User login
COVID pandemic associated with anorexia in Canadian youth
, data suggest.
Preliminary results of the Canadian Paediatric Surveillance Program (CPSP) indicate that the pandemic has been a precipitating factor in the development of anorexia nervosa in almost half of children and adolescents studied. The pandemic also has precipitated hospitalizations for anorexia in more than one-third of cases.
“Data globally, and certainly our data here in Canada, have shown a real increase in health care utilization with the onset of the COVID-19 pandemic,” study author Debra Katzman, MD, professor of pediatrics at the Hospital for Sick Children in Toronto and the University of Toronto, said in an interview. “And when I talk about health care utilization, I’m talking about hospitalizations for eating disorders.”
The data were included in the 2021 results of the CPSP.
Focus on appearance
CPSP is a collaboration between the Public Health Agency of Canada and the Canadian Pediatric Society that consists of a network of 2,800 pediatricians and pediatric subspecialists across Canada. The latest results include surveillance studies on 14 diseases and conditions, with data collected during various periods.
From April 2020 to May 2021, researchers identified 1,800 COVID-19 cases in children and collected detailed information on 1,456 of them, including 405 cases hospitalized with pediatric inflammatory multisystem syndrome (PIMS). The median age of hospitalized cases was 3.2 years for SARS-CoV-2 infection and 5.4 years for PIMS.
Dr. Katzman and colleagues observed 118 first-time hospitalizations for anorexia nervosa between Sept. 1 and Dec. 31, 2021. More than 90% of reported cases were female, with 66% of verified cases in teens aged 14-17 years and the remainder in adolescents aged 11-13 years.
In 49% of cases, the reporting physician identified the COVID-19 pandemic as a precipitating factor in the development of anorexia nervosa. In 37% of cases, the reporting physician identified the pandemic as having precipitated the anorexia-related hospitalization.
Last year, a cross-sectional analysis of children in Canada reported that monthly hospitalizations for anorexia nervosa increased from 7.5 to 20 from March through November 2020. The monthly rate in the CPSP study was closer to 30 for first-time hospitalizations.
Dr. Katzman said that the findings about anorexia nervosa didn’t surprise her. “There was so much disruption and [so many] restrictions to young peoples’ daily routines – closures of schools and recreational activities – they lost regular connection with their peers, and they lost extracurricular and social activities,” she said. “That led to heightened anxiety and depression and really a lack of control.”
Adolescents and teens were also spending more time on social media than they were before the pandemic, she noted. “They were looking at themselves all the time, so they were getting preoccupied with their body image. There was a heightened focus on appearance, and I think that things like public-health mitigation strategies – things like hand washing, social distancing, mask wearing – may have impacted the psychological well-being of young people.”
The closure of outpatient facilities, long waiting lists to get into facilities that were opened, and “coronaphobia” about going to physicians’ offices and emergency departments compounded the problem, Dr. Katzman added.
The long-term effects of COVID and eating disorders in children are unknown, Dr. Katzman said. “This is sort of a wake-up call for the health care system that during times of stress or pandemics or crises, these kinds of things can happen, and we need to be prepared to provide the resources for vulnerable populations moving forward,” she said.
Heightened anxiety
Commenting on the data, Margaret Thew, APNP, director of the eating disorders program at Children’s Wisconsin in Milwaukee, said that isolation due to school closures and negative social media messages created the “perfect storm” for eating disorders in adolescents and teenagers because of higher rates of anxiety and depression. Ms. Thew was not involved in the research.
The storm is not over yet, she said. “What everyone needs to keep in mind is that we still have this very heightened state of anxiety and depression ... for adolescents, teenagers, and preteens alike,” Ms. Thew said in an interview, “and we know that many of them are not coping with their anxiety very well.”
In her experience, since the start of the pandemic, the average age of pediatric patients with eating disorders declined from 16 to 15 years, and the youngest age declined from 12 to 11 years.
Overall, the CPSP results show that children are affected by mental health issues at an earlier age than before the pandemic, said Ms. Thew. “Years ago, we wouldn’t have thought that an 8-year-old needed to be screened for some of these risk factors, but now we’re definitely getting more younger children who are struggling, and I think it’s taking too long for them to get the care they need because it’s being overlooked,” she said.
The report was funded by the Public Health Agency of Canada, Health Canada, Alberta Children’s Hospital Research Institute, Bethanys Hope Foundation, CHEO Research Institute, and Children’s Hospital Research Institute of Manitoba. Dr. Katzman and Ms. Thew have no relevant disclosures.
A version of this article first appeared on Medscape.com.
, data suggest.
Preliminary results of the Canadian Paediatric Surveillance Program (CPSP) indicate that the pandemic has been a precipitating factor in the development of anorexia nervosa in almost half of children and adolescents studied. The pandemic also has precipitated hospitalizations for anorexia in more than one-third of cases.
“Data globally, and certainly our data here in Canada, have shown a real increase in health care utilization with the onset of the COVID-19 pandemic,” study author Debra Katzman, MD, professor of pediatrics at the Hospital for Sick Children in Toronto and the University of Toronto, said in an interview. “And when I talk about health care utilization, I’m talking about hospitalizations for eating disorders.”
The data were included in the 2021 results of the CPSP.
Focus on appearance
CPSP is a collaboration between the Public Health Agency of Canada and the Canadian Pediatric Society that consists of a network of 2,800 pediatricians and pediatric subspecialists across Canada. The latest results include surveillance studies on 14 diseases and conditions, with data collected during various periods.
From April 2020 to May 2021, researchers identified 1,800 COVID-19 cases in children and collected detailed information on 1,456 of them, including 405 cases hospitalized with pediatric inflammatory multisystem syndrome (PIMS). The median age of hospitalized cases was 3.2 years for SARS-CoV-2 infection and 5.4 years for PIMS.
Dr. Katzman and colleagues observed 118 first-time hospitalizations for anorexia nervosa between Sept. 1 and Dec. 31, 2021. More than 90% of reported cases were female, with 66% of verified cases in teens aged 14-17 years and the remainder in adolescents aged 11-13 years.
In 49% of cases, the reporting physician identified the COVID-19 pandemic as a precipitating factor in the development of anorexia nervosa. In 37% of cases, the reporting physician identified the pandemic as having precipitated the anorexia-related hospitalization.
Last year, a cross-sectional analysis of children in Canada reported that monthly hospitalizations for anorexia nervosa increased from 7.5 to 20 from March through November 2020. The monthly rate in the CPSP study was closer to 30 for first-time hospitalizations.
Dr. Katzman said that the findings about anorexia nervosa didn’t surprise her. “There was so much disruption and [so many] restrictions to young peoples’ daily routines – closures of schools and recreational activities – they lost regular connection with their peers, and they lost extracurricular and social activities,” she said. “That led to heightened anxiety and depression and really a lack of control.”
Adolescents and teens were also spending more time on social media than they were before the pandemic, she noted. “They were looking at themselves all the time, so they were getting preoccupied with their body image. There was a heightened focus on appearance, and I think that things like public-health mitigation strategies – things like hand washing, social distancing, mask wearing – may have impacted the psychological well-being of young people.”
The closure of outpatient facilities, long waiting lists to get into facilities that were opened, and “coronaphobia” about going to physicians’ offices and emergency departments compounded the problem, Dr. Katzman added.
The long-term effects of COVID and eating disorders in children are unknown, Dr. Katzman said. “This is sort of a wake-up call for the health care system that during times of stress or pandemics or crises, these kinds of things can happen, and we need to be prepared to provide the resources for vulnerable populations moving forward,” she said.
Heightened anxiety
Commenting on the data, Margaret Thew, APNP, director of the eating disorders program at Children’s Wisconsin in Milwaukee, said that isolation due to school closures and negative social media messages created the “perfect storm” for eating disorders in adolescents and teenagers because of higher rates of anxiety and depression. Ms. Thew was not involved in the research.
The storm is not over yet, she said. “What everyone needs to keep in mind is that we still have this very heightened state of anxiety and depression ... for adolescents, teenagers, and preteens alike,” Ms. Thew said in an interview, “and we know that many of them are not coping with their anxiety very well.”
In her experience, since the start of the pandemic, the average age of pediatric patients with eating disorders declined from 16 to 15 years, and the youngest age declined from 12 to 11 years.
Overall, the CPSP results show that children are affected by mental health issues at an earlier age than before the pandemic, said Ms. Thew. “Years ago, we wouldn’t have thought that an 8-year-old needed to be screened for some of these risk factors, but now we’re definitely getting more younger children who are struggling, and I think it’s taking too long for them to get the care they need because it’s being overlooked,” she said.
The report was funded by the Public Health Agency of Canada, Health Canada, Alberta Children’s Hospital Research Institute, Bethanys Hope Foundation, CHEO Research Institute, and Children’s Hospital Research Institute of Manitoba. Dr. Katzman and Ms. Thew have no relevant disclosures.
A version of this article first appeared on Medscape.com.
, data suggest.
Preliminary results of the Canadian Paediatric Surveillance Program (CPSP) indicate that the pandemic has been a precipitating factor in the development of anorexia nervosa in almost half of children and adolescents studied. The pandemic also has precipitated hospitalizations for anorexia in more than one-third of cases.
“Data globally, and certainly our data here in Canada, have shown a real increase in health care utilization with the onset of the COVID-19 pandemic,” study author Debra Katzman, MD, professor of pediatrics at the Hospital for Sick Children in Toronto and the University of Toronto, said in an interview. “And when I talk about health care utilization, I’m talking about hospitalizations for eating disorders.”
The data were included in the 2021 results of the CPSP.
Focus on appearance
CPSP is a collaboration between the Public Health Agency of Canada and the Canadian Pediatric Society that consists of a network of 2,800 pediatricians and pediatric subspecialists across Canada. The latest results include surveillance studies on 14 diseases and conditions, with data collected during various periods.
From April 2020 to May 2021, researchers identified 1,800 COVID-19 cases in children and collected detailed information on 1,456 of them, including 405 cases hospitalized with pediatric inflammatory multisystem syndrome (PIMS). The median age of hospitalized cases was 3.2 years for SARS-CoV-2 infection and 5.4 years for PIMS.
Dr. Katzman and colleagues observed 118 first-time hospitalizations for anorexia nervosa between Sept. 1 and Dec. 31, 2021. More than 90% of reported cases were female, with 66% of verified cases in teens aged 14-17 years and the remainder in adolescents aged 11-13 years.
In 49% of cases, the reporting physician identified the COVID-19 pandemic as a precipitating factor in the development of anorexia nervosa. In 37% of cases, the reporting physician identified the pandemic as having precipitated the anorexia-related hospitalization.
Last year, a cross-sectional analysis of children in Canada reported that monthly hospitalizations for anorexia nervosa increased from 7.5 to 20 from March through November 2020. The monthly rate in the CPSP study was closer to 30 for first-time hospitalizations.
Dr. Katzman said that the findings about anorexia nervosa didn’t surprise her. “There was so much disruption and [so many] restrictions to young peoples’ daily routines – closures of schools and recreational activities – they lost regular connection with their peers, and they lost extracurricular and social activities,” she said. “That led to heightened anxiety and depression and really a lack of control.”
Adolescents and teens were also spending more time on social media than they were before the pandemic, she noted. “They were looking at themselves all the time, so they were getting preoccupied with their body image. There was a heightened focus on appearance, and I think that things like public-health mitigation strategies – things like hand washing, social distancing, mask wearing – may have impacted the psychological well-being of young people.”
The closure of outpatient facilities, long waiting lists to get into facilities that were opened, and “coronaphobia” about going to physicians’ offices and emergency departments compounded the problem, Dr. Katzman added.
The long-term effects of COVID and eating disorders in children are unknown, Dr. Katzman said. “This is sort of a wake-up call for the health care system that during times of stress or pandemics or crises, these kinds of things can happen, and we need to be prepared to provide the resources for vulnerable populations moving forward,” she said.
Heightened anxiety
Commenting on the data, Margaret Thew, APNP, director of the eating disorders program at Children’s Wisconsin in Milwaukee, said that isolation due to school closures and negative social media messages created the “perfect storm” for eating disorders in adolescents and teenagers because of higher rates of anxiety and depression. Ms. Thew was not involved in the research.
The storm is not over yet, she said. “What everyone needs to keep in mind is that we still have this very heightened state of anxiety and depression ... for adolescents, teenagers, and preteens alike,” Ms. Thew said in an interview, “and we know that many of them are not coping with their anxiety very well.”
In her experience, since the start of the pandemic, the average age of pediatric patients with eating disorders declined from 16 to 15 years, and the youngest age declined from 12 to 11 years.
Overall, the CPSP results show that children are affected by mental health issues at an earlier age than before the pandemic, said Ms. Thew. “Years ago, we wouldn’t have thought that an 8-year-old needed to be screened for some of these risk factors, but now we’re definitely getting more younger children who are struggling, and I think it’s taking too long for them to get the care they need because it’s being overlooked,” she said.
The report was funded by the Public Health Agency of Canada, Health Canada, Alberta Children’s Hospital Research Institute, Bethanys Hope Foundation, CHEO Research Institute, and Children’s Hospital Research Institute of Manitoba. Dr. Katzman and Ms. Thew have no relevant disclosures.
A version of this article first appeared on Medscape.com.
Timing of food intake a novel strategy for treating mood disorders?
new research suggests.
Investigators at Brigham and Women’s Hospital, Boston, created a simulated nightwork schedule for 19 individuals in a laboratory setting. Participants then engaged in two different meal timing models – daytime-only meals (DMI), and meals taken during both daytime and nighttime (DNMC).
Depression- and anxiety-like mood levels increased by 26% and 16%, respectively, among the daytime and nighttime eaters, but there was no such increase in daytime-only eaters.
“Our findings provide evidence for the timing of food intake as a novel strategy to potentially minimize mood vulnerability in individuals experiencing circadian misalignment, such as people engaged in shift work, experiencing jet lag, or suffering from circadian rhythm disorders,” co–corresponding author Frank A.J.L. Scheer, PhD, director of the medical chronobiology program, Brigham and Women’s Hospital, Boston, said in a news release.
The study was published online in the Proceedings of the National Academy of Sciences.
Misaligned circadian clock
“Shift workers often experience a misalignment between their central circadian clock in the brain and daily behaviors, such as sleep/wake and fasting/eating cycles,” senior author Sarah Chellappa, MD, PhD, currently the Alexander Von Humboldt Experienced Fellow in the department of nuclear medicine, University of Cologne (Germany). Dr. Chellappa was a postdoctoral fellow at Brigham and Women’s Hospital when the study was conducted.
“They also have a 25%-40% higher risk of depression and anxiety,” she continued. “Since meal timing is important for physical health and diet is important for mood, we sought to find out whether meal timing can benefit mental health as well.”
Given that impaired glycemic control is a “risk factor for mood disruption,” the researchers tested the prediction that daytime eating “would prevent mood vulnerability, despite simulated night work.”
To investigate the question, they conducted a parallel-design, randomized clinical trial that included a 14-day circadian laboratory protocol with 19 healthy adults (12 men, 7 women; mean age, 26.5 ± 4.1 years) who underwent a forced desynchrony (FD) in dim light for 4 “days,” each of which consisted of 28 hours. Each 28-hour “day” resulted in an additional 4-hour misalignment between the central circadian clock and external behavioral/environmental cycles.
By the fourth day, the participants were misaligned by 12 hours, compared to baseline (that is, the first day). They were then randomly assigned to two groups.
The DNMC group – the control group – had a “typical 28-hour FD protocol,” with behavioral and environmental cycles (sleep/wake, rest/activity, supine/upright posture, dark during scheduled sleep/dim light during wakefulness) scheduled on a 28-hour cycle. Thus, they took their meals during both “daytime” and “nighttime,” which is the typical way that night workers eat.
The DMI group underwent a modified 28-hour FD protocol, with all cycles scheduled on a 28-hour basis, except for the fasting/eating cycle, which was scheduled on a 24-hour basis, resulting in meals consumed only during the “daytime.”
Depression- and anxiety-like mood (which “correspond to an amalgam of mood states typically observed in depression and anxiety) were assessed every hour during the 4 FD days, using computerized visual analogue scales.
Nutritional psychiatry
Participants in the DNMC group experienced an increase from baseline in depression- and anxiety-like mood levels of 26.2% (95% confidence interval, 21-31.5; P = .001; P value using false discovery rate, .01; effect-size r, 0.78) and 16.1% (95% CI, 8.5-23.6; P = .005; PFDR, .001; effect-size r, 0.47), respectively.
By contrast, a similar increase did not take place in the DMI group for either depression- or anxiety-like mood levels (95% CI, –5.7% to 7.4%, P not significant and 95% CI, –3.1% to 9.9%, P not significant, respectively).
The researchers tested “whether increase mood vulnerability during simulated night work was associated with the degree of internal circadian misalignment” — defined as “change in the phase difference between the acrophase of circadian glucose rhythms and the bathyphase of circadian body temperature rhythms.”
They found that a larger degree of internal circadian misalignment was “robustly associated” with more depression-like (r, 0.77; P = .001) and anxiety-like (r, 0.67; P = .002) mood levels during simulated night work.
The findings imply that meal timing had “moderate to large effects in depression-like and anxiety-like mood levels during night work, and that such effects were associated with the degree of internal circadian misalignment,” the authors wrote.
The laboratory protocol of both groups was identical except for the timing of meals. The authors noted that the “relevance of diet on sleep, circadian rhythms, and mental health is receiving growing awareness with the emergence of a new field, nutritional psychiatry.”
People who experience depression “often report poor-quality diets with high carbohydrate intake,” and there is evidence that adherence to the Mediterranean diet is associated “with lower odds of depression, anxiety, and psychological distress.”
They cautioned that although these emerging studies suggest an association between dietary factors and mental health, “experimental studies in individuals with depression and/or anxiety/anxiety-related disorders are required to determine causality and direction of effects.”
They described meal timing as “an emerging aspect of nutrition, with increasing research interest because of its influence on physical health.” However, they noted, “the causal role of the timing of food intake on mental health remains to be tested.”
Novel findings
Commenting for this article, Kathleen Merikangas, PhD, distinguished investigator and chief, genetic epidemiology research branch, intramural research program, National Institute of Mental Health, Bethesda, Md., described the research as important with novel findings.
