User login
Listen up: Birdsong may calm anxiety, paranoia
Investigators found that people who listened to recordings of birds singing experienced a significant reduction in anxiety and paranoia. In contrast, the researchers also found that recordings of traffic noises, including car engines, sirens, and construction, increased depressive states.
“The results suggest that it may be worthwhile to investigate the targeted use of natural sounds such as birdsong in a clinical setting – for example, in hospital waiting rooms or in psychiatric settings,” study investigator Emil Stobbe, MSc, a predoctoral fellow at the Max Planck Institute for Human Development, Berlin, said in an interview.
“If someone is seeking an easily accessible intervention to lower distress, listening to an audio clip of birds singing might be a great option,” he added.
The study was published online in Scientific Reports.
Nature’s calming effect
The aim of the research was “to investigate how the physical environment impact brain and mental health,” Mr. Stobbe said.
Mr. Stobbe said that there is significantly more research examining visual properties of the physical environment but that the auditory domain is not as well researched, although, he added, that the beneficial effects of interactions with nature are “well studied.”
He noted that anxiety and paranoia can be experienced by many individuals even though they may be unaware that they are experiencing these states.
“We wanted to investigate if the beneficial effects of nature can also exert their impact on these states. In theory, birds can be representational for natural and vital environment, which, in turn, transfer the positive effects of nature on birdsong listeners,” he said.
A previous study compared nature versus city soundscape conditions and showed that the nature soundscape improved participants’ cognitive performance but did not improve mood. The present study added diversity to the soundscapes and focused not only on cognition and general mood but also on state paranoia, “which can be measured in a change-sensitive manner” and “has been shown to increase in response to traffic noise.”
The researchers hypothesized that birdsong would have a greater beneficial effect on mood and paranoia and on cognitive performance compared with traffic noise. They also investigated whether greater versus lower diversity of bird species or noise sources within the soundscapes “would be a relevant factor modulating the effects.”
The researchers recruited participants (n = 295) from a crowdsourcing platform. Participants’ mean age was late 20s (standard deviations ranged from 6.30 to 7.72), with a greater proportion of male versus female participants.
To be included, participants were required to have no history of mental illness, hearing difficulties, substance/drug intake, or suicidal thoughts/tendencies.
The outcomes of interest (mood, paranoia, cognitive performance) were measured before and after soundscape exposure and each soundscape had a low- versus high-diversity version. This resulted in several analyses that compared two types of sounds (birdsongs vs. traffic noise) x two levels of diversity (low vs. high diversity) and two time points (pre- vs. post exposure).
The exposure to sounds lasted for 6 minutes, after which they were asked to report (on a 0-100 visual scale) how diverse/monotone, beautiful, and pleasant they perceived the soundscape to be.
Reduction in depressive symptoms
Participants were divided into four groups: low-diversity traffic noise soundscape (n = 83), high-diversity traffic noise soundscape (n = 60), low-diversity birdsong soundscape (n = 63), and high-diversity birdsong soundscape (n = 80)
In addition to listening to the sounds, participants completed questionnaires measuring mood (depression and anxiety) and paranoia as well as a test of digit span cognitive performance (both the forward and the backward versions).
The type, diversity, and type x diversity all revealed significant effect sizes (F[3, 276] = 78.6; P < .001; eta-squared = 0.461; F[3, 276] = 3.16; P = .025; eta-squared = 0.033; and F[3, 276] = 2.66; P = .028, respectively), “suggesting that all of these factors, as well as their interaction, had a significant impact on the perception of soundscapes (that is, ratings on monotony/diversity, beauty, and pleasantness).”
A post hoc examination showed that depressive symptoms significantly increased within the low- and high-diversity urban soundscapes but decreased significantly in the high-diversity birdsong soundscapes (T[1, 60] = –2.57; P = .012; d = –0.29).
For anxiety, the post hoc within-group analyses found no effects within low- and high-diversity traffic noise conditions (T[1, 82] = –1.37; P = .174; d = –0.15 and T[1, 68] = 0.49; P = .629; d = 0.06, respectively). By contrast, there were significant declines in both birdsong conditions (low diversity: T[1, 62] = –6.13; P < .001; d = –0.77; high diversity: T[1, 60] = –6.32; P < .001; d = –0.70).
Similarly, there were no changes in participants with paranoia when they listened to either low- or high-diversity traffic noises (T[1, 82] = –0.55; P = .583; d = –0.06 and T[1, 68] = 0.67; P = .507; d = 0.08, respectively). On the other hand, both birdsong conditions yielded reductions in paranoia (low diversity: T[1, 62] = –5.90; P < .001; d = –0.74; high diversity: T[1, 60] = –4.11; P < .001; d = –0.46).
None of the soundscapes had any effect on cognition.
“In theory, birds can be representational for natural and vital environments which, in turn, transfer the positive effects of nature on birdsong listeners,” said Mr. Stobbe.
“Taken together, the findings of the current study provide another facet of why interactions with nature can be beneficial for our mental health, and it is highly important to preserve nature,” he added.
Mr. Stobbe said that future research should focus on investigating mixed soundscapes including examining whether the presence of natural sounds in urban settings lower stressors such as traffic noise.
An understudied area
Commenting for this article, Ken Duckworth, MD, chief medical officer of the National Alliance on Mental Illness called the study “interesting but limited.”
Dr. Duckworth, who was not involved in the research said that the “benefits of nature are understudied” and agreed with the investigators that it is potentially important to study the use of birdsongs in psychiatric facilities. “Future studies could also correlate the role of birdsong with the mental health benefits/aspects of ‘being in nature,’ which has been found to have some effect.”
Open Access funding was enabled and organized by Projekt DEAL. The authors and Dr. Duckworth declared no competing interests.
A version of this article first appeared on Medscape.com.
Investigators found that people who listened to recordings of birds singing experienced a significant reduction in anxiety and paranoia. In contrast, the researchers also found that recordings of traffic noises, including car engines, sirens, and construction, increased depressive states.
“The results suggest that it may be worthwhile to investigate the targeted use of natural sounds such as birdsong in a clinical setting – for example, in hospital waiting rooms or in psychiatric settings,” study investigator Emil Stobbe, MSc, a predoctoral fellow at the Max Planck Institute for Human Development, Berlin, said in an interview.
“If someone is seeking an easily accessible intervention to lower distress, listening to an audio clip of birds singing might be a great option,” he added.
The study was published online in Scientific Reports.
Nature’s calming effect
The aim of the research was “to investigate how the physical environment impact brain and mental health,” Mr. Stobbe said.
Mr. Stobbe said that there is significantly more research examining visual properties of the physical environment but that the auditory domain is not as well researched, although, he added, that the beneficial effects of interactions with nature are “well studied.”
He noted that anxiety and paranoia can be experienced by many individuals even though they may be unaware that they are experiencing these states.
“We wanted to investigate if the beneficial effects of nature can also exert their impact on these states. In theory, birds can be representational for natural and vital environment, which, in turn, transfer the positive effects of nature on birdsong listeners,” he said.
A previous study compared nature versus city soundscape conditions and showed that the nature soundscape improved participants’ cognitive performance but did not improve mood. The present study added diversity to the soundscapes and focused not only on cognition and general mood but also on state paranoia, “which can be measured in a change-sensitive manner” and “has been shown to increase in response to traffic noise.”
The researchers hypothesized that birdsong would have a greater beneficial effect on mood and paranoia and on cognitive performance compared with traffic noise. They also investigated whether greater versus lower diversity of bird species or noise sources within the soundscapes “would be a relevant factor modulating the effects.”
The researchers recruited participants (n = 295) from a crowdsourcing platform. Participants’ mean age was late 20s (standard deviations ranged from 6.30 to 7.72), with a greater proportion of male versus female participants.
To be included, participants were required to have no history of mental illness, hearing difficulties, substance/drug intake, or suicidal thoughts/tendencies.
The outcomes of interest (mood, paranoia, cognitive performance) were measured before and after soundscape exposure and each soundscape had a low- versus high-diversity version. This resulted in several analyses that compared two types of sounds (birdsongs vs. traffic noise) x two levels of diversity (low vs. high diversity) and two time points (pre- vs. post exposure).
The exposure to sounds lasted for 6 minutes, after which they were asked to report (on a 0-100 visual scale) how diverse/monotone, beautiful, and pleasant they perceived the soundscape to be.
Reduction in depressive symptoms
Participants were divided into four groups: low-diversity traffic noise soundscape (n = 83), high-diversity traffic noise soundscape (n = 60), low-diversity birdsong soundscape (n = 63), and high-diversity birdsong soundscape (n = 80)
In addition to listening to the sounds, participants completed questionnaires measuring mood (depression and anxiety) and paranoia as well as a test of digit span cognitive performance (both the forward and the backward versions).
The type, diversity, and type x diversity all revealed significant effect sizes (F[3, 276] = 78.6; P < .001; eta-squared = 0.461; F[3, 276] = 3.16; P = .025; eta-squared = 0.033; and F[3, 276] = 2.66; P = .028, respectively), “suggesting that all of these factors, as well as their interaction, had a significant impact on the perception of soundscapes (that is, ratings on monotony/diversity, beauty, and pleasantness).”
A post hoc examination showed that depressive symptoms significantly increased within the low- and high-diversity urban soundscapes but decreased significantly in the high-diversity birdsong soundscapes (T[1, 60] = –2.57; P = .012; d = –0.29).
For anxiety, the post hoc within-group analyses found no effects within low- and high-diversity traffic noise conditions (T[1, 82] = –1.37; P = .174; d = –0.15 and T[1, 68] = 0.49; P = .629; d = 0.06, respectively). By contrast, there were significant declines in both birdsong conditions (low diversity: T[1, 62] = –6.13; P < .001; d = –0.77; high diversity: T[1, 60] = –6.32; P < .001; d = –0.70).
Similarly, there were no changes in participants with paranoia when they listened to either low- or high-diversity traffic noises (T[1, 82] = –0.55; P = .583; d = –0.06 and T[1, 68] = 0.67; P = .507; d = 0.08, respectively). On the other hand, both birdsong conditions yielded reductions in paranoia (low diversity: T[1, 62] = –5.90; P < .001; d = –0.74; high diversity: T[1, 60] = –4.11; P < .001; d = –0.46).
None of the soundscapes had any effect on cognition.
“In theory, birds can be representational for natural and vital environments which, in turn, transfer the positive effects of nature on birdsong listeners,” said Mr. Stobbe.
“Taken together, the findings of the current study provide another facet of why interactions with nature can be beneficial for our mental health, and it is highly important to preserve nature,” he added.
Mr. Stobbe said that future research should focus on investigating mixed soundscapes including examining whether the presence of natural sounds in urban settings lower stressors such as traffic noise.
An understudied area
Commenting for this article, Ken Duckworth, MD, chief medical officer of the National Alliance on Mental Illness called the study “interesting but limited.”
Dr. Duckworth, who was not involved in the research said that the “benefits of nature are understudied” and agreed with the investigators that it is potentially important to study the use of birdsongs in psychiatric facilities. “Future studies could also correlate the role of birdsong with the mental health benefits/aspects of ‘being in nature,’ which has been found to have some effect.”
Open Access funding was enabled and organized by Projekt DEAL. The authors and Dr. Duckworth declared no competing interests.
A version of this article first appeared on Medscape.com.
Investigators found that people who listened to recordings of birds singing experienced a significant reduction in anxiety and paranoia. In contrast, the researchers also found that recordings of traffic noises, including car engines, sirens, and construction, increased depressive states.
“The results suggest that it may be worthwhile to investigate the targeted use of natural sounds such as birdsong in a clinical setting – for example, in hospital waiting rooms or in psychiatric settings,” study investigator Emil Stobbe, MSc, a predoctoral fellow at the Max Planck Institute for Human Development, Berlin, said in an interview.
“If someone is seeking an easily accessible intervention to lower distress, listening to an audio clip of birds singing might be a great option,” he added.
The study was published online in Scientific Reports.
Nature’s calming effect
The aim of the research was “to investigate how the physical environment impact brain and mental health,” Mr. Stobbe said.
Mr. Stobbe said that there is significantly more research examining visual properties of the physical environment but that the auditory domain is not as well researched, although, he added, that the beneficial effects of interactions with nature are “well studied.”
He noted that anxiety and paranoia can be experienced by many individuals even though they may be unaware that they are experiencing these states.
“We wanted to investigate if the beneficial effects of nature can also exert their impact on these states. In theory, birds can be representational for natural and vital environment, which, in turn, transfer the positive effects of nature on birdsong listeners,” he said.
A previous study compared nature versus city soundscape conditions and showed that the nature soundscape improved participants’ cognitive performance but did not improve mood. The present study added diversity to the soundscapes and focused not only on cognition and general mood but also on state paranoia, “which can be measured in a change-sensitive manner” and “has been shown to increase in response to traffic noise.”
The researchers hypothesized that birdsong would have a greater beneficial effect on mood and paranoia and on cognitive performance compared with traffic noise. They also investigated whether greater versus lower diversity of bird species or noise sources within the soundscapes “would be a relevant factor modulating the effects.”
The researchers recruited participants (n = 295) from a crowdsourcing platform. Participants’ mean age was late 20s (standard deviations ranged from 6.30 to 7.72), with a greater proportion of male versus female participants.
To be included, participants were required to have no history of mental illness, hearing difficulties, substance/drug intake, or suicidal thoughts/tendencies.
The outcomes of interest (mood, paranoia, cognitive performance) were measured before and after soundscape exposure and each soundscape had a low- versus high-diversity version. This resulted in several analyses that compared two types of sounds (birdsongs vs. traffic noise) x two levels of diversity (low vs. high diversity) and two time points (pre- vs. post exposure).
The exposure to sounds lasted for 6 minutes, after which they were asked to report (on a 0-100 visual scale) how diverse/monotone, beautiful, and pleasant they perceived the soundscape to be.
Reduction in depressive symptoms
Participants were divided into four groups: low-diversity traffic noise soundscape (n = 83), high-diversity traffic noise soundscape (n = 60), low-diversity birdsong soundscape (n = 63), and high-diversity birdsong soundscape (n = 80)
In addition to listening to the sounds, participants completed questionnaires measuring mood (depression and anxiety) and paranoia as well as a test of digit span cognitive performance (both the forward and the backward versions).
The type, diversity, and type x diversity all revealed significant effect sizes (F[3, 276] = 78.6; P < .001; eta-squared = 0.461; F[3, 276] = 3.16; P = .025; eta-squared = 0.033; and F[3, 276] = 2.66; P = .028, respectively), “suggesting that all of these factors, as well as their interaction, had a significant impact on the perception of soundscapes (that is, ratings on monotony/diversity, beauty, and pleasantness).”
A post hoc examination showed that depressive symptoms significantly increased within the low- and high-diversity urban soundscapes but decreased significantly in the high-diversity birdsong soundscapes (T[1, 60] = –2.57; P = .012; d = –0.29).
For anxiety, the post hoc within-group analyses found no effects within low- and high-diversity traffic noise conditions (T[1, 82] = –1.37; P = .174; d = –0.15 and T[1, 68] = 0.49; P = .629; d = 0.06, respectively). By contrast, there were significant declines in both birdsong conditions (low diversity: T[1, 62] = –6.13; P < .001; d = –0.77; high diversity: T[1, 60] = –6.32; P < .001; d = –0.70).
Similarly, there were no changes in participants with paranoia when they listened to either low- or high-diversity traffic noises (T[1, 82] = –0.55; P = .583; d = –0.06 and T[1, 68] = 0.67; P = .507; d = 0.08, respectively). On the other hand, both birdsong conditions yielded reductions in paranoia (low diversity: T[1, 62] = –5.90; P < .001; d = –0.74; high diversity: T[1, 60] = –4.11; P < .001; d = –0.46).
None of the soundscapes had any effect on cognition.
“In theory, birds can be representational for natural and vital environments which, in turn, transfer the positive effects of nature on birdsong listeners,” said Mr. Stobbe.
“Taken together, the findings of the current study provide another facet of why interactions with nature can be beneficial for our mental health, and it is highly important to preserve nature,” he added.
Mr. Stobbe said that future research should focus on investigating mixed soundscapes including examining whether the presence of natural sounds in urban settings lower stressors such as traffic noise.
An understudied area
Commenting for this article, Ken Duckworth, MD, chief medical officer of the National Alliance on Mental Illness called the study “interesting but limited.”
Dr. Duckworth, who was not involved in the research said that the “benefits of nature are understudied” and agreed with the investigators that it is potentially important to study the use of birdsongs in psychiatric facilities. “Future studies could also correlate the role of birdsong with the mental health benefits/aspects of ‘being in nature,’ which has been found to have some effect.”
Open Access funding was enabled and organized by Projekt DEAL. The authors and Dr. Duckworth declared no competing interests.
A version of this article first appeared on Medscape.com.
FROM SCIENTIFIC REPORTS
Healthy diet, less news helped prevent anxiety, depression during COVID
VIENNA –
Results from a longitudinal Spanish survey study of more than 1,000 adults showed that being outside, relaxing, participating in physical activities, and drinking plenty of water were also beneficial. However, social contact with friends and relatives, following a routine, and pursuing hobbies had no significant impact.
“This was a little surprising,” lead author Joaquim Radua, MD, PhD, August Pi i Sunyer Biomedical Research Institute (IDIBAPS), Barcelona, said in a release.
“Like many people, we had assumed that personal contact would play a bigger part in avoiding anxiety and depression during stressful times,” he added.
However, Dr. Radua said that because the study was conducted during the COVID-19 pandemic, “people who socialized may also have been anxious about getting infected.”
Consequently, “it may be that this specific behavior cannot be extrapolated to other times, when there is no pandemic,” he said.
The findings were presented at the 35th European College of Neuropsychopharmacology (ECNP) Congress.
Correlational versus longitudinal studies
Dr. Radua emphasized that individuals “should socialize,” of course.
“We think it’s important that people continue to follow what works for them and that if you enjoy seeing friends or following a hobby, you continue to do so,” he said.
“Our work was centered on COVID, but we now need to see if these factors apply to other stressful circumstances. These simple behaviors may prevent anxiety and depression, and prevention is better than cure,” he added.
The researchers note that, in “times of uncertainty” such as the COVID-19 pandemic, many individuals experience increases in both anxiety and depressive symptoms.
Although a range of behaviors are recommended to help people cope, the investigators add that some of the recommendations are based on correlational studies.
Indeed, the researchers previously identified a correlation between following a healthy/balanced diet, among other measures, and lower anxiety and depressive symptoms during the pandemic.
However, it is unclear from cross-sectional studies whether the behavior alters the symptoms, in which case the behavior could be considered “helpful,” or conversely whether the symptoms alter an individual’s behavior, in which case the behaviors “may be useless,” the investigators note.
The investigative team therefore set out to provide more robust evidence for making recommendations and conducted a prospective longitudinal study.
They recruited 1,049 adults online via social networks, matching them to the regional, age and sex, and urbanicity distribution of the overall Spanish population.
Every 2 weeks for 12 months, the researchers administered the General Anxiety Disorder (GAD)-7, the Patient Health Questionnaire (PHQ)-9, and a two-item ecological momentary assessment to minimize recall bias, among other measures. They also asked about 10 self-report coping behaviors.
Significant coping behaviors
The study was completed by 942 individuals, indicating a retention of 90%.
Among both completers and non-completers there was an over-representation of individuals aged 18-34 years and women, compared with the general population, and fewer participants aged at least 65 years.
Pre-recruitment, the mean baseline GAD-7 score among completers was 7.4, falling to around 5.5 at the time of the first questionnaire. Scores on the PHQ-9 were 7.6 and 5.6, respectively.
Performing population-weighted autoregressive moving average models to analyze the relationship between the current frequency of the coping behaviors and future changes in anxiety and depressive symptoms, the investigators found that the greatest effect was from following a healthy, balanced diet, with an impact size of 0.95.
This was followed by avoiding too much stressful news (impact size, 0.91), staying outdoors or looking outside (0.40), doing relaxing activities (0.33), participating in physical exercise (0.32), and drinking water to hydrate (0.25).
Overall, these coping behaviors were associated with a significant reduction in anxiety and depressive symptoms (all, P < .001).
On the other hand, there was no impact on future symptoms from socializing with friends and relatives, whether or not they lived in the same household. There was also no effect from following a routine, pursuing hobbies, or performing home tasks.
The researchers note that similar results were obtained when excluding participants with hazardous alcohol consumption, defined as a score on the Alcohol Use Disorders Identification Test of 8 or higher.
However, they point out that despite its prospective design and large cohort, the study was not interventional. Therefore, they “cannot rule out the possibility that decreasing the frequency of a behavior is an early sign of some mechanism that later leads to increased anxiety and depression symptoms.”
Nevertheless, they believe that possibility “seems unlikely.”
Reflective of a unique time?
Commenting on the findings, Catherine Harmer, PhD, director of the Psychopharmacology and Emotional Research Lab, department of psychiatry, University of Oxford (England), said in the release this was an “interesting study” that “provides some important insights as to which behaviors may protect our mental health during times of significant stress.”
She said the finding that social contact was not beneficial was “surprising” but may reflect the fact that, during the pandemic, it was “stressful even to have those social contacts, even if we managed to meet a friend outside.”
The results of the study may therefore be “reflective of the unique experience” of the COVID-19 pandemic, said Dr. Harmer, who was not involved with the research.
“I wouldn’t think that reading too much news would generally be something that has a negative impact on depression and anxiety, but I think it was very much at the time,” she said.
With the pandemic overwhelming one country after another, “the more you read about it, the more frightening it was,” she added, noting that it is “easy to forget how frightened we were at the beginning.”
Dr. Harmer noted that “it would be interesting” if the study was repeated and the same factors came out – or if they were unique to that time.
This would be “useful to know, as these times may come again. And the more information we have to cope with a pandemic, the better,” she concluded.
The research was supported by the AXA Research Fund via an AXA Award granted to Dr. Radua from the call for projects “mitigating risk in the wake of the COVID-19 pandemic.” The investigators and Dr. Harmer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
VIENNA –
Results from a longitudinal Spanish survey study of more than 1,000 adults showed that being outside, relaxing, participating in physical activities, and drinking plenty of water were also beneficial. However, social contact with friends and relatives, following a routine, and pursuing hobbies had no significant impact.
“This was a little surprising,” lead author Joaquim Radua, MD, PhD, August Pi i Sunyer Biomedical Research Institute (IDIBAPS), Barcelona, said in a release.
“Like many people, we had assumed that personal contact would play a bigger part in avoiding anxiety and depression during stressful times,” he added.
However, Dr. Radua said that because the study was conducted during the COVID-19 pandemic, “people who socialized may also have been anxious about getting infected.”
Consequently, “it may be that this specific behavior cannot be extrapolated to other times, when there is no pandemic,” he said.
The findings were presented at the 35th European College of Neuropsychopharmacology (ECNP) Congress.
Correlational versus longitudinal studies
Dr. Radua emphasized that individuals “should socialize,” of course.
“We think it’s important that people continue to follow what works for them and that if you enjoy seeing friends or following a hobby, you continue to do so,” he said.
“Our work was centered on COVID, but we now need to see if these factors apply to other stressful circumstances. These simple behaviors may prevent anxiety and depression, and prevention is better than cure,” he added.
The researchers note that, in “times of uncertainty” such as the COVID-19 pandemic, many individuals experience increases in both anxiety and depressive symptoms.
Although a range of behaviors are recommended to help people cope, the investigators add that some of the recommendations are based on correlational studies.
Indeed, the researchers previously identified a correlation between following a healthy/balanced diet, among other measures, and lower anxiety and depressive symptoms during the pandemic.
However, it is unclear from cross-sectional studies whether the behavior alters the symptoms, in which case the behavior could be considered “helpful,” or conversely whether the symptoms alter an individual’s behavior, in which case the behaviors “may be useless,” the investigators note.
The investigative team therefore set out to provide more robust evidence for making recommendations and conducted a prospective longitudinal study.
They recruited 1,049 adults online via social networks, matching them to the regional, age and sex, and urbanicity distribution of the overall Spanish population.
Every 2 weeks for 12 months, the researchers administered the General Anxiety Disorder (GAD)-7, the Patient Health Questionnaire (PHQ)-9, and a two-item ecological momentary assessment to minimize recall bias, among other measures. They also asked about 10 self-report coping behaviors.
Significant coping behaviors
The study was completed by 942 individuals, indicating a retention of 90%.
Among both completers and non-completers there was an over-representation of individuals aged 18-34 years and women, compared with the general population, and fewer participants aged at least 65 years.
Pre-recruitment, the mean baseline GAD-7 score among completers was 7.4, falling to around 5.5 at the time of the first questionnaire. Scores on the PHQ-9 were 7.6 and 5.6, respectively.
Performing population-weighted autoregressive moving average models to analyze the relationship between the current frequency of the coping behaviors and future changes in anxiety and depressive symptoms, the investigators found that the greatest effect was from following a healthy, balanced diet, with an impact size of 0.95.
This was followed by avoiding too much stressful news (impact size, 0.91), staying outdoors or looking outside (0.40), doing relaxing activities (0.33), participating in physical exercise (0.32), and drinking water to hydrate (0.25).
Overall, these coping behaviors were associated with a significant reduction in anxiety and depressive symptoms (all, P < .001).
On the other hand, there was no impact on future symptoms from socializing with friends and relatives, whether or not they lived in the same household. There was also no effect from following a routine, pursuing hobbies, or performing home tasks.
The researchers note that similar results were obtained when excluding participants with hazardous alcohol consumption, defined as a score on the Alcohol Use Disorders Identification Test of 8 or higher.
However, they point out that despite its prospective design and large cohort, the study was not interventional. Therefore, they “cannot rule out the possibility that decreasing the frequency of a behavior is an early sign of some mechanism that later leads to increased anxiety and depression symptoms.”
Nevertheless, they believe that possibility “seems unlikely.”
Reflective of a unique time?
Commenting on the findings, Catherine Harmer, PhD, director of the Psychopharmacology and Emotional Research Lab, department of psychiatry, University of Oxford (England), said in the release this was an “interesting study” that “provides some important insights as to which behaviors may protect our mental health during times of significant stress.”
She said the finding that social contact was not beneficial was “surprising” but may reflect the fact that, during the pandemic, it was “stressful even to have those social contacts, even if we managed to meet a friend outside.”
The results of the study may therefore be “reflective of the unique experience” of the COVID-19 pandemic, said Dr. Harmer, who was not involved with the research.
“I wouldn’t think that reading too much news would generally be something that has a negative impact on depression and anxiety, but I think it was very much at the time,” she said.
With the pandemic overwhelming one country after another, “the more you read about it, the more frightening it was,” she added, noting that it is “easy to forget how frightened we were at the beginning.”
Dr. Harmer noted that “it would be interesting” if the study was repeated and the same factors came out – or if they were unique to that time.
This would be “useful to know, as these times may come again. And the more information we have to cope with a pandemic, the better,” she concluded.
The research was supported by the AXA Research Fund via an AXA Award granted to Dr. Radua from the call for projects “mitigating risk in the wake of the COVID-19 pandemic.” The investigators and Dr. Harmer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
VIENNA –
Results from a longitudinal Spanish survey study of more than 1,000 adults showed that being outside, relaxing, participating in physical activities, and drinking plenty of water were also beneficial. However, social contact with friends and relatives, following a routine, and pursuing hobbies had no significant impact.
“This was a little surprising,” lead author Joaquim Radua, MD, PhD, August Pi i Sunyer Biomedical Research Institute (IDIBAPS), Barcelona, said in a release.
“Like many people, we had assumed that personal contact would play a bigger part in avoiding anxiety and depression during stressful times,” he added.
However, Dr. Radua said that because the study was conducted during the COVID-19 pandemic, “people who socialized may also have been anxious about getting infected.”
Consequently, “it may be that this specific behavior cannot be extrapolated to other times, when there is no pandemic,” he said.
The findings were presented at the 35th European College of Neuropsychopharmacology (ECNP) Congress.
Correlational versus longitudinal studies
Dr. Radua emphasized that individuals “should socialize,” of course.
“We think it’s important that people continue to follow what works for them and that if you enjoy seeing friends or following a hobby, you continue to do so,” he said.
“Our work was centered on COVID, but we now need to see if these factors apply to other stressful circumstances. These simple behaviors may prevent anxiety and depression, and prevention is better than cure,” he added.
The researchers note that, in “times of uncertainty” such as the COVID-19 pandemic, many individuals experience increases in both anxiety and depressive symptoms.
