User login
The Right Choice? The importance of sometimes saying “no”
When I was a resident, one of the surgery faculty who often performed big, high-risk operations liked to say, “If the patient can tolerate a haircut, he can tolerate an operation.” By this, he meant that there were not patients who were too sick for surgery if the operation was indicated. However, over the last 2 decades, I have seen a handful of patients for whom the risks of the operation far outweigh the potential benefits and for whom I have said I am not offering surgery as an option.
Recently, I had a chance to discuss troubling ethics cases with group of thoughtful surgical residents. They raised concerns over the common scenario of being consulted in the middle of the night on the critically ill patient in the intensive care unit for whom the risks of surgery are extremely high. These residents asked the question of whether it is ever acceptable for surgeons to simply refuse to take such patients to the operating room if the alternative to surgery is virtually certain death. The overriding concern among the residents was whether saying “no” to a request for operative intervention in a critically ill patient can ever be justified since the surgeon is essentially “playing God” by not offering the possibility of intervention.
There is no question that there can be very sick patients who have a poor prognosis and the decision is appropriately made to recommend surgery even though the risks are very high. I also believe that there are patients for whom the risks of surgery are so high, and the prospects for a good outcome are so low, that surgery should not be recommended. However, it is important to distinguish two different scenarios. In one scenario, the surgical consultant decides that surgery is an option, but then tries to convince the surrogate decision makers (usually the patient’s family) to decline surgery because of the very high risks. In the second scenario, the surgeon decides that the risks to the patient are so high that it would be wrong to even take the patient to the operating room.
In both scenarios, the patient does not get an operation and in the vast majority of such cases, the patient will die in a short period of time. The question remains whether it is better to give families a choice or not. I believe that posing the question in this manner is misleading and presents a false dichotomy.
Although the distinctions can be subtle, it is critical for the surgeon to decide whether each patient has a high enough chance for survival that the operation is medically justifiable. If the answer is “yes,” then the next question will be one for the surrogate decision makers to decide whether to consent to the surgery or not. Based on the importance of respecting the autonomous choices of patients or their surrogates, it is important that surgeons respect the choice not to have an operation even if one is being recommended. If the answer to the question of whether the operation is medically justifiable is “no,” to offer surgery to family and then try to convince them to decline it by overstating the risks is misleading. Although such a strategy would give the family a sense of control over the situation, it would also give the false impression that surgery is truly an option. To act this way would allow the surgeon the ability to avoid “playing God” since the family is “making the decision”. However, I believe that taking that decision away from families when there is not really a reasonable choice for surgery is a better way to eliminate their potential guilt. Not only is it ethically acceptable to decline to offer an operation to an extremely high-risk patient, I would argue that such behavior is actually the ethical responsibility of the surgeon. We should take on the burden of saying “no” when surgery should NOT be performed. Forcing such a decision on families in the name of respecting autonomy is to shirk our responsibility and something that we must avoid doing whenever possible.
Dr. Angelos is an ACS Fellow; the Linda Kohler Anderson Professor of Surgery and Surgical Ethics; chief, endocrine surgery; and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago.
When I was a resident, one of the surgery faculty who often performed big, high-risk operations liked to say, “If the patient can tolerate a haircut, he can tolerate an operation.” By this, he meant that there were not patients who were too sick for surgery if the operation was indicated. However, over the last 2 decades, I have seen a handful of patients for whom the risks of the operation far outweigh the potential benefits and for whom I have said I am not offering surgery as an option.
Recently, I had a chance to discuss troubling ethics cases with group of thoughtful surgical residents. They raised concerns over the common scenario of being consulted in the middle of the night on the critically ill patient in the intensive care unit for whom the risks of surgery are extremely high. These residents asked the question of whether it is ever acceptable for surgeons to simply refuse to take such patients to the operating room if the alternative to surgery is virtually certain death. The overriding concern among the residents was whether saying “no” to a request for operative intervention in a critically ill patient can ever be justified since the surgeon is essentially “playing God” by not offering the possibility of intervention.
There is no question that there can be very sick patients who have a poor prognosis and the decision is appropriately made to recommend surgery even though the risks are very high. I also believe that there are patients for whom the risks of surgery are so high, and the prospects for a good outcome are so low, that surgery should not be recommended. However, it is important to distinguish two different scenarios. In one scenario, the surgical consultant decides that surgery is an option, but then tries to convince the surrogate decision makers (usually the patient’s family) to decline surgery because of the very high risks. In the second scenario, the surgeon decides that the risks to the patient are so high that it would be wrong to even take the patient to the operating room.
In both scenarios, the patient does not get an operation and in the vast majority of such cases, the patient will die in a short period of time. The question remains whether it is better to give families a choice or not. I believe that posing the question in this manner is misleading and presents a false dichotomy.
Although the distinctions can be subtle, it is critical for the surgeon to decide whether each patient has a high enough chance for survival that the operation is medically justifiable. If the answer is “yes,” then the next question will be one for the surrogate decision makers to decide whether to consent to the surgery or not. Based on the importance of respecting the autonomous choices of patients or their surrogates, it is important that surgeons respect the choice not to have an operation even if one is being recommended. If the answer to the question of whether the operation is medically justifiable is “no,” to offer surgery to family and then try to convince them to decline it by overstating the risks is misleading. Although such a strategy would give the family a sense of control over the situation, it would also give the false impression that surgery is truly an option. To act this way would allow the surgeon the ability to avoid “playing God” since the family is “making the decision”. However, I believe that taking that decision away from families when there is not really a reasonable choice for surgery is a better way to eliminate their potential guilt. Not only is it ethically acceptable to decline to offer an operation to an extremely high-risk patient, I would argue that such behavior is actually the ethical responsibility of the surgeon. We should take on the burden of saying “no” when surgery should NOT be performed. Forcing such a decision on families in the name of respecting autonomy is to shirk our responsibility and something that we must avoid doing whenever possible.
Dr. Angelos is an ACS Fellow; the Linda Kohler Anderson Professor of Surgery and Surgical Ethics; chief, endocrine surgery; and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago.
When I was a resident, one of the surgery faculty who often performed big, high-risk operations liked to say, “If the patient can tolerate a haircut, he can tolerate an operation.” By this, he meant that there were not patients who were too sick for surgery if the operation was indicated. However, over the last 2 decades, I have seen a handful of patients for whom the risks of the operation far outweigh the potential benefits and for whom I have said I am not offering surgery as an option.
Recently, I had a chance to discuss troubling ethics cases with group of thoughtful surgical residents. They raised concerns over the common scenario of being consulted in the middle of the night on the critically ill patient in the intensive care unit for whom the risks of surgery are extremely high. These residents asked the question of whether it is ever acceptable for surgeons to simply refuse to take such patients to the operating room if the alternative to surgery is virtually certain death. The overriding concern among the residents was whether saying “no” to a request for operative intervention in a critically ill patient can ever be justified since the surgeon is essentially “playing God” by not offering the possibility of intervention.
There is no question that there can be very sick patients who have a poor prognosis and the decision is appropriately made to recommend surgery even though the risks are very high. I also believe that there are patients for whom the risks of surgery are so high, and the prospects for a good outcome are so low, that surgery should not be recommended. However, it is important to distinguish two different scenarios. In one scenario, the surgical consultant decides that surgery is an option, but then tries to convince the surrogate decision makers (usually the patient’s family) to decline surgery because of the very high risks. In the second scenario, the surgeon decides that the risks to the patient are so high that it would be wrong to even take the patient to the operating room.
In both scenarios, the patient does not get an operation and in the vast majority of such cases, the patient will die in a short period of time. The question remains whether it is better to give families a choice or not. I believe that posing the question in this manner is misleading and presents a false dichotomy.
Although the distinctions can be subtle, it is critical for the surgeon to decide whether each patient has a high enough chance for survival that the operation is medically justifiable. If the answer is “yes,” then the next question will be one for the surrogate decision makers to decide whether to consent to the surgery or not. Based on the importance of respecting the autonomous choices of patients or their surrogates, it is important that surgeons respect the choice not to have an operation even if one is being recommended. If the answer to the question of whether the operation is medically justifiable is “no,” to offer surgery to family and then try to convince them to decline it by overstating the risks is misleading. Although such a strategy would give the family a sense of control over the situation, it would also give the false impression that surgery is truly an option. To act this way would allow the surgeon the ability to avoid “playing God” since the family is “making the decision”. However, I believe that taking that decision away from families when there is not really a reasonable choice for surgery is a better way to eliminate their potential guilt. Not only is it ethically acceptable to decline to offer an operation to an extremely high-risk patient, I would argue that such behavior is actually the ethical responsibility of the surgeon. We should take on the burden of saying “no” when surgery should NOT be performed. Forcing such a decision on families in the name of respecting autonomy is to shirk our responsibility and something that we must avoid doing whenever possible.
Dr. Angelos is an ACS Fellow; the Linda Kohler Anderson Professor of Surgery and Surgical Ethics; chief, endocrine surgery; and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago.
Has your bread become stale?
Diagnosing and treating illnesses are the bread and butter of hospitalist medicine. Has your bread become stale?
I used to be envious of older physicians who ‘grandfathered in’ and became exempt from the requirement to recertify every 10 years for the American Board of Internal Medicine. Preparing for the boards is extremely time consuming and, at times, incredibly stressful, but it’s what we have to do to prove that our medical knowledge is up to date, right?
Who hasn’t heard of at least one nightmare outcome after a physician treated a patient with out-of-date standards, probably the same ones he learned in medical school a long, long time ago? We may snicker at this scenario, but could we be guilty too? Could we be so set in our ways, so self-confident that we refuse to grow?
I was watching a hospital medicine CME DVD a few months ago and was shocked, as well as embarrassed, to learn that the way I was performing part of my neurological exam was antiquated. There was a new “gold standard” that I had never learned before. After all, I had been doing the exact same thing for years; too many years, it seems. I mistakenly assumed that all the physical examination skills I had learned in medical school were set in stone. But as in all aspects of medicine, even best practices for performing a basic examination have evolved over the years.
Then there is the old habit of ordering multiple blood tests on hospitalized patients every day. That’s just how many of us were trained during residency, but in real life it’s not always necessary. Sure, if there’s a reason to be concerned about specific parameters they should be followed closely, but most inpatients don’t really need chemistries and a CBC each and every day; if they weren’t already anemic, we could make them anemic with excessive blood draws. And how much of that knee-jerk reflex to order daily “routine labs” is really just defensive medicine anyway?
I recently started teaching residents and was a little apprehensive in the very beginning. After all, 2 decades later, I still remember the good (and bad) attendings, and to this very day I incorporate parts of what the good ones taught me into patient encounters. Now I would be the one who could leave a lasting, hopefully positive impression in brilliant young minds. I have found teaching residents to be motivating and eye-opening. I get to see what’s new on their burgeoning, technologically advanced horizons; and I am learning from them, too. It’s invigorating to grow in the field I love so much, to expand my mind and, sometimes, humbly acknowledge I need to switch gears and proceed in a different direction; I suspect many others would benefit from this revelation as well.
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
Diagnosing and treating illnesses are the bread and butter of hospitalist medicine. Has your bread become stale?
I used to be envious of older physicians who ‘grandfathered in’ and became exempt from the requirement to recertify every 10 years for the American Board of Internal Medicine. Preparing for the boards is extremely time consuming and, at times, incredibly stressful, but it’s what we have to do to prove that our medical knowledge is up to date, right?
Who hasn’t heard of at least one nightmare outcome after a physician treated a patient with out-of-date standards, probably the same ones he learned in medical school a long, long time ago? We may snicker at this scenario, but could we be guilty too? Could we be so set in our ways, so self-confident that we refuse to grow?
I was watching a hospital medicine CME DVD a few months ago and was shocked, as well as embarrassed, to learn that the way I was performing part of my neurological exam was antiquated. There was a new “gold standard” that I had never learned before. After all, I had been doing the exact same thing for years; too many years, it seems. I mistakenly assumed that all the physical examination skills I had learned in medical school were set in stone. But as in all aspects of medicine, even best practices for performing a basic examination have evolved over the years.
Then there is the old habit of ordering multiple blood tests on hospitalized patients every day. That’s just how many of us were trained during residency, but in real life it’s not always necessary. Sure, if there’s a reason to be concerned about specific parameters they should be followed closely, but most inpatients don’t really need chemistries and a CBC each and every day; if they weren’t already anemic, we could make them anemic with excessive blood draws. And how much of that knee-jerk reflex to order daily “routine labs” is really just defensive medicine anyway?
I recently started teaching residents and was a little apprehensive in the very beginning. After all, 2 decades later, I still remember the good (and bad) attendings, and to this very day I incorporate parts of what the good ones taught me into patient encounters. Now I would be the one who could leave a lasting, hopefully positive impression in brilliant young minds. I have found teaching residents to be motivating and eye-opening. I get to see what’s new on their burgeoning, technologically advanced horizons; and I am learning from them, too. It’s invigorating to grow in the field I love so much, to expand my mind and, sometimes, humbly acknowledge I need to switch gears and proceed in a different direction; I suspect many others would benefit from this revelation as well.
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
Diagnosing and treating illnesses are the bread and butter of hospitalist medicine. Has your bread become stale?
I used to be envious of older physicians who ‘grandfathered in’ and became exempt from the requirement to recertify every 10 years for the American Board of Internal Medicine. Preparing for the boards is extremely time consuming and, at times, incredibly stressful, but it’s what we have to do to prove that our medical knowledge is up to date, right?
Who hasn’t heard of at least one nightmare outcome after a physician treated a patient with out-of-date standards, probably the same ones he learned in medical school a long, long time ago? We may snicker at this scenario, but could we be guilty too? Could we be so set in our ways, so self-confident that we refuse to grow?
I was watching a hospital medicine CME DVD a few months ago and was shocked, as well as embarrassed, to learn that the way I was performing part of my neurological exam was antiquated. There was a new “gold standard” that I had never learned before. After all, I had been doing the exact same thing for years; too many years, it seems. I mistakenly assumed that all the physical examination skills I had learned in medical school were set in stone. But as in all aspects of medicine, even best practices for performing a basic examination have evolved over the years.
Then there is the old habit of ordering multiple blood tests on hospitalized patients every day. That’s just how many of us were trained during residency, but in real life it’s not always necessary. Sure, if there’s a reason to be concerned about specific parameters they should be followed closely, but most inpatients don’t really need chemistries and a CBC each and every day; if they weren’t already anemic, we could make them anemic with excessive blood draws. And how much of that knee-jerk reflex to order daily “routine labs” is really just defensive medicine anyway?
I recently started teaching residents and was a little apprehensive in the very beginning. After all, 2 decades later, I still remember the good (and bad) attendings, and to this very day I incorporate parts of what the good ones taught me into patient encounters. Now I would be the one who could leave a lasting, hopefully positive impression in brilliant young minds. I have found teaching residents to be motivating and eye-opening. I get to see what’s new on their burgeoning, technologically advanced horizons; and I am learning from them, too. It’s invigorating to grow in the field I love so much, to expand my mind and, sometimes, humbly acknowledge I need to switch gears and proceed in a different direction; I suspect many others would benefit from this revelation as well.
Dr. Hester is a hospitalist at Baltimore-Washington Medical Center in Glen Burnie, Md. She is the creator of the Patient Whiz, a patient-engagement app for iOS. Reach her at [email protected].
“If I had a hammer ... ”
Okay, it’s 4 o’clock in the afternoon. Do you know where your reflex hammer is? Do you even own one, or are reflex hammers just one of those things that should be part of the standard doctoring junk in the drawers of some (but, frustratingly not all) of the exam rooms in the clinic where you work? If you do own one, where did you get it? The last time you handled your reflex hammer, had the once-soft head ossified? And, now for the big question: Do you even care where your reflex hammer is hiding?
Several years ago, I wrote you about my long and deeply emotional relationship with tongue depressors. For 40 years, there was scarcely a waking hour that I wasn’t carrying at least one of these indispensable birch beauties over my heart in my shirt pocket. Throat sticks were a badge of my professional status, and I used them as much as a one-piece Leatherman (could be Swiss Army or multitool if you are uncomfortable with brand names) as I did for depressing tongues. Now that I no longer see patients, I always have a throat stick within reach to stir paint or shim the many poorly crafted D.I.Y. projects I have foolishly tackled.
On the other hand, I never grew very fond of my reflex hammer. In fact, I have never had much use for it. When I was a first-year medical student, most of us were short of money and even shorter on concerns about conflict of interest. Drug companies were eager to imprint their names on our pliable minds. We were offered nice black leather bags and stethoscopes. I still have and regularly used my Littman stethoscope. After many tubing replacements, the head no longer swivels to the bell position, which I never found very helpful anyway. In the bag was a reflex hammer with “Lilly” stamped on the silver-colored handle.
