User login
Who is in charge here?
My first patient of the afternoon was a simple hypertension follow-up, or so I thought as I was walking into the room. She was a healthy 50-year-old woman with no medical problems other than her blood pressure, which was measured at 130/76 in the office. Her heart and lungs were normal, she had no chest pain or shortness of breath, and she was taking her medications without any problem. All simple enough. I complimented her on how she was doing, told her to continue her medications, and return in 6 months.
She put up her hand and said, “Wait a minute.”
Then she pulled out her smartphone. She tapped open an app, and handed it to me so I could look at a graph of her home blood pressures. The graph had all of her readings from the last 4 months, taken 2-3 times a day. It had automatically labeled each blood pressure in green, yellow, or red to indicate whether they were normal, higher than normal, or elevated, respectively.
Of course, the app creators had determined that a ‘green’ (normal) systolic pressure was less than 120 mm Hg. Values above that were yellow (higher than normal), until a systolic pressure of 130, at which point they became red (elevated). This is consistent with the most recent American Heart Association guidelines, but these guidelines have been the subject of a lot of controversy. There are many, including myself, who believe that the correct systolic pressure to define hypertension should be 140 for many patients, rather than 130. The app disagrees, and patients using the app see the app’s definition of hypertension every time they enter a blood pressure. In the case of my patient, since normal was indicated only by a systolic of less than 120 (which is a relatively rare event), I had to explain the difference between normal blood pressure and her blood pressure goal, and why the two were not the same.
Later that afternoon I was seeing a 60-year-old male who had electrical cardioversion of his atrial fibrillation 2 weeks prior to the visit. He had been sent home, as is usually the case, on an antiarrhythmic and an oral anticoagulant. He was feeling fine and had not noticed any palpitations, chest discomfort, or shortness of breath. I listened to his heart and lungs, which sounded normal, and I told him it sounded like he was doing well. Then he said, “I have an Apple watch.” I had a feeling I knew what was coming next.
He handed me his iPhone and asked me if I could review his rhythm strips. For those unacquainted with the new Apple watch, all he had to do to obtain those strips was open an EKG app and touch the crown of his watch with a finger from his other hand. This essentially made an electrical connection from his left to right arm, allowing the watch to generate a one-lead EKG tracing. The device then provides a computer-generated rhythm strip and sends that image and an interpretation of it to an iPhone, which is connected to the watch via Bluetooth. These results can then be shared or printed out as a pdf document.
The patient wanted to know if the smartphone’s interpretation of those rhythm strips was correct, and if he was really having frequent asymptomatic recurrence of his atrial fibrillation. Unsurprising to me or anyone who has used one of these (or other) phone-based EKG devices, the watch-generated rhythm strips looked clean and clear and the interpretation was spot on. It correctly identified his frequent asymptomatic episodes of atrial fibrillation. This was important information, which markedly affected his medical care.
These two very different examples are early indications that the way that we will be collecting information will rapidly and radically change over the next few years. It has always been clear that making long-term decisions about the treatment of hypertension based on a single reading in the office setting is not optimal. It has been equally clear that a single office EKG provides a limited snapshot into the frequency of intermittent atrial fibrillation. Deciding how to treat patients has never been easy and many decisions are plagued with ambiguity. Having limited information is a blessing and a curse; it’s quick and easy to review a small amount of data, but there is a nagging recognition that those data are only a distant representation of a patient’s real health outside of the office.
As we move forward we will increasingly have the ability to see a patient’s physiologic parameters where and when those values are most important: during the countless hours when they are not in our offices. The new American Heart Association hypertension guideline, issued in late 2017, has placed increased emphasis on ambulatory blood pressure monitoring. Determining how to use all this new information will be a challenge. It will take time to become comfortable with interpreting and making sense of an incredible number of data points. For example, if a patient checks his blood pressure twice a day for 3 months, his efforts will generate 180 separate blood pressure readings! You can bet there is going to be a good deal of inconsistency in those readings, making interpretation challenging. There will also probably be a few high readings, such as the occasional 190/110, which are likely to cause concern and anxiety in patients. There is little question that the availability of such detailed information holds the potential to allow us to make better decisions. The challenge will be in deciding how to use it to actually improve – not just complicate – patient care.
What are your thoughts on this? Feel free to email us at [email protected].
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on twitter (@doctornotte).
My first patient of the afternoon was a simple hypertension follow-up, or so I thought as I was walking into the room. She was a healthy 50-year-old woman with no medical problems other than her blood pressure, which was measured at 130/76 in the office. Her heart and lungs were normal, she had no chest pain or shortness of breath, and she was taking her medications without any problem. All simple enough. I complimented her on how she was doing, told her to continue her medications, and return in 6 months.
She put up her hand and said, “Wait a minute.”
Then she pulled out her smartphone. She tapped open an app, and handed it to me so I could look at a graph of her home blood pressures. The graph had all of her readings from the last 4 months, taken 2-3 times a day. It had automatically labeled each blood pressure in green, yellow, or red to indicate whether they were normal, higher than normal, or elevated, respectively.
Of course, the app creators had determined that a ‘green’ (normal) systolic pressure was less than 120 mm Hg. Values above that were yellow (higher than normal), until a systolic pressure of 130, at which point they became red (elevated). This is consistent with the most recent American Heart Association guidelines, but these guidelines have been the subject of a lot of controversy. There are many, including myself, who believe that the correct systolic pressure to define hypertension should be 140 for many patients, rather than 130. The app disagrees, and patients using the app see the app’s definition of hypertension every time they enter a blood pressure. In the case of my patient, since normal was indicated only by a systolic of less than 120 (which is a relatively rare event), I had to explain the difference between normal blood pressure and her blood pressure goal, and why the two were not the same.
Later that afternoon I was seeing a 60-year-old male who had electrical cardioversion of his atrial fibrillation 2 weeks prior to the visit. He had been sent home, as is usually the case, on an antiarrhythmic and an oral anticoagulant. He was feeling fine and had not noticed any palpitations, chest discomfort, or shortness of breath. I listened to his heart and lungs, which sounded normal, and I told him it sounded like he was doing well. Then he said, “I have an Apple watch.” I had a feeling I knew what was coming next.
He handed me his iPhone and asked me if I could review his rhythm strips. For those unacquainted with the new Apple watch, all he had to do to obtain those strips was open an EKG app and touch the crown of his watch with a finger from his other hand. This essentially made an electrical connection from his left to right arm, allowing the watch to generate a one-lead EKG tracing. The device then provides a computer-generated rhythm strip and sends that image and an interpretation of it to an iPhone, which is connected to the watch via Bluetooth. These results can then be shared or printed out as a pdf document.
The patient wanted to know if the smartphone’s interpretation of those rhythm strips was correct, and if he was really having frequent asymptomatic recurrence of his atrial fibrillation. Unsurprising to me or anyone who has used one of these (or other) phone-based EKG devices, the watch-generated rhythm strips looked clean and clear and the interpretation was spot on. It correctly identified his frequent asymptomatic episodes of atrial fibrillation. This was important information, which markedly affected his medical care.
These two very different examples are early indications that the way that we will be collecting information will rapidly and radically change over the next few years. It has always been clear that making long-term decisions about the treatment of hypertension based on a single reading in the office setting is not optimal. It has been equally clear that a single office EKG provides a limited snapshot into the frequency of intermittent atrial fibrillation. Deciding how to treat patients has never been easy and many decisions are plagued with ambiguity. Having limited information is a blessing and a curse; it’s quick and easy to review a small amount of data, but there is a nagging recognition that those data are only a distant representation of a patient’s real health outside of the office.
As we move forward we will increasingly have the ability to see a patient’s physiologic parameters where and when those values are most important: during the countless hours when they are not in our offices. The new American Heart Association hypertension guideline, issued in late 2017, has placed increased emphasis on ambulatory blood pressure monitoring. Determining how to use all this new information will be a challenge. It will take time to become comfortable with interpreting and making sense of an incredible number of data points. For example, if a patient checks his blood pressure twice a day for 3 months, his efforts will generate 180 separate blood pressure readings! You can bet there is going to be a good deal of inconsistency in those readings, making interpretation challenging. There will also probably be a few high readings, such as the occasional 190/110, which are likely to cause concern and anxiety in patients. There is little question that the availability of such detailed information holds the potential to allow us to make better decisions. The challenge will be in deciding how to use it to actually improve – not just complicate – patient care.
What are your thoughts on this? Feel free to email us at [email protected].
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on twitter (@doctornotte).
My first patient of the afternoon was a simple hypertension follow-up, or so I thought as I was walking into the room. She was a healthy 50-year-old woman with no medical problems other than her blood pressure, which was measured at 130/76 in the office. Her heart and lungs were normal, she had no chest pain or shortness of breath, and she was taking her medications without any problem. All simple enough. I complimented her on how she was doing, told her to continue her medications, and return in 6 months.
She put up her hand and said, “Wait a minute.”
Then she pulled out her smartphone. She tapped open an app, and handed it to me so I could look at a graph of her home blood pressures. The graph had all of her readings from the last 4 months, taken 2-3 times a day. It had automatically labeled each blood pressure in green, yellow, or red to indicate whether they were normal, higher than normal, or elevated, respectively.
Of course, the app creators had determined that a ‘green’ (normal) systolic pressure was less than 120 mm Hg. Values above that were yellow (higher than normal), until a systolic pressure of 130, at which point they became red (elevated). This is consistent with the most recent American Heart Association guidelines, but these guidelines have been the subject of a lot of controversy. There are many, including myself, who believe that the correct systolic pressure to define hypertension should be 140 for many patients, rather than 130. The app disagrees, and patients using the app see the app’s definition of hypertension every time they enter a blood pressure. In the case of my patient, since normal was indicated only by a systolic of less than 120 (which is a relatively rare event), I had to explain the difference between normal blood pressure and her blood pressure goal, and why the two were not the same.
Later that afternoon I was seeing a 60-year-old male who had electrical cardioversion of his atrial fibrillation 2 weeks prior to the visit. He had been sent home, as is usually the case, on an antiarrhythmic and an oral anticoagulant. He was feeling fine and had not noticed any palpitations, chest discomfort, or shortness of breath. I listened to his heart and lungs, which sounded normal, and I told him it sounded like he was doing well. Then he said, “I have an Apple watch.” I had a feeling I knew what was coming next.
He handed me his iPhone and asked me if I could review his rhythm strips. For those unacquainted with the new Apple watch, all he had to do to obtain those strips was open an EKG app and touch the crown of his watch with a finger from his other hand. This essentially made an electrical connection from his left to right arm, allowing the watch to generate a one-lead EKG tracing. The device then provides a computer-generated rhythm strip and sends that image and an interpretation of it to an iPhone, which is connected to the watch via Bluetooth. These results can then be shared or printed out as a pdf document.
The patient wanted to know if the smartphone’s interpretation of those rhythm strips was correct, and if he was really having frequent asymptomatic recurrence of his atrial fibrillation. Unsurprising to me or anyone who has used one of these (or other) phone-based EKG devices, the watch-generated rhythm strips looked clean and clear and the interpretation was spot on. It correctly identified his frequent asymptomatic episodes of atrial fibrillation. This was important information, which markedly affected his medical care.
These two very different examples are early indications that the way that we will be collecting information will rapidly and radically change over the next few years. It has always been clear that making long-term decisions about the treatment of hypertension based on a single reading in the office setting is not optimal. It has been equally clear that a single office EKG provides a limited snapshot into the frequency of intermittent atrial fibrillation. Deciding how to treat patients has never been easy and many decisions are plagued with ambiguity. Having limited information is a blessing and a curse; it’s quick and easy to review a small amount of data, but there is a nagging recognition that those data are only a distant representation of a patient’s real health outside of the office.
As we move forward we will increasingly have the ability to see a patient’s physiologic parameters where and when those values are most important: during the countless hours when they are not in our offices. The new American Heart Association hypertension guideline, issued in late 2017, has placed increased emphasis on ambulatory blood pressure monitoring. Determining how to use all this new information will be a challenge. It will take time to become comfortable with interpreting and making sense of an incredible number of data points. For example, if a patient checks his blood pressure twice a day for 3 months, his efforts will generate 180 separate blood pressure readings! You can bet there is going to be a good deal of inconsistency in those readings, making interpretation challenging. There will also probably be a few high readings, such as the occasional 190/110, which are likely to cause concern and anxiety in patients. There is little question that the availability of such detailed information holds the potential to allow us to make better decisions. The challenge will be in deciding how to use it to actually improve – not just complicate – patient care.
What are your thoughts on this? Feel free to email us at [email protected].
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Jefferson Health. Follow him on twitter (@doctornotte).
Patients who want to make you retire, and how to cope
I was at a meeting in Orlando, sitting in the front row. The speaker was a former Disney executive who was telling us how to improve our offices. He kept walking very close to the edge of the stage – so close I was worried he might step off with the Klieg lights in his eyes. Then he got to the heart of his message, telling us that we need to make each patient encounter a marvelous experience, and how he and his staff had done so for millions of mouseketeers. “You need to make each customer feel special,” he said. He went on with saccharine examples of staff going above and beyond – for example, replacing toddlers’ dropped ice creams before they could cry.
That hit my trigger. From that point on, I was almost hoping he would fall off the stage.
Of course, there is a story behind my reaction.
One sunny day, while I was sitting at the most cluttered desk in the world, one of my staff came into my office to tell me a patient had called. The patient was very unhappy, I was told, and she planned to stink bomb me on social media. Concerned, I pulled the patient’s before-and-after photos. It looked as though she had a great result from her treatment, so I was perplexed. I phoned the patient, but she refused to tell me why she was unhappy. “I’m very unhappy, and I’m going to punish you,” she said. I urged her to come to the office and see me, at her convenience.
When we spoke face-to-face, I examined her nose and took a picture. I explained that her cancer was cured; her result was beautiful, the site was almost imperceptible. I added that I thought the appearance would continue to improve with time.
My patient refused to look at me, and refused to look at the site in the mirror. She shoved the preop defect photo away without giving it a glance. Instead, she told me how inconvenient it was for her to have had a skin cancer at all. Traffic had been terrible coming into the office on the morning of the procedure. There had been a 45-minute backup on the bridge on her way home. Her ex-husband had refused to help with her wound care. She continued in a similar vein for 15 minutes as I waited for her to accuse me of my transgressions. She concluded with a scowl and a whimper, “You just didn’t make me feel special.”
Everyone has difficult patients, and everyone has bad days, but I can’t recall ever being ambushed quite so adroitly in my 30 years of practice. I recognized my patient was being passive-aggressive and was playing a social media–augmented game of “Now I’ve got you, you S.O.B,” right out of Eric Berne’s book “Games People Play.” I’d say that this book should still be required reading for dealing with difficult patients.
There are ways to defuse such patients. One of the best is to slow things down and spread them around. The wider the array of interactions with people (the medical assistant, the nurse, the fellow, the Mohs surgeon, maybe the plastic surgeon), the more times the patient has to vent and the anger is defused across many targets. This also speaks to the value of requiring a preoperative consultation days before the procedure As I thought about this patient, I recalled that, because of the distance she was traveling, I had not done so.
I looked my patient in the eye and told her I was sorry she was unhappy. I told her I would be glad to see her again. I told her I realized how far she was driving and thought the traffic would not be a problem this early in the afternoon. I thanked her and showed her to the door. She stalked out of the office.
Technically and emotionally difficult patients are sometimes referred to you. They are patients who you might prefer not to take on but you do because, as a specialist, you may be at the end of the referral pipeline. Sometimes you can win the day, striking up a friendship or jollying them past their resentment at the world.
And The third law of surviving internship from Samuel Shem’s book “The House of God” is germane here. Remember, “the patient is the one with the disease.” And sometimes the disease is complicated by the patient’s emotional baggage. This is one of the reasons social media ratings can be so unfair. We have to realize that we are all going to be trashed unfairly at some point, and probably sued unfairly as well. As a malpractice attorney told me once, “You doctors shouldn’t take this so personally; it’s just business.”
And my patient? Despite my admonishments to you not to take things personally, I did feel bad for a week or so after our encounter. I did mail her a copy of her pre- and postoperative photographs. I have not seen her again. I did not look to see whether she burned me online.
But, by gosh, I’d really like to lock that Disney executive in a room with her for five minutes.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
I was at a meeting in Orlando, sitting in the front row. The speaker was a former Disney executive who was telling us how to improve our offices. He kept walking very close to the edge of the stage – so close I was worried he might step off with the Klieg lights in his eyes. Then he got to the heart of his message, telling us that we need to make each patient encounter a marvelous experience, and how he and his staff had done so for millions of mouseketeers. “You need to make each customer feel special,” he said. He went on with saccharine examples of staff going above and beyond – for example, replacing toddlers’ dropped ice creams before they could cry.
That hit my trigger. From that point on, I was almost hoping he would fall off the stage.
Of course, there is a story behind my reaction.
One sunny day, while I was sitting at the most cluttered desk in the world, one of my staff came into my office to tell me a patient had called. The patient was very unhappy, I was told, and she planned to stink bomb me on social media. Concerned, I pulled the patient’s before-and-after photos. It looked as though she had a great result from her treatment, so I was perplexed. I phoned the patient, but she refused to tell me why she was unhappy. “I’m very unhappy, and I’m going to punish you,” she said. I urged her to come to the office and see me, at her convenience.
When we spoke face-to-face, I examined her nose and took a picture. I explained that her cancer was cured; her result was beautiful, the site was almost imperceptible. I added that I thought the appearance would continue to improve with time.
My patient refused to look at me, and refused to look at the site in the mirror. She shoved the preop defect photo away without giving it a glance. Instead, she told me how inconvenient it was for her to have had a skin cancer at all. Traffic had been terrible coming into the office on the morning of the procedure. There had been a 45-minute backup on the bridge on her way home. Her ex-husband had refused to help with her wound care. She continued in a similar vein for 15 minutes as I waited for her to accuse me of my transgressions. She concluded with a scowl and a whimper, “You just didn’t make me feel special.”
Everyone has difficult patients, and everyone has bad days, but I can’t recall ever being ambushed quite so adroitly in my 30 years of practice. I recognized my patient was being passive-aggressive and was playing a social media–augmented game of “Now I’ve got you, you S.O.B,” right out of Eric Berne’s book “Games People Play.” I’d say that this book should still be required reading for dealing with difficult patients.
There are ways to defuse such patients. One of the best is to slow things down and spread them around. The wider the array of interactions with people (the medical assistant, the nurse, the fellow, the Mohs surgeon, maybe the plastic surgeon), the more times the patient has to vent and the anger is defused across many targets. This also speaks to the value of requiring a preoperative consultation days before the procedure As I thought about this patient, I recalled that, because of the distance she was traveling, I had not done so.
I looked my patient in the eye and told her I was sorry she was unhappy. I told her I would be glad to see her again. I told her I realized how far she was driving and thought the traffic would not be a problem this early in the afternoon. I thanked her and showed her to the door. She stalked out of the office.
Technically and emotionally difficult patients are sometimes referred to you. They are patients who you might prefer not to take on but you do because, as a specialist, you may be at the end of the referral pipeline. Sometimes you can win the day, striking up a friendship or jollying them past their resentment at the world.
And The third law of surviving internship from Samuel Shem’s book “The House of God” is germane here. Remember, “the patient is the one with the disease.” And sometimes the disease is complicated by the patient’s emotional baggage. This is one of the reasons social media ratings can be so unfair. We have to realize that we are all going to be trashed unfairly at some point, and probably sued unfairly as well. As a malpractice attorney told me once, “You doctors shouldn’t take this so personally; it’s just business.”
And my patient? Despite my admonishments to you not to take things personally, I did feel bad for a week or so after our encounter. I did mail her a copy of her pre- and postoperative photographs. I have not seen her again. I did not look to see whether she burned me online.
But, by gosh, I’d really like to lock that Disney executive in a room with her for five minutes.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
I was at a meeting in Orlando, sitting in the front row. The speaker was a former Disney executive who was telling us how to improve our offices. He kept walking very close to the edge of the stage – so close I was worried he might step off with the Klieg lights in his eyes. Then he got to the heart of his message, telling us that we need to make each patient encounter a marvelous experience, and how he and his staff had done so for millions of mouseketeers. “You need to make each customer feel special,” he said. He went on with saccharine examples of staff going above and beyond – for example, replacing toddlers’ dropped ice creams before they could cry.
That hit my trigger. From that point on, I was almost hoping he would fall off the stage.
Of course, there is a story behind my reaction.
One sunny day, while I was sitting at the most cluttered desk in the world, one of my staff came into my office to tell me a patient had called. The patient was very unhappy, I was told, and she planned to stink bomb me on social media. Concerned, I pulled the patient’s before-and-after photos. It looked as though she had a great result from her treatment, so I was perplexed. I phoned the patient, but she refused to tell me why she was unhappy. “I’m very unhappy, and I’m going to punish you,” she said. I urged her to come to the office and see me, at her convenience.
When we spoke face-to-face, I examined her nose and took a picture. I explained that her cancer was cured; her result was beautiful, the site was almost imperceptible. I added that I thought the appearance would continue to improve with time.
My patient refused to look at me, and refused to look at the site in the mirror. She shoved the preop defect photo away without giving it a glance. Instead, she told me how inconvenient it was for her to have had a skin cancer at all. Traffic had been terrible coming into the office on the morning of the procedure. There had been a 45-minute backup on the bridge on her way home. Her ex-husband had refused to help with her wound care. She continued in a similar vein for 15 minutes as I waited for her to accuse me of my transgressions. She concluded with a scowl and a whimper, “You just didn’t make me feel special.”
Everyone has difficult patients, and everyone has bad days, but I can’t recall ever being ambushed quite so adroitly in my 30 years of practice. I recognized my patient was being passive-aggressive and was playing a social media–augmented game of “Now I’ve got you, you S.O.B,” right out of Eric Berne’s book “Games People Play.” I’d say that this book should still be required reading for dealing with difficult patients.
There are ways to defuse such patients. One of the best is to slow things down and spread them around. The wider the array of interactions with people (the medical assistant, the nurse, the fellow, the Mohs surgeon, maybe the plastic surgeon), the more times the patient has to vent and the anger is defused across many targets. This also speaks to the value of requiring a preoperative consultation days before the procedure As I thought about this patient, I recalled that, because of the distance she was traveling, I had not done so.
I looked my patient in the eye and told her I was sorry she was unhappy. I told her I would be glad to see her again. I told her I realized how far she was driving and thought the traffic would not be a problem this early in the afternoon. I thanked her and showed her to the door. She stalked out of the office.
Technically and emotionally difficult patients are sometimes referred to you. They are patients who you might prefer not to take on but you do because, as a specialist, you may be at the end of the referral pipeline. Sometimes you can win the day, striking up a friendship or jollying them past their resentment at the world.
And The third law of surviving internship from Samuel Shem’s book “The House of God” is germane here. Remember, “the patient is the one with the disease.” And sometimes the disease is complicated by the patient’s emotional baggage. This is one of the reasons social media ratings can be so unfair. We have to realize that we are all going to be trashed unfairly at some point, and probably sued unfairly as well. As a malpractice attorney told me once, “You doctors shouldn’t take this so personally; it’s just business.”
And my patient? Despite my admonishments to you not to take things personally, I did feel bad for a week or so after our encounter. I did mail her a copy of her pre- and postoperative photographs. I have not seen her again. I did not look to see whether she burned me online.
But, by gosh, I’d really like to lock that Disney executive in a room with her for five minutes.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Workers’ compensation law
Question: Employee, a poorly controlled diabetic, accidentally stepped on a nail at work. Surrounding cellulitis and abscess formation set in, but because he was slow in getting to a doctor, the infection invaded the underlying bone, causing osteomyelitis. He ended up with a partial foot amputation. In a claim for workers’ compensation (WC) benefits, which of the following is best?
A. Employee has a claim under WC, a quasi no-fault system that requires an employer to compensate its employees only for accidents occurring in the workplace.
B. Employer may offer employee’s preexisting diabetic condition and his failure to promptly seek medical attention as substantial rebuttable evidence against compensability.
C. A similar no-fault system has been proposed as an alternative to medical tort litigation, but it has yet to be established in the developed world.
D. All are incorrect.
E. All are correct.
Answer: D. Fashioned after Europe’s Workers’ Accident Insurance system that was put into place by Germany’s Otto von Bismarck, workers’ compensation (WC) laws found their way into the United States by 1908. Today, all states have enacted such laws to effectuate the policy that work injuries are among the costs of production, which industry is required to bear. Such laws purport to do away with vexatious issues like contributory negligence, agency principles that negate an employment relationship, and assumption of risk defenses, all of which had previously been used to deny an injured worker compensatory benefits.
WC laws differ somewhat from state to state, both in statutory provisions and judicial interpretations. However, an illness or disease condition that is related to work conditions will suffice. The employer bears the burden of proof and is required to affirmatively rebut the presumption of compensability. This is usually a high bar to scale, and preexisting conditions and poor patient compliance are insufficient to negate a WC claim, although they are used in apportioning payments to the injured worker.
Take Hawaii, widely viewed as a proworker jurisdiction, as an example. Its key WC statutory language covers any employee who “suffers a personal injury either by accident arising out of and in the course of employment or by disease proximately caused by or resulting from the nature of the employment.”1 In Chung v. Animal Clinic Inc.,2 Dr. Chung suffered a heart attack after office hours while jogging around the Kalani High School track in Honolulu. One of the issues was whether his heart attack arose out of and in the course of his employment and, if so, whether the employer substantially rebutted the presumption that the heart attack was work connected.
The Supreme Court of Hawaii used the work-connection approach in interpreting the phrase “arising out of and in the course of employment,” thereby rejecting the necessity of establishing temporal, spatial, and circumstantial proximity between the injury and employment. It held that the work-connection approach simply requires the finding of a causal connection between the injury and any incidents or conditions of employment. The only relevant inquiry was whether Dr. Chung’s heart attack in fact was aggravated or accelerated by his work activity and whether there was substantial evidence to the contrary.
The employer provided expert testimony from a cardiologist attributing the heart attack to preexisting arteriosclerosis and physical exertion from jogging. On the other hand, another physician believed that Dr. Chung’s employment activities as principal veterinarian, administrator, and president of Animal Clinic, which engaged Dr. Chung for long hours, as well as his other business-related activities, generated a substantial amount of mental and emotional stress which was strongly linked to the production of heart disease. This was sufficient to establish a work connection. The Court also had this to say about legal versus medical causation: “... a medical man may give a generalized opinion that there was no connection between an incident at work and a heart attack, and, in his own mind, may mean thereby that a preexisting pathological condition was the overwhelming factor in bringing about the attack and that the part played by the work was insignificant. But, while it may be sound medically to say that the work did not ‘cause’ the attack, it may well be bad law, because, in general, existing law treats the slightest factor of aggravation as an adequate ‘cause.’ ”
In a recent seminal case,3 the same Court reiterated that, in order to be exonerated, the employer must adduce specific evidence to indicate why the work event did not or could not have caused, aggravated, or accelerated the injury. It ruled that the claim in question was compensable because all three experts had failed to explain why the industrial accident could not have caused the slightest aggravation or acceleration of an existing injury. The patient, previously asymptomatic, had sustained shoulder injuries at work. Notwithstanding X-ray evidence of preexisting degenerative changes, the Court found for the worker because the medical reports of the employer’s physicians did not provide a sufficient degree of specificity to constitute substantial rebuttable evidence since “under our workers’ compensation statute, the slightest aggravation or acceleration of an injury by the employment activity mandates compensation.”
WC’s quasi no-fault approach has been proposed as a model for adjudicating medical malpractice claims, which are currently decided by a fault-finding, adversarial system.4 The injured patient is randomly and unjustly compensated, and the combative nature of the proceedings traumatizes the doctor-patient relationship and promotes the wasteful practice of defensive medicine. In many instances, fault simply cannot be ascertained. Some of these same criticisms led to the introduction of the no-fault system for auto injuries and for workers’ compensation. However, injuries arising out of medical care differ in one essential aspect from all other injuries: They may be a natural and unavoidable consequence of the underlying illness or treatment. If all complications were deemed compensable, including those that are unavoidable, then a true comprehensive no-fault system would exist. However, it would prove prohibitively expensive.
No-fault medical injury systems are presently in place in countries like Sweden and New Zealand. The latter’s no-fault compensation scheme came into effect in 1974 under its Accident Compensation Act, which removed all accidental injuries including medical injuries from the tort system. Under the initial scheme, which has since undergone numerous major revisions, injured patients did not have to prove fault. All the claimant had to establish was “medical, surgical, dental, or first aid misadventure.” However, the revised Act of 1992 required the claimant to show “medical error,” which was defined (like negligence) as “the failure of a registered health professional to observe a standard of care and skill reasonably to be expected in the circumstances.” Now renamed the Accident Compensation Act 2001, it covers medical injuries that are “not a necessary part, or ordinary consequence, of the treatment.” The fact that the treatment did not achieve a desired result does not, of itself, constitute treatment injury.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Hawaii Revised Statutes (HRS) Section 386-3.
2. Chung v. Animal Clinic Inc., 636 P.2d 721 (1981).
3. Panoke v. Reef Development of Hawaii Inc., Supreme Court of Hawaii. No. SCWC–11–0000556. Decided: December 14, 2015.
4. Tan, SY. In Medical Malpractice: Understanding the Law, Managing the Risks. World Scientific Publishing Co. Pte Ltd., Singapore, 2006.
Question: Employee, a poorly controlled diabetic, accidentally stepped on a nail at work. Surrounding cellulitis and abscess formation set in, but because he was slow in getting to a doctor, the infection invaded the underlying bone, causing osteomyelitis. He ended up with a partial foot amputation. In a claim for workers’ compensation (WC) benefits, which of the following is best?
A. Employee has a claim under WC, a quasi no-fault system that requires an employer to compensate its employees only for accidents occurring in the workplace.
B. Employer may offer employee’s preexisting diabetic condition and his failure to promptly seek medical attention as substantial rebuttable evidence against compensability.
C. A similar no-fault system has been proposed as an alternative to medical tort litigation, but it has yet to be established in the developed world.
D. All are incorrect.
E. All are correct.
Answer: D. Fashioned after Europe’s Workers’ Accident Insurance system that was put into place by Germany’s Otto von Bismarck, workers’ compensation (WC) laws found their way into the United States by 1908. Today, all states have enacted such laws to effectuate the policy that work injuries are among the costs of production, which industry is required to bear. Such laws purport to do away with vexatious issues like contributory negligence, agency principles that negate an employment relationship, and assumption of risk defenses, all of which had previously been used to deny an injured worker compensatory benefits.
WC laws differ somewhat from state to state, both in statutory provisions and judicial interpretations. However, an illness or disease condition that is related to work conditions will suffice. The employer bears the burden of proof and is required to affirmatively rebut the presumption of compensability. This is usually a high bar to scale, and preexisting conditions and poor patient compliance are insufficient to negate a WC claim, although they are used in apportioning payments to the injured worker.
Take Hawaii, widely viewed as a proworker jurisdiction, as an example. Its key WC statutory language covers any employee who “suffers a personal injury either by accident arising out of and in the course of employment or by disease proximately caused by or resulting from the nature of the employment.”1 In Chung v. Animal Clinic Inc.,2 Dr. Chung suffered a heart attack after office hours while jogging around the Kalani High School track in Honolulu. One of the issues was whether his heart attack arose out of and in the course of his employment and, if so, whether the employer substantially rebutted the presumption that the heart attack was work connected.
The Supreme Court of Hawaii used the work-connection approach in interpreting the phrase “arising out of and in the course of employment,” thereby rejecting the necessity of establishing temporal, spatial, and circumstantial proximity between the injury and employment. It held that the work-connection approach simply requires the finding of a causal connection between the injury and any incidents or conditions of employment. The only relevant inquiry was whether Dr. Chung’s heart attack in fact was aggravated or accelerated by his work activity and whether there was substantial evidence to the contrary.
The employer provided expert testimony from a cardiologist attributing the heart attack to preexisting arteriosclerosis and physical exertion from jogging. On the other hand, another physician believed that Dr. Chung’s employment activities as principal veterinarian, administrator, and president of Animal Clinic, which engaged Dr. Chung for long hours, as well as his other business-related activities, generated a substantial amount of mental and emotional stress which was strongly linked to the production of heart disease. This was sufficient to establish a work connection. The Court also had this to say about legal versus medical causation: “... a medical man may give a generalized opinion that there was no connection between an incident at work and a heart attack, and, in his own mind, may mean thereby that a preexisting pathological condition was the overwhelming factor in bringing about the attack and that the part played by the work was insignificant. But, while it may be sound medically to say that the work did not ‘cause’ the attack, it may well be bad law, because, in general, existing law treats the slightest factor of aggravation as an adequate ‘cause.’ ”
In a recent seminal case,3 the same Court reiterated that, in order to be exonerated, the employer must adduce specific evidence to indicate why the work event did not or could not have caused, aggravated, or accelerated the injury. It ruled that the claim in question was compensable because all three experts had failed to explain why the industrial accident could not have caused the slightest aggravation or acceleration of an existing injury. The patient, previously asymptomatic, had sustained shoulder injuries at work. Notwithstanding X-ray evidence of preexisting degenerative changes, the Court found for the worker because the medical reports of the employer’s physicians did not provide a sufficient degree of specificity to constitute substantial rebuttable evidence since “under our workers’ compensation statute, the slightest aggravation or acceleration of an injury by the employment activity mandates compensation.”
WC’s quasi no-fault approach has been proposed as a model for adjudicating medical malpractice claims, which are currently decided by a fault-finding, adversarial system.4 The injured patient is randomly and unjustly compensated, and the combative nature of the proceedings traumatizes the doctor-patient relationship and promotes the wasteful practice of defensive medicine. In many instances, fault simply cannot be ascertained. Some of these same criticisms led to the introduction of the no-fault system for auto injuries and for workers’ compensation. However, injuries arising out of medical care differ in one essential aspect from all other injuries: They may be a natural and unavoidable consequence of the underlying illness or treatment. If all complications were deemed compensable, including those that are unavoidable, then a true comprehensive no-fault system would exist. However, it would prove prohibitively expensive.
No-fault medical injury systems are presently in place in countries like Sweden and New Zealand. The latter’s no-fault compensation scheme came into effect in 1974 under its Accident Compensation Act, which removed all accidental injuries including medical injuries from the tort system. Under the initial scheme, which has since undergone numerous major revisions, injured patients did not have to prove fault. All the claimant had to establish was “medical, surgical, dental, or first aid misadventure.” However, the revised Act of 1992 required the claimant to show “medical error,” which was defined (like negligence) as “the failure of a registered health professional to observe a standard of care and skill reasonably to be expected in the circumstances.” Now renamed the Accident Compensation Act 2001, it covers medical injuries that are “not a necessary part, or ordinary consequence, of the treatment.” The fact that the treatment did not achieve a desired result does not, of itself, constitute treatment injury.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Hawaii Revised Statutes (HRS) Section 386-3.
2. Chung v. Animal Clinic Inc., 636 P.2d 721 (1981).
3. Panoke v. Reef Development of Hawaii Inc., Supreme Court of Hawaii. No. SCWC–11–0000556. Decided: December 14, 2015.
4. Tan, SY. In Medical Malpractice: Understanding the Law, Managing the Risks. World Scientific Publishing Co. Pte Ltd., Singapore, 2006.
Question: Employee, a poorly controlled diabetic, accidentally stepped on a nail at work. Surrounding cellulitis and abscess formation set in, but because he was slow in getting to a doctor, the infection invaded the underlying bone, causing osteomyelitis. He ended up with a partial foot amputation. In a claim for workers’ compensation (WC) benefits, which of the following is best?
A. Employee has a claim under WC, a quasi no-fault system that requires an employer to compensate its employees only for accidents occurring in the workplace.
B. Employer may offer employee’s preexisting diabetic condition and his failure to promptly seek medical attention as substantial rebuttable evidence against compensability.
C. A similar no-fault system has been proposed as an alternative to medical tort litigation, but it has yet to be established in the developed world.
D. All are incorrect.
E. All are correct.
Answer: D. Fashioned after Europe’s Workers’ Accident Insurance system that was put into place by Germany’s Otto von Bismarck, workers’ compensation (WC) laws found their way into the United States by 1908. Today, all states have enacted such laws to effectuate the policy that work injuries are among the costs of production, which industry is required to bear. Such laws purport to do away with vexatious issues like contributory negligence, agency principles that negate an employment relationship, and assumption of risk defenses, all of which had previously been used to deny an injured worker compensatory benefits.
WC laws differ somewhat from state to state, both in statutory provisions and judicial interpretations. However, an illness or disease condition that is related to work conditions will suffice. The employer bears the burden of proof and is required to affirmatively rebut the presumption of compensability. This is usually a high bar to scale, and preexisting conditions and poor patient compliance are insufficient to negate a WC claim, although they are used in apportioning payments to the injured worker.
Take Hawaii, widely viewed as a proworker jurisdiction, as an example. Its key WC statutory language covers any employee who “suffers a personal injury either by accident arising out of and in the course of employment or by disease proximately caused by or resulting from the nature of the employment.”1 In Chung v. Animal Clinic Inc.,2 Dr. Chung suffered a heart attack after office hours while jogging around the Kalani High School track in Honolulu. One of the issues was whether his heart attack arose out of and in the course of his employment and, if so, whether the employer substantially rebutted the presumption that the heart attack was work connected.
The Supreme Court of Hawaii used the work-connection approach in interpreting the phrase “arising out of and in the course of employment,” thereby rejecting the necessity of establishing temporal, spatial, and circumstantial proximity between the injury and employment. It held that the work-connection approach simply requires the finding of a causal connection between the injury and any incidents or conditions of employment. The only relevant inquiry was whether Dr. Chung’s heart attack in fact was aggravated or accelerated by his work activity and whether there was substantial evidence to the contrary.
The employer provided expert testimony from a cardiologist attributing the heart attack to preexisting arteriosclerosis and physical exertion from jogging. On the other hand, another physician believed that Dr. Chung’s employment activities as principal veterinarian, administrator, and president of Animal Clinic, which engaged Dr. Chung for long hours, as well as his other business-related activities, generated a substantial amount of mental and emotional stress which was strongly linked to the production of heart disease. This was sufficient to establish a work connection. The Court also had this to say about legal versus medical causation: “... a medical man may give a generalized opinion that there was no connection between an incident at work and a heart attack, and, in his own mind, may mean thereby that a preexisting pathological condition was the overwhelming factor in bringing about the attack and that the part played by the work was insignificant. But, while it may be sound medically to say that the work did not ‘cause’ the attack, it may well be bad law, because, in general, existing law treats the slightest factor of aggravation as an adequate ‘cause.’ ”
In a recent seminal case,3 the same Court reiterated that, in order to be exonerated, the employer must adduce specific evidence to indicate why the work event did not or could not have caused, aggravated, or accelerated the injury. It ruled that the claim in question was compensable because all three experts had failed to explain why the industrial accident could not have caused the slightest aggravation or acceleration of an existing injury. The patient, previously asymptomatic, had sustained shoulder injuries at work. Notwithstanding X-ray evidence of preexisting degenerative changes, the Court found for the worker because the medical reports of the employer’s physicians did not provide a sufficient degree of specificity to constitute substantial rebuttable evidence since “under our workers’ compensation statute, the slightest aggravation or acceleration of an injury by the employment activity mandates compensation.”
WC’s quasi no-fault approach has been proposed as a model for adjudicating medical malpractice claims, which are currently decided by a fault-finding, adversarial system.4 The injured patient is randomly and unjustly compensated, and the combative nature of the proceedings traumatizes the doctor-patient relationship and promotes the wasteful practice of defensive medicine. In many instances, fault simply cannot be ascertained. Some of these same criticisms led to the introduction of the no-fault system for auto injuries and for workers’ compensation. However, injuries arising out of medical care differ in one essential aspect from all other injuries: They may be a natural and unavoidable consequence of the underlying illness or treatment. If all complications were deemed compensable, including those that are unavoidable, then a true comprehensive no-fault system would exist. However, it would prove prohibitively expensive.
No-fault medical injury systems are presently in place in countries like Sweden and New Zealand. The latter’s no-fault compensation scheme came into effect in 1974 under its Accident Compensation Act, which removed all accidental injuries including medical injuries from the tort system. Under the initial scheme, which has since undergone numerous major revisions, injured patients did not have to prove fault. All the claimant had to establish was “medical, surgical, dental, or first aid misadventure.” However, the revised Act of 1992 required the claimant to show “medical error,” which was defined (like negligence) as “the failure of a registered health professional to observe a standard of care and skill reasonably to be expected in the circumstances.” Now renamed the Accident Compensation Act 2001, it covers medical injuries that are “not a necessary part, or ordinary consequence, of the treatment.” The fact that the treatment did not achieve a desired result does not, of itself, constitute treatment injury.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. Hawaii Revised Statutes (HRS) Section 386-3.
2. Chung v. Animal Clinic Inc., 636 P.2d 721 (1981).
3. Panoke v. Reef Development of Hawaii Inc., Supreme Court of Hawaii. No. SCWC–11–0000556. Decided: December 14, 2015.
4. Tan, SY. In Medical Malpractice: Understanding the Law, Managing the Risks. World Scientific Publishing Co. Pte Ltd., Singapore, 2006.
Vaginal and Scrotal Rejuvenation: The Potential Role of Dermatologists in Genital Rejuvenation
To the Editor:
I read with interest the informative Cutis article by Hashim et al,1 which not only summarized the key features of vaginal rejuvenation but also concisely reviewed noninvasive treatments, including lasers and radiofrequency devices, that can be used to address this important issue. The authors emphasized that these treatments may represent a valuable addition to the cosmetic landscape. In addition, they also asserted that noninvasive vaginal rejuvenation is an expanding focus of cosmetic dermatology.1
Genital rejuvenation includes rejuvenation of the vagina in women and the scrotum in men. Since the term initially appeared in the literature in 2007,2 a PubMed search of articles indexed for MEDLINE yields an increasing number of articles on vaginal rejuvenation. More recently, the concept of scrotal rejuvenation was introduced in 2018.3
Similar to vaginal rejuvenation, scrotal rejuvenation includes procedures to remedy medical or cosmetic conditions of the scrotum. Hashim et al1 focused on morphology-associated vaginal changes for which rejuvenation techniques have been successful, such as excess clitoral hood; excess labia majora or minora; vaginal laxity; and vulvovaginal atrophy, which is considered to be a component of genitourinary syndrome of menopause. Morphology-associated changes of the scrotum include wrinkling (cutis scrotum gyratum or scrotum rugosum) and laxity (low-hanging or sagging scrotum or scrotomegaly
Intrinsic (aging) and extrinsic (trauma) alterations also can result in other changes that may be amenable to vaginal or scrotal rejuvenation; for example, in addition to changes in morphology, there are hair (eg, alopecia, hypertrichosis) and vascular (eg, angiokeratomas) conditions of the vagina and scrotum that may be suitable for rejuvenation.3-5 Dermatologists have the opportunity to provide treatment for the genital rejuvenation of their patients.
- Hashim PW, Nia JK, Zade J, et al. Noninvasive vaginal rejuvenation. Cutis. 2018;102:243-246.
- Committee on Gynecologic Practice, American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 378: vaginal “rejuvenation” and cosmetic vaginal procedures. Obstet Gynecol. 2007;110:737-738.
- Cohen PR. Scrotal rejuvenation. Cureus. 2018;10:e2316.
- Cohen PR. Genital rejuvenation: the next frontier in medical and cosmetic dermatology. Dermatol Online J. 2018:24. http://escholarship.org/uc/item/27v774t5. Accessed February 15, 2018.
- Cohen PR. A case report of scrotal rejuvenation: laser treatment of angiokeratomas of the scrotum [published online November 26, 2018]. Dermatol Ther (Heidelb). doi:10.1007/s13555-018-0272-z.
To the Editor:
I read with interest the informative Cutis article by Hashim et al,1 which not only summarized the key features of vaginal rejuvenation but also concisely reviewed noninvasive treatments, including lasers and radiofrequency devices, that can be used to address this important issue. The authors emphasized that these treatments may represent a valuable addition to the cosmetic landscape. In addition, they also asserted that noninvasive vaginal rejuvenation is an expanding focus of cosmetic dermatology.1
Genital rejuvenation includes rejuvenation of the vagina in women and the scrotum in men. Since the term initially appeared in the literature in 2007,2 a PubMed search of articles indexed for MEDLINE yields an increasing number of articles on vaginal rejuvenation. More recently, the concept of scrotal rejuvenation was introduced in 2018.3
Similar to vaginal rejuvenation, scrotal rejuvenation includes procedures to remedy medical or cosmetic conditions of the scrotum. Hashim et al1 focused on morphology-associated vaginal changes for which rejuvenation techniques have been successful, such as excess clitoral hood; excess labia majora or minora; vaginal laxity; and vulvovaginal atrophy, which is considered to be a component of genitourinary syndrome of menopause. Morphology-associated changes of the scrotum include wrinkling (cutis scrotum gyratum or scrotum rugosum) and laxity (low-hanging or sagging scrotum or scrotomegaly
Intrinsic (aging) and extrinsic (trauma) alterations also can result in other changes that may be amenable to vaginal or scrotal rejuvenation; for example, in addition to changes in morphology, there are hair (eg, alopecia, hypertrichosis) and vascular (eg, angiokeratomas) conditions of the vagina and scrotum that may be suitable for rejuvenation.3-5 Dermatologists have the opportunity to provide treatment for the genital rejuvenation of their patients.
To the Editor:
I read with interest the informative Cutis article by Hashim et al,1 which not only summarized the key features of vaginal rejuvenation but also concisely reviewed noninvasive treatments, including lasers and radiofrequency devices, that can be used to address this important issue. The authors emphasized that these treatments may represent a valuable addition to the cosmetic landscape. In addition, they also asserted that noninvasive vaginal rejuvenation is an expanding focus of cosmetic dermatology.1
Genital rejuvenation includes rejuvenation of the vagina in women and the scrotum in men. Since the term initially appeared in the literature in 2007,2 a PubMed search of articles indexed for MEDLINE yields an increasing number of articles on vaginal rejuvenation. More recently, the concept of scrotal rejuvenation was introduced in 2018.3
Similar to vaginal rejuvenation, scrotal rejuvenation includes procedures to remedy medical or cosmetic conditions of the scrotum. Hashim et al1 focused on morphology-associated vaginal changes for which rejuvenation techniques have been successful, such as excess clitoral hood; excess labia majora or minora; vaginal laxity; and vulvovaginal atrophy, which is considered to be a component of genitourinary syndrome of menopause. Morphology-associated changes of the scrotum include wrinkling (cutis scrotum gyratum or scrotum rugosum) and laxity (low-hanging or sagging scrotum or scrotomegaly
Intrinsic (aging) and extrinsic (trauma) alterations also can result in other changes that may be amenable to vaginal or scrotal rejuvenation; for example, in addition to changes in morphology, there are hair (eg, alopecia, hypertrichosis) and vascular (eg, angiokeratomas) conditions of the vagina and scrotum that may be suitable for rejuvenation.3-5 Dermatologists have the opportunity to provide treatment for the genital rejuvenation of their patients.
- Hashim PW, Nia JK, Zade J, et al. Noninvasive vaginal rejuvenation. Cutis. 2018;102:243-246.
- Committee on Gynecologic Practice, American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 378: vaginal “rejuvenation” and cosmetic vaginal procedures. Obstet Gynecol. 2007;110:737-738.
- Cohen PR. Scrotal rejuvenation. Cureus. 2018;10:e2316.
- Cohen PR. Genital rejuvenation: the next frontier in medical and cosmetic dermatology. Dermatol Online J. 2018:24. http://escholarship.org/uc/item/27v774t5. Accessed February 15, 2018.
- Cohen PR. A case report of scrotal rejuvenation: laser treatment of angiokeratomas of the scrotum [published online November 26, 2018]. Dermatol Ther (Heidelb). doi:10.1007/s13555-018-0272-z.
- Hashim PW, Nia JK, Zade J, et al. Noninvasive vaginal rejuvenation. Cutis. 2018;102:243-246.
- Committee on Gynecologic Practice, American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 378: vaginal “rejuvenation” and cosmetic vaginal procedures. Obstet Gynecol. 2007;110:737-738.
- Cohen PR. Scrotal rejuvenation. Cureus. 2018;10:e2316.
- Cohen PR. Genital rejuvenation: the next frontier in medical and cosmetic dermatology. Dermatol Online J. 2018:24. http://escholarship.org/uc/item/27v774t5. Accessed February 15, 2018.
- Cohen PR. A case report of scrotal rejuvenation: laser treatment of angiokeratomas of the scrotum [published online November 26, 2018]. Dermatol Ther (Heidelb). doi:10.1007/s13555-018-0272-z.
Recurrence of Elevated Intracranial Pressure Following Tetracycline Antibiotic Use
To the Editor:
In 1995, one of the authors (A.G.L.) reported the case of a 14-year-old boy who was diagnosed with pseudotumor cerebri following treatment with isotretinoin and tetracycline, both of which were implicated in the development of elevated intracranial pressure (ICP). The patient subsequently underwent optic nerve sheath fenestration for decompression due to progressive deterioration of the visual field despite discontinuation of both drugs.1
This patient recently returned to our office 28 years after his initial presentation with a recurrence of similar symptoms. He was subsequently diagnosed with elevated ICP after a single dose of doxycycline. His vision was 20/20 with correction for distance. Pupil size and extraocular motility were within normal limits. Physical examination was normal, and a dilated fundus examination showed a Frisen stage 1 disc edema in the right eye and a Frisen stage 3 disc edema in the left eye at presentation. The visual field showed enlarged blind spots in both eyes consistent with papilledema. Optical coherence tomography for optic nerve was 93 µm in the right eye and 124 µm in the left eye compared to earlier measures of 66 and 68 µm in the right and left eyes, respectively, indicating pseudonormalization of the parameters (disc edema in the setting of prior optic atrophy). In the setting of optic atrophy, when the nerve develops any swelling the thickness measured on optical coherence tomography may reach normal values, which are in fact abnormal and elevated in this case. Magnetic resonance imaging and magnetic resonance venography were within normal limits. Cerebrospinal fluid opening pressure was 26 cm of water, and analysis revealed high levels of West Nile virus antibodies (IgM and IgG), suggesting a recent viral infection. In addition to an established predisposition to develop elevated ICP on tetracycline antibiotics, this patient also had the precipitating factor of recent viral infection contributing to his raised ICP. Prior to his most recent presentation, his condition was stable with evidence of mild optic atrophy in both eyes and stable visual fields.
Various case reports have linked the use of tetracycline antibiotics to increased ICP. Gardner et al2 reported a case of fraternal twins who developed elevated ICP while on tetracycline for acne, suggesting a possible genetic susceptibility. In one nested case-control study, it was found that the relative risk (RR) of developing elevated ICP with tetracycline antibiotics was increased (RR=2.68 [95% CI, 0.89-8.11] for 15 days of current use; RR=3.64 [95% CI, 1.67-7.91] for 30 days of current use).3 Retrospective studies have demonstrated that 9% of the population (N=207) had prior treatment with tetracylines in a cohort of patients diagnosed with elevated ICP.4
In this group of drugs, minocycline has been closely associated with development of elevated ICP. One retrospective study showed that 75% of patients (9/12) with minocycline-associated ICP developed symptoms of elevated ICP within 8 weeks of starting therapy; however, half of the patients included in the study were obese. The inclusion of obese patients in this study is a confounding variable because idiopathic intracranial hypertension (IIH) is a disease that predominantly affects obese young females. The diagnosis of IIH, however, should be considered a diagnosis of exclusion, and it is uncommon in thin elderly or male patients.5
Tetracyclines have a half-life of 6 to 11 hours, and usually the elevated ICP decreases once the offending agent is discontinued, though papilledema could take months to resolve.
We describe an inadvertent rechallenge
- Lee AG. Pseudotumor cerebri after treatment with tetracycline and isotretinoin for acne. Cutis. 1995;55:165-168.
- Gardner K, Cox T, Digre KB. Idiopathic intracranial hypertension associated with tetracycline use in fraternal twins: case reports and review. Neurology. 1995;45:6-10.
- Sodhi M, Sheldon CA, Carleton B, et al. Oral fluoroquinolones and risk of secondary pseudotumor cerebri syndrome: nested case-control study. Neurology. 2017;89:792-795.
- Sundholm A, Burkill S, Sveinsson O, et al. Population‐based incidence and clinical characteristics of idiopathic intracranial hypertension. Acta Neurologica Scandinavica. 2017;136:427-433.
- Chiu AM, Chuenkongkaew WL, Cornblath WT, et al. Minocycline treatment and pseudotumor cerebri syndrome. Am J Ophthalmol. 1998;126:116-121.
To the Editor:
In 1995, one of the authors (A.G.L.) reported the case of a 14-year-old boy who was diagnosed with pseudotumor cerebri following treatment with isotretinoin and tetracycline, both of which were implicated in the development of elevated intracranial pressure (ICP). The patient subsequently underwent optic nerve sheath fenestration for decompression due to progressive deterioration of the visual field despite discontinuation of both drugs.1
This patient recently returned to our office 28 years after his initial presentation with a recurrence of similar symptoms. He was subsequently diagnosed with elevated ICP after a single dose of doxycycline. His vision was 20/20 with correction for distance. Pupil size and extraocular motility were within normal limits. Physical examination was normal, and a dilated fundus examination showed a Frisen stage 1 disc edema in the right eye and a Frisen stage 3 disc edema in the left eye at presentation. The visual field showed enlarged blind spots in both eyes consistent with papilledema. Optical coherence tomography for optic nerve was 93 µm in the right eye and 124 µm in the left eye compared to earlier measures of 66 and 68 µm in the right and left eyes, respectively, indicating pseudonormalization of the parameters (disc edema in the setting of prior optic atrophy). In the setting of optic atrophy, when the nerve develops any swelling the thickness measured on optical coherence tomography may reach normal values, which are in fact abnormal and elevated in this case. Magnetic resonance imaging and magnetic resonance venography were within normal limits. Cerebrospinal fluid opening pressure was 26 cm of water, and analysis revealed high levels of West Nile virus antibodies (IgM and IgG), suggesting a recent viral infection. In addition to an established predisposition to develop elevated ICP on tetracycline antibiotics, this patient also had the precipitating factor of recent viral infection contributing to his raised ICP. Prior to his most recent presentation, his condition was stable with evidence of mild optic atrophy in both eyes and stable visual fields.
Various case reports have linked the use of tetracycline antibiotics to increased ICP. Gardner et al2 reported a case of fraternal twins who developed elevated ICP while on tetracycline for acne, suggesting a possible genetic susceptibility. In one nested case-control study, it was found that the relative risk (RR) of developing elevated ICP with tetracycline antibiotics was increased (RR=2.68 [95% CI, 0.89-8.11] for 15 days of current use; RR=3.64 [95% CI, 1.67-7.91] for 30 days of current use).3 Retrospective studies have demonstrated that 9% of the population (N=207) had prior treatment with tetracylines in a cohort of patients diagnosed with elevated ICP.4
In this group of drugs, minocycline has been closely associated with development of elevated ICP. One retrospective study showed that 75% of patients (9/12) with minocycline-associated ICP developed symptoms of elevated ICP within 8 weeks of starting therapy; however, half of the patients included in the study were obese. The inclusion of obese patients in this study is a confounding variable because idiopathic intracranial hypertension (IIH) is a disease that predominantly affects obese young females. The diagnosis of IIH, however, should be considered a diagnosis of exclusion, and it is uncommon in thin elderly or male patients.5
Tetracyclines have a half-life of 6 to 11 hours, and usually the elevated ICP decreases once the offending agent is discontinued, though papilledema could take months to resolve.
We describe an inadvertent rechallenge
To the Editor:
In 1995, one of the authors (A.G.L.) reported the case of a 14-year-old boy who was diagnosed with pseudotumor cerebri following treatment with isotretinoin and tetracycline, both of which were implicated in the development of elevated intracranial pressure (ICP). The patient subsequently underwent optic nerve sheath fenestration for decompression due to progressive deterioration of the visual field despite discontinuation of both drugs.1
This patient recently returned to our office 28 years after his initial presentation with a recurrence of similar symptoms. He was subsequently diagnosed with elevated ICP after a single dose of doxycycline. His vision was 20/20 with correction for distance. Pupil size and extraocular motility were within normal limits. Physical examination was normal, and a dilated fundus examination showed a Frisen stage 1 disc edema in the right eye and a Frisen stage 3 disc edema in the left eye at presentation. The visual field showed enlarged blind spots in both eyes consistent with papilledema. Optical coherence tomography for optic nerve was 93 µm in the right eye and 124 µm in the left eye compared to earlier measures of 66 and 68 µm in the right and left eyes, respectively, indicating pseudonormalization of the parameters (disc edema in the setting of prior optic atrophy). In the setting of optic atrophy, when the nerve develops any swelling the thickness measured on optical coherence tomography may reach normal values, which are in fact abnormal and elevated in this case. Magnetic resonance imaging and magnetic resonance venography were within normal limits. Cerebrospinal fluid opening pressure was 26 cm of water, and analysis revealed high levels of West Nile virus antibodies (IgM and IgG), suggesting a recent viral infection. In addition to an established predisposition to develop elevated ICP on tetracycline antibiotics, this patient also had the precipitating factor of recent viral infection contributing to his raised ICP. Prior to his most recent presentation, his condition was stable with evidence of mild optic atrophy in both eyes and stable visual fields.
Various case reports have linked the use of tetracycline antibiotics to increased ICP. Gardner et al2 reported a case of fraternal twins who developed elevated ICP while on tetracycline for acne, suggesting a possible genetic susceptibility. In one nested case-control study, it was found that the relative risk (RR) of developing elevated ICP with tetracycline antibiotics was increased (RR=2.68 [95% CI, 0.89-8.11] for 15 days of current use; RR=3.64 [95% CI, 1.67-7.91] for 30 days of current use).3 Retrospective studies have demonstrated that 9% of the population (N=207) had prior treatment with tetracylines in a cohort of patients diagnosed with elevated ICP.4
In this group of drugs, minocycline has been closely associated with development of elevated ICP. One retrospective study showed that 75% of patients (9/12) with minocycline-associated ICP developed symptoms of elevated ICP within 8 weeks of starting therapy; however, half of the patients included in the study were obese. The inclusion of obese patients in this study is a confounding variable because idiopathic intracranial hypertension (IIH) is a disease that predominantly affects obese young females. The diagnosis of IIH, however, should be considered a diagnosis of exclusion, and it is uncommon in thin elderly or male patients.5
Tetracyclines have a half-life of 6 to 11 hours, and usually the elevated ICP decreases once the offending agent is discontinued, though papilledema could take months to resolve.
We describe an inadvertent rechallenge
- Lee AG. Pseudotumor cerebri after treatment with tetracycline and isotretinoin for acne. Cutis. 1995;55:165-168.
- Gardner K, Cox T, Digre KB. Idiopathic intracranial hypertension associated with tetracycline use in fraternal twins: case reports and review. Neurology. 1995;45:6-10.
- Sodhi M, Sheldon CA, Carleton B, et al. Oral fluoroquinolones and risk of secondary pseudotumor cerebri syndrome: nested case-control study. Neurology. 2017;89:792-795.
- Sundholm A, Burkill S, Sveinsson O, et al. Population‐based incidence and clinical characteristics of idiopathic intracranial hypertension. Acta Neurologica Scandinavica. 2017;136:427-433.
- Chiu AM, Chuenkongkaew WL, Cornblath WT, et al. Minocycline treatment and pseudotumor cerebri syndrome. Am J Ophthalmol. 1998;126:116-121.
- Lee AG. Pseudotumor cerebri after treatment with tetracycline and isotretinoin for acne. Cutis. 1995;55:165-168.
- Gardner K, Cox T, Digre KB. Idiopathic intracranial hypertension associated with tetracycline use in fraternal twins: case reports and review. Neurology. 1995;45:6-10.
- Sodhi M, Sheldon CA, Carleton B, et al. Oral fluoroquinolones and risk of secondary pseudotumor cerebri syndrome: nested case-control study. Neurology. 2017;89:792-795.
- Sundholm A, Burkill S, Sveinsson O, et al. Population‐based incidence and clinical characteristics of idiopathic intracranial hypertension. Acta Neurologica Scandinavica. 2017;136:427-433.
- Chiu AM, Chuenkongkaew WL, Cornblath WT, et al. Minocycline treatment and pseudotumor cerebri syndrome. Am J Ophthalmol. 1998;126:116-121.
A Closer Look at the New Biopsy Codes
Effective January 1, 2019, the 2 long-standing Current Procedural Terminology (CPT) biopsy codes 11100 (first lesion) and 11101 (each additional lesion biopsied on the same date of service) were replaced by a series of new biopsy codes that are specific to the method of removal, including tangential (11102, +11103), punch (11104, +11105), and incisional biopsies (11106, +11107)(Table).1,2 If a biopsy is performed using multiple techniques, only a single primary code of the highest value would be reported (ie, incisional>punch>tangential). The add-on codes are to be used for each additional lesion biopsied using the same or a different technique on the same day.
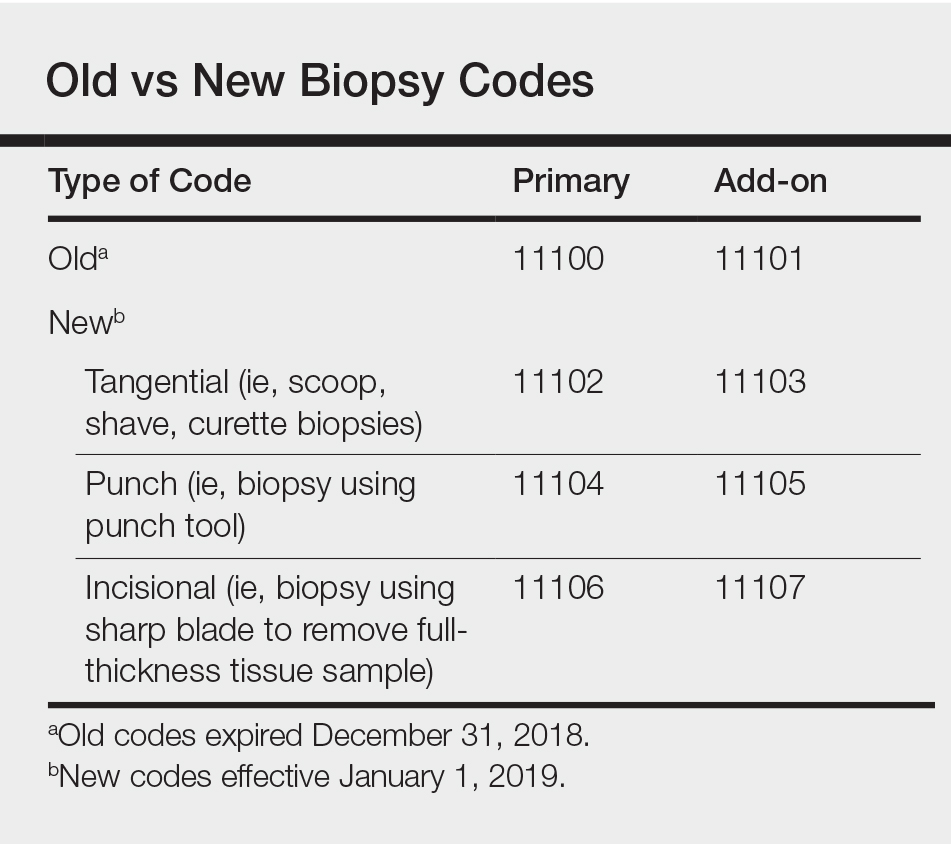
Tangential biopsies, performed with a sharp blade to remove epidermal tissue, include scoop, shave, and curette biopsies. Punch biopsies are performed using a punch tool, while incisional biopsies involve the use of a sharp blade to remove a full-thickness tissue sample.
Using Biopsy Codes Correctly
Only one primary biopsy code is to be reported on a given date. If 2 or more biopsies are performed using 2 or more techniques, then additional biopsies are to be reported using the relevant add-on codes. It is important to note that codes 11104 to 11107 include simple closures, which should not be coded separately.
In all cases, appropriate documentation is essential to support proper biopsy coding. Prior to any biopsy, patients should be educated on the associated risks, including bleeding, infection, and scarring, and patient consent should be obtained and documented in the medical record.
It bears noting the distinction between biopsies and excisions and their associated codes. Biopsies are performed for diagnostic purposes, with samples sent for histopathologic evaluation. Excisions are performed to entirely remove a lesion; it makes no difference whether or not the excised tissue is sent for histopathologic evaluation.
Reimbursement for biopsies has changed in 2019, with the rates for tangential biopsies decreasing relative to 2018 (−10.6%), while the rates for punch (+12.5%) and incisional (+35.5%) biopsies will be increasing.3
New Codes in Action
The following examples demonstrate how to use the new biopsy codes correctly in clinical practice.
A patient presents for evaluation of 3 lesions that he deems suspicious: 1 on the neck, 1 on the left upper arm, and 1 on the right lower arm. The dermatologist diagnoses the lesion on the neck as a seborrheic keratosis, a benign lesion, and the patient declines treatment. The lesions on each arm are suspicious for basal cell carcinoma, and the dermatologist performs shave biopsies at both sites to determine an accurate diagnosis. In this case, you would use CPT code 11102 (tangential biopsy of skin) for the first lesion and 11103 (tangential biopsy of skin, each additional lesion) for the second lesion.
A patient presents for evaluation of an itchy rash on both hands. On physical examination you observe small, firm, slightly erythematous papules in a ring formation on both hands. The patient says similar lesions have appeared and resolved in the past. She says she has sensitive skin and assumes the rash may have been caused by exposure to an irritating soap. The patient also points out a suspicious lesion on the right side of the upper back that seems to have grown in size over the last year. Based on the recurrence of the lesions on the hands and the characteristic formation of the papules, the dermatologist suspects granuloma annulare and performs a punch biopsy to confirm the diagnosis via histopathology. The lesion on the back is suspicious for melanoma, so the dermatologist performs an incisional biopsy of the lesion. For this patient, you would use CPT code 11106 (incisional biopsy) for the lesion on the back and 11105 (punch biopsy, each additional lesion) for the biopsy of the hand.
- Verhovshek J. CPT 2019 unveils tangential biopsy codes, more. American Academy of Professional Coders website. https://www.aapc.com/blog/44366-cpt-2019-unveils-tangential-biopsy-codes/. Published October 19, 2018. Accessed February 7, 2018.
- Grider D. 2019 CPT® coding for skin biopsies. ICD10 Monitor website. https://www.icd10monitor.com/2019-cpt-coding-for-skin-biopsies. Updated January 7, 2019. Accessed February 7, 2019.
- Kaufmann M. Coming soon: new biopsy codes. Practical Dermatol. 2018;15:18.
Effective January 1, 2019, the 2 long-standing Current Procedural Terminology (CPT) biopsy codes 11100 (first lesion) and 11101 (each additional lesion biopsied on the same date of service) were replaced by a series of new biopsy codes that are specific to the method of removal, including tangential (11102, +11103), punch (11104, +11105), and incisional biopsies (11106, +11107)(Table).1,2 If a biopsy is performed using multiple techniques, only a single primary code of the highest value would be reported (ie, incisional>punch>tangential). The add-on codes are to be used for each additional lesion biopsied using the same or a different technique on the same day.
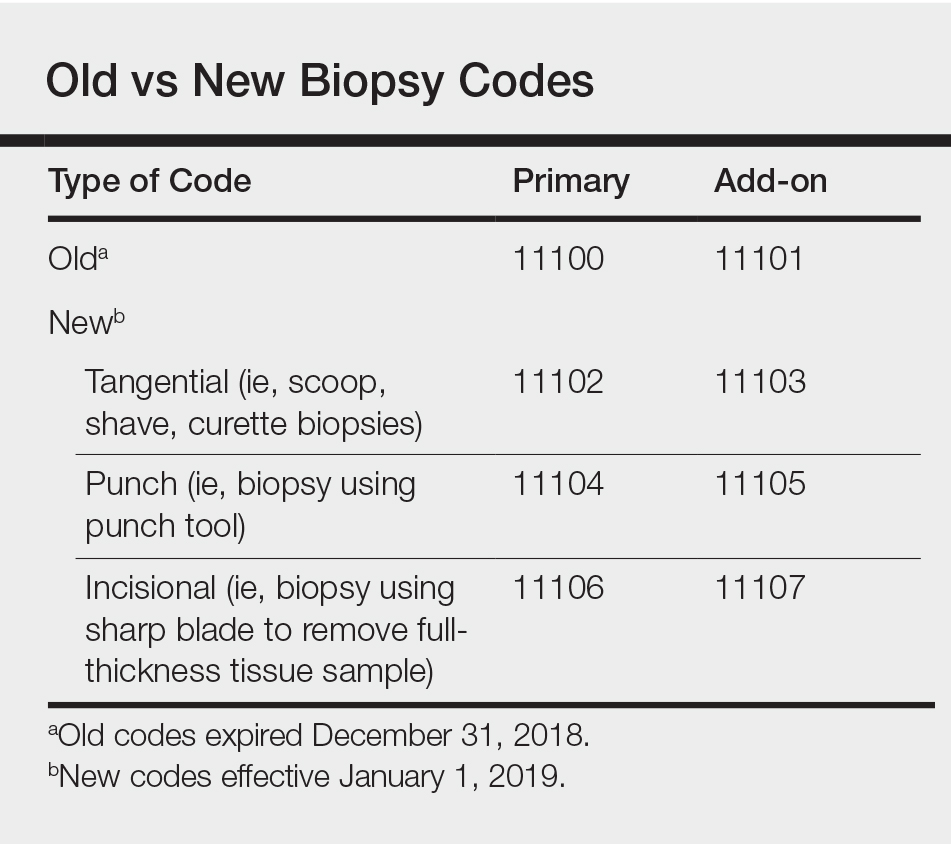
Tangential biopsies, performed with a sharp blade to remove epidermal tissue, include scoop, shave, and curette biopsies. Punch biopsies are performed using a punch tool, while incisional biopsies involve the use of a sharp blade to remove a full-thickness tissue sample.
Using Biopsy Codes Correctly
Only one primary biopsy code is to be reported on a given date. If 2 or more biopsies are performed using 2 or more techniques, then additional biopsies are to be reported using the relevant add-on codes. It is important to note that codes 11104 to 11107 include simple closures, which should not be coded separately.
In all cases, appropriate documentation is essential to support proper biopsy coding. Prior to any biopsy, patients should be educated on the associated risks, including bleeding, infection, and scarring, and patient consent should be obtained and documented in the medical record.
It bears noting the distinction between biopsies and excisions and their associated codes. Biopsies are performed for diagnostic purposes, with samples sent for histopathologic evaluation. Excisions are performed to entirely remove a lesion; it makes no difference whether or not the excised tissue is sent for histopathologic evaluation.
Reimbursement for biopsies has changed in 2019, with the rates for tangential biopsies decreasing relative to 2018 (−10.6%), while the rates for punch (+12.5%) and incisional (+35.5%) biopsies will be increasing.3
New Codes in Action
The following examples demonstrate how to use the new biopsy codes correctly in clinical practice.
A patient presents for evaluation of 3 lesions that he deems suspicious: 1 on the neck, 1 on the left upper arm, and 1 on the right lower arm. The dermatologist diagnoses the lesion on the neck as a seborrheic keratosis, a benign lesion, and the patient declines treatment. The lesions on each arm are suspicious for basal cell carcinoma, and the dermatologist performs shave biopsies at both sites to determine an accurate diagnosis. In this case, you would use CPT code 11102 (tangential biopsy of skin) for the first lesion and 11103 (tangential biopsy of skin, each additional lesion) for the second lesion.
A patient presents for evaluation of an itchy rash on both hands. On physical examination you observe small, firm, slightly erythematous papules in a ring formation on both hands. The patient says similar lesions have appeared and resolved in the past. She says she has sensitive skin and assumes the rash may have been caused by exposure to an irritating soap. The patient also points out a suspicious lesion on the right side of the upper back that seems to have grown in size over the last year. Based on the recurrence of the lesions on the hands and the characteristic formation of the papules, the dermatologist suspects granuloma annulare and performs a punch biopsy to confirm the diagnosis via histopathology. The lesion on the back is suspicious for melanoma, so the dermatologist performs an incisional biopsy of the lesion. For this patient, you would use CPT code 11106 (incisional biopsy) for the lesion on the back and 11105 (punch biopsy, each additional lesion) for the biopsy of the hand.
Effective January 1, 2019, the 2 long-standing Current Procedural Terminology (CPT) biopsy codes 11100 (first lesion) and 11101 (each additional lesion biopsied on the same date of service) were replaced by a series of new biopsy codes that are specific to the method of removal, including tangential (11102, +11103), punch (11104, +11105), and incisional biopsies (11106, +11107)(Table).1,2 If a biopsy is performed using multiple techniques, only a single primary code of the highest value would be reported (ie, incisional>punch>tangential). The add-on codes are to be used for each additional lesion biopsied using the same or a different technique on the same day.
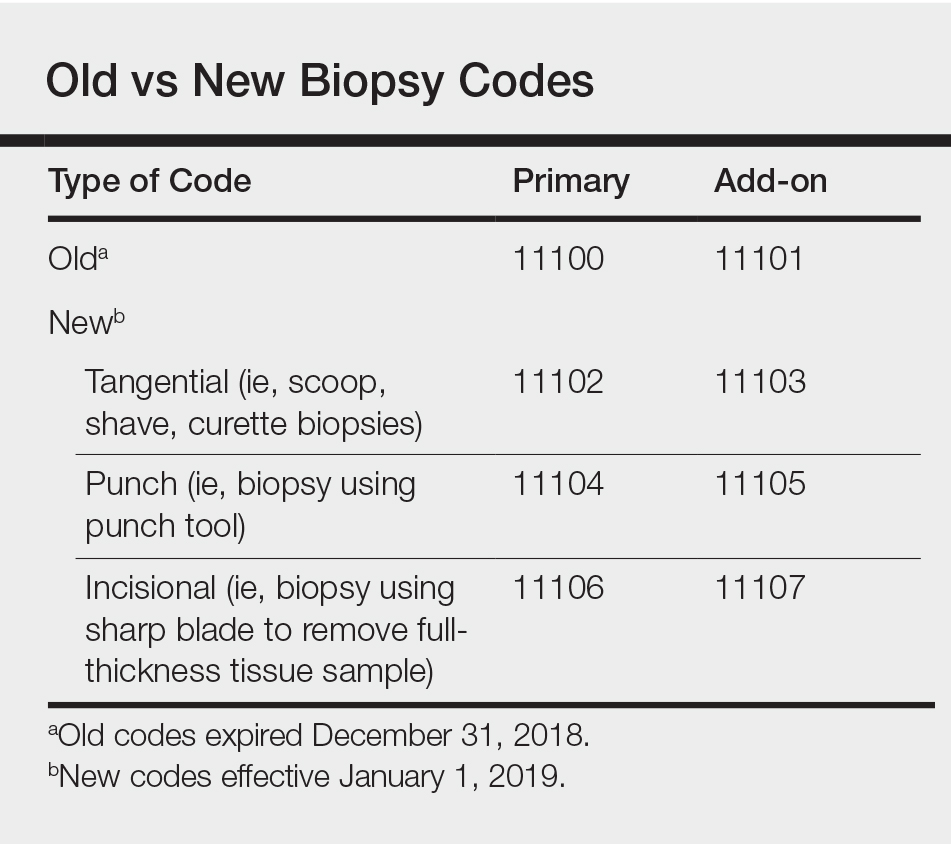
Tangential biopsies, performed with a sharp blade to remove epidermal tissue, include scoop, shave, and curette biopsies. Punch biopsies are performed using a punch tool, while incisional biopsies involve the use of a sharp blade to remove a full-thickness tissue sample.
Using Biopsy Codes Correctly
Only one primary biopsy code is to be reported on a given date. If 2 or more biopsies are performed using 2 or more techniques, then additional biopsies are to be reported using the relevant add-on codes. It is important to note that codes 11104 to 11107 include simple closures, which should not be coded separately.
In all cases, appropriate documentation is essential to support proper biopsy coding. Prior to any biopsy, patients should be educated on the associated risks, including bleeding, infection, and scarring, and patient consent should be obtained and documented in the medical record.
It bears noting the distinction between biopsies and excisions and their associated codes. Biopsies are performed for diagnostic purposes, with samples sent for histopathologic evaluation. Excisions are performed to entirely remove a lesion; it makes no difference whether or not the excised tissue is sent for histopathologic evaluation.
Reimbursement for biopsies has changed in 2019, with the rates for tangential biopsies decreasing relative to 2018 (−10.6%), while the rates for punch (+12.5%) and incisional (+35.5%) biopsies will be increasing.3
New Codes in Action
The following examples demonstrate how to use the new biopsy codes correctly in clinical practice.
A patient presents for evaluation of 3 lesions that he deems suspicious: 1 on the neck, 1 on the left upper arm, and 1 on the right lower arm. The dermatologist diagnoses the lesion on the neck as a seborrheic keratosis, a benign lesion, and the patient declines treatment. The lesions on each arm are suspicious for basal cell carcinoma, and the dermatologist performs shave biopsies at both sites to determine an accurate diagnosis. In this case, you would use CPT code 11102 (tangential biopsy of skin) for the first lesion and 11103 (tangential biopsy of skin, each additional lesion) for the second lesion.
A patient presents for evaluation of an itchy rash on both hands. On physical examination you observe small, firm, slightly erythematous papules in a ring formation on both hands. The patient says similar lesions have appeared and resolved in the past. She says she has sensitive skin and assumes the rash may have been caused by exposure to an irritating soap. The patient also points out a suspicious lesion on the right side of the upper back that seems to have grown in size over the last year. Based on the recurrence of the lesions on the hands and the characteristic formation of the papules, the dermatologist suspects granuloma annulare and performs a punch biopsy to confirm the diagnosis via histopathology. The lesion on the back is suspicious for melanoma, so the dermatologist performs an incisional biopsy of the lesion. For this patient, you would use CPT code 11106 (incisional biopsy) for the lesion on the back and 11105 (punch biopsy, each additional lesion) for the biopsy of the hand.
- Verhovshek J. CPT 2019 unveils tangential biopsy codes, more. American Academy of Professional Coders website. https://www.aapc.com/blog/44366-cpt-2019-unveils-tangential-biopsy-codes/. Published October 19, 2018. Accessed February 7, 2018.
- Grider D. 2019 CPT® coding for skin biopsies. ICD10 Monitor website. https://www.icd10monitor.com/2019-cpt-coding-for-skin-biopsies. Updated January 7, 2019. Accessed February 7, 2019.
- Kaufmann M. Coming soon: new biopsy codes. Practical Dermatol. 2018;15:18.
- Verhovshek J. CPT 2019 unveils tangential biopsy codes, more. American Academy of Professional Coders website. https://www.aapc.com/blog/44366-cpt-2019-unveils-tangential-biopsy-codes/. Published October 19, 2018. Accessed February 7, 2018.
- Grider D. 2019 CPT® coding for skin biopsies. ICD10 Monitor website. https://www.icd10monitor.com/2019-cpt-coding-for-skin-biopsies. Updated January 7, 2019. Accessed February 7, 2019.
- Kaufmann M. Coming soon: new biopsy codes. Practical Dermatol. 2018;15:18.
Cancer screening: A modest proposal for prevention
I have been assured by a very knowing American of my acquaintance in London, that a young healthy child well nursed is at a year old, a most delicious, nourishing, and wholesome food, whether stewed, roasted, baked, or boiled, and I make no doubt that it will equally serve in a fricassee, or ragout.
—Jonathan Swift, A Modest Proposal1
Large-scale cancer screening programs have the unintended consequences of false-positive results and overdiagnosis, leading to anxiety and overtreatment. The magnitude of these harms continues to be clarified after decades of screening.
Recognizing the trade-off between benefits and harms, the US Preventive Services Task Force (USPSTF) has changed several of its recommendations in recent years. Breast cancer screening recommendations have gone from yearly mammograms starting at age 40 to biennial mammograms starting at age 50 for women at average risk.2 Prostate cancer screening is no longer recommended for men age 70 and older, and even for men between 55 and 69, screening is now an individual decision.3
Newer screening programs are targeting high-risk groups rather than the general population, with the aim of increasing the likelihood of benefits and limiting the harms. For example, lung cancer screening is recommended only for current smokers or smokers who have quit within the past 15 years, are between 55 and 80, and have at least a 30 pack-year smoking history.4
The movement toward less-frequent screening and screening in a narrower population has evoked strong reactions from advocates of cancer screening. One professor of radiology writes, “It borders on unethical to suggest that the benefit of having your life saved by screening and living another 40 years can be balanced against the ‘harm’ of being recalled for additional mammographic views for what proves to not be a cancer.”5 Another notes, “It does not make any sense to throw away the lives saved by screening to avoid over-treating a small number of cancers.”6 Both of these authors defend the position that the goal of screening is to minimize cause-specific mortality, irrespective of overdiagnosis, overtreatment, or false-positive results. In other words, harm should have little to no weight in screening recommendations.
Although the debate on cancer screening is moving toward a more balanced discussion of benefits and harms, many patients are still subjected to screening that is more aggressive than the USPSTF recommends, which may be due to an underlying belief that no harm is greater than the benefit of saving a life.
IS MORE-AGGRESSIVE SCREENING THE ANSWER?
One may wonder if more-aggressive screening could prevent deaths that occur despite standard screening. For example, more-frequent screening or use of additional screening methods such as ultrasonography or magnetic resonance imaging has been suggested for patients at high risk of breast cancer.
A MODEST PROPOSAL
If one holds the view that benefits alone should be considered when writing recommendations about screening, the logical conclusion extends beyond screening. We would therefore like to propose a different approach to reducing cancer deaths in the general population:
Why not just remove everybody’s breasts, prostate gland, and colon before cancer arises?
TO CUT IS TO PREVENT
Currently, we offer prophylactic surgery to patients at high risk of cancer. For example, women with BRCA1/BRCA2 mutations are offered prophylactic mastectomy as one of several options for reducing risk of breast cancer. In 2013, the first case of prophylactic prostatectomy was performed in a man who had a BRCA1/BRCA2 mutation. Total colectomy is considered in men and women who have hereditary nonpolyposis colon cancer, instead of segmental resection, to prevent future cancer.
If prophylactic surgery were extended to the general population, it would greatly reduce the number of cancer deaths. Assuming that removing an organ almost always precludes development of cancer, we may predict that prophylactic mastectomy, prostatectomy, or colectomy would save the lives of most of the patients who are still dying of cancer of these organs. The effectiveness rates would approach, but not reach 100%; such is the case with prophylactic mastectomy.
Consider prostate-specific antigen (PSA) screening. Even using the favorable estimate of the impact of PSA screening, arising from the European Randomised Study of Screening for Prostate Cancer trial, 27 men have to be diagnosed, most undergoing local therapy (the trial was conducted before active surveillance became routine), to avert 1 death from prostate cancer over 13 years.9
Contrast this “number needed to diagnose” with the number needed to treat for a strategy of routine prostate removal at age 45 or 50. Given that the lifetime risk of death from prostate cancer approaches 3%, and few cases arise before this age, a prophylactic surgical strategy would avert 1 death per 33 operations. If proponents of screening are willing to accept a number needed to diagnose of 27 over a 13-year interval, they may be willing to consider a number needed to treat of 33 over a lifetime.
There may be harms such as perioperative and postoperative complications. Mastectomy could lead to emotional stress from altered body image. Prostatectomy can have long-term complications such as urinary incontinence and sexual dysfunction. Nevertheless, prophylactic organ removal would save far more lives than current screening practices. It also could decrease mental burden, as patients could rest assured that they will never develop cancer, whereas screening often involves ambiguous test results, follow-up tests, and interventions, increasing patient anxiety.
FINDING THE BALANCE BETWEEN BENEFITS AND HARMS
In truth, we do not really advocate universal mastectomy, prostatectomy, and colectomy to prevent cancer, no more than Swift1 really wanted to eat the children of Ireland to alleviate poverty and famine in that country. Rather, we use it as an extreme proposal to highlight the scope and depth of harms that inevitably arise from screening.
If proponents of aggressive screening believe that the goal is to reduce cause-specific mortality as much as possible, giving little weight or consideration to overdiagnosis and overtreatment, then they ought to embrace universal prophylactic surgery as well. Recognition of this logical consequence reminds us that we must make screening recommendations that balance benefits and harms.
Considering an extreme perspective can help in recognizing our bias toward saving lives from cancer and discounting the harms. Aggravating this bias, it is impossible to know whether an individual patient has avoided fatal cancer or undergone unnecessary treatment. Moreover, changing practice is more difficult if it involves rolling back interventions that were once the standard.
Balancing benefits and harms is especially difficult when trying to compare the benefit of preventing a single cancer death against a harm that is less serious but more common. Medicine has always involved difficult trade-offs, as seen in cost-benefit analysis of new treatments or balancing quality of life with quantity of life in a single patient. In addition, each individual may place different values on benefits of screening and avoiding possible harms.
There is an undeniable trade-off with screening, and we must make a conscious decision on where to draw the line when harms outweigh the benefits. We must proceed with caution when subjecting large numbers of men and women to the possibility of psychological burden and decreased quality of life.
Given the growing appreciation of the harms of screening, it is likely that future guidance will continue to move toward less- frequent screening or focusing resources on high-risk populations, where the absolute magnitude of benefit is greater. Cancer screening is also likely to become an individual decision based on personal values and informed decisions.
- Swift J. A Modest Proposal for Preventing the Children of Poor People in Ireland, from Being a Burden on Their Parents or Country, and for Making Them Beneficial to the Publick. Dublin: S. Harding, 1729.
- Nelson HD, Cantor A, Humphrey L, et al. Screening for breast cancer: a systematic review to update the 2009 US Preventive Services Task Force Recommendation. www.ncbi.nlm.nih.gov/books/NBK343819. Accessed February 13, 2019.
- US Preventive Services Task Force; Grossman DC, Curry SJ, Owens DK, et al. Screening for prostate cancer: US Preventive Services Task Force Recommendation Statement. JAMA 2018; 319(18):1901–1913. doi:10.1001/jama.2018.3710
- Humphrey L, Deffebach M, Pappas M, et al. Screening for lung cancer: systematic review to update the US Preventive Services Task Force Recommendation. www.ncbi.nlm.nih.gov/books/NBK154610. Accessed February 13, 2019.
- Kopans DB. A review of: “Tipping the balance of benefits and harms to favor screening mammography starting at age 40 years.” www.sbi-online.org/Portals/0/downloads/documents/pdfs/A%20review%20of%20Tipping%20the%20Balance%20of%20Benefits%20and%20Harms%20to%20Favor%20Screening%20Mammography%20Starting%20at%20Age%2040%20Years%20-%20Kopans.pdf. Accessed February 13, 2019.
- Yaffe M, Gordon, P. Routine mammograms do save lives: U of T expert. U of T News. www.utoronto.ca/news/routine-mammograms-do-save-lives-u-t-expert. Accessed February 13, 2019.
- Lin JS, Piper MA, Perdue LA, et al. Screening for colorectal cancer: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA 2016; 315(23):2576–2594. doi:10.1001/jama.2016.3332
- Knudsen AB, Zauber AG, Rutter CM, et al. Estimation of benefits, burden, and harms of colorectal cancer screening strategies: modeling study for the US Preventive Services Task Force. JAMA 2016; 315(23):2595–2609. doi:10.1001/jama.2016.6828
- Schröder FH, Hugosson J, Roobol MJ, et al; ERSPC Investigators. Screening and prostate cancer mortality: results of the European Randomised Study of Screening for Prostate Cancer (ERSPC) at 13 years of follow-up. Lancet 2014; 384(9959):2027–2035. doi:10.1016/S0140-6736(14)60525-0
I have been assured by a very knowing American of my acquaintance in London, that a young healthy child well nursed is at a year old, a most delicious, nourishing, and wholesome food, whether stewed, roasted, baked, or boiled, and I make no doubt that it will equally serve in a fricassee, or ragout.
—Jonathan Swift, A Modest Proposal1
Large-scale cancer screening programs have the unintended consequences of false-positive results and overdiagnosis, leading to anxiety and overtreatment. The magnitude of these harms continues to be clarified after decades of screening.
Recognizing the trade-off between benefits and harms, the US Preventive Services Task Force (USPSTF) has changed several of its recommendations in recent years. Breast cancer screening recommendations have gone from yearly mammograms starting at age 40 to biennial mammograms starting at age 50 for women at average risk.2 Prostate cancer screening is no longer recommended for men age 70 and older, and even for men between 55 and 69, screening is now an individual decision.3
Newer screening programs are targeting high-risk groups rather than the general population, with the aim of increasing the likelihood of benefits and limiting the harms. For example, lung cancer screening is recommended only for current smokers or smokers who have quit within the past 15 years, are between 55 and 80, and have at least a 30 pack-year smoking history.4
The movement toward less-frequent screening and screening in a narrower population has evoked strong reactions from advocates of cancer screening. One professor of radiology writes, “It borders on unethical to suggest that the benefit of having your life saved by screening and living another 40 years can be balanced against the ‘harm’ of being recalled for additional mammographic views for what proves to not be a cancer.”5 Another notes, “It does not make any sense to throw away the lives saved by screening to avoid over-treating a small number of cancers.”6 Both of these authors defend the position that the goal of screening is to minimize cause-specific mortality, irrespective of overdiagnosis, overtreatment, or false-positive results. In other words, harm should have little to no weight in screening recommendations.
Although the debate on cancer screening is moving toward a more balanced discussion of benefits and harms, many patients are still subjected to screening that is more aggressive than the USPSTF recommends, which may be due to an underlying belief that no harm is greater than the benefit of saving a life.
IS MORE-AGGRESSIVE SCREENING THE ANSWER?
One may wonder if more-aggressive screening could prevent deaths that occur despite standard screening. For example, more-frequent screening or use of additional screening methods such as ultrasonography or magnetic resonance imaging has been suggested for patients at high risk of breast cancer.
A MODEST PROPOSAL
If one holds the view that benefits alone should be considered when writing recommendations about screening, the logical conclusion extends beyond screening. We would therefore like to propose a different approach to reducing cancer deaths in the general population:
Why not just remove everybody’s breasts, prostate gland, and colon before cancer arises?
TO CUT IS TO PREVENT
Currently, we offer prophylactic surgery to patients at high risk of cancer. For example, women with BRCA1/BRCA2 mutations are offered prophylactic mastectomy as one of several options for reducing risk of breast cancer. In 2013, the first case of prophylactic prostatectomy was performed in a man who had a BRCA1/BRCA2 mutation. Total colectomy is considered in men and women who have hereditary nonpolyposis colon cancer, instead of segmental resection, to prevent future cancer.
If prophylactic surgery were extended to the general population, it would greatly reduce the number of cancer deaths. Assuming that removing an organ almost always precludes development of cancer, we may predict that prophylactic mastectomy, prostatectomy, or colectomy would save the lives of most of the patients who are still dying of cancer of these organs. The effectiveness rates would approach, but not reach 100%; such is the case with prophylactic mastectomy.
Consider prostate-specific antigen (PSA) screening. Even using the favorable estimate of the impact of PSA screening, arising from the European Randomised Study of Screening for Prostate Cancer trial, 27 men have to be diagnosed, most undergoing local therapy (the trial was conducted before active surveillance became routine), to avert 1 death from prostate cancer over 13 years.9
Contrast this “number needed to diagnose” with the number needed to treat for a strategy of routine prostate removal at age 45 or 50. Given that the lifetime risk of death from prostate cancer approaches 3%, and few cases arise before this age, a prophylactic surgical strategy would avert 1 death per 33 operations. If proponents of screening are willing to accept a number needed to diagnose of 27 over a 13-year interval, they may be willing to consider a number needed to treat of 33 over a lifetime.
There may be harms such as perioperative and postoperative complications. Mastectomy could lead to emotional stress from altered body image. Prostatectomy can have long-term complications such as urinary incontinence and sexual dysfunction. Nevertheless, prophylactic organ removal would save far more lives than current screening practices. It also could decrease mental burden, as patients could rest assured that they will never develop cancer, whereas screening often involves ambiguous test results, follow-up tests, and interventions, increasing patient anxiety.
FINDING THE BALANCE BETWEEN BENEFITS AND HARMS
In truth, we do not really advocate universal mastectomy, prostatectomy, and colectomy to prevent cancer, no more than Swift1 really wanted to eat the children of Ireland to alleviate poverty and famine in that country. Rather, we use it as an extreme proposal to highlight the scope and depth of harms that inevitably arise from screening.
If proponents of aggressive screening believe that the goal is to reduce cause-specific mortality as much as possible, giving little weight or consideration to overdiagnosis and overtreatment, then they ought to embrace universal prophylactic surgery as well. Recognition of this logical consequence reminds us that we must make screening recommendations that balance benefits and harms.
Considering an extreme perspective can help in recognizing our bias toward saving lives from cancer and discounting the harms. Aggravating this bias, it is impossible to know whether an individual patient has avoided fatal cancer or undergone unnecessary treatment. Moreover, changing practice is more difficult if it involves rolling back interventions that were once the standard.
Balancing benefits and harms is especially difficult when trying to compare the benefit of preventing a single cancer death against a harm that is less serious but more common. Medicine has always involved difficult trade-offs, as seen in cost-benefit analysis of new treatments or balancing quality of life with quantity of life in a single patient. In addition, each individual may place different values on benefits of screening and avoiding possible harms.
There is an undeniable trade-off with screening, and we must make a conscious decision on where to draw the line when harms outweigh the benefits. We must proceed with caution when subjecting large numbers of men and women to the possibility of psychological burden and decreased quality of life.
Given the growing appreciation of the harms of screening, it is likely that future guidance will continue to move toward less- frequent screening or focusing resources on high-risk populations, where the absolute magnitude of benefit is greater. Cancer screening is also likely to become an individual decision based on personal values and informed decisions.
I have been assured by a very knowing American of my acquaintance in London, that a young healthy child well nursed is at a year old, a most delicious, nourishing, and wholesome food, whether stewed, roasted, baked, or boiled, and I make no doubt that it will equally serve in a fricassee, or ragout.
—Jonathan Swift, A Modest Proposal1
Large-scale cancer screening programs have the unintended consequences of false-positive results and overdiagnosis, leading to anxiety and overtreatment. The magnitude of these harms continues to be clarified after decades of screening.
Recognizing the trade-off between benefits and harms, the US Preventive Services Task Force (USPSTF) has changed several of its recommendations in recent years. Breast cancer screening recommendations have gone from yearly mammograms starting at age 40 to biennial mammograms starting at age 50 for women at average risk.2 Prostate cancer screening is no longer recommended for men age 70 and older, and even for men between 55 and 69, screening is now an individual decision.3
Newer screening programs are targeting high-risk groups rather than the general population, with the aim of increasing the likelihood of benefits and limiting the harms. For example, lung cancer screening is recommended only for current smokers or smokers who have quit within the past 15 years, are between 55 and 80, and have at least a 30 pack-year smoking history.4
The movement toward less-frequent screening and screening in a narrower population has evoked strong reactions from advocates of cancer screening. One professor of radiology writes, “It borders on unethical to suggest that the benefit of having your life saved by screening and living another 40 years can be balanced against the ‘harm’ of being recalled for additional mammographic views for what proves to not be a cancer.”5 Another notes, “It does not make any sense to throw away the lives saved by screening to avoid over-treating a small number of cancers.”6 Both of these authors defend the position that the goal of screening is to minimize cause-specific mortality, irrespective of overdiagnosis, overtreatment, or false-positive results. In other words, harm should have little to no weight in screening recommendations.
Although the debate on cancer screening is moving toward a more balanced discussion of benefits and harms, many patients are still subjected to screening that is more aggressive than the USPSTF recommends, which may be due to an underlying belief that no harm is greater than the benefit of saving a life.
IS MORE-AGGRESSIVE SCREENING THE ANSWER?
One may wonder if more-aggressive screening could prevent deaths that occur despite standard screening. For example, more-frequent screening or use of additional screening methods such as ultrasonography or magnetic resonance imaging has been suggested for patients at high risk of breast cancer.
A MODEST PROPOSAL
If one holds the view that benefits alone should be considered when writing recommendations about screening, the logical conclusion extends beyond screening. We would therefore like to propose a different approach to reducing cancer deaths in the general population:
Why not just remove everybody’s breasts, prostate gland, and colon before cancer arises?
TO CUT IS TO PREVENT
Currently, we offer prophylactic surgery to patients at high risk of cancer. For example, women with BRCA1/BRCA2 mutations are offered prophylactic mastectomy as one of several options for reducing risk of breast cancer. In 2013, the first case of prophylactic prostatectomy was performed in a man who had a BRCA1/BRCA2 mutation. Total colectomy is considered in men and women who have hereditary nonpolyposis colon cancer, instead of segmental resection, to prevent future cancer.
If prophylactic surgery were extended to the general population, it would greatly reduce the number of cancer deaths. Assuming that removing an organ almost always precludes development of cancer, we may predict that prophylactic mastectomy, prostatectomy, or colectomy would save the lives of most of the patients who are still dying of cancer of these organs. The effectiveness rates would approach, but not reach 100%; such is the case with prophylactic mastectomy.
Consider prostate-specific antigen (PSA) screening. Even using the favorable estimate of the impact of PSA screening, arising from the European Randomised Study of Screening for Prostate Cancer trial, 27 men have to be diagnosed, most undergoing local therapy (the trial was conducted before active surveillance became routine), to avert 1 death from prostate cancer over 13 years.9
Contrast this “number needed to diagnose” with the number needed to treat for a strategy of routine prostate removal at age 45 or 50. Given that the lifetime risk of death from prostate cancer approaches 3%, and few cases arise before this age, a prophylactic surgical strategy would avert 1 death per 33 operations. If proponents of screening are willing to accept a number needed to diagnose of 27 over a 13-year interval, they may be willing to consider a number needed to treat of 33 over a lifetime.
There may be harms such as perioperative and postoperative complications. Mastectomy could lead to emotional stress from altered body image. Prostatectomy can have long-term complications such as urinary incontinence and sexual dysfunction. Nevertheless, prophylactic organ removal would save far more lives than current screening practices. It also could decrease mental burden, as patients could rest assured that they will never develop cancer, whereas screening often involves ambiguous test results, follow-up tests, and interventions, increasing patient anxiety.
FINDING THE BALANCE BETWEEN BENEFITS AND HARMS
In truth, we do not really advocate universal mastectomy, prostatectomy, and colectomy to prevent cancer, no more than Swift1 really wanted to eat the children of Ireland to alleviate poverty and famine in that country. Rather, we use it as an extreme proposal to highlight the scope and depth of harms that inevitably arise from screening.
If proponents of aggressive screening believe that the goal is to reduce cause-specific mortality as much as possible, giving little weight or consideration to overdiagnosis and overtreatment, then they ought to embrace universal prophylactic surgery as well. Recognition of this logical consequence reminds us that we must make screening recommendations that balance benefits and harms.
Considering an extreme perspective can help in recognizing our bias toward saving lives from cancer and discounting the harms. Aggravating this bias, it is impossible to know whether an individual patient has avoided fatal cancer or undergone unnecessary treatment. Moreover, changing practice is more difficult if it involves rolling back interventions that were once the standard.
Balancing benefits and harms is especially difficult when trying to compare the benefit of preventing a single cancer death against a harm that is less serious but more common. Medicine has always involved difficult trade-offs, as seen in cost-benefit analysis of new treatments or balancing quality of life with quantity of life in a single patient. In addition, each individual may place different values on benefits of screening and avoiding possible harms.
There is an undeniable trade-off with screening, and we must make a conscious decision on where to draw the line when harms outweigh the benefits. We must proceed with caution when subjecting large numbers of men and women to the possibility of psychological burden and decreased quality of life.
Given the growing appreciation of the harms of screening, it is likely that future guidance will continue to move toward less- frequent screening or focusing resources on high-risk populations, where the absolute magnitude of benefit is greater. Cancer screening is also likely to become an individual decision based on personal values and informed decisions.
- Swift J. A Modest Proposal for Preventing the Children of Poor People in Ireland, from Being a Burden on Their Parents or Country, and for Making Them Beneficial to the Publick. Dublin: S. Harding, 1729.
- Nelson HD, Cantor A, Humphrey L, et al. Screening for breast cancer: a systematic review to update the 2009 US Preventive Services Task Force Recommendation. www.ncbi.nlm.nih.gov/books/NBK343819. Accessed February 13, 2019.
- US Preventive Services Task Force; Grossman DC, Curry SJ, Owens DK, et al. Screening for prostate cancer: US Preventive Services Task Force Recommendation Statement. JAMA 2018; 319(18):1901–1913. doi:10.1001/jama.2018.3710
- Humphrey L, Deffebach M, Pappas M, et al. Screening for lung cancer: systematic review to update the US Preventive Services Task Force Recommendation. www.ncbi.nlm.nih.gov/books/NBK154610. Accessed February 13, 2019.
- Kopans DB. A review of: “Tipping the balance of benefits and harms to favor screening mammography starting at age 40 years.” www.sbi-online.org/Portals/0/downloads/documents/pdfs/A%20review%20of%20Tipping%20the%20Balance%20of%20Benefits%20and%20Harms%20to%20Favor%20Screening%20Mammography%20Starting%20at%20Age%2040%20Years%20-%20Kopans.pdf. Accessed February 13, 2019.
- Yaffe M, Gordon, P. Routine mammograms do save lives: U of T expert. U of T News. www.utoronto.ca/news/routine-mammograms-do-save-lives-u-t-expert. Accessed February 13, 2019.
- Lin JS, Piper MA, Perdue LA, et al. Screening for colorectal cancer: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA 2016; 315(23):2576–2594. doi:10.1001/jama.2016.3332
- Knudsen AB, Zauber AG, Rutter CM, et al. Estimation of benefits, burden, and harms of colorectal cancer screening strategies: modeling study for the US Preventive Services Task Force. JAMA 2016; 315(23):2595–2609. doi:10.1001/jama.2016.6828
- Schröder FH, Hugosson J, Roobol MJ, et al; ERSPC Investigators. Screening and prostate cancer mortality: results of the European Randomised Study of Screening for Prostate Cancer (ERSPC) at 13 years of follow-up. Lancet 2014; 384(9959):2027–2035. doi:10.1016/S0140-6736(14)60525-0
- Swift J. A Modest Proposal for Preventing the Children of Poor People in Ireland, from Being a Burden on Their Parents or Country, and for Making Them Beneficial to the Publick. Dublin: S. Harding, 1729.
- Nelson HD, Cantor A, Humphrey L, et al. Screening for breast cancer: a systematic review to update the 2009 US Preventive Services Task Force Recommendation. www.ncbi.nlm.nih.gov/books/NBK343819. Accessed February 13, 2019.
- US Preventive Services Task Force; Grossman DC, Curry SJ, Owens DK, et al. Screening for prostate cancer: US Preventive Services Task Force Recommendation Statement. JAMA 2018; 319(18):1901–1913. doi:10.1001/jama.2018.3710
- Humphrey L, Deffebach M, Pappas M, et al. Screening for lung cancer: systematic review to update the US Preventive Services Task Force Recommendation. www.ncbi.nlm.nih.gov/books/NBK154610. Accessed February 13, 2019.
- Kopans DB. A review of: “Tipping the balance of benefits and harms to favor screening mammography starting at age 40 years.” www.sbi-online.org/Portals/0/downloads/documents/pdfs/A%20review%20of%20Tipping%20the%20Balance%20of%20Benefits%20and%20Harms%20to%20Favor%20Screening%20Mammography%20Starting%20at%20Age%2040%20Years%20-%20Kopans.pdf. Accessed February 13, 2019.
- Yaffe M, Gordon, P. Routine mammograms do save lives: U of T expert. U of T News. www.utoronto.ca/news/routine-mammograms-do-save-lives-u-t-expert. Accessed February 13, 2019.
- Lin JS, Piper MA, Perdue LA, et al. Screening for colorectal cancer: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA 2016; 315(23):2576–2594. doi:10.1001/jama.2016.3332
- Knudsen AB, Zauber AG, Rutter CM, et al. Estimation of benefits, burden, and harms of colorectal cancer screening strategies: modeling study for the US Preventive Services Task Force. JAMA 2016; 315(23):2595–2609. doi:10.1001/jama.2016.6828
- Schröder FH, Hugosson J, Roobol MJ, et al; ERSPC Investigators. Screening and prostate cancer mortality: results of the European Randomised Study of Screening for Prostate Cancer (ERSPC) at 13 years of follow-up. Lancet 2014; 384(9959):2027–2035. doi:10.1016/S0140-6736(14)60525-0
Motherhood and the working psychiatrist
Raising a child is difficult. For working professional women, including doctors, that difficulty extends beyond bottles, bath time, and burping; it impacts day-to-day physiological function, time management, and emotional well-being.
The 1950s upheld a family model with traditional gender roles. By 1960, the family portrait of a breadwinner father and a stay-at-home mother with one or more children comprised 62% of American households.1 Precipitous changes occurred over the next decades as the housing market soared, education costs increased, and divorce rates rose. The 1980s ushered the arrival of women’s power suits and the notion of women “having it all.”1
Fast-forward to modern times. Medicine is changing, too. Women are slowly but surely starting to rise in this once male-led field. In 2017, for the first time more women than men enrolled in medical schools in the United States.2 In a 2015 report, the Association of American Medical Colleges found that 57% of residents who were pursuing psychiatry were women.3 And the median age of women applying to medical school who enrolled in 2017 or 2018 was 23 years.4
Choosing to parent as a physician poses challenges for women and men alike. As the rates of women in medicine and psychiatry are increasing, this article focuses on unique obstacles faced by mothers and aims to:
- explore the dueling duties of mothers who practice medicine
- consider the dilemma women face when returning to the workforce during the postpartum period
- discuss options for enhanced recognition and care of maternal and child well-being.
Duty: Being both parent and physician
The working psychiatrist mother has a duty to her patients and profession—not to mention a duty to her child. The demands are endless on both sides. No matter what stage of her professional career (medical school, residency, fellowship, or beyond) she chooses to begin motherhood, the responsibilities and expectations can be overwhelming. Doctor appointments, nausea and vomiting, fatigue, discomfort, and stress do not fit well within a schedule of intensive studying, working 24-hour shifts, navigating complex schedules, treating patients, and sorting out the financial heft of loan repayment, home ownership, contract negotiation, or relocation.5
Psychiatry carries a notable dichotomy of lecturing at length on the importance of maternal-infant attachment. John Bowlby argued that a child’s attachment to the mother is instinctual and primary, noting that early loss creates true mourning due to the primal ties of child to mother.6 Bowlby also asserted that personality development and psychopathology are rooted in the concept of attachment and the emotional security built through early childhood experiences.6
Continue to: Dr. Donald Winnnicott introduced the concept of...
Dr. Donald Winnicott introduced the concept of a “good-enough” mother in 1953.7 Today, although Winnicott’s teachings are explored in psychiatry training programs and practice, his concept does not resonate with many working mothers. Most physicians strive for perfection while struggling to balance their personal and professional lives.7
It’s no wonder that tales abound of female physicians being praised for their ability to take on grueling shifts up to their due date, forego lunch to pump breast milk, or cover shifts beyond child daycare closing times. This raises an interesting dilemma: Is the primary goal the efficiency of promoting commerce, patient numbers, and the workings of the health care system? Or is it the wellness of expecting mothers and the development and attachment of an infant to the parent? Is the goal to slowly and carefully craft our next generation of young humans? Or is there a way to “have it all”?
Dilemma: Misperceptions after returning to work
As they regain control of their bodies, sleep, and overall health, women who return to work during the postpartum period battle a myriad of misperceptions along with the logistical hurdles of breast-feeding. In a study of surgical residencies, 61% of program directors reported that female trainees’ work was negatively affected by becoming parents.8 But other evidence suggests there is a disparity between perception and reality.
As a result, misperceptions can negatively affect maternity leave or lactation time. Women often rightfully fear they may be viewed as taking leisure time or making convenient excuses to shirk responsibility, rather than focusing on the necessities for recovery, care, and bonding. Such pressures can lead to burnout and resentment. The struggle with breast-feeding is pervasive across all medical specialties. In a 2018 survey of 347 women who had children during surgical residency, 39% of respondents strongly considered leaving their training, 95.6% indicated that breast-feeding was important to them, and 58.1% stopped breast-feeding earlier than desired due to challenges faced in the workplace, such as poor access to lactation facilities and difficulty leaving the operating room to express milk.11
The American Academy of Pediatrics (AAP) recommends exclusive breast-feeding through 6 months of the postpartum period, and continued breast-feeding until the infant is at least 12 months old. Breast-feeding confers benefits to both the infant and mother, including positive impacts on the child’s cognitive development and health into adulthood, as well as higher productivity and lower absenteeism for breast-feeding mothers.12 By 2009, only 23 states had adopted laws to encourage breast-feeding in the workplace. In 2010, the United States government enacted the “reasonable break time” provision in Section 4207 of the Patient Protection and Affordable Care Act (ACA), which requires all employers to provide a period of time and private space other than a bathroom in which female employees can express milk for a child up to age 1.12
Continue to: In 2016...
In 2016, a follow-up national survey of employed women explored workplace changes after the ACA, and noted that only 40% of women had access to both break time and a private space for lactation.13 If the goal is to give working women a true choice of whether to continue breast-feeding after returning to work, these mothers need to be provided with the proper social and structural supports in order to allow for that personal decision.14
Discussion: Barriers to change
Breast-feeding, it has been argued, is the most enduring investment in women’s physical, cognitive, and social capacities, and provides protection for children against death, disease, and poverty.15 Research has shown that breast-feeding every child until age 1 would yield medical benefits, including fewer infections, increased intelligence in children, protection against breast cancer in mothers, and economic savings of $300 billion for the United States.15
We are no longer in the 1950s, but modern times still present challenges for mothers who are working as physicians. Although the AAP recommends that new parents receive 12 weeks leave from work, policies for faculty at the 12 top medical schools in the United States offer new mothers only approximately 2 months of paid leave.16 There also are problems of inconsistency among approaches to parenthood in graduate medical education (GME) training, different specialty clinical requirements, and different residency training programs. These factors all contribute to negative attitudes towards parenthood.17
We know the barriers for women.18 With more women entering the medical profession, we need to continue finding creative and workable solutions as these problems become more pressing.19 In a 2018 Time article, Lily Rothman wrote, “you can’t talk about breastfeeding in the United States without pointing out that every other wealthy country has found a way to accommodate breastfeeding mothers, and usually in the form of lengthy paid maternity leave.”20 However, maternity leave in the United States today dictates that mothers return to work while their children would still benefit from nursing.21
When it comes to GME and medical institutions, programs could look at barriers such as lack of accommodations for trainees who are pregnant or have young children. Addressing these barriers could include making private lactation rooms available and instituting flexible scheduling. It would be best if scheduling accommodations and policies were established by an institution’s administration, rather than leaving coverage up to the students or residents. Going further, institutions could consider offering flexible maternity leave and work schedules, allowing breaks for those who are breast-feeding, and creating lactation facilities.22 This could take the form of a breast-feeding support program that fits available budget resources.23
Continue to: Psychiatrists frequently discuss...
Psychiatrists frequently discuss Winnicott’s “good-enough mother” concept, with the mother transitioning from focusing on her baby’s needs to her own sense of personhood that is unable to respond to her baby’s every wish.6 This concept was established well before the shifting demographics of the nuclear family, the short maternity leaves and early returns to work, early separation of one’s infants to childcare settings, and experiences with pumped lactation milk that working mothers experience today. Is it any wonder childbearing female psychiatrists face a special kind of working-mother guilt?
1. Collins G. When everything changed: the amazing journey of American women from 1960 to the present. New York, NY: Little, Brown and Company; 2009;271, 301.
2. AAMCNews. More women than men enrolled in U.S. medical schools in 2017. Association of American Medical Colleges. https://news.aamc.org/press-releases/article/applicant-enrollment-2017/. Published December 18, 2017. Accessed November 21, 2018.
3. Vassar L. How medical specialties vary by gender. American Medical Association. https://wire.ama-assn.org/education/how-medical-specialties-vary-gender. Published February 18, 2015. Accessed November 21, 2018.
4. Association of American Medical Colleges. Table A-6: age of applicants to U.S. medical schools at anticipated matriculation by sex and race/ethnicity, 2014-2015 through 2017-2018. https://www.aamc.org/download/321468/data/factstablea6.pdf. Published November 30, 2017. Accessed February 7, 2019.
5. Jones V. Best time to have a baby as a physician? It depends. Doximity. https://opmed.doximity.com/articles/the-best-time-to-have-a-baby-as-a-physician-it-depends-c8064a92156c. Published September 11, 2017. Accessed November 21, 2018.
6. Mitchell SA, Black MJ. The British object relations school: W.R.D. Fairbairn and D.W. Winnicott. In: Freud and beyond: a history of modern psychoanalytic thought. New York, NY: Basic Books; 1995:125-126, 137.
7. Ratnapalan S, Batty H. To be good enough. Can Fam Physician. 2009;55(3):239-242.
8. Sandler BJ, Tackett JJ, Longo WE, et al. Pregnancy and parenthood among surgery residents: results of the first nationwide survey of general surgery residency program Directors. J Am Coll Surg. 2016;222(6):1090-1096.
9. Kmec JA. Are motherhood penalties and fatherhood bonuses warranted? Comparing pro-work behaviors and conditions of mothers, fathers, and non-parents. Social Science Research. 2011;40(2):444-459.
10. Hampton R. Working moms don’t deserve the blame for unfair work expectations. Slate. https://slate.com/human-interest/2018/05/working-moms-dont-deserve-blame-for-unfair-work-expectations.html. Published May 18, 2018. Accessed November 25, 2018.
11. Rangel EL, Smink DS, Castillo-Angeles M, et al. Pregnancy and motherhood during surgical training. JAMA Surgery. 2018;153(7):644-652.
12. Murtagh L, Moulton AD. Working mothers, breastfeeding, and the law. Am J Public Health. 2011;101(2):217-223.
13. Kozhimannil KB, Jou J, Gjerdingen DK, et al. Access to workplace accommodations to support breastfeeding after passage of the Affordable Care Act. Womens Health Issues. 2016;26(1):6-13.
14. Dinour LM, Bai YK. Breastfeeding: the illusion of choice. Womens Health Issues. 2016;26(5):479-482.
15. Hansen K. Breastfeeding: a smart investment in people and in economies. Lancet. 2016;387(10017):416.
16. Greenfield R. Even America’s top doctors aren’t getting the parental leave doctors recommend. Bloomberg. https://www.bloomberg.com/news/articles/2018-02-13/even-america-s-top-doctors-aren-t-getting-the-parental-leave-doctors-recommend. Published February 13, 2018. Accessed November 21, 2018.
17. Humphries LS, Lyon S, Garza R, et al. Parental leave policies in graduate medical education: a systematic review. American J Surg. 2017;214(4):634-639.
18. Raju TNK. Continued barriers for breast-feeding in public and the workplace. J Pediatr. 2006;148(5):677-679.
19. Stewart DE, Robinson GE. Combining motherhood with psychiatric training and practice. Can J Psychiatry. 1985;30(1):28-34.
20. Rothman L. D esperate women, desperate doctors and the surprising history behind the breastfeeding debate. Time. http://time.com/5353068/breastfeeding-debate-history/. Published July 31, 2018. Accessed November 21, 2018.
21. Livingston G. Among 41 nations, U.S. is the outlier when it comes to paid parental leave. Pew Research Center. http://www.pewresearch.org/fact-tank/2016/09/26/u-s-lacks-mandated-paid-parental-leave/. Published September 26, 2016. Accessed November 21, 2018.
22. McCluskey PD. Long hours, short leaves force moms to reconsider jobs as surgeons. Boston Globe. https://www.bostonglobe.com/metro/2018/03/21/new-survey-says-female-surgical-residents-struggle-balance-training-motherhood/2ENQU1aPZmIJYy20iaRlLL/story.html. Published March 21, 2018. Accessed November 21, 2018.
23. Dinour LM, Szaro JM. Employer-based programs to support breastfeeding among working mothers: a systematic review. Breastfeeding Med. 2017;12:131-141.
Raising a child is difficult. For working professional women, including doctors, that difficulty extends beyond bottles, bath time, and burping; it impacts day-to-day physiological function, time management, and emotional well-being.
The 1950s upheld a family model with traditional gender roles. By 1960, the family portrait of a breadwinner father and a stay-at-home mother with one or more children comprised 62% of American households.1 Precipitous changes occurred over the next decades as the housing market soared, education costs increased, and divorce rates rose. The 1980s ushered the arrival of women’s power suits and the notion of women “having it all.”1
Fast-forward to modern times. Medicine is changing, too. Women are slowly but surely starting to rise in this once male-led field. In 2017, for the first time more women than men enrolled in medical schools in the United States.2 In a 2015 report, the Association of American Medical Colleges found that 57% of residents who were pursuing psychiatry were women.3 And the median age of women applying to medical school who enrolled in 2017 or 2018 was 23 years.4
Choosing to parent as a physician poses challenges for women and men alike. As the rates of women in medicine and psychiatry are increasing, this article focuses on unique obstacles faced by mothers and aims to:
- explore the dueling duties of mothers who practice medicine
- consider the dilemma women face when returning to the workforce during the postpartum period
- discuss options for enhanced recognition and care of maternal and child well-being.
Duty: Being both parent and physician
The working psychiatrist mother has a duty to her patients and profession—not to mention a duty to her child. The demands are endless on both sides. No matter what stage of her professional career (medical school, residency, fellowship, or beyond) she chooses to begin motherhood, the responsibilities and expectations can be overwhelming. Doctor appointments, nausea and vomiting, fatigue, discomfort, and stress do not fit well within a schedule of intensive studying, working 24-hour shifts, navigating complex schedules, treating patients, and sorting out the financial heft of loan repayment, home ownership, contract negotiation, or relocation.5
Psychiatry carries a notable dichotomy of lecturing at length on the importance of maternal-infant attachment. John Bowlby argued that a child’s attachment to the mother is instinctual and primary, noting that early loss creates true mourning due to the primal ties of child to mother.6 Bowlby also asserted that personality development and psychopathology are rooted in the concept of attachment and the emotional security built through early childhood experiences.6
Continue to: Dr. Donald Winnnicott introduced the concept of...
Dr. Donald Winnicott introduced the concept of a “good-enough” mother in 1953.7 Today, although Winnicott’s teachings are explored in psychiatry training programs and practice, his concept does not resonate with many working mothers. Most physicians strive for perfection while struggling to balance their personal and professional lives.7
It’s no wonder that tales abound of female physicians being praised for their ability to take on grueling shifts up to their due date, forego lunch to pump breast milk, or cover shifts beyond child daycare closing times. This raises an interesting dilemma: Is the primary goal the efficiency of promoting commerce, patient numbers, and the workings of the health care system? Or is it the wellness of expecting mothers and the development and attachment of an infant to the parent? Is the goal to slowly and carefully craft our next generation of young humans? Or is there a way to “have it all”?
Dilemma: Misperceptions after returning to work
As they regain control of their bodies, sleep, and overall health, women who return to work during the postpartum period battle a myriad of misperceptions along with the logistical hurdles of breast-feeding. In a study of surgical residencies, 61% of program directors reported that female trainees’ work was negatively affected by becoming parents.8 But other evidence suggests there is a disparity between perception and reality.
As a result, misperceptions can negatively affect maternity leave or lactation time. Women often rightfully fear they may be viewed as taking leisure time or making convenient excuses to shirk responsibility, rather than focusing on the necessities for recovery, care, and bonding. Such pressures can lead to burnout and resentment. The struggle with breast-feeding is pervasive across all medical specialties. In a 2018 survey of 347 women who had children during surgical residency, 39% of respondents strongly considered leaving their training, 95.6% indicated that breast-feeding was important to them, and 58.1% stopped breast-feeding earlier than desired due to challenges faced in the workplace, such as poor access to lactation facilities and difficulty leaving the operating room to express milk.11
The American Academy of Pediatrics (AAP) recommends exclusive breast-feeding through 6 months of the postpartum period, and continued breast-feeding until the infant is at least 12 months old. Breast-feeding confers benefits to both the infant and mother, including positive impacts on the child’s cognitive development and health into adulthood, as well as higher productivity and lower absenteeism for breast-feeding mothers.12 By 2009, only 23 states had adopted laws to encourage breast-feeding in the workplace. In 2010, the United States government enacted the “reasonable break time” provision in Section 4207 of the Patient Protection and Affordable Care Act (ACA), which requires all employers to provide a period of time and private space other than a bathroom in which female employees can express milk for a child up to age 1.12
Continue to: In 2016...
In 2016, a follow-up national survey of employed women explored workplace changes after the ACA, and noted that only 40% of women had access to both break time and a private space for lactation.13 If the goal is to give working women a true choice of whether to continue breast-feeding after returning to work, these mothers need to be provided with the proper social and structural supports in order to allow for that personal decision.14
Discussion: Barriers to change
Breast-feeding, it has been argued, is the most enduring investment in women’s physical, cognitive, and social capacities, and provides protection for children against death, disease, and poverty.15 Research has shown that breast-feeding every child until age 1 would yield medical benefits, including fewer infections, increased intelligence in children, protection against breast cancer in mothers, and economic savings of $300 billion for the United States.15
We are no longer in the 1950s, but modern times still present challenges for mothers who are working as physicians. Although the AAP recommends that new parents receive 12 weeks leave from work, policies for faculty at the 12 top medical schools in the United States offer new mothers only approximately 2 months of paid leave.16 There also are problems of inconsistency among approaches to parenthood in graduate medical education (GME) training, different specialty clinical requirements, and different residency training programs. These factors all contribute to negative attitudes towards parenthood.17
We know the barriers for women.18 With more women entering the medical profession, we need to continue finding creative and workable solutions as these problems become more pressing.19 In a 2018 Time article, Lily Rothman wrote, “you can’t talk about breastfeeding in the United States without pointing out that every other wealthy country has found a way to accommodate breastfeeding mothers, and usually in the form of lengthy paid maternity leave.”20 However, maternity leave in the United States today dictates that mothers return to work while their children would still benefit from nursing.21
When it comes to GME and medical institutions, programs could look at barriers such as lack of accommodations for trainees who are pregnant or have young children. Addressing these barriers could include making private lactation rooms available and instituting flexible scheduling. It would be best if scheduling accommodations and policies were established by an institution’s administration, rather than leaving coverage up to the students or residents. Going further, institutions could consider offering flexible maternity leave and work schedules, allowing breaks for those who are breast-feeding, and creating lactation facilities.22 This could take the form of a breast-feeding support program that fits available budget resources.23
Continue to: Psychiatrists frequently discuss...
Psychiatrists frequently discuss Winnicott’s “good-enough mother” concept, with the mother transitioning from focusing on her baby’s needs to her own sense of personhood that is unable to respond to her baby’s every wish.6 This concept was established well before the shifting demographics of the nuclear family, the short maternity leaves and early returns to work, early separation of one’s infants to childcare settings, and experiences with pumped lactation milk that working mothers experience today. Is it any wonder childbearing female psychiatrists face a special kind of working-mother guilt?
Raising a child is difficult. For working professional women, including doctors, that difficulty extends beyond bottles, bath time, and burping; it impacts day-to-day physiological function, time management, and emotional well-being.
The 1950s upheld a family model with traditional gender roles. By 1960, the family portrait of a breadwinner father and a stay-at-home mother with one or more children comprised 62% of American households.1 Precipitous changes occurred over the next decades as the housing market soared, education costs increased, and divorce rates rose. The 1980s ushered the arrival of women’s power suits and the notion of women “having it all.”1
Fast-forward to modern times. Medicine is changing, too. Women are slowly but surely starting to rise in this once male-led field. In 2017, for the first time more women than men enrolled in medical schools in the United States.2 In a 2015 report, the Association of American Medical Colleges found that 57% of residents who were pursuing psychiatry were women.3 And the median age of women applying to medical school who enrolled in 2017 or 2018 was 23 years.4
Choosing to parent as a physician poses challenges for women and men alike. As the rates of women in medicine and psychiatry are increasing, this article focuses on unique obstacles faced by mothers and aims to:
- explore the dueling duties of mothers who practice medicine
- consider the dilemma women face when returning to the workforce during the postpartum period
- discuss options for enhanced recognition and care of maternal and child well-being.
Duty: Being both parent and physician
The working psychiatrist mother has a duty to her patients and profession—not to mention a duty to her child. The demands are endless on both sides. No matter what stage of her professional career (medical school, residency, fellowship, or beyond) she chooses to begin motherhood, the responsibilities and expectations can be overwhelming. Doctor appointments, nausea and vomiting, fatigue, discomfort, and stress do not fit well within a schedule of intensive studying, working 24-hour shifts, navigating complex schedules, treating patients, and sorting out the financial heft of loan repayment, home ownership, contract negotiation, or relocation.5
Psychiatry carries a notable dichotomy of lecturing at length on the importance of maternal-infant attachment. John Bowlby argued that a child’s attachment to the mother is instinctual and primary, noting that early loss creates true mourning due to the primal ties of child to mother.6 Bowlby also asserted that personality development and psychopathology are rooted in the concept of attachment and the emotional security built through early childhood experiences.6
Continue to: Dr. Donald Winnnicott introduced the concept of...
Dr. Donald Winnicott introduced the concept of a “good-enough” mother in 1953.7 Today, although Winnicott’s teachings are explored in psychiatry training programs and practice, his concept does not resonate with many working mothers. Most physicians strive for perfection while struggling to balance their personal and professional lives.7
It’s no wonder that tales abound of female physicians being praised for their ability to take on grueling shifts up to their due date, forego lunch to pump breast milk, or cover shifts beyond child daycare closing times. This raises an interesting dilemma: Is the primary goal the efficiency of promoting commerce, patient numbers, and the workings of the health care system? Or is it the wellness of expecting mothers and the development and attachment of an infant to the parent? Is the goal to slowly and carefully craft our next generation of young humans? Or is there a way to “have it all”?
Dilemma: Misperceptions after returning to work
As they regain control of their bodies, sleep, and overall health, women who return to work during the postpartum period battle a myriad of misperceptions along with the logistical hurdles of breast-feeding. In a study of surgical residencies, 61% of program directors reported that female trainees’ work was negatively affected by becoming parents.8 But other evidence suggests there is a disparity between perception and reality.
As a result, misperceptions can negatively affect maternity leave or lactation time. Women often rightfully fear they may be viewed as taking leisure time or making convenient excuses to shirk responsibility, rather than focusing on the necessities for recovery, care, and bonding. Such pressures can lead to burnout and resentment. The struggle with breast-feeding is pervasive across all medical specialties. In a 2018 survey of 347 women who had children during surgical residency, 39% of respondents strongly considered leaving their training, 95.6% indicated that breast-feeding was important to them, and 58.1% stopped breast-feeding earlier than desired due to challenges faced in the workplace, such as poor access to lactation facilities and difficulty leaving the operating room to express milk.11
The American Academy of Pediatrics (AAP) recommends exclusive breast-feeding through 6 months of the postpartum period, and continued breast-feeding until the infant is at least 12 months old. Breast-feeding confers benefits to both the infant and mother, including positive impacts on the child’s cognitive development and health into adulthood, as well as higher productivity and lower absenteeism for breast-feeding mothers.12 By 2009, only 23 states had adopted laws to encourage breast-feeding in the workplace. In 2010, the United States government enacted the “reasonable break time” provision in Section 4207 of the Patient Protection and Affordable Care Act (ACA), which requires all employers to provide a period of time and private space other than a bathroom in which female employees can express milk for a child up to age 1.12
Continue to: In 2016...
In 2016, a follow-up national survey of employed women explored workplace changes after the ACA, and noted that only 40% of women had access to both break time and a private space for lactation.13 If the goal is to give working women a true choice of whether to continue breast-feeding after returning to work, these mothers need to be provided with the proper social and structural supports in order to allow for that personal decision.14
Discussion: Barriers to change
Breast-feeding, it has been argued, is the most enduring investment in women’s physical, cognitive, and social capacities, and provides protection for children against death, disease, and poverty.15 Research has shown that breast-feeding every child until age 1 would yield medical benefits, including fewer infections, increased intelligence in children, protection against breast cancer in mothers, and economic savings of $300 billion for the United States.15
We are no longer in the 1950s, but modern times still present challenges for mothers who are working as physicians. Although the AAP recommends that new parents receive 12 weeks leave from work, policies for faculty at the 12 top medical schools in the United States offer new mothers only approximately 2 months of paid leave.16 There also are problems of inconsistency among approaches to parenthood in graduate medical education (GME) training, different specialty clinical requirements, and different residency training programs. These factors all contribute to negative attitudes towards parenthood.17
We know the barriers for women.18 With more women entering the medical profession, we need to continue finding creative and workable solutions as these problems become more pressing.19 In a 2018 Time article, Lily Rothman wrote, “you can’t talk about breastfeeding in the United States without pointing out that every other wealthy country has found a way to accommodate breastfeeding mothers, and usually in the form of lengthy paid maternity leave.”20 However, maternity leave in the United States today dictates that mothers return to work while their children would still benefit from nursing.21
When it comes to GME and medical institutions, programs could look at barriers such as lack of accommodations for trainees who are pregnant or have young children. Addressing these barriers could include making private lactation rooms available and instituting flexible scheduling. It would be best if scheduling accommodations and policies were established by an institution’s administration, rather than leaving coverage up to the students or residents. Going further, institutions could consider offering flexible maternity leave and work schedules, allowing breaks for those who are breast-feeding, and creating lactation facilities.22 This could take the form of a breast-feeding support program that fits available budget resources.23
Continue to: Psychiatrists frequently discuss...
Psychiatrists frequently discuss Winnicott’s “good-enough mother” concept, with the mother transitioning from focusing on her baby’s needs to her own sense of personhood that is unable to respond to her baby’s every wish.6 This concept was established well before the shifting demographics of the nuclear family, the short maternity leaves and early returns to work, early separation of one’s infants to childcare settings, and experiences with pumped lactation milk that working mothers experience today. Is it any wonder childbearing female psychiatrists face a special kind of working-mother guilt?
1. Collins G. When everything changed: the amazing journey of American women from 1960 to the present. New York, NY: Little, Brown and Company; 2009;271, 301.
2. AAMCNews. More women than men enrolled in U.S. medical schools in 2017. Association of American Medical Colleges. https://news.aamc.org/press-releases/article/applicant-enrollment-2017/. Published December 18, 2017. Accessed November 21, 2018.
3. Vassar L. How medical specialties vary by gender. American Medical Association. https://wire.ama-assn.org/education/how-medical-specialties-vary-gender. Published February 18, 2015. Accessed November 21, 2018.
4. Association of American Medical Colleges. Table A-6: age of applicants to U.S. medical schools at anticipated matriculation by sex and race/ethnicity, 2014-2015 through 2017-2018. https://www.aamc.org/download/321468/data/factstablea6.pdf. Published November 30, 2017. Accessed February 7, 2019.
5. Jones V. Best time to have a baby as a physician? It depends. Doximity. https://opmed.doximity.com/articles/the-best-time-to-have-a-baby-as-a-physician-it-depends-c8064a92156c. Published September 11, 2017. Accessed November 21, 2018.
6. Mitchell SA, Black MJ. The British object relations school: W.R.D. Fairbairn and D.W. Winnicott. In: Freud and beyond: a history of modern psychoanalytic thought. New York, NY: Basic Books; 1995:125-126, 137.
7. Ratnapalan S, Batty H. To be good enough. Can Fam Physician. 2009;55(3):239-242.
8. Sandler BJ, Tackett JJ, Longo WE, et al. Pregnancy and parenthood among surgery residents: results of the first nationwide survey of general surgery residency program Directors. J Am Coll Surg. 2016;222(6):1090-1096.
9. Kmec JA. Are motherhood penalties and fatherhood bonuses warranted? Comparing pro-work behaviors and conditions of mothers, fathers, and non-parents. Social Science Research. 2011;40(2):444-459.
10. Hampton R. Working moms don’t deserve the blame for unfair work expectations. Slate. https://slate.com/human-interest/2018/05/working-moms-dont-deserve-blame-for-unfair-work-expectations.html. Published May 18, 2018. Accessed November 25, 2018.
11. Rangel EL, Smink DS, Castillo-Angeles M, et al. Pregnancy and motherhood during surgical training. JAMA Surgery. 2018;153(7):644-652.
12. Murtagh L, Moulton AD. Working mothers, breastfeeding, and the law. Am J Public Health. 2011;101(2):217-223.
13. Kozhimannil KB, Jou J, Gjerdingen DK, et al. Access to workplace accommodations to support breastfeeding after passage of the Affordable Care Act. Womens Health Issues. 2016;26(1):6-13.
14. Dinour LM, Bai YK. Breastfeeding: the illusion of choice. Womens Health Issues. 2016;26(5):479-482.
15. Hansen K. Breastfeeding: a smart investment in people and in economies. Lancet. 2016;387(10017):416.
16. Greenfield R. Even America’s top doctors aren’t getting the parental leave doctors recommend. Bloomberg. https://www.bloomberg.com/news/articles/2018-02-13/even-america-s-top-doctors-aren-t-getting-the-parental-leave-doctors-recommend. Published February 13, 2018. Accessed November 21, 2018.
17. Humphries LS, Lyon S, Garza R, et al. Parental leave policies in graduate medical education: a systematic review. American J Surg. 2017;214(4):634-639.
18. Raju TNK. Continued barriers for breast-feeding in public and the workplace. J Pediatr. 2006;148(5):677-679.
19. Stewart DE, Robinson GE. Combining motherhood with psychiatric training and practice. Can J Psychiatry. 1985;30(1):28-34.
20. Rothman L. D esperate women, desperate doctors and the surprising history behind the breastfeeding debate. Time. http://time.com/5353068/breastfeeding-debate-history/. Published July 31, 2018. Accessed November 21, 2018.
21. Livingston G. Among 41 nations, U.S. is the outlier when it comes to paid parental leave. Pew Research Center. http://www.pewresearch.org/fact-tank/2016/09/26/u-s-lacks-mandated-paid-parental-leave/. Published September 26, 2016. Accessed November 21, 2018.
22. McCluskey PD. Long hours, short leaves force moms to reconsider jobs as surgeons. Boston Globe. https://www.bostonglobe.com/metro/2018/03/21/new-survey-says-female-surgical-residents-struggle-balance-training-motherhood/2ENQU1aPZmIJYy20iaRlLL/story.html. Published March 21, 2018. Accessed November 21, 2018.
23. Dinour LM, Szaro JM. Employer-based programs to support breastfeeding among working mothers: a systematic review. Breastfeeding Med. 2017;12:131-141.
1. Collins G. When everything changed: the amazing journey of American women from 1960 to the present. New York, NY: Little, Brown and Company; 2009;271, 301.
2. AAMCNews. More women than men enrolled in U.S. medical schools in 2017. Association of American Medical Colleges. https://news.aamc.org/press-releases/article/applicant-enrollment-2017/. Published December 18, 2017. Accessed November 21, 2018.
3. Vassar L. How medical specialties vary by gender. American Medical Association. https://wire.ama-assn.org/education/how-medical-specialties-vary-gender. Published February 18, 2015. Accessed November 21, 2018.
4. Association of American Medical Colleges. Table A-6: age of applicants to U.S. medical schools at anticipated matriculation by sex and race/ethnicity, 2014-2015 through 2017-2018. https://www.aamc.org/download/321468/data/factstablea6.pdf. Published November 30, 2017. Accessed February 7, 2019.
5. Jones V. Best time to have a baby as a physician? It depends. Doximity. https://opmed.doximity.com/articles/the-best-time-to-have-a-baby-as-a-physician-it-depends-c8064a92156c. Published September 11, 2017. Accessed November 21, 2018.
6. Mitchell SA, Black MJ. The British object relations school: W.R.D. Fairbairn and D.W. Winnicott. In: Freud and beyond: a history of modern psychoanalytic thought. New York, NY: Basic Books; 1995:125-126, 137.
7. Ratnapalan S, Batty H. To be good enough. Can Fam Physician. 2009;55(3):239-242.
8. Sandler BJ, Tackett JJ, Longo WE, et al. Pregnancy and parenthood among surgery residents: results of the first nationwide survey of general surgery residency program Directors. J Am Coll Surg. 2016;222(6):1090-1096.
9. Kmec JA. Are motherhood penalties and fatherhood bonuses warranted? Comparing pro-work behaviors and conditions of mothers, fathers, and non-parents. Social Science Research. 2011;40(2):444-459.
10. Hampton R. Working moms don’t deserve the blame for unfair work expectations. Slate. https://slate.com/human-interest/2018/05/working-moms-dont-deserve-blame-for-unfair-work-expectations.html. Published May 18, 2018. Accessed November 25, 2018.
11. Rangel EL, Smink DS, Castillo-Angeles M, et al. Pregnancy and motherhood during surgical training. JAMA Surgery. 2018;153(7):644-652.
12. Murtagh L, Moulton AD. Working mothers, breastfeeding, and the law. Am J Public Health. 2011;101(2):217-223.
13. Kozhimannil KB, Jou J, Gjerdingen DK, et al. Access to workplace accommodations to support breastfeeding after passage of the Affordable Care Act. Womens Health Issues. 2016;26(1):6-13.
14. Dinour LM, Bai YK. Breastfeeding: the illusion of choice. Womens Health Issues. 2016;26(5):479-482.
15. Hansen K. Breastfeeding: a smart investment in people and in economies. Lancet. 2016;387(10017):416.
16. Greenfield R. Even America’s top doctors aren’t getting the parental leave doctors recommend. Bloomberg. https://www.bloomberg.com/news/articles/2018-02-13/even-america-s-top-doctors-aren-t-getting-the-parental-leave-doctors-recommend. Published February 13, 2018. Accessed November 21, 2018.
17. Humphries LS, Lyon S, Garza R, et al. Parental leave policies in graduate medical education: a systematic review. American J Surg. 2017;214(4):634-639.
18. Raju TNK. Continued barriers for breast-feeding in public and the workplace. J Pediatr. 2006;148(5):677-679.
19. Stewart DE, Robinson GE. Combining motherhood with psychiatric training and practice. Can J Psychiatry. 1985;30(1):28-34.
20. Rothman L. D esperate women, desperate doctors and the surprising history behind the breastfeeding debate. Time. http://time.com/5353068/breastfeeding-debate-history/. Published July 31, 2018. Accessed November 21, 2018.
21. Livingston G. Among 41 nations, U.S. is the outlier when it comes to paid parental leave. Pew Research Center. http://www.pewresearch.org/fact-tank/2016/09/26/u-s-lacks-mandated-paid-parental-leave/. Published September 26, 2016. Accessed November 21, 2018.
22. McCluskey PD. Long hours, short leaves force moms to reconsider jobs as surgeons. Boston Globe. https://www.bostonglobe.com/metro/2018/03/21/new-survey-says-female-surgical-residents-struggle-balance-training-motherhood/2ENQU1aPZmIJYy20iaRlLL/story.html. Published March 21, 2018. Accessed November 21, 2018.
23. Dinour LM, Szaro JM. Employer-based programs to support breastfeeding among working mothers: a systematic review. Breastfeeding Med. 2017;12:131-141.
Shining a spotlight on physician well-being, more
Shining a spotlight on physician well-being
In “Physician impairment”1 (C
Dr. Farrell’s article does not acknowledge the rule of law. I do not understand why anyone wanting to help physicians would not want them to be aware of their employment rights under the ADA or advise that their ADA rights protect them from unwarranted medical inquiries and referrals to physician health programs (PHPs) or other entities for evaluation.
Dr. Farrell also claims that burnout, poor well-being, and mental disorders cause medical errors and low quality of patient care, but there are many reasons to doubt that this is the case.3,4 Readers should be wary of medical journal articles that cover topics related to physician well-being. Articles related to PHPs, in particular, typically paint an overly rosy picture of the effectiveness of these programs and fail to note important problematic aspects.5,6
Nicholas D. Lawson, MD
Georgetown University Law Center
Washington, DC
References
1. Lawson ND. Physician impairment. Current Psychiatry. 2017;16(10):8.
2. Farrell H. Physician impairment: a need for prevention. Current Psychiatry. 2018;17(9):41-44.
3. Lawson ND. Burnout is not associated with increased medical errors. Mayo Clin Proc. 2018;93(11):1683.
4. Tyssen R. What is the level of burnout that impairs functioning? J Intern Med. 2018;283(6):594-596.
5. Lawson ND, Boyd JW. Flaws in the methods and reporting of physician health program outcome studies. Gen Hosp Psychiatry. 2018;54:65-66.
6. Lawson ND, Boyd JW. Physician health program outcome data should be viewed with caution. Judges J. 2018;57(4):36.
The author responds
I thank Dr. Lawson for his interest in my article. In this extremely challenging work that we do as psychiatrists, which can sometimes be quite isolating, there is a long continuum of experience, reward, and challenge. Dr. Lawson’s research and publication on the topic of physician’s health issues are very much respected and appreciated. In fact, I see no conflict between Dr. Lawson’s letter and my 2018 column on the prevention of impairment.
Given the extensive continuum of our work, my article on physician’s health issues sought to shine a bright spotlight solely on the topic of prevention. As colleagues, there is significant value in supporting rather than reporting one another. Awareness of and sensitivity to physician vulnerability, early detection, and prevention will hopefully continue to gain traction in the future.
By putting the focus on proactively helping colleagues, my hope is that my article will spark an ongoing conversation about how we can work collaboratively to make well-being a priority.
Dr. Lawson’s thoughtful letter is much appreciated because it continues the discussion by shining a spotlight further down the continuum. He focuses on the aftermath of impairment and aptly points out the complications in reporting, confusion about duty, and the protections provided by the ADA. Also, I support Dr. Lawson’s cautions regarding PHPs—all the more reason to join together in shifting the dialogue from management of a crisis to prevention of it.
Helen M. Farrell, MD
Lecturer
Harvard Medical School
Psychiatrist
Beth Israel Deaconess Medical Center
Boston, Massachusetts
Continue to: Neuropolitics
Neuropolitics: Psychiatrists’ responsibility
Regarding Dr. Nasrallah’s editorial “Neuropolitics in the age of extremism: Brain regions involved in hatred” (C
I agree with Dr. Nasrallah that “even the most skillful psychiatrists” cannot “repair a nation caught up in poisonous emotional turmoil”—at least not by employing clinical skills alone. But that doesn’t mean we shouldn’t try, and the American Psychiatric Association (APA) ethics code (Sections 1.2, 3, and 7) compels us to speak out when our patients or the public are being harmed by public policy.1 We are much more likely to have an impact when we speak with one voice, as is the case with professional medical organizations such as the APA. In December 2018, APA President Dr. Altha J. Stewart issued a call to action addressing “the current climate of hateful and divisive rhetoric that leads to senseless violence and tragic loss of life,” stating “… we members must speak out, use our specialized training and expertise for the public’s benefit, and apply it to not only healing, but also preventing psychological trauma and senseless tragedies.”2
James L. Fleming, MD
Psychiatric Medical Care
Lee’s Summit, Missouri
References
1. American Psychiatric Association. The principles of medical ethics with annotations especially applicable to psychiatry, 2013 edition. https://www.psychiatry.org/psychiatrists/practice/ethics. Published 2013. Accessed February 5, 2019.
2. Stewart A, Pozios, V. Forget about staying in our lane: let’s connect the dots. American Psychiatric Association Publishing. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2018.12a20. Published December 3, 2018. Accessed February 3, 2019.
Shining a spotlight on physician well-being
In “Physician impairment”1 (C
Dr. Farrell’s article does not acknowledge the rule of law. I do not understand why anyone wanting to help physicians would not want them to be aware of their employment rights under the ADA or advise that their ADA rights protect them from unwarranted medical inquiries and referrals to physician health programs (PHPs) or other entities for evaluation.
Dr. Farrell also claims that burnout, poor well-being, and mental disorders cause medical errors and low quality of patient care, but there are many reasons to doubt that this is the case.3,4 Readers should be wary of medical journal articles that cover topics related to physician well-being. Articles related to PHPs, in particular, typically paint an overly rosy picture of the effectiveness of these programs and fail to note important problematic aspects.5,6
Nicholas D. Lawson, MD
Georgetown University Law Center
Washington, DC
References
1. Lawson ND. Physician impairment. Current Psychiatry. 2017;16(10):8.
2. Farrell H. Physician impairment: a need for prevention. Current Psychiatry. 2018;17(9):41-44.
3. Lawson ND. Burnout is not associated with increased medical errors. Mayo Clin Proc. 2018;93(11):1683.
4. Tyssen R. What is the level of burnout that impairs functioning? J Intern Med. 2018;283(6):594-596.
5. Lawson ND, Boyd JW. Flaws in the methods and reporting of physician health program outcome studies. Gen Hosp Psychiatry. 2018;54:65-66.
6. Lawson ND, Boyd JW. Physician health program outcome data should be viewed with caution. Judges J. 2018;57(4):36.
The author responds
I thank Dr. Lawson for his interest in my article. In this extremely challenging work that we do as psychiatrists, which can sometimes be quite isolating, there is a long continuum of experience, reward, and challenge. Dr. Lawson’s research and publication on the topic of physician’s health issues are very much respected and appreciated. In fact, I see no conflict between Dr. Lawson’s letter and my 2018 column on the prevention of impairment.
Given the extensive continuum of our work, my article on physician’s health issues sought to shine a bright spotlight solely on the topic of prevention. As colleagues, there is significant value in supporting rather than reporting one another. Awareness of and sensitivity to physician vulnerability, early detection, and prevention will hopefully continue to gain traction in the future.
By putting the focus on proactively helping colleagues, my hope is that my article will spark an ongoing conversation about how we can work collaboratively to make well-being a priority.
Dr. Lawson’s thoughtful letter is much appreciated because it continues the discussion by shining a spotlight further down the continuum. He focuses on the aftermath of impairment and aptly points out the complications in reporting, confusion about duty, and the protections provided by the ADA. Also, I support Dr. Lawson’s cautions regarding PHPs—all the more reason to join together in shifting the dialogue from management of a crisis to prevention of it.
Helen M. Farrell, MD
Lecturer
Harvard Medical School
Psychiatrist
Beth Israel Deaconess Medical Center
Boston, Massachusetts
Continue to: Neuropolitics
Neuropolitics: Psychiatrists’ responsibility
Regarding Dr. Nasrallah’s editorial “Neuropolitics in the age of extremism: Brain regions involved in hatred” (C
I agree with Dr. Nasrallah that “even the most skillful psychiatrists” cannot “repair a nation caught up in poisonous emotional turmoil”—at least not by employing clinical skills alone. But that doesn’t mean we shouldn’t try, and the American Psychiatric Association (APA) ethics code (Sections 1.2, 3, and 7) compels us to speak out when our patients or the public are being harmed by public policy.1 We are much more likely to have an impact when we speak with one voice, as is the case with professional medical organizations such as the APA. In December 2018, APA President Dr. Altha J. Stewart issued a call to action addressing “the current climate of hateful and divisive rhetoric that leads to senseless violence and tragic loss of life,” stating “… we members must speak out, use our specialized training and expertise for the public’s benefit, and apply it to not only healing, but also preventing psychological trauma and senseless tragedies.”2
James L. Fleming, MD
Psychiatric Medical Care
Lee’s Summit, Missouri
References
1. American Psychiatric Association. The principles of medical ethics with annotations especially applicable to psychiatry, 2013 edition. https://www.psychiatry.org/psychiatrists/practice/ethics. Published 2013. Accessed February 5, 2019.
2. Stewart A, Pozios, V. Forget about staying in our lane: let’s connect the dots. American Psychiatric Association Publishing. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2018.12a20. Published December 3, 2018. Accessed February 3, 2019.
Shining a spotlight on physician well-being
In “Physician impairment”1 (C
Dr. Farrell’s article does not acknowledge the rule of law. I do not understand why anyone wanting to help physicians would not want them to be aware of their employment rights under the ADA or advise that their ADA rights protect them from unwarranted medical inquiries and referrals to physician health programs (PHPs) or other entities for evaluation.
Dr. Farrell also claims that burnout, poor well-being, and mental disorders cause medical errors and low quality of patient care, but there are many reasons to doubt that this is the case.3,4 Readers should be wary of medical journal articles that cover topics related to physician well-being. Articles related to PHPs, in particular, typically paint an overly rosy picture of the effectiveness of these programs and fail to note important problematic aspects.5,6
Nicholas D. Lawson, MD
Georgetown University Law Center
Washington, DC
References
1. Lawson ND. Physician impairment. Current Psychiatry. 2017;16(10):8.
2. Farrell H. Physician impairment: a need for prevention. Current Psychiatry. 2018;17(9):41-44.
3. Lawson ND. Burnout is not associated with increased medical errors. Mayo Clin Proc. 2018;93(11):1683.
4. Tyssen R. What is the level of burnout that impairs functioning? J Intern Med. 2018;283(6):594-596.
5. Lawson ND, Boyd JW. Flaws in the methods and reporting of physician health program outcome studies. Gen Hosp Psychiatry. 2018;54:65-66.
6. Lawson ND, Boyd JW. Physician health program outcome data should be viewed with caution. Judges J. 2018;57(4):36.
The author responds
I thank Dr. Lawson for his interest in my article. In this extremely challenging work that we do as psychiatrists, which can sometimes be quite isolating, there is a long continuum of experience, reward, and challenge. Dr. Lawson’s research and publication on the topic of physician’s health issues are very much respected and appreciated. In fact, I see no conflict between Dr. Lawson’s letter and my 2018 column on the prevention of impairment.
Given the extensive continuum of our work, my article on physician’s health issues sought to shine a bright spotlight solely on the topic of prevention. As colleagues, there is significant value in supporting rather than reporting one another. Awareness of and sensitivity to physician vulnerability, early detection, and prevention will hopefully continue to gain traction in the future.
By putting the focus on proactively helping colleagues, my hope is that my article will spark an ongoing conversation about how we can work collaboratively to make well-being a priority.
Dr. Lawson’s thoughtful letter is much appreciated because it continues the discussion by shining a spotlight further down the continuum. He focuses on the aftermath of impairment and aptly points out the complications in reporting, confusion about duty, and the protections provided by the ADA. Also, I support Dr. Lawson’s cautions regarding PHPs—all the more reason to join together in shifting the dialogue from management of a crisis to prevention of it.
Helen M. Farrell, MD
Lecturer
Harvard Medical School
Psychiatrist
Beth Israel Deaconess Medical Center
Boston, Massachusetts
Continue to: Neuropolitics
Neuropolitics: Psychiatrists’ responsibility
Regarding Dr. Nasrallah’s editorial “Neuropolitics in the age of extremism: Brain regions involved in hatred” (C
I agree with Dr. Nasrallah that “even the most skillful psychiatrists” cannot “repair a nation caught up in poisonous emotional turmoil”—at least not by employing clinical skills alone. But that doesn’t mean we shouldn’t try, and the American Psychiatric Association (APA) ethics code (Sections 1.2, 3, and 7) compels us to speak out when our patients or the public are being harmed by public policy.1 We are much more likely to have an impact when we speak with one voice, as is the case with professional medical organizations such as the APA. In December 2018, APA President Dr. Altha J. Stewart issued a call to action addressing “the current climate of hateful and divisive rhetoric that leads to senseless violence and tragic loss of life,” stating “… we members must speak out, use our specialized training and expertise for the public’s benefit, and apply it to not only healing, but also preventing psychological trauma and senseless tragedies.”2
James L. Fleming, MD
Psychiatric Medical Care
Lee’s Summit, Missouri
References
1. American Psychiatric Association. The principles of medical ethics with annotations especially applicable to psychiatry, 2013 edition. https://www.psychiatry.org/psychiatrists/practice/ethics. Published 2013. Accessed February 5, 2019.
2. Stewart A, Pozios, V. Forget about staying in our lane: let’s connect the dots. American Psychiatric Association Publishing. https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2018.12a20. Published December 3, 2018. Accessed February 3, 2019.