The research “employs the elegant, carefully controlled laboratory procedures that have unraveled the influence of light and other environmental cues on sleep and circadian rhythms over the past 2 decades,” said Dr. Merikangas, who was not involved with the study.
“One of the most significant contributions of this work is its demonstration of the importance of investigating circadian rhythms of multiple systems rather than solely focusing on sleep, eating, or emotional states that have often been studied in isolation,” she pointed out.
“Growing evidence from basic research highlights the interdependence of multiple human systems that should be built into interventions that tend to focus on one or two domains.”
She recommended that this work be replicated “in more diverse samples ... in both controlled and naturalistic settings...to test both the generalizability and mechanism of these intriguing findings.”
The study was funded by the National Institutes of Health. Individual investigators were funded by the Alexander Von Humboldt Foundation and the American Diabetes Association. Dr. Chellappa disclosed no relevant financial relationships. Dr. Merikangas disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
Investigators at Brigham and Women’s Hospital, Boston, created a simulated nightwork schedule for 19 individuals in a laboratory setting. Participants then engaged in two different meal timing models – daytime-only meals (DMI), and meals taken during both daytime and nighttime (DNMC).
Depression- and anxiety-like mood levels increased by 26% and 16%, respectively, among the daytime and nighttime eaters, but there was no such increase in daytime-only eaters.
“Our findings provide evidence for the timing of food intake as a novel strategy to potentially minimize mood vulnerability in individuals experiencing circadian misalignment, such as people engaged in shift work, experiencing jet lag, or suffering from circadian rhythm disorders,” co–corresponding author Frank A.J.L. Scheer, PhD, director of the medical chronobiology program, Brigham and Women’s Hospital, Boston, said in a news release.
The study was published online in the Proceedings of the National Academy of Sciences.
Misaligned circadian clock
“Shift workers often experience a misalignment between their central circadian clock in the brain and daily behaviors, such as sleep/wake and fasting/eating cycles,” senior author Sarah Chellappa, MD, PhD, currently the Alexander Von Humboldt Experienced Fellow in the department of nuclear medicine, University of Cologne (Germany). Dr. Chellappa was a postdoctoral fellow at Brigham and Women’s Hospital when the study was conducted.
“They also have a 25%-40% higher risk of depression and anxiety,” she continued. “Since meal timing is important for physical health and diet is important for mood, we sought to find out whether meal timing can benefit mental health as well.”
Given that impaired glycemic control is a “risk factor for mood disruption,” the researchers tested the prediction that daytime eating “would prevent mood vulnerability, despite simulated night work.”
To investigate the question, they conducted a parallel-design, randomized clinical trial that included a 14-day circadian laboratory protocol with 19 healthy adults (12 men, 7 women; mean age, 26.5 ± 4.1 years) who underwent a forced desynchrony (FD) in dim light for 4 “days,” each of which consisted of 28 hours. Each 28-hour “day” resulted in an additional 4-hour misalignment between the central circadian clock and external behavioral/environmental cycles.
By the fourth day, the participants were misaligned by 12 hours, compared to baseline (that is, the first day). They were then randomly assigned to two groups.
The DNMC group – the control group – had a “typical 28-hour FD protocol,” with behavioral and environmental cycles (sleep/wake, rest/activity, supine/upright posture, dark during scheduled sleep/dim light during wakefulness) scheduled on a 28-hour cycle. Thus, they took their meals during both “daytime” and “nighttime,” which is the typical way that night workers eat.
The DMI group underwent a modified 28-hour FD protocol, with all cycles scheduled on a 28-hour basis, except for the fasting/eating cycle, which was scheduled on a 24-hour basis, resulting in meals consumed only during the “daytime.”
Depression- and anxiety-like mood (which “correspond to an amalgam of mood states typically observed in depression and anxiety) were assessed every hour during the 4 FD days, using computerized visual analogue scales.
Nutritional psychiatry
Participants in the DNMC group experienced an increase from baseline in depression- and anxiety-like mood levels of 26.2% (95% confidence interval, 21-31.5; P = .001; P value using false discovery rate, .01; effect-size r, 0.78) and 16.1% (95% CI, 8.5-23.6; P = .005; PFDR, .001; effect-size r, 0.47), respectively.
By contrast, a similar increase did not take place in the DMI group for either depression- or anxiety-like mood levels (95% CI, –5.7% to 7.4%, P not significant and 95% CI, –3.1% to 9.9%, P not significant, respectively).
The researchers tested “whether increase mood vulnerability during simulated night work was associated with the degree of internal circadian misalignment” — defined as “change in the phase difference between the acrophase of circadian glucose rhythms and the bathyphase of circadian body temperature rhythms.”
They found that a larger degree of internal circadian misalignment was “robustly associated” with more depression-like (r, 0.77; P = .001) and anxiety-like (r, 0.67; P = .002) mood levels during simulated night work.
The findings imply that meal timing had “moderate to large effects in depression-like and anxiety-like mood levels during night work, and that such effects were associated with the degree of internal circadian misalignment,” the authors wrote.
The laboratory protocol of both groups was identical except for the timing of meals. The authors noted that the “relevance of diet on sleep, circadian rhythms, and mental health is receiving growing awareness with the emergence of a new field, nutritional psychiatry.”
People who experience depression “often report poor-quality diets with high carbohydrate intake,” and there is evidence that adherence to the Mediterranean diet is associated “with lower odds of depression, anxiety, and psychological distress.”
They cautioned that although these emerging studies suggest an association between dietary factors and mental health, “experimental studies in individuals with depression and/or anxiety/anxiety-related disorders are required to determine causality and direction of effects.”
They described meal timing as “an emerging aspect of nutrition, with increasing research interest because of its influence on physical health.” However, they noted, “the causal role of the timing of food intake on mental health remains to be tested.”
Novel findings
Commenting for this article, Kathleen Merikangas, PhD, distinguished investigator and chief, genetic epidemiology research branch, intramural research program, National Institute of Mental Health, Bethesda, Md., described the research as important with novel findings.
The research “employs the elegant, carefully controlled laboratory procedures that have unraveled the influence of light and other environmental cues on sleep and circadian rhythms over the past 2 decades,” said Dr. Merikangas, who was not involved with the study.
“One of the most significant contributions of this work is its demonstration of the importance of investigating circadian rhythms of multiple systems rather than solely focusing on sleep, eating, or emotional states that have often been studied in isolation,” she pointed out.
“Growing evidence from basic research highlights the interdependence of multiple human systems that should be built into interventions that tend to focus on one or two domains.”
She recommended that this work be replicated “in more diverse samples ... in both controlled and naturalistic settings...to test both the generalizability and mechanism of these intriguing findings.”
The study was funded by the National Institutes of Health. Individual investigators were funded by the Alexander Von Humboldt Foundation and the American Diabetes Association. Dr. Chellappa disclosed no relevant financial relationships. Dr. Merikangas disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
Investigators at Brigham and Women’s Hospital, Boston, created a simulated nightwork schedule for 19 individuals in a laboratory setting. Participants then engaged in two different meal timing models – daytime-only meals (DMI), and meals taken during both daytime and nighttime (DNMC).
Depression- and anxiety-like mood levels increased by 26% and 16%, respectively, among the daytime and nighttime eaters, but there was no such increase in daytime-only eaters.
“Our findings provide evidence for the timing of food intake as a novel strategy to potentially minimize mood vulnerability in individuals experiencing circadian misalignment, such as people engaged in shift work, experiencing jet lag, or suffering from circadian rhythm disorders,” co–corresponding author Frank A.J.L. Scheer, PhD, director of the medical chronobiology program, Brigham and Women’s Hospital, Boston, said in a news release.
The study was published online in the Proceedings of the National Academy of Sciences.
Misaligned circadian clock
“Shift workers often experience a misalignment between their central circadian clock in the brain and daily behaviors, such as sleep/wake and fasting/eating cycles,” senior author Sarah Chellappa, MD, PhD, currently the Alexander Von Humboldt Experienced Fellow in the department of nuclear medicine, University of Cologne (Germany). Dr. Chellappa was a postdoctoral fellow at Brigham and Women’s Hospital when the study was conducted.
“They also have a 25%-40% higher risk of depression and anxiety,” she continued. “Since meal timing is important for physical health and diet is important for mood, we sought to find out whether meal timing can benefit mental health as well.”
Given that impaired glycemic control is a “risk factor for mood disruption,” the researchers tested the prediction that daytime eating “would prevent mood vulnerability, despite simulated night work.”
To investigate the question, they conducted a parallel-design, randomized clinical trial that included a 14-day circadian laboratory protocol with 19 healthy adults (12 men, 7 women; mean age, 26.5 ± 4.1 years) who underwent a forced desynchrony (FD) in dim light for 4 “days,” each of which consisted of 28 hours. Each 28-hour “day” resulted in an additional 4-hour misalignment between the central circadian clock and external behavioral/environmental cycles.
By the fourth day, the participants were misaligned by 12 hours, compared to baseline (that is, the first day). They were then randomly assigned to two groups.
The DNMC group – the control group – had a “typical 28-hour FD protocol,” with behavioral and environmental cycles (sleep/wake, rest/activity, supine/upright posture, dark during scheduled sleep/dim light during wakefulness) scheduled on a 28-hour cycle. Thus, they took their meals during both “daytime” and “nighttime,” which is the typical way that night workers eat.
The DMI group underwent a modified 28-hour FD protocol, with all cycles scheduled on a 28-hour basis, except for the fasting/eating cycle, which was scheduled on a 24-hour basis, resulting in meals consumed only during the “daytime.”
Depression- and anxiety-like mood (which “correspond to an amalgam of mood states typically observed in depression and anxiety) were assessed every hour during the 4 FD days, using computerized visual analogue scales.
Nutritional psychiatry
Participants in the DNMC group experienced an increase from baseline in depression- and anxiety-like mood levels of 26.2% (95% confidence interval, 21-31.5; P = .001; P value using false discovery rate, .01; effect-size r, 0.78) and 16.1% (95% CI, 8.5-23.6; P = .005; PFDR, .001; effect-size r, 0.47), respectively.
By contrast, a similar increase did not take place in the DMI group for either depression- or anxiety-like mood levels (95% CI, –5.7% to 7.4%, P not significant and 95% CI, –3.1% to 9.9%, P not significant, respectively).
The researchers tested “whether increase mood vulnerability during simulated night work was associated with the degree of internal circadian misalignment” — defined as “change in the phase difference between the acrophase of circadian glucose rhythms and the bathyphase of circadian body temperature rhythms.”
They found that a larger degree of internal circadian misalignment was “robustly associated” with more depression-like (r, 0.77; P = .001) and anxiety-like (r, 0.67; P = .002) mood levels during simulated night work.
The findings imply that meal timing had “moderate to large effects in depression-like and anxiety-like mood levels during night work, and that such effects were associated with the degree of internal circadian misalignment,” the authors wrote.
The laboratory protocol of both groups was identical except for the timing of meals. The authors noted that the “relevance of diet on sleep, circadian rhythms, and mental health is receiving growing awareness with the emergence of a new field, nutritional psychiatry.”
People who experience depression “often report poor-quality diets with high carbohydrate intake,” and there is evidence that adherence to the Mediterranean diet is associated “with lower odds of depression, anxiety, and psychological distress.”
They cautioned that although these emerging studies suggest an association between dietary factors and mental health, “experimental studies in individuals with depression and/or anxiety/anxiety-related disorders are required to determine causality and direction of effects.”
They described meal timing as “an emerging aspect of nutrition, with increasing research interest because of its influence on physical health.” However, they noted, “the causal role of the timing of food intake on mental health remains to be tested.”
Novel findings
Commenting for this article, Kathleen Merikangas, PhD, distinguished investigator and chief, genetic epidemiology research branch, intramural research program, National Institute of Mental Health, Bethesda, Md., described the research as important with novel findings.
The research “employs the elegant, carefully controlled laboratory procedures that have unraveled the influence of light and other environmental cues on sleep and circadian rhythms over the past 2 decades,” said Dr. Merikangas, who was not involved with the study.
“One of the most significant contributions of this work is its demonstration of the importance of investigating circadian rhythms of multiple systems rather than solely focusing on sleep, eating, or emotional states that have often been studied in isolation,” she pointed out.
“Growing evidence from basic research highlights the interdependence of multiple human systems that should be built into interventions that tend to focus on one or two domains.”
She recommended that this work be replicated “in more diverse samples ... in both controlled and naturalistic settings...to test both the generalizability and mechanism of these intriguing findings.”
The study was funded by the National Institutes of Health. Individual investigators were funded by the Alexander Von Humboldt Foundation and the American Diabetes Association. Dr. Chellappa disclosed no relevant financial relationships. Dr. Merikangas disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCE
‘Concerning’ rate of benzo/Z-drug use in IBD
Patients with inflammatory bowel disease (IBD) are 70% more likely to use benzodiazepines and “Z-drugs” than are the general population, a large study from Canada suggests.
Mood/anxiety disorders and sleep disorders are common in patients with IBD, but few studies have looked at use of benzodiazepines and Z-drugs (such as zolpidem, zaleplon, and eszopiclone) in this patient population.
The results are “concerning, and especially as the IBD population ages, these drugs are associated with health risks, including something as simple as falls,” first author Charles Bernstein, MD, of the IBD clinical and research centre, University of Manitoba, Winnipeg, told this news organization.
“Clinicians need to find better strategies to deal with anxiety disorders and sleep disorders in the IBD population,” Dr. Bernstein said.
The study was published online in the American Journal of Gastroenterology.
High burden of use
Using administrative data from Manitoba, Dr. Bernstein and colleagues identified 5,741 patients with IBD (2,381 with Crohn’s disease and 3,360 with ulcerative colitis) and matched them (1:5) to 28,661 population controls without IBD.
Over a 20-year period (1997-2017), there was a “high burden” of benzodiazepine and Z-drug use in the IBD population. In 2017, roughly 20% of Manitobans with IBD were using benzodiazepines, and 20% were using Z-drugs, the study team reports.
The benzodiazepine use rate (per 1,000) was 28.06 in the IBD cohort vs. 16.83 in the non-IBD population (adjusted rate ratio, 1.67). The use rate for Z-drugs was 21.07 in the IBD cohort vs. 11.26 in the non-IBD population (adjusted RR, 1.87).
Benzodiazepine use declined from 1997 to 2016, but it remained at least 50% higher in patients with IBD than in the general population over this period, the researchers found. The rate of Z-drug use also was higher in the IBD population than in the general population but remained stable over the 20-year study period.
Regardless of age, men and women had similarly high use rates for benzodiazepines, Z-drugs, and joint use of benzodiazepines and Z-drugs. The highest incidence rates for joint benzodiazepine and Z-drug use were in young adults (age 18-44 years), and these rates were similar among men and women.
Patients with IBD and a mood/anxiety disorder also were more likely to use benzodiazepines and Z-drugs and to be continuous users than were those without a mood/anxiety disorder.
Mental health and IBD go hand in hand
“The results are not very surprising, but they highlight the importance of mental health and mood disturbances in patients with IBD,” Ashwin Ananthakrishnan, MBBS, MPH, with Massachusetts General Hospital and Harvard Medical School in Boston, who wasn’t involved in the study, told this news organization.
“It is important for treating physicians to be aware of the important mental health implications of IBD diagnosis and disease activity, to screen patients for these disturbances, and to institute early effective interventions,” Dr. Ananthakrishnan said.
Also offering perspective, Laurie Keefer, PhD, academic health psychologist and director of psychobehavioral research within the division of gastroenterology, Mount Sinai Health System, New York, said that she is “concerned but not surprised” by the results of this study.
“One in three patients with IBD meets criteria for an anxiety disorder,” Dr. Keefer told this news organization.
And with the ongoing mental health crisis and shortage of mental health providers, “gastroenterologists are, unfortunately, in the position where they may have to manage these issues,” she said.
Dr. Keefer noted that when patients are first diagnosed with IBD, they will likely be on prednisone, and “an antidote” for the side effects of prednisone are benzodiazepines and sleeping medications because prednisone itself causes insomnia. “However, that’s really just a band-aid,” she said.
A major concern, said Dr. Keefer, is that young men and women who are diagnosed with IBD in their 20s may start using these drugs and become reliant on them.
“People do build up a tolerance to these drugs, so they need more and more to receive the same effect,” she said.
A better approach is to figure out why patients are so anxious and teach them skills to manage their anxiety and sleep problems so that they’re not dependent on these drugs, Dr. Keefer said.
“There are behavioral strategies that can help. These are harder to do, and they’re not a quick fix. However, they are skills you can learn in your 20s and so when you have an IBD flare at 50, you have the skills to deal with it,” she said.
“We just have to be a little more proactive in really encouraging patients to learn disease management skills,” Dr. Keefer added.
The study was funded by the Canadian Institutes of Health Research and Crohn’s and Colitis Canada. Dr. Bernstein has disclosed relationships with AbbVie Canada, Amgen Canada, Bristol-Myers Squibb Canada, Roche Canada, Janssen Canada, Sandoz Canada, Takeda and Takeda Canada, Pfizer Canada, Mylan Pharmaceuticals, and Medtronic Canada. Dr. Ananthakrishnan and Dr. Keefer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients with inflammatory bowel disease (IBD) are 70% more likely to use benzodiazepines and “Z-drugs” than are the general population, a large study from Canada suggests.
Mood/anxiety disorders and sleep disorders are common in patients with IBD, but few studies have looked at use of benzodiazepines and Z-drugs (such as zolpidem, zaleplon, and eszopiclone) in this patient population.
The results are “concerning, and especially as the IBD population ages, these drugs are associated with health risks, including something as simple as falls,” first author Charles Bernstein, MD, of the IBD clinical and research centre, University of Manitoba, Winnipeg, told this news organization.
“Clinicians need to find better strategies to deal with anxiety disorders and sleep disorders in the IBD population,” Dr. Bernstein said.
The study was published online in the American Journal of Gastroenterology.
High burden of use
Using administrative data from Manitoba, Dr. Bernstein and colleagues identified 5,741 patients with IBD (2,381 with Crohn’s disease and 3,360 with ulcerative colitis) and matched them (1:5) to 28,661 population controls without IBD.
Over a 20-year period (1997-2017), there was a “high burden” of benzodiazepine and Z-drug use in the IBD population. In 2017, roughly 20% of Manitobans with IBD were using benzodiazepines, and 20% were using Z-drugs, the study team reports.