I’m not sure how many years of unsuccessfully trying to consistently elicit deep tendon reflexes passed before I finally gave up. But it wasn’t many. In a general outpatient pediatric practice, there are very few situations that I felt I needed to know about the patient’s reflexes. Certainly, I didn’t see that they needed to be included as part of a health maintenance exam of a child with no complaints.
But every now and then a patient would complain, “Hey, you didn’t hit my knee with that hammer thing.” If they pleaded long enough, I would go hunting for one in a drawer. I didn’t want my patients to leave the office feeling that they had been cheated out of a full exam. If I couldn’t find a hammer, which happened more often than not, I would use the edge of my stethoscope as my tendon whacker. Maybe that’s why the old friend stopped rotating. If I had time, I would use the hammer or stethoscope edge to tap on the tendon of the forearm muscle that extends the middle finger. The result was particularly amusing to the preteen boys.
Of course, once every month or 3, I would encounter a clinical situation where knowing the status of the patient’s deep tendon reflexes might, just might, help me make a diagnosis. Obviously, if I had been a hospitalist, neurologist, or emergency department physician, I would have used a reflex hammer often enough to keep one handy. But, for me, the reflex hammer has been relegated to the drawer of miscellaneous stuff that is useful in eliciting memories, but that’s about it. Oh, by the way have you seen your head mirror lately?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping With a Picky Eater.”
Okay, it’s 4 o’clock in the afternoon. Do you know where your reflex hammer is? Do you even own one, or are reflex hammers just one of those things that should be part of the standard doctoring junk in the drawers of some (but, frustratingly not all) of the exam rooms in the clinic where you work? If you do own one, where did you get it? The last time you handled your reflex hammer, had the once-soft head ossified? And, now for the big question: Do you even care where your reflex hammer is hiding?
Several years ago, I wrote you about my long and deeply emotional relationship with tongue depressors. For 40 years, there was scarcely a waking hour that I wasn’t carrying at least one of these indispensable birch beauties over my heart in my shirt pocket. Throat sticks were a badge of my professional status, and I used them as much as a one-piece Leatherman (could be Swiss Army or multitool if you are uncomfortable with brand names) as I did for depressing tongues. Now that I no longer see patients, I always have a throat stick within reach to stir paint or shim the many poorly crafted D.I.Y. projects I have foolishly tackled.
On the other hand, I never grew very fond of my reflex hammer. In fact, I have never had much use for it. When I was a first-year medical student, most of us were short of money and even shorter on concerns about conflict of interest. Drug companies were eager to imprint their names on our pliable minds. We were offered nice black leather bags and stethoscopes. I still have and regularly used my Littman stethoscope. After many tubing replacements, the head no longer swivels to the bell position, which I never found very helpful anyway. In the bag was a reflex hammer with “Lilly” stamped on the silver-colored handle.
I’m not sure how many years of unsuccessfully trying to consistently elicit deep tendon reflexes passed before I finally gave up. But it wasn’t many. In a general outpatient pediatric practice, there are very few situations that I felt I needed to know about the patient’s reflexes. Certainly, I didn’t see that they needed to be included as part of a health maintenance exam of a child with no complaints.
But every now and then a patient would complain, “Hey, you didn’t hit my knee with that hammer thing.” If they pleaded long enough, I would go hunting for one in a drawer. I didn’t want my patients to leave the office feeling that they had been cheated out of a full exam. If I couldn’t find a hammer, which happened more often than not, I would use the edge of my stethoscope as my tendon whacker. Maybe that’s why the old friend stopped rotating. If I had time, I would use the hammer or stethoscope edge to tap on the tendon of the forearm muscle that extends the middle finger. The result was particularly amusing to the preteen boys.
Of course, once every month or 3, I would encounter a clinical situation where knowing the status of the patient’s deep tendon reflexes might, just might, help me make a diagnosis. Obviously, if I had been a hospitalist, neurologist, or emergency department physician, I would have used a reflex hammer often enough to keep one handy. But, for me, the reflex hammer has been relegated to the drawer of miscellaneous stuff that is useful in eliciting memories, but that’s about it. Oh, by the way have you seen your head mirror lately?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping With a Picky Eater.”
Okay, it’s 4 o’clock in the afternoon. Do you know where your reflex hammer is? Do you even own one, or are reflex hammers just one of those things that should be part of the standard doctoring junk in the drawers of some (but, frustratingly not all) of the exam rooms in the clinic where you work? If you do own one, where did you get it? The last time you handled your reflex hammer, had the once-soft head ossified? And, now for the big question: Do you even care where your reflex hammer is hiding?
Several years ago, I wrote you about my long and deeply emotional relationship with tongue depressors. For 40 years, there was scarcely a waking hour that I wasn’t carrying at least one of these indispensable birch beauties over my heart in my shirt pocket. Throat sticks were a badge of my professional status, and I used them as much as a one-piece Leatherman (could be Swiss Army or multitool if you are uncomfortable with brand names) as I did for depressing tongues. Now that I no longer see patients, I always have a throat stick within reach to stir paint or shim the many poorly crafted D.I.Y. projects I have foolishly tackled.
On the other hand, I never grew very fond of my reflex hammer. In fact, I have never had much use for it. When I was a first-year medical student, most of us were short of money and even shorter on concerns about conflict of interest. Drug companies were eager to imprint their names on our pliable minds. We were offered nice black leather bags and stethoscopes. I still have and regularly used my Littman stethoscope. After many tubing replacements, the head no longer swivels to the bell position, which I never found very helpful anyway. In the bag was a reflex hammer with “Lilly” stamped on the silver-colored handle.
I’m not sure how many years of unsuccessfully trying to consistently elicit deep tendon reflexes passed before I finally gave up. But it wasn’t many. In a general outpatient pediatric practice, there are very few situations that I felt I needed to know about the patient’s reflexes. Certainly, I didn’t see that they needed to be included as part of a health maintenance exam of a child with no complaints.
But every now and then a patient would complain, “Hey, you didn’t hit my knee with that hammer thing.” If they pleaded long enough, I would go hunting for one in a drawer. I didn’t want my patients to leave the office feeling that they had been cheated out of a full exam. If I couldn’t find a hammer, which happened more often than not, I would use the edge of my stethoscope as my tendon whacker. Maybe that’s why the old friend stopped rotating. If I had time, I would use the hammer or stethoscope edge to tap on the tendon of the forearm muscle that extends the middle finger. The result was particularly amusing to the preteen boys.
Of course, once every month or 3, I would encounter a clinical situation where knowing the status of the patient’s deep tendon reflexes might, just might, help me make a diagnosis. Obviously, if I had been a hospitalist, neurologist, or emergency department physician, I would have used a reflex hammer often enough to keep one handy. But, for me, the reflex hammer has been relegated to the drawer of miscellaneous stuff that is useful in eliciting memories, but that’s about it. Oh, by the way have you seen your head mirror lately?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping With a Picky Eater.”
Shyness vs. social anxiety
Many advocating for more attention to psychosocial issues by primary care pediatricians focus on serious conditions and the value of early recognition. For example, early recognition of autism spectrum disorder could lead to earlier intensive treatment that might impact the long-term course. Early diagnosis and appropriate treatment of attention-deficit/hyperactivity disorder very likely will lessen symptoms and also maintain self-esteem under the withering ordeal – often punctuated by teacher comments – of trying to pay attention hour after hour in school
Are there seemingly less serious conditions very likely worthy of early diagnosis, even those on the edge of normal developmental hurdles? One of the essential tasks of childhood is mastering the anxiety that emerges as children face the new challenges of each developmental stage, so parents, teachers, and clinicians are (or need to be) used to bearing anxiety in the children with whom they work. Intense shyness and anxiety around separation from parents are routine and healthy in infants and toddlers from 6-18 months. Anxiety in new social situations, such as the first day of preschool, is the rule, not the exception. School-age children commonly experience a surge of anxiety around performance and independence, as they are managing and mastering new skills in these domains every day. This anxiety can cause distress, but it should get better every time a child faces it, as they become better at managing the situation. When a child has an anxious temperament, poor coping skills, or parents who struggle to manage their own anxiety, children may have a harder time mastering new, anxiety-provoking challenges across settings. But, with time, and even just one adult who patiently models good coping, they will face and manage challenges. Social anxiety disorder is present when specific social or performance situations provoke the same intense anxiety and avoidance over and over, and for more than 6 months.
Most infants and young children who are more timid and fearful seem to grow into a normal range of social behavior, although few become extroverts. Some of these shy children are cautious in new situations for a period of time measured in minutes, but once the situations are familiar, these children are indistinguishable from their peers. However, some of these temperamentally timid children emerge consistently more anxious with greater likelihood to have phobias and to have social anxiety that can seriously impact long term happiness, achievement, and increase risk taking behaviors. A pediatrician should watch and note the emerging pattern of a timid toddler to see if the shyness eases or impacts social functioning; by bending the course of social interactions, social anxiety disorder critically affects developing social skills, self-regulation, affect tolerance, emerging identity, and confidence. Recognition and effective treatment of social anxiety will keep a child on the optimal developmental trajectory.
Anxiety disorders are the most common psychiatric illnesses in the United States, and social anxiety disorder (previously labeled as social phobia) is the third most common psychiatric disorder in U.S. adults (after depression and alcohol dependence). Most persistent anxiety disorders begin in childhood, and social anxiety is no exception. The mean age of onset for social anxiety is 13 years old, and it rarely begins after the age of 25, with an annual prevalence around 7% in childhood and adolescence (Psychiatr. Clin. North Am. 2009;32;483-524).The DSM-5 criteria for social anxiety disorder include, “a marked and persistent fear of one or more social or performance situations in which the person is exposed to unfamiliar people or to possible scrutiny by others,” and exposure to those situations provokes intense anxiety, which in children can be marked by severe or prolonged crying, freezing, tantrums, shrinking from social situations, refusing to speak, or clinging to parents. In adolescents, it may trigger panic attacks. The avoidance and distress interfere with the child’s function in school, social activities, or relationships, and must have lasted for at least 6 months. To ensure that there is not another problem of social relatedness, the child should have shown some capacity to have normal peer relationships.
Will social anxiety disorder be vividly apparent to teachers, parents, and clinicians? No. The feeling of anxiety is an internal experience, not easily observed, and anxious children and teens are rarely eager or comfortable communicators about their own anxiety. Indeed, in a 2007 survey of patients in treatment for anxiety, 36% of people with social anxiety disorder reported experiencing symptoms for 10 or more years before seeking help. It’s true that the distress children experience when feeling intensely anxious will probably be observable, but all of those behaviors (clinging, crying, tantrums) are common and normal expressions of distress in childhood. Even in adolescence, while having a panic attack may prompt the teenager to seek care, she may not connect it with the anxiety she was feeling about being called on in class or talking to peers, especially if that is an anxiety she has experienced for a long time as a daily part of her lives and routines.
Social anxiety disorder is treatable. The first-line treatment in mild to moderate cases, particularly with younger children, is cognitive-behavioral therapy. This is a practical variant of psychotherapy in which children develop and practice skills at recognizing and labeling their own feelings of anxiety, identifying the situations that trigger them, and practicing relaxation strategies that help them to face and manage the anxiety-provoking situations rather than avoiding them.
When symptoms or the degree of impairment are more severe, medications can become an important part of treatment. SSRIs are the first-line medications used to treat social anxiety disorder, and the effective doses are often higher than effective antidepressant doses, although we often titrate toward those doses more slowly with anxious patients to avoid side effects that might increase or exacerbate their anxiety.
Even with effective medication treatment, though, psychotherapy will be an essential part of treatment. These young patients need to build the essential skills of anxiety management, although it is in the nature of anxiety that such patients often wish to dissolve their anxiety by simply using a pill.
Anxiety disorders are typically chronic and will persist without effective treatment. Failure to recognize and treat social anxiety disorder can distort or even derail healthy development and may result in major psychiatric complications. As a pediatrician, you are trying to stop or modify a chain of potential events. Imagine a socially anxious young woman who enters puberty in high school. Will she withdraw from social activities? Will she avoid new opportunities or interests? Will alcohol become a necessary social lubricant? Will she be at increased risk for sexual assault at a party or poor grades in school? Will social anxiety affect her choice of college, fearful of leaving home? The incidence of secondary depression and substance abuse disorders is substantially higher in adolescents with untreated anxiety disorders. Although a depressed, alcohol-dependent teenager is more likely to be recognized as needing treatment, once they have developed those complications, effective treatment of the underlying anxiety will be much more complicated and slow to treat. Prevention starting before puberty is a much more desirable approach.
Pediatricians truly do have the opportunity to improve outcomes for these patients, by learning to recognize this sometimes-invisible disorder. Children suffering from anxiety disorders are more likely to identify a physical concern than a psychological one. (They have a lot of headaches and tummy aches!) When you are seeing a “shy” school-age child who has persistent crying spells around attending school on test days or before each sporting event despite loving practice, it is useful to gather more history. Is there a family history of anxiety or depression? What are the circumstances of their crying jags or persistent tantrums? Ask teenagers about episodes of shortness of breath, tachycardia, dizziness or sweating that leave them feeling like they are going to die (panic attacks). See if they can rank their anxiety on a scale from 1-10, and find out of there are consistent situations where their anxiety seems disproportionate. Children or teens may recognize that their anxiety is not merited, or they may not. If their parent also suffers from anxiety, they are less likely to recognize that this intense, persistent “shyness” in their child represents a treatable symptom. When you simply have a high index of suspicion, it is worth a referral to a mental health expert to evaluate their anxiety.
Reassuring parents and children that this is a common, treatable problem in childhood will go a long way to diminishing the secrecy and shame that can accompany paralyzing anxiety, and help your patients toward a track that optimizes their psychosocial development.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor of psychiatry and of pediatrics at Harvard Medical School, Boston.
Many advocating for more attention to psychosocial issues by primary care pediatricians focus on serious conditions and the value of early recognition. For example, early recognition of autism spectrum disorder could lead to earlier intensive treatment that might impact the long-term course. Early diagnosis and appropriate treatment of attention-deficit/hyperactivity disorder very likely will lessen symptoms and also maintain self-esteem under the withering ordeal – often punctuated by teacher comments – of trying to pay attention hour after hour in school
Are there seemingly less serious conditions very likely worthy of early diagnosis, even those on the edge of normal developmental hurdles? One of the essential tasks of childhood is mastering the anxiety that emerges as children face the new challenges of each developmental stage, so parents, teachers, and clinicians are (or need to be) used to bearing anxiety in the children with whom they work. Intense shyness and anxiety around separation from parents are routine and healthy in infants and toddlers from 6-18 months. Anxiety in new social situations, such as the first day of preschool, is the rule, not the exception. School-age children commonly experience a surge of anxiety around performance and independence, as they are managing and mastering new skills in these domains every day. This anxiety can cause distress, but it should get better every time a child faces it, as they become better at managing the situation. When a child has an anxious temperament, poor coping skills, or parents who struggle to manage their own anxiety, children may have a harder time mastering new, anxiety-provoking challenges across settings. But, with time, and even just one adult who patiently models good coping, they will face and manage challenges. Social anxiety disorder is present when specific social or performance situations provoke the same intense anxiety and avoidance over and over, and for more than 6 months.
Most infants and young children who are more timid and fearful seem to grow into a normal range of social behavior, although few become extroverts. Some of these shy children are cautious in new situations for a period of time measured in minutes, but once the situations are familiar, these children are indistinguishable from their peers. However, some of these temperamentally timid children emerge consistently more anxious with greater likelihood to have phobias and to have social anxiety that can seriously impact long term happiness, achievement, and increase risk taking behaviors. A pediatrician should watch and note the emerging pattern of a timid toddler to see if the shyness eases or impacts social functioning; by bending the course of social interactions, social anxiety disorder critically affects developing social skills, self-regulation, affect tolerance, emerging identity, and confidence. Recognition and effective treatment of social anxiety will keep a child on the optimal developmental trajectory.
Anxiety disorders are the most common psychiatric illnesses in the United States, and social anxiety disorder (previously labeled as social phobia) is the third most common psychiatric disorder in U.S. adults (after depression and alcohol dependence). Most persistent anxiety disorders begin in childhood, and social anxiety is no exception. The mean age of onset for social anxiety is 13 years old, and it rarely begins after the age of 25, with an annual prevalence around 7% in childhood and adolescence (Psychiatr. Clin. North Am. 2009;32;483-524).The DSM-5 criteria for social anxiety disorder include, “a marked and persistent fear of one or more social or performance situations in which the person is exposed to unfamiliar people or to possible scrutiny by others,” and exposure to those situations provokes intense anxiety, which in children can be marked by severe or prolonged crying, freezing, tantrums, shrinking from social situations, refusing to speak, or clinging to parents. In adolescents, it may trigger panic attacks. The avoidance and distress interfere with the child’s function in school, social activities, or relationships, and must have lasted for at least 6 months. To ensure that there is not another problem of social relatedness, the child should have shown some capacity to have normal peer relationships.
