User login
Looking for a healthy meat substitute? Consider the potato
Boil ‘em, mash ‘em, include ‘em in a balanced diet
It’s kind of funny that, even though potatoes are vegetables and vegetables are generally considered to be healthy foods, not many people think of potatoes as being particularly good for you. And that’s hardly surprising since we usually either consume them in the form of French fries or potato chips, neither of which are known for their healthiness.
In fact, some previous research shows that potatoes are a food to avoid, particularly for people with insulin resistance. However, a new study from England goes against the grain and asserts that the potato is perfectly fine for insulin-resistant individuals and filled with valuable nutrients and health benefits. Which is great news for the state of Idaho and the potato organization funding the research. Of course there’s a potato organization.
For the study, a group of obese, overweight, or insulin-resistant individuals received a diet of either beans, peas, and meat or fish or white potatoes with meat or fish for 8 weeks; both diets were heavy in fruits and vegetables and both diets replaced about 40% of typical meat consumption with either beans and peas or potatoes. By the end of the study, those on the potato diet experienced health benefits equivalent to those on the bean and pea diet, including losing roughly equivalent amounts of weight and similarly reducing the body’s insulin response.
The researchers noted that, because people tend to eat the same amount of food no matter what, replacing something like meat with dense, low-calorie potatoes meant study participants could eat normally yet consume much fewer calories. So you could make a delicious, healthy stew without the brace of conies and the nice fish, which would make Smeagol very happy.
You won’t have ‘monkeypox’ to kick around anymore
It’s true. No more monkeypox. It’s gone. It’s history. Adios. The World Health Organization said that the disease formerly known as monkeypox will now be called mpox. What? You didn’t think it had been cured, did you? You did? Really? Silly readers.
“Mpox will become a preferred term, replacing monkeypox, after a transition period of 1 year. This serves to mitigate the concerns raised by experts about confusion caused by a name change in the midst of a global outbreak,” WHO said in a statement announcing the change.
The stigma attached to the name was the main problem. New York City Health Commissioner Dr. Ashwin Vasan had sent a letter to WHO earlier this year, according to CNN, saying that there was “growing concern for the potentially devastating and stigmatizing effects that the messaging around the ‘monkeypox’ virus can have on … vulnerable communities.”
We here at LOTME applaud the fight against stigmas of any sort, but we sensed there was more to this name change business, so our dedicated team of investigative journalists went into action. Sure enough, while rooting through WHO Director-General Tedros Adhanom Ghebreyesus’s garbage, we found a list of the names that had been rejected in favor of mpox:
- K-pop (already taken)
- Keeping up with the Kardashi-pox
- Trumpox
- Pox the magic dragon
- Monkey plague (didn’t really solve the problem)
- Hockey pox
- Mission mpoxible
- Jurassic Pox
- The pox that refreshes
- Debbie
Feet catch what the ears miss
The spectrum of frequencies that can be heard by human ears varies from person to person. Then there’s the matter of personal taste in music and volume level. But what really gets people moving? A new study shows that it’s more about the frequency of the sound than the volume.
For the study, participants at a concert by electronic music duo Orphx at LIVELab – a research performance center on the McMaster University campus in Hamilton, Ont., that was specifically designed to study music and dance – filled out questionnaires before and after the show. They also wore motion-capture headbands to detect their movement throughout the concert. During the show the researchers turned very-low-frequency (VLF) sounds (8-37 Hz) on and off every 2.5 minutes. Movement speed was calculated during on and off periods.
Although the effects of subliminal messaging aren’t new, past studies have shown that participants were mostly aware of the messaging. In this study, the researchers found that the subjects’ movements increased by 11.8% when the VLF sounds were on, but without their awareness. The researchers and the participants attributed movement to the bass, as lower pitches tend to elicit stronger neural responses and thus movement, compared with higher pitches.
“Our whole sense of the beat is mediated by the vestibular system but nobody’s really, I think, effectively confirmed that,” Jonathan Cannon, an assistant professor of psychology, neuroscience, and behavior at McMaster who not involved in the study, told Live Science.
Not to say this study didn’t have its limitations, such as the effect of the surrounding crowd or vibrations of the floor influencing the need to dance. But it definitely makes you wonder about what’s actually playing in your favorite song.
Uncle Leonid wants you
Do you like to travel? Are you a bit of a thrill seeker? Do you have any extra socks? If you’re a physician who answered yes to those three questions, then we’ve got an opportunity for you.
Leonid Slutsky, leader of Russia’s populist Liberal Democratic Party and chairman of the foreign relations committee in the lower house of Russia’s parliament – yes, that Leonid Slutsky – recently made a bit of a recruiting pitch, although that’s not how ABC News described it.
Mr. Slutsky, a strong supporter of his country’s war against Ukraine, recently told the mothers of Russian soldiers “that the whole world is watching us. We are the largest state and when we do not have socks, shorts, doctors, intelligence, communications, or simply care for our children, questions arise that will be very difficult to answer.”
It’s probably not what he meant, but the lack of intelligence is pretty clear.
Boil ‘em, mash ‘em, include ‘em in a balanced diet
It’s kind of funny that, even though potatoes are vegetables and vegetables are generally considered to be healthy foods, not many people think of potatoes as being particularly good for you. And that’s hardly surprising since we usually either consume them in the form of French fries or potato chips, neither of which are known for their healthiness.
In fact, some previous research shows that potatoes are a food to avoid, particularly for people with insulin resistance. However, a new study from England goes against the grain and asserts that the potato is perfectly fine for insulin-resistant individuals and filled with valuable nutrients and health benefits. Which is great news for the state of Idaho and the potato organization funding the research. Of course there’s a potato organization.
For the study, a group of obese, overweight, or insulin-resistant individuals received a diet of either beans, peas, and meat or fish or white potatoes with meat or fish for 8 weeks; both diets were heavy in fruits and vegetables and both diets replaced about 40% of typical meat consumption with either beans and peas or potatoes. By the end of the study, those on the potato diet experienced health benefits equivalent to those on the bean and pea diet, including losing roughly equivalent amounts of weight and similarly reducing the body’s insulin response.
The researchers noted that, because people tend to eat the same amount of food no matter what, replacing something like meat with dense, low-calorie potatoes meant study participants could eat normally yet consume much fewer calories. So you could make a delicious, healthy stew without the brace of conies and the nice fish, which would make Smeagol very happy.
You won’t have ‘monkeypox’ to kick around anymore
It’s true. No more monkeypox. It’s gone. It’s history. Adios. The World Health Organization said that the disease formerly known as monkeypox will now be called mpox. What? You didn’t think it had been cured, did you? You did? Really? Silly readers.
“Mpox will become a preferred term, replacing monkeypox, after a transition period of 1 year. This serves to mitigate the concerns raised by experts about confusion caused by a name change in the midst of a global outbreak,” WHO said in a statement announcing the change.
The stigma attached to the name was the main problem. New York City Health Commissioner Dr. Ashwin Vasan had sent a letter to WHO earlier this year, according to CNN, saying that there was “growing concern for the potentially devastating and stigmatizing effects that the messaging around the ‘monkeypox’ virus can have on … vulnerable communities.”
We here at LOTME applaud the fight against stigmas of any sort, but we sensed there was more to this name change business, so our dedicated team of investigative journalists went into action. Sure enough, while rooting through WHO Director-General Tedros Adhanom Ghebreyesus’s garbage, we found a list of the names that had been rejected in favor of mpox:
- K-pop (already taken)
- Keeping up with the Kardashi-pox
- Trumpox
- Pox the magic dragon
- Monkey plague (didn’t really solve the problem)
- Hockey pox
- Mission mpoxible
- Jurassic Pox
- The pox that refreshes
- Debbie
Feet catch what the ears miss
The spectrum of frequencies that can be heard by human ears varies from person to person. Then there’s the matter of personal taste in music and volume level. But what really gets people moving? A new study shows that it’s more about the frequency of the sound than the volume.
For the study, participants at a concert by electronic music duo Orphx at LIVELab – a research performance center on the McMaster University campus in Hamilton, Ont., that was specifically designed to study music and dance – filled out questionnaires before and after the show. They also wore motion-capture headbands to detect their movement throughout the concert. During the show the researchers turned very-low-frequency (VLF) sounds (8-37 Hz) on and off every 2.5 minutes. Movement speed was calculated during on and off periods.
Although the effects of subliminal messaging aren’t new, past studies have shown that participants were mostly aware of the messaging. In this study, the researchers found that the subjects’ movements increased by 11.8% when the VLF sounds were on, but without their awareness. The researchers and the participants attributed movement to the bass, as lower pitches tend to elicit stronger neural responses and thus movement, compared with higher pitches.
“Our whole sense of the beat is mediated by the vestibular system but nobody’s really, I think, effectively confirmed that,” Jonathan Cannon, an assistant professor of psychology, neuroscience, and behavior at McMaster who not involved in the study, told Live Science.
Not to say this study didn’t have its limitations, such as the effect of the surrounding crowd or vibrations of the floor influencing the need to dance. But it definitely makes you wonder about what’s actually playing in your favorite song.
Uncle Leonid wants you
Do you like to travel? Are you a bit of a thrill seeker? Do you have any extra socks? If you’re a physician who answered yes to those three questions, then we’ve got an opportunity for you.
Leonid Slutsky, leader of Russia’s populist Liberal Democratic Party and chairman of the foreign relations committee in the lower house of Russia’s parliament – yes, that Leonid Slutsky – recently made a bit of a recruiting pitch, although that’s not how ABC News described it.
Mr. Slutsky, a strong supporter of his country’s war against Ukraine, recently told the mothers of Russian soldiers “that the whole world is watching us. We are the largest state and when we do not have socks, shorts, doctors, intelligence, communications, or simply care for our children, questions arise that will be very difficult to answer.”
It’s probably not what he meant, but the lack of intelligence is pretty clear.
Boil ‘em, mash ‘em, include ‘em in a balanced diet
It’s kind of funny that, even though potatoes are vegetables and vegetables are generally considered to be healthy foods, not many people think of potatoes as being particularly good for you. And that’s hardly surprising since we usually either consume them in the form of French fries or potato chips, neither of which are known for their healthiness.
In fact, some previous research shows that potatoes are a food to avoid, particularly for people with insulin resistance. However, a new study from England goes against the grain and asserts that the potato is perfectly fine for insulin-resistant individuals and filled with valuable nutrients and health benefits. Which is great news for the state of Idaho and the potato organization funding the research. Of course there’s a potato organization.
For the study, a group of obese, overweight, or insulin-resistant individuals received a diet of either beans, peas, and meat or fish or white potatoes with meat or fish for 8 weeks; both diets were heavy in fruits and vegetables and both diets replaced about 40% of typical meat consumption with either beans and peas or potatoes. By the end of the study, those on the potato diet experienced health benefits equivalent to those on the bean and pea diet, including losing roughly equivalent amounts of weight and similarly reducing the body’s insulin response.
The researchers noted that, because people tend to eat the same amount of food no matter what, replacing something like meat with dense, low-calorie potatoes meant study participants could eat normally yet consume much fewer calories. So you could make a delicious, healthy stew without the brace of conies and the nice fish, which would make Smeagol very happy.
You won’t have ‘monkeypox’ to kick around anymore
It’s true. No more monkeypox. It’s gone. It’s history. Adios. The World Health Organization said that the disease formerly known as monkeypox will now be called mpox. What? You didn’t think it had been cured, did you? You did? Really? Silly readers.
“Mpox will become a preferred term, replacing monkeypox, after a transition period of 1 year. This serves to mitigate the concerns raised by experts about confusion caused by a name change in the midst of a global outbreak,” WHO said in a statement announcing the change.
The stigma attached to the name was the main problem. New York City Health Commissioner Dr. Ashwin Vasan had sent a letter to WHO earlier this year, according to CNN, saying that there was “growing concern for the potentially devastating and stigmatizing effects that the messaging around the ‘monkeypox’ virus can have on … vulnerable communities.”
We here at LOTME applaud the fight against stigmas of any sort, but we sensed there was more to this name change business, so our dedicated team of investigative journalists went into action. Sure enough, while rooting through WHO Director-General Tedros Adhanom Ghebreyesus’s garbage, we found a list of the names that had been rejected in favor of mpox:
- K-pop (already taken)
- Keeping up with the Kardashi-pox
- Trumpox
- Pox the magic dragon
- Monkey plague (didn’t really solve the problem)
- Hockey pox
- Mission mpoxible
- Jurassic Pox
- The pox that refreshes
- Debbie
Feet catch what the ears miss
The spectrum of frequencies that can be heard by human ears varies from person to person. Then there’s the matter of personal taste in music and volume level. But what really gets people moving? A new study shows that it’s more about the frequency of the sound than the volume.
For the study, participants at a concert by electronic music duo Orphx at LIVELab – a research performance center on the McMaster University campus in Hamilton, Ont., that was specifically designed to study music and dance – filled out questionnaires before and after the show. They also wore motion-capture headbands to detect their movement throughout the concert. During the show the researchers turned very-low-frequency (VLF) sounds (8-37 Hz) on and off every 2.5 minutes. Movement speed was calculated during on and off periods.
Although the effects of subliminal messaging aren’t new, past studies have shown that participants were mostly aware of the messaging. In this study, the researchers found that the subjects’ movements increased by 11.8% when the VLF sounds were on, but without their awareness. The researchers and the participants attributed movement to the bass, as lower pitches tend to elicit stronger neural responses and thus movement, compared with higher pitches.
“Our whole sense of the beat is mediated by the vestibular system but nobody’s really, I think, effectively confirmed that,” Jonathan Cannon, an assistant professor of psychology, neuroscience, and behavior at McMaster who not involved in the study, told Live Science.
Not to say this study didn’t have its limitations, such as the effect of the surrounding crowd or vibrations of the floor influencing the need to dance. But it definitely makes you wonder about what’s actually playing in your favorite song.
Uncle Leonid wants you
Do you like to travel? Are you a bit of a thrill seeker? Do you have any extra socks? If you’re a physician who answered yes to those three questions, then we’ve got an opportunity for you.
Leonid Slutsky, leader of Russia’s populist Liberal Democratic Party and chairman of the foreign relations committee in the lower house of Russia’s parliament – yes, that Leonid Slutsky – recently made a bit of a recruiting pitch, although that’s not how ABC News described it.
Mr. Slutsky, a strong supporter of his country’s war against Ukraine, recently told the mothers of Russian soldiers “that the whole world is watching us. We are the largest state and when we do not have socks, shorts, doctors, intelligence, communications, or simply care for our children, questions arise that will be very difficult to answer.”
It’s probably not what he meant, but the lack of intelligence is pretty clear.
What is the genetic influence on the severity of COVID-19?
A striking characteristic of COVID-19 is that the severity of clinical outcomes is remarkably variable. Establishing a prognosis for individuals infected with COVID-19 remains a challenge.
Since the start of the COVID-19 pandemic, the heterogeneity of individuals who progress toward severe disease or death, along with the fact that individuals directly exposed to the virus do not necessarily become sick, supports the hypothesis that genetic risk or protective factors are at play.
In an interview with this news organization, Mayana Zatz, PhD, head professor of genetics and coordinator of the Human Genome and Stem Cell Study Center at the University of São Paulo, explained: “The first case that caught my eye was the case of my neighbors, a couple. He presented COVID-19 symptoms, but his wife, who took care of him, had absolutely no symptoms. I thought that it was strange, but we received 3,000 emails from people saying, ‘This happened to me, too.’”
Reports in the media about seven pairs of monozygotic (MZ) twins who died from COVID-19 within days of one another in Brazil also stood out, said the researcher.
, as well as their pathology. Dr. Zatz’s team analyzed the case of a 31-year-old Brazilian MZ twin brother pair who presented simultaneously with severe COVID-19 and the need for oxygen support, despite their age and good health conditions. Curiously, they were admitted and intubated on the same day, but neither of the twins knew about the other’s situation; they found out only when they were extubated.
The study was carried out at the USP with the collaboration of the State University of São Paulo. The authors mapped the genetic profile (by sequencing the genome responsible for coding proteins, or whole-exome sequencing) and the immune cell profile to evaluate innate and adaptive immunity.
The MZ twin brothers shared the same two rare genetic mutations, which may be associated with their increased risk of developing severe COVID-19. However, since these variants were not studied at the protein or functional level, their pathogenicity has yet to be determined. The twins also had [human leukocyte antigen (HLA)] alleles associated with severe COVID-19, which are important candidates for the mechanisms of innate and adaptive immunity and susceptibility to COVID-19 infection and manifestation.
But one particular oddity stood out to the researchers: One of the brothers required longer hospitalization, and only he reported symptoms of long COVID.
In the authors’ eyes, even though the patients shared genetic mutations potentially associated with the risk of developing severe COVID-19, the differences in clinical progression emphasize that, beyond genetic risk factors, continuous exposure to pathogens over a lifetime and other environmental factors mean that each individual’s immune response is unique, even in twins.
“There is no doubt that genetics contribute to the severity of COVID-19, and environmental factors sometimes give us the opportunity to study the disease, too. Such [is the case with] MZ twins who have genetic similarities, even with changes that take place over a lifetime,” José Eduardo Krieger, MD, PhD, professor of molecular medicine at the University of São Paulo Medical School (FMUSP), told this news organization. “Examining MZ twins is a strategy that may help, but, with n = 2, luck really needs to be on your side to get straight to the problem. You need to combine [these findings] with other studies to solve this conundrum,” said Dr. Krieger, who did not take part in the research.
Large cohorts
Genomic and computer resources allow for the study of large sets of data from thousands of individuals. In each of those sets of data, the signal offered by thousands of markers distributed throughout the genome can be studied. This is the possibility offered by various genomic studies of large cohorts of patients with different clinical manifestations.
“Researchers examine thousands of genetic variants throughout the genome from a large sample of individuals and have the chance, for example, to identify genetic variants that are more prevalent in patients who have presented with severe disease than in those who presented with milder disease,” said Dr. Krieger. “These associations highlight a chromosome region in which one or more genes explain, at least in part, the differences observed.”
Genomewide association studies have identified some genetic variants that indicate severity of COVID-19, with potential impact on the virus entering the cell, the immune response, or the development of cytokine storms.
One of these studies, COVID-19 Host Genetics Initiative (COVID-19 HGI), is an international, open-science collaboration for sharing scientific methods and resources with research groups across the world, with the goal of robustly mapping the host genetic determinants of SARS-CoV-2 infection and the severity of the resulting COVID-19 disease. At the start of 2021, the COVID-19 HGI combined genetic data from 49,562 cases and 2 million controls from 46 studies in 19 countries. A total of 853 samples from the BRACOVID study were included in the meta-analysis. The endeavor enabled the identification of 13 genomewide significant loci that are associated with SARS-CoV-2 infection or severe manifestations of COVID-19.
The BRACOVID study, in which Dr. Krieger participates, aims to identify host genetic factors that determine the severity of COVID-19. It is currently the largest project of its kind in Latin America. An article provides the analysis of the first 5,233 participants in the BRACOVID study, who were recruited in São Paulo. Of these participants, 3,533 had been infected with COVID-19 and hospitalized at either the Heart Institute or the Central Institute of the FMUSP General Hospital. The remaining 1,700 made up the control group, which included health care professionals and members of the general population. The controls were recruited through serology assays or PCR tests for SARS-CoV-2.
The researchers discovered a region of chromosome 1 that could play a role in modulating immune response and that could lead to an increase in the likelihood of hospitalization across a wide range of COVID-19 risk factors. This region of chromosome 1 was observed only in Brazilians with a strong European ancestry; however, this finding had not been mentioned in previous studies, suggesting that it could harbor a risk allele specific to the Brazilian population.
The study also confirmed most, but not all, of the regions recorded in the literature, which may be significant in identifying factors determining severity that are specific to a given population.
Including information from the BRACOVID study, other studies have enhanced the knowledge on affected organs. Combined data from 14,000 patients from nine countries evaluated a region of a single chromosome and found that carriers of a certain allele had a higher probability of experiencing various COVID-19 complications, such as severe respiratory failure, venous thromboembolism, and liver damage. The risk was even higher for individuals aged 60 years and over.
Discordant couples
Smaller sample sizes of underrepresented populations also provide relevant data for genomic studies. Dr. Zatz’s team carried out genomic studies on smaller groups, comparing serodiscordant couples (where one was infected and symptomatic while the partner remained asymptomatic and seronegative despite sharing the same bedroom during the infection). Their research found genetic variants related to immune response that were associated with susceptibility to infection and progression to severe COVID-19.
