User login
Medication pricing: So this is how it works
This is the second part in a series on medication pricing.
In my last column, I looked at the tremendous variation in prices among pharmacies for two psychotropic medications, aripiprazole and modafinil. The cash price variation could be as much as 45 times more from one pharmacy to the next, which I found to be both outrageous and incomprehensible.
To learn more about pharmaceutical pricing, I contacted Doug Hirsch, the cofounder of GoodRx, a firm based in Santa Monica, Calif., that offers deep discounts on some medications. The company sends discount cards to physicians’ offices – call me if you need some, I have many boxes of GoodRx cards – and has a website (www.GoodRx.com) and an app. It advertises that it is about transparency, and if you’ve ever tried the company’s site or app, the service it offers is remarkable and simple to use.
I approached Mr. Hirsch with two simple questions. The company offers “up to 90% discount” on the cash price of medications through its app, website, or discount card – all of which can be gotten for free. I wanted to know 1) Who pays for this difference in the medication cost, and 2) How does the company, with 95 employees, make any money? Mr. Hirsch was gracious enough (and patient enough!) to spend the next hour walking me through the steps of medication pricing. It was a lively conversation, so let me share with you what I have learned.
Medications are made by a pharmaceutical company or, for generics, there may be many manufacturers. The medications are sent to a pharmaceutical distributor, such as McKesson, and it, in turn, sells and delivers the products to pharmacy chains, as well as to smaller, independent pharmacies. The pharmacies pay an acquisition cost for medications then set a price for these medications that are considerably – or even astronomically – higher than the acquisition price. This is the cash retail price, or in medicine, what is called the Usual & Customary (U&C) cost of the medication. The price may be neither usual, customary, nor reasonable, and it’s not the price the pharmacy expects to recoup on sales.
Every major insurance company contracts with a pharmacy benefits manager (for example, Caremark, Express Scripts, and Optum) to negotiate the cost of medications with each major pharmacy chain. Physicians are familiar with PBMs, who intercede by requiring preauthorization procedures for certain medications or by instituting stepwise, fail-first, requirements before they will allow pharmacy benefits toward the purchase of medications. When the PBMs negotiate with the pharmacies, they will negotiate for a discount off the pharmacy’s U&C charge for medication, perhaps a discount as much as 75% or 80%. Mr. Hirsch noted, “The discount is not negotiated on a per-medication basis but as an across-the-board average, so for one medication, the insurance price may be 2% discount from the U&C cost, and on another medicine it may be 95%. There is a dramatic variation, more than you’d ever expect.”
GoodRx gathers prices from many places, including partnerships with a number of PBMs. In addition to providing discounted prices for insured customers, the PBMs also include in their negotiations a slightly less-discounted price for cash-paying patients who present with a GoodRx card or coupon. You might be surprised to learn that discounted prices can often be less than the typical patient copay. For patients with a high deductible, for medications that are not covered at all, or for times when the copay is higher than the cost of the medication, it will often be less expensive for patients to use a GoodRx discount instead of their insurance. And whether patients uses either their insurance or a GoodRx discount, part of the cost of the prescription includes an administrative fee that goes to the PBM. When GoodRx cards are used, the PBM pays GoodRx part of that fee. I hope you are still with me, because this is the part of the conversation where I started telling Mr. Hirsch that I was getting a headache.
I went back to the enormous cost discrepancy that I had discovered a couple of years ago with Provigil (modafinil). Thirty pills cost just under $35 at Costco, while all other pharmacies were charging close to $1,000. Mr. Hirsch explained, “From what I’ve been told, Costco bases their prices on their acquisition costs and then raises them a certain percent. It’s one way to provide a fair price, but that doesn’t mean they always have the lowest price. They are also the only major pharmacy that lists their drug prices on their website.”
I wanted to know what was in it for the PBMs. Why would Express Scripts be motivated to negotiate a discount in price for cash-paying customers outside of the insurance networks, and how did partnering with GoodRx benefit them? The answer, in part, lies with the fact that the website and app allow patients to comparison shop and go to pharmacies with lower prices. If patients use their insurance, the insurance company is paying less; if they don’t use their insurance because they learned the cash cost is less, then the cost burden has shifted from the insurance company entirely to the patient.
What’s in it for the pharmacies? Why would they be willing to accept less money from a patient bearing a discount card? Mr. Hirsch explained, “Pharmacies want to honor their contracts with PBMs, and the U&C prices are set high to enable negotiation so that they still make some profit. Most people couldn’t afford to pay the high U&C, but they can’t lower them for individual cash-pay customers because that would violate their agreements with PBMs, and Medicare and Medicaid, which is a felony. With the GoodRx price, they still make a profit, and people in drugstores buy other items as well.
GoodRx has 95 employees, and I was still left wondering how they generate income. Mr. Hirsch pinned it down to three sources: the portion of the administration fees the PBMs pay GoodRx, a small amount of advertising, and finally, GoodRx provides technology for the PBMs and charges for this service.
“We started asking how we could gather prices in this bizarre marketplace and address the pricing inefficiencies,” Mr. Hirsch said, “and now I get emails every day expressing gratitude.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
This is the second part in a series on medication pricing.
In my last column, I looked at the tremendous variation in prices among pharmacies for two psychotropic medications, aripiprazole and modafinil. The cash price variation could be as much as 45 times more from one pharmacy to the next, which I found to be both outrageous and incomprehensible.
To learn more about pharmaceutical pricing, I contacted Doug Hirsch, the cofounder of GoodRx, a firm based in Santa Monica, Calif., that offers deep discounts on some medications. The company sends discount cards to physicians’ offices – call me if you need some, I have many boxes of GoodRx cards – and has a website (www.GoodRx.com) and an app. It advertises that it is about transparency, and if you’ve ever tried the company’s site or app, the service it offers is remarkable and simple to use.
I approached Mr. Hirsch with two simple questions. The company offers “up to 90% discount” on the cash price of medications through its app, website, or discount card – all of which can be gotten for free. I wanted to know 1) Who pays for this difference in the medication cost, and 2) How does the company, with 95 employees, make any money? Mr. Hirsch was gracious enough (and patient enough!) to spend the next hour walking me through the steps of medication pricing. It was a lively conversation, so let me share with you what I have learned.
Medications are made by a pharmaceutical company or, for generics, there may be many manufacturers. The medications are sent to a pharmaceutical distributor, such as McKesson, and it, in turn, sells and delivers the products to pharmacy chains, as well as to smaller, independent pharmacies. The pharmacies pay an acquisition cost for medications then set a price for these medications that are considerably – or even astronomically – higher than the acquisition price. This is the cash retail price, or in medicine, what is called the Usual & Customary (U&C) cost of the medication. The price may be neither usual, customary, nor reasonable, and it’s not the price the pharmacy expects to recoup on sales.
Every major insurance company contracts with a pharmacy benefits manager (for example, Caremark, Express Scripts, and Optum) to negotiate the cost of medications with each major pharmacy chain. Physicians are familiar with PBMs, who intercede by requiring preauthorization procedures for certain medications or by instituting stepwise, fail-first, requirements before they will allow pharmacy benefits toward the purchase of medications. When the PBMs negotiate with the pharmacies, they will negotiate for a discount off the pharmacy’s U&C charge for medication, perhaps a discount as much as 75% or 80%. Mr. Hirsch noted, “The discount is not negotiated on a per-medication basis but as an across-the-board average, so for one medication, the insurance price may be 2% discount from the U&C cost, and on another medicine it may be 95%. There is a dramatic variation, more than you’d ever expect.”
GoodRx gathers prices from many places, including partnerships with a number of PBMs. In addition to providing discounted prices for insured customers, the PBMs also include in their negotiations a slightly less-discounted price for cash-paying patients who present with a GoodRx card or coupon. You might be surprised to learn that discounted prices can often be less than the typical patient copay. For patients with a high deductible, for medications that are not covered at all, or for times when the copay is higher than the cost of the medication, it will often be less expensive for patients to use a GoodRx discount instead of their insurance. And whether patients uses either their insurance or a GoodRx discount, part of the cost of the prescription includes an administrative fee that goes to the PBM. When GoodRx cards are used, the PBM pays GoodRx part of that fee. I hope you are still with me, because this is the part of the conversation where I started telling Mr. Hirsch that I was getting a headache.
I went back to the enormous cost discrepancy that I had discovered a couple of years ago with Provigil (modafinil). Thirty pills cost just under $35 at Costco, while all other pharmacies were charging close to $1,000. Mr. Hirsch explained, “From what I’ve been told, Costco bases their prices on their acquisition costs and then raises them a certain percent. It’s one way to provide a fair price, but that doesn’t mean they always have the lowest price. They are also the only major pharmacy that lists their drug prices on their website.”
I wanted to know what was in it for the PBMs. Why would Express Scripts be motivated to negotiate a discount in price for cash-paying customers outside of the insurance networks, and how did partnering with GoodRx benefit them? The answer, in part, lies with the fact that the website and app allow patients to comparison shop and go to pharmacies with lower prices. If patients use their insurance, the insurance company is paying less; if they don’t use their insurance because they learned the cash cost is less, then the cost burden has shifted from the insurance company entirely to the patient.
What’s in it for the pharmacies? Why would they be willing to accept less money from a patient bearing a discount card? Mr. Hirsch explained, “Pharmacies want to honor their contracts with PBMs, and the U&C prices are set high to enable negotiation so that they still make some profit. Most people couldn’t afford to pay the high U&C, but they can’t lower them for individual cash-pay customers because that would violate their agreements with PBMs, and Medicare and Medicaid, which is a felony. With the GoodRx price, they still make a profit, and people in drugstores buy other items as well.
GoodRx has 95 employees, and I was still left wondering how they generate income. Mr. Hirsch pinned it down to three sources: the portion of the administration fees the PBMs pay GoodRx, a small amount of advertising, and finally, GoodRx provides technology for the PBMs and charges for this service.
“We started asking how we could gather prices in this bizarre marketplace and address the pricing inefficiencies,” Mr. Hirsch said, “and now I get emails every day expressing gratitude.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
This is the second part in a series on medication pricing.
In my last column, I looked at the tremendous variation in prices among pharmacies for two psychotropic medications, aripiprazole and modafinil. The cash price variation could be as much as 45 times more from one pharmacy to the next, which I found to be both outrageous and incomprehensible.
To learn more about pharmaceutical pricing, I contacted Doug Hirsch, the cofounder of GoodRx, a firm based in Santa Monica, Calif., that offers deep discounts on some medications. The company sends discount cards to physicians’ offices – call me if you need some, I have many boxes of GoodRx cards – and has a website (www.GoodRx.com) and an app. It advertises that it is about transparency, and if you’ve ever tried the company’s site or app, the service it offers is remarkable and simple to use.
I approached Mr. Hirsch with two simple questions. The company offers “up to 90% discount” on the cash price of medications through its app, website, or discount card – all of which can be gotten for free. I wanted to know 1) Who pays for this difference in the medication cost, and 2) How does the company, with 95 employees, make any money? Mr. Hirsch was gracious enough (and patient enough!) to spend the next hour walking me through the steps of medication pricing. It was a lively conversation, so let me share with you what I have learned.
Medications are made by a pharmaceutical company or, for generics, there may be many manufacturers. The medications are sent to a pharmaceutical distributor, such as McKesson, and it, in turn, sells and delivers the products to pharmacy chains, as well as to smaller, independent pharmacies. The pharmacies pay an acquisition cost for medications then set a price for these medications that are considerably – or even astronomically – higher than the acquisition price. This is the cash retail price, or in medicine, what is called the Usual & Customary (U&C) cost of the medication. The price may be neither usual, customary, nor reasonable, and it’s not the price the pharmacy expects to recoup on sales.
Every major insurance company contracts with a pharmacy benefits manager (for example, Caremark, Express Scripts, and Optum) to negotiate the cost of medications with each major pharmacy chain. Physicians are familiar with PBMs, who intercede by requiring preauthorization procedures for certain medications or by instituting stepwise, fail-first, requirements before they will allow pharmacy benefits toward the purchase of medications. When the PBMs negotiate with the pharmacies, they will negotiate for a discount off the pharmacy’s U&C charge for medication, perhaps a discount as much as 75% or 80%. Mr. Hirsch noted, “The discount is not negotiated on a per-medication basis but as an across-the-board average, so for one medication, the insurance price may be 2% discount from the U&C cost, and on another medicine it may be 95%. There is a dramatic variation, more than you’d ever expect.”
GoodRx gathers prices from many places, including partnerships with a number of PBMs. In addition to providing discounted prices for insured customers, the PBMs also include in their negotiations a slightly less-discounted price for cash-paying patients who present with a GoodRx card or coupon. You might be surprised to learn that discounted prices can often be less than the typical patient copay. For patients with a high deductible, for medications that are not covered at all, or for times when the copay is higher than the cost of the medication, it will often be less expensive for patients to use a GoodRx discount instead of their insurance. And whether patients uses either their insurance or a GoodRx discount, part of the cost of the prescription includes an administrative fee that goes to the PBM. When GoodRx cards are used, the PBM pays GoodRx part of that fee. I hope you are still with me, because this is the part of the conversation where I started telling Mr. Hirsch that I was getting a headache.
I went back to the enormous cost discrepancy that I had discovered a couple of years ago with Provigil (modafinil). Thirty pills cost just under $35 at Costco, while all other pharmacies were charging close to $1,000. Mr. Hirsch explained, “From what I’ve been told, Costco bases their prices on their acquisition costs and then raises them a certain percent. It’s one way to provide a fair price, but that doesn’t mean they always have the lowest price. They are also the only major pharmacy that lists their drug prices on their website.”
I wanted to know what was in it for the PBMs. Why would Express Scripts be motivated to negotiate a discount in price for cash-paying customers outside of the insurance networks, and how did partnering with GoodRx benefit them? The answer, in part, lies with the fact that the website and app allow patients to comparison shop and go to pharmacies with lower prices. If patients use their insurance, the insurance company is paying less; if they don’t use their insurance because they learned the cash cost is less, then the cost burden has shifted from the insurance company entirely to the patient.
What’s in it for the pharmacies? Why would they be willing to accept less money from a patient bearing a discount card? Mr. Hirsch explained, “Pharmacies want to honor their contracts with PBMs, and the U&C prices are set high to enable negotiation so that they still make some profit. Most people couldn’t afford to pay the high U&C, but they can’t lower them for individual cash-pay customers because that would violate their agreements with PBMs, and Medicare and Medicaid, which is a felony. With the GoodRx price, they still make a profit, and people in drugstores buy other items as well.
GoodRx has 95 employees, and I was still left wondering how they generate income. Mr. Hirsch pinned it down to three sources: the portion of the administration fees the PBMs pay GoodRx, a small amount of advertising, and finally, GoodRx provides technology for the PBMs and charges for this service.
“We started asking how we could gather prices in this bizarre marketplace and address the pricing inefficiencies,” Mr. Hirsch said, “and now I get emails every day expressing gratitude.”
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016).
Mental health stressors still loom for Puerto Ricans after Maria
The physical and mental health needs of the people of Puerto Rico cannot be underestimated. Just think of what they have been through over the last few months.
When Hurricane Maria barreled onto the island on Sept. 20, 2017 – just 2 weeks after Hurricane Irma reportedly left more than 1 million residents without power – it ripped off roofs and left behind massive flooding, roads washed out, and utility poles and transmission lines knocked down. Whole forests were defoliated, a massive loss of flora and fauna occurred, and 80% of the crop value was destroyed, along with massive loss of stray dogs and cats, dairy cows, industrial chicken coops, and tropical birds, including endangered species. Beloved pets were displaced.
The official death toll as a result of Maria was 64 in December, but according to reporting by The New York Times, that number could be as high as 1,052. Most of the people who died reportedly were men and women over age 50 in hospitals and nursing homes suffering from illnesses such as diabetes, Alzheimer’s, kidney disease, hypertension, pneumonia, and other respiratory diseases.
