User login
Time to prescribe sauna bathing for cardiovascular health?
Is it time to start recommending regular sauna bathing to improve heart health?
While a post-workout sauna can compound the benefits of exercise, the hormetic effects of heat therapy alone can produce significant gains for microvascular and endothelial function, no workout required.
“There’s enough evidence to say that regular sauna use improves cardiovascular health,” Matthew S. Ganio, PhD, a professor of exercise science at the University of Arkansas in Fayetteville, who studies thermoregulatory responses and cardiovascular health, said.
“The more they used it, the greater the reduction in cardiovascular events like heart attack. But you don’t need to be in there more than 20-30 minutes. That’s where it seemed to have the best effect,” Dr. Ganio said, adding that studies have shown a dose-response.
A prospective cohort study published in 2015 in JAMA Internal Medicine included 20 years of data on more than 2,300 Finnish men who regularly sauna bathed. The researchers found that among participants who sat in saunas more frequently, rates of death from heart disease and stroke were lower than among those who did so less often.
Cutaneous vasodilation
The body experiences several physiologic changes when exposed to heat therapy of any kind, including sauna, hot water submerging, shortwave diathermy, and heat wrapping. Many of these changes involve elements of the cardiovascular system, said Earric Lee, PhD, an exercise physiologist and postdoctoral researcher at the University of Jyväskylä in Finland, who has studied the effects of sauna on cardiovascular health.
The mechanisms by which heat therapy improves cardiovascular fitness have not been determined, as few studies of sauna bathing have been conducted to this degree. One driver appears to be cutaneous vasodilation. To cool the body when exposed to extreme external heat, cutaneous vessels dilate and push blood to the skin, which lowers body temperature, increases heart rate, and delivers oxygen to muscles in the limbs in a way similar to aerobic exercise.
Sauna bathing has similar effects on heart rate and cardiac output. Studies have shown it can improve the circulation of blood through the body, as well as vascular endothelial function, which is closely tied to vascular tone.
“Increased cardiac output is one of the physiologic reasons sauna is good for heart health,” Dr. Ganio said.
During a sauna session, cardiac output can increase by as much as 70% in relation to elevated heart rate. And while heart rate and cardiac output rise, stroke volume remains stable. As stroke volume increases, the effort that muscle must exert increases. When heart rate rises, stroke volume often falls, which subjects the heart to less of a workout and reduces the amount of oxygen and blood circulating throughout the body.
Heat therapy also temporarily increases blood pressure, but in a way similar to exercise, which supports better long-term heart health, said Christopher Minson, PhD, the Kenneth M. and Kenda H. Singer Endowed Professor of Human Physiology at the University of Oregon in Eugene.
A small study of 19 healthy adults that was published in Complementary Therapies in Medicine in 2019 found that blood pressure and heart rate rose during a 25-minute sauna session as they might during moderate exercise, equivalent to an exercise load of about 60-100 watts. These parameters then steadily decreased for 30 minutes after the sauna. An earlier study found that in the long term, blood pressure was lower after a sauna than before a sauna.
Upregulated heat shock proteins
Both aerobic exercise and heat stress from sauna bathing increase the activity of heat shock proteins. A 2021 review published in Experimental Gerontology found that heat shock proteins become elevated in cells within 30 minutes of exposure to heat and remain elevated over time – an effect similar to exercise.
“Saunas increase heat shock proteins that break down old, dysfunctional proteins and then protect new proteins from becoming dysfunctional,” Hunter S. Waldman, PhD, an assistant professor of exercise science at the University of North Alabama in Florence, said. This effect is one way sauna bathing may quell systemic inflammation, Dr. Waldman said.
According to a 2018 review published in BioMed Research International, an abundance of heat shock proteins may increase exercise tolerance. The researchers concluded that the positive stress associated with elevated body temperature could help people be physically active for longer periods.
Added stress, especially heat-related strain, is not good for everyone, however. Dr. Waldman cautioned that heat exposure, be it through a sauna, hot tub, or other source, can be harmful for pregnant women and children and can be dangerous for people who have low blood pressure, since blood pressure often drops to rates that are lower than before taking a sauna. It also can impair semen quality for months after exposure, so people who are trying to conceive should avoid sauna bathing.
Anyone who has been diagnosed with a heart condition, including cardiac arrhythmia, coronary artery disease, and congestive heart failure, should always consult their physician prior to using sauna for the first time or before using it habitually, Dr. Lee said.
Effects compounded by exercise
Dr. Minson stressed that any type of heat therapy should be part of a lifestyle that includes mostly healthy habits overall, especially a regular exercise regime when possible.
“You have to have everything else working as well: finding time to relax, not being overly stressed, staying hydrated – all those things are critical with any exercise training and heat therapy program,” he said.
Dr. Lee said it’s easy to overhype the benefits of sauna bathing and agreed the practice should be used in tandem with other therapies, not as a replacement. So far, stacking research has shown it to be an effective extension of aerobic exercise.
A June 2023 review published in Mayo Clinic Proceedings found that while sauna bathing can produce benefits on its own, a post-workout sauna can extend the benefits of exercise. As a result, the researchers concluded, saunas likely provide the most benefit when combined with aerobic and strength training.
While some of the benefits of exercise overlap those associated with sauna bathing, “you’re going to get some benefits with exercise that you’re never going to get with sauna,” Dr. Ganio said.
For instance, strength training or aerobic exercise usually results in muscle contractions, which sauna bathing does not produce.
If a person is impaired in a way that makes exercise difficult, taking a sauna after aerobic activity can extend the cardiovascular benefits of the workout, even if muscle-building does not occur, Dr. Lee said.
“All other things considered, especially with aerobic exercise, it is very comparable, so we can look at adding sauna bathing post exercise as a way to lengthen the aerobic exercise workout,” he said. “It’s not to the same degree, but you can get many of the ranging benefits of exercising simply by going into the sauna.”
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Is it time to start recommending regular sauna bathing to improve heart health?
While a post-workout sauna can compound the benefits of exercise, the hormetic effects of heat therapy alone can produce significant gains for microvascular and endothelial function, no workout required.
“There’s enough evidence to say that regular sauna use improves cardiovascular health,” Matthew S. Ganio, PhD, a professor of exercise science at the University of Arkansas in Fayetteville, who studies thermoregulatory responses and cardiovascular health, said.
“The more they used it, the greater the reduction in cardiovascular events like heart attack. But you don’t need to be in there more than 20-30 minutes. That’s where it seemed to have the best effect,” Dr. Ganio said, adding that studies have shown a dose-response.
A prospective cohort study published in 2015 in JAMA Internal Medicine included 20 years of data on more than 2,300 Finnish men who regularly sauna bathed. The researchers found that among participants who sat in saunas more frequently, rates of death from heart disease and stroke were lower than among those who did so less often.
Cutaneous vasodilation
The body experiences several physiologic changes when exposed to heat therapy of any kind, including sauna, hot water submerging, shortwave diathermy, and heat wrapping. Many of these changes involve elements of the cardiovascular system, said Earric Lee, PhD, an exercise physiologist and postdoctoral researcher at the University of Jyväskylä in Finland, who has studied the effects of sauna on cardiovascular health.
The mechanisms by which heat therapy improves cardiovascular fitness have not been determined, as few studies of sauna bathing have been conducted to this degree. One driver appears to be cutaneous vasodilation. To cool the body when exposed to extreme external heat, cutaneous vessels dilate and push blood to the skin, which lowers body temperature, increases heart rate, and delivers oxygen to muscles in the limbs in a way similar to aerobic exercise.
Sauna bathing has similar effects on heart rate and cardiac output. Studies have shown it can improve the circulation of blood through the body, as well as vascular endothelial function, which is closely tied to vascular tone.
“Increased cardiac output is one of the physiologic reasons sauna is good for heart health,” Dr. Ganio said.
During a sauna session, cardiac output can increase by as much as 70% in relation to elevated heart rate. And while heart rate and cardiac output rise, stroke volume remains stable. As stroke volume increases, the effort that muscle must exert increases. When heart rate rises, stroke volume often falls, which subjects the heart to less of a workout and reduces the amount of oxygen and blood circulating throughout the body.
Heat therapy also temporarily increases blood pressure, but in a way similar to exercise, which supports better long-term heart health, said Christopher Minson, PhD, the Kenneth M. and Kenda H. Singer Endowed Professor of Human Physiology at the University of Oregon in Eugene.
A small study of 19 healthy adults that was published in Complementary Therapies in Medicine in 2019 found that blood pressure and heart rate rose during a 25-minute sauna session as they might during moderate exercise, equivalent to an exercise load of about 60-100 watts. These parameters then steadily decreased for 30 minutes after the sauna. An earlier study found that in the long term, blood pressure was lower after a sauna than before a sauna.
Upregulated heat shock proteins
Both aerobic exercise and heat stress from sauna bathing increase the activity of heat shock proteins. A 2021 review published in Experimental Gerontology found that heat shock proteins become elevated in cells within 30 minutes of exposure to heat and remain elevated over time – an effect similar to exercise.
“Saunas increase heat shock proteins that break down old, dysfunctional proteins and then protect new proteins from becoming dysfunctional,” Hunter S. Waldman, PhD, an assistant professor of exercise science at the University of North Alabama in Florence, said. This effect is one way sauna bathing may quell systemic inflammation, Dr. Waldman said.
According to a 2018 review published in BioMed Research International, an abundance of heat shock proteins may increase exercise tolerance. The researchers concluded that the positive stress associated with elevated body temperature could help people be physically active for longer periods.
Added stress, especially heat-related strain, is not good for everyone, however. Dr. Waldman cautioned that heat exposure, be it through a sauna, hot tub, or other source, can be harmful for pregnant women and children and can be dangerous for people who have low blood pressure, since blood pressure often drops to rates that are lower than before taking a sauna. It also can impair semen quality for months after exposure, so people who are trying to conceive should avoid sauna bathing.
Anyone who has been diagnosed with a heart condition, including cardiac arrhythmia, coronary artery disease, and congestive heart failure, should always consult their physician prior to using sauna for the first time or before using it habitually, Dr. Lee said.
Effects compounded by exercise
Dr. Minson stressed that any type of heat therapy should be part of a lifestyle that includes mostly healthy habits overall, especially a regular exercise regime when possible.
“You have to have everything else working as well: finding time to relax, not being overly stressed, staying hydrated – all those things are critical with any exercise training and heat therapy program,” he said.
Dr. Lee said it’s easy to overhype the benefits of sauna bathing and agreed the practice should be used in tandem with other therapies, not as a replacement. So far, stacking research has shown it to be an effective extension of aerobic exercise.
A June 2023 review published in Mayo Clinic Proceedings found that while sauna bathing can produce benefits on its own, a post-workout sauna can extend the benefits of exercise. As a result, the researchers concluded, saunas likely provide the most benefit when combined with aerobic and strength training.
While some of the benefits of exercise overlap those associated with sauna bathing, “you’re going to get some benefits with exercise that you’re never going to get with sauna,” Dr. Ganio said.
For instance, strength training or aerobic exercise usually results in muscle contractions, which sauna bathing does not produce.
If a person is impaired in a way that makes exercise difficult, taking a sauna after aerobic activity can extend the cardiovascular benefits of the workout, even if muscle-building does not occur, Dr. Lee said.
“All other things considered, especially with aerobic exercise, it is very comparable, so we can look at adding sauna bathing post exercise as a way to lengthen the aerobic exercise workout,” he said. “It’s not to the same degree, but you can get many of the ranging benefits of exercising simply by going into the sauna.”
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Is it time to start recommending regular sauna bathing to improve heart health?
While a post-workout sauna can compound the benefits of exercise, the hormetic effects of heat therapy alone can produce significant gains for microvascular and endothelial function, no workout required.
“There’s enough evidence to say that regular sauna use improves cardiovascular health,” Matthew S. Ganio, PhD, a professor of exercise science at the University of Arkansas in Fayetteville, who studies thermoregulatory responses and cardiovascular health, said.
“The more they used it, the greater the reduction in cardiovascular events like heart attack. But you don’t need to be in there more than 20-30 minutes. That’s where it seemed to have the best effect,” Dr. Ganio said, adding that studies have shown a dose-response.
A prospective cohort study published in 2015 in JAMA Internal Medicine included 20 years of data on more than 2,300 Finnish men who regularly sauna bathed. The researchers found that among participants who sat in saunas more frequently, rates of death from heart disease and stroke were lower than among those who did so less often.
Cutaneous vasodilation
The body experiences several physiologic changes when exposed to heat therapy of any kind, including sauna, hot water submerging, shortwave diathermy, and heat wrapping. Many of these changes involve elements of the cardiovascular system, said Earric Lee, PhD, an exercise physiologist and postdoctoral researcher at the University of Jyväskylä in Finland, who has studied the effects of sauna on cardiovascular health.
The mechanisms by which heat therapy improves cardiovascular fitness have not been determined, as few studies of sauna bathing have been conducted to this degree. One driver appears to be cutaneous vasodilation. To cool the body when exposed to extreme external heat, cutaneous vessels dilate and push blood to the skin, which lowers body temperature, increases heart rate, and delivers oxygen to muscles in the limbs in a way similar to aerobic exercise.
Sauna bathing has similar effects on heart rate and cardiac output. Studies have shown it can improve the circulation of blood through the body, as well as vascular endothelial function, which is closely tied to vascular tone.
“Increased cardiac output is one of the physiologic reasons sauna is good for heart health,” Dr. Ganio said.
During a sauna session, cardiac output can increase by as much as 70% in relation to elevated heart rate. And while heart rate and cardiac output rise, stroke volume remains stable. As stroke volume increases, the effort that muscle must exert increases. When heart rate rises, stroke volume often falls, which subjects the heart to less of a workout and reduces the amount of oxygen and blood circulating throughout the body.
Heat therapy also temporarily increases blood pressure, but in a way similar to exercise, which supports better long-term heart health, said Christopher Minson, PhD, the Kenneth M. and Kenda H. Singer Endowed Professor of Human Physiology at the University of Oregon in Eugene.
A small study of 19 healthy adults that was published in Complementary Therapies in Medicine in 2019 found that blood pressure and heart rate rose during a 25-minute sauna session as they might during moderate exercise, equivalent to an exercise load of about 60-100 watts. These parameters then steadily decreased for 30 minutes after the sauna. An earlier study found that in the long term, blood pressure was lower after a sauna than before a sauna.
Upregulated heat shock proteins
Both aerobic exercise and heat stress from sauna bathing increase the activity of heat shock proteins. A 2021 review published in Experimental Gerontology found that heat shock proteins become elevated in cells within 30 minutes of exposure to heat and remain elevated over time – an effect similar to exercise.
“Saunas increase heat shock proteins that break down old, dysfunctional proteins and then protect new proteins from becoming dysfunctional,” Hunter S. Waldman, PhD, an assistant professor of exercise science at the University of North Alabama in Florence, said. This effect is one way sauna bathing may quell systemic inflammation, Dr. Waldman said.
According to a 2018 review published in BioMed Research International, an abundance of heat shock proteins may increase exercise tolerance. The researchers concluded that the positive stress associated with elevated body temperature could help people be physically active for longer periods.
Added stress, especially heat-related strain, is not good for everyone, however. Dr. Waldman cautioned that heat exposure, be it through a sauna, hot tub, or other source, can be harmful for pregnant women and children and can be dangerous for people who have low blood pressure, since blood pressure often drops to rates that are lower than before taking a sauna. It also can impair semen quality for months after exposure, so people who are trying to conceive should avoid sauna bathing.
Anyone who has been diagnosed with a heart condition, including cardiac arrhythmia, coronary artery disease, and congestive heart failure, should always consult their physician prior to using sauna for the first time or before using it habitually, Dr. Lee said.
Effects compounded by exercise
Dr. Minson stressed that any type of heat therapy should be part of a lifestyle that includes mostly healthy habits overall, especially a regular exercise regime when possible.
“You have to have everything else working as well: finding time to relax, not being overly stressed, staying hydrated – all those things are critical with any exercise training and heat therapy program,” he said.
Dr. Lee said it’s easy to overhype the benefits of sauna bathing and agreed the practice should be used in tandem with other therapies, not as a replacement. So far, stacking research has shown it to be an effective extension of aerobic exercise.
A June 2023 review published in Mayo Clinic Proceedings found that while sauna bathing can produce benefits on its own, a post-workout sauna can extend the benefits of exercise. As a result, the researchers concluded, saunas likely provide the most benefit when combined with aerobic and strength training.
While some of the benefits of exercise overlap those associated with sauna bathing, “you’re going to get some benefits with exercise that you’re never going to get with sauna,” Dr. Ganio said.
For instance, strength training or aerobic exercise usually results in muscle contractions, which sauna bathing does not produce.
If a person is impaired in a way that makes exercise difficult, taking a sauna after aerobic activity can extend the cardiovascular benefits of the workout, even if muscle-building does not occur, Dr. Lee said.
“All other things considered, especially with aerobic exercise, it is very comparable, so we can look at adding sauna bathing post exercise as a way to lengthen the aerobic exercise workout,” he said. “It’s not to the same degree, but you can get many of the ranging benefits of exercising simply by going into the sauna.”
