User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Everyone wins when losers get paid
Bribery really is the solution to all of life’s problems
Breaking news: The United States has a bit of an obesity epidemic. Okay, maybe not so breaking news. But it’s a problem we’ve been struggling with for a very long time. Part of the issue is that there really is no secret to weight loss. Pretty much anything can work if you’re committed. The millions of diets floating around are testament to this idea.
The problem of losing weight is amplified if you don’t rake in the big bucks. Lower-income individuals often can’t afford healthy superfoods, and they’re often too busy to spend time at classes, exercising, or following programs. A group of researchers at New York University has offered up an alternate solution to encourage weight loss in low-income people: Pay them.
Specifically, pay them for losing weight. A reward, if you will. The researchers recruited several hundred lower-income people and split them into three groups. All participants received a free 1-year membership to a gym and weight-loss program, as well as food journals and fitness devices, but one group received payment (on average, about $300 overall) for attending meetings, exercising a certain amount every week, or weighing themselves twice a week. About 40% of people in this group lost 5% of their body weight after 6 months, twice as many as in the group that did not receive payment for performing these tasks.
The big winners, however, were those in the third group. They also received the free stuff, but the researchers offered them a more simple and direct bribe: Lose 5% of your weight over 6 months and we’ll pay you. The reward? About $450 on average, and it worked very well, with half this group losing the weight after 6 months. That said, after a year something like a fifth of this group put the weight back on, bringing them in line with the group that was paid to perform tasks. Still, both groups outperformed the control group, which received no money.
The takeaway from this research is pretty obvious. Pay people a fair price to do something, and they’ll do it. This is a lesson that has absolutely no relevance in the modern world. Nope, none whatsoever. We all receive completely fair wages. We all have plenty of money to pay for things. Everything is fine.
More green space, less medicine
Have you heard of the 3-30-300 rule? Proposed by urban forester Cecil Konijnendijk, it’s become the rule of thumb for urban planners and other foresters into getting more green space in populated areas. A recent study has found that people who lived within this 3-30-300 rule had better mental health and less medication use.
If you’re not an urban forester, however, you may not know what the 3-30-300 rule is. But it’s pretty simple, people should be able to see at least three trees from their home, have 30% tree canopy in their neighborhood, and have 300 Spartans to defend against the Persian army.
We may have made that last one up. It’s actually have a green space or park within 300 meters of your home.
In the new study, only 4.7% of people surveyed lived in an area that followed all three rules. About 62% of the surveyed lived with a green space at least 300 meters away, 43% had at least three trees within 15 meters from their home, and a rather pitiful 9% had adequate tree canopy coverage in their neighborhood.
Greater adherence to the 3-30-300 rule was associated with fewer visits to the psychologist, with 8.3% of the participants reporting a psychologist visit in the last year. The data come from a sample of a little over 3,000 Barcelona residents aged 15-97 who were randomly selected to participate in the Barcelona Public Health Agency Survey.
“There is an urgent need to provide citizens with more green space,” said Mark Nieuwenhuijsen, lead author of the study. “We may need to tear out asphalt and plant more trees, which would not only improve health, but also reduce heat island effects and contribute to carbon capture.”
The main goal and message is that more green space is good for everyone. So if you’re feeling a little overwhelmed, take a breather and sit somewhere green. Or call those 300 Spartans and get them to start knocking some buildings down.
Said the toilet to the engineer: Do you hear what I hear?
A mythical hero’s journey took Dorothy along the yellow brick road to find the Wizard of Oz. Huckleberry Finn used a raft to float down the Mississippi River. Luke Skywalker did most of his traveling between planets. For the rest of us, the journey may be just a bit shorter.
Also a bit less heroic. Unless, of course, you’re prepping for a colonoscopy. Yup, we’re headed to the toilet, but not just any toilet. This toilet was the subject of a presentation at the annual meeting of the Acoustical Society of America, titled “The feces thesis: Using machine learning to detect diarrhea,” and that presentation was the hero’s journey of Maia Gatlin, PhD, a research engineer at the Georgia Institute of Technology.
She and her team attached a noninvasive microphone sensor to a toilet, and now they can identify bowel diseases without collecting any identifiable information.
The audio sample of an excretion event is “transformed into a spectrogram, which essentially captures the sound in an image. Different events produce different features in the audio and the spectrogram. For example, urination creates a consistent tone, while defecation may have a singular tone. In contrast, diarrhea is more random,” they explained in the written statement.
They used a machine learning algorithm to classify each spectrogram based on its features. “The algorithm’s performance was tested against data with and without background noises to make sure it was learning the right sound features, regardless of the sensor’s environment,” Dr. Gatlin and associates wrote.
Their goal is to use the toilet sensor in areas where cholera is common to prevent the spread of disease. After that, who knows? “Perhaps someday, our algorithm can be used with existing in-home smart devices to monitor one’s own bowel movements and health!” she suggested.
That would be a heroic toilet indeed.
Bribery really is the solution to all of life’s problems
Breaking news: The United States has a bit of an obesity epidemic. Okay, maybe not so breaking news. But it’s a problem we’ve been struggling with for a very long time. Part of the issue is that there really is no secret to weight loss. Pretty much anything can work if you’re committed. The millions of diets floating around are testament to this idea.
The problem of losing weight is amplified if you don’t rake in the big bucks. Lower-income individuals often can’t afford healthy superfoods, and they’re often too busy to spend time at classes, exercising, or following programs. A group of researchers at New York University has offered up an alternate solution to encourage weight loss in low-income people: Pay them.
Specifically, pay them for losing weight. A reward, if you will. The researchers recruited several hundred lower-income people and split them into three groups. All participants received a free 1-year membership to a gym and weight-loss program, as well as food journals and fitness devices, but one group received payment (on average, about $300 overall) for attending meetings, exercising a certain amount every week, or weighing themselves twice a week. About 40% of people in this group lost 5% of their body weight after 6 months, twice as many as in the group that did not receive payment for performing these tasks.
The big winners, however, were those in the third group. They also received the free stuff, but the researchers offered them a more simple and direct bribe: Lose 5% of your weight over 6 months and we’ll pay you. The reward? About $450 on average, and it worked very well, with half this group losing the weight after 6 months. That said, after a year something like a fifth of this group put the weight back on, bringing them in line with the group that was paid to perform tasks. Still, both groups outperformed the control group, which received no money.
The takeaway from this research is pretty obvious. Pay people a fair price to do something, and they’ll do it. This is a lesson that has absolutely no relevance in the modern world. Nope, none whatsoever. We all receive completely fair wages. We all have plenty of money to pay for things. Everything is fine.
More green space, less medicine
Have you heard of the 3-30-300 rule? Proposed by urban forester Cecil Konijnendijk, it’s become the rule of thumb for urban planners and other foresters into getting more green space in populated areas. A recent study has found that people who lived within this 3-30-300 rule had better mental health and less medication use.
If you’re not an urban forester, however, you may not know what the 3-30-300 rule is. But it’s pretty simple, people should be able to see at least three trees from their home, have 30% tree canopy in their neighborhood, and have 300 Spartans to defend against the Persian army.
We may have made that last one up. It’s actually have a green space or park within 300 meters of your home.
In the new study, only 4.7% of people surveyed lived in an area that followed all three rules. About 62% of the surveyed lived with a green space at least 300 meters away, 43% had at least three trees within 15 meters from their home, and a rather pitiful 9% had adequate tree canopy coverage in their neighborhood.
Greater adherence to the 3-30-300 rule was associated with fewer visits to the psychologist, with 8.3% of the participants reporting a psychologist visit in the last year. The data come from a sample of a little over 3,000 Barcelona residents aged 15-97 who were randomly selected to participate in the Barcelona Public Health Agency Survey.
“There is an urgent need to provide citizens with more green space,” said Mark Nieuwenhuijsen, lead author of the study. “We may need to tear out asphalt and plant more trees, which would not only improve health, but also reduce heat island effects and contribute to carbon capture.”
The main goal and message is that more green space is good for everyone. So if you’re feeling a little overwhelmed, take a breather and sit somewhere green. Or call those 300 Spartans and get them to start knocking some buildings down.
Said the toilet to the engineer: Do you hear what I hear?
A mythical hero’s journey took Dorothy along the yellow brick road to find the Wizard of Oz. Huckleberry Finn used a raft to float down the Mississippi River. Luke Skywalker did most of his traveling between planets. For the rest of us, the journey may be just a bit shorter.
Also a bit less heroic. Unless, of course, you’re prepping for a colonoscopy. Yup, we’re headed to the toilet, but not just any toilet. This toilet was the subject of a presentation at the annual meeting of the Acoustical Society of America, titled “The feces thesis: Using machine learning to detect diarrhea,” and that presentation was the hero’s journey of Maia Gatlin, PhD, a research engineer at the Georgia Institute of Technology.
She and her team attached a noninvasive microphone sensor to a toilet, and now they can identify bowel diseases without collecting any identifiable information.
The audio sample of an excretion event is “transformed into a spectrogram, which essentially captures the sound in an image. Different events produce different features in the audio and the spectrogram. For example, urination creates a consistent tone, while defecation may have a singular tone. In contrast, diarrhea is more random,” they explained in the written statement.
They used a machine learning algorithm to classify each spectrogram based on its features. “The algorithm’s performance was tested against data with and without background noises to make sure it was learning the right sound features, regardless of the sensor’s environment,” Dr. Gatlin and associates wrote.
Their goal is to use the toilet sensor in areas where cholera is common to prevent the spread of disease. After that, who knows? “Perhaps someday, our algorithm can be used with existing in-home smart devices to monitor one’s own bowel movements and health!” she suggested.
That would be a heroic toilet indeed.
Bribery really is the solution to all of life’s problems
Breaking news: The United States has a bit of an obesity epidemic. Okay, maybe not so breaking news. But it’s a problem we’ve been struggling with for a very long time. Part of the issue is that there really is no secret to weight loss. Pretty much anything can work if you’re committed. The millions of diets floating around are testament to this idea.
The problem of losing weight is amplified if you don’t rake in the big bucks. Lower-income individuals often can’t afford healthy superfoods, and they’re often too busy to spend time at classes, exercising, or following programs. A group of researchers at New York University has offered up an alternate solution to encourage weight loss in low-income people: Pay them.
Specifically, pay them for losing weight. A reward, if you will. The researchers recruited several hundred lower-income people and split them into three groups. All participants received a free 1-year membership to a gym and weight-loss program, as well as food journals and fitness devices, but one group received payment (on average, about $300 overall) for attending meetings, exercising a certain amount every week, or weighing themselves twice a week. About 40% of people in this group lost 5% of their body weight after 6 months, twice as many as in the group that did not receive payment for performing these tasks.
The big winners, however, were those in the third group. They also received the free stuff, but the researchers offered them a more simple and direct bribe: Lose 5% of your weight over 6 months and we’ll pay you. The reward? About $450 on average, and it worked very well, with half this group losing the weight after 6 months. That said, after a year something like a fifth of this group put the weight back on, bringing them in line with the group that was paid to perform tasks. Still, both groups outperformed the control group, which received no money.
The takeaway from this research is pretty obvious. Pay people a fair price to do something, and they’ll do it. This is a lesson that has absolutely no relevance in the modern world. Nope, none whatsoever. We all receive completely fair wages. We all have plenty of money to pay for things. Everything is fine.
More green space, less medicine
Have you heard of the 3-30-300 rule? Proposed by urban forester Cecil Konijnendijk, it’s become the rule of thumb for urban planners and other foresters into getting more green space in populated areas. A recent study has found that people who lived within this 3-30-300 rule had better mental health and less medication use.
If you’re not an urban forester, however, you may not know what the 3-30-300 rule is. But it’s pretty simple, people should be able to see at least three trees from their home, have 30% tree canopy in their neighborhood, and have 300 Spartans to defend against the Persian army.
We may have made that last one up. It’s actually have a green space or park within 300 meters of your home.
In the new study, only 4.7% of people surveyed lived in an area that followed all three rules. About 62% of the surveyed lived with a green space at least 300 meters away, 43% had at least three trees within 15 meters from their home, and a rather pitiful 9% had adequate tree canopy coverage in their neighborhood.
Greater adherence to the 3-30-300 rule was associated with fewer visits to the psychologist, with 8.3% of the participants reporting a psychologist visit in the last year. The data come from a sample of a little over 3,000 Barcelona residents aged 15-97 who were randomly selected to participate in the Barcelona Public Health Agency Survey.
“There is an urgent need to provide citizens with more green space,” said Mark Nieuwenhuijsen, lead author of the study. “We may need to tear out asphalt and plant more trees, which would not only improve health, but also reduce heat island effects and contribute to carbon capture.”
The main goal and message is that more green space is good for everyone. So if you’re feeling a little overwhelmed, take a breather and sit somewhere green. Or call those 300 Spartans and get them to start knocking some buildings down.
Said the toilet to the engineer: Do you hear what I hear?
A mythical hero’s journey took Dorothy along the yellow brick road to find the Wizard of Oz. Huckleberry Finn used a raft to float down the Mississippi River. Luke Skywalker did most of his traveling between planets. For the rest of us, the journey may be just a bit shorter.
Also a bit less heroic. Unless, of course, you’re prepping for a colonoscopy. Yup, we’re headed to the toilet, but not just any toilet. This toilet was the subject of a presentation at the annual meeting of the Acoustical Society of America, titled “The feces thesis: Using machine learning to detect diarrhea,” and that presentation was the hero’s journey of Maia Gatlin, PhD, a research engineer at the Georgia Institute of Technology.
She and her team attached a noninvasive microphone sensor to a toilet, and now they can identify bowel diseases without collecting any identifiable information.
The audio sample of an excretion event is “transformed into a spectrogram, which essentially captures the sound in an image. Different events produce different features in the audio and the spectrogram. For example, urination creates a consistent tone, while defecation may have a singular tone. In contrast, diarrhea is more random,” they explained in the written statement.
They used a machine learning algorithm to classify each spectrogram based on its features. “The algorithm’s performance was tested against data with and without background noises to make sure it was learning the right sound features, regardless of the sensor’s environment,” Dr. Gatlin and associates wrote.
Their goal is to use the toilet sensor in areas where cholera is common to prevent the spread of disease. After that, who knows? “Perhaps someday, our algorithm can be used with existing in-home smart devices to monitor one’s own bowel movements and health!” she suggested.
That would be a heroic toilet indeed.
FDA tweaks Impella indications on basis of postapproval study
The U.S. Food and Drug Administration has updated the Abiomed Impella RP System’s approved indications in a way that “better reflects the characteristics of the patients who may benefit the most from treatment with the device,” the agency has announced.
The revised language reflects the final results of a postapproval study in which survival rates for patients who met the premarket-study entry criteria were comparable to rates seen in the premarket studies, the FDA observed.
The postapproval study “further confirms that the device is safe and effective when used for the currently approved indication.” The indication’s added words, however, tighten the description of eligible patients in a way that more precisely reflects the premarket-study population.
The update states that the Impella RP System is “indicated for providing temporary right ventricular support for up to 14 days in patients with a body surface area ≥ 1.5 m2, who develop acute right heart failure or decompensation for less than 48 hours following left ventricular assist device implantation, myocardial infarction, heart transplant, or open heart surgery, without the presence of profound shock, end organ failure, or acute neurologic injury.”
The FDA “believes that when the device is used for the currently approved indication in appropriately selected patients, the benefits of the Impella RP System continue to outweigh the risks.”
The reworded indication is the latest among several updates to the agency’s February 2019 letter to clinicians noting a signal of increased mortality associated with the Impella RP device in an interim analysis of the same postapproval study. Ultimately, no such signal has emerged among the subset of postapproval patients who would have been eligible for the premarket study.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has updated the Abiomed Impella RP System’s approved indications in a way that “better reflects the characteristics of the patients who may benefit the most from treatment with the device,” the agency has announced.
The revised language reflects the final results of a postapproval study in which survival rates for patients who met the premarket-study entry criteria were comparable to rates seen in the premarket studies, the FDA observed.
The postapproval study “further confirms that the device is safe and effective when used for the currently approved indication.” The indication’s added words, however, tighten the description of eligible patients in a way that more precisely reflects the premarket-study population.
The update states that the Impella RP System is “indicated for providing temporary right ventricular support for up to 14 days in patients with a body surface area ≥ 1.5 m2, who develop acute right heart failure or decompensation for less than 48 hours following left ventricular assist device implantation, myocardial infarction, heart transplant, or open heart surgery, without the presence of profound shock, end organ failure, or acute neurologic injury.”
The FDA “believes that when the device is used for the currently approved indication in appropriately selected patients, the benefits of the Impella RP System continue to outweigh the risks.”
The reworded indication is the latest among several updates to the agency’s February 2019 letter to clinicians noting a signal of increased mortality associated with the Impella RP device in an interim analysis of the same postapproval study. Ultimately, no such signal has emerged among the subset of postapproval patients who would have been eligible for the premarket study.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has updated the Abiomed Impella RP System’s approved indications in a way that “better reflects the characteristics of the patients who may benefit the most from treatment with the device,” the agency has announced.
The revised language reflects the final results of a postapproval study in which survival rates for patients who met the premarket-study entry criteria were comparable to rates seen in the premarket studies, the FDA observed.
The postapproval study “further confirms that the device is safe and effective when used for the currently approved indication.” The indication’s added words, however, tighten the description of eligible patients in a way that more precisely reflects the premarket-study population.
The update states that the Impella RP System is “indicated for providing temporary right ventricular support for up to 14 days in patients with a body surface area ≥ 1.5 m2, who develop acute right heart failure or decompensation for less than 48 hours following left ventricular assist device implantation, myocardial infarction, heart transplant, or open heart surgery, without the presence of profound shock, end organ failure, or acute neurologic injury.”
The FDA “believes that when the device is used for the currently approved indication in appropriately selected patients, the benefits of the Impella RP System continue to outweigh the risks.”
The reworded indication is the latest among several updates to the agency’s February 2019 letter to clinicians noting a signal of increased mortality associated with the Impella RP device in an interim analysis of the same postapproval study. Ultimately, no such signal has emerged among the subset of postapproval patients who would have been eligible for the premarket study.
A version of this article first appeared on Medscape.com.
