User login
Who’s increasing health care costs? Not us!
Determining who is responsible for the increase in health care cost in the United States has seemingly limitless possibilities. There are enough culprits to go around, but a recent analysis points a finger at hospital-based care (Health Aff. 2019 Feb;38[2]:184-9).
The authors of the paper found that, during the period from 2007 to 2014, inpatient hospital care for surgical procedures increased 42% and outpatient hospital care increased 25%. In the same period, physician care increased only 6%. Much of this increase in hospital costs was associated with hospital consolidations and mergers.
We have been led to believe that hospital mergers will cut costs by eliminating duplication of both physical and personnel overhead costs. In fact that doesn’t seem to happen. It appears that hospital mergers were associated with increased per patient costs and is a result of decrease in competition in local health care markets. This observation has been made in the past (Am Econ Rev. 2015 Jan;105:172-203), and was reiterated by the most recent report. If there were decreases in overhead observed in the mergers, they were not passed on to the patients or insurers.
There was a time when community hospitals, large and small, were run by community leaders and local doctors, often under the aegis of religious and social groups. I can remember the medical and community leadership in Utica, N.Y., where I grew up and where I worked in a hospital as a summer intern. Their goal was to provide quality health care. The financial success or failures of the hospitals were the responsibility of the local community, and the profits and losses were kept at a minimum.
Fast forward to the 21st century and health care in general, and hospital care in particular, has become a “cash cow.” Community leadership has been minimized, and where it exists, it is under constant pressure to make a profit. Hospital mergers, arranged under the guise of economy of size, are now controlled by hedge funds and large health care corporations.
The community board of trustees has been replaced by investors, whose main concern is the return on their investments regardless of quality of care or need. If those profits fail to materialize, the hospitals are taken over by another investor group. So much for quality. As the corporations grow, they buy up the competition, particularly small community hospitals leaving many, particularly in rural America, without medical support.
There seems to be little recourse to consumers or insurers to mitigate this process. Investors have a right to a return on their investment, but until we have governmental control of competition, that incentive remains. We can see similar price increases in the pharmaceutical marketplace, where Congress has limited competition to preserve the drug monopoly. Americans will be asked to pay more to maintain a system that is inherently on the road to bankruptcy and fails to provide either quality or fair drug and hospital charges.
But what do we care, we can afford it.
Dr. Goldstein is professor of medicine at Wayne State University and the division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit.
Determining who is responsible for the increase in health care cost in the United States has seemingly limitless possibilities. There are enough culprits to go around, but a recent analysis points a finger at hospital-based care (Health Aff. 2019 Feb;38[2]:184-9).
The authors of the paper found that, during the period from 2007 to 2014, inpatient hospital care for surgical procedures increased 42% and outpatient hospital care increased 25%. In the same period, physician care increased only 6%. Much of this increase in hospital costs was associated with hospital consolidations and mergers.
We have been led to believe that hospital mergers will cut costs by eliminating duplication of both physical and personnel overhead costs. In fact that doesn’t seem to happen. It appears that hospital mergers were associated with increased per patient costs and is a result of decrease in competition in local health care markets. This observation has been made in the past (Am Econ Rev. 2015 Jan;105:172-203), and was reiterated by the most recent report. If there were decreases in overhead observed in the mergers, they were not passed on to the patients or insurers.
There was a time when community hospitals, large and small, were run by community leaders and local doctors, often under the aegis of religious and social groups. I can remember the medical and community leadership in Utica, N.Y., where I grew up and where I worked in a hospital as a summer intern. Their goal was to provide quality health care. The financial success or failures of the hospitals were the responsibility of the local community, and the profits and losses were kept at a minimum.
Fast forward to the 21st century and health care in general, and hospital care in particular, has become a “cash cow.” Community leadership has been minimized, and where it exists, it is under constant pressure to make a profit. Hospital mergers, arranged under the guise of economy of size, are now controlled by hedge funds and large health care corporations.
The community board of trustees has been replaced by investors, whose main concern is the return on their investments regardless of quality of care or need. If those profits fail to materialize, the hospitals are taken over by another investor group. So much for quality. As the corporations grow, they buy up the competition, particularly small community hospitals leaving many, particularly in rural America, without medical support.
There seems to be little recourse to consumers or insurers to mitigate this process. Investors have a right to a return on their investment, but until we have governmental control of competition, that incentive remains. We can see similar price increases in the pharmaceutical marketplace, where Congress has limited competition to preserve the drug monopoly. Americans will be asked to pay more to maintain a system that is inherently on the road to bankruptcy and fails to provide either quality or fair drug and hospital charges.
But what do we care, we can afford it.
Dr. Goldstein is professor of medicine at Wayne State University and the division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit.
Determining who is responsible for the increase in health care cost in the United States has seemingly limitless possibilities. There are enough culprits to go around, but a recent analysis points a finger at hospital-based care (Health Aff. 2019 Feb;38[2]:184-9).
The authors of the paper found that, during the period from 2007 to 2014, inpatient hospital care for surgical procedures increased 42% and outpatient hospital care increased 25%. In the same period, physician care increased only 6%. Much of this increase in hospital costs was associated with hospital consolidations and mergers.
We have been led to believe that hospital mergers will cut costs by eliminating duplication of both physical and personnel overhead costs. In fact that doesn’t seem to happen. It appears that hospital mergers were associated with increased per patient costs and is a result of decrease in competition in local health care markets. This observation has been made in the past (Am Econ Rev. 2015 Jan;105:172-203), and was reiterated by the most recent report. If there were decreases in overhead observed in the mergers, they were not passed on to the patients or insurers.
There was a time when community hospitals, large and small, were run by community leaders and local doctors, often under the aegis of religious and social groups. I can remember the medical and community leadership in Utica, N.Y., where I grew up and where I worked in a hospital as a summer intern. Their goal was to provide quality health care. The financial success or failures of the hospitals were the responsibility of the local community, and the profits and losses were kept at a minimum.
Fast forward to the 21st century and health care in general, and hospital care in particular, has become a “cash cow.” Community leadership has been minimized, and where it exists, it is under constant pressure to make a profit. Hospital mergers, arranged under the guise of economy of size, are now controlled by hedge funds and large health care corporations.
The community board of trustees has been replaced by investors, whose main concern is the return on their investments regardless of quality of care or need. If those profits fail to materialize, the hospitals are taken over by another investor group. So much for quality. As the corporations grow, they buy up the competition, particularly small community hospitals leaving many, particularly in rural America, without medical support.
There seems to be little recourse to consumers or insurers to mitigate this process. Investors have a right to a return on their investment, but until we have governmental control of competition, that incentive remains. We can see similar price increases in the pharmaceutical marketplace, where Congress has limited competition to preserve the drug monopoly. Americans will be asked to pay more to maintain a system that is inherently on the road to bankruptcy and fails to provide either quality or fair drug and hospital charges.
But what do we care, we can afford it.
Dr. Goldstein is professor of medicine at Wayne State University and the division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit.
The paclitaxel paradox
As medical editor of Vascular Specialist, it has always been my hope to use our excellent reporters and rapid production schedule to keep readers abreast of the latest news in vascular surgery. While my colleagues at the Journal of Vascular Surgery publish studies that will drive treatment, my goal is to drive discussion.
With topics like burnout, workforce shortages, and electronic medical records, I feel we have been successful. The downside of staying current is we sometimes find ourselves publishing contradictory stories. This has been the case with paclitaxel. Let’s take a break from the fray and review where we are, and where we might go from here.
In 2012, the Zilver PTX became the first drug-eluting stent (DES) to gain Food and Drug Administration approval for the treatment of peripheral vascular disease. Two years later, the FDA approved the Lutonix 035 as the first drug-coated balloon (DCB) for use in the femoral-popliteal arteries. The Lutonix would also gain a second indication for failing dialysis fistulas. Medtronic and Spectranetics received authorizations for their DCBs in 2015 and 2017, respectively.
While the safety of paclitaxel-coated devices in the coronary system had previously been called into question, the drug was generally considered safe and effective in the peripheral arterial system. The controversy began in December 2018, when Katsanos et al.1 published a meta-analysis of 28 randomized, controlled trials (RCTs) investigating paclitaxel-coated devices in the femoral-popliteal arteries. While all-cause patient mortality was similar at 1 year between paclitaxel-coated devices and controls (2.3% in each), at 2 years the risk of death was significantly higher in those treated with paclitaxel (7.2% vs. 3.8%). The 5-year data were available for three trials where there was a continued significantly increased risk of mortality with paclitaxel (14.7% vs. 8.1%).
Opposition to these findings was prompt from both physicians and industry. Weaknesses of the analysis, both perceived and real, were hammered. The meta-analysis did not include individual patient data, and the actual cause of death was unknown in most of the included trials. The study was not adequately powered to eliminate the risk of type 1 error when comparing mortality after 2 years. Individuals assigned to the control group may have received paclitaxel treatment at some point in their follow-up. The DCB and DES treatment groups were combined. The methods employed by the authors, however, stood up reasonably well to scrutiny.
On Jan. 17, 2019, the FDA issued their first response stating, “the FDA believes that the benefits continue to outweigh the risks for approved paclitaxel-coated balloons and paclitaxel-eluting stents when used in accordance with their indications for use.”2
Later that month, Peter Schneider, MD, and associates published a patient-level meta-analysis in the Journal of the American College of Cardiology.3 The study included 1,980 patients and found no statistically significant difference in all-cause mortality between DCB (9.3%) and percutaneous transluminal angioplasty (PTA) (11.2%) through 5 years. Shortly after that, however, a correction was issued.
On Feb. 15, 2019, Medtronic reported an error in the 2- and 3-year follow-up periods for the IN.PACT Global postmarket study. The company stated, “Due to a programming error, mortality data were inadvertently omitted from the summary tables included in the statistical analysis.” The mortality in the DCB cohort was corrected from 9.30% to 15.12%. The authors stated that this new mortality rate was still not significantly higher than the PTA group (P = .09).4
Less than 1 week later, another device company issued a correction. And once again, the error had been made in favor of the paclitaxel-treated group. In 2016, the 5-year data from Cook Medical’s Zilver PTX trial were published in Circulation. The study reported a mortality of 10.2% in the DES group and 16.9% in the PTA cohort. Regrettably, these numbers were reversed and significantly higher in the paclitaxel-treated group (16.9% vs. 10.2%, P = .03).5
On Feb. 12, 2019, another response to the Katsanos meta-analysis was published in JAMA Cardiology.6 In this study, Secemsky et al. analyzed patient-level data from a Medicare database. The authors reported finding no evidence of paclitaxel- related deaths in 16,560 patients. Unfortunately, the mean follow-up time was only 389 days, which may have been insufficient to detect the late mortality reported in the Katsanos meta-analysis.
On March 15, 2019, the FDA issued a second statement, this time with a much stronger tone.7 The agency reported an ongoing analysis of the long-term survival data from the pivotal randomized trials. In the three studies with 5-year data available, each showed a significantly higher mortality in the paclitaxel group.
When pooled, there were 975 patients, and the risk of death was 20.1% in the paclitaxel group versus 13.4 % in the controls. The FDA recommended discussing the increased risk of mortality with all patients receiving paclitaxel therapy as part of the informed consent process. They also stated that for most patients alternative options should generally be used until additional analysis of the mortality risk is performed.
Industry bristled at this new, strongly worded statement. Becton Dickinson, makers of the Lutonix balloon, asserted that the FDA recommendation was based on “a limited review of data from less than 1,000 patients.”8 The company noted that its LEVANT 2 trial did not see a signal of increased mortality at 5 years. Although they did acknowledge that, among the randomized patients, there was a significantly higher mortality at 5 years for those treated with paclitaxel.
How do we make sense of this? Pac-litaxel is a cytotoxic drug. Its pharmacokinetics vary significantly based on the preparation and administration. The FDA label for the injectable form (Taxol) warns of anaphylaxis and severe hypersensitivity reactions, but there is no mention of long-term mortality. In the coronary vessels, paclitaxel-coated devices have been associated with myocardial infarction and death. Obviously it is easy to comprehend how local vessel effects in the coronary system can lead to increased mortality. The pathway is less clear with femoral-popliteal interventions. If the association of paclitaxel with death is truly causation there must be some systemic effects. The dose delivered with femoral- popliteal interventions is much higher than that seen with coronary devices.
The mortality may be associated with the platform used or even the formulation (crystalline formularies have a longer half-life). Could it be something more benign? Paclitaxel-treated patients see less recurrence of their femoral-popliteal disease. Are the control group patients with more recurrences seeing their interventionalist more often and therefore receiving more frequent reminders to comply with medical therapy?
At this point, we have few answers. After an all-day town hall at the recent Cardiovascular Research Technologies conference,9 one moderator said, “I came in with uncertainty and now I’m going away with uncertainty, but we made tremendous progress.” His comoderator added, “I know I don’t know.” Well then, glad we cleared that up!
In any event, changes are coming. The BASIL-3 trial has suspended recruitment. Physicians using paclitaxel-coated devices are now advised by the FDA to inform patients of the increased risk of death and to use alternatives in most cases. Therefore, if you employ these devices routinely in the femoral-popliteal vessels you are seemingly doing so in opposition to the recommendations of the FDA. Legal peril may follow.
The time for nitpicking the Katsanos analysis has ended. Our industry partners must be compelled to supply the data and finances needed to settle this issue. The signal seems real and it is time to find answers. Research initiatives are underway through the SVS, the VIVA group, the UK Medicines and Healthcare Products Regulatory Agency, and the FDA.
Going forward, the SVS has formed a Paclitaxel Safety Task Force under the leadership of President-elect Kim Hodgson. Their mission is to facilitate the performance and interpretation of an Individual Patient Data meta-analysis using patient-level RCT data from industry partners. The task force states: “We remain troubled by the recent reports of reanalysis of existing datasets, pooled analyses of RCTs, and other ‘series’, as we believe that the findings of these statistically inferior analyses bring no additional clarity, cannot be relied upon for guidance, and distract us from the analysis that needs to be performed.”
References
1. J Am Heart Assoc. 2018 Dec 18;7(24):e011245.
2. www.fda.gov/medicaldevices/safety/letterstohealthcareproviders/ucm629589.htm.
3. J Am Coll Cardiol. Jan 2019. doi: 10.1016/j.jacc.2019.01.013.
4. Circulation. 2019;139:e42.
5. https://evtoday.com/2019/02/20/zilver-ptx-trial-5-year-mortality-data-corrected-in-circulation.
6. JAMA Cardiol. 2019 Feb 12. doi:10.1001/jamacardio.2019.0325.
7. www.fda.gov/MedicalDevices/Safety/LetterstoHealthCareProviders/ucm633614.htm.
8. www.med-technews.com/news/bud-defends-safety-of-drug-coated-device-following-fda-warnin/.
9. www.crtonline.org/news-detail/paclitaxel-device-safety-thoroughly-discussed-at-c.
As medical editor of Vascular Specialist, it has always been my hope to use our excellent reporters and rapid production schedule to keep readers abreast of the latest news in vascular surgery. While my colleagues at the Journal of Vascular Surgery publish studies that will drive treatment, my goal is to drive discussion.
With topics like burnout, workforce shortages, and electronic medical records, I feel we have been successful. The downside of staying current is we sometimes find ourselves publishing contradictory stories. This has been the case with paclitaxel. Let’s take a break from the fray and review where we are, and where we might go from here.
In 2012, the Zilver PTX became the first drug-eluting stent (DES) to gain Food and Drug Administration approval for the treatment of peripheral vascular disease. Two years later, the FDA approved the Lutonix 035 as the first drug-coated balloon (DCB) for use in the femoral-popliteal arteries. The Lutonix would also gain a second indication for failing dialysis fistulas. Medtronic and Spectranetics received authorizations for their DCBs in 2015 and 2017, respectively.
While the safety of paclitaxel-coated devices in the coronary system had previously been called into question, the drug was generally considered safe and effective in the peripheral arterial system. The controversy began in December 2018, when Katsanos et al.1 published a meta-analysis of 28 randomized, controlled trials (RCTs) investigating paclitaxel-coated devices in the femoral-popliteal arteries. While all-cause patient mortality was similar at 1 year between paclitaxel-coated devices and controls (2.3% in each), at 2 years the risk of death was significantly higher in those treated with paclitaxel (7.2% vs. 3.8%). The 5-year data were available for three trials where there was a continued significantly increased risk of mortality with paclitaxel (14.7% vs. 8.1%).
Opposition to these findings was prompt from both physicians and industry. Weaknesses of the analysis, both perceived and real, were hammered. The meta-analysis did not include individual patient data, and the actual cause of death was unknown in most of the included trials. The study was not adequately powered to eliminate the risk of type 1 error when comparing mortality after 2 years. Individuals assigned to the control group may have received paclitaxel treatment at some point in their follow-up. The DCB and DES treatment groups were combined. The methods employed by the authors, however, stood up reasonably well to scrutiny.
On Jan. 17, 2019, the FDA issued their first response stating, “the FDA believes that the benefits continue to outweigh the risks for approved paclitaxel-coated balloons and paclitaxel-eluting stents when used in accordance with their indications for use.”2
Later that month, Peter Schneider, MD, and associates published a patient-level meta-analysis in the Journal of the American College of Cardiology.3 The study included 1,980 patients and found no statistically significant difference in all-cause mortality between DCB (9.3%) and percutaneous transluminal angioplasty (PTA) (11.2%) through 5 years. Shortly after that, however, a correction was issued.
On Feb. 15, 2019, Medtronic reported an error in the 2- and 3-year follow-up periods for the IN.PACT Global postmarket study. The company stated, “Due to a programming error, mortality data were inadvertently omitted from the summary tables included in the statistical analysis.” The mortality in the DCB cohort was corrected from 9.30% to 15.12%. The authors stated that this new mortality rate was still not significantly higher than the PTA group (P = .09).4
Less than 1 week later, another device company issued a correction. And once again, the error had been made in favor of the paclitaxel-treated group. In 2016, the 5-year data from Cook Medical’s Zilver PTX trial were published in Circulation. The study reported a mortality of 10.2% in the DES group and 16.9% in the PTA cohort. Regrettably, these numbers were reversed and significantly higher in the paclitaxel-treated group (16.9% vs. 10.2%, P = .03).5
On Feb. 12, 2019, another response to the Katsanos meta-analysis was published in JAMA Cardiology.6 In this study, Secemsky et al. analyzed patient-level data from a Medicare database. The authors reported finding no evidence of paclitaxel- related deaths in 16,560 patients. Unfortunately, the mean follow-up time was only 389 days, which may have been insufficient to detect the late mortality reported in the Katsanos meta-analysis.
On March 15, 2019, the FDA issued a second statement, this time with a much stronger tone.7 The agency reported an ongoing analysis of the long-term survival data from the pivotal randomized trials. In the three studies with 5-year data available, each showed a significantly higher mortality in the paclitaxel group.
When pooled, there were 975 patients, and the risk of death was 20.1% in the paclitaxel group versus 13.4 % in the controls. The FDA recommended discussing the increased risk of mortality with all patients receiving paclitaxel therapy as part of the informed consent process. They also stated that for most patients alternative options should generally be used until additional analysis of the mortality risk is performed.
Industry bristled at this new, strongly worded statement. Becton Dickinson, makers of the Lutonix balloon, asserted that the FDA recommendation was based on “a limited review of data from less than 1,000 patients.”8 The company noted that its LEVANT 2 trial did not see a signal of increased mortality at 5 years. Although they did acknowledge that, among the randomized patients, there was a significantly higher mortality at 5 years for those treated with paclitaxel.
How do we make sense of this? Pac-litaxel is a cytotoxic drug. Its pharmacokinetics vary significantly based on the preparation and administration. The FDA label for the injectable form (Taxol) warns of anaphylaxis and severe hypersensitivity reactions, but there is no mention of long-term mortality. In the coronary vessels, paclitaxel-coated devices have been associated with myocardial infarction and death. Obviously it is easy to comprehend how local vessel effects in the coronary system can lead to increased mortality. The pathway is less clear with femoral-popliteal interventions. If the association of paclitaxel with death is truly causation there must be some systemic effects. The dose delivered with femoral- popliteal interventions is much higher than that seen with coronary devices.
