User login
Folic acid tied to a reduction in suicide attempts
new research suggests.
After adjusting for multiple factors, results from a large pharmaco-epidemiological study showed taking folic acid was associated with a 44% reduction in suicide events.
“These results are really putting folic acid squarely on the map as a potential for large-scale, population-level prevention,” lead author Robert D. Gibbons, PhD, professor of biostatistics, Center for Health Statistics, University of Chicago, said in an interview.
“Folic acid is safe, inexpensive, and generally available, and if future randomized controlled trials show this association is beyond a shadow of a doubt causal, we have a new tool in the arsenal,” Dr. Gibbons said.
Having such a tool would be extremely important given that suicide is such a significant public health crisis worldwide, he added.
The findings were published online in JAMA Psychiatry.
Previous research ‘fairly thin’
Folate, the naturally occurring form of B9, is essential for neurogenesis, nucleotide synthesis, and methylation of homocysteine. Past research has suggested that taking folate can prevent neural tube and heart defects in the fetus during pregnancy – and may prevent strokes and reduce age-related hearing loss in adults.
In psychiatry, the role of folate has been recognized for more than a decade. It may enhance the effects of antidepressants; and folate deficiency can predict poorer response to SSRIs.
This has led to recommendations for folate augmentation in patients with low or normal levels at the start of depression treatment.
Although previous research has shown a link between folic acid and suicidality, the findings have been “fairly thin,” with studies being “generally small, and many are case series,” Dr. Gibbons said.
The current study follows an earlier analysis that used a novel statistical methodology for generating drug safety signals that was developed by Dr. Gibbons and colleagues. That study compared rates of suicide attempts before and after initiation of 922 drugs with at least 3,000 prescriptions.
Its results showed 10 drugs were associated with increased risk after exposure, with the strongest associations for alprazolam, butalbital, hydrocodone, and combination codeine/promethazine. In addition, 44 drugs were associated with decreased risk, many of which were antidepressants and antipsychotics.
“One of the most interesting findings in terms of the decreased risk was for folic acid,” said Dr. Gibbons.
He and his colleagues initially thought this was because of women taking folic acid during pregnancy. But when restricting the analysis to men, they found the same effect.
Their next step was to carry out the current large-scale pharmaco-epidemiological study.
Prescriptions for pain
The researchers used a health claims database that included 164 million enrollees. The study cohort was comprised of 866,586 adults with private health insurance (81.3% women; 10.4% aged 60 years and older) who filled a folic acid prescription between 2012 and 2017.
More than half of the folic acid prescriptions were associated with pain disorders. About 48% were for a single agent at a dosage of 1 mg/d, which is the upper tolerable limit for adults – including in pregnancy and lactation.
Other single-agent daily dosages ranging from 0.4 mg to 5 mg accounted for 0.11% of prescriptions. The remainder were multivitamins.
The participants were followed for 24 months. The within-person analysis compared suicide attempts or self-harm events resulting in an outpatient visit or inpatient admission during periods of folic acid treatment versus during periods without treatment.
During the study period, the overall suicidal event rate was 133 per 100,000 population, which is one-fourth the national rate reported by the National Institutes of Health of 600 per 100,000.
After adjusting for age, sex, diagnoses related to suicidal behavior and folic acid deficiency, history of folate-reducing medications, and history of suicidal events, the estimated hazard ratio for suicide events when taking folic acid was 0.56 (95% confidence interal, 0.48-0.65) – which indicates a 44% reduction in suicide events.
“This is a very large decrease and is extremely significant and exciting,” Dr. Gibbons said.
He noted the decrease in suicidal events may have been even greater considering the study captured only prescription folic acid, and participants may also have also taken over-the-counter products.
“The 44% reduction in suicide attempts may actually be an underestimate,” said Dr. Gibbons.
Age and sex did not moderate the association between folic acid and suicide attempts, and a similar association was found in women of childbearing age.
Provocative results?
The investigators also assessed a negative control group of 236,610 individuals using cyanocobalamin during the study period. Cyanocobalamin is a form of vitamin B12 that is essential for metabolism, blood cell synthesis, and the nervous system. It does not contain folic acid and is commonly used to treat anemia.
Results showed no association between cyanocobalamin and suicidal events in the adjusted analysis (HR, 1.01; 95% CI, 0.80-1.27) or unadjusted analysis (HR, 1.02; 95% CI, 0.80-1.28).
Dr. Gibbons noted this result boosts the argument that the association between folic acid and reduced suicidal attempts “isn’t just about health-seeking behavior like taking vitamin supplements.”
Another sensitivity analysis showed every additional month of treatment was associated with a 5% reduction in the suicidal event rate.
“This means the longer you take folic acid, the greater the benefit, which is what you would expect to see if there was a real association between a treatment and an outcome,” said Dr. Gibbons.
The new results “are so provocative that they really mandate the need for a well-controlled randomized controlled trial of folic acid and suicide events,” possibly in a high-risk population such as veterans, he noted.
Such a study could use longitudinal assessments of suicidal events, such as the validated Computerized Adaptive Test Suicide Scale, he added. This continuous scale of suicidality ranges from subclinical, signifying helplessness, hopelessness, and loss of pleasure, to suicide attempts and completion.
As for study limitations, the investigators noted that this study was observational, so there could be selection effects. And using claims data likely underrepresented the number of suicidal events because of incomplete reporting. As the researchers pointed out, the rate of suicidal events in this study was much lower than the national rate.
Other limitations cited were that the association between folic acid and suicidal events may be explained by healthy user bias; and although the investigators conducted a sensitivity analysis in women of childbearing age, they did not have data on women actively planning for a pregnancy.
‘Impressive, encouraging’
In a comment, Shirley Yen, PhD, associate professor of psychology, Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, described the new findings as “quite impressive” and “extremely encouraging.”
However, she noted “it’s too premature” to suggest widespread use of folic acid in patients with depressive symptoms.
Dr. Yen, who has researched suicide risks previously, was not involved with the current study.
She did agree with the investigators that the results call for “more robustly controlled studies. These could include double-blind, randomized, controlled trials that could “more formally assess” all folic acid usage as opposed to prescriptions only, Dr. Yen said.
The study was funded by the NIH, the Agency for Healthcare Research and Quality, and the Center of Excellence for Suicide Prevention. Dr. Gibbons reported serving as an expert witness in cases for the Department of Justice; receiving expert witness fees from Merck, GlaxoSmithKline, Pfizer, and Wyeth; and having founded Adaptive Testing Technologies, which distributes the Computerized Adaptive Test Suicide Scale. Dr. Yen reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
After adjusting for multiple factors, results from a large pharmaco-epidemiological study showed taking folic acid was associated with a 44% reduction in suicide events.
“These results are really putting folic acid squarely on the map as a potential for large-scale, population-level prevention,” lead author Robert D. Gibbons, PhD, professor of biostatistics, Center for Health Statistics, University of Chicago, said in an interview.
“Folic acid is safe, inexpensive, and generally available, and if future randomized controlled trials show this association is beyond a shadow of a doubt causal, we have a new tool in the arsenal,” Dr. Gibbons said.
Having such a tool would be extremely important given that suicide is such a significant public health crisis worldwide, he added.
The findings were published online in JAMA Psychiatry.
Previous research ‘fairly thin’
Folate, the naturally occurring form of B9, is essential for neurogenesis, nucleotide synthesis, and methylation of homocysteine. Past research has suggested that taking folate can prevent neural tube and heart defects in the fetus during pregnancy – and may prevent strokes and reduce age-related hearing loss in adults.
In psychiatry, the role of folate has been recognized for more than a decade. It may enhance the effects of antidepressants; and folate deficiency can predict poorer response to SSRIs.
This has led to recommendations for folate augmentation in patients with low or normal levels at the start of depression treatment.
Although previous research has shown a link between folic acid and suicidality, the findings have been “fairly thin,” with studies being “generally small, and many are case series,” Dr. Gibbons said.
The current study follows an earlier analysis that used a novel statistical methodology for generating drug safety signals that was developed by Dr. Gibbons and colleagues. That study compared rates of suicide attempts before and after initiation of 922 drugs with at least 3,000 prescriptions.
Its results showed 10 drugs were associated with increased risk after exposure, with the strongest associations for alprazolam, butalbital, hydrocodone, and combination codeine/promethazine. In addition, 44 drugs were associated with decreased risk, many of which were antidepressants and antipsychotics.
“One of the most interesting findings in terms of the decreased risk was for folic acid,” said Dr. Gibbons.
He and his colleagues initially thought this was because of women taking folic acid during pregnancy. But when restricting the analysis to men, they found the same effect.
Their next step was to carry out the current large-scale pharmaco-epidemiological study.
Prescriptions for pain
The researchers used a health claims database that included 164 million enrollees. The study cohort was comprised of 866,586 adults with private health insurance (81.3% women; 10.4% aged 60 years and older) who filled a folic acid prescription between 2012 and 2017.
More than half of the folic acid prescriptions were associated with pain disorders. About 48% were for a single agent at a dosage of 1 mg/d, which is the upper tolerable limit for adults – including in pregnancy and lactation.
Other single-agent daily dosages ranging from 0.4 mg to 5 mg accounted for 0.11% of prescriptions. The remainder were multivitamins.
The participants were followed for 24 months. The within-person analysis compared suicide attempts or self-harm events resulting in an outpatient visit or inpatient admission during periods of folic acid treatment versus during periods without treatment.
During the study period, the overall suicidal event rate was 133 per 100,000 population, which is one-fourth the national rate reported by the National Institutes of Health of 600 per 100,000.
After adjusting for age, sex, diagnoses related to suicidal behavior and folic acid deficiency, history of folate-reducing medications, and history of suicidal events, the estimated hazard ratio for suicide events when taking folic acid was 0.56 (95% confidence interal, 0.48-0.65) – which indicates a 44% reduction in suicide events.
“This is a very large decrease and is extremely significant and exciting,” Dr. Gibbons said.
He noted the decrease in suicidal events may have been even greater considering the study captured only prescription folic acid, and participants may also have also taken over-the-counter products.
“The 44% reduction in suicide attempts may actually be an underestimate,” said Dr. Gibbons.
Age and sex did not moderate the association between folic acid and suicide attempts, and a similar association was found in women of childbearing age.
Provocative results?
The investigators also assessed a negative control group of 236,610 individuals using cyanocobalamin during the study period. Cyanocobalamin is a form of vitamin B12 that is essential for metabolism, blood cell synthesis, and the nervous system. It does not contain folic acid and is commonly used to treat anemia.
Results showed no association between cyanocobalamin and suicidal events in the adjusted analysis (HR, 1.01; 95% CI, 0.80-1.27) or unadjusted analysis (HR, 1.02; 95% CI, 0.80-1.28).
Dr. Gibbons noted this result boosts the argument that the association between folic acid and reduced suicidal attempts “isn’t just about health-seeking behavior like taking vitamin supplements.”
Another sensitivity analysis showed every additional month of treatment was associated with a 5% reduction in the suicidal event rate.
“This means the longer you take folic acid, the greater the benefit, which is what you would expect to see if there was a real association between a treatment and an outcome,” said Dr. Gibbons.
The new results “are so provocative that they really mandate the need for a well-controlled randomized controlled trial of folic acid and suicide events,” possibly in a high-risk population such as veterans, he noted.
Such a study could use longitudinal assessments of suicidal events, such as the validated Computerized Adaptive Test Suicide Scale, he added. This continuous scale of suicidality ranges from subclinical, signifying helplessness, hopelessness, and loss of pleasure, to suicide attempts and completion.
As for study limitations, the investigators noted that this study was observational, so there could be selection effects. And using claims data likely underrepresented the number of suicidal events because of incomplete reporting. As the researchers pointed out, the rate of suicidal events in this study was much lower than the national rate.
Other limitations cited were that the association between folic acid and suicidal events may be explained by healthy user bias; and although the investigators conducted a sensitivity analysis in women of childbearing age, they did not have data on women actively planning for a pregnancy.
‘Impressive, encouraging’
In a comment, Shirley Yen, PhD, associate professor of psychology, Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, described the new findings as “quite impressive” and “extremely encouraging.”
However, she noted “it’s too premature” to suggest widespread use of folic acid in patients with depressive symptoms.
Dr. Yen, who has researched suicide risks previously, was not involved with the current study.
She did agree with the investigators that the results call for “more robustly controlled studies. These could include double-blind, randomized, controlled trials that could “more formally assess” all folic acid usage as opposed to prescriptions only, Dr. Yen said.
The study was funded by the NIH, the Agency for Healthcare Research and Quality, and the Center of Excellence for Suicide Prevention. Dr. Gibbons reported serving as an expert witness in cases for the Department of Justice; receiving expert witness fees from Merck, GlaxoSmithKline, Pfizer, and Wyeth; and having founded Adaptive Testing Technologies, which distributes the Computerized Adaptive Test Suicide Scale. Dr. Yen reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
After adjusting for multiple factors, results from a large pharmaco-epidemiological study showed taking folic acid was associated with a 44% reduction in suicide events.
“These results are really putting folic acid squarely on the map as a potential for large-scale, population-level prevention,” lead author Robert D. Gibbons, PhD, professor of biostatistics, Center for Health Statistics, University of Chicago, said in an interview.
“Folic acid is safe, inexpensive, and generally available, and if future randomized controlled trials show this association is beyond a shadow of a doubt causal, we have a new tool in the arsenal,” Dr. Gibbons said.
Having such a tool would be extremely important given that suicide is such a significant public health crisis worldwide, he added.
The findings were published online in JAMA Psychiatry.
Previous research ‘fairly thin’
Folate, the naturally occurring form of B9, is essential for neurogenesis, nucleotide synthesis, and methylation of homocysteine. Past research has suggested that taking folate can prevent neural tube and heart defects in the fetus during pregnancy – and may prevent strokes and reduce age-related hearing loss in adults.
In psychiatry, the role of folate has been recognized for more than a decade. It may enhance the effects of antidepressants; and folate deficiency can predict poorer response to SSRIs.
This has led to recommendations for folate augmentation in patients with low or normal levels at the start of depression treatment.
Although previous research has shown a link between folic acid and suicidality, the findings have been “fairly thin,” with studies being “generally small, and many are case series,” Dr. Gibbons said.
The current study follows an earlier analysis that used a novel statistical methodology for generating drug safety signals that was developed by Dr. Gibbons and colleagues. That study compared rates of suicide attempts before and after initiation of 922 drugs with at least 3,000 prescriptions.
Its results showed 10 drugs were associated with increased risk after exposure, with the strongest associations for alprazolam, butalbital, hydrocodone, and combination codeine/promethazine. In addition, 44 drugs were associated with decreased risk, many of which were antidepressants and antipsychotics.
“One of the most interesting findings in terms of the decreased risk was for folic acid,” said Dr. Gibbons.
He and his colleagues initially thought this was because of women taking folic acid during pregnancy. But when restricting the analysis to men, they found the same effect.
Their next step was to carry out the current large-scale pharmaco-epidemiological study.
Prescriptions for pain
The researchers used a health claims database that included 164 million enrollees. The study cohort was comprised of 866,586 adults with private health insurance (81.3% women; 10.4% aged 60 years and older) who filled a folic acid prescription between 2012 and 2017.
More than half of the folic acid prescriptions were associated with pain disorders. About 48% were for a single agent at a dosage of 1 mg/d, which is the upper tolerable limit for adults – including in pregnancy and lactation.
Other single-agent daily dosages ranging from 0.4 mg to 5 mg accounted for 0.11% of prescriptions. The remainder were multivitamins.
The participants were followed for 24 months. The within-person analysis compared suicide attempts or self-harm events resulting in an outpatient visit or inpatient admission during periods of folic acid treatment versus during periods without treatment.
During the study period, the overall suicidal event rate was 133 per 100,000 population, which is one-fourth the national rate reported by the National Institutes of Health of 600 per 100,000.
After adjusting for age, sex, diagnoses related to suicidal behavior and folic acid deficiency, history of folate-reducing medications, and history of suicidal events, the estimated hazard ratio for suicide events when taking folic acid was 0.56 (95% confidence interal, 0.48-0.65) – which indicates a 44% reduction in suicide events.
“This is a very large decrease and is extremely significant and exciting,” Dr. Gibbons said.
He noted the decrease in suicidal events may have been even greater considering the study captured only prescription folic acid, and participants may also have also taken over-the-counter products.
“The 44% reduction in suicide attempts may actually be an underestimate,” said Dr. Gibbons.
Age and sex did not moderate the association between folic acid and suicide attempts, and a similar association was found in women of childbearing age.
Provocative results?
The investigators also assessed a negative control group of 236,610 individuals using cyanocobalamin during the study period. Cyanocobalamin is a form of vitamin B12 that is essential for metabolism, blood cell synthesis, and the nervous system. It does not contain folic acid and is commonly used to treat anemia.
Results showed no association between cyanocobalamin and suicidal events in the adjusted analysis (HR, 1.01; 95% CI, 0.80-1.27) or unadjusted analysis (HR, 1.02; 95% CI, 0.80-1.28).
Dr. Gibbons noted this result boosts the argument that the association between folic acid and reduced suicidal attempts “isn’t just about health-seeking behavior like taking vitamin supplements.”
Another sensitivity analysis showed every additional month of treatment was associated with a 5% reduction in the suicidal event rate.
“This means the longer you take folic acid, the greater the benefit, which is what you would expect to see if there was a real association between a treatment and an outcome,” said Dr. Gibbons.
The new results “are so provocative that they really mandate the need for a well-controlled randomized controlled trial of folic acid and suicide events,” possibly in a high-risk population such as veterans, he noted.
Such a study could use longitudinal assessments of suicidal events, such as the validated Computerized Adaptive Test Suicide Scale, he added. This continuous scale of suicidality ranges from subclinical, signifying helplessness, hopelessness, and loss of pleasure, to suicide attempts and completion.
As for study limitations, the investigators noted that this study was observational, so there could be selection effects. And using claims data likely underrepresented the number of suicidal events because of incomplete reporting. As the researchers pointed out, the rate of suicidal events in this study was much lower than the national rate.
Other limitations cited were that the association between folic acid and suicidal events may be explained by healthy user bias; and although the investigators conducted a sensitivity analysis in women of childbearing age, they did not have data on women actively planning for a pregnancy.
‘Impressive, encouraging’
In a comment, Shirley Yen, PhD, associate professor of psychology, Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, described the new findings as “quite impressive” and “extremely encouraging.”
However, she noted “it’s too premature” to suggest widespread use of folic acid in patients with depressive symptoms.
Dr. Yen, who has researched suicide risks previously, was not involved with the current study.
She did agree with the investigators that the results call for “more robustly controlled studies. These could include double-blind, randomized, controlled trials that could “more formally assess” all folic acid usage as opposed to prescriptions only, Dr. Yen said.
The study was funded by the NIH, the Agency for Healthcare Research and Quality, and the Center of Excellence for Suicide Prevention. Dr. Gibbons reported serving as an expert witness in cases for the Department of Justice; receiving expert witness fees from Merck, GlaxoSmithKline, Pfizer, and Wyeth; and having founded Adaptive Testing Technologies, which distributes the Computerized Adaptive Test Suicide Scale. Dr. Yen reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Had my patient come in today, we may have had other options
Decades ago I saw a patient with non–small cell lung cancer (NSCLC) whose tumor was sent out for next-generation sequencing only to find a HER2 mutation. What to do? Had my patient come in today, we may have had other options.
Multiple studies have shown that trastuzumab (Herceptin, Genentech), as assessed by HER2 overexpression or amplification, has been shown to have essentially no efficacy benefit in NSCLC alone or in combination with chemotherapy. In fact, a randomized, phase 2 study of gemcitabine-cisplatin with or without trastuzumab in HER2 mutation–positive NSCLC essentially showed no difference between gemcitabine-cisplatin or gemcitabine-cisplatin with trastuzumab.
NSCLC has become the poster child for targeted therapies. After all, NSCLC makes up about 85% of all lung cancer cases, some of which are driven by gene mutations or other genetic abnormalities like translocation, fusion, or amplification. Seven of these genetic alterations have Food and Drug Administration–approved targeted drugs: EGFR, ALK, ROS1, BRAF V6006, RET, KRAS, MET, and NTRK fusions. And, now we have a new one: HER2.
In August, the FDA granted accelerated approval of trastuzumab deruxtecan (T-DXd) (Enhertu, Daiichi Sankyo) for the second-line treatment of NSCLC patients with HER alterations. T-DXd is a humanized anti-HER antibody linked to a topoisomerase 1 inhibitor. When given intravenously, the antibody portion of the molecule binds to cells with a mutated HER2 on the surface. The molecule is taken up by the cancer cell and the linker between the antibody and the chemotherapy drug is broken, so the drug will be delivered very specifically only to cancer cells that have a mutated HER2. In theory, they will only target cells with HER alterations and thus should have less toxicity.
Unlike other driver mutations, HER mutations are relatively rare. Roughly 3% of nonsquamous NSCLC tumors carry mutations in the HER2 gene, and they are associated with female sex, never-smokers, and a poor prognosis. Accelerated approved by the FDA was based on data from the DESTINY-Lung 02 phase 2 trial. An interim efficacy analysis of this trial reported an overall response rate to trastuzumab deruxtecan (at 5.4 mg/kg every 3 weeks) of 57.7% in 52 patients. Median duration of response was 8.7 months. Data are also available from the DESTINY-Lung-01 clinical trial, published in the New England Journal of Medicine, in which 91 patients with metastatic HER2-mutant NSCLC that was refractory to standard treatment were treated with T-DXd (at 6.4 mg/kg every 3 weeks). The investigators reported a 55% objective response rate, a median duration of response of 9.3 months, a median progression-free survival (PFS) of 8.2 months, and a median overall survival of almost 18 months.
Companion tests
Biomarker testing is obviously a must in these cases. The FDA-approved companion diagnostic tests to detect HER2 mutations: Life Companion tests, Technologies Corporation’s Oncomine Dx Target Test for use in lung tissue, and Guardant Health’s Guardant360 CDx for use on plasma samples. The agency notes that, if no mutation is detected in a plasma specimen, the tumor tissue should be tested.