‘Game changer’: Thyroid cancer recurrence no higher with lobectomy
Patients with intermediate-risk papillary thyroid cancer and lymph node metastasis show no significant increase in tumor recurrence when undergoing lobectomy compared with a total thyroidectomy, new research shows.
“Results of this cohort study suggest that patients with ipsilateral clinical lateral neck metastasis (cN1b) papillary thyroid cancer who underwent lobectomy exhibited recurrence-free survival rates similar to those who underwent total thyroidectomy after controlling for major prognostic factors,” the authors conclude in the study published online in JAMA Surgery.
“These findings suggest that cN1b alone should not be an absolute indication for total thyroidectomy,” they note.
The study, involving the largest cohort to date to compare patients with intermediate-risk papillary thyroid cancer treated with lobectomy versus total thyroidectomy, “challenged the current guidelines and pushed the boundary of limited surgical treatment even further,” say Michelle B. Mulder, MD, and Quan-Yang Duh, MD, of the department of surgery, University of California, San Francisco, in an accompanying editorial.
“It can be a game changer if confirmed by future prospective and multicenter studies,” they add.
Guidelines still recommend total thyroidectomy with subsequent RAI
While lower-intensity treatment options, with a lower risk of complications, have gained favor in the treatment of low-risk papillary thyroid cancer, guidelines still recommend the consideration of total thyroidectomy and subsequent radioactive iodine ablation (RAI) for intermediate-risk cancers because of the higher chance of recurrence, particularly among those with clinically positive nodes.
However, data on the superiority of a total thyroidectomy, with or without RAI, versus lobectomy is inconsistent, prompting first author Siyuan Xu, MD, of the department of head and neck surgical oncology, National Cancer Center, Beijing, and colleagues to compare the risk of recurrence with the two approaches.
For the study, patients with intermediate-risk papillary thyroid cancer treated at the Chinese Academy of Medical Sciences Cancer Hospital in Beijing between January 2000 and December 2017, who had a lobectomy or total thyroidectomy, were paired 1:1 in a propensity score matching analysis.
Other than treatment type, the 265 pairs of patients were matched based on all other potential prognostic factors, including age, sex, primary tumor size, minor extrathyroidal extension, multifocality, number of lymph node metastases, and lymph node ratio.
Participants were a mean age of 37 years and 66% were female.
With a median follow-up of 60 months in the lobectomy group and 58 months in the total thyroidectomy group, structural recurrences occurred in 7.9% (21) and 6.4% (17) of patients, respectively, which was not significantly different.
The primary endpoint, 5-year rate of recurrence-free survival, was also not significantly different between the lobectomy (92.3%) and total thyroidectomy groups (93.7%) (adjusted hazard ratio, 1.10; P = .77).
In a further stratified analysis of patients treated with total thyroidectomy along with RAI (n = 75), the lack of a significant difference in recurrence-free survival versus lobectomy remained (aHR, 0.59; P = .46).
The results were similar in unadjusted as well as adjusted analyses, and a power analysis indicated that the study had a 90% power to detect a more than 4.9% difference in recurrence-free survival.
“Given the lower complication rate of lobectomy, a maximal 4.9% recurrence-free survival difference is acceptable, which enhances the reliability of the study results,” the authors say.
They conclude that “our findings call into question whether cN1b alone [ipsilateral clinical lateral neck metastasis papillary thyroid cancer] should be an absolute determinant for deciding the optimal extent of thyroid surgery for papillary thyroid cancer.”
With total thyroidectomy, RAI can be given
An important argument in favor of total thyroidectomy is that with the complete resection of thyroid tissue, RAI ablation can then be used for postoperative detection of residual or metastatic disease, as well as for treatment, the authors note.
Indeed, a study using the Surveillance, Epidemiology, and End Results (SEER) database showed RAI ablation is associated with a 29% reduction in the risk of death in patients with intermediate-risk papillary thyroid cancer, with a hazard risk of 0.71.
However, conflicting data from Memorial Sloan-Kettering Cancer Center, New York, suggests no significant benefit with total thyroidectomy and RAI ablation.
The current study’s analysis of patients treated with RAI, though limited in size, supports the latter study’s findings, the authors note.
“When we performed further stratified analyses in patients treated with total thyroidectomy plus RAI ablation and their counterparts, no significant difference was found, which conformed with [the] result from the whole cohort.”
“Certainly, the stratified comparison did not have enough power to examine the effect of RAI ablation on tumor recurrence subject to the limitation of sample size and case selection [and] further study is needed on this topic,” they write.
Some limitations warrant cautious interpretation
In their editorial, Dr. Mulder and Dr. Duh note that while some previous studies have shown similar outcomes relating to tumor size, thyroid hormone suppression therapy, and multifocality, “few have addressed lateral neck involvement.”
They suggest cautious interpretation, however, due to limitations, acknowledged by the authors, including the single-center nature of the study.
“Appropriate propensity matching may mitigate selection bias but cannot eliminate it entirely and their findings may not be replicated in other institutions by other surgeons,” they note.
Other limitations include that changes in clinical practice and patient selection were likely over the course of the study because of significant changes in American Thyroid Association (ATA) guidelines between 2009 and 2017, and characteristics including molecular genetic testing, which could have influenced final results, were not taken into consideration.
Furthermore, for patients with intermediate-risk cancer, modifications in postoperative follow-up are necessary following lobectomy versus total thyroidectomy; “the role of radioiodine is limited and the levels of thyroglobulin more complicated to interpret,” they note.
The study and editorial authors had no disclosures to report.
A version of this article first appeared on Medscape.com.
Patients with intermediate-risk papillary thyroid cancer and lymph node metastasis show no significant increase in tumor recurrence when undergoing lobectomy compared with a total thyroidectomy, new research shows.
“Results of this cohort study suggest that patients with ipsilateral clinical lateral neck metastasis (cN1b) papillary thyroid cancer who underwent lobectomy exhibited recurrence-free survival rates similar to those who underwent total thyroidectomy after controlling for major prognostic factors,” the authors conclude in the study published online in JAMA Surgery.
“These findings suggest that cN1b alone should not be an absolute indication for total thyroidectomy,” they note.
The study, involving the largest cohort to date to compare patients with intermediate-risk papillary thyroid cancer treated with lobectomy versus total thyroidectomy, “challenged the current guidelines and pushed the boundary of limited surgical treatment even further,” say Michelle B. Mulder, MD, and Quan-Yang Duh, MD, of the department of surgery, University of California, San Francisco, in an accompanying editorial.
“It can be a game changer if confirmed by future prospective and multicenter studies,” they add.
Guidelines still recommend total thyroidectomy with subsequent RAI
While lower-intensity treatment options, with a lower risk of complications, have gained favor in the treatment of low-risk papillary thyroid cancer, guidelines still recommend the consideration of total thyroidectomy and subsequent radioactive iodine ablation (RAI) for intermediate-risk cancers because of the higher chance of recurrence, particularly among those with clinically positive nodes.
However, data on the superiority of a total thyroidectomy, with or without RAI, versus lobectomy is inconsistent, prompting first author Siyuan Xu, MD, of the department of head and neck surgical oncology, National Cancer Center, Beijing, and colleagues to compare the risk of recurrence with the two approaches.
For the study, patients with intermediate-risk papillary thyroid cancer treated at the Chinese Academy of Medical Sciences Cancer Hospital in Beijing between January 2000 and December 2017, who had a lobectomy or total thyroidectomy, were paired 1:1 in a propensity score matching analysis.
Other than treatment type, the 265 pairs of patients were matched based on all other potential prognostic factors, including age, sex, primary tumor size, minor extrathyroidal extension, multifocality, number of lymph node metastases, and lymph node ratio.
Participants were a mean age of 37 years and 66% were female.
With a median follow-up of 60 months in the lobectomy group and 58 months in the total thyroidectomy group, structural recurrences occurred in 7.9% (21) and 6.4% (17) of patients, respectively, which was not significantly different.
The primary endpoint, 5-year rate of recurrence-free survival, was also not significantly different between the lobectomy (92.3%) and total thyroidectomy groups (93.7%) (adjusted hazard ratio, 1.10; P = .77).
In a further stratified analysis of patients treated with total thyroidectomy along with RAI (n = 75), the lack of a significant difference in recurrence-free survival versus lobectomy remained (aHR, 0.59; P = .46).
The results were similar in unadjusted as well as adjusted analyses, and a power analysis indicated that the study had a 90% power to detect a more than 4.9% difference in recurrence-free survival.
“Given the lower complication rate of lobectomy, a maximal 4.9% recurrence-free survival difference is acceptable, which enhances the reliability of the study results,” the authors say.
They conclude that “our findings call into question whether cN1b alone [ipsilateral clinical lateral neck metastasis papillary thyroid cancer] should be an absolute determinant for deciding the optimal extent of thyroid surgery for papillary thyroid cancer.”
With total thyroidectomy, RAI can be given
An important argument in favor of total thyroidectomy is that with the complete resection of thyroid tissue, RAI ablation can then be used for postoperative detection of residual or metastatic disease, as well as for treatment, the authors note.
Indeed, a study using the Surveillance, Epidemiology, and End Results (SEER) database showed RAI ablation is associated with a 29% reduction in the risk of death in patients with intermediate-risk papillary thyroid cancer, with a hazard risk of 0.71.
However, conflicting data from Memorial Sloan-Kettering Cancer Center, New York, suggests no significant benefit with total thyroidectomy and RAI ablation.
The current study’s analysis of patients treated with RAI, though limited in size, supports the latter study’s findings, the authors note.
“When we performed further stratified analyses in patients treated with total thyroidectomy plus RAI ablation and their counterparts, no significant difference was found, which conformed with [the] result from the whole cohort.”
“Certainly, the stratified comparison did not have enough power to examine the effect of RAI ablation on tumor recurrence subject to the limitation of sample size and case selection [and] further study is needed on this topic,” they write.
Some limitations warrant cautious interpretation
In their editorial, Dr. Mulder and Dr. Duh note that while some previous studies have shown similar outcomes relating to tumor size, thyroid hormone suppression therapy, and multifocality, “few have addressed lateral neck involvement.”
They suggest cautious interpretation, however, due to limitations, acknowledged by the authors, including the single-center nature of the study.
“Appropriate propensity matching may mitigate selection bias but cannot eliminate it entirely and their findings may not be replicated in other institutions by other surgeons,” they note.
Other limitations include that changes in clinical practice and patient selection were likely over the course of the study because of significant changes in American Thyroid Association (ATA) guidelines between 2009 and 2017, and characteristics including molecular genetic testing, which could have influenced final results, were not taken into consideration.
Furthermore, for patients with intermediate-risk cancer, modifications in postoperative follow-up are necessary following lobectomy versus total thyroidectomy; “the role of radioiodine is limited and the levels of thyroglobulin more complicated to interpret,” they note.
The study and editorial authors had no disclosures to report.
A version of this article first appeared on Medscape.com.
Patients with intermediate-risk papillary thyroid cancer and lymph node metastasis show no significant increase in tumor recurrence when undergoing lobectomy compared with a total thyroidectomy, new research shows.
“Results of this cohort study suggest that patients with ipsilateral clinical lateral neck metastasis (cN1b) papillary thyroid cancer who underwent lobectomy exhibited recurrence-free survival rates similar to those who underwent total thyroidectomy after controlling for major prognostic factors,” the authors conclude in the study published online in JAMA Surgery.
“These findings suggest that cN1b alone should not be an absolute indication for total thyroidectomy,” they note.
The study, involving the largest cohort to date to compare patients with intermediate-risk papillary thyroid cancer treated with lobectomy versus total thyroidectomy, “challenged the current guidelines and pushed the boundary of limited surgical treatment even further,” say Michelle B. Mulder, MD, and Quan-Yang Duh, MD, of the department of surgery, University of California, San Francisco, in an accompanying editorial.
“It can be a game changer if confirmed by future prospective and multicenter studies,” they add.
Guidelines still recommend total thyroidectomy with subsequent RAI
While lower-intensity treatment options, with a lower risk of complications, have gained favor in the treatment of low-risk papillary thyroid cancer, guidelines still recommend the consideration of total thyroidectomy and subsequent radioactive iodine ablation (RAI) for intermediate-risk cancers because of the higher chance of recurrence, particularly among those with clinically positive nodes.
However, data on the superiority of a total thyroidectomy, with or without RAI, versus lobectomy is inconsistent, prompting first author Siyuan Xu, MD, of the department of head and neck surgical oncology, National Cancer Center, Beijing, and colleagues to compare the risk of recurrence with the two approaches.
For the study, patients with intermediate-risk papillary thyroid cancer treated at the Chinese Academy of Medical Sciences Cancer Hospital in Beijing between January 2000 and December 2017, who had a lobectomy or total thyroidectomy, were paired 1:1 in a propensity score matching analysis.
Other than treatment type, the 265 pairs of patients were matched based on all other potential prognostic factors, including age, sex, primary tumor size, minor extrathyroidal extension, multifocality, number of lymph node metastases, and lymph node ratio.
Participants were a mean age of 37 years and 66% were female.
With a median follow-up of 60 months in the lobectomy group and 58 months in the total thyroidectomy group, structural recurrences occurred in 7.9% (21) and 6.4% (17) of patients, respectively, which was not significantly different.
The primary endpoint, 5-year rate of recurrence-free survival, was also not significantly different between the lobectomy (92.3%) and total thyroidectomy groups (93.7%) (adjusted hazard ratio, 1.10; P = .77).
In a further stratified analysis of patients treated with total thyroidectomy along with RAI (n = 75), the lack of a significant difference in recurrence-free survival versus lobectomy remained (aHR, 0.59; P = .46).
The results were similar in unadjusted as well as adjusted analyses, and a power analysis indicated that the study had a 90% power to detect a more than 4.9% difference in recurrence-free survival.
“Given the lower complication rate of lobectomy, a maximal 4.9% recurrence-free survival difference is acceptable, which enhances the reliability of the study results,” the authors say.
They conclude that “our findings call into question whether cN1b alone [ipsilateral clinical lateral neck metastasis papillary thyroid cancer] should be an absolute determinant for deciding the optimal extent of thyroid surgery for papillary thyroid cancer.”
With total thyroidectomy, RAI can be given
An important argument in favor of total thyroidectomy is that with the complete resection of thyroid tissue, RAI ablation can then be used for postoperative detection of residual or metastatic disease, as well as for treatment, the authors note.
Indeed, a study using the Surveillance, Epidemiology, and End Results (SEER) database showed RAI ablation is associated with a 29% reduction in the risk of death in patients with intermediate-risk papillary thyroid cancer, with a hazard risk of 0.71.
However, conflicting data from Memorial Sloan-Kettering Cancer Center, New York, suggests no significant benefit with total thyroidectomy and RAI ablation.
The current study’s analysis of patients treated with RAI, though limited in size, supports the latter study’s findings, the authors note.
“When we performed further stratified analyses in patients treated with total thyroidectomy plus RAI ablation and their counterparts, no significant difference was found, which conformed with [the] result from the whole cohort.”
“Certainly, the stratified comparison did not have enough power to examine the effect of RAI ablation on tumor recurrence subject to the limitation of sample size and case selection [and] further study is needed on this topic,” they write.
Some limitations warrant cautious interpretation
In their editorial, Dr. Mulder and Dr. Duh note that while some previous studies have shown similar outcomes relating to tumor size, thyroid hormone suppression therapy, and multifocality, “few have addressed lateral neck involvement.”
They suggest cautious interpretation, however, due to limitations, acknowledged by the authors, including the single-center nature of the study.
“Appropriate propensity matching may mitigate selection bias but cannot eliminate it entirely and their findings may not be replicated in other institutions by other surgeons,” they note.
Other limitations include that changes in clinical practice and patient selection were likely over the course of the study because of significant changes in American Thyroid Association (ATA) guidelines between 2009 and 2017, and characteristics including molecular genetic testing, which could have influenced final results, were not taken into consideration.
Furthermore, for patients with intermediate-risk cancer, modifications in postoperative follow-up are necessary following lobectomy versus total thyroidectomy; “the role of radioiodine is limited and the levels of thyroglobulin more complicated to interpret,” they note.
The study and editorial authors had no disclosures to report.
A version of this article first appeared on Medscape.com.
FROM JAMA SURGERY
Joint replacements: Should there be BMI cutoffs?
For patients with severe arthritis, joint replacement is considered when more conservative treatments have failed. Because patients with obesity have a higher risk of complications during and after surgery, some surgeons, hospitals, and insurance companies have adopted body mass index cutoffs as a basis for deciding whether to offer patients these elective surgeries. But some experts argue that these cutoffs are arbitrary, exclude patients who can still benefit from the surgery, and can increase disparities in care.
“By enforcing cutoffs in general, you’re losing the ability for each surgeon to determine who they want to operate on,” said Daniel Wiznia, MD, assistant professor of orthopedic surgery at Yale University, New Haven, Conn. He is on the leadership committee of the Movement Is Life Caucus, a nonprofit group focused on eliminating disparities in musculoskeletal health. “For every surgeon, it’s up to them to decide if they feel comfortable doing the surgery,” he noted in an interview. “My guidance for that would be, don’t just say no because of the number – look at the patient’s entire medical profile.”
According to the Centers for Disease Control and Prevention, nearly 42% of adults in the United States have a BMI over 30, and 9.2% of adults have a BMI over 40. This excess weight puts additional stress on joints: When a person is walking, experts estimate that the force on the knees can be two to three times someone’s body weight. Over time, this pressure can wear down the cartilage on joints.
As a result, people who are overweight or obese are more likely to develop osteoarthritis and to need joint replacements. According to a Canadian study, patients with a BMI of 30-35 are 3.4 times as likely to require a hip replacement and are 8.5 times as likely to require a knee replacement compared to individuals with a BMI in the “healthy weight” range. With a BMI above 40, individuals were 8.5 times more likely to need a hip replacement and were 32.7 times as likely to need a knee replacement.
More complications, greater expense
While there are no universally recommended BMI cutoffs for joint replacement surgery, it is not uncommon for institutions to require that patients have a BMI below a certain value (usually 35-40) to proceed with surgery. A 2013 survey of physicians from the American Association of Hip and Knee Surgeons found that 52% of surgeons required a BMI below 40 to qualify for surgery.
