User login
Missed visits during pandemic cause ‘detrimental ripple effects’
according to a new report from the Urban Institute.
Among the adults who postponed or missed care, 32.6% said the gap worsened one or more health conditions or limited their ability to work or perform daily activities. The findings highlight “the detrimental ripple effects of delaying or forgoing care on overall health, functioning, and well-being,” researchers write.
The survey, conducted among 4,007 U.S. adults aged 18-64 in September 2020, found that adults with one or more chronic conditions were more likely than adults without chronic conditions to have delayed or missed care (40.7% vs. 26.4%). Adults with a mental health condition were particularly likely to have delayed or gone without care, write Dulce Gonzalez, MPP, a research associate in the Health Policy Center at the Urban Institute, and colleagues.
Doctors are already seeing the consequences of the missed visits, says Jacqueline W. Fincher, MD, president of the American College of Physicians.
Two of her patients with chronic conditions missed appointments last year. By the time they resumed care in 2021, their previsit lab tests showed significant kidney deterioration.
“Lo and behold, their kidneys were in failure. … One was in the hospital for 3 days and the other one was in for 5 days,” said Dr. Fincher, who practices general internal medicine in Georgia.
Dr. Fincher’s office has been proactive about calling patients with chronic diseases who missed follow-up visits or laboratory testing or who may have run out of medication, she said.
In her experience, delays mainly have been because of patients postponing visits. “We have stayed open the whole time now,” Dr. Fincher said. Her office offers telemedicine visits and in-person visits with safety precautions.
Still, some patients have decided to postpone care during the pandemic instead of asking their primary care doctor what they should do.
“We do know that chronic problems left without appropriate follow-up can create worse problems for them in terms of stroke, heart attack, and end organ damage,” Dr. Fincher said.
Lost lives
Future studies may help researchers understand the effects of delayed and missed care during the pandemic, said Russell S. Phillips, MD, director of the Center for Primary Care at Harvard Medical School, Boston.
“Although it is still early, and more data on patient outcomes will need to be collected, I anticipate that the ... delays in diagnosis, in cancer screening, and in management of chronic illness will result in lost lives and will emphasize the important role that primary care plays in saving lives,” Dr. Phillips said.
During the first several months of the pandemic, there were fewer diagnoses of hypertension, diabetes, and depression, Dr. Phillips said.
“In addition, and most importantly, the mortality rate for non-COVID conditions increased, suggesting that patients were not seeking care for symptoms of stroke or heart attack, which can be fatal if untreated,” he said. “We have also seen substantial decreases in cancer screening tests such as colonoscopy, and modeling studies suggest this will cost more lives based on delayed diagnoses of cancer.”
Vaccinating patients against COVID-19 may help primary care practices and patients get back on track, Dr. Phillips suggested.
In the meantime, some patients remain reluctant to come in. “Volumes are still lower than prepandemic, so it is challenging to overcome what is likely to be pent-up demand,” he told this news organization in an email. “Additionally, the continued burden of evaluating, testing, and monitoring patients with COVID or COVID-like symptoms makes it difficult to focus on chronic illness.”
Care most often skipped
The Urban Institute survey asked respondents about delays in prescription drugs, general doctor and specialist visits, going to a hospital, preventive health screenings or medical tests, treatment or follow-up care, dental care, mental health care or counseling, treatment or counseling for alcohol or drug use, and other types of medical care.
Dental care was the most common type of care that adults delayed or did not receive because of the pandemic (25.3%), followed by general doctor or specialist visits (20.6%) and preventive health screenings or medical tests (15.5%).
Black adults were more likely than White or Hispanic/Latinx adults to have delayed or forgone care (39.7% vs. 34.3% and 35.5%), the researchers found. Compared with adults with higher incomes, adults with lower incomes were more likely to have missed multiple types of care (26.6% vs. 20.3%).
The report by the Urban Institute researchers was supported by the Robert Wood Johnson Foundation. Dr. Phillips is an adviser to two telemedicine companies, Bicycle Health and Grow Health. Dr. Fincher has disclosed no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
according to a new report from the Urban Institute.
Among the adults who postponed or missed care, 32.6% said the gap worsened one or more health conditions or limited their ability to work or perform daily activities. The findings highlight “the detrimental ripple effects of delaying or forgoing care on overall health, functioning, and well-being,” researchers write.
The survey, conducted among 4,007 U.S. adults aged 18-64 in September 2020, found that adults with one or more chronic conditions were more likely than adults without chronic conditions to have delayed or missed care (40.7% vs. 26.4%). Adults with a mental health condition were particularly likely to have delayed or gone without care, write Dulce Gonzalez, MPP, a research associate in the Health Policy Center at the Urban Institute, and colleagues.
Doctors are already seeing the consequences of the missed visits, says Jacqueline W. Fincher, MD, president of the American College of Physicians.
Two of her patients with chronic conditions missed appointments last year. By the time they resumed care in 2021, their previsit lab tests showed significant kidney deterioration.
“Lo and behold, their kidneys were in failure. … One was in the hospital for 3 days and the other one was in for 5 days,” said Dr. Fincher, who practices general internal medicine in Georgia.
Dr. Fincher’s office has been proactive about calling patients with chronic diseases who missed follow-up visits or laboratory testing or who may have run out of medication, she said.
In her experience, delays mainly have been because of patients postponing visits. “We have stayed open the whole time now,” Dr. Fincher said. Her office offers telemedicine visits and in-person visits with safety precautions.
Still, some patients have decided to postpone care during the pandemic instead of asking their primary care doctor what they should do.
“We do know that chronic problems left without appropriate follow-up can create worse problems for them in terms of stroke, heart attack, and end organ damage,” Dr. Fincher said.
Lost lives
Future studies may help researchers understand the effects of delayed and missed care during the pandemic, said Russell S. Phillips, MD, director of the Center for Primary Care at Harvard Medical School, Boston.
“Although it is still early, and more data on patient outcomes will need to be collected, I anticipate that the ... delays in diagnosis, in cancer screening, and in management of chronic illness will result in lost lives and will emphasize the important role that primary care plays in saving lives,” Dr. Phillips said.
During the first several months of the pandemic, there were fewer diagnoses of hypertension, diabetes, and depression, Dr. Phillips said.
“In addition, and most importantly, the mortality rate for non-COVID conditions increased, suggesting that patients were not seeking care for symptoms of stroke or heart attack, which can be fatal if untreated,” he said. “We have also seen substantial decreases in cancer screening tests such as colonoscopy, and modeling studies suggest this will cost more lives based on delayed diagnoses of cancer.”
Vaccinating patients against COVID-19 may help primary care practices and patients get back on track, Dr. Phillips suggested.
In the meantime, some patients remain reluctant to come in. “Volumes are still lower than prepandemic, so it is challenging to overcome what is likely to be pent-up demand,” he told this news organization in an email. “Additionally, the continued burden of evaluating, testing, and monitoring patients with COVID or COVID-like symptoms makes it difficult to focus on chronic illness.”
Care most often skipped
The Urban Institute survey asked respondents about delays in prescription drugs, general doctor and specialist visits, going to a hospital, preventive health screenings or medical tests, treatment or follow-up care, dental care, mental health care or counseling, treatment or counseling for alcohol or drug use, and other types of medical care.
Dental care was the most common type of care that adults delayed or did not receive because of the pandemic (25.3%), followed by general doctor or specialist visits (20.6%) and preventive health screenings or medical tests (15.5%).
Black adults were more likely than White or Hispanic/Latinx adults to have delayed or forgone care (39.7% vs. 34.3% and 35.5%), the researchers found. Compared with adults with higher incomes, adults with lower incomes were more likely to have missed multiple types of care (26.6% vs. 20.3%).
The report by the Urban Institute researchers was supported by the Robert Wood Johnson Foundation. Dr. Phillips is an adviser to two telemedicine companies, Bicycle Health and Grow Health. Dr. Fincher has disclosed no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
according to a new report from the Urban Institute.
Among the adults who postponed or missed care, 32.6% said the gap worsened one or more health conditions or limited their ability to work or perform daily activities. The findings highlight “the detrimental ripple effects of delaying or forgoing care on overall health, functioning, and well-being,” researchers write.
The survey, conducted among 4,007 U.S. adults aged 18-64 in September 2020, found that adults with one or more chronic conditions were more likely than adults without chronic conditions to have delayed or missed care (40.7% vs. 26.4%). Adults with a mental health condition were particularly likely to have delayed or gone without care, write Dulce Gonzalez, MPP, a research associate in the Health Policy Center at the Urban Institute, and colleagues.
Doctors are already seeing the consequences of the missed visits, says Jacqueline W. Fincher, MD, president of the American College of Physicians.
Two of her patients with chronic conditions missed appointments last year. By the time they resumed care in 2021, their previsit lab tests showed significant kidney deterioration.
“Lo and behold, their kidneys were in failure. … One was in the hospital for 3 days and the other one was in for 5 days,” said Dr. Fincher, who practices general internal medicine in Georgia.
Dr. Fincher’s office has been proactive about calling patients with chronic diseases who missed follow-up visits or laboratory testing or who may have run out of medication, she said.
In her experience, delays mainly have been because of patients postponing visits. “We have stayed open the whole time now,” Dr. Fincher said. Her office offers telemedicine visits and in-person visits with safety precautions.
Still, some patients have decided to postpone care during the pandemic instead of asking their primary care doctor what they should do.
“We do know that chronic problems left without appropriate follow-up can create worse problems for them in terms of stroke, heart attack, and end organ damage,” Dr. Fincher said.
Lost lives
Future studies may help researchers understand the effects of delayed and missed care during the pandemic, said Russell S. Phillips, MD, director of the Center for Primary Care at Harvard Medical School, Boston.
“Although it is still early, and more data on patient outcomes will need to be collected, I anticipate that the ... delays in diagnosis, in cancer screening, and in management of chronic illness will result in lost lives and will emphasize the important role that primary care plays in saving lives,” Dr. Phillips said.
During the first several months of the pandemic, there were fewer diagnoses of hypertension, diabetes, and depression, Dr. Phillips said.
“In addition, and most importantly, the mortality rate for non-COVID conditions increased, suggesting that patients were not seeking care for symptoms of stroke or heart attack, which can be fatal if untreated,” he said. “We have also seen substantial decreases in cancer screening tests such as colonoscopy, and modeling studies suggest this will cost more lives based on delayed diagnoses of cancer.”
Vaccinating patients against COVID-19 may help primary care practices and patients get back on track, Dr. Phillips suggested.
In the meantime, some patients remain reluctant to come in. “Volumes are still lower than prepandemic, so it is challenging to overcome what is likely to be pent-up demand,” he told this news organization in an email. “Additionally, the continued burden of evaluating, testing, and monitoring patients with COVID or COVID-like symptoms makes it difficult to focus on chronic illness.”
Care most often skipped
The Urban Institute survey asked respondents about delays in prescription drugs, general doctor and specialist visits, going to a hospital, preventive health screenings or medical tests, treatment or follow-up care, dental care, mental health care or counseling, treatment or counseling for alcohol or drug use, and other types of medical care.
Dental care was the most common type of care that adults delayed or did not receive because of the pandemic (25.3%), followed by general doctor or specialist visits (20.6%) and preventive health screenings or medical tests (15.5%).
Black adults were more likely than White or Hispanic/Latinx adults to have delayed or forgone care (39.7% vs. 34.3% and 35.5%), the researchers found. Compared with adults with higher incomes, adults with lower incomes were more likely to have missed multiple types of care (26.6% vs. 20.3%).
The report by the Urban Institute researchers was supported by the Robert Wood Johnson Foundation. Dr. Phillips is an adviser to two telemedicine companies, Bicycle Health and Grow Health. Dr. Fincher has disclosed no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
How to make resident mental health care stigma free
Sarah Sofka, MD, FACP, noticed a pattern. As program director for the internal medicine (IM) residency at West Virginia University, Morgantown, she was informed when residents were sent to counseling because they were affected by burnout, depression, or anxiety. When trainees returned from these visits, many told her the same thing: They wished they had sought help sooner.
IM residents and their families had access to free counseling at WVU, but few used the resource, says Dr. Sofka. “So, we thought, let’s just schedule all of our residents for a therapy visit so they can go and see what it’s like,” she said. “This will hopefully decrease the stigma for seeking mental health care. If everybody’s going, it’s not a big deal.”
In July 2015, Dr. Sofka and her colleagues launched a universal well-being assessment program for the IM residents at WVU. The program leaders automatically scheduled first- and second-year residents for a visit to the faculty staff assistance program counselors. The visits were not mandatory, and residents could choose not to go; but if they did go, they received the entire day of their visit off from work.
Five and a half years after launching their program, Dr. Sofka and her colleagues conducted one of the first studies of the efficacy of an opt-out approach for resident mental wellness. They found that , suggesting that residents were seeking help proactively after having to at least consider it.
Opt-out counseling is a recent concept in residency programs – one that’s attracting interest from training programs across the country. Brown University, Providence, R.I.; the University of Colorado at Denver, Aurora; University of Pennsylvania, Philadelphia; and the University of California, San Francisco have at least one residency program that uses the approach.
Lisa Meeks, PhD, an assistant professor of family medicine at Michigan Medicine, in Ann Arbor, and other experts also believe opt-out counseling could decrease stigma and help normalize seeking care for mental health problems in the medical community while lowering the barriers for trainees who need help.
No time, no access, plenty of stigma
Burnout and mental health are known to be major concerns for health care workers, especially trainees. College graduates starting medical education have lower rates of burnout and depression, compared with demographically matched peers; however, once they’ve started training, medical students, residents, and fellows are more likely to be burned out and exhibit symptoms of depression. The ongoing COVID-19 pandemic is further fraying the well-being of overworked and traumatized health care professionals, and experts predict a mental health crisis will follow the viral crisis.
The Accreditation Council for Graduate Medical Education recently mandated that programs offer wellness services to trainees. Yet this doesn’t mean they are always used; well-known barriers stand between residents, medical students, and physicians and their receiving effective mental health treatment.
Two of the most obvious are access and time, given the grueling and often inflexible schedules of most trainees, says Jessica Gold, MD, a psychiatrist at Washington University, St. Louis, who specializes in treating medical professionals. Dr. Gold also points out that, to be done correctly, these programs require institutional support and investment – resources that aren’t always adequate.
“A lack of transparency and clear messaging around what is available, who provides the services, and how to access these services can be a major barrier,” says Erene Stergiopoulos, MD, a second-year psychiatry resident at the University of Toronto. In addition, there can be considerable lag between when a resident realizes they need help and when they manage to find a provider and schedule an appointment, says Dr. Meeks.
Even when these logistical barriers are overcome, trainees and physicians have to contend with the persistent stigma associated with mental health treatment in the culture of medicine, says Dr. Gold. A recent survey by the American College of Emergency Physicians found that 73% of surveyed physicians feel there is stigma in their workplace about seeking mental health treatment. Many state medical licensing boards still require physicians to disclose mental health treatment, which discourages many trainees and providers from seeking proactive care, says Mary Moffit, PhD, associate professor of psychiatry and director of the resident and faculty wellness program at Oregon Health & Science University, Portland.
How the opt-out approach works
“The idea is by making it opt-out, you really normalize it,” says Maneesh Batra, MD, MPH, associate director of the University of Washington, Seattle, Children’s Hospital residency program. Similar approaches have proven effective at shaping human behavior in other health care settings, including boosting testing rates for HIV and increasing immunization rates for childhood vaccines, Dr. Batra says.
In general, opt-out programs acknowledge that people are busy and won’t take that extra step or click that extra button if they don’t have to, says Oana Tomescu, MD, PhD, associate professor of clinical medicine and pediatrics at the University of Pennsylvania, Philadelphia.
In 2018, Dr. Sofka and her colleagues at WVU conducted a survey that showed that a majority of residents thought favorably of their opt-out program and said they would return to counseling for follow-up care. In their most recent study, published in the Journal of Graduate Medical Education in 2021, Dr. Sofka and her colleagues found that residents did just that – only 8 of 239 opted out of universally scheduled visits. Resident-initiated visits increased significantly from zero during the 2014-2015 academic year to 23 in 2018-2019. Between those periods, program-mandated visits decreased significantly from 12 to 3.
The initiative has succeeded in creating a culture of openness and caring at WVU, says 2nd-year internal medicine resident Nistha Modi, MD. “It sets the tone for the program – we talk about mental health openly,” says Dr. Modi.
Crucially, the counselors work out of a different building than the hospital where Dr. Modi and her fellow residents work and use a separate electronic medical record system to protect resident privacy. This is hugely important for medical trainees, note Dr. Tomescu, Dr. Gold, and many other experts. The therapists understand residency and medical education, and there is no limit to the number of visits a resident or fellow can make with the program counselors, says Dr. Modi.
Opt-out programs offer a counterbalance to many negative tendencies in residency, says Dr. Meeks. “We’ve normalized so many things that are not healthy and productive. ... We need to counterbalance that with normalizing help seeking. And it’s really difficult to normalize something that’s not part of a system.”
Costs, concerns, and systematic support
Providing unlimited, free counseling for trainees can be very beneficial, but it requires adequate funding and personnel resources. Offering unlimited access means that an institution has to follow through in making this degree of care available while also ensuring that the system doesn’t get overwhelmed or is unable to accommodate very sick individuals, says Dr. Gold.
Another concern that experts like Dr. Batra, Dr. Moffit, and Dr. Gold share is that residents who go to their scheduled appointments may not completely buy into the experience because it wasn’t their idea in the first place. Participation alone doesn’t necessarily indicate full acceptance. Program personnel don’t intend for these appointments to be thought of as mandatory, yet residents may still experience them that way. Several leading resident well-being programs instead emphasize outreach to trainees, institutional support, and accessible mental health resources that are – and feel – entirely voluntary.
“If I tell someone that they have to do something, it’s very different than if they arrive at that conclusion for themselves,” says Dr. Batra. “That’s how life works.”
When it comes to cost, a recent study published in Academic Medicine provides encouraging data. At the University of Colorado, an opt-out pilot program for IM and pediatrics interns during the 2017-2018 academic year cost just $940 total, equal to $11.75 per intern. As in West Virginia, the program in Colorado covered the cost of the visit, interns were provided a half day off (whether they attended their appointment or not), and the visits and surveys were entirely optional and confidential. During the 1-year pilot program, 29% of 80 interns attended the scheduled appointment, 56% opted out in advance, and 15% didn’t show up. The majority of interns who were surveyed (85%), however, thought the program should continue and that it had a positive effect on their wellness even if they didn’t attend their appointment.
