User login
Part 1: The Study in Question
Recently, my colleague Randy D. Danielsen, PhD, DFAAPA, PA-C Emeritus, shared a study from the American Journal of Emergency Medicine that focused on “the involvement of NPs and PAs who billed independently” in emergency departments (EDs).1 In casual conversation, several of us agreed the findings didn’t “pass the sniff test,” so I decided to do some investigating.
The context: Data from 2006-2009 indicate that in two-thirds of all EDs, NPs and PAs are involved in the care of 13.7% of all patients.2 Further analysis of Medicare Public Use Files from 2014 reveal that of 58,641 unique emergency medicine clinicians, 14,360 (24.5%) are advanced practice providers.3 All interesting statistics.
The American Journal of Emergency Medicine article, however, gave me (and several colleagues) pause. In it, the authors presented their analysis of Medicare provider utilization and payment data from 2012-2016.1 The researchers documented billing increases of 65% for NPs and 35% for PAs.
But what stopped me in my tracks was that the researchers emphasized an increase—from 18% to 24%—in NP/PA treatment of patients with the highest severity illness or injury (CPT code 99285).1 I discussed this finding with ED-based colleagues, and they too questioned its accuracy.
In fact, the more we parsed this study, the more questions we had … and the higher our eyebrows raised. What were the researchers examining and drawing conclusions on— independent billing by NPs and PAs, or independent practice? These are two very different measures. Were the authors in fact grousing about the increase in NP/PA providers in EDs?
There is a paucity of research on billing by NPs and PAs, and the discussion surrounding this particular study will undoubtedly prompt additional questions. Over the next 3 weeks, we invite you to join us on Thursdays as we continue our examination of this data—and encourage you to share your thoughts with us along the way!
1. Bai G, Kelen GD, Frick KD, Anderson GF. Nurse practitioners and physician assistants in emergency medical services who billed independently, 2012-2016. Am J Emerg Med. https://doi.org/10.1016/j.ajem.2019.01.052. Accessed April 1, 2019.
2. Wilder JL, Rooks, SP, Ginde AA. Update on midlevel provider utilization in US emergency departments, 2006 to 2009. Academic Emerg Med. 2012;19(8):986-989.
3. Hall MK, Burns K, Carius M, et al. State of the national emergency department workforce: who provides care where? Ann Emerg Med. 2018;72(3):302-307.
Recently, my colleague Randy D. Danielsen, PhD, DFAAPA, PA-C Emeritus, shared a study from the American Journal of Emergency Medicine that focused on “the involvement of NPs and PAs who billed independently” in emergency departments (EDs).1 In casual conversation, several of us agreed the findings didn’t “pass the sniff test,” so I decided to do some investigating.
The context: Data from 2006-2009 indicate that in two-thirds of all EDs, NPs and PAs are involved in the care of 13.7% of all patients.2 Further analysis of Medicare Public Use Files from 2014 reveal that of 58,641 unique emergency medicine clinicians, 14,360 (24.5%) are advanced practice providers.3 All interesting statistics.
The American Journal of Emergency Medicine article, however, gave me (and several colleagues) pause. In it, the authors presented their analysis of Medicare provider utilization and payment data from 2012-2016.1 The researchers documented billing increases of 65% for NPs and 35% for PAs.
But what stopped me in my tracks was that the researchers emphasized an increase—from 18% to 24%—in NP/PA treatment of patients with the highest severity illness or injury (CPT code 99285).1 I discussed this finding with ED-based colleagues, and they too questioned its accuracy.
In fact, the more we parsed this study, the more questions we had … and the higher our eyebrows raised. What were the researchers examining and drawing conclusions on— independent billing by NPs and PAs, or independent practice? These are two very different measures. Were the authors in fact grousing about the increase in NP/PA providers in EDs?
There is a paucity of research on billing by NPs and PAs, and the discussion surrounding this particular study will undoubtedly prompt additional questions. Over the next 3 weeks, we invite you to join us on Thursdays as we continue our examination of this data—and encourage you to share your thoughts with us along the way!
Recently, my colleague Randy D. Danielsen, PhD, DFAAPA, PA-C Emeritus, shared a study from the American Journal of Emergency Medicine that focused on “the involvement of NPs and PAs who billed independently” in emergency departments (EDs).1 In casual conversation, several of us agreed the findings didn’t “pass the sniff test,” so I decided to do some investigating.
The context: Data from 2006-2009 indicate that in two-thirds of all EDs, NPs and PAs are involved in the care of 13.7% of all patients.2 Further analysis of Medicare Public Use Files from 2014 reveal that of 58,641 unique emergency medicine clinicians, 14,360 (24.5%) are advanced practice providers.3 All interesting statistics.
The American Journal of Emergency Medicine article, however, gave me (and several colleagues) pause. In it, the authors presented their analysis of Medicare provider utilization and payment data from 2012-2016.1 The researchers documented billing increases of 65% for NPs and 35% for PAs.
But what stopped me in my tracks was that the researchers emphasized an increase—from 18% to 24%—in NP/PA treatment of patients with the highest severity illness or injury (CPT code 99285).1 I discussed this finding with ED-based colleagues, and they too questioned its accuracy.
In fact, the more we parsed this study, the more questions we had … and the higher our eyebrows raised. What were the researchers examining and drawing conclusions on— independent billing by NPs and PAs, or independent practice? These are two very different measures. Were the authors in fact grousing about the increase in NP/PA providers in EDs?
There is a paucity of research on billing by NPs and PAs, and the discussion surrounding this particular study will undoubtedly prompt additional questions. Over the next 3 weeks, we invite you to join us on Thursdays as we continue our examination of this data—and encourage you to share your thoughts with us along the way!
1. Bai G, Kelen GD, Frick KD, Anderson GF. Nurse practitioners and physician assistants in emergency medical services who billed independently, 2012-2016. Am J Emerg Med. https://doi.org/10.1016/j.ajem.2019.01.052. Accessed April 1, 2019.
2. Wilder JL, Rooks, SP, Ginde AA. Update on midlevel provider utilization in US emergency departments, 2006 to 2009. Academic Emerg Med. 2012;19(8):986-989.
3. Hall MK, Burns K, Carius M, et al. State of the national emergency department workforce: who provides care where? Ann Emerg Med. 2018;72(3):302-307.
1. Bai G, Kelen GD, Frick KD, Anderson GF. Nurse practitioners and physician assistants in emergency medical services who billed independently, 2012-2016. Am J Emerg Med. https://doi.org/10.1016/j.ajem.2019.01.052. Accessed April 1, 2019.
2. Wilder JL, Rooks, SP, Ginde AA. Update on midlevel provider utilization in US emergency departments, 2006 to 2009. Academic Emerg Med. 2012;19(8):986-989.
3. Hall MK, Burns K, Carius M, et al. State of the national emergency department workforce: who provides care where? Ann Emerg Med. 2018;72(3):302-307.
Thoughts for Thursday
Email Marie-Eileen Onieal, PhD, CPNP, FAANP, at: [email protected]
Email Randy D. Danielsen, PhD, DFAAPA, PA-C Emeritus, at: [email protected]
Email Marie-Eileen Onieal, PhD, CPNP, FAANP, at: [email protected]
Email Randy D. Danielsen, PhD, DFAAPA, PA-C Emeritus, at: [email protected]
Email Marie-Eileen Onieal, PhD, CPNP, FAANP, at: [email protected]
Email Randy D. Danielsen, PhD, DFAAPA, PA-C Emeritus, at: [email protected]
Reframing the conversation around the ‘gender-reveal’ ultrasound
How revealing fetal anatomy, not gender, is inclusive
Every ob.gyn. expects that the topic of gender will come up at some point in a patient’s pregnancy. “When will I find out the gender?” asks the 24-year-old at her first prenatal visit. “We want the gender to be a surprise!” exclaims the couple at their anatomy scan for their second in vitro fertilization pregnancy. “Do you know what you’re having?” asks the obstetrician anticipating an imminent delivery.
The topic of gender is in fact so ingrained in our practice that we don’t bat an eye when approached with questions about fetal gender. But what exactly are we talking about when we discuss the gender of an unborn baby?
As we established in our previous column, gender identity is an internal experience of gender that one feels to be a part of oneself. So, then, what does an ultrasound actually reveal? Objectively, ultrasound can show the provider the presence or absence of a hyperechoic anatomical structure between the fetal legs that may become a penis, a vagina, or an ambiguous form of genitalia. While ultrasound is an incredible tool for anatomical and other forms of antenatal testing, ultrasound cannot detect identity characteristics because identities are, by definition, socially and internally experienced without respect to anatomy.
The distinction between gender identity and sex assigned at birth in discussions of antenatal ultrasonography is more than just a simple problem of semantics or vocabulary. To describe a fetus as a boy or a girl based on the presence/absence of a projection between the fetal legs seen on ultrasound is to reinforce the idea that gender identity and sex assigned at birth are equivalent. This conflation also erases nonbinary, genderqueer, and many other groups that identify with genders other than “boy” or “girl.” To be clear, unborn fetuses do not have a gender identity. Studies have shown that children begin to self-label their gender as early as 18-24 months of age, and similarly those who grow up to inhabit gender-nonconforming identities usually already are starting to show signs of their nonconformity starting at age 2 years.1 Some of the deepest traumas that trans and gender-nonconforming people experience are rated to the enforcement of unwritten gender laws during early childhood that are applied based on the sex assigned at birth.
Obstetricians can help to break the cycle of inappropriate gender assignment by correctly using the terms “gender” and “sex assigned at birth.” One opportunity for addressing patients’ questions about fetal gender might be to avoid the term “gender” altogether when discussing fetal sex assigned at birth, emphasizing instead what fetal ultrasound is actually able to do: Give us information about the appearance of external genitalia to help predict what sex will be assigned at birth.2 We have used this strategy when performing anatomy scans, and our experience has been that patients often will make their own assumptions about what it means to see certain external genitalia on ultrasound between the fetal legs. Motivated providers who want to go the extra mile may use a patient’s exclamation about their understanding of the fetus’s gender as an opportunity to educate the patient on the distinction between gender and sex assigned at birth, but even just smiling and moving onto the next part of the scan is an appropriate way of maintaining an atmosphere of inclusion and respect.
One of the roots of gender-based violence and gender dysphoria later in life is the conflation of gender and sex assigned at birth. While there is an entire social and political framework that enforces and polices gender after birth, the obstetrician can take steps to break the cycle starting before the birth has even occurred. Obstetricians are tasked with the unique challenge of providing care for the mother-fetus dyad, and much of the work is in setting up the fetus for the best possible life. Our scope of inclusion should be sufficiently wide to account for nonanatomical variations that could develop later in life in the infants we deliver.
Dr. Bahng is a PGY-1 resident physician in the gynecology & obstetrics residency program at Emory University, Atlanta. Dr. Bahng identifies as nonbinary and uses they/them/their as their personal pronouns. Dr. Joyner is an assistant professor at Emory University and is the director of gynecologic services in the Gender Center at Grady Memorial Hospital in Atlanta. Dr. Joyner identifies as a cisgender female and uses she/hers/her as her personal pronouns. Dr. Bahng and Dr. Joyner reported no financial disclosures.
References
1. Horm Behav. 2013 Jul;64(2):288-97.
2. Obstet Gynecol Surv. 2009 Jan;64(1):50-7.
How revealing fetal anatomy, not gender, is inclusive
How revealing fetal anatomy, not gender, is inclusive
Every ob.gyn. expects that the topic of gender will come up at some point in a patient’s pregnancy. “When will I find out the gender?” asks the 24-year-old at her first prenatal visit. “We want the gender to be a surprise!” exclaims the couple at their anatomy scan for their second in vitro fertilization pregnancy. “Do you know what you’re having?” asks the obstetrician anticipating an imminent delivery.
The topic of gender is in fact so ingrained in our practice that we don’t bat an eye when approached with questions about fetal gender. But what exactly are we talking about when we discuss the gender of an unborn baby?
As we established in our previous column, gender identity is an internal experience of gender that one feels to be a part of oneself. So, then, what does an ultrasound actually reveal? Objectively, ultrasound can show the provider the presence or absence of a hyperechoic anatomical structure between the fetal legs that may become a penis, a vagina, or an ambiguous form of genitalia. While ultrasound is an incredible tool for anatomical and other forms of antenatal testing, ultrasound cannot detect identity characteristics because identities are, by definition, socially and internally experienced without respect to anatomy.
The distinction between gender identity and sex assigned at birth in discussions of antenatal ultrasonography is more than just a simple problem of semantics or vocabulary. To describe a fetus as a boy or a girl based on the presence/absence of a projection between the fetal legs seen on ultrasound is to reinforce the idea that gender identity and sex assigned at birth are equivalent. This conflation also erases nonbinary, genderqueer, and many other groups that identify with genders other than “boy” or “girl.” To be clear, unborn fetuses do not have a gender identity. Studies have shown that children begin to self-label their gender as early as 18-24 months of age, and similarly those who grow up to inhabit gender-nonconforming identities usually already are starting to show signs of their nonconformity starting at age 2 years.1 Some of the deepest traumas that trans and gender-nonconforming people experience are rated to the enforcement of unwritten gender laws during early childhood that are applied based on the sex assigned at birth.
Obstetricians can help to break the cycle of inappropriate gender assignment by correctly using the terms “gender” and “sex assigned at birth.” One opportunity for addressing patients’ questions about fetal gender might be to avoid the term “gender” altogether when discussing fetal sex assigned at birth, emphasizing instead what fetal ultrasound is actually able to do: Give us information about the appearance of external genitalia to help predict what sex will be assigned at birth.2 We have used this strategy when performing anatomy scans, and our experience has been that patients often will make their own assumptions about what it means to see certain external genitalia on ultrasound between the fetal legs. Motivated providers who want to go the extra mile may use a patient’s exclamation about their understanding of the fetus’s gender as an opportunity to educate the patient on the distinction between gender and sex assigned at birth, but even just smiling and moving onto the next part of the scan is an appropriate way of maintaining an atmosphere of inclusion and respect.
One of the roots of gender-based violence and gender dysphoria later in life is the conflation of gender and sex assigned at birth. While there is an entire social and political framework that enforces and polices gender after birth, the obstetrician can take steps to break the cycle starting before the birth has even occurred. Obstetricians are tasked with the unique challenge of providing care for the mother-fetus dyad, and much of the work is in setting up the fetus for the best possible life. Our scope of inclusion should be sufficiently wide to account for nonanatomical variations that could develop later in life in the infants we deliver.
Dr. Bahng is a PGY-1 resident physician in the gynecology & obstetrics residency program at Emory University, Atlanta. Dr. Bahng identifies as nonbinary and uses they/them/their as their personal pronouns. Dr. Joyner is an assistant professor at Emory University and is the director of gynecologic services in the Gender Center at Grady Memorial Hospital in Atlanta. Dr. Joyner identifies as a cisgender female and uses she/hers/her as her personal pronouns. Dr. Bahng and Dr. Joyner reported no financial disclosures.
References
1. Horm Behav. 2013 Jul;64(2):288-97.
2. Obstet Gynecol Surv. 2009 Jan;64(1):50-7.
Every ob.gyn. expects that the topic of gender will come up at some point in a patient’s pregnancy. “When will I find out the gender?” asks the 24-year-old at her first prenatal visit. “We want the gender to be a surprise!” exclaims the couple at their anatomy scan for their second in vitro fertilization pregnancy. “Do you know what you’re having?” asks the obstetrician anticipating an imminent delivery.
The topic of gender is in fact so ingrained in our practice that we don’t bat an eye when approached with questions about fetal gender. But what exactly are we talking about when we discuss the gender of an unborn baby?
As we established in our previous column, gender identity is an internal experience of gender that one feels to be a part of oneself. So, then, what does an ultrasound actually reveal? Objectively, ultrasound can show the provider the presence or absence of a hyperechoic anatomical structure between the fetal legs that may become a penis, a vagina, or an ambiguous form of genitalia. While ultrasound is an incredible tool for anatomical and other forms of antenatal testing, ultrasound cannot detect identity characteristics because identities are, by definition, socially and internally experienced without respect to anatomy.
The distinction between gender identity and sex assigned at birth in discussions of antenatal ultrasonography is more than just a simple problem of semantics or vocabulary. To describe a fetus as a boy or a girl based on the presence/absence of a projection between the fetal legs seen on ultrasound is to reinforce the idea that gender identity and sex assigned at birth are equivalent. This conflation also erases nonbinary, genderqueer, and many other groups that identify with genders other than “boy” or “girl.” To be clear, unborn fetuses do not have a gender identity. Studies have shown that children begin to self-label their gender as early as 18-24 months of age, and similarly those who grow up to inhabit gender-nonconforming identities usually already are starting to show signs of their nonconformity starting at age 2 years.1 Some of the deepest traumas that trans and gender-nonconforming people experience are rated to the enforcement of unwritten gender laws during early childhood that are applied based on the sex assigned at birth.
Obstetricians can help to break the cycle of inappropriate gender assignment by correctly using the terms “gender” and “sex assigned at birth.” One opportunity for addressing patients’ questions about fetal gender might be to avoid the term “gender” altogether when discussing fetal sex assigned at birth, emphasizing instead what fetal ultrasound is actually able to do: Give us information about the appearance of external genitalia to help predict what sex will be assigned at birth.2 We have used this strategy when performing anatomy scans, and our experience has been that patients often will make their own assumptions about what it means to see certain external genitalia on ultrasound between the fetal legs. Motivated providers who want to go the extra mile may use a patient’s exclamation about their understanding of the fetus’s gender as an opportunity to educate the patient on the distinction between gender and sex assigned at birth, but even just smiling and moving onto the next part of the scan is an appropriate way of maintaining an atmosphere of inclusion and respect.
One of the roots of gender-based violence and gender dysphoria later in life is the conflation of gender and sex assigned at birth. While there is an entire social and political framework that enforces and polices gender after birth, the obstetrician can take steps to break the cycle starting before the birth has even occurred. Obstetricians are tasked with the unique challenge of providing care for the mother-fetus dyad, and much of the work is in setting up the fetus for the best possible life. Our scope of inclusion should be sufficiently wide to account for nonanatomical variations that could develop later in life in the infants we deliver.
Dr. Bahng is a PGY-1 resident physician in the gynecology & obstetrics residency program at Emory University, Atlanta. Dr. Bahng identifies as nonbinary and uses they/them/their as their personal pronouns. Dr. Joyner is an assistant professor at Emory University and is the director of gynecologic services in the Gender Center at Grady Memorial Hospital in Atlanta. Dr. Joyner identifies as a cisgender female and uses she/hers/her as her personal pronouns. Dr. Bahng and Dr. Joyner reported no financial disclosures.
References
1. Horm Behav. 2013 Jul;64(2):288-97.
2. Obstet Gynecol Surv. 2009 Jan;64(1):50-7.
Personalizing guideline-driven cancer screening
Reports of cancer date back thousands of years to Egyptian texts. Its existence baffled scientists until the 1950s, when Watson, Crick, and Franklin discovered the structure of DNA, laying the groundwork for identifying the genetic pathways leading to cancer. Currently, cancer is a leading global cause of death and the second leading cause of death in the United States.1,2
In an effort to curtail cancer and its related morbidity and mortality, population-based screening programs have been implemented with tests that identify precancerous lesions and, preferably, early-stage rather than late-stage cancer.
Screening for cancer can lead to early diagnosis and prevent death from cancer, but the topic continues to provoke controversy.
VALUE OF SCREENING QUESTIONED
In a commentary in the March 2019 Cleveland Clinic Journal of Medicine, Kim et al3 argued that cancer screening is not very effective and that we need to find the balance between the potential benefit and harm.
Using data from the US Preventive Services Task Force (USPSTF) and various studies, the authors showed that although screening can prevent some deaths from breast, colon, prostate, and lung cancer, at least 3 times as many people who are screened still die of those diseases. Given that screening does not eliminate all cancer deaths, has not been definitely shown to decrease the all-cause mortality rate, and has the potential to harm through false-positive results, overdiagnosis, and overtreatment, the authors questioned the utility of screening and encouraged us to discuss the benefits and harms with our patients.