One of the main reasons for these cutoffs is the elevated risk of complications during and after surgery. Research suggests that obesity is associated with higher rates of wound dehiscence, prosthetic joint infection (PJI), and revision total joint arthroplasty. One 2016 study suggests that patients with a BMI of 35-39.9 are twice as likely to experience PJI compared to patients with a BMI below 35. For patients with a BMI of 40 or higher, PJI is four times as likely.
Another study found that patients whose BMI is 35-40 and who undergo total joint arthroplasty have a 6.4-fold greater risk of deep incision infection. For those with a BMI over 40, that rises to a 12.9-fold increased risk compared to patients with a BMI of 18.5-25. Patients with obesity tend to have other comorbidities that can increase the risk of complications during surgery, such as type 2 diabetes, coronary artery disease, and chronic kidney disease.
Because of the increased risk of complications, health care costs tend to be higher for patients with obesity. The growing popularity of bundled health payments can discourage operating on patients who are more likely to experience complications, such as patients with high BMIs, noted Dr. Wiznia.
Research suggests that minorities and people with lower socioeconomic status are disproportionately affected by these cutoffs. According to the CDC, among non-Hispanic Black Americans and Hispanic Americans, rates of obesity are higher than among their White counterparts, and these patients are less likely to undergo joint replacement. Strictly enforcing this eligibility criterion can worsen those disparities. A study involving 21,294 adults over age 50 from the National Health and Nutrition Examination Survey (NHANES) found that requiring a BMI of under 35 for total joint arthroplasty resulted in Black patients being 39% less likely to be eligible for surgery than White patients. And individuals with an annual household income under $45,000 were 19% less likely to qualify for surgery than those with a household income above $45,000.
BMI no better than other risk factors
Although high BMI is independently associated with a higher risk of complications, the increased risk of complications conferred by a BMI at or above 40 is similar to or lower than those of other comorbidities that surgeons generally accept, said Nicholas Giori, MD, PhD, professor of orthopedic surgery at Stanford (Calif.) University, and chief of orthopedic surgery at the VA Palo Alto Health Care System. These other comorbidities include age older than 75, hypertension that requires medication, and insulin-controlled diabetes. “The independent risk of just having the diagnosis of insulin-dependent diabetes is actually comparable to the independent risk of having obesity by itself,” he told this news organization, “and all of us operate on [patients with] diabetes.”
Also, there is no BMI at which the risk of complications suddenly increases, according to the American Academy of Orthopaedic Surgeons. “It’s a rising complication rate as you go into higher BMIs,” Dr. Giori said. “If you operate on someone with a BMI of 39 vs. 41, you’re not going to find that much of a difference [in risk].” But if a medical system enforced a hard BMI cutoff of 40, one patient would qualify for surgery while the other would be barred.
Weight not as “modifiable” as previously thought
Weight is often considered a “modifiable factor” for a person considering undergoing total joint arthroplasty, but research suggests that the issue is more complicated. “Obesity is tricky, because some people are successful [in weight loss],” said Dr. Giori. Those tend to be the more memorable stories. “But a large majority have a really hard time losing substantial weight – enough to make a difference in risk,” he continued.
A study conducted in North Carolina found that restricting patients with a BMI over 40 from having elective total joint arthroplasty procedures until their weight was optimized did not result in successful weight loss. Only 20% of patients who originally presented with a BMI above this limit eventually underwent surgery after 2 years, and fewer than half of these patients had achieved a BMI of less than 40 at the time of their surgery. A third of all patients in the study did not return to the orthopedic office after their first visit.
“To hold a hard cutoff when it’s very, very hard to modify ... is essentially telling people that they are not going to ever have surgery,” Dr. Giori said; “I think that can be unfair to some patients.”
Bariatric surgery is often suggested for patients with obesity who have not experienced successful weight loss with diet and lifestyle changes alone, but bariatric surgery comes with its own complications. Research on outcomes from total joint arthroplasty among patients with who have lost weight with bariatric surgery has yielded mixed results. “I rarely push anyone hard to go that route but present it as an option for certain patients,” said Benjamin M. Stronach, MD, an orthopedic surgeon at the University of Arkansas for Medical Sciences, in Little Rock. He usually brings up bariatric surgery with patients with a BMI in the high 40s or higher to gauge their interest. If patients are already considering weight loss surgery, his office provides referrals.
But even bariatric surgery does not result in successful long-term weight loss for every patient, Dr. Stronach said. He’s seeing more and more patients who come for consultations after having undergone bariatric surgery 10 to 15 years ago. These patients lost a significant amount of weight, but then gained the weight back. He noted that bariatric surgery can be very successful for some patients who adhere to their postbariatric regimen. “We typically see fairly impressive results in the short term,” he said.
Patients with obesity benefit from joint replacement
Although patients with obesity are at higher risk for complications from joint replacement surgery, research suggests that these patients can still benefit greatly from these surgeries and that these surgeries remain cost-effective. Some studies have found that patients with obesity tend to have worse outcomes after surgery than patients who are not obese, but often, patients with high BMIs are starting from a lower point, with greater joint pain and limited mobility, Dr. Giori said. But the improvements – that is, net change in measured outcomes – can be greater for obese patients.
“Several studies have shown equal or greater improvements in validated outcome scores, function, and satisfaction compared with nonobese patients after surgery,” authors wrote in a recent review article in which they discuss how to optimize joint replacement surgery for patients with obesity. The article, published in the November 2022 issue of the Journal of the American Academy of Orthopaedic Surgeon (JAAOS), is part of a collection of review articles by the Movement Is Life Caucus.
Encourage weight loss, but look beyond the number
Rather than adhering to strict BMI cutoffs, some experts urge surgeons to consider the patient as a whole and to evaluate each individual’s overall health and potential risk. Dr. Giori generally considers high BMI as just another comorbidity when assessing a patient’s overall risk. “For a person who only has a high BMI but is otherwise healthy, I see no reason not to go ahead and schedule that person for surgery, because reducing the patient’s BMI will not substantially reduce the patient’s complication risk, and a delay in surgery may adversely affect the patient’s quality of life and ability to earn a living,” he said.
“If someone is between a BMI of 40 and 45, we are definitely going to have a discussion about weight,” Dr. Stronach said. He generally counsels against surgery for any patient with a BMI at 45 or above. He wants patients to have a BMI below 40 before surgery but considers individual cases for exceptions. “We will still move forward at times with someone with a BMI of 41, as an example, who is otherwise healthy,” he said. Similarly, if a patient has lost a significant amount of weight (e.g., the patient’s BMI was reduced from 50 to 41), the patient is actively engaged in improving their health, and surgeons believe the patient has significantly reduced their risk, “a lot of time, we’re not going to draw a line in the sand right at [a BMI of] 40,” he said.
While using a BMI of under 35 or 40 as a guideline when starting to work with patients is reasonable, working toward a weight loss of 5%-10% of total body weight is another goal to consider, authors advise in the JAAOS obesity review article. Research suggests that even a 5% reduction in overall body weight can reduce surgical complications and can improve a patient’s glucose and lipid levels and cardiac profile. Referrals to dietitians and weight loss programs, as well as behavioral counseling, can also be useful in initiating weight loss and keeping patients engaged in the process, the authors wrote.
Consider a patient’s comorbidities
Many patients with obesity have comorbidities, such as type 2 diabetes and hypertension, that can also be optimized for surgery so as to lower a patient’s overall risk profile. For patients with diabetes, achieving an A1c of 8% or lower can be a reasonable goal and can reduce risk. “We’ve found that an HbA1c level of 8% or less is something that virtually all diabetics (though not everybody) can reach, and it’s something that can be reached in a reasonable amount of time,” Dr. Giori said. Preoperative use of beta-blockers, continued use of ACE inhibitors or angiotensin receptor blockers, and behavioral modifications can improve a patient’s cardiac health before surgery.
Malnutrition can be a correctable problem for patients, regardless of BMI. In the Movement Is Life collection of optimization articles, experts recommend that orthopedists screen for malnutrition with blood tests for albumin, vitamin D, transferrin, and total lymphocyte count. Patients with malnutrition should be screened for food insecurity, experts advise, and surgical candidates with deficiencies can be given supplements of omega-3 fatty acids, arginine, and protein shakes.
Surgeon comfort and shared decision-making
Dr. Wiznia emphasized that the patient and surgeon need to discuss the risks of surgery, concerns about potential complications, and how a complication could affect the patient’s life moving forward. “Ultimately, the surgeon needs to make the decision [of whether or not to proceed [with surgery] with the patient,” he said, “but not every surgeon is going to feel comfortable operating on these patients, and not every medical institution is going to have the equipment and the investments to support surgeons doing it.”
Dr. Giori agreed that surgeons should proceed only with surgical cases they feel comfortable with. Certain surgeons may decide not to operate on individuals with higher BMIs because of the potential complications and can refer these patients to more specialized care centers. Operating on larger patients is more difficult and requires surgical skills and expertise that the surgeon may not have, he noted. “What I do object to is a system-wide BMI cutoff – for example, if an insurance company won’t pay for you to have a joint replacement, regardless of where you go or who your surgeon is,” Dr. Giori added. “I think that’s wrong, because it’s not patient centered and it’s basically excluding people from having a life-altering operation.”
Dr. Giori and Dr. Wiznia report no relevant financial relationships. Dr. Stronach is a consultant for DJ Orthopaedics, Johnson & Johnson, and MiCare Path.
A version of this article first appeared on Medscape.com.
For patients with severe arthritis, joint replacement is considered when more conservative treatments have failed. Because patients with obesity have a higher risk of complications during and after surgery, some surgeons, hospitals, and insurance companies have adopted body mass index cutoffs as a basis for deciding whether to offer patients these elective surgeries. But some experts argue that these cutoffs are arbitrary, exclude patients who can still benefit from the surgery, and can increase disparities in care.
“By enforcing cutoffs in general, you’re losing the ability for each surgeon to determine who they want to operate on,” said Daniel Wiznia, MD, assistant professor of orthopedic surgery at Yale University, New Haven, Conn. He is on the leadership committee of the Movement Is Life Caucus, a nonprofit group focused on eliminating disparities in musculoskeletal health. “For every surgeon, it’s up to them to decide if they feel comfortable doing the surgery,” he noted in an interview. “My guidance for that would be, don’t just say no because of the number – look at the patient’s entire medical profile.”
According to the Centers for Disease Control and Prevention, nearly 42% of adults in the United States have a BMI over 30, and 9.2% of adults have a BMI over 40. This excess weight puts additional stress on joints: When a person is walking, experts estimate that the force on the knees can be two to three times someone’s body weight. Over time, this pressure can wear down the cartilage on joints.
As a result, people who are overweight or obese are more likely to develop osteoarthritis and to need joint replacements. According to a Canadian study, patients with a BMI of 30-35 are 3.4 times as likely to require a hip replacement and are 8.5 times as likely to require a knee replacement compared to individuals with a BMI in the “healthy weight” range. With a BMI above 40, individuals were 8.5 times more likely to need a hip replacement and were 32.7 times as likely to need a knee replacement.
More complications, greater expense
While there are no universally recommended BMI cutoffs for joint replacement surgery, it is not uncommon for institutions to require that patients have a BMI below a certain value (usually 35-40) to proceed with surgery. A 2013 survey of physicians from the American Association of Hip and Knee Surgeons found that 52% of surgeons required a BMI below 40 to qualify for surgery.
One of the main reasons for these cutoffs is the elevated risk of complications during and after surgery. Research suggests that obesity is associated with higher rates of wound dehiscence, prosthetic joint infection (PJI), and revision total joint arthroplasty. One 2016 study suggests that patients with a BMI of 35-39.9 are twice as likely to experience PJI compared to patients with a BMI below 35. For patients with a BMI of 40 or higher, PJI is four times as likely.
Another study found that patients whose BMI is 35-40 and who undergo total joint arthroplasty have a 6.4-fold greater risk of deep incision infection. For those with a BMI over 40, that rises to a 12.9-fold increased risk compared to patients with a BMI of 18.5-25. Patients with obesity tend to have other comorbidities that can increase the risk of complications during surgery, such as type 2 diabetes, coronary artery disease, and chronic kidney disease.
Because of the increased risk of complications, health care costs tend to be higher for patients with obesity. The growing popularity of bundled health payments can discourage operating on patients who are more likely to experience complications, such as patients with high BMIs, noted Dr. Wiznia.
Research suggests that minorities and people with lower socioeconomic status are disproportionately affected by these cutoffs. According to the CDC, among non-Hispanic Black Americans and Hispanic Americans, rates of obesity are higher than among their White counterparts, and these patients are less likely to undergo joint replacement. Strictly enforcing this eligibility criterion can worsen those disparities. A study involving 21,294 adults over age 50 from the National Health and Nutrition Examination Survey (NHANES) found that requiring a BMI of under 35 for total joint arthroplasty resulted in Black patients being 39% less likely to be eligible for surgery than White patients. And individuals with an annual household income under $45,000 were 19% less likely to qualify for surgery than those with a household income above $45,000.
BMI no better than other risk factors
Although high BMI is independently associated with a higher risk of complications, the increased risk of complications conferred by a BMI at or above 40 is similar to or lower than those of other comorbidities that surgeons generally accept, said Nicholas Giori, MD, PhD, professor of orthopedic surgery at Stanford (Calif.) University, and chief of orthopedic surgery at the VA Palo Alto Health Care System. These other comorbidities include age older than 75, hypertension that requires medication, and insulin-controlled diabetes. “The independent risk of just having the diagnosis of insulin-dependent diabetes is actually comparable to the independent risk of having obesity by itself,” he told this news organization, “and all of us operate on [patients with] diabetes.”
Also, there is no BMI at which the risk of complications suddenly increases, according to the American Academy of Orthopaedic Surgeons. “It’s a rising complication rate as you go into higher BMIs,” Dr. Giori said. “If you operate on someone with a BMI of 39 vs. 41, you’re not going to find that much of a difference [in risk].” But if a medical system enforced a hard BMI cutoff of 40, one patient would qualify for surgery while the other would be barred.
Weight not as “modifiable” as previously thought
Weight is often considered a “modifiable factor” for a person considering undergoing total joint arthroplasty, but research suggests that the issue is more complicated. “Obesity is tricky, because some people are successful [in weight loss],” said Dr. Giori. Those tend to be the more memorable stories. “But a large majority have a really hard time losing substantial weight – enough to make a difference in risk,” he continued.
A study conducted in North Carolina found that restricting patients with a BMI over 40 from having elective total joint arthroplasty procedures until their weight was optimized did not result in successful weight loss. Only 20% of patients who originally presented with a BMI above this limit eventually underwent surgery after 2 years, and fewer than half of these patients had achieved a BMI of less than 40 at the time of their surgery. A third of all patients in the study did not return to the orthopedic office after their first visit.
“To hold a hard cutoff when it’s very, very hard to modify ... is essentially telling people that they are not going to ever have surgery,” Dr. Giori said; “I think that can be unfair to some patients.”
Bariatric surgery is often suggested for patients with obesity who have not experienced successful weight loss with diet and lifestyle changes alone, but bariatric surgery comes with its own complications. Research on outcomes from total joint arthroplasty among patients with who have lost weight with bariatric surgery has yielded mixed results. “I rarely push anyone hard to go that route but present it as an option for certain patients,” said Benjamin M. Stronach, MD, an orthopedic surgeon at the University of Arkansas for Medical Sciences, in Little Rock. He usually brings up bariatric surgery with patients with a BMI in the high 40s or higher to gauge their interest. If patients are already considering weight loss surgery, his office provides referrals.
But even bariatric surgery does not result in successful long-term weight loss for every patient, Dr. Stronach said. He’s seeing more and more patients who come for consultations after having undergone bariatric surgery 10 to 15 years ago. These patients lost a significant amount of weight, but then gained the weight back. He noted that bariatric surgery can be very successful for some patients who adhere to their postbariatric regimen. “We typically see fairly impressive results in the short term,” he said.
Patients with obesity benefit from joint replacement
Although patients with obesity are at higher risk for complications from joint replacement surgery, research suggests that these patients can still benefit greatly from these surgeries and that these surgeries remain cost-effective. Some studies have found that patients with obesity tend to have worse outcomes after surgery than patients who are not obese, but often, patients with high BMIs are starting from a lower point, with greater joint pain and limited mobility, Dr. Giori said. But the improvements – that is, net change in measured outcomes – can be greater for obese patients.
“Several studies have shown equal or greater improvements in validated outcome scores, function, and satisfaction compared with nonobese patients after surgery,” authors wrote in a recent review article in which they discuss how to optimize joint replacement surgery for patients with obesity. The article, published in the November 2022 issue of the Journal of the American Academy of Orthopaedic Surgeon (JAAOS), is part of a collection of review articles by the Movement Is Life Caucus.
Encourage weight loss, but look beyond the number
Rather than adhering to strict BMI cutoffs, some experts urge surgeons to consider the patient as a whole and to evaluate each individual’s overall health and potential risk. Dr. Giori generally considers high BMI as just another comorbidity when assessing a patient’s overall risk. “For a person who only has a high BMI but is otherwise healthy, I see no reason not to go ahead and schedule that person for surgery, because reducing the patient’s BMI will not substantially reduce the patient’s complication risk, and a delay in surgery may adversely affect the patient’s quality of life and ability to earn a living,” he said.
“If someone is between a BMI of 40 and 45, we are definitely going to have a discussion about weight,” Dr. Stronach said. He generally counsels against surgery for any patient with a BMI at 45 or above. He wants patients to have a BMI below 40 before surgery but considers individual cases for exceptions. “We will still move forward at times with someone with a BMI of 41, as an example, who is otherwise healthy,” he said. Similarly, if a patient has lost a significant amount of weight (e.g., the patient’s BMI was reduced from 50 to 41), the patient is actively engaged in improving their health, and surgeons believe the patient has significantly reduced their risk, “a lot of time, we’re not going to draw a line in the sand right at [a BMI of] 40,” he said.