One grassroots organization that mobilized to provide supplies and medical assistance was Doctoras Boricuas, a group of all-female doctors in the United States and Puerto Rico that formed after the hurricanes to coordinate the delivery and distribution of supplies directly to Puerto Rico and the Virgin Islands. Two groups affiliated with the University of Missouri at Columbia joined forces to help: Global First Responder or GFR, a nonprofit, secular international medical relief organization founded in 2011 by Adam Beckett, MD, and the International Center for Psychosocial Trauma, or ICPT, a group established in 1995 by Syed Arshad Husain, MD, to help war-traumatized children in Bosnia. I joined Dr. Husain’s group of professionals – Kathryn Dewein, PhD; Andra Ferguson, PhD; and Cathy Grigg, PsyD, – all of whom have traveled broadly in the field of disaster psychiatry – to see how we could help the people of Puerto Rico in Maria’s aftermath.
What we did
ICPT and GFR were a combined team, but we served different functions. As part of ICPT, I focused on the mental health component and helped to train doctors, psychologists, social workers, and other mental health workers in both San Juan and Ponce. All told, we worked with about 50 people using the model of “Training the Trainers.” Many of our students were participants in the outreach teams. Our hope is that they will be able to train their peers to recognize and alleviate symptoms of acute and chronic stress disorders. Some of the techniques taught include patient education, relaxation training, breath work, visualization techniques, mindfulness training, narrative therapy, art therapy, and other expressive techniques.
What the PMSF did
Before Maria, the Ponce Medical School Foundation was in the process of facilitating the transfer of medical records into an electronic format. After the hurricane hit, however, PMSF’s program director, Antonio Fernandez, led a shift to disaster recovery work. PMSF got involved in airlifting dialysis patients off the island to safety, provided health care, and also collaborated with the Primary Care Psychology Program at Ponce Health Services University to assist in locating patients, identifying their health needs – including mental health – and providing for those needs to the extent possible.
At the time of our visit, Puerto Rico’s network of more than 90 largely rural federally funded primary care clinics mostly had reopened, but nearly half remained on back-up generators. Even with the medical centers open, patients were not coming in for one reason or another. People had medical problems, but the daily reality of survival, obtaining food and water, took precedence. Some patients were not showing up because they had left the country, or they were in shelters without transportation. Some people did not have fuel. Some could not keep track of their appointments without cell phones and electricity allowing them to access electronic planners. Some, having been without their medications since the storms, were too sick to travel. Outreach teams were necessary to locate patients, identify their needs, and provide medical and psychological care.
Community outreach
Nydia M. Cappas, PsyD, director of the Primary Care Psychology Program, told us that the outreach teams – consisting of doctors or other medical professionals, social workers, and psychologists, were being sent out to communities once a week. They visited homes for the elderly, orphans’ homes, and children in foster care, as well as individual patients. A similar service was provided by Vargas Medicine (VARMED) in the San Juan area.
Team members found that many people were suffering symptoms of posttraumatic stress disorder, even people who did not have prior psychiatric symptoms. They were having flashbacks and nightmares. Those flashbacks and nightmares were being triggered by clouds, by rain, by supplies beginning to run out.
Another trend we observed is that terrain changes prompted by Maria triggered PTSD symptoms among many veterans. The defoliated trees and brown earth were causing them to have flashbacks to the deserts of Afghanistan and Iraq. Children were showing regressive behaviors, loss of developmental milestones, and symptoms of separation anxiety such as wanting to sleep with their parents. In severe cases, they were having psychotic symptoms and auditory hallucinations. The children were grieving the loss of their homes, toys, pets, and family members, in some cases. , including medications, food, toiletries, and other household goods.
Puerto Rico’s future
Two and a half months after Maria, we learned from our students that things gradually had begun to improve. For example, the public schools had just reopened, and that change was expected to have a stabilizing effect on the children. We also learned that, of the 80 shelters that had been set up housing about 12,500 people, 40 shelters had closed. The five medical shelters that had been set up and funded by FEMA also were in the process of closing, and private donations were beginning to slow down. People were slowly returning to their tarped or otherwise repaired homes, albeit all too often without power.
During the storm, nearly 500,000* homes were destroyed. FEMA offered to airlift about 3,000 people who had no home 2 months past Maria to the U.S. mainland – either Florida or New York.
According to our students, people living in the mountains, mainly coffee growers and retired people and comprising about one-third of the population, remain in acute crisis. Part of the challenge is being able to reach this population: Some roads are still impassable, and supplies – such as drinking water – can be delivered only by helicopter. Despite current conditions, FEMA reportedly has announced that it would end emergency operations on the island.
Our team is currently involved in applying for grant funding that will enable us to return to provide additional training to physicians’ and teachers’ groups. Over the course of the next year, we would like to make six trips to Puerto Rico and focus each trip on a different region and different group of professionals so that the entire island has resources. In addition, we will offer follow-up consultations to professionals we trained previously. The regions to be trained would be San Juan, Ponce, Utuado, Mayagüez, Guayama, and a sixth to be determined upon need. We also would like to address the needs of any ongoing relief workers so that they will be more effective in their ongoing role. Meanwhile, financial assistance from the mainland remains uneven.
Many months after Maria (and Irma), the physical and mental health needs of the Puerto Rican people remain great. However, as mental health professionals, we have the tools to help them move forward.
Judith R. Milner, MD, MEd, SpecEd, is a general, child, and adolescent psychiatrist in private practice in Everett, Wash. She has traveled with various groups over the years in an effort to alleviate some of the suffering caused by war and natural disaster. Her predominant association has been with the International Center for Psychosocial Trauma. She also has worked with Step Up Rwanda Women and Pygmy Survival Alliance, as well as on the Committee for Women at the American Psychiatric Association and the Consumer Issues Committee and Membership Committee for the American Academy of Child and Adolescent Psychiatry.
*Correction, 2/12/2018: An earlier version of this story misstated the number of homes reportedly destroyed by Hurricane Maria.
The physical and mental health needs of the people of Puerto Rico cannot be underestimated. Just think of what they have been through over the last few months.
When Hurricane Maria barreled onto the island on Sept. 20, 2017 – just 2 weeks after Hurricane Irma reportedly left more than 1 million residents without power – it ripped off roofs and left behind massive flooding, roads washed out, and utility poles and transmission lines knocked down. Whole forests were defoliated, a massive loss of flora and fauna occurred, and 80% of the crop value was destroyed, along with massive loss of stray dogs and cats, dairy cows, industrial chicken coops, and tropical birds, including endangered species. Beloved pets were displaced.
The official death toll as a result of Maria was 64 in December, but according to reporting by The New York Times, that number could be as high as 1,052. Most of the people who died reportedly were men and women over age 50 in hospitals and nursing homes suffering from illnesses such as diabetes, Alzheimer’s, kidney disease, hypertension, pneumonia, and other respiratory diseases.
One grassroots organization that mobilized to provide supplies and medical assistance was Doctoras Boricuas, a group of all-female doctors in the United States and Puerto Rico that formed after the hurricanes to coordinate the delivery and distribution of supplies directly to Puerto Rico and the Virgin Islands. Two groups affiliated with the University of Missouri at Columbia joined forces to help: Global First Responder or GFR, a nonprofit, secular international medical relief organization founded in 2011 by Adam Beckett, MD, and the International Center for Psychosocial Trauma, or ICPT, a group established in 1995 by Syed Arshad Husain, MD, to help war-traumatized children in Bosnia. I joined Dr. Husain’s group of professionals – Kathryn Dewein, PhD; Andra Ferguson, PhD; and Cathy Grigg, PsyD, – all of whom have traveled broadly in the field of disaster psychiatry – to see how we could help the people of Puerto Rico in Maria’s aftermath.
What we did
ICPT and GFR were a combined team, but we served different functions. As part of ICPT, I focused on the mental health component and helped to train doctors, psychologists, social workers, and other mental health workers in both San Juan and Ponce. All told, we worked with about 50 people using the model of “Training the Trainers.” Many of our students were participants in the outreach teams. Our hope is that they will be able to train their peers to recognize and alleviate symptoms of acute and chronic stress disorders. Some of the techniques taught include patient education, relaxation training, breath work, visualization techniques, mindfulness training, narrative therapy, art therapy, and other expressive techniques.
What the PMSF did
Before Maria, the Ponce Medical School Foundation was in the process of facilitating the transfer of medical records into an electronic format. After the hurricane hit, however, PMSF’s program director, Antonio Fernandez, led a shift to disaster recovery work. PMSF got involved in airlifting dialysis patients off the island to safety, provided health care, and also collaborated with the Primary Care Psychology Program at Ponce Health Services University to assist in locating patients, identifying their health needs – including mental health – and providing for those needs to the extent possible.
At the time of our visit, Puerto Rico’s network of more than 90 largely rural federally funded primary care clinics mostly had reopened, but nearly half remained on back-up generators. Even with the medical centers open, patients were not coming in for one reason or another. People had medical problems, but the daily reality of survival, obtaining food and water, took precedence. Some patients were not showing up because they had left the country, or they were in shelters without transportation. Some people did not have fuel. Some could not keep track of their appointments without cell phones and electricity allowing them to access electronic planners. Some, having been without their medications since the storms, were too sick to travel. Outreach teams were necessary to locate patients, identify their needs, and provide medical and psychological care.
Community outreach
Nydia M. Cappas, PsyD, director of the Primary Care Psychology Program, told us that the outreach teams – consisting of doctors or other medical professionals, social workers, and psychologists, were being sent out to communities once a week. They visited homes for the elderly, orphans’ homes, and children in foster care, as well as individual patients. A similar service was provided by Vargas Medicine (VARMED) in the San Juan area.
Team members found that many people were suffering symptoms of posttraumatic stress disorder, even people who did not have prior psychiatric symptoms. They were having flashbacks and nightmares. Those flashbacks and nightmares were being triggered by clouds, by rain, by supplies beginning to run out.
Another trend we observed is that terrain changes prompted by Maria triggered PTSD symptoms among many veterans. The defoliated trees and brown earth were causing them to have flashbacks to the deserts of Afghanistan and Iraq. Children were showing regressive behaviors, loss of developmental milestones, and symptoms of separation anxiety such as wanting to sleep with their parents. In severe cases, they were having psychotic symptoms and auditory hallucinations. The children were grieving the loss of their homes, toys, pets, and family members, in some cases. , including medications, food, toiletries, and other household goods.
Puerto Rico’s future
Two and a half months after Maria, we learned from our students that things gradually had begun to improve. For example, the public schools had just reopened, and that change was expected to have a stabilizing effect on the children. We also learned that, of the 80 shelters that had been set up housing about 12,500 people, 40 shelters had closed. The five medical shelters that had been set up and funded by FEMA also were in the process of closing, and private donations were beginning to slow down. People were slowly returning to their tarped or otherwise repaired homes, albeit all too often without power.
During the storm, nearly 500,000* homes were destroyed. FEMA offered to airlift about 3,000 people who had no home 2 months past Maria to the U.S. mainland – either Florida or New York.
According to our students, people living in the mountains, mainly coffee growers and retired people and comprising about one-third of the population, remain in acute crisis. Part of the challenge is being able to reach this population: Some roads are still impassable, and supplies – such as drinking water – can be delivered only by helicopter. Despite current conditions, FEMA reportedly has announced that it would end emergency operations on the island.
Our team is currently involved in applying for grant funding that will enable us to return to provide additional training to physicians’ and teachers’ groups. Over the course of the next year, we would like to make six trips to Puerto Rico and focus each trip on a different region and different group of professionals so that the entire island has resources. In addition, we will offer follow-up consultations to professionals we trained previously. The regions to be trained would be San Juan, Ponce, Utuado, Mayagüez, Guayama, and a sixth to be determined upon need. We also would like to address the needs of any ongoing relief workers so that they will be more effective in their ongoing role. Meanwhile, financial assistance from the mainland remains uneven.
Many months after Maria (and Irma), the physical and mental health needs of the Puerto Rican people remain great. However, as mental health professionals, we have the tools to help them move forward.
Judith R. Milner, MD, MEd, SpecEd, is a general, child, and adolescent psychiatrist in private practice in Everett, Wash. She has traveled with various groups over the years in an effort to alleviate some of the suffering caused by war and natural disaster. Her predominant association has been with the International Center for Psychosocial Trauma. She also has worked with Step Up Rwanda Women and Pygmy Survival Alliance, as well as on the Committee for Women at the American Psychiatric Association and the Consumer Issues Committee and Membership Committee for the American Academy of Child and Adolescent Psychiatry.
*Correction, 2/12/2018: An earlier version of this story misstated the number of homes reportedly destroyed by Hurricane Maria.
The physical and mental health needs of the people of Puerto Rico cannot be underestimated. Just think of what they have been through over the last few months.
When Hurricane Maria barreled onto the island on Sept. 20, 2017 – just 2 weeks after Hurricane Irma reportedly left more than 1 million residents without power – it ripped off roofs and left behind massive flooding, roads washed out, and utility poles and transmission lines knocked down. Whole forests were defoliated, a massive loss of flora and fauna occurred, and 80% of the crop value was destroyed, along with massive loss of stray dogs and cats, dairy cows, industrial chicken coops, and tropical birds, including endangered species. Beloved pets were displaced.
The official death toll as a result of Maria was 64 in December, but according to reporting by The New York Times, that number could be as high as 1,052. Most of the people who died reportedly were men and women over age 50 in hospitals and nursing homes suffering from illnesses such as diabetes, Alzheimer’s, kidney disease, hypertension, pneumonia, and other respiratory diseases.
One grassroots organization that mobilized to provide supplies and medical assistance was Doctoras Boricuas, a group of all-female doctors in the United States and Puerto Rico that formed after the hurricanes to coordinate the delivery and distribution of supplies directly to Puerto Rico and the Virgin Islands. Two groups affiliated with the University of Missouri at Columbia joined forces to help: Global First Responder or GFR, a nonprofit, secular international medical relief organization founded in 2011 by Adam Beckett, MD, and the International Center for Psychosocial Trauma, or ICPT, a group established in 1995 by Syed Arshad Husain, MD, to help war-traumatized children in Bosnia. I joined Dr. Husain’s group of professionals – Kathryn Dewein, PhD; Andra Ferguson, PhD; and Cathy Grigg, PsyD, – all of whom have traveled broadly in the field of disaster psychiatry – to see how we could help the people of Puerto Rico in Maria’s aftermath.
What we did
ICPT and GFR were a combined team, but we served different functions. As part of ICPT, I focused on the mental health component and helped to train doctors, psychologists, social workers, and other mental health workers in both San Juan and Ponce. All told, we worked with about 50 people using the model of “Training the Trainers.” Many of our students were participants in the outreach teams. Our hope is that they will be able to train their peers to recognize and alleviate symptoms of acute and chronic stress disorders. Some of the techniques taught include patient education, relaxation training, breath work, visualization techniques, mindfulness training, narrative therapy, art therapy, and other expressive techniques.
What the PMSF did
Before Maria, the Ponce Medical School Foundation was in the process of facilitating the transfer of medical records into an electronic format. After the hurricane hit, however, PMSF’s program director, Antonio Fernandez, led a shift to disaster recovery work. PMSF got involved in airlifting dialysis patients off the island to safety, provided health care, and also collaborated with the Primary Care Psychology Program at Ponce Health Services University to assist in locating patients, identifying their health needs – including mental health – and providing for those needs to the extent possible.
At the time of our visit, Puerto Rico’s network of more than 90 largely rural federally funded primary care clinics mostly had reopened, but nearly half remained on back-up generators. Even with the medical centers open, patients were not coming in for one reason or another. People had medical problems, but the daily reality of survival, obtaining food and water, took precedence. Some patients were not showing up because they had left the country, or they were in shelters without transportation. Some people did not have fuel. Some could not keep track of their appointments without cell phones and electricity allowing them to access electronic planners. Some, having been without their medications since the storms, were too sick to travel. Outreach teams were necessary to locate patients, identify their needs, and provide medical and psychological care.
Community outreach
Nydia M. Cappas, PsyD, director of the Primary Care Psychology Program, told us that the outreach teams – consisting of doctors or other medical professionals, social workers, and psychologists, were being sent out to communities once a week. They visited homes for the elderly, orphans’ homes, and children in foster care, as well as individual patients. A similar service was provided by Vargas Medicine (VARMED) in the San Juan area.