Although a range of behaviors are recommended to help people cope, the investigators add that some of the recommendations are based on correlational studies.
Indeed, the researchers previously identified a correlation between following a healthy/balanced diet, among other measures, and lower anxiety and depressive symptoms during the pandemic.
However, it is unclear from cross-sectional studies whether the behavior alters the symptoms, in which case the behavior could be considered “helpful,” or conversely whether the symptoms alter an individual’s behavior, in which case the behaviors “may be useless,” the investigators note.
The investigative team therefore set out to provide more robust evidence for making recommendations and conducted a prospective longitudinal study.
They recruited 1,049 adults online via social networks, matching them to the regional, age and sex, and urbanicity distribution of the overall Spanish population.
Every 2 weeks for 12 months, the researchers administered the General Anxiety Disorder (GAD)-7, the Patient Health Questionnaire (PHQ)-9, and a two-item ecological momentary assessment to minimize recall bias, among other measures. They also asked about 10 self-report coping behaviors.
Significant coping behaviors
The study was completed by 942 individuals, indicating a retention of 90%.
Among both completers and non-completers there was an over-representation of individuals aged 18-34 years and women, compared with the general population, and fewer participants aged at least 65 years.
Pre-recruitment, the mean baseline GAD-7 score among completers was 7.4, falling to around 5.5 at the time of the first questionnaire. Scores on the PHQ-9 were 7.6 and 5.6, respectively.
Performing population-weighted autoregressive moving average models to analyze the relationship between the current frequency of the coping behaviors and future changes in anxiety and depressive symptoms, the investigators found that the greatest effect was from following a healthy, balanced diet, with an impact size of 0.95.
This was followed by avoiding too much stressful news (impact size, 0.91), staying outdoors or looking outside (0.40), doing relaxing activities (0.33), participating in physical exercise (0.32), and drinking water to hydrate (0.25).
Overall, these coping behaviors were associated with a significant reduction in anxiety and depressive symptoms (all, P < .001).
On the other hand, there was no impact on future symptoms from socializing with friends and relatives, whether or not they lived in the same household. There was also no effect from following a routine, pursuing hobbies, or performing home tasks.
The researchers note that similar results were obtained when excluding participants with hazardous alcohol consumption, defined as a score on the Alcohol Use Disorders Identification Test of 8 or higher.
However, they point out that despite its prospective design and large cohort, the study was not interventional. Therefore, they “cannot rule out the possibility that decreasing the frequency of a behavior is an early sign of some mechanism that later leads to increased anxiety and depression symptoms.”
Nevertheless, they believe that possibility “seems unlikely.”
Reflective of a unique time?
Commenting on the findings, Catherine Harmer, PhD, director of the Psychopharmacology and Emotional Research Lab, department of psychiatry, University of Oxford (England), said in the release this was an “interesting study” that “provides some important insights as to which behaviors may protect our mental health during times of significant stress.”
She said the finding that social contact was not beneficial was “surprising” but may reflect the fact that, during the pandemic, it was “stressful even to have those social contacts, even if we managed to meet a friend outside.”
The results of the study may therefore be “reflective of the unique experience” of the COVID-19 pandemic, said Dr. Harmer, who was not involved with the research.
“I wouldn’t think that reading too much news would generally be something that has a negative impact on depression and anxiety, but I think it was very much at the time,” she said.
With the pandemic overwhelming one country after another, “the more you read about it, the more frightening it was,” she added, noting that it is “easy to forget how frightened we were at the beginning.”
Dr. Harmer noted that “it would be interesting” if the study was repeated and the same factors came out – or if they were unique to that time.
This would be “useful to know, as these times may come again. And the more information we have to cope with a pandemic, the better,” she concluded.
The research was supported by the AXA Research Fund via an AXA Award granted to Dr. Radua from the call for projects “mitigating risk in the wake of the COVID-19 pandemic.” The investigators and Dr. Harmer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ECNP 2022
Preexisting mental illness symptoms spiked during pandemic
“Those with preexisting mental health conditions may be particularly vulnerable to these effects because they are more susceptible to experiencing high levels of stress during a crisis and are more likely to experience isolation/despair during confinement compared to the general population,” wrote Danna Ramirez of The Menninger Clinic, Houston, and colleagues.
In a study published in Psychiatry Research , the investigators compared data from 142 adolescents aged 12-17 years and 470 adults aged 18-79 years who were admitted to an inpatient psychiatric hospital in Houston. Of these, 65 adolescents and 235 adults were admitted before the pandemic, and 77 adolescents and 235 adults were admitted during the pandemic.
Clinical outcomes were scores on the Generalized Anxiety Disorder Scale (GAD-7), the Patient Health Questionnaire (PHQ-9), the Patient Health Questionnaire for Adolescents (PHQ-A), the Difficulties in Emotion Regulation Scale–Short Form (DERS-SF), the World Health Organization Disability Assessment Scale (WHODAS), the World Health Organization Alcohol, Smoking, and Substance Involvement Screening Test (WHOASSIST), the Pittsburgh Sleep Quality Index (PSQI), the Disturbing Dream and Nightmare Severity Index (DDNSI), and the Suicide Behaviors Questionnaire–Revised (SBQ-R).
Overall, adults admitted during the pandemic had significantly higher levels of anxiety, depression, emotional dysregulation, and disability (P < .001 for all) as well as nightmares (P = .013) compared to those admitted prior to the pandemic.
Among adolescents, measures of anxiety, depression, and sleep quality were significantly higher at admission during the pandemic compared to prior to the pandemic (P = .005, P = .005, and P = .011, respectively)
Reasons for the increase in symptom severity remain unclear, but include the possibility that individuals with preexisting mental illness simply became more ill; or that individuals with symptoms delayed hospital admission out of fear of exposure to COVID-19, which resulted in more severe symptoms at admission, the researchers wrote in their discussion.
The findings were limited by several factors, including the primarily White population and the reliance on self-reports, the researchers noted. Another limitation was the lack of differentiation between patients who may have had COVID-19 before hospitalization and those who did not, so the researchers could not determine whether the virus itself played a biological role in symptom severity.
However, the results support data from previous studies and identify increased psychiatry symptom severity for patients admitted for inpatient psychiatry care during the pandemic, they said. Although resources are scarce, the findings emphasize that mental health needs, especially for those with preexisting conditions, should not be overlooked, and continuity and expansion of access to mental health care for all should be prioritized, they concluded.
The study was supported by The Menninger Clinic and The Menninger Clinic Foundation. The researchers had no financial conflicts to disclose.
“Those with preexisting mental health conditions may be particularly vulnerable to these effects because they are more susceptible to experiencing high levels of stress during a crisis and are more likely to experience isolation/despair during confinement compared to the general population,” wrote Danna Ramirez of The Menninger Clinic, Houston, and colleagues.
In a study published in Psychiatry Research , the investigators compared data from 142 adolescents aged 12-17 years and 470 adults aged 18-79 years who were admitted to an inpatient psychiatric hospital in Houston. Of these, 65 adolescents and 235 adults were admitted before the pandemic, and 77 adolescents and 235 adults were admitted during the pandemic.
Clinical outcomes were scores on the Generalized Anxiety Disorder Scale (GAD-7), the Patient Health Questionnaire (PHQ-9), the Patient Health Questionnaire for Adolescents (PHQ-A), the Difficulties in Emotion Regulation Scale–Short Form (DERS-SF), the World Health Organization Disability Assessment Scale (WHODAS), the World Health Organization Alcohol, Smoking, and Substance Involvement Screening Test (WHOASSIST), the Pittsburgh Sleep Quality Index (PSQI), the Disturbing Dream and Nightmare Severity Index (DDNSI), and the Suicide Behaviors Questionnaire–Revised (SBQ-R).
Overall, adults admitted during the pandemic had significantly higher levels of anxiety, depression, emotional dysregulation, and disability (P < .001 for all) as well as nightmares (P = .013) compared to those admitted prior to the pandemic.
Among adolescents, measures of anxiety, depression, and sleep quality were significantly higher at admission during the pandemic compared to prior to the pandemic (P = .005, P = .005, and P = .011, respectively)
Reasons for the increase in symptom severity remain unclear, but include the possibility that individuals with preexisting mental illness simply became more ill; or that individuals with symptoms delayed hospital admission out of fear of exposure to COVID-19, which resulted in more severe symptoms at admission, the researchers wrote in their discussion.
The findings were limited by several factors, including the primarily White population and the reliance on self-reports, the researchers noted. Another limitation was the lack of differentiation between patients who may have had COVID-19 before hospitalization and those who did not, so the researchers could not determine whether the virus itself played a biological role in symptom severity.
However, the results support data from previous studies and identify increased psychiatry symptom severity for patients admitted for inpatient psychiatry care during the pandemic, they said. Although resources are scarce, the findings emphasize that mental health needs, especially for those with preexisting conditions, should not be overlooked, and continuity and expansion of access to mental health care for all should be prioritized, they concluded.
The study was supported by The Menninger Clinic and The Menninger Clinic Foundation. The researchers had no financial conflicts to disclose.
“Those with preexisting mental health conditions may be particularly vulnerable to these effects because they are more susceptible to experiencing high levels of stress during a crisis and are more likely to experience isolation/despair during confinement compared to the general population,” wrote Danna Ramirez of The Menninger Clinic, Houston, and colleagues.
In a study published in Psychiatry Research , the investigators compared data from 142 adolescents aged 12-17 years and 470 adults aged 18-79 years who were admitted to an inpatient psychiatric hospital in Houston. Of these, 65 adolescents and 235 adults were admitted before the pandemic, and 77 adolescents and 235 adults were admitted during the pandemic.
Clinical outcomes were scores on the Generalized Anxiety Disorder Scale (GAD-7), the Patient Health Questionnaire (PHQ-9), the Patient Health Questionnaire for Adolescents (PHQ-A), the Difficulties in Emotion Regulation Scale–Short Form (DERS-SF), the World Health Organization Disability Assessment Scale (WHODAS), the World Health Organization Alcohol, Smoking, and Substance Involvement Screening Test (WHOASSIST), the Pittsburgh Sleep Quality Index (PSQI), the Disturbing Dream and Nightmare Severity Index (DDNSI), and the Suicide Behaviors Questionnaire–Revised (SBQ-R).
Overall, adults admitted during the pandemic had significantly higher levels of anxiety, depression, emotional dysregulation, and disability (P < .001 for all) as well as nightmares (P = .013) compared to those admitted prior to the pandemic.
Among adolescents, measures of anxiety, depression, and sleep quality were significantly higher at admission during the pandemic compared to prior to the pandemic (P = .005, P = .005, and P = .011, respectively)
Reasons for the increase in symptom severity remain unclear, but include the possibility that individuals with preexisting mental illness simply became more ill; or that individuals with symptoms delayed hospital admission out of fear of exposure to COVID-19, which resulted in more severe symptoms at admission, the researchers wrote in their discussion.
The findings were limited by several factors, including the primarily White population and the reliance on self-reports, the researchers noted. Another limitation was the lack of differentiation between patients who may have had COVID-19 before hospitalization and those who did not, so the researchers could not determine whether the virus itself played a biological role in symptom severity.
However, the results support data from previous studies and identify increased psychiatry symptom severity for patients admitted for inpatient psychiatry care during the pandemic, they said. Although resources are scarce, the findings emphasize that mental health needs, especially for those with preexisting conditions, should not be overlooked, and continuity and expansion of access to mental health care for all should be prioritized, they concluded.
The study was supported by The Menninger Clinic and The Menninger Clinic Foundation. The researchers had no financial conflicts to disclose.
FROM PSYCHIATRY RESEARCH
E-health program improves perinatal depression
Patients with perinatal depression who used a specialized online tool showed improvement in symptoms, compared with controls who received routine care, based on data from 191 individuals.
Although perinatal depression affects approximately 17% of pregnant women and 13% of postpartum women, the condition is often underrecognized and undertreated, Brian Danaher, PhD, of Influents Innovations, Eugene, Ore., and colleagues wrote. Meta-analyses have shown that e-health interventions based on cognitive-behavioral therapy (CBT) can improve depression in general and perinatal depression in particular.
An e-health program known as the MomMoodBooster has demonstrated effectiveness at reducing postpartum depression, and the researchers evaluated the effectiveness of a perinatal version.
In a study published in the American Journal of Obstetrics & Gynecology, the researchers randomized 95 pregnant women and 96 postpartum women who met screening criteria for depression to routine care for perinatal depression, which included a 24/7 crisis hotline and a referral network or PDP plus a version of the MomMoodBooster with a perinatal depression component (MMB2). Participants were aged 18 and older, with no active suicidal ideation. The average age was 32 years; 84% were non-Hispanic, 67% were White, and 94% were married or in a long-term relationship. During the 12 weeks, each of six sessions became accessible online in sequence.
The primary endpoint was the change in outcomes at 12 weeks after the start of the program, with depressive symptom severity measured using the Patient Health Questionnaire (PHQ-9). Anxiety was assessed as a secondary outcome by using the Depression Anxiety Stress Scale. The minimal clinically important difference (MCID) was used to evaluate clinical significance, and was defined as a reduction in PHQ-9 of at least 5 points from baseline.
After controlling for perinatal status at baseline and assessment time, the MMB2 group had significantly greater decreases in depression severity and stress compared with the routine care group. In addition, based on MCID, significantly more women in the MMB2 group showed improvements in depression, compared with the routine care group (43% vs. 26%; odds ratio, 2.12; P = .015).
A total of 88 of the 89 women in the MMB2 group accessed the sessions, and approximately half (49%) viewed all six sessions.
Of the women who used the MMB2 program, 96% said that it was easy to use, 93% said they would recommend it, and 83% said it was helpful to them.
The study findings were limited by several factors including the lack of long-term follow-up data and inability to determine the durability of the treatment effects, the researchers noted. Another key limitation is the demographics of the study population (slightly older and a greater proportion of White individuals than the national average), which may not be representative of all perinatal women in the United States.
However, the results are consistent with findings from previous studies, including meta-analyses of CBT-based programs, the researchers wrote.
“When used in a largely self-directed approach, MMB2 could fill the gap when in-person treatment options are limited as well as for women whose circumstances (COVID) and/or concerns (stigma, costs) reduce the acceptability of in-person help,” they said. Use of e-health programs such as MMB2 could increase the scope of treatment for perinatal depression.
Expanding e-health options may improve outcomes and reduce disparities
Perinatal and postpartum depression is one of the most common conditions affecting pregnancy, Lisette D. Tanner, MD, of Emory University, Atlanta, said in an interview. “Depression can have serious consequences for both maternal and neonatal well-being, including preterm birth, low birth weight, and poor bonding, as well as delayed emotional and cognitive development of the newborn.
“While clinicians are encouraged to screen patients during and after pregnancy for signs and symptoms of depression, once identified, the availability of effective treatment is limited. Access to mental health resources is a long-standing disparity in medicine, and therefore research investigating readily available e-health treatment strategies is critically important,” said Dr. Tanner, who was not involved in the study.
In the current study, “I was surprised by the number of patients who saw a clinically significant improvement in depression scores in such a short period of time. An average of only 20 days elapsed between baseline and post-test scores and almost 43% of patients showed improvement. Mental health interventions typically take longer to demonstrate an effect, both medication and talk therapies,” she said.
“The largest barrier to adoption of any e-health modality into clinical practice is often the cost of implementation and maintaining infrastructure,” said Dr. Tanner. “A cost-effectiveness analysis of this intervention would be helpful to better delineate the value of such of program in comparison to more traditional treatments.”
More research is needed on the effectiveness of the intervention for specific populations, such as groups with lower socioeconomic status and patients with chronic mood disorders, Dr. Tanner said. “Additionally, introducing the program in locations with limited access to mental health resources would support more widespread implementation.”
The study was supported by the National Institutes of Mental Health. The researchers had no financial conflicts to disclose. Dr. Tanner had no financial conflicts to disclose.
Patients with perinatal depression who used a specialized online tool showed improvement in symptoms, compared with controls who received routine care, based on data from 191 individuals.
Although perinatal depression affects approximately 17% of pregnant women and 13% of postpartum women, the condition is often underrecognized and undertreated, Brian Danaher, PhD, of Influents Innovations, Eugene, Ore., and colleagues wrote. Meta-analyses have shown that e-health interventions based on cognitive-behavioral therapy (CBT) can improve depression in general and perinatal depression in particular.
An e-health program known as the MomMoodBooster has demonstrated effectiveness at reducing postpartum depression, and the researchers evaluated the effectiveness of a perinatal version.
In a study published in the American Journal of Obstetrics & Gynecology, the researchers randomized 95 pregnant women and 96 postpartum women who met screening criteria for depression to routine care for perinatal depression, which included a 24/7 crisis hotline and a referral network or PDP plus a version of the MomMoodBooster with a perinatal depression component (MMB2). Participants were aged 18 and older, with no active suicidal ideation. The average age was 32 years; 84% were non-Hispanic, 67% were White, and 94% were married or in a long-term relationship. During the 12 weeks, each of six sessions became accessible online in sequence.
The primary endpoint was the change in outcomes at 12 weeks after the start of the program, with depressive symptom severity measured using the Patient Health Questionnaire (PHQ-9). Anxiety was assessed as a secondary outcome by using the Depression Anxiety Stress Scale. The minimal clinically important difference (MCID) was used to evaluate clinical significance, and was defined as a reduction in PHQ-9 of at least 5 points from baseline.
After controlling for perinatal status at baseline and assessment time, the MMB2 group had significantly greater decreases in depression severity and stress compared with the routine care group. In addition, based on MCID, significantly more women in the MMB2 group showed improvements in depression, compared with the routine care group (43% vs. 26%; odds ratio, 2.12; P = .015).
A total of 88 of the 89 women in the MMB2 group accessed the sessions, and approximately half (49%) viewed all six sessions.
Of the women who used the MMB2 program, 96% said that it was easy to use, 93% said they would recommend it, and 83% said it was helpful to them.
The study findings were limited by several factors including the lack of long-term follow-up data and inability to determine the durability of the treatment effects, the researchers noted. Another key limitation is the demographics of the study population (slightly older and a greater proportion of White individuals than the national average), which may not be representative of all perinatal women in the United States.
However, the results are consistent with findings from previous studies, including meta-analyses of CBT-based programs, the researchers wrote.
“When used in a largely self-directed approach, MMB2 could fill the gap when in-person treatment options are limited as well as for women whose circumstances (COVID) and/or concerns (stigma, costs) reduce the acceptability of in-person help,” they said. Use of e-health programs such as MMB2 could increase the scope of treatment for perinatal depression.
Expanding e-health options may improve outcomes and reduce disparities
Perinatal and postpartum depression is one of the most common conditions affecting pregnancy, Lisette D. Tanner, MD, of Emory University, Atlanta, said in an interview. “Depression can have serious consequences for both maternal and neonatal well-being, including preterm birth, low birth weight, and poor bonding, as well as delayed emotional and cognitive development of the newborn.
“While clinicians are encouraged to screen patients during and after pregnancy for signs and symptoms of depression, once identified, the availability of effective treatment is limited. Access to mental health resources is a long-standing disparity in medicine, and therefore research investigating readily available e-health treatment strategies is critically important,” said Dr. Tanner, who was not involved in the study.
In the current study, “I was surprised by the number of patients who saw a clinically significant improvement in depression scores in such a short period of time. An average of only 20 days elapsed between baseline and post-test scores and almost 43% of patients showed improvement. Mental health interventions typically take longer to demonstrate an effect, both medication and talk therapies,” she said.
“The largest barrier to adoption of any e-health modality into clinical practice is often the cost of implementation and maintaining infrastructure,” said Dr. Tanner. “A cost-effectiveness analysis of this intervention would be helpful to better delineate the value of such of program in comparison to more traditional treatments.”
More research is needed on the effectiveness of the intervention for specific populations, such as groups with lower socioeconomic status and patients with chronic mood disorders, Dr. Tanner said. “Additionally, introducing the program in locations with limited access to mental health resources would support more widespread implementation.”
The study was supported by the National Institutes of Mental Health. The researchers had no financial conflicts to disclose. Dr. Tanner had no financial conflicts to disclose.
Patients with perinatal depression who used a specialized online tool showed improvement in symptoms, compared with controls who received routine care, based on data from 191 individuals.
Although perinatal depression affects approximately 17% of pregnant women and 13% of postpartum women, the condition is often underrecognized and undertreated, Brian Danaher, PhD, of Influents Innovations, Eugene, Ore., and colleagues wrote. Meta-analyses have shown that e-health interventions based on cognitive-behavioral therapy (CBT) can improve depression in general and perinatal depression in particular.
An e-health program known as the MomMoodBooster has demonstrated effectiveness at reducing postpartum depression, and the researchers evaluated the effectiveness of a perinatal version.
In a study published in the American Journal of Obstetrics & Gynecology, the researchers randomized 95 pregnant women and 96 postpartum women who met screening criteria for depression to routine care for perinatal depression, which included a 24/7 crisis hotline and a referral network or PDP plus a version of the MomMoodBooster with a perinatal depression component (MMB2). Participants were aged 18 and older, with no active suicidal ideation. The average age was 32 years; 84% were non-Hispanic, 67% were White, and 94% were married or in a long-term relationship. During the 12 weeks, each of six sessions became accessible online in sequence.
The primary endpoint was the change in outcomes at 12 weeks after the start of the program, with depressive symptom severity measured using the Patient Health Questionnaire (PHQ-9). Anxiety was assessed as a secondary outcome by using the Depression Anxiety Stress Scale. The minimal clinically important difference (MCID) was used to evaluate clinical significance, and was defined as a reduction in PHQ-9 of at least 5 points from baseline.
After controlling for perinatal status at baseline and assessment time, the MMB2 group had significantly greater decreases in depression severity and stress compared with the routine care group. In addition, based on MCID, significantly more women in the MMB2 group showed improvements in depression, compared with the routine care group (43% vs. 26%; odds ratio, 2.12; P = .015).
A total of 88 of the 89 women in the MMB2 group accessed the sessions, and approximately half (49%) viewed all six sessions.
Of the women who used the MMB2 program, 96% said that it was easy to use, 93% said they would recommend it, and 83% said it was helpful to them.
The study findings were limited by several factors including the lack of long-term follow-up data and inability to determine the durability of the treatment effects, the researchers noted. Another key limitation is the demographics of the study population (slightly older and a greater proportion of White individuals than the national average), which may not be representative of all perinatal women in the United States.
However, the results are consistent with findings from previous studies, including meta-analyses of CBT-based programs, the researchers wrote.
“When used in a largely self-directed approach, MMB2 could fill the gap when in-person treatment options are limited as well as for women whose circumstances (COVID) and/or concerns (stigma, costs) reduce the acceptability of in-person help,” they said. Use of e-health programs such as MMB2 could increase the scope of treatment for perinatal depression.
Expanding e-health options may improve outcomes and reduce disparities
Perinatal and postpartum depression is one of the most common conditions affecting pregnancy, Lisette D. Tanner, MD, of Emory University, Atlanta, said in an interview. “Depression can have serious consequences for both maternal and neonatal well-being, including preterm birth, low birth weight, and poor bonding, as well as delayed emotional and cognitive development of the newborn.
“While clinicians are encouraged to screen patients during and after pregnancy for signs and symptoms of depression, once identified, the availability of effective treatment is limited. Access to mental health resources is a long-standing disparity in medicine, and therefore research investigating readily available e-health treatment strategies is critically important,” said Dr. Tanner, who was not involved in the study.
In the current study, “I was surprised by the number of patients who saw a clinically significant improvement in depression scores in such a short period of time. An average of only 20 days elapsed between baseline and post-test scores and almost 43% of patients showed improvement. Mental health interventions typically take longer to demonstrate an effect, both medication and talk therapies,” she said.
“The largest barrier to adoption of any e-health modality into clinical practice is often the cost of implementation and maintaining infrastructure,” said Dr. Tanner. “A cost-effectiveness analysis of this intervention would be helpful to better delineate the value of such of program in comparison to more traditional treatments.”
More research is needed on the effectiveness of the intervention for specific populations, such as groups with lower socioeconomic status and patients with chronic mood disorders, Dr. Tanner said. “Additionally, introducing the program in locations with limited access to mental health resources would support more widespread implementation.”
The study was supported by the National Institutes of Mental Health. The researchers had no financial conflicts to disclose. Dr. Tanner had no financial conflicts to disclose.
FROM THE AMERICAN JOURNAL OF OBSTETRICS & GYNECOLOGY
Keep menstrual cramps away the dietary prevention way
Foods for thought: Menstrual cramp prevention
For those who menstruate, it’s typical for that time of the month to bring cravings for things that may give a serotonin boost that eases the rise in stress hormones. Chocolate and other foods high in sugar fall into that category, but they could actually be adding to the problem.
About 90% of adolescent girls have menstrual pain, and it’s the leading cause of school absences for the demographic. Muscle relaxers and PMS pills are usually the recommended solution to alleviating menstrual cramps, but what if the patient doesn’t want to take any medicine?
Serah Sannoh of Rutgers University wanted to find another way to relieve her menstrual pains. The literature review she presented at the annual meeting of the North American Menopause Society found multiple studies that examined dietary patterns that resulted in menstrual pain.
In Ms. Sannoh’s analysis, she looked at how certain foods have an effect on cramps. Do they contribute to the pain or reduce it? Diets high in processed foods, oils, sugars, salt, and omega-6 fatty acids promote inflammation in the muscles around the uterus. Thus, cramps.
The answer, sometimes, is not to add a medicine but to change our daily practices, she suggested. Foods high in omega-3 fatty acids helped reduce pain, and those who practiced a vegan diet had the lowest muscle inflammation rates. So more salmon and fewer Swedish Fish.
Stage 1 of the robot apocalypse is already upon us
The mere mention of a robot apocalypse is enough to conjure images of terrifying robot soldiers with Austrian accents harvesting and killing humanity while the survivors live blissfully in a simulation and do low-gravity kung fu with high-profile Hollywood actors. They’ll even take over the navy.
Reality is often less exciting than the movies, but rest assured, the robots will not be denied their dominion of Earth. Our future robot overlords are simply taking a more subtle, less dramatic route toward their ultimate subjugation of mankind: They’re making us all sad and burned out.
The research pulls from work conducted in multiple countries to paint a picture of a humanity filled with anxiety about jobs as robotic automation grows more common. In India, a survey of automobile manufacturing works showed that working alongside industrial robots was linked with greater reports of burnout and workplace incivility. In Singapore, a group of college students randomly assigned to read one of three articles – one about the use of robots in business, a generic article about robots, or an article unrelated to robots – were then surveyed about their job security concerns. Three guesses as to which group was most worried.
In addition, the researchers analyzed 185 U.S. metropolitan areas for robot prevalence alongside use of job-recruiting websites and found that the more robots a city used, the more common job searches were. Unemployment rates weren’t affected, suggesting people had job insecurity because of robots. Sure, there could be other, nonrobotic reasons for this, but that’s no fun. We’re here because we fear our future android rulers.
It’s not all doom and gloom, fortunately. In an online experiment, the study authors found that self-affirmation exercises, such as writing down characteristics or values important to us, can overcome the existential fears and lessen concern about robots in the workplace. One of the authors noted that, while some fear is justified, “media reports on new technologies like robots and algorithms tend to be apocalyptic in nature, so people may develop an irrational fear about them.”
Oops. Our bad.
Apocalypse, stage 2: Leaping oral superorganisms
The terms of our secret agreement with the shadowy-but-powerful dental-industrial complex stipulate that LOTME can only cover tooth-related news once a year. This is that once a year.
Since we’ve already dealt with a robot apocalypse, how about a sci-fi horror story? A story with a “cross-kingdom partnership” in which assemblages of bacteria and fungi perform feats greater than either could achieve on its own. A story in which new microscopy technologies allow “scientists to visualize the behavior of living microbes in real time,” according to a statement from the University of Pennsylvania, Philadelphia.
While looking at saliva samples from toddlers with severe tooth decay, lead author Zhi Ren and associates “noticed the bacteria and fungi forming these assemblages and developing motions we never thought they would possess: a ‘walking-like’ and ‘leaping-like’ mobility. … It’s almost like a new organism – a superorganism – with new functions,” said senior author Hyun Koo, DDS, PhD, of Penn Dental Medicine.
Did he say “mobility”? He did, didn’t he?
To study these alleged superorganisms, they set up a laboratory system “using the bacteria, fungi, and a tooth-like material, all incubated in human saliva,” the university explained.