While using a BMI of under 35 or 40 as a guideline when starting to work with patients is reasonable, working toward a weight loss of 5%-10% of total body weight is another goal to consider, authors advise in the JAAOS obesity review article. Research suggests that even a 5% reduction in overall body weight can reduce surgical complications and can improve a patient’s glucose and lipid levels and cardiac profile. Referrals to dietitians and weight loss programs, as well as behavioral counseling, can also be useful in initiating weight loss and keeping patients engaged in the process, the authors wrote.
Consider a patient’s comorbidities
Many patients with obesity have comorbidities, such as type 2 diabetes and hypertension, that can also be optimized for surgery so as to lower a patient’s overall risk profile. For patients with diabetes, achieving an A1c of 8% or lower can be a reasonable goal and can reduce risk. “We’ve found that an HbA1c level of 8% or less is something that virtually all diabetics (though not everybody) can reach, and it’s something that can be reached in a reasonable amount of time,” Dr. Giori said. Preoperative use of beta-blockers, continued use of ACE inhibitors or angiotensin receptor blockers, and behavioral modifications can improve a patient’s cardiac health before surgery.
Malnutrition can be a correctable problem for patients, regardless of BMI. In the Movement Is Life collection of optimization articles, experts recommend that orthopedists screen for malnutrition with blood tests for albumin, vitamin D, transferrin, and total lymphocyte count. Patients with malnutrition should be screened for food insecurity, experts advise, and surgical candidates with deficiencies can be given supplements of omega-3 fatty acids, arginine, and protein shakes.
Surgeon comfort and shared decision-making
Dr. Wiznia emphasized that the patient and surgeon need to discuss the risks of surgery, concerns about potential complications, and how a complication could affect the patient’s life moving forward. “Ultimately, the surgeon needs to make the decision [of whether or not to proceed [with surgery] with the patient,” he said, “but not every surgeon is going to feel comfortable operating on these patients, and not every medical institution is going to have the equipment and the investments to support surgeons doing it.”
Dr. Giori agreed that surgeons should proceed only with surgical cases they feel comfortable with. Certain surgeons may decide not to operate on individuals with higher BMIs because of the potential complications and can refer these patients to more specialized care centers. Operating on larger patients is more difficult and requires surgical skills and expertise that the surgeon may not have, he noted. “What I do object to is a system-wide BMI cutoff – for example, if an insurance company won’t pay for you to have a joint replacement, regardless of where you go or who your surgeon is,” Dr. Giori added. “I think that’s wrong, because it’s not patient centered and it’s basically excluding people from having a life-altering operation.”
Dr. Giori and Dr. Wiznia report no relevant financial relationships. Dr. Stronach is a consultant for DJ Orthopaedics, Johnson & Johnson, and MiCare Path.
A version of this article first appeared on Medscape.com.
For patients with severe arthritis, joint replacement is considered when more conservative treatments have failed. Because patients with obesity have a higher risk of complications during and after surgery, some surgeons, hospitals, and insurance companies have adopted body mass index cutoffs as a basis for deciding whether to offer patients these elective surgeries. But some experts argue that these cutoffs are arbitrary, exclude patients who can still benefit from the surgery, and can increase disparities in care.
“By enforcing cutoffs in general, you’re losing the ability for each surgeon to determine who they want to operate on,” said Daniel Wiznia, MD, assistant professor of orthopedic surgery at Yale University, New Haven, Conn. He is on the leadership committee of the Movement Is Life Caucus, a nonprofit group focused on eliminating disparities in musculoskeletal health. “For every surgeon, it’s up to them to decide if they feel comfortable doing the surgery,” he noted in an interview. “My guidance for that would be, don’t just say no because of the number – look at the patient’s entire medical profile.”
According to the Centers for Disease Control and Prevention, nearly 42% of adults in the United States have a BMI over 30, and 9.2% of adults have a BMI over 40. This excess weight puts additional stress on joints: When a person is walking, experts estimate that the force on the knees can be two to three times someone’s body weight. Over time, this pressure can wear down the cartilage on joints.
As a result, people who are overweight or obese are more likely to develop osteoarthritis and to need joint replacements. According to a Canadian study, patients with a BMI of 30-35 are 3.4 times as likely to require a hip replacement and are 8.5 times as likely to require a knee replacement compared to individuals with a BMI in the “healthy weight” range. With a BMI above 40, individuals were 8.5 times more likely to need a hip replacement and were 32.7 times as likely to need a knee replacement.
More complications, greater expense
While there are no universally recommended BMI cutoffs for joint replacement surgery, it is not uncommon for institutions to require that patients have a BMI below a certain value (usually 35-40) to proceed with surgery. A 2013 survey of physicians from the American Association of Hip and Knee Surgeons found that 52% of surgeons required a BMI below 40 to qualify for surgery.
One of the main reasons for these cutoffs is the elevated risk of complications during and after surgery. Research suggests that obesity is associated with higher rates of wound dehiscence, prosthetic joint infection (PJI), and revision total joint arthroplasty. One 2016 study suggests that patients with a BMI of 35-39.9 are twice as likely to experience PJI compared to patients with a BMI below 35. For patients with a BMI of 40 or higher, PJI is four times as likely.
Another study found that patients whose BMI is 35-40 and who undergo total joint arthroplasty have a 6.4-fold greater risk of deep incision infection. For those with a BMI over 40, that rises to a 12.9-fold increased risk compared to patients with a BMI of 18.5-25. Patients with obesity tend to have other comorbidities that can increase the risk of complications during surgery, such as type 2 diabetes, coronary artery disease, and chronic kidney disease.
Because of the increased risk of complications, health care costs tend to be higher for patients with obesity. The growing popularity of bundled health payments can discourage operating on patients who are more likely to experience complications, such as patients with high BMIs, noted Dr. Wiznia.
Research suggests that minorities and people with lower socioeconomic status are disproportionately affected by these cutoffs. According to the CDC, among non-Hispanic Black Americans and Hispanic Americans, rates of obesity are higher than among their White counterparts, and these patients are less likely to undergo joint replacement. Strictly enforcing this eligibility criterion can worsen those disparities. A study involving 21,294 adults over age 50 from the National Health and Nutrition Examination Survey (NHANES) found that requiring a BMI of under 35 for total joint arthroplasty resulted in Black patients being 39% less likely to be eligible for surgery than White patients. And individuals with an annual household income under $45,000 were 19% less likely to qualify for surgery than those with a household income above $45,000.
BMI no better than other risk factors
Although high BMI is independently associated with a higher risk of complications, the increased risk of complications conferred by a BMI at or above 40 is similar to or lower than those of other comorbidities that surgeons generally accept, said Nicholas Giori, MD, PhD, professor of orthopedic surgery at Stanford (Calif.) University, and chief of orthopedic surgery at the VA Palo Alto Health Care System. These other comorbidities include age older than 75, hypertension that requires medication, and insulin-controlled diabetes. “The independent risk of just having the diagnosis of insulin-dependent diabetes is actually comparable to the independent risk of having obesity by itself,” he told this news organization, “and all of us operate on [patients with] diabetes.”
Also, there is no BMI at which the risk of complications suddenly increases, according to the American Academy of Orthopaedic Surgeons. “It’s a rising complication rate as you go into higher BMIs,” Dr. Giori said. “If you operate on someone with a BMI of 39 vs. 41, you’re not going to find that much of a difference [in risk].” But if a medical system enforced a hard BMI cutoff of 40, one patient would qualify for surgery while the other would be barred.
Weight not as “modifiable” as previously thought
Weight is often considered a “modifiable factor” for a person considering undergoing total joint arthroplasty, but research suggests that the issue is more complicated. “Obesity is tricky, because some people are successful [in weight loss],” said Dr. Giori. Those tend to be the more memorable stories. “But a large majority have a really hard time losing substantial weight – enough to make a difference in risk,” he continued.
A study conducted in North Carolina found that restricting patients with a BMI over 40 from having elective total joint arthroplasty procedures until their weight was optimized did not result in successful weight loss. Only 20% of patients who originally presented with a BMI above this limit eventually underwent surgery after 2 years, and fewer than half of these patients had achieved a BMI of less than 40 at the time of their surgery. A third of all patients in the study did not return to the orthopedic office after their first visit.
“To hold a hard cutoff when it’s very, very hard to modify ... is essentially telling people that they are not going to ever have surgery,” Dr. Giori said; “I think that can be unfair to some patients.”
Bariatric surgery is often suggested for patients with obesity who have not experienced successful weight loss with diet and lifestyle changes alone, but bariatric surgery comes with its own complications. Research on outcomes from total joint arthroplasty among patients with who have lost weight with bariatric surgery has yielded mixed results. “I rarely push anyone hard to go that route but present it as an option for certain patients,” said Benjamin M. Stronach, MD, an orthopedic surgeon at the University of Arkansas for Medical Sciences, in Little Rock. He usually brings up bariatric surgery with patients with a BMI in the high 40s or higher to gauge their interest. If patients are already considering weight loss surgery, his office provides referrals.
But even bariatric surgery does not result in successful long-term weight loss for every patient, Dr. Stronach said. He’s seeing more and more patients who come for consultations after having undergone bariatric surgery 10 to 15 years ago. These patients lost a significant amount of weight, but then gained the weight back. He noted that bariatric surgery can be very successful for some patients who adhere to their postbariatric regimen. “We typically see fairly impressive results in the short term,” he said.
Patients with obesity benefit from joint replacement
Although patients with obesity are at higher risk for complications from joint replacement surgery, research suggests that these patients can still benefit greatly from these surgeries and that these surgeries remain cost-effective. Some studies have found that patients with obesity tend to have worse outcomes after surgery than patients who are not obese, but often, patients with high BMIs are starting from a lower point, with greater joint pain and limited mobility, Dr. Giori said. But the improvements – that is, net change in measured outcomes – can be greater for obese patients.
“Several studies have shown equal or greater improvements in validated outcome scores, function, and satisfaction compared with nonobese patients after surgery,” authors wrote in a recent review article in which they discuss how to optimize joint replacement surgery for patients with obesity. The article, published in the November 2022 issue of the Journal of the American Academy of Orthopaedic Surgeon (JAAOS), is part of a collection of review articles by the Movement Is Life Caucus.
Encourage weight loss, but look beyond the number
Rather than adhering to strict BMI cutoffs, some experts urge surgeons to consider the patient as a whole and to evaluate each individual’s overall health and potential risk. Dr. Giori generally considers high BMI as just another comorbidity when assessing a patient’s overall risk. “For a person who only has a high BMI but is otherwise healthy, I see no reason not to go ahead and schedule that person for surgery, because reducing the patient’s BMI will not substantially reduce the patient’s complication risk, and a delay in surgery may adversely affect the patient’s quality of life and ability to earn a living,” he said.
“If someone is between a BMI of 40 and 45, we are definitely going to have a discussion about weight,” Dr. Stronach said. He generally counsels against surgery for any patient with a BMI at 45 or above. He wants patients to have a BMI below 40 before surgery but considers individual cases for exceptions. “We will still move forward at times with someone with a BMI of 41, as an example, who is otherwise healthy,” he said. Similarly, if a patient has lost a significant amount of weight (e.g., the patient’s BMI was reduced from 50 to 41), the patient is actively engaged in improving their health, and surgeons believe the patient has significantly reduced their risk, “a lot of time, we’re not going to draw a line in the sand right at [a BMI of] 40,” he said.
While using a BMI of under 35 or 40 as a guideline when starting to work with patients is reasonable, working toward a weight loss of 5%-10% of total body weight is another goal to consider, authors advise in the JAAOS obesity review article. Research suggests that even a 5% reduction in overall body weight can reduce surgical complications and can improve a patient’s glucose and lipid levels and cardiac profile. Referrals to dietitians and weight loss programs, as well as behavioral counseling, can also be useful in initiating weight loss and keeping patients engaged in the process, the authors wrote.
Consider a patient’s comorbidities
Many patients with obesity have comorbidities, such as type 2 diabetes and hypertension, that can also be optimized for surgery so as to lower a patient’s overall risk profile. For patients with diabetes, achieving an A1c of 8% or lower can be a reasonable goal and can reduce risk. “We’ve found that an HbA1c level of 8% or less is something that virtually all diabetics (though not everybody) can reach, and it’s something that can be reached in a reasonable amount of time,” Dr. Giori said. Preoperative use of beta-blockers, continued use of ACE inhibitors or angiotensin receptor blockers, and behavioral modifications can improve a patient’s cardiac health before surgery.
Malnutrition can be a correctable problem for patients, regardless of BMI. In the Movement Is Life collection of optimization articles, experts recommend that orthopedists screen for malnutrition with blood tests for albumin, vitamin D, transferrin, and total lymphocyte count. Patients with malnutrition should be screened for food insecurity, experts advise, and surgical candidates with deficiencies can be given supplements of omega-3 fatty acids, arginine, and protein shakes.
Surgeon comfort and shared decision-making
Dr. Wiznia emphasized that the patient and surgeon need to discuss the risks of surgery, concerns about potential complications, and how a complication could affect the patient’s life moving forward. “Ultimately, the surgeon needs to make the decision [of whether or not to proceed [with surgery] with the patient,” he said, “but not every surgeon is going to feel comfortable operating on these patients, and not every medical institution is going to have the equipment and the investments to support surgeons doing it.”
Dr. Giori agreed that surgeons should proceed only with surgical cases they feel comfortable with. Certain surgeons may decide not to operate on individuals with higher BMIs because of the potential complications and can refer these patients to more specialized care centers. Operating on larger patients is more difficult and requires surgical skills and expertise that the surgeon may not have, he noted. “What I do object to is a system-wide BMI cutoff – for example, if an insurance company won’t pay for you to have a joint replacement, regardless of where you go or who your surgeon is,” Dr. Giori added. “I think that’s wrong, because it’s not patient centered and it’s basically excluding people from having a life-altering operation.”
Dr. Giori and Dr. Wiznia report no relevant financial relationships. Dr. Stronach is a consultant for DJ Orthopaedics, Johnson & Johnson, and MiCare Path.
A version of this article first appeared on Medscape.com.
Florida doc dies by suicide after allegedly drugging and raping patients
according to a police statement.
A week later, a Collier County Sheriff’s deputy found Dr. Salata’s body near his Naples home with a gunshot wound to the head, according to police. The medical examiner later ruled it a suicide.
Dr. Salata co-owned Pura Vida Medical Spa in Naples with his wife Jill Salata, a certified family nurse practitioner. They specialized in cosmetic treatment and surgery.
Naples police said that they arrested Dr. Salata after two female patients accused the doctor of allegedly drugging and raping them while they were still unconscious.
Both victims described being given nitrous oxide, also called laughing gas, for sedation and pain from the cosmetic procedure. The first victim, age 51, said Dr. Salata prescribed alprazolam (Xanax) to take before the procedure and then also gave her nitrous oxide and tequila, causing her to black out, according to NBC2 News.
The second victim, age 72, told police that as the nitrous oxide was wearing off, she found Dr. Salata performing sexual intercourse. The victim felt shocked after the sedation subsided about what had taken place, contacted police, and submitted to a sexual assault examination, according to the police statement.
At Dr. Salata’s November 22 hearing before Judge Michael Provost, a prosecutor asked the judge whether Dr. Salata should surrender his firearms; Provost reportedly dismissed the idea.
“It is disappointing and frustrating that Dr. Salata has escaped justice,” said one victim’s attorney, Adam Horowitz, in a blog post. “Yet, we are relieved that no other women will be assaulted by Dr. Salata again. It took tremendous courage for my client to tell her truth. She was ready to hold him accountable in court.”
Horowitz says he plans to file a civil lawsuit on behalf of his client against Dr. Salata’s estate. The Naples police are continuing their investigation into the victims’ cases, which now includes a third woman, said spokesman Lt. Bryan McGinn.
Meanwhile, the Pura Vida Medical Spa has closed permanently and its website has been deleted. One reviewer named Soul F. wrote on the spa’s Yelp page: “And now may God have mercy on this rapist’s soul. Amen.”
A version of this article first appeared on Medscape.com.
according to a police statement.
A week later, a Collier County Sheriff’s deputy found Dr. Salata’s body near his Naples home with a gunshot wound to the head, according to police. The medical examiner later ruled it a suicide.
Dr. Salata co-owned Pura Vida Medical Spa in Naples with his wife Jill Salata, a certified family nurse practitioner. They specialized in cosmetic treatment and surgery.
Naples police said that they arrested Dr. Salata after two female patients accused the doctor of allegedly drugging and raping them while they were still unconscious.
Both victims described being given nitrous oxide, also called laughing gas, for sedation and pain from the cosmetic procedure. The first victim, age 51, said Dr. Salata prescribed alprazolam (Xanax) to take before the procedure and then also gave her nitrous oxide and tequila, causing her to black out, according to NBC2 News.
The second victim, age 72, told police that as the nitrous oxide was wearing off, she found Dr. Salata performing sexual intercourse. The victim felt shocked after the sedation subsided about what had taken place, contacted police, and submitted to a sexual assault examination, according to the police statement.
At Dr. Salata’s November 22 hearing before Judge Michael Provost, a prosecutor asked the judge whether Dr. Salata should surrender his firearms; Provost reportedly dismissed the idea.
“It is disappointing and frustrating that Dr. Salata has escaped justice,” said one victim’s attorney, Adam Horowitz, in a blog post. “Yet, we are relieved that no other women will be assaulted by Dr. Salata again. It took tremendous courage for my client to tell her truth. She was ready to hold him accountable in court.”
Horowitz says he plans to file a civil lawsuit on behalf of his client against Dr. Salata’s estate. The Naples police are continuing their investigation into the victims’ cases, which now includes a third woman, said spokesman Lt. Bryan McGinn.
Meanwhile, the Pura Vida Medical Spa has closed permanently and its website has been deleted. One reviewer named Soul F. wrote on the spa’s Yelp page: “And now may God have mercy on this rapist’s soul. Amen.”
A version of this article first appeared on Medscape.com.
according to a police statement.
A week later, a Collier County Sheriff’s deputy found Dr. Salata’s body near his Naples home with a gunshot wound to the head, according to police. The medical examiner later ruled it a suicide.
Dr. Salata co-owned Pura Vida Medical Spa in Naples with his wife Jill Salata, a certified family nurse practitioner. They specialized in cosmetic treatment and surgery.
Naples police said that they arrested Dr. Salata after two female patients accused the doctor of allegedly drugging and raping them while they were still unconscious.