Other approvals
T-DXd is also approved for advanced breast and gastric patients who are HER-2 positive. Of note, the majority of HER2-positive NSCLC have HER2 mutations, whereas the majority of HER2-positive breast and gastric cancers have HER2 amplification (increased copy number) or overexpression (increased protein expression).
T-DXd is approved for unresectable or metastatic HER2-positive breast cancer patients who have received a prior anti-HER2–based regimen in the metastatic setting, or in the neoadjuvant or adjuvant setting and have developed disease recurrence during or within 6 months of completing therapy. DESTINY-Breast01 enrolled breast cancer patients who had received two or more prior anti-HER2 therapies in the metastatic setting, and reported a response rate of 60.3% with a median duration of response of 14.8 months.
For patients with locally advanced or metastatic HER2-positive gastric cancer who have received two or more prior therapies, including a trastuzumab-based regimen, approval was based on a randomized, phase 3 study comparing 6.4 mg/kg of T-DXd with physician’s choice – either irinotecan or paclitaxel. Overall survival was 12.5 months in the T-DXd arm, compared with 8.4 months in the irinotecan or paclitaxel arm (hazard ratio, 0.59). Response rates were 40.5% and 11.3%, respectively. Median PFS was 5.6 months in the T-DXd arm, compared with a median PFS of 3.5 months in the chemotherapy arm.
Trastuzumab emtansine vs. trastuzumab deruxtecan
Trastuzumab emtansine (T-DM1, ado-trastuzumab emtansine, Kadcyla) is another antibody-drug conjugate consisting of the humanized monoclonal antibody trastuzumab covalently linked to the antimicrotubule agent DM1. It is also approved for advanced breast cancer patients with HER2-positive disease. Although no studies comparing T-DXd with trastuzumab emtansine have been conducted in lung cancer patients, a randomized, phase 3 trial in patients with HER2-positive advanced breast cancer comparing the two reported an overall response rate of 79.7% of the patients who received trastuzumab deruxtecan and 34.2% of those who received trastuzumab emtansine. Drug-related interstitial lung disease (ILD) occurred in 10.5% of the patients in the trastuzumab deruxtecan group and in 1.9% of those in the trastuzumab emtansine group; at 12 months, 75.8% of the patients in the trastuzumab deruxtecan were alive without progression, compared with 34.1% of those receiving trastuzumab emtansine.
ILDs
In DESTINY-Lung01, ILD occurred in 26% of patients and resulted in death in two patients. Increased rates of ILD were more commonly observed at higher dose levels. Of 491 patients with unresectable or metastatic HER2-positive breast cancer treated with 5.4 mg/kg of T-TDx, ILD occurred in 13% of patients. Fatal outcomes caused by ILD and/or pneumonitis occurred in 1.4% of patients. Median time to first onset was 5.5 months (range, 1.1-20.8 months). In DESTINY-Gastric01, of the 125 patients with locally advanced or metastatic HER2-positive gastric or gastroesophageal junction adenocarcinoma treated with 6.4 mg/kg, T-DXd ILD occurred in 10% of patients. Median time to first onset was 2.8 months (range, 1.2-21.0 months).
Chemotherapy-like adverse effects
Other adverse events are more typically seen with cytotoxic agents and are presumably related to the release of the topoisomerase inhibitor into the blood stream. Although common (occurring in 97% of patients), these adverse events are generally mild (grade 1 or 2). Nausea was reported in about two-thirds of patients. Other side effects occurring in 20% or more of patients included vomiting, decreased appetite, alopecia, and constipation and diarrhea, musculoskeletal pain, and respiratory infections. Laboratory abnormalities occurred in 20% or more of patients included myelosuppression, increased AST, ALT, alkaline phosphatase, and hypokalemia (28%). Grade 3 or higher drug-related adverse events were observed in 46% of patients, with the most common being neutropenia and anemia which was observed in 19% and 10% of patients in the DESTINY-LUNG-01 trial.
Dr. Schiller is a medical oncologist and founding member of Oncologists United for Climate and Health. She is a former board member of the International Association for the Study of Lung Cancer and a current board member of the Lung Cancer Research Foundation.
Decades ago I saw a patient with non–small cell lung cancer (NSCLC) whose tumor was sent out for next-generation sequencing only to find a HER2 mutation. What to do? Had my patient come in today, we may have had other options.
Multiple studies have shown that trastuzumab (Herceptin, Genentech), as assessed by HER2 overexpression or amplification, has been shown to have essentially no efficacy benefit in NSCLC alone or in combination with chemotherapy. In fact, a randomized, phase 2 study of gemcitabine-cisplatin with or without trastuzumab in HER2 mutation–positive NSCLC essentially showed no difference between gemcitabine-cisplatin or gemcitabine-cisplatin with trastuzumab.
NSCLC has become the poster child for targeted therapies. After all, NSCLC makes up about 85% of all lung cancer cases, some of which are driven by gene mutations or other genetic abnormalities like translocation, fusion, or amplification. Seven of these genetic alterations have Food and Drug Administration–approved targeted drugs: EGFR, ALK, ROS1, BRAF V6006, RET, KRAS, MET, and NTRK fusions. And, now we have a new one: HER2.
In August, the FDA granted accelerated approval of trastuzumab deruxtecan (T-DXd) (Enhertu, Daiichi Sankyo) for the second-line treatment of NSCLC patients with HER alterations. T-DXd is a humanized anti-HER antibody linked to a topoisomerase 1 inhibitor. When given intravenously, the antibody portion of the molecule binds to cells with a mutated HER2 on the surface. The molecule is taken up by the cancer cell and the linker between the antibody and the chemotherapy drug is broken, so the drug will be delivered very specifically only to cancer cells that have a mutated HER2. In theory, they will only target cells with HER alterations and thus should have less toxicity.
Unlike other driver mutations, HER mutations are relatively rare. Roughly 3% of nonsquamous NSCLC tumors carry mutations in the HER2 gene, and they are associated with female sex, never-smokers, and a poor prognosis. Accelerated approved by the FDA was based on data from the DESTINY-Lung 02 phase 2 trial. An interim efficacy analysis of this trial reported an overall response rate to trastuzumab deruxtecan (at 5.4 mg/kg every 3 weeks) of 57.7% in 52 patients. Median duration of response was 8.7 months. Data are also available from the DESTINY-Lung-01 clinical trial, published in the New England Journal of Medicine, in which 91 patients with metastatic HER2-mutant NSCLC that was refractory to standard treatment were treated with T-DXd (at 6.4 mg/kg every 3 weeks). The investigators reported a 55% objective response rate, a median duration of response of 9.3 months, a median progression-free survival (PFS) of 8.2 months, and a median overall survival of almost 18 months.
Companion tests
Biomarker testing is obviously a must in these cases. The FDA-approved companion diagnostic tests to detect HER2 mutations: Life Companion tests, Technologies Corporation’s Oncomine Dx Target Test for use in lung tissue, and Guardant Health’s Guardant360 CDx for use on plasma samples. The agency notes that, if no mutation is detected in a plasma specimen, the tumor tissue should be tested.
Other approvals
T-DXd is also approved for advanced breast and gastric patients who are HER-2 positive. Of note, the majority of HER2-positive NSCLC have HER2 mutations, whereas the majority of HER2-positive breast and gastric cancers have HER2 amplification (increased copy number) or overexpression (increased protein expression).
T-DXd is approved for unresectable or metastatic HER2-positive breast cancer patients who have received a prior anti-HER2–based regimen in the metastatic setting, or in the neoadjuvant or adjuvant setting and have developed disease recurrence during or within 6 months of completing therapy. DESTINY-Breast01 enrolled breast cancer patients who had received two or more prior anti-HER2 therapies in the metastatic setting, and reported a response rate of 60.3% with a median duration of response of 14.8 months.
For patients with locally advanced or metastatic HER2-positive gastric cancer who have received two or more prior therapies, including a trastuzumab-based regimen, approval was based on a randomized, phase 3 study comparing 6.4 mg/kg of T-DXd with physician’s choice – either irinotecan or paclitaxel. Overall survival was 12.5 months in the T-DXd arm, compared with 8.4 months in the irinotecan or paclitaxel arm (hazard ratio, 0.59). Response rates were 40.5% and 11.3%, respectively. Median PFS was 5.6 months in the T-DXd arm, compared with a median PFS of 3.5 months in the chemotherapy arm.
Trastuzumab emtansine vs. trastuzumab deruxtecan
Trastuzumab emtansine (T-DM1, ado-trastuzumab emtansine, Kadcyla) is another antibody-drug conjugate consisting of the humanized monoclonal antibody trastuzumab covalently linked to the antimicrotubule agent DM1. It is also approved for advanced breast cancer patients with HER2-positive disease. Although no studies comparing T-DXd with trastuzumab emtansine have been conducted in lung cancer patients, a randomized, phase 3 trial in patients with HER2-positive advanced breast cancer comparing the two reported an overall response rate of 79.7% of the patients who received trastuzumab deruxtecan and 34.2% of those who received trastuzumab emtansine. Drug-related interstitial lung disease (ILD) occurred in 10.5% of the patients in the trastuzumab deruxtecan group and in 1.9% of those in the trastuzumab emtansine group; at 12 months, 75.8% of the patients in the trastuzumab deruxtecan were alive without progression, compared with 34.1% of those receiving trastuzumab emtansine.
ILDs
In DESTINY-Lung01, ILD occurred in 26% of patients and resulted in death in two patients. Increased rates of ILD were more commonly observed at higher dose levels. Of 491 patients with unresectable or metastatic HER2-positive breast cancer treated with 5.4 mg/kg of T-TDx, ILD occurred in 13% of patients. Fatal outcomes caused by ILD and/or pneumonitis occurred in 1.4% of patients. Median time to first onset was 5.5 months (range, 1.1-20.8 months). In DESTINY-Gastric01, of the 125 patients with locally advanced or metastatic HER2-positive gastric or gastroesophageal junction adenocarcinoma treated with 6.4 mg/kg, T-DXd ILD occurred in 10% of patients. Median time to first onset was 2.8 months (range, 1.2-21.0 months).
Chemotherapy-like adverse effects
Other adverse events are more typically seen with cytotoxic agents and are presumably related to the release of the topoisomerase inhibitor into the blood stream. Although common (occurring in 97% of patients), these adverse events are generally mild (grade 1 or 2). Nausea was reported in about two-thirds of patients. Other side effects occurring in 20% or more of patients included vomiting, decreased appetite, alopecia, and constipation and diarrhea, musculoskeletal pain, and respiratory infections. Laboratory abnormalities occurred in 20% or more of patients included myelosuppression, increased AST, ALT, alkaline phosphatase, and hypokalemia (28%). Grade 3 or higher drug-related adverse events were observed in 46% of patients, with the most common being neutropenia and anemia which was observed in 19% and 10% of patients in the DESTINY-LUNG-01 trial.
Dr. Schiller is a medical oncologist and founding member of Oncologists United for Climate and Health. She is a former board member of the International Association for the Study of Lung Cancer and a current board member of the Lung Cancer Research Foundation.
Decades ago I saw a patient with non–small cell lung cancer (NSCLC) whose tumor was sent out for next-generation sequencing only to find a HER2 mutation. What to do? Had my patient come in today, we may have had other options.
Multiple studies have shown that trastuzumab (Herceptin, Genentech), as assessed by HER2 overexpression or amplification, has been shown to have essentially no efficacy benefit in NSCLC alone or in combination with chemotherapy. In fact, a randomized, phase 2 study of gemcitabine-cisplatin with or without trastuzumab in HER2 mutation–positive NSCLC essentially showed no difference between gemcitabine-cisplatin or gemcitabine-cisplatin with trastuzumab.
NSCLC has become the poster child for targeted therapies. After all, NSCLC makes up about 85% of all lung cancer cases, some of which are driven by gene mutations or other genetic abnormalities like translocation, fusion, or amplification. Seven of these genetic alterations have Food and Drug Administration–approved targeted drugs: EGFR, ALK, ROS1, BRAF V6006, RET, KRAS, MET, and NTRK fusions. And, now we have a new one: HER2.
In August, the FDA granted accelerated approval of trastuzumab deruxtecan (T-DXd) (Enhertu, Daiichi Sankyo) for the second-line treatment of NSCLC patients with HER alterations. T-DXd is a humanized anti-HER antibody linked to a topoisomerase 1 inhibitor. When given intravenously, the antibody portion of the molecule binds to cells with a mutated HER2 on the surface. The molecule is taken up by the cancer cell and the linker between the antibody and the chemotherapy drug is broken, so the drug will be delivered very specifically only to cancer cells that have a mutated HER2. In theory, they will only target cells with HER alterations and thus should have less toxicity.
Unlike other driver mutations, HER mutations are relatively rare. Roughly 3% of nonsquamous NSCLC tumors carry mutations in the HER2 gene, and they are associated with female sex, never-smokers, and a poor prognosis. Accelerated approved by the FDA was based on data from the DESTINY-Lung 02 phase 2 trial. An interim efficacy analysis of this trial reported an overall response rate to trastuzumab deruxtecan (at 5.4 mg/kg every 3 weeks) of 57.7% in 52 patients. Median duration of response was 8.7 months. Data are also available from the DESTINY-Lung-01 clinical trial, published in the New England Journal of Medicine, in which 91 patients with metastatic HER2-mutant NSCLC that was refractory to standard treatment were treated with T-DXd (at 6.4 mg/kg every 3 weeks). The investigators reported a 55% objective response rate, a median duration of response of 9.3 months, a median progression-free survival (PFS) of 8.2 months, and a median overall survival of almost 18 months.
Companion tests
Biomarker testing is obviously a must in these cases. The FDA-approved companion diagnostic tests to detect HER2 mutations: Life Companion tests, Technologies Corporation’s Oncomine Dx Target Test for use in lung tissue, and Guardant Health’s Guardant360 CDx for use on plasma samples. The agency notes that, if no mutation is detected in a plasma specimen, the tumor tissue should be tested.
Other approvals
T-DXd is also approved for advanced breast and gastric patients who are HER-2 positive. Of note, the majority of HER2-positive NSCLC have HER2 mutations, whereas the majority of HER2-positive breast and gastric cancers have HER2 amplification (increased copy number) or overexpression (increased protein expression).
T-DXd is approved for unresectable or metastatic HER2-positive breast cancer patients who have received a prior anti-HER2–based regimen in the metastatic setting, or in the neoadjuvant or adjuvant setting and have developed disease recurrence during or within 6 months of completing therapy. DESTINY-Breast01 enrolled breast cancer patients who had received two or more prior anti-HER2 therapies in the metastatic setting, and reported a response rate of 60.3% with a median duration of response of 14.8 months.
For patients with locally advanced or metastatic HER2-positive gastric cancer who have received two or more prior therapies, including a trastuzumab-based regimen, approval was based on a randomized, phase 3 study comparing 6.4 mg/kg of T-DXd with physician’s choice – either irinotecan or paclitaxel. Overall survival was 12.5 months in the T-DXd arm, compared with 8.4 months in the irinotecan or paclitaxel arm (hazard ratio, 0.59). Response rates were 40.5% and 11.3%, respectively. Median PFS was 5.6 months in the T-DXd arm, compared with a median PFS of 3.5 months in the chemotherapy arm.
Trastuzumab emtansine vs. trastuzumab deruxtecan
Trastuzumab emtansine (T-DM1, ado-trastuzumab emtansine, Kadcyla) is another antibody-drug conjugate consisting of the humanized monoclonal antibody trastuzumab covalently linked to the antimicrotubule agent DM1. It is also approved for advanced breast cancer patients with HER2-positive disease. Although no studies comparing T-DXd with trastuzumab emtansine have been conducted in lung cancer patients, a randomized, phase 3 trial in patients with HER2-positive advanced breast cancer comparing the two reported an overall response rate of 79.7% of the patients who received trastuzumab deruxtecan and 34.2% of those who received trastuzumab emtansine. Drug-related interstitial lung disease (ILD) occurred in 10.5% of the patients in the trastuzumab deruxtecan group and in 1.9% of those in the trastuzumab emtansine group; at 12 months, 75.8% of the patients in the trastuzumab deruxtecan were alive without progression, compared with 34.1% of those receiving trastuzumab emtansine.
ILDs
In DESTINY-Lung01, ILD occurred in 26% of patients and resulted in death in two patients. Increased rates of ILD were more commonly observed at higher dose levels. Of 491 patients with unresectable or metastatic HER2-positive breast cancer treated with 5.4 mg/kg of T-TDx, ILD occurred in 13% of patients. Fatal outcomes caused by ILD and/or pneumonitis occurred in 1.4% of patients. Median time to first onset was 5.5 months (range, 1.1-20.8 months). In DESTINY-Gastric01, of the 125 patients with locally advanced or metastatic HER2-positive gastric or gastroesophageal junction adenocarcinoma treated with 6.4 mg/kg, T-DXd ILD occurred in 10% of patients. Median time to first onset was 2.8 months (range, 1.2-21.0 months).
Chemotherapy-like adverse effects
Other adverse events are more typically seen with cytotoxic agents and are presumably related to the release of the topoisomerase inhibitor into the blood stream. Although common (occurring in 97% of patients), these adverse events are generally mild (grade 1 or 2). Nausea was reported in about two-thirds of patients. Other side effects occurring in 20% or more of patients included vomiting, decreased appetite, alopecia, and constipation and diarrhea, musculoskeletal pain, and respiratory infections. Laboratory abnormalities occurred in 20% or more of patients included myelosuppression, increased AST, ALT, alkaline phosphatase, and hypokalemia (28%). Grade 3 or higher drug-related adverse events were observed in 46% of patients, with the most common being neutropenia and anemia which was observed in 19% and 10% of patients in the DESTINY-LUNG-01 trial.
Dr. Schiller is a medical oncologist and founding member of Oncologists United for Climate and Health. She is a former board member of the International Association for the Study of Lung Cancer and a current board member of the Lung Cancer Research Foundation.
SMART-CHOICE 3-year results support dropping aspirin after PCI
Shortening the duration of dual-antiplatelet therapy (DAPT) and continuing with a P2Y12 inhibitor alone after percutaneous coronary intervention (PCI) was associated with a similar rate of ischemic events but with less bleeding than prolonged DAPT after 3 years of follow-up in the SMART-CHOICE trial.
“The current the investigators, with lead author Ki Hong Choi, MD, division of cardiology, department of medicine, Samsung Medical Center, Sungkyunkwan University, Seoul, South Korea, conclude.
The 3-year results from the study were published online in JAMA Cardiology.
The authors explain that although dual therapy with aspirin and a P2Y12 inhibitor after PCI with a drug-eluting stent (DES) is crucial to reduce the risk of ischemic events, it raises concerns about increased risk of bleeding, and the antiplatelet strategy after PCI is currently shifting to reduce the duration of DAPT.
Several recent randomized studies have consistently shown that a short duration of DAPT (1-3 months) followed by P2Y12 inhibitor monotherapy had ischemia protection effects comparable with that of DAPT of longer duration, and it was associated with a significantly reduced risk of bleeding events in patients who underwent PCI, they note. However, these studies have so far reported only 1-year outcomes, and long-term results are not yet available.
The SMART-CHOICE trial compared two antiplatelet strategies – 3 months of DAPT followed by long-term P2Y12 inhibitor monotherapy (mainly with clopidogrel) or prolonged DAPT for 12 months or longer – in 2,993 patients who had undergone PCI with a drug-eluting stent. Results at 12 months showed a similar rate of ischemic events with both strategies but a lower rate of bleeding in the group that received shortened DAPT.
The SMART-CHOICE investigators now report the 3-year results showing similar outcomes.
At 3 years, the primary endpoint, a composite of all-cause death, myocardial infarction, or stroke, had occurred in 6.3% of the shortened DAPT group and 6.1% in the prolonged DAPT group, giving a hazard ratio of 1.06 (95% confidence interval, 0.79-1.44).
But in the shortened DAPT group, the risk of bleeding was reduced. Bleeding Academic Research Consortium (BARC) types 2-5 bleeding had occurred in 3.2% of the shortened DAPT group and in 8.2% of the prolonged DAPT group (hazard ratio, 0.39; 95% CI, 0.28-0.55). Major bleeding, BARC types 3-5, occurred in 1.2% of the shortened DAPT group and in 2.4% of the prolonged DAPT group (HR, 0.56; 95% CI 0.31-0.99).
The landmark analyses between 3 months and 3 years and per-protocol analyses showed consistent results.
The researchers point out that this is the first trial to report on the long-term safety and efficacy of P2Y12-inhibitor monotherapy as long-term maintenance therapy for stable patients treated with PCI.
“Especially considering that extended DAPT significantly reduced the risks of ischemic events compared with aspirin monotherapy in a couple of trials, comparison between P2Y12-inhibitor monotherapy and prolonged DAPT for recurrent ischemic events over a longer period beyond 1 year is of great importance,” they say.
They cite two other trials – HOST-EXAM and GLOBAL LEADERS – which have shown P2Y12-inhibitor monotherapy to be superior to aspirin monotherapy in preventing both ischemic and bleeding events during the long-term maintenance period after PCI.
“Combining the results of the current study, HOST-EXAM trial, and landmark analysis of the GLOBAL LEADERS trial, long-term P2Y12-inhibitor monotherapy after a minimum period of DAPT might be the most reliable option from among aspirin monotherapy, P2Y12 monotherapy, and extended DAPT for maintenance therapy after stabilizing patients who have undergone PCI with a current-generation DES,” they conclude.
They note that the American College of Cardiology/American Heart Association/Society for Cardiovascular Angiography and Interventions guidelines for coronary artery revascularization newly recommends a shorter course of DAPT followed by P2Y12 monotherapy as a class IIa indication. The recommendation is based on results of five large, randomized clinical trials, including SMART-CHOICE, TWILIGHT, STOPDAPT-2, TICO, and GLOBAL LEADERS.