The mortality may be associated with the platform used or even the formulation (crystalline formularies have a longer half-life). Could it be something more benign? Paclitaxel-treated patients see less recurrence of their femoral-popliteal disease. Are the control group patients with more recurrences seeing their interventionalist more often and therefore receiving more frequent reminders to comply with medical therapy?
At this point, we have few answers. After an all-day town hall at the recent Cardiovascular Research Technologies conference,9 one moderator said, “I came in with uncertainty and now I’m going away with uncertainty, but we made tremendous progress.” His comoderator added, “I know I don’t know.” Well then, glad we cleared that up!
In any event, changes are coming. The BASIL-3 trial has suspended recruitment. Physicians using paclitaxel-coated devices are now advised by the FDA to inform patients of the increased risk of death and to use alternatives in most cases. Therefore, if you employ these devices routinely in the femoral-popliteal vessels you are seemingly doing so in opposition to the recommendations of the FDA. Legal peril may follow.
The time for nitpicking the Katsanos analysis has ended. Our industry partners must be compelled to supply the data and finances needed to settle this issue. The signal seems real and it is time to find answers. Research initiatives are underway through the SVS, the VIVA group, the UK Medicines and Healthcare Products Regulatory Agency, and the FDA.
Going forward, the SVS has formed a Paclitaxel Safety Task Force under the leadership of President-elect Kim Hodgson. Their mission is to facilitate the performance and interpretation of an Individual Patient Data meta-analysis using patient-level RCT data from industry partners. The task force states: “We remain troubled by the recent reports of reanalysis of existing datasets, pooled analyses of RCTs, and other ‘series’, as we believe that the findings of these statistically inferior analyses bring no additional clarity, cannot be relied upon for guidance, and distract us from the analysis that needs to be performed.”
References
1. J Am Heart Assoc. 2018 Dec 18;7(24):e011245.
2. www.fda.gov/medicaldevices/safety/letterstohealthcareproviders/ucm629589.htm.
3. J Am Coll Cardiol. Jan 2019. doi: 10.1016/j.jacc.2019.01.013.
4. Circulation. 2019;139:e42.
5. https://evtoday.com/2019/02/20/zilver-ptx-trial-5-year-mortality-data-corrected-in-circulation.
6. JAMA Cardiol. 2019 Feb 12. doi:10.1001/jamacardio.2019.0325.
7. www.fda.gov/MedicalDevices/Safety/LetterstoHealthCareProviders/ucm633614.htm.
8. www.med-technews.com/news/bud-defends-safety-of-drug-coated-device-following-fda-warnin/.
9. www.crtonline.org/news-detail/paclitaxel-device-safety-thoroughly-discussed-at-c.
As medical editor of Vascular Specialist, it has always been my hope to use our excellent reporters and rapid production schedule to keep readers abreast of the latest news in vascular surgery. While my colleagues at the Journal of Vascular Surgery publish studies that will drive treatment, my goal is to drive discussion.
With topics like burnout, workforce shortages, and electronic medical records, I feel we have been successful. The downside of staying current is we sometimes find ourselves publishing contradictory stories. This has been the case with paclitaxel. Let’s take a break from the fray and review where we are, and where we might go from here.
In 2012, the Zilver PTX became the first drug-eluting stent (DES) to gain Food and Drug Administration approval for the treatment of peripheral vascular disease. Two years later, the FDA approved the Lutonix 035 as the first drug-coated balloon (DCB) for use in the femoral-popliteal arteries. The Lutonix would also gain a second indication for failing dialysis fistulas. Medtronic and Spectranetics received authorizations for their DCBs in 2015 and 2017, respectively.
While the safety of paclitaxel-coated devices in the coronary system had previously been called into question, the drug was generally considered safe and effective in the peripheral arterial system. The controversy began in December 2018, when Katsanos et al.1 published a meta-analysis of 28 randomized, controlled trials (RCTs) investigating paclitaxel-coated devices in the femoral-popliteal arteries. While all-cause patient mortality was similar at 1 year between paclitaxel-coated devices and controls (2.3% in each), at 2 years the risk of death was significantly higher in those treated with paclitaxel (7.2% vs. 3.8%). The 5-year data were available for three trials where there was a continued significantly increased risk of mortality with paclitaxel (14.7% vs. 8.1%).
Opposition to these findings was prompt from both physicians and industry. Weaknesses of the analysis, both perceived and real, were hammered. The meta-analysis did not include individual patient data, and the actual cause of death was unknown in most of the included trials. The study was not adequately powered to eliminate the risk of type 1 error when comparing mortality after 2 years. Individuals assigned to the control group may have received paclitaxel treatment at some point in their follow-up. The DCB and DES treatment groups were combined. The methods employed by the authors, however, stood up reasonably well to scrutiny.
On Jan. 17, 2019, the FDA issued their first response stating, “the FDA believes that the benefits continue to outweigh the risks for approved paclitaxel-coated balloons and paclitaxel-eluting stents when used in accordance with their indications for use.”2
Later that month, Peter Schneider, MD, and associates published a patient-level meta-analysis in the Journal of the American College of Cardiology.3 The study included 1,980 patients and found no statistically significant difference in all-cause mortality between DCB (9.3%) and percutaneous transluminal angioplasty (PTA) (11.2%) through 5 years. Shortly after that, however, a correction was issued.
On Feb. 15, 2019, Medtronic reported an error in the 2- and 3-year follow-up periods for the IN.PACT Global postmarket study. The company stated, “Due to a programming error, mortality data were inadvertently omitted from the summary tables included in the statistical analysis.” The mortality in the DCB cohort was corrected from 9.30% to 15.12%. The authors stated that this new mortality rate was still not significantly higher than the PTA group (P = .09).4
Less than 1 week later, another device company issued a correction. And once again, the error had been made in favor of the paclitaxel-treated group. In 2016, the 5-year data from Cook Medical’s Zilver PTX trial were published in Circulation. The study reported a mortality of 10.2% in the DES group and 16.9% in the PTA cohort. Regrettably, these numbers were reversed and significantly higher in the paclitaxel-treated group (16.9% vs. 10.2%, P = .03).5
On Feb. 12, 2019, another response to the Katsanos meta-analysis was published in JAMA Cardiology.6 In this study, Secemsky et al. analyzed patient-level data from a Medicare database. The authors reported finding no evidence of paclitaxel- related deaths in 16,560 patients. Unfortunately, the mean follow-up time was only 389 days, which may have been insufficient to detect the late mortality reported in the Katsanos meta-analysis.
On March 15, 2019, the FDA issued a second statement, this time with a much stronger tone.7 The agency reported an ongoing analysis of the long-term survival data from the pivotal randomized trials. In the three studies with 5-year data available, each showed a significantly higher mortality in the paclitaxel group.
When pooled, there were 975 patients, and the risk of death was 20.1% in the paclitaxel group versus 13.4 % in the controls. The FDA recommended discussing the increased risk of mortality with all patients receiving paclitaxel therapy as part of the informed consent process. They also stated that for most patients alternative options should generally be used until additional analysis of the mortality risk is performed.
Industry bristled at this new, strongly worded statement. Becton Dickinson, makers of the Lutonix balloon, asserted that the FDA recommendation was based on “a limited review of data from less than 1,000 patients.”8 The company noted that its LEVANT 2 trial did not see a signal of increased mortality at 5 years. Although they did acknowledge that, among the randomized patients, there was a significantly higher mortality at 5 years for those treated with paclitaxel.
How do we make sense of this? Pac-litaxel is a cytotoxic drug. Its pharmacokinetics vary significantly based on the preparation and administration. The FDA label for the injectable form (Taxol) warns of anaphylaxis and severe hypersensitivity reactions, but there is no mention of long-term mortality. In the coronary vessels, paclitaxel-coated devices have been associated with myocardial infarction and death. Obviously it is easy to comprehend how local vessel effects in the coronary system can lead to increased mortality. The pathway is less clear with femoral-popliteal interventions. If the association of paclitaxel with death is truly causation there must be some systemic effects. The dose delivered with femoral- popliteal interventions is much higher than that seen with coronary devices.
The mortality may be associated with the platform used or even the formulation (crystalline formularies have a longer half-life). Could it be something more benign? Paclitaxel-treated patients see less recurrence of their femoral-popliteal disease. Are the control group patients with more recurrences seeing their interventionalist more often and therefore receiving more frequent reminders to comply with medical therapy?
At this point, we have few answers. After an all-day town hall at the recent Cardiovascular Research Technologies conference,9 one moderator said, “I came in with uncertainty and now I’m going away with uncertainty, but we made tremendous progress.” His comoderator added, “I know I don’t know.” Well then, glad we cleared that up!
In any event, changes are coming. The BASIL-3 trial has suspended recruitment. Physicians using paclitaxel-coated devices are now advised by the FDA to inform patients of the increased risk of death and to use alternatives in most cases. Therefore, if you employ these devices routinely in the femoral-popliteal vessels you are seemingly doing so in opposition to the recommendations of the FDA. Legal peril may follow.
The time for nitpicking the Katsanos analysis has ended. Our industry partners must be compelled to supply the data and finances needed to settle this issue. The signal seems real and it is time to find answers. Research initiatives are underway through the SVS, the VIVA group, the UK Medicines and Healthcare Products Regulatory Agency, and the FDA.
Going forward, the SVS has formed a Paclitaxel Safety Task Force under the leadership of President-elect Kim Hodgson. Their mission is to facilitate the performance and interpretation of an Individual Patient Data meta-analysis using patient-level RCT data from industry partners. The task force states: “We remain troubled by the recent reports of reanalysis of existing datasets, pooled analyses of RCTs, and other ‘series’, as we believe that the findings of these statistically inferior analyses bring no additional clarity, cannot be relied upon for guidance, and distract us from the analysis that needs to be performed.”
References
1. J Am Heart Assoc. 2018 Dec 18;7(24):e011245.
2. www.fda.gov/medicaldevices/safety/letterstohealthcareproviders/ucm629589.htm.
3. J Am Coll Cardiol. Jan 2019. doi: 10.1016/j.jacc.2019.01.013.
4. Circulation. 2019;139:e42.
5. https://evtoday.com/2019/02/20/zilver-ptx-trial-5-year-mortality-data-corrected-in-circulation.
6. JAMA Cardiol. 2019 Feb 12. doi:10.1001/jamacardio.2019.0325.
7. www.fda.gov/MedicalDevices/Safety/LetterstoHealthCareProviders/ucm633614.htm.
8. www.med-technews.com/news/bud-defends-safety-of-drug-coated-device-following-fda-warnin/.
9. www.crtonline.org/news-detail/paclitaxel-device-safety-thoroughly-discussed-at-c.
Too much to lose from office visit recording or filming
A common phrase you see on inspirational posters is “sing like nobody’s listening, dance like nobody’s watching.”
In medicine, it should be “speak as if everyone is recording, behave as if everyone is filming.”
In this day and age, you’d think that would be obvious. Every few hours there’s a viral video of someone getting upset, then losing their temper and saying something most of us would regret. A few years ago it would be a private matter, but today things are rapidly spread over Facebook and Twitter. Even if it’s entirely false, that doesn’t matter. It’s easy for anyone with a smartphone and apps to edit the clip to make it entirely different from what really happened. People go with their first reaction. By the time the facts come out, they’ve moved on and don’t care about the truth.
Occasionally, I get a request to record what I’m saying. In most cases I decline, and never allow myself to be filmed. I do this because anything can be altered, and unless I go to the effort to record it myself, I have no way to prove who’s telling the truth. So it’s easier just to not do it at all.
Unfortunately, this is often taken as “proof” of me trying to hide something. I’m certainly not. Being open and honest with patients is always something I focus on. But the truth of what happened in a 30- to 60-minute visit can be misconstrued in an edited, and possibly altered, sound bite of 5-10 seconds. People who want to do such things have their own motives and aren’t interested in reason or honesty.
Doctors, like everyone else, are susceptible to human emotions and reactions, but a big part of the job is keeping them controlled and hidden when working with patients. It’s the best way to make reasoned decisions and work with someone who’s frightened, angry, or irrational.
If you find yourself losing the battle to stay in control, sometimes it’s good to remember that your words and actions could be being recorded and posted on Facebook in an hour, whether you permitted it or not. Because you don’t want to learn the hard way.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A common phrase you see on inspirational posters is “sing like nobody’s listening, dance like nobody’s watching.”
In medicine, it should be “speak as if everyone is recording, behave as if everyone is filming.”
In this day and age, you’d think that would be obvious. Every few hours there’s a viral video of someone getting upset, then losing their temper and saying something most of us would regret. A few years ago it would be a private matter, but today things are rapidly spread over Facebook and Twitter. Even if it’s entirely false, that doesn’t matter. It’s easy for anyone with a smartphone and apps to edit the clip to make it entirely different from what really happened. People go with their first reaction. By the time the facts come out, they’ve moved on and don’t care about the truth.
Occasionally, I get a request to record what I’m saying. In most cases I decline, and never allow myself to be filmed. I do this because anything can be altered, and unless I go to the effort to record it myself, I have no way to prove who’s telling the truth. So it’s easier just to not do it at all.
Unfortunately, this is often taken as “proof” of me trying to hide something. I’m certainly not. Being open and honest with patients is always something I focus on. But the truth of what happened in a 30- to 60-minute visit can be misconstrued in an edited, and possibly altered, sound bite of 5-10 seconds. People who want to do such things have their own motives and aren’t interested in reason or honesty.
Doctors, like everyone else, are susceptible to human emotions and reactions, but a big part of the job is keeping them controlled and hidden when working with patients. It’s the best way to make reasoned decisions and work with someone who’s frightened, angry, or irrational.
If you find yourself losing the battle to stay in control, sometimes it’s good to remember that your words and actions could be being recorded and posted on Facebook in an hour, whether you permitted it or not. Because you don’t want to learn the hard way.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A common phrase you see on inspirational posters is “sing like nobody’s listening, dance like nobody’s watching.”
In medicine, it should be “speak as if everyone is recording, behave as if everyone is filming.”
In this day and age, you’d think that would be obvious. Every few hours there’s a viral video of someone getting upset, then losing their temper and saying something most of us would regret. A few years ago it would be a private matter, but today things are rapidly spread over Facebook and Twitter. Even if it’s entirely false, that doesn’t matter. It’s easy for anyone with a smartphone and apps to edit the clip to make it entirely different from what really happened. People go with their first reaction. By the time the facts come out, they’ve moved on and don’t care about the truth.
Occasionally, I get a request to record what I’m saying. In most cases I decline, and never allow myself to be filmed. I do this because anything can be altered, and unless I go to the effort to record it myself, I have no way to prove who’s telling the truth. So it’s easier just to not do it at all.
Unfortunately, this is often taken as “proof” of me trying to hide something. I’m certainly not. Being open and honest with patients is always something I focus on. But the truth of what happened in a 30- to 60-minute visit can be misconstrued in an edited, and possibly altered, sound bite of 5-10 seconds. People who want to do such things have their own motives and aren’t interested in reason or honesty.
Doctors, like everyone else, are susceptible to human emotions and reactions, but a big part of the job is keeping them controlled and hidden when working with patients. It’s the best way to make reasoned decisions and work with someone who’s frightened, angry, or irrational.
If you find yourself losing the battle to stay in control, sometimes it’s good to remember that your words and actions could be being recorded and posted on Facebook in an hour, whether you permitted it or not. Because you don’t want to learn the hard way.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
2018 FDA-approved new drugs
In 2018, the Food and Drug Administration approved a record 58 new drugs for humans. One of these agents, Annovera (segesterone acetate and ethinyl estradiol), is a vaginal ring to prevent pregnancy and is not relevant in this article. A second drug, Asparlas (calaspargase pegol-mknl), indicated to treat acute lymphoblastic leukemia, has not yet been released by its manufacturer. The agents with molecular weights (MW) less than 1,000 probably cross the placenta, but nearly all, regardless of MW, will cross in the second half of pregnancy.
There is no human pregnancy data for these agents, but there are five drugs included in pregnancy registries. However, it will take some time before the outcomes of these drugs are published. The routine absence of pregnancy data for most drugs was pointed out in a reference that I coauthored (“Should pregnant women be included in phase 4 clinical drug trials?” Am J Obstet Gynecol. 2015 Dec;213[6]:810-5). The article makes a strong argument for including some drugs in these trials.
Amyloidosis
Onpattro (patisiran) is indicated for the treatment of the polyneuropathy of hereditary transthyretin-mediated amyloidosis in adults. The drug caused embryo-fetal death and reduced fetal body weight in rabbits at doses also associated with maternal toxicity. No developmental toxicity was observed in rats.
Anti-infectives
Aemcolo (rifamycin), which has a MW of 720, is indicated for treatment of travelers’ diarrhea caused by noninvasive strains of Escherichia coli. No adverse fetal effects were observed in rats and rabbits that received close to human doses.
Krintafel (tafenoquine) is an antimalarial agent that is used to prevent relapse in patients who are receiving appropriate antimalarial therapy for Plasmodium vivax infection. The drug may cause hemolytic anemia in a fetus deficient in glucose-6-phosphate dehydrogenase. In rabbits, the drug caused dose-related abortions and maternal toxicity was observed in rabbits and rats. Treatment with this drug in pregnancy is not recommended, according to the manufacturer.
Tpoxx (tecovirimat monohydrate), which has a MW of about 394, is indicated for the treatment of smallpox disease. The drug did not cause embryo-fetal toxicity in pregnant mice and rabbits, but the maximum exposure in rabbits was only 0.4 times the human exposure.
Xofluza (baloxavir marboxil), which has a MW of about 572, is a prodrug that is converted by hydrolysis to baloxavir. It is indicated for the treatment of acute uncomplicated influenza. No adverse developmental effects were observed in rats and rabbits.
Zemdri (plazomicin), which has a MW of about 593, is an aminoglycoside indicated for the treatment of complicated urinary tract infections including pyelonephritis. The drug did not cause fetal harm in rats and rabbits at doses that did not cause maternal toxicity; however, prolonged use of an aminoglycoside (such as streptomycin) has caused irreversible, bilateral congenital deafness in children exposed in utero to prolonged use and is a potential complication.
Three new drugs in 2018 are indicated for treating HIV-1:
Biktarvy is a three-drug combination that includes bictegravir, emtricitabine, and tenofovir. The latter two drugs are included in the 11th edition of my book (“Drugs in Pregnancy and Lactation,” 11th ed. [Riverwoods, Ill.: Wolters Kluwer, 2017) and are not included here. Both are classified as compatible in pregnancy. Bictegravir has a MW of about 471. No adverse embryo-fetal effects in rats and rabbits were observed with this agent.
Trogarzo (ibalizumab-uiyk), which has a MW of about 150,000, is a monoclonal antibody antiretroviral agent used in combination with other antiretrovirals. There are no animal data. Although the MW is very high, monoclonal antibodies are transported across the placenta as pregnancy progresses.
Pifeltro (doravirine), which has a MW of about 426, is a nonnucleoside reverse transcriptase inhibitor used in combination with other antiretroviral agents for the treatment of HIV-1. The drug caused no significant toxicologic effects on embryo-fetal rats and rabbits.
If Biktarvy, Pifeltro, or Trogarzo are used in pregnancy, health care providers are encouraged to register the patient in the Antiretroviral Pregnancy Registry by calling 1-800-258-4263.
There are three new agents in the tetracycline class.
Nuzyra (omadacycline), which has a MW of about 729, is for community-acquired bacterial pneumonia and acute bacterial skin and skin structure infections.
Seysara (sarecycline), which has a MW of about 524, is for inflammatory lesions of nonnodular, moderate to severe acne vulgaris.
Xerava (eravacycline), which has a MW of about 632, is for complicated intra-abdominal infection.