The team also went on to study a group of patients older than 90 years who recovered from COVID-19 with mild symptoms or who remained asymptomatic following a positive test for SARS-CoV-2. They compared these patients with a sample of elderly patients from the same city (São Paulo), sampled before the current pandemic. The researchers identified a genetic variant related to mucin production. “In individuals with mild COVID-19, the degradation of these mucins would be more efficient,” said Dr. Zatz. It is possible for this variant to interfere not only with the production of mucus, but also in its composition, as there is an exchange of amino acids in the protein.
“We continued the study by comparing the extremes, i.e., those in their 90s with mild COVID-19 and younger patients with severe COVID-19, including several who died,” said Dr. Zatz.
More personalized medicine
The specialists agreed that a genetic test to predict COVID-19 severity is still a long way away. The genetic component is too little understood to enable the evaluation of individual risk. It has been possible to identify several important areas but, as Dr. Krieger pointed out, a variant identified in a certain chromosome interval may not be just one gene. There may be various candidate genes, or there may be a regulatory sequence for a distant gene. Furthermore, there are regions with genes that make sense as moderators of COVID-19 severity, because they regulate an inflammatory or immunologic reaction, but evidence is still lacking.
Reaching the molecular mechanism would, in future, allow a medicine to be chosen for a given patient, as already happens with other diseases. It also could enable the discovery of new medicines following as-yet-unexplored lines of research. Dr. Zatz also considers the possibility of genetic therapy.
Even with the knowledge of human genetics, one part of the equation is missing: viral genetics. “Many of the individuals who were resistant to the Delta variant were later affected by Omicron,” she pointed out.
Significance of Brazil
“We have an infinite amount of genomic data worldwide, but the vast majority originates from White Americans of European origin,” said Dr. Krieger. Moreover, genomic associations of COVID-19 severity discovered in the Chinese population were not significant in the European population. Besides underscoring the importance of collaborating with international studies, this situation supports scientists’ interest in carrying out genetic studies within Brazil, he added.
“In the genomic study of the Brazilian population, we found 2 million variants that were not present in the European populations,” said Dr. Zatz.
Dr. Krieger mentioned a technical advantage that Brazil has. “Having been colonized by different ethnic groups and mixed many generations ago, Brazil has a population with a unique genetic structure; the recombinations are different. When preparing the samples, the regions break differently.” This factor could help to separate, in a candidate region, the gene that is significant from those that might not be.
In general, severe COVID-19 would be a complex phenomenon involving several genes and interactions with environmental factors. The Brazilian studies tried to find a factor that was unique to Brazil, but the significance of the differences remained unclear. “We found some signs that were specific to our population,” concluded Dr. Krieger. “But the reason that more people in Brazil died as a result of COVID-19 was not genetic,” he added.
Dr. Zatz and Dr. Krieger reported no conflicts of interest. This article was translated from the Medscape Portuguese edition.
A version of this article first appeared on Medscape.com.
A striking characteristic of COVID-19 is that the severity of clinical outcomes is remarkably variable. Establishing a prognosis for individuals infected with COVID-19 remains a challenge.
Since the start of the COVID-19 pandemic, the heterogeneity of individuals who progress toward severe disease or death, along with the fact that individuals directly exposed to the virus do not necessarily become sick, supports the hypothesis that genetic risk or protective factors are at play.
In an interview with this news organization, Mayana Zatz, PhD, head professor of genetics and coordinator of the Human Genome and Stem Cell Study Center at the University of São Paulo, explained: “The first case that caught my eye was the case of my neighbors, a couple. He presented COVID-19 symptoms, but his wife, who took care of him, had absolutely no symptoms. I thought that it was strange, but we received 3,000 emails from people saying, ‘This happened to me, too.’”
Reports in the media about seven pairs of monozygotic (MZ) twins who died from COVID-19 within days of one another in Brazil also stood out, said the researcher.
, as well as their pathology. Dr. Zatz’s team analyzed the case of a 31-year-old Brazilian MZ twin brother pair who presented simultaneously with severe COVID-19 and the need for oxygen support, despite their age and good health conditions. Curiously, they were admitted and intubated on the same day, but neither of the twins knew about the other’s situation; they found out only when they were extubated.
The study was carried out at the USP with the collaboration of the State University of São Paulo. The authors mapped the genetic profile (by sequencing the genome responsible for coding proteins, or whole-exome sequencing) and the immune cell profile to evaluate innate and adaptive immunity.
The MZ twin brothers shared the same two rare genetic mutations, which may be associated with their increased risk of developing severe COVID-19. However, since these variants were not studied at the protein or functional level, their pathogenicity has yet to be determined. The twins also had [human leukocyte antigen (HLA)] alleles associated with severe COVID-19, which are important candidates for the mechanisms of innate and adaptive immunity and susceptibility to COVID-19 infection and manifestation.
But one particular oddity stood out to the researchers: One of the brothers required longer hospitalization, and only he reported symptoms of long COVID.
In the authors’ eyes, even though the patients shared genetic mutations potentially associated with the risk of developing severe COVID-19, the differences in clinical progression emphasize that, beyond genetic risk factors, continuous exposure to pathogens over a lifetime and other environmental factors mean that each individual’s immune response is unique, even in twins.
“There is no doubt that genetics contribute to the severity of COVID-19, and environmental factors sometimes give us the opportunity to study the disease, too. Such [is the case with] MZ twins who have genetic similarities, even with changes that take place over a lifetime,” José Eduardo Krieger, MD, PhD, professor of molecular medicine at the University of São Paulo Medical School (FMUSP), told this news organization. “Examining MZ twins is a strategy that may help, but, with n = 2, luck really needs to be on your side to get straight to the problem. You need to combine [these findings] with other studies to solve this conundrum,” said Dr. Krieger, who did not take part in the research.
Large cohorts
Genomic and computer resources allow for the study of large sets of data from thousands of individuals. In each of those sets of data, the signal offered by thousands of markers distributed throughout the genome can be studied. This is the possibility offered by various genomic studies of large cohorts of patients with different clinical manifestations.
“Researchers examine thousands of genetic variants throughout the genome from a large sample of individuals and have the chance, for example, to identify genetic variants that are more prevalent in patients who have presented with severe disease than in those who presented with milder disease,” said Dr. Krieger. “These associations highlight a chromosome region in which one or more genes explain, at least in part, the differences observed.”
Genomewide association studies have identified some genetic variants that indicate severity of COVID-19, with potential impact on the virus entering the cell, the immune response, or the development of cytokine storms.
One of these studies, COVID-19 Host Genetics Initiative (COVID-19 HGI), is an international, open-science collaboration for sharing scientific methods and resources with research groups across the world, with the goal of robustly mapping the host genetic determinants of SARS-CoV-2 infection and the severity of the resulting COVID-19 disease. At the start of 2021, the COVID-19 HGI combined genetic data from 49,562 cases and 2 million controls from 46 studies in 19 countries. A total of 853 samples from the BRACOVID study were included in the meta-analysis. The endeavor enabled the identification of 13 genomewide significant loci that are associated with SARS-CoV-2 infection or severe manifestations of COVID-19.
The BRACOVID study, in which Dr. Krieger participates, aims to identify host genetic factors that determine the severity of COVID-19. It is currently the largest project of its kind in Latin America. An article provides the analysis of the first 5,233 participants in the BRACOVID study, who were recruited in São Paulo. Of these participants, 3,533 had been infected with COVID-19 and hospitalized at either the Heart Institute or the Central Institute of the FMUSP General Hospital. The remaining 1,700 made up the control group, which included health care professionals and members of the general population. The controls were recruited through serology assays or PCR tests for SARS-CoV-2.
The researchers discovered a region of chromosome 1 that could play a role in modulating immune response and that could lead to an increase in the likelihood of hospitalization across a wide range of COVID-19 risk factors. This region of chromosome 1 was observed only in Brazilians with a strong European ancestry; however, this finding had not been mentioned in previous studies, suggesting that it could harbor a risk allele specific to the Brazilian population.
The study also confirmed most, but not all, of the regions recorded in the literature, which may be significant in identifying factors determining severity that are specific to a given population.
Including information from the BRACOVID study, other studies have enhanced the knowledge on affected organs. Combined data from 14,000 patients from nine countries evaluated a region of a single chromosome and found that carriers of a certain allele had a higher probability of experiencing various COVID-19 complications, such as severe respiratory failure, venous thromboembolism, and liver damage. The risk was even higher for individuals aged 60 years and over.
Discordant couples
Smaller sample sizes of underrepresented populations also provide relevant data for genomic studies. Dr. Zatz’s team carried out genomic studies on smaller groups, comparing serodiscordant couples (where one was infected and symptomatic while the partner remained asymptomatic and seronegative despite sharing the same bedroom during the infection). Their research found genetic variants related to immune response that were associated with susceptibility to infection and progression to severe COVID-19.
The team also went on to study a group of patients older than 90 years who recovered from COVID-19 with mild symptoms or who remained asymptomatic following a positive test for SARS-CoV-2. They compared these patients with a sample of elderly patients from the same city (São Paulo), sampled before the current pandemic. The researchers identified a genetic variant related to mucin production. “In individuals with mild COVID-19, the degradation of these mucins would be more efficient,” said Dr. Zatz. It is possible for this variant to interfere not only with the production of mucus, but also in its composition, as there is an exchange of amino acids in the protein.
“We continued the study by comparing the extremes, i.e., those in their 90s with mild COVID-19 and younger patients with severe COVID-19, including several who died,” said Dr. Zatz.
More personalized medicine
The specialists agreed that a genetic test to predict COVID-19 severity is still a long way away. The genetic component is too little understood to enable the evaluation of individual risk. It has been possible to identify several important areas but, as Dr. Krieger pointed out, a variant identified in a certain chromosome interval may not be just one gene. There may be various candidate genes, or there may be a regulatory sequence for a distant gene. Furthermore, there are regions with genes that make sense as moderators of COVID-19 severity, because they regulate an inflammatory or immunologic reaction, but evidence is still lacking.
Reaching the molecular mechanism would, in future, allow a medicine to be chosen for a given patient, as already happens with other diseases. It also could enable the discovery of new medicines following as-yet-unexplored lines of research. Dr. Zatz also considers the possibility of genetic therapy.
Even with the knowledge of human genetics, one part of the equation is missing: viral genetics. “Many of the individuals who were resistant to the Delta variant were later affected by Omicron,” she pointed out.
Significance of Brazil
“We have an infinite amount of genomic data worldwide, but the vast majority originates from White Americans of European origin,” said Dr. Krieger. Moreover, genomic associations of COVID-19 severity discovered in the Chinese population were not significant in the European population. Besides underscoring the importance of collaborating with international studies, this situation supports scientists’ interest in carrying out genetic studies within Brazil, he added.
“In the genomic study of the Brazilian population, we found 2 million variants that were not present in the European populations,” said Dr. Zatz.
Dr. Krieger mentioned a technical advantage that Brazil has. “Having been colonized by different ethnic groups and mixed many generations ago, Brazil has a population with a unique genetic structure; the recombinations are different. When preparing the samples, the regions break differently.” This factor could help to separate, in a candidate region, the gene that is significant from those that might not be.
In general, severe COVID-19 would be a complex phenomenon involving several genes and interactions with environmental factors. The Brazilian studies tried to find a factor that was unique to Brazil, but the significance of the differences remained unclear. “We found some signs that were specific to our population,” concluded Dr. Krieger. “But the reason that more people in Brazil died as a result of COVID-19 was not genetic,” he added.
Dr. Zatz and Dr. Krieger reported no conflicts of interest. This article was translated from the Medscape Portuguese edition.
A version of this article first appeared on Medscape.com.
A striking characteristic of COVID-19 is that the severity of clinical outcomes is remarkably variable. Establishing a prognosis for individuals infected with COVID-19 remains a challenge.
Since the start of the COVID-19 pandemic, the heterogeneity of individuals who progress toward severe disease or death, along with the fact that individuals directly exposed to the virus do not necessarily become sick, supports the hypothesis that genetic risk or protective factors are at play.
In an interview with this news organization, Mayana Zatz, PhD, head professor of genetics and coordinator of the Human Genome and Stem Cell Study Center at the University of São Paulo, explained: “The first case that caught my eye was the case of my neighbors, a couple. He presented COVID-19 symptoms, but his wife, who took care of him, had absolutely no symptoms. I thought that it was strange, but we received 3,000 emails from people saying, ‘This happened to me, too.’”
Reports in the media about seven pairs of monozygotic (MZ) twins who died from COVID-19 within days of one another in Brazil also stood out, said the researcher.
, as well as their pathology. Dr. Zatz’s team analyzed the case of a 31-year-old Brazilian MZ twin brother pair who presented simultaneously with severe COVID-19 and the need for oxygen support, despite their age and good health conditions. Curiously, they were admitted and intubated on the same day, but neither of the twins knew about the other’s situation; they found out only when they were extubated.
The study was carried out at the USP with the collaboration of the State University of São Paulo. The authors mapped the genetic profile (by sequencing the genome responsible for coding proteins, or whole-exome sequencing) and the immune cell profile to evaluate innate and adaptive immunity.
The MZ twin brothers shared the same two rare genetic mutations, which may be associated with their increased risk of developing severe COVID-19. However, since these variants were not studied at the protein or functional level, their pathogenicity has yet to be determined. The twins also had [human leukocyte antigen (HLA)] alleles associated with severe COVID-19, which are important candidates for the mechanisms of innate and adaptive immunity and susceptibility to COVID-19 infection and manifestation.
But one particular oddity stood out to the researchers: One of the brothers required longer hospitalization, and only he reported symptoms of long COVID.
In the authors’ eyes, even though the patients shared genetic mutations potentially associated with the risk of developing severe COVID-19, the differences in clinical progression emphasize that, beyond genetic risk factors, continuous exposure to pathogens over a lifetime and other environmental factors mean that each individual’s immune response is unique, even in twins.
“There is no doubt that genetics contribute to the severity of COVID-19, and environmental factors sometimes give us the opportunity to study the disease, too. Such [is the case with] MZ twins who have genetic similarities, even with changes that take place over a lifetime,” José Eduardo Krieger, MD, PhD, professor of molecular medicine at the University of São Paulo Medical School (FMUSP), told this news organization. “Examining MZ twins is a strategy that may help, but, with n = 2, luck really needs to be on your side to get straight to the problem. You need to combine [these findings] with other studies to solve this conundrum,” said Dr. Krieger, who did not take part in the research.
Large cohorts
Genomic and computer resources allow for the study of large sets of data from thousands of individuals. In each of those sets of data, the signal offered by thousands of markers distributed throughout the genome can be studied. This is the possibility offered by various genomic studies of large cohorts of patients with different clinical manifestations.
“Researchers examine thousands of genetic variants throughout the genome from a large sample of individuals and have the chance, for example, to identify genetic variants that are more prevalent in patients who have presented with severe disease than in those who presented with milder disease,” said Dr. Krieger. “These associations highlight a chromosome region in which one or more genes explain, at least in part, the differences observed.”
Genomewide association studies have identified some genetic variants that indicate severity of COVID-19, with potential impact on the virus entering the cell, the immune response, or the development of cytokine storms.
One of these studies, COVID-19 Host Genetics Initiative (COVID-19 HGI), is an international, open-science collaboration for sharing scientific methods and resources with research groups across the world, with the goal of robustly mapping the host genetic determinants of SARS-CoV-2 infection and the severity of the resulting COVID-19 disease. At the start of 2021, the COVID-19 HGI combined genetic data from 49,562 cases and 2 million controls from 46 studies in 19 countries. A total of 853 samples from the BRACOVID study were included in the meta-analysis. The endeavor enabled the identification of 13 genomewide significant loci that are associated with SARS-CoV-2 infection or severe manifestations of COVID-19.
The BRACOVID study, in which Dr. Krieger participates, aims to identify host genetic factors that determine the severity of COVID-19. It is currently the largest project of its kind in Latin America. An article provides the analysis of the first 5,233 participants in the BRACOVID study, who were recruited in São Paulo. Of these participants, 3,533 had been infected with COVID-19 and hospitalized at either the Heart Institute or the Central Institute of the FMUSP General Hospital. The remaining 1,700 made up the control group, which included health care professionals and members of the general population. The controls were recruited through serology assays or PCR tests for SARS-CoV-2.
The researchers discovered a region of chromosome 1 that could play a role in modulating immune response and that could lead to an increase in the likelihood of hospitalization across a wide range of COVID-19 risk factors. This region of chromosome 1 was observed only in Brazilians with a strong European ancestry; however, this finding had not been mentioned in previous studies, suggesting that it could harbor a risk allele specific to the Brazilian population.
The study also confirmed most, but not all, of the regions recorded in the literature, which may be significant in identifying factors determining severity that are specific to a given population.
Including information from the BRACOVID study, other studies have enhanced the knowledge on affected organs. Combined data from 14,000 patients from nine countries evaluated a region of a single chromosome and found that carriers of a certain allele had a higher probability of experiencing various COVID-19 complications, such as severe respiratory failure, venous thromboembolism, and liver damage. The risk was even higher for individuals aged 60 years and over.
Discordant couples
Smaller sample sizes of underrepresented populations also provide relevant data for genomic studies. Dr. Zatz’s team carried out genomic studies on smaller groups, comparing serodiscordant couples (where one was infected and symptomatic while the partner remained asymptomatic and seronegative despite sharing the same bedroom during the infection). Their research found genetic variants related to immune response that were associated with susceptibility to infection and progression to severe COVID-19.
The team also went on to study a group of patients older than 90 years who recovered from COVID-19 with mild symptoms or who remained asymptomatic following a positive test for SARS-CoV-2. They compared these patients with a sample of elderly patients from the same city (São Paulo), sampled before the current pandemic. The researchers identified a genetic variant related to mucin production. “In individuals with mild COVID-19, the degradation of these mucins would be more efficient,” said Dr. Zatz. It is possible for this variant to interfere not only with the production of mucus, but also in its composition, as there is an exchange of amino acids in the protein.
“We continued the study by comparing the extremes, i.e., those in their 90s with mild COVID-19 and younger patients with severe COVID-19, including several who died,” said Dr. Zatz.
More personalized medicine
The specialists agreed that a genetic test to predict COVID-19 severity is still a long way away. The genetic component is too little understood to enable the evaluation of individual risk. It has been possible to identify several important areas but, as Dr. Krieger pointed out, a variant identified in a certain chromosome interval may not be just one gene. There may be various candidate genes, or there may be a regulatory sequence for a distant gene. Furthermore, there are regions with genes that make sense as moderators of COVID-19 severity, because they regulate an inflammatory or immunologic reaction, but evidence is still lacking.
Reaching the molecular mechanism would, in future, allow a medicine to be chosen for a given patient, as already happens with other diseases. It also could enable the discovery of new medicines following as-yet-unexplored lines of research. Dr. Zatz also considers the possibility of genetic therapy.
Even with the knowledge of human genetics, one part of the equation is missing: viral genetics. “Many of the individuals who were resistant to the Delta variant were later affected by Omicron,” she pointed out.
Significance of Brazil
“We have an infinite amount of genomic data worldwide, but the vast majority originates from White Americans of European origin,” said Dr. Krieger. Moreover, genomic associations of COVID-19 severity discovered in the Chinese population were not significant in the European population. Besides underscoring the importance of collaborating with international studies, this situation supports scientists’ interest in carrying out genetic studies within Brazil, he added.
“In the genomic study of the Brazilian population, we found 2 million variants that were not present in the European populations,” said Dr. Zatz.
Dr. Krieger mentioned a technical advantage that Brazil has. “Having been colonized by different ethnic groups and mixed many generations ago, Brazil has a population with a unique genetic structure; the recombinations are different. When preparing the samples, the regions break differently.” This factor could help to separate, in a candidate region, the gene that is significant from those that might not be.
In general, severe COVID-19 would be a complex phenomenon involving several genes and interactions with environmental factors. The Brazilian studies tried to find a factor that was unique to Brazil, but the significance of the differences remained unclear. “We found some signs that were specific to our population,” concluded Dr. Krieger. “But the reason that more people in Brazil died as a result of COVID-19 was not genetic,” he added.
Dr. Zatz and Dr. Krieger reported no conflicts of interest. This article was translated from the Medscape Portuguese edition.
A version of this article first appeared on Medscape.com.
Migraine in children and teens: managing the pain
By the time Mira Halker started high school, hardly a day passed that she wasn’t either getting a migraine attack or recovering from one. She missed volleyball team practice. She missed classes. She missed social events. And few people understood. After all, she looked healthy.
“A lot of times, people think I’m faking it,” said Mira, now 16, who lives in Phoenix. Friends called her flaky; her volleyball coaches questioned her dedication to the team. “I’m like, ‘I’m not trying to get out of this. This is not what this is about,’ ” she said.
