User login
Odds Are
I’ve always wondered what kind of irresponsible, misguided parent brings children to Las Vegas. Now I have the answer, right in the mirror. Don’t judge: My sister lives there, so if the kids are ever going to see their cousins, they have to share the road with trucks that say, “Girls! Girls! Girls!” (We told the 9-year-old that these were advertisements for clothing, which the women pictured seemed to need.)
It’s true that Las Vegas has become more family friendly...for the Kardashians. We did, however, manage to make the trip educational. In psychology, the kids found that after 10:00 p.m., everyone’s tempers are shorter than a 9-year-old boy lost in a crowd. In chemistry, they discovered that no substance yet synthesized can mask the smell of cigarette smoke. And in meteorology, they learned never to step in a puddle on The Strip; whatever it is, it’s not rain.
Hope falls
Is there anything we wouldn’t do to prevent someone from dying of cancer? We will ride bikes 150 miles, run marathons, and wear endless seas of pink, even though honestly it’s not everyone’s color (you know who you are). So if there were, say, a safe and effective means of preventing up to 4,000 cancer deaths a year, certainly doctors would be first in line to make sure everyone is protected, right?
Sure...between half and two-thirds of the time, according to a new analysis from the Centers for Disease Control and Prevention. That’s how often providers recommend human papillomavirus (HPV) vaccine to their eligible female and male patients. Maybe cervical, anal, penile, and oropharyngeal cancers need to get together and claim a color that looks good on everyone: Is cerulean taken?
I know we all get frustrated with vaccine deniers, but why aren’t we at least recommending HPV vaccine to 100% of our patients? Is it because they won’t be our patients by the time they get cancer? Is it because the vaccine is more expensive and more painful than some (both true, but again, y’all, cancer)? Is it because it’s awkward to talk to parents about how their cherubic 11-year-old is one day going to grow up into an adult who is likely to have, you know, S-E-X?
Whatever the reason, I share Assistant Surgeon General Dr. Anne Schuchat’s disappointment that only 37.6% of eligible girls and 13.6% of eligible boys got vaccinated against HPV last year. When poor parental uptake is the problem, we need to work on education. But when we as providers are not even recommending the vaccine, you can color me embarrassed.
Yellow-bellied?
Parents look at me like I’m crazy all the time, which I resent, because I’m only crazy most of the time. For the first 3 months of their baby's life, I tell parents to call me at the first sign of a fever; then I tell them fever is a nothing to worry about. I say that sleeping face-down can be deadly until their baby learns to roll back-to-front; then I tell them not to worry. And for the first 7 days of life, I tell them that newborn jaundice can cause severe brain damage, until I start saying it’s normal, especially in breastfed infants. I flip-flop more than a candidate for Congress.
A new study may reassure some mothers of nursing infants who look a little orange (the infants, that is; orange mothers should still be concerned). We’ve always known that breastfed infants tend to keep high levels of indirect bilirubin in their bloodstreams long after the first week in life, but no one yet had bothered to establish the typical range and time course. Dr. M. Jeffrey Maisels and a team from Oakland University William Beaumont School of Medicine changed all that with the use of transcutaneous bilirubin (TCB) monitors and 1,044 predominately breastfeeding infants.
Not only did they determine that at age 3-4 weeks between 34% and 43% of these infants still had TCB measurements over 5 mg/dL, they also reaffirmed that we doctors are really bad at guessing bilirubin levels from looking at babies. They asked trained clinicians to guess the “jaundice zone scores” of the infants, which sound like a customer loyalty program at a sporting goods store but are really just an estimate of how far down the infant’s body it looks yellow. The scores were so far off that a baby with a score of 0 could have a bilirubin level as high as 12.8 mg/dL. I can only hope that with his expertise in ferreting out bad human judgment, Dr. Maisels’s next study will investigate candidates for Congress.
Inattention
A complex society cannot function without some degree of trust; there’s all sorts of scary stuff I’d like to know, and I’m happy to pay a few dollars in taxes to make sure someone more qualified than I am is checking. Does this bridge I’m crossing have severe erosion? Is there another plane in our airspace? What was my 14-year-old daughter texting to her “boyfriend” last night? (Thanks, National Security Agency!)
Drug safety is one of those things, especially when many of my patients and one of my own children are taking said drug. A new study from researchers at Boston Children’s Hospital suggests that perhaps when it comes to the long-term safety of attention-deficit/hyperactivity disorder (ADHD) medications, the U.S. Food and Drug Administration has not looked as hard as it might. Paging Dr. Edward Snowden!
One might assume that since up to 10% of U.S. children now carry a diagnosis of ADHD, and since those children start medications as young as age 4 and continue to use them for many years, the safety studies that got these drugs approved would have been especially rigorous. Yeah, no. Only 5 of 32 preapproval trials focused on safety, these trials enrolled an average of 75 patients (as opposed to the recommended 1,500), and few lasted as long as 12 months, with approval sometimes granted after only 8 weeks of study and some older drugs being “grandfathered” in with essentially no safety data whatsoever.
I see one bright spot in this desert of data. Whenever I prescribe a stimulant for ADHD, I’ll understand that I’m taking a gamble, and I’ll fondly remember our family trip to Las Vegas.
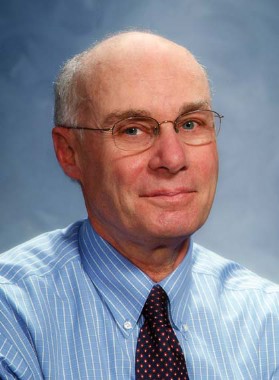
David L. Hill, M.D., FAAP, is the author of Dad to Dad: Parenting Like a Pro (AAP Publishing, 2012). He is also vice president of Cape Fear Pediatrics in Wilmington, N.C., and adjunct assistant professor of pediatrics at the University of North Carolina at Chapel Hill. He serves as Program Director for the AAP Council on Communications and Media and as an executive committee member of the North Carolina Pediatric Society. He has recorded commentaries for NPR's All Things Considered and provided content for various print, television, and Internet outlets.
I’ve always wondered what kind of irresponsible, misguided parent brings children to Las Vegas. Now I have the answer, right in the mirror. Don’t judge: My sister lives there, so if the kids are ever going to see their cousins, they have to share the road with trucks that say, “Girls! Girls! Girls!” (We told the 9-year-old that these were advertisements for clothing, which the women pictured seemed to need.)
It’s true that Las Vegas has become more family friendly...for the Kardashians. We did, however, manage to make the trip educational. In psychology, the kids found that after 10:00 p.m., everyone’s tempers are shorter than a 9-year-old boy lost in a crowd. In chemistry, they discovered that no substance yet synthesized can mask the smell of cigarette smoke. And in meteorology, they learned never to step in a puddle on The Strip; whatever it is, it’s not rain.
Hope falls
Is there anything we wouldn’t do to prevent someone from dying of cancer? We will ride bikes 150 miles, run marathons, and wear endless seas of pink, even though honestly it’s not everyone’s color (you know who you are). So if there were, say, a safe and effective means of preventing up to 4,000 cancer deaths a year, certainly doctors would be first in line to make sure everyone is protected, right?
Sure...between half and two-thirds of the time, according to a new analysis from the Centers for Disease Control and Prevention. That’s how often providers recommend human papillomavirus (HPV) vaccine to their eligible female and male patients. Maybe cervical, anal, penile, and oropharyngeal cancers need to get together and claim a color that looks good on everyone: Is cerulean taken?
I know we all get frustrated with vaccine deniers, but why aren’t we at least recommending HPV vaccine to 100% of our patients? Is it because they won’t be our patients by the time they get cancer? Is it because the vaccine is more expensive and more painful than some (both true, but again, y’all, cancer)? Is it because it’s awkward to talk to parents about how their cherubic 11-year-old is one day going to grow up into an adult who is likely to have, you know, S-E-X?
Whatever the reason, I share Assistant Surgeon General Dr. Anne Schuchat’s disappointment that only 37.6% of eligible girls and 13.6% of eligible boys got vaccinated against HPV last year. When poor parental uptake is the problem, we need to work on education. But when we as providers are not even recommending the vaccine, you can color me embarrassed.
Yellow-bellied?
Parents look at me like I’m crazy all the time, which I resent, because I’m only crazy most of the time. For the first 3 months of their baby's life, I tell parents to call me at the first sign of a fever; then I tell them fever is a nothing to worry about. I say that sleeping face-down can be deadly until their baby learns to roll back-to-front; then I tell them not to worry. And for the first 7 days of life, I tell them that newborn jaundice can cause severe brain damage, until I start saying it’s normal, especially in breastfed infants. I flip-flop more than a candidate for Congress.
A new study may reassure some mothers of nursing infants who look a little orange (the infants, that is; orange mothers should still be concerned). We’ve always known that breastfed infants tend to keep high levels of indirect bilirubin in their bloodstreams long after the first week in life, but no one yet had bothered to establish the typical range and time course. Dr. M. Jeffrey Maisels and a team from Oakland University William Beaumont School of Medicine changed all that with the use of transcutaneous bilirubin (TCB) monitors and 1,044 predominately breastfeeding infants.
Not only did they determine that at age 3-4 weeks between 34% and 43% of these infants still had TCB measurements over 5 mg/dL, they also reaffirmed that we doctors are really bad at guessing bilirubin levels from looking at babies. They asked trained clinicians to guess the “jaundice zone scores” of the infants, which sound like a customer loyalty program at a sporting goods store but are really just an estimate of how far down the infant’s body it looks yellow. The scores were so far off that a baby with a score of 0 could have a bilirubin level as high as 12.8 mg/dL. I can only hope that with his expertise in ferreting out bad human judgment, Dr. Maisels’s next study will investigate candidates for Congress.
Inattention
A complex society cannot function without some degree of trust; there’s all sorts of scary stuff I’d like to know, and I’m happy to pay a few dollars in taxes to make sure someone more qualified than I am is checking. Does this bridge I’m crossing have severe erosion? Is there another plane in our airspace? What was my 14-year-old daughter texting to her “boyfriend” last night? (Thanks, National Security Agency!)
Drug safety is one of those things, especially when many of my patients and one of my own children are taking said drug. A new study from researchers at Boston Children’s Hospital suggests that perhaps when it comes to the long-term safety of attention-deficit/hyperactivity disorder (ADHD) medications, the U.S. Food and Drug Administration has not looked as hard as it might. Paging Dr. Edward Snowden!
One might assume that since up to 10% of U.S. children now carry a diagnosis of ADHD, and since those children start medications as young as age 4 and continue to use them for many years, the safety studies that got these drugs approved would have been especially rigorous. Yeah, no. Only 5 of 32 preapproval trials focused on safety, these trials enrolled an average of 75 patients (as opposed to the recommended 1,500), and few lasted as long as 12 months, with approval sometimes granted after only 8 weeks of study and some older drugs being “grandfathered” in with essentially no safety data whatsoever.
I see one bright spot in this desert of data. Whenever I prescribe a stimulant for ADHD, I’ll understand that I’m taking a gamble, and I’ll fondly remember our family trip to Las Vegas.
David L. Hill, M.D., FAAP, is the author of Dad to Dad: Parenting Like a Pro (AAP Publishing, 2012). He is also vice president of Cape Fear Pediatrics in Wilmington, N.C., and adjunct assistant professor of pediatrics at the University of North Carolina at Chapel Hill. He serves as Program Director for the AAP Council on Communications and Media and as an executive committee member of the North Carolina Pediatric Society. He has recorded commentaries for NPR's All Things Considered and provided content for various print, television, and Internet outlets.
I’ve always wondered what kind of irresponsible, misguided parent brings children to Las Vegas. Now I have the answer, right in the mirror. Don’t judge: My sister lives there, so if the kids are ever going to see their cousins, they have to share the road with trucks that say, “Girls! Girls! Girls!” (We told the 9-year-old that these were advertisements for clothing, which the women pictured seemed to need.)
It’s true that Las Vegas has become more family friendly...for the Kardashians. We did, however, manage to make the trip educational. In psychology, the kids found that after 10:00 p.m., everyone’s tempers are shorter than a 9-year-old boy lost in a crowd. In chemistry, they discovered that no substance yet synthesized can mask the smell of cigarette smoke. And in meteorology, they learned never to step in a puddle on The Strip; whatever it is, it’s not rain.
Hope falls
Is there anything we wouldn’t do to prevent someone from dying of cancer? We will ride bikes 150 miles, run marathons, and wear endless seas of pink, even though honestly it’s not everyone’s color (you know who you are). So if there were, say, a safe and effective means of preventing up to 4,000 cancer deaths a year, certainly doctors would be first in line to make sure everyone is protected, right?
Sure...between half and two-thirds of the time, according to a new analysis from the Centers for Disease Control and Prevention. That’s how often providers recommend human papillomavirus (HPV) vaccine to their eligible female and male patients. Maybe cervical, anal, penile, and oropharyngeal cancers need to get together and claim a color that looks good on everyone: Is cerulean taken?
I know we all get frustrated with vaccine deniers, but why aren’t we at least recommending HPV vaccine to 100% of our patients? Is it because they won’t be our patients by the time they get cancer? Is it because the vaccine is more expensive and more painful than some (both true, but again, y’all, cancer)? Is it because it’s awkward to talk to parents about how their cherubic 11-year-old is one day going to grow up into an adult who is likely to have, you know, S-E-X?
Whatever the reason, I share Assistant Surgeon General Dr. Anne Schuchat’s disappointment that only 37.6% of eligible girls and 13.6% of eligible boys got vaccinated against HPV last year. When poor parental uptake is the problem, we need to work on education. But when we as providers are not even recommending the vaccine, you can color me embarrassed.
Yellow-bellied?
Parents look at me like I’m crazy all the time, which I resent, because I’m only crazy most of the time. For the first 3 months of their baby's life, I tell parents to call me at the first sign of a fever; then I tell them fever is a nothing to worry about. I say that sleeping face-down can be deadly until their baby learns to roll back-to-front; then I tell them not to worry. And for the first 7 days of life, I tell them that newborn jaundice can cause severe brain damage, until I start saying it’s normal, especially in breastfed infants. I flip-flop more than a candidate for Congress.
A new study may reassure some mothers of nursing infants who look a little orange (the infants, that is; orange mothers should still be concerned). We’ve always known that breastfed infants tend to keep high levels of indirect bilirubin in their bloodstreams long after the first week in life, but no one yet had bothered to establish the typical range and time course. Dr. M. Jeffrey Maisels and a team from Oakland University William Beaumont School of Medicine changed all that with the use of transcutaneous bilirubin (TCB) monitors and 1,044 predominately breastfeeding infants.
Not only did they determine that at age 3-4 weeks between 34% and 43% of these infants still had TCB measurements over 5 mg/dL, they also reaffirmed that we doctors are really bad at guessing bilirubin levels from looking at babies. They asked trained clinicians to guess the “jaundice zone scores” of the infants, which sound like a customer loyalty program at a sporting goods store but are really just an estimate of how far down the infant’s body it looks yellow. The scores were so far off that a baby with a score of 0 could have a bilirubin level as high as 12.8 mg/dL. I can only hope that with his expertise in ferreting out bad human judgment, Dr. Maisels’s next study will investigate candidates for Congress.
Inattention
A complex society cannot function without some degree of trust; there’s all sorts of scary stuff I’d like to know, and I’m happy to pay a few dollars in taxes to make sure someone more qualified than I am is checking. Does this bridge I’m crossing have severe erosion? Is there another plane in our airspace? What was my 14-year-old daughter texting to her “boyfriend” last night? (Thanks, National Security Agency!)
Drug safety is one of those things, especially when many of my patients and one of my own children are taking said drug. A new study from researchers at Boston Children’s Hospital suggests that perhaps when it comes to the long-term safety of attention-deficit/hyperactivity disorder (ADHD) medications, the U.S. Food and Drug Administration has not looked as hard as it might. Paging Dr. Edward Snowden!
One might assume that since up to 10% of U.S. children now carry a diagnosis of ADHD, and since those children start medications as young as age 4 and continue to use them for many years, the safety studies that got these drugs approved would have been especially rigorous. Yeah, no. Only 5 of 32 preapproval trials focused on safety, these trials enrolled an average of 75 patients (as opposed to the recommended 1,500), and few lasted as long as 12 months, with approval sometimes granted after only 8 weeks of study and some older drugs being “grandfathered” in with essentially no safety data whatsoever.
I see one bright spot in this desert of data. Whenever I prescribe a stimulant for ADHD, I’ll understand that I’m taking a gamble, and I’ll fondly remember our family trip to Las Vegas.
David L. Hill, M.D., FAAP, is the author of Dad to Dad: Parenting Like a Pro (AAP Publishing, 2012). He is also vice president of Cape Fear Pediatrics in Wilmington, N.C., and adjunct assistant professor of pediatrics at the University of North Carolina at Chapel Hill. He serves as Program Director for the AAP Council on Communications and Media and as an executive committee member of the North Carolina Pediatric Society. He has recorded commentaries for NPR's All Things Considered and provided content for various print, television, and Internet outlets.
Is it time for telemedicine?
In the constantly advancing world of health information technology, the buzzwords are always changing. In the 90s, HIPAA dominated the literature. In the past few years, meaningful use took over. Most recently, a great deal of attention has been paid to telemedicine. For the uninitiated, telemedicine, a.k.a. telehealth, is not simply returning patient phone calls after hours. Telemedicine is the idea of substituting in-person patient encounters with virtual ones, typically using a secure video interface. In this column, we will explore a general overview of telemedicine and consider how this new medium fits into the ever-changing landscape of patient care.
The patient will ‘see’ you now
As evidenced by the feedback we have received on previous columns, many of our readers are still reeling from the arduous task of implementing an EHR and shudder at the thought of introducing even more technology into their office workflow. Others who enjoy being on the cutting edge of medicine are eager to embrace these virtual visits. We’ve spoken to several early adopters and have learned that it can be a rewarding way to handle certain patient interactions, but telemedicine obviously isn’t right for every patient or condition. Some feel that the lack of physical presence is not conducive to handling personal conversations or conveying sensitive information. Others have met with resistance from patients who just can’t get used to the idea of hands-free care. As with anything else, there will be patients who remain skeptical, but there will also be those who prefer it.
One patient we engaged saw his physician’s choice to offer virtual visits as a huge benefit, saying that "the idea of saving the 30 minutes of driving in each direction to visit the doctor, along with avoiding the hassle of taking time off work, makes [telehealth] a perfect way to handle my blood pressure control." In this case, as with others, patients use information from devices such as home blood pressure monitors or glucometers to supplement the visit and provide objective data. As home technology advances, connected devices are becoming more sophisticated and allowing more complicated diagnostics to be done remotely. Smartphone-connected otoscopes and ECG machines are just two examples of what’s to come, and we plan to highlight some of these in an upcoming column.
Getting started: Is it safe?
There are several things to consider when getting started in telemedicine in your practice. First is hardware. In general, this is fairly straightforward as most practices are now set up with broadband Internet and computers or tablets. Obviously, a good quality webcam is essential to ensure quality communication with patients. Beyond this, it’s critical to think about the security of the video interaction.
Standard consumer video-conferencing software such as Skype and Apple’s FaceTime are not HIPAA-compliant and can’t be used for patient communications. An encrypted video portal is essential to maintain patient privacy and make sure the patient interaction remains secure. The good news is that several easy-to-use software packages exist to allow this, if the functionality is not already built in to your EHR. A quick web search for "HIPAA-compliant video conferencing" returned several low-cost examples – some that are even free for a few interactions per month. This may be a good way to see if there is interest from patients prior to a large outlay of money. But what about the question of liability?
Unfortunately, physicians in the 21st century are wired to always be concerned about the threat of litigation, and there is no question that telemedicine offers a new opportunity for scrutiny of our clinical decisions. In addition, many rightfully fear the idea of diagnosis and treatment without the laying on of hands. As of now, there is little-to-no legal precedent for the malpractice implications of telehealth visits, but Teledoc, the country’s largest purveyor of telemedicine, advertises 7.5 million members and zero malpractice claims. Whether or not this is enough to convince the skeptics remains to be seen, but so far telemedicine has seemingly managed to fly below the radar of the courts. Following the pattern of all areas of medicine, this is likely to change, but it may be prevented if physicians limit the kinds of services offered through virtual visits. Many providers, such as Teledoc, for example, do not prescribe Drug Enforcement Administration–controlled or so-called nontherapeutic medications. (If you’re wondering, Viagra and Cialis are both on this list.) In this way, they are able to avoid becoming confused with illegitimate drug fulfillment warehouses and limit encounters that might raise questions of legality.
Can I get paid for this?
Although there are many conceivable benefits to telemedicine, such as access to patients who are homebound or live in isolated rural areas, it is hard to imagine setting off down the virtual path without the promise of reimbursement. According to the American Telemedicine Association, 21 states and Washington, D.C., require coverage of telemedicine services with reimbursement at a rate on par with in-person visits, while providers in the others are left wanting. Currently, 120 members of the U.S. Congress support various bills to expand the reach and acceptance of telemedicine, according to the telemedicine association, but it’s clear there is a long way to go before telemedicine receives the full support of insurers. In the meantime, its only financial benefit may be as a marketing advantage for practices. Those who leverage this may be able to draw new business from patients seeking more options in the delivery of their care.
Are you ready?
As with all burgeoning areas of health IT, telemedicine in its early stages appears at best like science fiction and at worst like just another headache. Unlike the other buzzwords of the past few years, adoption of telemedicine seems to be less of a requirement and more of an option. It may or may not work in your practice or for your patient population. Most importantly, though, it represents one point on the continuum of care that will take on an increasingly prominent role in the consumer-driven health care market, and it may represent a boon to both patients and providers alike.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
In the constantly advancing world of health information technology, the buzzwords are always changing. In the 90s, HIPAA dominated the literature. In the past few years, meaningful use took over. Most recently, a great deal of attention has been paid to telemedicine. For the uninitiated, telemedicine, a.k.a. telehealth, is not simply returning patient phone calls after hours. Telemedicine is the idea of substituting in-person patient encounters with virtual ones, typically using a secure video interface. In this column, we will explore a general overview of telemedicine and consider how this new medium fits into the ever-changing landscape of patient care.
The patient will ‘see’ you now
As evidenced by the feedback we have received on previous columns, many of our readers are still reeling from the arduous task of implementing an EHR and shudder at the thought of introducing even more technology into their office workflow. Others who enjoy being on the cutting edge of medicine are eager to embrace these virtual visits. We’ve spoken to several early adopters and have learned that it can be a rewarding way to handle certain patient interactions, but telemedicine obviously isn’t right for every patient or condition. Some feel that the lack of physical presence is not conducive to handling personal conversations or conveying sensitive information. Others have met with resistance from patients who just can’t get used to the idea of hands-free care. As with anything else, there will be patients who remain skeptical, but there will also be those who prefer it.
One patient we engaged saw his physician’s choice to offer virtual visits as a huge benefit, saying that "the idea of saving the 30 minutes of driving in each direction to visit the doctor, along with avoiding the hassle of taking time off work, makes [telehealth] a perfect way to handle my blood pressure control." In this case, as with others, patients use information from devices such as home blood pressure monitors or glucometers to supplement the visit and provide objective data. As home technology advances, connected devices are becoming more sophisticated and allowing more complicated diagnostics to be done remotely. Smartphone-connected otoscopes and ECG machines are just two examples of what’s to come, and we plan to highlight some of these in an upcoming column.
Getting started: Is it safe?
There are several things to consider when getting started in telemedicine in your practice. First is hardware. In general, this is fairly straightforward as most practices are now set up with broadband Internet and computers or tablets. Obviously, a good quality webcam is essential to ensure quality communication with patients. Beyond this, it’s critical to think about the security of the video interaction.
Standard consumer video-conferencing software such as Skype and Apple’s FaceTime are not HIPAA-compliant and can’t be used for patient communications. An encrypted video portal is essential to maintain patient privacy and make sure the patient interaction remains secure. The good news is that several easy-to-use software packages exist to allow this, if the functionality is not already built in to your EHR. A quick web search for "HIPAA-compliant video conferencing" returned several low-cost examples – some that are even free for a few interactions per month. This may be a good way to see if there is interest from patients prior to a large outlay of money. But what about the question of liability?
Unfortunately, physicians in the 21st century are wired to always be concerned about the threat of litigation, and there is no question that telemedicine offers a new opportunity for scrutiny of our clinical decisions. In addition, many rightfully fear the idea of diagnosis and treatment without the laying on of hands. As of now, there is little-to-no legal precedent for the malpractice implications of telehealth visits, but Teledoc, the country’s largest purveyor of telemedicine, advertises 7.5 million members and zero malpractice claims. Whether or not this is enough to convince the skeptics remains to be seen, but so far telemedicine has seemingly managed to fly below the radar of the courts. Following the pattern of all areas of medicine, this is likely to change, but it may be prevented if physicians limit the kinds of services offered through virtual visits. Many providers, such as Teledoc, for example, do not prescribe Drug Enforcement Administration–controlled or so-called nontherapeutic medications. (If you’re wondering, Viagra and Cialis are both on this list.) In this way, they are able to avoid becoming confused with illegitimate drug fulfillment warehouses and limit encounters that might raise questions of legality.
Can I get paid for this?
Although there are many conceivable benefits to telemedicine, such as access to patients who are homebound or live in isolated rural areas, it is hard to imagine setting off down the virtual path without the promise of reimbursement. According to the American Telemedicine Association, 21 states and Washington, D.C., require coverage of telemedicine services with reimbursement at a rate on par with in-person visits, while providers in the others are left wanting. Currently, 120 members of the U.S. Congress support various bills to expand the reach and acceptance of telemedicine, according to the telemedicine association, but it’s clear there is a long way to go before telemedicine receives the full support of insurers. In the meantime, its only financial benefit may be as a marketing advantage for practices. Those who leverage this may be able to draw new business from patients seeking more options in the delivery of their care.
Are you ready?
As with all burgeoning areas of health IT, telemedicine in its early stages appears at best like science fiction and at worst like just another headache. Unlike the other buzzwords of the past few years, adoption of telemedicine seems to be less of a requirement and more of an option. It may or may not work in your practice or for your patient population. Most importantly, though, it represents one point on the continuum of care that will take on an increasingly prominent role in the consumer-driven health care market, and it may represent a boon to both patients and providers alike.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
In the constantly advancing world of health information technology, the buzzwords are always changing. In the 90s, HIPAA dominated the literature. In the past few years, meaningful use took over. Most recently, a great deal of attention has been paid to telemedicine. For the uninitiated, telemedicine, a.k.a. telehealth, is not simply returning patient phone calls after hours. Telemedicine is the idea of substituting in-person patient encounters with virtual ones, typically using a secure video interface. In this column, we will explore a general overview of telemedicine and consider how this new medium fits into the ever-changing landscape of patient care.
The patient will ‘see’ you now
As evidenced by the feedback we have received on previous columns, many of our readers are still reeling from the arduous task of implementing an EHR and shudder at the thought of introducing even more technology into their office workflow. Others who enjoy being on the cutting edge of medicine are eager to embrace these virtual visits. We’ve spoken to several early adopters and have learned that it can be a rewarding way to handle certain patient interactions, but telemedicine obviously isn’t right for every patient or condition. Some feel that the lack of physical presence is not conducive to handling personal conversations or conveying sensitive information. Others have met with resistance from patients who just can’t get used to the idea of hands-free care. As with anything else, there will be patients who remain skeptical, but there will also be those who prefer it.
One patient we engaged saw his physician’s choice to offer virtual visits as a huge benefit, saying that "the idea of saving the 30 minutes of driving in each direction to visit the doctor, along with avoiding the hassle of taking time off work, makes [telehealth] a perfect way to handle my blood pressure control." In this case, as with others, patients use information from devices such as home blood pressure monitors or glucometers to supplement the visit and provide objective data. As home technology advances, connected devices are becoming more sophisticated and allowing more complicated diagnostics to be done remotely. Smartphone-connected otoscopes and ECG machines are just two examples of what’s to come, and we plan to highlight some of these in an upcoming column.
Getting started: Is it safe?
There are several things to consider when getting started in telemedicine in your practice. First is hardware. In general, this is fairly straightforward as most practices are now set up with broadband Internet and computers or tablets. Obviously, a good quality webcam is essential to ensure quality communication with patients. Beyond this, it’s critical to think about the security of the video interaction.
Standard consumer video-conferencing software such as Skype and Apple’s FaceTime are not HIPAA-compliant and can’t be used for patient communications. An encrypted video portal is essential to maintain patient privacy and make sure the patient interaction remains secure. The good news is that several easy-to-use software packages exist to allow this, if the functionality is not already built in to your EHR. A quick web search for "HIPAA-compliant video conferencing" returned several low-cost examples – some that are even free for a few interactions per month. This may be a good way to see if there is interest from patients prior to a large outlay of money. But what about the question of liability?
Unfortunately, physicians in the 21st century are wired to always be concerned about the threat of litigation, and there is no question that telemedicine offers a new opportunity for scrutiny of our clinical decisions. In addition, many rightfully fear the idea of diagnosis and treatment without the laying on of hands. As of now, there is little-to-no legal precedent for the malpractice implications of telehealth visits, but Teledoc, the country’s largest purveyor of telemedicine, advertises 7.5 million members and zero malpractice claims. Whether or not this is enough to convince the skeptics remains to be seen, but so far telemedicine has seemingly managed to fly below the radar of the courts. Following the pattern of all areas of medicine, this is likely to change, but it may be prevented if physicians limit the kinds of services offered through virtual visits. Many providers, such as Teledoc, for example, do not prescribe Drug Enforcement Administration–controlled or so-called nontherapeutic medications. (If you’re wondering, Viagra and Cialis are both on this list.) In this way, they are able to avoid becoming confused with illegitimate drug fulfillment warehouses and limit encounters that might raise questions of legality.
Can I get paid for this?
Although there are many conceivable benefits to telemedicine, such as access to patients who are homebound or live in isolated rural areas, it is hard to imagine setting off down the virtual path without the promise of reimbursement. According to the American Telemedicine Association, 21 states and Washington, D.C., require coverage of telemedicine services with reimbursement at a rate on par with in-person visits, while providers in the others are left wanting. Currently, 120 members of the U.S. Congress support various bills to expand the reach and acceptance of telemedicine, according to the telemedicine association, but it’s clear there is a long way to go before telemedicine receives the full support of insurers. In the meantime, its only financial benefit may be as a marketing advantage for practices. Those who leverage this may be able to draw new business from patients seeking more options in the delivery of their care.
Are you ready?
As with all burgeoning areas of health IT, telemedicine in its early stages appears at best like science fiction and at worst like just another headache. Unlike the other buzzwords of the past few years, adoption of telemedicine seems to be less of a requirement and more of an option. It may or may not work in your practice or for your patient population. Most importantly, though, it represents one point on the continuum of care that will take on an increasingly prominent role in the consumer-driven health care market, and it may represent a boon to both patients and providers alike.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
When ‘normal’ just isn’t normal
As pediatricians, we are constantly evaluating children of all ages. We make determinations of normal and abnormal all the time. But, sometimes determining normal can be a challenge because children come in all shapes, sizes, and complexions, so "normal" can appear in a variety of ways.
When it comes to the adolescent, this is an even greater challenge because the onset of puberty is so varied that children of the same age can look vastly different, and pubertal changes only widen the variety. Obesity also has impacted the appearance of normal because it makes children look older, pubertal changes more advanced, and a thorough exam more difficult. So when is it okay to say, "They will just grow out of it?" Well, the best answer is when all the serious illnesses have been considered and ruled out.
Gynecomastia is a common finding in the adolescent wellness exam; 50%-60% of adolescent males experience some degree of breast enlargement starting at the age of 10 years. This peaks at ages 13-14, then regresses over a period of 18 months (N. Engl. J. Med. 2007;357:1229-37). For approximately 25% of children, the breast tissue persists, which leads to significant anxiety and insecurities among adolescent males. Even when asked if they have concerns, few will admit to it because the thought of the evaluation is more than they can handle.
Gynecomastia is caused from the increased ratio of estrogen to androgen. Antiandrogens, drugs, and weight gain have all been implicated. But in the evaluation of increased breast tissue, normal as well as abnormal causes have to be considered.
Exogenous causes include herbal products, such as tea tree oil, or medications. The most common drugs are cimetidine, ranitidine, and omeprazole, as well spirolactone and ketoconazole. With the exception of spirolactone, these are all drugs that are used commonly for minor illness in children, but have been identified as a cause for gynecomastia. Discontinuation of these products usually resolves the issue within a few months (Pharmacotherapy 1993;13:37-45).
Obesity can cause a pseudogynecomastia as well as a true gynecomastia because aromatase enzyme increases with the increase in fat tissue, which converts testosterone to estradiol. Clinically, pseudogynecomastia can be distinguished from true gynecomastia by doing a breast exam. True gynecomastia is a concentric, rubbery firm mass greater than 0.5cm, and directly below the areola, where pseudogynecomastia has diffuse enlargement and no discernable glandular tissue.
Abnormal causes of gynecomastia are much less common, but do occur. A careful physical examination and a detailed review of systems can be very helpful in ruling in or out serious causes.
An imbalance of estrogen and testosterone can result from estrogen or testosterone going up or down. These changes can be caused by other hormonal stimulation. Human chorionic gonadotropin (HGC) is increased with germ cell tumors, which can be found in abdominal or testicular masses, resulting in secondary hypogonadism. Elevated estradiol is found with testicular tumors and adrenal tumors.
Hyperthyroidism can cause gynecomastia. Additional symptoms include palpitations, weight loss, and anxiety. Physical findings include a goiter, exophthalmoses, and tremors.
Klinefelter’s syndrome, a condition that occurs in men who have an extra X chromosome, includes gynecomastia and hypogonadism. There is a 20%-60% increased risk of breast cancer in these patients, who tend to have less facial and body hair, reduced muscle tone, and narrower shoulders and wider hips (N. Engl. J. Med. 2007;357:1229-37). Suspicion of breast cancer should increase if the mass is unilateral, nontender, and eccentric to the areola.
Although the vast majority of patients with gynecomastia will resolve spontaneously, careful evaluation and consideration of abnormal causes can lead to early diagnosis and treatment.
Experienced pediatricians know it’s never "nothing" unless all the possible "somethings" have been ruled out!
Dr. Pearce is a pediatrician in Frankfort, Ill. E-mail her at [email protected].
As pediatricians, we are constantly evaluating children of all ages. We make determinations of normal and abnormal all the time. But, sometimes determining normal can be a challenge because children come in all shapes, sizes, and complexions, so "normal" can appear in a variety of ways.
When it comes to the adolescent, this is an even greater challenge because the onset of puberty is so varied that children of the same age can look vastly different, and pubertal changes only widen the variety. Obesity also has impacted the appearance of normal because it makes children look older, pubertal changes more advanced, and a thorough exam more difficult. So when is it okay to say, "They will just grow out of it?" Well, the best answer is when all the serious illnesses have been considered and ruled out.
Gynecomastia is a common finding in the adolescent wellness exam; 50%-60% of adolescent males experience some degree of breast enlargement starting at the age of 10 years. This peaks at ages 13-14, then regresses over a period of 18 months (N. Engl. J. Med. 2007;357:1229-37). For approximately 25% of children, the breast tissue persists, which leads to significant anxiety and insecurities among adolescent males. Even when asked if they have concerns, few will admit to it because the thought of the evaluation is more than they can handle.