The various dose-related toxicities observed with the three drugs in rats and rabbits included maternal deaths; increased postimplantation loss; reduced fetal body weights; delays in skeletal ossification; and fetal malformations of the skeleton, heart, and lung. Use of these drugs in the last half of pregnancy may cause permanent discoloration of the teeth and enamel hypoplasia, as well as inhibition of bone growth.
Antilipemic agents
Crysvita (burosumab-twza), which has a MW of about 147,000, is a fibroblast growth factor–blocking antibody indicated for the treatment of X-linked hypophosphatemia. In pregnant cynomolgus monkeys, doses slightly higher than the human dose were not teratogenic. The drug was detected in fetal serum indicating that it crossed the monkey placenta.
Tegsedi (inotersen), which has a MW of about 7,601, is an amyloidosis inhibitor used for polyneuropathy of hereditary transthyretin-mediated amyloidosis. It is available only through a restricted program. The drug was not teratogenic in mice and rabbits; however, it does decrease vitamin A levels, so supplementation with the vitamin is recommended.
Antineoplastics
The manufacturers recommend avoiding these drugs during pregnancy. Effective contraception should be used.
Daurismo (glasdegib), which has a MW of about 491, is a hedgehog pathway inhibitor indicated in combination with low-dose cytarabine for newly diagnosed acute myeloid leukemia (AML). The drug caused embryotoxicity, fetotoxicity, and teratogenicity in rats and rabbits at doses less than the human dose.
Erleada (apalutamide), which has a MW of about 477, is an androgen receptor inhibitor indicated for nonmetastatic, castration-resistant prostate cancer. Animal studies were not conducted because the drug should not be used in females.
Elzonris (tagraxofusp-erzs), which has a MW of 57,695, is a cytotoxin indicated for the treatment of blastic plasmacytoid dendritic cell neoplasm. Animal studies have not been conducted.
Lumoxiti (moxetumomab pasudotox–tdfk) which as a MW of about 63,000, is indicated for relapsed or refractory hairy cell leukemia. Studies have not been conducted in pregnant animals. Two life-threatening outcomes have occurred with the drug: capillary leak syndrome and hemolytic uremic syndrome. The drug should be discontinued if either occurs.
Lutathera (lutetium Lu 177 dotatate), which has a MW of about 1,610, is a radiolabeled somatostatin analogue given as a single intravenous dose every 8 weeks for four doses for the treatment of gastroenteropancreatic neuroendocrine tumors. Reproductive studies in animals have not been conducted. However, all radiopharmaceuticals have the potential to cause embryo-fetal harm. They also can cause infertility in males and females.
Talzenna (talazoparib), which has a MW of about 553, is a poly (ADP-ribose) polymerase inhibitor indicated for the treatment of certain types of breast cancer. At doses much less then the human dose, the drug caused fetal malformations and embryo-fetal death in rats.
Tibsovo (ivosidenib), which has a MW of 583, is an isocitrate dehydrogenase 1 inhibitor used for patients with relapsed or refractory AML. The drug caused embryo-fetal toxicity in rats and rabbits at doses slighter higher than the human dose.
There are seven new kinase inhibitors.
Braftovi (encorafenib), which has a MW of 540, is indicated in combination with Mektovi for patients with a specific type of metastatic melanoma. The drug caused embryo-fetal toxicity in rats and rabbits.
Copiktra (duvelisib), which has a MW of about 435, is indicated for treatment of chronic lymphocytic leukemia and follicular lymphoma. In rats and rabbits, the drug caused embryo-fetal death, lower fetal weights, and malformations.
Lorbrena (lorlatinib), which has a MW of about 406, is given for the treatment of metastatic non–small cell lung cancer. In rats and rabbits, the drug caused abortions, decreased fetal body weight, and major malformations.
Mektovi (binimetinib), which has a MW of about 441, is used in combination with Braftovi for patients with a specific type of melanoma. The drug was embryotoxic and abortifacient in rabbits.
Vitrakvi (larotrectinib), which has a MW of about 527, is used for patients with solid tumors. Studies in rats revealed fetal anasarca (extreme generalized edema) and omphalocele in rabbits.
Vizimpro (dacomitinib), which has a MW of about 488, is indicated for metastatic non–small cell lung cancer. The drug caused embryo-fetal toxicity in rats and mice.
Xospata (gilteritinib), which has a MW of about 1,222, is indicated for relapsed or refractory AML. In rats, the drug caused embryo-fetal death, suppressed fetal growth, and caused multiple malformations.
Three drugs are classified as monoclonal antibodies.
Gamifant (emapalumab), which has a MW of about 148,000, is indicated for primary hemophagocytic lymphohistiocytosis. A murine surrogate antimouse antibody was given to pregnant mice throughout gestation and no fetal harm was observed.
Libtayo (cemiplimab-rwlc), which has a MW of 146,000, is indicated for patients with metastatic or locally advanced cutaneous squamous cell carcinoma. Animal reproduction studies have not been conducted; however, based on its mechanism, increased rates of abortion or stillbirth may occur if the drug is used in human pregnancy.
Poteligeo (mogamulizumab-kpkc), which has a MW of about 149,000, is given for relapsed/refractory mycosis fungoides or Sézary syndrome. In pregnant monkeys, there was no embryo-fetal lethality, teratogenicity, fetal growth restriction, spontaneous abortion, or increased fetal death.
Central nervous system
There are three antimigraine agents that are monoclonal antibodies given as a subcutaneous injection.
Aimovig (erenumab-aooe), which has a MW of about 150,000, caused no adverse effects in monkey offspring.
Ajovy (fremanezumab-vfrm), which has a MW of about 148,000, had no adverse effect in rat and rabbit offspring.
Emgality (galcanezumab-gnlm), which has a MW of about 147,000, produced no adverse effects in rat and rabbit offspring.
Diacomit (stiripentol), which has a MW of about 234, is an anticonvulsant used to treat seizures associated with Dravet syndrome. The drug caused severe embryo-fetal toxicity in mice, rabbits, and rats. The drug is included in the North American Antiepileptic Drug (NAAED) Pregnancy Registry. Patients can enroll themselves by calling the toll-free number 1-888-233-2334 or visiting http://aedpregnancyregistry.org/.
Epidiolex (cannabidiol), which has a MW of about 314, is an anticonvulsant indicated for the treatment of seizures associated with Lennox-Gastaut syndrome or Dravet syndrome. In pregnant rats, doses up to about 16 times the recommended human dose (RHD) caused no embryo-fetal adverse effects. The drug caused decreased fetal body weights, increased fetal structural variations, and maternal toxicity when the drug was given to pregnant rabbits throughout organogenesis. The no-effect dose for embryo-fetal toxicity was less than the human dose. Patients can enroll themselves in the NAAED Pregnancy Registry by calling the toll-free number 1-888-233-2334 or visiting http://aedpregnancyregistry.org/.
Firdapse (amifampridine), a potassium channel blocker with a MW of about 201, is used for the treatment of Lambert-Eaton myasthenic syndrome. No adverse effects on embryo-fetal development were observed in rats and rabbits given the drug throughout organogenesis. However, in rats given the drug throughout pregnancy and lactation, there was an increase in stillbirths and pup deaths, reduced pup weight, and delayed sexual development in female pups.
Lucemyra (lofexidine), which has a MW of about 296, is used to mitigate opioid withdrawal symptoms to facilitate abrupt opioid discontinuation in adults. The drug caused severe toxicity in the fetuses of rats and rabbits.
Olumiant (baricitinib), which has a MW of about 371, is a Janus kinase inhibitor indicated for the treatment of rheumatoid arthritis. The drug was teratogenic in pregnant rats given doses about 20 times greater than the maximum RHD based on area under the curve. In rabbits, embryo death and rib anomalies were observed with doses 84 times greater than the maximum RHD, but no developmental toxicity was seen with doses 12 times greater than the maximum RHD.
Orilissa (elagolix), which has a MW of about 654, is a gonadotropin-releasing hormone receptor antagonist indicated for the management of pain associated with endometriosis. The drug caused abortions in rats and rabbits. Because the drug may increase the risk of early pregnancy loss, the manufacturer classifies it as contraindicated in pregnancy.
Dermatologic agents
Ilumya (tildrakizumab), which has a MW of about 147,000, is given by subcutaneous injection for the treatment of moderate to severe plaque psoriasis. When given during organogenesis in monkeys, no maternal or embryo-fetal toxicities were observed. However, when given throughout pregnancy a few neonatal deaths occurred, but the clinical significance of these nonclinical findings were unknown.
Fabry disease
Galafold (migalastat), which has a MW of about 200, is an alpha-galactosidase A pharmacologic chaperone indicated for the treatment of Fabry disease. Three pregnant women with Fabry disease were exposed to the drug in clinical studies but no information was provided on the pregnancy outcomes. No adverse developmental effects were observed in pregnant rats and rabbits.
Gastrointestinal agents
Akynzeo (netupitant or fosnetupitant palonosetron), which have MWs of about 579, 333, and 762, respectively, is available as an oral capsule (netupitant + palonosetron) and as an intravenous formulation (fosnetupitant + palonosetron). They are indicated, in combination with dexamethasone, for the prevention of nausea and vomiting related to cancer chemotherapy. Netupitant and fosnetupitant produced no embryo-fetal adverse effects in rats but were toxic to rabbit embryos. Palonosetron caused no embryo-fetal adverse effects in rats and rabbits.
Motegrity (prucalopride), which has a MW of about 486, is indicated for chronic idiopathic constipation. No adverse embryo-fetal developmental effects were observed in rats and rabbits.
Hematologic agents
Doptelet (avatrombopag), which has a MW of about 766, is indicated for the treatment of thrombocytopenia in adult patients with chronic liver disease who are scheduled to undergo a procedure. No embryo-fetal effects were observed in rats, but in rabbits the drug was associated with spontaneous abortions.
Lokelma (sodium zirconium cyclosilicate) is a nonabsorbed zirconium silicate that exchanges potassium for hydrogen and sodium. Animal studies have not been conducted. Because it is not absorbed, it is not expected to result in fetal exposure to the drug.
Mulpleta (lusutrombopag), which has a MW of about 592, a thrombopoietin receptor agonist, is indicated for the treatment of thrombocytopenia in patients with chronic liver disease. High levels of the drug in pregnant rats were associated with adverse developmental outcomes. No adverse embryo-fetal effects were seen in pregnant rabbits.
Palynziq (pegvaliase-pqpz), which has a MW of about 1,000,000, is a phenylalanine-metabolizing enzyme indicated to reduce blood phenylalanine concentrations in patients with phenylketonuria. In pregnant rats, the drug caused an increase in skeletal variations. In rabbits, the drug caused a high incidence of multiple malformations.
Takhzyro (lanadelumab-flyo), which has a MW of about 49,000, is a monoclonal antibody indicated for prophylaxis to prevent attacks of hereditary angioedema. The drug caused no fetal harm in monkeys.
Tavalisse (fostamatinib disodium hexahydrate), which has a MW of about 733, is a kinase inhibitor used for the treatment of thrombocytopenia. In pregnant rats and rabbits, the drug caused adverse developmental outcomes including embryo-fetal mortality, lower fetal weights, and structural anomalies.
Ultomiris (ravulizumab), which has a MW of about 148,000, is a humanized monoclonal antibody indicated for adult patients with paroxysmal nocturnal hemoglobinuria. In mice, the drug was associated with increased rates of developmental abnormalities and an increased rate of dead and moribund offspring.
Immunologic agent
Revcovi (elapegademase-lvlr), which has a MW of about 113,000, is a recombinant adenosine deaminase indicated for the treatment of adenosine deaminase severe combined immune deficiency. Animal studies in pregnancy have not been conducted.
Nutrient/Nutritional supplement
Fish oil is indicated as a source of calories and fatty acids in pediatric patients with parenteral nutrition-associated cholestasis. Animal reproduction studies have not been conducted. It is doubtful if this product will be used in pregnancy.
Ophthalmic – nerve growth factor
Oxervate (cenegermin-bkbj), which has a MW of 13,266, is a solution that contains 118 amino acids. It is a recombinant human nerve growth factor indicated for neurotrophic keratitis. In rats and rabbits given the drug during organogenesis, there was a slight increase in postimplantation loss at doses greater than or equal to 267 times the human dose.
Respiratory drugs
Symdeko (tezacaftor + ivacaftor), which have MWs of about 521 and 392, is indicated for the treatment of patients with cystic fibrosis who are homozygous for the F508del mutation or who have at least one mutation in the cystic fibrosis transmembrane conductance regulator gene. There were no adverse developmental effects in pregnant rats and rabbits when the drugs were used separately or combined.
Yupelri (revefenacin), which has a MW of about 598, is an anticholinergic drug. It is an inhaled solution for the maintenance treatment of chronic obstructive pulmonary disease. In rats and rabbits, doses that were about 209 times the RHD produced no evidence of fetal harm.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs reported no relevant financial disclosures. Email him at [email protected].
In 2018, the Food and Drug Administration approved a record 58 new drugs for humans. One of these agents, Annovera (segesterone acetate and ethinyl estradiol), is a vaginal ring to prevent pregnancy and is not relevant in this article. A second drug, Asparlas (calaspargase pegol-mknl), indicated to treat acute lymphoblastic leukemia, has not yet been released by its manufacturer. The agents with molecular weights (MW) less than 1,000 probably cross the placenta, but nearly all, regardless of MW, will cross in the second half of pregnancy.
There is no human pregnancy data for these agents, but there are five drugs included in pregnancy registries. However, it will take some time before the outcomes of these drugs are published. The routine absence of pregnancy data for most drugs was pointed out in a reference that I coauthored (“Should pregnant women be included in phase 4 clinical drug trials?” Am J Obstet Gynecol. 2015 Dec;213[6]:810-5). The article makes a strong argument for including some drugs in these trials.
Amyloidosis
Onpattro (patisiran) is indicated for the treatment of the polyneuropathy of hereditary transthyretin-mediated amyloidosis in adults. The drug caused embryo-fetal death and reduced fetal body weight in rabbits at doses also associated with maternal toxicity. No developmental toxicity was observed in rats.
Anti-infectives
Aemcolo (rifamycin), which has a MW of 720, is indicated for treatment of travelers’ diarrhea caused by noninvasive strains of Escherichia coli. No adverse fetal effects were observed in rats and rabbits that received close to human doses.
Krintafel (tafenoquine) is an antimalarial agent that is used to prevent relapse in patients who are receiving appropriate antimalarial therapy for Plasmodium vivax infection. The drug may cause hemolytic anemia in a fetus deficient in glucose-6-phosphate dehydrogenase. In rabbits, the drug caused dose-related abortions and maternal toxicity was observed in rabbits and rats. Treatment with this drug in pregnancy is not recommended, according to the manufacturer.
Tpoxx (tecovirimat monohydrate), which has a MW of about 394, is indicated for the treatment of smallpox disease. The drug did not cause embryo-fetal toxicity in pregnant mice and rabbits, but the maximum exposure in rabbits was only 0.4 times the human exposure.
Xofluza (baloxavir marboxil), which has a MW of about 572, is a prodrug that is converted by hydrolysis to baloxavir. It is indicated for the treatment of acute uncomplicated influenza. No adverse developmental effects were observed in rats and rabbits.
Zemdri (plazomicin), which has a MW of about 593, is an aminoglycoside indicated for the treatment of complicated urinary tract infections including pyelonephritis. The drug did not cause fetal harm in rats and rabbits at doses that did not cause maternal toxicity; however, prolonged use of an aminoglycoside (such as streptomycin) has caused irreversible, bilateral congenital deafness in children exposed in utero to prolonged use and is a potential complication.
Three new drugs in 2018 are indicated for treating HIV-1:
Biktarvy is a three-drug combination that includes bictegravir, emtricitabine, and tenofovir. The latter two drugs are included in the 11th edition of my book (“Drugs in Pregnancy and Lactation,” 11th ed. [Riverwoods, Ill.: Wolters Kluwer, 2017) and are not included here. Both are classified as compatible in pregnancy. Bictegravir has a MW of about 471. No adverse embryo-fetal effects in rats and rabbits were observed with this agent.
Trogarzo (ibalizumab-uiyk), which has a MW of about 150,000, is a monoclonal antibody antiretroviral agent used in combination with other antiretrovirals. There are no animal data. Although the MW is very high, monoclonal antibodies are transported across the placenta as pregnancy progresses.
Pifeltro (doravirine), which has a MW of about 426, is a nonnucleoside reverse transcriptase inhibitor used in combination with other antiretroviral agents for the treatment of HIV-1. The drug caused no significant toxicologic effects on embryo-fetal rats and rabbits.
If Biktarvy, Pifeltro, or Trogarzo are used in pregnancy, health care providers are encouraged to register the patient in the Antiretroviral Pregnancy Registry by calling 1-800-258-4263.
There are three new agents in the tetracycline class.
Nuzyra (omadacycline), which has a MW of about 729, is for community-acquired bacterial pneumonia and acute bacterial skin and skin structure infections.
Seysara (sarecycline), which has a MW of about 524, is for inflammatory lesions of nonnodular, moderate to severe acne vulgaris.
Xerava (eravacycline), which has a MW of about 632, is for complicated intra-abdominal infection.
The various dose-related toxicities observed with the three drugs in rats and rabbits included maternal deaths; increased postimplantation loss; reduced fetal body weights; delays in skeletal ossification; and fetal malformations of the skeleton, heart, and lung. Use of these drugs in the last half of pregnancy may cause permanent discoloration of the teeth and enamel hypoplasia, as well as inhibition of bone growth.
Antilipemic agents
Crysvita (burosumab-twza), which has a MW of about 147,000, is a fibroblast growth factor–blocking antibody indicated for the treatment of X-linked hypophosphatemia. In pregnant cynomolgus monkeys, doses slightly higher than the human dose were not teratogenic. The drug was detected in fetal serum indicating that it crossed the monkey placenta.
Tegsedi (inotersen), which has a MW of about 7,601, is an amyloidosis inhibitor used for polyneuropathy of hereditary transthyretin-mediated amyloidosis. It is available only through a restricted program. The drug was not teratogenic in mice and rabbits; however, it does decrease vitamin A levels, so supplementation with the vitamin is recommended.
Antineoplastics
The manufacturers recommend avoiding these drugs during pregnancy. Effective contraception should be used.
Daurismo (glasdegib), which has a MW of about 491, is a hedgehog pathway inhibitor indicated in combination with low-dose cytarabine for newly diagnosed acute myeloid leukemia (AML). The drug caused embryotoxicity, fetotoxicity, and teratogenicity in rats and rabbits at doses less than the human dose.
Erleada (apalutamide), which has a MW of about 477, is an androgen receptor inhibitor indicated for nonmetastatic, castration-resistant prostate cancer. Animal studies were not conducted because the drug should not be used in females.
Elzonris (tagraxofusp-erzs), which has a MW of 57,695, is a cytotoxin indicated for the treatment of blastic plasmacytoid dendritic cell neoplasm. Animal studies have not been conducted.
Lumoxiti (moxetumomab pasudotox–tdfk) which as a MW of about 63,000, is indicated for relapsed or refractory hairy cell leukemia. Studies have not been conducted in pregnant animals. Two life-threatening outcomes have occurred with the drug: capillary leak syndrome and hemolytic uremic syndrome. The drug should be discontinued if either occurs.
Lutathera (lutetium Lu 177 dotatate), which has a MW of about 1,610, is a radiolabeled somatostatin analogue given as a single intravenous dose every 8 weeks for four doses for the treatment of gastroenteropancreatic neuroendocrine tumors. Reproductive studies in animals have not been conducted. However, all radiopharmaceuticals have the potential to cause embryo-fetal harm. They also can cause infertility in males and females.
Talzenna (talazoparib), which has a MW of about 553, is a poly (ADP-ribose) polymerase inhibitor indicated for the treatment of certain types of breast cancer. At doses much less then the human dose, the drug caused fetal malformations and embryo-fetal death in rats.