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FDA OKs low-dose colchicine for broad CV indication
The Food and Drug Administration has approved the anti-inflammatory drug colchicine 0.5 mg tablets (Lodoco) as the first specific anti-inflammatory drug demonstrated to reduce the risk for myocardial infarction, stroke, coronary revascularization, and cardiovascular death in adult patients with established atherosclerotic disease or with multiple risk factors for cardiovascular disease.
The drug, which targets residual inflammation as an underlying cause of atherosclerotic cardiovascular disease, has a dosage of 0.5 mg once daily, and can be used alone or in combination with cholesterol-lowering medications.
The drug’s manufacturer, Agepha Pharma, said it anticipates that Lodoco will be available for prescription in the second half of 2023.
Colchicine has been available for many years and used at higher doses for the acute treatment of gout and pericarditis, but the current formulation is a much lower dose for long-term use in patients with atherosclerotic heart disease.
Data supporting the approval has come from two major randomized trials, LoDoCo-2 and COLCOT.
In the LoDoCo-2 trial, the anti-inflammatory drug cut the risk of cardiovascular events by one third when added to standard prevention therapies in patients with chronic coronary disease. And in the COLCOT study, use of colchicine reduced cardiovascular events by 23% compared with placebo in patients with a recent MI.
Paul Ridker, MD, director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital in Boston, who has been a pioneer in establishing inflammation as an underlying cause of atherosclerotic cardiovascular disease, welcomed the Lodoco approval.
‘A very big day for cardiology’
“This is a very big day for cardiology,” Dr. Ridker said in an interview.
“The FDA approval of colchicine for patients with atherosclerotic disease is a huge signal that physicians need to be aware of inflammation as a key player in cardiovascular disease,” he said.
Dr. Ridker was the lead author of a recent study showing that among patients receiving contemporary statins, inflammation assessed by high-sensitivity C-reactive protein (hsCRP) was a stronger predictor for risk of future cardiovascular events and death than LDL cholesterol.
He pointed out that
“That is virtually identical to the indication approved for statin therapy. That shows just how important the FDA thinks this is,” he commented.
But Dr. Ridker added that, while the label does not specify that Lodoco has to be used in addition to statin therapy, he believes that it will be used as additional therapy to statins in the vast majority of patients.
“This is not an alternative to statin therapy. In the randomized trials, the benefits were seen on top of statins,” he stressed.
Dr. Ridker believes that physicians will need time to feel comfortable with this new approach.
“Initially, I think, it will be used mainly by cardiologists who know about inflammation, but I believe over time it will be widely prescribed by internists, in much the same way as statins are used today,” he commented.
Dr. Ridker said he already uses low dose colchicine in his high-risk patients who have high levels of inflammation as seen on hsCRP testing. He believes this is where the drug will mostly be used initially, as this is where it is likely to be most effective.
The prescribing information states that Lodoco is contraindicated in patients who are taking strong CYP3A4 inhibitors or P-glycoprotein inhibitors, such as ketoconazole, fluconazole, and clarithromycin, and in patients with preexisting blood dyscrasias, renal failure, and severe hepatic impairment.
Common side effects reported in published clinical studies and literature with the use of colchicine are gastrointestinal symptoms (diarrhea, vomiting, abdominal cramping) and myalgia.
More serious adverse effects are listed as blood dyscrasias such as myelosuppression, leukopenia, granulocytopenia, thrombocytopenia, pancytopenia, and aplastic anemia; and neuromuscular toxicity in the form of myotoxicity including rhabdomyolysis, which may occur, especially in combination with other drugs known to cause this effect. If these adverse effects occur, it is recommended that the drug be stopped.
The prescribing information also notes that Lodoco may rarely and transiently impair fertility in males; and that patients with renal or hepatic impairment should be monitored closely for adverse effects of colchicine.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved the anti-inflammatory drug colchicine 0.5 mg tablets (Lodoco) as the first specific anti-inflammatory drug demonstrated to reduce the risk for myocardial infarction, stroke, coronary revascularization, and cardiovascular death in adult patients with established atherosclerotic disease or with multiple risk factors for cardiovascular disease.
The drug, which targets residual inflammation as an underlying cause of atherosclerotic cardiovascular disease, has a dosage of 0.5 mg once daily, and can be used alone or in combination with cholesterol-lowering medications.
The drug’s manufacturer, Agepha Pharma, said it anticipates that Lodoco will be available for prescription in the second half of 2023.
Colchicine has been available for many years and used at higher doses for the acute treatment of gout and pericarditis, but the current formulation is a much lower dose for long-term use in patients with atherosclerotic heart disease.
Data supporting the approval has come from two major randomized trials, LoDoCo-2 and COLCOT.
In the LoDoCo-2 trial, the anti-inflammatory drug cut the risk of cardiovascular events by one third when added to standard prevention therapies in patients with chronic coronary disease. And in the COLCOT study, use of colchicine reduced cardiovascular events by 23% compared with placebo in patients with a recent MI.
Paul Ridker, MD, director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital in Boston, who has been a pioneer in establishing inflammation as an underlying cause of atherosclerotic cardiovascular disease, welcomed the Lodoco approval.
‘A very big day for cardiology’
“This is a very big day for cardiology,” Dr. Ridker said in an interview.
“The FDA approval of colchicine for patients with atherosclerotic disease is a huge signal that physicians need to be aware of inflammation as a key player in cardiovascular disease,” he said.
Dr. Ridker was the lead author of a recent study showing that among patients receiving contemporary statins, inflammation assessed by high-sensitivity C-reactive protein (hsCRP) was a stronger predictor for risk of future cardiovascular events and death than LDL cholesterol.
He pointed out that
“That is virtually identical to the indication approved for statin therapy. That shows just how important the FDA thinks this is,” he commented.
But Dr. Ridker added that, while the label does not specify that Lodoco has to be used in addition to statin therapy, he believes that it will be used as additional therapy to statins in the vast majority of patients.
“This is not an alternative to statin therapy. In the randomized trials, the benefits were seen on top of statins,” he stressed.
Dr. Ridker believes that physicians will need time to feel comfortable with this new approach.
“Initially, I think, it will be used mainly by cardiologists who know about inflammation, but I believe over time it will be widely prescribed by internists, in much the same way as statins are used today,” he commented.
Dr. Ridker said he already uses low dose colchicine in his high-risk patients who have high levels of inflammation as seen on hsCRP testing. He believes this is where the drug will mostly be used initially, as this is where it is likely to be most effective.
The prescribing information states that Lodoco is contraindicated in patients who are taking strong CYP3A4 inhibitors or P-glycoprotein inhibitors, such as ketoconazole, fluconazole, and clarithromycin, and in patients with preexisting blood dyscrasias, renal failure, and severe hepatic impairment.
Common side effects reported in published clinical studies and literature with the use of colchicine are gastrointestinal symptoms (diarrhea, vomiting, abdominal cramping) and myalgia.
More serious adverse effects are listed as blood dyscrasias such as myelosuppression, leukopenia, granulocytopenia, thrombocytopenia, pancytopenia, and aplastic anemia; and neuromuscular toxicity in the form of myotoxicity including rhabdomyolysis, which may occur, especially in combination with other drugs known to cause this effect. If these adverse effects occur, it is recommended that the drug be stopped.
The prescribing information also notes that Lodoco may rarely and transiently impair fertility in males; and that patients with renal or hepatic impairment should be monitored closely for adverse effects of colchicine.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved the anti-inflammatory drug colchicine 0.5 mg tablets (Lodoco) as the first specific anti-inflammatory drug demonstrated to reduce the risk for myocardial infarction, stroke, coronary revascularization, and cardiovascular death in adult patients with established atherosclerotic disease or with multiple risk factors for cardiovascular disease.
The drug, which targets residual inflammation as an underlying cause of atherosclerotic cardiovascular disease, has a dosage of 0.5 mg once daily, and can be used alone or in combination with cholesterol-lowering medications.
The drug’s manufacturer, Agepha Pharma, said it anticipates that Lodoco will be available for prescription in the second half of 2023.
Colchicine has been available for many years and used at higher doses for the acute treatment of gout and pericarditis, but the current formulation is a much lower dose for long-term use in patients with atherosclerotic heart disease.
Data supporting the approval has come from two major randomized trials, LoDoCo-2 and COLCOT.
In the LoDoCo-2 trial, the anti-inflammatory drug cut the risk of cardiovascular events by one third when added to standard prevention therapies in patients with chronic coronary disease. And in the COLCOT study, use of colchicine reduced cardiovascular events by 23% compared with placebo in patients with a recent MI.
Paul Ridker, MD, director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital in Boston, who has been a pioneer in establishing inflammation as an underlying cause of atherosclerotic cardiovascular disease, welcomed the Lodoco approval.
‘A very big day for cardiology’
“This is a very big day for cardiology,” Dr. Ridker said in an interview.
“The FDA approval of colchicine for patients with atherosclerotic disease is a huge signal that physicians need to be aware of inflammation as a key player in cardiovascular disease,” he said.
Dr. Ridker was the lead author of a recent study showing that among patients receiving contemporary statins, inflammation assessed by high-sensitivity C-reactive protein (hsCRP) was a stronger predictor for risk of future cardiovascular events and death than LDL cholesterol.
He pointed out that
“That is virtually identical to the indication approved for statin therapy. That shows just how important the FDA thinks this is,” he commented.
But Dr. Ridker added that, while the label does not specify that Lodoco has to be used in addition to statin therapy, he believes that it will be used as additional therapy to statins in the vast majority of patients.
“This is not an alternative to statin therapy. In the randomized trials, the benefits were seen on top of statins,” he stressed.
Dr. Ridker believes that physicians will need time to feel comfortable with this new approach.
“Initially, I think, it will be used mainly by cardiologists who know about inflammation, but I believe over time it will be widely prescribed by internists, in much the same way as statins are used today,” he commented.
Dr. Ridker said he already uses low dose colchicine in his high-risk patients who have high levels of inflammation as seen on hsCRP testing. He believes this is where the drug will mostly be used initially, as this is where it is likely to be most effective.
The prescribing information states that Lodoco is contraindicated in patients who are taking strong CYP3A4 inhibitors or P-glycoprotein inhibitors, such as ketoconazole, fluconazole, and clarithromycin, and in patients with preexisting blood dyscrasias, renal failure, and severe hepatic impairment.
Common side effects reported in published clinical studies and literature with the use of colchicine are gastrointestinal symptoms (diarrhea, vomiting, abdominal cramping) and myalgia.
More serious adverse effects are listed as blood dyscrasias such as myelosuppression, leukopenia, granulocytopenia, thrombocytopenia, pancytopenia, and aplastic anemia; and neuromuscular toxicity in the form of myotoxicity including rhabdomyolysis, which may occur, especially in combination with other drugs known to cause this effect. If these adverse effects occur, it is recommended that the drug be stopped.
The prescribing information also notes that Lodoco may rarely and transiently impair fertility in males; and that patients with renal or hepatic impairment should be monitored closely for adverse effects of colchicine.
A version of this article first appeared on Medscape.com.
Aspirin warning: Anemia may increase with daily use
, according to results from a new randomized controlled trial.
In the study, which was published in Annals of Internal Medicine, investigators analyzed data from the Aspirin in Reducing Events in the Elderly (ASPREE) trial and examined hemoglobin concentrations among 19,114 healthy, community-dwelling older patients.
“We knew from large clinical trials, including our ASPREE trial, that daily low-dose aspirin increased the risk of clinically significant bleeding,” said Zoe McQuilten, MBBS, PhD, a hematologist at Monash University in Australia and the study’s lead author. “From our study, we found that low-dose aspirin also increased the risk of anemia during the trial, and this was most likely due to bleeding that was not clinically apparent.”
Anemia is common among elderly patients. It can cause fatigue, fast or irregular heartbeat, headache, chest pain, and pounding or whooshing sounds in the ear, according to the Cleveland Clinic. It can also worsen conditions such as heart failure, cognitive impairment, and depression in people aged 65 and older.
The U.S. Preventive Services Task Force changed its recommendation on aspirin for the primary prevention of cardiovascular disease in 2022, recommending against initiating low-dose aspirin for adults aged 60 years or older. For adults aged 40-59 who have a 10% or greater 10-year risk for cardiovascular disease, the agency recommends that patients and clinicians make the decision to initiate low-dose aspirin use on a case-by-case basis, as the net benefit is small.
Dr. McQuilten said she spent the last 5 years designing substages of anemia and conditions such as blood cancer. In many cases of anemia, doctors are unable to determine the underlying cause, she said. One study published in the Journal of American Geriatrics Society in 2021 found that in about one-third of anemia cases, the etiology was not clear.
About 50% of people older than 60 who were involved in the latest study took aspirin for prevention from 2011 to 2018. That number likely dropped after changes were made to the guidelines in 2022, according to Dr. McQuilten, but long-term use may have continued among older patients. The researchers also examined ferritin levels, which serve as a proxy for iron levels, at baseline and after 3 years.
The incidence of anemia was 51 events per 1,000 person-years in the aspirin group compared with 43 events per 1,000 person-years in the placebo group, according to the researchers. The estimated probability of experiencing anemia within 5 years was 23.5% (95% confidence interval [CI], 22.4%-24.6%) in the aspirin group and 20.3% (95% CI: 19.3% to 21.4%) in the placebo group. Aspirin therapy resulted in a 20% increase in the risk for anemia (95% CI, 1.12-1.29).
People who took aspirin were more likely to have lower serum levels of ferritin at the 3-year mark than were those who received placebo. The average decrease in ferritin among participants who took aspirin was 11.5% greater (95% CI, 9.3%-13.7%) than among those who took placebo.
Basil Eldadah, MD, PhD, supervisory medical officer at the National Institute on Aging, part of the National Institutes of Health, said the findings should encourage clinicians to pay closer attention to hemoglobin levels and have conversations with patients to discuss their need for taking aspirin.
“If somebody is already taking aspirin for any reason, keep an eye on hemoglobin,” said Dr. Eldadah, who was not involved in the study. “For somebody who’s taking aspirin and who’s older, and it’s not for an indication like cardiovascular disease, consider seriously whether that’s the best treatment option.”
The study did not examine the functional consequences of anemia on participants, which Dr. Eldadah said could be fodder for future research. The researchers said one limitation was that it was not clear whether anemia was sufficient to cause symptoms that affected participants’ quality of life or whether occult bleeding caused the anemia. The researchers also did not document whether patients saw their regular physicians and received treatment for anemia over the course of the trial.
The study was funded through grants from the National Health and Medical Research Council and the Bill and Melinda Gates Foundation. The authors reported receiving consulting fees, honoraria, and stock options, and have participated on data monitoring boards not related to the study for Vifor Pharma, ITL Biomedical, Pfizer, Boehringer Ingelheim, Bayer Healthcare, AbbVie, and Abbott Diagnostics.
A version of this article originally appeared on Medscape.com.
, according to results from a new randomized controlled trial.
In the study, which was published in Annals of Internal Medicine, investigators analyzed data from the Aspirin in Reducing Events in the Elderly (ASPREE) trial and examined hemoglobin concentrations among 19,114 healthy, community-dwelling older patients.
“We knew from large clinical trials, including our ASPREE trial, that daily low-dose aspirin increased the risk of clinically significant bleeding,” said Zoe McQuilten, MBBS, PhD, a hematologist at Monash University in Australia and the study’s lead author. “From our study, we found that low-dose aspirin also increased the risk of anemia during the trial, and this was most likely due to bleeding that was not clinically apparent.”
Anemia is common among elderly patients. It can cause fatigue, fast or irregular heartbeat, headache, chest pain, and pounding or whooshing sounds in the ear, according to the Cleveland Clinic. It can also worsen conditions such as heart failure, cognitive impairment, and depression in people aged 65 and older.
The U.S. Preventive Services Task Force changed its recommendation on aspirin for the primary prevention of cardiovascular disease in 2022, recommending against initiating low-dose aspirin for adults aged 60 years or older. For adults aged 40-59 who have a 10% or greater 10-year risk for cardiovascular disease, the agency recommends that patients and clinicians make the decision to initiate low-dose aspirin use on a case-by-case basis, as the net benefit is small.
Dr. McQuilten said she spent the last 5 years designing substages of anemia and conditions such as blood cancer. In many cases of anemia, doctors are unable to determine the underlying cause, she said. One study published in the Journal of American Geriatrics Society in 2021 found that in about one-third of anemia cases, the etiology was not clear.
About 50% of people older than 60 who were involved in the latest study took aspirin for prevention from 2011 to 2018. That number likely dropped after changes were made to the guidelines in 2022, according to Dr. McQuilten, but long-term use may have continued among older patients. The researchers also examined ferritin levels, which serve as a proxy for iron levels, at baseline and after 3 years.
The incidence of anemia was 51 events per 1,000 person-years in the aspirin group compared with 43 events per 1,000 person-years in the placebo group, according to the researchers. The estimated probability of experiencing anemia within 5 years was 23.5% (95% confidence interval [CI], 22.4%-24.6%) in the aspirin group and 20.3% (95% CI: 19.3% to 21.4%) in the placebo group. Aspirin therapy resulted in a 20% increase in the risk for anemia (95% CI, 1.12-1.29).