Her mother, Rashmi B. Halker Singh, MD, is a neurologist at Mayo Clinic who happens to specialize in migraine. Even so, finding a solution was not easy. Neither ibuprofen nor triptans, nor various preventive measures such as a daily prescription for topiramate controlled the pain and associated symptoms. Mira was barely making it through her school day and had to quit volleyball. Then, in the spring of 10th grade, Mira told her mother that she couldn’t go to prom because the loud noises and lights could give her a migraine attack.
Mother and daughter decided it was time to get even more aggressive. “There are these key moments in life that you can’t get back,” Dr. Singh said. “Migraine steals so much from you.”
Diagnosis
One of the challenges Mira’s physicians faced was deciding which medications and other therapies to prescribe to a teenager. Drug companies have been releasing a steady stream of new treatments for migraine headaches, and researchers promise more are on the way soon. Here’s what works for children, what hasn’t yet been approved for use with minors, and how to diagnose migraines in the first place, from experts at some of the nation’s leading pediatric headache centers.
Migraine affects about 10% of children, according to the American Migraine Foundation. The headaches can strike children as early as age 3 or 4 years, said Robert Little, MD, a pediatric neurologist at Phoenix Children’s Hospital.
Before puberty, boys report more migraine attacks than girls, according to the American Academy of Pediatrics. But that reverses in adolescence: By age 17, as many as 8% of boys and 23% of girls have had migraine. To diagnose migraine, Juliana H. VanderPluym, MD, associate professor of neurology at Mayo Clinic in Phoenix, said she uses the criteria published in the latest edition of the International Classification of Headache Disorders (ICHD): A patient must have had at least five attacks in their life; and in children and adolescents, the attacks must last no less than 2 hours.
In addition, the headaches should exhibit at least two out of four features:
1. Occur more on one side of the head than the other (although Dr. VanderPluym said in children and adolescents headaches often are bilateral).
2. Be of moderate to severe intensity.
3. Have a pounding or throbbing quality.
4. Grow worse with activity or cause an avoidance of activity.
If the attacks meet those criteria, clinicians should check to see if they meet at least one out of the two following:
1. Are sensitive to light and sounds.
2. Are associated with nausea and/or vomiting.
A clinician should consider whether the headaches are not better accounted for by another diagnosis, according to the ICHD criteria. But, Dr. VanderPluym warned that does not necessarily mean running a slew of tests.
“In the absence of red flag features, it is more than likely going to be migraine headache,” she said. That’s especially true if a child has a family history of migraine, as the condition is often passed down from parent to child.
Ultimately, the diagnosis is fairly simple and can be made in a minute or less, said Jack Gladstein, MD, a pediatrician at the University of Maryland whose research focuses on the clinical care of children and adolescents with headache.
“Migraine is acute,” Dr. Gladstein said. “It’s really bad. And it’s recurrent.”
First line of treatment
Whatever a patient takes to treat a migraine, they should hit it early and hard, Dr. Gladstein said.
“The first thing you say, as a primary care physician, is treat your migraine at first twinge, whatever you use. Don’t wait, don’t wish it away,” he said. “The longer you wait, the less chance anything will work.”
The second piece of advice, Dr. Gladstein said, is that whatever drug a patient is taking, they should be on the highest feasible dose. “Work as fast as you can to treat them. You want the brain to reset as quickly as you can,” he said.
Patients should begin with over-the-counter pain relievers, Dr. Little said. If those prove insufficient, they can try a triptan. Rizatriptan is the only such agent that the Food and Drug Administration has approved for children aged 6-17 years. Other drugs in the class – sumatriptan/naproxen, almotriptan, and zolmitriptan – are approved for children 12 and older.
Another migraine therapy recently approved for children aged 12 and older is the use of neurostimulators. “It’s helpful to be aware of them,” Dr. VanderPluym said.
However, if neurostimulators and acute medications prove insufficient, clinicians should warn patients not to up their doses of triptans. Rebound headaches can occur if patients take triptans more than twice a week, or a maximum 10 days per month.
Another possibility is to add a preventive therapy. One mild, first option is nutraceuticals, like riboflavin (vitamin B2) or magnesium, said Anisa F. Kelley, MD, a neurologist and associate director of the headache program at the Ann and Robert H. Lurie Children’s Hospital of Chicago.
“We don’t have definitive evidence, but they’re probably doing more benefit than they are harm,” Dr. Kelley said of these therapies. “In patients who have anywhere from 4 to 8 migraine days a month, where you’re in that in-between period where you don’t necessarily need a [prescription] prophylactic, I will often start with a nutraceutical,” Dr. Kelley said.
For those patients who don’t respond to nutraceuticals, or who need more support, clinicians can prescribe amitriptyline or topiramate. Dr. VanderPluym said.
A 2017 study found such prophylactics to be no more effective than placebo in pediatric migraine patients, but experts caution the results should not be considered definitive.
For one thing, the study enrolled a highly selective group of participants, with milder forms of migraine who may have improved anyway, Dr. VanderPluym said. All participants also received lifestyle counseling.
Every time participants came in for a follow-up, they were asked questions such as how much water were they drinking and how much sleep were they getting, Dr. Kelley noted. The takeaway, she said: “Pediatric and adolescent migraine [management] is very, very much reliant on lifestyle factors.”
Lifestyle triggers
Clinicians should counsel their migraine patients about lifestyle changes, experts said. Getting adequate sleep, staying hydrated, and managing stress can help reduce the intensity and frequency of attacks.
Migraine patients should also be mindful of their screen time, Dr. Kelley added.
“I’ve had lots and lots of patients who find excessive screen time will trigger or worsen migraine,” she said.
As for other potential triggers of attacks, the evidence is mixed.
“There’s clearly an association with disrupted sleep and migraine, and that has been very well established,” Dr. Little said. “And there is some modest amount of evidence that regular exercise can be helpful.” But for reported food triggers, he said, there have been very inconclusive results.
Commonly reported triggers include MSG, red wine, chocolate, and aged cheese. When Dr. Little’s patients keep headache diaries, tracking their meals alongside when they got migraine attacks, they often discover individualized triggers – strawberries, for instance, in one case, he said.
Scientists believe migraines result from the inappropriate activation of the trigeminal ganglion. “The question is, what causes it to get triggered? And how does it get triggered?” Dr. Gladstein said. “And that’s where there’s a lot of difference of opinion and no conclusive evidence.” Clinicians also should make sure that something else – usually depression, anxiety, insomnia, and dizziness – is not hindering effective migraine management. “If someone has terrible insomnia, until you treat the insomnia, the headaches aren’t going to get better,” he said.
As for Mira, her migraine attacks did not significantly improve, despite trying triptans, prophylactics, lifestyle changes, and shots to block nerve pain. When the headaches threatened Mira’s chance to go to her prom, her neurologist suggested trying something different. The physician persuaded the family’s insurance to cover a calcitonin gene-related peptide antagonist, an injectable monoclonal antibody treatment for migraine that the FDA has currently approved only for use in adults.
The difference for Mira has been extraordinary.
“I can do so much more than I was able to do,” said Mira, who attended the dance migraine free. “I feel liberated.”
It’s only migraine
One of the greatest challenges in diagnosing migraine can be reassuring the patient, the parents, even clinicians themselves that migraine really is the cause of all this pain and discomfort, experts said.
“A lot of migraine treatment actually comes down to migraine education,” Dr. VanderPluym said.
Patients and their parents often wonder how they can be sure that this pain is not resulting from something more dangerous than migraine, Dr. Little said. In these cases, he cites practice guidelines published by the American Academy of Neurology.
“The gist of those guidelines is that most pediatric patients do not need further workup,” he said. “But I think that there’s always a fear that you’re missing something because we don’t have a test that we can do” for migraine.
Some warning signs that further tests might be warranted, Dr. Kelley said, include:
- Headaches that wake a patient up in the middle of the night.
- Headaches that start first thing in the morning, especially those that include vomiting.
- A headache pattern that suddenly gets much worse.
- Certain symptoms that accompany the headache, such as tingling, numbness or double vision.
Although all of these signs can still stem from migraines – tingling or numbness, for instance, can be signs of migraine aura – running additional tests can rule out more serious concerns, she said.
By the time Mira Halker started high school, hardly a day passed that she wasn’t either getting a migraine attack or recovering from one. She missed volleyball team practice. She missed classes. She missed social events. And few people understood. After all, she looked healthy.
“A lot of times, people think I’m faking it,” said Mira, now 16, who lives in Phoenix. Friends called her flaky; her volleyball coaches questioned her dedication to the team. “I’m like, ‘I’m not trying to get out of this. This is not what this is about,’ ” she said.
Her mother, Rashmi B. Halker Singh, MD, is a neurologist at Mayo Clinic who happens to specialize in migraine. Even so, finding a solution was not easy. Neither ibuprofen nor triptans, nor various preventive measures such as a daily prescription for topiramate controlled the pain and associated symptoms. Mira was barely making it through her school day and had to quit volleyball. Then, in the spring of 10th grade, Mira told her mother that she couldn’t go to prom because the loud noises and lights could give her a migraine attack.
Mother and daughter decided it was time to get even more aggressive. “There are these key moments in life that you can’t get back,” Dr. Singh said. “Migraine steals so much from you.”
Diagnosis
One of the challenges Mira’s physicians faced was deciding which medications and other therapies to prescribe to a teenager. Drug companies have been releasing a steady stream of new treatments for migraine headaches, and researchers promise more are on the way soon. Here’s what works for children, what hasn’t yet been approved for use with minors, and how to diagnose migraines in the first place, from experts at some of the nation’s leading pediatric headache centers.
Migraine affects about 10% of children, according to the American Migraine Foundation. The headaches can strike children as early as age 3 or 4 years, said Robert Little, MD, a pediatric neurologist at Phoenix Children’s Hospital.
Before puberty, boys report more migraine attacks than girls, according to the American Academy of Pediatrics. But that reverses in adolescence: By age 17, as many as 8% of boys and 23% of girls have had migraine. To diagnose migraine, Juliana H. VanderPluym, MD, associate professor of neurology at Mayo Clinic in Phoenix, said she uses the criteria published in the latest edition of the International Classification of Headache Disorders (ICHD): A patient must have had at least five attacks in their life; and in children and adolescents, the attacks must last no less than 2 hours.
In addition, the headaches should exhibit at least two out of four features:
1. Occur more on one side of the head than the other (although Dr. VanderPluym said in children and adolescents headaches often are bilateral).
2. Be of moderate to severe intensity.
3. Have a pounding or throbbing quality.
4. Grow worse with activity or cause an avoidance of activity.
If the attacks meet those criteria, clinicians should check to see if they meet at least one out of the two following:
1. Are sensitive to light and sounds.
2. Are associated with nausea and/or vomiting.
A clinician should consider whether the headaches are not better accounted for by another diagnosis, according to the ICHD criteria. But, Dr. VanderPluym warned that does not necessarily mean running a slew of tests.
“In the absence of red flag features, it is more than likely going to be migraine headache,” she said. That’s especially true if a child has a family history of migraine, as the condition is often passed down from parent to child.
Ultimately, the diagnosis is fairly simple and can be made in a minute or less, said Jack Gladstein, MD, a pediatrician at the University of Maryland whose research focuses on the clinical care of children and adolescents with headache.
“Migraine is acute,” Dr. Gladstein said. “It’s really bad. And it’s recurrent.”
First line of treatment
Whatever a patient takes to treat a migraine, they should hit it early and hard, Dr. Gladstein said.
“The first thing you say, as a primary care physician, is treat your migraine at first twinge, whatever you use. Don’t wait, don’t wish it away,” he said. “The longer you wait, the less chance anything will work.”
The second piece of advice, Dr. Gladstein said, is that whatever drug a patient is taking, they should be on the highest feasible dose. “Work as fast as you can to treat them. You want the brain to reset as quickly as you can,” he said.
Patients should begin with over-the-counter pain relievers, Dr. Little said. If those prove insufficient, they can try a triptan. Rizatriptan is the only such agent that the Food and Drug Administration has approved for children aged 6-17 years. Other drugs in the class – sumatriptan/naproxen, almotriptan, and zolmitriptan – are approved for children 12 and older.
Another migraine therapy recently approved for children aged 12 and older is the use of neurostimulators. “It’s helpful to be aware of them,” Dr. VanderPluym said.
However, if neurostimulators and acute medications prove insufficient, clinicians should warn patients not to up their doses of triptans. Rebound headaches can occur if patients take triptans more than twice a week, or a maximum 10 days per month.
Another possibility is to add a preventive therapy. One mild, first option is nutraceuticals, like riboflavin (vitamin B2) or magnesium, said Anisa F. Kelley, MD, a neurologist and associate director of the headache program at the Ann and Robert H. Lurie Children’s Hospital of Chicago.
“We don’t have definitive evidence, but they’re probably doing more benefit than they are harm,” Dr. Kelley said of these therapies. “In patients who have anywhere from 4 to 8 migraine days a month, where you’re in that in-between period where you don’t necessarily need a [prescription] prophylactic, I will often start with a nutraceutical,” Dr. Kelley said.
For those patients who don’t respond to nutraceuticals, or who need more support, clinicians can prescribe amitriptyline or topiramate. Dr. VanderPluym said.
A 2017 study found such prophylactics to be no more effective than placebo in pediatric migraine patients, but experts caution the results should not be considered definitive.
For one thing, the study enrolled a highly selective group of participants, with milder forms of migraine who may have improved anyway, Dr. VanderPluym said. All participants also received lifestyle counseling.
Every time participants came in for a follow-up, they were asked questions such as how much water were they drinking and how much sleep were they getting, Dr. Kelley noted. The takeaway, she said: “Pediatric and adolescent migraine [management] is very, very much reliant on lifestyle factors.”
Lifestyle triggers
Clinicians should counsel their migraine patients about lifestyle changes, experts said. Getting adequate sleep, staying hydrated, and managing stress can help reduce the intensity and frequency of attacks.
Migraine patients should also be mindful of their screen time, Dr. Kelley added.
“I’ve had lots and lots of patients who find excessive screen time will trigger or worsen migraine,” she said.
As for other potential triggers of attacks, the evidence is mixed.
“There’s clearly an association with disrupted sleep and migraine, and that has been very well established,” Dr. Little said. “And there is some modest amount of evidence that regular exercise can be helpful.” But for reported food triggers, he said, there have been very inconclusive results.
Commonly reported triggers include MSG, red wine, chocolate, and aged cheese. When Dr. Little’s patients keep headache diaries, tracking their meals alongside when they got migraine attacks, they often discover individualized triggers – strawberries, for instance, in one case, he said.
Scientists believe migraines result from the inappropriate activation of the trigeminal ganglion. “The question is, what causes it to get triggered? And how does it get triggered?” Dr. Gladstein said. “And that’s where there’s a lot of difference of opinion and no conclusive evidence.” Clinicians also should make sure that something else – usually depression, anxiety, insomnia, and dizziness – is not hindering effective migraine management. “If someone has terrible insomnia, until you treat the insomnia, the headaches aren’t going to get better,” he said.
As for Mira, her migraine attacks did not significantly improve, despite trying triptans, prophylactics, lifestyle changes, and shots to block nerve pain. When the headaches threatened Mira’s chance to go to her prom, her neurologist suggested trying something different. The physician persuaded the family’s insurance to cover a calcitonin gene-related peptide antagonist, an injectable monoclonal antibody treatment for migraine that the FDA has currently approved only for use in adults.
The difference for Mira has been extraordinary.
“I can do so much more than I was able to do,” said Mira, who attended the dance migraine free. “I feel liberated.”
It’s only migraine
One of the greatest challenges in diagnosing migraine can be reassuring the patient, the parents, even clinicians themselves that migraine really is the cause of all this pain and discomfort, experts said.
“A lot of migraine treatment actually comes down to migraine education,” Dr. VanderPluym said.
Patients and their parents often wonder how they can be sure that this pain is not resulting from something more dangerous than migraine, Dr. Little said. In these cases, he cites practice guidelines published by the American Academy of Neurology.
“The gist of those guidelines is that most pediatric patients do not need further workup,” he said. “But I think that there’s always a fear that you’re missing something because we don’t have a test that we can do” for migraine.
Some warning signs that further tests might be warranted, Dr. Kelley said, include:
- Headaches that wake a patient up in the middle of the night.
- Headaches that start first thing in the morning, especially those that include vomiting.
- A headache pattern that suddenly gets much worse.
- Certain symptoms that accompany the headache, such as tingling, numbness or double vision.
Although all of these signs can still stem from migraines – tingling or numbness, for instance, can be signs of migraine aura – running additional tests can rule out more serious concerns, she said.
By the time Mira Halker started high school, hardly a day passed that she wasn’t either getting a migraine attack or recovering from one. She missed volleyball team practice. She missed classes. She missed social events. And few people understood. After all, she looked healthy.
“A lot of times, people think I’m faking it,” said Mira, now 16, who lives in Phoenix. Friends called her flaky; her volleyball coaches questioned her dedication to the team. “I’m like, ‘I’m not trying to get out of this. This is not what this is about,’ ” she said.
Her mother, Rashmi B. Halker Singh, MD, is a neurologist at Mayo Clinic who happens to specialize in migraine. Even so, finding a solution was not easy. Neither ibuprofen nor triptans, nor various preventive measures such as a daily prescription for topiramate controlled the pain and associated symptoms. Mira was barely making it through her school day and had to quit volleyball. Then, in the spring of 10th grade, Mira told her mother that she couldn’t go to prom because the loud noises and lights could give her a migraine attack.
Mother and daughter decided it was time to get even more aggressive. “There are these key moments in life that you can’t get back,” Dr. Singh said. “Migraine steals so much from you.”
Diagnosis
One of the challenges Mira’s physicians faced was deciding which medications and other therapies to prescribe to a teenager. Drug companies have been releasing a steady stream of new treatments for migraine headaches, and researchers promise more are on the way soon. Here’s what works for children, what hasn’t yet been approved for use with minors, and how to diagnose migraines in the first place, from experts at some of the nation’s leading pediatric headache centers.
Migraine affects about 10% of children, according to the American Migraine Foundation. The headaches can strike children as early as age 3 or 4 years, said Robert Little, MD, a pediatric neurologist at Phoenix Children’s Hospital.
Before puberty, boys report more migraine attacks than girls, according to the American Academy of Pediatrics. But that reverses in adolescence: By age 17, as many as 8% of boys and 23% of girls have had migraine. To diagnose migraine, Juliana H. VanderPluym, MD, associate professor of neurology at Mayo Clinic in Phoenix, said she uses the criteria published in the latest edition of the International Classification of Headache Disorders (ICHD): A patient must have had at least five attacks in their life; and in children and adolescents, the attacks must last no less than 2 hours.
In addition, the headaches should exhibit at least two out of four features:
1. Occur more on one side of the head than the other (although Dr. VanderPluym said in children and adolescents headaches often are bilateral).
2. Be of moderate to severe intensity.
3. Have a pounding or throbbing quality.
4. Grow worse with activity or cause an avoidance of activity.
If the attacks meet those criteria, clinicians should check to see if they meet at least one out of the two following:
1. Are sensitive to light and sounds.
2. Are associated with nausea and/or vomiting.
A clinician should consider whether the headaches are not better accounted for by another diagnosis, according to the ICHD criteria. But, Dr. VanderPluym warned that does not necessarily mean running a slew of tests.
“In the absence of red flag features, it is more than likely going to be migraine headache,” she said. That’s especially true if a child has a family history of migraine, as the condition is often passed down from parent to child.
Ultimately, the diagnosis is fairly simple and can be made in a minute or less, said Jack Gladstein, MD, a pediatrician at the University of Maryland whose research focuses on the clinical care of children and adolescents with headache.
“Migraine is acute,” Dr. Gladstein said. “It’s really bad. And it’s recurrent.”
First line of treatment
Whatever a patient takes to treat a migraine, they should hit it early and hard, Dr. Gladstein said.
“The first thing you say, as a primary care physician, is treat your migraine at first twinge, whatever you use. Don’t wait, don’t wish it away,” he said. “The longer you wait, the less chance anything will work.”
The second piece of advice, Dr. Gladstein said, is that whatever drug a patient is taking, they should be on the highest feasible dose. “Work as fast as you can to treat them. You want the brain to reset as quickly as you can,” he said.
Patients should begin with over-the-counter pain relievers, Dr. Little said. If those prove insufficient, they can try a triptan. Rizatriptan is the only such agent that the Food and Drug Administration has approved for children aged 6-17 years. Other drugs in the class – sumatriptan/naproxen, almotriptan, and zolmitriptan – are approved for children 12 and older.
Another migraine therapy recently approved for children aged 12 and older is the use of neurostimulators. “It’s helpful to be aware of them,” Dr. VanderPluym said.
However, if neurostimulators and acute medications prove insufficient, clinicians should warn patients not to up their doses of triptans. Rebound headaches can occur if patients take triptans more than twice a week, or a maximum 10 days per month.