Tibsovo (ivosidenib), which has a MW of 583, is an isocitrate dehydrogenase 1 inhibitor used for patients with relapsed or refractory AML. The drug caused embryo-fetal toxicity in rats and rabbits at doses slighter higher than the human dose.
There are seven new kinase inhibitors.
Braftovi (encorafenib), which has a MW of 540, is indicated in combination with Mektovi for patients with a specific type of metastatic melanoma. The drug caused embryo-fetal toxicity in rats and rabbits.
Copiktra (duvelisib), which has a MW of about 435, is indicated for treatment of chronic lymphocytic leukemia and follicular lymphoma. In rats and rabbits, the drug caused embryo-fetal death, lower fetal weights, and malformations.
Lorbrena (lorlatinib), which has a MW of about 406, is given for the treatment of metastatic non–small cell lung cancer. In rats and rabbits, the drug caused abortions, decreased fetal body weight, and major malformations.
Mektovi (binimetinib), which has a MW of about 441, is used in combination with Braftovi for patients with a specific type of melanoma. The drug was embryotoxic and abortifacient in rabbits.
Vitrakvi (larotrectinib), which has a MW of about 527, is used for patients with solid tumors. Studies in rats revealed fetal anasarca (extreme generalized edema) and omphalocele in rabbits.
Vizimpro (dacomitinib), which has a MW of about 488, is indicated for metastatic non–small cell lung cancer. The drug caused embryo-fetal toxicity in rats and mice.
Xospata (gilteritinib), which has a MW of about 1,222, is indicated for relapsed or refractory AML. In rats, the drug caused embryo-fetal death, suppressed fetal growth, and caused multiple malformations.
Three drugs are classified as monoclonal antibodies.
Gamifant (emapalumab), which has a MW of about 148,000, is indicated for primary hemophagocytic lymphohistiocytosis. A murine surrogate antimouse antibody was given to pregnant mice throughout gestation and no fetal harm was observed.
Libtayo (cemiplimab-rwlc), which has a MW of 146,000, is indicated for patients with metastatic or locally advanced cutaneous squamous cell carcinoma. Animal reproduction studies have not been conducted; however, based on its mechanism, increased rates of abortion or stillbirth may occur if the drug is used in human pregnancy.
Poteligeo (mogamulizumab-kpkc), which has a MW of about 149,000, is given for relapsed/refractory mycosis fungoides or Sézary syndrome. In pregnant monkeys, there was no embryo-fetal lethality, teratogenicity, fetal growth restriction, spontaneous abortion, or increased fetal death.
Central nervous system
There are three antimigraine agents that are monoclonal antibodies given as a subcutaneous injection.
Aimovig (erenumab-aooe), which has a MW of about 150,000, caused no adverse effects in monkey offspring.
Ajovy (fremanezumab-vfrm), which has a MW of about 148,000, had no adverse effect in rat and rabbit offspring.
Emgality (galcanezumab-gnlm), which has a MW of about 147,000, produced no adverse effects in rat and rabbit offspring.
Diacomit (stiripentol), which has a MW of about 234, is an anticonvulsant used to treat seizures associated with Dravet syndrome. The drug caused severe embryo-fetal toxicity in mice, rabbits, and rats. The drug is included in the North American Antiepileptic Drug (NAAED) Pregnancy Registry. Patients can enroll themselves by calling the toll-free number 1-888-233-2334 or visiting http://aedpregnancyregistry.org/.
Epidiolex (cannabidiol), which has a MW of about 314, is an anticonvulsant indicated for the treatment of seizures associated with Lennox-Gastaut syndrome or Dravet syndrome. In pregnant rats, doses up to about 16 times the recommended human dose (RHD) caused no embryo-fetal adverse effects. The drug caused decreased fetal body weights, increased fetal structural variations, and maternal toxicity when the drug was given to pregnant rabbits throughout organogenesis. The no-effect dose for embryo-fetal toxicity was less than the human dose. Patients can enroll themselves in the NAAED Pregnancy Registry by calling the toll-free number 1-888-233-2334 or visiting http://aedpregnancyregistry.org/.
Firdapse (amifampridine), a potassium channel blocker with a MW of about 201, is used for the treatment of Lambert-Eaton myasthenic syndrome. No adverse effects on embryo-fetal development were observed in rats and rabbits given the drug throughout organogenesis. However, in rats given the drug throughout pregnancy and lactation, there was an increase in stillbirths and pup deaths, reduced pup weight, and delayed sexual development in female pups.
Lucemyra (lofexidine), which has a MW of about 296, is used to mitigate opioid withdrawal symptoms to facilitate abrupt opioid discontinuation in adults. The drug caused severe toxicity in the fetuses of rats and rabbits.
Olumiant (baricitinib), which has a MW of about 371, is a Janus kinase inhibitor indicated for the treatment of rheumatoid arthritis. The drug was teratogenic in pregnant rats given doses about 20 times greater than the maximum RHD based on area under the curve. In rabbits, embryo death and rib anomalies were observed with doses 84 times greater than the maximum RHD, but no developmental toxicity was seen with doses 12 times greater than the maximum RHD.
Orilissa (elagolix), which has a MW of about 654, is a gonadotropin-releasing hormone receptor antagonist indicated for the management of pain associated with endometriosis. The drug caused abortions in rats and rabbits. Because the drug may increase the risk of early pregnancy loss, the manufacturer classifies it as contraindicated in pregnancy.
Dermatologic agents
Ilumya (tildrakizumab), which has a MW of about 147,000, is given by subcutaneous injection for the treatment of moderate to severe plaque psoriasis. When given during organogenesis in monkeys, no maternal or embryo-fetal toxicities were observed. However, when given throughout pregnancy a few neonatal deaths occurred, but the clinical significance of these nonclinical findings were unknown.
Fabry disease
Galafold (migalastat), which has a MW of about 200, is an alpha-galactosidase A pharmacologic chaperone indicated for the treatment of Fabry disease. Three pregnant women with Fabry disease were exposed to the drug in clinical studies but no information was provided on the pregnancy outcomes. No adverse developmental effects were observed in pregnant rats and rabbits.
Gastrointestinal agents
Akynzeo (netupitant or fosnetupitant palonosetron), which have MWs of about 579, 333, and 762, respectively, is available as an oral capsule (netupitant + palonosetron) and as an intravenous formulation (fosnetupitant + palonosetron). They are indicated, in combination with dexamethasone, for the prevention of nausea and vomiting related to cancer chemotherapy. Netupitant and fosnetupitant produced no embryo-fetal adverse effects in rats but were toxic to rabbit embryos. Palonosetron caused no embryo-fetal adverse effects in rats and rabbits.
Motegrity (prucalopride), which has a MW of about 486, is indicated for chronic idiopathic constipation. No adverse embryo-fetal developmental effects were observed in rats and rabbits.
Hematologic agents
Doptelet (avatrombopag), which has a MW of about 766, is indicated for the treatment of thrombocytopenia in adult patients with chronic liver disease who are scheduled to undergo a procedure. No embryo-fetal effects were observed in rats, but in rabbits the drug was associated with spontaneous abortions.
Lokelma (sodium zirconium cyclosilicate) is a nonabsorbed zirconium silicate that exchanges potassium for hydrogen and sodium. Animal studies have not been conducted. Because it is not absorbed, it is not expected to result in fetal exposure to the drug.
Mulpleta (lusutrombopag), which has a MW of about 592, a thrombopoietin receptor agonist, is indicated for the treatment of thrombocytopenia in patients with chronic liver disease. High levels of the drug in pregnant rats were associated with adverse developmental outcomes. No adverse embryo-fetal effects were seen in pregnant rabbits.
Palynziq (pegvaliase-pqpz), which has a MW of about 1,000,000, is a phenylalanine-metabolizing enzyme indicated to reduce blood phenylalanine concentrations in patients with phenylketonuria. In pregnant rats, the drug caused an increase in skeletal variations. In rabbits, the drug caused a high incidence of multiple malformations.
Takhzyro (lanadelumab-flyo), which has a MW of about 49,000, is a monoclonal antibody indicated for prophylaxis to prevent attacks of hereditary angioedema. The drug caused no fetal harm in monkeys.
Tavalisse (fostamatinib disodium hexahydrate), which has a MW of about 733, is a kinase inhibitor used for the treatment of thrombocytopenia. In pregnant rats and rabbits, the drug caused adverse developmental outcomes including embryo-fetal mortality, lower fetal weights, and structural anomalies.
Ultomiris (ravulizumab), which has a MW of about 148,000, is a humanized monoclonal antibody indicated for adult patients with paroxysmal nocturnal hemoglobinuria. In mice, the drug was associated with increased rates of developmental abnormalities and an increased rate of dead and moribund offspring.
Immunologic agent
Revcovi (elapegademase-lvlr), which has a MW of about 113,000, is a recombinant adenosine deaminase indicated for the treatment of adenosine deaminase severe combined immune deficiency. Animal studies in pregnancy have not been conducted.
Nutrient/Nutritional supplement
Fish oil is indicated as a source of calories and fatty acids in pediatric patients with parenteral nutrition-associated cholestasis. Animal reproduction studies have not been conducted. It is doubtful if this product will be used in pregnancy.
Ophthalmic – nerve growth factor
Oxervate (cenegermin-bkbj), which has a MW of 13,266, is a solution that contains 118 amino acids. It is a recombinant human nerve growth factor indicated for neurotrophic keratitis. In rats and rabbits given the drug during organogenesis, there was a slight increase in postimplantation loss at doses greater than or equal to 267 times the human dose.
Respiratory drugs
Symdeko (tezacaftor + ivacaftor), which have MWs of about 521 and 392, is indicated for the treatment of patients with cystic fibrosis who are homozygous for the F508del mutation or who have at least one mutation in the cystic fibrosis transmembrane conductance regulator gene. There were no adverse developmental effects in pregnant rats and rabbits when the drugs were used separately or combined.
Yupelri (revefenacin), which has a MW of about 598, is an anticholinergic drug. It is an inhaled solution for the maintenance treatment of chronic obstructive pulmonary disease. In rats and rabbits, doses that were about 209 times the RHD produced no evidence of fetal harm.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs reported no relevant financial disclosures. Email him at [email protected].
In 2018, the Food and Drug Administration approved a record 58 new drugs for humans. One of these agents, Annovera (segesterone acetate and ethinyl estradiol), is a vaginal ring to prevent pregnancy and is not relevant in this article. A second drug, Asparlas (calaspargase pegol-mknl), indicated to treat acute lymphoblastic leukemia, has not yet been released by its manufacturer. The agents with molecular weights (MW) less than 1,000 probably cross the placenta, but nearly all, regardless of MW, will cross in the second half of pregnancy.
There is no human pregnancy data for these agents, but there are five drugs included in pregnancy registries. However, it will take some time before the outcomes of these drugs are published. The routine absence of pregnancy data for most drugs was pointed out in a reference that I coauthored (“Should pregnant women be included in phase 4 clinical drug trials?” Am J Obstet Gynecol. 2015 Dec;213[6]:810-5). The article makes a strong argument for including some drugs in these trials.
Amyloidosis
Onpattro (patisiran) is indicated for the treatment of the polyneuropathy of hereditary transthyretin-mediated amyloidosis in adults. The drug caused embryo-fetal death and reduced fetal body weight in rabbits at doses also associated with maternal toxicity. No developmental toxicity was observed in rats.
Anti-infectives
Aemcolo (rifamycin), which has a MW of 720, is indicated for treatment of travelers’ diarrhea caused by noninvasive strains of Escherichia coli. No adverse fetal effects were observed in rats and rabbits that received close to human doses.
Krintafel (tafenoquine) is an antimalarial agent that is used to prevent relapse in patients who are receiving appropriate antimalarial therapy for Plasmodium vivax infection. The drug may cause hemolytic anemia in a fetus deficient in glucose-6-phosphate dehydrogenase. In rabbits, the drug caused dose-related abortions and maternal toxicity was observed in rabbits and rats. Treatment with this drug in pregnancy is not recommended, according to the manufacturer.
Tpoxx (tecovirimat monohydrate), which has a MW of about 394, is indicated for the treatment of smallpox disease. The drug did not cause embryo-fetal toxicity in pregnant mice and rabbits, but the maximum exposure in rabbits was only 0.4 times the human exposure.
Xofluza (baloxavir marboxil), which has a MW of about 572, is a prodrug that is converted by hydrolysis to baloxavir. It is indicated for the treatment of acute uncomplicated influenza. No adverse developmental effects were observed in rats and rabbits.
Zemdri (plazomicin), which has a MW of about 593, is an aminoglycoside indicated for the treatment of complicated urinary tract infections including pyelonephritis. The drug did not cause fetal harm in rats and rabbits at doses that did not cause maternal toxicity; however, prolonged use of an aminoglycoside (such as streptomycin) has caused irreversible, bilateral congenital deafness in children exposed in utero to prolonged use and is a potential complication.
Three new drugs in 2018 are indicated for treating HIV-1:
Biktarvy is a three-drug combination that includes bictegravir, emtricitabine, and tenofovir. The latter two drugs are included in the 11th edition of my book (“Drugs in Pregnancy and Lactation,” 11th ed. [Riverwoods, Ill.: Wolters Kluwer, 2017) and are not included here. Both are classified as compatible in pregnancy. Bictegravir has a MW of about 471. No adverse embryo-fetal effects in rats and rabbits were observed with this agent.
Trogarzo (ibalizumab-uiyk), which has a MW of about 150,000, is a monoclonal antibody antiretroviral agent used in combination with other antiretrovirals. There are no animal data. Although the MW is very high, monoclonal antibodies are transported across the placenta as pregnancy progresses.
Pifeltro (doravirine), which has a MW of about 426, is a nonnucleoside reverse transcriptase inhibitor used in combination with other antiretroviral agents for the treatment of HIV-1. The drug caused no significant toxicologic effects on embryo-fetal rats and rabbits.
If Biktarvy, Pifeltro, or Trogarzo are used in pregnancy, health care providers are encouraged to register the patient in the Antiretroviral Pregnancy Registry by calling 1-800-258-4263.
There are three new agents in the tetracycline class.
Nuzyra (omadacycline), which has a MW of about 729, is for community-acquired bacterial pneumonia and acute bacterial skin and skin structure infections.
Seysara (sarecycline), which has a MW of about 524, is for inflammatory lesions of nonnodular, moderate to severe acne vulgaris.
Xerava (eravacycline), which has a MW of about 632, is for complicated intra-abdominal infection.
The various dose-related toxicities observed with the three drugs in rats and rabbits included maternal deaths; increased postimplantation loss; reduced fetal body weights; delays in skeletal ossification; and fetal malformations of the skeleton, heart, and lung. Use of these drugs in the last half of pregnancy may cause permanent discoloration of the teeth and enamel hypoplasia, as well as inhibition of bone growth.
Antilipemic agents
Crysvita (burosumab-twza), which has a MW of about 147,000, is a fibroblast growth factor–blocking antibody indicated for the treatment of X-linked hypophosphatemia. In pregnant cynomolgus monkeys, doses slightly higher than the human dose were not teratogenic. The drug was detected in fetal serum indicating that it crossed the monkey placenta.
Tegsedi (inotersen), which has a MW of about 7,601, is an amyloidosis inhibitor used for polyneuropathy of hereditary transthyretin-mediated amyloidosis. It is available only through a restricted program. The drug was not teratogenic in mice and rabbits; however, it does decrease vitamin A levels, so supplementation with the vitamin is recommended.
Antineoplastics
The manufacturers recommend avoiding these drugs during pregnancy. Effective contraception should be used.
Daurismo (glasdegib), which has a MW of about 491, is a hedgehog pathway inhibitor indicated in combination with low-dose cytarabine for newly diagnosed acute myeloid leukemia (AML). The drug caused embryotoxicity, fetotoxicity, and teratogenicity in rats and rabbits at doses less than the human dose.
Erleada (apalutamide), which has a MW of about 477, is an androgen receptor inhibitor indicated for nonmetastatic, castration-resistant prostate cancer. Animal studies were not conducted because the drug should not be used in females.
Elzonris (tagraxofusp-erzs), which has a MW of 57,695, is a cytotoxin indicated for the treatment of blastic plasmacytoid dendritic cell neoplasm. Animal studies have not been conducted.
Lumoxiti (moxetumomab pasudotox–tdfk) which as a MW of about 63,000, is indicated for relapsed or refractory hairy cell leukemia. Studies have not been conducted in pregnant animals. Two life-threatening outcomes have occurred with the drug: capillary leak syndrome and hemolytic uremic syndrome. The drug should be discontinued if either occurs.
Lutathera (lutetium Lu 177 dotatate), which has a MW of about 1,610, is a radiolabeled somatostatin analogue given as a single intravenous dose every 8 weeks for four doses for the treatment of gastroenteropancreatic neuroendocrine tumors. Reproductive studies in animals have not been conducted. However, all radiopharmaceuticals have the potential to cause embryo-fetal harm. They also can cause infertility in males and females.
Talzenna (talazoparib), which has a MW of about 553, is a poly (ADP-ribose) polymerase inhibitor indicated for the treatment of certain types of breast cancer. At doses much less then the human dose, the drug caused fetal malformations and embryo-fetal death in rats.
Tibsovo (ivosidenib), which has a MW of 583, is an isocitrate dehydrogenase 1 inhibitor used for patients with relapsed or refractory AML. The drug caused embryo-fetal toxicity in rats and rabbits at doses slighter higher than the human dose.
There are seven new kinase inhibitors.
Braftovi (encorafenib), which has a MW of 540, is indicated in combination with Mektovi for patients with a specific type of metastatic melanoma. The drug caused embryo-fetal toxicity in rats and rabbits.
Copiktra (duvelisib), which has a MW of about 435, is indicated for treatment of chronic lymphocytic leukemia and follicular lymphoma. In rats and rabbits, the drug caused embryo-fetal death, lower fetal weights, and malformations.
Lorbrena (lorlatinib), which has a MW of about 406, is given for the treatment of metastatic non–small cell lung cancer. In rats and rabbits, the drug caused abortions, decreased fetal body weight, and major malformations.
Mektovi (binimetinib), which has a MW of about 441, is used in combination with Braftovi for patients with a specific type of melanoma. The drug was embryotoxic and abortifacient in rabbits.
Vitrakvi (larotrectinib), which has a MW of about 527, is used for patients with solid tumors. Studies in rats revealed fetal anasarca (extreme generalized edema) and omphalocele in rabbits.
Vizimpro (dacomitinib), which has a MW of about 488, is indicated for metastatic non–small cell lung cancer. The drug caused embryo-fetal toxicity in rats and mice.
Xospata (gilteritinib), which has a MW of about 1,222, is indicated for relapsed or refractory AML. In rats, the drug caused embryo-fetal death, suppressed fetal growth, and caused multiple malformations.
Three drugs are classified as monoclonal antibodies.
Gamifant (emapalumab), which has a MW of about 148,000, is indicated for primary hemophagocytic lymphohistiocytosis. A murine surrogate antimouse antibody was given to pregnant mice throughout gestation and no fetal harm was observed.
Libtayo (cemiplimab-rwlc), which has a MW of 146,000, is indicated for patients with metastatic or locally advanced cutaneous squamous cell carcinoma. Animal reproduction studies have not been conducted; however, based on its mechanism, increased rates of abortion or stillbirth may occur if the drug is used in human pregnancy.
Poteligeo (mogamulizumab-kpkc), which has a MW of about 149,000, is given for relapsed/refractory mycosis fungoides or Sézary syndrome. In pregnant monkeys, there was no embryo-fetal lethality, teratogenicity, fetal growth restriction, spontaneous abortion, or increased fetal death.
Central nervous system
There are three antimigraine agents that are monoclonal antibodies given as a subcutaneous injection.
Aimovig (erenumab-aooe), which has a MW of about 150,000, caused no adverse effects in monkey offspring.
Ajovy (fremanezumab-vfrm), which has a MW of about 148,000, had no adverse effect in rat and rabbit offspring.