Both victims described being given nitrous oxide, also called laughing gas, for sedation and pain from the cosmetic procedure. The first victim, age 51, said Dr. Salata prescribed alprazolam (Xanax) to take before the procedure and then also gave her nitrous oxide and tequila, causing her to black out, according to NBC2 News.
The second victim, age 72, told police that as the nitrous oxide was wearing off, she found Dr. Salata performing sexual intercourse. The victim felt shocked after the sedation subsided about what had taken place, contacted police, and submitted to a sexual assault examination, according to the police statement.
At Dr. Salata’s November 22 hearing before Judge Michael Provost, a prosecutor asked the judge whether Dr. Salata should surrender his firearms; Provost reportedly dismissed the idea.
“It is disappointing and frustrating that Dr. Salata has escaped justice,” said one victim’s attorney, Adam Horowitz, in a blog post. “Yet, we are relieved that no other women will be assaulted by Dr. Salata again. It took tremendous courage for my client to tell her truth. She was ready to hold him accountable in court.”
Horowitz says he plans to file a civil lawsuit on behalf of his client against Dr. Salata’s estate. The Naples police are continuing their investigation into the victims’ cases, which now includes a third woman, said spokesman Lt. Bryan McGinn.
Meanwhile, the Pura Vida Medical Spa has closed permanently and its website has been deleted. One reviewer named Soul F. wrote on the spa’s Yelp page: “And now may God have mercy on this rapist’s soul. Amen.”
A version of this article first appeared on Medscape.com.
How blunt is too blunt for informed consent?
Sitting across from a patient explaining a complicated treatment proposal, protocol, or medication may be one of the most complex yet crucial tasks you have as a physician. Although informed consent is at the forefront of shared decisions between you and your patient, there’s a fine line between providing enough information on the risks and benefits of a particular treatment and knowing you’ve explained it well enough to fully educate your patient about their choices.
“It is a bit of a fine line because unless your patient happens to be a health care provider, medicine is complicated for patients to understand,” said David L. Feldman, MD, chief medical officer at The Doctors Company, the nation’s largest medical malpractice insurer in New York.
In addition, documenting the interaction is critical, said James Giordano, PhD, MPhil, professor in the departments of neurology and biochemistry and chief of the neuroethics studies program at the Pellegrino Center for Clinical Bioethics at Georgetown University Medical Center, Washington.
“As with anything in medicine, the key rule is that if it’s not documented, it’s not done,” he said. “This also means diligent documentation in all aspects of the medical record, including the electronic medical record and the written one.”
That said, it’s important to know what’s enough and what’s too granular when you discuss a procedure with your patients, said Erum N. Ilyas, MD, a board-certified dermatologist at Schweiger Dermatology and a bioethicist near Philadelphia.
“One of the most challenging aspects of informed consent, especially for young physicians, is how to discuss a procedure or a medication in a manner that is both relevant and concise,” Dr. llyas said. “I’ve had residents about to perform a skin biopsy spend several minutes covering every aspect of every potential outcome of a routine skin biopsy. The patient is left traumatized and confused as to whether they should proceed with the small procedure.”
Instead, the goal of informed consent is to ensure that the patient has a general overview of the procedure and is empowered, knowing that the decision to proceed is, indeed, part of their decision-making process.
How long an informed consent discussion takes depends on the procedure.
“When I was in practice as a plastic surgeon, the conversations varied from the straightforward ‘I’m taking this mole off your cheek, and there’s a risk of scarring and bleeding’ to talking about a mastectomy and breast reconstruction, which could take an hour or more to discuss,” Dr. Feldman said.
Ultimately, it’s as essential for doctors to explain the risks associated with a procedure as it is for patients to understand precisely what’s involved, Dr. Ilyas added.
She also recommends creating a flow to the conversation that places the discussion of risks within the context of why the procedure is being performed. This way, clarity about both the risks and the need for the treatment or procedure can be achieved.
When doing so, it’s critical to make sure you’re speaking your patient’s language – literally.
“Have a translator in the room if needed,” Dr. Feldman added. “If your patient is hearing or sight impaired, you need to have every contingency ready to ensure that everyone is in complete communication.”
Document, document, document!
To best protect yourself, the patient must consent to each procedure and intervention via active, informed consent, said Dr. Giordano.
“It’s not enough to hand a patient a piece of paper and say sign it,” he said. “There should be some documented evidence that the patient has not only read the document but that the key parts of the document have been explained and that the patient’s level of comprehension has been assessed and verified.”
It is vital if the patient has a disability, a neurological impairment, or a neurocognitive or psychiatric condition that might impede his or her ability to understand the consent that’s being sought.
In addition, it’s best if a ‘clinical proxy’ handles the consent (for example, a nurse, office worker, or case manager).
“This can be very helpful because it means you’ve had third-party documentation of informed consent,” Dr. Giordano said. “It should then be re-documented with you as the clinician and stated that the patient has affirmatively and actively agreed to treatment.”
What happens when things go wrong?
If you’re sued over informed consent, with the patient claiming that you didn’t fully explain the potential risks, the first thing to consider is why this happened.
“Very often, these situations occur if there was some difficulty or competency of communication,” Dr. Giordano said. “You may have done everything right, but somehow the patient hasn’t gained an understanding of the procedure required.”
Physicians must take a hard look at how they’re explaining risks and possible side effects. For doctors who perform these procedures regularly, the risks may seem small, and they may unconsciously minimize them to the patient. But when something goes wrong, the patient may then feel that they didn’t fully understand the frequency of poor outcomes, or the potential severity.
Next, it’s important to perform a ‘gap analysis’ to assess why something went awry. That means, look at all the potential factors involved to identify which one was the weak link.
“It might be that the patient was on a signing frenzy and signed away but didn’t receive active and informed content,” Dr. Giordano said. “The goal is to learn how to close the gap for this case and for future cases.”
To protect yourself, consider using technology to your advantage, especially since lawsuits over informed consent usually happen several years after the procedure. This is when a patient might argue that you didn’t tell them about possible complications and that they might have opted out of the procedure if they had known about those issues ahead of time.
“Even before the statute of limitations is up for a lawsuit, it could be five years from the time the procedure occurred due to the length of time a lawsuit can take,” Dr. Feldman said. “That’s why it’s important to take a video of your conversation or make a recording of the informed consent conversation. This way if there’s a question of what you said, there’s a video of it.”
For many physicians, this would be a big change – to video record and then store all their informed consent conversations. It could most likely help you if a lawsuit occurs, but some physicians may feel that process to be cumbersome and time-consuming, and they’d rather find another way to ensure that patients understand the risks.
Ultimately, however, if there’s a legal question involved with informed consent, the general thinking is that the effect on the patient must be harmful for it to stand up.
“The question becomes whether the outcome rendered that gap in the consenting process forgivable,” Dr. Giordano said. “The hope is that there was nothing harmful to the patient and that the benefit of the procedure was demonstrable despite any gaps in the informed consent process.”
In the end, informed consent should be a matter of good communication before, during, and after any treatment or procedure.
“When you form a relationship with a patient who needs any procedure, small or large, you’re going to be guiding them through a very scary thing,” Dr. Feldman said. “You want to make patients feel like you care about them and that, while neither you nor the system is perfect, you’ll take care of them. That’s the bottom line.”
A version of this article first appeared on Medscape.com.
Sitting across from a patient explaining a complicated treatment proposal, protocol, or medication may be one of the most complex yet crucial tasks you have as a physician. Although informed consent is at the forefront of shared decisions between you and your patient, there’s a fine line between providing enough information on the risks and benefits of a particular treatment and knowing you’ve explained it well enough to fully educate your patient about their choices.
“It is a bit of a fine line because unless your patient happens to be a health care provider, medicine is complicated for patients to understand,” said David L. Feldman, MD, chief medical officer at The Doctors Company, the nation’s largest medical malpractice insurer in New York.
In addition, documenting the interaction is critical, said James Giordano, PhD, MPhil, professor in the departments of neurology and biochemistry and chief of the neuroethics studies program at the Pellegrino Center for Clinical Bioethics at Georgetown University Medical Center, Washington.
“As with anything in medicine, the key rule is that if it’s not documented, it’s not done,” he said. “This also means diligent documentation in all aspects of the medical record, including the electronic medical record and the written one.”
That said, it’s important to know what’s enough and what’s too granular when you discuss a procedure with your patients, said Erum N. Ilyas, MD, a board-certified dermatologist at Schweiger Dermatology and a bioethicist near Philadelphia.
“One of the most challenging aspects of informed consent, especially for young physicians, is how to discuss a procedure or a medication in a manner that is both relevant and concise,” Dr. llyas said. “I’ve had residents about to perform a skin biopsy spend several minutes covering every aspect of every potential outcome of a routine skin biopsy. The patient is left traumatized and confused as to whether they should proceed with the small procedure.”
Instead, the goal of informed consent is to ensure that the patient has a general overview of the procedure and is empowered, knowing that the decision to proceed is, indeed, part of their decision-making process.
How long an informed consent discussion takes depends on the procedure.
“When I was in practice as a plastic surgeon, the conversations varied from the straightforward ‘I’m taking this mole off your cheek, and there’s a risk of scarring and bleeding’ to talking about a mastectomy and breast reconstruction, which could take an hour or more to discuss,” Dr. Feldman said.
Ultimately, it’s as essential for doctors to explain the risks associated with a procedure as it is for patients to understand precisely what’s involved, Dr. Ilyas added.
She also recommends creating a flow to the conversation that places the discussion of risks within the context of why the procedure is being performed. This way, clarity about both the risks and the need for the treatment or procedure can be achieved.
When doing so, it’s critical to make sure you’re speaking your patient’s language – literally.
“Have a translator in the room if needed,” Dr. Feldman added. “If your patient is hearing or sight impaired, you need to have every contingency ready to ensure that everyone is in complete communication.”
Document, document, document!
To best protect yourself, the patient must consent to each procedure and intervention via active, informed consent, said Dr. Giordano.
“It’s not enough to hand a patient a piece of paper and say sign it,” he said. “There should be some documented evidence that the patient has not only read the document but that the key parts of the document have been explained and that the patient’s level of comprehension has been assessed and verified.”
It is vital if the patient has a disability, a neurological impairment, or a neurocognitive or psychiatric condition that might impede his or her ability to understand the consent that’s being sought.
In addition, it’s best if a ‘clinical proxy’ handles the consent (for example, a nurse, office worker, or case manager).
“This can be very helpful because it means you’ve had third-party documentation of informed consent,” Dr. Giordano said. “It should then be re-documented with you as the clinician and stated that the patient has affirmatively and actively agreed to treatment.”
What happens when things go wrong?
If you’re sued over informed consent, with the patient claiming that you didn’t fully explain the potential risks, the first thing to consider is why this happened.
“Very often, these situations occur if there was some difficulty or competency of communication,” Dr. Giordano said. “You may have done everything right, but somehow the patient hasn’t gained an understanding of the procedure required.”
Physicians must take a hard look at how they’re explaining risks and possible side effects. For doctors who perform these procedures regularly, the risks may seem small, and they may unconsciously minimize them to the patient. But when something goes wrong, the patient may then feel that they didn’t fully understand the frequency of poor outcomes, or the potential severity.
Next, it’s important to perform a ‘gap analysis’ to assess why something went awry. That means, look at all the potential factors involved to identify which one was the weak link.
“It might be that the patient was on a signing frenzy and signed away but didn’t receive active and informed content,” Dr. Giordano said. “The goal is to learn how to close the gap for this case and for future cases.”
To protect yourself, consider using technology to your advantage, especially since lawsuits over informed consent usually happen several years after the procedure. This is when a patient might argue that you didn’t tell them about possible complications and that they might have opted out of the procedure if they had known about those issues ahead of time.
“Even before the statute of limitations is up for a lawsuit, it could be five years from the time the procedure occurred due to the length of time a lawsuit can take,” Dr. Feldman said. “That’s why it’s important to take a video of your conversation or make a recording of the informed consent conversation. This way if there’s a question of what you said, there’s a video of it.”
For many physicians, this would be a big change – to video record and then store all their informed consent conversations. It could most likely help you if a lawsuit occurs, but some physicians may feel that process to be cumbersome and time-consuming, and they’d rather find another way to ensure that patients understand the risks.
Ultimately, however, if there’s a legal question involved with informed consent, the general thinking is that the effect on the patient must be harmful for it to stand up.
“The question becomes whether the outcome rendered that gap in the consenting process forgivable,” Dr. Giordano said. “The hope is that there was nothing harmful to the patient and that the benefit of the procedure was demonstrable despite any gaps in the informed consent process.”
In the end, informed consent should be a matter of good communication before, during, and after any treatment or procedure.
“When you form a relationship with a patient who needs any procedure, small or large, you’re going to be guiding them through a very scary thing,” Dr. Feldman said. “You want to make patients feel like you care about them and that, while neither you nor the system is perfect, you’ll take care of them. That’s the bottom line.”
A version of this article first appeared on Medscape.com.
Sitting across from a patient explaining a complicated treatment proposal, protocol, or medication may be one of the most complex yet crucial tasks you have as a physician. Although informed consent is at the forefront of shared decisions between you and your patient, there’s a fine line between providing enough information on the risks and benefits of a particular treatment and knowing you’ve explained it well enough to fully educate your patient about their choices.
“It is a bit of a fine line because unless your patient happens to be a health care provider, medicine is complicated for patients to understand,” said David L. Feldman, MD, chief medical officer at The Doctors Company, the nation’s largest medical malpractice insurer in New York.
In addition, documenting the interaction is critical, said James Giordano, PhD, MPhil, professor in the departments of neurology and biochemistry and chief of the neuroethics studies program at the Pellegrino Center for Clinical Bioethics at Georgetown University Medical Center, Washington.
“As with anything in medicine, the key rule is that if it’s not documented, it’s not done,” he said. “This also means diligent documentation in all aspects of the medical record, including the electronic medical record and the written one.”
That said, it’s important to know what’s enough and what’s too granular when you discuss a procedure with your patients, said Erum N. Ilyas, MD, a board-certified dermatologist at Schweiger Dermatology and a bioethicist near Philadelphia.
“One of the most challenging aspects of informed consent, especially for young physicians, is how to discuss a procedure or a medication in a manner that is both relevant and concise,” Dr. llyas said. “I’ve had residents about to perform a skin biopsy spend several minutes covering every aspect of every potential outcome of a routine skin biopsy. The patient is left traumatized and confused as to whether they should proceed with the small procedure.”
Instead, the goal of informed consent is to ensure that the patient has a general overview of the procedure and is empowered, knowing that the decision to proceed is, indeed, part of their decision-making process.
How long an informed consent discussion takes depends on the procedure.
“When I was in practice as a plastic surgeon, the conversations varied from the straightforward ‘I’m taking this mole off your cheek, and there’s a risk of scarring and bleeding’ to talking about a mastectomy and breast reconstruction, which could take an hour or more to discuss,” Dr. Feldman said.
Ultimately, it’s as essential for doctors to explain the risks associated with a procedure as it is for patients to understand precisely what’s involved, Dr. Ilyas added.
She also recommends creating a flow to the conversation that places the discussion of risks within the context of why the procedure is being performed. This way, clarity about both the risks and the need for the treatment or procedure can be achieved.
When doing so, it’s critical to make sure you’re speaking your patient’s language – literally.
“Have a translator in the room if needed,” Dr. Feldman added. “If your patient is hearing or sight impaired, you need to have every contingency ready to ensure that everyone is in complete communication.”
Document, document, document!
To best protect yourself, the patient must consent to each procedure and intervention via active, informed consent, said Dr. Giordano.
“It’s not enough to hand a patient a piece of paper and say sign it,” he said. “There should be some documented evidence that the patient has not only read the document but that the key parts of the document have been explained and that the patient’s level of comprehension has been assessed and verified.”
It is vital if the patient has a disability, a neurological impairment, or a neurocognitive or psychiatric condition that might impede his or her ability to understand the consent that’s being sought.
In addition, it’s best if a ‘clinical proxy’ handles the consent (for example, a nurse, office worker, or case manager).
“This can be very helpful because it means you’ve had third-party documentation of informed consent,” Dr. Giordano said. “It should then be re-documented with you as the clinician and stated that the patient has affirmatively and actively agreed to treatment.”
What happens when things go wrong?
If you’re sued over informed consent, with the patient claiming that you didn’t fully explain the potential risks, the first thing to consider is why this happened.
“Very often, these situations occur if there was some difficulty or competency of communication,” Dr. Giordano said. “You may have done everything right, but somehow the patient hasn’t gained an understanding of the procedure required.”
Physicians must take a hard look at how they’re explaining risks and possible side effects. For doctors who perform these procedures regularly, the risks may seem small, and they may unconsciously minimize them to the patient. But when something goes wrong, the patient may then feel that they didn’t fully understand the frequency of poor outcomes, or the potential severity.
Next, it’s important to perform a ‘gap analysis’ to assess why something went awry. That means, look at all the potential factors involved to identify which one was the weak link.
“It might be that the patient was on a signing frenzy and signed away but didn’t receive active and informed content,” Dr. Giordano said. “The goal is to learn how to close the gap for this case and for future cases.”
To protect yourself, consider using technology to your advantage, especially since lawsuits over informed consent usually happen several years after the procedure. This is when a patient might argue that you didn’t tell them about possible complications and that they might have opted out of the procedure if they had known about those issues ahead of time.
“Even before the statute of limitations is up for a lawsuit, it could be five years from the time the procedure occurred due to the length of time a lawsuit can take,” Dr. Feldman said. “That’s why it’s important to take a video of your conversation or make a recording of the informed consent conversation. This way if there’s a question of what you said, there’s a video of it.”
For many physicians, this would be a big change – to video record and then store all their informed consent conversations. It could most likely help you if a lawsuit occurs, but some physicians may feel that process to be cumbersome and time-consuming, and they’d rather find another way to ensure that patients understand the risks.
Ultimately, however, if there’s a legal question involved with informed consent, the general thinking is that the effect on the patient must be harmful for it to stand up.
“The question becomes whether the outcome rendered that gap in the consenting process forgivable,” Dr. Giordano said. “The hope is that there was nothing harmful to the patient and that the benefit of the procedure was demonstrable despite any gaps in the informed consent process.”