Another possibility is to add a preventive therapy. One mild, first option is nutraceuticals, like riboflavin (vitamin B2) or magnesium, said Anisa F. Kelley, MD, a neurologist and associate director of the headache program at the Ann and Robert H. Lurie Children’s Hospital of Chicago.
“We don’t have definitive evidence, but they’re probably doing more benefit than they are harm,” Dr. Kelley said of these therapies. “In patients who have anywhere from 4 to 8 migraine days a month, where you’re in that in-between period where you don’t necessarily need a [prescription] prophylactic, I will often start with a nutraceutical,” Dr. Kelley said.
For those patients who don’t respond to nutraceuticals, or who need more support, clinicians can prescribe amitriptyline or topiramate. Dr. VanderPluym said.
A 2017 study found such prophylactics to be no more effective than placebo in pediatric migraine patients, but experts caution the results should not be considered definitive.
For one thing, the study enrolled a highly selective group of participants, with milder forms of migraine who may have improved anyway, Dr. VanderPluym said. All participants also received lifestyle counseling.
Every time participants came in for a follow-up, they were asked questions such as how much water were they drinking and how much sleep were they getting, Dr. Kelley noted. The takeaway, she said: “Pediatric and adolescent migraine [management] is very, very much reliant on lifestyle factors.”
Lifestyle triggers
Clinicians should counsel their migraine patients about lifestyle changes, experts said. Getting adequate sleep, staying hydrated, and managing stress can help reduce the intensity and frequency of attacks.
Migraine patients should also be mindful of their screen time, Dr. Kelley added.
“I’ve had lots and lots of patients who find excessive screen time will trigger or worsen migraine,” she said.
As for other potential triggers of attacks, the evidence is mixed.
“There’s clearly an association with disrupted sleep and migraine, and that has been very well established,” Dr. Little said. “And there is some modest amount of evidence that regular exercise can be helpful.” But for reported food triggers, he said, there have been very inconclusive results.
Commonly reported triggers include MSG, red wine, chocolate, and aged cheese. When Dr. Little’s patients keep headache diaries, tracking their meals alongside when they got migraine attacks, they often discover individualized triggers – strawberries, for instance, in one case, he said.
Scientists believe migraines result from the inappropriate activation of the trigeminal ganglion. “The question is, what causes it to get triggered? And how does it get triggered?” Dr. Gladstein said. “And that’s where there’s a lot of difference of opinion and no conclusive evidence.” Clinicians also should make sure that something else – usually depression, anxiety, insomnia, and dizziness – is not hindering effective migraine management. “If someone has terrible insomnia, until you treat the insomnia, the headaches aren’t going to get better,” he said.
As for Mira, her migraine attacks did not significantly improve, despite trying triptans, prophylactics, lifestyle changes, and shots to block nerve pain. When the headaches threatened Mira’s chance to go to her prom, her neurologist suggested trying something different. The physician persuaded the family’s insurance to cover a calcitonin gene-related peptide antagonist, an injectable monoclonal antibody treatment for migraine that the FDA has currently approved only for use in adults.
The difference for Mira has been extraordinary.
“I can do so much more than I was able to do,” said Mira, who attended the dance migraine free. “I feel liberated.”
It’s only migraine
One of the greatest challenges in diagnosing migraine can be reassuring the patient, the parents, even clinicians themselves that migraine really is the cause of all this pain and discomfort, experts said.
“A lot of migraine treatment actually comes down to migraine education,” Dr. VanderPluym said.
Patients and their parents often wonder how they can be sure that this pain is not resulting from something more dangerous than migraine, Dr. Little said. In these cases, he cites practice guidelines published by the American Academy of Neurology.
“The gist of those guidelines is that most pediatric patients do not need further workup,” he said. “But I think that there’s always a fear that you’re missing something because we don’t have a test that we can do” for migraine.
Some warning signs that further tests might be warranted, Dr. Kelley said, include:
- Headaches that wake a patient up in the middle of the night.
- Headaches that start first thing in the morning, especially those that include vomiting.
- A headache pattern that suddenly gets much worse.
- Certain symptoms that accompany the headache, such as tingling, numbness or double vision.
Although all of these signs can still stem from migraines – tingling or numbness, for instance, can be signs of migraine aura – running additional tests can rule out more serious concerns, she said.
U.S. flu activity already at mid-season levels
according to the Centers of Disease Control and Prevention.
Nationally, 6% of all outpatient visits were because of flu or flu-like illness for the week of Nov. 13-19, up from 5.8% the previous week, the CDC’s Influenza Division said in its weekly FluView report.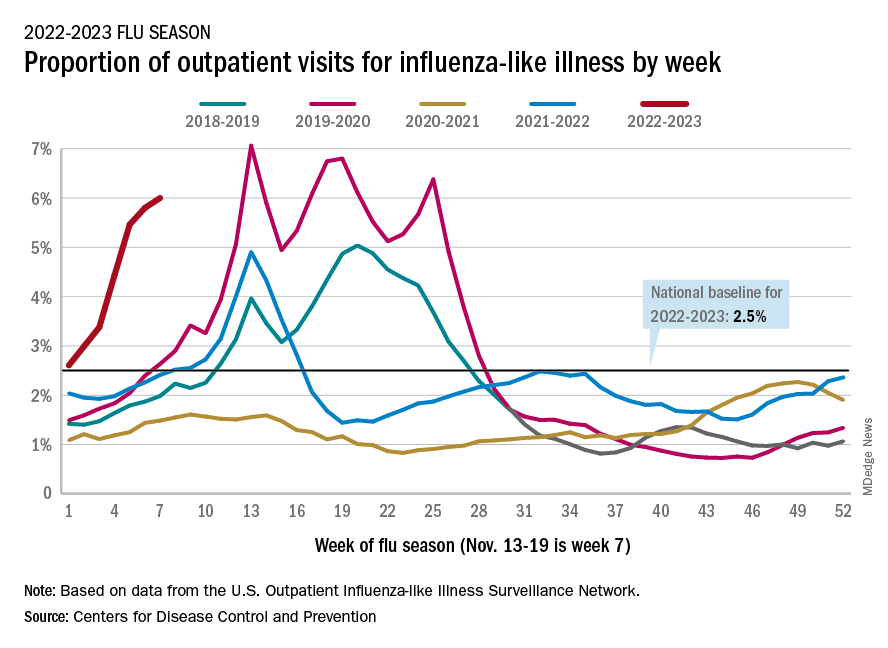
Those figures are the highest recorded in November since 2009, but the peak of the 2009-10 flu season occurred even earlier – the week of Oct. 18-24 – and the rate of flu-like illness had already dropped to just over 4.0% by Nov. 15-21 that year and continued to drop thereafter.
Although COVID-19 and respiratory syncytial virus (RSV) are included in the data from the CDC’s Outpatient Influenza-like Illness Surveillance Network, the agency did note that “seasonal influenza activity is elevated across the country” and estimated that “there have been at least 6.2 million illnesses, 53,000 hospitalizations, and 2,900 deaths from flu” during the 2022-23 season.
Total flu deaths include 11 reported in children as of Nov. 19, and children ages 0-4 had a higher proportion of visits for flu like-illness than other age groups.
The agency also said the cumulative hospitalization rate of 11.3 per 100,000 population “is higher than the rate observed in [the corresponding week of] every previous season since 2010-2011.” Adults 65 years and older have the highest cumulative rate, 25.9 per 100,000, for this year, compared with 20.7 for children 0-4; 11.1 for adults 50-64; 10.3 for children 5-17; and 5.6 for adults 18-49 years old, the CDC said.
A version of this article first appeared on WebMD.com.
according to the Centers of Disease Control and Prevention.
Nationally, 6% of all outpatient visits were because of flu or flu-like illness for the week of Nov. 13-19, up from 5.8% the previous week, the CDC’s Influenza Division said in its weekly FluView report.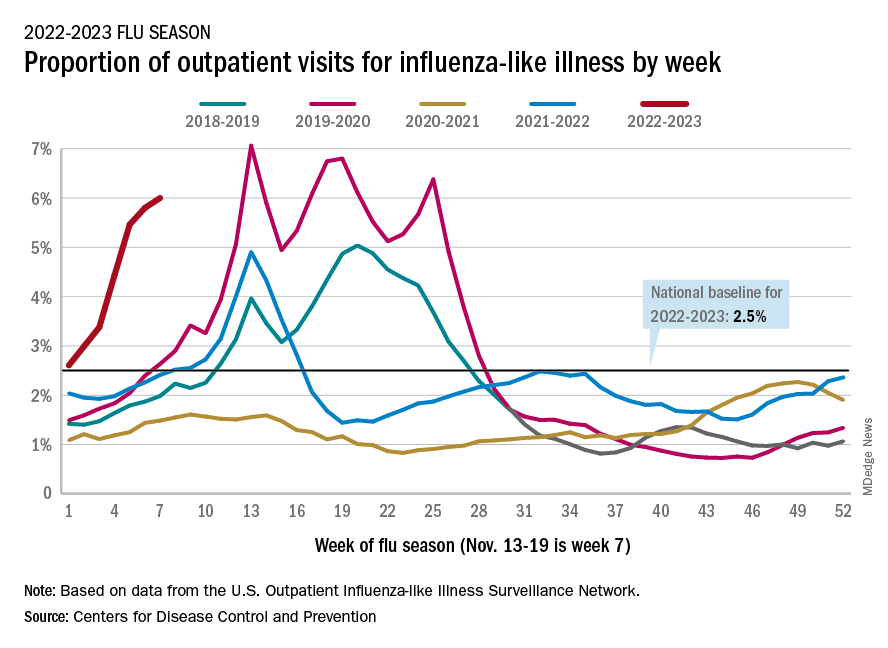
Those figures are the highest recorded in November since 2009, but the peak of the 2009-10 flu season occurred even earlier – the week of Oct. 18-24 – and the rate of flu-like illness had already dropped to just over 4.0% by Nov. 15-21 that year and continued to drop thereafter.
Although COVID-19 and respiratory syncytial virus (RSV) are included in the data from the CDC’s Outpatient Influenza-like Illness Surveillance Network, the agency did note that “seasonal influenza activity is elevated across the country” and estimated that “there have been at least 6.2 million illnesses, 53,000 hospitalizations, and 2,900 deaths from flu” during the 2022-23 season.
Total flu deaths include 11 reported in children as of Nov. 19, and children ages 0-4 had a higher proportion of visits for flu like-illness than other age groups.
The agency also said the cumulative hospitalization rate of 11.3 per 100,000 population “is higher than the rate observed in [the corresponding week of] every previous season since 2010-2011.” Adults 65 years and older have the highest cumulative rate, 25.9 per 100,000, for this year, compared with 20.7 for children 0-4; 11.1 for adults 50-64; 10.3 for children 5-17; and 5.6 for adults 18-49 years old, the CDC said.
A version of this article first appeared on WebMD.com.
according to the Centers of Disease Control and Prevention.
Nationally, 6% of all outpatient visits were because of flu or flu-like illness for the week of Nov. 13-19, up from 5.8% the previous week, the CDC’s Influenza Division said in its weekly FluView report.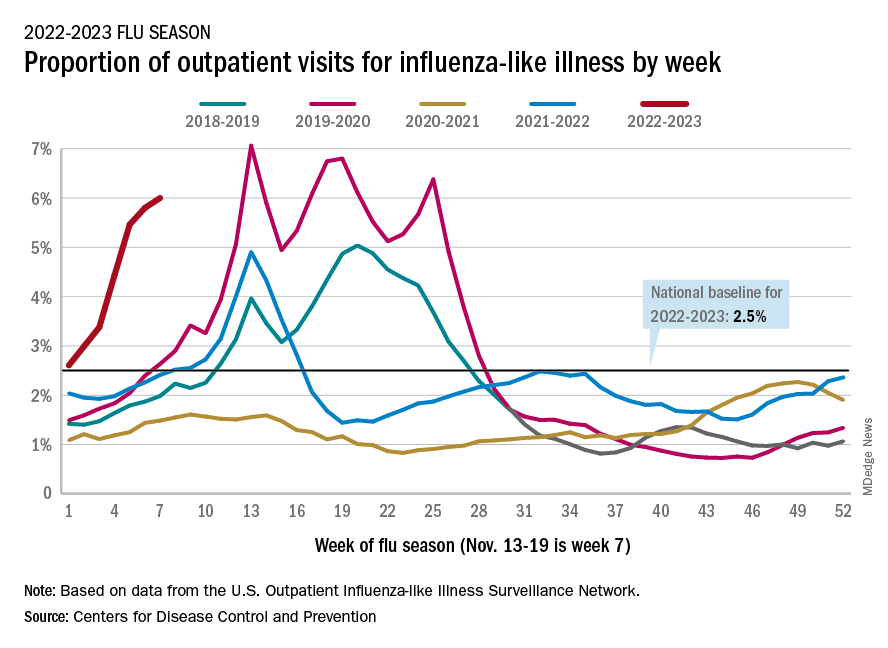
Those figures are the highest recorded in November since 2009, but the peak of the 2009-10 flu season occurred even earlier – the week of Oct. 18-24 – and the rate of flu-like illness had already dropped to just over 4.0% by Nov. 15-21 that year and continued to drop thereafter.
Although COVID-19 and respiratory syncytial virus (RSV) are included in the data from the CDC’s Outpatient Influenza-like Illness Surveillance Network, the agency did note that “seasonal influenza activity is elevated across the country” and estimated that “there have been at least 6.2 million illnesses, 53,000 hospitalizations, and 2,900 deaths from flu” during the 2022-23 season.
Total flu deaths include 11 reported in children as of Nov. 19, and children ages 0-4 had a higher proportion of visits for flu like-illness than other age groups.
The agency also said the cumulative hospitalization rate of 11.3 per 100,000 population “is higher than the rate observed in [the corresponding week of] every previous season since 2010-2011.” Adults 65 years and older have the highest cumulative rate, 25.9 per 100,000, for this year, compared with 20.7 for children 0-4; 11.1 for adults 50-64; 10.3 for children 5-17; and 5.6 for adults 18-49 years old, the CDC said.
A version of this article first appeared on WebMD.com.
Just 8 minutes of exercise a day is all you need
according to a new study in the European Heart Journal.
Just 54 minutes of vigorous exercise per week provides the most bang for your buck, researchers found, lowering the risk of early death from any cause by 36%, and your chances of getting heart disease by 35%.
Scientists examined data from fitness trackers worn by more than 71,000 people studied in the United Kingdom, then analyzed their health over the next several years.
While more time spent exercising unsurprisingly led to better health, the protective effects of exercise start to plateau after a certain point, according to the study.
A tough, short workout improves blood pressure, shrinks artery-clogging plaques, and boosts your overall fitness.
Vigorous exercise helps your body adapt better than moderate exercise does, leading to more notable benefits, says study author Matthew Ahmadi, PhD, a postdoctoral research fellow at the University of Sydney.
“Collectively, these will lower a person’s risk of cardiovascular disease. Exercise can also lower body inflammation, which will in turn lower the risk for certain cancers,” he says.
The CDC recommends at least 150 minutes of “moderate intensity” exercise each week, such as walking at a brisk pace. Or you could spend 75 minutes each week doing vigorous exercise, like running, it says. The CDC also recommends muscle strengthening activities, like lifting weights, at least 2 days per week.
But only 54% of Americans actually manage to get their 150 minutes of aerobic activity in each week, according to the most recent data from the National Center for Health Statistics. Even fewer – just 24% – also squeeze in the two recommended strength workouts.
So 8 minutes a day instead of 30 minutes could persuade busy people to get the exercise they need.
“Lack of time is one of the main reasons people have reported for not engaging in exercise,” says Dr. Ahmadi.
Vigorous exercise doesn’t mean you have to run, bike, or lift weights. Scientists consider a physical activity “vigorous” if it’s greater than 6 times your resting metabolic rate, or MET. That includes all kinds of strenuous movement, including dancing in a nightclub or carrying groceries upstairs.
“All of these activities are equally beneficial,” says Dr. Ahmadi.
He recommends aiming for 2-minute bouts of a heart-pumping activity, spread throughout the day for the most benefit in the least amount of time. If you wear a smartwatch or other device that tracks your heart rate, you’ll be above the threshold if your heart is pumping at 77% or more of your max heart rate (which most fitness trackers help you calculate).
No smartwatch? “The easiest way a person can infer if they are doing vigorous activity is if they are breathing hard enough that it’s difficult to have a conversation or speak in a full sentence while doing the activity,” Dr. Ahmadi says. In other words, if you’re huffing and puffing, then you’re in the zone.
A version of this article first appeared on WebMD.com.
according to a new study in the European Heart Journal.
Just 54 minutes of vigorous exercise per week provides the most bang for your buck, researchers found, lowering the risk of early death from any cause by 36%, and your chances of getting heart disease by 35%.
Scientists examined data from fitness trackers worn by more than 71,000 people studied in the United Kingdom, then analyzed their health over the next several years.
While more time spent exercising unsurprisingly led to better health, the protective effects of exercise start to plateau after a certain point, according to the study.
A tough, short workout improves blood pressure, shrinks artery-clogging plaques, and boosts your overall fitness.
Vigorous exercise helps your body adapt better than moderate exercise does, leading to more notable benefits, says study author Matthew Ahmadi, PhD, a postdoctoral research fellow at the University of Sydney.
“Collectively, these will lower a person’s risk of cardiovascular disease. Exercise can also lower body inflammation, which will in turn lower the risk for certain cancers,” he says.
The CDC recommends at least 150 minutes of “moderate intensity” exercise each week, such as walking at a brisk pace. Or you could spend 75 minutes each week doing vigorous exercise, like running, it says. The CDC also recommends muscle strengthening activities, like lifting weights, at least 2 days per week.
But only 54% of Americans actually manage to get their 150 minutes of aerobic activity in each week, according to the most recent data from the National Center for Health Statistics. Even fewer – just 24% – also squeeze in the two recommended strength workouts.
So 8 minutes a day instead of 30 minutes could persuade busy people to get the exercise they need.
“Lack of time is one of the main reasons people have reported for not engaging in exercise,” says Dr. Ahmadi.
Vigorous exercise doesn’t mean you have to run, bike, or lift weights. Scientists consider a physical activity “vigorous” if it’s greater than 6 times your resting metabolic rate, or MET. That includes all kinds of strenuous movement, including dancing in a nightclub or carrying groceries upstairs.
“All of these activities are equally beneficial,” says Dr. Ahmadi.
He recommends aiming for 2-minute bouts of a heart-pumping activity, spread throughout the day for the most benefit in the least amount of time. If you wear a smartwatch or other device that tracks your heart rate, you’ll be above the threshold if your heart is pumping at 77% or more of your max heart rate (which most fitness trackers help you calculate).
No smartwatch? “The easiest way a person can infer if they are doing vigorous activity is if they are breathing hard enough that it’s difficult to have a conversation or speak in a full sentence while doing the activity,” Dr. Ahmadi says. In other words, if you’re huffing and puffing, then you’re in the zone.
A version of this article first appeared on WebMD.com.
according to a new study in the European Heart Journal.
Just 54 minutes of vigorous exercise per week provides the most bang for your buck, researchers found, lowering the risk of early death from any cause by 36%, and your chances of getting heart disease by 35%.
Scientists examined data from fitness trackers worn by more than 71,000 people studied in the United Kingdom, then analyzed their health over the next several years.
While more time spent exercising unsurprisingly led to better health, the protective effects of exercise start to plateau after a certain point, according to the study.
A tough, short workout improves blood pressure, shrinks artery-clogging plaques, and boosts your overall fitness.
Vigorous exercise helps your body adapt better than moderate exercise does, leading to more notable benefits, says study author Matthew Ahmadi, PhD, a postdoctoral research fellow at the University of Sydney.
“Collectively, these will lower a person’s risk of cardiovascular disease. Exercise can also lower body inflammation, which will in turn lower the risk for certain cancers,” he says.
The CDC recommends at least 150 minutes of “moderate intensity” exercise each week, such as walking at a brisk pace. Or you could spend 75 minutes each week doing vigorous exercise, like running, it says. The CDC also recommends muscle strengthening activities, like lifting weights, at least 2 days per week.
But only 54% of Americans actually manage to get their 150 minutes of aerobic activity in each week, according to the most recent data from the National Center for Health Statistics. Even fewer – just 24% – also squeeze in the two recommended strength workouts.
So 8 minutes a day instead of 30 minutes could persuade busy people to get the exercise they need.
“Lack of time is one of the main reasons people have reported for not engaging in exercise,” says Dr. Ahmadi.
