User login
TIPP the scales in managing stress
The past year presented unprecedented challenges for many. In addition, mental health services have also been stretched to capacity. Anecdotally, some hospitals and emergency departments note that more youth have been presenting in mental health crises, and the severity of symptoms has also been higher. Safety planning is important, including working with patients to identify skills they can use in distress. Even those who do not experience suicidal thoughts may struggle with dysregulation or may use coping strategies that may not be the healthiest in the long term.
Within my practice, I see some families who are still waiting for an available therapist, or some may not wish to participate in therapy despite its being recommended. For these families, supporting them in using strategies that they may be willing and able to use in the moment to help them get through the moment of crisis can been helpful:
Case example (identifying details have been changed)
Emily is a 17-year-old girl who has a history of generalized anxiety disorder and obsessive-compulsive disorder. She has had multiple medication trials and a course of cognitive behavioral therapy when younger, with significant improvement in symptoms. She returns to clinic because of increased anxiety related to stressors of the pandemic. She wishes to not return to therapy because of feeling that she received maximal benefit and that further sessions would not be fruitful. However, she struggles with identifying what skills she can use, and her anxiety heightens significantly to near-panic and hyperventilating with even cursory exploration of triggers for her symptoms. Medications are also discussed during this appointment, and it is noted that it may take some time to see therapeutic effect. Of note, she reports no acute safety concerns. She has engaged in skin picking. No reported substance use. As she hyperventilates, she was asked to identify items in the room matching the colors of the rainbow in order. She was able to quickly do this, and then was asked to do it again. Afterward, she noted feeling much less anxious because it distracted her from her thoughts.
Distress tolerance skills can be very helpful to navigate getting through a crisis. When under stress, some may be more likely to engage in behaviors that are not helpful in the long term such as using avoidance; procrastinating; consuming tobacco, alcohol, or other substances; spending too much time on screens; or engaging in self-harm behaviors. While some of these activities may be okay in moderation, others are always harmful. At times, when encouraging patients to use skills with which they may be more familiar, e.g., deep breathing, progressive muscle relaxation, the response may be, “these don’t work!” It can be important to distinguish that the function of these skills is not to make someone feel good or to eliminate the stressor, but to “take some of the edge off” so they are less likely to slide into problematic behaviors. It can be beneficial to have multiple tools at one’s disposal because not all skills will always be effective or available.
TIPP skills (temperature, intense exercise, paced breathing, progressive muscle relaxation) are distress tolerance skills from dialectical behavioral therapy (DBT),1 which was initially developed to treat individuals with borderline personality disorder. More recently, the therapy modality has been applied to individuals who may struggle with emotion regulation for a variety of reasons. TIPP skills work quickly (within seconds to minutes) with the aim to decrease physiological arousal. They do not require a lot of thinking, and many are portable or easy to use. Given the speed of effect, these skills can also be used in lieu of p.r.n. medications or patients can be counseled about trying these instead of turning to substance use. The effect is brief (5-20 minutes), although this may lower the affective temperature sufficiently for someone to get through the intense moment or to be able to then utilize other skills that may require more cognitive reserves.
T – Temperature
Holding one’s breath and placing one’s face in cold water (above 50°) for 10-20 seconds to stimulate the diving response and decrease heart rate. Patients can repeat this up to 3 times. Alternatively, cold compresses or gel eye masks can be used.
I – Intense exercise
Aerobic exercise for 10-20 minutes. This can include running, jumping jacks, dancing to loud music in a way that feels intense. The parasympathetic nervous system (PNS) is activated for approximately 20 minutes after cessation of intense exercise.
P – Paced breathing
Decreasing rate of breathing, with each inhalation/exhalation cycle lasting 10-12 seconds and the exhale being longer than the inhale also activates the PNS.
P – Progressive muscle relaxation (PMR)
Sequentially tensing and relaxing muscles from head to toes. Having at least 5-10 minutes to perform this exercise is preferred.2 Children’s Hospital of Philadelphia offerssample PMR recordings.
Body scans can also be helpful. This practice differs from PMR in that it is a mindfulness practice noting body sensations without trying to change them. The University of Vermont offers some sample exercises.3
These skills were described to Emily. She noted that dunking her face in cold water was effective and it was reassuring knowing she had a tool to help her anxiety. She started to push herself to go outside to exercise. We additionally incorporated other distraction techniques such as identifying items from colors of the rainbow that were around her. She appreciated that she could even do this discreetly while at school. At times she had to do a couple of rounds, but this could help stop her repetitive thoughts so she could use other skills.
Helping patients identify skills that can help in the moment can help them feel supported and gain traction in other areas.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. She has no relevant financial disclosures
References
1. Rathus JH, Miller AL. DBT® Skills manual for adolescents. 2015. Guilford Press.
2. Guided Relaxation Exercises, Children’s Hospital of Philadelphia.
3. Vermont Center for Children, Youth, and Families: Staying Close While Keeping Your Distance.
The past year presented unprecedented challenges for many. In addition, mental health services have also been stretched to capacity. Anecdotally, some hospitals and emergency departments note that more youth have been presenting in mental health crises, and the severity of symptoms has also been higher. Safety planning is important, including working with patients to identify skills they can use in distress. Even those who do not experience suicidal thoughts may struggle with dysregulation or may use coping strategies that may not be the healthiest in the long term.
Within my practice, I see some families who are still waiting for an available therapist, or some may not wish to participate in therapy despite its being recommended. For these families, supporting them in using strategies that they may be willing and able to use in the moment to help them get through the moment of crisis can been helpful:
Case example (identifying details have been changed)
Emily is a 17-year-old girl who has a history of generalized anxiety disorder and obsessive-compulsive disorder. She has had multiple medication trials and a course of cognitive behavioral therapy when younger, with significant improvement in symptoms. She returns to clinic because of increased anxiety related to stressors of the pandemic. She wishes to not return to therapy because of feeling that she received maximal benefit and that further sessions would not be fruitful. However, she struggles with identifying what skills she can use, and her anxiety heightens significantly to near-panic and hyperventilating with even cursory exploration of triggers for her symptoms. Medications are also discussed during this appointment, and it is noted that it may take some time to see therapeutic effect. Of note, she reports no acute safety concerns. She has engaged in skin picking. No reported substance use. As she hyperventilates, she was asked to identify items in the room matching the colors of the rainbow in order. She was able to quickly do this, and then was asked to do it again. Afterward, she noted feeling much less anxious because it distracted her from her thoughts.
Distress tolerance skills can be very helpful to navigate getting through a crisis. When under stress, some may be more likely to engage in behaviors that are not helpful in the long term such as using avoidance; procrastinating; consuming tobacco, alcohol, or other substances; spending too much time on screens; or engaging in self-harm behaviors. While some of these activities may be okay in moderation, others are always harmful. At times, when encouraging patients to use skills with which they may be more familiar, e.g., deep breathing, progressive muscle relaxation, the response may be, “these don’t work!” It can be important to distinguish that the function of these skills is not to make someone feel good or to eliminate the stressor, but to “take some of the edge off” so they are less likely to slide into problematic behaviors. It can be beneficial to have multiple tools at one’s disposal because not all skills will always be effective or available.
TIPP skills (temperature, intense exercise, paced breathing, progressive muscle relaxation) are distress tolerance skills from dialectical behavioral therapy (DBT),1 which was initially developed to treat individuals with borderline personality disorder. More recently, the therapy modality has been applied to individuals who may struggle with emotion regulation for a variety of reasons. TIPP skills work quickly (within seconds to minutes) with the aim to decrease physiological arousal. They do not require a lot of thinking, and many are portable or easy to use. Given the speed of effect, these skills can also be used in lieu of p.r.n. medications or patients can be counseled about trying these instead of turning to substance use. The effect is brief (5-20 minutes), although this may lower the affective temperature sufficiently for someone to get through the intense moment or to be able to then utilize other skills that may require more cognitive reserves.
T – Temperature
Holding one’s breath and placing one’s face in cold water (above 50°) for 10-20 seconds to stimulate the diving response and decrease heart rate. Patients can repeat this up to 3 times. Alternatively, cold compresses or gel eye masks can be used.
I – Intense exercise
Aerobic exercise for 10-20 minutes. This can include running, jumping jacks, dancing to loud music in a way that feels intense. The parasympathetic nervous system (PNS) is activated for approximately 20 minutes after cessation of intense exercise.
P – Paced breathing
Decreasing rate of breathing, with each inhalation/exhalation cycle lasting 10-12 seconds and the exhale being longer than the inhale also activates the PNS.
P – Progressive muscle relaxation (PMR)
Sequentially tensing and relaxing muscles from head to toes. Having at least 5-10 minutes to perform this exercise is preferred.2 Children’s Hospital of Philadelphia offerssample PMR recordings.
Body scans can also be helpful. This practice differs from PMR in that it is a mindfulness practice noting body sensations without trying to change them. The University of Vermont offers some sample exercises.3
These skills were described to Emily. She noted that dunking her face in cold water was effective and it was reassuring knowing she had a tool to help her anxiety. She started to push herself to go outside to exercise. We additionally incorporated other distraction techniques such as identifying items from colors of the rainbow that were around her. She appreciated that she could even do this discreetly while at school. At times she had to do a couple of rounds, but this could help stop her repetitive thoughts so she could use other skills.
Helping patients identify skills that can help in the moment can help them feel supported and gain traction in other areas.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. She has no relevant financial disclosures
References
1. Rathus JH, Miller AL. DBT® Skills manual for adolescents. 2015. Guilford Press.
2. Guided Relaxation Exercises, Children’s Hospital of Philadelphia.
3. Vermont Center for Children, Youth, and Families: Staying Close While Keeping Your Distance.
The past year presented unprecedented challenges for many. In addition, mental health services have also been stretched to capacity. Anecdotally, some hospitals and emergency departments note that more youth have been presenting in mental health crises, and the severity of symptoms has also been higher. Safety planning is important, including working with patients to identify skills they can use in distress. Even those who do not experience suicidal thoughts may struggle with dysregulation or may use coping strategies that may not be the healthiest in the long term.
Within my practice, I see some families who are still waiting for an available therapist, or some may not wish to participate in therapy despite its being recommended. For these families, supporting them in using strategies that they may be willing and able to use in the moment to help them get through the moment of crisis can been helpful:
Case example (identifying details have been changed)
Emily is a 17-year-old girl who has a history of generalized anxiety disorder and obsessive-compulsive disorder. She has had multiple medication trials and a course of cognitive behavioral therapy when younger, with significant improvement in symptoms. She returns to clinic because of increased anxiety related to stressors of the pandemic. She wishes to not return to therapy because of feeling that she received maximal benefit and that further sessions would not be fruitful. However, she struggles with identifying what skills she can use, and her anxiety heightens significantly to near-panic and hyperventilating with even cursory exploration of triggers for her symptoms. Medications are also discussed during this appointment, and it is noted that it may take some time to see therapeutic effect. Of note, she reports no acute safety concerns. She has engaged in skin picking. No reported substance use. As she hyperventilates, she was asked to identify items in the room matching the colors of the rainbow in order. She was able to quickly do this, and then was asked to do it again. Afterward, she noted feeling much less anxious because it distracted her from her thoughts.
Distress tolerance skills can be very helpful to navigate getting through a crisis. When under stress, some may be more likely to engage in behaviors that are not helpful in the long term such as using avoidance; procrastinating; consuming tobacco, alcohol, or other substances; spending too much time on screens; or engaging in self-harm behaviors. While some of these activities may be okay in moderation, others are always harmful. At times, when encouraging patients to use skills with which they may be more familiar, e.g., deep breathing, progressive muscle relaxation, the response may be, “these don’t work!” It can be important to distinguish that the function of these skills is not to make someone feel good or to eliminate the stressor, but to “take some of the edge off” so they are less likely to slide into problematic behaviors. It can be beneficial to have multiple tools at one’s disposal because not all skills will always be effective or available.
TIPP skills (temperature, intense exercise, paced breathing, progressive muscle relaxation) are distress tolerance skills from dialectical behavioral therapy (DBT),1 which was initially developed to treat individuals with borderline personality disorder. More recently, the therapy modality has been applied to individuals who may struggle with emotion regulation for a variety of reasons. TIPP skills work quickly (within seconds to minutes) with the aim to decrease physiological arousal. They do not require a lot of thinking, and many are portable or easy to use. Given the speed of effect, these skills can also be used in lieu of p.r.n. medications or patients can be counseled about trying these instead of turning to substance use. The effect is brief (5-20 minutes), although this may lower the affective temperature sufficiently for someone to get through the intense moment or to be able to then utilize other skills that may require more cognitive reserves.
T – Temperature
Holding one’s breath and placing one’s face in cold water (above 50°) for 10-20 seconds to stimulate the diving response and decrease heart rate. Patients can repeat this up to 3 times. Alternatively, cold compresses or gel eye masks can be used.
I – Intense exercise
Aerobic exercise for 10-20 minutes. This can include running, jumping jacks, dancing to loud music in a way that feels intense. The parasympathetic nervous system (PNS) is activated for approximately 20 minutes after cessation of intense exercise.
P – Paced breathing
Decreasing rate of breathing, with each inhalation/exhalation cycle lasting 10-12 seconds and the exhale being longer than the inhale also activates the PNS.
P – Progressive muscle relaxation (PMR)
Sequentially tensing and relaxing muscles from head to toes. Having at least 5-10 minutes to perform this exercise is preferred.2 Children’s Hospital of Philadelphia offerssample PMR recordings.
Body scans can also be helpful. This practice differs from PMR in that it is a mindfulness practice noting body sensations without trying to change them. The University of Vermont offers some sample exercises.3
These skills were described to Emily. She noted that dunking her face in cold water was effective and it was reassuring knowing she had a tool to help her anxiety. She started to push herself to go outside to exercise. We additionally incorporated other distraction techniques such as identifying items from colors of the rainbow that were around her. She appreciated that she could even do this discreetly while at school. At times she had to do a couple of rounds, but this could help stop her repetitive thoughts so she could use other skills.
Helping patients identify skills that can help in the moment can help them feel supported and gain traction in other areas.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. She has no relevant financial disclosures
References
1. Rathus JH, Miller AL. DBT® Skills manual for adolescents. 2015. Guilford Press.
2. Guided Relaxation Exercises, Children’s Hospital of Philadelphia.
3. Vermont Center for Children, Youth, and Families: Staying Close While Keeping Your Distance.
Focus on youth concerns at well visits
Taking teens’ strengths, values, and dreams, into account through a previsit questionnaire was acceptable to them and may promote discussions with providers, based on data from 91 adolescents.
The American Academy of Pediatrics’ Bright Futures initiative recommends the use of a strength-based approach for adolescent well visits, but the extensive positive psychology inventories to identify teen strengths and values are impractical for the clinical visit setting, wrote Yidan Cao, MPH, of the Child Development through Primary Care at the University of Michigan, Ann Arbor, and colleagues. However, 76% of youth participating in focus groups responded that “using a confidential questionnaire about a teen’s strengths and goals before checkup visits would be a good addition to health care for teens,” the researchers said.
In a study presented in a poster session (#515) at the Pediatric Academic Societies annual meeting, the researchers recruited 91 community youth to participate in 13 focus groups related to teen depression and substance use. The age of the focus group participants ranged from 12 to 18 years, with an average of 15 years, 61.5% were female, and 1.1% identified as transgender. The racial breakdown was 51.6% White, 27.5% African American, 8.8% Asian, 2.2% Native American, 3.3% biracial, and 6.6% unknown.
The participants provided information on potential questionnaire items for an online previsit screening for well visits to assess strengths and identify values, goals, dream jobs, and life wishes.
Suggestions from the participants informed changes to the questionnaire, which included five categories: personal/social goals, goals for academics/training, strengths, values, and dream jobs.
The top endorsed personal goal of “to be happy” was chosen by 13.1% of the participants. The top academic goal was “get good grades” (45.5%). The top endorsed strength was “fitness/coordination/sports/physical activity” (22.9%), while the top value was caring and kindness (25.8%), and the top dream job category was health/medical (30.8%).
Key comments made by the youth participants for improving the previsit questionnaire included adding an option for “I can’t decide,” and allowing for multiple responses to avoid feeling pinned down or judged, the researchers noted.
The researchers highlighted one teen comment: “While I understand the purpose of limiting the participants to two answers, it is incredibly difficult to only choose two. Being limited to two very much restricts your understanding of our values. For example, I would’ve also liked to select ‘to do well in school’ and ‘to make a difference,’ but ‘being happy’ and ‘being loving to all those around me’ had to take precedent.”
The study was limited by not being fully generalizable to all teens, as other teens may hold views and beliefs that differ from those of the focus group participants, the researchers noted.
However, the findings support the value of a strength-based previsit questionnaire for adolescents, they said.
“Structured previsit data could facilitate relationship building and be actionable for assigning strength and resiliency building resources,” they noted. “A final strengths and goals questionnaire is now being piloted in computerized form contributing to decision supports for suggested teleprompters and associated resource options,” and future research may show the value of such previsit data for improved clinical process and outcomes of youth well visits, they concluded.
Recognize the uncertainty of adolescence
“Adolescents are at crossroads of identity, trying to figure out who they are, their goals and values,” said Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, in an interview. “Adolescence is also a critical time when teens have more control and choice over behaviors that impact their health, such as diet, exercise, substance use, and sexual activity. In this critical time period, clinicians can intervene on health-related behaviors and shape the trajectory of a teen’s life. However, to promote teen health, pediatricians need to have their patients’ trust, which can be hard to gain,” she emphasized.
“In my practice, I’ve found that teens often just want to be seen and heard,” said Dr. Curran. “Teens often have many adults in their life who focus on the ‘don’ts’ – don’t use drugs, don’t have sex, for example – and few that praise healthy behaviors or strengths, or seek to understand what is important to them. By listening to teens and understanding what’s important to them, we can then use motivational interviewing techniques to help create meaningful change in health-related behaviors. However, this takes time and investment, which is often in conflict with time pressures in the modern medical system.
“This study is useful because it examined the acceptability of a positive psychology questionnaire to be used at well visits when reviewed by youth, that could be used to streamline this important process,” said Dr. Curran.
“From my practice, I know that understanding a teen’s goals, values, and strengths is important – we do this daily in our practice when working with patients – but it was exciting to see that youth found it acceptable to do this via a previsit survey, which can potentially streamline well visits,” she noted.
