain lasting longer than 3 weeks who sought care at an emergency department were asked to rate their pain intensity on an 11-point numerical scale before and after randomization to receive either 30 mg intramuscular ketorolac or a 5-minute OMT session. Both groups experienced a reduction in pain, 1.7±1.6 (95% CI, 1.1-2.3; P<.001) and 2.8 ±1.7 (95% CI, 2.1-3.4; P<.002), respectively. However, patients receiving OMT showed a significantly greater reduction in pain intensity compared with those receiving ketorolac (95% CI, 0.2-1.9; P=.02).17
Otitis media
One study examined the role of OMT in children who had experienced 3 episodes of acute otitis media (AOM) in the 6 months before study enrollment, or 4 episodes in the prior 12 months. Fifty-seven children ages 6 months to 6 years were randomized to receive usual care or usual care plus 7 OMT sessions over 6 months. The OMT group showed a significantly reduced number of AOM episodes and reduced referral for myringotomy/ ventilation tube placement compared with the control group. Additionally, final tympanograms showed an increased frequency of more normal tympanogram types in the OMT group (95% CI, 0.08-1.02; P=.02).18
Pediatric asthma
Using the registry of an asthma clinic, 1 study selected 140 subjects ages 5 to 17 years and randomized them to receive 1 OMT or 1 sham session, with peak expiratory flows (PEF) measured before and after treatment. The OMT group showed a significant mean increase in PEF from 364 to 377 L/min (95% CI, 7.3-18.7) compared with no change in the sham group.19
In the same year (2005), a Cochrane review analyzed 3 previous trials including 156 children and adults and found no significant difference in lung function measures with OMT or other manipulative or sham treatments.20
Infantile colic
One study randomized 28 infants ages 1 to 12 weeks diagnosed with colic to receive 4 weekly OMT sessions or no treatment. At 4 weeks’ follow-up, the OMT group showed a significant reduction in parent-reported daily number of hours their infants spent crying, from 2.39 to 0.89 hours (P<.001), and a significant increase in the daily number of hours infants spent sleeping, from 11.55 to 12.9 hours (P<.002). The control group showed a nonsignificant reduction in daily number of hours infants spent crying, from 2.06 to 1.56 hours, and a nonsignificant increase in daily number of hours spent sleeping, from 11.86 to 12.04 hours.21
IBS, fibromyalgia …
A number of very small RCTs with equivocal results, pilot studies, and retrospective reviews have investigated the use of OMT in postsurgical functionality, irritable bowel syndrome, fibromyalgia, infantile torticollis, muscle spasticity, joint pain, labor pain, back pain during pregnancy, adult asthma, chronic obstructive pulmonary disease, and other medical conditions. Results to date have not been meaningful enough to recommend a place for OMT in the management of these disorders.
Limitations of evidence for OMT
Studies of OMT and other forms of spinal manipulation and manual modalities have been criticized for inconsistent quality.22 Sample sizes of published studies tend to be small, rendering statistical analysis problematic.
Pretrial bias of participants may also influence outcome measures. Patients tend to have preformed opinions regarding the efficacy of manual modalities.22
The lack of validation of a placebo control has historically been problematic, and the use of sham treatment is an attempt to overcome this.23 Some studies lack objective parameters for outcomes, relying on subjective patient ratings. Finally, severity of illness in chronic conditions such as back pain varies over time, affecting study results in follow-up.24
CORRESPONDENCE Sarah Cole, DO, 12680 olive Boulevard, Suite 300, St. Louis, MO 63141; [email protected]
1. Leosho E. An overview of osteopathic medicine. Arch Fam Med. 1999;8:477-484.
2. Hart AC. ICD-9-CM Expert for Physicians. Vols 1 & 2. Eden Prairie, Minn: Ingenix; 2010.
3. Ward RC. ed. Foundations for Osteopathic Medicine. Baltimore, Md: Williams & Wilkins; 1997:3–14.
4. Salamon E, Zhu W, Stefano G. Nitric oxide as a possible mechanism for understanding the therapeutic effects of osteopathic manipulative medicine. Int J Mol Med. 2004;14:443-449.
5. McPartland JM, Giuffrida A, King J, et al. Cannabimimetic effects of osteopathic manipulative treatment. J Am Osteopath Assoc. 2005;105:283-291.
6. Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-491.
7. Low back pain, adult (guideline). Institute for Clinical Systems Improvement. November 2008. Available at: http://www.icsi.org/guidelines_and_more/gl_os_prot/ musculo-skeletal/low_back_pain/low_back_pain__adult_5. html. Accessed April 8, 2010.
8. Johnson SM, Kurtz ME. Conditions and diagnoses for which osteopathic primary care physicians and specialists use osteopathic manipulative treatment. J Am Osteopath Assoc. 2002;102:527-532.
9. Licciardone J, Brimhall A, King L. Osteopathic manipulative treatment for low back pain: a systematic review and meta-analysis of randomized controlled trials. BMC Musculoskel Dis. 2005;6:43-55.
10. Andersson GB, Lucente T, Davis AM, et al. A comparison of osteopathic spinal manipulation with standard care for patients with low back pain. N Engl J Med. 1999;341:1426-1431.
11. Licciardone J, Stoll ST, Fulda KG, et al. Osteopathic manipulative treatment for chronic low back pain: a randomized controlled trial. Spine. 2003;28:1355-1362.
12. Williams NH, Wilkinson C, Russell I, et al. Randomized osteopathic manipulation study (ROMANS): pragmatic trial for spinal pain in primary care. Fam Pract. 2003;20:662-669.
13. Williams N, Edwards RT, Linck P, et al. Cost-utility analysis of osteopathy in primary care: results from a pragmatic randomized controlled trial. Fam Pract. 2004;21:643-650.
14. Gamber R, Holland S, Russo DP, et al. Cost-effective osteopathic manipulative medicine: a literature review of cost-effectiveness analysis for osteopathic manipulative treatment. J Am Osteopath Assoc. 2005;105:357-367.
15. Hoyt WH, Shaffer F, Bard DA, et al. Osteopathic manipulation in the treatment of muscle-contraction headache. J Am Osteopath Assoc. 1979;78:49-52.
16. Anderson R, Seniscal C. A comparison of selected osteopathic treatment and relaxation for tension-type headaches. Headache. 2006;46:1273-1280.
17. McReynolds T, Sheridan B. Intramuscular ketorolac vs. osteopathic manipulative treatment in the management of acute neck pain in the emergency department: a randomized clinical trial. J Am Osteopath Assoc. 2005;105:57-67.
18. Mills MV, Henley CE, Barnes LL, et al. The use of osteopathic manipulative treatment as adjuvant therapy in children with recurrent acute otitis media. Arch Pediatr Adolesc Med. 2003;157:861-866.
19. Guiney PA, Chou R, Vianna A, et al. Effects of osteopathic manipulative treatment on pediatric patients with asthma: a randomized controlled trial. J Am Osteopath Assoc. 2005;105:7-12.
20. Hondras MA, Linde K, Jones AP. Manual therapy for asthma. Cochrane Database Syst Rev. 2005;(2):CD001002.-
21. Hayden C, Mullinger B. A preliminary assessment of the impact of cranial osteopathy for the relief of infantile colic. Compl Ther Clin Pract. 2006;12:83-90.
22. Mein EA, Greenman PE, McMillin DL, et al. Manual medicine diversity: research pitfalls and the emerging medical paradigm. J Am Osteopath Assoc. 2001;101:441-446.
23. Noll DR, Degenhardt BF, Stuart M, et al. Effectiveness of a sham protocol and adverse effects in a clinical trial of osteopathic manipulative treatment in nursing home patients. J Am Osteopath Assoc. 2004;104:107-113.
24. Licciardone J, Russo D. Blinding protocols, treatment credibility and expectancy: methodologic issues in clinical trials of osteopathic manipulative treatment. J Am Osteopath Assoc. 2006;106:457-463.
• Consider osteopathic manipulation for low back pain that has not responded to customary care, and other musculoskeletal pain such as headache or neck pain. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A patient of yours has nonspecific back pain that fails to improve with the usual self-care measures. He asks you whether osteopathic manipulation might help. Would you be prepared to discuss the relevant clinical evidence?
For a patient such as this, expert guidelines do recommend referral for osteopathic spinal manipulation, which, if performed by a qualified physician, may be efficacious and cost effective. Limited data show that osteopathic manipulation may also be effective for nonspinal disorders.
We conducted a systematic review of the evidence for osteopathic manipulative treatment (OMT) as applied to several conditions. Specifically, we searched PubMed for English language articles published between 1970 and December 2007, using the keywords osteopathy, osteopathic medicine, osteopathic manipulation, spinal manipulation, and somatic dysfunction. Our findings follow.
How OMT contributes to wellness
Osteopathic manipulative procedures are based on the premise that the neuromuscular system is vital to maintaining homeostasis. Changes in the musculoskeletal system can affect other organs (somatovisceral reflex), and visceral pathology can manifest as abnormalities in musculoskeletal tissue texture and articular motion (viscerosomatic reflex).1 These musculoskeletal changes are diagnosed as somatic dysfunction and are assigned International Statistical Classification of Diseases and Related Health Problems (ICD-9) codes corresponding to the area of the body in which these changes are palpated.2 Similarly, OMT therapeutic procedures are assigned Evaluation and Management (E&M) codes corresponding to the number of body areas treated.
OMT comprises more than 100 different techniques used to treat somatic dysfunction. Some techniques are similar to those used by chiropractors and physical or massage therapists; others are unique to osteopathically trained physicians.
OMT has multiple physiologic effects. Mechanically, OMT causes articular release, freeing joint motion. Neuromuscularly, OMT generates afferent input into the dorsal root ganglion, diminishing motor neuron discharge and relaxing muscle fibers.3 Vascularly, OMT may increase nitric oxide concentration in the blood, promoting vasodilatation and increasing blood flow to peripheral vascular tissue.4 Neurochemically, OMT can transiently increase serum levels of anandamide, stimulating cannabinoid receptors in the brain.5
What the evidence says about OMT for back pain
Joint clinical practice guidelines issued in 2007 by the American College of Physicians and the American Pain Society give a weak recommendation based on moderate-quality evidence that manipulation is an appropriate nonpharmacologic modality for treating nonspecific acute and chronic low back pain that fails to improve with self-care.6
The Institute for Clinical Systems Improvement guidelines for back pain, updated in 2008, recommend referral to a spine therapy professional for manipulative treatment of nonspecific low back pain that has failed to improve with self-care after 2 weeks, or for a patient experiencing incapacitating pain. The guidelines suggest that referred patients usually demonstrate improvement within 3 to 4 visits and typically require no more than 6 visits.7
DO family practitioners appear to use OMT more often for pain in the back than for pain in other areas of the body.8 Although a large number of randomized controlled trials (RCTs) have examined the role of spinal manipulation for adults with back pain, regardless of the type of practitioner, fewer trials have focused on manipulation specifically performed by osteopathically trained physicians.
Pain reduction is significant. A meta-analysis was conducted on 8 RCTs involving patients with back pain of at least 3 weeks’ duration, with 318 patients assigned to receive OMT vs 231 controls. Subjects in the OMT group received a variable number of OMT sessions over a given time frame per study protocol, while subjects in the control group were allowed to pursue standard care for back pain, including nonsteroidal anti-inflammatory agents (NSAIDs), muscle relaxants, narcotics, physical therapy, and home exercises. The authors found a significant (30%) overall reduction in pain rating in the OMT group compared with various control therapies at 4 and 12 weeks’ follow-up (95% confidence interval [CI], -0.47 to -0.13; P=.001).9
Another study randomized 155 patients with subacute low back pain to receive standard care or standard care plus 8 sessions of OMT over 2 months. At follow-up, both groups had similar pain ratings on a visual analog scale, but participants in the OMT group required significantly less NSAIDs, muscle relaxants, and physical therapy.10
A few RCTs have investigated the role of OMT in adults with chronic low back pain. One study randomized 91 patients with non-specific back pain of more than 3 months’ duration to receive 7 sessions of OMT, 7 sessions of sham manipulative therapy, or usual care. (Sham manipulation consisted of range of motion and light touch without therapeutic intention.) Both OMT and sham therapy significantly decreased back pain at 1 month (P=.01 and P=.003, respectively), 3 months (P=.001, P=.01), and 6 months (P=.02, P=.02) compared with usual care.11
A study conducted in the United Kingdom randomized 201 patients with spinal pain of 2 to 12 weeks’ duration to receive usual care or usual care plus 3 OMT sessions. At 2 months’ follow-up, the OMT group, compared with the usual care group, exhibited a significant reduction in spinal pain levels (95% CI, 0.7-9.8; P=.02) and in psychological distress secondary to spinal pain (95% CI, 2.7-10.7; P=.001). Both measures were rated on a scale of 0 to 100.12
A follow-up cost analysis between the usual care and usual care/OMT group found a nonsignificant difference in mean health care costs due to spinal pain for the duration of the study, estimated to be 58 £ ($88.13 US) in the usual care group and 47 £ ($71.42 US) in the OMT group.13 Authors of other studies have inferred potential health care cost savings associated with OMT for back pain based on workers’ compensation claims, lost work time, provider services, medication use, or length of hospital stay.14
Evidence basis for OMT in other disorders
Headache
One study randomized 22 subjects with tension-type headaches lasting longer than 6 months to 10-minute sessions of OMT, sham therapy, or supine rest. Participants rated their discomfort on a scale of 0 (absence of headache) to 7 (debilitating headache) before and after study intervention. Only the OMT group showed a significant immediate post-treatment reduction in patient-rated headache severity (P<.003).15
A more recent study examined 26 patients with tension headaches of similar severity and frequency at baseline. All 26 subjects received training in progressive muscular relaxation home exercises, while 14 subjects also received 3 OMT sessions over 3 weeks. At 6 weeks’ follow-up, the OMT group noted 1.79 headache-free days per week, compared with 0.21 headache-free days per week in the control group (P=.016).16
Neck pain
Fifty-eight patients with neck pain lasting longer than 3 weeks who sought care at an emergency department were asked to rate their pain intensity on an 11-point numerical scale before and after randomization to receive either 30 mg intramuscular ketorolac or a 5-minute OMT session. Both groups experienced a reduction in pain, 1.7±1.6 (95% CI, 1.1-2.3; P<.001) and 2.8 ±1.7 (95% CI, 2.1-3.4; P<.002), respectively. However, patients receiving OMT showed a significantly greater reduction in pain intensity compared with those receiving ketorolac (95% CI, 0.2-1.9; P=.02).17
Otitis media
One study examined the role of OMT in children who had experienced 3 episodes of acute otitis media (AOM) in the 6 months before study enrollment, or 4 episodes in the prior 12 months. Fifty-seven children ages 6 months to 6 years were randomized to receive usual care or usual care plus 7 OMT sessions over 6 months. The OMT group showed a significantly reduced number of AOM episodes and reduced referral for myringotomy/ ventilation tube placement compared with the control group. Additionally, final tympanograms showed an increased frequency of more normal tympanogram types in the OMT group (95% CI, 0.08-1.02; P=.02).18
Pediatric asthma
Using the registry of an asthma clinic, 1 study selected 140 subjects ages 5 to 17 years and randomized them to receive 1 OMT or 1 sham session, with peak expiratory flows (PEF) measured before and after treatment. The OMT group showed a significant mean increase in PEF from 364 to 377 L/min (95% CI, 7.3-18.7) compared with no change in the sham group.19
In the same year (2005), a Cochrane review analyzed 3 previous trials including 156 children and adults and found no significant difference in lung function measures with OMT or other manipulative or sham treatments.20
Infantile colic
One study randomized 28 infants ages 1 to 12 weeks diagnosed with colic to receive 4 weekly OMT sessions or no treatment. At 4 weeks’ follow-up, the OMT group showed a significant reduction in parent-reported daily number of hours their infants spent crying, from 2.39 to 0.89 hours (P<.001), and a significant increase in the daily number of hours infants spent sleeping, from 11.55 to 12.9 hours (P<.002). The control group showed a nonsignificant reduction in daily number of hours infants spent crying, from 2.06 to 1.56 hours, and a nonsignificant increase in daily number of hours spent sleeping, from 11.86 to 12.04 hours.21
IBS, fibromyalgia …
A number of very small RCTs with equivocal results, pilot studies, and retrospective reviews have investigated the use of OMT in postsurgical functionality, irritable bowel syndrome, fibromyalgia, infantile torticollis, muscle spasticity, joint pain, labor pain, back pain during pregnancy, adult asthma, chronic obstructive pulmonary disease, and other medical conditions. Results to date have not been meaningful enough to recommend a place for OMT in the management of these disorders.
Limitations of evidence for OMT
Studies of OMT and other forms of spinal manipulation and manual modalities have been criticized for inconsistent quality.22 Sample sizes of published studies tend to be small, rendering statistical analysis problematic.
Pretrial bias of participants may also influence outcome measures. Patients tend to have preformed opinions regarding the efficacy of manual modalities.22
The lack of validation of a placebo control has historically been problematic, and the use of sham treatment is an attempt to overcome this.23 Some studies lack objective parameters for outcomes, relying on subjective patient ratings. Finally, severity of illness in chronic conditions such as back pain varies over time, affecting study results in follow-up.24
CORRESPONDENCE Sarah Cole, DO, 12680 olive Boulevard, Suite 300, St. Louis, MO 63141; [email protected]
• Consider osteopathic manipulation for low back pain that has not responded to customary care, and other musculoskeletal pain such as headache or neck pain. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
A patient of yours has nonspecific back pain that fails to improve with the usual self-care measures. He asks you whether osteopathic manipulation might help. Would you be prepared to discuss the relevant clinical evidence?
For a patient such as this, expert guidelines do recommend referral for osteopathic spinal manipulation, which, if performed by a qualified physician, may be efficacious and cost effective. Limited data show that osteopathic manipulation may also be effective for nonspinal disorders.
We conducted a systematic review of the evidence for osteopathic manipulative treatment (OMT) as applied to several conditions. Specifically, we searched PubMed for English language articles published between 1970 and December 2007, using the keywords osteopathy, osteopathic medicine, osteopathic manipulation, spinal manipulation, and somatic dysfunction. Our findings follow.
How OMT contributes to wellness
Osteopathic manipulative procedures are based on the premise that the neuromuscular system is vital to maintaining homeostasis. Changes in the musculoskeletal system can affect other organs (somatovisceral reflex), and visceral pathology can manifest as abnormalities in musculoskeletal tissue texture and articular motion (viscerosomatic reflex).1 These musculoskeletal changes are diagnosed as somatic dysfunction and are assigned International Statistical Classification of Diseases and Related Health Problems (ICD-9) codes corresponding to the area of the body in which these changes are palpated.2 Similarly, OMT therapeutic procedures are assigned Evaluation and Management (E&M) codes corresponding to the number of body areas treated.
OMT comprises more than 100 different techniques used to treat somatic dysfunction. Some techniques are similar to those used by chiropractors and physical or massage therapists; others are unique to osteopathically trained physicians.
OMT has multiple physiologic effects. Mechanically, OMT causes articular release, freeing joint motion. Neuromuscularly, OMT generates afferent input into the dorsal root ganglion, diminishing motor neuron discharge and relaxing muscle fibers.3 Vascularly, OMT may increase nitric oxide concentration in the blood, promoting vasodilatation and increasing blood flow to peripheral vascular tissue.4 Neurochemically, OMT can transiently increase serum levels of anandamide, stimulating cannabinoid receptors in the brain.5
What the evidence says about OMT for back pain
Joint clinical practice guidelines issued in 2007 by the American College of Physicians and the American Pain Society give a weak recommendation based on moderate-quality evidence that manipulation is an appropriate nonpharmacologic modality for treating nonspecific acute and chronic low back pain that fails to improve with self-care.6
The Institute for Clinical Systems Improvement guidelines for back pain, updated in 2008, recommend referral to a spine therapy professional for manipulative treatment of nonspecific low back pain that has failed to improve with self-care after 2 weeks, or for a patient experiencing incapacitating pain. The guidelines suggest that referred patients usually demonstrate improvement within 3 to 4 visits and typically require no more than 6 visits.7
DO family practitioners appear to use OMT more often for pain in the back than for pain in other areas of the body.8 Although a large number of randomized controlled trials (RCTs) have examined the role of spinal manipulation for adults with back pain, regardless of the type of practitioner, fewer trials have focused on manipulation specifically performed by osteopathically trained physicians.
Pain reduction is significant. A meta-analysis was conducted on 8 RCTs involving patients with back pain of at least 3 weeks’ duration, with 318 patients assigned to receive OMT vs 231 controls. Subjects in the OMT group received a variable number of OMT sessions over a given time frame per study protocol, while subjects in the control group were allowed to pursue standard care for back pain, including nonsteroidal anti-inflammatory agents (NSAIDs), muscle relaxants, narcotics, physical therapy, and home exercises. The authors found a significant (30%) overall reduction in pain rating in the OMT group compared with various control therapies at 4 and 12 weeks’ follow-up (95% confidence interval [CI], -0.47 to -0.13; P=.001).9
Another study randomized 155 patients with subacute low back pain to receive standard care or standard care plus 8 sessions of OMT over 2 months. At follow-up, both groups had similar pain ratings on a visual analog scale, but participants in the OMT group required significantly less NSAIDs, muscle relaxants, and physical therapy.10
A few RCTs have investigated the role of OMT in adults with chronic low back pain. One study randomized 91 patients with non-specific back pain of more than 3 months’ duration to receive 7 sessions of OMT, 7 sessions of sham manipulative therapy, or usual care. (Sham manipulation consisted of range of motion and light touch without therapeutic intention.) Both OMT and sham therapy significantly decreased back pain at 1 month (P=.01 and P=.003, respectively), 3 months (P=.001, P=.01), and 6 months (P=.02, P=.02) compared with usual care.11
A study conducted in the United Kingdom randomized 201 patients with spinal pain of 2 to 12 weeks’ duration to receive usual care or usual care plus 3 OMT sessions. At 2 months’ follow-up, the OMT group, compared with the usual care group, exhibited a significant reduction in spinal pain levels (95% CI, 0.7-9.8; P=.02) and in psychological distress secondary to spinal pain (95% CI, 2.7-10.7; P=.001). Both measures were rated on a scale of 0 to 100.12
A follow-up cost analysis between the usual care and usual care/OMT group found a nonsignificant difference in mean health care costs due to spinal pain for the duration of the study, estimated to be 58 £ ($88.13 US) in the usual care group and 47 £ ($71.42 US) in the OMT group.13 Authors of other studies have inferred potential health care cost savings associated with OMT for back pain based on workers’ compensation claims, lost work time, provider services, medication use, or length of hospital stay.14
Evidence basis for OMT in other disorders
Headache
One study randomized 22 subjects with tension-type headaches lasting longer than 6 months to 10-minute sessions of OMT, sham therapy, or supine rest. Participants rated their discomfort on a scale of 0 (absence of headache) to 7 (debilitating headache) before and after study intervention. Only the OMT group showed a significant immediate post-treatment reduction in patient-rated headache severity (P<.003).15
A more recent study examined 26 patients with tension headaches of similar severity and frequency at baseline. All 26 subjects received training in progressive muscular relaxation home exercises, while 14 subjects also received 3 OMT sessions over 3 weeks. At 6 weeks’ follow-up, the OMT group noted 1.79 headache-free days per week, compared with 0.21 headache-free days per week in the control group (P=.016).16
Neck pain
Fifty-eight patients with neck pain lasting longer than 3 weeks who sought care at an emergency department were asked to rate their pain intensity on an 11-point numerical scale before and after randomization to receive either 30 mg intramuscular ketorolac or a 5-minute OMT session. Both groups experienced a reduction in pain, 1.7±1.6 (95% CI, 1.1-2.3; P<.001) and 2.8 ±1.7 (95% CI, 2.1-3.4; P<.002), respectively. However, patients receiving OMT showed a significantly greater reduction in pain intensity compared with those receiving ketorolac (95% CI, 0.2-1.9; P=.02).17
Otitis media
One study examined the role of OMT in children who had experienced 3 episodes of acute otitis media (AOM) in the 6 months before study enrollment, or 4 episodes in the prior 12 months. Fifty-seven children ages 6 months to 6 years were randomized to receive usual care or usual care plus 7 OMT sessions over 6 months. The OMT group showed a significantly reduced number of AOM episodes and reduced referral for myringotomy/ ventilation tube placement compared with the control group. Additionally, final tympanograms showed an increased frequency of more normal tympanogram types in the OMT group (95% CI, 0.08-1.02; P=.02).18
Pediatric asthma
Using the registry of an asthma clinic, 1 study selected 140 subjects ages 5 to 17 years and randomized them to receive 1 OMT or 1 sham session, with peak expiratory flows (PEF) measured before and after treatment. The OMT group showed a significant mean increase in PEF from 364 to 377 L/min (95% CI, 7.3-18.7) compared with no change in the sham group.19
In the same year (2005), a Cochrane review analyzed 3 previous trials including 156 children and adults and found no significant difference in lung function measures with OMT or other manipulative or sham treatments.20
Infantile colic
One study randomized 28 infants ages 1 to 12 weeks diagnosed with colic to receive 4 weekly OMT sessions or no treatment. At 4 weeks’ follow-up, the OMT group showed a significant reduction in parent-reported daily number of hours their infants spent crying, from 2.39 to 0.89 hours (P<.001), and a significant increase in the daily number of hours infants spent sleeping, from 11.55 to 12.9 hours (P<.002). The control group showed a nonsignificant reduction in daily number of hours infants spent crying, from 2.06 to 1.56 hours, and a nonsignificant increase in daily number of hours spent sleeping, from 11.86 to 12.04 hours.21
IBS, fibromyalgia …
A number of very small RCTs with equivocal results, pilot studies, and retrospective reviews have investigated the use of OMT in postsurgical functionality, irritable bowel syndrome, fibromyalgia, infantile torticollis, muscle spasticity, joint pain, labor pain, back pain during pregnancy, adult asthma, chronic obstructive pulmonary disease, and other medical conditions. Results to date have not been meaningful enough to recommend a place for OMT in the management of these disorders.
Limitations of evidence for OMT
Studies of OMT and other forms of spinal manipulation and manual modalities have been criticized for inconsistent quality.22 Sample sizes of published studies tend to be small, rendering statistical analysis problematic.
Pretrial bias of participants may also influence outcome measures. Patients tend to have preformed opinions regarding the efficacy of manual modalities.22
The lack of validation of a placebo control has historically been problematic, and the use of sham treatment is an attempt to overcome this.23 Some studies lack objective parameters for outcomes, relying on subjective patient ratings. Finally, severity of illness in chronic conditions such as back pain varies over time, affecting study results in follow-up.24
CORRESPONDENCE Sarah Cole, DO, 12680 olive Boulevard, Suite 300, St. Louis, MO 63141; [email protected]
1. Leosho E. An overview of osteopathic medicine. Arch Fam Med. 1999;8:477-484.
2. Hart AC. ICD-9-CM Expert for Physicians. Vols 1 & 2. Eden Prairie, Minn: Ingenix; 2010.
3. Ward RC. ed. Foundations for Osteopathic Medicine. Baltimore, Md: Williams & Wilkins; 1997:3–14.
4. Salamon E, Zhu W, Stefano G. Nitric oxide as a possible mechanism for understanding the therapeutic effects of osteopathic manipulative medicine. Int J Mol Med. 2004;14:443-449.
5. McPartland JM, Giuffrida A, King J, et al. Cannabimimetic effects of osteopathic manipulative treatment. J Am Osteopath Assoc. 2005;105:283-291.
6. Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-491.
7. Low back pain, adult (guideline). Institute for Clinical Systems Improvement. November 2008. Available at: http://www.icsi.org/guidelines_and_more/gl_os_prot/ musculo-skeletal/low_back_pain/low_back_pain__adult_5. html. Accessed April 8, 2010.
8. Johnson SM, Kurtz ME. Conditions and diagnoses for which osteopathic primary care physicians and specialists use osteopathic manipulative treatment. J Am Osteopath Assoc. 2002;102:527-532.
9. Licciardone J, Brimhall A, King L. Osteopathic manipulative treatment for low back pain: a systematic review and meta-analysis of randomized controlled trials. BMC Musculoskel Dis. 2005;6:43-55.
10. Andersson GB, Lucente T, Davis AM, et al. A comparison of osteopathic spinal manipulation with standard care for patients with low back pain. N Engl J Med. 1999;341:1426-1431.
11. Licciardone J, Stoll ST, Fulda KG, et al. Osteopathic manipulative treatment for chronic low back pain: a randomized controlled trial. Spine. 2003;28:1355-1362.
12. Williams NH, Wilkinson C, Russell I, et al. Randomized osteopathic manipulation study (ROMANS): pragmatic trial for spinal pain in primary care. Fam Pract. 2003;20:662-669.
13. Williams N, Edwards RT, Linck P, et al. Cost-utility analysis of osteopathy in primary care: results from a pragmatic randomized controlled trial. Fam Pract. 2004;21:643-650.
14. Gamber R, Holland S, Russo DP, et al. Cost-effective osteopathic manipulative medicine: a literature review of cost-effectiveness analysis for osteopathic manipulative treatment. J Am Osteopath Assoc. 2005;105:357-367.
15. Hoyt WH, Shaffer F, Bard DA, et al. Osteopathic manipulation in the treatment of muscle-contraction headache. J Am Osteopath Assoc. 1979;78:49-52.
16. Anderson R, Seniscal C. A comparison of selected osteopathic treatment and relaxation for tension-type headaches. Headache. 2006;46:1273-1280.
17. McReynolds T, Sheridan B. Intramuscular ketorolac vs. osteopathic manipulative treatment in the management of acute neck pain in the emergency department: a randomized clinical trial. J Am Osteopath Assoc. 2005;105:57-67.
18. Mills MV, Henley CE, Barnes LL, et al. The use of osteopathic manipulative treatment as adjuvant therapy in children with recurrent acute otitis media. Arch Pediatr Adolesc Med. 2003;157:861-866.
19. Guiney PA, Chou R, Vianna A, et al. Effects of osteopathic manipulative treatment on pediatric patients with asthma: a randomized controlled trial. J Am Osteopath Assoc. 2005;105:7-12.
20. Hondras MA, Linde K, Jones AP. Manual therapy for asthma. Cochrane Database Syst Rev. 2005;(2):CD001002.-
21. Hayden C, Mullinger B. A preliminary assessment of the impact of cranial osteopathy for the relief of infantile colic. Compl Ther Clin Pract. 2006;12:83-90.
22. Mein EA, Greenman PE, McMillin DL, et al. Manual medicine diversity: research pitfalls and the emerging medical paradigm. J Am Osteopath Assoc. 2001;101:441-446.
23. Noll DR, Degenhardt BF, Stuart M, et al. Effectiveness of a sham protocol and adverse effects in a clinical trial of osteopathic manipulative treatment in nursing home patients. J Am Osteopath Assoc. 2004;104:107-113.
24. Licciardone J, Russo D. Blinding protocols, treatment credibility and expectancy: methodologic issues in clinical trials of osteopathic manipulative treatment. J Am Osteopath Assoc. 2006;106:457-463.
1. Leosho E. An overview of osteopathic medicine. Arch Fam Med. 1999;8:477-484.
2. Hart AC. ICD-9-CM Expert for Physicians. Vols 1 & 2. Eden Prairie, Minn: Ingenix; 2010.
3. Ward RC. ed. Foundations for Osteopathic Medicine. Baltimore, Md: Williams & Wilkins; 1997:3–14.
4. Salamon E, Zhu W, Stefano G. Nitric oxide as a possible mechanism for understanding the therapeutic effects of osteopathic manipulative medicine. Int J Mol Med. 2004;14:443-449.
5. McPartland JM, Giuffrida A, King J, et al. Cannabimimetic effects of osteopathic manipulative treatment. J Am Osteopath Assoc. 2005;105:283-291.
6. Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-491.
7. Low back pain, adult (guideline). Institute for Clinical Systems Improvement. November 2008. Available at: http://www.icsi.org/guidelines_and_more/gl_os_prot/ musculo-skeletal/low_back_pain/low_back_pain__adult_5. html. Accessed April 8, 2010.
8. Johnson SM, Kurtz ME. Conditions and diagnoses for which osteopathic primary care physicians and specialists use osteopathic manipulative treatment. J Am Osteopath Assoc. 2002;102:527-532.
9. Licciardone J, Brimhall A, King L. Osteopathic manipulative treatment for low back pain: a systematic review and meta-analysis of randomized controlled trials. BMC Musculoskel Dis. 2005;6:43-55.
10. Andersson GB, Lucente T, Davis AM, et al. A comparison of osteopathic spinal manipulation with standard care for patients with low back pain. N Engl J Med. 1999;341:1426-1431.
11. Licciardone J, Stoll ST, Fulda KG, et al. Osteopathic manipulative treatment for chronic low back pain: a randomized controlled trial. Spine. 2003;28:1355-1362.
12. Williams NH, Wilkinson C, Russell I, et al. Randomized osteopathic manipulation study (ROMANS): pragmatic trial for spinal pain in primary care. Fam Pract. 2003;20:662-669.
13. Williams N, Edwards RT, Linck P, et al. Cost-utility analysis of osteopathy in primary care: results from a pragmatic randomized controlled trial. Fam Pract. 2004;21:643-650.
14. Gamber R, Holland S, Russo DP, et al. Cost-effective osteopathic manipulative medicine: a literature review of cost-effectiveness analysis for osteopathic manipulative treatment. J Am Osteopath Assoc. 2005;105:357-367.
15. Hoyt WH, Shaffer F, Bard DA, et al. Osteopathic manipulation in the treatment of muscle-contraction headache. J Am Osteopath Assoc. 1979;78:49-52.
16. Anderson R, Seniscal C. A comparison of selected osteopathic treatment and relaxation for tension-type headaches. Headache. 2006;46:1273-1280.
17. McReynolds T, Sheridan B. Intramuscular ketorolac vs. osteopathic manipulative treatment in the management of acute neck pain in the emergency department: a randomized clinical trial. J Am Osteopath Assoc. 2005;105:57-67.
18. Mills MV, Henley CE, Barnes LL, et al. The use of osteopathic manipulative treatment as adjuvant therapy in children with recurrent acute otitis media. Arch Pediatr Adolesc Med. 2003;157:861-866.
19. Guiney PA, Chou R, Vianna A, et al. Effects of osteopathic manipulative treatment on pediatric patients with asthma: a randomized controlled trial. J Am Osteopath Assoc. 2005;105:7-12.
20. Hondras MA, Linde K, Jones AP. Manual therapy for asthma. Cochrane Database Syst Rev. 2005;(2):CD001002.-
21. Hayden C, Mullinger B. A preliminary assessment of the impact of cranial osteopathy for the relief of infantile colic. Compl Ther Clin Pract. 2006;12:83-90.
22. Mein EA, Greenman PE, McMillin DL, et al. Manual medicine diversity: research pitfalls and the emerging medical paradigm. J Am Osteopath Assoc. 2001;101:441-446.
23. Noll DR, Degenhardt BF, Stuart M, et al. Effectiveness of a sham protocol and adverse effects in a clinical trial of osteopathic manipulative treatment in nursing home patients. J Am Osteopath Assoc. 2004;104:107-113.
24. Licciardone J, Russo D. Blinding protocols, treatment credibility and expectancy: methodologic issues in clinical trials of osteopathic manipulative treatment. J Am Osteopath Assoc. 2006;106:457-463.
Test your skills: A worsening rash
A mother brings her 5-year-old boy in to your office because she is concerned about a rash on his legs that seems to be worsening. She tells you that he had a runny nose and a mild cough a week earlier, but that those symptoms resolved before the rash developed. He has also complained of “belly pain.”
The boy’s mother says he’s been less active and more irritable since the onset of the rash, and that he is hardly eating. She also tells you that earlier in the day, her son told her that it hurts to walk.
You dig deeper…
A complete review of systems is otherwise negative. The 5-year-old was born at term without complication. He has met all developmental milestones and his immunizations are up to date. He takes no medications.
The boy’s vital signs are normal. He has an erythematous maculopapular rash distributed on his legs symmetrically; it is palpable, nontender, and nonblanching. You detect no abnormalities in abdominal, neurologic, or musculoskeletal examinations.
A complete blood count (CBC) and basic metabolic panel (BMP) reveal mild leukocytosis with a normal differential. Urinalysis shows moderate blood and trace protein. Laboratory results are otherwise normal.
WHAT IS YOUR DIAGNOSIS?
A classic presentation revealed: Henoch-Schönlein purpura
The combination of rash (FIGURE), abdominal pain, arthralgia, and evidence of renal involvement are the classic symptoms for Henoch-Schönlein purpura (HSP),1 the most common systemic vasculitis of childhood.2 Fever may also be present. Boys are affected nearly twice as often as girls. HSP occurs only rarely among adults, and men and women are affected equally. The estimated annual incidence in children is 20 cases per 100,000, with most cases occurring in those between the ages of 4 and 6 years.3
Although the exact cause of HSP is unknown, 75% of cases follow an upper respiratory infection. Streptococcus, Mycoplasma, adenovirus, parvovirus, Epstein-Barr virus, and varicella have all been implicated as offending pathogens. A number of case reports have also described the disease after the use of certain drugs, including penicillin, ampicillin, and quinine; and after the administration of vaccines, including those for typhoid, measles, yellow fever, and cholera. In all cases, the underlying mechanism is thought to be a systemic rise in immunoglobulin A (IgA), which forms immune complexes deposited in arterioles, capillaries, and venules.4 The precise interactions in the mechanism of disease are yet to be determined.
FIGURE
Rash and leg pain
Like the patient described in the text, this 11-year-old girl had a similar rash on her legs, as well as leg and abdominal pain.
HSP is usually benign, self-limited
HSP signs and symptoms may occur in any order over a period of days to weeks. Symptoms tend to be less severe in younger children than in older children and adults. Besides abdominal and renal systems, the lungs and central nervous system (CNS) may be affected, although rarely in children. Pulmonary involvement, if it does occur, usually manifests as diffuse alveolar hemorrhage or interstitial pneumonia or fibrosis.5 CNS vasculitis may lead to cerebral hemorrhage.6
HSP usually is a benign, self-limited disorder. The average disease course is 4 weeks, although it may be as brief as 3 days or as long as 2 years. Up to 94% of children (and 89% of adults) recover fully.7 However, the potential for chronic renal disease does exist.8
The recurrence rate of HSP is generally reported as 40%;8 patients who develop nephritis have higher recurrence rates.9
Rash is almost always present
Nearly all of those affected with HSP exhibit a rash. In children, it may begin as urticarial or maculopapular skin lesions. The rash typically is a palpable purpura, with lesions measuring 2 to 10 mm in diameter. Classically, the rash appears symmetrically on the extensor surfaces of the arms, legs, and buttocks. Lesions may also occur on the face and ears; however, the rash usually spares the trunk.2 The rash generally fades over several days and gives way to darkened pigment. The purpuric lesions resolve more quickly with bed rest and tend to reappear when the patient resumes activity.
Bullous or necrotic lesions—although reported to occur in up to 60% of affected adults—are uncommon in children. If you had noted such lesions in this case, you would have had to rule out toxic vasculitides and meningococcal septicemia or other septic emboli.10
Arthralgia affects lower extremities
Arthralgia is the second most common clinical manifestation of HSP, occurring in approximately 82% of patients. Joint pain associated with HSP is likely due to periarticular soft tissue edema, and most commonly occurs in the hips, knees, or ankles.1,11 The arthralgia of HSP is transient and self-limited and does not cause permanent damage to the joints. Like the rash, joint pain tends to decrease with bed rest and increase with activity.11
Gastrointestinal involvement is rarely serious
Gastrointestinal involvement has been reported in 63% of patients with HSP. Symptoms typically include a colicky abdominal pain, associated with nausea and vomiting. These symptoms probably arise secondary to edema of the bowel wall and vasculitis of the gastrointestinal tract. The pain most often develops within 8 days of the appearance of the rash, but it has been reported to appear within weeks to months of cutaneous changes.12
Intussusception is the most common gastrointestinal complication in patients with HSP, with a reported overall incidence of 3.5% in hospitalized patients with severe abdominal pain. Gastrointestinal bleeding, presenting as either melena or hematochezia, has been reported in 25% of patients with HSP. Occult bleeding may occur in up to 50% of patients.12
More serious complications are rare, and they include bowel infarction and perforation, usually in the jejunum or ileum, and pancreatitis, cholecystitis, or protein-losing enteropathy secondary to HSP.
Renal involvement may require close follow-up
Renal disease has been reported to affect 30% to 70% of all HSP patients.13 Onset occurs within weeks to months after other symptoms of HSP. Most patients with renal involvement have only mild disease, such as asymptomatic hematuria and proteinuria.1,7,13 HSP is thought to account for approximately 15% of all glomerulopathies in childhood.13
Although renal disease in HSP is generally benign, such complications as nephrotic syndrome, hypertension, and acute and chronic renal failure may occur. Adults are much more susceptible to the latter complication.
When the diagnosis is unclear, renal biopsy may help confirm the presence of disease. Evidence of HSP is identical to that seen with IgA nephropathy.11,13 The percentage of glomeruli showing crescents on renal biopsy seems to be the most important prognostic finding, with crescent formation involving more than 50% of the glomeruli carrying a poor prognosis.14
Diagnosis is mainly clinical
Clinical diagnosis is not difficult with the classic 4 symptoms present (rash, abdominal pain, arthralgia, and evidence of renal involvement). However, when the presentation is less straightforward, confirmation of the diagnosis may depend on biopsy of the affected organ (eg, skin, kidney) demonstrating leukocytoclastic vasculitis with IgA deposition.
The differential diagnosis of HSP is large, and includes acute abdomen, meningococcal meningitis or septicemia, rheumatoid arthritis, idiopathic thrombocytopenic purpura, and systemic lupus erythematosus.15
Lab tests are minimally helpful. No lab test or imaging study is sensitive or specific for HSP. An elevated serum IgA level suggests the disease. A CBC may show leukocytosis and thrombocytosis, but test results may also be normal. The erythrocyte sedimentation rate may be elevated. On a BMP, blood urea nitrogen and creatinine levels may be elevated secondary to renal involvement or dehydration associated with HSP. Finally, hematuria or proteinuria show up on urinalysis in 30% to 70% of patients with HSP.2,12,13
What treatment is indicated?
Most patients with HSP recover completely without any specific intervention other than reassurance, bed rest, and supportive care. Arthralgia usually responds to nonsteroidal anti-inflammatory drugs and corticosteroids. Hospitalization is warranted when patients have a depleted volume status or inadequately controlled pain. With an otherwise un-complicated illness, watchful management suffices. Gastrointestinal and renal complications may require more aggressive therapy.
Gastrointestinal complications. As noted earlier, the most common gastrointestinal complication is intussusception. No definite measures for preventing intussusception appear in the literature. Some evidence supports the use of corticosteroids for severe abdominal symptoms,16,17 but in general, corticosteroids are not indicated for extrarenal manifestations. More serious complications such as bowel infarction or perforation, pancreatitis, or cholecystitis are rare.
Renal disease. Much research has focused on treatment options for patients with renal complications, due to the possibility of long-term debilitating effects. Although no evidence supports corticosteroid use for patients with mild renal involvement,16 for patients with severe renal disease—defined as crescenteric nephritis on biopsy, usually complicated by oliguria and hypertension—corticosteroids may help prevent irreversible glomerular injury.
Other agents that have been used for severe renal disease include azathioprine, cyclophosphamide, and dipyridamole. These drugs have shown some success in resolving symptoms, but their use remains controversial.16,18 Finally, plasmapheresis has led to significant clinical improvement for a small number of patients with severe, rapidly progressing HSP.
Caveat. The effectiveness of all treatments for HSP remains in question, given that patients’ symptoms may simply resolve spontaneously. A clear answer will depend on further research.
Rest, fluids, and ibuprofen for your patient
You send your patient home with his mother, and advise her to provide him with supportive care, including oral hydration. You tell her to encourage rest and to give symptomatic pain relief with an over-the-counter medication such as ibuprofen.