Vigorous exercise doesn’t mean you have to run, bike, or lift weights. Scientists consider a physical activity “vigorous” if it’s greater than 6 times your resting metabolic rate, or MET. That includes all kinds of strenuous movement, including dancing in a nightclub or carrying groceries upstairs.
“All of these activities are equally beneficial,” says Dr. Ahmadi.
He recommends aiming for 2-minute bouts of a heart-pumping activity, spread throughout the day for the most benefit in the least amount of time. If you wear a smartwatch or other device that tracks your heart rate, you’ll be above the threshold if your heart is pumping at 77% or more of your max heart rate (which most fitness trackers help you calculate).
No smartwatch? “The easiest way a person can infer if they are doing vigorous activity is if they are breathing hard enough that it’s difficult to have a conversation or speak in a full sentence while doing the activity,” Dr. Ahmadi says. In other words, if you’re huffing and puffing, then you’re in the zone.
A version of this article first appeared on WebMD.com.
FROM EUROPEAN HEART JOURNAL
More vaccinated people dying of COVID as fewer get booster shots
“We can no longer say this is a pandemic of the unvaccinated,” Kaiser Family Foundation Vice President Cynthia Cox, who conducted the analysis, told The Washington Post.
People who had been vaccinated or boosted made up 58% of COVID-19 deaths in August, the analysis showed. The rate has been on the rise: 23% of coronavirus deaths were among vaccinated people in September 2021, and the vaccinated made up 42% of deaths in January and February 2022, the Post reported.
Research continues to show that people who are vaccinated or boosted have a lower risk of death. The rise in deaths among the vaccinated is the result of three factors, Ms. Cox said.
- A large majority of people in the United States have been vaccinated (267 million people, the said).
- People who are at the greatest risk of dying from COVID-19 are more likely to be vaccinated and boosted, such as the elderly.
- Vaccines lose their effectiveness over time; the virus changes to avoid vaccines; and people need to choose to get boosters to continue to be protected.
The case for the effectiveness of vaccines and boosters versus skipping the shots remains strong. People age 6 months and older who are unvaccinated are six times more likely to die of COVID-19, compared to those who got the primary series of shots, the Post reported. Survival rates were even better with additional booster shots, particularly among older people.
“I feel very confident that if people continue to get vaccinated at good numbers, if people get boosted, we can absolutely have a very safe and healthy holiday season,” Ashish Jha, White House coronavirus czar, said on Nov. 22.
The number of Americans who have gotten the most recent booster has been increasing ahead of the holidays. CDC data show that 12% of the U.S. population age 5 and older has received a booster.
A new study by a team of researchers from Harvard University and Yale University estimates that 94% of the U.S. population has been infected with COVID-19 at least once, leaving just 1 in 20 people who have never had the virus.
“Despite these high exposure numbers, there is still substantial population susceptibility to infection with an Omicron variant,” the authors wrote.
They said that if all states achieved the vaccination levels of Vermont, where 55% of people had at least one booster and 22% got a second one, there would be “an appreciable improvement in population immunity, with greater relative impact for protection against infection versus severe disease. This additional protection results from both the recovery of immunity lost due to waning and the increased effectiveness of the bivalent booster against Omicron infections.”
A version of this article first appeared on WebMD.com.
“We can no longer say this is a pandemic of the unvaccinated,” Kaiser Family Foundation Vice President Cynthia Cox, who conducted the analysis, told The Washington Post.
People who had been vaccinated or boosted made up 58% of COVID-19 deaths in August, the analysis showed. The rate has been on the rise: 23% of coronavirus deaths were among vaccinated people in September 2021, and the vaccinated made up 42% of deaths in January and February 2022, the Post reported.
Research continues to show that people who are vaccinated or boosted have a lower risk of death. The rise in deaths among the vaccinated is the result of three factors, Ms. Cox said.
- A large majority of people in the United States have been vaccinated (267 million people, the said).
- People who are at the greatest risk of dying from COVID-19 are more likely to be vaccinated and boosted, such as the elderly.
- Vaccines lose their effectiveness over time; the virus changes to avoid vaccines; and people need to choose to get boosters to continue to be protected.
The case for the effectiveness of vaccines and boosters versus skipping the shots remains strong. People age 6 months and older who are unvaccinated are six times more likely to die of COVID-19, compared to those who got the primary series of shots, the Post reported. Survival rates were even better with additional booster shots, particularly among older people.
“I feel very confident that if people continue to get vaccinated at good numbers, if people get boosted, we can absolutely have a very safe and healthy holiday season,” Ashish Jha, White House coronavirus czar, said on Nov. 22.
The number of Americans who have gotten the most recent booster has been increasing ahead of the holidays. CDC data show that 12% of the U.S. population age 5 and older has received a booster.
A new study by a team of researchers from Harvard University and Yale University estimates that 94% of the U.S. population has been infected with COVID-19 at least once, leaving just 1 in 20 people who have never had the virus.
“Despite these high exposure numbers, there is still substantial population susceptibility to infection with an Omicron variant,” the authors wrote.
They said that if all states achieved the vaccination levels of Vermont, where 55% of people had at least one booster and 22% got a second one, there would be “an appreciable improvement in population immunity, with greater relative impact for protection against infection versus severe disease. This additional protection results from both the recovery of immunity lost due to waning and the increased effectiveness of the bivalent booster against Omicron infections.”
A version of this article first appeared on WebMD.com.
“We can no longer say this is a pandemic of the unvaccinated,” Kaiser Family Foundation Vice President Cynthia Cox, who conducted the analysis, told The Washington Post.
People who had been vaccinated or boosted made up 58% of COVID-19 deaths in August, the analysis showed. The rate has been on the rise: 23% of coronavirus deaths were among vaccinated people in September 2021, and the vaccinated made up 42% of deaths in January and February 2022, the Post reported.
Research continues to show that people who are vaccinated or boosted have a lower risk of death. The rise in deaths among the vaccinated is the result of three factors, Ms. Cox said.
- A large majority of people in the United States have been vaccinated (267 million people, the said).
- People who are at the greatest risk of dying from COVID-19 are more likely to be vaccinated and boosted, such as the elderly.
- Vaccines lose their effectiveness over time; the virus changes to avoid vaccines; and people need to choose to get boosters to continue to be protected.
The case for the effectiveness of vaccines and boosters versus skipping the shots remains strong. People age 6 months and older who are unvaccinated are six times more likely to die of COVID-19, compared to those who got the primary series of shots, the Post reported. Survival rates were even better with additional booster shots, particularly among older people.
“I feel very confident that if people continue to get vaccinated at good numbers, if people get boosted, we can absolutely have a very safe and healthy holiday season,” Ashish Jha, White House coronavirus czar, said on Nov. 22.
The number of Americans who have gotten the most recent booster has been increasing ahead of the holidays. CDC data show that 12% of the U.S. population age 5 and older has received a booster.
A new study by a team of researchers from Harvard University and Yale University estimates that 94% of the U.S. population has been infected with COVID-19 at least once, leaving just 1 in 20 people who have never had the virus.
“Despite these high exposure numbers, there is still substantial population susceptibility to infection with an Omicron variant,” the authors wrote.
They said that if all states achieved the vaccination levels of Vermont, where 55% of people had at least one booster and 22% got a second one, there would be “an appreciable improvement in population immunity, with greater relative impact for protection against infection versus severe disease. This additional protection results from both the recovery of immunity lost due to waning and the increased effectiveness of the bivalent booster against Omicron infections.”
A version of this article first appeared on WebMD.com.
Don’t call me ‘Dr.,’ say some physicians – but most prefer the title
When Mark Cucuzzella, MD, meets a new patient at the West Virginia Medical School clinic, he introduces himself as “Mark.” For one thing, says Dr. Cucuzzella, his last name is a mouthful. For another, the 56-year-old general practitioner asserts that getting on a first-name basis with his patients is integral to delivering the best care.
“I’m trying to break down the old paternalistic barriers of the doctor/patient relationship,” he says. “Titles create an environment where the doctors are making all the decisions and not involving the patient in any course of action.”
Aniruddh Setya, MD, has a different take on informality between patients and doctors: It’s not OK. “I am not your friend,” says the 35-year-old pediatrician from Florida-based KIDZ Medical Services. “There has to be a level of respect for the education and accomplishment of being a physician.”
published in JAMA Network Open. But that doesn’t mean most physicians support the practice. In fact, some doctors contend that it can be harmful, particularly to female physicians.
“My concern is that untitling (so termed by Amy Diehl, PhD, and Leanne Dzubinski, PhD) intrudes upon important professional boundaries and might be correlated with diminishing the value of someone’s time,” says Leah Witt, MD, a geriatrician at UCSF Health, San Francisco. Dr. Witt, along with colleague Lekshmi Santhosh, MD, a pulmonologist, offered commentary on the study results. “Studies have shown that women physicians get more patient portal messages, spend more time in the electronic health record, and have longer visits,” Dr. Witt said. “Dr. Santhosh and I wonder if untitling is a signifier of this diminished value of our time, and an assumption of increased ease of access leading to this higher workload.”
To compile the results reported in JAMA Network Open, Mayo Clinic researchers analyzed more than 90,000 emails from patients to doctors over the course of 3 years, beginning in 2018. Of those emails, more than 32% included the physician’s first name in greeting or salutation. For women physicians, the odds were twice as high that their titles would be omitted in the correspondence. The same holds true for doctors of osteopathic medicine (DOs) compared with MDs, and primary care physicians had similar odds for a title drop compared with specialists.
Dr. Witt says the findings are not surprising. “They match my experience as a woman in medicine, as Dr. Santhosh and I write in our commentary,” she says. “We think the findings could easily be replicated at other centers.”
Indeed, research on 321 speaker introductions at a medical rounds found that when female physicians introduced other physicians, they usually applied the doctor title. When the job of introducing colleagues fell to male physicians, however, the stats fell to 72.4% for male peers and only 49.2% when introducing female peers.
The Mayo Clinic study authors identified the pitfalls of patients who informally address their doctors. They wrote, “Untitling may have a negative impact on physicians, demonstrate lack of respect, and can lead to reduction in formality of the physician/patient relationship or workplace.”
Physician preferences vary
Although the results of the Mayo Clinic analysis didn’t and couldn’t address physician sentiments on patient informality, Dr. Setya observes that American culture is becoming less formal. “I’ve been practicing for over 10 years, and the number of people who consider doctors as equals is growing,” he says. “This has been particularly true over the last couple of years.”
This change was documented in 2015. Add in the pandemic and an entire society that is now accustomed to working from home in sweats, and it’s not a stretch to understand why some patients have become less formal in many settings. The 2015 article noted, however, that most physicians prefer to keep titles in the mix.
Perhaps most troublesome, says Dr. Setya, is that patients forgo asking whether it’s OK to use his first name and simply assume it’s acceptable. “It bothers me,” he says. “I became a doctor for more than the money.”
He suspects that his cultural background (Dr. Setya is of Indian descent) plays a role in how strongly he feels about patient-doctor informality. “As a British colony, Indian culture dictates that you pay respect to elders and to accomplishment,” he points out. “America is far looser when it comes to salutations.”
Dr. Cucuzzella largely agrees with Dr. Setya, but has a different view of the role culture plays in how physicians prefer to be addressed. “If your last name is difficult to pronounce, it can put the patient at ease if you give them an option,” he says. “I like my patients to feel comfortable and have a friendly conversation, so I don’t ask them to try to manage my last name.”
When patients revert to using Dr. Cucuzzella’s last name and title, this often breaks down along generational lines, Dr. Cucuzzella has found: Older patients might drop his title, whereas younger patients might keep it as a sign of respect. In some cases, Dr. Cucuzzella tries to bridge this gap, and offers the option of “Dr. Mark.” In his small West Virginia community, this is how people often refer to him.
Dr. Setya says that most of the older physicians he works with still prefer that patients and younger colleagues use their title, but he has witnessed exceptions to this. “My boss in residence hated to be called ‘Sir’ or ‘Doctor,’ ” he says. “In a situation like that, it is reasonable to ask, ‘How can I address you?’ But it has to be mutually agreed upon.”
Dr. Cucuzzella cites informality as the preferred mode for older patients. “If I have a 70-year-old patient, it seems natural they shouldn’t use my title,” he says. “They are worthy of equality in the community. If I’m talking to a retired CEO or state delegate, it’s uncomfortable if they call me doctor.”
Moreover, Dr. Cucuzzella maintains that establishing a less formal environment with patients leads to better outcomes. “Shared decision-making is a basic human right,” he says. “In 2022, doctors shouldn’t make decisions without patient input, unless it’s an emergency situation. Removing the title barriers makes that easier.”
How to handle informality
If you fall more in line with Dr. Setya, there are strategies you can use to try to keep formality in your doctor-patient relationships. Dr. Setya’s approach is indirect. “I don’t correct a patient if they use my first name, because that might seem hostile,” he says. “But I alert them in the way I address them back. A Sir, a Mrs., or a Mr. needs to go both ways.”
This particularly holds true in pediatrics, Dr. Setya has found. He has witnessed many colleagues addressing parents as “Mommy and Daddy,” something he says lacks respect and sets too informal a tone. “It’s almost universal that parents don’t like that, and we need to act accordingly.”
Dr. Witt also avoids directly correcting patients, but struggles when they drop her title. “The standard signature I use to sign every patient portal message I respond to includes my first and last name and credentials,” she says. “I maintain formality in most circumstances with that standard reply.”
Beneath the surface, however, Dr. Witt wishes it were easier. “I have struggled with answering the question, ‘Is it OK if I call you Leah?’ she says. “I want to keep our interaction anchored in professionalism without sacrificing the warmth I think is important to a productive patient-physician relationship. For this reason, I tend to say yes to this request, even though I’d rather patients didn’t make such requests.”
In the Fast Company article by Amy Diehl, PhD, and Leanne Dzubinski, PhD, on the topic of untitling professional women, the authors suggest several actions, beginning with leadership that sets expectations on the topic. They also suggest that physicians use polite corrections if patients untitle them. Supplying positive reinforcement when patients include your title can help, too. If all else fails, you can call out the offensive untitling. More often than not, especially with female physicians, the patient is demonstrating an unconscious bias rather than something deliberate.
Opinions vary on the topic of untitling, and ultimately each physician must make the decision for themselves. But creating informal cultures in an organization can have unintended consequences, especially for female peers.
Says Dr. Witt, “We all want to give our patients the best care we can, but professional boundaries are critical to time management, equitable care, and maintaining work-life balance. I would love to see a study that examines untitling by self-reported race and/or ethnicity of physicians, because we know that women of color experience higher rates of burnout and depression, and I wonder if untitling may be part of this.”
A version of this article first appeared on Medscape.com.
When Mark Cucuzzella, MD, meets a new patient at the West Virginia Medical School clinic, he introduces himself as “Mark.” For one thing, says Dr. Cucuzzella, his last name is a mouthful. For another, the 56-year-old general practitioner asserts that getting on a first-name basis with his patients is integral to delivering the best care.
“I’m trying to break down the old paternalistic barriers of the doctor/patient relationship,” he says. “Titles create an environment where the doctors are making all the decisions and not involving the patient in any course of action.”
Aniruddh Setya, MD, has a different take on informality between patients and doctors: It’s not OK. “I am not your friend,” says the 35-year-old pediatrician from Florida-based KIDZ Medical Services. “There has to be a level of respect for the education and accomplishment of being a physician.”
published in JAMA Network Open. But that doesn’t mean most physicians support the practice. In fact, some doctors contend that it can be harmful, particularly to female physicians.
“My concern is that untitling (so termed by Amy Diehl, PhD, and Leanne Dzubinski, PhD) intrudes upon important professional boundaries and might be correlated with diminishing the value of someone’s time,” says Leah Witt, MD, a geriatrician at UCSF Health, San Francisco. Dr. Witt, along with colleague Lekshmi Santhosh, MD, a pulmonologist, offered commentary on the study results. “Studies have shown that women physicians get more patient portal messages, spend more time in the electronic health record, and have longer visits,” Dr. Witt said. “Dr. Santhosh and I wonder if untitling is a signifier of this diminished value of our time, and an assumption of increased ease of access leading to this higher workload.”
To compile the results reported in JAMA Network Open, Mayo Clinic researchers analyzed more than 90,000 emails from patients to doctors over the course of 3 years, beginning in 2018. Of those emails, more than 32% included the physician’s first name in greeting or salutation. For women physicians, the odds were twice as high that their titles would be omitted in the correspondence. The same holds true for doctors of osteopathic medicine (DOs) compared with MDs, and primary care physicians had similar odds for a title drop compared with specialists.
Dr. Witt says the findings are not surprising. “They match my experience as a woman in medicine, as Dr. Santhosh and I write in our commentary,” she says. “We think the findings could easily be replicated at other centers.”
Indeed, research on 321 speaker introductions at a medical rounds found that when female physicians introduced other physicians, they usually applied the doctor title. When the job of introducing colleagues fell to male physicians, however, the stats fell to 72.4% for male peers and only 49.2% when introducing female peers.
The Mayo Clinic study authors identified the pitfalls of patients who informally address their doctors. They wrote, “Untitling may have a negative impact on physicians, demonstrate lack of respect, and can lead to reduction in formality of the physician/patient relationship or workplace.”
Physician preferences vary
Although the results of the Mayo Clinic analysis didn’t and couldn’t address physician sentiments on patient informality, Dr. Setya observes that American culture is becoming less formal. “I’ve been practicing for over 10 years, and the number of people who consider doctors as equals is growing,” he says. “This has been particularly true over the last couple of years.”
This change was documented in 2015. Add in the pandemic and an entire society that is now accustomed to working from home in sweats, and it’s not a stretch to understand why some patients have become less formal in many settings. The 2015 article noted, however, that most physicians prefer to keep titles in the mix.
Perhaps most troublesome, says Dr. Setya, is that patients forgo asking whether it’s OK to use his first name and simply assume it’s acceptable. “It bothers me,” he says. “I became a doctor for more than the money.”
He suspects that his cultural background (Dr. Setya is of Indian descent) plays a role in how strongly he feels about patient-doctor informality. “As a British colony, Indian culture dictates that you pay respect to elders and to accomplishment,” he points out. “America is far looser when it comes to salutations.”
Dr. Cucuzzella largely agrees with Dr. Setya, but has a different view of the role culture plays in how physicians prefer to be addressed. “If your last name is difficult to pronounce, it can put the patient at ease if you give them an option,” he says. “I like my patients to feel comfortable and have a friendly conversation, so I don’t ask them to try to manage my last name.”
When patients revert to using Dr. Cucuzzella’s last name and title, this often breaks down along generational lines, Dr. Cucuzzella has found: Older patients might drop his title, whereas younger patients might keep it as a sign of respect. In some cases, Dr. Cucuzzella tries to bridge this gap, and offers the option of “Dr. Mark.” In his small West Virginia community, this is how people often refer to him.
Dr. Setya says that most of the older physicians he works with still prefer that patients and younger colleagues use their title, but he has witnessed exceptions to this. “My boss in residence hated to be called ‘Sir’ or ‘Doctor,’ ” he says. “In a situation like that, it is reasonable to ask, ‘How can I address you?’ But it has to be mutually agreed upon.”
Dr. Cucuzzella cites informality as the preferred mode for older patients. “If I have a 70-year-old patient, it seems natural they shouldn’t use my title,” he says. “They are worthy of equality in the community. If I’m talking to a retired CEO or state delegate, it’s uncomfortable if they call me doctor.”
Moreover, Dr. Cucuzzella maintains that establishing a less formal environment with patients leads to better outcomes. “Shared decision-making is a basic human right,” he says. “In 2022, doctors shouldn’t make decisions without patient input, unless it’s an emergency situation. Removing the title barriers makes that easier.”
How to handle informality
If you fall more in line with Dr. Setya, there are strategies you can use to try to keep formality in your doctor-patient relationships. Dr. Setya’s approach is indirect. “I don’t correct a patient if they use my first name, because that might seem hostile,” he says. “But I alert them in the way I address them back. A Sir, a Mrs., or a Mr. needs to go both ways.”
This particularly holds true in pediatrics, Dr. Setya has found. He has witnessed many colleagues addressing parents as “Mommy and Daddy,” something he says lacks respect and sets too informal a tone. “It’s almost universal that parents don’t like that, and we need to act accordingly.”
Dr. Witt also avoids directly correcting patients, but struggles when they drop her title. “The standard signature I use to sign every patient portal message I respond to includes my first and last name and credentials,” she says. “I maintain formality in most circumstances with that standard reply.”
Beneath the surface, however, Dr. Witt wishes it were easier. “I have struggled with answering the question, ‘Is it OK if I call you Leah?’ she says. “I want to keep our interaction anchored in professionalism without sacrificing the warmth I think is important to a productive patient-physician relationship. For this reason, I tend to say yes to this request, even though I’d rather patients didn’t make such requests.”