Emgality (galcanezumab-gnlm), which has a MW of about 147,000, produced no adverse effects in rat and rabbit offspring.
Diacomit (stiripentol), which has a MW of about 234, is an anticonvulsant used to treat seizures associated with Dravet syndrome. The drug caused severe embryo-fetal toxicity in mice, rabbits, and rats. The drug is included in the North American Antiepileptic Drug (NAAED) Pregnancy Registry. Patients can enroll themselves by calling the toll-free number 1-888-233-2334 or visiting http://aedpregnancyregistry.org/.
Epidiolex (cannabidiol), which has a MW of about 314, is an anticonvulsant indicated for the treatment of seizures associated with Lennox-Gastaut syndrome or Dravet syndrome. In pregnant rats, doses up to about 16 times the recommended human dose (RHD) caused no embryo-fetal adverse effects. The drug caused decreased fetal body weights, increased fetal structural variations, and maternal toxicity when the drug was given to pregnant rabbits throughout organogenesis. The no-effect dose for embryo-fetal toxicity was less than the human dose. Patients can enroll themselves in the NAAED Pregnancy Registry by calling the toll-free number 1-888-233-2334 or visiting http://aedpregnancyregistry.org/.
Firdapse (amifampridine), a potassium channel blocker with a MW of about 201, is used for the treatment of Lambert-Eaton myasthenic syndrome. No adverse effects on embryo-fetal development were observed in rats and rabbits given the drug throughout organogenesis. However, in rats given the drug throughout pregnancy and lactation, there was an increase in stillbirths and pup deaths, reduced pup weight, and delayed sexual development in female pups.
Lucemyra (lofexidine), which has a MW of about 296, is used to mitigate opioid withdrawal symptoms to facilitate abrupt opioid discontinuation in adults. The drug caused severe toxicity in the fetuses of rats and rabbits.
Olumiant (baricitinib), which has a MW of about 371, is a Janus kinase inhibitor indicated for the treatment of rheumatoid arthritis. The drug was teratogenic in pregnant rats given doses about 20 times greater than the maximum RHD based on area under the curve. In rabbits, embryo death and rib anomalies were observed with doses 84 times greater than the maximum RHD, but no developmental toxicity was seen with doses 12 times greater than the maximum RHD.
Orilissa (elagolix), which has a MW of about 654, is a gonadotropin-releasing hormone receptor antagonist indicated for the management of pain associated with endometriosis. The drug caused abortions in rats and rabbits. Because the drug may increase the risk of early pregnancy loss, the manufacturer classifies it as contraindicated in pregnancy.
Dermatologic agents
Ilumya (tildrakizumab), which has a MW of about 147,000, is given by subcutaneous injection for the treatment of moderate to severe plaque psoriasis. When given during organogenesis in monkeys, no maternal or embryo-fetal toxicities were observed. However, when given throughout pregnancy a few neonatal deaths occurred, but the clinical significance of these nonclinical findings were unknown.
Fabry disease
Galafold (migalastat), which has a MW of about 200, is an alpha-galactosidase A pharmacologic chaperone indicated for the treatment of Fabry disease. Three pregnant women with Fabry disease were exposed to the drug in clinical studies but no information was provided on the pregnancy outcomes. No adverse developmental effects were observed in pregnant rats and rabbits.
Gastrointestinal agents
Akynzeo (netupitant or fosnetupitant palonosetron), which have MWs of about 579, 333, and 762, respectively, is available as an oral capsule (netupitant + palonosetron) and as an intravenous formulation (fosnetupitant + palonosetron). They are indicated, in combination with dexamethasone, for the prevention of nausea and vomiting related to cancer chemotherapy. Netupitant and fosnetupitant produced no embryo-fetal adverse effects in rats but were toxic to rabbit embryos. Palonosetron caused no embryo-fetal adverse effects in rats and rabbits.
Motegrity (prucalopride), which has a MW of about 486, is indicated for chronic idiopathic constipation. No adverse embryo-fetal developmental effects were observed in rats and rabbits.
Hematologic agents
Doptelet (avatrombopag), which has a MW of about 766, is indicated for the treatment of thrombocytopenia in adult patients with chronic liver disease who are scheduled to undergo a procedure. No embryo-fetal effects were observed in rats, but in rabbits the drug was associated with spontaneous abortions.
Lokelma (sodium zirconium cyclosilicate) is a nonabsorbed zirconium silicate that exchanges potassium for hydrogen and sodium. Animal studies have not been conducted. Because it is not absorbed, it is not expected to result in fetal exposure to the drug.
Mulpleta (lusutrombopag), which has a MW of about 592, a thrombopoietin receptor agonist, is indicated for the treatment of thrombocytopenia in patients with chronic liver disease. High levels of the drug in pregnant rats were associated with adverse developmental outcomes. No adverse embryo-fetal effects were seen in pregnant rabbits.
Palynziq (pegvaliase-pqpz), which has a MW of about 1,000,000, is a phenylalanine-metabolizing enzyme indicated to reduce blood phenylalanine concentrations in patients with phenylketonuria. In pregnant rats, the drug caused an increase in skeletal variations. In rabbits, the drug caused a high incidence of multiple malformations.
Takhzyro (lanadelumab-flyo), which has a MW of about 49,000, is a monoclonal antibody indicated for prophylaxis to prevent attacks of hereditary angioedema. The drug caused no fetal harm in monkeys.
Tavalisse (fostamatinib disodium hexahydrate), which has a MW of about 733, is a kinase inhibitor used for the treatment of thrombocytopenia. In pregnant rats and rabbits, the drug caused adverse developmental outcomes including embryo-fetal mortality, lower fetal weights, and structural anomalies.
Ultomiris (ravulizumab), which has a MW of about 148,000, is a humanized monoclonal antibody indicated for adult patients with paroxysmal nocturnal hemoglobinuria. In mice, the drug was associated with increased rates of developmental abnormalities and an increased rate of dead and moribund offspring.
Immunologic agent
Revcovi (elapegademase-lvlr), which has a MW of about 113,000, is a recombinant adenosine deaminase indicated for the treatment of adenosine deaminase severe combined immune deficiency. Animal studies in pregnancy have not been conducted.
Nutrient/Nutritional supplement
Fish oil is indicated as a source of calories and fatty acids in pediatric patients with parenteral nutrition-associated cholestasis. Animal reproduction studies have not been conducted. It is doubtful if this product will be used in pregnancy.
Ophthalmic – nerve growth factor
Oxervate (cenegermin-bkbj), which has a MW of 13,266, is a solution that contains 118 amino acids. It is a recombinant human nerve growth factor indicated for neurotrophic keratitis. In rats and rabbits given the drug during organogenesis, there was a slight increase in postimplantation loss at doses greater than or equal to 267 times the human dose.
Respiratory drugs
Symdeko (tezacaftor + ivacaftor), which have MWs of about 521 and 392, is indicated for the treatment of patients with cystic fibrosis who are homozygous for the F508del mutation or who have at least one mutation in the cystic fibrosis transmembrane conductance regulator gene. There were no adverse developmental effects in pregnant rats and rabbits when the drugs were used separately or combined.
Yupelri (revefenacin), which has a MW of about 598, is an anticholinergic drug. It is an inhaled solution for the maintenance treatment of chronic obstructive pulmonary disease. In rats and rabbits, doses that were about 209 times the RHD produced no evidence of fetal harm.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs reported no relevant financial disclosures. Email him at [email protected].
Postpartum hypertension
When managing our pregnant patients, we often might be tempted to view the delivery of the baby as the conclusion of prenatal care. For many women, the baby’s birth coincides with a resolution of health conditions that they may have experienced during pregnancy, including edema, gestational diabetes, and hypertensive disorders. However, the postpartum period remains a critical time in the health of the mother. Indeed, the weeks immediately following parturition often are colloquially referred to as the fourth trimester, further emphasizing the importance of appropriate patient management and care during this time.
One of the key health conditions we must monitor in the immediate postpartum period is hypertension. According to a 2018 report compiling data from nine of the Centers for Disease Control and Prevention’s Maternal Mortality Review Committees, hypertensive disorders accounted for approximately 9.3% of pregnancy-related maternal deaths within 42 days after delivery (http://reviewtoaction.org/Report_from_Nine_MMRCs). Although women who have hypertensive disorders during pregnancy are at risk for complications after giving birth, women without gestational hypertension, preeclampsia, or eclampsia can experience these conditions post partum at a rate between 0.3% and 27.5% (Am J Obstet Gynecol 2012 Jun;206[6]:470-5). Therefore, we cannot assume that a patient with an uncomplicated pregnancy is completely “in the clear” after delivery.
Despite these somewhat grim statistics, With vigilant monitoring and strong communication with our patients, ob.gyns. can reduce the risks of these complications from occurring, more quickly resolve symptoms as they might arise, and significantly improve the health and well-being of new mothers in the fourth trimester.
The importance of caring for all of our patients along the continuum of pregnancy, especially as it pertains to monitoring and preventing postpartum hypertension, is the focus of the third and final installment of this Master Class series on hypertension in pregnancy authored by Dr. Baha Sibai, professor of obstetrics, gynecology, and reproductive sciences at the University of Texas McGovern Medical School, Houston.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
When managing our pregnant patients, we often might be tempted to view the delivery of the baby as the conclusion of prenatal care. For many women, the baby’s birth coincides with a resolution of health conditions that they may have experienced during pregnancy, including edema, gestational diabetes, and hypertensive disorders. However, the postpartum period remains a critical time in the health of the mother. Indeed, the weeks immediately following parturition often are colloquially referred to as the fourth trimester, further emphasizing the importance of appropriate patient management and care during this time.
One of the key health conditions we must monitor in the immediate postpartum period is hypertension. According to a 2018 report compiling data from nine of the Centers for Disease Control and Prevention’s Maternal Mortality Review Committees, hypertensive disorders accounted for approximately 9.3% of pregnancy-related maternal deaths within 42 days after delivery (http://reviewtoaction.org/Report_from_Nine_MMRCs). Although women who have hypertensive disorders during pregnancy are at risk for complications after giving birth, women without gestational hypertension, preeclampsia, or eclampsia can experience these conditions post partum at a rate between 0.3% and 27.5% (Am J Obstet Gynecol 2012 Jun;206[6]:470-5). Therefore, we cannot assume that a patient with an uncomplicated pregnancy is completely “in the clear” after delivery.
Despite these somewhat grim statistics, With vigilant monitoring and strong communication with our patients, ob.gyns. can reduce the risks of these complications from occurring, more quickly resolve symptoms as they might arise, and significantly improve the health and well-being of new mothers in the fourth trimester.
The importance of caring for all of our patients along the continuum of pregnancy, especially as it pertains to monitoring and preventing postpartum hypertension, is the focus of the third and final installment of this Master Class series on hypertension in pregnancy authored by Dr. Baha Sibai, professor of obstetrics, gynecology, and reproductive sciences at the University of Texas McGovern Medical School, Houston.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
When managing our pregnant patients, we often might be tempted to view the delivery of the baby as the conclusion of prenatal care. For many women, the baby’s birth coincides with a resolution of health conditions that they may have experienced during pregnancy, including edema, gestational diabetes, and hypertensive disorders. However, the postpartum period remains a critical time in the health of the mother. Indeed, the weeks immediately following parturition often are colloquially referred to as the fourth trimester, further emphasizing the importance of appropriate patient management and care during this time.
One of the key health conditions we must monitor in the immediate postpartum period is hypertension. According to a 2018 report compiling data from nine of the Centers for Disease Control and Prevention’s Maternal Mortality Review Committees, hypertensive disorders accounted for approximately 9.3% of pregnancy-related maternal deaths within 42 days after delivery (http://reviewtoaction.org/Report_from_Nine_MMRCs). Although women who have hypertensive disorders during pregnancy are at risk for complications after giving birth, women without gestational hypertension, preeclampsia, or eclampsia can experience these conditions post partum at a rate between 0.3% and 27.5% (Am J Obstet Gynecol 2012 Jun;206[6]:470-5). Therefore, we cannot assume that a patient with an uncomplicated pregnancy is completely “in the clear” after delivery.
Despite these somewhat grim statistics, With vigilant monitoring and strong communication with our patients, ob.gyns. can reduce the risks of these complications from occurring, more quickly resolve symptoms as they might arise, and significantly improve the health and well-being of new mothers in the fourth trimester.
The importance of caring for all of our patients along the continuum of pregnancy, especially as it pertains to monitoring and preventing postpartum hypertension, is the focus of the third and final installment of this Master Class series on hypertension in pregnancy authored by Dr. Baha Sibai, professor of obstetrics, gynecology, and reproductive sciences at the University of Texas McGovern Medical School, Houston.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
Recognition, evaluation, and management of postpartum hypertension
Postpartum hypertension has a host of potential causes, some of which may be benign (such as the persistence of mild gestational hypertension or mild chronic hypertension) whereas others (such as severe de novo preeclampsia-eclampsia and HELLP syndrome [a complication of pregnancy characterized by hemolysis, elevated liver enzymes, and a low platelet count]) can be life threatening.
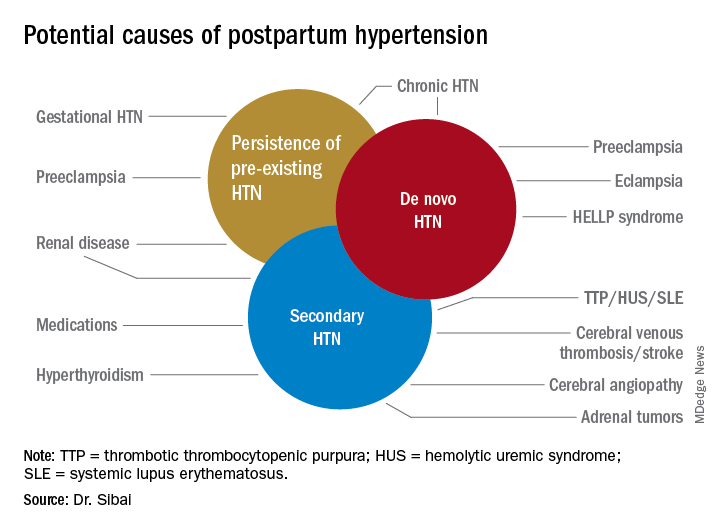
Postpartum hypertension may occur secondary to lupus, hyperthyroidism, hemolytic uremic syndrome, stroke, and other conditions, which means that we must have a high index of suspicion for secondary dangerous causes of hypertension when evaluating such women.
With monitoring, reporting, and prompt evaluation of symptoms in the postpartum period – and with patient education on signs and symptoms of severe hypertension and preeclampsia (PE) – we can expect to avoid a range of potential maternal complications, from hypertensive encephalopathy, liver hemorrhage, renal failure, and the development of eclampsia, ischemic stroke/cerebral hemorrhage, pulmonary edema, and cardiomyopathy.
Most women with gestational hypertension (GHTN) become normotensive during the first week post partum, but in women who develop PE during pregnancy, hypertension often takes longer to resolve. Some of these women may have an initial decrease in blood pressure immediately post partum followed by development of hypertension again between days 3 and 6. Therefore, This can be achieved either in-hospital, through home BP monitoring, or with in-office visits.
In addition, all women – including those who did not have hypertension during their pregnancies – should be educated about the signs and symptoms of severe hypertension or PE and instructed to report these to a medical provider in a timely fashion. Severe hypertension or PE with severe features may develop for the first time during the postpartum period either before or after hospital discharge. It is important to appreciate, moreover, that approximately 25%-40% of cases of eclampsia develop in the postpartum period with onset ranging from 2 days to 6 weeks after delivery. Moreover, almost one-third of women who develop the HELLP syndrome do so during the postpartum period.
Management of persistent hypertension
The most common causes for persistent hypertension beyond 48 hours after delivery are GHTN, PE, or chronic hypertension. Initial management will depend on history, clinical findings, presence or absence of associated symptoms, results of laboratory findings (urine protein, platelet count, liver enzymes, serum creatinine, and electrolytes), and response to prior treatment of hypertension.
Certain medications that frequently are prescribed in the postpartum period, such as ergonovine and decongestants, should be discontinued if they are being used. These agents can aggravate preexisting hypertension or result in new-onset hypertension if used in large or frequent doses. Their use also may be associated with cerebral symptoms, nausea, and vomiting.
Subsequent management includes close observation until resolution of hypertension and associated symptoms. If the patient has hypertension only with no symptoms, no proteinuria, and normal laboratory findings, BP control is the focus; antihypertensives are used if systolic BP remains persistently greater than or equal to 150 mm Hg and/or if diastolic BP persists at greater than or equal to 100 mm Hg. Intravenous boluses of either labetalol or hydralazine or oral rapid-acting nifedipine are used initially if systolic BP is greater than or equal to 160 mm Hg or diastolic BP greater than or equal to 110 mm Hg persists for at least 30 minutes. This is followed by oral medication to keep systolic BP less than 150 mg Hg and diastolic BP less than 100 mm Hg.
For patients with persistent hypertension after GHTN or PE, I recommend oral long-acting nifedipine XL (30 mg every 12 hours) or oral labetalol (200 mg every 8-12 hours). Compared with labetalol, oral nifedipine is associated with improved renal blood flow with resultant diuresis, which makes it the drug of choice in women with volume overload. In some, it is necessary to switch to a new agent such as an angiotensin-converting enzyme (ACE) inhibitor; an ACE inhibitor is the drug of choice in those with pregestational diabetes mellitus, renal disease, or cardiomyopathy. In addition, thiazide or loop diuretics may be needed in women with circulatory overload and in those with pulmonary edema. Antihypertensives such as nifedipine, labetalol, furosemide, captopril, and enalapril are compatible with breastfeeding.
If the BP remains less than 150 mm Hg (systolic) and/or less than 100 mm Hg (diastolic) for 24 hours, and there are no maternal symptoms, the patient may be discharged home with instructions for daily BP measurements (self or by a visiting nurse) and the reporting of symptoms until her next visit in 1 week. Antihypertensives then are discontinued if the BP remains below the hypertensive levels for at least 48 hours. This may take 1 or several weeks to achieve.
Women with PE with severe features should receive close monitoring of BP and of symptoms during the immediate postpartum period, as well as accurate measurements of fluid intake, urinary output, and weight gain. These women often have received large amounts of IV fluids during labor as a result of prehydration before epidural analgesia, as well as IV fluids administered during the use of oxytocin and magnesium sulfate in labor and post partum. Mobilization of extracellular fluid also leads to increased intravascular volume. As a result, women who have PE with severe features – particularly those with abnormal renal function, capillary leak, or early-onset disease – are at increased risk for pulmonary edema and exacerbation of severe hypertension.
Careful evaluation of the volume of IV fluids, oral intake, blood products, urine output, respiratory symptoms, and vital signs is advised. Patients who develop tachycardia or respiratory symptoms such as dry cough, shortness of breath, or orthopnea also should be monitored with pulse oximetry and frequent chest auscultation, as well as chest x-ray.
New-onset severe symptoms
Because severe hypertension or PE with severe features may develop for the first time during the postpartum period, postpartum women – and the medical providers and personnel who respond to patient phone calls – should be well educated about the signs and symptoms of severe hypertension or PE. These include new-onset severe headaches that do not respond to maximum doses of analgesics, persistent severe visual changes, and new-onset epigastric pain with nausea and vomiting, dyspnea, orthopnea, shortness of breath, or palpitations. These women are at increased risk for eclampsia, pulmonary edema, stroke, and thromboembolism; these women require careful evaluation and potential hospitalization.
Severe new onset of persistent headaches and/or visual symptoms. Women with hypertension in association with new-onset persistent headaches and/or visual changes should be suspected to have severe PE. Patients who have hypertension with seizure should be initially treated as having eclampsia and should receive brain imaging to rule out other etiologies. Magnesium sulfate therapy must be initiated promptly for seizure prophylaxis and/or treatment. In addition, intravenous antihypertensive medications are recommended to lower BP to the desired goal while considering an alternative cause for the cerebral symptoms.