You see the child again in 3 days, by which time his arthralgias are improving. Repeat urinalysis shows continuing moderate blood and trace protein. You follow him biweekly for 2 weeks, and then weekly for 4 more weeks. Six weeks after his initial presentation, his symptoms completely resolve, and urinalysis shows no evidence of hematuria or proteinuria. His blood pressure is normal at all visits.
You see the patient monthly for the next 5 months. Symptoms do not recur, and urinalysis results are normal. You counsel the boy’s mother regarding the risk of recurrence, and advise her to contact the office immediately if symptoms return.
CORRESPONDENCE Shailendra K. Saxena, MD, PhD, Department of Family Medicine, 10828 John Galt Boulevard, Omaha, NE 68137; [email protected]
1. Roberts PF, Waller TA, Brinker TM, et al. Henoch-Schönlein purpura: a review article. South Med J. 2007;100:821-824.
2. Tizard EJ. Henoch-Schönlein purpura. Arch Dis Child. 1999;80:380-383.
3. Gardner-Medwin JM, Dolezalova P, Cummins C, et al. Incidence of Henoch-Schönlein purpura, Kawasaki disease, and rare vasculitides in children of different ethnic origins. Lancet. 2002;360:1197-1202.
4. Yang YH, Chuang YH, Wang LC, et al. The immunology of Henoch-Schönlein purpura. Autoimmun Rev. 2008;7:179-184.
5. Nadrous HF, Yu AC, Specks U, et al. Pulmonary involvement in Henoch-Schönlein purpura. Mayo Clin Proc. 2004;79:1151-1157.
6. Elinson P, Foster KW, Kaufman DB. Magnetic resonance imaging of central nervous system vasculitis: a case report of Henoch-Schönlein purpura. Acta Pediatr. 2008;79:710-713.
7. Blanco R, Martínez-Taboada VM, Rodríguez-Valverde V, et al. Henoch-Schönlein purpura in adulthood and childhood: two different expressions of the same syndrome. Arthritis Rheum. 1997;40:859-864.
8. Dillon MJ. Henoch-Schönlein purpura (treatment and outcome). Cleve Clin J Med. 2002;69(suppl):S121-S123.
9. Alfredo CS, Nunes NA, Len CA, et al. Henoch-Schönlein purpura: recurrence and chronicity. J Pediatr (Rio J). 2007;83:177-180.
10. Morelli JG. Vascular disorders. In: Kliegman RM, Behrman RE, Jensen HB, eds. Nelson Textbook of Pediatrics. 18th ed. Philadelphia, Pa: Saunders Elsevier; 2007:2667–2673.
11. Trapani S, Micheli A, Grisolia F, et al. Henoch-Schönlein purpura in childhood: epidemiological and clinical analysis of 150 cases over a 5-year period and review of literature. Semin Arthritis Rheum. 2005;35:143-153.
12. Chang WL, Yang YH, Lin YT, et al. Gastrointestinal manifestations in Henoch-Schönlein purpura: a review of 261 patients. Acta Pediatr. 2004;93:1427-1431.
13. Chang WL, Yang YH, Wang LC, et al. Renal manifestations in Henoch-Schönlein purpura: a 10-year clinical study. Pediatr Nephrol. 2005;20:1269-1272.
14. Bogdanovic R. Henoch-Schönlein purpura nephritis in children: risk factors, prevention and treatment. Acta Paediatr. 2009;98:1882-1889.
15. Kraft DM, Mckee D, Scott C. Henoch-Schönlein purpura: a review. Am Fam Phys. 1998;58:405-408,411.
16. Szer IS. Gastrointestinal and renal involvement in vasculitis: management strategies in Henoch-Schönlein purpura. Cleve Clin J Med. 1999;66:312-317.
17. Leung SP. Use of intravenous hydrocortisone in Henoch-Schönlein purpura. J Paediatr Child Health. 2001;37:309-310.
18. Zaffanello M, Brugnara M, Franchini M, et al. Therapy for children with Henoch-Schönlein purpura nephritis: a systematic review. ScientificWorldJournal. 2007;7:20-30.
A mother brings her 5-year-old boy in to your office because she is concerned about a rash on his legs that seems to be worsening. She tells you that he had a runny nose and a mild cough a week earlier, but that those symptoms resolved before the rash developed. He has also complained of “belly pain.”
The boy’s mother says he’s been less active and more irritable since the onset of the rash, and that he is hardly eating. She also tells you that earlier in the day, her son told her that it hurts to walk.
You dig deeper…
A complete review of systems is otherwise negative. The 5-year-old was born at term without complication. He has met all developmental milestones and his immunizations are up to date. He takes no medications.
The boy’s vital signs are normal. He has an erythematous maculopapular rash distributed on his legs symmetrically; it is palpable, nontender, and nonblanching. You detect no abnormalities in abdominal, neurologic, or musculoskeletal examinations.
A complete blood count (CBC) and basic metabolic panel (BMP) reveal mild leukocytosis with a normal differential. Urinalysis shows moderate blood and trace protein. Laboratory results are otherwise normal.
WHAT IS YOUR DIAGNOSIS?
A classic presentation revealed: Henoch-Schönlein purpura
The combination of rash (FIGURE), abdominal pain, arthralgia, and evidence of renal involvement are the classic symptoms for Henoch-Schönlein purpura (HSP),1 the most common systemic vasculitis of childhood.2 Fever may also be present. Boys are affected nearly twice as often as girls. HSP occurs only rarely among adults, and men and women are affected equally. The estimated annual incidence in children is 20 cases per 100,000, with most cases occurring in those between the ages of 4 and 6 years.3
Although the exact cause of HSP is unknown, 75% of cases follow an upper respiratory infection. Streptococcus, Mycoplasma, adenovirus, parvovirus, Epstein-Barr virus, and varicella have all been implicated as offending pathogens. A number of case reports have also described the disease after the use of certain drugs, including penicillin, ampicillin, and quinine; and after the administration of vaccines, including those for typhoid, measles, yellow fever, and cholera. In all cases, the underlying mechanism is thought to be a systemic rise in immunoglobulin A (IgA), which forms immune complexes deposited in arterioles, capillaries, and venules.4 The precise interactions in the mechanism of disease are yet to be determined.
FIGURE
Rash and leg pain
Like the patient described in the text, this 11-year-old girl had a similar rash on her legs, as well as leg and abdominal pain.
HSP is usually benign, self-limited
HSP signs and symptoms may occur in any order over a period of days to weeks. Symptoms tend to be less severe in younger children than in older children and adults. Besides abdominal and renal systems, the lungs and central nervous system (CNS) may be affected, although rarely in children. Pulmonary involvement, if it does occur, usually manifests as diffuse alveolar hemorrhage or interstitial pneumonia or fibrosis.5 CNS vasculitis may lead to cerebral hemorrhage.6
HSP usually is a benign, self-limited disorder. The average disease course is 4 weeks, although it may be as brief as 3 days or as long as 2 years. Up to 94% of children (and 89% of adults) recover fully.7 However, the potential for chronic renal disease does exist.8
The recurrence rate of HSP is generally reported as 40%;8 patients who develop nephritis have higher recurrence rates.9
Rash is almost always present
Nearly all of those affected with HSP exhibit a rash. In children, it may begin as urticarial or maculopapular skin lesions. The rash typically is a palpable purpura, with lesions measuring 2 to 10 mm in diameter. Classically, the rash appears symmetrically on the extensor surfaces of the arms, legs, and buttocks. Lesions may also occur on the face and ears; however, the rash usually spares the trunk.2 The rash generally fades over several days and gives way to darkened pigment. The purpuric lesions resolve more quickly with bed rest and tend to reappear when the patient resumes activity.
Bullous or necrotic lesions—although reported to occur in up to 60% of affected adults—are uncommon in children. If you had noted such lesions in this case, you would have had to rule out toxic vasculitides and meningococcal septicemia or other septic emboli.10
Arthralgia affects lower extremities
Arthralgia is the second most common clinical manifestation of HSP, occurring in approximately 82% of patients. Joint pain associated with HSP is likely due to periarticular soft tissue edema, and most commonly occurs in the hips, knees, or ankles.1,11 The arthralgia of HSP is transient and self-limited and does not cause permanent damage to the joints. Like the rash, joint pain tends to decrease with bed rest and increase with activity.11
Gastrointestinal involvement is rarely serious
Gastrointestinal involvement has been reported in 63% of patients with HSP. Symptoms typically include a colicky abdominal pain, associated with nausea and vomiting. These symptoms probably arise secondary to edema of the bowel wall and vasculitis of the gastrointestinal tract. The pain most often develops within 8 days of the appearance of the rash, but it has been reported to appear within weeks to months of cutaneous changes.12
Intussusception is the most common gastrointestinal complication in patients with HSP, with a reported overall incidence of 3.5% in hospitalized patients with severe abdominal pain. Gastrointestinal bleeding, presenting as either melena or hematochezia, has been reported in 25% of patients with HSP. Occult bleeding may occur in up to 50% of patients.12
More serious complications are rare, and they include bowel infarction and perforation, usually in the jejunum or ileum, and pancreatitis, cholecystitis, or protein-losing enteropathy secondary to HSP.
Renal involvement may require close follow-up
Renal disease has been reported to affect 30% to 70% of all HSP patients.13 Onset occurs within weeks to months after other symptoms of HSP. Most patients with renal involvement have only mild disease, such as asymptomatic hematuria and proteinuria.1,7,13 HSP is thought to account for approximately 15% of all glomerulopathies in childhood.13
Although renal disease in HSP is generally benign, such complications as nephrotic syndrome, hypertension, and acute and chronic renal failure may occur. Adults are much more susceptible to the latter complication.
When the diagnosis is unclear, renal biopsy may help confirm the presence of disease. Evidence of HSP is identical to that seen with IgA nephropathy.11,13 The percentage of glomeruli showing crescents on renal biopsy seems to be the most important prognostic finding, with crescent formation involving more than 50% of the glomeruli carrying a poor prognosis.14
Diagnosis is mainly clinical
Clinical diagnosis is not difficult with the classic 4 symptoms present (rash, abdominal pain, arthralgia, and evidence of renal involvement). However, when the presentation is less straightforward, confirmation of the diagnosis may depend on biopsy of the affected organ (eg, skin, kidney) demonstrating leukocytoclastic vasculitis with IgA deposition.
The differential diagnosis of HSP is large, and includes acute abdomen, meningococcal meningitis or septicemia, rheumatoid arthritis, idiopathic thrombocytopenic purpura, and systemic lupus erythematosus.15
Lab tests are minimally helpful. No lab test or imaging study is sensitive or specific for HSP. An elevated serum IgA level suggests the disease. A CBC may show leukocytosis and thrombocytosis, but test results may also be normal. The erythrocyte sedimentation rate may be elevated. On a BMP, blood urea nitrogen and creatinine levels may be elevated secondary to renal involvement or dehydration associated with HSP. Finally, hematuria or proteinuria show up on urinalysis in 30% to 70% of patients with HSP.2,12,13
What treatment is indicated?
Most patients with HSP recover completely without any specific intervention other than reassurance, bed rest, and supportive care. Arthralgia usually responds to nonsteroidal anti-inflammatory drugs and corticosteroids. Hospitalization is warranted when patients have a depleted volume status or inadequately controlled pain. With an otherwise un-complicated illness, watchful management suffices. Gastrointestinal and renal complications may require more aggressive therapy.
Gastrointestinal complications. As noted earlier, the most common gastrointestinal complication is intussusception. No definite measures for preventing intussusception appear in the literature. Some evidence supports the use of corticosteroids for severe abdominal symptoms,16,17 but in general, corticosteroids are not indicated for extrarenal manifestations. More serious complications such as bowel infarction or perforation, pancreatitis, or cholecystitis are rare.
Renal disease. Much research has focused on treatment options for patients with renal complications, due to the possibility of long-term debilitating effects. Although no evidence supports corticosteroid use for patients with mild renal involvement,16 for patients with severe renal disease—defined as crescenteric nephritis on biopsy, usually complicated by oliguria and hypertension—corticosteroids may help prevent irreversible glomerular injury.
Other agents that have been used for severe renal disease include azathioprine, cyclophosphamide, and dipyridamole. These drugs have shown some success in resolving symptoms, but their use remains controversial.16,18 Finally, plasmapheresis has led to significant clinical improvement for a small number of patients with severe, rapidly progressing HSP.
Caveat. The effectiveness of all treatments for HSP remains in question, given that patients’ symptoms may simply resolve spontaneously. A clear answer will depend on further research.
Rest, fluids, and ibuprofen for your patient
You send your patient home with his mother, and advise her to provide him with supportive care, including oral hydration. You tell her to encourage rest and to give symptomatic pain relief with an over-the-counter medication such as ibuprofen.
You see the child again in 3 days, by which time his arthralgias are improving. Repeat urinalysis shows continuing moderate blood and trace protein. You follow him biweekly for 2 weeks, and then weekly for 4 more weeks. Six weeks after his initial presentation, his symptoms completely resolve, and urinalysis shows no evidence of hematuria or proteinuria. His blood pressure is normal at all visits.
You see the patient monthly for the next 5 months. Symptoms do not recur, and urinalysis results are normal. You counsel the boy’s mother regarding the risk of recurrence, and advise her to contact the office immediately if symptoms return.
CORRESPONDENCE Shailendra K. Saxena, MD, PhD, Department of Family Medicine, 10828 John Galt Boulevard, Omaha, NE 68137; [email protected]
A mother brings her 5-year-old boy in to your office because she is concerned about a rash on his legs that seems to be worsening. She tells you that he had a runny nose and a mild cough a week earlier, but that those symptoms resolved before the rash developed. He has also complained of “belly pain.”
The boy’s mother says he’s been less active and more irritable since the onset of the rash, and that he is hardly eating. She also tells you that earlier in the day, her son told her that it hurts to walk.
You dig deeper…
A complete review of systems is otherwise negative. The 5-year-old was born at term without complication. He has met all developmental milestones and his immunizations are up to date. He takes no medications.
The boy’s vital signs are normal. He has an erythematous maculopapular rash distributed on his legs symmetrically; it is palpable, nontender, and nonblanching. You detect no abnormalities in abdominal, neurologic, or musculoskeletal examinations.
A complete blood count (CBC) and basic metabolic panel (BMP) reveal mild leukocytosis with a normal differential. Urinalysis shows moderate blood and trace protein. Laboratory results are otherwise normal.
WHAT IS YOUR DIAGNOSIS?
A classic presentation revealed: Henoch-Schönlein purpura
The combination of rash (FIGURE), abdominal pain, arthralgia, and evidence of renal involvement are the classic symptoms for Henoch-Schönlein purpura (HSP),1 the most common systemic vasculitis of childhood.2 Fever may also be present. Boys are affected nearly twice as often as girls. HSP occurs only rarely among adults, and men and women are affected equally. The estimated annual incidence in children is 20 cases per 100,000, with most cases occurring in those between the ages of 4 and 6 years.3
Although the exact cause of HSP is unknown, 75% of cases follow an upper respiratory infection. Streptococcus, Mycoplasma, adenovirus, parvovirus, Epstein-Barr virus, and varicella have all been implicated as offending pathogens. A number of case reports have also described the disease after the use of certain drugs, including penicillin, ampicillin, and quinine; and after the administration of vaccines, including those for typhoid, measles, yellow fever, and cholera. In all cases, the underlying mechanism is thought to be a systemic rise in immunoglobulin A (IgA), which forms immune complexes deposited in arterioles, capillaries, and venules.4 The precise interactions in the mechanism of disease are yet to be determined.
FIGURE
Rash and leg pain
Like the patient described in the text, this 11-year-old girl had a similar rash on her legs, as well as leg and abdominal pain.
HSP is usually benign, self-limited
HSP signs and symptoms may occur in any order over a period of days to weeks. Symptoms tend to be less severe in younger children than in older children and adults. Besides abdominal and renal systems, the lungs and central nervous system (CNS) may be affected, although rarely in children. Pulmonary involvement, if it does occur, usually manifests as diffuse alveolar hemorrhage or interstitial pneumonia or fibrosis.5 CNS vasculitis may lead to cerebral hemorrhage.6
HSP usually is a benign, self-limited disorder. The average disease course is 4 weeks, although it may be as brief as 3 days or as long as 2 years. Up to 94% of children (and 89% of adults) recover fully.7 However, the potential for chronic renal disease does exist.8
The recurrence rate of HSP is generally reported as 40%;8 patients who develop nephritis have higher recurrence rates.9
Rash is almost always present
Nearly all of those affected with HSP exhibit a rash. In children, it may begin as urticarial or maculopapular skin lesions. The rash typically is a palpable purpura, with lesions measuring 2 to 10 mm in diameter. Classically, the rash appears symmetrically on the extensor surfaces of the arms, legs, and buttocks. Lesions may also occur on the face and ears; however, the rash usually spares the trunk.2 The rash generally fades over several days and gives way to darkened pigment. The purpuric lesions resolve more quickly with bed rest and tend to reappear when the patient resumes activity.
Bullous or necrotic lesions—although reported to occur in up to 60% of affected adults—are uncommon in children. If you had noted such lesions in this case, you would have had to rule out toxic vasculitides and meningococcal septicemia or other septic emboli.10
Arthralgia affects lower extremities
Arthralgia is the second most common clinical manifestation of HSP, occurring in approximately 82% of patients. Joint pain associated with HSP is likely due to periarticular soft tissue edema, and most commonly occurs in the hips, knees, or ankles.1,11 The arthralgia of HSP is transient and self-limited and does not cause permanent damage to the joints. Like the rash, joint pain tends to decrease with bed rest and increase with activity.11
Gastrointestinal involvement is rarely serious
Gastrointestinal involvement has been reported in 63% of patients with HSP. Symptoms typically include a colicky abdominal pain, associated with nausea and vomiting. These symptoms probably arise secondary to edema of the bowel wall and vasculitis of the gastrointestinal tract. The pain most often develops within 8 days of the appearance of the rash, but it has been reported to appear within weeks to months of cutaneous changes.12
Intussusception is the most common gastrointestinal complication in patients with HSP, with a reported overall incidence of 3.5% in hospitalized patients with severe abdominal pain. Gastrointestinal bleeding, presenting as either melena or hematochezia, has been reported in 25% of patients with HSP. Occult bleeding may occur in up to 50% of patients.12
More serious complications are rare, and they include bowel infarction and perforation, usually in the jejunum or ileum, and pancreatitis, cholecystitis, or protein-losing enteropathy secondary to HSP.
Renal involvement may require close follow-up
Renal disease has been reported to affect 30% to 70% of all HSP patients.13 Onset occurs within weeks to months after other symptoms of HSP. Most patients with renal involvement have only mild disease, such as asymptomatic hematuria and proteinuria.1,7,13 HSP is thought to account for approximately 15% of all glomerulopathies in childhood.13
Although renal disease in HSP is generally benign, such complications as nephrotic syndrome, hypertension, and acute and chronic renal failure may occur. Adults are much more susceptible to the latter complication.
When the diagnosis is unclear, renal biopsy may help confirm the presence of disease. Evidence of HSP is identical to that seen with IgA nephropathy.11,13 The percentage of glomeruli showing crescents on renal biopsy seems to be the most important prognostic finding, with crescent formation involving more than 50% of the glomeruli carrying a poor prognosis.14
Diagnosis is mainly clinical
Clinical diagnosis is not difficult with the classic 4 symptoms present (rash, abdominal pain, arthralgia, and evidence of renal involvement). However, when the presentation is less straightforward, confirmation of the diagnosis may depend on biopsy of the affected organ (eg, skin, kidney) demonstrating leukocytoclastic vasculitis with IgA deposition.
The differential diagnosis of HSP is large, and includes acute abdomen, meningococcal meningitis or septicemia, rheumatoid arthritis, idiopathic thrombocytopenic purpura, and systemic lupus erythematosus.15
Lab tests are minimally helpful. No lab test or imaging study is sensitive or specific for HSP. An elevated serum IgA level suggests the disease. A CBC may show leukocytosis and thrombocytosis, but test results may also be normal. The erythrocyte sedimentation rate may be elevated. On a BMP, blood urea nitrogen and creatinine levels may be elevated secondary to renal involvement or dehydration associated with HSP. Finally, hematuria or proteinuria show up on urinalysis in 30% to 70% of patients with HSP.2,12,13
What treatment is indicated?
Most patients with HSP recover completely without any specific intervention other than reassurance, bed rest, and supportive care. Arthralgia usually responds to nonsteroidal anti-inflammatory drugs and corticosteroids. Hospitalization is warranted when patients have a depleted volume status or inadequately controlled pain. With an otherwise un-complicated illness, watchful management suffices. Gastrointestinal and renal complications may require more aggressive therapy.
Gastrointestinal complications. As noted earlier, the most common gastrointestinal complication is intussusception. No definite measures for preventing intussusception appear in the literature. Some evidence supports the use of corticosteroids for severe abdominal symptoms,16,17 but in general, corticosteroids are not indicated for extrarenal manifestations. More serious complications such as bowel infarction or perforation, pancreatitis, or cholecystitis are rare.
Renal disease. Much research has focused on treatment options for patients with renal complications, due to the possibility of long-term debilitating effects. Although no evidence supports corticosteroid use for patients with mild renal involvement,16 for patients with severe renal disease—defined as crescenteric nephritis on biopsy, usually complicated by oliguria and hypertension—corticosteroids may help prevent irreversible glomerular injury.
Other agents that have been used for severe renal disease include azathioprine, cyclophosphamide, and dipyridamole. These drugs have shown some success in resolving symptoms, but their use remains controversial.16,18 Finally, plasmapheresis has led to significant clinical improvement for a small number of patients with severe, rapidly progressing HSP.
Caveat. The effectiveness of all treatments for HSP remains in question, given that patients’ symptoms may simply resolve spontaneously. A clear answer will depend on further research.
Rest, fluids, and ibuprofen for your patient
You send your patient home with his mother, and advise her to provide him with supportive care, including oral hydration. You tell her to encourage rest and to give symptomatic pain relief with an over-the-counter medication such as ibuprofen.
You see the child again in 3 days, by which time his arthralgias are improving. Repeat urinalysis shows continuing moderate blood and trace protein. You follow him biweekly for 2 weeks, and then weekly for 4 more weeks. Six weeks after his initial presentation, his symptoms completely resolve, and urinalysis shows no evidence of hematuria or proteinuria. His blood pressure is normal at all visits.
You see the patient monthly for the next 5 months. Symptoms do not recur, and urinalysis results are normal. You counsel the boy’s mother regarding the risk of recurrence, and advise her to contact the office immediately if symptoms return.
CORRESPONDENCE Shailendra K. Saxena, MD, PhD, Department of Family Medicine, 10828 John Galt Boulevard, Omaha, NE 68137; [email protected]
1. Roberts PF, Waller TA, Brinker TM, et al. Henoch-Schönlein purpura: a review article. South Med J. 2007;100:821-824.
2. Tizard EJ. Henoch-Schönlein purpura. Arch Dis Child. 1999;80:380-383.
3. Gardner-Medwin JM, Dolezalova P, Cummins C, et al. Incidence of Henoch-Schönlein purpura, Kawasaki disease, and rare vasculitides in children of different ethnic origins. Lancet. 2002;360:1197-1202.
4. Yang YH, Chuang YH, Wang LC, et al. The immunology of Henoch-Schönlein purpura. Autoimmun Rev. 2008;7:179-184.
5. Nadrous HF, Yu AC, Specks U, et al. Pulmonary involvement in Henoch-Schönlein purpura. Mayo Clin Proc. 2004;79:1151-1157.
6. Elinson P, Foster KW, Kaufman DB. Magnetic resonance imaging of central nervous system vasculitis: a case report of Henoch-Schönlein purpura. Acta Pediatr. 2008;79:710-713.
7. Blanco R, Martínez-Taboada VM, Rodríguez-Valverde V, et al. Henoch-Schönlein purpura in adulthood and childhood: two different expressions of the same syndrome. Arthritis Rheum. 1997;40:859-864.
8. Dillon MJ. Henoch-Schönlein purpura (treatment and outcome). Cleve Clin J Med. 2002;69(suppl):S121-S123.
9. Alfredo CS, Nunes NA, Len CA, et al. Henoch-Schönlein purpura: recurrence and chronicity. J Pediatr (Rio J). 2007;83:177-180.
10. Morelli JG. Vascular disorders. In: Kliegman RM, Behrman RE, Jensen HB, eds. Nelson Textbook of Pediatrics. 18th ed. Philadelphia, Pa: Saunders Elsevier; 2007:2667–2673.
11. Trapani S, Micheli A, Grisolia F, et al. Henoch-Schönlein purpura in childhood: epidemiological and clinical analysis of 150 cases over a 5-year period and review of literature. Semin Arthritis Rheum. 2005;35:143-153.
12. Chang WL, Yang YH, Lin YT, et al. Gastrointestinal manifestations in Henoch-Schönlein purpura: a review of 261 patients. Acta Pediatr. 2004;93:1427-1431.
13. Chang WL, Yang YH, Wang LC, et al. Renal manifestations in Henoch-Schönlein purpura: a 10-year clinical study. Pediatr Nephrol. 2005;20:1269-1272.
14. Bogdanovic R. Henoch-Schönlein purpura nephritis in children: risk factors, prevention and treatment. Acta Paediatr. 2009;98:1882-1889.
15. Kraft DM, Mckee D, Scott C. Henoch-Schönlein purpura: a review. Am Fam Phys. 1998;58:405-408,411.
16. Szer IS. Gastrointestinal and renal involvement in vasculitis: management strategies in Henoch-Schönlein purpura. Cleve Clin J Med. 1999;66:312-317.
17. Leung SP. Use of intravenous hydrocortisone in Henoch-Schönlein purpura. J Paediatr Child Health. 2001;37:309-310.
18. Zaffanello M, Brugnara M, Franchini M, et al. Therapy for children with Henoch-Schönlein purpura nephritis: a systematic review. ScientificWorldJournal. 2007;7:20-30.
1. Roberts PF, Waller TA, Brinker TM, et al. Henoch-Schönlein purpura: a review article. South Med J. 2007;100:821-824.
2. Tizard EJ. Henoch-Schönlein purpura. Arch Dis Child. 1999;80:380-383.
3. Gardner-Medwin JM, Dolezalova P, Cummins C, et al. Incidence of Henoch-Schönlein purpura, Kawasaki disease, and rare vasculitides in children of different ethnic origins. Lancet. 2002;360:1197-1202.
4. Yang YH, Chuang YH, Wang LC, et al. The immunology of Henoch-Schönlein purpura. Autoimmun Rev. 2008;7:179-184.
5. Nadrous HF, Yu AC, Specks U, et al. Pulmonary involvement in Henoch-Schönlein purpura. Mayo Clin Proc. 2004;79:1151-1157.
6. Elinson P, Foster KW, Kaufman DB. Magnetic resonance imaging of central nervous system vasculitis: a case report of Henoch-Schönlein purpura. Acta Pediatr. 2008;79:710-713.
7. Blanco R, Martínez-Taboada VM, Rodríguez-Valverde V, et al. Henoch-Schönlein purpura in adulthood and childhood: two different expressions of the same syndrome. Arthritis Rheum. 1997;40:859-864.
8. Dillon MJ. Henoch-Schönlein purpura (treatment and outcome). Cleve Clin J Med. 2002;69(suppl):S121-S123.
9. Alfredo CS, Nunes NA, Len CA, et al. Henoch-Schönlein purpura: recurrence and chronicity. J Pediatr (Rio J). 2007;83:177-180.
10. Morelli JG. Vascular disorders. In: Kliegman RM, Behrman RE, Jensen HB, eds. Nelson Textbook of Pediatrics. 18th ed. Philadelphia, Pa: Saunders Elsevier; 2007:2667–2673.
11. Trapani S, Micheli A, Grisolia F, et al. Henoch-Schönlein purpura in childhood: epidemiological and clinical analysis of 150 cases over a 5-year period and review of literature. Semin Arthritis Rheum. 2005;35:143-153.
12. Chang WL, Yang YH, Lin YT, et al. Gastrointestinal manifestations in Henoch-Schönlein purpura: a review of 261 patients. Acta Pediatr. 2004;93:1427-1431.
13. Chang WL, Yang YH, Wang LC, et al. Renal manifestations in Henoch-Schönlein purpura: a 10-year clinical study. Pediatr Nephrol. 2005;20:1269-1272.
14. Bogdanovic R. Henoch-Schönlein purpura nephritis in children: risk factors, prevention and treatment. Acta Paediatr. 2009;98:1882-1889.
15. Kraft DM, Mckee D, Scott C. Henoch-Schönlein purpura: a review. Am Fam Phys. 1998;58:405-408,411.
16. Szer IS. Gastrointestinal and renal involvement in vasculitis: management strategies in Henoch-Schönlein purpura. Cleve Clin J Med. 1999;66:312-317.
17. Leung SP. Use of intravenous hydrocortisone in Henoch-Schönlein purpura. J Paediatr Child Health. 2001;37:309-310.
18. Zaffanello M, Brugnara M, Franchini M, et al. Therapy for children with Henoch-Schönlein purpura nephritis: a systematic review. ScientificWorldJournal. 2007;7:20-30.
Optimize your use of stress tests: A Q&A guide
Order exercise stress testing without imaging for patients with a low to intermediate probability of coronary artery disease (CAD), unless preexisting electrocardiographic (EKG) changes would render such a test nondiagnostic. C
Order stress testing with imaging for patients with preexisting EKG changes and/or a high probability of CAD. C
Do not use stress testing to screen asymptomatic patients for CAD. C
Consider pharmacologic testing for patients who are unable to exercise to an appropriate cardiac workload; it has the same predictive value as a nuclear exercise stress test. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Exercise has been used for cardiac stress testing for decades. But testing and imaging techniques and knowledge of the efficacy of this common diagnostic tool continue to evolve. Optimizing your use of stress testing requires that you familiarize yourself with the latest evidence. The evidence-based answers to these 6 questions will help you do just that.
1. How reliable are exercise stress tests?
That depends, of course, on any number of variables, including the protocol utilized, the number of stenotic vessels, the degree of stenosis, and even the sex of the patient.
False-negative and false-positive results are frequent in treadmill testing without imaging. (For more on the different protocols, see “Standard and nuclear exercise stress tests: A look at protocols”) Sensitivity is related to the number of stenotic vessels and the degree of stenosis. For a man with single-vessel disease and ≥70% stenosis, the likelihood of an abnormal test is only 50% to 60%. Even in a man with left main artery disease, the sensitivity is only about 85%.1
In some cases, failure to reach a cardiac workload sufficient to produce ischemia can lead to a false-negative test, and it is up to the physician performing the test to label it as nondiagnostic. Other reasons for false-positive or false-negative results include preexisting ST segment abnormalities, which can cause false-positive elevation of the ST segment during exercise; the use of digitalis, which affects the ST segment; and the presence of ventricular hypertrophy or cardiomyopathy.1 Patients with any of these conditions should undergo stress testing with imaging instead.
Nuclear stress testing is indicated for patients who have baseline EKG abnormalities, suspected false-positive or false-negative results from a stress test without imaging, known CAD or previous revascularization, a pacemaker, or a moderate to high likelihood of a CAD diagnosis. The addition of a tracer isotope and imaging boosts the test’s predictive value.1
The positive predictive value of nuclear stress testing is difficult to calculate because an abnormal test should lead to initiation of therapy designed to reduce the risk of cardiac death or myocardial infarction (MI). Numerous studies have found the rate of cardiac events after a negative radionuclide stress test to be less than 1% per year.2 The event rate after a negative test is lower in women than in men; after a positive test, however, the event rate in women is 2 to 3 times higher.2,3 Overall, stress testing is less sensitive in women than in men, at least in part because of their lower likelihood of CAD associated with any given symptom set.4
Exercise stress testing can be done with a number of treadmill protocols. The most widely used are:18,19
- the Bruce Protocol (the most common),1 which increases the slope of the treadmill and the speed of the belt in 3-minute intervals;
- the modified Bruce Protocol, a less aggressive format in which slope and speed are alternatively increased; and
- the naughton Protocol (typically reserved for patients whose ability to walk is limited), which starts with a very slow belt speed and a nearly flat slope and increases both elements slowly.
During the test, heart rate and BP are measured, along with continuous EKG monitoring, but the frequency of BP measurement and 12-lead EKG printouts varies among testing facilities.
Patients must attain a heart rate of 85% of their age-predicted maximum for the test to be considered diagnostic; they typically exercise until they’re unable to continue or they develop symptoms that prompt the clinician performing the test to stop it. Monitoring continues for some time after the patient stops exercising—usually 4 to 5 minutes in an asymptomatic patient, or until any symptoms and EKG changes that developed during the test resolve. If chest pain or EKG changes persist, the patient may need to be admitted to the hospital.
The procedure for nuclear stress testing is similar, except that the patient must estimate when he or she can only walk for 1 more minute. A tracer isotope is injected at that time.
For years, thallium was used for this purpose. However, thallium is taken up by the perfused myocardium and has the drawback of rapid redistribution with resolution of ischemia, which can lead to false-negative tests.20
Technetium (99mTc-labeled sestamibi), which is commonly used for other nuclide scans, is now the preferred isotope for nuclear stress tests.21 It is taken up by mitochondria in the perfused myocardium and does not redistribute, which results in fewer false-negative scans. Additionally, the energy emitted by 99mTc-labeled sestamibi is higher and produces cleaner pictures.21
Single photon emission computed tomography (SPECT) scans are taken in 3 planes as part of the nuclear stress test. A set of resting scans is taken before the exercise test. The isotope is then allowed to wash out and another dose is injected at peak cardiac workload so a second set of scans can be taken and compared with the resting images.
Perfusion defects that are present both at rest and with stress indicate an area of infarction, whereas defects that appear with stress but not at rest indicate ischemia. The probable location of the coronary artery lesions responsible for the ischemia can be inferred from the area in which the defects appear.
Gated imaging—serial images that are coupled with EKG changes, then reassembled to produce a moving image of the heart—is now usually part of the process. The result can be examined for areas of wall motion abnormalities and used to calculate an ejection fraction.22
2. When should you rule out stress testing?
Stress testing is unnecessary in asymptomatic patients. Numerous studies have documented the lack of benefit from screening asymptomatic people for CAD using exercise stress testing.5,6 The US Preventive Services Task Force gives this a Grade D recommendation—recommending against routine stress testing.7
There are also numerous contraindications, both absolute and relative (TABLE).8 Relative contraindications, which include severe hypertension, left main coronary stenosis, moderate stenotic valvular disease, electrolyte abnormalities, cardiomyopathy, serious mental or physical impairment, and atrioventricular block are conditions that are likely to interfere with test performance or reliability.
Absolute contraindications, generally related to unstable cardiopulmonary disease, pose a far more serious threat. Indeed, administering a treadmill stress test to a patient with 1 or more absolute contraindications greatly increases the risk of death associated with the test.8
Even if a patient does not have any relative or absolute contraindications, there is still some risk of moving forward with the test. There is about a 1 in 2500 risk of MI or death during, or related to, exercise stress testing.8 The greater the likelihood that a patient has CAD, the higher the risk.
There is also a risk of hospitalization after the test, usually related to persistent chest pain or arrhythmias. (I generally admit patients whose chest pain is unresponsive to 3 doses of nitroglycerine or who develop EKG changes that persist after 20 minutes at rest.) The test also raises the possibility of injury from the equipment, such as sprains or fractures caused by falling from the treadmill.
Nuclear stress testing also has a small risk of an allergic reaction to the isotope used as a tracer. The radiation dose is 8 to 9 mSV, comparable to a computed tomography (CT) scan of the chest and generally less than that of a coronary angiogram.9
TABLE
Stress testing: Absolute and relative contraindications8
| Absolute contraindications |
|---|
| Recent MI (<2 days) |
| Unstable angina |
| Uncontrolled ventricular arrhythmia |
| Uncontrolled atrial arrhythmia that compromises cardiac function |
| Symptomatic HF (uncontrolled) |
| Severe aortic stenosis (uncontrolled) |
| Dissecting aneurysm (suspected or confirmed) |
| Myocarditis (active) |
| Pulmonary or systemic embolus (recent) |
| Acute pericarditis |
| Relative contraindications* |
| Severe hypertension |
| Left main coronary stenosis |
| Moderate stenotic valvular disease |
| Electrolyte abnormalities |
| Cardiomyopathy, including hypertrophic cardiomyopathy |
| Mental or physical impairment that results in an inability to exercise adequately |
| high-degree atrioventricular block |
| HF, heart failure; MI, myocardial infarction. |
| *Relative contraindications are conditions that are likely to interfere with test performance or reliability. |
3. Does the evidence support the use of stress tests for asymptomatic patients with diabetes? Are preop stress tests advisable?
The jury is still out on both questions.
The question of asymptomatic testing for patients with diabetes mellitus, who are more likely than those without the disease to develop CAD, frequently arises. Although individuals with diabetes have higher rates of silent ischemia than the general population, however, estimates of this prevalence vary widely.10 There are no clear guidelines for evaluation of asymptomatic diabetic patients with exercise stress testing. (See “Test your skills with these 3 cases”)
The addition of nuclide imaging adds diagnostic value to the test, but it is still not clear that this should be the preferred test for patients with diabetes who have normal resting EKGs.10,11 A recent randomized controlled trial investigating screening with pharmacologic stress testing in asymptomatic patients with type 2 diabetes did not show a reduction in cardiac event rates in patients who were screened compared with those who were not screened.12
Similarly, preoperative stress testing is subject to debate.13 Many studies have been done to evaluate the utility of preoperative stress testing, with revascularization procedures done before the planned surgery when significant CAD is found. (See “Before surgery: Have you done enough to mitigate risk?” J Fam Pract. 2010;59:202-211.) And, while many demonstrate the predictive power of various parameters that stress tests measure, literature reviews show that—with the exception of patients with unstable CAD—postop event rates are about the same for patients who underwent stress testing and subsequent revascularization vs those who were treated medically instead.13,14
CASE 1 Daniel G, a 68-year-old whom you’ve been treating for hypertension for more than 10 years, is about 25 pounds overweight. He has decided to begin an exercise regimen, and the trainer he hired to work with him at the gym has asked for medical clearance.
CASE 2 Marge H, age 73, has peripheral neuropathy and spinal stenosis. She sees a neurologist regularly, but has come to see you today to report that for the last several nights, her heart has been racing and she’s felt an uncomfortable sensation in her chest.
CASE 3 Ed W, a trim 56-year-old, has been swimming 5 days a week for years. Last week, he experienced a tightening in his chest in the middle of his swim. The pain subsided shortly after he stopped swimming, but it returned as soon as he got up to full speed again. He asks whether you think it’s a pulled muscle or angina.
Should any—or all—of these patients undergo cardiac stress testing?
CASE 1 Daniel’s case highlights the discrepancy between commonly held beliefs and medical evidence. For decades, people have been told to get a medical evaluation before starting an exercise program, and a stress test has commonly been part of that evaluation. However, numerous studies have failed to show a benefit of stress testing in asymptomatic people. The US Preventive Services Task force recommends against routine stress testing in asymptomatic people.7 And, while the american heart association/american college of cardiology guidelines suggest that stress testing in men over the age of 45 with 1 or more risk factors may occasionally yield useful information, the organizations acknowledge that this opinion is based on weak information.23
You tell Daniel that moderate exercise is unlikely to provoke a serious cardiac event and that if symptoms arise during exercise, he should report them promptly so that appropriate testing can be ordered.
CASE 2 Marge’s primary complaint sounds more like an arrhythmia than angina. however, coronary ischemia cannot be excluded; ischemia could be caused by decreased cardiac output from an arrhythmia, or it could be the cause of an arrhythmia. A holter monitor would be a good initial test for this patient, followed by stress testing to determine if angina is the cause of her symptoms. Because of marge’s peripheral neuropathy and spinal stenosis, she may be a candidate for a pharmacologic stress test.
Given that stress testing is less sensitive in women than in men, there is a widespread belief that women should not be tested with exercise stress testing alone. however, the available literature suggests that this test has appropriate predictive value for women with an intermediate CAD risk.4
CASE 3 Ed presents with typical symptoms of angina pectoris. While some noncardiac diseases—esophageal spasm, for example—can cause nearly identical symptoms, the likelihood that this patient has symptomatic CAD is high. Thus, he should undergo stress testing with nuclide imaging. This patient is physically fit and therefore can take an exercise test, which will provide information—most notably, functional capacity and the level of exertion needed to cause symptoms—that a pharmacologic stress test would not.
4. If your patient requires a pharmacologic stress test, what are your options besides adenosine?
While adenosine is the agent of choice, dipyridamole and dobutamine are other options. When any of these agents are used, it’s important to consider the side effects of each, and which drugs your patient will need to avoid prior to the stress test.
Adenosine is a mediator of coronary vasodilation. The drug dilates normal coronary arteries preferentially to stenotic vessels and causes redistribution of blood flow away from areas of the myocardium with compromised circulation.
Dipyridamole, a mediator of adenosine release, is sometimes used instead. Both drugs are given as a 4-minute infusion, with injection of the tracer late in the infusion.
The adverse effects of adenosine occur early in the infusion, and include dyspnea, bronchospasm, chest pain, nausea, and headache. Bradycardia can be marked, and brief periods of complete heart block and long sinus pauses may occur. Hypotension can likewise be profound. Many of these effects are extremely disturbing to the patient under-going the test, but they disappear within 30 seconds of stopping the infusion.
Dipyridamole has similar adverse effects, although heart block is not part of its adverse effect profile. In addition, the drug’s adverse effects occur later in the infusion than those associated with adenosine and last well after it is finished. However, dipyridamole’s side effects can be reversed with intravenous aminophylline without compromising the accuracy of the test.
Drugs to avoid that day. Methylxanthines antagonize adenosine and dipyridamole, and thus must be avoided on the day of the test. Caffeine and theophylline are among the substances to be avoided, although the degree to which they affect test results has been questioned recently.15
Severe COPD and asthma—especially in patients with uncontrolled wheezing—are relative contraindications to the use of adenosine and dipyridamole.
Interestingly, the cardiovascular effects (and EKG changes) associated with these drugs are not necessarily indicative of CAD. Thus, the entire EKG portion of a pharmacologic stress test is not useful in interpreting the finding. One small study suggests that, unlike exercise stress testing, adenosine stress testing may be safe in patients with severe aortic stenosis.16
Dobutamine is another alternative for pharmacologic stress testing, for patients who cannot take adenosine or are unable to stop theophylline or similar medications. An infusion of dobutamine with an escalating dose, sometimes including atropine, is used to accelerate the heart rate to 85% of the patient’s age-predicted maximum. The stress is primarily due to the chronotropic effect of the drug, but dobutamine has some coronary vasodilatory activity and may also induce some redistribution of coronary blood flow, similar to the effect of adenosine.
The positive and negative predictive values of pharmacologic stress testing are the same as for nuclear stress testing. Unlike exercise testing, however, functional capacity cannot be inferred from a pharmacologic stress test.
About 10% of patients undergoing pharmacologic stress testing will have a nondiagnostic test. The sensitivity of the test varies among studies, but it is approximately 84%, 95%, and 100% for single-, double-, and triplevessel disease, respectively. Patients with negative tests have an event rate of less than 1% per year.17
5. Is stress echocardiography comparable to stress testing?
Yes. Stress echocardiography, which involves echocardiographic studies taken before and after stress, can substitute for either exercise or pharmacologic stress testing (the stress can be achieved either with exercise or an infusion of dobutamine), and it has certain advantages: Stress echocardiography is cheaper than nuclear stress testing, and there is no radiation involved. In addition, stress echocardiography yields positive and negative predictive values similar to those seen with nuclear stress testing.2,3 The presence of ischemia is inferred from localized wall motion abnormalities.
The primary disadvantage of stress echocardiography is that it can be administered only by a cardiologist who has been specially trained in this procedure. In contrast, any community hospital nuclear medicine department has the capacity to perform nuclear imaging, and most radiologists are able to interpret the nuclide scans. In my experience, decisions about whether to order nuclear cardiac stress testing or stress echocardiography are influenced not only by the availability of these modalities, but also by the skill of the physicians who will interpret the tests.