“Incubated in human saliva.” There’s a phrase you don’t see every day.
It only took a few hours for the investigators to observe the bacterial/fungal assemblages making leaps of more than 100 microns across the tooth-like material. “That is more than 200 times their own body length,” Dr. Ren said, “making them even better than most vertebrates, relative to body size. For example, tree frogs and grasshoppers can leap forward about 50 times and 20 times their own body length, respectively.”
So, will it be the robots or the evil superorganisms? Let us give you a word of advice: Always bet on bacteria.
Foods for thought: Menstrual cramp prevention
For those who menstruate, it’s typical for that time of the month to bring cravings for things that may give a serotonin boost that eases the rise in stress hormones. Chocolate and other foods high in sugar fall into that category, but they could actually be adding to the problem.
About 90% of adolescent girls have menstrual pain, and it’s the leading cause of school absences for the demographic. Muscle relaxers and PMS pills are usually the recommended solution to alleviating menstrual cramps, but what if the patient doesn’t want to take any medicine?
Serah Sannoh of Rutgers University wanted to find another way to relieve her menstrual pains. The literature review she presented at the annual meeting of the North American Menopause Society found multiple studies that examined dietary patterns that resulted in menstrual pain.
In Ms. Sannoh’s analysis, she looked at how certain foods have an effect on cramps. Do they contribute to the pain or reduce it? Diets high in processed foods, oils, sugars, salt, and omega-6 fatty acids promote inflammation in the muscles around the uterus. Thus, cramps.
The answer, sometimes, is not to add a medicine but to change our daily practices, she suggested. Foods high in omega-3 fatty acids helped reduce pain, and those who practiced a vegan diet had the lowest muscle inflammation rates. So more salmon and fewer Swedish Fish.
Stage 1 of the robot apocalypse is already upon us
The mere mention of a robot apocalypse is enough to conjure images of terrifying robot soldiers with Austrian accents harvesting and killing humanity while the survivors live blissfully in a simulation and do low-gravity kung fu with high-profile Hollywood actors. They’ll even take over the navy.
Reality is often less exciting than the movies, but rest assured, the robots will not be denied their dominion of Earth. Our future robot overlords are simply taking a more subtle, less dramatic route toward their ultimate subjugation of mankind: They’re making us all sad and burned out.
The research pulls from work conducted in multiple countries to paint a picture of a humanity filled with anxiety about jobs as robotic automation grows more common. In India, a survey of automobile manufacturing works showed that working alongside industrial robots was linked with greater reports of burnout and workplace incivility. In Singapore, a group of college students randomly assigned to read one of three articles – one about the use of robots in business, a generic article about robots, or an article unrelated to robots – were then surveyed about their job security concerns. Three guesses as to which group was most worried.
In addition, the researchers analyzed 185 U.S. metropolitan areas for robot prevalence alongside use of job-recruiting websites and found that the more robots a city used, the more common job searches were. Unemployment rates weren’t affected, suggesting people had job insecurity because of robots. Sure, there could be other, nonrobotic reasons for this, but that’s no fun. We’re here because we fear our future android rulers.
It’s not all doom and gloom, fortunately. In an online experiment, the study authors found that self-affirmation exercises, such as writing down characteristics or values important to us, can overcome the existential fears and lessen concern about robots in the workplace. One of the authors noted that, while some fear is justified, “media reports on new technologies like robots and algorithms tend to be apocalyptic in nature, so people may develop an irrational fear about them.”
Oops. Our bad.
Apocalypse, stage 2: Leaping oral superorganisms
The terms of our secret agreement with the shadowy-but-powerful dental-industrial complex stipulate that LOTME can only cover tooth-related news once a year. This is that once a year.
Since we’ve already dealt with a robot apocalypse, how about a sci-fi horror story? A story with a “cross-kingdom partnership” in which assemblages of bacteria and fungi perform feats greater than either could achieve on its own. A story in which new microscopy technologies allow “scientists to visualize the behavior of living microbes in real time,” according to a statement from the University of Pennsylvania, Philadelphia.
While looking at saliva samples from toddlers with severe tooth decay, lead author Zhi Ren and associates “noticed the bacteria and fungi forming these assemblages and developing motions we never thought they would possess: a ‘walking-like’ and ‘leaping-like’ mobility. … It’s almost like a new organism – a superorganism – with new functions,” said senior author Hyun Koo, DDS, PhD, of Penn Dental Medicine.
Did he say “mobility”? He did, didn’t he?
To study these alleged superorganisms, they set up a laboratory system “using the bacteria, fungi, and a tooth-like material, all incubated in human saliva,” the university explained.
“Incubated in human saliva.” There’s a phrase you don’t see every day.
It only took a few hours for the investigators to observe the bacterial/fungal assemblages making leaps of more than 100 microns across the tooth-like material. “That is more than 200 times their own body length,” Dr. Ren said, “making them even better than most vertebrates, relative to body size. For example, tree frogs and grasshoppers can leap forward about 50 times and 20 times their own body length, respectively.”
So, will it be the robots or the evil superorganisms? Let us give you a word of advice: Always bet on bacteria.
Foods for thought: Menstrual cramp prevention
For those who menstruate, it’s typical for that time of the month to bring cravings for things that may give a serotonin boost that eases the rise in stress hormones. Chocolate and other foods high in sugar fall into that category, but they could actually be adding to the problem.
About 90% of adolescent girls have menstrual pain, and it’s the leading cause of school absences for the demographic. Muscle relaxers and PMS pills are usually the recommended solution to alleviating menstrual cramps, but what if the patient doesn’t want to take any medicine?
Serah Sannoh of Rutgers University wanted to find another way to relieve her menstrual pains. The literature review she presented at the annual meeting of the North American Menopause Society found multiple studies that examined dietary patterns that resulted in menstrual pain.
In Ms. Sannoh’s analysis, she looked at how certain foods have an effect on cramps. Do they contribute to the pain or reduce it? Diets high in processed foods, oils, sugars, salt, and omega-6 fatty acids promote inflammation in the muscles around the uterus. Thus, cramps.
The answer, sometimes, is not to add a medicine but to change our daily practices, she suggested. Foods high in omega-3 fatty acids helped reduce pain, and those who practiced a vegan diet had the lowest muscle inflammation rates. So more salmon and fewer Swedish Fish.
Stage 1 of the robot apocalypse is already upon us
The mere mention of a robot apocalypse is enough to conjure images of terrifying robot soldiers with Austrian accents harvesting and killing humanity while the survivors live blissfully in a simulation and do low-gravity kung fu with high-profile Hollywood actors. They’ll even take over the navy.
Reality is often less exciting than the movies, but rest assured, the robots will not be denied their dominion of Earth. Our future robot overlords are simply taking a more subtle, less dramatic route toward their ultimate subjugation of mankind: They’re making us all sad and burned out.
The research pulls from work conducted in multiple countries to paint a picture of a humanity filled with anxiety about jobs as robotic automation grows more common. In India, a survey of automobile manufacturing works showed that working alongside industrial robots was linked with greater reports of burnout and workplace incivility. In Singapore, a group of college students randomly assigned to read one of three articles – one about the use of robots in business, a generic article about robots, or an article unrelated to robots – were then surveyed about their job security concerns. Three guesses as to which group was most worried.
In addition, the researchers analyzed 185 U.S. metropolitan areas for robot prevalence alongside use of job-recruiting websites and found that the more robots a city used, the more common job searches were. Unemployment rates weren’t affected, suggesting people had job insecurity because of robots. Sure, there could be other, nonrobotic reasons for this, but that’s no fun. We’re here because we fear our future android rulers.
It’s not all doom and gloom, fortunately. In an online experiment, the study authors found that self-affirmation exercises, such as writing down characteristics or values important to us, can overcome the existential fears and lessen concern about robots in the workplace. One of the authors noted that, while some fear is justified, “media reports on new technologies like robots and algorithms tend to be apocalyptic in nature, so people may develop an irrational fear about them.”
Oops. Our bad.
Apocalypse, stage 2: Leaping oral superorganisms
The terms of our secret agreement with the shadowy-but-powerful dental-industrial complex stipulate that LOTME can only cover tooth-related news once a year. This is that once a year.
Since we’ve already dealt with a robot apocalypse, how about a sci-fi horror story? A story with a “cross-kingdom partnership” in which assemblages of bacteria and fungi perform feats greater than either could achieve on its own. A story in which new microscopy technologies allow “scientists to visualize the behavior of living microbes in real time,” according to a statement from the University of Pennsylvania, Philadelphia.
While looking at saliva samples from toddlers with severe tooth decay, lead author Zhi Ren and associates “noticed the bacteria and fungi forming these assemblages and developing motions we never thought they would possess: a ‘walking-like’ and ‘leaping-like’ mobility. … It’s almost like a new organism – a superorganism – with new functions,” said senior author Hyun Koo, DDS, PhD, of Penn Dental Medicine.
Did he say “mobility”? He did, didn’t he?
To study these alleged superorganisms, they set up a laboratory system “using the bacteria, fungi, and a tooth-like material, all incubated in human saliva,” the university explained.
“Incubated in human saliva.” There’s a phrase you don’t see every day.
It only took a few hours for the investigators to observe the bacterial/fungal assemblages making leaps of more than 100 microns across the tooth-like material. “That is more than 200 times their own body length,” Dr. Ren said, “making them even better than most vertebrates, relative to body size. For example, tree frogs and grasshoppers can leap forward about 50 times and 20 times their own body length, respectively.”
So, will it be the robots or the evil superorganisms? Let us give you a word of advice: Always bet on bacteria.
Digital mental health training acceptable to boarding teens
ANAHEIM, CALIF. – A modular digital intervention to teach mental health skills to youth awaiting transfer to psychiatric care appeared feasible to implement and acceptable to teens and their parents, according to a study presented at the American Academy of Pediatrics National Conference.
“This program has the potential to teach evidence-based mental health skills to youth during boarding, providing a head start on recovery prior to psychiatric hospitalization,” study coauthor Samantha House, DO, MPH, section chief of pediatric hospital medicine at Dartmouth Hitchcock Medical Center, Lebanon, N.H., told attendees.
Mental health boarding has become increasingly common as psychiatric care resources have been stretched by a crisis in pediatric mental health that began even before the COVID pandemic. Since youth often don’t receive evidence-based therapies while boarding, Dr. House and her coauthor, JoAnna K. Leyenaar, MD, PhD, MPH, developed a pilot program called I-CARE, which stands for Improving Care, Accelerating Recovery and Education.
I-CARE is a digital health intervention that combines videos on a tablet with workbook exercises that teach mental health skills. The seven modules include an introduction and one each on schedule-making, safety planning, psychoeducation, behavioral activation, relaxation skills, and mindfulness skills. Licensed nursing assistants who have received a 6-hour training from a clinical psychologist administer the program and provide safety supervision during boarding.
“I-CARE was designed to be largely self-directed, supported by ‘coaches’ who are not mental health professionals,” Dr. Leyenaar, vice chair of research in the department of pediatrics and an associate professor of pediatrics at Geisel School of Medicine at Dartmouth, Hanover, N.H., said in an interview. With this model, the program requires minimal additional resources beyond the tablets and workbooks, and is designed for implementation in settings with few or no mental health professionals, she said.
Cora Breuner, MD, MPH, a professor of pediatrics at the University of Washington, Seattle, and an attending physician at Seattle Children’s Hospital, was not involved in the study but was excited to see it.
“I think it’s a really good idea, and I like that it’s being studied,” Dr. Breuner said in an interview. She said the health care and public health system has let down an entire population who data had shown were experiencing mental health problems.
“We knew before the pandemic that behavioral health issues were creeping up slowly with anxiety, depression, suicidal ideation, and, of course, substance use disorders and eating disorders, and not a lot was being done about it,” Dr. Breuner said, and the pandemic exacerbated those issues. ”I don’t know why no one realized that this was going to be the downstream effect of having no socialization for kids for 18 months and limited resources for those who we need desperately to provide care for,” especially BIPOC [Black, Indigenous, and people of color] kids and underresourced kids.
That sentiment is exactly what inspired the creation of the program, according to Dr. Leyenaar.
The I-CARE program was implemented at Dartmouth Hitchcock Medical Center in November 2021 for adolescents aged 12-17 who were boarding because of suicidality or self-harm. The program and study excluded youth with psychosis and other cognitive or behavioral conditions that didn’t fit with the skills taught by the module training.
The researchers qualitatively evaluated the I-CARE program in youth who were offered at least two I-CARE modules and with parents present during boarding.
Twenty-four youth, with a median age of 14, were offered the I-CARE program between November 2021 and April 2022 while boarding for a median 8 days. Most of the patients were female (79%), and a third were transgender or gender diverse. Most were White (83%), and about two-thirds had Medicaid (62.5%). The most common diagnoses among the participants were major depressive disorder (71%) and generalized anxiety disorder (46%). Others included PTSD (29%), restrictive eating disorder (21%), and bipolar disorder (12.5%).
All offered the program completed the first module, and 79% participated in additional modules. The main reason for discontinuation was transfer to another facility, but a few youth either refused to engage with the program or felt they knew the material well enough that they weren’t benefiting from it.
The evaluation involved 16 youth, seven parents, and 17 clinicians. On a Likert scale, the composite score for the program’s appropriateness – suitability, applicability, and meeting needs – was an average 3.7, with a higher rating from clinicians (4.3) and caregivers (3.5) than youth (2.8).
“Some youth felt the intervention was better suited for a younger audience or those with less familiarity with mental health skills, but they acknowledged that the intervention would be helpful and appropriate for others,” Dr. House, who is also an assistant professor of pediatrics at Geisel School of Medicine, said.
Youth rated the acceptability of the program more highly (3.6) and all three groups found it easy to use, with an average feasibility score of 4 across the board. The program’s acceptability received an average score of 4 from parents and clinicians.
”Teens seem to particularly value the psychoeducation module that explains the relationship between thoughts and feelings, as well as the opportunity to develop a personalized safety plan,” Dr. Leyenaar said.
Among the challenges expressed by the participating teens were that the loud sounds and beeping in the hospital made it difficult to practice mindfulness and that they often had to wait for staff to be available to do I-CARE.
“I feel like not many people have been trained yet,” one teen said, “so to have more nurses available to do I-CARE would be helpful.”
Another participant found the coaches helpful. “Sometimes they were my nurse, sometimes they were someone I never met before. … and also, they were all really, really nice,” the teen said.
Another teen regarded the material as “really surface-level mental health stuff” that they thought “could be helpful to other people who are here for the first time.” But others found the content more beneficial.
“The videos were helpful. … I was worried that they weren’t going to be very informative, but they did make sense to me,” one participant said. “They weren’t overcomplicating things. … They weren’t saying anything I didn’t understand, so that was good.”
The researchers next plan to conduct a multisite study to determine the program’s effectiveness in improving health outcomes and reducing suicidal ideation. Dr. House and Dr. Leyenaar are looking at ways to refine the program.
”We may narrow the age range for participants, with an upper age limit of 16, since some older teens said that the modules were best suited for a younger audience,” Dr. Leyenaar said. “We are also discussing how to best support youth who are readmitted to our hospital and have participated in I-CARE previously.”
Dr. Breuner said she would be interested to see, in future studies of the program, whether it reduced the likelihood of inpatient psychiatric stay, the length of psychiatric stay after admission, or the risk of readmission. She also wondered if the program might be offered in languages other than English, whether a version might be specifically designed for BIPOC youth, and whether the researchers had considered offering the intervention to caregivers as well.
The modules are teaching the kids but should they also be teaching the parents? Dr. Breuner wondered. A lot of times, she said, the parents are bringing these kids in because they don’t know what to do and can’t deal with them anymore. Offering modules on the same skills to caregivers would also enable the caregivers to reinforce and reteach the skills to their children, especially if the youth struggled to really take in what the modules were trying to teach.
Dr. Leyenaar said she expects buy-in for a program like this would be high at other institutions, but it’s premature to scale it up until they’ve conducted at least another clinical trial on its effectiveness. The biggest potential barrier to buy-in that Dr. Breuner perceived would be cost.
“It’s always difficult when it costs money” since the hospital needs to train the clinicians who provide the care, Dr. Breuner said, but it’s possible those costs could be offset if the program reduces the risk of readmission or return to the emergency department.
While the overall risk of harms from the intervention are low, Dr. Breuner said it is important to be conscious that the intervention may not necessarily be appropriate for all youth.
“There’s always risk when there’s a trauma background, and you have to be very careful, especially with mindfulness training,” Dr. Breuner said. For those with a history of abuse or other adverse childhood experiences “for someone to get into a very calm, still place can actually be counterproductive.”
Dr. Breuner especially appreciated that the researchers involved the youth and caregivers in the evaluation process. “That the parents expressed positive attitudes is really incredible,” she said.
Dr. House, Dr. Leyenaar, and Dr. Breuner had no disclosures. No external funding was noted for the study.
ANAHEIM, CALIF. – A modular digital intervention to teach mental health skills to youth awaiting transfer to psychiatric care appeared feasible to implement and acceptable to teens and their parents, according to a study presented at the American Academy of Pediatrics National Conference.
“This program has the potential to teach evidence-based mental health skills to youth during boarding, providing a head start on recovery prior to psychiatric hospitalization,” study coauthor Samantha House, DO, MPH, section chief of pediatric hospital medicine at Dartmouth Hitchcock Medical Center, Lebanon, N.H., told attendees.
Mental health boarding has become increasingly common as psychiatric care resources have been stretched by a crisis in pediatric mental health that began even before the COVID pandemic. Since youth often don’t receive evidence-based therapies while boarding, Dr. House and her coauthor, JoAnna K. Leyenaar, MD, PhD, MPH, developed a pilot program called I-CARE, which stands for Improving Care, Accelerating Recovery and Education.
I-CARE is a digital health intervention that combines videos on a tablet with workbook exercises that teach mental health skills. The seven modules include an introduction and one each on schedule-making, safety planning, psychoeducation, behavioral activation, relaxation skills, and mindfulness skills. Licensed nursing assistants who have received a 6-hour training from a clinical psychologist administer the program and provide safety supervision during boarding.
“I-CARE was designed to be largely self-directed, supported by ‘coaches’ who are not mental health professionals,” Dr. Leyenaar, vice chair of research in the department of pediatrics and an associate professor of pediatrics at Geisel School of Medicine at Dartmouth, Hanover, N.H., said in an interview. With this model, the program requires minimal additional resources beyond the tablets and workbooks, and is designed for implementation in settings with few or no mental health professionals, she said.
Cora Breuner, MD, MPH, a professor of pediatrics at the University of Washington, Seattle, and an attending physician at Seattle Children’s Hospital, was not involved in the study but was excited to see it.
“I think it’s a really good idea, and I like that it’s being studied,” Dr. Breuner said in an interview. She said the health care and public health system has let down an entire population who data had shown were experiencing mental health problems.
“We knew before the pandemic that behavioral health issues were creeping up slowly with anxiety, depression, suicidal ideation, and, of course, substance use disorders and eating disorders, and not a lot was being done about it,” Dr. Breuner said, and the pandemic exacerbated those issues. ”I don’t know why no one realized that this was going to be the downstream effect of having no socialization for kids for 18 months and limited resources for those who we need desperately to provide care for,” especially BIPOC [Black, Indigenous, and people of color] kids and underresourced kids.
That sentiment is exactly what inspired the creation of the program, according to Dr. Leyenaar.
The I-CARE program was implemented at Dartmouth Hitchcock Medical Center in November 2021 for adolescents aged 12-17 who were boarding because of suicidality or self-harm. The program and study excluded youth with psychosis and other cognitive or behavioral conditions that didn’t fit with the skills taught by the module training.
The researchers qualitatively evaluated the I-CARE program in youth who were offered at least two I-CARE modules and with parents present during boarding.
Twenty-four youth, with a median age of 14, were offered the I-CARE program between November 2021 and April 2022 while boarding for a median 8 days. Most of the patients were female (79%), and a third were transgender or gender diverse. Most were White (83%), and about two-thirds had Medicaid (62.5%). The most common diagnoses among the participants were major depressive disorder (71%) and generalized anxiety disorder (46%). Others included PTSD (29%), restrictive eating disorder (21%), and bipolar disorder (12.5%).
All offered the program completed the first module, and 79% participated in additional modules. The main reason for discontinuation was transfer to another facility, but a few youth either refused to engage with the program or felt they knew the material well enough that they weren’t benefiting from it.
The evaluation involved 16 youth, seven parents, and 17 clinicians. On a Likert scale, the composite score for the program’s appropriateness – suitability, applicability, and meeting needs – was an average 3.7, with a higher rating from clinicians (4.3) and caregivers (3.5) than youth (2.8).
“Some youth felt the intervention was better suited for a younger audience or those with less familiarity with mental health skills, but they acknowledged that the intervention would be helpful and appropriate for others,” Dr. House, who is also an assistant professor of pediatrics at Geisel School of Medicine, said.
Youth rated the acceptability of the program more highly (3.6) and all three groups found it easy to use, with an average feasibility score of 4 across the board. The program’s acceptability received an average score of 4 from parents and clinicians.
”Teens seem to particularly value the psychoeducation module that explains the relationship between thoughts and feelings, as well as the opportunity to develop a personalized safety plan,” Dr. Leyenaar said.
Among the challenges expressed by the participating teens were that the loud sounds and beeping in the hospital made it difficult to practice mindfulness and that they often had to wait for staff to be available to do I-CARE.
“I feel like not many people have been trained yet,” one teen said, “so to have more nurses available to do I-CARE would be helpful.”
Another participant found the coaches helpful. “Sometimes they were my nurse, sometimes they were someone I never met before. … and also, they were all really, really nice,” the teen said.
Another teen regarded the material as “really surface-level mental health stuff” that they thought “could be helpful to other people who are here for the first time.” But others found the content more beneficial.
“The videos were helpful. … I was worried that they weren’t going to be very informative, but they did make sense to me,” one participant said. “They weren’t overcomplicating things. … They weren’t saying anything I didn’t understand, so that was good.”
The researchers next plan to conduct a multisite study to determine the program’s effectiveness in improving health outcomes and reducing suicidal ideation. Dr. House and Dr. Leyenaar are looking at ways to refine the program.
”We may narrow the age range for participants, with an upper age limit of 16, since some older teens said that the modules were best suited for a younger audience,” Dr. Leyenaar said. “We are also discussing how to best support youth who are readmitted to our hospital and have participated in I-CARE previously.”
Dr. Breuner said she would be interested to see, in future studies of the program, whether it reduced the likelihood of inpatient psychiatric stay, the length of psychiatric stay after admission, or the risk of readmission. She also wondered if the program might be offered in languages other than English, whether a version might be specifically designed for BIPOC youth, and whether the researchers had considered offering the intervention to caregivers as well.
The modules are teaching the kids but should they also be teaching the parents? Dr. Breuner wondered. A lot of times, she said, the parents are bringing these kids in because they don’t know what to do and can’t deal with them anymore. Offering modules on the same skills to caregivers would also enable the caregivers to reinforce and reteach the skills to their children, especially if the youth struggled to really take in what the modules were trying to teach.
Dr. Leyenaar said she expects buy-in for a program like this would be high at other institutions, but it’s premature to scale it up until they’ve conducted at least another clinical trial on its effectiveness. The biggest potential barrier to buy-in that Dr. Breuner perceived would be cost.
“It’s always difficult when it costs money” since the hospital needs to train the clinicians who provide the care, Dr. Breuner said, but it’s possible those costs could be offset if the program reduces the risk of readmission or return to the emergency department.
While the overall risk of harms from the intervention are low, Dr. Breuner said it is important to be conscious that the intervention may not necessarily be appropriate for all youth.
“There’s always risk when there’s a trauma background, and you have to be very careful, especially with mindfulness training,” Dr. Breuner said. For those with a history of abuse or other adverse childhood experiences “for someone to get into a very calm, still place can actually be counterproductive.”
Dr. Breuner especially appreciated that the researchers involved the youth and caregivers in the evaluation process. “That the parents expressed positive attitudes is really incredible,” she said.
Dr. House, Dr. Leyenaar, and Dr. Breuner had no disclosures. No external funding was noted for the study.
ANAHEIM, CALIF. – A modular digital intervention to teach mental health skills to youth awaiting transfer to psychiatric care appeared feasible to implement and acceptable to teens and their parents, according to a study presented at the American Academy of Pediatrics National Conference.
“This program has the potential to teach evidence-based mental health skills to youth during boarding, providing a head start on recovery prior to psychiatric hospitalization,” study coauthor Samantha House, DO, MPH, section chief of pediatric hospital medicine at Dartmouth Hitchcock Medical Center, Lebanon, N.H., told attendees.
Mental health boarding has become increasingly common as psychiatric care resources have been stretched by a crisis in pediatric mental health that began even before the COVID pandemic. Since youth often don’t receive evidence-based therapies while boarding, Dr. House and her coauthor, JoAnna K. Leyenaar, MD, PhD, MPH, developed a pilot program called I-CARE, which stands for Improving Care, Accelerating Recovery and Education.
I-CARE is a digital health intervention that combines videos on a tablet with workbook exercises that teach mental health skills. The seven modules include an introduction and one each on schedule-making, safety planning, psychoeducation, behavioral activation, relaxation skills, and mindfulness skills. Licensed nursing assistants who have received a 6-hour training from a clinical psychologist administer the program and provide safety supervision during boarding.
“I-CARE was designed to be largely self-directed, supported by ‘coaches’ who are not mental health professionals,” Dr. Leyenaar, vice chair of research in the department of pediatrics and an associate professor of pediatrics at Geisel School of Medicine at Dartmouth, Hanover, N.H., said in an interview. With this model, the program requires minimal additional resources beyond the tablets and workbooks, and is designed for implementation in settings with few or no mental health professionals, she said.
Cora Breuner, MD, MPH, a professor of pediatrics at the University of Washington, Seattle, and an attending physician at Seattle Children’s Hospital, was not involved in the study but was excited to see it.
“I think it’s a really good idea, and I like that it’s being studied,” Dr. Breuner said in an interview. She said the health care and public health system has let down an entire population who data had shown were experiencing mental health problems.
“We knew before the pandemic that behavioral health issues were creeping up slowly with anxiety, depression, suicidal ideation, and, of course, substance use disorders and eating disorders, and not a lot was being done about it,” Dr. Breuner said, and the pandemic exacerbated those issues. ”I don’t know why no one realized that this was going to be the downstream effect of having no socialization for kids for 18 months and limited resources for those who we need desperately to provide care for,” especially BIPOC [Black, Indigenous, and people of color] kids and underresourced kids.
That sentiment is exactly what inspired the creation of the program, according to Dr. Leyenaar.
The I-CARE program was implemented at Dartmouth Hitchcock Medical Center in November 2021 for adolescents aged 12-17 who were boarding because of suicidality or self-harm. The program and study excluded youth with psychosis and other cognitive or behavioral conditions that didn’t fit with the skills taught by the module training.
The researchers qualitatively evaluated the I-CARE program in youth who were offered at least two I-CARE modules and with parents present during boarding.
Twenty-four youth, with a median age of 14, were offered the I-CARE program between November 2021 and April 2022 while boarding for a median 8 days. Most of the patients were female (79%), and a third were transgender or gender diverse. Most were White (83%), and about two-thirds had Medicaid (62.5%). The most common diagnoses among the participants were major depressive disorder (71%) and generalized anxiety disorder (46%). Others included PTSD (29%), restrictive eating disorder (21%), and bipolar disorder (12.5%).
All offered the program completed the first module, and 79% participated in additional modules. The main reason for discontinuation was transfer to another facility, but a few youth either refused to engage with the program or felt they knew the material well enough that they weren’t benefiting from it.
The evaluation involved 16 youth, seven parents, and 17 clinicians. On a Likert scale, the composite score for the program’s appropriateness – suitability, applicability, and meeting needs – was an average 3.7, with a higher rating from clinicians (4.3) and caregivers (3.5) than youth (2.8).
“Some youth felt the intervention was better suited for a younger audience or those with less familiarity with mental health skills, but they acknowledged that the intervention would be helpful and appropriate for others,” Dr. House, who is also an assistant professor of pediatrics at Geisel School of Medicine, said.
Youth rated the acceptability of the program more highly (3.6) and all three groups found it easy to use, with an average feasibility score of 4 across the board. The program’s acceptability received an average score of 4 from parents and clinicians.
”Teens seem to particularly value the psychoeducation module that explains the relationship between thoughts and feelings, as well as the opportunity to develop a personalized safety plan,” Dr. Leyenaar said.
