User login
Pediatric Nail Diseases: Clinical Pearls
Our dermatology department recently sponsored a pediatric dermatology lecture series for the pediatric residency program. Within this series, Antonella Tosti, MD, a professor at the University of Miami Health System, Florida, and a renowned expert in nail disorders and allergic contact dermatitis, presented her clinical expertise on the presentation and management of common pediatric nail diseases. This article highlights pearls from her unique and enlightening lecture.
Pearl: Hand-foot-and-mouth disease is a recognized trigger for onychomadesis
An arrest in nail matrix activity is responsible for onychomadesis, or shedding of the nail. Its presentation in children can be further divided based upon the degree of involvement. If a few nails are affected, trauma should be implicated. In contrast, if all nails are involved, a systemic etiology should be suspected. Hand-foot-and-mouth disease (HFMD) has been recognized as a trigger for onychomadesis in school-aged children. Onychomadesis presents with characteristic proximal nail detachment (Figure 1). The association of HFMD with onychomadesis and Beau lines was first reported in 2000. Five patients who resided within close proximity and shared a physician-diagnosed case of HFMD presented with representative nail findings 4 weeks after illness.1 Hypotheses for these changes include viral-induced nail pathology, inflammation from cutaneous lesions of HFMD, and systemic effects from the disease.2 Given the prevalence of HFMD and benign outcome, clinicians should be cognizant of this unique cutaneous manifestation.

Pearl: Management of pediatric melanonychia can take a wait-and-see approach
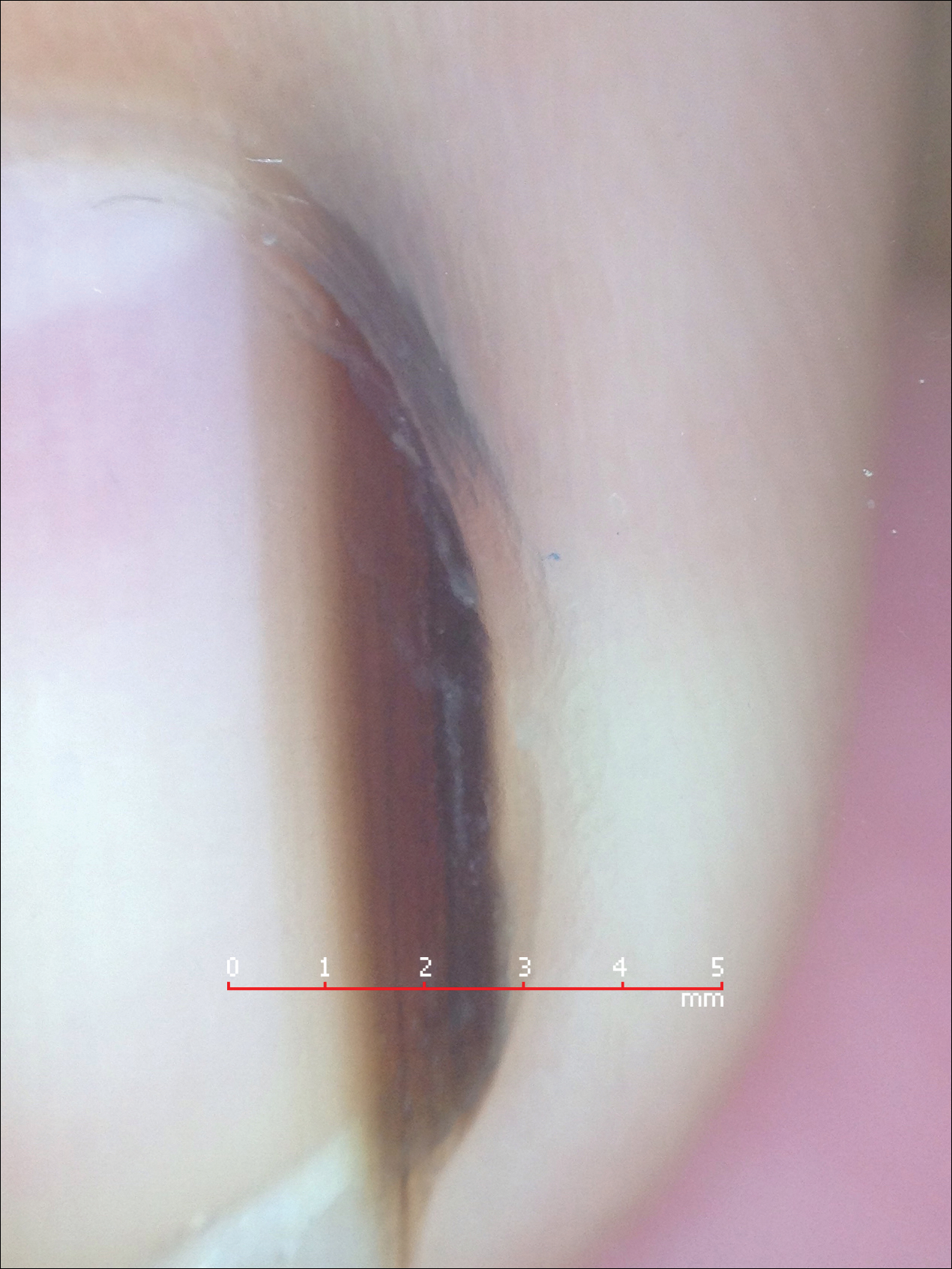
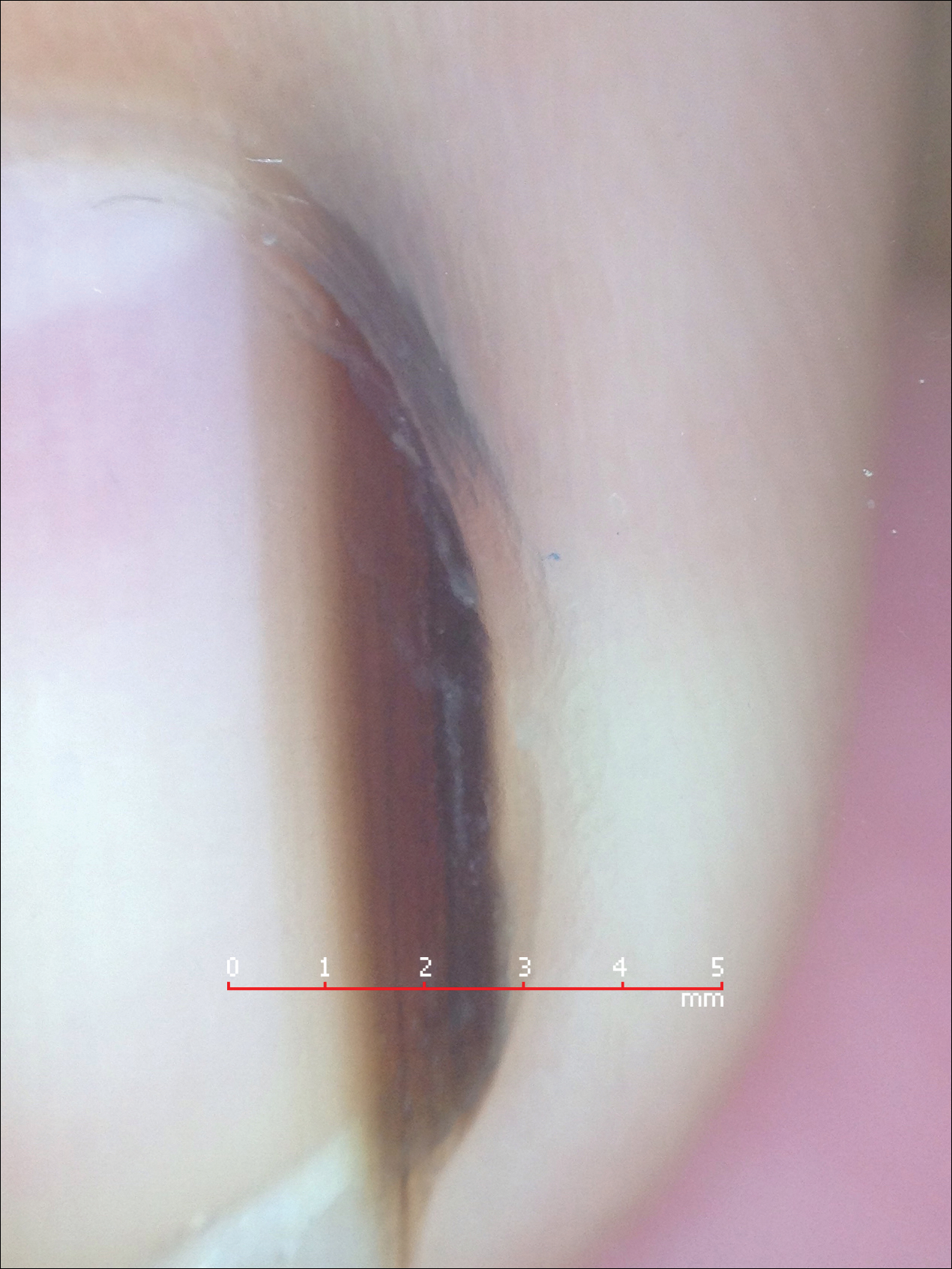
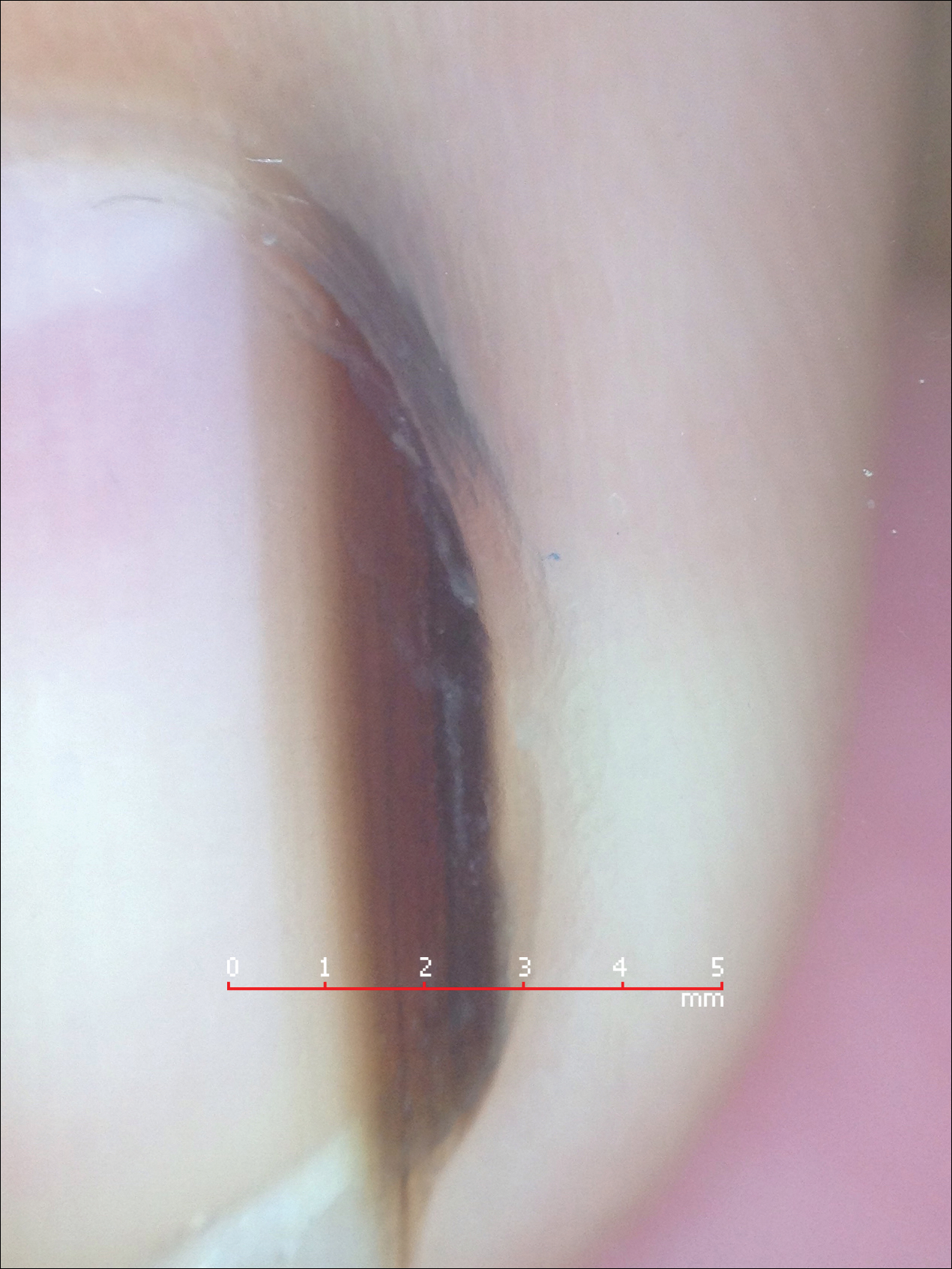
Melanonychia is the presence of a longitudinal brown-black band extending from the proximal nail fold. The cause of melanonychia can be due to either activation or hyperplasia. Activation is the less common etiology in children; however, if present, activation can be due to Laugier-Hunziker syndrome or trauma such as onychotillomania. Melanonychia in children usually is the result of hyperplasia of melanocytes and can manifest as a lentigo, nevus, or more rarely melanoma. Nail matrix nevi are typically exhibited on the fingernails, particularly the thumb, and frequently are junctional nevi (Figure 2). Spontaneous fading of nevi is expected with time due to decreased melanin production. Therapeutic options for melanonychia include regular clinical monitoring, biopsy, or excision. Dr. Tosti explained that one must be wary when pursuing a biopsy, as it can result in a false-negative finding due to missed pathology. If clinically indicated, a shave biopsy of the nail matrix can be performed to best analyze the lesion. She noted that if more than 3 mm of the matrix is removed, a resultant scar will ensue. Conservative management is recommended given the indolent clinical behavior of the majority of cases of melanonychia in children.3
Pearl: Congenital hypertrophy of the lateral nail folds can be treated with tape
Congenital hypertrophy of the lateral nail folds is relatively common in children and normally improves with age. Koilonychia may also occur simultaneously and can be viewed as a physiologic process in this age group. The etiology of the underlying disorder is due to anomalous periungual soft-tissue changes of the bilateral halluces; the resulting overgrowth can partially cover the nail plate. Although usually a self-limiting condition, the changes can cause inflammation and discomfort due to an ingrown nail.4 Dr. Tosti advised that by simply taping and retracting the bilateral overgrowth, the condition can be more readily resolved. This simple treatment can be demonstrated in the office and subsequently performed at home.
Pearl: Onychomycosis is uncommon in children
Onychomycosis occurs in less than 1% of children.5 Several factors are responsible for this decreased prevalence. More rapid nail growth and smaller nail surface area decreases the ability of the fungi to penetrate the nail plate.6 Furthermore, children have a diminished rate of tinea pedis, leading to less neighboring infection. When onychomycosis does affect this patient population, it commonly presents as distal subungual onychomycosis and favors the fingernails over the toenails. Treatment options usually parallel those of the adult population; however, all medications for children are considered off-label use by the US Food and Drug Administration. Dr. Tosti explained that oral granules of terbinafine can be sprinkled on food to help with pediatric ingestion. Topical therapies should also be considered; children usually respond better than their adult counterparts due to their thinner nails, which grant enhanced drug delivery and penetration.6
Pearl: Acute paronychia can be due to nail-biting and sucking
Acute paronychia is inflammation of the proximal nail fold. In children, it frequently is a result of mixed flora induced by nail-biting and sucking. Management involves culturing the affected lesions and is effectively treated with warm soaks alone. Dr. Tosti highlighted that Candida in the subungual space is a common colonizer and is typically self-limiting in nature if isolated. Candida can be cultured more readily in premature infants, immunosuppressed patients, and those with chronic mucocutaneous candidiasis. Patients with chronic mucocutaneous candidiasis can exhibit periungual inflammation involving several digits. The differential can include nail psoriasis, as both can demonstrate dystrophic changes. The differential for localized paronychia includes herpetic whitlow and can manifest as vesicles under the proximal nail fold.
Final Thoughts
These clinical pearls are shared to help deliver utmost care to our pediatric patients presenting with nail pathology. For example, a child exhibiting melanonychia can cause alarm due to the possibility of underlying melanoma; given the rarity of neoplasia in these patients, a conservative approach is favored to help avoid unnecessary biopsies and subsequent scarring. Similarly, it is important to be aware of the common colonizers of the subungual area, particularly Candida, to avoid unessential medications with potential side effects. The examples demonstrated help shed light on the management of pediatric nail diseases.
Acknowledgment
This article is possible thanks to the help of Antonella Tosti, MD (Miami, Florida), who contributed her time and expertise at the University of Miami Pediatric Grand Rounds to expand the foundation and knowledge of pediatric nail diseases.
- Clementz GC, Mancini AJ. Nail matrix arrest following hand-foot-mouth disease: a report of five children. Pediatr Dermatol. 2000;17:7-11.
- Yuksel S, Evrengul H, Ozhan B, et al. Onychomadesis-a late complication of hand-foot-mouth disease [published online May 2, 2016]. J Pediatr. 2016;174:274.
- Cooper C, Arva NC, Lee C, et al. A clinical, histopathologic, and outcome study of melanonychia striata in childhood. J Am Acad Dermatol. 2015;72:773-779.
- Piraccini BM, Parente GL, Varotti E, et al. Congenital hypertrophy of the lateral nail folds of the hallux: clinical features and follow-up of seven cases. Pediatr Dermatol. 2000;17:348-351.
- Totri CR, Feldstein S, Admani S, et al. Epidemiologic analysis of onychomycosis in the San Diego pediatric population [published online October 4, 2016]. Pediatr Dermatol. 2017;34:46-49.
- Feldstein S, Totri C, Friedlander SF. Antifungal therapy for onychomycosis in children. Clin Dermatol. 2015;33:333-339.
Our dermatology department recently sponsored a pediatric dermatology lecture series for the pediatric residency program. Within this series, Antonella Tosti, MD, a professor at the University of Miami Health System, Florida, and a renowned expert in nail disorders and allergic contact dermatitis, presented her clinical expertise on the presentation and management of common pediatric nail diseases. This article highlights pearls from her unique and enlightening lecture.
Pearl: Hand-foot-and-mouth disease is a recognized trigger for onychomadesis
An arrest in nail matrix activity is responsible for onychomadesis, or shedding of the nail. Its presentation in children can be further divided based upon the degree of involvement. If a few nails are affected, trauma should be implicated. In contrast, if all nails are involved, a systemic etiology should be suspected. Hand-foot-and-mouth disease (HFMD) has been recognized as a trigger for onychomadesis in school-aged children. Onychomadesis presents with characteristic proximal nail detachment (Figure 1). The association of HFMD with onychomadesis and Beau lines was first reported in 2000. Five patients who resided within close proximity and shared a physician-diagnosed case of HFMD presented with representative nail findings 4 weeks after illness.1 Hypotheses for these changes include viral-induced nail pathology, inflammation from cutaneous lesions of HFMD, and systemic effects from the disease.2 Given the prevalence of HFMD and benign outcome, clinicians should be cognizant of this unique cutaneous manifestation.

Pearl: Management of pediatric melanonychia can take a wait-and-see approach
Melanonychia is the presence of a longitudinal brown-black band extending from the proximal nail fold. The cause of melanonychia can be due to either activation or hyperplasia. Activation is the less common etiology in children; however, if present, activation can be due to Laugier-Hunziker syndrome or trauma such as onychotillomania. Melanonychia in children usually is the result of hyperplasia of melanocytes and can manifest as a lentigo, nevus, or more rarely melanoma. Nail matrix nevi are typically exhibited on the fingernails, particularly the thumb, and frequently are junctional nevi (Figure 2). Spontaneous fading of nevi is expected with time due to decreased melanin production. Therapeutic options for melanonychia include regular clinical monitoring, biopsy, or excision. Dr. Tosti explained that one must be wary when pursuing a biopsy, as it can result in a false-negative finding due to missed pathology. If clinically indicated, a shave biopsy of the nail matrix can be performed to best analyze the lesion. She noted that if more than 3 mm of the matrix is removed, a resultant scar will ensue. Conservative management is recommended given the indolent clinical behavior of the majority of cases of melanonychia in children.3
Pearl: Congenital hypertrophy of the lateral nail folds can be treated with tape
Congenital hypertrophy of the lateral nail folds is relatively common in children and normally improves with age. Koilonychia may also occur simultaneously and can be viewed as a physiologic process in this age group. The etiology of the underlying disorder is due to anomalous periungual soft-tissue changes of the bilateral halluces; the resulting overgrowth can partially cover the nail plate. Although usually a self-limiting condition, the changes can cause inflammation and discomfort due to an ingrown nail.4 Dr. Tosti advised that by simply taping and retracting the bilateral overgrowth, the condition can be more readily resolved. This simple treatment can be demonstrated in the office and subsequently performed at home.
