User login
How to talk with patients in ways that help them feel heard and understood
How do we become those professionals and make sure that we are doing a good job connecting and communicating with our patients?
Here are a few suggestions on how to do this.
Practice intent listening
When a patient shares their symptoms with you, show genuine curiosity and concern. Ask clarifying questions. Ask how the symptom or problem is affecting their day-to-day life. Avoid quick, rapid-fire questions back at the patient. Do not accept a patient self-diagnosis.
When a patient with a first-time headache says they are having a migraine headache, for example, ask many clarifying questions to make sure you can make a diagnosis of headache type, then use all the information you have gathered to educate the patient on what you believe they have.
It is easy to jump to treatment, but we always want to make sure we have the diagnosis correct first. By intently listening, it also makes it much easier to tell a patient you do not know what is causing their symptoms, but that you and the patient will be vigilant for any future clues that may lead to a diagnosis.
Use terminology that patients understand
Rachael Gotlieb, MD, and colleagues published an excellent study with eye-opening results on common phrases we use as health care providers and how often patients do not understand them.
Only 9% of patients understood what was meant when they were asked if they have been febrile. Only 2% understood what was meant by “I am concerned the patient has an occult infection.” Only 21% understood that “your xray findings were quite impressive” was bad news.
It is easy to avoid these medical language traps, we just have to check our doctor speak. Ask, “Do you have a fever?” Say, “I am concerned you may have an infection that is hard to find.”
Several other terms we use all the time in explaining things to patients that I have found most patients do not understand are the terms bilateral, systemic, and significant. Think carefully as you explain things to patients and check back to have them repeat to you what they think you said.
Be comfortable saying you don’t know
Many symptoms in medicine end up not being diagnosable. When a patient shares symptoms that do not fit a pattern of a disease, it is important to share with them why you think it is okay to wait and watch, even if you do not have a diagnosis.
Patients find it comforting that you are so honest with them. Doing this also has the benefit of gaining patients’ trust when you are sure about something, because it tells them you don’t have an answer for everything.
Ask your patients what they think is causing their symptoms
This way, you know what their big fear is. You can address what they are worried about, even if it isn’t something you are considering.
Patients are often fearful of a disease a close friend or relative has, so when they get new symptoms, they fear diseases that we might not think of. By knowing what they are fearful of, you can reassure when appropriate.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
How do we become those professionals and make sure that we are doing a good job connecting and communicating with our patients?
Here are a few suggestions on how to do this.
Practice intent listening
When a patient shares their symptoms with you, show genuine curiosity and concern. Ask clarifying questions. Ask how the symptom or problem is affecting their day-to-day life. Avoid quick, rapid-fire questions back at the patient. Do not accept a patient self-diagnosis.
When a patient with a first-time headache says they are having a migraine headache, for example, ask many clarifying questions to make sure you can make a diagnosis of headache type, then use all the information you have gathered to educate the patient on what you believe they have.
It is easy to jump to treatment, but we always want to make sure we have the diagnosis correct first. By intently listening, it also makes it much easier to tell a patient you do not know what is causing their symptoms, but that you and the patient will be vigilant for any future clues that may lead to a diagnosis.
Use terminology that patients understand
Rachael Gotlieb, MD, and colleagues published an excellent study with eye-opening results on common phrases we use as health care providers and how often patients do not understand them.
Only 9% of patients understood what was meant when they were asked if they have been febrile. Only 2% understood what was meant by “I am concerned the patient has an occult infection.” Only 21% understood that “your xray findings were quite impressive” was bad news.
It is easy to avoid these medical language traps, we just have to check our doctor speak. Ask, “Do you have a fever?” Say, “I am concerned you may have an infection that is hard to find.”
Several other terms we use all the time in explaining things to patients that I have found most patients do not understand are the terms bilateral, systemic, and significant. Think carefully as you explain things to patients and check back to have them repeat to you what they think you said.
Be comfortable saying you don’t know
Many symptoms in medicine end up not being diagnosable. When a patient shares symptoms that do not fit a pattern of a disease, it is important to share with them why you think it is okay to wait and watch, even if you do not have a diagnosis.
Patients find it comforting that you are so honest with them. Doing this also has the benefit of gaining patients’ trust when you are sure about something, because it tells them you don’t have an answer for everything.
Ask your patients what they think is causing their symptoms
This way, you know what their big fear is. You can address what they are worried about, even if it isn’t something you are considering.
Patients are often fearful of a disease a close friend or relative has, so when they get new symptoms, they fear diseases that we might not think of. By knowing what they are fearful of, you can reassure when appropriate.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
How do we become those professionals and make sure that we are doing a good job connecting and communicating with our patients?
Here are a few suggestions on how to do this.
Practice intent listening
When a patient shares their symptoms with you, show genuine curiosity and concern. Ask clarifying questions. Ask how the symptom or problem is affecting their day-to-day life. Avoid quick, rapid-fire questions back at the patient. Do not accept a patient self-diagnosis.
When a patient with a first-time headache says they are having a migraine headache, for example, ask many clarifying questions to make sure you can make a diagnosis of headache type, then use all the information you have gathered to educate the patient on what you believe they have.
It is easy to jump to treatment, but we always want to make sure we have the diagnosis correct first. By intently listening, it also makes it much easier to tell a patient you do not know what is causing their symptoms, but that you and the patient will be vigilant for any future clues that may lead to a diagnosis.
Use terminology that patients understand
Rachael Gotlieb, MD, and colleagues published an excellent study with eye-opening results on common phrases we use as health care providers and how often patients do not understand them.
Only 9% of patients understood what was meant when they were asked if they have been febrile. Only 2% understood what was meant by “I am concerned the patient has an occult infection.” Only 21% understood that “your xray findings were quite impressive” was bad news.
It is easy to avoid these medical language traps, we just have to check our doctor speak. Ask, “Do you have a fever?” Say, “I am concerned you may have an infection that is hard to find.”
Several other terms we use all the time in explaining things to patients that I have found most patients do not understand are the terms bilateral, systemic, and significant. Think carefully as you explain things to patients and check back to have them repeat to you what they think you said.
Be comfortable saying you don’t know
Many symptoms in medicine end up not being diagnosable. When a patient shares symptoms that do not fit a pattern of a disease, it is important to share with them why you think it is okay to wait and watch, even if you do not have a diagnosis.
Patients find it comforting that you are so honest with them. Doing this also has the benefit of gaining patients’ trust when you are sure about something, because it tells them you don’t have an answer for everything.
Ask your patients what they think is causing their symptoms
This way, you know what their big fear is. You can address what they are worried about, even if it isn’t something you are considering.
Patients are often fearful of a disease a close friend or relative has, so when they get new symptoms, they fear diseases that we might not think of. By knowing what they are fearful of, you can reassure when appropriate.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
Adverse events reported in one-quarter of inpatient admissions
as indicated from data from 2,809 admissions at 11 hospitals.
The 1991 Harvard Medical Practice Study, which focused on medical injury and litigation, documented an adverse event rate of 3.7 events per 100 admissions; 28% of those events were attributed to negligence, write David W. Bates, MD, of Brigham and Women’s Hospital, Boston, and colleagues.
Although patient safety has changed significantly since 1991, documenting improvements has been challenging, the researchers say. Several reports have shown a decrease in health care–associated infections. However, other aspects of safety – notably, adverse drug events, defined as injuries resulting from drugs taken – are not easily measured and tracked, the researchers say.
“We have not had good estimates of how much harm is being caused by care in hospitals in an ongoing way that looked across all types of adverse events,” and the current review is therefore important, Dr. Bates said in an interview.
In a study recently published in the New England Journal of Medicine, the researchers analyzed a random sample of 2,809 hospital admissions from 11 hospitals in Massachusetts during the 2018 calendar year. The hospitals ranged in size from fewer than 100 beds to more than 700 beds; all patients were aged 18 years and older. A panel of nine nurses reviewed the admissions records to identify potential adverse events, and eight physicians reviewed the adverse event summaries and either agreed or disagreed with the adverse event type. The severity of each event was ranked using a general severity scale into categories of significant, serious, life-threatening, or fatal.
Overall, at least one adverse event was identified in 23.6% of the hospital admissions. A total of 978 adverse events were deemed to have occurred during the index admission, and 222 of these (22.7%) were deemed preventable. Among the preventable adverse events, 19.7% were classified as serious, 3.3% as life-threatening, and 0.5% as fatal.
A total of 523 admissions (18.6%) involved at least one significant adverse event, defined as an event that caused unnecessary harm but from which recovery was rapid. A total of 211 admissions involved a serious adverse event, defined as harm resulting in substantial intervention or prolonged recovery; 34 included at least one life-threatening event; and seven admissions involved a fatal adverse event.
A total of 191 admissions involved at least one adverse event deemed preventable. Of those, 29 involved at least one preventable adverse event that was serious, life-threatening, or fatal, the researchers write. Of the seven deaths in the study population, one was deemed preventable.
The most common adverse events were adverse drug events, which accounted for 39.0% of the adverse events; surgical or other procedural events accounted for 30.4%; patient care events (including falls and pressure ulcers) accounted for 15.0%; and health care–associated infections accounted for 11.9%.
Overcoming barriers to better safety
“The overall level of harm, with nearly 1 in 4 patients suffering an adverse event, was higher than I expected it might be,” Dr. Bates told this news organization. However, techniques for identifying adverse events have improved, and “it is easier to find them in electronic records than in paper records,” he noted.
“Hospitals have many issues they are currently dealing with since COVID, and one issue is simply prioritization,” Dr. Bates said. “But it is now possible to measure harm for all patients using electronic tools, and if hospitals know how much harm they are having in specific areas, they can make choices about which ones to focus on.”
“We now have effective prevention strategies for most of the main kinds of harm,” he said. Generally, rates of harm are high because these strategies are not being used effectively, he said. “In addition, there are new tools that can be used – for example, to identify patients who are decompensating earlier,” he noted.
As for additional research, some specific types of harm that have been resistant to interventions, such as pressure ulcers, deserve more attention, said Dr. Bates. “In addition, diagnostic errors appear to cause a great deal of harm, but we don’t yet have good strategies for preventing these,” he said.
The study findings were limited by several factors, including the use of data from hospitals that might not represent hospitals at large and by the inclusion mainly of patients with private insurance, the researchers write. Other limitations include the likelihood that some adverse events were missed and the level of agreement on adverse events between adjudicators was only fair.
However, the findings serve as a reminder to health care professionals of the need for continued attention to improving patient safety, and measuring adverse events remains a critical part of guiding these improvements, the researchers conclude.
Timely reassessment and opportunities to improve
In the decades since the publication of the report, “To Err Is Human,” by the National Academies in 2000, significant attention has been paid to improving patient safety during hospitalizations, and health care systems have increased in both system and disease complexity, Said Suman Pal, MBBS, a specialist in hospital medicine at the University of New Mexico, Albuquerque, said in an interview. “Therefore, this study is important in reassessing the safety of inpatient care at the current time,” he said.
“The findings of this study showing preventable adverse events in approximately 7% of all admissions; while concerning, is not surprising, as it is consistent with other studies over time, as the authors have also noted in their discussion,” said Dr. Pal. The current findings “underscore the importance of continuous quality improvement efforts to increase the safety of patient care for hospitalized patients,” he noted.
“The increasing complexity of medical care, fragmentation of health care, structural inequities of health systems, and more recent widespread public health challenges such as the COVID-19 pandemic have been, in my opinion, barriers to improving patient safety,” Dr. Pal said. “The use of innovation and an interdisciplinary approach to patient safety and quality improvement in hospital-based care, such as the use of machine learning to monitor trends and predict the individualized risk of harm, could be a potential way out” to help reduce barriers and improve safety, he said.
“Additional research is needed to understand the key drivers of preventable harm for hospitalized patients in the United States,” said Dr. Pal. “When planning for change, keen attention must be paid to understanding how these [drivers] may differ for patients who have been historically marginalized or are otherwise underserved so as to not exacerbate health care inequities,” he added.
The study was funded by the Controlled Risk Insurance Company and the Risk Management Foundation of the Harvard Medical Institutions. Dr. Bates owns stock options with AESOP, Clew, FeelBetter, Guided Clinical Solutions, MDClone, and ValeraHealth and has grants/contracts from IBM Watson and EarlySense. He has also served as a consultant for CDI Negev. Dr. Pal has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
as indicated from data from 2,809 admissions at 11 hospitals.
The 1991 Harvard Medical Practice Study, which focused on medical injury and litigation, documented an adverse event rate of 3.7 events per 100 admissions; 28% of those events were attributed to negligence, write David W. Bates, MD, of Brigham and Women’s Hospital, Boston, and colleagues.
Although patient safety has changed significantly since 1991, documenting improvements has been challenging, the researchers say. Several reports have shown a decrease in health care–associated infections. However, other aspects of safety – notably, adverse drug events, defined as injuries resulting from drugs taken – are not easily measured and tracked, the researchers say.
“We have not had good estimates of how much harm is being caused by care in hospitals in an ongoing way that looked across all types of adverse events,” and the current review is therefore important, Dr. Bates said in an interview.
In a study recently published in the New England Journal of Medicine, the researchers analyzed a random sample of 2,809 hospital admissions from 11 hospitals in Massachusetts during the 2018 calendar year. The hospitals ranged in size from fewer than 100 beds to more than 700 beds; all patients were aged 18 years and older. A panel of nine nurses reviewed the admissions records to identify potential adverse events, and eight physicians reviewed the adverse event summaries and either agreed or disagreed with the adverse event type. The severity of each event was ranked using a general severity scale into categories of significant, serious, life-threatening, or fatal.
Overall, at least one adverse event was identified in 23.6% of the hospital admissions. A total of 978 adverse events were deemed to have occurred during the index admission, and 222 of these (22.7%) were deemed preventable. Among the preventable adverse events, 19.7% were classified as serious, 3.3% as life-threatening, and 0.5% as fatal.
A total of 523 admissions (18.6%) involved at least one significant adverse event, defined as an event that caused unnecessary harm but from which recovery was rapid. A total of 211 admissions involved a serious adverse event, defined as harm resulting in substantial intervention or prolonged recovery; 34 included at least one life-threatening event; and seven admissions involved a fatal adverse event.
A total of 191 admissions involved at least one adverse event deemed preventable. Of those, 29 involved at least one preventable adverse event that was serious, life-threatening, or fatal, the researchers write. Of the seven deaths in the study population, one was deemed preventable.
The most common adverse events were adverse drug events, which accounted for 39.0% of the adverse events; surgical or other procedural events accounted for 30.4%; patient care events (including falls and pressure ulcers) accounted for 15.0%; and health care–associated infections accounted for 11.9%.
Overcoming barriers to better safety
“The overall level of harm, with nearly 1 in 4 patients suffering an adverse event, was higher than I expected it might be,” Dr. Bates told this news organization. However, techniques for identifying adverse events have improved, and “it is easier to find them in electronic records than in paper records,” he noted.
“Hospitals have many issues they are currently dealing with since COVID, and one issue is simply prioritization,” Dr. Bates said. “But it is now possible to measure harm for all patients using electronic tools, and if hospitals know how much harm they are having in specific areas, they can make choices about which ones to focus on.”
“We now have effective prevention strategies for most of the main kinds of harm,” he said. Generally, rates of harm are high because these strategies are not being used effectively, he said. “In addition, there are new tools that can be used – for example, to identify patients who are decompensating earlier,” he noted.
As for additional research, some specific types of harm that have been resistant to interventions, such as pressure ulcers, deserve more attention, said Dr. Bates. “In addition, diagnostic errors appear to cause a great deal of harm, but we don’t yet have good strategies for preventing these,” he said.
The study findings were limited by several factors, including the use of data from hospitals that might not represent hospitals at large and by the inclusion mainly of patients with private insurance, the researchers write. Other limitations include the likelihood that some adverse events were missed and the level of agreement on adverse events between adjudicators was only fair.
However, the findings serve as a reminder to health care professionals of the need for continued attention to improving patient safety, and measuring adverse events remains a critical part of guiding these improvements, the researchers conclude.
Timely reassessment and opportunities to improve
In the decades since the publication of the report, “To Err Is Human,” by the National Academies in 2000, significant attention has been paid to improving patient safety during hospitalizations, and health care systems have increased in both system and disease complexity, Said Suman Pal, MBBS, a specialist in hospital medicine at the University of New Mexico, Albuquerque, said in an interview. “Therefore, this study is important in reassessing the safety of inpatient care at the current time,” he said.
“The findings of this study showing preventable adverse events in approximately 7% of all admissions; while concerning, is not surprising, as it is consistent with other studies over time, as the authors have also noted in their discussion,” said Dr. Pal. The current findings “underscore the importance of continuous quality improvement efforts to increase the safety of patient care for hospitalized patients,” he noted.
“The increasing complexity of medical care, fragmentation of health care, structural inequities of health systems, and more recent widespread public health challenges such as the COVID-19 pandemic have been, in my opinion, barriers to improving patient safety,” Dr. Pal said. “The use of innovation and an interdisciplinary approach to patient safety and quality improvement in hospital-based care, such as the use of machine learning to monitor trends and predict the individualized risk of harm, could be a potential way out” to help reduce barriers and improve safety, he said.
“Additional research is needed to understand the key drivers of preventable harm for hospitalized patients in the United States,” said Dr. Pal. “When planning for change, keen attention must be paid to understanding how these [drivers] may differ for patients who have been historically marginalized or are otherwise underserved so as to not exacerbate health care inequities,” he added.