People who took aspirin were more likely to have lower serum levels of ferritin at the 3-year mark than were those who received placebo. The average decrease in ferritin among participants who took aspirin was 11.5% greater (95% CI, 9.3%-13.7%) than among those who took placebo.
Basil Eldadah, MD, PhD, supervisory medical officer at the National Institute on Aging, part of the National Institutes of Health, said the findings should encourage clinicians to pay closer attention to hemoglobin levels and have conversations with patients to discuss their need for taking aspirin.
“If somebody is already taking aspirin for any reason, keep an eye on hemoglobin,” said Dr. Eldadah, who was not involved in the study. “For somebody who’s taking aspirin and who’s older, and it’s not for an indication like cardiovascular disease, consider seriously whether that’s the best treatment option.”
The study did not examine the functional consequences of anemia on participants, which Dr. Eldadah said could be fodder for future research. The researchers said one limitation was that it was not clear whether anemia was sufficient to cause symptoms that affected participants’ quality of life or whether occult bleeding caused the anemia. The researchers also did not document whether patients saw their regular physicians and received treatment for anemia over the course of the trial.
The study was funded through grants from the National Health and Medical Research Council and the Bill and Melinda Gates Foundation. The authors reported receiving consulting fees, honoraria, and stock options, and have participated on data monitoring boards not related to the study for Vifor Pharma, ITL Biomedical, Pfizer, Boehringer Ingelheim, Bayer Healthcare, AbbVie, and Abbott Diagnostics.
A version of this article originally appeared on Medscape.com.
, according to results from a new randomized controlled trial.
In the study, which was published in Annals of Internal Medicine, investigators analyzed data from the Aspirin in Reducing Events in the Elderly (ASPREE) trial and examined hemoglobin concentrations among 19,114 healthy, community-dwelling older patients.
“We knew from large clinical trials, including our ASPREE trial, that daily low-dose aspirin increased the risk of clinically significant bleeding,” said Zoe McQuilten, MBBS, PhD, a hematologist at Monash University in Australia and the study’s lead author. “From our study, we found that low-dose aspirin also increased the risk of anemia during the trial, and this was most likely due to bleeding that was not clinically apparent.”
Anemia is common among elderly patients. It can cause fatigue, fast or irregular heartbeat, headache, chest pain, and pounding or whooshing sounds in the ear, according to the Cleveland Clinic. It can also worsen conditions such as heart failure, cognitive impairment, and depression in people aged 65 and older.
The U.S. Preventive Services Task Force changed its recommendation on aspirin for the primary prevention of cardiovascular disease in 2022, recommending against initiating low-dose aspirin for adults aged 60 years or older. For adults aged 40-59 who have a 10% or greater 10-year risk for cardiovascular disease, the agency recommends that patients and clinicians make the decision to initiate low-dose aspirin use on a case-by-case basis, as the net benefit is small.
Dr. McQuilten said she spent the last 5 years designing substages of anemia and conditions such as blood cancer. In many cases of anemia, doctors are unable to determine the underlying cause, she said. One study published in the Journal of American Geriatrics Society in 2021 found that in about one-third of anemia cases, the etiology was not clear.
About 50% of people older than 60 who were involved in the latest study took aspirin for prevention from 2011 to 2018. That number likely dropped after changes were made to the guidelines in 2022, according to Dr. McQuilten, but long-term use may have continued among older patients. The researchers also examined ferritin levels, which serve as a proxy for iron levels, at baseline and after 3 years.
The incidence of anemia was 51 events per 1,000 person-years in the aspirin group compared with 43 events per 1,000 person-years in the placebo group, according to the researchers. The estimated probability of experiencing anemia within 5 years was 23.5% (95% confidence interval [CI], 22.4%-24.6%) in the aspirin group and 20.3% (95% CI: 19.3% to 21.4%) in the placebo group. Aspirin therapy resulted in a 20% increase in the risk for anemia (95% CI, 1.12-1.29).
People who took aspirin were more likely to have lower serum levels of ferritin at the 3-year mark than were those who received placebo. The average decrease in ferritin among participants who took aspirin was 11.5% greater (95% CI, 9.3%-13.7%) than among those who took placebo.
Basil Eldadah, MD, PhD, supervisory medical officer at the National Institute on Aging, part of the National Institutes of Health, said the findings should encourage clinicians to pay closer attention to hemoglobin levels and have conversations with patients to discuss their need for taking aspirin.
“If somebody is already taking aspirin for any reason, keep an eye on hemoglobin,” said Dr. Eldadah, who was not involved in the study. “For somebody who’s taking aspirin and who’s older, and it’s not for an indication like cardiovascular disease, consider seriously whether that’s the best treatment option.”
The study did not examine the functional consequences of anemia on participants, which Dr. Eldadah said could be fodder for future research. The researchers said one limitation was that it was not clear whether anemia was sufficient to cause symptoms that affected participants’ quality of life or whether occult bleeding caused the anemia. The researchers also did not document whether patients saw their regular physicians and received treatment for anemia over the course of the trial.
The study was funded through grants from the National Health and Medical Research Council and the Bill and Melinda Gates Foundation. The authors reported receiving consulting fees, honoraria, and stock options, and have participated on data monitoring boards not related to the study for Vifor Pharma, ITL Biomedical, Pfizer, Boehringer Ingelheim, Bayer Healthcare, AbbVie, and Abbott Diagnostics.
A version of this article originally appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
Upping CO2 does not benefit OHCA patients: TAME
The Targeted Therapeutic Mild Hypercapnia After Resuscitated Cardiac Arrest (TAME) study showed that the intervention failed to improve neurologic or functional outcomes or quality of life at 6 months. However, the researchers also found that slightly elevated CO2 levels were not associated with worse outcomes.
“I think these results show that our hypothesis – that raising CO2 levels as applied in this trial may be beneficial for these patients – was not effective, even though previous work suggested that it would be,” co–lead investigator Alistair Nichol, MD, said in an interview.
“This was a rigorous trial; the intervention was well delivered, and the results are pretty clear. Unfortunately, we have proved a null hypothesis – that this approach doesn’t seem to work,” Dr. Nichol, who is professor of critical care medicine at University College Dublin, said.
“However, we did find that hypercapnia was safe. This is an important finding, as sometimes in very sick patients such as those who develop pneumonia, we have to drive the ventilator less hard to minimize injury to the lungs, and this can lead to higher CO2 levels,” he added. “Our results show that this practice should not be harmful, which is reassuring.”
The TAME study was presented at the Critical Care Reviews 2023 Meeting (CCR23) held in Belfast, Northern Ireland.
It was simultaneously published online in the New England Journal of Medicine.
The researchers explain that after the return of spontaneous circulation, brain hypoperfusion may contribute to cerebral hypoxia, exacerbate brain damage, and lead to poor neurologic outcomes. The partial pressure of arterial carbon dioxide (PaCO2) is the major physiologic regulator of cerebrovascular tone, and increasing CO2 levels increases cerebral blood flow.
Two previous observational studies showed that exposure to hypercapnia was associated with an increase in the likelihood of being discharged home and better neurologic outcomes at 12 months, compared with hypocapnia or normocapnia.
In addition, a physiologic study showed that deliberate increases in PaCO2 induced higher cerebral oxygen saturations, compared with normocapnia. A phase 2 randomized trial showed that hypercapnia significantly attenuated the release of neuron-specific enolase, a biomarker of brain injury, and also suggested better 6-month neurologic recovery with hypercapnia compared with normocapnia.
The current TAME trial was conducted to try to confirm these results in a larger, more definitive study.
For the trial, 1,700 adults with coma who had been resuscitated after out-of-hospital cardiac arrest were randomly assigned to receive either 24 hours of mild hypercapnia (target PaCO2, 50-55 mm Hg) or normocapnia (target PaCO2, 35-45 mm Hg).
The primary outcome – a favorable neurologic outcome, defined as a score of 5 or higher on the Glasgow Outcome Scale–Extended at 6 months – occurred in 43.5% in the mild hypercapnia group and in 44.6% in the normocapnia group (relative risk, 0.98; P = .76).
By 6 months, 48.2% of those in the mild hypercapnia group and 45.9% in the normocapnia group had died (relative risk with mild hypercapnia, 1.05; 95% confidence interval, 0.94-1.16). In the mild hypercapnia group, 53.4% had a poor functional outcome, defined as a Modified Rankin Scale score of 4-6, compared with 51.3% in the normocapnia group.
Health-related quality of life, as assessed by the EQ Visual Analogue Scale component of the EuroQol-5D-5L, was similar in the two groups.
In terms of safety, results showed that mild hypercapnia did not increase the incidence of prespecified adverse events.
The authors note that there is concern that mild hypercapnia may worsen cerebral edema and elevate intracranial pressure; however, elevated intracranial pressure is uncommon in the first 72 hours after the return of spontaneous circulation.
In the TAME trial, there was one case of cerebral edema in the hypercapnia group. “This is a very low rate and would be expected in a group this size, so this does not indicate a safety concern,” Dr. Nichol commented.
The researchers are planning further analyses of biological samples to look for possible prognostic markers.
“These out-of-hospital cardiac arrest patients are a very diverse group, and it may be possible that some patients could have benefited from hypercapnia while others may have been harmed,” Dr. Nichol noted.
“Raising CO2 levels does improve overall delivery of oxygen to the brain, but this might not have occurred in the right areas. It may be possible that some patients benefited, and analysis of biological samples will help us look more closely at this.”
He added that other ongoing trials are investigating hypercapnia in patients with traumatic brain injury.
“These patients are managed differently and often have probes in their brain to measure the response to CO2, so more of a precision medicine approach is possible,” he explained.
He also noted that the TAME study, which was conducted in conjunction with the TTM-2 study investigating hypothermia in out-of-hospital cardiac arrest patients, has established a network of ICU teams around the world, providing an infrastructure for further trials to be performed in this patient population in the future.
The TAME trial was funded by the National Health and Medical Research Council of Australia, the Health Research Board of Ireland, and the Health Research Council of New Zealand.
A version of this article originally appeared on Medscape.com.
The Targeted Therapeutic Mild Hypercapnia After Resuscitated Cardiac Arrest (TAME) study showed that the intervention failed to improve neurologic or functional outcomes or quality of life at 6 months. However, the researchers also found that slightly elevated CO2 levels were not associated with worse outcomes.
“I think these results show that our hypothesis – that raising CO2 levels as applied in this trial may be beneficial for these patients – was not effective, even though previous work suggested that it would be,” co–lead investigator Alistair Nichol, MD, said in an interview.
“This was a rigorous trial; the intervention was well delivered, and the results are pretty clear. Unfortunately, we have proved a null hypothesis – that this approach doesn’t seem to work,” Dr. Nichol, who is professor of critical care medicine at University College Dublin, said.
“However, we did find that hypercapnia was safe. This is an important finding, as sometimes in very sick patients such as those who develop pneumonia, we have to drive the ventilator less hard to minimize injury to the lungs, and this can lead to higher CO2 levels,” he added. “Our results show that this practice should not be harmful, which is reassuring.”
The TAME study was presented at the Critical Care Reviews 2023 Meeting (CCR23) held in Belfast, Northern Ireland.
It was simultaneously published online in the New England Journal of Medicine.
The researchers explain that after the return of spontaneous circulation, brain hypoperfusion may contribute to cerebral hypoxia, exacerbate brain damage, and lead to poor neurologic outcomes. The partial pressure of arterial carbon dioxide (PaCO2) is the major physiologic regulator of cerebrovascular tone, and increasing CO2 levels increases cerebral blood flow.
Two previous observational studies showed that exposure to hypercapnia was associated with an increase in the likelihood of being discharged home and better neurologic outcomes at 12 months, compared with hypocapnia or normocapnia.
In addition, a physiologic study showed that deliberate increases in PaCO2 induced higher cerebral oxygen saturations, compared with normocapnia. A phase 2 randomized trial showed that hypercapnia significantly attenuated the release of neuron-specific enolase, a biomarker of brain injury, and also suggested better 6-month neurologic recovery with hypercapnia compared with normocapnia.
The current TAME trial was conducted to try to confirm these results in a larger, more definitive study.
For the trial, 1,700 adults with coma who had been resuscitated after out-of-hospital cardiac arrest were randomly assigned to receive either 24 hours of mild hypercapnia (target PaCO2, 50-55 mm Hg) or normocapnia (target PaCO2, 35-45 mm Hg).
The primary outcome – a favorable neurologic outcome, defined as a score of 5 or higher on the Glasgow Outcome Scale–Extended at 6 months – occurred in 43.5% in the mild hypercapnia group and in 44.6% in the normocapnia group (relative risk, 0.98; P = .76).
By 6 months, 48.2% of those in the mild hypercapnia group and 45.9% in the normocapnia group had died (relative risk with mild hypercapnia, 1.05; 95% confidence interval, 0.94-1.16). In the mild hypercapnia group, 53.4% had a poor functional outcome, defined as a Modified Rankin Scale score of 4-6, compared with 51.3% in the normocapnia group.
Health-related quality of life, as assessed by the EQ Visual Analogue Scale component of the EuroQol-5D-5L, was similar in the two groups.
In terms of safety, results showed that mild hypercapnia did not increase the incidence of prespecified adverse events.
The authors note that there is concern that mild hypercapnia may worsen cerebral edema and elevate intracranial pressure; however, elevated intracranial pressure is uncommon in the first 72 hours after the return of spontaneous circulation.
In the TAME trial, there was one case of cerebral edema in the hypercapnia group. “This is a very low rate and would be expected in a group this size, so this does not indicate a safety concern,” Dr. Nichol commented.
The researchers are planning further analyses of biological samples to look for possible prognostic markers.
“These out-of-hospital cardiac arrest patients are a very diverse group, and it may be possible that some patients could have benefited from hypercapnia while others may have been harmed,” Dr. Nichol noted.
“Raising CO2 levels does improve overall delivery of oxygen to the brain, but this might not have occurred in the right areas. It may be possible that some patients benefited, and analysis of biological samples will help us look more closely at this.”
He added that other ongoing trials are investigating hypercapnia in patients with traumatic brain injury.
“These patients are managed differently and often have probes in their brain to measure the response to CO2, so more of a precision medicine approach is possible,” he explained.
He also noted that the TAME study, which was conducted in conjunction with the TTM-2 study investigating hypothermia in out-of-hospital cardiac arrest patients, has established a network of ICU teams around the world, providing an infrastructure for further trials to be performed in this patient population in the future.
The TAME trial was funded by the National Health and Medical Research Council of Australia, the Health Research Board of Ireland, and the Health Research Council of New Zealand.
A version of this article originally appeared on Medscape.com.
The Targeted Therapeutic Mild Hypercapnia After Resuscitated Cardiac Arrest (TAME) study showed that the intervention failed to improve neurologic or functional outcomes or quality of life at 6 months. However, the researchers also found that slightly elevated CO2 levels were not associated with worse outcomes.
“I think these results show that our hypothesis – that raising CO2 levels as applied in this trial may be beneficial for these patients – was not effective, even though previous work suggested that it would be,” co–lead investigator Alistair Nichol, MD, said in an interview.
“This was a rigorous trial; the intervention was well delivered, and the results are pretty clear. Unfortunately, we have proved a null hypothesis – that this approach doesn’t seem to work,” Dr. Nichol, who is professor of critical care medicine at University College Dublin, said.
“However, we did find that hypercapnia was safe. This is an important finding, as sometimes in very sick patients such as those who develop pneumonia, we have to drive the ventilator less hard to minimize injury to the lungs, and this can lead to higher CO2 levels,” he added. “Our results show that this practice should not be harmful, which is reassuring.”
The TAME study was presented at the Critical Care Reviews 2023 Meeting (CCR23) held in Belfast, Northern Ireland.
It was simultaneously published online in the New England Journal of Medicine.
The researchers explain that after the return of spontaneous circulation, brain hypoperfusion may contribute to cerebral hypoxia, exacerbate brain damage, and lead to poor neurologic outcomes. The partial pressure of arterial carbon dioxide (PaCO2) is the major physiologic regulator of cerebrovascular tone, and increasing CO2 levels increases cerebral blood flow.
Two previous observational studies showed that exposure to hypercapnia was associated with an increase in the likelihood of being discharged home and better neurologic outcomes at 12 months, compared with hypocapnia or normocapnia.
In addition, a physiologic study showed that deliberate increases in PaCO2 induced higher cerebral oxygen saturations, compared with normocapnia. A phase 2 randomized trial showed that hypercapnia significantly attenuated the release of neuron-specific enolase, a biomarker of brain injury, and also suggested better 6-month neurologic recovery with hypercapnia compared with normocapnia.
The current TAME trial was conducted to try to confirm these results in a larger, more definitive study.
For the trial, 1,700 adults with coma who had been resuscitated after out-of-hospital cardiac arrest were randomly assigned to receive either 24 hours of mild hypercapnia (target PaCO2, 50-55 mm Hg) or normocapnia (target PaCO2, 35-45 mm Hg).
The primary outcome – a favorable neurologic outcome, defined as a score of 5 or higher on the Glasgow Outcome Scale–Extended at 6 months – occurred in 43.5% in the mild hypercapnia group and in 44.6% in the normocapnia group (relative risk, 0.98; P = .76).
By 6 months, 48.2% of those in the mild hypercapnia group and 45.9% in the normocapnia group had died (relative risk with mild hypercapnia, 1.05; 95% confidence interval, 0.94-1.16). In the mild hypercapnia group, 53.4% had a poor functional outcome, defined as a Modified Rankin Scale score of 4-6, compared with 51.3% in the normocapnia group.
Health-related quality of life, as assessed by the EQ Visual Analogue Scale component of the EuroQol-5D-5L, was similar in the two groups.
In terms of safety, results showed that mild hypercapnia did not increase the incidence of prespecified adverse events.
The authors note that there is concern that mild hypercapnia may worsen cerebral edema and elevate intracranial pressure; however, elevated intracranial pressure is uncommon in the first 72 hours after the return of spontaneous circulation.
In the TAME trial, there was one case of cerebral edema in the hypercapnia group. “This is a very low rate and would be expected in a group this size, so this does not indicate a safety concern,” Dr. Nichol commented.
The researchers are planning further analyses of biological samples to look for possible prognostic markers.
“These out-of-hospital cardiac arrest patients are a very diverse group, and it may be possible that some patients could have benefited from hypercapnia while others may have been harmed,” Dr. Nichol noted.
“Raising CO2 levels does improve overall delivery of oxygen to the brain, but this might not have occurred in the right areas. It may be possible that some patients benefited, and analysis of biological samples will help us look more closely at this.”
He added that other ongoing trials are investigating hypercapnia in patients with traumatic brain injury.
“These patients are managed differently and often have probes in their brain to measure the response to CO2, so more of a precision medicine approach is possible,” he explained.
He also noted that the TAME study, which was conducted in conjunction with the TTM-2 study investigating hypothermia in out-of-hospital cardiac arrest patients, has established a network of ICU teams around the world, providing an infrastructure for further trials to be performed in this patient population in the future.
The TAME trial was funded by the National Health and Medical Research Council of Australia, the Health Research Board of Ireland, and the Health Research Council of New Zealand.
A version of this article originally appeared on Medscape.com.
FROM CCR23
Syncope not associated with increased risk for car crash
In a case-crossover study that examined health and driving data for about 3,000 drivers in British Columbia, researchers found similar rates of ED visits for syncope before the dates of car crashes (1.6%) and before control dates (1.2%).
“An emergency visit for syncope did not appear to increase the risk of subsequent traffic crash,” lead author John A. Staples, MD, MPH, clinical associate professor of general internal medicine at the University of British Columbia, Vancouver, said in an interview.
The findings were published online in the Canadian Journal of Cardiology.
Case-crossover study
Syncope prompts more than 1 million visits to EDs in the United States each year. About 9% of patients with syncope have recurrence within 1 year.
Some jurisdictions legally require clinicians to advise patients at higher risk for syncope recurrence to stop driving temporarily. But guidelines about when and whom to restrict are not standardized, said Dr. Staples.
“I came to this topic because I work as a physician in a hospital and, a few years ago, I advised a young woman who suffered a serious injury after she passed out while driving and crashed her car,” he added. “She wanted to know if she could drive again and when. I found out that there wasn’t much evidence that could guide my advice to her. That is what planted the seed that eventually grew into this study.”
The researchers examined driving data from the Insurance Corporation of British Columbia and detailed ED visit data from regional health authorities. They included licensed drivers who were diagnosed with syncope and collapse at an ED between 2010 and 2015 in their study. The researchers focused on eligible participants who were involved in a motor vehicle collision between August 2011 and December 2015.
For each patient, the date of the crash was used to establish three control dates without crashes. The control dates were 26 weeks, 52 weeks, and 78 weeks before the crash. The investigators compared the rate of emergency visit for syncope in the 28 days before the crash with the rate of emergency visit for syncope in the 28 days before each control date.
An emergency visit for syncope occurred in 47 of 3,026 precrash intervals and 112 of 9,078 control intervals. This result indicated that syncope was not significantly associated with subsequent crash (adjusted odds ratio, 1.27; P = .18).
In addition, there was no significant association between syncope and crash in subgroups considered to be at higher risk for adverse outcomes after syncope, such as patients older than 65 years and patients with cardiovascular disease or cardiac syncope.
Gaps in data
“It’s a complicated study design but one that’s helpful to understand the temporal relationship between syncope and crash,” said Dr. Staples. “If we had found that the syncope visit was more likely to occur in the 4 weeks before the crash than in earlier matched 4-week control periods, we would have concluded that syncope transiently increases crash risk.”
Dr. Staples emphasized that this was a real-world study and that some patients with syncope at higher risk for a car crash likely stopped driving. “This study doesn’t say there’s no relationship between syncope and subsequent crash, just that our current practices, including current driving restrictions, seem to do an acceptable job of preventing some crashes.”
Limitations of the study influence the interpretation of the results. For example, the data sources did not indicate how patients modified their driving, said Dr. Staples.
Also lacking is information about how physicians identified which patients were at heightened risk for another syncope episode and advised those patients not to drive. “Now would be a good time to start to think about what other studies are needed to better tailor driving restrictions for the right patient,” said Dr. Staples.
‘A messy situation’
In a comment, Deepak L. Bhatt, MD, MPH, professor of cardiovascular medicine at Icahn School of Medicine at Mount Sinai, New York, called the conclusions “well thought out.” He said the study addressed a common, often perplexing problem in a practical way. Dr. Bhatt was not involved in the research.
“This study is trying to address the issue of what to do with people who have had syncope or fainting and have had a car crash. In general, we don’t really know what to do with those people, but there’s a lot of concern for many reasons, for both the patient and the public. There are potential legal liabilities, and the whole thing, generally speaking, tends to be a messy situation. Usually, the default position physicians take is to be very cautious and conservative, and restrict driving,” said Dr. Bhatt.
The study is reassuring, he added. “The authors have contextualized this risk very nicely. Physicians worry a lot about patients who have had an episode of syncope while driving and restrict their patients’ driving, at least temporarily. But as a society, we are much more permissive about people who drive drunk or under the influence, or who drive without seat belts, or who speed, or text while driving. So, within that larger context, we are extremely worried about this one source of risk that is probably less than these other sources of risk.”
Most of the time, the cause of the syncope is benign, said Dr. Bhatt. “We rule out the bad things, like a heart attack or cardiac arrest, seizure, and arrhythmia. Afterwards, the risk from driving is relatively small.” The study results support current practices and suggest “that we probably don’t need to be excessive with our restrictions.
“There is going to be a wide variation in practice, with some physicians wanting to be more restrictive, but there is a lot of subjectivity in how these recommendations are acted on in real life. That’s why I think this study really should reassure physicians that it’s okay to use common sense and good medical judgment when giving advice on driving to their patients,” Dr. Bhatt concluded.
The study was supported by the Canadian Institutes of Health Research and the Heart and Stroke Foundation Canada. Dr. Staples and Dr. Bhatt reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a case-crossover study that examined health and driving data for about 3,000 drivers in British Columbia, researchers found similar rates of ED visits for syncope before the dates of car crashes (1.6%) and before control dates (1.2%).
“An emergency visit for syncope did not appear to increase the risk of subsequent traffic crash,” lead author John A. Staples, MD, MPH, clinical associate professor of general internal medicine at the University of British Columbia, Vancouver, said in an interview.
The findings were published online in the Canadian Journal of Cardiology.
Case-crossover study
Syncope prompts more than 1 million visits to EDs in the United States each year. About 9% of patients with syncope have recurrence within 1 year.
Some jurisdictions legally require clinicians to advise patients at higher risk for syncope recurrence to stop driving temporarily. But guidelines about when and whom to restrict are not standardized, said Dr. Staples.
“I came to this topic because I work as a physician in a hospital and, a few years ago, I advised a young woman who suffered a serious injury after she passed out while driving and crashed her car,” he added. “She wanted to know if she could drive again and when. I found out that there wasn’t much evidence that could guide my advice to her. That is what planted the seed that eventually grew into this study.”
The researchers examined driving data from the Insurance Corporation of British Columbia and detailed ED visit data from regional health authorities. They included licensed drivers who were diagnosed with syncope and collapse at an ED between 2010 and 2015 in their study. The researchers focused on eligible participants who were involved in a motor vehicle collision between August 2011 and December 2015.
For each patient, the date of the crash was used to establish three control dates without crashes. The control dates were 26 weeks, 52 weeks, and 78 weeks before the crash. The investigators compared the rate of emergency visit for syncope in the 28 days before the crash with the rate of emergency visit for syncope in the 28 days before each control date.
An emergency visit for syncope occurred in 47 of 3,026 precrash intervals and 112 of 9,078 control intervals. This result indicated that syncope was not significantly associated with subsequent crash (adjusted odds ratio, 1.27; P = .18).
In addition, there was no significant association between syncope and crash in subgroups considered to be at higher risk for adverse outcomes after syncope, such as patients older than 65 years and patients with cardiovascular disease or cardiac syncope.
Gaps in data
“It’s a complicated study design but one that’s helpful to understand the temporal relationship between syncope and crash,” said Dr. Staples. “If we had found that the syncope visit was more likely to occur in the 4 weeks before the crash than in earlier matched 4-week control periods, we would have concluded that syncope transiently increases crash risk.”
Dr. Staples emphasized that this was a real-world study and that some patients with syncope at higher risk for a car crash likely stopped driving. “This study doesn’t say there’s no relationship between syncope and subsequent crash, just that our current practices, including current driving restrictions, seem to do an acceptable job of preventing some crashes.”
Limitations of the study influence the interpretation of the results. For example, the data sources did not indicate how patients modified their driving, said Dr. Staples.
Also lacking is information about how physicians identified which patients were at heightened risk for another syncope episode and advised those patients not to drive. “Now would be a good time to start to think about what other studies are needed to better tailor driving restrictions for the right patient,” said Dr. Staples.
‘A messy situation’
In a comment, Deepak L. Bhatt, MD, MPH, professor of cardiovascular medicine at Icahn School of Medicine at Mount Sinai, New York, called the conclusions “well thought out.” He said the study addressed a common, often perplexing problem in a practical way. Dr. Bhatt was not involved in the research.
“This study is trying to address the issue of what to do with people who have had syncope or fainting and have had a car crash. In general, we don’t really know what to do with those people, but there’s a lot of concern for many reasons, for both the patient and the public. There are potential legal liabilities, and the whole thing, generally speaking, tends to be a messy situation. Usually, the default position physicians take is to be very cautious and conservative, and restrict driving,” said Dr. Bhatt.
The study is reassuring, he added. “The authors have contextualized this risk very nicely. Physicians worry a lot about patients who have had an episode of syncope while driving and restrict their patients’ driving, at least temporarily. But as a society, we are much more permissive about people who drive drunk or under the influence, or who drive without seat belts, or who speed, or text while driving. So, within that larger context, we are extremely worried about this one source of risk that is probably less than these other sources of risk.”
Most of the time, the cause of the syncope is benign, said Dr. Bhatt. “We rule out the bad things, like a heart attack or cardiac arrest, seizure, and arrhythmia. Afterwards, the risk from driving is relatively small.” The study results support current practices and suggest “that we probably don’t need to be excessive with our restrictions.
“There is going to be a wide variation in practice, with some physicians wanting to be more restrictive, but there is a lot of subjectivity in how these recommendations are acted on in real life. That’s why I think this study really should reassure physicians that it’s okay to use common sense and good medical judgment when giving advice on driving to their patients,” Dr. Bhatt concluded.
The study was supported by the Canadian Institutes of Health Research and the Heart and Stroke Foundation Canada. Dr. Staples and Dr. Bhatt reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a case-crossover study that examined health and driving data for about 3,000 drivers in British Columbia, researchers found similar rates of ED visits for syncope before the dates of car crashes (1.6%) and before control dates (1.2%).
“An emergency visit for syncope did not appear to increase the risk of subsequent traffic crash,” lead author John A. Staples, MD, MPH, clinical associate professor of general internal medicine at the University of British Columbia, Vancouver, said in an interview.
The findings were published online in the Canadian Journal of Cardiology.
Case-crossover study
Syncope prompts more than 1 million visits to EDs in the United States each year. About 9% of patients with syncope have recurrence within 1 year.
Some jurisdictions legally require clinicians to advise patients at higher risk for syncope recurrence to stop driving temporarily. But guidelines about when and whom to restrict are not standardized, said Dr. Staples.
“I came to this topic because I work as a physician in a hospital and, a few years ago, I advised a young woman who suffered a serious injury after she passed out while driving and crashed her car,” he added. “She wanted to know if she could drive again and when. I found out that there wasn’t much evidence that could guide my advice to her. That is what planted the seed that eventually grew into this study.”
The researchers examined driving data from the Insurance Corporation of British Columbia and detailed ED visit data from regional health authorities. They included licensed drivers who were diagnosed with syncope and collapse at an ED between 2010 and 2015 in their study. The researchers focused on eligible participants who were involved in a motor vehicle collision between August 2011 and December 2015.
For each patient, the date of the crash was used to establish three control dates without crashes. The control dates were 26 weeks, 52 weeks, and 78 weeks before the crash. The investigators compared the rate of emergency visit for syncope in the 28 days before the crash with the rate of emergency visit for syncope in the 28 days before each control date.
An emergency visit for syncope occurred in 47 of 3,026 precrash intervals and 112 of 9,078 control intervals. This result indicated that syncope was not significantly associated with subsequent crash (adjusted odds ratio, 1.27; P = .18).
In addition, there was no significant association between syncope and crash in subgroups considered to be at higher risk for adverse outcomes after syncope, such as patients older than 65 years and patients with cardiovascular disease or cardiac syncope.
Gaps in data
“It’s a complicated study design but one that’s helpful to understand the temporal relationship between syncope and crash,” said Dr. Staples. “If we had found that the syncope visit was more likely to occur in the 4 weeks before the crash than in earlier matched 4-week control periods, we would have concluded that syncope transiently increases crash risk.”
Dr. Staples emphasized that this was a real-world study and that some patients with syncope at higher risk for a car crash likely stopped driving. “This study doesn’t say there’s no relationship between syncope and subsequent crash, just that our current practices, including current driving restrictions, seem to do an acceptable job of preventing some crashes.”
Limitations of the study influence the interpretation of the results. For example, the data sources did not indicate how patients modified their driving, said Dr. Staples.
Also lacking is information about how physicians identified which patients were at heightened risk for another syncope episode and advised those patients not to drive. “Now would be a good time to start to think about what other studies are needed to better tailor driving restrictions for the right patient,” said Dr. Staples.
‘A messy situation’
In a comment, Deepak L. Bhatt, MD, MPH, professor of cardiovascular medicine at Icahn School of Medicine at Mount Sinai, New York, called the conclusions “well thought out.” He said the study addressed a common, often perplexing problem in a practical way. Dr. Bhatt was not involved in the research.
“This study is trying to address the issue of what to do with people who have had syncope or fainting and have had a car crash. In general, we don’t really know what to do with those people, but there’s a lot of concern for many reasons, for both the patient and the public. There are potential legal liabilities, and the whole thing, generally speaking, tends to be a messy situation. Usually, the default position physicians take is to be very cautious and conservative, and restrict driving,” said Dr. Bhatt.
The study is reassuring, he added. “The authors have contextualized this risk very nicely. Physicians worry a lot about patients who have had an episode of syncope while driving and restrict their patients’ driving, at least temporarily. But as a society, we are much more permissive about people who drive drunk or under the influence, or who drive without seat belts, or who speed, or text while driving. So, within that larger context, we are extremely worried about this one source of risk that is probably less than these other sources of risk.”
Most of the time, the cause of the syncope is benign, said Dr. Bhatt. “We rule out the bad things, like a heart attack or cardiac arrest, seizure, and arrhythmia. Afterwards, the risk from driving is relatively small.” The study results support current practices and suggest “that we probably don’t need to be excessive with our restrictions.
“There is going to be a wide variation in practice, with some physicians wanting to be more restrictive, but there is a lot of subjectivity in how these recommendations are acted on in real life. That’s why I think this study really should reassure physicians that it’s okay to use common sense and good medical judgment when giving advice on driving to their patients,” Dr. Bhatt concluded.
The study was supported by the Canadian Institutes of Health Research and the Heart and Stroke Foundation Canada. Dr. Staples and Dr. Bhatt reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE CANADIAN JOURNAL OF CARDIOLOGY
Rehabilitation improves walk test results for post–pulmonary embolism patients with persistent dyspnea
In patients with persistent dyspnea following a pulmonary embolism, rehabilitation should be considered as a treatment option, according to findings from a randomized, controlled trial comparing usual care to a twice-weekly, 8-week physical exercise program.
The prevalence of persistent dyspnea, functional limitations, and reduced quality of life (QoL) after pulmonary embolism (PE) ranges from 30% to 50% in published studies. While the underlying mechanisms remain unclear and are likely multifactorial, Øyvind Jervan, MD, and colleagues reported, research suggests that deconditioning and psychological factors contribute substantially to post-PE impairment. Optimal management remains unknown.