Team members found that many people were suffering symptoms of posttraumatic stress disorder, even people who did not have prior psychiatric symptoms. They were having flashbacks and nightmares. Those flashbacks and nightmares were being triggered by clouds, by rain, by supplies beginning to run out.
Another trend we observed is that terrain changes prompted by Maria triggered PTSD symptoms among many veterans. The defoliated trees and brown earth were causing them to have flashbacks to the deserts of Afghanistan and Iraq. Children were showing regressive behaviors, loss of developmental milestones, and symptoms of separation anxiety such as wanting to sleep with their parents. In severe cases, they were having psychotic symptoms and auditory hallucinations. The children were grieving the loss of their homes, toys, pets, and family members, in some cases. , including medications, food, toiletries, and other household goods.
Puerto Rico’s future
Two and a half months after Maria, we learned from our students that things gradually had begun to improve. For example, the public schools had just reopened, and that change was expected to have a stabilizing effect on the children. We also learned that, of the 80 shelters that had been set up housing about 12,500 people, 40 shelters had closed. The five medical shelters that had been set up and funded by FEMA also were in the process of closing, and private donations were beginning to slow down. People were slowly returning to their tarped or otherwise repaired homes, albeit all too often without power.
During the storm, nearly 500,000* homes were destroyed. FEMA offered to airlift about 3,000 people who had no home 2 months past Maria to the U.S. mainland – either Florida or New York.
According to our students, people living in the mountains, mainly coffee growers and retired people and comprising about one-third of the population, remain in acute crisis. Part of the challenge is being able to reach this population: Some roads are still impassable, and supplies – such as drinking water – can be delivered only by helicopter. Despite current conditions, FEMA reportedly has announced that it would end emergency operations on the island.
Our team is currently involved in applying for grant funding that will enable us to return to provide additional training to physicians’ and teachers’ groups. Over the course of the next year, we would like to make six trips to Puerto Rico and focus each trip on a different region and different group of professionals so that the entire island has resources. In addition, we will offer follow-up consultations to professionals we trained previously. The regions to be trained would be San Juan, Ponce, Utuado, Mayagüez, Guayama, and a sixth to be determined upon need. We also would like to address the needs of any ongoing relief workers so that they will be more effective in their ongoing role. Meanwhile, financial assistance from the mainland remains uneven.
Many months after Maria (and Irma), the physical and mental health needs of the Puerto Rican people remain great. However, as mental health professionals, we have the tools to help them move forward.
Judith R. Milner, MD, MEd, SpecEd, is a general, child, and adolescent psychiatrist in private practice in Everett, Wash. She has traveled with various groups over the years in an effort to alleviate some of the suffering caused by war and natural disaster. Her predominant association has been with the International Center for Psychosocial Trauma. She also has worked with Step Up Rwanda Women and Pygmy Survival Alliance, as well as on the Committee for Women at the American Psychiatric Association and the Consumer Issues Committee and Membership Committee for the American Academy of Child and Adolescent Psychiatry.
*Correction, 2/12/2018: An earlier version of this story misstated the number of homes reportedly destroyed by Hurricane Maria.
The stigma toward BPD
In response to Dr. Mark Zimmerman’s article, “Improving the recognition of borderline personality disorder” (
Why all the stigma? Because mental health professionals don’t have complete information. The assumption used to be that BPD was “intractable” with no treatment. Even if this were true, it still would not be a reason to fail to disclose a diagnosis, because in other fields of medicine, the concept of “therapeutic privilege” fell by the wayside long ago. However, we now know that in many individuals with BPD, symptoms improve over time, and there are several effective treatments.
In DSM-II, published in 1968, obsessive-compulsive disorder (OCD) was characterized as an “obsessive compulsive neurosis.” It was not reclassified as the current OCD diagnosis until DSM-III-R was published in 1987, after the FDA approved clomipramine. Why is this important? Because once people realized that there was a treatment, they started acknowledging OCD more often.
The first step in addressing the stigma toward BPD is that mental health professionals must recognize their own bias toward this diagnosis. We must be re-educated that this diagnosis carries hope, symptoms improve, and that there are effective treatments. This is how professionals will increase the recognition of BPD.
Assistant Professor and Compliance Officer
Department of Psychiatry
University of Florida
Clinic Director
UF Child and Adolescent Psychiatry Clinic at Springhill Health Center
Gainesville, Florida
References
1. Unruh BT, Gunderson JG. “Good enough” psychiatric residency training in borderline personality disorder: challenges, choice points, and a model generalist curriculum. Harv Rev Psychiatry. 2016;24(5):367-377.
2. Sheehan L, Nieweglowski K, Corrigan P. The stigma of personality disorders. Curr Psychiatry Rep. 2016;18(1):11.
Continue to: The author responds
The author responds
I agree with Dr. Shapiro that stigma by mental health clinicians contributes to the underdiagnosis of BPD. Mental health professions often hold a negative view of patients with personality disorders, particularly those with BPD, and see these patients as being more difficult to treat.1-3 They are the patients that some clinicians are reluctant to treat.3,4 Clinicians perceive patients with personality disorders as less mentally ill, more manipulative, and more able to control their behavior than patients with other psychiatric disorders.3,5 Consistent with this, clinicians have less sympathetic attitudes and behave less empathically toward patients with BPD.5,6 The term “borderline” also is sometimes used pejoratively to describe patients.1
As I described in my article, there are several possible reasons BPD is underdiagnosed. Foremost is that mood disorders, anxiety disorders, and substance use disorders are common in patients with BPD, and the symptoms of these other disorders are typically patients’ chief concerns when they present for treatment. Patients with BPD do not usually report the features of BPD—such as abandonment fears, chronic feelings of emptiness, or an identity disturbance—as their chief concerns. If they did, BPD would likely be easier to recognize. On a related note, clinicians do not have the time, or do not take the time, to conduct a thorough enough evaluation to diagnose BPD when it occurs in a patient who presents for treatment of a mood disorder, anxiety disorder, or substance use disorder. Our clinical research group found that when psychiatrists are presented with the results of a semi-structured interview, BPD is much more frequently diagnosed.7 Such a finding would not be expected if stigma was the primary or sole reason for underdiagnosis.
Dr. Shapiro highlights the clinical consequence of underrecognition and underdiagnosis: the underutilization of empirically supported psychotherapies for BPD. A corollary of underdiagnosing BPD is overdiagnosis of bipolar disorder and overprescription of medication.8
There are other consequences of bias and stigma toward BPD. Despite the high levels of psychosocial morbidity, reduced health-related quality of life, high utilization of services, and excess mortality associated with BPD, this disorder is not included in the Global Burden of Disease Study. Thus, the public health significance of BPD is less fully appreciated. Finally, there is evidence that the level of funding for research from the National Institutes of Health is not commensurate with the level of psychosocial morbidity, mortality, and health expenditures associated with the disorder.9 Thus, the stigma toward BPD exists in both clinical and research communities.
Mark Zimmerman, MD
Professor of Psychiatry and Human Behavior
Warren Alpert Medical School of Brown University
Rhode Island Hospital
Providence, Rhode Island
References
1. Cleary M, Siegfried N, Walter G. Experience, knowledge and attitudes of mental health staff regarding clients with a borderline personality disorder. Int J Ment Health Nurs. 2002;11(3):186-191.
2. Gallop R, Lancee WJ, Garfinkel P. How nursing staff respond to the label “borderline personality disorder.” Hosp Community Psychiatry. 1989;40(8):815-819.
3. Lewis G, Appleby L. Personality disorder: the patients psychiatrists dislike. Br J Psychiatry. 1988;153:44-49.
4. Black DW, Pfohl B, Blum N, et al. Attitudes toward borderline personality disorder: a survey of 706 mental health clinicians. CNS Spectr. 2011;16(3):67-74.
5. Markham D, Trower P. The effects of the psychiatric label ‘borderline personality disorder’ on nursing staff’s perceptions and causal attributions for challenging behaviours. Br J Clin Psychol. 2003;42(pt 3):243-256.
6. Fraser K, Gallop R. Nurses’ confirming/disconfirming responses to patients diagnosed with borderline personality disorder. Arch Psychiatr Nurs. 1993;7(6):336-341.
7. Zimmerman M, Mattia JI. Differences between clinical and research practices in diagnosing borderline personality disorder. Am J Psychiatry. 1999;156(10):1570-1574.
8. Zimmerman M, Ruggero CJ, Chelminski I, et al. Is bipolar disorder overdiagnosed? J Clin Psychiatry. 2008;69(6):935-940.
9. Zimmerman M, Gazarian D. Is research on borderline personality disorder underfunded by the National Institute of Health? Psychiatry Res. 2014;220(3):941-944.
In response to Dr. Mark Zimmerman’s article, “Improving the recognition of borderline personality disorder” (
Why all the stigma? Because mental health professionals don’t have complete information. The assumption used to be that BPD was “intractable” with no treatment. Even if this were true, it still would not be a reason to fail to disclose a diagnosis, because in other fields of medicine, the concept of “therapeutic privilege” fell by the wayside long ago. However, we now know that in many individuals with BPD, symptoms improve over time, and there are several effective treatments.
In DSM-II, published in 1968, obsessive-compulsive disorder (OCD) was characterized as an “obsessive compulsive neurosis.” It was not reclassified as the current OCD diagnosis until DSM-III-R was published in 1987, after the FDA approved clomipramine. Why is this important? Because once people realized that there was a treatment, they started acknowledging OCD more often.
The first step in addressing the stigma toward BPD is that mental health professionals must recognize their own bias toward this diagnosis. We must be re-educated that this diagnosis carries hope, symptoms improve, and that there are effective treatments. This is how professionals will increase the recognition of BPD.
Assistant Professor and Compliance Officer
Department of Psychiatry
University of Florida
Clinic Director
UF Child and Adolescent Psychiatry Clinic at Springhill Health Center
Gainesville, Florida
References
1. Unruh BT, Gunderson JG. “Good enough” psychiatric residency training in borderline personality disorder: challenges, choice points, and a model generalist curriculum. Harv Rev Psychiatry. 2016;24(5):367-377.
2. Sheehan L, Nieweglowski K, Corrigan P. The stigma of personality disorders. Curr Psychiatry Rep. 2016;18(1):11.
Continue to: The author responds
The author responds
I agree with Dr. Shapiro that stigma by mental health clinicians contributes to the underdiagnosis of BPD. Mental health professions often hold a negative view of patients with personality disorders, particularly those with BPD, and see these patients as being more difficult to treat.1-3 They are the patients that some clinicians are reluctant to treat.3,4 Clinicians perceive patients with personality disorders as less mentally ill, more manipulative, and more able to control their behavior than patients with other psychiatric disorders.3,5 Consistent with this, clinicians have less sympathetic attitudes and behave less empathically toward patients with BPD.5,6 The term “borderline” also is sometimes used pejoratively to describe patients.1
As I described in my article, there are several possible reasons BPD is underdiagnosed. Foremost is that mood disorders, anxiety disorders, and substance use disorders are common in patients with BPD, and the symptoms of these other disorders are typically patients’ chief concerns when they present for treatment. Patients with BPD do not usually report the features of BPD—such as abandonment fears, chronic feelings of emptiness, or an identity disturbance—as their chief concerns. If they did, BPD would likely be easier to recognize. On a related note, clinicians do not have the time, or do not take the time, to conduct a thorough enough evaluation to diagnose BPD when it occurs in a patient who presents for treatment of a mood disorder, anxiety disorder, or substance use disorder. Our clinical research group found that when psychiatrists are presented with the results of a semi-structured interview, BPD is much more frequently diagnosed.7 Such a finding would not be expected if stigma was the primary or sole reason for underdiagnosis.
Dr. Shapiro highlights the clinical consequence of underrecognition and underdiagnosis: the underutilization of empirically supported psychotherapies for BPD. A corollary of underdiagnosing BPD is overdiagnosis of bipolar disorder and overprescription of medication.8
There are other consequences of bias and stigma toward BPD. Despite the high levels of psychosocial morbidity, reduced health-related quality of life, high utilization of services, and excess mortality associated with BPD, this disorder is not included in the Global Burden of Disease Study. Thus, the public health significance of BPD is less fully appreciated. Finally, there is evidence that the level of funding for research from the National Institutes of Health is not commensurate with the level of psychosocial morbidity, mortality, and health expenditures associated with the disorder.9 Thus, the stigma toward BPD exists in both clinical and research communities.
Mark Zimmerman, MD
Professor of Psychiatry and Human Behavior
Warren Alpert Medical School of Brown University
Rhode Island Hospital
Providence, Rhode Island
References
1. Cleary M, Siegfried N, Walter G. Experience, knowledge and attitudes of mental health staff regarding clients with a borderline personality disorder. Int J Ment Health Nurs. 2002;11(3):186-191.
2. Gallop R, Lancee WJ, Garfinkel P. How nursing staff respond to the label “borderline personality disorder.” Hosp Community Psychiatry. 1989;40(8):815-819.
3. Lewis G, Appleby L. Personality disorder: the patients psychiatrists dislike. Br J Psychiatry. 1988;153:44-49.
4. Black DW, Pfohl B, Blum N, et al. Attitudes toward borderline personality disorder: a survey of 706 mental health clinicians. CNS Spectr. 2011;16(3):67-74.
5. Markham D, Trower P. The effects of the psychiatric label ‘borderline personality disorder’ on nursing staff’s perceptions and causal attributions for challenging behaviours. Br J Clin Psychol. 2003;42(pt 3):243-256.
6. Fraser K, Gallop R. Nurses’ confirming/disconfirming responses to patients diagnosed with borderline personality disorder. Arch Psychiatr Nurs. 1993;7(6):336-341.
7. Zimmerman M, Mattia JI. Differences between clinical and research practices in diagnosing borderline personality disorder. Am J Psychiatry. 1999;156(10):1570-1574.
8. Zimmerman M, Ruggero CJ, Chelminski I, et al. Is bipolar disorder overdiagnosed? J Clin Psychiatry. 2008;69(6):935-940.
9. Zimmerman M, Gazarian D. Is research on borderline personality disorder underfunded by the National Institute of Health? Psychiatry Res. 2014;220(3):941-944.
In response to Dr. Mark Zimmerman’s article, “Improving the recognition of borderline personality disorder” (
Why all the stigma? Because mental health professionals don’t have complete information. The assumption used to be that BPD was “intractable” with no treatment. Even if this were true, it still would not be a reason to fail to disclose a diagnosis, because in other fields of medicine, the concept of “therapeutic privilege” fell by the wayside long ago. However, we now know that in many individuals with BPD, symptoms improve over time, and there are several effective treatments.
In DSM-II, published in 1968, obsessive-compulsive disorder (OCD) was characterized as an “obsessive compulsive neurosis.” It was not reclassified as the current OCD diagnosis until DSM-III-R was published in 1987, after the FDA approved clomipramine. Why is this important? Because once people realized that there was a treatment, they started acknowledging OCD more often.
The first step in addressing the stigma toward BPD is that mental health professionals must recognize their own bias toward this diagnosis. We must be re-educated that this diagnosis carries hope, symptoms improve, and that there are effective treatments. This is how professionals will increase the recognition of BPD.
Assistant Professor and Compliance Officer
Department of Psychiatry
University of Florida
Clinic Director
UF Child and Adolescent Psychiatry Clinic at Springhill Health Center
Gainesville, Florida
References
1. Unruh BT, Gunderson JG. “Good enough” psychiatric residency training in borderline personality disorder: challenges, choice points, and a model generalist curriculum. Harv Rev Psychiatry. 2016;24(5):367-377.
