User login
The COPD patient who couldn’t stop worrying
CASE A passive wish to die
Ms. M, age 76, has a history of major depressive disorder, unspecified anxiety disorder, and severe chronic obstructive pulmonary disease (COPD), for which she requires supplemental oxygen. She is admitted to a psychiatric hospital after several months of increased dysphoria, rumination, anhedonia, and a passive wish to die. She also has a decreased appetite and has lost 10 lb, experiences frequent daily episodes of shortness of breath and associated racing thoughts, and has a rapid heart rate.
HISTORY Past medication trials
In addition to COPD, Ms. M’s medical history includes hypertension. Past psychotropic medication trials used to treat her depression and anxiety have included aripiprazole, 5 mg/d; duloxetine, 60 mg/d; fluoxetine, 40 mg/d; mirtazapine, 30 mg nightly; buspirone, 10 mg twice daily; and clonazepam, 0.5 mg twice daily. She has no history of psychotherapy, and because of her uncontrolled anxiety and depression, she has never completed a pulmonary rehabilitation program.
Her current medications include salmeterol, 50 mcg inhaled twice daily, for COPD; amlodipine, 10 mg/d, for hypertension; buspirone, 10 mg twice daily, for anxiety; and duloxetine, 60 mg/d, for depression.
EXAMINATION No evidence of dementia
On examination, Ms. M is alert and oriented to person, place, date, and situation. Overall, she has mild difficulty with attention and short-term recall, which appears to be due to poor effort; intact long-term memory; and is able to abstract appropriately. There is no evidence of dementia.
A mental status exam reveals a frail, elderly woman with fair-to-poor hygiene, cooperative behavior, slowed motor activity, slowed speech with low volume, low mood, and depressed affect with constricted range. Her thought process is linear, her thought content includes passive death wishes, and she does not have hallucinations.
Bitemporal electroconvulsive therapy (ECT), 1.0 ms pulse width at 1.5 times Ms. M’s seizure threshold 3 times weekly, is initiated to treat her depression, with seizure duration averaging 45 seconds for each session. She receives a total of 8 treatments over the course of admission. Buspirone, 10 mg twice daily, is stopped shortly after admission, but she continues to receive duloxetine, 60 mg/d. Ms. M continues to have shortness of breath, palpitations, fearful ruminations about the future, and difficulty falling asleep.
[polldaddy:10673878]
The authors’ observations
The treatment team explores other options, such as benzodiazepines, psychotherapy modalities, and mindfulness exercises, to treat Ms. M’s anxiety and comorbid COPD. Lorazepam, 0.5 mg twice daily, was chosen to treat her acute anxiety. Due to Ms. M’s need for supplemental oxygen, the treatment team attempted to mitigate the risk of using a benzodiazepine by limiting its use to the minimum effective dose. The teams also looked for alternative therapies.
Continue to: Evalution of anxiety...
Evaluation of anxiety and depression in a patient with COPD is complicated by a high degree of symptom overlap. Patients with COPD may experience anxiety symptoms such as shortness of breath, rapid heart rate, numbness/tingling, and racing thoughts, and/or depressive symptoms such as decreased energy, impaired sleep, and impaired concentration. It can therefore be difficult to discern if a symptom is attributable to the physical diagnosis, the psychiatric diagnosis, or a combination of both. Catastrophic thinking about mild physical symptoms is common in patients with COPD. This can lead to hyperventilation and hypocapnia (manifested by lightheadedness, dizziness, paresthesia, and altered consciousness), with a reciprocally escalating cascade of anxiety and somatic symptoms.1
First-line therapy for anxiety disorders with comorbid COPD is CBT and other nonpharmacologic interventions.2,3
Although there is little evidence that traditional pharmacologic treatments (eg, antidepressants, benzodiazepines) have a statistically significant effect on anxiety and depression in COPD, studies have found that they have some clinical benefit.3 Risks, however, limit the utility of certain agents. Sedative-hypnotics potentially decrease respiratory drive and, particularly in older patients, antidepressants’ sedating effects can increase the risk of falls3 leading to increased morbidity, hospitalization, and mortality.
TREATMENT Mindfulness techniques and meditation
Ms. M’s symptoms show no improvement with the addition of lorazepam, 0.5 mg twice daily. A clinician teaches Ms. M mindfulness techniques, and she begins a trial of daily, individual, guided meditation using a meditation app. Respiratory therapists also instruct her on controlled breathing techniques such as pursed-lips breathing, diaphragmatic breathing, and deep breathing. They also encourage Ms. M to participate in the daily exercise group while on the unit.
[polldaddy:10673881]
The authors’ observations
Research indicates that low doses of opioids are safe and effective for refractory breathlessness in patients with severe COPD(those with an arterial partial pressure of oxygen ≤55 mm Hg or arterial oxygen saturation ≤88%).6,7
Continue to: The current opioid crisis...
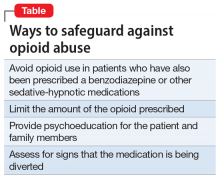
The current opioid crisis prompts additional caution in prescribing, especially when considering using short-acting, immediate-release opioids such as morphine, which have a greater potential for abuse and dependence.
Many patients with COPD in the end-of-life phase and in severe pain or discomfort due to the advanced stages of their illness receive opioids as part of palliative care. Patients with COPD whose medical care is predominantly palliative may benefit greatly from being prescribed opioids. Most patients with COPD who find relief from low-dose opioids usually have 6 to 12 months to live, and low-dose opioids may help them obtain the best possible quality of life.
Choosing opioids as a treatment involves the risk of physiologic dependence and opioid use disorder. For Ms. M, the potential benefits were thought to outweigh such risks.
OUTCOME Breathlessness improves, anxiety decreases
Ms. M’s lorazepam is discontinued, and immediate-release morphine is prescribed at a low dose of 1 mg/d on an as-needed basis for anxiety with good effect. Ms. M’s breathlessness improves, leading to an overall decrease in anxiety. She does not experience sedation, confusion, or adverse respiratory effects.
Ms. M’s anxiety and depression improve over the course of the hospitalization with this regimen. On hospital Day 25, she is discharged with a plan to continue duloxetine, 60 mg/d, ECT twice weekly, and low-dose morphine, 1 mg/d, as needed for anxiety. She is referred for pulmonary rehabilitation and CBT to maintain remission.
[polldaddy:10673882]
Continue to: The authors' observations
The authors’ observations
Ms. M’s case highlights several challenges associated with treating psychiatric illness in a patient with a chronic medical illness. The relationship between COPD, anxiety, and depression is complex, and is associated with reduced quality of life, increasing severity of pulmonary disease, increased dyspnea, a sense of loss and inability to cope, and decreased self-efficacy and adherence to treatment.9-11
Bottom Line
When traditional antidepressant and anxiolytic therapies have not sufficiently helped, consider low-dose, once-daily opioids to address refractory breathlessness in a patient with COPD with comorbid anxiety and depression. This treatment can lead patients to participate in rehabilitation therapies and improve their quality of life.
Related Resources
- Alexopoulos G, Kiosses D, Sirey J, et al. Untangling therapeutic ingredients of a personalized intervention for patients with depression and severe COPD. Am J Geriatr Psychiatry. 2014;22(11):1316-1324.
- Jackson D, Banerjee S, Sirey J, et al. Two interventions for patients with major depression and severe chronic obstructive pulmonary disease: impact on quality of life. Am J Geriatr Psychiatry. 2018;27(5):502-511.
Drug Brand Names
Amlodipine • Norvasc
Aripiprazole • Abilify
Buspirone • Buspar
Clonazepam • Klonopin
Duloxetine • Cymbalta
Fluoxetine • Prozac
Hydromorphone • Dilaudid
Levodopa • Sinemet
Lorazepam • Ativan
Mirtazapine • Remeron
Morphine • MS Contin
Naloxone • Narcan
Oxycodone • Oxycontin
Salmeterol • Serevent Diskus
1. Harnett D. The difficult-to-treat psychiatric patient with comorbid medical illness. In: Dewan M, Pies R, eds. The difficult-to-treat psychiatric patient. Washington, DC: American Psychiatric Association Publishing; 2001:325-357.
2. Panagioti M, Scott C, Blakemore A, et al. Overview of the prevalence, impact, and management of depression and anxiety in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2014;9:1289-1306.
3. Cafarella P, Effing T, Usmani ZA, et al. Treatments for anxiety and depression in patients with chronic obstructive pulmonary disease: a literature review. Respirology. 2012;17(4):627-638.
4. Heslop-Marshall K, Baker C, Carrick-Sen D, et al. Randomised controlled trial of cognitive behavioural therapy in COPD. ERJ Open Res. 2018;4:00094-2018. doi: 10.1183/23120541.00094-2018.
5. de Godoy DV, de Godoy RF. A randomized controlled trial of the effect of psychotherapy on anxiety and depression in chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2003;84(8):1154-1157.
6. Abernethy A, Currow D, Frith P, et al. Randomised, double blind, placebo controlled crossover trial of sustained release morphine for the management of refractory dyspnoea. BMJ. 2003;327(7414):523-528.
7. Janowiak P, Krajnik M, Podolec Z, et al. Dosimetrically administered nebulized morphine for breathlessness in very severe chronic obstructive pulmonary disease: a randomized, controlled trial. BMC Pulm Med. 2017;17:186.
8. Rocker G, Horton R, Currow D, et al. Palliation of dyspnoea in advanced COPD: revisiting a role for opioids. Thorax. 2009;64(10):910-915.
9. Pooler A, Beech R. Examining the relationship between anxiety and depression and exacerbations of COPD which result in hospital admission: a systematic review. Int J Chron Obstruct Pulmon Dis. 2014;9:315-330.
10. Carmen Valenza M, Valenza-Peña G, Torres-Sánchez I, et al. Effectiveness of controlled breathing techniques on anxiety and depression in hospitalized patients with COPD: a randomized clinical trial. Respir Care. 2014;59(2):209-215.
11. Pollok J, van Agteren J, Esterman A, et al. Psychological therapies for the treatment of depression in chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2019;3:CD012347. doi: 10.1002/14651858.CD012347.pub2.
12. Roberts N, Kidd L, Kirkwood K, et al. A systematic review of the content and delivery of education in pulmonary rehabilitation programmes. Respiratory Medicine. 2018;145:161-181.
13. Pumar M, Gray C, Walsh J, et al. Anxiety and depression-important psychological comorbidities of COPD. J Thorac Dis. 2014;6(11):1615-1631.
14. Alexopoulos G, Kiosses D, Sirey J, et al. Untangling therapeutic ingredients of a personalized intervention for patients with depression and severe COPD. Am J Geriatr Psychiatry. 2014;22(11):1316-1324.
15. Jackson D, Banerjee S, Sirey J, et al. Two interventions for patients with major depression and severe chronic obstructive pulmonary disease: impact on quality of life. Am J Geriatr Psychiatry. 2018;27(5):502-511.
CASE A passive wish to die
Ms. M, age 76, has a history of major depressive disorder, unspecified anxiety disorder, and severe chronic obstructive pulmonary disease (COPD), for which she requires supplemental oxygen. She is admitted to a psychiatric hospital after several months of increased dysphoria, rumination, anhedonia, and a passive wish to die. She also has a decreased appetite and has lost 10 lb, experiences frequent daily episodes of shortness of breath and associated racing thoughts, and has a rapid heart rate.
HISTORY Past medication trials
In addition to COPD, Ms. M’s medical history includes hypertension. Past psychotropic medication trials used to treat her depression and anxiety have included aripiprazole, 5 mg/d; duloxetine, 60 mg/d; fluoxetine, 40 mg/d; mirtazapine, 30 mg nightly; buspirone, 10 mg twice daily; and clonazepam, 0.5 mg twice daily. She has no history of psychotherapy, and because of her uncontrolled anxiety and depression, she has never completed a pulmonary rehabilitation program.
Her current medications include salmeterol, 50 mcg inhaled twice daily, for COPD; amlodipine, 10 mg/d, for hypertension; buspirone, 10 mg twice daily, for anxiety; and duloxetine, 60 mg/d, for depression.
EXAMINATION No evidence of dementia
On examination, Ms. M is alert and oriented to person, place, date, and situation. Overall, she has mild difficulty with attention and short-term recall, which appears to be due to poor effort; intact long-term memory; and is able to abstract appropriately. There is no evidence of dementia.
A mental status exam reveals a frail, elderly woman with fair-to-poor hygiene, cooperative behavior, slowed motor activity, slowed speech with low volume, low mood, and depressed affect with constricted range. Her thought process is linear, her thought content includes passive death wishes, and she does not have hallucinations.
Bitemporal electroconvulsive therapy (ECT), 1.0 ms pulse width at 1.5 times Ms. M’s seizure threshold 3 times weekly, is initiated to treat her depression, with seizure duration averaging 45 seconds for each session. She receives a total of 8 treatments over the course of admission. Buspirone, 10 mg twice daily, is stopped shortly after admission, but she continues to receive duloxetine, 60 mg/d. Ms. M continues to have shortness of breath, palpitations, fearful ruminations about the future, and difficulty falling asleep.
[polldaddy:10673878]
The authors’ observations
The treatment team explores other options, such as benzodiazepines, psychotherapy modalities, and mindfulness exercises, to treat Ms. M’s anxiety and comorbid COPD. Lorazepam, 0.5 mg twice daily, was chosen to treat her acute anxiety. Due to Ms. M’s need for supplemental oxygen, the treatment team attempted to mitigate the risk of using a benzodiazepine by limiting its use to the minimum effective dose. The teams also looked for alternative therapies.
Continue to: Evalution of anxiety...
Evaluation of anxiety and depression in a patient with COPD is complicated by a high degree of symptom overlap. Patients with COPD may experience anxiety symptoms such as shortness of breath, rapid heart rate, numbness/tingling, and racing thoughts, and/or depressive symptoms such as decreased energy, impaired sleep, and impaired concentration. It can therefore be difficult to discern if a symptom is attributable to the physical diagnosis, the psychiatric diagnosis, or a combination of both. Catastrophic thinking about mild physical symptoms is common in patients with COPD. This can lead to hyperventilation and hypocapnia (manifested by lightheadedness, dizziness, paresthesia, and altered consciousness), with a reciprocally escalating cascade of anxiety and somatic symptoms.1
First-line therapy for anxiety disorders with comorbid COPD is CBT and other nonpharmacologic interventions.2,3
Although there is little evidence that traditional pharmacologic treatments (eg, antidepressants, benzodiazepines) have a statistically significant effect on anxiety and depression in COPD, studies have found that they have some clinical benefit.3 Risks, however, limit the utility of certain agents. Sedative-hypnotics potentially decrease respiratory drive and, particularly in older patients, antidepressants’ sedating effects can increase the risk of falls3 leading to increased morbidity, hospitalization, and mortality.
TREATMENT Mindfulness techniques and meditation
Ms. M’s symptoms show no improvement with the addition of lorazepam, 0.5 mg twice daily. A clinician teaches Ms. M mindfulness techniques, and she begins a trial of daily, individual, guided meditation using a meditation app. Respiratory therapists also instruct her on controlled breathing techniques such as pursed-lips breathing, diaphragmatic breathing, and deep breathing. They also encourage Ms. M to participate in the daily exercise group while on the unit.
[polldaddy:10673881]
The authors’ observations
Research indicates that low doses of opioids are safe and effective for refractory breathlessness in patients with severe COPD(those with an arterial partial pressure of oxygen ≤55 mm Hg or arterial oxygen saturation ≤88%).6,7
Continue to: The current opioid crisis...
The current opioid crisis prompts additional caution in prescribing, especially when considering using short-acting, immediate-release opioids such as morphine, which have a greater potential for abuse and dependence.
Many patients with COPD in the end-of-life phase and in severe pain or discomfort due to the advanced stages of their illness receive opioids as part of palliative care. Patients with COPD whose medical care is predominantly palliative may benefit greatly from being prescribed opioids. Most patients with COPD who find relief from low-dose opioids usually have 6 to 12 months to live, and low-dose opioids may help them obtain the best possible quality of life.
Choosing opioids as a treatment involves the risk of physiologic dependence and opioid use disorder. For Ms. M, the potential benefits were thought to outweigh such risks.
OUTCOME Breathlessness improves, anxiety decreases
Ms. M’s lorazepam is discontinued, and immediate-release morphine is prescribed at a low dose of 1 mg/d on an as-needed basis for anxiety with good effect. Ms. M’s breathlessness improves, leading to an overall decrease in anxiety. She does not experience sedation, confusion, or adverse respiratory effects.
Ms. M’s anxiety and depression improve over the course of the hospitalization with this regimen. On hospital Day 25, she is discharged with a plan to continue duloxetine, 60 mg/d, ECT twice weekly, and low-dose morphine, 1 mg/d, as needed for anxiety. She is referred for pulmonary rehabilitation and CBT to maintain remission.
[polldaddy:10673882]
Continue to: The authors' observations
The authors’ observations
Ms. M’s case highlights several challenges associated with treating psychiatric illness in a patient with a chronic medical illness. The relationship between COPD, anxiety, and depression is complex, and is associated with reduced quality of life, increasing severity of pulmonary disease, increased dyspnea, a sense of loss and inability to cope, and decreased self-efficacy and adherence to treatment.9-11
Bottom Line
When traditional antidepressant and anxiolytic therapies have not sufficiently helped, consider low-dose, once-daily opioids to address refractory breathlessness in a patient with COPD with comorbid anxiety and depression. This treatment can lead patients to participate in rehabilitation therapies and improve their quality of life.
Related Resources
- Alexopoulos G, Kiosses D, Sirey J, et al. Untangling therapeutic ingredients of a personalized intervention for patients with depression and severe COPD. Am J Geriatr Psychiatry. 2014;22(11):1316-1324.
- Jackson D, Banerjee S, Sirey J, et al. Two interventions for patients with major depression and severe chronic obstructive pulmonary disease: impact on quality of life. Am J Geriatr Psychiatry. 2018;27(5):502-511.
Drug Brand Names
Amlodipine • Norvasc
Aripiprazole • Abilify
Buspirone • Buspar
Clonazepam • Klonopin
Duloxetine • Cymbalta
Fluoxetine • Prozac
Hydromorphone • Dilaudid
Levodopa • Sinemet
Lorazepam • Ativan
Mirtazapine • Remeron
Morphine • MS Contin
Naloxone • Narcan
Oxycodone • Oxycontin
Salmeterol • Serevent Diskus
CASE A passive wish to die
Ms. M, age 76, has a history of major depressive disorder, unspecified anxiety disorder, and severe chronic obstructive pulmonary disease (COPD), for which she requires supplemental oxygen. She is admitted to a psychiatric hospital after several months of increased dysphoria, rumination, anhedonia, and a passive wish to die. She also has a decreased appetite and has lost 10 lb, experiences frequent daily episodes of shortness of breath and associated racing thoughts, and has a rapid heart rate.
HISTORY Past medication trials
In addition to COPD, Ms. M’s medical history includes hypertension. Past psychotropic medication trials used to treat her depression and anxiety have included aripiprazole, 5 mg/d; duloxetine, 60 mg/d; fluoxetine, 40 mg/d; mirtazapine, 30 mg nightly; buspirone, 10 mg twice daily; and clonazepam, 0.5 mg twice daily. She has no history of psychotherapy, and because of her uncontrolled anxiety and depression, she has never completed a pulmonary rehabilitation program.
Her current medications include salmeterol, 50 mcg inhaled twice daily, for COPD; amlodipine, 10 mg/d, for hypertension; buspirone, 10 mg twice daily, for anxiety; and duloxetine, 60 mg/d, for depression.
EXAMINATION No evidence of dementia
On examination, Ms. M is alert and oriented to person, place, date, and situation. Overall, she has mild difficulty with attention and short-term recall, which appears to be due to poor effort; intact long-term memory; and is able to abstract appropriately. There is no evidence of dementia.
A mental status exam reveals a frail, elderly woman with fair-to-poor hygiene, cooperative behavior, slowed motor activity, slowed speech with low volume, low mood, and depressed affect with constricted range. Her thought process is linear, her thought content includes passive death wishes, and she does not have hallucinations.
Bitemporal electroconvulsive therapy (ECT), 1.0 ms pulse width at 1.5 times Ms. M’s seizure threshold 3 times weekly, is initiated to treat her depression, with seizure duration averaging 45 seconds for each session. She receives a total of 8 treatments over the course of admission. Buspirone, 10 mg twice daily, is stopped shortly after admission, but she continues to receive duloxetine, 60 mg/d. Ms. M continues to have shortness of breath, palpitations, fearful ruminations about the future, and difficulty falling asleep.
[polldaddy:10673878]
The authors’ observations
The treatment team explores other options, such as benzodiazepines, psychotherapy modalities, and mindfulness exercises, to treat Ms. M’s anxiety and comorbid COPD. Lorazepam, 0.5 mg twice daily, was chosen to treat her acute anxiety. Due to Ms. M’s need for supplemental oxygen, the treatment team attempted to mitigate the risk of using a benzodiazepine by limiting its use to the minimum effective dose. The teams also looked for alternative therapies.
Continue to: Evalution of anxiety...
Evaluation of anxiety and depression in a patient with COPD is complicated by a high degree of symptom overlap. Patients with COPD may experience anxiety symptoms such as shortness of breath, rapid heart rate, numbness/tingling, and racing thoughts, and/or depressive symptoms such as decreased energy, impaired sleep, and impaired concentration. It can therefore be difficult to discern if a symptom is attributable to the physical diagnosis, the psychiatric diagnosis, or a combination of both. Catastrophic thinking about mild physical symptoms is common in patients with COPD. This can lead to hyperventilation and hypocapnia (manifested by lightheadedness, dizziness, paresthesia, and altered consciousness), with a reciprocally escalating cascade of anxiety and somatic symptoms.1
First-line therapy for anxiety disorders with comorbid COPD is CBT and other nonpharmacologic interventions.2,3
Although there is little evidence that traditional pharmacologic treatments (eg, antidepressants, benzodiazepines) have a statistically significant effect on anxiety and depression in COPD, studies have found that they have some clinical benefit.3 Risks, however, limit the utility of certain agents. Sedative-hypnotics potentially decrease respiratory drive and, particularly in older patients, antidepressants’ sedating effects can increase the risk of falls3 leading to increased morbidity, hospitalization, and mortality.