In West Virginia, program costs are higher. The program has $20,000 in annual funding to cover the opt-out program and unlimited counseling visits for residents and fellows. With that funding, Dr. Sofka and her colleagues were also able to expand the program slightly last year to schedule all the critical care faculty for counseling visits. Cost is a barrier to expanding these services to the entire institution, which Dr. Sofka says she hopes to do one day.
Research in this area is still preliminary. The WVU and Colorado studies provide some of the first evidence in support of an opt-out approach. Eventually, it would be beneficial for multicenter studies and longitudinal research to track the effects of such programs over time, say Dr. Sofka and Ajay Major, MD, MBA, one of the study’s coauthors and a hematology/oncology fellow at the University of Chicago.
Whether a program goes with an opt-out approach or not, the systematic supports – protecting resident privacy, providing flexible scheduling, and more – are crucial.
As Dr. Tomescu notes, wellness shouldn’t be just something trainees have to do. “The key with really working on burnout at a huge level is for all programs and schools to recognize that it’s a shared responsibility.”
“I felt very fortunate that I was able to get some help throughout residency,” says Dr. Modi. “About how to be a better daughter. How to be content with things I have in life. How to be happy, and grateful. With the kind of job we have, I think we sometimes forget to be grateful.”
A version of this article first appeared on Medscape.com.
Sarah Sofka, MD, FACP, noticed a pattern. As program director for the internal medicine (IM) residency at West Virginia University, Morgantown, she was informed when residents were sent to counseling because they were affected by burnout, depression, or anxiety. When trainees returned from these visits, many told her the same thing: They wished they had sought help sooner.
IM residents and their families had access to free counseling at WVU, but few used the resource, says Dr. Sofka. “So, we thought, let’s just schedule all of our residents for a therapy visit so they can go and see what it’s like,” she said. “This will hopefully decrease the stigma for seeking mental health care. If everybody’s going, it’s not a big deal.”
In July 2015, Dr. Sofka and her colleagues launched a universal well-being assessment program for the IM residents at WVU. The program leaders automatically scheduled first- and second-year residents for a visit to the faculty staff assistance program counselors. The visits were not mandatory, and residents could choose not to go; but if they did go, they received the entire day of their visit off from work.
Five and a half years after launching their program, Dr. Sofka and her colleagues conducted one of the first studies of the efficacy of an opt-out approach for resident mental wellness. They found that , suggesting that residents were seeking help proactively after having to at least consider it.
Opt-out counseling is a recent concept in residency programs – one that’s attracting interest from training programs across the country. Brown University, Providence, R.I.; the University of Colorado at Denver, Aurora; University of Pennsylvania, Philadelphia; and the University of California, San Francisco have at least one residency program that uses the approach.
Lisa Meeks, PhD, an assistant professor of family medicine at Michigan Medicine, in Ann Arbor, and other experts also believe opt-out counseling could decrease stigma and help normalize seeking care for mental health problems in the medical community while lowering the barriers for trainees who need help.
No time, no access, plenty of stigma
Burnout and mental health are known to be major concerns for health care workers, especially trainees. College graduates starting medical education have lower rates of burnout and depression, compared with demographically matched peers; however, once they’ve started training, medical students, residents, and fellows are more likely to be burned out and exhibit symptoms of depression. The ongoing COVID-19 pandemic is further fraying the well-being of overworked and traumatized health care professionals, and experts predict a mental health crisis will follow the viral crisis.
The Accreditation Council for Graduate Medical Education recently mandated that programs offer wellness services to trainees. Yet this doesn’t mean they are always used; well-known barriers stand between residents, medical students, and physicians and their receiving effective mental health treatment.
Two of the most obvious are access and time, given the grueling and often inflexible schedules of most trainees, says Jessica Gold, MD, a psychiatrist at Washington University, St. Louis, who specializes in treating medical professionals. Dr. Gold also points out that, to be done correctly, these programs require institutional support and investment – resources that aren’t always adequate.
“A lack of transparency and clear messaging around what is available, who provides the services, and how to access these services can be a major barrier,” says Erene Stergiopoulos, MD, a second-year psychiatry resident at the University of Toronto. In addition, there can be considerable lag between when a resident realizes they need help and when they manage to find a provider and schedule an appointment, says Dr. Meeks.
Even when these logistical barriers are overcome, trainees and physicians have to contend with the persistent stigma associated with mental health treatment in the culture of medicine, says Dr. Gold. A recent survey by the American College of Emergency Physicians found that 73% of surveyed physicians feel there is stigma in their workplace about seeking mental health treatment. Many state medical licensing boards still require physicians to disclose mental health treatment, which discourages many trainees and providers from seeking proactive care, says Mary Moffit, PhD, associate professor of psychiatry and director of the resident and faculty wellness program at Oregon Health & Science University, Portland.
How the opt-out approach works
“The idea is by making it opt-out, you really normalize it,” says Maneesh Batra, MD, MPH, associate director of the University of Washington, Seattle, Children’s Hospital residency program. Similar approaches have proven effective at shaping human behavior in other health care settings, including boosting testing rates for HIV and increasing immunization rates for childhood vaccines, Dr. Batra says.
In general, opt-out programs acknowledge that people are busy and won’t take that extra step or click that extra button if they don’t have to, says Oana Tomescu, MD, PhD, associate professor of clinical medicine and pediatrics at the University of Pennsylvania, Philadelphia.
In 2018, Dr. Sofka and her colleagues at WVU conducted a survey that showed that a majority of residents thought favorably of their opt-out program and said they would return to counseling for follow-up care. In their most recent study, published in the Journal of Graduate Medical Education in 2021, Dr. Sofka and her colleagues found that residents did just that – only 8 of 239 opted out of universally scheduled visits. Resident-initiated visits increased significantly from zero during the 2014-2015 academic year to 23 in 2018-2019. Between those periods, program-mandated visits decreased significantly from 12 to 3.
The initiative has succeeded in creating a culture of openness and caring at WVU, says 2nd-year internal medicine resident Nistha Modi, MD. “It sets the tone for the program – we talk about mental health openly,” says Dr. Modi.
Crucially, the counselors work out of a different building than the hospital where Dr. Modi and her fellow residents work and use a separate electronic medical record system to protect resident privacy. This is hugely important for medical trainees, note Dr. Tomescu, Dr. Gold, and many other experts. The therapists understand residency and medical education, and there is no limit to the number of visits a resident or fellow can make with the program counselors, says Dr. Modi.
Opt-out programs offer a counterbalance to many negative tendencies in residency, says Dr. Meeks. “We’ve normalized so many things that are not healthy and productive. ... We need to counterbalance that with normalizing help seeking. And it’s really difficult to normalize something that’s not part of a system.”
Costs, concerns, and systematic support
Providing unlimited, free counseling for trainees can be very beneficial, but it requires adequate funding and personnel resources. Offering unlimited access means that an institution has to follow through in making this degree of care available while also ensuring that the system doesn’t get overwhelmed or is unable to accommodate very sick individuals, says Dr. Gold.
Another concern that experts like Dr. Batra, Dr. Moffit, and Dr. Gold share is that residents who go to their scheduled appointments may not completely buy into the experience because it wasn’t their idea in the first place. Participation alone doesn’t necessarily indicate full acceptance. Program personnel don’t intend for these appointments to be thought of as mandatory, yet residents may still experience them that way. Several leading resident well-being programs instead emphasize outreach to trainees, institutional support, and accessible mental health resources that are – and feel – entirely voluntary.
“If I tell someone that they have to do something, it’s very different than if they arrive at that conclusion for themselves,” says Dr. Batra. “That’s how life works.”
When it comes to cost, a recent study published in Academic Medicine provides encouraging data. At the University of Colorado, an opt-out pilot program for IM and pediatrics interns during the 2017-2018 academic year cost just $940 total, equal to $11.75 per intern. As in West Virginia, the program in Colorado covered the cost of the visit, interns were provided a half day off (whether they attended their appointment or not), and the visits and surveys were entirely optional and confidential. During the 1-year pilot program, 29% of 80 interns attended the scheduled appointment, 56% opted out in advance, and 15% didn’t show up. The majority of interns who were surveyed (85%), however, thought the program should continue and that it had a positive effect on their wellness even if they didn’t attend their appointment.
In West Virginia, program costs are higher. The program has $20,000 in annual funding to cover the opt-out program and unlimited counseling visits for residents and fellows. With that funding, Dr. Sofka and her colleagues were also able to expand the program slightly last year to schedule all the critical care faculty for counseling visits. Cost is a barrier to expanding these services to the entire institution, which Dr. Sofka says she hopes to do one day.
Research in this area is still preliminary. The WVU and Colorado studies provide some of the first evidence in support of an opt-out approach. Eventually, it would be beneficial for multicenter studies and longitudinal research to track the effects of such programs over time, say Dr. Sofka and Ajay Major, MD, MBA, one of the study’s coauthors and a hematology/oncology fellow at the University of Chicago.
Whether a program goes with an opt-out approach or not, the systematic supports – protecting resident privacy, providing flexible scheduling, and more – are crucial.
As Dr. Tomescu notes, wellness shouldn’t be just something trainees have to do. “The key with really working on burnout at a huge level is for all programs and schools to recognize that it’s a shared responsibility.”
“I felt very fortunate that I was able to get some help throughout residency,” says Dr. Modi. “About how to be a better daughter. How to be content with things I have in life. How to be happy, and grateful. With the kind of job we have, I think we sometimes forget to be grateful.”
A version of this article first appeared on Medscape.com.
Sarah Sofka, MD, FACP, noticed a pattern. As program director for the internal medicine (IM) residency at West Virginia University, Morgantown, she was informed when residents were sent to counseling because they were affected by burnout, depression, or anxiety. When trainees returned from these visits, many told her the same thing: They wished they had sought help sooner.
IM residents and their families had access to free counseling at WVU, but few used the resource, says Dr. Sofka. “So, we thought, let’s just schedule all of our residents for a therapy visit so they can go and see what it’s like,” she said. “This will hopefully decrease the stigma for seeking mental health care. If everybody’s going, it’s not a big deal.”
In July 2015, Dr. Sofka and her colleagues launched a universal well-being assessment program for the IM residents at WVU. The program leaders automatically scheduled first- and second-year residents for a visit to the faculty staff assistance program counselors. The visits were not mandatory, and residents could choose not to go; but if they did go, they received the entire day of their visit off from work.
Five and a half years after launching their program, Dr. Sofka and her colleagues conducted one of the first studies of the efficacy of an opt-out approach for resident mental wellness. They found that , suggesting that residents were seeking help proactively after having to at least consider it.
Opt-out counseling is a recent concept in residency programs – one that’s attracting interest from training programs across the country. Brown University, Providence, R.I.; the University of Colorado at Denver, Aurora; University of Pennsylvania, Philadelphia; and the University of California, San Francisco have at least one residency program that uses the approach.
Lisa Meeks, PhD, an assistant professor of family medicine at Michigan Medicine, in Ann Arbor, and other experts also believe opt-out counseling could decrease stigma and help normalize seeking care for mental health problems in the medical community while lowering the barriers for trainees who need help.
No time, no access, plenty of stigma
Burnout and mental health are known to be major concerns for health care workers, especially trainees. College graduates starting medical education have lower rates of burnout and depression, compared with demographically matched peers; however, once they’ve started training, medical students, residents, and fellows are more likely to be burned out and exhibit symptoms of depression. The ongoing COVID-19 pandemic is further fraying the well-being of overworked and traumatized health care professionals, and experts predict a mental health crisis will follow the viral crisis.
The Accreditation Council for Graduate Medical Education recently mandated that programs offer wellness services to trainees. Yet this doesn’t mean they are always used; well-known barriers stand between residents, medical students, and physicians and their receiving effective mental health treatment.
Two of the most obvious are access and time, given the grueling and often inflexible schedules of most trainees, says Jessica Gold, MD, a psychiatrist at Washington University, St. Louis, who specializes in treating medical professionals. Dr. Gold also points out that, to be done correctly, these programs require institutional support and investment – resources that aren’t always adequate.
“A lack of transparency and clear messaging around what is available, who provides the services, and how to access these services can be a major barrier,” says Erene Stergiopoulos, MD, a second-year psychiatry resident at the University of Toronto. In addition, there can be considerable lag between when a resident realizes they need help and when they manage to find a provider and schedule an appointment, says Dr. Meeks.
Even when these logistical barriers are overcome, trainees and physicians have to contend with the persistent stigma associated with mental health treatment in the culture of medicine, says Dr. Gold. A recent survey by the American College of Emergency Physicians found that 73% of surveyed physicians feel there is stigma in their workplace about seeking mental health treatment. Many state medical licensing boards still require physicians to disclose mental health treatment, which discourages many trainees and providers from seeking proactive care, says Mary Moffit, PhD, associate professor of psychiatry and director of the resident and faculty wellness program at Oregon Health & Science University, Portland.
How the opt-out approach works
“The idea is by making it opt-out, you really normalize it,” says Maneesh Batra, MD, MPH, associate director of the University of Washington, Seattle, Children’s Hospital residency program. Similar approaches have proven effective at shaping human behavior in other health care settings, including boosting testing rates for HIV and increasing immunization rates for childhood vaccines, Dr. Batra says.
In general, opt-out programs acknowledge that people are busy and won’t take that extra step or click that extra button if they don’t have to, says Oana Tomescu, MD, PhD, associate professor of clinical medicine and pediatrics at the University of Pennsylvania, Philadelphia.
In 2018, Dr. Sofka and her colleagues at WVU conducted a survey that showed that a majority of residents thought favorably of their opt-out program and said they would return to counseling for follow-up care. In their most recent study, published in the Journal of Graduate Medical Education in 2021, Dr. Sofka and her colleagues found that residents did just that – only 8 of 239 opted out of universally scheduled visits. Resident-initiated visits increased significantly from zero during the 2014-2015 academic year to 23 in 2018-2019. Between those periods, program-mandated visits decreased significantly from 12 to 3.
The initiative has succeeded in creating a culture of openness and caring at WVU, says 2nd-year internal medicine resident Nistha Modi, MD. “It sets the tone for the program – we talk about mental health openly,” says Dr. Modi.
Crucially, the counselors work out of a different building than the hospital where Dr. Modi and her fellow residents work and use a separate electronic medical record system to protect resident privacy. This is hugely important for medical trainees, note Dr. Tomescu, Dr. Gold, and many other experts. The therapists understand residency and medical education, and there is no limit to the number of visits a resident or fellow can make with the program counselors, says Dr. Modi.
Opt-out programs offer a counterbalance to many negative tendencies in residency, says Dr. Meeks. “We’ve normalized so many things that are not healthy and productive. ... We need to counterbalance that with normalizing help seeking. And it’s really difficult to normalize something that’s not part of a system.”
Costs, concerns, and systematic support
Providing unlimited, free counseling for trainees can be very beneficial, but it requires adequate funding and personnel resources. Offering unlimited access means that an institution has to follow through in making this degree of care available while also ensuring that the system doesn’t get overwhelmed or is unable to accommodate very sick individuals, says Dr. Gold.
Another concern that experts like Dr. Batra, Dr. Moffit, and Dr. Gold share is that residents who go to their scheduled appointments may not completely buy into the experience because it wasn’t their idea in the first place. Participation alone doesn’t necessarily indicate full acceptance. Program personnel don’t intend for these appointments to be thought of as mandatory, yet residents may still experience them that way. Several leading resident well-being programs instead emphasize outreach to trainees, institutional support, and accessible mental health resources that are – and feel – entirely voluntary.
“If I tell someone that they have to do something, it’s very different than if they arrive at that conclusion for themselves,” says Dr. Batra. “That’s how life works.”
When it comes to cost, a recent study published in Academic Medicine provides encouraging data. At the University of Colorado, an opt-out pilot program for IM and pediatrics interns during the 2017-2018 academic year cost just $940 total, equal to $11.75 per intern. As in West Virginia, the program in Colorado covered the cost of the visit, interns were provided a half day off (whether they attended their appointment or not), and the visits and surveys were entirely optional and confidential. During the 1-year pilot program, 29% of 80 interns attended the scheduled appointment, 56% opted out in advance, and 15% didn’t show up. The majority of interns who were surveyed (85%), however, thought the program should continue and that it had a positive effect on their wellness even if they didn’t attend their appointment.
In West Virginia, program costs are higher. The program has $20,000 in annual funding to cover the opt-out program and unlimited counseling visits for residents and fellows. With that funding, Dr. Sofka and her colleagues were also able to expand the program slightly last year to schedule all the critical care faculty for counseling visits. Cost is a barrier to expanding these services to the entire institution, which Dr. Sofka says she hopes to do one day.
Research in this area is still preliminary. The WVU and Colorado studies provide some of the first evidence in support of an opt-out approach. Eventually, it would be beneficial for multicenter studies and longitudinal research to track the effects of such programs over time, say Dr. Sofka and Ajay Major, MD, MBA, one of the study’s coauthors and a hematology/oncology fellow at the University of Chicago.
Whether a program goes with an opt-out approach or not, the systematic supports – protecting resident privacy, providing flexible scheduling, and more – are crucial.
As Dr. Tomescu notes, wellness shouldn’t be just something trainees have to do. “The key with really working on burnout at a huge level is for all programs and schools to recognize that it’s a shared responsibility.”
“I felt very fortunate that I was able to get some help throughout residency,” says Dr. Modi. “About how to be a better daughter. How to be content with things I have in life. How to be happy, and grateful. With the kind of job we have, I think we sometimes forget to be grateful.”
A version of this article first appeared on Medscape.com.
Is board recertification worth it?
I passed the neurology boards, for the first time, in 1998. Then again in 2009, and most recently in 2019.
So I’m up again in 2029. Regrettably, I missed grandfathering in for life by a few years.
Some people don’t study for them, but I’m a little too compulsive not to. I’d guess I put 40-50 hours into doing so in the 3 months beforehand. I didn’t want to fail and have to pay a hefty fee to retake them (the test fee for once is enough as it is).