Among the challenges expressed by the participating teens were that the loud sounds and beeping in the hospital made it difficult to practice mindfulness and that they often had to wait for staff to be available to do I-CARE.
“I feel like not many people have been trained yet,” one teen said, “so to have more nurses available to do I-CARE would be helpful.”
Another participant found the coaches helpful. “Sometimes they were my nurse, sometimes they were someone I never met before. … and also, they were all really, really nice,” the teen said.
Another teen regarded the material as “really surface-level mental health stuff” that they thought “could be helpful to other people who are here for the first time.” But others found the content more beneficial.
“The videos were helpful. … I was worried that they weren’t going to be very informative, but they did make sense to me,” one participant said. “They weren’t overcomplicating things. … They weren’t saying anything I didn’t understand, so that was good.”
The researchers next plan to conduct a multisite study to determine the program’s effectiveness in improving health outcomes and reducing suicidal ideation. Dr. House and Dr. Leyenaar are looking at ways to refine the program.
”We may narrow the age range for participants, with an upper age limit of 16, since some older teens said that the modules were best suited for a younger audience,” Dr. Leyenaar said. “We are also discussing how to best support youth who are readmitted to our hospital and have participated in I-CARE previously.”
Dr. Breuner said she would be interested to see, in future studies of the program, whether it reduced the likelihood of inpatient psychiatric stay, the length of psychiatric stay after admission, or the risk of readmission. She also wondered if the program might be offered in languages other than English, whether a version might be specifically designed for BIPOC youth, and whether the researchers had considered offering the intervention to caregivers as well.
The modules are teaching the kids but should they also be teaching the parents? Dr. Breuner wondered. A lot of times, she said, the parents are bringing these kids in because they don’t know what to do and can’t deal with them anymore. Offering modules on the same skills to caregivers would also enable the caregivers to reinforce and reteach the skills to their children, especially if the youth struggled to really take in what the modules were trying to teach.
Dr. Leyenaar said she expects buy-in for a program like this would be high at other institutions, but it’s premature to scale it up until they’ve conducted at least another clinical trial on its effectiveness. The biggest potential barrier to buy-in that Dr. Breuner perceived would be cost.
“It’s always difficult when it costs money” since the hospital needs to train the clinicians who provide the care, Dr. Breuner said, but it’s possible those costs could be offset if the program reduces the risk of readmission or return to the emergency department.
While the overall risk of harms from the intervention are low, Dr. Breuner said it is important to be conscious that the intervention may not necessarily be appropriate for all youth.
“There’s always risk when there’s a trauma background, and you have to be very careful, especially with mindfulness training,” Dr. Breuner said. For those with a history of abuse or other adverse childhood experiences “for someone to get into a very calm, still place can actually be counterproductive.”
Dr. Breuner especially appreciated that the researchers involved the youth and caregivers in the evaluation process. “That the parents expressed positive attitudes is really incredible,” she said.
Dr. House, Dr. Leyenaar, and Dr. Breuner had no disclosures. No external funding was noted for the study.
AT AAP 2022
Older diabetes drugs linked to dementia risk -- one lower, one higher
a new observational study in patients with type 2 diabetes suggests.
The data, obtained from nationwide electronic medical records from the Department of Veterans Affairs, yielded a 22% lower risk of dementia with TZD monotherapy and a 12% elevated risk with sulfonylurea monotherapy, compared with metformin monotherapy. The apparent protective effects of TZDs were greater among individuals with overweight or obesity.
“Our findings provide additional information to aid clinicians’ selection of [glucose-lowering medications] for patients with mild or moderate type 2 diabetes and [who] are at high risk of dementia,” Xin Tang and colleagues wrote in their article, published online in BMJ Open Diabetes Research & Care.
The results “add substantially to the literature concerning the effects of [glucose-lowering medications] on dementia where previous findings have been inconsistent. Studies with a follow-up time of less than 3 years have mainly reported null associations, while studies with longer a follow-up time typically yielded protective findings. With a mean follow-up time of 6.8 years, we had a sufficient duration to detect treatment differences,” the investigators wrote.
“Supplementing [a] sulfonylurea with either metformin or [a] TZD may partially offset its prodementia effects. These findings may help inform medication selection for elderly patients with T2D at high risk of dementia,” they added.
Randomized trials needed to determine cause and effect
Ivan Koychev, PhD, a senior clinical researcher in the department of psychiatry at the University of Oxford (England), told the UK Science Media Centre: “This is a large, well-conducted real-world data study that highlights the importance of checking whether already prescribed medications may be useful for preventing dementia.”
The findings regarding TZDs, also known as glitazones, are in line with existing literature suggesting dementia protection with other drugs prescribed for type 2 diabetes that weren’t examined in the current study, such as newer agents like glucagonlike peptide–1 (GLP-1) agonists and sodium-glucose cotransporter 2 (SGLT2) inhibitors, Dr. Koychev said.
“The main limitations of this study is that following the initial 2-year period the authors were interested in, the participants may have been prescribed one of the other type 2 diabetes drugs [GLP-1 agonists or SGLT2 inhibitors] that have been found to reduce dementia risk, thus potentially making the direct glitazone [TZD] effect more difficult to discern,” Dr. Koychev noted.
And, he pointed out that the study design limits attribution of causality. “It is also important to note that people with type 2 diabetes do run a higher risk of both dementia and cognitive deficits and that these medications are only prescribed in these patients, so all this data is from this patient group rather than the general population.”
James Connell, PhD, head of translational science at Alzheimer’s Research UK, agreed. “While this observational study found that those with type 2 diabetes taking thiazolidinedione had a lower dementia risk than those on the most common medication for type 2 diabetes, it only shows an association between taking the drug and dementia risk and not a causal relationship.
“Double-blind and placebo-controlled clinical trials are needed to see whether the drug [TDZ] could help lower dementia risk in people with and without diabetes. Anyone with any questions about what treatments they are receiving should speak to their doctor,” he told the UK Science Media Centre.
Opposite effects of sulfonylureas, TZDs versus metformin
The study authors analyzed 559,106 VA patients with type 2 diabetes who initiated glucose-lowering medication during 2001-2017 and took it for at least a year. They were aged 60 years or older and did not have dementia at baseline. Most were White (76.8%) and male (96.9%), two-thirds (63.1%) had obesity, and mean hemoglobin A1c was 6.8%.
Overall, 31,125 developed all-cause dementia. The incidence rate was 8.2 cases per 1,000 person-years, ranging from 6.2 cases per 1,000 person-years among those taking metformin monotherapy to 13.4 cases per 1,000 person-years in those taking both sulfonylurea and a TZD.
Compared with metformin monotherapy, the hazard ratio for all-cause dementia for sulfonylurea monotherapy was a significant 1.12. The increased risk was also seen for vascular dementia, with an HR of 1.14.
In contrast, TZD monotherapy was associated with a significantly lower risk for all-cause dementia (HR, 0.78), as well as for Alzheimer’s disease (HR, 0.89) and vascular dementia (HR, 0.43), compared with metformin monotherapy.
The combination of metformin and TZD also lowered the risk of all-cause dementia, while regimens including sulfonylureas raised the risks for all-cause and vascular dementia.
Most of the results didn’t change significantly when the drug exposure window was extended to 2 years.
Effects more pronounced in those with obesity
The protective 1-year effects of TZD monotherapy and of metformin plus TZD, compared with metformin alone, were more significant among participants aged 75 or younger and with a body mass index above 25 kg/m2, compared with those who were older than 75 years and with normal BMIs, respectively.
On the other hand, the greater risk for dementia incurred with sulfonylureas was further increased among those with higher BMI.
This research was partially funded by grants from the National Human Genome Research Institute, the National Science Foundation, the National Institute of Diabetes and Digestive and Kidney Disease, and the National Heart, Lung, and Blood Institute. Dr. Koychev is chief investigator for a trial, sponsored by Oxford University and funded by Novo Nordisk, testing whether the GLP-1 agonist semaglutide reduces the risk for dementia in aging adults.
A version of this article first appeared on Medscape.com.
a new observational study in patients with type 2 diabetes suggests.
The data, obtained from nationwide electronic medical records from the Department of Veterans Affairs, yielded a 22% lower risk of dementia with TZD monotherapy and a 12% elevated risk with sulfonylurea monotherapy, compared with metformin monotherapy. The apparent protective effects of TZDs were greater among individuals with overweight or obesity.
“Our findings provide additional information to aid clinicians’ selection of [glucose-lowering medications] for patients with mild or moderate type 2 diabetes and [who] are at high risk of dementia,” Xin Tang and colleagues wrote in their article, published online in BMJ Open Diabetes Research & Care.
The results “add substantially to the literature concerning the effects of [glucose-lowering medications] on dementia where previous findings have been inconsistent. Studies with a follow-up time of less than 3 years have mainly reported null associations, while studies with longer a follow-up time typically yielded protective findings. With a mean follow-up time of 6.8 years, we had a sufficient duration to detect treatment differences,” the investigators wrote.
“Supplementing [a] sulfonylurea with either metformin or [a] TZD may partially offset its prodementia effects. These findings may help inform medication selection for elderly patients with T2D at high risk of dementia,” they added.
Randomized trials needed to determine cause and effect
Ivan Koychev, PhD, a senior clinical researcher in the department of psychiatry at the University of Oxford (England), told the UK Science Media Centre: “This is a large, well-conducted real-world data study that highlights the importance of checking whether already prescribed medications may be useful for preventing dementia.”
The findings regarding TZDs, also known as glitazones, are in line with existing literature suggesting dementia protection with other drugs prescribed for type 2 diabetes that weren’t examined in the current study, such as newer agents like glucagonlike peptide–1 (GLP-1) agonists and sodium-glucose cotransporter 2 (SGLT2) inhibitors, Dr. Koychev said.
“The main limitations of this study is that following the initial 2-year period the authors were interested in, the participants may have been prescribed one of the other type 2 diabetes drugs [GLP-1 agonists or SGLT2 inhibitors] that have been found to reduce dementia risk, thus potentially making the direct glitazone [TZD] effect more difficult to discern,” Dr. Koychev noted.
And, he pointed out that the study design limits attribution of causality. “It is also important to note that people with type 2 diabetes do run a higher risk of both dementia and cognitive deficits and that these medications are only prescribed in these patients, so all this data is from this patient group rather than the general population.”
James Connell, PhD, head of translational science at Alzheimer’s Research UK, agreed. “While this observational study found that those with type 2 diabetes taking thiazolidinedione had a lower dementia risk than those on the most common medication for type 2 diabetes, it only shows an association between taking the drug and dementia risk and not a causal relationship.
“Double-blind and placebo-controlled clinical trials are needed to see whether the drug [TDZ] could help lower dementia risk in people with and without diabetes. Anyone with any questions about what treatments they are receiving should speak to their doctor,” he told the UK Science Media Centre.
Opposite effects of sulfonylureas, TZDs versus metformin
The study authors analyzed 559,106 VA patients with type 2 diabetes who initiated glucose-lowering medication during 2001-2017 and took it for at least a year. They were aged 60 years or older and did not have dementia at baseline. Most were White (76.8%) and male (96.9%), two-thirds (63.1%) had obesity, and mean hemoglobin A1c was 6.8%.
Overall, 31,125 developed all-cause dementia. The incidence rate was 8.2 cases per 1,000 person-years, ranging from 6.2 cases per 1,000 person-years among those taking metformin monotherapy to 13.4 cases per 1,000 person-years in those taking both sulfonylurea and a TZD.
Compared with metformin monotherapy, the hazard ratio for all-cause dementia for sulfonylurea monotherapy was a significant 1.12. The increased risk was also seen for vascular dementia, with an HR of 1.14.
In contrast, TZD monotherapy was associated with a significantly lower risk for all-cause dementia (HR, 0.78), as well as for Alzheimer’s disease (HR, 0.89) and vascular dementia (HR, 0.43), compared with metformin monotherapy.
The combination of metformin and TZD also lowered the risk of all-cause dementia, while regimens including sulfonylureas raised the risks for all-cause and vascular dementia.
Most of the results didn’t change significantly when the drug exposure window was extended to 2 years.
Effects more pronounced in those with obesity
The protective 1-year effects of TZD monotherapy and of metformin plus TZD, compared with metformin alone, were more significant among participants aged 75 or younger and with a body mass index above 25 kg/m2, compared with those who were older than 75 years and with normal BMIs, respectively.
On the other hand, the greater risk for dementia incurred with sulfonylureas was further increased among those with higher BMI.
This research was partially funded by grants from the National Human Genome Research Institute, the National Science Foundation, the National Institute of Diabetes and Digestive and Kidney Disease, and the National Heart, Lung, and Blood Institute. Dr. Koychev is chief investigator for a trial, sponsored by Oxford University and funded by Novo Nordisk, testing whether the GLP-1 agonist semaglutide reduces the risk for dementia in aging adults.
A version of this article first appeared on Medscape.com.
a new observational study in patients with type 2 diabetes suggests.
The data, obtained from nationwide electronic medical records from the Department of Veterans Affairs, yielded a 22% lower risk of dementia with TZD monotherapy and a 12% elevated risk with sulfonylurea monotherapy, compared with metformin monotherapy. The apparent protective effects of TZDs were greater among individuals with overweight or obesity.
“Our findings provide additional information to aid clinicians’ selection of [glucose-lowering medications] for patients with mild or moderate type 2 diabetes and [who] are at high risk of dementia,” Xin Tang and colleagues wrote in their article, published online in BMJ Open Diabetes Research & Care.
The results “add substantially to the literature concerning the effects of [glucose-lowering medications] on dementia where previous findings have been inconsistent. Studies with a follow-up time of less than 3 years have mainly reported null associations, while studies with longer a follow-up time typically yielded protective findings. With a mean follow-up time of 6.8 years, we had a sufficient duration to detect treatment differences,” the investigators wrote.
“Supplementing [a] sulfonylurea with either metformin or [a] TZD may partially offset its prodementia effects. These findings may help inform medication selection for elderly patients with T2D at high risk of dementia,” they added.
Randomized trials needed to determine cause and effect
Ivan Koychev, PhD, a senior clinical researcher in the department of psychiatry at the University of Oxford (England), told the UK Science Media Centre: “This is a large, well-conducted real-world data study that highlights the importance of checking whether already prescribed medications may be useful for preventing dementia.”
The findings regarding TZDs, also known as glitazones, are in line with existing literature suggesting dementia protection with other drugs prescribed for type 2 diabetes that weren’t examined in the current study, such as newer agents like glucagonlike peptide–1 (GLP-1) agonists and sodium-glucose cotransporter 2 (SGLT2) inhibitors, Dr. Koychev said.
“The main limitations of this study is that following the initial 2-year period the authors were interested in, the participants may have been prescribed one of the other type 2 diabetes drugs [GLP-1 agonists or SGLT2 inhibitors] that have been found to reduce dementia risk, thus potentially making the direct glitazone [TZD] effect more difficult to discern,” Dr. Koychev noted.
And, he pointed out that the study design limits attribution of causality. “It is also important to note that people with type 2 diabetes do run a higher risk of both dementia and cognitive deficits and that these medications are only prescribed in these patients, so all this data is from this patient group rather than the general population.”
James Connell, PhD, head of translational science at Alzheimer’s Research UK, agreed. “While this observational study found that those with type 2 diabetes taking thiazolidinedione had a lower dementia risk than those on the most common medication for type 2 diabetes, it only shows an association between taking the drug and dementia risk and not a causal relationship.
“Double-blind and placebo-controlled clinical trials are needed to see whether the drug [TDZ] could help lower dementia risk in people with and without diabetes. Anyone with any questions about what treatments they are receiving should speak to their doctor,” he told the UK Science Media Centre.
Opposite effects of sulfonylureas, TZDs versus metformin
The study authors analyzed 559,106 VA patients with type 2 diabetes who initiated glucose-lowering medication during 2001-2017 and took it for at least a year. They were aged 60 years or older and did not have dementia at baseline. Most were White (76.8%) and male (96.9%), two-thirds (63.1%) had obesity, and mean hemoglobin A1c was 6.8%.
Overall, 31,125 developed all-cause dementia. The incidence rate was 8.2 cases per 1,000 person-years, ranging from 6.2 cases per 1,000 person-years among those taking metformin monotherapy to 13.4 cases per 1,000 person-years in those taking both sulfonylurea and a TZD.
Compared with metformin monotherapy, the hazard ratio for all-cause dementia for sulfonylurea monotherapy was a significant 1.12. The increased risk was also seen for vascular dementia, with an HR of 1.14.
In contrast, TZD monotherapy was associated with a significantly lower risk for all-cause dementia (HR, 0.78), as well as for Alzheimer’s disease (HR, 0.89) and vascular dementia (HR, 0.43), compared with metformin monotherapy.
The combination of metformin and TZD also lowered the risk of all-cause dementia, while regimens including sulfonylureas raised the risks for all-cause and vascular dementia.
Most of the results didn’t change significantly when the drug exposure window was extended to 2 years.
Effects more pronounced in those with obesity
The protective 1-year effects of TZD monotherapy and of metformin plus TZD, compared with metformin alone, were more significant among participants aged 75 or younger and with a body mass index above 25 kg/m2, compared with those who were older than 75 years and with normal BMIs, respectively.
On the other hand, the greater risk for dementia incurred with sulfonylureas was further increased among those with higher BMI.
This research was partially funded by grants from the National Human Genome Research Institute, the National Science Foundation, the National Institute of Diabetes and Digestive and Kidney Disease, and the National Heart, Lung, and Blood Institute. Dr. Koychev is chief investigator for a trial, sponsored by Oxford University and funded by Novo Nordisk, testing whether the GLP-1 agonist semaglutide reduces the risk for dementia in aging adults.
A version of this article first appeared on Medscape.com.
FROM BMJ OPEN DIABETES RESEARCH & CARE
USPSTF calls for universal anxiety screening in children 8-18, jury out on suicide screening
For the first time, the task force recommended screening for anxiety in children aged 8-18 years who do not have a diagnosed anxiety disorder and are not showing signs or symptoms of anxiety.
This “B” recommendation reflects “moderate certainty” evidence that screening for anxiety in 8- to 18-year-olds has a moderate net benefit, the task force said.
However, the task force found “insufficient” evidence to weigh the balance of benefits and harms of screening for anxiety in children aged 7 and younger and therefore issued an “I” statement.
The task force also recommended screening for children aged 12-18 years for major depressive disorder (“B” recommendation) but said there is insufficient evidence to weigh the balance of benefits and harms of screening for depression in children aged 11 and younger (“I” statement).
These recommendations are in line with the 2016 recommendations on depression screening from the USPSTF.
“Fortunately, screening older children for anxiety and depression can identify these conditions so children and teens can receive the care that they need,” task force member Martha Kubik, PhD, RN, with George Mason University, Fairfax, Va., said in a statement.
“Unfortunately, there are key evidence gaps related to screening for anxiety and depression in younger children and screening for suicide risk in all youth,” added task force member Lori Pbert, PhD, University of Massachusetts, Worcester.
“We are calling for more research in these critical areas so we can provide health care professionals with evidence-based ways to keep their young patients healthy,” Dr. Pbert said.
Suicide screening
Turning to suicide, the task force says there is not enough evidence to recommend for or against screening for suicide risk in children and adolescents, and therefore issued an “I” statement – in line with the 2014 recommendation statement from the task force.
The task force acknowledged that the American Academy of Pediatrics, the American Foundation for Suicide Prevention, and experts from the National Institute of Mental Health have released a “Blueprint for Youth Suicide Prevention” that recommends universal screening for suicide risk in youth 12 years or older, while children aged 8-11 years should be screened as clinically indicated.
The task force’s final recommendation statements and corresponding evidence summaries on screening children and adolescents for anxiety, depression and suicide were published online Oct. 11, 2022, in JAMA and the USPSTF website.
The final recommendations are consistent with the 2022 draft recommendation statements on these topics.
The task force emphasized that screening is only the first step in helping children and adolescents with anxiety and depression. Youth who screen positive need further evaluation to determine if they have anxiety or depression.
After diagnosis, youth should participate in shared decision-making with their parents and healthcare professional to identify the best treatment or combination of treatments.
Only a first step
In an accompanying editorial, John Walkup, MD, with Ann and Robert H. Lurie Children’s Hospital, Chicago, and coauthors made the point that, for the potential of screening for pediatric anxiety disorders to be fully realized, research focused on the process of screening from evaluation to treatment needs to be a priority.
“Perhaps most critical is developing a smart and sophisticated process of screening aligned with evidence-based treatment strategies that brings added value to routine pediatric medical care and that improves physical and mental health outcomes for children and adolescents,” they wrote.
Members of the USPSTF disclosed no relevant financial relationships. Dr. Walkup reported serving as an unpaid member of the scientific council of the Anxiety and Depression Association of America, receiving royalties for anxiety-related continuing medical education activities from Wolters Kluwer and honoraria for anxiety presentations from the American Academy of Child and Adolescent Psychiatry and the American Academy of Pediatrics.
A version of this article first appeared on Medscape.com.
For the first time, the task force recommended screening for anxiety in children aged 8-18 years who do not have a diagnosed anxiety disorder and are not showing signs or symptoms of anxiety.
This “B” recommendation reflects “moderate certainty” evidence that screening for anxiety in 8- to 18-year-olds has a moderate net benefit, the task force said.
However, the task force found “insufficient” evidence to weigh the balance of benefits and harms of screening for anxiety in children aged 7 and younger and therefore issued an “I” statement.
The task force also recommended screening for children aged 12-18 years for major depressive disorder (“B” recommendation) but said there is insufficient evidence to weigh the balance of benefits and harms of screening for depression in children aged 11 and younger (“I” statement).
These recommendations are in line with the 2016 recommendations on depression screening from the USPSTF.
“Fortunately, screening older children for anxiety and depression can identify these conditions so children and teens can receive the care that they need,” task force member Martha Kubik, PhD, RN, with George Mason University, Fairfax, Va., said in a statement.
“Unfortunately, there are key evidence gaps related to screening for anxiety and depression in younger children and screening for suicide risk in all youth,” added task force member Lori Pbert, PhD, University of Massachusetts, Worcester.
“We are calling for more research in these critical areas so we can provide health care professionals with evidence-based ways to keep their young patients healthy,” Dr. Pbert said.
Suicide screening
Turning to suicide, the task force says there is not enough evidence to recommend for or against screening for suicide risk in children and adolescents, and therefore issued an “I” statement – in line with the 2014 recommendation statement from the task force.
The task force acknowledged that the American Academy of Pediatrics, the American Foundation for Suicide Prevention, and experts from the National Institute of Mental Health have released a “Blueprint for Youth Suicide Prevention” that recommends universal screening for suicide risk in youth 12 years or older, while children aged 8-11 years should be screened as clinically indicated.
The task force’s final recommendation statements and corresponding evidence summaries on screening children and adolescents for anxiety, depression and suicide were published online Oct. 11, 2022, in JAMA and the USPSTF website.
The final recommendations are consistent with the 2022 draft recommendation statements on these topics.
The task force emphasized that screening is only the first step in helping children and adolescents with anxiety and depression. Youth who screen positive need further evaluation to determine if they have anxiety or depression.
After diagnosis, youth should participate in shared decision-making with their parents and healthcare professional to identify the best treatment or combination of treatments.
Only a first step
In an accompanying editorial, John Walkup, MD, with Ann and Robert H. Lurie Children’s Hospital, Chicago, and coauthors made the point that, for the potential of screening for pediatric anxiety disorders to be fully realized, research focused on the process of screening from evaluation to treatment needs to be a priority.
“Perhaps most critical is developing a smart and sophisticated process of screening aligned with evidence-based treatment strategies that brings added value to routine pediatric medical care and that improves physical and mental health outcomes for children and adolescents,” they wrote.
Members of the USPSTF disclosed no relevant financial relationships. Dr. Walkup reported serving as an unpaid member of the scientific council of the Anxiety and Depression Association of America, receiving royalties for anxiety-related continuing medical education activities from Wolters Kluwer and honoraria for anxiety presentations from the American Academy of Child and Adolescent Psychiatry and the American Academy of Pediatrics.
A version of this article first appeared on Medscape.com.
For the first time, the task force recommended screening for anxiety in children aged 8-18 years who do not have a diagnosed anxiety disorder and are not showing signs or symptoms of anxiety.
This “B” recommendation reflects “moderate certainty” evidence that screening for anxiety in 8- to 18-year-olds has a moderate net benefit, the task force said.
However, the task force found “insufficient” evidence to weigh the balance of benefits and harms of screening for anxiety in children aged 7 and younger and therefore issued an “I” statement.
The task force also recommended screening for children aged 12-18 years for major depressive disorder (“B” recommendation) but said there is insufficient evidence to weigh the balance of benefits and harms of screening for depression in children aged 11 and younger (“I” statement).
These recommendations are in line with the 2016 recommendations on depression screening from the USPSTF.
“Fortunately, screening older children for anxiety and depression can identify these conditions so children and teens can receive the care that they need,” task force member Martha Kubik, PhD, RN, with George Mason University, Fairfax, Va., said in a statement.
“Unfortunately, there are key evidence gaps related to screening for anxiety and depression in younger children and screening for suicide risk in all youth,” added task force member Lori Pbert, PhD, University of Massachusetts, Worcester.
“We are calling for more research in these critical areas so we can provide health care professionals with evidence-based ways to keep their young patients healthy,” Dr. Pbert said.
Suicide screening
Turning to suicide, the task force says there is not enough evidence to recommend for or against screening for suicide risk in children and adolescents, and therefore issued an “I” statement – in line with the 2014 recommendation statement from the task force.
The task force acknowledged that the American Academy of Pediatrics, the American Foundation for Suicide Prevention, and experts from the National Institute of Mental Health have released a “Blueprint for Youth Suicide Prevention” that recommends universal screening for suicide risk in youth 12 years or older, while children aged 8-11 years should be screened as clinically indicated.
The task force’s final recommendation statements and corresponding evidence summaries on screening children and adolescents for anxiety, depression and suicide were published online Oct. 11, 2022, in JAMA and the USPSTF website.
The final recommendations are consistent with the 2022 draft recommendation statements on these topics.
The task force emphasized that screening is only the first step in helping children and adolescents with anxiety and depression. Youth who screen positive need further evaluation to determine if they have anxiety or depression.
After diagnosis, youth should participate in shared decision-making with their parents and healthcare professional to identify the best treatment or combination of treatments.
Only a first step
In an accompanying editorial, John Walkup, MD, with Ann and Robert H. Lurie Children’s Hospital, Chicago, and coauthors made the point that, for the potential of screening for pediatric anxiety disorders to be fully realized, research focused on the process of screening from evaluation to treatment needs to be a priority.
“Perhaps most critical is developing a smart and sophisticated process of screening aligned with evidence-based treatment strategies that brings added value to routine pediatric medical care and that improves physical and mental health outcomes for children and adolescents,” they wrote.
Members of the USPSTF disclosed no relevant financial relationships. Dr. Walkup reported serving as an unpaid member of the scientific council of the Anxiety and Depression Association of America, receiving royalties for anxiety-related continuing medical education activities from Wolters Kluwer and honoraria for anxiety presentations from the American Academy of Child and Adolescent Psychiatry and the American Academy of Pediatrics.
A version of this article first appeared on Medscape.com.
FROM JAMA
Clinical psychoeconomics: Accounting for money matters in psychiatric assessment and treatment
Despite money’s central role in our psychic lives, many trainees – and some seasoned practitioners – skirt around financial issues. Some clinicians confess that inquiring about patients’ finances feels “too personal.” They fear that asking about money could suggest that the clinician is primarily concerned with getting paid. Some clinicians feel that looking into patients’ finances might be unprofessional, outside one’s scope of practice. But it is not.
Trainees often receive little guidance concerning money matters in patients’ lives and treatments, considerations we have labeled clinical psychoeconomics. Considerable evidence suggests that financial concerns often provoke emotional distress and dysfunctional behaviors, and directly influence patient’s health care decisions. Financial issues also influence how clinicians view and react to patients.
We have recently reviewed (and illustrated through case vignettes) how money matters might impact psychiatric assessment, case formulation, treatment planning, and ongoing psychiatric treatments including psychotherapies.1 Consider how money affects people’s lives: Money helps people meet multiple practical, psychological, and social needs by enabling them to obtain food, clothing, shelter, other material goods, services, discretionary time, and opportunities. And money strongly influences relationships. Regardless of poverty or wealth, thoughts and behaviors connected to acquiring, possessing, and disposing of money, and feelings accompanying these processes such as greed, neediness, envy, pride, shame, guilt, and self-satisfaction often underly intrapsychic and interpersonal conflicts.