The study was funded by the Controlled Risk Insurance Company and the Risk Management Foundation of the Harvard Medical Institutions. Dr. Bates owns stock options with AESOP, Clew, FeelBetter, Guided Clinical Solutions, MDClone, and ValeraHealth and has grants/contracts from IBM Watson and EarlySense. He has also served as a consultant for CDI Negev. Dr. Pal has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
as indicated from data from 2,809 admissions at 11 hospitals.
The 1991 Harvard Medical Practice Study, which focused on medical injury and litigation, documented an adverse event rate of 3.7 events per 100 admissions; 28% of those events were attributed to negligence, write David W. Bates, MD, of Brigham and Women’s Hospital, Boston, and colleagues.
Although patient safety has changed significantly since 1991, documenting improvements has been challenging, the researchers say. Several reports have shown a decrease in health care–associated infections. However, other aspects of safety – notably, adverse drug events, defined as injuries resulting from drugs taken – are not easily measured and tracked, the researchers say.
“We have not had good estimates of how much harm is being caused by care in hospitals in an ongoing way that looked across all types of adverse events,” and the current review is therefore important, Dr. Bates said in an interview.
In a study recently published in the New England Journal of Medicine, the researchers analyzed a random sample of 2,809 hospital admissions from 11 hospitals in Massachusetts during the 2018 calendar year. The hospitals ranged in size from fewer than 100 beds to more than 700 beds; all patients were aged 18 years and older. A panel of nine nurses reviewed the admissions records to identify potential adverse events, and eight physicians reviewed the adverse event summaries and either agreed or disagreed with the adverse event type. The severity of each event was ranked using a general severity scale into categories of significant, serious, life-threatening, or fatal.
Overall, at least one adverse event was identified in 23.6% of the hospital admissions. A total of 978 adverse events were deemed to have occurred during the index admission, and 222 of these (22.7%) were deemed preventable. Among the preventable adverse events, 19.7% were classified as serious, 3.3% as life-threatening, and 0.5% as fatal.
A total of 523 admissions (18.6%) involved at least one significant adverse event, defined as an event that caused unnecessary harm but from which recovery was rapid. A total of 211 admissions involved a serious adverse event, defined as harm resulting in substantial intervention or prolonged recovery; 34 included at least one life-threatening event; and seven admissions involved a fatal adverse event.
A total of 191 admissions involved at least one adverse event deemed preventable. Of those, 29 involved at least one preventable adverse event that was serious, life-threatening, or fatal, the researchers write. Of the seven deaths in the study population, one was deemed preventable.
The most common adverse events were adverse drug events, which accounted for 39.0% of the adverse events; surgical or other procedural events accounted for 30.4%; patient care events (including falls and pressure ulcers) accounted for 15.0%; and health care–associated infections accounted for 11.9%.
Overcoming barriers to better safety
“The overall level of harm, with nearly 1 in 4 patients suffering an adverse event, was higher than I expected it might be,” Dr. Bates told this news organization. However, techniques for identifying adverse events have improved, and “it is easier to find them in electronic records than in paper records,” he noted.
“Hospitals have many issues they are currently dealing with since COVID, and one issue is simply prioritization,” Dr. Bates said. “But it is now possible to measure harm for all patients using electronic tools, and if hospitals know how much harm they are having in specific areas, they can make choices about which ones to focus on.”
“We now have effective prevention strategies for most of the main kinds of harm,” he said. Generally, rates of harm are high because these strategies are not being used effectively, he said. “In addition, there are new tools that can be used – for example, to identify patients who are decompensating earlier,” he noted.
As for additional research, some specific types of harm that have been resistant to interventions, such as pressure ulcers, deserve more attention, said Dr. Bates. “In addition, diagnostic errors appear to cause a great deal of harm, but we don’t yet have good strategies for preventing these,” he said.
The study findings were limited by several factors, including the use of data from hospitals that might not represent hospitals at large and by the inclusion mainly of patients with private insurance, the researchers write. Other limitations include the likelihood that some adverse events were missed and the level of agreement on adverse events between adjudicators was only fair.
However, the findings serve as a reminder to health care professionals of the need for continued attention to improving patient safety, and measuring adverse events remains a critical part of guiding these improvements, the researchers conclude.
Timely reassessment and opportunities to improve
In the decades since the publication of the report, “To Err Is Human,” by the National Academies in 2000, significant attention has been paid to improving patient safety during hospitalizations, and health care systems have increased in both system and disease complexity, Said Suman Pal, MBBS, a specialist in hospital medicine at the University of New Mexico, Albuquerque, said in an interview. “Therefore, this study is important in reassessing the safety of inpatient care at the current time,” he said.
“The findings of this study showing preventable adverse events in approximately 7% of all admissions; while concerning, is not surprising, as it is consistent with other studies over time, as the authors have also noted in their discussion,” said Dr. Pal. The current findings “underscore the importance of continuous quality improvement efforts to increase the safety of patient care for hospitalized patients,” he noted.
“The increasing complexity of medical care, fragmentation of health care, structural inequities of health systems, and more recent widespread public health challenges such as the COVID-19 pandemic have been, in my opinion, barriers to improving patient safety,” Dr. Pal said. “The use of innovation and an interdisciplinary approach to patient safety and quality improvement in hospital-based care, such as the use of machine learning to monitor trends and predict the individualized risk of harm, could be a potential way out” to help reduce barriers and improve safety, he said.
“Additional research is needed to understand the key drivers of preventable harm for hospitalized patients in the United States,” said Dr. Pal. “When planning for change, keen attention must be paid to understanding how these [drivers] may differ for patients who have been historically marginalized or are otherwise underserved so as to not exacerbate health care inequities,” he added.
The study was funded by the Controlled Risk Insurance Company and the Risk Management Foundation of the Harvard Medical Institutions. Dr. Bates owns stock options with AESOP, Clew, FeelBetter, Guided Clinical Solutions, MDClone, and ValeraHealth and has grants/contracts from IBM Watson and EarlySense. He has also served as a consultant for CDI Negev. Dr. Pal has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Unintended consequences of perfectly good programs and policies
Some of our worst decisions seemed like really good ideas at the time. We wouldn’t make them otherwise; but often we fall into the unintended consequence of “the cure being worse than the poison.” We have seen this when government is trying to fix a problem, often an emotionally charged problem, without considering the long-term consequences of the “fix.” We have seen the unintended consequences of certain health care policies and programs lead to abuse and negative downstream effects on the same population that they were intended to protect.
It has been postulated that unintended consequences fall into a framework that’s “based upon level of knowledge and the scope for avoidance.” Essentially, that means these consequences fall into one of four categories: knowable and avoidable, knowable and unavoidable, unknowable and avoidable, and unknowable and unavoidable.
What category do the following policies fall into?
Pharmacy benefit managers’ safe harbor from the Anti-Kickback Statute
Let’s start with the “safe harbor” from the Anti-Kickback Statute (AKS) for payments from drug companies to health insurance companies and pharmacy benefit managers (PBMs). The AKS was created in 1972 and its “main purpose is to protect patients and the federal health care programs from fraud and abuse by curtailing the corrupting influence of money on health care decisions.” During the 1990s, a number of safe harbor provisions under the AKS were instituted for certain payments to health insurance companies, PBMs, and other providers. The thinking was that these payments needed a safe harbor because, although they might meet the statutory definition of “kickbacks,” they were beneficial because they would reduce the cost of care and, more specifically, the prices of drugs.
While well-intentioned, those safe harbors now protect a system of such perverse incentives that patients are whipsawed back and forth onto drugs that are the most profitable for the PBMs, who create the annual list of insurance covered drugs (i.e., the formulary). It is clear now that protected kickbacks ($$), in the form of rebates and fees paid by pharmaceutical manufacturers to PBMs, determine what drugs will be on the formulary. PBMs then use utilization management tools such as step therapy to force patients to take those drugs first. Consequently, safe harbor protection from the AKS allows manufacturers to buy market share at the expense of patient’s health. Because these protected kickbacks are based on a percentage of the list price of the drugs, PBMs profit more from higher priced drugs, which PBMs call the lowest cost medications (for them, that is). These bids from various manufacturers can change over the course of a year, allowing PBMs to change formulary coverage (even mid-year) and nonmedically switch stable patients to the drug that is the most profitable. Much of this happens as a result of the unintended consequence of this particular safe harbor from the AKS. Ironically, the safe harbor has helped to create the very behavior that the law was supposed to prevent and has harmed the patients it was supposed to protect. Health care decisions are being corrupted by the influence of profits allowed by safe harbor from the AKS.
340B drug program lacks oversight
Helping hospitals pay for care of the indigent: What could go wrong with that? The 340B Drug Pricing Program was created in 1992 to help low-income patients have better access to outpatient medications. The program requires drug companies to offer deep discounts to safety-net providers and qualified “disproportionate share hospitals,” which have a minimum percentage threshold of Medicare and Medicaid patients. The idea was that these qualified entities would pass these savings through to their low-income patients who needed the medications. Sounds like a great idea!
Apparently, there is a lot of money to be made under the 340B program because what started in 1992 with 90 covered entities had expanded by 2017 to more than 12,000 covered entities. The program became a profit center in part because reimbursement for 340B-acquired drugs far exceeds the acquisition costs. Over the years, in order to increase profits, qualified entities, such as disproportionate share hospitals, added for-profit contracted outpatient pharmacies, significantly increasing the amount of 340B drugs dispensed to commercial patients. From 2010 to 2020, the number of contract pharmacy arrangements increased from 2,000 to over 100,000, massively increasing profits for the qualified hospitals and their for-profit contracted pharmacies, which included a number of Fortune 25 companies.
Unfortunately, there is no oversight of 340B programs, and there are no requirements that the 340B drug profits be used for charitable care. In fact, nearly 10 years ago, two experts stated in Health Affairs that, “our findings support the criticism that the 340B program is being converted from one that serves vulnerable patient populations to one that enriches hospitals and their affiliated clinics.” In spite of the immense profits generated at 340B hospitals, an analysis by Avalere Health revealed that “65 percent of 340B hospitals provide less charity care than the national average for all short-term acute care hospitals, including for-profit hospitals.”
I have seen this dynamic at work in my own community in south Louisiana. There is a major expanding 340B hospital system that refuses Medicaid patients into its clinics once the hospital has reached its minimum disproportionate share of Medicaid patients. Our community has many young female African American patients with lupus, many of whom are covered by Medicaid. Even though this 340B hospital system has rheumatology fellows, it closes its rheumatology clinic doors to patients with lupus who have Medicaid as soon as it has reached its 11.75% of Medicaid patients. Clearly, this is an abuse of a program instituted specifically to take care of those in need – and here in our community, it creates inequitable access to rheumatologic care for patients with lupus.
The statute that created 340B specifically listed certain nonhospital providers who need – and should continue to receive – access to 340B discounts, such as Federally Qualified Health Centers and others. There are many deserving safety net providers and special disease clinics that are taking care of the truly needy and deserve to get the 340B highly discounted drug pricing. However, many so-called nonprofit hospital systems are spreading into wealthy neighborhoods with contracted pharmacies making large profits without caring for those in need. Five years ago, the U.S. Government Accountability Office stated that more oversight of the 340B program was needed, but that still hasn’t happened. The combination of vague statutory language and a lack of oversight has led to unintended consequences of fraud and abuse of the system, with indigent patients not realizing the benefit of the steep discounts, being sued when they can’t pay their bills, and even turned away from clinics when the qualified hospital reaches it mandated minimum of Medicaid patients.
Knowable and avoidable?
Should it have been known that these abuses would result from these policies and programs? And if so, could guardrails have been put in place from the start to avoid these abuses? Maybe the answers to these questions are irrelevant: All we can do now is fix what is not working, which will require changes and oversight to ensure that the safe harbor policy and 340B drug discount program are achieving the desired ends. At this point, unfortunately, it is clear that they’re not. In fact, it looks like they have enabled “profits over patients” all the way.
As recently stated by Dr. Megan Ranney of Brown University: “In this country, we continually forget that the profit motive is not sufficient for the public’s health.” Yes, hindsight is 20/20. But now we need to take off our blinders, see what is happening, and act to finally put “patients over profits.”
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s Vice President of Advocacy and Government Affairs and its immediate Past President, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
Some of our worst decisions seemed like really good ideas at the time. We wouldn’t make them otherwise; but often we fall into the unintended consequence of “the cure being worse than the poison.” We have seen this when government is trying to fix a problem, often an emotionally charged problem, without considering the long-term consequences of the “fix.” We have seen the unintended consequences of certain health care policies and programs lead to abuse and negative downstream effects on the same population that they were intended to protect.
It has been postulated that unintended consequences fall into a framework that’s “based upon level of knowledge and the scope for avoidance.” Essentially, that means these consequences fall into one of four categories: knowable and avoidable, knowable and unavoidable, unknowable and avoidable, and unknowable and unavoidable.
What category do the following policies fall into?
Pharmacy benefit managers’ safe harbor from the Anti-Kickback Statute
Let’s start with the “safe harbor” from the Anti-Kickback Statute (AKS) for payments from drug companies to health insurance companies and pharmacy benefit managers (PBMs). The AKS was created in 1972 and its “main purpose is to protect patients and the federal health care programs from fraud and abuse by curtailing the corrupting influence of money on health care decisions.” During the 1990s, a number of safe harbor provisions under the AKS were instituted for certain payments to health insurance companies, PBMs, and other providers. The thinking was that these payments needed a safe harbor because, although they might meet the statutory definition of “kickbacks,” they were beneficial because they would reduce the cost of care and, more specifically, the prices of drugs.
While well-intentioned, those safe harbors now protect a system of such perverse incentives that patients are whipsawed back and forth onto drugs that are the most profitable for the PBMs, who create the annual list of insurance covered drugs (i.e., the formulary). It is clear now that protected kickbacks ($$), in the form of rebates and fees paid by pharmaceutical manufacturers to PBMs, determine what drugs will be on the formulary. PBMs then use utilization management tools such as step therapy to force patients to take those drugs first. Consequently, safe harbor protection from the AKS allows manufacturers to buy market share at the expense of patient’s health. Because these protected kickbacks are based on a percentage of the list price of the drugs, PBMs profit more from higher priced drugs, which PBMs call the lowest cost medications (for them, that is). These bids from various manufacturers can change over the course of a year, allowing PBMs to change formulary coverage (even mid-year) and nonmedically switch stable patients to the drug that is the most profitable. Much of this happens as a result of the unintended consequence of this particular safe harbor from the AKS. Ironically, the safe harbor has helped to create the very behavior that the law was supposed to prevent and has harmed the patients it was supposed to protect. Health care decisions are being corrupted by the influence of profits allowed by safe harbor from the AKS.
340B drug program lacks oversight
Helping hospitals pay for care of the indigent: What could go wrong with that? The 340B Drug Pricing Program was created in 1992 to help low-income patients have better access to outpatient medications. The program requires drug companies to offer deep discounts to safety-net providers and qualified “disproportionate share hospitals,” which have a minimum percentage threshold of Medicare and Medicaid patients. The idea was that these qualified entities would pass these savings through to their low-income patients who needed the medications. Sounds like a great idea!
Apparently, there is a lot of money to be made under the 340B program because what started in 1992 with 90 covered entities had expanded by 2017 to more than 12,000 covered entities. The program became a profit center in part because reimbursement for 340B-acquired drugs far exceeds the acquisition costs. Over the years, in order to increase profits, qualified entities, such as disproportionate share hospitals, added for-profit contracted outpatient pharmacies, significantly increasing the amount of 340B drugs dispensed to commercial patients. From 2010 to 2020, the number of contract pharmacy arrangements increased from 2,000 to over 100,000, massively increasing profits for the qualified hospitals and their for-profit contracted pharmacies, which included a number of Fortune 25 companies.
Unfortunately, there is no oversight of 340B programs, and there are no requirements that the 340B drug profits be used for charitable care. In fact, nearly 10 years ago, two experts stated in Health Affairs that, “our findings support the criticism that the 340B program is being converted from one that serves vulnerable patient populations to one that enriches hospitals and their affiliated clinics.” In spite of the immense profits generated at 340B hospitals, an analysis by Avalere Health revealed that “65 percent of 340B hospitals provide less charity care than the national average for all short-term acute care hospitals, including for-profit hospitals.”
I have seen this dynamic at work in my own community in south Louisiana. There is a major expanding 340B hospital system that refuses Medicaid patients into its clinics once the hospital has reached its minimum disproportionate share of Medicaid patients. Our community has many young female African American patients with lupus, many of whom are covered by Medicaid. Even though this 340B hospital system has rheumatology fellows, it closes its rheumatology clinic doors to patients with lupus who have Medicaid as soon as it has reached its 11.75% of Medicaid patients. Clearly, this is an abuse of a program instituted specifically to take care of those in need – and here in our community, it creates inequitable access to rheumatologic care for patients with lupus.
The statute that created 340B specifically listed certain nonhospital providers who need – and should continue to receive – access to 340B discounts, such as Federally Qualified Health Centers and others. There are many deserving safety net providers and special disease clinics that are taking care of the truly needy and deserve to get the 340B highly discounted drug pricing. However, many so-called nonprofit hospital systems are spreading into wealthy neighborhoods with contracted pharmacies making large profits without caring for those in need. Five years ago, the U.S. Government Accountability Office stated that more oversight of the 340B program was needed, but that still hasn’t happened. The combination of vague statutory language and a lack of oversight has led to unintended consequences of fraud and abuse of the system, with indigent patients not realizing the benefit of the steep discounts, being sued when they can’t pay their bills, and even turned away from clinics when the qualified hospital reaches it mandated minimum of Medicaid patients.