The investigators randomized adult patients 1:1 from two hospitals (Osfold Hospital and Akershus University Hospital) with PE identified via computed tomography pulmonary angiography 6-72 months prior to study inclusion to either a supervised outpatient exercise program or usual care. The once- or twice-weekly home-based program was tailored to each participant and included a 90-minute educational session on the cardiopulmonary system, diagnosis and treatment of PE and its possible long-term effects, the benefits of exercise and physical activity, and the management of breathlessness. Also during the intervention period, participants were given a simple home-based exercise program to be performed once or twice weekly. Differences between groups in the Incremental Shuttle Walk Test (ISWT), a standardized walking test that assesses exercise capacity, was the primary endpoint. Secondary endpoints included an endurance walk test (ESWT) and measures of symptoms and QoL.
Among 211 participants (median age 57 years; 56% men), the median time from diagnosis to inclusion was 10.3 months. Median baseline walking distance on the ISWT was 695 m with 21% achieving the 1,020-m maximum distance. At follow-up, a between-group difference of 53.0 m favored the rehabilitation group (89 evaluable subjects; 87 in usual care) (P = .0035). While subgroup analysis revealed a greater difference for those with shorter time from diagnosis (6-12 months vs. 12.1-72 months), the between-group differences were nonsignificant. Also, no ISWT differences between the intervention and control group were found for those with higher pulmonary embolism severity and dyspnea scores. The walk endurance test revealed no between-group differences.
Scores at follow-up on the Pulmonary Embolism-QoL questionnaire favored the rehabilitation group (mean difference –4%; P = .041), but there were no differences in generic QoL, dyspnea scores, or the ESWT.
“The present study adds to the growing evidence of the benefits of rehabilitation after PE,” the researchers stated. Although several recent studies have shown rehabilitation after PE results that were promising, the authors pointed out that most of these studies have been small or have lacked a control group, with great variations between them with respect to time, mode, and duration of intervention. In addition, the current study is the largest one addressing the effect of rehabilitation after PE to demonstrate in subjects with persistent dyspnea a positive effect on exercise capacity and QoL.
The researchers also commented that the small detected mean difference of 53 m in walking distance was lower than has been considered a worthwhile improvement by some, and its clinical relevance can be debated. Other studies, however, have used mean group differences of 40-62 m as clinically meaningful. The authors underscored also that the ISWT data were subject to a considerable ceiling effect which may underestimate the effect size.
Addressing study limitations, the researchers added that: “The rehabilitation program in the present study consisted mainly of exercise training. It is unknown whether the addition of occupational therapy, psychology, or dietary therapy would provide additional benefits for the participants. Most participants had mild symptoms, which may have limited the potential benefits of our rehabilitation program.”
The project was funded by Østfold Hospital Trust. Dr. Jervan reported no relevant conflicts of interest.
In patients with persistent dyspnea following a pulmonary embolism, rehabilitation should be considered as a treatment option, according to findings from a randomized, controlled trial comparing usual care to a twice-weekly, 8-week physical exercise program.
The prevalence of persistent dyspnea, functional limitations, and reduced quality of life (QoL) after pulmonary embolism (PE) ranges from 30% to 50% in published studies. While the underlying mechanisms remain unclear and are likely multifactorial, Øyvind Jervan, MD, and colleagues reported, research suggests that deconditioning and psychological factors contribute substantially to post-PE impairment. Optimal management remains unknown.
The investigators randomized adult patients 1:1 from two hospitals (Osfold Hospital and Akershus University Hospital) with PE identified via computed tomography pulmonary angiography 6-72 months prior to study inclusion to either a supervised outpatient exercise program or usual care. The once- or twice-weekly home-based program was tailored to each participant and included a 90-minute educational session on the cardiopulmonary system, diagnosis and treatment of PE and its possible long-term effects, the benefits of exercise and physical activity, and the management of breathlessness. Also during the intervention period, participants were given a simple home-based exercise program to be performed once or twice weekly. Differences between groups in the Incremental Shuttle Walk Test (ISWT), a standardized walking test that assesses exercise capacity, was the primary endpoint. Secondary endpoints included an endurance walk test (ESWT) and measures of symptoms and QoL.
Among 211 participants (median age 57 years; 56% men), the median time from diagnosis to inclusion was 10.3 months. Median baseline walking distance on the ISWT was 695 m with 21% achieving the 1,020-m maximum distance. At follow-up, a between-group difference of 53.0 m favored the rehabilitation group (89 evaluable subjects; 87 in usual care) (P = .0035). While subgroup analysis revealed a greater difference for those with shorter time from diagnosis (6-12 months vs. 12.1-72 months), the between-group differences were nonsignificant. Also, no ISWT differences between the intervention and control group were found for those with higher pulmonary embolism severity and dyspnea scores. The walk endurance test revealed no between-group differences.
Scores at follow-up on the Pulmonary Embolism-QoL questionnaire favored the rehabilitation group (mean difference –4%; P = .041), but there were no differences in generic QoL, dyspnea scores, or the ESWT.
“The present study adds to the growing evidence of the benefits of rehabilitation after PE,” the researchers stated. Although several recent studies have shown rehabilitation after PE results that were promising, the authors pointed out that most of these studies have been small or have lacked a control group, with great variations between them with respect to time, mode, and duration of intervention. In addition, the current study is the largest one addressing the effect of rehabilitation after PE to demonstrate in subjects with persistent dyspnea a positive effect on exercise capacity and QoL.
The researchers also commented that the small detected mean difference of 53 m in walking distance was lower than has been considered a worthwhile improvement by some, and its clinical relevance can be debated. Other studies, however, have used mean group differences of 40-62 m as clinically meaningful. The authors underscored also that the ISWT data were subject to a considerable ceiling effect which may underestimate the effect size.
Addressing study limitations, the researchers added that: “The rehabilitation program in the present study consisted mainly of exercise training. It is unknown whether the addition of occupational therapy, psychology, or dietary therapy would provide additional benefits for the participants. Most participants had mild symptoms, which may have limited the potential benefits of our rehabilitation program.”
The project was funded by Østfold Hospital Trust. Dr. Jervan reported no relevant conflicts of interest.
In patients with persistent dyspnea following a pulmonary embolism, rehabilitation should be considered as a treatment option, according to findings from a randomized, controlled trial comparing usual care to a twice-weekly, 8-week physical exercise program.
The prevalence of persistent dyspnea, functional limitations, and reduced quality of life (QoL) after pulmonary embolism (PE) ranges from 30% to 50% in published studies. While the underlying mechanisms remain unclear and are likely multifactorial, Øyvind Jervan, MD, and colleagues reported, research suggests that deconditioning and psychological factors contribute substantially to post-PE impairment. Optimal management remains unknown.
The investigators randomized adult patients 1:1 from two hospitals (Osfold Hospital and Akershus University Hospital) with PE identified via computed tomography pulmonary angiography 6-72 months prior to study inclusion to either a supervised outpatient exercise program or usual care. The once- or twice-weekly home-based program was tailored to each participant and included a 90-minute educational session on the cardiopulmonary system, diagnosis and treatment of PE and its possible long-term effects, the benefits of exercise and physical activity, and the management of breathlessness. Also during the intervention period, participants were given a simple home-based exercise program to be performed once or twice weekly. Differences between groups in the Incremental Shuttle Walk Test (ISWT), a standardized walking test that assesses exercise capacity, was the primary endpoint. Secondary endpoints included an endurance walk test (ESWT) and measures of symptoms and QoL.
Among 211 participants (median age 57 years; 56% men), the median time from diagnosis to inclusion was 10.3 months. Median baseline walking distance on the ISWT was 695 m with 21% achieving the 1,020-m maximum distance. At follow-up, a between-group difference of 53.0 m favored the rehabilitation group (89 evaluable subjects; 87 in usual care) (P = .0035). While subgroup analysis revealed a greater difference for those with shorter time from diagnosis (6-12 months vs. 12.1-72 months), the between-group differences were nonsignificant. Also, no ISWT differences between the intervention and control group were found for those with higher pulmonary embolism severity and dyspnea scores. The walk endurance test revealed no between-group differences.
Scores at follow-up on the Pulmonary Embolism-QoL questionnaire favored the rehabilitation group (mean difference –4%; P = .041), but there were no differences in generic QoL, dyspnea scores, or the ESWT.
“The present study adds to the growing evidence of the benefits of rehabilitation after PE,” the researchers stated. Although several recent studies have shown rehabilitation after PE results that were promising, the authors pointed out that most of these studies have been small or have lacked a control group, with great variations between them with respect to time, mode, and duration of intervention. In addition, the current study is the largest one addressing the effect of rehabilitation after PE to demonstrate in subjects with persistent dyspnea a positive effect on exercise capacity and QoL.
The researchers also commented that the small detected mean difference of 53 m in walking distance was lower than has been considered a worthwhile improvement by some, and its clinical relevance can be debated. Other studies, however, have used mean group differences of 40-62 m as clinically meaningful. The authors underscored also that the ISWT data were subject to a considerable ceiling effect which may underestimate the effect size.
Addressing study limitations, the researchers added that: “The rehabilitation program in the present study consisted mainly of exercise training. It is unknown whether the addition of occupational therapy, psychology, or dietary therapy would provide additional benefits for the participants. Most participants had mild symptoms, which may have limited the potential benefits of our rehabilitation program.”
The project was funded by Østfold Hospital Trust. Dr. Jervan reported no relevant conflicts of interest.
FROM THE JOURNAL CHEST
Depression drives metabolic syndrome
Previous research has established a connection between metabolic syndrome and depression, but data on the increased risk for depressed individuals to develop metabolic syndrome (MetS) are lacking, wrote Lara Onofre Ferriani, PhD, of Federal University of Espírito Santo, Vitoria, Brazil, and colleagues.
“Individuals with MetS and depression have increased levels of inflammatory markers, and it is speculated that inflammation could mediate this comorbidity,” they said.
In a study published in the Journal of Psychiatric Research, the investigators reviewed data from 13,883 participants in the Brazilian Longitudinal Study of Adult Health; all were civil servants at universities in Brazil. The participants ranged from 35 to 74 years of age, with a mean age of 51.9 years; 54.3% were women; and 52.4% were white; the mean follow-up period was 3.8 years.
The primary outcome was the association between depression diagnosis and severity on components of MetS at baseline and over a 4-year period. Participants were classified by MetS trajectory as recovered, incident, or persistent, and classified by depression status as without depression or with a mild, moderate, or severe current depressive episode. Depression status was based on the Clinical Interview Schedule Revised. MetS components and diagnosis were based on the National Cholesterol Education Program Adult Treatment Panel III.
In a logistic regression analysis, baseline depression was positively associated with recovered, incident, and persistent MetS (odds ratios, 1.59, 1.45, and 1.70, respectively).
Depression at baseline also was significantly associated with separate components of MetS: large waist circumference, high triglycerides, low high-density lipoprotein cholesterol, and hyperglycemia, with odds ratios of 1.47, 1.23, 1.30, and 1.38, respectively.
Although not seen at baseline, a significant positive association between baseline depression and the presence of three or more MetS components was noted at follow-up, with a positive dose-response effect, the researchers wrote in their discussion.
Not all associations were statistically significant, but this was mainly because of the small number of cases of moderate and severe depression, they said. However, the magnitude of associations was greater in severe depression, when compared with moderate and mild, which suggests that the risk of MetS may be higher in this population, they added.
The study findings were limited by several factors including the possible misclassification of depression, inability to differentiate among depressive subtypes, and the potential lack of generalizability to other populations beyond Brazilian civil servants, the researchers noted.
However, the results were strengthened by the large sample size and support the role of depression as a risk factor for MetS, they said. More research is needed to determine a bidirectional relationship and to assess the trajectory of depression after MetS develops, but the findings “highlight the need to investigate and manage metabolic and cardiovascular alterations in the presence of depression in clinical settings,” they concluded.
The study was supported by the Brazilian Ministry of Health (Science and Technology Department) and the Brazilian Ministry of Science, Technology and Innovation FINEP and CNPq, and by the Coordenaçaõ de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES). The researchers had no financial conflicts to disclose.
Previous research has established a connection between metabolic syndrome and depression, but data on the increased risk for depressed individuals to develop metabolic syndrome (MetS) are lacking, wrote Lara Onofre Ferriani, PhD, of Federal University of Espírito Santo, Vitoria, Brazil, and colleagues.
“Individuals with MetS and depression have increased levels of inflammatory markers, and it is speculated that inflammation could mediate this comorbidity,” they said.
In a study published in the Journal of Psychiatric Research, the investigators reviewed data from 13,883 participants in the Brazilian Longitudinal Study of Adult Health; all were civil servants at universities in Brazil. The participants ranged from 35 to 74 years of age, with a mean age of 51.9 years; 54.3% were women; and 52.4% were white; the mean follow-up period was 3.8 years.
The primary outcome was the association between depression diagnosis and severity on components of MetS at baseline and over a 4-year period. Participants were classified by MetS trajectory as recovered, incident, or persistent, and classified by depression status as without depression or with a mild, moderate, or severe current depressive episode. Depression status was based on the Clinical Interview Schedule Revised. MetS components and diagnosis were based on the National Cholesterol Education Program Adult Treatment Panel III.
In a logistic regression analysis, baseline depression was positively associated with recovered, incident, and persistent MetS (odds ratios, 1.59, 1.45, and 1.70, respectively).
Depression at baseline also was significantly associated with separate components of MetS: large waist circumference, high triglycerides, low high-density lipoprotein cholesterol, and hyperglycemia, with odds ratios of 1.47, 1.23, 1.30, and 1.38, respectively.
Although not seen at baseline, a significant positive association between baseline depression and the presence of three or more MetS components was noted at follow-up, with a positive dose-response effect, the researchers wrote in their discussion.
Not all associations were statistically significant, but this was mainly because of the small number of cases of moderate and severe depression, they said. However, the magnitude of associations was greater in severe depression, when compared with moderate and mild, which suggests that the risk of MetS may be higher in this population, they added.
The study findings were limited by several factors including the possible misclassification of depression, inability to differentiate among depressive subtypes, and the potential lack of generalizability to other populations beyond Brazilian civil servants, the researchers noted.
However, the results were strengthened by the large sample size and support the role of depression as a risk factor for MetS, they said. More research is needed to determine a bidirectional relationship and to assess the trajectory of depression after MetS develops, but the findings “highlight the need to investigate and manage metabolic and cardiovascular alterations in the presence of depression in clinical settings,” they concluded.
The study was supported by the Brazilian Ministry of Health (Science and Technology Department) and the Brazilian Ministry of Science, Technology and Innovation FINEP and CNPq, and by the Coordenaçaõ de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES). The researchers had no financial conflicts to disclose.
Previous research has established a connection between metabolic syndrome and depression, but data on the increased risk for depressed individuals to develop metabolic syndrome (MetS) are lacking, wrote Lara Onofre Ferriani, PhD, of Federal University of Espírito Santo, Vitoria, Brazil, and colleagues.
“Individuals with MetS and depression have increased levels of inflammatory markers, and it is speculated that inflammation could mediate this comorbidity,” they said.
In a study published in the Journal of Psychiatric Research, the investigators reviewed data from 13,883 participants in the Brazilian Longitudinal Study of Adult Health; all were civil servants at universities in Brazil. The participants ranged from 35 to 74 years of age, with a mean age of 51.9 years; 54.3% were women; and 52.4% were white; the mean follow-up period was 3.8 years.
The primary outcome was the association between depression diagnosis and severity on components of MetS at baseline and over a 4-year period. Participants were classified by MetS trajectory as recovered, incident, or persistent, and classified by depression status as without depression or with a mild, moderate, or severe current depressive episode. Depression status was based on the Clinical Interview Schedule Revised. MetS components and diagnosis were based on the National Cholesterol Education Program Adult Treatment Panel III.
In a logistic regression analysis, baseline depression was positively associated with recovered, incident, and persistent MetS (odds ratios, 1.59, 1.45, and 1.70, respectively).
Depression at baseline also was significantly associated with separate components of MetS: large waist circumference, high triglycerides, low high-density lipoprotein cholesterol, and hyperglycemia, with odds ratios of 1.47, 1.23, 1.30, and 1.38, respectively.
Although not seen at baseline, a significant positive association between baseline depression and the presence of three or more MetS components was noted at follow-up, with a positive dose-response effect, the researchers wrote in their discussion.
Not all associations were statistically significant, but this was mainly because of the small number of cases of moderate and severe depression, they said. However, the magnitude of associations was greater in severe depression, when compared with moderate and mild, which suggests that the risk of MetS may be higher in this population, they added.
The study findings were limited by several factors including the possible misclassification of depression, inability to differentiate among depressive subtypes, and the potential lack of generalizability to other populations beyond Brazilian civil servants, the researchers noted.
However, the results were strengthened by the large sample size and support the role of depression as a risk factor for MetS, they said. More research is needed to determine a bidirectional relationship and to assess the trajectory of depression after MetS develops, but the findings “highlight the need to investigate and manage metabolic and cardiovascular alterations in the presence of depression in clinical settings,” they concluded.
The study was supported by the Brazilian Ministry of Health (Science and Technology Department) and the Brazilian Ministry of Science, Technology and Innovation FINEP and CNPq, and by the Coordenaçaõ de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES). The researchers had no financial conflicts to disclose.
FROM THE JOURNAL OF PSYCHIATRIC RESEARCH
Support for minimally invasive mitral valve repair: Mini Mitral published
The trial, which was first presented earlier this year at the American College of Cardiology meeting, showed that minimally invasive mitral valve repair does not improve physical function at 12 weeks, compared with sternotomy, but outcomes at 1 year show minimally invasive repair is as safe and effective as sternotomy for degenerative mitral regurgitation.
The full results are now published online in JAMA.
The authors, led by Enoch Akowuah, MD, South Tees Hospitals NHS Foundation Trust, Middlesbrough, United Kingdom, explain that mitral valve repair surgery is the preferred treatment for patients with degenerative mitral regurgitation and is routinely performed via full sternotomy, enabling easy access to the heart, flexibility in myocardial protection strategies, and multiple ways of accessing the mitral valve and easing de-airing to prevent air emboli, which cause cerebrovascular accidents.
However, the invasiveness of sternotomy is associated with delayed return to presurgery physical function levels and an increase in postoperative complications.
An alternative new video-guided minimally invasive approach involving a 4- to 7-cm lateral thoracotomy, completely avoiding sternotomy, has been developed, with the hope that it should speed physical recovery function after surgery and reduce postoperative complications and costs by reducing hospital stay.
Dr. Akowuah et al. note that uptake of minithoracotomy is variable, with low rates in the United States and the United Kingdom but high rates in Germany. They say that this variation is attributable to the absence of high-quality evidence from randomized trials demonstrating equivalent or superior benefits, compared with sternotomy, and there are also concerns that the increased technical complexity of minithoracotomy may impair the ability to repair complex valve lesions or increase perioperative complications, particularly vascular injuries and stroke.
The U.K. Mini Mitral trial was therefore conducted to compare the effectiveness and safety of minithoracotomy versus sternotomy mitral valve repair.
For the trial, 330 patients with degenerative mitral regurgitation were randomized to receive either minithoracotomy or sternotomy mitral valve repair performed by an expert surgeon.
The primary outcome was physical functioning and associated return to usual activities measured by change from baseline in the 36-Item Short Form Health Survey (SF-36) physical functioning scale 12 weeks after the surgery.
This failed to show superiority of minithoracotomy, with a mean difference of 0.68 (95% confidence interval, −1.89 to 3.26) between the two groups.
Analysis of secondary outcomes demonstrated that time spent undertaking moderate to vigorous physical activity was higher among participants receiving minithoracotomy at 6 weeks, although the treatment effect was small at an average of 9 minutes and was not different at 12 weeks.
Postoperative length of hospital stay was reduced after minithoracotomy by 1 day, with a median of 5 days, compared with 6 days after sternotomy.
Although repair techniques were at the discretion of the surgeons and differed between the two procedures, high rates of valve repair and low rates of recurrent mitral regurgitation were observed in both groups. Cardiopulmonary bypass times were longer with minithoracotomy, but postoperative complications and adverse events were similar.
There was no difference between the two groups with respect to the prespecified safety outcome of death, repeat mitral valve surgery, or heart failure hospitalization up to 1 year, which occurred in 5.4% of patients undergoing minithoracotomy and 6.1% of those undergoing sternotomy.
“These findings can inform shared decision-making and treatment guidelines,” the authors conclude.
Approach ‘may appeal to patients’
In an editorial accompanying the publication of the study in JAMA, Maurice Enriquez-Sarano, MD, Minneapolis Heart Institute, Minnesota, says the results should be integrated into patient management.
“Mini-thoracotomy mitral repair carried low risk and was highly effective compared with sternotomy. It can thus be applied successfully by surgeons who achieve the necessary expertise,” he notes.
“Mini-thoracotomy may appeal to patients because the procedure is less disfiguring than sternotomy. The early (6-week) benefit, albeit small and transient, is important to patients,” he adds.
The study was funded by the United Kingdom’s National Institute for Health and Care Research. Dr. Akowuah reports no relevant financial relationships with industry. Dr. Enriquez-Sarano reports receiving consulting fees from Edwards Lifesciences, Artivion, ChemImage, HighLife, and Corcym.
A version of this article first appeared on Medscape.com.
The trial, which was first presented earlier this year at the American College of Cardiology meeting, showed that minimally invasive mitral valve repair does not improve physical function at 12 weeks, compared with sternotomy, but outcomes at 1 year show minimally invasive repair is as safe and effective as sternotomy for degenerative mitral regurgitation.
The full results are now published online in JAMA.
The authors, led by Enoch Akowuah, MD, South Tees Hospitals NHS Foundation Trust, Middlesbrough, United Kingdom, explain that mitral valve repair surgery is the preferred treatment for patients with degenerative mitral regurgitation and is routinely performed via full sternotomy, enabling easy access to the heart, flexibility in myocardial protection strategies, and multiple ways of accessing the mitral valve and easing de-airing to prevent air emboli, which cause cerebrovascular accidents.
However, the invasiveness of sternotomy is associated with delayed return to presurgery physical function levels and an increase in postoperative complications.
An alternative new video-guided minimally invasive approach involving a 4- to 7-cm lateral thoracotomy, completely avoiding sternotomy, has been developed, with the hope that it should speed physical recovery function after surgery and reduce postoperative complications and costs by reducing hospital stay.
Dr. Akowuah et al. note that uptake of minithoracotomy is variable, with low rates in the United States and the United Kingdom but high rates in Germany. They say that this variation is attributable to the absence of high-quality evidence from randomized trials demonstrating equivalent or superior benefits, compared with sternotomy, and there are also concerns that the increased technical complexity of minithoracotomy may impair the ability to repair complex valve lesions or increase perioperative complications, particularly vascular injuries and stroke.
The U.K. Mini Mitral trial was therefore conducted to compare the effectiveness and safety of minithoracotomy versus sternotomy mitral valve repair.
For the trial, 330 patients with degenerative mitral regurgitation were randomized to receive either minithoracotomy or sternotomy mitral valve repair performed by an expert surgeon.
The primary outcome was physical functioning and associated return to usual activities measured by change from baseline in the 36-Item Short Form Health Survey (SF-36) physical functioning scale 12 weeks after the surgery.
This failed to show superiority of minithoracotomy, with a mean difference of 0.68 (95% confidence interval, −1.89 to 3.26) between the two groups.
Analysis of secondary outcomes demonstrated that time spent undertaking moderate to vigorous physical activity was higher among participants receiving minithoracotomy at 6 weeks, although the treatment effect was small at an average of 9 minutes and was not different at 12 weeks.
Postoperative length of hospital stay was reduced after minithoracotomy by 1 day, with a median of 5 days, compared with 6 days after sternotomy.
Although repair techniques were at the discretion of the surgeons and differed between the two procedures, high rates of valve repair and low rates of recurrent mitral regurgitation were observed in both groups. Cardiopulmonary bypass times were longer with minithoracotomy, but postoperative complications and adverse events were similar.
There was no difference between the two groups with respect to the prespecified safety outcome of death, repeat mitral valve surgery, or heart failure hospitalization up to 1 year, which occurred in 5.4% of patients undergoing minithoracotomy and 6.1% of those undergoing sternotomy.
“These findings can inform shared decision-making and treatment guidelines,” the authors conclude.
Approach ‘may appeal to patients’
In an editorial accompanying the publication of the study in JAMA, Maurice Enriquez-Sarano, MD, Minneapolis Heart Institute, Minnesota, says the results should be integrated into patient management.
“Mini-thoracotomy mitral repair carried low risk and was highly effective compared with sternotomy. It can thus be applied successfully by surgeons who achieve the necessary expertise,” he notes.
“Mini-thoracotomy may appeal to patients because the procedure is less disfiguring than sternotomy. The early (6-week) benefit, albeit small and transient, is important to patients,” he adds.
The study was funded by the United Kingdom’s National Institute for Health and Care Research. Dr. Akowuah reports no relevant financial relationships with industry. Dr. Enriquez-Sarano reports receiving consulting fees from Edwards Lifesciences, Artivion, ChemImage, HighLife, and Corcym.
A version of this article first appeared on Medscape.com.
The trial, which was first presented earlier this year at the American College of Cardiology meeting, showed that minimally invasive mitral valve repair does not improve physical function at 12 weeks, compared with sternotomy, but outcomes at 1 year show minimally invasive repair is as safe and effective as sternotomy for degenerative mitral regurgitation.
The full results are now published online in JAMA.
The authors, led by Enoch Akowuah, MD, South Tees Hospitals NHS Foundation Trust, Middlesbrough, United Kingdom, explain that mitral valve repair surgery is the preferred treatment for patients with degenerative mitral regurgitation and is routinely performed via full sternotomy, enabling easy access to the heart, flexibility in myocardial protection strategies, and multiple ways of accessing the mitral valve and easing de-airing to prevent air emboli, which cause cerebrovascular accidents.
However, the invasiveness of sternotomy is associated with delayed return to presurgery physical function levels and an increase in postoperative complications.
An alternative new video-guided minimally invasive approach involving a 4- to 7-cm lateral thoracotomy, completely avoiding sternotomy, has been developed, with the hope that it should speed physical recovery function after surgery and reduce postoperative complications and costs by reducing hospital stay.
Dr. Akowuah et al. note that uptake of minithoracotomy is variable, with low rates in the United States and the United Kingdom but high rates in Germany. They say that this variation is attributable to the absence of high-quality evidence from randomized trials demonstrating equivalent or superior benefits, compared with sternotomy, and there are also concerns that the increased technical complexity of minithoracotomy may impair the ability to repair complex valve lesions or increase perioperative complications, particularly vascular injuries and stroke.
The U.K. Mini Mitral trial was therefore conducted to compare the effectiveness and safety of minithoracotomy versus sternotomy mitral valve repair.
For the trial, 330 patients with degenerative mitral regurgitation were randomized to receive either minithoracotomy or sternotomy mitral valve repair performed by an expert surgeon.
The primary outcome was physical functioning and associated return to usual activities measured by change from baseline in the 36-Item Short Form Health Survey (SF-36) physical functioning scale 12 weeks after the surgery.
This failed to show superiority of minithoracotomy, with a mean difference of 0.68 (95% confidence interval, −1.89 to 3.26) between the two groups.
Analysis of secondary outcomes demonstrated that time spent undertaking moderate to vigorous physical activity was higher among participants receiving minithoracotomy at 6 weeks, although the treatment effect was small at an average of 9 minutes and was not different at 12 weeks.
Postoperative length of hospital stay was reduced after minithoracotomy by 1 day, with a median of 5 days, compared with 6 days after sternotomy.
Although repair techniques were at the discretion of the surgeons and differed between the two procedures, high rates of valve repair and low rates of recurrent mitral regurgitation were observed in both groups. Cardiopulmonary bypass times were longer with minithoracotomy, but postoperative complications and adverse events were similar.
There was no difference between the two groups with respect to the prespecified safety outcome of death, repeat mitral valve surgery, or heart failure hospitalization up to 1 year, which occurred in 5.4% of patients undergoing minithoracotomy and 6.1% of those undergoing sternotomy.
“These findings can inform shared decision-making and treatment guidelines,” the authors conclude.
Approach ‘may appeal to patients’
In an editorial accompanying the publication of the study in JAMA, Maurice Enriquez-Sarano, MD, Minneapolis Heart Institute, Minnesota, says the results should be integrated into patient management.
“Mini-thoracotomy mitral repair carried low risk and was highly effective compared with sternotomy. It can thus be applied successfully by surgeons who achieve the necessary expertise,” he notes.
“Mini-thoracotomy may appeal to patients because the procedure is less disfiguring than sternotomy. The early (6-week) benefit, albeit small and transient, is important to patients,” he adds.
The study was funded by the United Kingdom’s National Institute for Health and Care Research. Dr. Akowuah reports no relevant financial relationships with industry. Dr. Enriquez-Sarano reports receiving consulting fees from Edwards Lifesciences, Artivion, ChemImage, HighLife, and Corcym.
A version of this article first appeared on Medscape.com.
Alcohol may curb stress signaling in brain to protect heart
The study shows that light to moderate drinking was associated with lower major adverse cardiovascular events (MACE), and this was partly mediated by decreased stress signaling in the brain.
In addition, the benefit of light to moderate drinking with respect to MACE was most pronounced among people with a history of anxiety, a condition known to be associated with higher stress signaling in the brain.
However, the apparent CVD benefits of light to moderate drinking were counterbalanced by an increased risk of cancer.
“There is no safe level of alcohol consumption,” senior author and cardiologist Ahmed Tawakol, MD, codirector of the Cardiovascular Imaging Research Center at Massachusetts General Hospital, Boston, said in an interview.
“We see cancer risk even at the level that we see some protection from heart disease. And higher amounts of alcohol clearly increase heart disease risk,” Dr. Tawakol said.
The study was published online in the Journal of the American College of Cardiology.
Clear mechanistic link
Chronic stress is associated with MACE via stress-related neural network activity (SNA). Light to moderate alcohol consumption has been linked to lower MACE risk, but the mechanisms behind this connection remain unclear.
“We know that when the neural centers of stress are activated, they trigger downstream changes that result in heart disease. And we’ve long appreciated that alcohol in the short term reduces stress, so we hypothesized that maybe alcohol impacts those stress systems chronically and that might explain its cardiovascular effects,” Dr. Tawakol explained.
The study included roughly 53,000 adults (mean age, 60 years; 60% women) from the Mass General Brigham Biobank. The researchers first evaluated the relationship between light to moderate alcohol consumption and MACE after adjusting for a range of genetic, clinical, lifestyle, and socioeconomic factors.
During mean follow-up of 3.4 years, 1,914 individuals experienced MACE. Light to moderate alcohol consumption (compared to none/minimal) was associated with lower MACE risk (hazard ratio [HR], 0.786; 95% confidence interval [CI], 0.717-0.862; P < .0001) after adjustment for cardiovascular risk factors.
The researchers then studied a subset of 713 individuals who had undergone previous PET/CT brain imaging (primarily for cancer surveillance) to determine the effect of light to moderate alcohol consumption on resting SNA.
They found that light to moderate alcohol consumption correlated with decreased SNA (standardized beta, –0.192; 95% CI, –0.338 to 0.046; P = .01). Lower SNA partially mediated the beneficial effect of light to moderate alcohol intake on MACE risk (odds ratio [OR], –0.040; 95% CI, –0.097 to –0.003; P < .05).
Light to moderate alcohol consumption was associated with larger decreases in MACE risk among individuals with a history of anxiety (HR, 0.60; 95% CI, 0.50-0.72, vs. HR, 1.78; 95% CI, 0.73-0.80; P = .003).
The coauthors of an editorial say the discovery of a “new possible mechanism of action” for why light to moderate alcohol consumption might protect the heart “deserves closer attention in future investigations.”
However, Giovanni de Gaetano, MD, PhD, department of epidemiology and prevention, IRCCS NEUROMED, Pozzilli, Italy, one of the authors, emphasized that individuals who consume alcohol should not “exceed the recommended daily dose limits suggested in many countries and that no abstainer should start to drink, even in moderation, solely for the purpose of improving his/her health outcomes.”
Dr. Tawakol and colleagues said that, given alcohol’s adverse health effects, such as heightened cancer risk, new interventions that have positive effects on the neurobiology of stress but without the harmful effects of alcohol are needed.
To that end, they are studying the effect of exercise, stress-reduction interventions such as meditation, and pharmacologic therapies on stress-associated neural networks, and how they might induce CV benefits.
Dr. Tawakol said in an interview that one “additional important message is that anxiety and other related conditions like depression have really substantial health consequences, including increased MACE. Safer interventions that reduce anxiety may yet prove to reduce the risk of heart disease very nicely.”
The study was supported by the National Institutes of Health. Dr. Tawakol and Dr. de Gaetano have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The study shows that light to moderate drinking was associated with lower major adverse cardiovascular events (MACE), and this was partly mediated by decreased stress signaling in the brain.
In addition, the benefit of light to moderate drinking with respect to MACE was most pronounced among people with a history of anxiety, a condition known to be associated with higher stress signaling in the brain.
However, the apparent CVD benefits of light to moderate drinking were counterbalanced by an increased risk of cancer.
“There is no safe level of alcohol consumption,” senior author and cardiologist Ahmed Tawakol, MD, codirector of the Cardiovascular Imaging Research Center at Massachusetts General Hospital, Boston, said in an interview.
“We see cancer risk even at the level that we see some protection from heart disease. And higher amounts of alcohol clearly increase heart disease risk,” Dr. Tawakol said.
The study was published online in the Journal of the American College of Cardiology.
Clear mechanistic link
Chronic stress is associated with MACE via stress-related neural network activity (SNA). Light to moderate alcohol consumption has been linked to lower MACE risk, but the mechanisms behind this connection remain unclear.
“We know that when the neural centers of stress are activated, they trigger downstream changes that result in heart disease. And we’ve long appreciated that alcohol in the short term reduces stress, so we hypothesized that maybe alcohol impacts those stress systems chronically and that might explain its cardiovascular effects,” Dr. Tawakol explained.
The study included roughly 53,000 adults (mean age, 60 years; 60% women) from the Mass General Brigham Biobank. The researchers first evaluated the relationship between light to moderate alcohol consumption and MACE after adjusting for a range of genetic, clinical, lifestyle, and socioeconomic factors.
During mean follow-up of 3.4 years, 1,914 individuals experienced MACE. Light to moderate alcohol consumption (compared to none/minimal) was associated with lower MACE risk (hazard ratio [HR], 0.786; 95% confidence interval [CI], 0.717-0.862; P < .0001) after adjustment for cardiovascular risk factors.
The researchers then studied a subset of 713 individuals who had undergone previous PET/CT brain imaging (primarily for cancer surveillance) to determine the effect of light to moderate alcohol consumption on resting SNA.
They found that light to moderate alcohol consumption correlated with decreased SNA (standardized beta, –0.192; 95% CI, –0.338 to 0.046; P = .01). Lower SNA partially mediated the beneficial effect of light to moderate alcohol intake on MACE risk (odds ratio [OR], –0.040; 95% CI, –0.097 to –0.003; P < .05).
Light to moderate alcohol consumption was associated with larger decreases in MACE risk among individuals with a history of anxiety (HR, 0.60; 95% CI, 0.50-0.72, vs. HR, 1.78; 95% CI, 0.73-0.80; P = .003).
The coauthors of an editorial say the discovery of a “new possible mechanism of action” for why light to moderate alcohol consumption might protect the heart “deserves closer attention in future investigations.”
However, Giovanni de Gaetano, MD, PhD, department of epidemiology and prevention, IRCCS NEUROMED, Pozzilli, Italy, one of the authors, emphasized that individuals who consume alcohol should not “exceed the recommended daily dose limits suggested in many countries and that no abstainer should start to drink, even in moderation, solely for the purpose of improving his/her health outcomes.”
Dr. Tawakol and colleagues said that, given alcohol’s adverse health effects, such as heightened cancer risk, new interventions that have positive effects on the neurobiology of stress but without the harmful effects of alcohol are needed.
To that end, they are studying the effect of exercise, stress-reduction interventions such as meditation, and pharmacologic therapies on stress-associated neural networks, and how they might induce CV benefits.
Dr. Tawakol said in an interview that one “additional important message is that anxiety and other related conditions like depression have really substantial health consequences, including increased MACE. Safer interventions that reduce anxiety may yet prove to reduce the risk of heart disease very nicely.”
The study was supported by the National Institutes of Health. Dr. Tawakol and Dr. de Gaetano have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The study shows that light to moderate drinking was associated with lower major adverse cardiovascular events (MACE), and this was partly mediated by decreased stress signaling in the brain.
In addition, the benefit of light to moderate drinking with respect to MACE was most pronounced among people with a history of anxiety, a condition known to be associated with higher stress signaling in the brain.
However, the apparent CVD benefits of light to moderate drinking were counterbalanced by an increased risk of cancer.
“There is no safe level of alcohol consumption,” senior author and cardiologist Ahmed Tawakol, MD, codirector of the Cardiovascular Imaging Research Center at Massachusetts General Hospital, Boston, said in an interview.
“We see cancer risk even at the level that we see some protection from heart disease. And higher amounts of alcohol clearly increase heart disease risk,” Dr. Tawakol said.
The study was published online in the Journal of the American College of Cardiology.
Clear mechanistic link
Chronic stress is associated with MACE via stress-related neural network activity (SNA). Light to moderate alcohol consumption has been linked to lower MACE risk, but the mechanisms behind this connection remain unclear.
“We know that when the neural centers of stress are activated, they trigger downstream changes that result in heart disease. And we’ve long appreciated that alcohol in the short term reduces stress, so we hypothesized that maybe alcohol impacts those stress systems chronically and that might explain its cardiovascular effects,” Dr. Tawakol explained.
The study included roughly 53,000 adults (mean age, 60 years; 60% women) from the Mass General Brigham Biobank. The researchers first evaluated the relationship between light to moderate alcohol consumption and MACE after adjusting for a range of genetic, clinical, lifestyle, and socioeconomic factors.
During mean follow-up of 3.4 years, 1,914 individuals experienced MACE. Light to moderate alcohol consumption (compared to none/minimal) was associated with lower MACE risk (hazard ratio [HR], 0.786; 95% confidence interval [CI], 0.717-0.862; P < .0001) after adjustment for cardiovascular risk factors.
The researchers then studied a subset of 713 individuals who had undergone previous PET/CT brain imaging (primarily for cancer surveillance) to determine the effect of light to moderate alcohol consumption on resting SNA.
They found that light to moderate alcohol consumption correlated with decreased SNA (standardized beta, –0.192; 95% CI, –0.338 to 0.046; P = .01). Lower SNA partially mediated the beneficial effect of light to moderate alcohol intake on MACE risk (odds ratio [OR], –0.040; 95% CI, –0.097 to –0.003; P < .05).
Light to moderate alcohol consumption was associated with larger decreases in MACE risk among individuals with a history of anxiety (HR, 0.60; 95% CI, 0.50-0.72, vs. HR, 1.78; 95% CI, 0.73-0.80; P = .003).
The coauthors of an editorial say the discovery of a “new possible mechanism of action” for why light to moderate alcohol consumption might protect the heart “deserves closer attention in future investigations.”
However, Giovanni de Gaetano, MD, PhD, department of epidemiology and prevention, IRCCS NEUROMED, Pozzilli, Italy, one of the authors, emphasized that individuals who consume alcohol should not “exceed the recommended daily dose limits suggested in many countries and that no abstainer should start to drink, even in moderation, solely for the purpose of improving his/her health outcomes.”
Dr. Tawakol and colleagues said that, given alcohol’s adverse health effects, such as heightened cancer risk, new interventions that have positive effects on the neurobiology of stress but without the harmful effects of alcohol are needed.
To that end, they are studying the effect of exercise, stress-reduction interventions such as meditation, and pharmacologic therapies on stress-associated neural networks, and how they might induce CV benefits.
Dr. Tawakol said in an interview that one “additional important message is that anxiety and other related conditions like depression have really substantial health consequences, including increased MACE. Safer interventions that reduce anxiety may yet prove to reduce the risk of heart disease very nicely.”
The study was supported by the National Institutes of Health. Dr. Tawakol and Dr. de Gaetano have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
The cardiopulmonary effects of mask wearing
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
There was a time when I would have had to explain to you what an N95 mask is, how it is designed to filter out 95% of fine particles, defined as stuff in the air less than 2.5 microns in size.
But of course, you know that now. The N95 had its moment – a moment that seemed to be passing as the concentration of airborne coronavirus particles decreased.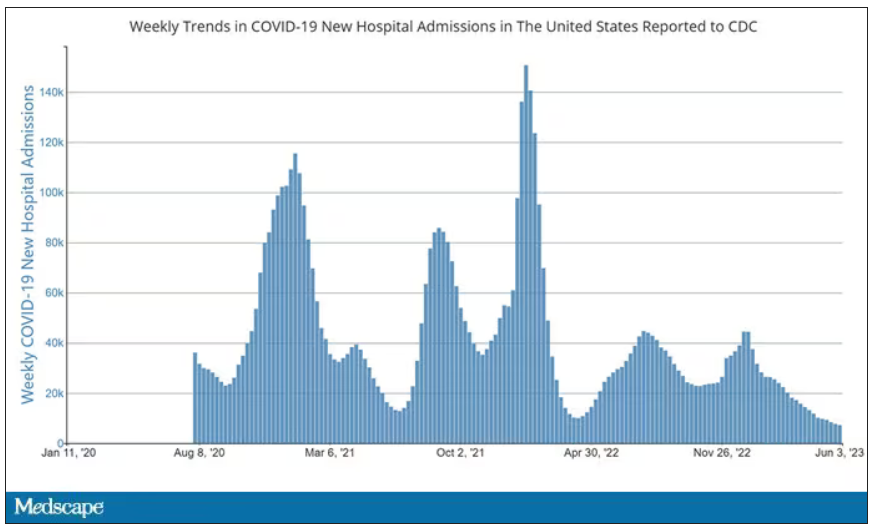
But, as the poet said, all that is less than 2.5 microns in size is not coronavirus. Wildfire smoke is also chock full of fine particulate matter. And so, N95s are having something of a comeback.
That’s why an article that took a deep look at what happens to our cardiovascular system when we wear N95 masks caught my eye.
Mask wearing has been the subject of intense debate around the country. While the vast majority of evidence, as well as the personal experience of thousands of doctors, suggests that wearing a mask has no significant physiologic effects, it’s not hard to find those who suggest that mask wearing depletes oxygen levels, or leads to infection, or has other bizarre effects.
In a world of conflicting opinions, a controlled study is a wonderful thing, and that’s what appeared in JAMA Network Open.
This isn’t a huge study, but it’s big enough to make some important conclusions. Thirty individuals, all young and healthy, half female, were enrolled. Each participant spent 3 days in a metabolic chamber; this is essentially a giant, airtight room where all the inputs (oxygen levels and so on) and outputs (carbon dioxide levels and so on) can be precisely measured.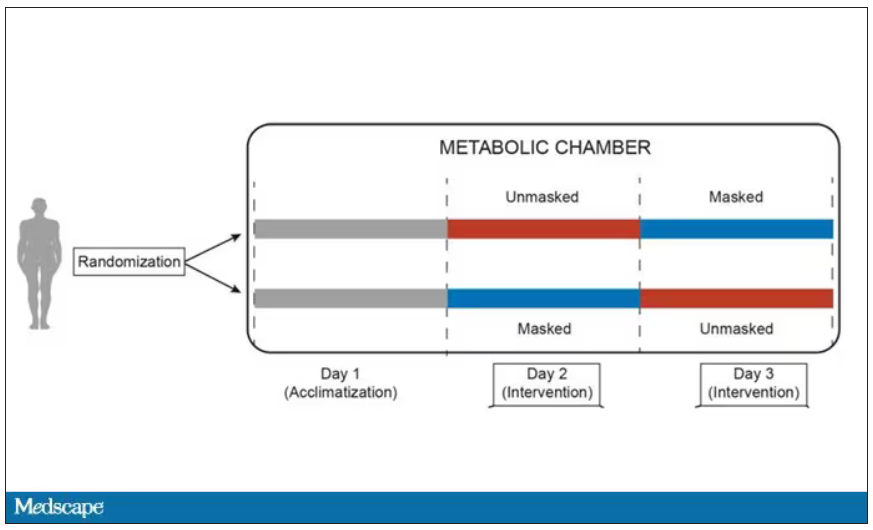
After a day of getting used to the environment, the participants spent a day either wearing an N95 mask or not for 16 waking hours. On the next day, they switched. Every other variable was controlled, from the calories in their diet to the temperature of the room itself.
They engaged in light exercise twice during the day – riding a stationary bike – and a host of physiologic parameters were measured. The question being, would the wearing of the mask for 16 hours straight change anything?
And the answer is yes, some things changed, but not by much.
Here’s a graph of the heart rate over time. You can see some separation, with higher heart rates during the mask-wearing day, particularly around 11 a.m. – when light exercise was scheduled.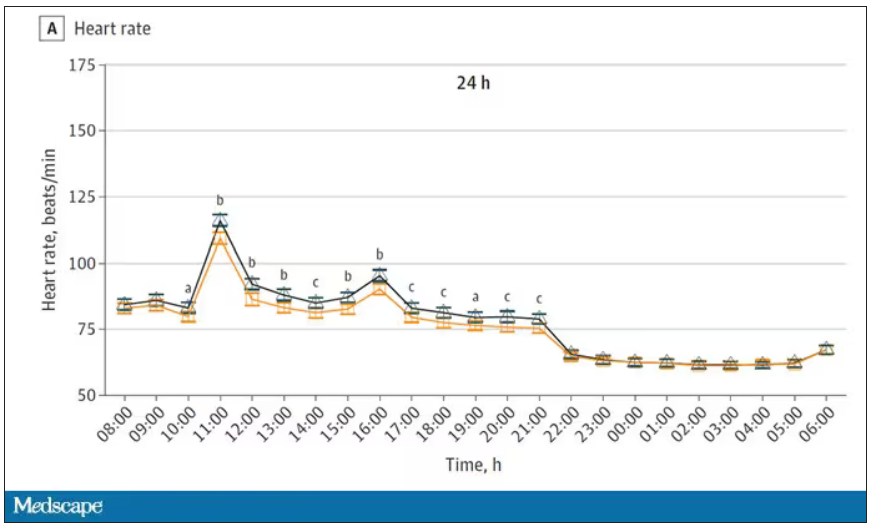
Zooming in on the exercise period makes the difference more clear. The heart rate was about eight beats/min higher while masked and engaging in exercise. Systolic blood pressure was about 6 mm Hg higher. Oxygen saturation was lower by 0.7%.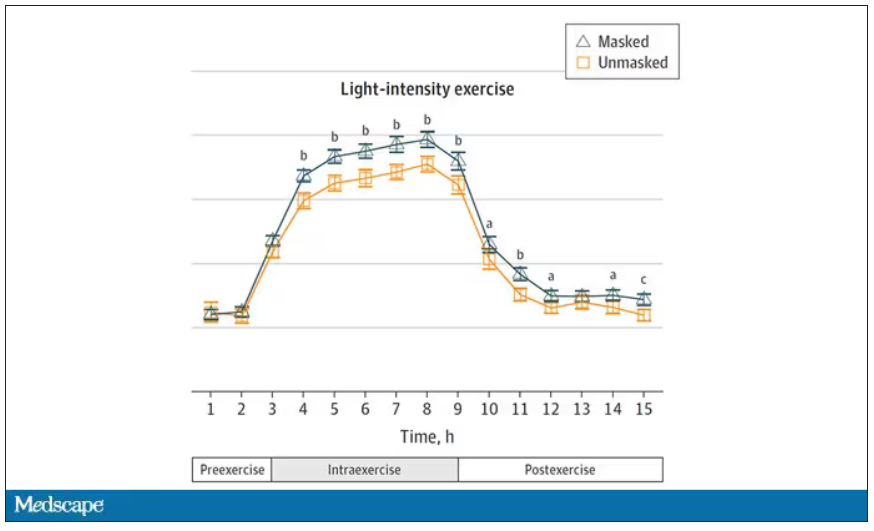
So yes, exercising while wearing an N95 mask might be different from exercising without an N95 mask. But nothing here looks dangerous to me. The 0.7% decrease in oxygen saturation is smaller than the typical measurement error of a pulse oximeter. The authors write that venous pH decreased during the masked day, which is of more interest to me as a nephrologist, but they don’t show that data even in the supplement. I suspect it didn’t decrease much.
They also showed that respiratory rate during exercise decreased in the masked condition. That doesn’t really make sense when you think about it in the context of the other findings, which are all suggestive of increased metabolic rate and sympathetic drive. Does that call the whole procedure into question? No, but it’s worth noting.
These were young, healthy people. You could certainly argue that those with more vulnerable cardiopulmonary status might have had different effects from mask wearing, but without a specific study in those people, it’s just conjecture. Clearly, this study lets us conclude that mask wearing at rest has less of an effect than mask wearing during exercise.
But remember that, in reality, we are wearing masks for a reason. One could imagine a study where this metabolic chamber was filled with wildfire smoke at a concentration similar to what we saw in New York. In that situation, we might find that wearing an N95 is quite helpful. The thing is, studying masks in isolation is useful because you can control so many variables. But masks aren’t used in isolation. In fact, that’s sort of their defining characteristic.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
There was a time when I would have had to explain to you what an N95 mask is, how it is designed to filter out 95% of fine particles, defined as stuff in the air less than 2.5 microns in size.
But of course, you know that now. The N95 had its moment – a moment that seemed to be passing as the concentration of airborne coronavirus particles decreased.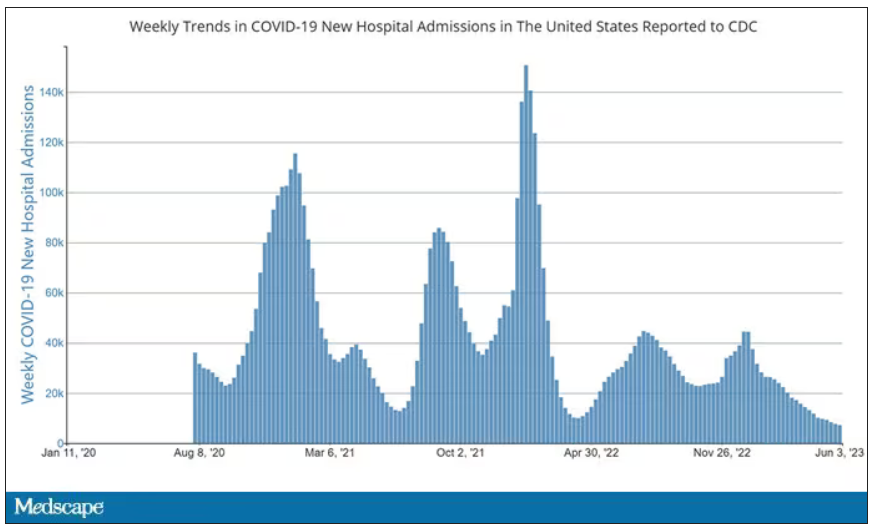
But, as the poet said, all that is less than 2.5 microns in size is not coronavirus. Wildfire smoke is also chock full of fine particulate matter. And so, N95s are having something of a comeback.
That’s why an article that took a deep look at what happens to our cardiovascular system when we wear N95 masks caught my eye.
Mask wearing has been the subject of intense debate around the country. While the vast majority of evidence, as well as the personal experience of thousands of doctors, suggests that wearing a mask has no significant physiologic effects, it’s not hard to find those who suggest that mask wearing depletes oxygen levels, or leads to infection, or has other bizarre effects.
In a world of conflicting opinions, a controlled study is a wonderful thing, and that’s what appeared in JAMA Network Open.
This isn’t a huge study, but it’s big enough to make some important conclusions. Thirty individuals, all young and healthy, half female, were enrolled. Each participant spent 3 days in a metabolic chamber; this is essentially a giant, airtight room where all the inputs (oxygen levels and so on) and outputs (carbon dioxide levels and so on) can be precisely measured.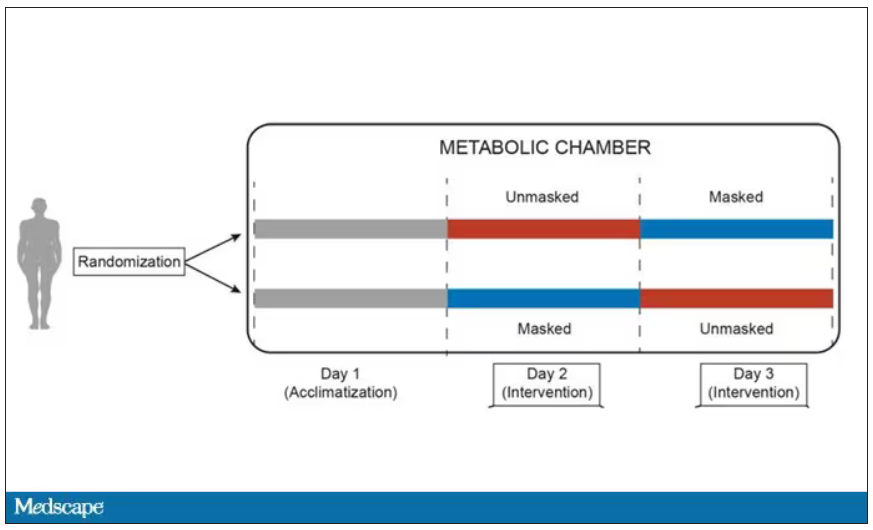
After a day of getting used to the environment, the participants spent a day either wearing an N95 mask or not for 16 waking hours. On the next day, they switched. Every other variable was controlled, from the calories in their diet to the temperature of the room itself.
They engaged in light exercise twice during the day – riding a stationary bike – and a host of physiologic parameters were measured. The question being, would the wearing of the mask for 16 hours straight change anything?
And the answer is yes, some things changed, but not by much.
Here’s a graph of the heart rate over time. You can see some separation, with higher heart rates during the mask-wearing day, particularly around 11 a.m. – when light exercise was scheduled.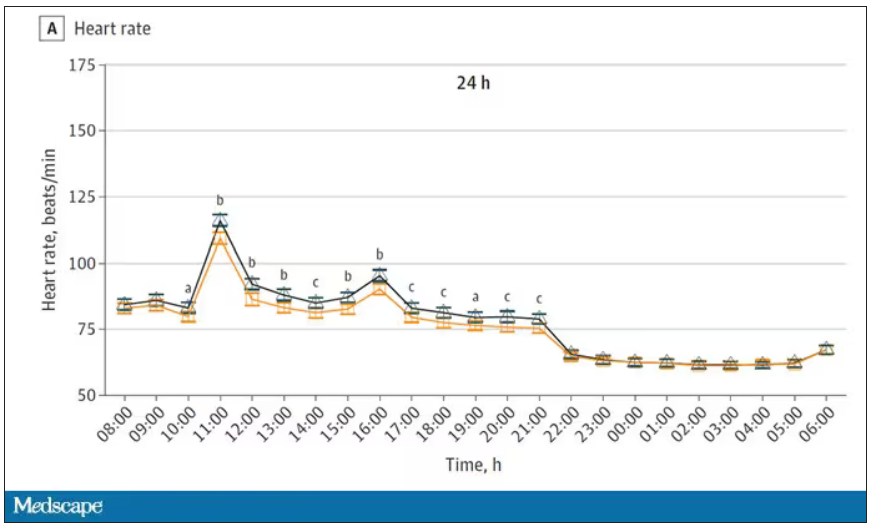
Zooming in on the exercise period makes the difference more clear. The heart rate was about eight beats/min higher while masked and engaging in exercise. Systolic blood pressure was about 6 mm Hg higher. Oxygen saturation was lower by 0.7%.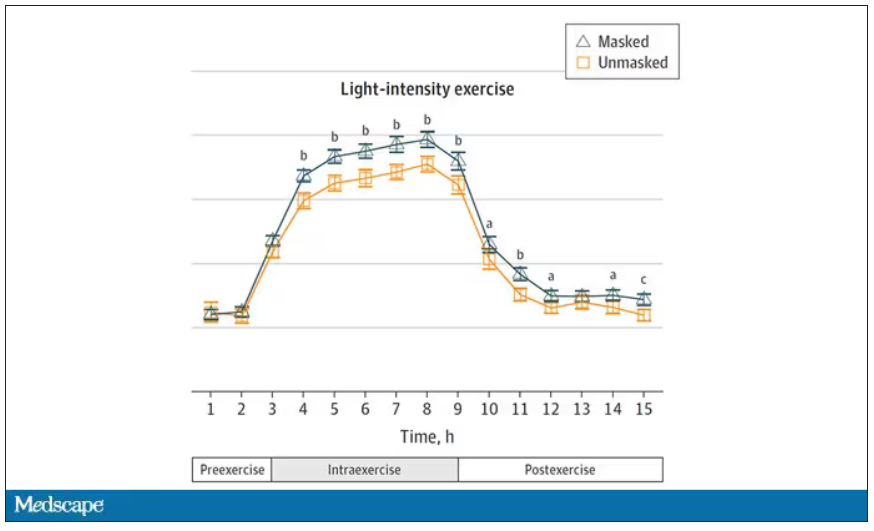
So yes, exercising while wearing an N95 mask might be different from exercising without an N95 mask. But nothing here looks dangerous to me. The 0.7% decrease in oxygen saturation is smaller than the typical measurement error of a pulse oximeter. The authors write that venous pH decreased during the masked day, which is of more interest to me as a nephrologist, but they don’t show that data even in the supplement. I suspect it didn’t decrease much.
They also showed that respiratory rate during exercise decreased in the masked condition. That doesn’t really make sense when you think about it in the context of the other findings, which are all suggestive of increased metabolic rate and sympathetic drive. Does that call the whole procedure into question? No, but it’s worth noting.
These were young, healthy people. You could certainly argue that those with more vulnerable cardiopulmonary status might have had different effects from mask wearing, but without a specific study in those people, it’s just conjecture. Clearly, this study lets us conclude that mask wearing at rest has less of an effect than mask wearing during exercise.
But remember that, in reality, we are wearing masks for a reason. One could imagine a study where this metabolic chamber was filled with wildfire smoke at a concentration similar to what we saw in New York. In that situation, we might find that wearing an N95 is quite helpful. The thing is, studying masks in isolation is useful because you can control so many variables. But masks aren’t used in isolation. In fact, that’s sort of their defining characteristic.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
There was a time when I would have had to explain to you what an N95 mask is, how it is designed to filter out 95% of fine particles, defined as stuff in the air less than 2.5 microns in size.
But of course, you know that now. The N95 had its moment – a moment that seemed to be passing as the concentration of airborne coronavirus particles decreased.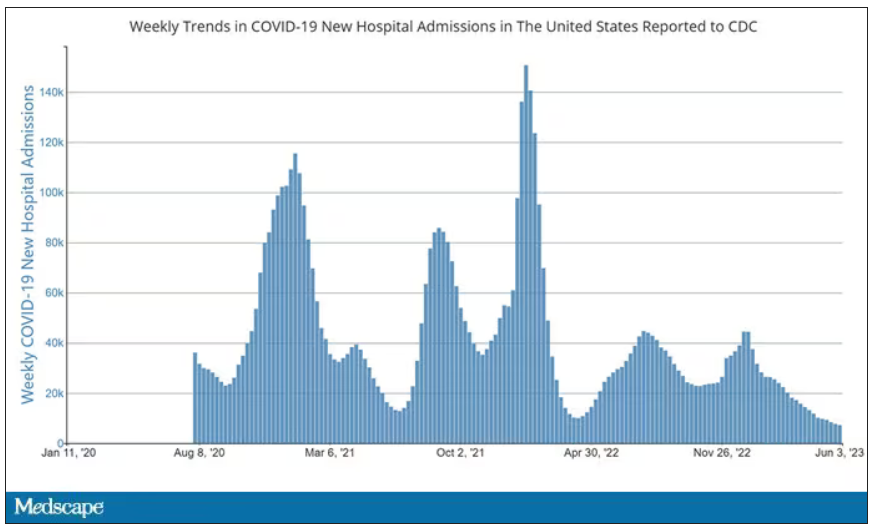
But, as the poet said, all that is less than 2.5 microns in size is not coronavirus. Wildfire smoke is also chock full of fine particulate matter. And so, N95s are having something of a comeback.
That’s why an article that took a deep look at what happens to our cardiovascular system when we wear N95 masks caught my eye.
Mask wearing has been the subject of intense debate around the country. While the vast majority of evidence, as well as the personal experience of thousands of doctors, suggests that wearing a mask has no significant physiologic effects, it’s not hard to find those who suggest that mask wearing depletes oxygen levels, or leads to infection, or has other bizarre effects.
In a world of conflicting opinions, a controlled study is a wonderful thing, and that’s what appeared in JAMA Network Open.
This isn’t a huge study, but it’s big enough to make some important conclusions. Thirty individuals, all young and healthy, half female, were enrolled. Each participant spent 3 days in a metabolic chamber; this is essentially a giant, airtight room where all the inputs (oxygen levels and so on) and outputs (carbon dioxide levels and so on) can be precisely measured.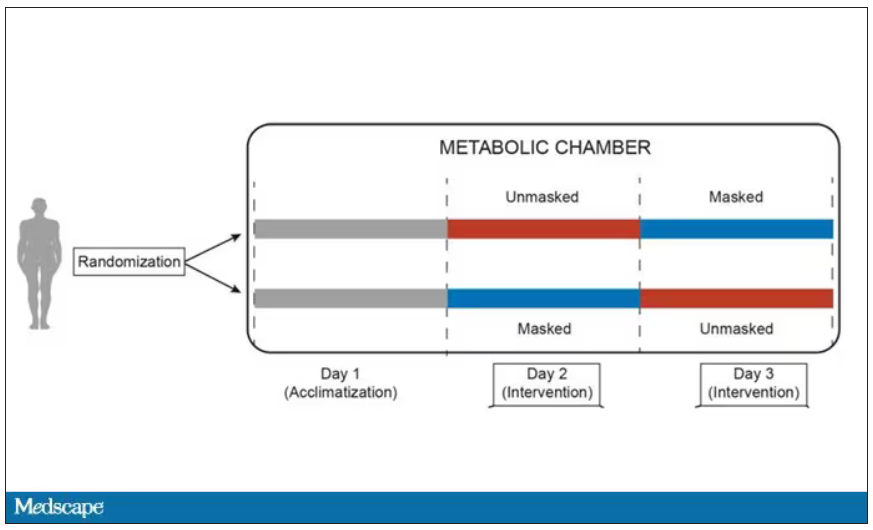
After a day of getting used to the environment, the participants spent a day either wearing an N95 mask or not for 16 waking hours. On the next day, they switched. Every other variable was controlled, from the calories in their diet to the temperature of the room itself.
They engaged in light exercise twice during the day – riding a stationary bike – and a host of physiologic parameters were measured. The question being, would the wearing of the mask for 16 hours straight change anything?
And the answer is yes, some things changed, but not by much.
Here’s a graph of the heart rate over time. You can see some separation, with higher heart rates during the mask-wearing day, particularly around 11 a.m. – when light exercise was scheduled.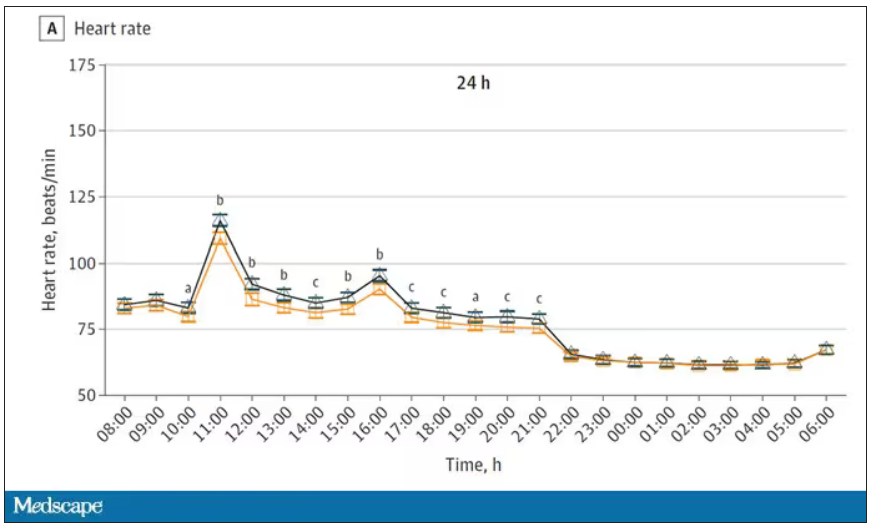
Zooming in on the exercise period makes the difference more clear. The heart rate was about eight beats/min higher while masked and engaging in exercise. Systolic blood pressure was about 6 mm Hg higher. Oxygen saturation was lower by 0.7%.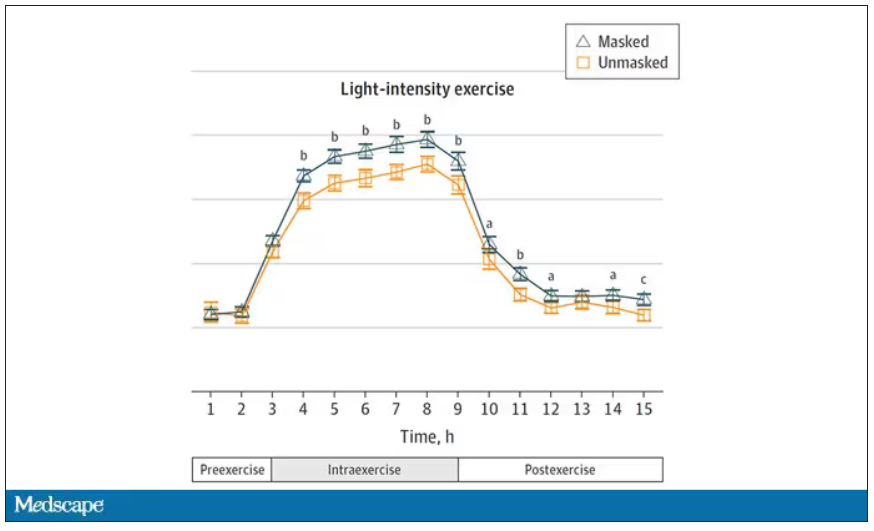
So yes, exercising while wearing an N95 mask might be different from exercising without an N95 mask. But nothing here looks dangerous to me. The 0.7% decrease in oxygen saturation is smaller than the typical measurement error of a pulse oximeter. The authors write that venous pH decreased during the masked day, which is of more interest to me as a nephrologist, but they don’t show that data even in the supplement. I suspect it didn’t decrease much.
They also showed that respiratory rate during exercise decreased in the masked condition. That doesn’t really make sense when you think about it in the context of the other findings, which are all suggestive of increased metabolic rate and sympathetic drive. Does that call the whole procedure into question? No, but it’s worth noting.
These were young, healthy people. You could certainly argue that those with more vulnerable cardiopulmonary status might have had different effects from mask wearing, but without a specific study in those people, it’s just conjecture. Clearly, this study lets us conclude that mask wearing at rest has less of an effect than mask wearing during exercise.
But remember that, in reality, we are wearing masks for a reason. One could imagine a study where this metabolic chamber was filled with wildfire smoke at a concentration similar to what we saw in New York. In that situation, we might find that wearing an N95 is quite helpful. The thing is, studying masks in isolation is useful because you can control so many variables. But masks aren’t used in isolation. In fact, that’s sort of their defining characteristic.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.