Individuals constantly engage in numerous simultaneous conscious, preconscious, and unconscious neuro-economic trade-offs that determine goals, efforts, and timing. Many are financially influenced. Money influences how virtually all patients seek, receive, and sustain their mental health care including psychotherapy.
Money problems can be associated with insecurity, impotence, feeling unloved, and lack of freedom or subjugation. Individuals may resent how they’re forced to acquire money, and feel shamed or morally injured by their jobs, financial dependence on other family members, public assistance, or their questionable ways of obtaining money.
Impoverished individuals may face choosing between food, housing, medications, and medical care. Domestically abused individuals may reluctantly remain with their abusers, risking physical harm or death rather than face destitution. Some families tolerate severely disabled individuals at home because they rely on their disability checks and caregiver payments. Suicides may turn on how individuals forecast financial repercussions affecting their families. Desires to avoid debt may lead to treatment avoidance.
Individuals with enough money to get by face daily financially related choices involving competing needs, desires, values, and loyalties. They may experience conflicts concerning spending on necessities vs. indulgences or spending on oneself vs. significant others.
Whereas some wealthy individuals may assume unwarranted airs of superiority and entitlement, others may feel guilty about wealth, or fearful that others like them only for their money. Individuals on the receiving end of wealth may feel emotionally and behaviorally manipulated by their benefactors.
Assessment
Assessments should consider how financial matters have shaped patients’ early psychological development as well their current lives. How do patients’ emotions, thoughts, and behaviors reflect money matters? What money-related pathologies are evident? What aspects of the patient’s “financial world” seem modifiable?
Financial questions should be posed colloquially. Screeners include: “Where do you live?”, “Who’s in the home?”, “How do you (all) manage financially?”, “What do you all do for a living?”, “How do you make ends meet?”, and “What financial problems are you facing?” Clinicians can quickly learn about patients’ financial self-sufficiencies, individuals for whom they bear financial responsibility, and others they rely on for support, for example, relatives. If patients avoid answering such questions forthrightly, particularly when financial arrangements are “complicated,” clinicians will want to revisit these issues later after establishing a firmer alliance but continue to wonder about the meaning of the patient’s reluctance.
When explicit, patients, families, and couples are fully aware of the conflicts but have difficulty resolving financial disputes. When conflicts are implicit, money problems may be unacknowledged, avoided, denied, or minimized. Conflicts concerning money are often transmitted trans-generationally.
Psychopathological conditions unequivocally linked to money include compulsive shopping, gambling disorders, miserly hoarding, impulse buying, and spending sprees during hypomanic and manic states. Mounting debts may create progressively insurmountable sources of distress. Money can be weaponized to sadistically create enticement, envy, or deprivation. Some monetarily antisocial individuals compromise interpersonal relationships as well as treatments. Individuals with alcohol/substance use disorders may spend so much on substances that little is left for necessities. Financially needy individuals may engage in morally questionable behaviors they might otherwise shun.
Case formulation and treatment planning
Incorporating money matters into case formulations entails demonstrating how financial concerns influenced maladaptive development and distort current attitudes, perceptions, and behaviors.
Concurrently, clinicians should acknowledge patients’ reality-based fiscal decisions, appreciating cultural and family value differences concerning how money should be acquired and spent. Since money often determines frequency and duration of treatment visits, clinicians are ethically obligated to discuss with patients what they might expect from different medications and psychotherapies, and their comparative costs.
Money matters’ impact on psychotherapies
Money matters often affect transference and countertransference reactions. Some reactions stem from how patients and clinicians compare their own financial situations with those of the other.
To help identify and ameliorate money-related countertransference responses, clinicians can reflect on questions such as: “How comfortable are you with people who are much poorer or richer than you are?” “How comfortable are you with impoverished individuals or with multimillionaires or their children?” And “why?” For trainees, all these reactions should be discussed in supervision.
Conclusions
To summarize, four clinical psychoeconomic issues should be routinely assessed and factored into psychiatric case formulations and treatment plans: how financial issues 1) have impacted patients’ psychological development; 2) impact patients’ current lives; 3) are likely to impact access, type, intensity, and duration of treatment visits; and 4) might provoke money-related transference and countertransference concerns.
In advising patients about treatment options, clinicians should discuss each treatment’s relative effectiveness and estimated costs of care. Patients’ decisions will likely be heavily influenced by financial considerations.
Dr. Yager is based in the department of psychiatry, University of Colorado at Denver, Aurora. Dr. Kay is based in the department of psychiatry, Wright State University, Dayton, Ohio. No external funds were received for this project, and the authors have no conflicts to disclose.
Reference
1. Yager J and Kay J. Money matters in psychiatric assessment, case formulation, treatment planning, and ongoing psychotherapy: Clinical psychoeconomics. J Nerv Ment Dis. 2022 Jun 10. doi: 10.1097/NMD.0000000000001552.
Despite money’s central role in our psychic lives, many trainees – and some seasoned practitioners – skirt around financial issues. Some clinicians confess that inquiring about patients’ finances feels “too personal.” They fear that asking about money could suggest that the clinician is primarily concerned with getting paid. Some clinicians feel that looking into patients’ finances might be unprofessional, outside one’s scope of practice. But it is not.
Trainees often receive little guidance concerning money matters in patients’ lives and treatments, considerations we have labeled clinical psychoeconomics. Considerable evidence suggests that financial concerns often provoke emotional distress and dysfunctional behaviors, and directly influence patient’s health care decisions. Financial issues also influence how clinicians view and react to patients.
We have recently reviewed (and illustrated through case vignettes) how money matters might impact psychiatric assessment, case formulation, treatment planning, and ongoing psychiatric treatments including psychotherapies.1 Consider how money affects people’s lives: Money helps people meet multiple practical, psychological, and social needs by enabling them to obtain food, clothing, shelter, other material goods, services, discretionary time, and opportunities. And money strongly influences relationships. Regardless of poverty or wealth, thoughts and behaviors connected to acquiring, possessing, and disposing of money, and feelings accompanying these processes such as greed, neediness, envy, pride, shame, guilt, and self-satisfaction often underly intrapsychic and interpersonal conflicts.
Individuals constantly engage in numerous simultaneous conscious, preconscious, and unconscious neuro-economic trade-offs that determine goals, efforts, and timing. Many are financially influenced. Money influences how virtually all patients seek, receive, and sustain their mental health care including psychotherapy.
Money problems can be associated with insecurity, impotence, feeling unloved, and lack of freedom or subjugation. Individuals may resent how they’re forced to acquire money, and feel shamed or morally injured by their jobs, financial dependence on other family members, public assistance, or their questionable ways of obtaining money.
Impoverished individuals may face choosing between food, housing, medications, and medical care. Domestically abused individuals may reluctantly remain with their abusers, risking physical harm or death rather than face destitution. Some families tolerate severely disabled individuals at home because they rely on their disability checks and caregiver payments. Suicides may turn on how individuals forecast financial repercussions affecting their families. Desires to avoid debt may lead to treatment avoidance.
Individuals with enough money to get by face daily financially related choices involving competing needs, desires, values, and loyalties. They may experience conflicts concerning spending on necessities vs. indulgences or spending on oneself vs. significant others.
Whereas some wealthy individuals may assume unwarranted airs of superiority and entitlement, others may feel guilty about wealth, or fearful that others like them only for their money. Individuals on the receiving end of wealth may feel emotionally and behaviorally manipulated by their benefactors.
Assessment
Assessments should consider how financial matters have shaped patients’ early psychological development as well their current lives. How do patients’ emotions, thoughts, and behaviors reflect money matters? What money-related pathologies are evident? What aspects of the patient’s “financial world” seem modifiable?
Financial questions should be posed colloquially. Screeners include: “Where do you live?”, “Who’s in the home?”, “How do you (all) manage financially?”, “What do you all do for a living?”, “How do you make ends meet?”, and “What financial problems are you facing?” Clinicians can quickly learn about patients’ financial self-sufficiencies, individuals for whom they bear financial responsibility, and others they rely on for support, for example, relatives. If patients avoid answering such questions forthrightly, particularly when financial arrangements are “complicated,” clinicians will want to revisit these issues later after establishing a firmer alliance but continue to wonder about the meaning of the patient’s reluctance.
When explicit, patients, families, and couples are fully aware of the conflicts but have difficulty resolving financial disputes. When conflicts are implicit, money problems may be unacknowledged, avoided, denied, or minimized. Conflicts concerning money are often transmitted trans-generationally.
Psychopathological conditions unequivocally linked to money include compulsive shopping, gambling disorders, miserly hoarding, impulse buying, and spending sprees during hypomanic and manic states. Mounting debts may create progressively insurmountable sources of distress. Money can be weaponized to sadistically create enticement, envy, or deprivation. Some monetarily antisocial individuals compromise interpersonal relationships as well as treatments. Individuals with alcohol/substance use disorders may spend so much on substances that little is left for necessities. Financially needy individuals may engage in morally questionable behaviors they might otherwise shun.
Case formulation and treatment planning
Incorporating money matters into case formulations entails demonstrating how financial concerns influenced maladaptive development and distort current attitudes, perceptions, and behaviors.
Concurrently, clinicians should acknowledge patients’ reality-based fiscal decisions, appreciating cultural and family value differences concerning how money should be acquired and spent. Since money often determines frequency and duration of treatment visits, clinicians are ethically obligated to discuss with patients what they might expect from different medications and psychotherapies, and their comparative costs.
Money matters’ impact on psychotherapies
Money matters often affect transference and countertransference reactions. Some reactions stem from how patients and clinicians compare their own financial situations with those of the other.
To help identify and ameliorate money-related countertransference responses, clinicians can reflect on questions such as: “How comfortable are you with people who are much poorer or richer than you are?” “How comfortable are you with impoverished individuals or with multimillionaires or their children?” And “why?” For trainees, all these reactions should be discussed in supervision.
Conclusions
To summarize, four clinical psychoeconomic issues should be routinely assessed and factored into psychiatric case formulations and treatment plans: how financial issues 1) have impacted patients’ psychological development; 2) impact patients’ current lives; 3) are likely to impact access, type, intensity, and duration of treatment visits; and 4) might provoke money-related transference and countertransference concerns.
In advising patients about treatment options, clinicians should discuss each treatment’s relative effectiveness and estimated costs of care. Patients’ decisions will likely be heavily influenced by financial considerations.
Dr. Yager is based in the department of psychiatry, University of Colorado at Denver, Aurora. Dr. Kay is based in the department of psychiatry, Wright State University, Dayton, Ohio. No external funds were received for this project, and the authors have no conflicts to disclose.
Reference
1. Yager J and Kay J. Money matters in psychiatric assessment, case formulation, treatment planning, and ongoing psychotherapy: Clinical psychoeconomics. J Nerv Ment Dis. 2022 Jun 10. doi: 10.1097/NMD.0000000000001552.
Despite money’s central role in our psychic lives, many trainees – and some seasoned practitioners – skirt around financial issues. Some clinicians confess that inquiring about patients’ finances feels “too personal.” They fear that asking about money could suggest that the clinician is primarily concerned with getting paid. Some clinicians feel that looking into patients’ finances might be unprofessional, outside one’s scope of practice. But it is not.
Trainees often receive little guidance concerning money matters in patients’ lives and treatments, considerations we have labeled clinical psychoeconomics. Considerable evidence suggests that financial concerns often provoke emotional distress and dysfunctional behaviors, and directly influence patient’s health care decisions. Financial issues also influence how clinicians view and react to patients.
We have recently reviewed (and illustrated through case vignettes) how money matters might impact psychiatric assessment, case formulation, treatment planning, and ongoing psychiatric treatments including psychotherapies.1 Consider how money affects people’s lives: Money helps people meet multiple practical, psychological, and social needs by enabling them to obtain food, clothing, shelter, other material goods, services, discretionary time, and opportunities. And money strongly influences relationships. Regardless of poverty or wealth, thoughts and behaviors connected to acquiring, possessing, and disposing of money, and feelings accompanying these processes such as greed, neediness, envy, pride, shame, guilt, and self-satisfaction often underly intrapsychic and interpersonal conflicts.
Individuals constantly engage in numerous simultaneous conscious, preconscious, and unconscious neuro-economic trade-offs that determine goals, efforts, and timing. Many are financially influenced. Money influences how virtually all patients seek, receive, and sustain their mental health care including psychotherapy.
Money problems can be associated with insecurity, impotence, feeling unloved, and lack of freedom or subjugation. Individuals may resent how they’re forced to acquire money, and feel shamed or morally injured by their jobs, financial dependence on other family members, public assistance, or their questionable ways of obtaining money.
Impoverished individuals may face choosing between food, housing, medications, and medical care. Domestically abused individuals may reluctantly remain with their abusers, risking physical harm or death rather than face destitution. Some families tolerate severely disabled individuals at home because they rely on their disability checks and caregiver payments. Suicides may turn on how individuals forecast financial repercussions affecting their families. Desires to avoid debt may lead to treatment avoidance.
Individuals with enough money to get by face daily financially related choices involving competing needs, desires, values, and loyalties. They may experience conflicts concerning spending on necessities vs. indulgences or spending on oneself vs. significant others.
Whereas some wealthy individuals may assume unwarranted airs of superiority and entitlement, others may feel guilty about wealth, or fearful that others like them only for their money. Individuals on the receiving end of wealth may feel emotionally and behaviorally manipulated by their benefactors.
Assessment
Assessments should consider how financial matters have shaped patients’ early psychological development as well their current lives. How do patients’ emotions, thoughts, and behaviors reflect money matters? What money-related pathologies are evident? What aspects of the patient’s “financial world” seem modifiable?
Financial questions should be posed colloquially. Screeners include: “Where do you live?”, “Who’s in the home?”, “How do you (all) manage financially?”, “What do you all do for a living?”, “How do you make ends meet?”, and “What financial problems are you facing?” Clinicians can quickly learn about patients’ financial self-sufficiencies, individuals for whom they bear financial responsibility, and others they rely on for support, for example, relatives. If patients avoid answering such questions forthrightly, particularly when financial arrangements are “complicated,” clinicians will want to revisit these issues later after establishing a firmer alliance but continue to wonder about the meaning of the patient’s reluctance.
When explicit, patients, families, and couples are fully aware of the conflicts but have difficulty resolving financial disputes. When conflicts are implicit, money problems may be unacknowledged, avoided, denied, or minimized. Conflicts concerning money are often transmitted trans-generationally.
Psychopathological conditions unequivocally linked to money include compulsive shopping, gambling disorders, miserly hoarding, impulse buying, and spending sprees during hypomanic and manic states. Mounting debts may create progressively insurmountable sources of distress. Money can be weaponized to sadistically create enticement, envy, or deprivation. Some monetarily antisocial individuals compromise interpersonal relationships as well as treatments. Individuals with alcohol/substance use disorders may spend so much on substances that little is left for necessities. Financially needy individuals may engage in morally questionable behaviors they might otherwise shun.
Case formulation and treatment planning
Incorporating money matters into case formulations entails demonstrating how financial concerns influenced maladaptive development and distort current attitudes, perceptions, and behaviors.
Concurrently, clinicians should acknowledge patients’ reality-based fiscal decisions, appreciating cultural and family value differences concerning how money should be acquired and spent. Since money often determines frequency and duration of treatment visits, clinicians are ethically obligated to discuss with patients what they might expect from different medications and psychotherapies, and their comparative costs.
Money matters’ impact on psychotherapies
Money matters often affect transference and countertransference reactions. Some reactions stem from how patients and clinicians compare their own financial situations with those of the other.
To help identify and ameliorate money-related countertransference responses, clinicians can reflect on questions such as: “How comfortable are you with people who are much poorer or richer than you are?” “How comfortable are you with impoverished individuals or with multimillionaires or their children?” And “why?” For trainees, all these reactions should be discussed in supervision.
Conclusions
To summarize, four clinical psychoeconomic issues should be routinely assessed and factored into psychiatric case formulations and treatment plans: how financial issues 1) have impacted patients’ psychological development; 2) impact patients’ current lives; 3) are likely to impact access, type, intensity, and duration of treatment visits; and 4) might provoke money-related transference and countertransference concerns.
In advising patients about treatment options, clinicians should discuss each treatment’s relative effectiveness and estimated costs of care. Patients’ decisions will likely be heavily influenced by financial considerations.
Dr. Yager is based in the department of psychiatry, University of Colorado at Denver, Aurora. Dr. Kay is based in the department of psychiatry, Wright State University, Dayton, Ohio. No external funds were received for this project, and the authors have no conflicts to disclose.
Reference
1. Yager J and Kay J. Money matters in psychiatric assessment, case formulation, treatment planning, and ongoing psychotherapy: Clinical psychoeconomics. J Nerv Ment Dis. 2022 Jun 10. doi: 10.1097/NMD.0000000000001552.
Generalized anxiety disorder: 8 studies of psychosocial interventions
SECOND OF 2 PARTS
For patients with generalized anxiety disorder (GAD), the intensity, duration, and frequency of an individual’s anxiety and worry are out of proportion to the actual likelihood or impact of an anticipated event, and they often find it difficult to prevent worrisome thoughts from interfering with daily life.1 Successful treatment for GAD is patient-specific and requires clinicians to consider all available psychotherapeutic and pharmacologic options.
In a 2020 meta-analysis of 79 randomized controlled trials (RCTs) with 11,002 participants diagnosed with GAD, Carl et al2 focused on pooled effect sizes of evidence-based psychotherapies and medications for GAD. Their analysis showed a medium to large effect size (Hedges g = 0.76) for psychotherapy, compared to a small effect size (Hedges g = 0.38) for medication on GAD outcomes. Other meta-analyses have shown that evidence-based psychotherapies have large effect sizes on GAD outcomes.3
However, in most of the studies included in these meta-analyses, the 2 treatment modalities—psychotherapy and pharmacotherapy—use different control types. The pharmacotherapy trials used a placebo, while psychotherapy studies often had a waitlist control. Thus, the findings of these meta-analyses should not lead to the conclusion that psychotherapy is necessarily more effective for GAD symptoms than pharmacotherapy. However, there is clear evidence that psychosocial interventions are at least as effective as medications for treating GAD. Also, patients often prefer psychosocial treatment over medication.
Part 1 (
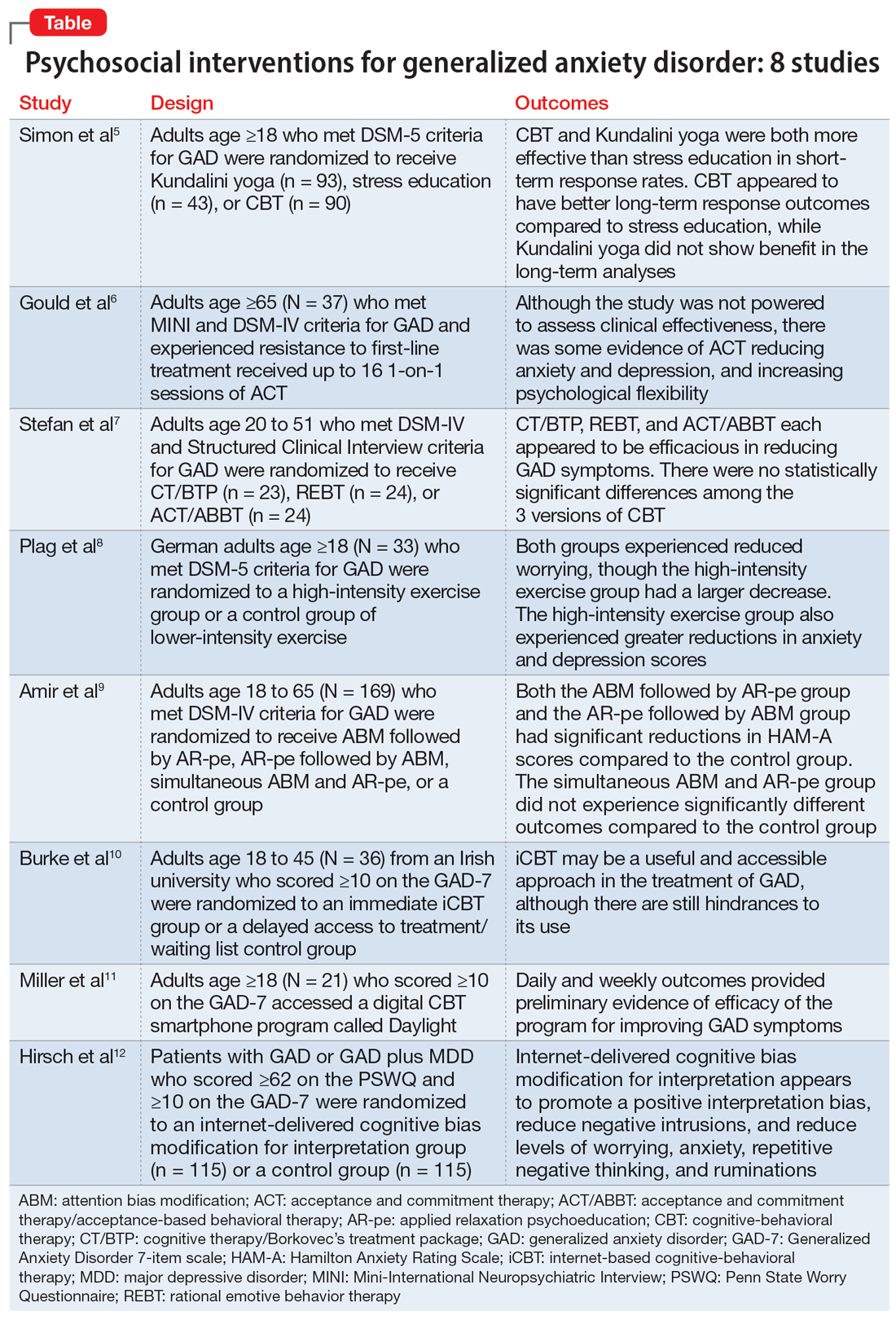
1. Simon NM, Hofmann SG, Rosenfield D, et al. Efficacy of yoga vs cognitive behavioral therapy vs stress education for the treatment of generalized anxiety disorder: a randomized clinical trial. JAMA Psychiatry. 2021;78(1):13-20. doi:10.1001/jamapsychiatry.2020.2496
Cognitive-behavioral therapy (CBT) is a first-line therapy for GAD.13 However, patients may not pursue CBT due to fiscal and logistical constraints, as well as the stigma associated with it. Yoga is a common complementary health practice used by adults in the United States,14 although evidence has been inconclusive for its use in treating anxiety. Simon et al5 examined the efficacy of Kundalini yoga (KY) vs stress education (SE) and CBT for treating GAD.
Study design
- A prospective, parallel-group, randomized-controlled, single-blind trial in 2 academic centers evaluated 226 adults age ≥18 who met DSM-5 criteria for GAD.
- Participants were randomized into 3 groups: KY (n = 93), SE (n = 43), or CBT (n = 90), and monitored for 12 weeks to determine the efficacy of each therapy.
- Exclusion criteria included current posttraumatic stress disorder, eating disorders, substance use disorders, significant suicidal ideation, mental disorder due to a medical or neurocognitive condition, lifetime psychosis, bipolar disorder (BD), developmental disorders, and having completed more than 5 yoga or CBT sessions in the past 5 years. Additionally, patients were either not taking medication for ≥2 weeks prior to the trial or had a stable regimen for ≥6 weeks.
- Each therapy was guided by 2 instructors during 12 120-minute sessions with 20 minutes of daily assignments and presented in cohorts of 4 to 6 participants.
- The primary outcome was an improvement in score on the Clinical Global Impression–Improvement scale from baseline at Week 12. Secondary measures included scores on the Meta-Cognitions Questionnaire and the Five Facet Mindfulness Questionnaire.
Outcomes
- A total of 155 participants finished the posttreatment assessment, with similar completion rates between the groups, and 123 participants completed the 6-month follow-up assessment.
- The KY group had a significantly higher response rate (54.2%) than the SE group (33%) at posttreatment, with a number needed to treat (NNT) of 4.59. At 6-month follow-up, the response rate in the KY group was not significantly higher than that of the SE group.
- The CBT group had a significantly higher response rate (70.8%) than the SE group (33%) at posttreatment, with a NNT of 2.62. At 6-month follow-up, the CBT response rate (76.7%) was significantly higher than the SE group (48%), with a NNT of 3.51.
- KY was not found to be as effective as CBT on noninferiority testing.
Continue to: Conclusions/limitations
Conclusions/limitations
- CBT and KY were both more effective than SE as assessed by short-term response rates.
- The authors did not find KY to be as effective as CBT at posttreatment or the 6-month follow-up. Additionally, CBT appeared to have better long-term response outcomes compared to SE, while KY did not display a benefit in follow-up analyses. Overall, KY appears to have a less robust efficacy compared to CBT in the treatment of GAD.
- These findings may not generalize to how CBT and yoga are approached in the community. Future studies can assess community-based methods.
2. Gould RL, Wetherell JL, Serfaty MA, et al. Acceptance and commitment therapy for older people with treatment-resistant generalised anxiety disorder: the FACTOID feasibility study. Health Technol Assess. 2021;25(54):1-150. doi:10.3310/hta25540
Older adults with GAD may experience treatment resistance to first-line therapies, such as selective serotonin reuptake inhibitors and CBT. Gould et al6 assessed whether acceptance and commitment therapy (ACT) could be a cost-effective option for older adults with treatment-resistant GAD (TR-GAD).
Study design
- In Stage 1 (intervention planning), individual interviews were conducted with 15 participants (11 female) with TR-GAD and 31 health care professionals, as well as 5 academic clinicians. The objective was to assess intervention preferences and priorities.
- Stage 2 included 37 participants, 8 clinicians, and 15 therapists, with the goal of assessing intervention design and feedback on the interventions.
- Participants were age ≥65 and met Mini-International Neuropsychiatric Interview (MINI) and DSM-IV criteria for GAD. They were living in the community and had not responded to the 3 steps of the stepped-care approach for GAD (ie, 6 weeks of an age-appropriate dose of antidepressant or a course of individual psychotherapy). Patients with dementia were excluded.
- Patients received ≤16 1-on-1 sessions of ACT.
- Self-reported outcomes were assessed at baseline and Week 20.
- The primary outcomes for Stage 2 were acceptability (attendance and satisfaction with ACT) and feasibility (recruitment and retention).
Outcomes
- ACT had high feasibility, with a recruitment rate of 93% and a retention rate of 81%.
- It also had high acceptability, with 70% of participants attending ≥10 sessions and 60% of participants showing satisfaction with therapy by scoring ≥21 points on the Satisfaction with Therapy subscale of the Satisfaction with Therapy and Therapist Scale-Revised. However, 80% of participants had not finished their ACT sessions when scores were collected.
- At Week 20, 13 patients showed reliable improvement on the Geriatric Anxiety Inventory, and 15 showed no reliable change. Seven participants showed reliable improvement in Geriatric Depression Scale-15 scores and 22 showed no reliable change. Seven participants showed improvement in the Action and Acceptance Questionnaire-II and 19 showed no reliable change.
Conclusions/limitations
- ACT had high levels of feasibility and acceptability, and large RCTs warrant further assessment of the benefits of this intervention.
- There was some evidence of reductions in anxiety and depression, as well as improvement with psychological flexibility.
- The study was not powered to assess clinical effectiveness, and recruitment for Stage 2 was limited to London.
Continue to: #3
3. Stefan S, Cristea IA, Szentagotai Tatar A, et al. Cognitive-behavioral therapy (CBT) for generalized anxiety disorder: contrasting various CBT approaches in a randomized clinical trial. J Clin Psychol. 2019;75(7):1188-1202. doi:10.1002/jclp.22779
Previous studies have demonstrated the efficacy of CBT for treating GAD.15,16 However, CBT involves varying approaches, which make it difficult to conclude which model of CBT is more effective. Stefan et al7 aimed to assess the efficacy of 3 versions of CBT for GAD.
Study design
- This RCT investigated 3 versions of CBT: cognitive therapy/Borkovec’s treatment package (CT/BTP), rational emotive behavior therapy (REBT), and acceptance and commitment therapy/acceptance-based behavioral therapy (ACT/ABBT).