I’ll be 63 when my next certification is due.
So I wonder (if I’m still in practice) will it even be worthwhile to do it all again? I like what I do, but certainly don’t plan on practicing forever.
Board certification looks good on paper, but certainly isn’t a requirement to practice. One of the best cardiologists I know has never bothered to get his board certification and I don’t think any less of him for it. He also isn’t wanting for patients, and those he has think he’s awesome.
That said, there are things, like being involved in research and legal work, where board certification is strongly recommended, if not mandatory. Since I do both, I certainly wouldn’t want to do anything that might affect my participating in them – if I’m still doing this in 8 years.
By the same token, my office lease runs out when I’m 62. At that point I’ll have been in the same place for 17 years. I don’t consider that a bad thing. I like my current office, and will be perfectly happy to wrap up my career here.
It brings up the same question, though, with logistics that are an even bigger PIA. The last thing I want to do is move my office as my career is winding down. But a lease extension for a few years can be negotiated, a board certification can’t.
I can’t help but wonder: If I’ve already passed it three times, hopefully that means I know what I’m doing. One side will argue that it’s purely greed, as the people who run the boards need money and a way to justify their existence. On the other side are those who argue that maintenance of certification, while not perfect, is the only way we have of making sure practicing physicians are staying up to snuff.
The truth, as always, is somewhere in between.
But it still raises a question that I, fortunately, have another 8 years to think about. Because I’m not in a position to debate if it’s right or wrong, I just have to play by the rules.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I passed the neurology boards, for the first time, in 1998. Then again in 2009, and most recently in 2019.
So I’m up again in 2029. Regrettably, I missed grandfathering in for life by a few years.
Some people don’t study for them, but I’m a little too compulsive not to. I’d guess I put 40-50 hours into doing so in the 3 months beforehand. I didn’t want to fail and have to pay a hefty fee to retake them (the test fee for once is enough as it is).
I’ll be 63 when my next certification is due.
So I wonder (if I’m still in practice) will it even be worthwhile to do it all again? I like what I do, but certainly don’t plan on practicing forever.
Board certification looks good on paper, but certainly isn’t a requirement to practice. One of the best cardiologists I know has never bothered to get his board certification and I don’t think any less of him for it. He also isn’t wanting for patients, and those he has think he’s awesome.
That said, there are things, like being involved in research and legal work, where board certification is strongly recommended, if not mandatory. Since I do both, I certainly wouldn’t want to do anything that might affect my participating in them – if I’m still doing this in 8 years.
By the same token, my office lease runs out when I’m 62. At that point I’ll have been in the same place for 17 years. I don’t consider that a bad thing. I like my current office, and will be perfectly happy to wrap up my career here.
It brings up the same question, though, with logistics that are an even bigger PIA. The last thing I want to do is move my office as my career is winding down. But a lease extension for a few years can be negotiated, a board certification can’t.
I can’t help but wonder: If I’ve already passed it three times, hopefully that means I know what I’m doing. One side will argue that it’s purely greed, as the people who run the boards need money and a way to justify their existence. On the other side are those who argue that maintenance of certification, while not perfect, is the only way we have of making sure practicing physicians are staying up to snuff.
The truth, as always, is somewhere in between.
But it still raises a question that I, fortunately, have another 8 years to think about. Because I’m not in a position to debate if it’s right or wrong, I just have to play by the rules.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I passed the neurology boards, for the first time, in 1998. Then again in 2009, and most recently in 2019.
So I’m up again in 2029. Regrettably, I missed grandfathering in for life by a few years.
Some people don’t study for them, but I’m a little too compulsive not to. I’d guess I put 40-50 hours into doing so in the 3 months beforehand. I didn’t want to fail and have to pay a hefty fee to retake them (the test fee for once is enough as it is).
I’ll be 63 when my next certification is due.
So I wonder (if I’m still in practice) will it even be worthwhile to do it all again? I like what I do, but certainly don’t plan on practicing forever.
Board certification looks good on paper, but certainly isn’t a requirement to practice. One of the best cardiologists I know has never bothered to get his board certification and I don’t think any less of him for it. He also isn’t wanting for patients, and those he has think he’s awesome.
That said, there are things, like being involved in research and legal work, where board certification is strongly recommended, if not mandatory. Since I do both, I certainly wouldn’t want to do anything that might affect my participating in them – if I’m still doing this in 8 years.
By the same token, my office lease runs out when I’m 62. At that point I’ll have been in the same place for 17 years. I don’t consider that a bad thing. I like my current office, and will be perfectly happy to wrap up my career here.
It brings up the same question, though, with logistics that are an even bigger PIA. The last thing I want to do is move my office as my career is winding down. But a lease extension for a few years can be negotiated, a board certification can’t.
I can’t help but wonder: If I’ve already passed it three times, hopefully that means I know what I’m doing. One side will argue that it’s purely greed, as the people who run the boards need money and a way to justify their existence. On the other side are those who argue that maintenance of certification, while not perfect, is the only way we have of making sure practicing physicians are staying up to snuff.
The truth, as always, is somewhere in between.
But it still raises a question that I, fortunately, have another 8 years to think about. Because I’m not in a position to debate if it’s right or wrong, I just have to play by the rules.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Docs become dog groomers and warehouse workers after COVID-19 work loss
One of the biggest conundrums of the COVID-19 pandemic has been the simultaneous panic-hiring of medical professionals in hot spots and significant downsizing of staff across the country. From huge hospital systems to private practices, the stoppage of breast reductions and knee replacements, not to mention the drops in motor vehicle accidents and bar fights, have quieted operating rooms and emergency departments and put doctors’ jobs on the chopping block. A widely cited survey suggests that 21% of doctors have had a work reduction due to COVID-19.
For many American doctors, this is their first extended period of unemployment. Unlike engineers or those with MBAs who might see their fortunes rise and fall with the whims of recessions and boom times, physicians are not exactly accustomed to being laid off. However, doctors were already smarting for years due to falling salaries and decreased autonomy, punctuated by endless clicks on electronic medical records software.
Stephanie Eschenbach Morgan, MD, a breast radiologist in North Carolina, trained for 10 years after college before earning a true physician’s salary.
“Being furloughed was awful. Initially, it was only going to be 2 weeks, and then it turned into 2 months with no pay,” she reflected.
Dr. Eschenbach Morgan and her surgeon husband, who lost a full quarter’s salary, had to ask for grace periods on their credit card and mortgage payments because they had paid a large tax bill right before the pandemic began. “We couldn’t get any stimulus help, so that added insult to injury,” she said.
With her time spent waiting in a holding pattern, Dr. Eschenbach Morgan homeschooled her two young children and started putting a home gym together. She went on a home organizing spree, started a garden, and, perhaps most impressively, caught up with 5 years of photo albums.
A bonus she noted: “I didn’t set an alarm for 2 months.”
Shella Farooki, MD, a radiologist in California, was also focused on homeschooling, itself a demanding job, and veered toward retirement. When one of her work contracts furloughed her (“at one point, I made $30K a month for [their business]”), she started saving money at home, teaching the kids, and applied for a Paycheck Protection Program loan. Her husband, a hospitalist, had had his shifts cut. Dr. Farooki tried a radiology artificial intelligence firm but backed out when she was asked to read 9,200 studies for them for $2,000 per month.
Now, she thinks about leaving medicine “every day.”
Some doctors are questioning whether they should be in medicine in the first place. Family medicine physician Jonathan Polak, MD, faced with his own pink slip, turned to pink T-shirts instead. His girlfriend manages an outlet of the teen fashion retailer Justice. Dr. Polak, who finished his residency just 2 years ago, didn’t hesitate to take a $10-an-hour gig as a stock doc, once even finding himself delivering a shelving unit from the shuttering store to a physician fleeing the city for rural New Hampshire to “escape.”
There’s no escape for him – yet. Saddled with “astronomical” student loans, he had considered grocery store work as well. Dr. Polak knows he can’t work part time or go into teaching long term, as he might like.
Even so, he’s doing everything he can to not be in patient care for the long haul – it’s just not what he thought it would be.
“The culture of medicine, bureaucracy, endless paperwork and charting, and threat of litigation sucks a lot of the joy out of it to the point that I don’t see myself doing it forever when imagining myself 5-10 years into it.”
Still, he recently took an 18-month hospital contract that will force him to move to Florida, but he’s also been turning himself into a veritable Renaissance man; composing music, training for an ultramarathon, studying the latest medical findings, roadtripping, and launching a podcast about dog grooming with a master groomer. “We found parallels between medicine and dog grooming,” he says, somewhat convincingly.
Also working the ruff life is Jen Tserng, MD, a former forensic pathologist who landed on news websites in recent years for becoming a professional dogwalker and housesitter without a permanent home. Dr. Tserng knows doctors were restless and unhappy before COVID-19, their thoughts wandering where the grass might be greener.
As her profile grew, she found her inbox gathering messages from disaffected medical minions: students with a fear of failing or staring down residency application season and employed doctors sick of the constant grind. As she recounted those de facto life coach conversations (“What do you really enjoy?” “Do you really like dogs?”) by phone from New York, she said matter-of-factly, “They don’t call because of COVID. They call because they hate their lives.”
Michelle Mudge-Riley, MD, a physician in Texas, has been seeing this shift for some time as well. She recently held a virtual version of her Physicians Helping Physicians conference, where doctors hear from their peers working successfully in fields like pharmaceuticals and real estate investing.
When COVID-19 hit, Dr. Mudge-Riley quickly pivoted to a virtual platform, where the MDs and DOs huddled in breakout rooms having honest chats about their fears and tentative hopes about their new careers.
“There has been increased interest in nonclinical exploration into full- and part-time careers, as well as side hustles, since COVID began,” she said. “Many physicians have had their hours or pay cut, and some have been laid off. Others are furloughed. Some just want out of an environment where they don’t feel safe.”
An ear, nose, and throat surgeon, Maansi Doshi, MD, from central California, didn’t feel safe – so she left. She had returned from India sick with a mystery virus right as the pandemic began (she said her COVID-19 tests were all negative) and was waiting to get well enough to go back to her private practice job. However, she said she clashed with Trump-supporting colleagues she feared might not be taking the pandemic seriously enough.
Finally getting over a relapse of her mystery virus, Dr. Doshi emailed her resignation in May. Her husband, family practice doctor Mark Mangiapane, MD, gave his job notice weeks later in solidarity because he worked in the same building. Together, they have embraced gardening, a Peloton splurge, and learning business skills to open private practices – solo primary care for him; ENT with a focus on her favorite surgery, rhinoplasty, for her.
Dr. Mangiapane had considered editing medical brochures and also tried to apply for a job as a county public health officer in rural California, but he received his own shock when he learned the county intended to open schools in the midst of the pandemic despite advisement to the contrary by the former health officer.
He retreated from job listings altogether after hearing his would-be peers were getting death threats – targeting their children.
Both doctors felt COVID-19 pushed them beyond their comfort zones. “If COVID hadn’t happened, I would be working. ... Be ‘owned.’ In a weird way, COVID made me more independent and take a risk with my career.”
Obstetrician Kwandaa Roberts, MD, certainly did; she took a budding interest in decorating dollhouses straight to Instagram and national news fame, and she is now a TV-show expert on “Sell This House.”
Like Dr. Doshi and Dr. Mangiapane, Dr. Polak wants to be more in control of his future – even if selling T-shirts at a mall means a certain loss of status along the way.
“Aside from my passion to learn and to have that connection with people, I went into medicine ... because of the job security I thought existed,” he said. “I would say that my getting furloughed has changed my view of the United States in a dramatic way. I do not feel as confident in the U.S. economy and general way of life as I did a year ago. And I am taking a number of steps to put myself in a more fluid, adaptable position in case another crisis like this occurs or if the current state of things worsens.”
A version of this article first appeared on Medscape.com.
One of the biggest conundrums of the COVID-19 pandemic has been the simultaneous panic-hiring of medical professionals in hot spots and significant downsizing of staff across the country. From huge hospital systems to private practices, the stoppage of breast reductions and knee replacements, not to mention the drops in motor vehicle accidents and bar fights, have quieted operating rooms and emergency departments and put doctors’ jobs on the chopping block. A widely cited survey suggests that 21% of doctors have had a work reduction due to COVID-19.
For many American doctors, this is their first extended period of unemployment. Unlike engineers or those with MBAs who might see their fortunes rise and fall with the whims of recessions and boom times, physicians are not exactly accustomed to being laid off. However, doctors were already smarting for years due to falling salaries and decreased autonomy, punctuated by endless clicks on electronic medical records software.
Stephanie Eschenbach Morgan, MD, a breast radiologist in North Carolina, trained for 10 years after college before earning a true physician’s salary.
“Being furloughed was awful. Initially, it was only going to be 2 weeks, and then it turned into 2 months with no pay,” she reflected.
Dr. Eschenbach Morgan and her surgeon husband, who lost a full quarter’s salary, had to ask for grace periods on their credit card and mortgage payments because they had paid a large tax bill right before the pandemic began. “We couldn’t get any stimulus help, so that added insult to injury,” she said.
With her time spent waiting in a holding pattern, Dr. Eschenbach Morgan homeschooled her two young children and started putting a home gym together. She went on a home organizing spree, started a garden, and, perhaps most impressively, caught up with 5 years of photo albums.
A bonus she noted: “I didn’t set an alarm for 2 months.”
Shella Farooki, MD, a radiologist in California, was also focused on homeschooling, itself a demanding job, and veered toward retirement. When one of her work contracts furloughed her (“at one point, I made $30K a month for [their business]”), she started saving money at home, teaching the kids, and applied for a Paycheck Protection Program loan. Her husband, a hospitalist, had had his shifts cut. Dr. Farooki tried a radiology artificial intelligence firm but backed out when she was asked to read 9,200 studies for them for $2,000 per month.
Now, she thinks about leaving medicine “every day.”
Some doctors are questioning whether they should be in medicine in the first place. Family medicine physician Jonathan Polak, MD, faced with his own pink slip, turned to pink T-shirts instead. His girlfriend manages an outlet of the teen fashion retailer Justice. Dr. Polak, who finished his residency just 2 years ago, didn’t hesitate to take a $10-an-hour gig as a stock doc, once even finding himself delivering a shelving unit from the shuttering store to a physician fleeing the city for rural New Hampshire to “escape.”
There’s no escape for him – yet. Saddled with “astronomical” student loans, he had considered grocery store work as well. Dr. Polak knows he can’t work part time or go into teaching long term, as he might like.
Even so, he’s doing everything he can to not be in patient care for the long haul – it’s just not what he thought it would be.
“The culture of medicine, bureaucracy, endless paperwork and charting, and threat of litigation sucks a lot of the joy out of it to the point that I don’t see myself doing it forever when imagining myself 5-10 years into it.”
Still, he recently took an 18-month hospital contract that will force him to move to Florida, but he’s also been turning himself into a veritable Renaissance man; composing music, training for an ultramarathon, studying the latest medical findings, roadtripping, and launching a podcast about dog grooming with a master groomer. “We found parallels between medicine and dog grooming,” he says, somewhat convincingly.
Also working the ruff life is Jen Tserng, MD, a former forensic pathologist who landed on news websites in recent years for becoming a professional dogwalker and housesitter without a permanent home. Dr. Tserng knows doctors were restless and unhappy before COVID-19, their thoughts wandering where the grass might be greener.
As her profile grew, she found her inbox gathering messages from disaffected medical minions: students with a fear of failing or staring down residency application season and employed doctors sick of the constant grind. As she recounted those de facto life coach conversations (“What do you really enjoy?” “Do you really like dogs?”) by phone from New York, she said matter-of-factly, “They don’t call because of COVID. They call because they hate their lives.”
Michelle Mudge-Riley, MD, a physician in Texas, has been seeing this shift for some time as well. She recently held a virtual version of her Physicians Helping Physicians conference, where doctors hear from their peers working successfully in fields like pharmaceuticals and real estate investing.
When COVID-19 hit, Dr. Mudge-Riley quickly pivoted to a virtual platform, where the MDs and DOs huddled in breakout rooms having honest chats about their fears and tentative hopes about their new careers.
“There has been increased interest in nonclinical exploration into full- and part-time careers, as well as side hustles, since COVID began,” she said. “Many physicians have had their hours or pay cut, and some have been laid off. Others are furloughed. Some just want out of an environment where they don’t feel safe.”
An ear, nose, and throat surgeon, Maansi Doshi, MD, from central California, didn’t feel safe – so she left. She had returned from India sick with a mystery virus right as the pandemic began (she said her COVID-19 tests were all negative) and was waiting to get well enough to go back to her private practice job. However, she said she clashed with Trump-supporting colleagues she feared might not be taking the pandemic seriously enough.
Finally getting over a relapse of her mystery virus, Dr. Doshi emailed her resignation in May. Her husband, family practice doctor Mark Mangiapane, MD, gave his job notice weeks later in solidarity because he worked in the same building. Together, they have embraced gardening, a Peloton splurge, and learning business skills to open private practices – solo primary care for him; ENT with a focus on her favorite surgery, rhinoplasty, for her.
Dr. Mangiapane had considered editing medical brochures and also tried to apply for a job as a county public health officer in rural California, but he received his own shock when he learned the county intended to open schools in the midst of the pandemic despite advisement to the contrary by the former health officer.
He retreated from job listings altogether after hearing his would-be peers were getting death threats – targeting their children.
Both doctors felt COVID-19 pushed them beyond their comfort zones. “If COVID hadn’t happened, I would be working. ... Be ‘owned.’ In a weird way, COVID made me more independent and take a risk with my career.”
Obstetrician Kwandaa Roberts, MD, certainly did; she took a budding interest in decorating dollhouses straight to Instagram and national news fame, and she is now a TV-show expert on “Sell This House.”
Like Dr. Doshi and Dr. Mangiapane, Dr. Polak wants to be more in control of his future – even if selling T-shirts at a mall means a certain loss of status along the way.
“Aside from my passion to learn and to have that connection with people, I went into medicine ... because of the job security I thought existed,” he said. “I would say that my getting furloughed has changed my view of the United States in a dramatic way. I do not feel as confident in the U.S. economy and general way of life as I did a year ago. And I am taking a number of steps to put myself in a more fluid, adaptable position in case another crisis like this occurs or if the current state of things worsens.”