Knowable and avoidable?
Should it have been known that these abuses would result from these policies and programs? And if so, could guardrails have been put in place from the start to avoid these abuses? Maybe the answers to these questions are irrelevant: All we can do now is fix what is not working, which will require changes and oversight to ensure that the safe harbor policy and 340B drug discount program are achieving the desired ends. At this point, unfortunately, it is clear that they’re not. In fact, it looks like they have enabled “profits over patients” all the way.
As recently stated by Dr. Megan Ranney of Brown University: “In this country, we continually forget that the profit motive is not sufficient for the public’s health.” Yes, hindsight is 20/20. But now we need to take off our blinders, see what is happening, and act to finally put “patients over profits.”
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s Vice President of Advocacy and Government Affairs and its immediate Past President, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
Some of our worst decisions seemed like really good ideas at the time. We wouldn’t make them otherwise; but often we fall into the unintended consequence of “the cure being worse than the poison.” We have seen this when government is trying to fix a problem, often an emotionally charged problem, without considering the long-term consequences of the “fix.” We have seen the unintended consequences of certain health care policies and programs lead to abuse and negative downstream effects on the same population that they were intended to protect.
It has been postulated that unintended consequences fall into a framework that’s “based upon level of knowledge and the scope for avoidance.” Essentially, that means these consequences fall into one of four categories: knowable and avoidable, knowable and unavoidable, unknowable and avoidable, and unknowable and unavoidable.
What category do the following policies fall into?
Pharmacy benefit managers’ safe harbor from the Anti-Kickback Statute
Let’s start with the “safe harbor” from the Anti-Kickback Statute (AKS) for payments from drug companies to health insurance companies and pharmacy benefit managers (PBMs). The AKS was created in 1972 and its “main purpose is to protect patients and the federal health care programs from fraud and abuse by curtailing the corrupting influence of money on health care decisions.” During the 1990s, a number of safe harbor provisions under the AKS were instituted for certain payments to health insurance companies, PBMs, and other providers. The thinking was that these payments needed a safe harbor because, although they might meet the statutory definition of “kickbacks,” they were beneficial because they would reduce the cost of care and, more specifically, the prices of drugs.
While well-intentioned, those safe harbors now protect a system of such perverse incentives that patients are whipsawed back and forth onto drugs that are the most profitable for the PBMs, who create the annual list of insurance covered drugs (i.e., the formulary). It is clear now that protected kickbacks ($$), in the form of rebates and fees paid by pharmaceutical manufacturers to PBMs, determine what drugs will be on the formulary. PBMs then use utilization management tools such as step therapy to force patients to take those drugs first. Consequently, safe harbor protection from the AKS allows manufacturers to buy market share at the expense of patient’s health. Because these protected kickbacks are based on a percentage of the list price of the drugs, PBMs profit more from higher priced drugs, which PBMs call the lowest cost medications (for them, that is). These bids from various manufacturers can change over the course of a year, allowing PBMs to change formulary coverage (even mid-year) and nonmedically switch stable patients to the drug that is the most profitable. Much of this happens as a result of the unintended consequence of this particular safe harbor from the AKS. Ironically, the safe harbor has helped to create the very behavior that the law was supposed to prevent and has harmed the patients it was supposed to protect. Health care decisions are being corrupted by the influence of profits allowed by safe harbor from the AKS.
340B drug program lacks oversight
Helping hospitals pay for care of the indigent: What could go wrong with that? The 340B Drug Pricing Program was created in 1992 to help low-income patients have better access to outpatient medications. The program requires drug companies to offer deep discounts to safety-net providers and qualified “disproportionate share hospitals,” which have a minimum percentage threshold of Medicare and Medicaid patients. The idea was that these qualified entities would pass these savings through to their low-income patients who needed the medications. Sounds like a great idea!
Apparently, there is a lot of money to be made under the 340B program because what started in 1992 with 90 covered entities had expanded by 2017 to more than 12,000 covered entities. The program became a profit center in part because reimbursement for 340B-acquired drugs far exceeds the acquisition costs. Over the years, in order to increase profits, qualified entities, such as disproportionate share hospitals, added for-profit contracted outpatient pharmacies, significantly increasing the amount of 340B drugs dispensed to commercial patients. From 2010 to 2020, the number of contract pharmacy arrangements increased from 2,000 to over 100,000, massively increasing profits for the qualified hospitals and their for-profit contracted pharmacies, which included a number of Fortune 25 companies.
Unfortunately, there is no oversight of 340B programs, and there are no requirements that the 340B drug profits be used for charitable care. In fact, nearly 10 years ago, two experts stated in Health Affairs that, “our findings support the criticism that the 340B program is being converted from one that serves vulnerable patient populations to one that enriches hospitals and their affiliated clinics.” In spite of the immense profits generated at 340B hospitals, an analysis by Avalere Health revealed that “65 percent of 340B hospitals provide less charity care than the national average for all short-term acute care hospitals, including for-profit hospitals.”
I have seen this dynamic at work in my own community in south Louisiana. There is a major expanding 340B hospital system that refuses Medicaid patients into its clinics once the hospital has reached its minimum disproportionate share of Medicaid patients. Our community has many young female African American patients with lupus, many of whom are covered by Medicaid. Even though this 340B hospital system has rheumatology fellows, it closes its rheumatology clinic doors to patients with lupus who have Medicaid as soon as it has reached its 11.75% of Medicaid patients. Clearly, this is an abuse of a program instituted specifically to take care of those in need – and here in our community, it creates inequitable access to rheumatologic care for patients with lupus.
The statute that created 340B specifically listed certain nonhospital providers who need – and should continue to receive – access to 340B discounts, such as Federally Qualified Health Centers and others. There are many deserving safety net providers and special disease clinics that are taking care of the truly needy and deserve to get the 340B highly discounted drug pricing. However, many so-called nonprofit hospital systems are spreading into wealthy neighborhoods with contracted pharmacies making large profits without caring for those in need. Five years ago, the U.S. Government Accountability Office stated that more oversight of the 340B program was needed, but that still hasn’t happened. The combination of vague statutory language and a lack of oversight has led to unintended consequences of fraud and abuse of the system, with indigent patients not realizing the benefit of the steep discounts, being sued when they can’t pay their bills, and even turned away from clinics when the qualified hospital reaches it mandated minimum of Medicaid patients.
Knowable and avoidable?
Should it have been known that these abuses would result from these policies and programs? And if so, could guardrails have been put in place from the start to avoid these abuses? Maybe the answers to these questions are irrelevant: All we can do now is fix what is not working, which will require changes and oversight to ensure that the safe harbor policy and 340B drug discount program are achieving the desired ends. At this point, unfortunately, it is clear that they’re not. In fact, it looks like they have enabled “profits over patients” all the way.
As recently stated by Dr. Megan Ranney of Brown University: “In this country, we continually forget that the profit motive is not sufficient for the public’s health.” Yes, hindsight is 20/20. But now we need to take off our blinders, see what is happening, and act to finally put “patients over profits.”
Dr. Feldman is a rheumatologist in private practice with The Rheumatology Group in New Orleans. She is the CSRO’s Vice President of Advocacy and Government Affairs and its immediate Past President, as well as past chair of the Alliance for Safe Biologic Medicines and a past member of the American College of Rheumatology insurance subcommittee. You can reach her at [email protected].
What the FTC’s proposed ban on noncompete agreements could mean for physicians, other clinicians
The proposed rule seeks to ban companies from enforcing noncompete clauses in employment contracts, a practice that represents an “unfair method of competition” with “exploitative and widespread” impacts, including suppression of wages, innovation, and entrepreneurial spirit, the FTC said. The public has 60 days to submit comments on the proposal before the FTC issues the final rule.
Employers often include noncompete clauses in physician contracts because they want to avoid having patients leave their health care system and follow a doctor to a competitor. A 2018 survey of primary care physicians found that about half of office-based physicians and 37% of physicians employed at hospitals or freestanding care centers were bound by restrictive covenants.
“A federal ban on noncompete agreements will ensure that physicians nationwide can finally change jobs without fear of being sued,” Erik B. Smith, MD, JD, clinical assistant professor of anesthesiology at the University of Southern California, Los Angeles, said in an interview.
Many doctors would like to see noncompete agreements vanish, but some physicians still favor them.
“As a small-practice owner, I am personally against this. The noncompete helps me take a risk and hire a physician. It typically takes 2-3 years for me to break even. I think this will further consolidate employment with large hospital systems unfortunately,” Texas cardiologist Rishin Shah, MD, recently tweeted in response to the FTC announcement.
Dr. Smith, who has advocated for noncompete reform, said about half of states currently allow the controversial clauses.
However, several states have recently passed laws restricting their use. California, North Dakota, and Oklahoma ban noncompetes, although some narrowly defined exceptions, such as the sale of a business, remain.
Other states, like Colorado, Illinois, and Oregon, broadly ban noncompete clauses, except for workers earning above a certain threshold. For example, in Colorado, noncompete agreements are permitted for highly compensated employees earning more than $101,250.
Despite additional restrictions on noncompete agreements for workers in the District of Columbia, the new legislation does not apply to physicians earning total compensation of $250,000 or more. However, their employers must define the geographic parameters of the noncompete and limit postemployment restrictions to 2 years.
Restrictive covenants are “uniquely challenging to family medicine’s emphasis on longitudinal care and the patient-physician relationship,” said Tochi Iroku-Malize, MD, MPH, president of the American Academy of Family Physicians. The limitations imposed by noncompete agreements “potentially reduce patient choice, lower the quality of care for patients, and ultimately harm the foundation of family medicine – our relationships with our patients.”
Although the proposed rule aligns with President Biden’s executive order promoting economic competition, Dr. Smith said a national ban on noncompete agreements may push the limits of FTC authority.
“This new rule will certainly result in a ‘major questions doctrine’ Supreme Court challenge,” said Dr. Smith, and possibly be struck down if the court determines an administrative overstep into areas of “vast economic or political significance.”
A controversial policy
The American Medical Association’s code of ethics discourages covenants that “unreasonably restrict” the ability of physicians to practice following contract termination. And in 2022, the AMA cited “overly broad” noncompete language as a red flag young physicians should watch out for during contract negotiations.
But in 2020, the AMA asked the FTC not to use its rulemaking authority to regulate noncompete clauses in physician employment contracts, and instead, relegate enforcement of such agreements to each state. The American Hospital Association expressed similar views.
Still, the FTC said that eliminating noncompete clauses will increase annual wages by $300 billion, allow 30 million Americans to pursue better job opportunities, and encourage hiring competition among employers. It will also save consumers up to $148 billion in health care costs annually.
“Noncompetes block workers from freely switching jobs, depriving them of higher wages and better working conditions, and depriving businesses of a talent pool that they need to build and expand,” Lina M. Khan, FTC chair, said in a press release about the proposal.
A national ban on noncompetes would keep more physicians in the industry and practicing in their communities, a win for patients and providers, said Dr. Smith. It could also compel employers to offer more competitive employment packages, including fair wages, better work conditions, and a culture of well-being and patient safety.
“Whatever the final rule is, I’m certain it will be legally challenged,” said Dr. Smith, adding that the nation’s most prominent business lobbying group, the Chamber of Commerce, has already issued a statement calling the rule “blatantly unlawful."
A version of this article first appeared on Medscape.com.
The proposed rule seeks to ban companies from enforcing noncompete clauses in employment contracts, a practice that represents an “unfair method of competition” with “exploitative and widespread” impacts, including suppression of wages, innovation, and entrepreneurial spirit, the FTC said. The public has 60 days to submit comments on the proposal before the FTC issues the final rule.
Employers often include noncompete clauses in physician contracts because they want to avoid having patients leave their health care system and follow a doctor to a competitor. A 2018 survey of primary care physicians found that about half of office-based physicians and 37% of physicians employed at hospitals or freestanding care centers were bound by restrictive covenants.
“A federal ban on noncompete agreements will ensure that physicians nationwide can finally change jobs without fear of being sued,” Erik B. Smith, MD, JD, clinical assistant professor of anesthesiology at the University of Southern California, Los Angeles, said in an interview.
Many doctors would like to see noncompete agreements vanish, but some physicians still favor them.
“As a small-practice owner, I am personally against this. The noncompete helps me take a risk and hire a physician. It typically takes 2-3 years for me to break even. I think this will further consolidate employment with large hospital systems unfortunately,” Texas cardiologist Rishin Shah, MD, recently tweeted in response to the FTC announcement.
Dr. Smith, who has advocated for noncompete reform, said about half of states currently allow the controversial clauses.
However, several states have recently passed laws restricting their use. California, North Dakota, and Oklahoma ban noncompetes, although some narrowly defined exceptions, such as the sale of a business, remain.
Other states, like Colorado, Illinois, and Oregon, broadly ban noncompete clauses, except for workers earning above a certain threshold. For example, in Colorado, noncompete agreements are permitted for highly compensated employees earning more than $101,250.
Despite additional restrictions on noncompete agreements for workers in the District of Columbia, the new legislation does not apply to physicians earning total compensation of $250,000 or more. However, their employers must define the geographic parameters of the noncompete and limit postemployment restrictions to 2 years.
Restrictive covenants are “uniquely challenging to family medicine’s emphasis on longitudinal care and the patient-physician relationship,” said Tochi Iroku-Malize, MD, MPH, president of the American Academy of Family Physicians. The limitations imposed by noncompete agreements “potentially reduce patient choice, lower the quality of care for patients, and ultimately harm the foundation of family medicine – our relationships with our patients.”
Although the proposed rule aligns with President Biden’s executive order promoting economic competition, Dr. Smith said a national ban on noncompete agreements may push the limits of FTC authority.
“This new rule will certainly result in a ‘major questions doctrine’ Supreme Court challenge,” said Dr. Smith, and possibly be struck down if the court determines an administrative overstep into areas of “vast economic or political significance.”
A controversial policy
The American Medical Association’s code of ethics discourages covenants that “unreasonably restrict” the ability of physicians to practice following contract termination. And in 2022, the AMA cited “overly broad” noncompete language as a red flag young physicians should watch out for during contract negotiations.
But in 2020, the AMA asked the FTC not to use its rulemaking authority to regulate noncompete clauses in physician employment contracts, and instead, relegate enforcement of such agreements to each state. The American Hospital Association expressed similar views.
Still, the FTC said that eliminating noncompete clauses will increase annual wages by $300 billion, allow 30 million Americans to pursue better job opportunities, and encourage hiring competition among employers. It will also save consumers up to $148 billion in health care costs annually.
“Noncompetes block workers from freely switching jobs, depriving them of higher wages and better working conditions, and depriving businesses of a talent pool that they need to build and expand,” Lina M. Khan, FTC chair, said in a press release about the proposal.
A national ban on noncompetes would keep more physicians in the industry and practicing in their communities, a win for patients and providers, said Dr. Smith. It could also compel employers to offer more competitive employment packages, including fair wages, better work conditions, and a culture of well-being and patient safety.
“Whatever the final rule is, I’m certain it will be legally challenged,” said Dr. Smith, adding that the nation’s most prominent business lobbying group, the Chamber of Commerce, has already issued a statement calling the rule “blatantly unlawful."
A version of this article first appeared on Medscape.com.
The proposed rule seeks to ban companies from enforcing noncompete clauses in employment contracts, a practice that represents an “unfair method of competition” with “exploitative and widespread” impacts, including suppression of wages, innovation, and entrepreneurial spirit, the FTC said. The public has 60 days to submit comments on the proposal before the FTC issues the final rule.
Employers often include noncompete clauses in physician contracts because they want to avoid having patients leave their health care system and follow a doctor to a competitor. A 2018 survey of primary care physicians found that about half of office-based physicians and 37% of physicians employed at hospitals or freestanding care centers were bound by restrictive covenants.
“A federal ban on noncompete agreements will ensure that physicians nationwide can finally change jobs without fear of being sued,” Erik B. Smith, MD, JD, clinical assistant professor of anesthesiology at the University of Southern California, Los Angeles, said in an interview.
Many doctors would like to see noncompete agreements vanish, but some physicians still favor them.
“As a small-practice owner, I am personally against this. The noncompete helps me take a risk and hire a physician. It typically takes 2-3 years for me to break even. I think this will further consolidate employment with large hospital systems unfortunately,” Texas cardiologist Rishin Shah, MD, recently tweeted in response to the FTC announcement.
Dr. Smith, who has advocated for noncompete reform, said about half of states currently allow the controversial clauses.
However, several states have recently passed laws restricting their use. California, North Dakota, and Oklahoma ban noncompetes, although some narrowly defined exceptions, such as the sale of a business, remain.
Other states, like Colorado, Illinois, and Oregon, broadly ban noncompete clauses, except for workers earning above a certain threshold. For example, in Colorado, noncompete agreements are permitted for highly compensated employees earning more than $101,250.
Despite additional restrictions on noncompete agreements for workers in the District of Columbia, the new legislation does not apply to physicians earning total compensation of $250,000 or more. However, their employers must define the geographic parameters of the noncompete and limit postemployment restrictions to 2 years.