2. Sheehan L, Nieweglowski K, Corrigan P. The stigma of personality disorders. Curr Psychiatry Rep. 2016;18(1):11.
Continue to: The author responds
The author responds
I agree with Dr. Shapiro that stigma by mental health clinicians contributes to the underdiagnosis of BPD. Mental health professions often hold a negative view of patients with personality disorders, particularly those with BPD, and see these patients as being more difficult to treat.1-3 They are the patients that some clinicians are reluctant to treat.3,4 Clinicians perceive patients with personality disorders as less mentally ill, more manipulative, and more able to control their behavior than patients with other psychiatric disorders.3,5 Consistent with this, clinicians have less sympathetic attitudes and behave less empathically toward patients with BPD.5,6 The term “borderline” also is sometimes used pejoratively to describe patients.1
As I described in my article, there are several possible reasons BPD is underdiagnosed. Foremost is that mood disorders, anxiety disorders, and substance use disorders are common in patients with BPD, and the symptoms of these other disorders are typically patients’ chief concerns when they present for treatment. Patients with BPD do not usually report the features of BPD—such as abandonment fears, chronic feelings of emptiness, or an identity disturbance—as their chief concerns. If they did, BPD would likely be easier to recognize. On a related note, clinicians do not have the time, or do not take the time, to conduct a thorough enough evaluation to diagnose BPD when it occurs in a patient who presents for treatment of a mood disorder, anxiety disorder, or substance use disorder. Our clinical research group found that when psychiatrists are presented with the results of a semi-structured interview, BPD is much more frequently diagnosed.7 Such a finding would not be expected if stigma was the primary or sole reason for underdiagnosis.
Dr. Shapiro highlights the clinical consequence of underrecognition and underdiagnosis: the underutilization of empirically supported psychotherapies for BPD. A corollary of underdiagnosing BPD is overdiagnosis of bipolar disorder and overprescription of medication.8
There are other consequences of bias and stigma toward BPD. Despite the high levels of psychosocial morbidity, reduced health-related quality of life, high utilization of services, and excess mortality associated with BPD, this disorder is not included in the Global Burden of Disease Study. Thus, the public health significance of BPD is less fully appreciated. Finally, there is evidence that the level of funding for research from the National Institutes of Health is not commensurate with the level of psychosocial morbidity, mortality, and health expenditures associated with the disorder.9 Thus, the stigma toward BPD exists in both clinical and research communities.
Mark Zimmerman, MD
Professor of Psychiatry and Human Behavior
Warren Alpert Medical School of Brown University
Rhode Island Hospital
Providence, Rhode Island
References
1. Cleary M, Siegfried N, Walter G. Experience, knowledge and attitudes of mental health staff regarding clients with a borderline personality disorder. Int J Ment Health Nurs. 2002;11(3):186-191.
2. Gallop R, Lancee WJ, Garfinkel P. How nursing staff respond to the label “borderline personality disorder.” Hosp Community Psychiatry. 1989;40(8):815-819.
3. Lewis G, Appleby L. Personality disorder: the patients psychiatrists dislike. Br J Psychiatry. 1988;153:44-49.
4. Black DW, Pfohl B, Blum N, et al. Attitudes toward borderline personality disorder: a survey of 706 mental health clinicians. CNS Spectr. 2011;16(3):67-74.
5. Markham D, Trower P. The effects of the psychiatric label ‘borderline personality disorder’ on nursing staff’s perceptions and causal attributions for challenging behaviours. Br J Clin Psychol. 2003;42(pt 3):243-256.
6. Fraser K, Gallop R. Nurses’ confirming/disconfirming responses to patients diagnosed with borderline personality disorder. Arch Psychiatr Nurs. 1993;7(6):336-341.
7. Zimmerman M, Mattia JI. Differences between clinical and research practices in diagnosing borderline personality disorder. Am J Psychiatry. 1999;156(10):1570-1574.
8. Zimmerman M, Ruggero CJ, Chelminski I, et al. Is bipolar disorder overdiagnosed? J Clin Psychiatry. 2008;69(6):935-940.
9. Zimmerman M, Gazarian D. Is research on borderline personality disorder underfunded by the National Institute of Health? Psychiatry Res. 2014;220(3):941-944.
Point-of-care ultrasound: Deploying in primary care
Two weeks ago, I saw a man with a swollen left leg in the office. It took me 2 days to get a Doppler study completed in my busy health care system. Point-of-care ultrasound (POCUS) would have been invaluable for this gentleman. As we know, though, POCUS has been “slow to grow” in primary care. However, as this month’s cover story suggests, things are changing.
Since the 1970s, ultrasound has been a standard diagnostic tool for many conditions. Initially considered the domain of radiologists and cardiologists with extensive training, technologic advances now allow accurate interpretation of ultrasound images by generalist physicians with a modest amount of training.
One of the first references to POCUS in general practice in the United States was published in 1988.1 Use of ultrasound in family medicine has developed slowly over the past 30 years, due to the high cost of equipment, a lack of training as a formal component of family medicine residency curricula, and a lack of evidence of its effectiveness in office practice. Only 6% of practicing family physicians (FPs) reported using non-obstetric POCUS in their practices in 2016, and only 2% of family medicine residency programs had established POCUS curricula in 2015.2,3
Ready for prime time. Although I had considered POCUS to be a relatively new and untested technology for primary care settings, my reading of the POCUS article has convinced me that POCUS is now ready for widespread deployment in family medicine office practice. Bornemann and colleagues review the evidence for the use of POCUS in 4 areas: the heart, the lung, screening for abdominal aortic aneurysm (AAA), and the diagnosis of deep vein thrombosis. They provide more than 30 references that support the accuracy and effectiveness of the use of POCUS by FPs for these areas. The equipment is affordable, there is ample evidence of accuracy and effectiveness, and, as they note, a curriculum for FP training has been published.
I certainly hope that POCUS continues to make its way into FPs’ offices. It would certainly help patients like the one I saw 2 weeks ago, and it would help us to screen for AAA in older male smokers, as recommended by the US Preventive Services Task Force.
I am delighted to see FP pioneers working to advance the use of POCUS in family medicine. Hopefully, it will become a standard part of family medicine training and practice sooner, rather than later.
1. Hahn RG, Davies TC, Rodney WM. Diagnostic ultrasound in general practice. J Fam Pract. 1988;5:129-135.
2. Clinical procedures performed by physicians at their practice. American Academy of Family Physicians Member Census, December 31, 2016. Available at: http://www.aafp.org/about/the-aafp/family-medicine-facts/table-12(rev).html. Accessed January 16, 2018.
3. Hall JW, Holman H, Bornemann P, et al. Point of care ultrasound in family medicine residency programs: a CERA study. Fam Med. 2015;47:706-711.
Two weeks ago, I saw a man with a swollen left leg in the office. It took me 2 days to get a Doppler study completed in my busy health care system. Point-of-care ultrasound (POCUS) would have been invaluable for this gentleman. As we know, though, POCUS has been “slow to grow” in primary care. However, as this month’s cover story suggests, things are changing.
Since the 1970s, ultrasound has been a standard diagnostic tool for many conditions. Initially considered the domain of radiologists and cardiologists with extensive training, technologic advances now allow accurate interpretation of ultrasound images by generalist physicians with a modest amount of training.
One of the first references to POCUS in general practice in the United States was published in 1988.1 Use of ultrasound in family medicine has developed slowly over the past 30 years, due to the high cost of equipment, a lack of training as a formal component of family medicine residency curricula, and a lack of evidence of its effectiveness in office practice. Only 6% of practicing family physicians (FPs) reported using non-obstetric POCUS in their practices in 2016, and only 2% of family medicine residency programs had established POCUS curricula in 2015.2,3
Ready for prime time. Although I had considered POCUS to be a relatively new and untested technology for primary care settings, my reading of the POCUS article has convinced me that POCUS is now ready for widespread deployment in family medicine office practice. Bornemann and colleagues review the evidence for the use of POCUS in 4 areas: the heart, the lung, screening for abdominal aortic aneurysm (AAA), and the diagnosis of deep vein thrombosis. They provide more than 30 references that support the accuracy and effectiveness of the use of POCUS by FPs for these areas. The equipment is affordable, there is ample evidence of accuracy and effectiveness, and, as they note, a curriculum for FP training has been published.
I certainly hope that POCUS continues to make its way into FPs’ offices. It would certainly help patients like the one I saw 2 weeks ago, and it would help us to screen for AAA in older male smokers, as recommended by the US Preventive Services Task Force.
I am delighted to see FP pioneers working to advance the use of POCUS in family medicine. Hopefully, it will become a standard part of family medicine training and practice sooner, rather than later.
Two weeks ago, I saw a man with a swollen left leg in the office. It took me 2 days to get a Doppler study completed in my busy health care system. Point-of-care ultrasound (POCUS) would have been invaluable for this gentleman. As we know, though, POCUS has been “slow to grow” in primary care. However, as this month’s cover story suggests, things are changing.
Since the 1970s, ultrasound has been a standard diagnostic tool for many conditions. Initially considered the domain of radiologists and cardiologists with extensive training, technologic advances now allow accurate interpretation of ultrasound images by generalist physicians with a modest amount of training.
One of the first references to POCUS in general practice in the United States was published in 1988.1 Use of ultrasound in family medicine has developed slowly over the past 30 years, due to the high cost of equipment, a lack of training as a formal component of family medicine residency curricula, and a lack of evidence of its effectiveness in office practice. Only 6% of practicing family physicians (FPs) reported using non-obstetric POCUS in their practices in 2016, and only 2% of family medicine residency programs had established POCUS curricula in 2015.2,3
Ready for prime time. Although I had considered POCUS to be a relatively new and untested technology for primary care settings, my reading of the POCUS article has convinced me that POCUS is now ready for widespread deployment in family medicine office practice. Bornemann and colleagues review the evidence for the use of POCUS in 4 areas: the heart, the lung, screening for abdominal aortic aneurysm (AAA), and the diagnosis of deep vein thrombosis. They provide more than 30 references that support the accuracy and effectiveness of the use of POCUS by FPs for these areas. The equipment is affordable, there is ample evidence of accuracy and effectiveness, and, as they note, a curriculum for FP training has been published.
I certainly hope that POCUS continues to make its way into FPs’ offices. It would certainly help patients like the one I saw 2 weeks ago, and it would help us to screen for AAA in older male smokers, as recommended by the US Preventive Services Task Force.
I am delighted to see FP pioneers working to advance the use of POCUS in family medicine. Hopefully, it will become a standard part of family medicine training and practice sooner, rather than later.
1. Hahn RG, Davies TC, Rodney WM. Diagnostic ultrasound in general practice. J Fam Pract. 1988;5:129-135.
2. Clinical procedures performed by physicians at their practice. American Academy of Family Physicians Member Census, December 31, 2016. Available at: http://www.aafp.org/about/the-aafp/family-medicine-facts/table-12(rev).html. Accessed January 16, 2018.
3. Hall JW, Holman H, Bornemann P, et al. Point of care ultrasound in family medicine residency programs: a CERA study. Fam Med. 2015;47:706-711.
1. Hahn RG, Davies TC, Rodney WM. Diagnostic ultrasound in general practice. J Fam Pract. 1988;5:129-135.
2. Clinical procedures performed by physicians at their practice. American Academy of Family Physicians Member Census, December 31, 2016. Available at: http://www.aafp.org/about/the-aafp/family-medicine-facts/table-12(rev).html. Accessed January 16, 2018.
3. Hall JW, Holman H, Bornemann P, et al. Point of care ultrasound in family medicine residency programs: a CERA study. Fam Med. 2015;47:706-711.
Preventive health: Getting rid of the middleman (uh-oh, that’s us!)
As physicians, we find that preventive health is, frankly, really difficult. It requires thinking about a changing list of recommendations unprompted by the symptoms for which patients present. Compounding that challenge is that, in doing preventive health well, we need to have personalized discussions with our patients and this requires they come into the office, which doesn’t always happen on a regular basis. Furthermore, when patients do come in, they usually are presenting for an acute care visit, so there is little time set aside to discuss preventive health.
For all these reasons and many others, the data suggest that we are not particularly good at performing preventive health maintenance. We are much better at figuring out diagnostic dilemmas and choosing among competing medications or procedures to most effectively address acute and chronic medical problems. Let’s examine the data to see if there is a shred of truth in what we are saying; then let’s look at a potential solution to the dilemma of preventive health that we all believe in and that we carry out less frequently than any of us would like.
First, let’s look at recent data on cancer screening reported by the CDC1:
- Mammography: 72% of women aged 50–74 years reported having had a mammogram within the past 2 years.
- Pap test: 83% of women reported being up to date with cervical cancer screening.
- Colorectal cancer screening: 62% of men and women reported colorectal cancer screening test use consistent with USPSTF recommendations.
Of note, colorectal cancer screening has improved dramatically over he last 15 years, while screening for breast and cervical cancer has largely plateaued.1
Our success with cancer screening – or lack thereof depending upon one’s perspective – looks quite good next to national vaccination rates for adults. The immunization rate for commonly recommended vaccines are as follows2:
- The Tdap vaccination rate is 20%.
- The tetanus-diphtheria vaccination rate is 62%.
- The herpes zoster vaccination rate is 28%.
- The influenza vaccination rate is 43%.
- The pneumococcal vaccination rate among high-risk persons aged 19-64 years is 20% and among adults aged greater than or equal to 65 years is 61%.
Of adults who had health insurance and at least 10 physician contacts within the past year, 23.8%-88.8% reported not having received vaccinations that were recommended.
In the business literature there is a great deal of disagreement about the value of the “middleman.” The term middleman describes someone who brings the product from the producer, or factory, to the consumer. On the one hand, if the factory can sell the product directly to the consumer, the consumer can save money and the factory can make more money. On the other hand, if the middleman can help the consumer make a better choice among the variety of products available, then the middleman provides value and the consumer benefits.3
Traditionally, clinicians have served the role of the middleman for preventive health activities, knowing what to recommend to patients and informing them of the correct preventive health choices that fit their needs. The problem with this concept is that preventive health recommendations are largely demographically based, are tied to population-based risk assessment, and usually require very little individual judgment.
We as physicians are good at – and I believe truly enjoy – exercising judgment. We love thinking things through and helping the person in front of us. We are not as good at remembering unprompted information in the middle of busy visits that are often made for unrelated reasons. Most of the people who have not had a colonoscopy or pneumococcal vaccine have not decided against the procedure after a detailed discussion with their physician. On the contrary, the service was never recommended, or it was recommended, but the patient did not follow up to have the procedure performed.
Let’s now imagine another approach. You’re a patient and once a year you click on an email that shows up in your inbox from your doctor with the words “Preventive Health” in the subject line. The EHR – based on your gender, age, and a query of what has been documented in your chart – has determined the preventive health activities that are recommended for you. You can choose to pursue, opt out, or get more information for each of the recommended preventive services as you read through them.
If you choose to have more information, it is provided in a structured format that allows you to drill down to the level of detail that you desire. In all probability, you will find a greater level of detail and accuracy of information about each preventive service than could possibly be provided during a routine office visit. Specifics about the risks and benefits of the procedure will also be more extensive, as it is unlikely your care providers are able to keep all of the details and risk ratios in their heads. If desired, you as a patient can take your time to read and digest the information, sleep on it, and come back to it to make an informed decision. This is not something you can do during a routine office visit.
If you choose to opt out of the procedure, just click the “declined” box. Otherwise, when you’ve made all of your decisions and indicate that you’re done, the necessary prescriptions for blood work and x-rays, as well as referrals to the appropriate specialists, will print out. An entry will also be made in the electronic record showing you’ve been provided preventive health recommendations that are appropriate for your age and sex and made your preferred choices. At any point, if you feel you’d like further discussion with your physician, you can make an appointment electronically through the interface.
The hurdles for implementing such a system are real, but they are solvable, and the development of such an approach is inevitable, enviable, and will ultimately be good for both patients and their providers. Patients will get more predictable and complete recommendations for preventive care and providers will have more time to do what we enjoy and are most skilled at – talking with patients to clarify diagnoses, decide upon treatment, and clarify questions that come up about preventive health recommendations.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
References
1. White A et al. Cancer screening test use – United States, 2015. MMWR Morb Mortal Wkly Rep. 2017 Mar 3;66(8):201-6.
2. Williams WW et al. Surveillance of vaccination coverage among adult populations – United States, 2014. MMWR Surveill Summ. 2016 Feb 5;65(1):1-36.
3. Conerly B. Don’t eliminate the middleman – He’s much too valuable. Forbes. Oct 28, 2015.
As physicians, we find that preventive health is, frankly, really difficult. It requires thinking about a changing list of recommendations unprompted by the symptoms for which patients present. Compounding that challenge is that, in doing preventive health well, we need to have personalized discussions with our patients and this requires they come into the office, which doesn’t always happen on a regular basis. Furthermore, when patients do come in, they usually are presenting for an acute care visit, so there is little time set aside to discuss preventive health.
