User login
Keeping office and home personas separate
When are you Dr. versus Mr./Mrs./Miss?
I try to keep a pretty solid wall between my two identities. When I’m outside the office, I’m not happy about suddenly having to change hats.
I run into patients at restaurants and stores, like everyone else. Most of the time, we just exchange waves or nods. (I’m sure some of them don’t want to acknowledge me, either.)
But there are always those who consider catching me in public as a chance to get their questions answered or meds refilled without having to call the office, and don’t care if the whole establishment hears them.
I’m pretty much blind without my glasses, so, unless asleep, I am never without them. My wife has learned that when I suddenly take them off in public, it means I’ve sighted a patient I don’t want seeing me. It’s the easiest way to quickly change my appearance.
Some will still recognize me and come over with questions, descriptions, new symptoms, or concerns about what they saw on TV, read on the Internet, or heard from a lady at the store. Provided that nothing is urgent, I tell them that, at the moment, I’m not Dr. Block. I’m Dad, or husband, or basketball fan. I suggest they call my office with their questions, and Dr. Block or his staff will get back to them. Most will, though I’ve had a few get angry and accuse me of being unreasonable or uncaring.
I don’t really care. Like everyone else, I have at least two personas (work and home) and try to keep them as separate as possible. Part of it is for practical reasons, but mostly, it’s personal. None of us want to be in the doctor role at home, or in the home persona while seeing patients.
I ask patients and family to respect this. I don’t like getting the non-urgent texts or calls from my kids when I’m at the office, either. There I’m trying to focus on patients and their problems, and distractions aren’t welcome.
We each draw this line somewhere, depending on our own comfort level. You can’t be both all the time. It’s bad for your sanity.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
When are you Dr. versus Mr./Mrs./Miss?
I try to keep a pretty solid wall between my two identities. When I’m outside the office, I’m not happy about suddenly having to change hats.
I run into patients at restaurants and stores, like everyone else. Most of the time, we just exchange waves or nods. (I’m sure some of them don’t want to acknowledge me, either.)
But there are always those who consider catching me in public as a chance to get their questions answered or meds refilled without having to call the office, and don’t care if the whole establishment hears them.
I’m pretty much blind without my glasses, so, unless asleep, I am never without them. My wife has learned that when I suddenly take them off in public, it means I’ve sighted a patient I don’t want seeing me. It’s the easiest way to quickly change my appearance.
Some will still recognize me and come over with questions, descriptions, new symptoms, or concerns about what they saw on TV, read on the Internet, or heard from a lady at the store. Provided that nothing is urgent, I tell them that, at the moment, I’m not Dr. Block. I’m Dad, or husband, or basketball fan. I suggest they call my office with their questions, and Dr. Block or his staff will get back to them. Most will, though I’ve had a few get angry and accuse me of being unreasonable or uncaring.
I don’t really care. Like everyone else, I have at least two personas (work and home) and try to keep them as separate as possible. Part of it is for practical reasons, but mostly, it’s personal. None of us want to be in the doctor role at home, or in the home persona while seeing patients.
I ask patients and family to respect this. I don’t like getting the non-urgent texts or calls from my kids when I’m at the office, either. There I’m trying to focus on patients and their problems, and distractions aren’t welcome.
We each draw this line somewhere, depending on our own comfort level. You can’t be both all the time. It’s bad for your sanity.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
When are you Dr. versus Mr./Mrs./Miss?
I try to keep a pretty solid wall between my two identities. When I’m outside the office, I’m not happy about suddenly having to change hats.
I run into patients at restaurants and stores, like everyone else. Most of the time, we just exchange waves or nods. (I’m sure some of them don’t want to acknowledge me, either.)
But there are always those who consider catching me in public as a chance to get their questions answered or meds refilled without having to call the office, and don’t care if the whole establishment hears them.
I’m pretty much blind without my glasses, so, unless asleep, I am never without them. My wife has learned that when I suddenly take them off in public, it means I’ve sighted a patient I don’t want seeing me. It’s the easiest way to quickly change my appearance.
Some will still recognize me and come over with questions, descriptions, new symptoms, or concerns about what they saw on TV, read on the Internet, or heard from a lady at the store. Provided that nothing is urgent, I tell them that, at the moment, I’m not Dr. Block. I’m Dad, or husband, or basketball fan. I suggest they call my office with their questions, and Dr. Block or his staff will get back to them. Most will, though I’ve had a few get angry and accuse me of being unreasonable or uncaring.
I don’t really care. Like everyone else, I have at least two personas (work and home) and try to keep them as separate as possible. Part of it is for practical reasons, but mostly, it’s personal. None of us want to be in the doctor role at home, or in the home persona while seeing patients.
I ask patients and family to respect this. I don’t like getting the non-urgent texts or calls from my kids when I’m at the office, either. There I’m trying to focus on patients and their problems, and distractions aren’t welcome.
We each draw this line somewhere, depending on our own comfort level. You can’t be both all the time. It’s bad for your sanity.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The mainstreaming of alternative therapies
In this issue, Dr. Onysko discusses “alternative” pharmacologic approaches to painful peripheral neuropathy. (See “Targeting neuropathic pain: Consider these alternatives.”) Because so many of our patients use alternative therapies, I contend that alternative therapies are no longer “alternative.” Even the federal government has officially recognized the widespread use of alternative therapies by changing the name of the National Center for Complementary and Alternative Medicine in December 2014 to the National Center for Complementary and Integrative Health.
Alternative medicine had a bad name in mainstream medicine until 1991, when the National Institutes of Health established the Office of Alternative Medicine, officially recognizing that some alternative treatments might have a scientific basis and true therapeutic effects beyond the placebo effect. Over the years, hundreds of randomized controlled trials (RCTs) have emerged to investigate the value of various herbal treatments, vitamin therapies, magnet therapy, acupuncture, tai chi, aromatherapy, and other physical medicine and medicinal treatment modalities.
Last spring, as I prepared an evidence-based medicine talk, I was struck by the solid evidence supporting numerous therapies we used to consider alternative. Many trials of acupuncture, for instance, have shown positive effects for various musculoskeletal problems. But acupuncture is also effective for functional dyspepsia, according to a well-designed RCT.1 In addition, it can relieve symptoms of irritable bowel syndrome (IBS), according to a Cochrane meta-analysis of 17 RCTs.2
One of the new kids on the block in alternative medicine is functional medicine, founded by nutritionist/biochemist Jeff Bland. According to the Institute of Functional Medicine Web site, functional medicine is a combination of holistic medicine principles and a belief that we can treat a wide variety of ailments with various dietary treatments, including supplements.3 Although research on the interaction between gut flora and human health is burgeoning, I’m wary of claims of effectiveness until we see evidence of improved patient-oriented outcomes from well-executed RCTs.
I’m keeping an open mind, however, about all forms of complementary and integrative therapies. After all, who would have guessed 30 years ago that peptic ulcer disease could be cured with antibiotics?
1. Ma TT, Yu SY, Li Y, et al. Randomised clinical trial: an assessment of acupuncture on specific meridian or specific acupoint vs. sham acupuncture for treating functional dyspepsia. Aliment Pharmacol Ther. 2012;35:552-561.
2. Manheimer E, Cheng K, Wieland LS, et al. Acupuncture for treatment of irritable bowel syndrome. Cochrane Database Syst Rev. 2012;5:CD005111.
3. Institute of Functional Medicine. What is functional medicine? Institute of Functional Medicine Web site. Available at: https://www.functionalmedicine.org/about/whatisfm/. Accessed July 20, 2015.
In this issue, Dr. Onysko discusses “alternative” pharmacologic approaches to painful peripheral neuropathy. (See “Targeting neuropathic pain: Consider these alternatives.”) Because so many of our patients use alternative therapies, I contend that alternative therapies are no longer “alternative.” Even the federal government has officially recognized the widespread use of alternative therapies by changing the name of the National Center for Complementary and Alternative Medicine in December 2014 to the National Center for Complementary and Integrative Health.
Alternative medicine had a bad name in mainstream medicine until 1991, when the National Institutes of Health established the Office of Alternative Medicine, officially recognizing that some alternative treatments might have a scientific basis and true therapeutic effects beyond the placebo effect. Over the years, hundreds of randomized controlled trials (RCTs) have emerged to investigate the value of various herbal treatments, vitamin therapies, magnet therapy, acupuncture, tai chi, aromatherapy, and other physical medicine and medicinal treatment modalities.
Last spring, as I prepared an evidence-based medicine talk, I was struck by the solid evidence supporting numerous therapies we used to consider alternative. Many trials of acupuncture, for instance, have shown positive effects for various musculoskeletal problems. But acupuncture is also effective for functional dyspepsia, according to a well-designed RCT.1 In addition, it can relieve symptoms of irritable bowel syndrome (IBS), according to a Cochrane meta-analysis of 17 RCTs.2
One of the new kids on the block in alternative medicine is functional medicine, founded by nutritionist/biochemist Jeff Bland. According to the Institute of Functional Medicine Web site, functional medicine is a combination of holistic medicine principles and a belief that we can treat a wide variety of ailments with various dietary treatments, including supplements.3 Although research on the interaction between gut flora and human health is burgeoning, I’m wary of claims of effectiveness until we see evidence of improved patient-oriented outcomes from well-executed RCTs.
I’m keeping an open mind, however, about all forms of complementary and integrative therapies. After all, who would have guessed 30 years ago that peptic ulcer disease could be cured with antibiotics?
In this issue, Dr. Onysko discusses “alternative” pharmacologic approaches to painful peripheral neuropathy. (See “Targeting neuropathic pain: Consider these alternatives.”) Because so many of our patients use alternative therapies, I contend that alternative therapies are no longer “alternative.” Even the federal government has officially recognized the widespread use of alternative therapies by changing the name of the National Center for Complementary and Alternative Medicine in December 2014 to the National Center for Complementary and Integrative Health.
Alternative medicine had a bad name in mainstream medicine until 1991, when the National Institutes of Health established the Office of Alternative Medicine, officially recognizing that some alternative treatments might have a scientific basis and true therapeutic effects beyond the placebo effect. Over the years, hundreds of randomized controlled trials (RCTs) have emerged to investigate the value of various herbal treatments, vitamin therapies, magnet therapy, acupuncture, tai chi, aromatherapy, and other physical medicine and medicinal treatment modalities.
Last spring, as I prepared an evidence-based medicine talk, I was struck by the solid evidence supporting numerous therapies we used to consider alternative. Many trials of acupuncture, for instance, have shown positive effects for various musculoskeletal problems. But acupuncture is also effective for functional dyspepsia, according to a well-designed RCT.1 In addition, it can relieve symptoms of irritable bowel syndrome (IBS), according to a Cochrane meta-analysis of 17 RCTs.2
One of the new kids on the block in alternative medicine is functional medicine, founded by nutritionist/biochemist Jeff Bland. According to the Institute of Functional Medicine Web site, functional medicine is a combination of holistic medicine principles and a belief that we can treat a wide variety of ailments with various dietary treatments, including supplements.3 Although research on the interaction between gut flora and human health is burgeoning, I’m wary of claims of effectiveness until we see evidence of improved patient-oriented outcomes from well-executed RCTs.
I’m keeping an open mind, however, about all forms of complementary and integrative therapies. After all, who would have guessed 30 years ago that peptic ulcer disease could be cured with antibiotics?