Will social anxiety disorder be vividly apparent to teachers, parents, and clinicians? No. The feeling of anxiety is an internal experience, not easily observed, and anxious children and teens are rarely eager or comfortable communicators about their own anxiety. Indeed, in a 2007 survey of patients in treatment for anxiety, 36% of people with social anxiety disorder reported experiencing symptoms for 10 or more years before seeking help. It’s true that the distress children experience when feeling intensely anxious will probably be observable, but all of those behaviors (clinging, crying, tantrums) are common and normal expressions of distress in childhood. Even in adolescence, while having a panic attack may prompt the teenager to seek care, she may not connect it with the anxiety she was feeling about being called on in class or talking to peers, especially if that is an anxiety she has experienced for a long time as a daily part of her lives and routines.
Social anxiety disorder is treatable. The first-line treatment in mild to moderate cases, particularly with younger children, is cognitive-behavioral therapy. This is a practical variant of psychotherapy in which children develop and practice skills at recognizing and labeling their own feelings of anxiety, identifying the situations that trigger them, and practicing relaxation strategies that help them to face and manage the anxiety-provoking situations rather than avoiding them.
When symptoms or the degree of impairment are more severe, medications can become an important part of treatment. SSRIs are the first-line medications used to treat social anxiety disorder, and the effective doses are often higher than effective antidepressant doses, although we often titrate toward those doses more slowly with anxious patients to avoid side effects that might increase or exacerbate their anxiety.
Even with effective medication treatment, though, psychotherapy will be an essential part of treatment. These young patients need to build the essential skills of anxiety management, although it is in the nature of anxiety that such patients often wish to dissolve their anxiety by simply using a pill.
Anxiety disorders are typically chronic and will persist without effective treatment. Failure to recognize and treat social anxiety disorder can distort or even derail healthy development and may result in major psychiatric complications. As a pediatrician, you are trying to stop or modify a chain of potential events. Imagine a socially anxious young woman who enters puberty in high school. Will she withdraw from social activities? Will she avoid new opportunities or interests? Will alcohol become a necessary social lubricant? Will she be at increased risk for sexual assault at a party or poor grades in school? Will social anxiety affect her choice of college, fearful of leaving home? The incidence of secondary depression and substance abuse disorders is substantially higher in adolescents with untreated anxiety disorders. Although a depressed, alcohol-dependent teenager is more likely to be recognized as needing treatment, once they have developed those complications, effective treatment of the underlying anxiety will be much more complicated and slow to treat. Prevention starting before puberty is a much more desirable approach.
Pediatricians truly do have the opportunity to improve outcomes for these patients, by learning to recognize this sometimes-invisible disorder. Children suffering from anxiety disorders are more likely to identify a physical concern than a psychological one. (They have a lot of headaches and tummy aches!) When you are seeing a “shy” school-age child who has persistent crying spells around attending school on test days or before each sporting event despite loving practice, it is useful to gather more history. Is there a family history of anxiety or depression? What are the circumstances of their crying jags or persistent tantrums? Ask teenagers about episodes of shortness of breath, tachycardia, dizziness or sweating that leave them feeling like they are going to die (panic attacks). See if they can rank their anxiety on a scale from 1-10, and find out of there are consistent situations where their anxiety seems disproportionate. Children or teens may recognize that their anxiety is not merited, or they may not. If their parent also suffers from anxiety, they are less likely to recognize that this intense, persistent “shyness” in their child represents a treatable symptom. When you simply have a high index of suspicion, it is worth a referral to a mental health expert to evaluate their anxiety.
Reassuring parents and children that this is a common, treatable problem in childhood will go a long way to diminishing the secrecy and shame that can accompany paralyzing anxiety, and help your patients toward a track that optimizes their psychosocial development.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor of psychiatry and of pediatrics at Harvard Medical School, Boston.
Many advocating for more attention to psychosocial issues by primary care pediatricians focus on serious conditions and the value of early recognition. For example, early recognition of autism spectrum disorder could lead to earlier intensive treatment that might impact the long-term course. Early diagnosis and appropriate treatment of attention-deficit/hyperactivity disorder very likely will lessen symptoms and also maintain self-esteem under the withering ordeal – often punctuated by teacher comments – of trying to pay attention hour after hour in school
Are there seemingly less serious conditions very likely worthy of early diagnosis, even those on the edge of normal developmental hurdles? One of the essential tasks of childhood is mastering the anxiety that emerges as children face the new challenges of each developmental stage, so parents, teachers, and clinicians are (or need to be) used to bearing anxiety in the children with whom they work. Intense shyness and anxiety around separation from parents are routine and healthy in infants and toddlers from 6-18 months. Anxiety in new social situations, such as the first day of preschool, is the rule, not the exception. School-age children commonly experience a surge of anxiety around performance and independence, as they are managing and mastering new skills in these domains every day. This anxiety can cause distress, but it should get better every time a child faces it, as they become better at managing the situation. When a child has an anxious temperament, poor coping skills, or parents who struggle to manage their own anxiety, children may have a harder time mastering new, anxiety-provoking challenges across settings. But, with time, and even just one adult who patiently models good coping, they will face and manage challenges. Social anxiety disorder is present when specific social or performance situations provoke the same intense anxiety and avoidance over and over, and for more than 6 months.
Most infants and young children who are more timid and fearful seem to grow into a normal range of social behavior, although few become extroverts. Some of these shy children are cautious in new situations for a period of time measured in minutes, but once the situations are familiar, these children are indistinguishable from their peers. However, some of these temperamentally timid children emerge consistently more anxious with greater likelihood to have phobias and to have social anxiety that can seriously impact long term happiness, achievement, and increase risk taking behaviors. A pediatrician should watch and note the emerging pattern of a timid toddler to see if the shyness eases or impacts social functioning; by bending the course of social interactions, social anxiety disorder critically affects developing social skills, self-regulation, affect tolerance, emerging identity, and confidence. Recognition and effective treatment of social anxiety will keep a child on the optimal developmental trajectory.
Anxiety disorders are the most common psychiatric illnesses in the United States, and social anxiety disorder (previously labeled as social phobia) is the third most common psychiatric disorder in U.S. adults (after depression and alcohol dependence). Most persistent anxiety disorders begin in childhood, and social anxiety is no exception. The mean age of onset for social anxiety is 13 years old, and it rarely begins after the age of 25, with an annual prevalence around 7% in childhood and adolescence (Psychiatr. Clin. North Am. 2009;32;483-524).The DSM-5 criteria for social anxiety disorder include, “a marked and persistent fear of one or more social or performance situations in which the person is exposed to unfamiliar people or to possible scrutiny by others,” and exposure to those situations provokes intense anxiety, which in children can be marked by severe or prolonged crying, freezing, tantrums, shrinking from social situations, refusing to speak, or clinging to parents. In adolescents, it may trigger panic attacks. The avoidance and distress interfere with the child’s function in school, social activities, or relationships, and must have lasted for at least 6 months. To ensure that there is not another problem of social relatedness, the child should have shown some capacity to have normal peer relationships.
Will social anxiety disorder be vividly apparent to teachers, parents, and clinicians? No. The feeling of anxiety is an internal experience, not easily observed, and anxious children and teens are rarely eager or comfortable communicators about their own anxiety. Indeed, in a 2007 survey of patients in treatment for anxiety, 36% of people with social anxiety disorder reported experiencing symptoms for 10 or more years before seeking help. It’s true that the distress children experience when feeling intensely anxious will probably be observable, but all of those behaviors (clinging, crying, tantrums) are common and normal expressions of distress in childhood. Even in adolescence, while having a panic attack may prompt the teenager to seek care, she may not connect it with the anxiety she was feeling about being called on in class or talking to peers, especially if that is an anxiety she has experienced for a long time as a daily part of her lives and routines.
Social anxiety disorder is treatable. The first-line treatment in mild to moderate cases, particularly with younger children, is cognitive-behavioral therapy. This is a practical variant of psychotherapy in which children develop and practice skills at recognizing and labeling their own feelings of anxiety, identifying the situations that trigger them, and practicing relaxation strategies that help them to face and manage the anxiety-provoking situations rather than avoiding them.
When symptoms or the degree of impairment are more severe, medications can become an important part of treatment. SSRIs are the first-line medications used to treat social anxiety disorder, and the effective doses are often higher than effective antidepressant doses, although we often titrate toward those doses more slowly with anxious patients to avoid side effects that might increase or exacerbate their anxiety.
Even with effective medication treatment, though, psychotherapy will be an essential part of treatment. These young patients need to build the essential skills of anxiety management, although it is in the nature of anxiety that such patients often wish to dissolve their anxiety by simply using a pill.
Anxiety disorders are typically chronic and will persist without effective treatment. Failure to recognize and treat social anxiety disorder can distort or even derail healthy development and may result in major psychiatric complications. As a pediatrician, you are trying to stop or modify a chain of potential events. Imagine a socially anxious young woman who enters puberty in high school. Will she withdraw from social activities? Will she avoid new opportunities or interests? Will alcohol become a necessary social lubricant? Will she be at increased risk for sexual assault at a party or poor grades in school? Will social anxiety affect her choice of college, fearful of leaving home? The incidence of secondary depression and substance abuse disorders is substantially higher in adolescents with untreated anxiety disorders. Although a depressed, alcohol-dependent teenager is more likely to be recognized as needing treatment, once they have developed those complications, effective treatment of the underlying anxiety will be much more complicated and slow to treat. Prevention starting before puberty is a much more desirable approach.
Pediatricians truly do have the opportunity to improve outcomes for these patients, by learning to recognize this sometimes-invisible disorder. Children suffering from anxiety disorders are more likely to identify a physical concern than a psychological one. (They have a lot of headaches and tummy aches!) When you are seeing a “shy” school-age child who has persistent crying spells around attending school on test days or before each sporting event despite loving practice, it is useful to gather more history. Is there a family history of anxiety or depression? What are the circumstances of their crying jags or persistent tantrums? Ask teenagers about episodes of shortness of breath, tachycardia, dizziness or sweating that leave them feeling like they are going to die (panic attacks). See if they can rank their anxiety on a scale from 1-10, and find out of there are consistent situations where their anxiety seems disproportionate. Children or teens may recognize that their anxiety is not merited, or they may not. If their parent also suffers from anxiety, they are less likely to recognize that this intense, persistent “shyness” in their child represents a treatable symptom. When you simply have a high index of suspicion, it is worth a referral to a mental health expert to evaluate their anxiety.
Reassuring parents and children that this is a common, treatable problem in childhood will go a long way to diminishing the secrecy and shame that can accompany paralyzing anxiety, and help your patients toward a track that optimizes their psychosocial development.
Dr. Swick is an attending psychiatrist in the division of child psychiatry at Massachusetts General Hospital, Boston, and director of the Parenting at a Challenging Time (PACT) Program at the Vernon Cancer Center at Newton Wellesley Hospital, also in Boston. Dr. Jellinek is professor of psychiatry and of pediatrics at Harvard Medical School, Boston.
Retire, Who Me?
Okay, so I didn’t last long as a VA retiree. My original plan was to hang it up entirely when I stepped down from my longstanding (27 years!) position as chief of medicine at the Phoenix VA Health Care System (VAHCS) at the end of June 2014. As some longtime readers may recall, my wife, Susan, has had a severe case of Sjögren’s syndrome for many years, and her symptoms have worsened progressively recently.
Our vacation home seemed a logical place to retire to, since it is in a more humid and oceanside California climate, and my wife could have some hope of breathing easier. As long as our youngest son was in high school in Phoenix, I had an excuse to stay in Arizona, but he graduated at the end of June.
Related: What's Wrong With My Wife?
Thus, all the stars aligned and I made my formal e-mail announcement to my troops in the Department of Medicine on February 14. The access scandal whose epicenter was the Phoenix VAHCS hit a couple of months later in April, and the horrendous press that ensued seemed to confirm that I should retire.
I mention these dates to counter the suspicion that I got out of Dodge because things got rough. Nothing could be further from the truth: I had to be practically dragged kicking and screaming from my office when the time arrived. I was not an enthusiastic retiree.
By early May I was already worrying about the idleness and boredom I assumed would be the hallmarks of true retirement. So I began to search frantically online for employment opportunities near our home. As it turned out, the best employment opportunity in the area was at a VA contract clinic in Oxnard. The clinic is a fully integrated part of the Greater Los Angeles VAHCS operated by Humana Government Services, not the VA.
I surprised myself by jumping at the opportunity to continue to work in a medical setting, especially one with a strong VA flavor. But I became increasingly apprehensive as the planned start date of August 4 approached. After all, for years I had had a vast array of hardworking medical helpers standing between me and the patients, including medical students, interns, residents, endocrine fellows, nurse practitioners, and physician assistants who would do almost all the direct patient care. I would occasionally visit with the patient who was not content to interact exclusively with my designated assistant or when an earnest trainee felt that I needed to assess a patient’s unique situation or concern.
Related: Keeping an Open Mind on HRT
But a small miracle has enveloped me since I began working at the Oxnard clinic. I have found that I enjoy taking care of the nonstop parade of dyslipidemic hypertensive diabetic patients who constitute the huge majority of those I see. Yes, there are many times when I wish I could sit back in my chair and unravel knotty organizational problems as I did at my previous job. And I also have persistent fantasies of sitting in my beach chair, drinking strong martinis while staring at the ever-fascinating waves of the nearby Pacific.
However, I have come to realize that I am truly a restless person. As long as there is some potential medical good to be achieved, I am hell- bent on making it happen if I can. While not all physicians share this philosophy, I strongly believe that the practice of medicine is a lifelong professional commitment that can be very difficult for many of us to walk away from. I certainly don’t know how long I’ll last in my new post. What could well drive me away is the almost-frantic pace of modern health care delivery, a pace that is largely determined by the tyranny of the electronic medical record, a monster who must be fed at all costs (more on this in the future). But for now, the need to contribute to the medical endeavor has proven considerably stronger than the countervailing desire for a quiet and comfortable retirement.
Related: Landmark Initiative Signed for Homeless Veterans
Don’t call me crazy just yet; instead, please follow the lead of my mostly grateful patients and call me doctor. That’s an honorific that’s still meaningful to me, and it keeps me slogging onward in spite of the many obstacles.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
Okay, so I didn’t last long as a VA retiree. My original plan was to hang it up entirely when I stepped down from my longstanding (27 years!) position as chief of medicine at the Phoenix VA Health Care System (VAHCS) at the end of June 2014. As some longtime readers may recall, my wife, Susan, has had a severe case of Sjögren’s syndrome for many years, and her symptoms have worsened progressively recently.
Our vacation home seemed a logical place to retire to, since it is in a more humid and oceanside California climate, and my wife could have some hope of breathing easier. As long as our youngest son was in high school in Phoenix, I had an excuse to stay in Arizona, but he graduated at the end of June.
Related: What's Wrong With My Wife?
Thus, all the stars aligned and I made my formal e-mail announcement to my troops in the Department of Medicine on February 14. The access scandal whose epicenter was the Phoenix VAHCS hit a couple of months later in April, and the horrendous press that ensued seemed to confirm that I should retire.
I mention these dates to counter the suspicion that I got out of Dodge because things got rough. Nothing could be further from the truth: I had to be practically dragged kicking and screaming from my office when the time arrived. I was not an enthusiastic retiree.
By early May I was already worrying about the idleness and boredom I assumed would be the hallmarks of true retirement. So I began to search frantically online for employment opportunities near our home. As it turned out, the best employment opportunity in the area was at a VA contract clinic in Oxnard. The clinic is a fully integrated part of the Greater Los Angeles VAHCS operated by Humana Government Services, not the VA.
I surprised myself by jumping at the opportunity to continue to work in a medical setting, especially one with a strong VA flavor. But I became increasingly apprehensive as the planned start date of August 4 approached. After all, for years I had had a vast array of hardworking medical helpers standing between me and the patients, including medical students, interns, residents, endocrine fellows, nurse practitioners, and physician assistants who would do almost all the direct patient care. I would occasionally visit with the patient who was not content to interact exclusively with my designated assistant or when an earnest trainee felt that I needed to assess a patient’s unique situation or concern.
Related: Keeping an Open Mind on HRT
But a small miracle has enveloped me since I began working at the Oxnard clinic. I have found that I enjoy taking care of the nonstop parade of dyslipidemic hypertensive diabetic patients who constitute the huge majority of those I see. Yes, there are many times when I wish I could sit back in my chair and unravel knotty organizational problems as I did at my previous job. And I also have persistent fantasies of sitting in my beach chair, drinking strong martinis while staring at the ever-fascinating waves of the nearby Pacific.