In the Fast Company article by Amy Diehl, PhD, and Leanne Dzubinski, PhD, on the topic of untitling professional women, the authors suggest several actions, beginning with leadership that sets expectations on the topic. They also suggest that physicians use polite corrections if patients untitle them. Supplying positive reinforcement when patients include your title can help, too. If all else fails, you can call out the offensive untitling. More often than not, especially with female physicians, the patient is demonstrating an unconscious bias rather than something deliberate.
Opinions vary on the topic of untitling, and ultimately each physician must make the decision for themselves. But creating informal cultures in an organization can have unintended consequences, especially for female peers.
Says Dr. Witt, “We all want to give our patients the best care we can, but professional boundaries are critical to time management, equitable care, and maintaining work-life balance. I would love to see a study that examines untitling by self-reported race and/or ethnicity of physicians, because we know that women of color experience higher rates of burnout and depression, and I wonder if untitling may be part of this.”
A version of this article first appeared on Medscape.com.
When Mark Cucuzzella, MD, meets a new patient at the West Virginia Medical School clinic, he introduces himself as “Mark.” For one thing, says Dr. Cucuzzella, his last name is a mouthful. For another, the 56-year-old general practitioner asserts that getting on a first-name basis with his patients is integral to delivering the best care.
“I’m trying to break down the old paternalistic barriers of the doctor/patient relationship,” he says. “Titles create an environment where the doctors are making all the decisions and not involving the patient in any course of action.”
Aniruddh Setya, MD, has a different take on informality between patients and doctors: It’s not OK. “I am not your friend,” says the 35-year-old pediatrician from Florida-based KIDZ Medical Services. “There has to be a level of respect for the education and accomplishment of being a physician.”
published in JAMA Network Open. But that doesn’t mean most physicians support the practice. In fact, some doctors contend that it can be harmful, particularly to female physicians.
“My concern is that untitling (so termed by Amy Diehl, PhD, and Leanne Dzubinski, PhD) intrudes upon important professional boundaries and might be correlated with diminishing the value of someone’s time,” says Leah Witt, MD, a geriatrician at UCSF Health, San Francisco. Dr. Witt, along with colleague Lekshmi Santhosh, MD, a pulmonologist, offered commentary on the study results. “Studies have shown that women physicians get more patient portal messages, spend more time in the electronic health record, and have longer visits,” Dr. Witt said. “Dr. Santhosh and I wonder if untitling is a signifier of this diminished value of our time, and an assumption of increased ease of access leading to this higher workload.”
To compile the results reported in JAMA Network Open, Mayo Clinic researchers analyzed more than 90,000 emails from patients to doctors over the course of 3 years, beginning in 2018. Of those emails, more than 32% included the physician’s first name in greeting or salutation. For women physicians, the odds were twice as high that their titles would be omitted in the correspondence. The same holds true for doctors of osteopathic medicine (DOs) compared with MDs, and primary care physicians had similar odds for a title drop compared with specialists.
Dr. Witt says the findings are not surprising. “They match my experience as a woman in medicine, as Dr. Santhosh and I write in our commentary,” she says. “We think the findings could easily be replicated at other centers.”
Indeed, research on 321 speaker introductions at a medical rounds found that when female physicians introduced other physicians, they usually applied the doctor title. When the job of introducing colleagues fell to male physicians, however, the stats fell to 72.4% for male peers and only 49.2% when introducing female peers.
The Mayo Clinic study authors identified the pitfalls of patients who informally address their doctors. They wrote, “Untitling may have a negative impact on physicians, demonstrate lack of respect, and can lead to reduction in formality of the physician/patient relationship or workplace.”
Physician preferences vary
Although the results of the Mayo Clinic analysis didn’t and couldn’t address physician sentiments on patient informality, Dr. Setya observes that American culture is becoming less formal. “I’ve been practicing for over 10 years, and the number of people who consider doctors as equals is growing,” he says. “This has been particularly true over the last couple of years.”
This change was documented in 2015. Add in the pandemic and an entire society that is now accustomed to working from home in sweats, and it’s not a stretch to understand why some patients have become less formal in many settings. The 2015 article noted, however, that most physicians prefer to keep titles in the mix.
Perhaps most troublesome, says Dr. Setya, is that patients forgo asking whether it’s OK to use his first name and simply assume it’s acceptable. “It bothers me,” he says. “I became a doctor for more than the money.”
He suspects that his cultural background (Dr. Setya is of Indian descent) plays a role in how strongly he feels about patient-doctor informality. “As a British colony, Indian culture dictates that you pay respect to elders and to accomplishment,” he points out. “America is far looser when it comes to salutations.”
Dr. Cucuzzella largely agrees with Dr. Setya, but has a different view of the role culture plays in how physicians prefer to be addressed. “If your last name is difficult to pronounce, it can put the patient at ease if you give them an option,” he says. “I like my patients to feel comfortable and have a friendly conversation, so I don’t ask them to try to manage my last name.”
When patients revert to using Dr. Cucuzzella’s last name and title, this often breaks down along generational lines, Dr. Cucuzzella has found: Older patients might drop his title, whereas younger patients might keep it as a sign of respect. In some cases, Dr. Cucuzzella tries to bridge this gap, and offers the option of “Dr. Mark.” In his small West Virginia community, this is how people often refer to him.
Dr. Setya says that most of the older physicians he works with still prefer that patients and younger colleagues use their title, but he has witnessed exceptions to this. “My boss in residence hated to be called ‘Sir’ or ‘Doctor,’ ” he says. “In a situation like that, it is reasonable to ask, ‘How can I address you?’ But it has to be mutually agreed upon.”
Dr. Cucuzzella cites informality as the preferred mode for older patients. “If I have a 70-year-old patient, it seems natural they shouldn’t use my title,” he says. “They are worthy of equality in the community. If I’m talking to a retired CEO or state delegate, it’s uncomfortable if they call me doctor.”
Moreover, Dr. Cucuzzella maintains that establishing a less formal environment with patients leads to better outcomes. “Shared decision-making is a basic human right,” he says. “In 2022, doctors shouldn’t make decisions without patient input, unless it’s an emergency situation. Removing the title barriers makes that easier.”
How to handle informality
If you fall more in line with Dr. Setya, there are strategies you can use to try to keep formality in your doctor-patient relationships. Dr. Setya’s approach is indirect. “I don’t correct a patient if they use my first name, because that might seem hostile,” he says. “But I alert them in the way I address them back. A Sir, a Mrs., or a Mr. needs to go both ways.”
This particularly holds true in pediatrics, Dr. Setya has found. He has witnessed many colleagues addressing parents as “Mommy and Daddy,” something he says lacks respect and sets too informal a tone. “It’s almost universal that parents don’t like that, and we need to act accordingly.”
Dr. Witt also avoids directly correcting patients, but struggles when they drop her title. “The standard signature I use to sign every patient portal message I respond to includes my first and last name and credentials,” she says. “I maintain formality in most circumstances with that standard reply.”
Beneath the surface, however, Dr. Witt wishes it were easier. “I have struggled with answering the question, ‘Is it OK if I call you Leah?’ she says. “I want to keep our interaction anchored in professionalism without sacrificing the warmth I think is important to a productive patient-physician relationship. For this reason, I tend to say yes to this request, even though I’d rather patients didn’t make such requests.”
In the Fast Company article by Amy Diehl, PhD, and Leanne Dzubinski, PhD, on the topic of untitling professional women, the authors suggest several actions, beginning with leadership that sets expectations on the topic. They also suggest that physicians use polite corrections if patients untitle them. Supplying positive reinforcement when patients include your title can help, too. If all else fails, you can call out the offensive untitling. More often than not, especially with female physicians, the patient is demonstrating an unconscious bias rather than something deliberate.
Opinions vary on the topic of untitling, and ultimately each physician must make the decision for themselves. But creating informal cultures in an organization can have unintended consequences, especially for female peers.
Says Dr. Witt, “We all want to give our patients the best care we can, but professional boundaries are critical to time management, equitable care, and maintaining work-life balance. I would love to see a study that examines untitling by self-reported race and/or ethnicity of physicians, because we know that women of color experience higher rates of burnout and depression, and I wonder if untitling may be part of this.”
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Study supports banning probiotics from the ICU
NASHVILLE, TENN. – Supported by several cases series, according to new findings presented at the annual meeting of the American College of Chest Physicians (CHEST).
According to data presented by Scott Mayer, MD, chief resident at HealthONE Denver, which is part of the HCA Healthcare chain of hospitals, the risk is increased by any probiotic exposure. However, the risk is particularly acute for powdered formulations, presumably because powder more easily disseminates to contaminate central venous catheters.
“We think that probiotics should be eliminated entirely from the ICU. If not, we encourage eliminating the powder formulations,” said Dr. Mayer, who led the study.
The data linking probiotics to ICU bacteremia were drawn from 23,533 ICU admissions over a 5-year period in the HCA hospital database. Bacteremia proven to be probiotic-related was uncommon (0.37%), but the consequences were serious.
For those with probiotic-related bacteremia, the mortality rate was 25.6% or essentially twofold greater than the 13.5% mortality rate among those without probiotic bacteremia. An odds ratio drawn from a regression analysis confirmed a significant difference (OR, 2.23; 95% confidence interval, 1.30-3.71; P < .01).
“The absolute risk of mortality is modest but not insignificant,” said Dr. Mayer. This suggests one probiotic-related mortality for about every 200 patients taking a probiotic in the ICU.
These deaths occur without any clear compensatory benefit from taking probiotics, according to Dr. Mayer. There is a long list of potential benefits from probiotics that might be relevant to patients in the ICU, particularly prophylaxis for Clostridioides difficile infection, but also including a variety of gastrointestinal disorders, such as irritable bowel syndrome; however, none of these are firmly established in general, and particularly for patients in the ICU.
“The American College of Gastroenterology currently recommends against probiotics for the prevention of C. diff.,” Dr. Mayer said. Although the American Gastroenterological Association has issued a “conditional recommendation” for prevention of C. diff. infection with probiotics, Dr. Mayer pointed out this is qualified by a “low quality of evidence” and it is not specific to the ICU setting.
“The evidence for benefit is weak or nonexistent, but the risks are real,” Dr. Mayer said.
To confirm that probiotic-associated ICU bacteremias in the HCA hospital database were, in fact, related to probiotics being taken by patients at time of admission, Dr. Mayer evaluated the record of each of the 86 patients with probiotic bacteremia–associated mortality.
“I identified the organism that grew from the blood cultures to confirm that it was contained in the probiotic the patient was taking,” explained Dr. Mayer, who said this information was available in the electronic medical records.
The risk of probiotic-associated bacteremia in ICU patients was consistent with a series of case series that prompted the study. Dr. Mayer explained that he became interested when he encountered patients on his ICU rounds who were taking probiotics. He knew very little about these agents and explored the medical literature to see what evidence was available.
“I found several case reports of ICU patients with probiotic-associated infections, several of which were suspected of being associated with contamination of the central lines,” Dr. Mayer said. In one case, the patient was not taking a probiotic, but a patient in an adjacent bed was receiving a powdered probiotic that was implicated. This prompted suspicion that the cause was central-line contamination.
This was evaluated in the HCA ICU database and also found to be a significant risk. Among the 67 patients in whom a capsule or tablet was used, the rate of probiotic-associated bacteremia was 0.33%. For those in which the probiotic was a powdered formulation, the rate was 0.76%, a significant difference (P < .01).
Dr. Mayer acknowledged that these data do not rule out all potential benefits from probiotics in the ICU. He believes an obstacle to proving benefit has been the heterogeneity of available products, which are likely to be relevant to any therapeutic role, including prevention of C. diff. infection.
“There are now a large number of products available, and they contain a large variety of strains of organisms, so this has been a difficult area to study,” he said. However, he maintains it is prudent at this point to avoid probiotics in the ICU because the risks are not confined to the patient making this choice.
“My concern is not just the lack of evidence of benefit relative to the risk for the patient but the potential for probiotics in the ICU to place other patients at risk,” Dr. Mayer said.
Others have also noted the potential benefits of probiotics in the ICU, but the promise remains elusive. In a 2018 review article published in the Journal of Emergency and Critical Care Medicine, the authors evaluated a series of potential applications of probiotics in critically ill patients. These included treatment of ventilator-associated pneumonia (VAP), catheter-associated urinary tract infections (CAUTI), and surgical-site infections (SSI). For each, the data were negative or inconclusive.
Over the 4 years that have passed since the review was published, several trials have further explored the potential benefits of probiotics in the ICU but none have changed this basic conclusion. For example, a 2021 multinational trial, published in The Lancet, randomized more than 2,600 patients to probiotics or placebo and showed no effect on VAP incidence (21.9% vs. 21.3%).
The lead author of the 2018 review, Heather A. Vitko, PhD, an associate professor in the department of acute and tertiary care, University of Pittsburgh School of Nursing, also emphasized that the potential for benefit cannot be considered without the potential for risk. She, like Dr. Mayer, cited the case studies implicating probiotics in systemic infections.
For administration, probiotic capsules or sachets “often need to be opened for administration through a feeding tube,” she noted. The risk of contamination comes from both the air and contaminated hands, the latter of which “can cause a translocation to a central line catheter where the microbes have direct entry into the systemic circulation.”
She did not call for a ban of probiotics in the ICU, but she did recommend “a precautionary approach,” encouraging clinicians to “distinguish between reality [of what has been proven] and what is presented in the marketing of antibiotics.”
Dr. Mayer and Dr. Vitko have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NASHVILLE, TENN. – Supported by several cases series, according to new findings presented at the annual meeting of the American College of Chest Physicians (CHEST).
According to data presented by Scott Mayer, MD, chief resident at HealthONE Denver, which is part of the HCA Healthcare chain of hospitals, the risk is increased by any probiotic exposure. However, the risk is particularly acute for powdered formulations, presumably because powder more easily disseminates to contaminate central venous catheters.
“We think that probiotics should be eliminated entirely from the ICU. If not, we encourage eliminating the powder formulations,” said Dr. Mayer, who led the study.
The data linking probiotics to ICU bacteremia were drawn from 23,533 ICU admissions over a 5-year period in the HCA hospital database. Bacteremia proven to be probiotic-related was uncommon (0.37%), but the consequences were serious.
For those with probiotic-related bacteremia, the mortality rate was 25.6% or essentially twofold greater than the 13.5% mortality rate among those without probiotic bacteremia. An odds ratio drawn from a regression analysis confirmed a significant difference (OR, 2.23; 95% confidence interval, 1.30-3.71; P < .01).
“The absolute risk of mortality is modest but not insignificant,” said Dr. Mayer. This suggests one probiotic-related mortality for about every 200 patients taking a probiotic in the ICU.
These deaths occur without any clear compensatory benefit from taking probiotics, according to Dr. Mayer. There is a long list of potential benefits from probiotics that might be relevant to patients in the ICU, particularly prophylaxis for Clostridioides difficile infection, but also including a variety of gastrointestinal disorders, such as irritable bowel syndrome; however, none of these are firmly established in general, and particularly for patients in the ICU.
“The American College of Gastroenterology currently recommends against probiotics for the prevention of C. diff.,” Dr. Mayer said. Although the American Gastroenterological Association has issued a “conditional recommendation” for prevention of C. diff. infection with probiotics, Dr. Mayer pointed out this is qualified by a “low quality of evidence” and it is not specific to the ICU setting.
“The evidence for benefit is weak or nonexistent, but the risks are real,” Dr. Mayer said.
To confirm that probiotic-associated ICU bacteremias in the HCA hospital database were, in fact, related to probiotics being taken by patients at time of admission, Dr. Mayer evaluated the record of each of the 86 patients with probiotic bacteremia–associated mortality.
“I identified the organism that grew from the blood cultures to confirm that it was contained in the probiotic the patient was taking,” explained Dr. Mayer, who said this information was available in the electronic medical records.
The risk of probiotic-associated bacteremia in ICU patients was consistent with a series of case series that prompted the study. Dr. Mayer explained that he became interested when he encountered patients on his ICU rounds who were taking probiotics. He knew very little about these agents and explored the medical literature to see what evidence was available.
“I found several case reports of ICU patients with probiotic-associated infections, several of which were suspected of being associated with contamination of the central lines,” Dr. Mayer said. In one case, the patient was not taking a probiotic, but a patient in an adjacent bed was receiving a powdered probiotic that was implicated. This prompted suspicion that the cause was central-line contamination.
This was evaluated in the HCA ICU database and also found to be a significant risk. Among the 67 patients in whom a capsule or tablet was used, the rate of probiotic-associated bacteremia was 0.33%. For those in which the probiotic was a powdered formulation, the rate was 0.76%, a significant difference (P < .01).
Dr. Mayer acknowledged that these data do not rule out all potential benefits from probiotics in the ICU. He believes an obstacle to proving benefit has been the heterogeneity of available products, which are likely to be relevant to any therapeutic role, including prevention of C. diff. infection.
“There are now a large number of products available, and they contain a large variety of strains of organisms, so this has been a difficult area to study,” he said. However, he maintains it is prudent at this point to avoid probiotics in the ICU because the risks are not confined to the patient making this choice.
“My concern is not just the lack of evidence of benefit relative to the risk for the patient but the potential for probiotics in the ICU to place other patients at risk,” Dr. Mayer said.
Others have also noted the potential benefits of probiotics in the ICU, but the promise remains elusive. In a 2018 review article published in the Journal of Emergency and Critical Care Medicine, the authors evaluated a series of potential applications of probiotics in critically ill patients. These included treatment of ventilator-associated pneumonia (VAP), catheter-associated urinary tract infections (CAUTI), and surgical-site infections (SSI). For each, the data were negative or inconclusive.
Over the 4 years that have passed since the review was published, several trials have further explored the potential benefits of probiotics in the ICU but none have changed this basic conclusion. For example, a 2021 multinational trial, published in The Lancet, randomized more than 2,600 patients to probiotics or placebo and showed no effect on VAP incidence (21.9% vs. 21.3%).
The lead author of the 2018 review, Heather A. Vitko, PhD, an associate professor in the department of acute and tertiary care, University of Pittsburgh School of Nursing, also emphasized that the potential for benefit cannot be considered without the potential for risk. She, like Dr. Mayer, cited the case studies implicating probiotics in systemic infections.
For administration, probiotic capsules or sachets “often need to be opened for administration through a feeding tube,” she noted. The risk of contamination comes from both the air and contaminated hands, the latter of which “can cause a translocation to a central line catheter where the microbes have direct entry into the systemic circulation.”
She did not call for a ban of probiotics in the ICU, but she did recommend “a precautionary approach,” encouraging clinicians to “distinguish between reality [of what has been proven] and what is presented in the marketing of antibiotics.”
Dr. Mayer and Dr. Vitko have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NASHVILLE, TENN. – Supported by several cases series, according to new findings presented at the annual meeting of the American College of Chest Physicians (CHEST).
According to data presented by Scott Mayer, MD, chief resident at HealthONE Denver, which is part of the HCA Healthcare chain of hospitals, the risk is increased by any probiotic exposure. However, the risk is particularly acute for powdered formulations, presumably because powder more easily disseminates to contaminate central venous catheters.
“We think that probiotics should be eliminated entirely from the ICU. If not, we encourage eliminating the powder formulations,” said Dr. Mayer, who led the study.
The data linking probiotics to ICU bacteremia were drawn from 23,533 ICU admissions over a 5-year period in the HCA hospital database. Bacteremia proven to be probiotic-related was uncommon (0.37%), but the consequences were serious.
For those with probiotic-related bacteremia, the mortality rate was 25.6% or essentially twofold greater than the 13.5% mortality rate among those without probiotic bacteremia. An odds ratio drawn from a regression analysis confirmed a significant difference (OR, 2.23; 95% confidence interval, 1.30-3.71; P < .01).
“The absolute risk of mortality is modest but not insignificant,” said Dr. Mayer. This suggests one probiotic-related mortality for about every 200 patients taking a probiotic in the ICU.
These deaths occur without any clear compensatory benefit from taking probiotics, according to Dr. Mayer. There is a long list of potential benefits from probiotics that might be relevant to patients in the ICU, particularly prophylaxis for Clostridioides difficile infection, but also including a variety of gastrointestinal disorders, such as irritable bowel syndrome; however, none of these are firmly established in general, and particularly for patients in the ICU.
“The American College of Gastroenterology currently recommends against probiotics for the prevention of C. diff.,” Dr. Mayer said. Although the American Gastroenterological Association has issued a “conditional recommendation” for prevention of C. diff. infection with probiotics, Dr. Mayer pointed out this is qualified by a “low quality of evidence” and it is not specific to the ICU setting.
“The evidence for benefit is weak or nonexistent, but the risks are real,” Dr. Mayer said.