For all these reasons and many others, the data suggest that we are not particularly good at performing preventive health maintenance. We are much better at figuring out diagnostic dilemmas and choosing among competing medications or procedures to most effectively address acute and chronic medical problems. Let’s examine the data to see if there is a shred of truth in what we are saying; then let’s look at a potential solution to the dilemma of preventive health that we all believe in and that we carry out less frequently than any of us would like.
First, let’s look at recent data on cancer screening reported by the CDC1:
- Mammography: 72% of women aged 50–74 years reported having had a mammogram within the past 2 years.
- Pap test: 83% of women reported being up to date with cervical cancer screening.
- Colorectal cancer screening: 62% of men and women reported colorectal cancer screening test use consistent with USPSTF recommendations.
Of note, colorectal cancer screening has improved dramatically over he last 15 years, while screening for breast and cervical cancer has largely plateaued.1
Our success with cancer screening – or lack thereof depending upon one’s perspective – looks quite good next to national vaccination rates for adults. The immunization rate for commonly recommended vaccines are as follows2:
- The Tdap vaccination rate is 20%.
- The tetanus-diphtheria vaccination rate is 62%.
- The herpes zoster vaccination rate is 28%.
- The influenza vaccination rate is 43%.
- The pneumococcal vaccination rate among high-risk persons aged 19-64 years is 20% and among adults aged greater than or equal to 65 years is 61%.
Of adults who had health insurance and at least 10 physician contacts within the past year, 23.8%-88.8% reported not having received vaccinations that were recommended.
In the business literature there is a great deal of disagreement about the value of the “middleman.” The term middleman describes someone who brings the product from the producer, or factory, to the consumer. On the one hand, if the factory can sell the product directly to the consumer, the consumer can save money and the factory can make more money. On the other hand, if the middleman can help the consumer make a better choice among the variety of products available, then the middleman provides value and the consumer benefits.3
Traditionally, clinicians have served the role of the middleman for preventive health activities, knowing what to recommend to patients and informing them of the correct preventive health choices that fit their needs. The problem with this concept is that preventive health recommendations are largely demographically based, are tied to population-based risk assessment, and usually require very little individual judgment.
We as physicians are good at – and I believe truly enjoy – exercising judgment. We love thinking things through and helping the person in front of us. We are not as good at remembering unprompted information in the middle of busy visits that are often made for unrelated reasons. Most of the people who have not had a colonoscopy or pneumococcal vaccine have not decided against the procedure after a detailed discussion with their physician. On the contrary, the service was never recommended, or it was recommended, but the patient did not follow up to have the procedure performed.
Let’s now imagine another approach. You’re a patient and once a year you click on an email that shows up in your inbox from your doctor with the words “Preventive Health” in the subject line. The EHR – based on your gender, age, and a query of what has been documented in your chart – has determined the preventive health activities that are recommended for you. You can choose to pursue, opt out, or get more information for each of the recommended preventive services as you read through them.
If you choose to have more information, it is provided in a structured format that allows you to drill down to the level of detail that you desire. In all probability, you will find a greater level of detail and accuracy of information about each preventive service than could possibly be provided during a routine office visit. Specifics about the risks and benefits of the procedure will also be more extensive, as it is unlikely your care providers are able to keep all of the details and risk ratios in their heads. If desired, you as a patient can take your time to read and digest the information, sleep on it, and come back to it to make an informed decision. This is not something you can do during a routine office visit.
If you choose to opt out of the procedure, just click the “declined” box. Otherwise, when you’ve made all of your decisions and indicate that you’re done, the necessary prescriptions for blood work and x-rays, as well as referrals to the appropriate specialists, will print out. An entry will also be made in the electronic record showing you’ve been provided preventive health recommendations that are appropriate for your age and sex and made your preferred choices. At any point, if you feel you’d like further discussion with your physician, you can make an appointment electronically through the interface.
The hurdles for implementing such a system are real, but they are solvable, and the development of such an approach is inevitable, enviable, and will ultimately be good for both patients and their providers. Patients will get more predictable and complete recommendations for preventive care and providers will have more time to do what we enjoy and are most skilled at – talking with patients to clarify diagnoses, decide upon treatment, and clarify questions that come up about preventive health recommendations.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
References
1. White A et al. Cancer screening test use – United States, 2015. MMWR Morb Mortal Wkly Rep. 2017 Mar 3;66(8):201-6.
2. Williams WW et al. Surveillance of vaccination coverage among adult populations – United States, 2014. MMWR Surveill Summ. 2016 Feb 5;65(1):1-36.
3. Conerly B. Don’t eliminate the middleman – He’s much too valuable. Forbes. Oct 28, 2015.
As physicians, we find that preventive health is, frankly, really difficult. It requires thinking about a changing list of recommendations unprompted by the symptoms for which patients present. Compounding that challenge is that, in doing preventive health well, we need to have personalized discussions with our patients and this requires they come into the office, which doesn’t always happen on a regular basis. Furthermore, when patients do come in, they usually are presenting for an acute care visit, so there is little time set aside to discuss preventive health.
For all these reasons and many others, the data suggest that we are not particularly good at performing preventive health maintenance. We are much better at figuring out diagnostic dilemmas and choosing among competing medications or procedures to most effectively address acute and chronic medical problems. Let’s examine the data to see if there is a shred of truth in what we are saying; then let’s look at a potential solution to the dilemma of preventive health that we all believe in and that we carry out less frequently than any of us would like.
First, let’s look at recent data on cancer screening reported by the CDC1:
- Mammography: 72% of women aged 50–74 years reported having had a mammogram within the past 2 years.
- Pap test: 83% of women reported being up to date with cervical cancer screening.
- Colorectal cancer screening: 62% of men and women reported colorectal cancer screening test use consistent with USPSTF recommendations.
Of note, colorectal cancer screening has improved dramatically over he last 15 years, while screening for breast and cervical cancer has largely plateaued.1
Our success with cancer screening – or lack thereof depending upon one’s perspective – looks quite good next to national vaccination rates for adults. The immunization rate for commonly recommended vaccines are as follows2:
- The Tdap vaccination rate is 20%.
- The tetanus-diphtheria vaccination rate is 62%.
- The herpes zoster vaccination rate is 28%.
- The influenza vaccination rate is 43%.
- The pneumococcal vaccination rate among high-risk persons aged 19-64 years is 20% and among adults aged greater than or equal to 65 years is 61%.
Of adults who had health insurance and at least 10 physician contacts within the past year, 23.8%-88.8% reported not having received vaccinations that were recommended.
In the business literature there is a great deal of disagreement about the value of the “middleman.” The term middleman describes someone who brings the product from the producer, or factory, to the consumer. On the one hand, if the factory can sell the product directly to the consumer, the consumer can save money and the factory can make more money. On the other hand, if the middleman can help the consumer make a better choice among the variety of products available, then the middleman provides value and the consumer benefits.3
Traditionally, clinicians have served the role of the middleman for preventive health activities, knowing what to recommend to patients and informing them of the correct preventive health choices that fit their needs. The problem with this concept is that preventive health recommendations are largely demographically based, are tied to population-based risk assessment, and usually require very little individual judgment.
We as physicians are good at – and I believe truly enjoy – exercising judgment. We love thinking things through and helping the person in front of us. We are not as good at remembering unprompted information in the middle of busy visits that are often made for unrelated reasons. Most of the people who have not had a colonoscopy or pneumococcal vaccine have not decided against the procedure after a detailed discussion with their physician. On the contrary, the service was never recommended, or it was recommended, but the patient did not follow up to have the procedure performed.
Let’s now imagine another approach. You’re a patient and once a year you click on an email that shows up in your inbox from your doctor with the words “Preventive Health” in the subject line. The EHR – based on your gender, age, and a query of what has been documented in your chart – has determined the preventive health activities that are recommended for you. You can choose to pursue, opt out, or get more information for each of the recommended preventive services as you read through them.
If you choose to have more information, it is provided in a structured format that allows you to drill down to the level of detail that you desire. In all probability, you will find a greater level of detail and accuracy of information about each preventive service than could possibly be provided during a routine office visit. Specifics about the risks and benefits of the procedure will also be more extensive, as it is unlikely your care providers are able to keep all of the details and risk ratios in their heads. If desired, you as a patient can take your time to read and digest the information, sleep on it, and come back to it to make an informed decision. This is not something you can do during a routine office visit.
If you choose to opt out of the procedure, just click the “declined” box. Otherwise, when you’ve made all of your decisions and indicate that you’re done, the necessary prescriptions for blood work and x-rays, as well as referrals to the appropriate specialists, will print out. An entry will also be made in the electronic record showing you’ve been provided preventive health recommendations that are appropriate for your age and sex and made your preferred choices. At any point, if you feel you’d like further discussion with your physician, you can make an appointment electronically through the interface.
The hurdles for implementing such a system are real, but they are solvable, and the development of such an approach is inevitable, enviable, and will ultimately be good for both patients and their providers. Patients will get more predictable and complete recommendations for preventive care and providers will have more time to do what we enjoy and are most skilled at – talking with patients to clarify diagnoses, decide upon treatment, and clarify questions that come up about preventive health recommendations.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
References
1. White A et al. Cancer screening test use – United States, 2015. MMWR Morb Mortal Wkly Rep. 2017 Mar 3;66(8):201-6.
2. Williams WW et al. Surveillance of vaccination coverage among adult populations – United States, 2014. MMWR Surveill Summ. 2016 Feb 5;65(1):1-36.
3. Conerly B. Don’t eliminate the middleman – He’s much too valuable. Forbes. Oct 28, 2015.
The care of ‘down there’
Let face it, it’s hard enough to get a teen girl to look up long enough to answer basic questions during an exam, let alone start a completely uncomfortable conversation about vaginal hygiene. Realistically, though, if we don’t have the conversation, who will? Sure, moms give some instructions on how to wipe properly and remind teens to change their pads frequently, but are they giving the correct advice? Are many women just suffering in silence, assuming it’s just something women deal with? Or are they continuing harmful practices that have been passed down through the generations?
Bacterial vaginosis
Bacterial vaginosis (BV) is a polymicrobial syndrome characterized by an imbalance of resident bacteria flora in the vagina.1 The normal flora is predominantly lactobacilli and produces hydrogen peroxide, which keeps the vaginal pH around 4.5. When normal flora is disrupted, other bacteria such as Gardnerella vaginalis, Mycoplasma hominis, and Prevotella bacteroides, to name just a few, can take over, resulting in an unpleasant odor, a watery discharge, and a lower pH. Although originally thought to be sexually transmitted, BV can occur at any age and without having intercourse.2
The incidence of BV varies among races, among socioeconomic classes, and with age. Cultural practices and resources play more of a role than physiologic differences.2 For example, African American women, particularly Caribbean blacks, have higher rates than white women, but douching also is more common among African American and Caribbean blacks than whites. Washing with harsh antiseptics or perfumed soaps also can increase risk, and BV can be sexually transmitted, so the number of partners a woman has can increase that risk.
The presence of BV also has significant social, interpersonal, and work effects and, for some women, is the source of extreme anxiety and distress, which is why many women turn to extreme measures such as douching to control it.3,5
Furthermore, BV is associated with preterm labor and low birth weight infants. Studies have shown that women who are culture positive in their second trimester are at greater risk for adverse outcomes.6
Douching
Douching began in the mid-1800s with the advent of the Eguisier irrigator, which was sold in French pharmacies and consisted of a plunger and a nozzle and was used to prevent pregnancy. Then, in the 1920’s, Lysol was used as the antiseptic, with claims that it acted as a spermicide. Rinsing out the vagina after coitus was believed to kill any sperm in the body and prevent pregnancy. It wasn’t until the 1980’s that the ill effects of Lysol on the vagina were acknowledged and the practice was discontinued.4
Although, generally, douching has fallen out of favor and most authorities advise against it,studies have shown that there can be a benefit when used for vaginosis or vaginitis in relieving symptoms.5,2 Those benefits do not outweigh the possible adverse effects. The process of douching allows for a pressurized solution to be injected into the vagina, thereby flushing bacteria throughout the vagina and into the uterus. In adolescence, the endothelial lining is more prone to adherence of the bacteria, so contracting a sexually transmitted infection is more likely and can increase the risk for ectopic pregnancy.2 The mucus lining of the vagina also tends to be thick; using harsh soaps thins the mucosa, again increasing the likelihood of infections. Furthermore, studies have confirmed that there also is a higher transmission rate of HIV and chlamydia when BV is present.2
Treating and preventing BV
The treatment of choice for BV is metronidazole taken orally or introduced vaginally. Studies have shown that recolonization of the lactobacilli can be slow, so the addition of lactic acid can be helpful. Clindamycin orally or vaginally also is a reasonable choice. Given that most of the bacteria causing BV have beta-lactamase, penicillin is not effective.7
Probiotics taken orally have a natural migration to the vaginal area and promote recolonization.7 Taking 250 mg of vitamin C 6 days/month for 6 months also has been shown to be helpful in recolonization and prevention of recurrence.8
A discussion of proper vaginal hygiene is important for adolescents and teens. Poor hygiene can significantly affect their social and interpersonal relationships, as well as their self-esteem. It puts them at greater risk for contracting sexually transmitted infections, and if they become pregnant, of having an adverse outcome.
In addition, inform them that douching with harsh or perfumed soaps changes the pH of the vagina, which can lead to bacterial overgrowth, so douching should be avoided. Advise them to change pads used during the menstrual cycle every 4-6 hours, and that cotton underwear and loose-fitting clothes also can reduce vaginal irritation. Lastly, advise teens to drink lots of fluids, eat yogurt, and take vitamin C and probiotics to reduce the risk of recurrence.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures.
References
1. Das P et al. PLoS One. 2015 Jun 30;10(6):e0130777.
2. Martino JL et al. Epidemiologic reviews. 2002;24(2):109-24.
3. Bilardi JE et al. PLoS ONE 2013;8(9):e74378.
4. www.Timeline.com/sexist-history-douching-bcc39f3d216c. 2016 Aug 14.
5. Fashemi B et al. Microb Ecol Health Dis. 2013 Feb 25. doi: 10.3402/mehd.v24i0.19703.
6. Hillier SL et al. N Engl J Med. 1995 Dec 28;333(26):1737-42.
7. Kumar N et al. J Pharm Bioallied Sci. 2011 Oct;3(4):496-503.
8. Krasnopolsky VN et al. J Clin Med Res. 2013 Aug;5(4):309-15..
Let face it, it’s hard enough to get a teen girl to look up long enough to answer basic questions during an exam, let alone start a completely uncomfortable conversation about vaginal hygiene. Realistically, though, if we don’t have the conversation, who will? Sure, moms give some instructions on how to wipe properly and remind teens to change their pads frequently, but are they giving the correct advice? Are many women just suffering in silence, assuming it’s just something women deal with? Or are they continuing harmful practices that have been passed down through the generations?
Bacterial vaginosis
Bacterial vaginosis (BV) is a polymicrobial syndrome characterized by an imbalance of resident bacteria flora in the vagina.1 The normal flora is predominantly lactobacilli and produces hydrogen peroxide, which keeps the vaginal pH around 4.5. When normal flora is disrupted, other bacteria such as Gardnerella vaginalis, Mycoplasma hominis, and Prevotella bacteroides, to name just a few, can take over, resulting in an unpleasant odor, a watery discharge, and a lower pH. Although originally thought to be sexually transmitted, BV can occur at any age and without having intercourse.2
The incidence of BV varies among races, among socioeconomic classes, and with age. Cultural practices and resources play more of a role than physiologic differences.2 For example, African American women, particularly Caribbean blacks, have higher rates than white women, but douching also is more common among African American and Caribbean blacks than whites. Washing with harsh antiseptics or perfumed soaps also can increase risk, and BV can be sexually transmitted, so the number of partners a woman has can increase that risk.
The presence of BV also has significant social, interpersonal, and work effects and, for some women, is the source of extreme anxiety and distress, which is why many women turn to extreme measures such as douching to control it.3,5
Furthermore, BV is associated with preterm labor and low birth weight infants. Studies have shown that women who are culture positive in their second trimester are at greater risk for adverse outcomes.6
Douching
Douching began in the mid-1800s with the advent of the Eguisier irrigator, which was sold in French pharmacies and consisted of a plunger and a nozzle and was used to prevent pregnancy. Then, in the 1920’s, Lysol was used as the antiseptic, with claims that it acted as a spermicide. Rinsing out the vagina after coitus was believed to kill any sperm in the body and prevent pregnancy. It wasn’t until the 1980’s that the ill effects of Lysol on the vagina were acknowledged and the practice was discontinued.4
Although, generally, douching has fallen out of favor and most authorities advise against it,studies have shown that there can be a benefit when used for vaginosis or vaginitis in relieving symptoms.5,2 Those benefits do not outweigh the possible adverse effects. The process of douching allows for a pressurized solution to be injected into the vagina, thereby flushing bacteria throughout the vagina and into the uterus. In adolescence, the endothelial lining is more prone to adherence of the bacteria, so contracting a sexually transmitted infection is more likely and can increase the risk for ectopic pregnancy.2 The mucus lining of the vagina also tends to be thick; using harsh soaps thins the mucosa, again increasing the likelihood of infections. Furthermore, studies have confirmed that there also is a higher transmission rate of HIV and chlamydia when BV is present.2
Treating and preventing BV
The treatment of choice for BV is metronidazole taken orally or introduced vaginally. Studies have shown that recolonization of the lactobacilli can be slow, so the addition of lactic acid can be helpful. Clindamycin orally or vaginally also is a reasonable choice. Given that most of the bacteria causing BV have beta-lactamase, penicillin is not effective.7
Probiotics taken orally have a natural migration to the vaginal area and promote recolonization.7 Taking 250 mg of vitamin C 6 days/month for 6 months also has been shown to be helpful in recolonization and prevention of recurrence.8
A discussion of proper vaginal hygiene is important for adolescents and teens. Poor hygiene can significantly affect their social and interpersonal relationships, as well as their self-esteem. It puts them at greater risk for contracting sexually transmitted infections, and if they become pregnant, of having an adverse outcome.
In addition, inform them that douching with harsh or perfumed soaps changes the pH of the vagina, which can lead to bacterial overgrowth, so douching should be avoided. Advise them to change pads used during the menstrual cycle every 4-6 hours, and that cotton underwear and loose-fitting clothes also can reduce vaginal irritation. Lastly, advise teens to drink lots of fluids, eat yogurt, and take vitamin C and probiotics to reduce the risk of recurrence.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures.
References
1. Das P et al. PLoS One. 2015 Jun 30;10(6):e0130777.
2. Martino JL et al. Epidemiologic reviews. 2002;24(2):109-24.
3. Bilardi JE et al. PLoS ONE 2013;8(9):e74378.
4. www.Timeline.com/sexist-history-douching-bcc39f3d216c. 2016 Aug 14.
5. Fashemi B et al. Microb Ecol Health Dis. 2013 Feb 25. doi: 10.3402/mehd.v24i0.19703.
6. Hillier SL et al. N Engl J Med. 1995 Dec 28;333(26):1737-42.
7. Kumar N et al. J Pharm Bioallied Sci. 2011 Oct;3(4):496-503.
8. Krasnopolsky VN et al. J Clin Med Res. 2013 Aug;5(4):309-15..
Let face it, it’s hard enough to get a teen girl to look up long enough to answer basic questions during an exam, let alone start a completely uncomfortable conversation about vaginal hygiene. Realistically, though, if we don’t have the conversation, who will? Sure, moms give some instructions on how to wipe properly and remind teens to change their pads frequently, but are they giving the correct advice? Are many women just suffering in silence, assuming it’s just something women deal with? Or are they continuing harmful practices that have been passed down through the generations?
Bacterial vaginosis
Bacterial vaginosis (BV) is a polymicrobial syndrome characterized by an imbalance of resident bacteria flora in the vagina.1 The normal flora is predominantly lactobacilli and produces hydrogen peroxide, which keeps the vaginal pH around 4.5. When normal flora is disrupted, other bacteria such as Gardnerella vaginalis, Mycoplasma hominis, and Prevotella bacteroides, to name just a few, can take over, resulting in an unpleasant odor, a watery discharge, and a lower pH. Although originally thought to be sexually transmitted, BV can occur at any age and without having intercourse.2
The incidence of BV varies among races, among socioeconomic classes, and with age. Cultural practices and resources play more of a role than physiologic differences.2 For example, African American women, particularly Caribbean blacks, have higher rates than white women, but douching also is more common among African American and Caribbean blacks than whites. Washing with harsh antiseptics or perfumed soaps also can increase risk, and BV can be sexually transmitted, so the number of partners a woman has can increase that risk.
The presence of BV also has significant social, interpersonal, and work effects and, for some women, is the source of extreme anxiety and distress, which is why many women turn to extreme measures such as douching to control it.3,5
Furthermore, BV is associated with preterm labor and low birth weight infants. Studies have shown that women who are culture positive in their second trimester are at greater risk for adverse outcomes.6
Douching
Douching began in the mid-1800s with the advent of the Eguisier irrigator, which was sold in French pharmacies and consisted of a plunger and a nozzle and was used to prevent pregnancy. Then, in the 1920’s, Lysol was used as the antiseptic, with claims that it acted as a spermicide. Rinsing out the vagina after coitus was believed to kill any sperm in the body and prevent pregnancy. It wasn’t until the 1980’s that the ill effects of Lysol on the vagina were acknowledged and the practice was discontinued.4
Although, generally, douching has fallen out of favor and most authorities advise against it,studies have shown that there can be a benefit when used for vaginosis or vaginitis in relieving symptoms.5,2 Those benefits do not outweigh the possible adverse effects. The process of douching allows for a pressurized solution to be injected into the vagina, thereby flushing bacteria throughout the vagina and into the uterus. In adolescence, the endothelial lining is more prone to adherence of the bacteria, so contracting a sexually transmitted infection is more likely and can increase the risk for ectopic pregnancy.2 The mucus lining of the vagina also tends to be thick; using harsh soaps thins the mucosa, again increasing the likelihood of infections. Furthermore, studies have confirmed that there also is a higher transmission rate of HIV and chlamydia when BV is present.2
Treating and preventing BV
The treatment of choice for BV is metronidazole taken orally or introduced vaginally. Studies have shown that recolonization of the lactobacilli can be slow, so the addition of lactic acid can be helpful. Clindamycin orally or vaginally also is a reasonable choice. Given that most of the bacteria causing BV have beta-lactamase, penicillin is not effective.7
Probiotics taken orally have a natural migration to the vaginal area and promote recolonization.7 Taking 250 mg of vitamin C 6 days/month for 6 months also has been shown to be helpful in recolonization and prevention of recurrence.8
A discussion of proper vaginal hygiene is important for adolescents and teens. Poor hygiene can significantly affect their social and interpersonal relationships, as well as their self-esteem. It puts them at greater risk for contracting sexually transmitted infections, and if they become pregnant, of having an adverse outcome.
In addition, inform them that douching with harsh or perfumed soaps changes the pH of the vagina, which can lead to bacterial overgrowth, so douching should be avoided. Advise them to change pads used during the menstrual cycle every 4-6 hours, and that cotton underwear and loose-fitting clothes also can reduce vaginal irritation. Lastly, advise teens to drink lots of fluids, eat yogurt, and take vitamin C and probiotics to reduce the risk of recurrence.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures.
References
1. Das P et al. PLoS One. 2015 Jun 30;10(6):e0130777.
2. Martino JL et al. Epidemiologic reviews. 2002;24(2):109-24.
3. Bilardi JE et al. PLoS ONE 2013;8(9):e74378.
4. www.Timeline.com/sexist-history-douching-bcc39f3d216c. 2016 Aug 14.
5. Fashemi B et al. Microb Ecol Health Dis. 2013 Feb 25. doi: 10.3402/mehd.v24i0.19703.
6. Hillier SL et al. N Engl J Med. 1995 Dec 28;333(26):1737-42.
7. Kumar N et al. J Pharm Bioallied Sci. 2011 Oct;3(4):496-503.
8. Krasnopolsky VN et al. J Clin Med Res. 2013 Aug;5(4):309-15..
Shoulder Arthroplasty in Cases of Significant Bone Loss: An Overview
Over the past few decades, there has been a dramatic increase in the number of shoulder arthroplasties performed around the world. This increase is the result of an aging and increasingly more active population, better implant technology, and the advent of reverse shoulder arthroplasty (RSA) for rotator cuff arthropathy. Additionally, as the indications for RSA have expanded to include pathologies such as rotator cuff insufficiency, chronic instabilities, trauma, and tumors, the number of arthroplasties will continue to increase. Although the results of most arthroplasties are good and predictable, any glenoid and/or humeral bone deficiencies can have detrimental effects on the clinical outcomes of these procedures. Bone loss becomes more of a problem in revision cases, and, as the number of primary arthroplasties increases, it follows that the number of revision procedures will also increase.
Many of the disease- or procedure-specific processes indicated for shoulder arthroplasty have predictable patterns of bone loss, especially on the glenoid side. Walch and colleagues1 and Bercik and colleagues2 made us aware that many patients with primary osteoarthritis have significant glenoid bone deformity. Similarly, there have been a number of first- and second-generation classification systems for delineating glenoid deformity in rotator cuff tear arthropathy and in revision settings. In revision settings, both glenoid and humeral bone deficiencies can occur as a result of implant removal, iatrogenic fracture, and even infection. Each of these bone loss patterns must be recognized and treated appropriately for the best surgical outcome.
The articles in this month of The American Journal of Orthopedics address the most up-to-date concepts and solutions regarding both humeral and glenoid bone loss in shoulder arthroplasty of all types.
HUMERAL BONE LOSS
Humeral bone loss is typically encountered in proximal humerus fractures, in revision surgery necessitating humeral component removal, and, less commonly, in tumors and infection.
In many displaced proximal humeral fractures indicated for shoulder arthroplasty, the bone is comminuted with displacement of the lesser and greater tuberosities. In these situations, failure of tuberosity healing may result in loss of rotator cuff function with loss of elevation, rotation, and even instability. Humeral shortening can also occur as a result of bone loss and can compromise deltoid function by loss of proper muscle tension, leading to instability, dysfunction, or both. In addition to possible instability, humeral shortening with metaphyseal bone loss can adversely affect long-term fixation of the humeral component, leading to stem loosening or failure. Cuff and colleagues3 showed significantly more rotational micromotion in cases lacking metaphyseal support, leading to aseptic loosening of the humeral stem.
Humeral bone loss can also result from humeral stem component removal in revision shoulder arthroplasty for infection, component failure or loosening, and even periprosthetic fracture resulting from surgery or trauma.
For the surgeon, humeral bone loss can create a complex set of circumstances related to rotator cuff attachment failure, soft-tissue balancing effects, and component fixation issues. Any such issue must be recognized and addressed for best outcomes. Best results can be obtained with preoperative imaging, planning, use of bone graft techniques, proximal humeral allografts, and, more recently, modular and patient-specific implants. All of these issues are discussed comprehensively in the articles this month.
Continue to: GLENOID BONE LOSS
GLENOID BONE LOSS
Proper glenoid component placement with durable fixation is crucial for success in anatomical total shoulder arthroplasty and RSA. Glenoid bone deformity and loss can result from intrinsic deformity characteristics seen in primary osteoarthritis, cuff tear arthropathy, or glenoid component removal in revision situations and infection. These bone deformity complications can be extremely difficult to treat and in some cases lead to catastrophic failure of the index arthroplasty.
We are now aware that one key to success in the face of moderate to severe deformity is proper recognition. Newer imaging techniques, including 2-dimensional (2-D) computed tomography (CT) and 3-dimensional (3-D) modeling and surgical planning software tools, which are outlined in an upcoming article, have given surgeons important new instruments that can help in treating these difficult cases.
Glenoid bone deformity in primary osteoarthritis was well delineated in the 1999 seminal study of CT changes by Walch and colleagues.1 The Walch classification system, which characterized glenoid morphology based on 2-D CT findings, was recently upgraded, based on 3-D imaging technology, to include Walch B3 and D patterns (Figure 1).2 Recognition of certain primary deformities in osteoarthritis has led to increased use of RSA in some cases of Walch B2, B3, and C deformities with substantial glenoid retroversion and/or humeral head subluxation.4
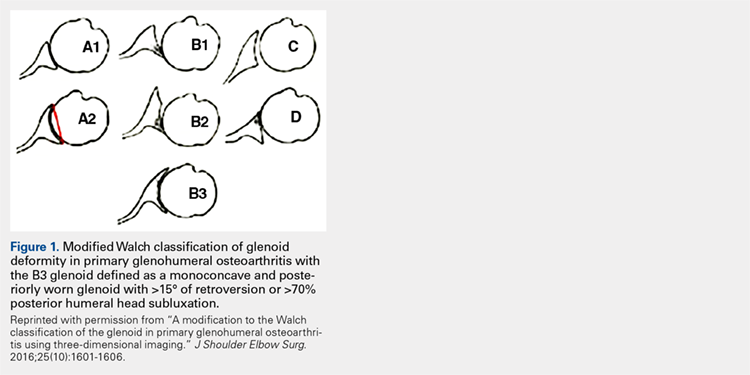
In cases of rotator cuff tear arthropathy, glenoid bone deformities are well described with several classification systems based on degree and dimension of bone insufficiency. The Hamada classification system defines the degree of medial glenoid erosion and superior bone loss, as well as acetabularization of the acromion in 5 grades; 5 Rispoli and colleagues6 defined and graded the degree of medicalization of the glenohumeral joint based on degree of subchondral plate erosion; and Visotsky and colleagues7 based their classification system on wear patterns of bone loss, alignment, and concomitant soft-tissue insufficiencies leading to instability and rotation loss.
In severe glenoid bone deficiency after glenoid component removal, Antuna and colleagues8 described the classic findings related to medial bone loss, anterior and posterior wall failure, and combinations thereof.
Continue to: All these classification systems...
All these classification systems are based on the 2-D appearance of the glenoid and should be considered cautiously. The glenoid is a complex 3-D structure that can be affected by any number of disease processes, trauma, and surgical intervention. Using more modern CT techniques and 3-D imaging, we now know that many deformities previously classified as unidirectional are, instead, complex and multidirectional.
Frankle and colleagues9 developed a classification based more 3-D CT models which has further classified severe glenoid vault deformities in relation to direction and degree of bone loss (Figures 2A-2E). Using this system, they were better able to determine degree and direction of deformity than in previous 2-D evaluations, and they were able to determine the amount of glenoid vault bone available for baseplate fixation. Scalise and colleagues10 further defined the influence of such 3-D planning in total shoulder arthroplasty.
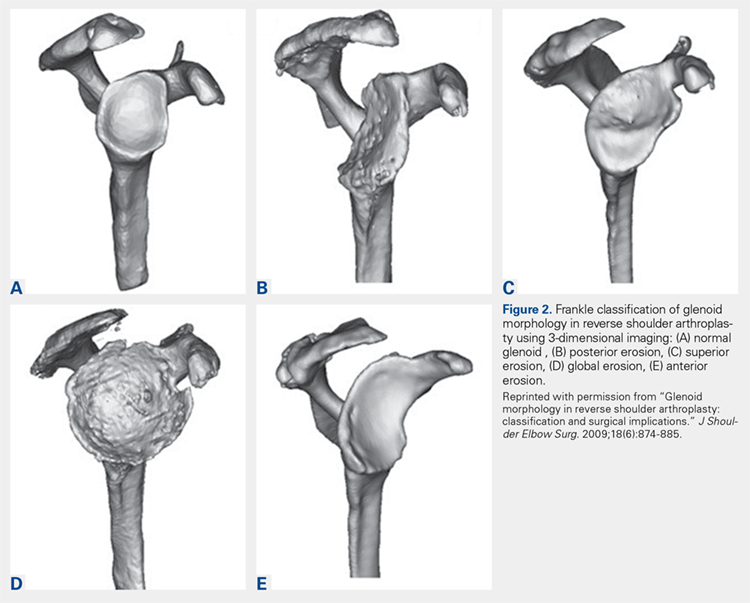
With knowledge of these classification systems and use of contemporary imaging systems, shoulder arthroplasty in cases of severe glenoid deficiency can be more successful. Potentially, we can improve outcomes even more in the more severe cases of bone loss with use of patient-specific planning tools, including the guides and patient-specific implants that are now readily available with many implant systems.11
Preoperative planning tools, bone-grafting techniques, augmented and specialized glenoid and humeral implants, and patient-specific implants are discussed this month to give our readers a comprehensive review of the latest concepts in shoulder arthroplasty in cases of significant bone loss or deformity.