The questionnaire is being developed as a pilot program, but more research is needed to determine the direct clinical impact, said Dr. Curran. “It will be important in the future to see if implementation of this questionnaire can be helpful in integrating this information into motivational interviewing and rapport building to help improve teens’ health outcomes.”
The study was supported in part by the National Institute on Drug Abuse and the National Institute of Mental Health. Two coauthors have a financial interest in the CHADIS online reporting program used in the study. Dr. Curran had no financial conflicts to disclose.
Taking teens’ strengths, values, and dreams, into account through a previsit questionnaire was acceptable to them and may promote discussions with providers, based on data from 91 adolescents.
The American Academy of Pediatrics’ Bright Futures initiative recommends the use of a strength-based approach for adolescent well visits, but the extensive positive psychology inventories to identify teen strengths and values are impractical for the clinical visit setting, wrote Yidan Cao, MPH, of the Child Development through Primary Care at the University of Michigan, Ann Arbor, and colleagues. However, 76% of youth participating in focus groups responded that “using a confidential questionnaire about a teen’s strengths and goals before checkup visits would be a good addition to health care for teens,” the researchers said.
In a study presented in a poster session (#515) at the Pediatric Academic Societies annual meeting, the researchers recruited 91 community youth to participate in 13 focus groups related to teen depression and substance use. The age of the focus group participants ranged from 12 to 18 years, with an average of 15 years, 61.5% were female, and 1.1% identified as transgender. The racial breakdown was 51.6% White, 27.5% African American, 8.8% Asian, 2.2% Native American, 3.3% biracial, and 6.6% unknown.
The participants provided information on potential questionnaire items for an online previsit screening for well visits to assess strengths and identify values, goals, dream jobs, and life wishes.
Suggestions from the participants informed changes to the questionnaire, which included five categories: personal/social goals, goals for academics/training, strengths, values, and dream jobs.
The top endorsed personal goal of “to be happy” was chosen by 13.1% of the participants. The top academic goal was “get good grades” (45.5%). The top endorsed strength was “fitness/coordination/sports/physical activity” (22.9%), while the top value was caring and kindness (25.8%), and the top dream job category was health/medical (30.8%).
Key comments made by the youth participants for improving the previsit questionnaire included adding an option for “I can’t decide,” and allowing for multiple responses to avoid feeling pinned down or judged, the researchers noted.
The researchers highlighted one teen comment: “While I understand the purpose of limiting the participants to two answers, it is incredibly difficult to only choose two. Being limited to two very much restricts your understanding of our values. For example, I would’ve also liked to select ‘to do well in school’ and ‘to make a difference,’ but ‘being happy’ and ‘being loving to all those around me’ had to take precedent.”
The study was limited by not being fully generalizable to all teens, as other teens may hold views and beliefs that differ from those of the focus group participants, the researchers noted.
However, the findings support the value of a strength-based previsit questionnaire for adolescents, they said.
“Structured previsit data could facilitate relationship building and be actionable for assigning strength and resiliency building resources,” they noted. “A final strengths and goals questionnaire is now being piloted in computerized form contributing to decision supports for suggested teleprompters and associated resource options,” and future research may show the value of such previsit data for improved clinical process and outcomes of youth well visits, they concluded.
Recognize the uncertainty of adolescence
“Adolescents are at crossroads of identity, trying to figure out who they are, their goals and values,” said Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, in an interview. “Adolescence is also a critical time when teens have more control and choice over behaviors that impact their health, such as diet, exercise, substance use, and sexual activity. In this critical time period, clinicians can intervene on health-related behaviors and shape the trajectory of a teen’s life. However, to promote teen health, pediatricians need to have their patients’ trust, which can be hard to gain,” she emphasized.
“In my practice, I’ve found that teens often just want to be seen and heard,” said Dr. Curran. “Teens often have many adults in their life who focus on the ‘don’ts’ – don’t use drugs, don’t have sex, for example – and few that praise healthy behaviors or strengths, or seek to understand what is important to them. By listening to teens and understanding what’s important to them, we can then use motivational interviewing techniques to help create meaningful change in health-related behaviors. However, this takes time and investment, which is often in conflict with time pressures in the modern medical system.
“This study is useful because it examined the acceptability of a positive psychology questionnaire to be used at well visits when reviewed by youth, that could be used to streamline this important process,” said Dr. Curran.
“From my practice, I know that understanding a teen’s goals, values, and strengths is important – we do this daily in our practice when working with patients – but it was exciting to see that youth found it acceptable to do this via a previsit survey, which can potentially streamline well visits,” she noted.
The questionnaire is being developed as a pilot program, but more research is needed to determine the direct clinical impact, said Dr. Curran. “It will be important in the future to see if implementation of this questionnaire can be helpful in integrating this information into motivational interviewing and rapport building to help improve teens’ health outcomes.”
The study was supported in part by the National Institute on Drug Abuse and the National Institute of Mental Health. Two coauthors have a financial interest in the CHADIS online reporting program used in the study. Dr. Curran had no financial conflicts to disclose.
Taking teens’ strengths, values, and dreams, into account through a previsit questionnaire was acceptable to them and may promote discussions with providers, based on data from 91 adolescents.
The American Academy of Pediatrics’ Bright Futures initiative recommends the use of a strength-based approach for adolescent well visits, but the extensive positive psychology inventories to identify teen strengths and values are impractical for the clinical visit setting, wrote Yidan Cao, MPH, of the Child Development through Primary Care at the University of Michigan, Ann Arbor, and colleagues. However, 76% of youth participating in focus groups responded that “using a confidential questionnaire about a teen’s strengths and goals before checkup visits would be a good addition to health care for teens,” the researchers said.
In a study presented in a poster session (#515) at the Pediatric Academic Societies annual meeting, the researchers recruited 91 community youth to participate in 13 focus groups related to teen depression and substance use. The age of the focus group participants ranged from 12 to 18 years, with an average of 15 years, 61.5% were female, and 1.1% identified as transgender. The racial breakdown was 51.6% White, 27.5% African American, 8.8% Asian, 2.2% Native American, 3.3% biracial, and 6.6% unknown.
The participants provided information on potential questionnaire items for an online previsit screening for well visits to assess strengths and identify values, goals, dream jobs, and life wishes.
Suggestions from the participants informed changes to the questionnaire, which included five categories: personal/social goals, goals for academics/training, strengths, values, and dream jobs.
The top endorsed personal goal of “to be happy” was chosen by 13.1% of the participants. The top academic goal was “get good grades” (45.5%). The top endorsed strength was “fitness/coordination/sports/physical activity” (22.9%), while the top value was caring and kindness (25.8%), and the top dream job category was health/medical (30.8%).
Key comments made by the youth participants for improving the previsit questionnaire included adding an option for “I can’t decide,” and allowing for multiple responses to avoid feeling pinned down or judged, the researchers noted.
The researchers highlighted one teen comment: “While I understand the purpose of limiting the participants to two answers, it is incredibly difficult to only choose two. Being limited to two very much restricts your understanding of our values. For example, I would’ve also liked to select ‘to do well in school’ and ‘to make a difference,’ but ‘being happy’ and ‘being loving to all those around me’ had to take precedent.”
The study was limited by not being fully generalizable to all teens, as other teens may hold views and beliefs that differ from those of the focus group participants, the researchers noted.
However, the findings support the value of a strength-based previsit questionnaire for adolescents, they said.
“Structured previsit data could facilitate relationship building and be actionable for assigning strength and resiliency building resources,” they noted. “A final strengths and goals questionnaire is now being piloted in computerized form contributing to decision supports for suggested teleprompters and associated resource options,” and future research may show the value of such previsit data for improved clinical process and outcomes of youth well visits, they concluded.
Recognize the uncertainty of adolescence
“Adolescents are at crossroads of identity, trying to figure out who they are, their goals and values,” said Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, in an interview. “Adolescence is also a critical time when teens have more control and choice over behaviors that impact their health, such as diet, exercise, substance use, and sexual activity. In this critical time period, clinicians can intervene on health-related behaviors and shape the trajectory of a teen’s life. However, to promote teen health, pediatricians need to have their patients’ trust, which can be hard to gain,” she emphasized.
“In my practice, I’ve found that teens often just want to be seen and heard,” said Dr. Curran. “Teens often have many adults in their life who focus on the ‘don’ts’ – don’t use drugs, don’t have sex, for example – and few that praise healthy behaviors or strengths, or seek to understand what is important to them. By listening to teens and understanding what’s important to them, we can then use motivational interviewing techniques to help create meaningful change in health-related behaviors. However, this takes time and investment, which is often in conflict with time pressures in the modern medical system.
“This study is useful because it examined the acceptability of a positive psychology questionnaire to be used at well visits when reviewed by youth, that could be used to streamline this important process,” said Dr. Curran.
“From my practice, I know that understanding a teen’s goals, values, and strengths is important – we do this daily in our practice when working with patients – but it was exciting to see that youth found it acceptable to do this via a previsit survey, which can potentially streamline well visits,” she noted.
The questionnaire is being developed as a pilot program, but more research is needed to determine the direct clinical impact, said Dr. Curran. “It will be important in the future to see if implementation of this questionnaire can be helpful in integrating this information into motivational interviewing and rapport building to help improve teens’ health outcomes.”
The study was supported in part by the National Institute on Drug Abuse and the National Institute of Mental Health. Two coauthors have a financial interest in the CHADIS online reporting program used in the study. Dr. Curran had no financial conflicts to disclose.
FROM PAS 2021
High body fat tied to slowed breast maturation in girls with obesity
Girls in late stages of puberty who had elevated levels of body fat showed unusually high levels of several hormones that could contribute to an earlier age of menarche and also slow breast development, according to data from 90 girls who spanned a wide range of body fat in the first longitudinal study to examine links between fat volume, levels of reproductive hormones, and clinical manifestations of hormone action during puberty.
The results showed that girls with greater body fat had higher levels of follicle stimulating hormone, inhibin B, estrone, and certain male-like reproductive hormones, and that this pattern “is specifically tied to body fat,” said Natalie D. Shaw, MD, senior investigator for the study, reported at the annual meeting of the Endocrine Society.
“We found that total body fat is associated with the timing of menarche, as others have reported for body weight,” she noted. The new findings showed that every 1% rise in percent total body fat linked with a significant 3% rise in the likelihood of menarche, menstrual onset. In the new study the average age of menarche was 11.7 years among the overweight or obese girls and 12.8 years among those with normal weights.
But the study’s unique use of an average of about three serial ultrasound breast examinations of each subject during an average 4 years of follow-up also showed that higher levels of body fat linked with slowed breast development in later stages, specifically maturation from stage D to stages D/E and E.
For example, girls with 33% body fat spent an average of 8.2 months in stage D, which stretched to an average of 11.2 months among girls with 38% body fat, reported Madison T. Ortega, a researcher with the Pediatric Endocrinology Group of the National Institute of Environmental Health Sciences in Research Triangle Park, N.C., who presented the report at the meeting.
Ultrasound shows what inspection can’t
Results from “several studies have shown earlier breast development in overweight and obese girls by inspection and palpation,” but the new findings from ultrasound examination provide more nuance about the structural breast changes actually occurring in these adolescents, said Dr. Shaw, who heads the Pediatric Endocrinology Group. The current study “was not designed to capture the onset of breast development,” and “it is possible that increased androgens or insulin resistance in girls with higher body fat interferes with normal breast development,” she explained in an interview.
“The authors showed that the timing and progress of early stages of puberty were not earlier in overweight or obese girls. Luteinizing hormone, the indicator of neuroendocrine pubertal onset, and timing of early stages of breast development were the same in all weight groups. The authors also discovered falsely advanced Turner breast stage designations with ultrasonography in some girls with obesity. This might suggest that prior findings in epidemiologic studies of an earlier start to puberty based mostly on breast development stages identified by self-reported inspection and, rarely, palpation, may have been biased by breast adipose tissue,” said Christine M. Burt Solorzano, MD, a pediatric endocrinologist at the University of Virginia in Charlottesville, who was not involved in the study.
“Development of increased follicle-stimulating hormone in late puberty suggests that pubertal tempo, not onset, may be increased in girls with obesity, and goes along with earlier menarche. Their finding of increased androgen levels during mid to late puberty with obesity are consistent with prior findings,” including work published Dr. Burt Solorzano and her associates, she noted. “Delayed timing of advanced breast morphology was unexpected and may reflect relatively lower levels of progesterone in girls with obesity,” a hormone necessary for later stages of breast maturation.
The findings “reinforce that early breast development in the setting of obesity may in fact reflect adipose tissue and not be a true representation of neuroendocrine precocious puberty,” Dr. Burt Solorzano said in an interview. The findings “also suggest that pubertal initiation may not happen earlier in girls with obesity, as has been thought, but rather the tempo of puberty may be more rapid, leading to earlier menarche.”
A possible step toward PCOS
The long-term clinical consequences of the hormonal state linked with overweight and obesity “are unknown,” said Dr. Shaw. However, she and her coworkers followed a few of their subjects with elevated testosterone levels during midpuberty, and several developed signs of early polycystic ovarian syndrome (PCOS) such as irregular menstrual cycles, acne, and hirsutism. “It may be possible to identify girls at high risk for PCOS before menarche,” she suggested.
Dr. Burt Solorzano agreed that delayed breast development in girls with high levels of body fat may reflect inadequate progesterone production, which when coupled with an obesity-related excess level of androgens could put girls at risk for chronic anovulation and later PCOS.
“Weight management during childhood and early puberty may mitigate the adverse effects of obesity on pubertal progression and avoid some of the lifetime complications related to early menarche,” Dr. Burt Solorzano said.
The Body Weight and Puberty Study enrolled 36 girls who were overweight or obese and 54 girls with normal weight. They averaged 11 years of age, with a range of 8.2-14.7 years. Average percent body fat was 41% among the overweight or obese girls and 27% among those with normal weight. The results reported by Ms. Ortega also appeared in a report published Feb 22, 2021 (J Clin Endocrinol Metab. doi: 10.1210/clinem/dgab092).
Dr. Shaw, Ms. Ortega, and Dr. Burt Solorzano had no disclosures.
Girls in late stages of puberty who had elevated levels of body fat showed unusually high levels of several hormones that could contribute to an earlier age of menarche and also slow breast development, according to data from 90 girls who spanned a wide range of body fat in the first longitudinal study to examine links between fat volume, levels of reproductive hormones, and clinical manifestations of hormone action during puberty.
The results showed that girls with greater body fat had higher levels of follicle stimulating hormone, inhibin B, estrone, and certain male-like reproductive hormones, and that this pattern “is specifically tied to body fat,” said Natalie D. Shaw, MD, senior investigator for the study, reported at the annual meeting of the Endocrine Society.
“We found that total body fat is associated with the timing of menarche, as others have reported for body weight,” she noted. The new findings showed that every 1% rise in percent total body fat linked with a significant 3% rise in the likelihood of menarche, menstrual onset. In the new study the average age of menarche was 11.7 years among the overweight or obese girls and 12.8 years among those with normal weights.
But the study’s unique use of an average of about three serial ultrasound breast examinations of each subject during an average 4 years of follow-up also showed that higher levels of body fat linked with slowed breast development in later stages, specifically maturation from stage D to stages D/E and E.
For example, girls with 33% body fat spent an average of 8.2 months in stage D, which stretched to an average of 11.2 months among girls with 38% body fat, reported Madison T. Ortega, a researcher with the Pediatric Endocrinology Group of the National Institute of Environmental Health Sciences in Research Triangle Park, N.C., who presented the report at the meeting.
Ultrasound shows what inspection can’t
Results from “several studies have shown earlier breast development in overweight and obese girls by inspection and palpation,” but the new findings from ultrasound examination provide more nuance about the structural breast changes actually occurring in these adolescents, said Dr. Shaw, who heads the Pediatric Endocrinology Group. The current study “was not designed to capture the onset of breast development,” and “it is possible that increased androgens or insulin resistance in girls with higher body fat interferes with normal breast development,” she explained in an interview.
“The authors showed that the timing and progress of early stages of puberty were not earlier in overweight or obese girls. Luteinizing hormone, the indicator of neuroendocrine pubertal onset, and timing of early stages of breast development were the same in all weight groups. The authors also discovered falsely advanced Turner breast stage designations with ultrasonography in some girls with obesity. This might suggest that prior findings in epidemiologic studies of an earlier start to puberty based mostly on breast development stages identified by self-reported inspection and, rarely, palpation, may have been biased by breast adipose tissue,” said Christine M. Burt Solorzano, MD, a pediatric endocrinologist at the University of Virginia in Charlottesville, who was not involved in the study.
“Development of increased follicle-stimulating hormone in late puberty suggests that pubertal tempo, not onset, may be increased in girls with obesity, and goes along with earlier menarche. Their finding of increased androgen levels during mid to late puberty with obesity are consistent with prior findings,” including work published Dr. Burt Solorzano and her associates, she noted. “Delayed timing of advanced breast morphology was unexpected and may reflect relatively lower levels of progesterone in girls with obesity,” a hormone necessary for later stages of breast maturation.
The findings “reinforce that early breast development in the setting of obesity may in fact reflect adipose tissue and not be a true representation of neuroendocrine precocious puberty,” Dr. Burt Solorzano said in an interview. The findings “also suggest that pubertal initiation may not happen earlier in girls with obesity, as has been thought, but rather the tempo of puberty may be more rapid, leading to earlier menarche.”
A possible step toward PCOS
The long-term clinical consequences of the hormonal state linked with overweight and obesity “are unknown,” said Dr. Shaw. However, she and her coworkers followed a few of their subjects with elevated testosterone levels during midpuberty, and several developed signs of early polycystic ovarian syndrome (PCOS) such as irregular menstrual cycles, acne, and hirsutism. “It may be possible to identify girls at high risk for PCOS before menarche,” she suggested.
Dr. Burt Solorzano agreed that delayed breast development in girls with high levels of body fat may reflect inadequate progesterone production, which when coupled with an obesity-related excess level of androgens could put girls at risk for chronic anovulation and later PCOS.
“Weight management during childhood and early puberty may mitigate the adverse effects of obesity on pubertal progression and avoid some of the lifetime complications related to early menarche,” Dr. Burt Solorzano said.