To confirm that probiotic-associated ICU bacteremias in the HCA hospital database were, in fact, related to probiotics being taken by patients at time of admission, Dr. Mayer evaluated the record of each of the 86 patients with probiotic bacteremia–associated mortality.
“I identified the organism that grew from the blood cultures to confirm that it was contained in the probiotic the patient was taking,” explained Dr. Mayer, who said this information was available in the electronic medical records.
The risk of probiotic-associated bacteremia in ICU patients was consistent with a series of case series that prompted the study. Dr. Mayer explained that he became interested when he encountered patients on his ICU rounds who were taking probiotics. He knew very little about these agents and explored the medical literature to see what evidence was available.
“I found several case reports of ICU patients with probiotic-associated infections, several of which were suspected of being associated with contamination of the central lines,” Dr. Mayer said. In one case, the patient was not taking a probiotic, but a patient in an adjacent bed was receiving a powdered probiotic that was implicated. This prompted suspicion that the cause was central-line contamination.
This was evaluated in the HCA ICU database and also found to be a significant risk. Among the 67 patients in whom a capsule or tablet was used, the rate of probiotic-associated bacteremia was 0.33%. For those in which the probiotic was a powdered formulation, the rate was 0.76%, a significant difference (P < .01).
Dr. Mayer acknowledged that these data do not rule out all potential benefits from probiotics in the ICU. He believes an obstacle to proving benefit has been the heterogeneity of available products, which are likely to be relevant to any therapeutic role, including prevention of C. diff. infection.
“There are now a large number of products available, and they contain a large variety of strains of organisms, so this has been a difficult area to study,” he said. However, he maintains it is prudent at this point to avoid probiotics in the ICU because the risks are not confined to the patient making this choice.
“My concern is not just the lack of evidence of benefit relative to the risk for the patient but the potential for probiotics in the ICU to place other patients at risk,” Dr. Mayer said.
Others have also noted the potential benefits of probiotics in the ICU, but the promise remains elusive. In a 2018 review article published in the Journal of Emergency and Critical Care Medicine, the authors evaluated a series of potential applications of probiotics in critically ill patients. These included treatment of ventilator-associated pneumonia (VAP), catheter-associated urinary tract infections (CAUTI), and surgical-site infections (SSI). For each, the data were negative or inconclusive.
Over the 4 years that have passed since the review was published, several trials have further explored the potential benefits of probiotics in the ICU but none have changed this basic conclusion. For example, a 2021 multinational trial, published in The Lancet, randomized more than 2,600 patients to probiotics or placebo and showed no effect on VAP incidence (21.9% vs. 21.3%).
The lead author of the 2018 review, Heather A. Vitko, PhD, an associate professor in the department of acute and tertiary care, University of Pittsburgh School of Nursing, also emphasized that the potential for benefit cannot be considered without the potential for risk. She, like Dr. Mayer, cited the case studies implicating probiotics in systemic infections.
For administration, probiotic capsules or sachets “often need to be opened for administration through a feeding tube,” she noted. The risk of contamination comes from both the air and contaminated hands, the latter of which “can cause a translocation to a central line catheter where the microbes have direct entry into the systemic circulation.”
She did not call for a ban of probiotics in the ICU, but she did recommend “a precautionary approach,” encouraging clinicians to “distinguish between reality [of what has been proven] and what is presented in the marketing of antibiotics.”
Dr. Mayer and Dr. Vitko have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CHEST 2022
Recommending exercise for migraine: Just do it
with high-intensity aerobics coming in second, and both beating top-line migraine medications topiramate and amitriptyline, new research suggests.
The new results should encourage clinicians to recommend patients with migraine engage in strength-training exercise whenever possible, study investigator Yohannes W. Woldeamanuel, MD, a physician-scientist and instructor, department of neurology and neurological sciences, Stanford (Calif.) University, told this news organization.
“Exercise is something patients can do all their lives and use it to prevent migraine attacks instead of taking daily medications or repetitive injections that have several adverse effects.”
The findings were published online in the Journal of Headache and Pain.
Head-to-head comparison
Several clinical trials have shown exercise is effective for migraine management, but to date, there have been no head-to-head comparisons of strength training and aerobic exercise, said Dr. Woldeamanuel.
This new study used a systematic review with network meta-analysis (NMA), which compares multiple interventions and ranks the efficacy of each one.
After a literature search, researchers included 21 clinical trials with an exercise regimen arm and a comparison control arm. All study data reported monthly frequency of migraine at baseline and at the end of the intervention.
The total combined sample size was 1,195 patients with migraine, who were a mean age of 35.5 years, with a female-to-male ratio of 6.7:1. All studies used International Classification of Headache Disorders (ICHD) criteria for migraine diagnosis.
The NMA provided 27 pairwise comparisons and 8 indirect comparisons. The pairwise comparisons provided direct evidence between the different interventions.
Researchers combined strength training, including weightlifting, with resistance training. Both modalities target muscles, while aerobic exercise targets cardiovascular health.
The average number of weeks was 9.3, 9.3, and 10.7, and the average number of hours per session for strength/resistance training, high-intensity aerobic exercise, and moderate-intensity aerobic exercise interventions was 50, 56, and 45.3, respectively.
The analysis showed all exercise interventions were more effective than the placebo groups in reducing the frequency of migraine. In terms of ranking, strength training came out on top, with a mean difference in monthly migraine days of −3.55 (95% confidence interval, −6.15 to −0.95) between the active and placebo groups.
Next was high-intensity aerobic exercise (−3.13; 95% CI, −5.28 to −0.97) and moderate-intensity aerobic exercise (−2.18; 95% CI, −3.25 to −1.11), followed by topiramate, placebo, and then amitriptyline.
Strength/resistance training was superior possibly because it targets muscle strengthening, particularly major muscles in the neck and shoulder area, which can be a source of the pain trigger, said Dr. Woldeamanuel. He added neck pain is highly comorbid with migraine.
Interestingly, patients doing exercises that focus on unaffected muscles – for example, squats – still get the benefits of less migraine burden, said Dr. Woldeamanuel.
Training recommendations
Strength training also increases or preserves lean muscle mass, which is associated with reduced migraine frequency. Research shows preservation of lean body mass combats central sensitization in various pain syndromes, said Dr. Woldeamanuel.
The superior effects of high- versus moderate-intensity aerobic exercise may be due to recruitment of endogenous molecules involved in exercise-mediated hypoalgesia (pain reduction).
The most common pathways are the opioid and endocannabinoid systems, although other systems are also likely involved, said Dr. Woldeamanuel. He noted migraine has been linked to a deficiency of both opioidergic and endocannabinoidergic signaling.
Dr. Woldeamanuel commented on the difficulty of comparing exercise interventions for patients with chronic versus episodic migraine, as many studies include both.
However, the two studies with moderate-intensity aerobic exercise exclusively involving patients with chronic migraine showed large effect sizes (Cohen’s d) of 0.80 and 1.10 in reducing monthly headache frequency.
Based on these new results and their own experience, the researchers recommend strength training start with 50% of repetition maximum (RM) with 2-3 sets of 12-15 repetitions three times a week along with 10 minutes of warm-up, stretching, and cool-down, totaling 45-60 minutes per session. Weight/resistance load can then be increased weekly by 5% of RM if the patient is capable of successfully completing three sets.
They also recommend including active recovery days (low-intensity exercise) between training days. All major muscles, including neck, shoulder, and upper limb muscles, should be trained in a rotation.
For high-intensity aerobic exercise, the authors recommend starting with interval training at 55% VO2max (maximum respiratory capacity), or 50% HRmax (maximal heart rate) for 45-60 minutes per session, including 10 minutes of warm-up and cool-down, three times per week. The intensity can then be increased by 5%-10% each week to reach a maximum target of 80%-90% by week 12.
It is best for patients to start with a trainer for guidance and supervision, but once they master the routines, they can do the exercises independently, said Dr. Woldeamanuel.
Managing flare-ups
Headache flare-ups are normal during exercise, which may be caused by “boom and bust cycles” – exercising excessively when feeling good then completely stopping when feeling bad, said Dr. Woldeamanuel. He noted these flare-ups don’t mean “there’s something wrong with the brain or there’s some injury to muscles.”
The best way to manage such flare-ups is to use a pacing strategy that involves “not going overboard on good days and avoiding excessive rest on bad days,” the investigators note.
Dr. Woldeamanuel noted exercise is a lifestyle-based intervention; it not only helps reduce migraine attacks but also helps control other known comorbidities such as obesity and hypertension.
In a comment, Elizabeth Loder, MD, vice-chair, academic affairs, department of neurology, Brigham and Women’s Hospital, and professor of neurology, Harvard Medical School, both in Boston, said, “It’s useful to collect and summarize all of these studies, and to focus on helping patients and doctors understand the possible value of different kinds of exercise.”
The review was “well done,” said Dr. Loder, adding the researchers “have looked carefully at the quality of included studies.”
The study received support from the National Institute of Neurological Disorders and Stroke of the National Institutes of Health. Dr. Woldeamanuel has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
with high-intensity aerobics coming in second, and both beating top-line migraine medications topiramate and amitriptyline, new research suggests.
The new results should encourage clinicians to recommend patients with migraine engage in strength-training exercise whenever possible, study investigator Yohannes W. Woldeamanuel, MD, a physician-scientist and instructor, department of neurology and neurological sciences, Stanford (Calif.) University, told this news organization.
“Exercise is something patients can do all their lives and use it to prevent migraine attacks instead of taking daily medications or repetitive injections that have several adverse effects.”
The findings were published online in the Journal of Headache and Pain.
Head-to-head comparison
Several clinical trials have shown exercise is effective for migraine management, but to date, there have been no head-to-head comparisons of strength training and aerobic exercise, said Dr. Woldeamanuel.
This new study used a systematic review with network meta-analysis (NMA), which compares multiple interventions and ranks the efficacy of each one.
After a literature search, researchers included 21 clinical trials with an exercise regimen arm and a comparison control arm. All study data reported monthly frequency of migraine at baseline and at the end of the intervention.
The total combined sample size was 1,195 patients with migraine, who were a mean age of 35.5 years, with a female-to-male ratio of 6.7:1. All studies used International Classification of Headache Disorders (ICHD) criteria for migraine diagnosis.
The NMA provided 27 pairwise comparisons and 8 indirect comparisons. The pairwise comparisons provided direct evidence between the different interventions.
Researchers combined strength training, including weightlifting, with resistance training. Both modalities target muscles, while aerobic exercise targets cardiovascular health.
The average number of weeks was 9.3, 9.3, and 10.7, and the average number of hours per session for strength/resistance training, high-intensity aerobic exercise, and moderate-intensity aerobic exercise interventions was 50, 56, and 45.3, respectively.
The analysis showed all exercise interventions were more effective than the placebo groups in reducing the frequency of migraine. In terms of ranking, strength training came out on top, with a mean difference in monthly migraine days of −3.55 (95% confidence interval, −6.15 to −0.95) between the active and placebo groups.
Next was high-intensity aerobic exercise (−3.13; 95% CI, −5.28 to −0.97) and moderate-intensity aerobic exercise (−2.18; 95% CI, −3.25 to −1.11), followed by topiramate, placebo, and then amitriptyline.
Strength/resistance training was superior possibly because it targets muscle strengthening, particularly major muscles in the neck and shoulder area, which can be a source of the pain trigger, said Dr. Woldeamanuel. He added neck pain is highly comorbid with migraine.
Interestingly, patients doing exercises that focus on unaffected muscles – for example, squats – still get the benefits of less migraine burden, said Dr. Woldeamanuel.
Training recommendations
Strength training also increases or preserves lean muscle mass, which is associated with reduced migraine frequency. Research shows preservation of lean body mass combats central sensitization in various pain syndromes, said Dr. Woldeamanuel.
The superior effects of high- versus moderate-intensity aerobic exercise may be due to recruitment of endogenous molecules involved in exercise-mediated hypoalgesia (pain reduction).
The most common pathways are the opioid and endocannabinoid systems, although other systems are also likely involved, said Dr. Woldeamanuel. He noted migraine has been linked to a deficiency of both opioidergic and endocannabinoidergic signaling.
Dr. Woldeamanuel commented on the difficulty of comparing exercise interventions for patients with chronic versus episodic migraine, as many studies include both.
However, the two studies with moderate-intensity aerobic exercise exclusively involving patients with chronic migraine showed large effect sizes (Cohen’s d) of 0.80 and 1.10 in reducing monthly headache frequency.
Based on these new results and their own experience, the researchers recommend strength training start with 50% of repetition maximum (RM) with 2-3 sets of 12-15 repetitions three times a week along with 10 minutes of warm-up, stretching, and cool-down, totaling 45-60 minutes per session. Weight/resistance load can then be increased weekly by 5% of RM if the patient is capable of successfully completing three sets.
They also recommend including active recovery days (low-intensity exercise) between training days. All major muscles, including neck, shoulder, and upper limb muscles, should be trained in a rotation.
For high-intensity aerobic exercise, the authors recommend starting with interval training at 55% VO2max (maximum respiratory capacity), or 50% HRmax (maximal heart rate) for 45-60 minutes per session, including 10 minutes of warm-up and cool-down, three times per week. The intensity can then be increased by 5%-10% each week to reach a maximum target of 80%-90% by week 12.
It is best for patients to start with a trainer for guidance and supervision, but once they master the routines, they can do the exercises independently, said Dr. Woldeamanuel.
Managing flare-ups
Headache flare-ups are normal during exercise, which may be caused by “boom and bust cycles” – exercising excessively when feeling good then completely stopping when feeling bad, said Dr. Woldeamanuel. He noted these flare-ups don’t mean “there’s something wrong with the brain or there’s some injury to muscles.”
The best way to manage such flare-ups is to use a pacing strategy that involves “not going overboard on good days and avoiding excessive rest on bad days,” the investigators note.
Dr. Woldeamanuel noted exercise is a lifestyle-based intervention; it not only helps reduce migraine attacks but also helps control other known comorbidities such as obesity and hypertension.
In a comment, Elizabeth Loder, MD, vice-chair, academic affairs, department of neurology, Brigham and Women’s Hospital, and professor of neurology, Harvard Medical School, both in Boston, said, “It’s useful to collect and summarize all of these studies, and to focus on helping patients and doctors understand the possible value of different kinds of exercise.”
The review was “well done,” said Dr. Loder, adding the researchers “have looked carefully at the quality of included studies.”
The study received support from the National Institute of Neurological Disorders and Stroke of the National Institutes of Health. Dr. Woldeamanuel has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
with high-intensity aerobics coming in second, and both beating top-line migraine medications topiramate and amitriptyline, new research suggests.
The new results should encourage clinicians to recommend patients with migraine engage in strength-training exercise whenever possible, study investigator Yohannes W. Woldeamanuel, MD, a physician-scientist and instructor, department of neurology and neurological sciences, Stanford (Calif.) University, told this news organization.
“Exercise is something patients can do all their lives and use it to prevent migraine attacks instead of taking daily medications or repetitive injections that have several adverse effects.”
The findings were published online in the Journal of Headache and Pain.
Head-to-head comparison
Several clinical trials have shown exercise is effective for migraine management, but to date, there have been no head-to-head comparisons of strength training and aerobic exercise, said Dr. Woldeamanuel.
This new study used a systematic review with network meta-analysis (NMA), which compares multiple interventions and ranks the efficacy of each one.
After a literature search, researchers included 21 clinical trials with an exercise regimen arm and a comparison control arm. All study data reported monthly frequency of migraine at baseline and at the end of the intervention.
The total combined sample size was 1,195 patients with migraine, who were a mean age of 35.5 years, with a female-to-male ratio of 6.7:1. All studies used International Classification of Headache Disorders (ICHD) criteria for migraine diagnosis.
The NMA provided 27 pairwise comparisons and 8 indirect comparisons. The pairwise comparisons provided direct evidence between the different interventions.
Researchers combined strength training, including weightlifting, with resistance training. Both modalities target muscles, while aerobic exercise targets cardiovascular health.
The average number of weeks was 9.3, 9.3, and 10.7, and the average number of hours per session for strength/resistance training, high-intensity aerobic exercise, and moderate-intensity aerobic exercise interventions was 50, 56, and 45.3, respectively.
The analysis showed all exercise interventions were more effective than the placebo groups in reducing the frequency of migraine. In terms of ranking, strength training came out on top, with a mean difference in monthly migraine days of −3.55 (95% confidence interval, −6.15 to −0.95) between the active and placebo groups.
Next was high-intensity aerobic exercise (−3.13; 95% CI, −5.28 to −0.97) and moderate-intensity aerobic exercise (−2.18; 95% CI, −3.25 to −1.11), followed by topiramate, placebo, and then amitriptyline.
Strength/resistance training was superior possibly because it targets muscle strengthening, particularly major muscles in the neck and shoulder area, which can be a source of the pain trigger, said Dr. Woldeamanuel. He added neck pain is highly comorbid with migraine.
Interestingly, patients doing exercises that focus on unaffected muscles – for example, squats – still get the benefits of less migraine burden, said Dr. Woldeamanuel.
Training recommendations
Strength training also increases or preserves lean muscle mass, which is associated with reduced migraine frequency. Research shows preservation of lean body mass combats central sensitization in various pain syndromes, said Dr. Woldeamanuel.
The superior effects of high- versus moderate-intensity aerobic exercise may be due to recruitment of endogenous molecules involved in exercise-mediated hypoalgesia (pain reduction).
The most common pathways are the opioid and endocannabinoid systems, although other systems are also likely involved, said Dr. Woldeamanuel. He noted migraine has been linked to a deficiency of both opioidergic and endocannabinoidergic signaling.
Dr. Woldeamanuel commented on the difficulty of comparing exercise interventions for patients with chronic versus episodic migraine, as many studies include both.
However, the two studies with moderate-intensity aerobic exercise exclusively involving patients with chronic migraine showed large effect sizes (Cohen’s d) of 0.80 and 1.10 in reducing monthly headache frequency.
Based on these new results and their own experience, the researchers recommend strength training start with 50% of repetition maximum (RM) with 2-3 sets of 12-15 repetitions three times a week along with 10 minutes of warm-up, stretching, and cool-down, totaling 45-60 minutes per session. Weight/resistance load can then be increased weekly by 5% of RM if the patient is capable of successfully completing three sets.
They also recommend including active recovery days (low-intensity exercise) between training days. All major muscles, including neck, shoulder, and upper limb muscles, should be trained in a rotation.
For high-intensity aerobic exercise, the authors recommend starting with interval training at 55% VO2max (maximum respiratory capacity), or 50% HRmax (maximal heart rate) for 45-60 minutes per session, including 10 minutes of warm-up and cool-down, three times per week. The intensity can then be increased by 5%-10% each week to reach a maximum target of 80%-90% by week 12.
It is best for patients to start with a trainer for guidance and supervision, but once they master the routines, they can do the exercises independently, said Dr. Woldeamanuel.
Managing flare-ups
Headache flare-ups are normal during exercise, which may be caused by “boom and bust cycles” – exercising excessively when feeling good then completely stopping when feeling bad, said Dr. Woldeamanuel. He noted these flare-ups don’t mean “there’s something wrong with the brain or there’s some injury to muscles.”
The best way to manage such flare-ups is to use a pacing strategy that involves “not going overboard on good days and avoiding excessive rest on bad days,” the investigators note.
Dr. Woldeamanuel noted exercise is a lifestyle-based intervention; it not only helps reduce migraine attacks but also helps control other known comorbidities such as obesity and hypertension.
In a comment, Elizabeth Loder, MD, vice-chair, academic affairs, department of neurology, Brigham and Women’s Hospital, and professor of neurology, Harvard Medical School, both in Boston, said, “It’s useful to collect and summarize all of these studies, and to focus on helping patients and doctors understand the possible value of different kinds of exercise.”
The review was “well done,” said Dr. Loder, adding the researchers “have looked carefully at the quality of included studies.”
The study received support from the National Institute of Neurological Disorders and Stroke of the National Institutes of Health. Dr. Woldeamanuel has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF HEADACHE AND PAIN
Highly processed foods ‘as addictive’ as tobacco
according to a new U.S. study that proposes a set of criteria to assess the addictive potential of some foods.
The research suggests that health care professionals are taking steps toward framing food addiction as a clinical entity in its own right; it currently lacks validated treatment protocols and recognition as a clinical diagnosis.
Meanwhile, other data, reported by researchers at the 2022 Diabetes Professional Care conference in London also add support to the clinical recognition of food addiction.
Clinical psychologist Jen Unwin, PhD, from Southport, England, showed that a 3-month online program of low-carbohydrate diet together with psychoeducational support significantly reduced food addiction symptoms among a varied group of individuals, not all of whom were overweight or had obesity.