This month of The American Journal of Orthopedics presents the most current and cutting-edge solutions for humeral and glenoid bone deformities and deficiencies in contemporary shoulder arthroplasties.
1. Walch G, Badet R, Boulahia A, Khoury A. Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplasty. 1999;14(6):756-760.
2. Bercik MJ, Kruse K 2nd, Yalizis M, Gauci MO, Chaoui J, Walch G. A modification to the Walch classification of the glenoid in primary glenohumeral osteoarthritis using three-dimensional imaging. J Shoulder Elbow Surg. 2016;25(10):1601-1606.
3. Cuff D, Levy JC, Gutiérrez S, Frankle M. Torsional stability of modular and non-modular reverse shoulder humeral components in a proximal humeral bone loss model. J Shoulder Elbow Surg. 2011;20(4):646-651.
4. Denard PJ, Walch G. Current concepts in the surgical management of primary glenohumeral arthritis with a biconcave glenoid. J Shoulder Elbow Surg. 2013;22(11):1589-1598.
5. Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res. 1990;(254):92-96.
6. Rispoli D, Sperling JW, Athwal GS, Schleck CD, Cofield RH. Humeral head replacement for the treatment of osteoarthritis. J Bone Joint Surg Am. 2006;88(12):2637-2644.
7. Visotsky JL, Basamania C, Seebauer L, Rockwood CA, Jensen KL. Cuff tear arthropathy: pathogenesis, classification, and algorithm for treatment. J Bone Joint Surg Am. 2004;86(suppl 2):35-40.
8. Antuna SA, Sperling JW, Cofield RH, Rowland CM. Glenoid revision surgery after total shoulder arthroplasty. J Shoulder Elbow Surg. 2001;10(3):217-224.
9. Frankle MA, Teramoto A, Luo ZP, Levy JC, Pupello D. Glenoid morphology in reverse shoulder arthroplasty: classification and surgical implications. J Shoulder Elbow Surg. 2009;18(6):874-885.
10. Scalise JJ, Codsi MJ, Bryan J, Brems JJ, Iannotti JP. The influence of three-dimensional computed tomography images of the shoulder in preoperative planning for total shoulder arthroplasty. J Bone Joint Surg Am. 2008;90(11):2438-2445.
11. Dines DM, Gulotta L, Craig EV, Dines JS. Novel solution for massive glenoid defects in shoulder arthroplasty: a patient-specific glenoid vault reconstruction system. Am J Orthop. 2017;46(2):104-108.
Over the past few decades, there has been a dramatic increase in the number of shoulder arthroplasties performed around the world. This increase is the result of an aging and increasingly more active population, better implant technology, and the advent of reverse shoulder arthroplasty (RSA) for rotator cuff arthropathy. Additionally, as the indications for RSA have expanded to include pathologies such as rotator cuff insufficiency, chronic instabilities, trauma, and tumors, the number of arthroplasties will continue to increase. Although the results of most arthroplasties are good and predictable, any glenoid and/or humeral bone deficiencies can have detrimental effects on the clinical outcomes of these procedures. Bone loss becomes more of a problem in revision cases, and, as the number of primary arthroplasties increases, it follows that the number of revision procedures will also increase.
Many of the disease- or procedure-specific processes indicated for shoulder arthroplasty have predictable patterns of bone loss, especially on the glenoid side. Walch and colleagues1 and Bercik and colleagues2 made us aware that many patients with primary osteoarthritis have significant glenoid bone deformity. Similarly, there have been a number of first- and second-generation classification systems for delineating glenoid deformity in rotator cuff tear arthropathy and in revision settings. In revision settings, both glenoid and humeral bone deficiencies can occur as a result of implant removal, iatrogenic fracture, and even infection. Each of these bone loss patterns must be recognized and treated appropriately for the best surgical outcome.
The articles in this month of The American Journal of Orthopedics address the most up-to-date concepts and solutions regarding both humeral and glenoid bone loss in shoulder arthroplasty of all types.
HUMERAL BONE LOSS
Humeral bone loss is typically encountered in proximal humerus fractures, in revision surgery necessitating humeral component removal, and, less commonly, in tumors and infection.
In many displaced proximal humeral fractures indicated for shoulder arthroplasty, the bone is comminuted with displacement of the lesser and greater tuberosities. In these situations, failure of tuberosity healing may result in loss of rotator cuff function with loss of elevation, rotation, and even instability. Humeral shortening can also occur as a result of bone loss and can compromise deltoid function by loss of proper muscle tension, leading to instability, dysfunction, or both. In addition to possible instability, humeral shortening with metaphyseal bone loss can adversely affect long-term fixation of the humeral component, leading to stem loosening or failure. Cuff and colleagues3 showed significantly more rotational micromotion in cases lacking metaphyseal support, leading to aseptic loosening of the humeral stem.
Humeral bone loss can also result from humeral stem component removal in revision shoulder arthroplasty for infection, component failure or loosening, and even periprosthetic fracture resulting from surgery or trauma.
For the surgeon, humeral bone loss can create a complex set of circumstances related to rotator cuff attachment failure, soft-tissue balancing effects, and component fixation issues. Any such issue must be recognized and addressed for best outcomes. Best results can be obtained with preoperative imaging, planning, use of bone graft techniques, proximal humeral allografts, and, more recently, modular and patient-specific implants. All of these issues are discussed comprehensively in the articles this month.
Continue to: GLENOID BONE LOSS
GLENOID BONE LOSS
Proper glenoid component placement with durable fixation is crucial for success in anatomical total shoulder arthroplasty and RSA. Glenoid bone deformity and loss can result from intrinsic deformity characteristics seen in primary osteoarthritis, cuff tear arthropathy, or glenoid component removal in revision situations and infection. These bone deformity complications can be extremely difficult to treat and in some cases lead to catastrophic failure of the index arthroplasty.
We are now aware that one key to success in the face of moderate to severe deformity is proper recognition. Newer imaging techniques, including 2-dimensional (2-D) computed tomography (CT) and 3-dimensional (3-D) modeling and surgical planning software tools, which are outlined in an upcoming article, have given surgeons important new instruments that can help in treating these difficult cases.
Glenoid bone deformity in primary osteoarthritis was well delineated in the 1999 seminal study of CT changes by Walch and colleagues.1 The Walch classification system, which characterized glenoid morphology based on 2-D CT findings, was recently upgraded, based on 3-D imaging technology, to include Walch B3 and D patterns (Figure 1).2 Recognition of certain primary deformities in osteoarthritis has led to increased use of RSA in some cases of Walch B2, B3, and C deformities with substantial glenoid retroversion and/or humeral head subluxation.4
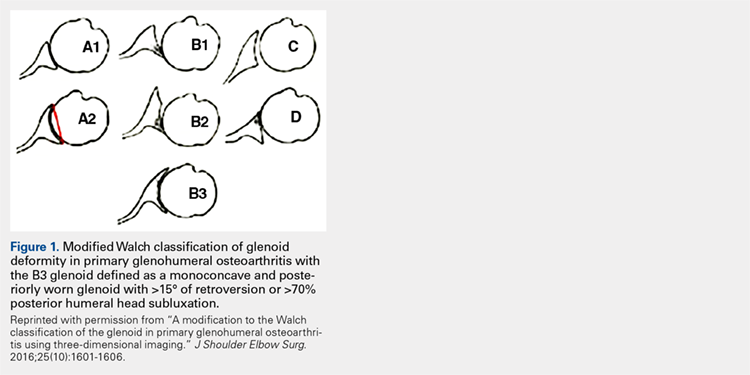
In cases of rotator cuff tear arthropathy, glenoid bone deformities are well described with several classification systems based on degree and dimension of bone insufficiency. The Hamada classification system defines the degree of medial glenoid erosion and superior bone loss, as well as acetabularization of the acromion in 5 grades; 5 Rispoli and colleagues6 defined and graded the degree of medicalization of the glenohumeral joint based on degree of subchondral plate erosion; and Visotsky and colleagues7 based their classification system on wear patterns of bone loss, alignment, and concomitant soft-tissue insufficiencies leading to instability and rotation loss.
In severe glenoid bone deficiency after glenoid component removal, Antuna and colleagues8 described the classic findings related to medial bone loss, anterior and posterior wall failure, and combinations thereof.
Continue to: All these classification systems...
All these classification systems are based on the 2-D appearance of the glenoid and should be considered cautiously. The glenoid is a complex 3-D structure that can be affected by any number of disease processes, trauma, and surgical intervention. Using more modern CT techniques and 3-D imaging, we now know that many deformities previously classified as unidirectional are, instead, complex and multidirectional.
Frankle and colleagues9 developed a classification based more 3-D CT models which has further classified severe glenoid vault deformities in relation to direction and degree of bone loss (Figures 2A-2E). Using this system, they were better able to determine degree and direction of deformity than in previous 2-D evaluations, and they were able to determine the amount of glenoid vault bone available for baseplate fixation. Scalise and colleagues10 further defined the influence of such 3-D planning in total shoulder arthroplasty.
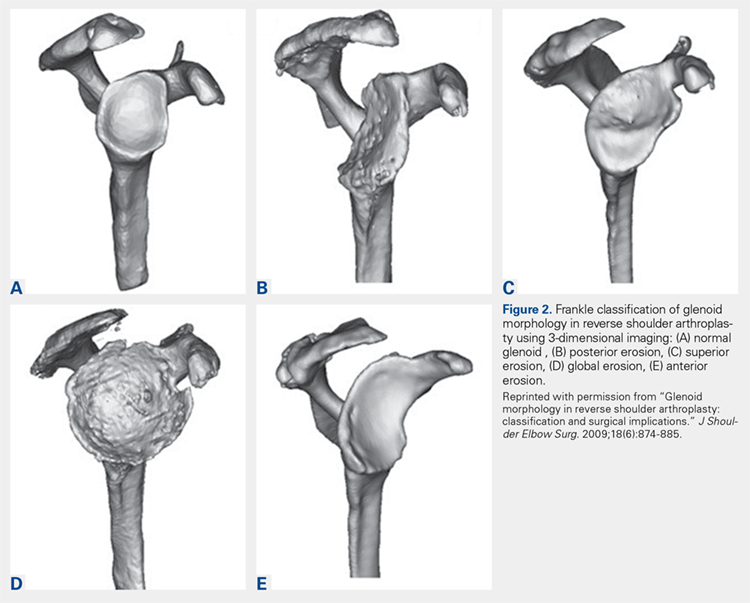
With knowledge of these classification systems and use of contemporary imaging systems, shoulder arthroplasty in cases of severe glenoid deficiency can be more successful. Potentially, we can improve outcomes even more in the more severe cases of bone loss with use of patient-specific planning tools, including the guides and patient-specific implants that are now readily available with many implant systems.11
Preoperative planning tools, bone-grafting techniques, augmented and specialized glenoid and humeral implants, and patient-specific implants are discussed this month to give our readers a comprehensive review of the latest concepts in shoulder arthroplasty in cases of significant bone loss or deformity.
This month of The American Journal of Orthopedics presents the most current and cutting-edge solutions for humeral and glenoid bone deformities and deficiencies in contemporary shoulder arthroplasties.
Over the past few decades, there has been a dramatic increase in the number of shoulder arthroplasties performed around the world. This increase is the result of an aging and increasingly more active population, better implant technology, and the advent of reverse shoulder arthroplasty (RSA) for rotator cuff arthropathy. Additionally, as the indications for RSA have expanded to include pathologies such as rotator cuff insufficiency, chronic instabilities, trauma, and tumors, the number of arthroplasties will continue to increase. Although the results of most arthroplasties are good and predictable, any glenoid and/or humeral bone deficiencies can have detrimental effects on the clinical outcomes of these procedures. Bone loss becomes more of a problem in revision cases, and, as the number of primary arthroplasties increases, it follows that the number of revision procedures will also increase.
Many of the disease- or procedure-specific processes indicated for shoulder arthroplasty have predictable patterns of bone loss, especially on the glenoid side. Walch and colleagues1 and Bercik and colleagues2 made us aware that many patients with primary osteoarthritis have significant glenoid bone deformity. Similarly, there have been a number of first- and second-generation classification systems for delineating glenoid deformity in rotator cuff tear arthropathy and in revision settings. In revision settings, both glenoid and humeral bone deficiencies can occur as a result of implant removal, iatrogenic fracture, and even infection. Each of these bone loss patterns must be recognized and treated appropriately for the best surgical outcome.
The articles in this month of The American Journal of Orthopedics address the most up-to-date concepts and solutions regarding both humeral and glenoid bone loss in shoulder arthroplasty of all types.
HUMERAL BONE LOSS
Humeral bone loss is typically encountered in proximal humerus fractures, in revision surgery necessitating humeral component removal, and, less commonly, in tumors and infection.
In many displaced proximal humeral fractures indicated for shoulder arthroplasty, the bone is comminuted with displacement of the lesser and greater tuberosities. In these situations, failure of tuberosity healing may result in loss of rotator cuff function with loss of elevation, rotation, and even instability. Humeral shortening can also occur as a result of bone loss and can compromise deltoid function by loss of proper muscle tension, leading to instability, dysfunction, or both. In addition to possible instability, humeral shortening with metaphyseal bone loss can adversely affect long-term fixation of the humeral component, leading to stem loosening or failure. Cuff and colleagues3 showed significantly more rotational micromotion in cases lacking metaphyseal support, leading to aseptic loosening of the humeral stem.
Humeral bone loss can also result from humeral stem component removal in revision shoulder arthroplasty for infection, component failure or loosening, and even periprosthetic fracture resulting from surgery or trauma.
For the surgeon, humeral bone loss can create a complex set of circumstances related to rotator cuff attachment failure, soft-tissue balancing effects, and component fixation issues. Any such issue must be recognized and addressed for best outcomes. Best results can be obtained with preoperative imaging, planning, use of bone graft techniques, proximal humeral allografts, and, more recently, modular and patient-specific implants. All of these issues are discussed comprehensively in the articles this month.
Continue to: GLENOID BONE LOSS
GLENOID BONE LOSS
Proper glenoid component placement with durable fixation is crucial for success in anatomical total shoulder arthroplasty and RSA. Glenoid bone deformity and loss can result from intrinsic deformity characteristics seen in primary osteoarthritis, cuff tear arthropathy, or glenoid component removal in revision situations and infection. These bone deformity complications can be extremely difficult to treat and in some cases lead to catastrophic failure of the index arthroplasty.
We are now aware that one key to success in the face of moderate to severe deformity is proper recognition. Newer imaging techniques, including 2-dimensional (2-D) computed tomography (CT) and 3-dimensional (3-D) modeling and surgical planning software tools, which are outlined in an upcoming article, have given surgeons important new instruments that can help in treating these difficult cases.
