User login
New hyperglycemia emergency guidance updates DKA definition
HAMBURG, GERMANY – along with many other updates to the last statement on the topic, published 14 years ago.
Based on extensive literature reviews and observations of current trends, the new document – due to be published soon – will cover diagnosis and management of the two most serious acute hyperglycemic emergencies seen in adults, DKA and hyperosmolar hyperglycemic state (HHS).
New to the 2023 version will be a strong emphasis on the excess morbidity and mortality risks associated with the increasingly common “hybrid” presentation of the two conditions together, now seen in about a third of cases.
The new report will also more strongly urge clinicians to investigate why the person experienced the emergency.
While new-onset diabetes and infection are recognized precipitating causes for DKA, insulin omission related to finances, mental health, and social determinants should be identified, and patients directed to appropriate resources, said experts previewing the upcoming new report at the annual meeting of the European Association for the Study of Diabetes.
“The challenge is, although we were making progress for a long time in terms of those hyperglycemic crises, we’ve really plateaued and there are still people being admitted in large numbers, and when you look more globally even more so,” said American Diabetes Association Chief Science and Medical Officer Robert A. Gabbay, MD, PhD.
The new consensus report will be jointly endorsed by the ADA, the EASD, the American Association of Clinical Endocrinology, the Diabetes Technology Society, and the Joint British Diabetes Societies for Inpatient Care. The previous consensus statement on the subject was published in 2009 by the ADA alone.
New DKA and HHS definitions reflect emerging trends
The statement will revise the definition of DKA, partly spurred by the increasing occurrence and recognition of euglycemic ketoacidosis arising from the use of sodium-glucose cotransporter 2 (SGLT2) inhibitors. For all patients with hyperglycemic crisis, the hyperglycemia cutoff is now lowered to 200 mg/dL (11.1 mmol/L) from the previous 250 mg/dL.
However, the glucose cutoff has been removed entirely for people with a history of diabetes.
“Both of these changes are recognizing the wide range of glucose levels at the presence of DKA. Approximately 10% of DKA occurs with euglycemia or near-normoglycemia,” noted coauthor Shivani Misra, MD, PhD, senior clinical lecturer and honorary consultant in Metabolic Medicine at Imperial College, London.
For assessing ketosis in DKA, the new statement strongly recommends use of beta-hydroxybutyrate – either via point-of-care test or serum level measured in a laboratory – with a low cutoff of ≥ 3.0 mmol/L. Alternatively, a urine ketone strip value of 2+ or greater can be used.
However, beta-hydroxybutyrate testing is more widely available now than it was in 2009 and is strongly preferred over urine ketone measurement because it’s the predominant ketone during acidosis. Moreover, urine acetoacetate – measured by the strips – paradoxically increases during resolution of DKA, and drug interferences can occur with urine ketone measurement, Dr. Misra noted.
Metabolic acidosis is now defined as a pH < 7.3 and/or a bicarbonate concentration < 18 mmol/L, up from 15 in some prior guidelines including the United Kingdom’s. Also, anion gap has been removed from the main definition but, the document will say, can still be used in settings where ketone testing is unavailable.
As previously, the new statement will classify DKA by mild, moderate, and severe but now for the first time there are recommendations of care for each of those levels, as well as for HHS.
For HHS, the glucose cutoff of ≥ 600 mg/dL will stay the same. But now, the effective serum osmolality has been lowered from > 320 to > 300 mOsml/L to account for the effect of dehydration, along with an alternative criteria of total serum osmolality > 320 mOsm/L. The same two changes as with DKA for both ketones and acidosis have also been included for HHS.
Asked to comment, session audience member and independent diabetes industry consultant Charles Alexander, MD, told this news organization, “I liked the proposal to eliminate the anion gap in decision-making and to focus on measurement of blood ketones, principally beta-hydroxybutyrate, in the diagnosis of DKA and monitoring the effect of treatment.
“If someone is on an SGLT2 inhibitor, there is no need to look at blood glucose levels, which may be normal or near normal in the setting of DKA.”
But Dr. Alexander thinks that they should have eliminated glucose levels entirely as part of the DKA/HHS definition even for people without diabetes.
“The problem is that medical education for many years has taught us that DKA is a condition of high blood glucose, but it may not be. It is good that they said blood glucose levels were not important if the patient had a history of diabetes. However, a glucose of 200mg/dL may not be low enough if someone is on an SGLT2 inhibitor. There needs to be a much lower threshold for measuring blood ketones in anyone with nausea, vomiting, and abdominal pain, regardless of the blood glucose level.”
Acute management: IV fluids, insulin, and potassium
Like the 2009 statement, the new one will include detailed management flowcharts for DKA and HHS, but this time in color. This new statement includes individual algorithms for management with intravenous fluids, insulin, and potassium. Bicarbonate has been removed and relegated to a note at the bottom saying that it should only be considered if pH is < 7.0.