TREATMENT Mindfulness techniques and meditation
Ms. M’s symptoms show no improvement with the addition of lorazepam, 0.5 mg twice daily. A clinician teaches Ms. M mindfulness techniques, and she begins a trial of daily, individual, guided meditation using a meditation app. Respiratory therapists also instruct her on controlled breathing techniques such as pursed-lips breathing, diaphragmatic breathing, and deep breathing. They also encourage Ms. M to participate in the daily exercise group while on the unit.
[polldaddy:10673881]
The authors’ observations
Research indicates that low doses of opioids are safe and effective for refractory breathlessness in patients with severe COPD(those with an arterial partial pressure of oxygen ≤55 mm Hg or arterial oxygen saturation ≤88%).6,7
Continue to: The current opioid crisis...
The current opioid crisis prompts additional caution in prescribing, especially when considering using short-acting, immediate-release opioids such as morphine, which have a greater potential for abuse and dependence.
Many patients with COPD in the end-of-life phase and in severe pain or discomfort due to the advanced stages of their illness receive opioids as part of palliative care. Patients with COPD whose medical care is predominantly palliative may benefit greatly from being prescribed opioids. Most patients with COPD who find relief from low-dose opioids usually have 6 to 12 months to live, and low-dose opioids may help them obtain the best possible quality of life.
Choosing opioids as a treatment involves the risk of physiologic dependence and opioid use disorder. For Ms. M, the potential benefits were thought to outweigh such risks.
OUTCOME Breathlessness improves, anxiety decreases
Ms. M’s lorazepam is discontinued, and immediate-release morphine is prescribed at a low dose of 1 mg/d on an as-needed basis for anxiety with good effect. Ms. M’s breathlessness improves, leading to an overall decrease in anxiety. She does not experience sedation, confusion, or adverse respiratory effects.
Ms. M’s anxiety and depression improve over the course of the hospitalization with this regimen. On hospital Day 25, she is discharged with a plan to continue duloxetine, 60 mg/d, ECT twice weekly, and low-dose morphine, 1 mg/d, as needed for anxiety. She is referred for pulmonary rehabilitation and CBT to maintain remission.
[polldaddy:10673882]
Continue to: The authors' observations
The authors’ observations
Ms. M’s case highlights several challenges associated with treating psychiatric illness in a patient with a chronic medical illness. The relationship between COPD, anxiety, and depression is complex, and is associated with reduced quality of life, increasing severity of pulmonary disease, increased dyspnea, a sense of loss and inability to cope, and decreased self-efficacy and adherence to treatment.9-11
Bottom Line
When traditional antidepressant and anxiolytic therapies have not sufficiently helped, consider low-dose, once-daily opioids to address refractory breathlessness in a patient with COPD with comorbid anxiety and depression. This treatment can lead patients to participate in rehabilitation therapies and improve their quality of life.
Related Resources
- Alexopoulos G, Kiosses D, Sirey J, et al. Untangling therapeutic ingredients of a personalized intervention for patients with depression and severe COPD. Am J Geriatr Psychiatry. 2014;22(11):1316-1324.
- Jackson D, Banerjee S, Sirey J, et al. Two interventions for patients with major depression and severe chronic obstructive pulmonary disease: impact on quality of life. Am J Geriatr Psychiatry. 2018;27(5):502-511.
Drug Brand Names
Amlodipine • Norvasc
Aripiprazole • Abilify
Buspirone • Buspar
Clonazepam • Klonopin
Duloxetine • Cymbalta
Fluoxetine • Prozac
Hydromorphone • Dilaudid
Levodopa • Sinemet
Lorazepam • Ativan
Mirtazapine • Remeron
Morphine • MS Contin
Naloxone • Narcan
Oxycodone • Oxycontin
Salmeterol • Serevent Diskus
1. Harnett D. The difficult-to-treat psychiatric patient with comorbid medical illness. In: Dewan M, Pies R, eds. The difficult-to-treat psychiatric patient. Washington, DC: American Psychiatric Association Publishing; 2001:325-357.
2. Panagioti M, Scott C, Blakemore A, et al. Overview of the prevalence, impact, and management of depression and anxiety in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2014;9:1289-1306.
3. Cafarella P, Effing T, Usmani ZA, et al. Treatments for anxiety and depression in patients with chronic obstructive pulmonary disease: a literature review. Respirology. 2012;17(4):627-638.
4. Heslop-Marshall K, Baker C, Carrick-Sen D, et al. Randomised controlled trial of cognitive behavioural therapy in COPD. ERJ Open Res. 2018;4:00094-2018. doi: 10.1183/23120541.00094-2018.
5. de Godoy DV, de Godoy RF. A randomized controlled trial of the effect of psychotherapy on anxiety and depression in chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2003;84(8):1154-1157.
6. Abernethy A, Currow D, Frith P, et al. Randomised, double blind, placebo controlled crossover trial of sustained release morphine for the management of refractory dyspnoea. BMJ. 2003;327(7414):523-528.
7. Janowiak P, Krajnik M, Podolec Z, et al. Dosimetrically administered nebulized morphine for breathlessness in very severe chronic obstructive pulmonary disease: a randomized, controlled trial. BMC Pulm Med. 2017;17:186.
8. Rocker G, Horton R, Currow D, et al. Palliation of dyspnoea in advanced COPD: revisiting a role for opioids. Thorax. 2009;64(10):910-915.
9. Pooler A, Beech R. Examining the relationship between anxiety and depression and exacerbations of COPD which result in hospital admission: a systematic review. Int J Chron Obstruct Pulmon Dis. 2014;9:315-330.
10. Carmen Valenza M, Valenza-Peña G, Torres-Sánchez I, et al. Effectiveness of controlled breathing techniques on anxiety and depression in hospitalized patients with COPD: a randomized clinical trial. Respir Care. 2014;59(2):209-215.
11. Pollok J, van Agteren J, Esterman A, et al. Psychological therapies for the treatment of depression in chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2019;3:CD012347. doi: 10.1002/14651858.CD012347.pub2.
12. Roberts N, Kidd L, Kirkwood K, et al. A systematic review of the content and delivery of education in pulmonary rehabilitation programmes. Respiratory Medicine. 2018;145:161-181.
13. Pumar M, Gray C, Walsh J, et al. Anxiety and depression-important psychological comorbidities of COPD. J Thorac Dis. 2014;6(11):1615-1631.
14. Alexopoulos G, Kiosses D, Sirey J, et al. Untangling therapeutic ingredients of a personalized intervention for patients with depression and severe COPD. Am J Geriatr Psychiatry. 2014;22(11):1316-1324.
15. Jackson D, Banerjee S, Sirey J, et al. Two interventions for patients with major depression and severe chronic obstructive pulmonary disease: impact on quality of life. Am J Geriatr Psychiatry. 2018;27(5):502-511.
1. Harnett D. The difficult-to-treat psychiatric patient with comorbid medical illness. In: Dewan M, Pies R, eds. The difficult-to-treat psychiatric patient. Washington, DC: American Psychiatric Association Publishing; 2001:325-357.
2. Panagioti M, Scott C, Blakemore A, et al. Overview of the prevalence, impact, and management of depression and anxiety in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2014;9:1289-1306.
3. Cafarella P, Effing T, Usmani ZA, et al. Treatments for anxiety and depression in patients with chronic obstructive pulmonary disease: a literature review. Respirology. 2012;17(4):627-638.
4. Heslop-Marshall K, Baker C, Carrick-Sen D, et al. Randomised controlled trial of cognitive behavioural therapy in COPD. ERJ Open Res. 2018;4:00094-2018. doi: 10.1183/23120541.00094-2018.
5. de Godoy DV, de Godoy RF. A randomized controlled trial of the effect of psychotherapy on anxiety and depression in chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2003;84(8):1154-1157.
6. Abernethy A, Currow D, Frith P, et al. Randomised, double blind, placebo controlled crossover trial of sustained release morphine for the management of refractory dyspnoea. BMJ. 2003;327(7414):523-528.
7. Janowiak P, Krajnik M, Podolec Z, et al. Dosimetrically administered nebulized morphine for breathlessness in very severe chronic obstructive pulmonary disease: a randomized, controlled trial. BMC Pulm Med. 2017;17:186.
8. Rocker G, Horton R, Currow D, et al. Palliation of dyspnoea in advanced COPD: revisiting a role for opioids. Thorax. 2009;64(10):910-915.
9. Pooler A, Beech R. Examining the relationship between anxiety and depression and exacerbations of COPD which result in hospital admission: a systematic review. Int J Chron Obstruct Pulmon Dis. 2014;9:315-330.
10. Carmen Valenza M, Valenza-Peña G, Torres-Sánchez I, et al. Effectiveness of controlled breathing techniques on anxiety and depression in hospitalized patients with COPD: a randomized clinical trial. Respir Care. 2014;59(2):209-215.
11. Pollok J, van Agteren J, Esterman A, et al. Psychological therapies for the treatment of depression in chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2019;3:CD012347. doi: 10.1002/14651858.CD012347.pub2.
12. Roberts N, Kidd L, Kirkwood K, et al. A systematic review of the content and delivery of education in pulmonary rehabilitation programmes. Respiratory Medicine. 2018;145:161-181.
13. Pumar M, Gray C, Walsh J, et al. Anxiety and depression-important psychological comorbidities of COPD. J Thorac Dis. 2014;6(11):1615-1631.
14. Alexopoulos G, Kiosses D, Sirey J, et al. Untangling therapeutic ingredients of a personalized intervention for patients with depression and severe COPD. Am J Geriatr Psychiatry. 2014;22(11):1316-1324.
15. Jackson D, Banerjee S, Sirey J, et al. Two interventions for patients with major depression and severe chronic obstructive pulmonary disease: impact on quality of life. Am J Geriatr Psychiatry. 2018;27(5):502-511.
What the Biden-Harris COVID-19 Advisory Board is missing
On Nov. 9, the Biden-Harris administration announced the members of its COVID-19 Advisory Board. Among them were many esteemed infectious disease and public health experts – encouraging, given that, for now, the COVID-19 pandemic shows no signs of slowing down. Not among them was a mental health professional.
As psychiatrists, we did not find this omission surprising, given the sidelined role our specialty too often plays among medical professionals. But we did find it disappointing. Not having a single behavioral health provider on the advisory board will prove to be a mistake that could affect millions of Americans.
Studies continue to roll in showing that patients with COVID-19 can present during and after infection with neuropsychiatric symptoms, including delirium, psychosis, and anxiety. In July, a meta-analysis published in The Lancet regarding the neuropsychological outcomes of earlier diseases caused by coronaviruses – severe acute respiratory syndrome and Middle East respiratory syndrome – suggested that, in the short term, close to one-quarter of patients experienced confusion representative of delirium. In the long term, following recovery, respondents frequently reported emotional lability, impaired concentration, and traumatic memories. Additionally, more recent research published in The Lancet suggests that rates of psychiatric disorders, dementia, and insomnia are significantly higher among survivors of COVID-19. This study echoes the findings of an article in JAMA from September that reported that, among patients who were hospitalized for COVID-19, mortality rates were higher for those who had previously been diagnosed with a psychiatric condition. And overall, the pandemic has been associated with significantly increased rates of anxiety and depression symptoms.
Although this research is preliminary,
This is especially true when you consider the following:
- It is very difficult to diagnose and treat mental health symptoms in a primary care setting that is already overburdened. Doing so results in delayed treatment and increased costs.
- In the long term, COVID-19 survivors will overburden the already underfunded mental healthcare system.
- Additional unforeseen psychological outcomes stem from the myriad traumas of events in 2020 (eg, racial unrest, children out of school, loss of jobs, the recent election).
Psychiatric disorders are notoriously difficult to diagnose and treat in the outpatient primary care setting, which is why mental health professionals will need to be a more integral part of the postpandemic treatment model and should be represented on the advisory board. Each year in the United States, there are more than 8 million doctors’ visits for depression, and more than half of these are in the primary care setting. Yet fewer than half of those patients leave with a diagnosis of depression or are treated for it.
Historically, screening for depression in the primary care setting is difficult given its broad presentation of symptoms, which include nonspecific physical complaints, such as digestive problems, headaches, insomnia, or general aches and pains. These shortcomings exist despite multiple changes in guidelines, such as regarding the use of self-screening tools and general screening for specific populations, such as postpartum women.
But screening alone has not been an effective strategy, especially when certain groups are less likely to be screened. These include older adults, Black persons, and men, all of whom are at higher risk for mortality after COVID-19. There is a failure to consistently apply standards of universal screening across all patient groups, and even if it occurs, there is a failure to establish reliable treatment and follow-up regimens. As clinicians, imagine how challenging diagnosis and treatment of more complicated psychiatric syndromes, such as somatoform disorder, will be in the primary care setting after the pandemic.
When almost two-thirds of symptoms in primary care are already “medically unexplained,” how do we expect primary care doctors to differentiate between those presenting with vague coronavirus-related “brain fog,” the run of the mill worrywart, and the 16%-34% with legitimate hypochondriasis of somatoform disorder who won’t improve without the involvement of a mental health provider?
A specialty in short supply
The mental health system we have now is inadequate for those who are currently diagnosed with mental disorders. Before the pandemic, emergency departments were boarding increasing numbers of patients with psychiatric illness because beds on inpatient units were unavailable. Individuals with insurance faced difficulty finding psychiatrists or psychotherapists who took insurance or who were availabile to accept new patients, given the growing shortage of providers in general. Community health centers continued to grapple with decreases in federal and state funding despite public political support for parity. Individuals with substance use faced few options for the outpatient, residential, or pharmacologic treatment that many needed to maintain sobriety.
Since the pandemic, we have seen rates of anxiety, depression, and suicidal thinking increase among adults and youth while many clinics have been forced to lay off employees, reduce services, or close their doors. As psychiatrists, we not only see the lack of treatment options for our patients but are forced to find creative solutions to meet their needs. How are we supposed to adapt (or feel confident) when individuals with or without previous mental illness face downstream consequences after COVID-19 when not one of our own is represented in the advisory board? How can we feel confident that downstream solutions acknowledge and address the intricacy of the behavioral health system that we, as mental health providers, know so intimately?
And what about the cumulative impact of everything else that has happened in 2020 in addition to the pandemic?! Although cataloging the various negative events that have happened this year is beyond the scope of this discussion, such lists have been compiled by the mainstream media and include the Australian brush fires, the crisis in Armenia, racial protests, economic uncertainties, and the run-up to and occurrence of the 2020 presidential election. Research is solid in its assertion that chronic stress can disturb our immune and cardiovascular systems, as well as mental health, leading to depression or anxiety. As a result of the pandemic itself, plus the events of this year, mental health providers are already warning not only of the current trauma underlying our day-to-day lives but also that of years to come.
More importantly, healthcare providers, both those represented by members of the advisory board and those who are not, are not immune to these issues. Before the pandemic, rates of suicide among doctors were already above average compared with other professions. After witnessing death repeatedly, self-isolation, the risk for infection to family, and dealing with the continued resistance to wearing masks, who knows what the eventual psychological toll our medical workforce will be?
Mental health providers have stepped up to the plate to provide care outside of traditional models to meet the needs that patients have now. One survey found that 81% of behavioral health providers began using telehealth for the first time in the past 6 months, owing to the COVID-19 pandemic. If not for the sake of the mental health of the Biden-Harris advisory board members themselves, who as doctors are likely to downplay the impact when struggling with mental health concerns in their own lives, a mental health provider deserves a seat at the table.
Plus, the outcomes speak for themselves when behavioral health providers collaborate with primary care providers to give treatment or when mental health experts are members of health crisis teams. Why wouldn’t the same be true for the Biden-Harris advisory board?
Kali Cyrus, MD, MPH, is an assistant professor of psychiatry and behavioral medicine at the Johns Hopkins School of Medicine, Baltimore, Maryland. She sees patients in private practice and offers consultation services in diversity strategy. Ranna Parekh, MD, MPH, is past deputy medical director and director of diversity and health equity for the American Psychiatric Association. She is currently a consultant psychiatrist at the Massachusetts General Hospital, Boston, and the chief diversity and inclusion officer at the American College of Cardiology.
A version of this article originally appeared on Medscape.com.
On Nov. 9, the Biden-Harris administration announced the members of its COVID-19 Advisory Board. Among them were many esteemed infectious disease and public health experts – encouraging, given that, for now, the COVID-19 pandemic shows no signs of slowing down. Not among them was a mental health professional.
As psychiatrists, we did not find this omission surprising, given the sidelined role our specialty too often plays among medical professionals. But we did find it disappointing. Not having a single behavioral health provider on the advisory board will prove to be a mistake that could affect millions of Americans.
Studies continue to roll in showing that patients with COVID-19 can present during and after infection with neuropsychiatric symptoms, including delirium, psychosis, and anxiety. In July, a meta-analysis published in The Lancet regarding the neuropsychological outcomes of earlier diseases caused by coronaviruses – severe acute respiratory syndrome and Middle East respiratory syndrome – suggested that, in the short term, close to one-quarter of patients experienced confusion representative of delirium. In the long term, following recovery, respondents frequently reported emotional lability, impaired concentration, and traumatic memories. Additionally, more recent research published in The Lancet suggests that rates of psychiatric disorders, dementia, and insomnia are significantly higher among survivors of COVID-19. This study echoes the findings of an article in JAMA from September that reported that, among patients who were hospitalized for COVID-19, mortality rates were higher for those who had previously been diagnosed with a psychiatric condition. And overall, the pandemic has been associated with significantly increased rates of anxiety and depression symptoms.
Although this research is preliminary,
This is especially true when you consider the following:
- It is very difficult to diagnose and treat mental health symptoms in a primary care setting that is already overburdened. Doing so results in delayed treatment and increased costs.
- In the long term, COVID-19 survivors will overburden the already underfunded mental healthcare system.
- Additional unforeseen psychological outcomes stem from the myriad traumas of events in 2020 (eg, racial unrest, children out of school, loss of jobs, the recent election).
Psychiatric disorders are notoriously difficult to diagnose and treat in the outpatient primary care setting, which is why mental health professionals will need to be a more integral part of the postpandemic treatment model and should be represented on the advisory board. Each year in the United States, there are more than 8 million doctors’ visits for depression, and more than half of these are in the primary care setting. Yet fewer than half of those patients leave with a diagnosis of depression or are treated for it.
Historically, screening for depression in the primary care setting is difficult given its broad presentation of symptoms, which include nonspecific physical complaints, such as digestive problems, headaches, insomnia, or general aches and pains. These shortcomings exist despite multiple changes in guidelines, such as regarding the use of self-screening tools and general screening for specific populations, such as postpartum women.
But screening alone has not been an effective strategy, especially when certain groups are less likely to be screened. These include older adults, Black persons, and men, all of whom are at higher risk for mortality after COVID-19. There is a failure to consistently apply standards of universal screening across all patient groups, and even if it occurs, there is a failure to establish reliable treatment and follow-up regimens. As clinicians, imagine how challenging diagnosis and treatment of more complicated psychiatric syndromes, such as somatoform disorder, will be in the primary care setting after the pandemic.
When almost two-thirds of symptoms in primary care are already “medically unexplained,” how do we expect primary care doctors to differentiate between those presenting with vague coronavirus-related “brain fog,” the run of the mill worrywart, and the 16%-34% with legitimate hypochondriasis of somatoform disorder who won’t improve without the involvement of a mental health provider?
A specialty in short supply
The mental health system we have now is inadequate for those who are currently diagnosed with mental disorders. Before the pandemic, emergency departments were boarding increasing numbers of patients with psychiatric illness because beds on inpatient units were unavailable. Individuals with insurance faced difficulty finding psychiatrists or psychotherapists who took insurance or who were availabile to accept new patients, given the growing shortage of providers in general. Community health centers continued to grapple with decreases in federal and state funding despite public political support for parity. Individuals with substance use faced few options for the outpatient, residential, or pharmacologic treatment that many needed to maintain sobriety.
Since the pandemic, we have seen rates of anxiety, depression, and suicidal thinking increase among adults and youth while many clinics have been forced to lay off employees, reduce services, or close their doors. As psychiatrists, we not only see the lack of treatment options for our patients but are forced to find creative solutions to meet their needs. How are we supposed to adapt (or feel confident) when individuals with or without previous mental illness face downstream consequences after COVID-19 when not one of our own is represented in the advisory board? How can we feel confident that downstream solutions acknowledge and address the intricacy of the behavioral health system that we, as mental health providers, know so intimately?
And what about the cumulative impact of everything else that has happened in 2020 in addition to the pandemic?! Although cataloging the various negative events that have happened this year is beyond the scope of this discussion, such lists have been compiled by the mainstream media and include the Australian brush fires, the crisis in Armenia, racial protests, economic uncertainties, and the run-up to and occurrence of the 2020 presidential election. Research is solid in its assertion that chronic stress can disturb our immune and cardiovascular systems, as well as mental health, leading to depression or anxiety. As a result of the pandemic itself, plus the events of this year, mental health providers are already warning not only of the current trauma underlying our day-to-day lives but also that of years to come.
More importantly, healthcare providers, both those represented by members of the advisory board and those who are not, are not immune to these issues. Before the pandemic, rates of suicide among doctors were already above average compared with other professions. After witnessing death repeatedly, self-isolation, the risk for infection to family, and dealing with the continued resistance to wearing masks, who knows what the eventual psychological toll our medical workforce will be?
Mental health providers have stepped up to the plate to provide care outside of traditional models to meet the needs that patients have now. One survey found that 81% of behavioral health providers began using telehealth for the first time in the past 6 months, owing to the COVID-19 pandemic. If not for the sake of the mental health of the Biden-Harris advisory board members themselves, who as doctors are likely to downplay the impact when struggling with mental health concerns in their own lives, a mental health provider deserves a seat at the table.