Women presenting with hypertension in association with refractory and/or thunderclap headaches, visual disturbances, or neurologic deficits should be evaluated for possible cerebrovascular complications such as reversible cerebral vasoconstriction syndrome (RCVS), cerebral venous thrombosis, or stroke. These women will require selective diagnostic neuroimaging and consultation with neurology and/or neurosurgery. Such an evaluation may include CT scan for hemorrhage, MRI for detection of vasogenic edema and/or ischemia or infarction, cerebral angiography for diagnosis of RCVS, and cerebral venography for detection of cerebral venous thrombosis. Subsequent treatment will depend on the etiology.
Severe new-onset epigastric/right upper quadrant pain with nausea and vomiting. Women with persistent nausea, vomiting, or epigastric pain should be evaluated for HELLP syndrome because up to 30% who develop the syndrome do so post partum. The time of onset of clinical and laboratory findings ranges from 1 to 7 days post partum. Women are managed as they are before delivery, with the use of magnesium sulfate, antihypertensives, and close monitoring of vital signs and laboratory values.
In general, patients with HELLP syndrome will demonstrate an improvement in clinical and laboratory findings within 72 hours after treatment. If there is either no improvement or a deterioration in these findings, then it is important to consult with appropriate specialists for evaluation and subsequent management of possible rare syndromes such as acute fatty liver, thrombotic thrombocytopenic purpura, hemolytic uremic syndrome, or exacerbation of lupus.
Severe new-onset shortness of breath, dyspnea, orthopnea, or palpitations. Women with these symptoms in the postpartum period should be evaluated for possible pulmonary edema, pulmonary embolism, or peripartum cardiomyopathy. Women with postpartum hypertension are at risk for pulmonary edema with onset at 3-6 days after delivery. Diagnosis is confirmed by physical exam (tachycardia, tachypnea), presence of rales on lung exam, pulse oximetry (oxygen saturation less than 93%), and chest x-ray, and echocardiography to exclude other etiologies. Treatment of pulmonary edema includes oxygen supplementation, 40 mg IV furosemide, control of severe hypertension, fluid restriction, and supportive care.
Pulmonary embolism usually is confirmed by chest CT angiography and managed with therapeutic anticoagulation. Peripartum cardiomyopathy is diagnosed by echocardiography revealing left ventricular systolic dysfunction (ejection fraction less than 45%, dilated left ventricle). Treatment includes IV furosemide, use of a vasodilator, and ACE inhibitor therapy.
Remote prognosis
Recent research suggests that women who develop PE may be at increased risk for future cardiovascular disease such as heart failure, coronary artery disease, and stroke later in life. Indeed, many of the risk factors and pathophysiologic abnormalities of PE are similar to those of coronary artery disease.
The American College of Obstetricians and Gynecologists and the American Heart Association recommend that women with PE receive close observation in the postpartum period and careful evaluation in the first year after delivery to identify those who could benefit from early intervention to prevent subsequent cardiovascular disease. In general, when pregnancies are complicated by PE, there are opportunities for lifestyle and risk factor modification.
Dr. Sibai is professor of obstetrics, gynecology, and reproductive sciences at the University of Texas McGovern Medical School, Houston
Postpartum hypertension has a host of potential causes, some of which may be benign (such as the persistence of mild gestational hypertension or mild chronic hypertension) whereas others (such as severe de novo preeclampsia-eclampsia and HELLP syndrome [a complication of pregnancy characterized by hemolysis, elevated liver enzymes, and a low platelet count]) can be life threatening.
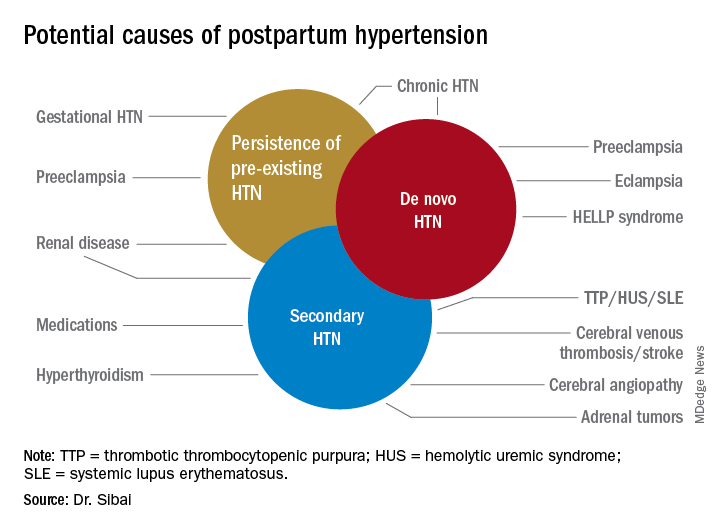
Postpartum hypertension may occur secondary to lupus, hyperthyroidism, hemolytic uremic syndrome, stroke, and other conditions, which means that we must have a high index of suspicion for secondary dangerous causes of hypertension when evaluating such women.
With monitoring, reporting, and prompt evaluation of symptoms in the postpartum period – and with patient education on signs and symptoms of severe hypertension and preeclampsia (PE) – we can expect to avoid a range of potential maternal complications, from hypertensive encephalopathy, liver hemorrhage, renal failure, and the development of eclampsia, ischemic stroke/cerebral hemorrhage, pulmonary edema, and cardiomyopathy.
Most women with gestational hypertension (GHTN) become normotensive during the first week post partum, but in women who develop PE during pregnancy, hypertension often takes longer to resolve. Some of these women may have an initial decrease in blood pressure immediately post partum followed by development of hypertension again between days 3 and 6. Therefore, This can be achieved either in-hospital, through home BP monitoring, or with in-office visits.
In addition, all women – including those who did not have hypertension during their pregnancies – should be educated about the signs and symptoms of severe hypertension or PE and instructed to report these to a medical provider in a timely fashion. Severe hypertension or PE with severe features may develop for the first time during the postpartum period either before or after hospital discharge. It is important to appreciate, moreover, that approximately 25%-40% of cases of eclampsia develop in the postpartum period with onset ranging from 2 days to 6 weeks after delivery. Moreover, almost one-third of women who develop the HELLP syndrome do so during the postpartum period.
Management of persistent hypertension
The most common causes for persistent hypertension beyond 48 hours after delivery are GHTN, PE, or chronic hypertension. Initial management will depend on history, clinical findings, presence or absence of associated symptoms, results of laboratory findings (urine protein, platelet count, liver enzymes, serum creatinine, and electrolytes), and response to prior treatment of hypertension.
Certain medications that frequently are prescribed in the postpartum period, such as ergonovine and decongestants, should be discontinued if they are being used. These agents can aggravate preexisting hypertension or result in new-onset hypertension if used in large or frequent doses. Their use also may be associated with cerebral symptoms, nausea, and vomiting.
Subsequent management includes close observation until resolution of hypertension and associated symptoms. If the patient has hypertension only with no symptoms, no proteinuria, and normal laboratory findings, BP control is the focus; antihypertensives are used if systolic BP remains persistently greater than or equal to 150 mm Hg and/or if diastolic BP persists at greater than or equal to 100 mm Hg. Intravenous boluses of either labetalol or hydralazine or oral rapid-acting nifedipine are used initially if systolic BP is greater than or equal to 160 mm Hg or diastolic BP greater than or equal to 110 mm Hg persists for at least 30 minutes. This is followed by oral medication to keep systolic BP less than 150 mg Hg and diastolic BP less than 100 mm Hg.
For patients with persistent hypertension after GHTN or PE, I recommend oral long-acting nifedipine XL (30 mg every 12 hours) or oral labetalol (200 mg every 8-12 hours). Compared with labetalol, oral nifedipine is associated with improved renal blood flow with resultant diuresis, which makes it the drug of choice in women with volume overload. In some, it is necessary to switch to a new agent such as an angiotensin-converting enzyme (ACE) inhibitor; an ACE inhibitor is the drug of choice in those with pregestational diabetes mellitus, renal disease, or cardiomyopathy. In addition, thiazide or loop diuretics may be needed in women with circulatory overload and in those with pulmonary edema. Antihypertensives such as nifedipine, labetalol, furosemide, captopril, and enalapril are compatible with breastfeeding.
If the BP remains less than 150 mm Hg (systolic) and/or less than 100 mm Hg (diastolic) for 24 hours, and there are no maternal symptoms, the patient may be discharged home with instructions for daily BP measurements (self or by a visiting nurse) and the reporting of symptoms until her next visit in 1 week. Antihypertensives then are discontinued if the BP remains below the hypertensive levels for at least 48 hours. This may take 1 or several weeks to achieve.
Women with PE with severe features should receive close monitoring of BP and of symptoms during the immediate postpartum period, as well as accurate measurements of fluid intake, urinary output, and weight gain. These women often have received large amounts of IV fluids during labor as a result of prehydration before epidural analgesia, as well as IV fluids administered during the use of oxytocin and magnesium sulfate in labor and post partum. Mobilization of extracellular fluid also leads to increased intravascular volume. As a result, women who have PE with severe features – particularly those with abnormal renal function, capillary leak, or early-onset disease – are at increased risk for pulmonary edema and exacerbation of severe hypertension.
Careful evaluation of the volume of IV fluids, oral intake, blood products, urine output, respiratory symptoms, and vital signs is advised. Patients who develop tachycardia or respiratory symptoms such as dry cough, shortness of breath, or orthopnea also should be monitored with pulse oximetry and frequent chest auscultation, as well as chest x-ray.
New-onset severe symptoms
Because severe hypertension or PE with severe features may develop for the first time during the postpartum period, postpartum women – and the medical providers and personnel who respond to patient phone calls – should be well educated about the signs and symptoms of severe hypertension or PE. These include new-onset severe headaches that do not respond to maximum doses of analgesics, persistent severe visual changes, and new-onset epigastric pain with nausea and vomiting, dyspnea, orthopnea, shortness of breath, or palpitations. These women are at increased risk for eclampsia, pulmonary edema, stroke, and thromboembolism; these women require careful evaluation and potential hospitalization.
Severe new onset of persistent headaches and/or visual symptoms. Women with hypertension in association with new-onset persistent headaches and/or visual changes should be suspected to have severe PE. Patients who have hypertension with seizure should be initially treated as having eclampsia and should receive brain imaging to rule out other etiologies. Magnesium sulfate therapy must be initiated promptly for seizure prophylaxis and/or treatment. In addition, intravenous antihypertensive medications are recommended to lower BP to the desired goal while considering an alternative cause for the cerebral symptoms.
Women presenting with hypertension in association with refractory and/or thunderclap headaches, visual disturbances, or neurologic deficits should be evaluated for possible cerebrovascular complications such as reversible cerebral vasoconstriction syndrome (RCVS), cerebral venous thrombosis, or stroke. These women will require selective diagnostic neuroimaging and consultation with neurology and/or neurosurgery. Such an evaluation may include CT scan for hemorrhage, MRI for detection of vasogenic edema and/or ischemia or infarction, cerebral angiography for diagnosis of RCVS, and cerebral venography for detection of cerebral venous thrombosis. Subsequent treatment will depend on the etiology.
Severe new-onset epigastric/right upper quadrant pain with nausea and vomiting. Women with persistent nausea, vomiting, or epigastric pain should be evaluated for HELLP syndrome because up to 30% who develop the syndrome do so post partum. The time of onset of clinical and laboratory findings ranges from 1 to 7 days post partum. Women are managed as they are before delivery, with the use of magnesium sulfate, antihypertensives, and close monitoring of vital signs and laboratory values.
In general, patients with HELLP syndrome will demonstrate an improvement in clinical and laboratory findings within 72 hours after treatment. If there is either no improvement or a deterioration in these findings, then it is important to consult with appropriate specialists for evaluation and subsequent management of possible rare syndromes such as acute fatty liver, thrombotic thrombocytopenic purpura, hemolytic uremic syndrome, or exacerbation of lupus.
Severe new-onset shortness of breath, dyspnea, orthopnea, or palpitations. Women with these symptoms in the postpartum period should be evaluated for possible pulmonary edema, pulmonary embolism, or peripartum cardiomyopathy. Women with postpartum hypertension are at risk for pulmonary edema with onset at 3-6 days after delivery. Diagnosis is confirmed by physical exam (tachycardia, tachypnea), presence of rales on lung exam, pulse oximetry (oxygen saturation less than 93%), and chest x-ray, and echocardiography to exclude other etiologies. Treatment of pulmonary edema includes oxygen supplementation, 40 mg IV furosemide, control of severe hypertension, fluid restriction, and supportive care.
Pulmonary embolism usually is confirmed by chest CT angiography and managed with therapeutic anticoagulation. Peripartum cardiomyopathy is diagnosed by echocardiography revealing left ventricular systolic dysfunction (ejection fraction less than 45%, dilated left ventricle). Treatment includes IV furosemide, use of a vasodilator, and ACE inhibitor therapy.
Remote prognosis
Recent research suggests that women who develop PE may be at increased risk for future cardiovascular disease such as heart failure, coronary artery disease, and stroke later in life. Indeed, many of the risk factors and pathophysiologic abnormalities of PE are similar to those of coronary artery disease.
The American College of Obstetricians and Gynecologists and the American Heart Association recommend that women with PE receive close observation in the postpartum period and careful evaluation in the first year after delivery to identify those who could benefit from early intervention to prevent subsequent cardiovascular disease. In general, when pregnancies are complicated by PE, there are opportunities for lifestyle and risk factor modification.
Dr. Sibai is professor of obstetrics, gynecology, and reproductive sciences at the University of Texas McGovern Medical School, Houston
Postpartum hypertension has a host of potential causes, some of which may be benign (such as the persistence of mild gestational hypertension or mild chronic hypertension) whereas others (such as severe de novo preeclampsia-eclampsia and HELLP syndrome [a complication of pregnancy characterized by hemolysis, elevated liver enzymes, and a low platelet count]) can be life threatening.
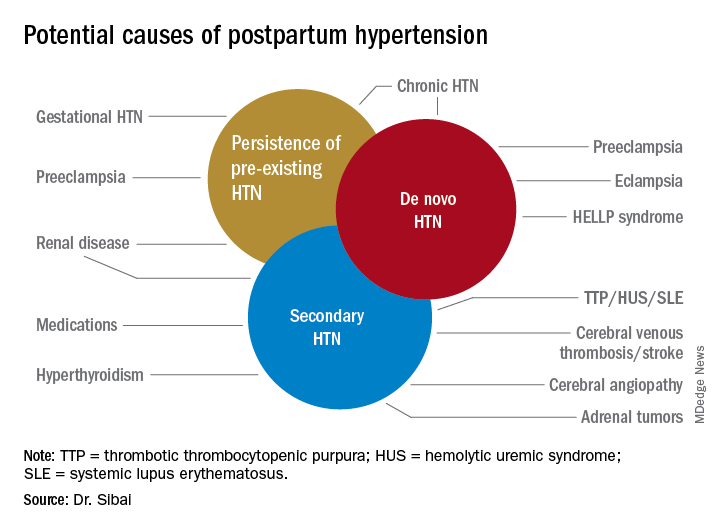
Postpartum hypertension may occur secondary to lupus, hyperthyroidism, hemolytic uremic syndrome, stroke, and other conditions, which means that we must have a high index of suspicion for secondary dangerous causes of hypertension when evaluating such women.
With monitoring, reporting, and prompt evaluation of symptoms in the postpartum period – and with patient education on signs and symptoms of severe hypertension and preeclampsia (PE) – we can expect to avoid a range of potential maternal complications, from hypertensive encephalopathy, liver hemorrhage, renal failure, and the development of eclampsia, ischemic stroke/cerebral hemorrhage, pulmonary edema, and cardiomyopathy.
Most women with gestational hypertension (GHTN) become normotensive during the first week post partum, but in women who develop PE during pregnancy, hypertension often takes longer to resolve. Some of these women may have an initial decrease in blood pressure immediately post partum followed by development of hypertension again between days 3 and 6. Therefore, This can be achieved either in-hospital, through home BP monitoring, or with in-office visits.
In addition, all women – including those who did not have hypertension during their pregnancies – should be educated about the signs and symptoms of severe hypertension or PE and instructed to report these to a medical provider in a timely fashion. Severe hypertension or PE with severe features may develop for the first time during the postpartum period either before or after hospital discharge. It is important to appreciate, moreover, that approximately 25%-40% of cases of eclampsia develop in the postpartum period with onset ranging from 2 days to 6 weeks after delivery. Moreover, almost one-third of women who develop the HELLP syndrome do so during the postpartum period.
Management of persistent hypertension
The most common causes for persistent hypertension beyond 48 hours after delivery are GHTN, PE, or chronic hypertension. Initial management will depend on history, clinical findings, presence or absence of associated symptoms, results of laboratory findings (urine protein, platelet count, liver enzymes, serum creatinine, and electrolytes), and response to prior treatment of hypertension.
Certain medications that frequently are prescribed in the postpartum period, such as ergonovine and decongestants, should be discontinued if they are being used. These agents can aggravate preexisting hypertension or result in new-onset hypertension if used in large or frequent doses. Their use also may be associated with cerebral symptoms, nausea, and vomiting.
Subsequent management includes close observation until resolution of hypertension and associated symptoms. If the patient has hypertension only with no symptoms, no proteinuria, and normal laboratory findings, BP control is the focus; antihypertensives are used if systolic BP remains persistently greater than or equal to 150 mm Hg and/or if diastolic BP persists at greater than or equal to 100 mm Hg. Intravenous boluses of either labetalol or hydralazine or oral rapid-acting nifedipine are used initially if systolic BP is greater than or equal to 160 mm Hg or diastolic BP greater than or equal to 110 mm Hg persists for at least 30 minutes. This is followed by oral medication to keep systolic BP less than 150 mg Hg and diastolic BP less than 100 mm Hg.
For patients with persistent hypertension after GHTN or PE, I recommend oral long-acting nifedipine XL (30 mg every 12 hours) or oral labetalol (200 mg every 8-12 hours). Compared with labetalol, oral nifedipine is associated with improved renal blood flow with resultant diuresis, which makes it the drug of choice in women with volume overload. In some, it is necessary to switch to a new agent such as an angiotensin-converting enzyme (ACE) inhibitor; an ACE inhibitor is the drug of choice in those with pregestational diabetes mellitus, renal disease, or cardiomyopathy. In addition, thiazide or loop diuretics may be needed in women with circulatory overload and in those with pulmonary edema. Antihypertensives such as nifedipine, labetalol, furosemide, captopril, and enalapril are compatible with breastfeeding.
If the BP remains less than 150 mm Hg (systolic) and/or less than 100 mm Hg (diastolic) for 24 hours, and there are no maternal symptoms, the patient may be discharged home with instructions for daily BP measurements (self or by a visiting nurse) and the reporting of symptoms until her next visit in 1 week. Antihypertensives then are discontinued if the BP remains below the hypertensive levels for at least 48 hours. This may take 1 or several weeks to achieve.
Women with PE with severe features should receive close monitoring of BP and of symptoms during the immediate postpartum period, as well as accurate measurements of fluid intake, urinary output, and weight gain. These women often have received large amounts of IV fluids during labor as a result of prehydration before epidural analgesia, as well as IV fluids administered during the use of oxytocin and magnesium sulfate in labor and post partum. Mobilization of extracellular fluid also leads to increased intravascular volume. As a result, women who have PE with severe features – particularly those with abnormal renal function, capillary leak, or early-onset disease – are at increased risk for pulmonary edema and exacerbation of severe hypertension.
Careful evaluation of the volume of IV fluids, oral intake, blood products, urine output, respiratory symptoms, and vital signs is advised. Patients who develop tachycardia or respiratory symptoms such as dry cough, shortness of breath, or orthopnea also should be monitored with pulse oximetry and frequent chest auscultation, as well as chest x-ray.