1. Ma TT, Yu SY, Li Y, et al. Randomised clinical trial: an assessment of acupuncture on specific meridian or specific acupoint vs. sham acupuncture for treating functional dyspepsia. Aliment Pharmacol Ther. 2012;35:552-561.
2. Manheimer E, Cheng K, Wieland LS, et al. Acupuncture for treatment of irritable bowel syndrome. Cochrane Database Syst Rev. 2012;5:CD005111.
3. Institute of Functional Medicine. What is functional medicine? Institute of Functional Medicine Web site. Available at: https://www.functionalmedicine.org/about/whatisfm/. Accessed July 20, 2015.
1. Ma TT, Yu SY, Li Y, et al. Randomised clinical trial: an assessment of acupuncture on specific meridian or specific acupoint vs. sham acupuncture for treating functional dyspepsia. Aliment Pharmacol Ther. 2012;35:552-561.
2. Manheimer E, Cheng K, Wieland LS, et al. Acupuncture for treatment of irritable bowel syndrome. Cochrane Database Syst Rev. 2012;5:CD005111.
3. Institute of Functional Medicine. What is functional medicine? Institute of Functional Medicine Web site. Available at: https://www.functionalmedicine.org/about/whatisfm/. Accessed July 20, 2015.
To Thine Own Health Be True
After 40 years as a PA (including 21 in academia), tucking myself safely into my seventh decade of life, I was feeling fairly invincible. Yes, I was experiencing increased fatigue and intermittent dizziness, but I attributed those to normal aging and my hectic schedule. Purely to get my colleagues and loved ones off my back, I agreed to see my primary care physician—but, feeling that I had little time for this and knowing that my health was just fine, thank you, I scheduled my appointment for a month later.
That appointment resulted in a referral to a cardiologist (which I didn’t think I needed) and a carotid ultrasound (which yielded negative results). I was still begrudging the time spent on these appointments, when my treadmill test revealed some ST changes in the lateral leads. OK, yes, I do have a positive family history for heart disease! But still, I was surprised.
This finding led to a nuclear treadmill test, which showed some ischemia. The cardiologist suggested an angiogram to rule out a probable false-positive result. Now, I really didn’t have time for this, either—but having gone this far, I felt it was important just to get it over with. Thank goodness I did!
During my angiogram (by the way, they give you great LaLa Land drugs), the interventional cardiologist discovered a 95% blockage of the circumflex, a 95% blockage of the right coronary artery, and a 60% blockage of the LAD. The big decision at that point, amidst the obvious shock of my mortality, was whether to opt for an open-heart bypass or stents. I chose stents (which, by the way, have had a significant impact on my energy level). My cardiologist tells me that, without the stents, if I had experienced a total occlusion event, I would not have survived. Quite a sobering thought!
My purpose in sharing this story is not to call attention to myself but rather to offer a wake-up call to those of us who think we are invincible. Many colleagues who have heard my story have decided to get their own long-delayed treadmill or other health-related tests. So here is my call to action to all of you: Take care of your health. The irony is that, for health care providers, this can be difficult.
Those who care for others often have a tough time caring for themselves. We know that physicians are notoriously bad patients, and I think PAs/NPs are no different. We deal with life-and-death issues all the time, and outward displays of distress are, at a minimum, discouraged. In general, our training and accumulated experience help us to develop good coping skills: We are taught to ignore basic human needs (like hunger and fatigue) and to remain capable, competent, and compassionate clinicians under highly stressful conditions.
Nonetheless, we experience these high levels of stress and seldom act to relieve them. As long ago as 1886, Dr William Ogle exposed clinicians’ vulnerability to high mortality risks, but to this day, the subject remains fairly neglected.1 Perhaps as a result of stigma—we worry about confidentiality, or that our colleagues will consider us inadequate or incompetent clinicians, or that a display of “weakness” means we have failed in some way—we often wait too long to seek treatment. Often, it takes a crisis before we stop to care for ourselves.
Continue for suggestions on how to take care of yourself >>
We promote the health of our patients, but we often forget that if health is to be sustained, those who provide the help must be capable of caring for both themselves and others.2 Without being overly prescriptive, I would like to share with you some suggestions for how you can take care of yourself:
1. Maintain a positive attitude. Yes, we often set ourselves up for failure, but we must have patience with ourselves. There are countless ways to practice reflection and find some time to think; it could entail an artistic outlet such as painting, sculpting, sewing, or singing. A colleague of mine listens to affirmations (now available by smartphone app) that she says help her succeed in her daily endeavors.
2. Identify your support systems. You know who they are: family, friends, and colleagues who bring positive support to your life. Spend more time with them. Clinicians with strong family or social connections are generally healthier than those who lack a support network. Make plans with supportive family members and friends, or seek out activities where you can meet new people.
3. Choose healthy, well-balanced meals. This is probably one of the most difficult tasks, due to our hectic and busy lifestyles. We should strive for low-fat, low-sugar, low-salt, high-fiber, and reasonably low-calorie meals. And drink more water—at least 6 to 8 glasses per day.
4. Get an appropriate amount of sleep. Restorative rest is one of the things you can control and should—no, must—give priority to. It is known that sleep is key to competent delivery of care. The National Sleep Foundation suggests seven to nine hours per night for those ages 26 to 64 and seven to eight hours per night for those older than 65.3 (In fact, some studies have suggested an increase in stroke linked to sleeping longer in older age.4)
5. Exercise. Schedule time for a sustainable exercise program. Put it on your calendar, and make that the one meeting that is essential. (This is another area in which technology can help, by providing reminders that you need to get up and move.) You don’t have to go to the gym twice a day or run a marathon. Walking for an hour three or four times a week will make a difference; even a 5-minute walk after a stressful meeting can help. Just do it!
6. Schedule time for R&R. Over the past decade, a staggering number of studies have demonstrated that our work performance plummets when we work prolonged periods without a break. Use your vacation time! A recent Harvard Business Review article reported that employees who take vacation are actually more productive.5 Make time for yourself—no one else will!
7. Take care of your mental health. Stress is a fact of life. Do what you can to relieve it; develop good coping skills and use them. You may find that keeping a journal in which you can vent your frustrations and fears or taking your dog for a long walk helps to relieve tension. Find what works for you. And make sure to laugh and find the humor in life. Laughter has been shown to boost the immune system and ease pain. It’s a great way to relax!
8. Take care of your physical health. Caring for your body is one of the best things you can do for yourself. Reduce or eliminate risk factors. Please get your routine health promotion procedures done (eg, colonoscopy, Pap smear, mammogram). And when you experience signs of illness, don’t ignore them! Seek advice early for anything out of the ordinary, be it intermittent dizziness, recurrent fatigue, unintended weight loss, feelings of despair—I could go on.
If even a handful of you heed these suggestions, and doing so makes a difference in your health and longevity, then I have completed my mission for this editorial.
We should be role models for our patients. The societal focus on healthy lifestyles is a challenge for all of us, but the benefits are enormous. I would love to hear from you regarding ways to enhance our physical and mental health and avoid early morbidity or mortality. You can reach me at [email protected].
REFERENCES
1. Woods R. Physician, heal thyself: the health and mortality of Victorian doctors. Soc Hist Med. 1966;9(1):1-30.
2. Borchardt GL. Role models for health promotion: the challenge for nurses. Nurs Forum. 2000;35(3):29-32.
3. Hershkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40-43.
4. Leng Y, Cappuccio FP, Wainwright NWJ, et al. Sleep duration and risk of fatal and nonfatal stroke: a prospective study and meta-analysis. Neurology. 2015;84(11):1072-1079.
5. Friedman R. Dear boss: your team wants you to go on vacation. Harvard Bus Rev. June 15, 2015.
After 40 years as a PA (including 21 in academia), tucking myself safely into my seventh decade of life, I was feeling fairly invincible. Yes, I was experiencing increased fatigue and intermittent dizziness, but I attributed those to normal aging and my hectic schedule. Purely to get my colleagues and loved ones off my back, I agreed to see my primary care physician—but, feeling that I had little time for this and knowing that my health was just fine, thank you, I scheduled my appointment for a month later.
That appointment resulted in a referral to a cardiologist (which I didn’t think I needed) and a carotid ultrasound (which yielded negative results). I was still begrudging the time spent on these appointments, when my treadmill test revealed some ST changes in the lateral leads. OK, yes, I do have a positive family history for heart disease! But still, I was surprised.
This finding led to a nuclear treadmill test, which showed some ischemia. The cardiologist suggested an angiogram to rule out a probable false-positive result. Now, I really didn’t have time for this, either—but having gone this far, I felt it was important just to get it over with. Thank goodness I did!
During my angiogram (by the way, they give you great LaLa Land drugs), the interventional cardiologist discovered a 95% blockage of the circumflex, a 95% blockage of the right coronary artery, and a 60% blockage of the LAD. The big decision at that point, amidst the obvious shock of my mortality, was whether to opt for an open-heart bypass or stents. I chose stents (which, by the way, have had a significant impact on my energy level). My cardiologist tells me that, without the stents, if I had experienced a total occlusion event, I would not have survived. Quite a sobering thought!
My purpose in sharing this story is not to call attention to myself but rather to offer a wake-up call to those of us who think we are invincible. Many colleagues who have heard my story have decided to get their own long-delayed treadmill or other health-related tests. So here is my call to action to all of you: Take care of your health. The irony is that, for health care providers, this can be difficult.
Those who care for others often have a tough time caring for themselves. We know that physicians are notoriously bad patients, and I think PAs/NPs are no different. We deal with life-and-death issues all the time, and outward displays of distress are, at a minimum, discouraged. In general, our training and accumulated experience help us to develop good coping skills: We are taught to ignore basic human needs (like hunger and fatigue) and to remain capable, competent, and compassionate clinicians under highly stressful conditions.
Nonetheless, we experience these high levels of stress and seldom act to relieve them. As long ago as 1886, Dr William Ogle exposed clinicians’ vulnerability to high mortality risks, but to this day, the subject remains fairly neglected.1 Perhaps as a result of stigma—we worry about confidentiality, or that our colleagues will consider us inadequate or incompetent clinicians, or that a display of “weakness” means we have failed in some way—we often wait too long to seek treatment. Often, it takes a crisis before we stop to care for ourselves.
Continue for suggestions on how to take care of yourself >>
We promote the health of our patients, but we often forget that if health is to be sustained, those who provide the help must be capable of caring for both themselves and others.2 Without being overly prescriptive, I would like to share with you some suggestions for how you can take care of yourself:
1. Maintain a positive attitude. Yes, we often set ourselves up for failure, but we must have patience with ourselves. There are countless ways to practice reflection and find some time to think; it could entail an artistic outlet such as painting, sculpting, sewing, or singing. A colleague of mine listens to affirmations (now available by smartphone app) that she says help her succeed in her daily endeavors.
2. Identify your support systems. You know who they are: family, friends, and colleagues who bring positive support to your life. Spend more time with them. Clinicians with strong family or social connections are generally healthier than those who lack a support network. Make plans with supportive family members and friends, or seek out activities where you can meet new people.
3. Choose healthy, well-balanced meals. This is probably one of the most difficult tasks, due to our hectic and busy lifestyles. We should strive for low-fat, low-sugar, low-salt, high-fiber, and reasonably low-calorie meals. And drink more water—at least 6 to 8 glasses per day.