Restrictive covenants are “uniquely challenging to family medicine’s emphasis on longitudinal care and the patient-physician relationship,” said Tochi Iroku-Malize, MD, MPH, president of the American Academy of Family Physicians. The limitations imposed by noncompete agreements “potentially reduce patient choice, lower the quality of care for patients, and ultimately harm the foundation of family medicine – our relationships with our patients.”
Although the proposed rule aligns with President Biden’s executive order promoting economic competition, Dr. Smith said a national ban on noncompete agreements may push the limits of FTC authority.
“This new rule will certainly result in a ‘major questions doctrine’ Supreme Court challenge,” said Dr. Smith, and possibly be struck down if the court determines an administrative overstep into areas of “vast economic or political significance.”
A controversial policy
The American Medical Association’s code of ethics discourages covenants that “unreasonably restrict” the ability of physicians to practice following contract termination. And in 2022, the AMA cited “overly broad” noncompete language as a red flag young physicians should watch out for during contract negotiations.
But in 2020, the AMA asked the FTC not to use its rulemaking authority to regulate noncompete clauses in physician employment contracts, and instead, relegate enforcement of such agreements to each state. The American Hospital Association expressed similar views.
Still, the FTC said that eliminating noncompete clauses will increase annual wages by $300 billion, allow 30 million Americans to pursue better job opportunities, and encourage hiring competition among employers. It will also save consumers up to $148 billion in health care costs annually.
“Noncompetes block workers from freely switching jobs, depriving them of higher wages and better working conditions, and depriving businesses of a talent pool that they need to build and expand,” Lina M. Khan, FTC chair, said in a press release about the proposal.
A national ban on noncompetes would keep more physicians in the industry and practicing in their communities, a win for patients and providers, said Dr. Smith. It could also compel employers to offer more competitive employment packages, including fair wages, better work conditions, and a culture of well-being and patient safety.
“Whatever the final rule is, I’m certain it will be legally challenged,” said Dr. Smith, adding that the nation’s most prominent business lobbying group, the Chamber of Commerce, has already issued a statement calling the rule “blatantly unlawful."
A version of this article first appeared on Medscape.com.
Diagnosing rare disorders
When I was a resident (back in the Cretaceous era), the idea of autoimmune encephalitis was just beginning to take hold. It was kind of like Bigfoot. A few reports, vague articles, the occasional sighting of what may or may not be a case. …
Unlike Bigfoot, however, the evidence quickly added up until there was no question that such a disorder existed. Then disorder became disorders, and now it seems a few more types are added to the list each year.
This doesn’t change the fact that they’re still, in the grand scheme of general neurology, relatively rare, though no one questions that they exist.
Today people still wishfully take pictures of Bigfoot, but they turn out to be images of bears or other animals, or tricks of light and shadow.
This is an issue with human thought. Many times we see what we want to see, especially if it’s more interesting than a mundane alternative.
An autoimmune encephalitis article in the January 2023 issue of JAMA Neurology looked into this. On reviewing 393 patients diagnosed with the disorder, the researchers found that 27% of them actually didn’t have it at all. Such things as functional disorders, neurodegenerative diseases, and primary psychiatric diagnoses were, instead, the culprits.
I’m not criticizing those who made an incorrect diagnosis. We all do. That’s the nature of medicine.
Which is worse? Missing the diagnosis entirely and not treating, or diagnosing a patient with something else and treating incorrectly? I guess it depends on the disease and nature of treatment.
Certainly, finding a case of autoimmune encephalitis is more interesting than, say toxic-metabolic encephalopathy from a bladder infection, just as getting a picture of Bigfoot is way more cool than one of a bear with mange.
But we need to be careful when faced with equivocal labs and data lest we read too much into them. There are too many gray zones in medicine to lead you astray. Not to say we won’t be.
But it’s not just rare diseases. In the early 1990s two different studies found that 24% of patients diagnosed with Parkinson’s disease were found to have something else on autopsy.
That was 30 years ago. Now we have DaT scans to help. Maybe our abilities as neurologists have also gotten better (though I don’t think the neurological exam has changed much since Charcot).
Our gadgets, labs, and treatments get better every year. We have tools available to us now that were unthinkable a generation ago. For that matter, they were unthinkable when I began my career.
But they don’t change the fact that human error never goes away. All of us are susceptible to it, and all of us make mistakes.
Such is the way of medicine now, and likely always. All we can do is our best and keep moving forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
When I was a resident (back in the Cretaceous era), the idea of autoimmune encephalitis was just beginning to take hold. It was kind of like Bigfoot. A few reports, vague articles, the occasional sighting of what may or may not be a case. …
Unlike Bigfoot, however, the evidence quickly added up until there was no question that such a disorder existed. Then disorder became disorders, and now it seems a few more types are added to the list each year.
This doesn’t change the fact that they’re still, in the grand scheme of general neurology, relatively rare, though no one questions that they exist.
Today people still wishfully take pictures of Bigfoot, but they turn out to be images of bears or other animals, or tricks of light and shadow.
This is an issue with human thought. Many times we see what we want to see, especially if it’s more interesting than a mundane alternative.
An autoimmune encephalitis article in the January 2023 issue of JAMA Neurology looked into this. On reviewing 393 patients diagnosed with the disorder, the researchers found that 27% of them actually didn’t have it at all. Such things as functional disorders, neurodegenerative diseases, and primary psychiatric diagnoses were, instead, the culprits.
I’m not criticizing those who made an incorrect diagnosis. We all do. That’s the nature of medicine.
Which is worse? Missing the diagnosis entirely and not treating, or diagnosing a patient with something else and treating incorrectly? I guess it depends on the disease and nature of treatment.
Certainly, finding a case of autoimmune encephalitis is more interesting than, say toxic-metabolic encephalopathy from a bladder infection, just as getting a picture of Bigfoot is way more cool than one of a bear with mange.
But we need to be careful when faced with equivocal labs and data lest we read too much into them. There are too many gray zones in medicine to lead you astray. Not to say we won’t be.
But it’s not just rare diseases. In the early 1990s two different studies found that 24% of patients diagnosed with Parkinson’s disease were found to have something else on autopsy.
That was 30 years ago. Now we have DaT scans to help. Maybe our abilities as neurologists have also gotten better (though I don’t think the neurological exam has changed much since Charcot).
Our gadgets, labs, and treatments get better every year. We have tools available to us now that were unthinkable a generation ago. For that matter, they were unthinkable when I began my career.
But they don’t change the fact that human error never goes away. All of us are susceptible to it, and all of us make mistakes.
Such is the way of medicine now, and likely always. All we can do is our best and keep moving forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
When I was a resident (back in the Cretaceous era), the idea of autoimmune encephalitis was just beginning to take hold. It was kind of like Bigfoot. A few reports, vague articles, the occasional sighting of what may or may not be a case. …
Unlike Bigfoot, however, the evidence quickly added up until there was no question that such a disorder existed. Then disorder became disorders, and now it seems a few more types are added to the list each year.
This doesn’t change the fact that they’re still, in the grand scheme of general neurology, relatively rare, though no one questions that they exist.
Today people still wishfully take pictures of Bigfoot, but they turn out to be images of bears or other animals, or tricks of light and shadow.
This is an issue with human thought. Many times we see what we want to see, especially if it’s more interesting than a mundane alternative.
An autoimmune encephalitis article in the January 2023 issue of JAMA Neurology looked into this. On reviewing 393 patients diagnosed with the disorder, the researchers found that 27% of them actually didn’t have it at all. Such things as functional disorders, neurodegenerative diseases, and primary psychiatric diagnoses were, instead, the culprits.
I’m not criticizing those who made an incorrect diagnosis. We all do. That’s the nature of medicine.
Which is worse? Missing the diagnosis entirely and not treating, or diagnosing a patient with something else and treating incorrectly? I guess it depends on the disease and nature of treatment.
Certainly, finding a case of autoimmune encephalitis is more interesting than, say toxic-metabolic encephalopathy from a bladder infection, just as getting a picture of Bigfoot is way more cool than one of a bear with mange.
But we need to be careful when faced with equivocal labs and data lest we read too much into them. There are too many gray zones in medicine to lead you astray. Not to say we won’t be.
But it’s not just rare diseases. In the early 1990s two different studies found that 24% of patients diagnosed with Parkinson’s disease were found to have something else on autopsy.
That was 30 years ago. Now we have DaT scans to help. Maybe our abilities as neurologists have also gotten better (though I don’t think the neurological exam has changed much since Charcot).
Our gadgets, labs, and treatments get better every year. We have tools available to us now that were unthinkable a generation ago. For that matter, they were unthinkable when I began my career.
But they don’t change the fact that human error never goes away. All of us are susceptible to it, and all of us make mistakes.
Such is the way of medicine now, and likely always. All we can do is our best and keep moving forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Pay an annual visit to your office
that your patients might see?
We tend not to notice gradual deterioration in the workplace we inhabit every day: Carpets fade and dull with constant traffic and cleaning; wallpaper and paint accumulate dirt, stains, and damage; furniture gets dirty and dented, fabric rips, hardware goes missing; laminate peels off the edges of desks and cabinets.
When did you last take a good look at your waiting room? How clean is it? Patients expect cleanliness in doctor’s offices, and they expect the reception area to be neat. How are the carpeting and upholstery holding up? Sit in your chairs; how do they feel? Patients don’t appreciate a sore back or bottom from any chairs, especially in a medical office. Consider investing in new furniture that will be attractive and comfortable for your patients.
Look at the decor itself; is it dated or just plain “old-looking?” Any interior designer will tell you they can determine quite accurately when a space was last decorated, simply by the color and style of the materials used. If your office is stuck in the ‘90s, it’s probably time for a change. Even if you don’t find anything obvious, it’s wise to check periodically for subtle evidence of age: Find some patches of protected carpeting and flooring under stationary furniture and compare them to exposed floors.
If your color scheme is hopelessly out of date and style, or if you are just tired of it, change it. Wallpaper and carpeting should be long-wearing industrial quality; paint should be high-quality “eggshell” finish to facilitate cleaning, and everything should be professionally applied. (This is neither the time nor place for do-it-yourself experiments.) Consider updating your overhead lighting. The harsh glow of fluorescent lights amid an uninspired decor creates a sterile, uninviting atmosphere.
During renovation, get your building’s maintenance crew to fix any nagging plumbing, electrical, or heating/air conditioning problems while pipes, ducts, and wires are more readily accessible. This is also a good time to clear out old textbooks, journals, and files that you will never open again, in this digital age.
If your wall decorations are dated and unattractive, now would be a good time to replace at least some of them. This need not be an expensive proposition; a few years ago, I redecorated my exam room walls with framed photos from my travel adventures – to very positive responses from patients and staff alike. If you’re not an artist or photographer, invite a family member, or local artists or talented patients, to display some of their creations on your walls. If you get too many contributions, you can rotate them on a periodic basis.
Plants are great aesthetic accents, yet many offices have little or no plant life. Plants naturally aerate an office suite and help make it feel less stuffy. Also, multiple studies have found that plants promote productivity among office staff and create a sense of calm for apprehensive patients. Improvements like this can make a big difference. They show an attention to detail and a willingness to make your practice as inviting as possible for patients and employees alike.
Spruce-up time is also an excellent opportunity to inventory your medical equipment. We’ve all seen “vintage” offices full of gadgets that were state-of-the-art decades ago. Nostalgia is nice; but would you want to be treated by a physician whose office could be a Smithsonian exhibit titled, “Doctor’s Office Circa 1975?” Neither would your patients, for the most part; many – particularly younger ones – assume that doctors who don’t keep up with technological innovations don’t keep up with anything else, either.
If you’re planning a vacation this year (and I hope you are), that would be the perfect time for a re-do. Your patients will be spared the dust and turmoil, tradespeople won’t have to work around your office hours, and you won’t have to cancel any hours that weren’t already canceled. Best of all, you’ll come back to a clean, fresh environment.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
that your patients might see?
We tend not to notice gradual deterioration in the workplace we inhabit every day: Carpets fade and dull with constant traffic and cleaning; wallpaper and paint accumulate dirt, stains, and damage; furniture gets dirty and dented, fabric rips, hardware goes missing; laminate peels off the edges of desks and cabinets.
When did you last take a good look at your waiting room? How clean is it? Patients expect cleanliness in doctor’s offices, and they expect the reception area to be neat. How are the carpeting and upholstery holding up? Sit in your chairs; how do they feel? Patients don’t appreciate a sore back or bottom from any chairs, especially in a medical office. Consider investing in new furniture that will be attractive and comfortable for your patients.
Look at the decor itself; is it dated or just plain “old-looking?” Any interior designer will tell you they can determine quite accurately when a space was last decorated, simply by the color and style of the materials used. If your office is stuck in the ‘90s, it’s probably time for a change. Even if you don’t find anything obvious, it’s wise to check periodically for subtle evidence of age: Find some patches of protected carpeting and flooring under stationary furniture and compare them to exposed floors.
If your color scheme is hopelessly out of date and style, or if you are just tired of it, change it. Wallpaper and carpeting should be long-wearing industrial quality; paint should be high-quality “eggshell” finish to facilitate cleaning, and everything should be professionally applied. (This is neither the time nor place for do-it-yourself experiments.) Consider updating your overhead lighting. The harsh glow of fluorescent lights amid an uninspired decor creates a sterile, uninviting atmosphere.
During renovation, get your building’s maintenance crew to fix any nagging plumbing, electrical, or heating/air conditioning problems while pipes, ducts, and wires are more readily accessible. This is also a good time to clear out old textbooks, journals, and files that you will never open again, in this digital age.
If your wall decorations are dated and unattractive, now would be a good time to replace at least some of them. This need not be an expensive proposition; a few years ago, I redecorated my exam room walls with framed photos from my travel adventures – to very positive responses from patients and staff alike. If you’re not an artist or photographer, invite a family member, or local artists or talented patients, to display some of their creations on your walls. If you get too many contributions, you can rotate them on a periodic basis.
Plants are great aesthetic accents, yet many offices have little or no plant life. Plants naturally aerate an office suite and help make it feel less stuffy. Also, multiple studies have found that plants promote productivity among office staff and create a sense of calm for apprehensive patients. Improvements like this can make a big difference. They show an attention to detail and a willingness to make your practice as inviting as possible for patients and employees alike.
Spruce-up time is also an excellent opportunity to inventory your medical equipment. We’ve all seen “vintage” offices full of gadgets that were state-of-the-art decades ago. Nostalgia is nice; but would you want to be treated by a physician whose office could be a Smithsonian exhibit titled, “Doctor’s Office Circa 1975?” Neither would your patients, for the most part; many – particularly younger ones – assume that doctors who don’t keep up with technological innovations don’t keep up with anything else, either.
If you’re planning a vacation this year (and I hope you are), that would be the perfect time for a re-do. Your patients will be spared the dust and turmoil, tradespeople won’t have to work around your office hours, and you won’t have to cancel any hours that weren’t already canceled. Best of all, you’ll come back to a clean, fresh environment.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
that your patients might see?
We tend not to notice gradual deterioration in the workplace we inhabit every day: Carpets fade and dull with constant traffic and cleaning; wallpaper and paint accumulate dirt, stains, and damage; furniture gets dirty and dented, fabric rips, hardware goes missing; laminate peels off the edges of desks and cabinets.
When did you last take a good look at your waiting room? How clean is it? Patients expect cleanliness in doctor’s offices, and they expect the reception area to be neat. How are the carpeting and upholstery holding up? Sit in your chairs; how do they feel? Patients don’t appreciate a sore back or bottom from any chairs, especially in a medical office. Consider investing in new furniture that will be attractive and comfortable for your patients.
Look at the decor itself; is it dated or just plain “old-looking?” Any interior designer will tell you they can determine quite accurately when a space was last decorated, simply by the color and style of the materials used. If your office is stuck in the ‘90s, it’s probably time for a change. Even if you don’t find anything obvious, it’s wise to check periodically for subtle evidence of age: Find some patches of protected carpeting and flooring under stationary furniture and compare them to exposed floors.
If your color scheme is hopelessly out of date and style, or if you are just tired of it, change it. Wallpaper and carpeting should be long-wearing industrial quality; paint should be high-quality “eggshell” finish to facilitate cleaning, and everything should be professionally applied. (This is neither the time nor place for do-it-yourself experiments.) Consider updating your overhead lighting. The harsh glow of fluorescent lights amid an uninspired decor creates a sterile, uninviting atmosphere.
During renovation, get your building’s maintenance crew to fix any nagging plumbing, electrical, or heating/air conditioning problems while pipes, ducts, and wires are more readily accessible. This is also a good time to clear out old textbooks, journals, and files that you will never open again, in this digital age.
If your wall decorations are dated and unattractive, now would be a good time to replace at least some of them. This need not be an expensive proposition; a few years ago, I redecorated my exam room walls with framed photos from my travel adventures – to very positive responses from patients and staff alike. If you’re not an artist or photographer, invite a family member, or local artists or talented patients, to display some of their creations on your walls. If you get too many contributions, you can rotate them on a periodic basis.
Plants are great aesthetic accents, yet many offices have little or no plant life. Plants naturally aerate an office suite and help make it feel less stuffy. Also, multiple studies have found that plants promote productivity among office staff and create a sense of calm for apprehensive patients. Improvements like this can make a big difference. They show an attention to detail and a willingness to make your practice as inviting as possible for patients and employees alike.