However, I have come to realize that I am truly a restless person. As long as there is some potential medical good to be achieved, I am hell- bent on making it happen if I can. While not all physicians share this philosophy, I strongly believe that the practice of medicine is a lifelong professional commitment that can be very difficult for many of us to walk away from. I certainly don’t know how long I’ll last in my new post. What could well drive me away is the almost-frantic pace of modern health care delivery, a pace that is largely determined by the tyranny of the electronic medical record, a monster who must be fed at all costs (more on this in the future). But for now, the need to contribute to the medical endeavor has proven considerably stronger than the countervailing desire for a quiet and comfortable retirement.
Related: Landmark Initiative Signed for Homeless Veterans
Don’t call me crazy just yet; instead, please follow the lead of my mostly grateful patients and call me doctor. That’s an honorific that’s still meaningful to me, and it keeps me slogging onward in spite of the many obstacles.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
Okay, so I didn’t last long as a VA retiree. My original plan was to hang it up entirely when I stepped down from my longstanding (27 years!) position as chief of medicine at the Phoenix VA Health Care System (VAHCS) at the end of June 2014. As some longtime readers may recall, my wife, Susan, has had a severe case of Sjögren’s syndrome for many years, and her symptoms have worsened progressively recently.
Our vacation home seemed a logical place to retire to, since it is in a more humid and oceanside California climate, and my wife could have some hope of breathing easier. As long as our youngest son was in high school in Phoenix, I had an excuse to stay in Arizona, but he graduated at the end of June.
Related: What's Wrong With My Wife?
Thus, all the stars aligned and I made my formal e-mail announcement to my troops in the Department of Medicine on February 14. The access scandal whose epicenter was the Phoenix VAHCS hit a couple of months later in April, and the horrendous press that ensued seemed to confirm that I should retire.
I mention these dates to counter the suspicion that I got out of Dodge because things got rough. Nothing could be further from the truth: I had to be practically dragged kicking and screaming from my office when the time arrived. I was not an enthusiastic retiree.
By early May I was already worrying about the idleness and boredom I assumed would be the hallmarks of true retirement. So I began to search frantically online for employment opportunities near our home. As it turned out, the best employment opportunity in the area was at a VA contract clinic in Oxnard. The clinic is a fully integrated part of the Greater Los Angeles VAHCS operated by Humana Government Services, not the VA.
I surprised myself by jumping at the opportunity to continue to work in a medical setting, especially one with a strong VA flavor. But I became increasingly apprehensive as the planned start date of August 4 approached. After all, for years I had had a vast array of hardworking medical helpers standing between me and the patients, including medical students, interns, residents, endocrine fellows, nurse practitioners, and physician assistants who would do almost all the direct patient care. I would occasionally visit with the patient who was not content to interact exclusively with my designated assistant or when an earnest trainee felt that I needed to assess a patient’s unique situation or concern.
Related: Keeping an Open Mind on HRT
But a small miracle has enveloped me since I began working at the Oxnard clinic. I have found that I enjoy taking care of the nonstop parade of dyslipidemic hypertensive diabetic patients who constitute the huge majority of those I see. Yes, there are many times when I wish I could sit back in my chair and unravel knotty organizational problems as I did at my previous job. And I also have persistent fantasies of sitting in my beach chair, drinking strong martinis while staring at the ever-fascinating waves of the nearby Pacific.
However, I have come to realize that I am truly a restless person. As long as there is some potential medical good to be achieved, I am hell- bent on making it happen if I can. While not all physicians share this philosophy, I strongly believe that the practice of medicine is a lifelong professional commitment that can be very difficult for many of us to walk away from. I certainly don’t know how long I’ll last in my new post. What could well drive me away is the almost-frantic pace of modern health care delivery, a pace that is largely determined by the tyranny of the electronic medical record, a monster who must be fed at all costs (more on this in the future). But for now, the need to contribute to the medical endeavor has proven considerably stronger than the countervailing desire for a quiet and comfortable retirement.
Related: Landmark Initiative Signed for Homeless Veterans
Don’t call me crazy just yet; instead, please follow the lead of my mostly grateful patients and call me doctor. That’s an honorific that’s still meaningful to me, and it keeps me slogging onward in spite of the many obstacles.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
Committed to Showing Results at the VA
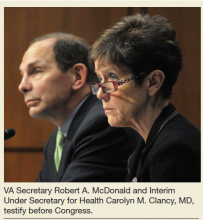
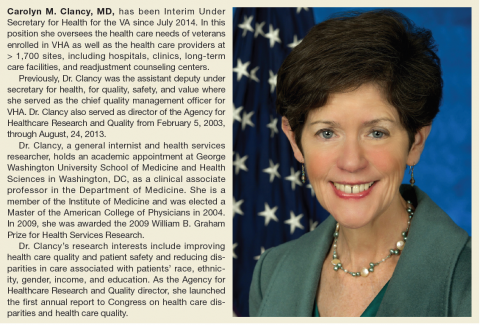
Carolyn M. Clancy, MD, was named Interim Under Secretary for Health for the VA on July 2, 2014, just as the wait time crisis seemed to be spinning out of control. Her appointment and the confirmation of Secretary Robert A. McDonald less than a month later proved essential to calming the furor but were admittedly just the first steps in a long-term process to increase veterans’ access to care and develop better systems and procedures across the agency.
Six months after her appointment, Federal Practitioner talked with Dr. Clancy about the pace of change and the role of health care providers in improving care for veterans. In the interview, Dr. Clancy clearly noted that many VA facilities already represent the best of U.S. health care and that the path forward requires sharing of best practices. Many other facilities, of course, will have to change, but Dr. Clancy insisted it is “an incredible opportunity” for the VA to learn as a system. Perhaps most heartening to VA practitioners, Dr. Clancy also recognized that “you can’t provide veteran-centered care without employees who are inspired to do their very, very best.”
To be sure, any successful change in VA procedures and culture will require buy-in not only from across the agency, but also from veterans and Congress. Dr. Clancy has already received 2 votes of confidence: The Paralyzed Veterans of America and the Vietnam Veterans of America jointly called on President Obama to make Dr. Clancy’s appointment permanent. The White House and congressional leaders, however, have yet to schedule hearings or comment publicly.
Below is an edited and condensed version of the interview. To hear the complete interview, including an in-depth discussion of the Blueprint for Excellence, visit http://www.fedprac.com/multimedia/multimedia-library.html.
Taking Measure of VA Strengths
Interim Under Secretary for Health Carolyn M. Clancy, MD. I came to this system in August of 2013 after more than 20 years at HHS, all working for an agency that had the lead charge for funding research to improve quality and safety in health care; and I had spent the last 10 years prior to coming here as the director of that agency. I came to VHA because I thought this system was unique among all systems, public and private, in this country and had the strongest foundation in place to deliver 21st century health care. And at least as important—probably more so—was the sense of mission among all of the employees I met. These were people I’ve known in academia, people I met on the interviews, people I’ve intersected with for a number of years in the research community. You can’t replicate it, and you can’t buy it; and I figured the combination of a strong foundation and mission meant that this was one of the best systems to work for.
I still think that. Some of our best facilities could compete head to head with any facilities in the private sector. There is no question about that. We have some systems, facilities, and clinics that are struggling as well, which is also very typical of the private sector.
What we have is an incredible opportunity, first, because we have a fabulous mission. We have highly committed and dedicated employees. We have an incredible opportunity to actually learn as a system. There has been a lot of discussion at a number of levels about how health care in the new century needs to be a learning health care system. We actually have the capability of delivering on that promise. So I’m very, very excited.
VA Clinical Staff and Recruitment
Dr. Clancy. I have often observed that change can be scary, but it’s also incredibly liberating. Some of our most dedicated employees, I know, can be frustrated, because they feel like they’re doing their part; but they aren’t always sure that the members of the team are as dedicated as they are or are going to catch the ball. And there’s no question that you don’t get to high-quality care without a good team. In other words, superb health care and exceptional veteran experience is a team sport by definition.
So I think it will actually help the vast majority of our frontline clinicians. It’ll be much, much easier for them to deliver the kind of care they want to deliver every single day but sometimes feel like they get stuck in workarounds.
As you have probably read and have heard me say, one of the biggest challenges of our crisis—now quite open to everyone—is how we had limited availability and limited capacity to meet the needs of the veterans we had the privilege of serving. So we are on a very, very big recruitment drive for all kinds of clinicians. And in addition to the incredible mission, we have taken some steps to make salaries a bit more competitive with the private sector. I want to underline a bit. You wouldn’t be coming to VA because you wanted to become wealthy, but we recognize that people have to pay student loans and so forth. And speaking of student loans, we have a variety of programs to help people pay down their educational debt.
And all of these things actually help, but the opportunity to deliver care that is really focused squarely on the needs of the individual veteran. That, I think, is what people will ultimately find far more exciting than any anxiety about change. …
The answer to the question about who are we recruiting is: yes. We’re recruiting all of those people [physicians and midlevel providers]. We often speak about the health care market in this country as if there were one health care market. And actually, U.S. health care, of which VA is very much a part, particularly now with the new law, is very much a series of local and regional markets. So to some extent, the ratios and the types of people that we’re going to need will depend on the specific community; but we’re looking for people in all of those areas.
Changing VA Culture
Dr. Clancy. There are a number of things that impact culture. Some of it is about stories. And I have to say that every day I get to be inspired by real-life stories of veterans and... their caregivers. Some of those caregivers are their family members or close friends: people who love them. And many of them are people who work for us in the Veterans Health Administration, people who just go the extra mile because it’s the right thing to do. Nobody said they had to do it. We don’t have a policy or a directive for it. To them, it’s as natural as gravity. …
Secretary McDonald often uses this diagram, an inverted pyramid that I love, where he starts off by having a regular pyramid; and he said, “This is how we think of a lot of organizations with the Secretary sitting right up here at the pinnacle, and veterans and everybody else are kind of down on the lowest tier.” And he said, “It’s exactly wrong. How I think about it is—” So, he flips it. We have people who provide direct care to veterans. We have people who help those people, and then we have people who help the people who are helping the people provide the care to veterans. And so that means that customer service is everybody’s job. It means that helping people on the front lines who are our colleagues—and we’re all in this together—make sure that they can deliver the care that veterans need. That is everybody’s job.
And I actually think it’s going to be a very, very easy sell. Reinforcing all of this is being transparent about data and how we’re doing. So we’re now starting to look internally at how our facilities compare with local counterparts in their particular community, and I think you will be seeing that become more public in the near future. We just have to make it a little more visually compelling.
This is how we learn. It isn’t to say, “Gee, look, you didn’t do as well as other facilities.” It’s to say, “Huh, you know, this facility actually has improved dramatically. Why don’t we go learn what they did?” which I think is consistent with [Federal Practitioner’s] focus on best practices. This is the big, big challenge and the opportunity for health care in general.
Blueprint for Excellence
In the wake of the wait time crisis, Carolyn M. Clancy, MD, has been tasked with implementing the Blueprint for Excellence. Its intent, according to the VA, is to “frame a set of activities that simultaneously address improving the performance of VHA health care now, developing a positive service culture, transitioning from ‘sick care’ to ‘health care’ in the broadest sense, and developing agile business systems and management processes that are efficient, transparent and accountable.”
All the changes at the VA will align with 10 strategies for sustained excellence, which focus on improving performance, promoting a positive culture of service, advancing health care innovation, and increasing operational effectiveness and accountability. The strategies include:
- Operate a health care network that anticipates and meets the unique needs of enrolled veterans, in general, and the service-disabled and most vulnerable veterans, in particular.
- Deliver high-quality, veteran-centered care that compares favorably to the best of the private sector in measured outcomes, value, efficiency, and patient experience.
- Leverage information technologies, analytics, and models of health care delivery to optimize individual and population health outcomes.
- Grow an organizational culture, rooted in VA’s core values and mission, that prioritizes the veteran first; engaging and inspiring employees to their highest possible level of performance and conduct.
- Foster an environment of continuous learning, responsible risk taking, and personal accountability.
- Advance health care that is personalized, proactive, and patient-driven and engages and inspires veterans to their highest possible level of health and well-being.
- Lead the nation in research and treatment of military service-related conditions.
- Become a model integrated health services network through innovative academic, intergovernmental, and community relationships, information exchange, and public-private partnerships.
- Operate and communicate with integrity, transparency, and accountability that earns and maintains the trust of veterans, stewards of the system (Congress, Veterans Service Organizations), and the public.
- Modernize management processes in human resources, procurement, payment, capital infrastructure, and information technology to operate with benchmark agility and efficiency.
To listen to Dr. Clancy’s in-depth discussion of the Blueprint for Excellence, visit http://www.fedprac.com/multimedia/multimedia-library/article/carolyn-clancy-on-implementing-the-blueprint-for-excellence-at-the-va/f7313e00ff18fcbcf4fcaead862c285a/ocregister.html.
Measuring Success or Failure
Dr. Clancy. We will be measuring this in a lot of different ways. First is that VA is, I believe, unique among federal departments in having a very deep all-employee survey. We also participate in the broad Federal Employee Viewpoint Survey. ... In addition to that, we field our own survey internally and take that very, very seriously.
So literally, as the electrons are rolling in, we have a National Center for Organization and Development, which is sharing their results with me and looking at [the data] across the entire system by network, by facility. How are we doing? Where are there challenges? Where are there opportunities? Who’s doing incredibly well that we might learn something about how they’re doing that in order to help those facilities that are having more challenges? That is a very, very current source of information.
And the reason it’s so important is you can’t provide veteran-centered care without employees who are inspired to do their very, very best. And people who are inspired to do their very best, by definition, are not terribly unhappy. So that’s a very, very important source.
And I’ll also say that in health care, in general, as well as here, we’re seeing very important correlations between responses to employee surveys and such indicators as avoidable patient harms, rates of hospital-associated infections or health care-associated infections, and so forth. So we know that the two are very highly correlated.
The other reason that the survey is incredibly important is that most service industries have known for a long time that the best source of innovation are the people who are providing the service and care every single day. So again, that gets back to people feeling motivated and empowered and inspired. …
Time Frame for Change
Dr. Clancy. I think that people are seeing changes already. Now I’m just judging from my own e-mails and other things that we get; and we touch base regularly with veterans service organizations, with many, many stakeholders and take that input very, very seriously, because they are incredible partners in helping us identify and solve problems, because what I really worry about are veterans who are encountering difficulties, who may be fearful or hesitant in some fashion to bring that to our attention.
So I think, in a qualitative sense, we are seeing some positive signals but also recognizing that the scale of changes we’re talking about will take some time. But we will continue to see qualitative differences and, I think, real, tangible differences in the care that veterans get as the months proceed from here. I remain very optimistic about the future of this system and the size of the opportunity that we have.
Our laserlike focus for this coming year is access and exceptional veteran experience. You know, navigating health care can be pretty challenging. I know this because I’m from a very, very large extended family; and nobody else is in health or medicine, so I get regular reports. And whether you’re enrolled in our system or get your care elsewhere, it is not always easy.
But we have the incredible privilege of serving people who essentially wrote a blank check on our behalf when they agreed to serve the country. And so access is not something that, for the most part, is monitored closely in the private sector. It is certainly not publicly reported. We are making a very, very strong commitment, not just to improving, but to being able to show people the results.
Carolyn M. Clancy, MD, was named Interim Under Secretary for Health for the VA on July 2, 2014, just as the wait time crisis seemed to be spinning out of control. Her appointment and the confirmation of Secretary Robert A. McDonald less than a month later proved essential to calming the furor but were admittedly just the first steps in a long-term process to increase veterans’ access to care and develop better systems and procedures across the agency.
Six months after her appointment, Federal Practitioner talked with Dr. Clancy about the pace of change and the role of health care providers in improving care for veterans. In the interview, Dr. Clancy clearly noted that many VA facilities already represent the best of U.S. health care and that the path forward requires sharing of best practices. Many other facilities, of course, will have to change, but Dr. Clancy insisted it is “an incredible opportunity” for the VA to learn as a system. Perhaps most heartening to VA practitioners, Dr. Clancy also recognized that “you can’t provide veteran-centered care without employees who are inspired to do their very, very best.”
To be sure, any successful change in VA procedures and culture will require buy-in not only from across the agency, but also from veterans and Congress. Dr. Clancy has already received 2 votes of confidence: The Paralyzed Veterans of America and the Vietnam Veterans of America jointly called on President Obama to make Dr. Clancy’s appointment permanent. The White House and congressional leaders, however, have yet to schedule hearings or comment publicly.
Below is an edited and condensed version of the interview. To hear the complete interview, including an in-depth discussion of the Blueprint for Excellence, visit http://www.fedprac.com/multimedia/multimedia-library.html.