4. Get an appropriate amount of sleep. Restorative rest is one of the things you can control and should—no, must—give priority to. It is known that sleep is key to competent delivery of care. The National Sleep Foundation suggests seven to nine hours per night for those ages 26 to 64 and seven to eight hours per night for those older than 65.3 (In fact, some studies have suggested an increase in stroke linked to sleeping longer in older age.4)
5. Exercise. Schedule time for a sustainable exercise program. Put it on your calendar, and make that the one meeting that is essential. (This is another area in which technology can help, by providing reminders that you need to get up and move.) You don’t have to go to the gym twice a day or run a marathon. Walking for an hour three or four times a week will make a difference; even a 5-minute walk after a stressful meeting can help. Just do it!
6. Schedule time for R&R. Over the past decade, a staggering number of studies have demonstrated that our work performance plummets when we work prolonged periods without a break. Use your vacation time! A recent Harvard Business Review article reported that employees who take vacation are actually more productive.5 Make time for yourself—no one else will!
7. Take care of your mental health. Stress is a fact of life. Do what you can to relieve it; develop good coping skills and use them. You may find that keeping a journal in which you can vent your frustrations and fears or taking your dog for a long walk helps to relieve tension. Find what works for you. And make sure to laugh and find the humor in life. Laughter has been shown to boost the immune system and ease pain. It’s a great way to relax!
8. Take care of your physical health. Caring for your body is one of the best things you can do for yourself. Reduce or eliminate risk factors. Please get your routine health promotion procedures done (eg, colonoscopy, Pap smear, mammogram). And when you experience signs of illness, don’t ignore them! Seek advice early for anything out of the ordinary, be it intermittent dizziness, recurrent fatigue, unintended weight loss, feelings of despair—I could go on.
If even a handful of you heed these suggestions, and doing so makes a difference in your health and longevity, then I have completed my mission for this editorial.
We should be role models for our patients. The societal focus on healthy lifestyles is a challenge for all of us, but the benefits are enormous. I would love to hear from you regarding ways to enhance our physical and mental health and avoid early morbidity or mortality. You can reach me at [email protected].
REFERENCES
1. Woods R. Physician, heal thyself: the health and mortality of Victorian doctors. Soc Hist Med. 1966;9(1):1-30.
2. Borchardt GL. Role models for health promotion: the challenge for nurses. Nurs Forum. 2000;35(3):29-32.
3. Hershkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40-43.
4. Leng Y, Cappuccio FP, Wainwright NWJ, et al. Sleep duration and risk of fatal and nonfatal stroke: a prospective study and meta-analysis. Neurology. 2015;84(11):1072-1079.
5. Friedman R. Dear boss: your team wants you to go on vacation. Harvard Bus Rev. June 15, 2015.
After 40 years as a PA (including 21 in academia), tucking myself safely into my seventh decade of life, I was feeling fairly invincible. Yes, I was experiencing increased fatigue and intermittent dizziness, but I attributed those to normal aging and my hectic schedule. Purely to get my colleagues and loved ones off my back, I agreed to see my primary care physician—but, feeling that I had little time for this and knowing that my health was just fine, thank you, I scheduled my appointment for a month later.
That appointment resulted in a referral to a cardiologist (which I didn’t think I needed) and a carotid ultrasound (which yielded negative results). I was still begrudging the time spent on these appointments, when my treadmill test revealed some ST changes in the lateral leads. OK, yes, I do have a positive family history for heart disease! But still, I was surprised.
This finding led to a nuclear treadmill test, which showed some ischemia. The cardiologist suggested an angiogram to rule out a probable false-positive result. Now, I really didn’t have time for this, either—but having gone this far, I felt it was important just to get it over with. Thank goodness I did!
During my angiogram (by the way, they give you great LaLa Land drugs), the interventional cardiologist discovered a 95% blockage of the circumflex, a 95% blockage of the right coronary artery, and a 60% blockage of the LAD. The big decision at that point, amidst the obvious shock of my mortality, was whether to opt for an open-heart bypass or stents. I chose stents (which, by the way, have had a significant impact on my energy level). My cardiologist tells me that, without the stents, if I had experienced a total occlusion event, I would not have survived. Quite a sobering thought!
My purpose in sharing this story is not to call attention to myself but rather to offer a wake-up call to those of us who think we are invincible. Many colleagues who have heard my story have decided to get their own long-delayed treadmill or other health-related tests. So here is my call to action to all of you: Take care of your health. The irony is that, for health care providers, this can be difficult.
Those who care for others often have a tough time caring for themselves. We know that physicians are notoriously bad patients, and I think PAs/NPs are no different. We deal with life-and-death issues all the time, and outward displays of distress are, at a minimum, discouraged. In general, our training and accumulated experience help us to develop good coping skills: We are taught to ignore basic human needs (like hunger and fatigue) and to remain capable, competent, and compassionate clinicians under highly stressful conditions.
Nonetheless, we experience these high levels of stress and seldom act to relieve them. As long ago as 1886, Dr William Ogle exposed clinicians’ vulnerability to high mortality risks, but to this day, the subject remains fairly neglected.1 Perhaps as a result of stigma—we worry about confidentiality, or that our colleagues will consider us inadequate or incompetent clinicians, or that a display of “weakness” means we have failed in some way—we often wait too long to seek treatment. Often, it takes a crisis before we stop to care for ourselves.
Continue for suggestions on how to take care of yourself >>
We promote the health of our patients, but we often forget that if health is to be sustained, those who provide the help must be capable of caring for both themselves and others.2 Without being overly prescriptive, I would like to share with you some suggestions for how you can take care of yourself:
1. Maintain a positive attitude. Yes, we often set ourselves up for failure, but we must have patience with ourselves. There are countless ways to practice reflection and find some time to think; it could entail an artistic outlet such as painting, sculpting, sewing, or singing. A colleague of mine listens to affirmations (now available by smartphone app) that she says help her succeed in her daily endeavors.
2. Identify your support systems. You know who they are: family, friends, and colleagues who bring positive support to your life. Spend more time with them. Clinicians with strong family or social connections are generally healthier than those who lack a support network. Make plans with supportive family members and friends, or seek out activities where you can meet new people.
3. Choose healthy, well-balanced meals. This is probably one of the most difficult tasks, due to our hectic and busy lifestyles. We should strive for low-fat, low-sugar, low-salt, high-fiber, and reasonably low-calorie meals. And drink more water—at least 6 to 8 glasses per day.
4. Get an appropriate amount of sleep. Restorative rest is one of the things you can control and should—no, must—give priority to. It is known that sleep is key to competent delivery of care. The National Sleep Foundation suggests seven to nine hours per night for those ages 26 to 64 and seven to eight hours per night for those older than 65.3 (In fact, some studies have suggested an increase in stroke linked to sleeping longer in older age.4)
5. Exercise. Schedule time for a sustainable exercise program. Put it on your calendar, and make that the one meeting that is essential. (This is another area in which technology can help, by providing reminders that you need to get up and move.) You don’t have to go to the gym twice a day or run a marathon. Walking for an hour three or four times a week will make a difference; even a 5-minute walk after a stressful meeting can help. Just do it!
6. Schedule time for R&R. Over the past decade, a staggering number of studies have demonstrated that our work performance plummets when we work prolonged periods without a break. Use your vacation time! A recent Harvard Business Review article reported that employees who take vacation are actually more productive.5 Make time for yourself—no one else will!
7. Take care of your mental health. Stress is a fact of life. Do what you can to relieve it; develop good coping skills and use them. You may find that keeping a journal in which you can vent your frustrations and fears or taking your dog for a long walk helps to relieve tension. Find what works for you. And make sure to laugh and find the humor in life. Laughter has been shown to boost the immune system and ease pain. It’s a great way to relax!
8. Take care of your physical health. Caring for your body is one of the best things you can do for yourself. Reduce or eliminate risk factors. Please get your routine health promotion procedures done (eg, colonoscopy, Pap smear, mammogram). And when you experience signs of illness, don’t ignore them! Seek advice early for anything out of the ordinary, be it intermittent dizziness, recurrent fatigue, unintended weight loss, feelings of despair—I could go on.
If even a handful of you heed these suggestions, and doing so makes a difference in your health and longevity, then I have completed my mission for this editorial.
We should be role models for our patients. The societal focus on healthy lifestyles is a challenge for all of us, but the benefits are enormous. I would love to hear from you regarding ways to enhance our physical and mental health and avoid early morbidity or mortality. You can reach me at [email protected].
REFERENCES
1. Woods R. Physician, heal thyself: the health and mortality of Victorian doctors. Soc Hist Med. 1966;9(1):1-30.
2. Borchardt GL. Role models for health promotion: the challenge for nurses. Nurs Forum. 2000;35(3):29-32.
3. Hershkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40-43.
4. Leng Y, Cappuccio FP, Wainwright NWJ, et al. Sleep duration and risk of fatal and nonfatal stroke: a prospective study and meta-analysis. Neurology. 2015;84(11):1072-1079.
5. Friedman R. Dear boss: your team wants you to go on vacation. Harvard Bus Rev. June 15, 2015.
Erratum
The article “How to do a 3-minute diabetic foot exam” (J Fam Pract. 2014;63:646-656) incorrectly stated in Table 4 that chronic venous insufficiency is a high priority indication for referral to a specialist. It is not. The correct indications for this category include: presence of diabetes with a previous history of ulcer, Charcot neuroarthropathy, or lower extremity amputation. This information has been corrected in the online version of the article.
The article “How to do a 3-minute diabetic foot exam” (J Fam Pract. 2014;63:646-656) incorrectly stated in Table 4 that chronic venous insufficiency is a high priority indication for referral to a specialist. It is not. The correct indications for this category include: presence of diabetes with a previous history of ulcer, Charcot neuroarthropathy, or lower extremity amputation. This information has been corrected in the online version of the article.
The article “How to do a 3-minute diabetic foot exam” (J Fam Pract. 2014;63:646-656) incorrectly stated in Table 4 that chronic venous insufficiency is a high priority indication for referral to a specialist. It is not. The correct indications for this category include: presence of diabetes with a previous history of ulcer, Charcot neuroarthropathy, or lower extremity amputation. This information has been corrected in the online version of the article.
Have we done enough to educate patients about e-cigarettes?
Electronic cigarettes (e-cigarettes) have become popular in the United States over the past decade.1 They have been widely marketed as an alternative to tobacco and as a way to quit smoking.
While the negative effects of smoking tobacco are well known (having as few as one to 4 cigarettes a day triples the risk of coronary artery disease and pulmonary neoplasia2), the potential risks of e-cigarettes are not as well known. There has been limited regulation and insufficient research into the harmful effects of inhaling their vapor.
The potentially harmful compounds within e-cigarette vapors include both organic and inorganic toxins.3 A study of the contents of numerous e-cigarette refills found formaldehyde and acrolein, along with several hydrocarbons.3 Lead, cadmium, and nickel were also found in e-cigarette refills and their inhaled vapors.1 Lead causes severe neurotoxicity,4 cadmium can cause organ damage,5 and inhaled nickel causes an inflammatory reaction in the lungs.6
The risk-to-benefit ratio of e-cigarettes as a means of tobacco cessation and the health consequences of breathing their vapors cannot be established until research is completed. What we do know is that the nicotine in e-cigarette vapors maintains continued addiction.