A version of this article first appeared on Medscape.com.
One of the biggest conundrums of the COVID-19 pandemic has been the simultaneous panic-hiring of medical professionals in hot spots and significant downsizing of staff across the country. From huge hospital systems to private practices, the stoppage of breast reductions and knee replacements, not to mention the drops in motor vehicle accidents and bar fights, have quieted operating rooms and emergency departments and put doctors’ jobs on the chopping block. A widely cited survey suggests that 21% of doctors have had a work reduction due to COVID-19.
For many American doctors, this is their first extended period of unemployment. Unlike engineers or those with MBAs who might see their fortunes rise and fall with the whims of recessions and boom times, physicians are not exactly accustomed to being laid off. However, doctors were already smarting for years due to falling salaries and decreased autonomy, punctuated by endless clicks on electronic medical records software.
Stephanie Eschenbach Morgan, MD, a breast radiologist in North Carolina, trained for 10 years after college before earning a true physician’s salary.
“Being furloughed was awful. Initially, it was only going to be 2 weeks, and then it turned into 2 months with no pay,” she reflected.
Dr. Eschenbach Morgan and her surgeon husband, who lost a full quarter’s salary, had to ask for grace periods on their credit card and mortgage payments because they had paid a large tax bill right before the pandemic began. “We couldn’t get any stimulus help, so that added insult to injury,” she said.
With her time spent waiting in a holding pattern, Dr. Eschenbach Morgan homeschooled her two young children and started putting a home gym together. She went on a home organizing spree, started a garden, and, perhaps most impressively, caught up with 5 years of photo albums.
A bonus she noted: “I didn’t set an alarm for 2 months.”
Shella Farooki, MD, a radiologist in California, was also focused on homeschooling, itself a demanding job, and veered toward retirement. When one of her work contracts furloughed her (“at one point, I made $30K a month for [their business]”), she started saving money at home, teaching the kids, and applied for a Paycheck Protection Program loan. Her husband, a hospitalist, had had his shifts cut. Dr. Farooki tried a radiology artificial intelligence firm but backed out when she was asked to read 9,200 studies for them for $2,000 per month.
Now, she thinks about leaving medicine “every day.”
Some doctors are questioning whether they should be in medicine in the first place. Family medicine physician Jonathan Polak, MD, faced with his own pink slip, turned to pink T-shirts instead. His girlfriend manages an outlet of the teen fashion retailer Justice. Dr. Polak, who finished his residency just 2 years ago, didn’t hesitate to take a $10-an-hour gig as a stock doc, once even finding himself delivering a shelving unit from the shuttering store to a physician fleeing the city for rural New Hampshire to “escape.”
There’s no escape for him – yet. Saddled with “astronomical” student loans, he had considered grocery store work as well. Dr. Polak knows he can’t work part time or go into teaching long term, as he might like.
Even so, he’s doing everything he can to not be in patient care for the long haul – it’s just not what he thought it would be.
“The culture of medicine, bureaucracy, endless paperwork and charting, and threat of litigation sucks a lot of the joy out of it to the point that I don’t see myself doing it forever when imagining myself 5-10 years into it.”
Still, he recently took an 18-month hospital contract that will force him to move to Florida, but he’s also been turning himself into a veritable Renaissance man; composing music, training for an ultramarathon, studying the latest medical findings, roadtripping, and launching a podcast about dog grooming with a master groomer. “We found parallels between medicine and dog grooming,” he says, somewhat convincingly.
Also working the ruff life is Jen Tserng, MD, a former forensic pathologist who landed on news websites in recent years for becoming a professional dogwalker and housesitter without a permanent home. Dr. Tserng knows doctors were restless and unhappy before COVID-19, their thoughts wandering where the grass might be greener.
As her profile grew, she found her inbox gathering messages from disaffected medical minions: students with a fear of failing or staring down residency application season and employed doctors sick of the constant grind. As she recounted those de facto life coach conversations (“What do you really enjoy?” “Do you really like dogs?”) by phone from New York, she said matter-of-factly, “They don’t call because of COVID. They call because they hate their lives.”
Michelle Mudge-Riley, MD, a physician in Texas, has been seeing this shift for some time as well. She recently held a virtual version of her Physicians Helping Physicians conference, where doctors hear from their peers working successfully in fields like pharmaceuticals and real estate investing.
When COVID-19 hit, Dr. Mudge-Riley quickly pivoted to a virtual platform, where the MDs and DOs huddled in breakout rooms having honest chats about their fears and tentative hopes about their new careers.
“There has been increased interest in nonclinical exploration into full- and part-time careers, as well as side hustles, since COVID began,” she said. “Many physicians have had their hours or pay cut, and some have been laid off. Others are furloughed. Some just want out of an environment where they don’t feel safe.”
An ear, nose, and throat surgeon, Maansi Doshi, MD, from central California, didn’t feel safe – so she left. She had returned from India sick with a mystery virus right as the pandemic began (she said her COVID-19 tests were all negative) and was waiting to get well enough to go back to her private practice job. However, she said she clashed with Trump-supporting colleagues she feared might not be taking the pandemic seriously enough.
Finally getting over a relapse of her mystery virus, Dr. Doshi emailed her resignation in May. Her husband, family practice doctor Mark Mangiapane, MD, gave his job notice weeks later in solidarity because he worked in the same building. Together, they have embraced gardening, a Peloton splurge, and learning business skills to open private practices – solo primary care for him; ENT with a focus on her favorite surgery, rhinoplasty, for her.
Dr. Mangiapane had considered editing medical brochures and also tried to apply for a job as a county public health officer in rural California, but he received his own shock when he learned the county intended to open schools in the midst of the pandemic despite advisement to the contrary by the former health officer.
He retreated from job listings altogether after hearing his would-be peers were getting death threats – targeting their children.
Both doctors felt COVID-19 pushed them beyond their comfort zones. “If COVID hadn’t happened, I would be working. ... Be ‘owned.’ In a weird way, COVID made me more independent and take a risk with my career.”
Obstetrician Kwandaa Roberts, MD, certainly did; she took a budding interest in decorating dollhouses straight to Instagram and national news fame, and she is now a TV-show expert on “Sell This House.”
Like Dr. Doshi and Dr. Mangiapane, Dr. Polak wants to be more in control of his future – even if selling T-shirts at a mall means a certain loss of status along the way.
“Aside from my passion to learn and to have that connection with people, I went into medicine ... because of the job security I thought existed,” he said. “I would say that my getting furloughed has changed my view of the United States in a dramatic way. I do not feel as confident in the U.S. economy and general way of life as I did a year ago. And I am taking a number of steps to put myself in a more fluid, adaptable position in case another crisis like this occurs or if the current state of things worsens.”
A version of this article first appeared on Medscape.com.
More competition for docs as insurers boost new telehealth plans?
Initially, the service will be part of some employer-sponsored insurance plans in 11 states. United intends to expand its footprint next year.
United is using the platform and the medical group of American Well, a telehealth service, to provide virtual primary care. Besides minor acute care, United’s virtual service covers annual wellness visits, routine follow-ups for chronic conditions, lab tests, and specialist referrals with little or no cost sharing.
The giant insurer is now offering its virtual primary care plan in Arizona, Colorado, Illinois, Maryland, North Carolina, Ohio, South Carolina, Texas, Virginia, Washington, D.C., and West Virginia.
Other insurers are offering similar virtual primary care plans. For example, Humana has partnered with Doctor on Demand, and Cigna is working with MDLive to offer virtual primary care plans. Both of these plans encourage consumers to form ongoing relationships with physicians hired by the telehealth services. Similarly, Harvard Pilgrim, which has also joined with Doctor on Demand, said that consumers get “virtual PCPs” along with a full care team.
Humana has priced the premiums for its virtual service at about half the cost of Humana’s most popular traditional plan. There are no copays for telehealth visits; there are $5 copays for common lab tests and prescriptions. Cigna said that its virtual plan makes coverage “more affordable,” but doesn’t provide any specifics.
According to United spokeswoman Maria Shydlo, the insurer’s virtual primary care service is not cheaper than its traditional products.
Increased telehealth adoption
When the COVID-19 pandemic first struck last year, telehealth was a lifesaver for primary care practices. Physicians were able to treat half or more of their patients through telehealth, including video and phone consultations.
That initial romance with telehealth did not last. Today, telehealth represents 9% of adult primary care visits. However, that’s still a much higher percentage than before 2020, and telehealth has become a fixture of primary care.
Prior to the pandemic, telehealth services dominated the virtual care space. Some large groups experimented with having their doctors conduct virtual consults with their patients. Other physicians dabbled with telehealth or stayed out of it entirely because health plans paid much less for virtual visits than for in-person visits.
That began to change as more and more states passed laws requiring payment parity. (Today, 36 states do.) Then as the pandemic took hold, Medicare loosened its regulations, allowing coverage of telehealth everywhere and establishing parity. But it’s unclear what will happen after the public health emergency ends.
United and other insurers portray their virtual primary care plans as an effort to connect more consumers with primary care physicians. Having a relationship with a primary care doctor, United noted in a press release, increases access to care, including preventive services. Moreover, a United survey found that a quarter of respondents preferred a virtual relationship with a primary care doctor.
Physician have mostly positive but mixed reactions
This news organization interviewed several physicians who practice in states where United has introduced its new offering. Only one doctor had heard about it, and another, solo family physician Will Sawyer, MD, of Cincinnati no longer contracts with United. Nevertheless, they all had strong opinions about virtual primary care plans from United and other insurers.
Dr. Sawyer is a big proponent of telehealth and notes that it’s “incredibly convenient” for older people, many of whom are afraid to come to the office out of fear they might contract COVID-19. He has found that telehealth can be useful for many kinds of acute and chronic care. But he believes (although he admits he does not have evidence) that United started its virtual primary care service mainly to save money.
Peter Basch, MD, an internist with MedStar Health in Washington, D.C., says he’s willing to give United the benefit of the doubt. Increasing access to care while lowering its cost, he says, is the right thing to do, and “it makes financial sense. So I wouldn’t question their motives.”
Dr. Basch is concerned, however, that insurers such as United might eventually cover some services virtually but not in the office. “I can imagine a situation where doctors feel their judgment is being disregarded and that this person really needs to come in. And there might be pressure from the employer or the manager of the medical group, telling the doctor that if you’re not careful about how you manage these visits, you may be losing money for the practice.”
Kenneth Kubitschek, MD, an internist in a medium-sized group in Asheville, N.C., was less enamored of telehealth than Dr. Basch and Dr. Sawyer are, although it currently accounts for 15%-20% of his group’s visits. “There’s definitely something you lose with telehealth in terms of the nuances of the interaction.”
No to some kinds of telehealth doctors
The physicians we spoke with were unified in their opposition to virtual primary care plans that mainly use physicians hired by telehealth services. Dr. Sawyer noted that one-off consultations with telehealth doctors might be okay for urgent care. “But what we’re trying to do with patients is change their behavior for better health outcomes, and that doesn’t happen in these one-off contacts,” he said.
Even if a patient were able to develop an online relationship with a telehealth doctor, Dr. Basch said, there are any number of situations in which an in-person visit might be necessary. “Whether it’s a urologic visit, a cardiac visit, or an allergy visit, do I need to listen to you or put my hands on you to palpate your liver? Or is this just a conversation with someone I know to see how they’re doing, how they’re managing their meds? Ninety percent of a diagnosis is history.”
Although the virtual plans allow a telehealth physician to refer a patient to an in-network specialist for an office visit, this isn’t the same as their primary care physician asking them to come in to be examined.
Moreover, Dr. Basch noted, people with chronic conditions can’t be treated only virtually. “I wouldn’t say that primary care should be done predominantly through virtual visits. It may be okay for young and healthy patients, but not for older people with chronic conditions. There are times when they should see their doctor in person.”
What can be done via telehealth
On the other hand, Dr. Basch heartily approves of conducting routine follow-up visits virtually for patients with chronic diseases, as long as the physician knows the patient’s history. Telehealth can also be used to coach patients on exercise, nutrition, and other lifestyle changes.
Dr. Kubitschek estimates that around 40%-50% of primary care can be delivered through telehealth. But the remainder encompasses potentially serious conditions that should be diagnosed and treated in face-to-face encounters, he said. “For example, if a patient has abdominal pain, you have to examine the person to get a clue of what they’re talking about. The pains are often diffuse, but they might be painful locally, which could indicate a mass or a bladder distension.”
For that reason, he doesn’t support the idea of patients depending on telehealth doctors in virtual primary care plans. “These doctors would not be available to care for the patient in an urgent situation without sending them to a costly emergency room or urgent care clinic. In those settings, excess testing is done because of a lack of familiarity with the patient and his or her history and exam. I think a combination of in-person and telehealth visits presents the best circumstance for the patient and the physician. Having said that, I do believe that telehealth alone is better than no interaction with a health care provider.”
United approach can help with prevention
Donny Aga, MD, an internist with Kelsey-Seybold, a multispecialty group in Houston, has been a member of United’s virtual health advisory group for the past 2 years. In his view, United’s virtual primary care service is moving in the right direction by covering preventive and chronic care. Noting that 25%-30% of patients nationally have put off wellness and chronic care visits out of fear of COVID-19, he said that,“if health plans like United are willing to cover preventive services through telehealth, that will allow us to catch up on a lot of the needed screening tests and exams. So it’s a very positive step forward.”
On the other hand, he said, virtual plans that depend solely on telehealth doctors are not the way to manage chronic conditions. “Primary care is best done by your own primary care physician, not by someone who doesn’t know you from a distance.”
Regarding the virtual plans in which patients can establish relationships with telehealth physicians, Dr. Aga said that this approach can benefit some patients, especially those who live in rural areas and don’t have access to primary care. But there are drawbacks, including the telehealth providers’ lack of knowledge about local specialists.
“The negative is that you don’t have a [primary care physicians] who’s local, who knows you, who has examined you before, and who has a good relationship with those specialists and knows who is the right specialist to see for your problem,” Dr. Aga said. “It’s very difficult, if you don’t live and work in that area, to know the best places to send people.”
Virtual visits cost less
Like Dr. Basch, Dr. Aga said it’s possible that some insurance companies might begin to cover office visits only for certain conditions or services if they can be managed more cheaply via telehealth. He hopes that doesn’t happen; if it does, he predicts that patients and doctors will push back hard.
Why would a virtual primary care visit cost a health plan less than an in-person visit if it’s paying doctors the same for both? Dr. Aga said it’s because fewer prescriptions and lab tests are ordered in telehealth encounters. He bases this assertion on the quarter of a million virtual visits that Kelsey-Seybold has conducted and also alludes to published studies.
The characteristics of telehealth visits might explain this phenomenon, he said. “These visits are typically much shorter, and it’s easy to be problem-centric and problem based. Physicians use more of their intuitive skills, rather than just lab everybody up and get an x-ray, because that patient’s not there, and it’s easier to draw blood or get an x-ray if somebody is there.”
Cutting practice overhead
From the perspective of Kelsey-Seybold, which is now conducting about a fifth of its visits virtually, “infrastructure costs are less” for telehealth, Aga notes. Although Dr. Kubitschek and Dr. Sawyer say it doesn’t take less time to conduct a telehealth visit than an office visit, other practice costs may decrease in relationship to the percentage of a doctor’s visits that are virtual.
“If implemented appropriately, telehealth consults should cost less in terms of the ancillary costs surrounding care,” said Dr. Basch. He recalls that, some years ago, a five-doctor primary care group in Portland, Ore., began charging small monthly fees to patients for full-service care that included email access. After a while, 40% of their patients were coming in, and the rest received care by email or phone. As a result, the doctors were able to downsize to a smaller office space because they didn’t need a waiting room.
Although Dr. Basch doesn’t believe it would be appropriate for practices to do something like this in the midst of a pandemic, he sees the possibility of it happening in the future. “Eventually, a group might be able to say: ‘Yes, our practice expenses can be lower if we do this smartly. We could do as well as we’ve done on whatever insurance pays for office visits, knowing that we can deliver care to the same patient panel at, say, 10% lower overhead with telehealth.’ ”
A version of this article first appeared on Medscape.com.
Initially, the service will be part of some employer-sponsored insurance plans in 11 states. United intends to expand its footprint next year.
United is using the platform and the medical group of American Well, a telehealth service, to provide virtual primary care. Besides minor acute care, United’s virtual service covers annual wellness visits, routine follow-ups for chronic conditions, lab tests, and specialist referrals with little or no cost sharing.
The giant insurer is now offering its virtual primary care plan in Arizona, Colorado, Illinois, Maryland, North Carolina, Ohio, South Carolina, Texas, Virginia, Washington, D.C., and West Virginia.
Other insurers are offering similar virtual primary care plans. For example, Humana has partnered with Doctor on Demand, and Cigna is working with MDLive to offer virtual primary care plans. Both of these plans encourage consumers to form ongoing relationships with physicians hired by the telehealth services. Similarly, Harvard Pilgrim, which has also joined with Doctor on Demand, said that consumers get “virtual PCPs” along with a full care team.
Humana has priced the premiums for its virtual service at about half the cost of Humana’s most popular traditional plan. There are no copays for telehealth visits; there are $5 copays for common lab tests and prescriptions. Cigna said that its virtual plan makes coverage “more affordable,” but doesn’t provide any specifics.
According to United spokeswoman Maria Shydlo, the insurer’s virtual primary care service is not cheaper than its traditional products.
Increased telehealth adoption
When the COVID-19 pandemic first struck last year, telehealth was a lifesaver for primary care practices. Physicians were able to treat half or more of their patients through telehealth, including video and phone consultations.
That initial romance with telehealth did not last. Today, telehealth represents 9% of adult primary care visits. However, that’s still a much higher percentage than before 2020, and telehealth has become a fixture of primary care.
Prior to the pandemic, telehealth services dominated the virtual care space. Some large groups experimented with having their doctors conduct virtual consults with their patients. Other physicians dabbled with telehealth or stayed out of it entirely because health plans paid much less for virtual visits than for in-person visits.
That began to change as more and more states passed laws requiring payment parity. (Today, 36 states do.) Then as the pandemic took hold, Medicare loosened its regulations, allowing coverage of telehealth everywhere and establishing parity. But it’s unclear what will happen after the public health emergency ends.