New-onset severe symptoms
Because severe hypertension or PE with severe features may develop for the first time during the postpartum period, postpartum women – and the medical providers and personnel who respond to patient phone calls – should be well educated about the signs and symptoms of severe hypertension or PE. These include new-onset severe headaches that do not respond to maximum doses of analgesics, persistent severe visual changes, and new-onset epigastric pain with nausea and vomiting, dyspnea, orthopnea, shortness of breath, or palpitations. These women are at increased risk for eclampsia, pulmonary edema, stroke, and thromboembolism; these women require careful evaluation and potential hospitalization.
Severe new onset of persistent headaches and/or visual symptoms. Women with hypertension in association with new-onset persistent headaches and/or visual changes should be suspected to have severe PE. Patients who have hypertension with seizure should be initially treated as having eclampsia and should receive brain imaging to rule out other etiologies. Magnesium sulfate therapy must be initiated promptly for seizure prophylaxis and/or treatment. In addition, intravenous antihypertensive medications are recommended to lower BP to the desired goal while considering an alternative cause for the cerebral symptoms.
Women presenting with hypertension in association with refractory and/or thunderclap headaches, visual disturbances, or neurologic deficits should be evaluated for possible cerebrovascular complications such as reversible cerebral vasoconstriction syndrome (RCVS), cerebral venous thrombosis, or stroke. These women will require selective diagnostic neuroimaging and consultation with neurology and/or neurosurgery. Such an evaluation may include CT scan for hemorrhage, MRI for detection of vasogenic edema and/or ischemia or infarction, cerebral angiography for diagnosis of RCVS, and cerebral venography for detection of cerebral venous thrombosis. Subsequent treatment will depend on the etiology.
Severe new-onset epigastric/right upper quadrant pain with nausea and vomiting. Women with persistent nausea, vomiting, or epigastric pain should be evaluated for HELLP syndrome because up to 30% who develop the syndrome do so post partum. The time of onset of clinical and laboratory findings ranges from 1 to 7 days post partum. Women are managed as they are before delivery, with the use of magnesium sulfate, antihypertensives, and close monitoring of vital signs and laboratory values.
In general, patients with HELLP syndrome will demonstrate an improvement in clinical and laboratory findings within 72 hours after treatment. If there is either no improvement or a deterioration in these findings, then it is important to consult with appropriate specialists for evaluation and subsequent management of possible rare syndromes such as acute fatty liver, thrombotic thrombocytopenic purpura, hemolytic uremic syndrome, or exacerbation of lupus.
Severe new-onset shortness of breath, dyspnea, orthopnea, or palpitations. Women with these symptoms in the postpartum period should be evaluated for possible pulmonary edema, pulmonary embolism, or peripartum cardiomyopathy. Women with postpartum hypertension are at risk for pulmonary edema with onset at 3-6 days after delivery. Diagnosis is confirmed by physical exam (tachycardia, tachypnea), presence of rales on lung exam, pulse oximetry (oxygen saturation less than 93%), and chest x-ray, and echocardiography to exclude other etiologies. Treatment of pulmonary edema includes oxygen supplementation, 40 mg IV furosemide, control of severe hypertension, fluid restriction, and supportive care.
Pulmonary embolism usually is confirmed by chest CT angiography and managed with therapeutic anticoagulation. Peripartum cardiomyopathy is diagnosed by echocardiography revealing left ventricular systolic dysfunction (ejection fraction less than 45%, dilated left ventricle). Treatment includes IV furosemide, use of a vasodilator, and ACE inhibitor therapy.
Remote prognosis
Recent research suggests that women who develop PE may be at increased risk for future cardiovascular disease such as heart failure, coronary artery disease, and stroke later in life. Indeed, many of the risk factors and pathophysiologic abnormalities of PE are similar to those of coronary artery disease.
The American College of Obstetricians and Gynecologists and the American Heart Association recommend that women with PE receive close observation in the postpartum period and careful evaluation in the first year after delivery to identify those who could benefit from early intervention to prevent subsequent cardiovascular disease. In general, when pregnancies are complicated by PE, there are opportunities for lifestyle and risk factor modification.
Dr. Sibai is professor of obstetrics, gynecology, and reproductive sciences at the University of Texas McGovern Medical School, Houston
Depression: a changing concept in the age of ketamine
What does it mean to define an amalgamation of symptoms as a “psychiatric disorder?” Are psychiatric disorders an extreme variation of normative human behavior? Is human behavior simply an output phenotype of some neurologic chemical processes that become disordered in mental illness? Can depression be localized in the brain and subsequently turned on or off? If depression were to be localized in the brain, would it be an excess of a neurotransmitter, the depletion of a receptor, a malfunctioning neuron, an overactive connectome, poorly processed genetic material, or something as yet undefined? Those questions always have been present in our minds and influenced our understanding of patients, but a recent development in psychiatry raises questions about one of the few things we were historically confident about.
A part of our foundational understanding of depression was that it is not sadness, per se. One can be sad for any amount of time. It is not uncommon to feel sad for any variety of reasons, such as watching an adorable 60-second commercial for dog food.1 Those fleeting moments of sadness can even be empowering; they remind us about the things we care about and would be sad to miss.
Sadness in oneself can demonstrate the experience of empathic sadness for others. On the contrary, depression appears to have little apparent purpose, and instead results in a maladaptive way of coping that is all-consuming and often very damaging. Depression is not a mood but a state of being, something that is not defined by how one feels but who one is or has become because of the disorder. So it comes as somewhat of a surprise when we heard that ketamine could alleviate depression in minutes.2,3 As described by a ketamine expert, symptoms are relieved in “no less than an hour.”4 The surprise is not so much that a treatment would work but that improvement could be defined in such a short time frame.
Psychiatry has debated the definition of depression for its entire existence. There are many ways to tackle the concept of depression. A lot of the debate has been about the causes of depression. One example of the continued evolution of our understanding of depression is our prior categorization of depression as “exogenous” or “endogenous.”5 Exogenous depression was described as happening in the context of social stressors and as best treated with therapy. Endogenous depression was a supposedly truer form of depression as a disorder and was more biologically based. Patients suffering from endogenous depression were thought to have chemical abnormalities in the brain that could be alleviated by tricyclic antidepressants and subsequently SSRIs. Like many prior debates about depression, this one appears to be little discussed nowadays. A review of the use of the term “endogenous depression” in books shows an onset in the 1930s, a peak in the 1980s, and a rapid decline since.6
More recently, psychiatrists have defined depression using the DSM-5 criteria. Depression is thought to be the presence of at least five out of nine symptoms listed in the manual for a period of 2 weeks that cause significant distress or impairment.7 The DSM attempts to address criticism by providing information on its limitations and best use, and encourages clinical interpretation of symptoms. The DSM does not portray itself as a gold standard but rather as a tool for treatment planning and effective communication between peers. Furthermore, the National Institute on Mental Health is promoting an alternative understanding of depression using its own Research Domain Criteria, which attempt to provide a more objective understanding of the disorder based on biological rather than subjective correlates.
The growing literature on ketamine partly hinges on the belief that depression is something that can be redefined and changed at any moment. Many trials ask patients whether their depression remains in remission in the subsequent hours, days, and weeks following administration of the drug. However, one wonders if that is even possible. If a patient’s depression is alleviated in an hour, was it really clinical depression? Is it truly in remission? Contrary to our previous understanding, is depression, in reality, a switch that can be turned off by an infusion of an N-methyl-D-aspartate (NMDA)–receptor antagonist? Without minimizing the suffering of patients seeking ketamine or the relief provided to patients who benefit from the treatment, we simply are pointing out that the definition of depression did not account for this reported phenomenon of relatively instantaneous relief. The seemingly miraculous effects of ketamine suggest a new paradigm where any intervention – whether chemical, social, or psychological – could turn off the devastating effects of depression in an instant.
After all, the most widely used scale of depression, the nine-item Patient Health Questionnaire (PHQ-9) asks patients, “Over the last 2 weeks, how often have you been bothered by any of the following problems?” The highest answer one can give is “Nearly every day.” Are we incorrect to think that if one were suicidal every minute of the past 2 weeks, one would still score, nearly every day, even if one’s symptoms were relieved for the past hour? Thus, a maximum score of 27 would remain a 27 no matter what happened in the past hour.
We do realize that we are being overly literal. Ketamine makes some people feel better quickly, and researchers try to capture that effect by asking patients about their symptoms within short intervals. Furthermore, one has to start somewhere. After the infusion is a reasonable time to ask patients how they feel. We are also cognizant that many ketamine researchers do more long-term follow-ups and/or have recommended longer-term studies. Nonetheless,
Expanding our definition of depression to encompass experiences with short time frames may have unintended consequences. As living circumstances rarely change in minutes, the emphasis on rapid recovery makes the patients more in control of their reported experiences and thus their diagnoses. One cannot assess a patient’s impairment or disability from minute to minute. One is left with emphasizing the patient’s subjective symptoms and deemphasizing their relationships, goals, and daily functioning. How could one measure eating habits, hygiene, or participation in hobbies every hour? Another consequence of this reduced time frame is the expansion of a diagnosis that no longer requires the presence of symptoms for 2 weeks. Considering the already vast number of people diagnosed with depression,9,10 this small change may further expand the number diagnosed with a mood disorder. Perhaps to many practitioners and patients these arguments seem obtuse and fastidious, but there is a core failure in modern psychiatry to clearly differentiate the human condition from mental illness. Said failure has vast implications for psychiatric epidemiology, the sociological understanding of psychic suffering and suicide, as well as the overprescribing of psychotropic medications.
Ketamine is an exciting prospect to many psychiatrists who feel like we have had little advancement and few novel treatments in a long time; advertised breakthroughs in the treatment of depression since fluoxetine have not been particularly impressive. Furthermore, the concerns about potential ketamine abuse are not theoretical but a very real problem in some parts of the world.11,12 The concerns about abuse are worsened considering recent evidence that suggests that ketamine’s effect may be driven by its opiate rather than NMDA effects.13 While some have discussed those concerns, we think that the field also needs to address the fact that the debate about ketamine is also changing our definition of depression.
References
1. https://www.youtube.com/watch?v=MpcUN6XvGmk.
2. J Clin Psychiatry. 2016 Jun;77(6):e719-25.
3. Emerg (Tehran). 2014 Winter;2(1):36-9.
4. “Is esketamine the game-changer for depression we want?” Rolling Stone. 2019 Mar 11.
5. Psychol Med. 1971;1(3):191-6.
6. https://books.google.com/ngrams.
7. Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5). American Psychiatric Association, 2013.
8. Am J Psychiatry. 2014 Apr;171(4):395-7.
9. “Many people taking antidepressants discover they cannot quit.” New York Times. 2018 Apr 7.
10. “Antidepressants show greatest increase in number of prescription items dispensed.” National Health Service. 2015 Jul 5.
11. “The ketamine connection.” BBC News. 2015 Jul 10.
12. Front Psychiatry. 2018 Jul 17. doi: 10.33389/fpsyt.2018.00313.
13. Am J Psychiatry. 2018 Dec 1;175(2):1205-15.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. Among his writings is Coercion and the critical psychiatrist, chapter 7 in the new book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer Nature Switzerland, 2019, pp. 155-77). Dr. Lehman is an associate professor of psychiatry at UCSD. He is codirector of all Acute and Intensive Psychiatric Treatment at the VA Medical Center in San Diego, where he practices clinical psychiatry. He also is the course director for the UCSD third-year medical student psychiatry clerkship.
*This article was updated 3/25/2019.
What does it mean to define an amalgamation of symptoms as a “psychiatric disorder?” Are psychiatric disorders an extreme variation of normative human behavior? Is human behavior simply an output phenotype of some neurologic chemical processes that become disordered in mental illness? Can depression be localized in the brain and subsequently turned on or off? If depression were to be localized in the brain, would it be an excess of a neurotransmitter, the depletion of a receptor, a malfunctioning neuron, an overactive connectome, poorly processed genetic material, or something as yet undefined? Those questions always have been present in our minds and influenced our understanding of patients, but a recent development in psychiatry raises questions about one of the few things we were historically confident about.
A part of our foundational understanding of depression was that it is not sadness, per se. One can be sad for any amount of time. It is not uncommon to feel sad for any variety of reasons, such as watching an adorable 60-second commercial for dog food.1 Those fleeting moments of sadness can even be empowering; they remind us about the things we care about and would be sad to miss.
Sadness in oneself can demonstrate the experience of empathic sadness for others. On the contrary, depression appears to have little apparent purpose, and instead results in a maladaptive way of coping that is all-consuming and often very damaging. Depression is not a mood but a state of being, something that is not defined by how one feels but who one is or has become because of the disorder. So it comes as somewhat of a surprise when we heard that ketamine could alleviate depression in minutes.2,3 As described by a ketamine expert, symptoms are relieved in “no less than an hour.”4 The surprise is not so much that a treatment would work but that improvement could be defined in such a short time frame.
Psychiatry has debated the definition of depression for its entire existence. There are many ways to tackle the concept of depression. A lot of the debate has been about the causes of depression. One example of the continued evolution of our understanding of depression is our prior categorization of depression as “exogenous” or “endogenous.”5 Exogenous depression was described as happening in the context of social stressors and as best treated with therapy. Endogenous depression was a supposedly truer form of depression as a disorder and was more biologically based. Patients suffering from endogenous depression were thought to have chemical abnormalities in the brain that could be alleviated by tricyclic antidepressants and subsequently SSRIs. Like many prior debates about depression, this one appears to be little discussed nowadays. A review of the use of the term “endogenous depression” in books shows an onset in the 1930s, a peak in the 1980s, and a rapid decline since.6
More recently, psychiatrists have defined depression using the DSM-5 criteria. Depression is thought to be the presence of at least five out of nine symptoms listed in the manual for a period of 2 weeks that cause significant distress or impairment.7 The DSM attempts to address criticism by providing information on its limitations and best use, and encourages clinical interpretation of symptoms. The DSM does not portray itself as a gold standard but rather as a tool for treatment planning and effective communication between peers. Furthermore, the National Institute on Mental Health is promoting an alternative understanding of depression using its own Research Domain Criteria, which attempt to provide a more objective understanding of the disorder based on biological rather than subjective correlates.
The growing literature on ketamine partly hinges on the belief that depression is something that can be redefined and changed at any moment. Many trials ask patients whether their depression remains in remission in the subsequent hours, days, and weeks following administration of the drug. However, one wonders if that is even possible. If a patient’s depression is alleviated in an hour, was it really clinical depression? Is it truly in remission? Contrary to our previous understanding, is depression, in reality, a switch that can be turned off by an infusion of an N-methyl-D-aspartate (NMDA)–receptor antagonist? Without minimizing the suffering of patients seeking ketamine or the relief provided to patients who benefit from the treatment, we simply are pointing out that the definition of depression did not account for this reported phenomenon of relatively instantaneous relief. The seemingly miraculous effects of ketamine suggest a new paradigm where any intervention – whether chemical, social, or psychological – could turn off the devastating effects of depression in an instant.
After all, the most widely used scale of depression, the nine-item Patient Health Questionnaire (PHQ-9) asks patients, “Over the last 2 weeks, how often have you been bothered by any of the following problems?” The highest answer one can give is “Nearly every day.” Are we incorrect to think that if one were suicidal every minute of the past 2 weeks, one would still score, nearly every day, even if one’s symptoms were relieved for the past hour? Thus, a maximum score of 27 would remain a 27 no matter what happened in the past hour.
We do realize that we are being overly literal. Ketamine makes some people feel better quickly, and researchers try to capture that effect by asking patients about their symptoms within short intervals. Furthermore, one has to start somewhere. After the infusion is a reasonable time to ask patients how they feel. We are also cognizant that many ketamine researchers do more long-term follow-ups and/or have recommended longer-term studies. Nonetheless,
Expanding our definition of depression to encompass experiences with short time frames may have unintended consequences. As living circumstances rarely change in minutes, the emphasis on rapid recovery makes the patients more in control of their reported experiences and thus their diagnoses. One cannot assess a patient’s impairment or disability from minute to minute. One is left with emphasizing the patient’s subjective symptoms and deemphasizing their relationships, goals, and daily functioning. How could one measure eating habits, hygiene, or participation in hobbies every hour? Another consequence of this reduced time frame is the expansion of a diagnosis that no longer requires the presence of symptoms for 2 weeks. Considering the already vast number of people diagnosed with depression,9,10 this small change may further expand the number diagnosed with a mood disorder. Perhaps to many practitioners and patients these arguments seem obtuse and fastidious, but there is a core failure in modern psychiatry to clearly differentiate the human condition from mental illness. Said failure has vast implications for psychiatric epidemiology, the sociological understanding of psychic suffering and suicide, as well as the overprescribing of psychotropic medications.
Ketamine is an exciting prospect to many psychiatrists who feel like we have had little advancement and few novel treatments in a long time; advertised breakthroughs in the treatment of depression since fluoxetine have not been particularly impressive. Furthermore, the concerns about potential ketamine abuse are not theoretical but a very real problem in some parts of the world.11,12 The concerns about abuse are worsened considering recent evidence that suggests that ketamine’s effect may be driven by its opiate rather than NMDA effects.13 While some have discussed those concerns, we think that the field also needs to address the fact that the debate about ketamine is also changing our definition of depression.
References
1. https://www.youtube.com/watch?v=MpcUN6XvGmk.
2. J Clin Psychiatry. 2016 Jun;77(6):e719-25.
3. Emerg (Tehran). 2014 Winter;2(1):36-9.
4. “Is esketamine the game-changer for depression we want?” Rolling Stone. 2019 Mar 11.
5. Psychol Med. 1971;1(3):191-6.
6. https://books.google.com/ngrams.
7. Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5). American Psychiatric Association, 2013.
8. Am J Psychiatry. 2014 Apr;171(4):395-7.
9. “Many people taking antidepressants discover they cannot quit.” New York Times. 2018 Apr 7.
10. “Antidepressants show greatest increase in number of prescription items dispensed.” National Health Service. 2015 Jul 5.
11. “The ketamine connection.” BBC News. 2015 Jul 10.
12. Front Psychiatry. 2018 Jul 17. doi: 10.33389/fpsyt.2018.00313.
13. Am J Psychiatry. 2018 Dec 1;175(2):1205-15.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. Among his writings is Coercion and the critical psychiatrist, chapter 7 in the new book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer Nature Switzerland, 2019, pp. 155-77). Dr. Lehman is an associate professor of psychiatry at UCSD. He is codirector of all Acute and Intensive Psychiatric Treatment at the VA Medical Center in San Diego, where he practices clinical psychiatry. He also is the course director for the UCSD third-year medical student psychiatry clerkship.
*This article was updated 3/25/2019.
What does it mean to define an amalgamation of symptoms as a “psychiatric disorder?” Are psychiatric disorders an extreme variation of normative human behavior? Is human behavior simply an output phenotype of some neurologic chemical processes that become disordered in mental illness? Can depression be localized in the brain and subsequently turned on or off? If depression were to be localized in the brain, would it be an excess of a neurotransmitter, the depletion of a receptor, a malfunctioning neuron, an overactive connectome, poorly processed genetic material, or something as yet undefined? Those questions always have been present in our minds and influenced our understanding of patients, but a recent development in psychiatry raises questions about one of the few things we were historically confident about.
A part of our foundational understanding of depression was that it is not sadness, per se. One can be sad for any amount of time. It is not uncommon to feel sad for any variety of reasons, such as watching an adorable 60-second commercial for dog food.1 Those fleeting moments of sadness can even be empowering; they remind us about the things we care about and would be sad to miss.
Sadness in oneself can demonstrate the experience of empathic sadness for others. On the contrary, depression appears to have little apparent purpose, and instead results in a maladaptive way of coping that is all-consuming and often very damaging. Depression is not a mood but a state of being, something that is not defined by how one feels but who one is or has become because of the disorder. So it comes as somewhat of a surprise when we heard that ketamine could alleviate depression in minutes.2,3 As described by a ketamine expert, symptoms are relieved in “no less than an hour.”4 The surprise is not so much that a treatment would work but that improvement could be defined in such a short time frame.