6. Which exercise-induced EKG changes are related to ischemia?
The only changes that correlate with myocardial ischemia are ST depression and ST elevation. J-point depression is almost universally seen with exercise. For this reason, the ST level is measured 80 milliseconds after the J point.
ST depression—the most common abnormal finding—indicates subendocardial ischemia. ST changes are most commonly seen in the inferior and lateral leads, but do not correlate with the location of ischemia. ST depression can be downsloping, horizontal, or upsloping. The first 2 are the most significant patterns, and 1 mm of ST depression is the minimum significant level. Upsloping ST depression is less significant, and 1.5 mm of depression is the minimum significant change.1 The greater the degree of ST depression, the higher the likelihood that significant occlusion will be seen on coronary angiography. ST depression that develops in the recovery period is a rare occurrence but of equal significance to ST depression that occurs with exercise, and is probably due to ischemia caused by shunting of blood into skeletal muscle and away from the heart.1
ST elevation is less common, but more ominous than ST depression, as it indicates transmural ischemia.1 This finding most often indicates high-grade left anterior descending (LAD) or left main CAD. It is most often seen in the anterior leads, and the location of ST changes correlates with the area of ischemia. Bear in mind, however, that the correlation between ST elevation and transmural ischemia is true only if the patient has no history of MI. ST elevation in leads in which Q waves are present at rest usually indicates ventricular dyskinesia or aneurysm and not ischemia.1
Premenopausal women and women who are taking estrogen supplements, in particular, are more likely than men to have false-positive ST changes, most likely because of a poorly understood effect of estrogen. The molecules of estrogen and of digitalis glycosides have some regions of structural similarity, and it is thought that both molecules can cause ST changes.10
And what about arrhythmias? Arrhythmias are often seen at rest and with exertion. Supraventricular arrhythmias, including supraventricular tachycardia, are not associated with CAD. Premature ventricular contractions (PVCs) are common at peak exertion. PVCs are probably related to catecholamine release and do not indicate ischemia. (See “A look at the stress test report”)
Ventricular tachycardia, however—defined as 3 or more consecutive PVCs—has a 90% correlation with significant coronary artery stenosis, as shown on angiography.1
Rate-dependent conduction disturbances, including 2-to-1 atrioventricular block and bundle-branch blocks, may also be seen. These may be associated with ischemia, but are not highly predictive of coronary artery stenosis. Further testing may be indicated to determine whether stenosis is present.1
The report from the physician who performs or reads the stress test should contain the following elements:
Heart rate achieved, including both the rate itself and the percentage of the patient’s age-predicted maximum that the heart rate represents. Failure to reach 85% of the maximum may be related to underlying cardiac or pulmonary disease, the use of beta-blockers, musculoskeletal disorders, or general deconditioning. However, it is obviously noteworthy if the patient develops chest pain or significant ST changes at a lower heart rate.
BP at peak exertion. There are no established levels for systolic BP at various ages. But failure of the systolic pressure to rise, or a drop in systolic pressure with exercise, indicates a lack of ventricular reserve and is a poor prognostic sign.
Functional capacity (METS). In addition to documenting the METS level itself, the report should compare it to the expected functional capacity based on the patient’s age and sex.
Chest pain (or its absence). In addition to noting whether or not chest pain developed, the report should detail the character and intensity of any pain that the patient experienced, the time into the test and the heart rate at which it developed, and the response to rest or nitroglycerine.
ST changes. Unless something in the patient’s condition changes, the workload required to produce symptoms or ST changes should be reproducible from test to test. The workload at which angina or ST changes occur is key to assessing disease severity.
Arrhythmias. Whether they’re seen at rest or develop with exertion, arrhythmias should be noted, as well.
The final report should also indicate whether the test is negative, positive, or nondiagnostic for findings consistent with CAD. Whenever possible, it should include a validated treadmill score, as well.
CORRESPONDENCE Mark A. Knox, MD, UPMC Shadyside Family Medicine Residency Program, 5230 Centre Avenue, Pittsburgh, PA 15232; [email protected]
1. Ellestad MH. Stress Testing: Principles and Practice. 3rd ed. Philadelphia: F.A. Davis Company; 1986.
2. Metz LD, Beattie M, Hom R, et al. The prognostic value of normal exercise myocardial perfusion imaging and exercise echocardiography. J Am Coll Cardiol. 2007;49:227-237.
3. Gibbons RJ. Noninvasive diagnosis and prognosis assessment in chronic coronary artery disease: stress testing with and without imaging perspective. Circ Cardiovasc Imaging. 2008;1:257-269
4. Mieres JH, Shaw LJ, Arai A, et al. Role of noninvasive testing in the clinical evaluation of women with suspected coronary artery disease: Consensus Statement From the Cardiac Imaging Committee, Council on Clinical Cardiology, and the Cardiovascular Imaging and Intervention Committee, Council on Cardiovascular Radiology and Intervention, American Heart Association. Circulation. 2005;111:682-696.
5. Scott IA. Evaluating cardiovascular risk assessment for asymptomatic people. BMJ. 2009;338:164-168.
6. Livschitz S, Sharabi Y, Yushin J, et al. Limited clinical value of exercise stress test for the screening of coronary artery disease in young, asymptomatic adult men. Am J Cardiol. 2000;86:462-464.
7. US Preventive Services Task Force. Screening for coronary heart disease: recommendation statement. Ann Intern Med. 2004;140:569-572.
8. Gibbons RJ, Balady GJ, Beasley JW, et al. ACC/AHA Guidelines for Exercise Testing: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). Circulation. 1997;96:345-354.
9. Health Physics Society. Doses from medical radiation sources. Available at: http://hps.org/hpspublications/articles/dosesfrommedicalradiation.html. Accessed April 9, 2010.
10. Albers AR, Krichavsky MZ, Balady GJ. Stress testing in patients with diabetes mellitus: diagnostic and prognostic value. Circulation. 2006;113:583-592.
11. Harris GD, White RD. Exercise stress testing in patients with type 2 diabetes: when are asymptomatic patients screened? Clin Diab. 2007;25:126-130.
12. Young LH, Wackers FJT, Chyun DA, et al. Cardiac outcomes after screening for asymptomatic coronary artery disease in patients with type 2 diabetes. The DIAD Study: a randomized controlled trial. JAMA. 2009;301:1547-1555.
13. Makaryus AN, Diamond JA. Nuclear stress testing in elderly persons: a review of its use in the assessment of cardiac risk, particularly in patients undergoing preoperative risk assessment. Drugs Aging. 2007;24:467-479.
14. McFalls EO, Ward HB, Moritz TE, et al. Coronary-artery revascularization before elective major vascular surgery. N Engl J Med 2004;351:2795-2804.
15. Kovacs D, Pivonka R, Khosla PG, et al. Effect of caffeine on myocardial perfusion imaging using single photon emission computed tomography during adenosine pharmacologic stress. Am J Ther 2008;15:431-434.
16. Samuels B, Kiat H, Friedman JD, et al. Adenosine pharmacologic stress myocardial perfusion tomographic imaging in patients with significant aortic stenosis: diagnostic effcacy and comparison of clinical, hemodynamic, and electrocardiographic variables with 100 age-matched control subjects. J Am Coll Cardiol. 1995;25:99-106.
17. Geleijnse ML, Elhendy A, Fioretti PM, et al. Dobutamine stress myocardial perfusion imaging. J Am Coll Cardiol. 2000;36:2017-2027.
18. Starling MR, Crawford MH, O’Rourke RA. Superiority of selected treadmill exercise protocols predischarge and six weeks postinfarction for detecting ischemic abnormalities. Am Heart J 1982;104:1054-1060.
19. Handler CE, Sowton E. A comparison of the Naughton and modified Bruce treadmill exercise protocols in their ability to detect ischaemic abnormalities six weeks after myocardial infarction. Eur Heart J. 1984;5:752-755.
20. Kahn JK, McGhie I, Akers MS, et al. Quantitative rotational tomography with 201T1 and 99mTc 2-methoxy-isobutyl-isonitrile. A direct comparison in normal individuals and patients with coronary artery disease. Circulation. 1989;79:1282-1293.
21. Vesely MR, Dilsizian V. Nuclear cardiac stress testing in the era of molecular medicine. J Nucl Med. 2008;49:399-413.
22. Avery P, Hudson N, Hubner P. Evaluation of changes in myocardial perfusion and function on exercise in patients with coronary artery disease by gated M1B1 scintigraphy. Br Heart J. 1993;70:22-26.
23. Gibbons RJ, Balady GJ, Bricker JT. ACC/AHA Guideline Update for Exercise Testing summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation. 2002;106:1883-1892.
Order exercise stress testing without imaging for patients with a low to intermediate probability of coronary artery disease (CAD), unless preexisting electrocardiographic (EKG) changes would render such a test nondiagnostic. C
Order stress testing with imaging for patients with preexisting EKG changes and/or a high probability of CAD. C
Do not use stress testing to screen asymptomatic patients for CAD. C
Consider pharmacologic testing for patients who are unable to exercise to an appropriate cardiac workload; it has the same predictive value as a nuclear exercise stress test. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Exercise has been used for cardiac stress testing for decades. But testing and imaging techniques and knowledge of the efficacy of this common diagnostic tool continue to evolve. Optimizing your use of stress testing requires that you familiarize yourself with the latest evidence. The evidence-based answers to these 6 questions will help you do just that.
1. How reliable are exercise stress tests?
That depends, of course, on any number of variables, including the protocol utilized, the number of stenotic vessels, the degree of stenosis, and even the sex of the patient.
False-negative and false-positive results are frequent in treadmill testing without imaging. (For more on the different protocols, see “Standard and nuclear exercise stress tests: A look at protocols”) Sensitivity is related to the number of stenotic vessels and the degree of stenosis. For a man with single-vessel disease and ≥70% stenosis, the likelihood of an abnormal test is only 50% to 60%. Even in a man with left main artery disease, the sensitivity is only about 85%.1
In some cases, failure to reach a cardiac workload sufficient to produce ischemia can lead to a false-negative test, and it is up to the physician performing the test to label it as nondiagnostic. Other reasons for false-positive or false-negative results include preexisting ST segment abnormalities, which can cause false-positive elevation of the ST segment during exercise; the use of digitalis, which affects the ST segment; and the presence of ventricular hypertrophy or cardiomyopathy.1 Patients with any of these conditions should undergo stress testing with imaging instead.
Nuclear stress testing is indicated for patients who have baseline EKG abnormalities, suspected false-positive or false-negative results from a stress test without imaging, known CAD or previous revascularization, a pacemaker, or a moderate to high likelihood of a CAD diagnosis. The addition of a tracer isotope and imaging boosts the test’s predictive value.1
The positive predictive value of nuclear stress testing is difficult to calculate because an abnormal test should lead to initiation of therapy designed to reduce the risk of cardiac death or myocardial infarction (MI). Numerous studies have found the rate of cardiac events after a negative radionuclide stress test to be less than 1% per year.2 The event rate after a negative test is lower in women than in men; after a positive test, however, the event rate in women is 2 to 3 times higher.2,3 Overall, stress testing is less sensitive in women than in men, at least in part because of their lower likelihood of CAD associated with any given symptom set.4
Exercise stress testing can be done with a number of treadmill protocols. The most widely used are:18,19
- the Bruce Protocol (the most common),1 which increases the slope of the treadmill and the speed of the belt in 3-minute intervals;
- the modified Bruce Protocol, a less aggressive format in which slope and speed are alternatively increased; and
- the naughton Protocol (typically reserved for patients whose ability to walk is limited), which starts with a very slow belt speed and a nearly flat slope and increases both elements slowly.
During the test, heart rate and BP are measured, along with continuous EKG monitoring, but the frequency of BP measurement and 12-lead EKG printouts varies among testing facilities.
Patients must attain a heart rate of 85% of their age-predicted maximum for the test to be considered diagnostic; they typically exercise until they’re unable to continue or they develop symptoms that prompt the clinician performing the test to stop it. Monitoring continues for some time after the patient stops exercising—usually 4 to 5 minutes in an asymptomatic patient, or until any symptoms and EKG changes that developed during the test resolve. If chest pain or EKG changes persist, the patient may need to be admitted to the hospital.
The procedure for nuclear stress testing is similar, except that the patient must estimate when he or she can only walk for 1 more minute. A tracer isotope is injected at that time.
For years, thallium was used for this purpose. However, thallium is taken up by the perfused myocardium and has the drawback of rapid redistribution with resolution of ischemia, which can lead to false-negative tests.20
Technetium (99mTc-labeled sestamibi), which is commonly used for other nuclide scans, is now the preferred isotope for nuclear stress tests.21 It is taken up by mitochondria in the perfused myocardium and does not redistribute, which results in fewer false-negative scans. Additionally, the energy emitted by 99mTc-labeled sestamibi is higher and produces cleaner pictures.21
Single photon emission computed tomography (SPECT) scans are taken in 3 planes as part of the nuclear stress test. A set of resting scans is taken before the exercise test. The isotope is then allowed to wash out and another dose is injected at peak cardiac workload so a second set of scans can be taken and compared with the resting images.
Perfusion defects that are present both at rest and with stress indicate an area of infarction, whereas defects that appear with stress but not at rest indicate ischemia. The probable location of the coronary artery lesions responsible for the ischemia can be inferred from the area in which the defects appear.
Gated imaging—serial images that are coupled with EKG changes, then reassembled to produce a moving image of the heart—is now usually part of the process. The result can be examined for areas of wall motion abnormalities and used to calculate an ejection fraction.22
2. When should you rule out stress testing?
Stress testing is unnecessary in asymptomatic patients. Numerous studies have documented the lack of benefit from screening asymptomatic people for CAD using exercise stress testing.5,6 The US Preventive Services Task Force gives this a Grade D recommendation—recommending against routine stress testing.7
There are also numerous contraindications, both absolute and relative (TABLE).8 Relative contraindications, which include severe hypertension, left main coronary stenosis, moderate stenotic valvular disease, electrolyte abnormalities, cardiomyopathy, serious mental or physical impairment, and atrioventricular block are conditions that are likely to interfere with test performance or reliability.
Absolute contraindications, generally related to unstable cardiopulmonary disease, pose a far more serious threat. Indeed, administering a treadmill stress test to a patient with 1 or more absolute contraindications greatly increases the risk of death associated with the test.8
Even if a patient does not have any relative or absolute contraindications, there is still some risk of moving forward with the test. There is about a 1 in 2500 risk of MI or death during, or related to, exercise stress testing.8 The greater the likelihood that a patient has CAD, the higher the risk.
There is also a risk of hospitalization after the test, usually related to persistent chest pain or arrhythmias. (I generally admit patients whose chest pain is unresponsive to 3 doses of nitroglycerine or who develop EKG changes that persist after 20 minutes at rest.) The test also raises the possibility of injury from the equipment, such as sprains or fractures caused by falling from the treadmill.
Nuclear stress testing also has a small risk of an allergic reaction to the isotope used as a tracer. The radiation dose is 8 to 9 mSV, comparable to a computed tomography (CT) scan of the chest and generally less than that of a coronary angiogram.9
TABLE
Stress testing: Absolute and relative contraindications8
| Absolute contraindications |
|---|
| Recent MI (<2 days) |
| Unstable angina |
| Uncontrolled ventricular arrhythmia |
| Uncontrolled atrial arrhythmia that compromises cardiac function |
| Symptomatic HF (uncontrolled) |
| Severe aortic stenosis (uncontrolled) |
| Dissecting aneurysm (suspected or confirmed) |
| Myocarditis (active) |
| Pulmonary or systemic embolus (recent) |
| Acute pericarditis |
| Relative contraindications* |
| Severe hypertension |
| Left main coronary stenosis |
| Moderate stenotic valvular disease |
| Electrolyte abnormalities |
| Cardiomyopathy, including hypertrophic cardiomyopathy |
| Mental or physical impairment that results in an inability to exercise adequately |
| high-degree atrioventricular block |
| HF, heart failure; MI, myocardial infarction. |
| *Relative contraindications are conditions that are likely to interfere with test performance or reliability. |
3. Does the evidence support the use of stress tests for asymptomatic patients with diabetes? Are preop stress tests advisable?
The jury is still out on both questions.
The question of asymptomatic testing for patients with diabetes mellitus, who are more likely than those without the disease to develop CAD, frequently arises. Although individuals with diabetes have higher rates of silent ischemia than the general population, however, estimates of this prevalence vary widely.10 There are no clear guidelines for evaluation of asymptomatic diabetic patients with exercise stress testing. (See “Test your skills with these 3 cases”)
The addition of nuclide imaging adds diagnostic value to the test, but it is still not clear that this should be the preferred test for patients with diabetes who have normal resting EKGs.10,11 A recent randomized controlled trial investigating screening with pharmacologic stress testing in asymptomatic patients with type 2 diabetes did not show a reduction in cardiac event rates in patients who were screened compared with those who were not screened.12
Similarly, preoperative stress testing is subject to debate.13 Many studies have been done to evaluate the utility of preoperative stress testing, with revascularization procedures done before the planned surgery when significant CAD is found. (See “Before surgery: Have you done enough to mitigate risk?” J Fam Pract. 2010;59:202-211.) And, while many demonstrate the predictive power of various parameters that stress tests measure, literature reviews show that—with the exception of patients with unstable CAD—postop event rates are about the same for patients who underwent stress testing and subsequent revascularization vs those who were treated medically instead.13,14
CASE 1 Daniel G, a 68-year-old whom you’ve been treating for hypertension for more than 10 years, is about 25 pounds overweight. He has decided to begin an exercise regimen, and the trainer he hired to work with him at the gym has asked for medical clearance.
CASE 2 Marge H, age 73, has peripheral neuropathy and spinal stenosis. She sees a neurologist regularly, but has come to see you today to report that for the last several nights, her heart has been racing and she’s felt an uncomfortable sensation in her chest.
CASE 3 Ed W, a trim 56-year-old, has been swimming 5 days a week for years. Last week, he experienced a tightening in his chest in the middle of his swim. The pain subsided shortly after he stopped swimming, but it returned as soon as he got up to full speed again. He asks whether you think it’s a pulled muscle or angina.
Should any—or all—of these patients undergo cardiac stress testing?
CASE 1 Daniel’s case highlights the discrepancy between commonly held beliefs and medical evidence. For decades, people have been told to get a medical evaluation before starting an exercise program, and a stress test has commonly been part of that evaluation. However, numerous studies have failed to show a benefit of stress testing in asymptomatic people. The US Preventive Services Task force recommends against routine stress testing in asymptomatic people.7 And, while the american heart association/american college of cardiology guidelines suggest that stress testing in men over the age of 45 with 1 or more risk factors may occasionally yield useful information, the organizations acknowledge that this opinion is based on weak information.23
You tell Daniel that moderate exercise is unlikely to provoke a serious cardiac event and that if symptoms arise during exercise, he should report them promptly so that appropriate testing can be ordered.
CASE 2 Marge’s primary complaint sounds more like an arrhythmia than angina. however, coronary ischemia cannot be excluded; ischemia could be caused by decreased cardiac output from an arrhythmia, or it could be the cause of an arrhythmia. A holter monitor would be a good initial test for this patient, followed by stress testing to determine if angina is the cause of her symptoms. Because of marge’s peripheral neuropathy and spinal stenosis, she may be a candidate for a pharmacologic stress test.
Given that stress testing is less sensitive in women than in men, there is a widespread belief that women should not be tested with exercise stress testing alone. however, the available literature suggests that this test has appropriate predictive value for women with an intermediate CAD risk.4
CASE 3 Ed presents with typical symptoms of angina pectoris. While some noncardiac diseases—esophageal spasm, for example—can cause nearly identical symptoms, the likelihood that this patient has symptomatic CAD is high. Thus, he should undergo stress testing with nuclide imaging. This patient is physically fit and therefore can take an exercise test, which will provide information—most notably, functional capacity and the level of exertion needed to cause symptoms—that a pharmacologic stress test would not.
4. If your patient requires a pharmacologic stress test, what are your options besides adenosine?
While adenosine is the agent of choice, dipyridamole and dobutamine are other options. When any of these agents are used, it’s important to consider the side effects of each, and which drugs your patient will need to avoid prior to the stress test.
Adenosine is a mediator of coronary vasodilation. The drug dilates normal coronary arteries preferentially to stenotic vessels and causes redistribution of blood flow away from areas of the myocardium with compromised circulation.
Dipyridamole, a mediator of adenosine release, is sometimes used instead. Both drugs are given as a 4-minute infusion, with injection of the tracer late in the infusion.
The adverse effects of adenosine occur early in the infusion, and include dyspnea, bronchospasm, chest pain, nausea, and headache. Bradycardia can be marked, and brief periods of complete heart block and long sinus pauses may occur. Hypotension can likewise be profound. Many of these effects are extremely disturbing to the patient under-going the test, but they disappear within 30 seconds of stopping the infusion.
Dipyridamole has similar adverse effects, although heart block is not part of its adverse effect profile. In addition, the drug’s adverse effects occur later in the infusion than those associated with adenosine and last well after it is finished. However, dipyridamole’s side effects can be reversed with intravenous aminophylline without compromising the accuracy of the test.
Drugs to avoid that day. Methylxanthines antagonize adenosine and dipyridamole, and thus must be avoided on the day of the test. Caffeine and theophylline are among the substances to be avoided, although the degree to which they affect test results has been questioned recently.15
Severe COPD and asthma—especially in patients with uncontrolled wheezing—are relative contraindications to the use of adenosine and dipyridamole.
Interestingly, the cardiovascular effects (and EKG changes) associated with these drugs are not necessarily indicative of CAD. Thus, the entire EKG portion of a pharmacologic stress test is not useful in interpreting the finding. One small study suggests that, unlike exercise stress testing, adenosine stress testing may be safe in patients with severe aortic stenosis.16
Dobutamine is another alternative for pharmacologic stress testing, for patients who cannot take adenosine or are unable to stop theophylline or similar medications. An infusion of dobutamine with an escalating dose, sometimes including atropine, is used to accelerate the heart rate to 85% of the patient’s age-predicted maximum. The stress is primarily due to the chronotropic effect of the drug, but dobutamine has some coronary vasodilatory activity and may also induce some redistribution of coronary blood flow, similar to the effect of adenosine.
The positive and negative predictive values of pharmacologic stress testing are the same as for nuclear stress testing. Unlike exercise testing, however, functional capacity cannot be inferred from a pharmacologic stress test.
About 10% of patients undergoing pharmacologic stress testing will have a nondiagnostic test. The sensitivity of the test varies among studies, but it is approximately 84%, 95%, and 100% for single-, double-, and triplevessel disease, respectively. Patients with negative tests have an event rate of less than 1% per year.17
5. Is stress echocardiography comparable to stress testing?
Yes. Stress echocardiography, which involves echocardiographic studies taken before and after stress, can substitute for either exercise or pharmacologic stress testing (the stress can be achieved either with exercise or an infusion of dobutamine), and it has certain advantages: Stress echocardiography is cheaper than nuclear stress testing, and there is no radiation involved. In addition, stress echocardiography yields positive and negative predictive values similar to those seen with nuclear stress testing.2,3 The presence of ischemia is inferred from localized wall motion abnormalities.
The primary disadvantage of stress echocardiography is that it can be administered only by a cardiologist who has been specially trained in this procedure. In contrast, any community hospital nuclear medicine department has the capacity to perform nuclear imaging, and most radiologists are able to interpret the nuclide scans. In my experience, decisions about whether to order nuclear cardiac stress testing or stress echocardiography are influenced not only by the availability of these modalities, but also by the skill of the physicians who will interpret the tests.
6. Which exercise-induced EKG changes are related to ischemia?
The only changes that correlate with myocardial ischemia are ST depression and ST elevation. J-point depression is almost universally seen with exercise. For this reason, the ST level is measured 80 milliseconds after the J point.
ST depression—the most common abnormal finding—indicates subendocardial ischemia. ST changes are most commonly seen in the inferior and lateral leads, but do not correlate with the location of ischemia. ST depression can be downsloping, horizontal, or upsloping. The first 2 are the most significant patterns, and 1 mm of ST depression is the minimum significant level. Upsloping ST depression is less significant, and 1.5 mm of depression is the minimum significant change.1 The greater the degree of ST depression, the higher the likelihood that significant occlusion will be seen on coronary angiography. ST depression that develops in the recovery period is a rare occurrence but of equal significance to ST depression that occurs with exercise, and is probably due to ischemia caused by shunting of blood into skeletal muscle and away from the heart.1
ST elevation is less common, but more ominous than ST depression, as it indicates transmural ischemia.1 This finding most often indicates high-grade left anterior descending (LAD) or left main CAD. It is most often seen in the anterior leads, and the location of ST changes correlates with the area of ischemia. Bear in mind, however, that the correlation between ST elevation and transmural ischemia is true only if the patient has no history of MI. ST elevation in leads in which Q waves are present at rest usually indicates ventricular dyskinesia or aneurysm and not ischemia.1
Premenopausal women and women who are taking estrogen supplements, in particular, are more likely than men to have false-positive ST changes, most likely because of a poorly understood effect of estrogen. The molecules of estrogen and of digitalis glycosides have some regions of structural similarity, and it is thought that both molecules can cause ST changes.10
And what about arrhythmias? Arrhythmias are often seen at rest and with exertion. Supraventricular arrhythmias, including supraventricular tachycardia, are not associated with CAD. Premature ventricular contractions (PVCs) are common at peak exertion. PVCs are probably related to catecholamine release and do not indicate ischemia. (See “A look at the stress test report”)
Ventricular tachycardia, however—defined as 3 or more consecutive PVCs—has a 90% correlation with significant coronary artery stenosis, as shown on angiography.1
Rate-dependent conduction disturbances, including 2-to-1 atrioventricular block and bundle-branch blocks, may also be seen. These may be associated with ischemia, but are not highly predictive of coronary artery stenosis. Further testing may be indicated to determine whether stenosis is present.1
The report from the physician who performs or reads the stress test should contain the following elements:
Heart rate achieved, including both the rate itself and the percentage of the patient’s age-predicted maximum that the heart rate represents. Failure to reach 85% of the maximum may be related to underlying cardiac or pulmonary disease, the use of beta-blockers, musculoskeletal disorders, or general deconditioning. However, it is obviously noteworthy if the patient develops chest pain or significant ST changes at a lower heart rate.
BP at peak exertion. There are no established levels for systolic BP at various ages. But failure of the systolic pressure to rise, or a drop in systolic pressure with exercise, indicates a lack of ventricular reserve and is a poor prognostic sign.
Functional capacity (METS). In addition to documenting the METS level itself, the report should compare it to the expected functional capacity based on the patient’s age and sex.
Chest pain (or its absence). In addition to noting whether or not chest pain developed, the report should detail the character and intensity of any pain that the patient experienced, the time into the test and the heart rate at which it developed, and the response to rest or nitroglycerine.
ST changes. Unless something in the patient’s condition changes, the workload required to produce symptoms or ST changes should be reproducible from test to test. The workload at which angina or ST changes occur is key to assessing disease severity.
Arrhythmias. Whether they’re seen at rest or develop with exertion, arrhythmias should be noted, as well.
The final report should also indicate whether the test is negative, positive, or nondiagnostic for findings consistent with CAD. Whenever possible, it should include a validated treadmill score, as well.
CORRESPONDENCE Mark A. Knox, MD, UPMC Shadyside Family Medicine Residency Program, 5230 Centre Avenue, Pittsburgh, PA 15232; [email protected]
Order exercise stress testing without imaging for patients with a low to intermediate probability of coronary artery disease (CAD), unless preexisting electrocardiographic (EKG) changes would render such a test nondiagnostic. C
Order stress testing with imaging for patients with preexisting EKG changes and/or a high probability of CAD. C
Do not use stress testing to screen asymptomatic patients for CAD. C
Consider pharmacologic testing for patients who are unable to exercise to an appropriate cardiac workload; it has the same predictive value as a nuclear exercise stress test. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Exercise has been used for cardiac stress testing for decades. But testing and imaging techniques and knowledge of the efficacy of this common diagnostic tool continue to evolve. Optimizing your use of stress testing requires that you familiarize yourself with the latest evidence. The evidence-based answers to these 6 questions will help you do just that.
1. How reliable are exercise stress tests?
That depends, of course, on any number of variables, including the protocol utilized, the number of stenotic vessels, the degree of stenosis, and even the sex of the patient.
False-negative and false-positive results are frequent in treadmill testing without imaging. (For more on the different protocols, see “Standard and nuclear exercise stress tests: A look at protocols”) Sensitivity is related to the number of stenotic vessels and the degree of stenosis. For a man with single-vessel disease and ≥70% stenosis, the likelihood of an abnormal test is only 50% to 60%. Even in a man with left main artery disease, the sensitivity is only about 85%.1
In some cases, failure to reach a cardiac workload sufficient to produce ischemia can lead to a false-negative test, and it is up to the physician performing the test to label it as nondiagnostic. Other reasons for false-positive or false-negative results include preexisting ST segment abnormalities, which can cause false-positive elevation of the ST segment during exercise; the use of digitalis, which affects the ST segment; and the presence of ventricular hypertrophy or cardiomyopathy.1 Patients with any of these conditions should undergo stress testing with imaging instead.
Nuclear stress testing is indicated for patients who have baseline EKG abnormalities, suspected false-positive or false-negative results from a stress test without imaging, known CAD or previous revascularization, a pacemaker, or a moderate to high likelihood of a CAD diagnosis. The addition of a tracer isotope and imaging boosts the test’s predictive value.1
The positive predictive value of nuclear stress testing is difficult to calculate because an abnormal test should lead to initiation of therapy designed to reduce the risk of cardiac death or myocardial infarction (MI). Numerous studies have found the rate of cardiac events after a negative radionuclide stress test to be less than 1% per year.2 The event rate after a negative test is lower in women than in men; after a positive test, however, the event rate in women is 2 to 3 times higher.2,3 Overall, stress testing is less sensitive in women than in men, at least in part because of their lower likelihood of CAD associated with any given symptom set.4
Exercise stress testing can be done with a number of treadmill protocols. The most widely used are:18,19
- the Bruce Protocol (the most common),1 which increases the slope of the treadmill and the speed of the belt in 3-minute intervals;
- the modified Bruce Protocol, a less aggressive format in which slope and speed are alternatively increased; and
- the naughton Protocol (typically reserved for patients whose ability to walk is limited), which starts with a very slow belt speed and a nearly flat slope and increases both elements slowly.
During the test, heart rate and BP are measured, along with continuous EKG monitoring, but the frequency of BP measurement and 12-lead EKG printouts varies among testing facilities.
Patients must attain a heart rate of 85% of their age-predicted maximum for the test to be considered diagnostic; they typically exercise until they’re unable to continue or they develop symptoms that prompt the clinician performing the test to stop it. Monitoring continues for some time after the patient stops exercising—usually 4 to 5 minutes in an asymptomatic patient, or until any symptoms and EKG changes that developed during the test resolve. If chest pain or EKG changes persist, the patient may need to be admitted to the hospital.
The procedure for nuclear stress testing is similar, except that the patient must estimate when he or she can only walk for 1 more minute. A tracer isotope is injected at that time.
For years, thallium was used for this purpose. However, thallium is taken up by the perfused myocardium and has the drawback of rapid redistribution with resolution of ischemia, which can lead to false-negative tests.20
Technetium (99mTc-labeled sestamibi), which is commonly used for other nuclide scans, is now the preferred isotope for nuclear stress tests.21 It is taken up by mitochondria in the perfused myocardium and does not redistribute, which results in fewer false-negative scans. Additionally, the energy emitted by 99mTc-labeled sestamibi is higher and produces cleaner pictures.21
Single photon emission computed tomography (SPECT) scans are taken in 3 planes as part of the nuclear stress test. A set of resting scans is taken before the exercise test. The isotope is then allowed to wash out and another dose is injected at peak cardiac workload so a second set of scans can be taken and compared with the resting images.
Perfusion defects that are present both at rest and with stress indicate an area of infarction, whereas defects that appear with stress but not at rest indicate ischemia. The probable location of the coronary artery lesions responsible for the ischemia can be inferred from the area in which the defects appear.
Gated imaging—serial images that are coupled with EKG changes, then reassembled to produce a moving image of the heart—is now usually part of the process. The result can be examined for areas of wall motion abnormalities and used to calculate an ejection fraction.22
2. When should you rule out stress testing?
Stress testing is unnecessary in asymptomatic patients. Numerous studies have documented the lack of benefit from screening asymptomatic people for CAD using exercise stress testing.5,6 The US Preventive Services Task Force gives this a Grade D recommendation—recommending against routine stress testing.7
There are also numerous contraindications, both absolute and relative (TABLE).8 Relative contraindications, which include severe hypertension, left main coronary stenosis, moderate stenotic valvular disease, electrolyte abnormalities, cardiomyopathy, serious mental or physical impairment, and atrioventricular block are conditions that are likely to interfere with test performance or reliability.
Absolute contraindications, generally related to unstable cardiopulmonary disease, pose a far more serious threat. Indeed, administering a treadmill stress test to a patient with 1 or more absolute contraindications greatly increases the risk of death associated with the test.8
Even if a patient does not have any relative or absolute contraindications, there is still some risk of moving forward with the test. There is about a 1 in 2500 risk of MI or death during, or related to, exercise stress testing.8 The greater the likelihood that a patient has CAD, the higher the risk.
There is also a risk of hospitalization after the test, usually related to persistent chest pain or arrhythmias. (I generally admit patients whose chest pain is unresponsive to 3 doses of nitroglycerine or who develop EKG changes that persist after 20 minutes at rest.) The test also raises the possibility of injury from the equipment, such as sprains or fractures caused by falling from the treadmill.
Nuclear stress testing also has a small risk of an allergic reaction to the isotope used as a tracer. The radiation dose is 8 to 9 mSV, comparable to a computed tomography (CT) scan of the chest and generally less than that of a coronary angiogram.9
TABLE
Stress testing: Absolute and relative contraindications8
| Absolute contraindications |
|---|
| Recent MI (<2 days) |
| Unstable angina |
| Uncontrolled ventricular arrhythmia |
| Uncontrolled atrial arrhythmia that compromises cardiac function |
| Symptomatic HF (uncontrolled) |
| Severe aortic stenosis (uncontrolled) |
| Dissecting aneurysm (suspected or confirmed) |
| Myocarditis (active) |
| Pulmonary or systemic embolus (recent) |
| Acute pericarditis |
| Relative contraindications* |
| Severe hypertension |
| Left main coronary stenosis |
| Moderate stenotic valvular disease |
| Electrolyte abnormalities |
| Cardiomyopathy, including hypertrophic cardiomyopathy |
| Mental or physical impairment that results in an inability to exercise adequately |
| high-degree atrioventricular block |
| HF, heart failure; MI, myocardial infarction. |
| *Relative contraindications are conditions that are likely to interfere with test performance or reliability. |
3. Does the evidence support the use of stress tests for asymptomatic patients with diabetes? Are preop stress tests advisable?
The jury is still out on both questions.
The question of asymptomatic testing for patients with diabetes mellitus, who are more likely than those without the disease to develop CAD, frequently arises. Although individuals with diabetes have higher rates of silent ischemia than the general population, however, estimates of this prevalence vary widely.10 There are no clear guidelines for evaluation of asymptomatic diabetic patients with exercise stress testing. (See “Test your skills with these 3 cases”)
The addition of nuclide imaging adds diagnostic value to the test, but it is still not clear that this should be the preferred test for patients with diabetes who have normal resting EKGs.10,11 A recent randomized controlled trial investigating screening with pharmacologic stress testing in asymptomatic patients with type 2 diabetes did not show a reduction in cardiac event rates in patients who were screened compared with those who were not screened.12
Similarly, preoperative stress testing is subject to debate.13 Many studies have been done to evaluate the utility of preoperative stress testing, with revascularization procedures done before the planned surgery when significant CAD is found. (See “Before surgery: Have you done enough to mitigate risk?” J Fam Pract. 2010;59:202-211.) And, while many demonstrate the predictive power of various parameters that stress tests measure, literature reviews show that—with the exception of patients with unstable CAD—postop event rates are about the same for patients who underwent stress testing and subsequent revascularization vs those who were treated medically instead.13,14
CASE 1 Daniel G, a 68-year-old whom you’ve been treating for hypertension for more than 10 years, is about 25 pounds overweight. He has decided to begin an exercise regimen, and the trainer he hired to work with him at the gym has asked for medical clearance.
CASE 2 Marge H, age 73, has peripheral neuropathy and spinal stenosis. She sees a neurologist regularly, but has come to see you today to report that for the last several nights, her heart has been racing and she’s felt an uncomfortable sensation in her chest.
CASE 3 Ed W, a trim 56-year-old, has been swimming 5 days a week for years. Last week, he experienced a tightening in his chest in the middle of his swim. The pain subsided shortly after he stopped swimming, but it returned as soon as he got up to full speed again. He asks whether you think it’s a pulled muscle or angina.
Should any—or all—of these patients undergo cardiac stress testing?
CASE 1 Daniel’s case highlights the discrepancy between commonly held beliefs and medical evidence. For decades, people have been told to get a medical evaluation before starting an exercise program, and a stress test has commonly been part of that evaluation. However, numerous studies have failed to show a benefit of stress testing in asymptomatic people. The US Preventive Services Task force recommends against routine stress testing in asymptomatic people.7 And, while the american heart association/american college of cardiology guidelines suggest that stress testing in men over the age of 45 with 1 or more risk factors may occasionally yield useful information, the organizations acknowledge that this opinion is based on weak information.23
You tell Daniel that moderate exercise is unlikely to provoke a serious cardiac event and that if symptoms arise during exercise, he should report them promptly so that appropriate testing can be ordered.
CASE 2 Marge’s primary complaint sounds more like an arrhythmia than angina. however, coronary ischemia cannot be excluded; ischemia could be caused by decreased cardiac output from an arrhythmia, or it could be the cause of an arrhythmia. A holter monitor would be a good initial test for this patient, followed by stress testing to determine if angina is the cause of her symptoms. Because of marge’s peripheral neuropathy and spinal stenosis, she may be a candidate for a pharmacologic stress test.
Given that stress testing is less sensitive in women than in men, there is a widespread belief that women should not be tested with exercise stress testing alone. however, the available literature suggests that this test has appropriate predictive value for women with an intermediate CAD risk.4
CASE 3 Ed presents with typical symptoms of angina pectoris. While some noncardiac diseases—esophageal spasm, for example—can cause nearly identical symptoms, the likelihood that this patient has symptomatic CAD is high. Thus, he should undergo stress testing with nuclide imaging. This patient is physically fit and therefore can take an exercise test, which will provide information—most notably, functional capacity and the level of exertion needed to cause symptoms—that a pharmacologic stress test would not.
4. If your patient requires a pharmacologic stress test, what are your options besides adenosine?
While adenosine is the agent of choice, dipyridamole and dobutamine are other options. When any of these agents are used, it’s important to consider the side effects of each, and which drugs your patient will need to avoid prior to the stress test.
Adenosine is a mediator of coronary vasodilation. The drug dilates normal coronary arteries preferentially to stenotic vessels and causes redistribution of blood flow away from areas of the myocardium with compromised circulation.
Dipyridamole, a mediator of adenosine release, is sometimes used instead. Both drugs are given as a 4-minute infusion, with injection of the tracer late in the infusion.
The adverse effects of adenosine occur early in the infusion, and include dyspnea, bronchospasm, chest pain, nausea, and headache. Bradycardia can be marked, and brief periods of complete heart block and long sinus pauses may occur. Hypotension can likewise be profound. Many of these effects are extremely disturbing to the patient under-going the test, but they disappear within 30 seconds of stopping the infusion.
Dipyridamole has similar adverse effects, although heart block is not part of its adverse effect profile. In addition, the drug’s adverse effects occur later in the infusion than those associated with adenosine and last well after it is finished. However, dipyridamole’s side effects can be reversed with intravenous aminophylline without compromising the accuracy of the test.
Drugs to avoid that day. Methylxanthines antagonize adenosine and dipyridamole, and thus must be avoided on the day of the test. Caffeine and theophylline are among the substances to be avoided, although the degree to which they affect test results has been questioned recently.15
Severe COPD and asthma—especially in patients with uncontrolled wheezing—are relative contraindications to the use of adenosine and dipyridamole.
Interestingly, the cardiovascular effects (and EKG changes) associated with these drugs are not necessarily indicative of CAD. Thus, the entire EKG portion of a pharmacologic stress test is not useful in interpreting the finding. One small study suggests that, unlike exercise stress testing, adenosine stress testing may be safe in patients with severe aortic stenosis.16
Dobutamine is another alternative for pharmacologic stress testing, for patients who cannot take adenosine or are unable to stop theophylline or similar medications. An infusion of dobutamine with an escalating dose, sometimes including atropine, is used to accelerate the heart rate to 85% of the patient’s age-predicted maximum. The stress is primarily due to the chronotropic effect of the drug, but dobutamine has some coronary vasodilatory activity and may also induce some redistribution of coronary blood flow, similar to the effect of adenosine.
The positive and negative predictive values of pharmacologic stress testing are the same as for nuclear stress testing. Unlike exercise testing, however, functional capacity cannot be inferred from a pharmacologic stress test.
About 10% of patients undergoing pharmacologic stress testing will have a nondiagnostic test. The sensitivity of the test varies among studies, but it is approximately 84%, 95%, and 100% for single-, double-, and triplevessel disease, respectively. Patients with negative tests have an event rate of less than 1% per year.17
5. Is stress echocardiography comparable to stress testing?
Yes. Stress echocardiography, which involves echocardiographic studies taken before and after stress, can substitute for either exercise or pharmacologic stress testing (the stress can be achieved either with exercise or an infusion of dobutamine), and it has certain advantages: Stress echocardiography is cheaper than nuclear stress testing, and there is no radiation involved. In addition, stress echocardiography yields positive and negative predictive values similar to those seen with nuclear stress testing.2,3 The presence of ischemia is inferred from localized wall motion abnormalities.
The primary disadvantage of stress echocardiography is that it can be administered only by a cardiologist who has been specially trained in this procedure. In contrast, any community hospital nuclear medicine department has the capacity to perform nuclear imaging, and most radiologists are able to interpret the nuclide scans. In my experience, decisions about whether to order nuclear cardiac stress testing or stress echocardiography are influenced not only by the availability of these modalities, but also by the skill of the physicians who will interpret the tests.
6. Which exercise-induced EKG changes are related to ischemia?
The only changes that correlate with myocardial ischemia are ST depression and ST elevation. J-point depression is almost universally seen with exercise. For this reason, the ST level is measured 80 milliseconds after the J point.
ST depression—the most common abnormal finding—indicates subendocardial ischemia. ST changes are most commonly seen in the inferior and lateral leads, but do not correlate with the location of ischemia. ST depression can be downsloping, horizontal, or upsloping. The first 2 are the most significant patterns, and 1 mm of ST depression is the minimum significant level. Upsloping ST depression is less significant, and 1.5 mm of depression is the minimum significant change.1 The greater the degree of ST depression, the higher the likelihood that significant occlusion will be seen on coronary angiography. ST depression that develops in the recovery period is a rare occurrence but of equal significance to ST depression that occurs with exercise, and is probably due to ischemia caused by shunting of blood into skeletal muscle and away from the heart.1
ST elevation is less common, but more ominous than ST depression, as it indicates transmural ischemia.1 This finding most often indicates high-grade left anterior descending (LAD) or left main CAD. It is most often seen in the anterior leads, and the location of ST changes correlates with the area of ischemia. Bear in mind, however, that the correlation between ST elevation and transmural ischemia is true only if the patient has no history of MI. ST elevation in leads in which Q waves are present at rest usually indicates ventricular dyskinesia or aneurysm and not ischemia.1
Premenopausal women and women who are taking estrogen supplements, in particular, are more likely than men to have false-positive ST changes, most likely because of a poorly understood effect of estrogen. The molecules of estrogen and of digitalis glycosides have some regions of structural similarity, and it is thought that both molecules can cause ST changes.10
And what about arrhythmias? Arrhythmias are often seen at rest and with exertion. Supraventricular arrhythmias, including supraventricular tachycardia, are not associated with CAD. Premature ventricular contractions (PVCs) are common at peak exertion. PVCs are probably related to catecholamine release and do not indicate ischemia. (See “A look at the stress test report”)
Ventricular tachycardia, however—defined as 3 or more consecutive PVCs—has a 90% correlation with significant coronary artery stenosis, as shown on angiography.1
Rate-dependent conduction disturbances, including 2-to-1 atrioventricular block and bundle-branch blocks, may also be seen. These may be associated with ischemia, but are not highly predictive of coronary artery stenosis. Further testing may be indicated to determine whether stenosis is present.1
The report from the physician who performs or reads the stress test should contain the following elements:
Heart rate achieved, including both the rate itself and the percentage of the patient’s age-predicted maximum that the heart rate represents. Failure to reach 85% of the maximum may be related to underlying cardiac or pulmonary disease, the use of beta-blockers, musculoskeletal disorders, or general deconditioning. However, it is obviously noteworthy if the patient develops chest pain or significant ST changes at a lower heart rate.