Dr. Unwin said her new data represent the first wide-scale clinical audit of its kind, other than a prior report of three patients with food addiction who were successfully treated with a ketogenic diet.
“Food addiction explains so much of what we see in clinical practice, where intelligent people understand what we tell them about the physiology associated with a low-carb diet, and they follow it for a while, but then they relapse,” said Dr. Unwin, explaining the difficulties faced by around 20% of her patients who are considered to have food addiction.
Meanwhile, the authors of the U.S. study, led by Ashley N. Gearhardt, PhD, a psychologist from the University of Michigan, Ann Arbor, wrote that the ability of highly processed foods (HPFs) “to rapidly deliver high doses of refined carbohydrates and/or fat appear key to their addictive potential. Thus, we conclude that HPFs can be considered addictive substances based on scientifically established criteria.”
They asserted that the contribution to preventable deaths by a diet dominated by highly processed foods is comparable with that of tobacco products, and as such, like Dr. Unwin, the authors sought clinical recognition and a more formalized protocol to manage food addiction.
“Understanding whether addiction contributes to HPF intake may lead to new treatments, as preliminary research finds that behavioral and pharmacological interventions that target addictive mechanisms may reduce compulsive HPF intake,” they stated.
The study led by Dr. Gearhardt was published in the journal Addiction, and the study led by Unwin was also recently published in Frontiers in Psychiatry.
Addiction criteria similar to tobacco
HPFs can be associated with an eating phenotype “that reflects the hallmarks of addiction,” said Dr. Gearhardt and coauthors; typically, loss of control over intake, intense cravings, inability to cut down, and continued use despite negative consequences.
Acknowledging the lack of a single addictive agent, they explain that food addiction reflects mechanisms implicated in other addictive disorders such as smoking.
As such, in their study, Dr. Gearhardt and colleagues proposed a set of scientifically based criteria for the evaluation of whether certain foods are addictive. “Specifically, we propose the primary criteria used to resolve one of the last major controversies over whether a substance, tobacco products, was addictive.”
They consider certain foods according to the primary criteria that have stood the test of time after being proposed in 1988 by the U.S. Surgeon General to establish the addictive potential of tobacco: they trigger compulsive use, they have psychoactive effects, and they are reinforcing.
They have updated these criteria to include the ability to trigger urges and cravings, and added that “both these products [tobacco and HPFs] are legal, easily accessible, inexpensive, lack an intoxication syndrome, and are major causes of preventable death.”
For example, with compulsive use, tobacco meets this criterion because evidence suggests that most smokers would like to quit but are unable to do so.
Likewise, wrote Dr. Gearhardt and colleagues, even “in the face of significant diet-related health consequences (e.g., diabetes and cardiovascular disease), the majority of patients are unable to adhere to medically recommended dietary plans that require a reduction in HPF intake.”
Reinforcement, through tobacco use, is demonstrated by its ‘being sufficiently rewarding to maintain self-administration” because of its ability to deliver nicotine, they said, quoting the Surgeon General’s report, and likewise, with food addiction, “both adults and children will self-administer HPFs (e.g., potato chips, candy, and cookies) even when satiated.”
Online group food addiction intervention study
Dr. Unwin and coauthors want people with food addiction to be able to access a validated treatment protocol. Their study aimed to evaluate an online group intervention across multiple sites in the United States, Canada, and the United Kingdom, involving an abstinent, low-carbohydrate diet and biopsychosocial education focused on addiction and recovery in people self-identifying as having food addiction.
“Lots of people with food addiction go to GPs who don’t clinically recognize this, or if they attend addiction services and psychiatry, then they tend to only specialize in drugs, alcohol, and gambling. Eating disorder services are linked but their programs mostly don’t work for a food addict,” Dr. Unwin remarked in an interview.
“We feel running groups, as well as training professionals to run groups, is the best way to manage food addiction,” she said, reflecting on the scale of the problem, with around 10% of adults in the U.K. general population considered to have food addiction. In Dr. Unwin’s study, some people had type 2 diabetes and some overweight/obesity, but she added that some participants were underweight or of normal weight.
Initially, the 103 participants received weekly group (8-24 people) sessions for 10-14 weeks, and then monthly maintenance comprising follow-up that involved coaching participants on how to cope with relapse and get back on track.
Food addiction symptoms were assessed pre- and post program using the modified Yale Food Addiction Scale (mYFAS) 2.0; ICD-10 symptoms of food-related substance use disorder (CRAVED); and mental health well-being measured using the short version of the Warwick Edinburgh Mental Wellbeing scale and body weight.
“The program eliminates processed foods with a personalized, abstinence food plan that involves education around mechanisms involved,” said Dr. Unwin, who explained that processed foods deliver a dopamine high, and in response to this, the brain lowers the number of dopamine receptors to effectively counteract the increase in dopamine. This drop in dopamine receptors explains the depression often associated with food addiction.
Dr. Unwin reported that food addiction symptoms were significantly reduced, with the mYFAS dropping by 1.52, the CRAVED score by 1.53, and body weight by 2.34 kg (5.2 lb). Mental health, as measured by the Warwick Edinburgh Mental Wellbeing scale, improved by 2.37 points.
“We were very interested in mental health and well-being because it impacts so much across our lives, and we saw significant improvements here, but we were less interested in weight because food addicts come in all shapes and sizes with some people underweight,” said Dr. Unwin. “Food addiction symptoms were significantly improved in the group, but we now need to look at the longer-term outcomes.”
Dr. Unwin runs a low-carbohydrate program for type 2 diabetes with her husband David Unwin, MD, who is a GP in Southport, England. She said that they ask patients if they think they have food addiction, and most say they do.
“I always try to explain to patients about the dopamine high, and how this starts the craving which makes people wonder when and where they can find the next sugar hit. Just thinking about the next chocolate bar gets the dopamine running for many people, and the more they tread this path then the worse it gets because the dopamine receptors keep reducing.”
Lorraine Avery, RN, a diabetes nurse specialist for Solent NHS Trust, who attended the DPC conference, welcomed Dr. Unwin’s presentation.
“My concern as a diabetes nurse specialist is that I’m unsure all our patients recognize their food addiction, and there are often more drivers to eating than just the food in front of them,” she said in an interview. “I think there’s an emotional element, too. These people are often ‘yo-yo’ dieters, and they join lots of expert companies to help them lose weight, but these companies want them to regain and re-join their programs,” she said.
“I think there is something about helping patients recognize they have a food addiction and they need to consider that other approaches might be helpful.”
Dr. Unwin reported no relevant financial relationships; some other authors have fee-paying clients with food addiction. Dr. Gearhardt and Ms. Avery reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new U.S. study that proposes a set of criteria to assess the addictive potential of some foods.
The research suggests that health care professionals are taking steps toward framing food addiction as a clinical entity in its own right; it currently lacks validated treatment protocols and recognition as a clinical diagnosis.
Meanwhile, other data, reported by researchers at the 2022 Diabetes Professional Care conference in London also add support to the clinical recognition of food addiction.
Clinical psychologist Jen Unwin, PhD, from Southport, England, showed that a 3-month online program of low-carbohydrate diet together with psychoeducational support significantly reduced food addiction symptoms among a varied group of individuals, not all of whom were overweight or had obesity.
Dr. Unwin said her new data represent the first wide-scale clinical audit of its kind, other than a prior report of three patients with food addiction who were successfully treated with a ketogenic diet.
“Food addiction explains so much of what we see in clinical practice, where intelligent people understand what we tell them about the physiology associated with a low-carb diet, and they follow it for a while, but then they relapse,” said Dr. Unwin, explaining the difficulties faced by around 20% of her patients who are considered to have food addiction.
Meanwhile, the authors of the U.S. study, led by Ashley N. Gearhardt, PhD, a psychologist from the University of Michigan, Ann Arbor, wrote that the ability of highly processed foods (HPFs) “to rapidly deliver high doses of refined carbohydrates and/or fat appear key to their addictive potential. Thus, we conclude that HPFs can be considered addictive substances based on scientifically established criteria.”
They asserted that the contribution to preventable deaths by a diet dominated by highly processed foods is comparable with that of tobacco products, and as such, like Dr. Unwin, the authors sought clinical recognition and a more formalized protocol to manage food addiction.
“Understanding whether addiction contributes to HPF intake may lead to new treatments, as preliminary research finds that behavioral and pharmacological interventions that target addictive mechanisms may reduce compulsive HPF intake,” they stated.
The study led by Dr. Gearhardt was published in the journal Addiction, and the study led by Unwin was also recently published in Frontiers in Psychiatry.
Addiction criteria similar to tobacco
HPFs can be associated with an eating phenotype “that reflects the hallmarks of addiction,” said Dr. Gearhardt and coauthors; typically, loss of control over intake, intense cravings, inability to cut down, and continued use despite negative consequences.
Acknowledging the lack of a single addictive agent, they explain that food addiction reflects mechanisms implicated in other addictive disorders such as smoking.
As such, in their study, Dr. Gearhardt and colleagues proposed a set of scientifically based criteria for the evaluation of whether certain foods are addictive. “Specifically, we propose the primary criteria used to resolve one of the last major controversies over whether a substance, tobacco products, was addictive.”
They consider certain foods according to the primary criteria that have stood the test of time after being proposed in 1988 by the U.S. Surgeon General to establish the addictive potential of tobacco: they trigger compulsive use, they have psychoactive effects, and they are reinforcing.
They have updated these criteria to include the ability to trigger urges and cravings, and added that “both these products [tobacco and HPFs] are legal, easily accessible, inexpensive, lack an intoxication syndrome, and are major causes of preventable death.”
For example, with compulsive use, tobacco meets this criterion because evidence suggests that most smokers would like to quit but are unable to do so.
Likewise, wrote Dr. Gearhardt and colleagues, even “in the face of significant diet-related health consequences (e.g., diabetes and cardiovascular disease), the majority of patients are unable to adhere to medically recommended dietary plans that require a reduction in HPF intake.”
Reinforcement, through tobacco use, is demonstrated by its ‘being sufficiently rewarding to maintain self-administration” because of its ability to deliver nicotine, they said, quoting the Surgeon General’s report, and likewise, with food addiction, “both adults and children will self-administer HPFs (e.g., potato chips, candy, and cookies) even when satiated.”
Online group food addiction intervention study
Dr. Unwin and coauthors want people with food addiction to be able to access a validated treatment protocol. Their study aimed to evaluate an online group intervention across multiple sites in the United States, Canada, and the United Kingdom, involving an abstinent, low-carbohydrate diet and biopsychosocial education focused on addiction and recovery in people self-identifying as having food addiction.
“Lots of people with food addiction go to GPs who don’t clinically recognize this, or if they attend addiction services and psychiatry, then they tend to only specialize in drugs, alcohol, and gambling. Eating disorder services are linked but their programs mostly don’t work for a food addict,” Dr. Unwin remarked in an interview.
“We feel running groups, as well as training professionals to run groups, is the best way to manage food addiction,” she said, reflecting on the scale of the problem, with around 10% of adults in the U.K. general population considered to have food addiction. In Dr. Unwin’s study, some people had type 2 diabetes and some overweight/obesity, but she added that some participants were underweight or of normal weight.
Initially, the 103 participants received weekly group (8-24 people) sessions for 10-14 weeks, and then monthly maintenance comprising follow-up that involved coaching participants on how to cope with relapse and get back on track.
Food addiction symptoms were assessed pre- and post program using the modified Yale Food Addiction Scale (mYFAS) 2.0; ICD-10 symptoms of food-related substance use disorder (CRAVED); and mental health well-being measured using the short version of the Warwick Edinburgh Mental Wellbeing scale and body weight.
“The program eliminates processed foods with a personalized, abstinence food plan that involves education around mechanisms involved,” said Dr. Unwin, who explained that processed foods deliver a dopamine high, and in response to this, the brain lowers the number of dopamine receptors to effectively counteract the increase in dopamine. This drop in dopamine receptors explains the depression often associated with food addiction.
Dr. Unwin reported that food addiction symptoms were significantly reduced, with the mYFAS dropping by 1.52, the CRAVED score by 1.53, and body weight by 2.34 kg (5.2 lb). Mental health, as measured by the Warwick Edinburgh Mental Wellbeing scale, improved by 2.37 points.
“We were very interested in mental health and well-being because it impacts so much across our lives, and we saw significant improvements here, but we were less interested in weight because food addicts come in all shapes and sizes with some people underweight,” said Dr. Unwin. “Food addiction symptoms were significantly improved in the group, but we now need to look at the longer-term outcomes.”
Dr. Unwin runs a low-carbohydrate program for type 2 diabetes with her husband David Unwin, MD, who is a GP in Southport, England. She said that they ask patients if they think they have food addiction, and most say they do.
“I always try to explain to patients about the dopamine high, and how this starts the craving which makes people wonder when and where they can find the next sugar hit. Just thinking about the next chocolate bar gets the dopamine running for many people, and the more they tread this path then the worse it gets because the dopamine receptors keep reducing.”
Lorraine Avery, RN, a diabetes nurse specialist for Solent NHS Trust, who attended the DPC conference, welcomed Dr. Unwin’s presentation.
“My concern as a diabetes nurse specialist is that I’m unsure all our patients recognize their food addiction, and there are often more drivers to eating than just the food in front of them,” she said in an interview. “I think there’s an emotional element, too. These people are often ‘yo-yo’ dieters, and they join lots of expert companies to help them lose weight, but these companies want them to regain and re-join their programs,” she said.
“I think there is something about helping patients recognize they have a food addiction and they need to consider that other approaches might be helpful.”
Dr. Unwin reported no relevant financial relationships; some other authors have fee-paying clients with food addiction. Dr. Gearhardt and Ms. Avery reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new U.S. study that proposes a set of criteria to assess the addictive potential of some foods.
The research suggests that health care professionals are taking steps toward framing food addiction as a clinical entity in its own right; it currently lacks validated treatment protocols and recognition as a clinical diagnosis.
Meanwhile, other data, reported by researchers at the 2022 Diabetes Professional Care conference in London also add support to the clinical recognition of food addiction.
Clinical psychologist Jen Unwin, PhD, from Southport, England, showed that a 3-month online program of low-carbohydrate diet together with psychoeducational support significantly reduced food addiction symptoms among a varied group of individuals, not all of whom were overweight or had obesity.
Dr. Unwin said her new data represent the first wide-scale clinical audit of its kind, other than a prior report of three patients with food addiction who were successfully treated with a ketogenic diet.
“Food addiction explains so much of what we see in clinical practice, where intelligent people understand what we tell them about the physiology associated with a low-carb diet, and they follow it for a while, but then they relapse,” said Dr. Unwin, explaining the difficulties faced by around 20% of her patients who are considered to have food addiction.
Meanwhile, the authors of the U.S. study, led by Ashley N. Gearhardt, PhD, a psychologist from the University of Michigan, Ann Arbor, wrote that the ability of highly processed foods (HPFs) “to rapidly deliver high doses of refined carbohydrates and/or fat appear key to their addictive potential. Thus, we conclude that HPFs can be considered addictive substances based on scientifically established criteria.”
They asserted that the contribution to preventable deaths by a diet dominated by highly processed foods is comparable with that of tobacco products, and as such, like Dr. Unwin, the authors sought clinical recognition and a more formalized protocol to manage food addiction.
“Understanding whether addiction contributes to HPF intake may lead to new treatments, as preliminary research finds that behavioral and pharmacological interventions that target addictive mechanisms may reduce compulsive HPF intake,” they stated.
The study led by Dr. Gearhardt was published in the journal Addiction, and the study led by Unwin was also recently published in Frontiers in Psychiatry.
Addiction criteria similar to tobacco
HPFs can be associated with an eating phenotype “that reflects the hallmarks of addiction,” said Dr. Gearhardt and coauthors; typically, loss of control over intake, intense cravings, inability to cut down, and continued use despite negative consequences.
Acknowledging the lack of a single addictive agent, they explain that food addiction reflects mechanisms implicated in other addictive disorders such as smoking.
As such, in their study, Dr. Gearhardt and colleagues proposed a set of scientifically based criteria for the evaluation of whether certain foods are addictive. “Specifically, we propose the primary criteria used to resolve one of the last major controversies over whether a substance, tobacco products, was addictive.”
They consider certain foods according to the primary criteria that have stood the test of time after being proposed in 1988 by the U.S. Surgeon General to establish the addictive potential of tobacco: they trigger compulsive use, they have psychoactive effects, and they are reinforcing.
They have updated these criteria to include the ability to trigger urges and cravings, and added that “both these products [tobacco and HPFs] are legal, easily accessible, inexpensive, lack an intoxication syndrome, and are major causes of preventable death.”
For example, with compulsive use, tobacco meets this criterion because evidence suggests that most smokers would like to quit but are unable to do so.
Likewise, wrote Dr. Gearhardt and colleagues, even “in the face of significant diet-related health consequences (e.g., diabetes and cardiovascular disease), the majority of patients are unable to adhere to medically recommended dietary plans that require a reduction in HPF intake.”
Reinforcement, through tobacco use, is demonstrated by its ‘being sufficiently rewarding to maintain self-administration” because of its ability to deliver nicotine, they said, quoting the Surgeon General’s report, and likewise, with food addiction, “both adults and children will self-administer HPFs (e.g., potato chips, candy, and cookies) even when satiated.”
Online group food addiction intervention study
Dr. Unwin and coauthors want people with food addiction to be able to access a validated treatment protocol. Their study aimed to evaluate an online group intervention across multiple sites in the United States, Canada, and the United Kingdom, involving an abstinent, low-carbohydrate diet and biopsychosocial education focused on addiction and recovery in people self-identifying as having food addiction.
“Lots of people with food addiction go to GPs who don’t clinically recognize this, or if they attend addiction services and psychiatry, then they tend to only specialize in drugs, alcohol, and gambling. Eating disorder services are linked but their programs mostly don’t work for a food addict,” Dr. Unwin remarked in an interview.
“We feel running groups, as well as training professionals to run groups, is the best way to manage food addiction,” she said, reflecting on the scale of the problem, with around 10% of adults in the U.K. general population considered to have food addiction. In Dr. Unwin’s study, some people had type 2 diabetes and some overweight/obesity, but she added that some participants were underweight or of normal weight.
Initially, the 103 participants received weekly group (8-24 people) sessions for 10-14 weeks, and then monthly maintenance comprising follow-up that involved coaching participants on how to cope with relapse and get back on track.
Food addiction symptoms were assessed pre- and post program using the modified Yale Food Addiction Scale (mYFAS) 2.0; ICD-10 symptoms of food-related substance use disorder (CRAVED); and mental health well-being measured using the short version of the Warwick Edinburgh Mental Wellbeing scale and body weight.
“The program eliminates processed foods with a personalized, abstinence food plan that involves education around mechanisms involved,” said Dr. Unwin, who explained that processed foods deliver a dopamine high, and in response to this, the brain lowers the number of dopamine receptors to effectively counteract the increase in dopamine. This drop in dopamine receptors explains the depression often associated with food addiction.
Dr. Unwin reported that food addiction symptoms were significantly reduced, with the mYFAS dropping by 1.52, the CRAVED score by 1.53, and body weight by 2.34 kg (5.2 lb). Mental health, as measured by the Warwick Edinburgh Mental Wellbeing scale, improved by 2.37 points.
“We were very interested in mental health and well-being because it impacts so much across our lives, and we saw significant improvements here, but we were less interested in weight because food addicts come in all shapes and sizes with some people underweight,” said Dr. Unwin. “Food addiction symptoms were significantly improved in the group, but we now need to look at the longer-term outcomes.”
Dr. Unwin runs a low-carbohydrate program for type 2 diabetes with her husband David Unwin, MD, who is a GP in Southport, England. She said that they ask patients if they think they have food addiction, and most say they do.
“I always try to explain to patients about the dopamine high, and how this starts the craving which makes people wonder when and where they can find the next sugar hit. Just thinking about the next chocolate bar gets the dopamine running for many people, and the more they tread this path then the worse it gets because the dopamine receptors keep reducing.”
Lorraine Avery, RN, a diabetes nurse specialist for Solent NHS Trust, who attended the DPC conference, welcomed Dr. Unwin’s presentation.
“My concern as a diabetes nurse specialist is that I’m unsure all our patients recognize their food addiction, and there are often more drivers to eating than just the food in front of them,” she said in an interview. “I think there’s an emotional element, too. These people are often ‘yo-yo’ dieters, and they join lots of expert companies to help them lose weight, but these companies want them to regain and re-join their programs,” she said.
“I think there is something about helping patients recognize they have a food addiction and they need to consider that other approaches might be helpful.”
Dr. Unwin reported no relevant financial relationships; some other authors have fee-paying clients with food addiction. Dr. Gearhardt and Ms. Avery reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.