The benzodiazepine use rate (per 1,000) was 28.06 in the IBD cohort vs. 16.83 in the non-IBD population (adjusted rate ratio, 1.67). The use rate for Z-drugs was 21.07 in the IBD cohort vs. 11.26 in the non-IBD population (adjusted RR, 1.87).
Benzodiazepine use declined from 1997 to 2016, but it remained at least 50% higher in patients with IBD than in the general population over this period, the researchers found. The rate of Z-drug use also was higher in the IBD population than in the general population but remained stable over the 20-year study period.
Regardless of age, men and women had similarly high use rates for benzodiazepines, Z-drugs, and joint use of benzodiazepines and Z-drugs. The highest incidence rates for joint benzodiazepine and Z-drug use were in young adults (age 18-44 years), and these rates were similar among men and women.
Patients with IBD and a mood/anxiety disorder also were more likely to use benzodiazepines and Z-drugs and to be continuous users than were those without a mood/anxiety disorder.
Mental health and IBD go hand in hand
“The results are not very surprising, but they highlight the importance of mental health and mood disturbances in patients with IBD,” Ashwin Ananthakrishnan, MBBS, MPH, with Massachusetts General Hospital and Harvard Medical School in Boston, who wasn’t involved in the study, told this news organization.
“It is important for treating physicians to be aware of the important mental health implications of IBD diagnosis and disease activity, to screen patients for these disturbances, and to institute early effective interventions,” Dr. Ananthakrishnan said.
Also offering perspective, Laurie Keefer, PhD, academic health psychologist and director of psychobehavioral research within the division of gastroenterology, Mount Sinai Health System, New York, said that she is “concerned but not surprised” by the results of this study.
“One in three patients with IBD meets criteria for an anxiety disorder,” Dr. Keefer told this news organization.
And with the ongoing mental health crisis and shortage of mental health providers, “gastroenterologists are, unfortunately, in the position where they may have to manage these issues,” she said.
Dr. Keefer noted that when patients are first diagnosed with IBD, they will likely be on prednisone, and “an antidote” for the side effects of prednisone are benzodiazepines and sleeping medications because prednisone itself causes insomnia. “However, that’s really just a band-aid,” she said.
A major concern, said Dr. Keefer, is that young men and women who are diagnosed with IBD in their 20s may start using these drugs and become reliant on them.
“People do build up a tolerance to these drugs, so they need more and more to receive the same effect,” she said.
A better approach is to figure out why patients are so anxious and teach them skills to manage their anxiety and sleep problems so that they’re not dependent on these drugs, Dr. Keefer said.
“There are behavioral strategies that can help. These are harder to do, and they’re not a quick fix. However, they are skills you can learn in your 20s and so when you have an IBD flare at 50, you have the skills to deal with it,” she said.
“We just have to be a little more proactive in really encouraging patients to learn disease management skills,” Dr. Keefer added.
The study was funded by the Canadian Institutes of Health Research and Crohn’s and Colitis Canada. Dr. Bernstein has disclosed relationships with AbbVie Canada, Amgen Canada, Bristol-Myers Squibb Canada, Roche Canada, Janssen Canada, Sandoz Canada, Takeda and Takeda Canada, Pfizer Canada, Mylan Pharmaceuticals, and Medtronic Canada. Dr. Ananthakrishnan and Dr. Keefer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients with inflammatory bowel disease (IBD) are 70% more likely to use benzodiazepines and “Z-drugs” than are the general population, a large study from Canada suggests.
Mood/anxiety disorders and sleep disorders are common in patients with IBD, but few studies have looked at use of benzodiazepines and Z-drugs (such as zolpidem, zaleplon, and eszopiclone) in this patient population.
The results are “concerning, and especially as the IBD population ages, these drugs are associated with health risks, including something as simple as falls,” first author Charles Bernstein, MD, of the IBD clinical and research centre, University of Manitoba, Winnipeg, told this news organization.
“Clinicians need to find better strategies to deal with anxiety disorders and sleep disorders in the IBD population,” Dr. Bernstein said.
The study was published online in the American Journal of Gastroenterology.
High burden of use
Using administrative data from Manitoba, Dr. Bernstein and colleagues identified 5,741 patients with IBD (2,381 with Crohn’s disease and 3,360 with ulcerative colitis) and matched them (1:5) to 28,661 population controls without IBD.
Over a 20-year period (1997-2017), there was a “high burden” of benzodiazepine and Z-drug use in the IBD population. In 2017, roughly 20% of Manitobans with IBD were using benzodiazepines, and 20% were using Z-drugs, the study team reports.
The benzodiazepine use rate (per 1,000) was 28.06 in the IBD cohort vs. 16.83 in the non-IBD population (adjusted rate ratio, 1.67). The use rate for Z-drugs was 21.07 in the IBD cohort vs. 11.26 in the non-IBD population (adjusted RR, 1.87).
Benzodiazepine use declined from 1997 to 2016, but it remained at least 50% higher in patients with IBD than in the general population over this period, the researchers found. The rate of Z-drug use also was higher in the IBD population than in the general population but remained stable over the 20-year study period.
Regardless of age, men and women had similarly high use rates for benzodiazepines, Z-drugs, and joint use of benzodiazepines and Z-drugs. The highest incidence rates for joint benzodiazepine and Z-drug use were in young adults (age 18-44 years), and these rates were similar among men and women.
Patients with IBD and a mood/anxiety disorder also were more likely to use benzodiazepines and Z-drugs and to be continuous users than were those without a mood/anxiety disorder.
Mental health and IBD go hand in hand
“The results are not very surprising, but they highlight the importance of mental health and mood disturbances in patients with IBD,” Ashwin Ananthakrishnan, MBBS, MPH, with Massachusetts General Hospital and Harvard Medical School in Boston, who wasn’t involved in the study, told this news organization.
“It is important for treating physicians to be aware of the important mental health implications of IBD diagnosis and disease activity, to screen patients for these disturbances, and to institute early effective interventions,” Dr. Ananthakrishnan said.
Also offering perspective, Laurie Keefer, PhD, academic health psychologist and director of psychobehavioral research within the division of gastroenterology, Mount Sinai Health System, New York, said that she is “concerned but not surprised” by the results of this study.
“One in three patients with IBD meets criteria for an anxiety disorder,” Dr. Keefer told this news organization.
And with the ongoing mental health crisis and shortage of mental health providers, “gastroenterologists are, unfortunately, in the position where they may have to manage these issues,” she said.
Dr. Keefer noted that when patients are first diagnosed with IBD, they will likely be on prednisone, and “an antidote” for the side effects of prednisone are benzodiazepines and sleeping medications because prednisone itself causes insomnia. “However, that’s really just a band-aid,” she said.
A major concern, said Dr. Keefer, is that young men and women who are diagnosed with IBD in their 20s may start using these drugs and become reliant on them.
“People do build up a tolerance to these drugs, so they need more and more to receive the same effect,” she said.
A better approach is to figure out why patients are so anxious and teach them skills to manage their anxiety and sleep problems so that they’re not dependent on these drugs, Dr. Keefer said.
“There are behavioral strategies that can help. These are harder to do, and they’re not a quick fix. However, they are skills you can learn in your 20s and so when you have an IBD flare at 50, you have the skills to deal with it,” she said.
“We just have to be a little more proactive in really encouraging patients to learn disease management skills,” Dr. Keefer added.
The study was funded by the Canadian Institutes of Health Research and Crohn’s and Colitis Canada. Dr. Bernstein has disclosed relationships with AbbVie Canada, Amgen Canada, Bristol-Myers Squibb Canada, Roche Canada, Janssen Canada, Sandoz Canada, Takeda and Takeda Canada, Pfizer Canada, Mylan Pharmaceuticals, and Medtronic Canada. Dr. Ananthakrishnan and Dr. Keefer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AMERICAN JOURNAL OF GASTROENTEROLOGY
USPSTF recommends anxiety screening in adults younger than 65
For the first time, the task force is recommending screening all adults aged 64 and younger for anxiety – including pregnant and postpartum women.
This “B” recommendation reflects “moderate certainty” evidence that screening for anxiety in this population has a moderate net benefit, the task force notes in a draft recommendation statement posted on its website.
The recommendation applies to adults aged 19-64 years who do not have a diagnosed mental health disorder or are not showing recognized signs or symptoms of anxiety.
Anxiety disorders are common and often go unrecognized in primary care, leading to long delays in treatment, the task force writes. They add that more evidence is needed to identify ideal screening intervals for all populations.
“A pragmatic approach in the absence of data might include screening all adults who have not been screened previously and using clinical judgment in consideration of risk factors, comorbid conditions, and life events to determine if additional screening of high-risk patients is warranted,” they write.
For adults aged 65 and older, the task force found “insufficient” evidence on the benefits and potential harms of screening for anxiety.
“Evidence on the accuracy of screening tools and the benefits and harms of screening and treatment of screen-detected anxiety in older adults is lacking, and the balance of benefits and harms cannot be determined,” they write.
Jury out on screening for suicide risk
The task force is continuing to recommend screening all adults for depression. This “B” recommendation reflects moderate-certainty evidence that screening for major depression in adults has a moderate net benefit.
However, they note there is not enough evidence to recommend for or against screening for suicide risk in all adults.
They therefore issued an “I” statement, indicating that the balance of benefits and harms cannot be determined at present.
“To address the critical need for supporting the mental health of adults in primary care, the Task Force reviewed the evidence on screening for anxiety, depression, and suicide risk,” task force member Lori Pbert, PhD, University of Massachusetts, Worcester, said in a news release.
“The good news is that screening all adults for depression, including those who are pregnant and postpartum, and screening adults younger than 65 for anxiety can help identify these conditions early so people can be connected to care,” Dr. Pbert said.
“Unfortunately, evidence is limited on screening adults 65 or older for anxiety and screening all adults for suicide risk, so we are urgently calling for more research,” added task force member Gbenga Ogedegbe, MD, MPH, founding director of the Institute for Excellence in Health Equity at NYU Langone Health.
Dr. Ogedegbe, also a professor at New York University, noted that “in the absence of evidence, health care professionals should use their judgment based on individual patient circumstances when determining whether or not to screen.”
The public comment period for the draft recommendations runs until Oct. 17.
A version of this article first appeared on Medscape.com.
For the first time, the task force is recommending screening all adults aged 64 and younger for anxiety – including pregnant and postpartum women.
This “B” recommendation reflects “moderate certainty” evidence that screening for anxiety in this population has a moderate net benefit, the task force notes in a draft recommendation statement posted on its website.
The recommendation applies to adults aged 19-64 years who do not have a diagnosed mental health disorder or are not showing recognized signs or symptoms of anxiety.
Anxiety disorders are common and often go unrecognized in primary care, leading to long delays in treatment, the task force writes. They add that more evidence is needed to identify ideal screening intervals for all populations.
“A pragmatic approach in the absence of data might include screening all adults who have not been screened previously and using clinical judgment in consideration of risk factors, comorbid conditions, and life events to determine if additional screening of high-risk patients is warranted,” they write.
For adults aged 65 and older, the task force found “insufficient” evidence on the benefits and potential harms of screening for anxiety.
“Evidence on the accuracy of screening tools and the benefits and harms of screening and treatment of screen-detected anxiety in older adults is lacking, and the balance of benefits and harms cannot be determined,” they write.
Jury out on screening for suicide risk
The task force is continuing to recommend screening all adults for depression. This “B” recommendation reflects moderate-certainty evidence that screening for major depression in adults has a moderate net benefit.
However, they note there is not enough evidence to recommend for or against screening for suicide risk in all adults.
They therefore issued an “I” statement, indicating that the balance of benefits and harms cannot be determined at present.
“To address the critical need for supporting the mental health of adults in primary care, the Task Force reviewed the evidence on screening for anxiety, depression, and suicide risk,” task force member Lori Pbert, PhD, University of Massachusetts, Worcester, said in a news release.
“The good news is that screening all adults for depression, including those who are pregnant and postpartum, and screening adults younger than 65 for anxiety can help identify these conditions early so people can be connected to care,” Dr. Pbert said.
“Unfortunately, evidence is limited on screening adults 65 or older for anxiety and screening all adults for suicide risk, so we are urgently calling for more research,” added task force member Gbenga Ogedegbe, MD, MPH, founding director of the Institute for Excellence in Health Equity at NYU Langone Health.
Dr. Ogedegbe, also a professor at New York University, noted that “in the absence of evidence, health care professionals should use their judgment based on individual patient circumstances when determining whether or not to screen.”
The public comment period for the draft recommendations runs until Oct. 17.
A version of this article first appeared on Medscape.com.
For the first time, the task force is recommending screening all adults aged 64 and younger for anxiety – including pregnant and postpartum women.
This “B” recommendation reflects “moderate certainty” evidence that screening for anxiety in this population has a moderate net benefit, the task force notes in a draft recommendation statement posted on its website.
The recommendation applies to adults aged 19-64 years who do not have a diagnosed mental health disorder or are not showing recognized signs or symptoms of anxiety.
Anxiety disorders are common and often go unrecognized in primary care, leading to long delays in treatment, the task force writes. They add that more evidence is needed to identify ideal screening intervals for all populations.
“A pragmatic approach in the absence of data might include screening all adults who have not been screened previously and using clinical judgment in consideration of risk factors, comorbid conditions, and life events to determine if additional screening of high-risk patients is warranted,” they write.
For adults aged 65 and older, the task force found “insufficient” evidence on the benefits and potential harms of screening for anxiety.
“Evidence on the accuracy of screening tools and the benefits and harms of screening and treatment of screen-detected anxiety in older adults is lacking, and the balance of benefits and harms cannot be determined,” they write.
Jury out on screening for suicide risk
The task force is continuing to recommend screening all adults for depression. This “B” recommendation reflects moderate-certainty evidence that screening for major depression in adults has a moderate net benefit.
However, they note there is not enough evidence to recommend for or against screening for suicide risk in all adults.
They therefore issued an “I” statement, indicating that the balance of benefits and harms cannot be determined at present.
“To address the critical need for supporting the mental health of adults in primary care, the Task Force reviewed the evidence on screening for anxiety, depression, and suicide risk,” task force member Lori Pbert, PhD, University of Massachusetts, Worcester, said in a news release.
“The good news is that screening all adults for depression, including those who are pregnant and postpartum, and screening adults younger than 65 for anxiety can help identify these conditions early so people can be connected to care,” Dr. Pbert said.
“Unfortunately, evidence is limited on screening adults 65 or older for anxiety and screening all adults for suicide risk, so we are urgently calling for more research,” added task force member Gbenga Ogedegbe, MD, MPH, founding director of the Institute for Excellence in Health Equity at NYU Langone Health.
Dr. Ogedegbe, also a professor at New York University, noted that “in the absence of evidence, health care professionals should use their judgment based on individual patient circumstances when determining whether or not to screen.”
The public comment period for the draft recommendations runs until Oct. 17.
A version of this article first appeared on Medscape.com.
Ketamine linked to reduced suicidal thoughts, depression, anxiety
, new research suggests.
Results from a retrospective chart review analysis, which included more than 400 participants with TRD, illustrate that ketamine is a safe and rapid treatment in a real-world patient population, lead author Patrick A. Oliver, MD, founder and medical director, MindPeace Clinics, Richmond, Va., told this news organization.
The effect was perhaps most notable for reducing suicidal ideation, he said.
“In 2 weeks, we can take somebody from being suicidal to nonsuicidal. It’s a total game changer,” Dr. Oliver added.
Every year in the United States, about 12 million individuals think about suicide, 3.2 million make a plan to kill themselves, and more than 46,000 succeed, the investigators note.
The findings were published online in the Journal of Clinical Psychiatry.
Molecule mixture
Primarily used as an anesthetic in hospitals, ketamine is also taken illegally as a recreational drug. Users may aim for an intense high or feeling of dissociation, or an out-of-body–type experience.
Ketamine is a mixture of two mirror-image molecules. An intranasal version of one of these molecules (esketamine) is approved by the U.S. Food and Drug Administration for TRD. Both esketamine and ketamine are believed to increase neurotrophic signaling that affects synaptic function.
The study included 424 patients (mean age, 41.7 years) with major depressive disorder or another mood disorder and who received at least one ketamine infusion at a specialty clinic. Most participants had failed prior medication trials.
Patients in the study were typically started on 0.5 mg/kg of ketamine, with the dose titrated to achieve symptoms of partial dissociation. The median dose administered after titration was 0.93 mg/kg over 40 minutes.
The main treatment course of at least six infusions within 21 days was completed by 70% of the patients.
At each clinic visit, all participants completed the Patient Health Questionnaire-9 (PHQ-9) and the Generalized Anxiety Disorder-7 (GAD-7).
The primary outcome was PHQ-9 total scores, for which researchers looked at seven time periods: 1 week, 2-3 weeks, 4-6 weeks, 7-12 weeks, 13-24 weeks, 25-51 weeks, and 52+ weeks.
‘Blows it out of the water’
Results showed PHQ-9 total scores declined by 50% throughout the course of treatment, with much of the improvement gained within 4-6 weeks. There was a significant difference between week 1 and all later time periods (all P values < .001) and between weeks 2 and 3 and all later periods (all P values < .001).
Other measures included treatment response, defined as at least a 50% improvement on the PHQ-9, and depression remission, defined as a PHQ-9 score of less than 5. After three infusions, 14% of the patients responded and 7% were in remission. After 10 infusions, 72% responded and 38% were in remission.
These results compare favorably to other depression treatments, said Dr. Oliver. “Truthfully, with the exception of ECT [electroconvulsive therapy], this blows it all out of the water,” he added.
Dr. Oliver noted that the success rate for repetitive transcranial magnetic stimulation is 40%-60% depending on the modality; and for selective serotonin reuptake inhibitors, the success rate “is somewhere between the mid-20s and low-30s percent range.”
Another outcome measure was the self-harm/suicidal ideation item of the PHQ-9 questionnaire, which asks about “thoughts that you would be better off dead, or of hurting yourself in some way.” About 22% of the study participants no longer reported suicidal ideation after 3 infusions, 50% by 6 infusions, and 75% by 10 infusions.
By 15 infusions, 85% no longer reported these thoughts. “Nothing else has shown that, ever,” said Dr. Oliver.
Symptoms of generalized anxiety were also substantially improved. There was about a 30% reduction in the GAD-7 score during treatment and, again, most of the response occurred by 4-6 weeks.