BP at peak exertion. There are no established levels for systolic BP at various ages. But failure of the systolic pressure to rise, or a drop in systolic pressure with exercise, indicates a lack of ventricular reserve and is a poor prognostic sign.
Functional capacity (METS). In addition to documenting the METS level itself, the report should compare it to the expected functional capacity based on the patient’s age and sex.
Chest pain (or its absence). In addition to noting whether or not chest pain developed, the report should detail the character and intensity of any pain that the patient experienced, the time into the test and the heart rate at which it developed, and the response to rest or nitroglycerine.
ST changes. Unless something in the patient’s condition changes, the workload required to produce symptoms or ST changes should be reproducible from test to test. The workload at which angina or ST changes occur is key to assessing disease severity.
Arrhythmias. Whether they’re seen at rest or develop with exertion, arrhythmias should be noted, as well.
The final report should also indicate whether the test is negative, positive, or nondiagnostic for findings consistent with CAD. Whenever possible, it should include a validated treadmill score, as well.
CORRESPONDENCE Mark A. Knox, MD, UPMC Shadyside Family Medicine Residency Program, 5230 Centre Avenue, Pittsburgh, PA 15232; [email protected]
1. Ellestad MH. Stress Testing: Principles and Practice. 3rd ed. Philadelphia: F.A. Davis Company; 1986.
2. Metz LD, Beattie M, Hom R, et al. The prognostic value of normal exercise myocardial perfusion imaging and exercise echocardiography. J Am Coll Cardiol. 2007;49:227-237.
3. Gibbons RJ. Noninvasive diagnosis and prognosis assessment in chronic coronary artery disease: stress testing with and without imaging perspective. Circ Cardiovasc Imaging. 2008;1:257-269
4. Mieres JH, Shaw LJ, Arai A, et al. Role of noninvasive testing in the clinical evaluation of women with suspected coronary artery disease: Consensus Statement From the Cardiac Imaging Committee, Council on Clinical Cardiology, and the Cardiovascular Imaging and Intervention Committee, Council on Cardiovascular Radiology and Intervention, American Heart Association. Circulation. 2005;111:682-696.
5. Scott IA. Evaluating cardiovascular risk assessment for asymptomatic people. BMJ. 2009;338:164-168.
6. Livschitz S, Sharabi Y, Yushin J, et al. Limited clinical value of exercise stress test for the screening of coronary artery disease in young, asymptomatic adult men. Am J Cardiol. 2000;86:462-464.
7. US Preventive Services Task Force. Screening for coronary heart disease: recommendation statement. Ann Intern Med. 2004;140:569-572.
8. Gibbons RJ, Balady GJ, Beasley JW, et al. ACC/AHA Guidelines for Exercise Testing: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). Circulation. 1997;96:345-354.
9. Health Physics Society. Doses from medical radiation sources. Available at: http://hps.org/hpspublications/articles/dosesfrommedicalradiation.html. Accessed April 9, 2010.
10. Albers AR, Krichavsky MZ, Balady GJ. Stress testing in patients with diabetes mellitus: diagnostic and prognostic value. Circulation. 2006;113:583-592.
11. Harris GD, White RD. Exercise stress testing in patients with type 2 diabetes: when are asymptomatic patients screened? Clin Diab. 2007;25:126-130.
12. Young LH, Wackers FJT, Chyun DA, et al. Cardiac outcomes after screening for asymptomatic coronary artery disease in patients with type 2 diabetes. The DIAD Study: a randomized controlled trial. JAMA. 2009;301:1547-1555.
13. Makaryus AN, Diamond JA. Nuclear stress testing in elderly persons: a review of its use in the assessment of cardiac risk, particularly in patients undergoing preoperative risk assessment. Drugs Aging. 2007;24:467-479.
14. McFalls EO, Ward HB, Moritz TE, et al. Coronary-artery revascularization before elective major vascular surgery. N Engl J Med 2004;351:2795-2804.
15. Kovacs D, Pivonka R, Khosla PG, et al. Effect of caffeine on myocardial perfusion imaging using single photon emission computed tomography during adenosine pharmacologic stress. Am J Ther 2008;15:431-434.
16. Samuels B, Kiat H, Friedman JD, et al. Adenosine pharmacologic stress myocardial perfusion tomographic imaging in patients with significant aortic stenosis: diagnostic effcacy and comparison of clinical, hemodynamic, and electrocardiographic variables with 100 age-matched control subjects. J Am Coll Cardiol. 1995;25:99-106.
17. Geleijnse ML, Elhendy A, Fioretti PM, et al. Dobutamine stress myocardial perfusion imaging. J Am Coll Cardiol. 2000;36:2017-2027.
18. Starling MR, Crawford MH, O’Rourke RA. Superiority of selected treadmill exercise protocols predischarge and six weeks postinfarction for detecting ischemic abnormalities. Am Heart J 1982;104:1054-1060.
19. Handler CE, Sowton E. A comparison of the Naughton and modified Bruce treadmill exercise protocols in their ability to detect ischaemic abnormalities six weeks after myocardial infarction. Eur Heart J. 1984;5:752-755.
20. Kahn JK, McGhie I, Akers MS, et al. Quantitative rotational tomography with 201T1 and 99mTc 2-methoxy-isobutyl-isonitrile. A direct comparison in normal individuals and patients with coronary artery disease. Circulation. 1989;79:1282-1293.
21. Vesely MR, Dilsizian V. Nuclear cardiac stress testing in the era of molecular medicine. J Nucl Med. 2008;49:399-413.
22. Avery P, Hudson N, Hubner P. Evaluation of changes in myocardial perfusion and function on exercise in patients with coronary artery disease by gated M1B1 scintigraphy. Br Heart J. 1993;70:22-26.
23. Gibbons RJ, Balady GJ, Bricker JT. ACC/AHA Guideline Update for Exercise Testing summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation. 2002;106:1883-1892.
1. Ellestad MH. Stress Testing: Principles and Practice. 3rd ed. Philadelphia: F.A. Davis Company; 1986.
2. Metz LD, Beattie M, Hom R, et al. The prognostic value of normal exercise myocardial perfusion imaging and exercise echocardiography. J Am Coll Cardiol. 2007;49:227-237.
3. Gibbons RJ. Noninvasive diagnosis and prognosis assessment in chronic coronary artery disease: stress testing with and without imaging perspective. Circ Cardiovasc Imaging. 2008;1:257-269
4. Mieres JH, Shaw LJ, Arai A, et al. Role of noninvasive testing in the clinical evaluation of women with suspected coronary artery disease: Consensus Statement From the Cardiac Imaging Committee, Council on Clinical Cardiology, and the Cardiovascular Imaging and Intervention Committee, Council on Cardiovascular Radiology and Intervention, American Heart Association. Circulation. 2005;111:682-696.
5. Scott IA. Evaluating cardiovascular risk assessment for asymptomatic people. BMJ. 2009;338:164-168.
6. Livschitz S, Sharabi Y, Yushin J, et al. Limited clinical value of exercise stress test for the screening of coronary artery disease in young, asymptomatic adult men. Am J Cardiol. 2000;86:462-464.
7. US Preventive Services Task Force. Screening for coronary heart disease: recommendation statement. Ann Intern Med. 2004;140:569-572.
8. Gibbons RJ, Balady GJ, Beasley JW, et al. ACC/AHA Guidelines for Exercise Testing: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). Circulation. 1997;96:345-354.
9. Health Physics Society. Doses from medical radiation sources. Available at: http://hps.org/hpspublications/articles/dosesfrommedicalradiation.html. Accessed April 9, 2010.
10. Albers AR, Krichavsky MZ, Balady GJ. Stress testing in patients with diabetes mellitus: diagnostic and prognostic value. Circulation. 2006;113:583-592.
11. Harris GD, White RD. Exercise stress testing in patients with type 2 diabetes: when are asymptomatic patients screened? Clin Diab. 2007;25:126-130.
12. Young LH, Wackers FJT, Chyun DA, et al. Cardiac outcomes after screening for asymptomatic coronary artery disease in patients with type 2 diabetes. The DIAD Study: a randomized controlled trial. JAMA. 2009;301:1547-1555.
13. Makaryus AN, Diamond JA. Nuclear stress testing in elderly persons: a review of its use in the assessment of cardiac risk, particularly in patients undergoing preoperative risk assessment. Drugs Aging. 2007;24:467-479.
14. McFalls EO, Ward HB, Moritz TE, et al. Coronary-artery revascularization before elective major vascular surgery. N Engl J Med 2004;351:2795-2804.
15. Kovacs D, Pivonka R, Khosla PG, et al. Effect of caffeine on myocardial perfusion imaging using single photon emission computed tomography during adenosine pharmacologic stress. Am J Ther 2008;15:431-434.
16. Samuels B, Kiat H, Friedman JD, et al. Adenosine pharmacologic stress myocardial perfusion tomographic imaging in patients with significant aortic stenosis: diagnostic effcacy and comparison of clinical, hemodynamic, and electrocardiographic variables with 100 age-matched control subjects. J Am Coll Cardiol. 1995;25:99-106.
17. Geleijnse ML, Elhendy A, Fioretti PM, et al. Dobutamine stress myocardial perfusion imaging. J Am Coll Cardiol. 2000;36:2017-2027.
18. Starling MR, Crawford MH, O’Rourke RA. Superiority of selected treadmill exercise protocols predischarge and six weeks postinfarction for detecting ischemic abnormalities. Am Heart J 1982;104:1054-1060.
19. Handler CE, Sowton E. A comparison of the Naughton and modified Bruce treadmill exercise protocols in their ability to detect ischaemic abnormalities six weeks after myocardial infarction. Eur Heart J. 1984;5:752-755.
20. Kahn JK, McGhie I, Akers MS, et al. Quantitative rotational tomography with 201T1 and 99mTc 2-methoxy-isobutyl-isonitrile. A direct comparison in normal individuals and patients with coronary artery disease. Circulation. 1989;79:1282-1293.
21. Vesely MR, Dilsizian V. Nuclear cardiac stress testing in the era of molecular medicine. J Nucl Med. 2008;49:399-413.
22. Avery P, Hudson N, Hubner P. Evaluation of changes in myocardial perfusion and function on exercise in patients with coronary artery disease by gated M1B1 scintigraphy. Br Heart J. 1993;70:22-26.
23. Gibbons RJ, Balady GJ, Bricker JT. ACC/AHA Guideline Update for Exercise Testing summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation. 2002;106:1883-1892.
Determining suicide risk (Hint: A screen is not enough)
• An individualized assessment is essential to identifying relevant risk factors. C
• Use direct questions, such as, “Have you had any thoughts about killing yourself?” to screen for suicidal ideation. B
• Ask a family member or close friend to ensure that any guns or other lethal means of suicide are inaccessible to the patient at risk. C
• Avoid the use of “no harm” contracts, which are controversial and lack demonstrated effectiveness. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE When Dr. A, a 68-year-old retired gastroenterologist with a history of hypertension and hypertriglyceridemia, sees his family physician (FP) for a routine check-up, his blood pressure, at 146/88 mm Hg, is uncharacteristically high. When the physician questions him about it, the patient reports taking his hydrochlorothiazide intermittently.
Dr. A, whom the FP treated for depression 5 years ago, appears downcast. in response to queries about his current mood, the patient describes a full depressive syndrome that has progressively worsened over the past month or so. The FP decides to assess his risk of suicide. But how best to proceed?
Assessing suicide risk is an essential skill for a primary care physician. It is also a daunting task, complicated by the fact that, while mental illness often predisposes patients to suicide, large numbers of people who suffer from major depression or other mental disorders are at low risk for suicide. Yet FPs, who are often the first health care practitioners patients turn to for treatment of mental health problems1 and who frequently care for the same patients for years, are well positioned to recognize when something is seriously amiss.
The difficulty comes in knowing what the next step should be. Many researchers have attempted to develop algorithms, questionnaires, and scales to facilitate rapid screening for suicide risk. But the validity and utility of such tools are questionable. Most have a low positive predictive value and generate large numbers of false-positive results.2-4 Thus, while a standard short screen or set of questions may be included in a suicide risk assessment, these measures alone are inadequate.2,3
What’s needed is an individualized approach that focuses on evaluating patients within the context of their health status, personal strengths, unique vulnerabilities, and specific circumstances. Here’s what we recommend.
Identify patients in need
Consider an individualized suicide risk assessment for patients with any of the following:
- A presentation suggestive of a mental disorder or substance abuse5-8
- the onset of, change in, or worsening of a serious medical condition
- a recent (or anticipated) major loss or psychosocial stressor9
- an expression of hopelessness10
- an acknowledgement of suicidal ideation.
CASE Dr. A fits more than 1 of the criteria: in addition to the recurrence of his depressive symptoms, he expresses hopelessness—noting that he stopped taking his medication 2 weeks ago because ”it just doesn’t matter.”
Dig deeper to assess risk
There are 4 key components of the assessment and documentation of suicide risk: (1) An overall assessment of risk, eg, low, moderate, or high; (2) a summary of the most salient risk factors and protective factors; (3) a plan to address modifiable risk factors; and (4) a rationale for the level of care and treatment provided. A thorough evaluation is the core element of the suicide risk assessment.2,11
The depth of the evaluation depends on the apparent risk, with more effort required for those at moderate or higher risk. (For high-risk patients, severe symptoms may impede a lengthy interview, and the need for hospitalization may be obvious.)
Some of the information needed may be available from the patient’s prior history. The rest can be obtained from a current medical history, including a discussion of factors known to exacerbate—or mitigate—risk (TABLE 1). The most robust predictors of suicide include being male,12 single or living alone;13 inpatient psychiatric treatment;10,14 hopelessness;10,13 and a suicide plan or a prior suicide attempt (although most “successful” suicides are completed on the first try14,15). In addition, suicide is often precipitated by a crisis, including financial, legal, or interpersonal difficulties, housing problems, educational failure, or job loss.
Sex and age considerations. For women, the incidence of suicide is highest for those in their late 40s. For men, who have a higher risk overall, the incidence increases dramatically in adolescence and remains elevated through adulthood, with a second large increase occurring after the age of 70.12
Does the patient have a psychiatric diagnosis? Mental illness has been found to be present in more than 90% of suicides,5-7 and a psychiatric diagnosis—or psychiatric symptoms such as agitation, aggression, or severe sleep disturbance2,10,16—is a key risk factor. Substance abuse is another significant risk.8,17 The risk of suicide may be especially high after discharge from a psychiatric hospital.
Is there a lack of support? The absence of a support system is a significant risk factor; conversely, marriage and children are commonly reported protective factors. In questioning patients about family and social ties, however, keep in mind that a situation that is protective for many, or most, people—eg, marriage—may represent an added stressor and risk factor for a particular patient.18
TABLE 1
Suicide assessment: Major risks vs protective factors
| Risk factors |
|---|
| Suicidality (ideation, intent, plan) |
| Prior suicide attempts2,13 |
| Hopelessness10,13 |
| Mental illness* 5-7 |
| Recent loss or crisis9 |
| Negativity, rigidity |
| Alcohol intoxication/abuse8,17 |
| Elderly12 |
| Male12 |
| Single/living alone13 |
| Gay/bisexual orientation13,25 |
| Psychiatric symptoms†10,14 |
| Impulsivity or violent/aggressive behavior |
| Family history of suicide26 |
| Unemployment2 |
| Protective factors |
| Female |
| Marriage |
| Children‡27,28 |
| Pregnancy29 |
| Interpersonal support |
| Positive coping skills30,31 |
| Religious activity32 |
| Life satisfaction33 |
| *Especially with recent psychiatric hospitalization. |
| † Including, but not limited to, anxiety, agitation, and impulsivity. |
| ‡ This includes any patient who feels responsible for children. |
Ask about suicidal ideation
The nature of suicidality, which may be the most relevant predictor of risk, can be assessed through a number of questions (TABLE 2).15 Not surprisingly, you are most likely to elicit information if you adopt an empathic, nonjudgmental, and direct communication style.
TABLE 2
Assessing suicidality: Sample questions
|
Whenever possible, begin with open-ended questions, and use follow-up questions or other cues to encourage elaboration. Ask patients whether they have thought about self-harm. If a patient acknowledges thoughts of suicide, ask additional questions to determine whether he or she has a plan and the means to carry it out. If so, what has prevented the patient from acting on it thus far?
Patients often require time to respond to such difficult questions, so resist the urge to rush through this portion of the suicide risk assessment. Simply waiting patiently may encourage a response.
CASE When directly questioned about suicidal ideation, Dr. A acknowledges that he has had thoughts of wanting to fall asleep and not wake up. Asked whether he has considered actually hurting himself, he pauses, looks away, sighs, and utters an unconvincing denial. When his FP observes, “you paused before answering that question and then looked away,” Dr. A re-establishes eye contact and admits that he has had thoughts of taking his life.
It is not uncommon for patients with suicidal ideation to initially deny it or simply fail to respond to questions, then later to open up in response to requests for clarification or further questions. This may be partly due to the patient’s own ambivalence. It may also have to do with the way the questions are presented. In order to get an accurate answer, avoid questions leading toward a negative response. Ask: ”Have you thought about killing yourself?” not “You’re not thinking about killing yourself, are you?”
Does the patient have a plan?
Suicidal ideation is defined as passive (having thoughts of wanting to die) or active (having thoughts of actually killing oneself). It is crucial to assess the level of intent and the lethality of any plan. Too often, physicians fail to probe enough to find out whether the patient has access to a lethal means of suicide, including, but not limited to, firearms or large quantities of pills that could be used as a potentially fatal overdose.
CASE Dr. A admits that he has had suicidal thoughts for the past 2 weeks, and that these thoughts have become more frequent and intense. He also says that while drinking last weekend, he thought about shooting himself.
Although Dr. A occasionally hunts and has access to guns, he denies having any intent or plan to act on his thoughts. He adds that he would never kill himself because he doesn’t want his wife and adult children to suffer.
Follow up with family or friends
For patients like Dr. A, who appear to be at significant risk, an interview with a family member or close friend may be helpful—or even necessary—to adequately gauge the extent of the danger. Patients usually consent to a physician’s request to obtain information from a loved one, particularly if the request is presented as routine or as an action taken on the patient’s behalf. A patient’s inability to name a close contact is a red flag, as individuals who are more isolated tend to be at higher risk than people with a supportive social network.19
A refusal to grant your request to contact a loved one is also worrisome, and it may still be appropriate to contact others for collateral information or notification if the patient appears to be at considerable risk.20 In such cases, be aware of local laws, and document the rationale for gathering clinical information. Focus on obtaining information needed for risk assessment. Ethical guidelines state that when “the risk of danger is deemed to be significant,” confidential information may be revealed.21
CASE Dr. A is initially reluctant to allow you to call his wife, but consents after being told that this is a routine action and for his benefit. His wife confirms his history of depressive symptoms and recalls that he became more withdrawn than usual several months ago. She has been worried about him and is glad he is finally getting help. although she is not concerned about her husband’s safety, she agrees to remove the gun from their home— and to follow up with the FP to verify that she has done so. She accepts the FP’s explanation of this as routine and is not overly alarmed by the request.
Further questioning of Dr. A and his wife, along with the FP’s knowledge of the patient, makes it clear that he has previously demonstrated good coping skills. Dr. A cannot identify a recent stressor to explain his symptoms, but acknowledges that he has become more pessimistic about the future and intermittently feels hopeless.
Dr. A generally believes his depression will resolve, as it did in the past. he has no history of psychiatric hospitalizations or suicide attempts. Nor does he have a history of problem drinking, although he admits he has been drinking alcohol more frequently than usual in the past several weeks. He identifies his wife as his primary support, although he’s aware that he has been isolating more from her and his many other supports in the past month.
Estimate risk, decide on next steps
For experienced clinicians, a determinatiuon of whether an individual is at low, moderate, or high risk is often based on both an analytical assessment and an intuitive sense of risk. In some cases, it may be useful to distinguish between acute and chronic or baseline risk.3
Patients judged to be at the highest risk may warrant immediate transport to the emergency department.22 If a patient at this level of risk does not agree to go to the hospital, involuntary admission may be necessary, depending on the laws in your state. (For patients at moderate or moderate-to-high risk, especially if acutely elevated from baseline, hospitalization may still be offered or recommended— and the recommendation documented.)
Pay particular attention to risk factors that can be modified. Access to firearms can be restricted. Treatment of mental disorders, which can generally be considered modifiable risk factors, should be a primary focus. FPs may be able to successfully treat depression, for instance, with medication and close follow-up. Counseling or psychotherapy may also be helpful; provide a referral to an alcohol or drug treatment program, as needed.
Consider a psychiatric consultation or referral if you do not feel comfortable managing a patient who has expressed any suicidal ideation.23 Psychiatric referral should also be considered when the patient does not respond to treatment with close follow-up, when psychotic symptoms are present, when hospitalization may be warranted, or when the patient has a history of suicidal thoughts or an articulated suicide plan.
Avoid suicide prevention contracts.2,24 Asking a patient to sign a “no harm,” or suicide prevention, contract is not recommended. While such contracts may lower the anxiety of physicians, they have not been found to reduce patients’ risk and are not an adequate substitute for a suicide risk assessment.
Develop a crisis response plan. Collaboratively developed safety or crisis response plans may be written on a card. Such plans can provide steps for self-management (eg, a distracting activity) and steps for external intervention if needed, such as seeking the company of a loved one or accessing emergency services.
CASE Dr. A appears to be at moderate to high risk of suicide. Salient risk factors include his age, sex, occupation (health care providers and agriculture workers are at elevated risk12,13), depression, increased use of alcohol, and suicidal ideation. He denies any intent of acting on these thoughts, however, and has a number of protective factors, including the lack of a prior attempt, his expectation that the depression will resolve, demonstrated good coping skills, and a supportive marriage.
The patient declines an offer of hospitalization. He does, however, agree to quit drinking, and to begin a regimen of antidepressants with more frequent visits to his FP. His FP offers him a referral for psychotherapy, and he agrees to seek immediate help, should he feel unsafe.
CORRESPONDENCE Jess G. Fiedorowicz, MD, 200 Hawkins Drive W278 GH, Iowa City, IA 52242; [email protected]
1. Brody DS, Thompson TL, 2nd, Larson DB, et al. Recognizing and managing depression in primary care. Gen Hosp Psychiatry. 1995;17:93-107.
2. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Am J Psychiatry. 2003;160(11 suppl):s1-s60.
3. Bryan CJ, Rudd MD. Advances in the assessment of suicide risk. J Clin Psychol. 2006;62:185-200.
4. Gaynes BN, West SL, Ford CA, et al. Screening for suicide risk in adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140:822-835.
5. Foster T, Gillespie K, McClelland R. Mental disorders and suicide in Northern Ireland. Br J Psychiatry. 1997;170:447-452.
6. Henriksson MM, Aro HM, Marttunen MJ, et al. Mental disorders and comorbidity in suicide. Am J Psychiatry. 1993;150:935-940.
7. Rich CL, Young D, Fowler RC. San Diego suicide study. I. Young vs old subjects. Arch Gen Psychiatry. 1986;43:577-582.
8. Fiedorowicz JG, Black DW, Coryell WH. Suicide and mental morbidity. In: Shrivastava A, ed. Handbook of Suicide Behaviour. London: Royal College of Psychiatrists; In Press.
9. Beautrais AL. Suicide and serious suicide attempts in youth: a multiple-group comparison study. Am J Psychiatry. 2003;160:1093-1099.
10. Conner KR, Duberstein PR, Conwell Y, et al. Psychological vulnerability to completed suicide: a review of empirical studies. Suicide Life Threat Behav. 2001;31:367-385.
11. Jacobs DG, Brewer ML. Application of The APA practice guidelines on suicide to clinical practice. CNS Spectr. 2006;11:447-454.
12. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS). Updated 2005. Available at: www.cdc.gov/ncipc/wisqars. Accessed December 20, 2008.
13. Coryell WH. Clinical assessment of suicide risk in depressive disorder. CNS Spectr. 2006;11:455-461.
14. Isometsa ET, Lonnqvist JK. Suicide attempts preceding completed suicide. Br J Psychiatry. 1998;173:531-535.
15. Coryell W, Young EA. Clinical predictors of suicide in primary major depressive disorder. J Clin Psychiatry. 2005;66:412-417.
16. Goldstein TR, Bridge JA, Brent DA. Sleep disturbance preceding completed suicide in adolescents. J Consult Clin Psychol. 2008;76:84-91.
17. Murphy GE, Wetzel RD, Robins E, et al. Multiple risk factors predict suicide in alcoholism. Arch Gen Psychiatry. 1992;49:459-463.
18. Russell Ramsay J, Newman CF. After the attempt: maintaining the therapeutic alliance following a patient’s suicide attempt. Suicide Life Threat Behav. 2005;35:413-424.
19. Beautrais AL. A case control study of suicide and attempted suicide in older adults. Suicide Life Threat Behav. 2002;32:1-9.
20. Simon RI. Assessing and Managing Suicide Risk: Guidelines for Clinically Based Risk Management. Washington, DC: American Psychiatric Publishing, Inc; 2005:54.
21. American Psychiatric Association. The Principles of Medical Ethics with Annotations Especially Applicable to Psychiatry. Washington, DC:2009. Available at: http://www.psych.org/MainMenu/PsychiatricPractice/Ethics/ResourcesStandards/ PrinciplesofMedicalEthics.aspx. Accessed April 23, 2010.
22. Raue PJ, Brown EL, Meyers BS, et al. Does every allusion to possible suicide require the same response? J Fam Pract. 2006;55:605-612.
23. Bronheim HE, Fulop G, Kunkel EJ, et al. The Academy of Psychosomatic Medicine practice guidelines for psychiatric consultation in the general medical setting. The Academy of Psychosomatic Medicine. Psychosomatics. 1998;39:S8-30.
24. Simon RI. The suicide prevention contract: clinical, legal, and risk management issues. J Am Acad Psychiatry Law. 1999;27:445-450.
25. Remafedi G, French S, Story M, et al. The relationship between suicide risk and sexual orientation: results of a population-based study. Am J Public Health. 1998;88:57-60.
26. Runeson B, Asberg M. Family history of suicide among suicide victims. Am J Psychiatry. 2003;160:1525-1526.
27. Hoyer G, Lund E. Suicide among women related to number of children in marriage. Arch Gen Psychiatry. 1993;50:134-137.
28. Clark DC, Fawcett J. The relation of parenthood to suicide. Arch Gen Psychiatry. 1994;51:160.-
29. Appleby L. Suicide during pregnancy and in the first postnatal year. BMJ. 1991;302:137-140.
30. Josepho SA, Plutchik R. Stress, coping, and suicide risk in psychiatric inpatients. Suicide Life Threat Behav. 1994;24:48-57.
31. Hughes SL, Neimeyer RA. Cognitive predictors of suicide risk among hospitalized psychiatric patients: a prospective study. Death Stud. 1993;17:103-124.
32. Nisbet PA, Duberstein PR, Conwell Y, Seidlitz L. The effect of participation in religious activities on suicide versus natural death in adults 50 and older. J Nerv Ment Dis. 2000;188:543-546.
33. Chioqueta AP, Stiles TC. The relationship between psychological buffers, hopelessness, and suicidal ideation: identification of protective factors. Crisis. 2007;28:67-73.
• An individualized assessment is essential to identifying relevant risk factors. C
• Use direct questions, such as, “Have you had any thoughts about killing yourself?” to screen for suicidal ideation. B
• Ask a family member or close friend to ensure that any guns or other lethal means of suicide are inaccessible to the patient at risk. C
• Avoid the use of “no harm” contracts, which are controversial and lack demonstrated effectiveness. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE When Dr. A, a 68-year-old retired gastroenterologist with a history of hypertension and hypertriglyceridemia, sees his family physician (FP) for a routine check-up, his blood pressure, at 146/88 mm Hg, is uncharacteristically high. When the physician questions him about it, the patient reports taking his hydrochlorothiazide intermittently.
Dr. A, whom the FP treated for depression 5 years ago, appears downcast. in response to queries about his current mood, the patient describes a full depressive syndrome that has progressively worsened over the past month or so. The FP decides to assess his risk of suicide. But how best to proceed?
Assessing suicide risk is an essential skill for a primary care physician. It is also a daunting task, complicated by the fact that, while mental illness often predisposes patients to suicide, large numbers of people who suffer from major depression or other mental disorders are at low risk for suicide. Yet FPs, who are often the first health care practitioners patients turn to for treatment of mental health problems1 and who frequently care for the same patients for years, are well positioned to recognize when something is seriously amiss.
The difficulty comes in knowing what the next step should be. Many researchers have attempted to develop algorithms, questionnaires, and scales to facilitate rapid screening for suicide risk. But the validity and utility of such tools are questionable. Most have a low positive predictive value and generate large numbers of false-positive results.2-4 Thus, while a standard short screen or set of questions may be included in a suicide risk assessment, these measures alone are inadequate.2,3
What’s needed is an individualized approach that focuses on evaluating patients within the context of their health status, personal strengths, unique vulnerabilities, and specific circumstances. Here’s what we recommend.
Identify patients in need
Consider an individualized suicide risk assessment for patients with any of the following:
- A presentation suggestive of a mental disorder or substance abuse5-8
- the onset of, change in, or worsening of a serious medical condition
- a recent (or anticipated) major loss or psychosocial stressor9
- an expression of hopelessness10
- an acknowledgement of suicidal ideation.
CASE Dr. A fits more than 1 of the criteria: in addition to the recurrence of his depressive symptoms, he expresses hopelessness—noting that he stopped taking his medication 2 weeks ago because ”it just doesn’t matter.”
Dig deeper to assess risk
There are 4 key components of the assessment and documentation of suicide risk: (1) An overall assessment of risk, eg, low, moderate, or high; (2) a summary of the most salient risk factors and protective factors; (3) a plan to address modifiable risk factors; and (4) a rationale for the level of care and treatment provided. A thorough evaluation is the core element of the suicide risk assessment.2,11
The depth of the evaluation depends on the apparent risk, with more effort required for those at moderate or higher risk. (For high-risk patients, severe symptoms may impede a lengthy interview, and the need for hospitalization may be obvious.)
Some of the information needed may be available from the patient’s prior history. The rest can be obtained from a current medical history, including a discussion of factors known to exacerbate—or mitigate—risk (TABLE 1). The most robust predictors of suicide include being male,12 single or living alone;13 inpatient psychiatric treatment;10,14 hopelessness;10,13 and a suicide plan or a prior suicide attempt (although most “successful” suicides are completed on the first try14,15). In addition, suicide is often precipitated by a crisis, including financial, legal, or interpersonal difficulties, housing problems, educational failure, or job loss.
Sex and age considerations. For women, the incidence of suicide is highest for those in their late 40s. For men, who have a higher risk overall, the incidence increases dramatically in adolescence and remains elevated through adulthood, with a second large increase occurring after the age of 70.12
Does the patient have a psychiatric diagnosis? Mental illness has been found to be present in more than 90% of suicides,5-7 and a psychiatric diagnosis—or psychiatric symptoms such as agitation, aggression, or severe sleep disturbance2,10,16—is a key risk factor. Substance abuse is another significant risk.8,17 The risk of suicide may be especially high after discharge from a psychiatric hospital.
Is there a lack of support? The absence of a support system is a significant risk factor; conversely, marriage and children are commonly reported protective factors. In questioning patients about family and social ties, however, keep in mind that a situation that is protective for many, or most, people—eg, marriage—may represent an added stressor and risk factor for a particular patient.18
TABLE 1
Suicide assessment: Major risks vs protective factors
| Risk factors |
|---|
| Suicidality (ideation, intent, plan) |
| Prior suicide attempts2,13 |
| Hopelessness10,13 |
| Mental illness* 5-7 |
| Recent loss or crisis9 |
| Negativity, rigidity |
| Alcohol intoxication/abuse8,17 |
| Elderly12 |
| Male12 |
| Single/living alone13 |
| Gay/bisexual orientation13,25 |
| Psychiatric symptoms†10,14 |
| Impulsivity or violent/aggressive behavior |
| Family history of suicide26 |
| Unemployment2 |
| Protective factors |
| Female |
| Marriage |
| Children‡27,28 |
| Pregnancy29 |
| Interpersonal support |
| Positive coping skills30,31 |
| Religious activity32 |
| Life satisfaction33 |
| *Especially with recent psychiatric hospitalization. |
| † Including, but not limited to, anxiety, agitation, and impulsivity. |
| ‡ This includes any patient who feels responsible for children. |
Ask about suicidal ideation
The nature of suicidality, which may be the most relevant predictor of risk, can be assessed through a number of questions (TABLE 2).15 Not surprisingly, you are most likely to elicit information if you adopt an empathic, nonjudgmental, and direct communication style.
TABLE 2
Assessing suicidality: Sample questions
|
Whenever possible, begin with open-ended questions, and use follow-up questions or other cues to encourage elaboration. Ask patients whether they have thought about self-harm. If a patient acknowledges thoughts of suicide, ask additional questions to determine whether he or she has a plan and the means to carry it out. If so, what has prevented the patient from acting on it thus far?
Patients often require time to respond to such difficult questions, so resist the urge to rush through this portion of the suicide risk assessment. Simply waiting patiently may encourage a response.
CASE When directly questioned about suicidal ideation, Dr. A acknowledges that he has had thoughts of wanting to fall asleep and not wake up. Asked whether he has considered actually hurting himself, he pauses, looks away, sighs, and utters an unconvincing denial. When his FP observes, “you paused before answering that question and then looked away,” Dr. A re-establishes eye contact and admits that he has had thoughts of taking his life.
It is not uncommon for patients with suicidal ideation to initially deny it or simply fail to respond to questions, then later to open up in response to requests for clarification or further questions. This may be partly due to the patient’s own ambivalence. It may also have to do with the way the questions are presented. In order to get an accurate answer, avoid questions leading toward a negative response. Ask: ”Have you thought about killing yourself?” not “You’re not thinking about killing yourself, are you?”
Does the patient have a plan?
Suicidal ideation is defined as passive (having thoughts of wanting to die) or active (having thoughts of actually killing oneself). It is crucial to assess the level of intent and the lethality of any plan. Too often, physicians fail to probe enough to find out whether the patient has access to a lethal means of suicide, including, but not limited to, firearms or large quantities of pills that could be used as a potentially fatal overdose.
CASE Dr. A admits that he has had suicidal thoughts for the past 2 weeks, and that these thoughts have become more frequent and intense. He also says that while drinking last weekend, he thought about shooting himself.
Although Dr. A occasionally hunts and has access to guns, he denies having any intent or plan to act on his thoughts. He adds that he would never kill himself because he doesn’t want his wife and adult children to suffer.
Follow up with family or friends
For patients like Dr. A, who appear to be at significant risk, an interview with a family member or close friend may be helpful—or even necessary—to adequately gauge the extent of the danger. Patients usually consent to a physician’s request to obtain information from a loved one, particularly if the request is presented as routine or as an action taken on the patient’s behalf. A patient’s inability to name a close contact is a red flag, as individuals who are more isolated tend to be at higher risk than people with a supportive social network.19
A refusal to grant your request to contact a loved one is also worrisome, and it may still be appropriate to contact others for collateral information or notification if the patient appears to be at considerable risk.20 In such cases, be aware of local laws, and document the rationale for gathering clinical information. Focus on obtaining information needed for risk assessment. Ethical guidelines state that when “the risk of danger is deemed to be significant,” confidential information may be revealed.21
CASE Dr. A is initially reluctant to allow you to call his wife, but consents after being told that this is a routine action and for his benefit. His wife confirms his history of depressive symptoms and recalls that he became more withdrawn than usual several months ago. She has been worried about him and is glad he is finally getting help. although she is not concerned about her husband’s safety, she agrees to remove the gun from their home— and to follow up with the FP to verify that she has done so. She accepts the FP’s explanation of this as routine and is not overly alarmed by the request.
Further questioning of Dr. A and his wife, along with the FP’s knowledge of the patient, makes it clear that he has previously demonstrated good coping skills. Dr. A cannot identify a recent stressor to explain his symptoms, but acknowledges that he has become more pessimistic about the future and intermittently feels hopeless.
Dr. A generally believes his depression will resolve, as it did in the past. he has no history of psychiatric hospitalizations or suicide attempts. Nor does he have a history of problem drinking, although he admits he has been drinking alcohol more frequently than usual in the past several weeks. He identifies his wife as his primary support, although he’s aware that he has been isolating more from her and his many other supports in the past month.
Estimate risk, decide on next steps
For experienced clinicians, a determinatiuon of whether an individual is at low, moderate, or high risk is often based on both an analytical assessment and an intuitive sense of risk. In some cases, it may be useful to distinguish between acute and chronic or baseline risk.3
Patients judged to be at the highest risk may warrant immediate transport to the emergency department.22 If a patient at this level of risk does not agree to go to the hospital, involuntary admission may be necessary, depending on the laws in your state. (For patients at moderate or moderate-to-high risk, especially if acutely elevated from baseline, hospitalization may still be offered or recommended— and the recommendation documented.)
Pay particular attention to risk factors that can be modified. Access to firearms can be restricted. Treatment of mental disorders, which can generally be considered modifiable risk factors, should be a primary focus. FPs may be able to successfully treat depression, for instance, with medication and close follow-up. Counseling or psychotherapy may also be helpful; provide a referral to an alcohol or drug treatment program, as needed.
Consider a psychiatric consultation or referral if you do not feel comfortable managing a patient who has expressed any suicidal ideation.23 Psychiatric referral should also be considered when the patient does not respond to treatment with close follow-up, when psychotic symptoms are present, when hospitalization may be warranted, or when the patient has a history of suicidal thoughts or an articulated suicide plan.
Avoid suicide prevention contracts.2,24 Asking a patient to sign a “no harm,” or suicide prevention, contract is not recommended. While such contracts may lower the anxiety of physicians, they have not been found to reduce patients’ risk and are not an adequate substitute for a suicide risk assessment.
Develop a crisis response plan. Collaboratively developed safety or crisis response plans may be written on a card. Such plans can provide steps for self-management (eg, a distracting activity) and steps for external intervention if needed, such as seeking the company of a loved one or accessing emergency services.
CASE Dr. A appears to be at moderate to high risk of suicide. Salient risk factors include his age, sex, occupation (health care providers and agriculture workers are at elevated risk12,13), depression, increased use of alcohol, and suicidal ideation. He denies any intent of acting on these thoughts, however, and has a number of protective factors, including the lack of a prior attempt, his expectation that the depression will resolve, demonstrated good coping skills, and a supportive marriage.
The patient declines an offer of hospitalization. He does, however, agree to quit drinking, and to begin a regimen of antidepressants with more frequent visits to his FP. His FP offers him a referral for psychotherapy, and he agrees to seek immediate help, should he feel unsafe.
CORRESPONDENCE Jess G. Fiedorowicz, MD, 200 Hawkins Drive W278 GH, Iowa City, IA 52242; [email protected]
• An individualized assessment is essential to identifying relevant risk factors. C
• Use direct questions, such as, “Have you had any thoughts about killing yourself?” to screen for suicidal ideation. B
• Ask a family member or close friend to ensure that any guns or other lethal means of suicide are inaccessible to the patient at risk. C
• Avoid the use of “no harm” contracts, which are controversial and lack demonstrated effectiveness. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE When Dr. A, a 68-year-old retired gastroenterologist with a history of hypertension and hypertriglyceridemia, sees his family physician (FP) for a routine check-up, his blood pressure, at 146/88 mm Hg, is uncharacteristically high. When the physician questions him about it, the patient reports taking his hydrochlorothiazide intermittently.
Dr. A, whom the FP treated for depression 5 years ago, appears downcast. in response to queries about his current mood, the patient describes a full depressive syndrome that has progressively worsened over the past month or so. The FP decides to assess his risk of suicide. But how best to proceed?
Assessing suicide risk is an essential skill for a primary care physician. It is also a daunting task, complicated by the fact that, while mental illness often predisposes patients to suicide, large numbers of people who suffer from major depression or other mental disorders are at low risk for suicide. Yet FPs, who are often the first health care practitioners patients turn to for treatment of mental health problems1 and who frequently care for the same patients for years, are well positioned to recognize when something is seriously amiss.
The difficulty comes in knowing what the next step should be. Many researchers have attempted to develop algorithms, questionnaires, and scales to facilitate rapid screening for suicide risk. But the validity and utility of such tools are questionable. Most have a low positive predictive value and generate large numbers of false-positive results.2-4 Thus, while a standard short screen or set of questions may be included in a suicide risk assessment, these measures alone are inadequate.2,3
What’s needed is an individualized approach that focuses on evaluating patients within the context of their health status, personal strengths, unique vulnerabilities, and specific circumstances. Here’s what we recommend.
Identify patients in need
Consider an individualized suicide risk assessment for patients with any of the following:
- A presentation suggestive of a mental disorder or substance abuse5-8
- the onset of, change in, or worsening of a serious medical condition
- a recent (or anticipated) major loss or psychosocial stressor9
- an expression of hopelessness10
- an acknowledgement of suicidal ideation.
CASE Dr. A fits more than 1 of the criteria: in addition to the recurrence of his depressive symptoms, he expresses hopelessness—noting that he stopped taking his medication 2 weeks ago because ”it just doesn’t matter.”
Dig deeper to assess risk
There are 4 key components of the assessment and documentation of suicide risk: (1) An overall assessment of risk, eg, low, moderate, or high; (2) a summary of the most salient risk factors and protective factors; (3) a plan to address modifiable risk factors; and (4) a rationale for the level of care and treatment provided. A thorough evaluation is the core element of the suicide risk assessment.2,11
The depth of the evaluation depends on the apparent risk, with more effort required for those at moderate or higher risk. (For high-risk patients, severe symptoms may impede a lengthy interview, and the need for hospitalization may be obvious.)
Some of the information needed may be available from the patient’s prior history. The rest can be obtained from a current medical history, including a discussion of factors known to exacerbate—or mitigate—risk (TABLE 1). The most robust predictors of suicide include being male,12 single or living alone;13 inpatient psychiatric treatment;10,14 hopelessness;10,13 and a suicide plan or a prior suicide attempt (although most “successful” suicides are completed on the first try14,15). In addition, suicide is often precipitated by a crisis, including financial, legal, or interpersonal difficulties, housing problems, educational failure, or job loss.
Sex and age considerations. For women, the incidence of suicide is highest for those in their late 40s. For men, who have a higher risk overall, the incidence increases dramatically in adolescence and remains elevated through adulthood, with a second large increase occurring after the age of 70.12
Does the patient have a psychiatric diagnosis? Mental illness has been found to be present in more than 90% of suicides,5-7 and a psychiatric diagnosis—or psychiatric symptoms such as agitation, aggression, or severe sleep disturbance2,10,16—is a key risk factor. Substance abuse is another significant risk.8,17 The risk of suicide may be especially high after discharge from a psychiatric hospital.