Pearl: Onychomycosis is uncommon in children
Onychomycosis occurs in less than 1% of children.5 Several factors are responsible for this decreased prevalence. More rapid nail growth and smaller nail surface area decreases the ability of the fungi to penetrate the nail plate.6 Furthermore, children have a diminished rate of tinea pedis, leading to less neighboring infection. When onychomycosis does affect this patient population, it commonly presents as distal subungual onychomycosis and favors the fingernails over the toenails. Treatment options usually parallel those of the adult population; however, all medications for children are considered off-label use by the US Food and Drug Administration. Dr. Tosti explained that oral granules of terbinafine can be sprinkled on food to help with pediatric ingestion. Topical therapies should also be considered; children usually respond better than their adult counterparts due to their thinner nails, which grant enhanced drug delivery and penetration.6
Pearl: Acute paronychia can be due to nail-biting and sucking
Acute paronychia is inflammation of the proximal nail fold. In children, it frequently is a result of mixed flora induced by nail-biting and sucking. Management involves culturing the affected lesions and is effectively treated with warm soaks alone. Dr. Tosti highlighted that Candida in the subungual space is a common colonizer and is typically self-limiting in nature if isolated. Candida can be cultured more readily in premature infants, immunosuppressed patients, and those with chronic mucocutaneous candidiasis. Patients with chronic mucocutaneous candidiasis can exhibit periungual inflammation involving several digits. The differential can include nail psoriasis, as both can demonstrate dystrophic changes. The differential for localized paronychia includes herpetic whitlow and can manifest as vesicles under the proximal nail fold.
Final Thoughts
These clinical pearls are shared to help deliver utmost care to our pediatric patients presenting with nail pathology. For example, a child exhibiting melanonychia can cause alarm due to the possibility of underlying melanoma; given the rarity of neoplasia in these patients, a conservative approach is favored to help avoid unnecessary biopsies and subsequent scarring. Similarly, it is important to be aware of the common colonizers of the subungual area, particularly Candida, to avoid unessential medications with potential side effects. The examples demonstrated help shed light on the management of pediatric nail diseases.
Acknowledgment
This article is possible thanks to the help of Antonella Tosti, MD (Miami, Florida), who contributed her time and expertise at the University of Miami Pediatric Grand Rounds to expand the foundation and knowledge of pediatric nail diseases.
Our dermatology department recently sponsored a pediatric dermatology lecture series for the pediatric residency program. Within this series, Antonella Tosti, MD, a professor at the University of Miami Health System, Florida, and a renowned expert in nail disorders and allergic contact dermatitis, presented her clinical expertise on the presentation and management of common pediatric nail diseases. This article highlights pearls from her unique and enlightening lecture.
Pearl: Hand-foot-and-mouth disease is a recognized trigger for onychomadesis
An arrest in nail matrix activity is responsible for onychomadesis, or shedding of the nail. Its presentation in children can be further divided based upon the degree of involvement. If a few nails are affected, trauma should be implicated. In contrast, if all nails are involved, a systemic etiology should be suspected. Hand-foot-and-mouth disease (HFMD) has been recognized as a trigger for onychomadesis in school-aged children. Onychomadesis presents with characteristic proximal nail detachment (Figure 1). The association of HFMD with onychomadesis and Beau lines was first reported in 2000. Five patients who resided within close proximity and shared a physician-diagnosed case of HFMD presented with representative nail findings 4 weeks after illness.1 Hypotheses for these changes include viral-induced nail pathology, inflammation from cutaneous lesions of HFMD, and systemic effects from the disease.2 Given the prevalence of HFMD and benign outcome, clinicians should be cognizant of this unique cutaneous manifestation.

Pearl: Management of pediatric melanonychia can take a wait-and-see approach
Melanonychia is the presence of a longitudinal brown-black band extending from the proximal nail fold. The cause of melanonychia can be due to either activation or hyperplasia. Activation is the less common etiology in children; however, if present, activation can be due to Laugier-Hunziker syndrome or trauma such as onychotillomania. Melanonychia in children usually is the result of hyperplasia of melanocytes and can manifest as a lentigo, nevus, or more rarely melanoma. Nail matrix nevi are typically exhibited on the fingernails, particularly the thumb, and frequently are junctional nevi (Figure 2). Spontaneous fading of nevi is expected with time due to decreased melanin production. Therapeutic options for melanonychia include regular clinical monitoring, biopsy, or excision. Dr. Tosti explained that one must be wary when pursuing a biopsy, as it can result in a false-negative finding due to missed pathology. If clinically indicated, a shave biopsy of the nail matrix can be performed to best analyze the lesion. She noted that if more than 3 mm of the matrix is removed, a resultant scar will ensue. Conservative management is recommended given the indolent clinical behavior of the majority of cases of melanonychia in children.3
Pearl: Congenital hypertrophy of the lateral nail folds can be treated with tape
Congenital hypertrophy of the lateral nail folds is relatively common in children and normally improves with age. Koilonychia may also occur simultaneously and can be viewed as a physiologic process in this age group. The etiology of the underlying disorder is due to anomalous periungual soft-tissue changes of the bilateral halluces; the resulting overgrowth can partially cover the nail plate. Although usually a self-limiting condition, the changes can cause inflammation and discomfort due to an ingrown nail.4 Dr. Tosti advised that by simply taping and retracting the bilateral overgrowth, the condition can be more readily resolved. This simple treatment can be demonstrated in the office and subsequently performed at home.
Pearl: Onychomycosis is uncommon in children
Onychomycosis occurs in less than 1% of children.5 Several factors are responsible for this decreased prevalence. More rapid nail growth and smaller nail surface area decreases the ability of the fungi to penetrate the nail plate.6 Furthermore, children have a diminished rate of tinea pedis, leading to less neighboring infection. When onychomycosis does affect this patient population, it commonly presents as distal subungual onychomycosis and favors the fingernails over the toenails. Treatment options usually parallel those of the adult population; however, all medications for children are considered off-label use by the US Food and Drug Administration. Dr. Tosti explained that oral granules of terbinafine can be sprinkled on food to help with pediatric ingestion. Topical therapies should also be considered; children usually respond better than their adult counterparts due to their thinner nails, which grant enhanced drug delivery and penetration.6
Pearl: Acute paronychia can be due to nail-biting and sucking
Acute paronychia is inflammation of the proximal nail fold. In children, it frequently is a result of mixed flora induced by nail-biting and sucking. Management involves culturing the affected lesions and is effectively treated with warm soaks alone. Dr. Tosti highlighted that Candida in the subungual space is a common colonizer and is typically self-limiting in nature if isolated. Candida can be cultured more readily in premature infants, immunosuppressed patients, and those with chronic mucocutaneous candidiasis. Patients with chronic mucocutaneous candidiasis can exhibit periungual inflammation involving several digits. The differential can include nail psoriasis, as both can demonstrate dystrophic changes. The differential for localized paronychia includes herpetic whitlow and can manifest as vesicles under the proximal nail fold.
Final Thoughts
These clinical pearls are shared to help deliver utmost care to our pediatric patients presenting with nail pathology. For example, a child exhibiting melanonychia can cause alarm due to the possibility of underlying melanoma; given the rarity of neoplasia in these patients, a conservative approach is favored to help avoid unnecessary biopsies and subsequent scarring. Similarly, it is important to be aware of the common colonizers of the subungual area, particularly Candida, to avoid unessential medications with potential side effects. The examples demonstrated help shed light on the management of pediatric nail diseases.
Acknowledgment
This article is possible thanks to the help of Antonella Tosti, MD (Miami, Florida), who contributed her time and expertise at the University of Miami Pediatric Grand Rounds to expand the foundation and knowledge of pediatric nail diseases.
- Clementz GC, Mancini AJ. Nail matrix arrest following hand-foot-mouth disease: a report of five children. Pediatr Dermatol. 2000;17:7-11.
- Yuksel S, Evrengul H, Ozhan B, et al. Onychomadesis-a late complication of hand-foot-mouth disease [published online May 2, 2016]. J Pediatr. 2016;174:274.
- Cooper C, Arva NC, Lee C, et al. A clinical, histopathologic, and outcome study of melanonychia striata in childhood. J Am Acad Dermatol. 2015;72:773-779.
- Piraccini BM, Parente GL, Varotti E, et al. Congenital hypertrophy of the lateral nail folds of the hallux: clinical features and follow-up of seven cases. Pediatr Dermatol. 2000;17:348-351.
- Totri CR, Feldstein S, Admani S, et al. Epidemiologic analysis of onychomycosis in the San Diego pediatric population [published online October 4, 2016]. Pediatr Dermatol. 2017;34:46-49.
- Feldstein S, Totri C, Friedlander SF. Antifungal therapy for onychomycosis in children. Clin Dermatol. 2015;33:333-339.
- Clementz GC, Mancini AJ. Nail matrix arrest following hand-foot-mouth disease: a report of five children. Pediatr Dermatol. 2000;17:7-11.
- Yuksel S, Evrengul H, Ozhan B, et al. Onychomadesis-a late complication of hand-foot-mouth disease [published online May 2, 2016]. J Pediatr. 2016;174:274.
- Cooper C, Arva NC, Lee C, et al. A clinical, histopathologic, and outcome study of melanonychia striata in childhood. J Am Acad Dermatol. 2015;72:773-779.
- Piraccini BM, Parente GL, Varotti E, et al. Congenital hypertrophy of the lateral nail folds of the hallux: clinical features and follow-up of seven cases. Pediatr Dermatol. 2000;17:348-351.
- Totri CR, Feldstein S, Admani S, et al. Epidemiologic analysis of onychomycosis in the San Diego pediatric population [published online October 4, 2016]. Pediatr Dermatol. 2017;34:46-49.
- Feldstein S, Totri C, Friedlander SF. Antifungal therapy for onychomycosis in children. Clin Dermatol. 2015;33:333-339.
Developing a personal scale for evaluating agitation on inpatient units
Agitation. As a mental health professional, you know it when you see it. While technically, it is the behavior that precedes aggression and violence, every clinical setting has its own flavor, from the voluntary psychiatric unit where I see my most acutely ill patients to the state hospital where I witnessed the type of violence that sent another patient to the emergency department.
Over the past 2 years of residency, I have developed a personal scale for measuring and responding to patient agitation. Through experiences that have provided the lower, upper (and even more upper) bounds to this scale, I have evolved from a nervous first-year intern to become a resident conscious of the need for a cool demeanor and continued engagement with the patient with escalating agitation.
The 2003 Treatment of Behavioral Emergencies: A Summary of the Expert Consensus Guidelines1 provides an excellent visual scale to measure agitation. It begins with a patient’s refusal to cooperate and ascends stepwise toward motor restlessness, lability and loud speech, intimidation, aggression against property, and hostile verbal behavior, and it ends with directly threatening or assaultive behavior.2 Only when I witnessed signs of clinically significant agitation, hostile countenance, unpredictable anger, pacing, clenched fists, yelling, and threats, did I develop a personal understanding and approach for measuring agitation on the inpatient unit.
The upper bound for my scale initially was defined by my first incident of severe agitation and aggression while on call. I no longer remember if the patient was agitated and psychotic or just angry and agitated. Though schizophrenia and bipolar disorder often are the underlying causes of agitation, personality disorders and substance use complicate or contribute to agitation.3 The nurse called me, saying: “Can you come to the unit right now? Mr. X is agitated and has ripped the soap dispenser off the wall in his bathroom.” It was just after midnight, and already several nursing calls into this situation. Verbal de-escalation had failed with Mr. X, who moved from agitation to aggressive behavior. He already had received two doses of haloperidol and lorazepam since my evening shift began. I looked into his bedroom and saw him wrestling with the sink, which did not come off the wall as easily as the soap dispenser. The thought process of an inexperienced intern went like this: “How much haloperidol is too much haloperidol? Will this night never end?” I called my attending for help, and there was desperation in my voice as I explained: “The medications aren’t working.
These situations usually result in good clinical lessons: Medications take time to work, and in some individuals, the “standard cocktail” might not be the best option. Nonetheless, the lag time can be excruciating. As a more experienced resident, I now consider how certain medications may fail an individual, and there might be a better alternative to haloperidol and lorazepam. I’ve expanded my repertoire of pharmacological methods and opt often for second-generation antipsychotics, such as olanzapine or risperidone, without or without a benzodiazepine, when possible.2
Of course, not all agitation becomes a behavioral health emergency, and an integral part of my training as a resident has been watching an attending run an intervention smoothly. It requires coordination and experience, skills that I’m gaining. In these cases, the agitation is addressed before it escalates, nursing staff and the physicians collaborate to deliver treatment, and the patient responds to verbal redirection and, if offered, accepts oral medications. These types of patients help cement the lower bound for my agitation scale.
Nonetheless, the patients who challenge the positive archetype are the ones who cement lessons for physicians. I remember a man who with his history of serious mental illness had adverse reactions to haloperidol, aripiprazole, olanzapine, and fluphenazine. To address his agitation, the nurses prepared 2 mg of lorazepam and 50 mg of diphenhydramine. As the patient ramped up, I heard a nurse sigh, “Why can’t we add IM thorazine?” I commiserated with the nurse; the psychiatric unit is a dangerous place to work. Psychiatry and emergency department nurses, compared with their counterparts in other units, are the most likely to be assaulted at work.4,5 It is personal for me as well. Studies suggest that 30%-40% of psychiatric residents will be attacked during their 4-year training, and I am in that 70%-90% of residents who has been verbally threatened more than once.6
With time and training, my verbal de-escalation techniques have improved, as I’ve learned to avoid threatening and judgmental body language, avoiding a natural tendency to stand with my arms crossed over my chest or hands on my hips. I now more accurately and incisively inquire about a patient’s mental state. How can I address their frustration? In a nonaccusatory way, I let the patients know that they are behaving in a way that is frightening and that continued behavior may have consequences. Even when faced by the heat of agitation, I try to value the patients’ choice: This event will affect our therapeutic relationship in the longer term.
Whenever possible, I want the patients to choose their medication formulation or at least be able to ask them, “Would you be willing to take … ?” With time, I am earning that cool demeanor psychiatrists are known for. I can model calm behavior and effectively use my knowledge about mentalization to try to de-escalate the situation.
My scale of measuring of agitation and violence had its upper level increased significantly from just a soap dispenser being ripped off the wall. One patient really upped the ante by swiping a public telephone off the wall and then went tearing down the hallway to pull the fire extinguisher out of its supposed “safe” case and hurl it. So on a recent night shift, when I heard yelling through the door of the call room, it was with a sense of understanding rather than trepidation that my co-resident and I approached the patient, already being corralled to his room by nursing staff. He was an enormous man, angry, paranoid, pacing, and shouting about how the other patients wanted to attack him. Despite his size, his menacing posture, and that somewhere in his agitation he had ripped off his scrub shirt, I couldn’t help but think, “Well at least the phone and the fire extinguisher are still attached to the wall.”
References
1 J Psychiatr Pract. 2003 Jan;9(1):16-38. Treatment of behavioral emergencies: A summary of the expert consensus guidelines.
2 J Psychiatr Pract. 2005 Nov;11 Suppl 1:5-108; quiz 110-2. The expert consensus guideline series. Treatment of behavioral emergencies 2005.
3 Clin Pract Epidemiol Ment Health. 2016 Oct 27;12:75-86. State of acute agitation at psychiatric emergencies in Europe: The STAGE study.
4 J Emerg Nurs. 2014 May;40(3):218-28; quiz 295. Incidence and cost of nurse workplace violence perpetrated by hospital patients or patient visitors.
5 Work. 2010;35(2):191-200. Physical assault among nursing staff employed in acute care.
6 Psychiatr Serv. 1999 Mar;50(3):381-3. Assaults by patients on psychiatric residents: a survey and training recommendations.
Dr. Posada is a second-year resident in the psychiatry & behavioral sciences department at George Washington University, Washington. She completed a bachelor’s degree at the George Washington University. For 2 years after her undergraduate education, she worked at the National Institutes of Allergy and Infectious Diseases studying HIV pathogenesis. Dr. Posada completed her medical degree at the University of Texas Medical Branch in Galveston. Her interests include public psychiatry, health care policy, health disparities, and psychosomatic medicine.
Agitation. As a mental health professional, you know it when you see it. While technically, it is the behavior that precedes aggression and violence, every clinical setting has its own flavor, from the voluntary psychiatric unit where I see my most acutely ill patients to the state hospital where I witnessed the type of violence that sent another patient to the emergency department.
Over the past 2 years of residency, I have developed a personal scale for measuring and responding to patient agitation. Through experiences that have provided the lower, upper (and even more upper) bounds to this scale, I have evolved from a nervous first-year intern to become a resident conscious of the need for a cool demeanor and continued engagement with the patient with escalating agitation.
The 2003 Treatment of Behavioral Emergencies: A Summary of the Expert Consensus Guidelines1 provides an excellent visual scale to measure agitation. It begins with a patient’s refusal to cooperate and ascends stepwise toward motor restlessness, lability and loud speech, intimidation, aggression against property, and hostile verbal behavior, and it ends with directly threatening or assaultive behavior.2 Only when I witnessed signs of clinically significant agitation, hostile countenance, unpredictable anger, pacing, clenched fists, yelling, and threats, did I develop a personal understanding and approach for measuring agitation on the inpatient unit.
The upper bound for my scale initially was defined by my first incident of severe agitation and aggression while on call. I no longer remember if the patient was agitated and psychotic or just angry and agitated. Though schizophrenia and bipolar disorder often are the underlying causes of agitation, personality disorders and substance use complicate or contribute to agitation.3 The nurse called me, saying: “Can you come to the unit right now? Mr. X is agitated and has ripped the soap dispenser off the wall in his bathroom.” It was just after midnight, and already several nursing calls into this situation. Verbal de-escalation had failed with Mr. X, who moved from agitation to aggressive behavior. He already had received two doses of haloperidol and lorazepam since my evening shift began. I looked into his bedroom and saw him wrestling with the sink, which did not come off the wall as easily as the soap dispenser. The thought process of an inexperienced intern went like this: “How much haloperidol is too much haloperidol? Will this night never end?” I called my attending for help, and there was desperation in my voice as I explained: “The medications aren’t working.
These situations usually result in good clinical lessons: Medications take time to work, and in some individuals, the “standard cocktail” might not be the best option. Nonetheless, the lag time can be excruciating. As a more experienced resident, I now consider how certain medications may fail an individual, and there might be a better alternative to haloperidol and lorazepam. I’ve expanded my repertoire of pharmacological methods and opt often for second-generation antipsychotics, such as olanzapine or risperidone, without or without a benzodiazepine, when possible.2
Of course, not all agitation becomes a behavioral health emergency, and an integral part of my training as a resident has been watching an attending run an intervention smoothly. It requires coordination and experience, skills that I’m gaining. In these cases, the agitation is addressed before it escalates, nursing staff and the physicians collaborate to deliver treatment, and the patient responds to verbal redirection and, if offered, accepts oral medications. These types of patients help cement the lower bound for my agitation scale.
Nonetheless, the patients who challenge the positive archetype are the ones who cement lessons for physicians. I remember a man who with his history of serious mental illness had adverse reactions to haloperidol, aripiprazole, olanzapine, and fluphenazine. To address his agitation, the nurses prepared 2 mg of lorazepam and 50 mg of diphenhydramine. As the patient ramped up, I heard a nurse sigh, “Why can’t we add IM thorazine?” I commiserated with the nurse; the psychiatric unit is a dangerous place to work. Psychiatry and emergency department nurses, compared with their counterparts in other units, are the most likely to be assaulted at work.4,5 It is personal for me as well. Studies suggest that 30%-40% of psychiatric residents will be attacked during their 4-year training, and I am in that 70%-90% of residents who has been verbally threatened more than once.6
With time and training, my verbal de-escalation techniques have improved, as I’ve learned to avoid threatening and judgmental body language, avoiding a natural tendency to stand with my arms crossed over my chest or hands on my hips. I now more accurately and incisively inquire about a patient’s mental state. How can I address their frustration? In a nonaccusatory way, I let the patients know that they are behaving in a way that is frightening and that continued behavior may have consequences. Even when faced by the heat of agitation, I try to value the patients’ choice: This event will affect our therapeutic relationship in the longer term.
Whenever possible, I want the patients to choose their medication formulation or at least be able to ask them, “Would you be willing to take … ?” With time, I am earning that cool demeanor psychiatrists are known for. I can model calm behavior and effectively use my knowledge about mentalization to try to de-escalate the situation.
My scale of measuring of agitation and violence had its upper level increased significantly from just a soap dispenser being ripped off the wall. One patient really upped the ante by swiping a public telephone off the wall and then went tearing down the hallway to pull the fire extinguisher out of its supposed “safe” case and hurl it. So on a recent night shift, when I heard yelling through the door of the call room, it was with a sense of understanding rather than trepidation that my co-resident and I approached the patient, already being corralled to his room by nursing staff. He was an enormous man, angry, paranoid, pacing, and shouting about how the other patients wanted to attack him. Despite his size, his menacing posture, and that somewhere in his agitation he had ripped off his scrub shirt, I couldn’t help but think, “Well at least the phone and the fire extinguisher are still attached to the wall.”
References
1 J Psychiatr Pract. 2003 Jan;9(1):16-38. Treatment of behavioral emergencies: A summary of the expert consensus guidelines.
2 J Psychiatr Pract. 2005 Nov;11 Suppl 1:5-108; quiz 110-2. The expert consensus guideline series. Treatment of behavioral emergencies 2005.
3 Clin Pract Epidemiol Ment Health. 2016 Oct 27;12:75-86. State of acute agitation at psychiatric emergencies in Europe: The STAGE study.
4 J Emerg Nurs. 2014 May;40(3):218-28; quiz 295. Incidence and cost of nurse workplace violence perpetrated by hospital patients or patient visitors.
5 Work. 2010;35(2):191-200. Physical assault among nursing staff employed in acute care.
6 Psychiatr Serv. 1999 Mar;50(3):381-3. Assaults by patients on psychiatric residents: a survey and training recommendations.
Dr. Posada is a second-year resident in the psychiatry & behavioral sciences department at George Washington University, Washington. She completed a bachelor’s degree at the George Washington University. For 2 years after her undergraduate education, she worked at the National Institutes of Allergy and Infectious Diseases studying HIV pathogenesis. Dr. Posada completed her medical degree at the University of Texas Medical Branch in Galveston. Her interests include public psychiatry, health care policy, health disparities, and psychosomatic medicine.
Agitation. As a mental health professional, you know it when you see it. While technically, it is the behavior that precedes aggression and violence, every clinical setting has its own flavor, from the voluntary psychiatric unit where I see my most acutely ill patients to the state hospital where I witnessed the type of violence that sent another patient to the emergency department.
Over the past 2 years of residency, I have developed a personal scale for measuring and responding to patient agitation. Through experiences that have provided the lower, upper (and even more upper) bounds to this scale, I have evolved from a nervous first-year intern to become a resident conscious of the need for a cool demeanor and continued engagement with the patient with escalating agitation.
The 2003 Treatment of Behavioral Emergencies: A Summary of the Expert Consensus Guidelines1 provides an excellent visual scale to measure agitation. It begins with a patient’s refusal to cooperate and ascends stepwise toward motor restlessness, lability and loud speech, intimidation, aggression against property, and hostile verbal behavior, and it ends with directly threatening or assaultive behavior.2 Only when I witnessed signs of clinically significant agitation, hostile countenance, unpredictable anger, pacing, clenched fists, yelling, and threats, did I develop a personal understanding and approach for measuring agitation on the inpatient unit.
The upper bound for my scale initially was defined by my first incident of severe agitation and aggression while on call. I no longer remember if the patient was agitated and psychotic or just angry and agitated. Though schizophrenia and bipolar disorder often are the underlying causes of agitation, personality disorders and substance use complicate or contribute to agitation.3 The nurse called me, saying: “Can you come to the unit right now? Mr. X is agitated and has ripped the soap dispenser off the wall in his bathroom.” It was just after midnight, and already several nursing calls into this situation. Verbal de-escalation had failed with Mr. X, who moved from agitation to aggressive behavior. He already had received two doses of haloperidol and lorazepam since my evening shift began. I looked into his bedroom and saw him wrestling with the sink, which did not come off the wall as easily as the soap dispenser. The thought process of an inexperienced intern went like this: “How much haloperidol is too much haloperidol? Will this night never end?” I called my attending for help, and there was desperation in my voice as I explained: “The medications aren’t working.
These situations usually result in good clinical lessons: Medications take time to work, and in some individuals, the “standard cocktail” might not be the best option. Nonetheless, the lag time can be excruciating. As a more experienced resident, I now consider how certain medications may fail an individual, and there might be a better alternative to haloperidol and lorazepam. I’ve expanded my repertoire of pharmacological methods and opt often for second-generation antipsychotics, such as olanzapine or risperidone, without or without a benzodiazepine, when possible.2
Of course, not all agitation becomes a behavioral health emergency, and an integral part of my training as a resident has been watching an attending run an intervention smoothly. It requires coordination and experience, skills that I’m gaining. In these cases, the agitation is addressed before it escalates, nursing staff and the physicians collaborate to deliver treatment, and the patient responds to verbal redirection and, if offered, accepts oral medications. These types of patients help cement the lower bound for my agitation scale.
Nonetheless, the patients who challenge the positive archetype are the ones who cement lessons for physicians. I remember a man who with his history of serious mental illness had adverse reactions to haloperidol, aripiprazole, olanzapine, and fluphenazine. To address his agitation, the nurses prepared 2 mg of lorazepam and 50 mg of diphenhydramine. As the patient ramped up, I heard a nurse sigh, “Why can’t we add IM thorazine?” I commiserated with the nurse; the psychiatric unit is a dangerous place to work. Psychiatry and emergency department nurses, compared with their counterparts in other units, are the most likely to be assaulted at work.4,5 It is personal for me as well. Studies suggest that 30%-40% of psychiatric residents will be attacked during their 4-year training, and I am in that 70%-90% of residents who has been verbally threatened more than once.6
With time and training, my verbal de-escalation techniques have improved, as I’ve learned to avoid threatening and judgmental body language, avoiding a natural tendency to stand with my arms crossed over my chest or hands on my hips. I now more accurately and incisively inquire about a patient’s mental state. How can I address their frustration? In a nonaccusatory way, I let the patients know that they are behaving in a way that is frightening and that continued behavior may have consequences. Even when faced by the heat of agitation, I try to value the patients’ choice: This event will affect our therapeutic relationship in the longer term.
Whenever possible, I want the patients to choose their medication formulation or at least be able to ask them, “Would you be willing to take … ?” With time, I am earning that cool demeanor psychiatrists are known for. I can model calm behavior and effectively use my knowledge about mentalization to try to de-escalate the situation.
My scale of measuring of agitation and violence had its upper level increased significantly from just a soap dispenser being ripped off the wall. One patient really upped the ante by swiping a public telephone off the wall and then went tearing down the hallway to pull the fire extinguisher out of its supposed “safe” case and hurl it. So on a recent night shift, when I heard yelling through the door of the call room, it was with a sense of understanding rather than trepidation that my co-resident and I approached the patient, already being corralled to his room by nursing staff. He was an enormous man, angry, paranoid, pacing, and shouting about how the other patients wanted to attack him. Despite his size, his menacing posture, and that somewhere in his agitation he had ripped off his scrub shirt, I couldn’t help but think, “Well at least the phone and the fire extinguisher are still attached to the wall.”
References
1 J Psychiatr Pract. 2003 Jan;9(1):16-38. Treatment of behavioral emergencies: A summary of the expert consensus guidelines.
2 J Psychiatr Pract. 2005 Nov;11 Suppl 1:5-108; quiz 110-2. The expert consensus guideline series. Treatment of behavioral emergencies 2005.
3 Clin Pract Epidemiol Ment Health. 2016 Oct 27;12:75-86. State of acute agitation at psychiatric emergencies in Europe: The STAGE study.
4 J Emerg Nurs. 2014 May;40(3):218-28; quiz 295. Incidence and cost of nurse workplace violence perpetrated by hospital patients or patient visitors.
5 Work. 2010;35(2):191-200. Physical assault among nursing staff employed in acute care.
6 Psychiatr Serv. 1999 Mar;50(3):381-3. Assaults by patients on psychiatric residents: a survey and training recommendations.
Dr. Posada is a second-year resident in the psychiatry & behavioral sciences department at George Washington University, Washington. She completed a bachelor’s degree at the George Washington University. For 2 years after her undergraduate education, she worked at the National Institutes of Allergy and Infectious Diseases studying HIV pathogenesis. Dr. Posada completed her medical degree at the University of Texas Medical Branch in Galveston. Her interests include public psychiatry, health care policy, health disparities, and psychosomatic medicine.
Teledermatology in Tijuana, Mexico
The Health Frontiers in Tijuana (HFiT) clinic is a binational partnership between the University of California, San Diego School of Medicine (San Diego, California); the Universidad Autónoma de Baja California School of Medicine (Tijuana, Mexico); and Desayunador Salesiano Padre Chava, a community grassroots organization in Tijuana, Mexico. Health Frontiers in Tijuana provides accessible quality health care for the underserved in Tijuana's Zona Norte.1 This article is a narrative meant to share my clinical experience as a dermatology resident who worked with HFiT to establish teledermatology services at this clinic.
Teledermatology in Tijuana
The patient population served by the HFiT clinic includes substance users, sex workers, the homeless, deportees, indigent patients, and recently Haitian immigrants.1 We established teledermatology services under the faculty leadership of Casey Carlos, MD, who was awarded a SkinCare for Developing Countries grant from the American Academy of Dermatology in April 2015 to address the need for teledermatology support for the clinic.2
Over the last 2 years, we have worked closely with 2 medical students from the University of California, San Diego--Nicole Herrick, BS, and Nicole DeMartinis, BA--to apply for the grant and create a system whereby volunteer residents and faculty consultants at the University of California, San Diego, can provide teledermatology services on a weekly basis to support the HFiT staff as they see patients with dermatologic conditions. Initially, we purchased touch screen tablets to use the Africa Teledermatology Project (africa.telederm.org) web-based program. The clinic was already functioning with electronic medical records with volunteers who carried tablets and scribed for the providers as they saw patients. We felt this method would be a great way to incorporate teledermatology into the clinic, and it functioned moderately well for several weeks but was very labor intensive on our part, as we frequently had to travel to Tijuana to retrain rotating clinic volunteers on how to use the program. Often, the Internet connection was slow, which made pulling up the Africa Teledermatology Project website difficult, and photographs also would take too long to upload in the middle of a busy clinic.
We are now exploring how to use a more simple email format to send the teledermatology consultations while still being compliant with the Health Insurance Portability and Accountability Act. We currently use secure university email accounts. Although we are still working out the details, this email-based method seems to work well. It has been a simple solution to accommodate a slow Internet connection and many rotating volunteers without requiring additional training. The email format also allows the photographs to be saved in draft messages, even if the Internet connection times out.
Once the teledermatology consultation is sent, the medical students and I review them and then get an attending physician's input on our proposed working diagnosis and plan. We work to have this process complete within several days to return the answered consultation to the requesting provider.
Final Thoughts
The HFiT providers have shared a lot of positive verbal feedback about this project. One frequent comment is how helpful it is to have access to a dermatologist for challenging cases. We also have heard many times that this project has inspired medical students and volunteers to expand their knowledge of dermatology. We are continuing to form new collaborative relationships with physicians in Tijuana. We will soon have the ability to train primary care providers at HFiT on performing simple skin biopsies and managing basic dermatologic conditions. Through our support of these providers, we are creating a sustainable partnership that is mutually beneficial to the patients in Tijuana as well as the medical students and residents in the United States. It is highly rewarding to all those involved with this project, and I am excited to see what challenges this next year will bring as we welcome many new patients from Haiti into the HFiT patient population.
- About Health Frontiers in Tijuana. University of California, San Diego School of Medicine website. https://meded.ucsd.edu/index.cfm/groups/hfit/about/. Accessed November 29, 2016.
- SkinCare for developing countries. American Academy of Dermatology website. https://www.aad.org/members/awards/skincare-for-developing-countries#undefined. Accessed November 29, 2016.
The Health Frontiers in Tijuana (HFiT) clinic is a binational partnership between the University of California, San Diego School of Medicine (San Diego, California); the Universidad Autónoma de Baja California School of Medicine (Tijuana, Mexico); and Desayunador Salesiano Padre Chava, a community grassroots organization in Tijuana, Mexico. Health Frontiers in Tijuana provides accessible quality health care for the underserved in Tijuana's Zona Norte.1 This article is a narrative meant to share my clinical experience as a dermatology resident who worked with HFiT to establish teledermatology services at this clinic.
Teledermatology in Tijuana
The patient population served by the HFiT clinic includes substance users, sex workers, the homeless, deportees, indigent patients, and recently Haitian immigrants.1 We established teledermatology services under the faculty leadership of Casey Carlos, MD, who was awarded a SkinCare for Developing Countries grant from the American Academy of Dermatology in April 2015 to address the need for teledermatology support for the clinic.2
Over the last 2 years, we have worked closely with 2 medical students from the University of California, San Diego--Nicole Herrick, BS, and Nicole DeMartinis, BA--to apply for the grant and create a system whereby volunteer residents and faculty consultants at the University of California, San Diego, can provide teledermatology services on a weekly basis to support the HFiT staff as they see patients with dermatologic conditions. Initially, we purchased touch screen tablets to use the Africa Teledermatology Project (africa.telederm.org) web-based program. The clinic was already functioning with electronic medical records with volunteers who carried tablets and scribed for the providers as they saw patients. We felt this method would be a great way to incorporate teledermatology into the clinic, and it functioned moderately well for several weeks but was very labor intensive on our part, as we frequently had to travel to Tijuana to retrain rotating clinic volunteers on how to use the program. Often, the Internet connection was slow, which made pulling up the Africa Teledermatology Project website difficult, and photographs also would take too long to upload in the middle of a busy clinic.
We are now exploring how to use a more simple email format to send the teledermatology consultations while still being compliant with the Health Insurance Portability and Accountability Act. We currently use secure university email accounts. Although we are still working out the details, this email-based method seems to work well. It has been a simple solution to accommodate a slow Internet connection and many rotating volunteers without requiring additional training. The email format also allows the photographs to be saved in draft messages, even if the Internet connection times out.
Once the teledermatology consultation is sent, the medical students and I review them and then get an attending physician's input on our proposed working diagnosis and plan. We work to have this process complete within several days to return the answered consultation to the requesting provider.
Final Thoughts
The HFiT providers have shared a lot of positive verbal feedback about this project. One frequent comment is how helpful it is to have access to a dermatologist for challenging cases. We also have heard many times that this project has inspired medical students and volunteers to expand their knowledge of dermatology. We are continuing to form new collaborative relationships with physicians in Tijuana. We will soon have the ability to train primary care providers at HFiT on performing simple skin biopsies and managing basic dermatologic conditions. Through our support of these providers, we are creating a sustainable partnership that is mutually beneficial to the patients in Tijuana as well as the medical students and residents in the United States. It is highly rewarding to all those involved with this project, and I am excited to see what challenges this next year will bring as we welcome many new patients from Haiti into the HFiT patient population.
The Health Frontiers in Tijuana (HFiT) clinic is a binational partnership between the University of California, San Diego School of Medicine (San Diego, California); the Universidad Autónoma de Baja California School of Medicine (Tijuana, Mexico); and Desayunador Salesiano Padre Chava, a community grassroots organization in Tijuana, Mexico. Health Frontiers in Tijuana provides accessible quality health care for the underserved in Tijuana's Zona Norte.1 This article is a narrative meant to share my clinical experience as a dermatology resident who worked with HFiT to establish teledermatology services at this clinic.
Teledermatology in Tijuana
The patient population served by the HFiT clinic includes substance users, sex workers, the homeless, deportees, indigent patients, and recently Haitian immigrants.1 We established teledermatology services under the faculty leadership of Casey Carlos, MD, who was awarded a SkinCare for Developing Countries grant from the American Academy of Dermatology in April 2015 to address the need for teledermatology support for the clinic.2
Over the last 2 years, we have worked closely with 2 medical students from the University of California, San Diego--Nicole Herrick, BS, and Nicole DeMartinis, BA--to apply for the grant and create a system whereby volunteer residents and faculty consultants at the University of California, San Diego, can provide teledermatology services on a weekly basis to support the HFiT staff as they see patients with dermatologic conditions. Initially, we purchased touch screen tablets to use the Africa Teledermatology Project (africa.telederm.org) web-based program. The clinic was already functioning with electronic medical records with volunteers who carried tablets and scribed for the providers as they saw patients. We felt this method would be a great way to incorporate teledermatology into the clinic, and it functioned moderately well for several weeks but was very labor intensive on our part, as we frequently had to travel to Tijuana to retrain rotating clinic volunteers on how to use the program. Often, the Internet connection was slow, which made pulling up the Africa Teledermatology Project website difficult, and photographs also would take too long to upload in the middle of a busy clinic.
We are now exploring how to use a more simple email format to send the teledermatology consultations while still being compliant with the Health Insurance Portability and Accountability Act. We currently use secure university email accounts. Although we are still working out the details, this email-based method seems to work well. It has been a simple solution to accommodate a slow Internet connection and many rotating volunteers without requiring additional training. The email format also allows the photographs to be saved in draft messages, even if the Internet connection times out.
Once the teledermatology consultation is sent, the medical students and I review them and then get an attending physician's input on our proposed working diagnosis and plan. We work to have this process complete within several days to return the answered consultation to the requesting provider.
Final Thoughts
The HFiT providers have shared a lot of positive verbal feedback about this project. One frequent comment is how helpful it is to have access to a dermatologist for challenging cases. We also have heard many times that this project has inspired medical students and volunteers to expand their knowledge of dermatology. We are continuing to form new collaborative relationships with physicians in Tijuana. We will soon have the ability to train primary care providers at HFiT on performing simple skin biopsies and managing basic dermatologic conditions. Through our support of these providers, we are creating a sustainable partnership that is mutually beneficial to the patients in Tijuana as well as the medical students and residents in the United States. It is highly rewarding to all those involved with this project, and I am excited to see what challenges this next year will bring as we welcome many new patients from Haiti into the HFiT patient population.
- About Health Frontiers in Tijuana. University of California, San Diego School of Medicine website. https://meded.ucsd.edu/index.cfm/groups/hfit/about/. Accessed November 29, 2016.
- SkinCare for developing countries. American Academy of Dermatology website. https://www.aad.org/members/awards/skincare-for-developing-countries#undefined. Accessed November 29, 2016.
- About Health Frontiers in Tijuana. University of California, San Diego School of Medicine website. https://meded.ucsd.edu/index.cfm/groups/hfit/about/. Accessed November 29, 2016.
- SkinCare for developing countries. American Academy of Dermatology website. https://www.aad.org/members/awards/skincare-for-developing-countries#undefined. Accessed November 29, 2016.
Update on New Drugs in Dermatology
CenterWatch (http://www.centerwatch.com/) is an online resource that provides directories, analysis, and market research of medications that are either under clinical evaluation or available for use in patients. A list of currently approved drugs by the US Food and Drug Administration (FDA) also is available by specialty. It is important for dermatologists in-training to know about recently approved drugs and those that are in the pipeline, as these treatments may benefit patients who are unresponsive to other previously used medications. New drugs also may be useful for physicians who have a difficult time getting insurance to cover prescriptions for their patients, as most new medications have built-in patient assistance.
New Drugs in Dermatology
Actinic Keratosis
Ameluz (aminolevulinic acid hydrochloride)(Biofrontera AG) is a new drug that was approved in May 2016 for treatment of mild to moderate actinic keratosis on the face and scalp.1 It is only intended for in-office use on patients who may not be candidates for other treatment options for actinic keratosis. The product is a gel formulation that should be applied to cover the lesions and approximately 5 mm of the surrounding area with a film of approximately 1-mm thickness. The entire treatment area is then illuminated with a red light source, either with a narrow spectrum around 630 nm with a light dose of approximately 37 J/cm2 or a broader and continuous spectrum in the range of 570 to 670 nm with a light dose between 75 and 200 J/cm2.1 Similar to the previously used aminolevulinic acid treatment method for actinic keratosis, the patient may experience a burning stinging sensation throughout the treatment and the skin will then proceed to peel.
Psoriasis and Psoriatic Arthritis
Taltz (ixekizumab)(Eli Lilly and Company) was approved by the FDA in March 2016 for the treatment of moderate to severe plaque psoriasis.2 It is a humanized IL-17A antagonist that works when IgG4 monoclonal antibodies selectively bind with IL-17A cytokines and inhibit their interaction with the IL-17 receptor. Although this injectable medication is approved for the treatment of psoriasis, it also can potentially be used off label for the treatment of psoriatic arthritis and rheumatoid arthritis. The approved dosage is 160 mg (two 80-mg injections) at week 0, followed by 80 mg at weeks 2, 4, 6, 8, 10, and 12, then 80 mg every 4 weeks.2 Injectable immunomodulatory medications such as ixekizumab are ideal for patients in whom topical treatments and light therapy failed and they continue to have serious psoriatic discomfort as well as for those who have substantial body surface area coverage.
In January 2015, Cosentyx (secukinumab)(Novartis Corporation) was approved by the FDA.3 Similar to ixekizumab, this injectable is an IgG1 monoclonal antibody that selectively binds to the IL-17A cytokine and inhibits its interaction with the IL-17 receptor. It is approved for the treatment of moderate to severe plaque psoriasis and psoriatic arthritis. The approved dosage for plaque psoriasis is 300 mg (two 150-mg subcutaneous injections) at weeks 0 through 4 followed by 300 mg every 4 weeks as needed until clearance.3 Similar to ixekizumab, secukinumab may be used for the treatment of recalcitrant psoriasis or psoriasis with substantial body surface area involvement.
Melanoma
Cotellic (cobimetinib)(Genentech USA, Inc) was FDA approved in November 2015.4 Cobimetinib is a reversible inhibitor of mitogen-activated protein kinase (MAPK)/extracellular signal regulated kinase 1. Mitogen-activated protein kinase MEK1 and MEK2 are regulators of the extracellular signal-related kinase pathway, which promotes cellular proliferation. This pathway is key, as melanomas that have a BRAF V600E and kinase mutation continue to proliferate due to the constitutive activation of MEK1 and MEK2, further promoting cellular proliferation. Cobimetinib is approved for the treatment of melanoma in patients with unresectable or metastatic melanoma with a BRAF V600E or V600K mutation, in conjunction with vemurafenib. Zelboraf (vemurafenib)(Genentech USA, Inc), another inhibitor of BRAF V600E, also is used for the treatment of unresectable melanomas and was initially approved in 2011.5
BRAF is a serine/threonine protein kinase. When unregulated, it results in the deregulation of cell proliferation. According to Ascierto et al,6 50% of melanomas have a BRAF mutation, with nearly 90% of them with a V600E mutation. Hence, since the advent of direct chemotherapeutic agents such as BRAF inhibitors, clinical trials have shown notable reduction in mortality and morbidity of melanoma patients with BRAF mutations.6
Imlygic (talimogene laherparepvec)(Amgen, Inc) is a modified oncolytic viral therapy.7 This treatment was approved by the FDA in 2015 and replicates within tumors to produce granulocyte-macrophage colony-stimulating factor protein, which promotes an antitumor immune response within unresectable cutaneous, subcutaneous, and nodal melanoma lesions. Although it is not a gene-directed therapy, the melanoma does not require a specific mutation for treatment. Again, this medication is better served in conjunction with other melanoma chemotherapeutic and surgical interventions.
Submental Fat
Kybella (deoxycholic acid)(Allergan) is a nonhuman, nonanimal, synthetically created compound that is naturally found within the human body for the breakdown and absorption of dietary fat.8 This drug was FDA approved in 2015 for the improvement of the appearance of moderate subcutaneous fat under the chin. Patients are evaluated in clinic to determine if the submental fat would be responsive to an injectable or require more radical surgical intervention based on desired outcomes. The treatment is administered as 0.2-mL injections (up to a total of 10 mL) spaced 1-cm apart and ideally is repeated at regular intervals to evaluate for efficacy.
Basal Cell Carcinoma
Odomzo (sonidegib)(Novartis Corporation) was FDA approved in 2015 for locally advanced basal cell carcinoma.9 Odomzo is a smoothened antagonist that inhibits the hedgehog signaling pathway. Smoothened is a transmembrane protein that allows for signal transduction of hedgehog proteins.10 Protein patched homolog 1 binds to smoothened protein and prevents the signal transduction through the cell for Gli family zinc factor 1 to continue protein translation; however, when PTCH is mutated and can no longer bind to smoothened, tumor formation results, specifically basal cell carcinoma. Hence, sonidegib is for the treatment of basal cell carcinomas that have persisted despite radiation treatment and/or surgery as well as for patients who have multiple basal cell carcinomas that can no longer be treated with surgery or radiation.
Final Thoughts
Overall, although there are several medications that can be used in conjunction for treatment of dermatological conditions, it always is recommended to know what is in the pipeline as FDA-approved medications for dermatology.
- Ameluz [package insert]. Leverkusen, Germany: Biofrontera Bioscience GmbH; 2016.
- Taltz [package insert]. Indianapolis, IN: Eli Lilly and Company; 2016.
- Cosentyx [package insert]. East Hanover, NJ: Novartis Corporation; 2015.
- Cotellic [package insert]. San Francisco, CA: Genentech, Inc; 2016.
- Zelboraf [package insert]. San Francisco, CA: Genentech, Inc; 2016.
- Ascierto PA, Kirkwood JM, Grob JJ, et al. The role of BRAF V600 mutation in melanoma. J Transl Med. 2012;10:85.
- Imlygic (talimogene laherparepvec). Thousand Oaks, CA: Amgen Inc; 2015.
- Kybella [package insert]. West Lake Village, CA: Kythera Biopharmaceuticals, Inc; 2015.
- Odomzo [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2015.
- Villavicencio EH, Walterhouse DO, Iannaccone PM. The sonic hedgehog-patched-gli pathway in human development and disease. Am J Hum Genet. 2000;67:1047-1054.
CenterWatch (http://www.centerwatch.com/) is an online resource that provides directories, analysis, and market research of medications that are either under clinical evaluation or available for use in patients. A list of currently approved drugs by the US Food and Drug Administration (FDA) also is available by specialty. It is important for dermatologists in-training to know about recently approved drugs and those that are in the pipeline, as these treatments may benefit patients who are unresponsive to other previously used medications. New drugs also may be useful for physicians who have a difficult time getting insurance to cover prescriptions for their patients, as most new medications have built-in patient assistance.
New Drugs in Dermatology
Actinic Keratosis
Ameluz (aminolevulinic acid hydrochloride)(Biofrontera AG) is a new drug that was approved in May 2016 for treatment of mild to moderate actinic keratosis on the face and scalp.1 It is only intended for in-office use on patients who may not be candidates for other treatment options for actinic keratosis. The product is a gel formulation that should be applied to cover the lesions and approximately 5 mm of the surrounding area with a film of approximately 1-mm thickness. The entire treatment area is then illuminated with a red light source, either with a narrow spectrum around 630 nm with a light dose of approximately 37 J/cm2 or a broader and continuous spectrum in the range of 570 to 670 nm with a light dose between 75 and 200 J/cm2.1 Similar to the previously used aminolevulinic acid treatment method for actinic keratosis, the patient may experience a burning stinging sensation throughout the treatment and the skin will then proceed to peel.
Psoriasis and Psoriatic Arthritis
Taltz (ixekizumab)(Eli Lilly and Company) was approved by the FDA in March 2016 for the treatment of moderate to severe plaque psoriasis.2 It is a humanized IL-17A antagonist that works when IgG4 monoclonal antibodies selectively bind with IL-17A cytokines and inhibit their interaction with the IL-17 receptor. Although this injectable medication is approved for the treatment of psoriasis, it also can potentially be used off label for the treatment of psoriatic arthritis and rheumatoid arthritis. The approved dosage is 160 mg (two 80-mg injections) at week 0, followed by 80 mg at weeks 2, 4, 6, 8, 10, and 12, then 80 mg every 4 weeks.2 Injectable immunomodulatory medications such as ixekizumab are ideal for patients in whom topical treatments and light therapy failed and they continue to have serious psoriatic discomfort as well as for those who have substantial body surface area coverage.
In January 2015, Cosentyx (secukinumab)(Novartis Corporation) was approved by the FDA.3 Similar to ixekizumab, this injectable is an IgG1 monoclonal antibody that selectively binds to the IL-17A cytokine and inhibits its interaction with the IL-17 receptor. It is approved for the treatment of moderate to severe plaque psoriasis and psoriatic arthritis. The approved dosage for plaque psoriasis is 300 mg (two 150-mg subcutaneous injections) at weeks 0 through 4 followed by 300 mg every 4 weeks as needed until clearance.3 Similar to ixekizumab, secukinumab may be used for the treatment of recalcitrant psoriasis or psoriasis with substantial body surface area involvement.
Melanoma
Cotellic (cobimetinib)(Genentech USA, Inc) was FDA approved in November 2015.4 Cobimetinib is a reversible inhibitor of mitogen-activated protein kinase (MAPK)/extracellular signal regulated kinase 1. Mitogen-activated protein kinase MEK1 and MEK2 are regulators of the extracellular signal-related kinase pathway, which promotes cellular proliferation. This pathway is key, as melanomas that have a BRAF V600E and kinase mutation continue to proliferate due to the constitutive activation of MEK1 and MEK2, further promoting cellular proliferation. Cobimetinib is approved for the treatment of melanoma in patients with unresectable or metastatic melanoma with a BRAF V600E or V600K mutation, in conjunction with vemurafenib. Zelboraf (vemurafenib)(Genentech USA, Inc), another inhibitor of BRAF V600E, also is used for the treatment of unresectable melanomas and was initially approved in 2011.5
BRAF is a serine/threonine protein kinase. When unregulated, it results in the deregulation of cell proliferation. According to Ascierto et al,6 50% of melanomas have a BRAF mutation, with nearly 90% of them with a V600E mutation. Hence, since the advent of direct chemotherapeutic agents such as BRAF inhibitors, clinical trials have shown notable reduction in mortality and morbidity of melanoma patients with BRAF mutations.6
Imlygic (talimogene laherparepvec)(Amgen, Inc) is a modified oncolytic viral therapy.7 This treatment was approved by the FDA in 2015 and replicates within tumors to produce granulocyte-macrophage colony-stimulating factor protein, which promotes an antitumor immune response within unresectable cutaneous, subcutaneous, and nodal melanoma lesions. Although it is not a gene-directed therapy, the melanoma does not require a specific mutation for treatment. Again, this medication is better served in conjunction with other melanoma chemotherapeutic and surgical interventions.
Submental Fat
Kybella (deoxycholic acid)(Allergan) is a nonhuman, nonanimal, synthetically created compound that is naturally found within the human body for the breakdown and absorption of dietary fat.8 This drug was FDA approved in 2015 for the improvement of the appearance of moderate subcutaneous fat under the chin. Patients are evaluated in clinic to determine if the submental fat would be responsive to an injectable or require more radical surgical intervention based on desired outcomes. The treatment is administered as 0.2-mL injections (up to a total of 10 mL) spaced 1-cm apart and ideally is repeated at regular intervals to evaluate for efficacy.
Basal Cell Carcinoma
Odomzo (sonidegib)(Novartis Corporation) was FDA approved in 2015 for locally advanced basal cell carcinoma.9 Odomzo is a smoothened antagonist that inhibits the hedgehog signaling pathway. Smoothened is a transmembrane protein that allows for signal transduction of hedgehog proteins.10 Protein patched homolog 1 binds to smoothened protein and prevents the signal transduction through the cell for Gli family zinc factor 1 to continue protein translation; however, when PTCH is mutated and can no longer bind to smoothened, tumor formation results, specifically basal cell carcinoma. Hence, sonidegib is for the treatment of basal cell carcinomas that have persisted despite radiation treatment and/or surgery as well as for patients who have multiple basal cell carcinomas that can no longer be treated with surgery or radiation.
Final Thoughts
Overall, although there are several medications that can be used in conjunction for treatment of dermatological conditions, it always is recommended to know what is in the pipeline as FDA-approved medications for dermatology.
CenterWatch (http://www.centerwatch.com/) is an online resource that provides directories, analysis, and market research of medications that are either under clinical evaluation or available for use in patients. A list of currently approved drugs by the US Food and Drug Administration (FDA) also is available by specialty. It is important for dermatologists in-training to know about recently approved drugs and those that are in the pipeline, as these treatments may benefit patients who are unresponsive to other previously used medications. New drugs also may be useful for physicians who have a difficult time getting insurance to cover prescriptions for their patients, as most new medications have built-in patient assistance.
New Drugs in Dermatology
Actinic Keratosis
Ameluz (aminolevulinic acid hydrochloride)(Biofrontera AG) is a new drug that was approved in May 2016 for treatment of mild to moderate actinic keratosis on the face and scalp.1 It is only intended for in-office use on patients who may not be candidates for other treatment options for actinic keratosis. The product is a gel formulation that should be applied to cover the lesions and approximately 5 mm of the surrounding area with a film of approximately 1-mm thickness. The entire treatment area is then illuminated with a red light source, either with a narrow spectrum around 630 nm with a light dose of approximately 37 J/cm2 or a broader and continuous spectrum in the range of 570 to 670 nm with a light dose between 75 and 200 J/cm2.1 Similar to the previously used aminolevulinic acid treatment method for actinic keratosis, the patient may experience a burning stinging sensation throughout the treatment and the skin will then proceed to peel.
Psoriasis and Psoriatic Arthritis
Taltz (ixekizumab)(Eli Lilly and Company) was approved by the FDA in March 2016 for the treatment of moderate to severe plaque psoriasis.2 It is a humanized IL-17A antagonist that works when IgG4 monoclonal antibodies selectively bind with IL-17A cytokines and inhibit their interaction with the IL-17 receptor. Although this injectable medication is approved for the treatment of psoriasis, it also can potentially be used off label for the treatment of psoriatic arthritis and rheumatoid arthritis. The approved dosage is 160 mg (two 80-mg injections) at week 0, followed by 80 mg at weeks 2, 4, 6, 8, 10, and 12, then 80 mg every 4 weeks.2 Injectable immunomodulatory medications such as ixekizumab are ideal for patients in whom topical treatments and light therapy failed and they continue to have serious psoriatic discomfort as well as for those who have substantial body surface area coverage.
In January 2015, Cosentyx (secukinumab)(Novartis Corporation) was approved by the FDA.3 Similar to ixekizumab, this injectable is an IgG1 monoclonal antibody that selectively binds to the IL-17A cytokine and inhibits its interaction with the IL-17 receptor. It is approved for the treatment of moderate to severe plaque psoriasis and psoriatic arthritis. The approved dosage for plaque psoriasis is 300 mg (two 150-mg subcutaneous injections) at weeks 0 through 4 followed by 300 mg every 4 weeks as needed until clearance.3 Similar to ixekizumab, secukinumab may be used for the treatment of recalcitrant psoriasis or psoriasis with substantial body surface area involvement.
Melanoma
Cotellic (cobimetinib)(Genentech USA, Inc) was FDA approved in November 2015.4 Cobimetinib is a reversible inhibitor of mitogen-activated protein kinase (MAPK)/extracellular signal regulated kinase 1. Mitogen-activated protein kinase MEK1 and MEK2 are regulators of the extracellular signal-related kinase pathway, which promotes cellular proliferation. This pathway is key, as melanomas that have a BRAF V600E and kinase mutation continue to proliferate due to the constitutive activation of MEK1 and MEK2, further promoting cellular proliferation. Cobimetinib is approved for the treatment of melanoma in patients with unresectable or metastatic melanoma with a BRAF V600E or V600K mutation, in conjunction with vemurafenib. Zelboraf (vemurafenib)(Genentech USA, Inc), another inhibitor of BRAF V600E, also is used for the treatment of unresectable melanomas and was initially approved in 2011.5
BRAF is a serine/threonine protein kinase. When unregulated, it results in the deregulation of cell proliferation. According to Ascierto et al,6 50% of melanomas have a BRAF mutation, with nearly 90% of them with a V600E mutation. Hence, since the advent of direct chemotherapeutic agents such as BRAF inhibitors, clinical trials have shown notable reduction in mortality and morbidity of melanoma patients with BRAF mutations.6
Imlygic (talimogene laherparepvec)(Amgen, Inc) is a modified oncolytic viral therapy.7 This treatment was approved by the FDA in 2015 and replicates within tumors to produce granulocyte-macrophage colony-stimulating factor protein, which promotes an antitumor immune response within unresectable cutaneous, subcutaneous, and nodal melanoma lesions. Although it is not a gene-directed therapy, the melanoma does not require a specific mutation for treatment. Again, this medication is better served in conjunction with other melanoma chemotherapeutic and surgical interventions.
Submental Fat
Kybella (deoxycholic acid)(Allergan) is a nonhuman, nonanimal, synthetically created compound that is naturally found within the human body for the breakdown and absorption of dietary fat.8 This drug was FDA approved in 2015 for the improvement of the appearance of moderate subcutaneous fat under the chin. Patients are evaluated in clinic to determine if the submental fat would be responsive to an injectable or require more radical surgical intervention based on desired outcomes. The treatment is administered as 0.2-mL injections (up to a total of 10 mL) spaced 1-cm apart and ideally is repeated at regular intervals to evaluate for efficacy.
Basal Cell Carcinoma
Odomzo (sonidegib)(Novartis Corporation) was FDA approved in 2015 for locally advanced basal cell carcinoma.9 Odomzo is a smoothened antagonist that inhibits the hedgehog signaling pathway. Smoothened is a transmembrane protein that allows for signal transduction of hedgehog proteins.10 Protein patched homolog 1 binds to smoothened protein and prevents the signal transduction through the cell for Gli family zinc factor 1 to continue protein translation; however, when PTCH is mutated and can no longer bind to smoothened, tumor formation results, specifically basal cell carcinoma. Hence, sonidegib is for the treatment of basal cell carcinomas that have persisted despite radiation treatment and/or surgery as well as for patients who have multiple basal cell carcinomas that can no longer be treated with surgery or radiation.
Final Thoughts
Overall, although there are several medications that can be used in conjunction for treatment of dermatological conditions, it always is recommended to know what is in the pipeline as FDA-approved medications for dermatology.
- Ameluz [package insert]. Leverkusen, Germany: Biofrontera Bioscience GmbH; 2016.
- Taltz [package insert]. Indianapolis, IN: Eli Lilly and Company; 2016.
- Cosentyx [package insert]. East Hanover, NJ: Novartis Corporation; 2015.
- Cotellic [package insert]. San Francisco, CA: Genentech, Inc; 2016.
- Zelboraf [package insert]. San Francisco, CA: Genentech, Inc; 2016.
- Ascierto PA, Kirkwood JM, Grob JJ, et al. The role of BRAF V600 mutation in melanoma. J Transl Med. 2012;10:85.
- Imlygic (talimogene laherparepvec). Thousand Oaks, CA: Amgen Inc; 2015.
- Kybella [package insert]. West Lake Village, CA: Kythera Biopharmaceuticals, Inc; 2015.
- Odomzo [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2015.
- Villavicencio EH, Walterhouse DO, Iannaccone PM. The sonic hedgehog-patched-gli pathway in human development and disease. Am J Hum Genet. 2000;67:1047-1054.
- Ameluz [package insert]. Leverkusen, Germany: Biofrontera Bioscience GmbH; 2016.
- Taltz [package insert]. Indianapolis, IN: Eli Lilly and Company; 2016.
- Cosentyx [package insert]. East Hanover, NJ: Novartis Corporation; 2015.
- Cotellic [package insert]. San Francisco, CA: Genentech, Inc; 2016.
- Zelboraf [package insert]. San Francisco, CA: Genentech, Inc; 2016.
- Ascierto PA, Kirkwood JM, Grob JJ, et al. The role of BRAF V600 mutation in melanoma. J Transl Med. 2012;10:85.
- Imlygic (talimogene laherparepvec). Thousand Oaks, CA: Amgen Inc; 2015.
- Kybella [package insert]. West Lake Village, CA: Kythera Biopharmaceuticals, Inc; 2015.
- Odomzo [package insert]. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2015.
- Villavicencio EH, Walterhouse DO, Iannaccone PM. The sonic hedgehog-patched-gli pathway in human development and disease. Am J Hum Genet. 2000;67:1047-1054.
Is physician-assisted suicide compatible with the Hippocratic Oath?
Do we stand by our Hippocratic Oath when providing physician-assisted suicide?
Physician-assisted suicide (PAS) is a form of euthanasia in which a physician provides the patient with the pertinent information, and, in certain cases, a prescription for the necessary lethal drugs, so that the individual can willingly and successfully terminate his or her own life. The justification for PAS is the compassionate relief of intractable human suffering. Euthanasia and PAS are accepted practices in European countries such as the Netherlands, Belgium, and Luxembourg.
Such patients are mentally incapable of making the difficult decision to end their life and therefore should require a psychiatric evaluation to include counseling prior to making a decision to engage in PAS. For patients with mental illness, PAS is even more problematic than for terminally ill patients, because patients may lack the capacity to make rational and responsible decisions. Indeed, there are sizable loopholes where our medical system lacks safeguards and similarly lacks the requirements for a thorough, pre-PAS mental health examination, family notifications, and consultations, and for the minimally necessary legal pressure required to ensure patient cooperation.
Critical role of mental health workers
Although PAS has been legalized in those five U.S. states, its support and cases have stalled in recent years, indicating serious ethical concerns, mostly because of multileveled challenges of combating and delineating cultural stereotypes, quantifying mental capacity, gauging quality of life, and deciding where to situate psychiatrists in the PAS decision.
The psychiatrist’s role is being debated. In the United States, opponents take issue with current PAS-legal state’s legislation regarding psychiatric evaluations. For example, Oregon stipulates a psychiatrist referral only in cases where a physician other than a psychiatrist believes the patient’s judgment is impaired. It’s agreed that psychiatrists have the best skill set to assess a patient’s perceptions. Other PAS-legal states require a psychiatrist or psychologist assessment before making the decision. Unfortunately, though, physicians have rarely referred these patients to psychiatrists before offering PAS as an option.
PAS opponents target standards by which concepts like “quality of life” or “contributing member of society” are judged – specifically, that “unbearable suffering” and its ramifications are ill defined – people whose lives are deemed “not worth living” (including the terminally ill) would be susceptible to “sympathetic death” via PAS that might result from PAS legalization. Opponents also argue that recognizing a suicide “right” contradicts that a significant number of suicide attempters have mental illness and need help. They say that legalizing PAS would enable mentally incapacitated people to commit the irreversible act based on their distorted perceptions without providing them the expected assistance from their profession.1
The use of euthanasia or PAS gradually is trending from physically terminally ill patients toward psychiatrically complex patients. There are cases in which euthanasia or PAS was requested by psychiatric patients who had chronic psychiatric, medical, and psychosocial histories rather than purely physical ailment histories. In one study, Scott Y. H. Kim, MD, PhD, and his associates reviewed cases in the Netherlands in which either euthanasia or PAS for psychiatric disorders was deployed. The granted PAS requests appeared to involve physician judgment without psychiatric input.
The study reviewed 66 cases: 55% of patients had chronic severe conditions with extensive histories of attempted suicides and psychiatric hospitalizations, demonstrating that the granted euthanasia and PAS requests had involved extensive evaluations. However, 11% of cases had no independent psychiatric input, and 24% involved disagreement among the physicians.2 PAS proponents and opponents support the involvement and expertise of psychiatrists in all of this.
Psychiatrists have long contended that suicide attempts are often a “cry for help,” not an earnest act to end one’s life. Legalizing PAS tells suicidal individuals that society does not care whether they live or die – a truly un-Hippocratic stance. The stereotypes tossed around in the PAS debate, which could mean life or death, need to be unpacked with specific criteria attached, rather than preconceptions.
Autonomy of patients and implications of PAS
In the PAS debate, there are serious life concerns exhibited by terminally ill/psychiatrically ill patients over losing their autonomy and becoming a burden to their families and caregivers. Stereotypes must be deconstructed, yes, but such patients generally have been considered to be rendered, by the sum effect of their illnesses, mentally incapable of making the decision to end their lives. Addressing this order of patient life concerns generally has been the realm of social workers, psychologists, and, in the most desirable cases, psychiatrists. Therefore, even in keeping with established practice, some form of competent psychiatric evaluation should be required before considering PAS as a viable option.
The call for this requirement is backed up by a study, which reported that 47% of patients who had considered or committed suicide previously were diagnosed with psychiatric disorders, and 15% had undiagnosed psychiatric disorders.3 Also, inventories of thwarted suicide attempters reveal that most lack the conviction to end their lives, and this obverse phenomenon is backed by a study that revealed that 75% of 96 suicidal patients were found to be ambivalent in their intent to end their lives. Suicide attempters simply may be trying to communicate with people in their lives in order to test their love and care.4 This indicates that those who attempt suicide are predominantly psychiatrically ill and prone to distorted perceptions, impaired judgment, frustration, escapism, and manipulative guilt.
Suicide is abhorrent to most human beings’ sensibilities, because humanity has an innate will to live.5 It is wrong to offer patients life-ending options when they might rejuvenate or ease into death naturally. With the debilitated or elderly, PAS could violate their human rights. If the attitude that they are a burden to society persists, then a certain segment of society might be tempted to avoid their intergenerational obligations to elders, particularly those elders presenting with concurrent mental illnesses. PAS would additionally fuel that problem. This would represent a profound injustice and gross violation of human dignity, while also serving as a denial of basic human rights, particularly the right to life and care.6
Conclusion
The complex physical, psychological, and social challenges associated with PAS and the difficulty in enforcing its laws necessitate more adept alternatives. Instead of conditionally legalizing suicide, we should ease patient suffering with compassion and calibrated treatment.6,7
Terminally ill patients often suffer from depression, affecting their rationality. Adequate counseling, medical care, and psychological care should be the response to terminally ill patients considering suicide. If society accepts that ending a life is a reasonable response to human suffering that could otherwise be treated or reversed, then those with the most serious psychiatric conditions are destined to become more vulnerable. Therefore, physicians and psychiatrists should instead work harder to help patients recover, rather than participating in their quest for death.
Simplistic legal and regulatory oversight is insufficient, because the questions evoked by PAS are complicated by life, death, and ethics. Further research is needed to look into the mechanisms and morality of how psychiatrists and other physicians will make judgments and recommendations that are vital elements in developing regulatory oversight on PAS. Finally, future studies should look at which practices have been successful and which might be deemed unethical.
References
1. Clin Med (Lond). 2010 Aug;109(4):323-5.
2. JAMA Psychiatry. 2016;73(4):362-8.
3. “The Final Months: A Study of the Lives of 134 Persons Who Committed Suicide,” New York: Oxford University Press, 1981.
4. “Why We Shouldn’t Legalize Assisting Suicide, Part I.” Department of Medical Ethics, National Right to Life Committee.
5. “Working with Suicidal Individuals: A Guide to Providing Understanding, Assessment and Support,” Philadelphia: Jessica Kingsley Publishers, 2010.
6. “Always Care, Never Kill: How Physician-Assisted Suicide Endangers the Weak, Corrupts Medicine, Compromises the Family, and Violates Human Dignity and Equality,” Washington: The Heritage Foundation, 2015.
7. Ann Intern Med. 2012 Jan 3;156(1 Pt 2):73-104.
Dr. Ahmed is a 2nd-year resident in the psychiatry & behavioral sciences department at the Nassau University Medical Center, New York. Over the last 3 years, he has published and presented papers at national and international forums. His interests include public social psychiatry, health care policy, health disparities, mental health stigma, and undiagnosed and overdiagnosed psychiatric illnesses in children. Dr. Ahmed is a member of the American Psychiatric Association, the American Society of Clinical Psychopharmacology, and the American Association for Social Psychiatry.
Do we stand by our Hippocratic Oath when providing physician-assisted suicide?
Physician-assisted suicide (PAS) is a form of euthanasia in which a physician provides the patient with the pertinent information, and, in certain cases, a prescription for the necessary lethal drugs, so that the individual can willingly and successfully terminate his or her own life. The justification for PAS is the compassionate relief of intractable human suffering. Euthanasia and PAS are accepted practices in European countries such as the Netherlands, Belgium, and Luxembourg.
Such patients are mentally incapable of making the difficult decision to end their life and therefore should require a psychiatric evaluation to include counseling prior to making a decision to engage in PAS. For patients with mental illness, PAS is even more problematic than for terminally ill patients, because patients may lack the capacity to make rational and responsible decisions. Indeed, there are sizable loopholes where our medical system lacks safeguards and similarly lacks the requirements for a thorough, pre-PAS mental health examination, family notifications, and consultations, and for the minimally necessary legal pressure required to ensure patient cooperation.
Critical role of mental health workers
Although PAS has been legalized in those five U.S. states, its support and cases have stalled in recent years, indicating serious ethical concerns, mostly because of multileveled challenges of combating and delineating cultural stereotypes, quantifying mental capacity, gauging quality of life, and deciding where to situate psychiatrists in the PAS decision.
The psychiatrist’s role is being debated. In the United States, opponents take issue with current PAS-legal state’s legislation regarding psychiatric evaluations. For example, Oregon stipulates a psychiatrist referral only in cases where a physician other than a psychiatrist believes the patient’s judgment is impaired. It’s agreed that psychiatrists have the best skill set to assess a patient’s perceptions. Other PAS-legal states require a psychiatrist or psychologist assessment before making the decision. Unfortunately, though, physicians have rarely referred these patients to psychiatrists before offering PAS as an option.
PAS opponents target standards by which concepts like “quality of life” or “contributing member of society” are judged – specifically, that “unbearable suffering” and its ramifications are ill defined – people whose lives are deemed “not worth living” (including the terminally ill) would be susceptible to “sympathetic death” via PAS that might result from PAS legalization. Opponents also argue that recognizing a suicide “right” contradicts that a significant number of suicide attempters have mental illness and need help. They say that legalizing PAS would enable mentally incapacitated people to commit the irreversible act based on their distorted perceptions without providing them the expected assistance from their profession.1
The use of euthanasia or PAS gradually is trending from physically terminally ill patients toward psychiatrically complex patients. There are cases in which euthanasia or PAS was requested by psychiatric patients who had chronic psychiatric, medical, and psychosocial histories rather than purely physical ailment histories. In one study, Scott Y. H. Kim, MD, PhD, and his associates reviewed cases in the Netherlands in which either euthanasia or PAS for psychiatric disorders was deployed. The granted PAS requests appeared to involve physician judgment without psychiatric input.
The study reviewed 66 cases: 55% of patients had chronic severe conditions with extensive histories of attempted suicides and psychiatric hospitalizations, demonstrating that the granted euthanasia and PAS requests had involved extensive evaluations. However, 11% of cases had no independent psychiatric input, and 24% involved disagreement among the physicians.2 PAS proponents and opponents support the involvement and expertise of psychiatrists in all of this.
Psychiatrists have long contended that suicide attempts are often a “cry for help,” not an earnest act to end one’s life. Legalizing PAS tells suicidal individuals that society does not care whether they live or die – a truly un-Hippocratic stance. The stereotypes tossed around in the PAS debate, which could mean life or death, need to be unpacked with specific criteria attached, rather than preconceptions.
Autonomy of patients and implications of PAS
In the PAS debate, there are serious life concerns exhibited by terminally ill/psychiatrically ill patients over losing their autonomy and becoming a burden to their families and caregivers. Stereotypes must be deconstructed, yes, but such patients generally have been considered to be rendered, by the sum effect of their illnesses, mentally incapable of making the decision to end their lives. Addressing this order of patient life concerns generally has been the realm of social workers, psychologists, and, in the most desirable cases, psychiatrists. Therefore, even in keeping with established practice, some form of competent psychiatric evaluation should be required before considering PAS as a viable option.
The call for this requirement is backed up by a study, which reported that 47% of patients who had considered or committed suicide previously were diagnosed with psychiatric disorders, and 15% had undiagnosed psychiatric disorders.3 Also, inventories of thwarted suicide attempters reveal that most lack the conviction to end their lives, and this obverse phenomenon is backed by a study that revealed that 75% of 96 suicidal patients were found to be ambivalent in their intent to end their lives. Suicide attempters simply may be trying to communicate with people in their lives in order to test their love and care.4 This indicates that those who attempt suicide are predominantly psychiatrically ill and prone to distorted perceptions, impaired judgment, frustration, escapism, and manipulative guilt.
Suicide is abhorrent to most human beings’ sensibilities, because humanity has an innate will to live.5 It is wrong to offer patients life-ending options when they might rejuvenate or ease into death naturally. With the debilitated or elderly, PAS could violate their human rights. If the attitude that they are a burden to society persists, then a certain segment of society might be tempted to avoid their intergenerational obligations to elders, particularly those elders presenting with concurrent mental illnesses. PAS would additionally fuel that problem. This would represent a profound injustice and gross violation of human dignity, while also serving as a denial of basic human rights, particularly the right to life and care.6
Conclusion
The complex physical, psychological, and social challenges associated with PAS and the difficulty in enforcing its laws necessitate more adept alternatives. Instead of conditionally legalizing suicide, we should ease patient suffering with compassion and calibrated treatment.6,7
Terminally ill patients often suffer from depression, affecting their rationality. Adequate counseling, medical care, and psychological care should be the response to terminally ill patients considering suicide. If society accepts that ending a life is a reasonable response to human suffering that could otherwise be treated or reversed, then those with the most serious psychiatric conditions are destined to become more vulnerable. Therefore, physicians and psychiatrists should instead work harder to help patients recover, rather than participating in their quest for death.
Simplistic legal and regulatory oversight is insufficient, because the questions evoked by PAS are complicated by life, death, and ethics. Further research is needed to look into the mechanisms and morality of how psychiatrists and other physicians will make judgments and recommendations that are vital elements in developing regulatory oversight on PAS. Finally, future studies should look at which practices have been successful and which might be deemed unethical.
References
1. Clin Med (Lond). 2010 Aug;109(4):323-5.
2. JAMA Psychiatry. 2016;73(4):362-8.
3. “The Final Months: A Study of the Lives of 134 Persons Who Committed Suicide,” New York: Oxford University Press, 1981.
4. “Why We Shouldn’t Legalize Assisting Suicide, Part I.” Department of Medical Ethics, National Right to Life Committee.
5. “Working with Suicidal Individuals: A Guide to Providing Understanding, Assessment and Support,” Philadelphia: Jessica Kingsley Publishers, 2010.
6. “Always Care, Never Kill: How Physician-Assisted Suicide Endangers the Weak, Corrupts Medicine, Compromises the Family, and Violates Human Dignity and Equality,” Washington: The Heritage Foundation, 2015.
7. Ann Intern Med. 2012 Jan 3;156(1 Pt 2):73-104.
Dr. Ahmed is a 2nd-year resident in the psychiatry & behavioral sciences department at the Nassau University Medical Center, New York. Over the last 3 years, he has published and presented papers at national and international forums. His interests include public social psychiatry, health care policy, health disparities, mental health stigma, and undiagnosed and overdiagnosed psychiatric illnesses in children. Dr. Ahmed is a member of the American Psychiatric Association, the American Society of Clinical Psychopharmacology, and the American Association for Social Psychiatry.
Do we stand by our Hippocratic Oath when providing physician-assisted suicide?
Physician-assisted suicide (PAS) is a form of euthanasia in which a physician provides the patient with the pertinent information, and, in certain cases, a prescription for the necessary lethal drugs, so that the individual can willingly and successfully terminate his or her own life. The justification for PAS is the compassionate relief of intractable human suffering. Euthanasia and PAS are accepted practices in European countries such as the Netherlands, Belgium, and Luxembourg.
Such patients are mentally incapable of making the difficult decision to end their life and therefore should require a psychiatric evaluation to include counseling prior to making a decision to engage in PAS. For patients with mental illness, PAS is even more problematic than for terminally ill patients, because patients may lack the capacity to make rational and responsible decisions. Indeed, there are sizable loopholes where our medical system lacks safeguards and similarly lacks the requirements for a thorough, pre-PAS mental health examination, family notifications, and consultations, and for the minimally necessary legal pressure required to ensure patient cooperation.
Critical role of mental health workers
Although PAS has been legalized in those five U.S. states, its support and cases have stalled in recent years, indicating serious ethical concerns, mostly because of multileveled challenges of combating and delineating cultural stereotypes, quantifying mental capacity, gauging quality of life, and deciding where to situate psychiatrists in the PAS decision.
The psychiatrist’s role is being debated. In the United States, opponents take issue with current PAS-legal state’s legislation regarding psychiatric evaluations. For example, Oregon stipulates a psychiatrist referral only in cases where a physician other than a psychiatrist believes the patient’s judgment is impaired. It’s agreed that psychiatrists have the best skill set to assess a patient’s perceptions. Other PAS-legal states require a psychiatrist or psychologist assessment before making the decision. Unfortunately, though, physicians have rarely referred these patients to psychiatrists before offering PAS as an option.
PAS opponents target standards by which concepts like “quality of life” or “contributing member of society” are judged – specifically, that “unbearable suffering” and its ramifications are ill defined – people whose lives are deemed “not worth living” (including the terminally ill) would be susceptible to “sympathetic death” via PAS that might result from PAS legalization. Opponents also argue that recognizing a suicide “right” contradicts that a significant number of suicide attempters have mental illness and need help. They say that legalizing PAS would enable mentally incapacitated people to commit the irreversible act based on their distorted perceptions without providing them the expected assistance from their profession.1
The use of euthanasia or PAS gradually is trending from physically terminally ill patients toward psychiatrically complex patients. There are cases in which euthanasia or PAS was requested by psychiatric patients who had chronic psychiatric, medical, and psychosocial histories rather than purely physical ailment histories. In one study, Scott Y. H. Kim, MD, PhD, and his associates reviewed cases in the Netherlands in which either euthanasia or PAS for psychiatric disorders was deployed. The granted PAS requests appeared to involve physician judgment without psychiatric input.
The study reviewed 66 cases: 55% of patients had chronic severe conditions with extensive histories of attempted suicides and psychiatric hospitalizations, demonstrating that the granted euthanasia and PAS requests had involved extensive evaluations. However, 11% of cases had no independent psychiatric input, and 24% involved disagreement among the physicians.2 PAS proponents and opponents support the involvement and expertise of psychiatrists in all of this.
Psychiatrists have long contended that suicide attempts are often a “cry for help,” not an earnest act to end one’s life. Legalizing PAS tells suicidal individuals that society does not care whether they live or die – a truly un-Hippocratic stance. The stereotypes tossed around in the PAS debate, which could mean life or death, need to be unpacked with specific criteria attached, rather than preconceptions.
Autonomy of patients and implications of PAS
In the PAS debate, there are serious life concerns exhibited by terminally ill/psychiatrically ill patients over losing their autonomy and becoming a burden to their families and caregivers. Stereotypes must be deconstructed, yes, but such patients generally have been considered to be rendered, by the sum effect of their illnesses, mentally incapable of making the decision to end their lives. Addressing this order of patient life concerns generally has been the realm of social workers, psychologists, and, in the most desirable cases, psychiatrists. Therefore, even in keeping with established practice, some form of competent psychiatric evaluation should be required before considering PAS as a viable option.
The call for this requirement is backed up by a study, which reported that 47% of patients who had considered or committed suicide previously were diagnosed with psychiatric disorders, and 15% had undiagnosed psychiatric disorders.3 Also, inventories of thwarted suicide attempters reveal that most lack the conviction to end their lives, and this obverse phenomenon is backed by a study that revealed that 75% of 96 suicidal patients were found to be ambivalent in their intent to end their lives. Suicide attempters simply may be trying to communicate with people in their lives in order to test their love and care.4 This indicates that those who attempt suicide are predominantly psychiatrically ill and prone to distorted perceptions, impaired judgment, frustration, escapism, and manipulative guilt.
Suicide is abhorrent to most human beings’ sensibilities, because humanity has an innate will to live.5 It is wrong to offer patients life-ending options when they might rejuvenate or ease into death naturally. With the debilitated or elderly, PAS could violate their human rights. If the attitude that they are a burden to society persists, then a certain segment of society might be tempted to avoid their intergenerational obligations to elders, particularly those elders presenting with concurrent mental illnesses. PAS would additionally fuel that problem. This would represent a profound injustice and gross violation of human dignity, while also serving as a denial of basic human rights, particularly the right to life and care.6
Conclusion
The complex physical, psychological, and social challenges associated with PAS and the difficulty in enforcing its laws necessitate more adept alternatives. Instead of conditionally legalizing suicide, we should ease patient suffering with compassion and calibrated treatment.6,7
Terminally ill patients often suffer from depression, affecting their rationality. Adequate counseling, medical care, and psychological care should be the response to terminally ill patients considering suicide. If society accepts that ending a life is a reasonable response to human suffering that could otherwise be treated or reversed, then those with the most serious psychiatric conditions are destined to become more vulnerable. Therefore, physicians and psychiatrists should instead work harder to help patients recover, rather than participating in their quest for death.
Simplistic legal and regulatory oversight is insufficient, because the questions evoked by PAS are complicated by life, death, and ethics. Further research is needed to look into the mechanisms and morality of how psychiatrists and other physicians will make judgments and recommendations that are vital elements in developing regulatory oversight on PAS. Finally, future studies should look at which practices have been successful and which might be deemed unethical.
References
1. Clin Med (Lond). 2010 Aug;109(4):323-5.
2. JAMA Psychiatry. 2016;73(4):362-8.
3. “The Final Months: A Study of the Lives of 134 Persons Who Committed Suicide,” New York: Oxford University Press, 1981.
4. “Why We Shouldn’t Legalize Assisting Suicide, Part I.” Department of Medical Ethics, National Right to Life Committee.
5. “Working with Suicidal Individuals: A Guide to Providing Understanding, Assessment and Support,” Philadelphia: Jessica Kingsley Publishers, 2010.
6. “Always Care, Never Kill: How Physician-Assisted Suicide Endangers the Weak, Corrupts Medicine, Compromises the Family, and Violates Human Dignity and Equality,” Washington: The Heritage Foundation, 2015.
7. Ann Intern Med. 2012 Jan 3;156(1 Pt 2):73-104.
Dr. Ahmed is a 2nd-year resident in the psychiatry & behavioral sciences department at the Nassau University Medical Center, New York. Over the last 3 years, he has published and presented papers at national and international forums. His interests include public social psychiatry, health care policy, health disparities, mental health stigma, and undiagnosed and overdiagnosed psychiatric illnesses in children. Dr. Ahmed is a member of the American Psychiatric Association, the American Society of Clinical Psychopharmacology, and the American Association for Social Psychiatry.
How to Increase Patient Adherence to Therapy
How do we increase patient adherence to therapy? This question fascinates me. As dermatologists, we will see thousands of patients over the course of our careers, most with treatable conditions that will improve with therapy and others with chronic or genetic conditions that will at least be made more tolerable with therapy. Only 50% of patients with a chronic condition are adherent to therapy.1 Why some patients adhere to treatment and others do not can be difficult to understand. The emotional makeup, culture, family background, socioeconomic status, and motivation of each person is unique, which leads to complexity. This column is not meant to answer a question that is both complex and broad; rather, it is meant to survey and summarize the literature on this topic.
Education
Health literacy is defined as cognitive and social skills that determine the motivation and ability of individuals to gain access to, understand, and use information in ways that promote and maintain good health.2 Greater health literacy leads to improved compliance and health outcomes.3,4 When we take the time to educate patients about their condition, it improves health literacy, treatment compliance, and patient safety and satisfaction, factors that ultimately are linked to better health outcomes.3-8
There are many practical ways of educating patients. Interestingly, one meta-analysis found that no single strategy is more effective than another.6 This analysis found that "[c]omprehensive interventions combining cognitive, behavioral, and affective components were more effective than single-focus interventions."6 The Centers for Disease Control and Prevention (CDC) website is an excellent source of information on how to educate patients and increase patient treatment compliance.2 The CDC website offers a free tool kit on how to design educational information to your target audience, resources for children, a database of health-related educational images, an electronic textbook on teaching patients with low literacy skills, a summary of evidence-based ideas on how to improve patient adherence to medications used long-term, and more.2
Facilitating Adherence
The World Health Organization (WHO) emphasizes 5 dimensions of patient adherence: health system, socioeconomic, condition-related, therapy-related, and patient-related factors.9 Becker and Maiman5 summarized it eloquently when they wrote that we must take "clinically appropriate steps to reduce the cost, complexity, duration, and amount of behavioral change required by the regimen and increasing the regimen's convenience through 'tailoring' and other approaches." It is a broad ultimatum that will require creativity and persistence on the part of the dermatology community.
Some common patient-related factors associated with nonadherence to treatment are lack of information and skills as they pertain to self-management, difficulty with motivation and self-efficacy, and lack of support for behavioral changes.9 It is interesting that low socioeconomic status has not been consistently shown to portend low treatment adherence. It has been shown that children, especially adolescents, and elderly patients tend to be the least adherent.9-11
Dermatologists Take Action
As dermatologists, the WHO encourages us (physicians) to promote optimism, provide enthusiasm, and encourage maintenance of healthy behaviors.9 Comprehensive interventions that have had a positive impact on patient adherence to therapy for diseases such as diabetes mellitus, asthma, and hypertension may serve as motivating examples.9 Some specific dermatologic conditions that will benefit from increased patient adherence include acne, vesiculobullous disease, psoriasis, and atopic dermatitis. We can lend support to efforts to reduce the cost of dermatologic medications and be aware of the populations most at risk for low adherence to treatment.9-12
Final Thoughts
As we work to increase patient adherence to therapy in dermatology, we will help improve health literacy, patient safety, and patient satisfaction. These factors are ultimately linked to better health outcomes. The CDC and WHO websites are excellent sources of information on practical methods for doing so.2,9
- Haynes RB, McDonald H, Garg AX, et al. Interventions for helping patients to follow prescriptions for medications. Cochrane Database Syst Rev. 2002:CD000011.
- Centers for Disease Control and Prevention. Health literacy. http://www.cdc.gov/healthliteracy/index.html. Updated January 13, 2016. Accessed September 23, 2016.
- Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97-107.
- Pignone MP, DeWalt DA. Literacy and health outcomes: is adherence the missing link? J Gen Intern Med. 2006;21:896-897.
- Becker MH, Maiman LA. Strategies for enhancing patient compliance. J Community Health. 1980;6:113-135.
- Roter DL, Hall JA, Merisca R, et al. Effectiveness of interventions to improve patient compliance: a meta-analysis. Med Care. 1998;36:1138-1161.
- Renzi C, Abeni D, Picardi A, et al. Factors associated with patient satisfaction with care among dermatological outpatients. Br J Dermatol. 2001;145:617-623.
- Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152:1423-1433.
- World Health Organization. Adherence to long-term therapies: evidence for action. http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf. Posted 2003. Accessed September 23, 2016.
- Lee IA, Maibach HI. Pharmionics in dermatology: a review of topical medication adherence. Am J Clin Dermatol. 2006;7:231-236.
- Burkhart P, Dunbar-Jacob J. Adherence research in the pediatric and adolescent populations: a decade in review. In: Hayman L, Mahon M, Turner R, eds. Chronic Illness in Children: An Evidence-Based Approach. New York, NY: Springer Publishing Company; 2002:199-229.
- Rosenberg ME, Rosenberg SP. Changes in retail prices of prescription dermatologic drugs from 2009 to 2015. JAMA Dermatol. 2016;152:158-163.
How do we increase patient adherence to therapy? This question fascinates me. As dermatologists, we will see thousands of patients over the course of our careers, most with treatable conditions that will improve with therapy and others with chronic or genetic conditions that will at least be made more tolerable with therapy. Only 50% of patients with a chronic condition are adherent to therapy.1 Why some patients adhere to treatment and others do not can be difficult to understand. The emotional makeup, culture, family background, socioeconomic status, and motivation of each person is unique, which leads to complexity. This column is not meant to answer a question that is both complex and broad; rather, it is meant to survey and summarize the literature on this topic.
Education
Health literacy is defined as cognitive and social skills that determine the motivation and ability of individuals to gain access to, understand, and use information in ways that promote and maintain good health.2 Greater health literacy leads to improved compliance and health outcomes.3,4 When we take the time to educate patients about their condition, it improves health literacy, treatment compliance, and patient safety and satisfaction, factors that ultimately are linked to better health outcomes.3-8
There are many practical ways of educating patients. Interestingly, one meta-analysis found that no single strategy is more effective than another.6 This analysis found that "[c]omprehensive interventions combining cognitive, behavioral, and affective components were more effective than single-focus interventions."6 The Centers for Disease Control and Prevention (CDC) website is an excellent source of information on how to educate patients and increase patient treatment compliance.2 The CDC website offers a free tool kit on how to design educational information to your target audience, resources for children, a database of health-related educational images, an electronic textbook on teaching patients with low literacy skills, a summary of evidence-based ideas on how to improve patient adherence to medications used long-term, and more.2
Facilitating Adherence
The World Health Organization (WHO) emphasizes 5 dimensions of patient adherence: health system, socioeconomic, condition-related, therapy-related, and patient-related factors.9 Becker and Maiman5 summarized it eloquently when they wrote that we must take "clinically appropriate steps to reduce the cost, complexity, duration, and amount of behavioral change required by the regimen and increasing the regimen's convenience through 'tailoring' and other approaches." It is a broad ultimatum that will require creativity and persistence on the part of the dermatology community.
Some common patient-related factors associated with nonadherence to treatment are lack of information and skills as they pertain to self-management, difficulty with motivation and self-efficacy, and lack of support for behavioral changes.9 It is interesting that low socioeconomic status has not been consistently shown to portend low treatment adherence. It has been shown that children, especially adolescents, and elderly patients tend to be the least adherent.9-11
Dermatologists Take Action
As dermatologists, the WHO encourages us (physicians) to promote optimism, provide enthusiasm, and encourage maintenance of healthy behaviors.9 Comprehensive interventions that have had a positive impact on patient adherence to therapy for diseases such as diabetes mellitus, asthma, and hypertension may serve as motivating examples.9 Some specific dermatologic conditions that will benefit from increased patient adherence include acne, vesiculobullous disease, psoriasis, and atopic dermatitis. We can lend support to efforts to reduce the cost of dermatologic medications and be aware of the populations most at risk for low adherence to treatment.9-12
Final Thoughts
As we work to increase patient adherence to therapy in dermatology, we will help improve health literacy, patient safety, and patient satisfaction. These factors are ultimately linked to better health outcomes. The CDC and WHO websites are excellent sources of information on practical methods for doing so.2,9
How do we increase patient adherence to therapy? This question fascinates me. As dermatologists, we will see thousands of patients over the course of our careers, most with treatable conditions that will improve with therapy and others with chronic or genetic conditions that will at least be made more tolerable with therapy. Only 50% of patients with a chronic condition are adherent to therapy.1 Why some patients adhere to treatment and others do not can be difficult to understand. The emotional makeup, culture, family background, socioeconomic status, and motivation of each person is unique, which leads to complexity. This column is not meant to answer a question that is both complex and broad; rather, it is meant to survey and summarize the literature on this topic.
Education
Health literacy is defined as cognitive and social skills that determine the motivation and ability of individuals to gain access to, understand, and use information in ways that promote and maintain good health.2 Greater health literacy leads to improved compliance and health outcomes.3,4 When we take the time to educate patients about their condition, it improves health literacy, treatment compliance, and patient safety and satisfaction, factors that ultimately are linked to better health outcomes.3-8
There are many practical ways of educating patients. Interestingly, one meta-analysis found that no single strategy is more effective than another.6 This analysis found that "[c]omprehensive interventions combining cognitive, behavioral, and affective components were more effective than single-focus interventions."6 The Centers for Disease Control and Prevention (CDC) website is an excellent source of information on how to educate patients and increase patient treatment compliance.2 The CDC website offers a free tool kit on how to design educational information to your target audience, resources for children, a database of health-related educational images, an electronic textbook on teaching patients with low literacy skills, a summary of evidence-based ideas on how to improve patient adherence to medications used long-term, and more.2
Facilitating Adherence
The World Health Organization (WHO) emphasizes 5 dimensions of patient adherence: health system, socioeconomic, condition-related, therapy-related, and patient-related factors.9 Becker and Maiman5 summarized it eloquently when they wrote that we must take "clinically appropriate steps to reduce the cost, complexity, duration, and amount of behavioral change required by the regimen and increasing the regimen's convenience through 'tailoring' and other approaches." It is a broad ultimatum that will require creativity and persistence on the part of the dermatology community.
Some common patient-related factors associated with nonadherence to treatment are lack of information and skills as they pertain to self-management, difficulty with motivation and self-efficacy, and lack of support for behavioral changes.9 It is interesting that low socioeconomic status has not been consistently shown to portend low treatment adherence. It has been shown that children, especially adolescents, and elderly patients tend to be the least adherent.9-11
Dermatologists Take Action
As dermatologists, the WHO encourages us (physicians) to promote optimism, provide enthusiasm, and encourage maintenance of healthy behaviors.9 Comprehensive interventions that have had a positive impact on patient adherence to therapy for diseases such as diabetes mellitus, asthma, and hypertension may serve as motivating examples.9 Some specific dermatologic conditions that will benefit from increased patient adherence include acne, vesiculobullous disease, psoriasis, and atopic dermatitis. We can lend support to efforts to reduce the cost of dermatologic medications and be aware of the populations most at risk for low adherence to treatment.9-12
Final Thoughts
As we work to increase patient adherence to therapy in dermatology, we will help improve health literacy, patient safety, and patient satisfaction. These factors are ultimately linked to better health outcomes. The CDC and WHO websites are excellent sources of information on practical methods for doing so.2,9
- Haynes RB, McDonald H, Garg AX, et al. Interventions for helping patients to follow prescriptions for medications. Cochrane Database Syst Rev. 2002:CD000011.
- Centers for Disease Control and Prevention. Health literacy. http://www.cdc.gov/healthliteracy/index.html. Updated January 13, 2016. Accessed September 23, 2016.
- Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97-107.
- Pignone MP, DeWalt DA. Literacy and health outcomes: is adherence the missing link? J Gen Intern Med. 2006;21:896-897.
- Becker MH, Maiman LA. Strategies for enhancing patient compliance. J Community Health. 1980;6:113-135.
- Roter DL, Hall JA, Merisca R, et al. Effectiveness of interventions to improve patient compliance: a meta-analysis. Med Care. 1998;36:1138-1161.
- Renzi C, Abeni D, Picardi A, et al. Factors associated with patient satisfaction with care among dermatological outpatients. Br J Dermatol. 2001;145:617-623.
- Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152:1423-1433.
- World Health Organization. Adherence to long-term therapies: evidence for action. http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf. Posted 2003. Accessed September 23, 2016.
- Lee IA, Maibach HI. Pharmionics in dermatology: a review of topical medication adherence. Am J Clin Dermatol. 2006;7:231-236.
- Burkhart P, Dunbar-Jacob J. Adherence research in the pediatric and adolescent populations: a decade in review. In: Hayman L, Mahon M, Turner R, eds. Chronic Illness in Children: An Evidence-Based Approach. New York, NY: Springer Publishing Company; 2002:199-229.
- Rosenberg ME, Rosenberg SP. Changes in retail prices of prescription dermatologic drugs from 2009 to 2015. JAMA Dermatol. 2016;152:158-163.
- Haynes RB, McDonald H, Garg AX, et al. Interventions for helping patients to follow prescriptions for medications. Cochrane Database Syst Rev. 2002:CD000011.
- Centers for Disease Control and Prevention. Health literacy. http://www.cdc.gov/healthliteracy/index.html. Updated January 13, 2016. Accessed September 23, 2016.
- Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97-107.
- Pignone MP, DeWalt DA. Literacy and health outcomes: is adherence the missing link? J Gen Intern Med. 2006;21:896-897.
- Becker MH, Maiman LA. Strategies for enhancing patient compliance. J Community Health. 1980;6:113-135.
- Roter DL, Hall JA, Merisca R, et al. Effectiveness of interventions to improve patient compliance: a meta-analysis. Med Care. 1998;36:1138-1161.
- Renzi C, Abeni D, Picardi A, et al. Factors associated with patient satisfaction with care among dermatological outpatients. Br J Dermatol. 2001;145:617-623.
- Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152:1423-1433.
- World Health Organization. Adherence to long-term therapies: evidence for action. http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf. Posted 2003. Accessed September 23, 2016.
- Lee IA, Maibach HI. Pharmionics in dermatology: a review of topical medication adherence. Am J Clin Dermatol. 2006;7:231-236.
- Burkhart P, Dunbar-Jacob J. Adherence research in the pediatric and adolescent populations: a decade in review. In: Hayman L, Mahon M, Turner R, eds. Chronic Illness in Children: An Evidence-Based Approach. New York, NY: Springer Publishing Company; 2002:199-229.
- Rosenberg ME, Rosenberg SP. Changes in retail prices of prescription dermatologic drugs from 2009 to 2015. JAMA Dermatol. 2016;152:158-163.
Navigating the ambiguity around whether to admit or discharge
In my first week of intern year, I learned the criteria for admission to an inpatient psychiatric unit: imminent harm to self, imminent harm to others, or the inability to care for self.1 The standard risk assessment. In residency training, each patient encounter trains us in the challenging practice of risk assessment in potentially dangerous situations. One quickly learns the anxiety a moderate risk patient will cause.
Less discussed than the risk assessment, but certainly, a frequent challenge facing psychiatry residents is whether an admission is “good” or “bad.” The bad admission reflects the type of patient and situation, when you, the psychiatrist, basically know that inpatient admission is likely inappropriate.2 Usually, these occur when your hands are tied by structural and systemic pressures. Perhaps the patient is a known “high utilizer” whose admission is primarily motivated by homelessness or lack of community mental health resources.3 Or maybe the bad admission is a patient with a personality disorder who is consistently readmitted by each resident in the program with seemingly little improvement after each admission.4 Bad admissions are the type of patient who, as the overnight resident, you feel a touch embarrassed signing out to the fresh resident there to relieve you in the morning. In these cases, I find myself making various justifications: It was a busy night; there was no collateral; no family; no friends; no outpatient support. I tell myself, I just couldn’t manage a safe enough discharge. I couldn’t mitigate the risk enough.
If the situation allows in the midst of the tumult, I create an intimate space to interview my patient. I pull up a chair and lean in to listen. To maintain an empathetic stance, I must recognize and control my biases toward high utilizers, drug use, homelessness, noncompliance, and the other host of factors that may influence my judgment. Between the hours of 1 a.m. and 6 a.m., fatigue, in particular, will breed negative countertransference. Before I sit down to listen, I repeat my mantra to myself: The least I can offer is kindness. Then the assessment and the decision-making process that leads to an admission or a discharge begins.
When I’m on call, I am torn by my obligations: to the patient, their safety and well-being; to the health care system and distributive justice; to making the “right” decision to admit or discharge; to my nursing staff and their safety; to my supervisors and my fellow residents who will judge and must deal with my clinical decision to admit or discharge. Some of these obligations that I struggle to balance are outlined as core competencies by the Accreditation Council for Graduate Medical Education and the American Board of Psychiatry and Neurology, and called the Psychiatry Milestone Project.5 I am supposed to be thinking about these issues as I work up a patient, evaluating, and making purposeful trade-offs. The educational language of these core competencies does not capture the tensions of these complicated on-call experiences.
The most useful thing I have learned this year is that the decision to admit or discharge is not a binary decision. The very act of assessment through an interview and making a plan with the patient is valuable in itself as risk mitigation. Only recently as a second-year resident have I fully realized how my presence could have therapeutic effects. Even a brief interview in the emergency department can be generative. I try to bring calm to the chaos around the patient. I listen, elicit protective factors and coping skills, and try to mobilize hope and internal strength building capabilities just as we are taught in my residency program.
However, I admittedly continue to dread my overnight calls. As a second-year resident, I am still uncomfortable with the ambiguity in some decisions to admit or discharge. Nonetheless, I recognize these experiences are only helping me become a better psychiatrist with every night I spend running between the ED and the psychiatric unit. To get through this process of residency, I have formulated another mantra: Every call and every patient is a learning experience.
References
1. BMC Health Serv Res. 2006;6:150.
2. Health Policy. 2000 Oct;53(3):157-84.
3. Adm Policy Ment Health. 2012 May;39(3):200-9.
4. Psychiatr Serv. 2015 Jan 1;66(1):15-20.
5. “The Psychiatry Milestone Project”: Assessment Tools. A Joint Initiative of the Accreditation Council for Graduate Medical Education and the American Board of Psychiatry and Neurology.
Dr. Posada is a second-year resident in the psychiatry & behavioral sciences department at George Washington University, Washington. She completed a bachelor’s degree at the George Washington University. For 2 years after her undergraduate education, she worked at the National Institutes of Allergy and Infectious Diseases studying HIV pathogenesis. Dr. Posada completed her medical degree at the University of Texas Medical Branch in Galveston. Her interests include public psychiatry, health care policy, health disparities, and psychosomatic medicine.
In my first week of intern year, I learned the criteria for admission to an inpatient psychiatric unit: imminent harm to self, imminent harm to others, or the inability to care for self.1 The standard risk assessment. In residency training, each patient encounter trains us in the challenging practice of risk assessment in potentially dangerous situations. One quickly learns the anxiety a moderate risk patient will cause.
Less discussed than the risk assessment, but certainly, a frequent challenge facing psychiatry residents is whether an admission is “good” or “bad.” The bad admission reflects the type of patient and situation, when you, the psychiatrist, basically know that inpatient admission is likely inappropriate.2 Usually, these occur when your hands are tied by structural and systemic pressures. Perhaps the patient is a known “high utilizer” whose admission is primarily motivated by homelessness or lack of community mental health resources.3 Or maybe the bad admission is a patient with a personality disorder who is consistently readmitted by each resident in the program with seemingly little improvement after each admission.4 Bad admissions are the type of patient who, as the overnight resident, you feel a touch embarrassed signing out to the fresh resident there to relieve you in the morning. In these cases, I find myself making various justifications: It was a busy night; there was no collateral; no family; no friends; no outpatient support. I tell myself, I just couldn’t manage a safe enough discharge. I couldn’t mitigate the risk enough.
If the situation allows in the midst of the tumult, I create an intimate space to interview my patient. I pull up a chair and lean in to listen. To maintain an empathetic stance, I must recognize and control my biases toward high utilizers, drug use, homelessness, noncompliance, and the other host of factors that may influence my judgment. Between the hours of 1 a.m. and 6 a.m., fatigue, in particular, will breed negative countertransference. Before I sit down to listen, I repeat my mantra to myself: The least I can offer is kindness. Then the assessment and the decision-making process that leads to an admission or a discharge begins.
When I’m on call, I am torn by my obligations: to the patient, their safety and well-being; to the health care system and distributive justice; to making the “right” decision to admit or discharge; to my nursing staff and their safety; to my supervisors and my fellow residents who will judge and must deal with my clinical decision to admit or discharge. Some of these obligations that I struggle to balance are outlined as core competencies by the Accreditation Council for Graduate Medical Education and the American Board of Psychiatry and Neurology, and called the Psychiatry Milestone Project.5 I am supposed to be thinking about these issues as I work up a patient, evaluating, and making purposeful trade-offs. The educational language of these core competencies does not capture the tensions of these complicated on-call experiences.
The most useful thing I have learned this year is that the decision to admit or discharge is not a binary decision. The very act of assessment through an interview and making a plan with the patient is valuable in itself as risk mitigation. Only recently as a second-year resident have I fully realized how my presence could have therapeutic effects. Even a brief interview in the emergency department can be generative. I try to bring calm to the chaos around the patient. I listen, elicit protective factors and coping skills, and try to mobilize hope and internal strength building capabilities just as we are taught in my residency program.
However, I admittedly continue to dread my overnight calls. As a second-year resident, I am still uncomfortable with the ambiguity in some decisions to admit or discharge. Nonetheless, I recognize these experiences are only helping me become a better psychiatrist with every night I spend running between the ED and the psychiatric unit. To get through this process of residency, I have formulated another mantra: Every call and every patient is a learning experience.
References
1. BMC Health Serv Res. 2006;6:150.
2. Health Policy. 2000 Oct;53(3):157-84.
3. Adm Policy Ment Health. 2012 May;39(3):200-9.
4. Psychiatr Serv. 2015 Jan 1;66(1):15-20.
5. “The Psychiatry Milestone Project”: Assessment Tools. A Joint Initiative of the Accreditation Council for Graduate Medical Education and the American Board of Psychiatry and Neurology.
Dr. Posada is a second-year resident in the psychiatry & behavioral sciences department at George Washington University, Washington. She completed a bachelor’s degree at the George Washington University. For 2 years after her undergraduate education, she worked at the National Institutes of Allergy and Infectious Diseases studying HIV pathogenesis. Dr. Posada completed her medical degree at the University of Texas Medical Branch in Galveston. Her interests include public psychiatry, health care policy, health disparities, and psychosomatic medicine.
In my first week of intern year, I learned the criteria for admission to an inpatient psychiatric unit: imminent harm to self, imminent harm to others, or the inability to care for self.1 The standard risk assessment. In residency training, each patient encounter trains us in the challenging practice of risk assessment in potentially dangerous situations. One quickly learns the anxiety a moderate risk patient will cause.
Less discussed than the risk assessment, but certainly, a frequent challenge facing psychiatry residents is whether an admission is “good” or “bad.” The bad admission reflects the type of patient and situation, when you, the psychiatrist, basically know that inpatient admission is likely inappropriate.2 Usually, these occur when your hands are tied by structural and systemic pressures. Perhaps the patient is a known “high utilizer” whose admission is primarily motivated by homelessness or lack of community mental health resources.3 Or maybe the bad admission is a patient with a personality disorder who is consistently readmitted by each resident in the program with seemingly little improvement after each admission.4 Bad admissions are the type of patient who, as the overnight resident, you feel a touch embarrassed signing out to the fresh resident there to relieve you in the morning. In these cases, I find myself making various justifications: It was a busy night; there was no collateral; no family; no friends; no outpatient support. I tell myself, I just couldn’t manage a safe enough discharge. I couldn’t mitigate the risk enough.
If the situation allows in the midst of the tumult, I create an intimate space to interview my patient. I pull up a chair and lean in to listen. To maintain an empathetic stance, I must recognize and control my biases toward high utilizers, drug use, homelessness, noncompliance, and the other host of factors that may influence my judgment. Between the hours of 1 a.m. and 6 a.m., fatigue, in particular, will breed negative countertransference. Before I sit down to listen, I repeat my mantra to myself: The least I can offer is kindness. Then the assessment and the decision-making process that leads to an admission or a discharge begins.
When I’m on call, I am torn by my obligations: to the patient, their safety and well-being; to the health care system and distributive justice; to making the “right” decision to admit or discharge; to my nursing staff and their safety; to my supervisors and my fellow residents who will judge and must deal with my clinical decision to admit or discharge. Some of these obligations that I struggle to balance are outlined as core competencies by the Accreditation Council for Graduate Medical Education and the American Board of Psychiatry and Neurology, and called the Psychiatry Milestone Project.5 I am supposed to be thinking about these issues as I work up a patient, evaluating, and making purposeful trade-offs. The educational language of these core competencies does not capture the tensions of these complicated on-call experiences.
The most useful thing I have learned this year is that the decision to admit or discharge is not a binary decision. The very act of assessment through an interview and making a plan with the patient is valuable in itself as risk mitigation. Only recently as a second-year resident have I fully realized how my presence could have therapeutic effects. Even a brief interview in the emergency department can be generative. I try to bring calm to the chaos around the patient. I listen, elicit protective factors and coping skills, and try to mobilize hope and internal strength building capabilities just as we are taught in my residency program.
However, I admittedly continue to dread my overnight calls. As a second-year resident, I am still uncomfortable with the ambiguity in some decisions to admit or discharge. Nonetheless, I recognize these experiences are only helping me become a better psychiatrist with every night I spend running between the ED and the psychiatric unit. To get through this process of residency, I have formulated another mantra: Every call and every patient is a learning experience.
References
1. BMC Health Serv Res. 2006;6:150.
2. Health Policy. 2000 Oct;53(3):157-84.
3. Adm Policy Ment Health. 2012 May;39(3):200-9.
4. Psychiatr Serv. 2015 Jan 1;66(1):15-20.
5. “The Psychiatry Milestone Project”: Assessment Tools. A Joint Initiative of the Accreditation Council for Graduate Medical Education and the American Board of Psychiatry and Neurology.
Dr. Posada is a second-year resident in the psychiatry & behavioral sciences department at George Washington University, Washington. She completed a bachelor’s degree at the George Washington University. For 2 years after her undergraduate education, she worked at the National Institutes of Allergy and Infectious Diseases studying HIV pathogenesis. Dr. Posada completed her medical degree at the University of Texas Medical Branch in Galveston. Her interests include public psychiatry, health care policy, health disparities, and psychosomatic medicine.
Influence of Diet in Acne Vulgaris and Atopic Dermatitis
When I am in clinic, I often get at least 3 to 4 inquiries each day from patients about the necessity for dietary restrictions or alterations as well as the benefits of these changes in limiting their dermatological disease processes. I usually am restricted in my response because the research rarely indicates benefits of one diet versus another; however, this discussion has recently become a heavily researched area as patients have come to value natural nonpharmaceutical approaches to their holistic care. In this article, a few dietary restrictions and supplements are reviewed that may have a beneficial effect in managing patients with acne vulgaris and atopic dermatitis.
Acne Vulgaris
In 1969 Fulton et al1 conducted one of the first few trials on acne and diet management. In this crossover, patient-blinded, interventional study, patients were divided into 2 subgroups (N=65): 1 adolescent patient with moderate acne was compared to 1 male prisoner given a chocolate bar for 4 weeks or a control bar with equivalent caloric index. The results indicated no change in acne vulgaris lesions based on either intervention; however, there were obvious deficiencies in the study including small sample size, inappropriate grouping of an adolescent patient versus a prisoner, and limited study period.1
Since then, multiple studies have been conducted with parallel participants, large sample sizes, and at least a 12-week study period. In 2005, Adebamowo et al2 studied 47,355 women using a validated food frequency questionnaire that determined the amount of dairy consumed, specifically skim milk. The study showed a positive link between increased dairy consumption and acne formation; however, again due to the retrospective analysis and recall bias, it is difficult to determine if a link can truly be noted between acne and dairy in this study.2
More recently, LaRosa et al3 conducted a study that included 225 participants aged 14 to 19 years. Excluding participants with lactose intolerance and current use of oral contraceptives and isotretinoin, the study placed 120 participants in the test group versus 105 participants in the control group. The study was conducted using 3 telephone interviews and a 24-hour diet recall technique. The results supported a link between acne and skim milk consumption. Again, although the studied relied on participant self-reports of diet and followed a case-control design, a possible association was suspected but not validated.3 A longitudinal, questionnaire-based population study performed by Ulvestad et al4 included 2489 patients. This study further evaluated recall of dairy product consumption at 15 to 16 years of age and then 3 years later acne severity was self-assessed and reported at 18 to 19 years of age. Overall, this evaluation indicated that a high intake of dairy products and acne in adolescence have been positively associated. However, it was another retrospective study with recall bias.4 In 2009 Melnick and Schmitz5 concluded that milk causes the body to elevate both insulin and insulinlike growth factor 1 levels. In another study by Melnick6 in 2011, a definitive link between increased insulin and insulinlike growth factor 1 signaling in promoting comedogenesis was reported. Given the few studies that show the potential link between dairy products and acne, this dairy-free diet can be considered as a diet recommendation for acne patients.
Atopic Dermatitis
A Cochrane review conducted in 2012 regarding dietary supplements as a treatment of atopic dermatitis evaluated randomized controlled trials (N=596). Supplementation with vitamin D, fish oil, olive oil, zinc sulfate, selenium, vitamin E, pyridoxine, sea buckthorn seed oil, hempseed oil, sunflower oil (linoleic acid), and docosahexaenoic acid were evaluated among all the studies reviewed for atopic dermatitis.7 Bronsnick et al8 conducted a review of evidence supporting vitamin supplementation and atopic dermatitis, and for the most part determined that the studies had insufficient evidence. The only positive correlation was noted with prebiotics and probiotics in another Cochrane review in 2013, which evaluated 4 studies with 1428 infants showing prebiotic supplementation reduced atopic dermatitis.9 In 2014 Panduru et al10 evaluated 16 studies in a meta-analysis that showed how probiotics were possibly beneficial in both general and high-risk atopic populations. Specifically, a subgroup analysis showed that Lactobacillus and Lactobacillus with Bifidobacterium also can be protective against atopic dermatitis.10 Lastly, diet avoidance in pregnancy or during lactation in infants up to 18 months of age did not have any effect on improving the infant’s atopic dermatitis based on a 2012 Cochrane review that included 952 participants.11
Conclusion
Overall, there are some benefits to dietary restrictions and supplementation as indicated by the studies reviewed here; however, the extent to which these changes contribute to disease manifestation has only been linked, not definitively proven. Randomized controlled trials with large sample sizes, double-blind studies, and appropriately controlled studies with comparative patient populations are difficult to obtain, as diet cannot be completely restrictive for every patient. Patients should be provided with the latest data supporting a possible link between dairy consumption and acne production as well as prebiotics or probiotics during pregnancy and at infancy to reduce the risk for atopic dermatitis with the caveat of association. That said, future studies might prove that dietary and environmental alterations may prevent disease progression or appearance far more than previously assumed.
- Fulton JE Jr, Plewaig G, Kligman AM. Effect of chocolate on acne vulgaris. JAMA. 1969;210: 2071-2074.
- Adebamowo CA, Spiegelman D, Berkey CS, et al. High school dietary diary intake and teenage acne. J Am Acad Dermatol. 2005;52:207-214.
- LaRosa CL, Quach KA, Koons K, et al. Consumption of dairy in teenagers with and without acne. J Am Acad Dermatol. 2016;75:318-322.
- Ulvestad M, Bjertness E, Dalgard F, et al. Acne and dairy products in adolescence: results from a Norwegian longitudinal study [published online ahead of print July 16, 2016]. J Eur Acad Dermatol Venereol. doi:10.1111/jdv.13835.
- Melnick BC, Schmitz G. Role of insulin, insulin like growth factor 1, hyperglycemic food and milk consumption in the pathogenesis of acne vulgaris. Exp Dermatol. 2009;18:833-841.
- Melnick BC. Evidence for acne-promoting effect of milk and other insulinotropic dairy products. Nestle Nutr Worksop
Ser Pediatr Program. 2011;67:131-145. - Bath-Hextall FJ, Jenkinson C, Humphreys R, et al. Dietary supplements for established atopic eczema. Cochrane Database Syst Rev. 2012;2:CD005205.
- Bronsnick T, Murzaku EC, Rao BK. Diet in dermatology: part i. atopic dermatitis, acne, and nonmelanoma skin cancer [published online November 15, 2014]. J Am Acad Dermatol. 2014;71:1039.e1-1039.e12.
- Osborn DA, Sinn JKH. Prebiotics in infants for prevention of allergy. Cochrane Database Syst Rev. 2013;2:CD006474.
- Panduru M, Panduru NM, Saˇlaˇvaˇstru CM, et al. Probiotics and primary prevention of atopic dermatitis: a meta-analysis of randomized controlled studies [published online April 4, 2014]. J Eur Acad Dermatol Venereol. 2015;29:232-242.
- Kramer MS, Kakuma R. Maternal dietary antigen avoidance during pregnancy or lactation, or both, for preventing or treating atopic disease in the child. Cochrane Database Syst Rev. 2012;9:CD000133.
When I am in clinic, I often get at least 3 to 4 inquiries each day from patients about the necessity for dietary restrictions or alterations as well as the benefits of these changes in limiting their dermatological disease processes. I usually am restricted in my response because the research rarely indicates benefits of one diet versus another; however, this discussion has recently become a heavily researched area as patients have come to value natural nonpharmaceutical approaches to their holistic care. In this article, a few dietary restrictions and supplements are reviewed that may have a beneficial effect in managing patients with acne vulgaris and atopic dermatitis.
Acne Vulgaris
In 1969 Fulton et al1 conducted one of the first few trials on acne and diet management. In this crossover, patient-blinded, interventional study, patients were divided into 2 subgroups (N=65): 1 adolescent patient with moderate acne was compared to 1 male prisoner given a chocolate bar for 4 weeks or a control bar with equivalent caloric index. The results indicated no change in acne vulgaris lesions based on either intervention; however, there were obvious deficiencies in the study including small sample size, inappropriate grouping of an adolescent patient versus a prisoner, and limited study period.1
Since then, multiple studies have been conducted with parallel participants, large sample sizes, and at least a 12-week study period. In 2005, Adebamowo et al2 studied 47,355 women using a validated food frequency questionnaire that determined the amount of dairy consumed, specifically skim milk. The study showed a positive link between increased dairy consumption and acne formation; however, again due to the retrospective analysis and recall bias, it is difficult to determine if a link can truly be noted between acne and dairy in this study.2
More recently, LaRosa et al3 conducted a study that included 225 participants aged 14 to 19 years. Excluding participants with lactose intolerance and current use of oral contraceptives and isotretinoin, the study placed 120 participants in the test group versus 105 participants in the control group. The study was conducted using 3 telephone interviews and a 24-hour diet recall technique. The results supported a link between acne and skim milk consumption. Again, although the studied relied on participant self-reports of diet and followed a case-control design, a possible association was suspected but not validated.3 A longitudinal, questionnaire-based population study performed by Ulvestad et al4 included 2489 patients. This study further evaluated recall of dairy product consumption at 15 to 16 years of age and then 3 years later acne severity was self-assessed and reported at 18 to 19 years of age. Overall, this evaluation indicated that a high intake of dairy products and acne in adolescence have been positively associated. However, it was another retrospective study with recall bias.4 In 2009 Melnick and Schmitz5 concluded that milk causes the body to elevate both insulin and insulinlike growth factor 1 levels. In another study by Melnick6 in 2011, a definitive link between increased insulin and insulinlike growth factor 1 signaling in promoting comedogenesis was reported. Given the few studies that show the potential link between dairy products and acne, this dairy-free diet can be considered as a diet recommendation for acne patients.
Atopic Dermatitis
A Cochrane review conducted in 2012 regarding dietary supplements as a treatment of atopic dermatitis evaluated randomized controlled trials (N=596). Supplementation with vitamin D, fish oil, olive oil, zinc sulfate, selenium, vitamin E, pyridoxine, sea buckthorn seed oil, hempseed oil, sunflower oil (linoleic acid), and docosahexaenoic acid were evaluated among all the studies reviewed for atopic dermatitis.7 Bronsnick et al8 conducted a review of evidence supporting vitamin supplementation and atopic dermatitis, and for the most part determined that the studies had insufficient evidence. The only positive correlation was noted with prebiotics and probiotics in another Cochrane review in 2013, which evaluated 4 studies with 1428 infants showing prebiotic supplementation reduced atopic dermatitis.9 In 2014 Panduru et al10 evaluated 16 studies in a meta-analysis that showed how probiotics were possibly beneficial in both general and high-risk atopic populations. Specifically, a subgroup analysis showed that Lactobacillus and Lactobacillus with Bifidobacterium also can be protective against atopic dermatitis.10 Lastly, diet avoidance in pregnancy or during lactation in infants up to 18 months of age did not have any effect on improving the infant’s atopic dermatitis based on a 2012 Cochrane review that included 952 participants.11
Conclusion
Overall, there are some benefits to dietary restrictions and supplementation as indicated by the studies reviewed here; however, the extent to which these changes contribute to disease manifestation has only been linked, not definitively proven. Randomized controlled trials with large sample sizes, double-blind studies, and appropriately controlled studies with comparative patient populations are difficult to obtain, as diet cannot be completely restrictive for every patient. Patients should be provided with the latest data supporting a possible link between dairy consumption and acne production as well as prebiotics or probiotics during pregnancy and at infancy to reduce the risk for atopic dermatitis with the caveat of association. That said, future studies might prove that dietary and environmental alterations may prevent disease progression or appearance far more than previously assumed.
When I am in clinic, I often get at least 3 to 4 inquiries each day from patients about the necessity for dietary restrictions or alterations as well as the benefits of these changes in limiting their dermatological disease processes. I usually am restricted in my response because the research rarely indicates benefits of one diet versus another; however, this discussion has recently become a heavily researched area as patients have come to value natural nonpharmaceutical approaches to their holistic care. In this article, a few dietary restrictions and supplements are reviewed that may have a beneficial effect in managing patients with acne vulgaris and atopic dermatitis.
Acne Vulgaris
In 1969 Fulton et al1 conducted one of the first few trials on acne and diet management. In this crossover, patient-blinded, interventional study, patients were divided into 2 subgroups (N=65): 1 adolescent patient with moderate acne was compared to 1 male prisoner given a chocolate bar for 4 weeks or a control bar with equivalent caloric index. The results indicated no change in acne vulgaris lesions based on either intervention; however, there were obvious deficiencies in the study including small sample size, inappropriate grouping of an adolescent patient versus a prisoner, and limited study period.1
Since then, multiple studies have been conducted with parallel participants, large sample sizes, and at least a 12-week study period. In 2005, Adebamowo et al2 studied 47,355 women using a validated food frequency questionnaire that determined the amount of dairy consumed, specifically skim milk. The study showed a positive link between increased dairy consumption and acne formation; however, again due to the retrospective analysis and recall bias, it is difficult to determine if a link can truly be noted between acne and dairy in this study.2
More recently, LaRosa et al3 conducted a study that included 225 participants aged 14 to 19 years. Excluding participants with lactose intolerance and current use of oral contraceptives and isotretinoin, the study placed 120 participants in the test group versus 105 participants in the control group. The study was conducted using 3 telephone interviews and a 24-hour diet recall technique. The results supported a link between acne and skim milk consumption. Again, although the studied relied on participant self-reports of diet and followed a case-control design, a possible association was suspected but not validated.3 A longitudinal, questionnaire-based population study performed by Ulvestad et al4 included 2489 patients. This study further evaluated recall of dairy product consumption at 15 to 16 years of age and then 3 years later acne severity was self-assessed and reported at 18 to 19 years of age. Overall, this evaluation indicated that a high intake of dairy products and acne in adolescence have been positively associated. However, it was another retrospective study with recall bias.4 In 2009 Melnick and Schmitz5 concluded that milk causes the body to elevate both insulin and insulinlike growth factor 1 levels. In another study by Melnick6 in 2011, a definitive link between increased insulin and insulinlike growth factor 1 signaling in promoting comedogenesis was reported. Given the few studies that show the potential link between dairy products and acne, this dairy-free diet can be considered as a diet recommendation for acne patients.
Atopic Dermatitis
A Cochrane review conducted in 2012 regarding dietary supplements as a treatment of atopic dermatitis evaluated randomized controlled trials (N=596). Supplementation with vitamin D, fish oil, olive oil, zinc sulfate, selenium, vitamin E, pyridoxine, sea buckthorn seed oil, hempseed oil, sunflower oil (linoleic acid), and docosahexaenoic acid were evaluated among all the studies reviewed for atopic dermatitis.7 Bronsnick et al8 conducted a review of evidence supporting vitamin supplementation and atopic dermatitis, and for the most part determined that the studies had insufficient evidence. The only positive correlation was noted with prebiotics and probiotics in another Cochrane review in 2013, which evaluated 4 studies with 1428 infants showing prebiotic supplementation reduced atopic dermatitis.9 In 2014 Panduru et al10 evaluated 16 studies in a meta-analysis that showed how probiotics were possibly beneficial in both general and high-risk atopic populations. Specifically, a subgroup analysis showed that Lactobacillus and Lactobacillus with Bifidobacterium also can be protective against atopic dermatitis.10 Lastly, diet avoidance in pregnancy or during lactation in infants up to 18 months of age did not have any effect on improving the infant’s atopic dermatitis based on a 2012 Cochrane review that included 952 participants.11
Conclusion
Overall, there are some benefits to dietary restrictions and supplementation as indicated by the studies reviewed here; however, the extent to which these changes contribute to disease manifestation has only been linked, not definitively proven. Randomized controlled trials with large sample sizes, double-blind studies, and appropriately controlled studies with comparative patient populations are difficult to obtain, as diet cannot be completely restrictive for every patient. Patients should be provided with the latest data supporting a possible link between dairy consumption and acne production as well as prebiotics or probiotics during pregnancy and at infancy to reduce the risk for atopic dermatitis with the caveat of association. That said, future studies might prove that dietary and environmental alterations may prevent disease progression or appearance far more than previously assumed.
- Fulton JE Jr, Plewaig G, Kligman AM. Effect of chocolate on acne vulgaris. JAMA. 1969;210: 2071-2074.
- Adebamowo CA, Spiegelman D, Berkey CS, et al. High school dietary diary intake and teenage acne. J Am Acad Dermatol. 2005;52:207-214.
- LaRosa CL, Quach KA, Koons K, et al. Consumption of dairy in teenagers with and without acne. J Am Acad Dermatol. 2016;75:318-322.
- Ulvestad M, Bjertness E, Dalgard F, et al. Acne and dairy products in adolescence: results from a Norwegian longitudinal study [published online ahead of print July 16, 2016]. J Eur Acad Dermatol Venereol. doi:10.1111/jdv.13835.
- Melnick BC, Schmitz G. Role of insulin, insulin like growth factor 1, hyperglycemic food and milk consumption in the pathogenesis of acne vulgaris. Exp Dermatol. 2009;18:833-841.
- Melnick BC. Evidence for acne-promoting effect of milk and other insulinotropic dairy products. Nestle Nutr Worksop
Ser Pediatr Program. 2011;67:131-145. - Bath-Hextall FJ, Jenkinson C, Humphreys R, et al. Dietary supplements for established atopic eczema. Cochrane Database Syst Rev. 2012;2:CD005205.
- Bronsnick T, Murzaku EC, Rao BK. Diet in dermatology: part i. atopic dermatitis, acne, and nonmelanoma skin cancer [published online November 15, 2014]. J Am Acad Dermatol. 2014;71:1039.e1-1039.e12.
- Osborn DA, Sinn JKH. Prebiotics in infants for prevention of allergy. Cochrane Database Syst Rev. 2013;2:CD006474.
- Panduru M, Panduru NM, Saˇlaˇvaˇstru CM, et al. Probiotics and primary prevention of atopic dermatitis: a meta-analysis of randomized controlled studies [published online April 4, 2014]. J Eur Acad Dermatol Venereol. 2015;29:232-242.
- Kramer MS, Kakuma R. Maternal dietary antigen avoidance during pregnancy or lactation, or both, for preventing or treating atopic disease in the child. Cochrane Database Syst Rev. 2012;9:CD000133.
- Fulton JE Jr, Plewaig G, Kligman AM. Effect of chocolate on acne vulgaris. JAMA. 1969;210: 2071-2074.
- Adebamowo CA, Spiegelman D, Berkey CS, et al. High school dietary diary intake and teenage acne. J Am Acad Dermatol. 2005;52:207-214.
- LaRosa CL, Quach KA, Koons K, et al. Consumption of dairy in teenagers with and without acne. J Am Acad Dermatol. 2016;75:318-322.
- Ulvestad M, Bjertness E, Dalgard F, et al. Acne and dairy products in adolescence: results from a Norwegian longitudinal study [published online ahead of print July 16, 2016]. J Eur Acad Dermatol Venereol. doi:10.1111/jdv.13835.
- Melnick BC, Schmitz G. Role of insulin, insulin like growth factor 1, hyperglycemic food and milk consumption in the pathogenesis of acne vulgaris. Exp Dermatol. 2009;18:833-841.
- Melnick BC. Evidence for acne-promoting effect of milk and other insulinotropic dairy products. Nestle Nutr Worksop
Ser Pediatr Program. 2011;67:131-145. - Bath-Hextall FJ, Jenkinson C, Humphreys R, et al. Dietary supplements for established atopic eczema. Cochrane Database Syst Rev. 2012;2:CD005205.
- Bronsnick T, Murzaku EC, Rao BK. Diet in dermatology: part i. atopic dermatitis, acne, and nonmelanoma skin cancer [published online November 15, 2014]. J Am Acad Dermatol. 2014;71:1039.e1-1039.e12.
- Osborn DA, Sinn JKH. Prebiotics in infants for prevention of allergy. Cochrane Database Syst Rev. 2013;2:CD006474.
- Panduru M, Panduru NM, Saˇlaˇvaˇstru CM, et al. Probiotics and primary prevention of atopic dermatitis: a meta-analysis of randomized controlled studies [published online April 4, 2014]. J Eur Acad Dermatol Venereol. 2015;29:232-242.
- Kramer MS, Kakuma R. Maternal dietary antigen avoidance during pregnancy or lactation, or both, for preventing or treating atopic disease in the child. Cochrane Database Syst Rev. 2012;9:CD000133.
Preventing, Identifying, and Managing Cosmetic Procedure Complications, Part 2: Lasers and Chemical Peels
The primary cosmetic procedures that dermatology residents will perform or assist in performing during their training are soft-tissue augmentation, botulinum toxin injections, laser therapy, and chemical peels. Because complications can occur from these procedures, it is important for residents to learn how to prevent, identify, and manage them for optimal patient outcomes. In part 2 of this series, laser therapy and chemical peels are discussed.
Lasers
In dermatology, lasers are used to treat dyschromia, resurface scars, remove skin growths, and rejuvenate aging skin.1,2 Ablative resurfacing lasers such as the CO2 laser are the most likely to lead to unwanted side effects. There is a risk for herpes simplex virus reactivation, impetigo, persistent erythema, dyschromia, and scarring.1-3 Some patients who undergo facial ablative resurfacing may develop a visible hypopigmented line of demarcation between treated and untreated skin along the jawline.3 With the development of fractional resurfacing lasers, the risk for dyschromia, persistent erythema, and scarring was lessened.1-3
Regardless of the type of resurfacing laser used, patients should be given adequate prophylaxis with an antiviral and antibiotic. For skin of color, fractional resurfacing lasers should be set at lower density settings with a higher fluence.1-3 Sites with fewer adnexal structures (eg, neck, dorsal hands) also should be treated at lower densities.3 When using Q-switched lasers that target pigment, caution should be used to avoid vesicle formation and/or skin crusting, which may lead to scarring or dyschromia.1-3 Some tattoo inks may paradoxically darken when treated with lasers.3 A test spot is advised, especially prior to treatment of permanent makeup tattoos. A pigmented lesion should never be treated if the diagnosis is unclear (eg, a biopsy to establish the diagnosis may be the best appropriate step for some pigmented lesions). For laser hair removal, the Nd:YAG laser is the safest for skin of color.2,3
Lasers that target vascular structures may cause unwanted purpura, hypopigmentation, or thermal injury.1-3 A larger spot size may help decrease the risk for purpura. The skin should be cooled properly and caution should be used to avoid pulse stacking. For intense pulsed light devices, overlap pulses slightly to avoid a zebralike pattern of slivers of untreated skin.1-3 For all laser procedures, strict sun protection is advised before and after the procedure.
Chemical Peels
Chemical peels are versatile and varied in their composition. They are categorized based on the depth to which the skin is affected by the peel: superficial (stratum corneum), medium (full-thickness epidermis), or deep (mid reticular dermis).4 Peels are most commonly used to treat dyschromia, aging, rhytides, actinic damage, and superficial scars.4,5 The success of a chemical peel depends largely on patient selection and preprocedure preparation. Patients who tend to develop postinflammatory hyperpigmention, have an underlying inflammatory or scarring skin disorder, are on photosensitizing medications, or have continued work- or hobby-related sun exposure are generally poor peel candidates.4,5 Strict sun protection should be advised both before and after a chemical peel.
While in training, residents are unlikely to perform a medium or deep peel. Superficial peels can be accomplished with trichloroacetic acid 10%, glycolic acid (GA) 30% to 50%, salicylic acid (SA) 20% to 30%, Jessner solution (SA, lactic acid, and resorcinol with ethanol), and tretinoin 1% to 5%.4 Glycolic acid and SA are known to be safer for patients with skin of color.4,5
Care should always be taken to prepare the skin for an even peel. Mild peeling agents such as tretinoin or adapalene may be used to prepare the skin in the weeks before the procedure.4 Skin of color may benefit from hydroquinone used before and after a chemical peel.5 At the time of the peel, acetone can be used to degrease the skin for a more even, effective peel. If a peel needs to be neutralized (eg, GA), make sure to have the neutralization solution on hand, as leaving the peel solution on for too long can lead to severe epidermolysis, which can be visualized by a graying of the skin and will not be seen with a properly performed superficial peel.4 Care should be taken at all times to protect the patient’s eyes. Eye flushes should be readily available. The medial canthus and perinasal folds may be protected with petrolatum. For a superficial peel, some desquamation (less with GA) and erythema may be noted for a few days.
Final Thoughts
For any cosmetic procedure, the patient’s expectations should be discussed. The provider may adeptly guide the patient toward realistic expectations for the procedure. Pretreatment and posttreatment photographs should always be taken to help document treatment progress; it may be helpful to show the patient the photographs at each visit. The expected skin reactions, recovery time, and risks should be fully discussed. Full informed consent should be obtained. Complications from cosmetic procedures will inevitably arise. As residents, we can take the opportunity to learn how to prevent, identify, and manage them.
- Hirsch R, Stier M. Complications and their management in cosmetic dermatology. Dermatol Clin. 2009;27:507-520.
- Oliaei A, Nelson JS, Fitzpatrick R, et al. Laser treatment of scars. Facial Plast Surg. 2012;28:518-524.
- Al Nomair N, Nazarian R, Marmur E. Complications in lasers, lights, and radiofrequency devices. Facial Plast Surg. 2012;28:340-346.
- Khunger N, IADVL Task Force. Standard guidelines of care for chemical peels. Indian J Dermatol Venereol Leprol. 2008;74(suppl):S5-S12.
- Sarkar R, Bansal S, Garg VK. Chemical peels for melasma in dark-skinned patients. J Cutan Aesthet Surg. 2012;5:247-253.
The primary cosmetic procedures that dermatology residents will perform or assist in performing during their training are soft-tissue augmentation, botulinum toxin injections, laser therapy, and chemical peels. Because complications can occur from these procedures, it is important for residents to learn how to prevent, identify, and manage them for optimal patient outcomes. In part 2 of this series, laser therapy and chemical peels are discussed.
Lasers
In dermatology, lasers are used to treat dyschromia, resurface scars, remove skin growths, and rejuvenate aging skin.1,2 Ablative resurfacing lasers such as the CO2 laser are the most likely to lead to unwanted side effects. There is a risk for herpes simplex virus reactivation, impetigo, persistent erythema, dyschromia, and scarring.1-3 Some patients who undergo facial ablative resurfacing may develop a visible hypopigmented line of demarcation between treated and untreated skin along the jawline.3 With the development of fractional resurfacing lasers, the risk for dyschromia, persistent erythema, and scarring was lessened.1-3
Regardless of the type of resurfacing laser used, patients should be given adequate prophylaxis with an antiviral and antibiotic. For skin of color, fractional resurfacing lasers should be set at lower density settings with a higher fluence.1-3 Sites with fewer adnexal structures (eg, neck, dorsal hands) also should be treated at lower densities.3 When using Q-switched lasers that target pigment, caution should be used to avoid vesicle formation and/or skin crusting, which may lead to scarring or dyschromia.1-3 Some tattoo inks may paradoxically darken when treated with lasers.3 A test spot is advised, especially prior to treatment of permanent makeup tattoos. A pigmented lesion should never be treated if the diagnosis is unclear (eg, a biopsy to establish the diagnosis may be the best appropriate step for some pigmented lesions). For laser hair removal, the Nd:YAG laser is the safest for skin of color.2,3
Lasers that target vascular structures may cause unwanted purpura, hypopigmentation, or thermal injury.1-3 A larger spot size may help decrease the risk for purpura. The skin should be cooled properly and caution should be used to avoid pulse stacking. For intense pulsed light devices, overlap pulses slightly to avoid a zebralike pattern of slivers of untreated skin.1-3 For all laser procedures, strict sun protection is advised before and after the procedure.
Chemical Peels
Chemical peels are versatile and varied in their composition. They are categorized based on the depth to which the skin is affected by the peel: superficial (stratum corneum), medium (full-thickness epidermis), or deep (mid reticular dermis).4 Peels are most commonly used to treat dyschromia, aging, rhytides, actinic damage, and superficial scars.4,5 The success of a chemical peel depends largely on patient selection and preprocedure preparation. Patients who tend to develop postinflammatory hyperpigmention, have an underlying inflammatory or scarring skin disorder, are on photosensitizing medications, or have continued work- or hobby-related sun exposure are generally poor peel candidates.4,5 Strict sun protection should be advised both before and after a chemical peel.
While in training, residents are unlikely to perform a medium or deep peel. Superficial peels can be accomplished with trichloroacetic acid 10%, glycolic acid (GA) 30% to 50%, salicylic acid (SA) 20% to 30%, Jessner solution (SA, lactic acid, and resorcinol with ethanol), and tretinoin 1% to 5%.4 Glycolic acid and SA are known to be safer for patients with skin of color.4,5
Care should always be taken to prepare the skin for an even peel. Mild peeling agents such as tretinoin or adapalene may be used to prepare the skin in the weeks before the procedure.4 Skin of color may benefit from hydroquinone used before and after a chemical peel.5 At the time of the peel, acetone can be used to degrease the skin for a more even, effective peel. If a peel needs to be neutralized (eg, GA), make sure to have the neutralization solution on hand, as leaving the peel solution on for too long can lead to severe epidermolysis, which can be visualized by a graying of the skin and will not be seen with a properly performed superficial peel.4 Care should be taken at all times to protect the patient’s eyes. Eye flushes should be readily available. The medial canthus and perinasal folds may be protected with petrolatum. For a superficial peel, some desquamation (less with GA) and erythema may be noted for a few days.
Final Thoughts
For any cosmetic procedure, the patient’s expectations should be discussed. The provider may adeptly guide the patient toward realistic expectations for the procedure. Pretreatment and posttreatment photographs should always be taken to help document treatment progress; it may be helpful to show the patient the photographs at each visit. The expected skin reactions, recovery time, and risks should be fully discussed. Full informed consent should be obtained. Complications from cosmetic procedures will inevitably arise. As residents, we can take the opportunity to learn how to prevent, identify, and manage them.
The primary cosmetic procedures that dermatology residents will perform or assist in performing during their training are soft-tissue augmentation, botulinum toxin injections, laser therapy, and chemical peels. Because complications can occur from these procedures, it is important for residents to learn how to prevent, identify, and manage them for optimal patient outcomes. In part 2 of this series, laser therapy and chemical peels are discussed.
Lasers
In dermatology, lasers are used to treat dyschromia, resurface scars, remove skin growths, and rejuvenate aging skin.1,2 Ablative resurfacing lasers such as the CO2 laser are the most likely to lead to unwanted side effects. There is a risk for herpes simplex virus reactivation, impetigo, persistent erythema, dyschromia, and scarring.1-3 Some patients who undergo facial ablative resurfacing may develop a visible hypopigmented line of demarcation between treated and untreated skin along the jawline.3 With the development of fractional resurfacing lasers, the risk for dyschromia, persistent erythema, and scarring was lessened.1-3
Regardless of the type of resurfacing laser used, patients should be given adequate prophylaxis with an antiviral and antibiotic. For skin of color, fractional resurfacing lasers should be set at lower density settings with a higher fluence.1-3 Sites with fewer adnexal structures (eg, neck, dorsal hands) also should be treated at lower densities.3 When using Q-switched lasers that target pigment, caution should be used to avoid vesicle formation and/or skin crusting, which may lead to scarring or dyschromia.1-3 Some tattoo inks may paradoxically darken when treated with lasers.3 A test spot is advised, especially prior to treatment of permanent makeup tattoos. A pigmented lesion should never be treated if the diagnosis is unclear (eg, a biopsy to establish the diagnosis may be the best appropriate step for some pigmented lesions). For laser hair removal, the Nd:YAG laser is the safest for skin of color.2,3
Lasers that target vascular structures may cause unwanted purpura, hypopigmentation, or thermal injury.1-3 A larger spot size may help decrease the risk for purpura. The skin should be cooled properly and caution should be used to avoid pulse stacking. For intense pulsed light devices, overlap pulses slightly to avoid a zebralike pattern of slivers of untreated skin.1-3 For all laser procedures, strict sun protection is advised before and after the procedure.
Chemical Peels
Chemical peels are versatile and varied in their composition. They are categorized based on the depth to which the skin is affected by the peel: superficial (stratum corneum), medium (full-thickness epidermis), or deep (mid reticular dermis).4 Peels are most commonly used to treat dyschromia, aging, rhytides, actinic damage, and superficial scars.4,5 The success of a chemical peel depends largely on patient selection and preprocedure preparation. Patients who tend to develop postinflammatory hyperpigmention, have an underlying inflammatory or scarring skin disorder, are on photosensitizing medications, or have continued work- or hobby-related sun exposure are generally poor peel candidates.4,5 Strict sun protection should be advised both before and after a chemical peel.
While in training, residents are unlikely to perform a medium or deep peel. Superficial peels can be accomplished with trichloroacetic acid 10%, glycolic acid (GA) 30% to 50%, salicylic acid (SA) 20% to 30%, Jessner solution (SA, lactic acid, and resorcinol with ethanol), and tretinoin 1% to 5%.4 Glycolic acid and SA are known to be safer for patients with skin of color.4,5
Care should always be taken to prepare the skin for an even peel. Mild peeling agents such as tretinoin or adapalene may be used to prepare the skin in the weeks before the procedure.4 Skin of color may benefit from hydroquinone used before and after a chemical peel.5 At the time of the peel, acetone can be used to degrease the skin for a more even, effective peel. If a peel needs to be neutralized (eg, GA), make sure to have the neutralization solution on hand, as leaving the peel solution on for too long can lead to severe epidermolysis, which can be visualized by a graying of the skin and will not be seen with a properly performed superficial peel.4 Care should be taken at all times to protect the patient’s eyes. Eye flushes should be readily available. The medial canthus and perinasal folds may be protected with petrolatum. For a superficial peel, some desquamation (less with GA) and erythema may be noted for a few days.
Final Thoughts
For any cosmetic procedure, the patient’s expectations should be discussed. The provider may adeptly guide the patient toward realistic expectations for the procedure. Pretreatment and posttreatment photographs should always be taken to help document treatment progress; it may be helpful to show the patient the photographs at each visit. The expected skin reactions, recovery time, and risks should be fully discussed. Full informed consent should be obtained. Complications from cosmetic procedures will inevitably arise. As residents, we can take the opportunity to learn how to prevent, identify, and manage them.
- Hirsch R, Stier M. Complications and their management in cosmetic dermatology. Dermatol Clin. 2009;27:507-520.
- Oliaei A, Nelson JS, Fitzpatrick R, et al. Laser treatment of scars. Facial Plast Surg. 2012;28:518-524.
- Al Nomair N, Nazarian R, Marmur E. Complications in lasers, lights, and radiofrequency devices. Facial Plast Surg. 2012;28:340-346.
- Khunger N, IADVL Task Force. Standard guidelines of care for chemical peels. Indian J Dermatol Venereol Leprol. 2008;74(suppl):S5-S12.
- Sarkar R, Bansal S, Garg VK. Chemical peels for melasma in dark-skinned patients. J Cutan Aesthet Surg. 2012;5:247-253.
- Hirsch R, Stier M. Complications and their management in cosmetic dermatology. Dermatol Clin. 2009;27:507-520.
- Oliaei A, Nelson JS, Fitzpatrick R, et al. Laser treatment of scars. Facial Plast Surg. 2012;28:518-524.
- Al Nomair N, Nazarian R, Marmur E. Complications in lasers, lights, and radiofrequency devices. Facial Plast Surg. 2012;28:340-346.
- Khunger N, IADVL Task Force. Standard guidelines of care for chemical peels. Indian J Dermatol Venereol Leprol. 2008;74(suppl):S5-S12.
- Sarkar R, Bansal S, Garg VK. Chemical peels for melasma in dark-skinned patients. J Cutan Aesthet Surg. 2012;5:247-253.
After-hours texting and professional boundaries
Recently, I was out on a Friday night with a friend who is a resident in another program. I hadn’t seen her in a very long time because of our hectic schedules. Around 10 p.m., she received a text from her attending asking her if she had left the scripts ready for the patient who was leaving on Monday.
Much has been written about professional boundaries and bosses texting their employees. For most jobs, a boss texting after hours over nonurgent matters is completely out of line. But in the medical field, there are no limits. People say, “Oh well, it’s the physician life.” Well maybe if we had more professional boundaries, our quality of life would be better. Maybe there wouldn’t be such a huge rate of burnout.
I encourage physicians to remember to contact your resident and coworkers during business hours. If the matter is not placing patients in danger, it can wait till the next morning. Nobody wants to pick up his phone in the middle of dinner to deal with patient care–related expectations that can be addressed the next business day.
Receiving a text brings all the stress of work back in the middle of our time off in which we are trying to take care of ourselves and the rest of our lives. It adds unnecessary stress to the overall high stress level and undermines our attempt to have a social life and meet a friend. A quick Internet search shows many blogs, journals, and different websites discussing this issue, but the voices of doctors and other health care providers are strangely silent on this topic.
I consider emails a more professional way of communicating than a text. I check my email often during a 24-hour period, and when I do, I’m ready for any potential information I might receive. I do not get notifications on my phone from my work email. But like my friend, I can’t avoid texts. We should have the opportunity to use our right to disconnect.
Some may argue, “Put your phone on silent if you don’t want to deal with it.” But not only do I use my phone for my life outside of work (as a resident, I make an effort to have one), but I want to be available for my peers and juniors when they are in the hospital. I want to be a resident my coworkers can text when they have a question and appreciate my advice. That is a decision I have made about the type of resident I want to be, and I am comfortable with it. Now if they text me asking a question that can wait till business hours the following day, they are crossing boundaries.
It might seem like a gray line. Somebody – maybe residency programs or our professional organizations – should address this so we have clear guidelines to protect our off-work time. Doesn’t our culture need to change the “physician life” so that we don’t bring our work responsibilities out for dinner on a Friday night? If the issue doesn’t need to be resolved quickly, it should be a given that texting is inappropriate.
Dr. Serrano is a PGY3 psychiatry resident at the Einstein Medical Center in Philadelphia.
Recently, I was out on a Friday night with a friend who is a resident in another program. I hadn’t seen her in a very long time because of our hectic schedules. Around 10 p.m., she received a text from her attending asking her if she had left the scripts ready for the patient who was leaving on Monday.
Much has been written about professional boundaries and bosses texting their employees. For most jobs, a boss texting after hours over nonurgent matters is completely out of line. But in the medical field, there are no limits. People say, “Oh well, it’s the physician life.” Well maybe if we had more professional boundaries, our quality of life would be better. Maybe there wouldn’t be such a huge rate of burnout.
I encourage physicians to remember to contact your resident and coworkers during business hours. If the matter is not placing patients in danger, it can wait till the next morning. Nobody wants to pick up his phone in the middle of dinner to deal with patient care–related expectations that can be addressed the next business day.
Receiving a text brings all the stress of work back in the middle of our time off in which we are trying to take care of ourselves and the rest of our lives. It adds unnecessary stress to the overall high stress level and undermines our attempt to have a social life and meet a friend. A quick Internet search shows many blogs, journals, and different websites discussing this issue, but the voices of doctors and other health care providers are strangely silent on this topic.
I consider emails a more professional way of communicating than a text. I check my email often during a 24-hour period, and when I do, I’m ready for any potential information I might receive. I do not get notifications on my phone from my work email. But like my friend, I can’t avoid texts. We should have the opportunity to use our right to disconnect.
Some may argue, “Put your phone on silent if you don’t want to deal with it.” But not only do I use my phone for my life outside of work (as a resident, I make an effort to have one), but I want to be available for my peers and juniors when they are in the hospital. I want to be a resident my coworkers can text when they have a question and appreciate my advice. That is a decision I have made about the type of resident I want to be, and I am comfortable with it. Now if they text me asking a question that can wait till business hours the following day, they are crossing boundaries.
It might seem like a gray line. Somebody – maybe residency programs or our professional organizations – should address this so we have clear guidelines to protect our off-work time. Doesn’t our culture need to change the “physician life” so that we don’t bring our work responsibilities out for dinner on a Friday night? If the issue doesn’t need to be resolved quickly, it should be a given that texting is inappropriate.
Dr. Serrano is a PGY3 psychiatry resident at the Einstein Medical Center in Philadelphia.
Recently, I was out on a Friday night with a friend who is a resident in another program. I hadn’t seen her in a very long time because of our hectic schedules. Around 10 p.m., she received a text from her attending asking her if she had left the scripts ready for the patient who was leaving on Monday.
Much has been written about professional boundaries and bosses texting their employees. For most jobs, a boss texting after hours over nonurgent matters is completely out of line. But in the medical field, there are no limits. People say, “Oh well, it’s the physician life.” Well maybe if we had more professional boundaries, our quality of life would be better. Maybe there wouldn’t be such a huge rate of burnout.
I encourage physicians to remember to contact your resident and coworkers during business hours. If the matter is not placing patients in danger, it can wait till the next morning. Nobody wants to pick up his phone in the middle of dinner to deal with patient care–related expectations that can be addressed the next business day.
Receiving a text brings all the stress of work back in the middle of our time off in which we are trying to take care of ourselves and the rest of our lives. It adds unnecessary stress to the overall high stress level and undermines our attempt to have a social life and meet a friend. A quick Internet search shows many blogs, journals, and different websites discussing this issue, but the voices of doctors and other health care providers are strangely silent on this topic.
I consider emails a more professional way of communicating than a text. I check my email often during a 24-hour period, and when I do, I’m ready for any potential information I might receive. I do not get notifications on my phone from my work email. But like my friend, I can’t avoid texts. We should have the opportunity to use our right to disconnect.
Some may argue, “Put your phone on silent if you don’t want to deal with it.” But not only do I use my phone for my life outside of work (as a resident, I make an effort to have one), but I want to be available for my peers and juniors when they are in the hospital. I want to be a resident my coworkers can text when they have a question and appreciate my advice. That is a decision I have made about the type of resident I want to be, and I am comfortable with it. Now if they text me asking a question that can wait till business hours the following day, they are crossing boundaries.
It might seem like a gray line. Somebody – maybe residency programs or our professional organizations – should address this so we have clear guidelines to protect our off-work time. Doesn’t our culture need to change the “physician life” so that we don’t bring our work responsibilities out for dinner on a Friday night? If the issue doesn’t need to be resolved quickly, it should be a given that texting is inappropriate.
Dr. Serrano is a PGY3 psychiatry resident at the Einstein Medical Center in Philadelphia.