United and other insurers portray their virtual primary care plans as an effort to connect more consumers with primary care physicians. Having a relationship with a primary care doctor, United noted in a press release, increases access to care, including preventive services. Moreover, a United survey found that a quarter of respondents preferred a virtual relationship with a primary care doctor.
Physician have mostly positive but mixed reactions
This news organization interviewed several physicians who practice in states where United has introduced its new offering. Only one doctor had heard about it, and another, solo family physician Will Sawyer, MD, of Cincinnati no longer contracts with United. Nevertheless, they all had strong opinions about virtual primary care plans from United and other insurers.
Dr. Sawyer is a big proponent of telehealth and notes that it’s “incredibly convenient” for older people, many of whom are afraid to come to the office out of fear they might contract COVID-19. He has found that telehealth can be useful for many kinds of acute and chronic care. But he believes (although he admits he does not have evidence) that United started its virtual primary care service mainly to save money.
Peter Basch, MD, an internist with MedStar Health in Washington, D.C., says he’s willing to give United the benefit of the doubt. Increasing access to care while lowering its cost, he says, is the right thing to do, and “it makes financial sense. So I wouldn’t question their motives.”
Dr. Basch is concerned, however, that insurers such as United might eventually cover some services virtually but not in the office. “I can imagine a situation where doctors feel their judgment is being disregarded and that this person really needs to come in. And there might be pressure from the employer or the manager of the medical group, telling the doctor that if you’re not careful about how you manage these visits, you may be losing money for the practice.”
Kenneth Kubitschek, MD, an internist in a medium-sized group in Asheville, N.C., was less enamored of telehealth than Dr. Basch and Dr. Sawyer are, although it currently accounts for 15%-20% of his group’s visits. “There’s definitely something you lose with telehealth in terms of the nuances of the interaction.”
No to some kinds of telehealth doctors
The physicians we spoke with were unified in their opposition to virtual primary care plans that mainly use physicians hired by telehealth services. Dr. Sawyer noted that one-off consultations with telehealth doctors might be okay for urgent care. “But what we’re trying to do with patients is change their behavior for better health outcomes, and that doesn’t happen in these one-off contacts,” he said.
Even if a patient were able to develop an online relationship with a telehealth doctor, Dr. Basch said, there are any number of situations in which an in-person visit might be necessary. “Whether it’s a urologic visit, a cardiac visit, or an allergy visit, do I need to listen to you or put my hands on you to palpate your liver? Or is this just a conversation with someone I know to see how they’re doing, how they’re managing their meds? Ninety percent of a diagnosis is history.”
Although the virtual plans allow a telehealth physician to refer a patient to an in-network specialist for an office visit, this isn’t the same as their primary care physician asking them to come in to be examined.
Moreover, Dr. Basch noted, people with chronic conditions can’t be treated only virtually. “I wouldn’t say that primary care should be done predominantly through virtual visits. It may be okay for young and healthy patients, but not for older people with chronic conditions. There are times when they should see their doctor in person.”
What can be done via telehealth
On the other hand, Dr. Basch heartily approves of conducting routine follow-up visits virtually for patients with chronic diseases, as long as the physician knows the patient’s history. Telehealth can also be used to coach patients on exercise, nutrition, and other lifestyle changes.
Dr. Kubitschek estimates that around 40%-50% of primary care can be delivered through telehealth. But the remainder encompasses potentially serious conditions that should be diagnosed and treated in face-to-face encounters, he said. “For example, if a patient has abdominal pain, you have to examine the person to get a clue of what they’re talking about. The pains are often diffuse, but they might be painful locally, which could indicate a mass or a bladder distension.”
For that reason, he doesn’t support the idea of patients depending on telehealth doctors in virtual primary care plans. “These doctors would not be available to care for the patient in an urgent situation without sending them to a costly emergency room or urgent care clinic. In those settings, excess testing is done because of a lack of familiarity with the patient and his or her history and exam. I think a combination of in-person and telehealth visits presents the best circumstance for the patient and the physician. Having said that, I do believe that telehealth alone is better than no interaction with a health care provider.”
United approach can help with prevention
Donny Aga, MD, an internist with Kelsey-Seybold, a multispecialty group in Houston, has been a member of United’s virtual health advisory group for the past 2 years. In his view, United’s virtual primary care service is moving in the right direction by covering preventive and chronic care. Noting that 25%-30% of patients nationally have put off wellness and chronic care visits out of fear of COVID-19, he said that,“if health plans like United are willing to cover preventive services through telehealth, that will allow us to catch up on a lot of the needed screening tests and exams. So it’s a very positive step forward.”
On the other hand, he said, virtual plans that depend solely on telehealth doctors are not the way to manage chronic conditions. “Primary care is best done by your own primary care physician, not by someone who doesn’t know you from a distance.”
Regarding the virtual plans in which patients can establish relationships with telehealth physicians, Dr. Aga said that this approach can benefit some patients, especially those who live in rural areas and don’t have access to primary care. But there are drawbacks, including the telehealth providers’ lack of knowledge about local specialists.
“The negative is that you don’t have a [primary care physicians] who’s local, who knows you, who has examined you before, and who has a good relationship with those specialists and knows who is the right specialist to see for your problem,” Dr. Aga said. “It’s very difficult, if you don’t live and work in that area, to know the best places to send people.”
Virtual visits cost less
Like Dr. Basch, Dr. Aga said it’s possible that some insurance companies might begin to cover office visits only for certain conditions or services if they can be managed more cheaply via telehealth. He hopes that doesn’t happen; if it does, he predicts that patients and doctors will push back hard.
Why would a virtual primary care visit cost a health plan less than an in-person visit if it’s paying doctors the same for both? Dr. Aga said it’s because fewer prescriptions and lab tests are ordered in telehealth encounters. He bases this assertion on the quarter of a million virtual visits that Kelsey-Seybold has conducted and also alludes to published studies.
The characteristics of telehealth visits might explain this phenomenon, he said. “These visits are typically much shorter, and it’s easy to be problem-centric and problem based. Physicians use more of their intuitive skills, rather than just lab everybody up and get an x-ray, because that patient’s not there, and it’s easier to draw blood or get an x-ray if somebody is there.”
Cutting practice overhead
From the perspective of Kelsey-Seybold, which is now conducting about a fifth of its visits virtually, “infrastructure costs are less” for telehealth, Aga notes. Although Dr. Kubitschek and Dr. Sawyer say it doesn’t take less time to conduct a telehealth visit than an office visit, other practice costs may decrease in relationship to the percentage of a doctor’s visits that are virtual.
“If implemented appropriately, telehealth consults should cost less in terms of the ancillary costs surrounding care,” said Dr. Basch. He recalls that, some years ago, a five-doctor primary care group in Portland, Ore., began charging small monthly fees to patients for full-service care that included email access. After a while, 40% of their patients were coming in, and the rest received care by email or phone. As a result, the doctors were able to downsize to a smaller office space because they didn’t need a waiting room.
Although Dr. Basch doesn’t believe it would be appropriate for practices to do something like this in the midst of a pandemic, he sees the possibility of it happening in the future. “Eventually, a group might be able to say: ‘Yes, our practice expenses can be lower if we do this smartly. We could do as well as we’ve done on whatever insurance pays for office visits, knowing that we can deliver care to the same patient panel at, say, 10% lower overhead with telehealth.’ ”
A version of this article first appeared on Medscape.com.
Initially, the service will be part of some employer-sponsored insurance plans in 11 states. United intends to expand its footprint next year.
United is using the platform and the medical group of American Well, a telehealth service, to provide virtual primary care. Besides minor acute care, United’s virtual service covers annual wellness visits, routine follow-ups for chronic conditions, lab tests, and specialist referrals with little or no cost sharing.
The giant insurer is now offering its virtual primary care plan in Arizona, Colorado, Illinois, Maryland, North Carolina, Ohio, South Carolina, Texas, Virginia, Washington, D.C., and West Virginia.
Other insurers are offering similar virtual primary care plans. For example, Humana has partnered with Doctor on Demand, and Cigna is working with MDLive to offer virtual primary care plans. Both of these plans encourage consumers to form ongoing relationships with physicians hired by the telehealth services. Similarly, Harvard Pilgrim, which has also joined with Doctor on Demand, said that consumers get “virtual PCPs” along with a full care team.
Humana has priced the premiums for its virtual service at about half the cost of Humana’s most popular traditional plan. There are no copays for telehealth visits; there are $5 copays for common lab tests and prescriptions. Cigna said that its virtual plan makes coverage “more affordable,” but doesn’t provide any specifics.
According to United spokeswoman Maria Shydlo, the insurer’s virtual primary care service is not cheaper than its traditional products.
Increased telehealth adoption
When the COVID-19 pandemic first struck last year, telehealth was a lifesaver for primary care practices. Physicians were able to treat half or more of their patients through telehealth, including video and phone consultations.
That initial romance with telehealth did not last. Today, telehealth represents 9% of adult primary care visits. However, that’s still a much higher percentage than before 2020, and telehealth has become a fixture of primary care.
Prior to the pandemic, telehealth services dominated the virtual care space. Some large groups experimented with having their doctors conduct virtual consults with their patients. Other physicians dabbled with telehealth or stayed out of it entirely because health plans paid much less for virtual visits than for in-person visits.
That began to change as more and more states passed laws requiring payment parity. (Today, 36 states do.) Then as the pandemic took hold, Medicare loosened its regulations, allowing coverage of telehealth everywhere and establishing parity. But it’s unclear what will happen after the public health emergency ends.
United and other insurers portray their virtual primary care plans as an effort to connect more consumers with primary care physicians. Having a relationship with a primary care doctor, United noted in a press release, increases access to care, including preventive services. Moreover, a United survey found that a quarter of respondents preferred a virtual relationship with a primary care doctor.
Physician have mostly positive but mixed reactions
This news organization interviewed several physicians who practice in states where United has introduced its new offering. Only one doctor had heard about it, and another, solo family physician Will Sawyer, MD, of Cincinnati no longer contracts with United. Nevertheless, they all had strong opinions about virtual primary care plans from United and other insurers.
Dr. Sawyer is a big proponent of telehealth and notes that it’s “incredibly convenient” for older people, many of whom are afraid to come to the office out of fear they might contract COVID-19. He has found that telehealth can be useful for many kinds of acute and chronic care. But he believes (although he admits he does not have evidence) that United started its virtual primary care service mainly to save money.
Peter Basch, MD, an internist with MedStar Health in Washington, D.C., says he’s willing to give United the benefit of the doubt. Increasing access to care while lowering its cost, he says, is the right thing to do, and “it makes financial sense. So I wouldn’t question their motives.”
Dr. Basch is concerned, however, that insurers such as United might eventually cover some services virtually but not in the office. “I can imagine a situation where doctors feel their judgment is being disregarded and that this person really needs to come in. And there might be pressure from the employer or the manager of the medical group, telling the doctor that if you’re not careful about how you manage these visits, you may be losing money for the practice.”
Kenneth Kubitschek, MD, an internist in a medium-sized group in Asheville, N.C., was less enamored of telehealth than Dr. Basch and Dr. Sawyer are, although it currently accounts for 15%-20% of his group’s visits. “There’s definitely something you lose with telehealth in terms of the nuances of the interaction.”
No to some kinds of telehealth doctors
The physicians we spoke with were unified in their opposition to virtual primary care plans that mainly use physicians hired by telehealth services. Dr. Sawyer noted that one-off consultations with telehealth doctors might be okay for urgent care. “But what we’re trying to do with patients is change their behavior for better health outcomes, and that doesn’t happen in these one-off contacts,” he said.
Even if a patient were able to develop an online relationship with a telehealth doctor, Dr. Basch said, there are any number of situations in which an in-person visit might be necessary. “Whether it’s a urologic visit, a cardiac visit, or an allergy visit, do I need to listen to you or put my hands on you to palpate your liver? Or is this just a conversation with someone I know to see how they’re doing, how they’re managing their meds? Ninety percent of a diagnosis is history.”
Although the virtual plans allow a telehealth physician to refer a patient to an in-network specialist for an office visit, this isn’t the same as their primary care physician asking them to come in to be examined.
Moreover, Dr. Basch noted, people with chronic conditions can’t be treated only virtually. “I wouldn’t say that primary care should be done predominantly through virtual visits. It may be okay for young and healthy patients, but not for older people with chronic conditions. There are times when they should see their doctor in person.”
What can be done via telehealth
On the other hand, Dr. Basch heartily approves of conducting routine follow-up visits virtually for patients with chronic diseases, as long as the physician knows the patient’s history. Telehealth can also be used to coach patients on exercise, nutrition, and other lifestyle changes.
Dr. Kubitschek estimates that around 40%-50% of primary care can be delivered through telehealth. But the remainder encompasses potentially serious conditions that should be diagnosed and treated in face-to-face encounters, he said. “For example, if a patient has abdominal pain, you have to examine the person to get a clue of what they’re talking about. The pains are often diffuse, but they might be painful locally, which could indicate a mass or a bladder distension.”
For that reason, he doesn’t support the idea of patients depending on telehealth doctors in virtual primary care plans. “These doctors would not be available to care for the patient in an urgent situation without sending them to a costly emergency room or urgent care clinic. In those settings, excess testing is done because of a lack of familiarity with the patient and his or her history and exam. I think a combination of in-person and telehealth visits presents the best circumstance for the patient and the physician. Having said that, I do believe that telehealth alone is better than no interaction with a health care provider.”
United approach can help with prevention
Donny Aga, MD, an internist with Kelsey-Seybold, a multispecialty group in Houston, has been a member of United’s virtual health advisory group for the past 2 years. In his view, United’s virtual primary care service is moving in the right direction by covering preventive and chronic care. Noting that 25%-30% of patients nationally have put off wellness and chronic care visits out of fear of COVID-19, he said that,“if health plans like United are willing to cover preventive services through telehealth, that will allow us to catch up on a lot of the needed screening tests and exams. So it’s a very positive step forward.”
On the other hand, he said, virtual plans that depend solely on telehealth doctors are not the way to manage chronic conditions. “Primary care is best done by your own primary care physician, not by someone who doesn’t know you from a distance.”
Regarding the virtual plans in which patients can establish relationships with telehealth physicians, Dr. Aga said that this approach can benefit some patients, especially those who live in rural areas and don’t have access to primary care. But there are drawbacks, including the telehealth providers’ lack of knowledge about local specialists.
“The negative is that you don’t have a [primary care physicians] who’s local, who knows you, who has examined you before, and who has a good relationship with those specialists and knows who is the right specialist to see for your problem,” Dr. Aga said. “It’s very difficult, if you don’t live and work in that area, to know the best places to send people.”
Virtual visits cost less
Like Dr. Basch, Dr. Aga said it’s possible that some insurance companies might begin to cover office visits only for certain conditions or services if they can be managed more cheaply via telehealth. He hopes that doesn’t happen; if it does, he predicts that patients and doctors will push back hard.
Why would a virtual primary care visit cost a health plan less than an in-person visit if it’s paying doctors the same for both? Dr. Aga said it’s because fewer prescriptions and lab tests are ordered in telehealth encounters. He bases this assertion on the quarter of a million virtual visits that Kelsey-Seybold has conducted and also alludes to published studies.
The characteristics of telehealth visits might explain this phenomenon, he said. “These visits are typically much shorter, and it’s easy to be problem-centric and problem based. Physicians use more of their intuitive skills, rather than just lab everybody up and get an x-ray, because that patient’s not there, and it’s easier to draw blood or get an x-ray if somebody is there.”
Cutting practice overhead
From the perspective of Kelsey-Seybold, which is now conducting about a fifth of its visits virtually, “infrastructure costs are less” for telehealth, Aga notes. Although Dr. Kubitschek and Dr. Sawyer say it doesn’t take less time to conduct a telehealth visit than an office visit, other practice costs may decrease in relationship to the percentage of a doctor’s visits that are virtual.
“If implemented appropriately, telehealth consults should cost less in terms of the ancillary costs surrounding care,” said Dr. Basch. He recalls that, some years ago, a five-doctor primary care group in Portland, Ore., began charging small monthly fees to patients for full-service care that included email access. After a while, 40% of their patients were coming in, and the rest received care by email or phone. As a result, the doctors were able to downsize to a smaller office space because they didn’t need a waiting room.
Although Dr. Basch doesn’t believe it would be appropriate for practices to do something like this in the midst of a pandemic, he sees the possibility of it happening in the future. “Eventually, a group might be able to say: ‘Yes, our practice expenses can be lower if we do this smartly. We could do as well as we’ve done on whatever insurance pays for office visits, knowing that we can deliver care to the same patient panel at, say, 10% lower overhead with telehealth.’ ”
A version of this article first appeared on Medscape.com.
Fired for good judgment a sign of physicians’ lost respect
What happened to Hasan Gokal, MD, should stick painfully in the craws of all physicians. It should serve as a call to action, because Dr. Gokal is sitting at home today without a job and under threat of further legal action while we continue about our day.
Dr. Gokal’s “crime” is that he vaccinated 10 strangers and acquaintances with soon-to-expire doses of the Moderna COVID-19 vaccine. He drove to the homes of some in the dark of night and injected others on his Sugar Land, Texas, lawn. He spent hours in a frantic search for willing recipients to beat the expiration clock. With minutes to spare, he gave the last dose to his at-risk wife, who has symptomatic pulmonary sarcoidosis, but whose age meant she did not fall into a vaccine priority tier.
According to the New York Times, Dr. Gokal’s wife was hesitant, afraid he might get into trouble. But why would she be hesitant? He wasn’t doing anything immoral. Perhaps she knew how far physicians have fallen and how bitterly they both could suffer.
In Barren County, Ky., where I live, a state of emergency was declared by our judge executive because of inclement weather. This directive allows our emergency management to “waive procedures and formalities otherwise required by the law.” It’s too bad that the same courtesy was not afforded to Dr. Gokal in Texas. It’s a shame that ice and snow didn’t drive his actions. Perhaps that would have protected him against the harsh criticism. Rather, it was his oath to patients and dedication to his fellow humans that motivated him, and for that, he was made to suffer.
Dr. Gokal was right to think that pouring the last 10 vaccine doses down the toilet would be an egregious act. But he was wrong in thinking his decision to find takers for the vaccine would be viewed as expedient. Instead, he was accused of graft and even nepotism. And there is the rub. That he was fired and charged with the theft of $137 worth of vaccines says everything about how physicians are treated in the year 2021. Dr. Gokal’s lawyer says the charge carried a maximum penalty of 1 year in prison and a fine of nearly $4,000.
Thank God a sage judge threw out the case and “rebuked” the office of District Attorney Kim Ogg. That hasn’t stopped her from threatening to bring the case to a grand jury. That threat invites anyone faced with the same scenario to flush the extra vaccine doses into the septic system. It encourages us to choose the toilet handle to avoid a mug shot.
And we can’t ignore the racial slant to this story. The Times reported that Dr. Gokal asked the officials, “Are you suggesting that there were too many Indian names in this group?”
“Exactly” was the answer. Let that sink in.
None of this would have happened 20 years ago. Back then, no one would have questioned the wisdom a physician gains from all our years of training and residency. In an age when anyone who conducts an office visit is now called “doctor,” respect for the letters “MD” has been leveled. We physicians have lost our autonomy and been cowed into submission.
But whatever his profession, Hasan Gokal was fired for being a good human. Today, the sun rose on 10 individuals who now enjoy better protection against a deadly pandemic. They include a bed-bound nonagenarian. A woman in her 80s with dementia. A mother with a child who uses a ventilator. All now have antibodies against SARS-CoV2 because of the tireless actions of Dr. Gokal.
Yet Dr. Gokal’s future is uncertain. Will we help him, or will we leave him to the wolves? In an email exchange with his lawyer’s office, I learned that Dr. Gokal has received offers of employment but is unable to entertain them because the actions by the Harris County District Attorney triggered an automatic review by the Texas Medical Board. A GoFundMe page was launched, but an appreciative Dr. Gokal stated publicly that he’d rather the money go to a needy charity.
In the last paragraph of the Times article, Dr. Gokal asks, “How can I take it back?” referencing stories about “the Pakistani doctor in Houston who stole all those vaccines.”
Let’s help him take back his story. In helping him, perhaps we can take back a little control. We could start with letters of support that could be mailed to his lawyer, Paul Doyle, Esq., of Houston, or tweet, respectfully of course, to the district attorney @Kimoggforda.
We can also let the Harris County Public Health Department in Houston know what we think of their actions.
On Martin Luther King Day, Kim Ogg, the district attorney who charged Dr. Gokal, tweeted MLK’s famous quote: “Injustice anywhere is a threat to justice everywhere.”
Let that motivate us to action.
Melissa Walton-Shirley, MD, is a native Kentuckian who retired from full-time invasive cardiology. She enjoys locums work in Montana and is a champion of physician rights and patient safety. In addition to opinion writing, she enjoys spending time with her husband, daughters and parents, and sidelines as a backing vocalist for local rock bands. A version of this article first appeared on Medscape.com.
What happened to Hasan Gokal, MD, should stick painfully in the craws of all physicians. It should serve as a call to action, because Dr. Gokal is sitting at home today without a job and under threat of further legal action while we continue about our day.
Dr. Gokal’s “crime” is that he vaccinated 10 strangers and acquaintances with soon-to-expire doses of the Moderna COVID-19 vaccine. He drove to the homes of some in the dark of night and injected others on his Sugar Land, Texas, lawn. He spent hours in a frantic search for willing recipients to beat the expiration clock. With minutes to spare, he gave the last dose to his at-risk wife, who has symptomatic pulmonary sarcoidosis, but whose age meant she did not fall into a vaccine priority tier.
According to the New York Times, Dr. Gokal’s wife was hesitant, afraid he might get into trouble. But why would she be hesitant? He wasn’t doing anything immoral. Perhaps she knew how far physicians have fallen and how bitterly they both could suffer.
In Barren County, Ky., where I live, a state of emergency was declared by our judge executive because of inclement weather. This directive allows our emergency management to “waive procedures and formalities otherwise required by the law.” It’s too bad that the same courtesy was not afforded to Dr. Gokal in Texas. It’s a shame that ice and snow didn’t drive his actions. Perhaps that would have protected him against the harsh criticism. Rather, it was his oath to patients and dedication to his fellow humans that motivated him, and for that, he was made to suffer.
Dr. Gokal was right to think that pouring the last 10 vaccine doses down the toilet would be an egregious act. But he was wrong in thinking his decision to find takers for the vaccine would be viewed as expedient. Instead, he was accused of graft and even nepotism. And there is the rub. That he was fired and charged with the theft of $137 worth of vaccines says everything about how physicians are treated in the year 2021. Dr. Gokal’s lawyer says the charge carried a maximum penalty of 1 year in prison and a fine of nearly $4,000.
Thank God a sage judge threw out the case and “rebuked” the office of District Attorney Kim Ogg. That hasn’t stopped her from threatening to bring the case to a grand jury. That threat invites anyone faced with the same scenario to flush the extra vaccine doses into the septic system. It encourages us to choose the toilet handle to avoid a mug shot.
And we can’t ignore the racial slant to this story. The Times reported that Dr. Gokal asked the officials, “Are you suggesting that there were too many Indian names in this group?”
“Exactly” was the answer. Let that sink in.
None of this would have happened 20 years ago. Back then, no one would have questioned the wisdom a physician gains from all our years of training and residency. In an age when anyone who conducts an office visit is now called “doctor,” respect for the letters “MD” has been leveled. We physicians have lost our autonomy and been cowed into submission.
But whatever his profession, Hasan Gokal was fired for being a good human. Today, the sun rose on 10 individuals who now enjoy better protection against a deadly pandemic. They include a bed-bound nonagenarian. A woman in her 80s with dementia. A mother with a child who uses a ventilator. All now have antibodies against SARS-CoV2 because of the tireless actions of Dr. Gokal.
Yet Dr. Gokal’s future is uncertain. Will we help him, or will we leave him to the wolves? In an email exchange with his lawyer’s office, I learned that Dr. Gokal has received offers of employment but is unable to entertain them because the actions by the Harris County District Attorney triggered an automatic review by the Texas Medical Board. A GoFundMe page was launched, but an appreciative Dr. Gokal stated publicly that he’d rather the money go to a needy charity.
In the last paragraph of the Times article, Dr. Gokal asks, “How can I take it back?” referencing stories about “the Pakistani doctor in Houston who stole all those vaccines.”
Let’s help him take back his story. In helping him, perhaps we can take back a little control. We could start with letters of support that could be mailed to his lawyer, Paul Doyle, Esq., of Houston, or tweet, respectfully of course, to the district attorney @Kimoggforda.
We can also let the Harris County Public Health Department in Houston know what we think of their actions.
On Martin Luther King Day, Kim Ogg, the district attorney who charged Dr. Gokal, tweeted MLK’s famous quote: “Injustice anywhere is a threat to justice everywhere.”
Let that motivate us to action.
Melissa Walton-Shirley, MD, is a native Kentuckian who retired from full-time invasive cardiology. She enjoys locums work in Montana and is a champion of physician rights and patient safety. In addition to opinion writing, she enjoys spending time with her husband, daughters and parents, and sidelines as a backing vocalist for local rock bands. A version of this article first appeared on Medscape.com.
What happened to Hasan Gokal, MD, should stick painfully in the craws of all physicians. It should serve as a call to action, because Dr. Gokal is sitting at home today without a job and under threat of further legal action while we continue about our day.
Dr. Gokal’s “crime” is that he vaccinated 10 strangers and acquaintances with soon-to-expire doses of the Moderna COVID-19 vaccine. He drove to the homes of some in the dark of night and injected others on his Sugar Land, Texas, lawn. He spent hours in a frantic search for willing recipients to beat the expiration clock. With minutes to spare, he gave the last dose to his at-risk wife, who has symptomatic pulmonary sarcoidosis, but whose age meant she did not fall into a vaccine priority tier.
According to the New York Times, Dr. Gokal’s wife was hesitant, afraid he might get into trouble. But why would she be hesitant? He wasn’t doing anything immoral. Perhaps she knew how far physicians have fallen and how bitterly they both could suffer.
In Barren County, Ky., where I live, a state of emergency was declared by our judge executive because of inclement weather. This directive allows our emergency management to “waive procedures and formalities otherwise required by the law.” It’s too bad that the same courtesy was not afforded to Dr. Gokal in Texas. It’s a shame that ice and snow didn’t drive his actions. Perhaps that would have protected him against the harsh criticism. Rather, it was his oath to patients and dedication to his fellow humans that motivated him, and for that, he was made to suffer.
Dr. Gokal was right to think that pouring the last 10 vaccine doses down the toilet would be an egregious act. But he was wrong in thinking his decision to find takers for the vaccine would be viewed as expedient. Instead, he was accused of graft and even nepotism. And there is the rub. That he was fired and charged with the theft of $137 worth of vaccines says everything about how physicians are treated in the year 2021. Dr. Gokal’s lawyer says the charge carried a maximum penalty of 1 year in prison and a fine of nearly $4,000.
Thank God a sage judge threw out the case and “rebuked” the office of District Attorney Kim Ogg. That hasn’t stopped her from threatening to bring the case to a grand jury. That threat invites anyone faced with the same scenario to flush the extra vaccine doses into the septic system. It encourages us to choose the toilet handle to avoid a mug shot.
And we can’t ignore the racial slant to this story. The Times reported that Dr. Gokal asked the officials, “Are you suggesting that there were too many Indian names in this group?”
“Exactly” was the answer. Let that sink in.
None of this would have happened 20 years ago. Back then, no one would have questioned the wisdom a physician gains from all our years of training and residency. In an age when anyone who conducts an office visit is now called “doctor,” respect for the letters “MD” has been leveled. We physicians have lost our autonomy and been cowed into submission.
But whatever his profession, Hasan Gokal was fired for being a good human. Today, the sun rose on 10 individuals who now enjoy better protection against a deadly pandemic. They include a bed-bound nonagenarian. A woman in her 80s with dementia. A mother with a child who uses a ventilator. All now have antibodies against SARS-CoV2 because of the tireless actions of Dr. Gokal.
Yet Dr. Gokal’s future is uncertain. Will we help him, or will we leave him to the wolves? In an email exchange with his lawyer’s office, I learned that Dr. Gokal has received offers of employment but is unable to entertain them because the actions by the Harris County District Attorney triggered an automatic review by the Texas Medical Board. A GoFundMe page was launched, but an appreciative Dr. Gokal stated publicly that he’d rather the money go to a needy charity.
In the last paragraph of the Times article, Dr. Gokal asks, “How can I take it back?” referencing stories about “the Pakistani doctor in Houston who stole all those vaccines.”
Let’s help him take back his story. In helping him, perhaps we can take back a little control. We could start with letters of support that could be mailed to his lawyer, Paul Doyle, Esq., of Houston, or tweet, respectfully of course, to the district attorney @Kimoggforda.
We can also let the Harris County Public Health Department in Houston know what we think of their actions.
On Martin Luther King Day, Kim Ogg, the district attorney who charged Dr. Gokal, tweeted MLK’s famous quote: “Injustice anywhere is a threat to justice everywhere.”
Let that motivate us to action.
Melissa Walton-Shirley, MD, is a native Kentuckian who retired from full-time invasive cardiology. She enjoys locums work in Montana and is a champion of physician rights and patient safety. In addition to opinion writing, she enjoys spending time with her husband, daughters and parents, and sidelines as a backing vocalist for local rock bands. A version of this article first appeared on Medscape.com.
Journal to retract psych paper after plagiarism allegations, editor steps down
A medical journal is retracting a paper after a psychiatrist alleged that the managing editor closely copied and published her withdrawn work and claimed it for his own.
In addition, the managing editor, Gary VandenBos, PhD, has resigned at the journal’s request, according to an email sent to the paper’s original author, psychiatrist Amy Barnhorst, MD, vice chair for community mental health at the University of California, Davis, and coauthor and UC Davis colleague Rocco Pallin, MPH.
Dr. Barnhorst shared emails – from the journal’s publisher, Springer Publishing Company, and from the editor in chief, Morgan Sammons, PhD – with this news organization.
The retraction is the end of a saga that began when Dr. Barnhorst and Dr. Pallin submitted a paper, at Dr. VandenBos’s request, to the Journal of Health Service Psychology, published by Springer.
As previously reported by this news organization, Dr. Barnhorst and Dr. Pallin eventually decided to withdraw the paper and were later notified by Dr. VandenBos that he’d published a similar article under his own authorship. Michael O. Miller, a retired judge who trained as a psychologist, was listed as a coauthor.
The two women – acknowledged experts in the article’s subject matter on how physicians can talk to patients about gun violence – immediately notified Dr. Sammons and Springer Publishing when they saw the published piece, saying they believed it plagiarized their original submission.
According to the e-mail Springer sent to Dr. Barnhorst, the publisher investigated and said that it would “be retracting the article shortly.”
The retraction notice will state: “The Editor in Chief and the authors, Dr. VandenBos and Mr. Miller, have retracted this article, as it significantly overlaps with an unpublished manuscript by Amy Barnhorst and Rocco Pallin.” It also states that “[Dr.] VandenBos accepts full responsibility for the overlap.”
The original article will still be available, but it will be marked as “retracted” and feature a link to the retraction notice.
Dr. Barnhorst, who garnered at least 40,000 likes when she tweeted about the alleged theft of her work, said in an interview that she and Dr. Pallin are “glad to see that the investigation is complete and the retraction has been issued.”
“At least we can now submit it to a new journal in a version that appropriately represents our work and expertise,” said Dr. Barnhorst. “I still have no idea how or why this happened, nor how much of it was intentional and on whose part, but I guess I never will!”
Editor removed
When contacted by this news organization to comment on the retraction and removal of Dr. VandenBos as managing editor, Dr. Sammons said it was not possible because, “I treat such correspondence as confidential.”
Dr. Sammons said he could “confirm that our investigation is reaching its conclusion and my colleagues at Springer Nature would be happy to contact you when we can provide a further update.”
Springer spokesperson Anne Korn also would not comment beyond saying, “The conclusion of our investigation is still in progress and may take a little additional time.”
In the letter sent to Dr. Barnhorst and Dr. Pallin, Dr. Sammons said he had “asked for and accepted the resignation of Dr. VandenBos,” and that the resignation will be announced “in the upcoming print issue of our journal.”
Dr. Sammons said he also notified the dean of the University of Arizona College of Law that Mr. Miller, who held a position at the school, was not aware of the original submission by the two women. Even so, the school suspended Mr. Miller’s academic appointment, according to Dr. Sammons’ letter.
The editor in chief also said that, while “[Dr.] VandenBos’ errors were substantial and had substantial consequences, my investigation did not find any intent to plagiarize your work.”
He apologized again to Dr. Barnhorst and Dr. Pallin, though, adding, “I and my associate editors have initiated a revision of our publications processes to ensure that errors such as the above do not occur in the future, and I apologize again that this lapse affected you and your scholarly work.”
A version of this article first appeared on Medscape.com.
A medical journal is retracting a paper after a psychiatrist alleged that the managing editor closely copied and published her withdrawn work and claimed it for his own.
In addition, the managing editor, Gary VandenBos, PhD, has resigned at the journal’s request, according to an email sent to the paper’s original author, psychiatrist Amy Barnhorst, MD, vice chair for community mental health at the University of California, Davis, and coauthor and UC Davis colleague Rocco Pallin, MPH.
Dr. Barnhorst shared emails – from the journal’s publisher, Springer Publishing Company, and from the editor in chief, Morgan Sammons, PhD – with this news organization.
The retraction is the end of a saga that began when Dr. Barnhorst and Dr. Pallin submitted a paper, at Dr. VandenBos’s request, to the Journal of Health Service Psychology, published by Springer.
As previously reported by this news organization, Dr. Barnhorst and Dr. Pallin eventually decided to withdraw the paper and were later notified by Dr. VandenBos that he’d published a similar article under his own authorship. Michael O. Miller, a retired judge who trained as a psychologist, was listed as a coauthor.
The two women – acknowledged experts in the article’s subject matter on how physicians can talk to patients about gun violence – immediately notified Dr. Sammons and Springer Publishing when they saw the published piece, saying they believed it plagiarized their original submission.
According to the e-mail Springer sent to Dr. Barnhorst, the publisher investigated and said that it would “be retracting the article shortly.”
The retraction notice will state: “The Editor in Chief and the authors, Dr. VandenBos and Mr. Miller, have retracted this article, as it significantly overlaps with an unpublished manuscript by Amy Barnhorst and Rocco Pallin.” It also states that “[Dr.] VandenBos accepts full responsibility for the overlap.”
The original article will still be available, but it will be marked as “retracted” and feature a link to the retraction notice.
Dr. Barnhorst, who garnered at least 40,000 likes when she tweeted about the alleged theft of her work, said in an interview that she and Dr. Pallin are “glad to see that the investigation is complete and the retraction has been issued.”
“At least we can now submit it to a new journal in a version that appropriately represents our work and expertise,” said Dr. Barnhorst. “I still have no idea how or why this happened, nor how much of it was intentional and on whose part, but I guess I never will!”
Editor removed
When contacted by this news organization to comment on the retraction and removal of Dr. VandenBos as managing editor, Dr. Sammons said it was not possible because, “I treat such correspondence as confidential.”
Dr. Sammons said he could “confirm that our investigation is reaching its conclusion and my colleagues at Springer Nature would be happy to contact you when we can provide a further update.”
Springer spokesperson Anne Korn also would not comment beyond saying, “The conclusion of our investigation is still in progress and may take a little additional time.”
In the letter sent to Dr. Barnhorst and Dr. Pallin, Dr. Sammons said he had “asked for and accepted the resignation of Dr. VandenBos,” and that the resignation will be announced “in the upcoming print issue of our journal.”
Dr. Sammons said he also notified the dean of the University of Arizona College of Law that Mr. Miller, who held a position at the school, was not aware of the original submission by the two women. Even so, the school suspended Mr. Miller’s academic appointment, according to Dr. Sammons’ letter.
The editor in chief also said that, while “[Dr.] VandenBos’ errors were substantial and had substantial consequences, my investigation did not find any intent to plagiarize your work.”
He apologized again to Dr. Barnhorst and Dr. Pallin, though, adding, “I and my associate editors have initiated a revision of our publications processes to ensure that errors such as the above do not occur in the future, and I apologize again that this lapse affected you and your scholarly work.”
A version of this article first appeared on Medscape.com.
A medical journal is retracting a paper after a psychiatrist alleged that the managing editor closely copied and published her withdrawn work and claimed it for his own.
In addition, the managing editor, Gary VandenBos, PhD, has resigned at the journal’s request, according to an email sent to the paper’s original author, psychiatrist Amy Barnhorst, MD, vice chair for community mental health at the University of California, Davis, and coauthor and UC Davis colleague Rocco Pallin, MPH.
Dr. Barnhorst shared emails – from the journal’s publisher, Springer Publishing Company, and from the editor in chief, Morgan Sammons, PhD – with this news organization.
The retraction is the end of a saga that began when Dr. Barnhorst and Dr. Pallin submitted a paper, at Dr. VandenBos’s request, to the Journal of Health Service Psychology, published by Springer.
As previously reported by this news organization, Dr. Barnhorst and Dr. Pallin eventually decided to withdraw the paper and were later notified by Dr. VandenBos that he’d published a similar article under his own authorship. Michael O. Miller, a retired judge who trained as a psychologist, was listed as a coauthor.
The two women – acknowledged experts in the article’s subject matter on how physicians can talk to patients about gun violence – immediately notified Dr. Sammons and Springer Publishing when they saw the published piece, saying they believed it plagiarized their original submission.
According to the e-mail Springer sent to Dr. Barnhorst, the publisher investigated and said that it would “be retracting the article shortly.”
The retraction notice will state: “The Editor in Chief and the authors, Dr. VandenBos and Mr. Miller, have retracted this article, as it significantly overlaps with an unpublished manuscript by Amy Barnhorst and Rocco Pallin.” It also states that “[Dr.] VandenBos accepts full responsibility for the overlap.”
The original article will still be available, but it will be marked as “retracted” and feature a link to the retraction notice.
Dr. Barnhorst, who garnered at least 40,000 likes when she tweeted about the alleged theft of her work, said in an interview that she and Dr. Pallin are “glad to see that the investigation is complete and the retraction has been issued.”
“At least we can now submit it to a new journal in a version that appropriately represents our work and expertise,” said Dr. Barnhorst. “I still have no idea how or why this happened, nor how much of it was intentional and on whose part, but I guess I never will!”
Editor removed
When contacted by this news organization to comment on the retraction and removal of Dr. VandenBos as managing editor, Dr. Sammons said it was not possible because, “I treat such correspondence as confidential.”
Dr. Sammons said he could “confirm that our investigation is reaching its conclusion and my colleagues at Springer Nature would be happy to contact you when we can provide a further update.”
Springer spokesperson Anne Korn also would not comment beyond saying, “The conclusion of our investigation is still in progress and may take a little additional time.”
In the letter sent to Dr. Barnhorst and Dr. Pallin, Dr. Sammons said he had “asked for and accepted the resignation of Dr. VandenBos,” and that the resignation will be announced “in the upcoming print issue of our journal.”
Dr. Sammons said he also notified the dean of the University of Arizona College of Law that Mr. Miller, who held a position at the school, was not aware of the original submission by the two women. Even so, the school suspended Mr. Miller’s academic appointment, according to Dr. Sammons’ letter.
The editor in chief also said that, while “[Dr.] VandenBos’ errors were substantial and had substantial consequences, my investigation did not find any intent to plagiarize your work.”
He apologized again to Dr. Barnhorst and Dr. Pallin, though, adding, “I and my associate editors have initiated a revision of our publications processes to ensure that errors such as the above do not occur in the future, and I apologize again that this lapse affected you and your scholarly work.”
A version of this article first appeared on Medscape.com.
The fax that got under my skin
I got an interesting fax recently.
It started with how tough things have been for small practices during the pandemic (like I need reminding) and suggests it has solutions for my practice to stay afloat.
I’m used to all kinds of these approaches, and was going to toss the fax, but decided to read on out of curiosity. I assumed it was an advertisement for a loan company, or to sell vitamins out of my office.
This one, surprisingly, suggested I buy gadgets that would allow me to “balance uneven skin tones,” “shrink pores,” “eliminate freckles and stretch marks,” and do “laser vaginal resurfacing”
Are you kidding me?
First of all, I try very hard to stay in my lane. I’m a neurologist, hopefully a competent one, and have no desire to go beyond that. Imagine how bad this would look in a legal case: I’d be pretty hard pressed to convince a malpractice lawyer and jury that “eliminating stretch marks” and “laser vaginal resurfacing” are within the scope and training of your average neurologist.
Second, I don’t see this sort of thing as reflecting well on me. Patients come here to be treated for Parkinson’s disease, strokes, and epilepsy. If I tried to change the appointment’s topic to “those issues are minor, let’s talk about your stretch marks” I’m pretty sure they’d be looking for a new neurologist. And, when it got back to the physician who referred them, so would she.
Third, my patients are tightening their belts like everyone else in this pandemic-associated economic downturn. Suddenly trying to sell them on a pricey cash-pay procedure, let alone one that’s pretty far out of my field, isn’t going to fly. Like my own family they’re watching every penny right now and shrinking pores is at the bottom of their financial priorities. If they really want that done I’d to happy to refer them to a dermatologist.
Not surprisingly, I tossed the fax. Caring for my patients is challenging enough when I stick to what I do best.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I got an interesting fax recently.
It started with how tough things have been for small practices during the pandemic (like I need reminding) and suggests it has solutions for my practice to stay afloat.
I’m used to all kinds of these approaches, and was going to toss the fax, but decided to read on out of curiosity. I assumed it was an advertisement for a loan company, or to sell vitamins out of my office.
This one, surprisingly, suggested I buy gadgets that would allow me to “balance uneven skin tones,” “shrink pores,” “eliminate freckles and stretch marks,” and do “laser vaginal resurfacing”
Are you kidding me?
First of all, I try very hard to stay in my lane. I’m a neurologist, hopefully a competent one, and have no desire to go beyond that. Imagine how bad this would look in a legal case: I’d be pretty hard pressed to convince a malpractice lawyer and jury that “eliminating stretch marks” and “laser vaginal resurfacing” are within the scope and training of your average neurologist.
Second, I don’t see this sort of thing as reflecting well on me. Patients come here to be treated for Parkinson’s disease, strokes, and epilepsy. If I tried to change the appointment’s topic to “those issues are minor, let’s talk about your stretch marks” I’m pretty sure they’d be looking for a new neurologist. And, when it got back to the physician who referred them, so would she.
Third, my patients are tightening their belts like everyone else in this pandemic-associated economic downturn. Suddenly trying to sell them on a pricey cash-pay procedure, let alone one that’s pretty far out of my field, isn’t going to fly. Like my own family they’re watching every penny right now and shrinking pores is at the bottom of their financial priorities. If they really want that done I’d to happy to refer them to a dermatologist.
Not surprisingly, I tossed the fax. Caring for my patients is challenging enough when I stick to what I do best.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I got an interesting fax recently.
It started with how tough things have been for small practices during the pandemic (like I need reminding) and suggests it has solutions for my practice to stay afloat.
I’m used to all kinds of these approaches, and was going to toss the fax, but decided to read on out of curiosity. I assumed it was an advertisement for a loan company, or to sell vitamins out of my office.
This one, surprisingly, suggested I buy gadgets that would allow me to “balance uneven skin tones,” “shrink pores,” “eliminate freckles and stretch marks,” and do “laser vaginal resurfacing”
Are you kidding me?
First of all, I try very hard to stay in my lane. I’m a neurologist, hopefully a competent one, and have no desire to go beyond that. Imagine how bad this would look in a legal case: I’d be pretty hard pressed to convince a malpractice lawyer and jury that “eliminating stretch marks” and “laser vaginal resurfacing” are within the scope and training of your average neurologist.
Second, I don’t see this sort of thing as reflecting well on me. Patients come here to be treated for Parkinson’s disease, strokes, and epilepsy. If I tried to change the appointment’s topic to “those issues are minor, let’s talk about your stretch marks” I’m pretty sure they’d be looking for a new neurologist. And, when it got back to the physician who referred them, so would she.
Third, my patients are tightening their belts like everyone else in this pandemic-associated economic downturn. Suddenly trying to sell them on a pricey cash-pay procedure, let alone one that’s pretty far out of my field, isn’t going to fly. Like my own family they’re watching every penny right now and shrinking pores is at the bottom of their financial priorities. If they really want that done I’d to happy to refer them to a dermatologist.
Not surprisingly, I tossed the fax. Caring for my patients is challenging enough when I stick to what I do best.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
FPs need to remind patients they care for whole families
I think there are multiple factors explaining why the percentage of family physicians treating children declined again. Not the least of these is that pediatricians have a very limited scope of practice and need to market and attract patients, which they do quite a bit. There are even pediatric urgent care centers popping up all over the place now, some likely funded by venture capital just as other urgent care centers have been funded.
The loss of pediatric inpatient volume because of the effectiveness of vaccines that prevent many bacterial and viral illnesses means that fewer pediatric graduates are spending time in the hospital.
Family doctors used to retain their pediatric patients by delivering babies, seeing them in the newborn nursery, and beginning their relationship with the kids there. FPs are delivering fewer babies and the subsequent reduction in new kids in their practices has been a factor in this as well.
Finally, in multispecialty practices, pediatricians are employed there. Families immediately assume that their kids should be going to the pediatricians, not the family doctors. We need to keep talking up the fact that we take care of whole families to retain our pediatric practices.
Neil S. Calman, MD, is president and chief executive officer of the Institute for Family Health and is professor and chair of the Alfred and Gail Engelberg department of family medicine and community health at the Icahn School of Medicine at Mount Sinai and the Mount Sinai Health System, both in New York. Dr. Calman also serves on the editorial advisory board of Family Practice News.
I think there are multiple factors explaining why the percentage of family physicians treating children declined again. Not the least of these is that pediatricians have a very limited scope of practice and need to market and attract patients, which they do quite a bit. There are even pediatric urgent care centers popping up all over the place now, some likely funded by venture capital just as other urgent care centers have been funded.
The loss of pediatric inpatient volume because of the effectiveness of vaccines that prevent many bacterial and viral illnesses means that fewer pediatric graduates are spending time in the hospital.
Family doctors used to retain their pediatric patients by delivering babies, seeing them in the newborn nursery, and beginning their relationship with the kids there. FPs are delivering fewer babies and the subsequent reduction in new kids in their practices has been a factor in this as well.
Finally, in multispecialty practices, pediatricians are employed there. Families immediately assume that their kids should be going to the pediatricians, not the family doctors. We need to keep talking up the fact that we take care of whole families to retain our pediatric practices.
Neil S. Calman, MD, is president and chief executive officer of the Institute for Family Health and is professor and chair of the Alfred and Gail Engelberg department of family medicine and community health at the Icahn School of Medicine at Mount Sinai and the Mount Sinai Health System, both in New York. Dr. Calman also serves on the editorial advisory board of Family Practice News.
I think there are multiple factors explaining why the percentage of family physicians treating children declined again. Not the least of these is that pediatricians have a very limited scope of practice and need to market and attract patients, which they do quite a bit. There are even pediatric urgent care centers popping up all over the place now, some likely funded by venture capital just as other urgent care centers have been funded.
The loss of pediatric inpatient volume because of the effectiveness of vaccines that prevent many bacterial and viral illnesses means that fewer pediatric graduates are spending time in the hospital.
Family doctors used to retain their pediatric patients by delivering babies, seeing them in the newborn nursery, and beginning their relationship with the kids there. FPs are delivering fewer babies and the subsequent reduction in new kids in their practices has been a factor in this as well.
Finally, in multispecialty practices, pediatricians are employed there. Families immediately assume that their kids should be going to the pediatricians, not the family doctors. We need to keep talking up the fact that we take care of whole families to retain our pediatric practices.
Neil S. Calman, MD, is president and chief executive officer of the Institute for Family Health and is professor and chair of the Alfred and Gail Engelberg department of family medicine and community health at the Icahn School of Medicine at Mount Sinai and the Mount Sinai Health System, both in New York. Dr. Calman also serves on the editorial advisory board of Family Practice News.
Ob.gyns. report high burnout prior to pandemic
Among ob.gyns. who reported burnout in the past year, 82% say they felt burned out before the advent of the coronavirus pandemic, according the Medscape Obstetrician & Gynecologist Lifestyle, Happiness, & Burnout Report.
The past year brought unusual challenges to physicians in all specialties in different ways.
“Whether on the front lines of treating COVID-19 patients, pivoting from in-person to virtual care, or even having to shutter their practices, physicians faced an onslaught of crises, while political tensions, social unrest, and environmental concerns probably affected their lives outside of medicine,” wrote Keith L. Martin and Mary Lyn Koval, both of Medscape Business of Medicine, in the introduction to the report.
Although more physicians said their burnout began prior to the pandemic, 81% of ob.gyns. reported that they were happy outside of work prior to the pandemic. However, those reporting happiness outside of work dropped to 57% after the pandemic started.
“One does not have to do a ‘deep dive’ to understand the top reasons reported for burnout,” said Mark P. Trolice, MD, director of Fertility CARE: The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando, in an interview. “Many conversations I have with colleagues are about the frustration of learning and managing electronic health records, insurance reimbursements, and a work-life balance. In addition, more physician practices are being purchased by hospitals or private-equity networks [that are] reducing and/or eliminating the autonomy of physicians.
“While all [respondents] exhibited a dramatic decline in ‘happiness’ prepandemic, compared with our current situation, ob.gyns. were no exception,” he added.
Burnout and suicidal thoughts
Overall, 26% of ob.gyn. survey respondents reported being burned out, 6% reported being depressed, and 18% reported being both burned out and depressed. Of those who reported burnout, 52% said burnout had “a strong or severe impact on my life,” while 20% reported a moderate impact and 28% reported little or no impact.
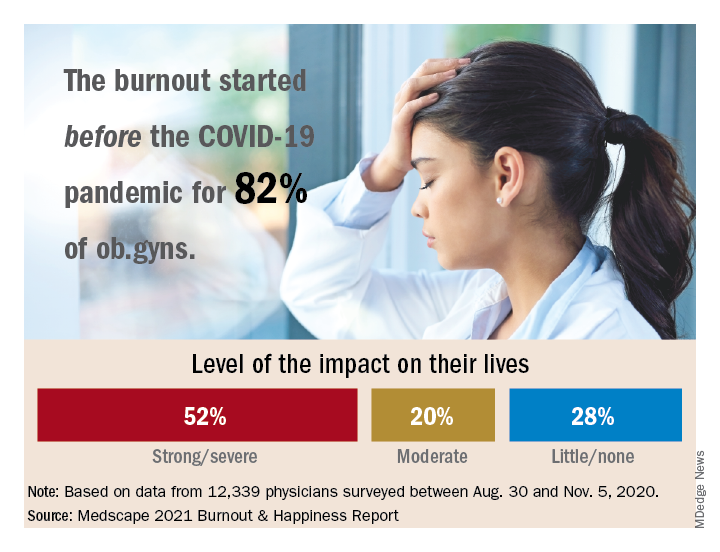
More than half (56%) of ob.gyns. who reported either depression or burnout said they had not sought professional help, although 17% reported receiving professional care in the past.
The main reason given for not seeking professional help was that burnout and depressive symptoms were not severe enough to merit it, according to 50% of respondents who reported burnout or depression but were not seeking help. In addition, 43% said they were too busy to seek help, 36% said they could deal with their symptoms without professional help, and 24% said they did not want to risk disclosure of their symptoms.
The most common cause of burnout was an overload of bureaucratic tasks, reported by 52% of respondents, followed by “lack of respect from administrators/employers, colleagues, or staff” (43%), and insufficient compensation or reimbursement (39%).
Notably, 19% of ob.gyns. reported suicidal thoughts, and 1% said they had attempted suicide.
“The most concerning statistic from this survey was in reference to suicidal ideation,” said Dr. Trolice. “Approximately one in five ob.gyns. have contemplated suicide, compared with 4.8% of adults age 18 and older in the U.S. reporting in 2019.”
Dr. Trolice said he was not surprised that relatively few ob.gyns. sought help for mental health issues. “Physicians are very private and usually do not seek help from colleagues, presumably from hubris. While this is unfortunate, all hospitals and health care organization should implement regular assessments of physicians’ health to ensure optimal performance from a professional and personal basis.”
Balance and self-care
The top workplace concern, by a large margin, was for work-life balance, reported by 44% of respondents, followed by compensation (19%), combining work and parenting (18%), and relationships with staff and colleagues (8%).
Approximately one-third (36%) of the ob.gyn. respondents said they made time to focus on personal well-being, compared with 35% of physicians overall. Although only 13% reported exercising every day, a total of 69% exercised at least twice a week, similar to the 70% of physicians overall who reported exercising at least twice a week.
“Work-life balance is high on the list of concerns, but physicians are split 50/50 on whether they would accept a salary reduction to improve this aspect of their lives,” Dr. Trolice said.
“Social relationships are a proven value to mental health, yet nearly 50% of ob.gyns. who reported feeling burnout use isolationism as their coping skill, citing a lack of severity to require treatment,” he noted. Nevertheless, more than 80% of responders were married and described their relationship as “good or very good.”
Address burnout at individual and organizational levels
“Sadly, the findings are not surprising,” said Iris Krisha, MD, of Emory University, Atlanta, in an interview. “Burnout rates have been steadily increasing among physicians across all specialties.” Barriers to reducing burnout exist at the organizational and individual level, therefore strategies to reduce burnout should address individual and organizational solutions, Dr. Krishna emphasized. “At the organizational level, solutions may include developing manageable workloads, creating fair productivity targets, encouraging physician engagement in work structure, supporting flexible work schedules, and allowing for protected time for education and exercise. On the individual level, physicians can work to develop stress management strategies, engage in mindfulness and self-care.”
To reduce the burden of bureaucratic tasks, “health care organizations can work toward optimizing electronic medical records and hire staff to offload clerical work, and physicians can seek training in efficiency,” said Dr. Krishna. In addition, “health care organizations can reduce the stigma that may surround burnout or mental health issues, as well as promote a culture of wellness and resilience,” to help reduce and prevent burnout.