Is there a lack of support? The absence of a support system is a significant risk factor; conversely, marriage and children are commonly reported protective factors. In questioning patients about family and social ties, however, keep in mind that a situation that is protective for many, or most, people—eg, marriage—may represent an added stressor and risk factor for a particular patient.18
TABLE 1
Suicide assessment: Major risks vs protective factors
| Risk factors |
|---|
| Suicidality (ideation, intent, plan) |
| Prior suicide attempts2,13 |
| Hopelessness10,13 |
| Mental illness* 5-7 |
| Recent loss or crisis9 |
| Negativity, rigidity |
| Alcohol intoxication/abuse8,17 |
| Elderly12 |
| Male12 |
| Single/living alone13 |
| Gay/bisexual orientation13,25 |
| Psychiatric symptoms†10,14 |
| Impulsivity or violent/aggressive behavior |
| Family history of suicide26 |
| Unemployment2 |
| Protective factors |
| Female |
| Marriage |
| Children‡27,28 |
| Pregnancy29 |
| Interpersonal support |
| Positive coping skills30,31 |
| Religious activity32 |
| Life satisfaction33 |
| *Especially with recent psychiatric hospitalization. |
| † Including, but not limited to, anxiety, agitation, and impulsivity. |
| ‡ This includes any patient who feels responsible for children. |
Ask about suicidal ideation
The nature of suicidality, which may be the most relevant predictor of risk, can be assessed through a number of questions (TABLE 2).15 Not surprisingly, you are most likely to elicit information if you adopt an empathic, nonjudgmental, and direct communication style.
TABLE 2
Assessing suicidality: Sample questions
|
Whenever possible, begin with open-ended questions, and use follow-up questions or other cues to encourage elaboration. Ask patients whether they have thought about self-harm. If a patient acknowledges thoughts of suicide, ask additional questions to determine whether he or she has a plan and the means to carry it out. If so, what has prevented the patient from acting on it thus far?
Patients often require time to respond to such difficult questions, so resist the urge to rush through this portion of the suicide risk assessment. Simply waiting patiently may encourage a response.
CASE When directly questioned about suicidal ideation, Dr. A acknowledges that he has had thoughts of wanting to fall asleep and not wake up. Asked whether he has considered actually hurting himself, he pauses, looks away, sighs, and utters an unconvincing denial. When his FP observes, “you paused before answering that question and then looked away,” Dr. A re-establishes eye contact and admits that he has had thoughts of taking his life.
It is not uncommon for patients with suicidal ideation to initially deny it or simply fail to respond to questions, then later to open up in response to requests for clarification or further questions. This may be partly due to the patient’s own ambivalence. It may also have to do with the way the questions are presented. In order to get an accurate answer, avoid questions leading toward a negative response. Ask: ”Have you thought about killing yourself?” not “You’re not thinking about killing yourself, are you?”
Does the patient have a plan?
Suicidal ideation is defined as passive (having thoughts of wanting to die) or active (having thoughts of actually killing oneself). It is crucial to assess the level of intent and the lethality of any plan. Too often, physicians fail to probe enough to find out whether the patient has access to a lethal means of suicide, including, but not limited to, firearms or large quantities of pills that could be used as a potentially fatal overdose.
CASE Dr. A admits that he has had suicidal thoughts for the past 2 weeks, and that these thoughts have become more frequent and intense. He also says that while drinking last weekend, he thought about shooting himself.
Although Dr. A occasionally hunts and has access to guns, he denies having any intent or plan to act on his thoughts. He adds that he would never kill himself because he doesn’t want his wife and adult children to suffer.
Follow up with family or friends
For patients like Dr. A, who appear to be at significant risk, an interview with a family member or close friend may be helpful—or even necessary—to adequately gauge the extent of the danger. Patients usually consent to a physician’s request to obtain information from a loved one, particularly if the request is presented as routine or as an action taken on the patient’s behalf. A patient’s inability to name a close contact is a red flag, as individuals who are more isolated tend to be at higher risk than people with a supportive social network.19
A refusal to grant your request to contact a loved one is also worrisome, and it may still be appropriate to contact others for collateral information or notification if the patient appears to be at considerable risk.20 In such cases, be aware of local laws, and document the rationale for gathering clinical information. Focus on obtaining information needed for risk assessment. Ethical guidelines state that when “the risk of danger is deemed to be significant,” confidential information may be revealed.21
CASE Dr. A is initially reluctant to allow you to call his wife, but consents after being told that this is a routine action and for his benefit. His wife confirms his history of depressive symptoms and recalls that he became more withdrawn than usual several months ago. She has been worried about him and is glad he is finally getting help. although she is not concerned about her husband’s safety, she agrees to remove the gun from their home— and to follow up with the FP to verify that she has done so. She accepts the FP’s explanation of this as routine and is not overly alarmed by the request.
Further questioning of Dr. A and his wife, along with the FP’s knowledge of the patient, makes it clear that he has previously demonstrated good coping skills. Dr. A cannot identify a recent stressor to explain his symptoms, but acknowledges that he has become more pessimistic about the future and intermittently feels hopeless.
Dr. A generally believes his depression will resolve, as it did in the past. he has no history of psychiatric hospitalizations or suicide attempts. Nor does he have a history of problem drinking, although he admits he has been drinking alcohol more frequently than usual in the past several weeks. He identifies his wife as his primary support, although he’s aware that he has been isolating more from her and his many other supports in the past month.
Estimate risk, decide on next steps
For experienced clinicians, a determinatiuon of whether an individual is at low, moderate, or high risk is often based on both an analytical assessment and an intuitive sense of risk. In some cases, it may be useful to distinguish between acute and chronic or baseline risk.3
Patients judged to be at the highest risk may warrant immediate transport to the emergency department.22 If a patient at this level of risk does not agree to go to the hospital, involuntary admission may be necessary, depending on the laws in your state. (For patients at moderate or moderate-to-high risk, especially if acutely elevated from baseline, hospitalization may still be offered or recommended— and the recommendation documented.)
Pay particular attention to risk factors that can be modified. Access to firearms can be restricted. Treatment of mental disorders, which can generally be considered modifiable risk factors, should be a primary focus. FPs may be able to successfully treat depression, for instance, with medication and close follow-up. Counseling or psychotherapy may also be helpful; provide a referral to an alcohol or drug treatment program, as needed.
Consider a psychiatric consultation or referral if you do not feel comfortable managing a patient who has expressed any suicidal ideation.23 Psychiatric referral should also be considered when the patient does not respond to treatment with close follow-up, when psychotic symptoms are present, when hospitalization may be warranted, or when the patient has a history of suicidal thoughts or an articulated suicide plan.
Avoid suicide prevention contracts.2,24 Asking a patient to sign a “no harm,” or suicide prevention, contract is not recommended. While such contracts may lower the anxiety of physicians, they have not been found to reduce patients’ risk and are not an adequate substitute for a suicide risk assessment.
Develop a crisis response plan. Collaboratively developed safety or crisis response plans may be written on a card. Such plans can provide steps for self-management (eg, a distracting activity) and steps for external intervention if needed, such as seeking the company of a loved one or accessing emergency services.
CASE Dr. A appears to be at moderate to high risk of suicide. Salient risk factors include his age, sex, occupation (health care providers and agriculture workers are at elevated risk12,13), depression, increased use of alcohol, and suicidal ideation. He denies any intent of acting on these thoughts, however, and has a number of protective factors, including the lack of a prior attempt, his expectation that the depression will resolve, demonstrated good coping skills, and a supportive marriage.
The patient declines an offer of hospitalization. He does, however, agree to quit drinking, and to begin a regimen of antidepressants with more frequent visits to his FP. His FP offers him a referral for psychotherapy, and he agrees to seek immediate help, should he feel unsafe.
CORRESPONDENCE Jess G. Fiedorowicz, MD, 200 Hawkins Drive W278 GH, Iowa City, IA 52242; [email protected]
1. Brody DS, Thompson TL, 2nd, Larson DB, et al. Recognizing and managing depression in primary care. Gen Hosp Psychiatry. 1995;17:93-107.
2. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Am J Psychiatry. 2003;160(11 suppl):s1-s60.
3. Bryan CJ, Rudd MD. Advances in the assessment of suicide risk. J Clin Psychol. 2006;62:185-200.
4. Gaynes BN, West SL, Ford CA, et al. Screening for suicide risk in adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140:822-835.
5. Foster T, Gillespie K, McClelland R. Mental disorders and suicide in Northern Ireland. Br J Psychiatry. 1997;170:447-452.
6. Henriksson MM, Aro HM, Marttunen MJ, et al. Mental disorders and comorbidity in suicide. Am J Psychiatry. 1993;150:935-940.
7. Rich CL, Young D, Fowler RC. San Diego suicide study. I. Young vs old subjects. Arch Gen Psychiatry. 1986;43:577-582.
8. Fiedorowicz JG, Black DW, Coryell WH. Suicide and mental morbidity. In: Shrivastava A, ed. Handbook of Suicide Behaviour. London: Royal College of Psychiatrists; In Press.
9. Beautrais AL. Suicide and serious suicide attempts in youth: a multiple-group comparison study. Am J Psychiatry. 2003;160:1093-1099.
10. Conner KR, Duberstein PR, Conwell Y, et al. Psychological vulnerability to completed suicide: a review of empirical studies. Suicide Life Threat Behav. 2001;31:367-385.
11. Jacobs DG, Brewer ML. Application of The APA practice guidelines on suicide to clinical practice. CNS Spectr. 2006;11:447-454.
12. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS). Updated 2005. Available at: www.cdc.gov/ncipc/wisqars. Accessed December 20, 2008.
13. Coryell WH. Clinical assessment of suicide risk in depressive disorder. CNS Spectr. 2006;11:455-461.
14. Isometsa ET, Lonnqvist JK. Suicide attempts preceding completed suicide. Br J Psychiatry. 1998;173:531-535.
15. Coryell W, Young EA. Clinical predictors of suicide in primary major depressive disorder. J Clin Psychiatry. 2005;66:412-417.
16. Goldstein TR, Bridge JA, Brent DA. Sleep disturbance preceding completed suicide in adolescents. J Consult Clin Psychol. 2008;76:84-91.
17. Murphy GE, Wetzel RD, Robins E, et al. Multiple risk factors predict suicide in alcoholism. Arch Gen Psychiatry. 1992;49:459-463.
18. Russell Ramsay J, Newman CF. After the attempt: maintaining the therapeutic alliance following a patient’s suicide attempt. Suicide Life Threat Behav. 2005;35:413-424.
19. Beautrais AL. A case control study of suicide and attempted suicide in older adults. Suicide Life Threat Behav. 2002;32:1-9.
20. Simon RI. Assessing and Managing Suicide Risk: Guidelines for Clinically Based Risk Management. Washington, DC: American Psychiatric Publishing, Inc; 2005:54.
21. American Psychiatric Association. The Principles of Medical Ethics with Annotations Especially Applicable to Psychiatry. Washington, DC:2009. Available at: http://www.psych.org/MainMenu/PsychiatricPractice/Ethics/ResourcesStandards/ PrinciplesofMedicalEthics.aspx. Accessed April 23, 2010.
22. Raue PJ, Brown EL, Meyers BS, et al. Does every allusion to possible suicide require the same response? J Fam Pract. 2006;55:605-612.
23. Bronheim HE, Fulop G, Kunkel EJ, et al. The Academy of Psychosomatic Medicine practice guidelines for psychiatric consultation in the general medical setting. The Academy of Psychosomatic Medicine. Psychosomatics. 1998;39:S8-30.
24. Simon RI. The suicide prevention contract: clinical, legal, and risk management issues. J Am Acad Psychiatry Law. 1999;27:445-450.
25. Remafedi G, French S, Story M, et al. The relationship between suicide risk and sexual orientation: results of a population-based study. Am J Public Health. 1998;88:57-60.
26. Runeson B, Asberg M. Family history of suicide among suicide victims. Am J Psychiatry. 2003;160:1525-1526.
27. Hoyer G, Lund E. Suicide among women related to number of children in marriage. Arch Gen Psychiatry. 1993;50:134-137.
28. Clark DC, Fawcett J. The relation of parenthood to suicide. Arch Gen Psychiatry. 1994;51:160.-
29. Appleby L. Suicide during pregnancy and in the first postnatal year. BMJ. 1991;302:137-140.
30. Josepho SA, Plutchik R. Stress, coping, and suicide risk in psychiatric inpatients. Suicide Life Threat Behav. 1994;24:48-57.
31. Hughes SL, Neimeyer RA. Cognitive predictors of suicide risk among hospitalized psychiatric patients: a prospective study. Death Stud. 1993;17:103-124.
32. Nisbet PA, Duberstein PR, Conwell Y, Seidlitz L. The effect of participation in religious activities on suicide versus natural death in adults 50 and older. J Nerv Ment Dis. 2000;188:543-546.
33. Chioqueta AP, Stiles TC. The relationship between psychological buffers, hopelessness, and suicidal ideation: identification of protective factors. Crisis. 2007;28:67-73.
1. Brody DS, Thompson TL, 2nd, Larson DB, et al. Recognizing and managing depression in primary care. Gen Hosp Psychiatry. 1995;17:93-107.
2. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Am J Psychiatry. 2003;160(11 suppl):s1-s60.
3. Bryan CJ, Rudd MD. Advances in the assessment of suicide risk. J Clin Psychol. 2006;62:185-200.
4. Gaynes BN, West SL, Ford CA, et al. Screening for suicide risk in adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140:822-835.
5. Foster T, Gillespie K, McClelland R. Mental disorders and suicide in Northern Ireland. Br J Psychiatry. 1997;170:447-452.
6. Henriksson MM, Aro HM, Marttunen MJ, et al. Mental disorders and comorbidity in suicide. Am J Psychiatry. 1993;150:935-940.
7. Rich CL, Young D, Fowler RC. San Diego suicide study. I. Young vs old subjects. Arch Gen Psychiatry. 1986;43:577-582.
8. Fiedorowicz JG, Black DW, Coryell WH. Suicide and mental morbidity. In: Shrivastava A, ed. Handbook of Suicide Behaviour. London: Royal College of Psychiatrists; In Press.
9. Beautrais AL. Suicide and serious suicide attempts in youth: a multiple-group comparison study. Am J Psychiatry. 2003;160:1093-1099.
10. Conner KR, Duberstein PR, Conwell Y, et al. Psychological vulnerability to completed suicide: a review of empirical studies. Suicide Life Threat Behav. 2001;31:367-385.
11. Jacobs DG, Brewer ML. Application of The APA practice guidelines on suicide to clinical practice. CNS Spectr. 2006;11:447-454.
12. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS). Updated 2005. Available at: www.cdc.gov/ncipc/wisqars. Accessed December 20, 2008.
13. Coryell WH. Clinical assessment of suicide risk in depressive disorder. CNS Spectr. 2006;11:455-461.
14. Isometsa ET, Lonnqvist JK. Suicide attempts preceding completed suicide. Br J Psychiatry. 1998;173:531-535.
15. Coryell W, Young EA. Clinical predictors of suicide in primary major depressive disorder. J Clin Psychiatry. 2005;66:412-417.
16. Goldstein TR, Bridge JA, Brent DA. Sleep disturbance preceding completed suicide in adolescents. J Consult Clin Psychol. 2008;76:84-91.
17. Murphy GE, Wetzel RD, Robins E, et al. Multiple risk factors predict suicide in alcoholism. Arch Gen Psychiatry. 1992;49:459-463.
18. Russell Ramsay J, Newman CF. After the attempt: maintaining the therapeutic alliance following a patient’s suicide attempt. Suicide Life Threat Behav. 2005;35:413-424.
19. Beautrais AL. A case control study of suicide and attempted suicide in older adults. Suicide Life Threat Behav. 2002;32:1-9.
20. Simon RI. Assessing and Managing Suicide Risk: Guidelines for Clinically Based Risk Management. Washington, DC: American Psychiatric Publishing, Inc; 2005:54.
21. American Psychiatric Association. The Principles of Medical Ethics with Annotations Especially Applicable to Psychiatry. Washington, DC:2009. Available at: http://www.psych.org/MainMenu/PsychiatricPractice/Ethics/ResourcesStandards/ PrinciplesofMedicalEthics.aspx. Accessed April 23, 2010.
22. Raue PJ, Brown EL, Meyers BS, et al. Does every allusion to possible suicide require the same response? J Fam Pract. 2006;55:605-612.
23. Bronheim HE, Fulop G, Kunkel EJ, et al. The Academy of Psychosomatic Medicine practice guidelines for psychiatric consultation in the general medical setting. The Academy of Psychosomatic Medicine. Psychosomatics. 1998;39:S8-30.
24. Simon RI. The suicide prevention contract: clinical, legal, and risk management issues. J Am Acad Psychiatry Law. 1999;27:445-450.
25. Remafedi G, French S, Story M, et al. The relationship between suicide risk and sexual orientation: results of a population-based study. Am J Public Health. 1998;88:57-60.
26. Runeson B, Asberg M. Family history of suicide among suicide victims. Am J Psychiatry. 2003;160:1525-1526.
27. Hoyer G, Lund E. Suicide among women related to number of children in marriage. Arch Gen Psychiatry. 1993;50:134-137.
28. Clark DC, Fawcett J. The relation of parenthood to suicide. Arch Gen Psychiatry. 1994;51:160.-
29. Appleby L. Suicide during pregnancy and in the first postnatal year. BMJ. 1991;302:137-140.
30. Josepho SA, Plutchik R. Stress, coping, and suicide risk in psychiatric inpatients. Suicide Life Threat Behav. 1994;24:48-57.
31. Hughes SL, Neimeyer RA. Cognitive predictors of suicide risk among hospitalized psychiatric patients: a prospective study. Death Stud. 1993;17:103-124.
32. Nisbet PA, Duberstein PR, Conwell Y, Seidlitz L. The effect of participation in religious activities on suicide versus natural death in adults 50 and older. J Nerv Ment Dis. 2000;188:543-546.
33. Chioqueta AP, Stiles TC. The relationship between psychological buffers, hopelessness, and suicidal ideation: identification of protective factors. Crisis. 2007;28:67-73.
Insulin therapy for type 2 diabetes: Making it work
• Inform patients with type 2 diabetes about the possible need for insulin therapy if diet, healthy lifestyle, and medications other than insulin do not achieve glycemic control. A
• Add basal insulin to oral medications as soon as needed to help patients reach fasting glycemic goals. If further adjustments are needed, add prandial insulin. B
• Choose basal and prandial insulin analogs to approximate normal physiologic insulin secretion. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Many patients with type 2 diabetes will eventually require insulin to reach glycemic targets that have been shown to protect against micro- and macro-vascular complications of the disease. But in the primary care setting, initiating and advancing insulin therapy for these patients can be challenging. This article discusses the barriers to initiating insulin therapy that family physicians often encounter and suggests strategies for addressing them. The goal should be to approximate normal physiologic insulin secretion as closely as possible. We will outline how that goal can best be achieved using combinations of long-acting and rapid-acting insulin analogs in a variety of basal-prandial regimens.
The evidence behind good glycemic control
Several landmark trials, including the United Kingdom Prospective Diabetes Study (UKPDS), the Diabetes Control and Complications Trial (DCCT), the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC), and the recent ADVANCE study, demonstrate the importance of good glycemic control in reducing the risk of microvascular complications of diabetes.1-4 These studies all show that lower glycosylated hemoglobin levels (hemoglobin A1C) are associated with a reduction in risk for the development or progression of microvascular complications of the disease.1-4
Setting glycemic targets
The American Diabetes Association (ADA) and the American Association of Clinical Endocrinologists (AACE) have established guidelines that provide physicians and patients with glycemic targets. The ADA recommends that hemoglobin A1C be maintained at <7.0% or as near normoglycemia (<6.0%) as possible without significant risk of hypoglycemia. Preprandial glucose targets are 70 to 130 mg/dL, and the postprandial target is <180 mg/dL.5 The AACE recommends even stricter glycemic control, with an A1C target of <6.5%, a preprandial target of ≤110 mg/dL, and peak postprandial glycemic target of ≤140 mg/dL.6 In clinical practice, it is best to aim for glycemic targets that are as close to ADA or AACE guidelines as possible, provided one can do so safely. In doing so, the clinician must recognize that glycemic goals should be individualized, to take into account the presence of comorbid conditions and the expected longevity of the patient.7
Glycemic control in type 2 diabetes. Diet, exercise, weight loss, and adoption of a healthy lifestyle are the cornerstones of care for patients at all stages of diabetes. As the disease progresses, most patients with diabetes will also require pharmacologic therapy that will need to be intensified over time.8
Oral agents are the place to begin. Typically, pharmacologic management of diabetes begins with oral agents.8 Several categories of oral medication can be used to treat type 2 diabetes, and more than 1 agent may be used for initial treatment of hyperglycemia. Insulin secretagogues (sulfonylureas and meglitinide analogs) are prescribed to treat the insulin secretory defect, whereas insulin sensitizers (metformin and thiazolidinediones) are used to address insulin resistance. Other agents include a-glucosidase inhibitors, which benefit patients with type 2 diabetes by slowing carbohydrate absorption, while glucagon-like peptide-1 (GLP-1) analogs and dipeptidyl peptidase-4 (DPP-4) inhibitors increase incretin levels, enhance insulin secretion in a glucose-dependent manner, and suppress pancreatic glucagon secretion.
When adding insulin becomes necessary
Even when combinations of these medications are used, many patients ultimately require the addition of exogenous insulin to achieve glycemic control.9 In clinical practice, however, insulin therapy is often delayed because physicians and patients alike are prey to misconceptions and fears about disease progression and the role of insulin.10 TABLE 1 presents some of the most common preconceptions held by patients about the initiation of insulin therapy, and suggests strategies for overcoming each of them.11
To help guide your decision making, you can follow the AACE/ACE Diabetes Algorithm for Glycemic Control, an updated guide for moving from oral medications to insulin therapy, depending on A1C levels. The algorithm is available at http://www.diabetesincontrol.com/images/issues/2012/04/aace_guidelines_for_glycemic_control.pdf.12
TABLE 1
“Insulin will make me fat,” and other patient concerns you’ll need to overcome
| Patient concern | How you can respond |
|---|---|
| Fear: “I’m afraid of needles.” | Insulin pens and smaller, thinner needles make injections almost painless. |
| Failure: “Going on insulin proves I can’t take control of my disease.” | The natural course of diabetes is to worsen over time, but controlling your blood glucose levels with insulin can slow that process down. |
| Stigma: “If people see me taking an insulin shot, they’ll think I’m a sick person.” | New injection devices like insulin pens are not very noticeable, and the needles are smaller and thinner than they used to be. |
| Weight gain: “Insulin will make me fat.” | I’ll help you find a nutritionist who can teach you how to eat healthier foods and develop an active lifestyle that helps keep you trim. And insulin is no more likely to make you fat than some of the oral agents you’ve been using. |
| Hypoglycemia: “I’ve heard that diabetics who use insulin can pass out suddenly, or even go into a coma. I think it’s called hypoglycemia, and it scares me.” | That’s less likely to happen with the newer forms of insulin we use now. And if you do have a hypoglycemic episode, it will probably be something mild you can treat yourself. I can teach you how to recognize what’s happening and what to do about it. |
| Complexity: “It all sounds too difficult for me to manage on my own.” | We have new, step-by-step instructions you can follow when you start insulin therapy and when you need to make changes. |
| Complications: “I know people on insulin who have serious complications like heart attacks and kidney disease. Will that happen to me?” | Diabetes-related complications are the result of inadequate control of blood sugar levels. Insulin provides more intensive glycemic control than you’ve been achieving, and that helps avoid the complications you’re concerned about. That’s why I recommend you start using insulin. |
| Source: Brunton S, et al. The role of basal insulin in type 2 diabetes management. J Fam Pract. 2005.11 | |
Early insulin gets results
Studies have demonstrated that the early use of intensive insulin improves beta-cell function and may enable patients to temporarily stop pharmacologic therapy for variable periods of time.13-15 In a Canadian study, 405 patients with type 2 diabetes receiving 0, 1, or 2 oral agents and with A1C levels between 7.5% and 11.0% were randomized to either a basal insulin or intensification of oral agents without adding insulin.16 Patients who were treated with insulin were 1.68 times more likely to achieve 2 consecutive A1C levels of 6.5% or less and achieved this endpoint sooner than those randomized to intensification of oral agents. Additionally, patients treated with insulin were able to achieve an adjusted mean A1C of 6.96%, compared with the 7.24% achieved by patients treated only with oral therapy. In addition to its glycemic benefits, insulin has also been shown to inhibit atherogenesis and improve triglyceride and high-density lipoprotein cholesterol levels.17,18
The next step: choosing the best insulin regimen
Long-acting basal insulin. Insulin glargine and insulin detemir are long-acting insulin analogs that were developed to approximate normal basal pancreatic secretion.19 Insulin glargine has a smooth, time-action pharmacokinetic profile without pronounced peaks.20 Several studies indicate that once-daily insulin glargine is as effective as twice-daily neutral protamine Hagedorn (NPH) insulin in controlling hyperglycemia, and is associated with reduced nocturnal hypoglycemia.20,21 Insulin detemir has also been shown to provide effective glycemic control with a reduced risk of hypoglycemia compared with NPH.22 This long-acting basal insulin is approved for once- or twice-daily subcutaneous administration and, like glargine, exhibits a dose-dependent duration of action of up to 24 hours.22,23
Prandial insulin may also be needed. If basal insulin plus antidiabetic drugs are not sufficient to control hyperglycemia, you can add prandial insulin to the treatment regimen. For guidance on initiating and advancing insulin therapy, consult the consensus algorithm from the ADA and the European Association for the Study of Diabetes at http://care.diabetesjournals.org/content/32/1/193.full.pdf+html.8 (See Figure 1 on page 198 of the pdf.) The rapid-acting insulin analogs—insulins aspart, lispro, and glulisine—have a more rapid onset and shorter duration of action than regular human insulin.24 The pharmacokinetic profiles of rapid-acting insulin analogs more closely resemble the prandial insulin response seen in individuals without diabetes.25 Rapid-acting analogs have an onset of action of 5 to 15 minutes—approximately twice as fast as regular insulin—and a duration of action of 2 to 5 hours, which is shorter than regular insulin.24-27 These attributes allow for greater dosing flexibility, as patients can inject insulin immediately before or after eating rather than having to inject regular insulin 30 to 45 minutes before the planned meal.24
Sometimes your patient needs to use both. Basal-prandial regimens, appropriate for all patients with type 1 diabetes, can also be used for some patients with newly diagnosed type 2 diabetes and for those who have not achieved glycemic targets with 1 or more oral agents or with prandial or premixed insulin regimens. Start newly diagnosed type 2 patients on a basal-prandial regimen if they have severe, symptomatic hyperglycemia. Such patients often have an A1C >10.0% or a fasting plasma glucose (FPG) >250 mg/dL. Oral agents alone are unlikely to reduce the A1C or FPG to target in such patients, and should be considered only after the extreme hyperglycemia has been reduced with an intensive insulin regimen.5
Premixed combinations are simpler, but have a downside
Premixed insulin combines an intermediate-acting insulin with a short- or rapid-acting insulin in a single injection. Premixed insulins are available in fixed-dose ratios to provide both basal and prandial insulin replacement. In addition to premixed regular-NPH combinations, 3 premixed insulin analog formulations are currently available: biphasic insulin lispro mix 75/25 (75% NPH and 25% lispro), biphasic insulin lispro mix 50/50 (50% NPH and 50% lispro), and biphasic insulin aspart 70/30 (70% NPH and 30% aspart).28
Premixed insulin is usually administered twice daily, before breakfast and supper.29 In some instances, a third injection at lunch is necessary to achieve glycemic goals.30 These regimens require patients to adhere to a consistent meal schedule and carbohydrate intake to avoid prandial hypo- and hyperglycemia.29
The disadvantage of a premixed insulin regimen is that the prandial and basal insulin components cannot be dosed independently. For example, if a patient who takes 75/25 insulin at breakfast has low blood sugars after breakfast but good glucose control at lunch-time and in the afternoon, it is not possible to reduce the amount of short-acting insulin without also reducing the dose of the NPH. Changing the dose of 75/25 to eliminate post-breakfast hypoglycemia may cause hyperglycemia in the afternoon, because the NPH dose will also be reduced. Separate injections of basal and prandial insulin provide a more physiologic regimen.
A subanalysis from the AT.LANTUS study examined glycemic parameters and safety over 24 weeks in 686 patients who switched from premixed insulin to once-daily insulin glargine.31 Patients were allowed to use oral agents as well, before and after the switch. After patients made the switch, A1C and FPG were significantly reduced, and the incidence of severe hypoglycemia was low. The addition of prandial insulin at 1 or more meals was associated with further improvements in glycemic control.31
A multifaceted, stepwise approach
Ideally, when a physician diagnoses a patient with diabetes, he or she has access to a diabetes care team that includes a dietitian or nutritionist, a certified diabetes nurse educator, a pharmacist, and an exercise physiologist. The team’s job is to educate the patient about the natural history of the disease and its complications and to teach diabetes self-management.
The real world. In practice, family physicians rarely have access to the kind of comprehensive diabetes care team that exists in specialty centers. You and your staff will need to provide the patient education that diabetes care requires, supplying patient-education handouts from online and print sources and making time to discuss food choices, meal planning, and daily exercise goals in follow-up visits. Written food and exercise logs are useful tools in this educational process.
Diabetes 101. At the time of diagnosis or at an early follow-up visit, be sure to inform the patient about all the treatment options— including insulin—that are available to treat the disease. Whenever possible, the discussion of insulin therapy should begin months or years before there is a need to initiate insulin treatment, so that when the time comes to start insulin, the patient will be more likely to accept the regimen. Patient education should include an introduction to carbohydrate content of different foods and the general principles of carbohydrate counting, home glucose monitoring, hypoglycemia awareness, and options for insulin delivery (syringe vs pen device).
When the time comes
To recognize the proper time to introduce insulin, evaluate A1C levels at least twice a year in patients who are meeting their glucose goals and every 3 months in those who are not meeting goals or whose treatment regimen has been changed.5 Additionally, patients should monitor their fasting, preprandial, and postprandial glucose levels regularly to be sure they are meeting glycemic targets and to minimize the risk of hypoglycemia. Glucose readings should be reviewed at every office visit.
Monitor glucose before and after meals
Both pre- and postprandial glucose levels should be monitored and managed in all patients with diabetes, whether or not they are treated with insulin. Some studies have suggested that home glucose monitoring may not improve glycemic control for patients taking oral agents. It is our view, however, that home glucose monitoring can facilitate changes in diet or exercise patterns and help physicians adjust or add treatment, based on pre- and postprandial glucose concentrations.
For some patients, focusing treatment initially on preprandial glucose may be sufficient, because elevated baseline preprandial glucose levels can lead to a higher overall plasma glucose profile and higher postprandial excursion.32 Basal insulin can be used to lower the fasting glucose levels and the overall glycemic profile for those patients.
Other patients, however, may have normal fasting and preprandial blood glucose levels with postprandial hyperglycemia. For these patients, modest postprandial glycemic excursions may be decreased initially by lowering the overall glycemic profile with basal insulin. In some cases, an injection of rapid-acting insulin before the meals that are associated with postprandial hyperglycemia is an effective treatment option.
Both pre- and postprandial glucose concentrations contribute to the A1C. At higher A1C concentrations (>7.5%) fasting glucose contributes more than postprandial glucose to the A1C. Below this concentration, the reverse holds true.33 As diabetes progresses, basal insulin can become insufficient to achieve glycemic control, and many patients eventually require the addition of prandial insulin at appropriate meals to control postprandial glucose excursions.32
The benefits of insulin treatment are most robust when both preprandial and postprandial glucose levels are taken into account. In a person with normal glucose homeostasis, about half the insulin released in a day is for basal regulation and the other half is meal related.34 Thus, most insulin treatment regimens are designed to provide approximately 50% of insulin as basal coverage and 50% at meals.34 Basal insulin suppresses gluconeogenesis between meals and overnight, whereas prandial insulin covers increases in blood glucose levels after meals.34
Use titration algorithms to balance glucose levels
Several simple titration algorithms can be used to initiate basal insulin. An initial dosage of 10 units daily (or 0.1 unit/kg) is a reasonable starting point for many patients with type 2 diabetes and moderate insulin resistance. This dose can be increased every 3 to 5 days until the target preprandial glucose level is achieved (TABLE 2).35,36 If a basal-prandial insulin regimen is started, then typically half the 24-hour insulin dosage is given as basal insulin.34 The remaining 50% is given as a rapid-acting insulin analog at meals. Dosages should be adjusted according to the patient’s self-monitored blood glucose values.35
Prandial insulin therapy is often initiated with a single injection administered either at the largest meal of the day or at the meal that most often increases postprandial glucose above target levels. The dose of prandial insulin is ideally based on the carbohydrate content of the meal and the pre-meal blood sugar, but for patients whose meals do not vary much in terms of carbohydrate content, it may be simpler to give fixed mealtime doses. Additional injections are added at other meals as necessary.
A patient’s 24-hour insulin dosage requirement can be estimated by multiplying the body weight (in kilograms) by a factor that takes the patient’s presumed insulin sensitivity into account. One strategy is to use a factor of 0.3 if the patient is insulin sensitive (usually lean), 0.5 if the patient is of average sensitivity (average weight to moderately overweight), and 0.6 if the patient is relatively insulin resistant (obese or morbidly obese).34 The total 24-hour insulin dose is the sum of the basal and prandial doses. It is crucial to take into account the oral agents a patient is using when calculating the total daily insulin requirements. In particular, patients who use insulin secretagogues may require less insulin if these medications are not stopped or reduced.
The effectiveness of a simple titration regimen was demonstrated in a study by Bergenstal and colleagues.37 They compared outcomes for patients with type 2 diabetes who calculated their dosage of a prandial, rapid-acting insulin analog (insulin glulisine) using a simple titration regimen with patients who based their dosage on carbohydrate counting. Carbohydrate counting involves adding the amount of carbohydrates in all the foods for a given meal and then dosing prandial insulin according to a ratio of units of insulin per gram of carbohydrate. For example, a meal containing 60 g of carbohydrate requires 6 units of insulin if a patient uses 1 unit of insulin per 10 g of carbohydrate. Patients on the simple regimen adjusted their weekly mealtime insulin dose by 1, 2, or 3 units, depending on their pre-meal glucose patterns.
When the 2 groups were compared, patients using a simple dosing algorithm did as well as those who based their dosage on carbohydrate counting. They achieved a similar degree of glycemic control (A1C reduction=~1.5%) and experienced fewer episodes of symptomatic hypoglycemia (defined as <50 mg/dL), 4.9 vs 8.0 events per patient year; P=.02).37 These findings support the use of a simple alternative method for prandial-dose titration and may allay concerns that basal-prandial insulin regimens are complicated and tedious to implement.
The recently published 4T study evaluated different insulin regimens for patients not achieving therapeutic goal on oral agents. Patients were started on basal insulin, prandial insulin, or premixed insulin. After 1 year, the insulin regimen was intensified in those who were still not achieving therapeutic goals, and the patients were evaluated after another 2 years. Prandial insulin was added for patients initially treated with basal insulin if they were not at A1C goal, basal insulin was added for those who started with prandial insulin, and a dose of rapid-acting insulin was given at lunch to those on twice-daily pre-mixed insulin who were not at goal. The A1C levels achieved at the end of the study did not differ among the treatment groups, and ranged from 6.8% to 7.1%.38
TABLE 2
Weekly insulin titration schedule
| Continue oral agent(s) at same dosage (eventually reduce) |
| Initiate insulin therapy If postprandial glucose levels are >140 mg/dL, add single insulin dose (about 10 U) in the evening. you can use:
|
Increase insulin dose every 3 to 5 days as needed, provided no nocturnal hypoglycemia occurs. Increase to:
|
| Treat to target level (usually FBG <120 mg/dL) |
| FBG, fasting blood glucose; NPH, neutral protamine Hagedorn. |
| Source: Chan JL et al. Mayo Clinic Proc. 2003.35 Adapted with permission. |
Overcoming reluctance
Despite convincing evidence that effective glycemic control can help delay or prevent diabetic complications, more than half the patients with type 2 diabetes do not achieve the treatment goal of A1C below 7.0%.39 Insulin therapy can help these patients reach glycemic targets rapidly and safely, but many patients and physicians are reluctant to start insulin for a variety of reasons.
For many, concern about hypoglycemia is at the top of the list. The way to address that concern is by educating patients to recognize symptoms of hypoglycemia and emphasizing the importance of frequent blood sugar monitoring, especially before driving and exercising. Insulin therapy does not increase the risk of hypoglycemic episodes. In fact, the risk of severe hypoglycemia in a patient with type 2 diabetes who has normal renal function and takes an appropriate dose of insulin is low.
Cost can also be a factor in the reluctance to start insulin therapy. The newer insulin analogs are more expensive than older formulations, but they more closely approximate physiologic insulin secretion and their use is associated with a reduced risk of hypoglycemia.
Finally, the perception that insulin regimens are complex and difficult to self-titrate is another common reason that physicians and patients are reluctant to begin insulin therapy or to progress from basal to basal/prandial regimens. In fact, insulin regimens are less complicated than patients fear. Several simple and practical algorithms are available to guide patients through a step-by-step process of initiating and advancing insulin therapy. Patients using these guidelines quickly become comfortable with insulin administration and savvy about interpreting blood glucose patterns based on meal content and exercise. Basal, premixed, and basal/prandial insulin regimens are all strategies that can help patients achieve their glycemic goals quickly and safely.
CORRESPONDENCE Jody Dushay, MD, Beth Israel Deaconess Medical Center, 330 Brookline Avenue, Boston, MA 02215; [email protected]
1. U.K. Prospective Diabetes Study 16. Overview of 6 years’ therapy of type II diabetes: a progressive disease. UK Prospective Diabetes Study Group. Diabetes. 1995;44:1249-1258.
2. The Diabetes Control and Complications Trial (DCCT). Design and methodologic considerations for the feasibility phase. Diabetes Control and Complications Trial Research Group. Diabetes. 1986;35:530-45.
3. Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643-2653.
4. Dluhy RG, McMahon GT. Intensive glycemic control in the ACCORD and ADVANCE trials. N Engl J Med. 2008;358:2630-2633.
5. American Diabetes Association. Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(suppl 1):S11-S61.
6. Rodbard HW, Blonde L, Braithwaite SS, et al. AACE Diabetes Mellitus Clinical Practice Guidelines Task Force. American Association of Clinical Endocrinologists medical guidelines for clinical practice for the management of diabetes mellitus. Endocr Pract. 2007;13(suppl 1):s1-s68.
7. Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. The Action to Control Cardiovascular Risk in Diabetes Study Group. N Engl J Med. 2008;358:2545-2559.
8. Nathan DM, Buse JB, Davidson MB, et al. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2009;32:193-203.
9. Riddle MC. Glycemic management of type 2 diabetes: an emerging strategy with oral agents, insulins, and combinations. Endocrinol Metab Clin North Am. 2005;34:77-98.
10. Riddle MC. The underuse of insulin therapy in North America. Diabetes Metab Res Rev. 2002;18(suppl 3):S42-S49.
11. Brunton SA, White JR, Renda SM. The role of basal insulin in type 2 diabetes management. J Fam Pract. 2005;54(suppl):S1-S8.
12. Rodbard HW, Jellinger PS, Davidson JA, et al. Statement by an American Association of Clinical Endocrinologists/American College of Endocrinology consensus panel on type 2 diabetes mellitus: an algorithm for glycemic control. Endocr Pract. 2009;15:540-559.
13. Li Y, Xu W, Liao Z. Induction of long-term glycemic control in newly diagnosed type 2 diabetic patients is associated with improvement of beta-cell function. Diabetes Care. 2004;27:2597-2602.
14. Ryan EA, Imes S, Wallace C. Short-term intensive insulin therapy in newly diagnosed type 2 diabetes. Diabetes Care. 2004;27:1028-1032.
15. McFarlane SI, Chaiken RL, Hirsch S, et al. Near-normoglycaemic remission in African-Americans with type 2 diabetes mellitus is associated with recovery of beta cell function. Diabet Med. 2001;18:10-16.
16. Gerstein HC, Yale JF, Harris SB, et al. A randomized trial of adding insulin glargine vs. avoidance of insulin in people with type 2 diabetes on either no oral glucose-lowering agents or submaximal doses of metformin and/or sulphonylureas. The Canadian INSIGHT (Implementing New Strategies with Insulin Glargine for Hyperglycaemia Treatment) Study. Diabet Med. 2006;23:736-742.
17. Dandona P, Aljada A, Chaudhuri A, et al. The potential influence of inflammation and insulin resistance on the pathogenesis and treatment of atherosclerosis-related complications in type 2 diabetes. J Clin Endocrinol Metab. 2003;88:2422-2429.
18. Nathan DM, Roussell A, Godine JE. Glyburide or insulin for metabolic control in non-insulin-dependent diabetes mellitus. A randomized, double-blind study. Ann Intern Med. 1988;108:334-340.
19. Mooradian AD, Bernbaum M, Albert SG. Narrative review: a rational approach to starting insulin therapy. Ann Intern Med. 2006;145:125-134.
20. Eliaschewitz FG, Calvo C, Valbuena H, et al. Therapy in type 2 diabetes: insulin glargine vs. NPH insulin both in combination with glimepiride. Arch Med Res. 2006;37:495-501.
21. Riddle MC, Rosenstock J, Gerich J. For the Insulin Glargine 4002 Study Investigators. The Treat-to-Target Trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care. 2003;26:3080-3086.
22. Hermansen K, Davies M, Derezinski T, et al. A 26-week, randomized, parallel, treat-to-target trial comparing insulin detemir with NPH insulin as add-on therapy to oral glucoselowering drugs in insulin-naive people with type 2 diabetes. Diabetes Care. 2006;29:1269-1274.
23. Ralová K, Bogoev M, Raz I, et al. Insulin detemir and insulin aspart: a promising basal-bolus regimen for type 2 diabetes. Diabetes Res Clin Pract. 2004;66:193-201.
24. Wittlin SD, Woehrle HJ, Gerich JE. Insulin pharmacokinetics. In: Leahy JL, Cefalu WT, eds. Insulin Therapy. New York, NY: Marcel Dekker, Inc.; 2002:73-85.
25. Hirsch IB. Insulin analogues. N Engl J Med. 2005;352:174-183.
26. Apidra [package insert]. Bridgewater, NJ: sanofi-aventis US LLC; 2009. Available at http://products.sanofi-aventis.us/apidra/apidra.pdf. Accessed February 1, 2010.
27. NovoLog [package insert]. Princeton, NJ; 2009. Available at: http://www.novolog.com/downloads/novolog-prescribinginformation.pdf. Accessed February 1, 2010.
28. Choe C, Edelman S. New therapeutic options for treating type-2 diabetes: a review of insulin analogs and premixed insulin analogs. J Natl Med Assoc. 2007;99:357-367.
29. Dailey G. A timely transition to insulin: identifying type 2 diabetes patients failing oral therapy. Formulary. 2005;40:114-130.
30. Garber AJ, Wahlen J, Wahl T, et al. Attainment of glycaemic goals in type 2 diabetes with once-, twice-, or thrice-daily dosing with biphasic insulin aspart 70/30 (The 1-2-3 study). Diabetes Obes Metab. 2006;8:58-66.
31. Davies M, Sinnassamy P, Storms F, et al. For the ATLANTUS Study Group. Insulin glargine-based therapy improves glycemic control in patients with type 2 diabetes sub-optimally controlled on premixed insulin therapies. Diabetes Res Clin Pract. 2008;79:368-375.
32. DeWitt DE, Hirsch IB. Outpatient insulin therapy in type 1 and type 2 diabetes mellitus: scientific review. JAMA. 2003;289:2254-2264.
33. Monnier L, Lapinski H, Colette C. Contributions of fasting and postprandial plasma glucose increments to the overall diurnal hyperglycemia of type 2 diabetic patients: variations with increasing levels of HbA(1c). Diabetes Care. 2003;26:881-885.
34. Leahy JL. Intensive insulin therapy in type 1 diabetes mellitus. In: Leahy JL, Cefalu WT, eds. Insulin Therapy. New York, NY: Marcel Dekker, Inc.; 2002:87-112.
35. Chan JL, Abrahamson MJ. Pharmacological management of type 2 diabetes mellitus: rationale for rational use of insulin. Mayo Clin Proc. 2003;78:459-467.
36. Levemir [package insert]. Princeton, NJ; Novo Nordisk Inc.; 2009. Available at: http://www.levemir-us.com/downloads/levemir-prescribing-information.pdf. Accessed February 2, 2010.
37. Bergenstal RM, Johnson M, Powers MA, et al. Adjust to target in type 2 diabetes: comparison of a simple algorithm to carbohydrate counting for adjustment of mealtime insulin glulisine. Diabetes Care. 2008;31:1305-1310.
38. Holman RR, Farmer AJ, Davies MJ, et al. Three-year efficacy of complex insulin regimens in type 2 diabetes. N Engl J Med. 2009;361:1736-1747.
39. Resnick HE, Foster GL, Bardsley J, et al. Achievement of American Diabetes Association Clinical Practice Recommendations among U.S. adults with diabetes, 1999-2002: the National Health and Nutrition Examination Survey. Diabetes Care. 2006;29:531-537.
• Inform patients with type 2 diabetes about the possible need for insulin therapy if diet, healthy lifestyle, and medications other than insulin do not achieve glycemic control. A
• Add basal insulin to oral medications as soon as needed to help patients reach fasting glycemic goals. If further adjustments are needed, add prandial insulin. B
• Choose basal and prandial insulin analogs to approximate normal physiologic insulin secretion. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Many patients with type 2 diabetes will eventually require insulin to reach glycemic targets that have been shown to protect against micro- and macro-vascular complications of the disease. But in the primary care setting, initiating and advancing insulin therapy for these patients can be challenging. This article discusses the barriers to initiating insulin therapy that family physicians often encounter and suggests strategies for addressing them. The goal should be to approximate normal physiologic insulin secretion as closely as possible. We will outline how that goal can best be achieved using combinations of long-acting and rapid-acting insulin analogs in a variety of basal-prandial regimens.
The evidence behind good glycemic control
Several landmark trials, including the United Kingdom Prospective Diabetes Study (UKPDS), the Diabetes Control and Complications Trial (DCCT), the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC), and the recent ADVANCE study, demonstrate the importance of good glycemic control in reducing the risk of microvascular complications of diabetes.1-4 These studies all show that lower glycosylated hemoglobin levels (hemoglobin A1C) are associated with a reduction in risk for the development or progression of microvascular complications of the disease.1-4
Setting glycemic targets
The American Diabetes Association (ADA) and the American Association of Clinical Endocrinologists (AACE) have established guidelines that provide physicians and patients with glycemic targets. The ADA recommends that hemoglobin A1C be maintained at <7.0% or as near normoglycemia (<6.0%) as possible without significant risk of hypoglycemia. Preprandial glucose targets are 70 to 130 mg/dL, and the postprandial target is <180 mg/dL.5 The AACE recommends even stricter glycemic control, with an A1C target of <6.5%, a preprandial target of ≤110 mg/dL, and peak postprandial glycemic target of ≤140 mg/dL.6 In clinical practice, it is best to aim for glycemic targets that are as close to ADA or AACE guidelines as possible, provided one can do so safely. In doing so, the clinician must recognize that glycemic goals should be individualized, to take into account the presence of comorbid conditions and the expected longevity of the patient.7
Glycemic control in type 2 diabetes. Diet, exercise, weight loss, and adoption of a healthy lifestyle are the cornerstones of care for patients at all stages of diabetes. As the disease progresses, most patients with diabetes will also require pharmacologic therapy that will need to be intensified over time.8
Oral agents are the place to begin. Typically, pharmacologic management of diabetes begins with oral agents.8 Several categories of oral medication can be used to treat type 2 diabetes, and more than 1 agent may be used for initial treatment of hyperglycemia. Insulin secretagogues (sulfonylureas and meglitinide analogs) are prescribed to treat the insulin secretory defect, whereas insulin sensitizers (metformin and thiazolidinediones) are used to address insulin resistance. Other agents include a-glucosidase inhibitors, which benefit patients with type 2 diabetes by slowing carbohydrate absorption, while glucagon-like peptide-1 (GLP-1) analogs and dipeptidyl peptidase-4 (DPP-4) inhibitors increase incretin levels, enhance insulin secretion in a glucose-dependent manner, and suppress pancreatic glucagon secretion.
When adding insulin becomes necessary
Even when combinations of these medications are used, many patients ultimately require the addition of exogenous insulin to achieve glycemic control.9 In clinical practice, however, insulin therapy is often delayed because physicians and patients alike are prey to misconceptions and fears about disease progression and the role of insulin.10 TABLE 1 presents some of the most common preconceptions held by patients about the initiation of insulin therapy, and suggests strategies for overcoming each of them.11
To help guide your decision making, you can follow the AACE/ACE Diabetes Algorithm for Glycemic Control, an updated guide for moving from oral medications to insulin therapy, depending on A1C levels. The algorithm is available at http://www.diabetesincontrol.com/images/issues/2012/04/aace_guidelines_for_glycemic_control.pdf.12
TABLE 1
“Insulin will make me fat,” and other patient concerns you’ll need to overcome
| Patient concern | How you can respond |
|---|---|
| Fear: “I’m afraid of needles.” | Insulin pens and smaller, thinner needles make injections almost painless. |
| Failure: “Going on insulin proves I can’t take control of my disease.” | The natural course of diabetes is to worsen over time, but controlling your blood glucose levels with insulin can slow that process down. |
| Stigma: “If people see me taking an insulin shot, they’ll think I’m a sick person.” | New injection devices like insulin pens are not very noticeable, and the needles are smaller and thinner than they used to be. |
| Weight gain: “Insulin will make me fat.” | I’ll help you find a nutritionist who can teach you how to eat healthier foods and develop an active lifestyle that helps keep you trim. And insulin is no more likely to make you fat than some of the oral agents you’ve been using. |
| Hypoglycemia: “I’ve heard that diabetics who use insulin can pass out suddenly, or even go into a coma. I think it’s called hypoglycemia, and it scares me.” | That’s less likely to happen with the newer forms of insulin we use now. And if you do have a hypoglycemic episode, it will probably be something mild you can treat yourself. I can teach you how to recognize what’s happening and what to do about it. |
| Complexity: “It all sounds too difficult for me to manage on my own.” | We have new, step-by-step instructions you can follow when you start insulin therapy and when you need to make changes. |
| Complications: “I know people on insulin who have serious complications like heart attacks and kidney disease. Will that happen to me?” | Diabetes-related complications are the result of inadequate control of blood sugar levels. Insulin provides more intensive glycemic control than you’ve been achieving, and that helps avoid the complications you’re concerned about. That’s why I recommend you start using insulin. |
| Source: Brunton S, et al. The role of basal insulin in type 2 diabetes management. J Fam Pract. 2005.11 | |
Early insulin gets results
Studies have demonstrated that the early use of intensive insulin improves beta-cell function and may enable patients to temporarily stop pharmacologic therapy for variable periods of time.13-15 In a Canadian study, 405 patients with type 2 diabetes receiving 0, 1, or 2 oral agents and with A1C levels between 7.5% and 11.0% were randomized to either a basal insulin or intensification of oral agents without adding insulin.16 Patients who were treated with insulin were 1.68 times more likely to achieve 2 consecutive A1C levels of 6.5% or less and achieved this endpoint sooner than those randomized to intensification of oral agents. Additionally, patients treated with insulin were able to achieve an adjusted mean A1C of 6.96%, compared with the 7.24% achieved by patients treated only with oral therapy. In addition to its glycemic benefits, insulin has also been shown to inhibit atherogenesis and improve triglyceride and high-density lipoprotein cholesterol levels.17,18
The next step: choosing the best insulin regimen
Long-acting basal insulin. Insulin glargine and insulin detemir are long-acting insulin analogs that were developed to approximate normal basal pancreatic secretion.19 Insulin glargine has a smooth, time-action pharmacokinetic profile without pronounced peaks.20 Several studies indicate that once-daily insulin glargine is as effective as twice-daily neutral protamine Hagedorn (NPH) insulin in controlling hyperglycemia, and is associated with reduced nocturnal hypoglycemia.20,21 Insulin detemir has also been shown to provide effective glycemic control with a reduced risk of hypoglycemia compared with NPH.22 This long-acting basal insulin is approved for once- or twice-daily subcutaneous administration and, like glargine, exhibits a dose-dependent duration of action of up to 24 hours.22,23
Prandial insulin may also be needed. If basal insulin plus antidiabetic drugs are not sufficient to control hyperglycemia, you can add prandial insulin to the treatment regimen. For guidance on initiating and advancing insulin therapy, consult the consensus algorithm from the ADA and the European Association for the Study of Diabetes at http://care.diabetesjournals.org/content/32/1/193.full.pdf+html.8 (See Figure 1 on page 198 of the pdf.) The rapid-acting insulin analogs—insulins aspart, lispro, and glulisine—have a more rapid onset and shorter duration of action than regular human insulin.24 The pharmacokinetic profiles of rapid-acting insulin analogs more closely resemble the prandial insulin response seen in individuals without diabetes.25 Rapid-acting analogs have an onset of action of 5 to 15 minutes—approximately twice as fast as regular insulin—and a duration of action of 2 to 5 hours, which is shorter than regular insulin.24-27 These attributes allow for greater dosing flexibility, as patients can inject insulin immediately before or after eating rather than having to inject regular insulin 30 to 45 minutes before the planned meal.24
Sometimes your patient needs to use both. Basal-prandial regimens, appropriate for all patients with type 1 diabetes, can also be used for some patients with newly diagnosed type 2 diabetes and for those who have not achieved glycemic targets with 1 or more oral agents or with prandial or premixed insulin regimens. Start newly diagnosed type 2 patients on a basal-prandial regimen if they have severe, symptomatic hyperglycemia. Such patients often have an A1C >10.0% or a fasting plasma glucose (FPG) >250 mg/dL. Oral agents alone are unlikely to reduce the A1C or FPG to target in such patients, and should be considered only after the extreme hyperglycemia has been reduced with an intensive insulin regimen.5
Premixed combinations are simpler, but have a downside
Premixed insulin combines an intermediate-acting insulin with a short- or rapid-acting insulin in a single injection. Premixed insulins are available in fixed-dose ratios to provide both basal and prandial insulin replacement. In addition to premixed regular-NPH combinations, 3 premixed insulin analog formulations are currently available: biphasic insulin lispro mix 75/25 (75% NPH and 25% lispro), biphasic insulin lispro mix 50/50 (50% NPH and 50% lispro), and biphasic insulin aspart 70/30 (70% NPH and 30% aspart).28
Premixed insulin is usually administered twice daily, before breakfast and supper.29 In some instances, a third injection at lunch is necessary to achieve glycemic goals.30 These regimens require patients to adhere to a consistent meal schedule and carbohydrate intake to avoid prandial hypo- and hyperglycemia.29
The disadvantage of a premixed insulin regimen is that the prandial and basal insulin components cannot be dosed independently. For example, if a patient who takes 75/25 insulin at breakfast has low blood sugars after breakfast but good glucose control at lunch-time and in the afternoon, it is not possible to reduce the amount of short-acting insulin without also reducing the dose of the NPH. Changing the dose of 75/25 to eliminate post-breakfast hypoglycemia may cause hyperglycemia in the afternoon, because the NPH dose will also be reduced. Separate injections of basal and prandial insulin provide a more physiologic regimen.
A subanalysis from the AT.LANTUS study examined glycemic parameters and safety over 24 weeks in 686 patients who switched from premixed insulin to once-daily insulin glargine.31 Patients were allowed to use oral agents as well, before and after the switch. After patients made the switch, A1C and FPG were significantly reduced, and the incidence of severe hypoglycemia was low. The addition of prandial insulin at 1 or more meals was associated with further improvements in glycemic control.31
A multifaceted, stepwise approach
Ideally, when a physician diagnoses a patient with diabetes, he or she has access to a diabetes care team that includes a dietitian or nutritionist, a certified diabetes nurse educator, a pharmacist, and an exercise physiologist. The team’s job is to educate the patient about the natural history of the disease and its complications and to teach diabetes self-management.
The real world. In practice, family physicians rarely have access to the kind of comprehensive diabetes care team that exists in specialty centers. You and your staff will need to provide the patient education that diabetes care requires, supplying patient-education handouts from online and print sources and making time to discuss food choices, meal planning, and daily exercise goals in follow-up visits. Written food and exercise logs are useful tools in this educational process.
Diabetes 101. At the time of diagnosis or at an early follow-up visit, be sure to inform the patient about all the treatment options— including insulin—that are available to treat the disease. Whenever possible, the discussion of insulin therapy should begin months or years before there is a need to initiate insulin treatment, so that when the time comes to start insulin, the patient will be more likely to accept the regimen. Patient education should include an introduction to carbohydrate content of different foods and the general principles of carbohydrate counting, home glucose monitoring, hypoglycemia awareness, and options for insulin delivery (syringe vs pen device).
When the time comes
To recognize the proper time to introduce insulin, evaluate A1C levels at least twice a year in patients who are meeting their glucose goals and every 3 months in those who are not meeting goals or whose treatment regimen has been changed.5 Additionally, patients should monitor their fasting, preprandial, and postprandial glucose levels regularly to be sure they are meeting glycemic targets and to minimize the risk of hypoglycemia. Glucose readings should be reviewed at every office visit.
Monitor glucose before and after meals
Both pre- and postprandial glucose levels should be monitored and managed in all patients with diabetes, whether or not they are treated with insulin. Some studies have suggested that home glucose monitoring may not improve glycemic control for patients taking oral agents. It is our view, however, that home glucose monitoring can facilitate changes in diet or exercise patterns and help physicians adjust or add treatment, based on pre- and postprandial glucose concentrations.
For some patients, focusing treatment initially on preprandial glucose may be sufficient, because elevated baseline preprandial glucose levels can lead to a higher overall plasma glucose profile and higher postprandial excursion.32 Basal insulin can be used to lower the fasting glucose levels and the overall glycemic profile for those patients.
Other patients, however, may have normal fasting and preprandial blood glucose levels with postprandial hyperglycemia. For these patients, modest postprandial glycemic excursions may be decreased initially by lowering the overall glycemic profile with basal insulin. In some cases, an injection of rapid-acting insulin before the meals that are associated with postprandial hyperglycemia is an effective treatment option.
Both pre- and postprandial glucose concentrations contribute to the A1C. At higher A1C concentrations (>7.5%) fasting glucose contributes more than postprandial glucose to the A1C. Below this concentration, the reverse holds true.33 As diabetes progresses, basal insulin can become insufficient to achieve glycemic control, and many patients eventually require the addition of prandial insulin at appropriate meals to control postprandial glucose excursions.32
The benefits of insulin treatment are most robust when both preprandial and postprandial glucose levels are taken into account. In a person with normal glucose homeostasis, about half the insulin released in a day is for basal regulation and the other half is meal related.34 Thus, most insulin treatment regimens are designed to provide approximately 50% of insulin as basal coverage and 50% at meals.34 Basal insulin suppresses gluconeogenesis between meals and overnight, whereas prandial insulin covers increases in blood glucose levels after meals.34
Use titration algorithms to balance glucose levels
Several simple titration algorithms can be used to initiate basal insulin. An initial dosage of 10 units daily (or 0.1 unit/kg) is a reasonable starting point for many patients with type 2 diabetes and moderate insulin resistance. This dose can be increased every 3 to 5 days until the target preprandial glucose level is achieved (TABLE 2).35,36 If a basal-prandial insulin regimen is started, then typically half the 24-hour insulin dosage is given as basal insulin.34 The remaining 50% is given as a rapid-acting insulin analog at meals. Dosages should be adjusted according to the patient’s self-monitored blood glucose values.35
Prandial insulin therapy is often initiated with a single injection administered either at the largest meal of the day or at the meal that most often increases postprandial glucose above target levels. The dose of prandial insulin is ideally based on the carbohydrate content of the meal and the pre-meal blood sugar, but for patients whose meals do not vary much in terms of carbohydrate content, it may be simpler to give fixed mealtime doses. Additional injections are added at other meals as necessary.
A patient’s 24-hour insulin dosage requirement can be estimated by multiplying the body weight (in kilograms) by a factor that takes the patient’s presumed insulin sensitivity into account. One strategy is to use a factor of 0.3 if the patient is insulin sensitive (usually lean), 0.5 if the patient is of average sensitivity (average weight to moderately overweight), and 0.6 if the patient is relatively insulin resistant (obese or morbidly obese).34 The total 24-hour insulin dose is the sum of the basal and prandial doses. It is crucial to take into account the oral agents a patient is using when calculating the total daily insulin requirements. In particular, patients who use insulin secretagogues may require less insulin if these medications are not stopped or reduced.
The effectiveness of a simple titration regimen was demonstrated in a study by Bergenstal and colleagues.37 They compared outcomes for patients with type 2 diabetes who calculated their dosage of a prandial, rapid-acting insulin analog (insulin glulisine) using a simple titration regimen with patients who based their dosage on carbohydrate counting. Carbohydrate counting involves adding the amount of carbohydrates in all the foods for a given meal and then dosing prandial insulin according to a ratio of units of insulin per gram of carbohydrate. For example, a meal containing 60 g of carbohydrate requires 6 units of insulin if a patient uses 1 unit of insulin per 10 g of carbohydrate. Patients on the simple regimen adjusted their weekly mealtime insulin dose by 1, 2, or 3 units, depending on their pre-meal glucose patterns.
When the 2 groups were compared, patients using a simple dosing algorithm did as well as those who based their dosage on carbohydrate counting. They achieved a similar degree of glycemic control (A1C reduction=~1.5%) and experienced fewer episodes of symptomatic hypoglycemia (defined as <50 mg/dL), 4.9 vs 8.0 events per patient year; P=.02).37 These findings support the use of a simple alternative method for prandial-dose titration and may allay concerns that basal-prandial insulin regimens are complicated and tedious to implement.
The recently published 4T study evaluated different insulin regimens for patients not achieving therapeutic goal on oral agents. Patients were started on basal insulin, prandial insulin, or premixed insulin. After 1 year, the insulin regimen was intensified in those who were still not achieving therapeutic goals, and the patients were evaluated after another 2 years. Prandial insulin was added for patients initially treated with basal insulin if they were not at A1C goal, basal insulin was added for those who started with prandial insulin, and a dose of rapid-acting insulin was given at lunch to those on twice-daily pre-mixed insulin who were not at goal. The A1C levels achieved at the end of the study did not differ among the treatment groups, and ranged from 6.8% to 7.1%.38
TABLE 2
Weekly insulin titration schedule
| Continue oral agent(s) at same dosage (eventually reduce) |
| Initiate insulin therapy If postprandial glucose levels are >140 mg/dL, add single insulin dose (about 10 U) in the evening. you can use:
|
Increase insulin dose every 3 to 5 days as needed, provided no nocturnal hypoglycemia occurs. Increase to:
|
| Treat to target level (usually FBG <120 mg/dL) |
| FBG, fasting blood glucose; NPH, neutral protamine Hagedorn. |
| Source: Chan JL et al. Mayo Clinic Proc. 2003.35 Adapted with permission. |
Overcoming reluctance
Despite convincing evidence that effective glycemic control can help delay or prevent diabetic complications, more than half the patients with type 2 diabetes do not achieve the treatment goal of A1C below 7.0%.39 Insulin therapy can help these patients reach glycemic targets rapidly and safely, but many patients and physicians are reluctant to start insulin for a variety of reasons.
For many, concern about hypoglycemia is at the top of the list. The way to address that concern is by educating patients to recognize symptoms of hypoglycemia and emphasizing the importance of frequent blood sugar monitoring, especially before driving and exercising. Insulin therapy does not increase the risk of hypoglycemic episodes. In fact, the risk of severe hypoglycemia in a patient with type 2 diabetes who has normal renal function and takes an appropriate dose of insulin is low.
Cost can also be a factor in the reluctance to start insulin therapy. The newer insulin analogs are more expensive than older formulations, but they more closely approximate physiologic insulin secretion and their use is associated with a reduced risk of hypoglycemia.
Finally, the perception that insulin regimens are complex and difficult to self-titrate is another common reason that physicians and patients are reluctant to begin insulin therapy or to progress from basal to basal/prandial regimens. In fact, insulin regimens are less complicated than patients fear. Several simple and practical algorithms are available to guide patients through a step-by-step process of initiating and advancing insulin therapy. Patients using these guidelines quickly become comfortable with insulin administration and savvy about interpreting blood glucose patterns based on meal content and exercise. Basal, premixed, and basal/prandial insulin regimens are all strategies that can help patients achieve their glycemic goals quickly and safely.
CORRESPONDENCE Jody Dushay, MD, Beth Israel Deaconess Medical Center, 330 Brookline Avenue, Boston, MA 02215; [email protected]
• Inform patients with type 2 diabetes about the possible need for insulin therapy if diet, healthy lifestyle, and medications other than insulin do not achieve glycemic control. A
• Add basal insulin to oral medications as soon as needed to help patients reach fasting glycemic goals. If further adjustments are needed, add prandial insulin. B
• Choose basal and prandial insulin analogs to approximate normal physiologic insulin secretion. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Many patients with type 2 diabetes will eventually require insulin to reach glycemic targets that have been shown to protect against micro- and macro-vascular complications of the disease. But in the primary care setting, initiating and advancing insulin therapy for these patients can be challenging. This article discusses the barriers to initiating insulin therapy that family physicians often encounter and suggests strategies for addressing them. The goal should be to approximate normal physiologic insulin secretion as closely as possible. We will outline how that goal can best be achieved using combinations of long-acting and rapid-acting insulin analogs in a variety of basal-prandial regimens.
The evidence behind good glycemic control
Several landmark trials, including the United Kingdom Prospective Diabetes Study (UKPDS), the Diabetes Control and Complications Trial (DCCT), the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC), and the recent ADVANCE study, demonstrate the importance of good glycemic control in reducing the risk of microvascular complications of diabetes.1-4 These studies all show that lower glycosylated hemoglobin levels (hemoglobin A1C) are associated with a reduction in risk for the development or progression of microvascular complications of the disease.1-4
Setting glycemic targets
The American Diabetes Association (ADA) and the American Association of Clinical Endocrinologists (AACE) have established guidelines that provide physicians and patients with glycemic targets. The ADA recommends that hemoglobin A1C be maintained at <7.0% or as near normoglycemia (<6.0%) as possible without significant risk of hypoglycemia. Preprandial glucose targets are 70 to 130 mg/dL, and the postprandial target is <180 mg/dL.5 The AACE recommends even stricter glycemic control, with an A1C target of <6.5%, a preprandial target of ≤110 mg/dL, and peak postprandial glycemic target of ≤140 mg/dL.6 In clinical practice, it is best to aim for glycemic targets that are as close to ADA or AACE guidelines as possible, provided one can do so safely. In doing so, the clinician must recognize that glycemic goals should be individualized, to take into account the presence of comorbid conditions and the expected longevity of the patient.7
Glycemic control in type 2 diabetes. Diet, exercise, weight loss, and adoption of a healthy lifestyle are the cornerstones of care for patients at all stages of diabetes. As the disease progresses, most patients with diabetes will also require pharmacologic therapy that will need to be intensified over time.8
Oral agents are the place to begin. Typically, pharmacologic management of diabetes begins with oral agents.8 Several categories of oral medication can be used to treat type 2 diabetes, and more than 1 agent may be used for initial treatment of hyperglycemia. Insulin secretagogues (sulfonylureas and meglitinide analogs) are prescribed to treat the insulin secretory defect, whereas insulin sensitizers (metformin and thiazolidinediones) are used to address insulin resistance. Other agents include a-glucosidase inhibitors, which benefit patients with type 2 diabetes by slowing carbohydrate absorption, while glucagon-like peptide-1 (GLP-1) analogs and dipeptidyl peptidase-4 (DPP-4) inhibitors increase incretin levels, enhance insulin secretion in a glucose-dependent manner, and suppress pancreatic glucagon secretion.
When adding insulin becomes necessary
Even when combinations of these medications are used, many patients ultimately require the addition of exogenous insulin to achieve glycemic control.9 In clinical practice, however, insulin therapy is often delayed because physicians and patients alike are prey to misconceptions and fears about disease progression and the role of insulin.10 TABLE 1 presents some of the most common preconceptions held by patients about the initiation of insulin therapy, and suggests strategies for overcoming each of them.11
To help guide your decision making, you can follow the AACE/ACE Diabetes Algorithm for Glycemic Control, an updated guide for moving from oral medications to insulin therapy, depending on A1C levels. The algorithm is available at http://www.diabetesincontrol.com/images/issues/2012/04/aace_guidelines_for_glycemic_control.pdf.12
TABLE 1
“Insulin will make me fat,” and other patient concerns you’ll need to overcome
| Patient concern | How you can respond |
|---|---|
| Fear: “I’m afraid of needles.” | Insulin pens and smaller, thinner needles make injections almost painless. |
| Failure: “Going on insulin proves I can’t take control of my disease.” | The natural course of diabetes is to worsen over time, but controlling your blood glucose levels with insulin can slow that process down. |
| Stigma: “If people see me taking an insulin shot, they’ll think I’m a sick person.” | New injection devices like insulin pens are not very noticeable, and the needles are smaller and thinner than they used to be. |
| Weight gain: “Insulin will make me fat.” | I’ll help you find a nutritionist who can teach you how to eat healthier foods and develop an active lifestyle that helps keep you trim. And insulin is no more likely to make you fat than some of the oral agents you’ve been using. |
| Hypoglycemia: “I’ve heard that diabetics who use insulin can pass out suddenly, or even go into a coma. I think it’s called hypoglycemia, and it scares me.” | That’s less likely to happen with the newer forms of insulin we use now. And if you do have a hypoglycemic episode, it will probably be something mild you can treat yourself. I can teach you how to recognize what’s happening and what to do about it. |
| Complexity: “It all sounds too difficult for me to manage on my own.” | We have new, step-by-step instructions you can follow when you start insulin therapy and when you need to make changes. |
| Complications: “I know people on insulin who have serious complications like heart attacks and kidney disease. Will that happen to me?” | Diabetes-related complications are the result of inadequate control of blood sugar levels. Insulin provides more intensive glycemic control than you’ve been achieving, and that helps avoid the complications you’re concerned about. That’s why I recommend you start using insulin. |
| Source: Brunton S, et al. The role of basal insulin in type 2 diabetes management. J Fam Pract. 2005.11 | |
Early insulin gets results
Studies have demonstrated that the early use of intensive insulin improves beta-cell function and may enable patients to temporarily stop pharmacologic therapy for variable periods of time.13-15 In a Canadian study, 405 patients with type 2 diabetes receiving 0, 1, or 2 oral agents and with A1C levels between 7.5% and 11.0% were randomized to either a basal insulin or intensification of oral agents without adding insulin.16 Patients who were treated with insulin were 1.68 times more likely to achieve 2 consecutive A1C levels of 6.5% or less and achieved this endpoint sooner than those randomized to intensification of oral agents. Additionally, patients treated with insulin were able to achieve an adjusted mean A1C of 6.96%, compared with the 7.24% achieved by patients treated only with oral therapy. In addition to its glycemic benefits, insulin has also been shown to inhibit atherogenesis and improve triglyceride and high-density lipoprotein cholesterol levels.17,18
The next step: choosing the best insulin regimen
Long-acting basal insulin. Insulin glargine and insulin detemir are long-acting insulin analogs that were developed to approximate normal basal pancreatic secretion.19 Insulin glargine has a smooth, time-action pharmacokinetic profile without pronounced peaks.20 Several studies indicate that once-daily insulin glargine is as effective as twice-daily neutral protamine Hagedorn (NPH) insulin in controlling hyperglycemia, and is associated with reduced nocturnal hypoglycemia.20,21 Insulin detemir has also been shown to provide effective glycemic control with a reduced risk of hypoglycemia compared with NPH.22 This long-acting basal insulin is approved for once- or twice-daily subcutaneous administration and, like glargine, exhibits a dose-dependent duration of action of up to 24 hours.22,23
Prandial insulin may also be needed. If basal insulin plus antidiabetic drugs are not sufficient to control hyperglycemia, you can add prandial insulin to the treatment regimen. For guidance on initiating and advancing insulin therapy, consult the consensus algorithm from the ADA and the European Association for the Study of Diabetes at http://care.diabetesjournals.org/content/32/1/193.full.pdf+html.8 (See Figure 1 on page 198 of the pdf.) The rapid-acting insulin analogs—insulins aspart, lispro, and glulisine—have a more rapid onset and shorter duration of action than regular human insulin.24 The pharmacokinetic profiles of rapid-acting insulin analogs more closely resemble the prandial insulin response seen in individuals without diabetes.25 Rapid-acting analogs have an onset of action of 5 to 15 minutes—approximately twice as fast as regular insulin—and a duration of action of 2 to 5 hours, which is shorter than regular insulin.24-27 These attributes allow for greater dosing flexibility, as patients can inject insulin immediately before or after eating rather than having to inject regular insulin 30 to 45 minutes before the planned meal.24
Sometimes your patient needs to use both. Basal-prandial regimens, appropriate for all patients with type 1 diabetes, can also be used for some patients with newly diagnosed type 2 diabetes and for those who have not achieved glycemic targets with 1 or more oral agents or with prandial or premixed insulin regimens. Start newly diagnosed type 2 patients on a basal-prandial regimen if they have severe, symptomatic hyperglycemia. Such patients often have an A1C >10.0% or a fasting plasma glucose (FPG) >250 mg/dL. Oral agents alone are unlikely to reduce the A1C or FPG to target in such patients, and should be considered only after the extreme hyperglycemia has been reduced with an intensive insulin regimen.5
Premixed combinations are simpler, but have a downside
Premixed insulin combines an intermediate-acting insulin with a short- or rapid-acting insulin in a single injection. Premixed insulins are available in fixed-dose ratios to provide both basal and prandial insulin replacement. In addition to premixed regular-NPH combinations, 3 premixed insulin analog formulations are currently available: biphasic insulin lispro mix 75/25 (75% NPH and 25% lispro), biphasic insulin lispro mix 50/50 (50% NPH and 50% lispro), and biphasic insulin aspart 70/30 (70% NPH and 30% aspart).28
Premixed insulin is usually administered twice daily, before breakfast and supper.29 In some instances, a third injection at lunch is necessary to achieve glycemic goals.30 These regimens require patients to adhere to a consistent meal schedule and carbohydrate intake to avoid prandial hypo- and hyperglycemia.29
The disadvantage of a premixed insulin regimen is that the prandial and basal insulin components cannot be dosed independently. For example, if a patient who takes 75/25 insulin at breakfast has low blood sugars after breakfast but good glucose control at lunch-time and in the afternoon, it is not possible to reduce the amount of short-acting insulin without also reducing the dose of the NPH. Changing the dose of 75/25 to eliminate post-breakfast hypoglycemia may cause hyperglycemia in the afternoon, because the NPH dose will also be reduced. Separate injections of basal and prandial insulin provide a more physiologic regimen.
A subanalysis from the AT.LANTUS study examined glycemic parameters and safety over 24 weeks in 686 patients who switched from premixed insulin to once-daily insulin glargine.31 Patients were allowed to use oral agents as well, before and after the switch. After patients made the switch, A1C and FPG were significantly reduced, and the incidence of severe hypoglycemia was low. The addition of prandial insulin at 1 or more meals was associated with further improvements in glycemic control.31
A multifaceted, stepwise approach
Ideally, when a physician diagnoses a patient with diabetes, he or she has access to a diabetes care team that includes a dietitian or nutritionist, a certified diabetes nurse educator, a pharmacist, and an exercise physiologist. The team’s job is to educate the patient about the natural history of the disease and its complications and to teach diabetes self-management.
The real world. In practice, family physicians rarely have access to the kind of comprehensive diabetes care team that exists in specialty centers. You and your staff will need to provide the patient education that diabetes care requires, supplying patient-education handouts from online and print sources and making time to discuss food choices, meal planning, and daily exercise goals in follow-up visits. Written food and exercise logs are useful tools in this educational process.
Diabetes 101. At the time of diagnosis or at an early follow-up visit, be sure to inform the patient about all the treatment options— including insulin—that are available to treat the disease. Whenever possible, the discussion of insulin therapy should begin months or years before there is a need to initiate insulin treatment, so that when the time comes to start insulin, the patient will be more likely to accept the regimen. Patient education should include an introduction to carbohydrate content of different foods and the general principles of carbohydrate counting, home glucose monitoring, hypoglycemia awareness, and options for insulin delivery (syringe vs pen device).
When the time comes
To recognize the proper time to introduce insulin, evaluate A1C levels at least twice a year in patients who are meeting their glucose goals and every 3 months in those who are not meeting goals or whose treatment regimen has been changed.5 Additionally, patients should monitor their fasting, preprandial, and postprandial glucose levels regularly to be sure they are meeting glycemic targets and to minimize the risk of hypoglycemia. Glucose readings should be reviewed at every office visit.
Monitor glucose before and after meals
Both pre- and postprandial glucose levels should be monitored and managed in all patients with diabetes, whether or not they are treated with insulin. Some studies have suggested that home glucose monitoring may not improve glycemic control for patients taking oral agents. It is our view, however, that home glucose monitoring can facilitate changes in diet or exercise patterns and help physicians adjust or add treatment, based on pre- and postprandial glucose concentrations.
For some patients, focusing treatment initially on preprandial glucose may be sufficient, because elevated baseline preprandial glucose levels can lead to a higher overall plasma glucose profile and higher postprandial excursion.32 Basal insulin can be used to lower the fasting glucose levels and the overall glycemic profile for those patients.
Other patients, however, may have normal fasting and preprandial blood glucose levels with postprandial hyperglycemia. For these patients, modest postprandial glycemic excursions may be decreased initially by lowering the overall glycemic profile with basal insulin. In some cases, an injection of rapid-acting insulin before the meals that are associated with postprandial hyperglycemia is an effective treatment option.
Both pre- and postprandial glucose concentrations contribute to the A1C. At higher A1C concentrations (>7.5%) fasting glucose contributes more than postprandial glucose to the A1C. Below this concentration, the reverse holds true.33 As diabetes progresses, basal insulin can become insufficient to achieve glycemic control, and many patients eventually require the addition of prandial insulin at appropriate meals to control postprandial glucose excursions.32
The benefits of insulin treatment are most robust when both preprandial and postprandial glucose levels are taken into account. In a person with normal glucose homeostasis, about half the insulin released in a day is for basal regulation and the other half is meal related.34 Thus, most insulin treatment regimens are designed to provide approximately 50% of insulin as basal coverage and 50% at meals.34 Basal insulin suppresses gluconeogenesis between meals and overnight, whereas prandial insulin covers increases in blood glucose levels after meals.34
Use titration algorithms to balance glucose levels
Several simple titration algorithms can be used to initiate basal insulin. An initial dosage of 10 units daily (or 0.1 unit/kg) is a reasonable starting point for many patients with type 2 diabetes and moderate insulin resistance. This dose can be increased every 3 to 5 days until the target preprandial glucose level is achieved (TABLE 2).35,36 If a basal-prandial insulin regimen is started, then typically half the 24-hour insulin dosage is given as basal insulin.34 The remaining 50% is given as a rapid-acting insulin analog at meals. Dosages should be adjusted according to the patient’s self-monitored blood glucose values.35
Prandial insulin therapy is often initiated with a single injection administered either at the largest meal of the day or at the meal that most often increases postprandial glucose above target levels. The dose of prandial insulin is ideally based on the carbohydrate content of the meal and the pre-meal blood sugar, but for patients whose meals do not vary much in terms of carbohydrate content, it may be simpler to give fixed mealtime doses. Additional injections are added at other meals as necessary.
A patient’s 24-hour insulin dosage requirement can be estimated by multiplying the body weight (in kilograms) by a factor that takes the patient’s presumed insulin sensitivity into account. One strategy is to use a factor of 0.3 if the patient is insulin sensitive (usually lean), 0.5 if the patient is of average sensitivity (average weight to moderately overweight), and 0.6 if the patient is relatively insulin resistant (obese or morbidly obese).34 The total 24-hour insulin dose is the sum of the basal and prandial doses. It is crucial to take into account the oral agents a patient is using when calculating the total daily insulin requirements. In particular, patients who use insulin secretagogues may require less insulin if these medications are not stopped or reduced.
The effectiveness of a simple titration regimen was demonstrated in a study by Bergenstal and colleagues.37 They compared outcomes for patients with type 2 diabetes who calculated their dosage of a prandial, rapid-acting insulin analog (insulin glulisine) using a simple titration regimen with patients who based their dosage on carbohydrate counting. Carbohydrate counting involves adding the amount of carbohydrates in all the foods for a given meal and then dosing prandial insulin according to a ratio of units of insulin per gram of carbohydrate. For example, a meal containing 60 g of carbohydrate requires 6 units of insulin if a patient uses 1 unit of insulin per 10 g of carbohydrate. Patients on the simple regimen adjusted their weekly mealtime insulin dose by 1, 2, or 3 units, depending on their pre-meal glucose patterns.
When the 2 groups were compared, patients using a simple dosing algorithm did as well as those who based their dosage on carbohydrate counting. They achieved a similar degree of glycemic control (A1C reduction=~1.5%) and experienced fewer episodes of symptomatic hypoglycemia (defined as <50 mg/dL), 4.9 vs 8.0 events per patient year; P=.02).37 These findings support the use of a simple alternative method for prandial-dose titration and may allay concerns that basal-prandial insulin regimens are complicated and tedious to implement.
The recently published 4T study evaluated different insulin regimens for patients not achieving therapeutic goal on oral agents. Patients were started on basal insulin, prandial insulin, or premixed insulin. After 1 year, the insulin regimen was intensified in those who were still not achieving therapeutic goals, and the patients were evaluated after another 2 years. Prandial insulin was added for patients initially treated with basal insulin if they were not at A1C goal, basal insulin was added for those who started with prandial insulin, and a dose of rapid-acting insulin was given at lunch to those on twice-daily pre-mixed insulin who were not at goal. The A1C levels achieved at the end of the study did not differ among the treatment groups, and ranged from 6.8% to 7.1%.38
TABLE 2
Weekly insulin titration schedule
| Continue oral agent(s) at same dosage (eventually reduce) |
| Initiate insulin therapy If postprandial glucose levels are >140 mg/dL, add single insulin dose (about 10 U) in the evening. you can use:
|
Increase insulin dose every 3 to 5 days as needed, provided no nocturnal hypoglycemia occurs. Increase to:
|
| Treat to target level (usually FBG <120 mg/dL) |
| FBG, fasting blood glucose; NPH, neutral protamine Hagedorn. |
| Source: Chan JL et al. Mayo Clinic Proc. 2003.35 Adapted with permission. |
Overcoming reluctance
Despite convincing evidence that effective glycemic control can help delay or prevent diabetic complications, more than half the patients with type 2 diabetes do not achieve the treatment goal of A1C below 7.0%.39 Insulin therapy can help these patients reach glycemic targets rapidly and safely, but many patients and physicians are reluctant to start insulin for a variety of reasons.
For many, concern about hypoglycemia is at the top of the list. The way to address that concern is by educating patients to recognize symptoms of hypoglycemia and emphasizing the importance of frequent blood sugar monitoring, especially before driving and exercising. Insulin therapy does not increase the risk of hypoglycemic episodes. In fact, the risk of severe hypoglycemia in a patient with type 2 diabetes who has normal renal function and takes an appropriate dose of insulin is low.
Cost can also be a factor in the reluctance to start insulin therapy. The newer insulin analogs are more expensive than older formulations, but they more closely approximate physiologic insulin secretion and their use is associated with a reduced risk of hypoglycemia.
Finally, the perception that insulin regimens are complex and difficult to self-titrate is another common reason that physicians and patients are reluctant to begin insulin therapy or to progress from basal to basal/prandial regimens. In fact, insulin regimens are less complicated than patients fear. Several simple and practical algorithms are available to guide patients through a step-by-step process of initiating and advancing insulin therapy. Patients using these guidelines quickly become comfortable with insulin administration and savvy about interpreting blood glucose patterns based on meal content and exercise. Basal, premixed, and basal/prandial insulin regimens are all strategies that can help patients achieve their glycemic goals quickly and safely.
CORRESPONDENCE Jody Dushay, MD, Beth Israel Deaconess Medical Center, 330 Brookline Avenue, Boston, MA 02215; [email protected]
1. U.K. Prospective Diabetes Study 16. Overview of 6 years’ therapy of type II diabetes: a progressive disease. UK Prospective Diabetes Study Group. Diabetes. 1995;44:1249-1258.
2. The Diabetes Control and Complications Trial (DCCT). Design and methodologic considerations for the feasibility phase. Diabetes Control and Complications Trial Research Group. Diabetes. 1986;35:530-45.
3. Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643-2653.
4. Dluhy RG, McMahon GT. Intensive glycemic control in the ACCORD and ADVANCE trials. N Engl J Med. 2008;358:2630-2633.
5. American Diabetes Association. Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(suppl 1):S11-S61.
6. Rodbard HW, Blonde L, Braithwaite SS, et al. AACE Diabetes Mellitus Clinical Practice Guidelines Task Force. American Association of Clinical Endocrinologists medical guidelines for clinical practice for the management of diabetes mellitus. Endocr Pract. 2007;13(suppl 1):s1-s68.
7. Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. The Action to Control Cardiovascular Risk in Diabetes Study Group. N Engl J Med. 2008;358:2545-2559.
8. Nathan DM, Buse JB, Davidson MB, et al. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2009;32:193-203.
9. Riddle MC. Glycemic management of type 2 diabetes: an emerging strategy with oral agents, insulins, and combinations. Endocrinol Metab Clin North Am. 2005;34:77-98.
10. Riddle MC. The underuse of insulin therapy in North America. Diabetes Metab Res Rev. 2002;18(suppl 3):S42-S49.
11. Brunton SA, White JR, Renda SM. The role of basal insulin in type 2 diabetes management. J Fam Pract. 2005;54(suppl):S1-S8.
12. Rodbard HW, Jellinger PS, Davidson JA, et al. Statement by an American Association of Clinical Endocrinologists/American College of Endocrinology consensus panel on type 2 diabetes mellitus: an algorithm for glycemic control. Endocr Pract. 2009;15:540-559.
13. Li Y, Xu W, Liao Z. Induction of long-term glycemic control in newly diagnosed type 2 diabetic patients is associated with improvement of beta-cell function. Diabetes Care. 2004;27:2597-2602.
14. Ryan EA, Imes S, Wallace C. Short-term intensive insulin therapy in newly diagnosed type 2 diabetes. Diabetes Care. 2004;27:1028-1032.
15. McFarlane SI, Chaiken RL, Hirsch S, et al. Near-normoglycaemic remission in African-Americans with type 2 diabetes mellitus is associated with recovery of beta cell function. Diabet Med. 2001;18:10-16.
16. Gerstein HC, Yale JF, Harris SB, et al. A randomized trial of adding insulin glargine vs. avoidance of insulin in people with type 2 diabetes on either no oral glucose-lowering agents or submaximal doses of metformin and/or sulphonylureas. The Canadian INSIGHT (Implementing New Strategies with Insulin Glargine for Hyperglycaemia Treatment) Study. Diabet Med. 2006;23:736-742.
17. Dandona P, Aljada A, Chaudhuri A, et al. The potential influence of inflammation and insulin resistance on the pathogenesis and treatment of atherosclerosis-related complications in type 2 diabetes. J Clin Endocrinol Metab. 2003;88:2422-2429.
18. Nathan DM, Roussell A, Godine JE. Glyburide or insulin for metabolic control in non-insulin-dependent diabetes mellitus. A randomized, double-blind study. Ann Intern Med. 1988;108:334-340.
19. Mooradian AD, Bernbaum M, Albert SG. Narrative review: a rational approach to starting insulin therapy. Ann Intern Med. 2006;145:125-134.
20. Eliaschewitz FG, Calvo C, Valbuena H, et al. Therapy in type 2 diabetes: insulin glargine vs. NPH insulin both in combination with glimepiride. Arch Med Res. 2006;37:495-501.
21. Riddle MC, Rosenstock J, Gerich J. For the Insulin Glargine 4002 Study Investigators. The Treat-to-Target Trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care. 2003;26:3080-3086.
22. Hermansen K, Davies M, Derezinski T, et al. A 26-week, randomized, parallel, treat-to-target trial comparing insulin detemir with NPH insulin as add-on therapy to oral glucoselowering drugs in insulin-naive people with type 2 diabetes. Diabetes Care. 2006;29:1269-1274.
23. Ralová K, Bogoev M, Raz I, et al. Insulin detemir and insulin aspart: a promising basal-bolus regimen for type 2 diabetes. Diabetes Res Clin Pract. 2004;66:193-201.
24. Wittlin SD, Woehrle HJ, Gerich JE. Insulin pharmacokinetics. In: Leahy JL, Cefalu WT, eds. Insulin Therapy. New York, NY: Marcel Dekker, Inc.; 2002:73-85.
25. Hirsch IB. Insulin analogues. N Engl J Med. 2005;352:174-183.
26. Apidra [package insert]. Bridgewater, NJ: sanofi-aventis US LLC; 2009. Available at http://products.sanofi-aventis.us/apidra/apidra.pdf. Accessed February 1, 2010.
27. NovoLog [package insert]. Princeton, NJ; 2009. Available at: http://www.novolog.com/downloads/novolog-prescribinginformation.pdf. Accessed February 1, 2010.
28. Choe C, Edelman S. New therapeutic options for treating type-2 diabetes: a review of insulin analogs and premixed insulin analogs. J Natl Med Assoc. 2007;99:357-367.
29. Dailey G. A timely transition to insulin: identifying type 2 diabetes patients failing oral therapy. Formulary. 2005;40:114-130.
30. Garber AJ, Wahlen J, Wahl T, et al. Attainment of glycaemic goals in type 2 diabetes with once-, twice-, or thrice-daily dosing with biphasic insulin aspart 70/30 (The 1-2-3 study). Diabetes Obes Metab. 2006;8:58-66.
31. Davies M, Sinnassamy P, Storms F, et al. For the ATLANTUS Study Group. Insulin glargine-based therapy improves glycemic control in patients with type 2 diabetes sub-optimally controlled on premixed insulin therapies. Diabetes Res Clin Pract. 2008;79:368-375.
32. DeWitt DE, Hirsch IB. Outpatient insulin therapy in type 1 and type 2 diabetes mellitus: scientific review. JAMA. 2003;289:2254-2264.
33. Monnier L, Lapinski H, Colette C. Contributions of fasting and postprandial plasma glucose increments to the overall diurnal hyperglycemia of type 2 diabetic patients: variations with increasing levels of HbA(1c). Diabetes Care. 2003;26:881-885.
34. Leahy JL. Intensive insulin therapy in type 1 diabetes mellitus. In: Leahy JL, Cefalu WT, eds. Insulin Therapy. New York, NY: Marcel Dekker, Inc.; 2002:87-112.
35. Chan JL, Abrahamson MJ. Pharmacological management of type 2 diabetes mellitus: rationale for rational use of insulin. Mayo Clin Proc. 2003;78:459-467.
36. Levemir [package insert]. Princeton, NJ; Novo Nordisk Inc.; 2009. Available at: http://www.levemir-us.com/downloads/levemir-prescribing-information.pdf. Accessed February 2, 2010.
37. Bergenstal RM, Johnson M, Powers MA, et al. Adjust to target in type 2 diabetes: comparison of a simple algorithm to carbohydrate counting for adjustment of mealtime insulin glulisine. Diabetes Care. 2008;31:1305-1310.
38. Holman RR, Farmer AJ, Davies MJ, et al. Three-year efficacy of complex insulin regimens in type 2 diabetes. N Engl J Med. 2009;361:1736-1747.
39. Resnick HE, Foster GL, Bardsley J, et al. Achievement of American Diabetes Association Clinical Practice Recommendations among U.S. adults with diabetes, 1999-2002: the National Health and Nutrition Examination Survey. Diabetes Care. 2006;29:531-537.
1. U.K. Prospective Diabetes Study 16. Overview of 6 years’ therapy of type II diabetes: a progressive disease. UK Prospective Diabetes Study Group. Diabetes. 1995;44:1249-1258.
2. The Diabetes Control and Complications Trial (DCCT). Design and methodologic considerations for the feasibility phase. Diabetes Control and Complications Trial Research Group. Diabetes. 1986;35:530-45.
3. Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643-2653.
4. Dluhy RG, McMahon GT. Intensive glycemic control in the ACCORD and ADVANCE trials. N Engl J Med. 2008;358:2630-2633.
5. American Diabetes Association. Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(suppl 1):S11-S61.
6. Rodbard HW, Blonde L, Braithwaite SS, et al. AACE Diabetes Mellitus Clinical Practice Guidelines Task Force. American Association of Clinical Endocrinologists medical guidelines for clinical practice for the management of diabetes mellitus. Endocr Pract. 2007;13(suppl 1):s1-s68.
7. Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. The Action to Control Cardiovascular Risk in Diabetes Study Group. N Engl J Med. 2008;358:2545-2559.
8. Nathan DM, Buse JB, Davidson MB, et al. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2009;32:193-203.
9. Riddle MC. Glycemic management of type 2 diabetes: an emerging strategy with oral agents, insulins, and combinations. Endocrinol Metab Clin North Am. 2005;34:77-98.
10. Riddle MC. The underuse of insulin therapy in North America. Diabetes Metab Res Rev. 2002;18(suppl 3):S42-S49.
11. Brunton SA, White JR, Renda SM. The role of basal insulin in type 2 diabetes management. J Fam Pract. 2005;54(suppl):S1-S8.
12. Rodbard HW, Jellinger PS, Davidson JA, et al. Statement by an American Association of Clinical Endocrinologists/American College of Endocrinology consensus panel on type 2 diabetes mellitus: an algorithm for glycemic control. Endocr Pract. 2009;15:540-559.
13. Li Y, Xu W, Liao Z. Induction of long-term glycemic control in newly diagnosed type 2 diabetic patients is associated with improvement of beta-cell function. Diabetes Care. 2004;27:2597-2602.
14. Ryan EA, Imes S, Wallace C. Short-term intensive insulin therapy in newly diagnosed type 2 diabetes. Diabetes Care. 2004;27:1028-1032.
15. McFarlane SI, Chaiken RL, Hirsch S, et al. Near-normoglycaemic remission in African-Americans with type 2 diabetes mellitus is associated with recovery of beta cell function. Diabet Med. 2001;18:10-16.
16. Gerstein HC, Yale JF, Harris SB, et al. A randomized trial of adding insulin glargine vs. avoidance of insulin in people with type 2 diabetes on either no oral glucose-lowering agents or submaximal doses of metformin and/or sulphonylureas. The Canadian INSIGHT (Implementing New Strategies with Insulin Glargine for Hyperglycaemia Treatment) Study. Diabet Med. 2006;23:736-742.
17. Dandona P, Aljada A, Chaudhuri A, et al. The potential influence of inflammation and insulin resistance on the pathogenesis and treatment of atherosclerosis-related complications in type 2 diabetes. J Clin Endocrinol Metab. 2003;88:2422-2429.
18. Nathan DM, Roussell A, Godine JE. Glyburide or insulin for metabolic control in non-insulin-dependent diabetes mellitus. A randomized, double-blind study. Ann Intern Med. 1988;108:334-340.
19. Mooradian AD, Bernbaum M, Albert SG. Narrative review: a rational approach to starting insulin therapy. Ann Intern Med. 2006;145:125-134.
20. Eliaschewitz FG, Calvo C, Valbuena H, et al. Therapy in type 2 diabetes: insulin glargine vs. NPH insulin both in combination with glimepiride. Arch Med Res. 2006;37:495-501.
21. Riddle MC, Rosenstock J, Gerich J. For the Insulin Glargine 4002 Study Investigators. The Treat-to-Target Trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care. 2003;26:3080-3086.
22. Hermansen K, Davies M, Derezinski T, et al. A 26-week, randomized, parallel, treat-to-target trial comparing insulin detemir with NPH insulin as add-on therapy to oral glucoselowering drugs in insulin-naive people with type 2 diabetes. Diabetes Care. 2006;29:1269-1274.
23. Ralová K, Bogoev M, Raz I, et al. Insulin detemir and insulin aspart: a promising basal-bolus regimen for type 2 diabetes. Diabetes Res Clin Pract. 2004;66:193-201.
24. Wittlin SD, Woehrle HJ, Gerich JE. Insulin pharmacokinetics. In: Leahy JL, Cefalu WT, eds. Insulin Therapy. New York, NY: Marcel Dekker, Inc.; 2002:73-85.
25. Hirsch IB. Insulin analogues. N Engl J Med. 2005;352:174-183.
26. Apidra [package insert]. Bridgewater, NJ: sanofi-aventis US LLC; 2009. Available at http://products.sanofi-aventis.us/apidra/apidra.pdf. Accessed February 1, 2010.
27. NovoLog [package insert]. Princeton, NJ; 2009. Available at: http://www.novolog.com/downloads/novolog-prescribinginformation.pdf. Accessed February 1, 2010.
28. Choe C, Edelman S. New therapeutic options for treating type-2 diabetes: a review of insulin analogs and premixed insulin analogs. J Natl Med Assoc. 2007;99:357-367.
29. Dailey G. A timely transition to insulin: identifying type 2 diabetes patients failing oral therapy. Formulary. 2005;40:114-130.
30. Garber AJ, Wahlen J, Wahl T, et al. Attainment of glycaemic goals in type 2 diabetes with once-, twice-, or thrice-daily dosing with biphasic insulin aspart 70/30 (The 1-2-3 study). Diabetes Obes Metab. 2006;8:58-66.
31. Davies M, Sinnassamy P, Storms F, et al. For the ATLANTUS Study Group. Insulin glargine-based therapy improves glycemic control in patients with type 2 diabetes sub-optimally controlled on premixed insulin therapies. Diabetes Res Clin Pract. 2008;79:368-375.
32. DeWitt DE, Hirsch IB. Outpatient insulin therapy in type 1 and type 2 diabetes mellitus: scientific review. JAMA. 2003;289:2254-2264.
33. Monnier L, Lapinski H, Colette C. Contributions of fasting and postprandial plasma glucose increments to the overall diurnal hyperglycemia of type 2 diabetic patients: variations with increasing levels of HbA(1c). Diabetes Care. 2003;26:881-885.
34. Leahy JL. Intensive insulin therapy in type 1 diabetes mellitus. In: Leahy JL, Cefalu WT, eds. Insulin Therapy. New York, NY: Marcel Dekker, Inc.; 2002:87-112.
35. Chan JL, Abrahamson MJ. Pharmacological management of type 2 diabetes mellitus: rationale for rational use of insulin. Mayo Clin Proc. 2003;78:459-467.
36. Levemir [package insert]. Princeton, NJ; Novo Nordisk Inc.; 2009. Available at: http://www.levemir-us.com/downloads/levemir-prescribing-information.pdf. Accessed February 2, 2010.
37. Bergenstal RM, Johnson M, Powers MA, et al. Adjust to target in type 2 diabetes: comparison of a simple algorithm to carbohydrate counting for adjustment of mealtime insulin glulisine. Diabetes Care. 2008;31:1305-1310.
38. Holman RR, Farmer AJ, Davies MJ, et al. Three-year efficacy of complex insulin regimens in type 2 diabetes. N Engl J Med. 2009;361:1736-1747.
39. Resnick HE, Foster GL, Bardsley J, et al. Achievement of American Diabetes Association Clinical Practice Recommendations among U.S. adults with diabetes, 1999-2002: the National Health and Nutrition Examination Survey. Diabetes Care. 2006;29:531-537.
Help patients with chronic kidney disease stave off dialysis
• Screen all patients for chronic kidney disease (CKD) by estimated glomerular filtration rate and persistent proteinuria. A
• Treat all CKD patients with angiotensin II receptor blockers or angiotensin-converting enzyme inhibitors, unless there is a contraindication. A
• Recommend a heart-healthy diet and refer patients with CKD to a registered dietitian for more intensive dietary modifications. A
• Integrate motivational interviewing into your care of CKD patients. This health coaching technique has been shown to be causally and independently associated with positive behavioral outcomes. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Over the last decade, the prevalence of chronic kidney disease (CKD) has grown approximately 20% to 25%, and current estimates are that the disease affects about 15% of the general population.1 All-cause hospitalization rates are almost 3 times higher among CKD patients than in those without the disease, and costs associated with CKD account for as much as 28% of the Medicare budget.1 Most disturbingly, the incidence at which patients diagnosed with CKD progress to end-stage renal disease (ESRD) continues to increase annually, reaching 354 cases per million population in 2007.1 By 2020, estimates are that more than 750,000 people in the United States will need dialysis for kidney failure.1
Guidelines exist, but awareness falls short
Several initiatives to increase awareness of CKD have been publicized. They include the Kidney Disease Outcome Quality Initiative (KDOQI) of the National Kidney Foundation (NKF), which issued clinical practice guidelines for treating chronic kidney disease in 2002, and Healthy People 2010, which includes specific measures to reduce the number of new cases and the complications, disability, economic costs, and mortality associated with the disease.2,3 Despite these efforts, studies show that many primary care providers are still unaware of these guidelines.4,5
Patients go undiagnosed until they reach the later stages of the disease, and many receive suboptimal care—even when they are identified—including lack of timely referral to a nephrologist and inadequate management of CKD comorbidities.6-13 (More on comorbidities, in a bit.)
Plus, there’s a lack of support … Care for these conditions is complex and difficult, and consultation or referral to a nephrologist may not be readily available, as the current pool of specialists is barely adequate to meet the needs of a growing population of CKD patients and the number of physicians-in-training entering the specialty is not adequate to meet the need.14 In this situation, primary care providers will have to assume an ever-enlarging share of the responsibility for care of CKD patients, including some clinical activities that are currently performed by specialists.
The first step: Screen all patients for CKD
Incorporating CKD screening into routine blood work for all patients facilitates earlier detection, evaluation, and treatment of the disease. Screening tests include the estimated glomerular filtration rate (GFR) based on serum creatinine as well as measurements of urine albumin and proteinuria. The persistence of proteinuria must be confirmed by 2 of 3 abnormal readings over a minimum of 3 months, because factors such as fever or exercise may affect test results. Measurement of albumin or total protein concentration in a spot sample avoids the need for timed collections. Factoring the concentration of total protein or albumin by urine creatinine concentration and using age/sex-specific thresholds eliminates most variations in measurement.15
Keep these comorbidities on your radar screen
Diabetes and hypertension are 2 of the most common causes of CKD in the United States, and the number of kidney failure cases due to these problems is increasing. The most important adverse outcomes of CKD are not only progression to ESRD, but also increased risk for cardiovascular disease (CVD). Studies show that the presence of albuminuria and a decreased estimated GFR consistently and incrementally increase the risk for CVD.16 Decreased GFR is an independent risk factor for CVD outcomes and for all-cause mortality, including sudden death in patients with existing coronary artery disease. Moreover, patients with CKD are 100 times more likely to die from CVD than to develop kidney failure.16
Depression is another prevalent, yet commonly overlooked, comorbid condition. Patients with any chronic disease are at risk for depression, with the incidence rising with the severity of the medical condition.17 CKD is no exception. Rates of depression as high as 29%, as well as rates of anxiety disorders as high as 46%, have been documented in patients on dialysis.18 Patients with depression are impaired in overall functioning and less able to follow medical regimens.17 In addition, low quality of life and depression predict higher morbidity and mortality rates in patients with ESRD.19 Because the diagnosis of depression is frequently missed in primary care settings, screening for depression should be a basic element in CKD management.20
Clinical management of kidney disease
The treatment goal for early-stage kidney disease is to address the risk factors that contribute to the progression of kidney disease: hypertension, heart disease, stroke, diabetes, and dyslipidemia. The TABLE reviews clinical management areas by disease stage.
Prescribe angiotensin antagonists. Angiotensin II receptor blockers (ARBs) and angiotensin-converting enzyme (ACE) inhibitors antagonize the toxic effects of increases in circulating angiotensin II and are therefore a key component of a therapeutic strategy to halt progressive kidney disease.2,21
Review medications, promote a healthier lifestyle. In addition to prescribing ARBs or ACE inhibitors, the family physician should review the CKD patient’s current medications to eliminate nephrotoxic drugs and adjust other medications on the basis of the patient’s creatinine clearance. Other measures include making sure vaccinations for influenza, pneumococcal pneumonia, and hepatitis B are up to date and emphasizing the importance of smoking cessation and exercise.
Treat comorbid conditions. Hypertension and diabetes must be treated aggressively. Patients with dyslipidemia should be managed with statins.2 Certain complications of progressive kidney disease, such as anemia, bone/mineral metabolic disease, and metabolic disorders, are typically treated by a nephrologist. Nevertheless, primary care providers need to understand these conditions in order to work together with the nephrologist in managing the CKD patient.
Check thyroid hormone and vitamin D levels. Understanding which factors predict disease progression or poor outcome is particularly useful. Most patients with CKD have low T3 syndrome, that is, low serum triiodothyronine levels in the absence of a thyroidal illness. In a recent paper, Song and colleagues showed that low T3 syndrome was common in early CKD and that estimated GFR was positively related with T3, independent of age and serum albumin.22
In another recent study, Ravani et al showed that plasma 25-hydroxyvitamin D is an independent, inverse predictor of disease progression and death in patients with stage 2 to 5 CKD.23 Vitamin D deficiency has been linked to CVD and early mortality in patients on hemodialysis.23 Checking for these 2 markers—low T3 syndrome and vitamin D deficiency—should therefore be part of your screening process for early stage CKD.
Refer to a dietitian. Dietary modification is another important component of the treatment plan. Dietary modifications are often needed to protect against CVD, help control blood pressure, reduce proteinuria, and improve metabolic control in patients with diabetes.2,24 Dietary modifications for CKD patients may go well beyond standard recommendations for a heart-healthy diet.2,24 Calcium, sodium, phosphorus, and potassium may need to be restricted according to laboratory values and stage of the disease.25 The KDOQI guidelines recommend referring CKD patients to a registered dietitian with experience in CKD for a complete nutritional assessment, comprehensive education on dietary restrictions and guidelines, and detailed dietary instruction.2
Manage CKD-associated anemia. Current guidelines do not propose normalizing hemoglobin in patients with renal disease, because lower levels of hemoglobin probably represent an adaptive response and correction to a “normal” level may disturb that response and lead to worse outcomes.26 For a discussion of management of anemia associated with CKD, see “Anemia and chronic kidney disease: What’s the connection?” in the January 2010 issue of this journal.27
Refer to a nephrologist early. A recent study by Chan et al demonstrates the beneficial effects of early referral to a nephrologist.28 There is no clear definition of early vs late referral and, at times, the only criterion is how much time elapsed before the patient was put on dialysis. Referral is considered “late” when management could have been improved by earlier contact with a specialist. It is probably prudent to refer stage 3 and 4 patients, at least for initial consultation. Chan’s meta-analysis found that patients referred late had nearly a 2-fold risk of death compared with those with early referrals. This risk persists at least up to 1 year after the initiation of renal replacement therapy.
Prepare patients for dialysis. It is very important that new hemodialysis patients present for initial treatment with an arteriovenous fistula in place, as first access for hemodialysis. Fistula placement is one of the most important reasons for timely referral to a nephrologist. Later referral is associated with a significantly prolonged hospital stay for initial renal replacement therapy. Late-referred patients are sicker, and many of the complications discussed here have not been optimally treated.
The optimal time to start preparing your patient for dialysis is when GFR measures between 15 and 29 mL/min/1.73 m2. Preparation includes counseling on nutrition and exercise, hepatitis B vaccination if needed, and scheduling for fistula placement.29
The hardest part: Changing habits
Effective CKD treatment must emphasize lifestyle management. You need to persuade smokers to quit and “couch potatoes” to start exercising regularly. Eating habits need to change, as well: This means fewer calories and restrictions on intake of salt and certain minerals. Medications for high blood pressure, diabetes, and kidney disease need to be taken consistently, as prescribed. The TABLE reviews the lifestyle issues that are particularly salient at each stage of CKD.
TABLE
Keying interventions to CKD stages
| Stage | Description | GFR (mL/min/1.73 m2) | Clinical action | Lifestyle management |
|---|---|---|---|---|
| At increased risk | ≥60 (with CKD risk factors) | Screening; CKD risk reduction | Healthy habits according to public health recommendations | |
| 1 | Kidney damage with normal or increased GFR | ≥90 | Diagnosis and treatment; treatment of comorbid conditions; slowing of progression; CVD risk reduction | Emphasis on heart health: physical activity, healthy diet, weight management, and stress management. Restricted sodium, potassium, calcium, phosphorus, and protein, with emphasis on plant vs animal food sources. Treatment adherence to medications and CV/diabetes/hypertension treatment plan if applicable. Assessment of depression and referral to treatment if appropriate. |
| 2 | Kidney damage with mildly decreased GFR | 60-89 | Same, plus estimation of progression | Same recommendations as stage 1 |
| 3 | Moderately decreased GFR | 30-59 | Same, plus evaluation and treatment of complications | Same recommendations as stage 1 |
| 4 | Severely decreased GFR | 15-29 | Preparation for kidney replacement therapy | Same as above, plus assessment of social support to prepare for dialysis treatment if appropriate |
| 5 | Kidney failure | <15 or dialysis | Replacement (if uremia present) | Same as above, plus restricted fluid intake and additional protein intake |
| Note: Shaded area identifies patients who have CKD; unshaded area designates individuals who are at increased risk for developing CKD. CKD is defined as either kidney damage or GFR <60 ml/min/1.73 m2 for ≥3 months. Kidney damage is defined as pathologic abnormalities or markers of damage, including abnormalities in blood or urine tests or imaging studies. | ||||
| CKD, chronic kidney disease; CVD, cardiovascular disease; GFR, glomerular filtration rate. | ||||
| Adapted from: Table 3: chronic kidney disease: a clinical action plan. National Kidney foundation. KDOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. 2002. | ||||
Lifestyle modifications like these are very difficult, and helping patients make them involves much more than simple patient education. In 1 study, Durose et al found that patients on hemodialysis failed to stay on their diets even when they knew which dietary restrictions they should follow and what the consequences of going off their diets would be.30
Update your persuasive techniques: take on the role of coach
Newer theories of behavior change no longer rely on simply providing information and advice, but rather address the complex interaction of motivations involved in attempts to change. These include cues to action, perception of benefits and consequences, environmental and cultural influences, sense of self-efficacy, ambivalence, and the intention to change.31
Unfortunately, health care providers are rarely trained in motivational techniques. Often, their approach to inducing change is authoritarian, confrontational, overly forceful, or guilt inducing. Such attitudes not only limit progress, but are actually correlated with negative behavioral and clinical outcomes.32,33 Recent research has verified the power of the patient–provider interaction in influencing treatment adherence and lifestyle change.33
To be successful in getting patients to adopt new behaviors, physicians need to move away from authoritarian modes and take on some of the attributes of a coach urging on the team.
How this coaching technique works
Motivational Interviewing is a health coaching technique that has been shown to be causally and independently associated with positive behavioral outcomes.34 The techniques used in the motivational interviewing approach are summarized in “The motivational interviewing tool kit”. Motivational interviewing is a goal-oriented, patient-centered counseling style for helping patients explore and resolve their ambivalence about behavior change.35 The approach has been used in diverse populations, settings, and medical conditions. Its efficacy was first demonstrated in the treatment of addictions to illegal drugs and alcohol.36 Continued research and 2 recent meta-analyses using rigorous methodology have validated the usefulness of this approach.37,38
Express empathy
Objective: To establish rapport and avoid resistance by demonstrating your understanding of the patient’s situation.
Example: “It’s not easy making all these changes.”
Follow-up: “But you also say you know these numbers put you at risk for more serious disease.”
Roll with resistance
Objective: To avoid magnifying resistance by allowing patients to explore their barriers in a nonjudgmental, supportive manner.
Example: “You really don’t want to take the medication anymore. It’s hard to remember and you don’t feel sick, so you don’t see why you need it.”
Follow-up: “I’m wondering where you see yourself in 6 months if you stop taking the medication?”
Elicit/provide reminder/elicit
Objective: To find out what the patient already knows, fill in the gaps or correct misconceptions, and explore how the change you suggest will fit into the patient’s life. This is a time-saving strategy that both validates patient knowledge and allows time to address barriers.
Example:
Elicit: “Mrs. Roberts, can you tell me what you know about managing your chronic kidney disease?”
Provide reminder: “That’s great. You’ve pretty much got it nailed. I’d just like to remind you about taking your statin medications and keeping close track of your blood pressure.”
Elicit: “What do you think the biggest barrier is for you right now in managing this condition?”
Support autonomy
Objective: To reduce resistance by assuring patients you know you can’t make them do anything—it’s their choice.
Example: “Of course, it’s your choice, but as your doctor, I’d be concerned if you decided not to try this medication.”
Follow-up: “Nobody can make you do anything that you don’t want to do. You need to consider all your options and make the choice that’s right for you at this time. If you do decide to try this medication, I assure you that we will monitor any side effects closely and adjust the dosage to minimize any problems.”
Explore ambivalence
Objective: To help the patient consider the pros and cons of change in a relaxed yet systematic manner.
Example: “So let’s talk about the pros and cons of trying to quit smoking at this time.”
Follow-up: “Let me see if I can summarize where you are. On the one hand, it’s pretty stressful for you right now and smoking helps you cope. You’ve tried to quit before and you couldn’t keep it up for very long. On the other hand, you really do understand the damage it’s doing to your body and how it is making it more difficult for us to treat your heart disease. Your wife is willing to quit with you and you’ve heard about this new quit medication that can help curb cravings. Did I get it all? What are you thinking you are going to do?”
Elicit change talk
Objective: To evoke the patient’s reasons, desire, ability, and need for change. This “change talk” predicts increased commitment to the lifestyle change, which, in turn, is correlated to a good clinical outcome.
Examples:
“What makes it important to you to start an exercise program?”
“What benefits would come from losing weight?”
“Why do you want to quit smoking?”
Follow-up: “You know that exercise will help you manage your stress, lose some weight, and lower your cholesterol levels. Plus, when you did it before, you had more energy and slept better. You also want to be a good role model for the kids and be able to play sports with them.”
Develop an action plan
Objective: To help the patient develop a plan that is realistic and fits into his or her life. When a patient “owns” the plan, he or she is more likely to follow through.
Examples:
“So what’s the next step for you?”
“What do you think you could do (and would be willing to do) for your health right now that would make the most difference?”
“What do you think your best option is?”
Follow-up: “You’ve outlined a great plan. You’re going to try to eat more vegetables and less meat, plus cut back on portion sizes. You’re also going to try and walk more. Lastly, you’re willing to try the pill box to see if it makes it easier to take your medications correctly.” (Pause). “So, are you going to do this?”
Motivational interviewing has been shown to be effective in improving general health status and sense of well-being, promoting physical activity, improving nutritional habits, encouraging medication adherence, and managing chronic conditions such as hypertension, hypercholesterolemia, obesity, and diabetes.35 A review of the literature on health behavior change demonstrates that motivational interviewing outperforms traditional advice-giving in the treatment of a broad range of behavioral problems and diseases.38
Motivational interviewing is focused on helping patients explore their ambivalence and identify individual barriers that are preventing change. The skill set that motivational interviewing provides can be modified for use in the brief patient encounters typically found in the primary care setting. For an example of how you might use motivational interviewing techniques with your CKD patients, see “Talking about change: A motivational interviewing conversation”.
Physician: Now that we’ve gone over your lab values and you don’t have any more questions, I’d like to take a few minutes to talk about how you’re doing with your treatment plan. Would that be okay with you?
Patient: Sure, doc.
Physician: You’re dealing with a lot of things all together—trying to change your diet, watching your weight, monitoring your blood sugar, and taking your medications.
Patient: It is a lot. Guess it’s obvious from my labs that I’m not doing so well. I feel like I get a handle on one thing but something else blows up.
Physician: Sounds like it feels a bit overwhelming right now.
Patient: Yeah, it really is…but I think I could do better.
Physician: Why don’t we start with reviewing what you’re doing well? you are getting your prescriptions filled, and it seems like you’re taking your medications regularly.
Patient: I really do, nearly all of the time.
Physician: What else are you doing well?
Patient: I’ve cut down on my salt intake. We’re using that salt substitute and it’s okay. Ummm…but I guess by the labs I’m not watching my potassium and phosphorus like I should.
Physician: What else are you doing well?
Patient: Well, my blood pressure is down from what it was. But my sugars are still out of whack and I can’t seem to lose weight.
Physician: Okay, so you’ve done a great job taking your medications and you’ve started to change your diet with the salt—both of which have really helped your blood pressure. As you say, there are some things we still need to tackle. But let’s break it down into small steps—forget the whole list. Can you think of just 1 or 2 more small things that you think you could do that would make a difference right now?
Patient: Well, my wife walks every evening after dinner. She’s been nagging me to walk with her. I guess I wouldn’t mind that so much as long as she doesn’t drag me too far. That would help me drop a few pounds and that might motivate me to be more careful with my diet. Plus, I know that exercise is also supposed to help my blood sugar.
Physician: So, a walk after dinner. Do you think you can do this?
Patient: Yes, I do.
Physician: When would you be willing to start?
Patient: Heck, I could start tomorrow. That’s something that wouldn’t be that big of a deal.
Physician: Great! Seems like a plan then. I’m confident that by taking these small steps like a walk every evening, you can get this under control. You have already improved in some important areas.
Patient: Thanks doc! I’ll see you next visit and hopefully my numbers will be better.
Your crucial role
CKD is well on its way to becoming a full-blown epidemic in the United States. Primary care providers carry the brunt of responsibility for the care of these patients, and with an increasing shortage of nephrologists, the scope of those activities will likely grow. Physicians in solo or small group practice must be prepared to deliver both the clinical and behavioral/lifestyle components of care themselves. While this is a challenging endeavor, we believe the framework outlined here will improve your ability to meet the complex needs of CKD patients.
CORRESPONDENCE Ariel Linden, DrPH, MS, Linden Consulting Group, 6208 NE Chestnut Street, Hillsboro, OR 97124; [email protected]
1. US Renal Data Systems. USRDS 2009 Annual Data Report: Atlas of Chronic Kidney Disease & End-Stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2009.
2. National Kidney Foundation. KDOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. 2002. Available at: http://www.kidney.org/professionals/kdoqi/guidelines_ckd/toc.htm. Accessed January 12, 2009.
3. U.S. Department of Health and Human Services. Healthy People 2010. (“Understanding and Improving Health” and “Objectives for Improving Health,” 2 volumes.) 2nd ed. Washington, DC: U.S. Government Printing Office, November 2000.
4. Fox CH, Brooks A, Zayas LE, et al. Primary care physicians’ knowledge and practice patterns in the treatment of chronic kidney disease: an Upstate New York Practice-based Research Network (UNYNET) study. J Am Board Fam Med. 2006;19:54-61.
5. Lea JP, McClellan WM, Melcher C, et al. CKD risk factors reported by primary care physicians: do guidelines make a difference? Am J Kidney Dis. 2006;47:72-77.
6. Foley RN, Murray AM, Li S, et al. Chronic kidney disease and the risk for cardiovascular disease, renal replacement, and death in the United States Medicare population, 1998 to 1999. J Am Soc Nephrol. 2005;16:489-495.
7. Nissenson AR, Collins AJ, Hurley J, et al. Opportunities for improving the care of patients with chronic renal insufficiency: current practice patterns. J Am Soc Nephrol. 2001;12:1713-1720.
8. McClellan WM, Knight DF, Karp H, et al. Early detection and treatment of renal disease in hospitalized diabetic and hypertensive patients: important differences between practice and published guidelines. Am J Kidney Dis. 1997;29:368-375.
9. Obrador GT, Ruthazer R, Arora P, et al. Prevalence of and factors associated with suboptimal care before initiation of dialysis in the United States. J Am Soc Nephrol. 1999;10:1793-1800.
10. Boulware LE, Troll MU, Jaar BG, et al. Identification and referral of patients with progressive CKD: a national study. Am J Kidney Dis. 2006;48:192-204.
11. John R, Webb M, Young A, et al. Unreferred chronic kidney disease: a longitudinal study. Am J Kidney Dis. 2004;43:825-835.
12. Wauters JP, Lameire N, Davison A, et al. Why patients with progressing kidney disease are referred late to the nephrologists: on causes and proposals for improvement. Nephrol Dial Transplant. 2005;20:490-496.
13. Ouseph R, Hendricks P, Hollon JA, et al. Under-recognition of chronic kidney disease in elderly outpatients. Clin Nephrol. 2007;68:373-378.
14. Himmelfarb J, Berns A, Szczech L, et al. Cost, quality, and value: the changing political economy of dialysis care. J Am Soc Nephrol. 2007;18:2021-2027.
15. Vassalotti JA, Stevens LA, Levey AS. Testing for chronic kidney disease: a position statement from the National Kidney Foundation. Am J Kidney Dis. 2007;50:169-180.
16. Saran AM, DuBose TD, Jr. Cardiovascular disease in chronic kidney disease. Ther Adv Cardiovasc Dis. 2008;2:425-434.
17. Mental Health America. Fact sheet: co-occurring disorders and depression. Available at: http://www.nmha.org/index.cfm?objectid=C7DF94C1-1372-4D20-C8FE4E509C20471B. Accessed January 25, 2009.
18. Cukor D, Coplan J, Brown C, et al. Course of depression and anxiety diagnosis in patients treated with hemodialysis: a 16-month follow-up. Am Soc Nephrol. 2008;3:1752-1758.
19. Lopez Revuelta K, Garcia Lopez FJ, de Alvaro Moreno F, et al. Perceived mental health at the start of dialysis as a predictor of morbidity and mortality in patients with end stage renal disease (CALVIDIA Study). Nephrol Dial Transplant. 2004;19:2347-2353.
20. Ford DE. A primary care approach: Managing depression in the face of chronic medical conditions. Am J Med. 2008;121(suppl 2):S38-S44.
21. Ferrari P. Prescribing angiotensin converting enzyme inhibitors and angiotensin receptor blockers in chronic kidney disease. Nephrol. 2007;12:81-89.
22. Song SH, Kwak IS, Lee DW, et al. The prevalence of low triiodothyronine according to the stage of chronic kidney disease in subjects with a normal thyroid-stimulating hormone. Nephrol Dial Transplant. 2009;24:1534-1538.
23. Ravani P, Malberti F, Tripepi G, et al. Vitamin D levels and patient outcome in chronic kidney disease. Kidney Int. 2009;75:88-95.
24. Cupisti A, Aparicio M, Barsotti G. Potential benefits of renal diets on cardiovascular risk factors in chronic kidney disease patients. Ren Fail. 2007;29:529-534.
25. Beto JA, Bansal VK. Medical nutrition therapy in chronic kidney failure: Integrating clinical practice guidelines. J Am Diet Assoc. 2004;104:404-409.
26. Al-Aly Z. The new role of calcimimetics as vasculotropic agents. Kidney Int. 2009;75:9-12.
27. Taliercio JJ. Anemia and chronic kidney disease: what’s the connection? J Fam Pract. 2010;59:14-18.
28. Chan MR, Dall AT, Fletcher KE, et al. Outcomes in patients with chronic kidney disease referred late to nephrologists: a meta-analysis. Am J Med. 2007;120:1063-1070.
29. Almaguer M, Herrera R, Alfonso J, et al. Primary health care strategies for the prevention of end-stage renal disease in Cuba. Kidney Int. 2005;68(suppl 97s):S4-S10.
30. Durose CL, Holdsworth M, Watson V, et al. Knowledge of dietary restrictions and the medical consequences of noncompliance by patients on hemodialysis are not predictive of dietary compliance. Am Diet Assoc. 2004;104:35-41.
31. Linden A, Butterworth SW, Roberts N. Disease management interventions II: what else is in the black box? Dis Manage. 2006;9:73-85.
32. Moyers TB, Martin T. Therapist influence on client language during motivational interviewing sessions. J Subst Abuse Treat. 2006;30:245-251.
33. Moyers TB, Martin T, Christopher PJ, et al. Client language as a mediator of motivational interviewing efficacy: where is the evidence? Alcohol Clin Exp Res. 2007;31(10 suppl):40s-47s.
34. Butterworth S, Linden A, McClay W. Health coaching as an intervention in health management programs. Dis Manage Health Outcomes. 2007;15:299-307.
35. Rollnick S, Miller WR, Butler CC. Motivational Interviewing in Health Care: Helping Patients Change Behavior. New York, NY: Guilford Press; 2008.
36. Miller WR. Motivational interviewing with problem drinkers. Behav Psychother. 1983;11:147-172.
37. Hettema J, Steele J, Miller WR. Motivational interviewing. Ann Rev Clin Psych. 2005;1:91-111.
38. Rubak S, Sandbaek A, Lauritzen T, et al. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55:305-312.
• Screen all patients for chronic kidney disease (CKD) by estimated glomerular filtration rate and persistent proteinuria. A
• Treat all CKD patients with angiotensin II receptor blockers or angiotensin-converting enzyme inhibitors, unless there is a contraindication. A
• Recommend a heart-healthy diet and refer patients with CKD to a registered dietitian for more intensive dietary modifications. A
• Integrate motivational interviewing into your care of CKD patients. This health coaching technique has been shown to be causally and independently associated with positive behavioral outcomes. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Over the last decade, the prevalence of chronic kidney disease (CKD) has grown approximately 20% to 25%, and current estimates are that the disease affects about 15% of the general population.1 All-cause hospitalization rates are almost 3 times higher among CKD patients than in those without the disease, and costs associated with CKD account for as much as 28% of the Medicare budget.1 Most disturbingly, the incidence at which patients diagnosed with CKD progress to end-stage renal disease (ESRD) continues to increase annually, reaching 354 cases per million population in 2007.1 By 2020, estimates are that more than 750,000 people in the United States will need dialysis for kidney failure.1
Guidelines exist, but awareness falls short
Several initiatives to increase awareness of CKD have been publicized. They include the Kidney Disease Outcome Quality Initiative (KDOQI) of the National Kidney Foundation (NKF), which issued clinical practice guidelines for treating chronic kidney disease in 2002, and Healthy People 2010, which includes specific measures to reduce the number of new cases and the complications, disability, economic costs, and mortality associated with the disease.2,3 Despite these efforts, studies show that many primary care providers are still unaware of these guidelines.4,5
Patients go undiagnosed until they reach the later stages of the disease, and many receive suboptimal care—even when they are identified—including lack of timely referral to a nephrologist and inadequate management of CKD comorbidities.6-13 (More on comorbidities, in a bit.)
Plus, there’s a lack of support … Care for these conditions is complex and difficult, and consultation or referral to a nephrologist may not be readily available, as the current pool of specialists is barely adequate to meet the needs of a growing population of CKD patients and the number of physicians-in-training entering the specialty is not adequate to meet the need.14 In this situation, primary care providers will have to assume an ever-enlarging share of the responsibility for care of CKD patients, including some clinical activities that are currently performed by specialists.
The first step: Screen all patients for CKD
Incorporating CKD screening into routine blood work for all patients facilitates earlier detection, evaluation, and treatment of the disease. Screening tests include the estimated glomerular filtration rate (GFR) based on serum creatinine as well as measurements of urine albumin and proteinuria. The persistence of proteinuria must be confirmed by 2 of 3 abnormal readings over a minimum of 3 months, because factors such as fever or exercise may affect test results. Measurement of albumin or total protein concentration in a spot sample avoids the need for timed collections. Factoring the concentration of total protein or albumin by urine creatinine concentration and using age/sex-specific thresholds eliminates most variations in measurement.15
Keep these comorbidities on your radar screen
Diabetes and hypertension are 2 of the most common causes of CKD in the United States, and the number of kidney failure cases due to these problems is increasing. The most important adverse outcomes of CKD are not only progression to ESRD, but also increased risk for cardiovascular disease (CVD). Studies show that the presence of albuminuria and a decreased estimated GFR consistently and incrementally increase the risk for CVD.16 Decreased GFR is an independent risk factor for CVD outcomes and for all-cause mortality, including sudden death in patients with existing coronary artery disease. Moreover, patients with CKD are 100 times more likely to die from CVD than to develop kidney failure.16
Depression is another prevalent, yet commonly overlooked, comorbid condition. Patients with any chronic disease are at risk for depression, with the incidence rising with the severity of the medical condition.17 CKD is no exception. Rates of depression as high as 29%, as well as rates of anxiety disorders as high as 46%, have been documented in patients on dialysis.18 Patients with depression are impaired in overall functioning and less able to follow medical regimens.17 In addition, low quality of life and depression predict higher morbidity and mortality rates in patients with ESRD.19 Because the diagnosis of depression is frequently missed in primary care settings, screening for depression should be a basic element in CKD management.20
Clinical management of kidney disease
The treatment goal for early-stage kidney disease is to address the risk factors that contribute to the progression of kidney disease: hypertension, heart disease, stroke, diabetes, and dyslipidemia. The TABLE reviews clinical management areas by disease stage.
Prescribe angiotensin antagonists. Angiotensin II receptor blockers (ARBs) and angiotensin-converting enzyme (ACE) inhibitors antagonize the toxic effects of increases in circulating angiotensin II and are therefore a key component of a therapeutic strategy to halt progressive kidney disease.2,21
Review medications, promote a healthier lifestyle. In addition to prescribing ARBs or ACE inhibitors, the family physician should review the CKD patient’s current medications to eliminate nephrotoxic drugs and adjust other medications on the basis of the patient’s creatinine clearance. Other measures include making sure vaccinations for influenza, pneumococcal pneumonia, and hepatitis B are up to date and emphasizing the importance of smoking cessation and exercise.
Treat comorbid conditions. Hypertension and diabetes must be treated aggressively. Patients with dyslipidemia should be managed with statins.2 Certain complications of progressive kidney disease, such as anemia, bone/mineral metabolic disease, and metabolic disorders, are typically treated by a nephrologist. Nevertheless, primary care providers need to understand these conditions in order to work together with the nephrologist in managing the CKD patient.
Check thyroid hormone and vitamin D levels. Understanding which factors predict disease progression or poor outcome is particularly useful. Most patients with CKD have low T3 syndrome, that is, low serum triiodothyronine levels in the absence of a thyroidal illness. In a recent paper, Song and colleagues showed that low T3 syndrome was common in early CKD and that estimated GFR was positively related with T3, independent of age and serum albumin.22
In another recent study, Ravani et al showed that plasma 25-hydroxyvitamin D is an independent, inverse predictor of disease progression and death in patients with stage 2 to 5 CKD.23 Vitamin D deficiency has been linked to CVD and early mortality in patients on hemodialysis.23 Checking for these 2 markers—low T3 syndrome and vitamin D deficiency—should therefore be part of your screening process for early stage CKD.