Study limitations
Sex, age, and other demographic characteristics did not predict response or remission, but suicide planning trended toward higher response rates (P = .083). This suggests that a more depressed subgroup can achieve greater benefit from the treatment than can less symptomatic patients, the investigators note.
A history of psychosis also trended toward better response to treatment (P = .086) but not remission.
The researchers note that study limitations include that it was retrospective, lacked a control group, and did not require patients to be hospitalized – so the study sample may have been less severely ill than in other studies.
In addition, most patients paid out of pocket for the treatment at $495 per infusion, and they self-reported their symptoms.
As well, the researchers did not assess adverse events, although nurses made follow-up calls to patients. Dr. Oliver noted the most common side effects of ketamine are nausea, vomiting, and anxiety.
Previous research has suggested that ketamine therapy is not linked to long-term side effects, such as sexual dysfunction, weight gain, lethargy, or cognitive issues, said Dr. Oliver.
The investigators point out another study limitation was lack of detailed demographic information, such as race, income, and education, which might affect its generalizability.
Concerns and questions
Pouya Movahed Rad, MD, PhD, senior consultant and researcher in psychiatry, Lund (Sweden) University, noted several concerns, including that the clinics treating the study participants with ketamine profited from it.
He also speculated about who can afford the treatment because only a few patients in the study were reimbursed through insurance.
Dr. Movahed Rad was not involved with the current research but was principal investigator for a recent study that compared intravenous ketamine to ECT.
He questioned whether the patient population in the new study really was “real world.” Well-designed randomized controlled trials have been carried out in a “naturalistic setting, [which] get closer to real-life patients,” he said.
He also noted that the median dose after clinician titration (0.93 mg/kg over 40 minutes) “may be considered very high.”
With regard to doses being titrated to achieve symptoms of partial dissociation, “there is no obvious evidence to my knowledge that patients need to develop dissociative symptoms in order to have antidepressant effect,” said Dr. Movahed Rad.
Finally, he noted that the finding that 28% of the participants were using illegal drugs “is worrying” and wondered what drugs they were taking; he also questioned why 81% of the study population needed to take antidepressants.
The study did not receive outside funding. Dr. Oliver is the founder of MindPeace Clinics, which specialize in ketamine therapeutics. Dr. Movahed Rad has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
Results from a retrospective chart review analysis, which included more than 400 participants with TRD, illustrate that ketamine is a safe and rapid treatment in a real-world patient population, lead author Patrick A. Oliver, MD, founder and medical director, MindPeace Clinics, Richmond, Va., told this news organization.
The effect was perhaps most notable for reducing suicidal ideation, he said.
“In 2 weeks, we can take somebody from being suicidal to nonsuicidal. It’s a total game changer,” Dr. Oliver added.
Every year in the United States, about 12 million individuals think about suicide, 3.2 million make a plan to kill themselves, and more than 46,000 succeed, the investigators note.
The findings were published online in the Journal of Clinical Psychiatry.
Molecule mixture
Primarily used as an anesthetic in hospitals, ketamine is also taken illegally as a recreational drug. Users may aim for an intense high or feeling of dissociation, or an out-of-body–type experience.
Ketamine is a mixture of two mirror-image molecules. An intranasal version of one of these molecules (esketamine) is approved by the U.S. Food and Drug Administration for TRD. Both esketamine and ketamine are believed to increase neurotrophic signaling that affects synaptic function.
The study included 424 patients (mean age, 41.7 years) with major depressive disorder or another mood disorder and who received at least one ketamine infusion at a specialty clinic. Most participants had failed prior medication trials.
Patients in the study were typically started on 0.5 mg/kg of ketamine, with the dose titrated to achieve symptoms of partial dissociation. The median dose administered after titration was 0.93 mg/kg over 40 minutes.
The main treatment course of at least six infusions within 21 days was completed by 70% of the patients.
At each clinic visit, all participants completed the Patient Health Questionnaire-9 (PHQ-9) and the Generalized Anxiety Disorder-7 (GAD-7).
The primary outcome was PHQ-9 total scores, for which researchers looked at seven time periods: 1 week, 2-3 weeks, 4-6 weeks, 7-12 weeks, 13-24 weeks, 25-51 weeks, and 52+ weeks.
‘Blows it out of the water’
Results showed PHQ-9 total scores declined by 50% throughout the course of treatment, with much of the improvement gained within 4-6 weeks. There was a significant difference between week 1 and all later time periods (all P values < .001) and between weeks 2 and 3 and all later periods (all P values < .001).
Other measures included treatment response, defined as at least a 50% improvement on the PHQ-9, and depression remission, defined as a PHQ-9 score of less than 5. After three infusions, 14% of the patients responded and 7% were in remission. After 10 infusions, 72% responded and 38% were in remission.
These results compare favorably to other depression treatments, said Dr. Oliver. “Truthfully, with the exception of ECT [electroconvulsive therapy], this blows it all out of the water,” he added.
Dr. Oliver noted that the success rate for repetitive transcranial magnetic stimulation is 40%-60% depending on the modality; and for selective serotonin reuptake inhibitors, the success rate “is somewhere between the mid-20s and low-30s percent range.”
Another outcome measure was the self-harm/suicidal ideation item of the PHQ-9 questionnaire, which asks about “thoughts that you would be better off dead, or of hurting yourself in some way.” About 22% of the study participants no longer reported suicidal ideation after 3 infusions, 50% by 6 infusions, and 75% by 10 infusions.
By 15 infusions, 85% no longer reported these thoughts. “Nothing else has shown that, ever,” said Dr. Oliver.
Symptoms of generalized anxiety were also substantially improved. There was about a 30% reduction in the GAD-7 score during treatment and, again, most of the response occurred by 4-6 weeks.
Study limitations
Sex, age, and other demographic characteristics did not predict response or remission, but suicide planning trended toward higher response rates (P = .083). This suggests that a more depressed subgroup can achieve greater benefit from the treatment than can less symptomatic patients, the investigators note.
A history of psychosis also trended toward better response to treatment (P = .086) but not remission.
The researchers note that study limitations include that it was retrospective, lacked a control group, and did not require patients to be hospitalized – so the study sample may have been less severely ill than in other studies.
In addition, most patients paid out of pocket for the treatment at $495 per infusion, and they self-reported their symptoms.
As well, the researchers did not assess adverse events, although nurses made follow-up calls to patients. Dr. Oliver noted the most common side effects of ketamine are nausea, vomiting, and anxiety.
Previous research has suggested that ketamine therapy is not linked to long-term side effects, such as sexual dysfunction, weight gain, lethargy, or cognitive issues, said Dr. Oliver.
The investigators point out another study limitation was lack of detailed demographic information, such as race, income, and education, which might affect its generalizability.
Concerns and questions
Pouya Movahed Rad, MD, PhD, senior consultant and researcher in psychiatry, Lund (Sweden) University, noted several concerns, including that the clinics treating the study participants with ketamine profited from it.
He also speculated about who can afford the treatment because only a few patients in the study were reimbursed through insurance.
Dr. Movahed Rad was not involved with the current research but was principal investigator for a recent study that compared intravenous ketamine to ECT.
He questioned whether the patient population in the new study really was “real world.” Well-designed randomized controlled trials have been carried out in a “naturalistic setting, [which] get closer to real-life patients,” he said.
He also noted that the median dose after clinician titration (0.93 mg/kg over 40 minutes) “may be considered very high.”
With regard to doses being titrated to achieve symptoms of partial dissociation, “there is no obvious evidence to my knowledge that patients need to develop dissociative symptoms in order to have antidepressant effect,” said Dr. Movahed Rad.
Finally, he noted that the finding that 28% of the participants were using illegal drugs “is worrying” and wondered what drugs they were taking; he also questioned why 81% of the study population needed to take antidepressants.
The study did not receive outside funding. Dr. Oliver is the founder of MindPeace Clinics, which specialize in ketamine therapeutics. Dr. Movahed Rad has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
Results from a retrospective chart review analysis, which included more than 400 participants with TRD, illustrate that ketamine is a safe and rapid treatment in a real-world patient population, lead author Patrick A. Oliver, MD, founder and medical director, MindPeace Clinics, Richmond, Va., told this news organization.
The effect was perhaps most notable for reducing suicidal ideation, he said.
“In 2 weeks, we can take somebody from being suicidal to nonsuicidal. It’s a total game changer,” Dr. Oliver added.
Every year in the United States, about 12 million individuals think about suicide, 3.2 million make a plan to kill themselves, and more than 46,000 succeed, the investigators note.
The findings were published online in the Journal of Clinical Psychiatry.
Molecule mixture
Primarily used as an anesthetic in hospitals, ketamine is also taken illegally as a recreational drug. Users may aim for an intense high or feeling of dissociation, or an out-of-body–type experience.
Ketamine is a mixture of two mirror-image molecules. An intranasal version of one of these molecules (esketamine) is approved by the U.S. Food and Drug Administration for TRD. Both esketamine and ketamine are believed to increase neurotrophic signaling that affects synaptic function.
The study included 424 patients (mean age, 41.7 years) with major depressive disorder or another mood disorder and who received at least one ketamine infusion at a specialty clinic. Most participants had failed prior medication trials.
Patients in the study were typically started on 0.5 mg/kg of ketamine, with the dose titrated to achieve symptoms of partial dissociation. The median dose administered after titration was 0.93 mg/kg over 40 minutes.
The main treatment course of at least six infusions within 21 days was completed by 70% of the patients.
At each clinic visit, all participants completed the Patient Health Questionnaire-9 (PHQ-9) and the Generalized Anxiety Disorder-7 (GAD-7).
The primary outcome was PHQ-9 total scores, for which researchers looked at seven time periods: 1 week, 2-3 weeks, 4-6 weeks, 7-12 weeks, 13-24 weeks, 25-51 weeks, and 52+ weeks.
‘Blows it out of the water’
Results showed PHQ-9 total scores declined by 50% throughout the course of treatment, with much of the improvement gained within 4-6 weeks. There was a significant difference between week 1 and all later time periods (all P values < .001) and between weeks 2 and 3 and all later periods (all P values < .001).
Other measures included treatment response, defined as at least a 50% improvement on the PHQ-9, and depression remission, defined as a PHQ-9 score of less than 5. After three infusions, 14% of the patients responded and 7% were in remission. After 10 infusions, 72% responded and 38% were in remission.
These results compare favorably to other depression treatments, said Dr. Oliver. “Truthfully, with the exception of ECT [electroconvulsive therapy], this blows it all out of the water,” he added.
Dr. Oliver noted that the success rate for repetitive transcranial magnetic stimulation is 40%-60% depending on the modality; and for selective serotonin reuptake inhibitors, the success rate “is somewhere between the mid-20s and low-30s percent range.”
Another outcome measure was the self-harm/suicidal ideation item of the PHQ-9 questionnaire, which asks about “thoughts that you would be better off dead, or of hurting yourself in some way.” About 22% of the study participants no longer reported suicidal ideation after 3 infusions, 50% by 6 infusions, and 75% by 10 infusions.
By 15 infusions, 85% no longer reported these thoughts. “Nothing else has shown that, ever,” said Dr. Oliver.
Symptoms of generalized anxiety were also substantially improved. There was about a 30% reduction in the GAD-7 score during treatment and, again, most of the response occurred by 4-6 weeks.
Study limitations
Sex, age, and other demographic characteristics did not predict response or remission, but suicide planning trended toward higher response rates (P = .083). This suggests that a more depressed subgroup can achieve greater benefit from the treatment than can less symptomatic patients, the investigators note.
A history of psychosis also trended toward better response to treatment (P = .086) but not remission.
The researchers note that study limitations include that it was retrospective, lacked a control group, and did not require patients to be hospitalized – so the study sample may have been less severely ill than in other studies.
In addition, most patients paid out of pocket for the treatment at $495 per infusion, and they self-reported their symptoms.
As well, the researchers did not assess adverse events, although nurses made follow-up calls to patients. Dr. Oliver noted the most common side effects of ketamine are nausea, vomiting, and anxiety.
Previous research has suggested that ketamine therapy is not linked to long-term side effects, such as sexual dysfunction, weight gain, lethargy, or cognitive issues, said Dr. Oliver.
The investigators point out another study limitation was lack of detailed demographic information, such as race, income, and education, which might affect its generalizability.
Concerns and questions
Pouya Movahed Rad, MD, PhD, senior consultant and researcher in psychiatry, Lund (Sweden) University, noted several concerns, including that the clinics treating the study participants with ketamine profited from it.
He also speculated about who can afford the treatment because only a few patients in the study were reimbursed through insurance.
Dr. Movahed Rad was not involved with the current research but was principal investigator for a recent study that compared intravenous ketamine to ECT.
He questioned whether the patient population in the new study really was “real world.” Well-designed randomized controlled trials have been carried out in a “naturalistic setting, [which] get closer to real-life patients,” he said.
He also noted that the median dose after clinician titration (0.93 mg/kg over 40 minutes) “may be considered very high.”
With regard to doses being titrated to achieve symptoms of partial dissociation, “there is no obvious evidence to my knowledge that patients need to develop dissociative symptoms in order to have antidepressant effect,” said Dr. Movahed Rad.
Finally, he noted that the finding that 28% of the participants were using illegal drugs “is worrying” and wondered what drugs they were taking; he also questioned why 81% of the study population needed to take antidepressants.
The study did not receive outside funding. Dr. Oliver is the founder of MindPeace Clinics, which specialize in ketamine therapeutics. Dr. Movahed Rad has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF CLINICAL PSYCHIATRY
Me, my spouse, and COVID
Managing family conflict and cohesion
I watched you in the garage, with your wipes and your mask, your gloves and bottles of sprays and potions. I admired your fealty to CNN’s Dr. Sanjay Gupta as he demonstrated the proper technique for disinfecting groceries. I watched sterile protocol being broken and quietly closed the garage door.
I listened to your descriptions of the agility of the virus with each exhalation of breath, and how far the virus could travel with a tailwind and in cold dry air. I listen as closely and with the same intention as I listen to my yoga teacher’s explication of the benefits of attention to the breath.
Relatives and friends came prepared to be entertained outdoors. Even masked, you eschewed the world. Your version of science clashes with my laissez-faire attitude. We blow up as a couple. Then we settle down and learn how to cope with the stress, as a team, together.
The COVID factor
In the first few months of any stressor, family and couple functioning must reorganize to manage well.
During lockdown, social scientists accessed an eager public ready to participate in their studies. With nowhere to go, many people, especially women, completed online COVID surveys. Community-based tools such as the Centers for Disease Control and Prevention’s Social Vulnerability Index identified populations of high social vulnerability (as caused by external stresses on human health, such as unemployment, overcrowding, presence of an individual with caregiving needs, and low educational attainment). It is assumed that such populations will experience more stress and have more difficulty coping and adjusting.
In a study by a team at the University of Miami, social vulnerability was associated with more disrupted family functioning, except when households with children (n = 2,666) were compared to households without children (n = 1,456).1 What allowed these families with children to enjoy better functioning?
Looking more closely at the Miami study, what can we find? It is a large survey study (n = 4,122), disseminated through professional networks and social media via purchased Facebook and Instagram ads. Data were logged in REDCap, and participants had the option of taking the survey in English or Spanish. Most participants were female (93.5%), 55.7% responded in English, and 44.3% in Spanish. There were few differences between the women who had and did not have children, in terms of their age, employment status, and education level. The number of children in the household did not affect the results.
This study used a new tool called the COVID-19 Household Environment Scale. This tool has 25 items measuring individual and household characteristics, and associated COVID-19 stressors. This tool also includes two family functioning measures: conflict and cohesion, asking the respondent to reflect on the change in “conflict” or “togetherness,” as it relates to household experiences and activities, compared with the period before social distancing.
The surprising finding was that even though households with children reported more conflict than before the start of the pandemic, they also reported more cohesion. This syncs with my experience. My niece and nephew found that having their teenage children at home brought them closer as a family, cut down on some of the extracurricular activities they did not support, and generally “slowed the world down.”
However, in a study in Germany, survey respondents (n = 1,042) noted that having children up to 17 years old was associated with decreases in satisfaction with family life, although this was not related to changes in family demands. The study assessed changes over 6 months and underscores the fact that perceptions of family demands and family well-being are independent of each other.2
These findings also resonate with prior research that measured burden and reward in couples. High burden is not associated with low reward; these two constructs are independent of each other.3
What about couples?
It is no surprise that poor relationships begat poor coping. In an online Belgian survey of 1,491 cohabiting couples during the shutdown, both men and women felt significantly more stress than before, because they felt restricted in their relationship.4
However, only women reported significantly more stress during the lockdown than before, because of relationship conflicts, such as feeling neglected by their partner. These feelings had predated lockdown.
In another lockdown online survey of 782 U.S. adults (89.8% White, 84.5% female), cohabitating intimate partners reported that there were higher thoughts of separation if the participants were younger, or if there was higher verbal aggression, higher relationship invalidation, and lower relationship satisfaction. Higher relationship satisfaction was reported when there was lower money stress, higher sexual fulfillment, lower relationship invalidation, and higher perceived fairness of relationship power. High relationship satisfaction was also reported where there were no children in the home.5
It should be noted that none of these relationship variables was measured in the Miami study discussed above, and this study did not measure perceived conflict or perceived cohesion, so we know less about these aspects of the family unit.
What about teens?
The COVID-19 lockdown had a positive effect on the dynamics in some families, according to a naturalistic study of adolescents (n = 155) who completed surveys at two time periods (initial and 8 weeks).6
These adolescents reported a reduction in perceived psychological control by their mothers, and no change in autonomy support. The changes did not vary according to gender or the mother’s employment situation. The decrease in psychological control was greater with higher initial levels of satisfaction with the mother, and lower levels of the teens disobeying their parents.
What about hospital settings?
The worst of the COVID experience was in the hospital. The pain was displayed on the faces of the staff as they labored to figure out how to care for the dying patients who had no contact with their families. Hospitals, out of fear of contamination and viral dissemination, excluded visitors. In those early days of uncertainty, the stress among staff, patients, and family members was high.
In response to family members feeling disconnected from the health care team and the psychological and moral distress of the staff, Nadine J. Kaslow and colleagues revised policies and procedures at Emory University, Atlanta, facilities to reprioritize patient- and family-centered care.7
The guiding principles focus on providing safe yet compassionate and ethical care, balancing community health and the mitigation of viral transmission, while appreciating family members as essential partners in care; fostering communication between patients and their families; and promoting interactions and decision-making among health care providers, patients, and families.