“The current results of extended follow-up from the SMART-CHOICE trial support evidence of aspirin-dropping strategy with indefinite use of P2Y12 inhibitor after minimum use of DAPT in patients who underwent PCI,” they say.
They point out that two further trials, A-CLOSE in high-risk patients and SMART-CHOICE III, will be helpful to confirm these findings.
P2Y12-inhibitor monotherapy ‘attractive concept’
In an accompanying editor’s note, Ajay Kirtane, MD, Columbia University Irving Medical Center/New York–Presbyterian Hospital, New York, and Roxana Mehran, MD, Icahn School of Medicine at Mount Sinai and the Cardiovascular Research Foundation, New York, note that current guidelines recommend 3-6 months of DAPT following PCI with current-generation drug-eluting stents in stable patients and 6-12 months or longer for those with acute coronary syndromes. For patients at higher risk of bleeding, even shorter DAPT durations can be considered on a case-by-case basis.
Historically, the component of DAPT subject to discontinuation decisions was the P2Y12 inhibitor (clopidogrel, prasugrel, or ticagrelor), but more recent trials have further explored whether discontinuation of the aspirin component of DAPT can mitigate bleeding while preserving anti-ischemic efficacy.
The editorialists explain that the concept of P2Y1-inhibitor monotherapy is attractive because it may optimize antiplatelet effects through a single agent that can avoid the gastrointestinal toxicity of aspirin as well as the increased bleeding that comes with combing multiple antithrombotic agents.
They suggest that the long-term results from the SMART-CHOICE trial “should lead clinicians to consider a strategy of monotherapy after a short period of DAPT as a viable one to mitigate bleeding risk,” although they also point out that SMART-CHOICE was underpowered to rigorously assess ischemic differences, so caution is warranted.
“For patients at greatest risk for recurrent ischemic events, the role of continued DAPT is always an option, but these data (and other consistent trials) give clinicians more options to pursue individualized treatment decisions,” they write.
“To some, the continually moving field of post-PCI antiplatelet therapy has provided too many choices, which can at times be dizzying. To us, every patient is different, and thoughtful evidence-based consideration is increasingly possible for many of our treatment decisions,” they conclude.
The SMART-CHOICE study was supported by unrestricted grants from the Korean Society of Interventional Cardiology, Abbott Vascular, Biotronik, and Boston Scientific.
A version of this article first appeared on Medscape.com.
Shortening the duration of dual-antiplatelet therapy (DAPT) and continuing with a P2Y12 inhibitor alone after percutaneous coronary intervention (PCI) was associated with a similar rate of ischemic events but with less bleeding than prolonged DAPT after 3 years of follow-up in the SMART-CHOICE trial.
“The current the investigators, with lead author Ki Hong Choi, MD, division of cardiology, department of medicine, Samsung Medical Center, Sungkyunkwan University, Seoul, South Korea, conclude.
The 3-year results from the study were published online in JAMA Cardiology.
The authors explain that although dual therapy with aspirin and a P2Y12 inhibitor after PCI with a drug-eluting stent (DES) is crucial to reduce the risk of ischemic events, it raises concerns about increased risk of bleeding, and the antiplatelet strategy after PCI is currently shifting to reduce the duration of DAPT.
Several recent randomized studies have consistently shown that a short duration of DAPT (1-3 months) followed by P2Y12 inhibitor monotherapy had ischemia protection effects comparable with that of DAPT of longer duration, and it was associated with a significantly reduced risk of bleeding events in patients who underwent PCI, they note. However, these studies have so far reported only 1-year outcomes, and long-term results are not yet available.
The SMART-CHOICE trial compared two antiplatelet strategies – 3 months of DAPT followed by long-term P2Y12 inhibitor monotherapy (mainly with clopidogrel) or prolonged DAPT for 12 months or longer – in 2,993 patients who had undergone PCI with a drug-eluting stent. Results at 12 months showed a similar rate of ischemic events with both strategies but a lower rate of bleeding in the group that received shortened DAPT.
The SMART-CHOICE investigators now report the 3-year results showing similar outcomes.
At 3 years, the primary endpoint, a composite of all-cause death, myocardial infarction, or stroke, had occurred in 6.3% of the shortened DAPT group and 6.1% in the prolonged DAPT group, giving a hazard ratio of 1.06 (95% confidence interval, 0.79-1.44).
But in the shortened DAPT group, the risk of bleeding was reduced. Bleeding Academic Research Consortium (BARC) types 2-5 bleeding had occurred in 3.2% of the shortened DAPT group and in 8.2% of the prolonged DAPT group (hazard ratio, 0.39; 95% CI, 0.28-0.55). Major bleeding, BARC types 3-5, occurred in 1.2% of the shortened DAPT group and in 2.4% of the prolonged DAPT group (HR, 0.56; 95% CI 0.31-0.99).
The landmark analyses between 3 months and 3 years and per-protocol analyses showed consistent results.
The researchers point out that this is the first trial to report on the long-term safety and efficacy of P2Y12-inhibitor monotherapy as long-term maintenance therapy for stable patients treated with PCI.
“Especially considering that extended DAPT significantly reduced the risks of ischemic events compared with aspirin monotherapy in a couple of trials, comparison between P2Y12-inhibitor monotherapy and prolonged DAPT for recurrent ischemic events over a longer period beyond 1 year is of great importance,” they say.
They cite two other trials – HOST-EXAM and GLOBAL LEADERS – which have shown P2Y12-inhibitor monotherapy to be superior to aspirin monotherapy in preventing both ischemic and bleeding events during the long-term maintenance period after PCI.
“Combining the results of the current study, HOST-EXAM trial, and landmark analysis of the GLOBAL LEADERS trial, long-term P2Y12-inhibitor monotherapy after a minimum period of DAPT might be the most reliable option from among aspirin monotherapy, P2Y12 monotherapy, and extended DAPT for maintenance therapy after stabilizing patients who have undergone PCI with a current-generation DES,” they conclude.
They note that the American College of Cardiology/American Heart Association/Society for Cardiovascular Angiography and Interventions guidelines for coronary artery revascularization newly recommends a shorter course of DAPT followed by P2Y12 monotherapy as a class IIa indication. The recommendation is based on results of five large, randomized clinical trials, including SMART-CHOICE, TWILIGHT, STOPDAPT-2, TICO, and GLOBAL LEADERS.
“The current results of extended follow-up from the SMART-CHOICE trial support evidence of aspirin-dropping strategy with indefinite use of P2Y12 inhibitor after minimum use of DAPT in patients who underwent PCI,” they say.
They point out that two further trials, A-CLOSE in high-risk patients and SMART-CHOICE III, will be helpful to confirm these findings.
P2Y12-inhibitor monotherapy ‘attractive concept’
In an accompanying editor’s note, Ajay Kirtane, MD, Columbia University Irving Medical Center/New York–Presbyterian Hospital, New York, and Roxana Mehran, MD, Icahn School of Medicine at Mount Sinai and the Cardiovascular Research Foundation, New York, note that current guidelines recommend 3-6 months of DAPT following PCI with current-generation drug-eluting stents in stable patients and 6-12 months or longer for those with acute coronary syndromes. For patients at higher risk of bleeding, even shorter DAPT durations can be considered on a case-by-case basis.
Historically, the component of DAPT subject to discontinuation decisions was the P2Y12 inhibitor (clopidogrel, prasugrel, or ticagrelor), but more recent trials have further explored whether discontinuation of the aspirin component of DAPT can mitigate bleeding while preserving anti-ischemic efficacy.
The editorialists explain that the concept of P2Y1-inhibitor monotherapy is attractive because it may optimize antiplatelet effects through a single agent that can avoid the gastrointestinal toxicity of aspirin as well as the increased bleeding that comes with combing multiple antithrombotic agents.
They suggest that the long-term results from the SMART-CHOICE trial “should lead clinicians to consider a strategy of monotherapy after a short period of DAPT as a viable one to mitigate bleeding risk,” although they also point out that SMART-CHOICE was underpowered to rigorously assess ischemic differences, so caution is warranted.
“For patients at greatest risk for recurrent ischemic events, the role of continued DAPT is always an option, but these data (and other consistent trials) give clinicians more options to pursue individualized treatment decisions,” they write.
“To some, the continually moving field of post-PCI antiplatelet therapy has provided too many choices, which can at times be dizzying. To us, every patient is different, and thoughtful evidence-based consideration is increasingly possible for many of our treatment decisions,” they conclude.
The SMART-CHOICE study was supported by unrestricted grants from the Korean Society of Interventional Cardiology, Abbott Vascular, Biotronik, and Boston Scientific.
A version of this article first appeared on Medscape.com.
Shortening the duration of dual-antiplatelet therapy (DAPT) and continuing with a P2Y12 inhibitor alone after percutaneous coronary intervention (PCI) was associated with a similar rate of ischemic events but with less bleeding than prolonged DAPT after 3 years of follow-up in the SMART-CHOICE trial.
“The current the investigators, with lead author Ki Hong Choi, MD, division of cardiology, department of medicine, Samsung Medical Center, Sungkyunkwan University, Seoul, South Korea, conclude.
The 3-year results from the study were published online in JAMA Cardiology.
The authors explain that although dual therapy with aspirin and a P2Y12 inhibitor after PCI with a drug-eluting stent (DES) is crucial to reduce the risk of ischemic events, it raises concerns about increased risk of bleeding, and the antiplatelet strategy after PCI is currently shifting to reduce the duration of DAPT.
Several recent randomized studies have consistently shown that a short duration of DAPT (1-3 months) followed by P2Y12 inhibitor monotherapy had ischemia protection effects comparable with that of DAPT of longer duration, and it was associated with a significantly reduced risk of bleeding events in patients who underwent PCI, they note. However, these studies have so far reported only 1-year outcomes, and long-term results are not yet available.
The SMART-CHOICE trial compared two antiplatelet strategies – 3 months of DAPT followed by long-term P2Y12 inhibitor monotherapy (mainly with clopidogrel) or prolonged DAPT for 12 months or longer – in 2,993 patients who had undergone PCI with a drug-eluting stent. Results at 12 months showed a similar rate of ischemic events with both strategies but a lower rate of bleeding in the group that received shortened DAPT.
The SMART-CHOICE investigators now report the 3-year results showing similar outcomes.
At 3 years, the primary endpoint, a composite of all-cause death, myocardial infarction, or stroke, had occurred in 6.3% of the shortened DAPT group and 6.1% in the prolonged DAPT group, giving a hazard ratio of 1.06 (95% confidence interval, 0.79-1.44).
But in the shortened DAPT group, the risk of bleeding was reduced. Bleeding Academic Research Consortium (BARC) types 2-5 bleeding had occurred in 3.2% of the shortened DAPT group and in 8.2% of the prolonged DAPT group (hazard ratio, 0.39; 95% CI, 0.28-0.55). Major bleeding, BARC types 3-5, occurred in 1.2% of the shortened DAPT group and in 2.4% of the prolonged DAPT group (HR, 0.56; 95% CI 0.31-0.99).
The landmark analyses between 3 months and 3 years and per-protocol analyses showed consistent results.
The researchers point out that this is the first trial to report on the long-term safety and efficacy of P2Y12-inhibitor monotherapy as long-term maintenance therapy for stable patients treated with PCI.
“Especially considering that extended DAPT significantly reduced the risks of ischemic events compared with aspirin monotherapy in a couple of trials, comparison between P2Y12-inhibitor monotherapy and prolonged DAPT for recurrent ischemic events over a longer period beyond 1 year is of great importance,” they say.
They cite two other trials – HOST-EXAM and GLOBAL LEADERS – which have shown P2Y12-inhibitor monotherapy to be superior to aspirin monotherapy in preventing both ischemic and bleeding events during the long-term maintenance period after PCI.
“Combining the results of the current study, HOST-EXAM trial, and landmark analysis of the GLOBAL LEADERS trial, long-term P2Y12-inhibitor monotherapy after a minimum period of DAPT might be the most reliable option from among aspirin monotherapy, P2Y12 monotherapy, and extended DAPT for maintenance therapy after stabilizing patients who have undergone PCI with a current-generation DES,” they conclude.
They note that the American College of Cardiology/American Heart Association/Society for Cardiovascular Angiography and Interventions guidelines for coronary artery revascularization newly recommends a shorter course of DAPT followed by P2Y12 monotherapy as a class IIa indication. The recommendation is based on results of five large, randomized clinical trials, including SMART-CHOICE, TWILIGHT, STOPDAPT-2, TICO, and GLOBAL LEADERS.
“The current results of extended follow-up from the SMART-CHOICE trial support evidence of aspirin-dropping strategy with indefinite use of P2Y12 inhibitor after minimum use of DAPT in patients who underwent PCI,” they say.
They point out that two further trials, A-CLOSE in high-risk patients and SMART-CHOICE III, will be helpful to confirm these findings.
P2Y12-inhibitor monotherapy ‘attractive concept’
In an accompanying editor’s note, Ajay Kirtane, MD, Columbia University Irving Medical Center/New York–Presbyterian Hospital, New York, and Roxana Mehran, MD, Icahn School of Medicine at Mount Sinai and the Cardiovascular Research Foundation, New York, note that current guidelines recommend 3-6 months of DAPT following PCI with current-generation drug-eluting stents in stable patients and 6-12 months or longer for those with acute coronary syndromes. For patients at higher risk of bleeding, even shorter DAPT durations can be considered on a case-by-case basis.
Historically, the component of DAPT subject to discontinuation decisions was the P2Y12 inhibitor (clopidogrel, prasugrel, or ticagrelor), but more recent trials have further explored whether discontinuation of the aspirin component of DAPT can mitigate bleeding while preserving anti-ischemic efficacy.
The editorialists explain that the concept of P2Y1-inhibitor monotherapy is attractive because it may optimize antiplatelet effects through a single agent that can avoid the gastrointestinal toxicity of aspirin as well as the increased bleeding that comes with combing multiple antithrombotic agents.
They suggest that the long-term results from the SMART-CHOICE trial “should lead clinicians to consider a strategy of monotherapy after a short period of DAPT as a viable one to mitigate bleeding risk,” although they also point out that SMART-CHOICE was underpowered to rigorously assess ischemic differences, so caution is warranted.
“For patients at greatest risk for recurrent ischemic events, the role of continued DAPT is always an option, but these data (and other consistent trials) give clinicians more options to pursue individualized treatment decisions,” they write.
“To some, the continually moving field of post-PCI antiplatelet therapy has provided too many choices, which can at times be dizzying. To us, every patient is different, and thoughtful evidence-based consideration is increasingly possible for many of our treatment decisions,” they conclude.
The SMART-CHOICE study was supported by unrestricted grants from the Korean Society of Interventional Cardiology, Abbott Vascular, Biotronik, and Boston Scientific.
A version of this article first appeared on Medscape.com.
FROM JAMA CARDIOLOGY
CAR T-cell therapy neurotoxicity linked to NfL elevations
“This is the first study to show NfL levels are elevated even before CAR T treatment is given,” first author Omar H. Butt, MD, PhD, of the Siteman Cancer Center at Barnes-Jewish Hospital and Washington University in St. Louis, said in an interview.
“While unlikely to be the sole driver of [the neurotoxicity], neural injury reflected by NfL may aid in identifying a high-risk subset of patients undergoing cellular therapy,” the authors concluded in the study, published in JAMA Oncology.
CAR T-cell therapy has gained favor for virtually revolutionizing the treatment of some leukemias and lymphomas, however, as many as 40%-60% of patients develop the neurotoxicity side effect, called immune effector cell–associated neurotoxicity syndrome (ICANS), which, though usually low grade, in more severe cases can cause substantial morbidity and even mortality.
Hence, “the early identification of patients at risk for ICANS is critical for preemptive management,” the authors noted.
NfL, an established marker of neuroaxonal injury in neurodegenerative diseases including multiple sclerosis and Alzheimer’s disease, has been shown in previous studies to be elevated following the development of ICANS and up to 5 days prior to its peak symptoms.
To further evaluate NfL elevations in relation to ICANS, Dr. Butt and colleagues identified 30 patients undergoing CD19 CART-cell therapy, including 77% for diffuse large B-cell lymphoma, at two U.S. centers: Washington University in St. Louis and Case Western Reserve University, Cleveland.
The patients had a median age of 64 and were 40% female.
Among them, four developed low-grade ICANS grade 1-2, and 7 developed ICANS grade 3 or higher.
Of those developing any-grade ICANS, baseline elevations of NfL prior to the CAR T-cell treatment, were significantly higher, compared with those who did not develop ICANs (mean 87.6 pg/mL vs. 29.4 pg/mL, P < .001), with no significant differences between the low-grade (1 and 2) and higher-grade (3 or higher) ICANS groups.
A receiver operating characteristic analysis showed baseline NfL levels significantly predicted the development of ICANS with high accuracy (area under the ROC curve, 0.96), as well as sensitivity (AUROC, 0.91) and specificity (AUROC, 0.95).
Notably, baseline NfL levels were associated with ICANS severity, but did not correlate with other factors including demographic, oncologic history, nononcologic neurologic history, or history of exposure to neurotoxic therapies.
However, Dr. Butt added, “it is important to note that our study was insufficiently powered to examine those relationships in earnest. Therefore, [a correlation between NfL and those factors] remains possible,” he said.
The elevated NfL levels observed prior to the development of ICANS remained high across the study’s seven time points, up to day 30 post infusion.
Interest in NfL levels on the rise
NfL assessment is currently only clinically validated in amyotrophic lateral sclerosis, where it is used to assess neuroaxonal health and integrity. However, testing is available as interest and evidence of NfL’s potential role in other settings grows.
Meanwhile, Dr. Butt and associates are themselves developing an assay to predict the development of ICANS, which will likely include NfL, if the role is validated in further studies.
“Future studies will explore validating NfL for ICANS and additional indications,” he said.
ICANS symptoms can range from headaches and confusion to seizures or strokes in more severe cases.
The current gold standard for treatment includes early intervention with high-dose steroids and careful monitoring, but there is reluctance to use such therapies because of concerns about their blunting the anticancer effects of the CAR T cells.
Importantly, if validated, elevations in NfL could signal the need for more precautionary measures with CAR T-cell therapy, Dr. Butt noted.
“Our data suggests patients with high NfL levels at baseline would benefit most from perhaps closer monitoring with frequent checks and possible early intervention at the first sign of symptoms, a period of time when it may be hard to distinguish ICANS from other causes of confusion, such as delirium,” he explained.
Limitations: Validation, preventive measures needed
Commenting on the study, Sattva S. Neelapu, MD, a professor and deputy chair of the department of lymphoma and myeloma at the University of Texas MD Anderson Cancer Center, Houston, agreed that the findings have potentially important implications.
“I think this is a very intriguing and novel finding that needs to be investigated further prospectively in a larger cohort and across different CAR T products in patients with lymphoma, leukemia, and myeloma,” Dr. Neelapu said in an interview.
The NfL elevations observed even before CAR T-cell therapy among those who went on to develop ICANS are notable, he added.
“This is the surprising finding in the study,” Dr. Neelapu said. “It raises the question whether neurologic injury is caused by prior therapies that these patients received or whether it is an age-related phenomenon, as we do see higher incidence and severity of ICANS in older patients or some other mechanisms.”
A key caveat, however, is that even if a risk is identified, options to prevent ICANS are currently limited, Dr. Neelapu noted.
“I think it is too early to implement this into clinical practice,” he said. In addition to needing further validation, “assessing NfL levels would be useful when there is an effective prophylactic or therapeutic strategy – both of which also need to be investigated.”
Dr. Butt and colleagues are developing a clinical assay for ICANS and reported a provisional patent pending on the use of plasma NfL as a predictive biomarker for ICANS. The study received support from the Washington University in St. Louis, the Paula and Rodger O. Riney Fund, the Daniel J. Brennan MD Fund, the Fred Simmons and Olga Mohan Fund; the National Cancer Institute, the National Multiple Sclerosis Society, and the National Institute of Neurological Disorders and Stroke. Dr. Neelapu reported conflicts of interest with numerous pharmaceutical companies.
“This is the first study to show NfL levels are elevated even before CAR T treatment is given,” first author Omar H. Butt, MD, PhD, of the Siteman Cancer Center at Barnes-Jewish Hospital and Washington University in St. Louis, said in an interview.
“While unlikely to be the sole driver of [the neurotoxicity], neural injury reflected by NfL may aid in identifying a high-risk subset of patients undergoing cellular therapy,” the authors concluded in the study, published in JAMA Oncology.
CAR T-cell therapy has gained favor for virtually revolutionizing the treatment of some leukemias and lymphomas, however, as many as 40%-60% of patients develop the neurotoxicity side effect, called immune effector cell–associated neurotoxicity syndrome (ICANS), which, though usually low grade, in more severe cases can cause substantial morbidity and even mortality.
Hence, “the early identification of patients at risk for ICANS is critical for preemptive management,” the authors noted.
NfL, an established marker of neuroaxonal injury in neurodegenerative diseases including multiple sclerosis and Alzheimer’s disease, has been shown in previous studies to be elevated following the development of ICANS and up to 5 days prior to its peak symptoms.
To further evaluate NfL elevations in relation to ICANS, Dr. Butt and colleagues identified 30 patients undergoing CD19 CART-cell therapy, including 77% for diffuse large B-cell lymphoma, at two U.S. centers: Washington University in St. Louis and Case Western Reserve University, Cleveland.
The patients had a median age of 64 and were 40% female.
Among them, four developed low-grade ICANS grade 1-2, and 7 developed ICANS grade 3 or higher.
Of those developing any-grade ICANS, baseline elevations of NfL prior to the CAR T-cell treatment, were significantly higher, compared with those who did not develop ICANs (mean 87.6 pg/mL vs. 29.4 pg/mL, P < .001), with no significant differences between the low-grade (1 and 2) and higher-grade (3 or higher) ICANS groups.
A receiver operating characteristic analysis showed baseline NfL levels significantly predicted the development of ICANS with high accuracy (area under the ROC curve, 0.96), as well as sensitivity (AUROC, 0.91) and specificity (AUROC, 0.95).
Notably, baseline NfL levels were associated with ICANS severity, but did not correlate with other factors including demographic, oncologic history, nononcologic neurologic history, or history of exposure to neurotoxic therapies.
However, Dr. Butt added, “it is important to note that our study was insufficiently powered to examine those relationships in earnest. Therefore, [a correlation between NfL and those factors] remains possible,” he said.
The elevated NfL levels observed prior to the development of ICANS remained high across the study’s seven time points, up to day 30 post infusion.
Interest in NfL levels on the rise
NfL assessment is currently only clinically validated in amyotrophic lateral sclerosis, where it is used to assess neuroaxonal health and integrity. However, testing is available as interest and evidence of NfL’s potential role in other settings grows.
Meanwhile, Dr. Butt and associates are themselves developing an assay to predict the development of ICANS, which will likely include NfL, if the role is validated in further studies.
“Future studies will explore validating NfL for ICANS and additional indications,” he said.
ICANS symptoms can range from headaches and confusion to seizures or strokes in more severe cases.
The current gold standard for treatment includes early intervention with high-dose steroids and careful monitoring, but there is reluctance to use such therapies because of concerns about their blunting the anticancer effects of the CAR T cells.
Importantly, if validated, elevations in NfL could signal the need for more precautionary measures with CAR T-cell therapy, Dr. Butt noted.
“Our data suggests patients with high NfL levels at baseline would benefit most from perhaps closer monitoring with frequent checks and possible early intervention at the first sign of symptoms, a period of time when it may be hard to distinguish ICANS from other causes of confusion, such as delirium,” he explained.
Limitations: Validation, preventive measures needed
Commenting on the study, Sattva S. Neelapu, MD, a professor and deputy chair of the department of lymphoma and myeloma at the University of Texas MD Anderson Cancer Center, Houston, agreed that the findings have potentially important implications.
“I think this is a very intriguing and novel finding that needs to be investigated further prospectively in a larger cohort and across different CAR T products in patients with lymphoma, leukemia, and myeloma,” Dr. Neelapu said in an interview.
The NfL elevations observed even before CAR T-cell therapy among those who went on to develop ICANS are notable, he added.
“This is the surprising finding in the study,” Dr. Neelapu said. “It raises the question whether neurologic injury is caused by prior therapies that these patients received or whether it is an age-related phenomenon, as we do see higher incidence and severity of ICANS in older patients or some other mechanisms.”
A key caveat, however, is that even if a risk is identified, options to prevent ICANS are currently limited, Dr. Neelapu noted.
“I think it is too early to implement this into clinical practice,” he said. In addition to needing further validation, “assessing NfL levels would be useful when there is an effective prophylactic or therapeutic strategy – both of which also need to be investigated.”
Dr. Butt and colleagues are developing a clinical assay for ICANS and reported a provisional patent pending on the use of plasma NfL as a predictive biomarker for ICANS. The study received support from the Washington University in St. Louis, the Paula and Rodger O. Riney Fund, the Daniel J. Brennan MD Fund, the Fred Simmons and Olga Mohan Fund; the National Cancer Institute, the National Multiple Sclerosis Society, and the National Institute of Neurological Disorders and Stroke. Dr. Neelapu reported conflicts of interest with numerous pharmaceutical companies.
“This is the first study to show NfL levels are elevated even before CAR T treatment is given,” first author Omar H. Butt, MD, PhD, of the Siteman Cancer Center at Barnes-Jewish Hospital and Washington University in St. Louis, said in an interview.
“While unlikely to be the sole driver of [the neurotoxicity], neural injury reflected by NfL may aid in identifying a high-risk subset of patients undergoing cellular therapy,” the authors concluded in the study, published in JAMA Oncology.
CAR T-cell therapy has gained favor for virtually revolutionizing the treatment of some leukemias and lymphomas, however, as many as 40%-60% of patients develop the neurotoxicity side effect, called immune effector cell–associated neurotoxicity syndrome (ICANS), which, though usually low grade, in more severe cases can cause substantial morbidity and even mortality.
Hence, “the early identification of patients at risk for ICANS is critical for preemptive management,” the authors noted.
NfL, an established marker of neuroaxonal injury in neurodegenerative diseases including multiple sclerosis and Alzheimer’s disease, has been shown in previous studies to be elevated following the development of ICANS and up to 5 days prior to its peak symptoms.
To further evaluate NfL elevations in relation to ICANS, Dr. Butt and colleagues identified 30 patients undergoing CD19 CART-cell therapy, including 77% for diffuse large B-cell lymphoma, at two U.S. centers: Washington University in St. Louis and Case Western Reserve University, Cleveland.
The patients had a median age of 64 and were 40% female.
Among them, four developed low-grade ICANS grade 1-2, and 7 developed ICANS grade 3 or higher.
Of those developing any-grade ICANS, baseline elevations of NfL prior to the CAR T-cell treatment, were significantly higher, compared with those who did not develop ICANs (mean 87.6 pg/mL vs. 29.4 pg/mL, P < .001), with no significant differences between the low-grade (1 and 2) and higher-grade (3 or higher) ICANS groups.
A receiver operating characteristic analysis showed baseline NfL levels significantly predicted the development of ICANS with high accuracy (area under the ROC curve, 0.96), as well as sensitivity (AUROC, 0.91) and specificity (AUROC, 0.95).
Notably, baseline NfL levels were associated with ICANS severity, but did not correlate with other factors including demographic, oncologic history, nononcologic neurologic history, or history of exposure to neurotoxic therapies.
However, Dr. Butt added, “it is important to note that our study was insufficiently powered to examine those relationships in earnest. Therefore, [a correlation between NfL and those factors] remains possible,” he said.
The elevated NfL levels observed prior to the development of ICANS remained high across the study’s seven time points, up to day 30 post infusion.
Interest in NfL levels on the rise
NfL assessment is currently only clinically validated in amyotrophic lateral sclerosis, where it is used to assess neuroaxonal health and integrity. However, testing is available as interest and evidence of NfL’s potential role in other settings grows.
Meanwhile, Dr. Butt and associates are themselves developing an assay to predict the development of ICANS, which will likely include NfL, if the role is validated in further studies.
“Future studies will explore validating NfL for ICANS and additional indications,” he said.
ICANS symptoms can range from headaches and confusion to seizures or strokes in more severe cases.
The current gold standard for treatment includes early intervention with high-dose steroids and careful monitoring, but there is reluctance to use such therapies because of concerns about their blunting the anticancer effects of the CAR T cells.
Importantly, if validated, elevations in NfL could signal the need for more precautionary measures with CAR T-cell therapy, Dr. Butt noted.
“Our data suggests patients with high NfL levels at baseline would benefit most from perhaps closer monitoring with frequent checks and possible early intervention at the first sign of symptoms, a period of time when it may be hard to distinguish ICANS from other causes of confusion, such as delirium,” he explained.
Limitations: Validation, preventive measures needed
Commenting on the study, Sattva S. Neelapu, MD, a professor and deputy chair of the department of lymphoma and myeloma at the University of Texas MD Anderson Cancer Center, Houston, agreed that the findings have potentially important implications.
“I think this is a very intriguing and novel finding that needs to be investigated further prospectively in a larger cohort and across different CAR T products in patients with lymphoma, leukemia, and myeloma,” Dr. Neelapu said in an interview.
The NfL elevations observed even before CAR T-cell therapy among those who went on to develop ICANS are notable, he added.
“This is the surprising finding in the study,” Dr. Neelapu said. “It raises the question whether neurologic injury is caused by prior therapies that these patients received or whether it is an age-related phenomenon, as we do see higher incidence and severity of ICANS in older patients or some other mechanisms.”
A key caveat, however, is that even if a risk is identified, options to prevent ICANS are currently limited, Dr. Neelapu noted.
“I think it is too early to implement this into clinical practice,” he said. In addition to needing further validation, “assessing NfL levels would be useful when there is an effective prophylactic or therapeutic strategy – both of which also need to be investigated.”
Dr. Butt and colleagues are developing a clinical assay for ICANS and reported a provisional patent pending on the use of plasma NfL as a predictive biomarker for ICANS. The study received support from the Washington University in St. Louis, the Paula and Rodger O. Riney Fund, the Daniel J. Brennan MD Fund, the Fred Simmons and Olga Mohan Fund; the National Cancer Institute, the National Multiple Sclerosis Society, and the National Institute of Neurological Disorders and Stroke. Dr. Neelapu reported conflicts of interest with numerous pharmaceutical companies.
FROM JAMA ONCOLOGY
Ezetimibe-statin combo lowers liver fat in open-label trial
Ezetimibe given in combination with rosuvastatin has a beneficial effect on liver fat in people with nonalcoholic fatty liver disease (NAFLD), according results of a randomized, active-controlled trial.
The findings, which come from the investigator-initiated ESSENTIAL trial, are likely to add to the debate over whether or not the lipid-lowering combination could be of benefit beyond its effects in the blood.
“We used magnetic resonance imaging-derived proton density fat fraction [MRI-PDFF], which is highly reliable method of assessing hepatic steatosis,” Youngjoon Kim, PhD, one of the study investigators, said at the annual meeting of the European Association for the Study of Diabetes in Barcelona.
“It enables accurate, repeatable and reproducible quantitative assessment of liver fat over the entire liver,” observed Dr. Kim, who works at Severance Hospital, part of Yonsei University in Seoul.
He reported that there was a significant 5.8% decrease in liver fat following 24 weeks’ treatment with ezetimibe and rosuvastatin comparing baseline with end of treatment MRI-PDFF values; a drop that was significant (18.2% vs. 12.3%, P < .001).
Rosuvastatin monotherapy also reduced liver fat from 15.0% at baseline to 12.4% after 24 weeks; this drop of 2.6% was also significant (P = .003).
This gave an absolute mean difference between the two study arms of 3.2% (P = .02).
Rationale for the ESSENTIAL study
Dr. Kim observed during his presentation that NAFLD is burgeoning problem around the world. Ezetimibe plus rosuvastatin was a combination treatment already used widely in clinical practice, and there had been some suggestion that ezetimibe might have an effect on liver fat.
“Although the effect of ezetimibe on hepatic steatosis is still controversial, ezetimibe has been reported to reduce visceral fat and improve insulin resistance in several studies” Dr. Kim said.
“Recently, our group reported that the use of ezetimibe affects autophagy of hepatocytes and the NLRP3 [NOD-like receptors containing pyrin domain 3] inflammasome,” he said.
Moreover, he added, “ezetimibe improved NASH [nonalcoholic steatohepatitis] in an animal model. However, the effects of ezetimibe have not been clearly shown in a human study.”
Dr. Kim also acknowledged a prior randomized control trial that had looked at the role of ezetimibe in 50 patients with NASH, but had not shown a benefit for the drug over placebo in terms of liver fat reduction.
Addressing the Hawthorne effect
“The size of the effect by that might actually be more modest due to the Hawthorne effect,” said session chair Onno Holleboom, MD, PhD, of Amsterdam UMC in the Netherlands.
“What we observe in the large clinical trials is an enormous Hawthorne effect – participating in a NAFLD trial makes people live healthier because they have health checks,” he said.
“That’s a major problem for showing efficacy for the intervention arm,” he added, but of course the open design meant that the trial only had intervention arms; “there was no placebo arm.”
A randomized, active-controlled, clinician-initiated trial
The main objective of the ESSENTIAL trial was therefore to take another look at the potential effect of ezetimibe on hepatic steatosis and doing so in the setting of statin therapy.
In all, 70 patients with NAFLD that had been confirmed via ultrasound were recruited into the prospective, single center, phase 4 trial. Participants were randomized 1:1 to received either ezetimibe 10 mg plus rosuvastatin 5 mg daily or rosuvastatin 5 mg for up to 24 weeks.
Change in liver fat was measured via MRI-PDFF, taking the average values in each of nine liver segments. Magnetic resonance elastography (MRE) was also used to measure liver fibrosis, although results did not show any differences either from baseline to end of treatment values in either group or when the two treatment groups were compared.
Dr. Kim reported that both treatment with the ezetimibe-rosuvastatin combination and rosuvastatin monotherapy reduced parameters that might be associated with a negative outcome in NAFLD, such as body mass index and waist circumference, triglycerides, and LDL cholesterol. There was also a reduction in C-reactive protein levels in the blood, and interleulin-18. There was no change in liver enzymes.
Several subgroup analyses were performed indicating that “individuals with higher BMI, type 2 diabetes, insulin resistance, and severe liver fibrosis were likely to be good responders to ezetimibe treatment,” Dr. Kim said.
“These data indicate that ezetimibe plus rosuvastatin is a safe and effective therapeutic option to treat patients with NAFLD and dyslipidemia,” he concluded.
The results of the ESSENTIAL study have been published in BMC Medicine.
The study was funded by the Yuhan Corporation. Dr. Kim had no conflicts of interest to report. Dr. Holleboom was not involved in the study and had no conflicts of interest.
Ezetimibe given in combination with rosuvastatin has a beneficial effect on liver fat in people with nonalcoholic fatty liver disease (NAFLD), according results of a randomized, active-controlled trial.
The findings, which come from the investigator-initiated ESSENTIAL trial, are likely to add to the debate over whether or not the lipid-lowering combination could be of benefit beyond its effects in the blood.
“We used magnetic resonance imaging-derived proton density fat fraction [MRI-PDFF], which is highly reliable method of assessing hepatic steatosis,” Youngjoon Kim, PhD, one of the study investigators, said at the annual meeting of the European Association for the Study of Diabetes in Barcelona.
“It enables accurate, repeatable and reproducible quantitative assessment of liver fat over the entire liver,” observed Dr. Kim, who works at Severance Hospital, part of Yonsei University in Seoul.
He reported that there was a significant 5.8% decrease in liver fat following 24 weeks’ treatment with ezetimibe and rosuvastatin comparing baseline with end of treatment MRI-PDFF values; a drop that was significant (18.2% vs. 12.3%, P < .001).
Rosuvastatin monotherapy also reduced liver fat from 15.0% at baseline to 12.4% after 24 weeks; this drop of 2.6% was also significant (P = .003).
This gave an absolute mean difference between the two study arms of 3.2% (P = .02).
Rationale for the ESSENTIAL study
Dr. Kim observed during his presentation that NAFLD is burgeoning problem around the world. Ezetimibe plus rosuvastatin was a combination treatment already used widely in clinical practice, and there had been some suggestion that ezetimibe might have an effect on liver fat.
“Although the effect of ezetimibe on hepatic steatosis is still controversial, ezetimibe has been reported to reduce visceral fat and improve insulin resistance in several studies” Dr. Kim said.
“Recently, our group reported that the use of ezetimibe affects autophagy of hepatocytes and the NLRP3 [NOD-like receptors containing pyrin domain 3] inflammasome,” he said.
Moreover, he added, “ezetimibe improved NASH [nonalcoholic steatohepatitis] in an animal model. However, the effects of ezetimibe have not been clearly shown in a human study.”
Dr. Kim also acknowledged a prior randomized control trial that had looked at the role of ezetimibe in 50 patients with NASH, but had not shown a benefit for the drug over placebo in terms of liver fat reduction.
Addressing the Hawthorne effect
“The size of the effect by that might actually be more modest due to the Hawthorne effect,” said session chair Onno Holleboom, MD, PhD, of Amsterdam UMC in the Netherlands.
“What we observe in the large clinical trials is an enormous Hawthorne effect – participating in a NAFLD trial makes people live healthier because they have health checks,” he said.
“That’s a major problem for showing efficacy for the intervention arm,” he added, but of course the open design meant that the trial only had intervention arms; “there was no placebo arm.”
A randomized, active-controlled, clinician-initiated trial
The main objective of the ESSENTIAL trial was therefore to take another look at the potential effect of ezetimibe on hepatic steatosis and doing so in the setting of statin therapy.
In all, 70 patients with NAFLD that had been confirmed via ultrasound were recruited into the prospective, single center, phase 4 trial. Participants were randomized 1:1 to received either ezetimibe 10 mg plus rosuvastatin 5 mg daily or rosuvastatin 5 mg for up to 24 weeks.
Change in liver fat was measured via MRI-PDFF, taking the average values in each of nine liver segments. Magnetic resonance elastography (MRE) was also used to measure liver fibrosis, although results did not show any differences either from baseline to end of treatment values in either group or when the two treatment groups were compared.
Dr. Kim reported that both treatment with the ezetimibe-rosuvastatin combination and rosuvastatin monotherapy reduced parameters that might be associated with a negative outcome in NAFLD, such as body mass index and waist circumference, triglycerides, and LDL cholesterol. There was also a reduction in C-reactive protein levels in the blood, and interleulin-18. There was no change in liver enzymes.
Several subgroup analyses were performed indicating that “individuals with higher BMI, type 2 diabetes, insulin resistance, and severe liver fibrosis were likely to be good responders to ezetimibe treatment,” Dr. Kim said.
“These data indicate that ezetimibe plus rosuvastatin is a safe and effective therapeutic option to treat patients with NAFLD and dyslipidemia,” he concluded.
The results of the ESSENTIAL study have been published in BMC Medicine.
The study was funded by the Yuhan Corporation. Dr. Kim had no conflicts of interest to report. Dr. Holleboom was not involved in the study and had no conflicts of interest.
Ezetimibe given in combination with rosuvastatin has a beneficial effect on liver fat in people with nonalcoholic fatty liver disease (NAFLD), according results of a randomized, active-controlled trial.
The findings, which come from the investigator-initiated ESSENTIAL trial, are likely to add to the debate over whether or not the lipid-lowering combination could be of benefit beyond its effects in the blood.
“We used magnetic resonance imaging-derived proton density fat fraction [MRI-PDFF], which is highly reliable method of assessing hepatic steatosis,” Youngjoon Kim, PhD, one of the study investigators, said at the annual meeting of the European Association for the Study of Diabetes in Barcelona.
“It enables accurate, repeatable and reproducible quantitative assessment of liver fat over the entire liver,” observed Dr. Kim, who works at Severance Hospital, part of Yonsei University in Seoul.
He reported that there was a significant 5.8% decrease in liver fat following 24 weeks’ treatment with ezetimibe and rosuvastatin comparing baseline with end of treatment MRI-PDFF values; a drop that was significant (18.2% vs. 12.3%, P < .001).
Rosuvastatin monotherapy also reduced liver fat from 15.0% at baseline to 12.4% after 24 weeks; this drop of 2.6% was also significant (P = .003).
This gave an absolute mean difference between the two study arms of 3.2% (P = .02).
Rationale for the ESSENTIAL study
Dr. Kim observed during his presentation that NAFLD is burgeoning problem around the world. Ezetimibe plus rosuvastatin was a combination treatment already used widely in clinical practice, and there had been some suggestion that ezetimibe might have an effect on liver fat.
“Although the effect of ezetimibe on hepatic steatosis is still controversial, ezetimibe has been reported to reduce visceral fat and improve insulin resistance in several studies” Dr. Kim said.
“Recently, our group reported that the use of ezetimibe affects autophagy of hepatocytes and the NLRP3 [NOD-like receptors containing pyrin domain 3] inflammasome,” he said.
Moreover, he added, “ezetimibe improved NASH [nonalcoholic steatohepatitis] in an animal model. However, the effects of ezetimibe have not been clearly shown in a human study.”
Dr. Kim also acknowledged a prior randomized control trial that had looked at the role of ezetimibe in 50 patients with NASH, but had not shown a benefit for the drug over placebo in terms of liver fat reduction.
Addressing the Hawthorne effect
“The size of the effect by that might actually be more modest due to the Hawthorne effect,” said session chair Onno Holleboom, MD, PhD, of Amsterdam UMC in the Netherlands.
“What we observe in the large clinical trials is an enormous Hawthorne effect – participating in a NAFLD trial makes people live healthier because they have health checks,” he said.
“That’s a major problem for showing efficacy for the intervention arm,” he added, but of course the open design meant that the trial only had intervention arms; “there was no placebo arm.”
A randomized, active-controlled, clinician-initiated trial
The main objective of the ESSENTIAL trial was therefore to take another look at the potential effect of ezetimibe on hepatic steatosis and doing so in the setting of statin therapy.
In all, 70 patients with NAFLD that had been confirmed via ultrasound were recruited into the prospective, single center, phase 4 trial. Participants were randomized 1:1 to received either ezetimibe 10 mg plus rosuvastatin 5 mg daily or rosuvastatin 5 mg for up to 24 weeks.
Change in liver fat was measured via MRI-PDFF, taking the average values in each of nine liver segments. Magnetic resonance elastography (MRE) was also used to measure liver fibrosis, although results did not show any differences either from baseline to end of treatment values in either group or when the two treatment groups were compared.
Dr. Kim reported that both treatment with the ezetimibe-rosuvastatin combination and rosuvastatin monotherapy reduced parameters that might be associated with a negative outcome in NAFLD, such as body mass index and waist circumference, triglycerides, and LDL cholesterol. There was also a reduction in C-reactive protein levels in the blood, and interleulin-18. There was no change in liver enzymes.
Several subgroup analyses were performed indicating that “individuals with higher BMI, type 2 diabetes, insulin resistance, and severe liver fibrosis were likely to be good responders to ezetimibe treatment,” Dr. Kim said.
“These data indicate that ezetimibe plus rosuvastatin is a safe and effective therapeutic option to treat patients with NAFLD and dyslipidemia,” he concluded.
The results of the ESSENTIAL study have been published in BMC Medicine.
The study was funded by the Yuhan Corporation. Dr. Kim had no conflicts of interest to report. Dr. Holleboom was not involved in the study and had no conflicts of interest.
FROM EASD 2022
Aspirin primary prevention benefit in those with raised Lp(a)?
Aspirin may be of specific benefit for the primary prevention of cardiovascular disease in individuals with raised Lp(a) levels, a new study has suggested.
The study analyzed data from the ASPREE (ASPirin in Reducing Events in the Elderly) trial, which randomized 19,000 individuals aged 70 years or older without a history of cardiovascular disease to aspirin (100 mg/day) or placebo. While the main results, reported previously, showed no net benefit of aspirin in the overall population, the current analysis suggests there may be a benefit in individuals with raised Lp(a) levels.