The Body Weight and Puberty Study enrolled 36 girls who were overweight or obese and 54 girls with normal weight. They averaged 11 years of age, with a range of 8.2-14.7 years. Average percent body fat was 41% among the overweight or obese girls and 27% among those with normal weight. The results reported by Ms. Ortega also appeared in a report published Feb 22, 2021 (J Clin Endocrinol Metab. doi: 10.1210/clinem/dgab092).
Dr. Shaw, Ms. Ortega, and Dr. Burt Solorzano had no disclosures.
Girls in late stages of puberty who had elevated levels of body fat showed unusually high levels of several hormones that could contribute to an earlier age of menarche and also slow breast development, according to data from 90 girls who spanned a wide range of body fat in the first longitudinal study to examine links between fat volume, levels of reproductive hormones, and clinical manifestations of hormone action during puberty.
The results showed that girls with greater body fat had higher levels of follicle stimulating hormone, inhibin B, estrone, and certain male-like reproductive hormones, and that this pattern “is specifically tied to body fat,” said Natalie D. Shaw, MD, senior investigator for the study, reported at the annual meeting of the Endocrine Society.
“We found that total body fat is associated with the timing of menarche, as others have reported for body weight,” she noted. The new findings showed that every 1% rise in percent total body fat linked with a significant 3% rise in the likelihood of menarche, menstrual onset. In the new study the average age of menarche was 11.7 years among the overweight or obese girls and 12.8 years among those with normal weights.
But the study’s unique use of an average of about three serial ultrasound breast examinations of each subject during an average 4 years of follow-up also showed that higher levels of body fat linked with slowed breast development in later stages, specifically maturation from stage D to stages D/E and E.
For example, girls with 33% body fat spent an average of 8.2 months in stage D, which stretched to an average of 11.2 months among girls with 38% body fat, reported Madison T. Ortega, a researcher with the Pediatric Endocrinology Group of the National Institute of Environmental Health Sciences in Research Triangle Park, N.C., who presented the report at the meeting.
Ultrasound shows what inspection can’t
Results from “several studies have shown earlier breast development in overweight and obese girls by inspection and palpation,” but the new findings from ultrasound examination provide more nuance about the structural breast changes actually occurring in these adolescents, said Dr. Shaw, who heads the Pediatric Endocrinology Group. The current study “was not designed to capture the onset of breast development,” and “it is possible that increased androgens or insulin resistance in girls with higher body fat interferes with normal breast development,” she explained in an interview.
“The authors showed that the timing and progress of early stages of puberty were not earlier in overweight or obese girls. Luteinizing hormone, the indicator of neuroendocrine pubertal onset, and timing of early stages of breast development were the same in all weight groups. The authors also discovered falsely advanced Turner breast stage designations with ultrasonography in some girls with obesity. This might suggest that prior findings in epidemiologic studies of an earlier start to puberty based mostly on breast development stages identified by self-reported inspection and, rarely, palpation, may have been biased by breast adipose tissue,” said Christine M. Burt Solorzano, MD, a pediatric endocrinologist at the University of Virginia in Charlottesville, who was not involved in the study.
“Development of increased follicle-stimulating hormone in late puberty suggests that pubertal tempo, not onset, may be increased in girls with obesity, and goes along with earlier menarche. Their finding of increased androgen levels during mid to late puberty with obesity are consistent with prior findings,” including work published Dr. Burt Solorzano and her associates, she noted. “Delayed timing of advanced breast morphology was unexpected and may reflect relatively lower levels of progesterone in girls with obesity,” a hormone necessary for later stages of breast maturation.
The findings “reinforce that early breast development in the setting of obesity may in fact reflect adipose tissue and not be a true representation of neuroendocrine precocious puberty,” Dr. Burt Solorzano said in an interview. The findings “also suggest that pubertal initiation may not happen earlier in girls with obesity, as has been thought, but rather the tempo of puberty may be more rapid, leading to earlier menarche.”
A possible step toward PCOS
The long-term clinical consequences of the hormonal state linked with overweight and obesity “are unknown,” said Dr. Shaw. However, she and her coworkers followed a few of their subjects with elevated testosterone levels during midpuberty, and several developed signs of early polycystic ovarian syndrome (PCOS) such as irregular menstrual cycles, acne, and hirsutism. “It may be possible to identify girls at high risk for PCOS before menarche,” she suggested.
Dr. Burt Solorzano agreed that delayed breast development in girls with high levels of body fat may reflect inadequate progesterone production, which when coupled with an obesity-related excess level of androgens could put girls at risk for chronic anovulation and later PCOS.
“Weight management during childhood and early puberty may mitigate the adverse effects of obesity on pubertal progression and avoid some of the lifetime complications related to early menarche,” Dr. Burt Solorzano said.
The Body Weight and Puberty Study enrolled 36 girls who were overweight or obese and 54 girls with normal weight. They averaged 11 years of age, with a range of 8.2-14.7 years. Average percent body fat was 41% among the overweight or obese girls and 27% among those with normal weight. The results reported by Ms. Ortega also appeared in a report published Feb 22, 2021 (J Clin Endocrinol Metab. doi: 10.1210/clinem/dgab092).
Dr. Shaw, Ms. Ortega, and Dr. Burt Solorzano had no disclosures.
FROM ENDO 2021
Are adolescents canaries in the coal mine?
Increasing youth suicides may be a warning about society’s psychosocial health.
Before COVID-19 pandemic, suicide rates were already increasing among adolescents.1 Loneliness, because of social isolation and loss of in-person community contacts, was recognized as one factor perhaps contributing to increasing adolescent suicide.2 Now, with the physical distancing measures vital to curbing the spread, the loneliness epidemic that preceded COVID-19 has only worsened, and suicidal thoughts in adolescents remain on the rise.3
Given the crucial role of interpersonal interactions and community in healthy adolescent development, these troubling trends provide insight not only into the psychosocial health of our teenagers but also into the psychosocial health of our society as a whole.
Over the past 8 months, our psychiatric crisis stabilization unit has experienced a surge in admissions for adolescents with suicidal ideation, often with accompanying attempts. Even more concerning, a significant percentage of these patients do not have additional symptoms of depression or premorbid risk factors for suicide. In many cases, there are no warning signs to alert parents of their adolescent’s imminent suicidal behavior.
Prior to COVID-19, most of our patients with suicidal ideations arrived withdrawn, irritable, and isolative. Interactions with these patients evoked poignant feelings of empathy and sadness, and these patients endorsed multiple additional symptoms consistent with criteria for a specified depressive disorder.
More recently, since COVID-19, we have observed patients who, mere hours earlier, were in an ED receiving medical interventions for a suicide attempt, now present on our unit smiling, laughing, and interacting contentedly with their peers. Upon integration into our milieu, they often report complete resolution of their suicidal thoughts. Interactions with these patients do not conjure feelings of sadness or despair. In fact, we often struggle with diagnostic specificity, because many of these patients do not meet criteria for a specified depressive disorder.
As observed in real time on our unit, meaningful interpersonal interactions are especially crucial to our adolescents’ psychosocial and emotional well-being. As their independence grows, their holding environment expands to incorporate the community. Nonparent family members, teachers, mentors, coaches, peers, parents, and most importantly, same-aged peers play a vital role in creating the environment necessary for healthy adolescent development.
The larger community is essential for adolescents to develop the skills and confidence to move into adulthood. When adolescents are lonely, with less contact with the community outside of their family, they lose the milieu in which they develop. Their fundamental psychological need of belonging becomes compromised; they fail to experience fidelity or a sense of self; and sometimes they no longer have the desire to live.
So what might the increasing suicide rate in adolescents indicate about the status of the psychosocial health of our society as a whole? Based on the vital necessity of community to support their development, Like the canary in the coal mines, this increase in suicidal ideations in our adolescent population may be a warning that our current lack of psychosocial supports have become toxic. If we cannot restore our relatedness and reconstruct our sense of community, societal psychosocial health may continue to decline.
References
1. National Center for Health Statistics Data Brief. 2019 Oct (352). https://www.cdc.gov/nchs/data/databriefs/db352-h.pdf
2. J Soc Pers Relationships. 2019 Mar 19. doi: 10.1177/0265407519836170.
3. Medscape.com. 2020 Sep 25. https://www.medscape.com/viewarticle/938065.
Dr. Loper is the team leader for inpatient psychiatric services at Prisma Health–Midlands in Columbia, S.C. He is an assistant professor in the department of neuropsychiatry and behavioral science at the University of South Carolina, Columbia. He has no conflicts of interest. Dr. Kaminstein is an adjunct assistant professor at the graduate school of education and affiliated faculty in the organizational dynamics program, School of Arts and Sciences, at the University of Pennsylvania, Philadelphia. He is a social psychologist who has been studying groups and organizations for more than 40 years. He has no conflicts of interest.
Increasing youth suicides may be a warning about society’s psychosocial health.
Increasing youth suicides may be a warning about society’s psychosocial health.
Before COVID-19 pandemic, suicide rates were already increasing among adolescents.1 Loneliness, because of social isolation and loss of in-person community contacts, was recognized as one factor perhaps contributing to increasing adolescent suicide.2 Now, with the physical distancing measures vital to curbing the spread, the loneliness epidemic that preceded COVID-19 has only worsened, and suicidal thoughts in adolescents remain on the rise.3
Given the crucial role of interpersonal interactions and community in healthy adolescent development, these troubling trends provide insight not only into the psychosocial health of our teenagers but also into the psychosocial health of our society as a whole.
Over the past 8 months, our psychiatric crisis stabilization unit has experienced a surge in admissions for adolescents with suicidal ideation, often with accompanying attempts. Even more concerning, a significant percentage of these patients do not have additional symptoms of depression or premorbid risk factors for suicide. In many cases, there are no warning signs to alert parents of their adolescent’s imminent suicidal behavior.
Prior to COVID-19, most of our patients with suicidal ideations arrived withdrawn, irritable, and isolative. Interactions with these patients evoked poignant feelings of empathy and sadness, and these patients endorsed multiple additional symptoms consistent with criteria for a specified depressive disorder.
More recently, since COVID-19, we have observed patients who, mere hours earlier, were in an ED receiving medical interventions for a suicide attempt, now present on our unit smiling, laughing, and interacting contentedly with their peers. Upon integration into our milieu, they often report complete resolution of their suicidal thoughts. Interactions with these patients do not conjure feelings of sadness or despair. In fact, we often struggle with diagnostic specificity, because many of these patients do not meet criteria for a specified depressive disorder.
As observed in real time on our unit, meaningful interpersonal interactions are especially crucial to our adolescents’ psychosocial and emotional well-being. As their independence grows, their holding environment expands to incorporate the community. Nonparent family members, teachers, mentors, coaches, peers, parents, and most importantly, same-aged peers play a vital role in creating the environment necessary for healthy adolescent development.
The larger community is essential for adolescents to develop the skills and confidence to move into adulthood. When adolescents are lonely, with less contact with the community outside of their family, they lose the milieu in which they develop. Their fundamental psychological need of belonging becomes compromised; they fail to experience fidelity or a sense of self; and sometimes they no longer have the desire to live.
So what might the increasing suicide rate in adolescents indicate about the status of the psychosocial health of our society as a whole? Based on the vital necessity of community to support their development, Like the canary in the coal mines, this increase in suicidal ideations in our adolescent population may be a warning that our current lack of psychosocial supports have become toxic. If we cannot restore our relatedness and reconstruct our sense of community, societal psychosocial health may continue to decline.
References
1. National Center for Health Statistics Data Brief. 2019 Oct (352). https://www.cdc.gov/nchs/data/databriefs/db352-h.pdf
2. J Soc Pers Relationships. 2019 Mar 19. doi: 10.1177/0265407519836170.
3. Medscape.com. 2020 Sep 25. https://www.medscape.com/viewarticle/938065.
Dr. Loper is the team leader for inpatient psychiatric services at Prisma Health–Midlands in Columbia, S.C. He is an assistant professor in the department of neuropsychiatry and behavioral science at the University of South Carolina, Columbia. He has no conflicts of interest. Dr. Kaminstein is an adjunct assistant professor at the graduate school of education and affiliated faculty in the organizational dynamics program, School of Arts and Sciences, at the University of Pennsylvania, Philadelphia. He is a social psychologist who has been studying groups and organizations for more than 40 years. He has no conflicts of interest.
Before COVID-19 pandemic, suicide rates were already increasing among adolescents.1 Loneliness, because of social isolation and loss of in-person community contacts, was recognized as one factor perhaps contributing to increasing adolescent suicide.2 Now, with the physical distancing measures vital to curbing the spread, the loneliness epidemic that preceded COVID-19 has only worsened, and suicidal thoughts in adolescents remain on the rise.3
Given the crucial role of interpersonal interactions and community in healthy adolescent development, these troubling trends provide insight not only into the psychosocial health of our teenagers but also into the psychosocial health of our society as a whole.
Over the past 8 months, our psychiatric crisis stabilization unit has experienced a surge in admissions for adolescents with suicidal ideation, often with accompanying attempts. Even more concerning, a significant percentage of these patients do not have additional symptoms of depression or premorbid risk factors for suicide. In many cases, there are no warning signs to alert parents of their adolescent’s imminent suicidal behavior.
Prior to COVID-19, most of our patients with suicidal ideations arrived withdrawn, irritable, and isolative. Interactions with these patients evoked poignant feelings of empathy and sadness, and these patients endorsed multiple additional symptoms consistent with criteria for a specified depressive disorder.
More recently, since COVID-19, we have observed patients who, mere hours earlier, were in an ED receiving medical interventions for a suicide attempt, now present on our unit smiling, laughing, and interacting contentedly with their peers. Upon integration into our milieu, they often report complete resolution of their suicidal thoughts. Interactions with these patients do not conjure feelings of sadness or despair. In fact, we often struggle with diagnostic specificity, because many of these patients do not meet criteria for a specified depressive disorder.
As observed in real time on our unit, meaningful interpersonal interactions are especially crucial to our adolescents’ psychosocial and emotional well-being. As their independence grows, their holding environment expands to incorporate the community. Nonparent family members, teachers, mentors, coaches, peers, parents, and most importantly, same-aged peers play a vital role in creating the environment necessary for healthy adolescent development.
The larger community is essential for adolescents to develop the skills and confidence to move into adulthood. When adolescents are lonely, with less contact with the community outside of their family, they lose the milieu in which they develop. Their fundamental psychological need of belonging becomes compromised; they fail to experience fidelity or a sense of self; and sometimes they no longer have the desire to live.
So what might the increasing suicide rate in adolescents indicate about the status of the psychosocial health of our society as a whole? Based on the vital necessity of community to support their development, Like the canary in the coal mines, this increase in suicidal ideations in our adolescent population may be a warning that our current lack of psychosocial supports have become toxic. If we cannot restore our relatedness and reconstruct our sense of community, societal psychosocial health may continue to decline.
References
1. National Center for Health Statistics Data Brief. 2019 Oct (352). https://www.cdc.gov/nchs/data/databriefs/db352-h.pdf
2. J Soc Pers Relationships. 2019 Mar 19. doi: 10.1177/0265407519836170.
3. Medscape.com. 2020 Sep 25. https://www.medscape.com/viewarticle/938065.
Dr. Loper is the team leader for inpatient psychiatric services at Prisma Health–Midlands in Columbia, S.C. He is an assistant professor in the department of neuropsychiatry and behavioral science at the University of South Carolina, Columbia. He has no conflicts of interest. Dr. Kaminstein is an adjunct assistant professor at the graduate school of education and affiliated faculty in the organizational dynamics program, School of Arts and Sciences, at the University of Pennsylvania, Philadelphia. He is a social psychologist who has been studying groups and organizations for more than 40 years. He has no conflicts of interest.
Marijuana vaping more common among Hispanic teens
Hispanic adolescents were more likely to use e-cigarettes to vape marijuana than were their Black and White counterparts in 2020, according to a recent study conducted by the Centers for Disease Control and Prevention and published in JAMA Pediatrics.
Researchers found that 25.6% of Hispanic students reported vaping marijuana, compared to 19.4% of Black students and 18.2% of White students. The study, which is an analysis of 2017, 2018, and 2020 results from the National Youth Tobacco Survey, also revealed that increases in this recreational practice occurred among all racial and ethnic groups within those 3 years, with Hispanic students having the largest percent increase, 11.6%, followed by Black students at 8.8% and White students at 7.4%.
“The initial motivation [to do this study] was to gain a better understanding of the prevalence of use of marijuana in e-cigarettes among youth, particularly given the context of the 2019 outbreak of e-cigarette, or vaping, product use–associated lung injury (EVALI),” study author Christina Vaughan Watson, DrPH, health scientist at the CDC’s National Center for Chronic Disease Prevention and Health Promotion, said in an interview.
The findings could help clinicians and physicians understand demographic variations among marijuana vapers and help inform targeted interventions for specific populations.
“Understanding demographic variations among those who are using marijuana in e-cigarettes can help inform evidenced-based interventions that may resonate with specific populations,” Dr. Watson explained.
Margaret Thew, DNP, medical director of adolescent medicine at Children’s Wisconsin in Milwaukee, who was not involved in the study, said in an interview that the findings were “eye opening” and revealed a pattern she hasn’t seen before in her adolescent clinic.
“I would have thought African-American or non-Hispanic Blacks would’ve been a higher group of use, because when we screen kids that’s what we tend to get from the population we see here,” Ms. Thew said.
Ms. Thew said the findings also had made her reconsider her clinic’s approach to screening adolescents for marijuana use as well as address possible language barriers.
“We are probably missing access to some of the kids that we may need to seek out,” she explained. “I also thought it sends a good message that we need to direct some of our education probably a little differently, especially if it’s a Hispanic population and English may not be the primary language.”
Dr. Watson said more research is needed to assess why differences in marijuana use in e-cigarettes exist among youth.
Marijuana use in e-cigarettes has become increasingly popular among U.S. teens, with one in five students in grades 10 and 12 reporting vaping marijuana within the past year in a 2019 study conducted by the National Institute on Drug Abuse.
Dr. Watson and colleagues also found statistically significant increases in vaping marijuana, with 19.5% of students reporting smoking marijuana via e-cigarettes in 2020, compared to 11.1% of them vaping the drug in 2017. They believe the rise in marijuana vaping among youth may be attributed to states increasingly legalizing adult marijuana sales, which could impact ease of access and social acceptance.