It’s up to us as physicians to educate our patients about the potential harm of e-cigarette chemical toxicity and encourage cessation of both tobacco products and e-cigarettes.
Kavitha Srinivasan, MD
Lee Smith, BA
Manasa Enja, MD
Steven Lippmann, MD
Louisville, Ky
1. Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation. 2014;129:1972-1986.
2. Bjartveit K, Tverdal A. Health consequences of smoking 1-4 cigarettes per day. Tob Control. 2005;14:315-320.
3. Varlet V, Farsalinos K, Augsburger M, et al. Toxicity assessment of refill liquids for electronic cigarettes. Int J Environ Res Public Health. 2015;12:4796-4815.
4. Skerfving S, Löfmark L, Lundh T, et al. Late effects of low blood lead concentrations in children on school performance and cognitive functions. Neurotoxicology. 2015;49:114-120.
5. Bernhoft RA. Cadmium toxicity and treatment. Scientific-World-Journal. 2013;2013:394652.
6. Das KK, Buchner V. Effect of nickel exposure on peripheral tissues: role of oxidative stress in toxicity and possible protection by ascorbic acid. Rev Environ Health. 2007;22:157-173.
Electronic cigarettes (e-cigarettes) have become popular in the United States over the past decade.1 They have been widely marketed as an alternative to tobacco and as a way to quit smoking.
While the negative effects of smoking tobacco are well known (having as few as one to 4 cigarettes a day triples the risk of coronary artery disease and pulmonary neoplasia2), the potential risks of e-cigarettes are not as well known. There has been limited regulation and insufficient research into the harmful effects of inhaling their vapor.
The potentially harmful compounds within e-cigarette vapors include both organic and inorganic toxins.3 A study of the contents of numerous e-cigarette refills found formaldehyde and acrolein, along with several hydrocarbons.3 Lead, cadmium, and nickel were also found in e-cigarette refills and their inhaled vapors.1 Lead causes severe neurotoxicity,4 cadmium can cause organ damage,5 and inhaled nickel causes an inflammatory reaction in the lungs.6
The risk-to-benefit ratio of e-cigarettes as a means of tobacco cessation and the health consequences of breathing their vapors cannot be established until research is completed. What we do know is that the nicotine in e-cigarette vapors maintains continued addiction.
It’s up to us as physicians to educate our patients about the potential harm of e-cigarette chemical toxicity and encourage cessation of both tobacco products and e-cigarettes.
Kavitha Srinivasan, MD
Lee Smith, BA
Manasa Enja, MD
Steven Lippmann, MD
Louisville, Ky
Electronic cigarettes (e-cigarettes) have become popular in the United States over the past decade.1 They have been widely marketed as an alternative to tobacco and as a way to quit smoking.
While the negative effects of smoking tobacco are well known (having as few as one to 4 cigarettes a day triples the risk of coronary artery disease and pulmonary neoplasia2), the potential risks of e-cigarettes are not as well known. There has been limited regulation and insufficient research into the harmful effects of inhaling their vapor.
The potentially harmful compounds within e-cigarette vapors include both organic and inorganic toxins.3 A study of the contents of numerous e-cigarette refills found formaldehyde and acrolein, along with several hydrocarbons.3 Lead, cadmium, and nickel were also found in e-cigarette refills and their inhaled vapors.1 Lead causes severe neurotoxicity,4 cadmium can cause organ damage,5 and inhaled nickel causes an inflammatory reaction in the lungs.6
The risk-to-benefit ratio of e-cigarettes as a means of tobacco cessation and the health consequences of breathing their vapors cannot be established until research is completed. What we do know is that the nicotine in e-cigarette vapors maintains continued addiction.
It’s up to us as physicians to educate our patients about the potential harm of e-cigarette chemical toxicity and encourage cessation of both tobacco products and e-cigarettes.
Kavitha Srinivasan, MD
Lee Smith, BA
Manasa Enja, MD
Steven Lippmann, MD
Louisville, Ky
1. Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation. 2014;129:1972-1986.
2. Bjartveit K, Tverdal A. Health consequences of smoking 1-4 cigarettes per day. Tob Control. 2005;14:315-320.
3. Varlet V, Farsalinos K, Augsburger M, et al. Toxicity assessment of refill liquids for electronic cigarettes. Int J Environ Res Public Health. 2015;12:4796-4815.
4. Skerfving S, Löfmark L, Lundh T, et al. Late effects of low blood lead concentrations in children on school performance and cognitive functions. Neurotoxicology. 2015;49:114-120.
5. Bernhoft RA. Cadmium toxicity and treatment. Scientific-World-Journal. 2013;2013:394652.
6. Das KK, Buchner V. Effect of nickel exposure on peripheral tissues: role of oxidative stress in toxicity and possible protection by ascorbic acid. Rev Environ Health. 2007;22:157-173.
1. Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation. 2014;129:1972-1986.
2. Bjartveit K, Tverdal A. Health consequences of smoking 1-4 cigarettes per day. Tob Control. 2005;14:315-320.
3. Varlet V, Farsalinos K, Augsburger M, et al. Toxicity assessment of refill liquids for electronic cigarettes. Int J Environ Res Public Health. 2015;12:4796-4815.
4. Skerfving S, Löfmark L, Lundh T, et al. Late effects of low blood lead concentrations in children on school performance and cognitive functions. Neurotoxicology. 2015;49:114-120.
5. Bernhoft RA. Cadmium toxicity and treatment. Scientific-World-Journal. 2013;2013:394652.
6. Das KK, Buchner V. Effect of nickel exposure on peripheral tissues: role of oxidative stress in toxicity and possible protection by ascorbic acid. Rev Environ Health. 2007;22:157-173.
Practice invites patients to run a 5K with their doctor
My new patient had just left his family doctor after 15 years. When I asked why, he said, “The doctor came into the room, looked at my chart, and told me I needed to lose weight, lower my cholesterol, and stop smoking. I looked at the 300-pound doctor who smelled of smoke and said, ‘Really?’ ”
How can we empower our patients to make healthy choices when we don’t always make these choices ourselves? Here’s one possibility: Invite them to join us in the struggle.
Last year, my practice created “Run 5K or Walk 1 Mile With Your Doctor” as a way to encourage both patients and medical professionals to get healthy. We also invited patients to join us in a walking/running club to prepare for the event. More than 200 people showed up, including physician assistants, nurses, nurse practitioners, medical assistants, respiratory therapists, family doctors, internists, office staff, cardiologists, orthopedists, and patients. In addition to raising heart rates, we also raised $7000 for the American Heart Association (AHA). This year we plan to merge the event with the annual AHA walk in September. I encourage all health care professionals to do the same.
As physicians, we can’t just talk the talk in the examining room. We should also walk the walk and show our patients that we’re right there in the trenches with them.
Elizabeth Khan, MD
Allentown, Pa
My new patient had just left his family doctor after 15 years. When I asked why, he said, “The doctor came into the room, looked at my chart, and told me I needed to lose weight, lower my cholesterol, and stop smoking. I looked at the 300-pound doctor who smelled of smoke and said, ‘Really?’ ”
How can we empower our patients to make healthy choices when we don’t always make these choices ourselves? Here’s one possibility: Invite them to join us in the struggle.
Last year, my practice created “Run 5K or Walk 1 Mile With Your Doctor” as a way to encourage both patients and medical professionals to get healthy. We also invited patients to join us in a walking/running club to prepare for the event. More than 200 people showed up, including physician assistants, nurses, nurse practitioners, medical assistants, respiratory therapists, family doctors, internists, office staff, cardiologists, orthopedists, and patients. In addition to raising heart rates, we also raised $7000 for the American Heart Association (AHA). This year we plan to merge the event with the annual AHA walk in September. I encourage all health care professionals to do the same.
As physicians, we can’t just talk the talk in the examining room. We should also walk the walk and show our patients that we’re right there in the trenches with them.
Elizabeth Khan, MD
Allentown, Pa
My new patient had just left his family doctor after 15 years. When I asked why, he said, “The doctor came into the room, looked at my chart, and told me I needed to lose weight, lower my cholesterol, and stop smoking. I looked at the 300-pound doctor who smelled of smoke and said, ‘Really?’ ”
How can we empower our patients to make healthy choices when we don’t always make these choices ourselves? Here’s one possibility: Invite them to join us in the struggle.
Last year, my practice created “Run 5K or Walk 1 Mile With Your Doctor” as a way to encourage both patients and medical professionals to get healthy. We also invited patients to join us in a walking/running club to prepare for the event. More than 200 people showed up, including physician assistants, nurses, nurse practitioners, medical assistants, respiratory therapists, family doctors, internists, office staff, cardiologists, orthopedists, and patients. In addition to raising heart rates, we also raised $7000 for the American Heart Association (AHA). This year we plan to merge the event with the annual AHA walk in September. I encourage all health care professionals to do the same.
As physicians, we can’t just talk the talk in the examining room. We should also walk the walk and show our patients that we’re right there in the trenches with them.
Elizabeth Khan, MD
Allentown, Pa
"The Times They Are A-Changin"
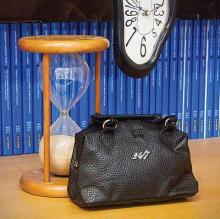
In April 1977, shortly after the new American Board of Emergency Medicine (ABEM) was constituted, it adopted the hourglass as its symbol for the unique nature of emergency medicine—a specialty in large part defined by the very brief time in which emergency physicians (EPs) must correctly identify and treat serious, life-threatening conditions. Incorporating the concept of the “golden hour” in which to prevent the irreversible consequences of serious trauma, and the frequently even shorter period to effectively intervene after cardiovascular and neurovascular catastrophes, the hourglass has become a powerful symbol that all emergency physicians are very, very proud of.
In the years since the American Board of Medical Specialties (ABMS) recognized Emergency Medicine as the 23rd specialty, though much about emergency medicine has remained the same, much has also changed. Currently, the time patients spend in EDs throughout the country is all too frequently determined, not by the time required to diagnose and initiate treatment for their illnesses, but by the time required for an inpatient bed to become available or for safe, reliable outpatient care to be arranged. In some hospitals, ED patients who are admitted and require inpatient care or “observation services” continue to be cared for by EPs and ED nurses, while in other hospitals the care and responsibility for such patients is transferred to the appropriate inpatient service—even as the patients remain for hours or days on ED stretchers on the ground floor of the hospital. In some cases, an entire “hospitalization” takes place in the ED.
Similarly, when the specialty of emergency medicine was first established, it faced not only time, but resource-limitations as well. Few CT scanners then were commonly available in close proximity to EDs; afterward, when CT scans did become easily accessible to ED patients and MRI scanners began to appear, no one considered MRI scans to be “ED procedures” because of the time required to complete the studies. This, of course, was before managed-care appeared on the scene and, more recently, Centers for Medicare & Medicaid Services (CMS) began to seriously question the need for some admissions and short hospital stays. The 2013 Rand Research Report on the “Evolving Role of Emergency Departments in the United States” (http://www.rand.org/content/dam/rand/pubs/research_reports/RR200/RR280/RAND_RR280.pdf) clearly describes the many other things that emergency medicine now encompasses.