Plus, the outcomes speak for themselves when behavioral health providers collaborate with primary care providers to give treatment or when mental health experts are members of health crisis teams. Why wouldn’t the same be true for the Biden-Harris advisory board?
Kali Cyrus, MD, MPH, is an assistant professor of psychiatry and behavioral medicine at the Johns Hopkins School of Medicine, Baltimore, Maryland. She sees patients in private practice and offers consultation services in diversity strategy. Ranna Parekh, MD, MPH, is past deputy medical director and director of diversity and health equity for the American Psychiatric Association. She is currently a consultant psychiatrist at the Massachusetts General Hospital, Boston, and the chief diversity and inclusion officer at the American College of Cardiology.
A version of this article originally appeared on Medscape.com.
On Nov. 9, the Biden-Harris administration announced the members of its COVID-19 Advisory Board. Among them were many esteemed infectious disease and public health experts – encouraging, given that, for now, the COVID-19 pandemic shows no signs of slowing down. Not among them was a mental health professional.
As psychiatrists, we did not find this omission surprising, given the sidelined role our specialty too often plays among medical professionals. But we did find it disappointing. Not having a single behavioral health provider on the advisory board will prove to be a mistake that could affect millions of Americans.
Studies continue to roll in showing that patients with COVID-19 can present during and after infection with neuropsychiatric symptoms, including delirium, psychosis, and anxiety. In July, a meta-analysis published in The Lancet regarding the neuropsychological outcomes of earlier diseases caused by coronaviruses – severe acute respiratory syndrome and Middle East respiratory syndrome – suggested that, in the short term, close to one-quarter of patients experienced confusion representative of delirium. In the long term, following recovery, respondents frequently reported emotional lability, impaired concentration, and traumatic memories. Additionally, more recent research published in The Lancet suggests that rates of psychiatric disorders, dementia, and insomnia are significantly higher among survivors of COVID-19. This study echoes the findings of an article in JAMA from September that reported that, among patients who were hospitalized for COVID-19, mortality rates were higher for those who had previously been diagnosed with a psychiatric condition. And overall, the pandemic has been associated with significantly increased rates of anxiety and depression symptoms.
Although this research is preliminary,
This is especially true when you consider the following:
- It is very difficult to diagnose and treat mental health symptoms in a primary care setting that is already overburdened. Doing so results in delayed treatment and increased costs.
- In the long term, COVID-19 survivors will overburden the already underfunded mental healthcare system.
- Additional unforeseen psychological outcomes stem from the myriad traumas of events in 2020 (eg, racial unrest, children out of school, loss of jobs, the recent election).
Psychiatric disorders are notoriously difficult to diagnose and treat in the outpatient primary care setting, which is why mental health professionals will need to be a more integral part of the postpandemic treatment model and should be represented on the advisory board. Each year in the United States, there are more than 8 million doctors’ visits for depression, and more than half of these are in the primary care setting. Yet fewer than half of those patients leave with a diagnosis of depression or are treated for it.
Historically, screening for depression in the primary care setting is difficult given its broad presentation of symptoms, which include nonspecific physical complaints, such as digestive problems, headaches, insomnia, or general aches and pains. These shortcomings exist despite multiple changes in guidelines, such as regarding the use of self-screening tools and general screening for specific populations, such as postpartum women.
But screening alone has not been an effective strategy, especially when certain groups are less likely to be screened. These include older adults, Black persons, and men, all of whom are at higher risk for mortality after COVID-19. There is a failure to consistently apply standards of universal screening across all patient groups, and even if it occurs, there is a failure to establish reliable treatment and follow-up regimens. As clinicians, imagine how challenging diagnosis and treatment of more complicated psychiatric syndromes, such as somatoform disorder, will be in the primary care setting after the pandemic.
When almost two-thirds of symptoms in primary care are already “medically unexplained,” how do we expect primary care doctors to differentiate between those presenting with vague coronavirus-related “brain fog,” the run of the mill worrywart, and the 16%-34% with legitimate hypochondriasis of somatoform disorder who won’t improve without the involvement of a mental health provider?
A specialty in short supply
The mental health system we have now is inadequate for those who are currently diagnosed with mental disorders. Before the pandemic, emergency departments were boarding increasing numbers of patients with psychiatric illness because beds on inpatient units were unavailable. Individuals with insurance faced difficulty finding psychiatrists or psychotherapists who took insurance or who were availabile to accept new patients, given the growing shortage of providers in general. Community health centers continued to grapple with decreases in federal and state funding despite public political support for parity. Individuals with substance use faced few options for the outpatient, residential, or pharmacologic treatment that many needed to maintain sobriety.
Since the pandemic, we have seen rates of anxiety, depression, and suicidal thinking increase among adults and youth while many clinics have been forced to lay off employees, reduce services, or close their doors. As psychiatrists, we not only see the lack of treatment options for our patients but are forced to find creative solutions to meet their needs. How are we supposed to adapt (or feel confident) when individuals with or without previous mental illness face downstream consequences after COVID-19 when not one of our own is represented in the advisory board? How can we feel confident that downstream solutions acknowledge and address the intricacy of the behavioral health system that we, as mental health providers, know so intimately?
And what about the cumulative impact of everything else that has happened in 2020 in addition to the pandemic?! Although cataloging the various negative events that have happened this year is beyond the scope of this discussion, such lists have been compiled by the mainstream media and include the Australian brush fires, the crisis in Armenia, racial protests, economic uncertainties, and the run-up to and occurrence of the 2020 presidential election. Research is solid in its assertion that chronic stress can disturb our immune and cardiovascular systems, as well as mental health, leading to depression or anxiety. As a result of the pandemic itself, plus the events of this year, mental health providers are already warning not only of the current trauma underlying our day-to-day lives but also that of years to come.
More importantly, healthcare providers, both those represented by members of the advisory board and those who are not, are not immune to these issues. Before the pandemic, rates of suicide among doctors were already above average compared with other professions. After witnessing death repeatedly, self-isolation, the risk for infection to family, and dealing with the continued resistance to wearing masks, who knows what the eventual psychological toll our medical workforce will be?
Mental health providers have stepped up to the plate to provide care outside of traditional models to meet the needs that patients have now. One survey found that 81% of behavioral health providers began using telehealth for the first time in the past 6 months, owing to the COVID-19 pandemic. If not for the sake of the mental health of the Biden-Harris advisory board members themselves, who as doctors are likely to downplay the impact when struggling with mental health concerns in their own lives, a mental health provider deserves a seat at the table.
Plus, the outcomes speak for themselves when behavioral health providers collaborate with primary care providers to give treatment or when mental health experts are members of health crisis teams. Why wouldn’t the same be true for the Biden-Harris advisory board?
Kali Cyrus, MD, MPH, is an assistant professor of psychiatry and behavioral medicine at the Johns Hopkins School of Medicine, Baltimore, Maryland. She sees patients in private practice and offers consultation services in diversity strategy. Ranna Parekh, MD, MPH, is past deputy medical director and director of diversity and health equity for the American Psychiatric Association. She is currently a consultant psychiatrist at the Massachusetts General Hospital, Boston, and the chief diversity and inclusion officer at the American College of Cardiology.
A version of this article originally appeared on Medscape.com.
Immunodeficiency strongly linked to mental illness, suicidal behavior
Patients with a primary humoral immunodeficiency (PID) are 91% more likely to have a psychiatric disorder and 84% more likely to exhibit suicidal behavior, compared against those without the condition, new research shows.
Results showed that this association, which was stronger in women, could not be fully explained by comorbid autoimmune diseases or by familial confounding.
These findings have important clinical implications, study investigator Josef Isung, MD, PhD, Centre for Psychiatry Research, Karolinska Institute, Stockholm, Sweden, told Medscape Medical News.
Clinicians managing patients with PID “should be aware of this increased association with psychiatric disorders and perhaps screen for them,” said Isung.
The study was published in the November issue of JAMA Psychiatry.
Registry study
Mounting evidence suggests immune disruption plays a role in psychiatric disorders through a range of mechanisms, including altered neurodevelopment. However, little is known about the neuropsychiatric consequences resulting from the underproduction of homeostatic antibodies.
They’re associated with an increased risk for recurrent infections and of developing autoimmune diseases.
The immunodeficiency can be severe, even life threatening, but can also be relatively mild. One of the less severe PID types is selective IgA deficiency, which is linked to increased infections within the mucosa-associated lymphoid tissue (MALT), an important immune barrier.
Experts have long suspected that infections within the MALT are associated with certain forms of psychopathology in children, particularly obsessive-compulsive disorder and chronic tic disorders.
While patients with this selective IgA subtype may be at some increased risk for infection and autoimmune disease, their overall health otherwise is good, said Isung.
The prevalence of PIDs ranges from about 1:250 to 1:20,000, depending on the type of humoral immunodeficiency, although most would fall into the relatively rare category, he added.
Using several linked national Swedish registries, researchers identified individuals with any PID diagnosis affecting immunoglobulin levels, their full siblings, and those with a lifetime diagnosis of selective IgA deficiency. In addition, they collected data on autoimmune diseases.
The study outcome was a lifetime record of a psychiatric disorder, a suicide attempt, or death by suicide.
Strong link to autism
Researchers identified 8378 patients (59% women) with PID affecting immunoglobulin levels (median age at first diagnosis, 47.8 years). They compared this group with almost 14.3 million subjects without PID.
In those with PID, 27.6% had an autoimmune disease vs 6.8% of those without PID, a statistically significant difference (P < .001).
About 20.5% of those with PID and 10.7% of unexposed subjects had at least one diagnosis of a psychiatric disorder.
In a model adjusted for year of birth, sex, and history of autoimmune disease, subjects with PID had a 91% higher likelihood of any psychiatric disorder (adjusted odds ratio [AOR] 1.91; 95% CI, 1.81 - 2.01; P < .001) vs their counterparts without PID.
The AORs for individual psychiatric disorders ranged from 1.34 (95% CI, 1.17 - 1.54; P < .001) for schizophrenia and other psychotic disorders to 2.99 (95% CI, 2.42 - 3.70; P < .001) for autism spectrum disorders (ASDs)
It’s unclear why the association with PID was strongest for autism, “but being a neurodevelopmental disorder, maybe autism is logically more associated with this type of disruption,” said Isung.
Research suggests that immunologic disruption may play a role in ASD, either through altered maternal immune function in utero or through immune disruption after birth, the researchers note.
Compared to those without PID, individuals with it had a significantly increased likelihood of any suicidal behavior (AOR, 1.84; 95% CI, 1.66 - 2.04, P < .001) as well as individual outcomes of death by suicide and suicide attempts.
The association with psychiatric disorders and suicidal behavior was markedly stronger for exposure to both PID and autoimmune disease than for exposure to either of these alone, which suggest an additive effect for these immune-related conditions.
Sex differences
“It was unclear to us why women seemed particularly vulnerable,” said Isung. He noted that PIDs are generally about as common in women as in men, but women tend to have higher rates of psychiatric disorders.
The analysis of the sibling cohort also revealed an elevated risk for psychiatric disorders, including ASD and suicidal behavior, but to a lesser degree.
“From this we could infer that at least part of the associations would be genetic, but part would be related to the disruption in itself,” said Isung.
An analysis examining selective IgA subtype also revealed a link with psychiatric disorders and suicidal behavior, suggesting this link is not exclusive to severe PID cases.
“Our conclusion here was that it seems like PID itself, or the immune disruption in itself, could explain the association rather than the burden of illness,” said Isung.
However, he acknowledged that the long-term stress and mental health fallout of having a chronic illness like PID may also explain some of the increased risk for psychiatric disorders.
This study, he said, provides more evidence that immune disruptions affect neurodevelopment and the brain. However, he added, the underlying mechanism still isn’t fully understood.
The results highlight the need to raise awareness of the association between immunodeficiency and mental illness, including suicidality among clinicians, patients, and advocates.
These findings may also have implications in patients with other immune deficiencies, said Isung, noting, “it would be interesting to further explore associations with other immunocompromised populations.”
No surprises
Commenting on the findings for Medscape Medical News, Igor Galynker, MD, professor of psychiatry at Icahn School of Medicine at Mount Sinai, New York City, said the study was “very well-done” and used “reliable and well-controlled” databases.
However, he added, the results “are neither particularly dramatic nor conclusive” as it makes sense that medical illnesses like PID would “increase risk of psychopathology,” said Galynker.
PID patients are much more likely to have contact with clinicians and to receive a psychiatric diagnosis, he said.
“People with a chronic illness are more stressed and generally have high incidences of depression, anxiety, and suicidal behavior. In addition to that, they may be more likely to be diagnosed with those conditions because they see a clinician more frequently.”
However, that reasoning doesn’t apply to autism, which manifests in early childhood and so is unlikely to be the result of stress, said Galynker, which is why he believes the finding that ASD is the psychiatric outcome most strongly associated with PID is “the most convincing.”
Galynker wasn’t surprised that the association between PID and psychiatric illnesses, and suicidal behaviors, was stronger among women.
“Women attempt suicide four times more often than men to begin with, so you would expect this to be more pronounced” in those with PID.
The study was supported by grants from the Centre for Psychiatry Research, Department of Clinical Neuroscience, Karolinska Institute; Stockholm Care Services; the Soderstrom Konig Foundation; and the Fredrik & Ingrid Thurings Foundation. Isung and Galynker have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Patients with a primary humoral immunodeficiency (PID) are 91% more likely to have a psychiatric disorder and 84% more likely to exhibit suicidal behavior, compared against those without the condition, new research shows.
Results showed that this association, which was stronger in women, could not be fully explained by comorbid autoimmune diseases or by familial confounding.
These findings have important clinical implications, study investigator Josef Isung, MD, PhD, Centre for Psychiatry Research, Karolinska Institute, Stockholm, Sweden, told Medscape Medical News.
Clinicians managing patients with PID “should be aware of this increased association with psychiatric disorders and perhaps screen for them,” said Isung.
The study was published in the November issue of JAMA Psychiatry.
Registry study
Mounting evidence suggests immune disruption plays a role in psychiatric disorders through a range of mechanisms, including altered neurodevelopment. However, little is known about the neuropsychiatric consequences resulting from the underproduction of homeostatic antibodies.
They’re associated with an increased risk for recurrent infections and of developing autoimmune diseases.
The immunodeficiency can be severe, even life threatening, but can also be relatively mild. One of the less severe PID types is selective IgA deficiency, which is linked to increased infections within the mucosa-associated lymphoid tissue (MALT), an important immune barrier.
Experts have long suspected that infections within the MALT are associated with certain forms of psychopathology in children, particularly obsessive-compulsive disorder and chronic tic disorders.
While patients with this selective IgA subtype may be at some increased risk for infection and autoimmune disease, their overall health otherwise is good, said Isung.
The prevalence of PIDs ranges from about 1:250 to 1:20,000, depending on the type of humoral immunodeficiency, although most would fall into the relatively rare category, he added.
Using several linked national Swedish registries, researchers identified individuals with any PID diagnosis affecting immunoglobulin levels, their full siblings, and those with a lifetime diagnosis of selective IgA deficiency. In addition, they collected data on autoimmune diseases.
The study outcome was a lifetime record of a psychiatric disorder, a suicide attempt, or death by suicide.
Strong link to autism
Researchers identified 8378 patients (59% women) with PID affecting immunoglobulin levels (median age at first diagnosis, 47.8 years). They compared this group with almost 14.3 million subjects without PID.
In those with PID, 27.6% had an autoimmune disease vs 6.8% of those without PID, a statistically significant difference (P < .001).
About 20.5% of those with PID and 10.7% of unexposed subjects had at least one diagnosis of a psychiatric disorder.
In a model adjusted for year of birth, sex, and history of autoimmune disease, subjects with PID had a 91% higher likelihood of any psychiatric disorder (adjusted odds ratio [AOR] 1.91; 95% CI, 1.81 - 2.01; P < .001) vs their counterparts without PID.
The AORs for individual psychiatric disorders ranged from 1.34 (95% CI, 1.17 - 1.54; P < .001) for schizophrenia and other psychotic disorders to 2.99 (95% CI, 2.42 - 3.70; P < .001) for autism spectrum disorders (ASDs)
It’s unclear why the association with PID was strongest for autism, “but being a neurodevelopmental disorder, maybe autism is logically more associated with this type of disruption,” said Isung.
Research suggests that immunologic disruption may play a role in ASD, either through altered maternal immune function in utero or through immune disruption after birth, the researchers note.
Compared to those without PID, individuals with it had a significantly increased likelihood of any suicidal behavior (AOR, 1.84; 95% CI, 1.66 - 2.04, P < .001) as well as individual outcomes of death by suicide and suicide attempts.
The association with psychiatric disorders and suicidal behavior was markedly stronger for exposure to both PID and autoimmune disease than for exposure to either of these alone, which suggest an additive effect for these immune-related conditions.
Sex differences
“It was unclear to us why women seemed particularly vulnerable,” said Isung. He noted that PIDs are generally about as common in women as in men, but women tend to have higher rates of psychiatric disorders.
The analysis of the sibling cohort also revealed an elevated risk for psychiatric disorders, including ASD and suicidal behavior, but to a lesser degree.
“From this we could infer that at least part of the associations would be genetic, but part would be related to the disruption in itself,” said Isung.
An analysis examining selective IgA subtype also revealed a link with psychiatric disorders and suicidal behavior, suggesting this link is not exclusive to severe PID cases.
“Our conclusion here was that it seems like PID itself, or the immune disruption in itself, could explain the association rather than the burden of illness,” said Isung.
However, he acknowledged that the long-term stress and mental health fallout of having a chronic illness like PID may also explain some of the increased risk for psychiatric disorders.
This study, he said, provides more evidence that immune disruptions affect neurodevelopment and the brain. However, he added, the underlying mechanism still isn’t fully understood.
The results highlight the need to raise awareness of the association between immunodeficiency and mental illness, including suicidality among clinicians, patients, and advocates.
These findings may also have implications in patients with other immune deficiencies, said Isung, noting, “it would be interesting to further explore associations with other immunocompromised populations.”
No surprises
Commenting on the findings for Medscape Medical News, Igor Galynker, MD, professor of psychiatry at Icahn School of Medicine at Mount Sinai, New York City, said the study was “very well-done” and used “reliable and well-controlled” databases.
However, he added, the results “are neither particularly dramatic nor conclusive” as it makes sense that medical illnesses like PID would “increase risk of psychopathology,” said Galynker.
PID patients are much more likely to have contact with clinicians and to receive a psychiatric diagnosis, he said.
“People with a chronic illness are more stressed and generally have high incidences of depression, anxiety, and suicidal behavior. In addition to that, they may be more likely to be diagnosed with those conditions because they see a clinician more frequently.”
However, that reasoning doesn’t apply to autism, which manifests in early childhood and so is unlikely to be the result of stress, said Galynker, which is why he believes the finding that ASD is the psychiatric outcome most strongly associated with PID is “the most convincing.”
Galynker wasn’t surprised that the association between PID and psychiatric illnesses, and suicidal behaviors, was stronger among women.
“Women attempt suicide four times more often than men to begin with, so you would expect this to be more pronounced” in those with PID.
The study was supported by grants from the Centre for Psychiatry Research, Department of Clinical Neuroscience, Karolinska Institute; Stockholm Care Services; the Soderstrom Konig Foundation; and the Fredrik & Ingrid Thurings Foundation. Isung and Galynker have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Patients with a primary humoral immunodeficiency (PID) are 91% more likely to have a psychiatric disorder and 84% more likely to exhibit suicidal behavior, compared against those without the condition, new research shows.
Results showed that this association, which was stronger in women, could not be fully explained by comorbid autoimmune diseases or by familial confounding.
These findings have important clinical implications, study investigator Josef Isung, MD, PhD, Centre for Psychiatry Research, Karolinska Institute, Stockholm, Sweden, told Medscape Medical News.
Clinicians managing patients with PID “should be aware of this increased association with psychiatric disorders and perhaps screen for them,” said Isung.
The study was published in the November issue of JAMA Psychiatry.
Registry study
Mounting evidence suggests immune disruption plays a role in psychiatric disorders through a range of mechanisms, including altered neurodevelopment. However, little is known about the neuropsychiatric consequences resulting from the underproduction of homeostatic antibodies.
They’re associated with an increased risk for recurrent infections and of developing autoimmune diseases.
The immunodeficiency can be severe, even life threatening, but can also be relatively mild. One of the less severe PID types is selective IgA deficiency, which is linked to increased infections within the mucosa-associated lymphoid tissue (MALT), an important immune barrier.
Experts have long suspected that infections within the MALT are associated with certain forms of psychopathology in children, particularly obsessive-compulsive disorder and chronic tic disorders.
While patients with this selective IgA subtype may be at some increased risk for infection and autoimmune disease, their overall health otherwise is good, said Isung.
The prevalence of PIDs ranges from about 1:250 to 1:20,000, depending on the type of humoral immunodeficiency, although most would fall into the relatively rare category, he added.
Using several linked national Swedish registries, researchers identified individuals with any PID diagnosis affecting immunoglobulin levels, their full siblings, and those with a lifetime diagnosis of selective IgA deficiency. In addition, they collected data on autoimmune diseases.
The study outcome was a lifetime record of a psychiatric disorder, a suicide attempt, or death by suicide.
Strong link to autism
Researchers identified 8378 patients (59% women) with PID affecting immunoglobulin levels (median age at first diagnosis, 47.8 years). They compared this group with almost 14.3 million subjects without PID.
In those with PID, 27.6% had an autoimmune disease vs 6.8% of those without PID, a statistically significant difference (P < .001).
About 20.5% of those with PID and 10.7% of unexposed subjects had at least one diagnosis of a psychiatric disorder.
In a model adjusted for year of birth, sex, and history of autoimmune disease, subjects with PID had a 91% higher likelihood of any psychiatric disorder (adjusted odds ratio [AOR] 1.91; 95% CI, 1.81 - 2.01; P < .001) vs their counterparts without PID.
The AORs for individual psychiatric disorders ranged from 1.34 (95% CI, 1.17 - 1.54; P < .001) for schizophrenia and other psychotic disorders to 2.99 (95% CI, 2.42 - 3.70; P < .001) for autism spectrum disorders (ASDs)
It’s unclear why the association with PID was strongest for autism, “but being a neurodevelopmental disorder, maybe autism is logically more associated with this type of disruption,” said Isung.
Research suggests that immunologic disruption may play a role in ASD, either through altered maternal immune function in utero or through immune disruption after birth, the researchers note.
Compared to those without PID, individuals with it had a significantly increased likelihood of any suicidal behavior (AOR, 1.84; 95% CI, 1.66 - 2.04, P < .001) as well as individual outcomes of death by suicide and suicide attempts.
The association with psychiatric disorders and suicidal behavior was markedly stronger for exposure to both PID and autoimmune disease than for exposure to either of these alone, which suggest an additive effect for these immune-related conditions.
Sex differences
“It was unclear to us why women seemed particularly vulnerable,” said Isung. He noted that PIDs are generally about as common in women as in men, but women tend to have higher rates of psychiatric disorders.
The analysis of the sibling cohort also revealed an elevated risk for psychiatric disorders, including ASD and suicidal behavior, but to a lesser degree.
“From this we could infer that at least part of the associations would be genetic, but part would be related to the disruption in itself,” said Isung.
An analysis examining selective IgA subtype also revealed a link with psychiatric disorders and suicidal behavior, suggesting this link is not exclusive to severe PID cases.
“Our conclusion here was that it seems like PID itself, or the immune disruption in itself, could explain the association rather than the burden of illness,” said Isung.
However, he acknowledged that the long-term stress and mental health fallout of having a chronic illness like PID may also explain some of the increased risk for psychiatric disorders.
This study, he said, provides more evidence that immune disruptions affect neurodevelopment and the brain. However, he added, the underlying mechanism still isn’t fully understood.
The results highlight the need to raise awareness of the association between immunodeficiency and mental illness, including suicidality among clinicians, patients, and advocates.
These findings may also have implications in patients with other immune deficiencies, said Isung, noting, “it would be interesting to further explore associations with other immunocompromised populations.”
No surprises
Commenting on the findings for Medscape Medical News, Igor Galynker, MD, professor of psychiatry at Icahn School of Medicine at Mount Sinai, New York City, said the study was “very well-done” and used “reliable and well-controlled” databases.
However, he added, the results “are neither particularly dramatic nor conclusive” as it makes sense that medical illnesses like PID would “increase risk of psychopathology,” said Galynker.
PID patients are much more likely to have contact with clinicians and to receive a psychiatric diagnosis, he said.
“People with a chronic illness are more stressed and generally have high incidences of depression, anxiety, and suicidal behavior. In addition to that, they may be more likely to be diagnosed with those conditions because they see a clinician more frequently.”
However, that reasoning doesn’t apply to autism, which manifests in early childhood and so is unlikely to be the result of stress, said Galynker, which is why he believes the finding that ASD is the psychiatric outcome most strongly associated with PID is “the most convincing.”
Galynker wasn’t surprised that the association between PID and psychiatric illnesses, and suicidal behaviors, was stronger among women.
“Women attempt suicide four times more often than men to begin with, so you would expect this to be more pronounced” in those with PID.
The study was supported by grants from the Centre for Psychiatry Research, Department of Clinical Neuroscience, Karolinska Institute; Stockholm Care Services; the Soderstrom Konig Foundation; and the Fredrik & Ingrid Thurings Foundation. Isung and Galynker have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Can mental health teams de-escalate crises in NYC?
“Defund the police”: It’s a slogan, or perhaps a battle cry, that has emerged from the Black Lives Matter movement as a response to race-related police brutality and concerns that people of color are profiled, targeted, arrested, charged, manhandled, and killed by law enforcement in a disproportionate and unjust manner. It crosses into our realm as psychiatrists as mental health emergency calls are handled by the police and not by mental health professionals. The result is sometimes tragic: As many as half of police shootings involve people with psychiatric disorders, and the hope is that many of the police shootings could be avoided if crises were handed by mental health clinicians instead of, or in cooperation with, the police.
At best, police officers receive a week of specialized, crisis intervention training about how to approach those with psychiatric disorders; most officers receive no training. This leaves psychiatry as the only field where medical crises are routinely handled by the police – it is demeaning and embarrassing for some of our patients and dangerous for others. The reality remains, however, that there are times when psychiatric disorders result in violent behavior, and patients being taken for involuntary treatment often resist transport, so either way there is risk, both to the patient and to anyone who responds to a call for assistance.
Early this month, the office of New York City Mayor Bill de Blasio announced that a major change would be made in how mental health calls to 911 are handled in two “high-need” areas. The mayor’s website states:
“Beginning in February 2021, new Mental Health Teams will use their physical and mental health expertise, and experience in crisis response to de-escalate emergency situations, will help reduce the number of times police will need to respond to 911 mental health calls in these precincts. These teams will have the expertise to respond to a range of behavioral health problems, such as suicide attempts, substance misuse, and serious mental illness, as well as physical health problems, which can be exacerbated by or mask mental health problems. NYC Health + Hospitals will train and provide ongoing technical assistance and support. In selecting team members for this program, FDNY will prioritize professionals with significant experience with mental health crises.”
The press release goes on to say that, in situations where there is a weapon or reason to believe there is a risk of violence, the police will be dispatched along with the new mental health team.
“This is the first time in our history that health professionals will be the default responders to mental health emergencies,” New York City First Lady Chirlane McCray said as she announced the new program. “Treating mental health crises as mental health challenges and not public safety ones is the modern and more appropriate approach.”
New York City is not the first city to employ this model. In the United States, the CAHOOTS (Crisis Assistance Helping Out on the Streets) program in Eugene, Ore., has been run by the White Bird Clinic since 1989 as part of a community policing initiative. Last year, the team responded to 24,000 calls and police backup was required on only 150 of those responses. The CAHOOTS website states:
“The CAHOOTS model has been in the spotlight recently as our nation struggles to reimagine public safety. The program mobilizes two-person teams consisting of a medic (a nurse, paramedic, or EMT) and a crisis worker who has substantial training and experience in the mental health field. The CAHOOTS teams deal with a wide range of mental health-related crises, including conflict resolution, welfare checks, substance abuse, suicide threats, and more, relying on trauma-informed de-escalation and harm reduction techniques. CAHOOTS staff are not law enforcement officers and do not carry weapons; their training and experience are the tools they use to ensure a non-violent resolution of crisis situations. They also handle non-emergent medical issues, avoiding costly ambulance transport and emergency room treatment.”
Other cities in the United States are also looking at implementing programs where mental health teams, and not the police, respond to emergency calls. Last year, Oakland, Calif.’s city council invested $40,000 in research to assess how they could best implement a program like the one in Eugene. They hope to begin the Mobile Assistance Community Responders of Oakland (MACROS) next year. Sigal Samuel writes in a Vox article, “The goal is to launch the pilot next year with funding from the city budget, and although supporters are not yet sure what its size and duration will be, they’re hopeful it’ll make a big difference to Oakland’s overpoliced community of people without homes. They were among those who first called for a non-policing approach.”
The model is not unique to the United States. In 2005, Stockholm started a program with a psychiatric ambulance – equipped with comfortable seating rather than a stretcher – to respond to mental health emergencies. The ambulance responds to 130 calls a month. It is staffed with a driver and two psychiatric nurses, and for half of the calls, the police also come. While the Swedish program was not about removing resources from the police, it has relieved the police of the responsibility for many psychiatric emergencies.
The New York City program will be modeled after the CAHOOTS initiative in Eugene. It differs from the mobile crisis response services in many other cities because CAHOOTS is hooked directly into the 911 emergency services system. Its website notes that the program has saved money:
“The cost savings are considerable. The CAHOOTS program budget is about $2.1 million annually, while the combined annual budgets for the Eugene and Springfield police departments are $90 million. In 2017, the CAHOOTS teams answered 17% of the Eugene Police Department’s overall call volume. The program saves the city of Eugene an estimated $8.5 million in public safety spending annually.”
Some worry there is an unpredictable aspect to calls for psychiatric emergencies, and the potential for mental health professions to be injured or killed. Annette Hanson, MD, a forensic psychiatrist at University of Maryland, Baltimore, voiced her concerns, “While multidisciplinary teams are useful, there have been rare cases of violence against responding mental health providers. People with serious mental illness are rarely violent but their dangerousness is unpredictable and cannot be predicted by case screening.”
Daniel Felts is a mental health crisis counselor who has worked at CAHOOTS for the past 4* years. He has responded to about 8,000 calls, and called for police backup only three times to request an immediate "Code 3 cover" when someone's safety has been in danger. Mr. Felts calls the police about once a month for concerns that do not require an immediate response for safety.* “Over the last 4 years, I am only aware of three instances when a team member’s safety was compromised because of a client’s violent behavior. No employee has been seriously physically harmed. In 30 years, with hundreds of thousands (millions?) of calls responded to, no CAHOOTS worker has ever been killed, shot, or stabbed in the line of duty,” Mr. Felts noted.
Emergency calls are screened. “It is not uncommon for CAHOOTS to be dispatched to ‘stage’ for calls involving active disputes or acutely suicidal individuals where means are present. “Staging” entails us parking roughly a mile away while police make first contact and advise whether it is safe for CAHOOTS to engage.”
Mr. Felts went on to discuss the program’s relationship with the community. “ and how we operate. Having operated in Eugene for 30 years, our service is well understood to be one that does not kill, harm, or violate personal boundaries or liberties.”
Would a program like the ones in Stockholm or in Eugene work in other places? Eugene is a city with a population of 172,000 with a low crime rate. Whether a program implemented in one city can be mimicked in another very different city is not clear.
Paul Appelbaum, MD, a forensic psychiatrist at Columbia University, New York, is optimistic about New York City’s forthcoming program.
“The proposed pilot project in NYC is a real step forward. Work that we’ve done looking at fatal encounters involving the police found that roughly 25% of all deaths at the hands of the police are of people with mental illness. In many of those cases, police were initially called to bring people who were clearly troubled for psychiatric evaluation, but as the situation escalated, the police turned to their weapons to control it, which led to a fatal outcome. Taking police out of the picture whenever possible in favor of trained mental health personnel is clearly a better approach. It will be important for the city to collect good outcome data to enable independent evaluation of the pilot project – not something that political entities are inclined toward, but a critical element in assessing the effectiveness of this approach.”
There are questions that remain about the new program. Mayor de Blasio’s office has not released information about which areas of the city are being chosen for the new program, how much the program will cost, or what the funding source will be. If it can be implemented safely and effectively, it has the potential to provide more sensitive care to patients in crisis, and to save lives.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
*Correction, 11/27/2020: An earlier version of this article misstated the number of years Daniel Felts has worked at CAHOOTS.
“Defund the police”: It’s a slogan, or perhaps a battle cry, that has emerged from the Black Lives Matter movement as a response to race-related police brutality and concerns that people of color are profiled, targeted, arrested, charged, manhandled, and killed by law enforcement in a disproportionate and unjust manner. It crosses into our realm as psychiatrists as mental health emergency calls are handled by the police and not by mental health professionals. The result is sometimes tragic: As many as half of police shootings involve people with psychiatric disorders, and the hope is that many of the police shootings could be avoided if crises were handed by mental health clinicians instead of, or in cooperation with, the police.
At best, police officers receive a week of specialized, crisis intervention training about how to approach those with psychiatric disorders; most officers receive no training. This leaves psychiatry as the only field where medical crises are routinely handled by the police – it is demeaning and embarrassing for some of our patients and dangerous for others. The reality remains, however, that there are times when psychiatric disorders result in violent behavior, and patients being taken for involuntary treatment often resist transport, so either way there is risk, both to the patient and to anyone who responds to a call for assistance.
Early this month, the office of New York City Mayor Bill de Blasio announced that a major change would be made in how mental health calls to 911 are handled in two “high-need” areas. The mayor’s website states:
“Beginning in February 2021, new Mental Health Teams will use their physical and mental health expertise, and experience in crisis response to de-escalate emergency situations, will help reduce the number of times police will need to respond to 911 mental health calls in these precincts. These teams will have the expertise to respond to a range of behavioral health problems, such as suicide attempts, substance misuse, and serious mental illness, as well as physical health problems, which can be exacerbated by or mask mental health problems. NYC Health + Hospitals will train and provide ongoing technical assistance and support. In selecting team members for this program, FDNY will prioritize professionals with significant experience with mental health crises.”
The press release goes on to say that, in situations where there is a weapon or reason to believe there is a risk of violence, the police will be dispatched along with the new mental health team.
“This is the first time in our history that health professionals will be the default responders to mental health emergencies,” New York City First Lady Chirlane McCray said as she announced the new program. “Treating mental health crises as mental health challenges and not public safety ones is the modern and more appropriate approach.”
New York City is not the first city to employ this model. In the United States, the CAHOOTS (Crisis Assistance Helping Out on the Streets) program in Eugene, Ore., has been run by the White Bird Clinic since 1989 as part of a community policing initiative. Last year, the team responded to 24,000 calls and police backup was required on only 150 of those responses. The CAHOOTS website states:
“The CAHOOTS model has been in the spotlight recently as our nation struggles to reimagine public safety. The program mobilizes two-person teams consisting of a medic (a nurse, paramedic, or EMT) and a crisis worker who has substantial training and experience in the mental health field. The CAHOOTS teams deal with a wide range of mental health-related crises, including conflict resolution, welfare checks, substance abuse, suicide threats, and more, relying on trauma-informed de-escalation and harm reduction techniques. CAHOOTS staff are not law enforcement officers and do not carry weapons; their training and experience are the tools they use to ensure a non-violent resolution of crisis situations. They also handle non-emergent medical issues, avoiding costly ambulance transport and emergency room treatment.”
Other cities in the United States are also looking at implementing programs where mental health teams, and not the police, respond to emergency calls. Last year, Oakland, Calif.’s city council invested $40,000 in research to assess how they could best implement a program like the one in Eugene. They hope to begin the Mobile Assistance Community Responders of Oakland (MACROS) next year. Sigal Samuel writes in a Vox article, “The goal is to launch the pilot next year with funding from the city budget, and although supporters are not yet sure what its size and duration will be, they’re hopeful it’ll make a big difference to Oakland’s overpoliced community of people without homes. They were among those who first called for a non-policing approach.”
The model is not unique to the United States. In 2005, Stockholm started a program with a psychiatric ambulance – equipped with comfortable seating rather than a stretcher – to respond to mental health emergencies. The ambulance responds to 130 calls a month. It is staffed with a driver and two psychiatric nurses, and for half of the calls, the police also come. While the Swedish program was not about removing resources from the police, it has relieved the police of the responsibility for many psychiatric emergencies.
The New York City program will be modeled after the CAHOOTS initiative in Eugene. It differs from the mobile crisis response services in many other cities because CAHOOTS is hooked directly into the 911 emergency services system. Its website notes that the program has saved money:
“The cost savings are considerable. The CAHOOTS program budget is about $2.1 million annually, while the combined annual budgets for the Eugene and Springfield police departments are $90 million. In 2017, the CAHOOTS teams answered 17% of the Eugene Police Department’s overall call volume. The program saves the city of Eugene an estimated $8.5 million in public safety spending annually.”
Some worry there is an unpredictable aspect to calls for psychiatric emergencies, and the potential for mental health professions to be injured or killed. Annette Hanson, MD, a forensic psychiatrist at University of Maryland, Baltimore, voiced her concerns, “While multidisciplinary teams are useful, there have been rare cases of violence against responding mental health providers. People with serious mental illness are rarely violent but their dangerousness is unpredictable and cannot be predicted by case screening.”
Daniel Felts is a mental health crisis counselor who has worked at CAHOOTS for the past 4* years. He has responded to about 8,000 calls, and called for police backup only three times to request an immediate "Code 3 cover" when someone's safety has been in danger. Mr. Felts calls the police about once a month for concerns that do not require an immediate response for safety.* “Over the last 4 years, I am only aware of three instances when a team member’s safety was compromised because of a client’s violent behavior. No employee has been seriously physically harmed. In 30 years, with hundreds of thousands (millions?) of calls responded to, no CAHOOTS worker has ever been killed, shot, or stabbed in the line of duty,” Mr. Felts noted.
Emergency calls are screened. “It is not uncommon for CAHOOTS to be dispatched to ‘stage’ for calls involving active disputes or acutely suicidal individuals where means are present. “Staging” entails us parking roughly a mile away while police make first contact and advise whether it is safe for CAHOOTS to engage.”
Mr. Felts went on to discuss the program’s relationship with the community. “ and how we operate. Having operated in Eugene for 30 years, our service is well understood to be one that does not kill, harm, or violate personal boundaries or liberties.”
Would a program like the ones in Stockholm or in Eugene work in other places? Eugene is a city with a population of 172,000 with a low crime rate. Whether a program implemented in one city can be mimicked in another very different city is not clear.
Paul Appelbaum, MD, a forensic psychiatrist at Columbia University, New York, is optimistic about New York City’s forthcoming program.
“The proposed pilot project in NYC is a real step forward. Work that we’ve done looking at fatal encounters involving the police found that roughly 25% of all deaths at the hands of the police are of people with mental illness. In many of those cases, police were initially called to bring people who were clearly troubled for psychiatric evaluation, but as the situation escalated, the police turned to their weapons to control it, which led to a fatal outcome. Taking police out of the picture whenever possible in favor of trained mental health personnel is clearly a better approach. It will be important for the city to collect good outcome data to enable independent evaluation of the pilot project – not something that political entities are inclined toward, but a critical element in assessing the effectiveness of this approach.”
There are questions that remain about the new program. Mayor de Blasio’s office has not released information about which areas of the city are being chosen for the new program, how much the program will cost, or what the funding source will be. If it can be implemented safely and effectively, it has the potential to provide more sensitive care to patients in crisis, and to save lives.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
*Correction, 11/27/2020: An earlier version of this article misstated the number of years Daniel Felts has worked at CAHOOTS.
“Defund the police”: It’s a slogan, or perhaps a battle cry, that has emerged from the Black Lives Matter movement as a response to race-related police brutality and concerns that people of color are profiled, targeted, arrested, charged, manhandled, and killed by law enforcement in a disproportionate and unjust manner. It crosses into our realm as psychiatrists as mental health emergency calls are handled by the police and not by mental health professionals. The result is sometimes tragic: As many as half of police shootings involve people with psychiatric disorders, and the hope is that many of the police shootings could be avoided if crises were handed by mental health clinicians instead of, or in cooperation with, the police.
At best, police officers receive a week of specialized, crisis intervention training about how to approach those with psychiatric disorders; most officers receive no training. This leaves psychiatry as the only field where medical crises are routinely handled by the police – it is demeaning and embarrassing for some of our patients and dangerous for others. The reality remains, however, that there are times when psychiatric disorders result in violent behavior, and patients being taken for involuntary treatment often resist transport, so either way there is risk, both to the patient and to anyone who responds to a call for assistance.
Early this month, the office of New York City Mayor Bill de Blasio announced that a major change would be made in how mental health calls to 911 are handled in two “high-need” areas. The mayor’s website states:
“Beginning in February 2021, new Mental Health Teams will use their physical and mental health expertise, and experience in crisis response to de-escalate emergency situations, will help reduce the number of times police will need to respond to 911 mental health calls in these precincts. These teams will have the expertise to respond to a range of behavioral health problems, such as suicide attempts, substance misuse, and serious mental illness, as well as physical health problems, which can be exacerbated by or mask mental health problems. NYC Health + Hospitals will train and provide ongoing technical assistance and support. In selecting team members for this program, FDNY will prioritize professionals with significant experience with mental health crises.”
The press release goes on to say that, in situations where there is a weapon or reason to believe there is a risk of violence, the police will be dispatched along with the new mental health team.
“This is the first time in our history that health professionals will be the default responders to mental health emergencies,” New York City First Lady Chirlane McCray said as she announced the new program. “Treating mental health crises as mental health challenges and not public safety ones is the modern and more appropriate approach.”
New York City is not the first city to employ this model. In the United States, the CAHOOTS (Crisis Assistance Helping Out on the Streets) program in Eugene, Ore., has been run by the White Bird Clinic since 1989 as part of a community policing initiative. Last year, the team responded to 24,000 calls and police backup was required on only 150 of those responses. The CAHOOTS website states:
“The CAHOOTS model has been in the spotlight recently as our nation struggles to reimagine public safety. The program mobilizes two-person teams consisting of a medic (a nurse, paramedic, or EMT) and a crisis worker who has substantial training and experience in the mental health field. The CAHOOTS teams deal with a wide range of mental health-related crises, including conflict resolution, welfare checks, substance abuse, suicide threats, and more, relying on trauma-informed de-escalation and harm reduction techniques. CAHOOTS staff are not law enforcement officers and do not carry weapons; their training and experience are the tools they use to ensure a non-violent resolution of crisis situations. They also handle non-emergent medical issues, avoiding costly ambulance transport and emergency room treatment.”
Other cities in the United States are also looking at implementing programs where mental health teams, and not the police, respond to emergency calls. Last year, Oakland, Calif.’s city council invested $40,000 in research to assess how they could best implement a program like the one in Eugene. They hope to begin the Mobile Assistance Community Responders of Oakland (MACROS) next year. Sigal Samuel writes in a Vox article, “The goal is to launch the pilot next year with funding from the city budget, and although supporters are not yet sure what its size and duration will be, they’re hopeful it’ll make a big difference to Oakland’s overpoliced community of people without homes. They were among those who first called for a non-policing approach.”
The model is not unique to the United States. In 2005, Stockholm started a program with a psychiatric ambulance – equipped with comfortable seating rather than a stretcher – to respond to mental health emergencies. The ambulance responds to 130 calls a month. It is staffed with a driver and two psychiatric nurses, and for half of the calls, the police also come. While the Swedish program was not about removing resources from the police, it has relieved the police of the responsibility for many psychiatric emergencies.
The New York City program will be modeled after the CAHOOTS initiative in Eugene. It differs from the mobile crisis response services in many other cities because CAHOOTS is hooked directly into the 911 emergency services system. Its website notes that the program has saved money:
“The cost savings are considerable. The CAHOOTS program budget is about $2.1 million annually, while the combined annual budgets for the Eugene and Springfield police departments are $90 million. In 2017, the CAHOOTS teams answered 17% of the Eugene Police Department’s overall call volume. The program saves the city of Eugene an estimated $8.5 million in public safety spending annually.”
Some worry there is an unpredictable aspect to calls for psychiatric emergencies, and the potential for mental health professions to be injured or killed. Annette Hanson, MD, a forensic psychiatrist at University of Maryland, Baltimore, voiced her concerns, “While multidisciplinary teams are useful, there have been rare cases of violence against responding mental health providers. People with serious mental illness are rarely violent but their dangerousness is unpredictable and cannot be predicted by case screening.”
Daniel Felts is a mental health crisis counselor who has worked at CAHOOTS for the past 4* years. He has responded to about 8,000 calls, and called for police backup only three times to request an immediate "Code 3 cover" when someone's safety has been in danger. Mr. Felts calls the police about once a month for concerns that do not require an immediate response for safety.* “Over the last 4 years, I am only aware of three instances when a team member’s safety was compromised because of a client’s violent behavior. No employee has been seriously physically harmed. In 30 years, with hundreds of thousands (millions?) of calls responded to, no CAHOOTS worker has ever been killed, shot, or stabbed in the line of duty,” Mr. Felts noted.
Emergency calls are screened. “It is not uncommon for CAHOOTS to be dispatched to ‘stage’ for calls involving active disputes or acutely suicidal individuals where means are present. “Staging” entails us parking roughly a mile away while police make first contact and advise whether it is safe for CAHOOTS to engage.”
Mr. Felts went on to discuss the program’s relationship with the community. “ and how we operate. Having operated in Eugene for 30 years, our service is well understood to be one that does not kill, harm, or violate personal boundaries or liberties.”
Would a program like the ones in Stockholm or in Eugene work in other places? Eugene is a city with a population of 172,000 with a low crime rate. Whether a program implemented in one city can be mimicked in another very different city is not clear.
Paul Appelbaum, MD, a forensic psychiatrist at Columbia University, New York, is optimistic about New York City’s forthcoming program.
“The proposed pilot project in NYC is a real step forward. Work that we’ve done looking at fatal encounters involving the police found that roughly 25% of all deaths at the hands of the police are of people with mental illness. In many of those cases, police were initially called to bring people who were clearly troubled for psychiatric evaluation, but as the situation escalated, the police turned to their weapons to control it, which led to a fatal outcome. Taking police out of the picture whenever possible in favor of trained mental health personnel is clearly a better approach. It will be important for the city to collect good outcome data to enable independent evaluation of the pilot project – not something that political entities are inclined toward, but a critical element in assessing the effectiveness of this approach.”
There are questions that remain about the new program. Mayor de Blasio’s office has not released information about which areas of the city are being chosen for the new program, how much the program will cost, or what the funding source will be. If it can be implemented safely and effectively, it has the potential to provide more sensitive care to patients in crisis, and to save lives.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2018). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins University, both in Baltimore.
*Correction, 11/27/2020: An earlier version of this article misstated the number of years Daniel Felts has worked at CAHOOTS.
Antidepressant shows early promise for mild COVID-19
Early treatment with the antidepressant fluvoxamine (Luvox) may help prevent respiratory deterioration in patients with mild symptomatic COVID-19, results of a preliminary randomized controlled trial suggest.
In the trial, none of the patients who took fluvoxamine within 7 days of first symptoms developed serious breathing difficulties or required hospitalization for respiratory deterioration.
“Most investigational treatments for COVID-19 have been aimed at the very sickest patients, but it’s also important to find therapies that prevent patients from getting sick enough to require supplemental oxygen or to have to go to the hospital,” study investigator Eric J. Lenze, MD, professor of psychiatry and director of the Healthy Mind Lab at Washington University, St. Louis, said in a statement.
“Our study suggests fluvoxamine may help fill that niche,” Lenze added.
The study was published online Nov. 12 in the JAMA.
Antiviral effects?
The study included 152 nonhospitalized adults (mean age, 46 years; 72% women) with confirmed SARS-CoV-2 infection and mild COVID-19 symptoms starting within 7 days and oxygen saturation of 92% or greater.
Eighty were randomly assigned to 100 mg of fluvoxamine three times daily for 15 days and 72 to matching placebo.
The primary outcome was clinical deterioration within 15 days of randomization defined by meeting two criteria. These included shortness of breath or hospitalization for shortness of breath or pneumonia and oxygen saturation <92% on room air or need for supplemental oxygen to achieve oxygen saturation of 92% or greater.
Clinical deterioration occurred in none of the 80 patients taking fluvoxamine compared with 6 of 72 (8.3%) patients taking placebo, an absolute difference of 8.7% (95% confidence interval, 1.8%-16.4%).
Clinical deterioration in the placebo group happened from 1 to 7 days after randomization and from 3 to 12 days after the onset of COVID-19 symptoms. Four of the 6 patients with clinical deterioration were admitted to the hospital for 4-21 days. One patient required mechanical ventilation for 10 days. No patients died.
Hypothesis generating
The authors cautioned that the study was small and with short follow-up and that the findings “need to be interpreted as hypothesis generating rather than as a demonstration of efficacy.”
However, they noted, if the drug turns out to be effective for COVID-19, the potential advantages of fluvoxamine for outpatient use include its safety, widespread availability, low cost, and oral administration.
Carolyn Machamer, PhD, member of the COVID-19 Early Treatment Fund (CETF) scientific advisory board, which funded the study, noted that there are several reasons fluvoxamine might be helpful in COVID-19.
“The preliminary data suggest the mechanism involves activation of the sigma-1 receptor, which has a number of documented activities. One strong possibility is that activation dampens cytokine release and thus the inflammatory response,” she said in an interview.
“Other possible mechanisms can include inhibition of platelet activation and modulation of autophagy. Coronaviruses usurp some autophagy machinery to remodel membranes for replicating their genomes, so this last mechanism might actually be antiviral,” said Dr. Machamer.
She added that a much larger trial is “crucial to see if the initial striking results can be reproduced, and the Healthy Mind Lab and CETF are currently coordinating these next steps.”
The editors of JAMA published an “Editor’s Note” with the study. In it, they wrote the pilot study addresses a “critically important question during the pandemic of how to prevent individuals who acquire COVID-19 from deteriorating to serious illness. If an effective treatment is found for this key gap in treatment, it will affect the health of millions of people worldwide.”
However, the study has “important limitations, and the findings should be interpreted as only hypothesis generating; they should not be used as the basis for current treatment decisions,” cautioned authors Christopher Seymour, MD, Howard Bauchner, MD, and Robert Golub, MD.
This study was supported by the Taylor Family Institute for Innovative Psychiatric Treatment at Washington University and the CETF. Additional support was provided by the Center for Brain Research in Mood Disorders at Washington University, the Bantly Foundation, and the National Institutes of Health.
Dr. Lenze has received grants from the Patient-Centered Outcomes Research Institute, Takeda, Alkermes, Janssen, Acadia, and the Barnes Jewish Hospital Foundation and has received consulting fees from Janssen and Jazz Pharmaceuticals. Dr. Machamer has disclosed no relevant financial relationships. Dr. Seymour has received grants from the National Institutes of Health and personal fees from Beckman Coulter and Edwards Lifesciences.
A version of this article originally appeared on Medscape.com.
Early treatment with the antidepressant fluvoxamine (Luvox) may help prevent respiratory deterioration in patients with mild symptomatic COVID-19, results of a preliminary randomized controlled trial suggest.
In the trial, none of the patients who took fluvoxamine within 7 days of first symptoms developed serious breathing difficulties or required hospitalization for respiratory deterioration.
“Most investigational treatments for COVID-19 have been aimed at the very sickest patients, but it’s also important to find therapies that prevent patients from getting sick enough to require supplemental oxygen or to have to go to the hospital,” study investigator Eric J. Lenze, MD, professor of psychiatry and director of the Healthy Mind Lab at Washington University, St. Louis, said in a statement.
“Our study suggests fluvoxamine may help fill that niche,” Lenze added.
The study was published online Nov. 12 in the JAMA.
Antiviral effects?
The study included 152 nonhospitalized adults (mean age, 46 years; 72% women) with confirmed SARS-CoV-2 infection and mild COVID-19 symptoms starting within 7 days and oxygen saturation of 92% or greater.
Eighty were randomly assigned to 100 mg of fluvoxamine three times daily for 15 days and 72 to matching placebo.
The primary outcome was clinical deterioration within 15 days of randomization defined by meeting two criteria. These included shortness of breath or hospitalization for shortness of breath or pneumonia and oxygen saturation <92% on room air or need for supplemental oxygen to achieve oxygen saturation of 92% or greater.
Clinical deterioration occurred in none of the 80 patients taking fluvoxamine compared with 6 of 72 (8.3%) patients taking placebo, an absolute difference of 8.7% (95% confidence interval, 1.8%-16.4%).
Clinical deterioration in the placebo group happened from 1 to 7 days after randomization and from 3 to 12 days after the onset of COVID-19 symptoms. Four of the 6 patients with clinical deterioration were admitted to the hospital for 4-21 days. One patient required mechanical ventilation for 10 days. No patients died.
Hypothesis generating
The authors cautioned that the study was small and with short follow-up and that the findings “need to be interpreted as hypothesis generating rather than as a demonstration of efficacy.”
However, they noted, if the drug turns out to be effective for COVID-19, the potential advantages of fluvoxamine for outpatient use include its safety, widespread availability, low cost, and oral administration.
Carolyn Machamer, PhD, member of the COVID-19 Early Treatment Fund (CETF) scientific advisory board, which funded the study, noted that there are several reasons fluvoxamine might be helpful in COVID-19.
“The preliminary data suggest the mechanism involves activation of the sigma-1 receptor, which has a number of documented activities. One strong possibility is that activation dampens cytokine release and thus the inflammatory response,” she said in an interview.
“Other possible mechanisms can include inhibition of platelet activation and modulation of autophagy. Coronaviruses usurp some autophagy machinery to remodel membranes for replicating their genomes, so this last mechanism might actually be antiviral,” said Dr. Machamer.
She added that a much larger trial is “crucial to see if the initial striking results can be reproduced, and the Healthy Mind Lab and CETF are currently coordinating these next steps.”
The editors of JAMA published an “Editor’s Note” with the study. In it, they wrote the pilot study addresses a “critically important question during the pandemic of how to prevent individuals who acquire COVID-19 from deteriorating to serious illness. If an effective treatment is found for this key gap in treatment, it will affect the health of millions of people worldwide.”
However, the study has “important limitations, and the findings should be interpreted as only hypothesis generating; they should not be used as the basis for current treatment decisions,” cautioned authors Christopher Seymour, MD, Howard Bauchner, MD, and Robert Golub, MD.
This study was supported by the Taylor Family Institute for Innovative Psychiatric Treatment at Washington University and the CETF. Additional support was provided by the Center for Brain Research in Mood Disorders at Washington University, the Bantly Foundation, and the National Institutes of Health.
Dr. Lenze has received grants from the Patient-Centered Outcomes Research Institute, Takeda, Alkermes, Janssen, Acadia, and the Barnes Jewish Hospital Foundation and has received consulting fees from Janssen and Jazz Pharmaceuticals. Dr. Machamer has disclosed no relevant financial relationships. Dr. Seymour has received grants from the National Institutes of Health and personal fees from Beckman Coulter and Edwards Lifesciences.
A version of this article originally appeared on Medscape.com.
Early treatment with the antidepressant fluvoxamine (Luvox) may help prevent respiratory deterioration in patients with mild symptomatic COVID-19, results of a preliminary randomized controlled trial suggest.
In the trial, none of the patients who took fluvoxamine within 7 days of first symptoms developed serious breathing difficulties or required hospitalization for respiratory deterioration.
“Most investigational treatments for COVID-19 have been aimed at the very sickest patients, but it’s also important to find therapies that prevent patients from getting sick enough to require supplemental oxygen or to have to go to the hospital,” study investigator Eric J. Lenze, MD, professor of psychiatry and director of the Healthy Mind Lab at Washington University, St. Louis, said in a statement.
“Our study suggests fluvoxamine may help fill that niche,” Lenze added.
The study was published online Nov. 12 in the JAMA.
Antiviral effects?
The study included 152 nonhospitalized adults (mean age, 46 years; 72% women) with confirmed SARS-CoV-2 infection and mild COVID-19 symptoms starting within 7 days and oxygen saturation of 92% or greater.
Eighty were randomly assigned to 100 mg of fluvoxamine three times daily for 15 days and 72 to matching placebo.
The primary outcome was clinical deterioration within 15 days of randomization defined by meeting two criteria. These included shortness of breath or hospitalization for shortness of breath or pneumonia and oxygen saturation <92% on room air or need for supplemental oxygen to achieve oxygen saturation of 92% or greater.
Clinical deterioration occurred in none of the 80 patients taking fluvoxamine compared with 6 of 72 (8.3%) patients taking placebo, an absolute difference of 8.7% (95% confidence interval, 1.8%-16.4%).
Clinical deterioration in the placebo group happened from 1 to 7 days after randomization and from 3 to 12 days after the onset of COVID-19 symptoms. Four of the 6 patients with clinical deterioration were admitted to the hospital for 4-21 days. One patient required mechanical ventilation for 10 days. No patients died.
Hypothesis generating
The authors cautioned that the study was small and with short follow-up and that the findings “need to be interpreted as hypothesis generating rather than as a demonstration of efficacy.”
However, they noted, if the drug turns out to be effective for COVID-19, the potential advantages of fluvoxamine for outpatient use include its safety, widespread availability, low cost, and oral administration.
Carolyn Machamer, PhD, member of the COVID-19 Early Treatment Fund (CETF) scientific advisory board, which funded the study, noted that there are several reasons fluvoxamine might be helpful in COVID-19.
“The preliminary data suggest the mechanism involves activation of the sigma-1 receptor, which has a number of documented activities. One strong possibility is that activation dampens cytokine release and thus the inflammatory response,” she said in an interview.
“Other possible mechanisms can include inhibition of platelet activation and modulation of autophagy. Coronaviruses usurp some autophagy machinery to remodel membranes for replicating their genomes, so this last mechanism might actually be antiviral,” said Dr. Machamer.
She added that a much larger trial is “crucial to see if the initial striking results can be reproduced, and the Healthy Mind Lab and CETF are currently coordinating these next steps.”
The editors of JAMA published an “Editor’s Note” with the study. In it, they wrote the pilot study addresses a “critically important question during the pandemic of how to prevent individuals who acquire COVID-19 from deteriorating to serious illness. If an effective treatment is found for this key gap in treatment, it will affect the health of millions of people worldwide.”
However, the study has “important limitations, and the findings should be interpreted as only hypothesis generating; they should not be used as the basis for current treatment decisions,” cautioned authors Christopher Seymour, MD, Howard Bauchner, MD, and Robert Golub, MD.
This study was supported by the Taylor Family Institute for Innovative Psychiatric Treatment at Washington University and the CETF. Additional support was provided by the Center for Brain Research in Mood Disorders at Washington University, the Bantly Foundation, and the National Institutes of Health.
Dr. Lenze has received grants from the Patient-Centered Outcomes Research Institute, Takeda, Alkermes, Janssen, Acadia, and the Barnes Jewish Hospital Foundation and has received consulting fees from Janssen and Jazz Pharmaceuticals. Dr. Machamer has disclosed no relevant financial relationships. Dr. Seymour has received grants from the National Institutes of Health and personal fees from Beckman Coulter and Edwards Lifesciences.
A version of this article originally appeared on Medscape.com.
Tips for physicians, patients to make the most of the holidays amid COVID
“We must accept finite disappointment, but never lose infinite hope,” Martin Luther King, Jr.
This holiday season will be like no other. We will remember it for the rest of our lives, and we will look back to see how we faced the holidays during a pandemic.
Like the rest of 2020, the holidays will need to be reimagined. Years and even decades of tradition will be broken as we place health above merriment.
Here are a few tips to help all of us and our patients make the most of this holiday season.
- Reprioritize: This holiday season will be about depth not breadth, quality not quantity, and less not more. Trips are canceled and gatherings have shrunk. We are not running from store to store or party to party. Instead, you will find yourself surrounded by fewer friends and family. Some will be alone to optimally protect their health and the health of others. Do your best to focus on the half-full portion.
- Embrace change: Don’t compare or try to make this year like previous years. Be creative and try to find ways to make a new format fun. Meeting during the day and limiting alcohol intake can assist in making sure everyone stays safe. It has been interesting to see how many of my patients have decreased their alcohol use during quarantine. I hope this pattern will continue over the next weeks and months.
- Practice self-care: As health care professionals, we must remember the old adage “physician, heal thyself.” This year has been so difficult for almost all of us. It was filled with unprecedented levels of personal and professional stress. Holidays are often about what we can do for others, but this year we may need to place self-care first. Do what brings you happiness.
Even though you aren’t traveling, you can still disconnect from work. Set up a schedule and stick to it making sure you take plenty of time to rest and enjoy. Many of us have been working extremely long hours and a break is so needed. Take it if you possibly can. Detox from your screen! Limit the news. Creativity and productivity will be enhanced in 2021 if we can come in recharged.
For those remaining on the front lines, be patient; the end is nearing. Take care of yourself when you are not working. We are all so grateful to those in our field who have sacrificed so much to care for others. Eat, drink, and rest well to keep your immune system strong.
- Acknowledge your negative emotions: As we all know, if you try to deny negative emotions, they continue to pop up. If we give them time and space to be felt, we will find they diminish in intensity. Long work hours may have prevented us from feeling our emotions, so don’t be surprised if they surface when we take a break.
Let yourself feel the sadness for what you have experienced this year. Be open about missing those who can’t be with you because of travel or other restrictions. Let yourself feel the disappointment about your holiday travel plans that you can’t embark upon.
You may elect to share these emotions with someone close to you or with a professional. To paraphrase Carl Jung, “what we resist, persists,” so don’t try to hide from your negative emotions. Most of us had lots of them in 2020, so don’t be shy about admitting it.
- Focus on growth: What have we learned from 2020 and how can we be better equipped in 2021 and beyond?
Trauma can bring growth not just disorder. This year has returned well-deserved prestige to our fields. We are being lauded as heroes as we have scarified our health and the health of our loved ones to serve others. Can we choose to celebrate our accomplishments?
We have become more resilient and learned to continue on in the face of great hardship. Many of us have gained confidence as we confronted this historic challenge. As we have been reminded of death daily, we learn to appreciate life more fully and not take any day for granted.
I am proud to be a physician during this pandemic, and I hope you are, too!
- Find joy: Often times, we find real happiness in smaller moments and experiences. For many, this time of year is filled with so much stress that it can be hard to carve out moments of joy. As we may be less busy socially this holiday season, might we find even more joy?
Joy can only be experienced in the present moment. Tap into all your senses. Eat slowly making sure to smell and taste every bite. Cherish those who can still gather at your table. If you find yourself alone, embrace that experience. Safety must continue to come first, and we can’t let down our guard now.
- Reflect: New Year’s Eve is always a time for reflection and hope for the future. Most of us will be glad to see 2020 in the rearview mirror. With multiple and very promising vaccines on the horizon, we can anticipate a brighter future. We must continue to work hard; remain patient; and be creative, resilient, and optimistic. Let’s try to fill our days with hope and purpose and work together to achieve a brighter future for all.
“Learn from yesterday, live for today, hope for tomorrow,” Albert Einstein
Wishing you health and happiness in this holiday season and beyond.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018). She also is founder of the Bekindr Global Initiative, a movement aimed at cultivating kindness in the world.
“We must accept finite disappointment, but never lose infinite hope,” Martin Luther King, Jr.
This holiday season will be like no other. We will remember it for the rest of our lives, and we will look back to see how we faced the holidays during a pandemic.
Like the rest of 2020, the holidays will need to be reimagined. Years and even decades of tradition will be broken as we place health above merriment.
Here are a few tips to help all of us and our patients make the most of this holiday season.
- Reprioritize: This holiday season will be about depth not breadth, quality not quantity, and less not more. Trips are canceled and gatherings have shrunk. We are not running from store to store or party to party. Instead, you will find yourself surrounded by fewer friends and family. Some will be alone to optimally protect their health and the health of others. Do your best to focus on the half-full portion.
- Embrace change: Don’t compare or try to make this year like previous years. Be creative and try to find ways to make a new format fun. Meeting during the day and limiting alcohol intake can assist in making sure everyone stays safe. It has been interesting to see how many of my patients have decreased their alcohol use during quarantine. I hope this pattern will continue over the next weeks and months.
- Practice self-care: As health care professionals, we must remember the old adage “physician, heal thyself.” This year has been so difficult for almost all of us. It was filled with unprecedented levels of personal and professional stress. Holidays are often about what we can do for others, but this year we may need to place self-care first. Do what brings you happiness.
Even though you aren’t traveling, you can still disconnect from work. Set up a schedule and stick to it making sure you take plenty of time to rest and enjoy. Many of us have been working extremely long hours and a break is so needed. Take it if you possibly can. Detox from your screen! Limit the news. Creativity and productivity will be enhanced in 2021 if we can come in recharged.
For those remaining on the front lines, be patient; the end is nearing. Take care of yourself when you are not working. We are all so grateful to those in our field who have sacrificed so much to care for others. Eat, drink, and rest well to keep your immune system strong.
- Acknowledge your negative emotions: As we all know, if you try to deny negative emotions, they continue to pop up. If we give them time and space to be felt, we will find they diminish in intensity. Long work hours may have prevented us from feeling our emotions, so don’t be surprised if they surface when we take a break.
Let yourself feel the sadness for what you have experienced this year. Be open about missing those who can’t be with you because of travel or other restrictions. Let yourself feel the disappointment about your holiday travel plans that you can’t embark upon.
You may elect to share these emotions with someone close to you or with a professional. To paraphrase Carl Jung, “what we resist, persists,” so don’t try to hide from your negative emotions. Most of us had lots of them in 2020, so don’t be shy about admitting it.
- Focus on growth: What have we learned from 2020 and how can we be better equipped in 2021 and beyond?
Trauma can bring growth not just disorder. This year has returned well-deserved prestige to our fields. We are being lauded as heroes as we have scarified our health and the health of our loved ones to serve others. Can we choose to celebrate our accomplishments?
We have become more resilient and learned to continue on in the face of great hardship. Many of us have gained confidence as we confronted this historic challenge. As we have been reminded of death daily, we learn to appreciate life more fully and not take any day for granted.
I am proud to be a physician during this pandemic, and I hope you are, too!
- Find joy: Often times, we find real happiness in smaller moments and experiences. For many, this time of year is filled with so much stress that it can be hard to carve out moments of joy. As we may be less busy socially this holiday season, might we find even more joy?
Joy can only be experienced in the present moment. Tap into all your senses. Eat slowly making sure to smell and taste every bite. Cherish those who can still gather at your table. If you find yourself alone, embrace that experience. Safety must continue to come first, and we can’t let down our guard now.
- Reflect: New Year’s Eve is always a time for reflection and hope for the future. Most of us will be glad to see 2020 in the rearview mirror. With multiple and very promising vaccines on the horizon, we can anticipate a brighter future. We must continue to work hard; remain patient; and be creative, resilient, and optimistic. Let’s try to fill our days with hope and purpose and work together to achieve a brighter future for all.
“Learn from yesterday, live for today, hope for tomorrow,” Albert Einstein
Wishing you health and happiness in this holiday season and beyond.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018). She also is founder of the Bekindr Global Initiative, a movement aimed at cultivating kindness in the world.
“We must accept finite disappointment, but never lose infinite hope,” Martin Luther King, Jr.
This holiday season will be like no other. We will remember it for the rest of our lives, and we will look back to see how we faced the holidays during a pandemic.
Like the rest of 2020, the holidays will need to be reimagined. Years and even decades of tradition will be broken as we place health above merriment.
Here are a few tips to help all of us and our patients make the most of this holiday season.
- Reprioritize: This holiday season will be about depth not breadth, quality not quantity, and less not more. Trips are canceled and gatherings have shrunk. We are not running from store to store or party to party. Instead, you will find yourself surrounded by fewer friends and family. Some will be alone to optimally protect their health and the health of others. Do your best to focus on the half-full portion.
- Embrace change: Don’t compare or try to make this year like previous years. Be creative and try to find ways to make a new format fun. Meeting during the day and limiting alcohol intake can assist in making sure everyone stays safe. It has been interesting to see how many of my patients have decreased their alcohol use during quarantine. I hope this pattern will continue over the next weeks and months.
- Practice self-care: As health care professionals, we must remember the old adage “physician, heal thyself.” This year has been so difficult for almost all of us. It was filled with unprecedented levels of personal and professional stress. Holidays are often about what we can do for others, but this year we may need to place self-care first. Do what brings you happiness.
Even though you aren’t traveling, you can still disconnect from work. Set up a schedule and stick to it making sure you take plenty of time to rest and enjoy. Many of us have been working extremely long hours and a break is so needed. Take it if you possibly can. Detox from your screen! Limit the news. Creativity and productivity will be enhanced in 2021 if we can come in recharged.
For those remaining on the front lines, be patient; the end is nearing. Take care of yourself when you are not working. We are all so grateful to those in our field who have sacrificed so much to care for others. Eat, drink, and rest well to keep your immune system strong.
- Acknowledge your negative emotions: As we all know, if you try to deny negative emotions, they continue to pop up. If we give them time and space to be felt, we will find they diminish in intensity. Long work hours may have prevented us from feeling our emotions, so don’t be surprised if they surface when we take a break.
Let yourself feel the sadness for what you have experienced this year. Be open about missing those who can’t be with you because of travel or other restrictions. Let yourself feel the disappointment about your holiday travel plans that you can’t embark upon.
You may elect to share these emotions with someone close to you or with a professional. To paraphrase Carl Jung, “what we resist, persists,” so don’t try to hide from your negative emotions. Most of us had lots of them in 2020, so don’t be shy about admitting it.
- Focus on growth: What have we learned from 2020 and how can we be better equipped in 2021 and beyond?
Trauma can bring growth not just disorder. This year has returned well-deserved prestige to our fields. We are being lauded as heroes as we have scarified our health and the health of our loved ones to serve others. Can we choose to celebrate our accomplishments?
We have become more resilient and learned to continue on in the face of great hardship. Many of us have gained confidence as we confronted this historic challenge. As we have been reminded of death daily, we learn to appreciate life more fully and not take any day for granted.
I am proud to be a physician during this pandemic, and I hope you are, too!
- Find joy: Often times, we find real happiness in smaller moments and experiences. For many, this time of year is filled with so much stress that it can be hard to carve out moments of joy. As we may be less busy socially this holiday season, might we find even more joy?
Joy can only be experienced in the present moment. Tap into all your senses. Eat slowly making sure to smell and taste every bite. Cherish those who can still gather at your table. If you find yourself alone, embrace that experience. Safety must continue to come first, and we can’t let down our guard now.
- Reflect: New Year’s Eve is always a time for reflection and hope for the future. Most of us will be glad to see 2020 in the rearview mirror. With multiple and very promising vaccines on the horizon, we can anticipate a brighter future. We must continue to work hard; remain patient; and be creative, resilient, and optimistic. Let’s try to fill our days with hope and purpose and work together to achieve a brighter future for all.
“Learn from yesterday, live for today, hope for tomorrow,” Albert Einstein
Wishing you health and happiness in this holiday season and beyond.
Dr. Ritvo, a psychiatrist with more than 25 years’ experience, practices in Miami Beach. She is the author of “Bekindr – The Transformative Power of Kindness” (Hellertown, Pa.: Momosa Publishing, 2018). She also is founder of the Bekindr Global Initiative, a movement aimed at cultivating kindness in the world.
Distinguish ‘sleepiness’ from ‘fatigue’ to help diagnose hypersomnia
, according to Ruth M. Benca, MD, PhD.
Fatigue, feeling tired, and lack of energy are common complaints that accompany insomnia and psychiatric disorders, but these patients do not fall asleep quickly in a restful setting and will have normal multiple sleep latency test (MSLT) in a laboratory. In contrast, excessive sleepiness, or hypersomnia, occurs when patients sleep more than 11 hours in a 24-hour period.
Patients with hypersomnia fall asleep in low stimulus situations and devote more energy to staying awake during situations. This excessive sleepiness can be dangerous in the context of activities such as driving, Dr. Benca said. These patients will also have low sleep latencies (< 8 minutes) when tested through MSLT in a laboratory, she added. Patients with hypersomnia may be irritable, have reduced attention or concentration, and have poor memory.
The primary cause of hypersomnia is sleep deprivation, but “both hypersomnia and fatigue are common complaints in psychiatric patients, including depression, bipolar disorder, seasonal affective disorder, [and] psychosis,” Dr. Benca explained. Other causes of hypersomnia include sleep disorders such as sleep apnea, circadian rhythm disorders and periodic limb movements, neurologic or degenerative disorders, mental disorders, and effects of medication. Idiopathic hypersomnia and narcolepsy are uncommon causes of hypersomnia and usually diagnosed in a sleep laboratory setting, she said.
In patients with depression, hypersomnia looks like patients having “nonimperative sleepiness,” Dr. Benca said. “They may spend a lot of time in bed; they may report long and nonrefreshing naps or long sleep time.”
There also is an issue with sleep inertia in patients with depression and hypersomnia, and with patients taking a long time to wake up and begin their day. In these patients, “when we put them in the sleep laboratory, the objective studies generally do not show that they are excessively sleepy, despite their reports of subjectively being sleepy,” she said.
There is not much objective MSLT or subjective measure data for hypersomnia in patients with schizophrenia despite these patients reporting daytime sleepiness or hypersomnolence, Dr. Benca admitted. Hypersomnia in patients with schizophrenia may be related to drug effects, poor sleep hygiene, circadian rhythm abnormalities, or comorbid sleep disorders. “Excessive sleepiness may also be related to the schizophrenia itself,” she said.
Treatments for hypersomnia
The first priority for patients with hypersomnia is to avoid sleep deprivation and practice good sleep hygiene – factors that are important both in insomnia and hypersomnia. “Make sure that patients are having adequate time in bed and having regular hours of sleep,” Dr. Benca said.
For patients with comorbid psychiatric, medical and sleep disorders, focus on getting rid of medications that may cause sleepiness, including sedating medications and antidepressants, and consider using stimulants if appropriate. While there are Food and Drug Administration–approved medications for narcolepsy and some are approved for hypersomnia in patients with obstructive sleep apnea (OSA), none are officially approved to treat hypersomnia in psychiatric patients.
“Whenever we use these drugs for those reasons, we’re using them off label,” Dr. Benca said.
Modafinil/armodafinil, approved for narcolepsy, shift-work disorder, and OSA in Ehlers-Danlos syndrome, is one off-label option for patients with hypersomnia. “They are lower potency and less addictive than the amphetamines, [with] fewer side effects,” Dr. Benca explained, but should be prescribed with caution in some women because of potential reduced efficacy of oral contraceptives. Side effects of modafinil include headache, nausea, eosinophilia, diarrhea, dry mouth, and anorexia.
Methylphenidate is another option for hypersomnia, available in racemic mixture, pure D-isomer, and time-release formulations.
Patients taking methylphenidate may experience nervousness, insomnia, anorexia, nausea, dizziness, hypertension, hypotension, hypersensitivity reactions, tachycardia, and headache as side effects.
For patients with central nervous system hypersomnias, amphetamines can be used, with methamphetamines having a “very similar profile” and similar side effects, including insomnia, restlessness, tachycardia, dizziness, diarrhea, constipation, hypertension, impotence, and rare cases of psychotic episodes.
Practice parameters released by the American Academy of Sleep Medicine in 2007 suggest that modafinil may have efficacy in idiopathic hypersomnia, Parkinson’s disease, myotonic dystrophy, and multiple sclerosis. The practice parameters also suggest hypersomnias of central origin can be treated with modafinil, amphetamine, methamphetamine, dextroamphetamine, and methylphenidate based on evidence or “long history of use” (Sleep. 2007;30:1705-11).
“Interestingly, there is no mention of psychiatric disorders in these practice parameters, and they report that there are mixed results using stimulants off label for sleepiness and fatigue in traumatic brain injury and poststroke fatigue,” Dr. Benca said.
Dr. Benca reported that she is a consultant to Eisai, Idorsia, Jazz, Merck, and Sunovion. Global Academy and this news organization are owned by the same parent company.
, according to Ruth M. Benca, MD, PhD.
Fatigue, feeling tired, and lack of energy are common complaints that accompany insomnia and psychiatric disorders, but these patients do not fall asleep quickly in a restful setting and will have normal multiple sleep latency test (MSLT) in a laboratory. In contrast, excessive sleepiness, or hypersomnia, occurs when patients sleep more than 11 hours in a 24-hour period.
Patients with hypersomnia fall asleep in low stimulus situations and devote more energy to staying awake during situations. This excessive sleepiness can be dangerous in the context of activities such as driving, Dr. Benca said. These patients will also have low sleep latencies (< 8 minutes) when tested through MSLT in a laboratory, she added. Patients with hypersomnia may be irritable, have reduced attention or concentration, and have poor memory.
The primary cause of hypersomnia is sleep deprivation, but “both hypersomnia and fatigue are common complaints in psychiatric patients, including depression, bipolar disorder, seasonal affective disorder, [and] psychosis,” Dr. Benca explained. Other causes of hypersomnia include sleep disorders such as sleep apnea, circadian rhythm disorders and periodic limb movements, neurologic or degenerative disorders, mental disorders, and effects of medication. Idiopathic hypersomnia and narcolepsy are uncommon causes of hypersomnia and usually diagnosed in a sleep laboratory setting, she said.
In patients with depression, hypersomnia looks like patients having “nonimperative sleepiness,” Dr. Benca said. “They may spend a lot of time in bed; they may report long and nonrefreshing naps or long sleep time.”
There also is an issue with sleep inertia in patients with depression and hypersomnia, and with patients taking a long time to wake up and begin their day. In these patients, “when we put them in the sleep laboratory, the objective studies generally do not show that they are excessively sleepy, despite their reports of subjectively being sleepy,” she said.
There is not much objective MSLT or subjective measure data for hypersomnia in patients with schizophrenia despite these patients reporting daytime sleepiness or hypersomnolence, Dr. Benca admitted. Hypersomnia in patients with schizophrenia may be related to drug effects, poor sleep hygiene, circadian rhythm abnormalities, or comorbid sleep disorders. “Excessive sleepiness may also be related to the schizophrenia itself,” she said.
Treatments for hypersomnia
The first priority for patients with hypersomnia is to avoid sleep deprivation and practice good sleep hygiene – factors that are important both in insomnia and hypersomnia. “Make sure that patients are having adequate time in bed and having regular hours of sleep,” Dr. Benca said.
For patients with comorbid psychiatric, medical and sleep disorders, focus on getting rid of medications that may cause sleepiness, including sedating medications and antidepressants, and consider using stimulants if appropriate. While there are Food and Drug Administration–approved medications for narcolepsy and some are approved for hypersomnia in patients with obstructive sleep apnea (OSA), none are officially approved to treat hypersomnia in psychiatric patients.
“Whenever we use these drugs for those reasons, we’re using them off label,” Dr. Benca said.
Modafinil/armodafinil, approved for narcolepsy, shift-work disorder, and OSA in Ehlers-Danlos syndrome, is one off-label option for patients with hypersomnia. “They are lower potency and less addictive than the amphetamines, [with] fewer side effects,” Dr. Benca explained, but should be prescribed with caution in some women because of potential reduced efficacy of oral contraceptives. Side effects of modafinil include headache, nausea, eosinophilia, diarrhea, dry mouth, and anorexia.
Methylphenidate is another option for hypersomnia, available in racemic mixture, pure D-isomer, and time-release formulations.
Patients taking methylphenidate may experience nervousness, insomnia, anorexia, nausea, dizziness, hypertension, hypotension, hypersensitivity reactions, tachycardia, and headache as side effects.
For patients with central nervous system hypersomnias, amphetamines can be used, with methamphetamines having a “very similar profile” and similar side effects, including insomnia, restlessness, tachycardia, dizziness, diarrhea, constipation, hypertension, impotence, and rare cases of psychotic episodes.
Practice parameters released by the American Academy of Sleep Medicine in 2007 suggest that modafinil may have efficacy in idiopathic hypersomnia, Parkinson’s disease, myotonic dystrophy, and multiple sclerosis. The practice parameters also suggest hypersomnias of central origin can be treated with modafinil, amphetamine, methamphetamine, dextroamphetamine, and methylphenidate based on evidence or “long history of use” (Sleep. 2007;30:1705-11).
“Interestingly, there is no mention of psychiatric disorders in these practice parameters, and they report that there are mixed results using stimulants off label for sleepiness and fatigue in traumatic brain injury and poststroke fatigue,” Dr. Benca said.
Dr. Benca reported that she is a consultant to Eisai, Idorsia, Jazz, Merck, and Sunovion. Global Academy and this news organization are owned by the same parent company.
, according to Ruth M. Benca, MD, PhD.
Fatigue, feeling tired, and lack of energy are common complaints that accompany insomnia and psychiatric disorders, but these patients do not fall asleep quickly in a restful setting and will have normal multiple sleep latency test (MSLT) in a laboratory. In contrast, excessive sleepiness, or hypersomnia, occurs when patients sleep more than 11 hours in a 24-hour period.
Patients with hypersomnia fall asleep in low stimulus situations and devote more energy to staying awake during situations. This excessive sleepiness can be dangerous in the context of activities such as driving, Dr. Benca said. These patients will also have low sleep latencies (< 8 minutes) when tested through MSLT in a laboratory, she added. Patients with hypersomnia may be irritable, have reduced attention or concentration, and have poor memory.
The primary cause of hypersomnia is sleep deprivation, but “both hypersomnia and fatigue are common complaints in psychiatric patients, including depression, bipolar disorder, seasonal affective disorder, [and] psychosis,” Dr. Benca explained. Other causes of hypersomnia include sleep disorders such as sleep apnea, circadian rhythm disorders and periodic limb movements, neurologic or degenerative disorders, mental disorders, and effects of medication. Idiopathic hypersomnia and narcolepsy are uncommon causes of hypersomnia and usually diagnosed in a sleep laboratory setting, she said.
In patients with depression, hypersomnia looks like patients having “nonimperative sleepiness,” Dr. Benca said. “They may spend a lot of time in bed; they may report long and nonrefreshing naps or long sleep time.”
There also is an issue with sleep inertia in patients with depression and hypersomnia, and with patients taking a long time to wake up and begin their day. In these patients, “when we put them in the sleep laboratory, the objective studies generally do not show that they are excessively sleepy, despite their reports of subjectively being sleepy,” she said.
There is not much objective MSLT or subjective measure data for hypersomnia in patients with schizophrenia despite these patients reporting daytime sleepiness or hypersomnolence, Dr. Benca admitted. Hypersomnia in patients with schizophrenia may be related to drug effects, poor sleep hygiene, circadian rhythm abnormalities, or comorbid sleep disorders. “Excessive sleepiness may also be related to the schizophrenia itself,” she said.
Treatments for hypersomnia
The first priority for patients with hypersomnia is to avoid sleep deprivation and practice good sleep hygiene – factors that are important both in insomnia and hypersomnia. “Make sure that patients are having adequate time in bed and having regular hours of sleep,” Dr. Benca said.
For patients with comorbid psychiatric, medical and sleep disorders, focus on getting rid of medications that may cause sleepiness, including sedating medications and antidepressants, and consider using stimulants if appropriate. While there are Food and Drug Administration–approved medications for narcolepsy and some are approved for hypersomnia in patients with obstructive sleep apnea (OSA), none are officially approved to treat hypersomnia in psychiatric patients.
“Whenever we use these drugs for those reasons, we’re using them off label,” Dr. Benca said.
Modafinil/armodafinil, approved for narcolepsy, shift-work disorder, and OSA in Ehlers-Danlos syndrome, is one off-label option for patients with hypersomnia. “They are lower potency and less addictive than the amphetamines, [with] fewer side effects,” Dr. Benca explained, but should be prescribed with caution in some women because of potential reduced efficacy of oral contraceptives. Side effects of modafinil include headache, nausea, eosinophilia, diarrhea, dry mouth, and anorexia.
Methylphenidate is another option for hypersomnia, available in racemic mixture, pure D-isomer, and time-release formulations.
Patients taking methylphenidate may experience nervousness, insomnia, anorexia, nausea, dizziness, hypertension, hypotension, hypersensitivity reactions, tachycardia, and headache as side effects.
For patients with central nervous system hypersomnias, amphetamines can be used, with methamphetamines having a “very similar profile” and similar side effects, including insomnia, restlessness, tachycardia, dizziness, diarrhea, constipation, hypertension, impotence, and rare cases of psychotic episodes.
Practice parameters released by the American Academy of Sleep Medicine in 2007 suggest that modafinil may have efficacy in idiopathic hypersomnia, Parkinson’s disease, myotonic dystrophy, and multiple sclerosis. The practice parameters also suggest hypersomnias of central origin can be treated with modafinil, amphetamine, methamphetamine, dextroamphetamine, and methylphenidate based on evidence or “long history of use” (Sleep. 2007;30:1705-11).
“Interestingly, there is no mention of psychiatric disorders in these practice parameters, and they report that there are mixed results using stimulants off label for sleepiness and fatigue in traumatic brain injury and poststroke fatigue,” Dr. Benca said.
Dr. Benca reported that she is a consultant to Eisai, Idorsia, Jazz, Merck, and Sunovion. Global Academy and this news organization are owned by the same parent company.
FROM PSYCHOPHARMACOLOGY UPDATE
Psilocybin delivers ‘remarkable’ relief in severe depression
Psilocybin, the psychedelic compound in “magic mushrooms,” rapidly improves symptoms and produces remission in as little as two sessions for patients with major depression, new research suggests.
Results of a small randomized trial showed that treatment with psilocybin was associated with a greater than 50% reduction in depressive symptoms in 67% of study participants. In addition, 71% showed improvement at 4-week follow-up, with more than 50% achieving remission.
“The finding that the majority of people whom we treated showed efficacy was quite a remarkable and gratifying finding and really sets the stage for psilocybin as a treatment for major depression,” senior investigator Roland Griffiths, PhD, Oliver Lee McCabe III Professor in the Neuropsychopharmacology of Consciousness, Johns Hopkins University, Baltimore, said in a statement.
“Perhaps the most exciting aspect of this as a new therapy is that psilocybin works as a therapeutic intervention with a single session or a few sessions, and then the effects are enduring. In contrast, most conventional treatments for depression ... are given chronically and also have chronic side effects,” added Dr. Griffiths, who is also director of the Johns Hopkins Center for Psychedelic and Consciousness Research.
The study was published online Nov.4 in JAMA Psychiatry.
Growing evidence base
As previously reported, psilocybin improves depressive symptoms for patients with cancer. However, these patients might be regarded as having a “reactive depression” to their life-threatening illness, said Dr. Griffiths.
“This study built on that previous research by asking the question, is psilocybin effective in patients who have major depressive disorder, [which is] a much larger population?” he said.
In addition, prior studies of psilocybin-assisted therapy had no control group, lead author Alan Davis, PhD, adjunct assistant professor in the psychedelic research unit, Johns Hopkins University, said in an interview.
The researchers created a control condition by randomly assigning 24 individuals (mean age, 39.8 years; 67% women) who were currently experiencing a moderate or severe major depressive episode to receive either immediate treatment (IT) (n = 13) or delayed treatment (DT) (n = 11).
Participants had longstanding depression, with a mean of 22.4 months in the current depressive episode. They were required to avoid using other antidepressants for 4 weeks prior to screening and up to 4 months following enrollment.
Patients were also required to be medically stable; have no personal/family history of psychotic or bipolar disorders; no past-year alcohol, substance, or nicotine use disorder; and no substantial lifetime or recent use of ketamine or classic hallucinogens.
Depression was measured using the Structured Clinical Interview for DSM-5 and the GRID-Hamilton Depression Rating Scale (GRID-HAMD). A baseline score of ≥17 was required for enrollment.
Participants received eight preparatory meetings with two session facilitators before the first psilocybin session and then 2-3 hours of follow-up meetings after the psilocybin sessions. In addition, they received 13 sessions of psychotherapy.
After completing these preparatory sessions, they underwent two psilocybin sessions, administered a mean of 1.6 weeks apart.
Participants in the DT group were assessed for depressive symptoms weekly for 8 weeks prior to entering the treatment protocol.
‘Surprising’ findings
Participants in the IT group exhibited significantly lower depression scores on the GRID-HAMD at 1 and 4 weeks after the second psilocybin session in comparison with patients in the DT group during the corresponding weeks.
Moreover, the effect sizes at weeks 5 and 8 were “large” (d = 2.2; 95% confidence interval, 1.4-3.0; and d = 2.6; 95% CI, 1.7-3.6, respectively).
An analysis of outcomes showed that, for all 24 participants, at 1 and at 4 weeks following the psilocybin intervention, 67% and 71% of participants, respectively, had a “clinically significant response” in depressive symptoms; 60% and 56%, respectively, met criteria for remission.
Within-subject T tests likewise revealed significant decreases in depression scores from baseline to 1- and 4-week follow-ups (P < .001; d = 3.6; 95% CI, 2.2-5.0; and P < .001; d = 3.6; 95% CI, 2.2-4.9, respectively).
Importantly, participants experienced no serious adverse effects.
Dr. Griffiths said he was “surprised” by the findings. “We knew that psilocybin would be effective in reactive depression of the type associated with illness, but we did not know that this would be the case in the large number of individuals who qualify for having [major depressive disorder].”
Dr. Davis said the finding “represents a large effect of this treatment among people with major depressive disorder – an approximately 4 times larger effect, compared to studies of antidepressant drugs.”
Dr. Davis noted that psychotherapy was an “essential” component of the study protocol. “ and that this treatment will always have a psychotherapy component and will not be Food and Drug Administration approved as a standalone medication.”
Tipping point
Collin Reiff, MD, clinical assistant professor in the department of psychiatry at New York University noted that because psychedelics are “still stigmatized,” the publication of this study in “one of the highest-impact journals in all of psychiatry suggests that research into psychedelics is now in the mainstream and that the academic psychiatry research community is paying close attention to what is happening.” He described this as a “tipping point.”
Dr. Reiff, who was not involved with the study, noted that research had been conducted on psychedelic compounds until the 1960s, “when they left the research lab and went mainstream, leading to the shutting down and subsequent dormancy of the research for the next 30-40 years.”
Psychedelic research is “undergoing a renaissance and no longer regarded with as much skepticism, but it is important to take our time doing this research so we do not repeat what happened in the 1960s,” said Dr. Reiff.
In an accompanying editorial, Charles F. Reynolds III, MD, endowed professor in geriatric psychiatry at the University of Pittsburgh Medical Center, Pennsylvania, questioned “for whom psychedelic-assisted psychotherapy is appropriate (or not), particularly in patients with depression who are suicidal of have a history of suicide attempt.”
Dr. Reynolds, who is also director of the Aging Institute of UPMC, who was not involved with the study, wrote that “personalizing the management of depression has to entail an understanding of the multiple contexts in which depression occurs, including genetic, developmental, psychosocial, cultural, medical, neurocognitive, and spiritual.”
The study was supported by a crowdsourcing campaign organized by Tim Ferris, as well as by grants from the Riverstyx Foundation. The Center for Psychedelic and Consciousness Research is funded by the Steven and Alexandra Cohen Foundation and receives support from Tim Ferriss, Matt Mullenweg, Craig Nerenberg, and Blake Mycoskie. It is also supported by grants from the National Institute on Drug Abuse. Dr. Davis received support from the NIDA. Dr. Griffiths was partially supported by a NIDA grant. Disclosures for the other authors are listed in the original article. Reiff reports owning stock in Compass Pathways. Dr. Reynolds reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Psilocybin, the psychedelic compound in “magic mushrooms,” rapidly improves symptoms and produces remission in as little as two sessions for patients with major depression, new research suggests.
Results of a small randomized trial showed that treatment with psilocybin was associated with a greater than 50% reduction in depressive symptoms in 67% of study participants. In addition, 71% showed improvement at 4-week follow-up, with more than 50% achieving remission.
“The finding that the majority of people whom we treated showed efficacy was quite a remarkable and gratifying finding and really sets the stage for psilocybin as a treatment for major depression,” senior investigator Roland Griffiths, PhD, Oliver Lee McCabe III Professor in the Neuropsychopharmacology of Consciousness, Johns Hopkins University, Baltimore, said in a statement.
“Perhaps the most exciting aspect of this as a new therapy is that psilocybin works as a therapeutic intervention with a single session or a few sessions, and then the effects are enduring. In contrast, most conventional treatments for depression ... are given chronically and also have chronic side effects,” added Dr. Griffiths, who is also director of the Johns Hopkins Center for Psychedelic and Consciousness Research.
The study was published online Nov.4 in JAMA Psychiatry.
Growing evidence base
As previously reported, psilocybin improves depressive symptoms for patients with cancer. However, these patients might be regarded as having a “reactive depression” to their life-threatening illness, said Dr. Griffiths.
“This study built on that previous research by asking the question, is psilocybin effective in patients who have major depressive disorder, [which is] a much larger population?” he said.
In addition, prior studies of psilocybin-assisted therapy had no control group, lead author Alan Davis, PhD, adjunct assistant professor in the psychedelic research unit, Johns Hopkins University, said in an interview.
The researchers created a control condition by randomly assigning 24 individuals (mean age, 39.8 years; 67% women) who were currently experiencing a moderate or severe major depressive episode to receive either immediate treatment (IT) (n = 13) or delayed treatment (DT) (n = 11).
Participants had longstanding depression, with a mean of 22.4 months in the current depressive episode. They were required to avoid using other antidepressants for 4 weeks prior to screening and up to 4 months following enrollment.
Patients were also required to be medically stable; have no personal/family history of psychotic or bipolar disorders; no past-year alcohol, substance, or nicotine use disorder; and no substantial lifetime or recent use of ketamine or classic hallucinogens.
Depression was measured using the Structured Clinical Interview for DSM-5 and the GRID-Hamilton Depression Rating Scale (GRID-HAMD). A baseline score of ≥17 was required for enrollment.
Participants received eight preparatory meetings with two session facilitators before the first psilocybin session and then 2-3 hours of follow-up meetings after the psilocybin sessions. In addition, they received 13 sessions of psychotherapy.
After completing these preparatory sessions, they underwent two psilocybin sessions, administered a mean of 1.6 weeks apart.
Participants in the DT group were assessed for depressive symptoms weekly for 8 weeks prior to entering the treatment protocol.
‘Surprising’ findings
Participants in the IT group exhibited significantly lower depression scores on the GRID-HAMD at 1 and 4 weeks after the second psilocybin session in comparison with patients in the DT group during the corresponding weeks.
Moreover, the effect sizes at weeks 5 and 8 were “large” (d = 2.2; 95% confidence interval, 1.4-3.0; and d = 2.6; 95% CI, 1.7-3.6, respectively).
An analysis of outcomes showed that, for all 24 participants, at 1 and at 4 weeks following the psilocybin intervention, 67% and 71% of participants, respectively, had a “clinically significant response” in depressive symptoms; 60% and 56%, respectively, met criteria for remission.
Within-subject T tests likewise revealed significant decreases in depression scores from baseline to 1- and 4-week follow-ups (P < .001; d = 3.6; 95% CI, 2.2-5.0; and P < .001; d = 3.6; 95% CI, 2.2-4.9, respectively).
Importantly, participants experienced no serious adverse effects.
Dr. Griffiths said he was “surprised” by the findings. “We knew that psilocybin would be effective in reactive depression of the type associated with illness, but we did not know that this would be the case in the large number of individuals who qualify for having [major depressive disorder].”
Dr. Davis said the finding “represents a large effect of this treatment among people with major depressive disorder – an approximately 4 times larger effect, compared to studies of antidepressant drugs.”
Dr. Davis noted that psychotherapy was an “essential” component of the study protocol. “ and that this treatment will always have a psychotherapy component and will not be Food and Drug Administration approved as a standalone medication.”
Tipping point
Collin Reiff, MD, clinical assistant professor in the department of psychiatry at New York University noted that because psychedelics are “still stigmatized,” the publication of this study in “one of the highest-impact journals in all of psychiatry suggests that research into psychedelics is now in the mainstream and that the academic psychiatry research community is paying close attention to what is happening.” He described this as a “tipping point.”
Dr. Reiff, who was not involved with the study, noted that research had been conducted on psychedelic compounds until the 1960s, “when they left the research lab and went mainstream, leading to the shutting down and subsequent dormancy of the research for the next 30-40 years.”
Psychedelic research is “undergoing a renaissance and no longer regarded with as much skepticism, but it is important to take our time doing this research so we do not repeat what happened in the 1960s,” said Dr. Reiff.
In an accompanying editorial, Charles F. Reynolds III, MD, endowed professor in geriatric psychiatry at the University of Pittsburgh Medical Center, Pennsylvania, questioned “for whom psychedelic-assisted psychotherapy is appropriate (or not), particularly in patients with depression who are suicidal of have a history of suicide attempt.”
Dr. Reynolds, who is also director of the Aging Institute of UPMC, who was not involved with the study, wrote that “personalizing the management of depression has to entail an understanding of the multiple contexts in which depression occurs, including genetic, developmental, psychosocial, cultural, medical, neurocognitive, and spiritual.”
The study was supported by a crowdsourcing campaign organized by Tim Ferris, as well as by grants from the Riverstyx Foundation. The Center for Psychedelic and Consciousness Research is funded by the Steven and Alexandra Cohen Foundation and receives support from Tim Ferriss, Matt Mullenweg, Craig Nerenberg, and Blake Mycoskie. It is also supported by grants from the National Institute on Drug Abuse. Dr. Davis received support from the NIDA. Dr. Griffiths was partially supported by a NIDA grant. Disclosures for the other authors are listed in the original article. Reiff reports owning stock in Compass Pathways. Dr. Reynolds reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Psilocybin, the psychedelic compound in “magic mushrooms,” rapidly improves symptoms and produces remission in as little as two sessions for patients with major depression, new research suggests.
Results of a small randomized trial showed that treatment with psilocybin was associated with a greater than 50% reduction in depressive symptoms in 67% of study participants. In addition, 71% showed improvement at 4-week follow-up, with more than 50% achieving remission.
“The finding that the majority of people whom we treated showed efficacy was quite a remarkable and gratifying finding and really sets the stage for psilocybin as a treatment for major depression,” senior investigator Roland Griffiths, PhD, Oliver Lee McCabe III Professor in the Neuropsychopharmacology of Consciousness, Johns Hopkins University, Baltimore, said in a statement.
“Perhaps the most exciting aspect of this as a new therapy is that psilocybin works as a therapeutic intervention with a single session or a few sessions, and then the effects are enduring. In contrast, most conventional treatments for depression ... are given chronically and also have chronic side effects,” added Dr. Griffiths, who is also director of the Johns Hopkins Center for Psychedelic and Consciousness Research.
The study was published online Nov.4 in JAMA Psychiatry.
Growing evidence base
As previously reported, psilocybin improves depressive symptoms for patients with cancer. However, these patients might be regarded as having a “reactive depression” to their life-threatening illness, said Dr. Griffiths.
“This study built on that previous research by asking the question, is psilocybin effective in patients who have major depressive disorder, [which is] a much larger population?” he said.
In addition, prior studies of psilocybin-assisted therapy had no control group, lead author Alan Davis, PhD, adjunct assistant professor in the psychedelic research unit, Johns Hopkins University, said in an interview.
The researchers created a control condition by randomly assigning 24 individuals (mean age, 39.8 years; 67% women) who were currently experiencing a moderate or severe major depressive episode to receive either immediate treatment (IT) (n = 13) or delayed treatment (DT) (n = 11).
Participants had longstanding depression, with a mean of 22.4 months in the current depressive episode. They were required to avoid using other antidepressants for 4 weeks prior to screening and up to 4 months following enrollment.
Patients were also required to be medically stable; have no personal/family history of psychotic or bipolar disorders; no past-year alcohol, substance, or nicotine use disorder; and no substantial lifetime or recent use of ketamine or classic hallucinogens.
Depression was measured using the Structured Clinical Interview for DSM-5 and the GRID-Hamilton Depression Rating Scale (GRID-HAMD). A baseline score of ≥17 was required for enrollment.
Participants received eight preparatory meetings with two session facilitators before the first psilocybin session and then 2-3 hours of follow-up meetings after the psilocybin sessions. In addition, they received 13 sessions of psychotherapy.
After completing these preparatory sessions, they underwent two psilocybin sessions, administered a mean of 1.6 weeks apart.
Participants in the DT group were assessed for depressive symptoms weekly for 8 weeks prior to entering the treatment protocol.
‘Surprising’ findings
Participants in the IT group exhibited significantly lower depression scores on the GRID-HAMD at 1 and 4 weeks after the second psilocybin session in comparison with patients in the DT group during the corresponding weeks.
Moreover, the effect sizes at weeks 5 and 8 were “large” (d = 2.2; 95% confidence interval, 1.4-3.0; and d = 2.6; 95% CI, 1.7-3.6, respectively).
An analysis of outcomes showed that, for all 24 participants, at 1 and at 4 weeks following the psilocybin intervention, 67% and 71% of participants, respectively, had a “clinically significant response” in depressive symptoms; 60% and 56%, respectively, met criteria for remission.
Within-subject T tests likewise revealed significant decreases in depression scores from baseline to 1- and 4-week follow-ups (P < .001; d = 3.6; 95% CI, 2.2-5.0; and P < .001; d = 3.6; 95% CI, 2.2-4.9, respectively).
Importantly, participants experienced no serious adverse effects.
Dr. Griffiths said he was “surprised” by the findings. “We knew that psilocybin would be effective in reactive depression of the type associated with illness, but we did not know that this would be the case in the large number of individuals who qualify for having [major depressive disorder].”
Dr. Davis said the finding “represents a large effect of this treatment among people with major depressive disorder – an approximately 4 times larger effect, compared to studies of antidepressant drugs.”
Dr. Davis noted that psychotherapy was an “essential” component of the study protocol. “ and that this treatment will always have a psychotherapy component and will not be Food and Drug Administration approved as a standalone medication.”
Tipping point
Collin Reiff, MD, clinical assistant professor in the department of psychiatry at New York University noted that because psychedelics are “still stigmatized,” the publication of this study in “one of the highest-impact journals in all of psychiatry suggests that research into psychedelics is now in the mainstream and that the academic psychiatry research community is paying close attention to what is happening.” He described this as a “tipping point.”
Dr. Reiff, who was not involved with the study, noted that research had been conducted on psychedelic compounds until the 1960s, “when they left the research lab and went mainstream, leading to the shutting down and subsequent dormancy of the research for the next 30-40 years.”
Psychedelic research is “undergoing a renaissance and no longer regarded with as much skepticism, but it is important to take our time doing this research so we do not repeat what happened in the 1960s,” said Dr. Reiff.
In an accompanying editorial, Charles F. Reynolds III, MD, endowed professor in geriatric psychiatry at the University of Pittsburgh Medical Center, Pennsylvania, questioned “for whom psychedelic-assisted psychotherapy is appropriate (or not), particularly in patients with depression who are suicidal of have a history of suicide attempt.”
Dr. Reynolds, who is also director of the Aging Institute of UPMC, who was not involved with the study, wrote that “personalizing the management of depression has to entail an understanding of the multiple contexts in which depression occurs, including genetic, developmental, psychosocial, cultural, medical, neurocognitive, and spiritual.”
The study was supported by a crowdsourcing campaign organized by Tim Ferris, as well as by grants from the Riverstyx Foundation. The Center for Psychedelic and Consciousness Research is funded by the Steven and Alexandra Cohen Foundation and receives support from Tim Ferriss, Matt Mullenweg, Craig Nerenberg, and Blake Mycoskie. It is also supported by grants from the National Institute on Drug Abuse. Dr. Davis received support from the NIDA. Dr. Griffiths was partially supported by a NIDA grant. Disclosures for the other authors are listed in the original article. Reiff reports owning stock in Compass Pathways. Dr. Reynolds reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Smartphones can differentiate bipolar from borderline personality disorder
There’s a reason they’re called smartphones.
Indeed, how patients use their smartphones and where they take them provides insight into what has been termed their “digital phenotype.” It’s information that, analyzed correctly, becomes useful in differentiating bipolar disorder from borderline personality disorder, a distinction that’s often challenging in clinical practice, Kate E.A. Saunders, MD, DPhil, said at the virtual congress of the European College of Neuropsychopharmacology.
Dr. Saunders, a psychiatrist at the University of Oxford (England), and colleagues have developed a smartphone app enabling patients to briefly characterize their current mood on a daily basis, as well as a machine learning model to analyze this data stream as patients’ moods evolve over time. In their prospective longitudinal Automated Monitoring of Symptom Severity (AMoSS) study of 48 patients with a confirmed diagnosis of bipolar disorder, 31 with borderline personality disorder, and 51 healthy volunteers, the tool correctly classified 75% of participants into the correct diagnostic category on the basis of 20 daily mood ratings (Transl Psychiatry. 2018 Dec 13;81:274. doi: 10.1038/s41398-018-0334-0).
The app also monitors activity via accelerometry and geolocation to assess an individual’s circadian rest-activity patterns, as well as telephone use and texting behavior. In another report from AMoSS, Dr. Saunders and coinvestigators showed that these patterns also distinguish persons with bipolar disorder from those with borderline personality disorder, who in turn differ from healthy controls (Transl Psychiatry. 2019 Aug 20;91:195. doi: 10.1038/s41398-019-0526-2).
It doesn’t replace doctors, but clearly it can add to diagnostic accuracy,” she said.
Borderline personality disorder and bipolar disorder are common diagnoses with quite different treatment approaches and prognoses. Studies have shown that rates of misdiagnosis of the two disorders are significant. The challenge is that they share overlapping diagnostic criteria, including prominent mood instability, which is difficult to assess reliably in clinical practice. That’s because the assessment relies on retrospective self-report of how patients felt in the past, which is often colored by their present mood state. The smartphone app sidesteps that limitation by having patients rate their mood daily digitally across six categories – anxiety, elation, sadness, anger, irritability, and energy – on a 1-7 scale.
The machine learning model that analyzes this information organizes the voluminous data into what Dr. Saunders called “signatures of mood” and breaks them down using rough path theory, a mathematical concept based upon differential equations. Dr. Saunders and colleagues have demonstrated that the shifting daily mood self-rating patterns can be used not only to sharpen the differential diagnosis between bipolar disorder and borderline personality disorder, but also to predict future mood. Automated analysis of the past 20 previous mood self-ratings predicted the next day’s mood in healthy controls with 89%-98% accuracy, depending upon which of the six mood categories was under scrutiny.
The predictive power in patients with bipolar disorder was also good, ranging from 82% accuracy for the energetic and anxious domains to 90% for the angry mood category. This ability to predict future mood states could have clinical value by assisting bipolar patients in enhancing proactive self-management and managing their mood stability to avoid depressive or manic relapse, although this has yet to be studied.
“For borderline personality disorder the predictive accuracy was not so good – 70%-78% – but perhaps that doesn’t matter,” Dr. Saunders said. “Perhaps that difficulty in predicting mood may actually be quite a useful diagnostic marker.”
‘Mr. Jones, the doctor is ready to see your phone now.’
The app’s accelerometry and geolocation capabilities can also enhance diagnostic accuracy, as has been shown in the AMoSS study.
The geolocation analysis generates data on the places a patient has gone and how much time was spent there. Feeding that information into the machine learning model predicted the presence or absence of depression with 85% accuracy for bipolar disorder, but couldn’t predict depression at all in borderline personality disorder.
“So we get a sense that people with bipolar disorder have behavioral manifestations of their mood symptoms which are much more consistent with one another and appear to change very consistently with their mood state, whereas borderline personality disorder seems to be characterized by something that’s much more unstable and unpredictable – and we can pick up these predictive variables using our smartphones,” Dr. Saunders said.
As depressive symptoms arise in patients with bipolar disorder, affected individuals display much less day-to-day variability in movement as measured by accelerometry. These changes predicted bipolar disorder with 76% specificity and 48% sensitivity.
“That’s OK. But we can’t do that at all in people with borderline personality disorder, again highlighting the fact that behavioral manifestations and symptoms in these groups are very, very different,” Dr. Saunders observed.
In AMoSS, analysis of activity, geolocation, and distal temperature rhythms showed that the individuals with borderline personality disorder displayed evidence of delayed circadian function, with a distinctive rest-activity pattern that differed from persons with bipolar disorder. This delayed circadian function might provide a novel therapeutic target in borderline personality disorder, a condition for which there is a notable lack of effective pharmacologic and psychotherapeutic interventions.
Phone use patterns were revealing. Patients with bipolar disorder had an increased total telephone call frequency relative to the healthy controls, whereas those with borderline personality disorder used text messaging much more frequently, consistent with the notion that borderline patients have difficulty in interpersonal communication.