Spruce-up time is also an excellent opportunity to inventory your medical equipment. We’ve all seen “vintage” offices full of gadgets that were state-of-the-art decades ago. Nostalgia is nice; but would you want to be treated by a physician whose office could be a Smithsonian exhibit titled, “Doctor’s Office Circa 1975?” Neither would your patients, for the most part; many – particularly younger ones – assume that doctors who don’t keep up with technological innovations don’t keep up with anything else, either.
If you’re planning a vacation this year (and I hope you are), that would be the perfect time for a re-do. Your patients will be spared the dust and turmoil, tradespeople won’t have to work around your office hours, and you won’t have to cancel any hours that weren’t already canceled. Best of all, you’ll come back to a clean, fresh environment.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Simulating psychoanalysis: A review of Freud’s Bones
While psychiatry has been the subject of many films, video games are not a medium commonly known for examining mental illness.1 There have been PC games over the years with psychiatric themes, such as Sanitarium (1998), Depression Quest (2013), Fran Bow (2015), and Night in the Woods (2017). Now for perhaps the first time a game has been developed with the practice of psychiatry as its primary focus.
Freud’s Bones is a 2022 game developed by independent Italian game studio Fortuna Imperatore. The result of a successful Kickstarter crowdfunding campaign, Freud’s Bones is advertised as “the first point & click narrative-drive game to pay homage to the birth of psychoanalysis and its founder, addressing the themes of sexuality and neuroses filled with existential doubts.”
In Freud’s Bones, you take control of Sigmund Freud and guide him through his daily tasks. Gameplay is of the simple point-and-click variety, modeled after classic LucasArts-style adventure games of the 1990s such as The Secret of Monkey Island or Day of the Tentacle. Prior to seeing your first patient, the game provides several documents the player can peruse to become familiar with basic concepts of psychoanalysis. Although the game was originally written in Italian (and translation gaffes occasionally arise), generally the English wording is easy to read. However, some players may feel intimidated or bored by the sheer quantity of text the game provides. All in-game text, including books and spoken words, are written and there is no recorded voice acting. Audio consists largely of unintrusive background music and occasional sound effects. The graphical style is simple and cartoonish but pleasant.
Freud’s personal life is a major focus of the game. His real life dog Jofi is a constant presence in Freud’s office. At various times the player will witness Freud’s dreams, act as a voice inside his head, and attempt to interpret mystical Egyptian messages he receives. Players are also tasked with managing Freud’s reputation in the scientific community. This is apparently intended as a reflection of in-game clinical acumen, but it was sometimes difficult to tell what direct influence my actions had on Freud’s reputation.
Freud’s energy may flag at various points during the game, and the player may choose to give him a cigar or a dose of cocaine to stimulate him. These options sound interesting on the surface, but I found the effect of these substances on the game’s actual outcome to be minimal. Some tasks are presented in a less than user-friendly manner. For example, on my initial playthrough I could not figure out how to complete several optional errands such as shopping for more tobacco or selecting a cover for Freud’s books. The player is also given the opportunity to make choices that affect Freud’s personal life, such as whether to pursue an extramarital affair. The game does have a few narrative surprises, including appearances from some of Freud’s well-known contemporaries. One particularly vivid sequence late in the game involves navigating Freud through a hallucination with some bizarre, but very Freudian, imagery.
By far the most interesting and enjoyable part of the game is the psychoanalysis sessions. The player guides Freud through multiple sessions with four different patients. Each of them has a unique story and associated symptoms, and the player can choose a variety of responses. For example, will you take a comforting, paternalistic approach to the patient uncomfortable with her first appointment? Or will you take the more stoic, quiet approach of the analyst and allow the patient to speak without prompting? Part of the player’s quest in guiding Freud through these sessions is to help patients bring their unconscious thoughts to conscious awareness. This is depicted graphically as the thought moves vertically through images representing the id, superego, and ego. Skillful questioning can bring these thoughts to the surface, but poor choices can leave valuable insights buried in the unconscious.
These therapy sessions were unique and engaging, and I wish they constituted a larger portion of the gameplay in Freud’s Bones. More patients, more sessions with each patient, and longer sessions would all have been welcome additions. These analytic sessions eventually culminate in an opportunity to offer a diagnosis, and the player’s accuracy in treatment can result in divergent outcomes for each patient. The game is not lengthy, as it can be played in its entirety in roughly 5-6 hours. Selecting different options for Freud’s personal life and the analysis sessions provides some replay value for subsequent playthroughs.
Overall, Freud’s Bones is a worthy effort for being uniquely designed as interactive entertainment simulating psychoanalysis. It provides an experience of interest to psychiatrists but is also accessible to the general public. While the game has flaws in that it can be overly text-heavy and goals are not always clear, it shines in the moments where it allows the player to participate directly in the process of psychoanalysis. Freud’s Bones is available for purchase on Steam (currently priced at $13.99) and can be played on Windows PCs.
Dr. Weber is a psychiatrist at Intermountain Logan Regional Hospital in Logan, Utah. He disclosed no relevant financial relationships.
References
1. See, for example, Gabbard GO, Gabbard K. Psychiatry and the Cinema, 2nd ed. American Psychiatric Press, Inc.; 1999.
While psychiatry has been the subject of many films, video games are not a medium commonly known for examining mental illness.1 There have been PC games over the years with psychiatric themes, such as Sanitarium (1998), Depression Quest (2013), Fran Bow (2015), and Night in the Woods (2017). Now for perhaps the first time a game has been developed with the practice of psychiatry as its primary focus.
Freud’s Bones is a 2022 game developed by independent Italian game studio Fortuna Imperatore. The result of a successful Kickstarter crowdfunding campaign, Freud’s Bones is advertised as “the first point & click narrative-drive game to pay homage to the birth of psychoanalysis and its founder, addressing the themes of sexuality and neuroses filled with existential doubts.”
In Freud’s Bones, you take control of Sigmund Freud and guide him through his daily tasks. Gameplay is of the simple point-and-click variety, modeled after classic LucasArts-style adventure games of the 1990s such as The Secret of Monkey Island or Day of the Tentacle. Prior to seeing your first patient, the game provides several documents the player can peruse to become familiar with basic concepts of psychoanalysis. Although the game was originally written in Italian (and translation gaffes occasionally arise), generally the English wording is easy to read. However, some players may feel intimidated or bored by the sheer quantity of text the game provides. All in-game text, including books and spoken words, are written and there is no recorded voice acting. Audio consists largely of unintrusive background music and occasional sound effects. The graphical style is simple and cartoonish but pleasant.
Freud’s personal life is a major focus of the game. His real life dog Jofi is a constant presence in Freud’s office. At various times the player will witness Freud’s dreams, act as a voice inside his head, and attempt to interpret mystical Egyptian messages he receives. Players are also tasked with managing Freud’s reputation in the scientific community. This is apparently intended as a reflection of in-game clinical acumen, but it was sometimes difficult to tell what direct influence my actions had on Freud’s reputation.
Freud’s energy may flag at various points during the game, and the player may choose to give him a cigar or a dose of cocaine to stimulate him. These options sound interesting on the surface, but I found the effect of these substances on the game’s actual outcome to be minimal. Some tasks are presented in a less than user-friendly manner. For example, on my initial playthrough I could not figure out how to complete several optional errands such as shopping for more tobacco or selecting a cover for Freud’s books. The player is also given the opportunity to make choices that affect Freud’s personal life, such as whether to pursue an extramarital affair. The game does have a few narrative surprises, including appearances from some of Freud’s well-known contemporaries. One particularly vivid sequence late in the game involves navigating Freud through a hallucination with some bizarre, but very Freudian, imagery.
By far the most interesting and enjoyable part of the game is the psychoanalysis sessions. The player guides Freud through multiple sessions with four different patients. Each of them has a unique story and associated symptoms, and the player can choose a variety of responses. For example, will you take a comforting, paternalistic approach to the patient uncomfortable with her first appointment? Or will you take the more stoic, quiet approach of the analyst and allow the patient to speak without prompting? Part of the player’s quest in guiding Freud through these sessions is to help patients bring their unconscious thoughts to conscious awareness. This is depicted graphically as the thought moves vertically through images representing the id, superego, and ego. Skillful questioning can bring these thoughts to the surface, but poor choices can leave valuable insights buried in the unconscious.
These therapy sessions were unique and engaging, and I wish they constituted a larger portion of the gameplay in Freud’s Bones. More patients, more sessions with each patient, and longer sessions would all have been welcome additions. These analytic sessions eventually culminate in an opportunity to offer a diagnosis, and the player’s accuracy in treatment can result in divergent outcomes for each patient. The game is not lengthy, as it can be played in its entirety in roughly 5-6 hours. Selecting different options for Freud’s personal life and the analysis sessions provides some replay value for subsequent playthroughs.
Overall, Freud’s Bones is a worthy effort for being uniquely designed as interactive entertainment simulating psychoanalysis. It provides an experience of interest to psychiatrists but is also accessible to the general public. While the game has flaws in that it can be overly text-heavy and goals are not always clear, it shines in the moments where it allows the player to participate directly in the process of psychoanalysis. Freud’s Bones is available for purchase on Steam (currently priced at $13.99) and can be played on Windows PCs.
Dr. Weber is a psychiatrist at Intermountain Logan Regional Hospital in Logan, Utah. He disclosed no relevant financial relationships.
References
1. See, for example, Gabbard GO, Gabbard K. Psychiatry and the Cinema, 2nd ed. American Psychiatric Press, Inc.; 1999.
While psychiatry has been the subject of many films, video games are not a medium commonly known for examining mental illness.1 There have been PC games over the years with psychiatric themes, such as Sanitarium (1998), Depression Quest (2013), Fran Bow (2015), and Night in the Woods (2017). Now for perhaps the first time a game has been developed with the practice of psychiatry as its primary focus.
Freud’s Bones is a 2022 game developed by independent Italian game studio Fortuna Imperatore. The result of a successful Kickstarter crowdfunding campaign, Freud’s Bones is advertised as “the first point & click narrative-drive game to pay homage to the birth of psychoanalysis and its founder, addressing the themes of sexuality and neuroses filled with existential doubts.”
In Freud’s Bones, you take control of Sigmund Freud and guide him through his daily tasks. Gameplay is of the simple point-and-click variety, modeled after classic LucasArts-style adventure games of the 1990s such as The Secret of Monkey Island or Day of the Tentacle. Prior to seeing your first patient, the game provides several documents the player can peruse to become familiar with basic concepts of psychoanalysis. Although the game was originally written in Italian (and translation gaffes occasionally arise), generally the English wording is easy to read. However, some players may feel intimidated or bored by the sheer quantity of text the game provides. All in-game text, including books and spoken words, are written and there is no recorded voice acting. Audio consists largely of unintrusive background music and occasional sound effects. The graphical style is simple and cartoonish but pleasant.
Freud’s personal life is a major focus of the game. His real life dog Jofi is a constant presence in Freud’s office. At various times the player will witness Freud’s dreams, act as a voice inside his head, and attempt to interpret mystical Egyptian messages he receives. Players are also tasked with managing Freud’s reputation in the scientific community. This is apparently intended as a reflection of in-game clinical acumen, but it was sometimes difficult to tell what direct influence my actions had on Freud’s reputation.
Freud’s energy may flag at various points during the game, and the player may choose to give him a cigar or a dose of cocaine to stimulate him. These options sound interesting on the surface, but I found the effect of these substances on the game’s actual outcome to be minimal. Some tasks are presented in a less than user-friendly manner. For example, on my initial playthrough I could not figure out how to complete several optional errands such as shopping for more tobacco or selecting a cover for Freud’s books. The player is also given the opportunity to make choices that affect Freud’s personal life, such as whether to pursue an extramarital affair. The game does have a few narrative surprises, including appearances from some of Freud’s well-known contemporaries. One particularly vivid sequence late in the game involves navigating Freud through a hallucination with some bizarre, but very Freudian, imagery.
By far the most interesting and enjoyable part of the game is the psychoanalysis sessions. The player guides Freud through multiple sessions with four different patients. Each of them has a unique story and associated symptoms, and the player can choose a variety of responses. For example, will you take a comforting, paternalistic approach to the patient uncomfortable with her first appointment? Or will you take the more stoic, quiet approach of the analyst and allow the patient to speak without prompting? Part of the player’s quest in guiding Freud through these sessions is to help patients bring their unconscious thoughts to conscious awareness. This is depicted graphically as the thought moves vertically through images representing the id, superego, and ego. Skillful questioning can bring these thoughts to the surface, but poor choices can leave valuable insights buried in the unconscious.
These therapy sessions were unique and engaging, and I wish they constituted a larger portion of the gameplay in Freud’s Bones. More patients, more sessions with each patient, and longer sessions would all have been welcome additions. These analytic sessions eventually culminate in an opportunity to offer a diagnosis, and the player’s accuracy in treatment can result in divergent outcomes for each patient. The game is not lengthy, as it can be played in its entirety in roughly 5-6 hours. Selecting different options for Freud’s personal life and the analysis sessions provides some replay value for subsequent playthroughs.
Overall, Freud’s Bones is a worthy effort for being uniquely designed as interactive entertainment simulating psychoanalysis. It provides an experience of interest to psychiatrists but is also accessible to the general public. While the game has flaws in that it can be overly text-heavy and goals are not always clear, it shines in the moments where it allows the player to participate directly in the process of psychoanalysis. Freud’s Bones is available for purchase on Steam (currently priced at $13.99) and can be played on Windows PCs.
Dr. Weber is a psychiatrist at Intermountain Logan Regional Hospital in Logan, Utah. He disclosed no relevant financial relationships.
References
1. See, for example, Gabbard GO, Gabbard K. Psychiatry and the Cinema, 2nd ed. American Psychiatric Press, Inc.; 1999.
By the numbers: Cardiology slow to add women, IMGs join more quickly
Despite Mark Twain’s assertion that “there are three kinds of lies: lies, damned lies, and statistics,” we’re going to dive into 20 years’ worth of data and, hopefully, come up with a few statistics that shed some light on the specialty’s workforce since Cardiology News published its first issue in February 2003.
We start with a major issue over these last 20 years: The participation of women in the specialty.
Back in July of 2002, just a few months before the first issue of Cardiology News was published, W. Bruce Fye, MD, then-president of the American College of Cardiology, wrote, “We need to do more to attract female medical graduates to our specialty because they represent almost one-half of the new doctors trained in this country. Cardiology needs to take full advantage of this large talent pool”
Data from the American Medical Association confirm that assertion: Of the nearly 20,000 postgraduate cardiologists in practice that year, only 7.8% were women. And that was at a time when more than 42% of medical school graduates were women, Dr. Fye noted, while also pointing out that “only 10% of cardiology trainees are female, and just 6% of ACC fellows are women.”
The gap between men and women has closed somewhat in the last 20 years, but the specialty continues to lag behind the profession as a whole. Women represented 16.7% of cardiologists in 2022, versus 37% of physicians overall, AMA data show. In 2019, for the first time, the majority of U.S. medical school students (50.5%) were women, according to the Association of American Medical Colleges.
A look at residency numbers from the Accreditation Council for Graduate Medical Education shows that continued slow improvement in the number of women can be expected, as 25.5% of cardiovascular disease residents were women during the 2021-2022 academic year. Only 2 of the 19 other internal medicine subspecialties were lower, and they happened to be interventional cardiology (20.1%) and clinical cardiac electrophysiology (14.5%).