Taking Measure of VA Strengths
Interim Under Secretary for Health Carolyn M. Clancy, MD. I came to this system in August of 2013 after more than 20 years at HHS, all working for an agency that had the lead charge for funding research to improve quality and safety in health care; and I had spent the last 10 years prior to coming here as the director of that agency. I came to VHA because I thought this system was unique among all systems, public and private, in this country and had the strongest foundation in place to deliver 21st century health care. And at least as important—probably more so—was the sense of mission among all of the employees I met. These were people I’ve known in academia, people I met on the interviews, people I’ve intersected with for a number of years in the research community. You can’t replicate it, and you can’t buy it; and I figured the combination of a strong foundation and mission meant that this was one of the best systems to work for.
I still think that. Some of our best facilities could compete head to head with any facilities in the private sector. There is no question about that. We have some systems, facilities, and clinics that are struggling as well, which is also very typical of the private sector.
What we have is an incredible opportunity, first, because we have a fabulous mission. We have highly committed and dedicated employees. We have an incredible opportunity to actually learn as a system. There has been a lot of discussion at a number of levels about how health care in the new century needs to be a learning health care system. We actually have the capability of delivering on that promise. So I’m very, very excited.
VA Clinical Staff and Recruitment
Dr. Clancy. I have often observed that change can be scary, but it’s also incredibly liberating. Some of our most dedicated employees, I know, can be frustrated, because they feel like they’re doing their part; but they aren’t always sure that the members of the team are as dedicated as they are or are going to catch the ball. And there’s no question that you don’t get to high-quality care without a good team. In other words, superb health care and exceptional veteran experience is a team sport by definition.
So I think it will actually help the vast majority of our frontline clinicians. It’ll be much, much easier for them to deliver the kind of care they want to deliver every single day but sometimes feel like they get stuck in workarounds.
As you have probably read and have heard me say, one of the biggest challenges of our crisis—now quite open to everyone—is how we had limited availability and limited capacity to meet the needs of the veterans we had the privilege of serving. So we are on a very, very big recruitment drive for all kinds of clinicians. And in addition to the incredible mission, we have taken some steps to make salaries a bit more competitive with the private sector. I want to underline a bit. You wouldn’t be coming to VA because you wanted to become wealthy, but we recognize that people have to pay student loans and so forth. And speaking of student loans, we have a variety of programs to help people pay down their educational debt.
And all of these things actually help, but the opportunity to deliver care that is really focused squarely on the needs of the individual veteran. That, I think, is what people will ultimately find far more exciting than any anxiety about change. …
The answer to the question about who are we recruiting is: yes. We’re recruiting all of those people [physicians and midlevel providers]. We often speak about the health care market in this country as if there were one health care market. And actually, U.S. health care, of which VA is very much a part, particularly now with the new law, is very much a series of local and regional markets. So to some extent, the ratios and the types of people that we’re going to need will depend on the specific community; but we’re looking for people in all of those areas.
Changing VA Culture
Dr. Clancy. There are a number of things that impact culture. Some of it is about stories. And I have to say that every day I get to be inspired by real-life stories of veterans and... their caregivers. Some of those caregivers are their family members or close friends: people who love them. And many of them are people who work for us in the Veterans Health Administration, people who just go the extra mile because it’s the right thing to do. Nobody said they had to do it. We don’t have a policy or a directive for it. To them, it’s as natural as gravity. …
Secretary McDonald often uses this diagram, an inverted pyramid that I love, where he starts off by having a regular pyramid; and he said, “This is how we think of a lot of organizations with the Secretary sitting right up here at the pinnacle, and veterans and everybody else are kind of down on the lowest tier.” And he said, “It’s exactly wrong. How I think about it is—” So, he flips it. We have people who provide direct care to veterans. We have people who help those people, and then we have people who help the people who are helping the people provide the care to veterans. And so that means that customer service is everybody’s job. It means that helping people on the front lines who are our colleagues—and we’re all in this together—make sure that they can deliver the care that veterans need. That is everybody’s job.
And I actually think it’s going to be a very, very easy sell. Reinforcing all of this is being transparent about data and how we’re doing. So we’re now starting to look internally at how our facilities compare with local counterparts in their particular community, and I think you will be seeing that become more public in the near future. We just have to make it a little more visually compelling.
This is how we learn. It isn’t to say, “Gee, look, you didn’t do as well as other facilities.” It’s to say, “Huh, you know, this facility actually has improved dramatically. Why don’t we go learn what they did?” which I think is consistent with [Federal Practitioner’s] focus on best practices. This is the big, big challenge and the opportunity for health care in general.
Blueprint for Excellence
In the wake of the wait time crisis, Carolyn M. Clancy, MD, has been tasked with implementing the Blueprint for Excellence. Its intent, according to the VA, is to “frame a set of activities that simultaneously address improving the performance of VHA health care now, developing a positive service culture, transitioning from ‘sick care’ to ‘health care’ in the broadest sense, and developing agile business systems and management processes that are efficient, transparent and accountable.”
All the changes at the VA will align with 10 strategies for sustained excellence, which focus on improving performance, promoting a positive culture of service, advancing health care innovation, and increasing operational effectiveness and accountability. The strategies include:
- Operate a health care network that anticipates and meets the unique needs of enrolled veterans, in general, and the service-disabled and most vulnerable veterans, in particular.
- Deliver high-quality, veteran-centered care that compares favorably to the best of the private sector in measured outcomes, value, efficiency, and patient experience.
- Leverage information technologies, analytics, and models of health care delivery to optimize individual and population health outcomes.
- Grow an organizational culture, rooted in VA’s core values and mission, that prioritizes the veteran first; engaging and inspiring employees to their highest possible level of performance and conduct.
- Foster an environment of continuous learning, responsible risk taking, and personal accountability.
- Advance health care that is personalized, proactive, and patient-driven and engages and inspires veterans to their highest possible level of health and well-being.
- Lead the nation in research and treatment of military service-related conditions.
- Become a model integrated health services network through innovative academic, intergovernmental, and community relationships, information exchange, and public-private partnerships.
- Operate and communicate with integrity, transparency, and accountability that earns and maintains the trust of veterans, stewards of the system (Congress, Veterans Service Organizations), and the public.
- Modernize management processes in human resources, procurement, payment, capital infrastructure, and information technology to operate with benchmark agility and efficiency.
To listen to Dr. Clancy’s in-depth discussion of the Blueprint for Excellence, visit http://www.fedprac.com/multimedia/multimedia-library/article/carolyn-clancy-on-implementing-the-blueprint-for-excellence-at-the-va/f7313e00ff18fcbcf4fcaead862c285a/ocregister.html.
Measuring Success or Failure
Dr. Clancy. We will be measuring this in a lot of different ways. First is that VA is, I believe, unique among federal departments in having a very deep all-employee survey. We also participate in the broad Federal Employee Viewpoint Survey. ... In addition to that, we field our own survey internally and take that very, very seriously.
So literally, as the electrons are rolling in, we have a National Center for Organization and Development, which is sharing their results with me and looking at [the data] across the entire system by network, by facility. How are we doing? Where are there challenges? Where are there opportunities? Who’s doing incredibly well that we might learn something about how they’re doing that in order to help those facilities that are having more challenges? That is a very, very current source of information.
And the reason it’s so important is you can’t provide veteran-centered care without employees who are inspired to do their very, very best. And people who are inspired to do their very best, by definition, are not terribly unhappy. So that’s a very, very important source.
And I’ll also say that in health care, in general, as well as here, we’re seeing very important correlations between responses to employee surveys and such indicators as avoidable patient harms, rates of hospital-associated infections or health care-associated infections, and so forth. So we know that the two are very highly correlated.
The other reason that the survey is incredibly important is that most service industries have known for a long time that the best source of innovation are the people who are providing the service and care every single day. So again, that gets back to people feeling motivated and empowered and inspired. …
Time Frame for Change
Dr. Clancy. I think that people are seeing changes already. Now I’m just judging from my own e-mails and other things that we get; and we touch base regularly with veterans service organizations, with many, many stakeholders and take that input very, very seriously, because they are incredible partners in helping us identify and solve problems, because what I really worry about are veterans who are encountering difficulties, who may be fearful or hesitant in some fashion to bring that to our attention.
So I think, in a qualitative sense, we are seeing some positive signals but also recognizing that the scale of changes we’re talking about will take some time. But we will continue to see qualitative differences and, I think, real, tangible differences in the care that veterans get as the months proceed from here. I remain very optimistic about the future of this system and the size of the opportunity that we have.
Our laserlike focus for this coming year is access and exceptional veteran experience. You know, navigating health care can be pretty challenging. I know this because I’m from a very, very large extended family; and nobody else is in health or medicine, so I get regular reports. And whether you’re enrolled in our system or get your care elsewhere, it is not always easy.
But we have the incredible privilege of serving people who essentially wrote a blank check on our behalf when they agreed to serve the country. And so access is not something that, for the most part, is monitored closely in the private sector. It is certainly not publicly reported. We are making a very, very strong commitment, not just to improving, but to being able to show people the results.
Carolyn M. Clancy, MD, was named Interim Under Secretary for Health for the VA on July 2, 2014, just as the wait time crisis seemed to be spinning out of control. Her appointment and the confirmation of Secretary Robert A. McDonald less than a month later proved essential to calming the furor but were admittedly just the first steps in a long-term process to increase veterans’ access to care and develop better systems and procedures across the agency.
Six months after her appointment, Federal Practitioner talked with Dr. Clancy about the pace of change and the role of health care providers in improving care for veterans. In the interview, Dr. Clancy clearly noted that many VA facilities already represent the best of U.S. health care and that the path forward requires sharing of best practices. Many other facilities, of course, will have to change, but Dr. Clancy insisted it is “an incredible opportunity” for the VA to learn as a system. Perhaps most heartening to VA practitioners, Dr. Clancy also recognized that “you can’t provide veteran-centered care without employees who are inspired to do their very, very best.”
To be sure, any successful change in VA procedures and culture will require buy-in not only from across the agency, but also from veterans and Congress. Dr. Clancy has already received 2 votes of confidence: The Paralyzed Veterans of America and the Vietnam Veterans of America jointly called on President Obama to make Dr. Clancy’s appointment permanent. The White House and congressional leaders, however, have yet to schedule hearings or comment publicly.
Below is an edited and condensed version of the interview. To hear the complete interview, including an in-depth discussion of the Blueprint for Excellence, visit http://www.fedprac.com/multimedia/multimedia-library.html.
Taking Measure of VA Strengths
Interim Under Secretary for Health Carolyn M. Clancy, MD. I came to this system in August of 2013 after more than 20 years at HHS, all working for an agency that had the lead charge for funding research to improve quality and safety in health care; and I had spent the last 10 years prior to coming here as the director of that agency. I came to VHA because I thought this system was unique among all systems, public and private, in this country and had the strongest foundation in place to deliver 21st century health care. And at least as important—probably more so—was the sense of mission among all of the employees I met. These were people I’ve known in academia, people I met on the interviews, people I’ve intersected with for a number of years in the research community. You can’t replicate it, and you can’t buy it; and I figured the combination of a strong foundation and mission meant that this was one of the best systems to work for.
I still think that. Some of our best facilities could compete head to head with any facilities in the private sector. There is no question about that. We have some systems, facilities, and clinics that are struggling as well, which is also very typical of the private sector.
What we have is an incredible opportunity, first, because we have a fabulous mission. We have highly committed and dedicated employees. We have an incredible opportunity to actually learn as a system. There has been a lot of discussion at a number of levels about how health care in the new century needs to be a learning health care system. We actually have the capability of delivering on that promise. So I’m very, very excited.
VA Clinical Staff and Recruitment
Dr. Clancy. I have often observed that change can be scary, but it’s also incredibly liberating. Some of our most dedicated employees, I know, can be frustrated, because they feel like they’re doing their part; but they aren’t always sure that the members of the team are as dedicated as they are or are going to catch the ball. And there’s no question that you don’t get to high-quality care without a good team. In other words, superb health care and exceptional veteran experience is a team sport by definition.
So I think it will actually help the vast majority of our frontline clinicians. It’ll be much, much easier for them to deliver the kind of care they want to deliver every single day but sometimes feel like they get stuck in workarounds.
As you have probably read and have heard me say, one of the biggest challenges of our crisis—now quite open to everyone—is how we had limited availability and limited capacity to meet the needs of the veterans we had the privilege of serving. So we are on a very, very big recruitment drive for all kinds of clinicians. And in addition to the incredible mission, we have taken some steps to make salaries a bit more competitive with the private sector. I want to underline a bit. You wouldn’t be coming to VA because you wanted to become wealthy, but we recognize that people have to pay student loans and so forth. And speaking of student loans, we have a variety of programs to help people pay down their educational debt.
And all of these things actually help, but the opportunity to deliver care that is really focused squarely on the needs of the individual veteran. That, I think, is what people will ultimately find far more exciting than any anxiety about change. …
The answer to the question about who are we recruiting is: yes. We’re recruiting all of those people [physicians and midlevel providers]. We often speak about the health care market in this country as if there were one health care market. And actually, U.S. health care, of which VA is very much a part, particularly now with the new law, is very much a series of local and regional markets. So to some extent, the ratios and the types of people that we’re going to need will depend on the specific community; but we’re looking for people in all of those areas.
Changing VA Culture
Dr. Clancy. There are a number of things that impact culture. Some of it is about stories. And I have to say that every day I get to be inspired by real-life stories of veterans and... their caregivers. Some of those caregivers are their family members or close friends: people who love them. And many of them are people who work for us in the Veterans Health Administration, people who just go the extra mile because it’s the right thing to do. Nobody said they had to do it. We don’t have a policy or a directive for it. To them, it’s as natural as gravity. …
Secretary McDonald often uses this diagram, an inverted pyramid that I love, where he starts off by having a regular pyramid; and he said, “This is how we think of a lot of organizations with the Secretary sitting right up here at the pinnacle, and veterans and everybody else are kind of down on the lowest tier.” And he said, “It’s exactly wrong. How I think about it is—” So, he flips it. We have people who provide direct care to veterans. We have people who help those people, and then we have people who help the people who are helping the people provide the care to veterans. And so that means that customer service is everybody’s job. It means that helping people on the front lines who are our colleagues—and we’re all in this together—make sure that they can deliver the care that veterans need. That is everybody’s job.
And I actually think it’s going to be a very, very easy sell. Reinforcing all of this is being transparent about data and how we’re doing. So we’re now starting to look internally at how our facilities compare with local counterparts in their particular community, and I think you will be seeing that become more public in the near future. We just have to make it a little more visually compelling.
This is how we learn. It isn’t to say, “Gee, look, you didn’t do as well as other facilities.” It’s to say, “Huh, you know, this facility actually has improved dramatically. Why don’t we go learn what they did?” which I think is consistent with [Federal Practitioner’s] focus on best practices. This is the big, big challenge and the opportunity for health care in general.
Blueprint for Excellence
In the wake of the wait time crisis, Carolyn M. Clancy, MD, has been tasked with implementing the Blueprint for Excellence. Its intent, according to the VA, is to “frame a set of activities that simultaneously address improving the performance of VHA health care now, developing a positive service culture, transitioning from ‘sick care’ to ‘health care’ in the broadest sense, and developing agile business systems and management processes that are efficient, transparent and accountable.”
All the changes at the VA will align with 10 strategies for sustained excellence, which focus on improving performance, promoting a positive culture of service, advancing health care innovation, and increasing operational effectiveness and accountability. The strategies include:
- Operate a health care network that anticipates and meets the unique needs of enrolled veterans, in general, and the service-disabled and most vulnerable veterans, in particular.
- Deliver high-quality, veteran-centered care that compares favorably to the best of the private sector in measured outcomes, value, efficiency, and patient experience.
- Leverage information technologies, analytics, and models of health care delivery to optimize individual and population health outcomes.
- Grow an organizational culture, rooted in VA’s core values and mission, that prioritizes the veteran first; engaging and inspiring employees to their highest possible level of performance and conduct.
- Foster an environment of continuous learning, responsible risk taking, and personal accountability.
- Advance health care that is personalized, proactive, and patient-driven and engages and inspires veterans to their highest possible level of health and well-being.
- Lead the nation in research and treatment of military service-related conditions.
- Become a model integrated health services network through innovative academic, intergovernmental, and community relationships, information exchange, and public-private partnerships.
- Operate and communicate with integrity, transparency, and accountability that earns and maintains the trust of veterans, stewards of the system (Congress, Veterans Service Organizations), and the public.
- Modernize management processes in human resources, procurement, payment, capital infrastructure, and information technology to operate with benchmark agility and efficiency.