In the end, informed consent should be a matter of good communication before, during, and after any treatment or procedure.
“When you form a relationship with a patient who needs any procedure, small or large, you’re going to be guiding them through a very scary thing,” Dr. Feldman said. “You want to make patients feel like you care about them and that, while neither you nor the system is perfect, you’ll take care of them. That’s the bottom line.”
A version of this article first appeared on Medscape.com.
Analysis of doctors’ EHR email finds infrequent but notable hostility
Among the emails, 43% were from patients; the remainder were mostly from other physicians or clinicians, or automated. The content of the messages wasn’t associated with doctor burnout, as the researchers had hypothesized. And only about 5% of the messages had negative sentiment.
But the researchers were struck by the hostility of that sentiment, displayed in messages like these that surely would be distressing for physicians to read:
“I hope and expect that you will spend eternity in he**. You are an abusive, nasty, cheap person.”
“Your office is full of liars, hypocrites and I will do everything in my power to prevent anyone from going to your bullsh** office again.”
About 5% of emails had an overall negative sentiment, with high-frequency words like “cancel,” “pain,” or “problem.” Among patient messages, 3% were negative and contained words and expletives suggesting hatred, hostility, or violence.
“F***” was the most common expletive used by patients.
Researchers provided examples of profanity-laced messages, including one patient who said, “I am so upset that I was told the blood work would include the gender of the baby. I have been waiting 5 [days] to find it, and it wasn’t even fu**ing tested!!!! What a disappointment in your office and the bullsh** I was told. I will be switching plans because this is sh**!”
Researchers also noted some high-frequency words associated with violence, such as “shoot,” “fight,” and “kill.”
“This is concerning, especially given documentation of patient-inflicted violence against physicians. Health systems should be proactive in ensuring that the in-basket does not become a venue for physician abuse and cyberbullying,” the researchers wrote in JAMA Network Open.
“Posting reminders in EHR patient portals to use kind language when sending messages, applying filters for expletives or threatening words, and creating frameworks for identifying patients who frequently send negative messages are potential strategies for mitigating this risk.”
Using a form of artificial intelligence technology called natural language processing (NLP), researchers at the University of California, San Diego, analyzed the characteristics of more than 1.4 million emails received by the university’s physicians, 43% of them from patients. They specifically looked at the volume of messages, word count, and overall sentiment.
Whereas other studies have examined the growing burden of EHR messaging for doctors, this type of email sentiment analysis could help in creating solutions. Researchers say that one such solution could involve applying filters for expletives or threatening words. It also could help identify fixable health system issues that make patients so angry, the researchers say.
Among the emails from physicians to physicians, just over half reported burnout, which correlated to the following phrases: “I am beginning to burn out and have one or more symptoms of burnout” and “I feel completely burned out [and] am at the point where I may need to seek help.”
On average, physicians who reported burnout received a greater volume of patient messages. The odds of burnout were significantly higher among Hispanic/Latinx physicians and females. Physicians with more than 15 years of clinical practice had markedly lower burnout.
Despite physicians now spending more time on EHR in-basket tasks than they did before the pandemic, the study found no significant associations between message characteristics and burnout.
Data for the cross-sectional study were collected from multiple specialties from April to September 2020. Physicians then completed a survey and assessed their burnout on a 5-point scale. Of the 609 physician responses, approximately 49% of participants were women, 56% were White, and 64% worked in outpatient settings. About 70% of the doctors had been in practice for 15 years or less.
The sentiment score was based on word content as well as the use of negation, punctuation, degree modifiers, all caps, emoticons, emojis, and acronyms. Positive patient messages were more likely to convey gratitude and thanks, along with casual expressions, such as “fyi” and “lol.”
A version of this article first appeared on Medscape.com.
Among the emails, 43% were from patients; the remainder were mostly from other physicians or clinicians, or automated. The content of the messages wasn’t associated with doctor burnout, as the researchers had hypothesized. And only about 5% of the messages had negative sentiment.
But the researchers were struck by the hostility of that sentiment, displayed in messages like these that surely would be distressing for physicians to read:
“I hope and expect that you will spend eternity in he**. You are an abusive, nasty, cheap person.”
“Your office is full of liars, hypocrites and I will do everything in my power to prevent anyone from going to your bullsh** office again.”
About 5% of emails had an overall negative sentiment, with high-frequency words like “cancel,” “pain,” or “problem.” Among patient messages, 3% were negative and contained words and expletives suggesting hatred, hostility, or violence.
“F***” was the most common expletive used by patients.
Researchers provided examples of profanity-laced messages, including one patient who said, “I am so upset that I was told the blood work would include the gender of the baby. I have been waiting 5 [days] to find it, and it wasn’t even fu**ing tested!!!! What a disappointment in your office and the bullsh** I was told. I will be switching plans because this is sh**!”
Researchers also noted some high-frequency words associated with violence, such as “shoot,” “fight,” and “kill.”
“This is concerning, especially given documentation of patient-inflicted violence against physicians. Health systems should be proactive in ensuring that the in-basket does not become a venue for physician abuse and cyberbullying,” the researchers wrote in JAMA Network Open.
“Posting reminders in EHR patient portals to use kind language when sending messages, applying filters for expletives or threatening words, and creating frameworks for identifying patients who frequently send negative messages are potential strategies for mitigating this risk.”
Using a form of artificial intelligence technology called natural language processing (NLP), researchers at the University of California, San Diego, analyzed the characteristics of more than 1.4 million emails received by the university’s physicians, 43% of them from patients. They specifically looked at the volume of messages, word count, and overall sentiment.
Whereas other studies have examined the growing burden of EHR messaging for doctors, this type of email sentiment analysis could help in creating solutions. Researchers say that one such solution could involve applying filters for expletives or threatening words. It also could help identify fixable health system issues that make patients so angry, the researchers say.
Among the emails from physicians to physicians, just over half reported burnout, which correlated to the following phrases: “I am beginning to burn out and have one or more symptoms of burnout” and “I feel completely burned out [and] am at the point where I may need to seek help.”
On average, physicians who reported burnout received a greater volume of patient messages. The odds of burnout were significantly higher among Hispanic/Latinx physicians and females. Physicians with more than 15 years of clinical practice had markedly lower burnout.
Despite physicians now spending more time on EHR in-basket tasks than they did before the pandemic, the study found no significant associations between message characteristics and burnout.
Data for the cross-sectional study were collected from multiple specialties from April to September 2020. Physicians then completed a survey and assessed their burnout on a 5-point scale. Of the 609 physician responses, approximately 49% of participants were women, 56% were White, and 64% worked in outpatient settings. About 70% of the doctors had been in practice for 15 years or less.
The sentiment score was based on word content as well as the use of negation, punctuation, degree modifiers, all caps, emoticons, emojis, and acronyms. Positive patient messages were more likely to convey gratitude and thanks, along with casual expressions, such as “fyi” and “lol.”
A version of this article first appeared on Medscape.com.
Among the emails, 43% were from patients; the remainder were mostly from other physicians or clinicians, or automated. The content of the messages wasn’t associated with doctor burnout, as the researchers had hypothesized. And only about 5% of the messages had negative sentiment.
But the researchers were struck by the hostility of that sentiment, displayed in messages like these that surely would be distressing for physicians to read:
“I hope and expect that you will spend eternity in he**. You are an abusive, nasty, cheap person.”
“Your office is full of liars, hypocrites and I will do everything in my power to prevent anyone from going to your bullsh** office again.”
About 5% of emails had an overall negative sentiment, with high-frequency words like “cancel,” “pain,” or “problem.” Among patient messages, 3% were negative and contained words and expletives suggesting hatred, hostility, or violence.
“F***” was the most common expletive used by patients.
Researchers provided examples of profanity-laced messages, including one patient who said, “I am so upset that I was told the blood work would include the gender of the baby. I have been waiting 5 [days] to find it, and it wasn’t even fu**ing tested!!!! What a disappointment in your office and the bullsh** I was told. I will be switching plans because this is sh**!”
Researchers also noted some high-frequency words associated with violence, such as “shoot,” “fight,” and “kill.”
“This is concerning, especially given documentation of patient-inflicted violence against physicians. Health systems should be proactive in ensuring that the in-basket does not become a venue for physician abuse and cyberbullying,” the researchers wrote in JAMA Network Open.
“Posting reminders in EHR patient portals to use kind language when sending messages, applying filters for expletives or threatening words, and creating frameworks for identifying patients who frequently send negative messages are potential strategies for mitigating this risk.”
Using a form of artificial intelligence technology called natural language processing (NLP), researchers at the University of California, San Diego, analyzed the characteristics of more than 1.4 million emails received by the university’s physicians, 43% of them from patients. They specifically looked at the volume of messages, word count, and overall sentiment.
Whereas other studies have examined the growing burden of EHR messaging for doctors, this type of email sentiment analysis could help in creating solutions. Researchers say that one such solution could involve applying filters for expletives or threatening words. It also could help identify fixable health system issues that make patients so angry, the researchers say.
Among the emails from physicians to physicians, just over half reported burnout, which correlated to the following phrases: “I am beginning to burn out and have one or more symptoms of burnout” and “I feel completely burned out [and] am at the point where I may need to seek help.”
On average, physicians who reported burnout received a greater volume of patient messages. The odds of burnout were significantly higher among Hispanic/Latinx physicians and females. Physicians with more than 15 years of clinical practice had markedly lower burnout.
Despite physicians now spending more time on EHR in-basket tasks than they did before the pandemic, the study found no significant associations between message characteristics and burnout.
Data for the cross-sectional study were collected from multiple specialties from April to September 2020. Physicians then completed a survey and assessed their burnout on a 5-point scale. Of the 609 physician responses, approximately 49% of participants were women, 56% were White, and 64% worked in outpatient settings. About 70% of the doctors had been in practice for 15 years or less.
The sentiment score was based on word content as well as the use of negation, punctuation, degree modifiers, all caps, emoticons, emojis, and acronyms. Positive patient messages were more likely to convey gratitude and thanks, along with casual expressions, such as “fyi” and “lol.”
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Looking for a healthy meat substitute? Consider the potato
Boil ‘em, mash ‘em, include ‘em in a balanced diet
It’s kind of funny that, even though potatoes are vegetables and vegetables are generally considered to be healthy foods, not many people think of potatoes as being particularly good for you. And that’s hardly surprising since we usually either consume them in the form of French fries or potato chips, neither of which are known for their healthiness.
In fact, some previous research shows that potatoes are a food to avoid, particularly for people with insulin resistance. However, a new study from England goes against the grain and asserts that the potato is perfectly fine for insulin-resistant individuals and filled with valuable nutrients and health benefits. Which is great news for the state of Idaho and the potato organization funding the research. Of course there’s a potato organization.
For the study, a group of obese, overweight, or insulin-resistant individuals received a diet of either beans, peas, and meat or fish or white potatoes with meat or fish for 8 weeks; both diets were heavy in fruits and vegetables and both diets replaced about 40% of typical meat consumption with either beans and peas or potatoes. By the end of the study, those on the potato diet experienced health benefits equivalent to those on the bean and pea diet, including losing roughly equivalent amounts of weight and similarly reducing the body’s insulin response.
The researchers noted that, because people tend to eat the same amount of food no matter what, replacing something like meat with dense, low-calorie potatoes meant study participants could eat normally yet consume much fewer calories. So you could make a delicious, healthy stew without the brace of conies and the nice fish, which would make Smeagol very happy.
You won’t have ‘monkeypox’ to kick around anymore
It’s true. No more monkeypox. It’s gone. It’s history. Adios. The World Health Organization said that the disease formerly known as monkeypox will now be called mpox. What? You didn’t think it had been cured, did you? You did? Really? Silly readers.
“Mpox will become a preferred term, replacing monkeypox, after a transition period of 1 year. This serves to mitigate the concerns raised by experts about confusion caused by a name change in the midst of a global outbreak,” WHO said in a statement announcing the change.
The stigma attached to the name was the main problem. New York City Health Commissioner Dr. Ashwin Vasan had sent a letter to WHO earlier this year, according to CNN, saying that there was “growing concern for the potentially devastating and stigmatizing effects that the messaging around the ‘monkeypox’ virus can have on … vulnerable communities.”
We here at LOTME applaud the fight against stigmas of any sort, but we sensed there was more to this name change business, so our dedicated team of investigative journalists went into action. Sure enough, while rooting through WHO Director-General Tedros Adhanom Ghebreyesus’s garbage, we found a list of the names that had been rejected in favor of mpox:
- K-pop (already taken)
- Keeping up with the Kardashi-pox
- Trumpox
- Pox the magic dragon
- Monkey plague (didn’t really solve the problem)
- Hockey pox
- Mission mpoxible
- Jurassic Pox
- The pox that refreshes
- Debbie
Feet catch what the ears miss
The spectrum of frequencies that can be heard by human ears varies from person to person. Then there’s the matter of personal taste in music and volume level. But what really gets people moving? A new study shows that it’s more about the frequency of the sound than the volume.
For the study, participants at a concert by electronic music duo Orphx at LIVELab – a research performance center on the McMaster University campus in Hamilton, Ont., that was specifically designed to study music and dance – filled out questionnaires before and after the show. They also wore motion-capture headbands to detect their movement throughout the concert. During the show the researchers turned very-low-frequency (VLF) sounds (8-37 Hz) on and off every 2.5 minutes. Movement speed was calculated during on and off periods.
Although the effects of subliminal messaging aren’t new, past studies have shown that participants were mostly aware of the messaging. In this study, the researchers found that the subjects’ movements increased by 11.8% when the VLF sounds were on, but without their awareness. The researchers and the participants attributed movement to the bass, as lower pitches tend to elicit stronger neural responses and thus movement, compared with higher pitches.
“Our whole sense of the beat is mediated by the vestibular system but nobody’s really, I think, effectively confirmed that,” Jonathan Cannon, an assistant professor of psychology, neuroscience, and behavior at McMaster who not involved in the study, told Live Science.
Not to say this study didn’t have its limitations, such as the effect of the surrounding crowd or vibrations of the floor influencing the need to dance. But it definitely makes you wonder about what’s actually playing in your favorite song.
Uncle Leonid wants you
Do you like to travel? Are you a bit of a thrill seeker? Do you have any extra socks? If you’re a physician who answered yes to those three questions, then we’ve got an opportunity for you.
Leonid Slutsky, leader of Russia’s populist Liberal Democratic Party and chairman of the foreign relations committee in the lower house of Russia’s parliament – yes, that Leonid Slutsky – recently made a bit of a recruiting pitch, although that’s not how ABC News described it.
Mr. Slutsky, a strong supporter of his country’s war against Ukraine, recently told the mothers of Russian soldiers “that the whole world is watching us. We are the largest state and when we do not have socks, shorts, doctors, intelligence, communications, or simply care for our children, questions arise that will be very difficult to answer.”
It’s probably not what he meant, but the lack of intelligence is pretty clear.
Boil ‘em, mash ‘em, include ‘em in a balanced diet
It’s kind of funny that, even though potatoes are vegetables and vegetables are generally considered to be healthy foods, not many people think of potatoes as being particularly good for you. And that’s hardly surprising since we usually either consume them in the form of French fries or potato chips, neither of which are known for their healthiness.
In fact, some previous research shows that potatoes are a food to avoid, particularly for people with insulin resistance. However, a new study from England goes against the grain and asserts that the potato is perfectly fine for insulin-resistant individuals and filled with valuable nutrients and health benefits. Which is great news for the state of Idaho and the potato organization funding the research. Of course there’s a potato organization.
For the study, a group of obese, overweight, or insulin-resistant individuals received a diet of either beans, peas, and meat or fish or white potatoes with meat or fish for 8 weeks; both diets were heavy in fruits and vegetables and both diets replaced about 40% of typical meat consumption with either beans and peas or potatoes. By the end of the study, those on the potato diet experienced health benefits equivalent to those on the bean and pea diet, including losing roughly equivalent amounts of weight and similarly reducing the body’s insulin response.
The researchers noted that, because people tend to eat the same amount of food no matter what, replacing something like meat with dense, low-calorie potatoes meant study participants could eat normally yet consume much fewer calories. So you could make a delicious, healthy stew without the brace of conies and the nice fish, which would make Smeagol very happy.
You won’t have ‘monkeypox’ to kick around anymore
It’s true. No more monkeypox. It’s gone. It’s history. Adios. The World Health Organization said that the disease formerly known as monkeypox will now be called mpox. What? You didn’t think it had been cured, did you? You did? Really? Silly readers.
“Mpox will become a preferred term, replacing monkeypox, after a transition period of 1 year. This serves to mitigate the concerns raised by experts about confusion caused by a name change in the midst of a global outbreak,” WHO said in a statement announcing the change.
The stigma attached to the name was the main problem. New York City Health Commissioner Dr. Ashwin Vasan had sent a letter to WHO earlier this year, according to CNN, saying that there was “growing concern for the potentially devastating and stigmatizing effects that the messaging around the ‘monkeypox’ virus can have on … vulnerable communities.”
We here at LOTME applaud the fight against stigmas of any sort, but we sensed there was more to this name change business, so our dedicated team of investigative journalists went into action. Sure enough, while rooting through WHO Director-General Tedros Adhanom Ghebreyesus’s garbage, we found a list of the names that had been rejected in favor of mpox:
- K-pop (already taken)
- Keeping up with the Kardashi-pox
- Trumpox
- Pox the magic dragon
- Monkey plague (didn’t really solve the problem)
- Hockey pox
- Mission mpoxible
- Jurassic Pox
- The pox that refreshes
- Debbie
Feet catch what the ears miss
The spectrum of frequencies that can be heard by human ears varies from person to person. Then there’s the matter of personal taste in music and volume level. But what really gets people moving? A new study shows that it’s more about the frequency of the sound than the volume.
For the study, participants at a concert by electronic music duo Orphx at LIVELab – a research performance center on the McMaster University campus in Hamilton, Ont., that was specifically designed to study music and dance – filled out questionnaires before and after the show. They also wore motion-capture headbands to detect their movement throughout the concert. During the show the researchers turned very-low-frequency (VLF) sounds (8-37 Hz) on and off every 2.5 minutes. Movement speed was calculated during on and off periods.