Gynecomastia is caused from the increased ratio of estrogen to androgen. Antiandrogens, drugs, and weight gain have all been implicated. But in the evaluation of increased breast tissue, normal as well as abnormal causes have to be considered.
Exogenous causes include herbal products, such as tea tree oil, or medications. The most common drugs are cimetidine, ranitidine, and omeprazole, as well spirolactone and ketoconazole. With the exception of spirolactone, these are all drugs that are used commonly for minor illness in children, but have been identified as a cause for gynecomastia. Discontinuation of these products usually resolves the issue within a few months (Pharmacotherapy 1993;13:37-45).
Obesity can cause a pseudogynecomastia as well as a true gynecomastia because aromatase enzyme increases with the increase in fat tissue, which converts testosterone to estradiol. Clinically, pseudogynecomastia can be distinguished from true gynecomastia by doing a breast exam. True gynecomastia is a concentric, rubbery firm mass greater than 0.5cm, and directly below the areola, where pseudogynecomastia has diffuse enlargement and no discernable glandular tissue.
Abnormal causes of gynecomastia are much less common, but do occur. A careful physical examination and a detailed review of systems can be very helpful in ruling in or out serious causes.
An imbalance of estrogen and testosterone can result from estrogen or testosterone going up or down. These changes can be caused by other hormonal stimulation. Human chorionic gonadotropin (HGC) is increased with germ cell tumors, which can be found in abdominal or testicular masses, resulting in secondary hypogonadism. Elevated estradiol is found with testicular tumors and adrenal tumors.
Hyperthyroidism can cause gynecomastia. Additional symptoms include palpitations, weight loss, and anxiety. Physical findings include a goiter, exophthalmoses, and tremors.
Klinefelter’s syndrome, a condition that occurs in men who have an extra X chromosome, includes gynecomastia and hypogonadism. There is a 20%-60% increased risk of breast cancer in these patients, who tend to have less facial and body hair, reduced muscle tone, and narrower shoulders and wider hips (N. Engl. J. Med. 2007;357:1229-37). Suspicion of breast cancer should increase if the mass is unilateral, nontender, and eccentric to the areola.
Although the vast majority of patients with gynecomastia will resolve spontaneously, careful evaluation and consideration of abnormal causes can lead to early diagnosis and treatment.
Experienced pediatricians know it’s never "nothing" unless all the possible "somethings" have been ruled out!
Dr. Pearce is a pediatrician in Frankfort, Ill. E-mail her at [email protected].
As pediatricians, we are constantly evaluating children of all ages. We make determinations of normal and abnormal all the time. But, sometimes determining normal can be a challenge because children come in all shapes, sizes, and complexions, so "normal" can appear in a variety of ways.
When it comes to the adolescent, this is an even greater challenge because the onset of puberty is so varied that children of the same age can look vastly different, and pubertal changes only widen the variety. Obesity also has impacted the appearance of normal because it makes children look older, pubertal changes more advanced, and a thorough exam more difficult. So when is it okay to say, "They will just grow out of it?" Well, the best answer is when all the serious illnesses have been considered and ruled out.
Gynecomastia is a common finding in the adolescent wellness exam; 50%-60% of adolescent males experience some degree of breast enlargement starting at the age of 10 years. This peaks at ages 13-14, then regresses over a period of 18 months (N. Engl. J. Med. 2007;357:1229-37). For approximately 25% of children, the breast tissue persists, which leads to significant anxiety and insecurities among adolescent males. Even when asked if they have concerns, few will admit to it because the thought of the evaluation is more than they can handle.
Gynecomastia is caused from the increased ratio of estrogen to androgen. Antiandrogens, drugs, and weight gain have all been implicated. But in the evaluation of increased breast tissue, normal as well as abnormal causes have to be considered.
Exogenous causes include herbal products, such as tea tree oil, or medications. The most common drugs are cimetidine, ranitidine, and omeprazole, as well spirolactone and ketoconazole. With the exception of spirolactone, these are all drugs that are used commonly for minor illness in children, but have been identified as a cause for gynecomastia. Discontinuation of these products usually resolves the issue within a few months (Pharmacotherapy 1993;13:37-45).
Obesity can cause a pseudogynecomastia as well as a true gynecomastia because aromatase enzyme increases with the increase in fat tissue, which converts testosterone to estradiol. Clinically, pseudogynecomastia can be distinguished from true gynecomastia by doing a breast exam. True gynecomastia is a concentric, rubbery firm mass greater than 0.5cm, and directly below the areola, where pseudogynecomastia has diffuse enlargement and no discernable glandular tissue.
Abnormal causes of gynecomastia are much less common, but do occur. A careful physical examination and a detailed review of systems can be very helpful in ruling in or out serious causes.
An imbalance of estrogen and testosterone can result from estrogen or testosterone going up or down. These changes can be caused by other hormonal stimulation. Human chorionic gonadotropin (HGC) is increased with germ cell tumors, which can be found in abdominal or testicular masses, resulting in secondary hypogonadism. Elevated estradiol is found with testicular tumors and adrenal tumors.
Hyperthyroidism can cause gynecomastia. Additional symptoms include palpitations, weight loss, and anxiety. Physical findings include a goiter, exophthalmoses, and tremors.
Klinefelter’s syndrome, a condition that occurs in men who have an extra X chromosome, includes gynecomastia and hypogonadism. There is a 20%-60% increased risk of breast cancer in these patients, who tend to have less facial and body hair, reduced muscle tone, and narrower shoulders and wider hips (N. Engl. J. Med. 2007;357:1229-37). Suspicion of breast cancer should increase if the mass is unilateral, nontender, and eccentric to the areola.
Although the vast majority of patients with gynecomastia will resolve spontaneously, careful evaluation and consideration of abnormal causes can lead to early diagnosis and treatment.
Experienced pediatricians know it’s never "nothing" unless all the possible "somethings" have been ruled out!
Dr. Pearce is a pediatrician in Frankfort, Ill. E-mail her at [email protected].
The Medical Roundtable: Pathophysiology of Headache Progression
DR. BURSTEIN: I am Rami Burstein. I am the academic director of the Headache Center at Beth Israel Deaconess Medical Center; Vice Chairman of Research in the Department of Anesthesia and Critical Care; and Professor of Anesthesia and Neuroscience at Harvard Medical School.
DR. CHARLES: I am Andrew Charles. I am a professor in the Department of Neurology at the UCLA School of Medicine and Director of the Headache Research and Treatment Program here.
DR. SCHOENEN: I’m Jean Schoenen. I’m a neurologist and professor at the University of Liege in Belgium and Director of the Headache Research Unit at the University hospital.
DR. GOADSBY: We are talking about the pathophysiology of headache progression, and in order to so, we should define at the start what we mean by “headache progression” so we’re all starting from the same point. Dr. Charles, when we talk about headache progression, what does it make you think about?
DR. CHARLES: It makes me think about a patient who has episodic migraine that occurs infrequently, let’s say once a month or once every other month, who at some point in the course of their life begins having headaches much more frequently, let’s say 2 or 3 or 4 times per week. Accompanying that, there may be a change in the quality of the headache, where it becomes somewhat less classic for episodic migraine and has fewer of the typical features that we consider associated with migraines.
DR. GOADSBY: That’s very helpful. What we’re really talking about and what we’re going to narrow ourselves down to is talking about the pathophysiology of migraine progression because we wouldn’t be able to cover all of the types of headaches. Dr. Schoenen, what is your comment on headache progression?
DR. SCHOENEN: I agree with what Dr. Charles said, although, clinically, I think that this disorder is quite heterogeneous between patients. Any migraineur has experienced, at some time in his life, progression of the disorder, where it becomes more frequent and then drops back again to its former frequency, but there seems to be a small population of patients in whom the disorder sometimes progress and then tips over into chronic migraine. That’s not the case for all migraineurs who progress, and many patients progress for some time and then do not progress up to what we call chronic migraines. So that may be something we have to consider from the pathophysiological point of view: What differs between those who progress to chronic migraine from those who do not?
DR. GOADSBY: Yes, you make a good point. Dr. Burstein?
DR. BURSTEIN: Maybe another aspect of the progression of headache is defined by treatment. When younger patients get a migraine, they go to sleep. When they wake up, their migraine is gone. They then progress to a point where they are unable to sleep off the migraine. They combine sleep with over-the-counter drugs such as nonsteroidal anti-inflammatory drugs (NSAIDs) in order to abort the migraine. As the disease progresses, they need something stronger than sleep and NSAIDs. As the disease continues to progress and they develop symptoms such as depression, anxiety, and fatigue, they benefit less from sleep and NSAIDs and seek alternative therapies, such as triptans.
Eventually, some aspects of the progression make them more and more resistant to conventional treatment and clearly define a pathophysiological or pathological change that makes it more difficult for them to become pain-free or respond to medication.
DR. GOADSBY: I think the other aspect of this, which is not often stated but may be incredibly informative if we understood it, is the basis for the regression of this progression. It seems that the population estimates for chronic migraine are stable, and that there’s clearly a group of people for whom the frequency of headaches can increase each year. There must be, clearly, a group of people in equal size who go from having more headache to less headache, and I wish I thought that was because we treated them properly, but I don’t think that’s the case on a population basis.
The resolution is almost as interesting as the induction. When we talk about progression, we’re talking about addition of burden, whether in terms of frequency, change in the type of headache, or, as Dr. Burstein just said, treatment. The other aspect of progression that’s discussed is whether there’s any progression of a consequent nature: Progression to acquisition of brain changes and, what have been, I think, erroneously been called brain lesions, progression in cognitive function. Dr. Schoenen, do you have a view about any of those things?
DR. SCHOENEN: I do not really believe that the majority of migraine patients accumulate brain lesions over their lifetime, even when they progress. Most patients who progress and experience chronic migraines have migraines without aura, very few or no white-matter lesions, and very little or no increased risk for stroke.1 Brain lesions on magnetic resonance imaging (MRI) were mainly reported in migraine-with-aura patients, and predominantly in females. The nature of these lesions is not known. In some studies, their prevalence was somewhat correlated with attack frequency, but the majority of subjects in the general population who suffer from migraine with aura experience low frequency of attacks. So, I do not believe that migraine without aura causes lesions in the brain, but I do believe that migraine without aura impairs, to some extent, cognitive performance, but that’s not related to the frequency of attacks, but likely due to the abnormal information processing that can be recorded in the brain of migraineurs between attacks.
DR. GOADSBY: Yes, exactly. Dr. Charles?
DR. CHARLES: The other imaging modalities that have shown changes are morphometric studies with MRI and functional MRI scans that show chronic changes in brain structure and function, particularly in areas related to pain processing, in patients with migraine. That is, I believe, something that may be occurring in patients who have progression of migraine, that there’s a plasticity of the brain that results in these structural and functional changes over time. I think that’s an area of great interest in terms of trying to understand how to reverse that process of progression.
DR. SCHOENEN: I agree completely with that. The problem is that many of these changes do not seem to be very specific to migraine. They are merely a consequence of the recurring head pain and also found in other pain disorders. Very few are specific to migraine. When patients develop chronic migraine, central sensitization occurs, and plastic changes appear in brain areas involved in pain processing and control. These areas are not specific to migraine. Taken together, I think brain changes seen in episodic migraine interictally are, for most cases, causally related to the disorder. In chronic migraine, these migraine-specific changes become overwhelmed by other brain modifications related to chronic pain, which have therapeutic implications.
DR. CHARLES: Yes, I agree.
DR. BURSTEIN: I think the biggest question that keeps coming up from all the imaging studies that show differences between migraine and non-migraine patients or migraine patients that progress and migraine patients that do not progress is what comes first: the changes that we see, which are responsible for the patient’s symptoms in the migraine, or the progression of the headache, which is causing the brain changes. For this, at least now, we don’t have a clear answer, although I think that most believe that progression of the migraine results in progressive changes and the beginning of brain malfunction. But the answer is not clear, and this belief somewhat conflicts with the concept of genetics, because if migraine patients do have genetic defects, you expect all changes to be there all along.
DR. GOADSBY: We currently have no clear data on what happens to migraineurs’ brains over time. Various changes in structure have been reported, but we do not know what happens, for example, if the migraine is controlled, do the brain changes revert? First, we must consider whether brain changes over time are linked with anything related to the headache. For example, if there’s high headache frequency or severity and then resolution, did changes occur? There don’t seem to be any long-term consequences of migraines. All the work done studying French people over the age of 70 on a population basis points to no untoward effect of a migraine on cognitive status,2 as do the data from the Women’s Health Study.3 Prospective examination of cognitive functions in that cohort identified absolutely no cognitive death attributable to migraine status. Whatever is happening in the brain can’t be all bad, since it doesn’t seem to have palpable consequences. I find that reassuring for patients.
DR. GOADSBY: I find the cognitive facts very reassuring for patients. I also find it reassuring to be able to tell them, even those with small changes, that as long as they live to even 75, they won’t have any particular problems.
I think we’ve probably come to the broad brush, that is, a group of migraineurs who have increased frequency and some change in quality. The treatment effects are perhaps most important for them. Before we go into the details of the pathophysiology, we should get some comments about the role of analgesic use, or the use of it in, as it is sometimes described, the evolution of migraines. Does analgesic use drive or follow the problem? I’ll start with Dr. Burstein.
DR. BURSTEIN: I belong to the group of people who believe that analgesics are overused, especially opiates and barbiturates, and contribute tremendously and significantly to the transition from acute to chronic pain, and from treatment that works to treatment that doesn’t work. They contribute on a molecular basis to sensitization; increase hyperexcitability; and add to the molecular aspects of the pathophysiology of increased excitability along the pain pathways in general, and in this case along the active trigeminovascular pain pathway.
DR. GOADSBY: We probably all agree that opioids are a problem, however, it’s how you look at it. Do you have in mind a particular site in the brain or particular pathways when you think about this process, or do you think “outside the brain” when you think about opioids and their role in this problem?
DR. BURSTEIN: I think that it will be in the first synapse between the peripheral and the central neuron. I think that the opioid’s ability to virtually bring to almost a complete stop the glutamate transporter and the inability of glutamate to clear itself out of the synapse contribute a lot to accessibility to susceptible pain neurons in the spinal cord, which is not where they eliminate pain. They eliminate pain in the brain stem, the rostral ventral inner medulla, the periaqueductal gray, and basal ganglia. When you eliminate the “off switch” by stopping medication, you’re left with a hyperexcitable spinal cord that has spinal glia that has a significantly reduced ability to clear glutamate from the synapse in the spinal cord.
DR. SCHOENEN: You’re right, but is that specific to migraine or not? Do you think that chronification due to medication overuse exists in other pain disorders?
DR. BURSTEIN: Yes, I think we have known that since 1988, when it first became clear in animal studies and then in human studies that opioids produced allodynia, hyperalgesia, and central sensitization.4
DR. SCHOENEN: I agree, but opioids are not a problem in Europe. Opioids are a problem in the United States. Analgesics containing opioids are very rarely overused in Europe right now because there are stricter limitations in their availability. The only one that still exists on the market is codeine combined with paracetamol. The most frequently overused preparations are non-opioid analgesics or NSAIDs combined with caffeine or triptans. The underlying process may be different between these molecules. Do you agree that it is possible that the daily intake of analgesics or NSAIDs by fibromyalgia patients, for instance, may play a role in chronifying their pain?
DR. BURSTEIN: Yes, I do. I think that whenever we prescribe opioids we make a big mistake, especially in the field of headache.
DR. GOADSBY: I will say one thing about Europe, when I was practicing there, the single biggest problem with overuse was codeine because codeine was available in the supermarkets. Medication overuse has regional and cultural dimensions, depending on what you have access to. Dr. Charles?
DR. CHARLES: I think with regard to the opioids, the other thing to keep in mind is that while they’re commonly viewed as having depressant or inhibitory actions, they in fact are excitatory in many areas of the brain, as well as the spinal cord. For example, most of the commonly used opioids can in fact cause seizures, and clearly have excitatory effects in the cortex. So it’s quite possible that in an episodic disorder of brain excitability, like migraine, they’re actually working not simply by changing pain, but also by changing some of the basic mechanisms until they reach a threshold that triggers migraine in the brain, even before the pain starts.
DR. GOADSBY: From that hypothesis, you might predict that patients with migraine with aura and opioid overuse would have more aura. You see where I’m headed with that?
DR. CHARLES: Sure. I wasn’t necessarily specifically referring to the visual cortex, but, in general, making the point that opioids have excitatory effects in the brain and using seizures as an example of a phenomenon, but not necessarily saying that it’s the cortex itself. Maybe it’s the hypothalamus or the thalamus or some other area of the brain in which they’re exerting excitatory effects.
DR. BURSTEIN: It can be the peripheral nervous system. Look, they produce itch, suggesting they are excitatory to certain classes of peripheral receptors.
DR. GOADSBY: Dr. Charles, do you agree that opioid-induced medication overuse problems precede as opposed to follow increased headache frequency, because there is this possibility that some medication overuse is simply because headache gets worse and patients just do what they need to do? I’m not sure lumping everyone together and saying everyone who overuses actually produces headache with the overuse so much as there’s more than one group.
DR. CHARLES: That’s right. Broadening the discussion to other medications, I think that it’s important to not lump all the acute medications for migraine into the same categories because they have such pharmacologically distinct properties that it isn’t plausible that they could all have the same effects. I think, as Dr. Schoenen mentioned, the combination analgesics, particularly those with caffeine, are particularly problematic. Recently in the United States, we’ve had a big uproar because of a shortage of one of the aspirin-and-caffeine-containing preparations. That, I think, is an example of how caffeine-containing preparations can be particularly problematic as a cause of medication-overuse headache.
DR. GOADSBY: Yes, I think the other component of this must be that there is some predisposition to it. The two studies that I’m aware of, the one that we were involved in in the rheumatology clinic and the one that Becker did in the gastro clinic, clearly show that there are people who overuse opioids by any standard definition who don’t have headache at all as a problem. So, there’s an important interaction, I think, between a genetic predisposition and these medicines. It’s something that would be wonderful to get at so we could be able to understand who are at risk and who aren’t at risk. One day I hope that we’ll be able to do that. Do you think that people who are at risk for one type of overuse are at risk for all? Let me ask Dr. Schoenen.
DR. SCHOENEN: I don’t know. I can only say that I see patients in whom overuse recurs and with a different drug. There are patients with overuse of a combined analgesic who return to an episodic form of migraine after drug withdrawal, but come back to my office 6 months or 1 year later with daily headache and daily use of a simple NSAID or analgesic. There may be a genetic predisposition to chronification by overuse of any anti-migraine drug, despite the fact that in practice simple NSAIDs are less likely to chronify the disorder.
Just to pick up what Andrew said, there is clearly a difference between the drugs and their effect on the brain. For example, looking at sensitivity in the somatosensory cortex with evoked potentials, there’s clearly a difference between patients overusing triptans and those taking NSAIDs, although their clinical phenotype is the same.
DR. SCHOENEN: Oh, yes. Well that was a study where we looked at metabolic changes with fluorodeoxyglucose positron emission tomography in brain areas that belong to the so-called pain matrix, but also in areas that are known to be involved in substance abuse.5 What we found was that metabolism was clearly decreased in several areas that are thought to belong to the pain matrix, but these changes were reversible after withdrawal of the drug 3 weeks later. The only area where hypometabolism was not reversible after drug withdrawal was the orbitofrontal cortex. The orbitofrontal hypoactivity was even worse after withdrawal, and it was more pronounced in those patients who were overusing combined analgesics. The orbitofrontal cortex has been shown to play a crucial role in substance dependence. Its hypofunction could predispose patients to recurrence of medication-overuse headache. To prove this, we’re completing a long-term follow-up study.
DR. GOADSBY: That is interesting because I think that’s one of the important contributions to the pathophysiological understanding in humans.
DR. SCHOENEN: A Swiss group just published similar results measuring the amount of brain tissue with MRI.6 They found decreased tissue density in the orbitofrontal cortex, as well as in the dorsal pons, where abnormal activity is known to occur during migraine attacks.
DR. GOADSBY: You brought up nonsteroidals, a slightly more vexed issue. I’ll start with Dr. Charles. Do you think nonsteroidals, and you don’t have to lump them all together if you don’t want to, have a role in medication overuse in terms of inducing headache?
DR. CHARLES: My own view is no. It’s only the nonsteroidals in combination with caffeine that are the cause of medication overuse. I think that view is supported by the study by Bigal and Lipton,7 which basically suggests that, at a population level, frequent use of nonsteroidals is not associated with progression of headache. In fact, there’s a slight trend in the opposite direction, which has led them to suggest that it may possibly be protective. So, no, I do not put nonsteroidal anti-inflammatory drugs in the same category as a cause, but I see them more as a consequence, or frequent use as a consequence of frequent headache rather than as a cause.
DR. GOADSBY: How do you see the difference in a mechanistic sense? I’ll give everyone a chance to weigh in on this.
DR. CHARLES: This is something that may have to do with agonism versus antagonism of receptors and specific mechanisms of analgesia. I think the things that we think about that are the significant players in terms of causing medication overuse are ones that are working on neurotransmitter receptors, like γ-aminobutyric acid receptors and opioid receptors, and, in the case of caffeine, maybe adenosine receptors. I think the issue with the nonsteroidals is harder to understand, particularly how they might pharmacologically actually cause medication overuse. So, I think that mechanistically, those are the questions that are before us now.
DR. GOADSBY: Dr. Burstein, you published on nonsteroidals and triptans in the context of sensitization.8 What’s your view about this, particularly at a mechanistic level?
DR. BURSTEIN: Mechanistically, the data suggest that triptans disrupt communication between peripheral and central trigeminovascular neurons and that NSAIDs inhibit both the peripheral and the central neurons.
Accordingly, it is reasonable to suggest that triptans do not reverse central sensitization because they do not inhibit central trigeminovascular neurons directly, not at the level of the spinal cord at least, and that NSAIDs reverse central sensitization indirectly, through their anti-inflammatory action in the spinal cord (mostly unknown mechanism).
I think, again, that in the context of the opioid treatment, it became apparent both in the animal data and in patient data that opioid treatment makes patients resistant to successful NSAID treatment. NSAIDs work much better in patients who do not have a history of favoring opioids. Once patients begin to use opioids, however, they see a noticeable decline in the potential benefit of NSAIDs or triptan treatments. Again, I think that the key to that is the spinal cord inability to clear glutamate from the synapse, although I don’t think that the NSAIDs target glutamate release in any way.
DR. SCHOENEN: I do partially agree with what has been said. I think clinically, we clearly see patients who with overuse of simple analgesics, like paracetamol or a single NSAID like ibuprofen, enter the vicious circle of chronification and reverse to episodic migraine after reducing intake of these drugs.
The second point is that in the electrophysiological studies of patients overusing simple NSAIDs, there is clearly indication of sensitization in sensory cortices. Thirdly, Dr. Charles was alluding to the Bigal et al. study showing that NSAIDs protect against migraine chronification contrary to triptans.6 In this study, however, the protective effect of NSAIDs was only seen with patients who had low frequency of headaches. In patients with high frequency of headaches at baseline, NSAIDs also had a deleterious effect.
DR. GOADSBY: In the last few minutes that we have, I’d like to get some views about whether you think that more aggressive treatment with preventives would be helpful in terms of restricting headache progression. When medical practitioners see people who experience 6 or 8 headaches a month, and a couple months later they have 10 or maybe 12 or 14, they want to help them get better before they get worse. So if we intervened earlier, do we think that we could do a better job? Is that mechanistically plausible? I’ll start with you, Dr. Charles.
DR. CHARLES: I think it’s an appealing concept, but unfortunately I think that in practice we don’t see that concept being realized. Taking a cynical view, I think in many cases, even with preventative therapy, migraine finds its way around them, and even patients on preventative therapy end up having progression. So I think until we better understand the process, we can’t really say with confidence that early preventive therapy is something that is going to prevent the progression of the disorder.
DR. GOADSBY: Dr. Schoenen?
DR. SCHOENEN: I fundamentally agree with that. I think we are very lousy in the prevention of migraine. Most of the drugs don’t reach 50% efficacy. The patients who respond to these drugs may be those who have a peculiar pathophysiological, possibly genetic, profile, and do not progress. Those who do not respond are probably those who are most prone to chronification of migraine and at last fail on all available preventative drugs. So, in addition to much better preventative treatments, we also really need many more treatments.
DR. GOADSBY: Yes. Dr. Burstein?
DR. BURSTEIN: Well, I want to take it in a slightly different direction. I am aware of the fact that there is no evidence for it because nobody has done the study, but the question that I would like to answer is whether migraine progression would look completely different in a group of patients whose migraine attacks were treated early from the first migraine attack in their life (ie, they didn’t let their migraine last more than a few hours). Comparing this "early-treatment" group to a group of patients who treat late (ie, they let themselves have a migraine for 8, 10, or 12 hours before it goes away by itself or before they treat it).
DR. GOADSBY: Well, that would be an interesting study, very expensive as well. But as you say, one of the things we lack very much in longitudinal study is what’s really a dreadful problem, because whatever we think about the pathophysiology of headache progression, we’d all agree it’s bad to have more headache, it’s bad to have worse headache, and it’s bad to have headaches that don’t respond to therapy. It’s a subject which deserves study.
FoxP2 Media LLC is the publisher of The Medical Roundtable.
DR. BURSTEIN: I am Rami Burstein. I am the academic director of the Headache Center at Beth Israel Deaconess Medical Center; Vice Chairman of Research in the Department of Anesthesia and Critical Care; and Professor of Anesthesia and Neuroscience at Harvard Medical School.
DR. CHARLES: I am Andrew Charles. I am a professor in the Department of Neurology at the UCLA School of Medicine and Director of the Headache Research and Treatment Program here.
DR. SCHOENEN: I’m Jean Schoenen. I’m a neurologist and professor at the University of Liege in Belgium and Director of the Headache Research Unit at the University hospital.
DR. GOADSBY: We are talking about the pathophysiology of headache progression, and in order to so, we should define at the start what we mean by “headache progression” so we’re all starting from the same point. Dr. Charles, when we talk about headache progression, what does it make you think about?
DR. CHARLES: It makes me think about a patient who has episodic migraine that occurs infrequently, let’s say once a month or once every other month, who at some point in the course of their life begins having headaches much more frequently, let’s say 2 or 3 or 4 times per week. Accompanying that, there may be a change in the quality of the headache, where it becomes somewhat less classic for episodic migraine and has fewer of the typical features that we consider associated with migraines.
DR. GOADSBY: That’s very helpful. What we’re really talking about and what we’re going to narrow ourselves down to is talking about the pathophysiology of migraine progression because we wouldn’t be able to cover all of the types of headaches. Dr. Schoenen, what is your comment on headache progression?
DR. SCHOENEN: I agree with what Dr. Charles said, although, clinically, I think that this disorder is quite heterogeneous between patients. Any migraineur has experienced, at some time in his life, progression of the disorder, where it becomes more frequent and then drops back again to its former frequency, but there seems to be a small population of patients in whom the disorder sometimes progress and then tips over into chronic migraine. That’s not the case for all migraineurs who progress, and many patients progress for some time and then do not progress up to what we call chronic migraines. So that may be something we have to consider from the pathophysiological point of view: What differs between those who progress to chronic migraine from those who do not?
DR. GOADSBY: Yes, you make a good point. Dr. Burstein?
DR. BURSTEIN: Maybe another aspect of the progression of headache is defined by treatment. When younger patients get a migraine, they go to sleep. When they wake up, their migraine is gone. They then progress to a point where they are unable to sleep off the migraine. They combine sleep with over-the-counter drugs such as nonsteroidal anti-inflammatory drugs (NSAIDs) in order to abort the migraine. As the disease progresses, they need something stronger than sleep and NSAIDs. As the disease continues to progress and they develop symptoms such as depression, anxiety, and fatigue, they benefit less from sleep and NSAIDs and seek alternative therapies, such as triptans.
Eventually, some aspects of the progression make them more and more resistant to conventional treatment and clearly define a pathophysiological or pathological change that makes it more difficult for them to become pain-free or respond to medication.
DR. GOADSBY: I think the other aspect of this, which is not often stated but may be incredibly informative if we understood it, is the basis for the regression of this progression. It seems that the population estimates for chronic migraine are stable, and that there’s clearly a group of people for whom the frequency of headaches can increase each year. There must be, clearly, a group of people in equal size who go from having more headache to less headache, and I wish I thought that was because we treated them properly, but I don’t think that’s the case on a population basis.
The resolution is almost as interesting as the induction. When we talk about progression, we’re talking about addition of burden, whether in terms of frequency, change in the type of headache, or, as Dr. Burstein just said, treatment. The other aspect of progression that’s discussed is whether there’s any progression of a consequent nature: Progression to acquisition of brain changes and, what have been, I think, erroneously been called brain lesions, progression in cognitive function. Dr. Schoenen, do you have a view about any of those things?
DR. SCHOENEN: I do not really believe that the majority of migraine patients accumulate brain lesions over their lifetime, even when they progress. Most patients who progress and experience chronic migraines have migraines without aura, very few or no white-matter lesions, and very little or no increased risk for stroke.1 Brain lesions on magnetic resonance imaging (MRI) were mainly reported in migraine-with-aura patients, and predominantly in females. The nature of these lesions is not known. In some studies, their prevalence was somewhat correlated with attack frequency, but the majority of subjects in the general population who suffer from migraine with aura experience low frequency of attacks. So, I do not believe that migraine without aura causes lesions in the brain, but I do believe that migraine without aura impairs, to some extent, cognitive performance, but that’s not related to the frequency of attacks, but likely due to the abnormal information processing that can be recorded in the brain of migraineurs between attacks.
DR. GOADSBY: Yes, exactly. Dr. Charles?
DR. CHARLES: The other imaging modalities that have shown changes are morphometric studies with MRI and functional MRI scans that show chronic changes in brain structure and function, particularly in areas related to pain processing, in patients with migraine. That is, I believe, something that may be occurring in patients who have progression of migraine, that there’s a plasticity of the brain that results in these structural and functional changes over time. I think that’s an area of great interest in terms of trying to understand how to reverse that process of progression.
DR. SCHOENEN: I agree completely with that. The problem is that many of these changes do not seem to be very specific to migraine. They are merely a consequence of the recurring head pain and also found in other pain disorders. Very few are specific to migraine. When patients develop chronic migraine, central sensitization occurs, and plastic changes appear in brain areas involved in pain processing and control. These areas are not specific to migraine. Taken together, I think brain changes seen in episodic migraine interictally are, for most cases, causally related to the disorder. In chronic migraine, these migraine-specific changes become overwhelmed by other brain modifications related to chronic pain, which have therapeutic implications.
DR. CHARLES: Yes, I agree.
DR. BURSTEIN: I think the biggest question that keeps coming up from all the imaging studies that show differences between migraine and non-migraine patients or migraine patients that progress and migraine patients that do not progress is what comes first: the changes that we see, which are responsible for the patient’s symptoms in the migraine, or the progression of the headache, which is causing the brain changes. For this, at least now, we don’t have a clear answer, although I think that most believe that progression of the migraine results in progressive changes and the beginning of brain malfunction. But the answer is not clear, and this belief somewhat conflicts with the concept of genetics, because if migraine patients do have genetic defects, you expect all changes to be there all along.
DR. GOADSBY: We currently have no clear data on what happens to migraineurs’ brains over time. Various changes in structure have been reported, but we do not know what happens, for example, if the migraine is controlled, do the brain changes revert? First, we must consider whether brain changes over time are linked with anything related to the headache. For example, if there’s high headache frequency or severity and then resolution, did changes occur? There don’t seem to be any long-term consequences of migraines. All the work done studying French people over the age of 70 on a population basis points to no untoward effect of a migraine on cognitive status,2 as do the data from the Women’s Health Study.3 Prospective examination of cognitive functions in that cohort identified absolutely no cognitive death attributable to migraine status. Whatever is happening in the brain can’t be all bad, since it doesn’t seem to have palpable consequences. I find that reassuring for patients.
DR. GOADSBY: I find the cognitive facts very reassuring for patients. I also find it reassuring to be able to tell them, even those with small changes, that as long as they live to even 75, they won’t have any particular problems.
I think we’ve probably come to the broad brush, that is, a group of migraineurs who have increased frequency and some change in quality. The treatment effects are perhaps most important for them. Before we go into the details of the pathophysiology, we should get some comments about the role of analgesic use, or the use of it in, as it is sometimes described, the evolution of migraines. Does analgesic use drive or follow the problem? I’ll start with Dr. Burstein.
DR. BURSTEIN: I belong to the group of people who believe that analgesics are overused, especially opiates and barbiturates, and contribute tremendously and significantly to the transition from acute to chronic pain, and from treatment that works to treatment that doesn’t work. They contribute on a molecular basis to sensitization; increase hyperexcitability; and add to the molecular aspects of the pathophysiology of increased excitability along the pain pathways in general, and in this case along the active trigeminovascular pain pathway.
DR. GOADSBY: We probably all agree that opioids are a problem, however, it’s how you look at it. Do you have in mind a particular site in the brain or particular pathways when you think about this process, or do you think “outside the brain” when you think about opioids and their role in this problem?
DR. BURSTEIN: I think that it will be in the first synapse between the peripheral and the central neuron. I think that the opioid’s ability to virtually bring to almost a complete stop the glutamate transporter and the inability of glutamate to clear itself out of the synapse contribute a lot to accessibility to susceptible pain neurons in the spinal cord, which is not where they eliminate pain. They eliminate pain in the brain stem, the rostral ventral inner medulla, the periaqueductal gray, and basal ganglia. When you eliminate the “off switch” by stopping medication, you’re left with a hyperexcitable spinal cord that has spinal glia that has a significantly reduced ability to clear glutamate from the synapse in the spinal cord.
DR. SCHOENEN: You’re right, but is that specific to migraine or not? Do you think that chronification due to medication overuse exists in other pain disorders?
DR. BURSTEIN: Yes, I think we have known that since 1988, when it first became clear in animal studies and then in human studies that opioids produced allodynia, hyperalgesia, and central sensitization.4
DR. SCHOENEN: I agree, but opioids are not a problem in Europe. Opioids are a problem in the United States. Analgesics containing opioids are very rarely overused in Europe right now because there are stricter limitations in their availability. The only one that still exists on the market is codeine combined with paracetamol. The most frequently overused preparations are non-opioid analgesics or NSAIDs combined with caffeine or triptans. The underlying process may be different between these molecules. Do you agree that it is possible that the daily intake of analgesics or NSAIDs by fibromyalgia patients, for instance, may play a role in chronifying their pain?
DR. BURSTEIN: Yes, I do. I think that whenever we prescribe opioids we make a big mistake, especially in the field of headache.
DR. GOADSBY: I will say one thing about Europe, when I was practicing there, the single biggest problem with overuse was codeine because codeine was available in the supermarkets. Medication overuse has regional and cultural dimensions, depending on what you have access to. Dr. Charles?
DR. CHARLES: I think with regard to the opioids, the other thing to keep in mind is that while they’re commonly viewed as having depressant or inhibitory actions, they in fact are excitatory in many areas of the brain, as well as the spinal cord. For example, most of the commonly used opioids can in fact cause seizures, and clearly have excitatory effects in the cortex. So it’s quite possible that in an episodic disorder of brain excitability, like migraine, they’re actually working not simply by changing pain, but also by changing some of the basic mechanisms until they reach a threshold that triggers migraine in the brain, even before the pain starts.
DR. GOADSBY: From that hypothesis, you might predict that patients with migraine with aura and opioid overuse would have more aura. You see where I’m headed with that?
DR. CHARLES: Sure. I wasn’t necessarily specifically referring to the visual cortex, but, in general, making the point that opioids have excitatory effects in the brain and using seizures as an example of a phenomenon, but not necessarily saying that it’s the cortex itself. Maybe it’s the hypothalamus or the thalamus or some other area of the brain in which they’re exerting excitatory effects.
DR. BURSTEIN: It can be the peripheral nervous system. Look, they produce itch, suggesting they are excitatory to certain classes of peripheral receptors.
DR. GOADSBY: Dr. Charles, do you agree that opioid-induced medication overuse problems precede as opposed to follow increased headache frequency, because there is this possibility that some medication overuse is simply because headache gets worse and patients just do what they need to do? I’m not sure lumping everyone together and saying everyone who overuses actually produces headache with the overuse so much as there’s more than one group.
DR. CHARLES: That’s right. Broadening the discussion to other medications, I think that it’s important to not lump all the acute medications for migraine into the same categories because they have such pharmacologically distinct properties that it isn’t plausible that they could all have the same effects. I think, as Dr. Schoenen mentioned, the combination analgesics, particularly those with caffeine, are particularly problematic. Recently in the United States, we’ve had a big uproar because of a shortage of one of the aspirin-and-caffeine-containing preparations. That, I think, is an example of how caffeine-containing preparations can be particularly problematic as a cause of medication-overuse headache.
DR. GOADSBY: Yes, I think the other component of this must be that there is some predisposition to it. The two studies that I’m aware of, the one that we were involved in in the rheumatology clinic and the one that Becker did in the gastro clinic, clearly show that there are people who overuse opioids by any standard definition who don’t have headache at all as a problem. So, there’s an important interaction, I think, between a genetic predisposition and these medicines. It’s something that would be wonderful to get at so we could be able to understand who are at risk and who aren’t at risk. One day I hope that we’ll be able to do that. Do you think that people who are at risk for one type of overuse are at risk for all? Let me ask Dr. Schoenen.
DR. SCHOENEN: I don’t know. I can only say that I see patients in whom overuse recurs and with a different drug. There are patients with overuse of a combined analgesic who return to an episodic form of migraine after drug withdrawal, but come back to my office 6 months or 1 year later with daily headache and daily use of a simple NSAID or analgesic. There may be a genetic predisposition to chronification by overuse of any anti-migraine drug, despite the fact that in practice simple NSAIDs are less likely to chronify the disorder.
Just to pick up what Andrew said, there is clearly a difference between the drugs and their effect on the brain. For example, looking at sensitivity in the somatosensory cortex with evoked potentials, there’s clearly a difference between patients overusing triptans and those taking NSAIDs, although their clinical phenotype is the same.
DR. SCHOENEN: Oh, yes. Well that was a study where we looked at metabolic changes with fluorodeoxyglucose positron emission tomography in brain areas that belong to the so-called pain matrix, but also in areas that are known to be involved in substance abuse.5 What we found was that metabolism was clearly decreased in several areas that are thought to belong to the pain matrix, but these changes were reversible after withdrawal of the drug 3 weeks later. The only area where hypometabolism was not reversible after drug withdrawal was the orbitofrontal cortex. The orbitofrontal hypoactivity was even worse after withdrawal, and it was more pronounced in those patients who were overusing combined analgesics. The orbitofrontal cortex has been shown to play a crucial role in substance dependence. Its hypofunction could predispose patients to recurrence of medication-overuse headache. To prove this, we’re completing a long-term follow-up study.
DR. GOADSBY: That is interesting because I think that’s one of the important contributions to the pathophysiological understanding in humans.
DR. SCHOENEN: A Swiss group just published similar results measuring the amount of brain tissue with MRI.6 They found decreased tissue density in the orbitofrontal cortex, as well as in the dorsal pons, where abnormal activity is known to occur during migraine attacks.
DR. GOADSBY: You brought up nonsteroidals, a slightly more vexed issue. I’ll start with Dr. Charles. Do you think nonsteroidals, and you don’t have to lump them all together if you don’t want to, have a role in medication overuse in terms of inducing headache?
DR. CHARLES: My own view is no. It’s only the nonsteroidals in combination with caffeine that are the cause of medication overuse. I think that view is supported by the study by Bigal and Lipton,7 which basically suggests that, at a population level, frequent use of nonsteroidals is not associated with progression of headache. In fact, there’s a slight trend in the opposite direction, which has led them to suggest that it may possibly be protective. So, no, I do not put nonsteroidal anti-inflammatory drugs in the same category as a cause, but I see them more as a consequence, or frequent use as a consequence of frequent headache rather than as a cause.
DR. GOADSBY: How do you see the difference in a mechanistic sense? I’ll give everyone a chance to weigh in on this.
DR. CHARLES: This is something that may have to do with agonism versus antagonism of receptors and specific mechanisms of analgesia. I think the things that we think about that are the significant players in terms of causing medication overuse are ones that are working on neurotransmitter receptors, like γ-aminobutyric acid receptors and opioid receptors, and, in the case of caffeine, maybe adenosine receptors. I think the issue with the nonsteroidals is harder to understand, particularly how they might pharmacologically actually cause medication overuse. So, I think that mechanistically, those are the questions that are before us now.
DR. GOADSBY: Dr. Burstein, you published on nonsteroidals and triptans in the context of sensitization.8 What’s your view about this, particularly at a mechanistic level?
DR. BURSTEIN: Mechanistically, the data suggest that triptans disrupt communication between peripheral and central trigeminovascular neurons and that NSAIDs inhibit both the peripheral and the central neurons.
Accordingly, it is reasonable to suggest that triptans do not reverse central sensitization because they do not inhibit central trigeminovascular neurons directly, not at the level of the spinal cord at least, and that NSAIDs reverse central sensitization indirectly, through their anti-inflammatory action in the spinal cord (mostly unknown mechanism).
I think, again, that in the context of the opioid treatment, it became apparent both in the animal data and in patient data that opioid treatment makes patients resistant to successful NSAID treatment. NSAIDs work much better in patients who do not have a history of favoring opioids. Once patients begin to use opioids, however, they see a noticeable decline in the potential benefit of NSAIDs or triptan treatments. Again, I think that the key to that is the spinal cord inability to clear glutamate from the synapse, although I don’t think that the NSAIDs target glutamate release in any way.
DR. SCHOENEN: I do partially agree with what has been said. I think clinically, we clearly see patients who with overuse of simple analgesics, like paracetamol or a single NSAID like ibuprofen, enter the vicious circle of chronification and reverse to episodic migraine after reducing intake of these drugs.
The second point is that in the electrophysiological studies of patients overusing simple NSAIDs, there is clearly indication of sensitization in sensory cortices. Thirdly, Dr. Charles was alluding to the Bigal et al. study showing that NSAIDs protect against migraine chronification contrary to triptans.6 In this study, however, the protective effect of NSAIDs was only seen with patients who had low frequency of headaches. In patients with high frequency of headaches at baseline, NSAIDs also had a deleterious effect.
DR. GOADSBY: In the last few minutes that we have, I’d like to get some views about whether you think that more aggressive treatment with preventives would be helpful in terms of restricting headache progression. When medical practitioners see people who experience 6 or 8 headaches a month, and a couple months later they have 10 or maybe 12 or 14, they want to help them get better before they get worse. So if we intervened earlier, do we think that we could do a better job? Is that mechanistically plausible? I’ll start with you, Dr. Charles.
DR. CHARLES: I think it’s an appealing concept, but unfortunately I think that in practice we don’t see that concept being realized. Taking a cynical view, I think in many cases, even with preventative therapy, migraine finds its way around them, and even patients on preventative therapy end up having progression. So I think until we better understand the process, we can’t really say with confidence that early preventive therapy is something that is going to prevent the progression of the disorder.
DR. GOADSBY: Dr. Schoenen?
DR. SCHOENEN: I fundamentally agree with that. I think we are very lousy in the prevention of migraine. Most of the drugs don’t reach 50% efficacy. The patients who respond to these drugs may be those who have a peculiar pathophysiological, possibly genetic, profile, and do not progress. Those who do not respond are probably those who are most prone to chronification of migraine and at last fail on all available preventative drugs. So, in addition to much better preventative treatments, we also really need many more treatments.
DR. GOADSBY: Yes. Dr. Burstein?
DR. BURSTEIN: Well, I want to take it in a slightly different direction. I am aware of the fact that there is no evidence for it because nobody has done the study, but the question that I would like to answer is whether migraine progression would look completely different in a group of patients whose migraine attacks were treated early from the first migraine attack in their life (ie, they didn’t let their migraine last more than a few hours). Comparing this "early-treatment" group to a group of patients who treat late (ie, they let themselves have a migraine for 8, 10, or 12 hours before it goes away by itself or before they treat it).
DR. GOADSBY: Well, that would be an interesting study, very expensive as well. But as you say, one of the things we lack very much in longitudinal study is what’s really a dreadful problem, because whatever we think about the pathophysiology of headache progression, we’d all agree it’s bad to have more headache, it’s bad to have worse headache, and it’s bad to have headaches that don’t respond to therapy. It’s a subject which deserves study.
FoxP2 Media LLC is the publisher of The Medical Roundtable.
DR. BURSTEIN: I am Rami Burstein. I am the academic director of the Headache Center at Beth Israel Deaconess Medical Center; Vice Chairman of Research in the Department of Anesthesia and Critical Care; and Professor of Anesthesia and Neuroscience at Harvard Medical School.
DR. CHARLES: I am Andrew Charles. I am a professor in the Department of Neurology at the UCLA School of Medicine and Director of the Headache Research and Treatment Program here.
DR. SCHOENEN: I’m Jean Schoenen. I’m a neurologist and professor at the University of Liege in Belgium and Director of the Headache Research Unit at the University hospital.
DR. GOADSBY: We are talking about the pathophysiology of headache progression, and in order to so, we should define at the start what we mean by “headache progression” so we’re all starting from the same point. Dr. Charles, when we talk about headache progression, what does it make you think about?
DR. CHARLES: It makes me think about a patient who has episodic migraine that occurs infrequently, let’s say once a month or once every other month, who at some point in the course of their life begins having headaches much more frequently, let’s say 2 or 3 or 4 times per week. Accompanying that, there may be a change in the quality of the headache, where it becomes somewhat less classic for episodic migraine and has fewer of the typical features that we consider associated with migraines.
DR. GOADSBY: That’s very helpful. What we’re really talking about and what we’re going to narrow ourselves down to is talking about the pathophysiology of migraine progression because we wouldn’t be able to cover all of the types of headaches. Dr. Schoenen, what is your comment on headache progression?
DR. SCHOENEN: I agree with what Dr. Charles said, although, clinically, I think that this disorder is quite heterogeneous between patients. Any migraineur has experienced, at some time in his life, progression of the disorder, where it becomes more frequent and then drops back again to its former frequency, but there seems to be a small population of patients in whom the disorder sometimes progress and then tips over into chronic migraine. That’s not the case for all migraineurs who progress, and many patients progress for some time and then do not progress up to what we call chronic migraines. So that may be something we have to consider from the pathophysiological point of view: What differs between those who progress to chronic migraine from those who do not?
DR. GOADSBY: Yes, you make a good point. Dr. Burstein?
DR. BURSTEIN: Maybe another aspect of the progression of headache is defined by treatment. When younger patients get a migraine, they go to sleep. When they wake up, their migraine is gone. They then progress to a point where they are unable to sleep off the migraine. They combine sleep with over-the-counter drugs such as nonsteroidal anti-inflammatory drugs (NSAIDs) in order to abort the migraine. As the disease progresses, they need something stronger than sleep and NSAIDs. As the disease continues to progress and they develop symptoms such as depression, anxiety, and fatigue, they benefit less from sleep and NSAIDs and seek alternative therapies, such as triptans.
Eventually, some aspects of the progression make them more and more resistant to conventional treatment and clearly define a pathophysiological or pathological change that makes it more difficult for them to become pain-free or respond to medication.
DR. GOADSBY: I think the other aspect of this, which is not often stated but may be incredibly informative if we understood it, is the basis for the regression of this progression. It seems that the population estimates for chronic migraine are stable, and that there’s clearly a group of people for whom the frequency of headaches can increase each year. There must be, clearly, a group of people in equal size who go from having more headache to less headache, and I wish I thought that was because we treated them properly, but I don’t think that’s the case on a population basis.
The resolution is almost as interesting as the induction. When we talk about progression, we’re talking about addition of burden, whether in terms of frequency, change in the type of headache, or, as Dr. Burstein just said, treatment. The other aspect of progression that’s discussed is whether there’s any progression of a consequent nature: Progression to acquisition of brain changes and, what have been, I think, erroneously been called brain lesions, progression in cognitive function. Dr. Schoenen, do you have a view about any of those things?
DR. SCHOENEN: I do not really believe that the majority of migraine patients accumulate brain lesions over their lifetime, even when they progress. Most patients who progress and experience chronic migraines have migraines without aura, very few or no white-matter lesions, and very little or no increased risk for stroke.1 Brain lesions on magnetic resonance imaging (MRI) were mainly reported in migraine-with-aura patients, and predominantly in females. The nature of these lesions is not known. In some studies, their prevalence was somewhat correlated with attack frequency, but the majority of subjects in the general population who suffer from migraine with aura experience low frequency of attacks. So, I do not believe that migraine without aura causes lesions in the brain, but I do believe that migraine without aura impairs, to some extent, cognitive performance, but that’s not related to the frequency of attacks, but likely due to the abnormal information processing that can be recorded in the brain of migraineurs between attacks.
DR. GOADSBY: Yes, exactly. Dr. Charles?
DR. CHARLES: The other imaging modalities that have shown changes are morphometric studies with MRI and functional MRI scans that show chronic changes in brain structure and function, particularly in areas related to pain processing, in patients with migraine. That is, I believe, something that may be occurring in patients who have progression of migraine, that there’s a plasticity of the brain that results in these structural and functional changes over time. I think that’s an area of great interest in terms of trying to understand how to reverse that process of progression.
DR. SCHOENEN: I agree completely with that. The problem is that many of these changes do not seem to be very specific to migraine. They are merely a consequence of the recurring head pain and also found in other pain disorders. Very few are specific to migraine. When patients develop chronic migraine, central sensitization occurs, and plastic changes appear in brain areas involved in pain processing and control. These areas are not specific to migraine. Taken together, I think brain changes seen in episodic migraine interictally are, for most cases, causally related to the disorder. In chronic migraine, these migraine-specific changes become overwhelmed by other brain modifications related to chronic pain, which have therapeutic implications.
DR. CHARLES: Yes, I agree.
DR. BURSTEIN: I think the biggest question that keeps coming up from all the imaging studies that show differences between migraine and non-migraine patients or migraine patients that progress and migraine patients that do not progress is what comes first: the changes that we see, which are responsible for the patient’s symptoms in the migraine, or the progression of the headache, which is causing the brain changes. For this, at least now, we don’t have a clear answer, although I think that most believe that progression of the migraine results in progressive changes and the beginning of brain malfunction. But the answer is not clear, and this belief somewhat conflicts with the concept of genetics, because if migraine patients do have genetic defects, you expect all changes to be there all along.
DR. GOADSBY: We currently have no clear data on what happens to migraineurs’ brains over time. Various changes in structure have been reported, but we do not know what happens, for example, if the migraine is controlled, do the brain changes revert? First, we must consider whether brain changes over time are linked with anything related to the headache. For example, if there’s high headache frequency or severity and then resolution, did changes occur? There don’t seem to be any long-term consequences of migraines. All the work done studying French people over the age of 70 on a population basis points to no untoward effect of a migraine on cognitive status,2 as do the data from the Women’s Health Study.3 Prospective examination of cognitive functions in that cohort identified absolutely no cognitive death attributable to migraine status. Whatever is happening in the brain can’t be all bad, since it doesn’t seem to have palpable consequences. I find that reassuring for patients.
DR. GOADSBY: I find the cognitive facts very reassuring for patients. I also find it reassuring to be able to tell them, even those with small changes, that as long as they live to even 75, they won’t have any particular problems.
I think we’ve probably come to the broad brush, that is, a group of migraineurs who have increased frequency and some change in quality. The treatment effects are perhaps most important for them. Before we go into the details of the pathophysiology, we should get some comments about the role of analgesic use, or the use of it in, as it is sometimes described, the evolution of migraines. Does analgesic use drive or follow the problem? I’ll start with Dr. Burstein.
DR. BURSTEIN: I belong to the group of people who believe that analgesics are overused, especially opiates and barbiturates, and contribute tremendously and significantly to the transition from acute to chronic pain, and from treatment that works to treatment that doesn’t work. They contribute on a molecular basis to sensitization; increase hyperexcitability; and add to the molecular aspects of the pathophysiology of increased excitability along the pain pathways in general, and in this case along the active trigeminovascular pain pathway.
DR. GOADSBY: We probably all agree that opioids are a problem, however, it’s how you look at it. Do you have in mind a particular site in the brain or particular pathways when you think about this process, or do you think “outside the brain” when you think about opioids and their role in this problem?
DR. BURSTEIN: I think that it will be in the first synapse between the peripheral and the central neuron. I think that the opioid’s ability to virtually bring to almost a complete stop the glutamate transporter and the inability of glutamate to clear itself out of the synapse contribute a lot to accessibility to susceptible pain neurons in the spinal cord, which is not where they eliminate pain. They eliminate pain in the brain stem, the rostral ventral inner medulla, the periaqueductal gray, and basal ganglia. When you eliminate the “off switch” by stopping medication, you’re left with a hyperexcitable spinal cord that has spinal glia that has a significantly reduced ability to clear glutamate from the synapse in the spinal cord.
DR. SCHOENEN: You’re right, but is that specific to migraine or not? Do you think that chronification due to medication overuse exists in other pain disorders?
DR. BURSTEIN: Yes, I think we have known that since 1988, when it first became clear in animal studies and then in human studies that opioids produced allodynia, hyperalgesia, and central sensitization.4
DR. SCHOENEN: I agree, but opioids are not a problem in Europe. Opioids are a problem in the United States. Analgesics containing opioids are very rarely overused in Europe right now because there are stricter limitations in their availability. The only one that still exists on the market is codeine combined with paracetamol. The most frequently overused preparations are non-opioid analgesics or NSAIDs combined with caffeine or triptans. The underlying process may be different between these molecules. Do you agree that it is possible that the daily intake of analgesics or NSAIDs by fibromyalgia patients, for instance, may play a role in chronifying their pain?
DR. BURSTEIN: Yes, I do. I think that whenever we prescribe opioids we make a big mistake, especially in the field of headache.
DR. GOADSBY: I will say one thing about Europe, when I was practicing there, the single biggest problem with overuse was codeine because codeine was available in the supermarkets. Medication overuse has regional and cultural dimensions, depending on what you have access to. Dr. Charles?
DR. CHARLES: I think with regard to the opioids, the other thing to keep in mind is that while they’re commonly viewed as having depressant or inhibitory actions, they in fact are excitatory in many areas of the brain, as well as the spinal cord. For example, most of the commonly used opioids can in fact cause seizures, and clearly have excitatory effects in the cortex. So it’s quite possible that in an episodic disorder of brain excitability, like migraine, they’re actually working not simply by changing pain, but also by changing some of the basic mechanisms until they reach a threshold that triggers migraine in the brain, even before the pain starts.
DR. GOADSBY: From that hypothesis, you might predict that patients with migraine with aura and opioid overuse would have more aura. You see where I’m headed with that?
DR. CHARLES: Sure. I wasn’t necessarily specifically referring to the visual cortex, but, in general, making the point that opioids have excitatory effects in the brain and using seizures as an example of a phenomenon, but not necessarily saying that it’s the cortex itself. Maybe it’s the hypothalamus or the thalamus or some other area of the brain in which they’re exerting excitatory effects.
DR. BURSTEIN: It can be the peripheral nervous system. Look, they produce itch, suggesting they are excitatory to certain classes of peripheral receptors.
DR. GOADSBY: Dr. Charles, do you agree that opioid-induced medication overuse problems precede as opposed to follow increased headache frequency, because there is this possibility that some medication overuse is simply because headache gets worse and patients just do what they need to do? I’m not sure lumping everyone together and saying everyone who overuses actually produces headache with the overuse so much as there’s more than one group.
DR. CHARLES: That’s right. Broadening the discussion to other medications, I think that it’s important to not lump all the acute medications for migraine into the same categories because they have such pharmacologically distinct properties that it isn’t plausible that they could all have the same effects. I think, as Dr. Schoenen mentioned, the combination analgesics, particularly those with caffeine, are particularly problematic. Recently in the United States, we’ve had a big uproar because of a shortage of one of the aspirin-and-caffeine-containing preparations. That, I think, is an example of how caffeine-containing preparations can be particularly problematic as a cause of medication-overuse headache.
DR. GOADSBY: Yes, I think the other component of this must be that there is some predisposition to it. The two studies that I’m aware of, the one that we were involved in in the rheumatology clinic and the one that Becker did in the gastro clinic, clearly show that there are people who overuse opioids by any standard definition who don’t have headache at all as a problem. So, there’s an important interaction, I think, between a genetic predisposition and these medicines. It’s something that would be wonderful to get at so we could be able to understand who are at risk and who aren’t at risk. One day I hope that we’ll be able to do that. Do you think that people who are at risk for one type of overuse are at risk for all? Let me ask Dr. Schoenen.
DR. SCHOENEN: I don’t know. I can only say that I see patients in whom overuse recurs and with a different drug. There are patients with overuse of a combined analgesic who return to an episodic form of migraine after drug withdrawal, but come back to my office 6 months or 1 year later with daily headache and daily use of a simple NSAID or analgesic. There may be a genetic predisposition to chronification by overuse of any anti-migraine drug, despite the fact that in practice simple NSAIDs are less likely to chronify the disorder.
Just to pick up what Andrew said, there is clearly a difference between the drugs and their effect on the brain. For example, looking at sensitivity in the somatosensory cortex with evoked potentials, there’s clearly a difference between patients overusing triptans and those taking NSAIDs, although their clinical phenotype is the same.
DR. SCHOENEN: Oh, yes. Well that was a study where we looked at metabolic changes with fluorodeoxyglucose positron emission tomography in brain areas that belong to the so-called pain matrix, but also in areas that are known to be involved in substance abuse.5 What we found was that metabolism was clearly decreased in several areas that are thought to belong to the pain matrix, but these changes were reversible after withdrawal of the drug 3 weeks later. The only area where hypometabolism was not reversible after drug withdrawal was the orbitofrontal cortex. The orbitofrontal hypoactivity was even worse after withdrawal, and it was more pronounced in those patients who were overusing combined analgesics. The orbitofrontal cortex has been shown to play a crucial role in substance dependence. Its hypofunction could predispose patients to recurrence of medication-overuse headache. To prove this, we’re completing a long-term follow-up study.
DR. GOADSBY: That is interesting because I think that’s one of the important contributions to the pathophysiological understanding in humans.
DR. SCHOENEN: A Swiss group just published similar results measuring the amount of brain tissue with MRI.6 They found decreased tissue density in the orbitofrontal cortex, as well as in the dorsal pons, where abnormal activity is known to occur during migraine attacks.
DR. GOADSBY: You brought up nonsteroidals, a slightly more vexed issue. I’ll start with Dr. Charles. Do you think nonsteroidals, and you don’t have to lump them all together if you don’t want to, have a role in medication overuse in terms of inducing headache?
DR. CHARLES: My own view is no. It’s only the nonsteroidals in combination with caffeine that are the cause of medication overuse. I think that view is supported by the study by Bigal and Lipton,7 which basically suggests that, at a population level, frequent use of nonsteroidals is not associated with progression of headache. In fact, there’s a slight trend in the opposite direction, which has led them to suggest that it may possibly be protective. So, no, I do not put nonsteroidal anti-inflammatory drugs in the same category as a cause, but I see them more as a consequence, or frequent use as a consequence of frequent headache rather than as a cause.
DR. GOADSBY: How do you see the difference in a mechanistic sense? I’ll give everyone a chance to weigh in on this.
DR. CHARLES: This is something that may have to do with agonism versus antagonism of receptors and specific mechanisms of analgesia. I think the things that we think about that are the significant players in terms of causing medication overuse are ones that are working on neurotransmitter receptors, like γ-aminobutyric acid receptors and opioid receptors, and, in the case of caffeine, maybe adenosine receptors. I think the issue with the nonsteroidals is harder to understand, particularly how they might pharmacologically actually cause medication overuse. So, I think that mechanistically, those are the questions that are before us now.
DR. GOADSBY: Dr. Burstein, you published on nonsteroidals and triptans in the context of sensitization.8 What’s your view about this, particularly at a mechanistic level?
DR. BURSTEIN: Mechanistically, the data suggest that triptans disrupt communication between peripheral and central trigeminovascular neurons and that NSAIDs inhibit both the peripheral and the central neurons.
Accordingly, it is reasonable to suggest that triptans do not reverse central sensitization because they do not inhibit central trigeminovascular neurons directly, not at the level of the spinal cord at least, and that NSAIDs reverse central sensitization indirectly, through their anti-inflammatory action in the spinal cord (mostly unknown mechanism).
I think, again, that in the context of the opioid treatment, it became apparent both in the animal data and in patient data that opioid treatment makes patients resistant to successful NSAID treatment. NSAIDs work much better in patients who do not have a history of favoring opioids. Once patients begin to use opioids, however, they see a noticeable decline in the potential benefit of NSAIDs or triptan treatments. Again, I think that the key to that is the spinal cord inability to clear glutamate from the synapse, although I don’t think that the NSAIDs target glutamate release in any way.
DR. SCHOENEN: I do partially agree with what has been said. I think clinically, we clearly see patients who with overuse of simple analgesics, like paracetamol or a single NSAID like ibuprofen, enter the vicious circle of chronification and reverse to episodic migraine after reducing intake of these drugs.
The second point is that in the electrophysiological studies of patients overusing simple NSAIDs, there is clearly indication of sensitization in sensory cortices. Thirdly, Dr. Charles was alluding to the Bigal et al. study showing that NSAIDs protect against migraine chronification contrary to triptans.6 In this study, however, the protective effect of NSAIDs was only seen with patients who had low frequency of headaches. In patients with high frequency of headaches at baseline, NSAIDs also had a deleterious effect.
DR. GOADSBY: In the last few minutes that we have, I’d like to get some views about whether you think that more aggressive treatment with preventives would be helpful in terms of restricting headache progression. When medical practitioners see people who experience 6 or 8 headaches a month, and a couple months later they have 10 or maybe 12 or 14, they want to help them get better before they get worse. So if we intervened earlier, do we think that we could do a better job? Is that mechanistically plausible? I’ll start with you, Dr. Charles.
DR. CHARLES: I think it’s an appealing concept, but unfortunately I think that in practice we don’t see that concept being realized. Taking a cynical view, I think in many cases, even with preventative therapy, migraine finds its way around them, and even patients on preventative therapy end up having progression. So I think until we better understand the process, we can’t really say with confidence that early preventive therapy is something that is going to prevent the progression of the disorder.
DR. GOADSBY: Dr. Schoenen?
DR. SCHOENEN: I fundamentally agree with that. I think we are very lousy in the prevention of migraine. Most of the drugs don’t reach 50% efficacy. The patients who respond to these drugs may be those who have a peculiar pathophysiological, possibly genetic, profile, and do not progress. Those who do not respond are probably those who are most prone to chronification of migraine and at last fail on all available preventative drugs. So, in addition to much better preventative treatments, we also really need many more treatments.
DR. GOADSBY: Yes. Dr. Burstein?
DR. BURSTEIN: Well, I want to take it in a slightly different direction. I am aware of the fact that there is no evidence for it because nobody has done the study, but the question that I would like to answer is whether migraine progression would look completely different in a group of patients whose migraine attacks were treated early from the first migraine attack in their life (ie, they didn’t let their migraine last more than a few hours). Comparing this "early-treatment" group to a group of patients who treat late (ie, they let themselves have a migraine for 8, 10, or 12 hours before it goes away by itself or before they treat it).
DR. GOADSBY: Well, that would be an interesting study, very expensive as well. But as you say, one of the things we lack very much in longitudinal study is what’s really a dreadful problem, because whatever we think about the pathophysiology of headache progression, we’d all agree it’s bad to have more headache, it’s bad to have worse headache, and it’s bad to have headaches that don’t respond to therapy. It’s a subject which deserves study.
FoxP2 Media LLC is the publisher of The Medical Roundtable.
FoxP2 Media LLC
The Medical Roundtable: Current Indications of Acupuncture
Acupuncture (a traditional Chinese medical practice systematically used for over 2000 years) involves insertion of thin stainless steel needles into specific points on the body to facilitate recovery and good health. This practice was first brought to Europe in the 17th Century,1 and the first journal article on acupuncture appeared in the 1820s.2 Not until recently has acupuncture been widely accepted because of the clash of east versus west paradigms.
Scientific advances in acupuncture research, coupled with the side effects of treating pain by conventional drugs, have dramatically promoted the use of acupuncture in the last 20 years. It is estimated that over 1 million practitioners (outside China) administer acupuncture treatments for chronic pain. Of these practitioners, over 300000 are physicians.3 An estimated 3 million American adults receive acupuncture treatments each year, and chronic pain is the most common presentation.4
One of the most significant events in the 1990s for acupuncture was the decision taken by the US Food and Drug Administration in March 1996 to reclassify the legal status of acupuncture as safe and effective medical devices.
Further, in November 1997, there was a consensus conference on acupuncture by the National Institutes of Health.5 This was a 2.5-day conference conducted to evaluate the scientific and medical data on the uses, risks, and benefits of acupuncture for a variety of conditions. The findings after reviewing approximately 2300 studies stated that “Promising results have emerged, for example, showing efficacy of acupuncture in adult postoperative and chemotherapy nausea and vomiting and postoperative dental pain.”
“There are other conditions such as stroke rehabilitation, headache, tennis elbow, osteoarthritis, lower back pain, carpal tunnel syndrome, and asthma, for which acupuncture may be useful as an adjunct treatment or could be included in a comprehensive management program. Although many issues remain to be clarified, there is sufficient evidence to prove the value of acupuncture in order to expand its use in conventional medicine and encourage further studies of its physiology and clinical value.”
Since the consensus conference in 1997, there has been a huge increase in the number of scientific studies conducted on acupuncture. The Cochrane Collaboration’s database includes now 6035 clinical trials and 53 systematic reviews on acupuncture in their database.6 This roundtable today will focus on the current indications for acupuncture, and we will discuss how it is used in clinical settings, its safety issues and clinical evidence, and how it works.
The other participants are Dr. Joseph Helms, Dr. Gary Kaplan, and Dr. Lixing Lao. Dr. Helms is the founding president of the American Academy of Medical Acupuncture. In 1980, Dr. Helms developed the Medical Acupuncture Physicians program as a continuing medical education course for the University of California, Los Angeles (UCLA), School of Medicine; has chaired the program since then through the Helms Medical Institute (HMI); and has trained over 6000 physicians during this period. Dr. Helms is professor of medical acupuncture on the adjunct clinical faculty of the Stanford Medical School and the author of Acupuncture Energetics: A Clinical Approach for Physicians.
Dr. Kaplan is the medical director of the Kaplan Center for Integrative Medicine in McLean, Virginia, and is an associate professor in the Department of Community and Family Medicine at Georgetown University, School of Medicine. He served on the board of the American Academy of Medical Acupuncture and was president of the Medical Acupuncture Research Foundation.
Our final participant, Dr. Lao, is a professor of Family Medicine and the director of Traditional Chinese Medicine Research program at the Center for Integrative Medicine, University of Maryland School of Medicine. Dr. Lao graduated from the Shanghai University in the Traditional Chinese Medicine Program, holds a PhD in physiology from the University of Maryland in Baltimore, and has practiced acupuncture for 30 years and conducted research for 20 years.
To begin this discussion, Dr. Helms, can you describe for us the different types of acupuncture, training, and how acupuncture is used in a clinical setting?
DR. HELMS: Thank you, Dr. Berman. Acupuncture is relatively new in the collection of American medical disciplines. It has been in constant evolution since President Nixon’s visit to China in 1972. This evolution is driven by public interest and demand as well as scientific evidence of its mechanism and clinical value. This started with linking the impact of acupuncture on pain to the endogenous opioid peptide cascade, which is currently being reinforced through functional magnetic resonance imaging studies that confirm an intracranial response to peripheral needling.
The 1997 Consensus Development Conference report5 that endorsed a handful of acupuncture applications was based on the quality of research design to evaluate acupuncture’s impact on different problems, rather than on the actual practice of acupuncture. Since that paper, over 400 randomized control trials have been published in peer review journals internationally. These studies demonstrate the favorable impact of acupuncture on a wide spectrum of medical problems, including, but not limited to, pain.
There are many different styles of acupuncture. This discipline has evolved through multiple cultures over the last 2000 years. Each culture and era of its blossoming has contributed its enduring quality and approach. Many of these styles of acupuncture were retained only in family traditions, while others were propagated nationally. It is only in the late 20th century and beginning of the 21st century that we have had the privilege to access many of the family and most of the national traditions of acupuncture training and practice.
The tradition, with which I’m most familiar with, is known as medical acupuncture. Medical acupuncture would best be described as a hybrid approach combining our understanding of acupuncture neuroanatomy and physiology with traditional precepts from the classics of acupuncture. Medical acupuncture is generally practiced by licensed practitioners of conventional biomedical medicine and is considered an additional qualification to their scope of practice. These would include doctors of medicine, doctors of osteopathy, doctors of dental surgery, and doctors of podiatric medicine.
Traditional Chinese Medicine is the approach most widely practiced in this country. It is an approach exported from post-Maoist China, having been developed to provide basic healthcare to the Chinese population as the country was transitioning from its revolutionary period in the 1950s and 1960s into a more stable political and social period. The Traditional Chinese Medicine model doesn’t contain the totality of the classics, but rather is an extraction that can be taught and absorbed by the western community. The Traditional Chinese Medicine approach covers internal medicine problems as well as pain problems.
Two additional, commonly used subdivisions of acupuncture are auricular acupuncture and Chinese scalp acupuncture. Auricular acupuncture was developed in France in the 1950s and 1960s and uses points exclusively on the ear to influence pain and organ function. Chinese scalp acupuncture is a recent development in Chinese medicine. It involves placing needles in the scalp overlying the cortical surfaces that relay pain signals.
DR. BERMAN: Could you elaborate on auricular acupuncture a little more and on what it is used for?
DR. HELMS: Auricular acupuncture is the least complex and most easily learned approach to acupuncture. It can be effective either as a standalone treatment or as an adjunct to body acupuncture. The scientific foundation of auricular acupuncture involves the ear’s complex innervation that links it to all 3 embryologic germ levels. Thus, with neurological representation of endoderm, mesoderm, and ectoderm, the ear manifests a homunculus of all body parts. Ear points that correspond to painful or disturbed structures demonstrate increased electrical conductivity, and thereby allow the ear to serve as a diagnostic tool and a therapeutic signal.
DR. BERMAN: I think in the past, auricular acupuncture was also used for problems of addiction but I don’t know if it’s still being used for this purpose.
DR. HELMS: There are several widely used acupuncture point combinations that have been shown to be useful in assisting a multidisciplinary approach to substance abuse problems, referred to as the “NADA protocol” that was developed by Michael Smith, MD. There is also a 5-point formula called battlefield acupuncture that is useful in dealing with acute traumatic pain.7
DR. BERMAN: Thank you, Dr. Helms. Dr. Kaplan and then Dr. Lao, could you comment about what’s being done in clinical settings and how acupuncture is used to treat certain diseases beyond what Dr. Helms has just explained?
DR. KAPLAN: We do a great deal of work for the treatment of pain and find acupuncture to be extremely effective for conditions such as headaches, back pain, and neck pain. We also find it useful for the treatment of peripheral neuropathies. In addition, because we deal with many chronic pain patients, we also see a lot of psychoemotional issues comorbid with the chronic pain. Acupuncture has proven to be very helpful as an adjunctive therapy dealing with the psychoemotional components that we see associated with chronic pain.
In my practice, approximately 20% of our pain population has posttraumatic stress syndrome, while approximately 60% has comorbid anxiety disorders or major depressive disorders. Acupuncture has been particularly unique as a therapeutic modality because it addresses both the pain and the psychological component of an individual’s illness at the same time. We’re able to talk about the totality of the individual as opposed to segmenting them into psychiatric versus pain versus sleep issues. From an acupuncture perspective, these conditions are not separate issues but different manifestations of a pattern of disharmony in the individual.
DR. LAO: I agree with Drs. Kaplan and Helms. In my practice, I see patients with a variety of complaints. In addition to pain, they also experience menstruation disorders, depression, and attention deficit disorder (ADD) (in children). A wide variety of diseases can be treated by acupuncture. Evidence of the effectiveness of acupuncture for the treatment of pain has recently been published by Vickers.4
Individual raw data show the full area of musculoskeletal pain, which includes neck pain, low back pain, headaches (migraine and tension headaches), osteoarthritis in the knees, and shoulder pain. There is a significant difference between acupuncture and conventional treatment in terms of their therapeutic effectiveness. There was also a significant difference between acupuncture and sham acupuncture, ie, placing of needles at points on the body that are not thought to be acupuncture points (off site points). Although the benefits were modest, they were highly significant.4
Dr. Berman, do you also want me to cover a little bit about the side effects or shall we save that for later?
DR. BERMAN: Let’s stick to the clinical use first, and then we’ll go to the side effects.
DR. KAPLAN: I’d like to chime in here. I’m boarded in family medicine and pain medicine and started my clinical practice in a general medical setting. As my practice evolved, I began seeing a greater number of individuals suffering with chronic pain and illness issues.
Over the last 30 years, acupuncture has heavily influenced my approach to patient care. Acupuncture is not simply a tool but a philosophy of care that has greatly enriched my western medical training. At times, when treating a patient, I believe the prism of a western approach will be more effective; there are also times when I rely exclusively on an acupuncture approach, but more commonly, I integrate the two in designing and implementing a care program.
Pain can be very effectively managed with acupuncture alone or as an adjunct. Many so-called functional or psychosomatic problems can be more effectively addressed using acupuncture in place of pharmaceutical agents. Likewise, the conventional approaches to organic problems can be reinforced and facilitated with acupuncture treatment.
Acupuncture covers a much broader range of clinical applications than simple neuromusculoskeletal pain or psychoemotional issues. It really covers the full spectrum of medicine.
DR. KAPLAN: We have used acupuncture successfully in women with hyperemesis gravidarum. Most of the medications are contraindicated because of the potential harm to the fetus. Acupuncture has been successful in at least providing these women with some level of relief in treating this condition.
I don’t have experience with acupuncture therapy for postoperative nausea/vomiting. We have used it a little bit in nausea/vomiting associated with chemotherapy, and again, we’ve been able to reduce the amount of medications that the patients require in order to control it; in some cases, we’ve actually been able to eliminate the need for medications.
Further, I want to go over what Dr. Helms was talking about—the importance of integrating acupuncture into a comprehensive treatment program. It is sometimes the main therapeutic modality that we use, but on many occasions, it is integrated into our medication regimes. In a comprehensive approach, we may use it in conjunction with physical therapy, and we will also be probing trigger points. We may also do prolotherapy with the patients.
Acupuncture gives us the ability to treat a wider range of conditions with fewer medications. We are frequently able to address irritable bowel syndrome (IBS), sleep disorders associated with the medical conditions, as well as the psychiatric conditions I was talking about earlier. Acupuncture is a beautiful adjunctive therapy and sometimes can be used as the sole therapeutic approach.
DR. BERMAN: In general, we’re now talking about acupuncture being part of a comprehensive approach to a number of chronic disorders.
DR. KAPLAN: That’s absolutely correct. You want to use all of the tools you have available, and acupuncture is a very powerful therapeutic modality in the treatment of these conditions.
DR. LAO: One of the nonpain areas that I think people should consider using acupuncture as a therapy is infertility. Many women now come to the clinic, particularly after the publication of the enhanced success rate of in vitro fertilization (IVF) in women receiving acupuncture treatment.8 Even those patients who elect to not go through IVF come for acupuncture treatment to enhance their chances of getting pregnant.
DR. BERMAN: Dr. Lao, is there evidence to support acupuncture for infertility?
DR. LAO: There’s a paper that was published a couple years ago through our center.8 The authors show a higher success rate of conventional IVF procedure when combined with acupuncture than with sham control. Current studies give clear evidence of the benefits of acupuncture to IVF patients.
DR. BERMAN: With the breathlessness COPD I was referring to, there was a study in the Archives of Internal Medicine just this past June 2012,9 which was a very well-done clinical trial aimed at studying COPD and using acupuncture in addition to conventional care, that showed clear outcomes of the benefits of acupuncture in this particular condition.
Dr. Helms, you have experienced acupuncture in the military setting. Can you talk a little bit about that?
DR. HELMS: In the last 5 years, 3 branches of the US Military have shown interest in pursuing acupuncture training for physicians to provide these services to their population. This interest reflects what’s happening in the civilian population and is more intensively motivated by the report of the Army’s pain management task force that identified some severe shortcomings in managing acute and chronic pain.
The feedback we’ve received from the military physicians we’ve trained has been very rewarding. The bulk of their treatments are for pain, ranging from headache to cervical, lumbar, and peripheral pain. Much of this pain is caused by the weight of their 75-pound protective gear, which they wear no matter where they are in the world, and of course, the physical trauma of battle. Interestingly, an almost equal percentage of treatments for active duty service members are for psychoemotional problems (anxiety, insomnia, depression, acute stress, and chronic stress) as for pain and physical trauma.
DR. BERMAN: Let me move on to the next subtopic. Dr. Lao, can you talk to us about how safe acupuncture is?
DR. LAO: There are few reported cases of complications in the English literature from 1965 to 1999, a 35-year span. There were a total of 202 case reports, which is about 5–6 cases per year.10 I have completed 2 reviews of case reports on adverse events associated with acupuncture. One was published in 200310 and the other one is accepted for publication.11 Events are divided into complications and adverse reactions. Complications such as injured organs or infections occur if acupuncture is not carefully performed. Adverse reactions include syncope and allergic reaction.
Infections constituted 50% of all complications. Needle infections may cause hepatitis. However, since the late 1980s, acupuncturists started using disposable needles, resulting in lower incidence of hepatitis and other infections.10 In recent years, another infection emerged that involves many different invasive procedures in medical settings such as methicillin-resistant Staphylococcus aureus (MRSA). This is likely due to the unsanitary conditions of these clinical settings, such as the use of contaminated disinfectant. It’s not the acupuncture needle itself that caused infection.
A larger survey12 showed that approximately 7% to 8% of the adverse events were classified as mild. These events include local site bleeding, pain in local needling site, nausea, or light-headedness. The occurrence of these mild adverse events is very low especially in the context of the large numbers of patients attended to acupuncture clinic every year.
In the last 10 years, 308 cases of side effects were noted from 26 countries.11 In the United States, only 17 cases have been reported, which is a very small percentage. I believe that this is due to extensive professional licensing requirement that is called Clean Needle Techniques (CNT) training. This requirement has dramatically decreased the risk of unnecessary side effects.
Other types of adverse events such as organ and tissue injuries are associated with knowledge of anatomy. Therefore, proper training of the acupuncturist could help reduce the occurrence of side effects due to acupuncture.
DR. BERMAN: From these prospective studies,10–12 we can conclude that serious adverse events are very rare with acupuncture and that there is, depending on the surveys, a 2% to 7% probability of occurrence of a mild side effect such as local site bleeding or occasional dizziness or localized pain to the area. Is there anything else on safety that either, Dr. Kaplan or Dr. Helms would like to add?
DR. HELMS: In addition to reinforcing that acupuncture is a very safe and forgiving therapeutic approach, I’d like to discourage readers from concluding that useful indications for acupuncture in medical practice are limited to what is published in the evidence-based literature. Acupuncture has been used for simple and complex problems by responsible practitioners in oriental and occidental cultures for much longer period than we have been documenting its efficacy. Acupuncture comes from a long tradition of the practice of medicine, albeit in cultures and eras quite distant from ours. Our hybrid medical acupuncture allows remarkable creativity in the hands of well-trained practitioners, to treat many problems that are not included among those already studied in the pharmaceutical model.
DR. BERMAN: I think that’s a very important point, but let’s talk a little bit about the research first, and then go back to this when we’re putting the research into the context of clinical practice. How should we take this into account?
DR. KAPLAN: Let’s briefly look at the clinical research, and then talk about some of the problems that we run into with research and what the research shows us in terms of how to better study procedures such as acupuncture, because studying procedures is different from studying drugs. The clinical studies roughly fall into 2 categories: effectiveness studies and efficacy studies, and many studies overlap and attempt to do both.
An effectiveness study looks at the extent to which a drug or procedure achieves its intended effect in the usual clinical setting. In these circumstances, you’re randomizing acupuncture against something such as a wait list control or usual care such as physical therapy or medications.
In 2009, a Cochrane database review studying acupuncture for prophylaxes of migraine showed that acupuncture was at least as effective, and possibly more effective, than prophylactic drugs with fewer adverse effects.13
In 2012, Andrew Vickers and his colleagues4 performed individualized patient data meta-analysis of 17,922 patients with a variety of back, neck, shoulder, osteoarthritic-related and headache pains and concluded that acupuncture was, in fact, effective for the treatment of chronic pain. Some effectiveness trials have shown acupuncture to be useful for some specific conditions, pain being the number one condition.
Efficacy is the extent to which a drug or procedure has the ability to bring about its intended effect under ideal circumstances, that is, acupuncture compared to a placebo. In the Vickers study,4 Vickers looked at the efficacy of acupuncture in the treatment of chronic pain and again concluded that true acupuncture was statistically slightly more efficacious than sham. Although this was not a big effect, it was nonetheless statistically significant.
From the 2012 Cochrane database review of IBS14 it was concluded that acupuncture was not efficacious as compared to a creditable sham, but there were several effectiveness trials where acupuncture tested better against 2 antispasmodic medications, which have some effect on both the severity and quality of life in patients with IBS.
While the Vickers study reported the efficacy as well as effectiveness of acupuncture, the IBS trial did not find any efficacy, when compared to the placebo, but did find evidence of the effectiveness of acupuncture.
What is particularly interesting about this study is that the natural history of carpal tunnel suggests that you will notice a 20% to 40% improvement over time. However, this study showed an 88% statistically significant improvement in both the true and sham acupuncture groups, which was maintained over 3 months of follow-up after the treatments ended.
The question that arises now is how you reconcile all of this, because it seems that the first piece of information that you come up with is that the sham may actually be a different form of active treatment. There’s an interesting study by Richard Harris and others in neuroimaging that was published in 2009.16 Harris’ team looked at the effects of true and sham acupuncture on the mu-opioid receptors in the central nervous system (CNS) using positron emission tomographic scanning in patients with fibromyalgia. Prior studies in patients with fibromyalgia have demonstrated increased levels of endogenous opioids in the cervical spinal fluid with decreased sensitivity in the mu-opioid receptors in the CNS regions known to be associated with the modulation of pain.
In the Harris study, the authors found that true acupuncture therapy evoked both short- and long-term increases in mu-opioid-binding potential receptors in the multiple pain areas and sensory processing areas associated with pain regulation. This was associated with clinical reports of pain reduction on the part of the subjects.
In the sham group, they also reported reduction in pain, though less than that in the true acupuncture group, and the positron emission tomographic scan showed no effect on the sensitivity of the mu-opioid receptors. The binding potential of these receptors did not improve as they did with the acupuncture treatments.
We know from prior studies that both true and sham acupuncture seem to increase the release of endogenous opioids, and we see that effect occurring in the ascending pathways and a segmental effect occurring in the spinal cord as well as in the descending modulating pathways mediated via dynorphins serotonin and norepinephrine. However, the effects of true acupuncture on the mu-opioid binding sensitivities are different from that of sham acupuncture.
In addition to this, we have imaging studies that have been conducted since the 1990s, and a recently published meta-analysis by Huang et al,17 which showed that while there is a problem with heterogeneity of these studies, they were able to conclude that the brain response to acupuncture encompasses a broad network of regions consistent with somatosensory affective and cognitive processing.
Overall, the neurophysiological evidence shows that acupuncture treatments affect the CNS in ways that are beneficial, long lasting, and unique to true acupuncture treatments. The neurophysiological evidence is also beginning to explain why we see different degrees of clinical effectiveness of acupuncture in conditions as diverse as gastrointestinal disorders, pain, and psychiatric conditions.
We have a lot more to learn and, far from being discouraged by this conflicting evidence in the literature, we should be excited by how much acupuncture has challenged and taught us about our understanding of human physiology. Does acupuncture work? Yes, according to the literature. Does acupuncture have unique and beneficial mechanisms of action on our neurophysiology? Again, I believe that the accumulative answer to that is yes.
The abovementioned discussion was about what’s going on in the CNS with acupuncture. There are a couple of other theories about how acupuncture may be effective. The one most commonly cited is work is that of Helen Langevin,18 where she writes about the network of acupuncture points and meridians viewed as representations of a network formed by interstitial connective tissue and that there has been an 80% correlation of the acupuncture points where the intramuscular connective tissue planes.
The needle grasp is a result of a winding of connective tissue and causes a tight mechanical coupling between the needle and the tissue, and there’s mounting evidence that this mechanical transduction can be translated into a variety of cellular and extracellular events. The 2 major models are the neurologic model, which is by far the most accepted and studied, and the connective tissue model.
Again, this is an evolving area. We have a lot more to learn, and I completely agree with Dr. Helms that we don’t want to be locked into the evidence-based approach that we fail to understand the true clinical benefits that acupuncture has shown repeatedly over thousand years of practice and that we see ourselves in day-to-day practice in our offices.
DR. BERMAN: Apart from summarizing the mechanisms, Dr. Kaplan, I think you mean that when we’re talking about evidence-based medicine, it’s not just about the efficacy shown by randomized control trials. There’s a wider range of methodologies and diseases to consider, depending on the question being asked. This is true of all medicine, including acupuncture, and if we narrow it down too much, we may fail to reap the benefits of using a very valuable tool as part of medicine.
DR. KAPLAN: I think you’re absolutely correct. The other thing that we need to keep in mind is that the evidence-based research itself is a very limiting concept because we keep finding new mechanisms and understanding new subtleties about how the nervous system is working, how our physiology works, and then we’re able to go back and say, “Ah, that’s the mechanism via which this is happening.” This whole topic about mu-opioid receptors is actually a breakthrough in terms of understanding how acupuncture may affect the CNS, which is unique and different from the way that sham does.
DR. BERMAN: What do you think are the cutting-edge research questions that still need to be answered as we go forward, questions that could not only inform us of how acupuncture works but could also affect clinical practice?
DR. KAPLAN: One of the areas that I’ve been particularly focused on is the microglial cells and their impact as the ultimate transducers between psychological stress, which gets translated into neurologic damage; and physical stress such as traumatic brain injury; as well as infectious stress, which also creates problems with neuroinflammation and neurodegeneration in conditions such as chronic pain and chronic illness.
We have seen evidence that acupuncture is actually neuroregenerative in some circumstances, certainly from some of the carpal tunnel studies that have been performed. We know that the microglia are involved in neuroregeneration; therefore, studying the effects of acupuncture on microglia may give us much more insight into how acupuncture works. This would be one area that I think should be focused on.
DR. BERMAN: Dr. Helms or Dr. Lao, any questions you think still need to be answered that can really make a difference?
DR. LAO: I agree with everything you have already said, but I think I’ll add one point: we need more translational studies on how to apply the scientific information to our daily practices in order to enhance the effectiveness of acupuncture treatment. We did some studies in which the effectiveness of a combination of conventional medication and acupuncture was evaluated. We found that the effectiveness of the combined therapy was much higher than that of acupuncture or the medication alone. Maybe, in the future, the research should be designed to answer the question of whether acupuncture reduces the side effects of a medication, resulting in enhanced effectiveness of both medicine and acupuncture.
DR. BERMAN: I would add one point that goes along with that: we need to get a better idea of the responders and nonresponders to acupuncture. We could begin to address this by setting up some pragmatic clinical trials with the idea of comparative effectiveness research in actual settings of clinical practice as well as cost effectiveness. Further, we could determine who responds, and we can include imaging and genomics assessments as part of the biomarkers that we’re analyzing.
Dr. Kaplan, do you have any final comments you want to add?
DR. KAPLAN: In terms of additional research, our thinking has been very much from a Bohr atom perspective [Bohr was a physicist who originally described the atom like a small solar system with electrons neatly orbiting the nucleus of the atom is a fixed orbit. This is a cartoon approximation of reality.] in terms of how the nervous system works, and we need to move toward a more quantum understanding. The whole field of neuroimaging is moving toward the concept of neuro-networking and trying to understand how the different regions of the brain interact with each other. I think that’s going to show a lot of promise even in terms of how acupuncture is affecting the system.
I also think that, as you mentioned briefly, the cost effectiveness research is extremely important. Integrating acupuncture into conventional medical practice has the potential, at least to significantly reduce cost to the patient and side effects of medications. I think studies need to be conducted on this issue. I’m optimistic these studies will confirm what we have witnessed in clinical practice.
DR. HELMS: Just a comment on that, Dr. Kaplan. You first need a model environment where acupuncture is fully integrated into a broad-based clinical setting, not individual practices. That’s the first hurdle to overcome before one looks at the impact of reducing reliance on pharmaceutical products or cutting back on the frequency of office visits and referrals to specialists.
DR. KAPLAN: I completely agree with you. I think that’s a challenge that we need to potentially take on in the future, but it’s something to be looking towards as we’re going to have to be more cost effective and more cost conscious in our treatment of a variety of diseases. I think acupuncture has a significant role to play here but we are not ready to perform those studies yet. We need to start to think about them and how they can be accomplished.
DR. HELMS: In the past, we have thought of acupuncture as a treatment for chronic conditions, but one of the biggest problems we face in the military today is trauma. It could be possible to compare management outcomes at military facilities that have integrated acupuncture into their trauma treatment with those that have not.
DR. BERMAN: Here is where the military comes into play. They have proposed a move towards expanding availability of acupuncture immediately following trauma and then follow that through with intermediate and long-term care facilities. If this approach succeeds, it would create an environment in which those issues of acute, sub-acute, and chronic consequences of trauma could be evaluated.
DR. LAO: In ancient literature, early acupuncture was largely used for emergency medicine, particularly in the ancient times when patients were unconscious or in conditions such as fainting or convulsions where they could not be treated with oral medicines. There is a large body of ancient literature that has documented this use.
DR. BERMAN: I want to thank all of you for participating in this discussion; it’s been a real pleasure.
FoxP2 Media LLC is the publisher of The Medical Roundtable.
Acupuncture (a traditional Chinese medical practice systematically used for over 2000 years) involves insertion of thin stainless steel needles into specific points on the body to facilitate recovery and good health. This practice was first brought to Europe in the 17th Century,1 and the first journal article on acupuncture appeared in the 1820s.2 Not until recently has acupuncture been widely accepted because of the clash of east versus west paradigms.
Scientific advances in acupuncture research, coupled with the side effects of treating pain by conventional drugs, have dramatically promoted the use of acupuncture in the last 20 years. It is estimated that over 1 million practitioners (outside China) administer acupuncture treatments for chronic pain. Of these practitioners, over 300000 are physicians.3 An estimated 3 million American adults receive acupuncture treatments each year, and chronic pain is the most common presentation.4
One of the most significant events in the 1990s for acupuncture was the decision taken by the US Food and Drug Administration in March 1996 to reclassify the legal status of acupuncture as safe and effective medical devices.
Further, in November 1997, there was a consensus conference on acupuncture by the National Institutes of Health.5 This was a 2.5-day conference conducted to evaluate the scientific and medical data on the uses, risks, and benefits of acupuncture for a variety of conditions. The findings after reviewing approximately 2300 studies stated that “Promising results have emerged, for example, showing efficacy of acupuncture in adult postoperative and chemotherapy nausea and vomiting and postoperative dental pain.”
“There are other conditions such as stroke rehabilitation, headache, tennis elbow, osteoarthritis, lower back pain, carpal tunnel syndrome, and asthma, for which acupuncture may be useful as an adjunct treatment or could be included in a comprehensive management program. Although many issues remain to be clarified, there is sufficient evidence to prove the value of acupuncture in order to expand its use in conventional medicine and encourage further studies of its physiology and clinical value.”
Since the consensus conference in 1997, there has been a huge increase in the number of scientific studies conducted on acupuncture. The Cochrane Collaboration’s database includes now 6035 clinical trials and 53 systematic reviews on acupuncture in their database.6 This roundtable today will focus on the current indications for acupuncture, and we will discuss how it is used in clinical settings, its safety issues and clinical evidence, and how it works.
The other participants are Dr. Joseph Helms, Dr. Gary Kaplan, and Dr. Lixing Lao. Dr. Helms is the founding president of the American Academy of Medical Acupuncture. In 1980, Dr. Helms developed the Medical Acupuncture Physicians program as a continuing medical education course for the University of California, Los Angeles (UCLA), School of Medicine; has chaired the program since then through the Helms Medical Institute (HMI); and has trained over 6000 physicians during this period. Dr. Helms is professor of medical acupuncture on the adjunct clinical faculty of the Stanford Medical School and the author of Acupuncture Energetics: A Clinical Approach for Physicians.
Dr. Kaplan is the medical director of the Kaplan Center for Integrative Medicine in McLean, Virginia, and is an associate professor in the Department of Community and Family Medicine at Georgetown University, School of Medicine. He served on the board of the American Academy of Medical Acupuncture and was president of the Medical Acupuncture Research Foundation.
Our final participant, Dr. Lao, is a professor of Family Medicine and the director of Traditional Chinese Medicine Research program at the Center for Integrative Medicine, University of Maryland School of Medicine. Dr. Lao graduated from the Shanghai University in the Traditional Chinese Medicine Program, holds a PhD in physiology from the University of Maryland in Baltimore, and has practiced acupuncture for 30 years and conducted research for 20 years.
To begin this discussion, Dr. Helms, can you describe for us the different types of acupuncture, training, and how acupuncture is used in a clinical setting?
DR. HELMS: Thank you, Dr. Berman. Acupuncture is relatively new in the collection of American medical disciplines. It has been in constant evolution since President Nixon’s visit to China in 1972. This evolution is driven by public interest and demand as well as scientific evidence of its mechanism and clinical value. This started with linking the impact of acupuncture on pain to the endogenous opioid peptide cascade, which is currently being reinforced through functional magnetic resonance imaging studies that confirm an intracranial response to peripheral needling.
The 1997 Consensus Development Conference report5 that endorsed a handful of acupuncture applications was based on the quality of research design to evaluate acupuncture’s impact on different problems, rather than on the actual practice of acupuncture. Since that paper, over 400 randomized control trials have been published in peer review journals internationally. These studies demonstrate the favorable impact of acupuncture on a wide spectrum of medical problems, including, but not limited to, pain.
There are many different styles of acupuncture. This discipline has evolved through multiple cultures over the last 2000 years. Each culture and era of its blossoming has contributed its enduring quality and approach. Many of these styles of acupuncture were retained only in family traditions, while others were propagated nationally. It is only in the late 20th century and beginning of the 21st century that we have had the privilege to access many of the family and most of the national traditions of acupuncture training and practice.
The tradition, with which I’m most familiar with, is known as medical acupuncture. Medical acupuncture would best be described as a hybrid approach combining our understanding of acupuncture neuroanatomy and physiology with traditional precepts from the classics of acupuncture. Medical acupuncture is generally practiced by licensed practitioners of conventional biomedical medicine and is considered an additional qualification to their scope of practice. These would include doctors of medicine, doctors of osteopathy, doctors of dental surgery, and doctors of podiatric medicine.
Traditional Chinese Medicine is the approach most widely practiced in this country. It is an approach exported from post-Maoist China, having been developed to provide basic healthcare to the Chinese population as the country was transitioning from its revolutionary period in the 1950s and 1960s into a more stable political and social period. The Traditional Chinese Medicine model doesn’t contain the totality of the classics, but rather is an extraction that can be taught and absorbed by the western community. The Traditional Chinese Medicine approach covers internal medicine problems as well as pain problems.
Two additional, commonly used subdivisions of acupuncture are auricular acupuncture and Chinese scalp acupuncture. Auricular acupuncture was developed in France in the 1950s and 1960s and uses points exclusively on the ear to influence pain and organ function. Chinese scalp acupuncture is a recent development in Chinese medicine. It involves placing needles in the scalp overlying the cortical surfaces that relay pain signals.
DR. BERMAN: Could you elaborate on auricular acupuncture a little more and on what it is used for?
DR. HELMS: Auricular acupuncture is the least complex and most easily learned approach to acupuncture. It can be effective either as a standalone treatment or as an adjunct to body acupuncture. The scientific foundation of auricular acupuncture involves the ear’s complex innervation that links it to all 3 embryologic germ levels. Thus, with neurological representation of endoderm, mesoderm, and ectoderm, the ear manifests a homunculus of all body parts. Ear points that correspond to painful or disturbed structures demonstrate increased electrical conductivity, and thereby allow the ear to serve as a diagnostic tool and a therapeutic signal.
DR. BERMAN: I think in the past, auricular acupuncture was also used for problems of addiction but I don’t know if it’s still being used for this purpose.
DR. HELMS: There are several widely used acupuncture point combinations that have been shown to be useful in assisting a multidisciplinary approach to substance abuse problems, referred to as the “NADA protocol” that was developed by Michael Smith, MD. There is also a 5-point formula called battlefield acupuncture that is useful in dealing with acute traumatic pain.7
DR. BERMAN: Thank you, Dr. Helms. Dr. Kaplan and then Dr. Lao, could you comment about what’s being done in clinical settings and how acupuncture is used to treat certain diseases beyond what Dr. Helms has just explained?
DR. KAPLAN: We do a great deal of work for the treatment of pain and find acupuncture to be extremely effective for conditions such as headaches, back pain, and neck pain. We also find it useful for the treatment of peripheral neuropathies. In addition, because we deal with many chronic pain patients, we also see a lot of psychoemotional issues comorbid with the chronic pain. Acupuncture has proven to be very helpful as an adjunctive therapy dealing with the psychoemotional components that we see associated with chronic pain.
In my practice, approximately 20% of our pain population has posttraumatic stress syndrome, while approximately 60% has comorbid anxiety disorders or major depressive disorders. Acupuncture has been particularly unique as a therapeutic modality because it addresses both the pain and the psychological component of an individual’s illness at the same time. We’re able to talk about the totality of the individual as opposed to segmenting them into psychiatric versus pain versus sleep issues. From an acupuncture perspective, these conditions are not separate issues but different manifestations of a pattern of disharmony in the individual.
DR. LAO: I agree with Drs. Kaplan and Helms. In my practice, I see patients with a variety of complaints. In addition to pain, they also experience menstruation disorders, depression, and attention deficit disorder (ADD) (in children). A wide variety of diseases can be treated by acupuncture. Evidence of the effectiveness of acupuncture for the treatment of pain has recently been published by Vickers.4
Individual raw data show the full area of musculoskeletal pain, which includes neck pain, low back pain, headaches (migraine and tension headaches), osteoarthritis in the knees, and shoulder pain. There is a significant difference between acupuncture and conventional treatment in terms of their therapeutic effectiveness. There was also a significant difference between acupuncture and sham acupuncture, ie, placing of needles at points on the body that are not thought to be acupuncture points (off site points). Although the benefits were modest, they were highly significant.4
Dr. Berman, do you also want me to cover a little bit about the side effects or shall we save that for later?
DR. BERMAN: Let’s stick to the clinical use first, and then we’ll go to the side effects.
DR. KAPLAN: I’d like to chime in here. I’m boarded in family medicine and pain medicine and started my clinical practice in a general medical setting. As my practice evolved, I began seeing a greater number of individuals suffering with chronic pain and illness issues.
Over the last 30 years, acupuncture has heavily influenced my approach to patient care. Acupuncture is not simply a tool but a philosophy of care that has greatly enriched my western medical training. At times, when treating a patient, I believe the prism of a western approach will be more effective; there are also times when I rely exclusively on an acupuncture approach, but more commonly, I integrate the two in designing and implementing a care program.
Pain can be very effectively managed with acupuncture alone or as an adjunct. Many so-called functional or psychosomatic problems can be more effectively addressed using acupuncture in place of pharmaceutical agents. Likewise, the conventional approaches to organic problems can be reinforced and facilitated with acupuncture treatment.
Acupuncture covers a much broader range of clinical applications than simple neuromusculoskeletal pain or psychoemotional issues. It really covers the full spectrum of medicine.
DR. KAPLAN: We have used acupuncture successfully in women with hyperemesis gravidarum. Most of the medications are contraindicated because of the potential harm to the fetus. Acupuncture has been successful in at least providing these women with some level of relief in treating this condition.
I don’t have experience with acupuncture therapy for postoperative nausea/vomiting. We have used it a little bit in nausea/vomiting associated with chemotherapy, and again, we’ve been able to reduce the amount of medications that the patients require in order to control it; in some cases, we’ve actually been able to eliminate the need for medications.
Further, I want to go over what Dr. Helms was talking about—the importance of integrating acupuncture into a comprehensive treatment program. It is sometimes the main therapeutic modality that we use, but on many occasions, it is integrated into our medication regimes. In a comprehensive approach, we may use it in conjunction with physical therapy, and we will also be probing trigger points. We may also do prolotherapy with the patients.
Acupuncture gives us the ability to treat a wider range of conditions with fewer medications. We are frequently able to address irritable bowel syndrome (IBS), sleep disorders associated with the medical conditions, as well as the psychiatric conditions I was talking about earlier. Acupuncture is a beautiful adjunctive therapy and sometimes can be used as the sole therapeutic approach.
DR. BERMAN: In general, we’re now talking about acupuncture being part of a comprehensive approach to a number of chronic disorders.
DR. KAPLAN: That’s absolutely correct. You want to use all of the tools you have available, and acupuncture is a very powerful therapeutic modality in the treatment of these conditions.
DR. LAO: One of the nonpain areas that I think people should consider using acupuncture as a therapy is infertility. Many women now come to the clinic, particularly after the publication of the enhanced success rate of in vitro fertilization (IVF) in women receiving acupuncture treatment.8 Even those patients who elect to not go through IVF come for acupuncture treatment to enhance their chances of getting pregnant.
DR. BERMAN: Dr. Lao, is there evidence to support acupuncture for infertility?
DR. LAO: There’s a paper that was published a couple years ago through our center.8 The authors show a higher success rate of conventional IVF procedure when combined with acupuncture than with sham control. Current studies give clear evidence of the benefits of acupuncture to IVF patients.
DR. BERMAN: With the breathlessness COPD I was referring to, there was a study in the Archives of Internal Medicine just this past June 2012,9 which was a very well-done clinical trial aimed at studying COPD and using acupuncture in addition to conventional care, that showed clear outcomes of the benefits of acupuncture in this particular condition.
Dr. Helms, you have experienced acupuncture in the military setting. Can you talk a little bit about that?
DR. HELMS: In the last 5 years, 3 branches of the US Military have shown interest in pursuing acupuncture training for physicians to provide these services to their population. This interest reflects what’s happening in the civilian population and is more intensively motivated by the report of the Army’s pain management task force that identified some severe shortcomings in managing acute and chronic pain.
The feedback we’ve received from the military physicians we’ve trained has been very rewarding. The bulk of their treatments are for pain, ranging from headache to cervical, lumbar, and peripheral pain. Much of this pain is caused by the weight of their 75-pound protective gear, which they wear no matter where they are in the world, and of course, the physical trauma of battle. Interestingly, an almost equal percentage of treatments for active duty service members are for psychoemotional problems (anxiety, insomnia, depression, acute stress, and chronic stress) as for pain and physical trauma.
DR. BERMAN: Let me move on to the next subtopic. Dr. Lao, can you talk to us about how safe acupuncture is?
DR. LAO: There are few reported cases of complications in the English literature from 1965 to 1999, a 35-year span. There were a total of 202 case reports, which is about 5–6 cases per year.10 I have completed 2 reviews of case reports on adverse events associated with acupuncture. One was published in 200310 and the other one is accepted for publication.11 Events are divided into complications and adverse reactions. Complications such as injured organs or infections occur if acupuncture is not carefully performed. Adverse reactions include syncope and allergic reaction.
Infections constituted 50% of all complications. Needle infections may cause hepatitis. However, since the late 1980s, acupuncturists started using disposable needles, resulting in lower incidence of hepatitis and other infections.10 In recent years, another infection emerged that involves many different invasive procedures in medical settings such as methicillin-resistant Staphylococcus aureus (MRSA). This is likely due to the unsanitary conditions of these clinical settings, such as the use of contaminated disinfectant. It’s not the acupuncture needle itself that caused infection.
A larger survey12 showed that approximately 7% to 8% of the adverse events were classified as mild. These events include local site bleeding, pain in local needling site, nausea, or light-headedness. The occurrence of these mild adverse events is very low especially in the context of the large numbers of patients attended to acupuncture clinic every year.
In the last 10 years, 308 cases of side effects were noted from 26 countries.11 In the United States, only 17 cases have been reported, which is a very small percentage. I believe that this is due to extensive professional licensing requirement that is called Clean Needle Techniques (CNT) training. This requirement has dramatically decreased the risk of unnecessary side effects.
Other types of adverse events such as organ and tissue injuries are associated with knowledge of anatomy. Therefore, proper training of the acupuncturist could help reduce the occurrence of side effects due to acupuncture.
DR. BERMAN: From these prospective studies,10–12 we can conclude that serious adverse events are very rare with acupuncture and that there is, depending on the surveys, a 2% to 7% probability of occurrence of a mild side effect such as local site bleeding or occasional dizziness or localized pain to the area. Is there anything else on safety that either, Dr. Kaplan or Dr. Helms would like to add?
DR. HELMS: In addition to reinforcing that acupuncture is a very safe and forgiving therapeutic approach, I’d like to discourage readers from concluding that useful indications for acupuncture in medical practice are limited to what is published in the evidence-based literature. Acupuncture has been used for simple and complex problems by responsible practitioners in oriental and occidental cultures for much longer period than we have been documenting its efficacy. Acupuncture comes from a long tradition of the practice of medicine, albeit in cultures and eras quite distant from ours. Our hybrid medical acupuncture allows remarkable creativity in the hands of well-trained practitioners, to treat many problems that are not included among those already studied in the pharmaceutical model.
DR. BERMAN: I think that’s a very important point, but let’s talk a little bit about the research first, and then go back to this when we’re putting the research into the context of clinical practice. How should we take this into account?
DR. KAPLAN: Let’s briefly look at the clinical research, and then talk about some of the problems that we run into with research and what the research shows us in terms of how to better study procedures such as acupuncture, because studying procedures is different from studying drugs. The clinical studies roughly fall into 2 categories: effectiveness studies and efficacy studies, and many studies overlap and attempt to do both.
An effectiveness study looks at the extent to which a drug or procedure achieves its intended effect in the usual clinical setting. In these circumstances, you’re randomizing acupuncture against something such as a wait list control or usual care such as physical therapy or medications.
In 2009, a Cochrane database review studying acupuncture for prophylaxes of migraine showed that acupuncture was at least as effective, and possibly more effective, than prophylactic drugs with fewer adverse effects.13
In 2012, Andrew Vickers and his colleagues4 performed individualized patient data meta-analysis of 17,922 patients with a variety of back, neck, shoulder, osteoarthritic-related and headache pains and concluded that acupuncture was, in fact, effective for the treatment of chronic pain. Some effectiveness trials have shown acupuncture to be useful for some specific conditions, pain being the number one condition.
Efficacy is the extent to which a drug or procedure has the ability to bring about its intended effect under ideal circumstances, that is, acupuncture compared to a placebo. In the Vickers study,4 Vickers looked at the efficacy of acupuncture in the treatment of chronic pain and again concluded that true acupuncture was statistically slightly more efficacious than sham. Although this was not a big effect, it was nonetheless statistically significant.
From the 2012 Cochrane database review of IBS14 it was concluded that acupuncture was not efficacious as compared to a creditable sham, but there were several effectiveness trials where acupuncture tested better against 2 antispasmodic medications, which have some effect on both the severity and quality of life in patients with IBS.
While the Vickers study reported the efficacy as well as effectiveness of acupuncture, the IBS trial did not find any efficacy, when compared to the placebo, but did find evidence of the effectiveness of acupuncture.
What is particularly interesting about this study is that the natural history of carpal tunnel suggests that you will notice a 20% to 40% improvement over time. However, this study showed an 88% statistically significant improvement in both the true and sham acupuncture groups, which was maintained over 3 months of follow-up after the treatments ended.
The question that arises now is how you reconcile all of this, because it seems that the first piece of information that you come up with is that the sham may actually be a different form of active treatment. There’s an interesting study by Richard Harris and others in neuroimaging that was published in 2009.16 Harris’ team looked at the effects of true and sham acupuncture on the mu-opioid receptors in the central nervous system (CNS) using positron emission tomographic scanning in patients with fibromyalgia. Prior studies in patients with fibromyalgia have demonstrated increased levels of endogenous opioids in the cervical spinal fluid with decreased sensitivity in the mu-opioid receptors in the CNS regions known to be associated with the modulation of pain.
In the Harris study, the authors found that true acupuncture therapy evoked both short- and long-term increases in mu-opioid-binding potential receptors in the multiple pain areas and sensory processing areas associated with pain regulation. This was associated with clinical reports of pain reduction on the part of the subjects.
In the sham group, they also reported reduction in pain, though less than that in the true acupuncture group, and the positron emission tomographic scan showed no effect on the sensitivity of the mu-opioid receptors. The binding potential of these receptors did not improve as they did with the acupuncture treatments.
We know from prior studies that both true and sham acupuncture seem to increase the release of endogenous opioids, and we see that effect occurring in the ascending pathways and a segmental effect occurring in the spinal cord as well as in the descending modulating pathways mediated via dynorphins serotonin and norepinephrine. However, the effects of true acupuncture on the mu-opioid binding sensitivities are different from that of sham acupuncture.
In addition to this, we have imaging studies that have been conducted since the 1990s, and a recently published meta-analysis by Huang et al,17 which showed that while there is a problem with heterogeneity of these studies, they were able to conclude that the brain response to acupuncture encompasses a broad network of regions consistent with somatosensory affective and cognitive processing.
Overall, the neurophysiological evidence shows that acupuncture treatments affect the CNS in ways that are beneficial, long lasting, and unique to true acupuncture treatments. The neurophysiological evidence is also beginning to explain why we see different degrees of clinical effectiveness of acupuncture in conditions as diverse as gastrointestinal disorders, pain, and psychiatric conditions.
We have a lot more to learn and, far from being discouraged by this conflicting evidence in the literature, we should be excited by how much acupuncture has challenged and taught us about our understanding of human physiology. Does acupuncture work? Yes, according to the literature. Does acupuncture have unique and beneficial mechanisms of action on our neurophysiology? Again, I believe that the accumulative answer to that is yes.
The abovementioned discussion was about what’s going on in the CNS with acupuncture. There are a couple of other theories about how acupuncture may be effective. The one most commonly cited is work is that of Helen Langevin,18 where she writes about the network of acupuncture points and meridians viewed as representations of a network formed by interstitial connective tissue and that there has been an 80% correlation of the acupuncture points where the intramuscular connective tissue planes.
The needle grasp is a result of a winding of connective tissue and causes a tight mechanical coupling between the needle and the tissue, and there’s mounting evidence that this mechanical transduction can be translated into a variety of cellular and extracellular events. The 2 major models are the neurologic model, which is by far the most accepted and studied, and the connective tissue model.
Again, this is an evolving area. We have a lot more to learn, and I completely agree with Dr. Helms that we don’t want to be locked into the evidence-based approach that we fail to understand the true clinical benefits that acupuncture has shown repeatedly over thousand years of practice and that we see ourselves in day-to-day practice in our offices.
DR. BERMAN: Apart from summarizing the mechanisms, Dr. Kaplan, I think you mean that when we’re talking about evidence-based medicine, it’s not just about the efficacy shown by randomized control trials. There’s a wider range of methodologies and diseases to consider, depending on the question being asked. This is true of all medicine, including acupuncture, and if we narrow it down too much, we may fail to reap the benefits of using a very valuable tool as part of medicine.
DR. KAPLAN: I think you’re absolutely correct. The other thing that we need to keep in mind is that the evidence-based research itself is a very limiting concept because we keep finding new mechanisms and understanding new subtleties about how the nervous system is working, how our physiology works, and then we’re able to go back and say, “Ah, that’s the mechanism via which this is happening.” This whole topic about mu-opioid receptors is actually a breakthrough in terms of understanding how acupuncture may affect the CNS, which is unique and different from the way that sham does.
DR. BERMAN: What do you think are the cutting-edge research questions that still need to be answered as we go forward, questions that could not only inform us of how acupuncture works but could also affect clinical practice?
DR. KAPLAN: One of the areas that I’ve been particularly focused on is the microglial cells and their impact as the ultimate transducers between psychological stress, which gets translated into neurologic damage; and physical stress such as traumatic brain injury; as well as infectious stress, which also creates problems with neuroinflammation and neurodegeneration in conditions such as chronic pain and chronic illness.
We have seen evidence that acupuncture is actually neuroregenerative in some circumstances, certainly from some of the carpal tunnel studies that have been performed. We know that the microglia are involved in neuroregeneration; therefore, studying the effects of acupuncture on microglia may give us much more insight into how acupuncture works. This would be one area that I think should be focused on.
DR. BERMAN: Dr. Helms or Dr. Lao, any questions you think still need to be answered that can really make a difference?
DR. LAO: I agree with everything you have already said, but I think I’ll add one point: we need more translational studies on how to apply the scientific information to our daily practices in order to enhance the effectiveness of acupuncture treatment. We did some studies in which the effectiveness of a combination of conventional medication and acupuncture was evaluated. We found that the effectiveness of the combined therapy was much higher than that of acupuncture or the medication alone. Maybe, in the future, the research should be designed to answer the question of whether acupuncture reduces the side effects of a medication, resulting in enhanced effectiveness of both medicine and acupuncture.
DR. BERMAN: I would add one point that goes along with that: we need to get a better idea of the responders and nonresponders to acupuncture. We could begin to address this by setting up some pragmatic clinical trials with the idea of comparative effectiveness research in actual settings of clinical practice as well as cost effectiveness. Further, we could determine who responds, and we can include imaging and genomics assessments as part of the biomarkers that we’re analyzing.
Dr. Kaplan, do you have any final comments you want to add?
DR. KAPLAN: In terms of additional research, our thinking has been very much from a Bohr atom perspective [Bohr was a physicist who originally described the atom like a small solar system with electrons neatly orbiting the nucleus of the atom is a fixed orbit. This is a cartoon approximation of reality.] in terms of how the nervous system works, and we need to move toward a more quantum understanding. The whole field of neuroimaging is moving toward the concept of neuro-networking and trying to understand how the different regions of the brain interact with each other. I think that’s going to show a lot of promise even in terms of how acupuncture is affecting the system.
I also think that, as you mentioned briefly, the cost effectiveness research is extremely important. Integrating acupuncture into conventional medical practice has the potential, at least to significantly reduce cost to the patient and side effects of medications. I think studies need to be conducted on this issue. I’m optimistic these studies will confirm what we have witnessed in clinical practice.
DR. HELMS: Just a comment on that, Dr. Kaplan. You first need a model environment where acupuncture is fully integrated into a broad-based clinical setting, not individual practices. That’s the first hurdle to overcome before one looks at the impact of reducing reliance on pharmaceutical products or cutting back on the frequency of office visits and referrals to specialists.
DR. KAPLAN: I completely agree with you. I think that’s a challenge that we need to potentially take on in the future, but it’s something to be looking towards as we’re going to have to be more cost effective and more cost conscious in our treatment of a variety of diseases. I think acupuncture has a significant role to play here but we are not ready to perform those studies yet. We need to start to think about them and how they can be accomplished.
DR. HELMS: In the past, we have thought of acupuncture as a treatment for chronic conditions, but one of the biggest problems we face in the military today is trauma. It could be possible to compare management outcomes at military facilities that have integrated acupuncture into their trauma treatment with those that have not.
DR. BERMAN: Here is where the military comes into play. They have proposed a move towards expanding availability of acupuncture immediately following trauma and then follow that through with intermediate and long-term care facilities. If this approach succeeds, it would create an environment in which those issues of acute, sub-acute, and chronic consequences of trauma could be evaluated.
DR. LAO: In ancient literature, early acupuncture was largely used for emergency medicine, particularly in the ancient times when patients were unconscious or in conditions such as fainting or convulsions where they could not be treated with oral medicines. There is a large body of ancient literature that has documented this use.
DR. BERMAN: I want to thank all of you for participating in this discussion; it’s been a real pleasure.
FoxP2 Media LLC is the publisher of The Medical Roundtable.
Acupuncture (a traditional Chinese medical practice systematically used for over 2000 years) involves insertion of thin stainless steel needles into specific points on the body to facilitate recovery and good health. This practice was first brought to Europe in the 17th Century,1 and the first journal article on acupuncture appeared in the 1820s.2 Not until recently has acupuncture been widely accepted because of the clash of east versus west paradigms.
Scientific advances in acupuncture research, coupled with the side effects of treating pain by conventional drugs, have dramatically promoted the use of acupuncture in the last 20 years. It is estimated that over 1 million practitioners (outside China) administer acupuncture treatments for chronic pain. Of these practitioners, over 300000 are physicians.3 An estimated 3 million American adults receive acupuncture treatments each year, and chronic pain is the most common presentation.4
One of the most significant events in the 1990s for acupuncture was the decision taken by the US Food and Drug Administration in March 1996 to reclassify the legal status of acupuncture as safe and effective medical devices.
Further, in November 1997, there was a consensus conference on acupuncture by the National Institutes of Health.5 This was a 2.5-day conference conducted to evaluate the scientific and medical data on the uses, risks, and benefits of acupuncture for a variety of conditions. The findings after reviewing approximately 2300 studies stated that “Promising results have emerged, for example, showing efficacy of acupuncture in adult postoperative and chemotherapy nausea and vomiting and postoperative dental pain.”
“There are other conditions such as stroke rehabilitation, headache, tennis elbow, osteoarthritis, lower back pain, carpal tunnel syndrome, and asthma, for which acupuncture may be useful as an adjunct treatment or could be included in a comprehensive management program. Although many issues remain to be clarified, there is sufficient evidence to prove the value of acupuncture in order to expand its use in conventional medicine and encourage further studies of its physiology and clinical value.”
Since the consensus conference in 1997, there has been a huge increase in the number of scientific studies conducted on acupuncture. The Cochrane Collaboration’s database includes now 6035 clinical trials and 53 systematic reviews on acupuncture in their database.6 This roundtable today will focus on the current indications for acupuncture, and we will discuss how it is used in clinical settings, its safety issues and clinical evidence, and how it works.
The other participants are Dr. Joseph Helms, Dr. Gary Kaplan, and Dr. Lixing Lao. Dr. Helms is the founding president of the American Academy of Medical Acupuncture. In 1980, Dr. Helms developed the Medical Acupuncture Physicians program as a continuing medical education course for the University of California, Los Angeles (UCLA), School of Medicine; has chaired the program since then through the Helms Medical Institute (HMI); and has trained over 6000 physicians during this period. Dr. Helms is professor of medical acupuncture on the adjunct clinical faculty of the Stanford Medical School and the author of Acupuncture Energetics: A Clinical Approach for Physicians.
Dr. Kaplan is the medical director of the Kaplan Center for Integrative Medicine in McLean, Virginia, and is an associate professor in the Department of Community and Family Medicine at Georgetown University, School of Medicine. He served on the board of the American Academy of Medical Acupuncture and was president of the Medical Acupuncture Research Foundation.
Our final participant, Dr. Lao, is a professor of Family Medicine and the director of Traditional Chinese Medicine Research program at the Center for Integrative Medicine, University of Maryland School of Medicine. Dr. Lao graduated from the Shanghai University in the Traditional Chinese Medicine Program, holds a PhD in physiology from the University of Maryland in Baltimore, and has practiced acupuncture for 30 years and conducted research for 20 years.
To begin this discussion, Dr. Helms, can you describe for us the different types of acupuncture, training, and how acupuncture is used in a clinical setting?
DR. HELMS: Thank you, Dr. Berman. Acupuncture is relatively new in the collection of American medical disciplines. It has been in constant evolution since President Nixon’s visit to China in 1972. This evolution is driven by public interest and demand as well as scientific evidence of its mechanism and clinical value. This started with linking the impact of acupuncture on pain to the endogenous opioid peptide cascade, which is currently being reinforced through functional magnetic resonance imaging studies that confirm an intracranial response to peripheral needling.
The 1997 Consensus Development Conference report5 that endorsed a handful of acupuncture applications was based on the quality of research design to evaluate acupuncture’s impact on different problems, rather than on the actual practice of acupuncture. Since that paper, over 400 randomized control trials have been published in peer review journals internationally. These studies demonstrate the favorable impact of acupuncture on a wide spectrum of medical problems, including, but not limited to, pain.
There are many different styles of acupuncture. This discipline has evolved through multiple cultures over the last 2000 years. Each culture and era of its blossoming has contributed its enduring quality and approach. Many of these styles of acupuncture were retained only in family traditions, while others were propagated nationally. It is only in the late 20th century and beginning of the 21st century that we have had the privilege to access many of the family and most of the national traditions of acupuncture training and practice.
The tradition, with which I’m most familiar with, is known as medical acupuncture. Medical acupuncture would best be described as a hybrid approach combining our understanding of acupuncture neuroanatomy and physiology with traditional precepts from the classics of acupuncture. Medical acupuncture is generally practiced by licensed practitioners of conventional biomedical medicine and is considered an additional qualification to their scope of practice. These would include doctors of medicine, doctors of osteopathy, doctors of dental surgery, and doctors of podiatric medicine.
Traditional Chinese Medicine is the approach most widely practiced in this country. It is an approach exported from post-Maoist China, having been developed to provide basic healthcare to the Chinese population as the country was transitioning from its revolutionary period in the 1950s and 1960s into a more stable political and social period. The Traditional Chinese Medicine model doesn’t contain the totality of the classics, but rather is an extraction that can be taught and absorbed by the western community. The Traditional Chinese Medicine approach covers internal medicine problems as well as pain problems.
Two additional, commonly used subdivisions of acupuncture are auricular acupuncture and Chinese scalp acupuncture. Auricular acupuncture was developed in France in the 1950s and 1960s and uses points exclusively on the ear to influence pain and organ function. Chinese scalp acupuncture is a recent development in Chinese medicine. It involves placing needles in the scalp overlying the cortical surfaces that relay pain signals.
DR. BERMAN: Could you elaborate on auricular acupuncture a little more and on what it is used for?
DR. HELMS: Auricular acupuncture is the least complex and most easily learned approach to acupuncture. It can be effective either as a standalone treatment or as an adjunct to body acupuncture. The scientific foundation of auricular acupuncture involves the ear’s complex innervation that links it to all 3 embryologic germ levels. Thus, with neurological representation of endoderm, mesoderm, and ectoderm, the ear manifests a homunculus of all body parts. Ear points that correspond to painful or disturbed structures demonstrate increased electrical conductivity, and thereby allow the ear to serve as a diagnostic tool and a therapeutic signal.
DR. BERMAN: I think in the past, auricular acupuncture was also used for problems of addiction but I don’t know if it’s still being used for this purpose.
DR. HELMS: There are several widely used acupuncture point combinations that have been shown to be useful in assisting a multidisciplinary approach to substance abuse problems, referred to as the “NADA protocol” that was developed by Michael Smith, MD. There is also a 5-point formula called battlefield acupuncture that is useful in dealing with acute traumatic pain.7
DR. BERMAN: Thank you, Dr. Helms. Dr. Kaplan and then Dr. Lao, could you comment about what’s being done in clinical settings and how acupuncture is used to treat certain diseases beyond what Dr. Helms has just explained?
DR. KAPLAN: We do a great deal of work for the treatment of pain and find acupuncture to be extremely effective for conditions such as headaches, back pain, and neck pain. We also find it useful for the treatment of peripheral neuropathies. In addition, because we deal with many chronic pain patients, we also see a lot of psychoemotional issues comorbid with the chronic pain. Acupuncture has proven to be very helpful as an adjunctive therapy dealing with the psychoemotional components that we see associated with chronic pain.
In my practice, approximately 20% of our pain population has posttraumatic stress syndrome, while approximately 60% has comorbid anxiety disorders or major depressive disorders. Acupuncture has been particularly unique as a therapeutic modality because it addresses both the pain and the psychological component of an individual’s illness at the same time. We’re able to talk about the totality of the individual as opposed to segmenting them into psychiatric versus pain versus sleep issues. From an acupuncture perspective, these conditions are not separate issues but different manifestations of a pattern of disharmony in the individual.
DR. LAO: I agree with Drs. Kaplan and Helms. In my practice, I see patients with a variety of complaints. In addition to pain, they also experience menstruation disorders, depression, and attention deficit disorder (ADD) (in children). A wide variety of diseases can be treated by acupuncture. Evidence of the effectiveness of acupuncture for the treatment of pain has recently been published by Vickers.4
Individual raw data show the full area of musculoskeletal pain, which includes neck pain, low back pain, headaches (migraine and tension headaches), osteoarthritis in the knees, and shoulder pain. There is a significant difference between acupuncture and conventional treatment in terms of their therapeutic effectiveness. There was also a significant difference between acupuncture and sham acupuncture, ie, placing of needles at points on the body that are not thought to be acupuncture points (off site points). Although the benefits were modest, they were highly significant.4
Dr. Berman, do you also want me to cover a little bit about the side effects or shall we save that for later?
DR. BERMAN: Let’s stick to the clinical use first, and then we’ll go to the side effects.
DR. KAPLAN: I’d like to chime in here. I’m boarded in family medicine and pain medicine and started my clinical practice in a general medical setting. As my practice evolved, I began seeing a greater number of individuals suffering with chronic pain and illness issues.
Over the last 30 years, acupuncture has heavily influenced my approach to patient care. Acupuncture is not simply a tool but a philosophy of care that has greatly enriched my western medical training. At times, when treating a patient, I believe the prism of a western approach will be more effective; there are also times when I rely exclusively on an acupuncture approach, but more commonly, I integrate the two in designing and implementing a care program.
Pain can be very effectively managed with acupuncture alone or as an adjunct. Many so-called functional or psychosomatic problems can be more effectively addressed using acupuncture in place of pharmaceutical agents. Likewise, the conventional approaches to organic problems can be reinforced and facilitated with acupuncture treatment.
Acupuncture covers a much broader range of clinical applications than simple neuromusculoskeletal pain or psychoemotional issues. It really covers the full spectrum of medicine.
DR. KAPLAN: We have used acupuncture successfully in women with hyperemesis gravidarum. Most of the medications are contraindicated because of the potential harm to the fetus. Acupuncture has been successful in at least providing these women with some level of relief in treating this condition.
I don’t have experience with acupuncture therapy for postoperative nausea/vomiting. We have used it a little bit in nausea/vomiting associated with chemotherapy, and again, we’ve been able to reduce the amount of medications that the patients require in order to control it; in some cases, we’ve actually been able to eliminate the need for medications.
Further, I want to go over what Dr. Helms was talking about—the importance of integrating acupuncture into a comprehensive treatment program. It is sometimes the main therapeutic modality that we use, but on many occasions, it is integrated into our medication regimes. In a comprehensive approach, we may use it in conjunction with physical therapy, and we will also be probing trigger points. We may also do prolotherapy with the patients.
Acupuncture gives us the ability to treat a wider range of conditions with fewer medications. We are frequently able to address irritable bowel syndrome (IBS), sleep disorders associated with the medical conditions, as well as the psychiatric conditions I was talking about earlier. Acupuncture is a beautiful adjunctive therapy and sometimes can be used as the sole therapeutic approach.
DR. BERMAN: In general, we’re now talking about acupuncture being part of a comprehensive approach to a number of chronic disorders.
DR. KAPLAN: That’s absolutely correct. You want to use all of the tools you have available, and acupuncture is a very powerful therapeutic modality in the treatment of these conditions.
DR. LAO: One of the nonpain areas that I think people should consider using acupuncture as a therapy is infertility. Many women now come to the clinic, particularly after the publication of the enhanced success rate of in vitro fertilization (IVF) in women receiving acupuncture treatment.8 Even those patients who elect to not go through IVF come for acupuncture treatment to enhance their chances of getting pregnant.
DR. BERMAN: Dr. Lao, is there evidence to support acupuncture for infertility?
DR. LAO: There’s a paper that was published a couple years ago through our center.8 The authors show a higher success rate of conventional IVF procedure when combined with acupuncture than with sham control. Current studies give clear evidence of the benefits of acupuncture to IVF patients.
DR. BERMAN: With the breathlessness COPD I was referring to, there was a study in the Archives of Internal Medicine just this past June 2012,9 which was a very well-done clinical trial aimed at studying COPD and using acupuncture in addition to conventional care, that showed clear outcomes of the benefits of acupuncture in this particular condition.
Dr. Helms, you have experienced acupuncture in the military setting. Can you talk a little bit about that?
DR. HELMS: In the last 5 years, 3 branches of the US Military have shown interest in pursuing acupuncture training for physicians to provide these services to their population. This interest reflects what’s happening in the civilian population and is more intensively motivated by the report of the Army’s pain management task force that identified some severe shortcomings in managing acute and chronic pain.
The feedback we’ve received from the military physicians we’ve trained has been very rewarding. The bulk of their treatments are for pain, ranging from headache to cervical, lumbar, and peripheral pain. Much of this pain is caused by the weight of their 75-pound protective gear, which they wear no matter where they are in the world, and of course, the physical trauma of battle. Interestingly, an almost equal percentage of treatments for active duty service members are for psychoemotional problems (anxiety, insomnia, depression, acute stress, and chronic stress) as for pain and physical trauma.
DR. BERMAN: Let me move on to the next subtopic. Dr. Lao, can you talk to us about how safe acupuncture is?
DR. LAO: There are few reported cases of complications in the English literature from 1965 to 1999, a 35-year span. There were a total of 202 case reports, which is about 5–6 cases per year.10 I have completed 2 reviews of case reports on adverse events associated with acupuncture. One was published in 200310 and the other one is accepted for publication.11 Events are divided into complications and adverse reactions. Complications such as injured organs or infections occur if acupuncture is not carefully performed. Adverse reactions include syncope and allergic reaction.
Infections constituted 50% of all complications. Needle infections may cause hepatitis. However, since the late 1980s, acupuncturists started using disposable needles, resulting in lower incidence of hepatitis and other infections.10 In recent years, another infection emerged that involves many different invasive procedures in medical settings such as methicillin-resistant Staphylococcus aureus (MRSA). This is likely due to the unsanitary conditions of these clinical settings, such as the use of contaminated disinfectant. It’s not the acupuncture needle itself that caused infection.
A larger survey12 showed that approximately 7% to 8% of the adverse events were classified as mild. These events include local site bleeding, pain in local needling site, nausea, or light-headedness. The occurrence of these mild adverse events is very low especially in the context of the large numbers of patients attended to acupuncture clinic every year.
In the last 10 years, 308 cases of side effects were noted from 26 countries.11 In the United States, only 17 cases have been reported, which is a very small percentage. I believe that this is due to extensive professional licensing requirement that is called Clean Needle Techniques (CNT) training. This requirement has dramatically decreased the risk of unnecessary side effects.
Other types of adverse events such as organ and tissue injuries are associated with knowledge of anatomy. Therefore, proper training of the acupuncturist could help reduce the occurrence of side effects due to acupuncture.
DR. BERMAN: From these prospective studies,10–12 we can conclude that serious adverse events are very rare with acupuncture and that there is, depending on the surveys, a 2% to 7% probability of occurrence of a mild side effect such as local site bleeding or occasional dizziness or localized pain to the area. Is there anything else on safety that either, Dr. Kaplan or Dr. Helms would like to add?
DR. HELMS: In addition to reinforcing that acupuncture is a very safe and forgiving therapeutic approach, I’d like to discourage readers from concluding that useful indications for acupuncture in medical practice are limited to what is published in the evidence-based literature. Acupuncture has been used for simple and complex problems by responsible practitioners in oriental and occidental cultures for much longer period than we have been documenting its efficacy. Acupuncture comes from a long tradition of the practice of medicine, albeit in cultures and eras quite distant from ours. Our hybrid medical acupuncture allows remarkable creativity in the hands of well-trained practitioners, to treat many problems that are not included among those already studied in the pharmaceutical model.
DR. BERMAN: I think that’s a very important point, but let’s talk a little bit about the research first, and then go back to this when we’re putting the research into the context of clinical practice. How should we take this into account?
DR. KAPLAN: Let’s briefly look at the clinical research, and then talk about some of the problems that we run into with research and what the research shows us in terms of how to better study procedures such as acupuncture, because studying procedures is different from studying drugs. The clinical studies roughly fall into 2 categories: effectiveness studies and efficacy studies, and many studies overlap and attempt to do both.
An effectiveness study looks at the extent to which a drug or procedure achieves its intended effect in the usual clinical setting. In these circumstances, you’re randomizing acupuncture against something such as a wait list control or usual care such as physical therapy or medications.
In 2009, a Cochrane database review studying acupuncture for prophylaxes of migraine showed that acupuncture was at least as effective, and possibly more effective, than prophylactic drugs with fewer adverse effects.13
In 2012, Andrew Vickers and his colleagues4 performed individualized patient data meta-analysis of 17,922 patients with a variety of back, neck, shoulder, osteoarthritic-related and headache pains and concluded that acupuncture was, in fact, effective for the treatment of chronic pain. Some effectiveness trials have shown acupuncture to be useful for some specific conditions, pain being the number one condition.
Efficacy is the extent to which a drug or procedure has the ability to bring about its intended effect under ideal circumstances, that is, acupuncture compared to a placebo. In the Vickers study,4 Vickers looked at the efficacy of acupuncture in the treatment of chronic pain and again concluded that true acupuncture was statistically slightly more efficacious than sham. Although this was not a big effect, it was nonetheless statistically significant.
From the 2012 Cochrane database review of IBS14 it was concluded that acupuncture was not efficacious as compared to a creditable sham, but there were several effectiveness trials where acupuncture tested better against 2 antispasmodic medications, which have some effect on both the severity and quality of life in patients with IBS.
While the Vickers study reported the efficacy as well as effectiveness of acupuncture, the IBS trial did not find any efficacy, when compared to the placebo, but did find evidence of the effectiveness of acupuncture.
What is particularly interesting about this study is that the natural history of carpal tunnel suggests that you will notice a 20% to 40% improvement over time. However, this study showed an 88% statistically significant improvement in both the true and sham acupuncture groups, which was maintained over 3 months of follow-up after the treatments ended.
The question that arises now is how you reconcile all of this, because it seems that the first piece of information that you come up with is that the sham may actually be a different form of active treatment. There’s an interesting study by Richard Harris and others in neuroimaging that was published in 2009.16 Harris’ team looked at the effects of true and sham acupuncture on the mu-opioid receptors in the central nervous system (CNS) using positron emission tomographic scanning in patients with fibromyalgia. Prior studies in patients with fibromyalgia have demonstrated increased levels of endogenous opioids in the cervical spinal fluid with decreased sensitivity in the mu-opioid receptors in the CNS regions known to be associated with the modulation of pain.
In the Harris study, the authors found that true acupuncture therapy evoked both short- and long-term increases in mu-opioid-binding potential receptors in the multiple pain areas and sensory processing areas associated with pain regulation. This was associated with clinical reports of pain reduction on the part of the subjects.
In the sham group, they also reported reduction in pain, though less than that in the true acupuncture group, and the positron emission tomographic scan showed no effect on the sensitivity of the mu-opioid receptors. The binding potential of these receptors did not improve as they did with the acupuncture treatments.
We know from prior studies that both true and sham acupuncture seem to increase the release of endogenous opioids, and we see that effect occurring in the ascending pathways and a segmental effect occurring in the spinal cord as well as in the descending modulating pathways mediated via dynorphins serotonin and norepinephrine. However, the effects of true acupuncture on the mu-opioid binding sensitivities are different from that of sham acupuncture.
In addition to this, we have imaging studies that have been conducted since the 1990s, and a recently published meta-analysis by Huang et al,17 which showed that while there is a problem with heterogeneity of these studies, they were able to conclude that the brain response to acupuncture encompasses a broad network of regions consistent with somatosensory affective and cognitive processing.
Overall, the neurophysiological evidence shows that acupuncture treatments affect the CNS in ways that are beneficial, long lasting, and unique to true acupuncture treatments. The neurophysiological evidence is also beginning to explain why we see different degrees of clinical effectiveness of acupuncture in conditions as diverse as gastrointestinal disorders, pain, and psychiatric conditions.
We have a lot more to learn and, far from being discouraged by this conflicting evidence in the literature, we should be excited by how much acupuncture has challenged and taught us about our understanding of human physiology. Does acupuncture work? Yes, according to the literature. Does acupuncture have unique and beneficial mechanisms of action on our neurophysiology? Again, I believe that the accumulative answer to that is yes.
The abovementioned discussion was about what’s going on in the CNS with acupuncture. There are a couple of other theories about how acupuncture may be effective. The one most commonly cited is work is that of Helen Langevin,18 where she writes about the network of acupuncture points and meridians viewed as representations of a network formed by interstitial connective tissue and that there has been an 80% correlation of the acupuncture points where the intramuscular connective tissue planes.
The needle grasp is a result of a winding of connective tissue and causes a tight mechanical coupling between the needle and the tissue, and there’s mounting evidence that this mechanical transduction can be translated into a variety of cellular and extracellular events. The 2 major models are the neurologic model, which is by far the most accepted and studied, and the connective tissue model.
Again, this is an evolving area. We have a lot more to learn, and I completely agree with Dr. Helms that we don’t want to be locked into the evidence-based approach that we fail to understand the true clinical benefits that acupuncture has shown repeatedly over thousand years of practice and that we see ourselves in day-to-day practice in our offices.
DR. BERMAN: Apart from summarizing the mechanisms, Dr. Kaplan, I think you mean that when we’re talking about evidence-based medicine, it’s not just about the efficacy shown by randomized control trials. There’s a wider range of methodologies and diseases to consider, depending on the question being asked. This is true of all medicine, including acupuncture, and if we narrow it down too much, we may fail to reap the benefits of using a very valuable tool as part of medicine.
DR. KAPLAN: I think you’re absolutely correct. The other thing that we need to keep in mind is that the evidence-based research itself is a very limiting concept because we keep finding new mechanisms and understanding new subtleties about how the nervous system is working, how our physiology works, and then we’re able to go back and say, “Ah, that’s the mechanism via which this is happening.” This whole topic about mu-opioid receptors is actually a breakthrough in terms of understanding how acupuncture may affect the CNS, which is unique and different from the way that sham does.
DR. BERMAN: What do you think are the cutting-edge research questions that still need to be answered as we go forward, questions that could not only inform us of how acupuncture works but could also affect clinical practice?
DR. KAPLAN: One of the areas that I’ve been particularly focused on is the microglial cells and their impact as the ultimate transducers between psychological stress, which gets translated into neurologic damage; and physical stress such as traumatic brain injury; as well as infectious stress, which also creates problems with neuroinflammation and neurodegeneration in conditions such as chronic pain and chronic illness.
We have seen evidence that acupuncture is actually neuroregenerative in some circumstances, certainly from some of the carpal tunnel studies that have been performed. We know that the microglia are involved in neuroregeneration; therefore, studying the effects of acupuncture on microglia may give us much more insight into how acupuncture works. This would be one area that I think should be focused on.
DR. BERMAN: Dr. Helms or Dr. Lao, any questions you think still need to be answered that can really make a difference?
DR. LAO: I agree with everything you have already said, but I think I’ll add one point: we need more translational studies on how to apply the scientific information to our daily practices in order to enhance the effectiveness of acupuncture treatment. We did some studies in which the effectiveness of a combination of conventional medication and acupuncture was evaluated. We found that the effectiveness of the combined therapy was much higher than that of acupuncture or the medication alone. Maybe, in the future, the research should be designed to answer the question of whether acupuncture reduces the side effects of a medication, resulting in enhanced effectiveness of both medicine and acupuncture.
DR. BERMAN: I would add one point that goes along with that: we need to get a better idea of the responders and nonresponders to acupuncture. We could begin to address this by setting up some pragmatic clinical trials with the idea of comparative effectiveness research in actual settings of clinical practice as well as cost effectiveness. Further, we could determine who responds, and we can include imaging and genomics assessments as part of the biomarkers that we’re analyzing.
Dr. Kaplan, do you have any final comments you want to add?
DR. KAPLAN: In terms of additional research, our thinking has been very much from a Bohr atom perspective [Bohr was a physicist who originally described the atom like a small solar system with electrons neatly orbiting the nucleus of the atom is a fixed orbit. This is a cartoon approximation of reality.] in terms of how the nervous system works, and we need to move toward a more quantum understanding. The whole field of neuroimaging is moving toward the concept of neuro-networking and trying to understand how the different regions of the brain interact with each other. I think that’s going to show a lot of promise even in terms of how acupuncture is affecting the system.
I also think that, as you mentioned briefly, the cost effectiveness research is extremely important. Integrating acupuncture into conventional medical practice has the potential, at least to significantly reduce cost to the patient and side effects of medications. I think studies need to be conducted on this issue. I’m optimistic these studies will confirm what we have witnessed in clinical practice.
DR. HELMS: Just a comment on that, Dr. Kaplan. You first need a model environment where acupuncture is fully integrated into a broad-based clinical setting, not individual practices. That’s the first hurdle to overcome before one looks at the impact of reducing reliance on pharmaceutical products or cutting back on the frequency of office visits and referrals to specialists.
DR. KAPLAN: I completely agree with you. I think that’s a challenge that we need to potentially take on in the future, but it’s something to be looking towards as we’re going to have to be more cost effective and more cost conscious in our treatment of a variety of diseases. I think acupuncture has a significant role to play here but we are not ready to perform those studies yet. We need to start to think about them and how they can be accomplished.
DR. HELMS: In the past, we have thought of acupuncture as a treatment for chronic conditions, but one of the biggest problems we face in the military today is trauma. It could be possible to compare management outcomes at military facilities that have integrated acupuncture into their trauma treatment with those that have not.
DR. BERMAN: Here is where the military comes into play. They have proposed a move towards expanding availability of acupuncture immediately following trauma and then follow that through with intermediate and long-term care facilities. If this approach succeeds, it would create an environment in which those issues of acute, sub-acute, and chronic consequences of trauma could be evaluated.
DR. LAO: In ancient literature, early acupuncture was largely used for emergency medicine, particularly in the ancient times when patients were unconscious or in conditions such as fainting or convulsions where they could not be treated with oral medicines. There is a large body of ancient literature that has documented this use.
DR. BERMAN: I want to thank all of you for participating in this discussion; it’s been a real pleasure.
FoxP2 Media LLC is the publisher of The Medical Roundtable.
FoxP2 Media LLC
Meet Dr. Leslie Baumann at the Summer AAD meeting
You love Dr. Baumann’s Cosmeceutical Critique column in Skin & Allergy News, and soon that content will be expanded in a new book entitled "Cosmeceuticals and Cosmetic Ingredients," available this November via Amazon.com. Meet Dr. Baumann at the Skin Disease Education Foundation (SDEF)/Skin & Allergy News Booth #1500 from 12:00-12:30 p.m. on Saturday, Aug. 9 at the 2014 Summer Academy Meeting in Chicago. And be sure to pick up a copy of her latest column from Skin & Allergy News, the leading news publication for aesthetic, medical, and surgical dermatology.
In addition, you can visit Dr. Baumann at her booth (#1716) during the meeting.
Read Dr. Baumann’s columns online at edermatologynews.com.
You love Dr. Baumann’s Cosmeceutical Critique column in Skin & Allergy News, and soon that content will be expanded in a new book entitled "Cosmeceuticals and Cosmetic Ingredients," available this November via Amazon.com. Meet Dr. Baumann at the Skin Disease Education Foundation (SDEF)/Skin & Allergy News Booth #1500 from 12:00-12:30 p.m. on Saturday, Aug. 9 at the 2014 Summer Academy Meeting in Chicago. And be sure to pick up a copy of her latest column from Skin & Allergy News, the leading news publication for aesthetic, medical, and surgical dermatology.
In addition, you can visit Dr. Baumann at her booth (#1716) during the meeting.
Read Dr. Baumann’s columns online at edermatologynews.com.
You love Dr. Baumann’s Cosmeceutical Critique column in Skin & Allergy News, and soon that content will be expanded in a new book entitled "Cosmeceuticals and Cosmetic Ingredients," available this November via Amazon.com. Meet Dr. Baumann at the Skin Disease Education Foundation (SDEF)/Skin & Allergy News Booth #1500 from 12:00-12:30 p.m. on Saturday, Aug. 9 at the 2014 Summer Academy Meeting in Chicago. And be sure to pick up a copy of her latest column from Skin & Allergy News, the leading news publication for aesthetic, medical, and surgical dermatology.
In addition, you can visit Dr. Baumann at her booth (#1716) during the meeting.
Read Dr. Baumann’s columns online at edermatologynews.com.
The Medical Roundtable: Nonconstipation Irritable Bowel Syndrome
Over the past several decades, our understanding of the function of the gastrointestinal (GI) tract, especially with regard to those controlled by the enteric nervous system, has increased dramatically. This increase in knowledge has been accompanied by an enhanced appreciation of the importance of the various functional GI disorders in terms of the pathophysiology and societal impact.
IBS is a prototypical functional GI disorder that affects more than 15% of the population1 and has been gaining increasing awareness in the press and media over the past decade. This period has also witnessed several diagnostic and therapeutic clinical trials with a more dichotomous approach to IBS, which separates the clinical presentations into IBS with constipation and IBS without constipation.
Investigators and clinicians alike have realized that the pragmatic approach, using the presence or absence of constipation as a symptom of IBS, may lend itself to the subsequent evaluation and management of the disorder. Additional insights of the role of inflammation and food intolerance have fundamentally altered the approach to IBS and its associated symptoms. Likewise, the development of targeted therapies for patients who have IBS with constipation and IBS without constipation has increased the number of options available to clinicians as well as the improved quality of life of patients.
My name is Brooks Cash, and I am Professor of Medicine at the Uniformed Services University of the Health Sciences, as well as a gastroenterologist and Deputy Commander for Medical Services at the Walter Reed National Military Medical Center in Bethesda, Maryland. I am joined by 3 world-renowned experts in the field of functional GI disorders and IBS in particular: Drs. Lin Chang, Lucinda Harris, and Brian Lacy.
Welcome everybody, and thank you for taking the time to discuss up-and-coming topics surrounding nonconstipation IBS. Why don’t you take a moment to introduce yourselves?
DR. CHANG: I’m Lin Chang. I’m a gastroenterologist and Professor of Medicine in the Division of Digestive Diseases at the David Geffen School of Medicine at UCLA.
DR. HARRIS: I’m Lucinda Harris. I am co-director of motility in the Division of Gastroenterology at the Mayo Clinic in Scottsdale and Associate Professor of Medicine in the Mayo School of Medicine.
DR. LACY: Hi, I’m Brian Lacy. I’m Professor of Medicine at the Geisel School of Medicine at Dartmouth and director of the GI Motility Laboratory at the Dartmouth-Hitchcock Medical Center in Lebanon, New Hampshire.
DR. CASH: Let’s start with a general overview. Dr. Lacy, will you describe the epidemiology and impact of nonconstipation IBS?
DR. LACY: When I think about the epidemiology of IBS, I like to break it down into both prevalence and incidence. The prevalence of IBS has been actively studied over the years, and it varies depending on how IBS was defined and where the study was performed.
In general, we consider IBS one of the most prevalent functional bowel disorders and certainly one of the most well studied ones as well. Some of the earlier criteria, as you know, involved the Manning criteria.2 These were a little bit more generous and less restrictive than the recent Rome criteria, but, in general, if we were to use a comprehensive review published in 2002 by Saito and colleagues3 from the Mayo Clinic, the prevalence of IBS in North America ranges from approximately 3% to 20%, and most studies quote the prevalence of IBS in about the 12% to 15% range.4–6 The incidence of IBS is slightly more difficult to calculate. That being said, the incidence ranges from about 200 to 400 in 100,000 people, or about 1% to 2% per year in the United States.6,7
DR. CASH: What about the impact in terms of quality of life and economics?
DR. LACY: In terms of the impact of IBS, I think there are a couple of different ways to analyze it. The first is to point out its prevalence, knowing that in primary care, about 10% to 15% of primary care visits are for IBS symptoms, and in the GI referral community, that number may be as high as 40% or 50%.8,9 We know that about two-thirds of those visits are for nonconstipated IBS patients.
Secondly, we can look at the impact on patients, and often, we measure that in terms of quality of life. We know that quality of life of patients with IBS is reduced similar to the case of patients with longstanding diabetes, and in terms of the physical score, it’s lower than that in patients with chronic acid reflux disease and even depression (using the SF-36). We also know from one study that IBS has been shown to increase the risk of suicide, and I think this points out how greatly this affects patients.10-12
Lastly, we can look at the economic impact of IBS. Again, we can either measure that in terms of the direct cost to patients or society. We know that this is one of the most common reasons for patients to skip school or work. We know that healthcare costs for patients with IBS are approximately 50% higher than that for age- and sex-matched controls without IBS.13-15
When we think about the impact on society, including lost healthcare costs, lost productivity, or medication use and procedures, IBS accounts for, on an average, about $20 billion to $30 billion per year of medical costs in the United States.14–17
DR. CHANG: The etiology of IBS is not really well understood, and I think the main issue is that it’s a multifactorial condition, and the clinical presentation can be very heterogeneous. That’s what makes it difficult to understand and makes the cause difficult to identify in each individual because the studies do not necessarily yield consistent results.
Now, it’s generally well accepted that IBS is due to an alteration in brain-gut communication or brain-gut interactions, and that leads to changes in GI motility, sensation, and secretion and increases the perception that the patient has of pain and other GI symptoms.
There are certain vulnerability factors that increase the risk of developing IBS, including genetic predisposition, because we know that IBS runs in families, and there seems to be some genetic component, although it’s still not very well understood. There’s also evidence that chronic stress early in life, or even as an adult, can increase the risk for developing IBS in addition to other chronic pain syndromes.
Then, there seems to be a trigger, which could be, for example, infection, with post-infectious IBS; that’s when a patient develops IBS after gastroenteritis, surgery, or a psychological stressor that’s more chronic and sustained. The patients could also develop symptoms of IBS that can wax and wane or can be chronic. IBS can vary in symptom presentation. Even after the trigger has passed, ie, the infection has cleared or the stressor is gone, the symptoms themselves can perpetuate the condition because of the possibility of symptom-associated anxiety, which would be very normal in patients with very bothersome symptoms.
There are also certain foods that may not really cause the onset of the IBS—unless it’s due to food poisoning—but can trigger the symptoms. There may also be some food intolerances or certain types of foods—such as fatty foods—or larger meals that don’t tend to sit well with patients.
Proposed mechanisms that may result in changes in GI function such as disturbed gut motility, secretion, and sensation and ultimately in the development of IBS symptoms include alterations in neuroimmune and neuroendocrine responses, intestinal permeability, central nervous system modulation of visceral stimuli and sensations, and serotonin signaling, and dysbiosis within the GI tract.18-22
DR. CASH: Dr. Chang, there are also other somatic comorbidities that patients with IBS often have. Can you tell us about those comorbidities, as well as the medical resource utilization that we might see in patients with IBS and those comorbidities? And finally, is it possible that there’s a shared pathophysiology with other somatic complaints or syndromes?
DR. CHANG: A number of studies have looked at the comorbidity of IBS with other functional somatic syndromes. I’m talking more about functional diseases. There is also evidence of IBS coexisting with gastroesophageal reflux disease or inflammatory bowel disease, but much of the literature on comorbidity with IBS is with other existing chronic pain syndromes or chronic somatic syndromes such as fibromyalgia, interstitial cystitis, temporomandibular joint disorder, migraine headaches, and chronic fatigue syndrome.
There are studies that look at the prevalence of these conditions in IBS, and there are studies that evaluate the prevalence of IBS in these conditions. It’s usually about 30% or a subgroup of IBS patients who have these other conditions.23 IBS and these other conditions are more prevalent in women.24
When you look at healthcare utilization—healthcare visits—what’s interesting is that studies show that IBS patients have a greater number of healthcare visits for GI symptoms than individuals without IBS. But many of their healthcare visits also are for non-GI complaints because many IBS patients report non-GI symptoms. Fatigue is one of the more common symptoms, and headaches or muscle aches are also common.
Sometimes, these symptom presentations don’t actually meet diagnostic criteria for other conditions such as migraine headaches, fibromyalgia, painful bladder syndrome, or interstitial cystitis. Interestingly, many IBS patients actually seek health care for those visits. In fact, when you look at the healthcare costs, there are more related costs due to diagnostic testing or medication or healthcare visits for non-GI complaints than there are for GI complaints. But for both types, the cost is higher than that for individuals without IBS.
I recently reviewed the literature on pathophysiologic mechanisms for IBS and other comorbidities, including functional dyspepsia, and there are a number of mechanisms that have been studied in IBS as well as these other conditions.23
Many abnormalities are very similar in IBS and the comorbid conditions. There’s evidence of increased pain perception and altered brain activation patterns in IBS and of these other conditions including fibromyalgia and temporomandibular joint disorder. The findings are very similar, and some of these brain areas that are abnormally activated are associated with either enhanced emotional arousal or altered pain processing.
There’s also evidence of immune changes such as increased numbers of mast cells, particularly in chronic fatigue syndrome and interstitial cystitis, and in some of the studies in functional dyspepsia and IBS. There’s also evidence of genetic factors and certain genetic polymorphisms that are associated with an increased prevalence of IBS or other chronic pain conditions.
Several different mechanisms appear to be shared among these different conditions.
DR. CASH: Dr. Harris, many consider the diagnosis of nonconstipation IBS one of exclusion, while others feel that the Rome criteria are sufficient to make the diagnosis. We heard Dr. Lacy refer to the Rome criteria earlier. What are the Rome criteria, and how valid are they in terms of making the diagnosis of IBS and in particular nonconstipation IBS?
DR. HARRIS: The Rome committee is a group of gastroenterologists that had met since 1997 to decide the diagnostic criteria of IBS, as well as other functional disorders. We are currently using the Rome III criteria,25 and they define IBS as recurrent abdominal pain or discomfort that occurs at least 3 days per months in the last 3 months and is associated with 2 or more of the following criteria: (1) the abdominal pain or discomfort improves with defecation, (2) the onset of symptoms is associated with a change in form of stool, and (3) the onset of symptoms is associated with a change in frequency of stool. Also, the symptom onset should be present for at least 6 months prior to diagnosis.
They have also further defined the criteria into IBS subtypes according to stool form so that IBS with constipation indicates that you have hard or lumpy stools ≥25% of the time and diarrhea (loose or mushy stools) <25% of the time. IBS with diarrhea means the stools are loose or mushy >25% of the time and hard or lumpy <25% of the time. Mixed type IBS is defined as hard and lumpy stools ≥25% of the time and loose or watery stools >25% of the time.25
Finally, there is IBS that can’t be subtyped, called IBS unsubtyped. These are people who we can’t be subtyped because they have insufficient abnormalities of stool subtype to meet the criteria above. But most patients, I think, when you speak to them, can give you an idea of how their bowel movements are and you can easily subtype them.
The other important factor in using the criteria is to make sure that there are no alarm symptoms such as age > 50 years during the onset of the symptoms, blood in the stool, nocturnal symptoms, unintentional weight loss, or a dramatic change in the pattern of symptoms. However, it is important to realize that the stool pattern can change.
It’s also important to make sure that there is no family history of organic GI diseases such as colon cancer, inflammatory bowel disease, or celiac disease, and that there’s no recent history of antibiotic intake.
If you use the red flag symptoms and look at the patient’s history of symptoms, a clinical diagnosis can be made.
DR. LACY: Let’s tackle the easy one first, and I think that’s the role of colonoscopy. Several studies have pointed out that if patients meet Rome III criteria in the absence of warning signs, the utility of a colonoscopy would be very, very low.
We all agree that if the patient is older than 50 years, and ≥45 years for African Americans, even if there are signs of IBS and you’re pretty confident about the diagnosis, a colonoscopy is still required for screening purposes.
The utility of a colonoscopy in a younger patient—younger than 45 years—with classic symptoms of IBS in the absence of warning signs is extremely low, and I don’t generally recommend that.
One caveat, of course, is that as clinicians, we’re always double-checking to make sure that our diagnosis is correct. We review the patient, see them in follow-up, and make sure that our treatments are appropriate in helping the patients. But if things aren’t making sense, and if the patients aren’t responding, we’ll always go back and question whether the diagnosis was correct, realizing that in some patients with nonconstipated IBS, what appears to be IBS might actually be microscopic colitis, including lymphocytic colitis or collagenous colitis, and celiac disease.
That’s a nice segue, and I think testing for celiac disease is really quite controversial. We know from the study published in Lancet in 2001 by Sanders and colleagues26 that patients with IBS were apparently 5 to 10 times more likely to have celiac disease than those who did not have the disease, and there was a real level of enthusiasm to test nearly all patients with IBS to look for celiac disease.
We also know from the American College of Gastroenterology (ACG) guidelines27 published in 2009 that for patients with diarrhea-predominant IBS or mixed IBS, meaning the nonconstipated IBS patterns, testing for celiac disease is recommended. Keep in mind, of course, that the prevalence in the United States is estimated at about 1%. That being said, I think the best recent investigations were the multicenter trials involving Bethesda Naval and Michigan.28 This multicenter trial involved nearly 500 patients with nonconstipated IBS and nearly the same number of healthy controls who were admitted for routine colonoscopies, and the prevalence of celiac disease was virtually identical. It was 0.41% for IBS patients and 0.44% for controls. Thus, I don’t routinely recommend testing for celiac disease, although if someone has nonconstipated IBS symptoms and they don’t respond to what I think is appropriate initial empiric therapy, at some point, I may check them.
DR. CASH: So, Drs. Harris and Chang, what’s your take on the celiac question and should we be testing for celiac disease in patients with symptoms consistent with nonconstipation IBS?
DR. HARRIS: I find that in patients in whom bloating is a disproportionate symptom, it might be worthwhile to check for celiac disease and review the family history. I think we’ll get into this discussion a little more detail when we discuss the diet, but we also have to think about gluten sensitivity. It’s become more challenging to sort out who truly has celiac disease and who may have gluten sensitivity, and I think those are important considerations.
DR. CHANG: I agree. At this point, the evidence suggests that we should still screen for celiac disease because it is cost effective, since the treatment is so different from that for IBS.
I think for microscopic colitis as well, it would be nice to do a similar cost analysis to determine whether we should be screening for it more than we do because it’s actually fairly prevalent in the population of IBS patients with diarrhea, particularly in middle-aged women, as Brooks’ study demonstrated.29
DR. HARRIS: The prevalence in the Western world is estimated to be 1 in 132 patients.30
That’s a fairly common occurrence for a disorder, so I think the jury is still out. A study previously suggested that celiac disease is more common in IBS patients, and one study suggested that it isn’t so.27,28,31–33 I think that that the decision to screen or not to screen is not clear yet.
DR. CASH: Yes, it’s still a very controversial issue. Dr. Chang, once the diagnosis has been made, what is the natural history of nonconstipation IBS in terms of surgery rates or the change in diagnosis, perhaps even the risk of developing other disease, which seems to be a common concern of our patients?
DR. CHANG: There was one study that evaluated the natural history of IBS many years ago.34 It reviewed multiple other studies where they followed patients from 6 months to 6 years after the original IBS diagnosis, and they found—consistent with the data that you and others have presented—that the prevalence of determining an alternative diagnosis to IBS is very small.35 It’s about 2% or slightly more than that.
Up to 50% of patients will actually have unchanged symptoms over the years. About 2% to 18% will have worse symptoms.34
If you follow-up the IBS symptoms over time, about a quarter to a third of patients will actually become symptom-free. And we know from post-infectious IBS longitudinal data that the prevalence of IBS declines over time.
In general—and this is something that I tell my patients—the symptoms usually fluctuate over time and much of what we do to treat or manage the symptoms can help to alleviate them to a certain extent. But even when the patients are working hard to manage their symptoms, they can still have symptom flares, although they may be less frequent or milder, and that’s just part of the natural history.
For the bowel habit subtypes, studies have shown that if you follow-up patients, over time, their subtype of IBS can actually change. One study by Doug Drossman and colleagues36 followed IBS patients for over 1 year. They evaluated the symptoms every 3 months in that 1 year and found that 75% of IBS patients actually had a change in their bowel habit subtype over the 1 year.
You would typically see the IBS constipation and the mixed IBS interchanging from one another, and the mixed IBS would also interchange with the IBS with diarrhea. It was less frequent for an IBS with diarrhea to change into an IBS with constipation.
DR. CASH: Certainly, the changing clinical picture of IBS is going to make the evaluation and management of those patients more challenging as well.
Let’s shift over to the topic of treatment. Dr. Harris, you mentioned a few moments ago the role of gluten and perhaps gluten sensitivity. So what role, if any, does diet play in the treatment of nonconstipation IBS?
DR. HARRIS: I think that diet is probably the forgotten factor. Patients have, for years, been telling us that when they eat certain foods, they seem to experience more severe symptoms. They tell us that onions, garlic, fatty, and richer meals cause the symptoms to appear. In fact, Albena Halpert did a study37 that looked at factors in diet that have helped patients, and patients reported that if they ate smaller or less fatty meals or avoid lactose, their IBS symptoms improved.
So, lactose intolerance is a fairly common symptom in the population, in general, and the 2009 ACG guidelines quote a study that showed that the prevalence in the population is about 25%, whereas in the IBS patient population, it’s somewhat higher, around 35% to 38%.38
Patients find that when they avoid lactose, sometimes, there is an improvement in their symptoms of bloating and diarrhea.
In practice, I’ve found that perhaps the symptoms may not persistently improve, but patients do tend to feel better. Besides lactose, I think that consuming smaller meals, more frequent meals, and less fatty meals are also helpful for patients.
Recently, many researchers have been interested in both gluten sensitivity and FODMAPS, which stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, and these are essentially a group of carbohydrates in the diet that can cause GI symptoms, particularly diarrhea and bloating.
There is a review on FODMAPS and food intolerances by Barrett and Gibson in the July 2012 issue of Therapeutic Advances in Gastroenterology,39 as well as one from 2011 called Food: The Forgotten Factor by Dr. Eswaran in the Gastroenterology Clinics of North America.40 So, I would refer people to those reviews.
Essentially, there seems to be a group of patients who have carbohydrate intolerance. Fructose breath testing can help screen some of those patients, but by no means is it a definitive test for intolerance to carbohydrates.
Gluten is one of those carbohydrates. Essentially, gluten is a fructan, and when people go on a low-FODMAP diet, they inadvertently decrease gluten in their diet, although I think there is a subset of patients who also have sensitivity to wheat that’s different from a food allergy.
So, I think we need to get a better understanding of carbohydrates in the diet because in some patients, they seem to play a role in their symptoms.
DR. CASH: It certainly seems like an easy place to start for our patients as well.
DR. HARRIS: I would urge you to first test patients for celiac disease before you put them on a fructose-restricted diet, because once you reduce gluten in the diet, you may decrease your ability to diagnose celiac disease. I think that is an important consideration, and 10% of patients who have negative celiac disease serology can still have celiac disease even with negative blood tests.41
DR. CASH: Dr. Chang, it seems like patients and practitioners want to use agents such as probiotics for a myriad of conditions these days. Are there any data that support the use of probiotics in patients with nonconstipation IBS, and, if so, what are the thoughts with regards to how these agents might work?
DR. CHANG: There have actually been a number of studies evaluating the efficacy of probiotics in IBS patients; however, most studies haven’t really focused on a particular bowel habit. There is at least one study where they evaluated IBS with constipation.42,43
Although there are a number of probiotic studies, most of them are not of high quality. The one probiotic that has been examined in high-quality studies—two different studies—was Bifidobacterium infantis, and this probiotic has been shown to reduce IBS symptoms.44,45
In one study where they evaluated the medication in caplet form, the improvement in symptoms was seen at 4 weeks.45
So one take-home message from that study is that you’d want to keep the patient on probiotics for at least a month to determine whether it’s really efficacious.
The other probiotic that has been studied for IBS and bloating and gas-related symptoms is Bifidobacterium lactis or animalis (it has different names), and this probiotic is present in yogurt available in grocery stores. That has been shown to have some efficacy in decreasing IBS symptoms. But there are several other probiotics that have been shown (albeit not in high-quality studies) to have efficacy in IBS.
There are a number of mechanisms of action that probiotics can help for both digestive health and GI disease, and these include modulating the signals in the gut and affecting immune modulation. By ingesting these probiotics, you may change the composition of the bacterial flora in the gut, which can yield beneficial effects.
There’s also evidence that probiotics maintain the barrier function of the intestinal lining that might be beneficial in IBS, because there is some evidence that IBS patients—or at least a subgroup of IBS patients—have increased intestinal permeability, which may play a role in symptom presentation.
DR. CASH: Dr. Lacy, what medications have evidence to support their use in nonconstipation IBS, and is there a tiered approach to their use?
DR. LACY: I think a good approach is to remind ourselves that we can’t cure IBS, and that our goal is to improve patients’ symptoms. With that in mind, when I see nonconstipated IBS patients, often, I start treatment with an antidiarrheal agent, which might include Imodium or Lomotil. These may improve diarrhea, but they won’t help pain or bloating, which are the most common reasons patients come to see a gastroenterologist.
I frequently use alosetron. This is the only Food and Drug Administration (FDA)-approved medication for women with IBS and diarrhea symptoms. It’s been shown to be safe and effective. I may use a bile acid-binding agent such as cholestyramine or colestipol or colesevelam, although there are very limited data to support their use. It doesn’t mean they don’t work; we just don’t have a lot of data on them.
There are limited data showing that smooth muscle anti-spasmodics, mostly due to their anticholinergic activity, may slow down the action of the GI tract and improve symptoms of pain. Some providers use low-dose tricyclic antidepressants to both slow the GI tract and improve pain. There are also limited data on clonidine and a small study evaluating the use of dextofisopam.
But that’s our armamentarium right now, and I think the art of this job is to try to find the right medication for the right patient while minimizing the side effects.
DR. CASH: Along those lines, Dr. Lacy, there were recently some data with regard to antibiotics for nonconstipation IBS and bloating. Can you describe the relevant data?
DR. LACY: This is a very exciting field, although I think the first thing we need to do is educate both patients and physicians that when we talk about antibiotics, we have to be very careful about how we frame the discussion, ie, we really need to focus on nonabsorbable antibiotics that remain in the GI tract. One of my concerns is that unless you know the area well, or unless you know the data well, you may randomly prescribe a number of different antibiotics for IBS, and this is not only potentially dangerous, but also unhelpful.
When I think about this topic, I think about the broad-spectrum antibiotic rifaximin, which is a nonabsorbable antibiotic that stays within the GI tract and focuses on typical gut bacteria, including gram-negative rods and anaerobic bacteria.
At present, there have been 5 randomized, double-blind, placebo-controlled studies looking at the effects of rifaximin in patients with nonconstipated IBS.46,47 In summary, these studies together include more than 2000 patients, and it’s been shown that rifaximin has improved not only global symptoms of IBS, but also individual symptoms of bloating, pain, discomfort, and diarrhea. Although it is not FDA-approved—and that is important to mention right now—there are ongoing studies that hopefully will lead to its approval.
If rifaximin isn’t available to your patient, another alternative would be neomycin. There is one small study48 showing that neomycin may be effective in IBS patients, but I am just mentioning it because it’s another nonabsorbable antibiotic that I think is safe and at least pathophysiologically makes sense.
DR. CASH: Dr. Harris, any thoughts regarding the use of complementary and alternative medicine for nonconstipation IBS?
DR. HARRIS: As we talk about that, I think we also need to mention some other basic concepts that I discuss with patients, and that is the benefit of exercise and sleep. There have been studies49,50 that have shown that when patients who have IBS don’t sleep well, they actually may have more pain the following day. So, I always try to emphasize on those important basic health concepts with my patients with IBS.
Additionally, there was one study last year that showed that exercise seems to improve abdominal pain as well in patients with IBS.51
As for complementary and alternative medicine, there are certain herbal medications, particularly peppermint oil, that can be used. There have been some small trials52 that have shown that peppermint oils works as a smooth muscle relaxant, although it’s best if it is in a form that gets digested further down the GI tract in the small bowel—so an encapsulated formulation is more useful—because otherwise, it can increase symptoms of gastroesophageal reflux disease.
Some patients find fennel tea and chamomile soothing, but there are no studies on their efficacy. There was one study that Bensoussan53 did a number of years ago that looked at Chinese herbal medicine, and I don’t know the components of the medicine, but the study did suggest that it had some benefit.
Lastly, these are not complementary therapies necessarily, but to address the mind-body connection of IBS patients, studies have shown that modalities such as mindfulness therapy and cognitive-behavioral therapy (CBT) can be helpful. There have also been some studies54–56 that have shown that using the CBT technique can help decrease the severity of abdominal pain and discomfort.
I believe there are also some studies with hypnotherapy, and Dr. Chang may be able to expand on those a little bit.
DR. CHANG: Those are more traditional behavioral therapies. There is a recent study57 showing that mindfulness meditation, which is becoming increasingly popular and used in other chronic illnesses, could be beneficial in reducing IBS symptoms.
There also have been acupuncture studies in IBS. If you look at uncontrolled studies, it seems that IBS is efficacious, but if you examine controlled studies with either sham acupuncture such as using needles that actually don’t penetrate deeply, the data are less robust and don’t really show much of a significant effect of IBS symptoms.58 The augmented interaction between the healthcare provider and patient is the beneficial component of these acupuncture therapy sessions.
DR. CASH: Dr. Chang, as a follow-up to that, what new and emerging therapeutics for IBS with constipation should we be looking toward in the next couple of years?
DR. CHANG: Well, there are 2 therapies that are currently being studied in either a phase II or phase III study. There’s an ongoing phase III study evaluating the efficacy of a kappa opioid receptor agonist, asimadoline, in relieving symptoms in patients with IBS with diarrhea. Asimadoline activates kappa opioid receptors, which are thought to become upregulated or increased in a sensitized chronic pain state such as in patients with particularly more severe symptoms.
A previous phase II study59 showed that asimadoline had particular efficacy in the IBS with diarrhea subgroup of patients who had more moderate pain. This is now being currently studied in a larger phase III trial.
There’s also an ongoing phase II trial with a tryptophan hydroxylase 1 inhibitor. This agent decreases the GI levels of serotonin. Basically, it works peripherally. There was a phase II trial where the higher dose of a tryptophan hydroxylase 1 inhibitor helped to decrease overall IBS symptoms and improve stool consistency in IBS with diarrhea.60
DR. LACY: There are 2 things I like to ask my patients as I finish the interview and examination: “What are you worried about? What are your fears and concerns?” And I try to address their concerns because data from our laboratory61 and from Dr. Chang’s laboratory62 showed that about 30% of patients are worried that their symptoms represent cancer, and I think it’s a good time to educate and reassure our patients about this.
The second thing I always ask is, “What are your goals.” I think we all see a lot of IBS patients each week, but it continues to strike me that everybody’s goals are very different, and some patients want to focus on just pain, some on just bloating, and some on altered bowel habits. So I’ve given up guessing what their goals are, and I just ask them point blank.
I think that’s very, very useful, and that lets a patient know that, once again, you’re focusing on them. It empowers them to choose the next step—whether they want to choose diet or medications and/or what type of medication.
DR. HARRIS: I would agree totally with Dr. Lacy’s excellent point. I do ask the patient, “What do you want to accomplish when you come to see me? What is your motivation for coming to see me? What problems or symptoms seem to be the most important to you?”
DR. CHANG: I agree with Dr. Lacy and Dr. Harris’s comments, and I would say that many patients, particularly in the clinic population, may have comorbid psychological symptoms, and some of the concerns and fears that were mentioned previously.
I think it’s important for healthcare providers to acknowledge that there may be an influence of the psychological symptoms on their disease or their symptoms, but they need not necessarily feel compelled to cure or fix them. I think that acknowledgment is helpful for patients and that reassurance and some education would be useful.
DR. CASH: I want to thank you all for taking the time to discuss this topic. It’s been very informative and a real pleasure.
FoxP2 Media LLC is the publisher of The Medical Roundtable.
Over the past several decades, our understanding of the function of the gastrointestinal (GI) tract, especially with regard to those controlled by the enteric nervous system, has increased dramatically. This increase in knowledge has been accompanied by an enhanced appreciation of the importance of the various functional GI disorders in terms of the pathophysiology and societal impact.
IBS is a prototypical functional GI disorder that affects more than 15% of the population1 and has been gaining increasing awareness in the press and media over the past decade. This period has also witnessed several diagnostic and therapeutic clinical trials with a more dichotomous approach to IBS, which separates the clinical presentations into IBS with constipation and IBS without constipation.
Investigators and clinicians alike have realized that the pragmatic approach, using the presence or absence of constipation as a symptom of IBS, may lend itself to the subsequent evaluation and management of the disorder. Additional insights of the role of inflammation and food intolerance have fundamentally altered the approach to IBS and its associated symptoms. Likewise, the development of targeted therapies for patients who have IBS with constipation and IBS without constipation has increased the number of options available to clinicians as well as the improved quality of life of patients.
My name is Brooks Cash, and I am Professor of Medicine at the Uniformed Services University of the Health Sciences, as well as a gastroenterologist and Deputy Commander for Medical Services at the Walter Reed National Military Medical Center in Bethesda, Maryland. I am joined by 3 world-renowned experts in the field of functional GI disorders and IBS in particular: Drs. Lin Chang, Lucinda Harris, and Brian Lacy.
Welcome everybody, and thank you for taking the time to discuss up-and-coming topics surrounding nonconstipation IBS. Why don’t you take a moment to introduce yourselves?
DR. CHANG: I’m Lin Chang. I’m a gastroenterologist and Professor of Medicine in the Division of Digestive Diseases at the David Geffen School of Medicine at UCLA.
DR. HARRIS: I’m Lucinda Harris. I am co-director of motility in the Division of Gastroenterology at the Mayo Clinic in Scottsdale and Associate Professor of Medicine in the Mayo School of Medicine.
DR. LACY: Hi, I’m Brian Lacy. I’m Professor of Medicine at the Geisel School of Medicine at Dartmouth and director of the GI Motility Laboratory at the Dartmouth-Hitchcock Medical Center in Lebanon, New Hampshire.
DR. CASH: Let’s start with a general overview. Dr. Lacy, will you describe the epidemiology and impact of nonconstipation IBS?
DR. LACY: When I think about the epidemiology of IBS, I like to break it down into both prevalence and incidence. The prevalence of IBS has been actively studied over the years, and it varies depending on how IBS was defined and where the study was performed.
In general, we consider IBS one of the most prevalent functional bowel disorders and certainly one of the most well studied ones as well. Some of the earlier criteria, as you know, involved the Manning criteria.2 These were a little bit more generous and less restrictive than the recent Rome criteria, but, in general, if we were to use a comprehensive review published in 2002 by Saito and colleagues3 from the Mayo Clinic, the prevalence of IBS in North America ranges from approximately 3% to 20%, and most studies quote the prevalence of IBS in about the 12% to 15% range.4–6 The incidence of IBS is slightly more difficult to calculate. That being said, the incidence ranges from about 200 to 400 in 100,000 people, or about 1% to 2% per year in the United States.6,7
DR. CASH: What about the impact in terms of quality of life and economics?
DR. LACY: In terms of the impact of IBS, I think there are a couple of different ways to analyze it. The first is to point out its prevalence, knowing that in primary care, about 10% to 15% of primary care visits are for IBS symptoms, and in the GI referral community, that number may be as high as 40% or 50%.8,9 We know that about two-thirds of those visits are for nonconstipated IBS patients.
Secondly, we can look at the impact on patients, and often, we measure that in terms of quality of life. We know that quality of life of patients with IBS is reduced similar to the case of patients with longstanding diabetes, and in terms of the physical score, it’s lower than that in patients with chronic acid reflux disease and even depression (using the SF-36). We also know from one study that IBS has been shown to increase the risk of suicide, and I think this points out how greatly this affects patients.10-12
Lastly, we can look at the economic impact of IBS. Again, we can either measure that in terms of the direct cost to patients or society. We know that this is one of the most common reasons for patients to skip school or work. We know that healthcare costs for patients with IBS are approximately 50% higher than that for age- and sex-matched controls without IBS.13-15
When we think about the impact on society, including lost healthcare costs, lost productivity, or medication use and procedures, IBS accounts for, on an average, about $20 billion to $30 billion per year of medical costs in the United States.14–17
DR. CHANG: The etiology of IBS is not really well understood, and I think the main issue is that it’s a multifactorial condition, and the clinical presentation can be very heterogeneous. That’s what makes it difficult to understand and makes the cause difficult to identify in each individual because the studies do not necessarily yield consistent results.
Now, it’s generally well accepted that IBS is due to an alteration in brain-gut communication or brain-gut interactions, and that leads to changes in GI motility, sensation, and secretion and increases the perception that the patient has of pain and other GI symptoms.
There are certain vulnerability factors that increase the risk of developing IBS, including genetic predisposition, because we know that IBS runs in families, and there seems to be some genetic component, although it’s still not very well understood. There’s also evidence that chronic stress early in life, or even as an adult, can increase the risk for developing IBS in addition to other chronic pain syndromes.
Then, there seems to be a trigger, which could be, for example, infection, with post-infectious IBS; that’s when a patient develops IBS after gastroenteritis, surgery, or a psychological stressor that’s more chronic and sustained. The patients could also develop symptoms of IBS that can wax and wane or can be chronic. IBS can vary in symptom presentation. Even after the trigger has passed, ie, the infection has cleared or the stressor is gone, the symptoms themselves can perpetuate the condition because of the possibility of symptom-associated anxiety, which would be very normal in patients with very bothersome symptoms.
There are also certain foods that may not really cause the onset of the IBS—unless it’s due to food poisoning—but can trigger the symptoms. There may also be some food intolerances or certain types of foods—such as fatty foods—or larger meals that don’t tend to sit well with patients.
Proposed mechanisms that may result in changes in GI function such as disturbed gut motility, secretion, and sensation and ultimately in the development of IBS symptoms include alterations in neuroimmune and neuroendocrine responses, intestinal permeability, central nervous system modulation of visceral stimuli and sensations, and serotonin signaling, and dysbiosis within the GI tract.18-22
DR. CASH: Dr. Chang, there are also other somatic comorbidities that patients with IBS often have. Can you tell us about those comorbidities, as well as the medical resource utilization that we might see in patients with IBS and those comorbidities? And finally, is it possible that there’s a shared pathophysiology with other somatic complaints or syndromes?
DR. CHANG: A number of studies have looked at the comorbidity of IBS with other functional somatic syndromes. I’m talking more about functional diseases. There is also evidence of IBS coexisting with gastroesophageal reflux disease or inflammatory bowel disease, but much of the literature on comorbidity with IBS is with other existing chronic pain syndromes or chronic somatic syndromes such as fibromyalgia, interstitial cystitis, temporomandibular joint disorder, migraine headaches, and chronic fatigue syndrome.
There are studies that look at the prevalence of these conditions in IBS, and there are studies that evaluate the prevalence of IBS in these conditions. It’s usually about 30% or a subgroup of IBS patients who have these other conditions.23 IBS and these other conditions are more prevalent in women.24
When you look at healthcare utilization—healthcare visits—what’s interesting is that studies show that IBS patients have a greater number of healthcare visits for GI symptoms than individuals without IBS. But many of their healthcare visits also are for non-GI complaints because many IBS patients report non-GI symptoms. Fatigue is one of the more common symptoms, and headaches or muscle aches are also common.
Sometimes, these symptom presentations don’t actually meet diagnostic criteria for other conditions such as migraine headaches, fibromyalgia, painful bladder syndrome, or interstitial cystitis. Interestingly, many IBS patients actually seek health care for those visits. In fact, when you look at the healthcare costs, there are more related costs due to diagnostic testing or medication or healthcare visits for non-GI complaints than there are for GI complaints. But for both types, the cost is higher than that for individuals without IBS.
I recently reviewed the literature on pathophysiologic mechanisms for IBS and other comorbidities, including functional dyspepsia, and there are a number of mechanisms that have been studied in IBS as well as these other conditions.23
Many abnormalities are very similar in IBS and the comorbid conditions. There’s evidence of increased pain perception and altered brain activation patterns in IBS and of these other conditions including fibromyalgia and temporomandibular joint disorder. The findings are very similar, and some of these brain areas that are abnormally activated are associated with either enhanced emotional arousal or altered pain processing.
There’s also evidence of immune changes such as increased numbers of mast cells, particularly in chronic fatigue syndrome and interstitial cystitis, and in some of the studies in functional dyspepsia and IBS. There’s also evidence of genetic factors and certain genetic polymorphisms that are associated with an increased prevalence of IBS or other chronic pain conditions.
Several different mechanisms appear to be shared among these different conditions.
DR. CASH: Dr. Harris, many consider the diagnosis of nonconstipation IBS one of exclusion, while others feel that the Rome criteria are sufficient to make the diagnosis. We heard Dr. Lacy refer to the Rome criteria earlier. What are the Rome criteria, and how valid are they in terms of making the diagnosis of IBS and in particular nonconstipation IBS?
DR. HARRIS: The Rome committee is a group of gastroenterologists that had met since 1997 to decide the diagnostic criteria of IBS, as well as other functional disorders. We are currently using the Rome III criteria,25 and they define IBS as recurrent abdominal pain or discomfort that occurs at least 3 days per months in the last 3 months and is associated with 2 or more of the following criteria: (1) the abdominal pain or discomfort improves with defecation, (2) the onset of symptoms is associated with a change in form of stool, and (3) the onset of symptoms is associated with a change in frequency of stool. Also, the symptom onset should be present for at least 6 months prior to diagnosis.
They have also further defined the criteria into IBS subtypes according to stool form so that IBS with constipation indicates that you have hard or lumpy stools ≥25% of the time and diarrhea (loose or mushy stools) <25% of the time. IBS with diarrhea means the stools are loose or mushy >25% of the time and hard or lumpy <25% of the time. Mixed type IBS is defined as hard and lumpy stools ≥25% of the time and loose or watery stools >25% of the time.25
Finally, there is IBS that can’t be subtyped, called IBS unsubtyped. These are people who we can’t be subtyped because they have insufficient abnormalities of stool subtype to meet the criteria above. But most patients, I think, when you speak to them, can give you an idea of how their bowel movements are and you can easily subtype them.
The other important factor in using the criteria is to make sure that there are no alarm symptoms such as age > 50 years during the onset of the symptoms, blood in the stool, nocturnal symptoms, unintentional weight loss, or a dramatic change in the pattern of symptoms. However, it is important to realize that the stool pattern can change.
It’s also important to make sure that there is no family history of organic GI diseases such as colon cancer, inflammatory bowel disease, or celiac disease, and that there’s no recent history of antibiotic intake.
If you use the red flag symptoms and look at the patient’s history of symptoms, a clinical diagnosis can be made.
DR. LACY: Let’s tackle the easy one first, and I think that’s the role of colonoscopy. Several studies have pointed out that if patients meet Rome III criteria in the absence of warning signs, the utility of a colonoscopy would be very, very low.
We all agree that if the patient is older than 50 years, and ≥45 years for African Americans, even if there are signs of IBS and you’re pretty confident about the diagnosis, a colonoscopy is still required for screening purposes.
The utility of a colonoscopy in a younger patient—younger than 45 years—with classic symptoms of IBS in the absence of warning signs is extremely low, and I don’t generally recommend that.
One caveat, of course, is that as clinicians, we’re always double-checking to make sure that our diagnosis is correct. We review the patient, see them in follow-up, and make sure that our treatments are appropriate in helping the patients. But if things aren’t making sense, and if the patients aren’t responding, we’ll always go back and question whether the diagnosis was correct, realizing that in some patients with nonconstipated IBS, what appears to be IBS might actually be microscopic colitis, including lymphocytic colitis or collagenous colitis, and celiac disease.
That’s a nice segue, and I think testing for celiac disease is really quite controversial. We know from the study published in Lancet in 2001 by Sanders and colleagues26 that patients with IBS were apparently 5 to 10 times more likely to have celiac disease than those who did not have the disease, and there was a real level of enthusiasm to test nearly all patients with IBS to look for celiac disease.
We also know from the American College of Gastroenterology (ACG) guidelines27 published in 2009 that for patients with diarrhea-predominant IBS or mixed IBS, meaning the nonconstipated IBS patterns, testing for celiac disease is recommended. Keep in mind, of course, that the prevalence in the United States is estimated at about 1%. That being said, I think the best recent investigations were the multicenter trials involving Bethesda Naval and Michigan.28 This multicenter trial involved nearly 500 patients with nonconstipated IBS and nearly the same number of healthy controls who were admitted for routine colonoscopies, and the prevalence of celiac disease was virtually identical. It was 0.41% for IBS patients and 0.44% for controls. Thus, I don’t routinely recommend testing for celiac disease, although if someone has nonconstipated IBS symptoms and they don’t respond to what I think is appropriate initial empiric therapy, at some point, I may check them.
DR. CASH: So, Drs. Harris and Chang, what’s your take on the celiac question and should we be testing for celiac disease in patients with symptoms consistent with nonconstipation IBS?
DR. HARRIS: I find that in patients in whom bloating is a disproportionate symptom, it might be worthwhile to check for celiac disease and review the family history. I think we’ll get into this discussion a little more detail when we discuss the diet, but we also have to think about gluten sensitivity. It’s become more challenging to sort out who truly has celiac disease and who may have gluten sensitivity, and I think those are important considerations.
DR. CHANG: I agree. At this point, the evidence suggests that we should still screen for celiac disease because it is cost effective, since the treatment is so different from that for IBS.
I think for microscopic colitis as well, it would be nice to do a similar cost analysis to determine whether we should be screening for it more than we do because it’s actually fairly prevalent in the population of IBS patients with diarrhea, particularly in middle-aged women, as Brooks’ study demonstrated.29
DR. HARRIS: The prevalence in the Western world is estimated to be 1 in 132 patients.30
That’s a fairly common occurrence for a disorder, so I think the jury is still out. A study previously suggested that celiac disease is more common in IBS patients, and one study suggested that it isn’t so.27,28,31–33 I think that that the decision to screen or not to screen is not clear yet.
DR. CASH: Yes, it’s still a very controversial issue. Dr. Chang, once the diagnosis has been made, what is the natural history of nonconstipation IBS in terms of surgery rates or the change in diagnosis, perhaps even the risk of developing other disease, which seems to be a common concern of our patients?
DR. CHANG: There was one study that evaluated the natural history of IBS many years ago.34 It reviewed multiple other studies where they followed patients from 6 months to 6 years after the original IBS diagnosis, and they found—consistent with the data that you and others have presented—that the prevalence of determining an alternative diagnosis to IBS is very small.35 It’s about 2% or slightly more than that.
Up to 50% of patients will actually have unchanged symptoms over the years. About 2% to 18% will have worse symptoms.34
If you follow-up the IBS symptoms over time, about a quarter to a third of patients will actually become symptom-free. And we know from post-infectious IBS longitudinal data that the prevalence of IBS declines over time.
In general—and this is something that I tell my patients—the symptoms usually fluctuate over time and much of what we do to treat or manage the symptoms can help to alleviate them to a certain extent. But even when the patients are working hard to manage their symptoms, they can still have symptom flares, although they may be less frequent or milder, and that’s just part of the natural history.
For the bowel habit subtypes, studies have shown that if you follow-up patients, over time, their subtype of IBS can actually change. One study by Doug Drossman and colleagues36 followed IBS patients for over 1 year. They evaluated the symptoms every 3 months in that 1 year and found that 75% of IBS patients actually had a change in their bowel habit subtype over the 1 year.
You would typically see the IBS constipation and the mixed IBS interchanging from one another, and the mixed IBS would also interchange with the IBS with diarrhea. It was less frequent for an IBS with diarrhea to change into an IBS with constipation.
DR. CASH: Certainly, the changing clinical picture of IBS is going to make the evaluation and management of those patients more challenging as well.
Let’s shift over to the topic of treatment. Dr. Harris, you mentioned a few moments ago the role of gluten and perhaps gluten sensitivity. So what role, if any, does diet play in the treatment of nonconstipation IBS?
DR. HARRIS: I think that diet is probably the forgotten factor. Patients have, for years, been telling us that when they eat certain foods, they seem to experience more severe symptoms. They tell us that onions, garlic, fatty, and richer meals cause the symptoms to appear. In fact, Albena Halpert did a study37 that looked at factors in diet that have helped patients, and patients reported that if they ate smaller or less fatty meals or avoid lactose, their IBS symptoms improved.
So, lactose intolerance is a fairly common symptom in the population, in general, and the 2009 ACG guidelines quote a study that showed that the prevalence in the population is about 25%, whereas in the IBS patient population, it’s somewhat higher, around 35% to 38%.38
Patients find that when they avoid lactose, sometimes, there is an improvement in their symptoms of bloating and diarrhea.
In practice, I’ve found that perhaps the symptoms may not persistently improve, but patients do tend to feel better. Besides lactose, I think that consuming smaller meals, more frequent meals, and less fatty meals are also helpful for patients.
Recently, many researchers have been interested in both gluten sensitivity and FODMAPS, which stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, and these are essentially a group of carbohydrates in the diet that can cause GI symptoms, particularly diarrhea and bloating.
There is a review on FODMAPS and food intolerances by Barrett and Gibson in the July 2012 issue of Therapeutic Advances in Gastroenterology,39 as well as one from 2011 called Food: The Forgotten Factor by Dr. Eswaran in the Gastroenterology Clinics of North America.40 So, I would refer people to those reviews.
Essentially, there seems to be a group of patients who have carbohydrate intolerance. Fructose breath testing can help screen some of those patients, but by no means is it a definitive test for intolerance to carbohydrates.
Gluten is one of those carbohydrates. Essentially, gluten is a fructan, and when people go on a low-FODMAP diet, they inadvertently decrease gluten in their diet, although I think there is a subset of patients who also have sensitivity to wheat that’s different from a food allergy.
So, I think we need to get a better understanding of carbohydrates in the diet because in some patients, they seem to play a role in their symptoms.
DR. CASH: It certainly seems like an easy place to start for our patients as well.
DR. HARRIS: I would urge you to first test patients for celiac disease before you put them on a fructose-restricted diet, because once you reduce gluten in the diet, you may decrease your ability to diagnose celiac disease. I think that is an important consideration, and 10% of patients who have negative celiac disease serology can still have celiac disease even with negative blood tests.41
DR. CASH: Dr. Chang, it seems like patients and practitioners want to use agents such as probiotics for a myriad of conditions these days. Are there any data that support the use of probiotics in patients with nonconstipation IBS, and, if so, what are the thoughts with regards to how these agents might work?
DR. CHANG: There have actually been a number of studies evaluating the efficacy of probiotics in IBS patients; however, most studies haven’t really focused on a particular bowel habit. There is at least one study where they evaluated IBS with constipation.42,43
Although there are a number of probiotic studies, most of them are not of high quality. The one probiotic that has been examined in high-quality studies—two different studies—was Bifidobacterium infantis, and this probiotic has been shown to reduce IBS symptoms.44,45
In one study where they evaluated the medication in caplet form, the improvement in symptoms was seen at 4 weeks.45
So one take-home message from that study is that you’d want to keep the patient on probiotics for at least a month to determine whether it’s really efficacious.
The other probiotic that has been studied for IBS and bloating and gas-related symptoms is Bifidobacterium lactis or animalis (it has different names), and this probiotic is present in yogurt available in grocery stores. That has been shown to have some efficacy in decreasing IBS symptoms. But there are several other probiotics that have been shown (albeit not in high-quality studies) to have efficacy in IBS.
There are a number of mechanisms of action that probiotics can help for both digestive health and GI disease, and these include modulating the signals in the gut and affecting immune modulation. By ingesting these probiotics, you may change the composition of the bacterial flora in the gut, which can yield beneficial effects.
There’s also evidence that probiotics maintain the barrier function of the intestinal lining that might be beneficial in IBS, because there is some evidence that IBS patients—or at least a subgroup of IBS patients—have increased intestinal permeability, which may play a role in symptom presentation.
DR. CASH: Dr. Lacy, what medications have evidence to support their use in nonconstipation IBS, and is there a tiered approach to their use?
DR. LACY: I think a good approach is to remind ourselves that we can’t cure IBS, and that our goal is to improve patients’ symptoms. With that in mind, when I see nonconstipated IBS patients, often, I start treatment with an antidiarrheal agent, which might include Imodium or Lomotil. These may improve diarrhea, but they won’t help pain or bloating, which are the most common reasons patients come to see a gastroenterologist.
I frequently use alosetron. This is the only Food and Drug Administration (FDA)-approved medication for women with IBS and diarrhea symptoms. It’s been shown to be safe and effective. I may use a bile acid-binding agent such as cholestyramine or colestipol or colesevelam, although there are very limited data to support their use. It doesn’t mean they don’t work; we just don’t have a lot of data on them.
There are limited data showing that smooth muscle anti-spasmodics, mostly due to their anticholinergic activity, may slow down the action of the GI tract and improve symptoms of pain. Some providers use low-dose tricyclic antidepressants to both slow the GI tract and improve pain. There are also limited data on clonidine and a small study evaluating the use of dextofisopam.
But that’s our armamentarium right now, and I think the art of this job is to try to find the right medication for the right patient while minimizing the side effects.
DR. CASH: Along those lines, Dr. Lacy, there were recently some data with regard to antibiotics for nonconstipation IBS and bloating. Can you describe the relevant data?
DR. LACY: This is a very exciting field, although I think the first thing we need to do is educate both patients and physicians that when we talk about antibiotics, we have to be very careful about how we frame the discussion, ie, we really need to focus on nonabsorbable antibiotics that remain in the GI tract. One of my concerns is that unless you know the area well, or unless you know the data well, you may randomly prescribe a number of different antibiotics for IBS, and this is not only potentially dangerous, but also unhelpful.
When I think about this topic, I think about the broad-spectrum antibiotic rifaximin, which is a nonabsorbable antibiotic that stays within the GI tract and focuses on typical gut bacteria, including gram-negative rods and anaerobic bacteria.
At present, there have been 5 randomized, double-blind, placebo-controlled studies looking at the effects of rifaximin in patients with nonconstipated IBS.46,47 In summary, these studies together include more than 2000 patients, and it’s been shown that rifaximin has improved not only global symptoms of IBS, but also individual symptoms of bloating, pain, discomfort, and diarrhea. Although it is not FDA-approved—and that is important to mention right now—there are ongoing studies that hopefully will lead to its approval.
If rifaximin isn’t available to your patient, another alternative would be neomycin. There is one small study48 showing that neomycin may be effective in IBS patients, but I am just mentioning it because it’s another nonabsorbable antibiotic that I think is safe and at least pathophysiologically makes sense.
DR. CASH: Dr. Harris, any thoughts regarding the use of complementary and alternative medicine for nonconstipation IBS?
DR. HARRIS: As we talk about that, I think we also need to mention some other basic concepts that I discuss with patients, and that is the benefit of exercise and sleep. There have been studies49,50 that have shown that when patients who have IBS don’t sleep well, they actually may have more pain the following day. So, I always try to emphasize on those important basic health concepts with my patients with IBS.
Additionally, there was one study last year that showed that exercise seems to improve abdominal pain as well in patients with IBS.51
As for complementary and alternative medicine, there are certain herbal medications, particularly peppermint oil, that can be used. There have been some small trials52 that have shown that peppermint oils works as a smooth muscle relaxant, although it’s best if it is in a form that gets digested further down the GI tract in the small bowel—so an encapsulated formulation is more useful—because otherwise, it can increase symptoms of gastroesophageal reflux disease.
Some patients find fennel tea and chamomile soothing, but there are no studies on their efficacy. There was one study that Bensoussan53 did a number of years ago that looked at Chinese herbal medicine, and I don’t know the components of the medicine, but the study did suggest that it had some benefit.
Lastly, these are not complementary therapies necessarily, but to address the mind-body connection of IBS patients, studies have shown that modalities such as mindfulness therapy and cognitive-behavioral therapy (CBT) can be helpful. There have also been some studies54–56 that have shown that using the CBT technique can help decrease the severity of abdominal pain and discomfort.
I believe there are also some studies with hypnotherapy, and Dr. Chang may be able to expand on those a little bit.
DR. CHANG: Those are more traditional behavioral therapies. There is a recent study57 showing that mindfulness meditation, which is becoming increasingly popular and used in other chronic illnesses, could be beneficial in reducing IBS symptoms.
There also have been acupuncture studies in IBS. If you look at uncontrolled studies, it seems that IBS is efficacious, but if you examine controlled studies with either sham acupuncture such as using needles that actually don’t penetrate deeply, the data are less robust and don’t really show much of a significant effect of IBS symptoms.58 The augmented interaction between the healthcare provider and patient is the beneficial component of these acupuncture therapy sessions.
DR. CASH: Dr. Chang, as a follow-up to that, what new and emerging therapeutics for IBS with constipation should we be looking toward in the next couple of years?
DR. CHANG: Well, there are 2 therapies that are currently being studied in either a phase II or phase III study. There’s an ongoing phase III study evaluating the efficacy of a kappa opioid receptor agonist, asimadoline, in relieving symptoms in patients with IBS with diarrhea. Asimadoline activates kappa opioid receptors, which are thought to become upregulated or increased in a sensitized chronic pain state such as in patients with particularly more severe symptoms.
A previous phase II study59 showed that asimadoline had particular efficacy in the IBS with diarrhea subgroup of patients who had more moderate pain. This is now being currently studied in a larger phase III trial.
There’s also an ongoing phase II trial with a tryptophan hydroxylase 1 inhibitor. This agent decreases the GI levels of serotonin. Basically, it works peripherally. There was a phase II trial where the higher dose of a tryptophan hydroxylase 1 inhibitor helped to decrease overall IBS symptoms and improve stool consistency in IBS with diarrhea.60
DR. LACY: There are 2 things I like to ask my patients as I finish the interview and examination: “What are you worried about? What are your fears and concerns?” And I try to address their concerns because data from our laboratory61 and from Dr. Chang’s laboratory62 showed that about 30% of patients are worried that their symptoms represent cancer, and I think it’s a good time to educate and reassure our patients about this.
The second thing I always ask is, “What are your goals.” I think we all see a lot of IBS patients each week, but it continues to strike me that everybody’s goals are very different, and some patients want to focus on just pain, some on just bloating, and some on altered bowel habits. So I’ve given up guessing what their goals are, and I just ask them point blank.
I think that’s very, very useful, and that lets a patient know that, once again, you’re focusing on them. It empowers them to choose the next step—whether they want to choose diet or medications and/or what type of medication.
DR. HARRIS: I would agree totally with Dr. Lacy’s excellent point. I do ask the patient, “What do you want to accomplish when you come to see me? What is your motivation for coming to see me? What problems or symptoms seem to be the most important to you?”
DR. CHANG: I agree with Dr. Lacy and Dr. Harris’s comments, and I would say that many patients, particularly in the clinic population, may have comorbid psychological symptoms, and some of the concerns and fears that were mentioned previously.
I think it’s important for healthcare providers to acknowledge that there may be an influence of the psychological symptoms on their disease or their symptoms, but they need not necessarily feel compelled to cure or fix them. I think that acknowledgment is helpful for patients and that reassurance and some education would be useful.
DR. CASH: I want to thank you all for taking the time to discuss this topic. It’s been very informative and a real pleasure.
FoxP2 Media LLC is the publisher of The Medical Roundtable.
Over the past several decades, our understanding of the function of the gastrointestinal (GI) tract, especially with regard to those controlled by the enteric nervous system, has increased dramatically. This increase in knowledge has been accompanied by an enhanced appreciation of the importance of the various functional GI disorders in terms of the pathophysiology and societal impact.
IBS is a prototypical functional GI disorder that affects more than 15% of the population1 and has been gaining increasing awareness in the press and media over the past decade. This period has also witnessed several diagnostic and therapeutic clinical trials with a more dichotomous approach to IBS, which separates the clinical presentations into IBS with constipation and IBS without constipation.
Investigators and clinicians alike have realized that the pragmatic approach, using the presence or absence of constipation as a symptom of IBS, may lend itself to the subsequent evaluation and management of the disorder. Additional insights of the role of inflammation and food intolerance have fundamentally altered the approach to IBS and its associated symptoms. Likewise, the development of targeted therapies for patients who have IBS with constipation and IBS without constipation has increased the number of options available to clinicians as well as the improved quality of life of patients.
My name is Brooks Cash, and I am Professor of Medicine at the Uniformed Services University of the Health Sciences, as well as a gastroenterologist and Deputy Commander for Medical Services at the Walter Reed National Military Medical Center in Bethesda, Maryland. I am joined by 3 world-renowned experts in the field of functional GI disorders and IBS in particular: Drs. Lin Chang, Lucinda Harris, and Brian Lacy.
Welcome everybody, and thank you for taking the time to discuss up-and-coming topics surrounding nonconstipation IBS. Why don’t you take a moment to introduce yourselves?
DR. CHANG: I’m Lin Chang. I’m a gastroenterologist and Professor of Medicine in the Division of Digestive Diseases at the David Geffen School of Medicine at UCLA.
DR. HARRIS: I’m Lucinda Harris. I am co-director of motility in the Division of Gastroenterology at the Mayo Clinic in Scottsdale and Associate Professor of Medicine in the Mayo School of Medicine.
DR. LACY: Hi, I’m Brian Lacy. I’m Professor of Medicine at the Geisel School of Medicine at Dartmouth and director of the GI Motility Laboratory at the Dartmouth-Hitchcock Medical Center in Lebanon, New Hampshire.
DR. CASH: Let’s start with a general overview. Dr. Lacy, will you describe the epidemiology and impact of nonconstipation IBS?
DR. LACY: When I think about the epidemiology of IBS, I like to break it down into both prevalence and incidence. The prevalence of IBS has been actively studied over the years, and it varies depending on how IBS was defined and where the study was performed.
In general, we consider IBS one of the most prevalent functional bowel disorders and certainly one of the most well studied ones as well. Some of the earlier criteria, as you know, involved the Manning criteria.2 These were a little bit more generous and less restrictive than the recent Rome criteria, but, in general, if we were to use a comprehensive review published in 2002 by Saito and colleagues3 from the Mayo Clinic, the prevalence of IBS in North America ranges from approximately 3% to 20%, and most studies quote the prevalence of IBS in about the 12% to 15% range.4–6 The incidence of IBS is slightly more difficult to calculate. That being said, the incidence ranges from about 200 to 400 in 100,000 people, or about 1% to 2% per year in the United States.6,7
DR. CASH: What about the impact in terms of quality of life and economics?
DR. LACY: In terms of the impact of IBS, I think there are a couple of different ways to analyze it. The first is to point out its prevalence, knowing that in primary care, about 10% to 15% of primary care visits are for IBS symptoms, and in the GI referral community, that number may be as high as 40% or 50%.8,9 We know that about two-thirds of those visits are for nonconstipated IBS patients.
Secondly, we can look at the impact on patients, and often, we measure that in terms of quality of life. We know that quality of life of patients with IBS is reduced similar to the case of patients with longstanding diabetes, and in terms of the physical score, it’s lower than that in patients with chronic acid reflux disease and even depression (using the SF-36). We also know from one study that IBS has been shown to increase the risk of suicide, and I think this points out how greatly this affects patients.10-12
Lastly, we can look at the economic impact of IBS. Again, we can either measure that in terms of the direct cost to patients or society. We know that this is one of the most common reasons for patients to skip school or work. We know that healthcare costs for patients with IBS are approximately 50% higher than that for age- and sex-matched controls without IBS.13-15
When we think about the impact on society, including lost healthcare costs, lost productivity, or medication use and procedures, IBS accounts for, on an average, about $20 billion to $30 billion per year of medical costs in the United States.14–17
DR. CHANG: The etiology of IBS is not really well understood, and I think the main issue is that it’s a multifactorial condition, and the clinical presentation can be very heterogeneous. That’s what makes it difficult to understand and makes the cause difficult to identify in each individual because the studies do not necessarily yield consistent results.
Now, it’s generally well accepted that IBS is due to an alteration in brain-gut communication or brain-gut interactions, and that leads to changes in GI motility, sensation, and secretion and increases the perception that the patient has of pain and other GI symptoms.
There are certain vulnerability factors that increase the risk of developing IBS, including genetic predisposition, because we know that IBS runs in families, and there seems to be some genetic component, although it’s still not very well understood. There’s also evidence that chronic stress early in life, or even as an adult, can increase the risk for developing IBS in addition to other chronic pain syndromes.
Then, there seems to be a trigger, which could be, for example, infection, with post-infectious IBS; that’s when a patient develops IBS after gastroenteritis, surgery, or a psychological stressor that’s more chronic and sustained. The patients could also develop symptoms of IBS that can wax and wane or can be chronic. IBS can vary in symptom presentation. Even after the trigger has passed, ie, the infection has cleared or the stressor is gone, the symptoms themselves can perpetuate the condition because of the possibility of symptom-associated anxiety, which would be very normal in patients with very bothersome symptoms.
There are also certain foods that may not really cause the onset of the IBS—unless it’s due to food poisoning—but can trigger the symptoms. There may also be some food intolerances or certain types of foods—such as fatty foods—or larger meals that don’t tend to sit well with patients.
Proposed mechanisms that may result in changes in GI function such as disturbed gut motility, secretion, and sensation and ultimately in the development of IBS symptoms include alterations in neuroimmune and neuroendocrine responses, intestinal permeability, central nervous system modulation of visceral stimuli and sensations, and serotonin signaling, and dysbiosis within the GI tract.18-22
DR. CASH: Dr. Chang, there are also other somatic comorbidities that patients with IBS often have. Can you tell us about those comorbidities, as well as the medical resource utilization that we might see in patients with IBS and those comorbidities? And finally, is it possible that there’s a shared pathophysiology with other somatic complaints or syndromes?
DR. CHANG: A number of studies have looked at the comorbidity of IBS with other functional somatic syndromes. I’m talking more about functional diseases. There is also evidence of IBS coexisting with gastroesophageal reflux disease or inflammatory bowel disease, but much of the literature on comorbidity with IBS is with other existing chronic pain syndromes or chronic somatic syndromes such as fibromyalgia, interstitial cystitis, temporomandibular joint disorder, migraine headaches, and chronic fatigue syndrome.
There are studies that look at the prevalence of these conditions in IBS, and there are studies that evaluate the prevalence of IBS in these conditions. It’s usually about 30% or a subgroup of IBS patients who have these other conditions.23 IBS and these other conditions are more prevalent in women.24
When you look at healthcare utilization—healthcare visits—what’s interesting is that studies show that IBS patients have a greater number of healthcare visits for GI symptoms than individuals without IBS. But many of their healthcare visits also are for non-GI complaints because many IBS patients report non-GI symptoms. Fatigue is one of the more common symptoms, and headaches or muscle aches are also common.
Sometimes, these symptom presentations don’t actually meet diagnostic criteria for other conditions such as migraine headaches, fibromyalgia, painful bladder syndrome, or interstitial cystitis. Interestingly, many IBS patients actually seek health care for those visits. In fact, when you look at the healthcare costs, there are more related costs due to diagnostic testing or medication or healthcare visits for non-GI complaints than there are for GI complaints. But for both types, the cost is higher than that for individuals without IBS.
I recently reviewed the literature on pathophysiologic mechanisms for IBS and other comorbidities, including functional dyspepsia, and there are a number of mechanisms that have been studied in IBS as well as these other conditions.23
Many abnormalities are very similar in IBS and the comorbid conditions. There’s evidence of increased pain perception and altered brain activation patterns in IBS and of these other conditions including fibromyalgia and temporomandibular joint disorder. The findings are very similar, and some of these brain areas that are abnormally activated are associated with either enhanced emotional arousal or altered pain processing.
There’s also evidence of immune changes such as increased numbers of mast cells, particularly in chronic fatigue syndrome and interstitial cystitis, and in some of the studies in functional dyspepsia and IBS. There’s also evidence of genetic factors and certain genetic polymorphisms that are associated with an increased prevalence of IBS or other chronic pain conditions.
Several different mechanisms appear to be shared among these different conditions.
DR. CASH: Dr. Harris, many consider the diagnosis of nonconstipation IBS one of exclusion, while others feel that the Rome criteria are sufficient to make the diagnosis. We heard Dr. Lacy refer to the Rome criteria earlier. What are the Rome criteria, and how valid are they in terms of making the diagnosis of IBS and in particular nonconstipation IBS?
DR. HARRIS: The Rome committee is a group of gastroenterologists that had met since 1997 to decide the diagnostic criteria of IBS, as well as other functional disorders. We are currently using the Rome III criteria,25 and they define IBS as recurrent abdominal pain or discomfort that occurs at least 3 days per months in the last 3 months and is associated with 2 or more of the following criteria: (1) the abdominal pain or discomfort improves with defecation, (2) the onset of symptoms is associated with a change in form of stool, and (3) the onset of symptoms is associated with a change in frequency of stool. Also, the symptom onset should be present for at least 6 months prior to diagnosis.
They have also further defined the criteria into IBS subtypes according to stool form so that IBS with constipation indicates that you have hard or lumpy stools ≥25% of the time and diarrhea (loose or mushy stools) <25% of the time. IBS with diarrhea means the stools are loose or mushy >25% of the time and hard or lumpy <25% of the time. Mixed type IBS is defined as hard and lumpy stools ≥25% of the time and loose or watery stools >25% of the time.25
Finally, there is IBS that can’t be subtyped, called IBS unsubtyped. These are people who we can’t be subtyped because they have insufficient abnormalities of stool subtype to meet the criteria above. But most patients, I think, when you speak to them, can give you an idea of how their bowel movements are and you can easily subtype them.
The other important factor in using the criteria is to make sure that there are no alarm symptoms such as age > 50 years during the onset of the symptoms, blood in the stool, nocturnal symptoms, unintentional weight loss, or a dramatic change in the pattern of symptoms. However, it is important to realize that the stool pattern can change.
It’s also important to make sure that there is no family history of organic GI diseases such as colon cancer, inflammatory bowel disease, or celiac disease, and that there’s no recent history of antibiotic intake.
If you use the red flag symptoms and look at the patient’s history of symptoms, a clinical diagnosis can be made.
DR. LACY: Let’s tackle the easy one first, and I think that’s the role of colonoscopy. Several studies have pointed out that if patients meet Rome III criteria in the absence of warning signs, the utility of a colonoscopy would be very, very low.
We all agree that if the patient is older than 50 years, and ≥45 years for African Americans, even if there are signs of IBS and you’re pretty confident about the diagnosis, a colonoscopy is still required for screening purposes.
The utility of a colonoscopy in a younger patient—younger than 45 years—with classic symptoms of IBS in the absence of warning signs is extremely low, and I don’t generally recommend that.
One caveat, of course, is that as clinicians, we’re always double-checking to make sure that our diagnosis is correct. We review the patient, see them in follow-up, and make sure that our treatments are appropriate in helping the patients. But if things aren’t making sense, and if the patients aren’t responding, we’ll always go back and question whether the diagnosis was correct, realizing that in some patients with nonconstipated IBS, what appears to be IBS might actually be microscopic colitis, including lymphocytic colitis or collagenous colitis, and celiac disease.
That’s a nice segue, and I think testing for celiac disease is really quite controversial. We know from the study published in Lancet in 2001 by Sanders and colleagues26 that patients with IBS were apparently 5 to 10 times more likely to have celiac disease than those who did not have the disease, and there was a real level of enthusiasm to test nearly all patients with IBS to look for celiac disease.
We also know from the American College of Gastroenterology (ACG) guidelines27 published in 2009 that for patients with diarrhea-predominant IBS or mixed IBS, meaning the nonconstipated IBS patterns, testing for celiac disease is recommended. Keep in mind, of course, that the prevalence in the United States is estimated at about 1%. That being said, I think the best recent investigations were the multicenter trials involving Bethesda Naval and Michigan.28 This multicenter trial involved nearly 500 patients with nonconstipated IBS and nearly the same number of healthy controls who were admitted for routine colonoscopies, and the prevalence of celiac disease was virtually identical. It was 0.41% for IBS patients and 0.44% for controls. Thus, I don’t routinely recommend testing for celiac disease, although if someone has nonconstipated IBS symptoms and they don’t respond to what I think is appropriate initial empiric therapy, at some point, I may check them.
DR. CASH: So, Drs. Harris and Chang, what’s your take on the celiac question and should we be testing for celiac disease in patients with symptoms consistent with nonconstipation IBS?
DR. HARRIS: I find that in patients in whom bloating is a disproportionate symptom, it might be worthwhile to check for celiac disease and review the family history. I think we’ll get into this discussion a little more detail when we discuss the diet, but we also have to think about gluten sensitivity. It’s become more challenging to sort out who truly has celiac disease and who may have gluten sensitivity, and I think those are important considerations.
DR. CHANG: I agree. At this point, the evidence suggests that we should still screen for celiac disease because it is cost effective, since the treatment is so different from that for IBS.
I think for microscopic colitis as well, it would be nice to do a similar cost analysis to determine whether we should be screening for it more than we do because it’s actually fairly prevalent in the population of IBS patients with diarrhea, particularly in middle-aged women, as Brooks’ study demonstrated.29
DR. HARRIS: The prevalence in the Western world is estimated to be 1 in 132 patients.30
That’s a fairly common occurrence for a disorder, so I think the jury is still out. A study previously suggested that celiac disease is more common in IBS patients, and one study suggested that it isn’t so.27,28,31–33 I think that that the decision to screen or not to screen is not clear yet.
DR. CASH: Yes, it’s still a very controversial issue. Dr. Chang, once the diagnosis has been made, what is the natural history of nonconstipation IBS in terms of surgery rates or the change in diagnosis, perhaps even the risk of developing other disease, which seems to be a common concern of our patients?
DR. CHANG: There was one study that evaluated the natural history of IBS many years ago.34 It reviewed multiple other studies where they followed patients from 6 months to 6 years after the original IBS diagnosis, and they found—consistent with the data that you and others have presented—that the prevalence of determining an alternative diagnosis to IBS is very small.35 It’s about 2% or slightly more than that.
Up to 50% of patients will actually have unchanged symptoms over the years. About 2% to 18% will have worse symptoms.34
If you follow-up the IBS symptoms over time, about a quarter to a third of patients will actually become symptom-free. And we know from post-infectious IBS longitudinal data that the prevalence of IBS declines over time.
In general—and this is something that I tell my patients—the symptoms usually fluctuate over time and much of what we do to treat or manage the symptoms can help to alleviate them to a certain extent. But even when the patients are working hard to manage their symptoms, they can still have symptom flares, although they may be less frequent or milder, and that’s just part of the natural history.
For the bowel habit subtypes, studies have shown that if you follow-up patients, over time, their subtype of IBS can actually change. One study by Doug Drossman and colleagues36 followed IBS patients for over 1 year. They evaluated the symptoms every 3 months in that 1 year and found that 75% of IBS patients actually had a change in their bowel habit subtype over the 1 year.
You would typically see the IBS constipation and the mixed IBS interchanging from one another, and the mixed IBS would also interchange with the IBS with diarrhea. It was less frequent for an IBS with diarrhea to change into an IBS with constipation.
DR. CASH: Certainly, the changing clinical picture of IBS is going to make the evaluation and management of those patients more challenging as well.
Let’s shift over to the topic of treatment. Dr. Harris, you mentioned a few moments ago the role of gluten and perhaps gluten sensitivity. So what role, if any, does diet play in the treatment of nonconstipation IBS?
DR. HARRIS: I think that diet is probably the forgotten factor. Patients have, for years, been telling us that when they eat certain foods, they seem to experience more severe symptoms. They tell us that onions, garlic, fatty, and richer meals cause the symptoms to appear. In fact, Albena Halpert did a study37 that looked at factors in diet that have helped patients, and patients reported that if they ate smaller or less fatty meals or avoid lactose, their IBS symptoms improved.
So, lactose intolerance is a fairly common symptom in the population, in general, and the 2009 ACG guidelines quote a study that showed that the prevalence in the population is about 25%, whereas in the IBS patient population, it’s somewhat higher, around 35% to 38%.38
Patients find that when they avoid lactose, sometimes, there is an improvement in their symptoms of bloating and diarrhea.
In practice, I’ve found that perhaps the symptoms may not persistently improve, but patients do tend to feel better. Besides lactose, I think that consuming smaller meals, more frequent meals, and less fatty meals are also helpful for patients.
Recently, many researchers have been interested in both gluten sensitivity and FODMAPS, which stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, and these are essentially a group of carbohydrates in the diet that can cause GI symptoms, particularly diarrhea and bloating.
There is a review on FODMAPS and food intolerances by Barrett and Gibson in the July 2012 issue of Therapeutic Advances in Gastroenterology,39 as well as one from 2011 called Food: The Forgotten Factor by Dr. Eswaran in the Gastroenterology Clinics of North America.40 So, I would refer people to those reviews.
Essentially, there seems to be a group of patients who have carbohydrate intolerance. Fructose breath testing can help screen some of those patients, but by no means is it a definitive test for intolerance to carbohydrates.
Gluten is one of those carbohydrates. Essentially, gluten is a fructan, and when people go on a low-FODMAP diet, they inadvertently decrease gluten in their diet, although I think there is a subset of patients who also have sensitivity to wheat that’s different from a food allergy.
So, I think we need to get a better understanding of carbohydrates in the diet because in some patients, they seem to play a role in their symptoms.
DR. CASH: It certainly seems like an easy place to start for our patients as well.
DR. HARRIS: I would urge you to first test patients for celiac disease before you put them on a fructose-restricted diet, because once you reduce gluten in the diet, you may decrease your ability to diagnose celiac disease. I think that is an important consideration, and 10% of patients who have negative celiac disease serology can still have celiac disease even with negative blood tests.41
DR. CASH: Dr. Chang, it seems like patients and practitioners want to use agents such as probiotics for a myriad of conditions these days. Are there any data that support the use of probiotics in patients with nonconstipation IBS, and, if so, what are the thoughts with regards to how these agents might work?
DR. CHANG: There have actually been a number of studies evaluating the efficacy of probiotics in IBS patients; however, most studies haven’t really focused on a particular bowel habit. There is at least one study where they evaluated IBS with constipation.42,43
Although there are a number of probiotic studies, most of them are not of high quality. The one probiotic that has been examined in high-quality studies—two different studies—was Bifidobacterium infantis, and this probiotic has been shown to reduce IBS symptoms.44,45
In one study where they evaluated the medication in caplet form, the improvement in symptoms was seen at 4 weeks.45
So one take-home message from that study is that you’d want to keep the patient on probiotics for at least a month to determine whether it’s really efficacious.
The other probiotic that has been studied for IBS and bloating and gas-related symptoms is Bifidobacterium lactis or animalis (it has different names), and this probiotic is present in yogurt available in grocery stores. That has been shown to have some efficacy in decreasing IBS symptoms. But there are several other probiotics that have been shown (albeit not in high-quality studies) to have efficacy in IBS.
There are a number of mechanisms of action that probiotics can help for both digestive health and GI disease, and these include modulating the signals in the gut and affecting immune modulation. By ingesting these probiotics, you may change the composition of the bacterial flora in the gut, which can yield beneficial effects.
There’s also evidence that probiotics maintain the barrier function of the intestinal lining that might be beneficial in IBS, because there is some evidence that IBS patients—or at least a subgroup of IBS patients—have increased intestinal permeability, which may play a role in symptom presentation.
DR. CASH: Dr. Lacy, what medications have evidence to support their use in nonconstipation IBS, and is there a tiered approach to their use?
DR. LACY: I think a good approach is to remind ourselves that we can’t cure IBS, and that our goal is to improve patients’ symptoms. With that in mind, when I see nonconstipated IBS patients, often, I start treatment with an antidiarrheal agent, which might include Imodium or Lomotil. These may improve diarrhea, but they won’t help pain or bloating, which are the most common reasons patients come to see a gastroenterologist.
I frequently use alosetron. This is the only Food and Drug Administration (FDA)-approved medication for women with IBS and diarrhea symptoms. It’s been shown to be safe and effective. I may use a bile acid-binding agent such as cholestyramine or colestipol or colesevelam, although there are very limited data to support their use. It doesn’t mean they don’t work; we just don’t have a lot of data on them.
There are limited data showing that smooth muscle anti-spasmodics, mostly due to their anticholinergic activity, may slow down the action of the GI tract and improve symptoms of pain. Some providers use low-dose tricyclic antidepressants to both slow the GI tract and improve pain. There are also limited data on clonidine and a small study evaluating the use of dextofisopam.
But that’s our armamentarium right now, and I think the art of this job is to try to find the right medication for the right patient while minimizing the side effects.
DR. CASH: Along those lines, Dr. Lacy, there were recently some data with regard to antibiotics for nonconstipation IBS and bloating. Can you describe the relevant data?
DR. LACY: This is a very exciting field, although I think the first thing we need to do is educate both patients and physicians that when we talk about antibiotics, we have to be very careful about how we frame the discussion, ie, we really need to focus on nonabsorbable antibiotics that remain in the GI tract. One of my concerns is that unless you know the area well, or unless you know the data well, you may randomly prescribe a number of different antibiotics for IBS, and this is not only potentially dangerous, but also unhelpful.
When I think about this topic, I think about the broad-spectrum antibiotic rifaximin, which is a nonabsorbable antibiotic that stays within the GI tract and focuses on typical gut bacteria, including gram-negative rods and anaerobic bacteria.
At present, there have been 5 randomized, double-blind, placebo-controlled studies looking at the effects of rifaximin in patients with nonconstipated IBS.46,47 In summary, these studies together include more than 2000 patients, and it’s been shown that rifaximin has improved not only global symptoms of IBS, but also individual symptoms of bloating, pain, discomfort, and diarrhea. Although it is not FDA-approved—and that is important to mention right now—there are ongoing studies that hopefully will lead to its approval.
If rifaximin isn’t available to your patient, another alternative would be neomycin. There is one small study48 showing that neomycin may be effective in IBS patients, but I am just mentioning it because it’s another nonabsorbable antibiotic that I think is safe and at least pathophysiologically makes sense.
DR. CASH: Dr. Harris, any thoughts regarding the use of complementary and alternative medicine for nonconstipation IBS?
DR. HARRIS: As we talk about that, I think we also need to mention some other basic concepts that I discuss with patients, and that is the benefit of exercise and sleep. There have been studies49,50 that have shown that when patients who have IBS don’t sleep well, they actually may have more pain the following day. So, I always try to emphasize on those important basic health concepts with my patients with IBS.
Additionally, there was one study last year that showed that exercise seems to improve abdominal pain as well in patients with IBS.51
As for complementary and alternative medicine, there are certain herbal medications, particularly peppermint oil, that can be used. There have been some small trials52 that have shown that peppermint oils works as a smooth muscle relaxant, although it’s best if it is in a form that gets digested further down the GI tract in the small bowel—so an encapsulated formulation is more useful—because otherwise, it can increase symptoms of gastroesophageal reflux disease.
Some patients find fennel tea and chamomile soothing, but there are no studies on their efficacy. There was one study that Bensoussan53 did a number of years ago that looked at Chinese herbal medicine, and I don’t know the components of the medicine, but the study did suggest that it had some benefit.
Lastly, these are not complementary therapies necessarily, but to address the mind-body connection of IBS patients, studies have shown that modalities such as mindfulness therapy and cognitive-behavioral therapy (CBT) can be helpful. There have also been some studies54–56 that have shown that using the CBT technique can help decrease the severity of abdominal pain and discomfort.
I believe there are also some studies with hypnotherapy, and Dr. Chang may be able to expand on those a little bit.
DR. CHANG: Those are more traditional behavioral therapies. There is a recent study57 showing that mindfulness meditation, which is becoming increasingly popular and used in other chronic illnesses, could be beneficial in reducing IBS symptoms.
There also have been acupuncture studies in IBS. If you look at uncontrolled studies, it seems that IBS is efficacious, but if you examine controlled studies with either sham acupuncture such as using needles that actually don’t penetrate deeply, the data are less robust and don’t really show much of a significant effect of IBS symptoms.58 The augmented interaction between the healthcare provider and patient is the beneficial component of these acupuncture therapy sessions.
DR. CASH: Dr. Chang, as a follow-up to that, what new and emerging therapeutics for IBS with constipation should we be looking toward in the next couple of years?
DR. CHANG: Well, there are 2 therapies that are currently being studied in either a phase II or phase III study. There’s an ongoing phase III study evaluating the efficacy of a kappa opioid receptor agonist, asimadoline, in relieving symptoms in patients with IBS with diarrhea. Asimadoline activates kappa opioid receptors, which are thought to become upregulated or increased in a sensitized chronic pain state such as in patients with particularly more severe symptoms.
A previous phase II study59 showed that asimadoline had particular efficacy in the IBS with diarrhea subgroup of patients who had more moderate pain. This is now being currently studied in a larger phase III trial.
There’s also an ongoing phase II trial with a tryptophan hydroxylase 1 inhibitor. This agent decreases the GI levels of serotonin. Basically, it works peripherally. There was a phase II trial where the higher dose of a tryptophan hydroxylase 1 inhibitor helped to decrease overall IBS symptoms and improve stool consistency in IBS with diarrhea.60
DR. LACY: There are 2 things I like to ask my patients as I finish the interview and examination: “What are you worried about? What are your fears and concerns?” And I try to address their concerns because data from our laboratory61 and from Dr. Chang’s laboratory62 showed that about 30% of patients are worried that their symptoms represent cancer, and I think it’s a good time to educate and reassure our patients about this.
The second thing I always ask is, “What are your goals.” I think we all see a lot of IBS patients each week, but it continues to strike me that everybody’s goals are very different, and some patients want to focus on just pain, some on just bloating, and some on altered bowel habits. So I’ve given up guessing what their goals are, and I just ask them point blank.
I think that’s very, very useful, and that lets a patient know that, once again, you’re focusing on them. It empowers them to choose the next step—whether they want to choose diet or medications and/or what type of medication.
DR. HARRIS: I would agree totally with Dr. Lacy’s excellent point. I do ask the patient, “What do you want to accomplish when you come to see me? What is your motivation for coming to see me? What problems or symptoms seem to be the most important to you?”
DR. CHANG: I agree with Dr. Lacy and Dr. Harris’s comments, and I would say that many patients, particularly in the clinic population, may have comorbid psychological symptoms, and some of the concerns and fears that were mentioned previously.
I think it’s important for healthcare providers to acknowledge that there may be an influence of the psychological symptoms on their disease or their symptoms, but they need not necessarily feel compelled to cure or fix them. I think that acknowledgment is helpful for patients and that reassurance and some education would be useful.
DR. CASH: I want to thank you all for taking the time to discuss this topic. It’s been very informative and a real pleasure.
FoxP2 Media LLC is the publisher of The Medical Roundtable.
FoxP2 Media LLC
Diabetes care: Whose goals are they?
Words are important, and the language of medicine is changing. Two words that have taken on great importance in health care are “goals” and “targets.” A portion of primary care physicians’ compensation for caring for patients with diabetes, hypertension, and hyperlipidemia depends on our patients achieving certain goals and targets for blood sugar, blood pressure (BP), and lipids, as summarized for type 2 diabetes in “Is your patient on target? Optimizing diabetes management” by Harmes and Cigolle. Based on randomized trials published during the past several years, the “official” US goal for glucose control should be customized to fit patients’ individual risk profiles, although 7% is still recommended for younger and healthier patients with diabetes. Based on randomized trial data, the BP target is less stringent than in the past—now 140/90 mm Hg for all patients with hypertension, including those with diabetes, although not all experts agree with this newer recommendation.
We have entered a confusing time regarding lipid control because of the new and controversial guidelines to treat patients based on risk of cardiovascular disease rather than treating to a specific low-density lipoprotein cholesterol target.
Whose goals and targets are these? We know they are goals for insurance companies and health plans because they send us reports and pay us incentives when enough of our patients hit the targets (or penalize us if they don’t).
They are our goals, too, because we know that, to some extent, our patient’s likelihood of bad things happening to them is linked to their blood sugar, BP, and lipid control.
Ultimately, these have to be our patients’ goals, because they are the ones who have to buy into taking medications, which have costs, risks, and side effects, and altering their lifestyles, which is difficult for most.
Goal setting is an effective method for helping people increase physical activity and improve their diets.1 This requires negotiating with patients about what they believe is achievable. In addition, these goals need not be the same as the targets proposed by the experts. Even the American Diabetes Association has come around to the idea that patients should have some flexibility and that one hemoglobin A1c target does not fit all. I like the idea of sharing a simple “report card” with patients at each visit that lists the A (A1c), B (BP), and C (cholesterol) targets and the patient’s most recent values. Point-of-care testing allows for immediate feedback and medication adjustment.
What tools do you use to help your patients achieve their diabetes goals?
REFERENCE
1. Greaves CJ, Sheppard KE, Abraham C, et al; IMAGE Study Group. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health. 2011;11:119.
Words are important, and the language of medicine is changing. Two words that have taken on great importance in health care are “goals” and “targets.” A portion of primary care physicians’ compensation for caring for patients with diabetes, hypertension, and hyperlipidemia depends on our patients achieving certain goals and targets for blood sugar, blood pressure (BP), and lipids, as summarized for type 2 diabetes in “Is your patient on target? Optimizing diabetes management” by Harmes and Cigolle. Based on randomized trials published during the past several years, the “official” US goal for glucose control should be customized to fit patients’ individual risk profiles, although 7% is still recommended for younger and healthier patients with diabetes. Based on randomized trial data, the BP target is less stringent than in the past—now 140/90 mm Hg for all patients with hypertension, including those with diabetes, although not all experts agree with this newer recommendation.
We have entered a confusing time regarding lipid control because of the new and controversial guidelines to treat patients based on risk of cardiovascular disease rather than treating to a specific low-density lipoprotein cholesterol target.
Whose goals and targets are these? We know they are goals for insurance companies and health plans because they send us reports and pay us incentives when enough of our patients hit the targets (or penalize us if they don’t).
They are our goals, too, because we know that, to some extent, our patient’s likelihood of bad things happening to them is linked to their blood sugar, BP, and lipid control.
Ultimately, these have to be our patients’ goals, because they are the ones who have to buy into taking medications, which have costs, risks, and side effects, and altering their lifestyles, which is difficult for most.
Goal setting is an effective method for helping people increase physical activity and improve their diets.1 This requires negotiating with patients about what they believe is achievable. In addition, these goals need not be the same as the targets proposed by the experts. Even the American Diabetes Association has come around to the idea that patients should have some flexibility and that one hemoglobin A1c target does not fit all. I like the idea of sharing a simple “report card” with patients at each visit that lists the A (A1c), B (BP), and C (cholesterol) targets and the patient’s most recent values. Point-of-care testing allows for immediate feedback and medication adjustment.
What tools do you use to help your patients achieve their diabetes goals?
Words are important, and the language of medicine is changing. Two words that have taken on great importance in health care are “goals” and “targets.” A portion of primary care physicians’ compensation for caring for patients with diabetes, hypertension, and hyperlipidemia depends on our patients achieving certain goals and targets for blood sugar, blood pressure (BP), and lipids, as summarized for type 2 diabetes in “Is your patient on target? Optimizing diabetes management” by Harmes and Cigolle. Based on randomized trials published during the past several years, the “official” US goal for glucose control should be customized to fit patients’ individual risk profiles, although 7% is still recommended for younger and healthier patients with diabetes. Based on randomized trial data, the BP target is less stringent than in the past—now 140/90 mm Hg for all patients with hypertension, including those with diabetes, although not all experts agree with this newer recommendation.
We have entered a confusing time regarding lipid control because of the new and controversial guidelines to treat patients based on risk of cardiovascular disease rather than treating to a specific low-density lipoprotein cholesterol target.
Whose goals and targets are these? We know they are goals for insurance companies and health plans because they send us reports and pay us incentives when enough of our patients hit the targets (or penalize us if they don’t).
They are our goals, too, because we know that, to some extent, our patient’s likelihood of bad things happening to them is linked to their blood sugar, BP, and lipid control.
Ultimately, these have to be our patients’ goals, because they are the ones who have to buy into taking medications, which have costs, risks, and side effects, and altering their lifestyles, which is difficult for most.
Goal setting is an effective method for helping people increase physical activity and improve their diets.1 This requires negotiating with patients about what they believe is achievable. In addition, these goals need not be the same as the targets proposed by the experts. Even the American Diabetes Association has come around to the idea that patients should have some flexibility and that one hemoglobin A1c target does not fit all. I like the idea of sharing a simple “report card” with patients at each visit that lists the A (A1c), B (BP), and C (cholesterol) targets and the patient’s most recent values. Point-of-care testing allows for immediate feedback and medication adjustment.
What tools do you use to help your patients achieve their diabetes goals?
REFERENCE
1. Greaves CJ, Sheppard KE, Abraham C, et al; IMAGE Study Group. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health. 2011;11:119.
REFERENCE
1. Greaves CJ, Sheppard KE, Abraham C, et al; IMAGE Study Group. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health. 2011;11:119.
When patients ask about medical marijuana
How often do your patients ask about medical marijuana? I suppose it depends on where you live, but here in Arizona, it’s legal. So they ask about using it for migraines, epilepsy, diabetic neuropathy pain, and others. I hear the question from many patients.
How do I answer it? It gets tricky. I have mixed feelings about it, with anecdotal evidence from patients who have tried it, medical journals, and the usual overhyped stories in the lay press. It’s often hard for doctors to see the answer clearly and even more so for patients.
I suspect a lot of the interest comes from the commonly held belief that if it comes from "natural" sources, it has to be better for you than "chemicals." Never mind that what my dog leaves in the backyard is also "natural" or that THC is a chemical. Pretty much everything in the human body (and universe in general) is technically a chemical.
So I tell them I don’t know for sure. At best, it may help them. At worst, it’s an expensive placebo that could lead to other health issues. I explain the treatments I have to offer and that nothing is 100% successful or completely free of side effects – even "natural" products.
I’ve learned that those who’ve decided to use it won’t be dissuaded by my arguments or any amount of equivocal data, so I try to keep an open mind.
I let them make their own decision and document it carefully. If they want to go find a medical dispensary, that’s their call in the end, not mine. I also tell them that, if it doesn’t work, I’ll still be here to do my best to help them. I don’t take offense at their decision, ever.
At our best, doctors are only advisers. We can’t make anyone do anything they don’t want to.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
How often do your patients ask about medical marijuana? I suppose it depends on where you live, but here in Arizona, it’s legal. So they ask about using it for migraines, epilepsy, diabetic neuropathy pain, and others. I hear the question from many patients.
How do I answer it? It gets tricky. I have mixed feelings about it, with anecdotal evidence from patients who have tried it, medical journals, and the usual overhyped stories in the lay press. It’s often hard for doctors to see the answer clearly and even more so for patients.
I suspect a lot of the interest comes from the commonly held belief that if it comes from "natural" sources, it has to be better for you than "chemicals." Never mind that what my dog leaves in the backyard is also "natural" or that THC is a chemical. Pretty much everything in the human body (and universe in general) is technically a chemical.
So I tell them I don’t know for sure. At best, it may help them. At worst, it’s an expensive placebo that could lead to other health issues. I explain the treatments I have to offer and that nothing is 100% successful or completely free of side effects – even "natural" products.
I’ve learned that those who’ve decided to use it won’t be dissuaded by my arguments or any amount of equivocal data, so I try to keep an open mind.
I let them make their own decision and document it carefully. If they want to go find a medical dispensary, that’s their call in the end, not mine. I also tell them that, if it doesn’t work, I’ll still be here to do my best to help them. I don’t take offense at their decision, ever.
At our best, doctors are only advisers. We can’t make anyone do anything they don’t want to.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
How often do your patients ask about medical marijuana? I suppose it depends on where you live, but here in Arizona, it’s legal. So they ask about using it for migraines, epilepsy, diabetic neuropathy pain, and others. I hear the question from many patients.
How do I answer it? It gets tricky. I have mixed feelings about it, with anecdotal evidence from patients who have tried it, medical journals, and the usual overhyped stories in the lay press. It’s often hard for doctors to see the answer clearly and even more so for patients.
I suspect a lot of the interest comes from the commonly held belief that if it comes from "natural" sources, it has to be better for you than "chemicals." Never mind that what my dog leaves in the backyard is also "natural" or that THC is a chemical. Pretty much everything in the human body (and universe in general) is technically a chemical.
So I tell them I don’t know for sure. At best, it may help them. At worst, it’s an expensive placebo that could lead to other health issues. I explain the treatments I have to offer and that nothing is 100% successful or completely free of side effects – even "natural" products.
I’ve learned that those who’ve decided to use it won’t be dissuaded by my arguments or any amount of equivocal data, so I try to keep an open mind.
I let them make their own decision and document it carefully. If they want to go find a medical dispensary, that’s their call in the end, not mine. I also tell them that, if it doesn’t work, I’ll still be here to do my best to help them. I don’t take offense at their decision, ever.
At our best, doctors are only advisers. We can’t make anyone do anything they don’t want to.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Freewheelin'
Two weeks ago, I received a few video clips of my granddaughter’s 5th birthday party. Although my daughter had loosely scripted a fairy-themed event, she was wise enough to have stepped back and let the children freewheel. What I watched was a half a dozen 4- and 5-year-old girls wearing their self-decorated fairy wings running and running and running in a tree-shaded park jumping (or in their minds flying) on and off a small stage yelling "Calling all fairies, calling all fairies." Forty minutes of nonstop running and jumping, a cupcake and small scoop of ice cream, and that was it ... the perfect party.
No one was coaching these little cherubs to run. No one had set up traffic cones or a finish line. No ribbons or plastic medals were awarded in recognition of their participation. They were running for the sheer pleasure of activity, driven by what is probably an inborn urge to move. Every toddler I have known functions like a tightly wound windup toy ready to hit the ground running when placed down on the straight flat surface of a shopping mall or airport concourse.
It appears that this drive to run is not unique to young Homo sapiens. Two Dutch scientists set up a small running wheel in a wooded setting and then using motion sensors and remote video recorders watched what happened (Proc. R. Soc. B 2014 [doi:10.1098/rspb.2014.0210]). It turns out that wild mice enjoy running, spending from 1 to 18 minutes freewheeling. Frogs also occasionally jumped on and off the wheel, but running was obviously not their thing.
While the drive to run seems to be bred into us, unfortunately it is an urge that is easily extinguished. One needs only to watch a physical education class of sixth graders being asked to do a 1-mile run/walk to become painfully aware that too many children can no longer run, let alone do it for the pure enjoyment. How did such a strong drive disappear?
I wonder what would have happened if the Dutch investigators had put a smart phone with a colorful app running next to the wheel. How many of the mice have chosen to sit down and watch the screen instead of climbing on for a run? If a small electric train running in a circle had been placed next in the environment, would some of the mice have preferred to hop on for a ride? Or suppose they had played a recording of an older mouse squeaking a warning call that was the rodent equivalent of "Don’t climb on that; you could hurt yourself"?
I certainly believe (and there is animal evidence to support) that certain individuals inherit a preference for a sedentary lifestyle. However, I am equally sure that we have created a society that provides an abundance of powerfully attractive sedentary options to remaining active. In my mind, first and foremost among these attractions is color television (I don’t recall black and white TV being all that exciting). The magnetic attraction of colorful and active video images is difficult for anyone to resist. As pediatricians, we must continue to preach the word about the health hazards associated with screen time. And, I would add again my plea for us to spend less energy on worrying about what’s on the screen and instead emphasize the need to keep the exposure time down.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including "How to Say No to Your Toddler." E-mail him at [email protected].
Two weeks ago, I received a few video clips of my granddaughter’s 5th birthday party. Although my daughter had loosely scripted a fairy-themed event, she was wise enough to have stepped back and let the children freewheel. What I watched was a half a dozen 4- and 5-year-old girls wearing their self-decorated fairy wings running and running and running in a tree-shaded park jumping (or in their minds flying) on and off a small stage yelling "Calling all fairies, calling all fairies." Forty minutes of nonstop running and jumping, a cupcake and small scoop of ice cream, and that was it ... the perfect party.
No one was coaching these little cherubs to run. No one had set up traffic cones or a finish line. No ribbons or plastic medals were awarded in recognition of their participation. They were running for the sheer pleasure of activity, driven by what is probably an inborn urge to move. Every toddler I have known functions like a tightly wound windup toy ready to hit the ground running when placed down on the straight flat surface of a shopping mall or airport concourse.
It appears that this drive to run is not unique to young Homo sapiens. Two Dutch scientists set up a small running wheel in a wooded setting and then using motion sensors and remote video recorders watched what happened (Proc. R. Soc. B 2014 [doi:10.1098/rspb.2014.0210]). It turns out that wild mice enjoy running, spending from 1 to 18 minutes freewheeling. Frogs also occasionally jumped on and off the wheel, but running was obviously not their thing.
While the drive to run seems to be bred into us, unfortunately it is an urge that is easily extinguished. One needs only to watch a physical education class of sixth graders being asked to do a 1-mile run/walk to become painfully aware that too many children can no longer run, let alone do it for the pure enjoyment. How did such a strong drive disappear?
I wonder what would have happened if the Dutch investigators had put a smart phone with a colorful app running next to the wheel. How many of the mice have chosen to sit down and watch the screen instead of climbing on for a run? If a small electric train running in a circle had been placed next in the environment, would some of the mice have preferred to hop on for a ride? Or suppose they had played a recording of an older mouse squeaking a warning call that was the rodent equivalent of "Don’t climb on that; you could hurt yourself"?
I certainly believe (and there is animal evidence to support) that certain individuals inherit a preference for a sedentary lifestyle. However, I am equally sure that we have created a society that provides an abundance of powerfully attractive sedentary options to remaining active. In my mind, first and foremost among these attractions is color television (I don’t recall black and white TV being all that exciting). The magnetic attraction of colorful and active video images is difficult for anyone to resist. As pediatricians, we must continue to preach the word about the health hazards associated with screen time. And, I would add again my plea for us to spend less energy on worrying about what’s on the screen and instead emphasize the need to keep the exposure time down.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including "How to Say No to Your Toddler." E-mail him at [email protected].
Two weeks ago, I received a few video clips of my granddaughter’s 5th birthday party. Although my daughter had loosely scripted a fairy-themed event, she was wise enough to have stepped back and let the children freewheel. What I watched was a half a dozen 4- and 5-year-old girls wearing their self-decorated fairy wings running and running and running in a tree-shaded park jumping (or in their minds flying) on and off a small stage yelling "Calling all fairies, calling all fairies." Forty minutes of nonstop running and jumping, a cupcake and small scoop of ice cream, and that was it ... the perfect party.
No one was coaching these little cherubs to run. No one had set up traffic cones or a finish line. No ribbons or plastic medals were awarded in recognition of their participation. They were running for the sheer pleasure of activity, driven by what is probably an inborn urge to move. Every toddler I have known functions like a tightly wound windup toy ready to hit the ground running when placed down on the straight flat surface of a shopping mall or airport concourse.
It appears that this drive to run is not unique to young Homo sapiens. Two Dutch scientists set up a small running wheel in a wooded setting and then using motion sensors and remote video recorders watched what happened (Proc. R. Soc. B 2014 [doi:10.1098/rspb.2014.0210]). It turns out that wild mice enjoy running, spending from 1 to 18 minutes freewheeling. Frogs also occasionally jumped on and off the wheel, but running was obviously not their thing.
While the drive to run seems to be bred into us, unfortunately it is an urge that is easily extinguished. One needs only to watch a physical education class of sixth graders being asked to do a 1-mile run/walk to become painfully aware that too many children can no longer run, let alone do it for the pure enjoyment. How did such a strong drive disappear?
I wonder what would have happened if the Dutch investigators had put a smart phone with a colorful app running next to the wheel. How many of the mice have chosen to sit down and watch the screen instead of climbing on for a run? If a small electric train running in a circle had been placed next in the environment, would some of the mice have preferred to hop on for a ride? Or suppose they had played a recording of an older mouse squeaking a warning call that was the rodent equivalent of "Don’t climb on that; you could hurt yourself"?
I certainly believe (and there is animal evidence to support) that certain individuals inherit a preference for a sedentary lifestyle. However, I am equally sure that we have created a society that provides an abundance of powerfully attractive sedentary options to remaining active. In my mind, first and foremost among these attractions is color television (I don’t recall black and white TV being all that exciting). The magnetic attraction of colorful and active video images is difficult for anyone to resist. As pediatricians, we must continue to preach the word about the health hazards associated with screen time. And, I would add again my plea for us to spend less energy on worrying about what’s on the screen and instead emphasize the need to keep the exposure time down.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics including "How to Say No to Your Toddler." E-mail him at [email protected].