Psychiatry has debated the definition of depression for its entire existence. There are many ways to tackle the concept of depression. A lot of the debate has been about the causes of depression. One example of the continued evolution of our understanding of depression is our prior categorization of depression as “exogenous” or “endogenous.”5 Exogenous depression was described as happening in the context of social stressors and as best treated with therapy. Endogenous depression was a supposedly truer form of depression as a disorder and was more biologically based. Patients suffering from endogenous depression were thought to have chemical abnormalities in the brain that could be alleviated by tricyclic antidepressants and subsequently SSRIs. Like many prior debates about depression, this one appears to be little discussed nowadays. A review of the use of the term “endogenous depression” in books shows an onset in the 1930s, a peak in the 1980s, and a rapid decline since.6
More recently, psychiatrists have defined depression using the DSM-5 criteria. Depression is thought to be the presence of at least five out of nine symptoms listed in the manual for a period of 2 weeks that cause significant distress or impairment.7 The DSM attempts to address criticism by providing information on its limitations and best use, and encourages clinical interpretation of symptoms. The DSM does not portray itself as a gold standard but rather as a tool for treatment planning and effective communication between peers. Furthermore, the National Institute on Mental Health is promoting an alternative understanding of depression using its own Research Domain Criteria, which attempt to provide a more objective understanding of the disorder based on biological rather than subjective correlates.
The growing literature on ketamine partly hinges on the belief that depression is something that can be redefined and changed at any moment. Many trials ask patients whether their depression remains in remission in the subsequent hours, days, and weeks following administration of the drug. However, one wonders if that is even possible. If a patient’s depression is alleviated in an hour, was it really clinical depression? Is it truly in remission? Contrary to our previous understanding, is depression, in reality, a switch that can be turned off by an infusion of an N-methyl-D-aspartate (NMDA)–receptor antagonist? Without minimizing the suffering of patients seeking ketamine or the relief provided to patients who benefit from the treatment, we simply are pointing out that the definition of depression did not account for this reported phenomenon of relatively instantaneous relief. The seemingly miraculous effects of ketamine suggest a new paradigm where any intervention – whether chemical, social, or psychological – could turn off the devastating effects of depression in an instant.
After all, the most widely used scale of depression, the nine-item Patient Health Questionnaire (PHQ-9) asks patients, “Over the last 2 weeks, how often have you been bothered by any of the following problems?” The highest answer one can give is “Nearly every day.” Are we incorrect to think that if one were suicidal every minute of the past 2 weeks, one would still score, nearly every day, even if one’s symptoms were relieved for the past hour? Thus, a maximum score of 27 would remain a 27 no matter what happened in the past hour.
We do realize that we are being overly literal. Ketamine makes some people feel better quickly, and researchers try to capture that effect by asking patients about their symptoms within short intervals. Furthermore, one has to start somewhere. After the infusion is a reasonable time to ask patients how they feel. We are also cognizant that many ketamine researchers do more long-term follow-ups and/or have recommended longer-term studies. Nonetheless,
Expanding our definition of depression to encompass experiences with short time frames may have unintended consequences. As living circumstances rarely change in minutes, the emphasis on rapid recovery makes the patients more in control of their reported experiences and thus their diagnoses. One cannot assess a patient’s impairment or disability from minute to minute. One is left with emphasizing the patient’s subjective symptoms and deemphasizing their relationships, goals, and daily functioning. How could one measure eating habits, hygiene, or participation in hobbies every hour? Another consequence of this reduced time frame is the expansion of a diagnosis that no longer requires the presence of symptoms for 2 weeks. Considering the already vast number of people diagnosed with depression,9,10 this small change may further expand the number diagnosed with a mood disorder. Perhaps to many practitioners and patients these arguments seem obtuse and fastidious, but there is a core failure in modern psychiatry to clearly differentiate the human condition from mental illness. Said failure has vast implications for psychiatric epidemiology, the sociological understanding of psychic suffering and suicide, as well as the overprescribing of psychotropic medications.
Ketamine is an exciting prospect to many psychiatrists who feel like we have had little advancement and few novel treatments in a long time; advertised breakthroughs in the treatment of depression since fluoxetine have not been particularly impressive. Furthermore, the concerns about potential ketamine abuse are not theoretical but a very real problem in some parts of the world.11,12 The concerns about abuse are worsened considering recent evidence that suggests that ketamine’s effect may be driven by its opiate rather than NMDA effects.13 While some have discussed those concerns, we think that the field also needs to address the fact that the debate about ketamine is also changing our definition of depression.
References
1. https://www.youtube.com/watch?v=MpcUN6XvGmk.
2. J Clin Psychiatry. 2016 Jun;77(6):e719-25.
3. Emerg (Tehran). 2014 Winter;2(1):36-9.
4. “Is esketamine the game-changer for depression we want?” Rolling Stone. 2019 Mar 11.
5. Psychol Med. 1971;1(3):191-6.
6. https://books.google.com/ngrams.
7. Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5). American Psychiatric Association, 2013.
8. Am J Psychiatry. 2014 Apr;171(4):395-7.
9. “Many people taking antidepressants discover they cannot quit.” New York Times. 2018 Apr 7.
10. “Antidepressants show greatest increase in number of prescription items dispensed.” National Health Service. 2015 Jul 5.
11. “The ketamine connection.” BBC News. 2015 Jul 10.
12. Front Psychiatry. 2018 Jul 17. doi: 10.33389/fpsyt.2018.00313.
13. Am J Psychiatry. 2018 Dec 1;175(2):1205-15.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. Among his writings is Coercion and the critical psychiatrist, chapter 7 in the new book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer Nature Switzerland, 2019, pp. 155-77). Dr. Lehman is an associate professor of psychiatry at UCSD. He is codirector of all Acute and Intensive Psychiatric Treatment at the VA Medical Center in San Diego, where he practices clinical psychiatry. He also is the course director for the UCSD third-year medical student psychiatry clerkship.
*This article was updated 3/25/2019.
Spring
There is little to want for living in San Diego, America’s Finest City. The weather here is 72 and sunny year round. Yet, there are shortcomings. For one, there are no Forsythia. Forsythia are the deciduous shrubs that act as the harbingers of spring, blooming brilliant yellow across cold gray damp parts of the United States right now.
I grew up in New England where Forsythia bushes flower this time of year – a most welcome sign that the winter’s worst was over. Along with the purple crocus plants popping up in the warm bits of grass that breaks through the snow, seeing the Forsythia bloom always evoked that most appealing of feelings, hope. Hope that the discomfort of winter has passed. Hope that the beauty of nature will return. A promise that this year’s cycle of life will continue.
. A future with less suffering or with more joy. And as their doctors, we can help them get there.
A newly insured patient came to see me today. She had severe psoriasis. Her face, masked with red scaly patches, was heavy with the burden of the long winter she had endured. She was itchy and flaky and so embarrassed as to struggle to make eye contact with me. When I told her that we could help her, that there are treatments for her that would clear up the psoriasis and relieve her symptoms, she started to cry. Her husband intervened, apologizing for her. “I’m sorry. She has had this for so long, and you are the first person to tell her that she can get better. You have given us hope.”
When I walked back to my office I noticed the Rhode Island flag that I have mounted. Under the stars and blue anchor on it is the word “hope.” In 1664, when the state seal was created, it was the most important of ideas. It is why the settlers of Rhode Island risked their lives to cross an ocean to start anew, why my ancestors came from Italy two centuries later, why my parents sent me to college, why I decided to try for medicine. It is what most of us give every day. Hope, the ability to see into the future and bring that feeling back to the present. The belief that whatever and wherever you are, soon it will be even better. It cannot, however, be commanded. You can’t insist a patient hope any more than you can make them love. You must first understand what they see and feel, then show them how things might be better through trust.
Throughout life, hope creates possibilities. It unites us. It motivates us. It is the destroyer of winter and of burnout and of disease. It is one of the most important gifts that we give patients, and we do it everyday. Tomorrow in your practice, notice how often you foster it. Pay attention to how your patient changes the moment you give it to them. Watch the Forsythia bloom as you reassure them that their spring will return again.
“We must accept finite disappointment, but never lose infinite hope.” – Martin Luther King Jr.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
There is little to want for living in San Diego, America’s Finest City. The weather here is 72 and sunny year round. Yet, there are shortcomings. For one, there are no Forsythia. Forsythia are the deciduous shrubs that act as the harbingers of spring, blooming brilliant yellow across cold gray damp parts of the United States right now.
I grew up in New England where Forsythia bushes flower this time of year – a most welcome sign that the winter’s worst was over. Along with the purple crocus plants popping up in the warm bits of grass that breaks through the snow, seeing the Forsythia bloom always evoked that most appealing of feelings, hope. Hope that the discomfort of winter has passed. Hope that the beauty of nature will return. A promise that this year’s cycle of life will continue.
. A future with less suffering or with more joy. And as their doctors, we can help them get there.
A newly insured patient came to see me today. She had severe psoriasis. Her face, masked with red scaly patches, was heavy with the burden of the long winter she had endured. She was itchy and flaky and so embarrassed as to struggle to make eye contact with me. When I told her that we could help her, that there are treatments for her that would clear up the psoriasis and relieve her symptoms, she started to cry. Her husband intervened, apologizing for her. “I’m sorry. She has had this for so long, and you are the first person to tell her that she can get better. You have given us hope.”
When I walked back to my office I noticed the Rhode Island flag that I have mounted. Under the stars and blue anchor on it is the word “hope.” In 1664, when the state seal was created, it was the most important of ideas. It is why the settlers of Rhode Island risked their lives to cross an ocean to start anew, why my ancestors came from Italy two centuries later, why my parents sent me to college, why I decided to try for medicine. It is what most of us give every day. Hope, the ability to see into the future and bring that feeling back to the present. The belief that whatever and wherever you are, soon it will be even better. It cannot, however, be commanded. You can’t insist a patient hope any more than you can make them love. You must first understand what they see and feel, then show them how things might be better through trust.
Throughout life, hope creates possibilities. It unites us. It motivates us. It is the destroyer of winter and of burnout and of disease. It is one of the most important gifts that we give patients, and we do it everyday. Tomorrow in your practice, notice how often you foster it. Pay attention to how your patient changes the moment you give it to them. Watch the Forsythia bloom as you reassure them that their spring will return again.
“We must accept finite disappointment, but never lose infinite hope.” – Martin Luther King Jr.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
There is little to want for living in San Diego, America’s Finest City. The weather here is 72 and sunny year round. Yet, there are shortcomings. For one, there are no Forsythia. Forsythia are the deciduous shrubs that act as the harbingers of spring, blooming brilliant yellow across cold gray damp parts of the United States right now.
I grew up in New England where Forsythia bushes flower this time of year – a most welcome sign that the winter’s worst was over. Along with the purple crocus plants popping up in the warm bits of grass that breaks through the snow, seeing the Forsythia bloom always evoked that most appealing of feelings, hope. Hope that the discomfort of winter has passed. Hope that the beauty of nature will return. A promise that this year’s cycle of life will continue.
. A future with less suffering or with more joy. And as their doctors, we can help them get there.
A newly insured patient came to see me today. She had severe psoriasis. Her face, masked with red scaly patches, was heavy with the burden of the long winter she had endured. She was itchy and flaky and so embarrassed as to struggle to make eye contact with me. When I told her that we could help her, that there are treatments for her that would clear up the psoriasis and relieve her symptoms, she started to cry. Her husband intervened, apologizing for her. “I’m sorry. She has had this for so long, and you are the first person to tell her that she can get better. You have given us hope.”
When I walked back to my office I noticed the Rhode Island flag that I have mounted. Under the stars and blue anchor on it is the word “hope.” In 1664, when the state seal was created, it was the most important of ideas. It is why the settlers of Rhode Island risked their lives to cross an ocean to start anew, why my ancestors came from Italy two centuries later, why my parents sent me to college, why I decided to try for medicine. It is what most of us give every day. Hope, the ability to see into the future and bring that feeling back to the present. The belief that whatever and wherever you are, soon it will be even better. It cannot, however, be commanded. You can’t insist a patient hope any more than you can make them love. You must first understand what they see and feel, then show them how things might be better through trust.
Throughout life, hope creates possibilities. It unites us. It motivates us. It is the destroyer of winter and of burnout and of disease. It is one of the most important gifts that we give patients, and we do it everyday. Tomorrow in your practice, notice how often you foster it. Pay attention to how your patient changes the moment you give it to them. Watch the Forsythia bloom as you reassure them that their spring will return again.
“We must accept finite disappointment, but never lose infinite hope.” – Martin Luther King Jr.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Unintended consequences in the drive to simplify computerized test ordering
“X marks the spot!”
It’s one of the classic pirate tropes, bringing to mind images of Long John Silver, buried treasure, and a secret map with an “X” to show the hidden gold.
Today that “X” (or, in some cases, a check mark or radio button) seems to be indicating where the money is to be lost, rather than found.
Hospital computer systems are increasingly reliant on preprogrammed order lists that you check off rather than the actual test itself. We’ve gone from having to write out the tests we want, to typing them into a box, to checking them off with a mouse.
I’ve seen systems where you’re offered a menu such as:
A. Brain MRI (noncontrast)
B. Brain MRI (w/wo contrast)
C. Head MRA (noncontrast)
D. Head MRA (with contrast)
E. Neck MRA (noncontrast)
F. Neck MRA (with contrast)
G. Brain MRI and head/neck MRA (noncontrast)
H. Brain MRI and head/neck MRA (w/wo contrast)
And that’s just for the brain and its vascular supply. Expand that to the rest of the nervous system, then to the whole body, then to other tests (labs) ... and you get the idea.
I suppose the driving force here is to make the system easier to use. Doctors are busy. It saves time just have to check a box if you want three tests, rather than note all of them individually.
But it’s really not that hard to check off three. Probably less than 5 seconds (as of my last time on call). And this is where, to me, X marks the spot where the money isn’t.
Humans, like most animals, are pretty good at defaulting to a low-energy setting. So if you only have to check off one box instead of three, or five, or whatever, why bother?
If the patient is being admitted for a stroke/TIA, then it makes sense to do the brain MRI and head/neck MRA. But what if it’s just headaches, or a new seizure, or a concussion? I see plenty of times when more tests are done than necessary, simply because the ordering physician either didn’t know what was really needed or because it was easier to just check the box.
This is not, in my experience, rare. I’d say anywhere from one-third to half of patients I’ve consulted on had an overkill neurological work-up, in which tests with no medical indications had been ordered. They’ve generally already been put in the system, or even done, before I get to the bedside.
I suppose one could say they should wait for the specialist to get there before any of the costly tests are ordered, but that opens up another can of worms. What if a critical finding that needed to be acted upon isn’t found in time because of such a rule? Not only that, but waiting for me to show up and order tests means it will take longer to get them done, adding onto the hospital stay, and (again) running up costs.
So that’s not an answer, either. There really isn’t one, unfortunately.
But, in our haste to make things easier, or faster, or even just flashier, the trend seems to be at the cost of doing things reasonably. At the same time that we’re trying to save money, the single “X” may be marking the spot where we’re actually throwing it away.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“X marks the spot!”
It’s one of the classic pirate tropes, bringing to mind images of Long John Silver, buried treasure, and a secret map with an “X” to show the hidden gold.
Today that “X” (or, in some cases, a check mark or radio button) seems to be indicating where the money is to be lost, rather than found.
Hospital computer systems are increasingly reliant on preprogrammed order lists that you check off rather than the actual test itself. We’ve gone from having to write out the tests we want, to typing them into a box, to checking them off with a mouse.
I’ve seen systems where you’re offered a menu such as:
A. Brain MRI (noncontrast)
B. Brain MRI (w/wo contrast)
C. Head MRA (noncontrast)
D. Head MRA (with contrast)
E. Neck MRA (noncontrast)
F. Neck MRA (with contrast)
G. Brain MRI and head/neck MRA (noncontrast)
H. Brain MRI and head/neck MRA (w/wo contrast)
And that’s just for the brain and its vascular supply. Expand that to the rest of the nervous system, then to the whole body, then to other tests (labs) ... and you get the idea.
I suppose the driving force here is to make the system easier to use. Doctors are busy. It saves time just have to check a box if you want three tests, rather than note all of them individually.
But it’s really not that hard to check off three. Probably less than 5 seconds (as of my last time on call). And this is where, to me, X marks the spot where the money isn’t.
Humans, like most animals, are pretty good at defaulting to a low-energy setting. So if you only have to check off one box instead of three, or five, or whatever, why bother?
If the patient is being admitted for a stroke/TIA, then it makes sense to do the brain MRI and head/neck MRA. But what if it’s just headaches, or a new seizure, or a concussion? I see plenty of times when more tests are done than necessary, simply because the ordering physician either didn’t know what was really needed or because it was easier to just check the box.
This is not, in my experience, rare. I’d say anywhere from one-third to half of patients I’ve consulted on had an overkill neurological work-up, in which tests with no medical indications had been ordered. They’ve generally already been put in the system, or even done, before I get to the bedside.
I suppose one could say they should wait for the specialist to get there before any of the costly tests are ordered, but that opens up another can of worms. What if a critical finding that needed to be acted upon isn’t found in time because of such a rule? Not only that, but waiting for me to show up and order tests means it will take longer to get them done, adding onto the hospital stay, and (again) running up costs.
So that’s not an answer, either. There really isn’t one, unfortunately.
But, in our haste to make things easier, or faster, or even just flashier, the trend seems to be at the cost of doing things reasonably. At the same time that we’re trying to save money, the single “X” may be marking the spot where we’re actually throwing it away.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“X marks the spot!”
It’s one of the classic pirate tropes, bringing to mind images of Long John Silver, buried treasure, and a secret map with an “X” to show the hidden gold.
Today that “X” (or, in some cases, a check mark or radio button) seems to be indicating where the money is to be lost, rather than found.
Hospital computer systems are increasingly reliant on preprogrammed order lists that you check off rather than the actual test itself. We’ve gone from having to write out the tests we want, to typing them into a box, to checking them off with a mouse.
I’ve seen systems where you’re offered a menu such as:
A. Brain MRI (noncontrast)
B. Brain MRI (w/wo contrast)
C. Head MRA (noncontrast)
D. Head MRA (with contrast)
E. Neck MRA (noncontrast)
F. Neck MRA (with contrast)
G. Brain MRI and head/neck MRA (noncontrast)
H. Brain MRI and head/neck MRA (w/wo contrast)
And that’s just for the brain and its vascular supply. Expand that to the rest of the nervous system, then to the whole body, then to other tests (labs) ... and you get the idea.
I suppose the driving force here is to make the system easier to use. Doctors are busy. It saves time just have to check a box if you want three tests, rather than note all of them individually.
But it’s really not that hard to check off three. Probably less than 5 seconds (as of my last time on call). And this is where, to me, X marks the spot where the money isn’t.
Humans, like most animals, are pretty good at defaulting to a low-energy setting. So if you only have to check off one box instead of three, or five, or whatever, why bother?
If the patient is being admitted for a stroke/TIA, then it makes sense to do the brain MRI and head/neck MRA. But what if it’s just headaches, or a new seizure, or a concussion? I see plenty of times when more tests are done than necessary, simply because the ordering physician either didn’t know what was really needed or because it was easier to just check the box.
This is not, in my experience, rare. I’d say anywhere from one-third to half of patients I’ve consulted on had an overkill neurological work-up, in which tests with no medical indications had been ordered. They’ve generally already been put in the system, or even done, before I get to the bedside.
I suppose one could say they should wait for the specialist to get there before any of the costly tests are ordered, but that opens up another can of worms. What if a critical finding that needed to be acted upon isn’t found in time because of such a rule? Not only that, but waiting for me to show up and order tests means it will take longer to get them done, adding onto the hospital stay, and (again) running up costs.
So that’s not an answer, either. There really isn’t one, unfortunately.
But, in our haste to make things easier, or faster, or even just flashier, the trend seems to be at the cost of doing things reasonably. At the same time that we’re trying to save money, the single “X” may be marking the spot where we’re actually throwing it away.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.





