- A total of 75 adults (60 women) age 20 to 51 and diagnosed with GAD by the Structured Clinical Interview for DSM-IV were initially randomized to one of the treatment arms for 20 sessions; 4 dropped out before receiving the allocated intervention. Exclusion criteria included panic disorder, severe major depressive disorder (MDD), BD, substance use or dependence, psychotic disorders, suicidal or homicidal ideation, organic brain syndrome, disabling medical conditions, intellectual disability, treatment with a psychotropic drug within the past 3 months, and psychotherapy provided outside the trial.
- The primary outcomes were scores on the Generalized Anxiety Disorder Questionnaire IV (GAD-Q-IV) and the Penn State Worry Questionnaire (PSWQ). A secondary outcome included assessing negative automatic thoughts by the Automatic Thoughts Questionnaire.
Outcomes
- There were no significant differences among the 3 treatment groups with regards to demographic data.
- Approximately 70% of patients (16 of 23) in the CT/BTP group had scores below the cutoff point for response (9) on the GAD-Q-IV, approximately 71% of patients (17 of 24) in the REBT group scored below the cutoff point, and approximately 79% of patients (19 of 24) in the ACT/ABBT group scored below the cutoff point.
- Approximately 83% of patients in the CT/BTP scored below the cutoff point for response (65) on the PSWQ, approximately 83% of patients in the REBT group scored below the cutoff point, and approximately 80% of patients in the ACT/ABBT group scored below the cutoff point.
- There were positive correlations between pre-post changes in GAD symptoms and dysfunctional automatic thoughts in each group.
- There was no statistically significant difference among the 3 versions of CBT.
Conclusions/limitations
- CT/BTP, REBT, and ACT/ABBT each appear to be efficacious in reducing GAD symptoms, allowing the choice of treatment to be determined by patient and clinician preference.
- The study’s small sample size may have prevented differences between the groups from being detected.
- There was no control group, and only 39 of 75 individuals completed the study in its entirety.
4. Plag J, Schmidt-Hellinger P, Klippstein T, et al. Working out the worries: a randomized controlled trial of high intensity interval training in generalized anxiety disorder. J Anxiety Disord. 2020;76:102311. doi:10.1016/j.janxdis.2020.10231
Research has shown the efficacy of aerobic exercise for various anxiety disorders,17-19 but differs regarding the type of exercise and its intensity, frequency, and duration. There is evidence that high-intensity interval training (HIIT) may be beneficial in treating serious mental illness.20 Plag et al8 examined the efficacy and acceptance of HIIT in patients with GAD.
Continue to: Study design
Study design
- A total of 33 German adults (24 women) age ≥18 who met DSM-5 criteria for GAD were enrolled in a parallel-group, assessor-blinded RCT. Participants were blinded to the hypotheses of the trial, but not to the intervention.
- Participants were randomized to a HIIT group (engaged in HIIT on a bicycle ergometer every second day within 12 days, with each session lasting 20 minutes and consisting of alternating sessions of 77% to 95% maximum heart rate and <70% maximum heart rate) or a control group of lower-intensity exercise (LIT; consisted of 6 30-minute sessions within 12 days involving stretching and adapted yoga positions with heart rate <70% maximum heart rate).
- Exclusion criteria included severe depression, schizophrenia, borderline personality disorder (BPD), substance use disorder, suicidality, epilepsy, severe respiratory or cardiovascular diseases, and current psychotherapy. The use of medications was allowed if the patient was stable ≥4 weeks prior to the trial and remained stable during the trial.
- The primary outcome of worrying was assessed by the PSWQ. Other assessment tools included the Hamilton Anxiety Rating Scale (HAM-A), Hamilton Depression Rating Scale (HAM-D), Anxiety Control Questionnaire, and Screening for Somatoform Symptoms-7 (SOMS-7).
Outcomes
- Baseline PSWQ scores in both groups were >60, indicating “high worriers.”
- Both groups experienced reductions in worrying as measured by PSWQ scores. However, the HIIT group had a larger decrease in worrying compared to the LIT group (P < .02). Post-hoc analyses showed significant reductions in symptom severity from baseline to poststudy (P < .01; d = 0.68), and at 30-day follow-up (P < .01; d = 0.62) in the HIIT group. There was no significant difference in the LIT group from baseline to poststudy or at follow-up.
- Secondary outcome measures included a greater reduction in anxiety and depression as determined by change in HAM-A and HAM-D scores in the HIIT group compared to the LIT group.
- All measures showed improvement in the HIIT group, whereas the LIT group showed improvement in HAM-A and HAM-D scores poststudy and at follow-up, as well as SOMS-7 scores at follow-up.
Conclusions/limitations
- HIIT demonstrated a large treatment effect for treating GAD, including somatic symptoms and worrying.
- HIIT displayed a fast onset of action and low cancellation rate, which suggests it is tolerable.
- This study had a small sample size consisting of participants from only 1 institution, which limits generalizability, and did not look at the long-term effects of the interventions.
5. Amir N, Taboas W, Montero M. Feasibility and dissemination of a computerized home-based treatment for generalized anxiety disorder: a randomized clinical trial. Behav Res Ther. 2019;120:103446. doi:10.1016/j.brat.2019.103446
Many patients with anxiety disorders do not receive treatment, and logistical factors such as limited time, expertise, and available resources hinder patients from obtaining quality CBT. Attention bias modification (ABM) is a computer-based approach in which patients complete tasks guiding their attention away from threat-relevant cues.21 Applied relaxation psychoeducation (AR-pe) is another empirically supported treatment that can be administered via computer. Amir et al9 examined the feasibility and effectiveness of a home-based computerized regimen of sequenced or simultaneous ABM and AR-pe in patients with GAD.
Study design
- A total of 169 adults age 18 to 65 who met DSM-IV criteria for GAD were randomized into 4 groups: ABM followed by AR-pe, AR-pe followed by ABM, simultaneous ABM and AR-pe, or a clinical monitoring assessment only control group (CM).
- Participants were expected to complete up to 24 30-minute sessions on their home computer over 12 weeks.
- Exclusion criteria included current psychotropic medications/CBT initiated 3 months prior to the study, BD, schizophrenia, or substance use disorder.
- The primary outcome measure was anxiety symptoms as assessed by the HAM-A (remission was defined as a score ≤7 at Week 13). Other measures included the PSWQ, Spielberger State-Trait Anxiety Inventory, Sheehan Disability Scale, and Beck Depression Inventory.
- Participants were assessed at Month 3, Month 6, and Month 12 poststudy.
Continue to: Outcomes
Outcomes
- Baseline characteristics did not significantly differ between groups.
- In the active groups, 41% of participants met remission criteria, compared to 19% in the CM group.
- The ABM followed by AR-pe group and the AR-pe followed by ABM group had significant reductions in HAM-A scores (P = .003 and P = .020) compared to the CM group.
- The simultaneous ABM and AR-pe group did not have a significant difference in outcomes compared to the CM group (P = .081).
- On the PSWQ, the CM group had a larger decrease in worry than all active cohorts combined, with follow-up analysis indicating the CM group surpassed the ABM group (P = .019).
Conclusions/limitations
- Sequential delivery of ABM and AR-pe may be a viable, easy-to-access treatment option for patients with GAD who have limited access to other therapies.
- Individuals assigned to receive simultaneous ABM and AR-pe appeared to complete fewer tasks compared to those in the sequential groups, which suggests that participants were less inclined to complete all tasks despite being allowed more time.
- This study did not examine the effects of ABM only or AR-pe only.
- This study was unable to accurately assess home usage of the program.
6. Burke J, Richards D, Timulak L. Helpful and hindering events in internet-delivered cognitive behavioural treatment for generalized anxiety. Behav Cogn Psychother. 2019;47(3):386-399. doi:10.1017/S1352465818000504
Patients with GAD may not be able to obtain adequate treatment due to financial or logistical constraints. Internet-delivered interventions are easily accessible and provide an opportunity for patients who cannot or do not want to seek traditional therapy options. Burke et al10 aimed to better understand the useful and impeding events of internet-based cognitive-behavioral therapy (iCBT).
Study design
- A total of 36 adults (25 women) age 18 to 45 from an Irish university were randomized to an immediate iCBT treatment group or a delayed access to treatment/waiting list control group. The iCBT program, called Calming Anxiety, involved 6 modules of CBT for GAD.
- Participants initially scored ≥10 on the Generalized Anxiety Disorder 7-item scale (GAD-7).
- The study employed the Helpful and Hindering Aspects of Therapy (HAT) questionnaire to assess the most useful and impeding events in therapy.
- The data were divided into 4 domains: helpful events, helpful impacts, hindering events, and hindering impacts.
Outcomes
- Of the 8 helpful events identified, the top 3 were psychoeducation, supporter interaction, and monitoring.
- Of the 5 helpful impacts identified, the top 3 were support and validation, applying coping strategies/behavioral change, and clarification, awareness, and insight.
- The 2 identified hindering events were treatment content/form and amount of work/technical issues.
- The 3 identified hindering impacts were frustration/irritation, increased anxiety, and isolation.
Continue to: Conclusions/limitations
Conclusions/limitations
- iCBT may be a useful and accessible approach for treating GAD, although there are still hindrances to its use.
- This study was qualitative and did not comment on the efficacy of the applied intervention.
- The benefits of iCBT may differ depending on the patient’s level of computer literacy.
7. Miller CB, Gu J, Henry AL, et al. Feasibility and efficacy of a digital CBT intervention for symptoms of generalized anxiety disorder: a randomized multiple-baseline study. J Behav Ther Exp Psychiatry. 2021;70:101609. doi:10.1016/j.jbtep.2020.101609
Access to CBT is limited due to cost, dearth of trained therapists, scheduling availability, stigma, and transportation. Digital CBT may help overcome these obstacles. Miller et al11 studied the feasibility and efficacy of a new automated, digital CBT intervention named Daylight.
Study design
- This randomized, multiple-baseline, single-case, experimental trial included 21 adults (20 women) age ≥18 who scored ≥10 on the GAD-7 and screened positive for GAD on MINI version 7 for DSM-5.
- Participants were not taking psychotropic medications or had been on a stable medication regimen for ≥4 weeks.
- Exclusion criteria included past or present psychosis, schizophrenia, BD, seizure disorder, substance use disorder, trauma to the head or brain damage, severe cognitive impairment, serious physical health concerns necessitating surgery or with prognosis <6 months, and pregnancy.
- Participants were randomized to 1 of 3 baseline durations: 2 weeks, 4 weeks, or 6 weeks. They then could access the smartphone program Daylight. The trial lasted for 12 to 16 weeks.
- Primary anxiety outcomes were assessed daily and weekly, while secondary outcomes (depressive symptoms, sleep) were measured weekly.
- Postintervention was defined as 6 weeks after the start of the intervention and follow-up was 10 weeks after the start of the intervention.
- Participants were deemed not to have clinically significant anxiety if they scored <10 on GAD-7; not to have significant depressive symptoms if they scored <10 on the Patient Health Questionnaire-9 (PHQ-9); and not to have sleep difficulty if they scored >16 on the Sleep Condition Indicator (SCI-8). The change was considered reliable if patients scored below the previously discussed thresholds and showed a difference in score greater than the known unreliability of the questionnaire (GAD-7 reductions ≥5, PHQ-9 reductions ≥6, SCI-8 increases ≥7).
Outcomes
- In terms of feasibility, 76% of participants completed all 4 modules, 81% completed 3 modules, 86% completed 2 modules, and all participants completed at least 1 module.
- No serious adverse events were observed, but 43% of participants reported unwanted symptoms such as agitation, fatigue, low mood, or reduced motivation.
- As evaluated by the Credibility/Expectancy Questionnaire, the program received moderate to high credibility scores. Participants indicated they were mostly satisfied with the program, although some expressed technical difficulties and a lack of specificity to their anxiety symptoms.
- Overall daily anxiety scores significantly decreased from baseline to postintervention (P < .001). Weekly anxiety scores significantly decreased from baseline to postintervention (P = .024), and follow-up (P = .017) as measured by the GAD-7.
- For participants with anxiety, 70% no longer had clinically significant anxiety symptoms postintervention, and 65% had both clinically significant and reliable change at postintervention. Eighty percent had clinically significant and reliable change at follow-up.
- For participants with depressive symptoms, 61% had clinical and reliable change at postintervention and 44% maintained both at follow-up.
- For participants with sleep disturbances, 35% had clinical and reliable improvement at postintervention and 40% had clinical and reliable change at follow-up.
Conclusions/limitations
- Daylight appears to be a feasible program with regards to acceptability, engagement, credibility, satisfaction, and safety.
- The daily and weekly outcomes support preliminary evidence of program efficacy in improving GAD symptoms.
- Most participants identified as female and were recruited online, which limits generalizability, and the study had a small sample size.
Continue to: #8
8. Hirsch CR, Krahé C, Whyte J, et al. Internet-delivered interpretation training reduces worry and anxiety in individuals with generalized anxiety disorder: a randomized controlled experiment. J Consult Clin Psychol. 2021;89(7):575-589. doi:10.1037/ccp0000660
The cognitive model of pathological worry posits that worry in GAD occurs due to various factors, including automatic cognitive bias in which ambiguous events are perceived as threatening to the individual.22 Cognitive bias modification for interpretation (CBM) is an approach that assesses an individual’s interpretation bias and resolves ambiguity through the individual’s reading or listening to multiple ambiguous situations.12 Hirsch et al12 examined if an internet-delivered CBM approach would promote positive interpretations and reduce worry and anxiety in patients with GAD.
Study design
- In this dual-arm, parallel group, single-blind RCT, adult participants were randomized to a CBM group (n = 115) or a control group (n = 115); only 186 participants were included in the analyses.
- Patients with GAD only and those with GAD comorbid with MDD who scored ≥62 on the PSWQ and ≥10 on the GAD-7 were recruited. Patients receiving psychotropic medication had to be stable on their regimen for ≥3 months prior to the trial.
- Exclusion criteria included residing outside the United Kingdom, severe depression as measured by a PHQ-9 score ≥23, self-harm in the past 12 months or suicide attempt in past 2 years, a PHQ-9 suicidal ideation score >1, concurrent psychosis, BD, BPD, substance abuse, and current or recent (within the past 6 months) psychological treatment.
- The groups completed up to 10 online training (CBM) or control (listened to ambiguous scenarios but not asked to resolve the ambiguity) sessions in 1 month.
- Primary outcome measures included the scrambled sentences test (SST) and a recognition test (RT) to assess interpretation bias.
- Secondary outcome measures included a breathing focus task (BFT), PSWQ and PSWQ-past week, Ruminative Response Scale (RRS), Repetitive Thinking Questionnaire-trait (RTQ-T), PHQ-9, and GAD-7.
- Scores were assessed preintervention (T0), postintervention (T1), 1 month postintervention (T2), and 3 months postintervention (T3).
Outcomes
- CBM was associated with a more positive interpretation at T1 than the control sessions (P < .001 on both SST and RT).
- CBM was associated with significantly reduced negative intrusions as per BFTs at T1.
- The CBM group had significant less worry as per PSWQ, and significantly less anxiety as per GAD-7 at T1, T2, and T3.
- The CBM group had significantly fewer depressive symptoms as per PHQ-9 at T1, T2, and T3.
- The CBM group had significantly lower levels of ruminations as per RRS at T1, T2, and T3.
- The CBM group had significantly lower levels of general repetitive negative thinking (RNT) as per RTQ-T at T1 and T2, but not T3.
Conclusions/limitations
- Digital CBM appears to promote a positive interpretation bias.
- CBM appears to reduce negative intrusions after the intervention, as well as reduced levels of worrying, anxiety, RNT, and ruminations, with effects lasting ≤3 months except for the RNT.
- CBM appears to be an efficacious, low-intensity, easily accessible intervention that can help individuals with GAD.
- The study recruited participants via advertisements rather than clinical services, and excluded individuals with severe depression.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed., text revision. American Psychiatric Association; 2022.
2. Carl E, Witcraft SM, Kauffman BY, et al. Psychological and pharmacological treatments for generalized anxiety disorder (GAD): a meta-analysis of randomized controlled trials. Cogn Behav Ther. 2020;49(1):1-21. doi:10.1080/16506073.2018.1560358
3. Cuijpers P, Cristea IA, Karyotaki E, et al. How effective are cognitive behavior therapies for major depression and anxiety disorders? A meta‐analytic update of the evidence. World Psychiatry. 2016;15(3):245-258. doi:10.1002/wps.20346
4. Saeed SA, Majarwitz DJ. Generalized anxiety disorder: 8 studies of biological interventions. Current Psychiatry. 2022;21(7):10-12,20,22-27. doi:10.12788/cp.02645
5. Simon NM, Hofmann SG, Rosenfield D, et al. Efficacy of yoga vs cognitive behavioral therapy vs stress education for the treatment of generalized anxiety disorder: a randomized clinical trial. JAMA Psychiatry. 2021;78(1):13-20. doi:10.1001/jamapsychiatry.2020.2496
6. Gould RL, Wetherell JL, Serfaty MA, et al. Acceptance and commitment therapy for older people with treatment-resistant generalised anxiety disorder: the FACTOID feasibility study. Health Technol Assess. 2021;25(54):1-150. doi:10.3310/hta25540
7. Stefan S, Cristea IA, Szentagotai Tatar A, et al. Cognitive-behavioral therapy (CBT) for generalized anxiety disorder: contrasting various CBT approaches in a randomized clinical trial. J Clin Psychol. 2019;75(7):1188-1202. doi:10.1002/jclp.22779
8. Plag J, Schmidt-Hellinger P, Klippstein T, et al. Working out the worries: a randomized controlled trial of high intensity interval training in generalized anxiety disorder. J Anxiety Disord. 2020;76:102311. doi:10.1016/j.janxdis.2020.102311
9. Amir N, Taboas W, Montero M. Feasibility and dissemination of a computerized home-based treatment for generalized anxiety disorder: a randomized clinical trial. Behav Res Ther. 2019;120:103446. doi:10.1016/j.brat.2019.103446
10. Burke J, Richards D, Timulak L. Helpful and hindering events in internet-delivered cognitive behavioural treatment for generalized anxiety. Behav Cogn Psychother. 2019;47(3):386-399. doi:10.1017/S1352465818000504
11. Miller CB, Gu J, Henry AL, et al. Feasibility and efficacy of a digital CBT intervention for symptoms of generalized anxiety disorder: a randomized multiple-baseline study. J Behav Ther Exp Psychiatry. 2021;70:101609. doi:10.1016/j.jbtep.2020.101609
12. Hirsch CR, Krahé C, Whyte J, et al. Internet-delivered interpretation training reduces worry and anxiety in individuals with generalized anxiety disorder: a randomized controlled experiment. J Consult Clin Psychol. 2021;89(7):575-589. doi:10.1037/ccp0000660
13. Hofmann SG, Smits JAJ. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621-632. doi:10.4088/jcp.v69n0415
14. Clarke TC, Barnes PM, Black LI, et al. Use of yoga, meditation, and chiropractors among U.S. adults aged 18 and over. NCHS Data Brief. 2018;(325):1-8.
15. Carpenter JK, Andrews LA, Witcraft SM, et al. Cognitive behavioral therapy for anxiety and related disorders: a meta-analysis of randomized placebo-controlled trials. Depress Anxiety. 2018;35(6):502-514. doi:10.1002/da.22728
16. Covin R, Ouimet AJ, Seeds PM, et al. A meta-analysis of CBT for pathological worry among clients with GAD. J Anxiety Disord. 2008;22(1):108-116. doi:10.1016/j.janxdis.2007.01.002
17. Merom D, Phongsavan P, Wagner R, et al. Promoting walking as an adjunct intervention to group cognitive behavioral therapy for anxiety disorders--a pilot group randomized trial. J Anxiety Disord. 2008;22(6):959-968. doi:10.1016/j.janxdis.2007.09.010
18. Herring MP, Jacob ML, Suveg C, et al. Feasibility of exercise training for the short-term treatment of generalized anxiety disorder: a randomized controlled trial. Psychother Psychosom. 2012;81(1):21-28. doi:10.1159/000327898
19. Bischoff S, Wieder G, Einsle F, et al. Running for extinction? Aerobic exercise as an augmentation of exposure therapy in panic disorder with agoraphobia. J Psychiatr Res. 2018;101:34-41. doi:10.1016/j.jpsychires.2018.03.001
20. Korman N, Armour M, Chapman J, et al. High Intensity Interval training (HIIT) for people with severe mental illness: a systematic review & meta-analysis of intervention studies- considering diverse approaches for mental and physical recovery. Psychiatry Res. 2020;284:112601. doi:10.1016/j.psychres.2019.112601
21. Amir N, Beard C, Cobb M, et al. Attention modification program in individuals with generalized anxiety disorder. J Abnorm Psychol. 2009;118(1):28-33. doi:10.1037/a0012589
22. Hirsh CR, Mathews A. A cognitive model of pathological worry. Behav Res Ther. 2012;50(10):636-646. doi:10.1016/j.brat.2012.007
SECOND OF 2 PARTS
For patients with generalized anxiety disorder (GAD), the intensity, duration, and frequency of an individual’s anxiety and worry are out of proportion to the actual likelihood or impact of an anticipated event, and they often find it difficult to prevent worrisome thoughts from interfering with daily life.1 Successful treatment for GAD is patient-specific and requires clinicians to consider all available psychotherapeutic and pharmacologic options.
In a 2020 meta-analysis of 79 randomized controlled trials (RCTs) with 11,002 participants diagnosed with GAD, Carl et al2 focused on pooled effect sizes of evidence-based psychotherapies and medications for GAD. Their analysis showed a medium to large effect size (Hedges g = 0.76) for psychotherapy, compared to a small effect size (Hedges g = 0.38) for medication on GAD outcomes. Other meta-analyses have shown that evidence-based psychotherapies have large effect sizes on GAD outcomes.3
However, in most of the studies included in these meta-analyses, the 2 treatment modalities—psychotherapy and pharmacotherapy—use different control types. The pharmacotherapy trials used a placebo, while psychotherapy studies often had a waitlist control. Thus, the findings of these meta-analyses should not lead to the conclusion that psychotherapy is necessarily more effective for GAD symptoms than pharmacotherapy. However, there is clear evidence that psychosocial interventions are at least as effective as medications for treating GAD. Also, patients often prefer psychosocial treatment over medication.
Part 1 (
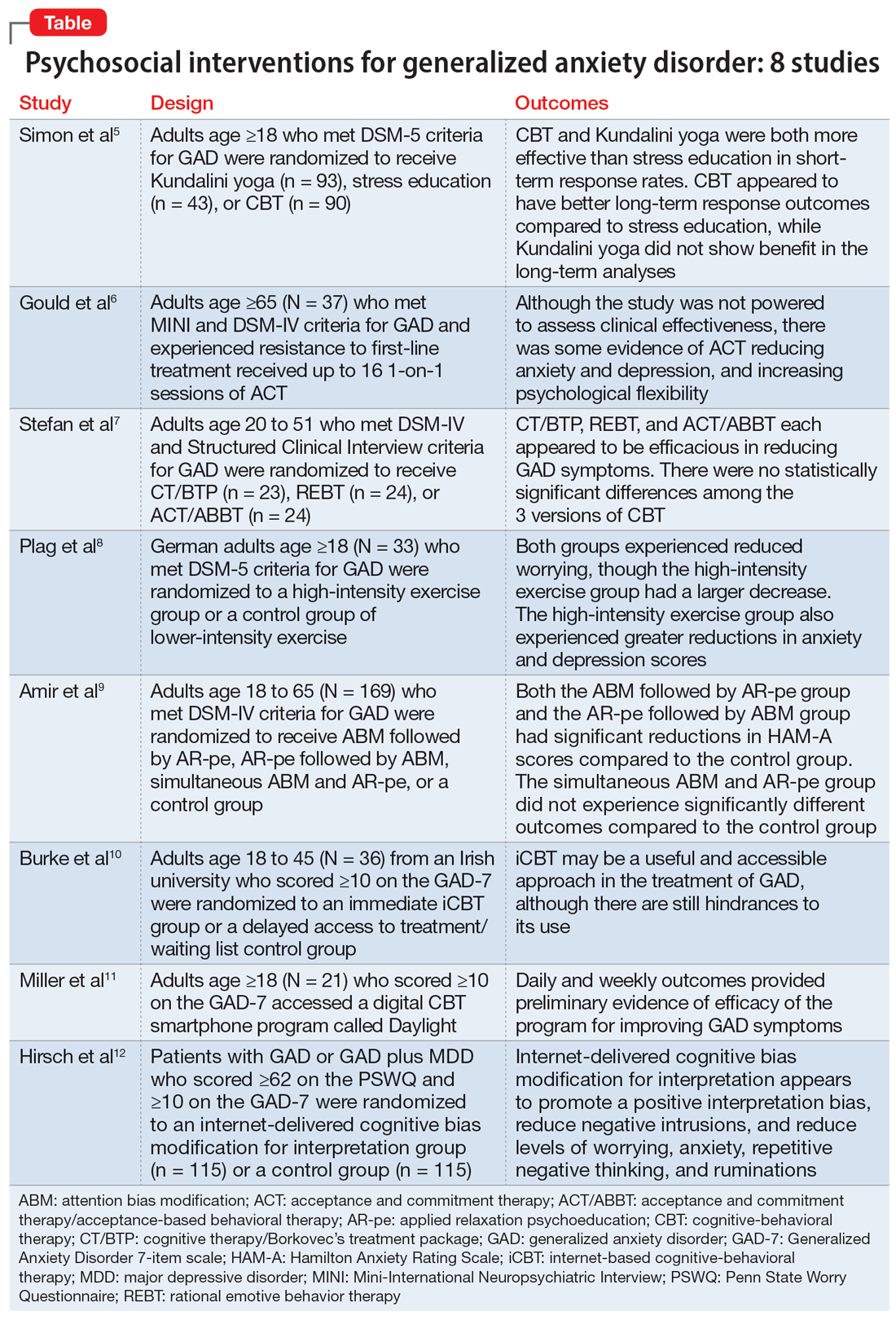
1. Simon NM, Hofmann SG, Rosenfield D, et al. Efficacy of yoga vs cognitive behavioral therapy vs stress education for the treatment of generalized anxiety disorder: a randomized clinical trial. JAMA Psychiatry. 2021;78(1):13-20. doi:10.1001/jamapsychiatry.2020.2496
Cognitive-behavioral therapy (CBT) is a first-line therapy for GAD.13 However, patients may not pursue CBT due to fiscal and logistical constraints, as well as the stigma associated with it. Yoga is a common complementary health practice used by adults in the United States,14 although evidence has been inconclusive for its use in treating anxiety. Simon et al5 examined the efficacy of Kundalini yoga (KY) vs stress education (SE) and CBT for treating GAD.
Study design
- A prospective, parallel-group, randomized-controlled, single-blind trial in 2 academic centers evaluated 226 adults age ≥18 who met DSM-5 criteria for GAD.
- Participants were randomized into 3 groups: KY (n = 93), SE (n = 43), or CBT (n = 90), and monitored for 12 weeks to determine the efficacy of each therapy.
- Exclusion criteria included current posttraumatic stress disorder, eating disorders, substance use disorders, significant suicidal ideation, mental disorder due to a medical or neurocognitive condition, lifetime psychosis, bipolar disorder (BD), developmental disorders, and having completed more than 5 yoga or CBT sessions in the past 5 years. Additionally, patients were either not taking medication for ≥2 weeks prior to the trial or had a stable regimen for ≥6 weeks.
- Each therapy was guided by 2 instructors during 12 120-minute sessions with 20 minutes of daily assignments and presented in cohorts of 4 to 6 participants.
- The primary outcome was an improvement in score on the Clinical Global Impression–Improvement scale from baseline at Week 12. Secondary measures included scores on the Meta-Cognitions Questionnaire and the Five Facet Mindfulness Questionnaire.
Outcomes
- A total of 155 participants finished the posttreatment assessment, with similar completion rates between the groups, and 123 participants completed the 6-month follow-up assessment.
- The KY group had a significantly higher response rate (54.2%) than the SE group (33%) at posttreatment, with a number needed to treat (NNT) of 4.59. At 6-month follow-up, the response rate in the KY group was not significantly higher than that of the SE group.
- The CBT group had a significantly higher response rate (70.8%) than the SE group (33%) at posttreatment, with a NNT of 2.62. At 6-month follow-up, the CBT response rate (76.7%) was significantly higher than the SE group (48%), with a NNT of 3.51.
- KY was not found to be as effective as CBT on noninferiority testing.
Continue to: Conclusions/limitations
Conclusions/limitations
- CBT and KY were both more effective than SE as assessed by short-term response rates.