The current analysis was published online in the Journal of the American College of Cardiology.
“Our study provides evidence that aspirin may specifically benefit older individuals with genotypes for elevated plasma Lp(a) in the setting of high-risk primary prevention of cardiovascular events and that overall benefit may outweigh harm related to major bleeding,” the authors, led by Paul Lacaze, PhD, Monash University, Melbourne, conclude.
They also point out that similar observations have been previously seen in another large aspirin primary prevention study conducted in younger women, the Women’s Health Study, and the current analysis provides validation of those findings.
“Our results provide new evidence to support the potential use of aspirin to target individuals with elevated Lp(a) for the primary prevention of cardiovascular events,” the researchers say.
They acknowledge that these results would be strengthened by the use of directly measured plasma Lp(a) levels, in addition to Lp(a) genotypes.
But they add: “Nonetheless, given the lack of any currently approved therapies for targeting elevated Lp(a), our findings may have widespread clinical implications, adding evidence to the rationale that aspirin may be a viable option for reducing Lp(a)-mediated cardiovascular risk.”
Dr. Lacaze and colleagues explain that elevated plasma Lp(a) levels confer up to fourfold increased risk of cardiovascular disease, with around 20%-30% of the general population affected. Despite the high burden and prevalence of elevated plasma Lp(a), there are currently no approved pharmacologic therapies targeting this lipoprotein. Although promising candidates are in development for the secondary prevention of Lp(a)-mediated cardiovascular disease, it will be many years before these candidates are assessed for primary prevention.
For the current study, researchers analyzed data from 12,815 ASPREE participants who had undergone genotyping and compared outcomes with aspirin versus placebo in those with and without genotypes associated with elevated Lp(a) levels.
Results showed that individuals with elevated Lp(a)-associated genotypes, defined in two different ways, showed a reduction in ischemic events with aspirin versus placebo, and this benefit was not outweighed by an increased bleeding risk.
Specifically, in the placebo group, individuals who carried the rs3798220-C allele, which is known to be associated with raised Lp(a) levels, making up 3.2% of the genotyped population in the study, had an almost twofold increased risk of major adverse cardiovascular events than those not carrying this genotype. However, the risk was attenuated in the aspirin group, with carriers of the rs3798220-C allele actually having a lower rate of cardiovascular events than noncarriers.
In addition, rs3798220-C carrier status was not significantly associated with increased risk of clinically significant bleeding events in the aspirin group.
Similar results were seen with the second way of identifying patients with a high risk of elevated Lp(a) levels using a 43-variant genetic risk score (LPA-GRS).
In the whole study population, aspirin reduced major adverse cardiovascular events by 1.7 events per 1,000 person-years and increased clinically significant bleeding events by 1.7 events per 1,000 person-years, suggesting parity between overall benefit versus harm.
However, in the rs3798220-C subgroup, aspirin reduced major adverse cardiovascular events by 11.4 events per 1,000 person-years (a more than sixfold higher magnitude of cardiovascular disease risk reduction than in the overall cohort), with a bleeding risk of 3.3 events per 1,000 person-years, the researchers report.
“Hence in rs3798220-C carriers, aspirin appeared to have a net benefit of 8.1 events per 1,000 person-years,” they state.
In the highest LPA-GRS quintile, aspirin reduced major adverse cardiovascular events by 3.3 events per 1,000 person-years (approximately twofold higher magnitude of risk reduction, compared with the overall cohort), with an increase in bleeding risk of 1.6 events per 1,000 person-years (almost identical bleeding risk to the overall cohort). This shifted the benefit versus harm balance in the highest LPA-GRS quintile to a net benefit of 1.7 events per 1,000 person-years.
Similar findings in the Women’s Health Study
Dr. Lacaze and colleagues point out that similar results have also been seen in another large aspirin primary prevention study – the Women’s Health Study (WHS).
The WHS compared aspirin 100 mg every other day with placebo in initially healthy younger women. Previously reported results showed that women carrying the rs3798220-C variant, associated with highly elevated Lp(a) levels, had a twofold higher risk of cardiovascular events than noncarrier women in the placebo group, but this risk was reduced in the aspirin group. And there was no increased risk of bleeding in women with elevated Lp(a).
“These results, in the absence of any other randomized controlled trial evidence or approved therapy for treating Lp(a)-associated risk, have been used by some physicians as justification for prescribing aspirin in patients with elevated Lp(a),” Dr. Lacaze and colleagues note.
“In the present study of the ASPREE trial population, our results were consistent with the WHS analysis, despite randomizing older individuals (both men and women),” they add.
They say this validation of the WHS result provides evidence that a very high-risk subgroup of individuals with highly elevated Lp(a) – those carrying the rs3798220-C allele – may benefit from low-dose aspirin for the primary prevention of cardiovascular events. Further, the benefits in this subgroup specifically may outweigh any bleeding risk.
But they point out that rs3798220-C carriers comprise only a small portion of all individuals with elevated Lp(a) in the general population, while the polygenic LPA-GRS explains about 60% of the variation in directly measured plasma Lp(a) levels and has the potential advantage of being able to identify a larger group of individuals at increased risk.
The researchers note, however, that it is not clear to what extent the LPA-GRS results add further evidence to suggest that individuals with elevated Lp(a), beyond rs3798220-C carriers, may be more likely to benefit from aspirin.
“If the benefit of aspirin extends beyond very high-risk rs3798220-C carriers alone, to the broader 20%-30% of individuals with elevated Lp(a), the potential utility of aspirin for the primary prevention of cardiovascular events would increase substantially,” they say.
‘Very high clinical relevance’
In an accompanying editorial, Ana Devesa, MD, Borja Ibanez, MD, PhD, and Valentin Fuster, MD, PhD, The National Center for Cardiovascular Research, Madrid, say that: “[Dr.] Lacaze et al. are to be congratulated for a study of very high clinical relevance that represents a first indication for primary prevention for patients at high cardiovascular risk.”
They explain that the pathogenic mechanism of Lp(a) is believed to be a combination of prothrombotic and proatherogenic effects, and the current findings support the hypothesis that the prothrombotic mechanism of Lp(a) is mediated by platelet aggregation.
This would explain the occurrence of thrombotic events in the presence of atherosclerosis in that elevated Lp(a) levels may induce platelet adhesion and aggregation to the activated atherosclerotic plaque, thus enhancing the atherothrombotic process. Moreover, activated platelets release several mediators that result in cell adhesion and attraction of chemokines and proinflammatory cytokines, driving an inflammatory response and mediating atherosclerosis progression, they add.
The editorialists highlight the limitations of the study already acknowledged by the authors: The analysis used genotypes rather than elevated Lp(a) levels and included only those of European ancestry, meaning the results are difficult to extrapolate to other populations.
“The next steps in clinical practice should be defined, and there are still questions to be answered,” they conclude. “Will every patient benefit from antithrombotic therapies? Should all patients who have elevated Lp(a) levels be treated with aspirin?”
The ASPREE Biobank is supported by grants from the Commonwealth Scientific and Industrial Research Organisation, Monash University, Menzies Research Institute, Australian National University, University of Melbourne, National Institutes of Health, National Health and Medical Research Council of Australia, and the Victorian Cancer Agency. Dr. Lacaze is supported by a National Heart Foundation Future Leader Fellowship.
A version of this article first appeared on Medscape.com.
Aspirin may be of specific benefit for the primary prevention of cardiovascular disease in individuals with raised Lp(a) levels, a new study has suggested.
The study analyzed data from the ASPREE (ASPirin in Reducing Events in the Elderly) trial, which randomized 19,000 individuals aged 70 years or older without a history of cardiovascular disease to aspirin (100 mg/day) or placebo. While the main results, reported previously, showed no net benefit of aspirin in the overall population, the current analysis suggests there may be a benefit in individuals with raised Lp(a) levels.
The current analysis was published online in the Journal of the American College of Cardiology.
“Our study provides evidence that aspirin may specifically benefit older individuals with genotypes for elevated plasma Lp(a) in the setting of high-risk primary prevention of cardiovascular events and that overall benefit may outweigh harm related to major bleeding,” the authors, led by Paul Lacaze, PhD, Monash University, Melbourne, conclude.
They also point out that similar observations have been previously seen in another large aspirin primary prevention study conducted in younger women, the Women’s Health Study, and the current analysis provides validation of those findings.
“Our results provide new evidence to support the potential use of aspirin to target individuals with elevated Lp(a) for the primary prevention of cardiovascular events,” the researchers say.
They acknowledge that these results would be strengthened by the use of directly measured plasma Lp(a) levels, in addition to Lp(a) genotypes.
But they add: “Nonetheless, given the lack of any currently approved therapies for targeting elevated Lp(a), our findings may have widespread clinical implications, adding evidence to the rationale that aspirin may be a viable option for reducing Lp(a)-mediated cardiovascular risk.”
Dr. Lacaze and colleagues explain that elevated plasma Lp(a) levels confer up to fourfold increased risk of cardiovascular disease, with around 20%-30% of the general population affected. Despite the high burden and prevalence of elevated plasma Lp(a), there are currently no approved pharmacologic therapies targeting this lipoprotein. Although promising candidates are in development for the secondary prevention of Lp(a)-mediated cardiovascular disease, it will be many years before these candidates are assessed for primary prevention.
For the current study, researchers analyzed data from 12,815 ASPREE participants who had undergone genotyping and compared outcomes with aspirin versus placebo in those with and without genotypes associated with elevated Lp(a) levels.
Results showed that individuals with elevated Lp(a)-associated genotypes, defined in two different ways, showed a reduction in ischemic events with aspirin versus placebo, and this benefit was not outweighed by an increased bleeding risk.
Specifically, in the placebo group, individuals who carried the rs3798220-C allele, which is known to be associated with raised Lp(a) levels, making up 3.2% of the genotyped population in the study, had an almost twofold increased risk of major adverse cardiovascular events than those not carrying this genotype. However, the risk was attenuated in the aspirin group, with carriers of the rs3798220-C allele actually having a lower rate of cardiovascular events than noncarriers.
In addition, rs3798220-C carrier status was not significantly associated with increased risk of clinically significant bleeding events in the aspirin group.
Similar results were seen with the second way of identifying patients with a high risk of elevated Lp(a) levels using a 43-variant genetic risk score (LPA-GRS).
In the whole study population, aspirin reduced major adverse cardiovascular events by 1.7 events per 1,000 person-years and increased clinically significant bleeding events by 1.7 events per 1,000 person-years, suggesting parity between overall benefit versus harm.
However, in the rs3798220-C subgroup, aspirin reduced major adverse cardiovascular events by 11.4 events per 1,000 person-years (a more than sixfold higher magnitude of cardiovascular disease risk reduction than in the overall cohort), with a bleeding risk of 3.3 events per 1,000 person-years, the researchers report.
“Hence in rs3798220-C carriers, aspirin appeared to have a net benefit of 8.1 events per 1,000 person-years,” they state.
In the highest LPA-GRS quintile, aspirin reduced major adverse cardiovascular events by 3.3 events per 1,000 person-years (approximately twofold higher magnitude of risk reduction, compared with the overall cohort), with an increase in bleeding risk of 1.6 events per 1,000 person-years (almost identical bleeding risk to the overall cohort). This shifted the benefit versus harm balance in the highest LPA-GRS quintile to a net benefit of 1.7 events per 1,000 person-years.
Similar findings in the Women’s Health Study
Dr. Lacaze and colleagues point out that similar results have also been seen in another large aspirin primary prevention study – the Women’s Health Study (WHS).
The WHS compared aspirin 100 mg every other day with placebo in initially healthy younger women. Previously reported results showed that women carrying the rs3798220-C variant, associated with highly elevated Lp(a) levels, had a twofold higher risk of cardiovascular events than noncarrier women in the placebo group, but this risk was reduced in the aspirin group. And there was no increased risk of bleeding in women with elevated Lp(a).
“These results, in the absence of any other randomized controlled trial evidence or approved therapy for treating Lp(a)-associated risk, have been used by some physicians as justification for prescribing aspirin in patients with elevated Lp(a),” Dr. Lacaze and colleagues note.
“In the present study of the ASPREE trial population, our results were consistent with the WHS analysis, despite randomizing older individuals (both men and women),” they add.
They say this validation of the WHS result provides evidence that a very high-risk subgroup of individuals with highly elevated Lp(a) – those carrying the rs3798220-C allele – may benefit from low-dose aspirin for the primary prevention of cardiovascular events. Further, the benefits in this subgroup specifically may outweigh any bleeding risk.
But they point out that rs3798220-C carriers comprise only a small portion of all individuals with elevated Lp(a) in the general population, while the polygenic LPA-GRS explains about 60% of the variation in directly measured plasma Lp(a) levels and has the potential advantage of being able to identify a larger group of individuals at increased risk.
The researchers note, however, that it is not clear to what extent the LPA-GRS results add further evidence to suggest that individuals with elevated Lp(a), beyond rs3798220-C carriers, may be more likely to benefit from aspirin.
“If the benefit of aspirin extends beyond very high-risk rs3798220-C carriers alone, to the broader 20%-30% of individuals with elevated Lp(a), the potential utility of aspirin for the primary prevention of cardiovascular events would increase substantially,” they say.
‘Very high clinical relevance’
In an accompanying editorial, Ana Devesa, MD, Borja Ibanez, MD, PhD, and Valentin Fuster, MD, PhD, The National Center for Cardiovascular Research, Madrid, say that: “[Dr.] Lacaze et al. are to be congratulated for a study of very high clinical relevance that represents a first indication for primary prevention for patients at high cardiovascular risk.”
They explain that the pathogenic mechanism of Lp(a) is believed to be a combination of prothrombotic and proatherogenic effects, and the current findings support the hypothesis that the prothrombotic mechanism of Lp(a) is mediated by platelet aggregation.
This would explain the occurrence of thrombotic events in the presence of atherosclerosis in that elevated Lp(a) levels may induce platelet adhesion and aggregation to the activated atherosclerotic plaque, thus enhancing the atherothrombotic process. Moreover, activated platelets release several mediators that result in cell adhesion and attraction of chemokines and proinflammatory cytokines, driving an inflammatory response and mediating atherosclerosis progression, they add.
The editorialists highlight the limitations of the study already acknowledged by the authors: The analysis used genotypes rather than elevated Lp(a) levels and included only those of European ancestry, meaning the results are difficult to extrapolate to other populations.
“The next steps in clinical practice should be defined, and there are still questions to be answered,” they conclude. “Will every patient benefit from antithrombotic therapies? Should all patients who have elevated Lp(a) levels be treated with aspirin?”
The ASPREE Biobank is supported by grants from the Commonwealth Scientific and Industrial Research Organisation, Monash University, Menzies Research Institute, Australian National University, University of Melbourne, National Institutes of Health, National Health and Medical Research Council of Australia, and the Victorian Cancer Agency. Dr. Lacaze is supported by a National Heart Foundation Future Leader Fellowship.
A version of this article first appeared on Medscape.com.
Aspirin may be of specific benefit for the primary prevention of cardiovascular disease in individuals with raised Lp(a) levels, a new study has suggested.
The study analyzed data from the ASPREE (ASPirin in Reducing Events in the Elderly) trial, which randomized 19,000 individuals aged 70 years or older without a history of cardiovascular disease to aspirin (100 mg/day) or placebo. While the main results, reported previously, showed no net benefit of aspirin in the overall population, the current analysis suggests there may be a benefit in individuals with raised Lp(a) levels.
The current analysis was published online in the Journal of the American College of Cardiology.
“Our study provides evidence that aspirin may specifically benefit older individuals with genotypes for elevated plasma Lp(a) in the setting of high-risk primary prevention of cardiovascular events and that overall benefit may outweigh harm related to major bleeding,” the authors, led by Paul Lacaze, PhD, Monash University, Melbourne, conclude.
They also point out that similar observations have been previously seen in another large aspirin primary prevention study conducted in younger women, the Women’s Health Study, and the current analysis provides validation of those findings.
“Our results provide new evidence to support the potential use of aspirin to target individuals with elevated Lp(a) for the primary prevention of cardiovascular events,” the researchers say.
They acknowledge that these results would be strengthened by the use of directly measured plasma Lp(a) levels, in addition to Lp(a) genotypes.
But they add: “Nonetheless, given the lack of any currently approved therapies for targeting elevated Lp(a), our findings may have widespread clinical implications, adding evidence to the rationale that aspirin may be a viable option for reducing Lp(a)-mediated cardiovascular risk.”
Dr. Lacaze and colleagues explain that elevated plasma Lp(a) levels confer up to fourfold increased risk of cardiovascular disease, with around 20%-30% of the general population affected. Despite the high burden and prevalence of elevated plasma Lp(a), there are currently no approved pharmacologic therapies targeting this lipoprotein. Although promising candidates are in development for the secondary prevention of Lp(a)-mediated cardiovascular disease, it will be many years before these candidates are assessed for primary prevention.
For the current study, researchers analyzed data from 12,815 ASPREE participants who had undergone genotyping and compared outcomes with aspirin versus placebo in those with and without genotypes associated with elevated Lp(a) levels.
Results showed that individuals with elevated Lp(a)-associated genotypes, defined in two different ways, showed a reduction in ischemic events with aspirin versus placebo, and this benefit was not outweighed by an increased bleeding risk.
Specifically, in the placebo group, individuals who carried the rs3798220-C allele, which is known to be associated with raised Lp(a) levels, making up 3.2% of the genotyped population in the study, had an almost twofold increased risk of major adverse cardiovascular events than those not carrying this genotype. However, the risk was attenuated in the aspirin group, with carriers of the rs3798220-C allele actually having a lower rate of cardiovascular events than noncarriers.
In addition, rs3798220-C carrier status was not significantly associated with increased risk of clinically significant bleeding events in the aspirin group.
Similar results were seen with the second way of identifying patients with a high risk of elevated Lp(a) levels using a 43-variant genetic risk score (LPA-GRS).
In the whole study population, aspirin reduced major adverse cardiovascular events by 1.7 events per 1,000 person-years and increased clinically significant bleeding events by 1.7 events per 1,000 person-years, suggesting parity between overall benefit versus harm.
However, in the rs3798220-C subgroup, aspirin reduced major adverse cardiovascular events by 11.4 events per 1,000 person-years (a more than sixfold higher magnitude of cardiovascular disease risk reduction than in the overall cohort), with a bleeding risk of 3.3 events per 1,000 person-years, the researchers report.
“Hence in rs3798220-C carriers, aspirin appeared to have a net benefit of 8.1 events per 1,000 person-years,” they state.
In the highest LPA-GRS quintile, aspirin reduced major adverse cardiovascular events by 3.3 events per 1,000 person-years (approximately twofold higher magnitude of risk reduction, compared with the overall cohort), with an increase in bleeding risk of 1.6 events per 1,000 person-years (almost identical bleeding risk to the overall cohort). This shifted the benefit versus harm balance in the highest LPA-GRS quintile to a net benefit of 1.7 events per 1,000 person-years.
Similar findings in the Women’s Health Study
Dr. Lacaze and colleagues point out that similar results have also been seen in another large aspirin primary prevention study – the Women’s Health Study (WHS).
The WHS compared aspirin 100 mg every other day with placebo in initially healthy younger women. Previously reported results showed that women carrying the rs3798220-C variant, associated with highly elevated Lp(a) levels, had a twofold higher risk of cardiovascular events than noncarrier women in the placebo group, but this risk was reduced in the aspirin group. And there was no increased risk of bleeding in women with elevated Lp(a).
“These results, in the absence of any other randomized controlled trial evidence or approved therapy for treating Lp(a)-associated risk, have been used by some physicians as justification for prescribing aspirin in patients with elevated Lp(a),” Dr. Lacaze and colleagues note.
“In the present study of the ASPREE trial population, our results were consistent with the WHS analysis, despite randomizing older individuals (both men and women),” they add.
They say this validation of the WHS result provides evidence that a very high-risk subgroup of individuals with highly elevated Lp(a) – those carrying the rs3798220-C allele – may benefit from low-dose aspirin for the primary prevention of cardiovascular events. Further, the benefits in this subgroup specifically may outweigh any bleeding risk.
But they point out that rs3798220-C carriers comprise only a small portion of all individuals with elevated Lp(a) in the general population, while the polygenic LPA-GRS explains about 60% of the variation in directly measured plasma Lp(a) levels and has the potential advantage of being able to identify a larger group of individuals at increased risk.
The researchers note, however, that it is not clear to what extent the LPA-GRS results add further evidence to suggest that individuals with elevated Lp(a), beyond rs3798220-C carriers, may be more likely to benefit from aspirin.
“If the benefit of aspirin extends beyond very high-risk rs3798220-C carriers alone, to the broader 20%-30% of individuals with elevated Lp(a), the potential utility of aspirin for the primary prevention of cardiovascular events would increase substantially,” they say.
‘Very high clinical relevance’
In an accompanying editorial, Ana Devesa, MD, Borja Ibanez, MD, PhD, and Valentin Fuster, MD, PhD, The National Center for Cardiovascular Research, Madrid, say that: “[Dr.] Lacaze et al. are to be congratulated for a study of very high clinical relevance that represents a first indication for primary prevention for patients at high cardiovascular risk.”
They explain that the pathogenic mechanism of Lp(a) is believed to be a combination of prothrombotic and proatherogenic effects, and the current findings support the hypothesis that the prothrombotic mechanism of Lp(a) is mediated by platelet aggregation.
This would explain the occurrence of thrombotic events in the presence of atherosclerosis in that elevated Lp(a) levels may induce platelet adhesion and aggregation to the activated atherosclerotic plaque, thus enhancing the atherothrombotic process. Moreover, activated platelets release several mediators that result in cell adhesion and attraction of chemokines and proinflammatory cytokines, driving an inflammatory response and mediating atherosclerosis progression, they add.
The editorialists highlight the limitations of the study already acknowledged by the authors: The analysis used genotypes rather than elevated Lp(a) levels and included only those of European ancestry, meaning the results are difficult to extrapolate to other populations.
“The next steps in clinical practice should be defined, and there are still questions to be answered,” they conclude. “Will every patient benefit from antithrombotic therapies? Should all patients who have elevated Lp(a) levels be treated with aspirin?”
The ASPREE Biobank is supported by grants from the Commonwealth Scientific and Industrial Research Organisation, Monash University, Menzies Research Institute, Australian National University, University of Melbourne, National Institutes of Health, National Health and Medical Research Council of Australia, and the Victorian Cancer Agency. Dr. Lacaze is supported by a National Heart Foundation Future Leader Fellowship.
A version of this article first appeared on Medscape.com.
Positive top-line phase 3 data for lecanemab in early Alzheimer’s
compared with placebo and decreased amyloid levels in the brain of adults enrolled in a phase 3 trial.
The Clarity AD trial included 1,795 adults with early AD and confirmed amyloid pathology in the brain. Treatment consisted of lecanemab 10 mg/kg biweekly or matching placebo.
Treatment with lecanemab met the primary endpoint, reducing clinical decline on the global cognitive and functional scale, the Clinical Dementia Rating–Sum of Boxes (CDR-SB), at 18 months by 27%, compared with placebo, with a treatment difference in the score change of –0.45 (P = .00005), the companies reported.
Starting as early as 6 months, across all time points, treatment with lecanemab yielded highly statistically significant changes in CDR-SB from baseline, compared with placebo (all P < .01).
The study also met all key secondary endpoints with highly statistically significant results, compared with placebo (P < .01).
Key secondary endpoints, in comparison with placebo, were change from baseline at 18 months in amyloid levels in the brain measured by amyloid PET, the AD Assessment Scale–cognitive subscale14 (ADAS-cog14), the AD Composite Score (ADCOMS), and the AD Cooperative Study–Activities of Daily Living Scale for Mild Cognitive Impairment (ADCS MCI-ADL).
Imaging abnormalities within expectations
Overall, rates of amyloid-related imaging abnormalities (ARIA) related to lecanemab were “within expectations,” the companies said.
The incidence of ARIA related to edema (ARIA-E) was 12.5% in the lecanemab group and 1.7% in the placebo group.
The incidence of symptomatic ARIA-E was 2.8% and 0.0%, respectively, and the rate of cerebral hemorrhage (ARIA-H) was 17.0% and 8.7%. The total incidence of ARIA (ARIA-E and/or ARIA-H) was 21.3% in the lecanemab group and 9.3% in the placebo group.
Full results of the Clarity AD trial will be presented in November at the Clinical Trials on Alzheimer’s Congress.
Incremental benefit
Responding to the findings, the Alzheimer’s Association said in a statement that it “enthusiastically welcomes” the positive findings. It noted that these are “the most encouraging results in clinical trials treating the underlying causes of Alzheimer’s to date.
“For people in the earliest stages of Alzheimer’s, this treatment has the potential to change the course of the disease in a clinically meaningful way. These results indicate lecanemab may give people more time at or near their full abilities to participate in daily life, remain independent and make future health care decisions,” the Alzheimer’s Association added.
Also weighing in, Howard Fillit, MD, cofounder and chief science officer at the Alzheimer’s Drug Discovery Foundation, said in a release that “the combination of the biomarker change – reduced amyloid – plus slowing of cognitive decline in this study is encouraging news for the 57 million patients around the world living with Alzheimer’s.
“However, amyloid-clearing drugs will provide an incremental benefit at best, and there is still a pressing need for the next generation of drugs focused on other targets based on our knowledge of the biology of aging,” Dr. Fillit cautioned.
“We are optimistic about the future as many of these drugs are in development, with 75% of drugs in the pipeline now targeting nonamyloid pathways of neurodegeneration,” he added.
In July 2022, the Food and Drug Administration accepted Eisai’s biologics license application for lecanemab under the accelerated approval pathway and granted priority review. Lecanemab has a prescription Drugs User Fee Act action date of Jan. 6, 2023.
A version of this article first appeared on Medscape.com.
compared with placebo and decreased amyloid levels in the brain of adults enrolled in a phase 3 trial.
The Clarity AD trial included 1,795 adults with early AD and confirmed amyloid pathology in the brain. Treatment consisted of lecanemab 10 mg/kg biweekly or matching placebo.
Treatment with lecanemab met the primary endpoint, reducing clinical decline on the global cognitive and functional scale, the Clinical Dementia Rating–Sum of Boxes (CDR-SB), at 18 months by 27%, compared with placebo, with a treatment difference in the score change of –0.45 (P = .00005), the companies reported.
Starting as early as 6 months, across all time points, treatment with lecanemab yielded highly statistically significant changes in CDR-SB from baseline, compared with placebo (all P < .01).
The study also met all key secondary endpoints with highly statistically significant results, compared with placebo (P < .01).
Key secondary endpoints, in comparison with placebo, were change from baseline at 18 months in amyloid levels in the brain measured by amyloid PET, the AD Assessment Scale–cognitive subscale14 (ADAS-cog14), the AD Composite Score (ADCOMS), and the AD Cooperative Study–Activities of Daily Living Scale for Mild Cognitive Impairment (ADCS MCI-ADL).
Imaging abnormalities within expectations
Overall, rates of amyloid-related imaging abnormalities (ARIA) related to lecanemab were “within expectations,” the companies said.
The incidence of ARIA related to edema (ARIA-E) was 12.5% in the lecanemab group and 1.7% in the placebo group.
The incidence of symptomatic ARIA-E was 2.8% and 0.0%, respectively, and the rate of cerebral hemorrhage (ARIA-H) was 17.0% and 8.7%. The total incidence of ARIA (ARIA-E and/or ARIA-H) was 21.3% in the lecanemab group and 9.3% in the placebo group.
Full results of the Clarity AD trial will be presented in November at the Clinical Trials on Alzheimer’s Congress.
Incremental benefit
Responding to the findings, the Alzheimer’s Association said in a statement that it “enthusiastically welcomes” the positive findings. It noted that these are “the most encouraging results in clinical trials treating the underlying causes of Alzheimer’s to date.
“For people in the earliest stages of Alzheimer’s, this treatment has the potential to change the course of the disease in a clinically meaningful way. These results indicate lecanemab may give people more time at or near their full abilities to participate in daily life, remain independent and make future health care decisions,” the Alzheimer’s Association added.
Also weighing in, Howard Fillit, MD, cofounder and chief science officer at the Alzheimer’s Drug Discovery Foundation, said in a release that “the combination of the biomarker change – reduced amyloid – plus slowing of cognitive decline in this study is encouraging news for the 57 million patients around the world living with Alzheimer’s.
“However, amyloid-clearing drugs will provide an incremental benefit at best, and there is still a pressing need for the next generation of drugs focused on other targets based on our knowledge of the biology of aging,” Dr. Fillit cautioned.
“We are optimistic about the future as many of these drugs are in development, with 75% of drugs in the pipeline now targeting nonamyloid pathways of neurodegeneration,” he added.
In July 2022, the Food and Drug Administration accepted Eisai’s biologics license application for lecanemab under the accelerated approval pathway and granted priority review. Lecanemab has a prescription Drugs User Fee Act action date of Jan. 6, 2023.
A version of this article first appeared on Medscape.com.
compared with placebo and decreased amyloid levels in the brain of adults enrolled in a phase 3 trial.
The Clarity AD trial included 1,795 adults with early AD and confirmed amyloid pathology in the brain. Treatment consisted of lecanemab 10 mg/kg biweekly or matching placebo.
Treatment with lecanemab met the primary endpoint, reducing clinical decline on the global cognitive and functional scale, the Clinical Dementia Rating–Sum of Boxes (CDR-SB), at 18 months by 27%, compared with placebo, with a treatment difference in the score change of –0.45 (P = .00005), the companies reported.
Starting as early as 6 months, across all time points, treatment with lecanemab yielded highly statistically significant changes in CDR-SB from baseline, compared with placebo (all P < .01).
The study also met all key secondary endpoints with highly statistically significant results, compared with placebo (P < .01).
Key secondary endpoints, in comparison with placebo, were change from baseline at 18 months in amyloid levels in the brain measured by amyloid PET, the AD Assessment Scale–cognitive subscale14 (ADAS-cog14), the AD Composite Score (ADCOMS), and the AD Cooperative Study–Activities of Daily Living Scale for Mild Cognitive Impairment (ADCS MCI-ADL).
Imaging abnormalities within expectations
Overall, rates of amyloid-related imaging abnormalities (ARIA) related to lecanemab were “within expectations,” the companies said.
The incidence of ARIA related to edema (ARIA-E) was 12.5% in the lecanemab group and 1.7% in the placebo group.
The incidence of symptomatic ARIA-E was 2.8% and 0.0%, respectively, and the rate of cerebral hemorrhage (ARIA-H) was 17.0% and 8.7%. The total incidence of ARIA (ARIA-E and/or ARIA-H) was 21.3% in the lecanemab group and 9.3% in the placebo group.
Full results of the Clarity AD trial will be presented in November at the Clinical Trials on Alzheimer’s Congress.
Incremental benefit
Responding to the findings, the Alzheimer’s Association said in a statement that it “enthusiastically welcomes” the positive findings. It noted that these are “the most encouraging results in clinical trials treating the underlying causes of Alzheimer’s to date.
“For people in the earliest stages of Alzheimer’s, this treatment has the potential to change the course of the disease in a clinically meaningful way. These results indicate lecanemab may give people more time at or near their full abilities to participate in daily life, remain independent and make future health care decisions,” the Alzheimer’s Association added.
Also weighing in, Howard Fillit, MD, cofounder and chief science officer at the Alzheimer’s Drug Discovery Foundation, said in a release that “the combination of the biomarker change – reduced amyloid – plus slowing of cognitive decline in this study is encouraging news for the 57 million patients around the world living with Alzheimer’s.
“However, amyloid-clearing drugs will provide an incremental benefit at best, and there is still a pressing need for the next generation of drugs focused on other targets based on our knowledge of the biology of aging,” Dr. Fillit cautioned.
“We are optimistic about the future as many of these drugs are in development, with 75% of drugs in the pipeline now targeting nonamyloid pathways of neurodegeneration,” he added.
In July 2022, the Food and Drug Administration accepted Eisai’s biologics license application for lecanemab under the accelerated approval pathway and granted priority review. Lecanemab has a prescription Drugs User Fee Act action date of Jan. 6, 2023.
A version of this article first appeared on Medscape.com.
Heart failure drug a new treatment option for alcoholism?
(AUD), new research suggests.
Researchers at the National Institute on Drug Abuse, the National Institute on Alcohol Abuse and Alcoholism, and Yale University, New Haven, Conn., investigated the impact of spironolactone on AUD.
Initially, they studied rodents and found that spironolactone reduced binge drinking in mice and reduced self-administration of alcohol in rats without adversely affecting food or water intake or causing motor or coordination problems.
They also analyzed electronic health records of patients drawn from the United States Veterans Affairs health care system to explore potential changes in alcohol use after spironolactone treatment was initiated for other conditions and found a significant link between spironolactone treatment and reduction in self-reported alcohol consumption, with the largest effects observed among those who reported hazardous/heavy episodic alcohol use prior to starting spironolactone treatment.
“Combining findings across three species and different types of research studies, and then seeing similarities in these data, gives us confidence that we are onto something potentially important scientifically and clinically,” senior coauthor Lorenzo Leggio, MD, PhD, senior investigator in the Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, a joint NIDA and NIAAA laboratory, said in a news release.
The study was published online in Molecular Psychiatry.
There is a “critical need to increase the armamentarium of pharmacotherapies to treat individuals with AUD,” the authors note, adding that neuroendocrine systems involved in alcohol craving and drinking “offer promising pharmacologic targets in this regard.”
“Both our team and others have observed that patients with AUD often present with changes in peripheral hormones, including aldosterone, which plays a key role in regulating blood pressure and electrolytes,” Dr. Leggio said in an interview.
Spironolactone is a nonselective mineralocorticoid receptor (MT) antagonist. In studies in animal models, investigators said they found “an inverse correlation between alcohol drinking and the expression of the MR in the amygdala, a key brain region in the development and maintenance of AUD and addiction in general.”
Taken together, this led them to hypothesize that blocking the MR, which is the mechanism of action of spironolactone, “could be a novel pharmacotherapeutic approach for AUD,” he said.
Previous research by the same group of researchers suggested spironolactone “may be a potential new medication to treat patients with AUD.” The present study expanded on those findings and consisted of a three-part investigation.
In the current study, the investigators tested different dosages of spironolactone on binge-like alcohol consumption in male and female mice and assessed food and water intake, blood alcohol levels, motor coordination, and spontaneous locomotion.
They then tested the effects of different dosages of spironolactone injections on operant alcohol self-administration in alcohol-dependent and nondependent male and female rats, also testing blood alcohol levels and motor coordination.
Finally, they analyzed health records of veterans to examine the association between at least 60 continuous days of spironolactone treatment and self-reported alcohol consumption (measured by the Alcohol Use Disorders Identification Test-Consumption [AUDIT-C]).
Each of the spironolactone-exposed patients was matched using propensity scores with up to five unexposed patients who had reported alcohol consumption in the 2 years prior to the index date.
The final analysis included a matched cohort of 10,726 spironolactone-exposed individuals who were matched to 34,461 unexposed individuals.
New targets
Spironolactone reduced alcohol intake in mice drinking a sweetened alcohol solution; a 2-way ANOVA revealed a main effect of dose (F 4,52 = 9.09; P < .0001) and sex, with female mice drinking more alcohol, compared to male mice (F 1,13 = 6.05; P = .02).
Post hoc comparisons showed that spironolactone at doses of 50, 100, and 200 mg/kg significantly reduced alcohol intake (P values = .007, .002, and .0001, respectively).
In mice drinking an unsweetened alcohol solution, the 2-way repeated measures ANOVA similarly found a main effect of dose (F 4,52 = 5.77; P = .0006), but not of sex (F 1,13 = 1.41; P = .25).
Spironolactone had no effect on the mice’s intake of a sweet solution without alcohol and had no impact on the consumption of food and water or on locomotion and coordination.
In rats, a 2-way ANOVA revealed a significant spironolactone effect of dose (F 3,66 = 43.95; P < .001), with a post hoc test indicating that spironolactone at 25, 50, and 75 mg/kg reduced alcohol self-administration in alcohol-dependent and nondependent rats (all P values = .0001).
In humans, among the exposed individuals in the matched cohort, 25%, 57%, and 18% received daily doses of spironolactone of less than 25 mg/day, 25-49 mg/day, and 50 mg/day or higher, respectively, with a median follow-up time of 542 (interquartile range, 337-730) days.
The AUDIT-C scores decreased during the study period in both treatment groups, with a larger decrease in average AUDIT-C scores among the exposed vs. unexposed individuals.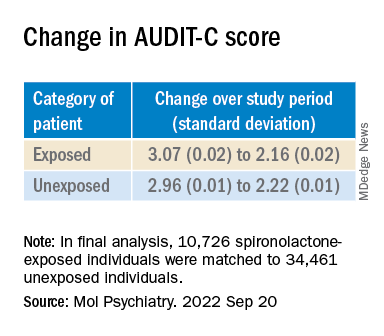
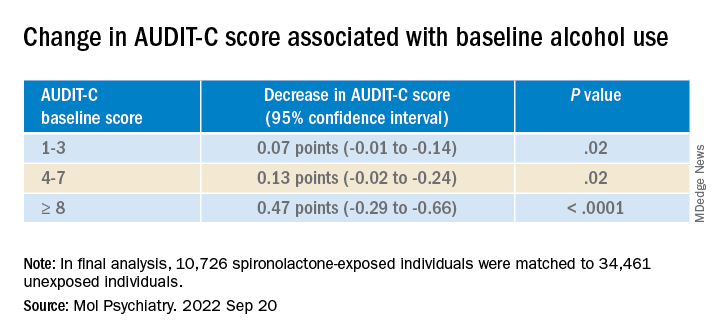
“These are very exciting times because, thanks to the progress in the addiction biomedical research field, we are increasing our understanding of the mechanisms how some people develop AUD; hence we can use this knowledge to identify new targets.” The current study “is an example of these ongoing efforts,” said Dr. Leggio.
“It is important to note that [these results] are important but preliminary.” At this juncture, “it would be too premature to think about prescribing spironolactone to treat AUD,” he added.
Exciting findings
Commenting on the study, Joyce Besheer, PhD, professor, department of psychiatry and Bowles Center for Alcohol Studies, University of North Carolina at Chapel Hill, called the study an “elegant demonstration of translational science.”
“While clinical trials will be needed to determine whether this medication is effective at reducing drinking in patients with AUD, these findings are exciting as they suggest that spironolactone may be a promising compound and new treatment options for AUD are much needed,” said Dr. Besheer, who was not involved with the current study.
Dr. Leggio agreed. “We now need prospective, placebo-controlled studies to assess the potential safety and efficacy of spironolactone in people with AUD,” he said.
This work was supported by the National Institutes of Health and the NIAAA. Dr. Leggio, study coauthors, and Dr. Besheer declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(AUD), new research suggests.
Researchers at the National Institute on Drug Abuse, the National Institute on Alcohol Abuse and Alcoholism, and Yale University, New Haven, Conn., investigated the impact of spironolactone on AUD.
Initially, they studied rodents and found that spironolactone reduced binge drinking in mice and reduced self-administration of alcohol in rats without adversely affecting food or water intake or causing motor or coordination problems.
They also analyzed electronic health records of patients drawn from the United States Veterans Affairs health care system to explore potential changes in alcohol use after spironolactone treatment was initiated for other conditions and found a significant link between spironolactone treatment and reduction in self-reported alcohol consumption, with the largest effects observed among those who reported hazardous/heavy episodic alcohol use prior to starting spironolactone treatment.
“Combining findings across three species and different types of research studies, and then seeing similarities in these data, gives us confidence that we are onto something potentially important scientifically and clinically,” senior coauthor Lorenzo Leggio, MD, PhD, senior investigator in the Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, a joint NIDA and NIAAA laboratory, said in a news release.
The study was published online in Molecular Psychiatry.
There is a “critical need to increase the armamentarium of pharmacotherapies to treat individuals with AUD,” the authors note, adding that neuroendocrine systems involved in alcohol craving and drinking “offer promising pharmacologic targets in this regard.”
“Both our team and others have observed that patients with AUD often present with changes in peripheral hormones, including aldosterone, which plays a key role in regulating blood pressure and electrolytes,” Dr. Leggio said in an interview.
Spironolactone is a nonselective mineralocorticoid receptor (MT) antagonist. In studies in animal models, investigators said they found “an inverse correlation between alcohol drinking and the expression of the MR in the amygdala, a key brain region in the development and maintenance of AUD and addiction in general.”
Taken together, this led them to hypothesize that blocking the MR, which is the mechanism of action of spironolactone, “could be a novel pharmacotherapeutic approach for AUD,” he said.
Previous research by the same group of researchers suggested spironolactone “may be a potential new medication to treat patients with AUD.” The present study expanded on those findings and consisted of a three-part investigation.
In the current study, the investigators tested different dosages of spironolactone on binge-like alcohol consumption in male and female mice and assessed food and water intake, blood alcohol levels, motor coordination, and spontaneous locomotion.
They then tested the effects of different dosages of spironolactone injections on operant alcohol self-administration in alcohol-dependent and nondependent male and female rats, also testing blood alcohol levels and motor coordination.
Finally, they analyzed health records of veterans to examine the association between at least 60 continuous days of spironolactone treatment and self-reported alcohol consumption (measured by the Alcohol Use Disorders Identification Test-Consumption [AUDIT-C]).
Each of the spironolactone-exposed patients was matched using propensity scores with up to five unexposed patients who had reported alcohol consumption in the 2 years prior to the index date.
The final analysis included a matched cohort of 10,726 spironolactone-exposed individuals who were matched to 34,461 unexposed individuals.
New targets
Spironolactone reduced alcohol intake in mice drinking a sweetened alcohol solution; a 2-way ANOVA revealed a main effect of dose (F 4,52 = 9.09; P < .0001) and sex, with female mice drinking more alcohol, compared to male mice (F 1,13 = 6.05; P = .02).
Post hoc comparisons showed that spironolactone at doses of 50, 100, and 200 mg/kg significantly reduced alcohol intake (P values = .007, .002, and .0001, respectively).
In mice drinking an unsweetened alcohol solution, the 2-way repeated measures ANOVA similarly found a main effect of dose (F 4,52 = 5.77; P = .0006), but not of sex (F 1,13 = 1.41; P = .25).
Spironolactone had no effect on the mice’s intake of a sweet solution without alcohol and had no impact on the consumption of food and water or on locomotion and coordination.
In rats, a 2-way ANOVA revealed a significant spironolactone effect of dose (F 3,66 = 43.95; P < .001), with a post hoc test indicating that spironolactone at 25, 50, and 75 mg/kg reduced alcohol self-administration in alcohol-dependent and nondependent rats (all P values = .0001).
In humans, among the exposed individuals in the matched cohort, 25%, 57%, and 18% received daily doses of spironolactone of less than 25 mg/day, 25-49 mg/day, and 50 mg/day or higher, respectively, with a median follow-up time of 542 (interquartile range, 337-730) days.
The AUDIT-C scores decreased during the study period in both treatment groups, with a larger decrease in average AUDIT-C scores among the exposed vs. unexposed individuals.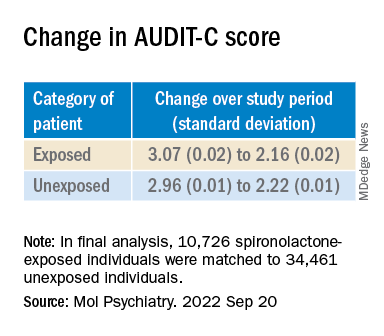
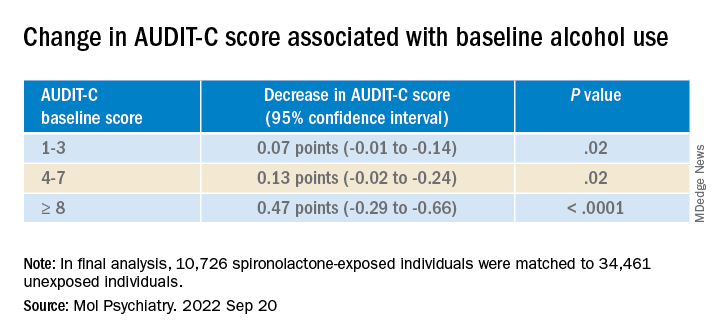
“These are very exciting times because, thanks to the progress in the addiction biomedical research field, we are increasing our understanding of the mechanisms how some people develop AUD; hence we can use this knowledge to identify new targets.” The current study “is an example of these ongoing efforts,” said Dr. Leggio.
“It is important to note that [these results] are important but preliminary.” At this juncture, “it would be too premature to think about prescribing spironolactone to treat AUD,” he added.
Exciting findings
Commenting on the study, Joyce Besheer, PhD, professor, department of psychiatry and Bowles Center for Alcohol Studies, University of North Carolina at Chapel Hill, called the study an “elegant demonstration of translational science.”
“While clinical trials will be needed to determine whether this medication is effective at reducing drinking in patients with AUD, these findings are exciting as they suggest that spironolactone may be a promising compound and new treatment options for AUD are much needed,” said Dr. Besheer, who was not involved with the current study.
Dr. Leggio agreed. “We now need prospective, placebo-controlled studies to assess the potential safety and efficacy of spironolactone in people with AUD,” he said.
This work was supported by the National Institutes of Health and the NIAAA. Dr. Leggio, study coauthors, and Dr. Besheer declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(AUD), new research suggests.
Researchers at the National Institute on Drug Abuse, the National Institute on Alcohol Abuse and Alcoholism, and Yale University, New Haven, Conn., investigated the impact of spironolactone on AUD.
Initially, they studied rodents and found that spironolactone reduced binge drinking in mice and reduced self-administration of alcohol in rats without adversely affecting food or water intake or causing motor or coordination problems.
They also analyzed electronic health records of patients drawn from the United States Veterans Affairs health care system to explore potential changes in alcohol use after spironolactone treatment was initiated for other conditions and found a significant link between spironolactone treatment and reduction in self-reported alcohol consumption, with the largest effects observed among those who reported hazardous/heavy episodic alcohol use prior to starting spironolactone treatment.
“Combining findings across three species and different types of research studies, and then seeing similarities in these data, gives us confidence that we are onto something potentially important scientifically and clinically,” senior coauthor Lorenzo Leggio, MD, PhD, senior investigator in the Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, a joint NIDA and NIAAA laboratory, said in a news release.
The study was published online in Molecular Psychiatry.
There is a “critical need to increase the armamentarium of pharmacotherapies to treat individuals with AUD,” the authors note, adding that neuroendocrine systems involved in alcohol craving and drinking “offer promising pharmacologic targets in this regard.”
“Both our team and others have observed that patients with AUD often present with changes in peripheral hormones, including aldosterone, which plays a key role in regulating blood pressure and electrolytes,” Dr. Leggio said in an interview.
Spironolactone is a nonselective mineralocorticoid receptor (MT) antagonist. In studies in animal models, investigators said they found “an inverse correlation between alcohol drinking and the expression of the MR in the amygdala, a key brain region in the development and maintenance of AUD and addiction in general.”
Taken together, this led them to hypothesize that blocking the MR, which is the mechanism of action of spironolactone, “could be a novel pharmacotherapeutic approach for AUD,” he said.
Previous research by the same group of researchers suggested spironolactone “may be a potential new medication to treat patients with AUD.” The present study expanded on those findings and consisted of a three-part investigation.
In the current study, the investigators tested different dosages of spironolactone on binge-like alcohol consumption in male and female mice and assessed food and water intake, blood alcohol levels, motor coordination, and spontaneous locomotion.
They then tested the effects of different dosages of spironolactone injections on operant alcohol self-administration in alcohol-dependent and nondependent male and female rats, also testing blood alcohol levels and motor coordination.
Finally, they analyzed health records of veterans to examine the association between at least 60 continuous days of spironolactone treatment and self-reported alcohol consumption (measured by the Alcohol Use Disorders Identification Test-Consumption [AUDIT-C]).
Each of the spironolactone-exposed patients was matched using propensity scores with up to five unexposed patients who had reported alcohol consumption in the 2 years prior to the index date.
The final analysis included a matched cohort of 10,726 spironolactone-exposed individuals who were matched to 34,461 unexposed individuals.
New targets
Spironolactone reduced alcohol intake in mice drinking a sweetened alcohol solution; a 2-way ANOVA revealed a main effect of dose (F 4,52 = 9.09; P < .0001) and sex, with female mice drinking more alcohol, compared to male mice (F 1,13 = 6.05; P = .02).
Post hoc comparisons showed that spironolactone at doses of 50, 100, and 200 mg/kg significantly reduced alcohol intake (P values = .007, .002, and .0001, respectively).
In mice drinking an unsweetened alcohol solution, the 2-way repeated measures ANOVA similarly found a main effect of dose (F 4,52 = 5.77; P = .0006), but not of sex (F 1,13 = 1.41; P = .25).
Spironolactone had no effect on the mice’s intake of a sweet solution without alcohol and had no impact on the consumption of food and water or on locomotion and coordination.
In rats, a 2-way ANOVA revealed a significant spironolactone effect of dose (F 3,66 = 43.95; P < .001), with a post hoc test indicating that spironolactone at 25, 50, and 75 mg/kg reduced alcohol self-administration in alcohol-dependent and nondependent rats (all P values = .0001).
In humans, among the exposed individuals in the matched cohort, 25%, 57%, and 18% received daily doses of spironolactone of less than 25 mg/day, 25-49 mg/day, and 50 mg/day or higher, respectively, with a median follow-up time of 542 (interquartile range, 337-730) days.
The AUDIT-C scores decreased during the study period in both treatment groups, with a larger decrease in average AUDIT-C scores among the exposed vs. unexposed individuals.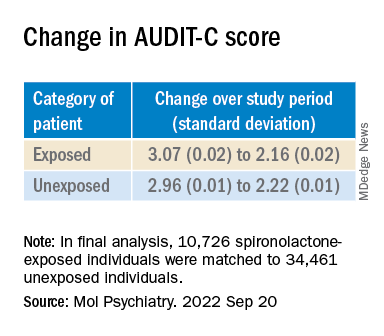
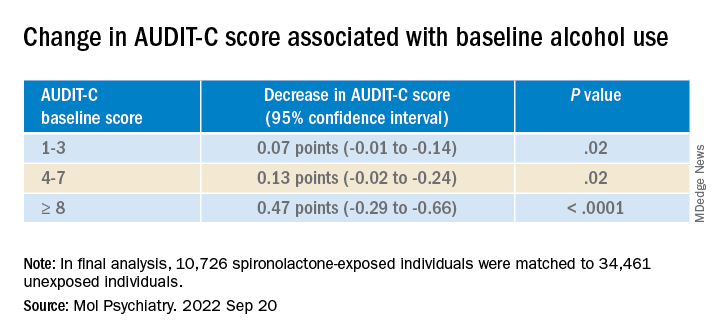
“These are very exciting times because, thanks to the progress in the addiction biomedical research field, we are increasing our understanding of the mechanisms how some people develop AUD; hence we can use this knowledge to identify new targets.” The current study “is an example of these ongoing efforts,” said Dr. Leggio.
“It is important to note that [these results] are important but preliminary.” At this juncture, “it would be too premature to think about prescribing spironolactone to treat AUD,” he added.
Exciting findings
Commenting on the study, Joyce Besheer, PhD, professor, department of psychiatry and Bowles Center for Alcohol Studies, University of North Carolina at Chapel Hill, called the study an “elegant demonstration of translational science.”
“While clinical trials will be needed to determine whether this medication is effective at reducing drinking in patients with AUD, these findings are exciting as they suggest that spironolactone may be a promising compound and new treatment options for AUD are much needed,” said Dr. Besheer, who was not involved with the current study.
Dr. Leggio agreed. “We now need prospective, placebo-controlled studies to assess the potential safety and efficacy of spironolactone in people with AUD,” he said.
This work was supported by the National Institutes of Health and the NIAAA. Dr. Leggio, study coauthors, and Dr. Besheer declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM MOLECULAR PSYCHIATRY
Apremilast may have some cardiometabolic benefits in patients with psoriasis
The trial, led by Joel M. Gelfand, MD, MSCE, professor of dermatology and epidemiology and vice chair of clinical research in dermatology at the University of Pennsylvania, Philadelphia, found that apremilast (Otezla) has a neutral effect on aortic vascular inflammation in patients with moderate to severe psoriasis.
It also had variable, but generally favorable, associations with 68 cardiometabolic biomarkers tested and associations with reductions in both visceral and subcutaneous fat. Findings of the study were published online in JAMA Dermatology.
Fat reductions maintained at 1-year mark
The researchers found a 5%-6% reduction in subcutaneous and visceral fat at week 16 of the study that was maintained at the 1-year mark. “The fact that it was rock stable a year later is pretty encouraging,” Dr. Gelfand told this news organization.
As for effects on vascular inflammation, Dr. Gelfand said, “The good news is we didn’t find any adverse effects on aortic vascular inflammation, but we didn’t find any beneficial effects either. That was a little disappointing.
“The most surprising thing was really the effects on visceral adiposity,” he added. “I’m not aware of any other drug having demonstrated that effect.”
Michael S. Garshick, MD, a cardiologist with NYU Langone Health in New York, who was not involved with the trial, told this news organization that despite seemingly good epidemiologic evidence in observational studies that by treating psoriasis surrogates of cardiovascular risk can be reduced, this trial, like others before it, failed to reduce aortic vascular inflammation.
The trial does help answer the question of whether apremilast can induce weight loss, he said, something that earlier trials suggested. “This trial confirms that, which is exciting,” he said. The reduction in both visceral and subcutaneous fat “deserves a lot further study.”
Several questions remain, Dr. Garshick said. Both he and Dr. Gelfand pointed to the need for large, placebo-controlled trials. “We still don’t know which medications may be preferrable in psoriasis to reduce [cardiovascular] risk if any at all,” Dr. Garshick said.
Seventy patients enrolled
In total, 70 patients with moderate to severe psoriasis were enrolled, 60 completed week 16, and 39 completed week 52 of the single-arm, open-label trial conducted between April 2017 and August 2021 at seven dermatology sites in the United States.
Participants took 30 mg of apremilast, an oral phosphodiesterase-4 (PDE-4) inhibitor approved for treating psoriasis and psoriatic arthritis, twice daily. Participants’ average age was 47.5 years; most were male (77.1%) and White (82.9%); almost 6% were Black. Average body mass index was 30 kg/m2. Patients could not have received biologics within 90 days of study baseline (or 180 days for ustekinumab [Stelara]).
There was no change in aortic vascular inflammation at week 16 (target to background ratio, −0.02; 95% confidence interval [CI], −0.08 to 0.05; P = .61) or week 52 (target to background ratio, −0.07; 95% CI, −0.15 to 0.01; P = .09) compared with baseline.
“At week 16, there were reductions in levels of interleukin-1b, fetuin A, valine, leucine, and isoleucine,” the authors wrote, adding that at week 52, compared with baseline, “there were reductions in levels of ferritin, cholesterol efflux capacity, beta-hydroxybutyrate, acetone, and ketone bodies, and an increase in levels of apolipoprotein A-1.”
This study highlights the importance of screening, Dr. Garshick said.
He and Dr. Gelfand said people with psoriatic disease tend to be vastly underscreened for cardiovascular risk factors.
Dr. Gelfand said, “If we did what we knew worked – meaning we screened them for diabetes, we screen their cholesterol, we check their blood pressure, and we adequately treated those traditional cardiovascular risk factors, we probably could narrow the gap quite a bit” in terms of the lower life expectancy people face when they have more significant psoriasis.
Celgene was the initial funding sponsor; sponsorship was then transferred to Amgen. The authors designed, executed, analyzed, and reported the study. Celgene provided nonbinding input into study design, and Amgen provided nonbinding input into the reporting of results. Dr. Gelfand reported numerous disclosures with various pharmaceutical companies and organizations. Dr. Garshick reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The trial, led by Joel M. Gelfand, MD, MSCE, professor of dermatology and epidemiology and vice chair of clinical research in dermatology at the University of Pennsylvania, Philadelphia, found that apremilast (Otezla) has a neutral effect on aortic vascular inflammation in patients with moderate to severe psoriasis.
It also had variable, but generally favorable, associations with 68 cardiometabolic biomarkers tested and associations with reductions in both visceral and subcutaneous fat. Findings of the study were published online in JAMA Dermatology.
Fat reductions maintained at 1-year mark
The researchers found a 5%-6% reduction in subcutaneous and visceral fat at week 16 of the study that was maintained at the 1-year mark. “The fact that it was rock stable a year later is pretty encouraging,” Dr. Gelfand told this news organization.
As for effects on vascular inflammation, Dr. Gelfand said, “The good news is we didn’t find any adverse effects on aortic vascular inflammation, but we didn’t find any beneficial effects either. That was a little disappointing.
“The most surprising thing was really the effects on visceral adiposity,” he added. “I’m not aware of any other drug having demonstrated that effect.”
Michael S. Garshick, MD, a cardiologist with NYU Langone Health in New York, who was not involved with the trial, told this news organization that despite seemingly good epidemiologic evidence in observational studies that by treating psoriasis surrogates of cardiovascular risk can be reduced, this trial, like others before it, failed to reduce aortic vascular inflammation.
The trial does help answer the question of whether apremilast can induce weight loss, he said, something that earlier trials suggested. “This trial confirms that, which is exciting,” he said. The reduction in both visceral and subcutaneous fat “deserves a lot further study.”
Several questions remain, Dr. Garshick said. Both he and Dr. Gelfand pointed to the need for large, placebo-controlled trials. “We still don’t know which medications may be preferrable in psoriasis to reduce [cardiovascular] risk if any at all,” Dr. Garshick said.
Seventy patients enrolled
In total, 70 patients with moderate to severe psoriasis were enrolled, 60 completed week 16, and 39 completed week 52 of the single-arm, open-label trial conducted between April 2017 and August 2021 at seven dermatology sites in the United States.
Participants took 30 mg of apremilast, an oral phosphodiesterase-4 (PDE-4) inhibitor approved for treating psoriasis and psoriatic arthritis, twice daily. Participants’ average age was 47.5 years; most were male (77.1%) and White (82.9%); almost 6% were Black. Average body mass index was 30 kg/m2. Patients could not have received biologics within 90 days of study baseline (or 180 days for ustekinumab [Stelara]).
There was no change in aortic vascular inflammation at week 16 (target to background ratio, −0.02; 95% confidence interval [CI], −0.08 to 0.05; P = .61) or week 52 (target to background ratio, −0.07; 95% CI, −0.15 to 0.01; P = .09) compared with baseline.
“At week 16, there were reductions in levels of interleukin-1b, fetuin A, valine, leucine, and isoleucine,” the authors wrote, adding that at week 52, compared with baseline, “there were reductions in levels of ferritin, cholesterol efflux capacity, beta-hydroxybutyrate, acetone, and ketone bodies, and an increase in levels of apolipoprotein A-1.”
This study highlights the importance of screening, Dr. Garshick said.
He and Dr. Gelfand said people with psoriatic disease tend to be vastly underscreened for cardiovascular risk factors.
Dr. Gelfand said, “If we did what we knew worked – meaning we screened them for diabetes, we screen their cholesterol, we check their blood pressure, and we adequately treated those traditional cardiovascular risk factors, we probably could narrow the gap quite a bit” in terms of the lower life expectancy people face when they have more significant psoriasis.
Celgene was the initial funding sponsor; sponsorship was then transferred to Amgen. The authors designed, executed, analyzed, and reported the study. Celgene provided nonbinding input into study design, and Amgen provided nonbinding input into the reporting of results. Dr. Gelfand reported numerous disclosures with various pharmaceutical companies and organizations. Dr. Garshick reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The trial, led by Joel M. Gelfand, MD, MSCE, professor of dermatology and epidemiology and vice chair of clinical research in dermatology at the University of Pennsylvania, Philadelphia, found that apremilast (Otezla) has a neutral effect on aortic vascular inflammation in patients with moderate to severe psoriasis.
It also had variable, but generally favorable, associations with 68 cardiometabolic biomarkers tested and associations with reductions in both visceral and subcutaneous fat. Findings of the study were published online in JAMA Dermatology.
Fat reductions maintained at 1-year mark
The researchers found a 5%-6% reduction in subcutaneous and visceral fat at week 16 of the study that was maintained at the 1-year mark. “The fact that it was rock stable a year later is pretty encouraging,” Dr. Gelfand told this news organization.
As for effects on vascular inflammation, Dr. Gelfand said, “The good news is we didn’t find any adverse effects on aortic vascular inflammation, but we didn’t find any beneficial effects either. That was a little disappointing.
“The most surprising thing was really the effects on visceral adiposity,” he added. “I’m not aware of any other drug having demonstrated that effect.”
Michael S. Garshick, MD, a cardiologist with NYU Langone Health in New York, who was not involved with the trial, told this news organization that despite seemingly good epidemiologic evidence in observational studies that by treating psoriasis surrogates of cardiovascular risk can be reduced, this trial, like others before it, failed to reduce aortic vascular inflammation.
The trial does help answer the question of whether apremilast can induce weight loss, he said, something that earlier trials suggested. “This trial confirms that, which is exciting,” he said. The reduction in both visceral and subcutaneous fat “deserves a lot further study.”
Several questions remain, Dr. Garshick said. Both he and Dr. Gelfand pointed to the need for large, placebo-controlled trials. “We still don’t know which medications may be preferrable in psoriasis to reduce [cardiovascular] risk if any at all,” Dr. Garshick said.
Seventy patients enrolled
In total, 70 patients with moderate to severe psoriasis were enrolled, 60 completed week 16, and 39 completed week 52 of the single-arm, open-label trial conducted between April 2017 and August 2021 at seven dermatology sites in the United States.
Participants took 30 mg of apremilast, an oral phosphodiesterase-4 (PDE-4) inhibitor approved for treating psoriasis and psoriatic arthritis, twice daily. Participants’ average age was 47.5 years; most were male (77.1%) and White (82.9%); almost 6% were Black. Average body mass index was 30 kg/m2. Patients could not have received biologics within 90 days of study baseline (or 180 days for ustekinumab [Stelara]).
There was no change in aortic vascular inflammation at week 16 (target to background ratio, −0.02; 95% confidence interval [CI], −0.08 to 0.05; P = .61) or week 52 (target to background ratio, −0.07; 95% CI, −0.15 to 0.01; P = .09) compared with baseline.
“At week 16, there were reductions in levels of interleukin-1b, fetuin A, valine, leucine, and isoleucine,” the authors wrote, adding that at week 52, compared with baseline, “there were reductions in levels of ferritin, cholesterol efflux capacity, beta-hydroxybutyrate, acetone, and ketone bodies, and an increase in levels of apolipoprotein A-1.”
This study highlights the importance of screening, Dr. Garshick said.
He and Dr. Gelfand said people with psoriatic disease tend to be vastly underscreened for cardiovascular risk factors.
Dr. Gelfand said, “If we did what we knew worked – meaning we screened them for diabetes, we screen their cholesterol, we check their blood pressure, and we adequately treated those traditional cardiovascular risk factors, we probably could narrow the gap quite a bit” in terms of the lower life expectancy people face when they have more significant psoriasis.
Celgene was the initial funding sponsor; sponsorship was then transferred to Amgen. The authors designed, executed, analyzed, and reported the study. Celgene provided nonbinding input into study design, and Amgen provided nonbinding input into the reporting of results. Dr. Gelfand reported numerous disclosures with various pharmaceutical companies and organizations. Dr. Garshick reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA DERMATOLOGY
Add PCSK9 inhibitor to high-intensity statin at primary PCI, proposes sham-controlled EPIC-STEMI
It’s best to have patients on aggressive lipid-lowering therapy before discharge after an acute ST-segment elevation myocardial infarction (STEMI), so why not start it right away – even in the cath lab – using some of the most potent LDL cholesterol–lowering agents available?
That was a main idea behind the randomized, sham-controlled EPIC-STEMI trial, in which STEMI patients were started on a PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitor immediately before direct percutaneous coronary intervention (PCI) and on top of high-intensity statins.
Those in the trial getting the active agent showed a 22% drop in LDL cholesterol levels by 6 weeks, compared with the control group given a sham injection along with high-intensity statins. They were also more likely to meet LDL cholesterol goals specified in some guidelines, including reduction by at least 50%. And those outcomes were achieved regardless of baseline LDL cholesterol levels or prior statin use.
Adoption of the trial’s early, aggressive LDL cholesterolreduction strategy in practice “has the potential to substantially reduce morbidity and mortality” in such cases “by further reducing LDL beyond statins in a much greater number of high-risk patients than are currently being treated with these agents,” suggested principal investigator Shamir R. Mehta, MD, MSc, when presenting the findings at the Transcatheter Cardiovascular Therapeutics annual meeting, sponsored by the Cardiovascular Research Foundation.
Adherence to secondary prevention measures in patients with acute coronary syndromes (ACS) is much better if they are started before hospital discharge, explained Dr. Mehta, senior scientist with Population Health Research Institute and professor of medicine at McMaster University, Hamilton, Ont. But “as soon as the patient has left the hospital, it is much more difficult to get these therapies on board.”
Routine adoption of such aggressive in-hospital, lipid-lowering therapy for the vast population with ACS would likely mean far fewer deaths and cardiovascular events “across a broader patient population.”
EPIC-STEMI is among the first studies to explore the strategy. “I think that’s the point of the trial that we wanted to make, that we don’t yet have data on this. We’re treading very carefully with PCSK9 inhibitors, and it’s just inching forward in populations. And I think we need a bold trial to see whether or not this changes things.”
The PCSK9 inhibitor alirocumab (Praluent) was used in EPIC-STEMI, which was published in EuroIntervention, with Dr. Mehta as lead author, the same day as his presentation. The drug and its sham injection were given on top of either atorvastatin 40-80 mg or rosuvastatin 40 mg.
Early initiation of statins in patients with acute STEMI has become standard, but there’s good evidence from intracoronary imaging studies suggesting that the addition of PCSK9 inhibitors might promote further stabilization of plaques that could potentially cause recurrent ischemic events.
Treatment with the injectable drugs plus statins led to significant coronary lesion regression in the GLAGOV trial of patients with stable coronary disease. And initiation of PCSK9 inhibitors with high-intensity statins soon after PCI for ACS improved atheroma shrinkage in non–infarct-related arteries over 1 year in the recent, placebo-controlled PACMAN-AMI trial.
Dr. Mehta pointed out that LDL reductions on PCSK9 inhibition, compared with the sham control, weren’t necessarily as impressive as might be expected from the major trials of long-term therapy with the drugs.
“You need longer [therapy] in order to see a difference in LDL levels when you use a PCSK9 inhibitor acutely. This is shown also on measures of infarct size.” There was no difference between treatment groups in infarct size as measured by levels of the MB fraction of creatine kinase, he reported.
“What this is telling us is that the acute use of a PCSK9 inhibitor did not modify the size or the severity of the baseline STEMI event.”
And EPIC-STEMI was too small and never intended to assess clinical outcomes; it was more about feasibility and what degree of LDL cholesterol lowering might be expected.
The trial was needed, Dr. Mehta said, because the PCSK9 inhibitors haven’t been extensively adopted into clinical practice and are not getting to the patients who could most benefit. One of the reasons for that is quite clear to him. “We are missing the high-risk patients because we are not treating them acutely,” Dr. Mehta said in an interview.
The strategy “has not yet been evaluated, and there have been barriers,” he observed. “Cost has been a barrier. Access to the drug has been a barrier. But in terms of the science, in terms of reducing cardiovascular events, this is a strategy that has to be tested.”
The aggressive, early LDL cholesterol reduction strategy should be evaluated for its effect on long-term outcomes, “especially knowing that in the first 30 days to 6 months post STEMI there’s a tremendous uptick in ischemic events, including recurrent myocardial infarction,” Roxana Mehran, MD, said at a media briefing on EPIC-STEMI held before Dr. Mehta’s formal presentation.
The “fantastic reduction acutely” with a PCSK9 inhibitor on top of statins, “hopefully reducing inflammation” similarly to what’s been observed in past trials, “absolutely warrants” a STEMI clinical outcomes trial, said Dr. Mehran, Icahn School of Medicine at Mount Sinai, New York, who isn’t connected with EPIC-STEMI.
If better post-discharge medication adherence is one of the acute strategy’s goals, it will be important to consider the potential influence of prescribing a periodically injected drug, proposed Eric A. Cohen, MD, Sunnybrook Health Sciences Center, Toronto, at the press conference.
“Keep in mind that STEMI patients typically come to the hospital on zero medications and leave 2 days later on five medications,” Dr. Cohen observed. “I’m curious whether having one of those as a sub-Q injection every 2 weeks, and reducing the pill burden, will help or deter adherence to therapy. I think it’s worth studying.”
The trial originally included 97 patients undergoing PCI for STEMI who were randomly assigned to receive the PCSK9 inhibitor or a sham injection on top of high-intensity statins, without regard to LDL cholesterol levels. Randomization took place after diagnostic angiography but before PCI.
The analysis, however, subsequently excluded 29 patients who could not continue with the study, “mainly because of hospital research clinic closure due to the COVID-19 pandemic,” the published report states.
That left 68 patients who had received at least one dose of PCSK9 inhibitor, alirocumab 150 mg subcutaneously, or the sham injection, and had at least one blood draw for LDL cholesterol response which, Dr. Mehta said, still left adequate statistical power for the LDL cholesterol–based primary endpoint.
By 6 weeks, LDL cholesterol levels had fallen 72.9% in the active-therapy group and by 48.1% in the control group (P < .001). Also, 92.1% and 56.7% of patients, respectively (P = .002), had achieved levels below the 1.4 mmol/L (54 mg/dL) goal in the European guidelines, Dr. Mehta reported.
Levels fell more than 50% compared with baseline in 89.5% of alirocumab patients and 60% (P = .007) of controls, respectively.
There was no significant difference in rates of attaining LDL cholesterol levels below the 70 mg/dL (1.8 mmol/L) threshold specified in U.S. guidelines for very high-risk patients: 94.7% of alirocumab patients and 83.4% of controls (P = .26).
Nor did the groups differ significantly in natriuretic peptide levels, which reflect ventricular remodeling; or in 6-week change in the inflammatory biomarker high-sensitivity C-reactive protein.
An open-label, randomized trial scheduled to launch before the end of 2022 will explore similarly early initiation of a PCSK9 inhibitor, compared with standard lipid management, in an estimated 4,000 patients hospitalized with STEMI or non-STEMI.
The EVOLVE MI trial is looking at the monoclonal antibody evolocumab (Repatha) for its effect on the primary endpoint of myocardial infarction, ischemic stroke, arterial revascularization, or death from any cause over an expected 3-4 years.
EPIC-STEMI was supported in part by Sanofi. Dr. Mehta reported an unrestricted grant from Sanofi to Hamilton Health Sciences for the present study and consulting fees from Amgen, Sanofi, and Novartis. Dr. Cohen disclosed receiving grant support from and holding research contracts with Abbott Vascular; and receiving fees for consulting, honoraria, or serving on a speaker’s bureau for Abbott Vascular, Medtronic, and Baylis. Dr. Mehran disclosed receiving grants or research support from numerous pharmaceutical companies; receiving consultant fee or honoraria or serving on a speaker’s bureau for Novartis, Abbott Vascular, Janssen, Medtronic, Medscape/WebMD, and Cine-Med Research; and holding equity, stock, or stock options with Control Rad, Applied Therapeutics, and Elixir Medical.
A version of this article first appeared on Medscape.com.
It’s best to have patients on aggressive lipid-lowering therapy before discharge after an acute ST-segment elevation myocardial infarction (STEMI), so why not start it right away – even in the cath lab – using some of the most potent LDL cholesterol–lowering agents available?
That was a main idea behind the randomized, sham-controlled EPIC-STEMI trial, in which STEMI patients were started on a PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitor immediately before direct percutaneous coronary intervention (PCI) and on top of high-intensity statins.
Those in the trial getting the active agent showed a 22% drop in LDL cholesterol levels by 6 weeks, compared with the control group given a sham injection along with high-intensity statins. They were also more likely to meet LDL cholesterol goals specified in some guidelines, including reduction by at least 50%. And those outcomes were achieved regardless of baseline LDL cholesterol levels or prior statin use.
Adoption of the trial’s early, aggressive LDL cholesterolreduction strategy in practice “has the potential to substantially reduce morbidity and mortality” in such cases “by further reducing LDL beyond statins in a much greater number of high-risk patients than are currently being treated with these agents,” suggested principal investigator Shamir R. Mehta, MD, MSc, when presenting the findings at the Transcatheter Cardiovascular Therapeutics annual meeting, sponsored by the Cardiovascular Research Foundation.
Adherence to secondary prevention measures in patients with acute coronary syndromes (ACS) is much better if they are started before hospital discharge, explained Dr. Mehta, senior scientist with Population Health Research Institute and professor of medicine at McMaster University, Hamilton, Ont. But “as soon as the patient has left the hospital, it is much more difficult to get these therapies on board.”
Routine adoption of such aggressive in-hospital, lipid-lowering therapy for the vast population with ACS would likely mean far fewer deaths and cardiovascular events “across a broader patient population.”
EPIC-STEMI is among the first studies to explore the strategy. “I think that’s the point of the trial that we wanted to make, that we don’t yet have data on this. We’re treading very carefully with PCSK9 inhibitors, and it’s just inching forward in populations. And I think we need a bold trial to see whether or not this changes things.”
The PCSK9 inhibitor alirocumab (Praluent) was used in EPIC-STEMI, which was published in EuroIntervention, with Dr. Mehta as lead author, the same day as his presentation. The drug and its sham injection were given on top of either atorvastatin 40-80 mg or rosuvastatin 40 mg.
Early initiation of statins in patients with acute STEMI has become standard, but there’s good evidence from intracoronary imaging studies suggesting that the addition of PCSK9 inhibitors might promote further stabilization of plaques that could potentially cause recurrent ischemic events.
Treatment with the injectable drugs plus statins led to significant coronary lesion regression in the GLAGOV trial of patients with stable coronary disease. And initiation of PCSK9 inhibitors with high-intensity statins soon after PCI for ACS improved atheroma shrinkage in non–infarct-related arteries over 1 year in the recent, placebo-controlled PACMAN-AMI trial.
Dr. Mehta pointed out that LDL reductions on PCSK9 inhibition, compared with the sham control, weren’t necessarily as impressive as might be expected from the major trials of long-term therapy with the drugs.
“You need longer [therapy] in order to see a difference in LDL levels when you use a PCSK9 inhibitor acutely. This is shown also on measures of infarct size.” There was no difference between treatment groups in infarct size as measured by levels of the MB fraction of creatine kinase, he reported.
“What this is telling us is that the acute use of a PCSK9 inhibitor did not modify the size or the severity of the baseline STEMI event.”
And EPIC-STEMI was too small and never intended to assess clinical outcomes; it was more about feasibility and what degree of LDL cholesterol lowering might be expected.
The trial was needed, Dr. Mehta said, because the PCSK9 inhibitors haven’t been extensively adopted into clinical practice and are not getting to the patients who could most benefit. One of the reasons for that is quite clear to him. “We are missing the high-risk patients because we are not treating them acutely,” Dr. Mehta said in an interview.
The strategy “has not yet been evaluated, and there have been barriers,” he observed. “Cost has been a barrier. Access to the drug has been a barrier. But in terms of the science, in terms of reducing cardiovascular events, this is a strategy that has to be tested.”
The aggressive, early LDL cholesterol reduction strategy should be evaluated for its effect on long-term outcomes, “especially knowing that in the first 30 days to 6 months post STEMI there’s a tremendous uptick in ischemic events, including recurrent myocardial infarction,” Roxana Mehran, MD, said at a media briefing on EPIC-STEMI held before Dr. Mehta’s formal presentation.
The “fantastic reduction acutely” with a PCSK9 inhibitor on top of statins, “hopefully reducing inflammation” similarly to what’s been observed in past trials, “absolutely warrants” a STEMI clinical outcomes trial, said Dr. Mehran, Icahn School of Medicine at Mount Sinai, New York, who isn’t connected with EPIC-STEMI.
If better post-discharge medication adherence is one of the acute strategy’s goals, it will be important to consider the potential influence of prescribing a periodically injected drug, proposed Eric A. Cohen, MD, Sunnybrook Health Sciences Center, Toronto, at the press conference.
“Keep in mind that STEMI patients typically come to the hospital on zero medications and leave 2 days later on five medications,” Dr. Cohen observed. “I’m curious whether having one of those as a sub-Q injection every 2 weeks, and reducing the pill burden, will help or deter adherence to therapy. I think it’s worth studying.”
The trial originally included 97 patients undergoing PCI for STEMI who were randomly assigned to receive the PCSK9 inhibitor or a sham injection on top of high-intensity statins, without regard to LDL cholesterol levels. Randomization took place after diagnostic angiography but before PCI.
The analysis, however, subsequently excluded 29 patients who could not continue with the study, “mainly because of hospital research clinic closure due to the COVID-19 pandemic,” the published report states.
That left 68 patients who had received at least one dose of PCSK9 inhibitor, alirocumab 150 mg subcutaneously, or the sham injection, and had at least one blood draw for LDL cholesterol response which, Dr. Mehta said, still left adequate statistical power for the LDL cholesterol–based primary endpoint.
By 6 weeks, LDL cholesterol levels had fallen 72.9% in the active-therapy group and by 48.1% in the control group (P < .001). Also, 92.1% and 56.7% of patients, respectively (P = .002), had achieved levels below the 1.4 mmol/L (54 mg/dL) goal in the European guidelines, Dr. Mehta reported.
Levels fell more than 50% compared with baseline in 89.5% of alirocumab patients and 60% (P = .007) of controls, respectively.
There was no significant difference in rates of attaining LDL cholesterol levels below the 70 mg/dL (1.8 mmol/L) threshold specified in U.S. guidelines for very high-risk patients: 94.7% of alirocumab patients and 83.4% of controls (P = .26).
Nor did the groups differ significantly in natriuretic peptide levels, which reflect ventricular remodeling; or in 6-week change in the inflammatory biomarker high-sensitivity C-reactive protein.
An open-label, randomized trial scheduled to launch before the end of 2022 will explore similarly early initiation of a PCSK9 inhibitor, compared with standard lipid management, in an estimated 4,000 patients hospitalized with STEMI or non-STEMI.
The EVOLVE MI trial is looking at the monoclonal antibody evolocumab (Repatha) for its effect on the primary endpoint of myocardial infarction, ischemic stroke, arterial revascularization, or death from any cause over an expected 3-4 years.
EPIC-STEMI was supported in part by Sanofi. Dr. Mehta reported an unrestricted grant from Sanofi to Hamilton Health Sciences for the present study and consulting fees from Amgen, Sanofi, and Novartis. Dr. Cohen disclosed receiving grant support from and holding research contracts with Abbott Vascular; and receiving fees for consulting, honoraria, or serving on a speaker’s bureau for Abbott Vascular, Medtronic, and Baylis. Dr. Mehran disclosed receiving grants or research support from numerous pharmaceutical companies; receiving consultant fee or honoraria or serving on a speaker’s bureau for Novartis, Abbott Vascular, Janssen, Medtronic, Medscape/WebMD, and Cine-Med Research; and holding equity, stock, or stock options with Control Rad, Applied Therapeutics, and Elixir Medical.
A version of this article first appeared on Medscape.com.
It’s best to have patients on aggressive lipid-lowering therapy before discharge after an acute ST-segment elevation myocardial infarction (STEMI), so why not start it right away – even in the cath lab – using some of the most potent LDL cholesterol–lowering agents available?
That was a main idea behind the randomized, sham-controlled EPIC-STEMI trial, in which STEMI patients were started on a PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitor immediately before direct percutaneous coronary intervention (PCI) and on top of high-intensity statins.
Those in the trial getting the active agent showed a 22% drop in LDL cholesterol levels by 6 weeks, compared with the control group given a sham injection along with high-intensity statins. They were also more likely to meet LDL cholesterol goals specified in some guidelines, including reduction by at least 50%. And those outcomes were achieved regardless of baseline LDL cholesterol levels or prior statin use.
Adoption of the trial’s early, aggressive LDL cholesterolreduction strategy in practice “has the potential to substantially reduce morbidity and mortality” in such cases “by further reducing LDL beyond statins in a much greater number of high-risk patients than are currently being treated with these agents,” suggested principal investigator Shamir R. Mehta, MD, MSc, when presenting the findings at the Transcatheter Cardiovascular Therapeutics annual meeting, sponsored by the Cardiovascular Research Foundation.
Adherence to secondary prevention measures in patients with acute coronary syndromes (ACS) is much better if they are started before hospital discharge, explained Dr. Mehta, senior scientist with Population Health Research Institute and professor of medicine at McMaster University, Hamilton, Ont. But “as soon as the patient has left the hospital, it is much more difficult to get these therapies on board.”
Routine adoption of such aggressive in-hospital, lipid-lowering therapy for the vast population with ACS would likely mean far fewer deaths and cardiovascular events “across a broader patient population.”
EPIC-STEMI is among the first studies to explore the strategy. “I think that’s the point of the trial that we wanted to make, that we don’t yet have data on this. We’re treading very carefully with PCSK9 inhibitors, and it’s just inching forward in populations. And I think we need a bold trial to see whether or not this changes things.”
The PCSK9 inhibitor alirocumab (Praluent) was used in EPIC-STEMI, which was published in EuroIntervention, with Dr. Mehta as lead author, the same day as his presentation. The drug and its sham injection were given on top of either atorvastatin 40-80 mg or rosuvastatin 40 mg.
Early initiation of statins in patients with acute STEMI has become standard, but there’s good evidence from intracoronary imaging studies suggesting that the addition of PCSK9 inhibitors might promote further stabilization of plaques that could potentially cause recurrent ischemic events.
Treatment with the injectable drugs plus statins led to significant coronary lesion regression in the GLAGOV trial of patients with stable coronary disease. And initiation of PCSK9 inhibitors with high-intensity statins soon after PCI for ACS improved atheroma shrinkage in non–infarct-related arteries over 1 year in the recent, placebo-controlled PACMAN-AMI trial.
Dr. Mehta pointed out that LDL reductions on PCSK9 inhibition, compared with the sham control, weren’t necessarily as impressive as might be expected from the major trials of long-term therapy with the drugs.
“You need longer [therapy] in order to see a difference in LDL levels when you use a PCSK9 inhibitor acutely. This is shown also on measures of infarct size.” There was no difference between treatment groups in infarct size as measured by levels of the MB fraction of creatine kinase, he reported.
“What this is telling us is that the acute use of a PCSK9 inhibitor did not modify the size or the severity of the baseline STEMI event.”
And EPIC-STEMI was too small and never intended to assess clinical outcomes; it was more about feasibility and what degree of LDL cholesterol lowering might be expected.
The trial was needed, Dr. Mehta said, because the PCSK9 inhibitors haven’t been extensively adopted into clinical practice and are not getting to the patients who could most benefit. One of the reasons for that is quite clear to him. “We are missing the high-risk patients because we are not treating them acutely,” Dr. Mehta said in an interview.
The strategy “has not yet been evaluated, and there have been barriers,” he observed. “Cost has been a barrier. Access to the drug has been a barrier. But in terms of the science, in terms of reducing cardiovascular events, this is a strategy that has to be tested.”
The aggressive, early LDL cholesterol reduction strategy should be evaluated for its effect on long-term outcomes, “especially knowing that in the first 30 days to 6 months post STEMI there’s a tremendous uptick in ischemic events, including recurrent myocardial infarction,” Roxana Mehran, MD, said at a media briefing on EPIC-STEMI held before Dr. Mehta’s formal presentation.
The “fantastic reduction acutely” with a PCSK9 inhibitor on top of statins, “hopefully reducing inflammation” similarly to what’s been observed in past trials, “absolutely warrants” a STEMI clinical outcomes trial, said Dr. Mehran, Icahn School of Medicine at Mount Sinai, New York, who isn’t connected with EPIC-STEMI.
If better post-discharge medication adherence is one of the acute strategy’s goals, it will be important to consider the potential influence of prescribing a periodically injected drug, proposed Eric A. Cohen, MD, Sunnybrook Health Sciences Center, Toronto, at the press conference.
“Keep in mind that STEMI patients typically come to the hospital on zero medications and leave 2 days later on five medications,” Dr. Cohen observed. “I’m curious whether having one of those as a sub-Q injection every 2 weeks, and reducing the pill burden, will help or deter adherence to therapy. I think it’s worth studying.”
The trial originally included 97 patients undergoing PCI for STEMI who were randomly assigned to receive the PCSK9 inhibitor or a sham injection on top of high-intensity statins, without regard to LDL cholesterol levels. Randomization took place after diagnostic angiography but before PCI.
The analysis, however, subsequently excluded 29 patients who could not continue with the study, “mainly because of hospital research clinic closure due to the COVID-19 pandemic,” the published report states.
That left 68 patients who had received at least one dose of PCSK9 inhibitor, alirocumab 150 mg subcutaneously, or the sham injection, and had at least one blood draw for LDL cholesterol response which, Dr. Mehta said, still left adequate statistical power for the LDL cholesterol–based primary endpoint.
By 6 weeks, LDL cholesterol levels had fallen 72.9% in the active-therapy group and by 48.1% in the control group (P < .001). Also, 92.1% and 56.7% of patients, respectively (P = .002), had achieved levels below the 1.4 mmol/L (54 mg/dL) goal in the European guidelines, Dr. Mehta reported.
Levels fell more than 50% compared with baseline in 89.5% of alirocumab patients and 60% (P = .007) of controls, respectively.
There was no significant difference in rates of attaining LDL cholesterol levels below the 70 mg/dL (1.8 mmol/L) threshold specified in U.S. guidelines for very high-risk patients: 94.7% of alirocumab patients and 83.4% of controls (P = .26).
Nor did the groups differ significantly in natriuretic peptide levels, which reflect ventricular remodeling; or in 6-week change in the inflammatory biomarker high-sensitivity C-reactive protein.
An open-label, randomized trial scheduled to launch before the end of 2022 will explore similarly early initiation of a PCSK9 inhibitor, compared with standard lipid management, in an estimated 4,000 patients hospitalized with STEMI or non-STEMI.
The EVOLVE MI trial is looking at the monoclonal antibody evolocumab (Repatha) for its effect on the primary endpoint of myocardial infarction, ischemic stroke, arterial revascularization, or death from any cause over an expected 3-4 years.
EPIC-STEMI was supported in part by Sanofi. Dr. Mehta reported an unrestricted grant from Sanofi to Hamilton Health Sciences for the present study and consulting fees from Amgen, Sanofi, and Novartis. Dr. Cohen disclosed receiving grant support from and holding research contracts with Abbott Vascular; and receiving fees for consulting, honoraria, or serving on a speaker’s bureau for Abbott Vascular, Medtronic, and Baylis. Dr. Mehran disclosed receiving grants or research support from numerous pharmaceutical companies; receiving consultant fee or honoraria or serving on a speaker’s bureau for Novartis, Abbott Vascular, Janssen, Medtronic, Medscape/WebMD, and Cine-Med Research; and holding equity, stock, or stock options with Control Rad, Applied Therapeutics, and Elixir Medical.
A version of this article first appeared on Medscape.com.
FROM TCT 2022