Although the effects of subliminal messaging aren’t new, past studies have shown that participants were mostly aware of the messaging. In this study, the researchers found that the subjects’ movements increased by 11.8% when the VLF sounds were on, but without their awareness. The researchers and the participants attributed movement to the bass, as lower pitches tend to elicit stronger neural responses and thus movement, compared with higher pitches.
“Our whole sense of the beat is mediated by the vestibular system but nobody’s really, I think, effectively confirmed that,” Jonathan Cannon, an assistant professor of psychology, neuroscience, and behavior at McMaster who not involved in the study, told Live Science.
Not to say this study didn’t have its limitations, such as the effect of the surrounding crowd or vibrations of the floor influencing the need to dance. But it definitely makes you wonder about what’s actually playing in your favorite song.
Uncle Leonid wants you
Do you like to travel? Are you a bit of a thrill seeker? Do you have any extra socks? If you’re a physician who answered yes to those three questions, then we’ve got an opportunity for you.
Leonid Slutsky, leader of Russia’s populist Liberal Democratic Party and chairman of the foreign relations committee in the lower house of Russia’s parliament – yes, that Leonid Slutsky – recently made a bit of a recruiting pitch, although that’s not how ABC News described it.
Mr. Slutsky, a strong supporter of his country’s war against Ukraine, recently told the mothers of Russian soldiers “that the whole world is watching us. We are the largest state and when we do not have socks, shorts, doctors, intelligence, communications, or simply care for our children, questions arise that will be very difficult to answer.”
It’s probably not what he meant, but the lack of intelligence is pretty clear.
Boil ‘em, mash ‘em, include ‘em in a balanced diet
It’s kind of funny that, even though potatoes are vegetables and vegetables are generally considered to be healthy foods, not many people think of potatoes as being particularly good for you. And that’s hardly surprising since we usually either consume them in the form of French fries or potato chips, neither of which are known for their healthiness.
In fact, some previous research shows that potatoes are a food to avoid, particularly for people with insulin resistance. However, a new study from England goes against the grain and asserts that the potato is perfectly fine for insulin-resistant individuals and filled with valuable nutrients and health benefits. Which is great news for the state of Idaho and the potato organization funding the research. Of course there’s a potato organization.
For the study, a group of obese, overweight, or insulin-resistant individuals received a diet of either beans, peas, and meat or fish or white potatoes with meat or fish for 8 weeks; both diets were heavy in fruits and vegetables and both diets replaced about 40% of typical meat consumption with either beans and peas or potatoes. By the end of the study, those on the potato diet experienced health benefits equivalent to those on the bean and pea diet, including losing roughly equivalent amounts of weight and similarly reducing the body’s insulin response.
The researchers noted that, because people tend to eat the same amount of food no matter what, replacing something like meat with dense, low-calorie potatoes meant study participants could eat normally yet consume much fewer calories. So you could make a delicious, healthy stew without the brace of conies and the nice fish, which would make Smeagol very happy.
You won’t have ‘monkeypox’ to kick around anymore
It’s true. No more monkeypox. It’s gone. It’s history. Adios. The World Health Organization said that the disease formerly known as monkeypox will now be called mpox. What? You didn’t think it had been cured, did you? You did? Really? Silly readers.
“Mpox will become a preferred term, replacing monkeypox, after a transition period of 1 year. This serves to mitigate the concerns raised by experts about confusion caused by a name change in the midst of a global outbreak,” WHO said in a statement announcing the change.
The stigma attached to the name was the main problem. New York City Health Commissioner Dr. Ashwin Vasan had sent a letter to WHO earlier this year, according to CNN, saying that there was “growing concern for the potentially devastating and stigmatizing effects that the messaging around the ‘monkeypox’ virus can have on … vulnerable communities.”
We here at LOTME applaud the fight against stigmas of any sort, but we sensed there was more to this name change business, so our dedicated team of investigative journalists went into action. Sure enough, while rooting through WHO Director-General Tedros Adhanom Ghebreyesus’s garbage, we found a list of the names that had been rejected in favor of mpox:
- K-pop (already taken)
- Keeping up with the Kardashi-pox
- Trumpox
- Pox the magic dragon
- Monkey plague (didn’t really solve the problem)
- Hockey pox
- Mission mpoxible
- Jurassic Pox
- The pox that refreshes
- Debbie
Feet catch what the ears miss
The spectrum of frequencies that can be heard by human ears varies from person to person. Then there’s the matter of personal taste in music and volume level. But what really gets people moving? A new study shows that it’s more about the frequency of the sound than the volume.
For the study, participants at a concert by electronic music duo Orphx at LIVELab – a research performance center on the McMaster University campus in Hamilton, Ont., that was specifically designed to study music and dance – filled out questionnaires before and after the show. They also wore motion-capture headbands to detect their movement throughout the concert. During the show the researchers turned very-low-frequency (VLF) sounds (8-37 Hz) on and off every 2.5 minutes. Movement speed was calculated during on and off periods.
Although the effects of subliminal messaging aren’t new, past studies have shown that participants were mostly aware of the messaging. In this study, the researchers found that the subjects’ movements increased by 11.8% when the VLF sounds were on, but without their awareness. The researchers and the participants attributed movement to the bass, as lower pitches tend to elicit stronger neural responses and thus movement, compared with higher pitches.
“Our whole sense of the beat is mediated by the vestibular system but nobody’s really, I think, effectively confirmed that,” Jonathan Cannon, an assistant professor of psychology, neuroscience, and behavior at McMaster who not involved in the study, told Live Science.
Not to say this study didn’t have its limitations, such as the effect of the surrounding crowd or vibrations of the floor influencing the need to dance. But it definitely makes you wonder about what’s actually playing in your favorite song.
Uncle Leonid wants you
Do you like to travel? Are you a bit of a thrill seeker? Do you have any extra socks? If you’re a physician who answered yes to those three questions, then we’ve got an opportunity for you.
Leonid Slutsky, leader of Russia’s populist Liberal Democratic Party and chairman of the foreign relations committee in the lower house of Russia’s parliament – yes, that Leonid Slutsky – recently made a bit of a recruiting pitch, although that’s not how ABC News described it.
Mr. Slutsky, a strong supporter of his country’s war against Ukraine, recently told the mothers of Russian soldiers “that the whole world is watching us. We are the largest state and when we do not have socks, shorts, doctors, intelligence, communications, or simply care for our children, questions arise that will be very difficult to answer.”
It’s probably not what he meant, but the lack of intelligence is pretty clear.
Rates of health care use after bariatric surgery in teens
Researchers found significantly lower rates of both emergency department (ED) use and hospitalization 5 years after sleeve gastrectomy compared with gastric bypass, and similarly low rates of adverse events.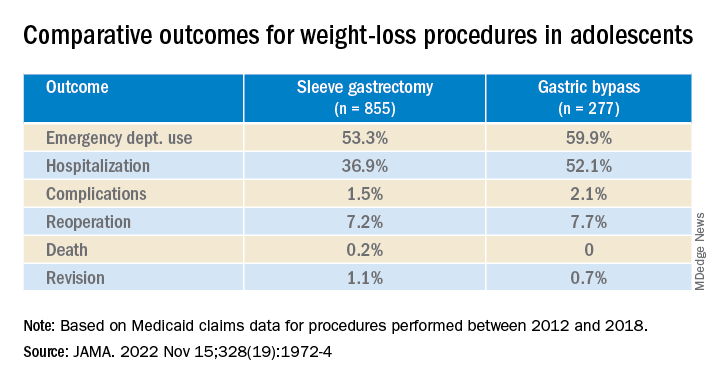
The study, by researchers with the department of surgery and Center for Health Outcomes and Policy, University of Michigan, Ann Arbor, was published in JAMA.
Studies have shown that sleeve gastrectomy and gastric bypass both lead to significant weight loss and are associated with low complication rates among adolescents with severe obesity.
Until now, however, comparative outcomes for these two weight-loss procedures have not been described for adolescents insured by Medicaid, the largest insurer of adolescents in the United States.
Using Medicaid claims data, Ryan Howard, MD, and colleagues identified 855 adolescents who underwent sleeve gastrectomy and 277 who underwent Roux-en-Y gastric bypass between 2012 and 2018.
Adolescents in both groups were about 18 years old on average at the time of surgery, and about three-quarters were female.
Sleeve gastrectomy became more common over the study period. The annual percentage of sleeve gastrectomy relative to gastric bypass increased from 48.8% in 2012 to 82.6% in 2018.
There was no significant difference in rates of complications (P = .31) or reoperation (P = .78), defined as abdominal operation potentially related to the index procedure, including biliary procedures and abdominal wall, internal, and paraesophageal hernia repair.
Researchers also found no difference between sleeve gastrectomy and gastric bypass in rates of death (P = .42) or revision (P = .63), which included any operation that directly modified the index procedure.
The results “may help inform the treatment of severe obesity in adolescents insured by Medicaid, although future studies should also evaluate long-term weight loss and comorbidity resolution in this population,” Dr. Howard and colleagues write.
They caution that their analysis is subject to selection bias because patient characteristics may influence the choice of procedure, although appropriate statistical adjustment was used.
Other limitations include the small sample size, which increases the possibility of type II error; the relatively short follow-up period; and the inability to directly attribute outcomes to the index procedure.
Funding for the study was provided by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers found significantly lower rates of both emergency department (ED) use and hospitalization 5 years after sleeve gastrectomy compared with gastric bypass, and similarly low rates of adverse events.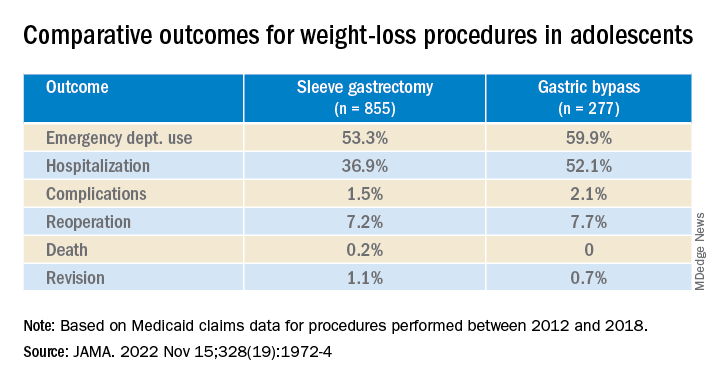
The study, by researchers with the department of surgery and Center for Health Outcomes and Policy, University of Michigan, Ann Arbor, was published in JAMA.
Studies have shown that sleeve gastrectomy and gastric bypass both lead to significant weight loss and are associated with low complication rates among adolescents with severe obesity.
Until now, however, comparative outcomes for these two weight-loss procedures have not been described for adolescents insured by Medicaid, the largest insurer of adolescents in the United States.
Using Medicaid claims data, Ryan Howard, MD, and colleagues identified 855 adolescents who underwent sleeve gastrectomy and 277 who underwent Roux-en-Y gastric bypass between 2012 and 2018.
Adolescents in both groups were about 18 years old on average at the time of surgery, and about three-quarters were female.
Sleeve gastrectomy became more common over the study period. The annual percentage of sleeve gastrectomy relative to gastric bypass increased from 48.8% in 2012 to 82.6% in 2018.
There was no significant difference in rates of complications (P = .31) or reoperation (P = .78), defined as abdominal operation potentially related to the index procedure, including biliary procedures and abdominal wall, internal, and paraesophageal hernia repair.
Researchers also found no difference between sleeve gastrectomy and gastric bypass in rates of death (P = .42) or revision (P = .63), which included any operation that directly modified the index procedure.
The results “may help inform the treatment of severe obesity in adolescents insured by Medicaid, although future studies should also evaluate long-term weight loss and comorbidity resolution in this population,” Dr. Howard and colleagues write.
They caution that their analysis is subject to selection bias because patient characteristics may influence the choice of procedure, although appropriate statistical adjustment was used.
Other limitations include the small sample size, which increases the possibility of type II error; the relatively short follow-up period; and the inability to directly attribute outcomes to the index procedure.
Funding for the study was provided by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers found significantly lower rates of both emergency department (ED) use and hospitalization 5 years after sleeve gastrectomy compared with gastric bypass, and similarly low rates of adverse events.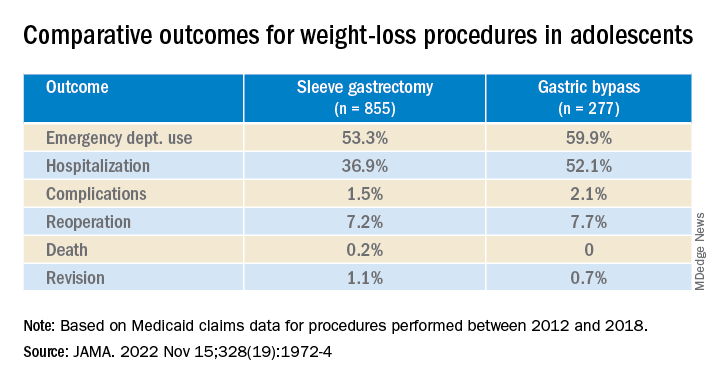
The study, by researchers with the department of surgery and Center for Health Outcomes and Policy, University of Michigan, Ann Arbor, was published in JAMA.
Studies have shown that sleeve gastrectomy and gastric bypass both lead to significant weight loss and are associated with low complication rates among adolescents with severe obesity.
Until now, however, comparative outcomes for these two weight-loss procedures have not been described for adolescents insured by Medicaid, the largest insurer of adolescents in the United States.
Using Medicaid claims data, Ryan Howard, MD, and colleagues identified 855 adolescents who underwent sleeve gastrectomy and 277 who underwent Roux-en-Y gastric bypass between 2012 and 2018.
Adolescents in both groups were about 18 years old on average at the time of surgery, and about three-quarters were female.
Sleeve gastrectomy became more common over the study period. The annual percentage of sleeve gastrectomy relative to gastric bypass increased from 48.8% in 2012 to 82.6% in 2018.
There was no significant difference in rates of complications (P = .31) or reoperation (P = .78), defined as abdominal operation potentially related to the index procedure, including biliary procedures and abdominal wall, internal, and paraesophageal hernia repair.
Researchers also found no difference between sleeve gastrectomy and gastric bypass in rates of death (P = .42) or revision (P = .63), which included any operation that directly modified the index procedure.
The results “may help inform the treatment of severe obesity in adolescents insured by Medicaid, although future studies should also evaluate long-term weight loss and comorbidity resolution in this population,” Dr. Howard and colleagues write.
They caution that their analysis is subject to selection bias because patient characteristics may influence the choice of procedure, although appropriate statistical adjustment was used.
Other limitations include the small sample size, which increases the possibility of type II error; the relatively short follow-up period; and the inability to directly attribute outcomes to the index procedure.
Funding for the study was provided by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA
Don’t call me ‘Dr.,’ say some physicians – but most prefer the title
When Mark Cucuzzella, MD, meets a new patient at the West Virginia Medical School clinic, he introduces himself as “Mark.” For one thing, says Dr. Cucuzzella, his last name is a mouthful. For another, the 56-year-old general practitioner asserts that getting on a first-name basis with his patients is integral to delivering the best care.
“I’m trying to break down the old paternalistic barriers of the doctor/patient relationship,” he says. “Titles create an environment where the doctors are making all the decisions and not involving the patient in any course of action.”
Aniruddh Setya, MD, has a different take on informality between patients and doctors: It’s not OK. “I am not your friend,” says the 35-year-old pediatrician from Florida-based KIDZ Medical Services. “There has to be a level of respect for the education and accomplishment of being a physician.”
published in JAMA Network Open. But that doesn’t mean most physicians support the practice. In fact, some doctors contend that it can be harmful, particularly to female physicians.
“My concern is that untitling (so termed by Amy Diehl, PhD, and Leanne Dzubinski, PhD) intrudes upon important professional boundaries and might be correlated with diminishing the value of someone’s time,” says Leah Witt, MD, a geriatrician at UCSF Health, San Francisco. Dr. Witt, along with colleague Lekshmi Santhosh, MD, a pulmonologist, offered commentary on the study results. “Studies have shown that women physicians get more patient portal messages, spend more time in the electronic health record, and have longer visits,” Dr. Witt said. “Dr. Santhosh and I wonder if untitling is a signifier of this diminished value of our time, and an assumption of increased ease of access leading to this higher workload.”
To compile the results reported in JAMA Network Open, Mayo Clinic researchers analyzed more than 90,000 emails from patients to doctors over the course of 3 years, beginning in 2018. Of those emails, more than 32% included the physician’s first name in greeting or salutation. For women physicians, the odds were twice as high that their titles would be omitted in the correspondence. The same holds true for doctors of osteopathic medicine (DOs) compared with MDs, and primary care physicians had similar odds for a title drop compared with specialists.
Dr. Witt says the findings are not surprising. “They match my experience as a woman in medicine, as Dr. Santhosh and I write in our commentary,” she says. “We think the findings could easily be replicated at other centers.”
Indeed, research on 321 speaker introductions at a medical rounds found that when female physicians introduced other physicians, they usually applied the doctor title. When the job of introducing colleagues fell to male physicians, however, the stats fell to 72.4% for male peers and only 49.2% when introducing female peers.
The Mayo Clinic study authors identified the pitfalls of patients who informally address their doctors. They wrote, “Untitling may have a negative impact on physicians, demonstrate lack of respect, and can lead to reduction in formality of the physician/patient relationship or workplace.”
Physician preferences vary
Although the results of the Mayo Clinic analysis didn’t and couldn’t address physician sentiments on patient informality, Dr. Setya observes that American culture is becoming less formal. “I’ve been practicing for over 10 years, and the number of people who consider doctors as equals is growing,” he says. “This has been particularly true over the last couple of years.”
This change was documented in 2015. Add in the pandemic and an entire society that is now accustomed to working from home in sweats, and it’s not a stretch to understand why some patients have become less formal in many settings. The 2015 article noted, however, that most physicians prefer to keep titles in the mix.
Perhaps most troublesome, says Dr. Setya, is that patients forgo asking whether it’s OK to use his first name and simply assume it’s acceptable. “It bothers me,” he says. “I became a doctor for more than the money.”