Refer to a dietitian. Dietary modification is another important component of the treatment plan. Dietary modifications are often needed to protect against CVD, help control blood pressure, reduce proteinuria, and improve metabolic control in patients with diabetes.2,24 Dietary modifications for CKD patients may go well beyond standard recommendations for a heart-healthy diet.2,24 Calcium, sodium, phosphorus, and potassium may need to be restricted according to laboratory values and stage of the disease.25 The KDOQI guidelines recommend referring CKD patients to a registered dietitian with experience in CKD for a complete nutritional assessment, comprehensive education on dietary restrictions and guidelines, and detailed dietary instruction.2
Manage CKD-associated anemia. Current guidelines do not propose normalizing hemoglobin in patients with renal disease, because lower levels of hemoglobin probably represent an adaptive response and correction to a “normal” level may disturb that response and lead to worse outcomes.26 For a discussion of management of anemia associated with CKD, see “Anemia and chronic kidney disease: What’s the connection?” in the January 2010 issue of this journal.27
Refer to a nephrologist early. A recent study by Chan et al demonstrates the beneficial effects of early referral to a nephrologist.28 There is no clear definition of early vs late referral and, at times, the only criterion is how much time elapsed before the patient was put on dialysis. Referral is considered “late” when management could have been improved by earlier contact with a specialist. It is probably prudent to refer stage 3 and 4 patients, at least for initial consultation. Chan’s meta-analysis found that patients referred late had nearly a 2-fold risk of death compared with those with early referrals. This risk persists at least up to 1 year after the initiation of renal replacement therapy.
Prepare patients for dialysis. It is very important that new hemodialysis patients present for initial treatment with an arteriovenous fistula in place, as first access for hemodialysis. Fistula placement is one of the most important reasons for timely referral to a nephrologist. Later referral is associated with a significantly prolonged hospital stay for initial renal replacement therapy. Late-referred patients are sicker, and many of the complications discussed here have not been optimally treated.
The optimal time to start preparing your patient for dialysis is when GFR measures between 15 and 29 mL/min/1.73 m2. Preparation includes counseling on nutrition and exercise, hepatitis B vaccination if needed, and scheduling for fistula placement.29
The hardest part: Changing habits
Effective CKD treatment must emphasize lifestyle management. You need to persuade smokers to quit and “couch potatoes” to start exercising regularly. Eating habits need to change, as well: This means fewer calories and restrictions on intake of salt and certain minerals. Medications for high blood pressure, diabetes, and kidney disease need to be taken consistently, as prescribed. The TABLE reviews the lifestyle issues that are particularly salient at each stage of CKD.
TABLE
Keying interventions to CKD stages
| Stage | Description | GFR (mL/min/1.73 m2) | Clinical action | Lifestyle management |
|---|---|---|---|---|
| At increased risk | ≥60 (with CKD risk factors) | Screening; CKD risk reduction | Healthy habits according to public health recommendations | |
| 1 | Kidney damage with normal or increased GFR | ≥90 | Diagnosis and treatment; treatment of comorbid conditions; slowing of progression; CVD risk reduction | Emphasis on heart health: physical activity, healthy diet, weight management, and stress management. Restricted sodium, potassium, calcium, phosphorus, and protein, with emphasis on plant vs animal food sources. Treatment adherence to medications and CV/diabetes/hypertension treatment plan if applicable. Assessment of depression and referral to treatment if appropriate. |
| 2 | Kidney damage with mildly decreased GFR | 60-89 | Same, plus estimation of progression | Same recommendations as stage 1 |
| 3 | Moderately decreased GFR | 30-59 | Same, plus evaluation and treatment of complications | Same recommendations as stage 1 |
| 4 | Severely decreased GFR | 15-29 | Preparation for kidney replacement therapy | Same as above, plus assessment of social support to prepare for dialysis treatment if appropriate |
| 5 | Kidney failure | <15 or dialysis | Replacement (if uremia present) | Same as above, plus restricted fluid intake and additional protein intake |
| Note: Shaded area identifies patients who have CKD; unshaded area designates individuals who are at increased risk for developing CKD. CKD is defined as either kidney damage or GFR <60 ml/min/1.73 m2 for ≥3 months. Kidney damage is defined as pathologic abnormalities or markers of damage, including abnormalities in blood or urine tests or imaging studies. | ||||
| CKD, chronic kidney disease; CVD, cardiovascular disease; GFR, glomerular filtration rate. | ||||
| Adapted from: Table 3: chronic kidney disease: a clinical action plan. National Kidney foundation. KDOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. 2002. | ||||
Lifestyle modifications like these are very difficult, and helping patients make them involves much more than simple patient education. In 1 study, Durose et al found that patients on hemodialysis failed to stay on their diets even when they knew which dietary restrictions they should follow and what the consequences of going off their diets would be.30
Update your persuasive techniques: take on the role of coach
Newer theories of behavior change no longer rely on simply providing information and advice, but rather address the complex interaction of motivations involved in attempts to change. These include cues to action, perception of benefits and consequences, environmental and cultural influences, sense of self-efficacy, ambivalence, and the intention to change.31
Unfortunately, health care providers are rarely trained in motivational techniques. Often, their approach to inducing change is authoritarian, confrontational, overly forceful, or guilt inducing. Such attitudes not only limit progress, but are actually correlated with negative behavioral and clinical outcomes.32,33 Recent research has verified the power of the patient–provider interaction in influencing treatment adherence and lifestyle change.33
To be successful in getting patients to adopt new behaviors, physicians need to move away from authoritarian modes and take on some of the attributes of a coach urging on the team.
How this coaching technique works
Motivational Interviewing is a health coaching technique that has been shown to be causally and independently associated with positive behavioral outcomes.34 The techniques used in the motivational interviewing approach are summarized in “The motivational interviewing tool kit”. Motivational interviewing is a goal-oriented, patient-centered counseling style for helping patients explore and resolve their ambivalence about behavior change.35 The approach has been used in diverse populations, settings, and medical conditions. Its efficacy was first demonstrated in the treatment of addictions to illegal drugs and alcohol.36 Continued research and 2 recent meta-analyses using rigorous methodology have validated the usefulness of this approach.37,38
Express empathy
Objective: To establish rapport and avoid resistance by demonstrating your understanding of the patient’s situation.
Example: “It’s not easy making all these changes.”
Follow-up: “But you also say you know these numbers put you at risk for more serious disease.”
Roll with resistance
Objective: To avoid magnifying resistance by allowing patients to explore their barriers in a nonjudgmental, supportive manner.
Example: “You really don’t want to take the medication anymore. It’s hard to remember and you don’t feel sick, so you don’t see why you need it.”
Follow-up: “I’m wondering where you see yourself in 6 months if you stop taking the medication?”
Elicit/provide reminder/elicit
Objective: To find out what the patient already knows, fill in the gaps or correct misconceptions, and explore how the change you suggest will fit into the patient’s life. This is a time-saving strategy that both validates patient knowledge and allows time to address barriers.
Example:
Elicit: “Mrs. Roberts, can you tell me what you know about managing your chronic kidney disease?”
Provide reminder: “That’s great. You’ve pretty much got it nailed. I’d just like to remind you about taking your statin medications and keeping close track of your blood pressure.”
Elicit: “What do you think the biggest barrier is for you right now in managing this condition?”
Support autonomy
Objective: To reduce resistance by assuring patients you know you can’t make them do anything—it’s their choice.
Example: “Of course, it’s your choice, but as your doctor, I’d be concerned if you decided not to try this medication.”
Follow-up: “Nobody can make you do anything that you don’t want to do. You need to consider all your options and make the choice that’s right for you at this time. If you do decide to try this medication, I assure you that we will monitor any side effects closely and adjust the dosage to minimize any problems.”
Explore ambivalence
Objective: To help the patient consider the pros and cons of change in a relaxed yet systematic manner.
Example: “So let’s talk about the pros and cons of trying to quit smoking at this time.”
Follow-up: “Let me see if I can summarize where you are. On the one hand, it’s pretty stressful for you right now and smoking helps you cope. You’ve tried to quit before and you couldn’t keep it up for very long. On the other hand, you really do understand the damage it’s doing to your body and how it is making it more difficult for us to treat your heart disease. Your wife is willing to quit with you and you’ve heard about this new quit medication that can help curb cravings. Did I get it all? What are you thinking you are going to do?”
Elicit change talk
Objective: To evoke the patient’s reasons, desire, ability, and need for change. This “change talk” predicts increased commitment to the lifestyle change, which, in turn, is correlated to a good clinical outcome.
Examples:
“What makes it important to you to start an exercise program?”
“What benefits would come from losing weight?”
“Why do you want to quit smoking?”
Follow-up: “You know that exercise will help you manage your stress, lose some weight, and lower your cholesterol levels. Plus, when you did it before, you had more energy and slept better. You also want to be a good role model for the kids and be able to play sports with them.”
Develop an action plan
Objective: To help the patient develop a plan that is realistic and fits into his or her life. When a patient “owns” the plan, he or she is more likely to follow through.
Examples:
“So what’s the next step for you?”
“What do you think you could do (and would be willing to do) for your health right now that would make the most difference?”
“What do you think your best option is?”
Follow-up: “You’ve outlined a great plan. You’re going to try to eat more vegetables and less meat, plus cut back on portion sizes. You’re also going to try and walk more. Lastly, you’re willing to try the pill box to see if it makes it easier to take your medications correctly.” (Pause). “So, are you going to do this?”
Motivational interviewing has been shown to be effective in improving general health status and sense of well-being, promoting physical activity, improving nutritional habits, encouraging medication adherence, and managing chronic conditions such as hypertension, hypercholesterolemia, obesity, and diabetes.35 A review of the literature on health behavior change demonstrates that motivational interviewing outperforms traditional advice-giving in the treatment of a broad range of behavioral problems and diseases.38
Motivational interviewing is focused on helping patients explore their ambivalence and identify individual barriers that are preventing change. The skill set that motivational interviewing provides can be modified for use in the brief patient encounters typically found in the primary care setting. For an example of how you might use motivational interviewing techniques with your CKD patients, see “Talking about change: A motivational interviewing conversation”.
Physician: Now that we’ve gone over your lab values and you don’t have any more questions, I’d like to take a few minutes to talk about how you’re doing with your treatment plan. Would that be okay with you?
Patient: Sure, doc.
Physician: You’re dealing with a lot of things all together—trying to change your diet, watching your weight, monitoring your blood sugar, and taking your medications.
Patient: It is a lot. Guess it’s obvious from my labs that I’m not doing so well. I feel like I get a handle on one thing but something else blows up.
Physician: Sounds like it feels a bit overwhelming right now.
Patient: Yeah, it really is…but I think I could do better.
Physician: Why don’t we start with reviewing what you’re doing well? you are getting your prescriptions filled, and it seems like you’re taking your medications regularly.
Patient: I really do, nearly all of the time.
Physician: What else are you doing well?
Patient: I’ve cut down on my salt intake. We’re using that salt substitute and it’s okay. Ummm…but I guess by the labs I’m not watching my potassium and phosphorus like I should.
Physician: What else are you doing well?
Patient: Well, my blood pressure is down from what it was. But my sugars are still out of whack and I can’t seem to lose weight.
Physician: Okay, so you’ve done a great job taking your medications and you’ve started to change your diet with the salt—both of which have really helped your blood pressure. As you say, there are some things we still need to tackle. But let’s break it down into small steps—forget the whole list. Can you think of just 1 or 2 more small things that you think you could do that would make a difference right now?
Patient: Well, my wife walks every evening after dinner. She’s been nagging me to walk with her. I guess I wouldn’t mind that so much as long as she doesn’t drag me too far. That would help me drop a few pounds and that might motivate me to be more careful with my diet. Plus, I know that exercise is also supposed to help my blood sugar.
Physician: So, a walk after dinner. Do you think you can do this?
Patient: Yes, I do.
Physician: When would you be willing to start?
Patient: Heck, I could start tomorrow. That’s something that wouldn’t be that big of a deal.
Physician: Great! Seems like a plan then. I’m confident that by taking these small steps like a walk every evening, you can get this under control. You have already improved in some important areas.
Patient: Thanks doc! I’ll see you next visit and hopefully my numbers will be better.
Your crucial role
CKD is well on its way to becoming a full-blown epidemic in the United States. Primary care providers carry the brunt of responsibility for the care of these patients, and with an increasing shortage of nephrologists, the scope of those activities will likely grow. Physicians in solo or small group practice must be prepared to deliver both the clinical and behavioral/lifestyle components of care themselves. While this is a challenging endeavor, we believe the framework outlined here will improve your ability to meet the complex needs of CKD patients.
CORRESPONDENCE Ariel Linden, DrPH, MS, Linden Consulting Group, 6208 NE Chestnut Street, Hillsboro, OR 97124; [email protected]
• Screen all patients for chronic kidney disease (CKD) by estimated glomerular filtration rate and persistent proteinuria. A
• Treat all CKD patients with angiotensin II receptor blockers or angiotensin-converting enzyme inhibitors, unless there is a contraindication. A
• Recommend a heart-healthy diet and refer patients with CKD to a registered dietitian for more intensive dietary modifications. A
• Integrate motivational interviewing into your care of CKD patients. This health coaching technique has been shown to be causally and independently associated with positive behavioral outcomes. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Over the last decade, the prevalence of chronic kidney disease (CKD) has grown approximately 20% to 25%, and current estimates are that the disease affects about 15% of the general population.1 All-cause hospitalization rates are almost 3 times higher among CKD patients than in those without the disease, and costs associated with CKD account for as much as 28% of the Medicare budget.1 Most disturbingly, the incidence at which patients diagnosed with CKD progress to end-stage renal disease (ESRD) continues to increase annually, reaching 354 cases per million population in 2007.1 By 2020, estimates are that more than 750,000 people in the United States will need dialysis for kidney failure.1
Guidelines exist, but awareness falls short
Several initiatives to increase awareness of CKD have been publicized. They include the Kidney Disease Outcome Quality Initiative (KDOQI) of the National Kidney Foundation (NKF), which issued clinical practice guidelines for treating chronic kidney disease in 2002, and Healthy People 2010, which includes specific measures to reduce the number of new cases and the complications, disability, economic costs, and mortality associated with the disease.2,3 Despite these efforts, studies show that many primary care providers are still unaware of these guidelines.4,5
Patients go undiagnosed until they reach the later stages of the disease, and many receive suboptimal care—even when they are identified—including lack of timely referral to a nephrologist and inadequate management of CKD comorbidities.6-13 (More on comorbidities, in a bit.)
Plus, there’s a lack of support … Care for these conditions is complex and difficult, and consultation or referral to a nephrologist may not be readily available, as the current pool of specialists is barely adequate to meet the needs of a growing population of CKD patients and the number of physicians-in-training entering the specialty is not adequate to meet the need.14 In this situation, primary care providers will have to assume an ever-enlarging share of the responsibility for care of CKD patients, including some clinical activities that are currently performed by specialists.
The first step: Screen all patients for CKD
Incorporating CKD screening into routine blood work for all patients facilitates earlier detection, evaluation, and treatment of the disease. Screening tests include the estimated glomerular filtration rate (GFR) based on serum creatinine as well as measurements of urine albumin and proteinuria. The persistence of proteinuria must be confirmed by 2 of 3 abnormal readings over a minimum of 3 months, because factors such as fever or exercise may affect test results. Measurement of albumin or total protein concentration in a spot sample avoids the need for timed collections. Factoring the concentration of total protein or albumin by urine creatinine concentration and using age/sex-specific thresholds eliminates most variations in measurement.15
Keep these comorbidities on your radar screen
Diabetes and hypertension are 2 of the most common causes of CKD in the United States, and the number of kidney failure cases due to these problems is increasing. The most important adverse outcomes of CKD are not only progression to ESRD, but also increased risk for cardiovascular disease (CVD). Studies show that the presence of albuminuria and a decreased estimated GFR consistently and incrementally increase the risk for CVD.16 Decreased GFR is an independent risk factor for CVD outcomes and for all-cause mortality, including sudden death in patients with existing coronary artery disease. Moreover, patients with CKD are 100 times more likely to die from CVD than to develop kidney failure.16
Depression is another prevalent, yet commonly overlooked, comorbid condition. Patients with any chronic disease are at risk for depression, with the incidence rising with the severity of the medical condition.17 CKD is no exception. Rates of depression as high as 29%, as well as rates of anxiety disorders as high as 46%, have been documented in patients on dialysis.18 Patients with depression are impaired in overall functioning and less able to follow medical regimens.17 In addition, low quality of life and depression predict higher morbidity and mortality rates in patients with ESRD.19 Because the diagnosis of depression is frequently missed in primary care settings, screening for depression should be a basic element in CKD management.20
Clinical management of kidney disease
The treatment goal for early-stage kidney disease is to address the risk factors that contribute to the progression of kidney disease: hypertension, heart disease, stroke, diabetes, and dyslipidemia. The TABLE reviews clinical management areas by disease stage.
Prescribe angiotensin antagonists. Angiotensin II receptor blockers (ARBs) and angiotensin-converting enzyme (ACE) inhibitors antagonize the toxic effects of increases in circulating angiotensin II and are therefore a key component of a therapeutic strategy to halt progressive kidney disease.2,21
Review medications, promote a healthier lifestyle. In addition to prescribing ARBs or ACE inhibitors, the family physician should review the CKD patient’s current medications to eliminate nephrotoxic drugs and adjust other medications on the basis of the patient’s creatinine clearance. Other measures include making sure vaccinations for influenza, pneumococcal pneumonia, and hepatitis B are up to date and emphasizing the importance of smoking cessation and exercise.
Treat comorbid conditions. Hypertension and diabetes must be treated aggressively. Patients with dyslipidemia should be managed with statins.2 Certain complications of progressive kidney disease, such as anemia, bone/mineral metabolic disease, and metabolic disorders, are typically treated by a nephrologist. Nevertheless, primary care providers need to understand these conditions in order to work together with the nephrologist in managing the CKD patient.
Check thyroid hormone and vitamin D levels. Understanding which factors predict disease progression or poor outcome is particularly useful. Most patients with CKD have low T3 syndrome, that is, low serum triiodothyronine levels in the absence of a thyroidal illness. In a recent paper, Song and colleagues showed that low T3 syndrome was common in early CKD and that estimated GFR was positively related with T3, independent of age and serum albumin.22
In another recent study, Ravani et al showed that plasma 25-hydroxyvitamin D is an independent, inverse predictor of disease progression and death in patients with stage 2 to 5 CKD.23 Vitamin D deficiency has been linked to CVD and early mortality in patients on hemodialysis.23 Checking for these 2 markers—low T3 syndrome and vitamin D deficiency—should therefore be part of your screening process for early stage CKD.
Refer to a dietitian. Dietary modification is another important component of the treatment plan. Dietary modifications are often needed to protect against CVD, help control blood pressure, reduce proteinuria, and improve metabolic control in patients with diabetes.2,24 Dietary modifications for CKD patients may go well beyond standard recommendations for a heart-healthy diet.2,24 Calcium, sodium, phosphorus, and potassium may need to be restricted according to laboratory values and stage of the disease.25 The KDOQI guidelines recommend referring CKD patients to a registered dietitian with experience in CKD for a complete nutritional assessment, comprehensive education on dietary restrictions and guidelines, and detailed dietary instruction.2
Manage CKD-associated anemia. Current guidelines do not propose normalizing hemoglobin in patients with renal disease, because lower levels of hemoglobin probably represent an adaptive response and correction to a “normal” level may disturb that response and lead to worse outcomes.26 For a discussion of management of anemia associated with CKD, see “Anemia and chronic kidney disease: What’s the connection?” in the January 2010 issue of this journal.27
Refer to a nephrologist early. A recent study by Chan et al demonstrates the beneficial effects of early referral to a nephrologist.28 There is no clear definition of early vs late referral and, at times, the only criterion is how much time elapsed before the patient was put on dialysis. Referral is considered “late” when management could have been improved by earlier contact with a specialist. It is probably prudent to refer stage 3 and 4 patients, at least for initial consultation. Chan’s meta-analysis found that patients referred late had nearly a 2-fold risk of death compared with those with early referrals. This risk persists at least up to 1 year after the initiation of renal replacement therapy.
Prepare patients for dialysis. It is very important that new hemodialysis patients present for initial treatment with an arteriovenous fistula in place, as first access for hemodialysis. Fistula placement is one of the most important reasons for timely referral to a nephrologist. Later referral is associated with a significantly prolonged hospital stay for initial renal replacement therapy. Late-referred patients are sicker, and many of the complications discussed here have not been optimally treated.
The optimal time to start preparing your patient for dialysis is when GFR measures between 15 and 29 mL/min/1.73 m2. Preparation includes counseling on nutrition and exercise, hepatitis B vaccination if needed, and scheduling for fistula placement.29
The hardest part: Changing habits
Effective CKD treatment must emphasize lifestyle management. You need to persuade smokers to quit and “couch potatoes” to start exercising regularly. Eating habits need to change, as well: This means fewer calories and restrictions on intake of salt and certain minerals. Medications for high blood pressure, diabetes, and kidney disease need to be taken consistently, as prescribed. The TABLE reviews the lifestyle issues that are particularly salient at each stage of CKD.
TABLE
Keying interventions to CKD stages
| Stage | Description | GFR (mL/min/1.73 m2) | Clinical action | Lifestyle management |
|---|---|---|---|---|
| At increased risk | ≥60 (with CKD risk factors) | Screening; CKD risk reduction | Healthy habits according to public health recommendations | |
| 1 | Kidney damage with normal or increased GFR | ≥90 | Diagnosis and treatment; treatment of comorbid conditions; slowing of progression; CVD risk reduction | Emphasis on heart health: physical activity, healthy diet, weight management, and stress management. Restricted sodium, potassium, calcium, phosphorus, and protein, with emphasis on plant vs animal food sources. Treatment adherence to medications and CV/diabetes/hypertension treatment plan if applicable. Assessment of depression and referral to treatment if appropriate. |
| 2 | Kidney damage with mildly decreased GFR | 60-89 | Same, plus estimation of progression | Same recommendations as stage 1 |
| 3 | Moderately decreased GFR | 30-59 | Same, plus evaluation and treatment of complications | Same recommendations as stage 1 |
| 4 | Severely decreased GFR | 15-29 | Preparation for kidney replacement therapy | Same as above, plus assessment of social support to prepare for dialysis treatment if appropriate |
| 5 | Kidney failure | <15 or dialysis | Replacement (if uremia present) | Same as above, plus restricted fluid intake and additional protein intake |
| Note: Shaded area identifies patients who have CKD; unshaded area designates individuals who are at increased risk for developing CKD. CKD is defined as either kidney damage or GFR <60 ml/min/1.73 m2 for ≥3 months. Kidney damage is defined as pathologic abnormalities or markers of damage, including abnormalities in blood or urine tests or imaging studies. | ||||
| CKD, chronic kidney disease; CVD, cardiovascular disease; GFR, glomerular filtration rate. | ||||
| Adapted from: Table 3: chronic kidney disease: a clinical action plan. National Kidney foundation. KDOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. 2002. | ||||
Lifestyle modifications like these are very difficult, and helping patients make them involves much more than simple patient education. In 1 study, Durose et al found that patients on hemodialysis failed to stay on their diets even when they knew which dietary restrictions they should follow and what the consequences of going off their diets would be.30
Update your persuasive techniques: take on the role of coach
Newer theories of behavior change no longer rely on simply providing information and advice, but rather address the complex interaction of motivations involved in attempts to change. These include cues to action, perception of benefits and consequences, environmental and cultural influences, sense of self-efficacy, ambivalence, and the intention to change.31
Unfortunately, health care providers are rarely trained in motivational techniques. Often, their approach to inducing change is authoritarian, confrontational, overly forceful, or guilt inducing. Such attitudes not only limit progress, but are actually correlated with negative behavioral and clinical outcomes.32,33 Recent research has verified the power of the patient–provider interaction in influencing treatment adherence and lifestyle change.33
To be successful in getting patients to adopt new behaviors, physicians need to move away from authoritarian modes and take on some of the attributes of a coach urging on the team.
How this coaching technique works
Motivational Interviewing is a health coaching technique that has been shown to be causally and independently associated with positive behavioral outcomes.34 The techniques used in the motivational interviewing approach are summarized in “The motivational interviewing tool kit”. Motivational interviewing is a goal-oriented, patient-centered counseling style for helping patients explore and resolve their ambivalence about behavior change.35 The approach has been used in diverse populations, settings, and medical conditions. Its efficacy was first demonstrated in the treatment of addictions to illegal drugs and alcohol.36 Continued research and 2 recent meta-analyses using rigorous methodology have validated the usefulness of this approach.37,38
Express empathy
Objective: To establish rapport and avoid resistance by demonstrating your understanding of the patient’s situation.
Example: “It’s not easy making all these changes.”
Follow-up: “But you also say you know these numbers put you at risk for more serious disease.”
Roll with resistance
Objective: To avoid magnifying resistance by allowing patients to explore their barriers in a nonjudgmental, supportive manner.
Example: “You really don’t want to take the medication anymore. It’s hard to remember and you don’t feel sick, so you don’t see why you need it.”
Follow-up: “I’m wondering where you see yourself in 6 months if you stop taking the medication?”
Elicit/provide reminder/elicit
Objective: To find out what the patient already knows, fill in the gaps or correct misconceptions, and explore how the change you suggest will fit into the patient’s life. This is a time-saving strategy that both validates patient knowledge and allows time to address barriers.
Example:
Elicit: “Mrs. Roberts, can you tell me what you know about managing your chronic kidney disease?”
Provide reminder: “That’s great. You’ve pretty much got it nailed. I’d just like to remind you about taking your statin medications and keeping close track of your blood pressure.”
Elicit: “What do you think the biggest barrier is for you right now in managing this condition?”
Support autonomy
Objective: To reduce resistance by assuring patients you know you can’t make them do anything—it’s their choice.
Example: “Of course, it’s your choice, but as your doctor, I’d be concerned if you decided not to try this medication.”
Follow-up: “Nobody can make you do anything that you don’t want to do. You need to consider all your options and make the choice that’s right for you at this time. If you do decide to try this medication, I assure you that we will monitor any side effects closely and adjust the dosage to minimize any problems.”
Explore ambivalence
Objective: To help the patient consider the pros and cons of change in a relaxed yet systematic manner.
Example: “So let’s talk about the pros and cons of trying to quit smoking at this time.”
Follow-up: “Let me see if I can summarize where you are. On the one hand, it’s pretty stressful for you right now and smoking helps you cope. You’ve tried to quit before and you couldn’t keep it up for very long. On the other hand, you really do understand the damage it’s doing to your body and how it is making it more difficult for us to treat your heart disease. Your wife is willing to quit with you and you’ve heard about this new quit medication that can help curb cravings. Did I get it all? What are you thinking you are going to do?”
Elicit change talk
Objective: To evoke the patient’s reasons, desire, ability, and need for change. This “change talk” predicts increased commitment to the lifestyle change, which, in turn, is correlated to a good clinical outcome.
Examples:
“What makes it important to you to start an exercise program?”
“What benefits would come from losing weight?”
“Why do you want to quit smoking?”
Follow-up: “You know that exercise will help you manage your stress, lose some weight, and lower your cholesterol levels. Plus, when you did it before, you had more energy and slept better. You also want to be a good role model for the kids and be able to play sports with them.”
Develop an action plan
Objective: To help the patient develop a plan that is realistic and fits into his or her life. When a patient “owns” the plan, he or she is more likely to follow through.
Examples:
“So what’s the next step for you?”
“What do you think you could do (and would be willing to do) for your health right now that would make the most difference?”
“What do you think your best option is?”
Follow-up: “You’ve outlined a great plan. You’re going to try to eat more vegetables and less meat, plus cut back on portion sizes. You’re also going to try and walk more. Lastly, you’re willing to try the pill box to see if it makes it easier to take your medications correctly.” (Pause). “So, are you going to do this?”
Motivational interviewing has been shown to be effective in improving general health status and sense of well-being, promoting physical activity, improving nutritional habits, encouraging medication adherence, and managing chronic conditions such as hypertension, hypercholesterolemia, obesity, and diabetes.35 A review of the literature on health behavior change demonstrates that motivational interviewing outperforms traditional advice-giving in the treatment of a broad range of behavioral problems and diseases.38
Motivational interviewing is focused on helping patients explore their ambivalence and identify individual barriers that are preventing change. The skill set that motivational interviewing provides can be modified for use in the brief patient encounters typically found in the primary care setting. For an example of how you might use motivational interviewing techniques with your CKD patients, see “Talking about change: A motivational interviewing conversation”.
Physician: Now that we’ve gone over your lab values and you don’t have any more questions, I’d like to take a few minutes to talk about how you’re doing with your treatment plan. Would that be okay with you?
Patient: Sure, doc.
Physician: You’re dealing with a lot of things all together—trying to change your diet, watching your weight, monitoring your blood sugar, and taking your medications.
Patient: It is a lot. Guess it’s obvious from my labs that I’m not doing so well. I feel like I get a handle on one thing but something else blows up.
Physician: Sounds like it feels a bit overwhelming right now.
Patient: Yeah, it really is…but I think I could do better.
Physician: Why don’t we start with reviewing what you’re doing well? you are getting your prescriptions filled, and it seems like you’re taking your medications regularly.
Patient: I really do, nearly all of the time.
Physician: What else are you doing well?
Patient: I’ve cut down on my salt intake. We’re using that salt substitute and it’s okay. Ummm…but I guess by the labs I’m not watching my potassium and phosphorus like I should.
Physician: What else are you doing well?
Patient: Well, my blood pressure is down from what it was. But my sugars are still out of whack and I can’t seem to lose weight.
Physician: Okay, so you’ve done a great job taking your medications and you’ve started to change your diet with the salt—both of which have really helped your blood pressure. As you say, there are some things we still need to tackle. But let’s break it down into small steps—forget the whole list. Can you think of just 1 or 2 more small things that you think you could do that would make a difference right now?
Patient: Well, my wife walks every evening after dinner. She’s been nagging me to walk with her. I guess I wouldn’t mind that so much as long as she doesn’t drag me too far. That would help me drop a few pounds and that might motivate me to be more careful with my diet. Plus, I know that exercise is also supposed to help my blood sugar.
Physician: So, a walk after dinner. Do you think you can do this?
Patient: Yes, I do.
Physician: When would you be willing to start?
Patient: Heck, I could start tomorrow. That’s something that wouldn’t be that big of a deal.
Physician: Great! Seems like a plan then. I’m confident that by taking these small steps like a walk every evening, you can get this under control. You have already improved in some important areas.
Patient: Thanks doc! I’ll see you next visit and hopefully my numbers will be better.
Your crucial role
CKD is well on its way to becoming a full-blown epidemic in the United States. Primary care providers carry the brunt of responsibility for the care of these patients, and with an increasing shortage of nephrologists, the scope of those activities will likely grow. Physicians in solo or small group practice must be prepared to deliver both the clinical and behavioral/lifestyle components of care themselves. While this is a challenging endeavor, we believe the framework outlined here will improve your ability to meet the complex needs of CKD patients.
CORRESPONDENCE Ariel Linden, DrPH, MS, Linden Consulting Group, 6208 NE Chestnut Street, Hillsboro, OR 97124; [email protected]
1. US Renal Data Systems. USRDS 2009 Annual Data Report: Atlas of Chronic Kidney Disease & End-Stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2009.
2. National Kidney Foundation. KDOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. 2002. Available at: http://www.kidney.org/professionals/kdoqi/guidelines_ckd/toc.htm. Accessed January 12, 2009.
3. U.S. Department of Health and Human Services. Healthy People 2010. (“Understanding and Improving Health” and “Objectives for Improving Health,” 2 volumes.) 2nd ed. Washington, DC: U.S. Government Printing Office, November 2000.
4. Fox CH, Brooks A, Zayas LE, et al. Primary care physicians’ knowledge and practice patterns in the treatment of chronic kidney disease: an Upstate New York Practice-based Research Network (UNYNET) study. J Am Board Fam Med. 2006;19:54-61.
5. Lea JP, McClellan WM, Melcher C, et al. CKD risk factors reported by primary care physicians: do guidelines make a difference? Am J Kidney Dis. 2006;47:72-77.
6. Foley RN, Murray AM, Li S, et al. Chronic kidney disease and the risk for cardiovascular disease, renal replacement, and death in the United States Medicare population, 1998 to 1999. J Am Soc Nephrol. 2005;16:489-495.
7. Nissenson AR, Collins AJ, Hurley J, et al. Opportunities for improving the care of patients with chronic renal insufficiency: current practice patterns. J Am Soc Nephrol. 2001;12:1713-1720.
8. McClellan WM, Knight DF, Karp H, et al. Early detection and treatment of renal disease in hospitalized diabetic and hypertensive patients: important differences between practice and published guidelines. Am J Kidney Dis. 1997;29:368-375.
9. Obrador GT, Ruthazer R, Arora P, et al. Prevalence of and factors associated with suboptimal care before initiation of dialysis in the United States. J Am Soc Nephrol. 1999;10:1793-1800.
10. Boulware LE, Troll MU, Jaar BG, et al. Identification and referral of patients with progressive CKD: a national study. Am J Kidney Dis. 2006;48:192-204.
11. John R, Webb M, Young A, et al. Unreferred chronic kidney disease: a longitudinal study. Am J Kidney Dis. 2004;43:825-835.
12. Wauters JP, Lameire N, Davison A, et al. Why patients with progressing kidney disease are referred late to the nephrologists: on causes and proposals for improvement. Nephrol Dial Transplant. 2005;20:490-496.
13. Ouseph R, Hendricks P, Hollon JA, et al. Under-recognition of chronic kidney disease in elderly outpatients. Clin Nephrol. 2007;68:373-378.
14. Himmelfarb J, Berns A, Szczech L, et al. Cost, quality, and value: the changing political economy of dialysis care. J Am Soc Nephrol. 2007;18:2021-2027.
15. Vassalotti JA, Stevens LA, Levey AS. Testing for chronic kidney disease: a position statement from the National Kidney Foundation. Am J Kidney Dis. 2007;50:169-180.
16. Saran AM, DuBose TD, Jr. Cardiovascular disease in chronic kidney disease. Ther Adv Cardiovasc Dis. 2008;2:425-434.
17. Mental Health America. Fact sheet: co-occurring disorders and depression. Available at: http://www.nmha.org/index.cfm?objectid=C7DF94C1-1372-4D20-C8FE4E509C20471B. Accessed January 25, 2009.
18. Cukor D, Coplan J, Brown C, et al. Course of depression and anxiety diagnosis in patients treated with hemodialysis: a 16-month follow-up. Am Soc Nephrol. 2008;3:1752-1758.
19. Lopez Revuelta K, Garcia Lopez FJ, de Alvaro Moreno F, et al. Perceived mental health at the start of dialysis as a predictor of morbidity and mortality in patients with end stage renal disease (CALVIDIA Study). Nephrol Dial Transplant. 2004;19:2347-2353.
20. Ford DE. A primary care approach: Managing depression in the face of chronic medical conditions. Am J Med. 2008;121(suppl 2):S38-S44.
21. Ferrari P. Prescribing angiotensin converting enzyme inhibitors and angiotensin receptor blockers in chronic kidney disease. Nephrol. 2007;12:81-89.
22. Song SH, Kwak IS, Lee DW, et al. The prevalence of low triiodothyronine according to the stage of chronic kidney disease in subjects with a normal thyroid-stimulating hormone. Nephrol Dial Transplant. 2009;24:1534-1538.
23. Ravani P, Malberti F, Tripepi G, et al. Vitamin D levels and patient outcome in chronic kidney disease. Kidney Int. 2009;75:88-95.
24. Cupisti A, Aparicio M, Barsotti G. Potential benefits of renal diets on cardiovascular risk factors in chronic kidney disease patients. Ren Fail. 2007;29:529-534.
25. Beto JA, Bansal VK. Medical nutrition therapy in chronic kidney failure: Integrating clinical practice guidelines. J Am Diet Assoc. 2004;104:404-409.
26. Al-Aly Z. The new role of calcimimetics as vasculotropic agents. Kidney Int. 2009;75:9-12.
27. Taliercio JJ. Anemia and chronic kidney disease: what’s the connection? J Fam Pract. 2010;59:14-18.
28. Chan MR, Dall AT, Fletcher KE, et al. Outcomes in patients with chronic kidney disease referred late to nephrologists: a meta-analysis. Am J Med. 2007;120:1063-1070.
29. Almaguer M, Herrera R, Alfonso J, et al. Primary health care strategies for the prevention of end-stage renal disease in Cuba. Kidney Int. 2005;68(suppl 97s):S4-S10.
30. Durose CL, Holdsworth M, Watson V, et al. Knowledge of dietary restrictions and the medical consequences of noncompliance by patients on hemodialysis are not predictive of dietary compliance. Am Diet Assoc. 2004;104:35-41.
31. Linden A, Butterworth SW, Roberts N. Disease management interventions II: what else is in the black box? Dis Manage. 2006;9:73-85.
32. Moyers TB, Martin T. Therapist influence on client language during motivational interviewing sessions. J Subst Abuse Treat. 2006;30:245-251.
33. Moyers TB, Martin T, Christopher PJ, et al. Client language as a mediator of motivational interviewing efficacy: where is the evidence? Alcohol Clin Exp Res. 2007;31(10 suppl):40s-47s.
34. Butterworth S, Linden A, McClay W. Health coaching as an intervention in health management programs. Dis Manage Health Outcomes. 2007;15:299-307.
35. Rollnick S, Miller WR, Butler CC. Motivational Interviewing in Health Care: Helping Patients Change Behavior. New York, NY: Guilford Press; 2008.
36. Miller WR. Motivational interviewing with problem drinkers. Behav Psychother. 1983;11:147-172.
37. Hettema J, Steele J, Miller WR. Motivational interviewing. Ann Rev Clin Psych. 2005;1:91-111.
38. Rubak S, Sandbaek A, Lauritzen T, et al. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55:305-312.
1. US Renal Data Systems. USRDS 2009 Annual Data Report: Atlas of Chronic Kidney Disease & End-Stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2009.
2. National Kidney Foundation. KDOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. 2002. Available at: http://www.kidney.org/professionals/kdoqi/guidelines_ckd/toc.htm. Accessed January 12, 2009.
3. U.S. Department of Health and Human Services. Healthy People 2010. (“Understanding and Improving Health” and “Objectives for Improving Health,” 2 volumes.) 2nd ed. Washington, DC: U.S. Government Printing Office, November 2000.
4. Fox CH, Brooks A, Zayas LE, et al. Primary care physicians’ knowledge and practice patterns in the treatment of chronic kidney disease: an Upstate New York Practice-based Research Network (UNYNET) study. J Am Board Fam Med. 2006;19:54-61.
5. Lea JP, McClellan WM, Melcher C, et al. CKD risk factors reported by primary care physicians: do guidelines make a difference? Am J Kidney Dis. 2006;47:72-77.
6. Foley RN, Murray AM, Li S, et al. Chronic kidney disease and the risk for cardiovascular disease, renal replacement, and death in the United States Medicare population, 1998 to 1999. J Am Soc Nephrol. 2005;16:489-495.
7. Nissenson AR, Collins AJ, Hurley J, et al. Opportunities for improving the care of patients with chronic renal insufficiency: current practice patterns. J Am Soc Nephrol. 2001;12:1713-1720.
8. McClellan WM, Knight DF, Karp H, et al. Early detection and treatment of renal disease in hospitalized diabetic and hypertensive patients: important differences between practice and published guidelines. Am J Kidney Dis. 1997;29:368-375.
9. Obrador GT, Ruthazer R, Arora P, et al. Prevalence of and factors associated with suboptimal care before initiation of dialysis in the United States. J Am Soc Nephrol. 1999;10:1793-1800.
10. Boulware LE, Troll MU, Jaar BG, et al. Identification and referral of patients with progressive CKD: a national study. Am J Kidney Dis. 2006;48:192-204.
11. John R, Webb M, Young A, et al. Unreferred chronic kidney disease: a longitudinal study. Am J Kidney Dis. 2004;43:825-835.
12. Wauters JP, Lameire N, Davison A, et al. Why patients with progressing kidney disease are referred late to the nephrologists: on causes and proposals for improvement. Nephrol Dial Transplant. 2005;20:490-496.
13. Ouseph R, Hendricks P, Hollon JA, et al. Under-recognition of chronic kidney disease in elderly outpatients. Clin Nephrol. 2007;68:373-378.
14. Himmelfarb J, Berns A, Szczech L, et al. Cost, quality, and value: the changing political economy of dialysis care. J Am Soc Nephrol. 2007;18:2021-2027.
15. Vassalotti JA, Stevens LA, Levey AS. Testing for chronic kidney disease: a position statement from the National Kidney Foundation. Am J Kidney Dis. 2007;50:169-180.
16. Saran AM, DuBose TD, Jr. Cardiovascular disease in chronic kidney disease. Ther Adv Cardiovasc Dis. 2008;2:425-434.
17. Mental Health America. Fact sheet: co-occurring disorders and depression. Available at: http://www.nmha.org/index.cfm?objectid=C7DF94C1-1372-4D20-C8FE4E509C20471B. Accessed January 25, 2009.
18. Cukor D, Coplan J, Brown C, et al. Course of depression and anxiety diagnosis in patients treated with hemodialysis: a 16-month follow-up. Am Soc Nephrol. 2008;3:1752-1758.
19. Lopez Revuelta K, Garcia Lopez FJ, de Alvaro Moreno F, et al. Perceived mental health at the start of dialysis as a predictor of morbidity and mortality in patients with end stage renal disease (CALVIDIA Study). Nephrol Dial Transplant. 2004;19:2347-2353.
20. Ford DE. A primary care approach: Managing depression in the face of chronic medical conditions. Am J Med. 2008;121(suppl 2):S38-S44.
21. Ferrari P. Prescribing angiotensin converting enzyme inhibitors and angiotensin receptor blockers in chronic kidney disease. Nephrol. 2007;12:81-89.
22. Song SH, Kwak IS, Lee DW, et al. The prevalence of low triiodothyronine according to the stage of chronic kidney disease in subjects with a normal thyroid-stimulating hormone. Nephrol Dial Transplant. 2009;24:1534-1538.
23. Ravani P, Malberti F, Tripepi G, et al. Vitamin D levels and patient outcome in chronic kidney disease. Kidney Int. 2009;75:88-95.
24. Cupisti A, Aparicio M, Barsotti G. Potential benefits of renal diets on cardiovascular risk factors in chronic kidney disease patients. Ren Fail. 2007;29:529-534.
25. Beto JA, Bansal VK. Medical nutrition therapy in chronic kidney failure: Integrating clinical practice guidelines. J Am Diet Assoc. 2004;104:404-409.
26. Al-Aly Z. The new role of calcimimetics as vasculotropic agents. Kidney Int. 2009;75:9-12.
27. Taliercio JJ. Anemia and chronic kidney disease: what’s the connection? J Fam Pract. 2010;59:14-18.
28. Chan MR, Dall AT, Fletcher KE, et al. Outcomes in patients with chronic kidney disease referred late to nephrologists: a meta-analysis. Am J Med. 2007;120:1063-1070.
29. Almaguer M, Herrera R, Alfonso J, et al. Primary health care strategies for the prevention of end-stage renal disease in Cuba. Kidney Int. 2005;68(suppl 97s):S4-S10.
30. Durose CL, Holdsworth M, Watson V, et al. Knowledge of dietary restrictions and the medical consequences of noncompliance by patients on hemodialysis are not predictive of dietary compliance. Am Diet Assoc. 2004;104:35-41.
31. Linden A, Butterworth SW, Roberts N. Disease management interventions II: what else is in the black box? Dis Manage. 2006;9:73-85.
32. Moyers TB, Martin T. Therapist influence on client language during motivational interviewing sessions. J Subst Abuse Treat. 2006;30:245-251.
33. Moyers TB, Martin T, Christopher PJ, et al. Client language as a mediator of motivational interviewing efficacy: where is the evidence? Alcohol Clin Exp Res. 2007;31(10 suppl):40s-47s.
34. Butterworth S, Linden A, McClay W. Health coaching as an intervention in health management programs. Dis Manage Health Outcomes. 2007;15:299-307.
35. Rollnick S, Miller WR, Butler CC. Motivational Interviewing in Health Care: Helping Patients Change Behavior. New York, NY: Guilford Press; 2008.
36. Miller WR. Motivational interviewing with problem drinkers. Behav Psychother. 1983;11:147-172.
37. Hettema J, Steele J, Miller WR. Motivational interviewing. Ann Rev Clin Psych. 2005;1:91-111.
38. Rubak S, Sandbaek A, Lauritzen T, et al. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55:305-312.
The Journal of Family Practice ©2010 Dowden Health Media