When men are added to the mix, cardiovascular disease had a total of 3,320 active residents training in 268 programs in 2021-2022, making it the largest of the IM subspecialties in both respects. The resident total is up 57% since 2003, when it came in at 2,117, while programs have increased 55% from the 173 that were operating 2 decades ago. During the year in the middle (2011-2012), there were 2,521 residents in 187 programs, so a larger share of the growth has occurred in the last 10 years, the ACGME data indicate.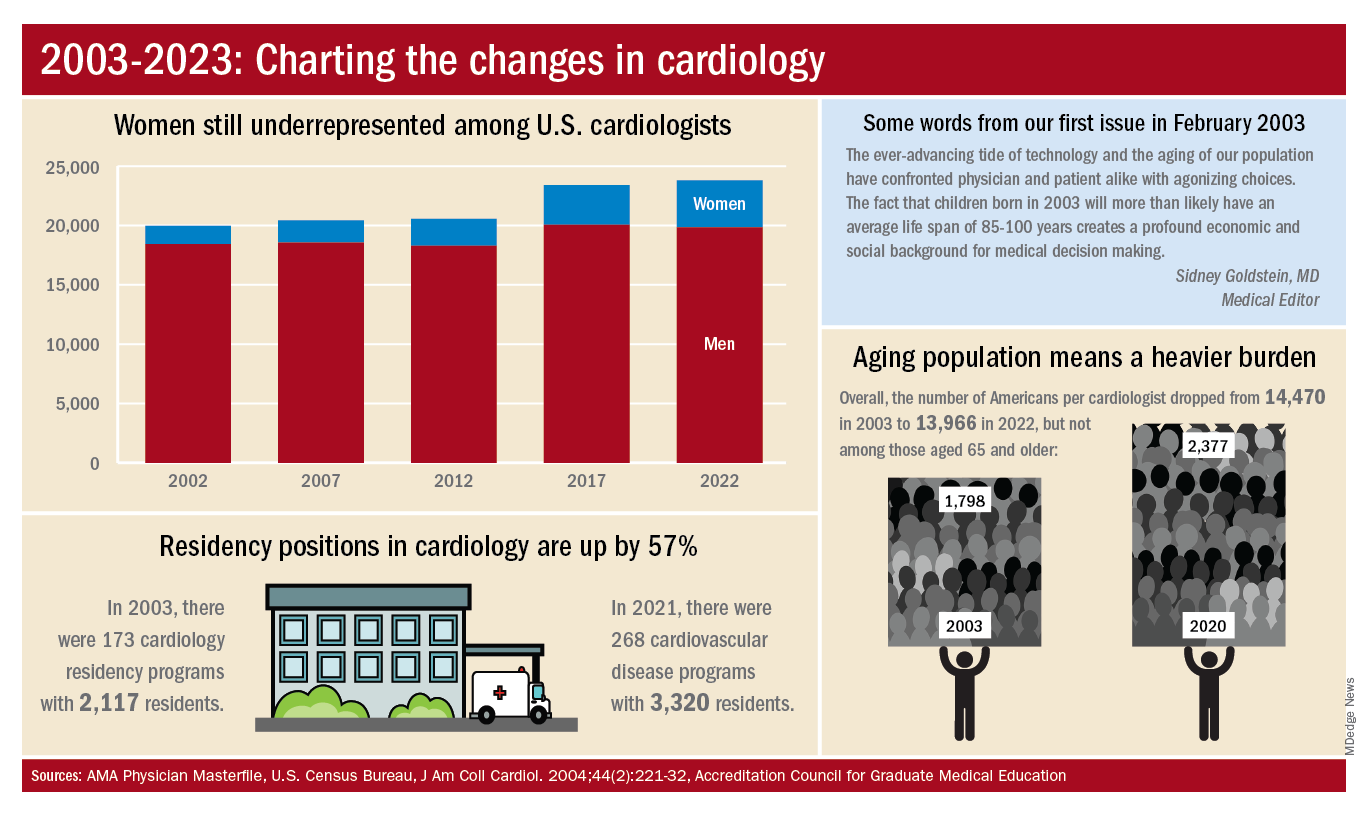
The shortage of cardiologists that Dr. Fye and others wrote about 20 years ago has not gone away. A 2018 report from health consulting firm PYA noted the increase in obesity and the low number of medical school graduates choosing the specialty. “Older and fewer physicians specializing in cardiology, coupled with the aging of baby boomers and gravitation toward practice in urban areas, will continue to exacerbate shortages in physician services in the specialty of cardiology, especially in rural areas, over the next decade,” PYA principal Lyle Oelrich wrote.
A little math appears to back up the claims of a cardiologist shortage. Based on census figures for the U.S. population in 2003, there were 14,470 Americans for each of the cardiologists reported by the AMA. That figure dropped to 13,966 by 2022, which seems like an improvement, but it comes with a caveat. The number of Americans aged 65 years and older increased from 1,798 to 2,377 per cardiologist as of 2020, the latest year for which population data were available by age.
One source of growth in the cardiology workforce has been perhaps its most significant minority: international medical graduates. Even by 2004, IMGs represented a much larger segment of all cardiologists (30.0%) than did women (9.3%), based on AMA data. To put it another way, there were more IMGs specializing in cardiovascular disease (6,615) in 2004 than there were women (3,963) in 2022.
The latest data on cardiology training programs – overall numbers were not available – put IMGs at 39.2% for the 2019-2020 academic year. The 2022 fellowship match provides a slightly smaller proportion of IMGs (37.4%) filling cardiovascular disease positions, according to the National Resident Matching Program.
Despite Mark Twain’s assertion that “there are three kinds of lies: lies, damned lies, and statistics,” we’re going to dive into 20 years’ worth of data and, hopefully, come up with a few statistics that shed some light on the specialty’s workforce since Cardiology News published its first issue in February 2003.
We start with a major issue over these last 20 years: The participation of women in the specialty.
Back in July of 2002, just a few months before the first issue of Cardiology News was published, W. Bruce Fye, MD, then-president of the American College of Cardiology, wrote, “We need to do more to attract female medical graduates to our specialty because they represent almost one-half of the new doctors trained in this country. Cardiology needs to take full advantage of this large talent pool”
Data from the American Medical Association confirm that assertion: Of the nearly 20,000 postgraduate cardiologists in practice that year, only 7.8% were women. And that was at a time when more than 42% of medical school graduates were women, Dr. Fye noted, while also pointing out that “only 10% of cardiology trainees are female, and just 6% of ACC fellows are women.”
The gap between men and women has closed somewhat in the last 20 years, but the specialty continues to lag behind the profession as a whole. Women represented 16.7% of cardiologists in 2022, versus 37% of physicians overall, AMA data show. In 2019, for the first time, the majority of U.S. medical school students (50.5%) were women, according to the Association of American Medical Colleges.
A look at residency numbers from the Accreditation Council for Graduate Medical Education shows that continued slow improvement in the number of women can be expected, as 25.5% of cardiovascular disease residents were women during the 2021-2022 academic year. Only 2 of the 19 other internal medicine subspecialties were lower, and they happened to be interventional cardiology (20.1%) and clinical cardiac electrophysiology (14.5%).
When men are added to the mix, cardiovascular disease had a total of 3,320 active residents training in 268 programs in 2021-2022, making it the largest of the IM subspecialties in both respects. The resident total is up 57% since 2003, when it came in at 2,117, while programs have increased 55% from the 173 that were operating 2 decades ago. During the year in the middle (2011-2012), there were 2,521 residents in 187 programs, so a larger share of the growth has occurred in the last 10 years, the ACGME data indicate.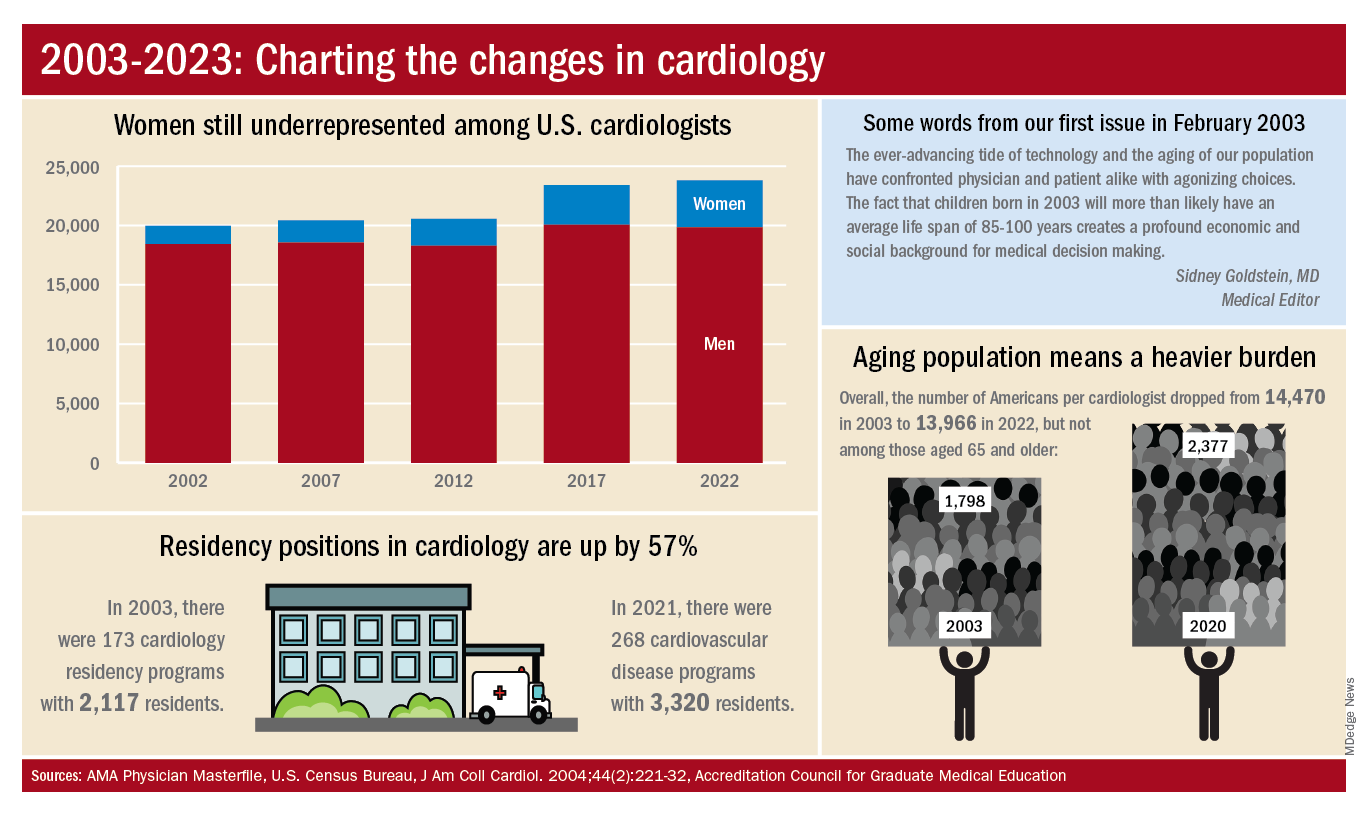
The shortage of cardiologists that Dr. Fye and others wrote about 20 years ago has not gone away. A 2018 report from health consulting firm PYA noted the increase in obesity and the low number of medical school graduates choosing the specialty. “Older and fewer physicians specializing in cardiology, coupled with the aging of baby boomers and gravitation toward practice in urban areas, will continue to exacerbate shortages in physician services in the specialty of cardiology, especially in rural areas, over the next decade,” PYA principal Lyle Oelrich wrote.
A little math appears to back up the claims of a cardiologist shortage. Based on census figures for the U.S. population in 2003, there were 14,470 Americans for each of the cardiologists reported by the AMA. That figure dropped to 13,966 by 2022, which seems like an improvement, but it comes with a caveat. The number of Americans aged 65 years and older increased from 1,798 to 2,377 per cardiologist as of 2020, the latest year for which population data were available by age.
One source of growth in the cardiology workforce has been perhaps its most significant minority: international medical graduates. Even by 2004, IMGs represented a much larger segment of all cardiologists (30.0%) than did women (9.3%), based on AMA data. To put it another way, there were more IMGs specializing in cardiovascular disease (6,615) in 2004 than there were women (3,963) in 2022.
The latest data on cardiology training programs – overall numbers were not available – put IMGs at 39.2% for the 2019-2020 academic year. The 2022 fellowship match provides a slightly smaller proportion of IMGs (37.4%) filling cardiovascular disease positions, according to the National Resident Matching Program.
Despite Mark Twain’s assertion that “there are three kinds of lies: lies, damned lies, and statistics,” we’re going to dive into 20 years’ worth of data and, hopefully, come up with a few statistics that shed some light on the specialty’s workforce since Cardiology News published its first issue in February 2003.
We start with a major issue over these last 20 years: The participation of women in the specialty.
Back in July of 2002, just a few months before the first issue of Cardiology News was published, W. Bruce Fye, MD, then-president of the American College of Cardiology, wrote, “We need to do more to attract female medical graduates to our specialty because they represent almost one-half of the new doctors trained in this country. Cardiology needs to take full advantage of this large talent pool”
Data from the American Medical Association confirm that assertion: Of the nearly 20,000 postgraduate cardiologists in practice that year, only 7.8% were women. And that was at a time when more than 42% of medical school graduates were women, Dr. Fye noted, while also pointing out that “only 10% of cardiology trainees are female, and just 6% of ACC fellows are women.”
The gap between men and women has closed somewhat in the last 20 years, but the specialty continues to lag behind the profession as a whole. Women represented 16.7% of cardiologists in 2022, versus 37% of physicians overall, AMA data show. In 2019, for the first time, the majority of U.S. medical school students (50.5%) were women, according to the Association of American Medical Colleges.
A look at residency numbers from the Accreditation Council for Graduate Medical Education shows that continued slow improvement in the number of women can be expected, as 25.5% of cardiovascular disease residents were women during the 2021-2022 academic year. Only 2 of the 19 other internal medicine subspecialties were lower, and they happened to be interventional cardiology (20.1%) and clinical cardiac electrophysiology (14.5%).
When men are added to the mix, cardiovascular disease had a total of 3,320 active residents training in 268 programs in 2021-2022, making it the largest of the IM subspecialties in both respects. The resident total is up 57% since 2003, when it came in at 2,117, while programs have increased 55% from the 173 that were operating 2 decades ago. During the year in the middle (2011-2012), there were 2,521 residents in 187 programs, so a larger share of the growth has occurred in the last 10 years, the ACGME data indicate.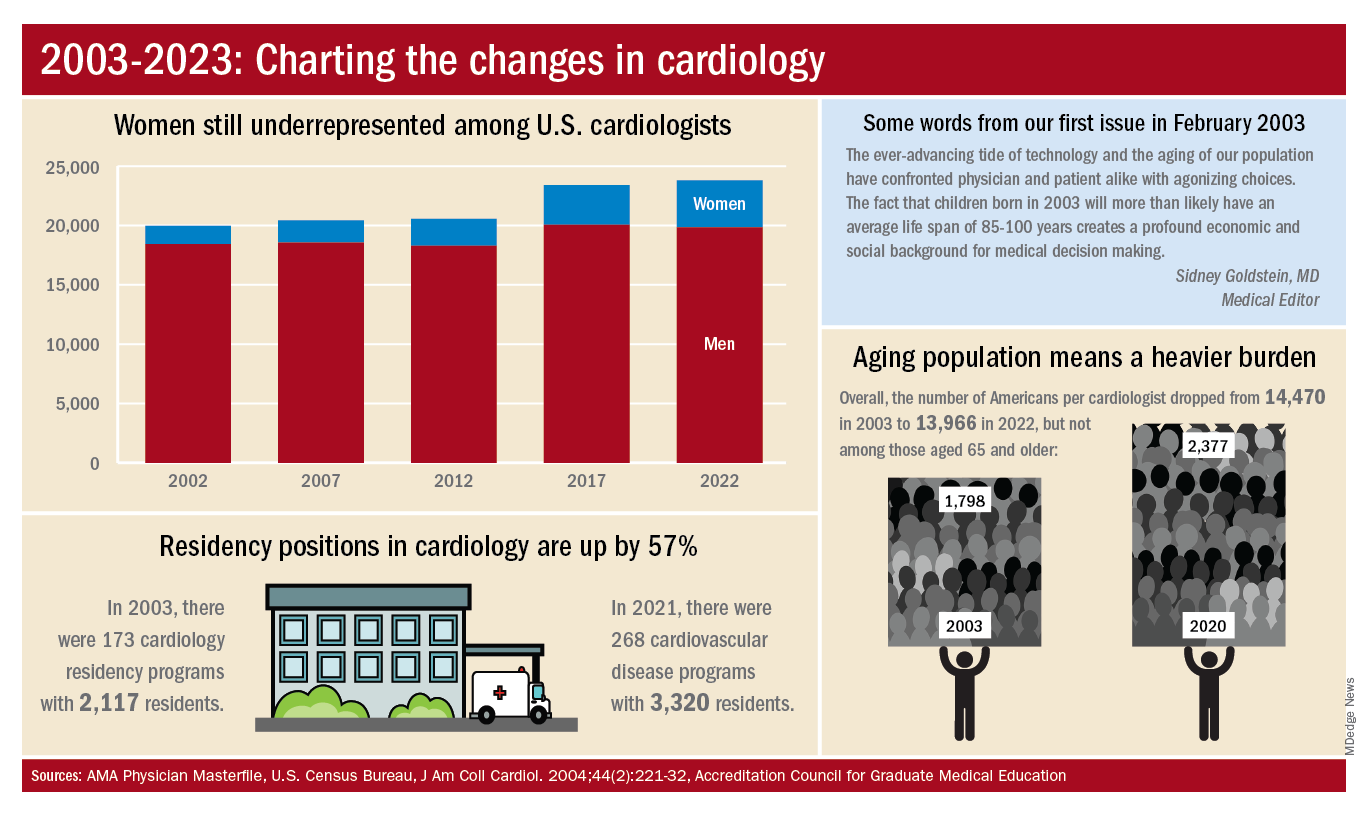
The shortage of cardiologists that Dr. Fye and others wrote about 20 years ago has not gone away. A 2018 report from health consulting firm PYA noted the increase in obesity and the low number of medical school graduates choosing the specialty. “Older and fewer physicians specializing in cardiology, coupled with the aging of baby boomers and gravitation toward practice in urban areas, will continue to exacerbate shortages in physician services in the specialty of cardiology, especially in rural areas, over the next decade,” PYA principal Lyle Oelrich wrote.
A little math appears to back up the claims of a cardiologist shortage. Based on census figures for the U.S. population in 2003, there were 14,470 Americans for each of the cardiologists reported by the AMA. That figure dropped to 13,966 by 2022, which seems like an improvement, but it comes with a caveat. The number of Americans aged 65 years and older increased from 1,798 to 2,377 per cardiologist as of 2020, the latest year for which population data were available by age.
One source of growth in the cardiology workforce has been perhaps its most significant minority: international medical graduates. Even by 2004, IMGs represented a much larger segment of all cardiologists (30.0%) than did women (9.3%), based on AMA data. To put it another way, there were more IMGs specializing in cardiovascular disease (6,615) in 2004 than there were women (3,963) in 2022.
The latest data on cardiology training programs – overall numbers were not available – put IMGs at 39.2% for the 2019-2020 academic year. The 2022 fellowship match provides a slightly smaller proportion of IMGs (37.4%) filling cardiovascular disease positions, according to the National Resident Matching Program.