Find positivity and purpose
Improving the workplace experience so physicians feel engaged and in control as they navigate their many responsibilities may help reduce burnout, said Dr. Trolice. On the individual level, “finding your purpose to give you more meaning at work, discovering the power of hope to embrace optimism, and building friendships at work for greater engagement with others,” can help as well.
“In the face of adversity and setbacks, people in happier workplaces tend to be better at coping with and recovering from work pressure and at reconciling conflict,” Dr. Trolice emphasized. “The practice of medicine has dramatically changed for many physicians compared with the original expectations when they applied to medical school. Nevertheless, it behooves physician to adapt to 21st century medical care as they remind themselves of their purpose.”
The report included responses from 12,339 physicians across 29 specialties who completed a 10-minute online survey between Aug. 30 and Nov. 5, 2020. Participants were required to be practicing U.S. physicians.
Among ob.gyns. who reported burnout in the past year, 82% say they felt burned out before the advent of the coronavirus pandemic, according the Medscape Obstetrician & Gynecologist Lifestyle, Happiness, & Burnout Report.
The past year brought unusual challenges to physicians in all specialties in different ways.
“Whether on the front lines of treating COVID-19 patients, pivoting from in-person to virtual care, or even having to shutter their practices, physicians faced an onslaught of crises, while political tensions, social unrest, and environmental concerns probably affected their lives outside of medicine,” wrote Keith L. Martin and Mary Lyn Koval, both of Medscape Business of Medicine, in the introduction to the report.
Although more physicians said their burnout began prior to the pandemic, 81% of ob.gyns. reported that they were happy outside of work prior to the pandemic. However, those reporting happiness outside of work dropped to 57% after the pandemic started.
“One does not have to do a ‘deep dive’ to understand the top reasons reported for burnout,” said Mark P. Trolice, MD, director of Fertility CARE: The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando, in an interview. “Many conversations I have with colleagues are about the frustration of learning and managing electronic health records, insurance reimbursements, and a work-life balance. In addition, more physician practices are being purchased by hospitals or private-equity networks [that are] reducing and/or eliminating the autonomy of physicians.
“While all [respondents] exhibited a dramatic decline in ‘happiness’ prepandemic, compared with our current situation, ob.gyns. were no exception,” he added.
Burnout and suicidal thoughts
Overall, 26% of ob.gyn. survey respondents reported being burned out, 6% reported being depressed, and 18% reported being both burned out and depressed. Of those who reported burnout, 52% said burnout had “a strong or severe impact on my life,” while 20% reported a moderate impact and 28% reported little or no impact.
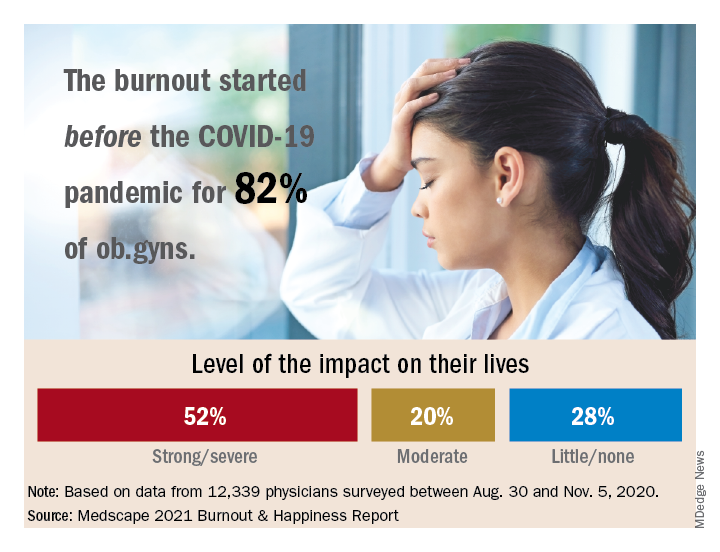
More than half (56%) of ob.gyns. who reported either depression or burnout said they had not sought professional help, although 17% reported receiving professional care in the past.
The main reason given for not seeking professional help was that burnout and depressive symptoms were not severe enough to merit it, according to 50% of respondents who reported burnout or depression but were not seeking help. In addition, 43% said they were too busy to seek help, 36% said they could deal with their symptoms without professional help, and 24% said they did not want to risk disclosure of their symptoms.
The most common cause of burnout was an overload of bureaucratic tasks, reported by 52% of respondents, followed by “lack of respect from administrators/employers, colleagues, or staff” (43%), and insufficient compensation or reimbursement (39%).
Notably, 19% of ob.gyns. reported suicidal thoughts, and 1% said they had attempted suicide.
“The most concerning statistic from this survey was in reference to suicidal ideation,” said Dr. Trolice. “Approximately one in five ob.gyns. have contemplated suicide, compared with 4.8% of adults age 18 and older in the U.S. reporting in 2019.”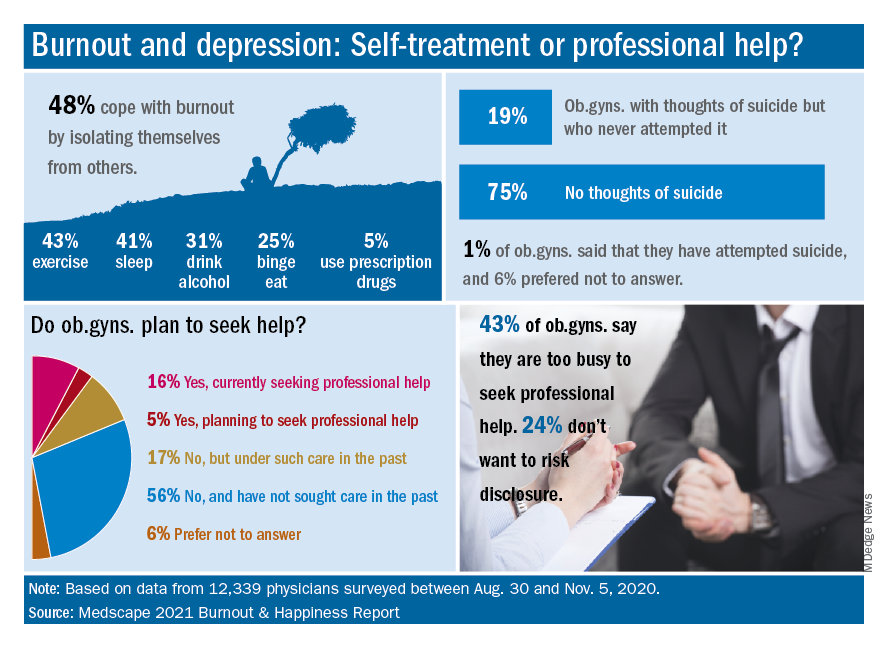
Dr. Trolice said he was not surprised that relatively few ob.gyns. sought help for mental health issues. “Physicians are very private and usually do not seek help from colleagues, presumably from hubris. While this is unfortunate, all hospitals and health care organization should implement regular assessments of physicians’ health to ensure optimal performance from a professional and personal basis.”
Balance and self-care
The top workplace concern, by a large margin, was for work-life balance, reported by 44% of respondents, followed by compensation (19%), combining work and parenting (18%), and relationships with staff and colleagues (8%).
Approximately one-third (36%) of the ob.gyn. respondents said they made time to focus on personal well-being, compared with 35% of physicians overall. Although only 13% reported exercising every day, a total of 69% exercised at least twice a week, similar to the 70% of physicians overall who reported exercising at least twice a week.
“Work-life balance is high on the list of concerns, but physicians are split 50/50 on whether they would accept a salary reduction to improve this aspect of their lives,” Dr. Trolice said.
“Social relationships are a proven value to mental health, yet nearly 50% of ob.gyns. who reported feeling burnout use isolationism as their coping skill, citing a lack of severity to require treatment,” he noted. Nevertheless, more than 80% of responders were married and described their relationship as “good or very good.”
Address burnout at individual and organizational levels
“Sadly, the findings are not surprising,” said Iris Krisha, MD, of Emory University, Atlanta, in an interview. “Burnout rates have been steadily increasing among physicians across all specialties.” Barriers to reducing burnout exist at the organizational and individual level, therefore strategies to reduce burnout should address individual and organizational solutions, Dr. Krishna emphasized. “At the organizational level, solutions may include developing manageable workloads, creating fair productivity targets, encouraging physician engagement in work structure, supporting flexible work schedules, and allowing for protected time for education and exercise. On the individual level, physicians can work to develop stress management strategies, engage in mindfulness and self-care.”
To reduce the burden of bureaucratic tasks, “health care organizations can work toward optimizing electronic medical records and hire staff to offload clerical work, and physicians can seek training in efficiency,” said Dr. Krishna. In addition, “health care organizations can reduce the stigma that may surround burnout or mental health issues, as well as promote a culture of wellness and resilience,” to help reduce and prevent burnout.
Find positivity and purpose
Improving the workplace experience so physicians feel engaged and in control as they navigate their many responsibilities may help reduce burnout, said Dr. Trolice. On the individual level, “finding your purpose to give you more meaning at work, discovering the power of hope to embrace optimism, and building friendships at work for greater engagement with others,” can help as well.
“In the face of adversity and setbacks, people in happier workplaces tend to be better at coping with and recovering from work pressure and at reconciling conflict,” Dr. Trolice emphasized. “The practice of medicine has dramatically changed for many physicians compared with the original expectations when they applied to medical school. Nevertheless, it behooves physician to adapt to 21st century medical care as they remind themselves of their purpose.”
The report included responses from 12,339 physicians across 29 specialties who completed a 10-minute online survey between Aug. 30 and Nov. 5, 2020. Participants were required to be practicing U.S. physicians.
Among ob.gyns. who reported burnout in the past year, 82% say they felt burned out before the advent of the coronavirus pandemic, according the Medscape Obstetrician & Gynecologist Lifestyle, Happiness, & Burnout Report.
The past year brought unusual challenges to physicians in all specialties in different ways.
“Whether on the front lines of treating COVID-19 patients, pivoting from in-person to virtual care, or even having to shutter their practices, physicians faced an onslaught of crises, while political tensions, social unrest, and environmental concerns probably affected their lives outside of medicine,” wrote Keith L. Martin and Mary Lyn Koval, both of Medscape Business of Medicine, in the introduction to the report.
Although more physicians said their burnout began prior to the pandemic, 81% of ob.gyns. reported that they were happy outside of work prior to the pandemic. However, those reporting happiness outside of work dropped to 57% after the pandemic started.
“One does not have to do a ‘deep dive’ to understand the top reasons reported for burnout,” said Mark P. Trolice, MD, director of Fertility CARE: The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando, in an interview. “Many conversations I have with colleagues are about the frustration of learning and managing electronic health records, insurance reimbursements, and a work-life balance. In addition, more physician practices are being purchased by hospitals or private-equity networks [that are] reducing and/or eliminating the autonomy of physicians.
“While all [respondents] exhibited a dramatic decline in ‘happiness’ prepandemic, compared with our current situation, ob.gyns. were no exception,” he added.
Burnout and suicidal thoughts
Overall, 26% of ob.gyn. survey respondents reported being burned out, 6% reported being depressed, and 18% reported being both burned out and depressed. Of those who reported burnout, 52% said burnout had “a strong or severe impact on my life,” while 20% reported a moderate impact and 28% reported little or no impact.
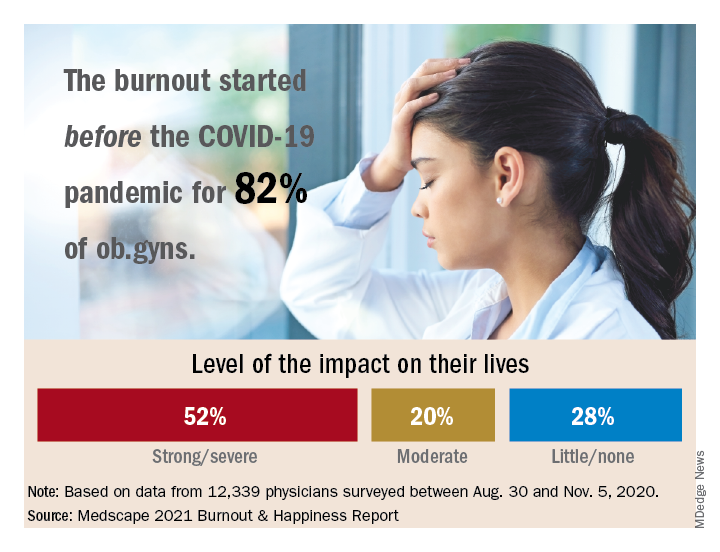
More than half (56%) of ob.gyns. who reported either depression or burnout said they had not sought professional help, although 17% reported receiving professional care in the past.
The main reason given for not seeking professional help was that burnout and depressive symptoms were not severe enough to merit it, according to 50% of respondents who reported burnout or depression but were not seeking help. In addition, 43% said they were too busy to seek help, 36% said they could deal with their symptoms without professional help, and 24% said they did not want to risk disclosure of their symptoms.
The most common cause of burnout was an overload of bureaucratic tasks, reported by 52% of respondents, followed by “lack of respect from administrators/employers, colleagues, or staff” (43%), and insufficient compensation or reimbursement (39%).
Notably, 19% of ob.gyns. reported suicidal thoughts, and 1% said they had attempted suicide.
“The most concerning statistic from this survey was in reference to suicidal ideation,” said Dr. Trolice. “Approximately one in five ob.gyns. have contemplated suicide, compared with 4.8% of adults age 18 and older in the U.S. reporting in 2019.”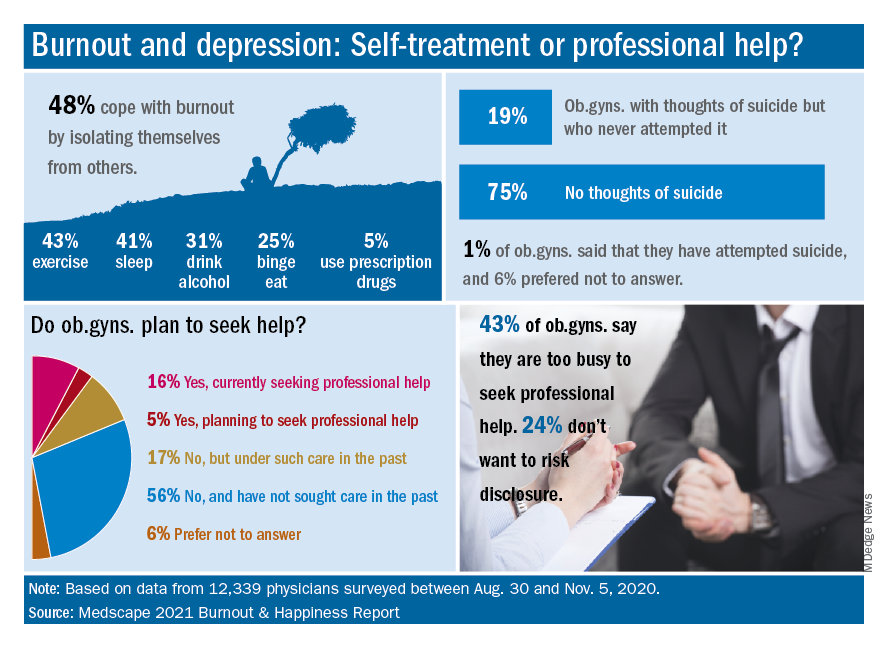
Dr. Trolice said he was not surprised that relatively few ob.gyns. sought help for mental health issues. “Physicians are very private and usually do not seek help from colleagues, presumably from hubris. While this is unfortunate, all hospitals and health care organization should implement regular assessments of physicians’ health to ensure optimal performance from a professional and personal basis.”
Balance and self-care
The top workplace concern, by a large margin, was for work-life balance, reported by 44% of respondents, followed by compensation (19%), combining work and parenting (18%), and relationships with staff and colleagues (8%).
Approximately one-third (36%) of the ob.gyn. respondents said they made time to focus on personal well-being, compared with 35% of physicians overall. Although only 13% reported exercising every day, a total of 69% exercised at least twice a week, similar to the 70% of physicians overall who reported exercising at least twice a week.
“Work-life balance is high on the list of concerns, but physicians are split 50/50 on whether they would accept a salary reduction to improve this aspect of their lives,” Dr. Trolice said.
“Social relationships are a proven value to mental health, yet nearly 50% of ob.gyns. who reported feeling burnout use isolationism as their coping skill, citing a lack of severity to require treatment,” he noted. Nevertheless, more than 80% of responders were married and described their relationship as “good or very good.”
Address burnout at individual and organizational levels
“Sadly, the findings are not surprising,” said Iris Krisha, MD, of Emory University, Atlanta, in an interview. “Burnout rates have been steadily increasing among physicians across all specialties.” Barriers to reducing burnout exist at the organizational and individual level, therefore strategies to reduce burnout should address individual and organizational solutions, Dr. Krishna emphasized. “At the organizational level, solutions may include developing manageable workloads, creating fair productivity targets, encouraging physician engagement in work structure, supporting flexible work schedules, and allowing for protected time for education and exercise. On the individual level, physicians can work to develop stress management strategies, engage in mindfulness and self-care.”
To reduce the burden of bureaucratic tasks, “health care organizations can work toward optimizing electronic medical records and hire staff to offload clerical work, and physicians can seek training in efficiency,” said Dr. Krishna. In addition, “health care organizations can reduce the stigma that may surround burnout or mental health issues, as well as promote a culture of wellness and resilience,” to help reduce and prevent burnout.
Find positivity and purpose
Improving the workplace experience so physicians feel engaged and in control as they navigate their many responsibilities may help reduce burnout, said Dr. Trolice. On the individual level, “finding your purpose to give you more meaning at work, discovering the power of hope to embrace optimism, and building friendships at work for greater engagement with others,” can help as well.
“In the face of adversity and setbacks, people in happier workplaces tend to be better at coping with and recovering from work pressure and at reconciling conflict,” Dr. Trolice emphasized. “The practice of medicine has dramatically changed for many physicians compared with the original expectations when they applied to medical school. Nevertheless, it behooves physician to adapt to 21st century medical care as they remind themselves of their purpose.”
The report included responses from 12,339 physicians across 29 specialties who completed a 10-minute online survey between Aug. 30 and Nov. 5, 2020. Participants were required to be practicing U.S. physicians.