- The authors did not find KY to be as effective as CBT at posttreatment or the 6-month follow-up. Additionally, CBT appeared to have better long-term response outcomes compared to SE, while KY did not display a benefit in follow-up analyses. Overall, KY appears to have a less robust efficacy compared to CBT in the treatment of GAD.
- These findings may not generalize to how CBT and yoga are approached in the community. Future studies can assess community-based methods.
2. Gould RL, Wetherell JL, Serfaty MA, et al. Acceptance and commitment therapy for older people with treatment-resistant generalised anxiety disorder: the FACTOID feasibility study. Health Technol Assess. 2021;25(54):1-150. doi:10.3310/hta25540
Older adults with GAD may experience treatment resistance to first-line therapies, such as selective serotonin reuptake inhibitors and CBT. Gould et al6 assessed whether acceptance and commitment therapy (ACT) could be a cost-effective option for older adults with treatment-resistant GAD (TR-GAD).
Study design
- In Stage 1 (intervention planning), individual interviews were conducted with 15 participants (11 female) with TR-GAD and 31 health care professionals, as well as 5 academic clinicians. The objective was to assess intervention preferences and priorities.
- Stage 2 included 37 participants, 8 clinicians, and 15 therapists, with the goal of assessing intervention design and feedback on the interventions.
- Participants were age ≥65 and met Mini-International Neuropsychiatric Interview (MINI) and DSM-IV criteria for GAD. They were living in the community and had not responded to the 3 steps of the stepped-care approach for GAD (ie, 6 weeks of an age-appropriate dose of antidepressant or a course of individual psychotherapy). Patients with dementia were excluded.
- Patients received ≤16 1-on-1 sessions of ACT.
- Self-reported outcomes were assessed at baseline and Week 20.
- The primary outcomes for Stage 2 were acceptability (attendance and satisfaction with ACT) and feasibility (recruitment and retention).
Outcomes
- ACT had high feasibility, with a recruitment rate of 93% and a retention rate of 81%.
- It also had high acceptability, with 70% of participants attending ≥10 sessions and 60% of participants showing satisfaction with therapy by scoring ≥21 points on the Satisfaction with Therapy subscale of the Satisfaction with Therapy and Therapist Scale-Revised. However, 80% of participants had not finished their ACT sessions when scores were collected.
- At Week 20, 13 patients showed reliable improvement on the Geriatric Anxiety Inventory, and 15 showed no reliable change. Seven participants showed reliable improvement in Geriatric Depression Scale-15 scores and 22 showed no reliable change. Seven participants showed improvement in the Action and Acceptance Questionnaire-II and 19 showed no reliable change.
Conclusions/limitations
- ACT had high levels of feasibility and acceptability, and large RCTs warrant further assessment of the benefits of this intervention.
- There was some evidence of reductions in anxiety and depression, as well as improvement with psychological flexibility.
- The study was not powered to assess clinical effectiveness, and recruitment for Stage 2 was limited to London.
Continue to: #3
3. Stefan S, Cristea IA, Szentagotai Tatar A, et al. Cognitive-behavioral therapy (CBT) for generalized anxiety disorder: contrasting various CBT approaches in a randomized clinical trial. J Clin Psychol. 2019;75(7):1188-1202. doi:10.1002/jclp.22779
Previous studies have demonstrated the efficacy of CBT for treating GAD.15,16 However, CBT involves varying approaches, which make it difficult to conclude which model of CBT is more effective. Stefan et al7 aimed to assess the efficacy of 3 versions of CBT for GAD.
Study design
- This RCT investigated 3 versions of CBT: cognitive therapy/Borkovec’s treatment package (CT/BTP), rational emotive behavior therapy (REBT), and acceptance and commitment therapy/acceptance-based behavioral therapy (ACT/ABBT).
- A total of 75 adults (60 women) age 20 to 51 and diagnosed with GAD by the Structured Clinical Interview for DSM-IV were initially randomized to one of the treatment arms for 20 sessions; 4 dropped out before receiving the allocated intervention. Exclusion criteria included panic disorder, severe major depressive disorder (MDD), BD, substance use or dependence, psychotic disorders, suicidal or homicidal ideation, organic brain syndrome, disabling medical conditions, intellectual disability, treatment with a psychotropic drug within the past 3 months, and psychotherapy provided outside the trial.
- The primary outcomes were scores on the Generalized Anxiety Disorder Questionnaire IV (GAD-Q-IV) and the Penn State Worry Questionnaire (PSWQ). A secondary outcome included assessing negative automatic thoughts by the Automatic Thoughts Questionnaire.
Outcomes
- There were no significant differences among the 3 treatment groups with regards to demographic data.
- Approximately 70% of patients (16 of 23) in the CT/BTP group had scores below the cutoff point for response (9) on the GAD-Q-IV, approximately 71% of patients (17 of 24) in the REBT group scored below the cutoff point, and approximately 79% of patients (19 of 24) in the ACT/ABBT group scored below the cutoff point.
- Approximately 83% of patients in the CT/BTP scored below the cutoff point for response (65) on the PSWQ, approximately 83% of patients in the REBT group scored below the cutoff point, and approximately 80% of patients in the ACT/ABBT group scored below the cutoff point.
- There were positive correlations between pre-post changes in GAD symptoms and dysfunctional automatic thoughts in each group.
- There was no statistically significant difference among the 3 versions of CBT.
Conclusions/limitations
- CT/BTP, REBT, and ACT/ABBT each appear to be efficacious in reducing GAD symptoms, allowing the choice of treatment to be determined by patient and clinician preference.
- The study’s small sample size may have prevented differences between the groups from being detected.
- There was no control group, and only 39 of 75 individuals completed the study in its entirety.
4. Plag J, Schmidt-Hellinger P, Klippstein T, et al. Working out the worries: a randomized controlled trial of high intensity interval training in generalized anxiety disorder. J Anxiety Disord. 2020;76:102311. doi:10.1016/j.janxdis.2020.10231
Research has shown the efficacy of aerobic exercise for various anxiety disorders,17-19 but differs regarding the type of exercise and its intensity, frequency, and duration. There is evidence that high-intensity interval training (HIIT) may be beneficial in treating serious mental illness.20 Plag et al8 examined the efficacy and acceptance of HIIT in patients with GAD.
Continue to: Study design
Study design
- A total of 33 German adults (24 women) age ≥18 who met DSM-5 criteria for GAD were enrolled in a parallel-group, assessor-blinded RCT. Participants were blinded to the hypotheses of the trial, but not to the intervention.
- Participants were randomized to a HIIT group (engaged in HIIT on a bicycle ergometer every second day within 12 days, with each session lasting 20 minutes and consisting of alternating sessions of 77% to 95% maximum heart rate and <70% maximum heart rate) or a control group of lower-intensity exercise (LIT; consisted of 6 30-minute sessions within 12 days involving stretching and adapted yoga positions with heart rate <70% maximum heart rate).
- Exclusion criteria included severe depression, schizophrenia, borderline personality disorder (BPD), substance use disorder, suicidality, epilepsy, severe respiratory or cardiovascular diseases, and current psychotherapy. The use of medications was allowed if the patient was stable ≥4 weeks prior to the trial and remained stable during the trial.
- The primary outcome of worrying was assessed by the PSWQ. Other assessment tools included the Hamilton Anxiety Rating Scale (HAM-A), Hamilton Depression Rating Scale (HAM-D), Anxiety Control Questionnaire, and Screening for Somatoform Symptoms-7 (SOMS-7).
Outcomes
- Baseline PSWQ scores in both groups were >60, indicating “high worriers.”
- Both groups experienced reductions in worrying as measured by PSWQ scores. However, the HIIT group had a larger decrease in worrying compared to the LIT group (P < .02). Post-hoc analyses showed significant reductions in symptom severity from baseline to poststudy (P < .01; d = 0.68), and at 30-day follow-up (P < .01; d = 0.62) in the HIIT group. There was no significant difference in the LIT group from baseline to poststudy or at follow-up.
- Secondary outcome measures included a greater reduction in anxiety and depression as determined by change in HAM-A and HAM-D scores in the HIIT group compared to the LIT group.
- All measures showed improvement in the HIIT group, whereas the LIT group showed improvement in HAM-A and HAM-D scores poststudy and at follow-up, as well as SOMS-7 scores at follow-up.
Conclusions/limitations
- HIIT demonstrated a large treatment effect for treating GAD, including somatic symptoms and worrying.
- HIIT displayed a fast onset of action and low cancellation rate, which suggests it is tolerable.
- This study had a small sample size consisting of participants from only 1 institution, which limits generalizability, and did not look at the long-term effects of the interventions.
5. Amir N, Taboas W, Montero M. Feasibility and dissemination of a computerized home-based treatment for generalized anxiety disorder: a randomized clinical trial. Behav Res Ther. 2019;120:103446. doi:10.1016/j.brat.2019.103446
Many patients with anxiety disorders do not receive treatment, and logistical factors such as limited time, expertise, and available resources hinder patients from obtaining quality CBT. Attention bias modification (ABM) is a computer-based approach in which patients complete tasks guiding their attention away from threat-relevant cues.21 Applied relaxation psychoeducation (AR-pe) is another empirically supported treatment that can be administered via computer. Amir et al9 examined the feasibility and effectiveness of a home-based computerized regimen of sequenced or simultaneous ABM and AR-pe in patients with GAD.
Study design
- A total of 169 adults age 18 to 65 who met DSM-IV criteria for GAD were randomized into 4 groups: ABM followed by AR-pe, AR-pe followed by ABM, simultaneous ABM and AR-pe, or a clinical monitoring assessment only control group (CM).
- Participants were expected to complete up to 24 30-minute sessions on their home computer over 12 weeks.
- Exclusion criteria included current psychotropic medications/CBT initiated 3 months prior to the study, BD, schizophrenia, or substance use disorder.
- The primary outcome measure was anxiety symptoms as assessed by the HAM-A (remission was defined as a score ≤7 at Week 13). Other measures included the PSWQ, Spielberger State-Trait Anxiety Inventory, Sheehan Disability Scale, and Beck Depression Inventory.
- Participants were assessed at Month 3, Month 6, and Month 12 poststudy.
Continue to: Outcomes
Outcomes
- Baseline characteristics did not significantly differ between groups.
- In the active groups, 41% of participants met remission criteria, compared to 19% in the CM group.
- The ABM followed by AR-pe group and the AR-pe followed by ABM group had significant reductions in HAM-A scores (P = .003 and P = .020) compared to the CM group.
- The simultaneous ABM and AR-pe group did not have a significant difference in outcomes compared to the CM group (P = .081).
- On the PSWQ, the CM group had a larger decrease in worry than all active cohorts combined, with follow-up analysis indicating the CM group surpassed the ABM group (P = .019).
Conclusions/limitations
- Sequential delivery of ABM and AR-pe may be a viable, easy-to-access treatment option for patients with GAD who have limited access to other therapies.
- Individuals assigned to receive simultaneous ABM and AR-pe appeared to complete fewer tasks compared to those in the sequential groups, which suggests that participants were less inclined to complete all tasks despite being allowed more time.
- This study did not examine the effects of ABM only or AR-pe only.
- This study was unable to accurately assess home usage of the program.
6. Burke J, Richards D, Timulak L. Helpful and hindering events in internet-delivered cognitive behavioural treatment for generalized anxiety. Behav Cogn Psychother. 2019;47(3):386-399. doi:10.1017/S1352465818000504
Patients with GAD may not be able to obtain adequate treatment due to financial or logistical constraints. Internet-delivered interventions are easily accessible and provide an opportunity for patients who cannot or do not want to seek traditional therapy options. Burke et al10 aimed to better understand the useful and impeding events of internet-based cognitive-behavioral therapy (iCBT).
Study design
- A total of 36 adults (25 women) age 18 to 45 from an Irish university were randomized to an immediate iCBT treatment group or a delayed access to treatment/waiting list control group. The iCBT program, called Calming Anxiety, involved 6 modules of CBT for GAD.
- Participants initially scored ≥10 on the Generalized Anxiety Disorder 7-item scale (GAD-7).
- The study employed the Helpful and Hindering Aspects of Therapy (HAT) questionnaire to assess the most useful and impeding events in therapy.
- The data were divided into 4 domains: helpful events, helpful impacts, hindering events, and hindering impacts.
Outcomes
- Of the 8 helpful events identified, the top 3 were psychoeducation, supporter interaction, and monitoring.
- Of the 5 helpful impacts identified, the top 3 were support and validation, applying coping strategies/behavioral change, and clarification, awareness, and insight.
- The 2 identified hindering events were treatment content/form and amount of work/technical issues.
- The 3 identified hindering impacts were frustration/irritation, increased anxiety, and isolation.
Continue to: Conclusions/limitations
Conclusions/limitations
- iCBT may be a useful and accessible approach for treating GAD, although there are still hindrances to its use.
- This study was qualitative and did not comment on the efficacy of the applied intervention.
- The benefits of iCBT may differ depending on the patient’s level of computer literacy.
7. Miller CB, Gu J, Henry AL, et al. Feasibility and efficacy of a digital CBT intervention for symptoms of generalized anxiety disorder: a randomized multiple-baseline study. J Behav Ther Exp Psychiatry. 2021;70:101609. doi:10.1016/j.jbtep.2020.101609
Access to CBT is limited due to cost, dearth of trained therapists, scheduling availability, stigma, and transportation. Digital CBT may help overcome these obstacles. Miller et al11 studied the feasibility and efficacy of a new automated, digital CBT intervention named Daylight.
Study design
- This randomized, multiple-baseline, single-case, experimental trial included 21 adults (20 women) age ≥18 who scored ≥10 on the GAD-7 and screened positive for GAD on MINI version 7 for DSM-5.
- Participants were not taking psychotropic medications or had been on a stable medication regimen for ≥4 weeks.
- Exclusion criteria included past or present psychosis, schizophrenia, BD, seizure disorder, substance use disorder, trauma to the head or brain damage, severe cognitive impairment, serious physical health concerns necessitating surgery or with prognosis <6 months, and pregnancy.
- Participants were randomized to 1 of 3 baseline durations: 2 weeks, 4 weeks, or 6 weeks. They then could access the smartphone program Daylight. The trial lasted for 12 to 16 weeks.
- Primary anxiety outcomes were assessed daily and weekly, while secondary outcomes (depressive symptoms, sleep) were measured weekly.
- Postintervention was defined as 6 weeks after the start of the intervention and follow-up was 10 weeks after the start of the intervention.
- Participants were deemed not to have clinically significant anxiety if they scored <10 on GAD-7; not to have significant depressive symptoms if they scored <10 on the Patient Health Questionnaire-9 (PHQ-9); and not to have sleep difficulty if they scored >16 on the Sleep Condition Indicator (SCI-8). The change was considered reliable if patients scored below the previously discussed thresholds and showed a difference in score greater than the known unreliability of the questionnaire (GAD-7 reductions ≥5, PHQ-9 reductions ≥6, SCI-8 increases ≥7).
Outcomes
- In terms of feasibility, 76% of participants completed all 4 modules, 81% completed 3 modules, 86% completed 2 modules, and all participants completed at least 1 module.
- No serious adverse events were observed, but 43% of participants reported unwanted symptoms such as agitation, fatigue, low mood, or reduced motivation.
- As evaluated by the Credibility/Expectancy Questionnaire, the program received moderate to high credibility scores. Participants indicated they were mostly satisfied with the program, although some expressed technical difficulties and a lack of specificity to their anxiety symptoms.
- Overall daily anxiety scores significantly decreased from baseline to postintervention (P < .001). Weekly anxiety scores significantly decreased from baseline to postintervention (P = .024), and follow-up (P = .017) as measured by the GAD-7.
- For participants with anxiety, 70% no longer had clinically significant anxiety symptoms postintervention, and 65% had both clinically significant and reliable change at postintervention. Eighty percent had clinically significant and reliable change at follow-up.
- For participants with depressive symptoms, 61% had clinical and reliable change at postintervention and 44% maintained both at follow-up.
- For participants with sleep disturbances, 35% had clinical and reliable improvement at postintervention and 40% had clinical and reliable change at follow-up.
Conclusions/limitations
- Daylight appears to be a feasible program with regards to acceptability, engagement, credibility, satisfaction, and safety.
- The daily and weekly outcomes support preliminary evidence of program efficacy in improving GAD symptoms.
- Most participants identified as female and were recruited online, which limits generalizability, and the study had a small sample size.
Continue to: #8
8. Hirsch CR, Krahé C, Whyte J, et al. Internet-delivered interpretation training reduces worry and anxiety in individuals with generalized anxiety disorder: a randomized controlled experiment. J Consult Clin Psychol. 2021;89(7):575-589. doi:10.1037/ccp0000660
The cognitive model of pathological worry posits that worry in GAD occurs due to various factors, including automatic cognitive bias in which ambiguous events are perceived as threatening to the individual.22 Cognitive bias modification for interpretation (CBM) is an approach that assesses an individual’s interpretation bias and resolves ambiguity through the individual’s reading or listening to multiple ambiguous situations.12 Hirsch et al12 examined if an internet-delivered CBM approach would promote positive interpretations and reduce worry and anxiety in patients with GAD.
Study design
- In this dual-arm, parallel group, single-blind RCT, adult participants were randomized to a CBM group (n = 115) or a control group (n = 115); only 186 participants were included in the analyses.
- Patients with GAD only and those with GAD comorbid with MDD who scored ≥62 on the PSWQ and ≥10 on the GAD-7 were recruited. Patients receiving psychotropic medication had to be stable on their regimen for ≥3 months prior to the trial.
- Exclusion criteria included residing outside the United Kingdom, severe depression as measured by a PHQ-9 score ≥23, self-harm in the past 12 months or suicide attempt in past 2 years, a PHQ-9 suicidal ideation score >1, concurrent psychosis, BD, BPD, substance abuse, and current or recent (within the past 6 months) psychological treatment.
- The groups completed up to 10 online training (CBM) or control (listened to ambiguous scenarios but not asked to resolve the ambiguity) sessions in 1 month.
- Primary outcome measures included the scrambled sentences test (SST) and a recognition test (RT) to assess interpretation bias.
- Secondary outcome measures included a breathing focus task (BFT), PSWQ and PSWQ-past week, Ruminative Response Scale (RRS), Repetitive Thinking Questionnaire-trait (RTQ-T), PHQ-9, and GAD-7.
- Scores were assessed preintervention (T0), postintervention (T1), 1 month postintervention (T2), and 3 months postintervention (T3).
Outcomes
- CBM was associated with a more positive interpretation at T1 than the control sessions (P < .001 on both SST and RT).
- CBM was associated with significantly reduced negative intrusions as per BFTs at T1.
- The CBM group had significant less worry as per PSWQ, and significantly less anxiety as per GAD-7 at T1, T2, and T3.
- The CBM group had significantly fewer depressive symptoms as per PHQ-9 at T1, T2, and T3.
- The CBM group had significantly lower levels of ruminations as per RRS at T1, T2, and T3.
- The CBM group had significantly lower levels of general repetitive negative thinking (RNT) as per RTQ-T at T1 and T2, but not T3.
Conclusions/limitations
- Digital CBM appears to promote a positive interpretation bias.
- CBM appears to reduce negative intrusions after the intervention, as well as reduced levels of worrying, anxiety, RNT, and ruminations, with effects lasting ≤3 months except for the RNT.
- CBM appears to be an efficacious, low-intensity, easily accessible intervention that can help individuals with GAD.
- The study recruited participants via advertisements rather than clinical services, and excluded individuals with severe depression.
SECOND OF 2 PARTS
For patients with generalized anxiety disorder (GAD), the intensity, duration, and frequency of an individual’s anxiety and worry are out of proportion to the actual likelihood or impact of an anticipated event, and they often find it difficult to prevent worrisome thoughts from interfering with daily life.1 Successful treatment for GAD is patient-specific and requires clinicians to consider all available psychotherapeutic and pharmacologic options.
In a 2020 meta-analysis of 79 randomized controlled trials (RCTs) with 11,002 participants diagnosed with GAD, Carl et al2 focused on pooled effect sizes of evidence-based psychotherapies and medications for GAD. Their analysis showed a medium to large effect size (Hedges g = 0.76) for psychotherapy, compared to a small effect size (Hedges g = 0.38) for medication on GAD outcomes. Other meta-analyses have shown that evidence-based psychotherapies have large effect sizes on GAD outcomes.3
However, in most of the studies included in these meta-analyses, the 2 treatment modalities—psychotherapy and pharmacotherapy—use different control types. The pharmacotherapy trials used a placebo, while psychotherapy studies often had a waitlist control. Thus, the findings of these meta-analyses should not lead to the conclusion that psychotherapy is necessarily more effective for GAD symptoms than pharmacotherapy. However, there is clear evidence that psychosocial interventions are at least as effective as medications for treating GAD. Also, patients often prefer psychosocial treatment over medication.
Part 1 (
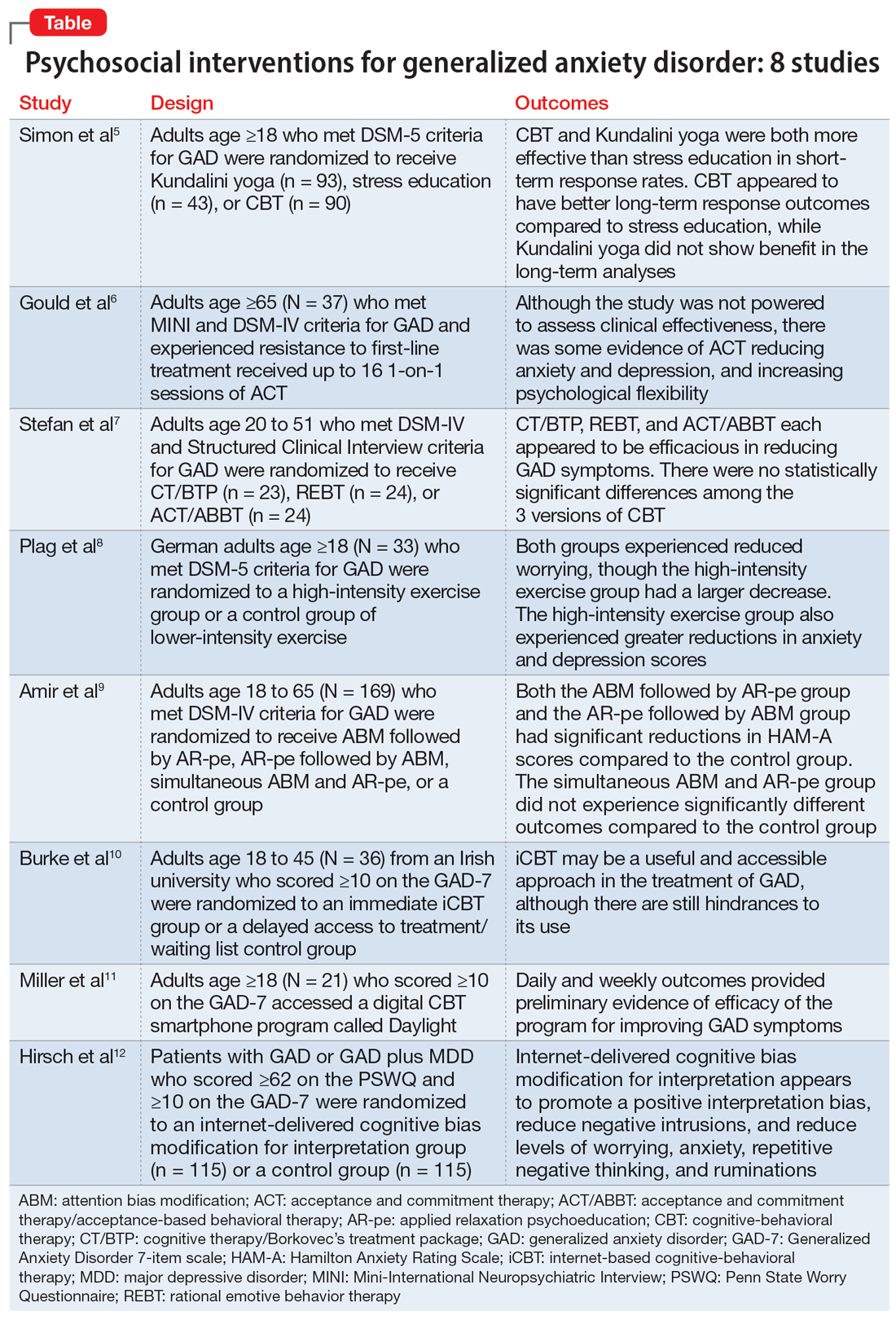
1. Simon NM, Hofmann SG, Rosenfield D, et al. Efficacy of yoga vs cognitive behavioral therapy vs stress education for the treatment of generalized anxiety disorder: a randomized clinical trial. JAMA Psychiatry. 2021;78(1):13-20. doi:10.1001/jamapsychiatry.2020.2496
Cognitive-behavioral therapy (CBT) is a first-line therapy for GAD.13 However, patients may not pursue CBT due to fiscal and logistical constraints, as well as the stigma associated with it. Yoga is a common complementary health practice used by adults in the United States,14 although evidence has been inconclusive for its use in treating anxiety. Simon et al5 examined the efficacy of Kundalini yoga (KY) vs stress education (SE) and CBT for treating GAD.
Study design
- A prospective, parallel-group, randomized-controlled, single-blind trial in 2 academic centers evaluated 226 adults age ≥18 who met DSM-5 criteria for GAD.
- Participants were randomized into 3 groups: KY (n = 93), SE (n = 43), or CBT (n = 90), and monitored for 12 weeks to determine the efficacy of each therapy.
- Exclusion criteria included current posttraumatic stress disorder, eating disorders, substance use disorders, significant suicidal ideation, mental disorder due to a medical or neurocognitive condition, lifetime psychosis, bipolar disorder (BD), developmental disorders, and having completed more than 5 yoga or CBT sessions in the past 5 years. Additionally, patients were either not taking medication for ≥2 weeks prior to the trial or had a stable regimen for ≥6 weeks.
- Each therapy was guided by 2 instructors during 12 120-minute sessions with 20 minutes of daily assignments and presented in cohorts of 4 to 6 participants.
- The primary outcome was an improvement in score on the Clinical Global Impression–Improvement scale from baseline at Week 12. Secondary measures included scores on the Meta-Cognitions Questionnaire and the Five Facet Mindfulness Questionnaire.
Outcomes
- A total of 155 participants finished the posttreatment assessment, with similar completion rates between the groups, and 123 participants completed the 6-month follow-up assessment.
- The KY group had a significantly higher response rate (54.2%) than the SE group (33%) at posttreatment, with a number needed to treat (NNT) of 4.59. At 6-month follow-up, the response rate in the KY group was not significantly higher than that of the SE group.
- The CBT group had a significantly higher response rate (70.8%) than the SE group (33%) at posttreatment, with a NNT of 2.62. At 6-month follow-up, the CBT response rate (76.7%) was significantly higher than the SE group (48%), with a NNT of 3.51.
- KY was not found to be as effective as CBT on noninferiority testing.
Continue to: Conclusions/limitations
Conclusions/limitations
- CBT and KY were both more effective than SE as assessed by short-term response rates.
- The authors did not find KY to be as effective as CBT at posttreatment or the 6-month follow-up. Additionally, CBT appeared to have better long-term response outcomes compared to SE, while KY did not display a benefit in follow-up analyses. Overall, KY appears to have a less robust efficacy compared to CBT in the treatment of GAD.
- These findings may not generalize to how CBT and yoga are approached in the community. Future studies can assess community-based methods.
2. Gould RL, Wetherell JL, Serfaty MA, et al. Acceptance and commitment therapy for older people with treatment-resistant generalised anxiety disorder: the FACTOID feasibility study. Health Technol Assess. 2021;25(54):1-150. doi:10.3310/hta25540
Older adults with GAD may experience treatment resistance to first-line therapies, such as selective serotonin reuptake inhibitors and CBT. Gould et al6 assessed whether acceptance and commitment therapy (ACT) could be a cost-effective option for older adults with treatment-resistant GAD (TR-GAD).
Study design
- In Stage 1 (intervention planning), individual interviews were conducted with 15 participants (11 female) with TR-GAD and 31 health care professionals, as well as 5 academic clinicians. The objective was to assess intervention preferences and priorities.
- Stage 2 included 37 participants, 8 clinicians, and 15 therapists, with the goal of assessing intervention design and feedback on the interventions.
- Participants were age ≥65 and met Mini-International Neuropsychiatric Interview (MINI) and DSM-IV criteria for GAD. They were living in the community and had not responded to the 3 steps of the stepped-care approach for GAD (ie, 6 weeks of an age-appropriate dose of antidepressant or a course of individual psychotherapy). Patients with dementia were excluded.
- Patients received ≤16 1-on-1 sessions of ACT.
- Self-reported outcomes were assessed at baseline and Week 20.
- The primary outcomes for Stage 2 were acceptability (attendance and satisfaction with ACT) and feasibility (recruitment and retention).
Outcomes
- ACT had high feasibility, with a recruitment rate of 93% and a retention rate of 81%.
- It also had high acceptability, with 70% of participants attending ≥10 sessions and 60% of participants showing satisfaction with therapy by scoring ≥21 points on the Satisfaction with Therapy subscale of the Satisfaction with Therapy and Therapist Scale-Revised. However, 80% of participants had not finished their ACT sessions when scores were collected.
- At Week 20, 13 patients showed reliable improvement on the Geriatric Anxiety Inventory, and 15 showed no reliable change. Seven participants showed reliable improvement in Geriatric Depression Scale-15 scores and 22 showed no reliable change. Seven participants showed improvement in the Action and Acceptance Questionnaire-II and 19 showed no reliable change.
Conclusions/limitations
- ACT had high levels of feasibility and acceptability, and large RCTs warrant further assessment of the benefits of this intervention.
- There was some evidence of reductions in anxiety and depression, as well as improvement with psychological flexibility.
- The study was not powered to assess clinical effectiveness, and recruitment for Stage 2 was limited to London.
Continue to: #3
3. Stefan S, Cristea IA, Szentagotai Tatar A, et al. Cognitive-behavioral therapy (CBT) for generalized anxiety disorder: contrasting various CBT approaches in a randomized clinical trial. J Clin Psychol. 2019;75(7):1188-1202. doi:10.1002/jclp.22779
Previous studies have demonstrated the efficacy of CBT for treating GAD.15,16 However, CBT involves varying approaches, which make it difficult to conclude which model of CBT is more effective. Stefan et al7 aimed to assess the efficacy of 3 versions of CBT for GAD.
Study design
- This RCT investigated 3 versions of CBT: cognitive therapy/Borkovec’s treatment package (CT/BTP), rational emotive behavior therapy (REBT), and acceptance and commitment therapy/acceptance-based behavioral therapy (ACT/ABBT).
- A total of 75 adults (60 women) age 20 to 51 and diagnosed with GAD by the Structured Clinical Interview for DSM-IV were initially randomized to one of the treatment arms for 20 sessions; 4 dropped out before receiving the allocated intervention. Exclusion criteria included panic disorder, severe major depressive disorder (MDD), BD, substance use or dependence, psychotic disorders, suicidal or homicidal ideation, organic brain syndrome, disabling medical conditions, intellectual disability, treatment with a psychotropic drug within the past 3 months, and psychotherapy provided outside the trial.
- The primary outcomes were scores on the Generalized Anxiety Disorder Questionnaire IV (GAD-Q-IV) and the Penn State Worry Questionnaire (PSWQ). A secondary outcome included assessing negative automatic thoughts by the Automatic Thoughts Questionnaire.
Outcomes
- There were no significant differences among the 3 treatment groups with regards to demographic data.
- Approximately 70% of patients (16 of 23) in the CT/BTP group had scores below the cutoff point for response (9) on the GAD-Q-IV, approximately 71% of patients (17 of 24) in the REBT group scored below the cutoff point, and approximately 79% of patients (19 of 24) in the ACT/ABBT group scored below the cutoff point.
- Approximately 83% of patients in the CT/BTP scored below the cutoff point for response (65) on the PSWQ, approximately 83% of patients in the REBT group scored below the cutoff point, and approximately 80% of patients in the ACT/ABBT group scored below the cutoff point.
- There were positive correlations between pre-post changes in GAD symptoms and dysfunctional automatic thoughts in each group.
- There was no statistically significant difference among the 3 versions of CBT.
Conclusions/limitations
- CT/BTP, REBT, and ACT/ABBT each appear to be efficacious in reducing GAD symptoms, allowing the choice of treatment to be determined by patient and clinician preference.
- The study’s small sample size may have prevented differences between the groups from being detected.
- There was no control group, and only 39 of 75 individuals completed the study in its entirety.
4. Plag J, Schmidt-Hellinger P, Klippstein T, et al. Working out the worries: a randomized controlled trial of high intensity interval training in generalized anxiety disorder. J Anxiety Disord. 2020;76:102311. doi:10.1016/j.janxdis.2020.10231
Research has shown the efficacy of aerobic exercise for various anxiety disorders,17-19 but differs regarding the type of exercise and its intensity, frequency, and duration. There is evidence that high-intensity interval training (HIIT) may be beneficial in treating serious mental illness.20 Plag et al8 examined the efficacy and acceptance of HIIT in patients with GAD.
Continue to: Study design
Study design
- A total of 33 German adults (24 women) age ≥18 who met DSM-5 criteria for GAD were enrolled in a parallel-group, assessor-blinded RCT. Participants were blinded to the hypotheses of the trial, but not to the intervention.
- Participants were randomized to a HIIT group (engaged in HIIT on a bicycle ergometer every second day within 12 days, with each session lasting 20 minutes and consisting of alternating sessions of 77% to 95% maximum heart rate and <70% maximum heart rate) or a control group of lower-intensity exercise (LIT; consisted of 6 30-minute sessions within 12 days involving stretching and adapted yoga positions with heart rate <70% maximum heart rate).
- Exclusion criteria included severe depression, schizophrenia, borderline personality disorder (BPD), substance use disorder, suicidality, epilepsy, severe respiratory or cardiovascular diseases, and current psychotherapy. The use of medications was allowed if the patient was stable ≥4 weeks prior to the trial and remained stable during the trial.
- The primary outcome of worrying was assessed by the PSWQ. Other assessment tools included the Hamilton Anxiety Rating Scale (HAM-A), Hamilton Depression Rating Scale (HAM-D), Anxiety Control Questionnaire, and Screening for Somatoform Symptoms-7 (SOMS-7).
Outcomes
- Baseline PSWQ scores in both groups were >60, indicating “high worriers.”
- Both groups experienced reductions in worrying as measured by PSWQ scores. However, the HIIT group had a larger decrease in worrying compared to the LIT group (P < .02). Post-hoc analyses showed significant reductions in symptom severity from baseline to poststudy (P < .01; d = 0.68), and at 30-day follow-up (P < .01; d = 0.62) in the HIIT group. There was no significant difference in the LIT group from baseline to poststudy or at follow-up.
- Secondary outcome measures included a greater reduction in anxiety and depression as determined by change in HAM-A and HAM-D scores in the HIIT group compared to the LIT group.
- All measures showed improvement in the HIIT group, whereas the LIT group showed improvement in HAM-A and HAM-D scores poststudy and at follow-up, as well as SOMS-7 scores at follow-up.
Conclusions/limitations
- HIIT demonstrated a large treatment effect for treating GAD, including somatic symptoms and worrying.
- HIIT displayed a fast onset of action and low cancellation rate, which suggests it is tolerable.
- This study had a small sample size consisting of participants from only 1 institution, which limits generalizability, and did not look at the long-term effects of the interventions.
5. Amir N, Taboas W, Montero M. Feasibility and dissemination of a computerized home-based treatment for generalized anxiety disorder: a randomized clinical trial. Behav Res Ther. 2019;120:103446. doi:10.1016/j.brat.2019.103446
Many patients with anxiety disorders do not receive treatment, and logistical factors such as limited time, expertise, and available resources hinder patients from obtaining quality CBT. Attention bias modification (ABM) is a computer-based approach in which patients complete tasks guiding their attention away from threat-relevant cues.21 Applied relaxation psychoeducation (AR-pe) is another empirically supported treatment that can be administered via computer. Amir et al9 examined the feasibility and effectiveness of a home-based computerized regimen of sequenced or simultaneous ABM and AR-pe in patients with GAD.
Study design
- A total of 169 adults age 18 to 65 who met DSM-IV criteria for GAD were randomized into 4 groups: ABM followed by AR-pe, AR-pe followed by ABM, simultaneous ABM and AR-pe, or a clinical monitoring assessment only control group (CM).
- Participants were expected to complete up to 24 30-minute sessions on their home computer over 12 weeks.
- Exclusion criteria included current psychotropic medications/CBT initiated 3 months prior to the study, BD, schizophrenia, or substance use disorder.
- The primary outcome measure was anxiety symptoms as assessed by the HAM-A (remission was defined as a score ≤7 at Week 13). Other measures included the PSWQ, Spielberger State-Trait Anxiety Inventory, Sheehan Disability Scale, and Beck Depression Inventory.
- Participants were assessed at Month 3, Month 6, and Month 12 poststudy.
Continue to: Outcomes
Outcomes
- Baseline characteristics did not significantly differ between groups.
- In the active groups, 41% of participants met remission criteria, compared to 19% in the CM group.
- The ABM followed by AR-pe group and the AR-pe followed by ABM group had significant reductions in HAM-A scores (P = .003 and P = .020) compared to the CM group.
- The simultaneous ABM and AR-pe group did not have a significant difference in outcomes compared to the CM group (P = .081).
- On the PSWQ, the CM group had a larger decrease in worry than all active cohorts combined, with follow-up analysis indicating the CM group surpassed the ABM group (P = .019).
Conclusions/limitations
- Sequential delivery of ABM and AR-pe may be a viable, easy-to-access treatment option for patients with GAD who have limited access to other therapies.
- Individuals assigned to receive simultaneous ABM and AR-pe appeared to complete fewer tasks compared to those in the sequential groups, which suggests that participants were less inclined to complete all tasks despite being allowed more time.
- This study did not examine the effects of ABM only or AR-pe only.
- This study was unable to accurately assess home usage of the program.
6. Burke J, Richards D, Timulak L. Helpful and hindering events in internet-delivered cognitive behavioural treatment for generalized anxiety. Behav Cogn Psychother. 2019;47(3):386-399. doi:10.1017/S1352465818000504
Patients with GAD may not be able to obtain adequate treatment due to financial or logistical constraints. Internet-delivered interventions are easily accessible and provide an opportunity for patients who cannot or do not want to seek traditional therapy options. Burke et al10 aimed to better understand the useful and impeding events of internet-based cognitive-behavioral therapy (iCBT).
Study design
- A total of 36 adults (25 women) age 18 to 45 from an Irish university were randomized to an immediate iCBT treatment group or a delayed access to treatment/waiting list control group. The iCBT program, called Calming Anxiety, involved 6 modules of CBT for GAD.
- Participants initially scored ≥10 on the Generalized Anxiety Disorder 7-item scale (GAD-7).
- The study employed the Helpful and Hindering Aspects of Therapy (HAT) questionnaire to assess the most useful and impeding events in therapy.
- The data were divided into 4 domains: helpful events, helpful impacts, hindering events, and hindering impacts.
Outcomes
- Of the 8 helpful events identified, the top 3 were psychoeducation, supporter interaction, and monitoring.
- Of the 5 helpful impacts identified, the top 3 were support and validation, applying coping strategies/behavioral change, and clarification, awareness, and insight.
- The 2 identified hindering events were treatment content/form and amount of work/technical issues.
- The 3 identified hindering impacts were frustration/irritation, increased anxiety, and isolation.
Continue to: Conclusions/limitations
Conclusions/limitations
- iCBT may be a useful and accessible approach for treating GAD, although there are still hindrances to its use.
- This study was qualitative and did not comment on the efficacy of the applied intervention.
- The benefits of iCBT may differ depending on the patient’s level of computer literacy.
7. Miller CB, Gu J, Henry AL, et al. Feasibility and efficacy of a digital CBT intervention for symptoms of generalized anxiety disorder: a randomized multiple-baseline study. J Behav Ther Exp Psychiatry. 2021;70:101609. doi:10.1016/j.jbtep.2020.101609
Access to CBT is limited due to cost, dearth of trained therapists, scheduling availability, stigma, and transportation. Digital CBT may help overcome these obstacles. Miller et al11 studied the feasibility and efficacy of a new automated, digital CBT intervention named Daylight.
Study design
- This randomized, multiple-baseline, single-case, experimental trial included 21 adults (20 women) age ≥18 who scored ≥10 on the GAD-7 and screened positive for GAD on MINI version 7 for DSM-5.
- Participants were not taking psychotropic medications or had been on a stable medication regimen for ≥4 weeks.
- Exclusion criteria included past or present psychosis, schizophrenia, BD, seizure disorder, substance use disorder, trauma to the head or brain damage, severe cognitive impairment, serious physical health concerns necessitating surgery or with prognosis <6 months, and pregnancy.
- Participants were randomized to 1 of 3 baseline durations: 2 weeks, 4 weeks, or 6 weeks. They then could access the smartphone program Daylight. The trial lasted for 12 to 16 weeks.
- Primary anxiety outcomes were assessed daily and weekly, while secondary outcomes (depressive symptoms, sleep) were measured weekly.
- Postintervention was defined as 6 weeks after the start of the intervention and follow-up was 10 weeks after the start of the intervention.
- Participants were deemed not to have clinically significant anxiety if they scored <10 on GAD-7; not to have significant depressive symptoms if they scored <10 on the Patient Health Questionnaire-9 (PHQ-9); and not to have sleep difficulty if they scored >16 on the Sleep Condition Indicator (SCI-8). The change was considered reliable if patients scored below the previously discussed thresholds and showed a difference in score greater than the known unreliability of the questionnaire (GAD-7 reductions ≥5, PHQ-9 reductions ≥6, SCI-8 increases ≥7).
Outcomes
- In terms of feasibility, 76% of participants completed all 4 modules, 81% completed 3 modules, 86% completed 2 modules, and all participants completed at least 1 module.
- No serious adverse events were observed, but 43% of participants reported unwanted symptoms such as agitation, fatigue, low mood, or reduced motivation.
- As evaluated by the Credibility/Expectancy Questionnaire, the program received moderate to high credibility scores. Participants indicated they were mostly satisfied with the program, although some expressed technical difficulties and a lack of specificity to their anxiety symptoms.
- Overall daily anxiety scores significantly decreased from baseline to postintervention (P < .001). Weekly anxiety scores significantly decreased from baseline to postintervention (P = .024), and follow-up (P = .017) as measured by the GAD-7.
- For participants with anxiety, 70% no longer had clinically significant anxiety symptoms postintervention, and 65% had both clinically significant and reliable change at postintervention. Eighty percent had clinically significant and reliable change at follow-up.
- For participants with depressive symptoms, 61% had clinical and reliable change at postintervention and 44% maintained both at follow-up.
- For participants with sleep disturbances, 35% had clinical and reliable improvement at postintervention and 40% had clinical and reliable change at follow-up.
Conclusions/limitations
- Daylight appears to be a feasible program with regards to acceptability, engagement, credibility, satisfaction, and safety.
- The daily and weekly outcomes support preliminary evidence of program efficacy in improving GAD symptoms.
- Most participants identified as female and were recruited online, which limits generalizability, and the study had a small sample size.
Continue to: #8
8. Hirsch CR, Krahé C, Whyte J, et al. Internet-delivered interpretation training reduces worry and anxiety in individuals with generalized anxiety disorder: a randomized controlled experiment. J Consult Clin Psychol. 2021;89(7):575-589. doi:10.1037/ccp0000660
The cognitive model of pathological worry posits that worry in GAD occurs due to various factors, including automatic cognitive bias in which ambiguous events are perceived as threatening to the individual.22 Cognitive bias modification for interpretation (CBM) is an approach that assesses an individual’s interpretation bias and resolves ambiguity through the individual’s reading or listening to multiple ambiguous situations.12 Hirsch et al12 examined if an internet-delivered CBM approach would promote positive interpretations and reduce worry and anxiety in patients with GAD.
Study design
- In this dual-arm, parallel group, single-blind RCT, adult participants were randomized to a CBM group (n = 115) or a control group (n = 115); only 186 participants were included in the analyses.
- Patients with GAD only and those with GAD comorbid with MDD who scored ≥62 on the PSWQ and ≥10 on the GAD-7 were recruited. Patients receiving psychotropic medication had to be stable on their regimen for ≥3 months prior to the trial.
- Exclusion criteria included residing outside the United Kingdom, severe depression as measured by a PHQ-9 score ≥23, self-harm in the past 12 months or suicide attempt in past 2 years, a PHQ-9 suicidal ideation score >1, concurrent psychosis, BD, BPD, substance abuse, and current or recent (within the past 6 months) psychological treatment.
- The groups completed up to 10 online training (CBM) or control (listened to ambiguous scenarios but not asked to resolve the ambiguity) sessions in 1 month.
- Primary outcome measures included the scrambled sentences test (SST) and a recognition test (RT) to assess interpretation bias.
- Secondary outcome measures included a breathing focus task (BFT), PSWQ and PSWQ-past week, Ruminative Response Scale (RRS), Repetitive Thinking Questionnaire-trait (RTQ-T), PHQ-9, and GAD-7.
- Scores were assessed preintervention (T0), postintervention (T1), 1 month postintervention (T2), and 3 months postintervention (T3).
Outcomes
- CBM was associated with a more positive interpretation at T1 than the control sessions (P < .001 on both SST and RT).
- CBM was associated with significantly reduced negative intrusions as per BFTs at T1.
- The CBM group had significant less worry as per PSWQ, and significantly less anxiety as per GAD-7 at T1, T2, and T3.
- The CBM group had significantly fewer depressive symptoms as per PHQ-9 at T1, T2, and T3.
- The CBM group had significantly lower levels of ruminations as per RRS at T1, T2, and T3.
- The CBM group had significantly lower levels of general repetitive negative thinking (RNT) as per RTQ-T at T1 and T2, but not T3.
Conclusions/limitations
- Digital CBM appears to promote a positive interpretation bias.
- CBM appears to reduce negative intrusions after the intervention, as well as reduced levels of worrying, anxiety, RNT, and ruminations, with effects lasting ≤3 months except for the RNT.
- CBM appears to be an efficacious, low-intensity, easily accessible intervention that can help individuals with GAD.
- The study recruited participants via advertisements rather than clinical services, and excluded individuals with severe depression.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed., text revision. American Psychiatric Association; 2022.
2. Carl E, Witcraft SM, Kauffman BY, et al. Psychological and pharmacological treatments for generalized anxiety disorder (GAD): a meta-analysis of randomized controlled trials. Cogn Behav Ther. 2020;49(1):1-21. doi:10.1080/16506073.2018.1560358
3. Cuijpers P, Cristea IA, Karyotaki E, et al. How effective are cognitive behavior therapies for major depression and anxiety disorders? A meta‐analytic update of the evidence. World Psychiatry. 2016;15(3):245-258. doi:10.1002/wps.20346
4. Saeed SA, Majarwitz DJ. Generalized anxiety disorder: 8 studies of biological interventions. Current Psychiatry. 2022;21(7):10-12,20,22-27. doi:10.12788/cp.02645
5. Simon NM, Hofmann SG, Rosenfield D, et al. Efficacy of yoga vs cognitive behavioral therapy vs stress education for the treatment of generalized anxiety disorder: a randomized clinical trial. JAMA Psychiatry. 2021;78(1):13-20. doi:10.1001/jamapsychiatry.2020.2496
6. Gould RL, Wetherell JL, Serfaty MA, et al. Acceptance and commitment therapy for older people with treatment-resistant generalised anxiety disorder: the FACTOID feasibility study. Health Technol Assess. 2021;25(54):1-150. doi:10.3310/hta25540
7. Stefan S, Cristea IA, Szentagotai Tatar A, et al. Cognitive-behavioral therapy (CBT) for generalized anxiety disorder: contrasting various CBT approaches in a randomized clinical trial. J Clin Psychol. 2019;75(7):1188-1202. doi:10.1002/jclp.22779
8. Plag J, Schmidt-Hellinger P, Klippstein T, et al. Working out the worries: a randomized controlled trial of high intensity interval training in generalized anxiety disorder. J Anxiety Disord. 2020;76:102311. doi:10.1016/j.janxdis.2020.102311
9. Amir N, Taboas W, Montero M. Feasibility and dissemination of a computerized home-based treatment for generalized anxiety disorder: a randomized clinical trial. Behav Res Ther. 2019;120:103446. doi:10.1016/j.brat.2019.103446
10. Burke J, Richards D, Timulak L. Helpful and hindering events in internet-delivered cognitive behavioural treatment for generalized anxiety. Behav Cogn Psychother. 2019;47(3):386-399. doi:10.1017/S1352465818000504
11. Miller CB, Gu J, Henry AL, et al. Feasibility and efficacy of a digital CBT intervention for symptoms of generalized anxiety disorder: a randomized multiple-baseline study. J Behav Ther Exp Psychiatry. 2021;70:101609. doi:10.1016/j.jbtep.2020.101609
12. Hirsch CR, Krahé C, Whyte J, et al. Internet-delivered interpretation training reduces worry and anxiety in individuals with generalized anxiety disorder: a randomized controlled experiment. J Consult Clin Psychol. 2021;89(7):575-589. doi:10.1037/ccp0000660
13. Hofmann SG, Smits JAJ. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621-632. doi:10.4088/jcp.v69n0415
14. Clarke TC, Barnes PM, Black LI, et al. Use of yoga, meditation, and chiropractors among U.S. adults aged 18 and over. NCHS Data Brief. 2018;(325):1-8.
15. Carpenter JK, Andrews LA, Witcraft SM, et al. Cognitive behavioral therapy for anxiety and related disorders: a meta-analysis of randomized placebo-controlled trials. Depress Anxiety. 2018;35(6):502-514. doi:10.1002/da.22728
16. Covin R, Ouimet AJ, Seeds PM, et al. A meta-analysis of CBT for pathological worry among clients with GAD. J Anxiety Disord. 2008;22(1):108-116. doi:10.1016/j.janxdis.2007.01.002
17. Merom D, Phongsavan P, Wagner R, et al. Promoting walking as an adjunct intervention to group cognitive behavioral therapy for anxiety disorders--a pilot group randomized trial. J Anxiety Disord. 2008;22(6):959-968. doi:10.1016/j.janxdis.2007.09.010
18. Herring MP, Jacob ML, Suveg C, et al. Feasibility of exercise training for the short-term treatment of generalized anxiety disorder: a randomized controlled trial. Psychother Psychosom. 2012;81(1):21-28. doi:10.1159/000327898
19. Bischoff S, Wieder G, Einsle F, et al. Running for extinction? Aerobic exercise as an augmentation of exposure therapy in panic disorder with agoraphobia. J Psychiatr Res. 2018;101:34-41. doi:10.1016/j.jpsychires.2018.03.001
20. Korman N, Armour M, Chapman J, et al. High Intensity Interval training (HIIT) for people with severe mental illness: a systematic review & meta-analysis of intervention studies- considering diverse approaches for mental and physical recovery. Psychiatry Res. 2020;284:112601. doi:10.1016/j.psychres.2019.112601
21. Amir N, Beard C, Cobb M, et al. Attention modification program in individuals with generalized anxiety disorder. J Abnorm Psychol. 2009;118(1):28-33. doi:10.1037/a0012589
22. Hirsh CR, Mathews A. A cognitive model of pathological worry. Behav Res Ther. 2012;50(10):636-646. doi:10.1016/j.brat.2012.007
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed., text revision. American Psychiatric Association; 2022.
2. Carl E, Witcraft SM, Kauffman BY, et al. Psychological and pharmacological treatments for generalized anxiety disorder (GAD): a meta-analysis of randomized controlled trials. Cogn Behav Ther. 2020;49(1):1-21. doi:10.1080/16506073.2018.1560358
3. Cuijpers P, Cristea IA, Karyotaki E, et al. How effective are cognitive behavior therapies for major depression and anxiety disorders? A meta‐analytic update of the evidence. World Psychiatry. 2016;15(3):245-258. doi:10.1002/wps.20346
4. Saeed SA, Majarwitz DJ. Generalized anxiety disorder: 8 studies of biological interventions. Current Psychiatry. 2022;21(7):10-12,20,22-27. doi:10.12788/cp.02645
5. Simon NM, Hofmann SG, Rosenfield D, et al. Efficacy of yoga vs cognitive behavioral therapy vs stress education for the treatment of generalized anxiety disorder: a randomized clinical trial. JAMA Psychiatry. 2021;78(1):13-20. doi:10.1001/jamapsychiatry.2020.2496
6. Gould RL, Wetherell JL, Serfaty MA, et al. Acceptance and commitment therapy for older people with treatment-resistant generalised anxiety disorder: the FACTOID feasibility study. Health Technol Assess. 2021;25(54):1-150. doi:10.3310/hta25540
7. Stefan S, Cristea IA, Szentagotai Tatar A, et al. Cognitive-behavioral therapy (CBT) for generalized anxiety disorder: contrasting various CBT approaches in a randomized clinical trial. J Clin Psychol. 2019;75(7):1188-1202. doi:10.1002/jclp.22779
8. Plag J, Schmidt-Hellinger P, Klippstein T, et al. Working out the worries: a randomized controlled trial of high intensity interval training in generalized anxiety disorder. J Anxiety Disord. 2020;76:102311. doi:10.1016/j.janxdis.2020.102311
9. Amir N, Taboas W, Montero M. Feasibility and dissemination of a computerized home-based treatment for generalized anxiety disorder: a randomized clinical trial. Behav Res Ther. 2019;120:103446. doi:10.1016/j.brat.2019.103446
10. Burke J, Richards D, Timulak L. Helpful and hindering events in internet-delivered cognitive behavioural treatment for generalized anxiety. Behav Cogn Psychother. 2019;47(3):386-399. doi:10.1017/S1352465818000504
11. Miller CB, Gu J, Henry AL, et al. Feasibility and efficacy of a digital CBT intervention for symptoms of generalized anxiety disorder: a randomized multiple-baseline study. J Behav Ther Exp Psychiatry. 2021;70:101609. doi:10.1016/j.jbtep.2020.101609
12. Hirsch CR, Krahé C, Whyte J, et al. Internet-delivered interpretation training reduces worry and anxiety in individuals with generalized anxiety disorder: a randomized controlled experiment. J Consult Clin Psychol. 2021;89(7):575-589. doi:10.1037/ccp0000660
13. Hofmann SG, Smits JAJ. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621-632. doi:10.4088/jcp.v69n0415
14. Clarke TC, Barnes PM, Black LI, et al. Use of yoga, meditation, and chiropractors among U.S. adults aged 18 and over. NCHS Data Brief. 2018;(325):1-8.
15. Carpenter JK, Andrews LA, Witcraft SM, et al. Cognitive behavioral therapy for anxiety and related disorders: a meta-analysis of randomized placebo-controlled trials. Depress Anxiety. 2018;35(6):502-514. doi:10.1002/da.22728
16. Covin R, Ouimet AJ, Seeds PM, et al. A meta-analysis of CBT for pathological worry among clients with GAD. J Anxiety Disord. 2008;22(1):108-116. doi:10.1016/j.janxdis.2007.01.002
17. Merom D, Phongsavan P, Wagner R, et al. Promoting walking as an adjunct intervention to group cognitive behavioral therapy for anxiety disorders--a pilot group randomized trial. J Anxiety Disord. 2008;22(6):959-968. doi:10.1016/j.janxdis.2007.09.010
18. Herring MP, Jacob ML, Suveg C, et al. Feasibility of exercise training for the short-term treatment of generalized anxiety disorder: a randomized controlled trial. Psychother Psychosom. 2012;81(1):21-28. doi:10.1159/000327898
19. Bischoff S, Wieder G, Einsle F, et al. Running for extinction? Aerobic exercise as an augmentation of exposure therapy in panic disorder with agoraphobia. J Psychiatr Res. 2018;101:34-41. doi:10.1016/j.jpsychires.2018.03.001
20. Korman N, Armour M, Chapman J, et al. High Intensity Interval training (HIIT) for people with severe mental illness: a systematic review & meta-analysis of intervention studies- considering diverse approaches for mental and physical recovery. Psychiatry Res. 2020;284:112601. doi:10.1016/j.psychres.2019.112601
21. Amir N, Beard C, Cobb M, et al. Attention modification program in individuals with generalized anxiety disorder. J Abnorm Psychol. 2009;118(1):28-33. doi:10.1037/a0012589
22. Hirsh CR, Mathews A. A cognitive model of pathological worry. Behav Res Ther. 2012;50(10):636-646. doi:10.1016/j.brat.2012.007