In view of the apparently meager benefit, the USPSTF has relaxed its recommendations for screening for breast and prostate cancer in average-risk populations in recent years, a move that has evoked strong reactions from some clinicians. Proponents of screening argue that preventing late-stage cancers can save money, as the direct and indirect costs of morbidity associated with late-stage cancers are substantial, and that patients prefer screening when a test is available. Current models of screening efficacy do not take these factors into account.4
Kim et al, in defending the USPSTF’s position, suggested that the motivation for aggressive testing may be a belief that no harm is greater than the benefit of saving a life. They illustrated this through a Swiftian “modest proposal,” ie, universal prophylactic organectomy to prevent cancer. This hypothetical extreme measure would nearly eliminate the risk of cancer in the removed organs and prevent overdiagnosis and overtreatment of malignancies, but at substantial harm and cost.
In response to this proposal, we would like to point out the alternative extreme: stop all cancer screening programs. The pendulum would swing from what was previously considered a benefit—cancer prevention—to a harm, ie, cancer.
IN DEFENSE OF CANCER SCREENING
Observational studies, systematic reviews, meta-analyses, and modeling studies show that screening for cervical, colorectal, breast, and prostate cancer decreases disease-specific mortality.5–11
For example, in lung cancer, the National Lung Screening Trial demonstrated reductions in disease-specific and overall mortality in patients at high risk who underwent low-dose screening computed tomography.12
In breast cancer, a systematic review demonstrated decreased disease-specific mortality for women ages 50 through 79 who underwent screening mammography.13
In cervical cancer, lower rates of cancer-related death and invasive cancer have also been shown with screening.14
In colorectal cancer, great strides have been made in reducing both the incidence of and mortality from this disease over the past 30 years through fecal occult blood testing. Early detection shifts the 5-year survival rate—14% for late-stage cancer—to over 90%.15 Colorectal cancer screening has also been shown to be cost-effective, with savings in excess of $30,000 per life-year gained from screening.16
Moreover, recent data from the Prostate, Lung, Colorectal, and Ovarian Cancer (PLCO) screening trial17 demonstrated a 2-fold higher overall non-cancer-related mortality rate in participants who did not adhere to screening compared with those who were fully adherent to all sex-specific PLCO screening tests when adjusted for age, sex, and ethnicity. Although a possible explanation is that people who adhere to screening recommendations are also likely to have a healthier lifestyle overall, the association persisted (although it was slightly attenuated) even after adjusting for medical risk and behavioral factors.
ON THIS WE CAN AGREE
Like Kim et al, we also believe an informed discussion of screening should occur with each patient—and challenge Kim et al to design an efficient and practical approach to allow providers to do so in a busy office visit aimed to address and manage other competing diseases.
In addition, medical science needs to improve. Methods to increase the efficacy of screening and decrease risks should be explored; these include improving test and operator performance, reducing nonadherence to screening, investigating novel biomarkers or precursors of cancer and pathways that escape current detection, and devising better risk-stratification tools.
Bodies such as the USPSTF should use models that account for factors not considered previously but important when informing patients of potential benefits and harm. Examples include varying sensitivities and specificities at different rounds of testing and accounting for the variability in risk or efficacy affected by race, ethnicity, sex, and patient preferences.
We practice in the era of evidence-based medicine. Guidelines and recommendations are based on the available evidence. As more studies are published, disease mechanisms are better understood, and the effects of previous recommendations are evaluated, cancer screening programs will be further refined or replaced. The balance between benefit and harm will be further delineated.
Kim et al knocked on the door of personalized medicine, where individual screening will be based on individual risk. Until that door is opened, screening should be personalized through the risk-benefit discussions we have with our patients. Ultimately, the choice to undergo screening is the patient’s.
- Torre LA, Siegel RL, Ward EM, Jemal A. Global cancer incidence and mortality rates and trends—an update. Cancer Epidemiol Biomarkers Prev 2016; 25(1):16–27. doi:10.1158/1055-9965.EPI-15-0578
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin 2018; 68(1):7–30. doi:10.3322/caac.21442
- Kim MS, Nishikawa G, Prasad V. Cancer screening: a modest proposal for prevention. Cleve Clin J Med 2019; 86(3):157–160. doi:10.3949/ccjm.86a.18092
- Knudsen AB, Zauber AG, Rutter CM, et al. Estimation of benefits, burden, and harms of colorectal cancer screening strategies: modeling study for the US Preventive Services Task Force. JAMA 2016; 315(23):2595–2609. doi:10.1001/jama.2016.6828
- Peirson L, Fitzpatrick-Lewis D, Ciliska D, Warren R. Screening for cervical cancer: a systematic review and meta-analysis. Syst Rev 2013; 2:35. doi:10.1186/2046-4053-2-35
- Whitlock EP, Vesco KK, Eder M, Lin JS, Senger CA, Burda BU. Liquid-based cytology and human papillomavirus testing to screen for cervical cancer: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med 2011; 155(10):687–697. doi:10.7326/0003-4819-155-10-201111150-00376
- Yang DX, Gross CP, Soulos PR, Yu JB. Estimating the magnitude of colorectal cancers prevented during the era of screening: 1976 to 2009. Cancer 2014; 120:2893–2901. doi:10.1002/cncr.28794
- Edwards BK, Ward E, Kohler BA, et al. Annual report to the nation on the status of cancer, 1975–2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer 2010; 116(3):544–573. doi:10.1002/cncr.24760
- Myers ER, Moorman P, Gierisch JM, et al. Benefits and harms of breast cancer screening: a systematic review. JAMA 2015; 314(15):1615–1634. doi:10.1001/jama.2015.13183
- Independent UK Panel on Breast Cancer Screening. The benefits and harms of breast cancer screening: an independent review. Lancet 2012; 380(9855):1778–1786. doi:10.1016/S0140-6736(12)61611-0
- Etzioni R, Tsodikov A, Mariotto A, et al. Quantifying the role of PSA screening in the US prostate cancer mortality decline. Cancer Causes Control 2008; 19(2):175–181. doi:10.1007/s10552-007-9083-8
- National Lung Screening Trial Research Team, Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011; 365(5):395–409. doi:10.1056/NEJMoa1102873
- Nelson HD, Fu R, Cantor A, et al. Effectiveness of breast cancer screening: systematic review and meta-analysis to update the 2009 U.S. Preventive Services Task Force recommendation. Ann Intern Med 2016; 164(4):244–255. doi:10.7326/M15-0969
- US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, et al. Screening for cervical cancer: US Preventive Services Task Force recommendation statement. JAMA 2018; 320(7):674–686. doi:10.1001/jama.2018.10897
- Kopetz S, Chang GJ, Overman MJ, et al. Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol 2009; 27(22):3677–3683. doi:10.1200/JCO.2008.20.5278
- Patel S, Kilgore M. Cost effectiveness of colorectal cancer screening strategies. Cancer Control 2015; 22(2):248–258. doi:10.1177/107327481502200219
- Pierre-Victor D, Pinsky PF. Association of nonadherence to cancer screening examinations with mortality from unrelated causes: a secondary analysis of the PLCO cancer screening trial. JAMA Intern Med 2019; 179(2):196–203. doi:10.1001/jamainternmed.2018.5982
Reports of cancer date back thousands of years to Egyptian texts. Its existence baffled scientists until the 1950s, when Watson, Crick, and Franklin discovered the structure of DNA, laying the groundwork for identifying the genetic pathways leading to cancer. Currently, cancer is a leading global cause of death and the second leading cause of death in the United States.1,2
In an effort to curtail cancer and its related morbidity and mortality, population-based screening programs have been implemented with tests that identify precancerous lesions and, preferably, early-stage rather than late-stage cancer.
Screening for cancer can lead to early diagnosis and prevent death from cancer, but the topic continues to provoke controversy.
VALUE OF SCREENING QUESTIONED
In a commentary in the March 2019 Cleveland Clinic Journal of Medicine, Kim et al3 argued that cancer screening is not very effective and that we need to find the balance between the potential benefit and harm.
Using data from the US Preventive Services Task Force (USPSTF) and various studies, the authors showed that although screening can prevent some deaths from breast, colon, prostate, and lung cancer, at least 3 times as many people who are screened still die of those diseases. Given that screening does not eliminate all cancer deaths, has not been definitely shown to decrease the all-cause mortality rate, and has the potential to harm through false-positive results, overdiagnosis, and overtreatment, the authors questioned the utility of screening and encouraged us to discuss the benefits and harms with our patients.
In view of the apparently meager benefit, the USPSTF has relaxed its recommendations for screening for breast and prostate cancer in average-risk populations in recent years, a move that has evoked strong reactions from some clinicians. Proponents of screening argue that preventing late-stage cancers can save money, as the direct and indirect costs of morbidity associated with late-stage cancers are substantial, and that patients prefer screening when a test is available. Current models of screening efficacy do not take these factors into account.4
Kim et al, in defending the USPSTF’s position, suggested that the motivation for aggressive testing may be a belief that no harm is greater than the benefit of saving a life. They illustrated this through a Swiftian “modest proposal,” ie, universal prophylactic organectomy to prevent cancer. This hypothetical extreme measure would nearly eliminate the risk of cancer in the removed organs and prevent overdiagnosis and overtreatment of malignancies, but at substantial harm and cost.
In response to this proposal, we would like to point out the alternative extreme: stop all cancer screening programs. The pendulum would swing from what was previously considered a benefit—cancer prevention—to a harm, ie, cancer.
IN DEFENSE OF CANCER SCREENING
Observational studies, systematic reviews, meta-analyses, and modeling studies show that screening for cervical, colorectal, breast, and prostate cancer decreases disease-specific mortality.5–11
For example, in lung cancer, the National Lung Screening Trial demonstrated reductions in disease-specific and overall mortality in patients at high risk who underwent low-dose screening computed tomography.12
In breast cancer, a systematic review demonstrated decreased disease-specific mortality for women ages 50 through 79 who underwent screening mammography.13
In cervical cancer, lower rates of cancer-related death and invasive cancer have also been shown with screening.14
In colorectal cancer, great strides have been made in reducing both the incidence of and mortality from this disease over the past 30 years through fecal occult blood testing. Early detection shifts the 5-year survival rate—14% for late-stage cancer—to over 90%.15 Colorectal cancer screening has also been shown to be cost-effective, with savings in excess of $30,000 per life-year gained from screening.16
Moreover, recent data from the Prostate, Lung, Colorectal, and Ovarian Cancer (PLCO) screening trial17 demonstrated a 2-fold higher overall non-cancer-related mortality rate in participants who did not adhere to screening compared with those who were fully adherent to all sex-specific PLCO screening tests when adjusted for age, sex, and ethnicity. Although a possible explanation is that people who adhere to screening recommendations are also likely to have a healthier lifestyle overall, the association persisted (although it was slightly attenuated) even after adjusting for medical risk and behavioral factors.
ON THIS WE CAN AGREE
Like Kim et al, we also believe an informed discussion of screening should occur with each patient—and challenge Kim et al to design an efficient and practical approach to allow providers to do so in a busy office visit aimed to address and manage other competing diseases.
In addition, medical science needs to improve. Methods to increase the efficacy of screening and decrease risks should be explored; these include improving test and operator performance, reducing nonadherence to screening, investigating novel biomarkers or precursors of cancer and pathways that escape current detection, and devising better risk-stratification tools.
Bodies such as the USPSTF should use models that account for factors not considered previously but important when informing patients of potential benefits and harm. Examples include varying sensitivities and specificities at different rounds of testing and accounting for the variability in risk or efficacy affected by race, ethnicity, sex, and patient preferences.
We practice in the era of evidence-based medicine. Guidelines and recommendations are based on the available evidence. As more studies are published, disease mechanisms are better understood, and the effects of previous recommendations are evaluated, cancer screening programs will be further refined or replaced. The balance between benefit and harm will be further delineated.
Kim et al knocked on the door of personalized medicine, where individual screening will be based on individual risk. Until that door is opened, screening should be personalized through the risk-benefit discussions we have with our patients. Ultimately, the choice to undergo screening is the patient’s.
Reports of cancer date back thousands of years to Egyptian texts. Its existence baffled scientists until the 1950s, when Watson, Crick, and Franklin discovered the structure of DNA, laying the groundwork for identifying the genetic pathways leading to cancer. Currently, cancer is a leading global cause of death and the second leading cause of death in the United States.1,2
In an effort to curtail cancer and its related morbidity and mortality, population-based screening programs have been implemented with tests that identify precancerous lesions and, preferably, early-stage rather than late-stage cancer.
Screening for cancer can lead to early diagnosis and prevent death from cancer, but the topic continues to provoke controversy.
VALUE OF SCREENING QUESTIONED
In a commentary in the March 2019 Cleveland Clinic Journal of Medicine, Kim et al3 argued that cancer screening is not very effective and that we need to find the balance between the potential benefit and harm.
Using data from the US Preventive Services Task Force (USPSTF) and various studies, the authors showed that although screening can prevent some deaths from breast, colon, prostate, and lung cancer, at least 3 times as many people who are screened still die of those diseases. Given that screening does not eliminate all cancer deaths, has not been definitely shown to decrease the all-cause mortality rate, and has the potential to harm through false-positive results, overdiagnosis, and overtreatment, the authors questioned the utility of screening and encouraged us to discuss the benefits and harms with our patients.
In view of the apparently meager benefit, the USPSTF has relaxed its recommendations for screening for breast and prostate cancer in average-risk populations in recent years, a move that has evoked strong reactions from some clinicians. Proponents of screening argue that preventing late-stage cancers can save money, as the direct and indirect costs of morbidity associated with late-stage cancers are substantial, and that patients prefer screening when a test is available. Current models of screening efficacy do not take these factors into account.4
Kim et al, in defending the USPSTF’s position, suggested that the motivation for aggressive testing may be a belief that no harm is greater than the benefit of saving a life. They illustrated this through a Swiftian “modest proposal,” ie, universal prophylactic organectomy to prevent cancer. This hypothetical extreme measure would nearly eliminate the risk of cancer in the removed organs and prevent overdiagnosis and overtreatment of malignancies, but at substantial harm and cost.
In response to this proposal, we would like to point out the alternative extreme: stop all cancer screening programs. The pendulum would swing from what was previously considered a benefit—cancer prevention—to a harm, ie, cancer.
IN DEFENSE OF CANCER SCREENING
Observational studies, systematic reviews, meta-analyses, and modeling studies show that screening for cervical, colorectal, breast, and prostate cancer decreases disease-specific mortality.5–11
For example, in lung cancer, the National Lung Screening Trial demonstrated reductions in disease-specific and overall mortality in patients at high risk who underwent low-dose screening computed tomography.12
In breast cancer, a systematic review demonstrated decreased disease-specific mortality for women ages 50 through 79 who underwent screening mammography.13
In cervical cancer, lower rates of cancer-related death and invasive cancer have also been shown with screening.14
In colorectal cancer, great strides have been made in reducing both the incidence of and mortality from this disease over the past 30 years through fecal occult blood testing. Early detection shifts the 5-year survival rate—14% for late-stage cancer—to over 90%.15 Colorectal cancer screening has also been shown to be cost-effective, with savings in excess of $30,000 per life-year gained from screening.16
Moreover, recent data from the Prostate, Lung, Colorectal, and Ovarian Cancer (PLCO) screening trial17 demonstrated a 2-fold higher overall non-cancer-related mortality rate in participants who did not adhere to screening compared with those who were fully adherent to all sex-specific PLCO screening tests when adjusted for age, sex, and ethnicity. Although a possible explanation is that people who adhere to screening recommendations are also likely to have a healthier lifestyle overall, the association persisted (although it was slightly attenuated) even after adjusting for medical risk and behavioral factors.
ON THIS WE CAN AGREE
Like Kim et al, we also believe an informed discussion of screening should occur with each patient—and challenge Kim et al to design an efficient and practical approach to allow providers to do so in a busy office visit aimed to address and manage other competing diseases.
In addition, medical science needs to improve. Methods to increase the efficacy of screening and decrease risks should be explored; these include improving test and operator performance, reducing nonadherence to screening, investigating novel biomarkers or precursors of cancer and pathways that escape current detection, and devising better risk-stratification tools.
Bodies such as the USPSTF should use models that account for factors not considered previously but important when informing patients of potential benefits and harm. Examples include varying sensitivities and specificities at different rounds of testing and accounting for the variability in risk or efficacy affected by race, ethnicity, sex, and patient preferences.
We practice in the era of evidence-based medicine. Guidelines and recommendations are based on the available evidence. As more studies are published, disease mechanisms are better understood, and the effects of previous recommendations are evaluated, cancer screening programs will be further refined or replaced. The balance between benefit and harm will be further delineated.
Kim et al knocked on the door of personalized medicine, where individual screening will be based on individual risk. Until that door is opened, screening should be personalized through the risk-benefit discussions we have with our patients. Ultimately, the choice to undergo screening is the patient’s.
- Torre LA, Siegel RL, Ward EM, Jemal A. Global cancer incidence and mortality rates and trends—an update. Cancer Epidemiol Biomarkers Prev 2016; 25(1):16–27. doi:10.1158/1055-9965.EPI-15-0578
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin 2018; 68(1):7–30. doi:10.3322/caac.21442
- Kim MS, Nishikawa G, Prasad V. Cancer screening: a modest proposal for prevention. Cleve Clin J Med 2019; 86(3):157–160. doi:10.3949/ccjm.86a.18092
- Knudsen AB, Zauber AG, Rutter CM, et al. Estimation of benefits, burden, and harms of colorectal cancer screening strategies: modeling study for the US Preventive Services Task Force. JAMA 2016; 315(23):2595–2609. doi:10.1001/jama.2016.6828
- Peirson L, Fitzpatrick-Lewis D, Ciliska D, Warren R. Screening for cervical cancer: a systematic review and meta-analysis. Syst Rev 2013; 2:35. doi:10.1186/2046-4053-2-35
- Whitlock EP, Vesco KK, Eder M, Lin JS, Senger CA, Burda BU. Liquid-based cytology and human papillomavirus testing to screen for cervical cancer: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med 2011; 155(10):687–697. doi:10.7326/0003-4819-155-10-201111150-00376
- Yang DX, Gross CP, Soulos PR, Yu JB. Estimating the magnitude of colorectal cancers prevented during the era of screening: 1976 to 2009. Cancer 2014; 120:2893–2901. doi:10.1002/cncr.28794
- Edwards BK, Ward E, Kohler BA, et al. Annual report to the nation on the status of cancer, 1975–2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer 2010; 116(3):544–573. doi:10.1002/cncr.24760
- Myers ER, Moorman P, Gierisch JM, et al. Benefits and harms of breast cancer screening: a systematic review. JAMA 2015; 314(15):1615–1634. doi:10.1001/jama.2015.13183
- Independent UK Panel on Breast Cancer Screening. The benefits and harms of breast cancer screening: an independent review. Lancet 2012; 380(9855):1778–1786. doi:10.1016/S0140-6736(12)61611-0
- Etzioni R, Tsodikov A, Mariotto A, et al. Quantifying the role of PSA screening in the US prostate cancer mortality decline. Cancer Causes Control 2008; 19(2):175–181. doi:10.1007/s10552-007-9083-8
- National Lung Screening Trial Research Team, Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011; 365(5):395–409. doi:10.1056/NEJMoa1102873
- Nelson HD, Fu R, Cantor A, et al. Effectiveness of breast cancer screening: systematic review and meta-analysis to update the 2009 U.S. Preventive Services Task Force recommendation. Ann Intern Med 2016; 164(4):244–255. doi:10.7326/M15-0969
- US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, et al. Screening for cervical cancer: US Preventive Services Task Force recommendation statement. JAMA 2018; 320(7):674–686. doi:10.1001/jama.2018.10897
- Kopetz S, Chang GJ, Overman MJ, et al. Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol 2009; 27(22):3677–3683. doi:10.1200/JCO.2008.20.5278
- Patel S, Kilgore M. Cost effectiveness of colorectal cancer screening strategies. Cancer Control 2015; 22(2):248–258. doi:10.1177/107327481502200219
- Pierre-Victor D, Pinsky PF. Association of nonadherence to cancer screening examinations with mortality from unrelated causes: a secondary analysis of the PLCO cancer screening trial. JAMA Intern Med 2019; 179(2):196–203. doi:10.1001/jamainternmed.2018.5982
- Torre LA, Siegel RL, Ward EM, Jemal A. Global cancer incidence and mortality rates and trends—an update. Cancer Epidemiol Biomarkers Prev 2016; 25(1):16–27. doi:10.1158/1055-9965.EPI-15-0578
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin 2018; 68(1):7–30. doi:10.3322/caac.21442
- Kim MS, Nishikawa G, Prasad V. Cancer screening: a modest proposal for prevention. Cleve Clin J Med 2019; 86(3):157–160. doi:10.3949/ccjm.86a.18092
- Knudsen AB, Zauber AG, Rutter CM, et al. Estimation of benefits, burden, and harms of colorectal cancer screening strategies: modeling study for the US Preventive Services Task Force. JAMA 2016; 315(23):2595–2609. doi:10.1001/jama.2016.6828
- Peirson L, Fitzpatrick-Lewis D, Ciliska D, Warren R. Screening for cervical cancer: a systematic review and meta-analysis. Syst Rev 2013; 2:35. doi:10.1186/2046-4053-2-35
- Whitlock EP, Vesco KK, Eder M, Lin JS, Senger CA, Burda BU. Liquid-based cytology and human papillomavirus testing to screen for cervical cancer: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med 2011; 155(10):687–697. doi:10.7326/0003-4819-155-10-201111150-00376
- Yang DX, Gross CP, Soulos PR, Yu JB. Estimating the magnitude of colorectal cancers prevented during the era of screening: 1976 to 2009. Cancer 2014; 120:2893–2901. doi:10.1002/cncr.28794
- Edwards BK, Ward E, Kohler BA, et al. Annual report to the nation on the status of cancer, 1975–2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer 2010; 116(3):544–573. doi:10.1002/cncr.24760
- Myers ER, Moorman P, Gierisch JM, et al. Benefits and harms of breast cancer screening: a systematic review. JAMA 2015; 314(15):1615–1634. doi:10.1001/jama.2015.13183
- Independent UK Panel on Breast Cancer Screening. The benefits and harms of breast cancer screening: an independent review. Lancet 2012; 380(9855):1778–1786. doi:10.1016/S0140-6736(12)61611-0
- Etzioni R, Tsodikov A, Mariotto A, et al. Quantifying the role of PSA screening in the US prostate cancer mortality decline. Cancer Causes Control 2008; 19(2):175–181. doi:10.1007/s10552-007-9083-8
- National Lung Screening Trial Research Team, Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011; 365(5):395–409. doi:10.1056/NEJMoa1102873
- Nelson HD, Fu R, Cantor A, et al. Effectiveness of breast cancer screening: systematic review and meta-analysis to update the 2009 U.S. Preventive Services Task Force recommendation. Ann Intern Med 2016; 164(4):244–255. doi:10.7326/M15-0969
- US Preventive Services Task Force, Curry SJ, Krist AH, Owens DK, et al. Screening for cervical cancer: US Preventive Services Task Force recommendation statement. JAMA 2018; 320(7):674–686. doi:10.1001/jama.2018.10897
- Kopetz S, Chang GJ, Overman MJ, et al. Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol 2009; 27(22):3677–3683. doi:10.1200/JCO.2008.20.5278
- Patel S, Kilgore M. Cost effectiveness of colorectal cancer screening strategies. Cancer Control 2015; 22(2):248–258. doi:10.1177/107327481502200219
- Pierre-Victor D, Pinsky PF. Association of nonadherence to cancer screening examinations with mortality from unrelated causes: a secondary analysis of the PLCO cancer screening trial. JAMA Intern Med 2019; 179(2):196–203. doi:10.1001/jamainternmed.2018.5982
The old humanities and the new science at 100: Osler’s enduring message
“Twin berries on one stem, grievous damage has been done to both in regarding the Humanities and Science in any other light than complemental.”
—Sir William Osler1
The year 2019 marks the 100th anniversary of Sir William Osler’s last public speech. Still reeling from the death of his only son in World War I, he had been asked to give the presidential inaugural address of the Classical Association at Oxford. It was the first time a physician had received the honor, and Osler took the assignment very seriously. He chose to speak about “The old humanities and the new science,” and to call for a reunification of the two fields. “Humanists have not enough Science” he warned, “and Science sadly lacks the Humanities…this unhappy divorce…should never have taken place.”1 Later, he said that it was the speech to which he had given the greatest thought and preparation. It was in fact Osler’s personal legacy: 2 months later he turned 70, and 7 months later he was dead.
Revisiting the address today, what can Osler teach the high-tech physician of today, when doctors have become “providers” and patients “consumers”? Is Osler’s message still relevant to our craft, or has he simply become an icon of professional nostalgia with little value for our times?
THE NEED FOR THE HUMANITIES IN MEDICINE
Medicine has certainly grown both powerful and successful. Yet it is also confronting hurdles that would have been unimaginable in Osler’s time. Physicians are now the professionals with the highest suicide rate,2 a burnout rate as high as 70%,3,4 rampant depression,5 dwindling empathy,6 a predominantly negative perception by the public,7,8 and a disturbing propensity to quit.9 These, of course, may just be symptoms of an increasingly meaningless environment wherein doctors have become small cogs in a medical-industrial complex they can’t control or even understand. Still, is it possible that something more personal may have been lost in the way we now select and educate physicians? Could this, in turn, make us less resilient?
In this regard, Osler’s last public speech serves as an enduring reminder of the need for the humanities in medicine. Osler not only believed it, but throughout his life never missed a chance to express in words, writings, and deeds that the humanities are indeed “the hormones” of the profession. In 1919 he warned against the risk of separating our humanistic tradition from the sciences, and urged us “to infect [anyone] with the spirit of the Humanities,” since to him that was “the greatest single gift in education.”1
Unfortunately, the humanities are slippery, not easily quantifiable, hard to define, and seemingly incompatible with an evidence-based approach. Quite understandably, today’s data-obsessed medicine views them with suspicion. But besides reminding us that in medicine not all that counts can be counted, and not all that can be counted counts, the humanities are in fact a fundamental component of the physician’s skill set.
In a multicenter survey of 5 medical schools,10 there was indeed a correlation between students’ exposure to the humanities and many of the personal qualities whose absence we lament in today’s medicine: empathy, tolerance for ambiguity, emotional intelligence, and prevention of burnout. Most significant was a strong correlation with wisdom, as measured by the 21-item Brief Wisdom Screening Scale.11 That all these traits may correlate with humanities exposure is intuitive, since the humanities not only teach tolerance and compassion, but also capture the collective experience of those who came before us. Hence, they teach us wisdom. Wisdom is not an ACGME competency, but it’s undoubtedly a prerequisite for the art of healing.12 In fact, wisdom may very well be the fundamental trait that characterizes a well-rounded physician, since it encompasses empathy, resilience, comfort with ambiguity, and the capacity to learn from the past. Not surprisingly, wisdom in the world was Osler’s closing wish in 1919.
The humanities can also nurture the very personal qualities we desire in physicians. For example, observing drama fosters empathy,13 as does taking an elective in medical humanities.14 Drawing enhances the reading of faces,15 and observing art improves the art of clinical observation.16 Reading good literature prompts better detection of emotions,17 and reflective writing improves students’ well-being.18 Playing a musical instrument reduces burnout.19 And an undergraduate major in the humanities correlates with greater tolerance for ambiguity,20 a highly desirable trait in physicians, since it means openness to new ideas and the capacity to better cope with difficult situations.21
In fact, some of the qualities fostered by the humanities even translate into better patient care. For instance, tolerance for ambiguity correlates with more positive attitudes towards patients who have frustrating complaints,22 with lower use of resources,23 and with a career choice in direct patient care.24 Hence, it has been suggested that it should be a prerequisite for medical school admission.25 Physicians’ empathy is also beneficial, since it correlates with a lower rate of complications and better outcomes in the care of diabetic patients.26 This should not come as a surprise. As Hippocrates put it 2,500 years ago, “some patients, though conscious that their condition is perilous, recover their health simply through their contentment with the goodness of the physician.”27
Lastly, studying the humanities may provide crucial antibodies against the pain and suffering that are unavoidable staples of the human condition. To paraphrase Osler, the humanities might vaccinate us against the difficulties of our profession. Hippocrates himself had suggested that “it is well to superintend the sick to make them well, to care for the healthy to keep them well, but also to care for one’s self…”27 That is why many institutions now require medical students to take humanities courses.28
MEDICINE: AN ART BASED ON SCIENCE
Yet this effort may amount to a rearguard action that arrives too late and provides too little. The humanities should probably be taught before medical school.29 After all, if it’s possible to make a scientist out of a humanist (Osler was living proof), the experience of the past decades seems to suggest that it’s considerably harder to make a humanist out of a scientist—hence the need to revisit undergraduate curricula and admission criteria to medical school, so that students can receive an adequate foundation in both arenas. Ironically, students express positive attitudes toward a liberal education and think it would actually help them as physicians.30 Yet they also understand that the selection process remains tilted towards the sciences.30–32
For Osler, scientific evidence was important but not a substitute for a humanistic approach. As he reminded students, “The practice of medicine is an art based on science,”33 whose main goals are to prevent disease, relieve suffering, and heal the sick. To do so, one ought to care more “for the individual patient than for the special features of the disease.”34 But he warned them, “It is much harder to acquire the art than the science.”35 In fact, “The practice of medicine is a calling in which your heart will be exercised equally with your head.”33 Hence the need to “cultivate equally well hearts and heads.”34 Almost foreseeing our infatuation with guidelines, he also warned against turning medicine into assembly-line work. There are “two great types of practitioners—the routinist and the rationalist,” he said in 1900, and “into the clutches of the demon routine the majority of us ultimately come.”36
Like most great people, Osler was a man of lights, shadows, and contradictions, probably not quite the saint we wish to believe. Yet he provides insights that are as valid today as they were for his own times, and possibly even more so. His 1919 speech is a paean to the humanities, but also a potential eulogy. As a Victorian physician, Osler was a blend of the new science and the old humanities. He knew that “the old art cannot possibly be replaced by, but must be absorbed in, the new science.”35 Yet he could also see the upcoming split between the two cultures, and he tried to warn us. He could in fact foresee the end of an entire way of life. As he said in his address, “there must be a very different civilization or there will be no civilization at all.”1
The crisis we face in medicine today may indeed be a symptom of a much larger cultural shift. As Osler himself put it, “The philosophies of one age have become the absurdities of the next, and the foolishness of yesterday has become the wisdom of tomorrow.”33 Like Osler, we live in times of transition that require us to act. If in 1910 Flexner gave us science,37 Osler in 1919 reminded us that medicine also needs the humanities. We ought to heed his message and reconcile the two fields. The alternative is a future full of tricorders and burned-out technicians, but sorely lacking in healers.
- Osler W. The old humanities and the new science: the presidential address delivered before the Classical Association at Oxford, May, 1919. Br Med J 1919; 2(3053):1–7. pmid:20769536
- Agerbo E, Gunnell D, Bonde JP, Mortensen PB, Nordentoft M. Suicide and occupation: the impact of socio-economic, demographic and psychiatric differences. Psychol Med 2007; 37(8):1131–1140. doi:10.1017/S0033291707000487
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc 2015; 90(12):1600–1613. doi:10.1016/j.mayocp.2015.08.023
- Dyrbye LN, Thomas MR, Massie FS, et al. Burnout and suicidal ideation among US medical students. Ann Intern Med 2008; 149(5):334–341. pmid:18765703
- Mata DA, Ramos MA, Bansal N, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA 2015; 314(22):2373–2383. doi:10.1001/jama.2015.15845
- Hojat M, Mangione S, Nasca TJ, et al. An empirical study of decline in empathy in medical school. Med Educ 2004; 38(9):934–941. doi:10.1111/j.1365-2929.2004.01911.x
- Flores G. Mad scientists, compassionate healers, and greedy egotists: the portrayal of physicians in the movies. J Natl Med Assoc 2002; 94(7):635–658. pmid:12126293
- Imber JB. Trusting Doctors: The Decline of Moral Authority in American Medicine. Princeton, NJ: Princeton University Press; 2008.
- Krauthammer, C. Why doctors quit. The Washington Post. May 28, 2015. https://www.washingtonpost.com/opinions/why-doctors-quit/2015/05/28/1e9d8e6e-056f-11e5-a428-c984eb077d4e_story.html?utm_term=.aa8804a518db. Accessed March 4, 2019.
- Mangione S, Chakraborti C, Staltari G, et al. Medical students' exposure to the humanities correlates with positive personal qualities and reduced burnout: a multi-institutional US survey. J Gen Intern Med 2018; 33(5):628–634. doi:10.1007/s11606-017-4275-8
- Glück J, König S, Naschenweng K, et al. How to measure wisdom: content, reliability, and validity of five measures. Front Psychol 2013; 4:405. doi:10.3389/fpsyg.2013.00405
- Papagiannis A. Eliot’s triad: information, knowledge and wisdom in medicine. Hektoen International. Spring 2014. https://hekint.org/2017/01/29/eliots-triad-information-knowledge-and-wisdom-in-medicine. Accessed March 4, 2019.
- Hojat M, Axelrod D, Spandorfer J, Mangione S. Enhancing and sustaining empathy in medical students. Med Teach 2013; 35(12):996–1001. doi:10.3109/0142159X.2013.802300
- Graham J, Benson LM, Swanson J, Potyk D, Daratha K, Roberts K. Medical humanities coursework is associated with greater measured empathy in medical students. Am J Med 2016; 129(12):1334–1337. doi:10.1016/j.amjmed.2016.08.005
- Brechet C, Baldy R, Picard D. How does Sam feel? Children's labelling and drawing of basic emotions. Br J Dev Psychol 2009; 27(Pt 3):587–606. pmid:19994570
- Naghshineh S, Hafler JP, Miller AR, et al. Formal art observation training improves medical students’ visual diagnostic skills. J Gen Intern Med 2008; 23(7):991–997. doi:10.1007/s11606-008-0667-0
- Kidd DC, Castano E. Reading literary fiction improves theory of mind. Science 2013; 342(6156):377–380. doi:10.1126/science.1239918
- Shapiro J, Kasman D, Shafer A. Words and wards: a model of reflective writing and its uses in medical education. J Med Humanit 2006; 27(4):231–244. doi:10.1007/s10912-006-9020-y
- Bittman BB, Snyder C, Bruhn KT, et al. Recreational music-making: an integrative group intervention for reducing burnout and improving mood states in first year associate degree nursing students: insights and economic impact. Int J Nurs Educ Scholarsh 2004;1:Article12. doi:10.2202/1548-923x.1044
- DeForge BR, Sobal J. Intolerance of ambiguity in students entering medical school. Soc Sci Med 1989; 28(8):869–874. pmid:2705020
- Ghosh AK. Understanding medical uncertainty: a primer for physicians. J Assoc Physicians India 2004; 52:739–742. pmid:15839454
- Merrill JM, Camacho Z, Laux LF, Thornby JI, Vallbona C. How medical school shapes students’ orientation to patients’ psychological problems. Acad Med 1991; 66(9 suppl):S4–S6. pmid:1930523
- Allison JJ, Kiefe CI, Cook EF, Gerrity MS, Orav EJ, Centor R. The association of physician attitudes about uncertainty and risk taking with resource use in a Medicare HMO. Med Decis Making 1998; 18(3):320–329. doi:10.1177/0272989X9801800310
- Gerrity MS, Earp JAL, DeVilles RF, DW Light. Uncertainty and professional work: perceptions of physicians in clinical practice. Am J Sociol 1992; 97(4):1022–1051. https://www.jstor.org/stable/2781505. Accessed March 6, 2019.
- Geller G. Tolerance for ambiguity: an ethics-based criterion for medical student selection. Acad Med 2013; 88(5):581–584. doi:10.1097/ACM.0b013e31828a4b8e
- Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med 2011; 86(3):359–364. doi:10.1097/ACM.0b013e3182086fe1
- Hippocrates. Precepts. Section 8, Part VI. Perseus Digital Library. http://perseus.uchicago.edu/perseus-cgi/citequery3.pl?dbname=GreekFeb2011&getid=1&query=Hipp.%20Praec.%208. Accessed March 4, 2019.
- Kidd MG, Connor JT. Striving to do good things: teaching humanities in Canadian medical schools. J Med Humanit 2008; 29(1):45–54. doi:10.1007/s10912-007-9049-6
- Thomas L. Notes of a biology-watcher. How to fix the premedical curriculum. N Engl J Med 1978; 298(21):1180–1181. doi:10.1056/NEJM197805252982106
- Simmons A. Beyond the premedical syndrome: premedical student attitudes toward liberal education and implications for advising. NACADA Journal 2005; 25(1):64–73.
- Kumar B, Swee ML and Suneja M. The premedical curriculum: we can do better for future physicians. South Med J 2017; 110(8):538–539. doi:10.14423/SMJ.0000000000000683
- Gunderman RB, Kanter SL. Perspective: “how to fix the premedical curriculum” revisited. Acad Med 2008; 83(12):1158–1161. doi:10.1097/ACM.0b013e31818c6515
- Osler W. Aequanimitas with Other Addresses to Medical Students, Nurses and Practitioners of Medicine. Philadelphia, PA: Blakiston; 1904.
- Osler W. Address to the students of the Albany Medical College. Albany Med Ann 1899; 20:307–309.
- Osler W. The reserves of life. St Mary’s Hosp Gaz 1907; 13:95–98.
- Osler W. An address on the importance of post-graduate study. Delivered at the opening of the Museums of the Medical Graduates College and Polyclinic, July 4th, 1900. Br Med J 1900; 2(2063):73–75. pmid:20759107
- Flexner A. Medical Education in the United States and Canada. New York, The Carnegie Foundation 1910.
“Twin berries on one stem, grievous damage has been done to both in regarding the Humanities and Science in any other light than complemental.”
—Sir William Osler1
The year 2019 marks the 100th anniversary of Sir William Osler’s last public speech. Still reeling from the death of his only son in World War I, he had been asked to give the presidential inaugural address of the Classical Association at Oxford. It was the first time a physician had received the honor, and Osler took the assignment very seriously. He chose to speak about “The old humanities and the new science,” and to call for a reunification of the two fields. “Humanists have not enough Science” he warned, “and Science sadly lacks the Humanities…this unhappy divorce…should never have taken place.”1 Later, he said that it was the speech to which he had given the greatest thought and preparation. It was in fact Osler’s personal legacy: 2 months later he turned 70, and 7 months later he was dead.
Revisiting the address today, what can Osler teach the high-tech physician of today, when doctors have become “providers” and patients “consumers”? Is Osler’s message still relevant to our craft, or has he simply become an icon of professional nostalgia with little value for our times?
THE NEED FOR THE HUMANITIES IN MEDICINE
Medicine has certainly grown both powerful and successful. Yet it is also confronting hurdles that would have been unimaginable in Osler’s time. Physicians are now the professionals with the highest suicide rate,2 a burnout rate as high as 70%,3,4 rampant depression,5 dwindling empathy,6 a predominantly negative perception by the public,7,8 and a disturbing propensity to quit.9 These, of course, may just be symptoms of an increasingly meaningless environment wherein doctors have become small cogs in a medical-industrial complex they can’t control or even understand. Still, is it possible that something more personal may have been lost in the way we now select and educate physicians? Could this, in turn, make us less resilient?
In this regard, Osler’s last public speech serves as an enduring reminder of the need for the humanities in medicine. Osler not only believed it, but throughout his life never missed a chance to express in words, writings, and deeds that the humanities are indeed “the hormones” of the profession. In 1919 he warned against the risk of separating our humanistic tradition from the sciences, and urged us “to infect [anyone] with the spirit of the Humanities,” since to him that was “the greatest single gift in education.”1
Unfortunately, the humanities are slippery, not easily quantifiable, hard to define, and seemingly incompatible with an evidence-based approach. Quite understandably, today’s data-obsessed medicine views them with suspicion. But besides reminding us that in medicine not all that counts can be counted, and not all that can be counted counts, the humanities are in fact a fundamental component of the physician’s skill set.