To listen to Dr. Clancy’s in-depth discussion of the Blueprint for Excellence, visit http://www.fedprac.com/multimedia/multimedia-library/article/carolyn-clancy-on-implementing-the-blueprint-for-excellence-at-the-va/f7313e00ff18fcbcf4fcaead862c285a/ocregister.html.
Measuring Success or Failure
Dr. Clancy. We will be measuring this in a lot of different ways. First is that VA is, I believe, unique among federal departments in having a very deep all-employee survey. We also participate in the broad Federal Employee Viewpoint Survey. ... In addition to that, we field our own survey internally and take that very, very seriously.
So literally, as the electrons are rolling in, we have a National Center for Organization and Development, which is sharing their results with me and looking at [the data] across the entire system by network, by facility. How are we doing? Where are there challenges? Where are there opportunities? Who’s doing incredibly well that we might learn something about how they’re doing that in order to help those facilities that are having more challenges? That is a very, very current source of information.
And the reason it’s so important is you can’t provide veteran-centered care without employees who are inspired to do their very, very best. And people who are inspired to do their very best, by definition, are not terribly unhappy. So that’s a very, very important source.
And I’ll also say that in health care, in general, as well as here, we’re seeing very important correlations between responses to employee surveys and such indicators as avoidable patient harms, rates of hospital-associated infections or health care-associated infections, and so forth. So we know that the two are very highly correlated.
The other reason that the survey is incredibly important is that most service industries have known for a long time that the best source of innovation are the people who are providing the service and care every single day. So again, that gets back to people feeling motivated and empowered and inspired. …
Time Frame for Change
Dr. Clancy. I think that people are seeing changes already. Now I’m just judging from my own e-mails and other things that we get; and we touch base regularly with veterans service organizations, with many, many stakeholders and take that input very, very seriously, because they are incredible partners in helping us identify and solve problems, because what I really worry about are veterans who are encountering difficulties, who may be fearful or hesitant in some fashion to bring that to our attention.
So I think, in a qualitative sense, we are seeing some positive signals but also recognizing that the scale of changes we’re talking about will take some time. But we will continue to see qualitative differences and, I think, real, tangible differences in the care that veterans get as the months proceed from here. I remain very optimistic about the future of this system and the size of the opportunity that we have.
Our laserlike focus for this coming year is access and exceptional veteran experience. You know, navigating health care can be pretty challenging. I know this because I’m from a very, very large extended family; and nobody else is in health or medicine, so I get regular reports. And whether you’re enrolled in our system or get your care elsewhere, it is not always easy.
But we have the incredible privilege of serving people who essentially wrote a blank check on our behalf when they agreed to serve the country. And so access is not something that, for the most part, is monitored closely in the private sector. It is certainly not publicly reported. We are making a very, very strong commitment, not just to improving, but to being able to show people the results.
Time-dependent decisions
Let’s talk about your average workday. Is it a long day? Or is it a half-day that feels like a two-thirds day? Does it start with early morning rounds or taking your daughter to day care … or both? Breakfast? Eaten at home or behind the wheel? Do you have a break at lunchtime? How do you invest that time? Or has someone invested it for you by scheduling a #$@%&*! department meeting?
When does your day end? After the last patient is seen? Or do you stay until your charting is done? Do you make end-of-the-day rounds? Does your office scheduling reasonably approximate the reality of when you would like to leave?
Even more importantly, how does your day end? Are you wasted physically and mentally? Is the last hour and a half a stress packed, clock-watching ordeal because you have to pick up your daughter from day care? And/or be home in time to prepare dinner? Or even just eat? Have you given up on sharing the meal with your family but have promised your son that you will be home to tuck him in and give him a good-night kiss? Did you stop promising to read him a story months ago because you were never there in time?
I suspect that once you have had a cup of coffee, negotiated your commute, and settled into your office routine, the mornings are less taxing than your afternoons. Particularly if your routine includes a drop-dead time commitment when you must leave to do after school pickups and make or join the family for dinner. Do you think the quality of your doctoring is as good in the afternoon as it was in the morning? Be honest! Because I have some data that shouldn’t surprise you.
In a study entitled “Time of day and the decision to prescribe antibiotics (JAMA Intern. Med. 2014;174:2029-31), a group of physicians at Brigham and Women’s Hospital in Boston analyzed the billing and electronic health records of 21,000 clinic visits of adults diagnosed with an acute respiratory illness. The investigators found that the likelihood that a patient would be prescribed antibiotics increased throughout both the morning and afternoon office visit sessions. By the end of each 4-hour session, 5% more patients received antibiotics than at the beginning of the session.
You could argue that, for some, an as-yet-undiscovered quirk of pulmonary bacterial pathogens prompts their victims to schedule appointments later in the day. The authors of the study, however, suggest that the physicians were suffering from “decision fatigue,” a phenomenon that has apparently been described in other professionals, including judges.
But what is decision fatigue? Isn’t it really just a description of one of the things that can happen when we get tired? Everyone with a job is making decisions. “Should I mop behind the toilet or just make a quick swipe where it’s obvious?” Or, “Is it really that important to make sure I have correctly tightened that bolt on that carburetor?”
If you are physically tired or squeezed by commitment to be out of the office at a specific time for another obligation, priority lists can reshuffle as the end of the day approaches. And the quality of care can suffer. Taking the extra time to explain to a patient why antibiotics aren’t appropriate for his or her situation may drop behind the speedier alternative of simply writing a prescription.
I’m sure that this study from a Harvard-affiliated hospital could be repeated using any one of a variety of quality of care measures. It should prompt all of us to rethink how we are structuring our lives. Are you staying up too late watching television or whatever? Has your decision of where to live locked you into a time-gobbling commute? Do you invest your lunch break in a restorative activity, such as a brisk walk outside? Is your office schedule realistic? Have you accepted inflexible commitments at the end of the day that make it impossible for you to spend extra time with a patient when it would probably improve the quality of his care?
Practicing good medicine boils down to making sure that we are in good physical and mental health and have fostered a work environment that fosters good decisions. Fatigue happens, but our patients shouldn’t have to suffer the consequences when it happens to us.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater.” E-mail him at [email protected].
Let’s talk about your average workday. Is it a long day? Or is it a half-day that feels like a two-thirds day? Does it start with early morning rounds or taking your daughter to day care … or both? Breakfast? Eaten at home or behind the wheel? Do you have a break at lunchtime? How do you invest that time? Or has someone invested it for you by scheduling a #$@%&*! department meeting?
When does your day end? After the last patient is seen? Or do you stay until your charting is done? Do you make end-of-the-day rounds? Does your office scheduling reasonably approximate the reality of when you would like to leave?
Even more importantly, how does your day end? Are you wasted physically and mentally? Is the last hour and a half a stress packed, clock-watching ordeal because you have to pick up your daughter from day care? And/or be home in time to prepare dinner? Or even just eat? Have you given up on sharing the meal with your family but have promised your son that you will be home to tuck him in and give him a good-night kiss? Did you stop promising to read him a story months ago because you were never there in time?
I suspect that once you have had a cup of coffee, negotiated your commute, and settled into your office routine, the mornings are less taxing than your afternoons. Particularly if your routine includes a drop-dead time commitment when you must leave to do after school pickups and make or join the family for dinner. Do you think the quality of your doctoring is as good in the afternoon as it was in the morning? Be honest! Because I have some data that shouldn’t surprise you.
In a study entitled “Time of day and the decision to prescribe antibiotics (JAMA Intern. Med. 2014;174:2029-31), a group of physicians at Brigham and Women’s Hospital in Boston analyzed the billing and electronic health records of 21,000 clinic visits of adults diagnosed with an acute respiratory illness. The investigators found that the likelihood that a patient would be prescribed antibiotics increased throughout both the morning and afternoon office visit sessions. By the end of each 4-hour session, 5% more patients received antibiotics than at the beginning of the session.
You could argue that, for some, an as-yet-undiscovered quirk of pulmonary bacterial pathogens prompts their victims to schedule appointments later in the day. The authors of the study, however, suggest that the physicians were suffering from “decision fatigue,” a phenomenon that has apparently been described in other professionals, including judges.
But what is decision fatigue? Isn’t it really just a description of one of the things that can happen when we get tired? Everyone with a job is making decisions. “Should I mop behind the toilet or just make a quick swipe where it’s obvious?” Or, “Is it really that important to make sure I have correctly tightened that bolt on that carburetor?”
If you are physically tired or squeezed by commitment to be out of the office at a specific time for another obligation, priority lists can reshuffle as the end of the day approaches. And the quality of care can suffer. Taking the extra time to explain to a patient why antibiotics aren’t appropriate for his or her situation may drop behind the speedier alternative of simply writing a prescription.
I’m sure that this study from a Harvard-affiliated hospital could be repeated using any one of a variety of quality of care measures. It should prompt all of us to rethink how we are structuring our lives. Are you staying up too late watching television or whatever? Has your decision of where to live locked you into a time-gobbling commute? Do you invest your lunch break in a restorative activity, such as a brisk walk outside? Is your office schedule realistic? Have you accepted inflexible commitments at the end of the day that make it impossible for you to spend extra time with a patient when it would probably improve the quality of his care?
Practicing good medicine boils down to making sure that we are in good physical and mental health and have fostered a work environment that fosters good decisions. Fatigue happens, but our patients shouldn’t have to suffer the consequences when it happens to us.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater.” E-mail him at [email protected].
Let’s talk about your average workday. Is it a long day? Or is it a half-day that feels like a two-thirds day? Does it start with early morning rounds or taking your daughter to day care … or both? Breakfast? Eaten at home or behind the wheel? Do you have a break at lunchtime? How do you invest that time? Or has someone invested it for you by scheduling a #$@%&*! department meeting?
When does your day end? After the last patient is seen? Or do you stay until your charting is done? Do you make end-of-the-day rounds? Does your office scheduling reasonably approximate the reality of when you would like to leave?
Even more importantly, how does your day end? Are you wasted physically and mentally? Is the last hour and a half a stress packed, clock-watching ordeal because you have to pick up your daughter from day care? And/or be home in time to prepare dinner? Or even just eat? Have you given up on sharing the meal with your family but have promised your son that you will be home to tuck him in and give him a good-night kiss? Did you stop promising to read him a story months ago because you were never there in time?
I suspect that once you have had a cup of coffee, negotiated your commute, and settled into your office routine, the mornings are less taxing than your afternoons. Particularly if your routine includes a drop-dead time commitment when you must leave to do after school pickups and make or join the family for dinner. Do you think the quality of your doctoring is as good in the afternoon as it was in the morning? Be honest! Because I have some data that shouldn’t surprise you.
In a study entitled “Time of day and the decision to prescribe antibiotics (JAMA Intern. Med. 2014;174:2029-31), a group of physicians at Brigham and Women’s Hospital in Boston analyzed the billing and electronic health records of 21,000 clinic visits of adults diagnosed with an acute respiratory illness. The investigators found that the likelihood that a patient would be prescribed antibiotics increased throughout both the morning and afternoon office visit sessions. By the end of each 4-hour session, 5% more patients received antibiotics than at the beginning of the session.
You could argue that, for some, an as-yet-undiscovered quirk of pulmonary bacterial pathogens prompts their victims to schedule appointments later in the day. The authors of the study, however, suggest that the physicians were suffering from “decision fatigue,” a phenomenon that has apparently been described in other professionals, including judges.
But what is decision fatigue? Isn’t it really just a description of one of the things that can happen when we get tired? Everyone with a job is making decisions. “Should I mop behind the toilet or just make a quick swipe where it’s obvious?” Or, “Is it really that important to make sure I have correctly tightened that bolt on that carburetor?”
If you are physically tired or squeezed by commitment to be out of the office at a specific time for another obligation, priority lists can reshuffle as the end of the day approaches. And the quality of care can suffer. Taking the extra time to explain to a patient why antibiotics aren’t appropriate for his or her situation may drop behind the speedier alternative of simply writing a prescription.
I’m sure that this study from a Harvard-affiliated hospital could be repeated using any one of a variety of quality of care measures. It should prompt all of us to rethink how we are structuring our lives. Are you staying up too late watching television or whatever? Has your decision of where to live locked you into a time-gobbling commute? Do you invest your lunch break in a restorative activity, such as a brisk walk outside? Is your office schedule realistic? Have you accepted inflexible commitments at the end of the day that make it impossible for you to spend extra time with a patient when it would probably improve the quality of his care?
Practicing good medicine boils down to making sure that we are in good physical and mental health and have fostered a work environment that fosters good decisions. Fatigue happens, but our patients shouldn’t have to suffer the consequences when it happens to us.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Coping with a Picky Eater.” E-mail him at [email protected].
New fatigue diagnosis is a valid disease
“It is all in your head.” Patients hate to hear that. I am not sure why physicians still say it.
Lots of “real disease” is in your head: multiple sclerosis, strokes, pain, and depression. That does not mean that there is not organic pathology.
The report from the evidence-heavy Institute of Medicine (IOM) validates what so many patients have known all along: Chronic fatigue syndrome is a valid diagnosis.
No, we do not have laboratory or radiologic markers of the disease. Of course, there are not biomarkers of many other diseases, including posttraumatic stress disorder, pain, and depression.
What is tremendously important about this report is that it scientifically validates the experiences of so many patients – patients who previously have been dismissed by their physicians, thereby adding to their misery.
To reiterate the conclusions of the report:
“Myalgic encephalomyelitis/chronic fatigue syndrome – commonly referred to as ME/CFS – is a legitimate, serious, and complex systemic disease that frequently and dramatically limits the activities of affected individuals.” In the report, the IOM developed new diagnostic criteria for the disorder that include five main symptoms. In addition, it recommended that the disorder be renamed “systemic exertion intolerance disease” and be assigned a new code in the International Classification of Diseases, Tenth Edition.
The report goes on to say that between 836,000 and 2.5 million Americans suffer from ME/CFS, and an estimated 84%-91% of people with ME/CFS are not diagnosed. The disease’s symptoms can be treated, even though a cure does not exist. Its cause remains unknown, although in some cases symptoms have been triggered by an infection.
Less than one-third of medical schools include ME/CFS-specific information in the curriculum. Most patients (67%-77%) said that it took more than a year to receive a diagnosis – about 29% of these patients said it took more than 5 years. The direct and indirect economic costs of ME/CFS to society have been estimated at $17 billion to $24 billion annually, $9.1 billion of which has been attributed to lost household and job productivity.
Clearly, it is a disorder that physicians should take seriously. Especially psychiatrists, who know many diseases are “all in the head.”
Dr. Ritchie serves as professor of psychiatry at the Uniformed Services University of the Health Sciences in Bethesda, Md., and at Georgetown University in Washington. She retired from the U.S. Army in 2010 after serving for 24 years and holding many leadership positions, including chief of psychiatry.
“It is all in your head.” Patients hate to hear that. I am not sure why physicians still say it.
Lots of “real disease” is in your head: multiple sclerosis, strokes, pain, and depression. That does not mean that there is not organic pathology.
The report from the evidence-heavy Institute of Medicine (IOM) validates what so many patients have known all along: Chronic fatigue syndrome is a valid diagnosis.
No, we do not have laboratory or radiologic markers of the disease. Of course, there are not biomarkers of many other diseases, including posttraumatic stress disorder, pain, and depression.
What is tremendously important about this report is that it scientifically validates the experiences of so many patients – patients who previously have been dismissed by their physicians, thereby adding to their misery.
To reiterate the conclusions of the report:
“Myalgic encephalomyelitis/chronic fatigue syndrome – commonly referred to as ME/CFS – is a legitimate, serious, and complex systemic disease that frequently and dramatically limits the activities of affected individuals.” In the report, the IOM developed new diagnostic criteria for the disorder that include five main symptoms. In addition, it recommended that the disorder be renamed “systemic exertion intolerance disease” and be assigned a new code in the International Classification of Diseases, Tenth Edition.
The report goes on to say that between 836,000 and 2.5 million Americans suffer from ME/CFS, and an estimated 84%-91% of people with ME/CFS are not diagnosed. The disease’s symptoms can be treated, even though a cure does not exist. Its cause remains unknown, although in some cases symptoms have been triggered by an infection.
Less than one-third of medical schools include ME/CFS-specific information in the curriculum. Most patients (67%-77%) said that it took more than a year to receive a diagnosis – about 29% of these patients said it took more than 5 years. The direct and indirect economic costs of ME/CFS to society have been estimated at $17 billion to $24 billion annually, $9.1 billion of which has been attributed to lost household and job productivity.
Clearly, it is a disorder that physicians should take seriously. Especially psychiatrists, who know many diseases are “all in the head.”
Dr. Ritchie serves as professor of psychiatry at the Uniformed Services University of the Health Sciences in Bethesda, Md., and at Georgetown University in Washington. She retired from the U.S. Army in 2010 after serving for 24 years and holding many leadership positions, including chief of psychiatry.
“It is all in your head.” Patients hate to hear that. I am not sure why physicians still say it.
Lots of “real disease” is in your head: multiple sclerosis, strokes, pain, and depression. That does not mean that there is not organic pathology.
The report from the evidence-heavy Institute of Medicine (IOM) validates what so many patients have known all along: Chronic fatigue syndrome is a valid diagnosis.
No, we do not have laboratory or radiologic markers of the disease. Of course, there are not biomarkers of many other diseases, including posttraumatic stress disorder, pain, and depression.
What is tremendously important about this report is that it scientifically validates the experiences of so many patients – patients who previously have been dismissed by their physicians, thereby adding to their misery.
To reiterate the conclusions of the report:
“Myalgic encephalomyelitis/chronic fatigue syndrome – commonly referred to as ME/CFS – is a legitimate, serious, and complex systemic disease that frequently and dramatically limits the activities of affected individuals.” In the report, the IOM developed new diagnostic criteria for the disorder that include five main symptoms. In addition, it recommended that the disorder be renamed “systemic exertion intolerance disease” and be assigned a new code in the International Classification of Diseases, Tenth Edition.
The report goes on to say that between 836,000 and 2.5 million Americans suffer from ME/CFS, and an estimated 84%-91% of people with ME/CFS are not diagnosed. The disease’s symptoms can be treated, even though a cure does not exist. Its cause remains unknown, although in some cases symptoms have been triggered by an infection.
Less than one-third of medical schools include ME/CFS-specific information in the curriculum. Most patients (67%-77%) said that it took more than a year to receive a diagnosis – about 29% of these patients said it took more than 5 years. The direct and indirect economic costs of ME/CFS to society have been estimated at $17 billion to $24 billion annually, $9.1 billion of which has been attributed to lost household and job productivity.
Clearly, it is a disorder that physicians should take seriously. Especially psychiatrists, who know many diseases are “all in the head.”
Dr. Ritchie serves as professor of psychiatry at the Uniformed Services University of the Health Sciences in Bethesda, Md., and at Georgetown University in Washington. She retired from the U.S. Army in 2010 after serving for 24 years and holding many leadership positions, including chief of psychiatry.
Can Dermatologists Influence the Political Process?
Can dermatologists influence the political process? This age-old question raises its head when things are happening that we do not like or that we believe could be done better. Even though dermatologists have skills and expertise that allow us to be effective in our medical practice, most of us feel incompetent when it comes to dealing with the government. The political process is not the primary focus of our time and energy, not a topic in continuing medical education, and definitely not a place of comfort. At my medical school commencement ceremony, Leon Jaworski, a special prosecutor during Watergate, gave an address in which he scolded the medical community for not being more involved in the political process, insisting that society would benefit from our participation. This message was a lightning bolt out of the blue for me. It was the first time in all my medical school years that any respected senior figure had broached the concept that a physician’s role includes engagement in the workings of government. Jaworski was insistent, and he was right.
Influencing the political process (ie, advocating effectively) requires skills and expertise that can be acquired with attention to 3 primary principles: interfacing with legislators, establishing credibility, and joining forces within professional societies.
How to Interface With Legislators
Interfacing with legislators is exactly that: interFACEing. Based on 4 online surveys of congressional staff members (2010-2013) by the Congressional Management Foundation, the most influential way to communicate with a senator or representative is an in-person visit.1 Successful politicians regard keeping in touch with their constituents to be the most critical factor in their effectiveness.
Getting face time with a legislator can be difficult. In the short-term, the most successful strategy is for the request to come from a constituent who is affiliated with an association or corporation that represents the interests of many constituents. In the long-term, personal visits, letters (e-mail is preferred for security reasons), and telephone calls are most important when they come from constituents who are well known, highly regarded, and have gone out of their way to be helpful to the legislator’s office, which means we need to pay attention to building a relationship with our legislators. For example, I had a long-standing, one-sided correspondence with former representative Barney Frank (Democrat, Massachusetts), writing him regularly on issues that concerned me. I once chided him for not showing up for a vote I thought was important and in return I received a 3-page handwritten letter from him concerning his absence. YES! He knew my name, he knew what was important to me, and he had enough regard for my opinion to answer me personally.
Building a relationship with a staffer can be as important or sometimes even more important than with the legislators themselves. Staffers have direct access to legislators and understand the best way to facilitate moving your information and concerns forward. Meet with them, keep their contact information on hand, and direct your questions and comments to them. Staffers know how you can be helpful to their office, whether it is by supplying information, providing feedback on a position or comment, or hosting a neighborhood coffee gathering in your home so the legislator can meet other constituents. Attending events in your district or offering a simple fundraiser in your home for local and state legislators is an excellent way to be involved with candidates in a way that promotes a future relationship. When the Stark exemption was being discussed in relation to anatomic pathology at an in-office laboratory, I offered a tour of my Mohs unit to a staffer so she could see how integral and important it is for surgeons to perform histology examinations to ensure proper patient care. She did not take me up on the offer, but she subsequently called me with a question concerning a similar issue.
It is not optimal to develop relationships solely with legislators from the political party with which you identify. Dermatologists’ professional interests of concern will likely require bipartisan support for resolution.
Establish Your Credibility
Do some homework on your key issues; find the facts that support your position and also be sure to understand the opposition’s concerns. Be able to present your viewpoint in a focused and concise way with a clear sense of what you are asking the legislator to do.
Keep in mind that you want to develop a long-term, trusted relationship. It is important to be respectful and leave general political feelings out of the meeting. Schedule a meeting with the intention of presenting only 2 or 3 concrete requests. During the visit, it helps to set the context for the conversation if you reference a particular bill. Staffers often ask questions about the bill if it is not one they are currently following, which allows you to become a dependable source of good information. You can engage with staffers or legislators by asking them directly and politely for their views and position on the issue. It often is effective to leave them with a 1- to 2-page summary for review and to follow up later with a formal thank you for their time.
Participate in Professional Societies
Join professional societies to acquire the information you need, refine and consolidate messaging, and represent a larger constituency. Most of the societies that dermatologists belong to, including the American Academy of Dermatology Association, the American Society for Dermatologic Surgery Association, and the American College of Mohs Surgery, have identified legislative priorities and promote coordinated visits to Congress. The American Academy of Dermatology Association organizes its annual Legislative Conference in Washington, DC, each fall, which includes an in-depth program of speakers, discussions, and information concerning priority issues. Messages are refined and appointments are made for visits with legislators and/or their staffers. Your small group will include experienced colleagues so that you develop your skills with their mentorship. Many state societies also train their members to be effective at advocacy at the State House. Finally and most importantly, a sizeable war chest (yes, your dollars are needed too) for SkinPAC, the American Academy of Dermatology Association Political Action Committee, creates notice and respect for dermatology’s commitment to the issues of importance to the profession.
Dermatologists Have Impacted Legislation
Interaction by individual dermatologists with legislators has had a direct impact on health care issues. A Medicare Advantage Participant Bill of Rights recently was introduced and has garnered bipartisan support in the Senate due to meetings between dermatologists and key members of Congress and the Obama administration about concerns with narrow physician networks. There is a robust bipartisan Congressional Skin Cancer Caucus that representatives have joined because of discussions with their constituent dermatologists. The strong testimonies of 2 dermatologists in Maryland has picked up 3 more yes votes for passing a bill that prohibits use of tanning devices in minors younger than 18 years in that state. California dermatologists also put enough pressure on their state senators to defeat the elimination of the in-office exception to self-referral for anatomic pathology services.
Final Thoughts
Dermatologists do have a voice. We do have influence. We must “sit at the table.”2 Build a relationship with your legislators. Develop your message and become a trusted voice. Join forces with other dermatologists. “Let’s grab the front seat together.”2
1. Face-to-face with congress: before, during, and after meetings with legislators. Congressional Management Foundation Web site. http://www.congressfoundation.org/projects/communicating-with-congress/face-to-face. Accessed January 9, 2015.
2. Sandberg S. Why we have too few women leaders. http://www.ted.com/talks/sheryl_sandberg_why_we_have_too_few_women_leaders. Accessed January 6, 2015.
Can dermatologists influence the political process? This age-old question raises its head when things are happening that we do not like or that we believe could be done better. Even though dermatologists have skills and expertise that allow us to be effective in our medical practice, most of us feel incompetent when it comes to dealing with the government. The political process is not the primary focus of our time and energy, not a topic in continuing medical education, and definitely not a place of comfort. At my medical school commencement ceremony, Leon Jaworski, a special prosecutor during Watergate, gave an address in which he scolded the medical community for not being more involved in the political process, insisting that society would benefit from our participation. This message was a lightning bolt out of the blue for me. It was the first time in all my medical school years that any respected senior figure had broached the concept that a physician’s role includes engagement in the workings of government. Jaworski was insistent, and he was right.
Influencing the political process (ie, advocating effectively) requires skills and expertise that can be acquired with attention to 3 primary principles: interfacing with legislators, establishing credibility, and joining forces within professional societies.
How to Interface With Legislators
Interfacing with legislators is exactly that: interFACEing. Based on 4 online surveys of congressional staff members (2010-2013) by the Congressional Management Foundation, the most influential way to communicate with a senator or representative is an in-person visit.1 Successful politicians regard keeping in touch with their constituents to be the most critical factor in their effectiveness.
Getting face time with a legislator can be difficult. In the short-term, the most successful strategy is for the request to come from a constituent who is affiliated with an association or corporation that represents the interests of many constituents. In the long-term, personal visits, letters (e-mail is preferred for security reasons), and telephone calls are most important when they come from constituents who are well known, highly regarded, and have gone out of their way to be helpful to the legislator’s office, which means we need to pay attention to building a relationship with our legislators. For example, I had a long-standing, one-sided correspondence with former representative Barney Frank (Democrat, Massachusetts), writing him regularly on issues that concerned me. I once chided him for not showing up for a vote I thought was important and in return I received a 3-page handwritten letter from him concerning his absence. YES! He knew my name, he knew what was important to me, and he had enough regard for my opinion to answer me personally.
Building a relationship with a staffer can be as important or sometimes even more important than with the legislators themselves. Staffers have direct access to legislators and understand the best way to facilitate moving your information and concerns forward. Meet with them, keep their contact information on hand, and direct your questions and comments to them. Staffers know how you can be helpful to their office, whether it is by supplying information, providing feedback on a position or comment, or hosting a neighborhood coffee gathering in your home so the legislator can meet other constituents. Attending events in your district or offering a simple fundraiser in your home for local and state legislators is an excellent way to be involved with candidates in a way that promotes a future relationship. When the Stark exemption was being discussed in relation to anatomic pathology at an in-office laboratory, I offered a tour of my Mohs unit to a staffer so she could see how integral and important it is for surgeons to perform histology examinations to ensure proper patient care. She did not take me up on the offer, but she subsequently called me with a question concerning a similar issue.
It is not optimal to develop relationships solely with legislators from the political party with which you identify. Dermatologists’ professional interests of concern will likely require bipartisan support for resolution.
Establish Your Credibility
Do some homework on your key issues; find the facts that support your position and also be sure to understand the opposition’s concerns. Be able to present your viewpoint in a focused and concise way with a clear sense of what you are asking the legislator to do.
Keep in mind that you want to develop a long-term, trusted relationship. It is important to be respectful and leave general political feelings out of the meeting. Schedule a meeting with the intention of presenting only 2 or 3 concrete requests. During the visit, it helps to set the context for the conversation if you reference a particular bill. Staffers often ask questions about the bill if it is not one they are currently following, which allows you to become a dependable source of good information. You can engage with staffers or legislators by asking them directly and politely for their views and position on the issue. It often is effective to leave them with a 1- to 2-page summary for review and to follow up later with a formal thank you for their time.
Participate in Professional Societies
Join professional societies to acquire the information you need, refine and consolidate messaging, and represent a larger constituency. Most of the societies that dermatologists belong to, including the American Academy of Dermatology Association, the American Society for Dermatologic Surgery Association, and the American College of Mohs Surgery, have identified legislative priorities and promote coordinated visits to Congress. The American Academy of Dermatology Association organizes its annual Legislative Conference in Washington, DC, each fall, which includes an in-depth program of speakers, discussions, and information concerning priority issues. Messages are refined and appointments are made for visits with legislators and/or their staffers. Your small group will include experienced colleagues so that you develop your skills with their mentorship. Many state societies also train their members to be effective at advocacy at the State House. Finally and most importantly, a sizeable war chest (yes, your dollars are needed too) for SkinPAC, the American Academy of Dermatology Association Political Action Committee, creates notice and respect for dermatology’s commitment to the issues of importance to the profession.
Dermatologists Have Impacted Legislation
Interaction by individual dermatologists with legislators has had a direct impact on health care issues. A Medicare Advantage Participant Bill of Rights recently was introduced and has garnered bipartisan support in the Senate due to meetings between dermatologists and key members of Congress and the Obama administration about concerns with narrow physician networks. There is a robust bipartisan Congressional Skin Cancer Caucus that representatives have joined because of discussions with their constituent dermatologists. The strong testimonies of 2 dermatologists in Maryland has picked up 3 more yes votes for passing a bill that prohibits use of tanning devices in minors younger than 18 years in that state. California dermatologists also put enough pressure on their state senators to defeat the elimination of the in-office exception to self-referral for anatomic pathology services.
Final Thoughts
Dermatologists do have a voice. We do have influence. We must “sit at the table.”2 Build a relationship with your legislators. Develop your message and become a trusted voice. Join forces with other dermatologists. “Let’s grab the front seat together.”2
Can dermatologists influence the political process? This age-old question raises its head when things are happening that we do not like or that we believe could be done better. Even though dermatologists have skills and expertise that allow us to be effective in our medical practice, most of us feel incompetent when it comes to dealing with the government. The political process is not the primary focus of our time and energy, not a topic in continuing medical education, and definitely not a place of comfort. At my medical school commencement ceremony, Leon Jaworski, a special prosecutor during Watergate, gave an address in which he scolded the medical community for not being more involved in the political process, insisting that society would benefit from our participation. This message was a lightning bolt out of the blue for me. It was the first time in all my medical school years that any respected senior figure had broached the concept that a physician’s role includes engagement in the workings of government. Jaworski was insistent, and he was right.
Influencing the political process (ie, advocating effectively) requires skills and expertise that can be acquired with attention to 3 primary principles: interfacing with legislators, establishing credibility, and joining forces within professional societies.
How to Interface With Legislators
Interfacing with legislators is exactly that: interFACEing. Based on 4 online surveys of congressional staff members (2010-2013) by the Congressional Management Foundation, the most influential way to communicate with a senator or representative is an in-person visit.1 Successful politicians regard keeping in touch with their constituents to be the most critical factor in their effectiveness.
Getting face time with a legislator can be difficult. In the short-term, the most successful strategy is for the request to come from a constituent who is affiliated with an association or corporation that represents the interests of many constituents. In the long-term, personal visits, letters (e-mail is preferred for security reasons), and telephone calls are most important when they come from constituents who are well known, highly regarded, and have gone out of their way to be helpful to the legislator’s office, which means we need to pay attention to building a relationship with our legislators. For example, I had a long-standing, one-sided correspondence with former representative Barney Frank (Democrat, Massachusetts), writing him regularly on issues that concerned me. I once chided him for not showing up for a vote I thought was important and in return I received a 3-page handwritten letter from him concerning his absence. YES! He knew my name, he knew what was important to me, and he had enough regard for my opinion to answer me personally.
Building a relationship with a staffer can be as important or sometimes even more important than with the legislators themselves. Staffers have direct access to legislators and understand the best way to facilitate moving your information and concerns forward. Meet with them, keep their contact information on hand, and direct your questions and comments to them. Staffers know how you can be helpful to their office, whether it is by supplying information, providing feedback on a position or comment, or hosting a neighborhood coffee gathering in your home so the legislator can meet other constituents. Attending events in your district or offering a simple fundraiser in your home for local and state legislators is an excellent way to be involved with candidates in a way that promotes a future relationship. When the Stark exemption was being discussed in relation to anatomic pathology at an in-office laboratory, I offered a tour of my Mohs unit to a staffer so she could see how integral and important it is for surgeons to perform histology examinations to ensure proper patient care. She did not take me up on the offer, but she subsequently called me with a question concerning a similar issue.
It is not optimal to develop relationships solely with legislators from the political party with which you identify. Dermatologists’ professional interests of concern will likely require bipartisan support for resolution.
Establish Your Credibility
Do some homework on your key issues; find the facts that support your position and also be sure to understand the opposition’s concerns. Be able to present your viewpoint in a focused and concise way with a clear sense of what you are asking the legislator to do.
Keep in mind that you want to develop a long-term, trusted relationship. It is important to be respectful and leave general political feelings out of the meeting. Schedule a meeting with the intention of presenting only 2 or 3 concrete requests. During the visit, it helps to set the context for the conversation if you reference a particular bill. Staffers often ask questions about the bill if it is not one they are currently following, which allows you to become a dependable source of good information. You can engage with staffers or legislators by asking them directly and politely for their views and position on the issue. It often is effective to leave them with a 1- to 2-page summary for review and to follow up later with a formal thank you for their time.
Participate in Professional Societies
Join professional societies to acquire the information you need, refine and consolidate messaging, and represent a larger constituency. Most of the societies that dermatologists belong to, including the American Academy of Dermatology Association, the American Society for Dermatologic Surgery Association, and the American College of Mohs Surgery, have identified legislative priorities and promote coordinated visits to Congress. The American Academy of Dermatology Association organizes its annual Legislative Conference in Washington, DC, each fall, which includes an in-depth program of speakers, discussions, and information concerning priority issues. Messages are refined and appointments are made for visits with legislators and/or their staffers. Your small group will include experienced colleagues so that you develop your skills with their mentorship. Many state societies also train their members to be effective at advocacy at the State House. Finally and most importantly, a sizeable war chest (yes, your dollars are needed too) for SkinPAC, the American Academy of Dermatology Association Political Action Committee, creates notice and respect for dermatology’s commitment to the issues of importance to the profession.
Dermatologists Have Impacted Legislation
Interaction by individual dermatologists with legislators has had a direct impact on health care issues. A Medicare Advantage Participant Bill of Rights recently was introduced and has garnered bipartisan support in the Senate due to meetings between dermatologists and key members of Congress and the Obama administration about concerns with narrow physician networks. There is a robust bipartisan Congressional Skin Cancer Caucus that representatives have joined because of discussions with their constituent dermatologists. The strong testimonies of 2 dermatologists in Maryland has picked up 3 more yes votes for passing a bill that prohibits use of tanning devices in minors younger than 18 years in that state. California dermatologists also put enough pressure on their state senators to defeat the elimination of the in-office exception to self-referral for anatomic pathology services.
Final Thoughts
Dermatologists do have a voice. We do have influence. We must “sit at the table.”2 Build a relationship with your legislators. Develop your message and become a trusted voice. Join forces with other dermatologists. “Let’s grab the front seat together.”2
1. Face-to-face with congress: before, during, and after meetings with legislators. Congressional Management Foundation Web site. http://www.congressfoundation.org/projects/communicating-with-congress/face-to-face. Accessed January 9, 2015.
2. Sandberg S. Why we have too few women leaders. http://www.ted.com/talks/sheryl_sandberg_why_we_have_too_few_women_leaders. Accessed January 6, 2015.
1. Face-to-face with congress: before, during, and after meetings with legislators. Congressional Management Foundation Web site. http://www.congressfoundation.org/projects/communicating-with-congress/face-to-face. Accessed January 9, 2015.
2. Sandberg S. Why we have too few women leaders. http://www.ted.com/talks/sheryl_sandberg_why_we_have_too_few_women_leaders. Accessed January 6, 2015.
2014 Meaningful Use postmortem: Lessons learned from year 1 of Stage 2
With 2014 behind us, we are finally able to assess the implications of Meaningful Use Stage 2 for Eligible Professionals. It is now clear – as anticipated – that the updated criteria have presented a significant challenge to many. In fact, it is predicted that only a fraction of those who attained Stage 1 of Meaningful Use will attest for Stage 2 for the 2014 year. As a result, physicians who have received financial incentives under the program will now face penalties, and may see a real impact on their bottom lines.
If it’s any consolation, there is hope (and even some evidence) that the Centers for Medicare & Medicaid Services will make a few amendments to the Meaningful Use program over the next few months. This will allow for additional flexibility for providers, and with any luck, will mean more people qualify in 2015. In this column, we’ll highlight the proposed changes and share a few observations from the first year of Stage 2.
Here’s what’s new
On Jan. 29, 2015, CMS released a proposed rule that would adjust the reporting period for 2015 – currently set for the entire year – to 90 days. While this is the same length as 2014, it would give providers an extra 9 months to upgrade software, systems, and work-flows to attest for Stage 2. For those who were able to take advantage of the CEHRT [certified EHR technology] Flexibility and continue Stage 1 in 2014, this may be just the reprieve needed to stay on track. For those who made an unsuccessful attempt at Stage 2 last year, this just makes the second try a bit easier.
In case you are wondering, if you “miss” a year of Meaningful Use, you simply continue as if you made it. In other words, under the current rule, if you are due to start a full year of Stage 2 reporting in 2015, you are still obligated to do so even if you were unsuccessful with 90 days of Stage 2 in 2014. The proposed rule would change that, and keep everyone’s reporting period at 90 days regardless of stage or year. (Remember: A 1% per year penalty is assessed for every year an eligible professional fails to meet the requirements, up to a maximum of 5%. These penalties continue indefinitely.)
CMS is considering other changes as well. Specifically, their press release states they are looking to “modify other aspects of the program to match long-term goals, reduce complexity, and lessen providers’ reporting burdens.” As of now, it is unclear what that might include, but a review of the challenges from 2014 may point to some strong possibilities. We’ll start with a principle we’ve dealt with previously:
Interoperability is hard
The most noteworthy changes from Stage 1 to Stage 2 are all requirements to pass information into and out of the EHR. These include: making records available through a secure patient portal, the ability to communicate with patients through electronic means, and the transmission of “summary of care” documents between providers. These requirements also happen to be the most challenging for physicians, because they rely on other systems and individuals to make the connections possible.
Up to this point, EHR vendors have not prioritized adopting established standards for data transmission, and Stage 2 really brought this shortcoming to light. So much so, that CMS considered it a valid reason to invoke the CEHRT Flexibility. By “limited exception” providers could continue with Stage 1 this past year if “their referral partners [did] not upgrade to 2014 Edition Certified EHR Technology” (i.e., doctors are given a pass on the need to send “summary of care” data if there’s no one around to receive it). But secure and reliable electronic communication with other physicians is just one area of struggle. Another that is arguably more difficult is communicating electronically with patients. Compared with the challenges of interoperability, we’ve observed that:
Patient care is even harder
It’s one thing to incentivize (or penalize) physicians for adopting Health Information Technology, but it is an entirely different thing to hold them responsible for whether or not their patients choose to embrace it. Unfortunately, the 2014 Meaningful Use measures seem to do just that. With quotas for providing “secure electronic access” through a patient portal, the MU program forces physicians to engage patients on a new virtual “playing field.” This may seem like a good thing on the surface, but it has been riddled with headaches for providers and patients alike.
With the dawn of EHR portals, physicians suddenly perceive a new level of exposure. Patients can now peer into their charts and uncover unfiltered diagnosis terminology or slightly abnormal lab values that may raise unwarranted concern. As a result, physicians have become much more conscientious about documentation, but most feel this is just one more layer of complexity to slow them down. Additionally, as patients discover the convenience and immediacy of secure e-mail, more care is now being delivered outside the context of an office visit. This requires a huge time commitment from physicians and, in most cases, provides no income – and this time demand is not limited to just the doctors! Office staff have the new and unwelcome task of providing technical support to patients for website problems, lost passwords, etc. All of these underscore this final observation:
This isn’t getting any easier
We realize this last point is self-evident, but its impact is hard to quantify. With every new stage of meaningful use, new requirements aimed at making care more efficient for patients only seem to make delivery of care much less efficient for physicians. As physicians become mired in regulations and visit volumes drop, care will ultimately become less efficient for everyone. In response to these and many other issues, we are hopeful to see some significant adjustments made to the timeline and requirements of meaningful use. In the meantime, we certainly acknowledge the challenges and as always invite your feedback and comments.
Dr. Notte is an FP and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
With 2014 behind us, we are finally able to assess the implications of Meaningful Use Stage 2 for Eligible Professionals. It is now clear – as anticipated – that the updated criteria have presented a significant challenge to many. In fact, it is predicted that only a fraction of those who attained Stage 1 of Meaningful Use will attest for Stage 2 for the 2014 year. As a result, physicians who have received financial incentives under the program will now face penalties, and may see a real impact on their bottom lines.
If it’s any consolation, there is hope (and even some evidence) that the Centers for Medicare & Medicaid Services will make a few amendments to the Meaningful Use program over the next few months. This will allow for additional flexibility for providers, and with any luck, will mean more people qualify in 2015. In this column, we’ll highlight the proposed changes and share a few observations from the first year of Stage 2.
Here’s what’s new
On Jan. 29, 2015, CMS released a proposed rule that would adjust the reporting period for 2015 – currently set for the entire year – to 90 days. While this is the same length as 2014, it would give providers an extra 9 months to upgrade software, systems, and work-flows to attest for Stage 2. For those who were able to take advantage of the CEHRT [certified EHR technology] Flexibility and continue Stage 1 in 2014, this may be just the reprieve needed to stay on track. For those who made an unsuccessful attempt at Stage 2 last year, this just makes the second try a bit easier.
In case you are wondering, if you “miss” a year of Meaningful Use, you simply continue as if you made it. In other words, under the current rule, if you are due to start a full year of Stage 2 reporting in 2015, you are still obligated to do so even if you were unsuccessful with 90 days of Stage 2 in 2014. The proposed rule would change that, and keep everyone’s reporting period at 90 days regardless of stage or year. (Remember: A 1% per year penalty is assessed for every year an eligible professional fails to meet the requirements, up to a maximum of 5%. These penalties continue indefinitely.)
CMS is considering other changes as well. Specifically, their press release states they are looking to “modify other aspects of the program to match long-term goals, reduce complexity, and lessen providers’ reporting burdens.” As of now, it is unclear what that might include, but a review of the challenges from 2014 may point to some strong possibilities. We’ll start with a principle we’ve dealt with previously:
Interoperability is hard
The most noteworthy changes from Stage 1 to Stage 2 are all requirements to pass information into and out of the EHR. These include: making records available through a secure patient portal, the ability to communicate with patients through electronic means, and the transmission of “summary of care” documents between providers. These requirements also happen to be the most challenging for physicians, because they rely on other systems and individuals to make the connections possible.
Up to this point, EHR vendors have not prioritized adopting established standards for data transmission, and Stage 2 really brought this shortcoming to light. So much so, that CMS considered it a valid reason to invoke the CEHRT Flexibility. By “limited exception” providers could continue with Stage 1 this past year if “their referral partners [did] not upgrade to 2014 Edition Certified EHR Technology” (i.e., doctors are given a pass on the need to send “summary of care” data if there’s no one around to receive it). But secure and reliable electronic communication with other physicians is just one area of struggle. Another that is arguably more difficult is communicating electronically with patients. Compared with the challenges of interoperability, we’ve observed that:
Patient care is even harder
It’s one thing to incentivize (or penalize) physicians for adopting Health Information Technology, but it is an entirely different thing to hold them responsible for whether or not their patients choose to embrace it. Unfortunately, the 2014 Meaningful Use measures seem to do just that. With quotas for providing “secure electronic access” through a patient portal, the MU program forces physicians to engage patients on a new virtual “playing field.” This may seem like a good thing on the surface, but it has been riddled with headaches for providers and patients alike.
With the dawn of EHR portals, physicians suddenly perceive a new level of exposure. Patients can now peer into their charts and uncover unfiltered diagnosis terminology or slightly abnormal lab values that may raise unwarranted concern. As a result, physicians have become much more conscientious about documentation, but most feel this is just one more layer of complexity to slow them down. Additionally, as patients discover the convenience and immediacy of secure e-mail, more care is now being delivered outside the context of an office visit. This requires a huge time commitment from physicians and, in most cases, provides no income – and this time demand is not limited to just the doctors! Office staff have the new and unwelcome task of providing technical support to patients for website problems, lost passwords, etc. All of these underscore this final observation:
This isn’t getting any easier
We realize this last point is self-evident, but its impact is hard to quantify. With every new stage of meaningful use, new requirements aimed at making care more efficient for patients only seem to make delivery of care much less efficient for physicians. As physicians become mired in regulations and visit volumes drop, care will ultimately become less efficient for everyone. In response to these and many other issues, we are hopeful to see some significant adjustments made to the timeline and requirements of meaningful use. In the meantime, we certainly acknowledge the challenges and as always invite your feedback and comments.
Dr. Notte is an FP and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
With 2014 behind us, we are finally able to assess the implications of Meaningful Use Stage 2 for Eligible Professionals. It is now clear – as anticipated – that the updated criteria have presented a significant challenge to many. In fact, it is predicted that only a fraction of those who attained Stage 1 of Meaningful Use will attest for Stage 2 for the 2014 year. As a result, physicians who have received financial incentives under the program will now face penalties, and may see a real impact on their bottom lines.
If it’s any consolation, there is hope (and even some evidence) that the Centers for Medicare & Medicaid Services will make a few amendments to the Meaningful Use program over the next few months. This will allow for additional flexibility for providers, and with any luck, will mean more people qualify in 2015. In this column, we’ll highlight the proposed changes and share a few observations from the first year of Stage 2.
Here’s what’s new
On Jan. 29, 2015, CMS released a proposed rule that would adjust the reporting period for 2015 – currently set for the entire year – to 90 days. While this is the same length as 2014, it would give providers an extra 9 months to upgrade software, systems, and work-flows to attest for Stage 2. For those who were able to take advantage of the CEHRT [certified EHR technology] Flexibility and continue Stage 1 in 2014, this may be just the reprieve needed to stay on track. For those who made an unsuccessful attempt at Stage 2 last year, this just makes the second try a bit easier.
In case you are wondering, if you “miss” a year of Meaningful Use, you simply continue as if you made it. In other words, under the current rule, if you are due to start a full year of Stage 2 reporting in 2015, you are still obligated to do so even if you were unsuccessful with 90 days of Stage 2 in 2014. The proposed rule would change that, and keep everyone’s reporting period at 90 days regardless of stage or year. (Remember: A 1% per year penalty is assessed for every year an eligible professional fails to meet the requirements, up to a maximum of 5%. These penalties continue indefinitely.)
CMS is considering other changes as well. Specifically, their press release states they are looking to “modify other aspects of the program to match long-term goals, reduce complexity, and lessen providers’ reporting burdens.” As of now, it is unclear what that might include, but a review of the challenges from 2014 may point to some strong possibilities. We’ll start with a principle we’ve dealt with previously:
Interoperability is hard
The most noteworthy changes from Stage 1 to Stage 2 are all requirements to pass information into and out of the EHR. These include: making records available through a secure patient portal, the ability to communicate with patients through electronic means, and the transmission of “summary of care” documents between providers. These requirements also happen to be the most challenging for physicians, because they rely on other systems and individuals to make the connections possible.
Up to this point, EHR vendors have not prioritized adopting established standards for data transmission, and Stage 2 really brought this shortcoming to light. So much so, that CMS considered it a valid reason to invoke the CEHRT Flexibility. By “limited exception” providers could continue with Stage 1 this past year if “their referral partners [did] not upgrade to 2014 Edition Certified EHR Technology” (i.e., doctors are given a pass on the need to send “summary of care” data if there’s no one around to receive it). But secure and reliable electronic communication with other physicians is just one area of struggle. Another that is arguably more difficult is communicating electronically with patients. Compared with the challenges of interoperability, we’ve observed that:
Patient care is even harder
It’s one thing to incentivize (or penalize) physicians for adopting Health Information Technology, but it is an entirely different thing to hold them responsible for whether or not their patients choose to embrace it. Unfortunately, the 2014 Meaningful Use measures seem to do just that. With quotas for providing “secure electronic access” through a patient portal, the MU program forces physicians to engage patients on a new virtual “playing field.” This may seem like a good thing on the surface, but it has been riddled with headaches for providers and patients alike.
With the dawn of EHR portals, physicians suddenly perceive a new level of exposure. Patients can now peer into their charts and uncover unfiltered diagnosis terminology or slightly abnormal lab values that may raise unwarranted concern. As a result, physicians have become much more conscientious about documentation, but most feel this is just one more layer of complexity to slow them down. Additionally, as patients discover the convenience and immediacy of secure e-mail, more care is now being delivered outside the context of an office visit. This requires a huge time commitment from physicians and, in most cases, provides no income – and this time demand is not limited to just the doctors! Office staff have the new and unwelcome task of providing technical support to patients for website problems, lost passwords, etc. All of these underscore this final observation:
This isn’t getting any easier
We realize this last point is self-evident, but its impact is hard to quantify. With every new stage of meaningful use, new requirements aimed at making care more efficient for patients only seem to make delivery of care much less efficient for physicians. As physicians become mired in regulations and visit volumes drop, care will ultimately become less efficient for everyone. In response to these and many other issues, we are hopeful to see some significant adjustments made to the timeline and requirements of meaningful use. In the meantime, we certainly acknowledge the challenges and as always invite your feedback and comments.
Dr. Notte is an FP and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.