Ms. Thew believes the rise in marijuana vaping among youth can be attributed to the legalization of marijuana, which may send “a message to adolescents that it must be safe for them to use,” as well as the increasing popularity of e-cigarettes.
In fact, as of April 2021, marijuana is legal for adults in 16 states and the District of Columbia. Meanwhile, medical marijuana is legal in 36 states, according to the National Conference of State Legislatures.
“I mean, there’s just definitely been a lot more use of [e-cigarettes]. Vaping and things like that definitely took off between 2019 and 2020,” Ms. Thew explained. “And I think marijuana use in itself is going up tremendously, I think more kids who would have used alcohol in the past use weed.”
Although public attitudes toward marijuana have relaxed, previous studies have linked it to memory dysfunction, as well as long-term cognitive effects that can interfere with perception of time and motor function. However, studies also have shown that cannabis use can combat age-related cognitive decline and help with pain reduction.
However, when it comes to adolescents, Dr. Watson and colleagues said e-cigarette use among youth and young adults is unsafe, regardless of the substances used in these products, including marijuana. Furthermore, they said marijuana use can lead to higher risks of more problematic use later in life, adding that evidence-based strategies to reduce marijuana use in e-cigarettes are important for protecting young people.
The study author and experts disclosed no relevant financial relationships.
Hispanic adolescents were more likely to use e-cigarettes to vape marijuana than were their Black and White counterparts in 2020, according to a recent study conducted by the Centers for Disease Control and Prevention and published in JAMA Pediatrics.
Researchers found that 25.6% of Hispanic students reported vaping marijuana, compared to 19.4% of Black students and 18.2% of White students. The study, which is an analysis of 2017, 2018, and 2020 results from the National Youth Tobacco Survey, also revealed that increases in this recreational practice occurred among all racial and ethnic groups within those 3 years, with Hispanic students having the largest percent increase, 11.6%, followed by Black students at 8.8% and White students at 7.4%.
“The initial motivation [to do this study] was to gain a better understanding of the prevalence of use of marijuana in e-cigarettes among youth, particularly given the context of the 2019 outbreak of e-cigarette, or vaping, product use–associated lung injury (EVALI),” study author Christina Vaughan Watson, DrPH, health scientist at the CDC’s National Center for Chronic Disease Prevention and Health Promotion, said in an interview.
The findings could help clinicians and physicians understand demographic variations among marijuana vapers and help inform targeted interventions for specific populations.
“Understanding demographic variations among those who are using marijuana in e-cigarettes can help inform evidenced-based interventions that may resonate with specific populations,” Dr. Watson explained.
Margaret Thew, DNP, medical director of adolescent medicine at Children’s Wisconsin in Milwaukee, who was not involved in the study, said in an interview that the findings were “eye opening” and revealed a pattern she hasn’t seen before in her adolescent clinic.
“I would have thought African-American or non-Hispanic Blacks would’ve been a higher group of use, because when we screen kids that’s what we tend to get from the population we see here,” Ms. Thew said.
Ms. Thew said the findings also had made her reconsider her clinic’s approach to screening adolescents for marijuana use as well as address possible language barriers.
“We are probably missing access to some of the kids that we may need to seek out,” she explained. “I also thought it sends a good message that we need to direct some of our education probably a little differently, especially if it’s a Hispanic population and English may not be the primary language.”
Dr. Watson said more research is needed to assess why differences in marijuana use in e-cigarettes exist among youth.
Marijuana use in e-cigarettes has become increasingly popular among U.S. teens, with one in five students in grades 10 and 12 reporting vaping marijuana within the past year in a 2019 study conducted by the National Institute on Drug Abuse.
Dr. Watson and colleagues also found statistically significant increases in vaping marijuana, with 19.5% of students reporting smoking marijuana via e-cigarettes in 2020, compared to 11.1% of them vaping the drug in 2017. They believe the rise in marijuana vaping among youth may be attributed to states increasingly legalizing adult marijuana sales, which could impact ease of access and social acceptance.
Ms. Thew believes the rise in marijuana vaping among youth can be attributed to the legalization of marijuana, which may send “a message to adolescents that it must be safe for them to use,” as well as the increasing popularity of e-cigarettes.
In fact, as of April 2021, marijuana is legal for adults in 16 states and the District of Columbia. Meanwhile, medical marijuana is legal in 36 states, according to the National Conference of State Legislatures.
“I mean, there’s just definitely been a lot more use of [e-cigarettes]. Vaping and things like that definitely took off between 2019 and 2020,” Ms. Thew explained. “And I think marijuana use in itself is going up tremendously, I think more kids who would have used alcohol in the past use weed.”
Although public attitudes toward marijuana have relaxed, previous studies have linked it to memory dysfunction, as well as long-term cognitive effects that can interfere with perception of time and motor function. However, studies also have shown that cannabis use can combat age-related cognitive decline and help with pain reduction.
However, when it comes to adolescents, Dr. Watson and colleagues said e-cigarette use among youth and young adults is unsafe, regardless of the substances used in these products, including marijuana. Furthermore, they said marijuana use can lead to higher risks of more problematic use later in life, adding that evidence-based strategies to reduce marijuana use in e-cigarettes are important for protecting young people.
The study author and experts disclosed no relevant financial relationships.
Hispanic adolescents were more likely to use e-cigarettes to vape marijuana than were their Black and White counterparts in 2020, according to a recent study conducted by the Centers for Disease Control and Prevention and published in JAMA Pediatrics.
Researchers found that 25.6% of Hispanic students reported vaping marijuana, compared to 19.4% of Black students and 18.2% of White students. The study, which is an analysis of 2017, 2018, and 2020 results from the National Youth Tobacco Survey, also revealed that increases in this recreational practice occurred among all racial and ethnic groups within those 3 years, with Hispanic students having the largest percent increase, 11.6%, followed by Black students at 8.8% and White students at 7.4%.
“The initial motivation [to do this study] was to gain a better understanding of the prevalence of use of marijuana in e-cigarettes among youth, particularly given the context of the 2019 outbreak of e-cigarette, or vaping, product use–associated lung injury (EVALI),” study author Christina Vaughan Watson, DrPH, health scientist at the CDC’s National Center for Chronic Disease Prevention and Health Promotion, said in an interview.
The findings could help clinicians and physicians understand demographic variations among marijuana vapers and help inform targeted interventions for specific populations.
“Understanding demographic variations among those who are using marijuana in e-cigarettes can help inform evidenced-based interventions that may resonate with specific populations,” Dr. Watson explained.
Margaret Thew, DNP, medical director of adolescent medicine at Children’s Wisconsin in Milwaukee, who was not involved in the study, said in an interview that the findings were “eye opening” and revealed a pattern she hasn’t seen before in her adolescent clinic.
“I would have thought African-American or non-Hispanic Blacks would’ve been a higher group of use, because when we screen kids that’s what we tend to get from the population we see here,” Ms. Thew said.
Ms. Thew said the findings also had made her reconsider her clinic’s approach to screening adolescents for marijuana use as well as address possible language barriers.
“We are probably missing access to some of the kids that we may need to seek out,” she explained. “I also thought it sends a good message that we need to direct some of our education probably a little differently, especially if it’s a Hispanic population and English may not be the primary language.”
Dr. Watson said more research is needed to assess why differences in marijuana use in e-cigarettes exist among youth.
Marijuana use in e-cigarettes has become increasingly popular among U.S. teens, with one in five students in grades 10 and 12 reporting vaping marijuana within the past year in a 2019 study conducted by the National Institute on Drug Abuse.
Dr. Watson and colleagues also found statistically significant increases in vaping marijuana, with 19.5% of students reporting smoking marijuana via e-cigarettes in 2020, compared to 11.1% of them vaping the drug in 2017. They believe the rise in marijuana vaping among youth may be attributed to states increasingly legalizing adult marijuana sales, which could impact ease of access and social acceptance.
Ms. Thew believes the rise in marijuana vaping among youth can be attributed to the legalization of marijuana, which may send “a message to adolescents that it must be safe for them to use,” as well as the increasing popularity of e-cigarettes.
In fact, as of April 2021, marijuana is legal for adults in 16 states and the District of Columbia. Meanwhile, medical marijuana is legal in 36 states, according to the National Conference of State Legislatures.
“I mean, there’s just definitely been a lot more use of [e-cigarettes]. Vaping and things like that definitely took off between 2019 and 2020,” Ms. Thew explained. “And I think marijuana use in itself is going up tremendously, I think more kids who would have used alcohol in the past use weed.”
Although public attitudes toward marijuana have relaxed, previous studies have linked it to memory dysfunction, as well as long-term cognitive effects that can interfere with perception of time and motor function. However, studies also have shown that cannabis use can combat age-related cognitive decline and help with pain reduction.
However, when it comes to adolescents, Dr. Watson and colleagues said e-cigarette use among youth and young adults is unsafe, regardless of the substances used in these products, including marijuana. Furthermore, they said marijuana use can lead to higher risks of more problematic use later in life, adding that evidence-based strategies to reduce marijuana use in e-cigarettes are important for protecting young people.
The study author and experts disclosed no relevant financial relationships.
Challenges persist in adolescents with rheumatic disease transitioning to adult care
The inadequacies and challenges of transitioning pediatric rheumatology patients to adult care were highlighted in several research studies shared at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance.
“Not surprisingly, these studies demonstrate that transition challenges remain pervasive,” Rebecca Sadun, MD, PhD, who was not involved in any of the research, said in an interview. Nevertheless, she pointed out that one of the studies showed that eight of nine sites participating in one of the studies had at least developed a formal transition policy, and three were able to fully integrate that policy into their health care system despite the ongoing pandemic.
In that study, Joyce Chang, MD, of the Children’s Hospital of Philadelphia and colleagues used structured interviews and then quantitative research to explore processes for transition polices across nine rheumatology sites. Aside from the three that had already implemented their policies, three others were preparing implementation. The other three withdrew because of COVID-19. None of the sites had reached sustainment phase. Six of the sites had access to a social work network, and two sites had fewer than four providers.
The authors found that a higher level of change efficacy or change commitment using the Organizational Readiness for Implementing Change framework did not correspond with reaching implementation.
“The first sites to reach implementation had access to [information technology] support and involved nursing, though this was not sufficient or necessary,” the authors wrote. They noted the need for strategies to reduce the burden of data collection to improve the resilience of implementation efforts against health care system stress.
Who more often transitions to adult care?
Effective transition policies can help reduce the likelihood of young patients falling through the cracks as they grow from adolescence into young adulthood, especially those at highest risk for losing continuity of care.
“Young adults who are both medically and socially complex are at highest risk,” said Dr. Sadun, an assistant professor of adult and pediatric rheumatology at Duke University, Durham, N.C. “This is especially true for patients with systemic illnesses, patients requiring biologic medications, and patients with custody, transportation, and financial barriers.”
Research led by Emily A. Smitherman, MD, an assistant professor of pediatric rheumatology at Children’s of Alabama in Birmingham, looked more closely at who is and is not transitioning their care. The researchers analyzed retrospective data from the CARRA Registry, including the Long-Term Follow-Up Call Registry, through December 2019. Among 1,311 patients with inactive status, 537 of these patients had juvenile idiopathic arthritis and were aged at least 18 years. Only 186 of those patients, however, had data in the Long-Term Follow-Up Registry. Patients who were Black or had lower income were less likely to have data in the Long-Term Follow-Up Registry.
Just over half the patients in the long-term registry had transferred their care to an adult rheumatologist, and 83% overall were under the care of any physician. Patients who transferred their care were significantly more likely to have private insurance (87% vs. 70%; P = .009) and were more likely to be full-time students (74% vs. 58%; P = .036).
The researchers found no association between patients’ disease status at their last CARRA Registry visit and a successful transition to adult care. However, those who had transferred care to an adult rheumatologist tended to have a higher median level of pain (4 vs. 2 on a scale of 0-10) and more disease activity (3 vs. 1 on 0-10 scale) than did those who had not transferred care (P = .022 and P = .011, respectively). A higher proportion of those who transferred care had also experienced morning stiffness over the past week (49% vs. 30%; P = .015).
How young adults prefer to learn transition skills
The third study aimed to better understand the experience and preferences of young adults themselves as they transitioned from pediatric to adult care. Kristine Carandang, PhD, a postdoctoral scholar at the University of California, San Diego, and colleagues first conducted focus groups with 39 adolescents and young adults, ages 16-28 years, who had rheumatic conditions. Using the qualitative data from the focus groups, they designed a survey to capture quantitative data on young patients’ experiences.
“What we’re always trying to work on is, how do we bring that youth voice more clearly into the research literature?” Courtney K. Wells, PhD, MSW, an assistant professor of social work at the University of Wisconsin–River Falls, said in an interview. She noted that both she and Dr. Carandang were patients with rheumatic diseases, so they had lived and grown up with disease themselves and then become researchers.
“We have the information that’s in the literature, but then we also both work with youth in a couple different ways, and what we hear from youth is what we heard in our paper, but it isn’t all represented in the literature,” Dr. Wells said. That disconnect is why they also included two young adults as coauthors in the study.
“As much as we appreciate the model of the six components [of health care transition], we recognize that the youth voice isn’t represented very well,” Dr. Wells said. “The way it’s written is more for doctors and policy makers and targeted for the health care system rather than the young people themselves.”
Their research bore that out. Among 137 survey respondents, aged 18-28 years, the vast majority (89%) were women and most (75%) were White. Half the patients (50%) had a diagnosis of lupus.
“For 9 out of 11 self-management and self-advocacy skills examined, there was a significant difference between how adolescent and young adult patients experienced learning self- management skills versus how they would have preferred to learn the skills,” the researchers concluded. “Overall, adolescent and young adult patients most frequently learned about transition skills from their parents. Most participants would have preferred to learn these skills from their rheumatology team.”
For example, 46.7% of the respondents learned how to communicate their medical history from their parents, but 48.5% would have preferred to learn that from their rheumatology team. Only a quarter (24.8%) had learned that skill from their health care team.
“For most of these skills, they were getting that information from their parents, which is concerning because their parents don’t necessarily have information that is accurate,” Dr. Wells said. “Their parents managed their health care, and they taught them to do it the way they were doing it.”
Just over one-third of respondents said they learned from their parents how to track their symptoms so they could answer the rheumatologists’ questions. Only one in five respondents (20.4%) had learned this skill from their rheumatology team, but 41.2% would have preferred hearing it from their health care team, compared with 22.1% who preferred learning it from their parents.
Nearly half the respondents reported learning from their parents how to advocate for themselves when dissatisfied with their care or symptoms (49.6%) and how to talk to the office staff to make appointments, fill out paperwork, and access health records (47.4%). Just over half (51.5%) would have preferred to learn about office communication from their health care team. Preferences on self-advocacy were split between learning from parents (36.8%) and learning from their health care team (31.6%).
An opportunity for other organizations to support transition
The researchers noted that education did not necessarily need to come only from rheumatologists. Other health care professionals, including nurses and social workers, could help young patients develop skills as well.
“They said they’re also open to talking to other people, but they want their rheumatologist to lead the whole process,” Dr. Wells said. While reimbursement gaps may have presented a barrier in the past, Dr. Wells said that current billing codes have removed that obstacle, allowing physicians to bill for discussing transition skills and care.
“Largely, it’s a time issue,” Dr. Wells said. “Rheumatologists are going to tell patients first about their disease, ask how their medication is working and how their health is. Then, if we have time, we’ll cover the transition pieces, and what it boils down to is that they just don’t have time.”
The respondents indicated an interest in technology that can help their education and transition, such as patient portals, telehealth, and smartphone apps.
While 66.4% of respondents said they would attend an in-person health care appointment to learn skills for transitioning to adult care, 74.5% would attend a telehealth appointment, and 77.2% would complete a structured program within a patient portal.
Dr. Wells said she doesn’t see many of the health care system pressures easing up to allow rheumatologists more time for transition care, but she sees an opportunity for organizations, such as the Arthritis Foundation or Lupus Foundation of America, to step in and help.
“It is a matter of being creative and that, ultimately, is the barrier: Whose job is it to make it happen?” she said. “That’s where some other groups are going to need to be advocates.”
Another notable set of findings from this research was the need for young patients’ access to mental health and sexual/reproductive health services. Just over two-thirds of respondents preferred to discuss these topics with their rheumatology team, but only 59.1% felt comfortable starting the conversation about mental health, and only 47.4% felt comfortable broaching the topic of reproductive/sexual health. Even more patients preferred discussing use of drugs and alcohol with their health care team (71.5%), but more patients also felt comfortable initiating that discussion (72.2%).
“It may be that somebody who’s trained to address those issues, especially the mental health piece, may be more appropriate to have that role, and that’s part of the transition, too, these other larger life issues,” Dr. Wells said. “One of the benefits of going to an adult rheumatologist is that they are the most knowledgeable and prepared to help you with those topics.”
None of the individuals quoted in this story had any disclosures to report.
The inadequacies and challenges of transitioning pediatric rheumatology patients to adult care were highlighted in several research studies shared at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance.
“Not surprisingly, these studies demonstrate that transition challenges remain pervasive,” Rebecca Sadun, MD, PhD, who was not involved in any of the research, said in an interview. Nevertheless, she pointed out that one of the studies showed that eight of nine sites participating in one of the studies had at least developed a formal transition policy, and three were able to fully integrate that policy into their health care system despite the ongoing pandemic.
In that study, Joyce Chang, MD, of the Children’s Hospital of Philadelphia and colleagues used structured interviews and then quantitative research to explore processes for transition polices across nine rheumatology sites. Aside from the three that had already implemented their policies, three others were preparing implementation. The other three withdrew because of COVID-19. None of the sites had reached sustainment phase. Six of the sites had access to a social work network, and two sites had fewer than four providers.
The authors found that a higher level of change efficacy or change commitment using the Organizational Readiness for Implementing Change framework did not correspond with reaching implementation.
“The first sites to reach implementation had access to [information technology] support and involved nursing, though this was not sufficient or necessary,” the authors wrote. They noted the need for strategies to reduce the burden of data collection to improve the resilience of implementation efforts against health care system stress.
Who more often transitions to adult care?
Effective transition policies can help reduce the likelihood of young patients falling through the cracks as they grow from adolescence into young adulthood, especially those at highest risk for losing continuity of care.
“Young adults who are both medically and socially complex are at highest risk,” said Dr. Sadun, an assistant professor of adult and pediatric rheumatology at Duke University, Durham, N.C. “This is especially true for patients with systemic illnesses, patients requiring biologic medications, and patients with custody, transportation, and financial barriers.”
Research led by Emily A. Smitherman, MD, an assistant professor of pediatric rheumatology at Children’s of Alabama in Birmingham, looked more closely at who is and is not transitioning their care. The researchers analyzed retrospective data from the CARRA Registry, including the Long-Term Follow-Up Call Registry, through December 2019. Among 1,311 patients with inactive status, 537 of these patients had juvenile idiopathic arthritis and were aged at least 18 years. Only 186 of those patients, however, had data in the Long-Term Follow-Up Registry. Patients who were Black or had lower income were less likely to have data in the Long-Term Follow-Up Registry.
Just over half the patients in the long-term registry had transferred their care to an adult rheumatologist, and 83% overall were under the care of any physician. Patients who transferred their care were significantly more likely to have private insurance (87% vs. 70%; P = .009) and were more likely to be full-time students (74% vs. 58%; P = .036).
The researchers found no association between patients’ disease status at their last CARRA Registry visit and a successful transition to adult care. However, those who had transferred care to an adult rheumatologist tended to have a higher median level of pain (4 vs. 2 on a scale of 0-10) and more disease activity (3 vs. 1 on 0-10 scale) than did those who had not transferred care (P = .022 and P = .011, respectively). A higher proportion of those who transferred care had also experienced morning stiffness over the past week (49% vs. 30%; P = .015).
How young adults prefer to learn transition skills
The third study aimed to better understand the experience and preferences of young adults themselves as they transitioned from pediatric to adult care. Kristine Carandang, PhD, a postdoctoral scholar at the University of California, San Diego, and colleagues first conducted focus groups with 39 adolescents and young adults, ages 16-28 years, who had rheumatic conditions. Using the qualitative data from the focus groups, they designed a survey to capture quantitative data on young patients’ experiences.
“What we’re always trying to work on is, how do we bring that youth voice more clearly into the research literature?” Courtney K. Wells, PhD, MSW, an assistant professor of social work at the University of Wisconsin–River Falls, said in an interview. She noted that both she and Dr. Carandang were patients with rheumatic diseases, so they had lived and grown up with disease themselves and then become researchers.
“We have the information that’s in the literature, but then we also both work with youth in a couple different ways, and what we hear from youth is what we heard in our paper, but it isn’t all represented in the literature,” Dr. Wells said. That disconnect is why they also included two young adults as coauthors in the study.
“As much as we appreciate the model of the six components [of health care transition], we recognize that the youth voice isn’t represented very well,” Dr. Wells said. “The way it’s written is more for doctors and policy makers and targeted for the health care system rather than the young people themselves.”
Their research bore that out. Among 137 survey respondents, aged 18-28 years, the vast majority (89%) were women and most (75%) were White. Half the patients (50%) had a diagnosis of lupus.
“For 9 out of 11 self-management and self-advocacy skills examined, there was a significant difference between how adolescent and young adult patients experienced learning self- management skills versus how they would have preferred to learn the skills,” the researchers concluded. “Overall, adolescent and young adult patients most frequently learned about transition skills from their parents. Most participants would have preferred to learn these skills from their rheumatology team.”
For example, 46.7% of the respondents learned how to communicate their medical history from their parents, but 48.5% would have preferred to learn that from their rheumatology team. Only a quarter (24.8%) had learned that skill from their health care team.
“For most of these skills, they were getting that information from their parents, which is concerning because their parents don’t necessarily have information that is accurate,” Dr. Wells said. “Their parents managed their health care, and they taught them to do it the way they were doing it.”
Just over one-third of respondents said they learned from their parents how to track their symptoms so they could answer the rheumatologists’ questions. Only one in five respondents (20.4%) had learned this skill from their rheumatology team, but 41.2% would have preferred hearing it from their health care team, compared with 22.1% who preferred learning it from their parents.
Nearly half the respondents reported learning from their parents how to advocate for themselves when dissatisfied with their care or symptoms (49.6%) and how to talk to the office staff to make appointments, fill out paperwork, and access health records (47.4%). Just over half (51.5%) would have preferred to learn about office communication from their health care team. Preferences on self-advocacy were split between learning from parents (36.8%) and learning from their health care team (31.6%).
An opportunity for other organizations to support transition
The researchers noted that education did not necessarily need to come only from rheumatologists. Other health care professionals, including nurses and social workers, could help young patients develop skills as well.
“They said they’re also open to talking to other people, but they want their rheumatologist to lead the whole process,” Dr. Wells said. While reimbursement gaps may have presented a barrier in the past, Dr. Wells said that current billing codes have removed that obstacle, allowing physicians to bill for discussing transition skills and care.
“Largely, it’s a time issue,” Dr. Wells said. “Rheumatologists are going to tell patients first about their disease, ask how their medication is working and how their health is. Then, if we have time, we’ll cover the transition pieces, and what it boils down to is that they just don’t have time.”
The respondents indicated an interest in technology that can help their education and transition, such as patient portals, telehealth, and smartphone apps.
While 66.4% of respondents said they would attend an in-person health care appointment to learn skills for transitioning to adult care, 74.5% would attend a telehealth appointment, and 77.2% would complete a structured program within a patient portal.
Dr. Wells said she doesn’t see many of the health care system pressures easing up to allow rheumatologists more time for transition care, but she sees an opportunity for organizations, such as the Arthritis Foundation or Lupus Foundation of America, to step in and help.
“It is a matter of being creative and that, ultimately, is the barrier: Whose job is it to make it happen?” she said. “That’s where some other groups are going to need to be advocates.”
Another notable set of findings from this research was the need for young patients’ access to mental health and sexual/reproductive health services. Just over two-thirds of respondents preferred to discuss these topics with their rheumatology team, but only 59.1% felt comfortable starting the conversation about mental health, and only 47.4% felt comfortable broaching the topic of reproductive/sexual health. Even more patients preferred discussing use of drugs and alcohol with their health care team (71.5%), but more patients also felt comfortable initiating that discussion (72.2%).
“It may be that somebody who’s trained to address those issues, especially the mental health piece, may be more appropriate to have that role, and that’s part of the transition, too, these other larger life issues,” Dr. Wells said. “One of the benefits of going to an adult rheumatologist is that they are the most knowledgeable and prepared to help you with those topics.”
None of the individuals quoted in this story had any disclosures to report.
The inadequacies and challenges of transitioning pediatric rheumatology patients to adult care were highlighted in several research studies shared at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance.
“Not surprisingly, these studies demonstrate that transition challenges remain pervasive,” Rebecca Sadun, MD, PhD, who was not involved in any of the research, said in an interview. Nevertheless, she pointed out that one of the studies showed that eight of nine sites participating in one of the studies had at least developed a formal transition policy, and three were able to fully integrate that policy into their health care system despite the ongoing pandemic.
In that study, Joyce Chang, MD, of the Children’s Hospital of Philadelphia and colleagues used structured interviews and then quantitative research to explore processes for transition polices across nine rheumatology sites. Aside from the three that had already implemented their policies, three others were preparing implementation. The other three withdrew because of COVID-19. None of the sites had reached sustainment phase. Six of the sites had access to a social work network, and two sites had fewer than four providers.
The authors found that a higher level of change efficacy or change commitment using the Organizational Readiness for Implementing Change framework did not correspond with reaching implementation.
“The first sites to reach implementation had access to [information technology] support and involved nursing, though this was not sufficient or necessary,” the authors wrote. They noted the need for strategies to reduce the burden of data collection to improve the resilience of implementation efforts against health care system stress.
Who more often transitions to adult care?
Effective transition policies can help reduce the likelihood of young patients falling through the cracks as they grow from adolescence into young adulthood, especially those at highest risk for losing continuity of care.
“Young adults who are both medically and socially complex are at highest risk,” said Dr. Sadun, an assistant professor of adult and pediatric rheumatology at Duke University, Durham, N.C. “This is especially true for patients with systemic illnesses, patients requiring biologic medications, and patients with custody, transportation, and financial barriers.”
Research led by Emily A. Smitherman, MD, an assistant professor of pediatric rheumatology at Children’s of Alabama in Birmingham, looked more closely at who is and is not transitioning their care. The researchers analyzed retrospective data from the CARRA Registry, including the Long-Term Follow-Up Call Registry, through December 2019. Among 1,311 patients with inactive status, 537 of these patients had juvenile idiopathic arthritis and were aged at least 18 years. Only 186 of those patients, however, had data in the Long-Term Follow-Up Registry. Patients who were Black or had lower income were less likely to have data in the Long-Term Follow-Up Registry.
Just over half the patients in the long-term registry had transferred their care to an adult rheumatologist, and 83% overall were under the care of any physician. Patients who transferred their care were significantly more likely to have private insurance (87% vs. 70%; P = .009) and were more likely to be full-time students (74% vs. 58%; P = .036).
The researchers found no association between patients’ disease status at their last CARRA Registry visit and a successful transition to adult care. However, those who had transferred care to an adult rheumatologist tended to have a higher median level of pain (4 vs. 2 on a scale of 0-10) and more disease activity (3 vs. 1 on 0-10 scale) than did those who had not transferred care (P = .022 and P = .011, respectively). A higher proportion of those who transferred care had also experienced morning stiffness over the past week (49% vs. 30%; P = .015).
How young adults prefer to learn transition skills
The third study aimed to better understand the experience and preferences of young adults themselves as they transitioned from pediatric to adult care. Kristine Carandang, PhD, a postdoctoral scholar at the University of California, San Diego, and colleagues first conducted focus groups with 39 adolescents and young adults, ages 16-28 years, who had rheumatic conditions. Using the qualitative data from the focus groups, they designed a survey to capture quantitative data on young patients’ experiences.
“What we’re always trying to work on is, how do we bring that youth voice more clearly into the research literature?” Courtney K. Wells, PhD, MSW, an assistant professor of social work at the University of Wisconsin–River Falls, said in an interview. She noted that both she and Dr. Carandang were patients with rheumatic diseases, so they had lived and grown up with disease themselves and then become researchers.
“We have the information that’s in the literature, but then we also both work with youth in a couple different ways, and what we hear from youth is what we heard in our paper, but it isn’t all represented in the literature,” Dr. Wells said. That disconnect is why they also included two young adults as coauthors in the study.
“As much as we appreciate the model of the six components [of health care transition], we recognize that the youth voice isn’t represented very well,” Dr. Wells said. “The way it’s written is more for doctors and policy makers and targeted for the health care system rather than the young people themselves.”
Their research bore that out. Among 137 survey respondents, aged 18-28 years, the vast majority (89%) were women and most (75%) were White. Half the patients (50%) had a diagnosis of lupus.
“For 9 out of 11 self-management and self-advocacy skills examined, there was a significant difference between how adolescent and young adult patients experienced learning self- management skills versus how they would have preferred to learn the skills,” the researchers concluded. “Overall, adolescent and young adult patients most frequently learned about transition skills from their parents. Most participants would have preferred to learn these skills from their rheumatology team.”
For example, 46.7% of the respondents learned how to communicate their medical history from their parents, but 48.5% would have preferred to learn that from their rheumatology team. Only a quarter (24.8%) had learned that skill from their health care team.
“For most of these skills, they were getting that information from their parents, which is concerning because their parents don’t necessarily have information that is accurate,” Dr. Wells said. “Their parents managed their health care, and they taught them to do it the way they were doing it.”
Just over one-third of respondents said they learned from their parents how to track their symptoms so they could answer the rheumatologists’ questions. Only one in five respondents (20.4%) had learned this skill from their rheumatology team, but 41.2% would have preferred hearing it from their health care team, compared with 22.1% who preferred learning it from their parents.
Nearly half the respondents reported learning from their parents how to advocate for themselves when dissatisfied with their care or symptoms (49.6%) and how to talk to the office staff to make appointments, fill out paperwork, and access health records (47.4%). Just over half (51.5%) would have preferred to learn about office communication from their health care team. Preferences on self-advocacy were split between learning from parents (36.8%) and learning from their health care team (31.6%).
An opportunity for other organizations to support transition
The researchers noted that education did not necessarily need to come only from rheumatologists. Other health care professionals, including nurses and social workers, could help young patients develop skills as well.
“They said they’re also open to talking to other people, but they want their rheumatologist to lead the whole process,” Dr. Wells said. While reimbursement gaps may have presented a barrier in the past, Dr. Wells said that current billing codes have removed that obstacle, allowing physicians to bill for discussing transition skills and care.
“Largely, it’s a time issue,” Dr. Wells said. “Rheumatologists are going to tell patients first about their disease, ask how their medication is working and how their health is. Then, if we have time, we’ll cover the transition pieces, and what it boils down to is that they just don’t have time.”
The respondents indicated an interest in technology that can help their education and transition, such as patient portals, telehealth, and smartphone apps.
While 66.4% of respondents said they would attend an in-person health care appointment to learn skills for transitioning to adult care, 74.5% would attend a telehealth appointment, and 77.2% would complete a structured program within a patient portal.
Dr. Wells said she doesn’t see many of the health care system pressures easing up to allow rheumatologists more time for transition care, but she sees an opportunity for organizations, such as the Arthritis Foundation or Lupus Foundation of America, to step in and help.
“It is a matter of being creative and that, ultimately, is the barrier: Whose job is it to make it happen?” she said. “That’s where some other groups are going to need to be advocates.”
Another notable set of findings from this research was the need for young patients’ access to mental health and sexual/reproductive health services. Just over two-thirds of respondents preferred to discuss these topics with their rheumatology team, but only 59.1% felt comfortable starting the conversation about mental health, and only 47.4% felt comfortable broaching the topic of reproductive/sexual health. Even more patients preferred discussing use of drugs and alcohol with their health care team (71.5%), but more patients also felt comfortable initiating that discussion (72.2%).
“It may be that somebody who’s trained to address those issues, especially the mental health piece, may be more appropriate to have that role, and that’s part of the transition, too, these other larger life issues,” Dr. Wells said. “One of the benefits of going to an adult rheumatologist is that they are the most knowledgeable and prepared to help you with those topics.”
None of the individuals quoted in this story had any disclosures to report.
FROM CARRA 2021
Teen tanning bed ban would prevent more than 15,000 melanoma cases
and cost less than other, well-established public health interventions, according to a microsimulation of that age group’s virtual life course.
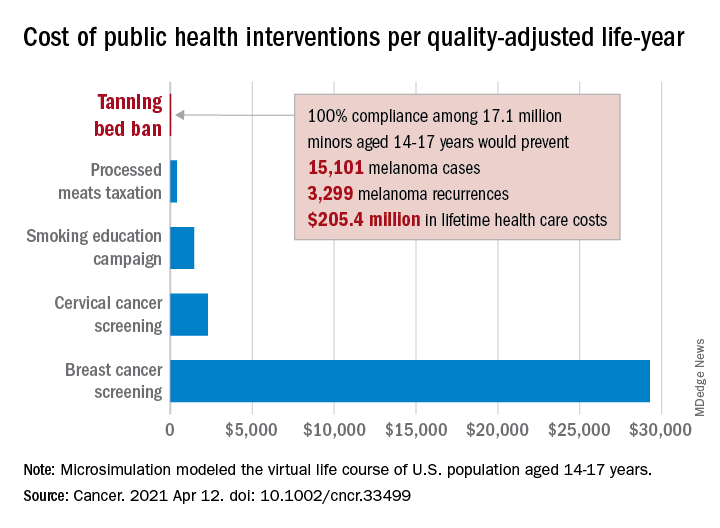
“Even with extensive sensitivity analyses on the costs of inspections, noncompliance with a ban, and the risk of developing melanoma in those who have used tanning beds, a ban can be considered highly cost effective,” Antoine Eskander, MD, ScM, of the University of Toronto, and associates said in Cancer.
Compared with no ban, such an intervention could save over $205 million in lifetime health care costs among the 17.1 million young people (based on the 2010 Census population) who would be affected, they said.
The more than 15,000 melanoma cases and 3,300 recurrences prevented would save $12 per average minor after adjusting for societal costs, such as lost productivity, formal and informal health care, economic losses to the tanning bed industry, and the need for monitoring, the investigators reported.
Switching to quality-adjusted life-years shows an improvement of 0.0002 QALYs per child for a ban, based on an overall cost of almost $24.9 per QALY, compared with no ban, they said, which makes it “more cost effective than many well-established public health interventions”:
- Processed meats taxation ($270/QALY).
- Smoking education campaign ($1,337/QALY).
- Cervical cancer screening ($2,166/QALY).
- Breast cancer screening ($29,284/QALY).
- Lung cancer screening ($49,200-$96,700/QALY).
Among the many parameters included in the microsimulation were the odds ratio of developing melanoma from exposure to tanning beds before age 25 (1.35), melanoma stage at presentation, risk of recurrence, and the cost of four annual inspections for each of the nation’s more than 13,000 tanning salons, Dr. Eskander and associates explained.
and cost less than other, well-established public health interventions, according to a microsimulation of that age group’s virtual life course.
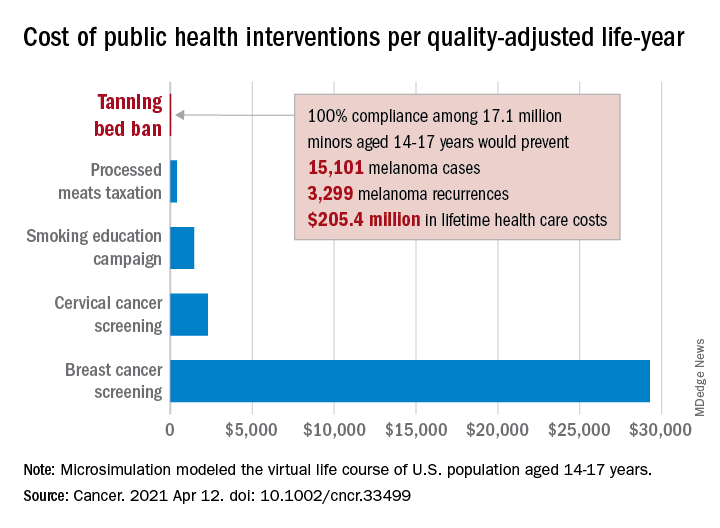
“Even with extensive sensitivity analyses on the costs of inspections, noncompliance with a ban, and the risk of developing melanoma in those who have used tanning beds, a ban can be considered highly cost effective,” Antoine Eskander, MD, ScM, of the University of Toronto, and associates said in Cancer.