He suspects that his cultural background (Dr. Setya is of Indian descent) plays a role in how strongly he feels about patient-doctor informality. “As a British colony, Indian culture dictates that you pay respect to elders and to accomplishment,” he points out. “America is far looser when it comes to salutations.”
Dr. Cucuzzella largely agrees with Dr. Setya, but has a different view of the role culture plays in how physicians prefer to be addressed. “If your last name is difficult to pronounce, it can put the patient at ease if you give them an option,” he says. “I like my patients to feel comfortable and have a friendly conversation, so I don’t ask them to try to manage my last name.”
When patients revert to using Dr. Cucuzzella’s last name and title, this often breaks down along generational lines, Dr. Cucuzzella has found: Older patients might drop his title, whereas younger patients might keep it as a sign of respect. In some cases, Dr. Cucuzzella tries to bridge this gap, and offers the option of “Dr. Mark.” In his small West Virginia community, this is how people often refer to him.
Dr. Setya says that most of the older physicians he works with still prefer that patients and younger colleagues use their title, but he has witnessed exceptions to this. “My boss in residence hated to be called ‘Sir’ or ‘Doctor,’ ” he says. “In a situation like that, it is reasonable to ask, ‘How can I address you?’ But it has to be mutually agreed upon.”
Dr. Cucuzzella cites informality as the preferred mode for older patients. “If I have a 70-year-old patient, it seems natural they shouldn’t use my title,” he says. “They are worthy of equality in the community. If I’m talking to a retired CEO or state delegate, it’s uncomfortable if they call me doctor.”
Moreover, Dr. Cucuzzella maintains that establishing a less formal environment with patients leads to better outcomes. “Shared decision-making is a basic human right,” he says. “In 2022, doctors shouldn’t make decisions without patient input, unless it’s an emergency situation. Removing the title barriers makes that easier.”
How to handle informality
If you fall more in line with Dr. Setya, there are strategies you can use to try to keep formality in your doctor-patient relationships. Dr. Setya’s approach is indirect. “I don’t correct a patient if they use my first name, because that might seem hostile,” he says. “But I alert them in the way I address them back. A Sir, a Mrs., or a Mr. needs to go both ways.”
This particularly holds true in pediatrics, Dr. Setya has found. He has witnessed many colleagues addressing parents as “Mommy and Daddy,” something he says lacks respect and sets too informal a tone. “It’s almost universal that parents don’t like that, and we need to act accordingly.”
Dr. Witt also avoids directly correcting patients, but struggles when they drop her title. “The standard signature I use to sign every patient portal message I respond to includes my first and last name and credentials,” she says. “I maintain formality in most circumstances with that standard reply.”
Beneath the surface, however, Dr. Witt wishes it were easier. “I have struggled with answering the question, ‘Is it OK if I call you Leah?’ she says. “I want to keep our interaction anchored in professionalism without sacrificing the warmth I think is important to a productive patient-physician relationship. For this reason, I tend to say yes to this request, even though I’d rather patients didn’t make such requests.”
In the Fast Company article by Amy Diehl, PhD, and Leanne Dzubinski, PhD, on the topic of untitling professional women, the authors suggest several actions, beginning with leadership that sets expectations on the topic. They also suggest that physicians use polite corrections if patients untitle them. Supplying positive reinforcement when patients include your title can help, too. If all else fails, you can call out the offensive untitling. More often than not, especially with female physicians, the patient is demonstrating an unconscious bias rather than something deliberate.
Opinions vary on the topic of untitling, and ultimately each physician must make the decision for themselves. But creating informal cultures in an organization can have unintended consequences, especially for female peers.
Says Dr. Witt, “We all want to give our patients the best care we can, but professional boundaries are critical to time management, equitable care, and maintaining work-life balance. I would love to see a study that examines untitling by self-reported race and/or ethnicity of physicians, because we know that women of color experience higher rates of burnout and depression, and I wonder if untitling may be part of this.”
A version of this article first appeared on Medscape.com.
When Mark Cucuzzella, MD, meets a new patient at the West Virginia Medical School clinic, he introduces himself as “Mark.” For one thing, says Dr. Cucuzzella, his last name is a mouthful. For another, the 56-year-old general practitioner asserts that getting on a first-name basis with his patients is integral to delivering the best care.
“I’m trying to break down the old paternalistic barriers of the doctor/patient relationship,” he says. “Titles create an environment where the doctors are making all the decisions and not involving the patient in any course of action.”
Aniruddh Setya, MD, has a different take on informality between patients and doctors: It’s not OK. “I am not your friend,” says the 35-year-old pediatrician from Florida-based KIDZ Medical Services. “There has to be a level of respect for the education and accomplishment of being a physician.”
published in JAMA Network Open. But that doesn’t mean most physicians support the practice. In fact, some doctors contend that it can be harmful, particularly to female physicians.
“My concern is that untitling (so termed by Amy Diehl, PhD, and Leanne Dzubinski, PhD) intrudes upon important professional boundaries and might be correlated with diminishing the value of someone’s time,” says Leah Witt, MD, a geriatrician at UCSF Health, San Francisco. Dr. Witt, along with colleague Lekshmi Santhosh, MD, a pulmonologist, offered commentary on the study results. “Studies have shown that women physicians get more patient portal messages, spend more time in the electronic health record, and have longer visits,” Dr. Witt said. “Dr. Santhosh and I wonder if untitling is a signifier of this diminished value of our time, and an assumption of increased ease of access leading to this higher workload.”
To compile the results reported in JAMA Network Open, Mayo Clinic researchers analyzed more than 90,000 emails from patients to doctors over the course of 3 years, beginning in 2018. Of those emails, more than 32% included the physician’s first name in greeting or salutation. For women physicians, the odds were twice as high that their titles would be omitted in the correspondence. The same holds true for doctors of osteopathic medicine (DOs) compared with MDs, and primary care physicians had similar odds for a title drop compared with specialists.
Dr. Witt says the findings are not surprising. “They match my experience as a woman in medicine, as Dr. Santhosh and I write in our commentary,” she says. “We think the findings could easily be replicated at other centers.”
Indeed, research on 321 speaker introductions at a medical rounds found that when female physicians introduced other physicians, they usually applied the doctor title. When the job of introducing colleagues fell to male physicians, however, the stats fell to 72.4% for male peers and only 49.2% when introducing female peers.
The Mayo Clinic study authors identified the pitfalls of patients who informally address their doctors. They wrote, “Untitling may have a negative impact on physicians, demonstrate lack of respect, and can lead to reduction in formality of the physician/patient relationship or workplace.”
Physician preferences vary
Although the results of the Mayo Clinic analysis didn’t and couldn’t address physician sentiments on patient informality, Dr. Setya observes that American culture is becoming less formal. “I’ve been practicing for over 10 years, and the number of people who consider doctors as equals is growing,” he says. “This has been particularly true over the last couple of years.”
This change was documented in 2015. Add in the pandemic and an entire society that is now accustomed to working from home in sweats, and it’s not a stretch to understand why some patients have become less formal in many settings. The 2015 article noted, however, that most physicians prefer to keep titles in the mix.
Perhaps most troublesome, says Dr. Setya, is that patients forgo asking whether it’s OK to use his first name and simply assume it’s acceptable. “It bothers me,” he says. “I became a doctor for more than the money.”
He suspects that his cultural background (Dr. Setya is of Indian descent) plays a role in how strongly he feels about patient-doctor informality. “As a British colony, Indian culture dictates that you pay respect to elders and to accomplishment,” he points out. “America is far looser when it comes to salutations.”
Dr. Cucuzzella largely agrees with Dr. Setya, but has a different view of the role culture plays in how physicians prefer to be addressed. “If your last name is difficult to pronounce, it can put the patient at ease if you give them an option,” he says. “I like my patients to feel comfortable and have a friendly conversation, so I don’t ask them to try to manage my last name.”
When patients revert to using Dr. Cucuzzella’s last name and title, this often breaks down along generational lines, Dr. Cucuzzella has found: Older patients might drop his title, whereas younger patients might keep it as a sign of respect. In some cases, Dr. Cucuzzella tries to bridge this gap, and offers the option of “Dr. Mark.” In his small West Virginia community, this is how people often refer to him.
Dr. Setya says that most of the older physicians he works with still prefer that patients and younger colleagues use their title, but he has witnessed exceptions to this. “My boss in residence hated to be called ‘Sir’ or ‘Doctor,’ ” he says. “In a situation like that, it is reasonable to ask, ‘How can I address you?’ But it has to be mutually agreed upon.”
Dr. Cucuzzella cites informality as the preferred mode for older patients. “If I have a 70-year-old patient, it seems natural they shouldn’t use my title,” he says. “They are worthy of equality in the community. If I’m talking to a retired CEO or state delegate, it’s uncomfortable if they call me doctor.”
Moreover, Dr. Cucuzzella maintains that establishing a less formal environment with patients leads to better outcomes. “Shared decision-making is a basic human right,” he says. “In 2022, doctors shouldn’t make decisions without patient input, unless it’s an emergency situation. Removing the title barriers makes that easier.”
How to handle informality
If you fall more in line with Dr. Setya, there are strategies you can use to try to keep formality in your doctor-patient relationships. Dr. Setya’s approach is indirect. “I don’t correct a patient if they use my first name, because that might seem hostile,” he says. “But I alert them in the way I address them back. A Sir, a Mrs., or a Mr. needs to go both ways.”
This particularly holds true in pediatrics, Dr. Setya has found. He has witnessed many colleagues addressing parents as “Mommy and Daddy,” something he says lacks respect and sets too informal a tone. “It’s almost universal that parents don’t like that, and we need to act accordingly.”
Dr. Witt also avoids directly correcting patients, but struggles when they drop her title. “The standard signature I use to sign every patient portal message I respond to includes my first and last name and credentials,” she says. “I maintain formality in most circumstances with that standard reply.”
Beneath the surface, however, Dr. Witt wishes it were easier. “I have struggled with answering the question, ‘Is it OK if I call you Leah?’ she says. “I want to keep our interaction anchored in professionalism without sacrificing the warmth I think is important to a productive patient-physician relationship. For this reason, I tend to say yes to this request, even though I’d rather patients didn’t make such requests.”
In the Fast Company article by Amy Diehl, PhD, and Leanne Dzubinski, PhD, on the topic of untitling professional women, the authors suggest several actions, beginning with leadership that sets expectations on the topic. They also suggest that physicians use polite corrections if patients untitle them. Supplying positive reinforcement when patients include your title can help, too. If all else fails, you can call out the offensive untitling. More often than not, especially with female physicians, the patient is demonstrating an unconscious bias rather than something deliberate.
Opinions vary on the topic of untitling, and ultimately each physician must make the decision for themselves. But creating informal cultures in an organization can have unintended consequences, especially for female peers.
Says Dr. Witt, “We all want to give our patients the best care we can, but professional boundaries are critical to time management, equitable care, and maintaining work-life balance. I would love to see a study that examines untitling by self-reported race and/or ethnicity of physicians, because we know that women of color experience higher rates of burnout and depression, and I wonder if untitling may be part of this.”
A version of this article first appeared on Medscape.com.
When Mark Cucuzzella, MD, meets a new patient at the West Virginia Medical School clinic, he introduces himself as “Mark.” For one thing, says Dr. Cucuzzella, his last name is a mouthful. For another, the 56-year-old general practitioner asserts that getting on a first-name basis with his patients is integral to delivering the best care.
“I’m trying to break down the old paternalistic barriers of the doctor/patient relationship,” he says. “Titles create an environment where the doctors are making all the decisions and not involving the patient in any course of action.”
Aniruddh Setya, MD, has a different take on informality between patients and doctors: It’s not OK. “I am not your friend,” says the 35-year-old pediatrician from Florida-based KIDZ Medical Services. “There has to be a level of respect for the education and accomplishment of being a physician.”
published in JAMA Network Open. But that doesn’t mean most physicians support the practice. In fact, some doctors contend that it can be harmful, particularly to female physicians.
“My concern is that untitling (so termed by Amy Diehl, PhD, and Leanne Dzubinski, PhD) intrudes upon important professional boundaries and might be correlated with diminishing the value of someone’s time,” says Leah Witt, MD, a geriatrician at UCSF Health, San Francisco. Dr. Witt, along with colleague Lekshmi Santhosh, MD, a pulmonologist, offered commentary on the study results. “Studies have shown that women physicians get more patient portal messages, spend more time in the electronic health record, and have longer visits,” Dr. Witt said. “Dr. Santhosh and I wonder if untitling is a signifier of this diminished value of our time, and an assumption of increased ease of access leading to this higher workload.”
To compile the results reported in JAMA Network Open, Mayo Clinic researchers analyzed more than 90,000 emails from patients to doctors over the course of 3 years, beginning in 2018. Of those emails, more than 32% included the physician’s first name in greeting or salutation. For women physicians, the odds were twice as high that their titles would be omitted in the correspondence. The same holds true for doctors of osteopathic medicine (DOs) compared with MDs, and primary care physicians had similar odds for a title drop compared with specialists.
Dr. Witt says the findings are not surprising. “They match my experience as a woman in medicine, as Dr. Santhosh and I write in our commentary,” she says. “We think the findings could easily be replicated at other centers.”
Indeed, research on 321 speaker introductions at a medical rounds found that when female physicians introduced other physicians, they usually applied the doctor title. When the job of introducing colleagues fell to male physicians, however, the stats fell to 72.4% for male peers and only 49.2% when introducing female peers.
The Mayo Clinic study authors identified the pitfalls of patients who informally address their doctors. They wrote, “Untitling may have a negative impact on physicians, demonstrate lack of respect, and can lead to reduction in formality of the physician/patient relationship or workplace.”
Physician preferences vary
Although the results of the Mayo Clinic analysis didn’t and couldn’t address physician sentiments on patient informality, Dr. Setya observes that American culture is becoming less formal. “I’ve been practicing for over 10 years, and the number of people who consider doctors as equals is growing,” he says. “This has been particularly true over the last couple of years.”
This change was documented in 2015. Add in the pandemic and an entire society that is now accustomed to working from home in sweats, and it’s not a stretch to understand why some patients have become less formal in many settings. The 2015 article noted, however, that most physicians prefer to keep titles in the mix.
Perhaps most troublesome, says Dr. Setya, is that patients forgo asking whether it’s OK to use his first name and simply assume it’s acceptable. “It bothers me,” he says. “I became a doctor for more than the money.”
He suspects that his cultural background (Dr. Setya is of Indian descent) plays a role in how strongly he feels about patient-doctor informality. “As a British colony, Indian culture dictates that you pay respect to elders and to accomplishment,” he points out. “America is far looser when it comes to salutations.”
Dr. Cucuzzella largely agrees with Dr. Setya, but has a different view of the role culture plays in how physicians prefer to be addressed. “If your last name is difficult to pronounce, it can put the patient at ease if you give them an option,” he says. “I like my patients to feel comfortable and have a friendly conversation, so I don’t ask them to try to manage my last name.”
When patients revert to using Dr. Cucuzzella’s last name and title, this often breaks down along generational lines, Dr. Cucuzzella has found: Older patients might drop his title, whereas younger patients might keep it as a sign of respect. In some cases, Dr. Cucuzzella tries to bridge this gap, and offers the option of “Dr. Mark.” In his small West Virginia community, this is how people often refer to him.
Dr. Setya says that most of the older physicians he works with still prefer that patients and younger colleagues use their title, but he has witnessed exceptions to this. “My boss in residence hated to be called ‘Sir’ or ‘Doctor,’ ” he says. “In a situation like that, it is reasonable to ask, ‘How can I address you?’ But it has to be mutually agreed upon.”
Dr. Cucuzzella cites informality as the preferred mode for older patients. “If I have a 70-year-old patient, it seems natural they shouldn’t use my title,” he says. “They are worthy of equality in the community. If I’m talking to a retired CEO or state delegate, it’s uncomfortable if they call me doctor.”
Moreover, Dr. Cucuzzella maintains that establishing a less formal environment with patients leads to better outcomes. “Shared decision-making is a basic human right,” he says. “In 2022, doctors shouldn’t make decisions without patient input, unless it’s an emergency situation. Removing the title barriers makes that easier.”
How to handle informality
If you fall more in line with Dr. Setya, there are strategies you can use to try to keep formality in your doctor-patient relationships. Dr. Setya’s approach is indirect. “I don’t correct a patient if they use my first name, because that might seem hostile,” he says. “But I alert them in the way I address them back. A Sir, a Mrs., or a Mr. needs to go both ways.”
This particularly holds true in pediatrics, Dr. Setya has found. He has witnessed many colleagues addressing parents as “Mommy and Daddy,” something he says lacks respect and sets too informal a tone. “It’s almost universal that parents don’t like that, and we need to act accordingly.”
Dr. Witt also avoids directly correcting patients, but struggles when they drop her title. “The standard signature I use to sign every patient portal message I respond to includes my first and last name and credentials,” she says. “I maintain formality in most circumstances with that standard reply.”
Beneath the surface, however, Dr. Witt wishes it were easier. “I have struggled with answering the question, ‘Is it OK if I call you Leah?’ she says. “I want to keep our interaction anchored in professionalism without sacrificing the warmth I think is important to a productive patient-physician relationship. For this reason, I tend to say yes to this request, even though I’d rather patients didn’t make such requests.”
In the Fast Company article by Amy Diehl, PhD, and Leanne Dzubinski, PhD, on the topic of untitling professional women, the authors suggest several actions, beginning with leadership that sets expectations on the topic. They also suggest that physicians use polite corrections if patients untitle them. Supplying positive reinforcement when patients include your title can help, too. If all else fails, you can call out the offensive untitling. More often than not, especially with female physicians, the patient is demonstrating an unconscious bias rather than something deliberate.
Opinions vary on the topic of untitling, and ultimately each physician must make the decision for themselves. But creating informal cultures in an organization can have unintended consequences, especially for female peers.
Says Dr. Witt, “We all want to give our patients the best care we can, but professional boundaries are critical to time management, equitable care, and maintaining work-life balance. I would love to see a study that examines untitling by self-reported race and/or ethnicity of physicians, because we know that women of color experience higher rates of burnout and depression, and I wonder if untitling may be part of this.”
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN












