User login
Teen girls are in crisis: A call to action resulting from 2021 CDC data
Case: “Where’s my mommy?”
A 13-year-old girl “D” appeared lifeless in her hospital bed, swallowed by tubes, gauze, and crisp white sheets. She seemed fragile next to the giant machines beeping all around her, as they churned and groaned to keep her alive. She was in the pediatric intensive care unit, a place she had only seen once or twice on TV. Her sleeping mother lay next to her in an uncomfortable-looking recliner chair, curled up in a ball. She abruptly woke up when I walked into the room, doing her best to wipe away 5 days’ worth of worry and sadness from her exhausted face. She saw “Child Psychiatrist” written on my hospital badge, desperately searching my face for answers or a sign of hope.
Her daughter – a straight-A middle school student who loved Taylor Swift and soccer – had overdosed on Tylenol after discovering that she did not make the cheerleading team. I reported that her daughter’s liver enzymes were finally trending down and that she would likely not require a liver transplant. She would survive. As tears welled up in this mother’s eyes, I heard a faint whisper from across the room. “Where’s my mommy?” D was awake and frantically searching the room for her mother, someone who could soothe her in this living nightmare. As the two embraced, I felt tears well up in my eyes as I couldn’t help but think of my own 3-year-old daughter at home. How could I protect her from the sadness and despair that this little girl was feeling? How can we collectively protect every little girl from wanting to end their life?
CDC data: Teen girls need help now
The latest biennial Centers for Disease Control and Prevention Youth Risk Behavior Survey, administered in the fall of 2021, resulted in alarming data showing that mental health has worsened for all adolescents, but especially for girls. The survey was administered to more than 17,000 students in 152 public and private schools throughout the United States, showing that “America’s teen girls are engulfed in a growing wave of sadness, violence, and trauma.”1 In particular, rates of sadness, suicidal ideation, suicide attempts, and mental health crisis ED visits among girls are the highest reported in a decade. Nearly 60% of girls felt persistent sadness or hopelessness during the past year, double the rate of boys. More than 25% of girls made a suicide plan; this percentage increased 60% over the past 10 years. Alarmingly, ED visits for suicide attempts for girls increased more than 50% in the past 2 years alone.
Even before the COVID-19 pandemic, experts were sounding the alarm on the growing rates of anxiety and depression in U.S. youth. The pandemic-driven isolation, lack of social connection, and missing of major milestones did not help the situation and only deepened the cracks in a faulty mental health care system. Further, civil unrest and social upheaval in the United States felt – and continues to feel – chaotic and unpredictable. For teens, the current cultural climate represents their not-too-distant future as adults, causing worry and anxiety.
In addition to securing their futures through performance in school and extracurricular activities, teenagers are forming their identities. Establishing a personal identity is a difficult task for all teens, though teenage girls face uniquely difficult challenges in our current society. In particular, teenage girls are expected to conform their behaviors to fit societal expectations that may clash with their desires and self-conceptualization. This conflict is further complicated by heightened beauty standards, online hate and competition, academic pressure, and self-doubt. CDC data show that girls experience sexual harassment and cyberbullying at roughly twice the rate of their male counterparts. Girls also experience higher levels of sexual violence and bullying. Alarmingly, 14% of girls reported being forced to have sex at some point in their lives. The sad truth is that, for every 10 teenage girls you know, at least one of them, and probably more, has likely been raped.
A call to action for providers
As providers, what can we do about these alarming statistics? It’s easy to become overwhelmed by data on a national level. However, regardless of our current clinical practice situation, we cannot lose sight of the humanity behind these numbers. Five extra minutes of truly listening to our patients, normalizing conversations about mental health, and looking for mental health warning signs (that is, increased isolation, declining function in school, maladaptive coping skills such as self-injurious behavior or substance use) can mean the difference between life and death.
As pediatric providers, formally screening for suicide risk is critical. Specifically, the American Academy of Pediatrics recommends that all youth aged 12 years or older be screened for suicide risk.2 In addition to asking families to reduce access to lethal means, it is important to utilize suicide-specific screeners to prevent suicide attempts and deaths in the pediatric community. Pediatric providers must feel prepared to counsel patients and families on suicide prevention and, if this skill set is underdeveloped, appropriate referrals and support must be provided.
At the same time, it is important to note the larger context. This national tragedy has been long-standing and further accelerated by the social isolation and stress of the pandemic. Madigan and colleagues recently showed that the lack of a social outlet resulting from COVID-19 caused an increase in screen time among all children.3 As a result, many teen girls turned to social media to recreate these social connections online.4 This dependence on social media for validation has contributed to increased rates of depression by intensifying unrealistic body standards, comparisons, and competition among peers.5 However, recent pediatric partnership programs have improved mental health access, reduced ED visits, and increased primary care physician’s comfort with managing mental health concerns.6 These programs are called Child Psychiatry Access Programs (CPAPs) and utilize a collaborative care model through which primary care clinicians consult with child and adolescent psychiatrists. CPAPs, while not the entire solution, offer a major step in the right direction toward tackling this mental health crisis in a sustainable, collaborative, and effective way.
As students return to in-person learning, connectedness at school is a powerful protective factor against depression and anxiety. We must infuse resources and support into our schools and teachers, as they stand on the front lines for our children. Specifically, bolstering schools with school counselors and appropriate mental health support staff will help rescue teachers from burnout while also explicitly identifying mental health care as a priority. Finally, modeling positive behavior for families and identifying safe adults at school can help at-risk youth feel more connected. To achieve meaningful improvement in children’s mental health, it is crucial to collaboratively remodel broken systems to ensure that all children are supported early, effectively, and equitably.
Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences, program director of the child and adolescent psychiatry fellowship, and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior in Los Angeles.
References
1. Centers for Disease Control and Prevention. YRBSS Data Summary & Trends. 2023 Feb 13. https://www.cdc.gov/healthyyouth/data/yrbs/yrbs_data_summary_and_trends.htm
2. American Academy of Pediatrics. Screening for Suicide Risk in Clinical Practice. 2023 Feb 22. https://www.aap.org/en/patient-care/blueprint-for-youth-suicide-prevention/strategies-for-clinical-settings-for-youth-suicide-prevention/screening-for-suicide-risk-in-clinical-practice/
3. Madigan S et al. JAMA Pediatr. 2022;176(12):1188-98. doi: 10.1001/JAMAPEDIATRICS.2022.4116
4. Pew Research Center. Teens, Social Media and Technology 2022. 2022 Aug 10. https://www.pewresearch.org/internet/2022/08/10/teens-social-media-and-technology-2022/
5. Hunt MG et al. J Social Clin Psychology. 2018;37(10):751-68. doi: 10.1521/JSCP.2018.37.10.751
6. Godoy L et al. J Pediatr Health Care. 2022 Dec 16. doi: 10.1016/j.pedhc.2022.11.009.
Case: “Where’s my mommy?”
A 13-year-old girl “D” appeared lifeless in her hospital bed, swallowed by tubes, gauze, and crisp white sheets. She seemed fragile next to the giant machines beeping all around her, as they churned and groaned to keep her alive. She was in the pediatric intensive care unit, a place she had only seen once or twice on TV. Her sleeping mother lay next to her in an uncomfortable-looking recliner chair, curled up in a ball. She abruptly woke up when I walked into the room, doing her best to wipe away 5 days’ worth of worry and sadness from her exhausted face. She saw “Child Psychiatrist” written on my hospital badge, desperately searching my face for answers or a sign of hope.
Her daughter – a straight-A middle school student who loved Taylor Swift and soccer – had overdosed on Tylenol after discovering that she did not make the cheerleading team. I reported that her daughter’s liver enzymes were finally trending down and that she would likely not require a liver transplant. She would survive. As tears welled up in this mother’s eyes, I heard a faint whisper from across the room. “Where’s my mommy?” D was awake and frantically searching the room for her mother, someone who could soothe her in this living nightmare. As the two embraced, I felt tears well up in my eyes as I couldn’t help but think of my own 3-year-old daughter at home. How could I protect her from the sadness and despair that this little girl was feeling? How can we collectively protect every little girl from wanting to end their life?
CDC data: Teen girls need help now
The latest biennial Centers for Disease Control and Prevention Youth Risk Behavior Survey, administered in the fall of 2021, resulted in alarming data showing that mental health has worsened for all adolescents, but especially for girls. The survey was administered to more than 17,000 students in 152 public and private schools throughout the United States, showing that “America’s teen girls are engulfed in a growing wave of sadness, violence, and trauma.”1 In particular, rates of sadness, suicidal ideation, suicide attempts, and mental health crisis ED visits among girls are the highest reported in a decade. Nearly 60% of girls felt persistent sadness or hopelessness during the past year, double the rate of boys. More than 25% of girls made a suicide plan; this percentage increased 60% over the past 10 years. Alarmingly, ED visits for suicide attempts for girls increased more than 50% in the past 2 years alone.
Even before the COVID-19 pandemic, experts were sounding the alarm on the growing rates of anxiety and depression in U.S. youth. The pandemic-driven isolation, lack of social connection, and missing of major milestones did not help the situation and only deepened the cracks in a faulty mental health care system. Further, civil unrest and social upheaval in the United States felt – and continues to feel – chaotic and unpredictable. For teens, the current cultural climate represents their not-too-distant future as adults, causing worry and anxiety.
In addition to securing their futures through performance in school and extracurricular activities, teenagers are forming their identities. Establishing a personal identity is a difficult task for all teens, though teenage girls face uniquely difficult challenges in our current society. In particular, teenage girls are expected to conform their behaviors to fit societal expectations that may clash with their desires and self-conceptualization. This conflict is further complicated by heightened beauty standards, online hate and competition, academic pressure, and self-doubt. CDC data show that girls experience sexual harassment and cyberbullying at roughly twice the rate of their male counterparts. Girls also experience higher levels of sexual violence and bullying. Alarmingly, 14% of girls reported being forced to have sex at some point in their lives. The sad truth is that, for every 10 teenage girls you know, at least one of them, and probably more, has likely been raped.
A call to action for providers
As providers, what can we do about these alarming statistics? It’s easy to become overwhelmed by data on a national level. However, regardless of our current clinical practice situation, we cannot lose sight of the humanity behind these numbers. Five extra minutes of truly listening to our patients, normalizing conversations about mental health, and looking for mental health warning signs (that is, increased isolation, declining function in school, maladaptive coping skills such as self-injurious behavior or substance use) can mean the difference between life and death.
As pediatric providers, formally screening for suicide risk is critical. Specifically, the American Academy of Pediatrics recommends that all youth aged 12 years or older be screened for suicide risk.2 In addition to asking families to reduce access to lethal means, it is important to utilize suicide-specific screeners to prevent suicide attempts and deaths in the pediatric community. Pediatric providers must feel prepared to counsel patients and families on suicide prevention and, if this skill set is underdeveloped, appropriate referrals and support must be provided.
At the same time, it is important to note the larger context. This national tragedy has been long-standing and further accelerated by the social isolation and stress of the pandemic. Madigan and colleagues recently showed that the lack of a social outlet resulting from COVID-19 caused an increase in screen time among all children.3 As a result, many teen girls turned to social media to recreate these social connections online.4 This dependence on social media for validation has contributed to increased rates of depression by intensifying unrealistic body standards, comparisons, and competition among peers.5 However, recent pediatric partnership programs have improved mental health access, reduced ED visits, and increased primary care physician’s comfort with managing mental health concerns.6 These programs are called Child Psychiatry Access Programs (CPAPs) and utilize a collaborative care model through which primary care clinicians consult with child and adolescent psychiatrists. CPAPs, while not the entire solution, offer a major step in the right direction toward tackling this mental health crisis in a sustainable, collaborative, and effective way.
As students return to in-person learning, connectedness at school is a powerful protective factor against depression and anxiety. We must infuse resources and support into our schools and teachers, as they stand on the front lines for our children. Specifically, bolstering schools with school counselors and appropriate mental health support staff will help rescue teachers from burnout while also explicitly identifying mental health care as a priority. Finally, modeling positive behavior for families and identifying safe adults at school can help at-risk youth feel more connected. To achieve meaningful improvement in children’s mental health, it is crucial to collaboratively remodel broken systems to ensure that all children are supported early, effectively, and equitably.
Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences, program director of the child and adolescent psychiatry fellowship, and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior in Los Angeles.
References
1. Centers for Disease Control and Prevention. YRBSS Data Summary & Trends. 2023 Feb 13. https://www.cdc.gov/healthyyouth/data/yrbs/yrbs_data_summary_and_trends.htm
2. American Academy of Pediatrics. Screening for Suicide Risk in Clinical Practice. 2023 Feb 22. https://www.aap.org/en/patient-care/blueprint-for-youth-suicide-prevention/strategies-for-clinical-settings-for-youth-suicide-prevention/screening-for-suicide-risk-in-clinical-practice/
3. Madigan S et al. JAMA Pediatr. 2022;176(12):1188-98. doi: 10.1001/JAMAPEDIATRICS.2022.4116
4. Pew Research Center. Teens, Social Media and Technology 2022. 2022 Aug 10. https://www.pewresearch.org/internet/2022/08/10/teens-social-media-and-technology-2022/
5. Hunt MG et al. J Social Clin Psychology. 2018;37(10):751-68. doi: 10.1521/JSCP.2018.37.10.751
6. Godoy L et al. J Pediatr Health Care. 2022 Dec 16. doi: 10.1016/j.pedhc.2022.11.009.
Case: “Where’s my mommy?”
A 13-year-old girl “D” appeared lifeless in her hospital bed, swallowed by tubes, gauze, and crisp white sheets. She seemed fragile next to the giant machines beeping all around her, as they churned and groaned to keep her alive. She was in the pediatric intensive care unit, a place she had only seen once or twice on TV. Her sleeping mother lay next to her in an uncomfortable-looking recliner chair, curled up in a ball. She abruptly woke up when I walked into the room, doing her best to wipe away 5 days’ worth of worry and sadness from her exhausted face. She saw “Child Psychiatrist” written on my hospital badge, desperately searching my face for answers or a sign of hope.
Her daughter – a straight-A middle school student who loved Taylor Swift and soccer – had overdosed on Tylenol after discovering that she did not make the cheerleading team. I reported that her daughter’s liver enzymes were finally trending down and that she would likely not require a liver transplant. She would survive. As tears welled up in this mother’s eyes, I heard a faint whisper from across the room. “Where’s my mommy?” D was awake and frantically searching the room for her mother, someone who could soothe her in this living nightmare. As the two embraced, I felt tears well up in my eyes as I couldn’t help but think of my own 3-year-old daughter at home. How could I protect her from the sadness and despair that this little girl was feeling? How can we collectively protect every little girl from wanting to end their life?
CDC data: Teen girls need help now
The latest biennial Centers for Disease Control and Prevention Youth Risk Behavior Survey, administered in the fall of 2021, resulted in alarming data showing that mental health has worsened for all adolescents, but especially for girls. The survey was administered to more than 17,000 students in 152 public and private schools throughout the United States, showing that “America’s teen girls are engulfed in a growing wave of sadness, violence, and trauma.”1 In particular, rates of sadness, suicidal ideation, suicide attempts, and mental health crisis ED visits among girls are the highest reported in a decade. Nearly 60% of girls felt persistent sadness or hopelessness during the past year, double the rate of boys. More than 25% of girls made a suicide plan; this percentage increased 60% over the past 10 years. Alarmingly, ED visits for suicide attempts for girls increased more than 50% in the past 2 years alone.
Even before the COVID-19 pandemic, experts were sounding the alarm on the growing rates of anxiety and depression in U.S. youth. The pandemic-driven isolation, lack of social connection, and missing of major milestones did not help the situation and only deepened the cracks in a faulty mental health care system. Further, civil unrest and social upheaval in the United States felt – and continues to feel – chaotic and unpredictable. For teens, the current cultural climate represents their not-too-distant future as adults, causing worry and anxiety.
In addition to securing their futures through performance in school and extracurricular activities, teenagers are forming their identities. Establishing a personal identity is a difficult task for all teens, though teenage girls face uniquely difficult challenges in our current society. In particular, teenage girls are expected to conform their behaviors to fit societal expectations that may clash with their desires and self-conceptualization. This conflict is further complicated by heightened beauty standards, online hate and competition, academic pressure, and self-doubt. CDC data show that girls experience sexual harassment and cyberbullying at roughly twice the rate of their male counterparts. Girls also experience higher levels of sexual violence and bullying. Alarmingly, 14% of girls reported being forced to have sex at some point in their lives. The sad truth is that, for every 10 teenage girls you know, at least one of them, and probably more, has likely been raped.
A call to action for providers
As providers, what can we do about these alarming statistics? It’s easy to become overwhelmed by data on a national level. However, regardless of our current clinical practice situation, we cannot lose sight of the humanity behind these numbers. Five extra minutes of truly listening to our patients, normalizing conversations about mental health, and looking for mental health warning signs (that is, increased isolation, declining function in school, maladaptive coping skills such as self-injurious behavior or substance use) can mean the difference between life and death.
As pediatric providers, formally screening for suicide risk is critical. Specifically, the American Academy of Pediatrics recommends that all youth aged 12 years or older be screened for suicide risk.2 In addition to asking families to reduce access to lethal means, it is important to utilize suicide-specific screeners to prevent suicide attempts and deaths in the pediatric community. Pediatric providers must feel prepared to counsel patients and families on suicide prevention and, if this skill set is underdeveloped, appropriate referrals and support must be provided.
At the same time, it is important to note the larger context. This national tragedy has been long-standing and further accelerated by the social isolation and stress of the pandemic. Madigan and colleagues recently showed that the lack of a social outlet resulting from COVID-19 caused an increase in screen time among all children.3 As a result, many teen girls turned to social media to recreate these social connections online.4 This dependence on social media for validation has contributed to increased rates of depression by intensifying unrealistic body standards, comparisons, and competition among peers.5 However, recent pediatric partnership programs have improved mental health access, reduced ED visits, and increased primary care physician’s comfort with managing mental health concerns.6 These programs are called Child Psychiatry Access Programs (CPAPs) and utilize a collaborative care model through which primary care clinicians consult with child and adolescent psychiatrists. CPAPs, while not the entire solution, offer a major step in the right direction toward tackling this mental health crisis in a sustainable, collaborative, and effective way.
As students return to in-person learning, connectedness at school is a powerful protective factor against depression and anxiety. We must infuse resources and support into our schools and teachers, as they stand on the front lines for our children. Specifically, bolstering schools with school counselors and appropriate mental health support staff will help rescue teachers from burnout while also explicitly identifying mental health care as a priority. Finally, modeling positive behavior for families and identifying safe adults at school can help at-risk youth feel more connected. To achieve meaningful improvement in children’s mental health, it is crucial to collaboratively remodel broken systems to ensure that all children are supported early, effectively, and equitably.
Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences, program director of the child and adolescent psychiatry fellowship, and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior in Los Angeles.
References
1. Centers for Disease Control and Prevention. YRBSS Data Summary & Trends. 2023 Feb 13. https://www.cdc.gov/healthyyouth/data/yrbs/yrbs_data_summary_and_trends.htm
2. American Academy of Pediatrics. Screening for Suicide Risk in Clinical Practice. 2023 Feb 22. https://www.aap.org/en/patient-care/blueprint-for-youth-suicide-prevention/strategies-for-clinical-settings-for-youth-suicide-prevention/screening-for-suicide-risk-in-clinical-practice/
3. Madigan S et al. JAMA Pediatr. 2022;176(12):1188-98. doi: 10.1001/JAMAPEDIATRICS.2022.4116
4. Pew Research Center. Teens, Social Media and Technology 2022. 2022 Aug 10. https://www.pewresearch.org/internet/2022/08/10/teens-social-media-and-technology-2022/
5. Hunt MG et al. J Social Clin Psychology. 2018;37(10):751-68. doi: 10.1521/JSCP.2018.37.10.751
6. Godoy L et al. J Pediatr Health Care. 2022 Dec 16. doi: 10.1016/j.pedhc.2022.11.009.
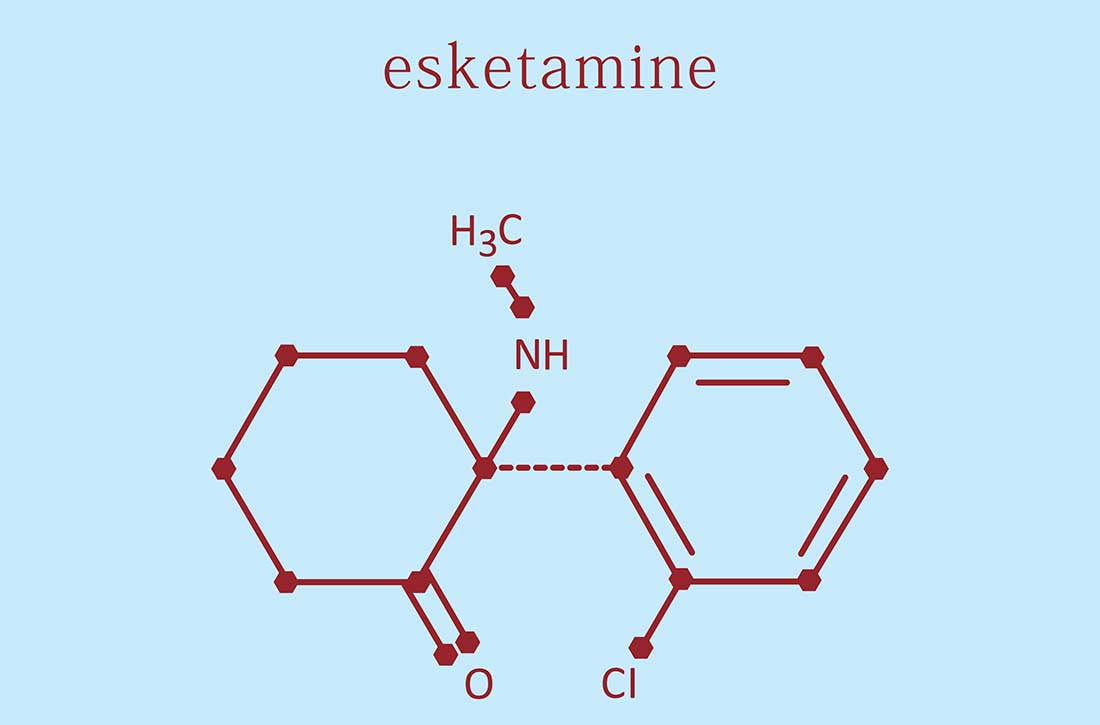
ECT vs. ketamine for major depressive disorder: New data
“Although ECT is superior to ketamine for patients with a major depressive episode, our findings suggest that the therapeutic advantage may be smaller than what was demonstrated in prior analyses,” first author Vikas Menon, MD, department of psychiatry, Jawaharlal Institute of Postgraduate Medical Education & Research, Puducherry, India, told this news organization.
“This supports a recommendation for a trial of ketamine before a trial of ECT for patients with MDE, though this recommendation is limited by the small size and number of existing trials,” Dr. Menon said.
The study was published online in JAMA Psychiatry.
Questions remain
The meta-analysis included five trials of 278 adults with MDE (141 treated with ketamine and 137 with ECT).
In the main analysis, posttreatment depression ratings showed a trend for lower scores with ECT, compared with ketamine (standardized mean difference, −0.39; 95% confidence interval, −0.81 to 0.02).
In a sensitivity analysis of the two methodologically stronger trials, ECT was superior to ketamine (pooled SMD, −0.45; 95% CI, −0.75 to −0.14).
ECT was also superior to ketamine in terms of response rates (risk ratio, 1.27; 95% CI, 1.06-1.53) and remission rates (RR, 1.43; 95% CI, 1.12-1.82).
There were no significant between-group differences for number of sessions to response and remission and for cognitive outcomes.
Key limitations of the analysis were the small number of studies with limited sample sizes and a high risk of bias in all trials.
“There is a need for more comparative studies with adequate sample size in non-inferiority designs, examining a wider range of benefits and side effects and followed up for longer durations to answer clinically relevant questions about the nature and durability of observed benefits with ketamine,” said Dr. Menon.
“In patients with MDE for whom the administration of ECT is limited by restricted availability of the treatment, concerns about its cognitive adverse effects, negative patient attitudes, and other issues, clinicians may consider a trial of ketamine,” he added.
‘Important research’
Several experts offered perspective on the analysis in a statement from the U.K.-based nonprofit Science Media Centre, which was not involved with the conduct of this study.
Rupert McShane, MD, psychiatrist at the University of Oxford (England), noted that ECT and ketamine are both “potent” treatments for depression, and this meta-analysis shows that they are, “broadly speaking, equally as good as each other with perhaps a slight advantage for ECT.”
“Whether or not there is a difference depends on exactly how you define it and how you cut the data. Despite the slight advantage for ECT in this analysis, the authors support using ketamine before ECT, especially in patients who are worried about the cognitive risks of ECT. This seems sensible,” Dr. McShane said.
Allan Young, MBChB, clinical psychiatrist at King’s College London, noted that both ketamine and ECT have been shown to help some patients with treatment-resistant depression.
“Clearly the relative benefits of these two treatments need to be understood better, but this review of the existing literature suggests that ECT may benefit some more than ketamine,” said Mr. Young.
“There is evidence that ketamine with ECT may add little extra benefit, but much more work needs to be done to fully understand how these treatments fit best into the treatment pathway for major depressive episodes. However, based on this evidence, ECT clearly still merits a place in the treatment pathway,” Mr. Young added.
George Kirov, PhD, clinical professor, division of psychological medicine and clinical neurosciences, Cardiff University (England), said while the study is conducted well, most of the evidence is coming from one large trial conducted in Sweden.
“The other studies add small numbers of patients and the authors even present a sensitivity analysis after removing studies of poor quality, thus leaving only two studies and exposing even further the dependence of the results on one single study,” Dr. Kirov noted.
“The small studies should not be blamed for their size, as this is very difficult research to perform. On the other hand, the trends were in the same direction,” he added.
With those caveats in mind, Dr. Kirov said he still thinks this is “important research. It establishes the superiority of ECT against an active comparator (ketamine) which is very popular now and accepted to be quite effective.”
The study had no specific funding. Dr. Menon reports no relevant financial relationships. Dr. McShane is former chair of the ECT and Related Treatments Committee, Royal College of Psychiatrists and runs a ketamine clinic and an ECT service. Mr. Young has received compensation for lectures and advisory boards for AstraZeneca, Eli Lilly, Lundbeck, Sunovion, Servier, Livanova, Janssen, Allergan, Bionomics, Sumitomo Dainippon Pharma, COMPASS, and Sage, and has served as principal investigator on a trial of intranasal esketamine in treatment-resistant depression. Dr. Kirov has no interest to declare other than running the ECT service in Cardiff.
A version of this article first appeared on Medscape.com.
“Although ECT is superior to ketamine for patients with a major depressive episode, our findings suggest that the therapeutic advantage may be smaller than what was demonstrated in prior analyses,” first author Vikas Menon, MD, department of psychiatry, Jawaharlal Institute of Postgraduate Medical Education & Research, Puducherry, India, told this news organization.
“This supports a recommendation for a trial of ketamine before a trial of ECT for patients with MDE, though this recommendation is limited by the small size and number of existing trials,” Dr. Menon said.
The study was published online in JAMA Psychiatry.
Questions remain
The meta-analysis included five trials of 278 adults with MDE (141 treated with ketamine and 137 with ECT).
In the main analysis, posttreatment depression ratings showed a trend for lower scores with ECT, compared with ketamine (standardized mean difference, −0.39; 95% confidence interval, −0.81 to 0.02).
In a sensitivity analysis of the two methodologically stronger trials, ECT was superior to ketamine (pooled SMD, −0.45; 95% CI, −0.75 to −0.14).
ECT was also superior to ketamine in terms of response rates (risk ratio, 1.27; 95% CI, 1.06-1.53) and remission rates (RR, 1.43; 95% CI, 1.12-1.82).
There were no significant between-group differences for number of sessions to response and remission and for cognitive outcomes.
Key limitations of the analysis were the small number of studies with limited sample sizes and a high risk of bias in all trials.
“There is a need for more comparative studies with adequate sample size in non-inferiority designs, examining a wider range of benefits and side effects and followed up for longer durations to answer clinically relevant questions about the nature and durability of observed benefits with ketamine,” said Dr. Menon.
“In patients with MDE for whom the administration of ECT is limited by restricted availability of the treatment, concerns about its cognitive adverse effects, negative patient attitudes, and other issues, clinicians may consider a trial of ketamine,” he added.
‘Important research’
Several experts offered perspective on the analysis in a statement from the U.K.-based nonprofit Science Media Centre, which was not involved with the conduct of this study.
Rupert McShane, MD, psychiatrist at the University of Oxford (England), noted that ECT and ketamine are both “potent” treatments for depression, and this meta-analysis shows that they are, “broadly speaking, equally as good as each other with perhaps a slight advantage for ECT.”
“Whether or not there is a difference depends on exactly how you define it and how you cut the data. Despite the slight advantage for ECT in this analysis, the authors support using ketamine before ECT, especially in patients who are worried about the cognitive risks of ECT. This seems sensible,” Dr. McShane said.
Allan Young, MBChB, clinical psychiatrist at King’s College London, noted that both ketamine and ECT have been shown to help some patients with treatment-resistant depression.
“Clearly the relative benefits of these two treatments need to be understood better, but this review of the existing literature suggests that ECT may benefit some more than ketamine,” said Mr. Young.
“There is evidence that ketamine with ECT may add little extra benefit, but much more work needs to be done to fully understand how these treatments fit best into the treatment pathway for major depressive episodes. However, based on this evidence, ECT clearly still merits a place in the treatment pathway,” Mr. Young added.
George Kirov, PhD, clinical professor, division of psychological medicine and clinical neurosciences, Cardiff University (England), said while the study is conducted well, most of the evidence is coming from one large trial conducted in Sweden.
“The other studies add small numbers of patients and the authors even present a sensitivity analysis after removing studies of poor quality, thus leaving only two studies and exposing even further the dependence of the results on one single study,” Dr. Kirov noted.
“The small studies should not be blamed for their size, as this is very difficult research to perform. On the other hand, the trends were in the same direction,” he added.
With those caveats in mind, Dr. Kirov said he still thinks this is “important research. It establishes the superiority of ECT against an active comparator (ketamine) which is very popular now and accepted to be quite effective.”
The study had no specific funding. Dr. Menon reports no relevant financial relationships. Dr. McShane is former chair of the ECT and Related Treatments Committee, Royal College of Psychiatrists and runs a ketamine clinic and an ECT service. Mr. Young has received compensation for lectures and advisory boards for AstraZeneca, Eli Lilly, Lundbeck, Sunovion, Servier, Livanova, Janssen, Allergan, Bionomics, Sumitomo Dainippon Pharma, COMPASS, and Sage, and has served as principal investigator on a trial of intranasal esketamine in treatment-resistant depression. Dr. Kirov has no interest to declare other than running the ECT service in Cardiff.
A version of this article first appeared on Medscape.com.
“Although ECT is superior to ketamine for patients with a major depressive episode, our findings suggest that the therapeutic advantage may be smaller than what was demonstrated in prior analyses,” first author Vikas Menon, MD, department of psychiatry, Jawaharlal Institute of Postgraduate Medical Education & Research, Puducherry, India, told this news organization.
“This supports a recommendation for a trial of ketamine before a trial of ECT for patients with MDE, though this recommendation is limited by the small size and number of existing trials,” Dr. Menon said.
The study was published online in JAMA Psychiatry.
Questions remain
The meta-analysis included five trials of 278 adults with MDE (141 treated with ketamine and 137 with ECT).
In the main analysis, posttreatment depression ratings showed a trend for lower scores with ECT, compared with ketamine (standardized mean difference, −0.39; 95% confidence interval, −0.81 to 0.02).
In a sensitivity analysis of the two methodologically stronger trials, ECT was superior to ketamine (pooled SMD, −0.45; 95% CI, −0.75 to −0.14).
ECT was also superior to ketamine in terms of response rates (risk ratio, 1.27; 95% CI, 1.06-1.53) and remission rates (RR, 1.43; 95% CI, 1.12-1.82).
There were no significant between-group differences for number of sessions to response and remission and for cognitive outcomes.
Key limitations of the analysis were the small number of studies with limited sample sizes and a high risk of bias in all trials.
“There is a need for more comparative studies with adequate sample size in non-inferiority designs, examining a wider range of benefits and side effects and followed up for longer durations to answer clinically relevant questions about the nature and durability of observed benefits with ketamine,” said Dr. Menon.
“In patients with MDE for whom the administration of ECT is limited by restricted availability of the treatment, concerns about its cognitive adverse effects, negative patient attitudes, and other issues, clinicians may consider a trial of ketamine,” he added.
‘Important research’
Several experts offered perspective on the analysis in a statement from the U.K.-based nonprofit Science Media Centre, which was not involved with the conduct of this study.
Rupert McShane, MD, psychiatrist at the University of Oxford (England), noted that ECT and ketamine are both “potent” treatments for depression, and this meta-analysis shows that they are, “broadly speaking, equally as good as each other with perhaps a slight advantage for ECT.”
“Whether or not there is a difference depends on exactly how you define it and how you cut the data. Despite the slight advantage for ECT in this analysis, the authors support using ketamine before ECT, especially in patients who are worried about the cognitive risks of ECT. This seems sensible,” Dr. McShane said.
Allan Young, MBChB, clinical psychiatrist at King’s College London, noted that both ketamine and ECT have been shown to help some patients with treatment-resistant depression.
“Clearly the relative benefits of these two treatments need to be understood better, but this review of the existing literature suggests that ECT may benefit some more than ketamine,” said Mr. Young.
“There is evidence that ketamine with ECT may add little extra benefit, but much more work needs to be done to fully understand how these treatments fit best into the treatment pathway for major depressive episodes. However, based on this evidence, ECT clearly still merits a place in the treatment pathway,” Mr. Young added.
George Kirov, PhD, clinical professor, division of psychological medicine and clinical neurosciences, Cardiff University (England), said while the study is conducted well, most of the evidence is coming from one large trial conducted in Sweden.
“The other studies add small numbers of patients and the authors even present a sensitivity analysis after removing studies of poor quality, thus leaving only two studies and exposing even further the dependence of the results on one single study,” Dr. Kirov noted.
“The small studies should not be blamed for their size, as this is very difficult research to perform. On the other hand, the trends were in the same direction,” he added.
With those caveats in mind, Dr. Kirov said he still thinks this is “important research. It establishes the superiority of ECT against an active comparator (ketamine) which is very popular now and accepted to be quite effective.”
The study had no specific funding. Dr. Menon reports no relevant financial relationships. Dr. McShane is former chair of the ECT and Related Treatments Committee, Royal College of Psychiatrists and runs a ketamine clinic and an ECT service. Mr. Young has received compensation for lectures and advisory boards for AstraZeneca, Eli Lilly, Lundbeck, Sunovion, Servier, Livanova, Janssen, Allergan, Bionomics, Sumitomo Dainippon Pharma, COMPASS, and Sage, and has served as principal investigator on a trial of intranasal esketamine in treatment-resistant depression. Dr. Kirov has no interest to declare other than running the ECT service in Cardiff.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Anger in adults a red flag for childhood trauma
PARIS –
Investigators examined data on more than 2,250 individuals who were asked about trauma during childhood and a subsequent tendency toward anger or angry outbursts 4 years later.
Results showed that emotional neglect during childhood was associated with approximately a 40% increased likelihood of subsequent anger, while psychological abuse was linked to a 30% increased likelihood.
Childhood physical abuse was also significantly associated with anger in adults, with an increased risk of approximately 40%. The researchers found no link between childhood sexual abuse and adult anger.
“We can’t definitively say that the trauma causes the anger, but the link is clear,” study investigator Nienke De Bles, PhD student, department of psychiatry, Leiden (the Netherlands) University Medical Center, said in a news release.
“Being easily angered can have several consequences,” she continued. “It can make personal interactions more difficult, and it can have consequences for your mental health and well-being, but people who get angry easily also have a greater tendency to discontinue psychiatric treatment, so this anger may mean that it reduces their chances of a better life,” she added.
Ms. De Bles believes that “it should be standard practice to ask depression and anxiety sufferers about anger and past trauma, even if the patient is not exhibiting current anger.”
The findings were presented at the European Psychiatric Association 2023 Congress.
A ‘red flag’ for abuse
“Psychiatric treatments for past trauma may differ from treatments for depression, so psychiatrists need to try to understand the cause so that they can offer the correct treatment to each patient,” said Ms. De Bles.
Ms. De Bles noted that childhood trauma has many negative consequences later in life and that it is associated with a higher prevalence of adult depression and anxiety.
“There are several potential mechanisms for psychopathology in the context of childhood trauma, and emotion regulation seems to be one of the key mechanisms,” she said.
The researchers previously found that anger was highly prevalent among patients with affective disorders. It was present in 30% of those with current anxiety or depressive disorder and in 40% of those with comorbid depression and anxiety with a tendency toward anger versus 5% of healthy control persons.
Other studies have shown that anger is associated with poor treatment outcomes and dropping out of treatment.
To further investigate the link between childhood trauma and anger in adulthood, the researchers examined data on 2,271 participants in the Netherlands Study of Depression and Anxiety (NESDA).
Childhood trauma was assessed at baseline using the semistructured Childhood Trauma Interview. Anger was measured at a 4-year follow-up using the Spielberger Trait Anger Subscale, the Anger Attacks Questionnaire, and the borderline and antisocial subscales of the Personality Disorder Questionnaire 4 to identify cluster B personality traits.
Results showed that emotional neglect during childhood was significantly associated with trait anger in adulthood, at an adjusted odds ratio of 1.42 (P < .001), anger attacks (OR, 1.35; P = .004), and borderline (OR, 1.76; P < .001) and antisocial (OR, 1.88; P = .001) personality traits.
Childhood psychological abuse was also significantly associated with later trait anger (OR, 1.28; P = .002), anger attacks (OR, 1.31; P = .024), and borderline (OR, 1.77; P < .001) and antisocial (OR, 1.69; P = .011) traits.
There was also a significant association between childhood psychical abuse and trait anger in adulthood (OR, 1.37; P < .001), anger attacks (OR, 1.48; P = .004), and borderline (OR, 1.71; P < .001) and antisocial (OR, 1.98; P = .002) traits.
There was no significant association between sexual abuse experienced in childhood and later anger or personality traits.
Ms. De Bles said the findings suggest “there is indeed a relationship between childhood trauma and anger in adulthood, and this is something that might be interesting for clinicians, as anger could be a red flag for a history of childhood trauma.”
She said in an interview that anger is a “very normal human emotion” but that it has not been as widely studied as sadness and anxiety.
She suggested that future research could examine the use of trauma-based therapies for patients with a history of childhood trauma and anger.
Overlooked, neglected
Commenting on the findings, Nur Hani Zainal, PhD, department of healthcare policy, Harvard Medical School, Boston, said the findings are “very consistent with the current biopsychosocial models in psychiatry and clinical psychology.”
Dr. Zainal, who was coauthor of a recent study that showed that anger appears to mediate the relationship between childhood trauma and adult psychopathology, said the current study offers a “good, incremental contribution” to the literature.
She noted there are “good uses” for the emotion of anger, as “sometimes we need anger to set healthy boundaries for ourselves.” However, she agreed that, as an aspect of depression, anxiety, and posttraumatic stress disorder, it is often “overlooked.”
Dr. Zainal said that the findings reinforce the importance of thoroughly evaluating adult patients’ experiences during childhood.
Julian Beezhold, MD, secretary general of the EPA and a consultant psychiatrist with the Norwich (England) Medical School, University of East Anglia, commented in the release that anger is a “somewhat neglected symptom.
“The findings are in line with what we see in day-to-day clinical practice and will hopefully help increase the awareness of the importance of both anger and associated childhood trauma.”
The infrastructure for the NESDA study is funded through the Geestkracht program of the Netherlands Organization for Health Research and Development and financial contributions by participating universities and mental health care organizations. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
PARIS –
Investigators examined data on more than 2,250 individuals who were asked about trauma during childhood and a subsequent tendency toward anger or angry outbursts 4 years later.
Results showed that emotional neglect during childhood was associated with approximately a 40% increased likelihood of subsequent anger, while psychological abuse was linked to a 30% increased likelihood.
Childhood physical abuse was also significantly associated with anger in adults, with an increased risk of approximately 40%. The researchers found no link between childhood sexual abuse and adult anger.
“We can’t definitively say that the trauma causes the anger, but the link is clear,” study investigator Nienke De Bles, PhD student, department of psychiatry, Leiden (the Netherlands) University Medical Center, said in a news release.
“Being easily angered can have several consequences,” she continued. “It can make personal interactions more difficult, and it can have consequences for your mental health and well-being, but people who get angry easily also have a greater tendency to discontinue psychiatric treatment, so this anger may mean that it reduces their chances of a better life,” she added.
Ms. De Bles believes that “it should be standard practice to ask depression and anxiety sufferers about anger and past trauma, even if the patient is not exhibiting current anger.”
The findings were presented at the European Psychiatric Association 2023 Congress.
A ‘red flag’ for abuse
“Psychiatric treatments for past trauma may differ from treatments for depression, so psychiatrists need to try to understand the cause so that they can offer the correct treatment to each patient,” said Ms. De Bles.
Ms. De Bles noted that childhood trauma has many negative consequences later in life and that it is associated with a higher prevalence of adult depression and anxiety.
“There are several potential mechanisms for psychopathology in the context of childhood trauma, and emotion regulation seems to be one of the key mechanisms,” she said.
The researchers previously found that anger was highly prevalent among patients with affective disorders. It was present in 30% of those with current anxiety or depressive disorder and in 40% of those with comorbid depression and anxiety with a tendency toward anger versus 5% of healthy control persons.
Other studies have shown that anger is associated with poor treatment outcomes and dropping out of treatment.
To further investigate the link between childhood trauma and anger in adulthood, the researchers examined data on 2,271 participants in the Netherlands Study of Depression and Anxiety (NESDA).
Childhood trauma was assessed at baseline using the semistructured Childhood Trauma Interview. Anger was measured at a 4-year follow-up using the Spielberger Trait Anger Subscale, the Anger Attacks Questionnaire, and the borderline and antisocial subscales of the Personality Disorder Questionnaire 4 to identify cluster B personality traits.
Results showed that emotional neglect during childhood was significantly associated with trait anger in adulthood, at an adjusted odds ratio of 1.42 (P < .001), anger attacks (OR, 1.35; P = .004), and borderline (OR, 1.76; P < .001) and antisocial (OR, 1.88; P = .001) personality traits.
Childhood psychological abuse was also significantly associated with later trait anger (OR, 1.28; P = .002), anger attacks (OR, 1.31; P = .024), and borderline (OR, 1.77; P < .001) and antisocial (OR, 1.69; P = .011) traits.
There was also a significant association between childhood psychical abuse and trait anger in adulthood (OR, 1.37; P < .001), anger attacks (OR, 1.48; P = .004), and borderline (OR, 1.71; P < .001) and antisocial (OR, 1.98; P = .002) traits.
There was no significant association between sexual abuse experienced in childhood and later anger or personality traits.
Ms. De Bles said the findings suggest “there is indeed a relationship between childhood trauma and anger in adulthood, and this is something that might be interesting for clinicians, as anger could be a red flag for a history of childhood trauma.”
She said in an interview that anger is a “very normal human emotion” but that it has not been as widely studied as sadness and anxiety.
She suggested that future research could examine the use of trauma-based therapies for patients with a history of childhood trauma and anger.
Overlooked, neglected
Commenting on the findings, Nur Hani Zainal, PhD, department of healthcare policy, Harvard Medical School, Boston, said the findings are “very consistent with the current biopsychosocial models in psychiatry and clinical psychology.”
Dr. Zainal, who was coauthor of a recent study that showed that anger appears to mediate the relationship between childhood trauma and adult psychopathology, said the current study offers a “good, incremental contribution” to the literature.
She noted there are “good uses” for the emotion of anger, as “sometimes we need anger to set healthy boundaries for ourselves.” However, she agreed that, as an aspect of depression, anxiety, and posttraumatic stress disorder, it is often “overlooked.”
Dr. Zainal said that the findings reinforce the importance of thoroughly evaluating adult patients’ experiences during childhood.
Julian Beezhold, MD, secretary general of the EPA and a consultant psychiatrist with the Norwich (England) Medical School, University of East Anglia, commented in the release that anger is a “somewhat neglected symptom.
“The findings are in line with what we see in day-to-day clinical practice and will hopefully help increase the awareness of the importance of both anger and associated childhood trauma.”
The infrastructure for the NESDA study is funded through the Geestkracht program of the Netherlands Organization for Health Research and Development and financial contributions by participating universities and mental health care organizations. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
PARIS –
Investigators examined data on more than 2,250 individuals who were asked about trauma during childhood and a subsequent tendency toward anger or angry outbursts 4 years later.
Results showed that emotional neglect during childhood was associated with approximately a 40% increased likelihood of subsequent anger, while psychological abuse was linked to a 30% increased likelihood.
Childhood physical abuse was also significantly associated with anger in adults, with an increased risk of approximately 40%. The researchers found no link between childhood sexual abuse and adult anger.
“We can’t definitively say that the trauma causes the anger, but the link is clear,” study investigator Nienke De Bles, PhD student, department of psychiatry, Leiden (the Netherlands) University Medical Center, said in a news release.
“Being easily angered can have several consequences,” she continued. “It can make personal interactions more difficult, and it can have consequences for your mental health and well-being, but people who get angry easily also have a greater tendency to discontinue psychiatric treatment, so this anger may mean that it reduces their chances of a better life,” she added.
Ms. De Bles believes that “it should be standard practice to ask depression and anxiety sufferers about anger and past trauma, even if the patient is not exhibiting current anger.”
The findings were presented at the European Psychiatric Association 2023 Congress.
A ‘red flag’ for abuse
“Psychiatric treatments for past trauma may differ from treatments for depression, so psychiatrists need to try to understand the cause so that they can offer the correct treatment to each patient,” said Ms. De Bles.
Ms. De Bles noted that childhood trauma has many negative consequences later in life and that it is associated with a higher prevalence of adult depression and anxiety.
“There are several potential mechanisms for psychopathology in the context of childhood trauma, and emotion regulation seems to be one of the key mechanisms,” she said.
The researchers previously found that anger was highly prevalent among patients with affective disorders. It was present in 30% of those with current anxiety or depressive disorder and in 40% of those with comorbid depression and anxiety with a tendency toward anger versus 5% of healthy control persons.
Other studies have shown that anger is associated with poor treatment outcomes and dropping out of treatment.
To further investigate the link between childhood trauma and anger in adulthood, the researchers examined data on 2,271 participants in the Netherlands Study of Depression and Anxiety (NESDA).
Childhood trauma was assessed at baseline using the semistructured Childhood Trauma Interview. Anger was measured at a 4-year follow-up using the Spielberger Trait Anger Subscale, the Anger Attacks Questionnaire, and the borderline and antisocial subscales of the Personality Disorder Questionnaire 4 to identify cluster B personality traits.
Results showed that emotional neglect during childhood was significantly associated with trait anger in adulthood, at an adjusted odds ratio of 1.42 (P < .001), anger attacks (OR, 1.35; P = .004), and borderline (OR, 1.76; P < .001) and antisocial (OR, 1.88; P = .001) personality traits.
Childhood psychological abuse was also significantly associated with later trait anger (OR, 1.28; P = .002), anger attacks (OR, 1.31; P = .024), and borderline (OR, 1.77; P < .001) and antisocial (OR, 1.69; P = .011) traits.
There was also a significant association between childhood psychical abuse and trait anger in adulthood (OR, 1.37; P < .001), anger attacks (OR, 1.48; P = .004), and borderline (OR, 1.71; P < .001) and antisocial (OR, 1.98; P = .002) traits.
There was no significant association between sexual abuse experienced in childhood and later anger or personality traits.
Ms. De Bles said the findings suggest “there is indeed a relationship between childhood trauma and anger in adulthood, and this is something that might be interesting for clinicians, as anger could be a red flag for a history of childhood trauma.”
She said in an interview that anger is a “very normal human emotion” but that it has not been as widely studied as sadness and anxiety.
She suggested that future research could examine the use of trauma-based therapies for patients with a history of childhood trauma and anger.
Overlooked, neglected
Commenting on the findings, Nur Hani Zainal, PhD, department of healthcare policy, Harvard Medical School, Boston, said the findings are “very consistent with the current biopsychosocial models in psychiatry and clinical psychology.”
Dr. Zainal, who was coauthor of a recent study that showed that anger appears to mediate the relationship between childhood trauma and adult psychopathology, said the current study offers a “good, incremental contribution” to the literature.
She noted there are “good uses” for the emotion of anger, as “sometimes we need anger to set healthy boundaries for ourselves.” However, she agreed that, as an aspect of depression, anxiety, and posttraumatic stress disorder, it is often “overlooked.”
Dr. Zainal said that the findings reinforce the importance of thoroughly evaluating adult patients’ experiences during childhood.
Julian Beezhold, MD, secretary general of the EPA and a consultant psychiatrist with the Norwich (England) Medical School, University of East Anglia, commented in the release that anger is a “somewhat neglected symptom.
“The findings are in line with what we see in day-to-day clinical practice and will hopefully help increase the awareness of the importance of both anger and associated childhood trauma.”
The infrastructure for the NESDA study is funded through the Geestkracht program of the Netherlands Organization for Health Research and Development and financial contributions by participating universities and mental health care organizations. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT EPA 2023
Single-dose psilocybin promising for resistant depression
PARIS –
Known as COMP360, the synthetic agent, a proprietary, purified form of psilocybin, improved symptoms related to mood and anhedonia while leaving aspects such as appetite and weight changes unaffected, reported investigators led by Guy M. Goodwin, PhD, emeritus professor of psychiatry, University of Oxford, England, and chief medical officer, COMPASS Pathways.
The study was presented at the European Psychiatric Association (EPA) 2023 Congress.
100 million affected
Affecting up to 100 million people globally, TRD is “not an official diagnosis,” although it is often defined as the failure to elicit a response with at least two antidepressant treatments, said Dr. Goodwin.
Compared to their counterparts with non-TRD, those with TRD experience higher relapse rates, higher rates of suicidal behavior, and more residual symptoms even when they do respond to treatment.
Previous results from the study known as P-TRD indicated that a single 25-mg dose of COMP360 significantly reduced depression scores for up to 12 weeks when given along with psychological support, although a later analysis suggested the effect subsequently dropped off.
The vast majority of the patients in the trial were naive to psychedelics, and so, Dr. Goodwin explained, they undergo a preparation phase during which they receive psychoeducation and have at least two visits with a therapist, who then stays with them during administration of the drug to offer support if they experience psychological distress.
Following the psilocybin session, participants go through a process known as integration, which involves two sessions with a therapist within 2 weeks.
“That, in our view, is essentially about safety, and about identifying problems that have arisen as a result of taking the drug,” said Dr. Goodwin.
The phase 2b trial examined changes in specific depression symptoms after psilocybin treatment in 233 patients with TRD. Participants were a mean age of 39.8 years and 59% were women. They were randomized to receive one of three doses of the drug: a 1-mg dose (n = 79), a 10-mg dose (n = 75), or a 25-mg dose (n = 79).
The primary outcome was changes in individual items on the Montgomery-Åsberg Depression Rating Scale (MADRS) and 16-item Quick Inventory of Depressive Symptomatology–Self Report (QIDS-SR-16) scale.
While the effect on overall depression scores is important, said Dr. Goodwin, many of the items included in the depression assessment scales are “uninformative.”
Reduction in ‘core’ symptoms
Participants were assessed by a blinded rater at baseline, day 1, day 2, and at 1, 2, 3, 6, 9, and 12 weeks after administration of COMP360. The primary endpoint was a reduction in individual items on MADRS and scores from baseline to 3 weeks. Individual items on the QIDS-SR-16 were rated by participants at the same time points.
Investigators found the largest mean changes from baseline were on reported and apparent sadness, lassitude, inability to feel, and concentration difficulties, with “very nice and clear dose-related differences,” Dr. Goodwin said.
The results indicate that the significant benefit with the largest dose at 3 weeks versus baseline was confined to items such as inability to feel and reported and apparent sadness on the MADRS and feeling sad and general interest on the QIDS-SR-16 (Table 1).
The results suggest the effect of COMP360 is “on the core symptoms of depression,” said Dr. Goodwin.
Results were similar for individual items on the QIDS-SR-16, with the greatest changes in items including feeling sad, general interest, energy level, falling asleep, view of myself, concentration/decision-making, and feeling down.
Other scale items, such as decreased appetite, feel restless, and weight changes, showed negligible changes in response to COMP360 therapy and were described by Dr. Goodwin as “inconsequential.”
“Essentially, these items are contributing nothing but noise to the signal,” he said.
He added the results of the study need to be replicated and that plans for phase 3 trials are underway. These studies, he said, are designed to convince the Food and Drug Administration that “this is not just a recreational drug, it’s a medicine.”
Enthusiasm running ahead of the data
Commenting on the findings, Bertha K. Madras, PhD, professor of psychobiology, department of psychiatry, Harvard Medical School, Boston, who was not involved in the study, said “hallucinogens are an intriguing class of drugs and I support ongoing high-quality research in this area.”
However, she told this news organization that the “breathtaking endorsement of this drug is far ahead of scientific data.”
She cited concerns such as the “narrow demographics” of participants, their previous experience with and expectations of hallucinogens, the “potential for symptom fluidity of enrollees,” such as depression evolving into psychosis, and the “undefined role” of the therapist during a hallucinogenic session.
“Finally, I am concerned that enthusiasm for therapeutic potential has been, and will continue to be, preempted and directed towards legalization and widespread access for vulnerable populations,” Dr. Madras said.
This, she said, “is occurring at breakneck speed in the U.S., with scant resistance or skepticism from the investigators engaged in therapeutic assessment.”
The study was funded by COMPASS Pathways. Dr. Goodwin has reported relationships with COMPASS Pathways, Buckley Psytech, Boehringer Ingelheim, Clerkenwell Health, EVA Pharma, Lundbeck, Janssen Global Services, Novartis, Ocean Neurosciences, P1vital, Sage Therapeutics, Servier, Takeda, and WebMD.
A version of this article first appeared on Medscape.com.
PARIS –
Known as COMP360, the synthetic agent, a proprietary, purified form of psilocybin, improved symptoms related to mood and anhedonia while leaving aspects such as appetite and weight changes unaffected, reported investigators led by Guy M. Goodwin, PhD, emeritus professor of psychiatry, University of Oxford, England, and chief medical officer, COMPASS Pathways.
The study was presented at the European Psychiatric Association (EPA) 2023 Congress.
100 million affected
Affecting up to 100 million people globally, TRD is “not an official diagnosis,” although it is often defined as the failure to elicit a response with at least two antidepressant treatments, said Dr. Goodwin.
Compared to their counterparts with non-TRD, those with TRD experience higher relapse rates, higher rates of suicidal behavior, and more residual symptoms even when they do respond to treatment.
Previous results from the study known as P-TRD indicated that a single 25-mg dose of COMP360 significantly reduced depression scores for up to 12 weeks when given along with psychological support, although a later analysis suggested the effect subsequently dropped off.
The vast majority of the patients in the trial were naive to psychedelics, and so, Dr. Goodwin explained, they undergo a preparation phase during which they receive psychoeducation and have at least two visits with a therapist, who then stays with them during administration of the drug to offer support if they experience psychological distress.
Following the psilocybin session, participants go through a process known as integration, which involves two sessions with a therapist within 2 weeks.
“That, in our view, is essentially about safety, and about identifying problems that have arisen as a result of taking the drug,” said Dr. Goodwin.
The phase 2b trial examined changes in specific depression symptoms after psilocybin treatment in 233 patients with TRD. Participants were a mean age of 39.8 years and 59% were women. They were randomized to receive one of three doses of the drug: a 1-mg dose (n = 79), a 10-mg dose (n = 75), or a 25-mg dose (n = 79).
The primary outcome was changes in individual items on the Montgomery-Åsberg Depression Rating Scale (MADRS) and 16-item Quick Inventory of Depressive Symptomatology–Self Report (QIDS-SR-16) scale.
While the effect on overall depression scores is important, said Dr. Goodwin, many of the items included in the depression assessment scales are “uninformative.”
Reduction in ‘core’ symptoms
Participants were assessed by a blinded rater at baseline, day 1, day 2, and at 1, 2, 3, 6, 9, and 12 weeks after administration of COMP360. The primary endpoint was a reduction in individual items on MADRS and scores from baseline to 3 weeks. Individual items on the QIDS-SR-16 were rated by participants at the same time points.
Investigators found the largest mean changes from baseline were on reported and apparent sadness, lassitude, inability to feel, and concentration difficulties, with “very nice and clear dose-related differences,” Dr. Goodwin said.
The results indicate that the significant benefit with the largest dose at 3 weeks versus baseline was confined to items such as inability to feel and reported and apparent sadness on the MADRS and feeling sad and general interest on the QIDS-SR-16 (Table 1).
The results suggest the effect of COMP360 is “on the core symptoms of depression,” said Dr. Goodwin.
Results were similar for individual items on the QIDS-SR-16, with the greatest changes in items including feeling sad, general interest, energy level, falling asleep, view of myself, concentration/decision-making, and feeling down.
Other scale items, such as decreased appetite, feel restless, and weight changes, showed negligible changes in response to COMP360 therapy and were described by Dr. Goodwin as “inconsequential.”
“Essentially, these items are contributing nothing but noise to the signal,” he said.
He added the results of the study need to be replicated and that plans for phase 3 trials are underway. These studies, he said, are designed to convince the Food and Drug Administration that “this is not just a recreational drug, it’s a medicine.”
Enthusiasm running ahead of the data
Commenting on the findings, Bertha K. Madras, PhD, professor of psychobiology, department of psychiatry, Harvard Medical School, Boston, who was not involved in the study, said “hallucinogens are an intriguing class of drugs and I support ongoing high-quality research in this area.”
However, she told this news organization that the “breathtaking endorsement of this drug is far ahead of scientific data.”
She cited concerns such as the “narrow demographics” of participants, their previous experience with and expectations of hallucinogens, the “potential for symptom fluidity of enrollees,” such as depression evolving into psychosis, and the “undefined role” of the therapist during a hallucinogenic session.
“Finally, I am concerned that enthusiasm for therapeutic potential has been, and will continue to be, preempted and directed towards legalization and widespread access for vulnerable populations,” Dr. Madras said.
This, she said, “is occurring at breakneck speed in the U.S., with scant resistance or skepticism from the investigators engaged in therapeutic assessment.”
The study was funded by COMPASS Pathways. Dr. Goodwin has reported relationships with COMPASS Pathways, Buckley Psytech, Boehringer Ingelheim, Clerkenwell Health, EVA Pharma, Lundbeck, Janssen Global Services, Novartis, Ocean Neurosciences, P1vital, Sage Therapeutics, Servier, Takeda, and WebMD.
A version of this article first appeared on Medscape.com.
PARIS –
Known as COMP360, the synthetic agent, a proprietary, purified form of psilocybin, improved symptoms related to mood and anhedonia while leaving aspects such as appetite and weight changes unaffected, reported investigators led by Guy M. Goodwin, PhD, emeritus professor of psychiatry, University of Oxford, England, and chief medical officer, COMPASS Pathways.
The study was presented at the European Psychiatric Association (EPA) 2023 Congress.
100 million affected
Affecting up to 100 million people globally, TRD is “not an official diagnosis,” although it is often defined as the failure to elicit a response with at least two antidepressant treatments, said Dr. Goodwin.
Compared to their counterparts with non-TRD, those with TRD experience higher relapse rates, higher rates of suicidal behavior, and more residual symptoms even when they do respond to treatment.
Previous results from the study known as P-TRD indicated that a single 25-mg dose of COMP360 significantly reduced depression scores for up to 12 weeks when given along with psychological support, although a later analysis suggested the effect subsequently dropped off.
The vast majority of the patients in the trial were naive to psychedelics, and so, Dr. Goodwin explained, they undergo a preparation phase during which they receive psychoeducation and have at least two visits with a therapist, who then stays with them during administration of the drug to offer support if they experience psychological distress.
Following the psilocybin session, participants go through a process known as integration, which involves two sessions with a therapist within 2 weeks.
“That, in our view, is essentially about safety, and about identifying problems that have arisen as a result of taking the drug,” said Dr. Goodwin.
The phase 2b trial examined changes in specific depression symptoms after psilocybin treatment in 233 patients with TRD. Participants were a mean age of 39.8 years and 59% were women. They were randomized to receive one of three doses of the drug: a 1-mg dose (n = 79), a 10-mg dose (n = 75), or a 25-mg dose (n = 79).
The primary outcome was changes in individual items on the Montgomery-Åsberg Depression Rating Scale (MADRS) and 16-item Quick Inventory of Depressive Symptomatology–Self Report (QIDS-SR-16) scale.
While the effect on overall depression scores is important, said Dr. Goodwin, many of the items included in the depression assessment scales are “uninformative.”
Reduction in ‘core’ symptoms
Participants were assessed by a blinded rater at baseline, day 1, day 2, and at 1, 2, 3, 6, 9, and 12 weeks after administration of COMP360. The primary endpoint was a reduction in individual items on MADRS and scores from baseline to 3 weeks. Individual items on the QIDS-SR-16 were rated by participants at the same time points.
Investigators found the largest mean changes from baseline were on reported and apparent sadness, lassitude, inability to feel, and concentration difficulties, with “very nice and clear dose-related differences,” Dr. Goodwin said.
The results indicate that the significant benefit with the largest dose at 3 weeks versus baseline was confined to items such as inability to feel and reported and apparent sadness on the MADRS and feeling sad and general interest on the QIDS-SR-16 (Table 1).
The results suggest the effect of COMP360 is “on the core symptoms of depression,” said Dr. Goodwin.
Results were similar for individual items on the QIDS-SR-16, with the greatest changes in items including feeling sad, general interest, energy level, falling asleep, view of myself, concentration/decision-making, and feeling down.
Other scale items, such as decreased appetite, feel restless, and weight changes, showed negligible changes in response to COMP360 therapy and were described by Dr. Goodwin as “inconsequential.”
“Essentially, these items are contributing nothing but noise to the signal,” he said.
He added the results of the study need to be replicated and that plans for phase 3 trials are underway. These studies, he said, are designed to convince the Food and Drug Administration that “this is not just a recreational drug, it’s a medicine.”
Enthusiasm running ahead of the data
Commenting on the findings, Bertha K. Madras, PhD, professor of psychobiology, department of psychiatry, Harvard Medical School, Boston, who was not involved in the study, said “hallucinogens are an intriguing class of drugs and I support ongoing high-quality research in this area.”
However, she told this news organization that the “breathtaking endorsement of this drug is far ahead of scientific data.”
She cited concerns such as the “narrow demographics” of participants, their previous experience with and expectations of hallucinogens, the “potential for symptom fluidity of enrollees,” such as depression evolving into psychosis, and the “undefined role” of the therapist during a hallucinogenic session.
“Finally, I am concerned that enthusiasm for therapeutic potential has been, and will continue to be, preempted and directed towards legalization and widespread access for vulnerable populations,” Dr. Madras said.
This, she said, “is occurring at breakneck speed in the U.S., with scant resistance or skepticism from the investigators engaged in therapeutic assessment.”
The study was funded by COMPASS Pathways. Dr. Goodwin has reported relationships with COMPASS Pathways, Buckley Psytech, Boehringer Ingelheim, Clerkenwell Health, EVA Pharma, Lundbeck, Janssen Global Services, Novartis, Ocean Neurosciences, P1vital, Sage Therapeutics, Servier, Takeda, and WebMD.
A version of this article first appeared on Medscape.com.
AT EPA 2023
Glutathione a potential biomarker for postpartum suicide
Approximately 10,000 suicide deaths are recorded in Brazil every year. The suicide risk is highest among patients with depressive disorders, particularly women (> 18% vs. 11% for men).
There are countless people who work to prevent suicide, and the challenges they face are many. But now, on the horizon, there are new tools that could prove invaluable to their efforts – tools such as biomarkers. In a study recently published in the journal Frontiers in Psychiatry, researchers from the Catholic University of Pelotas (UCPel), Brazil, reported an association of glutathione (GSH) with the degree of suicide risk in women at 18 months postpartum. Specifically, they found that reduced serum GSH levels were significantly lower for those with moderate to high suicide risk than for those without suicide risk. Their findings suggest that GSH may be a potential biomarker or etiologic factor among women at risk for suicide, with therapeutic implications.
This was a case-control study nested within a cohort study. From this cohort, 45 women were selected at 18 months postpartum. Thirty of them had mood disorders, such as major depression and bipolar disorder. The other 15 participants, none of whom had a mood disorder, made up the control group.
Depression and the risk for suicide were assessed using the Mini International Neuropsychiatric Interview Plus (MINI-Plus 5.0.0 Brazilian version), module A and module C, respectively. Blood samples were collected to evaluate serum levels of the following oxidative stress biomarkers: reactive oxygen species, superoxide dismutase, and GSH.
The prevalence of suicide risk observed in the women at 18 months postpartum was 24.4%. The prevalence of suicide risk in the mood disorder group was 36.7%.
In addition, the statistical analysis found that women with moderate to high suicide risk had cerebral redox imbalance, resulting in a decrease in blood GSH levels.
The study team was led by neuroscientist Adriano Martimbianco de Assis, PhD, the coordinator of UCPel’s postgraduate program in health and behavior. He said that the correlation identified between GSH serum levels and suicide risk gives rise to two possible applications: using GSH as a biomarker for suicide risk and using GSH therapeutically.
Regarding the former application, Dr. Martimbianco de Assis explained that additional studies are needed to take a step forward. “Although we believe that most of the GSH came from the brain – given that it’s the brain’s main antioxidant – as we analyze blood samples, we’re not yet able to rule out the possibility that it came from other organs,” he said in an interview. So, confirming that hypothesis will require studies that involve imaging brain tissue. According to Dr. Martimbianco de Assis, once there is confirmation, it will be possible to move to using the antioxidant as a biomarker for suicide risk.
He also shared his views about the second application: using GSH therapeutically. “We already know that there are very simple alternatives that can influence GSH levels, [and they] mostly have to do with exercise and [improving the quality of] the food one eats. But there are also drugs: for example, N-acetyl cysteine, which is a precursor of GSH.” Adopting strategies to increase the levels of this antioxidant in the body should reverse the imbalance identified in the study and, as a result, may lead to lowering the risk for suicide. But, he reiterated, “getting to a place where GSH [can be used] in clinical practice hinges on getting that confirmation that it did, in fact, come from the brain. Recall that our study found lower levels of GSH in women at risk for suicide.”
Even though the study evaluated postpartum women, it’s possible that the results can be extrapolated to other populations, said Dr. Martimbianco de Assis. This is because when the data were collected, 18 months had already passed since giving birth. The participants’ physiological condition at that point was more similar to the one prior to becoming pregnant.
The UCPel researchers continue to follow the cohort. “We intend to continue monitoring GSH levels at other times. Forty-eight months have now passed since the women gave birth, and the idea is to continue studying [the patients involved in the study],” said Dr. Martimbianco de Assis, adding that the team also intends to analyze brain tissue from in vitro studies using cell cultures.
This article was translated from the Medscape Portuguese Edition and a version appeared on Medscape.com.
Approximately 10,000 suicide deaths are recorded in Brazil every year. The suicide risk is highest among patients with depressive disorders, particularly women (> 18% vs. 11% for men).
There are countless people who work to prevent suicide, and the challenges they face are many. But now, on the horizon, there are new tools that could prove invaluable to their efforts – tools such as biomarkers. In a study recently published in the journal Frontiers in Psychiatry, researchers from the Catholic University of Pelotas (UCPel), Brazil, reported an association of glutathione (GSH) with the degree of suicide risk in women at 18 months postpartum. Specifically, they found that reduced serum GSH levels were significantly lower for those with moderate to high suicide risk than for those without suicide risk. Their findings suggest that GSH may be a potential biomarker or etiologic factor among women at risk for suicide, with therapeutic implications.
This was a case-control study nested within a cohort study. From this cohort, 45 women were selected at 18 months postpartum. Thirty of them had mood disorders, such as major depression and bipolar disorder. The other 15 participants, none of whom had a mood disorder, made up the control group.
Depression and the risk for suicide were assessed using the Mini International Neuropsychiatric Interview Plus (MINI-Plus 5.0.0 Brazilian version), module A and module C, respectively. Blood samples were collected to evaluate serum levels of the following oxidative stress biomarkers: reactive oxygen species, superoxide dismutase, and GSH.
The prevalence of suicide risk observed in the women at 18 months postpartum was 24.4%. The prevalence of suicide risk in the mood disorder group was 36.7%.
In addition, the statistical analysis found that women with moderate to high suicide risk had cerebral redox imbalance, resulting in a decrease in blood GSH levels.
The study team was led by neuroscientist Adriano Martimbianco de Assis, PhD, the coordinator of UCPel’s postgraduate program in health and behavior. He said that the correlation identified between GSH serum levels and suicide risk gives rise to two possible applications: using GSH as a biomarker for suicide risk and using GSH therapeutically.
Regarding the former application, Dr. Martimbianco de Assis explained that additional studies are needed to take a step forward. “Although we believe that most of the GSH came from the brain – given that it’s the brain’s main antioxidant – as we analyze blood samples, we’re not yet able to rule out the possibility that it came from other organs,” he said in an interview. So, confirming that hypothesis will require studies that involve imaging brain tissue. According to Dr. Martimbianco de Assis, once there is confirmation, it will be possible to move to using the antioxidant as a biomarker for suicide risk.
He also shared his views about the second application: using GSH therapeutically. “We already know that there are very simple alternatives that can influence GSH levels, [and they] mostly have to do with exercise and [improving the quality of] the food one eats. But there are also drugs: for example, N-acetyl cysteine, which is a precursor of GSH.” Adopting strategies to increase the levels of this antioxidant in the body should reverse the imbalance identified in the study and, as a result, may lead to lowering the risk for suicide. But, he reiterated, “getting to a place where GSH [can be used] in clinical practice hinges on getting that confirmation that it did, in fact, come from the brain. Recall that our study found lower levels of GSH in women at risk for suicide.”
Even though the study evaluated postpartum women, it’s possible that the results can be extrapolated to other populations, said Dr. Martimbianco de Assis. This is because when the data were collected, 18 months had already passed since giving birth. The participants’ physiological condition at that point was more similar to the one prior to becoming pregnant.
The UCPel researchers continue to follow the cohort. “We intend to continue monitoring GSH levels at other times. Forty-eight months have now passed since the women gave birth, and the idea is to continue studying [the patients involved in the study],” said Dr. Martimbianco de Assis, adding that the team also intends to analyze brain tissue from in vitro studies using cell cultures.
This article was translated from the Medscape Portuguese Edition and a version appeared on Medscape.com.
Approximately 10,000 suicide deaths are recorded in Brazil every year. The suicide risk is highest among patients with depressive disorders, particularly women (> 18% vs. 11% for men).
There are countless people who work to prevent suicide, and the challenges they face are many. But now, on the horizon, there are new tools that could prove invaluable to their efforts – tools such as biomarkers. In a study recently published in the journal Frontiers in Psychiatry, researchers from the Catholic University of Pelotas (UCPel), Brazil, reported an association of glutathione (GSH) with the degree of suicide risk in women at 18 months postpartum. Specifically, they found that reduced serum GSH levels were significantly lower for those with moderate to high suicide risk than for those without suicide risk. Their findings suggest that GSH may be a potential biomarker or etiologic factor among women at risk for suicide, with therapeutic implications.
This was a case-control study nested within a cohort study. From this cohort, 45 women were selected at 18 months postpartum. Thirty of them had mood disorders, such as major depression and bipolar disorder. The other 15 participants, none of whom had a mood disorder, made up the control group.
Depression and the risk for suicide were assessed using the Mini International Neuropsychiatric Interview Plus (MINI-Plus 5.0.0 Brazilian version), module A and module C, respectively. Blood samples were collected to evaluate serum levels of the following oxidative stress biomarkers: reactive oxygen species, superoxide dismutase, and GSH.
The prevalence of suicide risk observed in the women at 18 months postpartum was 24.4%. The prevalence of suicide risk in the mood disorder group was 36.7%.
In addition, the statistical analysis found that women with moderate to high suicide risk had cerebral redox imbalance, resulting in a decrease in blood GSH levels.
The study team was led by neuroscientist Adriano Martimbianco de Assis, PhD, the coordinator of UCPel’s postgraduate program in health and behavior. He said that the correlation identified between GSH serum levels and suicide risk gives rise to two possible applications: using GSH as a biomarker for suicide risk and using GSH therapeutically.
Regarding the former application, Dr. Martimbianco de Assis explained that additional studies are needed to take a step forward. “Although we believe that most of the GSH came from the brain – given that it’s the brain’s main antioxidant – as we analyze blood samples, we’re not yet able to rule out the possibility that it came from other organs,” he said in an interview. So, confirming that hypothesis will require studies that involve imaging brain tissue. According to Dr. Martimbianco de Assis, once there is confirmation, it will be possible to move to using the antioxidant as a biomarker for suicide risk.
He also shared his views about the second application: using GSH therapeutically. “We already know that there are very simple alternatives that can influence GSH levels, [and they] mostly have to do with exercise and [improving the quality of] the food one eats. But there are also drugs: for example, N-acetyl cysteine, which is a precursor of GSH.” Adopting strategies to increase the levels of this antioxidant in the body should reverse the imbalance identified in the study and, as a result, may lead to lowering the risk for suicide. But, he reiterated, “getting to a place where GSH [can be used] in clinical practice hinges on getting that confirmation that it did, in fact, come from the brain. Recall that our study found lower levels of GSH in women at risk for suicide.”
Even though the study evaluated postpartum women, it’s possible that the results can be extrapolated to other populations, said Dr. Martimbianco de Assis. This is because when the data were collected, 18 months had already passed since giving birth. The participants’ physiological condition at that point was more similar to the one prior to becoming pregnant.
The UCPel researchers continue to follow the cohort. “We intend to continue monitoring GSH levels at other times. Forty-eight months have now passed since the women gave birth, and the idea is to continue studying [the patients involved in the study],” said Dr. Martimbianco de Assis, adding that the team also intends to analyze brain tissue from in vitro studies using cell cultures.
This article was translated from the Medscape Portuguese Edition and a version appeared on Medscape.com.
Mindfulness-based CBT an ‘important’ option for moderate depression
The findings suggest that “offering practitioner-supported MBCT-SH as an intervention for mild to moderate depression would improve outcomes and save money compared with practitioner-supported CBT-SH,” noted the investigators, led by Clara Strauss, PhD, DClinPsy, with the University of Sussex School of Psychology in England.
Practitioner-supported CBT-SH is recommended in U.K. national treatment guidelines for mild to moderate depression. However, some patients’ conditions don’t respond, and dropout rates are high.
The Low-Intensity Guided Help Through Mindfulness (LIGHTMind) trial tested practitioner-supported MBCT-SH as an alternative.
The findings have “important implications” for the more than 100,000 people currently offered CBT-SH for depression in the Improving Access to Psychological Therapies (IAPT) program each year and in publicly funded services elsewhere, the researchers noted.
If translated into routine practice, “this would see many more people recovering from depression while costing health services less money,” they added.
The study was published online in JAMA Psychiatry .
Practice changing?
The trial included 410 adults (mean age, 32 years; 62% women) with mild to moderate depression who were recruited from 10 publicly funded psychological therapy services in England as part of the IAPT program.
Participants were given one of two established self-help workbooks – The Mindful Way Workbook: An 8-Week Program to Free Yourself from Depression and Emotional Distress, written by the pioneers of MBCT, or Overcoming Depression and Low Mood, 3rd Edition: A Five Areas Approach, which is a CBT-SH program widely used in IAPT.
Use of the self-help books was supported by six structured phone or in-person sessions with a trained psychological well-being practitioner.
The primary outcome was depression symptom severity at 16 weeks, which was determined on the basis of Patient Health Questionnaire 9 (PHQ-9) score.
At 16 weeks following randomization, MBCT-SH led to significantly greater reductions in depression symptom severity compared with CBT-SH (mean PHQ-9 score, 7.2 vs. 8.6; between-group difference, 1.5 points; P = .009; d = −0.36).
MBCT-SH also had superior effects on anxiety symptom severity at 16 weeks.
At the 42-week follow-up, between-group effects on depression and anxiety symptom severity remained in the hypothesized direction but were nonsignificant.
This could be due in part by the greater postintervention psychological therapy accessed by participants in the CBT-SH group, the investigators noted.
Practitioner-supported MBCT-SH was more cost-effective than supported CBT-SH.
On average, the CBT-SH intervention cost health services £526 ($631) more per participant than the MBCT-SH intervention over the 42-week follow-up. The probability of MBCT-SH being cost-effective compared with CBT-SH exceeded 95%, the researchers noted.
Useful model for the United States
Commenting for this news organization, Zindel Segal, PhD, professor of psychology, University of Toronto, Scarborough, cautioned against making too much of the differences between the groups, because CBT-SH “trended positive and had a pretty healthy effect size, it just never reached significance.
“I wouldn’t say mindfulness drastically outperformed cognitive therapy. But cognitive therapy is a robust treatment in its own right, and so doing a little bit better is significant,” Dr. Segal said.
He also noted that, appropriately, the trial enrolled adults who were experiencing moderate depression and were not acutely ill. “That’s one of the rationales for self-help compared to providing patients with a more resource-intensive group treatment.
“If you look at the needs of people with moderate depression, what you find is that for cognitive therapy to work, negative thoughts and feelings need to be pervasive in order to make use of the techniques,” Dr. Segal explained.
“With mindfulness, you don’t need any to have constant negative thoughts or feelings. Anything that arises in your experience serves as grist for mill in terms of concentration and focus,” Dr. Segal said.
He also noted that mindfulness-based intervention is “more optimized” for people who are experiencing some measure of recovery or remission.
“It’s well suited for that, as it trends towards the wellness spectrum. But for people who might have greater levels of acuity or severity, cognitive-behavioral therapy might be indicated,” said Dr. Segal.
He also said the U.K. study findings are relevant to U.S. patients with depression.
“While it’s not disseminated in the same way through any kind of national program, the self-help books that are used are widely available, and the support that people were offered, either in person, telephone, or email, could be easily delivered. This would be a very useful model,” Dr. Segal said.
The LIGHTMind trial was funded by the National Institute for Health and Care Research and the Brighton and Sussex Clinical Trials Unit. Dr. Strauss has received grants from Headspace, is research lead for Sussex Mindfulness Centre, and has been chief investigator on National Institute for Health and Care Research. Dr. Segal is one of the authors of the MBCT-SH workbooks used in the study.
A version of this article first appeared on Medscape.com.
The findings suggest that “offering practitioner-supported MBCT-SH as an intervention for mild to moderate depression would improve outcomes and save money compared with practitioner-supported CBT-SH,” noted the investigators, led by Clara Strauss, PhD, DClinPsy, with the University of Sussex School of Psychology in England.
Practitioner-supported CBT-SH is recommended in U.K. national treatment guidelines for mild to moderate depression. However, some patients’ conditions don’t respond, and dropout rates are high.
The Low-Intensity Guided Help Through Mindfulness (LIGHTMind) trial tested practitioner-supported MBCT-SH as an alternative.
The findings have “important implications” for the more than 100,000 people currently offered CBT-SH for depression in the Improving Access to Psychological Therapies (IAPT) program each year and in publicly funded services elsewhere, the researchers noted.
If translated into routine practice, “this would see many more people recovering from depression while costing health services less money,” they added.
The study was published online in JAMA Psychiatry .
Practice changing?
The trial included 410 adults (mean age, 32 years; 62% women) with mild to moderate depression who were recruited from 10 publicly funded psychological therapy services in England as part of the IAPT program.
Participants were given one of two established self-help workbooks – The Mindful Way Workbook: An 8-Week Program to Free Yourself from Depression and Emotional Distress, written by the pioneers of MBCT, or Overcoming Depression and Low Mood, 3rd Edition: A Five Areas Approach, which is a CBT-SH program widely used in IAPT.
Use of the self-help books was supported by six structured phone or in-person sessions with a trained psychological well-being practitioner.
The primary outcome was depression symptom severity at 16 weeks, which was determined on the basis of Patient Health Questionnaire 9 (PHQ-9) score.
At 16 weeks following randomization, MBCT-SH led to significantly greater reductions in depression symptom severity compared with CBT-SH (mean PHQ-9 score, 7.2 vs. 8.6; between-group difference, 1.5 points; P = .009; d = −0.36).
MBCT-SH also had superior effects on anxiety symptom severity at 16 weeks.
At the 42-week follow-up, between-group effects on depression and anxiety symptom severity remained in the hypothesized direction but were nonsignificant.
This could be due in part by the greater postintervention psychological therapy accessed by participants in the CBT-SH group, the investigators noted.
Practitioner-supported MBCT-SH was more cost-effective than supported CBT-SH.
On average, the CBT-SH intervention cost health services £526 ($631) more per participant than the MBCT-SH intervention over the 42-week follow-up. The probability of MBCT-SH being cost-effective compared with CBT-SH exceeded 95%, the researchers noted.
Useful model for the United States
Commenting for this news organization, Zindel Segal, PhD, professor of psychology, University of Toronto, Scarborough, cautioned against making too much of the differences between the groups, because CBT-SH “trended positive and had a pretty healthy effect size, it just never reached significance.
“I wouldn’t say mindfulness drastically outperformed cognitive therapy. But cognitive therapy is a robust treatment in its own right, and so doing a little bit better is significant,” Dr. Segal said.
He also noted that, appropriately, the trial enrolled adults who were experiencing moderate depression and were not acutely ill. “That’s one of the rationales for self-help compared to providing patients with a more resource-intensive group treatment.
“If you look at the needs of people with moderate depression, what you find is that for cognitive therapy to work, negative thoughts and feelings need to be pervasive in order to make use of the techniques,” Dr. Segal explained.
“With mindfulness, you don’t need any to have constant negative thoughts or feelings. Anything that arises in your experience serves as grist for mill in terms of concentration and focus,” Dr. Segal said.
He also noted that mindfulness-based intervention is “more optimized” for people who are experiencing some measure of recovery or remission.
“It’s well suited for that, as it trends towards the wellness spectrum. But for people who might have greater levels of acuity or severity, cognitive-behavioral therapy might be indicated,” said Dr. Segal.
He also said the U.K. study findings are relevant to U.S. patients with depression.
“While it’s not disseminated in the same way through any kind of national program, the self-help books that are used are widely available, and the support that people were offered, either in person, telephone, or email, could be easily delivered. This would be a very useful model,” Dr. Segal said.
The LIGHTMind trial was funded by the National Institute for Health and Care Research and the Brighton and Sussex Clinical Trials Unit. Dr. Strauss has received grants from Headspace, is research lead for Sussex Mindfulness Centre, and has been chief investigator on National Institute for Health and Care Research. Dr. Segal is one of the authors of the MBCT-SH workbooks used in the study.
A version of this article first appeared on Medscape.com.
The findings suggest that “offering practitioner-supported MBCT-SH as an intervention for mild to moderate depression would improve outcomes and save money compared with practitioner-supported CBT-SH,” noted the investigators, led by Clara Strauss, PhD, DClinPsy, with the University of Sussex School of Psychology in England.
Practitioner-supported CBT-SH is recommended in U.K. national treatment guidelines for mild to moderate depression. However, some patients’ conditions don’t respond, and dropout rates are high.
The Low-Intensity Guided Help Through Mindfulness (LIGHTMind) trial tested practitioner-supported MBCT-SH as an alternative.
The findings have “important implications” for the more than 100,000 people currently offered CBT-SH for depression in the Improving Access to Psychological Therapies (IAPT) program each year and in publicly funded services elsewhere, the researchers noted.
If translated into routine practice, “this would see many more people recovering from depression while costing health services less money,” they added.
The study was published online in JAMA Psychiatry .
Practice changing?
The trial included 410 adults (mean age, 32 years; 62% women) with mild to moderate depression who were recruited from 10 publicly funded psychological therapy services in England as part of the IAPT program.
Participants were given one of two established self-help workbooks – The Mindful Way Workbook: An 8-Week Program to Free Yourself from Depression and Emotional Distress, written by the pioneers of MBCT, or Overcoming Depression and Low Mood, 3rd Edition: A Five Areas Approach, which is a CBT-SH program widely used in IAPT.
Use of the self-help books was supported by six structured phone or in-person sessions with a trained psychological well-being practitioner.
The primary outcome was depression symptom severity at 16 weeks, which was determined on the basis of Patient Health Questionnaire 9 (PHQ-9) score.
At 16 weeks following randomization, MBCT-SH led to significantly greater reductions in depression symptom severity compared with CBT-SH (mean PHQ-9 score, 7.2 vs. 8.6; between-group difference, 1.5 points; P = .009; d = −0.36).
MBCT-SH also had superior effects on anxiety symptom severity at 16 weeks.
At the 42-week follow-up, between-group effects on depression and anxiety symptom severity remained in the hypothesized direction but were nonsignificant.
This could be due in part by the greater postintervention psychological therapy accessed by participants in the CBT-SH group, the investigators noted.
Practitioner-supported MBCT-SH was more cost-effective than supported CBT-SH.
On average, the CBT-SH intervention cost health services £526 ($631) more per participant than the MBCT-SH intervention over the 42-week follow-up. The probability of MBCT-SH being cost-effective compared with CBT-SH exceeded 95%, the researchers noted.
Useful model for the United States
Commenting for this news organization, Zindel Segal, PhD, professor of psychology, University of Toronto, Scarborough, cautioned against making too much of the differences between the groups, because CBT-SH “trended positive and had a pretty healthy effect size, it just never reached significance.
“I wouldn’t say mindfulness drastically outperformed cognitive therapy. But cognitive therapy is a robust treatment in its own right, and so doing a little bit better is significant,” Dr. Segal said.
He also noted that, appropriately, the trial enrolled adults who were experiencing moderate depression and were not acutely ill. “That’s one of the rationales for self-help compared to providing patients with a more resource-intensive group treatment.
“If you look at the needs of people with moderate depression, what you find is that for cognitive therapy to work, negative thoughts and feelings need to be pervasive in order to make use of the techniques,” Dr. Segal explained.
“With mindfulness, you don’t need any to have constant negative thoughts or feelings. Anything that arises in your experience serves as grist for mill in terms of concentration and focus,” Dr. Segal said.
He also noted that mindfulness-based intervention is “more optimized” for people who are experiencing some measure of recovery or remission.
“It’s well suited for that, as it trends towards the wellness spectrum. But for people who might have greater levels of acuity or severity, cognitive-behavioral therapy might be indicated,” said Dr. Segal.
He also said the U.K. study findings are relevant to U.S. patients with depression.
“While it’s not disseminated in the same way through any kind of national program, the self-help books that are used are widely available, and the support that people were offered, either in person, telephone, or email, could be easily delivered. This would be a very useful model,” Dr. Segal said.
The LIGHTMind trial was funded by the National Institute for Health and Care Research and the Brighton and Sussex Clinical Trials Unit. Dr. Strauss has received grants from Headspace, is research lead for Sussex Mindfulness Centre, and has been chief investigator on National Institute for Health and Care Research. Dr. Segal is one of the authors of the MBCT-SH workbooks used in the study.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Music at bedtime may aid depression-related insomnia
PARIS –
The Music to Improve Sleep Quality in Adults With Depression and Insomnia (MUSTAFI) trial randomly assigned more than 110 outpatients with depression to either a music intervention or a waiting list. Sleep quality and quality of life significantly improved after listening to music for half an hour at bedtime for 4 weeks.
“This is a low-cost, safe intervention that has no side effects and may easily be implemented in psychiatry” along with existing treatments, lead researcher Helle Nystrup Lund, PhD, unit for depression, Aalborg (Denmark) University Hospital, said in an interview.
The findings were presented at the European Psychiatric Association 2023 Congress, and recently published in the Nordic Journal of Psychiatry.
Difficult to resolve
The researchers noted that insomnia is common in patients with depression and is “difficult to resolve.”
They noted that, while music is commonly used as a sleep aid and a growing evidence base suggests it has positive effects, there have been few investigations into the effectiveness of music for patients with depression-related insomnia.
To fill this research gap, 112 outpatients with depression and comorbid insomnia who were receiving care at a single center were randomly assigned to either an intervention group or a wait list control group.
Participants in the intervention group listened to music for a minimum of 30 minutes at bedtime for 4 weeks. The music was delivered via the MusicStar app, which is available as a free download from the Apple and Android (Google Play) app stores. The app was developed by Dr. Lund and Lars Rye Bertelsen, a PhD student and music therapist at Aalborg University Hospital.
The app is designed as a multicolored star, with each arm of the star linking to a playlist lasting between 30 minutes and 1 hour. Each color of the star indicates a different tempo of music.
Blue playlists, Dr. Lund explained, offer the quietest music, green is more lively, and red is the most dynamic. Gray playlists linked to project-related soundtracks, such as summer rain.
Dr. Lund said organizing the playlists by stimuli and color code, instead of genre, allows users to regulate their level of arousal and makes the music choice intuitive and easy.
She said that the genres of music include New Age, folk, pop, classical, and film soundtracks, “but no hard rock.”
“There’s actually a quite large selection of music available, because studies show that individual choice is important, as are personal preferences,” she said, adding that the endless choices offered by streaming services can cause confusion.
“So we made curated playlists and designed them with well-known pieces, but also with newly composed music not associated with anything,” Dr. Lund said.
Participants were assessed using the Pittsburgh Sleep Quality Index (PSQI), the Hamilton Depression Rating Scale, and two World Health Organization well-being questionnaires (WHO-5, WHOQOL-BREF), as well as actigraphy.
Results showed that, at 4 weeks, participants in the intervention group experienced significant improvements in sleep quality in comparison with control persons. The effect size for the PSQI was –2.1, and for quality of life on the WHO-5, the effect size was 8.4.
A subanalysis revealed that the length of nocturnal sleep in the intervention group increased by an average of 18 minutes during the study from a baseline of approximately 5 hours per night, said Dr. Lund.
However, there were no changes in actigraphy measurements and no significant improvements in HAMD-17 scores.
Dr. Lund said that, on the basis of these positive findings, music intervention as a sleep aid is now offered at Aalborg University Hospital to patients with depression-related insomnia.
Clinically meaningful?
Commenting on the findings, Gerald J. Haeffel, PhD, department of psychology, University of Notre Dame, South Bend, Ind., said that overall, the study showed there was a change in sleep-quality and quality of life scores of “about 10% in each.”
“This, on the surface, would seem to be a meaningful change,” although it is less clear whether it is “clinically meaningful.” Perhaps it is, “but it would be nice to have more information.”
It would be useful, he said, to “show the means for each group pre- to postintervention, along with standard deviations,” he added.
Dr. Haeffel added that on the basis of current results, it isn’t possible to determine whether individuals’ control over music choice is important.
“We have no idea if ‘choice’ or length of playlist had any causal role in the results. One would need to run a study with the same playlist, but in one group people have to listen to whatever song comes on versus another condition in which they get to choose a song off the same list,” he said.
He noted that his group conducted a study in which highly popular music that was chosen by individual participants was found to have a positive effect. Even so, he said, “we could not determine if it was ‘choice’ or ‘popularity’ that caused the positive effects of music.”
In addition, he said, the reason music has a positive effect on insomnia remains unclear.
“It is not because it helped with depression, and it’s not because it’s actually changing objective sleep parameters. It could be that it improves mood right before bed or helps distract people right before bed. At the same time, it could also just be a placebo effect,” said Dr. Haeffel.
In addition, he said, it’s important to note that the music intervention had no comparator, so “maybe just doing something different or getting to talk with researchers created the effect and has nothing to do with music.”
Overall, he believes that there are “not enough data” to use the sleep intervention that was employed in the current study “as primary intervention, but future work could show its usefulness as a supplement.”
Dr. Lund and Mr. Bertelsen reported ownership and sales of the MusicStar app. Dr. Haeffel reported no relevant financial relationships.
PARIS –
The Music to Improve Sleep Quality in Adults With Depression and Insomnia (MUSTAFI) trial randomly assigned more than 110 outpatients with depression to either a music intervention or a waiting list. Sleep quality and quality of life significantly improved after listening to music for half an hour at bedtime for 4 weeks.
“This is a low-cost, safe intervention that has no side effects and may easily be implemented in psychiatry” along with existing treatments, lead researcher Helle Nystrup Lund, PhD, unit for depression, Aalborg (Denmark) University Hospital, said in an interview.
The findings were presented at the European Psychiatric Association 2023 Congress, and recently published in the Nordic Journal of Psychiatry.
Difficult to resolve
The researchers noted that insomnia is common in patients with depression and is “difficult to resolve.”
They noted that, while music is commonly used as a sleep aid and a growing evidence base suggests it has positive effects, there have been few investigations into the effectiveness of music for patients with depression-related insomnia.
To fill this research gap, 112 outpatients with depression and comorbid insomnia who were receiving care at a single center were randomly assigned to either an intervention group or a wait list control group.
Participants in the intervention group listened to music for a minimum of 30 minutes at bedtime for 4 weeks. The music was delivered via the MusicStar app, which is available as a free download from the Apple and Android (Google Play) app stores. The app was developed by Dr. Lund and Lars Rye Bertelsen, a PhD student and music therapist at Aalborg University Hospital.
The app is designed as a multicolored star, with each arm of the star linking to a playlist lasting between 30 minutes and 1 hour. Each color of the star indicates a different tempo of music.
Blue playlists, Dr. Lund explained, offer the quietest music, green is more lively, and red is the most dynamic. Gray playlists linked to project-related soundtracks, such as summer rain.
Dr. Lund said organizing the playlists by stimuli and color code, instead of genre, allows users to regulate their level of arousal and makes the music choice intuitive and easy.
She said that the genres of music include New Age, folk, pop, classical, and film soundtracks, “but no hard rock.”
“There’s actually a quite large selection of music available, because studies show that individual choice is important, as are personal preferences,” she said, adding that the endless choices offered by streaming services can cause confusion.
“So we made curated playlists and designed them with well-known pieces, but also with newly composed music not associated with anything,” Dr. Lund said.
Participants were assessed using the Pittsburgh Sleep Quality Index (PSQI), the Hamilton Depression Rating Scale, and two World Health Organization well-being questionnaires (WHO-5, WHOQOL-BREF), as well as actigraphy.
Results showed that, at 4 weeks, participants in the intervention group experienced significant improvements in sleep quality in comparison with control persons. The effect size for the PSQI was –2.1, and for quality of life on the WHO-5, the effect size was 8.4.
A subanalysis revealed that the length of nocturnal sleep in the intervention group increased by an average of 18 minutes during the study from a baseline of approximately 5 hours per night, said Dr. Lund.
However, there were no changes in actigraphy measurements and no significant improvements in HAMD-17 scores.
Dr. Lund said that, on the basis of these positive findings, music intervention as a sleep aid is now offered at Aalborg University Hospital to patients with depression-related insomnia.
Clinically meaningful?
Commenting on the findings, Gerald J. Haeffel, PhD, department of psychology, University of Notre Dame, South Bend, Ind., said that overall, the study showed there was a change in sleep-quality and quality of life scores of “about 10% in each.”
“This, on the surface, would seem to be a meaningful change,” although it is less clear whether it is “clinically meaningful.” Perhaps it is, “but it would be nice to have more information.”
It would be useful, he said, to “show the means for each group pre- to postintervention, along with standard deviations,” he added.
Dr. Haeffel added that on the basis of current results, it isn’t possible to determine whether individuals’ control over music choice is important.
“We have no idea if ‘choice’ or length of playlist had any causal role in the results. One would need to run a study with the same playlist, but in one group people have to listen to whatever song comes on versus another condition in which they get to choose a song off the same list,” he said.
He noted that his group conducted a study in which highly popular music that was chosen by individual participants was found to have a positive effect. Even so, he said, “we could not determine if it was ‘choice’ or ‘popularity’ that caused the positive effects of music.”
In addition, he said, the reason music has a positive effect on insomnia remains unclear.
“It is not because it helped with depression, and it’s not because it’s actually changing objective sleep parameters. It could be that it improves mood right before bed or helps distract people right before bed. At the same time, it could also just be a placebo effect,” said Dr. Haeffel.
In addition, he said, it’s important to note that the music intervention had no comparator, so “maybe just doing something different or getting to talk with researchers created the effect and has nothing to do with music.”
Overall, he believes that there are “not enough data” to use the sleep intervention that was employed in the current study “as primary intervention, but future work could show its usefulness as a supplement.”
Dr. Lund and Mr. Bertelsen reported ownership and sales of the MusicStar app. Dr. Haeffel reported no relevant financial relationships.
PARIS –
The Music to Improve Sleep Quality in Adults With Depression and Insomnia (MUSTAFI) trial randomly assigned more than 110 outpatients with depression to either a music intervention or a waiting list. Sleep quality and quality of life significantly improved after listening to music for half an hour at bedtime for 4 weeks.
“This is a low-cost, safe intervention that has no side effects and may easily be implemented in psychiatry” along with existing treatments, lead researcher Helle Nystrup Lund, PhD, unit for depression, Aalborg (Denmark) University Hospital, said in an interview.
The findings were presented at the European Psychiatric Association 2023 Congress, and recently published in the Nordic Journal of Psychiatry.
Difficult to resolve
The researchers noted that insomnia is common in patients with depression and is “difficult to resolve.”
They noted that, while music is commonly used as a sleep aid and a growing evidence base suggests it has positive effects, there have been few investigations into the effectiveness of music for patients with depression-related insomnia.
To fill this research gap, 112 outpatients with depression and comorbid insomnia who were receiving care at a single center were randomly assigned to either an intervention group or a wait list control group.
Participants in the intervention group listened to music for a minimum of 30 minutes at bedtime for 4 weeks. The music was delivered via the MusicStar app, which is available as a free download from the Apple and Android (Google Play) app stores. The app was developed by Dr. Lund and Lars Rye Bertelsen, a PhD student and music therapist at Aalborg University Hospital.
The app is designed as a multicolored star, with each arm of the star linking to a playlist lasting between 30 minutes and 1 hour. Each color of the star indicates a different tempo of music.
Blue playlists, Dr. Lund explained, offer the quietest music, green is more lively, and red is the most dynamic. Gray playlists linked to project-related soundtracks, such as summer rain.
Dr. Lund said organizing the playlists by stimuli and color code, instead of genre, allows users to regulate their level of arousal and makes the music choice intuitive and easy.
She said that the genres of music include New Age, folk, pop, classical, and film soundtracks, “but no hard rock.”
“There’s actually a quite large selection of music available, because studies show that individual choice is important, as are personal preferences,” she said, adding that the endless choices offered by streaming services can cause confusion.
“So we made curated playlists and designed them with well-known pieces, but also with newly composed music not associated with anything,” Dr. Lund said.
Participants were assessed using the Pittsburgh Sleep Quality Index (PSQI), the Hamilton Depression Rating Scale, and two World Health Organization well-being questionnaires (WHO-5, WHOQOL-BREF), as well as actigraphy.
Results showed that, at 4 weeks, participants in the intervention group experienced significant improvements in sleep quality in comparison with control persons. The effect size for the PSQI was –2.1, and for quality of life on the WHO-5, the effect size was 8.4.
A subanalysis revealed that the length of nocturnal sleep in the intervention group increased by an average of 18 minutes during the study from a baseline of approximately 5 hours per night, said Dr. Lund.
However, there were no changes in actigraphy measurements and no significant improvements in HAMD-17 scores.
Dr. Lund said that, on the basis of these positive findings, music intervention as a sleep aid is now offered at Aalborg University Hospital to patients with depression-related insomnia.
Clinically meaningful?
Commenting on the findings, Gerald J. Haeffel, PhD, department of psychology, University of Notre Dame, South Bend, Ind., said that overall, the study showed there was a change in sleep-quality and quality of life scores of “about 10% in each.”
“This, on the surface, would seem to be a meaningful change,” although it is less clear whether it is “clinically meaningful.” Perhaps it is, “but it would be nice to have more information.”
It would be useful, he said, to “show the means for each group pre- to postintervention, along with standard deviations,” he added.
Dr. Haeffel added that on the basis of current results, it isn’t possible to determine whether individuals’ control over music choice is important.
“We have no idea if ‘choice’ or length of playlist had any causal role in the results. One would need to run a study with the same playlist, but in one group people have to listen to whatever song comes on versus another condition in which they get to choose a song off the same list,” he said.
He noted that his group conducted a study in which highly popular music that was chosen by individual participants was found to have a positive effect. Even so, he said, “we could not determine if it was ‘choice’ or ‘popularity’ that caused the positive effects of music.”
In addition, he said, the reason music has a positive effect on insomnia remains unclear.
“It is not because it helped with depression, and it’s not because it’s actually changing objective sleep parameters. It could be that it improves mood right before bed or helps distract people right before bed. At the same time, it could also just be a placebo effect,” said Dr. Haeffel.
In addition, he said, it’s important to note that the music intervention had no comparator, so “maybe just doing something different or getting to talk with researchers created the effect and has nothing to do with music.”
Overall, he believes that there are “not enough data” to use the sleep intervention that was employed in the current study “as primary intervention, but future work could show its usefulness as a supplement.”
Dr. Lund and Mr. Bertelsen reported ownership and sales of the MusicStar app. Dr. Haeffel reported no relevant financial relationships.
AT EPA 2023
Intranasal esketamine: A primer
Intranasal esketamine is an FDA-approved ketamine molecule indicated for use together with an oral antidepressant for treatment-resistant depression (TRD) in patients age ≥18 who have had an inadequate response to ≥2 antidepressants, and for depressive symptoms in adults with major depressive disorder with suicidal thoughts or actions.¹ Since March 2019, we’ve been treating patients with intranasal esketamine. Based on our experiences, here is a summary of what we have learned.
REMS is required. Due to the potential risks resulting from sedation and dissociation caused by esketamine and the risk of abuse and misuse, esketamine is available only through a Risk Evaluation and Mitigation Strategy (REMS) program. The program links your office Drug Enforcement Administration number to the address where this schedule III medication will be stored and given to the patient for self-administration. Requirements and other details about the REMS are available at www.spravatorems.com.
Treatment. Start with the online REMS patient enrollment/consent form. Contraindications include having a history of aneurysmal vascular disease, intracerebral hemorrhage, or allergy to ketamine/esketamine. Adjunctive treatment with esketamine plus sertraline, escitalopram, venlafaxine, or duloxetine are comparably effective.¹ We have found that adding magnesium to block glutamate action at N-methyl-
Iatrogenic effects rarely lead to dropout. The first session is critical to allay anticipatory anxiety. Sedation, blood pressure increase, and dissociation are common but transient adverse effects that typically peak at 40 minutes and resolve by 90 minutes. Record blood pressure on a REMS monitoring form before treatment, at 40 minutes, and at 2 hours. Avoid administering sedative or prohypertensive medications together with esketamine.¹ Dissociation is more common in patients with a history of trauma. Combine music, guided imagery, or psychotherapy to harness this for therapeutic benefit. Sleepiness can last 4 hours; make sure the patient has arranged for a ride home, as they cannot drive until the next day. Verify normal blood pressure before starting treatment. Clonidine or labetalol for hypertension/severe dissociation and ondansetron or prochlorperazine for nausea are rarely needed. Advise patients to use the bathroom before treatment and keep a trash can nearby for vomiting. Other transient adverse effects found in TRD clinical trials that occurred >5% and twice that of placebo were dizziness, vertigo, numbness, and feeling drunk.¹
Reimbursement for treatment with esketamine is available through most insurances, including copay cards, rebates, deductible support, and free assistance programs. Coverage is either through pharmacy benefit, assignment of medical benefit (pharmacy handles the medical benefit), or medical benefit with remuneration above wholesale price.
Zeitgeist shift. Emergency departments are backlogged and patients languish waiting to feel the effects of oral antidepressants. Intranasal esketamine could help alleviate this situation by producing a more immediate response. We also have observed improvements in comorbid posttraumatic stress disorder and in cognitive deficits of dementia, possibly due to rapidly enhanced neuroplasticity, neurogenesis, and astrocyte functioning, which NMDA receptor antagonism, AMPA activation, and downstream mediators (eg, brain-derived neurotrophic factor) may promote.4
1. Spravato (esketamine nasal spray) medication guide. Accessed November 22, 2022. https://www.janssenlabels.com/package-insert/product-patient-information/SPRAVATO-medication-guide.pdf
2. Spravato Healthcare Professional Website. TRD safety & efficacy. Accessed November 22, 2022. https://www.spravatohcp.com/trd-long-term/efficacy
3. Popova V, Daly EJ, Trivedi M, et al. Efficacy and safety of flexibly dosed esketamine nasal spray combined with a newly initiated oral antidepressant in treatment-resistant depression: a randomized double-blind active-controlled study. Am J Psychiatry. 2019;176(6):428-438. doi:10.1176/appi.ajp.2019.19020172
4. Matveychuk D, Thomas RK, Swainson J, et al. Ketamine as an antidepressant: overview of its mechanisms of action and potential predictive biomarkers. Ther Adv Psychopharmacol. 2020;10:2045125320916657. doi:10.1177/2045125320916657
Intranasal esketamine is an FDA-approved ketamine molecule indicated for use together with an oral antidepressant for treatment-resistant depression (TRD) in patients age ≥18 who have had an inadequate response to ≥2 antidepressants, and for depressive symptoms in adults with major depressive disorder with suicidal thoughts or actions.¹ Since March 2019, we’ve been treating patients with intranasal esketamine. Based on our experiences, here is a summary of what we have learned.
REMS is required. Due to the potential risks resulting from sedation and dissociation caused by esketamine and the risk of abuse and misuse, esketamine is available only through a Risk Evaluation and Mitigation Strategy (REMS) program. The program links your office Drug Enforcement Administration number to the address where this schedule III medication will be stored and given to the patient for self-administration. Requirements and other details about the REMS are available at www.spravatorems.com.
Treatment. Start with the online REMS patient enrollment/consent form. Contraindications include having a history of aneurysmal vascular disease, intracerebral hemorrhage, or allergy to ketamine/esketamine. Adjunctive treatment with esketamine plus sertraline, escitalopram, venlafaxine, or duloxetine are comparably effective.¹ We have found that adding magnesium to block glutamate action at N-methyl-
Iatrogenic effects rarely lead to dropout. The first session is critical to allay anticipatory anxiety. Sedation, blood pressure increase, and dissociation are common but transient adverse effects that typically peak at 40 minutes and resolve by 90 minutes. Record blood pressure on a REMS monitoring form before treatment, at 40 minutes, and at 2 hours. Avoid administering sedative or prohypertensive medications together with esketamine.¹ Dissociation is more common in patients with a history of trauma. Combine music, guided imagery, or psychotherapy to harness this for therapeutic benefit. Sleepiness can last 4 hours; make sure the patient has arranged for a ride home, as they cannot drive until the next day. Verify normal blood pressure before starting treatment. Clonidine or labetalol for hypertension/severe dissociation and ondansetron or prochlorperazine for nausea are rarely needed. Advise patients to use the bathroom before treatment and keep a trash can nearby for vomiting. Other transient adverse effects found in TRD clinical trials that occurred >5% and twice that of placebo were dizziness, vertigo, numbness, and feeling drunk.¹
Reimbursement for treatment with esketamine is available through most insurances, including copay cards, rebates, deductible support, and free assistance programs. Coverage is either through pharmacy benefit, assignment of medical benefit (pharmacy handles the medical benefit), or medical benefit with remuneration above wholesale price.
Zeitgeist shift. Emergency departments are backlogged and patients languish waiting to feel the effects of oral antidepressants. Intranasal esketamine could help alleviate this situation by producing a more immediate response. We also have observed improvements in comorbid posttraumatic stress disorder and in cognitive deficits of dementia, possibly due to rapidly enhanced neuroplasticity, neurogenesis, and astrocyte functioning, which NMDA receptor antagonism, AMPA activation, and downstream mediators (eg, brain-derived neurotrophic factor) may promote.4
Intranasal esketamine is an FDA-approved ketamine molecule indicated for use together with an oral antidepressant for treatment-resistant depression (TRD) in patients age ≥18 who have had an inadequate response to ≥2 antidepressants, and for depressive symptoms in adults with major depressive disorder with suicidal thoughts or actions.¹ Since March 2019, we’ve been treating patients with intranasal esketamine. Based on our experiences, here is a summary of what we have learned.
REMS is required. Due to the potential risks resulting from sedation and dissociation caused by esketamine and the risk of abuse and misuse, esketamine is available only through a Risk Evaluation and Mitigation Strategy (REMS) program. The program links your office Drug Enforcement Administration number to the address where this schedule III medication will be stored and given to the patient for self-administration. Requirements and other details about the REMS are available at www.spravatorems.com.
Treatment. Start with the online REMS patient enrollment/consent form. Contraindications include having a history of aneurysmal vascular disease, intracerebral hemorrhage, or allergy to ketamine/esketamine. Adjunctive treatment with esketamine plus sertraline, escitalopram, venlafaxine, or duloxetine are comparably effective.¹ We have found that adding magnesium to block glutamate action at N-methyl-
Iatrogenic effects rarely lead to dropout. The first session is critical to allay anticipatory anxiety. Sedation, blood pressure increase, and dissociation are common but transient adverse effects that typically peak at 40 minutes and resolve by 90 minutes. Record blood pressure on a REMS monitoring form before treatment, at 40 minutes, and at 2 hours. Avoid administering sedative or prohypertensive medications together with esketamine.¹ Dissociation is more common in patients with a history of trauma. Combine music, guided imagery, or psychotherapy to harness this for therapeutic benefit. Sleepiness can last 4 hours; make sure the patient has arranged for a ride home, as they cannot drive until the next day. Verify normal blood pressure before starting treatment. Clonidine or labetalol for hypertension/severe dissociation and ondansetron or prochlorperazine for nausea are rarely needed. Advise patients to use the bathroom before treatment and keep a trash can nearby for vomiting. Other transient adverse effects found in TRD clinical trials that occurred >5% and twice that of placebo were dizziness, vertigo, numbness, and feeling drunk.¹
Reimbursement for treatment with esketamine is available through most insurances, including copay cards, rebates, deductible support, and free assistance programs. Coverage is either through pharmacy benefit, assignment of medical benefit (pharmacy handles the medical benefit), or medical benefit with remuneration above wholesale price.
Zeitgeist shift. Emergency departments are backlogged and patients languish waiting to feel the effects of oral antidepressants. Intranasal esketamine could help alleviate this situation by producing a more immediate response. We also have observed improvements in comorbid posttraumatic stress disorder and in cognitive deficits of dementia, possibly due to rapidly enhanced neuroplasticity, neurogenesis, and astrocyte functioning, which NMDA receptor antagonism, AMPA activation, and downstream mediators (eg, brain-derived neurotrophic factor) may promote.4
1. Spravato (esketamine nasal spray) medication guide. Accessed November 22, 2022. https://www.janssenlabels.com/package-insert/product-patient-information/SPRAVATO-medication-guide.pdf
2. Spravato Healthcare Professional Website. TRD safety & efficacy. Accessed November 22, 2022. https://www.spravatohcp.com/trd-long-term/efficacy
3. Popova V, Daly EJ, Trivedi M, et al. Efficacy and safety of flexibly dosed esketamine nasal spray combined with a newly initiated oral antidepressant in treatment-resistant depression: a randomized double-blind active-controlled study. Am J Psychiatry. 2019;176(6):428-438. doi:10.1176/appi.ajp.2019.19020172
4. Matveychuk D, Thomas RK, Swainson J, et al. Ketamine as an antidepressant: overview of its mechanisms of action and potential predictive biomarkers. Ther Adv Psychopharmacol. 2020;10:2045125320916657. doi:10.1177/2045125320916657
1. Spravato (esketamine nasal spray) medication guide. Accessed November 22, 2022. https://www.janssenlabels.com/package-insert/product-patient-information/SPRAVATO-medication-guide.pdf
2. Spravato Healthcare Professional Website. TRD safety & efficacy. Accessed November 22, 2022. https://www.spravatohcp.com/trd-long-term/efficacy
3. Popova V, Daly EJ, Trivedi M, et al. Efficacy and safety of flexibly dosed esketamine nasal spray combined with a newly initiated oral antidepressant in treatment-resistant depression: a randomized double-blind active-controlled study. Am J Psychiatry. 2019;176(6):428-438. doi:10.1176/appi.ajp.2019.19020172
4. Matveychuk D, Thomas RK, Swainson J, et al. Ketamine as an antidepressant: overview of its mechanisms of action and potential predictive biomarkers. Ther Adv Psychopharmacol. 2020;10:2045125320916657. doi:10.1177/2045125320916657
Are parents infecting their children with contagious negativity?
A couple of weeks ago I stumbled across a report of a Pew Research Center’s survey titled “Parenting in America today” (Pew Research Center. Jan. 24, 2023), which found that 40% of parents in the United States with children younger than 18 are “extremely or very worried” that at some point their children might struggle with anxiety or depression. Thirty-six percent replied that they were “somewhat” worried. This total of more than 75% represents a significant change from the 2015 Pew Center survey in which only 54% of parents were “somewhat” worried about their children’s mental health.
Prompted by these findings I began work on a column in which I planned to encourage pediatricians to think more like family physicians when we were working with children who were experiencing serious mental health problems. My primary message was going to be that we should turn more of our attention to the mental health of the anxious parents who must endure the often long and frustrating path toward effective psychiatric care for their children. This might come in the form of some simple suggestions about nonpharmacologic self-help strategies. Or, it could mean encouraging parents to seek psychiatric care or counseling for themselves as they wait for help for their child.
However, as I began that column, my thoughts kept drifting toward a broader consideration of the relationship between parents and pediatric mental health. If mental health of children is causing their parents to be anxious and depressed isn’t it just as likely that this is a bidirectional connection? This was not exactly an “aha” moment for me because it is a relationship I have considered for sometime. However, it is a concept that I have come to realize is receiving far too little attention.
There are exceptions. For example, a recent opinion piece in the New York Times by David French, “What if Kids Are Sad and Stressed Because Their Parents Are?” (March 19, 2023) echoes many of my concerns. Drawing on his experiences traveling around college campuses, Mr. French observes, “Just as parents are upset about their children’s anxiety and depression, children are anxious about their parent’s mental health.”
He notes that an August 2022 NBC News poll found that 58% of registered voters feel this country’s best days are behind it and joins me in imagining that this negative mind set is filtering down to the pediatric population. He acknowledges that there are other likely contributors to teen unhappiness including the ubiquity of smart phones, the secularization of society, and the media’s focus on the political divide. However, Mr. French wonders if the parenting style that results in childhood experiences that are dominated by adult supervision and protection may also be playing a large role.
In his conclusion, Mr. French asks us to consider “How much fear and anxiety should we import to our lives and homes?” as we adults search for an answer.
As I continued to drill down for other possible solutions, I encountered an avenue of psychological research that suggests that instead of, or in addition to, filtering out the anxiety-generating deluge of information, we begin to give some thought to how our beliefs may be coloring our perception of reality.
Jeremy D.W. Clifton, PhD, a psychologist at the University of Pennsylvania Positive Psychology Center has done extensive research on the relationship between our basic beliefs about the world (known as primal beliefs or simply primals in psychologist lingo) and how we interpret reality. For example, one of your primal beliefs may be that the world is a dangerous place. I, on the other hand, may see the world as a stimulating environment offering me endless opportunities to explore. I may see the world as an abundant resource limited only by my creativity. You, however, see it as a barren wasteland.
Dr. Clifton’s research has shown that our primals (at least those of adults) are relatively immutable through one’s lifetime and “do not appear to be the consequence of our experiences.” For example, living in a ZIP code with a high crime rate does not predict that you will see the world as a dangerous place. Nor does being affluent guarantee that an adult sees the world rich with opportunities.
It is unclear exactly when and by what process we develop our primal beliefs, but it is safe to say our parents probably play a large role. Exactly to what degree the tsunami of bad news we are allowing to inundate our children’s lives plays a role is unclear. However, it is reasonable to assume that news about climate change, school shootings, and the pandemic must be a contributor.
According to Dr. Clifton, there is some evidence that certain mind exercises, when applied diligently, can occasionally modify the primal beliefs of an individual who sees the world as dangerous and barren. Until such strategies become more readily accessible, the best we can do is acknowledge that our children are like canaries in a coal mine full of negative perceptions, then do our best to clear the air.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
A couple of weeks ago I stumbled across a report of a Pew Research Center’s survey titled “Parenting in America today” (Pew Research Center. Jan. 24, 2023), which found that 40% of parents in the United States with children younger than 18 are “extremely or very worried” that at some point their children might struggle with anxiety or depression. Thirty-six percent replied that they were “somewhat” worried. This total of more than 75% represents a significant change from the 2015 Pew Center survey in which only 54% of parents were “somewhat” worried about their children’s mental health.
Prompted by these findings I began work on a column in which I planned to encourage pediatricians to think more like family physicians when we were working with children who were experiencing serious mental health problems. My primary message was going to be that we should turn more of our attention to the mental health of the anxious parents who must endure the often long and frustrating path toward effective psychiatric care for their children. This might come in the form of some simple suggestions about nonpharmacologic self-help strategies. Or, it could mean encouraging parents to seek psychiatric care or counseling for themselves as they wait for help for their child.
However, as I began that column, my thoughts kept drifting toward a broader consideration of the relationship between parents and pediatric mental health. If mental health of children is causing their parents to be anxious and depressed isn’t it just as likely that this is a bidirectional connection? This was not exactly an “aha” moment for me because it is a relationship I have considered for sometime. However, it is a concept that I have come to realize is receiving far too little attention.
There are exceptions. For example, a recent opinion piece in the New York Times by David French, “What if Kids Are Sad and Stressed Because Their Parents Are?” (March 19, 2023) echoes many of my concerns. Drawing on his experiences traveling around college campuses, Mr. French observes, “Just as parents are upset about their children’s anxiety and depression, children are anxious about their parent’s mental health.”
He notes that an August 2022 NBC News poll found that 58% of registered voters feel this country’s best days are behind it and joins me in imagining that this negative mind set is filtering down to the pediatric population. He acknowledges that there are other likely contributors to teen unhappiness including the ubiquity of smart phones, the secularization of society, and the media’s focus on the political divide. However, Mr. French wonders if the parenting style that results in childhood experiences that are dominated by adult supervision and protection may also be playing a large role.
In his conclusion, Mr. French asks us to consider “How much fear and anxiety should we import to our lives and homes?” as we adults search for an answer.
As I continued to drill down for other possible solutions, I encountered an avenue of psychological research that suggests that instead of, or in addition to, filtering out the anxiety-generating deluge of information, we begin to give some thought to how our beliefs may be coloring our perception of reality.
Jeremy D.W. Clifton, PhD, a psychologist at the University of Pennsylvania Positive Psychology Center has done extensive research on the relationship between our basic beliefs about the world (known as primal beliefs or simply primals in psychologist lingo) and how we interpret reality. For example, one of your primal beliefs may be that the world is a dangerous place. I, on the other hand, may see the world as a stimulating environment offering me endless opportunities to explore. I may see the world as an abundant resource limited only by my creativity. You, however, see it as a barren wasteland.
Dr. Clifton’s research has shown that our primals (at least those of adults) are relatively immutable through one’s lifetime and “do not appear to be the consequence of our experiences.” For example, living in a ZIP code with a high crime rate does not predict that you will see the world as a dangerous place. Nor does being affluent guarantee that an adult sees the world rich with opportunities.
It is unclear exactly when and by what process we develop our primal beliefs, but it is safe to say our parents probably play a large role. Exactly to what degree the tsunami of bad news we are allowing to inundate our children’s lives plays a role is unclear. However, it is reasonable to assume that news about climate change, school shootings, and the pandemic must be a contributor.
According to Dr. Clifton, there is some evidence that certain mind exercises, when applied diligently, can occasionally modify the primal beliefs of an individual who sees the world as dangerous and barren. Until such strategies become more readily accessible, the best we can do is acknowledge that our children are like canaries in a coal mine full of negative perceptions, then do our best to clear the air.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
A couple of weeks ago I stumbled across a report of a Pew Research Center’s survey titled “Parenting in America today” (Pew Research Center. Jan. 24, 2023), which found that 40% of parents in the United States with children younger than 18 are “extremely or very worried” that at some point their children might struggle with anxiety or depression. Thirty-six percent replied that they were “somewhat” worried. This total of more than 75% represents a significant change from the 2015 Pew Center survey in which only 54% of parents were “somewhat” worried about their children’s mental health.
Prompted by these findings I began work on a column in which I planned to encourage pediatricians to think more like family physicians when we were working with children who were experiencing serious mental health problems. My primary message was going to be that we should turn more of our attention to the mental health of the anxious parents who must endure the often long and frustrating path toward effective psychiatric care for their children. This might come in the form of some simple suggestions about nonpharmacologic self-help strategies. Or, it could mean encouraging parents to seek psychiatric care or counseling for themselves as they wait for help for their child.
However, as I began that column, my thoughts kept drifting toward a broader consideration of the relationship between parents and pediatric mental health. If mental health of children is causing their parents to be anxious and depressed isn’t it just as likely that this is a bidirectional connection? This was not exactly an “aha” moment for me because it is a relationship I have considered for sometime. However, it is a concept that I have come to realize is receiving far too little attention.
There are exceptions. For example, a recent opinion piece in the New York Times by David French, “What if Kids Are Sad and Stressed Because Their Parents Are?” (March 19, 2023) echoes many of my concerns. Drawing on his experiences traveling around college campuses, Mr. French observes, “Just as parents are upset about their children’s anxiety and depression, children are anxious about their parent’s mental health.”
He notes that an August 2022 NBC News poll found that 58% of registered voters feel this country’s best days are behind it and joins me in imagining that this negative mind set is filtering down to the pediatric population. He acknowledges that there are other likely contributors to teen unhappiness including the ubiquity of smart phones, the secularization of society, and the media’s focus on the political divide. However, Mr. French wonders if the parenting style that results in childhood experiences that are dominated by adult supervision and protection may also be playing a large role.
In his conclusion, Mr. French asks us to consider “How much fear and anxiety should we import to our lives and homes?” as we adults search for an answer.
As I continued to drill down for other possible solutions, I encountered an avenue of psychological research that suggests that instead of, or in addition to, filtering out the anxiety-generating deluge of information, we begin to give some thought to how our beliefs may be coloring our perception of reality.
Jeremy D.W. Clifton, PhD, a psychologist at the University of Pennsylvania Positive Psychology Center has done extensive research on the relationship between our basic beliefs about the world (known as primal beliefs or simply primals in psychologist lingo) and how we interpret reality. For example, one of your primal beliefs may be that the world is a dangerous place. I, on the other hand, may see the world as a stimulating environment offering me endless opportunities to explore. I may see the world as an abundant resource limited only by my creativity. You, however, see it as a barren wasteland.
Dr. Clifton’s research has shown that our primals (at least those of adults) are relatively immutable through one’s lifetime and “do not appear to be the consequence of our experiences.” For example, living in a ZIP code with a high crime rate does not predict that you will see the world as a dangerous place. Nor does being affluent guarantee that an adult sees the world rich with opportunities.
It is unclear exactly when and by what process we develop our primal beliefs, but it is safe to say our parents probably play a large role. Exactly to what degree the tsunami of bad news we are allowing to inundate our children’s lives plays a role is unclear. However, it is reasonable to assume that news about climate change, school shootings, and the pandemic must be a contributor.
According to Dr. Clifton, there is some evidence that certain mind exercises, when applied diligently, can occasionally modify the primal beliefs of an individual who sees the world as dangerous and barren. Until such strategies become more readily accessible, the best we can do is acknowledge that our children are like canaries in a coal mine full of negative perceptions, then do our best to clear the air.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Impact of child abuse differs by gender
PARIS – , new research shows.
Investigators found childhood emotional and sexual abuse had a greater effect on women than men, whereas men were more adversely affected by emotional and physical neglect.
“Our findings indicate that exposure to childhood maltreatment increases the risk of having psychiatric symptoms in both men and women,” lead researcher Thanavadee Prachason, PhD, department of psychiatry and neuropsychology, Maastricht (the Netherlands) University Medical Center, said in a press release.
“Exposure to emotionally or sexually abusive experiences during childhood increases the risk of a variety of psychiatric symptoms, particularly in women. In contrast, a history of emotional or physical neglect in childhood increases the risk of having psychiatric symptoms more in men,” Dr. Prachason added.
The findings were presented at the European Psychiatric Association 2023 Congress.
A leading mental illness risk factor
Study presenter Laura Fusar-Poli, MD, PhD, from the department of brain and behavioral sciences, University of Pavia (Italy), said that the differential impact of trauma subtypes in men and women indicate that both gender and the type of childhood adversity experienced need to be taken into account in future studies.
Dr. Fusar-Poli began by highlighting that 13%-36% of individuals have experienced some kind of childhood trauma, with 30% exposed to at least two types of trauma.
Trauma has been identified as a risk factor for a range of mental health problems.
“It is estimated that, worldwide, around one third of all psychiatric disorders are related to childhood trauma,” senior researcher Sinan Gül
Consequently, “childhood trauma is a leading preventable risk factor for mental illness,” he added.
Previous research suggests the subtype of trauma has an impact on subsequent biological changes and clinical outcomes, and that there are gender differences in the effects of childhood trauma.
To investigate, the researchers examined data from TwinssCan, a Belgian cohort of twins and siblings aged 15-35 years without a diagnosis of pervasive mental disorders.
The study included 477 females and 314 males who had completed the Childhood Trauma Questionnaire–Short Form (CTQ) and the Symptom Checklist-90 SR (SCL-90) to determine exposure to childhood adversity and levels of psychopathology, respectively.
Results showed that total CTQ scores were significantly associated with total SCL-90 scores in both men and women, as well as with each of the nine symptom domains of the SCL-90 (P < .001 for all assessments). These included psychoticism, paranoid ideation, anxiety, depression, somatization, obsessive-compulsive, interpersonal sensitivity, hostility, and phobic anxiety.
There were no significant differences in the associations with total CTQ scores between men and women.
However, when the researchers examined trauma subtypes and psychopathology, clear gender differences emerged.
Investigators found a significant association between emotional abuse on the CTQ and total SCL-90 scores in both men (P < .023) and women (P < .001), but that the association was significantly stronger in women (P = .043).
Sexual abuse was significantly associated with total SCL-90 scores in women (P < .001), while emotional neglect and physical neglect were significantly associated with psychopathology scores in men (P = .026 and P < .001, respectively).
“Physical neglect may include experiences of not having enough to eat, wearing dirty clothes, not being taken care of, and not getting taken to the doctor when the person was growing up,” said Dr. Prachason.
“Emotional neglect may include childhood experiences like not feeling loved or important, and not feeling close to the family.”
In women, emotional abuse was significantly associated with all nine symptom domains of the SCL-90, while sexual abuse was associated with seven: psychoticism, paranoid ideation, anxiety, depression, somatization, obsessive-compulsive, and hostility.
Physical neglect, in men, was significantly associated with eight of the symptom domains (all but somatization), but emotional neglect was linked only to depression, Dr. Fusar-Poli reported.
“This study showed a very important consequence of childhood trauma, and not only in people with mental disorders. I would like to underline that this is a general population, composed of adolescents and young adults, which is the age in which the majority of mental disorders starts, Dr. Fusar-Poli said in an interview.
She emphasized that psychotic disorders are only a part of the “broad range” of conditions that may be related to childhood trauma, which “can have an impact on sub-threshold symptoms that can affect functioning and quality of life in the general population.”
Addressing the differential findings in men and women, Dr. Gül
However, he said, this is “something that we really need understand,” as there is likely an underlying mechanism, “and not only a biological mechanism but probably a societal one.”
Dr. Gül
Compromised cognitive, emotional function
Commenting on the findings for this news organization, Elaine F. Walker, PhD, professor of psychology and neuroscience at Emory University in Atlanta, said stress exposure in general, including childhood trauma, “has transdiagnostic effects on vulnerability to mental disorders.”
“The effects are primarily mediated by the hypothalamic-pituitary-adrenal axis, which triggers the release of cortisol. When persistently elevated, this can result in neurobiological processes that have adverse effects on brain structure and circuitry which, in turn, compromises cognitive and emotional functioning,” said Dr. Walker, who was not associated with the study.
She noted that, “while it is possible that there are sex differences in biological sensitivity to certain subtypes of childhood trauma, it may also be the case that sex differences in the likelihood of exposure to trauma subtypes is actually the key factor.”
“At the present time, there are not specific treatment protocols aimed at addressing childhood trauma subtypes, but most experienced therapists will incorporate information about the individual’s trauma history in their treatment,” Dr. Walker added.
Also commenting on the research, Philip Gorwood, MD, PhD, head of the Clinique des Maladies Mentales et de l’Encéphale at Centre Hospitalier Sainte Anne in Paris, said the results are “important … as childhood trauma has been clearly recognized as a major risk factor for the vast majority of psychiatric disorders, but with poor knowledge of gender specificities.”
“Understanding which aspects of trauma are more damaging according to gender will facilitate research on the resilience process. Many intervention strategies will indeed benefit from a more personalized approach,” he said in a statement. Dr. Gorwood was not involved with this study.
The study authors, Dr. Gorwood, and Dr. Walker report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
PARIS – , new research shows.
Investigators found childhood emotional and sexual abuse had a greater effect on women than men, whereas men were more adversely affected by emotional and physical neglect.
“Our findings indicate that exposure to childhood maltreatment increases the risk of having psychiatric symptoms in both men and women,” lead researcher Thanavadee Prachason, PhD, department of psychiatry and neuropsychology, Maastricht (the Netherlands) University Medical Center, said in a press release.
“Exposure to emotionally or sexually abusive experiences during childhood increases the risk of a variety of psychiatric symptoms, particularly in women. In contrast, a history of emotional or physical neglect in childhood increases the risk of having psychiatric symptoms more in men,” Dr. Prachason added.
The findings were presented at the European Psychiatric Association 2023 Congress.
A leading mental illness risk factor
Study presenter Laura Fusar-Poli, MD, PhD, from the department of brain and behavioral sciences, University of Pavia (Italy), said that the differential impact of trauma subtypes in men and women indicate that both gender and the type of childhood adversity experienced need to be taken into account in future studies.
Dr. Fusar-Poli began by highlighting that 13%-36% of individuals have experienced some kind of childhood trauma, with 30% exposed to at least two types of trauma.
Trauma has been identified as a risk factor for a range of mental health problems.
“It is estimated that, worldwide, around one third of all psychiatric disorders are related to childhood trauma,” senior researcher Sinan Gül
Consequently, “childhood trauma is a leading preventable risk factor for mental illness,” he added.
Previous research suggests the subtype of trauma has an impact on subsequent biological changes and clinical outcomes, and that there are gender differences in the effects of childhood trauma.
To investigate, the researchers examined data from TwinssCan, a Belgian cohort of twins and siblings aged 15-35 years without a diagnosis of pervasive mental disorders.
The study included 477 females and 314 males who had completed the Childhood Trauma Questionnaire–Short Form (CTQ) and the Symptom Checklist-90 SR (SCL-90) to determine exposure to childhood adversity and levels of psychopathology, respectively.
Results showed that total CTQ scores were significantly associated with total SCL-90 scores in both men and women, as well as with each of the nine symptom domains of the SCL-90 (P < .001 for all assessments). These included psychoticism, paranoid ideation, anxiety, depression, somatization, obsessive-compulsive, interpersonal sensitivity, hostility, and phobic anxiety.
There were no significant differences in the associations with total CTQ scores between men and women.
However, when the researchers examined trauma subtypes and psychopathology, clear gender differences emerged.
Investigators found a significant association between emotional abuse on the CTQ and total SCL-90 scores in both men (P < .023) and women (P < .001), but that the association was significantly stronger in women (P = .043).
Sexual abuse was significantly associated with total SCL-90 scores in women (P < .001), while emotional neglect and physical neglect were significantly associated with psychopathology scores in men (P = .026 and P < .001, respectively).
“Physical neglect may include experiences of not having enough to eat, wearing dirty clothes, not being taken care of, and not getting taken to the doctor when the person was growing up,” said Dr. Prachason.
“Emotional neglect may include childhood experiences like not feeling loved or important, and not feeling close to the family.”
In women, emotional abuse was significantly associated with all nine symptom domains of the SCL-90, while sexual abuse was associated with seven: psychoticism, paranoid ideation, anxiety, depression, somatization, obsessive-compulsive, and hostility.
Physical neglect, in men, was significantly associated with eight of the symptom domains (all but somatization), but emotional neglect was linked only to depression, Dr. Fusar-Poli reported.
“This study showed a very important consequence of childhood trauma, and not only in people with mental disorders. I would like to underline that this is a general population, composed of adolescents and young adults, which is the age in which the majority of mental disorders starts, Dr. Fusar-Poli said in an interview.
She emphasized that psychotic disorders are only a part of the “broad range” of conditions that may be related to childhood trauma, which “can have an impact on sub-threshold symptoms that can affect functioning and quality of life in the general population.”
Addressing the differential findings in men and women, Dr. Gül
However, he said, this is “something that we really need understand,” as there is likely an underlying mechanism, “and not only a biological mechanism but probably a societal one.”
Dr. Gül
Compromised cognitive, emotional function
Commenting on the findings for this news organization, Elaine F. Walker, PhD, professor of psychology and neuroscience at Emory University in Atlanta, said stress exposure in general, including childhood trauma, “has transdiagnostic effects on vulnerability to mental disorders.”
“The effects are primarily mediated by the hypothalamic-pituitary-adrenal axis, which triggers the release of cortisol. When persistently elevated, this can result in neurobiological processes that have adverse effects on brain structure and circuitry which, in turn, compromises cognitive and emotional functioning,” said Dr. Walker, who was not associated with the study.
She noted that, “while it is possible that there are sex differences in biological sensitivity to certain subtypes of childhood trauma, it may also be the case that sex differences in the likelihood of exposure to trauma subtypes is actually the key factor.”
“At the present time, there are not specific treatment protocols aimed at addressing childhood trauma subtypes, but most experienced therapists will incorporate information about the individual’s trauma history in their treatment,” Dr. Walker added.
Also commenting on the research, Philip Gorwood, MD, PhD, head of the Clinique des Maladies Mentales et de l’Encéphale at Centre Hospitalier Sainte Anne in Paris, said the results are “important … as childhood trauma has been clearly recognized as a major risk factor for the vast majority of psychiatric disorders, but with poor knowledge of gender specificities.”
“Understanding which aspects of trauma are more damaging according to gender will facilitate research on the resilience process. Many intervention strategies will indeed benefit from a more personalized approach,” he said in a statement. Dr. Gorwood was not involved with this study.
The study authors, Dr. Gorwood, and Dr. Walker report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
PARIS – , new research shows.
Investigators found childhood emotional and sexual abuse had a greater effect on women than men, whereas men were more adversely affected by emotional and physical neglect.
“Our findings indicate that exposure to childhood maltreatment increases the risk of having psychiatric symptoms in both men and women,” lead researcher Thanavadee Prachason, PhD, department of psychiatry and neuropsychology, Maastricht (the Netherlands) University Medical Center, said in a press release.
“Exposure to emotionally or sexually abusive experiences during childhood increases the risk of a variety of psychiatric symptoms, particularly in women. In contrast, a history of emotional or physical neglect in childhood increases the risk of having psychiatric symptoms more in men,” Dr. Prachason added.
The findings were presented at the European Psychiatric Association 2023 Congress.
A leading mental illness risk factor
Study presenter Laura Fusar-Poli, MD, PhD, from the department of brain and behavioral sciences, University of Pavia (Italy), said that the differential impact of trauma subtypes in men and women indicate that both gender and the type of childhood adversity experienced need to be taken into account in future studies.
Dr. Fusar-Poli began by highlighting that 13%-36% of individuals have experienced some kind of childhood trauma, with 30% exposed to at least two types of trauma.
Trauma has been identified as a risk factor for a range of mental health problems.
“It is estimated that, worldwide, around one third of all psychiatric disorders are related to childhood trauma,” senior researcher Sinan Gül
Consequently, “childhood trauma is a leading preventable risk factor for mental illness,” he added.
Previous research suggests the subtype of trauma has an impact on subsequent biological changes and clinical outcomes, and that there are gender differences in the effects of childhood trauma.
To investigate, the researchers examined data from TwinssCan, a Belgian cohort of twins and siblings aged 15-35 years without a diagnosis of pervasive mental disorders.
The study included 477 females and 314 males who had completed the Childhood Trauma Questionnaire–Short Form (CTQ) and the Symptom Checklist-90 SR (SCL-90) to determine exposure to childhood adversity and levels of psychopathology, respectively.
Results showed that total CTQ scores were significantly associated with total SCL-90 scores in both men and women, as well as with each of the nine symptom domains of the SCL-90 (P < .001 for all assessments). These included psychoticism, paranoid ideation, anxiety, depression, somatization, obsessive-compulsive, interpersonal sensitivity, hostility, and phobic anxiety.
There were no significant differences in the associations with total CTQ scores between men and women.
However, when the researchers examined trauma subtypes and psychopathology, clear gender differences emerged.
Investigators found a significant association between emotional abuse on the CTQ and total SCL-90 scores in both men (P < .023) and women (P < .001), but that the association was significantly stronger in women (P = .043).
Sexual abuse was significantly associated with total SCL-90 scores in women (P < .001), while emotional neglect and physical neglect were significantly associated with psychopathology scores in men (P = .026 and P < .001, respectively).
“Physical neglect may include experiences of not having enough to eat, wearing dirty clothes, not being taken care of, and not getting taken to the doctor when the person was growing up,” said Dr. Prachason.
“Emotional neglect may include childhood experiences like not feeling loved or important, and not feeling close to the family.”
In women, emotional abuse was significantly associated with all nine symptom domains of the SCL-90, while sexual abuse was associated with seven: psychoticism, paranoid ideation, anxiety, depression, somatization, obsessive-compulsive, and hostility.
Physical neglect, in men, was significantly associated with eight of the symptom domains (all but somatization), but emotional neglect was linked only to depression, Dr. Fusar-Poli reported.
“This study showed a very important consequence of childhood trauma, and not only in people with mental disorders. I would like to underline that this is a general population, composed of adolescents and young adults, which is the age in which the majority of mental disorders starts, Dr. Fusar-Poli said in an interview.
She emphasized that psychotic disorders are only a part of the “broad range” of conditions that may be related to childhood trauma, which “can have an impact on sub-threshold symptoms that can affect functioning and quality of life in the general population.”
Addressing the differential findings in men and women, Dr. Gül
However, he said, this is “something that we really need understand,” as there is likely an underlying mechanism, “and not only a biological mechanism but probably a societal one.”
Dr. Gül
Compromised cognitive, emotional function
Commenting on the findings for this news organization, Elaine F. Walker, PhD, professor of psychology and neuroscience at Emory University in Atlanta, said stress exposure in general, including childhood trauma, “has transdiagnostic effects on vulnerability to mental disorders.”
“The effects are primarily mediated by the hypothalamic-pituitary-adrenal axis, which triggers the release of cortisol. When persistently elevated, this can result in neurobiological processes that have adverse effects on brain structure and circuitry which, in turn, compromises cognitive and emotional functioning,” said Dr. Walker, who was not associated with the study.
She noted that, “while it is possible that there are sex differences in biological sensitivity to certain subtypes of childhood trauma, it may also be the case that sex differences in the likelihood of exposure to trauma subtypes is actually the key factor.”
“At the present time, there are not specific treatment protocols aimed at addressing childhood trauma subtypes, but most experienced therapists will incorporate information about the individual’s trauma history in their treatment,” Dr. Walker added.
Also commenting on the research, Philip Gorwood, MD, PhD, head of the Clinique des Maladies Mentales et de l’Encéphale at Centre Hospitalier Sainte Anne in Paris, said the results are “important … as childhood trauma has been clearly recognized as a major risk factor for the vast majority of psychiatric disorders, but with poor knowledge of gender specificities.”
“Understanding which aspects of trauma are more damaging according to gender will facilitate research on the resilience process. Many intervention strategies will indeed benefit from a more personalized approach,” he said in a statement. Dr. Gorwood was not involved with this study.
The study authors, Dr. Gorwood, and Dr. Walker report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT EPA 2023