COVID continues to intrude in many of our lives. Many people are mourning family members and friends who died after contracting the disease. Many people choose to ignore their risk and live their lives as before. Many people, like my spouse and me, continue to debate the merits of venturing into public spaces. Personally, COVID has given me time to read many more books than I could ever have imagined and allowed my spouse to explore the delicate nuances of cooking.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected].
References
1. Chavez JV et al. Assessing the impact of COVID-19 social distancing and social vulnerability on family functioning in an international sample of households with and without children. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 233-48. doi: 10.1037/cfp0000166.
2. Rudolph CW, Zacher H. Family demands and satisfaction with family life during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 249-59. doi: 10.1037/cfp0000170.
3. Heru AM et al. Family functioning in the caregivers of patients with dementia. Int J Geriatr Psychiatry. 2004 Jun;19(6):533-7. doi: 10.1002/gps.1119.
4. Schokkenbroek JM et al. Partners in lockdown: Relationship stress in men and women during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 149-57. doi: 10.1037/cfp0000172.
5. Eubanks Fleming CJ, Franzese AT. Should I stay or should I go? Evaluating intimate relationship outcomes during the 2020 pandemic shutdown. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 158-67. doi: 10.1037/cfp0000169.
6. Bacikova-Sleskova M,et al. Did perceived parenting in adolescence change as a result of the COVID-19 lockdown? A natural experiment. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 271-80. doi: 10.1037/cfp0000167.
7. Kaslow NJ et al. A roadmap for patient- and family-centered care during the pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 223-32. doi: 10.1037/cfp0000176.
Managing family conflict and cohesion
Managing family conflict and cohesion
I watched you in the garage, with your wipes and your mask, your gloves and bottles of sprays and potions. I admired your fealty to CNN’s Dr. Sanjay Gupta as he demonstrated the proper technique for disinfecting groceries. I watched sterile protocol being broken and quietly closed the garage door.
I listened to your descriptions of the agility of the virus with each exhalation of breath, and how far the virus could travel with a tailwind and in cold dry air. I listen as closely and with the same intention as I listen to my yoga teacher’s explication of the benefits of attention to the breath.
Relatives and friends came prepared to be entertained outdoors. Even masked, you eschewed the world. Your version of science clashes with my laissez-faire attitude. We blow up as a couple. Then we settle down and learn how to cope with the stress, as a team, together.
The COVID factor
In the first few months of any stressor, family and couple functioning must reorganize to manage well.
During lockdown, social scientists accessed an eager public ready to participate in their studies. With nowhere to go, many people, especially women, completed online COVID surveys. Community-based tools such as the Centers for Disease Control and Prevention’s Social Vulnerability Index identified populations of high social vulnerability (as caused by external stresses on human health, such as unemployment, overcrowding, presence of an individual with caregiving needs, and low educational attainment). It is assumed that such populations will experience more stress and have more difficulty coping and adjusting.
In a study by a team at the University of Miami, social vulnerability was associated with more disrupted family functioning, except when households with children (n = 2,666) were compared to households without children (n = 1,456).1 What allowed these families with children to enjoy better functioning?
Looking more closely at the Miami study, what can we find? It is a large survey study (n = 4,122), disseminated through professional networks and social media via purchased Facebook and Instagram ads. Data were logged in REDCap, and participants had the option of taking the survey in English or Spanish. Most participants were female (93.5%), 55.7% responded in English, and 44.3% in Spanish. There were few differences between the women who had and did not have children, in terms of their age, employment status, and education level. The number of children in the household did not affect the results.
This study used a new tool called the COVID-19 Household Environment Scale. This tool has 25 items measuring individual and household characteristics, and associated COVID-19 stressors. This tool also includes two family functioning measures: conflict and cohesion, asking the respondent to reflect on the change in “conflict” or “togetherness,” as it relates to household experiences and activities, compared with the period before social distancing.
The surprising finding was that even though households with children reported more conflict than before the start of the pandemic, they also reported more cohesion. This syncs with my experience. My niece and nephew found that having their teenage children at home brought them closer as a family, cut down on some of the extracurricular activities they did not support, and generally “slowed the world down.”
However, in a study in Germany, survey respondents (n = 1,042) noted that having children up to 17 years old was associated with decreases in satisfaction with family life, although this was not related to changes in family demands. The study assessed changes over 6 months and underscores the fact that perceptions of family demands and family well-being are independent of each other.2
These findings also resonate with prior research that measured burden and reward in couples. High burden is not associated with low reward; these two constructs are independent of each other.3
What about couples?
It is no surprise that poor relationships begat poor coping. In an online Belgian survey of 1,491 cohabiting couples during the shutdown, both men and women felt significantly more stress than before, because they felt restricted in their relationship.4
However, only women reported significantly more stress during the lockdown than before, because of relationship conflicts, such as feeling neglected by their partner. These feelings had predated lockdown.
In another lockdown online survey of 782 U.S. adults (89.8% White, 84.5% female), cohabitating intimate partners reported that there were higher thoughts of separation if the participants were younger, or if there was higher verbal aggression, higher relationship invalidation, and lower relationship satisfaction. Higher relationship satisfaction was reported when there was lower money stress, higher sexual fulfillment, lower relationship invalidation, and higher perceived fairness of relationship power. High relationship satisfaction was also reported where there were no children in the home.5
It should be noted that none of these relationship variables was measured in the Miami study discussed above, and this study did not measure perceived conflict or perceived cohesion, so we know less about these aspects of the family unit.
What about teens?
The COVID-19 lockdown had a positive effect on the dynamics in some families, according to a naturalistic study of adolescents (n = 155) who completed surveys at two time periods (initial and 8 weeks).6
These adolescents reported a reduction in perceived psychological control by their mothers, and no change in autonomy support. The changes did not vary according to gender or the mother’s employment situation. The decrease in psychological control was greater with higher initial levels of satisfaction with the mother, and lower levels of the teens disobeying their parents.
What about hospital settings?
The worst of the COVID experience was in the hospital. The pain was displayed on the faces of the staff as they labored to figure out how to care for the dying patients who had no contact with their families. Hospitals, out of fear of contamination and viral dissemination, excluded visitors. In those early days of uncertainty, the stress among staff, patients, and family members was high.
In response to family members feeling disconnected from the health care team and the psychological and moral distress of the staff, Nadine J. Kaslow and colleagues revised policies and procedures at Emory University, Atlanta, facilities to reprioritize patient- and family-centered care.7
The guiding principles focus on providing safe yet compassionate and ethical care, balancing community health and the mitigation of viral transmission, while appreciating family members as essential partners in care; fostering communication between patients and their families; and promoting interactions and decision-making among health care providers, patients, and families.
COVID continues to intrude in many of our lives. Many people are mourning family members and friends who died after contracting the disease. Many people choose to ignore their risk and live their lives as before. Many people, like my spouse and me, continue to debate the merits of venturing into public spaces. Personally, COVID has given me time to read many more books than I could ever have imagined and allowed my spouse to explore the delicate nuances of cooking.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected].
References
1. Chavez JV et al. Assessing the impact of COVID-19 social distancing and social vulnerability on family functioning in an international sample of households with and without children. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 233-48. doi: 10.1037/cfp0000166.
2. Rudolph CW, Zacher H. Family demands and satisfaction with family life during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 249-59. doi: 10.1037/cfp0000170.
3. Heru AM et al. Family functioning in the caregivers of patients with dementia. Int J Geriatr Psychiatry. 2004 Jun;19(6):533-7. doi: 10.1002/gps.1119.
4. Schokkenbroek JM et al. Partners in lockdown: Relationship stress in men and women during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 149-57. doi: 10.1037/cfp0000172.
5. Eubanks Fleming CJ, Franzese AT. Should I stay or should I go? Evaluating intimate relationship outcomes during the 2020 pandemic shutdown. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 158-67. doi: 10.1037/cfp0000169.
6. Bacikova-Sleskova M,et al. Did perceived parenting in adolescence change as a result of the COVID-19 lockdown? A natural experiment. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 271-80. doi: 10.1037/cfp0000167.
7. Kaslow NJ et al. A roadmap for patient- and family-centered care during the pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 223-32. doi: 10.1037/cfp0000176.
I watched you in the garage, with your wipes and your mask, your gloves and bottles of sprays and potions. I admired your fealty to CNN’s Dr. Sanjay Gupta as he demonstrated the proper technique for disinfecting groceries. I watched sterile protocol being broken and quietly closed the garage door.
I listened to your descriptions of the agility of the virus with each exhalation of breath, and how far the virus could travel with a tailwind and in cold dry air. I listen as closely and with the same intention as I listen to my yoga teacher’s explication of the benefits of attention to the breath.
Relatives and friends came prepared to be entertained outdoors. Even masked, you eschewed the world. Your version of science clashes with my laissez-faire attitude. We blow up as a couple. Then we settle down and learn how to cope with the stress, as a team, together.
The COVID factor
In the first few months of any stressor, family and couple functioning must reorganize to manage well.
During lockdown, social scientists accessed an eager public ready to participate in their studies. With nowhere to go, many people, especially women, completed online COVID surveys. Community-based tools such as the Centers for Disease Control and Prevention’s Social Vulnerability Index identified populations of high social vulnerability (as caused by external stresses on human health, such as unemployment, overcrowding, presence of an individual with caregiving needs, and low educational attainment). It is assumed that such populations will experience more stress and have more difficulty coping and adjusting.
In a study by a team at the University of Miami, social vulnerability was associated with more disrupted family functioning, except when households with children (n = 2,666) were compared to households without children (n = 1,456).1 What allowed these families with children to enjoy better functioning?
Looking more closely at the Miami study, what can we find? It is a large survey study (n = 4,122), disseminated through professional networks and social media via purchased Facebook and Instagram ads. Data were logged in REDCap, and participants had the option of taking the survey in English or Spanish. Most participants were female (93.5%), 55.7% responded in English, and 44.3% in Spanish. There were few differences between the women who had and did not have children, in terms of their age, employment status, and education level. The number of children in the household did not affect the results.
This study used a new tool called the COVID-19 Household Environment Scale. This tool has 25 items measuring individual and household characteristics, and associated COVID-19 stressors. This tool also includes two family functioning measures: conflict and cohesion, asking the respondent to reflect on the change in “conflict” or “togetherness,” as it relates to household experiences and activities, compared with the period before social distancing.
The surprising finding was that even though households with children reported more conflict than before the start of the pandemic, they also reported more cohesion. This syncs with my experience. My niece and nephew found that having their teenage children at home brought them closer as a family, cut down on some of the extracurricular activities they did not support, and generally “slowed the world down.”
However, in a study in Germany, survey respondents (n = 1,042) noted that having children up to 17 years old was associated with decreases in satisfaction with family life, although this was not related to changes in family demands. The study assessed changes over 6 months and underscores the fact that perceptions of family demands and family well-being are independent of each other.2
These findings also resonate with prior research that measured burden and reward in couples. High burden is not associated with low reward; these two constructs are independent of each other.3
What about couples?
It is no surprise that poor relationships begat poor coping. In an online Belgian survey of 1,491 cohabiting couples during the shutdown, both men and women felt significantly more stress than before, because they felt restricted in their relationship.4
However, only women reported significantly more stress during the lockdown than before, because of relationship conflicts, such as feeling neglected by their partner. These feelings had predated lockdown.
In another lockdown online survey of 782 U.S. adults (89.8% White, 84.5% female), cohabitating intimate partners reported that there were higher thoughts of separation if the participants were younger, or if there was higher verbal aggression, higher relationship invalidation, and lower relationship satisfaction. Higher relationship satisfaction was reported when there was lower money stress, higher sexual fulfillment, lower relationship invalidation, and higher perceived fairness of relationship power. High relationship satisfaction was also reported where there were no children in the home.5
It should be noted that none of these relationship variables was measured in the Miami study discussed above, and this study did not measure perceived conflict or perceived cohesion, so we know less about these aspects of the family unit.
What about teens?
The COVID-19 lockdown had a positive effect on the dynamics in some families, according to a naturalistic study of adolescents (n = 155) who completed surveys at two time periods (initial and 8 weeks).6
These adolescents reported a reduction in perceived psychological control by their mothers, and no change in autonomy support. The changes did not vary according to gender or the mother’s employment situation. The decrease in psychological control was greater with higher initial levels of satisfaction with the mother, and lower levels of the teens disobeying their parents.
What about hospital settings?
The worst of the COVID experience was in the hospital. The pain was displayed on the faces of the staff as they labored to figure out how to care for the dying patients who had no contact with their families. Hospitals, out of fear of contamination and viral dissemination, excluded visitors. In those early days of uncertainty, the stress among staff, patients, and family members was high.
In response to family members feeling disconnected from the health care team and the psychological and moral distress of the staff, Nadine J. Kaslow and colleagues revised policies and procedures at Emory University, Atlanta, facilities to reprioritize patient- and family-centered care.7
The guiding principles focus on providing safe yet compassionate and ethical care, balancing community health and the mitigation of viral transmission, while appreciating family members as essential partners in care; fostering communication between patients and their families; and promoting interactions and decision-making among health care providers, patients, and families.
COVID continues to intrude in many of our lives. Many people are mourning family members and friends who died after contracting the disease. Many people choose to ignore their risk and live their lives as before. Many people, like my spouse and me, continue to debate the merits of venturing into public spaces. Personally, COVID has given me time to read many more books than I could ever have imagined and allowed my spouse to explore the delicate nuances of cooking.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected].
References
1. Chavez JV et al. Assessing the impact of COVID-19 social distancing and social vulnerability on family functioning in an international sample of households with and without children. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 233-48. doi: 10.1037/cfp0000166.
2. Rudolph CW, Zacher H. Family demands and satisfaction with family life during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 249-59. doi: 10.1037/cfp0000170.
3. Heru AM et al. Family functioning in the caregivers of patients with dementia. Int J Geriatr Psychiatry. 2004 Jun;19(6):533-7. doi: 10.1002/gps.1119.
4. Schokkenbroek JM et al. Partners in lockdown: Relationship stress in men and women during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 149-57. doi: 10.1037/cfp0000172.
5. Eubanks Fleming CJ, Franzese AT. Should I stay or should I go? Evaluating intimate relationship outcomes during the 2020 pandemic shutdown. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 158-67. doi: 10.1037/cfp0000169.
6. Bacikova-Sleskova M,et al. Did perceived parenting in adolescence change as a result of the COVID-19 lockdown? A natural experiment. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 271-80. doi: 10.1037/cfp0000167.
7. Kaslow NJ et al. A roadmap for patient- and family-centered care during the pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 223-32. doi: 10.1037/cfp0000176.
Detachment predicts worse posttraumatic outcomes
The results highlight the importance of screening for dissociation in patients who have experienced trauma, study investigator Lauren A.M. Lebois, PhD, director of the dissociative disorders and trauma research program at McLean Hospital in Belmont, Mass., told this news organization.
“Clinicians could identify individuals potentially at risk of a chronic, more severe psychiatric course before these people go down that road, and they have the opportunity to connect folks with a phased trauma treatment approach to speed their recovery,” said Dr. Lebois, who is also an assistant professor of psychiatry at Harvard Medical School, Boston.
The study was published in the American Journal of Psychiatry.
Underdiagnosed
Feelings of detachment or derealization are a type of dissociation. Patients with the syndrome report feeling foggy or as if they are in a dream. Dissociative diagnoses are not rare and, in fact, are more prevalent than schizophrenia.
Research supports a powerful relationship between dissociation and traumatic experiences. However, dissociation is among the most stigmatized of psychiatric conditions. Even among clinicians and researchers, beliefs about dissociation are often not based on the scientific literature, said Dr. Lebois.
“For instance, skepticism, misunderstanding, and lack of professional education about dissociation all contribute to striking rates of underdiagnosis and misdiagnoses,” she said.
Dr. Lebois and colleagues used data from the larger Advancing Understanding of Recovery After Trauma (AURORA) study and included 1,464 adults, mean age 35 years, appearing at 22 U.S. emergency departments. Patients experienced a traumatic event such as a motor vehicle crash or physical or sexual assault.
About 2 weeks after the trauma, participants reported symptoms of derealization as measured by a two-item version of the Brief Dissociative Experiences Scale.
Brain imaging data
A subset of 145 patients underwent functional MRI (fMRI), during which they completed an emotion reactivity task (viewing fearful-looking human faces) and a resting-state scan.
In addition to measuring history of childhood maltreatment, researchers assessed posttraumatic stress symptom severity at 2 weeks and again at 3 months using the posttraumatic stress disorder checklist. Also at 3 months, they measured depression and anxiety symptoms, pain, and functional impairment.
About 55% of self-report participants and 50% of MRI participants endorsed some level of persistent derealization at 2 weeks.
After controlling for potential confounders, including sex, age, childhood maltreatment, and current posttraumatic stress symptoms, researchers found persistent derealization was associated with increased ventromedial prefrontal cortex (vmPFC) activity while viewing fearful faces.
The vmPFC helps to regulate emotional and physical reactions. “This region puts the ‘brakes’ on your emotional and physical reactivity – helping you to calm down” after a threatening or stressful experience has passed, said Dr. Lebois.
Researchers also found an association between higher self-reported derealization and decreased resting-state connectivity between the vmPFC and the orbitofrontal cortex and right lobule VIIIa – a region of the cerebellum involved in sensorimotor function.
“This may contribute to perceptual and affective distortions experienced during derealization – for example, feelings that surroundings are fading away, unreal, or strange,” said Dr. Lebois.
More pain, depression, anxiety
Higher levels of self-reported derealization at 2 weeks post trauma predicted higher levels of PTSD, anxiety, and depression as well as more bodily pain and impairment in work, family, and social life at 3 months.
“When we accounted for baseline levels of posttraumatic stress symptoms and trauma history, higher levels of self-reported derealization still predicted higher posttraumatic stress disorder and depression symptoms at 3 months,” said Dr. Lebois.
Additional adjusted analyses showed increased vmPFC activity during the fearful face task predicted 3-month self-reported PTSD symptoms.
Dr. Lebois “highly recommends” clinicians screen for dissociative symptoms, including derealization, in patients with trauma. Self-report screening tools are freely available online.
She noted patients with significant dissociative symptoms often do better with a “phase-oriented” approach to trauma treatment.
“In phase one, they learn emotional regulation skills to help them take more control over when they dissociate. Then they can successfully move on to trauma processing in phase two, which can involve exposure to trauma details.”
Although the field is not yet ready to use brain scans to diagnose dissociative symptoms, the new results “take us one step closer to being able to use objective neuroimaging biomarkers of derealization to augment subjective self-report measures,” said Dr. Lebois.
A limitation of the study was it could not determine a causal relationship, as some derealization may have been present before the traumatic event. The findings may not generalize to other types of dissociation, and the derealization assessment was measured only through a self-report 2 weeks after the trauma.
Another limitation was exclusion of patients with self-inflicted injuries or who were involved in domestic violence. The researchers noted the prevalence of derealization might have been even higher if such individuals were included.
An important investigation
In an accompanying editorial, Lisa M. Shin, PhD, department of psychology, Tufts University, and department of psychiatry, Massachusetts General Hospital and Harvard Medical School, Boston, notes having both clinical and neuroimaging variables as well as a large sample size makes the study “an important investigation” into predictors of psychiatric symptoms post-trauma.
Investigating a specific subtype of dissociation – persistent derealization – adds to the “novelty” of the study, she said.
The new findings “are certainly exciting for their potential clinical relevance and contributions to neurocircuitry models of PTSD,” she writes.
Some may argue administering a short, self-report measure of derealization “is far more efficient, cost-effective, and inclusive than conducting a specialized and expensive fMRI scan that is unlikely to be available to everyone,” notes Dr. Shin.
However, she added, a potential benefit of such a scan is identification of specific brain regions as potential targets for intervention. “For example, the results of this and other studies suggest that the vmPFC is a reasonable target for transcranial magnetic stimulation or its variants.”
The new results need to be replicated in a large, independent sample, said Dr. Shin. She added it would be helpful to know if other types of dissociation, and activation in other subregions of the vmPFC, also predict psychiatric outcomes after a trauma.
The study was supported by National Institute of Mental Health grants, the U.S. Army Medical Research and Material Command, One Mind, and the Mayday Fund. Dr. Lebois has received grant support from NIMH, and her spouse receives payments from Vanderbilt University for technology licensed to Acadia Pharmaceuticals. Dr. Shin receives textbook-related royalties from Pearson.
A version of this article first appeared on Medscape.com.
The results highlight the importance of screening for dissociation in patients who have experienced trauma, study investigator Lauren A.M. Lebois, PhD, director of the dissociative disorders and trauma research program at McLean Hospital in Belmont, Mass., told this news organization.
“Clinicians could identify individuals potentially at risk of a chronic, more severe psychiatric course before these people go down that road, and they have the opportunity to connect folks with a phased trauma treatment approach to speed their recovery,” said Dr. Lebois, who is also an assistant professor of psychiatry at Harvard Medical School, Boston.
The study was published in the American Journal of Psychiatry.
Underdiagnosed
Feelings of detachment or derealization are a type of dissociation. Patients with the syndrome report feeling foggy or as if they are in a dream. Dissociative diagnoses are not rare and, in fact, are more prevalent than schizophrenia.
Research supports a powerful relationship between dissociation and traumatic experiences. However, dissociation is among the most stigmatized of psychiatric conditions. Even among clinicians and researchers, beliefs about dissociation are often not based on the scientific literature, said Dr. Lebois.
“For instance, skepticism, misunderstanding, and lack of professional education about dissociation all contribute to striking rates of underdiagnosis and misdiagnoses,” she said.
Dr. Lebois and colleagues used data from the larger Advancing Understanding of Recovery After Trauma (AURORA) study and included 1,464 adults, mean age 35 years, appearing at 22 U.S. emergency departments. Patients experienced a traumatic event such as a motor vehicle crash or physical or sexual assault.
About 2 weeks after the trauma, participants reported symptoms of derealization as measured by a two-item version of the Brief Dissociative Experiences Scale.
Brain imaging data
A subset of 145 patients underwent functional MRI (fMRI), during which they completed an emotion reactivity task (viewing fearful-looking human faces) and a resting-state scan.
In addition to measuring history of childhood maltreatment, researchers assessed posttraumatic stress symptom severity at 2 weeks and again at 3 months using the posttraumatic stress disorder checklist. Also at 3 months, they measured depression and anxiety symptoms, pain, and functional impairment.
About 55% of self-report participants and 50% of MRI participants endorsed some level of persistent derealization at 2 weeks.
After controlling for potential confounders, including sex, age, childhood maltreatment, and current posttraumatic stress symptoms, researchers found persistent derealization was associated with increased ventromedial prefrontal cortex (vmPFC) activity while viewing fearful faces.
The vmPFC helps to regulate emotional and physical reactions. “This region puts the ‘brakes’ on your emotional and physical reactivity – helping you to calm down” after a threatening or stressful experience has passed, said Dr. Lebois.
Researchers also found an association between higher self-reported derealization and decreased resting-state connectivity between the vmPFC and the orbitofrontal cortex and right lobule VIIIa – a region of the cerebellum involved in sensorimotor function.
“This may contribute to perceptual and affective distortions experienced during derealization – for example, feelings that surroundings are fading away, unreal, or strange,” said Dr. Lebois.
More pain, depression, anxiety
Higher levels of self-reported derealization at 2 weeks post trauma predicted higher levels of PTSD, anxiety, and depression as well as more bodily pain and impairment in work, family, and social life at 3 months.
“When we accounted for baseline levels of posttraumatic stress symptoms and trauma history, higher levels of self-reported derealization still predicted higher posttraumatic stress disorder and depression symptoms at 3 months,” said Dr. Lebois.
Additional adjusted analyses showed increased vmPFC activity during the fearful face task predicted 3-month self-reported PTSD symptoms.
Dr. Lebois “highly recommends” clinicians screen for dissociative symptoms, including derealization, in patients with trauma. Self-report screening tools are freely available online.
She noted patients with significant dissociative symptoms often do better with a “phase-oriented” approach to trauma treatment.
“In phase one, they learn emotional regulation skills to help them take more control over when they dissociate. Then they can successfully move on to trauma processing in phase two, which can involve exposure to trauma details.”
Although the field is not yet ready to use brain scans to diagnose dissociative symptoms, the new results “take us one step closer to being able to use objective neuroimaging biomarkers of derealization to augment subjective self-report measures,” said Dr. Lebois.
A limitation of the study was it could not determine a causal relationship, as some derealization may have been present before the traumatic event. The findings may not generalize to other types of dissociation, and the derealization assessment was measured only through a self-report 2 weeks after the trauma.
Another limitation was exclusion of patients with self-inflicted injuries or who were involved in domestic violence. The researchers noted the prevalence of derealization might have been even higher if such individuals were included.
An important investigation
In an accompanying editorial, Lisa M. Shin, PhD, department of psychology, Tufts University, and department of psychiatry, Massachusetts General Hospital and Harvard Medical School, Boston, notes having both clinical and neuroimaging variables as well as a large sample size makes the study “an important investigation” into predictors of psychiatric symptoms post-trauma.
Investigating a specific subtype of dissociation – persistent derealization – adds to the “novelty” of the study, she said.
The new findings “are certainly exciting for their potential clinical relevance and contributions to neurocircuitry models of PTSD,” she writes.
Some may argue administering a short, self-report measure of derealization “is far more efficient, cost-effective, and inclusive than conducting a specialized and expensive fMRI scan that is unlikely to be available to everyone,” notes Dr. Shin.
However, she added, a potential benefit of such a scan is identification of specific brain regions as potential targets for intervention. “For example, the results of this and other studies suggest that the vmPFC is a reasonable target for transcranial magnetic stimulation or its variants.”
The new results need to be replicated in a large, independent sample, said Dr. Shin. She added it would be helpful to know if other types of dissociation, and activation in other subregions of the vmPFC, also predict psychiatric outcomes after a trauma.
The study was supported by National Institute of Mental Health grants, the U.S. Army Medical Research and Material Command, One Mind, and the Mayday Fund. Dr. Lebois has received grant support from NIMH, and her spouse receives payments from Vanderbilt University for technology licensed to Acadia Pharmaceuticals. Dr. Shin receives textbook-related royalties from Pearson.
A version of this article first appeared on Medscape.com.
The results highlight the importance of screening for dissociation in patients who have experienced trauma, study investigator Lauren A.M. Lebois, PhD, director of the dissociative disorders and trauma research program at McLean Hospital in Belmont, Mass., told this news organization.
“Clinicians could identify individuals potentially at risk of a chronic, more severe psychiatric course before these people go down that road, and they have the opportunity to connect folks with a phased trauma treatment approach to speed their recovery,” said Dr. Lebois, who is also an assistant professor of psychiatry at Harvard Medical School, Boston.
The study was published in the American Journal of Psychiatry.
Underdiagnosed
Feelings of detachment or derealization are a type of dissociation. Patients with the syndrome report feeling foggy or as if they are in a dream. Dissociative diagnoses are not rare and, in fact, are more prevalent than schizophrenia.
Research supports a powerful relationship between dissociation and traumatic experiences. However, dissociation is among the most stigmatized of psychiatric conditions. Even among clinicians and researchers, beliefs about dissociation are often not based on the scientific literature, said Dr. Lebois.
“For instance, skepticism, misunderstanding, and lack of professional education about dissociation all contribute to striking rates of underdiagnosis and misdiagnoses,” she said.
Dr. Lebois and colleagues used data from the larger Advancing Understanding of Recovery After Trauma (AURORA) study and included 1,464 adults, mean age 35 years, appearing at 22 U.S. emergency departments. Patients experienced a traumatic event such as a motor vehicle crash or physical or sexual assault.
About 2 weeks after the trauma, participants reported symptoms of derealization as measured by a two-item version of the Brief Dissociative Experiences Scale.
Brain imaging data
A subset of 145 patients underwent functional MRI (fMRI), during which they completed an emotion reactivity task (viewing fearful-looking human faces) and a resting-state scan.
In addition to measuring history of childhood maltreatment, researchers assessed posttraumatic stress symptom severity at 2 weeks and again at 3 months using the posttraumatic stress disorder checklist. Also at 3 months, they measured depression and anxiety symptoms, pain, and functional impairment.
About 55% of self-report participants and 50% of MRI participants endorsed some level of persistent derealization at 2 weeks.
After controlling for potential confounders, including sex, age, childhood maltreatment, and current posttraumatic stress symptoms, researchers found persistent derealization was associated with increased ventromedial prefrontal cortex (vmPFC) activity while viewing fearful faces.
The vmPFC helps to regulate emotional and physical reactions. “This region puts the ‘brakes’ on your emotional and physical reactivity – helping you to calm down” after a threatening or stressful experience has passed, said Dr. Lebois.
Researchers also found an association between higher self-reported derealization and decreased resting-state connectivity between the vmPFC and the orbitofrontal cortex and right lobule VIIIa – a region of the cerebellum involved in sensorimotor function.
“This may contribute to perceptual and affective distortions experienced during derealization – for example, feelings that surroundings are fading away, unreal, or strange,” said Dr. Lebois.
More pain, depression, anxiety
Higher levels of self-reported derealization at 2 weeks post trauma predicted higher levels of PTSD, anxiety, and depression as well as more bodily pain and impairment in work, family, and social life at 3 months.
“When we accounted for baseline levels of posttraumatic stress symptoms and trauma history, higher levels of self-reported derealization still predicted higher posttraumatic stress disorder and depression symptoms at 3 months,” said Dr. Lebois.
Additional adjusted analyses showed increased vmPFC activity during the fearful face task predicted 3-month self-reported PTSD symptoms.
Dr. Lebois “highly recommends” clinicians screen for dissociative symptoms, including derealization, in patients with trauma. Self-report screening tools are freely available online.
She noted patients with significant dissociative symptoms often do better with a “phase-oriented” approach to trauma treatment.
“In phase one, they learn emotional regulation skills to help them take more control over when they dissociate. Then they can successfully move on to trauma processing in phase two, which can involve exposure to trauma details.”
Although the field is not yet ready to use brain scans to diagnose dissociative symptoms, the new results “take us one step closer to being able to use objective neuroimaging biomarkers of derealization to augment subjective self-report measures,” said Dr. Lebois.
A limitation of the study was it could not determine a causal relationship, as some derealization may have been present before the traumatic event. The findings may not generalize to other types of dissociation, and the derealization assessment was measured only through a self-report 2 weeks after the trauma.
Another limitation was exclusion of patients with self-inflicted injuries or who were involved in domestic violence. The researchers noted the prevalence of derealization might have been even higher if such individuals were included.
An important investigation
In an accompanying editorial, Lisa M. Shin, PhD, department of psychology, Tufts University, and department of psychiatry, Massachusetts General Hospital and Harvard Medical School, Boston, notes having both clinical and neuroimaging variables as well as a large sample size makes the study “an important investigation” into predictors of psychiatric symptoms post-trauma.
Investigating a specific subtype of dissociation – persistent derealization – adds to the “novelty” of the study, she said.
The new findings “are certainly exciting for their potential clinical relevance and contributions to neurocircuitry models of PTSD,” she writes.
Some may argue administering a short, self-report measure of derealization “is far more efficient, cost-effective, and inclusive than conducting a specialized and expensive fMRI scan that is unlikely to be available to everyone,” notes Dr. Shin.
However, she added, a potential benefit of such a scan is identification of specific brain regions as potential targets for intervention. “For example, the results of this and other studies suggest that the vmPFC is a reasonable target for transcranial magnetic stimulation or its variants.”
The new results need to be replicated in a large, independent sample, said Dr. Shin. She added it would be helpful to know if other types of dissociation, and activation in other subregions of the vmPFC, also predict psychiatric outcomes after a trauma.
The study was supported by National Institute of Mental Health grants, the U.S. Army Medical Research and Material Command, One Mind, and the Mayday Fund. Dr. Lebois has received grant support from NIMH, and her spouse receives payments from Vanderbilt University for technology licensed to Acadia Pharmaceuticals. Dr. Shin receives textbook-related royalties from Pearson.
A version of this article first appeared on Medscape.com.
FROM AMERICAN JOURNAL OF PSYCHIATRY
Mental health in America: ‘The kids are not alright’
A new report shines a light on the toll the pandemic and other stressors have taken on the mental health of U.S. children and adolescents over the last 6 years.
The report shows a dramatic increase in use of acute care services for depression, anxiety, and other mental health conditions, especially among teens and preteens.
The report – The Kids Are Not Alright: Pediatric Mental Health Care Utilization from 2016-2021 – is the work of researchers at the Clarify Health Institute, the research arm of Clarify Health.
The results are “deeply concerning” and should “spark a conversation” around the need to improve access, utilization, and quality of pediatric behavioral health services, Niall Brennan, chief analytics and privacy officer for the Clarify Health Institute, told this news organization.
‘Startling’ trends
Leveraging an observational, national sample of insurance claims from more than 20 million children aged 1-19 years annually, the researchers observed several disturbing trends in mental health care.
From 2016 to 2021, inpatient (IP) admissions rose 61% (from 30 to 48 visits annually per 1,000) and emergency department visits rose 20% (from 55 to 66 visits annually per 1,000).
Mental health IP admissions ranged from a low of 27% in the West North Central region to a high of 137% in the Middle Atlantic region.
There were substantial increases from 2016 to 2021 in mental health IP admissions among children of all age groups, but particularly among adolescents 12 to 15 years old, increasing 84% among girls and 83% among boys in this age group.
There was also a sharp increase in mental health ED visits among girls and boys aged 12-15 years, increasing 20% overall during the study period.
Mental health IP use grew faster from 2016 to 2021 among children with commercial insurance than among those with Medicaid (103% vs. 40%).
In contrast, mental health–specific ED visits declined 10% among children with commercial insurance and increased by 20% among those with Medicaid.
ED utilization rates in 2021 were nearly twice as high in the Medicaid population, compared with those for children with commercial insurance.
These are “startling” increases, Mr. Brennan said in an interview.
These trends “reinforce health care leaders’ responsibility to address children’s mental health, especially when considering that half of all mental health conditions onset during adolescence and carry into adulthood,” Jean Drouin, MD, Clarify Health’s chief executive office and cofounder, adds in a news release.
“With a growing consensus that mental, behavioral, and physical health intersect, this research report aims to spark a conversation about the overall wellbeing of America’s next generation,” Dr. Drouin says.
Concern for the future
Commenting on the new report, Anish Dube, MD, chair of the American Psychiatric Association’s Council on Children, Adolescents, and their Families, said the findings are “concerning, though unsurprising.”
“They confirm what those of us in clinical practice have experienced in the last several years. The need for mental health services continues to rise every year, while access to adequate help remains lacking,” Dr. Dube said.
“With the recent COVID-19 pandemic, concerns about the effects of climate change, global political uncertainty, and a rapidly changing employment landscape, young people in particular are vulnerable to worries about their future and feelings of helplessness and hopelessness,” he added.
Dr. Dube said there is no one right solution, and addressing this problem must consider individual and local factors.
However, some of the broader interventions needed to tackle the problem include increasing access to care by enforcing mental health parity and increasing the number of trained and qualified mental health professionals, such as child and adolescent psychiatrists, who can assess and treat these conditions in young people before they become major crises and lead to acute interventions like inpatient hospitalization.
“Public health interventions aimed at schools and families in raising awareness of mental health and well-being, and simple, cost-effective interventions to practice mental wellness will also help reduce the burden of mental illness in young people,” Dr. Dube added.
“The APA continues to fight for mental health parity enforcement and for meaningful access to mental health care for children, adolescents, and their families,” Dr. Dube said.
This research was conducted by the Clarify Health Institute. Mr. Brennan and Dr. Dube report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new report shines a light on the toll the pandemic and other stressors have taken on the mental health of U.S. children and adolescents over the last 6 years.
The report shows a dramatic increase in use of acute care services for depression, anxiety, and other mental health conditions, especially among teens and preteens.
The report – The Kids Are Not Alright: Pediatric Mental Health Care Utilization from 2016-2021 – is the work of researchers at the Clarify Health Institute, the research arm of Clarify Health.
The results are “deeply concerning” and should “spark a conversation” around the need to improve access, utilization, and quality of pediatric behavioral health services, Niall Brennan, chief analytics and privacy officer for the Clarify Health Institute, told this news organization.
‘Startling’ trends
Leveraging an observational, national sample of insurance claims from more than 20 million children aged 1-19 years annually, the researchers observed several disturbing trends in mental health care.