If the venerable hourglass no longer depicts all that emergency medicine has become, is it time to freshen the image or adopt a new symbol? One other extremely significant time-related feature of emergency medicine that has endured is the recognition that the hours during which the human body gets sick or injured are not restricted to typical work hours or work days, and that, as the title of Brian Zink’s book suggests, EPs are trained to care for “Anyone, Anything, Anytime” (Anyone, Anything, Anytime: A History of Emergency Medicine. Philadelphia, PA: Mosby, Inc; 2006). Perhaps, the time has come to add “24/7” to the hourglass symbol. This suggestion is not as frivolous as it may sound, as increasingly federal and state governments and private insurers are using the availability of care 24 hours a day, 7 days a week as a principal characteristic that differentiates emergency medicine, and the higher reimbursement rates it commands, from the care provided by urgent care and “convenient care” centers.
In April 1977, shortly after the new American Board of Emergency Medicine (ABEM) was constituted, it adopted the hourglass as its symbol for the unique nature of emergency medicine—a specialty in large part defined by the very brief time in which emergency physicians (EPs) must correctly identify and treat serious, life-threatening conditions. Incorporating the concept of the “golden hour” in which to prevent the irreversible consequences of serious trauma, and the frequently even shorter period to effectively intervene after cardiovascular and neurovascular catastrophes, the hourglass has become a powerful symbol that all emergency physicians are very, very proud of.
In the years since the American Board of Medical Specialties (ABMS) recognized Emergency Medicine as the 23rd specialty, though much about emergency medicine has remained the same, much has also changed. Currently, the time patients spend in EDs throughout the country is all too frequently determined, not by the time required to diagnose and initiate treatment for their illnesses, but by the time required for an inpatient bed to become available or for safe, reliable outpatient care to be arranged. In some hospitals, ED patients who are admitted and require inpatient care or “observation services” continue to be cared for by EPs and ED nurses, while in other hospitals the care and responsibility for such patients is transferred to the appropriate inpatient service—even as the patients remain for hours or days on ED stretchers on the ground floor of the hospital. In some cases, an entire “hospitalization” takes place in the ED.
Similarly, when the specialty of emergency medicine was first established, it faced not only time, but resource-limitations as well. Few CT scanners then were commonly available in close proximity to EDs; afterward, when CT scans did become easily accessible to ED patients and MRI scanners began to appear, no one considered MRI scans to be “ED procedures” because of the time required to complete the studies. This, of course, was before managed-care appeared on the scene and, more recently, Centers for Medicare & Medicaid Services (CMS) began to seriously question the need for some admissions and short hospital stays. The 2013 Rand Research Report on the “Evolving Role of Emergency Departments in the United States” (http://www.rand.org/content/dam/rand/pubs/research_reports/RR200/RR280/RAND_RR280.pdf) clearly describes the many other things that emergency medicine now encompasses.
If the venerable hourglass no longer depicts all that emergency medicine has become, is it time to freshen the image or adopt a new symbol? One other extremely significant time-related feature of emergency medicine that has endured is the recognition that the hours during which the human body gets sick or injured are not restricted to typical work hours or work days, and that, as the title of Brian Zink’s book suggests, EPs are trained to care for “Anyone, Anything, Anytime” (Anyone, Anything, Anytime: A History of Emergency Medicine. Philadelphia, PA: Mosby, Inc; 2006). Perhaps, the time has come to add “24/7” to the hourglass symbol. This suggestion is not as frivolous as it may sound, as increasingly federal and state governments and private insurers are using the availability of care 24 hours a day, 7 days a week as a principal characteristic that differentiates emergency medicine, and the higher reimbursement rates it commands, from the care provided by urgent care and “convenient care” centers.
In April 1977, shortly after the new American Board of Emergency Medicine (ABEM) was constituted, it adopted the hourglass as its symbol for the unique nature of emergency medicine—a specialty in large part defined by the very brief time in which emergency physicians (EPs) must correctly identify and treat serious, life-threatening conditions. Incorporating the concept of the “golden hour” in which to prevent the irreversible consequences of serious trauma, and the frequently even shorter period to effectively intervene after cardiovascular and neurovascular catastrophes, the hourglass has become a powerful symbol that all emergency physicians are very, very proud of.
In the years since the American Board of Medical Specialties (ABMS) recognized Emergency Medicine as the 23rd specialty, though much about emergency medicine has remained the same, much has also changed. Currently, the time patients spend in EDs throughout the country is all too frequently determined, not by the time required to diagnose and initiate treatment for their illnesses, but by the time required for an inpatient bed to become available or for safe, reliable outpatient care to be arranged. In some hospitals, ED patients who are admitted and require inpatient care or “observation services” continue to be cared for by EPs and ED nurses, while in other hospitals the care and responsibility for such patients is transferred to the appropriate inpatient service—even as the patients remain for hours or days on ED stretchers on the ground floor of the hospital. In some cases, an entire “hospitalization” takes place in the ED.
Similarly, when the specialty of emergency medicine was first established, it faced not only time, but resource-limitations as well. Few CT scanners then were commonly available in close proximity to EDs; afterward, when CT scans did become easily accessible to ED patients and MRI scanners began to appear, no one considered MRI scans to be “ED procedures” because of the time required to complete the studies. This, of course, was before managed-care appeared on the scene and, more recently, Centers for Medicare & Medicaid Services (CMS) began to seriously question the need for some admissions and short hospital stays. The 2013 Rand Research Report on the “Evolving Role of Emergency Departments in the United States” (http://www.rand.org/content/dam/rand/pubs/research_reports/RR200/RR280/RAND_RR280.pdf) clearly describes the many other things that emergency medicine now encompasses.
If the venerable hourglass no longer depicts all that emergency medicine has become, is it time to freshen the image or adopt a new symbol? One other extremely significant time-related feature of emergency medicine that has endured is the recognition that the hours during which the human body gets sick or injured are not restricted to typical work hours or work days, and that, as the title of Brian Zink’s book suggests, EPs are trained to care for “Anyone, Anything, Anytime” (Anyone, Anything, Anytime: A History of Emergency Medicine. Philadelphia, PA: Mosby, Inc; 2006). Perhaps, the time has come to add “24/7” to the hourglass symbol. This suggestion is not as frivolous as it may sound, as increasingly federal and state governments and private insurers are using the availability of care 24 hours a day, 7 days a week as a principal characteristic that differentiates emergency medicine, and the higher reimbursement rates it commands, from the care provided by urgent care and “convenient care” centers.
Update on informed consent
Question: Which of the following statements regarding the doctrine of informed consent is best?
A. All jurisdictions now require disclosure geared toward the reasonable patient rather than the reasonable doctor.
B. Disclosures are less important and sometimes unnecessary in global clinical research protocols.
C. The trend is toward the use of simplified and personalized consent forms.
D. A and C.
Answer: C. An important development in the doctrine of informed consent deals with the typical consent form, which is lengthy (going on 14 pages in one report), largely incomprehensible, and densely legalistic. Worse, the physician may misconstrue the form as a proxy for risk disclosure, whereas in fact the duly signed form merely purports to indicate that meaningful discussion of risks, benefits, and alternatives had taken place – if indeed that has been the case.
A review of more than 500 separate informed consent forms revealed these documents have limited educational value, go mostly unread, and are frequently misunderstood by patients (Arch. Surg. 2000;135:26-33).Thus, there is much to recommend the recent move toward shorter forms that use simpler language, bigger type fonts, and even graphics to improve patient and family understanding.
For example, a novel personalized approach currently being tested offers evidence-based benefits and risks to patients undergoing elective percutaneous coronary intervention. The consent document draws on the American College of Cardiology’s National Cardiovascular Data Registry to offer individualized risk estimates, and lists the experience of the health care team and the anticipated financial costs (JAMA 2010;303:1190-1).
Such approaches are consonant with the notion of patient-centered care, which the Institute of Medicine has identified as a core attribute of high-quality health care systems.
One of the continuing controversies in informed consent is the requisite standard of disclosure.
Historically, what needed to be disclosed was judged by what was ordinarily expected of the reasonable physician in the community. However, in 1972, Canterbury v. Spence (464 F.2d 772 [D.C. Cir. 1972]) persuasively argued for replacing such a professional standard (what doctors customarily would disclose) with a patient-oriented standard, i.e., what a reasonable patient would want to know.
California quickly followed, and an increasing number of jurisdictions such as Alaska, Hawaii, Massachusetts, Minnesota, Texas, West Virginia, and Wisconsin have since embraced this patient-centered standard. However, a number of other jurisdictions, including Arkansas, Indiana, Michigan, Montana, Nebraska, Nevada, and Wyoming, continue to adhere to the professional or physician-centered standard.
The momentum toward patient-centered disclosure appears to be growing, and has spread to other common-law jurisdictions abroad such as Canada and Australia. The United Kingdom was a steadfast opponent of patient-centric consent since Sidaway v. Board of Governors of the Bethlem Royal Hospital and the Maudsley Hospital ([1985] AC 871), its seminal House of Lords decision in the 1980s.
However, it finally abandoned its opposition on March 11, 2015, when its Supreme Court decided the case of a baby boy who sustained brain injury and arm paralysis at birth as a result of shoulder dystocia (Montgomery v. Lanarkshire Health Board [2015] UKSC 11).
The plaintiff alleged that being a diabetic mother, she should have been warned of the risks of shoulder dystocia and offered the alternative of a cesarean section. The obstetrician said she did not warn because the risks of a serious problem were very small. The court sided with the plaintiff, overturned Sidaway’s professional standard, and adopted the patient standard of disclosure as the new law.
What needs to be disclosed continues to plague the practitioner. The term “material risks” merely begs the question of the definition of “material.” It has been said that the crucial factor is the patient’s need.
The vexing issue surrounding the scope of risk disclosure is compounded by court decisions allowing inquiry outside the medical condition itself, such as a physician’s alcoholism or HIV status, and financial incentives amounting to a breach of fiduciary responsibility. However, courts have tended to reject requiring disclosure of practitioner experience or patient prognosis.
Novel issues continue to surface. For example, a recent Wisconsin Supreme Court case dealt with whether it was necessary for a physician to disclose the availability of a collateral test not directly linked to a patient’s diagnosis.
In Jandre v. Wis. Injured Patients & Families Comp. Fund (813 N.W.2d 627 [Wis. 2012]), a doctor diagnosed Bell’s palsy as the cause of a patient’s neurologic symptoms, because she heard no carotid bruits and the head CT scan was normal. Shortly thereafter, the patient developed a stroke. Although the doctor was found not negligent for the misdiagnosis, the plaintiff then proceeded on a lack of informed consent theory, asserting that the doctor should have advised him of the availability of a carotid ultrasound test to rule out a TIA.
In a momentous decision, the Wisconsin Supreme Court affirmed the lower court’s judgment in finding the physician liable for failing to disclose the availability of the ultrasound procedure.
Another area where informed consent is under renewed scrutiny is in research. Doctors in practice are increasingly participating as coinvestigators in industry-sponsored drug trials, and should be familiar with what is expected in the research context.
Augmented rules regarding informed consent govern all clinical research, with patient safety and free meaningful choice being paramount considerations. Federal and state regulations, implemented and monitored by institutional review boards, serve to enforce compliance and safeguard the safety of experimental subjects.
Still, as predicted nearly 50 years ago by Dr. Henry K. Beecher, “In any precise sense, statements regarding consent are meaningless unless one knows how fully the patient was informed of all risks, and if these are not known, that fact should also be made clear. A far more dependable safeguard than consent is the presence of a truly responsible investigator” (N. Engl. J. Med. 1966;274:1354-60).
Scandals in human research led by or in collaboration with U.S. investigators in foreign countries have been in the news. Global clinical trials are supposed to be carried out in compliance with the Nuremberg Code and the Declaration of Helsinki, but there may be occasional lapses or disregard for such international laws. A recent example is the trial using the antibiotic trovafloxacin, administered orally, versus FDA-approved parenteral ceftriaxone, during a meningitis outbreak in Nigeria (N. Engl. J. Med. 2009;360:2050-3).
Finally, the politics of abortion and first amendment rights have managed to insinuate themselves into the informed consent debate. Can states mandate disclosure in the name of securing meaningful informed consent, e.g., requiring physicians to provide information that might encourage a woman to reconsider her decision to have an abortion?
In 1992, the U.S. Supreme Court decided that this passes constitutional muster, because it did not place an undue burden on the woman. However, the Fourth Circuit Appellate Court recently ruled unconstitutional a North Carolina statute called Display of Real-Time View Requirement. The statute requires physicians to display ultrasound images of the unborn child to a mother contemplating an abortion, which the court ruled violated the First Amendment’s prohibition on state-compelled speech (N. Engl. J. Med. 2015;372:1285-7).
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: Which of the following statements regarding the doctrine of informed consent is best?
A. All jurisdictions now require disclosure geared toward the reasonable patient rather than the reasonable doctor.
B. Disclosures are less important and sometimes unnecessary in global clinical research protocols.
C. The trend is toward the use of simplified and personalized consent forms.
D. A and C.
Answer: C. An important development in the doctrine of informed consent deals with the typical consent form, which is lengthy (going on 14 pages in one report), largely incomprehensible, and densely legalistic. Worse, the physician may misconstrue the form as a proxy for risk disclosure, whereas in fact the duly signed form merely purports to indicate that meaningful discussion of risks, benefits, and alternatives had taken place – if indeed that has been the case.
A review of more than 500 separate informed consent forms revealed these documents have limited educational value, go mostly unread, and are frequently misunderstood by patients (Arch. Surg. 2000;135:26-33).Thus, there is much to recommend the recent move toward shorter forms that use simpler language, bigger type fonts, and even graphics to improve patient and family understanding.
For example, a novel personalized approach currently being tested offers evidence-based benefits and risks to patients undergoing elective percutaneous coronary intervention. The consent document draws on the American College of Cardiology’s National Cardiovascular Data Registry to offer individualized risk estimates, and lists the experience of the health care team and the anticipated financial costs (JAMA 2010;303:1190-1).
Such approaches are consonant with the notion of patient-centered care, which the Institute of Medicine has identified as a core attribute of high-quality health care systems.
One of the continuing controversies in informed consent is the requisite standard of disclosure.
Historically, what needed to be disclosed was judged by what was ordinarily expected of the reasonable physician in the community. However, in 1972, Canterbury v. Spence (464 F.2d 772 [D.C. Cir. 1972]) persuasively argued for replacing such a professional standard (what doctors customarily would disclose) with a patient-oriented standard, i.e., what a reasonable patient would want to know.
California quickly followed, and an increasing number of jurisdictions such as Alaska, Hawaii, Massachusetts, Minnesota, Texas, West Virginia, and Wisconsin have since embraced this patient-centered standard. However, a number of other jurisdictions, including Arkansas, Indiana, Michigan, Montana, Nebraska, Nevada, and Wyoming, continue to adhere to the professional or physician-centered standard.
The momentum toward patient-centered disclosure appears to be growing, and has spread to other common-law jurisdictions abroad such as Canada and Australia. The United Kingdom was a steadfast opponent of patient-centric consent since Sidaway v. Board of Governors of the Bethlem Royal Hospital and the Maudsley Hospital ([1985] AC 871), its seminal House of Lords decision in the 1980s.
However, it finally abandoned its opposition on March 11, 2015, when its Supreme Court decided the case of a baby boy who sustained brain injury and arm paralysis at birth as a result of shoulder dystocia (Montgomery v. Lanarkshire Health Board [2015] UKSC 11).
The plaintiff alleged that being a diabetic mother, she should have been warned of the risks of shoulder dystocia and offered the alternative of a cesarean section. The obstetrician said she did not warn because the risks of a serious problem were very small. The court sided with the plaintiff, overturned Sidaway’s professional standard, and adopted the patient standard of disclosure as the new law.
What needs to be disclosed continues to plague the practitioner. The term “material risks” merely begs the question of the definition of “material.” It has been said that the crucial factor is the patient’s need.
The vexing issue surrounding the scope of risk disclosure is compounded by court decisions allowing inquiry outside the medical condition itself, such as a physician’s alcoholism or HIV status, and financial incentives amounting to a breach of fiduciary responsibility. However, courts have tended to reject requiring disclosure of practitioner experience or patient prognosis.
Novel issues continue to surface. For example, a recent Wisconsin Supreme Court case dealt with whether it was necessary for a physician to disclose the availability of a collateral test not directly linked to a patient’s diagnosis.
In Jandre v. Wis. Injured Patients & Families Comp. Fund (813 N.W.2d 627 [Wis. 2012]), a doctor diagnosed Bell’s palsy as the cause of a patient’s neurologic symptoms, because she heard no carotid bruits and the head CT scan was normal. Shortly thereafter, the patient developed a stroke. Although the doctor was found not negligent for the misdiagnosis, the plaintiff then proceeded on a lack of informed consent theory, asserting that the doctor should have advised him of the availability of a carotid ultrasound test to rule out a TIA.
In a momentous decision, the Wisconsin Supreme Court affirmed the lower court’s judgment in finding the physician liable for failing to disclose the availability of the ultrasound procedure.
Another area where informed consent is under renewed scrutiny is in research. Doctors in practice are increasingly participating as coinvestigators in industry-sponsored drug trials, and should be familiar with what is expected in the research context.
Augmented rules regarding informed consent govern all clinical research, with patient safety and free meaningful choice being paramount considerations. Federal and state regulations, implemented and monitored by institutional review boards, serve to enforce compliance and safeguard the safety of experimental subjects.
Still, as predicted nearly 50 years ago by Dr. Henry K. Beecher, “In any precise sense, statements regarding consent are meaningless unless one knows how fully the patient was informed of all risks, and if these are not known, that fact should also be made clear. A far more dependable safeguard than consent is the presence of a truly responsible investigator” (N. Engl. J. Med. 1966;274:1354-60).
Scandals in human research led by or in collaboration with U.S. investigators in foreign countries have been in the news. Global clinical trials are supposed to be carried out in compliance with the Nuremberg Code and the Declaration of Helsinki, but there may be occasional lapses or disregard for such international laws. A recent example is the trial using the antibiotic trovafloxacin, administered orally, versus FDA-approved parenteral ceftriaxone, during a meningitis outbreak in Nigeria (N. Engl. J. Med. 2009;360:2050-3).
Finally, the politics of abortion and first amendment rights have managed to insinuate themselves into the informed consent debate. Can states mandate disclosure in the name of securing meaningful informed consent, e.g., requiring physicians to provide information that might encourage a woman to reconsider her decision to have an abortion?
In 1992, the U.S. Supreme Court decided that this passes constitutional muster, because it did not place an undue burden on the woman. However, the Fourth Circuit Appellate Court recently ruled unconstitutional a North Carolina statute called Display of Real-Time View Requirement. The statute requires physicians to display ultrasound images of the unborn child to a mother contemplating an abortion, which the court ruled violated the First Amendment’s prohibition on state-compelled speech (N. Engl. J. Med. 2015;372:1285-7).
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Question: Which of the following statements regarding the doctrine of informed consent is best?
A. All jurisdictions now require disclosure geared toward the reasonable patient rather than the reasonable doctor.
B. Disclosures are less important and sometimes unnecessary in global clinical research protocols.
C. The trend is toward the use of simplified and personalized consent forms.
D. A and C.
Answer: C. An important development in the doctrine of informed consent deals with the typical consent form, which is lengthy (going on 14 pages in one report), largely incomprehensible, and densely legalistic. Worse, the physician may misconstrue the form as a proxy for risk disclosure, whereas in fact the duly signed form merely purports to indicate that meaningful discussion of risks, benefits, and alternatives had taken place – if indeed that has been the case.
A review of more than 500 separate informed consent forms revealed these documents have limited educational value, go mostly unread, and are frequently misunderstood by patients (Arch. Surg. 2000;135:26-33).Thus, there is much to recommend the recent move toward shorter forms that use simpler language, bigger type fonts, and even graphics to improve patient and family understanding.
For example, a novel personalized approach currently being tested offers evidence-based benefits and risks to patients undergoing elective percutaneous coronary intervention. The consent document draws on the American College of Cardiology’s National Cardiovascular Data Registry to offer individualized risk estimates, and lists the experience of the health care team and the anticipated financial costs (JAMA 2010;303:1190-1).
Such approaches are consonant with the notion of patient-centered care, which the Institute of Medicine has identified as a core attribute of high-quality health care systems.
One of the continuing controversies in informed consent is the requisite standard of disclosure.
Historically, what needed to be disclosed was judged by what was ordinarily expected of the reasonable physician in the community. However, in 1972, Canterbury v. Spence (464 F.2d 772 [D.C. Cir. 1972]) persuasively argued for replacing such a professional standard (what doctors customarily would disclose) with a patient-oriented standard, i.e., what a reasonable patient would want to know.
California quickly followed, and an increasing number of jurisdictions such as Alaska, Hawaii, Massachusetts, Minnesota, Texas, West Virginia, and Wisconsin have since embraced this patient-centered standard. However, a number of other jurisdictions, including Arkansas, Indiana, Michigan, Montana, Nebraska, Nevada, and Wyoming, continue to adhere to the professional or physician-centered standard.
The momentum toward patient-centered disclosure appears to be growing, and has spread to other common-law jurisdictions abroad such as Canada and Australia. The United Kingdom was a steadfast opponent of patient-centric consent since Sidaway v. Board of Governors of the Bethlem Royal Hospital and the Maudsley Hospital ([1985] AC 871), its seminal House of Lords decision in the 1980s.
However, it finally abandoned its opposition on March 11, 2015, when its Supreme Court decided the case of a baby boy who sustained brain injury and arm paralysis at birth as a result of shoulder dystocia (Montgomery v. Lanarkshire Health Board [2015] UKSC 11).
The plaintiff alleged that being a diabetic mother, she should have been warned of the risks of shoulder dystocia and offered the alternative of a cesarean section. The obstetrician said she did not warn because the risks of a serious problem were very small. The court sided with the plaintiff, overturned Sidaway’s professional standard, and adopted the patient standard of disclosure as the new law.
What needs to be disclosed continues to plague the practitioner. The term “material risks” merely begs the question of the definition of “material.” It has been said that the crucial factor is the patient’s need.
The vexing issue surrounding the scope of risk disclosure is compounded by court decisions allowing inquiry outside the medical condition itself, such as a physician’s alcoholism or HIV status, and financial incentives amounting to a breach of fiduciary responsibility. However, courts have tended to reject requiring disclosure of practitioner experience or patient prognosis.
Novel issues continue to surface. For example, a recent Wisconsin Supreme Court case dealt with whether it was necessary for a physician to disclose the availability of a collateral test not directly linked to a patient’s diagnosis.
In Jandre v. Wis. Injured Patients & Families Comp. Fund (813 N.W.2d 627 [Wis. 2012]), a doctor diagnosed Bell’s palsy as the cause of a patient’s neurologic symptoms, because she heard no carotid bruits and the head CT scan was normal. Shortly thereafter, the patient developed a stroke. Although the doctor was found not negligent for the misdiagnosis, the plaintiff then proceeded on a lack of informed consent theory, asserting that the doctor should have advised him of the availability of a carotid ultrasound test to rule out a TIA.
In a momentous decision, the Wisconsin Supreme Court affirmed the lower court’s judgment in finding the physician liable for failing to disclose the availability of the ultrasound procedure.
Another area where informed consent is under renewed scrutiny is in research. Doctors in practice are increasingly participating as coinvestigators in industry-sponsored drug trials, and should be familiar with what is expected in the research context.
Augmented rules regarding informed consent govern all clinical research, with patient safety and free meaningful choice being paramount considerations. Federal and state regulations, implemented and monitored by institutional review boards, serve to enforce compliance and safeguard the safety of experimental subjects.
Still, as predicted nearly 50 years ago by Dr. Henry K. Beecher, “In any precise sense, statements regarding consent are meaningless unless one knows how fully the patient was informed of all risks, and if these are not known, that fact should also be made clear. A far more dependable safeguard than consent is the presence of a truly responsible investigator” (N. Engl. J. Med. 1966;274:1354-60).
Scandals in human research led by or in collaboration with U.S. investigators in foreign countries have been in the news. Global clinical trials are supposed to be carried out in compliance with the Nuremberg Code and the Declaration of Helsinki, but there may be occasional lapses or disregard for such international laws. A recent example is the trial using the antibiotic trovafloxacin, administered orally, versus FDA-approved parenteral ceftriaxone, during a meningitis outbreak in Nigeria (N. Engl. J. Med. 2009;360:2050-3).
Finally, the politics of abortion and first amendment rights have managed to insinuate themselves into the informed consent debate. Can states mandate disclosure in the name of securing meaningful informed consent, e.g., requiring physicians to provide information that might encourage a woman to reconsider her decision to have an abortion?
In 1992, the U.S. Supreme Court decided that this passes constitutional muster, because it did not place an undue burden on the woman. However, the Fourth Circuit Appellate Court recently ruled unconstitutional a North Carolina statute called Display of Real-Time View Requirement. The statute requires physicians to display ultrasound images of the unborn child to a mother contemplating an abortion, which the court ruled violated the First Amendment’s prohibition on state-compelled speech (N. Engl. J. Med. 2015;372:1285-7).
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, and currently directs the St. Francis International Center for Healthcare Ethics in Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. Some of the articles in this series are adapted from the author’s 2006 book, “Medical Malpractice: Understanding the Law, Managing the Risk,” and his 2012 Halsbury treatise, “Medical Negligence and Professional Misconduct.” For additional information, readers may contact the author at [email protected].
Feeling weird
In January, I purchased the newly published second edition of “The Anthropology of Childhood: Cherubs, Chattel, Changelings,” by David F. Lancy (New York: Cambridge University Press, 2015), hoping it would provide me with some food for thought on the cold, dark winter nights. When the crocuses sprouted in April, I had slogged only halfway through its 533 pages (of which 104 are a list of references) and set it aside.
It has the heft of college text, but it is really more of a heavily referenced opinion piece. The author is an emeritus professor of anthropology at Utah State University, Logan, and his primary message is that how we value our children and how we choose to raise them here in North America should not be considered a benchmark against which to judge the way other societies treat their children. To emphasize his contention that we should not consider ourselves the norm, he refers to us as part of the WEIRD world (Western, Educated, Industrialized, Rich, Democracies).
Nearly every page includes at least one observation by an anthropologist that illustrates how different we are from many other societies. Not everyone values young children as cherubs the way we do. In some cultures, children are barely tolerated until they are old enough to contribute to the group. In some cultures, they are treated as no more than chattel.
While we believe that parents, certainly mothers, should play a critical role in the raising of children, there are many societies in which mothers are considered essential only for birthing and providing nutrition until the child is weaned. Children are left to be raised by other members of the society. Often, it is older siblings or cousins who assume the role we associate with parenthood.
The diversity of attitudes and child-rearing practices that Professor Lancy lays out in his tome is fascinating, even shocking at times, but after a few hundred pages one gets the message. But what I and every other parent want to know is if there is a common thread in these diverse cultures that can help us define the “natural” or the “best” or the “correct” way to parent our children. This question is particularly vexing for us in the WEIRD as we have become more heterogeneous, diverse, and multicultural. Most new millennium parents have no cultural tradition to fall back on, or if they have one it is likely to be very different from their partner in parenting. The result is that many parents find themselves on a constant, anxiety-driven search for the proper way to raise their child.
It’s not entirely clear to me how he arrives at it, but Professor Lancy offers his opinion on how we WEIRDs should raise our children. He feels we are taking the job of parenting far too seriously, and as a result, are meddling in a process that is best left to play out on its own. He observes, as do I, that children learn best by doing and imitating, not by being taught. Parents, specifically “involved” parents, are not a necessary requirement of successful child rearing. This message may come as an ego-busting shock to some parents. On the other hand, it should be liberating and guilt assuaging for parents whose careers and lifestyles limit the time they can spend with their children.
While I agree with Professor Lancy’s observation that much of the parenting that is done our society is unnecessary, and even at times counterproductive, the problem is that our society doesn’t offer many alternatives that provide the children an environment in which they can learn by doing and imitating. For example, grouping child care and preschool by age isolates young children from older children who can provide powerful role models for skill development. Unrealistic parental and provider fears about injury build barriers that rob children of opportunities to learn and grow.
The fact that here in the WEIRD families tend to have low birth rates makes it unlikely that parents will back off from overfocusing on their children. However, with help from knowledgeable and experienced experts in child health and behavior – pediatricians – there may be hope that some parents can learn to step back and let their children learn and develop in a more natural way.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater.” Email him at [email protected].
In January, I purchased the newly published second edition of “The Anthropology of Childhood: Cherubs, Chattel, Changelings,” by David F. Lancy (New York: Cambridge University Press, 2015), hoping it would provide me with some food for thought on the cold, dark winter nights. When the crocuses sprouted in April, I had slogged only halfway through its 533 pages (of which 104 are a list of references) and set it aside.
It has the heft of college text, but it is really more of a heavily referenced opinion piece. The author is an emeritus professor of anthropology at Utah State University, Logan, and his primary message is that how we value our children and how we choose to raise them here in North America should not be considered a benchmark against which to judge the way other societies treat their children. To emphasize his contention that we should not consider ourselves the norm, he refers to us as part of the WEIRD world (Western, Educated, Industrialized, Rich, Democracies).
Nearly every page includes at least one observation by an anthropologist that illustrates how different we are from many other societies. Not everyone values young children as cherubs the way we do. In some cultures, children are barely tolerated until they are old enough to contribute to the group. In some cultures, they are treated as no more than chattel.
While we believe that parents, certainly mothers, should play a critical role in the raising of children, there are many societies in which mothers are considered essential only for birthing and providing nutrition until the child is weaned. Children are left to be raised by other members of the society. Often, it is older siblings or cousins who assume the role we associate with parenthood.
The diversity of attitudes and child-rearing practices that Professor Lancy lays out in his tome is fascinating, even shocking at times, but after a few hundred pages one gets the message. But what I and every other parent want to know is if there is a common thread in these diverse cultures that can help us define the “natural” or the “best” or the “correct” way to parent our children. This question is particularly vexing for us in the WEIRD as we have become more heterogeneous, diverse, and multicultural. Most new millennium parents have no cultural tradition to fall back on, or if they have one it is likely to be very different from their partner in parenting. The result is that many parents find themselves on a constant, anxiety-driven search for the proper way to raise their child.
It’s not entirely clear to me how he arrives at it, but Professor Lancy offers his opinion on how we WEIRDs should raise our children. He feels we are taking the job of parenting far too seriously, and as a result, are meddling in a process that is best left to play out on its own. He observes, as do I, that children learn best by doing and imitating, not by being taught. Parents, specifically “involved” parents, are not a necessary requirement of successful child rearing. This message may come as an ego-busting shock to some parents. On the other hand, it should be liberating and guilt assuaging for parents whose careers and lifestyles limit the time they can spend with their children.
While I agree with Professor Lancy’s observation that much of the parenting that is done our society is unnecessary, and even at times counterproductive, the problem is that our society doesn’t offer many alternatives that provide the children an environment in which they can learn by doing and imitating. For example, grouping child care and preschool by age isolates young children from older children who can provide powerful role models for skill development. Unrealistic parental and provider fears about injury build barriers that rob children of opportunities to learn and grow.
The fact that here in the WEIRD families tend to have low birth rates makes it unlikely that parents will back off from overfocusing on their children. However, with help from knowledgeable and experienced experts in child health and behavior – pediatricians – there may be hope that some parents can learn to step back and let their children learn and develop in a more natural way.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater.” Email him at [email protected].
In January, I purchased the newly published second edition of “The Anthropology of Childhood: Cherubs, Chattel, Changelings,” by David F. Lancy (New York: Cambridge University Press, 2015), hoping it would provide me with some food for thought on the cold, dark winter nights. When the crocuses sprouted in April, I had slogged only halfway through its 533 pages (of which 104 are a list of references) and set it aside.
It has the heft of college text, but it is really more of a heavily referenced opinion piece. The author is an emeritus professor of anthropology at Utah State University, Logan, and his primary message is that how we value our children and how we choose to raise them here in North America should not be considered a benchmark against which to judge the way other societies treat their children. To emphasize his contention that we should not consider ourselves the norm, he refers to us as part of the WEIRD world (Western, Educated, Industrialized, Rich, Democracies).
Nearly every page includes at least one observation by an anthropologist that illustrates how different we are from many other societies. Not everyone values young children as cherubs the way we do. In some cultures, children are barely tolerated until they are old enough to contribute to the group. In some cultures, they are treated as no more than chattel.
While we believe that parents, certainly mothers, should play a critical role in the raising of children, there are many societies in which mothers are considered essential only for birthing and providing nutrition until the child is weaned. Children are left to be raised by other members of the society. Often, it is older siblings or cousins who assume the role we associate with parenthood.
The diversity of attitudes and child-rearing practices that Professor Lancy lays out in his tome is fascinating, even shocking at times, but after a few hundred pages one gets the message. But what I and every other parent want to know is if there is a common thread in these diverse cultures that can help us define the “natural” or the “best” or the “correct” way to parent our children. This question is particularly vexing for us in the WEIRD as we have become more heterogeneous, diverse, and multicultural. Most new millennium parents have no cultural tradition to fall back on, or if they have one it is likely to be very different from their partner in parenting. The result is that many parents find themselves on a constant, anxiety-driven search for the proper way to raise their child.
It’s not entirely clear to me how he arrives at it, but Professor Lancy offers his opinion on how we WEIRDs should raise our children. He feels we are taking the job of parenting far too seriously, and as a result, are meddling in a process that is best left to play out on its own. He observes, as do I, that children learn best by doing and imitating, not by being taught. Parents, specifically “involved” parents, are not a necessary requirement of successful child rearing. This message may come as an ego-busting shock to some parents. On the other hand, it should be liberating and guilt assuaging for parents whose careers and lifestyles limit the time they can spend with their children.