Vision screening at well-child visits cost-effective for detecting amblyopia
Screening for amblyopia during primary care visits is more cost-effective than screening in school settings and optometric examinations in kindergarten-aged children in Toronto, data suggest.
Because of the low prevalence of amblyopia among young children, a population-based screening program may not warrant the resources required, despite the added health benefits of a universal program, according to the researchers.
“Amblyopia is a public health problem. For this reason, population-wide approaches to detect and treat amblyopia are critical, and approaches such as school screening and mandated optometry exams have been recommended and introduced in some jurisdictions,” study author Afua Oteng Asare, OD, PhD, a research assistant professor at the University of Utah in Salt Lake City, told this news organization. Dr. Asare conducted the study as a PhD student at the University of Toronto.
“With increasing budgeting constraints and limited resources, policymakers are relying more on economic analyses that measure value-for-money to inform their decisions on programming,” she said. “Evidence comparing the cost-effectiveness of vision-testing approaches to the status quo is, however, limited.”
The study was published in JAMA Network Open.
Analyzing costs
Despite recommendations for routine testing, a notable percentage of children in Canada and the United States don’t receive an annual vision exam. The percentage is even higher among children from low-income households, said Dr. Asare. Universal screening in schools and mandatory optometric examinations may improve vision care. But the cost-effectiveness of these measures is unknown for certain conditions, such as amblyopia, the prevalence of which ranges between 3% and 5% in young children.
In Ontario, Canada’s largest province with about 3 million children, universal funding for children’s annual comprehensive eye exams and vision screening during well-child visits is provided through provincial health insurance.
In 2018, the Ontario Ministry of Health introduced guidelines for administering vision screening in kindergartens by public health departments. However, school-based screening has been difficult to introduce because of increasing costs and budgeting constraints, the authors wrote. As an alternative to underfunded programs, optometric associations in Canada have advocated for physicians to recommend early childhood optometric exams.
The investigators analyzed the incremental costs and health benefits, from the perspective of the Ontario government, of public health school screening and optometrist-based vision exams, compared with standard vision screening conducted during well-child visits with primary care physicians. They focused on the aim of detecting amblyopia and amblyopia-related risk factors in children between ages 3 and 5 years in Toronto.
For the analysis, the research team simulated a hypothetical cohort of 25,000 children over 15 years in a probabilistic health state transition model. They incorporated various assumptions, including that children had irreversible vision impairment if not diagnosed by an optometrist. In addition, incremental costs were adjusted to favor the standard screening strategy during well-child visits.
In the school-based and primary care scenarios, children with a positive or inconclusive test result were referred to an optometrist for diagnosis and treatment, which would incur the cost of an optometric evaluation. If positive, children were treated with prescription glasses and additional patching for amblyopia.
The research team measured outcomes as incremental quality-adjusted life-years (QALYs), and health utilities were derived from data on adults, because of the lack of data on children under age 6 years with amblyopia or amblyopia risk factors. The researchers also estimated direct costs to the Ontario government, including visits with primary care doctors, optometrists, public health nurses, and contract screeners, as well as prescription glasses for children with vision impairment who receive social assistance. Costs were expressed in Canadian dollars (CAD).
Overall, compared with the primary care screening strategy, the school screening and optometric examination strategies were generally less costly and had more health benefits. The incremental difference in cost was a savings per child of $84.09 CAD for school screening and $74.47 CAD for optometric examinations. Optometric examinations yielded the largest gain in QALYs, compared with the primary care screening strategy, producing average QALYs of 0.0508 per child.
However, only 20% of school screening iterations and 29% of optometric exam iterations were cost-effective, relative to the primary care screening strategy, at a willingness-to-pay threshold of $50,000 CAD per QALY gained. For instance, when comparing optometric exams with primary care screenings, if the cost of vision screening was $11.50 CAD, the incremental cost-effectiveness ratio would be $77.95 CAD per QALY gained.
Results ‘make sense’
“We were initially surprised that the alternative screening programs were not cost-effective, compared to status quo vision screening in well-child visits,” said Dr. Asare. “However, the results make sense, considering the study’s universal approach (screening all children regardless of their vision status) and the study’s consideration only of amblyopia, and not of refractive errors, which are even more common in kindergarten children.”
Dr. Asare noted the lack of current data on the rate of vision screenings conducted in childhood by primary care practitioners and on referrals to eye care providers for children with abnormal screenings. Data on vision health disparities and barriers to accessing vision care in young children also are scarce.
“My ultimate research goal is to create and evaluate evidence-based, cost-effective interventions to be used at the point of care by pediatric primary care providers to improve the quality of vision care for children, especially those from socioeconomically deprived backgrounds,” she said. “The take-home message is that school vision screening and mandated eye exams are excellent programs, but they may not be suitable for all contexts.”
Additional studies are needed to look at the cost-effectiveness of the different screening strategies for other aspects included in childhood vision tests, including binocular vision problems, refractive disorders, myopia, allergies, and rare eye diseases.
Significant underestimation?
Susan Leat, PhD, a researcher and professor emerita at the University of Waterloo (Ont.) School of Optometry and Vision Science, said, “This study only considers amblyopia, and not all eye diseases and disorders, which significantly underestimates the cost-effectiveness of optometric eye exams.”
Dr. Leat, who wasn’t involved with this study, has researched pediatric optometry and visual development. She and colleagues are developing new tools to test visual acuity in young children.
“If all disorders were taken into account, then optometric testing would be by far the most cost-effective,” she said. “Optometrists can detect all disorders, including more subtle disorders, which if uncorrected or untreated, can impact a child’s early learning.”
The study authors reported no funding for the study. Dr. Asare and Dr. Leat reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Screening for amblyopia during primary care visits is more cost-effective than screening in school settings and optometric examinations in kindergarten-aged children in Toronto, data suggest.
Because of the low prevalence of amblyopia among young children, a population-based screening program may not warrant the resources required, despite the added health benefits of a universal program, according to the researchers.
“Amblyopia is a public health problem. For this reason, population-wide approaches to detect and treat amblyopia are critical, and approaches such as school screening and mandated optometry exams have been recommended and introduced in some jurisdictions,” study author Afua Oteng Asare, OD, PhD, a research assistant professor at the University of Utah in Salt Lake City, told this news organization. Dr. Asare conducted the study as a PhD student at the University of Toronto.
“With increasing budgeting constraints and limited resources, policymakers are relying more on economic analyses that measure value-for-money to inform their decisions on programming,” she said. “Evidence comparing the cost-effectiveness of vision-testing approaches to the status quo is, however, limited.”
The study was published in JAMA Network Open.
Analyzing costs
Despite recommendations for routine testing, a notable percentage of children in Canada and the United States don’t receive an annual vision exam. The percentage is even higher among children from low-income households, said Dr. Asare. Universal screening in schools and mandatory optometric examinations may improve vision care. But the cost-effectiveness of these measures is unknown for certain conditions, such as amblyopia, the prevalence of which ranges between 3% and 5% in young children.
In Ontario, Canada’s largest province with about 3 million children, universal funding for children’s annual comprehensive eye exams and vision screening during well-child visits is provided through provincial health insurance.
In 2018, the Ontario Ministry of Health introduced guidelines for administering vision screening in kindergartens by public health departments. However, school-based screening has been difficult to introduce because of increasing costs and budgeting constraints, the authors wrote. As an alternative to underfunded programs, optometric associations in Canada have advocated for physicians to recommend early childhood optometric exams.
The investigators analyzed the incremental costs and health benefits, from the perspective of the Ontario government, of public health school screening and optometrist-based vision exams, compared with standard vision screening conducted during well-child visits with primary care physicians. They focused on the aim of detecting amblyopia and amblyopia-related risk factors in children between ages 3 and 5 years in Toronto.
For the analysis, the research team simulated a hypothetical cohort of 25,000 children over 15 years in a probabilistic health state transition model. They incorporated various assumptions, including that children had irreversible vision impairment if not diagnosed by an optometrist. In addition, incremental costs were adjusted to favor the standard screening strategy during well-child visits.
In the school-based and primary care scenarios, children with a positive or inconclusive test result were referred to an optometrist for diagnosis and treatment, which would incur the cost of an optometric evaluation. If positive, children were treated with prescription glasses and additional patching for amblyopia.
The research team measured outcomes as incremental quality-adjusted life-years (QALYs), and health utilities were derived from data on adults, because of the lack of data on children under age 6 years with amblyopia or amblyopia risk factors. The researchers also estimated direct costs to the Ontario government, including visits with primary care doctors, optometrists, public health nurses, and contract screeners, as well as prescription glasses for children with vision impairment who receive social assistance. Costs were expressed in Canadian dollars (CAD).
Overall, compared with the primary care screening strategy, the school screening and optometric examination strategies were generally less costly and had more health benefits. The incremental difference in cost was a savings per child of $84.09 CAD for school screening and $74.47 CAD for optometric examinations. Optometric examinations yielded the largest gain in QALYs, compared with the primary care screening strategy, producing average QALYs of 0.0508 per child.
However, only 20% of school screening iterations and 29% of optometric exam iterations were cost-effective, relative to the primary care screening strategy, at a willingness-to-pay threshold of $50,000 CAD per QALY gained. For instance, when comparing optometric exams with primary care screenings, if the cost of vision screening was $11.50 CAD, the incremental cost-effectiveness ratio would be $77.95 CAD per QALY gained.
Results ‘make sense’
“We were initially surprised that the alternative screening programs were not cost-effective, compared to status quo vision screening in well-child visits,” said Dr. Asare. “However, the results make sense, considering the study’s universal approach (screening all children regardless of their vision status) and the study’s consideration only of amblyopia, and not of refractive errors, which are even more common in kindergarten children.”
Dr. Asare noted the lack of current data on the rate of vision screenings conducted in childhood by primary care practitioners and on referrals to eye care providers for children with abnormal screenings. Data on vision health disparities and barriers to accessing vision care in young children also are scarce.
“My ultimate research goal is to create and evaluate evidence-based, cost-effective interventions to be used at the point of care by pediatric primary care providers to improve the quality of vision care for children, especially those from socioeconomically deprived backgrounds,” she said. “The take-home message is that school vision screening and mandated eye exams are excellent programs, but they may not be suitable for all contexts.”
Additional studies are needed to look at the cost-effectiveness of the different screening strategies for other aspects included in childhood vision tests, including binocular vision problems, refractive disorders, myopia, allergies, and rare eye diseases.
Significant underestimation?
Susan Leat, PhD, a researcher and professor emerita at the University of Waterloo (Ont.) School of Optometry and Vision Science, said, “This study only considers amblyopia, and not all eye diseases and disorders, which significantly underestimates the cost-effectiveness of optometric eye exams.”
Dr. Leat, who wasn’t involved with this study, has researched pediatric optometry and visual development. She and colleagues are developing new tools to test visual acuity in young children.
“If all disorders were taken into account, then optometric testing would be by far the most cost-effective,” she said. “Optometrists can detect all disorders, including more subtle disorders, which if uncorrected or untreated, can impact a child’s early learning.”
The study authors reported no funding for the study. Dr. Asare and Dr. Leat reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Screening for amblyopia during primary care visits is more cost-effective than screening in school settings and optometric examinations in kindergarten-aged children in Toronto, data suggest.
Because of the low prevalence of amblyopia among young children, a population-based screening program may not warrant the resources required, despite the added health benefits of a universal program, according to the researchers.
“Amblyopia is a public health problem. For this reason, population-wide approaches to detect and treat amblyopia are critical, and approaches such as school screening and mandated optometry exams have been recommended and introduced in some jurisdictions,” study author Afua Oteng Asare, OD, PhD, a research assistant professor at the University of Utah in Salt Lake City, told this news organization. Dr. Asare conducted the study as a PhD student at the University of Toronto.
“With increasing budgeting constraints and limited resources, policymakers are relying more on economic analyses that measure value-for-money to inform their decisions on programming,” she said. “Evidence comparing the cost-effectiveness of vision-testing approaches to the status quo is, however, limited.”
The study was published in JAMA Network Open.
Analyzing costs
Despite recommendations for routine testing, a notable percentage of children in Canada and the United States don’t receive an annual vision exam. The percentage is even higher among children from low-income households, said Dr. Asare. Universal screening in schools and mandatory optometric examinations may improve vision care. But the cost-effectiveness of these measures is unknown for certain conditions, such as amblyopia, the prevalence of which ranges between 3% and 5% in young children.
In Ontario, Canada’s largest province with about 3 million children, universal funding for children’s annual comprehensive eye exams and vision screening during well-child visits is provided through provincial health insurance.
In 2018, the Ontario Ministry of Health introduced guidelines for administering vision screening in kindergartens by public health departments. However, school-based screening has been difficult to introduce because of increasing costs and budgeting constraints, the authors wrote. As an alternative to underfunded programs, optometric associations in Canada have advocated for physicians to recommend early childhood optometric exams.
The investigators analyzed the incremental costs and health benefits, from the perspective of the Ontario government, of public health school screening and optometrist-based vision exams, compared with standard vision screening conducted during well-child visits with primary care physicians. They focused on the aim of detecting amblyopia and amblyopia-related risk factors in children between ages 3 and 5 years in Toronto.
For the analysis, the research team simulated a hypothetical cohort of 25,000 children over 15 years in a probabilistic health state transition model. They incorporated various assumptions, including that children had irreversible vision impairment if not diagnosed by an optometrist. In addition, incremental costs were adjusted to favor the standard screening strategy during well-child visits.
In the school-based and primary care scenarios, children with a positive or inconclusive test result were referred to an optometrist for diagnosis and treatment, which would incur the cost of an optometric evaluation. If positive, children were treated with prescription glasses and additional patching for amblyopia.
The research team measured outcomes as incremental quality-adjusted life-years (QALYs), and health utilities were derived from data on adults, because of the lack of data on children under age 6 years with amblyopia or amblyopia risk factors. The researchers also estimated direct costs to the Ontario government, including visits with primary care doctors, optometrists, public health nurses, and contract screeners, as well as prescription glasses for children with vision impairment who receive social assistance. Costs were expressed in Canadian dollars (CAD).
Overall, compared with the primary care screening strategy, the school screening and optometric examination strategies were generally less costly and had more health benefits. The incremental difference in cost was a savings per child of $84.09 CAD for school screening and $74.47 CAD for optometric examinations. Optometric examinations yielded the largest gain in QALYs, compared with the primary care screening strategy, producing average QALYs of 0.0508 per child.
However, only 20% of school screening iterations and 29% of optometric exam iterations were cost-effective, relative to the primary care screening strategy, at a willingness-to-pay threshold of $50,000 CAD per QALY gained. For instance, when comparing optometric exams with primary care screenings, if the cost of vision screening was $11.50 CAD, the incremental cost-effectiveness ratio would be $77.95 CAD per QALY gained.
Results ‘make sense’
“We were initially surprised that the alternative screening programs were not cost-effective, compared to status quo vision screening in well-child visits,” said Dr. Asare. “However, the results make sense, considering the study’s universal approach (screening all children regardless of their vision status) and the study’s consideration only of amblyopia, and not of refractive errors, which are even more common in kindergarten children.”
Dr. Asare noted the lack of current data on the rate of vision screenings conducted in childhood by primary care practitioners and on referrals to eye care providers for children with abnormal screenings. Data on vision health disparities and barriers to accessing vision care in young children also are scarce.
“My ultimate research goal is to create and evaluate evidence-based, cost-effective interventions to be used at the point of care by pediatric primary care providers to improve the quality of vision care for children, especially those from socioeconomically deprived backgrounds,” she said. “The take-home message is that school vision screening and mandated eye exams are excellent programs, but they may not be suitable for all contexts.”
Additional studies are needed to look at the cost-effectiveness of the different screening strategies for other aspects included in childhood vision tests, including binocular vision problems, refractive disorders, myopia, allergies, and rare eye diseases.
Significant underestimation?
Susan Leat, PhD, a researcher and professor emerita at the University of Waterloo (Ont.) School of Optometry and Vision Science, said, “This study only considers amblyopia, and not all eye diseases and disorders, which significantly underestimates the cost-effectiveness of optometric eye exams.”
Dr. Leat, who wasn’t involved with this study, has researched pediatric optometry and visual development. She and colleagues are developing new tools to test visual acuity in young children.
“If all disorders were taken into account, then optometric testing would be by far the most cost-effective,” she said. “Optometrists can detect all disorders, including more subtle disorders, which if uncorrected or untreated, can impact a child’s early learning.”
The study authors reported no funding for the study. Dr. Asare and Dr. Leat reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Singer is paralyzed after delay in care; hospital must pay
Delay in treatment will cost hospital millions
according to a report on WFAA.com, among other news sites.
On March 21, 2019, Judy “Jessie” Adams, then part of a singing-songwriting duo with her husband, Richard, went to Premier Interventional Pain Management, in Flower Mound, Tex., prior to the couple’s drive to Ohio for a funeral. At Premier, Jesse received an epidural steroid injection (ESI) that she hoped would ease her back pain during the long drive.
Instead, the injection ended up increasing her pain.
“He [the pain physician] gave me the shot, but I couldn’t feel my legs. They were tingling, but I couldn’t feel them,” Mrs. Adams explained. “The pain was so bad in my back.” In their suit, Adams and her husband alleged that the doctor had probably “nicked a blood vessel during the ESI procedure, causing Jessie to hemorrhage.” (The couple’s suit against the doctor was settled prior to trial.)