From 2016 to 2021, inpatient (IP) admissions rose 61% (from 30 to 48 visits annually per 1,000) and emergency department visits rose 20% (from 55 to 66 visits annually per 1,000).
Mental health IP admissions ranged from a low of 27% in the West North Central region to a high of 137% in the Middle Atlantic region.
There were substantial increases from 2016 to 2021 in mental health IP admissions among children of all age groups, but particularly among adolescents 12 to 15 years old, increasing 84% among girls and 83% among boys in this age group.
There was also a sharp increase in mental health ED visits among girls and boys aged 12-15 years, increasing 20% overall during the study period.
Mental health IP use grew faster from 2016 to 2021 among children with commercial insurance than among those with Medicaid (103% vs. 40%).
In contrast, mental health–specific ED visits declined 10% among children with commercial insurance and increased by 20% among those with Medicaid.
ED utilization rates in 2021 were nearly twice as high in the Medicaid population, compared with those for children with commercial insurance.
These are “startling” increases, Mr. Brennan said in an interview.
These trends “reinforce health care leaders’ responsibility to address children’s mental health, especially when considering that half of all mental health conditions onset during adolescence and carry into adulthood,” Jean Drouin, MD, Clarify Health’s chief executive office and cofounder, adds in a news release.
“With a growing consensus that mental, behavioral, and physical health intersect, this research report aims to spark a conversation about the overall wellbeing of America’s next generation,” Dr. Drouin says.
Concern for the future
Commenting on the new report, Anish Dube, MD, chair of the American Psychiatric Association’s Council on Children, Adolescents, and their Families, said the findings are “concerning, though unsurprising.”
“They confirm what those of us in clinical practice have experienced in the last several years. The need for mental health services continues to rise every year, while access to adequate help remains lacking,” Dr. Dube said.
“With the recent COVID-19 pandemic, concerns about the effects of climate change, global political uncertainty, and a rapidly changing employment landscape, young people in particular are vulnerable to worries about their future and feelings of helplessness and hopelessness,” he added.
Dr. Dube said there is no one right solution, and addressing this problem must consider individual and local factors.
However, some of the broader interventions needed to tackle the problem include increasing access to care by enforcing mental health parity and increasing the number of trained and qualified mental health professionals, such as child and adolescent psychiatrists, who can assess and treat these conditions in young people before they become major crises and lead to acute interventions like inpatient hospitalization.
“Public health interventions aimed at schools and families in raising awareness of mental health and well-being, and simple, cost-effective interventions to practice mental wellness will also help reduce the burden of mental illness in young people,” Dr. Dube added.
“The APA continues to fight for mental health parity enforcement and for meaningful access to mental health care for children, adolescents, and their families,” Dr. Dube said.
This research was conducted by the Clarify Health Institute. Mr. Brennan and Dr. Dube report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new report shines a light on the toll the pandemic and other stressors have taken on the mental health of U.S. children and adolescents over the last 6 years.
The report shows a dramatic increase in use of acute care services for depression, anxiety, and other mental health conditions, especially among teens and preteens.
The report – The Kids Are Not Alright: Pediatric Mental Health Care Utilization from 2016-2021 – is the work of researchers at the Clarify Health Institute, the research arm of Clarify Health.
The results are “deeply concerning” and should “spark a conversation” around the need to improve access, utilization, and quality of pediatric behavioral health services, Niall Brennan, chief analytics and privacy officer for the Clarify Health Institute, told this news organization.
‘Startling’ trends
Leveraging an observational, national sample of insurance claims from more than 20 million children aged 1-19 years annually, the researchers observed several disturbing trends in mental health care.
From 2016 to 2021, inpatient (IP) admissions rose 61% (from 30 to 48 visits annually per 1,000) and emergency department visits rose 20% (from 55 to 66 visits annually per 1,000).
Mental health IP admissions ranged from a low of 27% in the West North Central region to a high of 137% in the Middle Atlantic region.
There were substantial increases from 2016 to 2021 in mental health IP admissions among children of all age groups, but particularly among adolescents 12 to 15 years old, increasing 84% among girls and 83% among boys in this age group.
There was also a sharp increase in mental health ED visits among girls and boys aged 12-15 years, increasing 20% overall during the study period.
Mental health IP use grew faster from 2016 to 2021 among children with commercial insurance than among those with Medicaid (103% vs. 40%).
In contrast, mental health–specific ED visits declined 10% among children with commercial insurance and increased by 20% among those with Medicaid.
ED utilization rates in 2021 were nearly twice as high in the Medicaid population, compared with those for children with commercial insurance.
These are “startling” increases, Mr. Brennan said in an interview.
These trends “reinforce health care leaders’ responsibility to address children’s mental health, especially when considering that half of all mental health conditions onset during adolescence and carry into adulthood,” Jean Drouin, MD, Clarify Health’s chief executive office and cofounder, adds in a news release.
“With a growing consensus that mental, behavioral, and physical health intersect, this research report aims to spark a conversation about the overall wellbeing of America’s next generation,” Dr. Drouin says.
Concern for the future
Commenting on the new report, Anish Dube, MD, chair of the American Psychiatric Association’s Council on Children, Adolescents, and their Families, said the findings are “concerning, though unsurprising.”
“They confirm what those of us in clinical practice have experienced in the last several years. The need for mental health services continues to rise every year, while access to adequate help remains lacking,” Dr. Dube said.
“With the recent COVID-19 pandemic, concerns about the effects of climate change, global political uncertainty, and a rapidly changing employment landscape, young people in particular are vulnerable to worries about their future and feelings of helplessness and hopelessness,” he added.
Dr. Dube said there is no one right solution, and addressing this problem must consider individual and local factors.
However, some of the broader interventions needed to tackle the problem include increasing access to care by enforcing mental health parity and increasing the number of trained and qualified mental health professionals, such as child and adolescent psychiatrists, who can assess and treat these conditions in young people before they become major crises and lead to acute interventions like inpatient hospitalization.
“Public health interventions aimed at schools and families in raising awareness of mental health and well-being, and simple, cost-effective interventions to practice mental wellness will also help reduce the burden of mental illness in young people,” Dr. Dube added.
“The APA continues to fight for mental health parity enforcement and for meaningful access to mental health care for children, adolescents, and their families,” Dr. Dube said.
This research was conducted by the Clarify Health Institute. Mr. Brennan and Dr. Dube report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Psychedelics may ease fear of death and dying
Psychedelics can produce positive changes in attitudes about death and dying – and may be a way to help ease anxiety and depression toward the end of life, new research suggests.
In a retrospective study of more than 3,000 participants,
“Individuals with existential anxiety and depression at end of life account for substantial suffering and significantly increased health care expenses from desperate and often futile seeking of intensive and expensive medical treatments,” co-investigator Roland Griffiths, PhD, Center for Psychedelics and Consciousness Research at Johns Hopkins Medicine, Baltimore, told this news organization.
“The present findings, which show that both psychedelic and non–drug-occasioned experiences can produce positive and enduring changes in attitudes about death, suggest the importance of future prospective experimental and clinical observational studies to better understand mechanisms of such changes as well as their potential clinical utility in ameliorating suffering related to fear of death,” Dr. Griffiths said.
The results were published online Aug. 24 in PLOS ONE.
Direct comparisons
Both psychedelic drug experiences and near-death experiences can alter perspectives on death and dying, but there have been few direct comparisons of these phenomena, the investigators note.
In the current study, they directly compared psychedelic-occasioned and nondrug experiences, which altered individuals’ beliefs about death.
The researchers surveyed 3,192 mostly White adults from the United States, including 933 who had a natural, nondrug near-death experience and 2,259 who had psychedelic near-death experiences induced with lysergic acid diethylamide, psilocybin, ayahuasca, or N,N-dimethyltryptamine.
The psychedelic group had more men than women and tended to be younger at the time of the experience than was the nondrug group.
Nearly 90% of individuals in both groups said that they were less afraid of death than they were before their experiences.
About half of both groups said they’d encountered something they might call “God” during the experience.
Three-quarters of the psychedelic group and 85% of the nondrug group rated their experiences as among the top five most personally meaningful and spiritually significant events of their life.
Individuals in both groups also reported moderate- to strong-lasting positive changes in personal well-being and life purpose and meaning after their experiences.
However, there were some differences between the groups.
More research needed
Compared with the psychedelic group, the nondrug group was more likely to report being unconscious, clinically dead, or that their life was in imminent danger.
The nonpsychedelic group was also more likely to report that their experience was very brief, lasting 5 minutes or less.
Both the psychedelic and nondrug participants showed robust increases on standardized measures of mystical and near-death experiences, but these measures were significantly greater in the psychedelic group.
The survey findings are in line with several recent clinical trials showing that a single treatment with the psychedelic psilocybin produced sustained decreases in anxiety and depression among patients with a life-threatening cancer diagnosis.
This includes a 2016 study by Dr. Griffiths and colleagues, which included 51 patients with late-stage cancer. As reported at the time, results showed a single, high dose of psilocybin had rapid, clinically significant, and lasting effects on mood and anxiety.
Limitations of the current survey cited by the researchers include the use of retrospective self-report to describe changes in death attitudes and the subjective features of the experiences. Also, respondents were a self-selected study population that may not be representative of all psychedelic or near-death experiences.
In addition, the study did not attempt to document worldview and other belief changes, such as increased belief in afterlife, that might help explain why death attitudes changed.
Looking ahead, the researchers note that future studies are needed to better understand the potential clinical use of psychedelics in ameliorating suffering related to fear of death.
Support through the Johns Hopkins Center for Psychedelic and Consciousness Research was provided by Tim Ferriss, Matt Mullenweg, Blake Mycoskie, Craig Nerenberg, and the Steven and Alexandra Cohen Foundation. Funding was also provided by the Y.C. Ho/Helen and Michael Chiang Foundation. The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Psychedelics can produce positive changes in attitudes about death and dying – and may be a way to help ease anxiety and depression toward the end of life, new research suggests.
In a retrospective study of more than 3,000 participants,
“Individuals with existential anxiety and depression at end of life account for substantial suffering and significantly increased health care expenses from desperate and often futile seeking of intensive and expensive medical treatments,” co-investigator Roland Griffiths, PhD, Center for Psychedelics and Consciousness Research at Johns Hopkins Medicine, Baltimore, told this news organization.
“The present findings, which show that both psychedelic and non–drug-occasioned experiences can produce positive and enduring changes in attitudes about death, suggest the importance of future prospective experimental and clinical observational studies to better understand mechanisms of such changes as well as their potential clinical utility in ameliorating suffering related to fear of death,” Dr. Griffiths said.
The results were published online Aug. 24 in PLOS ONE.
Direct comparisons
Both psychedelic drug experiences and near-death experiences can alter perspectives on death and dying, but there have been few direct comparisons of these phenomena, the investigators note.
In the current study, they directly compared psychedelic-occasioned and nondrug experiences, which altered individuals’ beliefs about death.
The researchers surveyed 3,192 mostly White adults from the United States, including 933 who had a natural, nondrug near-death experience and 2,259 who had psychedelic near-death experiences induced with lysergic acid diethylamide, psilocybin, ayahuasca, or N,N-dimethyltryptamine.
The psychedelic group had more men than women and tended to be younger at the time of the experience than was the nondrug group.
Nearly 90% of individuals in both groups said that they were less afraid of death than they were before their experiences.
About half of both groups said they’d encountered something they might call “God” during the experience.
Three-quarters of the psychedelic group and 85% of the nondrug group rated their experiences as among the top five most personally meaningful and spiritually significant events of their life.
Individuals in both groups also reported moderate- to strong-lasting positive changes in personal well-being and life purpose and meaning after their experiences.
However, there were some differences between the groups.
More research needed
Compared with the psychedelic group, the nondrug group was more likely to report being unconscious, clinically dead, or that their life was in imminent danger.
The nonpsychedelic group was also more likely to report that their experience was very brief, lasting 5 minutes or less.
Both the psychedelic and nondrug participants showed robust increases on standardized measures of mystical and near-death experiences, but these measures were significantly greater in the psychedelic group.
The survey findings are in line with several recent clinical trials showing that a single treatment with the psychedelic psilocybin produced sustained decreases in anxiety and depression among patients with a life-threatening cancer diagnosis.
This includes a 2016 study by Dr. Griffiths and colleagues, which included 51 patients with late-stage cancer. As reported at the time, results showed a single, high dose of psilocybin had rapid, clinically significant, and lasting effects on mood and anxiety.
Limitations of the current survey cited by the researchers include the use of retrospective self-report to describe changes in death attitudes and the subjective features of the experiences. Also, respondents were a self-selected study population that may not be representative of all psychedelic or near-death experiences.
In addition, the study did not attempt to document worldview and other belief changes, such as increased belief in afterlife, that might help explain why death attitudes changed.
Looking ahead, the researchers note that future studies are needed to better understand the potential clinical use of psychedelics in ameliorating suffering related to fear of death.
Support through the Johns Hopkins Center for Psychedelic and Consciousness Research was provided by Tim Ferriss, Matt Mullenweg, Blake Mycoskie, Craig Nerenberg, and the Steven and Alexandra Cohen Foundation. Funding was also provided by the Y.C. Ho/Helen and Michael Chiang Foundation. The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Psychedelics can produce positive changes in attitudes about death and dying – and may be a way to help ease anxiety and depression toward the end of life, new research suggests.
In a retrospective study of more than 3,000 participants,
“Individuals with existential anxiety and depression at end of life account for substantial suffering and significantly increased health care expenses from desperate and often futile seeking of intensive and expensive medical treatments,” co-investigator Roland Griffiths, PhD, Center for Psychedelics and Consciousness Research at Johns Hopkins Medicine, Baltimore, told this news organization.
“The present findings, which show that both psychedelic and non–drug-occasioned experiences can produce positive and enduring changes in attitudes about death, suggest the importance of future prospective experimental and clinical observational studies to better understand mechanisms of such changes as well as their potential clinical utility in ameliorating suffering related to fear of death,” Dr. Griffiths said.
The results were published online Aug. 24 in PLOS ONE.
Direct comparisons
Both psychedelic drug experiences and near-death experiences can alter perspectives on death and dying, but there have been few direct comparisons of these phenomena, the investigators note.
In the current study, they directly compared psychedelic-occasioned and nondrug experiences, which altered individuals’ beliefs about death.
The researchers surveyed 3,192 mostly White adults from the United States, including 933 who had a natural, nondrug near-death experience and 2,259 who had psychedelic near-death experiences induced with lysergic acid diethylamide, psilocybin, ayahuasca, or N,N-dimethyltryptamine.
The psychedelic group had more men than women and tended to be younger at the time of the experience than was the nondrug group.
Nearly 90% of individuals in both groups said that they were less afraid of death than they were before their experiences.
About half of both groups said they’d encountered something they might call “God” during the experience.
Three-quarters of the psychedelic group and 85% of the nondrug group rated their experiences as among the top five most personally meaningful and spiritually significant events of their life.
Individuals in both groups also reported moderate- to strong-lasting positive changes in personal well-being and life purpose and meaning after their experiences.
However, there were some differences between the groups.
More research needed
Compared with the psychedelic group, the nondrug group was more likely to report being unconscious, clinically dead, or that their life was in imminent danger.
The nonpsychedelic group was also more likely to report that their experience was very brief, lasting 5 minutes or less.
Both the psychedelic and nondrug participants showed robust increases on standardized measures of mystical and near-death experiences, but these measures were significantly greater in the psychedelic group.
The survey findings are in line with several recent clinical trials showing that a single treatment with the psychedelic psilocybin produced sustained decreases in anxiety and depression among patients with a life-threatening cancer diagnosis.
This includes a 2016 study by Dr. Griffiths and colleagues, which included 51 patients with late-stage cancer. As reported at the time, results showed a single, high dose of psilocybin had rapid, clinically significant, and lasting effects on mood and anxiety.
Limitations of the current survey cited by the researchers include the use of retrospective self-report to describe changes in death attitudes and the subjective features of the experiences. Also, respondents were a self-selected study population that may not be representative of all psychedelic or near-death experiences.
In addition, the study did not attempt to document worldview and other belief changes, such as increased belief in afterlife, that might help explain why death attitudes changed.
Looking ahead, the researchers note that future studies are needed to better understand the potential clinical use of psychedelics in ameliorating suffering related to fear of death.
Support through the Johns Hopkins Center for Psychedelic and Consciousness Research was provided by Tim Ferriss, Matt Mullenweg, Blake Mycoskie, Craig Nerenberg, and the Steven and Alexandra Cohen Foundation. Funding was also provided by the Y.C. Ho/Helen and Michael Chiang Foundation. The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PLOS ONE
Prior psychological distress tied to ‘long-COVID’ conditions
In an analysis of almost 55,000 adult participants in three ongoing studies, having depression, anxiety, worry, perceived stress, or loneliness early in the pandemic, before SARS-CoV-2 infection, was associated with a 50% increased risk for developing long COVID. These types of psychological distress were also associated with a 15% to 51% greater risk for impairment in daily life among individuals with long COVID.
Psychological distress was even more strongly associated with developing long COVID than were physical health risk factors, and the increased risk was not explained by health behaviors such as smoking or physical comorbidities, researchers note.
“Our findings suggest the need to consider psychological health in addition to physical health as risk factors of long COVID-19,” lead author Siwen Wang, MD, postdoctoral fellow, department of nutrition, Harvard T. H. Chan School of Public Health, Boston, said in an interview.
“We need to increase public awareness of the importance of mental health and focus on getting mental health care for people who need it, increasing the supply of mental health clinicians and improving access to care,” she said.
The findings were published online in JAMA Psychiatry.
‘Poorly understood’
Postacute sequelae of SARS-CoV-2 (“long COVID”), which are “signs and symptoms consistent with COVID-19 that extend beyond 4 weeks from onset of infection” constitute “an emerging health issue,” the investigators write.
Dr. Wang noted that it has been estimated that 8-23 million Americans have developed long COVID. However, “despite the high prevalence and daily life impairment associated with long COVID, it is still poorly understood, and few risk factors have been established,” she said.
Although psychological distress may be implicated in long COVID, only three previous studies investigated psychological factors as potential contributors, the researchers note. Also, no study has investigated the potential role of other common manifestations of distress that have increased during the pandemic, such as loneliness and perceived stress, they add.
To investigate these issues, the researchers turned to three large ongoing longitudinal studies: the Nurses’ Health Study II (NSHII), the Nurses’ Health study 3 (NHS3), and the Growing Up Today Study (GUTS).
They analyzed data on 54,960 total participants (96.6% women; mean age, 57.5 years). Of the full group, 38% were active health care workers.
Participants completed an online COVID-19 questionnaire from April 2020 to Sept. 1, 2020 (baseline), and monthly surveys thereafter. Beginning in August 2020, surveys were administered quarterly. The end of follow-up was in November 2021.
The COVID questionnaires included questions about positive SARS-CoV-2 test results, COVID symptoms and hospitalization since March 1, 2020, and the presence of long-term COVID symptoms, such as fatigue, respiratory problems, persistent cough, muscle/joint/chest pain, smell/taste problems, confusion/disorientation/brain fog, depression/anxiety/changes in mood, headache, and memory problems.
Participants who reported these post-COVID conditions were asked about the frequency of symptoms and the degree of impairment in daily life.
Inflammation, immune dysregulation implicated?
The Patient Health Questionnaire–4 (PHQ-4) was used to assess for anxiety and depressive symptoms in the past 2 weeks. It consists of a two-item depression measure (PHQ-2) and a two-item Generalized Anxiety Disorder Scale (GAD-2).
Non–health care providers completed two additional assessments of psychological distress: the four-item Perceived Stress Scale and the three-item UCLA Loneliness Scale.
The researchers included demographic factors, weight, smoking status, marital status, and medical conditions, including diabetes, hypertension, hypercholesterolemia, asthma, and cancer, and socioeconomic factors as covariates.
For each participant, the investigators calculated the number of types of distress experienced at a high level, including probable depression, probable anxiety, worry about COVID-19, being in the top quartile of perceived stress, and loneliness.
During the 19 months of follow-up (1-47 weeks after baseline), 6% of respondents reported a positive result on a SARS-CoV-2 antibody, antigen, or polymerase chain reaction test.
Of these, 43.9% reported long-COVID conditions, with most reporting that symptoms lasted 2 months or longer; 55.8% reported at least occasional daily life impairment.
The most common post-COVID conditions were fatigue (reported by 56%), loss of smell or taste problems (44.6%), shortness of breath (25.5%), confusion/disorientation/ brain fog (24.5%), and memory issues (21.8%).
Among patients who had been infected, there was a considerably higher rate of preinfection psychological distress after adjusting for sociodemographic factors, health behaviors, and comorbidities. Each type of distress was associated with post-COVID conditions.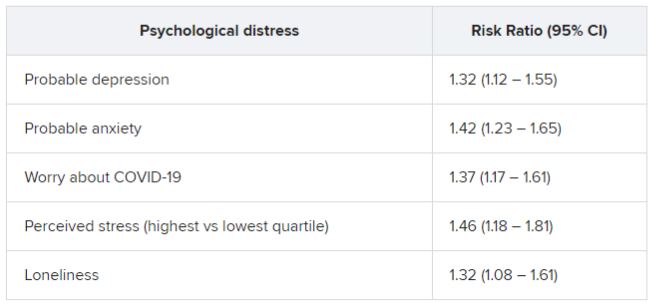
In addition, participants who had experienced at least two types of distress prior to infection were at nearly 50% increased risk for post–COVID conditions (risk ratio, 1.49; 95% confidence interval, 1.23-1.80).
Among those with post-COVID conditions, all types of distress were associated with increased risk for daily life impairment (RR range, 1.15-1.51).
Senior author Andrea Roberts, PhD, senior research scientist at the Harvard T. H. Chan School of Public Health, Boston, noted that the investigators did not examine biological mechanisms potentially underlying the association they found.
However, “based on prior research, it may be that inflammation and immune dysregulation related to psychological distress play a role in the association of distress with long COVID, but we can’t be sure,” Dr. Roberts said.
Contributes to the field
Commenting for this article, Yapeng Su, PhD, a postdoctoral researcher at the Fred Hutchinson Cancer Research Center in Seattle, called the study “great work contributing to the long-COVID research field and revealing important connections” with psychological stress prior to infection.
Dr. Su, who was not involved with the study, was previously at the Institute for Systems Biology, also in Seattle, and has written about long COVID.
He noted that the “biological mechanism of such intriguing linkage is definitely the important next step, which will likely require deep phenotyping of biological specimens from these patients longitudinally.”
Dr. Wang pointed to past research suggesting that some patients with mental illness “sometimes develop autoantibodies that have also been associated with increased risk of long COVID.” In addition, depression “affects the brain in ways that may explain certain cognitive symptoms in long COVID,” she added.
More studies are now needed to understand how psychological distress increases the risk for long COVID, said Dr. Wang.
The research was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institutes of Health, the Dean’s Fund for Scientific Advancement Acceleration Award from the Harvard T. H. Chan School of Public Health, the Massachusetts Consortium on Pathogen Readiness Evergrande COVID-19 Response Fund Award, and the Veterans Affairs Health Services Research and Development Service funds. Dr. Wang and Dr. Roberts have reported no relevant financial relationships. The other investigators’ disclosures are listed in the original article. Dr. Su reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In an analysis of almost 55,000 adult participants in three ongoing studies, having depression, anxiety, worry, perceived stress, or loneliness early in the pandemic, before SARS-CoV-2 infection, was associated with a 50% increased risk for developing long COVID. These types of psychological distress were also associated with a 15% to 51% greater risk for impairment in daily life among individuals with long COVID.
Psychological distress was even more strongly associated with developing long COVID than were physical health risk factors, and the increased risk was not explained by health behaviors such as smoking or physical comorbidities, researchers note.
“Our findings suggest the need to consider psychological health in addition to physical health as risk factors of long COVID-19,” lead author Siwen Wang, MD, postdoctoral fellow, department of nutrition, Harvard T. H. Chan School of Public Health, Boston, said in an interview.
“We need to increase public awareness of the importance of mental health and focus on getting mental health care for people who need it, increasing the supply of mental health clinicians and improving access to care,” she said.
The findings were published online in JAMA Psychiatry.
‘Poorly understood’
Postacute sequelae of SARS-CoV-2 (“long COVID”), which are “signs and symptoms consistent with COVID-19 that extend beyond 4 weeks from onset of infection” constitute “an emerging health issue,” the investigators write.
Dr. Wang noted that it has been estimated that 8-23 million Americans have developed long COVID. However, “despite the high prevalence and daily life impairment associated with long COVID, it is still poorly understood, and few risk factors have been established,” she said.
Although psychological distress may be implicated in long COVID, only three previous studies investigated psychological factors as potential contributors, the researchers note. Also, no study has investigated the potential role of other common manifestations of distress that have increased during the pandemic, such as loneliness and perceived stress, they add.
To investigate these issues, the researchers turned to three large ongoing longitudinal studies: the Nurses’ Health Study II (NSHII), the Nurses’ Health study 3 (NHS3), and the Growing Up Today Study (GUTS).
They analyzed data on 54,960 total participants (96.6% women; mean age, 57.5 years). Of the full group, 38% were active health care workers.
Participants completed an online COVID-19 questionnaire from April 2020 to Sept. 1, 2020 (baseline), and monthly surveys thereafter. Beginning in August 2020, surveys were administered quarterly. The end of follow-up was in November 2021.
The COVID questionnaires included questions about positive SARS-CoV-2 test results, COVID symptoms and hospitalization since March 1, 2020, and the presence of long-term COVID symptoms, such as fatigue, respiratory problems, persistent cough, muscle/joint/chest pain, smell/taste problems, confusion/disorientation/brain fog, depression/anxiety/changes in mood, headache, and memory problems.
Participants who reported these post-COVID conditions were asked about the frequency of symptoms and the degree of impairment in daily life.
Inflammation, immune dysregulation implicated?
The Patient Health Questionnaire–4 (PHQ-4) was used to assess for anxiety and depressive symptoms in the past 2 weeks. It consists of a two-item depression measure (PHQ-2) and a two-item Generalized Anxiety Disorder Scale (GAD-2).
Non–health care providers completed two additional assessments of psychological distress: the four-item Perceived Stress Scale and the three-item UCLA Loneliness Scale.
The researchers included demographic factors, weight, smoking status, marital status, and medical conditions, including diabetes, hypertension, hypercholesterolemia, asthma, and cancer, and socioeconomic factors as covariates.
For each participant, the investigators calculated the number of types of distress experienced at a high level, including probable depression, probable anxiety, worry about COVID-19, being in the top quartile of perceived stress, and loneliness.
During the 19 months of follow-up (1-47 weeks after baseline), 6% of respondents reported a positive result on a SARS-CoV-2 antibody, antigen, or polymerase chain reaction test.
Of these, 43.9% reported long-COVID conditions, with most reporting that symptoms lasted 2 months or longer; 55.8% reported at least occasional daily life impairment.
The most common post-COVID conditions were fatigue (reported by 56%), loss of smell or taste problems (44.6%), shortness of breath (25.5%), confusion/disorientation/ brain fog (24.5%), and memory issues (21.8%).
Among patients who had been infected, there was a considerably higher rate of preinfection psychological distress after adjusting for sociodemographic factors, health behaviors, and comorbidities. Each type of distress was associated with post-COVID conditions.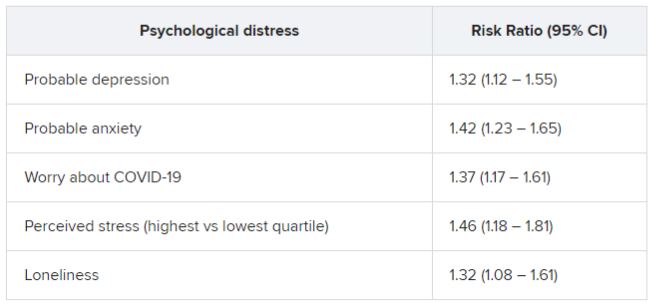
In addition, participants who had experienced at least two types of distress prior to infection were at nearly 50% increased risk for post–COVID conditions (risk ratio, 1.49; 95% confidence interval, 1.23-1.80).
Among those with post-COVID conditions, all types of distress were associated with increased risk for daily life impairment (RR range, 1.15-1.51).
Senior author Andrea Roberts, PhD, senior research scientist at the Harvard T. H. Chan School of Public Health, Boston, noted that the investigators did not examine biological mechanisms potentially underlying the association they found.
However, “based on prior research, it may be that inflammation and immune dysregulation related to psychological distress play a role in the association of distress with long COVID, but we can’t be sure,” Dr. Roberts said.
Contributes to the field
Commenting for this article, Yapeng Su, PhD, a postdoctoral researcher at the Fred Hutchinson Cancer Research Center in Seattle, called the study “great work contributing to the long-COVID research field and revealing important connections” with psychological stress prior to infection.
Dr. Su, who was not involved with the study, was previously at the Institute for Systems Biology, also in Seattle, and has written about long COVID.
He noted that the “biological mechanism of such intriguing linkage is definitely the important next step, which will likely require deep phenotyping of biological specimens from these patients longitudinally.”
Dr. Wang pointed to past research suggesting that some patients with mental illness “sometimes develop autoantibodies that have also been associated with increased risk of long COVID.” In addition, depression “affects the brain in ways that may explain certain cognitive symptoms in long COVID,” she added.
More studies are now needed to understand how psychological distress increases the risk for long COVID, said Dr. Wang.
The research was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institutes of Health, the Dean’s Fund for Scientific Advancement Acceleration Award from the Harvard T. H. Chan School of Public Health, the Massachusetts Consortium on Pathogen Readiness Evergrande COVID-19 Response Fund Award, and the Veterans Affairs Health Services Research and Development Service funds. Dr. Wang and Dr. Roberts have reported no relevant financial relationships. The other investigators’ disclosures are listed in the original article. Dr. Su reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In an analysis of almost 55,000 adult participants in three ongoing studies, having depression, anxiety, worry, perceived stress, or loneliness early in the pandemic, before SARS-CoV-2 infection, was associated with a 50% increased risk for developing long COVID. These types of psychological distress were also associated with a 15% to 51% greater risk for impairment in daily life among individuals with long COVID.
Psychological distress was even more strongly associated with developing long COVID than were physical health risk factors, and the increased risk was not explained by health behaviors such as smoking or physical comorbidities, researchers note.
“Our findings suggest the need to consider psychological health in addition to physical health as risk factors of long COVID-19,” lead author Siwen Wang, MD, postdoctoral fellow, department of nutrition, Harvard T. H. Chan School of Public Health, Boston, said in an interview.
“We need to increase public awareness of the importance of mental health and focus on getting mental health care for people who need it, increasing the supply of mental health clinicians and improving access to care,” she said.
The findings were published online in JAMA Psychiatry.
‘Poorly understood’
Postacute sequelae of SARS-CoV-2 (“long COVID”), which are “signs and symptoms consistent with COVID-19 that extend beyond 4 weeks from onset of infection” constitute “an emerging health issue,” the investigators write.
Dr. Wang noted that it has been estimated that 8-23 million Americans have developed long COVID. However, “despite the high prevalence and daily life impairment associated with long COVID, it is still poorly understood, and few risk factors have been established,” she said.
Although psychological distress may be implicated in long COVID, only three previous studies investigated psychological factors as potential contributors, the researchers note. Also, no study has investigated the potential role of other common manifestations of distress that have increased during the pandemic, such as loneliness and perceived stress, they add.
To investigate these issues, the researchers turned to three large ongoing longitudinal studies: the Nurses’ Health Study II (NSHII), the Nurses’ Health study 3 (NHS3), and the Growing Up Today Study (GUTS).
They analyzed data on 54,960 total participants (96.6% women; mean age, 57.5 years). Of the full group, 38% were active health care workers.
Participants completed an online COVID-19 questionnaire from April 2020 to Sept. 1, 2020 (baseline), and monthly surveys thereafter. Beginning in August 2020, surveys were administered quarterly. The end of follow-up was in November 2021.
The COVID questionnaires included questions about positive SARS-CoV-2 test results, COVID symptoms and hospitalization since March 1, 2020, and the presence of long-term COVID symptoms, such as fatigue, respiratory problems, persistent cough, muscle/joint/chest pain, smell/taste problems, confusion/disorientation/brain fog, depression/anxiety/changes in mood, headache, and memory problems.
Participants who reported these post-COVID conditions were asked about the frequency of symptoms and the degree of impairment in daily life.
Inflammation, immune dysregulation implicated?
The Patient Health Questionnaire–4 (PHQ-4) was used to assess for anxiety and depressive symptoms in the past 2 weeks. It consists of a two-item depression measure (PHQ-2) and a two-item Generalized Anxiety Disorder Scale (GAD-2).
Non–health care providers completed two additional assessments of psychological distress: the four-item Perceived Stress Scale and the three-item UCLA Loneliness Scale.
The researchers included demographic factors, weight, smoking status, marital status, and medical conditions, including diabetes, hypertension, hypercholesterolemia, asthma, and cancer, and socioeconomic factors as covariates.
For each participant, the investigators calculated the number of types of distress experienced at a high level, including probable depression, probable anxiety, worry about COVID-19, being in the top quartile of perceived stress, and loneliness.
During the 19 months of follow-up (1-47 weeks after baseline), 6% of respondents reported a positive result on a SARS-CoV-2 antibody, antigen, or polymerase chain reaction test.
Of these, 43.9% reported long-COVID conditions, with most reporting that symptoms lasted 2 months or longer; 55.8% reported at least occasional daily life impairment.
The most common post-COVID conditions were fatigue (reported by 56%), loss of smell or taste problems (44.6%), shortness of breath (25.5%), confusion/disorientation/ brain fog (24.5%), and memory issues (21.8%).
Among patients who had been infected, there was a considerably higher rate of preinfection psychological distress after adjusting for sociodemographic factors, health behaviors, and comorbidities. Each type of distress was associated with post-COVID conditions.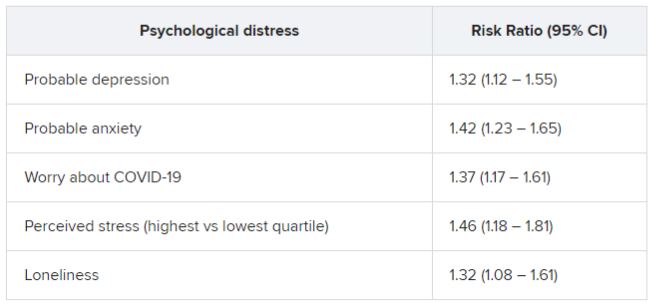
In addition, participants who had experienced at least two types of distress prior to infection were at nearly 50% increased risk for post–COVID conditions (risk ratio, 1.49; 95% confidence interval, 1.23-1.80).
Among those with post-COVID conditions, all types of distress were associated with increased risk for daily life impairment (RR range, 1.15-1.51).
Senior author Andrea Roberts, PhD, senior research scientist at the Harvard T. H. Chan School of Public Health, Boston, noted that the investigators did not examine biological mechanisms potentially underlying the association they found.
However, “based on prior research, it may be that inflammation and immune dysregulation related to psychological distress play a role in the association of distress with long COVID, but we can’t be sure,” Dr. Roberts said.
Contributes to the field
Commenting for this article, Yapeng Su, PhD, a postdoctoral researcher at the Fred Hutchinson Cancer Research Center in Seattle, called the study “great work contributing to the long-COVID research field and revealing important connections” with psychological stress prior to infection.
Dr. Su, who was not involved with the study, was previously at the Institute for Systems Biology, also in Seattle, and has written about long COVID.
He noted that the “biological mechanism of such intriguing linkage is definitely the important next step, which will likely require deep phenotyping of biological specimens from these patients longitudinally.”
Dr. Wang pointed to past research suggesting that some patients with mental illness “sometimes develop autoantibodies that have also been associated with increased risk of long COVID.” In addition, depression “affects the brain in ways that may explain certain cognitive symptoms in long COVID,” she added.
More studies are now needed to understand how psychological distress increases the risk for long COVID, said Dr. Wang.
The research was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institutes of Health, the Dean’s Fund for Scientific Advancement Acceleration Award from the Harvard T. H. Chan School of Public Health, the Massachusetts Consortium on Pathogen Readiness Evergrande COVID-19 Response Fund Award, and the Veterans Affairs Health Services Research and Development Service funds. Dr. Wang and Dr. Roberts have reported no relevant financial relationships. The other investigators’ disclosures are listed in the original article. Dr. Su reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY