User login
Interventional psychiatry (Part 1)
Advances in the understanding of neurobiological and neuropsychiatric pathophysiology have opened new avenues of treatment for psychiatric patients. Historically, with a few exceptions, most psychiatric medications have been administered orally. However, many of the newer treatments require some form of specialized administration because they cannot be taken orally due to their chemical property (such as aducanumab); because there is the need to produce stable blood levels of the medication (such as brexanolone); because oral administration greatly diminished efficacy (such as oral vs IV magnesium or scopolamine), or because the treatment is focused on specific brain structures. This need for specialized administration has created a subspecialty called interventional psychiatry.
Part 1 of this 2-part article provides an overview of 1 type of interventional psychiatry: parenterally administered medications, including those administered via IV. We also describe 3 other interventional approaches to treatment: stellate ganglion blocks, glabellar botulinum toxin (BT) injections, and trigger point injections. In Part 2 we will review interventional approaches that involve neuromodulation.
Parenteral medications in psychiatry
In general, IV and IM medications can be more potent that oral medications due to their overall faster onset of action and higher blood concentrations. These more invasive forms of administration can have significant limitations, such as a risk of infection at the injection site, the need to be administered in a medical setting, additional time, and patient discomfort.
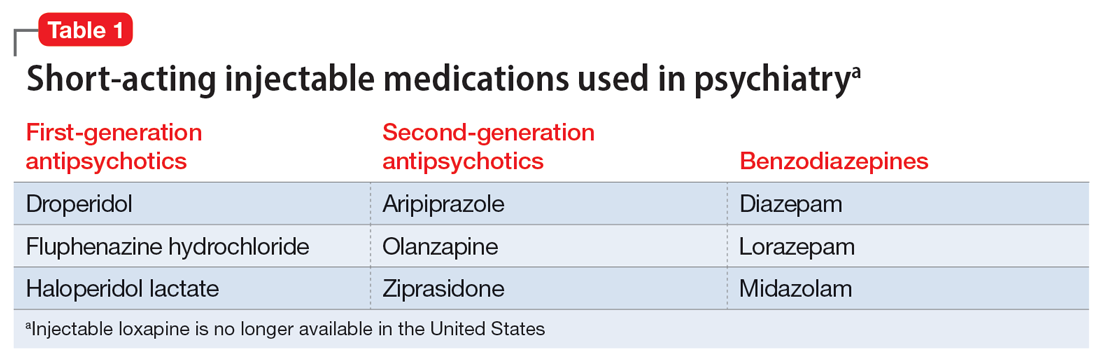
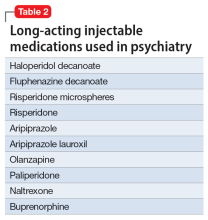
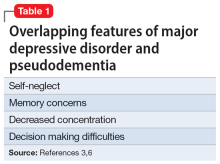
Table 1 lists short-acting injectable medications used in psychiatry, and Table 2 lists long-acting injectable medications. Parenteral administration of antipsychotics is performed to alleviate acute agitation or for chronic symptom control. These medications generally are not considered interventional treatments, but could be classified as such due to their invasive nature.1 Furthermore, inhalable loxapine—which is indicated for managing acute agitation—requires a Risk Evaluation and Mitigation Strategy program consisting of 2 hours observation and monitoring of respiratory status.2,3 Other indications for parenteral treatments include IM naltrexone extended release4 and subcutaneous injections of buprenorphine extended release5 and risperidone.6
IV administration
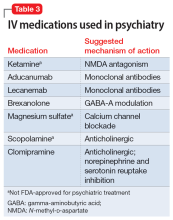
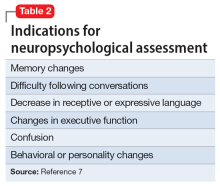
Most IV treatments described in this article are not FDA-approved for psychiatric treatment. Despite this, many interventional psychiatric treatments are part of clinical practice. IV infusion of ketamine is the most widely known and most researched of these. Table 3 lists other IV treatments that could be used as psychiatric treatment.
Ketamine
Since the early 1960s, ketamine has been used as a surgical anesthetic for animals. In the United States, it was approved for human surgical anesthesia in 1970. It was widely used during the Vietnam War due to its lack of inhibition of respiratory drive; medical staff first noticed an improvement in depressive symptoms and the resolution of suicidal ideation in patients who received ketamine. This led to further research on ketamine, particularly to determine its application in treatment-resistant depression (TRD) and other conditions.7 IV ketamine administration is most widely researched, but IM injections, intranasal sprays, and lozenges are also available. The dissociative properties of ketamine have led to its recreational use.8
Hypotheses for the mechanism of action of ketamine as an antidepressant include direct synaptic or extrasynaptic (GluN2B-selective), N-methyl-
Continue to: Ketamine is a schedule...
Ketamine is a schedule III medication with addictive properties. Delirium, panic attacks, hallucinations, nightmares, dysphoria, and paranoia may occur during and after use.13 Premedication with benzodiazepines, most notably lorazepam, is occasionally used to minimize ketamine’s adverse effects, but this generally is not recommended because doing so reduces ketamine’s antidepressant effects.14 Driving and operating heavy machinery is contraindicated after IV infusion. The usual protocol involves an IV infusion of ketamine 0.4 mg/kg to 1 mg/kg dosing over 1 hour. Doses between 0.4 mg/kg and 0.6 mg/kg are most common. Ketamine has a therapeutic window; doses >0.5 mg/kg are progressively less effective.15 Unlike the recommendation after esketamine administration, after receiving ketamine, patients remain in the care of their treatment team for <2 hours.
Esketamine, the S enantiomer of ketamine, was FDA-approved for TRD as an intranasal formulation. Esketamine is more commonly used than IV ketamine because it is FDA-approved and typically covered by insurance, but it may not be as effective.16 An economic analysis by Brendle et al17 suggested insurance companies would lower costs if they covered ketamine infusions vs intranasal esketamine.
Aducanumab and lecanemab
The most recent FDA-approved interventional agents are aducanumab and lecanemab, which are indicated for treating Alzheimer disease.18,19 Both are human monoclonal antibodies that bind selectively and with high affinity to amyloid beta plaque aggregates and promote their removal by Fc receptor–mediated phagocytosis.20
FDA approval of aducanumab and lecanemab was controversial. Initially, aducanumab’s safety monitoring board performed a futility analysis that suggested aducanumab was unlikely to separate from placebo, and the research was stopped.21 The manufacturer petitioned the FDA to consider the medication for accelerated approval on the basis of biomarker data showing that amyloid beta plaque aggregates become smaller. Current FDA approval is temporary to allow patients access to this potentially beneficial agent, but the manufacturer must supply clinical evidence that the reduction of amyloid beta plaques is associated with desirable changes in the course of Alzheimer disease, or risk losing the approval.
Lecanemab is also a human monoclonal antibody intended to remove amyloid beta plaques that was FDA-approved under the accelerated approval pathway.22 Unlike aducanumab, lecanemab demonstrated a statistically significant (although clinically imperceptible) reduction in the rate of cognitive decline; it did not show cognitive improvement.23 Lecanemab also significantly reduced amyloid beta plaques.23
Continue to: Aducanumab and lecanemab are generally...
Aducanumab and lecanemab are generally not covered by insurance and typically cost >$26,000 annually. Both are administered by IV infusion once a month. More monoclonal antibody medications for treating early Alzheimer disease are in the late stages of development, most notably donanebab.24 Observations during clinical trials found that in the later stages of Alzheimer disease, forceful removal of plaques by the autoimmune process damages neurons, while in less dense deposits of early dementia such removal is not harmful to the cells and prevents amyloid buildup.
Brexanolone is an aqueous formulation of allopregnanolone, a major metabolite of progesterone and a positive allosteric modulator of GABA-A receptors.25 Its levels are maximal at the end of the third trimester of pregnancy and fall rapidly following delivery. Research showed a 3-day infusion was rapidly and significantly effective for treating postpartum depression26 and brexanolone received FDA approval for this indication in March 2019.27 However, various administrative, economic, insurance, and other hurdles make it difficult for patients to access this treatment. Despite its rapid onset of action (usually 48 hours), brexanolone takes an average of 15 days to go through the prior authorization process.28 In addition to the need for prior authorization, the main impediment to the use of brexanolone is the 3-day infusion schedule, which greatly magnifies the cost but is partially circumvented by the availability of dedicated outpatient centers.
Magnesium
Magnesium is on the World Health Organization’s Model List of Essential Medicines.29 There has been extensive research on the use of magnesium sulfate for psychiatric indications, especially for depression.30 Magnesium functions similarly to calcium channel blockers by competitively blocking intracellular calcium channels, decreasing calcium availability, and inhibiting smooth muscle contractility.31 It also competes with calcium at the motor end plate, reducing excitation by inhibiting the release of acetylcholine.32 This property is used for high-dose IV magnesium treatment of impending preterm labor in obstetrics. Magnesium sulfate is the drug of choice in treating eclamptic seizures and preventing seizures in severe preeclampsia or gestational hypertension with severe features.33 It is also used to treat torsade de pointes, severe asthma exacerbations, constipation, and barium poisoning.34 Beneficial use in asthma treatment35 and the treatment of migraine36 have also been reported.
IV magnesium in myocardial infarction may be harmful,37 though outside of acute cardiac events, magnesium is found to be safe.38
Oral magnesium sulfate is a common over-the-counter anxiety remedy. As a general cell stabilizer (mediated by the reduction of intracellular calcium), magnesium is potentially beneficial outside of its muscle-relaxing properties, although muscle relaxing can benefit anxious patients. It is used to treat anxiety,39 alcohol withdrawal,40 and fear.41 Low magnesium blood levels are found in patients with depression, schizophrenia,42 and attention-deficit/hyperactivity disorder.43 However, it is important to note that the therapeutic effect of magnesium when treating anxiety and headache is independent of preinfusion magnesium blood levels.43
Continue to: The efficacy of oral magnesium...
The efficacy of oral magnesium is not robust. However, IV administration has a pronounced beneficial effect as an abortive and preventative treatment in many patients with anxiety.44
IV administration of magnesium can produce adverse effects, including flushing, sweating, hypotension, depressed reflexes, flaccid paralysis, hypothermia, circulatory collapse, and cardiac and CNS depression. These complications are very rare and dose-dependent.45 Magnesium is excreted by the kidneys, and dosing must be decreased in patients with kidney failure. The most common adverse effect is local burning along the vein upon infusion; small doses of IV lidocaine can remedy this. Hot flashes are also common.45
Various dosing strategies are available. In patients with anxiety, application dosing is based on the recommended preeclampsia IV dose of 4 g diluted in 250 mL of 5% dextrose. Much higher doses may be used in obstetrics. Unlike in obstetrics, for psychiatric indications, magnesium is administered over 60 to 90 minutes. Heart monitoring is recommended.
Scopolamine
Scopolamine is primarily used to relieve nausea, vomiting, and dizziness associated with motion sickness and recovery from anesthesia. It is also used in ophthalmology and in patients with excessive sweating. In off-label and experimental applications, scopolamine has been used in patients with TRD.46
Scopolamine is an anticholinergic medication. It is a nonselective antagonist at muscarinic receptors.47 Tricyclic antidepressants (TCAs) possess strong anticholinergic function. Newer generations of antidepressants were designed specifically not to have this function because it was believed to be an unwanted and potentially dangerous adverse effect. However, data suggest that anticholinergic action is important in decreasing depressive symptoms. Several hypotheses of anticholinergic effects on depression have been published since the 1970s. They include the cholinergic-adrenergic hypothesis,48 acetylcholine predominance relative to adrenergic action hypothesis,49 and insecticide poisoning observations.50 Centrally acting physostigmine (but not peripherally acting neostigmine) was reported to control mania.48,51 A genetic connection between the M2 acetylcholine receptor in patients with major depressive disorder (MDD) and alcohol use disorder is also suggestive.52
Continue to: Multiple animal studies show...
Multiple animal studies show direct improvement in mobility and a decrease in despair upon introducing anticholinergic substances.53-55 The cholinergic theory of depression has been studied in several controlled clinical human studies.56,57 Use of a short-acting anticholinergic glycopyrrolate during electroconvulsive therapy (ECT) may contribute to the procedure’s efficacy.
Human research shows scopolamine has a higher efficacy as an antidepressant and anti-anxiety medication in women than in men,58 possibly because estrogen increases the activity of choline acetyltransferase and release of acetylcholine.59,60 M2 receptors mediate estrogen influence on the NMDAR, which may explain the anticholinergic effects of depression treatments in women.61
Another proposed mechanism of action of scopolamine is a potent inhibition of the NMDAR.62 Rapid treatments of depression may be based on this mechanism. Examples of such treatments include IV ketamine and sleep deprivation.63 IV scopolamine shows potency in treating MDD and bipolar depression. This treatment should be reserved for patients who do not respond to or are not candidates for other usual treatment modalities of MDD and for the most severe cases. Scopolamine is 30 times more potent than amitriptyline in anticholinergic effect and reportedly produces sustained improvement in MDD.64
Scopolamine has no black-box warnings. It has not been studied in pregnant women and is not recommended for use during pregnancy. Due to possible negative cardiovascular effects, a normal electrocardiogram is required before the start of treatment. Exercise caution in patients with glaucoma, benign prostatic enlargement, gastroparesis, unstable cardiovascular status, or severe renal impairment.
Treatment with scopolamine is not indicated for patients with myasthenia gravis, psychosis, or seizures. Patients must be off potassium for 3 days before beginning scopolamine treatment. Patients should consult with their cardiologist before having a scopolamine infusion. Adverse reactions may include psychosis, tachycardia, seizures, paralytic ileus, and glaucoma exacerbation. The most common adverse effects of scopolamine infusion treatment include drowsiness, dry mouth, blurred vision, lightheadedness, and dizziness. Due to possible drowsiness, operating motor vehicles or heavy machinery must be avoided on the day of treatment.65 Overall, the adverse effects of scopolamine are preventable and manageable, and its antidepressant efficacy is noteworthy.66
Continue to: Treatment typically consists of 3 consecutive infusions...
Treatment typically consists of 3 consecutive infusions of 4 mcg/kg separated by 3 to 5 days.56 It is possible to have a longer treatment course if the patient experiences only partial improvement. Repeated courses or maintenance treatment (similar to ECT maintenance) are utilized in some patients if indicated. Cardiac monitoring is mandatory.
Clomipramine
Clomipramine, a TCA, acts as a preferential inhibitor of 5-hydroxytryptamine uptake and has proven effective in managing depression, TRD, and obsessive-compulsive disorder (OCD).67 Although this medication has reported treatment benefits for patients with phobia, panic disorder,15 chronic pain,68 Tourette syndrome,69 premature ejaculation, anorexia nervosa,70 cataplexy,49 and enuresis,71 it is FDA-approved only for the treatment of OCD.72 Clomipramine may also be beneficial for pain and headache, possibly because of its anti-inflammatory action.73 The anticholinergic effects of clomipramine may add to its efficacy in depression.
The pathophysiology of MDD is connected to hyperactivity of the HPA axis and elevated cortisol levels. Higher clomipramine plasma levels show a linear correlation with lower cortisol secretion and levels, possibly aiding in the treatment of MDD and anxiety.74 The higher the blood level, the more pronounced clomipramine’s therapeutic effect across multiple domains.75
IV infusion of clomipramine produces the highest concentration in the shortest time, but overall, research does not necessarily support increased efficacy of IV over oral administration. There is evidence suggesting that subgroups of patients with severe, treatment-refractory OCD may benefit from IV agents and research suggests a faster onset of action.76 Faster onset of symptom relief is the basis for IV clomipramine use. In patients with OCD, it can take several months for oral medications to produce therapeutic benefits; not all patients can tolerate this. In such scenarios, IV administration may be considered, though it is not appropriate for routine use until more research is available. Patients with treatment-resistant OCD who have exhausted other means of symptom relief may also be candidates for IV treatment.
The adverse effects of IV clomipramine are no different from oral use, though they may be more pronounced. A pretreatment cardiac exam is desirable because clomipramine, like other TCAs, may be cardiotoxic. The anticholinergic adverse effects of TCAs are well known to clinicians77 and partially explained in the scopolamine section of this article. It is not advisable to combine clomipramine with other TCAs or serotonin reuptake inhibitors. Clomipramine also should not be combined with monoamine oxidase inhibitors, though such a combination was reported in medical literature.78 Combination with antiarrhythmics such as lidocaine or opioids such as fentanyl or and tramadol is highly discouraged (fentanyl and tramadol also have serotonergic effects).79
Continue to: Clomipramine for IV use is not commercially available...
Clomipramine for IV use is not commercially available and must be sterilely compounded. The usual course of treatment is a series of 3 infusions: 150 mg on Day 1, 200 mg on Day 2 or Day 3, and 250 mg on Day 3, Day 4, or Day 5, depending on tolerability. A protocol with a 50 mg/d starting dose and titration up to a maximum dose of 225 mg/d over 5 to 7 days has been suggested for inpatient settings.67 Titration to 250 mg is more common.80
A longer series may be performed, but this increases the likelihood of adverse effects. Booster and maintenance treatments are also completed when required. Cardiac monitoring is mandatory.
Vortioxetine and citalopram
IV treatment of depression with
Injections and blocks
Three interventional approaches to treatment that possess psychotherapeutic potential include stellate ganglion blocks (SGBs), glabellar BT injections, and trigger point injections (TPIs). None of these are FDA-approved for psychiatric treatment.
Stellate ganglion blocks
The sympathetic nervous system is involved in autonomic hyperarousal and is at the core of posttraumatic symptomatology.83 Insomnia, anxiety, irritability, hypervigilance, and other excitatory CNS events are connected to the sympathetic nervous system and amygdala activation is commonly observed in those exposed to extreme stress or traumatic events.84
Continue to: SGBs were first performed 100 years ago...
SGBs were first performed 100 years ago and reported to have beneficial psychiatric effects at the end of the 1940s. In 1998 in Finland, improvement of posttraumatic stress disorder (PTSD) symptoms was observed accidentally via thoracic level spine blocks.85 In 2006, cervical level sympathetic blocks were shown to be effective for PTSD symptom control.86 By the end of 2010, Veterans Administration hospitals adopted SGBs to treat veterans with PTSD.87,88 The first multisite, randomized clinical trial of
Since the stellate ganglion is connected to the amygdala, SGB has also been assessed for treating anxiety and depression.89,90 Outside of PTSD, SGBs are used to treat complex regional pain syndrome,91 phantom limb pain, trigeminal neuralgia,92 intractable angina,93 and postherpetic neuralgia in the head, neck, upper chest, or arms.94 The procedure consists of an injection of a local anesthetic through a 25-gauge needle into the stellate sympathetic ganglion at the C6 or C7 vertebral levels. An injection into C6 is considered safer because of specific cervical spine anatomy. Ideally, fluoroscopic guidance or ultrasound is used to guide needle insertion.95
A severe drop in blood pressure may be associated with SGBs and is mitigated by IV hydration. Other adverse effects include red eyes, drooping of the eyelids, nasal congestion, hoarseness, difficulty swallowing, a sensation of a “lump” in the throat, and a sensation of warmth or tingling in the arm or hand. Bilateral SGB is contraindicated due to the danger of respiratory arrest.96
Glabellar BT injections
OnabotulinumtoxinA (BT) injection was first approved for therapeutic use in 1989 for eye muscle disorders such as strabismus97 and blepharospasm.98 It was later approved for several other indications, including cosmetic use, hyperhidrosis, migraine prevention, neurogenic bladder disorder, overactive bladder, urinary incontinence, and spasticity.99-104 BT is used off-label for achalasia and sialorrhea.105,106 Its mechanism of action is primarily attributed to muscle paralysis by blocking presynaptic acetylcholine release into neuromuscular junctions.107
Facial BT injections are usually administered for cosmetic purposes, but smoothing forehead wrinkles and frown lines (the glabellar region of the face) both have antidepressant effects.108 BT injections into the glabellar region also demonstrate antidepressant effects, particularly in patients with comorbid migraines and MDD.109 Early case observations supported the independent benefit of the toxin on MDD when the toxin was injected into the glabellar region.110,111 The most frequent protocol involves injections in the procerus and corrugator muscles.
Continue to: The facial feedback/emotional proprioception hypothesis...
The facial feedback/emotional proprioception hypothesis has dominated thinking about the mood-improving effects of BT. The theory is that blocking muscular expression of sadness (especially in the face) interrupts the experience of sadness; therefore, depression subsides.112,113 However, BT injections in the muscles involved in the smile and an expression of positive emotions (lateral part of the musculus orbicularis oculi) have been associated with increased MDD scores.114 Thus, the mechanism clearly involves more than the cosmetic effect, since facial muscle injections in rats also have antidepressant effects.115
The use of progressive muscle relaxation is well-established in psychiatric treatment. The investigated conditions of increased muscle tone, especially torticollis and blepharospasm, are associated with MDD, and it may be speculated that proprioceptive feedback from the affected muscles may be causally involved in this association.116-118 Activity of the corrugator muscle has been positively associated with increased amygdala activity.119 This suggests a potential similar mechanism to that hypothesized for SGB.
Alternatively, BT is commonly used to treat chronic conditions that may contribute to depression; its success in relieving the underlying problem may indirectly relieve MDD. Thus, in a postmarketing safety evaluation of BT, MDD was demonstrated 40% to 88% less often by patients treated with BT for 6 of the 8 conditions and injection sites, such as in spasms and spasticity of arms and legs, torticollis and neck pain, and axilla and palm injections for hyperhidrosis. In a parotid and submandibular glands BT injection subcohort, no patients experienced depressive symptoms.120
Medicinal BT is generally considered safe. The most common adverse effects are hypersensitivity, injection site reactions, and other adverse effects specific to the injection site.121 Additionally, the cosmetic effects are transient, given the nature of the medication.
Trigger point injections
TPIs in the neck and shoulders are frequently used to treat tension headaches and various referred pain locations in the face and arms. Tension and depression frequently overlap in clinical practice.122 Relieving muscle tension (with resulting trigger points) improves muscle function and mood.
Continue to: The higher the number of active...
The higher the number of active trigger points (TPs), the greater the physical burden of headache and the higher the anxiety level. Gender differences in TP prevalence and TPI efficacy have been described in the literature. For example, the number of active TPs seems directly associated with anxiety levels in women but not in men.123 Although TPs appear to be more closely associated with anxiety than depression,124 depression associated with muscle tension does improve with TPIs. European studies have demonstrated a decrease in scores on the Hamilton Depression Rating Scale and Hamilton Anxiety Rating Scale following TPI treatment.125 The effect may be indirect, as when a patient’s pain is relieved, sleep and other psychiatric symptoms improve.126
A randomized controlled trial by Castro Sánchez et al127 demonstrated that dry needling therapy in patients with fibromyalgia syndrome (FMS) showed improvements in pain pressure thresholds, body pain, vitality, and social function, as well as total FMS symptoms, quality of sleep, anxiety, hospital anxiety and depression, general pain intensity, and fatigue.
Myofascial pain syndrome, catastrophizing, and muscle tension are common in patients with depression, anxiety, and somatization. Local TPI therapy aimed at inactivating pain generators is supported by moderate quality evidence. All manner of therapies have been described, including injection of saline, corticosteroids, local anesthetic agents, and dry needling. BT injections in chronic TPs are also practiced, though no specific injection therapy has been reliably shown to be more advantageous than another. The benefits of TPIs may be derived from the needle itself rather than from any specific substance injected. Stimulation of a local twitch response with direct needling of the TP appears of importance. There is no established consensus regarding the number of injection points, frequency of administration, and volume or type of injectate.128
Adverse effects of TPIs relate to the nature of the invasive therapy, with the risk of tissue damage and bleeding. Pneumothorax risk is present with needle insertion at the neck and thorax.129 Patients with diabetes may experience variations in blood sugar control if steroids are used.
Bottom Line
Interventional treatment modalities that may have a role in psychiatric treatment include IV administration of ketamine, aducanumab, lecanemab, brexanolone, magnesium, scopolamine, and clomipramine. Other interventional approaches include stellate ganglion blocks, glabellar botulinum toxin injections, and trigger point injections.
Related Resources
- Dokucu ME, Janicak PG. Nontraditional therapies for treatment-resistant depression. Current Psychiatry. 2021; 20(9):38-43,49. doi:10.12788/cp.0166
- Kim J, Khoury R, Grossberg GT. Botulinum toxin: emerging psychiatric indications. Current Psychiatry. 2018;17(12):8-18.
Drug Brand Names
Aducanumab • Aduhelm
Aripiprazole • Abilify
Aripiprazole lauroxil • Aristada
Brexanolone • Zulresso
Buprenorphine • Sublocade
Citalopram • Celexa
Clomipramine • Anafranil
Diazepam • Valium
Droperidol • Inapsine
Esketamine • Spravato
Fentanyl • Actiq
Fluphenazine decanoate • Modecate
Fluphenazine hydrochloride • Prolixin
Haloperidol decanoate • Haldol decanoate
Haloperidol lactate • Haldol
Ketamine • Ketalar
Lecanemab • Leqembi
Lidocaine • Xylocaine
Lorazepam • Ativan
Loxapine inhaled • Adasuve
Naltrexone • Vivitrol
Magnesium sulfate • Sulfamag
Midazolam • Versed
Olanzapine • Zyprexa
OnabotulinumtoxinA injection • Botox
Paliperidone • Invega Hafyera, Invega Sustenna, Invega Trinza
Rapamycin • Rapamune, Sirolimus
Risperidone • Perseris
Risperidone microspheres • Risperdal Consta, Rykindo
Scopolamine • Hyoscine
Tramadol • Conzip
Vortioxetine • Trintellix
Ziprasidone • Geodon
1. Vincent KM, Ryan M, Palmer E, et al. Interventional psychiatry. Postgrad Med. 2020;132(7):573-574.
2. Allen MH, Feifel D, Lesem MD, et al. Efficacy and safety of loxapine for inhalation in the treatment of agitation in patients with schizophrenia: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2011;72(10):1313-1321.
3. Kwentus J, Riesenberg RA, Marandi M, et al. Rapid acute treatment of agitation in patients with bipolar I disorder: a multicenter, randomized, placebo-controlled clinical trial with inhaled loxapine. Bipolar Disord. 2012;14(1):31-40.
4. Lee JD, Nunes EV Jr, Novo P, et al. Comparative effectiveness of extended-release naltrexone versus buprenorphine-naloxone for opioid relapse prevention (X:BOT): a multicentre, open-label, randomised controlled trial. Lancet. 2018;391(10118):309-318.
5. Haight BR, Learned SM, Laffont CM, et al. Efficacy and safety of a monthly buprenorphine depot injection for opioid use disorder: a multicentre, randomised, double‐blind, placebo‐controlled, phase 3 trial. Lancet. 2019;393(10173):778-790.
6. Andorn A, Graham J, Csernansky J, et al. Monthly extended-release risperidone (RBP-7000) in the treatment of schizophrenia: results from the phase 3 program. J Clin Psychopharmacol. 2019;39(5):428-433.
7. Dundee TW. Twenty-five years of ketamine. A report of an international meeting. Anaesthesia. 1990;45(2):159. doi:10.1111/j.1365-2044.1990.tb14287.x
8. White PF, Way WL, Trevor AJ. Ketamine--its pharmacology and therapeutic uses. Anesthesiology. 1982;56(2):119-136. doi:10.1097/00000542-198202000-00007
9. Zanos P, Gould TD. Mechanisms of ketamine action as an antidepressant. Mol Psychiatry. 2018;23(4):801-811.
10. Molero P, Ramos-Quiroga JA, Martin-Santos R, et al. Antidepressant efficacy and tolerability of ketamine and esketamine: a critical review. CNS Drugs. 2018;32(5):411-420. doi:10.1007/s40263-018-0519-3
11. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215.
12. Witkin JM, Martin AE, Golani LK, et al. Rapid-acting antidepressants. Adv Pharmacol. 2019;86:47-96.
13. Strayer RJ, Nelson LS. Adverse events associated with ketamine for procedural sedation in adults. Am J Emerg Med. 2008;26(9):985-1028. doi:10.1016/j.ajem.2007.12.005
14. Frye MA, Blier P, Tye SJ. Concomitant benzodiazepine use attenuates ketamine response: implications for large scale study design and clinical development. J Clin Psychopharmacol. 2015;35(3):334-336.
15. Fava M, Freeman MP, Flynn M, et al. Double-blind, placebo-controlled, dose-ranging trial of intravenous ketamine as adjunctive therapy in treatment-resistant depression (TRD). Mol Psychiatry. 2020;25(7):1592-1603.
16. Bahji A, Vazquez GH, Zarate CA Jr. Comparative efficacy of racemic ketamine and esketamine for depression: a systematic review and meta-analysis. J Affect Disord. 2021;278:542-555. Erratum in: J Affect Disord. 2021;281:1001.
17. Brendle M, Robison R, Malone DC. Cost-effectiveness of esketamine nasal spray compared to intravenous ketamine for patients with treatment-resistant depression in the US utilizing clinical trial efficacy and real-world effectiveness estimates. J Affect Disord. 2022;319:388-396.
18. Dhillon S. Aducanumab: first approval. Drugs. 2021;81(12):1437-1443. Erratum in: Drugs. 2021;81(14):1701.
19. van Dyck CH, Swanson CJ, Aisen P, et al. Lecanemab in early Alzheimer’s disease. N Engl J Med. 2023;388(1):9-21. doi:10.1056/NEJMoa2212948
20. Sevigny J, Chiao P, Bussière T, et al. The antibody aducanumab reduces Aβ plaques in Alzheimer’s disease. Nature. 2016;537(7618):50-56. Update in: Nature. 2017;546(7659):564.
21. Fillit H, Green A. Aducanumab and the FDA – where are we now? Nat Rev Neurol. 2021;17(3):129-130.
22. Reardon S. FDA approves Alzheimer’s drug lecanemab amid safety concerns. Nature. 2023;613(7943):227-228. doi:10.1038/d41586-023-00030-3
23. McDade E, Cummings JL, Dhadda S, et al. Lecanemab in patients with early Alzheimer’s disease: detailed results on biomarker, cognitive, and clinical effects from the randomized and open-label extension of the phase 2 proof-of-concept study. Alzheimers Res Ther. 2022;14(1):191. doi:10.1186/s13195-022-01124-2
24. Mintun MA, Lo AC, Evans CD, et al. Donanemab in early Alzheimer’s disease. N Engl J Med. 2021;384(18):1691-1704.
25. Luisi S, Petraglia F, Benedetto C, et al. Serum allopregnanolone levels in pregnant women: changes during pregnancy, at delivery, and in hypertensive patients. J Clin Endocrinol Metab. 2000;85(7):2429-2433.
26. Meltzer-Brody S, Colquhoun H, Riesenberg R, et al. Brexanolone injection in post-partum depression: two multicentre, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet. 2018;392(10152):1058-1070.
27. Powell JG, Garland S, Preston K, et al. Brexanolone (Zulresso): finally, an FDA-approved treatment for postpartum depression. Ann Pharmacother. 2020;54(2):157-163.
28. Patterson R, Krohn H, Richardson E, et al. A brexanolone treatment program at an academic medical center: patient selection, 90-day posttreatment outcomes, and lessons learned. J Acad Consult Liaison Psychiatry. 2022;63(1):14-22.
29. World Health Organization. WHO model list of essential medicines - 22nd list (2021). World Health Organization. September 30, 2021. Accessed April 7, 2023. https://www.who.int/publications/i/item/WHO-MHP-HPS-EML-2021.02
30. Eby GA, Eby KL, Mruk H. Magnesium and major depression. In: Vink R, Nechifor M, eds. Magnesium in the Central Nervous System. University of Adelaide Press; 2011.
31. Plant TM, Zeleznik AJ. Knobil and Neill’s Physiology of Reproduction. 4th ed. Elsevier Inc.; 2015:2503-2550.
32. Sidebotham D, Le Grice IJ. Physiology and pathophysiology. In: Sidebotham D, McKee A, Gillham M, Levy J. Cardiothoracic Critical Care. Elsevier, Inc.; 2007:3-27.
33. Duley L, Gülmezoglu AM, Henderson-Smart DJ, et al. Magnesium sulphate and other anticonvulsants for women with pre-eclampsia. Cochrane Database Syst Rev. 2010;2010(11):CD000025.
34. Emergency supply of medicines. In: British National Formulary. British Medical Association, Royal Pharmaceutical Society; 2015:6. Accessed April 7, 2023. https://www.academia.edu/35076015/british_national_formulary_2015_pdf
35. Kwofie K, Wolfson AB. Intravenous magnesium sulfate for acute asthma exacerbation in children and adults. Am Fam Physician. 2021;103(4):245-246.
36. Patniyot IR, Gelfand AA. Acute treatment therapies for pediatric migraine: a qualitative systematic review. Headache. 2016;56(1):49-70.
37. Wang X, Du X, Yang H, et al. Use of intravenous magnesium sulfate among patients with acute myocardial infarction in China from 2001 to 2015: China PEACE-Retrospective AMI Study. BMJ Open. 2020;10(3):e033269.
38. Karhu E, Atlas SE, Jinrun G, et al. Intravenous infusion of magnesium sulfate is not associated with cardiovascular, liver, kidney, and metabolic toxicity in adults. J Clin Transl Res. 2018;4(1):47-55.
39. Noah L, Pickering G, Mazur A, et al. Impact of magnesium supplementation, in combination with vitamin B6, on stress and magnesium status: secondary data from a randomized controlled trial. Magnes Res. 2020;33(3):45-57.
40. Erstad BL, Cotugno CL. Management of alcohol withdrawal. Am J Health Syst Pharm. 1995;52(7):697-709.
41. Abumaria N, Luo L, Ahn M, et al. Magnesium supplement enhances spatial-context pattern separation and prevents fear overgeneralization. Behav Pharmacol. 2013;24(4):255-263.
42. Kirov GK, Tsachev KN. Magnesium, schizophrenia and manic-depressive disease. Neuropsychobiology. 1990;23(2):79-81.
43. Botturi A, Ciappolino V, Delvecchio G, et al. The role and the effect of magnesium in mental disorders: a systematic review. Nutrients. 2020;12(6):1661.
44. Kirkland AE, Sarlo GL, Holton KF. The role of magnesium in neurological disorders. Nutrients. 2018;10(6):730.
45. Magnesium sulfate intravenous side effects by likelihood and severity. WebMD. Accessed April 9, 2023. https://www.webmd.com/drugs/2/drug-149570/magnesium-sulfate-intravenous/details/list-sideeffects
46. Scopolamine base transdermal system – uses, side effects, and more. WebMD. Accessed April 9, 2023. https://www.webmd.com/drugs/2/drug-14032/scopolamine-transdermal/details
47. Bolden C, Cusack B, Richelson E. Antagonism by antimuscarinic and neuroleptic compounds at the five cloned human muscarinic cholinergic receptors expressed in Chinese hamster ovary cells. J Pharmacol Exp Ther. 1992;260(2):576-580.
48. Janowsky DS, el-Yousef MK, Davis JM, et al. A cholinergic-adrenergic hypothesis of mania and depression. Lancet. 1972;2(7778):632-635.
49. Janowsky DS, Risch SC, Gillin JC. Adrenergic-cholinergic balance and the treatment of affective disorders. Prog Neuropsychopharmacol Biol Psychiatry. 1983;7(2-3):297-307.
50. Gershon S, Shaw FH. Psychiatric sequelae of chronic exposure to organophosphorous insecticides. Lancet. 1972;1(7191):1371-1374.
51. Davis KL, Berger PA, Hollister LE, et al. Physostigmine in mania. Arch Gen Psychiatry. 1978;35(1):119-122.
52. Wang JC, Hinrichs AL, Stock H, et al. Evidence of common and specific genetic effects: association of the muscarinic acetylcholine receptor M2 (CHRM2) gene with alcohol dependence and major depressive syndrome. Hum Mol Genet. 2004;13(17):1903-1911.
53. Brown RG. Effects of antidepressants and anticholinergics in a mouse “behavioral despair” test. Eur J Pharmacol. 1979;58(3):331-334.
54. Porsolt RD, Le Pichon M, Jalfre M. Depression: a new animal model sensitive to antidepressant treatments. Nature. 1977;266(5604):730-732.
55. Ji CX, Zhang JJ. Effect of scopolamine on depression in mice. Abstract in English. Yao Xue Xue Bao. 2011;46(4):400-405.
56. Furey ML, Drevets WC. Antidepressant efficacy of the antimuscarinic drug scopolamine: a randomized, placebo-controlled clinical trial. Arch Gen Psychiatry. 2006;63(10):1121-1129.
57. Drevets WC, Furey ML. Replication of scopolamine’s antidepressant efficacy in major depressive disorder: a randomized, placebo-controlled clinical trial. Biol Psychiatry. 2010;67(5):432-438.
58. Furey ML, Khanna A, Hoffman EM, et al. Scopolamine produces larger antidepressant and antianxiety effects in women than in men. Neuropsychopharmacology. 2010;35(12):2479-2488.
59. Gibbs RB, Gabor R, Cox T, et al. Effects of raloxifene and estradiol on hippocampal acetylcholine release and spatial learning in the rat. Psychoneuroendocrinology. 2004;29(6):741-748.
60. Pongrac JL, Gibbs RB, Defranco DB. Estrogen-mediated regulation of cholinergic expression in basal forebrain neurons requires extracellular-signal-regulated kinase activity. Neuroscience. 2004;124(4):809-816.
61. Daniel JM, Dohanich GP. Acetylcholine mediates the estrogen-induced increase in NMDA receptor binding in CA1 of the hippocampus and the associated improvement in working memory. J Neurosci. 2001;21(17):6949-6956.
62. Gerhard DM, Wohleb ES, Duman RS. Emerging treatment mechanisms for depression: focus on glutamate and synaptic plasticity. Drug Discov Today. 2016;21(3):454-464.
63. Voderholzer U. Sleep deprivation and antidepressant treatment. Dialogues Clin Neurosci. 2003;5(4):366-369.
64. Hasselmann H. Scopolamine and depression: a role for muscarinic antagonism? CNS Neurol Disord Drug Targets. 2014;13(4):673-683.
65. Transderm scopolamine [prescribing information]. Warren, NJ: GSK Consumer Healthcare; 2019.
66. Jaffe RJ, Novakovic V, Peselow ED. Scopolamine as an antidepressant: a systematic review. Clin Neuropharmacol. 2013;36(1):24-26.
67. Karameh WK, Khani M. Intravenous clomipramine for treatment-resistant obsessive-compulsive disorder. Int J Neuropsychopharmacol. 2015;19(2):pyv084.
68. Andrews ET, Beattie RM, Tighe MP. Functional abdominal pain: what clinicians need to know. Arch Dis Child. 2020;105(10):938-944. doi:10.1136/archdischild-2020-318825
69. Aliane V, Pérez S, Bohren Y, et al. Key role of striatal cholinergic interneurons in processes leading to arrest of motor stereotypies. Brain. 2011;134(Pt 1):110-118. doi:10.1093/brain/awq285
70. Tzavara ET, Bymaster FP, Davis RJ, et al. M4 muscarinic receptors regulate the dynamics of cholinergic and dopaminergic neurotransmission: relevance to the pathophysiology and treatment of related CNS pathologies. FASEB J. 2004;18(12):1410-1412. doi:10.1096/fj.04-1575fje
71. Korczyn AD, Kish I. The mechanism of imipramine in enuresis nocturna. Clin Exp Pharmacol Physiol. 1979;6(1):31-35. doi:10.1111/j.1440-1681.1979.tb00004.x
72. Trimble MR. Worldwide use of clomipramine. J Clin Psychiatry. 1990;51(Suppl):51-54; discussion 55-58.
73. Gong W, Zhang S, Zong Y, et al. Involvement of the microglial NLRP3 inflammasome in the anti-inflammatory effect of the antidepressant clomipramine. J Affect Disord. 2019;254:15-25.
74. Piwowarska J, Wrzosek M, Radziwon’-Zaleska M. Serum cortisol concentration in patients with major depression after treatment with clomipramine. Pharmacol Rep. 2009;61(4):604-611.
75. Danish University Antidepressant Group (DUAG). Clomipramine dose-effect study in patients with depression: clinical end points and pharmacokinetics. Clin Pharmacol Ther. 1999;66(2):152-165.
76. Moukaddam NJ, Hirschfeld RMA. Intravenous antidepressants: a review. Depress Anxiety. 2004;19(1):1-9.
77. Gerretsen P, Pollock BG. Rediscovering adverse anticholinergic effects. J Clin Psychiatry. 2011;72(6):869-870. doi:10.4088/JCP.11ac07093
78. Thomas SJ, Shin M, McInnis MG, et al. Combination therapy with monoamine oxidase inhibitors and other antidepressants or stimulants: strategies for the management of treatment-resistant depression. Pharmacotherapy. 2015;35(4):433-449. doi:10.1002/phar.1576
79. Robles LA. Serotonin syndrome induced by fentanyl in a child: case report. Clin Neuropharmacol. 2015;38(5):206-208. doi:10.1097/WNF.0000000000000100
80. Fallon BA, Liebowitz MR, Campeas R, et al. Intravenous clomipramine for obsessive-compulsive disorder refractory to oral clomipramine: a placebo-controlled study. Arch Gen Psychiatry. 1998;55(10):918-924.
81. Vieta E, Florea I, Schmidt SN, et al. Intravenous vortioxetine to accelerate onset of effect in major depressive disorder: a 2-week, randomized, double-blind, placebo-controlled study. Int Clin Psychopharmacol. 2019;34(4):153-160.
82. Kasper S, Müller-Spahn F. Intravenous antidepressant treatment: focus on citalopram. Eur Arch Psychiatry Clin Neurosci. 2002;252(3):105-109.
83. Togay B, El-Mallakh RS. Posttraumatic stress disorder: from pathophysiology to pharmacology. Current Psychiatry. 2020;19(5):33-39.
84. Adhikari A, Lerner TN, Finkelstein J, et al. Basomedial amygdala mediates top-down control of anxiety and fear. Nature. 2015;527(7577):179-185. doi:10.1038/nature15698
85. Lipov E. In search of an effective treatment for combat-related post-traumatic stress disorder (PTSD): can the stellate ganglion block be the answer? Pain Pract. 2010;10(4):265-266.
86. Lipov E, Ritchie EC. A review of the use of stellate ganglion block in the treatment of PTSD. Curr Psychiatry Rep. 2015;17(8):599.
87. Olmsted KLR, Bartoszek M, McLean B, et al. Effect of stellate ganglion block treatment on posttraumatic stress disorder symptoms: a randomized clinical trial. JAMA Psychiatry. 2020;77(2):130-138.
88. Lipov E, Candido K. The successful use of left-sided stellate ganglion block in patients that fail to respond to right-sided stellate ganglion block for the treatment of post-traumatic stress disorder symptoms: a retrospective analysis of 205 patients. Mil Med. 2021;186(11-12):319-320.
89. Li Y, Loshak H. Stellate ganglion block for the treatment of post-traumatic stress disorder, depression, and anxiety. Canadian J Health Technol. 2021;1(3):1-30.
90. Kerzner J, Liu H, Demchenko I, et al. Stellate ganglion block for psychiatric disorders: a systematic review of the clinical research landscape. Chronic Stress (Thousand Oaks). 2021;5:24705470211055176.
91. Wie C, Gupta R, Maloney J, et al. Interventional modalities to treat complex regional pain syndrome. Curr Pain Headache Rep. 2021;25(2):10. doi:10.1007/s11916-020-00904-5
92. Chaturvedi A, Dash HH. Sympathetic blockade for the relief of chronic pain. J Indian Med Assoc. 2001;99(12):698-703.
93. Chester M, Hammond C. Leach A. Long-term benefits of stellate ganglion block in severe chronic refractory angina. Pain. 2000;87(1):103-105. doi:10.1016/S0304-3959(00)00270-0
94. Jeon Y. Therapeutic potential of stellate ganglion block in orofacial pain: a mini review. J Dent Anesth Pain Med. 2016;16(3):159-163. doi:10.17245/jdapm.2016.16.3.159
95. Shan HH, Chen HF, Ni Y, et al. Effects of stellate ganglion block through different approaches under guidance of ultrasound. Front Surg. 2022;8:797793. doi:10.3389/fsurg.2021.797793
96. Goel V, Patwardhan AM, Ibrahim M, et al. Complications associated with stellate ganglion nerve block: a systematic review. Reg Anesth Pain Med. 2019;rapm-2018-100127. doi:10.1136/rapm-2018-100127
97. Rowe FJ, Noonan CP. Botulinum toxin for the treatment of strabismus. Cochrane Database Syst Rev. 2017;3(3):CD006499.
98. Roggenkämper P, Jost WH, Bihari K, et al. Efficacy and safety of a new botulinum toxin type A free of complexing proteins in the treatment of blepharospasm. J Neural Transm (Vienna). 2006;113(3):303-312.
99. Heckmann M, Ceballos-Baumann AO, Plewig G; Hyperhidrosis Study Group. Botulinum toxin A for axillary hyperhidrosis (excessive sweating). N Engl J Med. 2001;344(7):488-493.
100. Carruthers JA, Lowe NJ, Menter MA, et al. A multicenter, double-blind, randomized, placebo-controlled study of the efficacy and safety of botulinum toxin type A in the treatment of glabellar lines. J Am Acad Dermatol. 2002;46(6):840-849.
101. Schurch B, de Sèze M, Denys P, et al. Botulinum toxin type A is a safe and effective treatment for neurogenic urinary incontinence: results of a single treatment, randomized, placebo controlled 6-month study. J Urol. 2005;174:196–200.
102. Aurora SK, Winner P, Freeman MC, et al. OnabotulinumtoxinA for treatment of chronic migraine: Pooled analyses of the 56-week PREEMPT clinical program. Headache. 2011;51(9):1358-1373.
103. Dashtipour K, Chen JJ, Walker HW, et al. Systematic literature review of abobotulinumtoxinA in clinical trials for adult upper limb spasticity. Am J Phys Med Rehabil. 2015;94(3):229-238.
104. Nitti VW, Dmochowski R, Herschorn S, et al. OnabotulinumtoxinA for the treatment of patients with overactive bladder and urinary incontinence: results of a phase 3, randomized, placebo-controlled trial. J Urol. 2017;197(2S):S216-S223.
105. Jongerius PH, van den Hoogen FJA, van Limbeek J, et al. Effect of botulinum toxin in the treatment of drooling: a controlled clinical trial. Pediatrics. 2004;114(3):620-627.
106. Zaninotto, G. Annese V, Costantini M, et al. Randomized controlled trial of botulinum toxin versus laparoscopic heller myotomy for esophageal achalasia. Ann Surg. 2004;239(3):364-370.
107. Dressler D, Adib Saberi F. Botulinum toxin: mechanisms of action. Eur Neurol. 2005;53:3-9.
108. Lewis MB, Bowler PJ. Botulinum toxin cosmetic therapy correlates with a more positive mood. J Cosmet Dermatol. 2009;8(1):24-26.
109. Affatato O, Moulin TC, Pisanu C, et al. High efficacy of onabotulinumtoxinA treatment in patients with comorbid migraine and depression: a meta-analysis. J Transl Med. 2021;19(1):133.
110. Finzi E, Wasserman E. Treatment of depression with botulinum toxin A: a case series. Dermatol Surg. 2006;32(5):645-649; discussion 649-650.
111. Schulze J, Neumann I, Magid M, et al. Botulinum toxin for the management of depression: an updated review of the evidence and meta-analysis. J Psychiatr Res. 2021;135:332-340.
112. Finzi E, Rosenthal NE. Emotional proprioception: treatment of depression with afferent facial feedback. J Psychiatr Res. 2016;80:93-96.
113. Söderkvist S, Ohlén K, Dimberg U. How the experience of emotion is modulated by facial feedback. J Nonverbal Behav. 2018;42(1):129-151.
114. Lewis, MB. The interactions between botulinum-toxin-based facial treatments and embodied emotions. Sci Rep. 2018;8(1):14720.
115. Li Y, Liu J, Liu X, et al. Antidepressant-like action of single facial injection of botulinum neurotoxin A is associated with augmented 5-HT levels and BDNF/ERK/CREB pathways in mouse brain. Neurosci Bull. 2019;35(4):661-672. Erratum in: Neurosci Bull. 2019;35(4):779-780.
116. Gündel H, Wolf A, Xidara V, et al. High psychiatric comorbidity in spasmodic torticollis: a controlled study. J Nerv Ment Dis. 2003;191(7):465-473.
117. Hall TA, McGwin G Jr, Searcey K, et al. Health-related quality of life and psychosocial characteristics of patients with benign essential blepharospasm. Arch Ophthalmol. 2006;124(1):116-119.
118. Ceylan D, Erer S, Zarifog˘lu M, et al. Evaluation of anxiety and depression scales and quality of life in cervical dystonia patients on botulinum toxin therapy and their relatives. Neurol Sci. 2019;40(4):725-731.
119. Heller AS, Lapate RC, Mayer KE, et al. The face of negative affect: trial-by-trial corrugator responses to negative pictures are positively associated with amygdala and negatively associated with ventromedial prefrontal cortex activity. J Cogn Neurosci. 2014;26(9):2102-2110.
120. Makunts T, Wollmer MA, Abagyan R. Postmarketing safety surveillance data reveals antidepressant effects of botulinum toxin across various indications and injection sites. Sci Rep. 2020;10(1):12851.
121. Ahsanuddin S, Roy S, Nasser W, et al. Adverse events associated with botox as reported in a Food and Drug Administration database. Aesthetic Plast Surg. 2021;45(3):1201-1209. doi:10.1007/s00266-020-02027-z
122. Kashif M, Tahir S, Ashfaq F, et al. Association of myofascial trigger points in neck and shoulder region with depression, anxiety, and stress among university students. J Pak Med Assoc. 2021;71(9):2139-2142.
123. Cigarán-Méndez M, Jiménez-Antona C, Parás-Bravo P, et al. Active trigger points are associated with anxiety and widespread pressure pain sensitivity in women, but not men, with tension type headache. Pain Pract. 2019;19(5):522-529.
124. Palacios-Ceña M, Castaldo M, Wang K, et al. Relationship of active trigger points with related disability and anxiety in people with tension-type headache. Medicine (Baltimore). 2017;96(13):e6548.
125. Karadas Ö, Inan LE, Ulas Ü, et al. Efficacy of local lidocaine application on anxiety and depression and its curative effect on patients with chronic tension-type headache. Eur Neurol. 2013;70(1-2):95-101.
126. Gerwin RD. Classification, epidemiology and natural history of myofascial pain syndrome. Curr Pain Headache Rep. 2001;5(5):412-420.
127. Castro Sánchez AM, García López H, Fernández Sánchez M, et al. Improvement in clinical outcomes after dry needling versus myofascial release on pain pressure thresholds, quality of life, fatigue, pain intensity, quality of sleep, anxiety, and depression in patients with fibromyalgia syndrome. Disabil Rehabil. 2019;41(19):2235-2246.
128. Healy GM, Finn DP, O’Gorman DA, et al. Pretreatment anxiety and pain acceptance are associated with response to trigger point injection therapy for chronic myofascial pain. Pain Med. 2015;16(10):1955-1966.
129. Morjaria JB, Lakshminarayana UB, Liu-Shiu-Cheong P, et al. Pneumothorax: a tale of pain or spontaneity. Ther Adv Chronic Dis. 2014;5(6):269-273.
Advances in the understanding of neurobiological and neuropsychiatric pathophysiology have opened new avenues of treatment for psychiatric patients. Historically, with a few exceptions, most psychiatric medications have been administered orally. However, many of the newer treatments require some form of specialized administration because they cannot be taken orally due to their chemical property (such as aducanumab); because there is the need to produce stable blood levels of the medication (such as brexanolone); because oral administration greatly diminished efficacy (such as oral vs IV magnesium or scopolamine), or because the treatment is focused on specific brain structures. This need for specialized administration has created a subspecialty called interventional psychiatry.
Part 1 of this 2-part article provides an overview of 1 type of interventional psychiatry: parenterally administered medications, including those administered via IV. We also describe 3 other interventional approaches to treatment: stellate ganglion blocks, glabellar botulinum toxin (BT) injections, and trigger point injections. In Part 2 we will review interventional approaches that involve neuromodulation.
Parenteral medications in psychiatry
In general, IV and IM medications can be more potent that oral medications due to their overall faster onset of action and higher blood concentrations. These more invasive forms of administration can have significant limitations, such as a risk of infection at the injection site, the need to be administered in a medical setting, additional time, and patient discomfort.
Table 1 lists short-acting injectable medications used in psychiatry, and Table 2 lists long-acting injectable medications. Parenteral administration of antipsychotics is performed to alleviate acute agitation or for chronic symptom control. These medications generally are not considered interventional treatments, but could be classified as such due to their invasive nature.1 Furthermore, inhalable loxapine—which is indicated for managing acute agitation—requires a Risk Evaluation and Mitigation Strategy program consisting of 2 hours observation and monitoring of respiratory status.2,3 Other indications for parenteral treatments include IM naltrexone extended release4 and subcutaneous injections of buprenorphine extended release5 and risperidone.6
IV administration
Most IV treatments described in this article are not FDA-approved for psychiatric treatment. Despite this, many interventional psychiatric treatments are part of clinical practice. IV infusion of ketamine is the most widely known and most researched of these. Table 3 lists other IV treatments that could be used as psychiatric treatment.
Ketamine
Since the early 1960s, ketamine has been used as a surgical anesthetic for animals. In the United States, it was approved for human surgical anesthesia in 1970. It was widely used during the Vietnam War due to its lack of inhibition of respiratory drive; medical staff first noticed an improvement in depressive symptoms and the resolution of suicidal ideation in patients who received ketamine. This led to further research on ketamine, particularly to determine its application in treatment-resistant depression (TRD) and other conditions.7 IV ketamine administration is most widely researched, but IM injections, intranasal sprays, and lozenges are also available. The dissociative properties of ketamine have led to its recreational use.8
Hypotheses for the mechanism of action of ketamine as an antidepressant include direct synaptic or extrasynaptic (GluN2B-selective), N-methyl-
Continue to: Ketamine is a schedule...
Ketamine is a schedule III medication with addictive properties. Delirium, panic attacks, hallucinations, nightmares, dysphoria, and paranoia may occur during and after use.13 Premedication with benzodiazepines, most notably lorazepam, is occasionally used to minimize ketamine’s adverse effects, but this generally is not recommended because doing so reduces ketamine’s antidepressant effects.14 Driving and operating heavy machinery is contraindicated after IV infusion. The usual protocol involves an IV infusion of ketamine 0.4 mg/kg to 1 mg/kg dosing over 1 hour. Doses between 0.4 mg/kg and 0.6 mg/kg are most common. Ketamine has a therapeutic window; doses >0.5 mg/kg are progressively less effective.15 Unlike the recommendation after esketamine administration, after receiving ketamine, patients remain in the care of their treatment team for <2 hours.
Esketamine, the S enantiomer of ketamine, was FDA-approved for TRD as an intranasal formulation. Esketamine is more commonly used than IV ketamine because it is FDA-approved and typically covered by insurance, but it may not be as effective.16 An economic analysis by Brendle et al17 suggested insurance companies would lower costs if they covered ketamine infusions vs intranasal esketamine.
Aducanumab and lecanemab
The most recent FDA-approved interventional agents are aducanumab and lecanemab, which are indicated for treating Alzheimer disease.18,19 Both are human monoclonal antibodies that bind selectively and with high affinity to amyloid beta plaque aggregates and promote their removal by Fc receptor–mediated phagocytosis.20
FDA approval of aducanumab and lecanemab was controversial. Initially, aducanumab’s safety monitoring board performed a futility analysis that suggested aducanumab was unlikely to separate from placebo, and the research was stopped.21 The manufacturer petitioned the FDA to consider the medication for accelerated approval on the basis of biomarker data showing that amyloid beta plaque aggregates become smaller. Current FDA approval is temporary to allow patients access to this potentially beneficial agent, but the manufacturer must supply clinical evidence that the reduction of amyloid beta plaques is associated with desirable changes in the course of Alzheimer disease, or risk losing the approval.
Lecanemab is also a human monoclonal antibody intended to remove amyloid beta plaques that was FDA-approved under the accelerated approval pathway.22 Unlike aducanumab, lecanemab demonstrated a statistically significant (although clinically imperceptible) reduction in the rate of cognitive decline; it did not show cognitive improvement.23 Lecanemab also significantly reduced amyloid beta plaques.23
Continue to: Aducanumab and lecanemab are generally...
Aducanumab and lecanemab are generally not covered by insurance and typically cost >$26,000 annually. Both are administered by IV infusion once a month. More monoclonal antibody medications for treating early Alzheimer disease are in the late stages of development, most notably donanebab.24 Observations during clinical trials found that in the later stages of Alzheimer disease, forceful removal of plaques by the autoimmune process damages neurons, while in less dense deposits of early dementia such removal is not harmful to the cells and prevents amyloid buildup.
Brexanolone is an aqueous formulation of allopregnanolone, a major metabolite of progesterone and a positive allosteric modulator of GABA-A receptors.25 Its levels are maximal at the end of the third trimester of pregnancy and fall rapidly following delivery. Research showed a 3-day infusion was rapidly and significantly effective for treating postpartum depression26 and brexanolone received FDA approval for this indication in March 2019.27 However, various administrative, economic, insurance, and other hurdles make it difficult for patients to access this treatment. Despite its rapid onset of action (usually 48 hours), brexanolone takes an average of 15 days to go through the prior authorization process.28 In addition to the need for prior authorization, the main impediment to the use of brexanolone is the 3-day infusion schedule, which greatly magnifies the cost but is partially circumvented by the availability of dedicated outpatient centers.
Magnesium
Magnesium is on the World Health Organization’s Model List of Essential Medicines.29 There has been extensive research on the use of magnesium sulfate for psychiatric indications, especially for depression.30 Magnesium functions similarly to calcium channel blockers by competitively blocking intracellular calcium channels, decreasing calcium availability, and inhibiting smooth muscle contractility.31 It also competes with calcium at the motor end plate, reducing excitation by inhibiting the release of acetylcholine.32 This property is used for high-dose IV magnesium treatment of impending preterm labor in obstetrics. Magnesium sulfate is the drug of choice in treating eclamptic seizures and preventing seizures in severe preeclampsia or gestational hypertension with severe features.33 It is also used to treat torsade de pointes, severe asthma exacerbations, constipation, and barium poisoning.34 Beneficial use in asthma treatment35 and the treatment of migraine36 have also been reported.
IV magnesium in myocardial infarction may be harmful,37 though outside of acute cardiac events, magnesium is found to be safe.38
Oral magnesium sulfate is a common over-the-counter anxiety remedy. As a general cell stabilizer (mediated by the reduction of intracellular calcium), magnesium is potentially beneficial outside of its muscle-relaxing properties, although muscle relaxing can benefit anxious patients. It is used to treat anxiety,39 alcohol withdrawal,40 and fear.41 Low magnesium blood levels are found in patients with depression, schizophrenia,42 and attention-deficit/hyperactivity disorder.43 However, it is important to note that the therapeutic effect of magnesium when treating anxiety and headache is independent of preinfusion magnesium blood levels.43
Continue to: The efficacy of oral magnesium...
The efficacy of oral magnesium is not robust. However, IV administration has a pronounced beneficial effect as an abortive and preventative treatment in many patients with anxiety.44
IV administration of magnesium can produce adverse effects, including flushing, sweating, hypotension, depressed reflexes, flaccid paralysis, hypothermia, circulatory collapse, and cardiac and CNS depression. These complications are very rare and dose-dependent.45 Magnesium is excreted by the kidneys, and dosing must be decreased in patients with kidney failure. The most common adverse effect is local burning along the vein upon infusion; small doses of IV lidocaine can remedy this. Hot flashes are also common.45
Various dosing strategies are available. In patients with anxiety, application dosing is based on the recommended preeclampsia IV dose of 4 g diluted in 250 mL of 5% dextrose. Much higher doses may be used in obstetrics. Unlike in obstetrics, for psychiatric indications, magnesium is administered over 60 to 90 minutes. Heart monitoring is recommended.
Scopolamine
Scopolamine is primarily used to relieve nausea, vomiting, and dizziness associated with motion sickness and recovery from anesthesia. It is also used in ophthalmology and in patients with excessive sweating. In off-label and experimental applications, scopolamine has been used in patients with TRD.46
Scopolamine is an anticholinergic medication. It is a nonselective antagonist at muscarinic receptors.47 Tricyclic antidepressants (TCAs) possess strong anticholinergic function. Newer generations of antidepressants were designed specifically not to have this function because it was believed to be an unwanted and potentially dangerous adverse effect. However, data suggest that anticholinergic action is important in decreasing depressive symptoms. Several hypotheses of anticholinergic effects on depression have been published since the 1970s. They include the cholinergic-adrenergic hypothesis,48 acetylcholine predominance relative to adrenergic action hypothesis,49 and insecticide poisoning observations.50 Centrally acting physostigmine (but not peripherally acting neostigmine) was reported to control mania.48,51 A genetic connection between the M2 acetylcholine receptor in patients with major depressive disorder (MDD) and alcohol use disorder is also suggestive.52
Continue to: Multiple animal studies show...
Multiple animal studies show direct improvement in mobility and a decrease in despair upon introducing anticholinergic substances.53-55 The cholinergic theory of depression has been studied in several controlled clinical human studies.56,57 Use of a short-acting anticholinergic glycopyrrolate during electroconvulsive therapy (ECT) may contribute to the procedure’s efficacy.
Human research shows scopolamine has a higher efficacy as an antidepressant and anti-anxiety medication in women than in men,58 possibly because estrogen increases the activity of choline acetyltransferase and release of acetylcholine.59,60 M2 receptors mediate estrogen influence on the NMDAR, which may explain the anticholinergic effects of depression treatments in women.61
Another proposed mechanism of action of scopolamine is a potent inhibition of the NMDAR.62 Rapid treatments of depression may be based on this mechanism. Examples of such treatments include IV ketamine and sleep deprivation.63 IV scopolamine shows potency in treating MDD and bipolar depression. This treatment should be reserved for patients who do not respond to or are not candidates for other usual treatment modalities of MDD and for the most severe cases. Scopolamine is 30 times more potent than amitriptyline in anticholinergic effect and reportedly produces sustained improvement in MDD.64
Scopolamine has no black-box warnings. It has not been studied in pregnant women and is not recommended for use during pregnancy. Due to possible negative cardiovascular effects, a normal electrocardiogram is required before the start of treatment. Exercise caution in patients with glaucoma, benign prostatic enlargement, gastroparesis, unstable cardiovascular status, or severe renal impairment.
Treatment with scopolamine is not indicated for patients with myasthenia gravis, psychosis, or seizures. Patients must be off potassium for 3 days before beginning scopolamine treatment. Patients should consult with their cardiologist before having a scopolamine infusion. Adverse reactions may include psychosis, tachycardia, seizures, paralytic ileus, and glaucoma exacerbation. The most common adverse effects of scopolamine infusion treatment include drowsiness, dry mouth, blurred vision, lightheadedness, and dizziness. Due to possible drowsiness, operating motor vehicles or heavy machinery must be avoided on the day of treatment.65 Overall, the adverse effects of scopolamine are preventable and manageable, and its antidepressant efficacy is noteworthy.66
Continue to: Treatment typically consists of 3 consecutive infusions...
Treatment typically consists of 3 consecutive infusions of 4 mcg/kg separated by 3 to 5 days.56 It is possible to have a longer treatment course if the patient experiences only partial improvement. Repeated courses or maintenance treatment (similar to ECT maintenance) are utilized in some patients if indicated. Cardiac monitoring is mandatory.
Clomipramine
Clomipramine, a TCA, acts as a preferential inhibitor of 5-hydroxytryptamine uptake and has proven effective in managing depression, TRD, and obsessive-compulsive disorder (OCD).67 Although this medication has reported treatment benefits for patients with phobia, panic disorder,15 chronic pain,68 Tourette syndrome,69 premature ejaculation, anorexia nervosa,70 cataplexy,49 and enuresis,71 it is FDA-approved only for the treatment of OCD.72 Clomipramine may also be beneficial for pain and headache, possibly because of its anti-inflammatory action.73 The anticholinergic effects of clomipramine may add to its efficacy in depression.
The pathophysiology of MDD is connected to hyperactivity of the HPA axis and elevated cortisol levels. Higher clomipramine plasma levels show a linear correlation with lower cortisol secretion and levels, possibly aiding in the treatment of MDD and anxiety.74 The higher the blood level, the more pronounced clomipramine’s therapeutic effect across multiple domains.75
IV infusion of clomipramine produces the highest concentration in the shortest time, but overall, research does not necessarily support increased efficacy of IV over oral administration. There is evidence suggesting that subgroups of patients with severe, treatment-refractory OCD may benefit from IV agents and research suggests a faster onset of action.76 Faster onset of symptom relief is the basis for IV clomipramine use. In patients with OCD, it can take several months for oral medications to produce therapeutic benefits; not all patients can tolerate this. In such scenarios, IV administration may be considered, though it is not appropriate for routine use until more research is available. Patients with treatment-resistant OCD who have exhausted other means of symptom relief may also be candidates for IV treatment.
The adverse effects of IV clomipramine are no different from oral use, though they may be more pronounced. A pretreatment cardiac exam is desirable because clomipramine, like other TCAs, may be cardiotoxic. The anticholinergic adverse effects of TCAs are well known to clinicians77 and partially explained in the scopolamine section of this article. It is not advisable to combine clomipramine with other TCAs or serotonin reuptake inhibitors. Clomipramine also should not be combined with monoamine oxidase inhibitors, though such a combination was reported in medical literature.78 Combination with antiarrhythmics such as lidocaine or opioids such as fentanyl or and tramadol is highly discouraged (fentanyl and tramadol also have serotonergic effects).79
Continue to: Clomipramine for IV use is not commercially available...
Clomipramine for IV use is not commercially available and must be sterilely compounded. The usual course of treatment is a series of 3 infusions: 150 mg on Day 1, 200 mg on Day 2 or Day 3, and 250 mg on Day 3, Day 4, or Day 5, depending on tolerability. A protocol with a 50 mg/d starting dose and titration up to a maximum dose of 225 mg/d over 5 to 7 days has been suggested for inpatient settings.67 Titration to 250 mg is more common.80
A longer series may be performed, but this increases the likelihood of adverse effects. Booster and maintenance treatments are also completed when required. Cardiac monitoring is mandatory.
Vortioxetine and citalopram
IV treatment of depression with
Injections and blocks
Three interventional approaches to treatment that possess psychotherapeutic potential include stellate ganglion blocks (SGBs), glabellar BT injections, and trigger point injections (TPIs). None of these are FDA-approved for psychiatric treatment.
Stellate ganglion blocks
The sympathetic nervous system is involved in autonomic hyperarousal and is at the core of posttraumatic symptomatology.83 Insomnia, anxiety, irritability, hypervigilance, and other excitatory CNS events are connected to the sympathetic nervous system and amygdala activation is commonly observed in those exposed to extreme stress or traumatic events.84
Continue to: SGBs were first performed 100 years ago...
SGBs were first performed 100 years ago and reported to have beneficial psychiatric effects at the end of the 1940s. In 1998 in Finland, improvement of posttraumatic stress disorder (PTSD) symptoms was observed accidentally via thoracic level spine blocks.85 In 2006, cervical level sympathetic blocks were shown to be effective for PTSD symptom control.86 By the end of 2010, Veterans Administration hospitals adopted SGBs to treat veterans with PTSD.87,88 The first multisite, randomized clinical trial of
Since the stellate ganglion is connected to the amygdala, SGB has also been assessed for treating anxiety and depression.89,90 Outside of PTSD, SGBs are used to treat complex regional pain syndrome,91 phantom limb pain, trigeminal neuralgia,92 intractable angina,93 and postherpetic neuralgia in the head, neck, upper chest, or arms.94 The procedure consists of an injection of a local anesthetic through a 25-gauge needle into the stellate sympathetic ganglion at the C6 or C7 vertebral levels. An injection into C6 is considered safer because of specific cervical spine anatomy. Ideally, fluoroscopic guidance or ultrasound is used to guide needle insertion.95
A severe drop in blood pressure may be associated with SGBs and is mitigated by IV hydration. Other adverse effects include red eyes, drooping of the eyelids, nasal congestion, hoarseness, difficulty swallowing, a sensation of a “lump” in the throat, and a sensation of warmth or tingling in the arm or hand. Bilateral SGB is contraindicated due to the danger of respiratory arrest.96
Glabellar BT injections
OnabotulinumtoxinA (BT) injection was first approved for therapeutic use in 1989 for eye muscle disorders such as strabismus97 and blepharospasm.98 It was later approved for several other indications, including cosmetic use, hyperhidrosis, migraine prevention, neurogenic bladder disorder, overactive bladder, urinary incontinence, and spasticity.99-104 BT is used off-label for achalasia and sialorrhea.105,106 Its mechanism of action is primarily attributed to muscle paralysis by blocking presynaptic acetylcholine release into neuromuscular junctions.107
Facial BT injections are usually administered for cosmetic purposes, but smoothing forehead wrinkles and frown lines (the glabellar region of the face) both have antidepressant effects.108 BT injections into the glabellar region also demonstrate antidepressant effects, particularly in patients with comorbid migraines and MDD.109 Early case observations supported the independent benefit of the toxin on MDD when the toxin was injected into the glabellar region.110,111 The most frequent protocol involves injections in the procerus and corrugator muscles.
Continue to: The facial feedback/emotional proprioception hypothesis...
The facial feedback/emotional proprioception hypothesis has dominated thinking about the mood-improving effects of BT. The theory is that blocking muscular expression of sadness (especially in the face) interrupts the experience of sadness; therefore, depression subsides.112,113 However, BT injections in the muscles involved in the smile and an expression of positive emotions (lateral part of the musculus orbicularis oculi) have been associated with increased MDD scores.114 Thus, the mechanism clearly involves more than the cosmetic effect, since facial muscle injections in rats also have antidepressant effects.115
The use of progressive muscle relaxation is well-established in psychiatric treatment. The investigated conditions of increased muscle tone, especially torticollis and blepharospasm, are associated with MDD, and it may be speculated that proprioceptive feedback from the affected muscles may be causally involved in this association.116-118 Activity of the corrugator muscle has been positively associated with increased amygdala activity.119 This suggests a potential similar mechanism to that hypothesized for SGB.
Alternatively, BT is commonly used to treat chronic conditions that may contribute to depression; its success in relieving the underlying problem may indirectly relieve MDD. Thus, in a postmarketing safety evaluation of BT, MDD was demonstrated 40% to 88% less often by patients treated with BT for 6 of the 8 conditions and injection sites, such as in spasms and spasticity of arms and legs, torticollis and neck pain, and axilla and palm injections for hyperhidrosis. In a parotid and submandibular glands BT injection subcohort, no patients experienced depressive symptoms.120
Medicinal BT is generally considered safe. The most common adverse effects are hypersensitivity, injection site reactions, and other adverse effects specific to the injection site.121 Additionally, the cosmetic effects are transient, given the nature of the medication.
Trigger point injections
TPIs in the neck and shoulders are frequently used to treat tension headaches and various referred pain locations in the face and arms. Tension and depression frequently overlap in clinical practice.122 Relieving muscle tension (with resulting trigger points) improves muscle function and mood.
Continue to: The higher the number of active...
The higher the number of active trigger points (TPs), the greater the physical burden of headache and the higher the anxiety level. Gender differences in TP prevalence and TPI efficacy have been described in the literature. For example, the number of active TPs seems directly associated with anxiety levels in women but not in men.123 Although TPs appear to be more closely associated with anxiety than depression,124 depression associated with muscle tension does improve with TPIs. European studies have demonstrated a decrease in scores on the Hamilton Depression Rating Scale and Hamilton Anxiety Rating Scale following TPI treatment.125 The effect may be indirect, as when a patient’s pain is relieved, sleep and other psychiatric symptoms improve.126
A randomized controlled trial by Castro Sánchez et al127 demonstrated that dry needling therapy in patients with fibromyalgia syndrome (FMS) showed improvements in pain pressure thresholds, body pain, vitality, and social function, as well as total FMS symptoms, quality of sleep, anxiety, hospital anxiety and depression, general pain intensity, and fatigue.
Myofascial pain syndrome, catastrophizing, and muscle tension are common in patients with depression, anxiety, and somatization. Local TPI therapy aimed at inactivating pain generators is supported by moderate quality evidence. All manner of therapies have been described, including injection of saline, corticosteroids, local anesthetic agents, and dry needling. BT injections in chronic TPs are also practiced, though no specific injection therapy has been reliably shown to be more advantageous than another. The benefits of TPIs may be derived from the needle itself rather than from any specific substance injected. Stimulation of a local twitch response with direct needling of the TP appears of importance. There is no established consensus regarding the number of injection points, frequency of administration, and volume or type of injectate.128
Adverse effects of TPIs relate to the nature of the invasive therapy, with the risk of tissue damage and bleeding. Pneumothorax risk is present with needle insertion at the neck and thorax.129 Patients with diabetes may experience variations in blood sugar control if steroids are used.
Bottom Line
Interventional treatment modalities that may have a role in psychiatric treatment include IV administration of ketamine, aducanumab, lecanemab, brexanolone, magnesium, scopolamine, and clomipramine. Other interventional approaches include stellate ganglion blocks, glabellar botulinum toxin injections, and trigger point injections.
Related Resources
- Dokucu ME, Janicak PG. Nontraditional therapies for treatment-resistant depression. Current Psychiatry. 2021; 20(9):38-43,49. doi:10.12788/cp.0166
- Kim J, Khoury R, Grossberg GT. Botulinum toxin: emerging psychiatric indications. Current Psychiatry. 2018;17(12):8-18.
Drug Brand Names
Aducanumab • Aduhelm
Aripiprazole • Abilify
Aripiprazole lauroxil • Aristada
Brexanolone • Zulresso
Buprenorphine • Sublocade
Citalopram • Celexa
Clomipramine • Anafranil
Diazepam • Valium
Droperidol • Inapsine
Esketamine • Spravato
Fentanyl • Actiq
Fluphenazine decanoate • Modecate
Fluphenazine hydrochloride • Prolixin
Haloperidol decanoate • Haldol decanoate
Haloperidol lactate • Haldol
Ketamine • Ketalar
Lecanemab • Leqembi
Lidocaine • Xylocaine
Lorazepam • Ativan
Loxapine inhaled • Adasuve
Naltrexone • Vivitrol
Magnesium sulfate • Sulfamag
Midazolam • Versed
Olanzapine • Zyprexa
OnabotulinumtoxinA injection • Botox
Paliperidone • Invega Hafyera, Invega Sustenna, Invega Trinza
Rapamycin • Rapamune, Sirolimus
Risperidone • Perseris
Risperidone microspheres • Risperdal Consta, Rykindo
Scopolamine • Hyoscine
Tramadol • Conzip
Vortioxetine • Trintellix
Ziprasidone • Geodon
Advances in the understanding of neurobiological and neuropsychiatric pathophysiology have opened new avenues of treatment for psychiatric patients. Historically, with a few exceptions, most psychiatric medications have been administered orally. However, many of the newer treatments require some form of specialized administration because they cannot be taken orally due to their chemical property (such as aducanumab); because there is the need to produce stable blood levels of the medication (such as brexanolone); because oral administration greatly diminished efficacy (such as oral vs IV magnesium or scopolamine), or because the treatment is focused on specific brain structures. This need for specialized administration has created a subspecialty called interventional psychiatry.
Part 1 of this 2-part article provides an overview of 1 type of interventional psychiatry: parenterally administered medications, including those administered via IV. We also describe 3 other interventional approaches to treatment: stellate ganglion blocks, glabellar botulinum toxin (BT) injections, and trigger point injections. In Part 2 we will review interventional approaches that involve neuromodulation.
Parenteral medications in psychiatry
In general, IV and IM medications can be more potent that oral medications due to their overall faster onset of action and higher blood concentrations. These more invasive forms of administration can have significant limitations, such as a risk of infection at the injection site, the need to be administered in a medical setting, additional time, and patient discomfort.
Table 1 lists short-acting injectable medications used in psychiatry, and Table 2 lists long-acting injectable medications. Parenteral administration of antipsychotics is performed to alleviate acute agitation or for chronic symptom control. These medications generally are not considered interventional treatments, but could be classified as such due to their invasive nature.1 Furthermore, inhalable loxapine—which is indicated for managing acute agitation—requires a Risk Evaluation and Mitigation Strategy program consisting of 2 hours observation and monitoring of respiratory status.2,3 Other indications for parenteral treatments include IM naltrexone extended release4 and subcutaneous injections of buprenorphine extended release5 and risperidone.6
IV administration
Most IV treatments described in this article are not FDA-approved for psychiatric treatment. Despite this, many interventional psychiatric treatments are part of clinical practice. IV infusion of ketamine is the most widely known and most researched of these. Table 3 lists other IV treatments that could be used as psychiatric treatment.
Ketamine
Since the early 1960s, ketamine has been used as a surgical anesthetic for animals. In the United States, it was approved for human surgical anesthesia in 1970. It was widely used during the Vietnam War due to its lack of inhibition of respiratory drive; medical staff first noticed an improvement in depressive symptoms and the resolution of suicidal ideation in patients who received ketamine. This led to further research on ketamine, particularly to determine its application in treatment-resistant depression (TRD) and other conditions.7 IV ketamine administration is most widely researched, but IM injections, intranasal sprays, and lozenges are also available. The dissociative properties of ketamine have led to its recreational use.8
Hypotheses for the mechanism of action of ketamine as an antidepressant include direct synaptic or extrasynaptic (GluN2B-selective), N-methyl-
Continue to: Ketamine is a schedule...
Ketamine is a schedule III medication with addictive properties. Delirium, panic attacks, hallucinations, nightmares, dysphoria, and paranoia may occur during and after use.13 Premedication with benzodiazepines, most notably lorazepam, is occasionally used to minimize ketamine’s adverse effects, but this generally is not recommended because doing so reduces ketamine’s antidepressant effects.14 Driving and operating heavy machinery is contraindicated after IV infusion. The usual protocol involves an IV infusion of ketamine 0.4 mg/kg to 1 mg/kg dosing over 1 hour. Doses between 0.4 mg/kg and 0.6 mg/kg are most common. Ketamine has a therapeutic window; doses >0.5 mg/kg are progressively less effective.15 Unlike the recommendation after esketamine administration, after receiving ketamine, patients remain in the care of their treatment team for <2 hours.
Esketamine, the S enantiomer of ketamine, was FDA-approved for TRD as an intranasal formulation. Esketamine is more commonly used than IV ketamine because it is FDA-approved and typically covered by insurance, but it may not be as effective.16 An economic analysis by Brendle et al17 suggested insurance companies would lower costs if they covered ketamine infusions vs intranasal esketamine.
Aducanumab and lecanemab
The most recent FDA-approved interventional agents are aducanumab and lecanemab, which are indicated for treating Alzheimer disease.18,19 Both are human monoclonal antibodies that bind selectively and with high affinity to amyloid beta plaque aggregates and promote their removal by Fc receptor–mediated phagocytosis.20
FDA approval of aducanumab and lecanemab was controversial. Initially, aducanumab’s safety monitoring board performed a futility analysis that suggested aducanumab was unlikely to separate from placebo, and the research was stopped.21 The manufacturer petitioned the FDA to consider the medication for accelerated approval on the basis of biomarker data showing that amyloid beta plaque aggregates become smaller. Current FDA approval is temporary to allow patients access to this potentially beneficial agent, but the manufacturer must supply clinical evidence that the reduction of amyloid beta plaques is associated with desirable changes in the course of Alzheimer disease, or risk losing the approval.
Lecanemab is also a human monoclonal antibody intended to remove amyloid beta plaques that was FDA-approved under the accelerated approval pathway.22 Unlike aducanumab, lecanemab demonstrated a statistically significant (although clinically imperceptible) reduction in the rate of cognitive decline; it did not show cognitive improvement.23 Lecanemab also significantly reduced amyloid beta plaques.23
Continue to: Aducanumab and lecanemab are generally...
Aducanumab and lecanemab are generally not covered by insurance and typically cost >$26,000 annually. Both are administered by IV infusion once a month. More monoclonal antibody medications for treating early Alzheimer disease are in the late stages of development, most notably donanebab.24 Observations during clinical trials found that in the later stages of Alzheimer disease, forceful removal of plaques by the autoimmune process damages neurons, while in less dense deposits of early dementia such removal is not harmful to the cells and prevents amyloid buildup.
Brexanolone is an aqueous formulation of allopregnanolone, a major metabolite of progesterone and a positive allosteric modulator of GABA-A receptors.25 Its levels are maximal at the end of the third trimester of pregnancy and fall rapidly following delivery. Research showed a 3-day infusion was rapidly and significantly effective for treating postpartum depression26 and brexanolone received FDA approval for this indication in March 2019.27 However, various administrative, economic, insurance, and other hurdles make it difficult for patients to access this treatment. Despite its rapid onset of action (usually 48 hours), brexanolone takes an average of 15 days to go through the prior authorization process.28 In addition to the need for prior authorization, the main impediment to the use of brexanolone is the 3-day infusion schedule, which greatly magnifies the cost but is partially circumvented by the availability of dedicated outpatient centers.
Magnesium
Magnesium is on the World Health Organization’s Model List of Essential Medicines.29 There has been extensive research on the use of magnesium sulfate for psychiatric indications, especially for depression.30 Magnesium functions similarly to calcium channel blockers by competitively blocking intracellular calcium channels, decreasing calcium availability, and inhibiting smooth muscle contractility.31 It also competes with calcium at the motor end plate, reducing excitation by inhibiting the release of acetylcholine.32 This property is used for high-dose IV magnesium treatment of impending preterm labor in obstetrics. Magnesium sulfate is the drug of choice in treating eclamptic seizures and preventing seizures in severe preeclampsia or gestational hypertension with severe features.33 It is also used to treat torsade de pointes, severe asthma exacerbations, constipation, and barium poisoning.34 Beneficial use in asthma treatment35 and the treatment of migraine36 have also been reported.
IV magnesium in myocardial infarction may be harmful,37 though outside of acute cardiac events, magnesium is found to be safe.38
Oral magnesium sulfate is a common over-the-counter anxiety remedy. As a general cell stabilizer (mediated by the reduction of intracellular calcium), magnesium is potentially beneficial outside of its muscle-relaxing properties, although muscle relaxing can benefit anxious patients. It is used to treat anxiety,39 alcohol withdrawal,40 and fear.41 Low magnesium blood levels are found in patients with depression, schizophrenia,42 and attention-deficit/hyperactivity disorder.43 However, it is important to note that the therapeutic effect of magnesium when treating anxiety and headache is independent of preinfusion magnesium blood levels.43
Continue to: The efficacy of oral magnesium...
The efficacy of oral magnesium is not robust. However, IV administration has a pronounced beneficial effect as an abortive and preventative treatment in many patients with anxiety.44
IV administration of magnesium can produce adverse effects, including flushing, sweating, hypotension, depressed reflexes, flaccid paralysis, hypothermia, circulatory collapse, and cardiac and CNS depression. These complications are very rare and dose-dependent.45 Magnesium is excreted by the kidneys, and dosing must be decreased in patients with kidney failure. The most common adverse effect is local burning along the vein upon infusion; small doses of IV lidocaine can remedy this. Hot flashes are also common.45
Various dosing strategies are available. In patients with anxiety, application dosing is based on the recommended preeclampsia IV dose of 4 g diluted in 250 mL of 5% dextrose. Much higher doses may be used in obstetrics. Unlike in obstetrics, for psychiatric indications, magnesium is administered over 60 to 90 minutes. Heart monitoring is recommended.
Scopolamine
Scopolamine is primarily used to relieve nausea, vomiting, and dizziness associated with motion sickness and recovery from anesthesia. It is also used in ophthalmology and in patients with excessive sweating. In off-label and experimental applications, scopolamine has been used in patients with TRD.46
Scopolamine is an anticholinergic medication. It is a nonselective antagonist at muscarinic receptors.47 Tricyclic antidepressants (TCAs) possess strong anticholinergic function. Newer generations of antidepressants were designed specifically not to have this function because it was believed to be an unwanted and potentially dangerous adverse effect. However, data suggest that anticholinergic action is important in decreasing depressive symptoms. Several hypotheses of anticholinergic effects on depression have been published since the 1970s. They include the cholinergic-adrenergic hypothesis,48 acetylcholine predominance relative to adrenergic action hypothesis,49 and insecticide poisoning observations.50 Centrally acting physostigmine (but not peripherally acting neostigmine) was reported to control mania.48,51 A genetic connection between the M2 acetylcholine receptor in patients with major depressive disorder (MDD) and alcohol use disorder is also suggestive.52
Continue to: Multiple animal studies show...
Multiple animal studies show direct improvement in mobility and a decrease in despair upon introducing anticholinergic substances.53-55 The cholinergic theory of depression has been studied in several controlled clinical human studies.56,57 Use of a short-acting anticholinergic glycopyrrolate during electroconvulsive therapy (ECT) may contribute to the procedure’s efficacy.
Human research shows scopolamine has a higher efficacy as an antidepressant and anti-anxiety medication in women than in men,58 possibly because estrogen increases the activity of choline acetyltransferase and release of acetylcholine.59,60 M2 receptors mediate estrogen influence on the NMDAR, which may explain the anticholinergic effects of depression treatments in women.61
Another proposed mechanism of action of scopolamine is a potent inhibition of the NMDAR.62 Rapid treatments of depression may be based on this mechanism. Examples of such treatments include IV ketamine and sleep deprivation.63 IV scopolamine shows potency in treating MDD and bipolar depression. This treatment should be reserved for patients who do not respond to or are not candidates for other usual treatment modalities of MDD and for the most severe cases. Scopolamine is 30 times more potent than amitriptyline in anticholinergic effect and reportedly produces sustained improvement in MDD.64
Scopolamine has no black-box warnings. It has not been studied in pregnant women and is not recommended for use during pregnancy. Due to possible negative cardiovascular effects, a normal electrocardiogram is required before the start of treatment. Exercise caution in patients with glaucoma, benign prostatic enlargement, gastroparesis, unstable cardiovascular status, or severe renal impairment.
Treatment with scopolamine is not indicated for patients with myasthenia gravis, psychosis, or seizures. Patients must be off potassium for 3 days before beginning scopolamine treatment. Patients should consult with their cardiologist before having a scopolamine infusion. Adverse reactions may include psychosis, tachycardia, seizures, paralytic ileus, and glaucoma exacerbation. The most common adverse effects of scopolamine infusion treatment include drowsiness, dry mouth, blurred vision, lightheadedness, and dizziness. Due to possible drowsiness, operating motor vehicles or heavy machinery must be avoided on the day of treatment.65 Overall, the adverse effects of scopolamine are preventable and manageable, and its antidepressant efficacy is noteworthy.66
Continue to: Treatment typically consists of 3 consecutive infusions...
Treatment typically consists of 3 consecutive infusions of 4 mcg/kg separated by 3 to 5 days.56 It is possible to have a longer treatment course if the patient experiences only partial improvement. Repeated courses or maintenance treatment (similar to ECT maintenance) are utilized in some patients if indicated. Cardiac monitoring is mandatory.
Clomipramine
Clomipramine, a TCA, acts as a preferential inhibitor of 5-hydroxytryptamine uptake and has proven effective in managing depression, TRD, and obsessive-compulsive disorder (OCD).67 Although this medication has reported treatment benefits for patients with phobia, panic disorder,15 chronic pain,68 Tourette syndrome,69 premature ejaculation, anorexia nervosa,70 cataplexy,49 and enuresis,71 it is FDA-approved only for the treatment of OCD.72 Clomipramine may also be beneficial for pain and headache, possibly because of its anti-inflammatory action.73 The anticholinergic effects of clomipramine may add to its efficacy in depression.
The pathophysiology of MDD is connected to hyperactivity of the HPA axis and elevated cortisol levels. Higher clomipramine plasma levels show a linear correlation with lower cortisol secretion and levels, possibly aiding in the treatment of MDD and anxiety.74 The higher the blood level, the more pronounced clomipramine’s therapeutic effect across multiple domains.75
IV infusion of clomipramine produces the highest concentration in the shortest time, but overall, research does not necessarily support increased efficacy of IV over oral administration. There is evidence suggesting that subgroups of patients with severe, treatment-refractory OCD may benefit from IV agents and research suggests a faster onset of action.76 Faster onset of symptom relief is the basis for IV clomipramine use. In patients with OCD, it can take several months for oral medications to produce therapeutic benefits; not all patients can tolerate this. In such scenarios, IV administration may be considered, though it is not appropriate for routine use until more research is available. Patients with treatment-resistant OCD who have exhausted other means of symptom relief may also be candidates for IV treatment.
The adverse effects of IV clomipramine are no different from oral use, though they may be more pronounced. A pretreatment cardiac exam is desirable because clomipramine, like other TCAs, may be cardiotoxic. The anticholinergic adverse effects of TCAs are well known to clinicians77 and partially explained in the scopolamine section of this article. It is not advisable to combine clomipramine with other TCAs or serotonin reuptake inhibitors. Clomipramine also should not be combined with monoamine oxidase inhibitors, though such a combination was reported in medical literature.78 Combination with antiarrhythmics such as lidocaine or opioids such as fentanyl or and tramadol is highly discouraged (fentanyl and tramadol also have serotonergic effects).79
Continue to: Clomipramine for IV use is not commercially available...
Clomipramine for IV use is not commercially available and must be sterilely compounded. The usual course of treatment is a series of 3 infusions: 150 mg on Day 1, 200 mg on Day 2 or Day 3, and 250 mg on Day 3, Day 4, or Day 5, depending on tolerability. A protocol with a 50 mg/d starting dose and titration up to a maximum dose of 225 mg/d over 5 to 7 days has been suggested for inpatient settings.67 Titration to 250 mg is more common.80
A longer series may be performed, but this increases the likelihood of adverse effects. Booster and maintenance treatments are also completed when required. Cardiac monitoring is mandatory.
Vortioxetine and citalopram
IV treatment of depression with
Injections and blocks
Three interventional approaches to treatment that possess psychotherapeutic potential include stellate ganglion blocks (SGBs), glabellar BT injections, and trigger point injections (TPIs). None of these are FDA-approved for psychiatric treatment.
Stellate ganglion blocks
The sympathetic nervous system is involved in autonomic hyperarousal and is at the core of posttraumatic symptomatology.83 Insomnia, anxiety, irritability, hypervigilance, and other excitatory CNS events are connected to the sympathetic nervous system and amygdala activation is commonly observed in those exposed to extreme stress or traumatic events.84
Continue to: SGBs were first performed 100 years ago...
SGBs were first performed 100 years ago and reported to have beneficial psychiatric effects at the end of the 1940s. In 1998 in Finland, improvement of posttraumatic stress disorder (PTSD) symptoms was observed accidentally via thoracic level spine blocks.85 In 2006, cervical level sympathetic blocks were shown to be effective for PTSD symptom control.86 By the end of 2010, Veterans Administration hospitals adopted SGBs to treat veterans with PTSD.87,88 The first multisite, randomized clinical trial of
Since the stellate ganglion is connected to the amygdala, SGB has also been assessed for treating anxiety and depression.89,90 Outside of PTSD, SGBs are used to treat complex regional pain syndrome,91 phantom limb pain, trigeminal neuralgia,92 intractable angina,93 and postherpetic neuralgia in the head, neck, upper chest, or arms.94 The procedure consists of an injection of a local anesthetic through a 25-gauge needle into the stellate sympathetic ganglion at the C6 or C7 vertebral levels. An injection into C6 is considered safer because of specific cervical spine anatomy. Ideally, fluoroscopic guidance or ultrasound is used to guide needle insertion.95
A severe drop in blood pressure may be associated with SGBs and is mitigated by IV hydration. Other adverse effects include red eyes, drooping of the eyelids, nasal congestion, hoarseness, difficulty swallowing, a sensation of a “lump” in the throat, and a sensation of warmth or tingling in the arm or hand. Bilateral SGB is contraindicated due to the danger of respiratory arrest.96
Glabellar BT injections
OnabotulinumtoxinA (BT) injection was first approved for therapeutic use in 1989 for eye muscle disorders such as strabismus97 and blepharospasm.98 It was later approved for several other indications, including cosmetic use, hyperhidrosis, migraine prevention, neurogenic bladder disorder, overactive bladder, urinary incontinence, and spasticity.99-104 BT is used off-label for achalasia and sialorrhea.105,106 Its mechanism of action is primarily attributed to muscle paralysis by blocking presynaptic acetylcholine release into neuromuscular junctions.107
Facial BT injections are usually administered for cosmetic purposes, but smoothing forehead wrinkles and frown lines (the glabellar region of the face) both have antidepressant effects.108 BT injections into the glabellar region also demonstrate antidepressant effects, particularly in patients with comorbid migraines and MDD.109 Early case observations supported the independent benefit of the toxin on MDD when the toxin was injected into the glabellar region.110,111 The most frequent protocol involves injections in the procerus and corrugator muscles.
Continue to: The facial feedback/emotional proprioception hypothesis...
The facial feedback/emotional proprioception hypothesis has dominated thinking about the mood-improving effects of BT. The theory is that blocking muscular expression of sadness (especially in the face) interrupts the experience of sadness; therefore, depression subsides.112,113 However, BT injections in the muscles involved in the smile and an expression of positive emotions (lateral part of the musculus orbicularis oculi) have been associated with increased MDD scores.114 Thus, the mechanism clearly involves more than the cosmetic effect, since facial muscle injections in rats also have antidepressant effects.115
The use of progressive muscle relaxation is well-established in psychiatric treatment. The investigated conditions of increased muscle tone, especially torticollis and blepharospasm, are associated with MDD, and it may be speculated that proprioceptive feedback from the affected muscles may be causally involved in this association.116-118 Activity of the corrugator muscle has been positively associated with increased amygdala activity.119 This suggests a potential similar mechanism to that hypothesized for SGB.
Alternatively, BT is commonly used to treat chronic conditions that may contribute to depression; its success in relieving the underlying problem may indirectly relieve MDD. Thus, in a postmarketing safety evaluation of BT, MDD was demonstrated 40% to 88% less often by patients treated with BT for 6 of the 8 conditions and injection sites, such as in spasms and spasticity of arms and legs, torticollis and neck pain, and axilla and palm injections for hyperhidrosis. In a parotid and submandibular glands BT injection subcohort, no patients experienced depressive symptoms.120
Medicinal BT is generally considered safe. The most common adverse effects are hypersensitivity, injection site reactions, and other adverse effects specific to the injection site.121 Additionally, the cosmetic effects are transient, given the nature of the medication.
Trigger point injections
TPIs in the neck and shoulders are frequently used to treat tension headaches and various referred pain locations in the face and arms. Tension and depression frequently overlap in clinical practice.122 Relieving muscle tension (with resulting trigger points) improves muscle function and mood.
Continue to: The higher the number of active...
The higher the number of active trigger points (TPs), the greater the physical burden of headache and the higher the anxiety level. Gender differences in TP prevalence and TPI efficacy have been described in the literature. For example, the number of active TPs seems directly associated with anxiety levels in women but not in men.123 Although TPs appear to be more closely associated with anxiety than depression,124 depression associated with muscle tension does improve with TPIs. European studies have demonstrated a decrease in scores on the Hamilton Depression Rating Scale and Hamilton Anxiety Rating Scale following TPI treatment.125 The effect may be indirect, as when a patient’s pain is relieved, sleep and other psychiatric symptoms improve.126
A randomized controlled trial by Castro Sánchez et al127 demonstrated that dry needling therapy in patients with fibromyalgia syndrome (FMS) showed improvements in pain pressure thresholds, body pain, vitality, and social function, as well as total FMS symptoms, quality of sleep, anxiety, hospital anxiety and depression, general pain intensity, and fatigue.
Myofascial pain syndrome, catastrophizing, and muscle tension are common in patients with depression, anxiety, and somatization. Local TPI therapy aimed at inactivating pain generators is supported by moderate quality evidence. All manner of therapies have been described, including injection of saline, corticosteroids, local anesthetic agents, and dry needling. BT injections in chronic TPs are also practiced, though no specific injection therapy has been reliably shown to be more advantageous than another. The benefits of TPIs may be derived from the needle itself rather than from any specific substance injected. Stimulation of a local twitch response with direct needling of the TP appears of importance. There is no established consensus regarding the number of injection points, frequency of administration, and volume or type of injectate.128
Adverse effects of TPIs relate to the nature of the invasive therapy, with the risk of tissue damage and bleeding. Pneumothorax risk is present with needle insertion at the neck and thorax.129 Patients with diabetes may experience variations in blood sugar control if steroids are used.
Bottom Line
Interventional treatment modalities that may have a role in psychiatric treatment include IV administration of ketamine, aducanumab, lecanemab, brexanolone, magnesium, scopolamine, and clomipramine. Other interventional approaches include stellate ganglion blocks, glabellar botulinum toxin injections, and trigger point injections.
Related Resources
- Dokucu ME, Janicak PG. Nontraditional therapies for treatment-resistant depression. Current Psychiatry. 2021; 20(9):38-43,49. doi:10.12788/cp.0166
- Kim J, Khoury R, Grossberg GT. Botulinum toxin: emerging psychiatric indications. Current Psychiatry. 2018;17(12):8-18.
Drug Brand Names
Aducanumab • Aduhelm
Aripiprazole • Abilify
Aripiprazole lauroxil • Aristada
Brexanolone • Zulresso
Buprenorphine • Sublocade
Citalopram • Celexa
Clomipramine • Anafranil
Diazepam • Valium
Droperidol • Inapsine
Esketamine • Spravato
Fentanyl • Actiq
Fluphenazine decanoate • Modecate
Fluphenazine hydrochloride • Prolixin
Haloperidol decanoate • Haldol decanoate
Haloperidol lactate • Haldol
Ketamine • Ketalar
Lecanemab • Leqembi
Lidocaine • Xylocaine
Lorazepam • Ativan
Loxapine inhaled • Adasuve
Naltrexone • Vivitrol
Magnesium sulfate • Sulfamag
Midazolam • Versed
Olanzapine • Zyprexa
OnabotulinumtoxinA injection • Botox
Paliperidone • Invega Hafyera, Invega Sustenna, Invega Trinza
Rapamycin • Rapamune, Sirolimus
Risperidone • Perseris
Risperidone microspheres • Risperdal Consta, Rykindo
Scopolamine • Hyoscine
Tramadol • Conzip
Vortioxetine • Trintellix
Ziprasidone • Geodon
1. Vincent KM, Ryan M, Palmer E, et al. Interventional psychiatry. Postgrad Med. 2020;132(7):573-574.
2. Allen MH, Feifel D, Lesem MD, et al. Efficacy and safety of loxapine for inhalation in the treatment of agitation in patients with schizophrenia: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2011;72(10):1313-1321.
3. Kwentus J, Riesenberg RA, Marandi M, et al. Rapid acute treatment of agitation in patients with bipolar I disorder: a multicenter, randomized, placebo-controlled clinical trial with inhaled loxapine. Bipolar Disord. 2012;14(1):31-40.
4. Lee JD, Nunes EV Jr, Novo P, et al. Comparative effectiveness of extended-release naltrexone versus buprenorphine-naloxone for opioid relapse prevention (X:BOT): a multicentre, open-label, randomised controlled trial. Lancet. 2018;391(10118):309-318.
5. Haight BR, Learned SM, Laffont CM, et al. Efficacy and safety of a monthly buprenorphine depot injection for opioid use disorder: a multicentre, randomised, double‐blind, placebo‐controlled, phase 3 trial. Lancet. 2019;393(10173):778-790.
6. Andorn A, Graham J, Csernansky J, et al. Monthly extended-release risperidone (RBP-7000) in the treatment of schizophrenia: results from the phase 3 program. J Clin Psychopharmacol. 2019;39(5):428-433.
7. Dundee TW. Twenty-five years of ketamine. A report of an international meeting. Anaesthesia. 1990;45(2):159. doi:10.1111/j.1365-2044.1990.tb14287.x
8. White PF, Way WL, Trevor AJ. Ketamine--its pharmacology and therapeutic uses. Anesthesiology. 1982;56(2):119-136. doi:10.1097/00000542-198202000-00007
9. Zanos P, Gould TD. Mechanisms of ketamine action as an antidepressant. Mol Psychiatry. 2018;23(4):801-811.
10. Molero P, Ramos-Quiroga JA, Martin-Santos R, et al. Antidepressant efficacy and tolerability of ketamine and esketamine: a critical review. CNS Drugs. 2018;32(5):411-420. doi:10.1007/s40263-018-0519-3
11. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215.
12. Witkin JM, Martin AE, Golani LK, et al. Rapid-acting antidepressants. Adv Pharmacol. 2019;86:47-96.
13. Strayer RJ, Nelson LS. Adverse events associated with ketamine for procedural sedation in adults. Am J Emerg Med. 2008;26(9):985-1028. doi:10.1016/j.ajem.2007.12.005
14. Frye MA, Blier P, Tye SJ. Concomitant benzodiazepine use attenuates ketamine response: implications for large scale study design and clinical development. J Clin Psychopharmacol. 2015;35(3):334-336.
15. Fava M, Freeman MP, Flynn M, et al. Double-blind, placebo-controlled, dose-ranging trial of intravenous ketamine as adjunctive therapy in treatment-resistant depression (TRD). Mol Psychiatry. 2020;25(7):1592-1603.
16. Bahji A, Vazquez GH, Zarate CA Jr. Comparative efficacy of racemic ketamine and esketamine for depression: a systematic review and meta-analysis. J Affect Disord. 2021;278:542-555. Erratum in: J Affect Disord. 2021;281:1001.
17. Brendle M, Robison R, Malone DC. Cost-effectiveness of esketamine nasal spray compared to intravenous ketamine for patients with treatment-resistant depression in the US utilizing clinical trial efficacy and real-world effectiveness estimates. J Affect Disord. 2022;319:388-396.
18. Dhillon S. Aducanumab: first approval. Drugs. 2021;81(12):1437-1443. Erratum in: Drugs. 2021;81(14):1701.
19. van Dyck CH, Swanson CJ, Aisen P, et al. Lecanemab in early Alzheimer’s disease. N Engl J Med. 2023;388(1):9-21. doi:10.1056/NEJMoa2212948
20. Sevigny J, Chiao P, Bussière T, et al. The antibody aducanumab reduces Aβ plaques in Alzheimer’s disease. Nature. 2016;537(7618):50-56. Update in: Nature. 2017;546(7659):564.
21. Fillit H, Green A. Aducanumab and the FDA – where are we now? Nat Rev Neurol. 2021;17(3):129-130.
22. Reardon S. FDA approves Alzheimer’s drug lecanemab amid safety concerns. Nature. 2023;613(7943):227-228. doi:10.1038/d41586-023-00030-3
23. McDade E, Cummings JL, Dhadda S, et al. Lecanemab in patients with early Alzheimer’s disease: detailed results on biomarker, cognitive, and clinical effects from the randomized and open-label extension of the phase 2 proof-of-concept study. Alzheimers Res Ther. 2022;14(1):191. doi:10.1186/s13195-022-01124-2
24. Mintun MA, Lo AC, Evans CD, et al. Donanemab in early Alzheimer’s disease. N Engl J Med. 2021;384(18):1691-1704.
25. Luisi S, Petraglia F, Benedetto C, et al. Serum allopregnanolone levels in pregnant women: changes during pregnancy, at delivery, and in hypertensive patients. J Clin Endocrinol Metab. 2000;85(7):2429-2433.
26. Meltzer-Brody S, Colquhoun H, Riesenberg R, et al. Brexanolone injection in post-partum depression: two multicentre, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet. 2018;392(10152):1058-1070.
27. Powell JG, Garland S, Preston K, et al. Brexanolone (Zulresso): finally, an FDA-approved treatment for postpartum depression. Ann Pharmacother. 2020;54(2):157-163.
28. Patterson R, Krohn H, Richardson E, et al. A brexanolone treatment program at an academic medical center: patient selection, 90-day posttreatment outcomes, and lessons learned. J Acad Consult Liaison Psychiatry. 2022;63(1):14-22.
29. World Health Organization. WHO model list of essential medicines - 22nd list (2021). World Health Organization. September 30, 2021. Accessed April 7, 2023. https://www.who.int/publications/i/item/WHO-MHP-HPS-EML-2021.02
30. Eby GA, Eby KL, Mruk H. Magnesium and major depression. In: Vink R, Nechifor M, eds. Magnesium in the Central Nervous System. University of Adelaide Press; 2011.
31. Plant TM, Zeleznik AJ. Knobil and Neill’s Physiology of Reproduction. 4th ed. Elsevier Inc.; 2015:2503-2550.
32. Sidebotham D, Le Grice IJ. Physiology and pathophysiology. In: Sidebotham D, McKee A, Gillham M, Levy J. Cardiothoracic Critical Care. Elsevier, Inc.; 2007:3-27.
33. Duley L, Gülmezoglu AM, Henderson-Smart DJ, et al. Magnesium sulphate and other anticonvulsants for women with pre-eclampsia. Cochrane Database Syst Rev. 2010;2010(11):CD000025.
34. Emergency supply of medicines. In: British National Formulary. British Medical Association, Royal Pharmaceutical Society; 2015:6. Accessed April 7, 2023. https://www.academia.edu/35076015/british_national_formulary_2015_pdf
35. Kwofie K, Wolfson AB. Intravenous magnesium sulfate for acute asthma exacerbation in children and adults. Am Fam Physician. 2021;103(4):245-246.
36. Patniyot IR, Gelfand AA. Acute treatment therapies for pediatric migraine: a qualitative systematic review. Headache. 2016;56(1):49-70.
37. Wang X, Du X, Yang H, et al. Use of intravenous magnesium sulfate among patients with acute myocardial infarction in China from 2001 to 2015: China PEACE-Retrospective AMI Study. BMJ Open. 2020;10(3):e033269.
38. Karhu E, Atlas SE, Jinrun G, et al. Intravenous infusion of magnesium sulfate is not associated with cardiovascular, liver, kidney, and metabolic toxicity in adults. J Clin Transl Res. 2018;4(1):47-55.
39. Noah L, Pickering G, Mazur A, et al. Impact of magnesium supplementation, in combination with vitamin B6, on stress and magnesium status: secondary data from a randomized controlled trial. Magnes Res. 2020;33(3):45-57.
40. Erstad BL, Cotugno CL. Management of alcohol withdrawal. Am J Health Syst Pharm. 1995;52(7):697-709.
41. Abumaria N, Luo L, Ahn M, et al. Magnesium supplement enhances spatial-context pattern separation and prevents fear overgeneralization. Behav Pharmacol. 2013;24(4):255-263.
42. Kirov GK, Tsachev KN. Magnesium, schizophrenia and manic-depressive disease. Neuropsychobiology. 1990;23(2):79-81.
43. Botturi A, Ciappolino V, Delvecchio G, et al. The role and the effect of magnesium in mental disorders: a systematic review. Nutrients. 2020;12(6):1661.
44. Kirkland AE, Sarlo GL, Holton KF. The role of magnesium in neurological disorders. Nutrients. 2018;10(6):730.
45. Magnesium sulfate intravenous side effects by likelihood and severity. WebMD. Accessed April 9, 2023. https://www.webmd.com/drugs/2/drug-149570/magnesium-sulfate-intravenous/details/list-sideeffects
46. Scopolamine base transdermal system – uses, side effects, and more. WebMD. Accessed April 9, 2023. https://www.webmd.com/drugs/2/drug-14032/scopolamine-transdermal/details
47. Bolden C, Cusack B, Richelson E. Antagonism by antimuscarinic and neuroleptic compounds at the five cloned human muscarinic cholinergic receptors expressed in Chinese hamster ovary cells. J Pharmacol Exp Ther. 1992;260(2):576-580.
48. Janowsky DS, el-Yousef MK, Davis JM, et al. A cholinergic-adrenergic hypothesis of mania and depression. Lancet. 1972;2(7778):632-635.
49. Janowsky DS, Risch SC, Gillin JC. Adrenergic-cholinergic balance and the treatment of affective disorders. Prog Neuropsychopharmacol Biol Psychiatry. 1983;7(2-3):297-307.
50. Gershon S, Shaw FH. Psychiatric sequelae of chronic exposure to organophosphorous insecticides. Lancet. 1972;1(7191):1371-1374.
51. Davis KL, Berger PA, Hollister LE, et al. Physostigmine in mania. Arch Gen Psychiatry. 1978;35(1):119-122.
52. Wang JC, Hinrichs AL, Stock H, et al. Evidence of common and specific genetic effects: association of the muscarinic acetylcholine receptor M2 (CHRM2) gene with alcohol dependence and major depressive syndrome. Hum Mol Genet. 2004;13(17):1903-1911.
53. Brown RG. Effects of antidepressants and anticholinergics in a mouse “behavioral despair” test. Eur J Pharmacol. 1979;58(3):331-334.
54. Porsolt RD, Le Pichon M, Jalfre M. Depression: a new animal model sensitive to antidepressant treatments. Nature. 1977;266(5604):730-732.
55. Ji CX, Zhang JJ. Effect of scopolamine on depression in mice. Abstract in English. Yao Xue Xue Bao. 2011;46(4):400-405.
56. Furey ML, Drevets WC. Antidepressant efficacy of the antimuscarinic drug scopolamine: a randomized, placebo-controlled clinical trial. Arch Gen Psychiatry. 2006;63(10):1121-1129.
57. Drevets WC, Furey ML. Replication of scopolamine’s antidepressant efficacy in major depressive disorder: a randomized, placebo-controlled clinical trial. Biol Psychiatry. 2010;67(5):432-438.
58. Furey ML, Khanna A, Hoffman EM, et al. Scopolamine produces larger antidepressant and antianxiety effects in women than in men. Neuropsychopharmacology. 2010;35(12):2479-2488.
59. Gibbs RB, Gabor R, Cox T, et al. Effects of raloxifene and estradiol on hippocampal acetylcholine release and spatial learning in the rat. Psychoneuroendocrinology. 2004;29(6):741-748.
60. Pongrac JL, Gibbs RB, Defranco DB. Estrogen-mediated regulation of cholinergic expression in basal forebrain neurons requires extracellular-signal-regulated kinase activity. Neuroscience. 2004;124(4):809-816.
61. Daniel JM, Dohanich GP. Acetylcholine mediates the estrogen-induced increase in NMDA receptor binding in CA1 of the hippocampus and the associated improvement in working memory. J Neurosci. 2001;21(17):6949-6956.
62. Gerhard DM, Wohleb ES, Duman RS. Emerging treatment mechanisms for depression: focus on glutamate and synaptic plasticity. Drug Discov Today. 2016;21(3):454-464.
63. Voderholzer U. Sleep deprivation and antidepressant treatment. Dialogues Clin Neurosci. 2003;5(4):366-369.
64. Hasselmann H. Scopolamine and depression: a role for muscarinic antagonism? CNS Neurol Disord Drug Targets. 2014;13(4):673-683.
65. Transderm scopolamine [prescribing information]. Warren, NJ: GSK Consumer Healthcare; 2019.
66. Jaffe RJ, Novakovic V, Peselow ED. Scopolamine as an antidepressant: a systematic review. Clin Neuropharmacol. 2013;36(1):24-26.
67. Karameh WK, Khani M. Intravenous clomipramine for treatment-resistant obsessive-compulsive disorder. Int J Neuropsychopharmacol. 2015;19(2):pyv084.
68. Andrews ET, Beattie RM, Tighe MP. Functional abdominal pain: what clinicians need to know. Arch Dis Child. 2020;105(10):938-944. doi:10.1136/archdischild-2020-318825
69. Aliane V, Pérez S, Bohren Y, et al. Key role of striatal cholinergic interneurons in processes leading to arrest of motor stereotypies. Brain. 2011;134(Pt 1):110-118. doi:10.1093/brain/awq285
70. Tzavara ET, Bymaster FP, Davis RJ, et al. M4 muscarinic receptors regulate the dynamics of cholinergic and dopaminergic neurotransmission: relevance to the pathophysiology and treatment of related CNS pathologies. FASEB J. 2004;18(12):1410-1412. doi:10.1096/fj.04-1575fje
71. Korczyn AD, Kish I. The mechanism of imipramine in enuresis nocturna. Clin Exp Pharmacol Physiol. 1979;6(1):31-35. doi:10.1111/j.1440-1681.1979.tb00004.x
72. Trimble MR. Worldwide use of clomipramine. J Clin Psychiatry. 1990;51(Suppl):51-54; discussion 55-58.
73. Gong W, Zhang S, Zong Y, et al. Involvement of the microglial NLRP3 inflammasome in the anti-inflammatory effect of the antidepressant clomipramine. J Affect Disord. 2019;254:15-25.
74. Piwowarska J, Wrzosek M, Radziwon’-Zaleska M. Serum cortisol concentration in patients with major depression after treatment with clomipramine. Pharmacol Rep. 2009;61(4):604-611.
75. Danish University Antidepressant Group (DUAG). Clomipramine dose-effect study in patients with depression: clinical end points and pharmacokinetics. Clin Pharmacol Ther. 1999;66(2):152-165.
76. Moukaddam NJ, Hirschfeld RMA. Intravenous antidepressants: a review. Depress Anxiety. 2004;19(1):1-9.
77. Gerretsen P, Pollock BG. Rediscovering adverse anticholinergic effects. J Clin Psychiatry. 2011;72(6):869-870. doi:10.4088/JCP.11ac07093
78. Thomas SJ, Shin M, McInnis MG, et al. Combination therapy with monoamine oxidase inhibitors and other antidepressants or stimulants: strategies for the management of treatment-resistant depression. Pharmacotherapy. 2015;35(4):433-449. doi:10.1002/phar.1576
79. Robles LA. Serotonin syndrome induced by fentanyl in a child: case report. Clin Neuropharmacol. 2015;38(5):206-208. doi:10.1097/WNF.0000000000000100
80. Fallon BA, Liebowitz MR, Campeas R, et al. Intravenous clomipramine for obsessive-compulsive disorder refractory to oral clomipramine: a placebo-controlled study. Arch Gen Psychiatry. 1998;55(10):918-924.
81. Vieta E, Florea I, Schmidt SN, et al. Intravenous vortioxetine to accelerate onset of effect in major depressive disorder: a 2-week, randomized, double-blind, placebo-controlled study. Int Clin Psychopharmacol. 2019;34(4):153-160.
82. Kasper S, Müller-Spahn F. Intravenous antidepressant treatment: focus on citalopram. Eur Arch Psychiatry Clin Neurosci. 2002;252(3):105-109.
83. Togay B, El-Mallakh RS. Posttraumatic stress disorder: from pathophysiology to pharmacology. Current Psychiatry. 2020;19(5):33-39.
84. Adhikari A, Lerner TN, Finkelstein J, et al. Basomedial amygdala mediates top-down control of anxiety and fear. Nature. 2015;527(7577):179-185. doi:10.1038/nature15698
85. Lipov E. In search of an effective treatment for combat-related post-traumatic stress disorder (PTSD): can the stellate ganglion block be the answer? Pain Pract. 2010;10(4):265-266.
86. Lipov E, Ritchie EC. A review of the use of stellate ganglion block in the treatment of PTSD. Curr Psychiatry Rep. 2015;17(8):599.
87. Olmsted KLR, Bartoszek M, McLean B, et al. Effect of stellate ganglion block treatment on posttraumatic stress disorder symptoms: a randomized clinical trial. JAMA Psychiatry. 2020;77(2):130-138.
88. Lipov E, Candido K. The successful use of left-sided stellate ganglion block in patients that fail to respond to right-sided stellate ganglion block for the treatment of post-traumatic stress disorder symptoms: a retrospective analysis of 205 patients. Mil Med. 2021;186(11-12):319-320.
89. Li Y, Loshak H. Stellate ganglion block for the treatment of post-traumatic stress disorder, depression, and anxiety. Canadian J Health Technol. 2021;1(3):1-30.
90. Kerzner J, Liu H, Demchenko I, et al. Stellate ganglion block for psychiatric disorders: a systematic review of the clinical research landscape. Chronic Stress (Thousand Oaks). 2021;5:24705470211055176.
91. Wie C, Gupta R, Maloney J, et al. Interventional modalities to treat complex regional pain syndrome. Curr Pain Headache Rep. 2021;25(2):10. doi:10.1007/s11916-020-00904-5
92. Chaturvedi A, Dash HH. Sympathetic blockade for the relief of chronic pain. J Indian Med Assoc. 2001;99(12):698-703.
93. Chester M, Hammond C. Leach A. Long-term benefits of stellate ganglion block in severe chronic refractory angina. Pain. 2000;87(1):103-105. doi:10.1016/S0304-3959(00)00270-0
94. Jeon Y. Therapeutic potential of stellate ganglion block in orofacial pain: a mini review. J Dent Anesth Pain Med. 2016;16(3):159-163. doi:10.17245/jdapm.2016.16.3.159
95. Shan HH, Chen HF, Ni Y, et al. Effects of stellate ganglion block through different approaches under guidance of ultrasound. Front Surg. 2022;8:797793. doi:10.3389/fsurg.2021.797793
96. Goel V, Patwardhan AM, Ibrahim M, et al. Complications associated with stellate ganglion nerve block: a systematic review. Reg Anesth Pain Med. 2019;rapm-2018-100127. doi:10.1136/rapm-2018-100127
97. Rowe FJ, Noonan CP. Botulinum toxin for the treatment of strabismus. Cochrane Database Syst Rev. 2017;3(3):CD006499.
98. Roggenkämper P, Jost WH, Bihari K, et al. Efficacy and safety of a new botulinum toxin type A free of complexing proteins in the treatment of blepharospasm. J Neural Transm (Vienna). 2006;113(3):303-312.
99. Heckmann M, Ceballos-Baumann AO, Plewig G; Hyperhidrosis Study Group. Botulinum toxin A for axillary hyperhidrosis (excessive sweating). N Engl J Med. 2001;344(7):488-493.
100. Carruthers JA, Lowe NJ, Menter MA, et al. A multicenter, double-blind, randomized, placebo-controlled study of the efficacy and safety of botulinum toxin type A in the treatment of glabellar lines. J Am Acad Dermatol. 2002;46(6):840-849.
101. Schurch B, de Sèze M, Denys P, et al. Botulinum toxin type A is a safe and effective treatment for neurogenic urinary incontinence: results of a single treatment, randomized, placebo controlled 6-month study. J Urol. 2005;174:196–200.
102. Aurora SK, Winner P, Freeman MC, et al. OnabotulinumtoxinA for treatment of chronic migraine: Pooled analyses of the 56-week PREEMPT clinical program. Headache. 2011;51(9):1358-1373.
103. Dashtipour K, Chen JJ, Walker HW, et al. Systematic literature review of abobotulinumtoxinA in clinical trials for adult upper limb spasticity. Am J Phys Med Rehabil. 2015;94(3):229-238.
104. Nitti VW, Dmochowski R, Herschorn S, et al. OnabotulinumtoxinA for the treatment of patients with overactive bladder and urinary incontinence: results of a phase 3, randomized, placebo-controlled trial. J Urol. 2017;197(2S):S216-S223.
105. Jongerius PH, van den Hoogen FJA, van Limbeek J, et al. Effect of botulinum toxin in the treatment of drooling: a controlled clinical trial. Pediatrics. 2004;114(3):620-627.
106. Zaninotto, G. Annese V, Costantini M, et al. Randomized controlled trial of botulinum toxin versus laparoscopic heller myotomy for esophageal achalasia. Ann Surg. 2004;239(3):364-370.
107. Dressler D, Adib Saberi F. Botulinum toxin: mechanisms of action. Eur Neurol. 2005;53:3-9.
108. Lewis MB, Bowler PJ. Botulinum toxin cosmetic therapy correlates with a more positive mood. J Cosmet Dermatol. 2009;8(1):24-26.
109. Affatato O, Moulin TC, Pisanu C, et al. High efficacy of onabotulinumtoxinA treatment in patients with comorbid migraine and depression: a meta-analysis. J Transl Med. 2021;19(1):133.
110. Finzi E, Wasserman E. Treatment of depression with botulinum toxin A: a case series. Dermatol Surg. 2006;32(5):645-649; discussion 649-650.
111. Schulze J, Neumann I, Magid M, et al. Botulinum toxin for the management of depression: an updated review of the evidence and meta-analysis. J Psychiatr Res. 2021;135:332-340.
112. Finzi E, Rosenthal NE. Emotional proprioception: treatment of depression with afferent facial feedback. J Psychiatr Res. 2016;80:93-96.
113. Söderkvist S, Ohlén K, Dimberg U. How the experience of emotion is modulated by facial feedback. J Nonverbal Behav. 2018;42(1):129-151.
114. Lewis, MB. The interactions between botulinum-toxin-based facial treatments and embodied emotions. Sci Rep. 2018;8(1):14720.
115. Li Y, Liu J, Liu X, et al. Antidepressant-like action of single facial injection of botulinum neurotoxin A is associated with augmented 5-HT levels and BDNF/ERK/CREB pathways in mouse brain. Neurosci Bull. 2019;35(4):661-672. Erratum in: Neurosci Bull. 2019;35(4):779-780.
116. Gündel H, Wolf A, Xidara V, et al. High psychiatric comorbidity in spasmodic torticollis: a controlled study. J Nerv Ment Dis. 2003;191(7):465-473.
117. Hall TA, McGwin G Jr, Searcey K, et al. Health-related quality of life and psychosocial characteristics of patients with benign essential blepharospasm. Arch Ophthalmol. 2006;124(1):116-119.
118. Ceylan D, Erer S, Zarifog˘lu M, et al. Evaluation of anxiety and depression scales and quality of life in cervical dystonia patients on botulinum toxin therapy and their relatives. Neurol Sci. 2019;40(4):725-731.
119. Heller AS, Lapate RC, Mayer KE, et al. The face of negative affect: trial-by-trial corrugator responses to negative pictures are positively associated with amygdala and negatively associated with ventromedial prefrontal cortex activity. J Cogn Neurosci. 2014;26(9):2102-2110.
120. Makunts T, Wollmer MA, Abagyan R. Postmarketing safety surveillance data reveals antidepressant effects of botulinum toxin across various indications and injection sites. Sci Rep. 2020;10(1):12851.
121. Ahsanuddin S, Roy S, Nasser W, et al. Adverse events associated with botox as reported in a Food and Drug Administration database. Aesthetic Plast Surg. 2021;45(3):1201-1209. doi:10.1007/s00266-020-02027-z
122. Kashif M, Tahir S, Ashfaq F, et al. Association of myofascial trigger points in neck and shoulder region with depression, anxiety, and stress among university students. J Pak Med Assoc. 2021;71(9):2139-2142.
123. Cigarán-Méndez M, Jiménez-Antona C, Parás-Bravo P, et al. Active trigger points are associated with anxiety and widespread pressure pain sensitivity in women, but not men, with tension type headache. Pain Pract. 2019;19(5):522-529.
124. Palacios-Ceña M, Castaldo M, Wang K, et al. Relationship of active trigger points with related disability and anxiety in people with tension-type headache. Medicine (Baltimore). 2017;96(13):e6548.
125. Karadas Ö, Inan LE, Ulas Ü, et al. Efficacy of local lidocaine application on anxiety and depression and its curative effect on patients with chronic tension-type headache. Eur Neurol. 2013;70(1-2):95-101.
126. Gerwin RD. Classification, epidemiology and natural history of myofascial pain syndrome. Curr Pain Headache Rep. 2001;5(5):412-420.
127. Castro Sánchez AM, García López H, Fernández Sánchez M, et al. Improvement in clinical outcomes after dry needling versus myofascial release on pain pressure thresholds, quality of life, fatigue, pain intensity, quality of sleep, anxiety, and depression in patients with fibromyalgia syndrome. Disabil Rehabil. 2019;41(19):2235-2246.
128. Healy GM, Finn DP, O’Gorman DA, et al. Pretreatment anxiety and pain acceptance are associated with response to trigger point injection therapy for chronic myofascial pain. Pain Med. 2015;16(10):1955-1966.
129. Morjaria JB, Lakshminarayana UB, Liu-Shiu-Cheong P, et al. Pneumothorax: a tale of pain or spontaneity. Ther Adv Chronic Dis. 2014;5(6):269-273.
1. Vincent KM, Ryan M, Palmer E, et al. Interventional psychiatry. Postgrad Med. 2020;132(7):573-574.
2. Allen MH, Feifel D, Lesem MD, et al. Efficacy and safety of loxapine for inhalation in the treatment of agitation in patients with schizophrenia: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2011;72(10):1313-1321.
3. Kwentus J, Riesenberg RA, Marandi M, et al. Rapid acute treatment of agitation in patients with bipolar I disorder: a multicenter, randomized, placebo-controlled clinical trial with inhaled loxapine. Bipolar Disord. 2012;14(1):31-40.
4. Lee JD, Nunes EV Jr, Novo P, et al. Comparative effectiveness of extended-release naltrexone versus buprenorphine-naloxone for opioid relapse prevention (X:BOT): a multicentre, open-label, randomised controlled trial. Lancet. 2018;391(10118):309-318.
5. Haight BR, Learned SM, Laffont CM, et al. Efficacy and safety of a monthly buprenorphine depot injection for opioid use disorder: a multicentre, randomised, double‐blind, placebo‐controlled, phase 3 trial. Lancet. 2019;393(10173):778-790.
6. Andorn A, Graham J, Csernansky J, et al. Monthly extended-release risperidone (RBP-7000) in the treatment of schizophrenia: results from the phase 3 program. J Clin Psychopharmacol. 2019;39(5):428-433.
7. Dundee TW. Twenty-five years of ketamine. A report of an international meeting. Anaesthesia. 1990;45(2):159. doi:10.1111/j.1365-2044.1990.tb14287.x
8. White PF, Way WL, Trevor AJ. Ketamine--its pharmacology and therapeutic uses. Anesthesiology. 1982;56(2):119-136. doi:10.1097/00000542-198202000-00007
9. Zanos P, Gould TD. Mechanisms of ketamine action as an antidepressant. Mol Psychiatry. 2018;23(4):801-811.
10. Molero P, Ramos-Quiroga JA, Martin-Santos R, et al. Antidepressant efficacy and tolerability of ketamine and esketamine: a critical review. CNS Drugs. 2018;32(5):411-420. doi:10.1007/s40263-018-0519-3
11. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215.
12. Witkin JM, Martin AE, Golani LK, et al. Rapid-acting antidepressants. Adv Pharmacol. 2019;86:47-96.
13. Strayer RJ, Nelson LS. Adverse events associated with ketamine for procedural sedation in adults. Am J Emerg Med. 2008;26(9):985-1028. doi:10.1016/j.ajem.2007.12.005
14. Frye MA, Blier P, Tye SJ. Concomitant benzodiazepine use attenuates ketamine response: implications for large scale study design and clinical development. J Clin Psychopharmacol. 2015;35(3):334-336.
15. Fava M, Freeman MP, Flynn M, et al. Double-blind, placebo-controlled, dose-ranging trial of intravenous ketamine as adjunctive therapy in treatment-resistant depression (TRD). Mol Psychiatry. 2020;25(7):1592-1603.
16. Bahji A, Vazquez GH, Zarate CA Jr. Comparative efficacy of racemic ketamine and esketamine for depression: a systematic review and meta-analysis. J Affect Disord. 2021;278:542-555. Erratum in: J Affect Disord. 2021;281:1001.
17. Brendle M, Robison R, Malone DC. Cost-effectiveness of esketamine nasal spray compared to intravenous ketamine for patients with treatment-resistant depression in the US utilizing clinical trial efficacy and real-world effectiveness estimates. J Affect Disord. 2022;319:388-396.
18. Dhillon S. Aducanumab: first approval. Drugs. 2021;81(12):1437-1443. Erratum in: Drugs. 2021;81(14):1701.
19. van Dyck CH, Swanson CJ, Aisen P, et al. Lecanemab in early Alzheimer’s disease. N Engl J Med. 2023;388(1):9-21. doi:10.1056/NEJMoa2212948
20. Sevigny J, Chiao P, Bussière T, et al. The antibody aducanumab reduces Aβ plaques in Alzheimer’s disease. Nature. 2016;537(7618):50-56. Update in: Nature. 2017;546(7659):564.
21. Fillit H, Green A. Aducanumab and the FDA – where are we now? Nat Rev Neurol. 2021;17(3):129-130.
22. Reardon S. FDA approves Alzheimer’s drug lecanemab amid safety concerns. Nature. 2023;613(7943):227-228. doi:10.1038/d41586-023-00030-3
23. McDade E, Cummings JL, Dhadda S, et al. Lecanemab in patients with early Alzheimer’s disease: detailed results on biomarker, cognitive, and clinical effects from the randomized and open-label extension of the phase 2 proof-of-concept study. Alzheimers Res Ther. 2022;14(1):191. doi:10.1186/s13195-022-01124-2
24. Mintun MA, Lo AC, Evans CD, et al. Donanemab in early Alzheimer’s disease. N Engl J Med. 2021;384(18):1691-1704.
25. Luisi S, Petraglia F, Benedetto C, et al. Serum allopregnanolone levels in pregnant women: changes during pregnancy, at delivery, and in hypertensive patients. J Clin Endocrinol Metab. 2000;85(7):2429-2433.
26. Meltzer-Brody S, Colquhoun H, Riesenberg R, et al. Brexanolone injection in post-partum depression: two multicentre, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet. 2018;392(10152):1058-1070.
27. Powell JG, Garland S, Preston K, et al. Brexanolone (Zulresso): finally, an FDA-approved treatment for postpartum depression. Ann Pharmacother. 2020;54(2):157-163.
28. Patterson R, Krohn H, Richardson E, et al. A brexanolone treatment program at an academic medical center: patient selection, 90-day posttreatment outcomes, and lessons learned. J Acad Consult Liaison Psychiatry. 2022;63(1):14-22.
29. World Health Organization. WHO model list of essential medicines - 22nd list (2021). World Health Organization. September 30, 2021. Accessed April 7, 2023. https://www.who.int/publications/i/item/WHO-MHP-HPS-EML-2021.02
30. Eby GA, Eby KL, Mruk H. Magnesium and major depression. In: Vink R, Nechifor M, eds. Magnesium in the Central Nervous System. University of Adelaide Press; 2011.
31. Plant TM, Zeleznik AJ. Knobil and Neill’s Physiology of Reproduction. 4th ed. Elsevier Inc.; 2015:2503-2550.
32. Sidebotham D, Le Grice IJ. Physiology and pathophysiology. In: Sidebotham D, McKee A, Gillham M, Levy J. Cardiothoracic Critical Care. Elsevier, Inc.; 2007:3-27.
33. Duley L, Gülmezoglu AM, Henderson-Smart DJ, et al. Magnesium sulphate and other anticonvulsants for women with pre-eclampsia. Cochrane Database Syst Rev. 2010;2010(11):CD000025.
34. Emergency supply of medicines. In: British National Formulary. British Medical Association, Royal Pharmaceutical Society; 2015:6. Accessed April 7, 2023. https://www.academia.edu/35076015/british_national_formulary_2015_pdf
35. Kwofie K, Wolfson AB. Intravenous magnesium sulfate for acute asthma exacerbation in children and adults. Am Fam Physician. 2021;103(4):245-246.
36. Patniyot IR, Gelfand AA. Acute treatment therapies for pediatric migraine: a qualitative systematic review. Headache. 2016;56(1):49-70.
37. Wang X, Du X, Yang H, et al. Use of intravenous magnesium sulfate among patients with acute myocardial infarction in China from 2001 to 2015: China PEACE-Retrospective AMI Study. BMJ Open. 2020;10(3):e033269.
38. Karhu E, Atlas SE, Jinrun G, et al. Intravenous infusion of magnesium sulfate is not associated with cardiovascular, liver, kidney, and metabolic toxicity in adults. J Clin Transl Res. 2018;4(1):47-55.
39. Noah L, Pickering G, Mazur A, et al. Impact of magnesium supplementation, in combination with vitamin B6, on stress and magnesium status: secondary data from a randomized controlled trial. Magnes Res. 2020;33(3):45-57.
40. Erstad BL, Cotugno CL. Management of alcohol withdrawal. Am J Health Syst Pharm. 1995;52(7):697-709.
41. Abumaria N, Luo L, Ahn M, et al. Magnesium supplement enhances spatial-context pattern separation and prevents fear overgeneralization. Behav Pharmacol. 2013;24(4):255-263.
42. Kirov GK, Tsachev KN. Magnesium, schizophrenia and manic-depressive disease. Neuropsychobiology. 1990;23(2):79-81.
43. Botturi A, Ciappolino V, Delvecchio G, et al. The role and the effect of magnesium in mental disorders: a systematic review. Nutrients. 2020;12(6):1661.
44. Kirkland AE, Sarlo GL, Holton KF. The role of magnesium in neurological disorders. Nutrients. 2018;10(6):730.
45. Magnesium sulfate intravenous side effects by likelihood and severity. WebMD. Accessed April 9, 2023. https://www.webmd.com/drugs/2/drug-149570/magnesium-sulfate-intravenous/details/list-sideeffects
46. Scopolamine base transdermal system – uses, side effects, and more. WebMD. Accessed April 9, 2023. https://www.webmd.com/drugs/2/drug-14032/scopolamine-transdermal/details
47. Bolden C, Cusack B, Richelson E. Antagonism by antimuscarinic and neuroleptic compounds at the five cloned human muscarinic cholinergic receptors expressed in Chinese hamster ovary cells. J Pharmacol Exp Ther. 1992;260(2):576-580.
48. Janowsky DS, el-Yousef MK, Davis JM, et al. A cholinergic-adrenergic hypothesis of mania and depression. Lancet. 1972;2(7778):632-635.
49. Janowsky DS, Risch SC, Gillin JC. Adrenergic-cholinergic balance and the treatment of affective disorders. Prog Neuropsychopharmacol Biol Psychiatry. 1983;7(2-3):297-307.
50. Gershon S, Shaw FH. Psychiatric sequelae of chronic exposure to organophosphorous insecticides. Lancet. 1972;1(7191):1371-1374.
51. Davis KL, Berger PA, Hollister LE, et al. Physostigmine in mania. Arch Gen Psychiatry. 1978;35(1):119-122.
52. Wang JC, Hinrichs AL, Stock H, et al. Evidence of common and specific genetic effects: association of the muscarinic acetylcholine receptor M2 (CHRM2) gene with alcohol dependence and major depressive syndrome. Hum Mol Genet. 2004;13(17):1903-1911.
53. Brown RG. Effects of antidepressants and anticholinergics in a mouse “behavioral despair” test. Eur J Pharmacol. 1979;58(3):331-334.
54. Porsolt RD, Le Pichon M, Jalfre M. Depression: a new animal model sensitive to antidepressant treatments. Nature. 1977;266(5604):730-732.
55. Ji CX, Zhang JJ. Effect of scopolamine on depression in mice. Abstract in English. Yao Xue Xue Bao. 2011;46(4):400-405.
56. Furey ML, Drevets WC. Antidepressant efficacy of the antimuscarinic drug scopolamine: a randomized, placebo-controlled clinical trial. Arch Gen Psychiatry. 2006;63(10):1121-1129.
57. Drevets WC, Furey ML. Replication of scopolamine’s antidepressant efficacy in major depressive disorder: a randomized, placebo-controlled clinical trial. Biol Psychiatry. 2010;67(5):432-438.
58. Furey ML, Khanna A, Hoffman EM, et al. Scopolamine produces larger antidepressant and antianxiety effects in women than in men. Neuropsychopharmacology. 2010;35(12):2479-2488.
59. Gibbs RB, Gabor R, Cox T, et al. Effects of raloxifene and estradiol on hippocampal acetylcholine release and spatial learning in the rat. Psychoneuroendocrinology. 2004;29(6):741-748.
60. Pongrac JL, Gibbs RB, Defranco DB. Estrogen-mediated regulation of cholinergic expression in basal forebrain neurons requires extracellular-signal-regulated kinase activity. Neuroscience. 2004;124(4):809-816.
61. Daniel JM, Dohanich GP. Acetylcholine mediates the estrogen-induced increase in NMDA receptor binding in CA1 of the hippocampus and the associated improvement in working memory. J Neurosci. 2001;21(17):6949-6956.
62. Gerhard DM, Wohleb ES, Duman RS. Emerging treatment mechanisms for depression: focus on glutamate and synaptic plasticity. Drug Discov Today. 2016;21(3):454-464.
63. Voderholzer U. Sleep deprivation and antidepressant treatment. Dialogues Clin Neurosci. 2003;5(4):366-369.
64. Hasselmann H. Scopolamine and depression: a role for muscarinic antagonism? CNS Neurol Disord Drug Targets. 2014;13(4):673-683.
65. Transderm scopolamine [prescribing information]. Warren, NJ: GSK Consumer Healthcare; 2019.
66. Jaffe RJ, Novakovic V, Peselow ED. Scopolamine as an antidepressant: a systematic review. Clin Neuropharmacol. 2013;36(1):24-26.
67. Karameh WK, Khani M. Intravenous clomipramine for treatment-resistant obsessive-compulsive disorder. Int J Neuropsychopharmacol. 2015;19(2):pyv084.
68. Andrews ET, Beattie RM, Tighe MP. Functional abdominal pain: what clinicians need to know. Arch Dis Child. 2020;105(10):938-944. doi:10.1136/archdischild-2020-318825
69. Aliane V, Pérez S, Bohren Y, et al. Key role of striatal cholinergic interneurons in processes leading to arrest of motor stereotypies. Brain. 2011;134(Pt 1):110-118. doi:10.1093/brain/awq285
70. Tzavara ET, Bymaster FP, Davis RJ, et al. M4 muscarinic receptors regulate the dynamics of cholinergic and dopaminergic neurotransmission: relevance to the pathophysiology and treatment of related CNS pathologies. FASEB J. 2004;18(12):1410-1412. doi:10.1096/fj.04-1575fje
71. Korczyn AD, Kish I. The mechanism of imipramine in enuresis nocturna. Clin Exp Pharmacol Physiol. 1979;6(1):31-35. doi:10.1111/j.1440-1681.1979.tb00004.x
72. Trimble MR. Worldwide use of clomipramine. J Clin Psychiatry. 1990;51(Suppl):51-54; discussion 55-58.
73. Gong W, Zhang S, Zong Y, et al. Involvement of the microglial NLRP3 inflammasome in the anti-inflammatory effect of the antidepressant clomipramine. J Affect Disord. 2019;254:15-25.
74. Piwowarska J, Wrzosek M, Radziwon’-Zaleska M. Serum cortisol concentration in patients with major depression after treatment with clomipramine. Pharmacol Rep. 2009;61(4):604-611.
75. Danish University Antidepressant Group (DUAG). Clomipramine dose-effect study in patients with depression: clinical end points and pharmacokinetics. Clin Pharmacol Ther. 1999;66(2):152-165.
76. Moukaddam NJ, Hirschfeld RMA. Intravenous antidepressants: a review. Depress Anxiety. 2004;19(1):1-9.
77. Gerretsen P, Pollock BG. Rediscovering adverse anticholinergic effects. J Clin Psychiatry. 2011;72(6):869-870. doi:10.4088/JCP.11ac07093
78. Thomas SJ, Shin M, McInnis MG, et al. Combination therapy with monoamine oxidase inhibitors and other antidepressants or stimulants: strategies for the management of treatment-resistant depression. Pharmacotherapy. 2015;35(4):433-449. doi:10.1002/phar.1576
79. Robles LA. Serotonin syndrome induced by fentanyl in a child: case report. Clin Neuropharmacol. 2015;38(5):206-208. doi:10.1097/WNF.0000000000000100
80. Fallon BA, Liebowitz MR, Campeas R, et al. Intravenous clomipramine for obsessive-compulsive disorder refractory to oral clomipramine: a placebo-controlled study. Arch Gen Psychiatry. 1998;55(10):918-924.
81. Vieta E, Florea I, Schmidt SN, et al. Intravenous vortioxetine to accelerate onset of effect in major depressive disorder: a 2-week, randomized, double-blind, placebo-controlled study. Int Clin Psychopharmacol. 2019;34(4):153-160.
82. Kasper S, Müller-Spahn F. Intravenous antidepressant treatment: focus on citalopram. Eur Arch Psychiatry Clin Neurosci. 2002;252(3):105-109.
83. Togay B, El-Mallakh RS. Posttraumatic stress disorder: from pathophysiology to pharmacology. Current Psychiatry. 2020;19(5):33-39.
84. Adhikari A, Lerner TN, Finkelstein J, et al. Basomedial amygdala mediates top-down control of anxiety and fear. Nature. 2015;527(7577):179-185. doi:10.1038/nature15698
85. Lipov E. In search of an effective treatment for combat-related post-traumatic stress disorder (PTSD): can the stellate ganglion block be the answer? Pain Pract. 2010;10(4):265-266.
86. Lipov E, Ritchie EC. A review of the use of stellate ganglion block in the treatment of PTSD. Curr Psychiatry Rep. 2015;17(8):599.
87. Olmsted KLR, Bartoszek M, McLean B, et al. Effect of stellate ganglion block treatment on posttraumatic stress disorder symptoms: a randomized clinical trial. JAMA Psychiatry. 2020;77(2):130-138.
88. Lipov E, Candido K. The successful use of left-sided stellate ganglion block in patients that fail to respond to right-sided stellate ganglion block for the treatment of post-traumatic stress disorder symptoms: a retrospective analysis of 205 patients. Mil Med. 2021;186(11-12):319-320.
89. Li Y, Loshak H. Stellate ganglion block for the treatment of post-traumatic stress disorder, depression, and anxiety. Canadian J Health Technol. 2021;1(3):1-30.
90. Kerzner J, Liu H, Demchenko I, et al. Stellate ganglion block for psychiatric disorders: a systematic review of the clinical research landscape. Chronic Stress (Thousand Oaks). 2021;5:24705470211055176.
91. Wie C, Gupta R, Maloney J, et al. Interventional modalities to treat complex regional pain syndrome. Curr Pain Headache Rep. 2021;25(2):10. doi:10.1007/s11916-020-00904-5
92. Chaturvedi A, Dash HH. Sympathetic blockade for the relief of chronic pain. J Indian Med Assoc. 2001;99(12):698-703.
93. Chester M, Hammond C. Leach A. Long-term benefits of stellate ganglion block in severe chronic refractory angina. Pain. 2000;87(1):103-105. doi:10.1016/S0304-3959(00)00270-0
94. Jeon Y. Therapeutic potential of stellate ganglion block in orofacial pain: a mini review. J Dent Anesth Pain Med. 2016;16(3):159-163. doi:10.17245/jdapm.2016.16.3.159
95. Shan HH, Chen HF, Ni Y, et al. Effects of stellate ganglion block through different approaches under guidance of ultrasound. Front Surg. 2022;8:797793. doi:10.3389/fsurg.2021.797793
96. Goel V, Patwardhan AM, Ibrahim M, et al. Complications associated with stellate ganglion nerve block: a systematic review. Reg Anesth Pain Med. 2019;rapm-2018-100127. doi:10.1136/rapm-2018-100127
97. Rowe FJ, Noonan CP. Botulinum toxin for the treatment of strabismus. Cochrane Database Syst Rev. 2017;3(3):CD006499.
98. Roggenkämper P, Jost WH, Bihari K, et al. Efficacy and safety of a new botulinum toxin type A free of complexing proteins in the treatment of blepharospasm. J Neural Transm (Vienna). 2006;113(3):303-312.
99. Heckmann M, Ceballos-Baumann AO, Plewig G; Hyperhidrosis Study Group. Botulinum toxin A for axillary hyperhidrosis (excessive sweating). N Engl J Med. 2001;344(7):488-493.
100. Carruthers JA, Lowe NJ, Menter MA, et al. A multicenter, double-blind, randomized, placebo-controlled study of the efficacy and safety of botulinum toxin type A in the treatment of glabellar lines. J Am Acad Dermatol. 2002;46(6):840-849.
101. Schurch B, de Sèze M, Denys P, et al. Botulinum toxin type A is a safe and effective treatment for neurogenic urinary incontinence: results of a single treatment, randomized, placebo controlled 6-month study. J Urol. 2005;174:196–200.
102. Aurora SK, Winner P, Freeman MC, et al. OnabotulinumtoxinA for treatment of chronic migraine: Pooled analyses of the 56-week PREEMPT clinical program. Headache. 2011;51(9):1358-1373.
103. Dashtipour K, Chen JJ, Walker HW, et al. Systematic literature review of abobotulinumtoxinA in clinical trials for adult upper limb spasticity. Am J Phys Med Rehabil. 2015;94(3):229-238.
104. Nitti VW, Dmochowski R, Herschorn S, et al. OnabotulinumtoxinA for the treatment of patients with overactive bladder and urinary incontinence: results of a phase 3, randomized, placebo-controlled trial. J Urol. 2017;197(2S):S216-S223.
105. Jongerius PH, van den Hoogen FJA, van Limbeek J, et al. Effect of botulinum toxin in the treatment of drooling: a controlled clinical trial. Pediatrics. 2004;114(3):620-627.
106. Zaninotto, G. Annese V, Costantini M, et al. Randomized controlled trial of botulinum toxin versus laparoscopic heller myotomy for esophageal achalasia. Ann Surg. 2004;239(3):364-370.
107. Dressler D, Adib Saberi F. Botulinum toxin: mechanisms of action. Eur Neurol. 2005;53:3-9.
108. Lewis MB, Bowler PJ. Botulinum toxin cosmetic therapy correlates with a more positive mood. J Cosmet Dermatol. 2009;8(1):24-26.
109. Affatato O, Moulin TC, Pisanu C, et al. High efficacy of onabotulinumtoxinA treatment in patients with comorbid migraine and depression: a meta-analysis. J Transl Med. 2021;19(1):133.
110. Finzi E, Wasserman E. Treatment of depression with botulinum toxin A: a case series. Dermatol Surg. 2006;32(5):645-649; discussion 649-650.
111. Schulze J, Neumann I, Magid M, et al. Botulinum toxin for the management of depression: an updated review of the evidence and meta-analysis. J Psychiatr Res. 2021;135:332-340.
112. Finzi E, Rosenthal NE. Emotional proprioception: treatment of depression with afferent facial feedback. J Psychiatr Res. 2016;80:93-96.
113. Söderkvist S, Ohlén K, Dimberg U. How the experience of emotion is modulated by facial feedback. J Nonverbal Behav. 2018;42(1):129-151.
114. Lewis, MB. The interactions between botulinum-toxin-based facial treatments and embodied emotions. Sci Rep. 2018;8(1):14720.
115. Li Y, Liu J, Liu X, et al. Antidepressant-like action of single facial injection of botulinum neurotoxin A is associated with augmented 5-HT levels and BDNF/ERK/CREB pathways in mouse brain. Neurosci Bull. 2019;35(4):661-672. Erratum in: Neurosci Bull. 2019;35(4):779-780.
116. Gündel H, Wolf A, Xidara V, et al. High psychiatric comorbidity in spasmodic torticollis: a controlled study. J Nerv Ment Dis. 2003;191(7):465-473.
117. Hall TA, McGwin G Jr, Searcey K, et al. Health-related quality of life and psychosocial characteristics of patients with benign essential blepharospasm. Arch Ophthalmol. 2006;124(1):116-119.
118. Ceylan D, Erer S, Zarifog˘lu M, et al. Evaluation of anxiety and depression scales and quality of life in cervical dystonia patients on botulinum toxin therapy and their relatives. Neurol Sci. 2019;40(4):725-731.
119. Heller AS, Lapate RC, Mayer KE, et al. The face of negative affect: trial-by-trial corrugator responses to negative pictures are positively associated with amygdala and negatively associated with ventromedial prefrontal cortex activity. J Cogn Neurosci. 2014;26(9):2102-2110.
120. Makunts T, Wollmer MA, Abagyan R. Postmarketing safety surveillance data reveals antidepressant effects of botulinum toxin across various indications and injection sites. Sci Rep. 2020;10(1):12851.
121. Ahsanuddin S, Roy S, Nasser W, et al. Adverse events associated with botox as reported in a Food and Drug Administration database. Aesthetic Plast Surg. 2021;45(3):1201-1209. doi:10.1007/s00266-020-02027-z
122. Kashif M, Tahir S, Ashfaq F, et al. Association of myofascial trigger points in neck and shoulder region with depression, anxiety, and stress among university students. J Pak Med Assoc. 2021;71(9):2139-2142.
123. Cigarán-Méndez M, Jiménez-Antona C, Parás-Bravo P, et al. Active trigger points are associated with anxiety and widespread pressure pain sensitivity in women, but not men, with tension type headache. Pain Pract. 2019;19(5):522-529.
124. Palacios-Ceña M, Castaldo M, Wang K, et al. Relationship of active trigger points with related disability and anxiety in people with tension-type headache. Medicine (Baltimore). 2017;96(13):e6548.
125. Karadas Ö, Inan LE, Ulas Ü, et al. Efficacy of local lidocaine application on anxiety and depression and its curative effect on patients with chronic tension-type headache. Eur Neurol. 2013;70(1-2):95-101.
126. Gerwin RD. Classification, epidemiology and natural history of myofascial pain syndrome. Curr Pain Headache Rep. 2001;5(5):412-420.
127. Castro Sánchez AM, García López H, Fernández Sánchez M, et al. Improvement in clinical outcomes after dry needling versus myofascial release on pain pressure thresholds, quality of life, fatigue, pain intensity, quality of sleep, anxiety, and depression in patients with fibromyalgia syndrome. Disabil Rehabil. 2019;41(19):2235-2246.
128. Healy GM, Finn DP, O’Gorman DA, et al. Pretreatment anxiety and pain acceptance are associated with response to trigger point injection therapy for chronic myofascial pain. Pain Med. 2015;16(10):1955-1966.
129. Morjaria JB, Lakshminarayana UB, Liu-Shiu-Cheong P, et al. Pneumothorax: a tale of pain or spontaneity. Ther Adv Chronic Dis. 2014;5(6):269-273.
Antidepressants for patients who are breastfeeding: What to consider
Ms. D, age 32, recently gave birth to her second child. Her psychiatric history includes major depressive disorder. She had been stable on mirtazapine 30 mg at bedtime for 3 years. Based on clinical stability and patient preference, Ms. D elected to taper off mirtazapine 1 month prior to delivery. Now at 1 month postdelivery, Ms. D notes the reemergence of her depressive symptoms; during her child’s latest pediatrician visit, she scores 15 on the Edinburgh Postnatal Depression Scale (EPDS). She breastfeeds her baby and wants more information on the safety of taking an antidepressant while breastfeeding.
Ms. D discusses her previous use of mirtazapine with her treatment team. The team reviews the available resources with Ms. D and together they plan to make a shared decision regarding treatment of her depression at her next appointment.
The American Academy of Pediatrics1 and World Health Organization2 recommend exclusive breastfeeding of infants for their first 6 months of life and support it as a complement to other foods through and beyond age 2. Untreated conditions such as postpartum depression impact maternal well-being and may interfere with parenting and child development. In fact, untreated maternal mental health leads to an increased risk of suicide, reduced maternal economic productivity, and worsened health for both mother and child.3
Because many women experience psychiatric symptoms before they become pregnant as well as during the perinatal period, questions often arise regardingthe use of psychiatric medications—specifically antidepressants—and their safety in patients who are breastfeeding. Key considerations regarding medication management should include the patient’s previous response to medications, the risks of untreated maternal mental illness, and evidence regarding risks and benefits in lactation. This article summarizes where to find evidence-based lactation information, how to interpret that information, and what information is available for select antidepressants.
Locating lactation information
Start by checking the manufacturer’s medication labeling (“prescribing information”) and medication information resources such as Micromedex (www.micromedexsolutions.com) and Lexicomp (www.wolterskluwer.com/en/solutions/lexicomp). The updated labeling includes a risk/benefit assessment of available data on the risk for continued use of a medication during pregnancy compared to the risk if a medication is discontinued and the disorder goes untreated.4 The “breastfeeding considerations” section of medication labeling include details regarding the presence of the medication and the amount of it in breastmilk, adverse events in infants exposed to the medication through breastmilk, and additional pertinent data as applicable. Lexicomp includes information regarding breastfeeding considerations, and a subscription may also include access to Briggs Drugs in Pregnancy and Lactation’s information pages. Micromedex includes its own lactation safety rating scale score.
Several other resources can help guide clinicians toward patient-specific recommendations. From the National Library of Medicine, LactMed (https://www.ncbi.nlm.nih.gov/books/NBK501922/) allows clinicians to search for specific medications to see what information exists pertaining to medication levels in breastmilk and infant blood as well as potential adverse effects in the nursing infant and/or on lactation and breastmilk.5 LactMed provides information regarding alternative medications to consider and references from which the information was gathered.
Another helpful resource is the InfantRisk Center from Texas Tech University Health Sciences Center, which includes a free call center for parents and clinicians who have questions about medications and breastfeeding (806-352-2519; Monday through Friday, 8
Continue to: How to interpret the information
How to interpret the information
Medication levels in breastmilk are affected by several properties, such as the medication’s molecular weight, protein binding, pKa, and volume of distribution. A few commonly used terms in lactation literature for medications include the relative infant dose (RID) and milk/plasma (M/P) ratio.
RID provides information about relative medication exposure for the infant. It is calculated by dividing the infant’s dose of a medication via breastmilk (mg/kg/d) by the mother’s dose (mg/kg/d).7 Most consider an RID <10% to be safe.7
M/P is the ratio of medication concentration in the mother’s milk divided by the medication concentration in the mother’s plasma. A ratio <1 is preferable and generally indicates that a low level of medication has been transferred to human milk.7
Another factor that can be evaluated is protein binding. Medications that are highly protein-bound do not tend to pass as easily into breastmilk and can minimize infant exposure.
Several risk categorization systems are available, depending upon the resource used to obtain lactation information. One common system is Hale’s Lactation Risk Categories, with 5 safety levels ranging from L1 (breastfeeding compatible) to L5 (hazardous) (Table 17). Briggs et al8 utilize 7 categories to summarize recommendations ranging from breastfeeding-compatible to contraindicated; however, it is important to read the full medication monograph in the context of the rating provided. Table 27,8 provides breastfeeding information from Hale’s7 and from Briggs et al8 for some commonly used antidepressants.
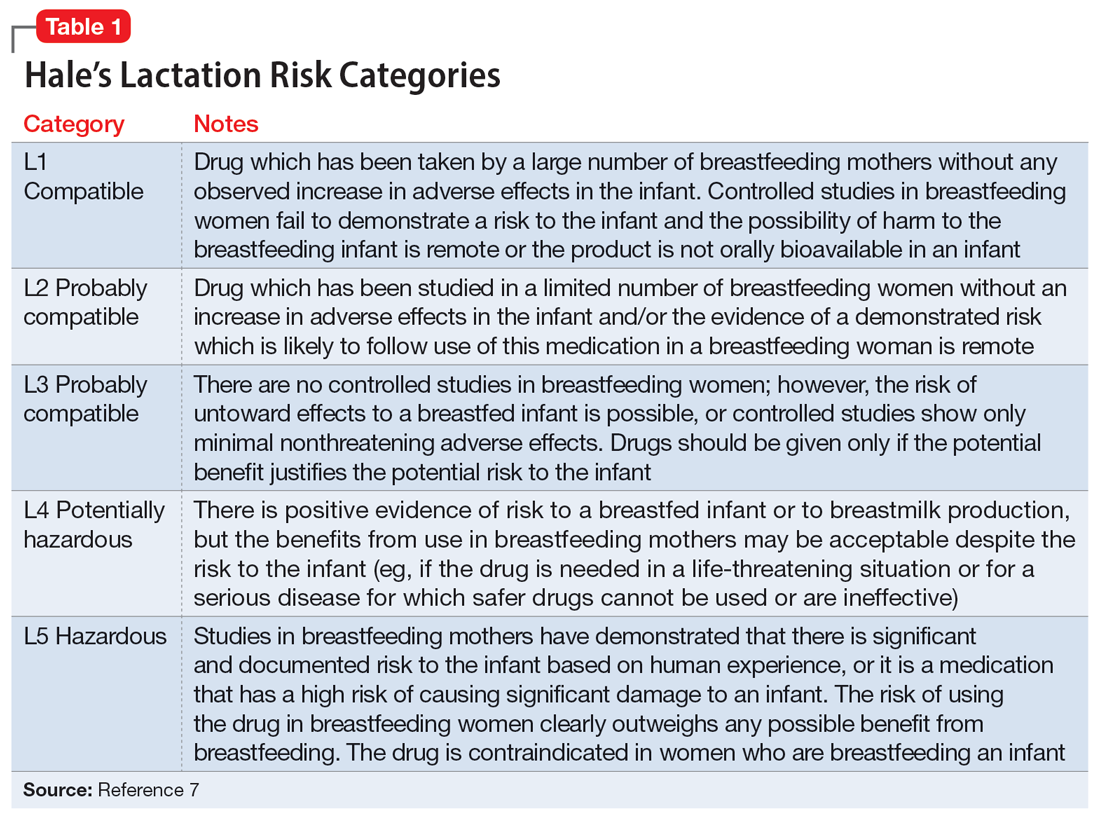
In addition to interpreting available literature, it is also important to consider patient-specific factors, including (but not limited to) the severity of the patient’s psychiatric disorder and their previous response to medication. If a mother achieved remission on a particular antidepressant in the past, it may be preferable to restart that agent rather than trial a new medication.
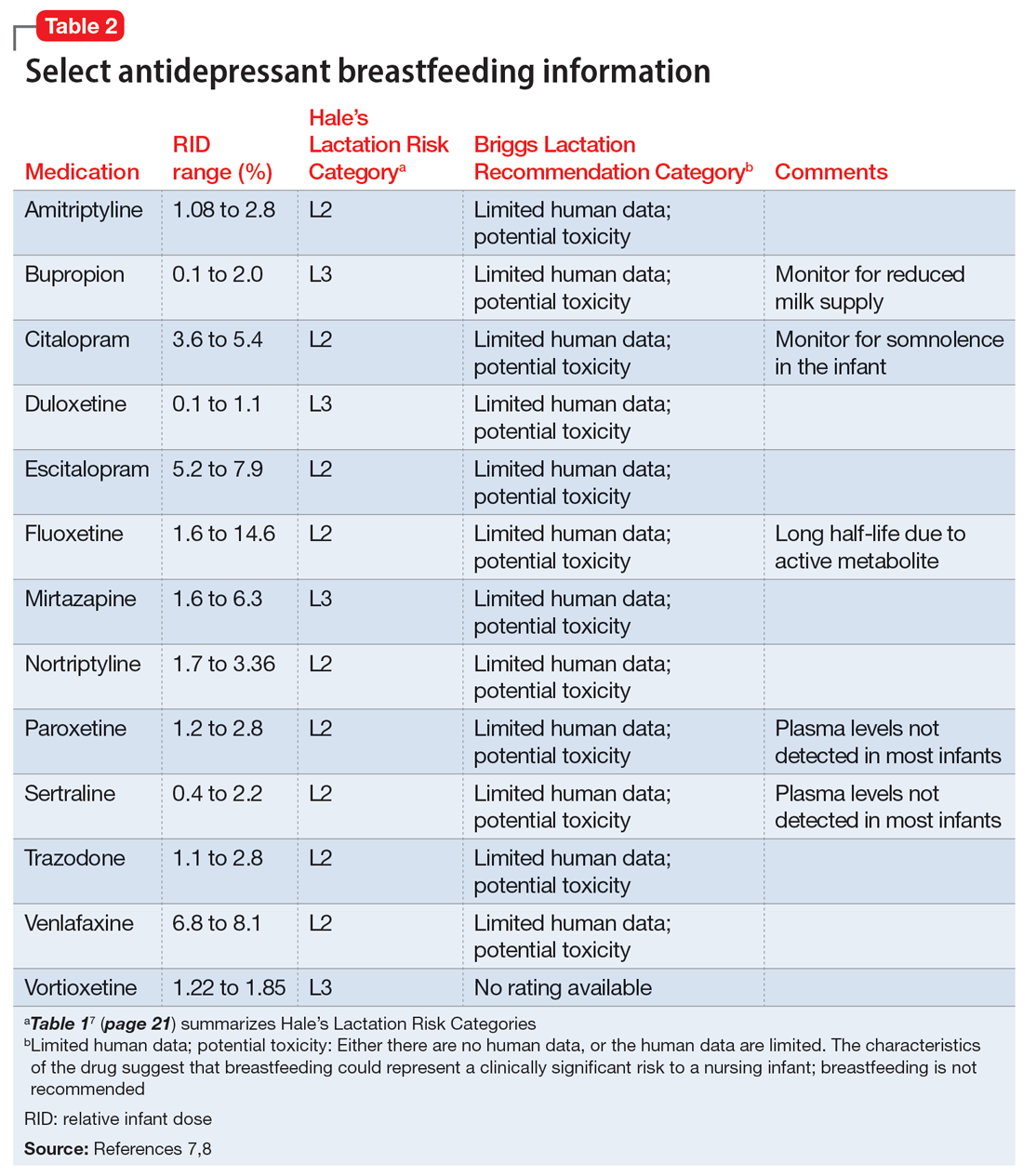
CASE CONTINUED
Two weeks later and following the use of a variety of resources, Ms. D’s treatment team finds that mirtazapine is rated Probably Compatible (L3 in Hale’s Lactation Risk Categories), with an M/P ratio of 0.76.7 The RID of mirtazapine ranges from 1.6% to 6.3%, and limited data from infants exposed to maternal use of mirtazapine during breastfeeding have not shown adverse effects.5 The treatment team administers the EDPS to Ms. D again and she scores 18. Given Ms. D’s previous remission with mirtazapine, current severity of depressive symptoms, and the risk/benefit assessment from lactation resources, the decision is made to restart mirtazapine 15 mg/d at bedtime with the option to titrate up if indicated. Ms. D plans to continue breastfeeding and will monitor for signs of any adverse effects in her infant. The Figure provides a summary of navigating this individualized decision with patients.
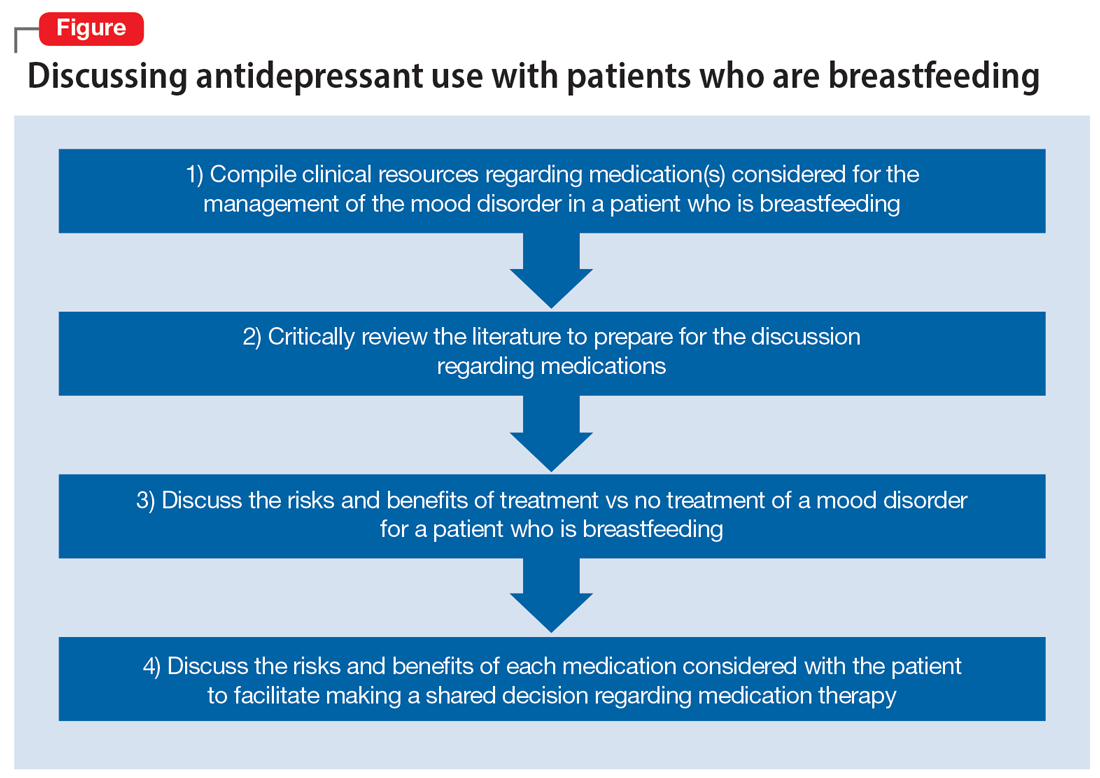
Related Resources
- MotherToBaby. Medication fact sheets, option to contact for no-charge consultation, free patient education information materials. www.mothertobaby.org
- Reprotox. Summaries on effects of medications on pregnancy, reproduction, and development (subscription required). www.reprotox.org
Drug Brand Names
Bupropion • Wellbutrin
Citalopram • Celexa
Duloxetine • Cymbalta
Escitalopram • Lexapro
Fluoxetine • Prozac
Mirtazapine • Remeron
Nortriptyline • Pamelor
Paroxetine • Paxil
Sertraline • Zoloft
Trazodone • Oleptro
Venlafaxine • Effexor
Vortioxetine • Trintellix
1. American Academy of Pediatrics. American Academy of Pediatrics calls for more support for breastfeeding mothers within updated policy recommendations. June 27, 2022. Accessed April 7, 2023. https://www.aap.org/en/news-room/news-releases/aap/2022/american-academy-of-pediatrics-calls-for-more-support-for-breastfeeding-mothers-within-updated-policy-recommendations
2. World Health Organization. Breastfeeding recommendations. Accessed April 7, 2023. https://www.who.int/health-topics/breastfeeding#tab=tab_2
3. Margiotta C, Gao J, O’Neil S, et al. The economic impact of untreated maternal mental health conditions in Texas. BMC Pregnancy Childbirth. 2022;22(1):700. doi:10.1186/s12884-022-05001-6
4. Freeman MP, Farchione T, Yao L, et al. Psychiatric medications and reproductive safety: scientific and clinical perspectives pertaining to the US FDA pregnancy and lactation labeling rule. J Clin Psychiatry. 2018;79(4):18ah38120.
5. Drugs and Lactation Database (LactMed). National Library of Medicine (US); 2011. Updated April 18, 2016. Accessed September 29, 2022. https://www.ncbi.nlm.nih.gov/books/NBK501922/
6. InfantRisk Center Resources. InfantRisk Center at Texas Tech University Health Sciences Center. Accessed September 29, 2022. https://www.infantrisk.com/infantrisk-center-resources
7. Hale TW, Krutsch K. Hale’s Medications and Mother’s Milk 2023: A Manual of Lactational Pharmacology. Springer Publishing; 2023.
8. Briggs GG, Freeman RK, Towers CV, et al. Briggs Drugs in Pregnancy and Lactation: A Reference Guide to Fetal and Neonatal Risk. 12th ed. Lippincott Williams & Wilkins; 2021.
Ms. D, age 32, recently gave birth to her second child. Her psychiatric history includes major depressive disorder. She had been stable on mirtazapine 30 mg at bedtime for 3 years. Based on clinical stability and patient preference, Ms. D elected to taper off mirtazapine 1 month prior to delivery. Now at 1 month postdelivery, Ms. D notes the reemergence of her depressive symptoms; during her child’s latest pediatrician visit, she scores 15 on the Edinburgh Postnatal Depression Scale (EPDS). She breastfeeds her baby and wants more information on the safety of taking an antidepressant while breastfeeding.
Ms. D discusses her previous use of mirtazapine with her treatment team. The team reviews the available resources with Ms. D and together they plan to make a shared decision regarding treatment of her depression at her next appointment.
The American Academy of Pediatrics1 and World Health Organization2 recommend exclusive breastfeeding of infants for their first 6 months of life and support it as a complement to other foods through and beyond age 2. Untreated conditions such as postpartum depression impact maternal well-being and may interfere with parenting and child development. In fact, untreated maternal mental health leads to an increased risk of suicide, reduced maternal economic productivity, and worsened health for both mother and child.3
Because many women experience psychiatric symptoms before they become pregnant as well as during the perinatal period, questions often arise regardingthe use of psychiatric medications—specifically antidepressants—and their safety in patients who are breastfeeding. Key considerations regarding medication management should include the patient’s previous response to medications, the risks of untreated maternal mental illness, and evidence regarding risks and benefits in lactation. This article summarizes where to find evidence-based lactation information, how to interpret that information, and what information is available for select antidepressants.
Locating lactation information
Start by checking the manufacturer’s medication labeling (“prescribing information”) and medication information resources such as Micromedex (www.micromedexsolutions.com) and Lexicomp (www.wolterskluwer.com/en/solutions/lexicomp). The updated labeling includes a risk/benefit assessment of available data on the risk for continued use of a medication during pregnancy compared to the risk if a medication is discontinued and the disorder goes untreated.4 The “breastfeeding considerations” section of medication labeling include details regarding the presence of the medication and the amount of it in breastmilk, adverse events in infants exposed to the medication through breastmilk, and additional pertinent data as applicable. Lexicomp includes information regarding breastfeeding considerations, and a subscription may also include access to Briggs Drugs in Pregnancy and Lactation’s information pages. Micromedex includes its own lactation safety rating scale score.
Several other resources can help guide clinicians toward patient-specific recommendations. From the National Library of Medicine, LactMed (https://www.ncbi.nlm.nih.gov/books/NBK501922/) allows clinicians to search for specific medications to see what information exists pertaining to medication levels in breastmilk and infant blood as well as potential adverse effects in the nursing infant and/or on lactation and breastmilk.5 LactMed provides information regarding alternative medications to consider and references from which the information was gathered.
Another helpful resource is the InfantRisk Center from Texas Tech University Health Sciences Center, which includes a free call center for parents and clinicians who have questions about medications and breastfeeding (806-352-2519; Monday through Friday, 8
Continue to: How to interpret the information
How to interpret the information
Medication levels in breastmilk are affected by several properties, such as the medication’s molecular weight, protein binding, pKa, and volume of distribution. A few commonly used terms in lactation literature for medications include the relative infant dose (RID) and milk/plasma (M/P) ratio.
RID provides information about relative medication exposure for the infant. It is calculated by dividing the infant’s dose of a medication via breastmilk (mg/kg/d) by the mother’s dose (mg/kg/d).7 Most consider an RID <10% to be safe.7
M/P is the ratio of medication concentration in the mother’s milk divided by the medication concentration in the mother’s plasma. A ratio <1 is preferable and generally indicates that a low level of medication has been transferred to human milk.7
Another factor that can be evaluated is protein binding. Medications that are highly protein-bound do not tend to pass as easily into breastmilk and can minimize infant exposure.
Several risk categorization systems are available, depending upon the resource used to obtain lactation information. One common system is Hale’s Lactation Risk Categories, with 5 safety levels ranging from L1 (breastfeeding compatible) to L5 (hazardous) (Table 17). Briggs et al8 utilize 7 categories to summarize recommendations ranging from breastfeeding-compatible to contraindicated; however, it is important to read the full medication monograph in the context of the rating provided. Table 27,8 provides breastfeeding information from Hale’s7 and from Briggs et al8 for some commonly used antidepressants.
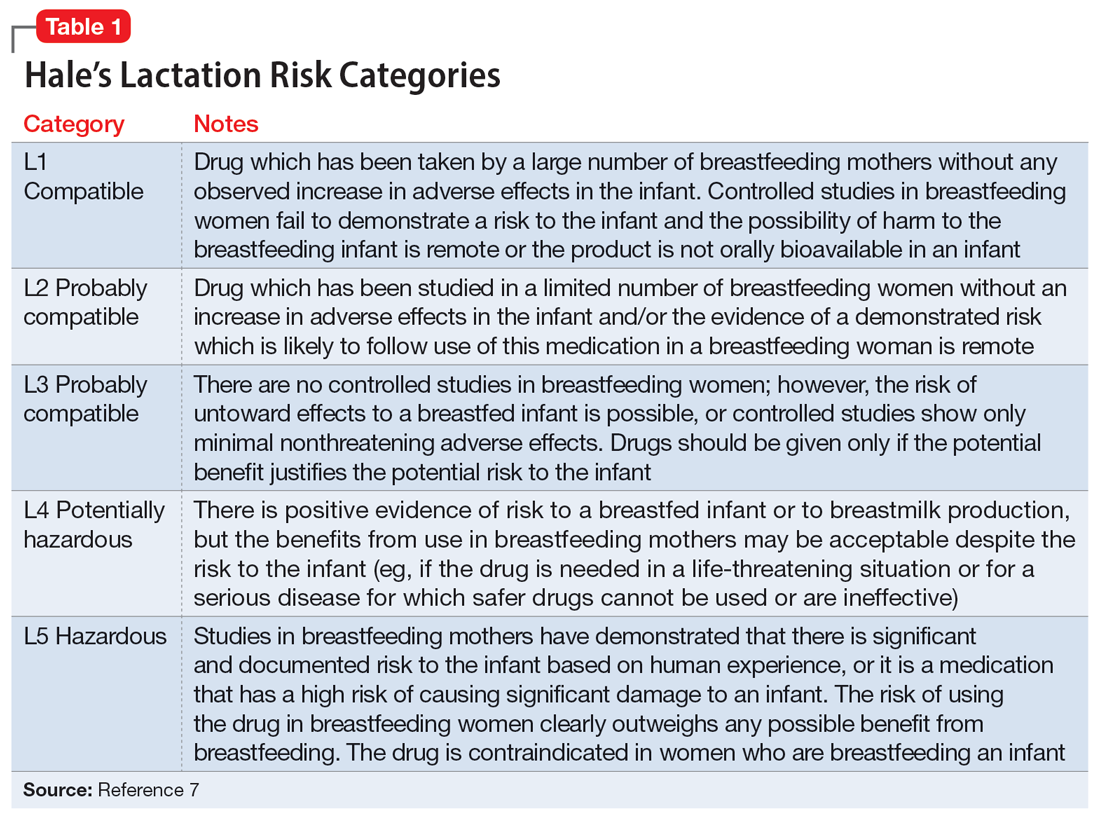
In addition to interpreting available literature, it is also important to consider patient-specific factors, including (but not limited to) the severity of the patient’s psychiatric disorder and their previous response to medication. If a mother achieved remission on a particular antidepressant in the past, it may be preferable to restart that agent rather than trial a new medication.
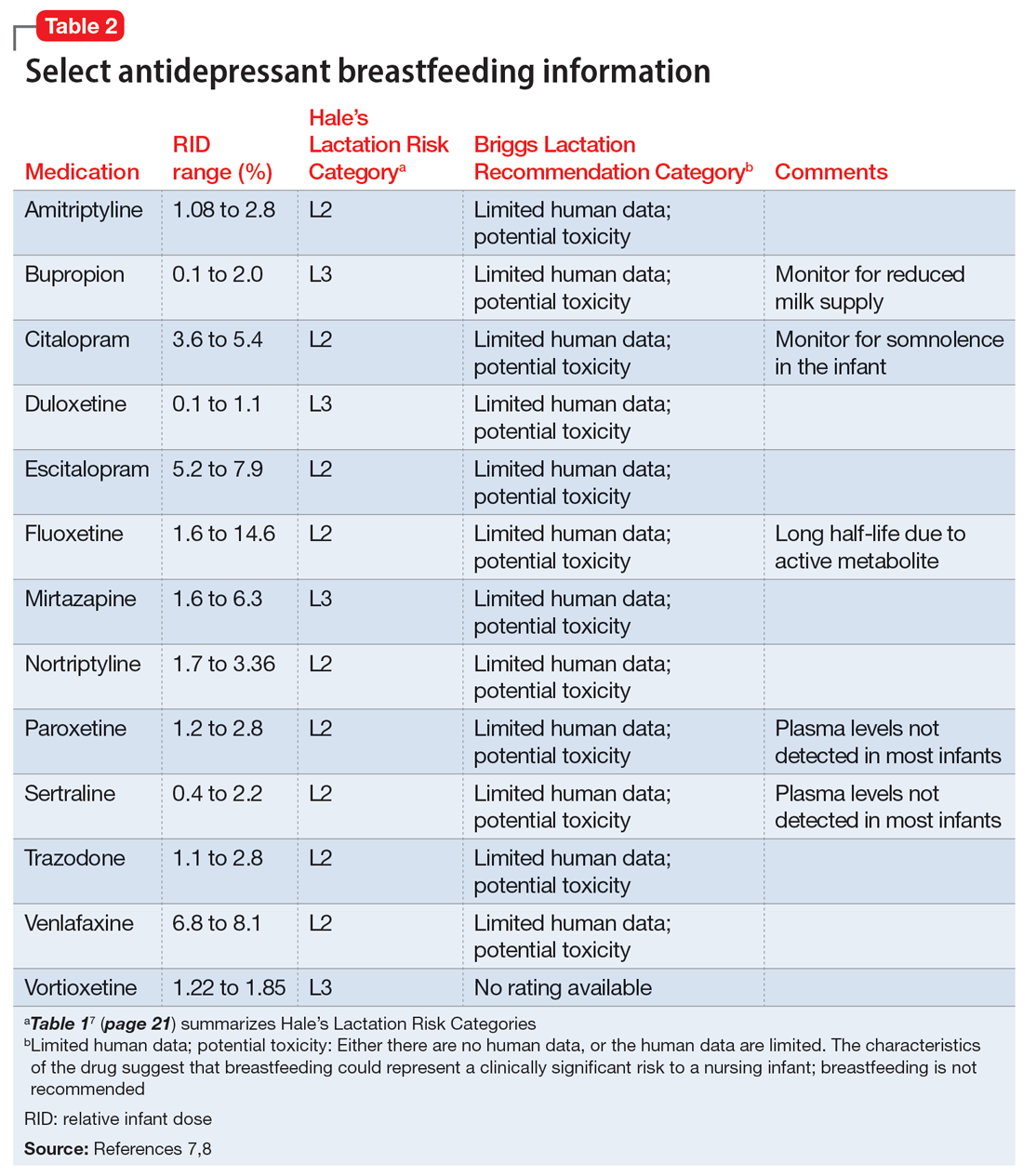
CASE CONTINUED
Two weeks later and following the use of a variety of resources, Ms. D’s treatment team finds that mirtazapine is rated Probably Compatible (L3 in Hale’s Lactation Risk Categories), with an M/P ratio of 0.76.7 The RID of mirtazapine ranges from 1.6% to 6.3%, and limited data from infants exposed to maternal use of mirtazapine during breastfeeding have not shown adverse effects.5 The treatment team administers the EDPS to Ms. D again and she scores 18. Given Ms. D’s previous remission with mirtazapine, current severity of depressive symptoms, and the risk/benefit assessment from lactation resources, the decision is made to restart mirtazapine 15 mg/d at bedtime with the option to titrate up if indicated. Ms. D plans to continue breastfeeding and will monitor for signs of any adverse effects in her infant. The Figure provides a summary of navigating this individualized decision with patients.
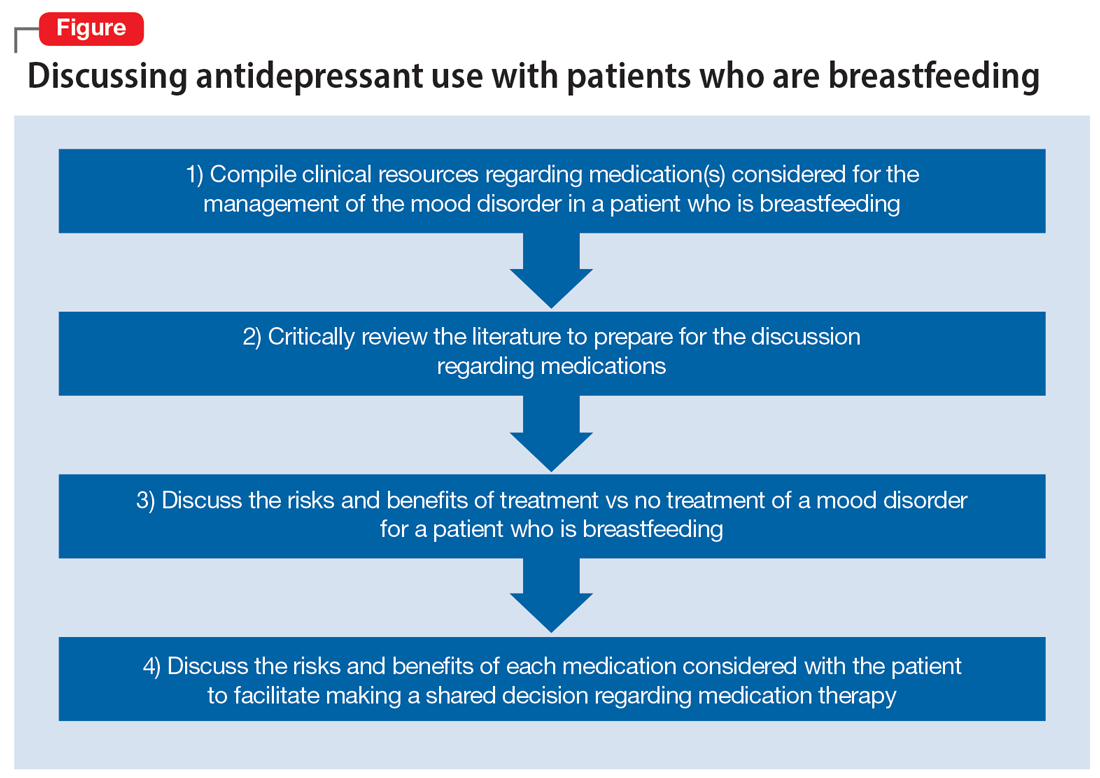
Related Resources
- MotherToBaby. Medication fact sheets, option to contact for no-charge consultation, free patient education information materials. www.mothertobaby.org
- Reprotox. Summaries on effects of medications on pregnancy, reproduction, and development (subscription required). www.reprotox.org
Drug Brand Names
Bupropion • Wellbutrin
Citalopram • Celexa
Duloxetine • Cymbalta
Escitalopram • Lexapro
Fluoxetine • Prozac
Mirtazapine • Remeron
Nortriptyline • Pamelor
Paroxetine • Paxil
Sertraline • Zoloft
Trazodone • Oleptro
Venlafaxine • Effexor
Vortioxetine • Trintellix
Ms. D, age 32, recently gave birth to her second child. Her psychiatric history includes major depressive disorder. She had been stable on mirtazapine 30 mg at bedtime for 3 years. Based on clinical stability and patient preference, Ms. D elected to taper off mirtazapine 1 month prior to delivery. Now at 1 month postdelivery, Ms. D notes the reemergence of her depressive symptoms; during her child’s latest pediatrician visit, she scores 15 on the Edinburgh Postnatal Depression Scale (EPDS). She breastfeeds her baby and wants more information on the safety of taking an antidepressant while breastfeeding.
Ms. D discusses her previous use of mirtazapine with her treatment team. The team reviews the available resources with Ms. D and together they plan to make a shared decision regarding treatment of her depression at her next appointment.
The American Academy of Pediatrics1 and World Health Organization2 recommend exclusive breastfeeding of infants for their first 6 months of life and support it as a complement to other foods through and beyond age 2. Untreated conditions such as postpartum depression impact maternal well-being and may interfere with parenting and child development. In fact, untreated maternal mental health leads to an increased risk of suicide, reduced maternal economic productivity, and worsened health for both mother and child.3
Because many women experience psychiatric symptoms before they become pregnant as well as during the perinatal period, questions often arise regardingthe use of psychiatric medications—specifically antidepressants—and their safety in patients who are breastfeeding. Key considerations regarding medication management should include the patient’s previous response to medications, the risks of untreated maternal mental illness, and evidence regarding risks and benefits in lactation. This article summarizes where to find evidence-based lactation information, how to interpret that information, and what information is available for select antidepressants.
Locating lactation information
Start by checking the manufacturer’s medication labeling (“prescribing information”) and medication information resources such as Micromedex (www.micromedexsolutions.com) and Lexicomp (www.wolterskluwer.com/en/solutions/lexicomp). The updated labeling includes a risk/benefit assessment of available data on the risk for continued use of a medication during pregnancy compared to the risk if a medication is discontinued and the disorder goes untreated.4 The “breastfeeding considerations” section of medication labeling include details regarding the presence of the medication and the amount of it in breastmilk, adverse events in infants exposed to the medication through breastmilk, and additional pertinent data as applicable. Lexicomp includes information regarding breastfeeding considerations, and a subscription may also include access to Briggs Drugs in Pregnancy and Lactation’s information pages. Micromedex includes its own lactation safety rating scale score.
Several other resources can help guide clinicians toward patient-specific recommendations. From the National Library of Medicine, LactMed (https://www.ncbi.nlm.nih.gov/books/NBK501922/) allows clinicians to search for specific medications to see what information exists pertaining to medication levels in breastmilk and infant blood as well as potential adverse effects in the nursing infant and/or on lactation and breastmilk.5 LactMed provides information regarding alternative medications to consider and references from which the information was gathered.
Another helpful resource is the InfantRisk Center from Texas Tech University Health Sciences Center, which includes a free call center for parents and clinicians who have questions about medications and breastfeeding (806-352-2519; Monday through Friday, 8
Continue to: How to interpret the information
How to interpret the information
Medication levels in breastmilk are affected by several properties, such as the medication’s molecular weight, protein binding, pKa, and volume of distribution. A few commonly used terms in lactation literature for medications include the relative infant dose (RID) and milk/plasma (M/P) ratio.
RID provides information about relative medication exposure for the infant. It is calculated by dividing the infant’s dose of a medication via breastmilk (mg/kg/d) by the mother’s dose (mg/kg/d).7 Most consider an RID <10% to be safe.7
M/P is the ratio of medication concentration in the mother’s milk divided by the medication concentration in the mother’s plasma. A ratio <1 is preferable and generally indicates that a low level of medication has been transferred to human milk.7
Another factor that can be evaluated is protein binding. Medications that are highly protein-bound do not tend to pass as easily into breastmilk and can minimize infant exposure.
Several risk categorization systems are available, depending upon the resource used to obtain lactation information. One common system is Hale’s Lactation Risk Categories, with 5 safety levels ranging from L1 (breastfeeding compatible) to L5 (hazardous) (Table 17). Briggs et al8 utilize 7 categories to summarize recommendations ranging from breastfeeding-compatible to contraindicated; however, it is important to read the full medication monograph in the context of the rating provided. Table 27,8 provides breastfeeding information from Hale’s7 and from Briggs et al8 for some commonly used antidepressants.
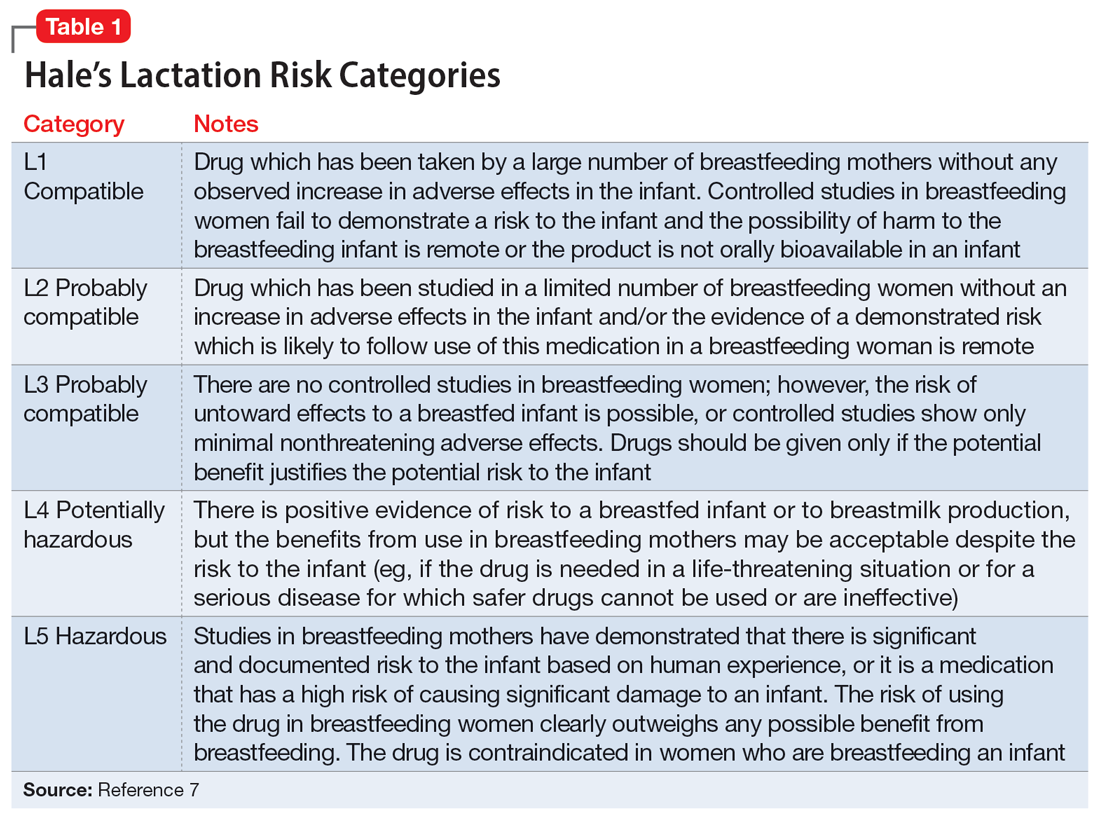
In addition to interpreting available literature, it is also important to consider patient-specific factors, including (but not limited to) the severity of the patient’s psychiatric disorder and their previous response to medication. If a mother achieved remission on a particular antidepressant in the past, it may be preferable to restart that agent rather than trial a new medication.
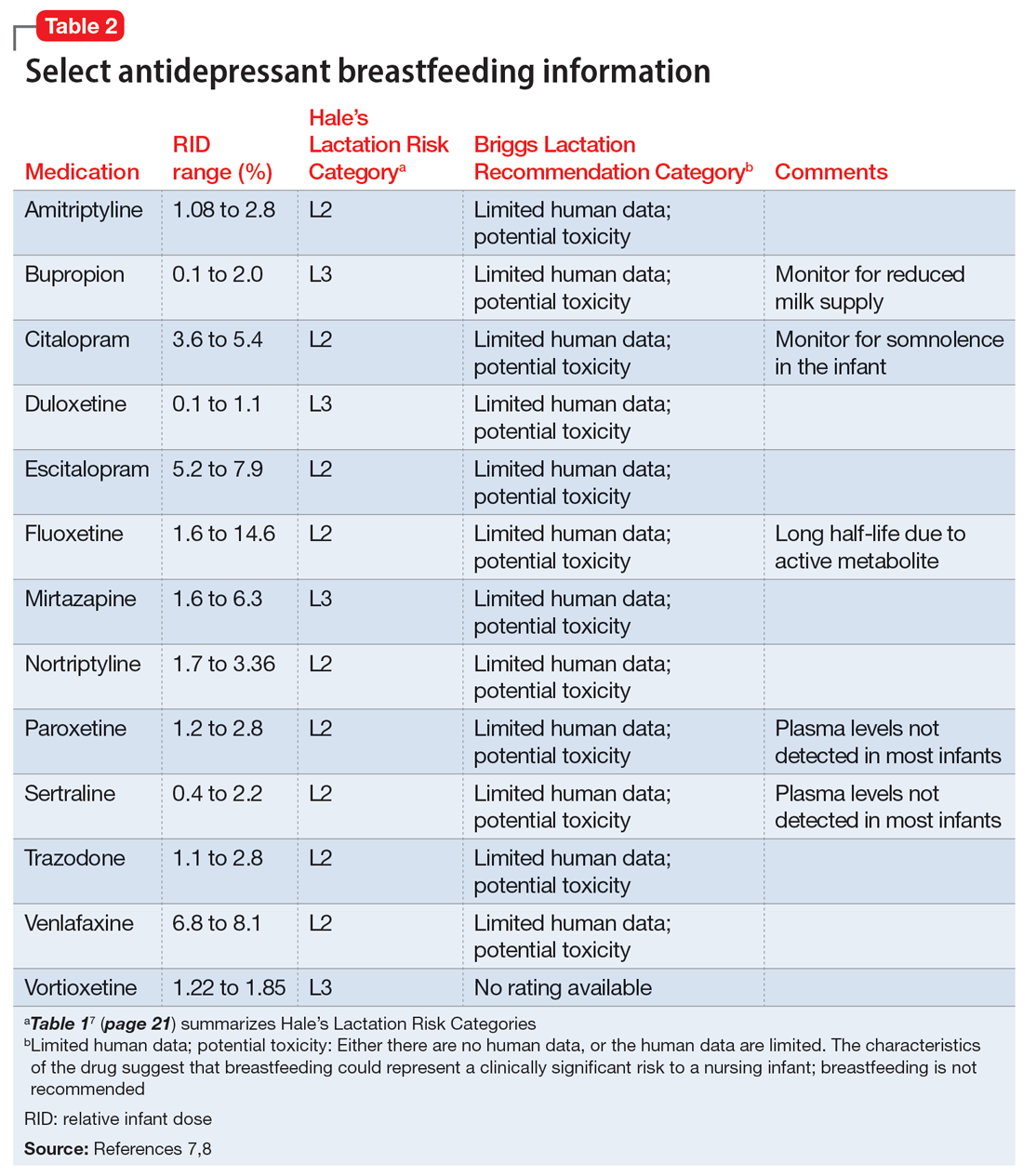
CASE CONTINUED
Two weeks later and following the use of a variety of resources, Ms. D’s treatment team finds that mirtazapine is rated Probably Compatible (L3 in Hale’s Lactation Risk Categories), with an M/P ratio of 0.76.7 The RID of mirtazapine ranges from 1.6% to 6.3%, and limited data from infants exposed to maternal use of mirtazapine during breastfeeding have not shown adverse effects.5 The treatment team administers the EDPS to Ms. D again and she scores 18. Given Ms. D’s previous remission with mirtazapine, current severity of depressive symptoms, and the risk/benefit assessment from lactation resources, the decision is made to restart mirtazapine 15 mg/d at bedtime with the option to titrate up if indicated. Ms. D plans to continue breastfeeding and will monitor for signs of any adverse effects in her infant. The Figure provides a summary of navigating this individualized decision with patients.
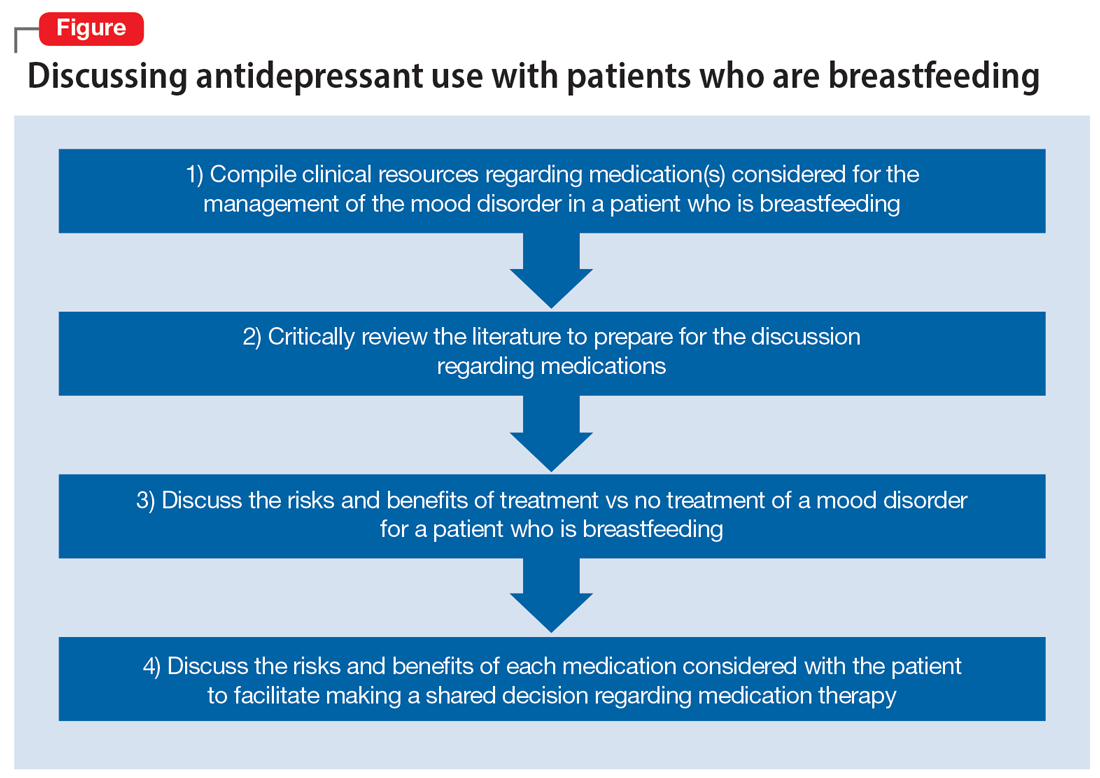
Related Resources
- MotherToBaby. Medication fact sheets, option to contact for no-charge consultation, free patient education information materials. www.mothertobaby.org
- Reprotox. Summaries on effects of medications on pregnancy, reproduction, and development (subscription required). www.reprotox.org
Drug Brand Names
Bupropion • Wellbutrin
Citalopram • Celexa
Duloxetine • Cymbalta
Escitalopram • Lexapro
Fluoxetine • Prozac
Mirtazapine • Remeron
Nortriptyline • Pamelor
Paroxetine • Paxil
Sertraline • Zoloft
Trazodone • Oleptro
Venlafaxine • Effexor
Vortioxetine • Trintellix
1. American Academy of Pediatrics. American Academy of Pediatrics calls for more support for breastfeeding mothers within updated policy recommendations. June 27, 2022. Accessed April 7, 2023. https://www.aap.org/en/news-room/news-releases/aap/2022/american-academy-of-pediatrics-calls-for-more-support-for-breastfeeding-mothers-within-updated-policy-recommendations
2. World Health Organization. Breastfeeding recommendations. Accessed April 7, 2023. https://www.who.int/health-topics/breastfeeding#tab=tab_2
3. Margiotta C, Gao J, O’Neil S, et al. The economic impact of untreated maternal mental health conditions in Texas. BMC Pregnancy Childbirth. 2022;22(1):700. doi:10.1186/s12884-022-05001-6
4. Freeman MP, Farchione T, Yao L, et al. Psychiatric medications and reproductive safety: scientific and clinical perspectives pertaining to the US FDA pregnancy and lactation labeling rule. J Clin Psychiatry. 2018;79(4):18ah38120.
5. Drugs and Lactation Database (LactMed). National Library of Medicine (US); 2011. Updated April 18, 2016. Accessed September 29, 2022. https://www.ncbi.nlm.nih.gov/books/NBK501922/
6. InfantRisk Center Resources. InfantRisk Center at Texas Tech University Health Sciences Center. Accessed September 29, 2022. https://www.infantrisk.com/infantrisk-center-resources
7. Hale TW, Krutsch K. Hale’s Medications and Mother’s Milk 2023: A Manual of Lactational Pharmacology. Springer Publishing; 2023.
8. Briggs GG, Freeman RK, Towers CV, et al. Briggs Drugs in Pregnancy and Lactation: A Reference Guide to Fetal and Neonatal Risk. 12th ed. Lippincott Williams & Wilkins; 2021.
1. American Academy of Pediatrics. American Academy of Pediatrics calls for more support for breastfeeding mothers within updated policy recommendations. June 27, 2022. Accessed April 7, 2023. https://www.aap.org/en/news-room/news-releases/aap/2022/american-academy-of-pediatrics-calls-for-more-support-for-breastfeeding-mothers-within-updated-policy-recommendations
2. World Health Organization. Breastfeeding recommendations. Accessed April 7, 2023. https://www.who.int/health-topics/breastfeeding#tab=tab_2
3. Margiotta C, Gao J, O’Neil S, et al. The economic impact of untreated maternal mental health conditions in Texas. BMC Pregnancy Childbirth. 2022;22(1):700. doi:10.1186/s12884-022-05001-6
4. Freeman MP, Farchione T, Yao L, et al. Psychiatric medications and reproductive safety: scientific and clinical perspectives pertaining to the US FDA pregnancy and lactation labeling rule. J Clin Psychiatry. 2018;79(4):18ah38120.
5. Drugs and Lactation Database (LactMed). National Library of Medicine (US); 2011. Updated April 18, 2016. Accessed September 29, 2022. https://www.ncbi.nlm.nih.gov/books/NBK501922/
6. InfantRisk Center Resources. InfantRisk Center at Texas Tech University Health Sciences Center. Accessed September 29, 2022. https://www.infantrisk.com/infantrisk-center-resources
7. Hale TW, Krutsch K. Hale’s Medications and Mother’s Milk 2023: A Manual of Lactational Pharmacology. Springer Publishing; 2023.
8. Briggs GG, Freeman RK, Towers CV, et al. Briggs Drugs in Pregnancy and Lactation: A Reference Guide to Fetal and Neonatal Risk. 12th ed. Lippincott Williams & Wilkins; 2021.
Depressed and cognitively impaired
CASE Depressed and anxious
Five years ago, Ms. X, age 60, was diagnosed with treatment-resistant major depressive disorder (MDD) with anxiety. This diagnosis was established by a previous psychiatrist. She presents to a clinic for a second opinion.
Since her diagnosis, Ms. X has experienced sad mood, anhedonia, difficulty falling asleep, increased appetite and weight, and decreased concentration and attention. Her anxiety stems from her inability to work, which causes her to worry about her children. In the clinic, the treatment team conducts the Patient Health Questionnaire-9 (PHQ-9) and Generalized Anxiety Disorder-7 item scale (GAD-7) with Ms. X. She scores 16 on the PHQ-9, indicating moderately severe depression, and scores 12 on the GAD-7, indicating moderate anxiety.
Ms. X’s current medication regimen consists of venlafaxine extended-release (XR) 225 mg/d, trazodone 100 mg/d at bedtime, and clonazepam 1 mg twice daily. She reports no significant improvement of her symptoms from these medications. Additionally, Ms. X reports that in the past she had been prescribed fluoxetine, citalopram, and duloxetine, but she cannot recall the dosages.
Ms. X appears appropriately groomed, maintains appropriate eye contact, has clear speech, and does not show evidence of internal stimulation; however, she has difficulty following instructions. She makes negative comments about herself such as “I’m worthless” and “Nobody cares about me.” The treatment team decides to taper Ms. X off venlafaxine XR and initiates sertraline 50 mg/d, while continuing trazodone 50 mg/d at bedtime and clonazepam 1 mg twice daily. The team refers her for cognitive-behavioral therapy (CBT) to address her cognitive distortions, sad mood, and anxiety. Ms. X is asked to follow up with Psychiatry in 1 week.
EVALUATION Unusual behavior
At her CBT intake, Ms. X endorses depression and anxiety. Her PHQ-9 score at this visit is 19 (moderately severe depression) and GAD-7 score is 16 (severe anxiety). The psychologist notes that Ms. X is able to complete activities of daily living and instrumental activities of daily living without assistance. Ms. X denies any use of illicit substances or alcohol. No gross memory impairment is noted during this appointment, though Ms. X exhibits unusual behavior, including exiting and re-entering the clinic multiple times to repeatedly ask about follow-up appointments. The psychologist concludes that Ms. X’s presentation and behavior can be explained by MDD and pseudodementia.
[polldaddy:12189562]
The authors’ observations
Pseudodementia gained recognition in clinical research >100 years ago.1 Officially coined by Kiloh in 1961, the term was used broadly to categorize psychiatric cases that present like dementia but are the result of reversible causes. More recently, it has been used to describe older adults who present with cognitive deficits in the context of depressive symptoms.2 The goal of evaluation is to determine if the primary issue is a cognitive disorder or a depressive episode. DSM-5-TR does not classify pseudodementia as a distinct diagnosis, but instead categorizes its symptoms as components under other major diagnostic categories. Patients can present with MDD and associated cognitive symptoms, or with a cognitive disorder with depressive symptoms, which would be diagnosed as a cognitive disorder with a major depressive-like episode.3
Pseudodementia is rare. Brodaty et al4 found the prevalence of pseudodementia in primary care settings was 0.6%. Older adults (age >65) who live alone are at increased risk of developing pseudodementia, which can be worsened by poor social support and acute psychosocial and environmental changes.5 A key characteristic of this disorder is that as the patient’s depressed mood improves, their memory and cognition also improve.6 Table 13,6 outlines overlapping features of MDD and pseudodementia.
Continue to: EVALUATION Worsening depression
EVALUATION Worsening depression
At her Psychiatry follow-up appointment, Ms. X reports that her mood is worse since she ended the relationship with her partner and she feels anxious because the partner was financially supporting her. Her PHQ-9 score is 24 (severe depression) and her GAD-7 score is 12 (moderate anxiety). Ms. X reports tolerating her transition from venlafaxine XR 225 mg/d to sertraline 50 mg/d well.
Additionally, Ms. X reports her children have called her “useless” since she continues to have difficulties following through on household tasks, even though she has no physical impairments that prevent her from completing them. The Psychiatry team observes that Ms. X has no problems walking or moving her arms or legs.
The Psychiatry team administers the Montreal Cognitive Assessment (MoCA). Ms. X scores 22, indicating mild impairment.
The team recommends a neuropsychological assessment to determine if this MoCA score is due to a cognitive disorder or is rooted in her mood symptoms. The team also recommends an MRI of the brain, complete blood count (CBC), comprehensive metabolic panel (CMP), and urinalysis (UA).
[polldaddy:12189567]
Continue to: The authors' observations
The authors’ observations
Neuropsychological assessments are important tools for exploring the behavioral manifestations of brain dysfunction (Table 2).7 These assessments factor in elements of neurology, psychiatry, and psychology to provide information about the diagnosis, prognosis, and functional status of patients with medical conditions, especially those with neurocognitive and psychiatric disorders. They combine information from the patient and collateral interviews, behavioral observations, a review of patient records, and objective tests of motor, emotional, and cognitive function.
Among other uses, neuropsychological assessments can help identify depression in patients with neurologic impairment, determine the diagnosis and plan of care for patients with concussions, determine the risk of a motor vehicle crash in patients with cognitive impairment, and distinguish Alzheimer disease from vascular dementia.8 Components of such assessments include the Beck Anxiety Inventory (BAI) to assess anxiety, the Dementia Rating Scale-2 and Neuropsychological Assessment Battery-Screening Module to assess dementia, and the Beck Depression Inventory (BDI) to assess depression.9
EVALUATION Continued cognitive decline
A different psychologist performs the neuropsychological assessment, who conducts the Repeatable Battery for the Assessment of Neuropsychological Status Update to determine if Ms. X is experiencing cognitive impairment. Her immediate memory, visuospatial/constructions, language, attention, and delayed memory are significantly impaired for someone her age. The psychologist also administers the Wechsler Adult Intelligence Scale IV and finds Ms. X’s general cognitive ability is within the low average range of intellectual functioning as measured by Full-Scale IQ. Ms. X scores 29 on the BDI-II, indicating significant depressive symptoms, and 13 on the BAI, indicating mild anxiety symptoms.
Ms. X is diagnosed with MDD and an unspecified neurocognitive disorder. The psychologist recommends she start CBT to address her mood and anxiety symptoms.
Upon reviewing the results with Ms. X, the treatment team again recommends a brain MRI, CBC, CMP, and UA to rule out organic causes of her cognitive decline. Ms. X decides against the MRI and laboratory workup and elects to continue her present medication regimen and CBT.
Several weeks later, Ms. X’s family brings her to the emergency department (ED) for evaluation of worsening mood, decreased personal hygiene, increased irritability, and further cognitive decline. They report she is having an increasingly difficult time remembering things such as where she parked her car. The ED team decides to discontinue clonazepam but continues sertraline and trazodone.
Continue to: CBC, CMP, and UA...
CBC, CMP, and UA are unremarkable. Ms. X undergoes a brain CT scan without contrast, which reveals hyperdense lesions in the inferior left tentorium, posterior fossa. A subsequent brain MRI with contrast reveals a dural-based enhancing mass, inferior to the left tentorium, in the left posterior fossa measuring 2.2 cm x 2.1 cm, suggestive of a meningioma. The team orders a Neurosurgery consult.
[polldaddy:12189571]
The authors’ observations
While most brain tumors are secondary to metastasis, meningiomas are the most common primary CNS tumor. Typically, they are asymptomatic; their diagnosis is often delayed until the patient presents with psychiatric symptoms without any focal neurologic findings. The frontal lobe is the most common location of meningioma. Data from 48 case reports of patients with meningiomas and psychiatric symptoms suggest symptoms do not always correlate with specific brain regions.10,11
Indications for neuroimaging in cases such as Ms. X include an abrupt change in behavior or personality, lack of response to psychiatric treatment, presence of focal neurologic signs, and an unusual psychiatric presentation and development of symptoms.11
TREATMENT Neurosurgery
Neurosurgery recommends and performs a suboccipital craniotomy for biopsy and resection. Ms. X tolerates the procedure well. A meningioma is found in the posterior fossa, near the cerebellar convexity. A biopsy finds no evidence of malignancies.
At her postoperative follow-up appointment several days after the procedure, Ms. X reports new-onset hearing loss and tinnitus.
[polldaddy:12189747]
Continue to: The authors' observations
The authors’ observations
Patients who require neurosurgery typically already carry a heavy psychiatric burden, which makes it challenging to determine the exact psychiatric consequences of neurosurgery.12-14 For example, research shows that temporal lobe resection and temporal lobectomy for treatment-resistant epilepsy can lead to an exacerbation of baseline psychiatric symptoms and the development of new symptoms (31% to 34%).15,16 However, Bommakanti et al13 found no new psychiatric symptoms after resection of meningiomas, and surgery seemed to play a role in ameliorating psychiatric symptoms in patients with intracranial tumors. Research attempting to document the psychiatric sequelae of neurosurgery has had mixed results, and it is difficult to determine what effects brain surgery has on mental health.
OUTCOME Minimal improvement
Several weeks after neurosurgery, Ms. X and her family report her mood is improved. Her PHQ-9 score improves to 15, but her GAD-7 score increases to 13, 1 point above her previous score.
The treatment team recommends Ms. X continue taking sertraline 50 mg/d and trazodone 50 mg/d at bedtime. Ms. X’s family reports her cognition and memory have not improved; her MoCA score increases by 1 point to 23. The treatment team discusses with Ms. X and her family the possibility that her cognitive problems maybe better explained as a neurocognitive disorder rather than as a result of the meningioma, since her MoCA score has not significantly improved. Ms. X and her family decide to seek a second opinion from a neurologist.
Bottom Line
Pseudodementia is a term used to describe older adults who present with cognitive issues in the context of depressive symptoms. Even in the absence of focal findings, neuroimaging should be considered as part of the workup in patients who continue to experience a progressive decline in mood and cognitive function.
Related Resources
- Moller MD, Parmenter BA, Lane DW. Neuropsychological testing: a useful but underutilized resource. Current Psychiatry. 2019;18(11):40-46,51.
- Pollak J. Psychological/neuropsychological testing: when to refer for reexamination. Current Psychiatry. 2021;20(9):18- 19,30-31,37. doi:10.12788/cp.0157
Drug Brand Names
Citalopram • Celexa
Clonazepam • Klonopin
Duloxetine • Cymbalta
Fluoxetine • Prozac
Sertraline • Zoloft
Trazodone • Oleptro
Venlafaxine extended- release • Effexor XR
1. Nussbaum PD. (1994). Pseudodementia: a slow death. Neuropsychol Rev. 1994;4(2):71-90. doi:10.1007/BF01874829
2. Kang H, Zhao F, You L, et al. (2014). Pseudo-dementia: a neuropsychological review. Ann Indian Acad Neurol. 17(2):147-154. doi:10.4103/0972-2327.132613
3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed, text revision. American Psychiatric Association; 2022.
4. Brodaty H, Connors MH. Pseudodementia, pseudo-pseudodementia, and pseudodepression. Alzheimers Dement (Amst). 2020;12(1):e12027. doi:10.1002/dad2.12027
5. Sekhon S, Marwaha R. Depressive Cognitive Disorders. StatPearls Publishing; 2022. https://www.ncbi.nlm.nih.gov/books/NBK559256/
6. Brown WA. Pseudodementia: issues in diagnosis. Psychiatric Times. April 9, 2005. Accessed February 3, 2023. www.psychiatrictimes.com/view/pseudodementia-issues-diagnosis
7. Kulas JF, Naugle RI. (2003). Indications for neuropsychological assessment. Cleve Clin J Med. 2003;70(9):785-792.
8. Braun M, Tupper D, Kaufmann P, et al. Neuropsychological assessment: a valuable tool in the diagnosis and management of neurological, neurodevelopmental, medical, and psychiatric disorders. Cogn Behav Neurol. 2011;24(3):107-114.
9. Michels TC, Tiu AY, Graver CJ. Neuropsychological evaluation in primary care. Am Fam Physician. 2010;82(5):495-502.
10. Wiemels J, Wrensch M, Claus EB. Epidemiology and etiology of meningioma. J Neurooncol. 2010;99(3):307-314. doi:10.1007/s11060-010-0386-3
11. Gyawali S, Sharma P, Mahapatra A. Meningioma and psychiatric symptoms: an individual patient data analysis. Asian J Psychiatr. 2019;42:94-103. doi:10.1016/j.ajp.2019.03.029
12. McAllister TW. Neurobehavioral sequelae of traumatic brain injury: evaluation and management. World Psychiatry. 2008;7(1):3-10. doi:10.1002/j.2051-5545.2008.tb00139.x
13. Bommakanti K, Gaddamanugu P, Alladi S, et al. Pre-operative and post-operative psychiatric manifestations in patients with supratentorial meningiomas. Clin Neurol Neurosurg. 2016;147:24-29. doi:10.1016/j.clineuro.2016.05.018
14. Devinsky O, Barr WB, Vickrey BG, et al. Changes in depression and anxiety after resective surgery for epilepsy. Neurology. 2005;65(11):1744-1749. doi:10.1212/01.wnl.0000187114.71524.c3
15. Blumer D, Wakhlu S, Davies K, et al. Psychiatric outcome of temporal lobectomy for epilepsy: incidence and treatment of psychiatric complications. Epilepsia. 1998;39(5):478-486. doi:10.1111/j.1528-1157.1998.tb01409.x
16. Glosser G, Zwil AS, Glosser DS, et al. Psychiatric aspects of temporal lobe epilepsy before and after anterior temporal lobectomy. J Neurol Neurosurg Psychiatry. 2000;68(1):53-58. doi:10.1136/jnnp.68.1.53
CASE Depressed and anxious
Five years ago, Ms. X, age 60, was diagnosed with treatment-resistant major depressive disorder (MDD) with anxiety. This diagnosis was established by a previous psychiatrist. She presents to a clinic for a second opinion.
Since her diagnosis, Ms. X has experienced sad mood, anhedonia, difficulty falling asleep, increased appetite and weight, and decreased concentration and attention. Her anxiety stems from her inability to work, which causes her to worry about her children. In the clinic, the treatment team conducts the Patient Health Questionnaire-9 (PHQ-9) and Generalized Anxiety Disorder-7 item scale (GAD-7) with Ms. X. She scores 16 on the PHQ-9, indicating moderately severe depression, and scores 12 on the GAD-7, indicating moderate anxiety.
Ms. X’s current medication regimen consists of venlafaxine extended-release (XR) 225 mg/d, trazodone 100 mg/d at bedtime, and clonazepam 1 mg twice daily. She reports no significant improvement of her symptoms from these medications. Additionally, Ms. X reports that in the past she had been prescribed fluoxetine, citalopram, and duloxetine, but she cannot recall the dosages.
Ms. X appears appropriately groomed, maintains appropriate eye contact, has clear speech, and does not show evidence of internal stimulation; however, she has difficulty following instructions. She makes negative comments about herself such as “I’m worthless” and “Nobody cares about me.” The treatment team decides to taper Ms. X off venlafaxine XR and initiates sertraline 50 mg/d, while continuing trazodone 50 mg/d at bedtime and clonazepam 1 mg twice daily. The team refers her for cognitive-behavioral therapy (CBT) to address her cognitive distortions, sad mood, and anxiety. Ms. X is asked to follow up with Psychiatry in 1 week.
EVALUATION Unusual behavior
At her CBT intake, Ms. X endorses depression and anxiety. Her PHQ-9 score at this visit is 19 (moderately severe depression) and GAD-7 score is 16 (severe anxiety). The psychologist notes that Ms. X is able to complete activities of daily living and instrumental activities of daily living without assistance. Ms. X denies any use of illicit substances or alcohol. No gross memory impairment is noted during this appointment, though Ms. X exhibits unusual behavior, including exiting and re-entering the clinic multiple times to repeatedly ask about follow-up appointments. The psychologist concludes that Ms. X’s presentation and behavior can be explained by MDD and pseudodementia.
[polldaddy:12189562]
The authors’ observations
Pseudodementia gained recognition in clinical research >100 years ago.1 Officially coined by Kiloh in 1961, the term was used broadly to categorize psychiatric cases that present like dementia but are the result of reversible causes. More recently, it has been used to describe older adults who present with cognitive deficits in the context of depressive symptoms.2 The goal of evaluation is to determine if the primary issue is a cognitive disorder or a depressive episode. DSM-5-TR does not classify pseudodementia as a distinct diagnosis, but instead categorizes its symptoms as components under other major diagnostic categories. Patients can present with MDD and associated cognitive symptoms, or with a cognitive disorder with depressive symptoms, which would be diagnosed as a cognitive disorder with a major depressive-like episode.3
Pseudodementia is rare. Brodaty et al4 found the prevalence of pseudodementia in primary care settings was 0.6%. Older adults (age >65) who live alone are at increased risk of developing pseudodementia, which can be worsened by poor social support and acute psychosocial and environmental changes.5 A key characteristic of this disorder is that as the patient’s depressed mood improves, their memory and cognition also improve.6 Table 13,6 outlines overlapping features of MDD and pseudodementia.
Continue to: EVALUATION Worsening depression
EVALUATION Worsening depression
At her Psychiatry follow-up appointment, Ms. X reports that her mood is worse since she ended the relationship with her partner and she feels anxious because the partner was financially supporting her. Her PHQ-9 score is 24 (severe depression) and her GAD-7 score is 12 (moderate anxiety). Ms. X reports tolerating her transition from venlafaxine XR 225 mg/d to sertraline 50 mg/d well.
Additionally, Ms. X reports her children have called her “useless” since she continues to have difficulties following through on household tasks, even though she has no physical impairments that prevent her from completing them. The Psychiatry team observes that Ms. X has no problems walking or moving her arms or legs.
The Psychiatry team administers the Montreal Cognitive Assessment (MoCA). Ms. X scores 22, indicating mild impairment.
The team recommends a neuropsychological assessment to determine if this MoCA score is due to a cognitive disorder or is rooted in her mood symptoms. The team also recommends an MRI of the brain, complete blood count (CBC), comprehensive metabolic panel (CMP), and urinalysis (UA).
[polldaddy:12189567]
Continue to: The authors' observations
The authors’ observations
Neuropsychological assessments are important tools for exploring the behavioral manifestations of brain dysfunction (Table 2).7 These assessments factor in elements of neurology, psychiatry, and psychology to provide information about the diagnosis, prognosis, and functional status of patients with medical conditions, especially those with neurocognitive and psychiatric disorders. They combine information from the patient and collateral interviews, behavioral observations, a review of patient records, and objective tests of motor, emotional, and cognitive function.
Among other uses, neuropsychological assessments can help identify depression in patients with neurologic impairment, determine the diagnosis and plan of care for patients with concussions, determine the risk of a motor vehicle crash in patients with cognitive impairment, and distinguish Alzheimer disease from vascular dementia.8 Components of such assessments include the Beck Anxiety Inventory (BAI) to assess anxiety, the Dementia Rating Scale-2 and Neuropsychological Assessment Battery-Screening Module to assess dementia, and the Beck Depression Inventory (BDI) to assess depression.9
EVALUATION Continued cognitive decline
A different psychologist performs the neuropsychological assessment, who conducts the Repeatable Battery for the Assessment of Neuropsychological Status Update to determine if Ms. X is experiencing cognitive impairment. Her immediate memory, visuospatial/constructions, language, attention, and delayed memory are significantly impaired for someone her age. The psychologist also administers the Wechsler Adult Intelligence Scale IV and finds Ms. X’s general cognitive ability is within the low average range of intellectual functioning as measured by Full-Scale IQ. Ms. X scores 29 on the BDI-II, indicating significant depressive symptoms, and 13 on the BAI, indicating mild anxiety symptoms.
Ms. X is diagnosed with MDD and an unspecified neurocognitive disorder. The psychologist recommends she start CBT to address her mood and anxiety symptoms.
Upon reviewing the results with Ms. X, the treatment team again recommends a brain MRI, CBC, CMP, and UA to rule out organic causes of her cognitive decline. Ms. X decides against the MRI and laboratory workup and elects to continue her present medication regimen and CBT.
Several weeks later, Ms. X’s family brings her to the emergency department (ED) for evaluation of worsening mood, decreased personal hygiene, increased irritability, and further cognitive decline. They report she is having an increasingly difficult time remembering things such as where she parked her car. The ED team decides to discontinue clonazepam but continues sertraline and trazodone.
Continue to: CBC, CMP, and UA...
CBC, CMP, and UA are unremarkable. Ms. X undergoes a brain CT scan without contrast, which reveals hyperdense lesions in the inferior left tentorium, posterior fossa. A subsequent brain MRI with contrast reveals a dural-based enhancing mass, inferior to the left tentorium, in the left posterior fossa measuring 2.2 cm x 2.1 cm, suggestive of a meningioma. The team orders a Neurosurgery consult.
[polldaddy:12189571]
The authors’ observations
While most brain tumors are secondary to metastasis, meningiomas are the most common primary CNS tumor. Typically, they are asymptomatic; their diagnosis is often delayed until the patient presents with psychiatric symptoms without any focal neurologic findings. The frontal lobe is the most common location of meningioma. Data from 48 case reports of patients with meningiomas and psychiatric symptoms suggest symptoms do not always correlate with specific brain regions.10,11
Indications for neuroimaging in cases such as Ms. X include an abrupt change in behavior or personality, lack of response to psychiatric treatment, presence of focal neurologic signs, and an unusual psychiatric presentation and development of symptoms.11
TREATMENT Neurosurgery
Neurosurgery recommends and performs a suboccipital craniotomy for biopsy and resection. Ms. X tolerates the procedure well. A meningioma is found in the posterior fossa, near the cerebellar convexity. A biopsy finds no evidence of malignancies.
At her postoperative follow-up appointment several days after the procedure, Ms. X reports new-onset hearing loss and tinnitus.
[polldaddy:12189747]
Continue to: The authors' observations
The authors’ observations
Patients who require neurosurgery typically already carry a heavy psychiatric burden, which makes it challenging to determine the exact psychiatric consequences of neurosurgery.12-14 For example, research shows that temporal lobe resection and temporal lobectomy for treatment-resistant epilepsy can lead to an exacerbation of baseline psychiatric symptoms and the development of new symptoms (31% to 34%).15,16 However, Bommakanti et al13 found no new psychiatric symptoms after resection of meningiomas, and surgery seemed to play a role in ameliorating psychiatric symptoms in patients with intracranial tumors. Research attempting to document the psychiatric sequelae of neurosurgery has had mixed results, and it is difficult to determine what effects brain surgery has on mental health.
OUTCOME Minimal improvement
Several weeks after neurosurgery, Ms. X and her family report her mood is improved. Her PHQ-9 score improves to 15, but her GAD-7 score increases to 13, 1 point above her previous score.
The treatment team recommends Ms. X continue taking sertraline 50 mg/d and trazodone 50 mg/d at bedtime. Ms. X’s family reports her cognition and memory have not improved; her MoCA score increases by 1 point to 23. The treatment team discusses with Ms. X and her family the possibility that her cognitive problems maybe better explained as a neurocognitive disorder rather than as a result of the meningioma, since her MoCA score has not significantly improved. Ms. X and her family decide to seek a second opinion from a neurologist.
Bottom Line
Pseudodementia is a term used to describe older adults who present with cognitive issues in the context of depressive symptoms. Even in the absence of focal findings, neuroimaging should be considered as part of the workup in patients who continue to experience a progressive decline in mood and cognitive function.
Related Resources
- Moller MD, Parmenter BA, Lane DW. Neuropsychological testing: a useful but underutilized resource. Current Psychiatry. 2019;18(11):40-46,51.
- Pollak J. Psychological/neuropsychological testing: when to refer for reexamination. Current Psychiatry. 2021;20(9):18- 19,30-31,37. doi:10.12788/cp.0157
Drug Brand Names
Citalopram • Celexa
Clonazepam • Klonopin
Duloxetine • Cymbalta
Fluoxetine • Prozac
Sertraline • Zoloft
Trazodone • Oleptro
Venlafaxine extended- release • Effexor XR
CASE Depressed and anxious
Five years ago, Ms. X, age 60, was diagnosed with treatment-resistant major depressive disorder (MDD) with anxiety. This diagnosis was established by a previous psychiatrist. She presents to a clinic for a second opinion.
Since her diagnosis, Ms. X has experienced sad mood, anhedonia, difficulty falling asleep, increased appetite and weight, and decreased concentration and attention. Her anxiety stems from her inability to work, which causes her to worry about her children. In the clinic, the treatment team conducts the Patient Health Questionnaire-9 (PHQ-9) and Generalized Anxiety Disorder-7 item scale (GAD-7) with Ms. X. She scores 16 on the PHQ-9, indicating moderately severe depression, and scores 12 on the GAD-7, indicating moderate anxiety.
Ms. X’s current medication regimen consists of venlafaxine extended-release (XR) 225 mg/d, trazodone 100 mg/d at bedtime, and clonazepam 1 mg twice daily. She reports no significant improvement of her symptoms from these medications. Additionally, Ms. X reports that in the past she had been prescribed fluoxetine, citalopram, and duloxetine, but she cannot recall the dosages.
Ms. X appears appropriately groomed, maintains appropriate eye contact, has clear speech, and does not show evidence of internal stimulation; however, she has difficulty following instructions. She makes negative comments about herself such as “I’m worthless” and “Nobody cares about me.” The treatment team decides to taper Ms. X off venlafaxine XR and initiates sertraline 50 mg/d, while continuing trazodone 50 mg/d at bedtime and clonazepam 1 mg twice daily. The team refers her for cognitive-behavioral therapy (CBT) to address her cognitive distortions, sad mood, and anxiety. Ms. X is asked to follow up with Psychiatry in 1 week.
EVALUATION Unusual behavior
At her CBT intake, Ms. X endorses depression and anxiety. Her PHQ-9 score at this visit is 19 (moderately severe depression) and GAD-7 score is 16 (severe anxiety). The psychologist notes that Ms. X is able to complete activities of daily living and instrumental activities of daily living without assistance. Ms. X denies any use of illicit substances or alcohol. No gross memory impairment is noted during this appointment, though Ms. X exhibits unusual behavior, including exiting and re-entering the clinic multiple times to repeatedly ask about follow-up appointments. The psychologist concludes that Ms. X’s presentation and behavior can be explained by MDD and pseudodementia.
[polldaddy:12189562]
The authors’ observations
Pseudodementia gained recognition in clinical research >100 years ago.1 Officially coined by Kiloh in 1961, the term was used broadly to categorize psychiatric cases that present like dementia but are the result of reversible causes. More recently, it has been used to describe older adults who present with cognitive deficits in the context of depressive symptoms.2 The goal of evaluation is to determine if the primary issue is a cognitive disorder or a depressive episode. DSM-5-TR does not classify pseudodementia as a distinct diagnosis, but instead categorizes its symptoms as components under other major diagnostic categories. Patients can present with MDD and associated cognitive symptoms, or with a cognitive disorder with depressive symptoms, which would be diagnosed as a cognitive disorder with a major depressive-like episode.3
Pseudodementia is rare. Brodaty et al4 found the prevalence of pseudodementia in primary care settings was 0.6%. Older adults (age >65) who live alone are at increased risk of developing pseudodementia, which can be worsened by poor social support and acute psychosocial and environmental changes.5 A key characteristic of this disorder is that as the patient’s depressed mood improves, their memory and cognition also improve.6 Table 13,6 outlines overlapping features of MDD and pseudodementia.
Continue to: EVALUATION Worsening depression
EVALUATION Worsening depression
At her Psychiatry follow-up appointment, Ms. X reports that her mood is worse since she ended the relationship with her partner and she feels anxious because the partner was financially supporting her. Her PHQ-9 score is 24 (severe depression) and her GAD-7 score is 12 (moderate anxiety). Ms. X reports tolerating her transition from venlafaxine XR 225 mg/d to sertraline 50 mg/d well.
Additionally, Ms. X reports her children have called her “useless” since she continues to have difficulties following through on household tasks, even though she has no physical impairments that prevent her from completing them. The Psychiatry team observes that Ms. X has no problems walking or moving her arms or legs.
The Psychiatry team administers the Montreal Cognitive Assessment (MoCA). Ms. X scores 22, indicating mild impairment.
The team recommends a neuropsychological assessment to determine if this MoCA score is due to a cognitive disorder or is rooted in her mood symptoms. The team also recommends an MRI of the brain, complete blood count (CBC), comprehensive metabolic panel (CMP), and urinalysis (UA).
[polldaddy:12189567]
Continue to: The authors' observations
The authors’ observations
Neuropsychological assessments are important tools for exploring the behavioral manifestations of brain dysfunction (Table 2).7 These assessments factor in elements of neurology, psychiatry, and psychology to provide information about the diagnosis, prognosis, and functional status of patients with medical conditions, especially those with neurocognitive and psychiatric disorders. They combine information from the patient and collateral interviews, behavioral observations, a review of patient records, and objective tests of motor, emotional, and cognitive function.
Among other uses, neuropsychological assessments can help identify depression in patients with neurologic impairment, determine the diagnosis and plan of care for patients with concussions, determine the risk of a motor vehicle crash in patients with cognitive impairment, and distinguish Alzheimer disease from vascular dementia.8 Components of such assessments include the Beck Anxiety Inventory (BAI) to assess anxiety, the Dementia Rating Scale-2 and Neuropsychological Assessment Battery-Screening Module to assess dementia, and the Beck Depression Inventory (BDI) to assess depression.9
EVALUATION Continued cognitive decline
A different psychologist performs the neuropsychological assessment, who conducts the Repeatable Battery for the Assessment of Neuropsychological Status Update to determine if Ms. X is experiencing cognitive impairment. Her immediate memory, visuospatial/constructions, language, attention, and delayed memory are significantly impaired for someone her age. The psychologist also administers the Wechsler Adult Intelligence Scale IV and finds Ms. X’s general cognitive ability is within the low average range of intellectual functioning as measured by Full-Scale IQ. Ms. X scores 29 on the BDI-II, indicating significant depressive symptoms, and 13 on the BAI, indicating mild anxiety symptoms.
Ms. X is diagnosed with MDD and an unspecified neurocognitive disorder. The psychologist recommends she start CBT to address her mood and anxiety symptoms.
Upon reviewing the results with Ms. X, the treatment team again recommends a brain MRI, CBC, CMP, and UA to rule out organic causes of her cognitive decline. Ms. X decides against the MRI and laboratory workup and elects to continue her present medication regimen and CBT.
Several weeks later, Ms. X’s family brings her to the emergency department (ED) for evaluation of worsening mood, decreased personal hygiene, increased irritability, and further cognitive decline. They report she is having an increasingly difficult time remembering things such as where she parked her car. The ED team decides to discontinue clonazepam but continues sertraline and trazodone.
Continue to: CBC, CMP, and UA...
CBC, CMP, and UA are unremarkable. Ms. X undergoes a brain CT scan without contrast, which reveals hyperdense lesions in the inferior left tentorium, posterior fossa. A subsequent brain MRI with contrast reveals a dural-based enhancing mass, inferior to the left tentorium, in the left posterior fossa measuring 2.2 cm x 2.1 cm, suggestive of a meningioma. The team orders a Neurosurgery consult.
[polldaddy:12189571]
The authors’ observations
While most brain tumors are secondary to metastasis, meningiomas are the most common primary CNS tumor. Typically, they are asymptomatic; their diagnosis is often delayed until the patient presents with psychiatric symptoms without any focal neurologic findings. The frontal lobe is the most common location of meningioma. Data from 48 case reports of patients with meningiomas and psychiatric symptoms suggest symptoms do not always correlate with specific brain regions.10,11
Indications for neuroimaging in cases such as Ms. X include an abrupt change in behavior or personality, lack of response to psychiatric treatment, presence of focal neurologic signs, and an unusual psychiatric presentation and development of symptoms.11
TREATMENT Neurosurgery
Neurosurgery recommends and performs a suboccipital craniotomy for biopsy and resection. Ms. X tolerates the procedure well. A meningioma is found in the posterior fossa, near the cerebellar convexity. A biopsy finds no evidence of malignancies.
At her postoperative follow-up appointment several days after the procedure, Ms. X reports new-onset hearing loss and tinnitus.
[polldaddy:12189747]
Continue to: The authors' observations
The authors’ observations
Patients who require neurosurgery typically already carry a heavy psychiatric burden, which makes it challenging to determine the exact psychiatric consequences of neurosurgery.12-14 For example, research shows that temporal lobe resection and temporal lobectomy for treatment-resistant epilepsy can lead to an exacerbation of baseline psychiatric symptoms and the development of new symptoms (31% to 34%).15,16 However, Bommakanti et al13 found no new psychiatric symptoms after resection of meningiomas, and surgery seemed to play a role in ameliorating psychiatric symptoms in patients with intracranial tumors. Research attempting to document the psychiatric sequelae of neurosurgery has had mixed results, and it is difficult to determine what effects brain surgery has on mental health.
OUTCOME Minimal improvement
Several weeks after neurosurgery, Ms. X and her family report her mood is improved. Her PHQ-9 score improves to 15, but her GAD-7 score increases to 13, 1 point above her previous score.
The treatment team recommends Ms. X continue taking sertraline 50 mg/d and trazodone 50 mg/d at bedtime. Ms. X’s family reports her cognition and memory have not improved; her MoCA score increases by 1 point to 23. The treatment team discusses with Ms. X and her family the possibility that her cognitive problems maybe better explained as a neurocognitive disorder rather than as a result of the meningioma, since her MoCA score has not significantly improved. Ms. X and her family decide to seek a second opinion from a neurologist.
Bottom Line
Pseudodementia is a term used to describe older adults who present with cognitive issues in the context of depressive symptoms. Even in the absence of focal findings, neuroimaging should be considered as part of the workup in patients who continue to experience a progressive decline in mood and cognitive function.
Related Resources
- Moller MD, Parmenter BA, Lane DW. Neuropsychological testing: a useful but underutilized resource. Current Psychiatry. 2019;18(11):40-46,51.
- Pollak J. Psychological/neuropsychological testing: when to refer for reexamination. Current Psychiatry. 2021;20(9):18- 19,30-31,37. doi:10.12788/cp.0157
Drug Brand Names
Citalopram • Celexa
Clonazepam • Klonopin
Duloxetine • Cymbalta
Fluoxetine • Prozac
Sertraline • Zoloft
Trazodone • Oleptro
Venlafaxine extended- release • Effexor XR
1. Nussbaum PD. (1994). Pseudodementia: a slow death. Neuropsychol Rev. 1994;4(2):71-90. doi:10.1007/BF01874829
2. Kang H, Zhao F, You L, et al. (2014). Pseudo-dementia: a neuropsychological review. Ann Indian Acad Neurol. 17(2):147-154. doi:10.4103/0972-2327.132613
3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed, text revision. American Psychiatric Association; 2022.
4. Brodaty H, Connors MH. Pseudodementia, pseudo-pseudodementia, and pseudodepression. Alzheimers Dement (Amst). 2020;12(1):e12027. doi:10.1002/dad2.12027
5. Sekhon S, Marwaha R. Depressive Cognitive Disorders. StatPearls Publishing; 2022. https://www.ncbi.nlm.nih.gov/books/NBK559256/
6. Brown WA. Pseudodementia: issues in diagnosis. Psychiatric Times. April 9, 2005. Accessed February 3, 2023. www.psychiatrictimes.com/view/pseudodementia-issues-diagnosis
7. Kulas JF, Naugle RI. (2003). Indications for neuropsychological assessment. Cleve Clin J Med. 2003;70(9):785-792.
8. Braun M, Tupper D, Kaufmann P, et al. Neuropsychological assessment: a valuable tool in the diagnosis and management of neurological, neurodevelopmental, medical, and psychiatric disorders. Cogn Behav Neurol. 2011;24(3):107-114.
9. Michels TC, Tiu AY, Graver CJ. Neuropsychological evaluation in primary care. Am Fam Physician. 2010;82(5):495-502.
10. Wiemels J, Wrensch M, Claus EB. Epidemiology and etiology of meningioma. J Neurooncol. 2010;99(3):307-314. doi:10.1007/s11060-010-0386-3
11. Gyawali S, Sharma P, Mahapatra A. Meningioma and psychiatric symptoms: an individual patient data analysis. Asian J Psychiatr. 2019;42:94-103. doi:10.1016/j.ajp.2019.03.029
12. McAllister TW. Neurobehavioral sequelae of traumatic brain injury: evaluation and management. World Psychiatry. 2008;7(1):3-10. doi:10.1002/j.2051-5545.2008.tb00139.x
13. Bommakanti K, Gaddamanugu P, Alladi S, et al. Pre-operative and post-operative psychiatric manifestations in patients with supratentorial meningiomas. Clin Neurol Neurosurg. 2016;147:24-29. doi:10.1016/j.clineuro.2016.05.018
14. Devinsky O, Barr WB, Vickrey BG, et al. Changes in depression and anxiety after resective surgery for epilepsy. Neurology. 2005;65(11):1744-1749. doi:10.1212/01.wnl.0000187114.71524.c3
15. Blumer D, Wakhlu S, Davies K, et al. Psychiatric outcome of temporal lobectomy for epilepsy: incidence and treatment of psychiatric complications. Epilepsia. 1998;39(5):478-486. doi:10.1111/j.1528-1157.1998.tb01409.x
16. Glosser G, Zwil AS, Glosser DS, et al. Psychiatric aspects of temporal lobe epilepsy before and after anterior temporal lobectomy. J Neurol Neurosurg Psychiatry. 2000;68(1):53-58. doi:10.1136/jnnp.68.1.53
1. Nussbaum PD. (1994). Pseudodementia: a slow death. Neuropsychol Rev. 1994;4(2):71-90. doi:10.1007/BF01874829
2. Kang H, Zhao F, You L, et al. (2014). Pseudo-dementia: a neuropsychological review. Ann Indian Acad Neurol. 17(2):147-154. doi:10.4103/0972-2327.132613
3. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed, text revision. American Psychiatric Association; 2022.
4. Brodaty H, Connors MH. Pseudodementia, pseudo-pseudodementia, and pseudodepression. Alzheimers Dement (Amst). 2020;12(1):e12027. doi:10.1002/dad2.12027
5. Sekhon S, Marwaha R. Depressive Cognitive Disorders. StatPearls Publishing; 2022. https://www.ncbi.nlm.nih.gov/books/NBK559256/
6. Brown WA. Pseudodementia: issues in diagnosis. Psychiatric Times. April 9, 2005. Accessed February 3, 2023. www.psychiatrictimes.com/view/pseudodementia-issues-diagnosis
7. Kulas JF, Naugle RI. (2003). Indications for neuropsychological assessment. Cleve Clin J Med. 2003;70(9):785-792.
8. Braun M, Tupper D, Kaufmann P, et al. Neuropsychological assessment: a valuable tool in the diagnosis and management of neurological, neurodevelopmental, medical, and psychiatric disorders. Cogn Behav Neurol. 2011;24(3):107-114.
9. Michels TC, Tiu AY, Graver CJ. Neuropsychological evaluation in primary care. Am Fam Physician. 2010;82(5):495-502.
10. Wiemels J, Wrensch M, Claus EB. Epidemiology and etiology of meningioma. J Neurooncol. 2010;99(3):307-314. doi:10.1007/s11060-010-0386-3
11. Gyawali S, Sharma P, Mahapatra A. Meningioma and psychiatric symptoms: an individual patient data analysis. Asian J Psychiatr. 2019;42:94-103. doi:10.1016/j.ajp.2019.03.029
12. McAllister TW. Neurobehavioral sequelae of traumatic brain injury: evaluation and management. World Psychiatry. 2008;7(1):3-10. doi:10.1002/j.2051-5545.2008.tb00139.x
13. Bommakanti K, Gaddamanugu P, Alladi S, et al. Pre-operative and post-operative psychiatric manifestations in patients with supratentorial meningiomas. Clin Neurol Neurosurg. 2016;147:24-29. doi:10.1016/j.clineuro.2016.05.018
14. Devinsky O, Barr WB, Vickrey BG, et al. Changes in depression and anxiety after resective surgery for epilepsy. Neurology. 2005;65(11):1744-1749. doi:10.1212/01.wnl.0000187114.71524.c3
15. Blumer D, Wakhlu S, Davies K, et al. Psychiatric outcome of temporal lobectomy for epilepsy: incidence and treatment of psychiatric complications. Epilepsia. 1998;39(5):478-486. doi:10.1111/j.1528-1157.1998.tb01409.x
16. Glosser G, Zwil AS, Glosser DS, et al. Psychiatric aspects of temporal lobe epilepsy before and after anterior temporal lobectomy. J Neurol Neurosurg Psychiatry. 2000;68(1):53-58. doi:10.1136/jnnp.68.1.53
Disrupted gut microbiome a key driver of major depression?
Investigators found that MDD had specific metabolic “signatures” consisting of 124 metabolites that spanned energy and lipid pathways, with some involving the tricarboxylic acid cycle in particular. These changes in metabolites were consistent with differences in composition of several gut microbiota.
The researchers found that fatty acids and intermediate and very large lipoproteins changed in association with the depressive disease process. However, high-density lipoproteins and metabolites in the tricarboxylic acid cycle did not.
“As we wait to establish causal influences through clinical trials, clinicians should advise patients suffering from mood disorders to modify their diet by increasing the intake of fresh fruits, vegetables, and whole grains, as these provide the required fuel/fiber to the gut microbiota for their enrichment, and more short-chain fatty acids are produced for the optimal functioning of the body,” study investigator Najaf Amin, PhD, DSc, senior researcher, Nuffield Department of Population Health, Oxford University, England, told this news organization.
“At the same time, patients should be advised to minimize the intake of sugars and processed foods, which are known to have an inverse impact on the gut microbiome and are associated with higher inflammation,” she said.
The study was published online in JAMA Psychiatry.
MDD poorly understood
Although most antidepressants target the monoamine pathway, “evidence is increasing for a more complex interplay of multiple pathways involving a wide range of metabolic alterations spanning energy and lipid metabolism,” the authors wrote.
Previous research using the Nightingale proton nuclear magnetic resonance (NMR) metabolomics platform showed a “shift” toward decreased levels of high-density lipoproteins (HDLs) and increased levels of very low-density lipoproteins (VLDLs) and triglycerides among patients with depression.
The gut microbiome, which is primarily modulated by diet, “has been shown to be a major determinant of circulating lipids, specifically triglycerides and HDLs, and to regulate mitochondrial function,” the investigators noted. Patients with MDD are known to have disruptions in the gut microbiome.
The gut microbiome may “explain part of the shift in VLDL and HDL levels observed in patients with depression and if the metabolic signatures of the disease based on Nightingale metabolites can be used as a tool to infer the association between gut microbiome and depression.”
Dr. Amin called depression “one of the most poorly understood diseases, as underlying mechanisms remain elusive.”
Large-scale genetic studies “have shown that the contribution of genetics to depression is modest,” she continued. On the other hand, initial animal studies suggest the gut microbiome “may potentially have a causal influence on depression.”
Several studies have evaluated the influence of gut microbiome on depression, “but, due to small sample sizes and inadequate control for confounding factors, most of their findings were not reproducible.”
Harnessing the power of the UK Biobank, the investigators studied 58,257 individuals who were between the ages of 37 and 73 years at recruitment. They used data on NMR spectroscopy–based plasma metabolites in depression. Individuals who didn’t report depression at baseline served as controls.
Logistic regression analysis was used to test the association of metabolite levels with depression in four models, each with an increasing number of covariates.
To identify patterns of correlation in the “metabolic signatures of MDD and the human gut biome,” they regressed the metabolic signatures of MDD on the metabolic signatures of the gut microbiota and then regressed the metabolic signature of gut microbiota on the metabolic signatures of MDD.
Bidirectional 2-sample Mendelian randomization was used to ascertain the direction of the association observed between metabolites and MDD.
Individuals with lifetime and recurrent MDD were compared with controls (6,811 vs. 51,446 and 4,370 vs. 62,508, respectively).
Participants with lifetime MDD were significantly younger (median [IQR] age, 56 [49-62] years vs. 58 [51-64] years) and were more likely to be female in comparison with controls (54% vs. 35%).
‘Novel findings’
In the fully adjusted analysis, metabolic signatures of MDD were found to consist of 124 metabolites that spanned energy and lipid metabolism pathways.
The investigators noted that these “novel findings” included 49 metabolites encompassing those involved in the tricarboxylic acid cycle – citrate and pyruvate.
The findings revealed that fatty acids and intermediate and VLDL changed in association with the disease process. On the other hand, HDL and the metabolites in the tricarboxylic acid cycle did not.
“We observed that the genera Sellimonas, Eggerthella, Hungatella, and Lachnoclostridium were more abundant, while genera Ruminococcaceae ... Coprococcus, Lachnospiraceae ... Eubacterium ventriosum, Subdoligranulum, and family Ruminococcaceae were depleted in the guts of individuals with more symptoms of depression,” said Dr. Amin. “Of these, genus Eggerthella showed statistical evidence of being involved in the causal pathway.”
These microbes are involved in the synthesis of important neurotransmitters, such as gamma aminobutyric acid, butyrate, glutamate, and serotonin, she noted.
Butyrate produced by the gut can cross the blood-brain barrier, enter the brain, and affect transcriptional and translational activity or be used by the cells for generating energy, she added. “So basically, butyrate can influence depression through several routes – i.e., via immune regulation, genomic transcript/translation, and/or affecting energy metabolism.”
No causality
Commenting on the study, Emeran Mayer, MD, distinguished research professor of medicine, G. Oppenheimer Center for Neurobiology of Stress and Resilience and UCLA Brain Gut Microbiome Center, called it the “largest, most comprehensive and best validated association study to date providing further evidence for an association between gut microbial taxa, previously identified in patients with MDD, blood metabolites (generated by host and by microbes) and questionnaire data.”
However, “despite its strengths, the study does not allow [us] to identify a causal role of the microbiome alterations in the observed microbial and metabolic changes (fatty acids, Krebs cycle components),” cautioned Dr. Mayer, who was not involved with the study.
Moreover, “causality of gut microbial changes on the behavioral phenotype of depression cannot been inferred,” he concluded.
Metabolomics data were provided by the Alzheimer’s Disease Metabolomics Consortium. The study was funded wholly or in part by grants from the National Institute on Aging and Foundation for the National Institutes of Health. It was further supported by a grant from ZonMW Memorabel. Dr. Amin reports no relevant financial relationships. The other authors’ disclosures are listed oin the original article. Dr. Mayer is a scientific advisory board member of Danone, Axial Therapeutics, Viome, Amare, Mahana Therapeutics, Pendulum, Bloom Biosciences, and APC Microbiome Ireland.
A version of this article originally appeared on Medscape.com.
Investigators found that MDD had specific metabolic “signatures” consisting of 124 metabolites that spanned energy and lipid pathways, with some involving the tricarboxylic acid cycle in particular. These changes in metabolites were consistent with differences in composition of several gut microbiota.
The researchers found that fatty acids and intermediate and very large lipoproteins changed in association with the depressive disease process. However, high-density lipoproteins and metabolites in the tricarboxylic acid cycle did not.
“As we wait to establish causal influences through clinical trials, clinicians should advise patients suffering from mood disorders to modify their diet by increasing the intake of fresh fruits, vegetables, and whole grains, as these provide the required fuel/fiber to the gut microbiota for their enrichment, and more short-chain fatty acids are produced for the optimal functioning of the body,” study investigator Najaf Amin, PhD, DSc, senior researcher, Nuffield Department of Population Health, Oxford University, England, told this news organization.
“At the same time, patients should be advised to minimize the intake of sugars and processed foods, which are known to have an inverse impact on the gut microbiome and are associated with higher inflammation,” she said.
The study was published online in JAMA Psychiatry.
MDD poorly understood
Although most antidepressants target the monoamine pathway, “evidence is increasing for a more complex interplay of multiple pathways involving a wide range of metabolic alterations spanning energy and lipid metabolism,” the authors wrote.
Previous research using the Nightingale proton nuclear magnetic resonance (NMR) metabolomics platform showed a “shift” toward decreased levels of high-density lipoproteins (HDLs) and increased levels of very low-density lipoproteins (VLDLs) and triglycerides among patients with depression.
The gut microbiome, which is primarily modulated by diet, “has been shown to be a major determinant of circulating lipids, specifically triglycerides and HDLs, and to regulate mitochondrial function,” the investigators noted. Patients with MDD are known to have disruptions in the gut microbiome.
The gut microbiome may “explain part of the shift in VLDL and HDL levels observed in patients with depression and if the metabolic signatures of the disease based on Nightingale metabolites can be used as a tool to infer the association between gut microbiome and depression.”
Dr. Amin called depression “one of the most poorly understood diseases, as underlying mechanisms remain elusive.”
Large-scale genetic studies “have shown that the contribution of genetics to depression is modest,” she continued. On the other hand, initial animal studies suggest the gut microbiome “may potentially have a causal influence on depression.”
Several studies have evaluated the influence of gut microbiome on depression, “but, due to small sample sizes and inadequate control for confounding factors, most of their findings were not reproducible.”
Harnessing the power of the UK Biobank, the investigators studied 58,257 individuals who were between the ages of 37 and 73 years at recruitment. They used data on NMR spectroscopy–based plasma metabolites in depression. Individuals who didn’t report depression at baseline served as controls.
Logistic regression analysis was used to test the association of metabolite levels with depression in four models, each with an increasing number of covariates.
To identify patterns of correlation in the “metabolic signatures of MDD and the human gut biome,” they regressed the metabolic signatures of MDD on the metabolic signatures of the gut microbiota and then regressed the metabolic signature of gut microbiota on the metabolic signatures of MDD.
Bidirectional 2-sample Mendelian randomization was used to ascertain the direction of the association observed between metabolites and MDD.
Individuals with lifetime and recurrent MDD were compared with controls (6,811 vs. 51,446 and 4,370 vs. 62,508, respectively).
Participants with lifetime MDD were significantly younger (median [IQR] age, 56 [49-62] years vs. 58 [51-64] years) and were more likely to be female in comparison with controls (54% vs. 35%).
‘Novel findings’
In the fully adjusted analysis, metabolic signatures of MDD were found to consist of 124 metabolites that spanned energy and lipid metabolism pathways.
The investigators noted that these “novel findings” included 49 metabolites encompassing those involved in the tricarboxylic acid cycle – citrate and pyruvate.
The findings revealed that fatty acids and intermediate and VLDL changed in association with the disease process. On the other hand, HDL and the metabolites in the tricarboxylic acid cycle did not.
“We observed that the genera Sellimonas, Eggerthella, Hungatella, and Lachnoclostridium were more abundant, while genera Ruminococcaceae ... Coprococcus, Lachnospiraceae ... Eubacterium ventriosum, Subdoligranulum, and family Ruminococcaceae were depleted in the guts of individuals with more symptoms of depression,” said Dr. Amin. “Of these, genus Eggerthella showed statistical evidence of being involved in the causal pathway.”
These microbes are involved in the synthesis of important neurotransmitters, such as gamma aminobutyric acid, butyrate, glutamate, and serotonin, she noted.
Butyrate produced by the gut can cross the blood-brain barrier, enter the brain, and affect transcriptional and translational activity or be used by the cells for generating energy, she added. “So basically, butyrate can influence depression through several routes – i.e., via immune regulation, genomic transcript/translation, and/or affecting energy metabolism.”
No causality
Commenting on the study, Emeran Mayer, MD, distinguished research professor of medicine, G. Oppenheimer Center for Neurobiology of Stress and Resilience and UCLA Brain Gut Microbiome Center, called it the “largest, most comprehensive and best validated association study to date providing further evidence for an association between gut microbial taxa, previously identified in patients with MDD, blood metabolites (generated by host and by microbes) and questionnaire data.”
However, “despite its strengths, the study does not allow [us] to identify a causal role of the microbiome alterations in the observed microbial and metabolic changes (fatty acids, Krebs cycle components),” cautioned Dr. Mayer, who was not involved with the study.
Moreover, “causality of gut microbial changes on the behavioral phenotype of depression cannot been inferred,” he concluded.
Metabolomics data were provided by the Alzheimer’s Disease Metabolomics Consortium. The study was funded wholly or in part by grants from the National Institute on Aging and Foundation for the National Institutes of Health. It was further supported by a grant from ZonMW Memorabel. Dr. Amin reports no relevant financial relationships. The other authors’ disclosures are listed oin the original article. Dr. Mayer is a scientific advisory board member of Danone, Axial Therapeutics, Viome, Amare, Mahana Therapeutics, Pendulum, Bloom Biosciences, and APC Microbiome Ireland.
A version of this article originally appeared on Medscape.com.
Investigators found that MDD had specific metabolic “signatures” consisting of 124 metabolites that spanned energy and lipid pathways, with some involving the tricarboxylic acid cycle in particular. These changes in metabolites were consistent with differences in composition of several gut microbiota.
The researchers found that fatty acids and intermediate and very large lipoproteins changed in association with the depressive disease process. However, high-density lipoproteins and metabolites in the tricarboxylic acid cycle did not.
“As we wait to establish causal influences through clinical trials, clinicians should advise patients suffering from mood disorders to modify their diet by increasing the intake of fresh fruits, vegetables, and whole grains, as these provide the required fuel/fiber to the gut microbiota for their enrichment, and more short-chain fatty acids are produced for the optimal functioning of the body,” study investigator Najaf Amin, PhD, DSc, senior researcher, Nuffield Department of Population Health, Oxford University, England, told this news organization.
“At the same time, patients should be advised to minimize the intake of sugars and processed foods, which are known to have an inverse impact on the gut microbiome and are associated with higher inflammation,” she said.
The study was published online in JAMA Psychiatry.
MDD poorly understood
Although most antidepressants target the monoamine pathway, “evidence is increasing for a more complex interplay of multiple pathways involving a wide range of metabolic alterations spanning energy and lipid metabolism,” the authors wrote.
Previous research using the Nightingale proton nuclear magnetic resonance (NMR) metabolomics platform showed a “shift” toward decreased levels of high-density lipoproteins (HDLs) and increased levels of very low-density lipoproteins (VLDLs) and triglycerides among patients with depression.
The gut microbiome, which is primarily modulated by diet, “has been shown to be a major determinant of circulating lipids, specifically triglycerides and HDLs, and to regulate mitochondrial function,” the investigators noted. Patients with MDD are known to have disruptions in the gut microbiome.
The gut microbiome may “explain part of the shift in VLDL and HDL levels observed in patients with depression and if the metabolic signatures of the disease based on Nightingale metabolites can be used as a tool to infer the association between gut microbiome and depression.”
Dr. Amin called depression “one of the most poorly understood diseases, as underlying mechanisms remain elusive.”
Large-scale genetic studies “have shown that the contribution of genetics to depression is modest,” she continued. On the other hand, initial animal studies suggest the gut microbiome “may potentially have a causal influence on depression.”
Several studies have evaluated the influence of gut microbiome on depression, “but, due to small sample sizes and inadequate control for confounding factors, most of their findings were not reproducible.”
Harnessing the power of the UK Biobank, the investigators studied 58,257 individuals who were between the ages of 37 and 73 years at recruitment. They used data on NMR spectroscopy–based plasma metabolites in depression. Individuals who didn’t report depression at baseline served as controls.
Logistic regression analysis was used to test the association of metabolite levels with depression in four models, each with an increasing number of covariates.
To identify patterns of correlation in the “metabolic signatures of MDD and the human gut biome,” they regressed the metabolic signatures of MDD on the metabolic signatures of the gut microbiota and then regressed the metabolic signature of gut microbiota on the metabolic signatures of MDD.
Bidirectional 2-sample Mendelian randomization was used to ascertain the direction of the association observed between metabolites and MDD.
Individuals with lifetime and recurrent MDD were compared with controls (6,811 vs. 51,446 and 4,370 vs. 62,508, respectively).
Participants with lifetime MDD were significantly younger (median [IQR] age, 56 [49-62] years vs. 58 [51-64] years) and were more likely to be female in comparison with controls (54% vs. 35%).
‘Novel findings’
In the fully adjusted analysis, metabolic signatures of MDD were found to consist of 124 metabolites that spanned energy and lipid metabolism pathways.
The investigators noted that these “novel findings” included 49 metabolites encompassing those involved in the tricarboxylic acid cycle – citrate and pyruvate.
The findings revealed that fatty acids and intermediate and VLDL changed in association with the disease process. On the other hand, HDL and the metabolites in the tricarboxylic acid cycle did not.
“We observed that the genera Sellimonas, Eggerthella, Hungatella, and Lachnoclostridium were more abundant, while genera Ruminococcaceae ... Coprococcus, Lachnospiraceae ... Eubacterium ventriosum, Subdoligranulum, and family Ruminococcaceae were depleted in the guts of individuals with more symptoms of depression,” said Dr. Amin. “Of these, genus Eggerthella showed statistical evidence of being involved in the causal pathway.”
These microbes are involved in the synthesis of important neurotransmitters, such as gamma aminobutyric acid, butyrate, glutamate, and serotonin, she noted.
Butyrate produced by the gut can cross the blood-brain barrier, enter the brain, and affect transcriptional and translational activity or be used by the cells for generating energy, she added. “So basically, butyrate can influence depression through several routes – i.e., via immune regulation, genomic transcript/translation, and/or affecting energy metabolism.”
No causality
Commenting on the study, Emeran Mayer, MD, distinguished research professor of medicine, G. Oppenheimer Center for Neurobiology of Stress and Resilience and UCLA Brain Gut Microbiome Center, called it the “largest, most comprehensive and best validated association study to date providing further evidence for an association between gut microbial taxa, previously identified in patients with MDD, blood metabolites (generated by host and by microbes) and questionnaire data.”
However, “despite its strengths, the study does not allow [us] to identify a causal role of the microbiome alterations in the observed microbial and metabolic changes (fatty acids, Krebs cycle components),” cautioned Dr. Mayer, who was not involved with the study.
Moreover, “causality of gut microbial changes on the behavioral phenotype of depression cannot been inferred,” he concluded.
Metabolomics data were provided by the Alzheimer’s Disease Metabolomics Consortium. The study was funded wholly or in part by grants from the National Institute on Aging and Foundation for the National Institutes of Health. It was further supported by a grant from ZonMW Memorabel. Dr. Amin reports no relevant financial relationships. The other authors’ disclosures are listed oin the original article. Dr. Mayer is a scientific advisory board member of Danone, Axial Therapeutics, Viome, Amare, Mahana Therapeutics, Pendulum, Bloom Biosciences, and APC Microbiome Ireland.
A version of this article originally appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Psilocybin promising for body dysmorphic disorder
WASHINGTON – Psilocybin is safe and effective in patients with body dysmorphic disorder (BDD), preliminary findings of a small pilot study show.
“The results suggest that psilocybin appears to be relatively safe and potentially helpful for people with BDD, and that it has a broader scope than just depression,” study investigator Franklin Schneier, MD, codirector of the Anxiety Disorders Clinic, New York State Psychiatric Institute, and special lecturer in psychiatry at Columbia University Medical Center in New York City, told this news organization.
So far, psilocybin has mostly been examined in clinical trials among patients with major depression. Dr. Schneier said he is aware of only a single case in the literature of its use in BDD: a patient who self-treated with psilocybin and reported symptom improvement.
The current study was presented as part of the Anxiety and Depression Association of America Anxiety & Depression conference.
Few treatment options
Patients with BDD are preoccupied with a body part they perceive as ugly or defective, “and not just mildly so,” said Dr. Schneier. “It bothers them to the extreme such that they may obsess about it on and off all day long.”
Such patients may engage in compulsive behaviors like constantly checking themselves in the mirror, and going to great lengths to conceal the body part they feel is defective. “They often seek out cosmetic procedures that objectively aren’t warranted,” said Dr. Schneier.
BDD patients often have comorbid depression, and many attempt suicide. As with other anxiety and depressive disorders, BDD is twice as prevalent in women vs. men, said Dr. Schneier.
Selective serotonin reuptake inhibitors (SSRIs) and cognitive behavioral therapy (CBT) are the only approved therapies for BDD.
The investigators thought there may be a good chance BDD patients could benefit from psilocybin. Psilocybin alters bodily self-awareness, which “might shake up people’s beliefs about their abnormal body perceptions,” said Dr. Schneier.
There’s also some suggestion that psilocybin relaxes inflexible thinking, he added. “People with BDD have very rigid beliefs about their body distortions that aren’t easily swayed by logic.”
The study included 12 adults (8 women, 4 men) with a mean age of 34 years and moderate to severe BDD who failed at least one SSRI course and had had BDD for an average of 21 years.
Participants had preliminary sessions with a therapist familiar with psilocybin who prepared them psychologically and discussed what to expect from the experience. On the day of the intervention, subjects took a single 25 mg oral dose of synthetic psilocybin in a comfortable setting.
Therapists were present for the next 8 hours to answer questions and support subjects through the experience.
High response rate
The primary efficacy outcome was change in the BDD Yale-Brown Obsessive Compulsive Disorder Scale Modified (BDD-YBOCS) total score.
The mean baseline BDD-YBOCS score was 29.17. Researchers regularly assessed this score in the following weeks.
At 12 weeks, BDD-YBOCS scores decreased significantly from baseline (P < .001) with a large effect size (partial eta squared = .54).
However, said Dr. Schneier, what really stood out was the proportion of responders. At week 12, seven (58%) of the 12 participants were responders, as defined by a 30% or greater decrease in the BDD-YBOCS score. Of these, three were “almost symptom-free,” he added.
A number of secondary outcomes, including conviction of belief, disability, and negative affect, also significantly improved.
It’s too early to determine if additional treatment is required. The investigators plan to follow-up with the cohort at 1 year.
Although exciting, these early results warrant caution, said Dr. Schneier. “On the one hand, this is a sample of people who have struggled for a long time and have failed previous therapies, so that’s good. But on the other hand, it’s an open trial with no placebo group, and everyone has high expectations, so we don’t know how much of a placebo effect there was.”
Most adverse events, including headaches and fatigue, were mild and resolved within the first week after dosing, and there were no serious adverse events.
Based on these findings, Dr. Schneier said controlled trials of psilocybin in BDD are warranted.
Need for scientific rigor
Commenting on the research, Charles B. Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, University of Texas at Austin, said while promising, psilocybin is “not for everyone” and patients need to be closely screened.
“We want to know their medical history and if they have a family history of schizophrenia or bipolar disorder. We don’t know whether these [psychedelic] medicines might trigger an episode.”
Dr. Nemeroff also noted there’s a risk of “troubling” side effects from the drug.
“My view is psilocybin clearly has therapeutic effects and we need to apply scientific rigor as we would any medicine in order to determine the risk/benefit ratio,” said Dr. Nemeroff, who was not associated with this psilocybin trial.
In addition, psilocybin is being tested in conditions other than BDD and major depression, including anorexia nervosa, postpartum depression, and alcohol use disorder, he added.
The study received funding from COMPASS Pathways PLC.
Dr. Nemeroff reports he has received research support from the NIH and Stanley Medical Research Institute; served as a consultant for Bracket (Clintara), Fortress Biotech, Intra-Cellular Therapies, Janssen Research and Development, Magstim, Navitor Pharmaceuticals, Sunovion Pharmaceuticals, Taisho Pharmaceuticals, Takeda, TC MSO, and Xhale; served on scientific advisory boards for the American Foundation for Suicide Prevention, the Anxiety and Depression Association of America, Bracket (Clintara), Brain and Behavior Research Foundation, Laureate Institute for Brain Research, Skyland Trail, and Xhale; is a stockholder in AbbVie, Antares, BI Gen Holdings, Celgene, OPKO Health, Seattle Genetics, and Xhale; serves on the board of directors for the American Foundation for Suicide Prevention, Anxiety and Depression Association of America, and Gratitude America; has received income or equity of $10,000 or more from American Psychiatric Publishing, Bracket (Clintara), Magstim, CME Outfitters, and Intra-Cellular Therapies; and holds patents on a method and devices for transdermal delivery of lithium and a method of assessing antidepressant drug therapy via transport inhibition of monoamine neurotransmitters by ex vivo assay.
A version of this article first appeared on Medscape.com.
WASHINGTON – Psilocybin is safe and effective in patients with body dysmorphic disorder (BDD), preliminary findings of a small pilot study show.
“The results suggest that psilocybin appears to be relatively safe and potentially helpful for people with BDD, and that it has a broader scope than just depression,” study investigator Franklin Schneier, MD, codirector of the Anxiety Disorders Clinic, New York State Psychiatric Institute, and special lecturer in psychiatry at Columbia University Medical Center in New York City, told this news organization.
So far, psilocybin has mostly been examined in clinical trials among patients with major depression. Dr. Schneier said he is aware of only a single case in the literature of its use in BDD: a patient who self-treated with psilocybin and reported symptom improvement.
The current study was presented as part of the Anxiety and Depression Association of America Anxiety & Depression conference.
Few treatment options
Patients with BDD are preoccupied with a body part they perceive as ugly or defective, “and not just mildly so,” said Dr. Schneier. “It bothers them to the extreme such that they may obsess about it on and off all day long.”
Such patients may engage in compulsive behaviors like constantly checking themselves in the mirror, and going to great lengths to conceal the body part they feel is defective. “They often seek out cosmetic procedures that objectively aren’t warranted,” said Dr. Schneier.
BDD patients often have comorbid depression, and many attempt suicide. As with other anxiety and depressive disorders, BDD is twice as prevalent in women vs. men, said Dr. Schneier.
Selective serotonin reuptake inhibitors (SSRIs) and cognitive behavioral therapy (CBT) are the only approved therapies for BDD.
The investigators thought there may be a good chance BDD patients could benefit from psilocybin. Psilocybin alters bodily self-awareness, which “might shake up people’s beliefs about their abnormal body perceptions,” said Dr. Schneier.
There’s also some suggestion that psilocybin relaxes inflexible thinking, he added. “People with BDD have very rigid beliefs about their body distortions that aren’t easily swayed by logic.”
The study included 12 adults (8 women, 4 men) with a mean age of 34 years and moderate to severe BDD who failed at least one SSRI course and had had BDD for an average of 21 years.
Participants had preliminary sessions with a therapist familiar with psilocybin who prepared them psychologically and discussed what to expect from the experience. On the day of the intervention, subjects took a single 25 mg oral dose of synthetic psilocybin in a comfortable setting.
Therapists were present for the next 8 hours to answer questions and support subjects through the experience.
High response rate
The primary efficacy outcome was change in the BDD Yale-Brown Obsessive Compulsive Disorder Scale Modified (BDD-YBOCS) total score.
The mean baseline BDD-YBOCS score was 29.17. Researchers regularly assessed this score in the following weeks.
At 12 weeks, BDD-YBOCS scores decreased significantly from baseline (P < .001) with a large effect size (partial eta squared = .54).
However, said Dr. Schneier, what really stood out was the proportion of responders. At week 12, seven (58%) of the 12 participants were responders, as defined by a 30% or greater decrease in the BDD-YBOCS score. Of these, three were “almost symptom-free,” he added.
A number of secondary outcomes, including conviction of belief, disability, and negative affect, also significantly improved.
It’s too early to determine if additional treatment is required. The investigators plan to follow-up with the cohort at 1 year.
Although exciting, these early results warrant caution, said Dr. Schneier. “On the one hand, this is a sample of people who have struggled for a long time and have failed previous therapies, so that’s good. But on the other hand, it’s an open trial with no placebo group, and everyone has high expectations, so we don’t know how much of a placebo effect there was.”
Most adverse events, including headaches and fatigue, were mild and resolved within the first week after dosing, and there were no serious adverse events.
Based on these findings, Dr. Schneier said controlled trials of psilocybin in BDD are warranted.
Need for scientific rigor
Commenting on the research, Charles B. Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, University of Texas at Austin, said while promising, psilocybin is “not for everyone” and patients need to be closely screened.
“We want to know their medical history and if they have a family history of schizophrenia or bipolar disorder. We don’t know whether these [psychedelic] medicines might trigger an episode.”
Dr. Nemeroff also noted there’s a risk of “troubling” side effects from the drug.
“My view is psilocybin clearly has therapeutic effects and we need to apply scientific rigor as we would any medicine in order to determine the risk/benefit ratio,” said Dr. Nemeroff, who was not associated with this psilocybin trial.
In addition, psilocybin is being tested in conditions other than BDD and major depression, including anorexia nervosa, postpartum depression, and alcohol use disorder, he added.
The study received funding from COMPASS Pathways PLC.
Dr. Nemeroff reports he has received research support from the NIH and Stanley Medical Research Institute; served as a consultant for Bracket (Clintara), Fortress Biotech, Intra-Cellular Therapies, Janssen Research and Development, Magstim, Navitor Pharmaceuticals, Sunovion Pharmaceuticals, Taisho Pharmaceuticals, Takeda, TC MSO, and Xhale; served on scientific advisory boards for the American Foundation for Suicide Prevention, the Anxiety and Depression Association of America, Bracket (Clintara), Brain and Behavior Research Foundation, Laureate Institute for Brain Research, Skyland Trail, and Xhale; is a stockholder in AbbVie, Antares, BI Gen Holdings, Celgene, OPKO Health, Seattle Genetics, and Xhale; serves on the board of directors for the American Foundation for Suicide Prevention, Anxiety and Depression Association of America, and Gratitude America; has received income or equity of $10,000 or more from American Psychiatric Publishing, Bracket (Clintara), Magstim, CME Outfitters, and Intra-Cellular Therapies; and holds patents on a method and devices for transdermal delivery of lithium and a method of assessing antidepressant drug therapy via transport inhibition of monoamine neurotransmitters by ex vivo assay.
A version of this article first appeared on Medscape.com.
WASHINGTON – Psilocybin is safe and effective in patients with body dysmorphic disorder (BDD), preliminary findings of a small pilot study show.
“The results suggest that psilocybin appears to be relatively safe and potentially helpful for people with BDD, and that it has a broader scope than just depression,” study investigator Franklin Schneier, MD, codirector of the Anxiety Disorders Clinic, New York State Psychiatric Institute, and special lecturer in psychiatry at Columbia University Medical Center in New York City, told this news organization.
So far, psilocybin has mostly been examined in clinical trials among patients with major depression. Dr. Schneier said he is aware of only a single case in the literature of its use in BDD: a patient who self-treated with psilocybin and reported symptom improvement.
The current study was presented as part of the Anxiety and Depression Association of America Anxiety & Depression conference.
Few treatment options
Patients with BDD are preoccupied with a body part they perceive as ugly or defective, “and not just mildly so,” said Dr. Schneier. “It bothers them to the extreme such that they may obsess about it on and off all day long.”
Such patients may engage in compulsive behaviors like constantly checking themselves in the mirror, and going to great lengths to conceal the body part they feel is defective. “They often seek out cosmetic procedures that objectively aren’t warranted,” said Dr. Schneier.
BDD patients often have comorbid depression, and many attempt suicide. As with other anxiety and depressive disorders, BDD is twice as prevalent in women vs. men, said Dr. Schneier.
Selective serotonin reuptake inhibitors (SSRIs) and cognitive behavioral therapy (CBT) are the only approved therapies for BDD.
The investigators thought there may be a good chance BDD patients could benefit from psilocybin. Psilocybin alters bodily self-awareness, which “might shake up people’s beliefs about their abnormal body perceptions,” said Dr. Schneier.
There’s also some suggestion that psilocybin relaxes inflexible thinking, he added. “People with BDD have very rigid beliefs about their body distortions that aren’t easily swayed by logic.”
The study included 12 adults (8 women, 4 men) with a mean age of 34 years and moderate to severe BDD who failed at least one SSRI course and had had BDD for an average of 21 years.
Participants had preliminary sessions with a therapist familiar with psilocybin who prepared them psychologically and discussed what to expect from the experience. On the day of the intervention, subjects took a single 25 mg oral dose of synthetic psilocybin in a comfortable setting.
Therapists were present for the next 8 hours to answer questions and support subjects through the experience.
High response rate
The primary efficacy outcome was change in the BDD Yale-Brown Obsessive Compulsive Disorder Scale Modified (BDD-YBOCS) total score.
The mean baseline BDD-YBOCS score was 29.17. Researchers regularly assessed this score in the following weeks.
At 12 weeks, BDD-YBOCS scores decreased significantly from baseline (P < .001) with a large effect size (partial eta squared = .54).
However, said Dr. Schneier, what really stood out was the proportion of responders. At week 12, seven (58%) of the 12 participants were responders, as defined by a 30% or greater decrease in the BDD-YBOCS score. Of these, three were “almost symptom-free,” he added.
A number of secondary outcomes, including conviction of belief, disability, and negative affect, also significantly improved.
It’s too early to determine if additional treatment is required. The investigators plan to follow-up with the cohort at 1 year.
Although exciting, these early results warrant caution, said Dr. Schneier. “On the one hand, this is a sample of people who have struggled for a long time and have failed previous therapies, so that’s good. But on the other hand, it’s an open trial with no placebo group, and everyone has high expectations, so we don’t know how much of a placebo effect there was.”
Most adverse events, including headaches and fatigue, were mild and resolved within the first week after dosing, and there were no serious adverse events.
Based on these findings, Dr. Schneier said controlled trials of psilocybin in BDD are warranted.
Need for scientific rigor
Commenting on the research, Charles B. Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, University of Texas at Austin, said while promising, psilocybin is “not for everyone” and patients need to be closely screened.
“We want to know their medical history and if they have a family history of schizophrenia or bipolar disorder. We don’t know whether these [psychedelic] medicines might trigger an episode.”
Dr. Nemeroff also noted there’s a risk of “troubling” side effects from the drug.
“My view is psilocybin clearly has therapeutic effects and we need to apply scientific rigor as we would any medicine in order to determine the risk/benefit ratio,” said Dr. Nemeroff, who was not associated with this psilocybin trial.
In addition, psilocybin is being tested in conditions other than BDD and major depression, including anorexia nervosa, postpartum depression, and alcohol use disorder, he added.
The study received funding from COMPASS Pathways PLC.
Dr. Nemeroff reports he has received research support from the NIH and Stanley Medical Research Institute; served as a consultant for Bracket (Clintara), Fortress Biotech, Intra-Cellular Therapies, Janssen Research and Development, Magstim, Navitor Pharmaceuticals, Sunovion Pharmaceuticals, Taisho Pharmaceuticals, Takeda, TC MSO, and Xhale; served on scientific advisory boards for the American Foundation for Suicide Prevention, the Anxiety and Depression Association of America, Bracket (Clintara), Brain and Behavior Research Foundation, Laureate Institute for Brain Research, Skyland Trail, and Xhale; is a stockholder in AbbVie, Antares, BI Gen Holdings, Celgene, OPKO Health, Seattle Genetics, and Xhale; serves on the board of directors for the American Foundation for Suicide Prevention, Anxiety and Depression Association of America, and Gratitude America; has received income or equity of $10,000 or more from American Psychiatric Publishing, Bracket (Clintara), Magstim, CME Outfitters, and Intra-Cellular Therapies; and holds patents on a method and devices for transdermal delivery of lithium and a method of assessing antidepressant drug therapy via transport inhibition of monoamine neurotransmitters by ex vivo assay.
A version of this article first appeared on Medscape.com.
AT ADAA 2023
Meditation curbs stress, depression as adjunct to CAD rehab
Regular meditation reduced depression by roughly 44% in adults with coronary artery disease who were involved in a cardiovascular rehabilitation program.
An increasing body of research supports the impact of psychological risk factors including stress, personality type, anger, and hostility on conditions such as depression and anxiety, but also social isolation and low socioeconomic status, Ana Luisa Vitorino Monteiro, MD, of the University of Lisbon said in a presentation at the annual congress of the European Association of Preventive Cardiology. In addition, “stress, anxiety, and depression deteriorate the cardiovascular (CV) system through psycho-neuro-immunoendocrinology system and behavioral pathways.”
Meditation as a tool for stress management has been gaining popularity, but its use as part of a CV rehabilitation program as a complementary therapy has not been well studied, she added.
Dr. Monteiro and colleagues recruited 80 adults with CAD who were undergoing CV rehabilitation to join a meditation program. Of these, 48 accepted (60%) and 40% declined. Those who accepted were part of an exercise-based CV rehabilitation program that met three times a week for at least 6 months. The mean age of the participants was 65 years, and 80% were male.
Participants were randomized to an intervention group with a weekly 90-minute session that included breathing and meditation for 1 month in addition to usual care, or to usual care in the rehabilitation program. Over the next 3 months, the intervention patients were encouraged to practice daily meditation for 20 minutes alone or using video support material, with a weekly follow-up phone call. Assessments of stress, anxiety, and depression took place at baseline and after 4 months using the Perceived Stress Scale, Beck Anxiety Inventory, Beck Depression Inventory, and HeartQoL questionnaire.
At 4 months, individuals in the meditation group had reduced depression levels significantly, by 44%, compared with controls (P < .001). Anxiety and stress decreased significantly, by 30% (P = .04) and 31% (P = .05), respectively. After 4 months, individuals in the control group were offered the opportunity to follow the meditation protocol.
In addition, “the emotional dimension of quality of life increased by 60% in the intervention group,” Dr. Monteiro noted. However, physical QoL did not change between groups.
The study was limited by the small sample size, and more research is needed in larger and more diverse populations, Dr. Monteiro said. However, the results support the value of meditation as an adjunct component of care for CAD patients in a long-term rehabilitation program.
Motivation makes a difference
The current study is important as an exploration of “a straightforward, simple, low-risk approach that could be an adjunct to benefit patients with serious cardiovascular disease,” Brian Olshansky, MD, a cardiologist at the University of Iowa, Iowa City, said in an interview.
“We have moved into a time of polypharmacy and multiple interventions for patients with underlying cardiovascular disease which, in many cases, have proven benefit but also potential adverse effects,” he said. “Engaging patients to participate in their health care, when there is serious underlying cardiovascular disease, has potential beneficial impact in many ways. Meditation is a low-risk, low-cost, potentially beneficial adjunct to standard medical therapy that may enhance psychological outcomes as shown here in this small study.”
However, “patients often rely on high-cost, potentially high-risk therapeutic interventions, expecting complete control of their problems without their own collaborative intervention,” he noted.
Dr. Olshansky said he was not surprised by any of the findings, and would have been surprised if meditation had failed to show any benefit for the study population.
“I am very pleased to see these results and would encourage meditation practice to be part of cardiovascular rehabilitation for motivated individuals,” he said. “What did surprise me was the adherence to the meditation protocol for those who participated. This represents a highly motivated group and it may be difficult to expect the same results in less motivated individuals.”
The current study has several strengths, including the use of controls and high rates of adherence to the protocol, said Dr. Olshansky. Other strengths include the standardized approach and the reasonable quality of the outcome measures, which showed a substantial benefit.
However, “this is a small study of motivated individuals of whom 80% were male,” and generalizability to other populations is unclear, Dr. Olshansky said. In addition, the racial mix was not described, and the severity of the underlying coronary artery disease and the therapies provided to these individuals is not detailed. A sicker population may not fare as well.”
The reasons for the benefits of meditation remain uncertain, Dr. Olshansky said. “It could be, specifically, that the meditation itself has physiological effects that ultimately translate into psychosocial benefit. However, those who enrolled and were interested may have derived a placebo effect. In any case, benefit was achieved, but the crossover benefit to the control group is unclear.
“In other words, the statistical approach to benefit is uncertain as to when it was measured, but presumably before the control group was allowed to engage in a meditation practice,” and the follow-up was short term, said Dr. Olshansky.
Data support patient engagement
The message to clinicians and patients: “Patients should be engaged in their own health care when it comes to rehabilitation for cardiovascular disease,” said Dr. Olshansky. “Motivated individuals who are educated about a meditative practice performed in a standardized way will have improvement most likely in their quality of life, and when it comes to measurements of depression, stress and anxiety.”
Although the mechanisms behind the benefits remain unclear, “having a standardized credible prescription for which patients can become intimately engaged is beneficial,” he added.
The study received no outside funding. Neither Dr. Monteiro nor Dr. Olshansky had any financial conflicts to disclose.
Regular meditation reduced depression by roughly 44% in adults with coronary artery disease who were involved in a cardiovascular rehabilitation program.
An increasing body of research supports the impact of psychological risk factors including stress, personality type, anger, and hostility on conditions such as depression and anxiety, but also social isolation and low socioeconomic status, Ana Luisa Vitorino Monteiro, MD, of the University of Lisbon said in a presentation at the annual congress of the European Association of Preventive Cardiology. In addition, “stress, anxiety, and depression deteriorate the cardiovascular (CV) system through psycho-neuro-immunoendocrinology system and behavioral pathways.”
Meditation as a tool for stress management has been gaining popularity, but its use as part of a CV rehabilitation program as a complementary therapy has not been well studied, she added.
Dr. Monteiro and colleagues recruited 80 adults with CAD who were undergoing CV rehabilitation to join a meditation program. Of these, 48 accepted (60%) and 40% declined. Those who accepted were part of an exercise-based CV rehabilitation program that met three times a week for at least 6 months. The mean age of the participants was 65 years, and 80% were male.
Participants were randomized to an intervention group with a weekly 90-minute session that included breathing and meditation for 1 month in addition to usual care, or to usual care in the rehabilitation program. Over the next 3 months, the intervention patients were encouraged to practice daily meditation for 20 minutes alone or using video support material, with a weekly follow-up phone call. Assessments of stress, anxiety, and depression took place at baseline and after 4 months using the Perceived Stress Scale, Beck Anxiety Inventory, Beck Depression Inventory, and HeartQoL questionnaire.
At 4 months, individuals in the meditation group had reduced depression levels significantly, by 44%, compared with controls (P < .001). Anxiety and stress decreased significantly, by 30% (P = .04) and 31% (P = .05), respectively. After 4 months, individuals in the control group were offered the opportunity to follow the meditation protocol.
In addition, “the emotional dimension of quality of life increased by 60% in the intervention group,” Dr. Monteiro noted. However, physical QoL did not change between groups.
The study was limited by the small sample size, and more research is needed in larger and more diverse populations, Dr. Monteiro said. However, the results support the value of meditation as an adjunct component of care for CAD patients in a long-term rehabilitation program.
Motivation makes a difference
The current study is important as an exploration of “a straightforward, simple, low-risk approach that could be an adjunct to benefit patients with serious cardiovascular disease,” Brian Olshansky, MD, a cardiologist at the University of Iowa, Iowa City, said in an interview.
“We have moved into a time of polypharmacy and multiple interventions for patients with underlying cardiovascular disease which, in many cases, have proven benefit but also potential adverse effects,” he said. “Engaging patients to participate in their health care, when there is serious underlying cardiovascular disease, has potential beneficial impact in many ways. Meditation is a low-risk, low-cost, potentially beneficial adjunct to standard medical therapy that may enhance psychological outcomes as shown here in this small study.”
However, “patients often rely on high-cost, potentially high-risk therapeutic interventions, expecting complete control of their problems without their own collaborative intervention,” he noted.
Dr. Olshansky said he was not surprised by any of the findings, and would have been surprised if meditation had failed to show any benefit for the study population.
“I am very pleased to see these results and would encourage meditation practice to be part of cardiovascular rehabilitation for motivated individuals,” he said. “What did surprise me was the adherence to the meditation protocol for those who participated. This represents a highly motivated group and it may be difficult to expect the same results in less motivated individuals.”
The current study has several strengths, including the use of controls and high rates of adherence to the protocol, said Dr. Olshansky. Other strengths include the standardized approach and the reasonable quality of the outcome measures, which showed a substantial benefit.
However, “this is a small study of motivated individuals of whom 80% were male,” and generalizability to other populations is unclear, Dr. Olshansky said. In addition, the racial mix was not described, and the severity of the underlying coronary artery disease and the therapies provided to these individuals is not detailed. A sicker population may not fare as well.”
The reasons for the benefits of meditation remain uncertain, Dr. Olshansky said. “It could be, specifically, that the meditation itself has physiological effects that ultimately translate into psychosocial benefit. However, those who enrolled and were interested may have derived a placebo effect. In any case, benefit was achieved, but the crossover benefit to the control group is unclear.
“In other words, the statistical approach to benefit is uncertain as to when it was measured, but presumably before the control group was allowed to engage in a meditation practice,” and the follow-up was short term, said Dr. Olshansky.
Data support patient engagement
The message to clinicians and patients: “Patients should be engaged in their own health care when it comes to rehabilitation for cardiovascular disease,” said Dr. Olshansky. “Motivated individuals who are educated about a meditative practice performed in a standardized way will have improvement most likely in their quality of life, and when it comes to measurements of depression, stress and anxiety.”
Although the mechanisms behind the benefits remain unclear, “having a standardized credible prescription for which patients can become intimately engaged is beneficial,” he added.
The study received no outside funding. Neither Dr. Monteiro nor Dr. Olshansky had any financial conflicts to disclose.
Regular meditation reduced depression by roughly 44% in adults with coronary artery disease who were involved in a cardiovascular rehabilitation program.
An increasing body of research supports the impact of psychological risk factors including stress, personality type, anger, and hostility on conditions such as depression and anxiety, but also social isolation and low socioeconomic status, Ana Luisa Vitorino Monteiro, MD, of the University of Lisbon said in a presentation at the annual congress of the European Association of Preventive Cardiology. In addition, “stress, anxiety, and depression deteriorate the cardiovascular (CV) system through psycho-neuro-immunoendocrinology system and behavioral pathways.”
Meditation as a tool for stress management has been gaining popularity, but its use as part of a CV rehabilitation program as a complementary therapy has not been well studied, she added.
Dr. Monteiro and colleagues recruited 80 adults with CAD who were undergoing CV rehabilitation to join a meditation program. Of these, 48 accepted (60%) and 40% declined. Those who accepted were part of an exercise-based CV rehabilitation program that met three times a week for at least 6 months. The mean age of the participants was 65 years, and 80% were male.
Participants were randomized to an intervention group with a weekly 90-minute session that included breathing and meditation for 1 month in addition to usual care, or to usual care in the rehabilitation program. Over the next 3 months, the intervention patients were encouraged to practice daily meditation for 20 minutes alone or using video support material, with a weekly follow-up phone call. Assessments of stress, anxiety, and depression took place at baseline and after 4 months using the Perceived Stress Scale, Beck Anxiety Inventory, Beck Depression Inventory, and HeartQoL questionnaire.
At 4 months, individuals in the meditation group had reduced depression levels significantly, by 44%, compared with controls (P < .001). Anxiety and stress decreased significantly, by 30% (P = .04) and 31% (P = .05), respectively. After 4 months, individuals in the control group were offered the opportunity to follow the meditation protocol.
In addition, “the emotional dimension of quality of life increased by 60% in the intervention group,” Dr. Monteiro noted. However, physical QoL did not change between groups.
The study was limited by the small sample size, and more research is needed in larger and more diverse populations, Dr. Monteiro said. However, the results support the value of meditation as an adjunct component of care for CAD patients in a long-term rehabilitation program.
Motivation makes a difference
The current study is important as an exploration of “a straightforward, simple, low-risk approach that could be an adjunct to benefit patients with serious cardiovascular disease,” Brian Olshansky, MD, a cardiologist at the University of Iowa, Iowa City, said in an interview.
“We have moved into a time of polypharmacy and multiple interventions for patients with underlying cardiovascular disease which, in many cases, have proven benefit but also potential adverse effects,” he said. “Engaging patients to participate in their health care, when there is serious underlying cardiovascular disease, has potential beneficial impact in many ways. Meditation is a low-risk, low-cost, potentially beneficial adjunct to standard medical therapy that may enhance psychological outcomes as shown here in this small study.”
However, “patients often rely on high-cost, potentially high-risk therapeutic interventions, expecting complete control of their problems without their own collaborative intervention,” he noted.
Dr. Olshansky said he was not surprised by any of the findings, and would have been surprised if meditation had failed to show any benefit for the study population.
“I am very pleased to see these results and would encourage meditation practice to be part of cardiovascular rehabilitation for motivated individuals,” he said. “What did surprise me was the adherence to the meditation protocol for those who participated. This represents a highly motivated group and it may be difficult to expect the same results in less motivated individuals.”
The current study has several strengths, including the use of controls and high rates of adherence to the protocol, said Dr. Olshansky. Other strengths include the standardized approach and the reasonable quality of the outcome measures, which showed a substantial benefit.
However, “this is a small study of motivated individuals of whom 80% were male,” and generalizability to other populations is unclear, Dr. Olshansky said. In addition, the racial mix was not described, and the severity of the underlying coronary artery disease and the therapies provided to these individuals is not detailed. A sicker population may not fare as well.”
The reasons for the benefits of meditation remain uncertain, Dr. Olshansky said. “It could be, specifically, that the meditation itself has physiological effects that ultimately translate into psychosocial benefit. However, those who enrolled and were interested may have derived a placebo effect. In any case, benefit was achieved, but the crossover benefit to the control group is unclear.
“In other words, the statistical approach to benefit is uncertain as to when it was measured, but presumably before the control group was allowed to engage in a meditation practice,” and the follow-up was short term, said Dr. Olshansky.
Data support patient engagement
The message to clinicians and patients: “Patients should be engaged in their own health care when it comes to rehabilitation for cardiovascular disease,” said Dr. Olshansky. “Motivated individuals who are educated about a meditative practice performed in a standardized way will have improvement most likely in their quality of life, and when it comes to measurements of depression, stress and anxiety.”
Although the mechanisms behind the benefits remain unclear, “having a standardized credible prescription for which patients can become intimately engaged is beneficial,” he added.
The study received no outside funding. Neither Dr. Monteiro nor Dr. Olshansky had any financial conflicts to disclose.
FROM ESC PREVENTIVE CARDIOLOGY 2023
Steep rise in cannabis-related suicide attempts
The increases were notable both during and after the pandemic and were highest among children and female persons.
Investigators examined closed cases of cannabis-related human exposures that were coded as intentional-suspected suicidal.
Of note, there was a statistically significant increase in cannabis poisonings in young children (5-13 years) in 2021, during the pandemic, compared with 2019, a prepandemic year (3.1% vs. 1.3%; P < .001), the researchers report.
“This may speak to both increased access to cannabis as well as poor mental health status during the pandemic period,” study investigator Tracy Klein, PhD, assistant director, Center for Cannabis Policy, Research and Outreach, Washington State University Vancouver, Mount Vista, said in an interview.
The study was published online in JAMA Network Open.
Reports of intentional poisonings with cannabis increased by roughly 17% annually over the study period. Most cases occurred in recent years and involved individuals aged 14-64 years. Nearly all (96.5%) cases involved more than one substance.
“The resemblance of cannabis edibles, implicated in the majority of poisonings to candy, vitamins, and food products, is a risk to patients across the life span who may not fully understand what they are consuming or how potent it is,” Dr. Klein said in an interview.
Overall, nearly 1 in 10 exposures resulted in death or other major outcomes (life-threatening outcomes or outcomes involving major residual disability or disfigurement). For older adults, 19.4% of exposures led to death or other major harm.
“Elderly patients may also have comorbid conditions and polypharmacy, which contributes to their much more serious outcomes from cannabis poisoning,” Dr. Klein said.
The researchers caution that, owing to the cross-sectional nature of the data, they could not identify a causal association between cannabis use and suicide attempt.
With more states legalizing cannabis use by adults, increases in cannabis use will likely persist.
“It is important to further examine the suspected association between cannabis use and suicidal behaviors and how risks can be prevented or mitigated,” the researchers note.
Dr. Klein encourages health care providers to ask patients whether they are using cannabis and how they obtain and store it.
“As with all medications and substances, storage is a key safety issue that is elicited during a careful history,” said Dr. Klein.
Support for the study was provided in part by funds provided for medical and biological research by the State of Washington Initiative Measure No. 171. Dr. Klein has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The increases were notable both during and after the pandemic and were highest among children and female persons.
Investigators examined closed cases of cannabis-related human exposures that were coded as intentional-suspected suicidal.
Of note, there was a statistically significant increase in cannabis poisonings in young children (5-13 years) in 2021, during the pandemic, compared with 2019, a prepandemic year (3.1% vs. 1.3%; P < .001), the researchers report.
“This may speak to both increased access to cannabis as well as poor mental health status during the pandemic period,” study investigator Tracy Klein, PhD, assistant director, Center for Cannabis Policy, Research and Outreach, Washington State University Vancouver, Mount Vista, said in an interview.
The study was published online in JAMA Network Open.
Reports of intentional poisonings with cannabis increased by roughly 17% annually over the study period. Most cases occurred in recent years and involved individuals aged 14-64 years. Nearly all (96.5%) cases involved more than one substance.
“The resemblance of cannabis edibles, implicated in the majority of poisonings to candy, vitamins, and food products, is a risk to patients across the life span who may not fully understand what they are consuming or how potent it is,” Dr. Klein said in an interview.
Overall, nearly 1 in 10 exposures resulted in death or other major outcomes (life-threatening outcomes or outcomes involving major residual disability or disfigurement). For older adults, 19.4% of exposures led to death or other major harm.
“Elderly patients may also have comorbid conditions and polypharmacy, which contributes to their much more serious outcomes from cannabis poisoning,” Dr. Klein said.
The researchers caution that, owing to the cross-sectional nature of the data, they could not identify a causal association between cannabis use and suicide attempt.
With more states legalizing cannabis use by adults, increases in cannabis use will likely persist.
“It is important to further examine the suspected association between cannabis use and suicidal behaviors and how risks can be prevented or mitigated,” the researchers note.
Dr. Klein encourages health care providers to ask patients whether they are using cannabis and how they obtain and store it.
“As with all medications and substances, storage is a key safety issue that is elicited during a careful history,” said Dr. Klein.
Support for the study was provided in part by funds provided for medical and biological research by the State of Washington Initiative Measure No. 171. Dr. Klein has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The increases were notable both during and after the pandemic and were highest among children and female persons.
Investigators examined closed cases of cannabis-related human exposures that were coded as intentional-suspected suicidal.
Of note, there was a statistically significant increase in cannabis poisonings in young children (5-13 years) in 2021, during the pandemic, compared with 2019, a prepandemic year (3.1% vs. 1.3%; P < .001), the researchers report.
“This may speak to both increased access to cannabis as well as poor mental health status during the pandemic period,” study investigator Tracy Klein, PhD, assistant director, Center for Cannabis Policy, Research and Outreach, Washington State University Vancouver, Mount Vista, said in an interview.
The study was published online in JAMA Network Open.
Reports of intentional poisonings with cannabis increased by roughly 17% annually over the study period. Most cases occurred in recent years and involved individuals aged 14-64 years. Nearly all (96.5%) cases involved more than one substance.
“The resemblance of cannabis edibles, implicated in the majority of poisonings to candy, vitamins, and food products, is a risk to patients across the life span who may not fully understand what they are consuming or how potent it is,” Dr. Klein said in an interview.
Overall, nearly 1 in 10 exposures resulted in death or other major outcomes (life-threatening outcomes or outcomes involving major residual disability or disfigurement). For older adults, 19.4% of exposures led to death or other major harm.
“Elderly patients may also have comorbid conditions and polypharmacy, which contributes to their much more serious outcomes from cannabis poisoning,” Dr. Klein said.
The researchers caution that, owing to the cross-sectional nature of the data, they could not identify a causal association between cannabis use and suicide attempt.
With more states legalizing cannabis use by adults, increases in cannabis use will likely persist.
“It is important to further examine the suspected association between cannabis use and suicidal behaviors and how risks can be prevented or mitigated,” the researchers note.
Dr. Klein encourages health care providers to ask patients whether they are using cannabis and how they obtain and store it.
“As with all medications and substances, storage is a key safety issue that is elicited during a careful history,” said Dr. Klein.
Support for the study was provided in part by funds provided for medical and biological research by the State of Washington Initiative Measure No. 171. Dr. Klein has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Telehealth suicide prevention program safe, acceptable
WASHINGTON –
Skeptics had worried that participating in the program through telehealth would exacerbate safety and other issues veterans had about discussing suicide in a group setting, study investigator Sarah Sullivan, PhD student, Health Psychology & Clinical Science, City University of New York, told this news organization.
“But that for us was not really true. People opened up about their suicidal thoughts and triggers even on this telehealth format, and that’s really important for providers to know,” she said.
The findings were presented as part of the Anxiety and Depression Association of America Anxiety & Depression conference.
Trial run
Suicide is a major public health issue, particularly for veterans. Recent data from the Veterans Administration show 17 veterans die by suicide every day.
The current study included 15 male and 2 female veterans (29.4% White, 70.6% Hispanic) from New York City and Philadelphia. Participants had an average age of 50 and all were either deemed by a clinician to be at extremely high risk for suicide or were hospitalized for this reason.
The individuals completed an online version of the Project Life Force (PLF) program, which uses dialectical behavioral therapy and psychoeducational approaches. The program includes the brief Safety Planning intervention (SPI), aimed at reducing short-term suicide risk.
Considered a best practice, the SPI includes a written list of personal suicide warning signs or triggers, internal coping strategies, social contacts who offer support and distraction from suicidal thoughts, contact information for professionals, a suicide crisis hotline, and nearby emergency services.
In addition to these steps, the PLF program focuses on sleep, exercise, and making the safety plan accessible.
The telehealth platform for the program was WebEx software. Participants were offered a “trial run” to orient them to the technology, said Ms. Sullivan.
Group sessions were held once weekly for 10 weeks, with optional “booster” sessions if needed. Each session included about five participants.
To ensure privacy, participants were provided with headphones and laptops. This was especially important for those sharing a living space, including spouses and children, said Ms. Sullivan.
High ratings
Participants completed the Acceptability of Intervention Measure (AIM), Intervention Appropriateness Measure (IAM), and Feasibility of Intervention Measure (FIM). Each of these yields scores from four items rated on a Likert scale of 1-5, for a total score ranging from 5 to 20, with higher scores indicating higher ratings.
Veterans rated PLF-T as highly acceptable (mean AIM, 17.50), appropriate (mean IAM, 17.25), and feasible (mean FIM, 18).
Study participants reported the program was convenient and noted that it decreased the burden of traveling to sessions, especially during the COVID-19 pandemic.
They also reported the program was less likely to compete with other demands such as childcare and other appointments, said Ms. Sullivan.
In addition, it helped those with comorbidities such as posttraumatic stress disorder, she added. She noted veterans with PTSD may be triggered on subways or buses when traveling to in-person treatment sessions.
“That can take away from addressing the suicidal triggers,” said Ms. Sullivan. “So, this program allows them to fully concentrate on the safety plan.”
Results showed that study participants “enjoyed the group and would recommend it to others,” said Ms. Sullivan. “I think that signifies the group was effective in its goal of mitigating loneliness, which was exacerbated during the COVID-19 pandemic, and creating a socially supportive environment, especially for the vets living alone.”
Veterans also reported that the program helped them understand the connection between depression or PTSD and suicidal thoughts, urges, and plans. In addition, they appreciated the group dynamics, where they felt connected to other veterans experiencing similar challenges.
Hopeful results
Commenting on the study, Paul E. Holtzheimer, MD, deputy director for research at the National Center for PTSD, praised the study for focusing on a very high-risk group.
“This gets you closer to the population you’re probably going to have an impact on in terms of preventing suicide,” said Dr. Holtzheimer, a professor of psychiatry and surgery at Dartmouth College’s Geisel School of Medicine, Hanover, N.H.
The fact that many of the participants had attempted suicide in the last year underlines that this was a very high-risk population, said Dr. Holtzheimer. “Not only are they thinking about suicide, but almost two-thirds had actually attempted or tried something.”
This kind of program “would be great for rural environments where people may be living like four hours away from the VA or a clinic,” said Dr. Holtzheimer, noting that many veterans are often quite isolated.
“One of the very positive outcomes of the COVID-19 pandemic was helping us strengthen our ability to do telehealth,” he said.
However, Dr. Holtzheimer noted the study was small and qualitative. “The next step ideally would be a controlled trial looking at not just ideation but at risky behavior or clear suicide attempts or preparation, like buying a gun or hoarding medication, to help determine efficacy.”
The researchers and Dr. Holtzheimer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
WASHINGTON –
Skeptics had worried that participating in the program through telehealth would exacerbate safety and other issues veterans had about discussing suicide in a group setting, study investigator Sarah Sullivan, PhD student, Health Psychology & Clinical Science, City University of New York, told this news organization.
“But that for us was not really true. People opened up about their suicidal thoughts and triggers even on this telehealth format, and that’s really important for providers to know,” she said.
The findings were presented as part of the Anxiety and Depression Association of America Anxiety & Depression conference.
Trial run
Suicide is a major public health issue, particularly for veterans. Recent data from the Veterans Administration show 17 veterans die by suicide every day.
The current study included 15 male and 2 female veterans (29.4% White, 70.6% Hispanic) from New York City and Philadelphia. Participants had an average age of 50 and all were either deemed by a clinician to be at extremely high risk for suicide or were hospitalized for this reason.
The individuals completed an online version of the Project Life Force (PLF) program, which uses dialectical behavioral therapy and psychoeducational approaches. The program includes the brief Safety Planning intervention (SPI), aimed at reducing short-term suicide risk.
Considered a best practice, the SPI includes a written list of personal suicide warning signs or triggers, internal coping strategies, social contacts who offer support and distraction from suicidal thoughts, contact information for professionals, a suicide crisis hotline, and nearby emergency services.
In addition to these steps, the PLF program focuses on sleep, exercise, and making the safety plan accessible.
The telehealth platform for the program was WebEx software. Participants were offered a “trial run” to orient them to the technology, said Ms. Sullivan.
Group sessions were held once weekly for 10 weeks, with optional “booster” sessions if needed. Each session included about five participants.
To ensure privacy, participants were provided with headphones and laptops. This was especially important for those sharing a living space, including spouses and children, said Ms. Sullivan.
High ratings
Participants completed the Acceptability of Intervention Measure (AIM), Intervention Appropriateness Measure (IAM), and Feasibility of Intervention Measure (FIM). Each of these yields scores from four items rated on a Likert scale of 1-5, for a total score ranging from 5 to 20, with higher scores indicating higher ratings.
Veterans rated PLF-T as highly acceptable (mean AIM, 17.50), appropriate (mean IAM, 17.25), and feasible (mean FIM, 18).
Study participants reported the program was convenient and noted that it decreased the burden of traveling to sessions, especially during the COVID-19 pandemic.
They also reported the program was less likely to compete with other demands such as childcare and other appointments, said Ms. Sullivan.
In addition, it helped those with comorbidities such as posttraumatic stress disorder, she added. She noted veterans with PTSD may be triggered on subways or buses when traveling to in-person treatment sessions.
“That can take away from addressing the suicidal triggers,” said Ms. Sullivan. “So, this program allows them to fully concentrate on the safety plan.”
Results showed that study participants “enjoyed the group and would recommend it to others,” said Ms. Sullivan. “I think that signifies the group was effective in its goal of mitigating loneliness, which was exacerbated during the COVID-19 pandemic, and creating a socially supportive environment, especially for the vets living alone.”
Veterans also reported that the program helped them understand the connection between depression or PTSD and suicidal thoughts, urges, and plans. In addition, they appreciated the group dynamics, where they felt connected to other veterans experiencing similar challenges.
Hopeful results
Commenting on the study, Paul E. Holtzheimer, MD, deputy director for research at the National Center for PTSD, praised the study for focusing on a very high-risk group.
“This gets you closer to the population you’re probably going to have an impact on in terms of preventing suicide,” said Dr. Holtzheimer, a professor of psychiatry and surgery at Dartmouth College’s Geisel School of Medicine, Hanover, N.H.
The fact that many of the participants had attempted suicide in the last year underlines that this was a very high-risk population, said Dr. Holtzheimer. “Not only are they thinking about suicide, but almost two-thirds had actually attempted or tried something.”
This kind of program “would be great for rural environments where people may be living like four hours away from the VA or a clinic,” said Dr. Holtzheimer, noting that many veterans are often quite isolated.
“One of the very positive outcomes of the COVID-19 pandemic was helping us strengthen our ability to do telehealth,” he said.
However, Dr. Holtzheimer noted the study was small and qualitative. “The next step ideally would be a controlled trial looking at not just ideation but at risky behavior or clear suicide attempts or preparation, like buying a gun or hoarding medication, to help determine efficacy.”
The researchers and Dr. Holtzheimer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
WASHINGTON –
Skeptics had worried that participating in the program through telehealth would exacerbate safety and other issues veterans had about discussing suicide in a group setting, study investigator Sarah Sullivan, PhD student, Health Psychology & Clinical Science, City University of New York, told this news organization.
“But that for us was not really true. People opened up about their suicidal thoughts and triggers even on this telehealth format, and that’s really important for providers to know,” she said.
The findings were presented as part of the Anxiety and Depression Association of America Anxiety & Depression conference.
Trial run
Suicide is a major public health issue, particularly for veterans. Recent data from the Veterans Administration show 17 veterans die by suicide every day.
The current study included 15 male and 2 female veterans (29.4% White, 70.6% Hispanic) from New York City and Philadelphia. Participants had an average age of 50 and all were either deemed by a clinician to be at extremely high risk for suicide or were hospitalized for this reason.
The individuals completed an online version of the Project Life Force (PLF) program, which uses dialectical behavioral therapy and psychoeducational approaches. The program includes the brief Safety Planning intervention (SPI), aimed at reducing short-term suicide risk.
Considered a best practice, the SPI includes a written list of personal suicide warning signs or triggers, internal coping strategies, social contacts who offer support and distraction from suicidal thoughts, contact information for professionals, a suicide crisis hotline, and nearby emergency services.
In addition to these steps, the PLF program focuses on sleep, exercise, and making the safety plan accessible.
The telehealth platform for the program was WebEx software. Participants were offered a “trial run” to orient them to the technology, said Ms. Sullivan.
Group sessions were held once weekly for 10 weeks, with optional “booster” sessions if needed. Each session included about five participants.
To ensure privacy, participants were provided with headphones and laptops. This was especially important for those sharing a living space, including spouses and children, said Ms. Sullivan.
High ratings
Participants completed the Acceptability of Intervention Measure (AIM), Intervention Appropriateness Measure (IAM), and Feasibility of Intervention Measure (FIM). Each of these yields scores from four items rated on a Likert scale of 1-5, for a total score ranging from 5 to 20, with higher scores indicating higher ratings.
Veterans rated PLF-T as highly acceptable (mean AIM, 17.50), appropriate (mean IAM, 17.25), and feasible (mean FIM, 18).
Study participants reported the program was convenient and noted that it decreased the burden of traveling to sessions, especially during the COVID-19 pandemic.
They also reported the program was less likely to compete with other demands such as childcare and other appointments, said Ms. Sullivan.
In addition, it helped those with comorbidities such as posttraumatic stress disorder, she added. She noted veterans with PTSD may be triggered on subways or buses when traveling to in-person treatment sessions.
“That can take away from addressing the suicidal triggers,” said Ms. Sullivan. “So, this program allows them to fully concentrate on the safety plan.”
Results showed that study participants “enjoyed the group and would recommend it to others,” said Ms. Sullivan. “I think that signifies the group was effective in its goal of mitigating loneliness, which was exacerbated during the COVID-19 pandemic, and creating a socially supportive environment, especially for the vets living alone.”
Veterans also reported that the program helped them understand the connection between depression or PTSD and suicidal thoughts, urges, and plans. In addition, they appreciated the group dynamics, where they felt connected to other veterans experiencing similar challenges.
Hopeful results
Commenting on the study, Paul E. Holtzheimer, MD, deputy director for research at the National Center for PTSD, praised the study for focusing on a very high-risk group.
“This gets you closer to the population you’re probably going to have an impact on in terms of preventing suicide,” said Dr. Holtzheimer, a professor of psychiatry and surgery at Dartmouth College’s Geisel School of Medicine, Hanover, N.H.
The fact that many of the participants had attempted suicide in the last year underlines that this was a very high-risk population, said Dr. Holtzheimer. “Not only are they thinking about suicide, but almost two-thirds had actually attempted or tried something.”
This kind of program “would be great for rural environments where people may be living like four hours away from the VA or a clinic,” said Dr. Holtzheimer, noting that many veterans are often quite isolated.
“One of the very positive outcomes of the COVID-19 pandemic was helping us strengthen our ability to do telehealth,” he said.
However, Dr. Holtzheimer noted the study was small and qualitative. “The next step ideally would be a controlled trial looking at not just ideation but at risky behavior or clear suicide attempts or preparation, like buying a gun or hoarding medication, to help determine efficacy.”
The researchers and Dr. Holtzheimer report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ADAA 2023
Neuropsychiatric side effects of hormonal contraceptives: More common than you think!
Since its introduction in 1950, the combined oral contraceptive pill has been used by countless women as a method for birth control (Liao P. Can Fam Physician. 2012 Dec; 58[12]:e757-e760).
Hormonal contraception (HC) provides women with both contraceptive and noncontraceptive benefits, most notably a method for avoiding unintended pregnancy. In addition to being an effective method of contraception, oral contraceptive pills (OCPs) are well established for treating conditions such as hirsutism, pain symptoms associated with endometriosis and adenomyosis, and pelvic inflammatory disease, among others (Schindler A. Int J Endocrinol Metab. 2013 Winter;11[1]:41-7).
Combined hormonal contraceptives are also first-line treatment for women with menstrual disorders, and in women with polycystic ovary syndrome, can offer an effective long-term method to regulate their menstrual cycle, decrease androgens, clear up oily skin and acne, and reduce facial hair while also providing them with effective contraception (de Melo et al. Open Access J Contracept. 2017;8:13-23).
Associations between ‘the pill’ and mood effects remain controversial
More than 100 million women worldwide use hormonal contraceptives today, yet despite this, the data are mixed regarding the prevalence and extent of neuropsychiatric symptoms and mood changes associated with use of “the pill.” Some studies show combined oral contraceptives are associated with a decrease in general well-being, but had no effect on depression, in women compared with placebo (Zethraeus N et al. Fertil Steril. 2017 May;107[5]:1238-45).
However, a large Danish study published in JAMA Psychiatry of more than 1 million women found a significant association between use of hormonal contraception and antidepressant use or first diagnosis of depression, with adolescents having a higher rate of first depression diagnosis and antidepressant use compared with women 20–30 years old (Skovlund C et al. JAMA Psychiatry. 2016 Nov 1;73[11]:1154-62).
Studies have also shown long-term exposure to levonorgestrel is significantly associated with anxiety and sleep problems in women without a history of these issues (Slattery J et al. Drug Saf. 2018 Oct;41[10]:951-8). A recent small nationwide cohort study in France suggests this may also be true of levonorgestrel delivered by intrauterine devices (IUD) and the association may be dose-dependent (Roland N et al. JAMA. 2023;329[3]:257-9).
Of note, a study published in the American Journal of Psychiatry found a nearly twofold risk of suicide attempt and over threefold risk of suicide among women taking hormonal contraception compared with women who had never used hormonal contraceptives (Skovlund et al. Am J Psychiatry. 2017 Nov 17:appiajp201717060616).
Knowledge gaps make drawing conclusions difficult
The latest information on use of antidepressant and antianxiety medications in women of reproductive age (18-44 years) is sparse and, in some cases, outdated. According to data from the National Health and Nutrition Examination Survey, 18.6% of adult women 18 years or older reported using antidepressant medications within the last 30 days in 2017-2018, an increase from 13.8% in 2009-2010. Among women aged 15-44 year with private employer–sponsored insurance surveyed during 2008-2013, the results showed 15.4% of women filled a prescription for an antidepressant. We must look back further to find data on antianxiety medication use among women aged 18-44 years where use of antianxiety drugs (anxiolytics, sedatives, and hypnotics) was 4.3% between 2005 and 2008.
A lack of literature in this area is likely due to significant underreporting, and an inability to select patients who are sensitive to or at risk of developing neuropsychiatric symptoms resulting from hormonal contraception use because the true pathophysiology is unknown. Existing studies tend to use varying methods to assess mood changes, and do not usually specify hormonal contraceptive use type in their analyses (Schaffir J et al. Eur J Contracept Reprod Health Care. 2016 Oct;21[5]:347-55).
Studies of this nature also require large sample sizes, but the percentage of women who develop neuropsychiatric symptoms from hormonal contraceptive use has historically been relatively small. In the late 1990s, Rosenberg and colleagues found 46% of 1,657 women discontinued oral contraceptives due to side effects within 6 months of starting a new prescription; of these women, 5% reported mood changes as their reason for discontinuing oral contraceptives (Rosenberg M et al. Am J Obstet Gynecol. 1998 Sep;179[3 Pt 1]:577-82).
One might expect that, as lower dosage combined hormonal contraceptives were developed in the 1980s, that the rate of reporting psychological side effects would continue to decrease as well. Yet greater awareness of the potential for mood changes while on “the pill” as outlined by the lay press and social media may be leading to increased reporting of neuropsychiatric effects in women. In a recent cross-sectional survey of 188 women in New York, 43.6% said they experienced mood changes while on hormonal contraceptives, and 61.2% of women with histories of psychiatric illness reported mood changes they attributed to hormonal contraceptives (Martell S et al. Contracept Reprod Med. 2023;8:9).
Martell and colleagues found 48.3% of women cited side effects as a reason for discontinuing hormonal contraception, and 43 participants mentioned psychological side effects unprompted, including 2 patients with suicidal thoughts. The authors said this suggests “psychological side effects, at least in part, may have impacted” HC users’ decisions to switch from OCPs to an alternative method of contraception.
It is also not clear what risk factors exist for women who develop neuropsychiatric symptoms from hormonal contraceptive use. First, it is important to note that both progestin-only contraceptives and combined hormonal contraceptives are classified by the Centers for Disease Control and Prevention’s US Medical Eligibility Criteria for Contraceptive Use, 2016 as having no restrictions for use, including among patients with depression. While women in a smaller subgroup have significant neuropsychiatric symptoms related to their hormonal contraceptives, the underlying mechanism is unknown, and is thought to be largely related to the progestogen component of combined hormonal contraceptives or progestogen-only contraceptives (Mu E. Aust Prescr. 2022 Jun; 45[3]:75-9). We know that some women are hormone sensitive, while others are less so, and some not at all. Progestogens could affect mood as a direct action of the progestogen, because progestogens can be neurosteroids, or the progestogen effect could be mediated secondarily through a change in that woman’s own production of or bioavailability of androgens or naturally occurring estrogens (Giatti S. J Mol Endocrinol. 2016 Aug;57[2]:R109-26).
Here, we also find that currently available evidence limits our ability to draw firm conclusions. A study by Berry-Bibee and colleagues found a “low concern for clinically significant interactions” between hormonal contraception and psychotropic drugs, but was limited by quality/quantity of evidence (Berry-Bibee E et al. Contraception. 2016 Dec;94[6]:650-67). Interestingly, a study by Robinson and colleagues from the mid-2000s posited based on low evidence that “psychological response to the practice of contraception” was a potential explanation for the side effect profile of hormonal contraception (Robinson S et al. Med Hypotheses. 2004;63[2]:268-73).
Further, it may be that women with premenstrual dysphoric disorder (PMDD) might be selected for oral contraceptives, and they are predisposed to other neuropsychiatric problems. Estimates have placed the prevalence of comorbid psychiatric disorders such as anxiety, major depression, bipolar disorder, and posttraumatic stress disorder as high as 70% for women with PMDD (Sepede G et al. Neuropsychiatr Dis Treat. 2020;16:415-26). This phenomenon is not new, having been characterized in the lay literature nearly 20 years ago, by endocrinologist Geoffrey P. Redmond, MD (Redmond GP. The Hormonally Vulnerable Woman. New York: HarperCollins; 2005).
While the cause is not exactly idiosyncratic, They tend to have an entire spectrum of responses to the progestogens in combined or progestin-only contraceptives, ranging from just a flattened affect – which could easily be explained by their flattened level of endogenous hormones – to frank depression. Their frank depression, in turn, can be demonstrated to include suicidal ideation and actual suicide.
Compounding this issue is a woman’s perception of her sexuality. Some women with low sexual desire or sexual problems who are younger may have more distress about their problems compared with women of older reproductive age. While the reason for that is not clear, it may be that in the sexual arena, it is more important for some younger women to be a sexual person than in perimenopausal women, or that women who are younger are more likely to be partnered than women of older reproductive age. While the European Society of Sexual Medicine concluded in a 2019 position statement that there is inconclusive evidence whether hormonal contraception may be contributing to changes in sexual desire and sexual dysfunction, it appears that “a minority of women” experience “better or worse sexual functioning” from taking combined oral contraceptives (Both S et al. J Sex Med. 2019 Nov;16[11]:1681-95), suggesting that the majority of women report no significant changes.
Practitioners should discuss mood effects during consultation
An ob.gyn., primary care physicians, or others with prescriptive authority (i.e. nurse practitioners and physician assistants) in clinical practice may encounter a patient who seems to have mood side effects owing to progestogen-containing contraceptives that they prescribe. However, many ob.gyns. are likely unaware of the prevalence, or that some of those same patients can have such significant mood effects that they would become or are suicidal.
I believe questioning patients about mood effects during consultation and particularly during follow-up following the initiation of any hormonal contraceptive is worth a passing comment for every patient, which should include mood effects in broader discussion for anyone currently using an antidepressant, patients with a history of antidepressant use, and patients who have considered suicide. As we do with other drugs, these questions can be posed in the form of a questionnaire followed up by the practitioner in counseling.
Practitioners who encounter a patient with mood changes as a result of hormonal contraceptive use can consider changing to a nonhormonal method of birth control, or recommending the patient use a barrier method during sexual activity, as none of these options have neuropsychiatric side effects.
Ultimately, practitioners of all types need to engage in shared decision-making to identify the key benefits and risks of hormonal contraceptive use for each patient, which may involve trial and error to determine the ideal treatment. It is critical that practitioners of all types strike a balance between alleviating patient concerns about potential mood changes, monitoring patients with an appreciable risk of mood changes, and continuing patients on hormonal contraception for whom the benefits outweigh the risks.
Dr. Simon is a clinical professor at George Washington University and the medical director and founder of IntimMedicine Specialists in Washington, which provides patient-focused care for women across the reproductive life cycle. He is a past president of the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Dr. Simon has been a consultant to, received grant and research support from, and served on the speakers bureau for various pharmaceutical companies that develop combination hormonal contraceptives. Email Dr. Simon at [email protected].
Since its introduction in 1950, the combined oral contraceptive pill has been used by countless women as a method for birth control (Liao P. Can Fam Physician. 2012 Dec; 58[12]:e757-e760).
Hormonal contraception (HC) provides women with both contraceptive and noncontraceptive benefits, most notably a method for avoiding unintended pregnancy. In addition to being an effective method of contraception, oral contraceptive pills (OCPs) are well established for treating conditions such as hirsutism, pain symptoms associated with endometriosis and adenomyosis, and pelvic inflammatory disease, among others (Schindler A. Int J Endocrinol Metab. 2013 Winter;11[1]:41-7).
Combined hormonal contraceptives are also first-line treatment for women with menstrual disorders, and in women with polycystic ovary syndrome, can offer an effective long-term method to regulate their menstrual cycle, decrease androgens, clear up oily skin and acne, and reduce facial hair while also providing them with effective contraception (de Melo et al. Open Access J Contracept. 2017;8:13-23).
Associations between ‘the pill’ and mood effects remain controversial
More than 100 million women worldwide use hormonal contraceptives today, yet despite this, the data are mixed regarding the prevalence and extent of neuropsychiatric symptoms and mood changes associated with use of “the pill.” Some studies show combined oral contraceptives are associated with a decrease in general well-being, but had no effect on depression, in women compared with placebo (Zethraeus N et al. Fertil Steril. 2017 May;107[5]:1238-45).
However, a large Danish study published in JAMA Psychiatry of more than 1 million women found a significant association between use of hormonal contraception and antidepressant use or first diagnosis of depression, with adolescents having a higher rate of first depression diagnosis and antidepressant use compared with women 20–30 years old (Skovlund C et al. JAMA Psychiatry. 2016 Nov 1;73[11]:1154-62).
Studies have also shown long-term exposure to levonorgestrel is significantly associated with anxiety and sleep problems in women without a history of these issues (Slattery J et al. Drug Saf. 2018 Oct;41[10]:951-8). A recent small nationwide cohort study in France suggests this may also be true of levonorgestrel delivered by intrauterine devices (IUD) and the association may be dose-dependent (Roland N et al. JAMA. 2023;329[3]:257-9).
Of note, a study published in the American Journal of Psychiatry found a nearly twofold risk of suicide attempt and over threefold risk of suicide among women taking hormonal contraception compared with women who had never used hormonal contraceptives (Skovlund et al. Am J Psychiatry. 2017 Nov 17:appiajp201717060616).
Knowledge gaps make drawing conclusions difficult
The latest information on use of antidepressant and antianxiety medications in women of reproductive age (18-44 years) is sparse and, in some cases, outdated. According to data from the National Health and Nutrition Examination Survey, 18.6% of adult women 18 years or older reported using antidepressant medications within the last 30 days in 2017-2018, an increase from 13.8% in 2009-2010. Among women aged 15-44 year with private employer–sponsored insurance surveyed during 2008-2013, the results showed 15.4% of women filled a prescription for an antidepressant. We must look back further to find data on antianxiety medication use among women aged 18-44 years where use of antianxiety drugs (anxiolytics, sedatives, and hypnotics) was 4.3% between 2005 and 2008.
A lack of literature in this area is likely due to significant underreporting, and an inability to select patients who are sensitive to or at risk of developing neuropsychiatric symptoms resulting from hormonal contraception use because the true pathophysiology is unknown. Existing studies tend to use varying methods to assess mood changes, and do not usually specify hormonal contraceptive use type in their analyses (Schaffir J et al. Eur J Contracept Reprod Health Care. 2016 Oct;21[5]:347-55).
Studies of this nature also require large sample sizes, but the percentage of women who develop neuropsychiatric symptoms from hormonal contraceptive use has historically been relatively small. In the late 1990s, Rosenberg and colleagues found 46% of 1,657 women discontinued oral contraceptives due to side effects within 6 months of starting a new prescription; of these women, 5% reported mood changes as their reason for discontinuing oral contraceptives (Rosenberg M et al. Am J Obstet Gynecol. 1998 Sep;179[3 Pt 1]:577-82).
One might expect that, as lower dosage combined hormonal contraceptives were developed in the 1980s, that the rate of reporting psychological side effects would continue to decrease as well. Yet greater awareness of the potential for mood changes while on “the pill” as outlined by the lay press and social media may be leading to increased reporting of neuropsychiatric effects in women. In a recent cross-sectional survey of 188 women in New York, 43.6% said they experienced mood changes while on hormonal contraceptives, and 61.2% of women with histories of psychiatric illness reported mood changes they attributed to hormonal contraceptives (Martell S et al. Contracept Reprod Med. 2023;8:9).
Martell and colleagues found 48.3% of women cited side effects as a reason for discontinuing hormonal contraception, and 43 participants mentioned psychological side effects unprompted, including 2 patients with suicidal thoughts. The authors said this suggests “psychological side effects, at least in part, may have impacted” HC users’ decisions to switch from OCPs to an alternative method of contraception.
It is also not clear what risk factors exist for women who develop neuropsychiatric symptoms from hormonal contraceptive use. First, it is important to note that both progestin-only contraceptives and combined hormonal contraceptives are classified by the Centers for Disease Control and Prevention’s US Medical Eligibility Criteria for Contraceptive Use, 2016 as having no restrictions for use, including among patients with depression. While women in a smaller subgroup have significant neuropsychiatric symptoms related to their hormonal contraceptives, the underlying mechanism is unknown, and is thought to be largely related to the progestogen component of combined hormonal contraceptives or progestogen-only contraceptives (Mu E. Aust Prescr. 2022 Jun; 45[3]:75-9). We know that some women are hormone sensitive, while others are less so, and some not at all. Progestogens could affect mood as a direct action of the progestogen, because progestogens can be neurosteroids, or the progestogen effect could be mediated secondarily through a change in that woman’s own production of or bioavailability of androgens or naturally occurring estrogens (Giatti S. J Mol Endocrinol. 2016 Aug;57[2]:R109-26).
Here, we also find that currently available evidence limits our ability to draw firm conclusions. A study by Berry-Bibee and colleagues found a “low concern for clinically significant interactions” between hormonal contraception and psychotropic drugs, but was limited by quality/quantity of evidence (Berry-Bibee E et al. Contraception. 2016 Dec;94[6]:650-67). Interestingly, a study by Robinson and colleagues from the mid-2000s posited based on low evidence that “psychological response to the practice of contraception” was a potential explanation for the side effect profile of hormonal contraception (Robinson S et al. Med Hypotheses. 2004;63[2]:268-73).
Further, it may be that women with premenstrual dysphoric disorder (PMDD) might be selected for oral contraceptives, and they are predisposed to other neuropsychiatric problems. Estimates have placed the prevalence of comorbid psychiatric disorders such as anxiety, major depression, bipolar disorder, and posttraumatic stress disorder as high as 70% for women with PMDD (Sepede G et al. Neuropsychiatr Dis Treat. 2020;16:415-26). This phenomenon is not new, having been characterized in the lay literature nearly 20 years ago, by endocrinologist Geoffrey P. Redmond, MD (Redmond GP. The Hormonally Vulnerable Woman. New York: HarperCollins; 2005).
While the cause is not exactly idiosyncratic, They tend to have an entire spectrum of responses to the progestogens in combined or progestin-only contraceptives, ranging from just a flattened affect – which could easily be explained by their flattened level of endogenous hormones – to frank depression. Their frank depression, in turn, can be demonstrated to include suicidal ideation and actual suicide.
Compounding this issue is a woman’s perception of her sexuality. Some women with low sexual desire or sexual problems who are younger may have more distress about their problems compared with women of older reproductive age. While the reason for that is not clear, it may be that in the sexual arena, it is more important for some younger women to be a sexual person than in perimenopausal women, or that women who are younger are more likely to be partnered than women of older reproductive age. While the European Society of Sexual Medicine concluded in a 2019 position statement that there is inconclusive evidence whether hormonal contraception may be contributing to changes in sexual desire and sexual dysfunction, it appears that “a minority of women” experience “better or worse sexual functioning” from taking combined oral contraceptives (Both S et al. J Sex Med. 2019 Nov;16[11]:1681-95), suggesting that the majority of women report no significant changes.
Practitioners should discuss mood effects during consultation
An ob.gyn., primary care physicians, or others with prescriptive authority (i.e. nurse practitioners and physician assistants) in clinical practice may encounter a patient who seems to have mood side effects owing to progestogen-containing contraceptives that they prescribe. However, many ob.gyns. are likely unaware of the prevalence, or that some of those same patients can have such significant mood effects that they would become or are suicidal.
I believe questioning patients about mood effects during consultation and particularly during follow-up following the initiation of any hormonal contraceptive is worth a passing comment for every patient, which should include mood effects in broader discussion for anyone currently using an antidepressant, patients with a history of antidepressant use, and patients who have considered suicide. As we do with other drugs, these questions can be posed in the form of a questionnaire followed up by the practitioner in counseling.
Practitioners who encounter a patient with mood changes as a result of hormonal contraceptive use can consider changing to a nonhormonal method of birth control, or recommending the patient use a barrier method during sexual activity, as none of these options have neuropsychiatric side effects.
Ultimately, practitioners of all types need to engage in shared decision-making to identify the key benefits and risks of hormonal contraceptive use for each patient, which may involve trial and error to determine the ideal treatment. It is critical that practitioners of all types strike a balance between alleviating patient concerns about potential mood changes, monitoring patients with an appreciable risk of mood changes, and continuing patients on hormonal contraception for whom the benefits outweigh the risks.
Dr. Simon is a clinical professor at George Washington University and the medical director and founder of IntimMedicine Specialists in Washington, which provides patient-focused care for women across the reproductive life cycle. He is a past president of the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Dr. Simon has been a consultant to, received grant and research support from, and served on the speakers bureau for various pharmaceutical companies that develop combination hormonal contraceptives. Email Dr. Simon at [email protected].
Since its introduction in 1950, the combined oral contraceptive pill has been used by countless women as a method for birth control (Liao P. Can Fam Physician. 2012 Dec; 58[12]:e757-e760).
Hormonal contraception (HC) provides women with both contraceptive and noncontraceptive benefits, most notably a method for avoiding unintended pregnancy. In addition to being an effective method of contraception, oral contraceptive pills (OCPs) are well established for treating conditions such as hirsutism, pain symptoms associated with endometriosis and adenomyosis, and pelvic inflammatory disease, among others (Schindler A. Int J Endocrinol Metab. 2013 Winter;11[1]:41-7).
Combined hormonal contraceptives are also first-line treatment for women with menstrual disorders, and in women with polycystic ovary syndrome, can offer an effective long-term method to regulate their menstrual cycle, decrease androgens, clear up oily skin and acne, and reduce facial hair while also providing them with effective contraception (de Melo et al. Open Access J Contracept. 2017;8:13-23).
Associations between ‘the pill’ and mood effects remain controversial
More than 100 million women worldwide use hormonal contraceptives today, yet despite this, the data are mixed regarding the prevalence and extent of neuropsychiatric symptoms and mood changes associated with use of “the pill.” Some studies show combined oral contraceptives are associated with a decrease in general well-being, but had no effect on depression, in women compared with placebo (Zethraeus N et al. Fertil Steril. 2017 May;107[5]:1238-45).
However, a large Danish study published in JAMA Psychiatry of more than 1 million women found a significant association between use of hormonal contraception and antidepressant use or first diagnosis of depression, with adolescents having a higher rate of first depression diagnosis and antidepressant use compared with women 20–30 years old (Skovlund C et al. JAMA Psychiatry. 2016 Nov 1;73[11]:1154-62).
Studies have also shown long-term exposure to levonorgestrel is significantly associated with anxiety and sleep problems in women without a history of these issues (Slattery J et al. Drug Saf. 2018 Oct;41[10]:951-8). A recent small nationwide cohort study in France suggests this may also be true of levonorgestrel delivered by intrauterine devices (IUD) and the association may be dose-dependent (Roland N et al. JAMA. 2023;329[3]:257-9).
Of note, a study published in the American Journal of Psychiatry found a nearly twofold risk of suicide attempt and over threefold risk of suicide among women taking hormonal contraception compared with women who had never used hormonal contraceptives (Skovlund et al. Am J Psychiatry. 2017 Nov 17:appiajp201717060616).
Knowledge gaps make drawing conclusions difficult
The latest information on use of antidepressant and antianxiety medications in women of reproductive age (18-44 years) is sparse and, in some cases, outdated. According to data from the National Health and Nutrition Examination Survey, 18.6% of adult women 18 years or older reported using antidepressant medications within the last 30 days in 2017-2018, an increase from 13.8% in 2009-2010. Among women aged 15-44 year with private employer–sponsored insurance surveyed during 2008-2013, the results showed 15.4% of women filled a prescription for an antidepressant. We must look back further to find data on antianxiety medication use among women aged 18-44 years where use of antianxiety drugs (anxiolytics, sedatives, and hypnotics) was 4.3% between 2005 and 2008.
A lack of literature in this area is likely due to significant underreporting, and an inability to select patients who are sensitive to or at risk of developing neuropsychiatric symptoms resulting from hormonal contraception use because the true pathophysiology is unknown. Existing studies tend to use varying methods to assess mood changes, and do not usually specify hormonal contraceptive use type in their analyses (Schaffir J et al. Eur J Contracept Reprod Health Care. 2016 Oct;21[5]:347-55).
Studies of this nature also require large sample sizes, but the percentage of women who develop neuropsychiatric symptoms from hormonal contraceptive use has historically been relatively small. In the late 1990s, Rosenberg and colleagues found 46% of 1,657 women discontinued oral contraceptives due to side effects within 6 months of starting a new prescription; of these women, 5% reported mood changes as their reason for discontinuing oral contraceptives (Rosenberg M et al. Am J Obstet Gynecol. 1998 Sep;179[3 Pt 1]:577-82).
One might expect that, as lower dosage combined hormonal contraceptives were developed in the 1980s, that the rate of reporting psychological side effects would continue to decrease as well. Yet greater awareness of the potential for mood changes while on “the pill” as outlined by the lay press and social media may be leading to increased reporting of neuropsychiatric effects in women. In a recent cross-sectional survey of 188 women in New York, 43.6% said they experienced mood changes while on hormonal contraceptives, and 61.2% of women with histories of psychiatric illness reported mood changes they attributed to hormonal contraceptives (Martell S et al. Contracept Reprod Med. 2023;8:9).
Martell and colleagues found 48.3% of women cited side effects as a reason for discontinuing hormonal contraception, and 43 participants mentioned psychological side effects unprompted, including 2 patients with suicidal thoughts. The authors said this suggests “psychological side effects, at least in part, may have impacted” HC users’ decisions to switch from OCPs to an alternative method of contraception.
It is also not clear what risk factors exist for women who develop neuropsychiatric symptoms from hormonal contraceptive use. First, it is important to note that both progestin-only contraceptives and combined hormonal contraceptives are classified by the Centers for Disease Control and Prevention’s US Medical Eligibility Criteria for Contraceptive Use, 2016 as having no restrictions for use, including among patients with depression. While women in a smaller subgroup have significant neuropsychiatric symptoms related to their hormonal contraceptives, the underlying mechanism is unknown, and is thought to be largely related to the progestogen component of combined hormonal contraceptives or progestogen-only contraceptives (Mu E. Aust Prescr. 2022 Jun; 45[3]:75-9). We know that some women are hormone sensitive, while others are less so, and some not at all. Progestogens could affect mood as a direct action of the progestogen, because progestogens can be neurosteroids, or the progestogen effect could be mediated secondarily through a change in that woman’s own production of or bioavailability of androgens or naturally occurring estrogens (Giatti S. J Mol Endocrinol. 2016 Aug;57[2]:R109-26).
Here, we also find that currently available evidence limits our ability to draw firm conclusions. A study by Berry-Bibee and colleagues found a “low concern for clinically significant interactions” between hormonal contraception and psychotropic drugs, but was limited by quality/quantity of evidence (Berry-Bibee E et al. Contraception. 2016 Dec;94[6]:650-67). Interestingly, a study by Robinson and colleagues from the mid-2000s posited based on low evidence that “psychological response to the practice of contraception” was a potential explanation for the side effect profile of hormonal contraception (Robinson S et al. Med Hypotheses. 2004;63[2]:268-73).
Further, it may be that women with premenstrual dysphoric disorder (PMDD) might be selected for oral contraceptives, and they are predisposed to other neuropsychiatric problems. Estimates have placed the prevalence of comorbid psychiatric disorders such as anxiety, major depression, bipolar disorder, and posttraumatic stress disorder as high as 70% for women with PMDD (Sepede G et al. Neuropsychiatr Dis Treat. 2020;16:415-26). This phenomenon is not new, having been characterized in the lay literature nearly 20 years ago, by endocrinologist Geoffrey P. Redmond, MD (Redmond GP. The Hormonally Vulnerable Woman. New York: HarperCollins; 2005).
While the cause is not exactly idiosyncratic, They tend to have an entire spectrum of responses to the progestogens in combined or progestin-only contraceptives, ranging from just a flattened affect – which could easily be explained by their flattened level of endogenous hormones – to frank depression. Their frank depression, in turn, can be demonstrated to include suicidal ideation and actual suicide.
Compounding this issue is a woman’s perception of her sexuality. Some women with low sexual desire or sexual problems who are younger may have more distress about their problems compared with women of older reproductive age. While the reason for that is not clear, it may be that in the sexual arena, it is more important for some younger women to be a sexual person than in perimenopausal women, or that women who are younger are more likely to be partnered than women of older reproductive age. While the European Society of Sexual Medicine concluded in a 2019 position statement that there is inconclusive evidence whether hormonal contraception may be contributing to changes in sexual desire and sexual dysfunction, it appears that “a minority of women” experience “better or worse sexual functioning” from taking combined oral contraceptives (Both S et al. J Sex Med. 2019 Nov;16[11]:1681-95), suggesting that the majority of women report no significant changes.
Practitioners should discuss mood effects during consultation
An ob.gyn., primary care physicians, or others with prescriptive authority (i.e. nurse practitioners and physician assistants) in clinical practice may encounter a patient who seems to have mood side effects owing to progestogen-containing contraceptives that they prescribe. However, many ob.gyns. are likely unaware of the prevalence, or that some of those same patients can have such significant mood effects that they would become or are suicidal.
I believe questioning patients about mood effects during consultation and particularly during follow-up following the initiation of any hormonal contraceptive is worth a passing comment for every patient, which should include mood effects in broader discussion for anyone currently using an antidepressant, patients with a history of antidepressant use, and patients who have considered suicide. As we do with other drugs, these questions can be posed in the form of a questionnaire followed up by the practitioner in counseling.
Practitioners who encounter a patient with mood changes as a result of hormonal contraceptive use can consider changing to a nonhormonal method of birth control, or recommending the patient use a barrier method during sexual activity, as none of these options have neuropsychiatric side effects.
Ultimately, practitioners of all types need to engage in shared decision-making to identify the key benefits and risks of hormonal contraceptive use for each patient, which may involve trial and error to determine the ideal treatment. It is critical that practitioners of all types strike a balance between alleviating patient concerns about potential mood changes, monitoring patients with an appreciable risk of mood changes, and continuing patients on hormonal contraception for whom the benefits outweigh the risks.
Dr. Simon is a clinical professor at George Washington University and the medical director and founder of IntimMedicine Specialists in Washington, which provides patient-focused care for women across the reproductive life cycle. He is a past president of the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Dr. Simon has been a consultant to, received grant and research support from, and served on the speakers bureau for various pharmaceutical companies that develop combination hormonal contraceptives. Email Dr. Simon at [email protected].
Physical exercise tied to a reduction in suicide attempts
A meta-analysis of 17 randomized controlled trials (RCTs), which included more than 1,000 participants with mental or physical illnesses, showed there was a significant reduction in suicide attempts in participants randomly assigned to receive exercise interventions, compared with inactive controls. However, there were no differences between the exercise and the control groups in suicidal ideation or mortality.
On the other hand, there was also no significant difference in dropout rates between those randomly assigned to exercise versus inactive controls, suggesting that people with mental or physical impairments are able to adhere to exercise regimens.
“A common misconception is that patients, particularly those suffering from mental of physical illness, are not willing or motivated enough to participate in an exercise [regimen], and this has led to primary care providers underprescribing exercise to those with mental or physical illness,” lead author Nicholas Fabiano, MD, a resident in the department of psychiatry at the University of Ottawa, told this news organization.
As a result of the study findings, “we recommend that providers do not have apprehension about prescribing exercise to patients with physical or mental illness. Exercise may be an effective way to reduce suicidal behaviors” in these patients, he said.
The study was published online in the Journal of Affective Disorders.
Physical, mental health strongly linked
Existing literature has “demonstrated a protective effect of physical activity on suicidal ideation in the general population,” but to date there have been no systematic reviews or meta-analyses investigating its impact on suicide-related outcomes in patients with physical or mental illness, the authors write.
“Those with mental or physical illness are at increased risk of suicide, compared to the general population,” Dr. Fabiano commented.
“We often split up ‘mental health’ and ‘physical health’ in medicine; however, I believe that the two are more on a continuum and a holistic term, such as ‘health,’ should be used instead,” he added.
He noted that mental and physical health are “inexorably intertwined” and those with physical illness are more prone to developing mental illness, whereas those with mental illness are more likely to suffer from a variety of other medical conditions. “Therefore, when treating those with mental illness, it is also imperative that we bolster one’s physical health through easily accessible activities such as exercise,” he said.
The goal of the study was to determine whether individuals with “any mental, physical, clinical, or subclinical condition” might benefit from exercise, particularly in relation to suicide-related outcomes. They searched multiple databases from inception to June 2022 to identify RCTs investigating exercise and suicidal ideation in participants with physical or mental conditions.
Of 673 studies, 17 met the inclusion criteria (total of 1,021 participants). Participants’ mean age was 42.7 years, 82% were female, and 54% were randomly assigned to an exercise intervention.
Most studies (82%) focused on clinical versus subclinical outcomes. Depression was the most commonly included condition (59%). Aerobic exercise (53%) was the most common form of exercise used in the active study groups. This was followed by mind-body exercise and strength training (53%, 17.6%, and 17.6%, respectively). The mean follow-up time was 10 weeks.
Reduced impulsivity
The researchers found a difference in post-intervention suicidal ideation when they compared exercise participants to all control and inactive control participants (standardized mean difference, –1.09; 95% confidence interval, –3.08 to 0.90; P = .20, k = 5). However, the difference was not statistically significant.
Similarly, there was no significant difference (P = .60) in suicidal ideation incidence for subgroup analyses that stratified data among participants with depression, sickle cell disease, and suicidality.
All-cause discontinuation also did not significantly differ between participants who were randomly assigned to exercise interventions versus all controls or inactive controls (odds ratio, 0.85; 95% CI, 0.38-1.94; P = .86, k = 12 and OR, 0.81; 95% CI, 0.25-2.68; P = .70). All-cause discontinuation also did not differ between participants randomized to exercise versus active controls (OR, 0.94; 95% CI, 0.38-2.32; P = .79, k = 3).
Likewise, there were nonsignificant differences between participants who underwent aerobic exercise and strength training (P = .20).
However, there were some nonsignificant differences when comparing participants with depression and stress who received the exercise intervention versus controls (P = .46).
There was a significant reduction in suicide attempts in individuals who participated in exercise interventions versus inactive controls (OR, 0.23; 95% CI, 0.09-0.67; P = .04, k = 2). On the other hand, there was no significant difference in mortality (P = .70).
Most of the studies (82%) were “at high risk of bias,” the authors note. In addition, the analysis was limited because the included studies were “few, underpowered, and heterogeneous.”
Dr. Fabiano hypothesized that the lack of effect on suicidal ideation or mortality is “likely due to the limited sample size.” As additional RCTs are conducted, Dr. Fabiano expects to see decreases in both suicidal ideation and suicide attempts.
The findings may “be explained by the ideation-to-action framework, which suggests that the development of suicidal ideation and the progression to suicide attempts are distinct processes with different influential factors,” he said.
Increased levels of exercise have been “shown to reduce emotional impulsivity and, as it has been shown that most suicide attempts are characterized by impulsivity and low lethality, we hypothesize that regular exercise serves as a protective factor against suicide attempts,” he said.
Not useful?
Commenting on the study, Fabien Legrand, PhD, a lecturer in clinical psychology, University of Reims Champagne-Ardenne, Reims, France, said that the impact of physical activity is of “particular interest” to him because it is closely linked to his research activity, where he has “been exploring the antidepressant effects of exercise for more than 15 years.”
A small pilot study conducted by Dr. Legrand and colleagues found rigorous physical activity to be helpful in reducing hopelessness in psychiatric patients, compared with controls. “This result is of particular relevance for suicidal patients, since it has long been documented that hopelessness is one of the main triggers of suicide ideation and suicide attempts,” he said.
Initially, Dr. Legrand “warmly welcomed” the current review and meta-analysis on the exercise and suicide. However, he felt that the paper fell short in accomplishing its intended goal. “After a thorough reading of the paper, I don’t think that the information provided can be used in any way,” he stated.
“The paper’s title – ‘Effects of Physical Exercise on Suicidal Ideation and Behavior’ – does not do justice to its content, since 9 of the included 17 RCTs did not measure changes in suicidal ideation and/or suicidal behavior following participation in an exercise program,” noted Dr. Legrand, who was not involved with authorship or the current analysis.
The study was funded by the University of Ottawa department of psychiatry. Dr. Fabiano declares no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. Legrand declares no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A meta-analysis of 17 randomized controlled trials (RCTs), which included more than 1,000 participants with mental or physical illnesses, showed there was a significant reduction in suicide attempts in participants randomly assigned to receive exercise interventions, compared with inactive controls. However, there were no differences between the exercise and the control groups in suicidal ideation or mortality.
On the other hand, there was also no significant difference in dropout rates between those randomly assigned to exercise versus inactive controls, suggesting that people with mental or physical impairments are able to adhere to exercise regimens.
“A common misconception is that patients, particularly those suffering from mental of physical illness, are not willing or motivated enough to participate in an exercise [regimen], and this has led to primary care providers underprescribing exercise to those with mental or physical illness,” lead author Nicholas Fabiano, MD, a resident in the department of psychiatry at the University of Ottawa, told this news organization.
As a result of the study findings, “we recommend that providers do not have apprehension about prescribing exercise to patients with physical or mental illness. Exercise may be an effective way to reduce suicidal behaviors” in these patients, he said.
The study was published online in the Journal of Affective Disorders.
Physical, mental health strongly linked
Existing literature has “demonstrated a protective effect of physical activity on suicidal ideation in the general population,” but to date there have been no systematic reviews or meta-analyses investigating its impact on suicide-related outcomes in patients with physical or mental illness, the authors write.
“Those with mental or physical illness are at increased risk of suicide, compared to the general population,” Dr. Fabiano commented.
“We often split up ‘mental health’ and ‘physical health’ in medicine; however, I believe that the two are more on a continuum and a holistic term, such as ‘health,’ should be used instead,” he added.
He noted that mental and physical health are “inexorably intertwined” and those with physical illness are more prone to developing mental illness, whereas those with mental illness are more likely to suffer from a variety of other medical conditions. “Therefore, when treating those with mental illness, it is also imperative that we bolster one’s physical health through easily accessible activities such as exercise,” he said.
The goal of the study was to determine whether individuals with “any mental, physical, clinical, or subclinical condition” might benefit from exercise, particularly in relation to suicide-related outcomes. They searched multiple databases from inception to June 2022 to identify RCTs investigating exercise and suicidal ideation in participants with physical or mental conditions.
Of 673 studies, 17 met the inclusion criteria (total of 1,021 participants). Participants’ mean age was 42.7 years, 82% were female, and 54% were randomly assigned to an exercise intervention.
Most studies (82%) focused on clinical versus subclinical outcomes. Depression was the most commonly included condition (59%). Aerobic exercise (53%) was the most common form of exercise used in the active study groups. This was followed by mind-body exercise and strength training (53%, 17.6%, and 17.6%, respectively). The mean follow-up time was 10 weeks.
Reduced impulsivity
The researchers found a difference in post-intervention suicidal ideation when they compared exercise participants to all control and inactive control participants (standardized mean difference, –1.09; 95% confidence interval, –3.08 to 0.90; P = .20, k = 5). However, the difference was not statistically significant.
Similarly, there was no significant difference (P = .60) in suicidal ideation incidence for subgroup analyses that stratified data among participants with depression, sickle cell disease, and suicidality.
All-cause discontinuation also did not significantly differ between participants who were randomly assigned to exercise interventions versus all controls or inactive controls (odds ratio, 0.85; 95% CI, 0.38-1.94; P = .86, k = 12 and OR, 0.81; 95% CI, 0.25-2.68; P = .70). All-cause discontinuation also did not differ between participants randomized to exercise versus active controls (OR, 0.94; 95% CI, 0.38-2.32; P = .79, k = 3).
Likewise, there were nonsignificant differences between participants who underwent aerobic exercise and strength training (P = .20).
However, there were some nonsignificant differences when comparing participants with depression and stress who received the exercise intervention versus controls (P = .46).
There was a significant reduction in suicide attempts in individuals who participated in exercise interventions versus inactive controls (OR, 0.23; 95% CI, 0.09-0.67; P = .04, k = 2). On the other hand, there was no significant difference in mortality (P = .70).
Most of the studies (82%) were “at high risk of bias,” the authors note. In addition, the analysis was limited because the included studies were “few, underpowered, and heterogeneous.”
Dr. Fabiano hypothesized that the lack of effect on suicidal ideation or mortality is “likely due to the limited sample size.” As additional RCTs are conducted, Dr. Fabiano expects to see decreases in both suicidal ideation and suicide attempts.
The findings may “be explained by the ideation-to-action framework, which suggests that the development of suicidal ideation and the progression to suicide attempts are distinct processes with different influential factors,” he said.
Increased levels of exercise have been “shown to reduce emotional impulsivity and, as it has been shown that most suicide attempts are characterized by impulsivity and low lethality, we hypothesize that regular exercise serves as a protective factor against suicide attempts,” he said.
Not useful?
Commenting on the study, Fabien Legrand, PhD, a lecturer in clinical psychology, University of Reims Champagne-Ardenne, Reims, France, said that the impact of physical activity is of “particular interest” to him because it is closely linked to his research activity, where he has “been exploring the antidepressant effects of exercise for more than 15 years.”
A small pilot study conducted by Dr. Legrand and colleagues found rigorous physical activity to be helpful in reducing hopelessness in psychiatric patients, compared with controls. “This result is of particular relevance for suicidal patients, since it has long been documented that hopelessness is one of the main triggers of suicide ideation and suicide attempts,” he said.
Initially, Dr. Legrand “warmly welcomed” the current review and meta-analysis on the exercise and suicide. However, he felt that the paper fell short in accomplishing its intended goal. “After a thorough reading of the paper, I don’t think that the information provided can be used in any way,” he stated.
“The paper’s title – ‘Effects of Physical Exercise on Suicidal Ideation and Behavior’ – does not do justice to its content, since 9 of the included 17 RCTs did not measure changes in suicidal ideation and/or suicidal behavior following participation in an exercise program,” noted Dr. Legrand, who was not involved with authorship or the current analysis.
The study was funded by the University of Ottawa department of psychiatry. Dr. Fabiano declares no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. Legrand declares no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A meta-analysis of 17 randomized controlled trials (RCTs), which included more than 1,000 participants with mental or physical illnesses, showed there was a significant reduction in suicide attempts in participants randomly assigned to receive exercise interventions, compared with inactive controls. However, there were no differences between the exercise and the control groups in suicidal ideation or mortality.
On the other hand, there was also no significant difference in dropout rates between those randomly assigned to exercise versus inactive controls, suggesting that people with mental or physical impairments are able to adhere to exercise regimens.
“A common misconception is that patients, particularly those suffering from mental of physical illness, are not willing or motivated enough to participate in an exercise [regimen], and this has led to primary care providers underprescribing exercise to those with mental or physical illness,” lead author Nicholas Fabiano, MD, a resident in the department of psychiatry at the University of Ottawa, told this news organization.
As a result of the study findings, “we recommend that providers do not have apprehension about prescribing exercise to patients with physical or mental illness. Exercise may be an effective way to reduce suicidal behaviors” in these patients, he said.
The study was published online in the Journal of Affective Disorders.
Physical, mental health strongly linked
Existing literature has “demonstrated a protective effect of physical activity on suicidal ideation in the general population,” but to date there have been no systematic reviews or meta-analyses investigating its impact on suicide-related outcomes in patients with physical or mental illness, the authors write.
“Those with mental or physical illness are at increased risk of suicide, compared to the general population,” Dr. Fabiano commented.
“We often split up ‘mental health’ and ‘physical health’ in medicine; however, I believe that the two are more on a continuum and a holistic term, such as ‘health,’ should be used instead,” he added.
He noted that mental and physical health are “inexorably intertwined” and those with physical illness are more prone to developing mental illness, whereas those with mental illness are more likely to suffer from a variety of other medical conditions. “Therefore, when treating those with mental illness, it is also imperative that we bolster one’s physical health through easily accessible activities such as exercise,” he said.
The goal of the study was to determine whether individuals with “any mental, physical, clinical, or subclinical condition” might benefit from exercise, particularly in relation to suicide-related outcomes. They searched multiple databases from inception to June 2022 to identify RCTs investigating exercise and suicidal ideation in participants with physical or mental conditions.
Of 673 studies, 17 met the inclusion criteria (total of 1,021 participants). Participants’ mean age was 42.7 years, 82% were female, and 54% were randomly assigned to an exercise intervention.
Most studies (82%) focused on clinical versus subclinical outcomes. Depression was the most commonly included condition (59%). Aerobic exercise (53%) was the most common form of exercise used in the active study groups. This was followed by mind-body exercise and strength training (53%, 17.6%, and 17.6%, respectively). The mean follow-up time was 10 weeks.
Reduced impulsivity
The researchers found a difference in post-intervention suicidal ideation when they compared exercise participants to all control and inactive control participants (standardized mean difference, –1.09; 95% confidence interval, –3.08 to 0.90; P = .20, k = 5). However, the difference was not statistically significant.
Similarly, there was no significant difference (P = .60) in suicidal ideation incidence for subgroup analyses that stratified data among participants with depression, sickle cell disease, and suicidality.
All-cause discontinuation also did not significantly differ between participants who were randomly assigned to exercise interventions versus all controls or inactive controls (odds ratio, 0.85; 95% CI, 0.38-1.94; P = .86, k = 12 and OR, 0.81; 95% CI, 0.25-2.68; P = .70). All-cause discontinuation also did not differ between participants randomized to exercise versus active controls (OR, 0.94; 95% CI, 0.38-2.32; P = .79, k = 3).
Likewise, there were nonsignificant differences between participants who underwent aerobic exercise and strength training (P = .20).
However, there were some nonsignificant differences when comparing participants with depression and stress who received the exercise intervention versus controls (P = .46).
There was a significant reduction in suicide attempts in individuals who participated in exercise interventions versus inactive controls (OR, 0.23; 95% CI, 0.09-0.67; P = .04, k = 2). On the other hand, there was no significant difference in mortality (P = .70).
Most of the studies (82%) were “at high risk of bias,” the authors note. In addition, the analysis was limited because the included studies were “few, underpowered, and heterogeneous.”
Dr. Fabiano hypothesized that the lack of effect on suicidal ideation or mortality is “likely due to the limited sample size.” As additional RCTs are conducted, Dr. Fabiano expects to see decreases in both suicidal ideation and suicide attempts.
The findings may “be explained by the ideation-to-action framework, which suggests that the development of suicidal ideation and the progression to suicide attempts are distinct processes with different influential factors,” he said.
Increased levels of exercise have been “shown to reduce emotional impulsivity and, as it has been shown that most suicide attempts are characterized by impulsivity and low lethality, we hypothesize that regular exercise serves as a protective factor against suicide attempts,” he said.
Not useful?
Commenting on the study, Fabien Legrand, PhD, a lecturer in clinical psychology, University of Reims Champagne-Ardenne, Reims, France, said that the impact of physical activity is of “particular interest” to him because it is closely linked to his research activity, where he has “been exploring the antidepressant effects of exercise for more than 15 years.”
A small pilot study conducted by Dr. Legrand and colleagues found rigorous physical activity to be helpful in reducing hopelessness in psychiatric patients, compared with controls. “This result is of particular relevance for suicidal patients, since it has long been documented that hopelessness is one of the main triggers of suicide ideation and suicide attempts,” he said.
Initially, Dr. Legrand “warmly welcomed” the current review and meta-analysis on the exercise and suicide. However, he felt that the paper fell short in accomplishing its intended goal. “After a thorough reading of the paper, I don’t think that the information provided can be used in any way,” he stated.
“The paper’s title – ‘Effects of Physical Exercise on Suicidal Ideation and Behavior’ – does not do justice to its content, since 9 of the included 17 RCTs did not measure changes in suicidal ideation and/or suicidal behavior following participation in an exercise program,” noted Dr. Legrand, who was not involved with authorship or the current analysis.
The study was funded by the University of Ottawa department of psychiatry. Dr. Fabiano declares no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. Legrand declares no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF AFFECTIVE DISORDERS