Mrs. Adams remained under observation at the pain facility for about 1½ hours, at which point she was taken by ambulance to nearby Texas Health Presbyterian Hospital. There, in the emergency department, staff ordered a “STAT MRI” in preparation for an emergency laminectomy.
For reasons that remain murky, the MRI wasn’t performed for 1 hour and 37 minutes. The emergency laminectomy itself wasn’t started until more than 5 hours after Adams had been admitted to the ED. This was a direct violation of hospital protocol, which required that emergency surgeries be performed within 1 hour of admittance in the first available surgical suite. (At trial, Mrs. Adams’s attorneys from Lyons & Simmons offered evidence that a suite became available 49 minutes after Adams had arrived at the ED.)
During the wait, Mrs. Adams continued to experience excruciating pain. “I kept screaming: ‘Help me,’ ” she recalled. At trial, her attorneys argued that the hospital’s delay in addressing her spinal emergency led directly to her current paralysis, which keeps her confined to a wheelchair and renders her incontinent.
The hospital disagreed. In court, it maintained that Mrs. Adams was already paralyzed when she arrived at the ED and that there was no delay in care.
The jury saw things differently, however. Siding with the plaintiffs, it awarded Mrs. Adams and her husband $10.1 million, including $500,000 for Mr. Adams’s loss of future earnings and $1 million for his “loss of consortium” with his wife.
Their music career now effectively over, Mr. Adams spends most of his time taking care of Mrs. Adams.
“Music was our lifeblood for so many years, and he can’t do it anymore,” Mrs. Adams said. “He goes upstairs to play his guitar and write, and suddenly I need him to come and cath me. I just feel like I’m going to wake up from this bad dream, but it’s the same routine.”
Two doctors are absolved in woman’s sudden death
In a 3-2 decision in December 2022, the Pennsylvania Supreme Court ruled that the state’s 2-year statute of limitations in wrongful-death cases applies even in cases in which plaintiffs fail to identify the cause of death in a timely manner, as a report in the Claims Journal indicates.
The decision stems from a lawsuit filed by Linda Reibenstein on behalf of her mother, Mary Ann Whitman, who died in late April 2010 from a ruptured aortic aneurysm.
On April 12, 2010, Ms. Whitman visited Patrick D. Conaboy, MD, a Scranton family physician, complaining of a persistent cough, fever, and lower-back pain. Following an initial examination, Dr. Conaboy ordered an aortic duplex ultrasound scan and a CT scan of the patient’s abdomen.
The ultrasound was performed by radiologist Charles Barax, MD, who reviewed both scans. He identified a “poorly visualized aortic aneurysm.” At this point, Dr. Conaboy referred Ms. Whitman to a vascular surgeon. But before this visit could take place, Whitman’s aneurysm ruptured, killing her. This was listed as the medical cause of death on the patient’s death certificate.
In April 2011, Ms. Reibenstein filed a claim against Dr. Barax, alleging that he had failed to gauge the severity of her mother’s condition. Ms. Reibenstein’s attorney wasn’t able to question Dr. Barax on the record until well after the state’s 2-year statute of limitations had elapsed. When he did testify, Dr. Barax explained that the scans’ image quality prevented him from determining whether Whitman’s aneurysm was rupturing or simply bleeding. Despite this, he insisted that he had warned Dr. Conaboy of the potential for Ms. Whitman’s aneurysm to rupture.
In March 2016, nearly 6 years after her mother’s death, Ms. Reibenstein filed a new lawsuit, this one against Dr. Conaboy, whom she alleged had failed to properly treat her mother’s condition. Dr. Conaboy, in turn, asked the court for summary judgment – that is, a judgment in his favor without a full trial – arguing that the state’s window for filing a wrongful-death claim had long since closed. For their part, Ms. Reibenstein and her attorney argued that the state’s 2-year statute of limitations didn’t start until the plaintiff had discovered the cause of her mother’s death.
Initially refusing to dismiss the case, a lower court reconsidered Dr. Conaboy’s motion for summary judgment and ruled that Ms. Reibenstein had failed to present any evidence of “affirmative misrepresentation or fraudulent concealment.” In other words, in the absence of any willful attempt on the part of the defendant to hide the legal cause of death, which includes “acts, omissions, or events having some causative connection with the death,” the statute of limitations remained in effect, and the defendant’s motion was thereby granted.
Continuing the legal seesaw, a state appeals court reversed the lower-court ruling. Noting that the Pennsylvania malpractice statute was ambiguous, the court argued that it should be interpreted in a way that protects plaintiffs who seek “fair compensation” but encounter willfully erected obstacles in pursuit of their claim.
Dr. Conaboy then took his case to the state’s highest court. In its majority decision, the Pennsylvania Supreme Court staked out a narrow definition of cause of death – one based on the death certificate – and ruled that only willful fraud in that document would constitute the necessary condition for halting the claim’s clock. Furthermore, the high court said, when lawmakers adopted the Medical Care Availability and Reduction of Error Act in 2002, they did so with no guarantee “that all of the information necessary to sustain a claim will be gathered in the limitations period.”
Similarly, the court ruled, “at some point the clock must run out, lest health care providers remain subject to liability exposure indefinitely, with the prospect of a trial marred by the death or diminished memory of material witnesses or the loss of critical evidence.”
A version of this article first appeared on Medscape.com.
Delay in treatment will cost hospital millions
according to a report on WFAA.com, among other news sites.
On March 21, 2019, Judy “Jessie” Adams, then part of a singing-songwriting duo with her husband, Richard, went to Premier Interventional Pain Management, in Flower Mound, Tex., prior to the couple’s drive to Ohio for a funeral. At Premier, Jesse received an epidural steroid injection (ESI) that she hoped would ease her back pain during the long drive.
Instead, the injection ended up increasing her pain.
“He [the pain physician] gave me the shot, but I couldn’t feel my legs. They were tingling, but I couldn’t feel them,” Mrs. Adams explained. “The pain was so bad in my back.” In their suit, Adams and her husband alleged that the doctor had probably “nicked a blood vessel during the ESI procedure, causing Jessie to hemorrhage.” (The couple’s suit against the doctor was settled prior to trial.)
Mrs. Adams remained under observation at the pain facility for about 1½ hours, at which point she was taken by ambulance to nearby Texas Health Presbyterian Hospital. There, in the emergency department, staff ordered a “STAT MRI” in preparation for an emergency laminectomy.
For reasons that remain murky, the MRI wasn’t performed for 1 hour and 37 minutes. The emergency laminectomy itself wasn’t started until more than 5 hours after Adams had been admitted to the ED. This was a direct violation of hospital protocol, which required that emergency surgeries be performed within 1 hour of admittance in the first available surgical suite. (At trial, Mrs. Adams’s attorneys from Lyons & Simmons offered evidence that a suite became available 49 minutes after Adams had arrived at the ED.)
During the wait, Mrs. Adams continued to experience excruciating pain. “I kept screaming: ‘Help me,’ ” she recalled. At trial, her attorneys argued that the hospital’s delay in addressing her spinal emergency led directly to her current paralysis, which keeps her confined to a wheelchair and renders her incontinent.
The hospital disagreed. In court, it maintained that Mrs. Adams was already paralyzed when she arrived at the ED and that there was no delay in care.
The jury saw things differently, however. Siding with the plaintiffs, it awarded Mrs. Adams and her husband $10.1 million, including $500,000 for Mr. Adams’s loss of future earnings and $1 million for his “loss of consortium” with his wife.
Their music career now effectively over, Mr. Adams spends most of his time taking care of Mrs. Adams.
“Music was our lifeblood for so many years, and he can’t do it anymore,” Mrs. Adams said. “He goes upstairs to play his guitar and write, and suddenly I need him to come and cath me. I just feel like I’m going to wake up from this bad dream, but it’s the same routine.”
Two doctors are absolved in woman’s sudden death
In a 3-2 decision in December 2022, the Pennsylvania Supreme Court ruled that the state’s 2-year statute of limitations in wrongful-death cases applies even in cases in which plaintiffs fail to identify the cause of death in a timely manner, as a report in the Claims Journal indicates.
The decision stems from a lawsuit filed by Linda Reibenstein on behalf of her mother, Mary Ann Whitman, who died in late April 2010 from a ruptured aortic aneurysm.
On April 12, 2010, Ms. Whitman visited Patrick D. Conaboy, MD, a Scranton family physician, complaining of a persistent cough, fever, and lower-back pain. Following an initial examination, Dr. Conaboy ordered an aortic duplex ultrasound scan and a CT scan of the patient’s abdomen.
The ultrasound was performed by radiologist Charles Barax, MD, who reviewed both scans. He identified a “poorly visualized aortic aneurysm.” At this point, Dr. Conaboy referred Ms. Whitman to a vascular surgeon. But before this visit could take place, Whitman’s aneurysm ruptured, killing her. This was listed as the medical cause of death on the patient’s death certificate.
In April 2011, Ms. Reibenstein filed a claim against Dr. Barax, alleging that he had failed to gauge the severity of her mother’s condition. Ms. Reibenstein’s attorney wasn’t able to question Dr. Barax on the record until well after the state’s 2-year statute of limitations had elapsed. When he did testify, Dr. Barax explained that the scans’ image quality prevented him from determining whether Whitman’s aneurysm was rupturing or simply bleeding. Despite this, he insisted that he had warned Dr. Conaboy of the potential for Ms. Whitman’s aneurysm to rupture.
In March 2016, nearly 6 years after her mother’s death, Ms. Reibenstein filed a new lawsuit, this one against Dr. Conaboy, whom she alleged had failed to properly treat her mother’s condition. Dr. Conaboy, in turn, asked the court for summary judgment – that is, a judgment in his favor without a full trial – arguing that the state’s window for filing a wrongful-death claim had long since closed. For their part, Ms. Reibenstein and her attorney argued that the state’s 2-year statute of limitations didn’t start until the plaintiff had discovered the cause of her mother’s death.
Initially refusing to dismiss the case, a lower court reconsidered Dr. Conaboy’s motion for summary judgment and ruled that Ms. Reibenstein had failed to present any evidence of “affirmative misrepresentation or fraudulent concealment.” In other words, in the absence of any willful attempt on the part of the defendant to hide the legal cause of death, which includes “acts, omissions, or events having some causative connection with the death,” the statute of limitations remained in effect, and the defendant’s motion was thereby granted.
Continuing the legal seesaw, a state appeals court reversed the lower-court ruling. Noting that the Pennsylvania malpractice statute was ambiguous, the court argued that it should be interpreted in a way that protects plaintiffs who seek “fair compensation” but encounter willfully erected obstacles in pursuit of their claim.
Dr. Conaboy then took his case to the state’s highest court. In its majority decision, the Pennsylvania Supreme Court staked out a narrow definition of cause of death – one based on the death certificate – and ruled that only willful fraud in that document would constitute the necessary condition for halting the claim’s clock. Furthermore, the high court said, when lawmakers adopted the Medical Care Availability and Reduction of Error Act in 2002, they did so with no guarantee “that all of the information necessary to sustain a claim will be gathered in the limitations period.”
Similarly, the court ruled, “at some point the clock must run out, lest health care providers remain subject to liability exposure indefinitely, with the prospect of a trial marred by the death or diminished memory of material witnesses or the loss of critical evidence.”
A version of this article first appeared on Medscape.com.
Delay in treatment will cost hospital millions
according to a report on WFAA.com, among other news sites.
On March 21, 2019, Judy “Jessie” Adams, then part of a singing-songwriting duo with her husband, Richard, went to Premier Interventional Pain Management, in Flower Mound, Tex., prior to the couple’s drive to Ohio for a funeral. At Premier, Jesse received an epidural steroid injection (ESI) that she hoped would ease her back pain during the long drive.
Instead, the injection ended up increasing her pain.
“He [the pain physician] gave me the shot, but I couldn’t feel my legs. They were tingling, but I couldn’t feel them,” Mrs. Adams explained. “The pain was so bad in my back.” In their suit, Adams and her husband alleged that the doctor had probably “nicked a blood vessel during the ESI procedure, causing Jessie to hemorrhage.” (The couple’s suit against the doctor was settled prior to trial.)
Mrs. Adams remained under observation at the pain facility for about 1½ hours, at which point she was taken by ambulance to nearby Texas Health Presbyterian Hospital. There, in the emergency department, staff ordered a “STAT MRI” in preparation for an emergency laminectomy.
For reasons that remain murky, the MRI wasn’t performed for 1 hour and 37 minutes. The emergency laminectomy itself wasn’t started until more than 5 hours after Adams had been admitted to the ED. This was a direct violation of hospital protocol, which required that emergency surgeries be performed within 1 hour of admittance in the first available surgical suite. (At trial, Mrs. Adams’s attorneys from Lyons & Simmons offered evidence that a suite became available 49 minutes after Adams had arrived at the ED.)
During the wait, Mrs. Adams continued to experience excruciating pain. “I kept screaming: ‘Help me,’ ” she recalled. At trial, her attorneys argued that the hospital’s delay in addressing her spinal emergency led directly to her current paralysis, which keeps her confined to a wheelchair and renders her incontinent.
The hospital disagreed. In court, it maintained that Mrs. Adams was already paralyzed when she arrived at the ED and that there was no delay in care.
The jury saw things differently, however. Siding with the plaintiffs, it awarded Mrs. Adams and her husband $10.1 million, including $500,000 for Mr. Adams’s loss of future earnings and $1 million for his “loss of consortium” with his wife.
Their music career now effectively over, Mr. Adams spends most of his time taking care of Mrs. Adams.
“Music was our lifeblood for so many years, and he can’t do it anymore,” Mrs. Adams said. “He goes upstairs to play his guitar and write, and suddenly I need him to come and cath me. I just feel like I’m going to wake up from this bad dream, but it’s the same routine.”
Two doctors are absolved in woman’s sudden death
In a 3-2 decision in December 2022, the Pennsylvania Supreme Court ruled that the state’s 2-year statute of limitations in wrongful-death cases applies even in cases in which plaintiffs fail to identify the cause of death in a timely manner, as a report in the Claims Journal indicates.
The decision stems from a lawsuit filed by Linda Reibenstein on behalf of her mother, Mary Ann Whitman, who died in late April 2010 from a ruptured aortic aneurysm.
On April 12, 2010, Ms. Whitman visited Patrick D. Conaboy, MD, a Scranton family physician, complaining of a persistent cough, fever, and lower-back pain. Following an initial examination, Dr. Conaboy ordered an aortic duplex ultrasound scan and a CT scan of the patient’s abdomen.
The ultrasound was performed by radiologist Charles Barax, MD, who reviewed both scans. He identified a “poorly visualized aortic aneurysm.” At this point, Dr. Conaboy referred Ms. Whitman to a vascular surgeon. But before this visit could take place, Whitman’s aneurysm ruptured, killing her. This was listed as the medical cause of death on the patient’s death certificate.
In April 2011, Ms. Reibenstein filed a claim against Dr. Barax, alleging that he had failed to gauge the severity of her mother’s condition. Ms. Reibenstein’s attorney wasn’t able to question Dr. Barax on the record until well after the state’s 2-year statute of limitations had elapsed. When he did testify, Dr. Barax explained that the scans’ image quality prevented him from determining whether Whitman’s aneurysm was rupturing or simply bleeding. Despite this, he insisted that he had warned Dr. Conaboy of the potential for Ms. Whitman’s aneurysm to rupture.
In March 2016, nearly 6 years after her mother’s death, Ms. Reibenstein filed a new lawsuit, this one against Dr. Conaboy, whom she alleged had failed to properly treat her mother’s condition. Dr. Conaboy, in turn, asked the court for summary judgment – that is, a judgment in his favor without a full trial – arguing that the state’s window for filing a wrongful-death claim had long since closed. For their part, Ms. Reibenstein and her attorney argued that the state’s 2-year statute of limitations didn’t start until the plaintiff had discovered the cause of her mother’s death.
Initially refusing to dismiss the case, a lower court reconsidered Dr. Conaboy’s motion for summary judgment and ruled that Ms. Reibenstein had failed to present any evidence of “affirmative misrepresentation or fraudulent concealment.” In other words, in the absence of any willful attempt on the part of the defendant to hide the legal cause of death, which includes “acts, omissions, or events having some causative connection with the death,” the statute of limitations remained in effect, and the defendant’s motion was thereby granted.
Continuing the legal seesaw, a state appeals court reversed the lower-court ruling. Noting that the Pennsylvania malpractice statute was ambiguous, the court argued that it should be interpreted in a way that protects plaintiffs who seek “fair compensation” but encounter willfully erected obstacles in pursuit of their claim.
Dr. Conaboy then took his case to the state’s highest court. In its majority decision, the Pennsylvania Supreme Court staked out a narrow definition of cause of death – one based on the death certificate – and ruled that only willful fraud in that document would constitute the necessary condition for halting the claim’s clock. Furthermore, the high court said, when lawmakers adopted the Medical Care Availability and Reduction of Error Act in 2002, they did so with no guarantee “that all of the information necessary to sustain a claim will be gathered in the limitations period.”
Similarly, the court ruled, “at some point the clock must run out, lest health care providers remain subject to liability exposure indefinitely, with the prospect of a trial marred by the death or diminished memory of material witnesses or the loss of critical evidence.”
A version of this article first appeared on Medscape.com.