Compared with no ban, such an intervention could save over $205 million in lifetime health care costs among the 17.1 million young people (based on the 2010 Census population) who would be affected, they said.
The more than 15,000 melanoma cases and 3,300 recurrences prevented would save $12 per average minor after adjusting for societal costs, such as lost productivity, formal and informal health care, economic losses to the tanning bed industry, and the need for monitoring, the investigators reported.
Switching to quality-adjusted life-years shows an improvement of 0.0002 QALYs per child for a ban, based on an overall cost of almost $24.9 per QALY, compared with no ban, they said, which makes it “more cost effective than many well-established public health interventions”:
- Processed meats taxation ($270/QALY).
- Smoking education campaign ($1,337/QALY).
- Cervical cancer screening ($2,166/QALY).
- Breast cancer screening ($29,284/QALY).
- Lung cancer screening ($49,200-$96,700/QALY).
Among the many parameters included in the microsimulation were the odds ratio of developing melanoma from exposure to tanning beds before age 25 (1.35), melanoma stage at presentation, risk of recurrence, and the cost of four annual inspections for each of the nation’s more than 13,000 tanning salons, Dr. Eskander and associates explained.
and cost less than other, well-established public health interventions, according to a microsimulation of that age group’s virtual life course.
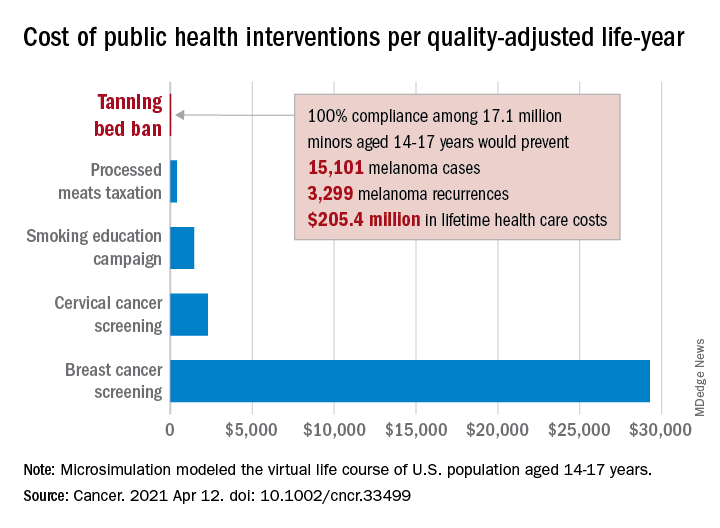
“Even with extensive sensitivity analyses on the costs of inspections, noncompliance with a ban, and the risk of developing melanoma in those who have used tanning beds, a ban can be considered highly cost effective,” Antoine Eskander, MD, ScM, of the University of Toronto, and associates said in Cancer.
Compared with no ban, such an intervention could save over $205 million in lifetime health care costs among the 17.1 million young people (based on the 2010 Census population) who would be affected, they said.
The more than 15,000 melanoma cases and 3,300 recurrences prevented would save $12 per average minor after adjusting for societal costs, such as lost productivity, formal and informal health care, economic losses to the tanning bed industry, and the need for monitoring, the investigators reported.
Switching to quality-adjusted life-years shows an improvement of 0.0002 QALYs per child for a ban, based on an overall cost of almost $24.9 per QALY, compared with no ban, they said, which makes it “more cost effective than many well-established public health interventions”:
- Processed meats taxation ($270/QALY).
- Smoking education campaign ($1,337/QALY).
- Cervical cancer screening ($2,166/QALY).
- Breast cancer screening ($29,284/QALY).
- Lung cancer screening ($49,200-$96,700/QALY).
Among the many parameters included in the microsimulation were the odds ratio of developing melanoma from exposure to tanning beds before age 25 (1.35), melanoma stage at presentation, risk of recurrence, and the cost of four annual inspections for each of the nation’s more than 13,000 tanning salons, Dr. Eskander and associates explained.
FROM CANCER
Family psychoeducation is critical in care of children with disabilities
Dr. Margaret G. Klitzke is a board-certified child and adolescent psychiatrist who has worked across all settings of the Center for Autism and Developmental Disabilities at Bradley Hospital in East Providence, R.I.
I spoke with Dr. Klitzke recently about her work as an outpatient psychiatrist at the center and about the important role of families in the treatment it provides. The center offers highly specialized clinical services for children and adolescents between the ages of 2 and 18 who show signs of serious emotional and behavioral problems in addition to a developmental disability, such as autism, Asperger’s, or intellectual disability.
The center’s model of care emphasizes family involvement. Dr. Klitzke was trained in family interventions by Nathan B. Epstein, MD, and Duane S. Bishop, MD, the originators of the McMaster approach and the problem-centered systems therapy of the family. This training informs much of her work with families.
ALISON M. HERU, MD: Hello, Dr. Klitzke and thank you for agreeing to this interview.
MARGARET G. KLITZKE, DO: My pleasure.
AMH: I admire your dedication to this population of children and adolescents. To me, it seems very hard to work with patients and families where there is significant disability and there is little hope of the patient “getting better.”
MGK: When parents come to us, they have great hopes their children can be helped. They often express understanding and acceptance of the child’s disability, and seek to understand the psychiatric or behavioral issues. These parents are often very dedicated to their children, giving up careers to care for them. But as professionals, we must be sensitive to the role each parent can play and how they can support each other and the family.
AMH: So much of your work focuses on family inclusion and family psychoeducation?
MGK: Yes. An example that stands out is a couple where the mother had become the voice for the family in dealing with professionals, but she was overwhelmed in this role. So, we invited the father in. He explained that medical professionals and school personnel would address their remarks to his wife and that he felt marginalized. We worked with the couple, now always including the father, and he has gone on to become a vocal advocate for children with disabilities. It is inspiring to watch families become advocates – to insist that others see the child’s strengths – not just weaknesses.
AMH: Do you feel that the families ever come to you with too high expectations of what you can do to help their child?
MGK: As a child psychiatrist, one must put oneself in the parents’ shoes. Charlie Zeanah Jr., MD, and others have done wonderful work in attachment. They have identified that parents have fantasies and beliefs about what the child will be like before the child is born. We all have fantasies about our babies before they come to us! For many families, they quickly come to understand that their child is not like other children. This new world of parenting is not what they expected. A mother once gave me a short piece called “Welcome to Holland,” written by a mother whose child has Down syndrome.
AMH: How do you begin to work with these families? There must be such a sense of loss and tragedy in their lives.
MGK: My first goal is to understand what it is like to have a child with developmental disability, not just for the parents but for the siblings, too. I strive to understand what the parents want for their child and how they see themselves as a family. I see us, the health care team, as agents to help the child and the family be the very best they can be.
AMH: How do you deal with parents who are not be on the same page?
MGK: It is important that parents are consistent and are able to work together. Even if they are divorced, I have seen families able to unite around the care of their child with a disability. This is quite an achievement given the high rates of divorce – although most of the families that I have worked with are intact. As in all families, each member has a role in helping the family function well. It means using the strength of each parent to help them become a parenting team.
AMH: What if the parents have unrealistic expectations of their child?
MGK: Yes, there are parents who come to us with unrealistic expectations, such as believing their nonverbal child will talk some day. In such a case, we must be certain that we have exhausted all methods to help this child communicate, and once we have done all we can, then we must accept where that child is; to accept and help the family accept, the child’s weaknesses and acknowledge their strengths. Change what you can and be a support for everything else.
AMH: I find it hard to imagine caring for a severely disabled child. How do these parents do this?
MGK: These are children who are nonverbal, and children who can be very fragile, even medically. What I see are parents who want to connect, who want to find that something inside that child, that special place where there is connection. That place of reciprocity. That is important to us all, helping the family find that place of reciprocal connection.
AMH: What language do you use to discuss this with families?
MGK: I say, “This is the child’s strength and this is the child’s weakness; capitalize on the strengths and let’s shore up their weaknesses.”
AMH: How do you approach the families? Where do you start?
MGK: I meet the family where they are. One cannot with these families or any families stand rigidly 10 feet away, and demand that they change. This never works, and we will be of no help to them. We must understand the family system and how they have arrived at their current place of functioning.
AMH: Can you give an example?
MGK: Yes, for example if a parent is drinking excessively, I help them understand why they are coping that way and see if they are willing to change.
AMH: What keeps you going ?
MGK: I think it comes back to the family work. For me, I believe the families are doing the very best they can. If the family is really impaired in some way, I see it as my job to figure out why that is their pattern of behavior, and I do what I can to help them facilitate change.
AMH: What inspires you about these families?
MGK: These families are able to recognize the strengths and beauty that their children bring them – the strength of these children, their personalities and their wills of steel! They are able to communicate what they need. Siblings, too, make life decisions based on their experiences. They often end up going down the path of caring for such children as professionals.
AMH: Do you have any recommendations for a young child psychiatrist who might be considering working with this population?
MGK: Developmental disabilities in child psychiatry is where medicine, neurology, and child development meet. The advances in genetics and neurology are major gifts to the field. It used to be that I would have to sell the field to medical students and residents. Now they are coming to me saying that they want to work in this area. It is an intellectually rich field in which to work. There is a real change happening. But the place where it becomes really magical is in working with the families.
AMH: What other changes have you seen?
MGK: With the closure of big institutions, it is less of an option for families to walk away. The families now feel that they need to take care of the child.
AMH: What has your career taught you?
MGK: It has taught me patience, to enter every situation without preconceived notions, and that there is something new to learn every day.
References
J Child Adolesc Psychiatry. 1975 Jun 1;14(3):387-421.
Evaluation and Treating Families: The McMaster Approach. Routledge/Taylor & Francis Group, 2005.
Movies to watch
Lorenzo’s Oil, 1992.
My Left Foot, 1989.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest.
Dr. Klitkze is a 1983 graduate of the Texas College of Osteopathic Medicine, and completed her residency and fellowship training at Brown University, Providence, R.I. She is a member of the American Psychiatric Association, the American Academy of Child and Adolescent Psychiatry, and the Rhode Island Medical Society, where she serves on the Physicians’ Health Committee. She is actively involved in teaching medical students, residents, and fellows, and has received several teaching awards from the department of psychiatry and human behavior at Brown.
Dr. Margaret G. Klitzke is a board-certified child and adolescent psychiatrist who has worked across all settings of the Center for Autism and Developmental Disabilities at Bradley Hospital in East Providence, R.I.
I spoke with Dr. Klitzke recently about her work as an outpatient psychiatrist at the center and about the important role of families in the treatment it provides. The center offers highly specialized clinical services for children and adolescents between the ages of 2 and 18 who show signs of serious emotional and behavioral problems in addition to a developmental disability, such as autism, Asperger’s, or intellectual disability.
The center’s model of care emphasizes family involvement. Dr. Klitzke was trained in family interventions by Nathan B. Epstein, MD, and Duane S. Bishop, MD, the originators of the McMaster approach and the problem-centered systems therapy of the family. This training informs much of her work with families.
ALISON M. HERU, MD: Hello, Dr. Klitzke and thank you for agreeing to this interview.
MARGARET G. KLITZKE, DO: My pleasure.
AMH: I admire your dedication to this population of children and adolescents. To me, it seems very hard to work with patients and families where there is significant disability and there is little hope of the patient “getting better.”
MGK: When parents come to us, they have great hopes their children can be helped. They often express understanding and acceptance of the child’s disability, and seek to understand the psychiatric or behavioral issues. These parents are often very dedicated to their children, giving up careers to care for them. But as professionals, we must be sensitive to the role each parent can play and how they can support each other and the family.
AMH: So much of your work focuses on family inclusion and family psychoeducation?
MGK: Yes. An example that stands out is a couple where the mother had become the voice for the family in dealing with professionals, but she was overwhelmed in this role. So, we invited the father in. He explained that medical professionals and school personnel would address their remarks to his wife and that he felt marginalized. We worked with the couple, now always including the father, and he has gone on to become a vocal advocate for children with disabilities. It is inspiring to watch families become advocates – to insist that others see the child’s strengths – not just weaknesses.
AMH: Do you feel that the families ever come to you with too high expectations of what you can do to help their child?
MGK: As a child psychiatrist, one must put oneself in the parents’ shoes. Charlie Zeanah Jr., MD, and others have done wonderful work in attachment. They have identified that parents have fantasies and beliefs about what the child will be like before the child is born. We all have fantasies about our babies before they come to us! For many families, they quickly come to understand that their child is not like other children. This new world of parenting is not what they expected. A mother once gave me a short piece called “Welcome to Holland,” written by a mother whose child has Down syndrome.
AMH: How do you begin to work with these families? There must be such a sense of loss and tragedy in their lives.
MGK: My first goal is to understand what it is like to have a child with developmental disability, not just for the parents but for the siblings, too. I strive to understand what the parents want for their child and how they see themselves as a family. I see us, the health care team, as agents to help the child and the family be the very best they can be.
AMH: How do you deal with parents who are not be on the same page?
MGK: It is important that parents are consistent and are able to work together. Even if they are divorced, I have seen families able to unite around the care of their child with a disability. This is quite an achievement given the high rates of divorce – although most of the families that I have worked with are intact. As in all families, each member has a role in helping the family function well. It means using the strength of each parent to help them become a parenting team.
AMH: What if the parents have unrealistic expectations of their child?
MGK: Yes, there are parents who come to us with unrealistic expectations, such as believing their nonverbal child will talk some day. In such a case, we must be certain that we have exhausted all methods to help this child communicate, and once we have done all we can, then we must accept where that child is; to accept and help the family accept, the child’s weaknesses and acknowledge their strengths. Change what you can and be a support for everything else.
AMH: I find it hard to imagine caring for a severely disabled child. How do these parents do this?
MGK: These are children who are nonverbal, and children who can be very fragile, even medically. What I see are parents who want to connect, who want to find that something inside that child, that special place where there is connection. That place of reciprocity. That is important to us all, helping the family find that place of reciprocal connection.
AMH: What language do you use to discuss this with families?
MGK: I say, “This is the child’s strength and this is the child’s weakness; capitalize on the strengths and let’s shore up their weaknesses.”
AMH: How do you approach the families? Where do you start?
MGK: I meet the family where they are. One cannot with these families or any families stand rigidly 10 feet away, and demand that they change. This never works, and we will be of no help to them. We must understand the family system and how they have arrived at their current place of functioning.
AMH: Can you give an example?
MGK: Yes, for example if a parent is drinking excessively, I help them understand why they are coping that way and see if they are willing to change.
AMH: What keeps you going ?
MGK: I think it comes back to the family work. For me, I believe the families are doing the very best they can. If the family is really impaired in some way, I see it as my job to figure out why that is their pattern of behavior, and I do what I can to help them facilitate change.
AMH: What inspires you about these families?
MGK: These families are able to recognize the strengths and beauty that their children bring them – the strength of these children, their personalities and their wills of steel! They are able to communicate what they need. Siblings, too, make life decisions based on their experiences. They often end up going down the path of caring for such children as professionals.
AMH: Do you have any recommendations for a young child psychiatrist who might be considering working with this population?
MGK: Developmental disabilities in child psychiatry is where medicine, neurology, and child development meet. The advances in genetics and neurology are major gifts to the field. It used to be that I would have to sell the field to medical students and residents. Now they are coming to me saying that they want to work in this area. It is an intellectually rich field in which to work. There is a real change happening. But the place where it becomes really magical is in working with the families.
AMH: What other changes have you seen?
MGK: With the closure of big institutions, it is less of an option for families to walk away. The families now feel that they need to take care of the child.
AMH: What has your career taught you?
MGK: It has taught me patience, to enter every situation without preconceived notions, and that there is something new to learn every day.
References
J Child Adolesc Psychiatry. 1975 Jun 1;14(3):387-421.
Evaluation and Treating Families: The McMaster Approach. Routledge/Taylor & Francis Group, 2005.
Movies to watch
Lorenzo’s Oil, 1992.
My Left Foot, 1989.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest.
Dr. Klitkze is a 1983 graduate of the Texas College of Osteopathic Medicine, and completed her residency and fellowship training at Brown University, Providence, R.I. She is a member of the American Psychiatric Association, the American Academy of Child and Adolescent Psychiatry, and the Rhode Island Medical Society, where she serves on the Physicians’ Health Committee. She is actively involved in teaching medical students, residents, and fellows, and has received several teaching awards from the department of psychiatry and human behavior at Brown.
Dr. Margaret G. Klitzke is a board-certified child and adolescent psychiatrist who has worked across all settings of the Center for Autism and Developmental Disabilities at Bradley Hospital in East Providence, R.I.
I spoke with Dr. Klitzke recently about her work as an outpatient psychiatrist at the center and about the important role of families in the treatment it provides. The center offers highly specialized clinical services for children and adolescents between the ages of 2 and 18 who show signs of serious emotional and behavioral problems in addition to a developmental disability, such as autism, Asperger’s, or intellectual disability.
The center’s model of care emphasizes family involvement. Dr. Klitzke was trained in family interventions by Nathan B. Epstein, MD, and Duane S. Bishop, MD, the originators of the McMaster approach and the problem-centered systems therapy of the family. This training informs much of her work with families.
ALISON M. HERU, MD: Hello, Dr. Klitzke and thank you for agreeing to this interview.
MARGARET G. KLITZKE, DO: My pleasure.
AMH: I admire your dedication to this population of children and adolescents. To me, it seems very hard to work with patients and families where there is significant disability and there is little hope of the patient “getting better.”
MGK: When parents come to us, they have great hopes their children can be helped. They often express understanding and acceptance of the child’s disability, and seek to understand the psychiatric or behavioral issues. These parents are often very dedicated to their children, giving up careers to care for them. But as professionals, we must be sensitive to the role each parent can play and how they can support each other and the family.
AMH: So much of your work focuses on family inclusion and family psychoeducation?
MGK: Yes. An example that stands out is a couple where the mother had become the voice for the family in dealing with professionals, but she was overwhelmed in this role. So, we invited the father in. He explained that medical professionals and school personnel would address their remarks to his wife and that he felt marginalized. We worked with the couple, now always including the father, and he has gone on to become a vocal advocate for children with disabilities. It is inspiring to watch families become advocates – to insist that others see the child’s strengths – not just weaknesses.
AMH: Do you feel that the families ever come to you with too high expectations of what you can do to help their child?
MGK: As a child psychiatrist, one must put oneself in the parents’ shoes. Charlie Zeanah Jr., MD, and others have done wonderful work in attachment. They have identified that parents have fantasies and beliefs about what the child will be like before the child is born. We all have fantasies about our babies before they come to us! For many families, they quickly come to understand that their child is not like other children. This new world of parenting is not what they expected. A mother once gave me a short piece called “Welcome to Holland,” written by a mother whose child has Down syndrome.
AMH: How do you begin to work with these families? There must be such a sense of loss and tragedy in their lives.
MGK: My first goal is to understand what it is like to have a child with developmental disability, not just for the parents but for the siblings, too. I strive to understand what the parents want for their child and how they see themselves as a family. I see us, the health care team, as agents to help the child and the family be the very best they can be.
AMH: How do you deal with parents who are not be on the same page?
MGK: It is important that parents are consistent and are able to work together. Even if they are divorced, I have seen families able to unite around the care of their child with a disability. This is quite an achievement given the high rates of divorce – although most of the families that I have worked with are intact. As in all families, each member has a role in helping the family function well. It means using the strength of each parent to help them become a parenting team.
AMH: What if the parents have unrealistic expectations of their child?
MGK: Yes, there are parents who come to us with unrealistic expectations, such as believing their nonverbal child will talk some day. In such a case, we must be certain that we have exhausted all methods to help this child communicate, and once we have done all we can, then we must accept where that child is; to accept and help the family accept, the child’s weaknesses and acknowledge their strengths. Change what you can and be a support for everything else.
AMH: I find it hard to imagine caring for a severely disabled child. How do these parents do this?
MGK: These are children who are nonverbal, and children who can be very fragile, even medically. What I see are parents who want to connect, who want to find that something inside that child, that special place where there is connection. That place of reciprocity. That is important to us all, helping the family find that place of reciprocal connection.
AMH: What language do you use to discuss this with families?
MGK: I say, “This is the child’s strength and this is the child’s weakness; capitalize on the strengths and let’s shore up their weaknesses.”
AMH: How do you approach the families? Where do you start?
MGK: I meet the family where they are. One cannot with these families or any families stand rigidly 10 feet away, and demand that they change. This never works, and we will be of no help to them. We must understand the family system and how they have arrived at their current place of functioning.
AMH: Can you give an example?
MGK: Yes, for example if a parent is drinking excessively, I help them understand why they are coping that way and see if they are willing to change.
AMH: What keeps you going ?
MGK: I think it comes back to the family work. For me, I believe the families are doing the very best they can. If the family is really impaired in some way, I see it as my job to figure out why that is their pattern of behavior, and I do what I can to help them facilitate change.
AMH: What inspires you about these families?
MGK: These families are able to recognize the strengths and beauty that their children bring them – the strength of these children, their personalities and their wills of steel! They are able to communicate what they need. Siblings, too, make life decisions based on their experiences. They often end up going down the path of caring for such children as professionals.
AMH: Do you have any recommendations for a young child psychiatrist who might be considering working with this population?
MGK: Developmental disabilities in child psychiatry is where medicine, neurology, and child development meet. The advances in genetics and neurology are major gifts to the field. It used to be that I would have to sell the field to medical students and residents. Now they are coming to me saying that they want to work in this area. It is an intellectually rich field in which to work. There is a real change happening. But the place where it becomes really magical is in working with the families.
AMH: What other changes have you seen?
MGK: With the closure of big institutions, it is less of an option for families to walk away. The families now feel that they need to take care of the child.
AMH: What has your career taught you?
MGK: It has taught me patience, to enter every situation without preconceived notions, and that there is something new to learn every day.
References
J Child Adolesc Psychiatry. 1975 Jun 1;14(3):387-421.
Evaluation and Treating Families: The McMaster Approach. Routledge/Taylor & Francis Group, 2005.
Movies to watch
Lorenzo’s Oil, 1992.
My Left Foot, 1989.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest.
Dr. Klitkze is a 1983 graduate of the Texas College of Osteopathic Medicine, and completed her residency and fellowship training at Brown University, Providence, R.I. She is a member of the American Psychiatric Association, the American Academy of Child and Adolescent Psychiatry, and the Rhode Island Medical Society, where she serves on the Physicians’ Health Committee. She is actively involved in teaching medical students, residents, and fellows, and has received several teaching awards from the department of psychiatry and human behavior at Brown.
Hyperphagia, anxiety eased with carbetocin in patients with Prader-Willi syndrome
Children and adolescents with Prader-Willi syndrome (PWS) who received three daily, intranasal doses of carbetocin, an investigational, long-acting oxytocin analogue, had significant improvement in hyperphagia and anxiety during 8 weeks on treatment, compared with placebo in a multicenter, phase 3 trial with 119 patients.
The treatment also appeared safe during up to 56 additional weeks on active treatment, with no serious adverse effects nor “unexpected” events, and once completing the study about 95% of enrolled patients opted to remain on active treatment, Cheri L. Deal, MD, PhD, said at the annual meeting of the Endocrine Society.
Based on “the significant results for the placebo-controlled period, as well as for those finishing the 56-week extension, we may well have a new armament for helping these kids and their families deal with the unrelenting hunger of patients with PWS as well as some of the behavioral symptoms,” Dr. Deal, chief of endocrinology and diabetes at the Sainte-Justine Mother-Child University of Montreal Hospital, said in an interview. No treatment currently has labeling for addressing the hyperphagia or anxiety that is characteristic and often problematic for children and adolescents with PWS, an autosomal dominant genetic disease with an incidence of about 1 in 15,000 births and an estimated U.S. prevalence of about 9,000 cases, or about 1 case for every 37,000 people.
‘Gorgeous’ safety
“The results looked pretty positive, and we’re encouraged by what appears to be a good safety profile, so overall I think the PWS community is very excited by the results and is very interested in getting access to this drug,” commented Theresa V. Strong, PhD, director of research programs for the Foundation for Prader-Willi Research in Walnut, Calif., a group not involved with the study. Currently, “we have no effective treatments for these difficult behaviors” of hyperphagia and anxiety. Surveys and studies run by the foundation have documented that hyperphagia and anxiety “were the two most important symptoms that families would like to see treated,” Dr. Strong added in an interview.
PWS “is complex and affects almost every aspect of the lives of affected people and their families. Any treatment that can chip away at some of the problems these patients have can be a huge benefit to the patients and their families,” said Jennifer L. Miller, MD, a professor of pediatric endocrinology at the University of Florida, Gainesville, and a coinvestigator on the study.
But the finding that carbetocin appeared to address, at least in part, this unmet need while compiling a safety record that Dr. Miller called “gorgeous” and “remarkable,” also came with a few limitations.
Fewer patients than planned, and muddled outcomes
The CARE-PWS trial aimed to enroll 175 patients, but fell short once the COVID-19 pandemic hit. Plus the trial had two prespecified primary endpoints – improvements in a measure of hyperphagia, and in a measure of obsessive and compulsive behaviors – specifically in the 40 patients who received the higher of the two dosages studied, 9.6 mg t.i.d. intranasally. Neither endpoint showed significant improvement among the patients on this dosage, compared with the 40 patients who received placebo, although both outcomes trended in the right direction in the actively treated patients.
The study’s positive results came in a secondary treatment group, 39 patients who received 3.2 mg t.i.d., also intranasally. This subgroup had significant benefit, compared with placebo, for reducing hyperphagia symptoms as measured on the Hyperphagia Questionnaire for Clinical Trials (HQ-CT) Total Score. After the first 8 weeks on treatment, patients on the lower carbetocin dosage had an average reduction in their HQ-CT score of greater than 5 points, more than double the reduction seen among control patients who received placebo.
Those on the 3.2-mg t.i.d. dosage also showed significant improvements, compared with placebo, for anxiety, measured by the PWS Anxiety and Distress Questionnaire Total Score, as well as on measures of clinical global impression of severity, and of clinical global impression of change. Like the higher-dosage patients the lower-dosage subgroup did not show a significant difference compared with placebo for the other primary endpoint, change in obsessive and compulsive behaviors as measured by the Children’s Yale-Brown Obsessive-Compulsive Scale Total Score, although also like the higher dosage the effect from the lower dosage trended toward benefit.
A further limitation was that, at the time of her report, presented in abstract OR16-3 at the meeting, Dr. Deal could only present complete 64-week follow-up for 72 patients, although this reassuringly showed that, as time on the 9.6-mg t.i.d. dosage continued beyond 8 weeks, patients gradually improved their HQ-CT response so that by 64 weeks on treatment their hyperphagia score had improved as much as in the patients who received the lower dosage.
In short, documented benefits occurred on the lower dosage, especially for clinically meaningful symptoms like hyperphagia and anxiety, but the study’s overall results were not fully consistent by statistical criteria.
Benefiting an unmet need?
“While it is regrettable that we did not get to 175 patients because of COVID-19, the dataset is significant enough for me to feel that the FDA [Food and Drug Administration] needs to take a very serious look and consider approval,” Dr. Deal said in an interview. “Once safety is assured, which I think it is, I can only hope that regulatory officials understand their unmet needs of this rare disease community and will allow the drug to move to the next stage.”
“This is a very rare disease, and having families participate in trials is really challenging,” especially while the COVID-19 pandemic continues, Dr. Strong said. For the pediatric and adolescent patients targeted in this study “it will take a while for COVID to go away and for families to feel safe again being in a trial, so a real concern is that a need for more clinical trials is not terribly feasible now. Given that the safety profile looked good and one dose seemed to have good efficacy, as long as the long-term data continue to look good we’d love for the FDA to look at the existing data and see whether there is a path forward.”
Dr. Miller highlighted the limitations of what the CARE-PWS findings show.
“Given that it was only an 8-week trial of drug against placebo, and the fact that the primary outcomes weren’t met for the higher dose, my thought is that potentially we need to study more patients for a longer period at the 3.2-mg dose,” she said. She acknowledged that the metric used in the study to assess obsessive and compulsive behaviors is “very difficult” to apply to patients with PWS because of uncertainties in scoring obsessions in patients “who are not very good at telling you what they’re thinking.” Plus, “it’s absolutely not a problem that we did not see an effect on obsession and compulsions if the treatment potentially improves anxiety and hyperphagia, which are very common.” A treatment that reliably reduces these symptoms “would be amazing,” Dr. Miller added.
“PWS is very rare, so it’s very hard to do trials. Maybe the FDA will approve carbetocin because it was safe and gave a signal of efficacy at the lower dose. But my thought is that additional treatment trials are needed with only the lower dose and with longer duration,” she said.
CARE-PWS enrolled patients with nutritional phase 3 PWS who were aged 7-18 years at any of 24 sites in the United States, Canada, or Australia during 2018-2020. They averaged about 12 years of age, and 56% were girls.
The most common adverse effect from carbetocin was flushing, occurring in 14% of those on the lower dose and 21% on the higher dose, but not in any placebo patient. Other adverse effects more common on the lower dose than in the placebo group included headache in 16%, and diarrhea in 9%.
Carbetocin is not only long-lasting in circulation, it also has better affinity for oxytocin receptors than for vasopressin receptors, reducing the potential for causing hyponatremia. The idea to use it in patients with PWS followed prior studies with oxytocin, which had shown dopamine interactions that reduced anxiety and influenced food ingestion behavior. Brain autopsy studies had shown that patients with Prader-Willi syndrome have substantially fewer neurons than usual producing oxytocin. Treatment with intranasal carbetocin had shown efficacy for improving hyperphagia and behavior in a controlled phase 2 study with 37 patients.
Carbetocin is approved for use in reducing excessive bleeding after childbirth, particularly cesarean, in more than 20 countries outside the United States.
CARE-PWS was sponsored by Levo Therapeutics, the company developing carbetocin. Dr. Deal has been an adviser to Levo Therapeutics. Dr. Strong is an employee of the Foundation for Prader-Willi Research, which has received support from Levo Therapeutics as well as from other drug companies, but which receives most of its funding from individuals. Dr. Miller has received research funding from Levo Therapeutics and also from Harmony Biosciences, Rhythm Pharmaceuticals, and Soleno Therapeutics.
Children and adolescents with Prader-Willi syndrome (PWS) who received three daily, intranasal doses of carbetocin, an investigational, long-acting oxytocin analogue, had significant improvement in hyperphagia and anxiety during 8 weeks on treatment, compared with placebo in a multicenter, phase 3 trial with 119 patients.
The treatment also appeared safe during up to 56 additional weeks on active treatment, with no serious adverse effects nor “unexpected” events, and once completing the study about 95% of enrolled patients opted to remain on active treatment, Cheri L. Deal, MD, PhD, said at the annual meeting of the Endocrine Society.
Based on “the significant results for the placebo-controlled period, as well as for those finishing the 56-week extension, we may well have a new armament for helping these kids and their families deal with the unrelenting hunger of patients with PWS as well as some of the behavioral symptoms,” Dr. Deal, chief of endocrinology and diabetes at the Sainte-Justine Mother-Child University of Montreal Hospital, said in an interview. No treatment currently has labeling for addressing the hyperphagia or anxiety that is characteristic and often problematic for children and adolescents with PWS, an autosomal dominant genetic disease with an incidence of about 1 in 15,000 births and an estimated U.S. prevalence of about 9,000 cases, or about 1 case for every 37,000 people.
‘Gorgeous’ safety
“The results looked pretty positive, and we’re encouraged by what appears to be a good safety profile, so overall I think the PWS community is very excited by the results and is very interested in getting access to this drug,” commented Theresa V. Strong, PhD, director of research programs for the Foundation for Prader-Willi Research in Walnut, Calif., a group not involved with the study. Currently, “we have no effective treatments for these difficult behaviors” of hyperphagia and anxiety. Surveys and studies run by the foundation have documented that hyperphagia and anxiety “were the two most important symptoms that families would like to see treated,” Dr. Strong added in an interview.
PWS “is complex and affects almost every aspect of the lives of affected people and their families. Any treatment that can chip away at some of the problems these patients have can be a huge benefit to the patients and their families,” said Jennifer L. Miller, MD, a professor of pediatric endocrinology at the University of Florida, Gainesville, and a coinvestigator on the study.
But the finding that carbetocin appeared to address, at least in part, this unmet need while compiling a safety record that Dr. Miller called “gorgeous” and “remarkable,” also came with a few limitations.
Fewer patients than planned, and muddled outcomes
The CARE-PWS trial aimed to enroll 175 patients, but fell short once the COVID-19 pandemic hit. Plus the trial had two prespecified primary endpoints – improvements in a measure of hyperphagia, and in a measure of obsessive and compulsive behaviors – specifically in the 40 patients who received the higher of the two dosages studied, 9.6 mg t.i.d. intranasally. Neither endpoint showed significant improvement among the patients on this dosage, compared with the 40 patients who received placebo, although both outcomes trended in the right direction in the actively treated patients.
The study’s positive results came in a secondary treatment group, 39 patients who received 3.2 mg t.i.d., also intranasally. This subgroup had significant benefit, compared with placebo, for reducing hyperphagia symptoms as measured on the Hyperphagia Questionnaire for Clinical Trials (HQ-CT) Total Score. After the first 8 weeks on treatment, patients on the lower carbetocin dosage had an average reduction in their HQ-CT score of greater than 5 points, more than double the reduction seen among control patients who received placebo.
Those on the 3.2-mg t.i.d. dosage also showed significant improvements, compared with placebo, for anxiety, measured by the PWS Anxiety and Distress Questionnaire Total Score, as well as on measures of clinical global impression of severity, and of clinical global impression of change. Like the higher-dosage patients the lower-dosage subgroup did not show a significant difference compared with placebo for the other primary endpoint, change in obsessive and compulsive behaviors as measured by the Children’s Yale-Brown Obsessive-Compulsive Scale Total Score, although also like the higher dosage the effect from the lower dosage trended toward benefit.
A further limitation was that, at the time of her report, presented in abstract OR16-3 at the meeting, Dr. Deal could only present complete 64-week follow-up for 72 patients, although this reassuringly showed that, as time on the 9.6-mg t.i.d. dosage continued beyond 8 weeks, patients gradually improved their HQ-CT response so that by 64 weeks on treatment their hyperphagia score had improved as much as in the patients who received the lower dosage.
In short, documented benefits occurred on the lower dosage, especially for clinically meaningful symptoms like hyperphagia and anxiety, but the study’s overall results were not fully consistent by statistical criteria.
Benefiting an unmet need?
“While it is regrettable that we did not get to 175 patients because of COVID-19, the dataset is significant enough for me to feel that the FDA [Food and Drug Administration] needs to take a very serious look and consider approval,” Dr. Deal said in an interview. “Once safety is assured, which I think it is, I can only hope that regulatory officials understand their unmet needs of this rare disease community and will allow the drug to move to the next stage.”
“This is a very rare disease, and having families participate in trials is really challenging,” especially while the COVID-19 pandemic continues, Dr. Strong said. For the pediatric and adolescent patients targeted in this study “it will take a while for COVID to go away and for families to feel safe again being in a trial, so a real concern is that a need for more clinical trials is not terribly feasible now. Given that the safety profile looked good and one dose seemed to have good efficacy, as long as the long-term data continue to look good we’d love for the FDA to look at the existing data and see whether there is a path forward.”
Dr. Miller highlighted the limitations of what the CARE-PWS findings show.
“Given that it was only an 8-week trial of drug against placebo, and the fact that the primary outcomes weren’t met for the higher dose, my thought is that potentially we need to study more patients for a longer period at the 3.2-mg dose,” she said. She acknowledged that the metric used in the study to assess obsessive and compulsive behaviors is “very difficult” to apply to patients with PWS because of uncertainties in scoring obsessions in patients “who are not very good at telling you what they’re thinking.” Plus, “it’s absolutely not a problem that we did not see an effect on obsession and compulsions if the treatment potentially improves anxiety and hyperphagia, which are very common.” A treatment that reliably reduces these symptoms “would be amazing,” Dr. Miller added.
“PWS is very rare, so it’s very hard to do trials. Maybe the FDA will approve carbetocin because it was safe and gave a signal of efficacy at the lower dose. But my thought is that additional treatment trials are needed with only the lower dose and with longer duration,” she said.
CARE-PWS enrolled patients with nutritional phase 3 PWS who were aged 7-18 years at any of 24 sites in the United States, Canada, or Australia during 2018-2020. They averaged about 12 years of age, and 56% were girls.
The most common adverse effect from carbetocin was flushing, occurring in 14% of those on the lower dose and 21% on the higher dose, but not in any placebo patient. Other adverse effects more common on the lower dose than in the placebo group included headache in 16%, and diarrhea in 9%.
Carbetocin is not only long-lasting in circulation, it also has better affinity for oxytocin receptors than for vasopressin receptors, reducing the potential for causing hyponatremia. The idea to use it in patients with PWS followed prior studies with oxytocin, which had shown dopamine interactions that reduced anxiety and influenced food ingestion behavior. Brain autopsy studies had shown that patients with Prader-Willi syndrome have substantially fewer neurons than usual producing oxytocin. Treatment with intranasal carbetocin had shown efficacy for improving hyperphagia and behavior in a controlled phase 2 study with 37 patients.
Carbetocin is approved for use in reducing excessive bleeding after childbirth, particularly cesarean, in more than 20 countries outside the United States.
CARE-PWS was sponsored by Levo Therapeutics, the company developing carbetocin. Dr. Deal has been an adviser to Levo Therapeutics. Dr. Strong is an employee of the Foundation for Prader-Willi Research, which has received support from Levo Therapeutics as well as from other drug companies, but which receives most of its funding from individuals. Dr. Miller has received research funding from Levo Therapeutics and also from Harmony Biosciences, Rhythm Pharmaceuticals, and Soleno Therapeutics.
Children and adolescents with Prader-Willi syndrome (PWS) who received three daily, intranasal doses of carbetocin, an investigational, long-acting oxytocin analogue, had significant improvement in hyperphagia and anxiety during 8 weeks on treatment, compared with placebo in a multicenter, phase 3 trial with 119 patients.
The treatment also appeared safe during up to 56 additional weeks on active treatment, with no serious adverse effects nor “unexpected” events, and once completing the study about 95% of enrolled patients opted to remain on active treatment, Cheri L. Deal, MD, PhD, said at the annual meeting of the Endocrine Society.
Based on “the significant results for the placebo-controlled period, as well as for those finishing the 56-week extension, we may well have a new armament for helping these kids and their families deal with the unrelenting hunger of patients with PWS as well as some of the behavioral symptoms,” Dr. Deal, chief of endocrinology and diabetes at the Sainte-Justine Mother-Child University of Montreal Hospital, said in an interview. No treatment currently has labeling for addressing the hyperphagia or anxiety that is characteristic and often problematic for children and adolescents with PWS, an autosomal dominant genetic disease with an incidence of about 1 in 15,000 births and an estimated U.S. prevalence of about 9,000 cases, or about 1 case for every 37,000 people.
‘Gorgeous’ safety
“The results looked pretty positive, and we’re encouraged by what appears to be a good safety profile, so overall I think the PWS community is very excited by the results and is very interested in getting access to this drug,” commented Theresa V. Strong, PhD, director of research programs for the Foundation for Prader-Willi Research in Walnut, Calif., a group not involved with the study. Currently, “we have no effective treatments for these difficult behaviors” of hyperphagia and anxiety. Surveys and studies run by the foundation have documented that hyperphagia and anxiety “were the two most important symptoms that families would like to see treated,” Dr. Strong added in an interview.
PWS “is complex and affects almost every aspect of the lives of affected people and their families. Any treatment that can chip away at some of the problems these patients have can be a huge benefit to the patients and their families,” said Jennifer L. Miller, MD, a professor of pediatric endocrinology at the University of Florida, Gainesville, and a coinvestigator on the study.
But the finding that carbetocin appeared to address, at least in part, this unmet need while compiling a safety record that Dr. Miller called “gorgeous” and “remarkable,” also came with a few limitations.
Fewer patients than planned, and muddled outcomes
The CARE-PWS trial aimed to enroll 175 patients, but fell short once the COVID-19 pandemic hit. Plus the trial had two prespecified primary endpoints – improvements in a measure of hyperphagia, and in a measure of obsessive and compulsive behaviors – specifically in the 40 patients who received the higher of the two dosages studied, 9.6 mg t.i.d. intranasally. Neither endpoint showed significant improvement among the patients on this dosage, compared with the 40 patients who received placebo, although both outcomes trended in the right direction in the actively treated patients.
The study’s positive results came in a secondary treatment group, 39 patients who received 3.2 mg t.i.d., also intranasally. This subgroup had significant benefit, compared with placebo, for reducing hyperphagia symptoms as measured on the Hyperphagia Questionnaire for Clinical Trials (HQ-CT) Total Score. After the first 8 weeks on treatment, patients on the lower carbetocin dosage had an average reduction in their HQ-CT score of greater than 5 points, more than double the reduction seen among control patients who received placebo.
Those on the 3.2-mg t.i.d. dosage also showed significant improvements, compared with placebo, for anxiety, measured by the PWS Anxiety and Distress Questionnaire Total Score, as well as on measures of clinical global impression of severity, and of clinical global impression of change. Like the higher-dosage patients the lower-dosage subgroup did not show a significant difference compared with placebo for the other primary endpoint, change in obsessive and compulsive behaviors as measured by the Children’s Yale-Brown Obsessive-Compulsive Scale Total Score, although also like the higher dosage the effect from the lower dosage trended toward benefit.
A further limitation was that, at the time of her report, presented in abstract OR16-3 at the meeting, Dr. Deal could only present complete 64-week follow-up for 72 patients, although this reassuringly showed that, as time on the 9.6-mg t.i.d. dosage continued beyond 8 weeks, patients gradually improved their HQ-CT response so that by 64 weeks on treatment their hyperphagia score had improved as much as in the patients who received the lower dosage.
In short, documented benefits occurred on the lower dosage, especially for clinically meaningful symptoms like hyperphagia and anxiety, but the study’s overall results were not fully consistent by statistical criteria.
Benefiting an unmet need?
“While it is regrettable that we did not get to 175 patients because of COVID-19, the dataset is significant enough for me to feel that the FDA [Food and Drug Administration] needs to take a very serious look and consider approval,” Dr. Deal said in an interview. “Once safety is assured, which I think it is, I can only hope that regulatory officials understand their unmet needs of this rare disease community and will allow the drug to move to the next stage.”
“This is a very rare disease, and having families participate in trials is really challenging,” especially while the COVID-19 pandemic continues, Dr. Strong said. For the pediatric and adolescent patients targeted in this study “it will take a while for COVID to go away and for families to feel safe again being in a trial, so a real concern is that a need for more clinical trials is not terribly feasible now. Given that the safety profile looked good and one dose seemed to have good efficacy, as long as the long-term data continue to look good we’d love for the FDA to look at the existing data and see whether there is a path forward.”
Dr. Miller highlighted the limitations of what the CARE-PWS findings show.
“Given that it was only an 8-week trial of drug against placebo, and the fact that the primary outcomes weren’t met for the higher dose, my thought is that potentially we need to study more patients for a longer period at the 3.2-mg dose,” she said. She acknowledged that the metric used in the study to assess obsessive and compulsive behaviors is “very difficult” to apply to patients with PWS because of uncertainties in scoring obsessions in patients “who are not very good at telling you what they’re thinking.” Plus, “it’s absolutely not a problem that we did not see an effect on obsession and compulsions if the treatment potentially improves anxiety and hyperphagia, which are very common.” A treatment that reliably reduces these symptoms “would be amazing,” Dr. Miller added.
“PWS is very rare, so it’s very hard to do trials. Maybe the FDA will approve carbetocin because it was safe and gave a signal of efficacy at the lower dose. But my thought is that additional treatment trials are needed with only the lower dose and with longer duration,” she said.
CARE-PWS enrolled patients with nutritional phase 3 PWS who were aged 7-18 years at any of 24 sites in the United States, Canada, or Australia during 2018-2020. They averaged about 12 years of age, and 56% were girls.
The most common adverse effect from carbetocin was flushing, occurring in 14% of those on the lower dose and 21% on the higher dose, but not in any placebo patient. Other adverse effects more common on the lower dose than in the placebo group included headache in 16%, and diarrhea in 9%.
Carbetocin is not only long-lasting in circulation, it also has better affinity for oxytocin receptors than for vasopressin receptors, reducing the potential for causing hyponatremia. The idea to use it in patients with PWS followed prior studies with oxytocin, which had shown dopamine interactions that reduced anxiety and influenced food ingestion behavior. Brain autopsy studies had shown that patients with Prader-Willi syndrome have substantially fewer neurons than usual producing oxytocin. Treatment with intranasal carbetocin had shown efficacy for improving hyperphagia and behavior in a controlled phase 2 study with 37 patients.
Carbetocin is approved for use in reducing excessive bleeding after childbirth, particularly cesarean, in more than 20 countries outside the United States.
CARE-PWS was sponsored by Levo Therapeutics, the company developing carbetocin. Dr. Deal has been an adviser to Levo Therapeutics. Dr. Strong is an employee of the Foundation for Prader-Willi Research, which has received support from Levo Therapeutics as well as from other drug companies, but which receives most of its funding from individuals. Dr. Miller has received research funding from Levo Therapeutics and also from Harmony Biosciences, Rhythm Pharmaceuticals, and Soleno Therapeutics.
FROM ENDO 2021
Nonfatal opioid overdose rises in teen girls
More adolescent girls than boys experienced nonfatal opioid overdose and reported baseline levels of anxiety, depression, and self-harm, according to data from a retrospective cohort study of more than 20,000 youth in the United States.
Previous studies have identified sex-based differences in opioid overdose such as a higher prevalence of co-occurring psychiatric disorders in women compared with men, wrote Sarah M. Bagley, MD, of Boston University, and colleagues. “However, few studies have examined whether such sex-based differences in opioid overdose risk extend to the population of adolescents and young adults,” they said.
In a retrospective cohort study published in JAMA Network Open, the researchers identified 20,312 commercially insured youth aged 11-24 years who experienced a nonfatal opioid overdose between Jan. 1, 2006, and Dec. 31, 2017, and reviewed data using the IBM MarketScan Commercial Database. The average age of the study population was 20 years and approximately 42% were female.
Females aged 11-16 years had a significantly higher incidence of nonfatal opioid overdose (60%) compared with males, but this trend reversed at age 17 years, after which the incidence of nonfatal opioid overdose became significantly higher in males. “Our finding that females younger than 17 years had a higher incidence of NFOD is consistent with epidemiologic data that have indicated changes in alcohol and drug prevalence among female youths,” the researchers wrote.
Overall, 57.8% of the cohort had mood and anxiety disorders, 12.8% had trauma- or stress-related disorders, and 11.7% had attention-deficit/hyperactivity disorder.
When analyzed by sex, females had a significantly higher prevalence than that of males of mood or anxiety disorders (65.5% vs. 51.9%) trauma or stress-related disorders (16.4% vs. 10.1%) and attempts at suicide or self-harm (14.6% vs. 9.9%). Males had significantly higher prevalence than that of females of opioid use disorder (44.7% vs. 29.2%), cannabis use disorder (18.3% vs. 11.3%), and alcohol use disorder (20.3% vs. 14.4%).
“Although in our study, female youths had a lower prevalence of all substance use disorders, including OUD [opioid use disorder], and a higher prevalence of mood and trauma-associated disorders, both male and female youths had a higher prevalence of psychiatric illness and substance use disorder than youths in the general population,” the researchers noted.
The study findings were limited by several factors including the inclusion only of youth with commercial insurance, with no uninsured or publicly insured youth, and only those youth who sought health care after a nonfatal opioid overdose, the researchers noted. The prevalence of substance use and mental health disorders may be over- or underdiagnosed, and race was not included as a variable because of unreliable data, they added. The database also did not allow for gender identity beyond sex as listed by the insurance carrier, they said.
However, the results indicate significant differences in the incidence of nonfatal opioid overdose and accompanying mental health and substance use disorders based on age and sex, they said.
“These differences may have important implications for developing effective interventions to prevent first-time NFOD and to engage youths in care after an NFOD,” they concluded.
The study was supported by grants to several researchers from the National Institute on Drug Abuse, National Institutes of Health, and the Charles A. King Trust. The researchers had no financial conflicts to disclose.
More adolescent girls than boys experienced nonfatal opioid overdose and reported baseline levels of anxiety, depression, and self-harm, according to data from a retrospective cohort study of more than 20,000 youth in the United States.
Previous studies have identified sex-based differences in opioid overdose such as a higher prevalence of co-occurring psychiatric disorders in women compared with men, wrote Sarah M. Bagley, MD, of Boston University, and colleagues. “However, few studies have examined whether such sex-based differences in opioid overdose risk extend to the population of adolescents and young adults,” they said.
In a retrospective cohort study published in JAMA Network Open, the researchers identified 20,312 commercially insured youth aged 11-24 years who experienced a nonfatal opioid overdose between Jan. 1, 2006, and Dec. 31, 2017, and reviewed data using the IBM MarketScan Commercial Database. The average age of the study population was 20 years and approximately 42% were female.
Females aged 11-16 years had a significantly higher incidence of nonfatal opioid overdose (60%) compared with males, but this trend reversed at age 17 years, after which the incidence of nonfatal opioid overdose became significantly higher in males. “Our finding that females younger than 17 years had a higher incidence of NFOD is consistent with epidemiologic data that have indicated changes in alcohol and drug prevalence among female youths,” the researchers wrote.
Overall, 57.8% of the cohort had mood and anxiety disorders, 12.8% had trauma- or stress-related disorders, and 11.7% had attention-deficit/hyperactivity disorder.
When analyzed by sex, females had a significantly higher prevalence than that of males of mood or anxiety disorders (65.5% vs. 51.9%) trauma or stress-related disorders (16.4% vs. 10.1%) and attempts at suicide or self-harm (14.6% vs. 9.9%). Males had significantly higher prevalence than that of females of opioid use disorder (44.7% vs. 29.2%), cannabis use disorder (18.3% vs. 11.3%), and alcohol use disorder (20.3% vs. 14.4%).
“Although in our study, female youths had a lower prevalence of all substance use disorders, including OUD [opioid use disorder], and a higher prevalence of mood and trauma-associated disorders, both male and female youths had a higher prevalence of psychiatric illness and substance use disorder than youths in the general population,” the researchers noted.
The study findings were limited by several factors including the inclusion only of youth with commercial insurance, with no uninsured or publicly insured youth, and only those youth who sought health care after a nonfatal opioid overdose, the researchers noted. The prevalence of substance use and mental health disorders may be over- or underdiagnosed, and race was not included as a variable because of unreliable data, they added. The database also did not allow for gender identity beyond sex as listed by the insurance carrier, they said.
However, the results indicate significant differences in the incidence of nonfatal opioid overdose and accompanying mental health and substance use disorders based on age and sex, they said.
“These differences may have important implications for developing effective interventions to prevent first-time NFOD and to engage youths in care after an NFOD,” they concluded.
The study was supported by grants to several researchers from the National Institute on Drug Abuse, National Institutes of Health, and the Charles A. King Trust. The researchers had no financial conflicts to disclose.
More adolescent girls than boys experienced nonfatal opioid overdose and reported baseline levels of anxiety, depression, and self-harm, according to data from a retrospective cohort study of more than 20,000 youth in the United States.
Previous studies have identified sex-based differences in opioid overdose such as a higher prevalence of co-occurring psychiatric disorders in women compared with men, wrote Sarah M. Bagley, MD, of Boston University, and colleagues. “However, few studies have examined whether such sex-based differences in opioid overdose risk extend to the population of adolescents and young adults,” they said.
In a retrospective cohort study published in JAMA Network Open, the researchers identified 20,312 commercially insured youth aged 11-24 years who experienced a nonfatal opioid overdose between Jan. 1, 2006, and Dec. 31, 2017, and reviewed data using the IBM MarketScan Commercial Database. The average age of the study population was 20 years and approximately 42% were female.
Females aged 11-16 years had a significantly higher incidence of nonfatal opioid overdose (60%) compared with males, but this trend reversed at age 17 years, after which the incidence of nonfatal opioid overdose became significantly higher in males. “Our finding that females younger than 17 years had a higher incidence of NFOD is consistent with epidemiologic data that have indicated changes in alcohol and drug prevalence among female youths,” the researchers wrote.
Overall, 57.8% of the cohort had mood and anxiety disorders, 12.8% had trauma- or stress-related disorders, and 11.7% had attention-deficit/hyperactivity disorder.
When analyzed by sex, females had a significantly higher prevalence than that of males of mood or anxiety disorders (65.5% vs. 51.9%) trauma or stress-related disorders (16.4% vs. 10.1%) and attempts at suicide or self-harm (14.6% vs. 9.9%). Males had significantly higher prevalence than that of females of opioid use disorder (44.7% vs. 29.2%), cannabis use disorder (18.3% vs. 11.3%), and alcohol use disorder (20.3% vs. 14.4%).
“Although in our study, female youths had a lower prevalence of all substance use disorders, including OUD [opioid use disorder], and a higher prevalence of mood and trauma-associated disorders, both male and female youths had a higher prevalence of psychiatric illness and substance use disorder than youths in the general population,” the researchers noted.
The study findings were limited by several factors including the inclusion only of youth with commercial insurance, with no uninsured or publicly insured youth, and only those youth who sought health care after a nonfatal opioid overdose, the researchers noted. The prevalence of substance use and mental health disorders may be over- or underdiagnosed, and race was not included as a variable because of unreliable data, they added. The database also did not allow for gender identity beyond sex as listed by the insurance carrier, they said.
However, the results indicate significant differences in the incidence of nonfatal opioid overdose and accompanying mental health and substance use disorders based on age and sex, they said.
“These differences may have important implications for developing effective interventions to prevent first-time NFOD and to engage youths in care after an NFOD,” they concluded.
The study was supported by grants to several researchers from the National Institute on Drug Abuse, National Institutes of Health, and the Charles A. King Trust. The researchers had no financial conflicts to disclose.
FROM JAMA NETWORK OPEN