Glenoid bone deformity in primary osteoarthritis was well delineated in the 1999 seminal study of CT changes by Walch and colleagues.1 The Walch classification system, which characterized glenoid morphology based on 2-D CT findings, was recently upgraded, based on 3-D imaging technology, to include Walch B3 and D patterns (Figure 1).2 Recognition of certain primary deformities in osteoarthritis has led to increased use of RSA in some cases of Walch B2, B3, and C deformities with substantial glenoid retroversion and/or humeral head subluxation.4
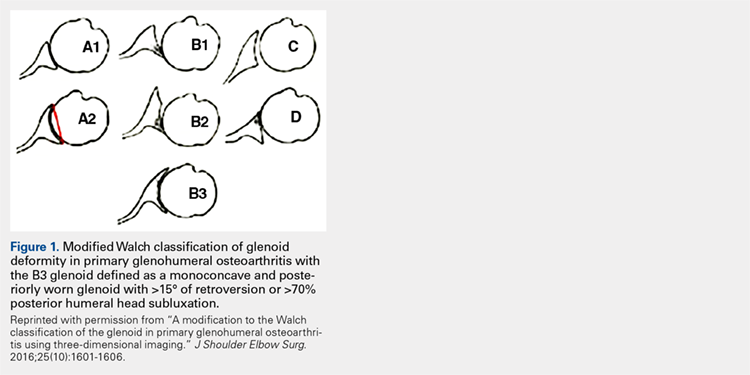
In cases of rotator cuff tear arthropathy, glenoid bone deformities are well described with several classification systems based on degree and dimension of bone insufficiency. The Hamada classification system defines the degree of medial glenoid erosion and superior bone loss, as well as acetabularization of the acromion in 5 grades; 5 Rispoli and colleagues6 defined and graded the degree of medicalization of the glenohumeral joint based on degree of subchondral plate erosion; and Visotsky and colleagues7 based their classification system on wear patterns of bone loss, alignment, and concomitant soft-tissue insufficiencies leading to instability and rotation loss.
In severe glenoid bone deficiency after glenoid component removal, Antuna and colleagues8 described the classic findings related to medial bone loss, anterior and posterior wall failure, and combinations thereof.
Continue to: All these classification systems...
All these classification systems are based on the 2-D appearance of the glenoid and should be considered cautiously. The glenoid is a complex 3-D structure that can be affected by any number of disease processes, trauma, and surgical intervention. Using more modern CT techniques and 3-D imaging, we now know that many deformities previously classified as unidirectional are, instead, complex and multidirectional.
Frankle and colleagues9 developed a classification based more 3-D CT models which has further classified severe glenoid vault deformities in relation to direction and degree of bone loss (Figures 2A-2E). Using this system, they were better able to determine degree and direction of deformity than in previous 2-D evaluations, and they were able to determine the amount of glenoid vault bone available for baseplate fixation. Scalise and colleagues10 further defined the influence of such 3-D planning in total shoulder arthroplasty.
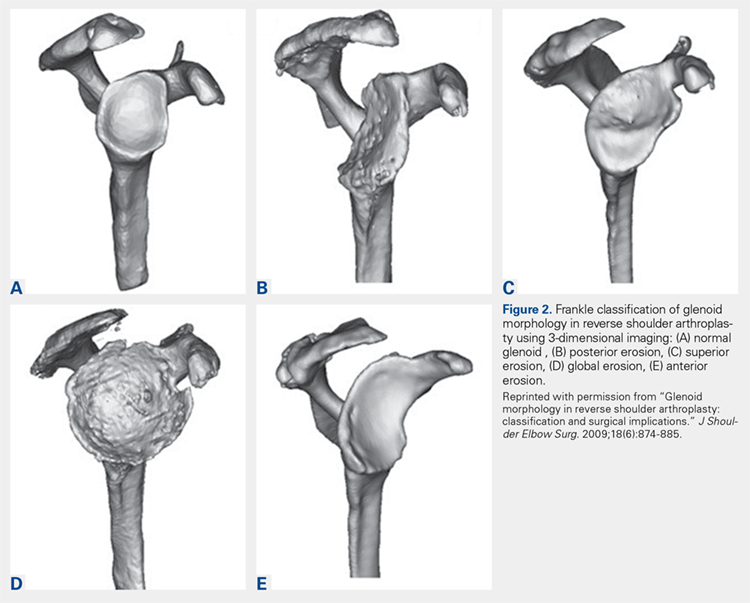
With knowledge of these classification systems and use of contemporary imaging systems, shoulder arthroplasty in cases of severe glenoid deficiency can be more successful. Potentially, we can improve outcomes even more in the more severe cases of bone loss with use of patient-specific planning tools, including the guides and patient-specific implants that are now readily available with many implant systems.11
Preoperative planning tools, bone-grafting techniques, augmented and specialized glenoid and humeral implants, and patient-specific implants are discussed this month to give our readers a comprehensive review of the latest concepts in shoulder arthroplasty in cases of significant bone loss or deformity.
This month of The American Journal of Orthopedics presents the most current and cutting-edge solutions for humeral and glenoid bone deformities and deficiencies in contemporary shoulder arthroplasties.
1. Walch G, Badet R, Boulahia A, Khoury A. Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplasty. 1999;14(6):756-760.
2. Bercik MJ, Kruse K 2nd, Yalizis M, Gauci MO, Chaoui J, Walch G. A modification to the Walch classification of the glenoid in primary glenohumeral osteoarthritis using three-dimensional imaging. J Shoulder Elbow Surg. 2016;25(10):1601-1606.
3. Cuff D, Levy JC, Gutiérrez S, Frankle M. Torsional stability of modular and non-modular reverse shoulder humeral components in a proximal humeral bone loss model. J Shoulder Elbow Surg. 2011;20(4):646-651.
4. Denard PJ, Walch G. Current concepts in the surgical management of primary glenohumeral arthritis with a biconcave glenoid. J Shoulder Elbow Surg. 2013;22(11):1589-1598.
5. Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res. 1990;(254):92-96.
6. Rispoli D, Sperling JW, Athwal GS, Schleck CD, Cofield RH. Humeral head replacement for the treatment of osteoarthritis. J Bone Joint Surg Am. 2006;88(12):2637-2644.
7. Visotsky JL, Basamania C, Seebauer L, Rockwood CA, Jensen KL. Cuff tear arthropathy: pathogenesis, classification, and algorithm for treatment. J Bone Joint Surg Am. 2004;86(suppl 2):35-40.
8. Antuna SA, Sperling JW, Cofield RH, Rowland CM. Glenoid revision surgery after total shoulder arthroplasty. J Shoulder Elbow Surg. 2001;10(3):217-224.
9. Frankle MA, Teramoto A, Luo ZP, Levy JC, Pupello D. Glenoid morphology in reverse shoulder arthroplasty: classification and surgical implications. J Shoulder Elbow Surg. 2009;18(6):874-885.
10. Scalise JJ, Codsi MJ, Bryan J, Brems JJ, Iannotti JP. The influence of three-dimensional computed tomography images of the shoulder in preoperative planning for total shoulder arthroplasty. J Bone Joint Surg Am. 2008;90(11):2438-2445.
11. Dines DM, Gulotta L, Craig EV, Dines JS. Novel solution for massive glenoid defects in shoulder arthroplasty: a patient-specific glenoid vault reconstruction system. Am J Orthop. 2017;46(2):104-108.
1. Walch G, Badet R, Boulahia A, Khoury A. Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplasty. 1999;14(6):756-760.
2. Bercik MJ, Kruse K 2nd, Yalizis M, Gauci MO, Chaoui J, Walch G. A modification to the Walch classification of the glenoid in primary glenohumeral osteoarthritis using three-dimensional imaging. J Shoulder Elbow Surg. 2016;25(10):1601-1606.
3. Cuff D, Levy JC, Gutiérrez S, Frankle M. Torsional stability of modular and non-modular reverse shoulder humeral components in a proximal humeral bone loss model. J Shoulder Elbow Surg. 2011;20(4):646-651.
4. Denard PJ, Walch G. Current concepts in the surgical management of primary glenohumeral arthritis with a biconcave glenoid. J Shoulder Elbow Surg. 2013;22(11):1589-1598.
5. Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res. 1990;(254):92-96.
6. Rispoli D, Sperling JW, Athwal GS, Schleck CD, Cofield RH. Humeral head replacement for the treatment of osteoarthritis. J Bone Joint Surg Am. 2006;88(12):2637-2644.
7. Visotsky JL, Basamania C, Seebauer L, Rockwood CA, Jensen KL. Cuff tear arthropathy: pathogenesis, classification, and algorithm for treatment. J Bone Joint Surg Am. 2004;86(suppl 2):35-40.
8. Antuna SA, Sperling JW, Cofield RH, Rowland CM. Glenoid revision surgery after total shoulder arthroplasty. J Shoulder Elbow Surg. 2001;10(3):217-224.
9. Frankle MA, Teramoto A, Luo ZP, Levy JC, Pupello D. Glenoid morphology in reverse shoulder arthroplasty: classification and surgical implications. J Shoulder Elbow Surg. 2009;18(6):874-885.
10. Scalise JJ, Codsi MJ, Bryan J, Brems JJ, Iannotti JP. The influence of three-dimensional computed tomography images of the shoulder in preoperative planning for total shoulder arthroplasty. J Bone Joint Surg Am. 2008;90(11):2438-2445.
11. Dines DM, Gulotta L, Craig EV, Dines JS. Novel solution for massive glenoid defects in shoulder arthroplasty: a patient-specific glenoid vault reconstruction system. Am J Orthop. 2017;46(2):104-108.
Warn patients about the risk of misusing OTC pain meds
Roughly 8 in 10 Americans routinely reach for over-the-counter (OTC) pain pills to relieve headaches, backaches, sore muscles, fevers, or colds, according to a national poll by the American Gastroenterological Association (AGA). Most are unaware that these medications, if used incorrectly, can be just as dangerous as prescription drugs.
In my GI practice, I often see cases of accidental OTC pain medicine overdose that have caused stomach bleeding, ulcers, liver damage, and even liver failure. And, I am not alone – the poll found that gastroenterologists see, on average, nearly two patients per week with complications from OTC pain pills.
As the nation’s attention is focused on the opioid crisis, and with good reason, we cannot forget about the risks associated with OTC pain medicines. While it may seem harmless to take more OTC medications than indicated, the body is not capable of absorbing higher doses of pain medicine ingredients at a faster rate.
According to the AGA’s survey, many people are confident they can manage symptoms on their own, without consulting a doctor. Yet, the same poll found that 39% of Americans knowingly took more than the recommended dosage. In most cases, they falsely believed that taking more OTC pain medicine than what was indicated on the label would help them “feel better faster.”
A short time ago, I treated a woman in her 20s who recently had dental surgery. She was taking Lortab, which is a combination of acetaminophen and hydrocodone, an opioid. But when she still felt pain, she took additional OTC acetaminophen to try to find faster relief. When I saw her, her liver tests were abnormal, her acetaminophen level was elevated, and she was feeling very nauseated. In trying to get faster pain relief, she unintentionally overdosed on OTC pain medicine.
To help patients avoid this kind of medication mishap, it’s vital that health care providers initiate conversations at every visit about the dangers of OTC pain medicine overdose. The following tips have helped me advise my patients and educate them on the associated risks:
• Encourage your patients to read and follow all medicine labels, even on OTC drugs – every time they reach for something in the medicine cabinet.
• Talk to your patients about the two main types of oral OTC pain medicines and make sure they know to take only one product at a time containing the same type of active ingredient.
• Ask about all medicines your patients take, including OTC medicines, as they may not know to tell you.
• Patients may not realize that their current health situation, age, and/or medical history can impact their risk for OTC pain medicine overdose. Let them know that products that worked in the past may no longer be the right choice for them now.
If more health care providers emphasized the dangers of incorrect usage of OTC pain medicines, we could easily help patients avoid the dangerous side effects of taking too much.
Dr. Wilcox is professor of medicine in the division of gastroenterology and hepatology at the University of Alabama at Birmingham and a chair of AGA’s Gut Check: Know Your Medicine campaign.
Roughly 8 in 10 Americans routinely reach for over-the-counter (OTC) pain pills to relieve headaches, backaches, sore muscles, fevers, or colds, according to a national poll by the American Gastroenterological Association (AGA). Most are unaware that these medications, if used incorrectly, can be just as dangerous as prescription drugs.
In my GI practice, I often see cases of accidental OTC pain medicine overdose that have caused stomach bleeding, ulcers, liver damage, and even liver failure. And, I am not alone – the poll found that gastroenterologists see, on average, nearly two patients per week with complications from OTC pain pills.
As the nation’s attention is focused on the opioid crisis, and with good reason, we cannot forget about the risks associated with OTC pain medicines. While it may seem harmless to take more OTC medications than indicated, the body is not capable of absorbing higher doses of pain medicine ingredients at a faster rate.
According to the AGA’s survey, many people are confident they can manage symptoms on their own, without consulting a doctor. Yet, the same poll found that 39% of Americans knowingly took more than the recommended dosage. In most cases, they falsely believed that taking more OTC pain medicine than what was indicated on the label would help them “feel better faster.”
A short time ago, I treated a woman in her 20s who recently had dental surgery. She was taking Lortab, which is a combination of acetaminophen and hydrocodone, an opioid. But when she still felt pain, she took additional OTC acetaminophen to try to find faster relief. When I saw her, her liver tests were abnormal, her acetaminophen level was elevated, and she was feeling very nauseated. In trying to get faster pain relief, she unintentionally overdosed on OTC pain medicine.
To help patients avoid this kind of medication mishap, it’s vital that health care providers initiate conversations at every visit about the dangers of OTC pain medicine overdose. The following tips have helped me advise my patients and educate them on the associated risks:
• Encourage your patients to read and follow all medicine labels, even on OTC drugs – every time they reach for something in the medicine cabinet.
• Talk to your patients about the two main types of oral OTC pain medicines and make sure they know to take only one product at a time containing the same type of active ingredient.
• Ask about all medicines your patients take, including OTC medicines, as they may not know to tell you.
• Patients may not realize that their current health situation, age, and/or medical history can impact their risk for OTC pain medicine overdose. Let them know that products that worked in the past may no longer be the right choice for them now.
If more health care providers emphasized the dangers of incorrect usage of OTC pain medicines, we could easily help patients avoid the dangerous side effects of taking too much.
Dr. Wilcox is professor of medicine in the division of gastroenterology and hepatology at the University of Alabama at Birmingham and a chair of AGA’s Gut Check: Know Your Medicine campaign.
Roughly 8 in 10 Americans routinely reach for over-the-counter (OTC) pain pills to relieve headaches, backaches, sore muscles, fevers, or colds, according to a national poll by the American Gastroenterological Association (AGA). Most are unaware that these medications, if used incorrectly, can be just as dangerous as prescription drugs.
In my GI practice, I often see cases of accidental OTC pain medicine overdose that have caused stomach bleeding, ulcers, liver damage, and even liver failure. And, I am not alone – the poll found that gastroenterologists see, on average, nearly two patients per week with complications from OTC pain pills.
As the nation’s attention is focused on the opioid crisis, and with good reason, we cannot forget about the risks associated with OTC pain medicines. While it may seem harmless to take more OTC medications than indicated, the body is not capable of absorbing higher doses of pain medicine ingredients at a faster rate.
According to the AGA’s survey, many people are confident they can manage symptoms on their own, without consulting a doctor. Yet, the same poll found that 39% of Americans knowingly took more than the recommended dosage. In most cases, they falsely believed that taking more OTC pain medicine than what was indicated on the label would help them “feel better faster.”
A short time ago, I treated a woman in her 20s who recently had dental surgery. She was taking Lortab, which is a combination of acetaminophen and hydrocodone, an opioid. But when she still felt pain, she took additional OTC acetaminophen to try to find faster relief. When I saw her, her liver tests were abnormal, her acetaminophen level was elevated, and she was feeling very nauseated. In trying to get faster pain relief, she unintentionally overdosed on OTC pain medicine.
To help patients avoid this kind of medication mishap, it’s vital that health care providers initiate conversations at every visit about the dangers of OTC pain medicine overdose. The following tips have helped me advise my patients and educate them on the associated risks:
• Encourage your patients to read and follow all medicine labels, even on OTC drugs – every time they reach for something in the medicine cabinet.
• Talk to your patients about the two main types of oral OTC pain medicines and make sure they know to take only one product at a time containing the same type of active ingredient.
• Ask about all medicines your patients take, including OTC medicines, as they may not know to tell you.
• Patients may not realize that their current health situation, age, and/or medical history can impact their risk for OTC pain medicine overdose. Let them know that products that worked in the past may no longer be the right choice for them now.
If more health care providers emphasized the dangers of incorrect usage of OTC pain medicines, we could easily help patients avoid the dangerous side effects of taking too much.
Dr. Wilcox is professor of medicine in the division of gastroenterology and hepatology at the University of Alabama at Birmingham and a chair of AGA’s Gut Check: Know Your Medicine campaign.