In a multicenter survey of 5 medical schools,10 there was indeed a correlation between students’ exposure to the humanities and many of the personal qualities whose absence we lament in today’s medicine: empathy, tolerance for ambiguity, emotional intelligence, and prevention of burnout. Most significant was a strong correlation with wisdom, as measured by the 21-item Brief Wisdom Screening Scale.11 That all these traits may correlate with humanities exposure is intuitive, since the humanities not only teach tolerance and compassion, but also capture the collective experience of those who came before us. Hence, they teach us wisdom. Wisdom is not an ACGME competency, but it’s undoubtedly a prerequisite for the art of healing.12 In fact, wisdom may very well be the fundamental trait that characterizes a well-rounded physician, since it encompasses empathy, resilience, comfort with ambiguity, and the capacity to learn from the past. Not surprisingly, wisdom in the world was Osler’s closing wish in 1919.
The humanities can also nurture the very personal qualities we desire in physicians. For example, observing drama fosters empathy,13 as does taking an elective in medical humanities.14 Drawing enhances the reading of faces,15 and observing art improves the art of clinical observation.16 Reading good literature prompts better detection of emotions,17 and reflective writing improves students’ well-being.18 Playing a musical instrument reduces burnout.19 And an undergraduate major in the humanities correlates with greater tolerance for ambiguity,20 a highly desirable trait in physicians, since it means openness to new ideas and the capacity to better cope with difficult situations.21
In fact, some of the qualities fostered by the humanities even translate into better patient care. For instance, tolerance for ambiguity correlates with more positive attitudes towards patients who have frustrating complaints,22 with lower use of resources,23 and with a career choice in direct patient care.24 Hence, it has been suggested that it should be a prerequisite for medical school admission.25 Physicians’ empathy is also beneficial, since it correlates with a lower rate of complications and better outcomes in the care of diabetic patients.26 This should not come as a surprise. As Hippocrates put it 2,500 years ago, “some patients, though conscious that their condition is perilous, recover their health simply through their contentment with the goodness of the physician.”27
Lastly, studying the humanities may provide crucial antibodies against the pain and suffering that are unavoidable staples of the human condition. To paraphrase Osler, the humanities might vaccinate us against the difficulties of our profession. Hippocrates himself had suggested that “it is well to superintend the sick to make them well, to care for the healthy to keep them well, but also to care for one’s self…”27 That is why many institutions now require medical students to take humanities courses.28
MEDICINE: AN ART BASED ON SCIENCE
Yet this effort may amount to a rearguard action that arrives too late and provides too little. The humanities should probably be taught before medical school.29 After all, if it’s possible to make a scientist out of a humanist (Osler was living proof), the experience of the past decades seems to suggest that it’s considerably harder to make a humanist out of a scientist—hence the need to revisit undergraduate curricula and admission criteria to medical school, so that students can receive an adequate foundation in both arenas. Ironically, students express positive attitudes toward a liberal education and think it would actually help them as physicians.30 Yet they also understand that the selection process remains tilted towards the sciences.30–32
For Osler, scientific evidence was important but not a substitute for a humanistic approach. As he reminded students, “The practice of medicine is an art based on science,”33 whose main goals are to prevent disease, relieve suffering, and heal the sick. To do so, one ought to care more “for the individual patient than for the special features of the disease.”34 But he warned them, “It is much harder to acquire the art than the science.”35 In fact, “The practice of medicine is a calling in which your heart will be exercised equally with your head.”33 Hence the need to “cultivate equally well hearts and heads.”34 Almost foreseeing our infatuation with guidelines, he also warned against turning medicine into assembly-line work. There are “two great types of practitioners—the routinist and the rationalist,” he said in 1900, and “into the clutches of the demon routine the majority of us ultimately come.”36
Like most great people, Osler was a man of lights, shadows, and contradictions, probably not quite the saint we wish to believe. Yet he provides insights that are as valid today as they were for his own times, and possibly even more so. His 1919 speech is a paean to the humanities, but also a potential eulogy. As a Victorian physician, Osler was a blend of the new science and the old humanities. He knew that “the old art cannot possibly be replaced by, but must be absorbed in, the new science.”35 Yet he could also see the upcoming split between the two cultures, and he tried to warn us. He could in fact foresee the end of an entire way of life. As he said in his address, “there must be a very different civilization or there will be no civilization at all.”1
The crisis we face in medicine today may indeed be a symptom of a much larger cultural shift. As Osler himself put it, “The philosophies of one age have become the absurdities of the next, and the foolishness of yesterday has become the wisdom of tomorrow.”33 Like Osler, we live in times of transition that require us to act. If in 1910 Flexner gave us science,37 Osler in 1919 reminded us that medicine also needs the humanities. We ought to heed his message and reconcile the two fields. The alternative is a future full of tricorders and burned-out technicians, but sorely lacking in healers.
“Twin berries on one stem, grievous damage has been done to both in regarding the Humanities and Science in any other light than complemental.”
—Sir William Osler1
The year 2019 marks the 100th anniversary of Sir William Osler’s last public speech. Still reeling from the death of his only son in World War I, he had been asked to give the presidential inaugural address of the Classical Association at Oxford. It was the first time a physician had received the honor, and Osler took the assignment very seriously. He chose to speak about “The old humanities and the new science,” and to call for a reunification of the two fields. “Humanists have not enough Science” he warned, “and Science sadly lacks the Humanities…this unhappy divorce…should never have taken place.”1 Later, he said that it was the speech to which he had given the greatest thought and preparation. It was in fact Osler’s personal legacy: 2 months later he turned 70, and 7 months later he was dead.
Revisiting the address today, what can Osler teach the high-tech physician of today, when doctors have become “providers” and patients “consumers”? Is Osler’s message still relevant to our craft, or has he simply become an icon of professional nostalgia with little value for our times?
THE NEED FOR THE HUMANITIES IN MEDICINE
Medicine has certainly grown both powerful and successful. Yet it is also confronting hurdles that would have been unimaginable in Osler’s time. Physicians are now the professionals with the highest suicide rate,2 a burnout rate as high as 70%,3,4 rampant depression,5 dwindling empathy,6 a predominantly negative perception by the public,7,8 and a disturbing propensity to quit.9 These, of course, may just be symptoms of an increasingly meaningless environment wherein doctors have become small cogs in a medical-industrial complex they can’t control or even understand. Still, is it possible that something more personal may have been lost in the way we now select and educate physicians? Could this, in turn, make us less resilient?
In this regard, Osler’s last public speech serves as an enduring reminder of the need for the humanities in medicine. Osler not only believed it, but throughout his life never missed a chance to express in words, writings, and deeds that the humanities are indeed “the hormones” of the profession. In 1919 he warned against the risk of separating our humanistic tradition from the sciences, and urged us “to infect [anyone] with the spirit of the Humanities,” since to him that was “the greatest single gift in education.”1
Unfortunately, the humanities are slippery, not easily quantifiable, hard to define, and seemingly incompatible with an evidence-based approach. Quite understandably, today’s data-obsessed medicine views them with suspicion. But besides reminding us that in medicine not all that counts can be counted, and not all that can be counted counts, the humanities are in fact a fundamental component of the physician’s skill set.
In a multicenter survey of 5 medical schools,10 there was indeed a correlation between students’ exposure to the humanities and many of the personal qualities whose absence we lament in today’s medicine: empathy, tolerance for ambiguity, emotional intelligence, and prevention of burnout. Most significant was a strong correlation with wisdom, as measured by the 21-item Brief Wisdom Screening Scale.11 That all these traits may correlate with humanities exposure is intuitive, since the humanities not only teach tolerance and compassion, but also capture the collective experience of those who came before us. Hence, they teach us wisdom. Wisdom is not an ACGME competency, but it’s undoubtedly a prerequisite for the art of healing.12 In fact, wisdom may very well be the fundamental trait that characterizes a well-rounded physician, since it encompasses empathy, resilience, comfort with ambiguity, and the capacity to learn from the past. Not surprisingly, wisdom in the world was Osler’s closing wish in 1919.
The humanities can also nurture the very personal qualities we desire in physicians. For example, observing drama fosters empathy,13 as does taking an elective in medical humanities.14 Drawing enhances the reading of faces,15 and observing art improves the art of clinical observation.16 Reading good literature prompts better detection of emotions,17 and reflective writing improves students’ well-being.18 Playing a musical instrument reduces burnout.19 And an undergraduate major in the humanities correlates with greater tolerance for ambiguity,20 a highly desirable trait in physicians, since it means openness to new ideas and the capacity to better cope with difficult situations.21
In fact, some of the qualities fostered by the humanities even translate into better patient care. For instance, tolerance for ambiguity correlates with more positive attitudes towards patients who have frustrating complaints,22 with lower use of resources,23 and with a career choice in direct patient care.24 Hence, it has been suggested that it should be a prerequisite for medical school admission.25 Physicians’ empathy is also beneficial, since it correlates with a lower rate of complications and better outcomes in the care of diabetic patients.26 This should not come as a surprise. As Hippocrates put it 2,500 years ago, “some patients, though conscious that their condition is perilous, recover their health simply through their contentment with the goodness of the physician.”27
Lastly, studying the humanities may provide crucial antibodies against the pain and suffering that are unavoidable staples of the human condition. To paraphrase Osler, the humanities might vaccinate us against the difficulties of our profession. Hippocrates himself had suggested that “it is well to superintend the sick to make them well, to care for the healthy to keep them well, but also to care for one’s self…”27 That is why many institutions now require medical students to take humanities courses.28
MEDICINE: AN ART BASED ON SCIENCE
Yet this effort may amount to a rearguard action that arrives too late and provides too little. The humanities should probably be taught before medical school.29 After all, if it’s possible to make a scientist out of a humanist (Osler was living proof), the experience of the past decades seems to suggest that it’s considerably harder to make a humanist out of a scientist—hence the need to revisit undergraduate curricula and admission criteria to medical school, so that students can receive an adequate foundation in both arenas. Ironically, students express positive attitudes toward a liberal education and think it would actually help them as physicians.30 Yet they also understand that the selection process remains tilted towards the sciences.30–32
For Osler, scientific evidence was important but not a substitute for a humanistic approach. As he reminded students, “The practice of medicine is an art based on science,”33 whose main goals are to prevent disease, relieve suffering, and heal the sick. To do so, one ought to care more “for the individual patient than for the special features of the disease.”34 But he warned them, “It is much harder to acquire the art than the science.”35 In fact, “The practice of medicine is a calling in which your heart will be exercised equally with your head.”33 Hence the need to “cultivate equally well hearts and heads.”34 Almost foreseeing our infatuation with guidelines, he also warned against turning medicine into assembly-line work. There are “two great types of practitioners—the routinist and the rationalist,” he said in 1900, and “into the clutches of the demon routine the majority of us ultimately come.”36
Like most great people, Osler was a man of lights, shadows, and contradictions, probably not quite the saint we wish to believe. Yet he provides insights that are as valid today as they were for his own times, and possibly even more so. His 1919 speech is a paean to the humanities, but also a potential eulogy. As a Victorian physician, Osler was a blend of the new science and the old humanities. He knew that “the old art cannot possibly be replaced by, but must be absorbed in, the new science.”35 Yet he could also see the upcoming split between the two cultures, and he tried to warn us. He could in fact foresee the end of an entire way of life. As he said in his address, “there must be a very different civilization or there will be no civilization at all.”1
The crisis we face in medicine today may indeed be a symptom of a much larger cultural shift. As Osler himself put it, “The philosophies of one age have become the absurdities of the next, and the foolishness of yesterday has become the wisdom of tomorrow.”33 Like Osler, we live in times of transition that require us to act. If in 1910 Flexner gave us science,37 Osler in 1919 reminded us that medicine also needs the humanities. We ought to heed his message and reconcile the two fields. The alternative is a future full of tricorders and burned-out technicians, but sorely lacking in healers.
- Osler W. The old humanities and the new science: the presidential address delivered before the Classical Association at Oxford, May, 1919. Br Med J 1919; 2(3053):1–7. pmid:20769536
- Agerbo E, Gunnell D, Bonde JP, Mortensen PB, Nordentoft M. Suicide and occupation: the impact of socio-economic, demographic and psychiatric differences. Psychol Med 2007; 37(8):1131–1140. doi:10.1017/S0033291707000487
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc 2015; 90(12):1600–1613. doi:10.1016/j.mayocp.2015.08.023
- Dyrbye LN, Thomas MR, Massie FS, et al. Burnout and suicidal ideation among US medical students. Ann Intern Med 2008; 149(5):334–341. pmid:18765703
- Mata DA, Ramos MA, Bansal N, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA 2015; 314(22):2373–2383. doi:10.1001/jama.2015.15845
- Hojat M, Mangione S, Nasca TJ, et al. An empirical study of decline in empathy in medical school. Med Educ 2004; 38(9):934–941. doi:10.1111/j.1365-2929.2004.01911.x
- Flores G. Mad scientists, compassionate healers, and greedy egotists: the portrayal of physicians in the movies. J Natl Med Assoc 2002; 94(7):635–658. pmid:12126293
- Imber JB. Trusting Doctors: The Decline of Moral Authority in American Medicine. Princeton, NJ: Princeton University Press; 2008.
- Krauthammer, C. Why doctors quit. The Washington Post. May 28, 2015. https://www.washingtonpost.com/opinions/why-doctors-quit/2015/05/28/1e9d8e6e-056f-11e5-a428-c984eb077d4e_story.html?utm_term=.aa8804a518db. Accessed March 4, 2019.
- Mangione S, Chakraborti C, Staltari G, et al. Medical students' exposure to the humanities correlates with positive personal qualities and reduced burnout: a multi-institutional US survey. J Gen Intern Med 2018; 33(5):628–634. doi:10.1007/s11606-017-4275-8
- Glück J, König S, Naschenweng K, et al. How to measure wisdom: content, reliability, and validity of five measures. Front Psychol 2013; 4:405. doi:10.3389/fpsyg.2013.00405
- Papagiannis A. Eliot’s triad: information, knowledge and wisdom in medicine. Hektoen International. Spring 2014. https://hekint.org/2017/01/29/eliots-triad-information-knowledge-and-wisdom-in-medicine. Accessed March 4, 2019.
- Hojat M, Axelrod D, Spandorfer J, Mangione S. Enhancing and sustaining empathy in medical students. Med Teach 2013; 35(12):996–1001. doi:10.3109/0142159X.2013.802300
- Graham J, Benson LM, Swanson J, Potyk D, Daratha K, Roberts K. Medical humanities coursework is associated with greater measured empathy in medical students. Am J Med 2016; 129(12):1334–1337. doi:10.1016/j.amjmed.2016.08.005
- Brechet C, Baldy R, Picard D. How does Sam feel? Children's labelling and drawing of basic emotions. Br J Dev Psychol 2009; 27(Pt 3):587–606. pmid:19994570
- Naghshineh S, Hafler JP, Miller AR, et al. Formal art observation training improves medical students’ visual diagnostic skills. J Gen Intern Med 2008; 23(7):991–997. doi:10.1007/s11606-008-0667-0
- Kidd DC, Castano E. Reading literary fiction improves theory of mind. Science 2013; 342(6156):377–380. doi:10.1126/science.1239918
- Shapiro J, Kasman D, Shafer A. Words and wards: a model of reflective writing and its uses in medical education. J Med Humanit 2006; 27(4):231–244. doi:10.1007/s10912-006-9020-y
- Bittman BB, Snyder C, Bruhn KT, et al. Recreational music-making: an integrative group intervention for reducing burnout and improving mood states in first year associate degree nursing students: insights and economic impact. Int J Nurs Educ Scholarsh 2004;1:Article12. doi:10.2202/1548-923x.1044
- DeForge BR, Sobal J. Intolerance of ambiguity in students entering medical school. Soc Sci Med 1989; 28(8):869–874. pmid:2705020
- Ghosh AK. Understanding medical uncertainty: a primer for physicians. J Assoc Physicians India 2004; 52:739–742. pmid:15839454
- Merrill JM, Camacho Z, Laux LF, Thornby JI, Vallbona C. How medical school shapes students’ orientation to patients’ psychological problems. Acad Med 1991; 66(9 suppl):S4–S6. pmid:1930523
- Allison JJ, Kiefe CI, Cook EF, Gerrity MS, Orav EJ, Centor R. The association of physician attitudes about uncertainty and risk taking with resource use in a Medicare HMO. Med Decis Making 1998; 18(3):320–329. doi:10.1177/0272989X9801800310
- Gerrity MS, Earp JAL, DeVilles RF, DW Light. Uncertainty and professional work: perceptions of physicians in clinical practice. Am J Sociol 1992; 97(4):1022–1051. https://www.jstor.org/stable/2781505. Accessed March 6, 2019.
- Geller G. Tolerance for ambiguity: an ethics-based criterion for medical student selection. Acad Med 2013; 88(5):581–584. doi:10.1097/ACM.0b013e31828a4b8e
- Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med 2011; 86(3):359–364. doi:10.1097/ACM.0b013e3182086fe1
- Hippocrates. Precepts. Section 8, Part VI. Perseus Digital Library. http://perseus.uchicago.edu/perseus-cgi/citequery3.pl?dbname=GreekFeb2011&getid=1&query=Hipp.%20Praec.%208. Accessed March 4, 2019.
- Kidd MG, Connor JT. Striving to do good things: teaching humanities in Canadian medical schools. J Med Humanit 2008; 29(1):45–54. doi:10.1007/s10912-007-9049-6
- Thomas L. Notes of a biology-watcher. How to fix the premedical curriculum. N Engl J Med 1978; 298(21):1180–1181. doi:10.1056/NEJM197805252982106
- Simmons A. Beyond the premedical syndrome: premedical student attitudes toward liberal education and implications for advising. NACADA Journal 2005; 25(1):64–73.
- Kumar B, Swee ML and Suneja M. The premedical curriculum: we can do better for future physicians. South Med J 2017; 110(8):538–539. doi:10.14423/SMJ.0000000000000683
- Gunderman RB, Kanter SL. Perspective: “how to fix the premedical curriculum” revisited. Acad Med 2008; 83(12):1158–1161. doi:10.1097/ACM.0b013e31818c6515
- Osler W. Aequanimitas with Other Addresses to Medical Students, Nurses and Practitioners of Medicine. Philadelphia, PA: Blakiston; 1904.
- Osler W. Address to the students of the Albany Medical College. Albany Med Ann 1899; 20:307–309.
- Osler W. The reserves of life. St Mary’s Hosp Gaz 1907; 13:95–98.
- Osler W. An address on the importance of post-graduate study. Delivered at the opening of the Museums of the Medical Graduates College and Polyclinic, July 4th, 1900. Br Med J 1900; 2(2063):73–75. pmid:20759107
- Flexner A. Medical Education in the United States and Canada. New York, The Carnegie Foundation 1910.
- Osler W. The old humanities and the new science: the presidential address delivered before the Classical Association at Oxford, May, 1919. Br Med J 1919; 2(3053):1–7. pmid:20769536
- Agerbo E, Gunnell D, Bonde JP, Mortensen PB, Nordentoft M. Suicide and occupation: the impact of socio-economic, demographic and psychiatric differences. Psychol Med 2007; 37(8):1131–1140. doi:10.1017/S0033291707000487
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc 2015; 90(12):1600–1613. doi:10.1016/j.mayocp.2015.08.023
- Dyrbye LN, Thomas MR, Massie FS, et al. Burnout and suicidal ideation among US medical students. Ann Intern Med 2008; 149(5):334–341. pmid:18765703
- Mata DA, Ramos MA, Bansal N, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA 2015; 314(22):2373–2383. doi:10.1001/jama.2015.15845
- Hojat M, Mangione S, Nasca TJ, et al. An empirical study of decline in empathy in medical school. Med Educ 2004; 38(9):934–941. doi:10.1111/j.1365-2929.2004.01911.x
- Flores G. Mad scientists, compassionate healers, and greedy egotists: the portrayal of physicians in the movies. J Natl Med Assoc 2002; 94(7):635–658. pmid:12126293
- Imber JB. Trusting Doctors: The Decline of Moral Authority in American Medicine. Princeton, NJ: Princeton University Press; 2008.
- Krauthammer, C. Why doctors quit. The Washington Post. May 28, 2015. https://www.washingtonpost.com/opinions/why-doctors-quit/2015/05/28/1e9d8e6e-056f-11e5-a428-c984eb077d4e_story.html?utm_term=.aa8804a518db. Accessed March 4, 2019.
- Mangione S, Chakraborti C, Staltari G, et al. Medical students' exposure to the humanities correlates with positive personal qualities and reduced burnout: a multi-institutional US survey. J Gen Intern Med 2018; 33(5):628–634. doi:10.1007/s11606-017-4275-8
- Glück J, König S, Naschenweng K, et al. How to measure wisdom: content, reliability, and validity of five measures. Front Psychol 2013; 4:405. doi:10.3389/fpsyg.2013.00405
- Papagiannis A. Eliot’s triad: information, knowledge and wisdom in medicine. Hektoen International. Spring 2014. https://hekint.org/2017/01/29/eliots-triad-information-knowledge-and-wisdom-in-medicine. Accessed March 4, 2019.
- Hojat M, Axelrod D, Spandorfer J, Mangione S. Enhancing and sustaining empathy in medical students. Med Teach 2013; 35(12):996–1001. doi:10.3109/0142159X.2013.802300
- Graham J, Benson LM, Swanson J, Potyk D, Daratha K, Roberts K. Medical humanities coursework is associated with greater measured empathy in medical students. Am J Med 2016; 129(12):1334–1337. doi:10.1016/j.amjmed.2016.08.005
- Brechet C, Baldy R, Picard D. How does Sam feel? Children's labelling and drawing of basic emotions. Br J Dev Psychol 2009; 27(Pt 3):587–606. pmid:19994570
- Naghshineh S, Hafler JP, Miller AR, et al. Formal art observation training improves medical students’ visual diagnostic skills. J Gen Intern Med 2008; 23(7):991–997. doi:10.1007/s11606-008-0667-0
- Kidd DC, Castano E. Reading literary fiction improves theory of mind. Science 2013; 342(6156):377–380. doi:10.1126/science.1239918
- Shapiro J, Kasman D, Shafer A. Words and wards: a model of reflective writing and its uses in medical education. J Med Humanit 2006; 27(4):231–244. doi:10.1007/s10912-006-9020-y
- Bittman BB, Snyder C, Bruhn KT, et al. Recreational music-making: an integrative group intervention for reducing burnout and improving mood states in first year associate degree nursing students: insights and economic impact. Int J Nurs Educ Scholarsh 2004;1:Article12. doi:10.2202/1548-923x.1044
- DeForge BR, Sobal J. Intolerance of ambiguity in students entering medical school. Soc Sci Med 1989; 28(8):869–874. pmid:2705020
- Ghosh AK. Understanding medical uncertainty: a primer for physicians. J Assoc Physicians India 2004; 52:739–742. pmid:15839454
- Merrill JM, Camacho Z, Laux LF, Thornby JI, Vallbona C. How medical school shapes students’ orientation to patients’ psychological problems. Acad Med 1991; 66(9 suppl):S4–S6. pmid:1930523
- Allison JJ, Kiefe CI, Cook EF, Gerrity MS, Orav EJ, Centor R. The association of physician attitudes about uncertainty and risk taking with resource use in a Medicare HMO. Med Decis Making 1998; 18(3):320–329. doi:10.1177/0272989X9801800310
- Gerrity MS, Earp JAL, DeVilles RF, DW Light. Uncertainty and professional work: perceptions of physicians in clinical practice. Am J Sociol 1992; 97(4):1022–1051. https://www.jstor.org/stable/2781505. Accessed March 6, 2019.
- Geller G. Tolerance for ambiguity: an ethics-based criterion for medical student selection. Acad Med 2013; 88(5):581–584. doi:10.1097/ACM.0b013e31828a4b8e
- Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med 2011; 86(3):359–364. doi:10.1097/ACM.0b013e3182086fe1
- Hippocrates. Precepts. Section 8, Part VI. Perseus Digital Library. http://perseus.uchicago.edu/perseus-cgi/citequery3.pl?dbname=GreekFeb2011&getid=1&query=Hipp.%20Praec.%208. Accessed March 4, 2019.
- Kidd MG, Connor JT. Striving to do good things: teaching humanities in Canadian medical schools. J Med Humanit 2008; 29(1):45–54. doi:10.1007/s10912-007-9049-6
- Thomas L. Notes of a biology-watcher. How to fix the premedical curriculum. N Engl J Med 1978; 298(21):1180–1181. doi:10.1056/NEJM197805252982106
- Simmons A. Beyond the premedical syndrome: premedical student attitudes toward liberal education and implications for advising. NACADA Journal 2005; 25(1):64–73.
- Kumar B, Swee ML and Suneja M. The premedical curriculum: we can do better for future physicians. South Med J 2017; 110(8):538–539. doi:10.14423/SMJ.0000000000000683
- Gunderman RB, Kanter SL. Perspective: “how to fix the premedical curriculum” revisited. Acad Med 2008; 83(12):1158–1161. doi:10.1097/ACM.0b013e31818c6515
- Osler W. Aequanimitas with Other Addresses to Medical Students, Nurses and Practitioners of Medicine. Philadelphia, PA: Blakiston; 1904.
- Osler W. Address to the students of the Albany Medical College. Albany Med Ann 1899; 20:307–309.
- Osler W. The reserves of life. St Mary’s Hosp Gaz 1907; 13:95–98.
- Osler W. An address on the importance of post-graduate study. Delivered at the opening of the Museums of the Medical Graduates College and Polyclinic, July 4th, 1900. Br Med J 1900; 2(2063):73–75. pmid:20759107
- Flexner A. Medical Education in the United States and Canada. New York, The Carnegie Foundation 1910.
More cost compression coming
In mid-March, the President released his FY2020 budget proposal. Traditionally, the White House budget has little relation to the ultimate budget since Congress actually creates the final iteration (assuming the government can pass a budget at all). This budget cuts funding for the NIH, Medicare, Medicaid, and most agencies not related to defense, border security, or the TSA. No matter what the final version looks like, the federal deficit will balloon as a result of last year’s tax cuts that were combined with relentless increases in entitlement program spending. The message for health care leaders is clear: Since we are responsible for an enormous percentage of committed federal and state spending, we will be in the cross-hairs of cost compression.
As we enter the 2020 election cycle in earnest, politicians will argue about “Medicare for All” versus government overreach. We will wrestle with competing philosophies of States’ Rights versus Federalism. As physicians, we must advocate for a system of funds flow and regulatory power that we believe best serves our patients within a financially sustainable framework.
On to this month’s issue – there are two stories on early-age colon cancer. A page one story adds to our understanding of the molecular pathways involved (microsatellite instability) and tumor location. Another story points out that younger CRC patients often go undiagnosed or are misdiagnosed. The AGA has published important clinical guidance about pregnancy and IBD and switching from biologic medications to biosimilars. Finally, an enormously important study, published in The Lancet, confirmed that hepatitis C treatment with direct-acting antiviral medications reduces mortality and cancer risk – something we suspected but needed confirmed.
I hope to see everyone at DDW next month.
John I. Allen, MD, MBA, AGAF
Editor in Chief
In mid-March, the President released his FY2020 budget proposal. Traditionally, the White House budget has little relation to the ultimate budget since Congress actually creates the final iteration (assuming the government can pass a budget at all). This budget cuts funding for the NIH, Medicare, Medicaid, and most agencies not related to defense, border security, or the TSA. No matter what the final version looks like, the federal deficit will balloon as a result of last year’s tax cuts that were combined with relentless increases in entitlement program spending. The message for health care leaders is clear: Since we are responsible for an enormous percentage of committed federal and state spending, we will be in the cross-hairs of cost compression.
As we enter the 2020 election cycle in earnest, politicians will argue about “Medicare for All” versus government overreach. We will wrestle with competing philosophies of States’ Rights versus Federalism. As physicians, we must advocate for a system of funds flow and regulatory power that we believe best serves our patients within a financially sustainable framework.
On to this month’s issue – there are two stories on early-age colon cancer. A page one story adds to our understanding of the molecular pathways involved (microsatellite instability) and tumor location. Another story points out that younger CRC patients often go undiagnosed or are misdiagnosed. The AGA has published important clinical guidance about pregnancy and IBD and switching from biologic medications to biosimilars. Finally, an enormously important study, published in The Lancet, confirmed that hepatitis C treatment with direct-acting antiviral medications reduces mortality and cancer risk – something we suspected but needed confirmed.
I hope to see everyone at DDW next month.
John I. Allen, MD, MBA, AGAF
Editor in Chief
In mid-March, the President released his FY2020 budget proposal. Traditionally, the White House budget has little relation to the ultimate budget since Congress actually creates the final iteration (assuming the government can pass a budget at all). This budget cuts funding for the NIH, Medicare, Medicaid, and most agencies not related to defense, border security, or the TSA. No matter what the final version looks like, the federal deficit will balloon as a result of last year’s tax cuts that were combined with relentless increases in entitlement program spending. The message for health care leaders is clear: Since we are responsible for an enormous percentage of committed federal and state spending, we will be in the cross-hairs of cost compression.
As we enter the 2020 election cycle in earnest, politicians will argue about “Medicare for All” versus government overreach. We will wrestle with competing philosophies of States’ Rights versus Federalism. As physicians, we must advocate for a system of funds flow and regulatory power that we believe best serves our patients within a financially sustainable framework.
On to this month’s issue – there are two stories on early-age colon cancer. A page one story adds to our understanding of the molecular pathways involved (microsatellite instability) and tumor location. Another story points out that younger CRC patients often go undiagnosed or are misdiagnosed. The AGA has published important clinical guidance about pregnancy and IBD and switching from biologic medications to biosimilars. Finally, an enormously important study, published in The Lancet, confirmed that hepatitis C treatment with direct-acting antiviral medications reduces mortality and cancer risk – something we suspected but needed confirmed.
I hope to see everyone at DDW next month.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Paraphilic disorders: A better understanding
In my role as the Director of The Johns Hopkins Sex and Gender Clinic, I have had the opportunity to provide care to 3 broad categories of patients: patients with sexual dysfunctions, patients experiencing gender dysphoria, and patients manifesting a paraphilic disorder. This article will not address sexual dysfunctions or gender dysphoria, but these terms are defined in the Box1-3 to clearly distinguish them from paraphilic disorders.
Box
Individuals with a sexual dysfunction (eg, erectile dysfunction or anorgasmia) generally experience conventional sexual feelings, but they may have difficulty performing sexually.1 Although ordinarily capable of adequate sexual performance, persons with a paraphilic disorder experience atypical erotic cravings.2 Such cravings can either be for an atypical or unacceptable category of potential partner (eg, animals or children), or for an atypical or unacceptable type of behavior (eg, crossdressing or public exhibitionism). Individuals with gender dysphoria frequently experience distress because their internal sense of feeling either male or female is not congruent with their external physical anatomy.3 The primary concerns of individuals experiencing gender dysphoria relate to feelings of gender identity, as opposed to problems involving erotic arousal.
Persons with paraphilic disorders (predominantly males) experience recurrent atypical sexual fantasies and urges that cause clinically significant impairment or distress.1 Those atypical fantasies and urges may be directed towards unacceptable partners such as animals or children, or towards unacceptable behaviors such as public exhibitionism. Table 11 lists the paraphilic disorders identified in DSM-5. This article focuses primarily, though not exclusively, upon pedophilic disorder, and its pharmacologic treatment. However, the rationale underlying such treatment is applicable across the paraphilic spectrum. Before providing such treatment, it is important for clinicians to have a clear conceptual understanding of paraphilic disorders.
When is a difference a disorder?
Cancer and respiration are 2 different biologic phenomenon. Cancer causes suffering and impairment, and as a consequence, we label it a disorder. We do so in the hope of learning more about it, and being able to successfully treat it. We do not classify respiration as a disorder because we do not consider it to be harmful.
The spectrum of human sexuality is quite broad, and psychiatry is generally not concerned with private sexual thoughts and behaviors involving consenting adults that do not cause suffering or impairment. When adults choose to engage in “kinky sex” that causes neither harm nor distress, so be it.
Some individuals may be privately aware of experiencing either an exclusive or nonexclusive sexual attraction to children. Some of these individuals may not be distressed by experiencing such attractions, and may be fully capable of resisting the temptation to enact them. In such an instance, even though an individual may be experiencing sexual attractions that are different from the norm, there may not be a sufficient basis for diagnosing pedophilic disorder. However, that difference in sexual phenomenology (ie, mental experience) could rise to the level of a diagnosable disorder if the individual in question expresses distress about experiencing such attractions, and/or if his capacity to resist acting upon them is impaired.4 Under such circumstances, treatment would be warranted.
Patients with paraphilic disorders deserve treatment
Prior to establishment of the Betty Ford Clinic in 1982, individuals who were drug- or alcohol-dependent were often portrayed in a negative light and referred to by derogatory pejoratives such as “bum” or “pothead.”5 Over time, society came to appreciate that good people, deserving of treatment, can become dependent upon substances, and in recent years there has been considerable support for related research initiatives and humane care. However, there has not been analogous support for individuals who manifest paraphilic disorders, especially those with pedophilic disorder. Instead, such individuals are often perceived as undeserving of mental health care and resources. This has been the case, even though successful treatment of a pedophilic disorder could help prevent the serious consequences of child molestation from occurring.
In contemporary society, the term pedophilia, which is a psychiatric specifier intended to guide research and treatment, has been hijacked by the nonmedical community and turned into a demeaning pejorative. In the collective consciousness of the public, the term pedophilia is routinely and mistakenly equated with the behavior of child molestation. Just as all alcoholics are not drunk drivers, all individuals with pedophilic disorder are not “child molesters.” Conversely, not all “child molesters” have pedophilic disorder.
Continue to: Individuals with other types...
Individuals with other types of paraphilic disorders are frequently similarly maligned and referred to as “perverts” or “deviants.” Public service announcements are frequently aired to reach out to individuals who are depressed, or drug- or alcohol-dependent, or suffering with other forms of mental disorders. When does one hear a public service announcement that encourages young people who may be experiencing disturbing or unacceptable sexual feelings to seek psychiatric treatment? There is a support group on the internet called Virtuous Pedophiles.6 That organization is unequivocally opposed to child molestation, while supporting efforts to improve the mental well-being of individuals who, through no fault of their own, experience unwanted pedophilic feelings.
Causes and noncauses
In attempting to elucidate etiology, researchers typically investigate nature (biology) and/or nurture (life experiences). In terms of the development of pedophilic disorder, there is evidence that both nature and nurture can play a role. Researchers have found that boys who are sexually abused are at increased risk for developing pedophilic disorder, and evidence of temporal lobe disturbances has also been documented in some instances.7,8
From clinical, societal, and forensic perspectives, it may be equally important to identify noncausal factors. Paraphilic disorders, including pedophilic disorder, do not develop as a consequence of volitional choice.9 For example, none of us decide which category, or categories, of potential partners are going to attract us sexually. Rather, in maturing we discover the nature of our own sexuality. Children do not ponder their options, somehow deciding while growing up to be attracted to the opposite sex (heterosexuality), the same sex (homosexuality), or both sexes (bisexuality). Similarly, in maturing into adulthood, individuals do not decide to become sexually attracted to prepubescent children. Who would decide to do that? Instead, unlike most of us, some individuals discover this about themselves; this often is a deeply disturbing insight.
It is not an individual’s fault that he or she has a paraphilic disorder. It is, however, his or her responsibility to do something about it. This may require accessing appropriate psychiatric care.
Why treatment may be needed
Sex is a powerful, biologically based appetite that recurrently craves satiation. God or nature has put that drive into all of us to ensure the survival of humanity. Even when that powerful biologic drive becomes misdirected (for example, towards children, or towards a desire to engage in public exhibitionism), it still recurrently craves satisfaction. It does not require mental health expertise to appreciate what a problematic situation this could become.
Continue to: Some individuals need help...
Some individuals need help in overcoming cravings related to nonsexual appetites. For example, Americans spend millions of dollars each year trying to diet; they often require some form of assistance in order to succeed. Individuals who crave drugs or alcohol often require mental health interventions to abstain because they are unable to consistently resist through willpower alone the powerful biologic urges that drive their actions.
The fundamental mental characteristic of any paraphilic disorder is the presence of intense, recurrent, sexual urges of an atypical nature. In the case of a pedophilic disorder, those urges involve sexual feelings about children.2 In the case of an exhibitionistic disorder, the afflicted individual experiences intense, recurrent sexual fantasies/urges related to exposing his genitals in public.1 Clearly, most men do not have to recurrently fight off the urge to act in such a fashion. Given the driven nature of intense erotic cravings, individuals who experience such cravings will frequently require access to competent mental health care.
Pharmacologic treatment of paraphilic disorders
In the future, we may develop a scientifically based understanding of the biologic factors that underlie qualitative differences in sexuality. At that point, it may become possible to intervene pharmacologically, changing the qualitative nature of a sexual urge with pharmacologic interventions. This cannot yet be done. H
In 1939, a Nobel Prize in Chemistry was awarded for the identification and isolation of the hormone testosterone, which energizes sexual drive.10 If an individual is hungering sexually to expose himself, to view child pornography, or to engage in sexual acts with children, the intensity of such hungers can be significantly reduced by lowering testosterone, thereby enhancing the capacity for successful sexual self-control.
A large body of scientific data has documented a marked decrease in sexually motivated behaviors when testosterone levels are significantly diminished.11 There is also evidence that recidivism rates of sexually motivated crimes can be significantly reduced when testosterone-lowering interventions are used.12
Continue to: Historically, removal of the testes...
Historically, removal of the testes (surgical castration) had been the only effective way to reliably lower testosterone. Today, this can be achieved pharmacologically. Use of a sex drive–lowering medication should be considered when either the clinician or the patient is concerned that a nonpharmacologic approach may be inadequate. In all instances, a patient with a paraphilic disorder should be informed that pharmacologic treatment is an option. A protocol for the pharmacologic treatment of paraphilic disorders that is based on my clinical experience is summarized in Table 2.
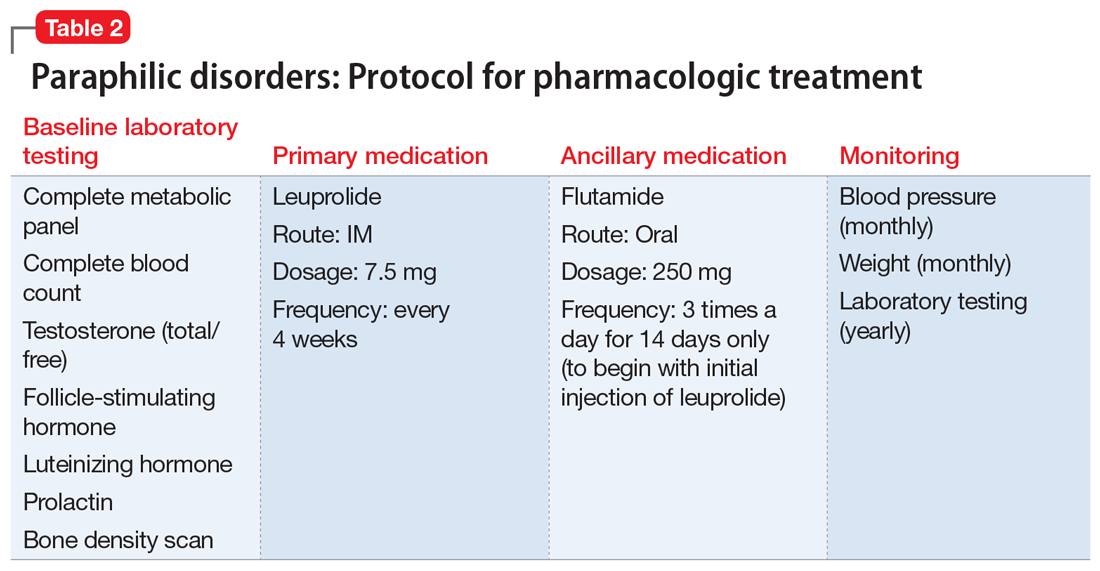
Leuprolide. A depot form of leuprolide is the most commonly employed agent to pharmacologically lower testosterone to treat a paraphilic disorder.13 When injected into muscle, leuprolide binds to it before gradually being released into the bloodstream. Previously, a depot medroxyprogesterone (a form of progesterone) had been used to treat paraphilic disorders.14 However, that had required weekly rather than monthly injections, and carried an increased risk of thrombotic emboli.
Prescribing leuprolide to treat a paraphilic disorder falls under FDA guidelines regarding the use of an approved drug for an “off-label” indication, and therefore is not considered investigational. For treating a paraphilic disorder, an effective dosage of leuprolide is 7.5 mg IM every 4 weeks. Long-term treatment is generally required, analogous to the management of diabetes. Because the initial injection of the series can cause a transient increase in testosterone (prior to its sustained decline), flutamide, a testosterone receptor blocking agent, is ordinarily prescribed for the first 14 days only, following initiation of treatment with depot leuprolide.15 Using flutamide in this fashion prevents the transient increase in testosterone from transiently increasing sexual drive. Flutamide should be discontinued after 14 days because long-term use can result in liver toxicity.
Some clinicians have been hesitant to prescribe leuprolide because of negative connotations associated with the term “chemical castration.” Unlike surgical castration, use of leuprolide is not a physically irreversible intervention, and does not result in sterility (although there may be an increase of atypical sperm and a decrease in total sperm production). The dosage can sometimes be titrated without a loss of efficacy.
In general, leuprolide’s safety protocol is well within the range associated with psychotropic medications.13 Low-risk adverse effects, such as hot flashes or cold sweats, may occur, especially during the period when hormone levels are in transition. There are no absolute contraindications to the use of leuprolide.
Continue to: Other medications
Other medications. Some researchers have suggested treating paraphilic disorders with psychotropic medications known to lower libido, such as selective serotonin reuptake inhibitors (SSRIs).16 However, leuprolide is far more reliable in consistently lowering testosterone and lowering the frequency and intensity of sexual urges. Although psychiatrists unfamiliar with treating paraphilic disorders may feel more comfortable initiating treatment with an SSRI, in my clinical experience, SSRIs have often proven inadequate for this purpose. When it comes to those paraphilic disorders in which treatment failure can result in significant harm (eg, pedophilic disorder), in my judgment, leuprolide should be the pharmacologic treatment of choice.
The opioid antagonist naltrexone has been used clinically to reduce cravings, primarily cravings for alcohol or drugs.17 However, I have not seen convincing evidence that it can be reliably beneficial in treating paraphilic disorders.
Tests to order before starting leuprolide
Long-term use of leuprolide can increase the risk of osteoporosis. Therefore, a baseline bone density scan should be performed before starting a patient on leuprolide. Baseline levels of testosterone, follicle-stimulating hormone, and luteinizing hormone also should be obtained. Patients should have yearly physical examinations, with accompanying laboratory testing. Hematocrit levels are often marginally low after beginning treatment, but not in a clinically significant way. Patients should also undergo routine monitoring for possible weight gain and the potential for associated hypertension. Treatment is predicated upon the known testosterone-suppressing effects of leuprolide, not upon routine monitoring of blood androgen levels.
Pharmacologic treatment of a paraphilic disorder should ordinarily occur in conjunction with nonpharmacologic modalities. One such modality would be group therapy, similar to the type frequently used to treat other craving disorders, such as drug or alcohol dependency.
In recent years, I have seen increasing numbers of patients presenting with a history of accessing and viewing child pornography. Once they have become more aware of the serious consequences of this behavior, most patients have been able to discontinue doing so without pharmacologic treatment. However, for patients in whom that behavior has seemed more driven (suggestive of a variant of voyeuristic disorder), prescription of leuprolide has been beneficial. Under such circumstances, I have diagnosed the patient’s condition as “other specified paraphilic disorder” with elements of pedophilia and voyeurism—the associated behaviors restricted to the voyeuristic viewing of child pornography.18
Continue to: Can treated patients still be sexual?
Can treated patients still be sexual?
If pharmacologic treatment of a paraphilic disorder results in erectile dysfunction, prescription of a medication such as sildenafil can be considered for patients who are in a consenting adult relationship, generally with the knowledge of their partner. Sildenafil can facilitate erectile capacity without increasing sexual drive. It can be helpful to explain to a patient that the purpose of pharmacologic treatment is not to prevent the enjoyment of sexual feelings within the context of a healthy, consenting, adult relationship, but instead to lower the intensity of problematic sexual urges, thereby facilitating sexual self-control. Just as lowering the appetite for food can make it easier to diet but not impossible to eat, lowering sexual appetite can facilitate successful self-control without necessarily interfering with erotic feelings experienced during sexual intimacy.
Bottom Line
Paraphilic disorders are not manifestations of a character flaw, but manifestations of unchosen qualitative differences in the nature of one’s sexual cravings. Not enough is yet known about the biology of sex to be able to pharmacologically alter its qualitative nature. However, pharmacologically lowering the intensity of a patient’s sexual drive can facilitate successful sexual self-regulation.
Related Resources
- LeVay S. Gay, straight and the reason why: the science of sexual orientation. London, UK: Oxford University Press; 2011.
- Rosler A, Witztum E. Treatment of men with paraphilia with a long-acting analogue of gonadotropin-releasing hormone. N Engl J Med. 1998;338(7):416-422.
- Brown GR. Overview of paraphilic disorders (paraphilias). https://www.merckmanuals.com/professional/psychiatricdisorders/sexuality,-gender-dysphoria,-and-paraphilias/overview-of-paraphilic-disorders.
Drug Brand Names
Flutamide • Eulexin
Leuprolide injection •
Eligard, Lupron Depot
Medroxyprogesterone •
Provera
Naltrexone • Revia, Vivitrol
Progesterone • Prometrium
Sildenafil • Viagra
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:423-450.
2. Berlin FS. Pedophilia: criminal mind-set or mental disorder? A conceptual review. American Journal of Forensic Psychiatry. 2001;32(2):3-25.
3. Berlin FS. A conceptual overview and commentary on gender dysphoria. J Am Acad Psychiatry Law. 2016;44(2):246-252
4. Berlin FS. Pedophilia: when is a difference a disorder: Peer commentaries on Green (2002) and Schmidt (2002). Arch Sex Behav. 2002;31:1-2.
5. Ford B, Chase C. Betty: a glad awakening. New York, NY: Doubleday; 1987.
6. Virtuous Pedophiles. https://www.virped.org/. Accessed September 28, 2018.
7. Freund K, Kuban M. The basis of the abused abuser theory of pedophilia: A further elaboration of an earlier study. Arch Sex Behav. 1994;23(5):553-563.
8. Mendes MF, Chow T, Ringman T, et al. Pedophilia and temporal lobe disturbances. J Neuropsychiatry Clin Neurosci. 2000;12(1):71-76.
9. Money J. Love and love sickness: The science of sex, gender differences, and pair bonding. Baltimore, MD: Johns Hopkins University Press; 1980.
10. The Nobel Prize in Chemistry 1939. https://www.nobelprize.org/prizes/chemistry/1939/summary/. Accessed September 29, 2018.
11. Berlin FS. Commentary: The impact of surgical castration on sexual recidivism risk among civilly committed sex offenders. J Am Acad Psychiatry Law. 2005;33(1):37-41.
12. Hansen H. Treatment of dangerous sexual offenders. In: Seminar on Prison Health Services in Tampere, Finland. Helsinki, Finland: Ministry of Justice, Government Printing Centre; 1991:33-38.
13. Berlin FS. Risk/benefit ratio of androgen deprivation treatment for sex offenders. J Am Acad Psychiatry Law. 2009;37(1):59-62.
14. Berlin FS, Meinecke CF. Treatment of sex offenders with antiandrogenic medication: conceptualization, review of treatment modalities, and preliminary findings. Am J Psychiatry. 1981;138(5):601-607.
15. Neri R. Pharmacology and pharmacokinetics of flutamide. Urology. 1989;34(suppl 4):19-21; discussion 46-56.
16. Adi Y, Ashcroft D, Browne K, et al. Clinical effectiveness and cost consequences of selective serotonin receptor reuptake inhibitors in the treatment of sex offenders. Health Technol Assess. 2002;6(28):1-66.
17. Anton RF. Naltrexone for the management of alcohol dependence. N Engl J Med. 2008;359(7):715-721.
18. Berlin FS. Commentary on pedophilia diagnostic criteria in DSM-5. J Am Acad Psychiatry Law. 2011;39(2):242-244.
In my role as the Director of The Johns Hopkins Sex and Gender Clinic, I have had the opportunity to provide care to 3 broad categories of patients: patients with sexual dysfunctions, patients experiencing gender dysphoria, and patients manifesting a paraphilic disorder. This article will not address sexual dysfunctions or gender dysphoria, but these terms are defined in the Box1-3 to clearly distinguish them from paraphilic disorders.
Box
Individuals with a sexual dysfunction (eg, erectile dysfunction or anorgasmia) generally experience conventional sexual feelings, but they may have difficulty performing sexually.1 Although ordinarily capable of adequate sexual performance, persons with a paraphilic disorder experience atypical erotic cravings.2 Such cravings can either be for an atypical or unacceptable category of potential partner (eg, animals or children), or for an atypical or unacceptable type of behavior (eg, crossdressing or public exhibitionism). Individuals with gender dysphoria frequently experience distress because their internal sense of feeling either male or female is not congruent with their external physical anatomy.3 The primary concerns of individuals experiencing gender dysphoria relate to feelings of gender identity, as opposed to problems involving erotic arousal.
Persons with paraphilic disorders (predominantly males) experience recurrent atypical sexual fantasies and urges that cause clinically significant impairment or distress.1 Those atypical fantasies and urges may be directed towards unacceptable partners such as animals or children, or towards unacceptable behaviors such as public exhibitionism. Table 11 lists the paraphilic disorders identified in DSM-5. This article focuses primarily, though not exclusively, upon pedophilic disorder, and its pharmacologic treatment. However, the rationale underlying such treatment is applicable across the paraphilic spectrum. Before providing such treatment, it is important for clinicians to have a clear conceptual understanding of paraphilic disorders.
When is a difference a disorder?
Cancer and respiration are 2 different biologic phenomenon. Cancer causes suffering and impairment, and as a consequence, we label it a disorder. We do so in the hope of learning more about it, and being able to successfully treat it. We do not classify respiration as a disorder because we do not consider it to be harmful.
The spectrum of human sexuality is quite broad, and psychiatry is generally not concerned with private sexual thoughts and behaviors involving consenting adults that do not cause suffering or impairment. When adults choose to engage in “kinky sex” that causes neither harm nor distress, so be it.
Some individuals may be privately aware of experiencing either an exclusive or nonexclusive sexual attraction to children. Some of these individuals may not be distressed by experiencing such attractions, and may be fully capable of resisting the temptation to enact them. In such an instance, even though an individual may be experiencing sexual attractions that are different from the norm, there may not be a sufficient basis for diagnosing pedophilic disorder. However, that difference in sexual phenomenology (ie, mental experience) could rise to the level of a diagnosable disorder if the individual in question expresses distress about experiencing such attractions, and/or if his capacity to resist acting upon them is impaired.4 Under such circumstances, treatment would be warranted.
Patients with paraphilic disorders deserve treatment
Prior to establishment of the Betty Ford Clinic in 1982, individuals who were drug- or alcohol-dependent were often portrayed in a negative light and referred to by derogatory pejoratives such as “bum” or “pothead.”5 Over time, society came to appreciate that good people, deserving of treatment, can become dependent upon substances, and in recent years there has been considerable support for related research initiatives and humane care. However, there has not been analogous support for individuals who manifest paraphilic disorders, especially those with pedophilic disorder. Instead, such individuals are often perceived as undeserving of mental health care and resources. This has been the case, even though successful treatment of a pedophilic disorder could help prevent the serious consequences of child molestation from occurring.
In contemporary society, the term pedophilia, which is a psychiatric specifier intended to guide research and treatment, has been hijacked by the nonmedical community and turned into a demeaning pejorative. In the collective consciousness of the public, the term pedophilia is routinely and mistakenly equated with the behavior of child molestation. Just as all alcoholics are not drunk drivers, all individuals with pedophilic disorder are not “child molesters.” Conversely, not all “child molesters” have pedophilic disorder.
Continue to: Individuals with other types...
Individuals with other types of paraphilic disorders are frequently similarly maligned and referred to as “perverts” or “deviants.” Public service announcements are frequently aired to reach out to individuals who are depressed, or drug- or alcohol-dependent, or suffering with other forms of mental disorders. When does one hear a public service announcement that encourages young people who may be experiencing disturbing or unacceptable sexual feelings to seek psychiatric treatment? There is a support group on the internet called Virtuous Pedophiles.6 That organization is unequivocally opposed to child molestation, while supporting efforts to improve the mental well-being of individuals who, through no fault of their own, experience unwanted pedophilic feelings.
Causes and noncauses
In attempting to elucidate etiology, researchers typically investigate nature (biology) and/or nurture (life experiences). In terms of the development of pedophilic disorder, there is evidence that both nature and nurture can play a role. Researchers have found that boys who are sexually abused are at increased risk for developing pedophilic disorder, and evidence of temporal lobe disturbances has also been documented in some instances.7,8
From clinical, societal, and forensic perspectives, it may be equally important to identify noncausal factors. Paraphilic disorders, including pedophilic disorder, do not develop as a consequence of volitional choice.9 For example, none of us decide which category, or categories, of potential partners are going to attract us sexually. Rather, in maturing we discover the nature of our own sexuality. Children do not ponder their options, somehow deciding while growing up to be attracted to the opposite sex (heterosexuality), the same sex (homosexuality), or both sexes (bisexuality). Similarly, in maturing into adulthood, individuals do not decide to become sexually attracted to prepubescent children. Who would decide to do that? Instead, unlike most of us, some individuals discover this about themselves; this often is a deeply disturbing insight.
It is not an individual’s fault that he or she has a paraphilic disorder. It is, however, his or her responsibility to do something about it. This may require accessing appropriate psychiatric care.
Why treatment may be needed
Sex is a powerful, biologically based appetite that recurrently craves satiation. God or nature has put that drive into all of us to ensure the survival of humanity. Even when that powerful biologic drive becomes misdirected (for example, towards children, or towards a desire to engage in public exhibitionism), it still recurrently craves satisfaction. It does not require mental health expertise to appreciate what a problematic situation this could become.
Continue to: Some individuals need help...
Some individuals need help in overcoming cravings related to nonsexual appetites. For example, Americans spend millions of dollars each year trying to diet; they often require some form of assistance in order to succeed. Individuals who crave drugs or alcohol often require mental health interventions to abstain because they are unable to consistently resist through willpower alone the powerful biologic urges that drive their actions.
The fundamental mental characteristic of any paraphilic disorder is the presence of intense, recurrent, sexual urges of an atypical nature. In the case of a pedophilic disorder, those urges involve sexual feelings about children.2 In the case of an exhibitionistic disorder, the afflicted individual experiences intense, recurrent sexual fantasies/urges related to exposing his genitals in public.1 Clearly, most men do not have to recurrently fight off the urge to act in such a fashion. Given the driven nature of intense erotic cravings, individuals who experience such cravings will frequently require access to competent mental health care.
Pharmacologic treatment of paraphilic disorders
In the future, we may develop a scientifically based understanding of the biologic factors that underlie qualitative differences in sexuality. At that point, it may become possible to intervene pharmacologically, changing the qualitative nature of a sexual urge with pharmacologic interventions. This cannot yet be done. H
In 1939, a Nobel Prize in Chemistry was awarded for the identification and isolation of the hormone testosterone, which energizes sexual drive.10 If an individual is hungering sexually to expose himself, to view child pornography, or to engage in sexual acts with children, the intensity of such hungers can be significantly reduced by lowering testosterone, thereby enhancing the capacity for successful sexual self-control.
A large body of scientific data has documented a marked decrease in sexually motivated behaviors when testosterone levels are significantly diminished.11 There is also evidence that recidivism rates of sexually motivated crimes can be significantly reduced when testosterone-lowering interventions are used.12
Continue to: Historically, removal of the testes...
Historically, removal of the testes (surgical castration) had been the only effective way to reliably lower testosterone. Today, this can be achieved pharmacologically. Use of a sex drive–lowering medication should be considered when either the clinician or the patient is concerned that a nonpharmacologic approach may be inadequate. In all instances, a patient with a paraphilic disorder should be informed that pharmacologic treatment is an option. A protocol for the pharmacologic treatment of paraphilic disorders that is based on my clinical experience is summarized in Table 2.
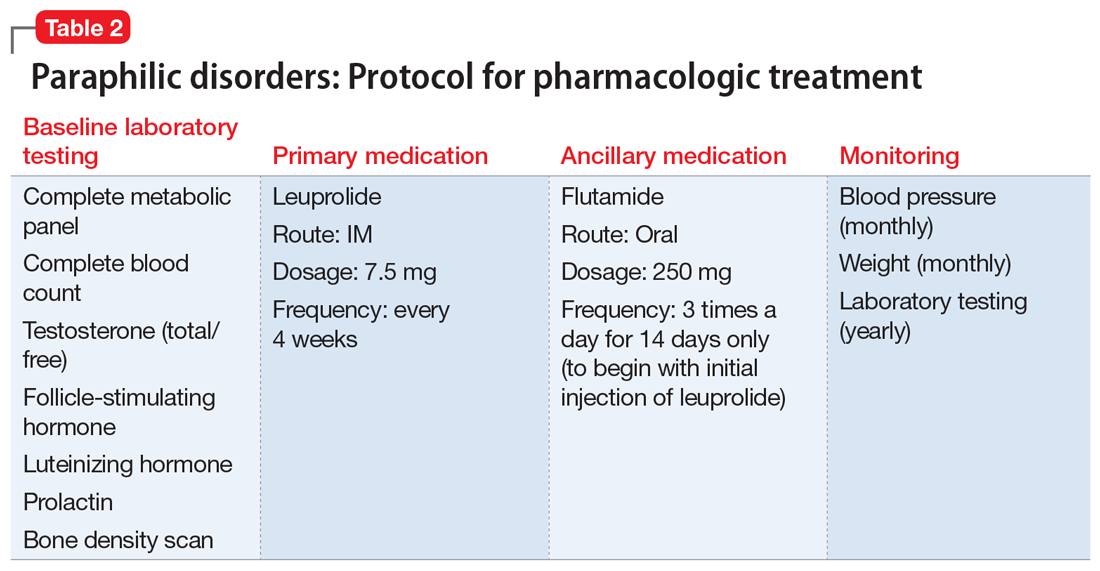
Leuprolide. A depot form of leuprolide is the most commonly employed agent to pharmacologically lower testosterone to treat a paraphilic disorder.13 When injected into muscle, leuprolide binds to it before gradually being released into the bloodstream. Previously, a depot medroxyprogesterone (a form of progesterone) had been used to treat paraphilic disorders.14 However, that had required weekly rather than monthly injections, and carried an increased risk of thrombotic emboli.
Prescribing leuprolide to treat a paraphilic disorder falls under FDA guidelines regarding the use of an approved drug for an “off-label” indication, and therefore is not considered investigational. For treating a paraphilic disorder, an effective dosage of leuprolide is 7.5 mg IM every 4 weeks. Long-term treatment is generally required, analogous to the management of diabetes. Because the initial injection of the series can cause a transient increase in testosterone (prior to its sustained decline), flutamide, a testosterone receptor blocking agent, is ordinarily prescribed for the first 14 days only, following initiation of treatment with depot leuprolide.15 Using flutamide in this fashion prevents the transient increase in testosterone from transiently increasing sexual drive. Flutamide should be discontinued after 14 days because long-term use can result in liver toxicity.
Some clinicians have been hesitant to prescribe leuprolide because of negative connotations associated with the term “chemical castration.” Unlike surgical castration, use of leuprolide is not a physically irreversible intervention, and does not result in sterility (although there may be an increase of atypical sperm and a decrease in total sperm production). The dosage can sometimes be titrated without a loss of efficacy.
In general, leuprolide’s safety protocol is well within the range associated with psychotropic medications.13 Low-risk adverse effects, such as hot flashes or cold sweats, may occur, especially during the period when hormone levels are in transition. There are no absolute contraindications to the use of leuprolide.
Continue to: Other medications
Other medications. Some researchers have suggested treating paraphilic disorders with psychotropic medications known to lower libido, such as selective serotonin reuptake inhibitors (SSRIs).16 However, leuprolide is far more reliable in consistently lowering testosterone and lowering the frequency and intensity of sexual urges. Although psychiatrists unfamiliar with treating paraphilic disorders may feel more comfortable initiating treatment with an SSRI, in my clinical experience, SSRIs have often proven inadequate for this purpose. When it comes to those paraphilic disorders in which treatment failure can result in significant harm (eg, pedophilic disorder), in my judgment, leuprolide should be the pharmacologic treatment of choice.
The opioid antagonist naltrexone has been used clinically to reduce cravings, primarily cravings for alcohol or drugs.17 However, I have not seen convincing evidence that it can be reliably beneficial in treating paraphilic disorders.
Tests to order before starting leuprolide
Long-term use of leuprolide can increase the risk of osteoporosis. Therefore, a baseline bone density scan should be performed before starting a patient on leuprolide. Baseline levels of testosterone, follicle-stimulating hormone, and luteinizing hormone also should be obtained. Patients should have yearly physical examinations, with accompanying laboratory testing. Hematocrit levels are often marginally low after beginning treatment, but not in a clinically significant way. Patients should also undergo routine monitoring for possible weight gain and the potential for associated hypertension. Treatment is predicated upon the known testosterone-suppressing effects of leuprolide, not upon routine monitoring of blood androgen levels.
Pharmacologic treatment of a paraphilic disorder should ordinarily occur in conjunction with nonpharmacologic modalities. One such modality would be group therapy, similar to the type frequently used to treat other craving disorders, such as drug or alcohol dependency.
In recent years, I have seen increasing numbers of patients presenting with a history of accessing and viewing child pornography. Once they have become more aware of the serious consequences of this behavior, most patients have been able to discontinue doing so without pharmacologic treatment. However, for patients in whom that behavior has seemed more driven (suggestive of a variant of voyeuristic disorder), prescription of leuprolide has been beneficial. Under such circumstances, I have diagnosed the patient’s condition as “other specified paraphilic disorder” with elements of pedophilia and voyeurism—the associated behaviors restricted to the voyeuristic viewing of child pornography.18
Continue to: Can treated patients still be sexual?
Can treated patients still be sexual?
If pharmacologic treatment of a paraphilic disorder results in erectile dysfunction, prescription of a medication such as sildenafil can be considered for patients who are in a consenting adult relationship, generally with the knowledge of their partner. Sildenafil can facilitate erectile capacity without increasing sexual drive. It can be helpful to explain to a patient that the purpose of pharmacologic treatment is not to prevent the enjoyment of sexual feelings within the context of a healthy, consenting, adult relationship, but instead to lower the intensity of problematic sexual urges, thereby facilitating sexual self-control. Just as lowering the appetite for food can make it easier to diet but not impossible to eat, lowering sexual appetite can facilitate successful self-control without necessarily interfering with erotic feelings experienced during sexual intimacy.
Bottom Line
Paraphilic disorders are not manifestations of a character flaw, but manifestations of unchosen qualitative differences in the nature of one’s sexual cravings. Not enough is yet known about the biology of sex to be able to pharmacologically alter its qualitative nature. However, pharmacologically lowering the intensity of a patient’s sexual drive can facilitate successful sexual self-regulation.
Related Resources
- LeVay S. Gay, straight and the reason why: the science of sexual orientation. London, UK: Oxford University Press; 2011.
- Rosler A, Witztum E. Treatment of men with paraphilia with a long-acting analogue of gonadotropin-releasing hormone. N Engl J Med. 1998;338(7):416-422.
- Brown GR. Overview of paraphilic disorders (paraphilias). https://www.merckmanuals.com/professional/psychiatricdisorders/sexuality,-gender-dysphoria,-and-paraphilias/overview-of-paraphilic-disorders.
Drug Brand Names
Flutamide • Eulexin
Leuprolide injection •
Eligard, Lupron Depot
Medroxyprogesterone •
Provera
Naltrexone • Revia, Vivitrol
Progesterone • Prometrium
Sildenafil • Viagra
In my role as the Director of The Johns Hopkins Sex and Gender Clinic, I have had the opportunity to provide care to 3 broad categories of patients: patients with sexual dysfunctions, patients experiencing gender dysphoria, and patients manifesting a paraphilic disorder. This article will not address sexual dysfunctions or gender dysphoria, but these terms are defined in the Box1-3 to clearly distinguish them from paraphilic disorders.
Box
Individuals with a sexual dysfunction (eg, erectile dysfunction or anorgasmia) generally experience conventional sexual feelings, but they may have difficulty performing sexually.1 Although ordinarily capable of adequate sexual performance, persons with a paraphilic disorder experience atypical erotic cravings.2 Such cravings can either be for an atypical or unacceptable category of potential partner (eg, animals or children), or for an atypical or unacceptable type of behavior (eg, crossdressing or public exhibitionism). Individuals with gender dysphoria frequently experience distress because their internal sense of feeling either male or female is not congruent with their external physical anatomy.3 The primary concerns of individuals experiencing gender dysphoria relate to feelings of gender identity, as opposed to problems involving erotic arousal.
Persons with paraphilic disorders (predominantly males) experience recurrent atypical sexual fantasies and urges that cause clinically significant impairment or distress.1 Those atypical fantasies and urges may be directed towards unacceptable partners such as animals or children, or towards unacceptable behaviors such as public exhibitionism. Table 11 lists the paraphilic disorders identified in DSM-5. This article focuses primarily, though not exclusively, upon pedophilic disorder, and its pharmacologic treatment. However, the rationale underlying such treatment is applicable across the paraphilic spectrum. Before providing such treatment, it is important for clinicians to have a clear conceptual understanding of paraphilic disorders.
When is a difference a disorder?
Cancer and respiration are 2 different biologic phenomenon. Cancer causes suffering and impairment, and as a consequence, we label it a disorder. We do so in the hope of learning more about it, and being able to successfully treat it. We do not classify respiration as a disorder because we do not consider it to be harmful.
The spectrum of human sexuality is quite broad, and psychiatry is generally not concerned with private sexual thoughts and behaviors involving consenting adults that do not cause suffering or impairment. When adults choose to engage in “kinky sex” that causes neither harm nor distress, so be it.
Some individuals may be privately aware of experiencing either an exclusive or nonexclusive sexual attraction to children. Some of these individuals may not be distressed by experiencing such attractions, and may be fully capable of resisting the temptation to enact them. In such an instance, even though an individual may be experiencing sexual attractions that are different from the norm, there may not be a sufficient basis for diagnosing pedophilic disorder. However, that difference in sexual phenomenology (ie, mental experience) could rise to the level of a diagnosable disorder if the individual in question expresses distress about experiencing such attractions, and/or if his capacity to resist acting upon them is impaired.4 Under such circumstances, treatment would be warranted.
Patients with paraphilic disorders deserve treatment
Prior to establishment of the Betty Ford Clinic in 1982, individuals who were drug- or alcohol-dependent were often portrayed in a negative light and referred to by derogatory pejoratives such as “bum” or “pothead.”5 Over time, society came to appreciate that good people, deserving of treatment, can become dependent upon substances, and in recent years there has been considerable support for related research initiatives and humane care. However, there has not been analogous support for individuals who manifest paraphilic disorders, especially those with pedophilic disorder. Instead, such individuals are often perceived as undeserving of mental health care and resources. This has been the case, even though successful treatment of a pedophilic disorder could help prevent the serious consequences of child molestation from occurring.
In contemporary society, the term pedophilia, which is a psychiatric specifier intended to guide research and treatment, has been hijacked by the nonmedical community and turned into a demeaning pejorative. In the collective consciousness of the public, the term pedophilia is routinely and mistakenly equated with the behavior of child molestation. Just as all alcoholics are not drunk drivers, all individuals with pedophilic disorder are not “child molesters.” Conversely, not all “child molesters” have pedophilic disorder.
Continue to: Individuals with other types...
Individuals with other types of paraphilic disorders are frequently similarly maligned and referred to as “perverts” or “deviants.” Public service announcements are frequently aired to reach out to individuals who are depressed, or drug- or alcohol-dependent, or suffering with other forms of mental disorders. When does one hear a public service announcement that encourages young people who may be experiencing disturbing or unacceptable sexual feelings to seek psychiatric treatment? There is a support group on the internet called Virtuous Pedophiles.6 That organization is unequivocally opposed to child molestation, while supporting efforts to improve the mental well-being of individuals who, through no fault of their own, experience unwanted pedophilic feelings.
Causes and noncauses
In attempting to elucidate etiology, researchers typically investigate nature (biology) and/or nurture (life experiences). In terms of the development of pedophilic disorder, there is evidence that both nature and nurture can play a role. Researchers have found that boys who are sexually abused are at increased risk for developing pedophilic disorder, and evidence of temporal lobe disturbances has also been documented in some instances.7,8
From clinical, societal, and forensic perspectives, it may be equally important to identify noncausal factors. Paraphilic disorders, including pedophilic disorder, do not develop as a consequence of volitional choice.9 For example, none of us decide which category, or categories, of potential partners are going to attract us sexually. Rather, in maturing we discover the nature of our own sexuality. Children do not ponder their options, somehow deciding while growing up to be attracted to the opposite sex (heterosexuality), the same sex (homosexuality), or both sexes (bisexuality). Similarly, in maturing into adulthood, individuals do not decide to become sexually attracted to prepubescent children. Who would decide to do that? Instead, unlike most of us, some individuals discover this about themselves; this often is a deeply disturbing insight.
It is not an individual’s fault that he or she has a paraphilic disorder. It is, however, his or her responsibility to do something about it. This may require accessing appropriate psychiatric care.
Why treatment may be needed
Sex is a powerful, biologically based appetite that recurrently craves satiation. God or nature has put that drive into all of us to ensure the survival of humanity. Even when that powerful biologic drive becomes misdirected (for example, towards children, or towards a desire to engage in public exhibitionism), it still recurrently craves satisfaction. It does not require mental health expertise to appreciate what a problematic situation this could become.
Continue to: Some individuals need help...
Some individuals need help in overcoming cravings related to nonsexual appetites. For example, Americans spend millions of dollars each year trying to diet; they often require some form of assistance in order to succeed. Individuals who crave drugs or alcohol often require mental health interventions to abstain because they are unable to consistently resist through willpower alone the powerful biologic urges that drive their actions.
The fundamental mental characteristic of any paraphilic disorder is the presence of intense, recurrent, sexual urges of an atypical nature. In the case of a pedophilic disorder, those urges involve sexual feelings about children.2 In the case of an exhibitionistic disorder, the afflicted individual experiences intense, recurrent sexual fantasies/urges related to exposing his genitals in public.1 Clearly, most men do not have to recurrently fight off the urge to act in such a fashion. Given the driven nature of intense erotic cravings, individuals who experience such cravings will frequently require access to competent mental health care.
Pharmacologic treatment of paraphilic disorders
In the future, we may develop a scientifically based understanding of the biologic factors that underlie qualitative differences in sexuality. At that point, it may become possible to intervene pharmacologically, changing the qualitative nature of a sexual urge with pharmacologic interventions. This cannot yet be done. H
In 1939, a Nobel Prize in Chemistry was awarded for the identification and isolation of the hormone testosterone, which energizes sexual drive.10 If an individual is hungering sexually to expose himself, to view child pornography, or to engage in sexual acts with children, the intensity of such hungers can be significantly reduced by lowering testosterone, thereby enhancing the capacity for successful sexual self-control.
A large body of scientific data has documented a marked decrease in sexually motivated behaviors when testosterone levels are significantly diminished.11 There is also evidence that recidivism rates of sexually motivated crimes can be significantly reduced when testosterone-lowering interventions are used.12
Continue to: Historically, removal of the testes...
Historically, removal of the testes (surgical castration) had been the only effective way to reliably lower testosterone. Today, this can be achieved pharmacologically. Use of a sex drive–lowering medication should be considered when either the clinician or the patient is concerned that a nonpharmacologic approach may be inadequate. In all instances, a patient with a paraphilic disorder should be informed that pharmacologic treatment is an option. A protocol for the pharmacologic treatment of paraphilic disorders that is based on my clinical experience is summarized in Table 2.
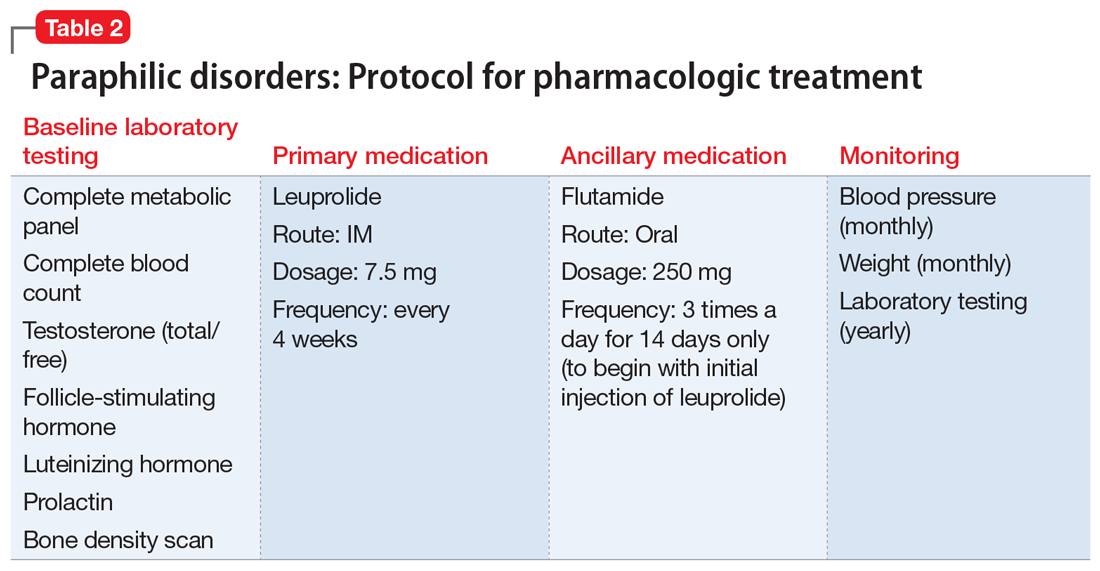
Leuprolide. A depot form of leuprolide is the most commonly employed agent to pharmacologically lower testosterone to treat a paraphilic disorder.13 When injected into muscle, leuprolide binds to it before gradually being released into the bloodstream. Previously, a depot medroxyprogesterone (a form of progesterone) had been used to treat paraphilic disorders.14 However, that had required weekly rather than monthly injections, and carried an increased risk of thrombotic emboli.
Prescribing leuprolide to treat a paraphilic disorder falls under FDA guidelines regarding the use of an approved drug for an “off-label” indication, and therefore is not considered investigational. For treating a paraphilic disorder, an effective dosage of leuprolide is 7.5 mg IM every 4 weeks. Long-term treatment is generally required, analogous to the management of diabetes. Because the initial injection of the series can cause a transient increase in testosterone (prior to its sustained decline), flutamide, a testosterone receptor blocking agent, is ordinarily prescribed for the first 14 days only, following initiation of treatment with depot leuprolide.15 Using flutamide in this fashion prevents the transient increase in testosterone from transiently increasing sexual drive. Flutamide should be discontinued after 14 days because long-term use can result in liver toxicity.
Some clinicians have been hesitant to prescribe leuprolide because of negative connotations associated with the term “chemical castration.” Unlike surgical castration, use of leuprolide is not a physically irreversible intervention, and does not result in sterility (although there may be an increase of atypical sperm and a decrease in total sperm production). The dosage can sometimes be titrated without a loss of efficacy.
In general, leuprolide’s safety protocol is well within the range associated with psychotropic medications.13 Low-risk adverse effects, such as hot flashes or cold sweats, may occur, especially during the period when hormone levels are in transition. There are no absolute contraindications to the use of leuprolide.
Continue to: Other medications
Other medications. Some researchers have suggested treating paraphilic disorders with psychotropic medications known to lower libido, such as selective serotonin reuptake inhibitors (SSRIs).16 However, leuprolide is far more reliable in consistently lowering testosterone and lowering the frequency and intensity of sexual urges. Although psychiatrists unfamiliar with treating paraphilic disorders may feel more comfortable initiating treatment with an SSRI, in my clinical experience, SSRIs have often proven inadequate for this purpose. When it comes to those paraphilic disorders in which treatment failure can result in significant harm (eg, pedophilic disorder), in my judgment, leuprolide should be the pharmacologic treatment of choice.
The opioid antagonist naltrexone has been used clinically to reduce cravings, primarily cravings for alcohol or drugs.17 However, I have not seen convincing evidence that it can be reliably beneficial in treating paraphilic disorders.
Tests to order before starting leuprolide
Long-term use of leuprolide can increase the risk of osteoporosis. Therefore, a baseline bone density scan should be performed before starting a patient on leuprolide. Baseline levels of testosterone, follicle-stimulating hormone, and luteinizing hormone also should be obtained. Patients should have yearly physical examinations, with accompanying laboratory testing. Hematocrit levels are often marginally low after beginning treatment, but not in a clinically significant way. Patients should also undergo routine monitoring for possible weight gain and the potential for associated hypertension. Treatment is predicated upon the known testosterone-suppressing effects of leuprolide, not upon routine monitoring of blood androgen levels.
Pharmacologic treatment of a paraphilic disorder should ordinarily occur in conjunction with nonpharmacologic modalities. One such modality would be group therapy, similar to the type frequently used to treat other craving disorders, such as drug or alcohol dependency.
In recent years, I have seen increasing numbers of patients presenting with a history of accessing and viewing child pornography. Once they have become more aware of the serious consequences of this behavior, most patients have been able to discontinue doing so without pharmacologic treatment. However, for patients in whom that behavior has seemed more driven (suggestive of a variant of voyeuristic disorder), prescription of leuprolide has been beneficial. Under such circumstances, I have diagnosed the patient’s condition as “other specified paraphilic disorder” with elements of pedophilia and voyeurism—the associated behaviors restricted to the voyeuristic viewing of child pornography.18
Continue to: Can treated patients still be sexual?
Can treated patients still be sexual?
If pharmacologic treatment of a paraphilic disorder results in erectile dysfunction, prescription of a medication such as sildenafil can be considered for patients who are in a consenting adult relationship, generally with the knowledge of their partner. Sildenafil can facilitate erectile capacity without increasing sexual drive. It can be helpful to explain to a patient that the purpose of pharmacologic treatment is not to prevent the enjoyment of sexual feelings within the context of a healthy, consenting, adult relationship, but instead to lower the intensity of problematic sexual urges, thereby facilitating sexual self-control. Just as lowering the appetite for food can make it easier to diet but not impossible to eat, lowering sexual appetite can facilitate successful self-control without necessarily interfering with erotic feelings experienced during sexual intimacy.
Bottom Line
Paraphilic disorders are not manifestations of a character flaw, but manifestations of unchosen qualitative differences in the nature of one’s sexual cravings. Not enough is yet known about the biology of sex to be able to pharmacologically alter its qualitative nature. However, pharmacologically lowering the intensity of a patient’s sexual drive can facilitate successful sexual self-regulation.
Related Resources
- LeVay S. Gay, straight and the reason why: the science of sexual orientation. London, UK: Oxford University Press; 2011.
- Rosler A, Witztum E. Treatment of men with paraphilia with a long-acting analogue of gonadotropin-releasing hormone. N Engl J Med. 1998;338(7):416-422.
- Brown GR. Overview of paraphilic disorders (paraphilias). https://www.merckmanuals.com/professional/psychiatricdisorders/sexuality,-gender-dysphoria,-and-paraphilias/overview-of-paraphilic-disorders.
Drug Brand Names
Flutamide • Eulexin
Leuprolide injection •
Eligard, Lupron Depot
Medroxyprogesterone •
Provera
Naltrexone • Revia, Vivitrol
Progesterone • Prometrium
Sildenafil • Viagra
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:423-450.
2. Berlin FS. Pedophilia: criminal mind-set or mental disorder? A conceptual review. American Journal of Forensic Psychiatry. 2001;32(2):3-25.
3. Berlin FS. A conceptual overview and commentary on gender dysphoria. J Am Acad Psychiatry Law. 2016;44(2):246-252
4. Berlin FS. Pedophilia: when is a difference a disorder: Peer commentaries on Green (2002) and Schmidt (2002). Arch Sex Behav. 2002;31:1-2.
5. Ford B, Chase C. Betty: a glad awakening. New York, NY: Doubleday; 1987.
6. Virtuous Pedophiles. https://www.virped.org/. Accessed September 28, 2018.
7. Freund K, Kuban M. The basis of the abused abuser theory of pedophilia: A further elaboration of an earlier study. Arch Sex Behav. 1994;23(5):553-563.
8. Mendes MF, Chow T, Ringman T, et al. Pedophilia and temporal lobe disturbances. J Neuropsychiatry Clin Neurosci. 2000;12(1):71-76.
9. Money J. Love and love sickness: The science of sex, gender differences, and pair bonding. Baltimore, MD: Johns Hopkins University Press; 1980.
10. The Nobel Prize in Chemistry 1939. https://www.nobelprize.org/prizes/chemistry/1939/summary/. Accessed September 29, 2018.
11. Berlin FS. Commentary: The impact of surgical castration on sexual recidivism risk among civilly committed sex offenders. J Am Acad Psychiatry Law. 2005;33(1):37-41.
12. Hansen H. Treatment of dangerous sexual offenders. In: Seminar on Prison Health Services in Tampere, Finland. Helsinki, Finland: Ministry of Justice, Government Printing Centre; 1991:33-38.
13. Berlin FS. Risk/benefit ratio of androgen deprivation treatment for sex offenders. J Am Acad Psychiatry Law. 2009;37(1):59-62.
14. Berlin FS, Meinecke CF. Treatment of sex offenders with antiandrogenic medication: conceptualization, review of treatment modalities, and preliminary findings. Am J Psychiatry. 1981;138(5):601-607.
15. Neri R. Pharmacology and pharmacokinetics of flutamide. Urology. 1989;34(suppl 4):19-21; discussion 46-56.
16. Adi Y, Ashcroft D, Browne K, et al. Clinical effectiveness and cost consequences of selective serotonin receptor reuptake inhibitors in the treatment of sex offenders. Health Technol Assess. 2002;6(28):1-66.
17. Anton RF. Naltrexone for the management of alcohol dependence. N Engl J Med. 2008;359(7):715-721.
18. Berlin FS. Commentary on pedophilia diagnostic criteria in DSM-5. J Am Acad Psychiatry Law. 2011;39(2):242-244.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:423-450.
2. Berlin FS. Pedophilia: criminal mind-set or mental disorder? A conceptual review. American Journal of Forensic Psychiatry. 2001;32(2):3-25.
3. Berlin FS. A conceptual overview and commentary on gender dysphoria. J Am Acad Psychiatry Law. 2016;44(2):246-252
4. Berlin FS. Pedophilia: when is a difference a disorder: Peer commentaries on Green (2002) and Schmidt (2002). Arch Sex Behav. 2002;31:1-2.
5. Ford B, Chase C. Betty: a glad awakening. New York, NY: Doubleday; 1987.
6. Virtuous Pedophiles. https://www.virped.org/. Accessed September 28, 2018.
7. Freund K, Kuban M. The basis of the abused abuser theory of pedophilia: A further elaboration of an earlier study. Arch Sex Behav. 1994;23(5):553-563.
8. Mendes MF, Chow T, Ringman T, et al. Pedophilia and temporal lobe disturbances. J Neuropsychiatry Clin Neurosci. 2000;12(1):71-76.
9. Money J. Love and love sickness: The science of sex, gender differences, and pair bonding. Baltimore, MD: Johns Hopkins University Press; 1980.
10. The Nobel Prize in Chemistry 1939. https://www.nobelprize.org/prizes/chemistry/1939/summary/. Accessed September 29, 2018.
11. Berlin FS. Commentary: The impact of surgical castration on sexual recidivism risk among civilly committed sex offenders. J Am Acad Psychiatry Law. 2005;33(1):37-41.
12. Hansen H. Treatment of dangerous sexual offenders. In: Seminar on Prison Health Services in Tampere, Finland. Helsinki, Finland: Ministry of Justice, Government Printing Centre; 1991:33-38.
13. Berlin FS. Risk/benefit ratio of androgen deprivation treatment for sex offenders. J Am Acad Psychiatry Law. 2009;37(1):59-62.
14. Berlin FS, Meinecke CF. Treatment of sex offenders with antiandrogenic medication: conceptualization, review of treatment modalities, and preliminary findings. Am J Psychiatry. 1981;138(5):601-607.
15. Neri R. Pharmacology and pharmacokinetics of flutamide. Urology. 1989;34(suppl 4):19-21; discussion 46-56.
16. Adi Y, Ashcroft D, Browne K, et al. Clinical effectiveness and cost consequences of selective serotonin receptor reuptake inhibitors in the treatment of sex offenders. Health Technol Assess. 2002;6(28):1-66.
17. Anton RF. Naltrexone for the management of alcohol dependence. N Engl J Med. 2008;359(7):715-721.
18. Berlin FS. Commentary on pedophilia diagnostic criteria in DSM-5. J Am Acad Psychiatry Law. 2011;39(2):242-244.
A.I. and U 2
In a previous Letter from Maine I wrote about a study performed in China in which more than half a million patients were diagnosed by an artificial intelligence (A.I.) system that was able to extract and analyze information from their electronic medical records. The system was at least as accurate as physicians who had access to the same data (“A.I. Shows Promise Assisting Physicians,” by Cade Metz, The New York Times, Feb. 11, 2019). I ended my column with the hopeful assumption that despite incredible advances in A.I., the practice of medicine always would include a human element. However, I left unexplained exactly how physicians would fit into the post-A.I. revolution. In the weeks since I submitted that column, I have been searching for roles that might remain for physicians after A.I. has snatched their bread and butter of diagnosis and management.
I easily can envision a system in which the patient enters her chief complaint and current symptoms into her smartphone or tablet. Using its database of the patient’s past, family, and social history, the system generates a list of laboratory and imaging studies, some of which the patient may be able to submit directly from her handheld device. For example, the system may be able to use the patient’s phone to “examine” her. The A.I. system then generates a diagnosis.
If the diagnosed condition and management is simple and straightforward, such as a rash, the information could be communicated to the patient directly, with a short paragraph of explanation and list of persistent symptoms that would indicate that the condition was not improving as expected. A contact dermatitis comes to mind here.
However, suppose the A.I. system determines that the patient has a 90% chance of having stage IV pancreatic cancer, with a life expectancy of 6 months. Is this the kind of information you would like to learn about yourself by clicking “Your Diagnosis” box on your phone while you were having lunch with a friend? Obviously, a diagnosis of this severity should be communicated human to human, even though it was generated by a highly accurate computer system. And this communication would best be done in the form of a dialogue with someone who knows the patient and has some understanding of how she might understand and cope with the information. In the absence of a prior relationship, the dialogue should occur in real time and face to face at a minimum. I guess we have to acknowledge that FaceTime or Skype might be acceptable here.
Fortunately, stage IV cancers are rare, but there are a bazillion other conditions that, while not serious, require a nuanced explanation as part of a successful management plan that takes into account the patient’s level of anxiety and cognitive abilities. A boilerplate paragraph or two spit out by an A.I. system isn’t good health care. Although I know many physicians do rely on printed handouts for conditions they feel is a no-brainer.
The bottom line is that even when a machine may be better than we are at making some diagnoses, there always will be a role for a human to help other humans understand and cope with those diagnoses. At this point, physicians would appear be the obvious choice to fill that role. How we will get reimbursed for our communication skills is unclear.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
In a previous Letter from Maine I wrote about a study performed in China in which more than half a million patients were diagnosed by an artificial intelligence (A.I.) system that was able to extract and analyze information from their electronic medical records. The system was at least as accurate as physicians who had access to the same data (“A.I. Shows Promise Assisting Physicians,” by Cade Metz, The New York Times, Feb. 11, 2019). I ended my column with the hopeful assumption that despite incredible advances in A.I., the practice of medicine always would include a human element. However, I left unexplained exactly how physicians would fit into the post-A.I. revolution. In the weeks since I submitted that column, I have been searching for roles that might remain for physicians after A.I. has snatched their bread and butter of diagnosis and management.
I easily can envision a system in which the patient enters her chief complaint and current symptoms into her smartphone or tablet. Using its database of the patient’s past, family, and social history, the system generates a list of laboratory and imaging studies, some of which the patient may be able to submit directly from her handheld device. For example, the system may be able to use the patient’s phone to “examine” her. The A.I. system then generates a diagnosis.
If the diagnosed condition and management is simple and straightforward, such as a rash, the information could be communicated to the patient directly, with a short paragraph of explanation and list of persistent symptoms that would indicate that the condition was not improving as expected. A contact dermatitis comes to mind here.
However, suppose the A.I. system determines that the patient has a 90% chance of having stage IV pancreatic cancer, with a life expectancy of 6 months. Is this the kind of information you would like to learn about yourself by clicking “Your Diagnosis” box on your phone while you were having lunch with a friend? Obviously, a diagnosis of this severity should be communicated human to human, even though it was generated by a highly accurate computer system. And this communication would best be done in the form of a dialogue with someone who knows the patient and has some understanding of how she might understand and cope with the information. In the absence of a prior relationship, the dialogue should occur in real time and face to face at a minimum. I guess we have to acknowledge that FaceTime or Skype might be acceptable here.
Fortunately, stage IV cancers are rare, but there are a bazillion other conditions that, while not serious, require a nuanced explanation as part of a successful management plan that takes into account the patient’s level of anxiety and cognitive abilities. A boilerplate paragraph or two spit out by an A.I. system isn’t good health care. Although I know many physicians do rely on printed handouts for conditions they feel is a no-brainer.
The bottom line is that even when a machine may be better than we are at making some diagnoses, there always will be a role for a human to help other humans understand and cope with those diagnoses. At this point, physicians would appear be the obvious choice to fill that role. How we will get reimbursed for our communication skills is unclear.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
In a previous Letter from Maine I wrote about a study performed in China in which more than half a million patients were diagnosed by an artificial intelligence (A.I.) system that was able to extract and analyze information from their electronic medical records. The system was at least as accurate as physicians who had access to the same data (“A.I. Shows Promise Assisting Physicians,” by Cade Metz, The New York Times, Feb. 11, 2019). I ended my column with the hopeful assumption that despite incredible advances in A.I., the practice of medicine always would include a human element. However, I left unexplained exactly how physicians would fit into the post-A.I. revolution. In the weeks since I submitted that column, I have been searching for roles that might remain for physicians after A.I. has snatched their bread and butter of diagnosis and management.
I easily can envision a system in which the patient enters her chief complaint and current symptoms into her smartphone or tablet. Using its database of the patient’s past, family, and social history, the system generates a list of laboratory and imaging studies, some of which the patient may be able to submit directly from her handheld device. For example, the system may be able to use the patient’s phone to “examine” her. The A.I. system then generates a diagnosis.
If the diagnosed condition and management is simple and straightforward, such as a rash, the information could be communicated to the patient directly, with a short paragraph of explanation and list of persistent symptoms that would indicate that the condition was not improving as expected. A contact dermatitis comes to mind here.
However, suppose the A.I. system determines that the patient has a 90% chance of having stage IV pancreatic cancer, with a life expectancy of 6 months. Is this the kind of information you would like to learn about yourself by clicking “Your Diagnosis” box on your phone while you were having lunch with a friend? Obviously, a diagnosis of this severity should be communicated human to human, even though it was generated by a highly accurate computer system. And this communication would best be done in the form of a dialogue with someone who knows the patient and has some understanding of how she might understand and cope with the information. In the absence of a prior relationship, the dialogue should occur in real time and face to face at a minimum. I guess we have to acknowledge that FaceTime or Skype might be acceptable here.
Fortunately, stage IV cancers are rare, but there are a bazillion other conditions that, while not serious, require a nuanced explanation as part of a successful management plan that takes into account the patient’s level of anxiety and cognitive abilities. A boilerplate paragraph or two spit out by an A.I. system isn’t good health care. Although I know many physicians do rely on printed handouts for conditions they feel is a no-brainer.
The bottom line is that even when a machine may be better than we are at making some diagnoses, there always will be a role for a human to help other humans understand and cope with those diagnoses. At this point, physicians would appear be the obvious choice to fill that role. How we will get reimbursed for our communication skills is unclear.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Sleeping poorly may mean itching more
Study results showing an association between active atopic dermatitis (AD) and poor sleep quality were published in JAMA Pediatrics by a group of dermatologists at the University of California, San Francisco (JAMA Pediatr. 2019 Mar 4. doi: 10.1001/jamapediatrics.2019.0025). The data on the sleep quality and quantity of nearly 14,000 children were collected over span of 11 years. Of these children, slightly fewer than 5,000 met the researchers’ definition of atopic dermatitis.
Although the sleep duration of children with and without AD was not statistically different, the reports of poor sleep quality and sleep disturbances by children with AD were dramatically more frequent – a nearly 50% higher chance of having more sleep-quality disturbances. In addition, children with more severe active disease were even more likely to report poor sleep quality – almost 80%.
I suspect that you’re not surprised by these findings. You have probably heard numerous tales of poor sleep from families who have children with AD. It just makes sense that a child whose skin is dry and itchy will have trouble sleeping. I’m sure you have struggled to help parents be more diligent about applying moisturizing creams and lotions, and have been aggressive with steroid creams during flare-ups. You may have added sleep onset-promoting antihistamines when topical treatments haven’t been as effective as you had hoped.
Has your working assumption always been that if you can get the child’s skin settled down, the itching will improve and the child will have an easier time falling asleep? But have you ever considered flipping the equation over and tried to be more aggressive in managing the child’s sleep problems?
Like many other folks with psoriasis, I have noticed that my itching is worse when I am tired, and particularly worse in that evil interval between crawling into bed and falling asleep. As the grandparent of a child with AD, I have observed a similar phenomenon. While I am not going to claim that sleep deprivation causes psoriasis or AD, I think that we need to consider the association between poor sleep quality and itching as a feedback loop that must be interrupted. This means that in addition to recommending topicals and moisturizing strategies, we must learn more about our patients’ sleep habits and suggest appropriate sleep hygiene practices.
Many parents aren’t aware of the cruel paradox that an overtired child is more likely to have trouble falling asleep. Has the child been allowed to give up his nap prematurely? Is bedtime at an appropriate hour, and does it consist of a limited number of sleep-promoting rituals? Is the bedroom dark enough, cool enough, and free of electronic distractions?
Providing effective counseling on sleep hygiene is time consuming and requires that you have first convinced the parents that the child’s itching is being aggravated by his sleep deprivation and not just the other way around. Successful management may require a close working relationship between the child’s pediatrician and his dermatologist, with both physicians reinforcing each other’s message that atopic dermatitis isn’t just skin deep.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Is My Child Overtired?: The Sleep Solution for Raising Happier, Healthier Children.” Email him at [email protected].
Study results showing an association between active atopic dermatitis (AD) and poor sleep quality were published in JAMA Pediatrics by a group of dermatologists at the University of California, San Francisco (JAMA Pediatr. 2019 Mar 4. doi: 10.1001/jamapediatrics.2019.0025). The data on the sleep quality and quantity of nearly 14,000 children were collected over span of 11 years. Of these children, slightly fewer than 5,000 met the researchers’ definition of atopic dermatitis.
Although the sleep duration of children with and without AD was not statistically different, the reports of poor sleep quality and sleep disturbances by children with AD were dramatically more frequent – a nearly 50% higher chance of having more sleep-quality disturbances. In addition, children with more severe active disease were even more likely to report poor sleep quality – almost 80%.
I suspect that you’re not surprised by these findings. You have probably heard numerous tales of poor sleep from families who have children with AD. It just makes sense that a child whose skin is dry and itchy will have trouble sleeping. I’m sure you have struggled to help parents be more diligent about applying moisturizing creams and lotions, and have been aggressive with steroid creams during flare-ups. You may have added sleep onset-promoting antihistamines when topical treatments haven’t been as effective as you had hoped.
Has your working assumption always been that if you can get the child’s skin settled down, the itching will improve and the child will have an easier time falling asleep? But have you ever considered flipping the equation over and tried to be more aggressive in managing the child’s sleep problems?
Like many other folks with psoriasis, I have noticed that my itching is worse when I am tired, and particularly worse in that evil interval between crawling into bed and falling asleep. As the grandparent of a child with AD, I have observed a similar phenomenon. While I am not going to claim that sleep deprivation causes psoriasis or AD, I think that we need to consider the association between poor sleep quality and itching as a feedback loop that must be interrupted. This means that in addition to recommending topicals and moisturizing strategies, we must learn more about our patients’ sleep habits and suggest appropriate sleep hygiene practices.
Many parents aren’t aware of the cruel paradox that an overtired child is more likely to have trouble falling asleep. Has the child been allowed to give up his nap prematurely? Is bedtime at an appropriate hour, and does it consist of a limited number of sleep-promoting rituals? Is the bedroom dark enough, cool enough, and free of electronic distractions?
Providing effective counseling on sleep hygiene is time consuming and requires that you have first convinced the parents that the child’s itching is being aggravated by his sleep deprivation and not just the other way around. Successful management may require a close working relationship between the child’s pediatrician and his dermatologist, with both physicians reinforcing each other’s message that atopic dermatitis isn’t just skin deep.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Is My Child Overtired?: The Sleep Solution for Raising Happier, Healthier Children.” Email him at [email protected].
Study results showing an association between active atopic dermatitis (AD) and poor sleep quality were published in JAMA Pediatrics by a group of dermatologists at the University of California, San Francisco (JAMA Pediatr. 2019 Mar 4. doi: 10.1001/jamapediatrics.2019.0025). The data on the sleep quality and quantity of nearly 14,000 children were collected over span of 11 years. Of these children, slightly fewer than 5,000 met the researchers’ definition of atopic dermatitis.
Although the sleep duration of children with and without AD was not statistically different, the reports of poor sleep quality and sleep disturbances by children with AD were dramatically more frequent – a nearly 50% higher chance of having more sleep-quality disturbances. In addition, children with more severe active disease were even more likely to report poor sleep quality – almost 80%.
I suspect that you’re not surprised by these findings. You have probably heard numerous tales of poor sleep from families who have children with AD. It just makes sense that a child whose skin is dry and itchy will have trouble sleeping. I’m sure you have struggled to help parents be more diligent about applying moisturizing creams and lotions, and have been aggressive with steroid creams during flare-ups. You may have added sleep onset-promoting antihistamines when topical treatments haven’t been as effective as you had hoped.
Has your working assumption always been that if you can get the child’s skin settled down, the itching will improve and the child will have an easier time falling asleep? But have you ever considered flipping the equation over and tried to be more aggressive in managing the child’s sleep problems?
Like many other folks with psoriasis, I have noticed that my itching is worse when I am tired, and particularly worse in that evil interval between crawling into bed and falling asleep. As the grandparent of a child with AD, I have observed a similar phenomenon. While I am not going to claim that sleep deprivation causes psoriasis or AD, I think that we need to consider the association between poor sleep quality and itching as a feedback loop that must be interrupted. This means that in addition to recommending topicals and moisturizing strategies, we must learn more about our patients’ sleep habits and suggest appropriate sleep hygiene practices.
Many parents aren’t aware of the cruel paradox that an overtired child is more likely to have trouble falling asleep. Has the child been allowed to give up his nap prematurely? Is bedtime at an appropriate hour, and does it consist of a limited number of sleep-promoting rituals? Is the bedroom dark enough, cool enough, and free of electronic distractions?
Providing effective counseling on sleep hygiene is time consuming and requires that you have first convinced the parents that the child’s itching is being aggravated by his sleep deprivation and not just the other way around. Successful management may require a close working relationship between the child’s pediatrician and his dermatologist, with both physicians reinforcing each other’s message that atopic dermatitis isn’t just skin deep.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Is My Child Overtired?: The Sleep Solution for Raising Happier, Healthier Children.” Email him at [email protected].