Smartphone-based diagnostic differentiation between bipolar disorder and borderline personality disorder isn’t ready for prime time use in clinical practice, Dr. Saunders said. This is groundbreaking work that needs to be refined and replicated in larger studies. There are important ethical and data protection issues that require attention. But patients are gung-ho. Dr. Saunders noted that participant compliance in AMoSS was “extraordinarily good,” at 82%. Moreover, even though the study lasted for 3 months, more than 60% of subjects continued filing mood reports for 12 months.
“Smartphones may also give us an improved understanding of the lived experience of people with mental health problems. That’s certainly the feedback we got a lot from patients. They enjoy using this technology. They feel it’s helpful to be able to show their clinician this is what it’s like for them,” Dr. Saunders said.
Clinical usefulness is limited
The study was interesting as a pilot, and it is technologically very innovative. However, at this stage, it is unclear how the results can be used clinically, said Igor Galynker, MD, PhD, when asked about the findings.
There is a place for using this type of technology for patients living in remote areas, for example. However, Dr. Galynker, director of the Richard and Cynthia Zirinsky Center for Bipolar Disorder in New York, said such technology should be viewed as augmentation rather than as a substitute for face-to-face treatment.
“Typically, if clinicians have enough time to speak to the patient and to take history, they can differentiate between bipolar disorder and borderline personality disorder: The former is cyclical, the latter is less so. However, this is hard to do without face-to-face contact, or when you only have 10 minutes,” said Dr. Galynker, professor of psychiatry at the Icahn School of Medicine and director of the Galynker Research and Prevention Laboratory, both at Mount Sinai in New York.
Dr. Saunders’ work is funded by the Wellcome Trust and the National Institute for Health Research. Dr. Galynker reported receiving funding from the National Institute of Mental Health and the American Foundation for Suicide Prevention. He has no other disclosures.
SOURCE: ECNP 2020. Session S21.
There’s a reason they’re called smartphones.
Indeed, how patients use their smartphones and where they take them provides insight into what has been termed their “digital phenotype.” It’s information that, analyzed correctly, becomes useful in differentiating bipolar disorder from borderline personality disorder, a distinction that’s often challenging in clinical practice, Kate E.A. Saunders, MD, DPhil, said at the virtual congress of the European College of Neuropsychopharmacology.
Dr. Saunders, a psychiatrist at the University of Oxford (England), and colleagues have developed a smartphone app enabling patients to briefly characterize their current mood on a daily basis, as well as a machine learning model to analyze this data stream as patients’ moods evolve over time. In their prospective longitudinal Automated Monitoring of Symptom Severity (AMoSS) study of 48 patients with a confirmed diagnosis of bipolar disorder, 31 with borderline personality disorder, and 51 healthy volunteers, the tool correctly classified 75% of participants into the correct diagnostic category on the basis of 20 daily mood ratings (Transl Psychiatry. 2018 Dec 13;81:274. doi: 10.1038/s41398-018-0334-0).
The app also monitors activity via accelerometry and geolocation to assess an individual’s circadian rest-activity patterns, as well as telephone use and texting behavior. In another report from AMoSS, Dr. Saunders and coinvestigators showed that these patterns also distinguish persons with bipolar disorder from those with borderline personality disorder, who in turn differ from healthy controls (Transl Psychiatry. 2019 Aug 20;91:195. doi: 10.1038/s41398-019-0526-2).
It doesn’t replace doctors, but clearly it can add to diagnostic accuracy,” she said.
Borderline personality disorder and bipolar disorder are common diagnoses with quite different treatment approaches and prognoses. Studies have shown that rates of misdiagnosis of the two disorders are significant. The challenge is that they share overlapping diagnostic criteria, including prominent mood instability, which is difficult to assess reliably in clinical practice. That’s because the assessment relies on retrospective self-report of how patients felt in the past, which is often colored by their present mood state. The smartphone app sidesteps that limitation by having patients rate their mood daily digitally across six categories – anxiety, elation, sadness, anger, irritability, and energy – on a 1-7 scale.
The machine learning model that analyzes this information organizes the voluminous data into what Dr. Saunders called “signatures of mood” and breaks them down using rough path theory, a mathematical concept based upon differential equations. Dr. Saunders and colleagues have demonstrated that the shifting daily mood self-rating patterns can be used not only to sharpen the differential diagnosis between bipolar disorder and borderline personality disorder, but also to predict future mood. Automated analysis of the past 20 previous mood self-ratings predicted the next day’s mood in healthy controls with 89%-98% accuracy, depending upon which of the six mood categories was under scrutiny.
The predictive power in patients with bipolar disorder was also good, ranging from 82% accuracy for the energetic and anxious domains to 90% for the angry mood category. This ability to predict future mood states could have clinical value by assisting bipolar patients in enhancing proactive self-management and managing their mood stability to avoid depressive or manic relapse, although this has yet to be studied.
“For borderline personality disorder the predictive accuracy was not so good – 70%-78% – but perhaps that doesn’t matter,” Dr. Saunders said. “Perhaps that difficulty in predicting mood may actually be quite a useful diagnostic marker.”
‘Mr. Jones, the doctor is ready to see your phone now.’
The app’s accelerometry and geolocation capabilities can also enhance diagnostic accuracy, as has been shown in the AMoSS study.
The geolocation analysis generates data on the places a patient has gone and how much time was spent there. Feeding that information into the machine learning model predicted the presence or absence of depression with 85% accuracy for bipolar disorder, but couldn’t predict depression at all in borderline personality disorder.
“So we get a sense that people with bipolar disorder have behavioral manifestations of their mood symptoms which are much more consistent with one another and appear to change very consistently with their mood state, whereas borderline personality disorder seems to be characterized by something that’s much more unstable and unpredictable – and we can pick up these predictive variables using our smartphones,” Dr. Saunders said.
As depressive symptoms arise in patients with bipolar disorder, affected individuals display much less day-to-day variability in movement as measured by accelerometry. These changes predicted bipolar disorder with 76% specificity and 48% sensitivity.
“That’s OK. But we can’t do that at all in people with borderline personality disorder, again highlighting the fact that behavioral manifestations and symptoms in these groups are very, very different,” Dr. Saunders observed.
In AMoSS, analysis of activity, geolocation, and distal temperature rhythms showed that the individuals with borderline personality disorder displayed evidence of delayed circadian function, with a distinctive rest-activity pattern that differed from persons with bipolar disorder. This delayed circadian function might provide a novel therapeutic target in borderline personality disorder, a condition for which there is a notable lack of effective pharmacologic and psychotherapeutic interventions.
Phone use patterns were revealing. Patients with bipolar disorder had an increased total telephone call frequency relative to the healthy controls, whereas those with borderline personality disorder used text messaging much more frequently, consistent with the notion that borderline patients have difficulty in interpersonal communication.
Smartphone-based diagnostic differentiation between bipolar disorder and borderline personality disorder isn’t ready for prime time use in clinical practice, Dr. Saunders said. This is groundbreaking work that needs to be refined and replicated in larger studies. There are important ethical and data protection issues that require attention. But patients are gung-ho. Dr. Saunders noted that participant compliance in AMoSS was “extraordinarily good,” at 82%. Moreover, even though the study lasted for 3 months, more than 60% of subjects continued filing mood reports for 12 months.
“Smartphones may also give us an improved understanding of the lived experience of people with mental health problems. That’s certainly the feedback we got a lot from patients. They enjoy using this technology. They feel it’s helpful to be able to show their clinician this is what it’s like for them,” Dr. Saunders said.
Clinical usefulness is limited
The study was interesting as a pilot, and it is technologically very innovative. However, at this stage, it is unclear how the results can be used clinically, said Igor Galynker, MD, PhD, when asked about the findings.
There is a place for using this type of technology for patients living in remote areas, for example. However, Dr. Galynker, director of the Richard and Cynthia Zirinsky Center for Bipolar Disorder in New York, said such technology should be viewed as augmentation rather than as a substitute for face-to-face treatment.
“Typically, if clinicians have enough time to speak to the patient and to take history, they can differentiate between bipolar disorder and borderline personality disorder: The former is cyclical, the latter is less so. However, this is hard to do without face-to-face contact, or when you only have 10 minutes,” said Dr. Galynker, professor of psychiatry at the Icahn School of Medicine and director of the Galynker Research and Prevention Laboratory, both at Mount Sinai in New York.
Dr. Saunders’ work is funded by the Wellcome Trust and the National Institute for Health Research. Dr. Galynker reported receiving funding from the National Institute of Mental Health and the American Foundation for Suicide Prevention. He has no other disclosures.
SOURCE: ECNP 2020. Session S21.
There’s a reason they’re called smartphones.
Indeed, how patients use their smartphones and where they take them provides insight into what has been termed their “digital phenotype.” It’s information that, analyzed correctly, becomes useful in differentiating bipolar disorder from borderline personality disorder, a distinction that’s often challenging in clinical practice, Kate E.A. Saunders, MD, DPhil, said at the virtual congress of the European College of Neuropsychopharmacology.
Dr. Saunders, a psychiatrist at the University of Oxford (England), and colleagues have developed a smartphone app enabling patients to briefly characterize their current mood on a daily basis, as well as a machine learning model to analyze this data stream as patients’ moods evolve over time. In their prospective longitudinal Automated Monitoring of Symptom Severity (AMoSS) study of 48 patients with a confirmed diagnosis of bipolar disorder, 31 with borderline personality disorder, and 51 healthy volunteers, the tool correctly classified 75% of participants into the correct diagnostic category on the basis of 20 daily mood ratings (Transl Psychiatry. 2018 Dec 13;81:274. doi: 10.1038/s41398-018-0334-0).
The app also monitors activity via accelerometry and geolocation to assess an individual’s circadian rest-activity patterns, as well as telephone use and texting behavior. In another report from AMoSS, Dr. Saunders and coinvestigators showed that these patterns also distinguish persons with bipolar disorder from those with borderline personality disorder, who in turn differ from healthy controls (Transl Psychiatry. 2019 Aug 20;91:195. doi: 10.1038/s41398-019-0526-2).
It doesn’t replace doctors, but clearly it can add to diagnostic accuracy,” she said.
Borderline personality disorder and bipolar disorder are common diagnoses with quite different treatment approaches and prognoses. Studies have shown that rates of misdiagnosis of the two disorders are significant. The challenge is that they share overlapping diagnostic criteria, including prominent mood instability, which is difficult to assess reliably in clinical practice. That’s because the assessment relies on retrospective self-report of how patients felt in the past, which is often colored by their present mood state. The smartphone app sidesteps that limitation by having patients rate their mood daily digitally across six categories – anxiety, elation, sadness, anger, irritability, and energy – on a 1-7 scale.
The machine learning model that analyzes this information organizes the voluminous data into what Dr. Saunders called “signatures of mood” and breaks them down using rough path theory, a mathematical concept based upon differential equations. Dr. Saunders and colleagues have demonstrated that the shifting daily mood self-rating patterns can be used not only to sharpen the differential diagnosis between bipolar disorder and borderline personality disorder, but also to predict future mood. Automated analysis of the past 20 previous mood self-ratings predicted the next day’s mood in healthy controls with 89%-98% accuracy, depending upon which of the six mood categories was under scrutiny.
The predictive power in patients with bipolar disorder was also good, ranging from 82% accuracy for the energetic and anxious domains to 90% for the angry mood category. This ability to predict future mood states could have clinical value by assisting bipolar patients in enhancing proactive self-management and managing their mood stability to avoid depressive or manic relapse, although this has yet to be studied.
“For borderline personality disorder the predictive accuracy was not so good – 70%-78% – but perhaps that doesn’t matter,” Dr. Saunders said. “Perhaps that difficulty in predicting mood may actually be quite a useful diagnostic marker.”
‘Mr. Jones, the doctor is ready to see your phone now.’
The app’s accelerometry and geolocation capabilities can also enhance diagnostic accuracy, as has been shown in the AMoSS study.
The geolocation analysis generates data on the places a patient has gone and how much time was spent there. Feeding that information into the machine learning model predicted the presence or absence of depression with 85% accuracy for bipolar disorder, but couldn’t predict depression at all in borderline personality disorder.
“So we get a sense that people with bipolar disorder have behavioral manifestations of their mood symptoms which are much more consistent with one another and appear to change very consistently with their mood state, whereas borderline personality disorder seems to be characterized by something that’s much more unstable and unpredictable – and we can pick up these predictive variables using our smartphones,” Dr. Saunders said.
As depressive symptoms arise in patients with bipolar disorder, affected individuals display much less day-to-day variability in movement as measured by accelerometry. These changes predicted bipolar disorder with 76% specificity and 48% sensitivity.
“That’s OK. But we can’t do that at all in people with borderline personality disorder, again highlighting the fact that behavioral manifestations and symptoms in these groups are very, very different,” Dr. Saunders observed.
In AMoSS, analysis of activity, geolocation, and distal temperature rhythms showed that the individuals with borderline personality disorder displayed evidence of delayed circadian function, with a distinctive rest-activity pattern that differed from persons with bipolar disorder. This delayed circadian function might provide a novel therapeutic target in borderline personality disorder, a condition for which there is a notable lack of effective pharmacologic and psychotherapeutic interventions.
Phone use patterns were revealing. Patients with bipolar disorder had an increased total telephone call frequency relative to the healthy controls, whereas those with borderline personality disorder used text messaging much more frequently, consistent with the notion that borderline patients have difficulty in interpersonal communication.
Smartphone-based diagnostic differentiation between bipolar disorder and borderline personality disorder isn’t ready for prime time use in clinical practice, Dr. Saunders said. This is groundbreaking work that needs to be refined and replicated in larger studies. There are important ethical and data protection issues that require attention. But patients are gung-ho. Dr. Saunders noted that participant compliance in AMoSS was “extraordinarily good,” at 82%. Moreover, even though the study lasted for 3 months, more than 60% of subjects continued filing mood reports for 12 months.
“Smartphones may also give us an improved understanding of the lived experience of people with mental health problems. That’s certainly the feedback we got a lot from patients. They enjoy using this technology. They feel it’s helpful to be able to show their clinician this is what it’s like for them,” Dr. Saunders said.
Clinical usefulness is limited
The study was interesting as a pilot, and it is technologically very innovative. However, at this stage, it is unclear how the results can be used clinically, said Igor Galynker, MD, PhD, when asked about the findings.
There is a place for using this type of technology for patients living in remote areas, for example. However, Dr. Galynker, director of the Richard and Cynthia Zirinsky Center for Bipolar Disorder in New York, said such technology should be viewed as augmentation rather than as a substitute for face-to-face treatment.
“Typically, if clinicians have enough time to speak to the patient and to take history, they can differentiate between bipolar disorder and borderline personality disorder: The former is cyclical, the latter is less so. However, this is hard to do without face-to-face contact, or when you only have 10 minutes,” said Dr. Galynker, professor of psychiatry at the Icahn School of Medicine and director of the Galynker Research and Prevention Laboratory, both at Mount Sinai in New York.
Dr. Saunders’ work is funded by the Wellcome Trust and the National Institute for Health Research. Dr. Galynker reported receiving funding from the National Institute of Mental Health and the American Foundation for Suicide Prevention. He has no other disclosures.
SOURCE: ECNP 2020. Session S21.
FROM ECNP 2020
Who’s at risk for depression on isotretinoin?
A Sanaa Butt, MD, reported at the virtual annual congress of the European Academy of Dermatology and Venereology.
This was, however, the sole identifiable risk factor for treatment-limiting depressive symptoms in acne patients on isotretinoin in the study of 3,151 consecutive acne patients taking isotretinoin. There was no significant difference between those who did or did not develop depression on the oral retinoid in terms of age, gender, or daily dose of the drug at the time it was discontinued.
“Depressive symptoms occurred at any time from the date of initiation of isotretinoin up to 6 months into therapy, with no identifiable peak time period,” said Dr. Butt, a dermatologist with the U.K. National Health Service Tayside district at Ninewells Hospital, Dundee, Scotland. “Lower doses appear not to be protective,” she added.
The Tayside district has a catchment of roughly 450,000 people. The local population tends to stay put because Tayside is an economically disadvantaged and remote part of Scotland. There are very few private practice dermatologists in the area, so Dr. Butt and coinvestigators are confident their observational study of NHS patients captured the great majority of isotretinoin users in northern Scotland.
The investigators utilized software to analyze the contents of more than 8,000 digitized letters exchanged between NHS Tayside dermatologists and general practitioners during 2005-2018, zeroing in on 3,151 consecutive patients on isotretinoin for acne and 158 on the drug for other conditions, most often rosacea or folliculitis. They then drilled down further through the letters, electronically searching for key words such as suicide, depression, and anxiety. In this way, they ultimately identified 30 patients who discontinued the drug because they developed depressive symptoms. All 30 were on the drug for acne.
The annual incidence of treatment-limiting depressive mood changes was 0.96%, a figure that remained steady over the 13-year study period, even though prescribing of isotretinoin increased over time. This flat incidence rate effectively rules out the potential for confounding because of assessor bias, especially since many different NHS dermatologists were prescribing the drug, Dr. Butt said.
Half of acne patients prescribed isotretinoin were female and 50% were male. And 15 cases of treatment discontinuation caused by development of depressive symptoms occurred in females, 15 in males. A history of past depressive illness was present in 9.3% of females who started on isotretinoin and in 4.5% of the males. The relative risk of treatment-limiting depressive mood changes was increased 790% among females with a prior history of depressive illness and 440% in males with such a history.
Dr. Butt reported having no financial conflicts regarding her NHS-funded study.
A Sanaa Butt, MD, reported at the virtual annual congress of the European Academy of Dermatology and Venereology.
This was, however, the sole identifiable risk factor for treatment-limiting depressive symptoms in acne patients on isotretinoin in the study of 3,151 consecutive acne patients taking isotretinoin. There was no significant difference between those who did or did not develop depression on the oral retinoid in terms of age, gender, or daily dose of the drug at the time it was discontinued.
“Depressive symptoms occurred at any time from the date of initiation of isotretinoin up to 6 months into therapy, with no identifiable peak time period,” said Dr. Butt, a dermatologist with the U.K. National Health Service Tayside district at Ninewells Hospital, Dundee, Scotland. “Lower doses appear not to be protective,” she added.
The Tayside district has a catchment of roughly 450,000 people. The local population tends to stay put because Tayside is an economically disadvantaged and remote part of Scotland. There are very few private practice dermatologists in the area, so Dr. Butt and coinvestigators are confident their observational study of NHS patients captured the great majority of isotretinoin users in northern Scotland.
The investigators utilized software to analyze the contents of more than 8,000 digitized letters exchanged between NHS Tayside dermatologists and general practitioners during 2005-2018, zeroing in on 3,151 consecutive patients on isotretinoin for acne and 158 on the drug for other conditions, most often rosacea or folliculitis. They then drilled down further through the letters, electronically searching for key words such as suicide, depression, and anxiety. In this way, they ultimately identified 30 patients who discontinued the drug because they developed depressive symptoms. All 30 were on the drug for acne.
The annual incidence of treatment-limiting depressive mood changes was 0.96%, a figure that remained steady over the 13-year study period, even though prescribing of isotretinoin increased over time. This flat incidence rate effectively rules out the potential for confounding because of assessor bias, especially since many different NHS dermatologists were prescribing the drug, Dr. Butt said.
Half of acne patients prescribed isotretinoin were female and 50% were male. And 15 cases of treatment discontinuation caused by development of depressive symptoms occurred in females, 15 in males. A history of past depressive illness was present in 9.3% of females who started on isotretinoin and in 4.5% of the males. The relative risk of treatment-limiting depressive mood changes was increased 790% among females with a prior history of depressive illness and 440% in males with such a history.
Dr. Butt reported having no financial conflicts regarding her NHS-funded study.
A Sanaa Butt, MD, reported at the virtual annual congress of the European Academy of Dermatology and Venereology.
This was, however, the sole identifiable risk factor for treatment-limiting depressive symptoms in acne patients on isotretinoin in the study of 3,151 consecutive acne patients taking isotretinoin. There was no significant difference between those who did or did not develop depression on the oral retinoid in terms of age, gender, or daily dose of the drug at the time it was discontinued.
“Depressive symptoms occurred at any time from the date of initiation of isotretinoin up to 6 months into therapy, with no identifiable peak time period,” said Dr. Butt, a dermatologist with the U.K. National Health Service Tayside district at Ninewells Hospital, Dundee, Scotland. “Lower doses appear not to be protective,” she added.
The Tayside district has a catchment of roughly 450,000 people. The local population tends to stay put because Tayside is an economically disadvantaged and remote part of Scotland. There are very few private practice dermatologists in the area, so Dr. Butt and coinvestigators are confident their observational study of NHS patients captured the great majority of isotretinoin users in northern Scotland.
The investigators utilized software to analyze the contents of more than 8,000 digitized letters exchanged between NHS Tayside dermatologists and general practitioners during 2005-2018, zeroing in on 3,151 consecutive patients on isotretinoin for acne and 158 on the drug for other conditions, most often rosacea or folliculitis. They then drilled down further through the letters, electronically searching for key words such as suicide, depression, and anxiety. In this way, they ultimately identified 30 patients who discontinued the drug because they developed depressive symptoms. All 30 were on the drug for acne.
The annual incidence of treatment-limiting depressive mood changes was 0.96%, a figure that remained steady over the 13-year study period, even though prescribing of isotretinoin increased over time. This flat incidence rate effectively rules out the potential for confounding because of assessor bias, especially since many different NHS dermatologists were prescribing the drug, Dr. Butt said.
Half of acne patients prescribed isotretinoin were female and 50% were male. And 15 cases of treatment discontinuation caused by development of depressive symptoms occurred in females, 15 in males. A history of past depressive illness was present in 9.3% of females who started on isotretinoin and in 4.5% of the males. The relative risk of treatment-limiting depressive mood changes was increased 790% among females with a prior history of depressive illness and 440% in males with such a history.
Dr. Butt reported having no financial conflicts regarding her NHS-funded study.
FROM THE EADV CONGRESS