While I agree with Professor Lancy’s observation that much of the parenting that is done our society is unnecessary, and even at times counterproductive, the problem is that our society doesn’t offer many alternatives that provide the children an environment in which they can learn by doing and imitating. For example, grouping child care and preschool by age isolates young children from older children who can provide powerful role models for skill development. Unrealistic parental and provider fears about injury build barriers that rob children of opportunities to learn and grow.
The fact that here in the WEIRD families tend to have low birth rates makes it unlikely that parents will back off from overfocusing on their children. However, with help from knowledgeable and experienced experts in child health and behavior – pediatricians – there may be hope that some parents can learn to step back and let their children learn and develop in a more natural way.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater.” Email him at [email protected].
Safe driver
Reducing morbidity and mortality is the focus of medicine, and much of our day is spent focusing on this, but how much do we as pediatricians address on the leading cause of death in teens? Motor vehicle accidents are the leading cause of death among 15- to 20-year-olds. In 2011, about 2,650 teens in the United States aged 16-19 years were killed and almost 292,000 were treated in emergency departments for injuries suffered in motor vehicle crashes, according to the Centers for Disease Control and Prevention. In 2010, the American Academy of Pediatrics reaffirmed its statement that was published on teen drivers in 2006, which encouraged pediatricians to be active participants in the education and lobbying for laws that promote of safe driving.
It may appear to be out of the scope of treatment to educate on safe driving, but the reality is that many parents are unaware of the risk factors that contribute to unsafe driving, as well the conditions that can be managed to improve their driving ability.
The major risk factors for increased injury among teens are immaturity, which leads to increased risk taking; inexperience; and distractions. Immaturity is the leading risk factor, clearly demonstrated in the number of crashes involving 16-year-old drivers, which is two times greater when compared with 17-year-olds and three times greater when compared with 25- to 29-year-olds.
Although distracted driving is not a problem limited to just teens, that compounded with inexperience certainly explains why they account for 14% of fatal accidents despite being only 6% of drivers. It has been statistically shown that the greater the number of teens in a vehicle, the more likely they are to have an accident. Talking on the phone also increases the risk of an accident, but “hands-free” driving shows little improvement in risk. Texting and driving is the leading cause of death among teens, accounting for 3,000 deaths annually according to a study by Cohen Children’s Medical Center, in New Hyde Park, N.Y., which surpasses drinking and driving; www.teendriversource.org reports the statistics on teen driving and stated that brain activity needed for driving is reduced by 37%. Many teens self-report texting and driving and “near accidents.”
Attention-deficit/hyperactivity disorder (ADHD) also has been shown to put teen drivers at increased risk. Teens with ADHD show two to four times the increased risk of crashes.Psychostimulants have been shown to significantly improve their attention during driving, and long-acting methylphenidate has been shown to more effective, even for nighttime driving, over the short-acting methylphenidate (Pediatrics 2006;118:2570-81).
Fairly recent changes in laws and driver education has shown significant improvement in accident rates. Graduated driver laws started in 1996, and now is the law in every state. The minimum requirements include a learner’s permit of 2 months of longer, night restriction, and passenger restriction; states vary in their requirements. Optimally, graduated driver laws include a three-phase program that starts with the learner’s permit, vision screen, and driver’s test. Phase two is supervised driving, which also requires 6 months of no violations, 12 months of no crashes, and the road test. Phase three is a full license without restrictions.
Analysis of this program by state showed a significant reduction in crashes among the 15- to 19-year-olds. The reduction was mostly attributed to the restriction in nighttime driving, restricted number of passengers, and the extend period of supervised driving. In 1997, Florida’s first full year of its graduated driver law system, there was a 9% reduction in fatal and injury crashes for 15- to 17-year-olds, compared with 1995. All of these are important teaching points for parents; the National Highway Traffic Safety Administration is an excellent resource for statistics on the distracted driver to encourage teens to put the phones down.
Motor vehicle accidents are the No. 1 cause of death for teens, according to the Centers for Disease Control and Prevention. If our role as a pediatrician is to prevent morbidity and mortality, then we must play an active role in educating our patients on seriousness of safe driving. Just as we promote vaccines for the prevention of illness, we must promote the rules of the road to prevent an early and avoidable death.
Dr. Pearce is a pediatrician in Frankfort, Ill. E-mail her at [email protected].
Reducing morbidity and mortality is the focus of medicine, and much of our day is spent focusing on this, but how much do we as pediatricians address on the leading cause of death in teens? Motor vehicle accidents are the leading cause of death among 15- to 20-year-olds. In 2011, about 2,650 teens in the United States aged 16-19 years were killed and almost 292,000 were treated in emergency departments for injuries suffered in motor vehicle crashes, according to the Centers for Disease Control and Prevention. In 2010, the American Academy of Pediatrics reaffirmed its statement that was published on teen drivers in 2006, which encouraged pediatricians to be active participants in the education and lobbying for laws that promote of safe driving.
It may appear to be out of the scope of treatment to educate on safe driving, but the reality is that many parents are unaware of the risk factors that contribute to unsafe driving, as well the conditions that can be managed to improve their driving ability.
The major risk factors for increased injury among teens are immaturity, which leads to increased risk taking; inexperience; and distractions. Immaturity is the leading risk factor, clearly demonstrated in the number of crashes involving 16-year-old drivers, which is two times greater when compared with 17-year-olds and three times greater when compared with 25- to 29-year-olds.
Although distracted driving is not a problem limited to just teens, that compounded with inexperience certainly explains why they account for 14% of fatal accidents despite being only 6% of drivers. It has been statistically shown that the greater the number of teens in a vehicle, the more likely they are to have an accident. Talking on the phone also increases the risk of an accident, but “hands-free” driving shows little improvement in risk. Texting and driving is the leading cause of death among teens, accounting for 3,000 deaths annually according to a study by Cohen Children’s Medical Center, in New Hyde Park, N.Y., which surpasses drinking and driving; www.teendriversource.org reports the statistics on teen driving and stated that brain activity needed for driving is reduced by 37%. Many teens self-report texting and driving and “near accidents.”
Attention-deficit/hyperactivity disorder (ADHD) also has been shown to put teen drivers at increased risk. Teens with ADHD show two to four times the increased risk of crashes.Psychostimulants have been shown to significantly improve their attention during driving, and long-acting methylphenidate has been shown to more effective, even for nighttime driving, over the short-acting methylphenidate (Pediatrics 2006;118:2570-81).
Fairly recent changes in laws and driver education has shown significant improvement in accident rates. Graduated driver laws started in 1996, and now is the law in every state. The minimum requirements include a learner’s permit of 2 months of longer, night restriction, and passenger restriction; states vary in their requirements. Optimally, graduated driver laws include a three-phase program that starts with the learner’s permit, vision screen, and driver’s test. Phase two is supervised driving, which also requires 6 months of no violations, 12 months of no crashes, and the road test. Phase three is a full license without restrictions.
Analysis of this program by state showed a significant reduction in crashes among the 15- to 19-year-olds. The reduction was mostly attributed to the restriction in nighttime driving, restricted number of passengers, and the extend period of supervised driving. In 1997, Florida’s first full year of its graduated driver law system, there was a 9% reduction in fatal and injury crashes for 15- to 17-year-olds, compared with 1995. All of these are important teaching points for parents; the National Highway Traffic Safety Administration is an excellent resource for statistics on the distracted driver to encourage teens to put the phones down.
Motor vehicle accidents are the No. 1 cause of death for teens, according to the Centers for Disease Control and Prevention. If our role as a pediatrician is to prevent morbidity and mortality, then we must play an active role in educating our patients on seriousness of safe driving. Just as we promote vaccines for the prevention of illness, we must promote the rules of the road to prevent an early and avoidable death.
Dr. Pearce is a pediatrician in Frankfort, Ill. E-mail her at [email protected].
Reducing morbidity and mortality is the focus of medicine, and much of our day is spent focusing on this, but how much do we as pediatricians address on the leading cause of death in teens? Motor vehicle accidents are the leading cause of death among 15- to 20-year-olds. In 2011, about 2,650 teens in the United States aged 16-19 years were killed and almost 292,000 were treated in emergency departments for injuries suffered in motor vehicle crashes, according to the Centers for Disease Control and Prevention. In 2010, the American Academy of Pediatrics reaffirmed its statement that was published on teen drivers in 2006, which encouraged pediatricians to be active participants in the education and lobbying for laws that promote of safe driving.
It may appear to be out of the scope of treatment to educate on safe driving, but the reality is that many parents are unaware of the risk factors that contribute to unsafe driving, as well the conditions that can be managed to improve their driving ability.
The major risk factors for increased injury among teens are immaturity, which leads to increased risk taking; inexperience; and distractions. Immaturity is the leading risk factor, clearly demonstrated in the number of crashes involving 16-year-old drivers, which is two times greater when compared with 17-year-olds and three times greater when compared with 25- to 29-year-olds.
Although distracted driving is not a problem limited to just teens, that compounded with inexperience certainly explains why they account for 14% of fatal accidents despite being only 6% of drivers. It has been statistically shown that the greater the number of teens in a vehicle, the more likely they are to have an accident. Talking on the phone also increases the risk of an accident, but “hands-free” driving shows little improvement in risk. Texting and driving is the leading cause of death among teens, accounting for 3,000 deaths annually according to a study by Cohen Children’s Medical Center, in New Hyde Park, N.Y., which surpasses drinking and driving; www.teendriversource.org reports the statistics on teen driving and stated that brain activity needed for driving is reduced by 37%. Many teens self-report texting and driving and “near accidents.”
Attention-deficit/hyperactivity disorder (ADHD) also has been shown to put teen drivers at increased risk. Teens with ADHD show two to four times the increased risk of crashes.Psychostimulants have been shown to significantly improve their attention during driving, and long-acting methylphenidate has been shown to more effective, even for nighttime driving, over the short-acting methylphenidate (Pediatrics 2006;118:2570-81).
Fairly recent changes in laws and driver education has shown significant improvement in accident rates. Graduated driver laws started in 1996, and now is the law in every state. The minimum requirements include a learner’s permit of 2 months of longer, night restriction, and passenger restriction; states vary in their requirements. Optimally, graduated driver laws include a three-phase program that starts with the learner’s permit, vision screen, and driver’s test. Phase two is supervised driving, which also requires 6 months of no violations, 12 months of no crashes, and the road test. Phase three is a full license without restrictions.
Analysis of this program by state showed a significant reduction in crashes among the 15- to 19-year-olds. The reduction was mostly attributed to the restriction in nighttime driving, restricted number of passengers, and the extend period of supervised driving. In 1997, Florida’s first full year of its graduated driver law system, there was a 9% reduction in fatal and injury crashes for 15- to 17-year-olds, compared with 1995. All of these are important teaching points for parents; the National Highway Traffic Safety Administration is an excellent resource for statistics on the distracted driver to encourage teens to put the phones down.
Motor vehicle accidents are the No. 1 cause of death for teens, according to the Centers for Disease Control and Prevention. If our role as a pediatrician is to prevent morbidity and mortality, then we must play an active role in educating our patients on seriousness of safe driving. Just as we promote vaccines for the prevention of illness, we must promote the rules of the road to prevent an early and avoidable death.
Dr. Pearce is a pediatrician in Frankfort, Ill. E-mail her at [email protected].