Under fluid treatment, the new statement offers more information about using crystalloids to treat dehydration and a recommendation to add dextrose to IV fluid therapy as a substrate when the glucose drops below 250 mg/dL, in order to prevent hypoglycemia. For euglycemic DKA, the recommendation is to include dextrose and normal saline simultaneously.
And for the first time, subcutaneous rather than IV insulin is considered acceptable for mild, but not moderate or severe, DKA.
Two options are suggested for IV insulin in HHS: The fluid can be given first and low-dose fixed-rate insulin infusion added, or fluids and insulin can be given at the same time.
Criteria for resolution of DKA are a venous pH of ≥ 7.3 or bicarbonate > 18 mmol/L, ketones < 0.6 mmol/L, and glucose ideally < 200 mg/dL (11.0 mmol/L). For HHS, resolution is suggested when the measured or calculated serum osmolality falls to < 300 mosm/kg, blood glucose is < 250mg/dL (13.9 mmol/L), urine output > 0.5 mL/kg/hour, and cognitive status is improved.
The statement also will provide detailed recommended options for transitioning from IV to subcutaneous insulin, but defers to clinical judgment for deciding when the patient can be discharged. The initiation or continuation of SGLT2 inhibitors is not recommended at any time during hospitalization for hyperglycemic crises.
Mitigating complications, preventing recurrence
In addition to listing potential complications of treating hyperglycemic crises, just as the 2009 statement did, the new one will offer mitigation strategies for some of the more common ones. For preventing hypoglycemia, frequent blood glucose monitoring is advised along with adding dextrose to the IV fluids when glucose drops below 250 mg/dL.
For prevention of hypokalemia, which occurs in about half of patients treated for DKA and HHS, the statement recommends potassium monitoring every 4 hours and replacement added to fluids.
Acute kidney injury, also occurring in about half of people treated for DKA and/or HHS, usually resolves with hydration. Daily renal function monitoring is advised.
Preventing recurrence: Many factors beyond clinical
Prevention of recurrence with readmission for DKA and/or HHS, occurring in up to 22% of U.S. patients within 30 days, entails close follow-up within 2-4 weeks after discharge (including via telemedicine), and assessment of possible causes, including mental health disorders and social determinants of health.
Appropriate education should be provided, including “structured education” involving problem-solving, sick day rules, injection techniques, a review of insulin doses, consideration of continuous glucose monitoring (CGM), and home ketone testing.
Patients should be provided with an adequate supply of insulin and durable diabetes equipment, along with contact information for health care professionals who can assist them. Social service professionals can be helpful for patients who lack reliable access.
Dr. Gabbay told this news organization, “The eye-opening thing is we tend to typically think of DKA as how people tend to get diagnosed with diabetes and, yes, that’s true, but that’s only a minority of people. Those might be preventable by early screening, but all these other people and the number of recurrent episodes, that’s an area where it’s really a failure of the system where we can do better in ensuring that doesn’t happen.”
Education is only part of it, he stressed. “It’s not just an intelligence thing. It’s social factors, and there can be complex psychological issues and mental health issues. We need to screen for those things when we see someone coming back the second, third, fifth, or sixth time. We’ve all seen that. Just educating them to take their insulin is not the answer. …You’ve got to ask the questions and engage them to go a little deeper.”
Dr. Gabbay is an employee of the ADA. Dr. Alexander has reported being a nonpaid advisor for diaTribe and a consultant for Kinexum. Dr. Misra has received speaker fees from Sanofi and ABCD and an investigator-initiated research grant from Dexcom, and is a trustee for the Diabetes Research and Wellness Foundation in the United Kingdom.
A version of this article appeared on Medscape.com.
HAMBURG, GERMANY – along with many other updates to the last statement on the topic, published 14 years ago.
Based on extensive literature reviews and observations of current trends, the new document – due to be published soon – will cover diagnosis and management of the two most serious acute hyperglycemic emergencies seen in adults, DKA and hyperosmolar hyperglycemic state (HHS).
New to the 2023 version will be a strong emphasis on the excess morbidity and mortality risks associated with the increasingly common “hybrid” presentation of the two conditions together, now seen in about a third of cases.
The new report will also more strongly urge clinicians to investigate why the person experienced the emergency.
While new-onset diabetes and infection are recognized precipitating causes for DKA, insulin omission related to finances, mental health, and social determinants should be identified, and patients directed to appropriate resources, said experts previewing the upcoming new report at the annual meeting of the European Association for the Study of Diabetes.
“The challenge is, although we were making progress for a long time in terms of those hyperglycemic crises, we’ve really plateaued and there are still people being admitted in large numbers, and when you look more globally even more so,” said American Diabetes Association Chief Science and Medical Officer Robert A. Gabbay, MD, PhD.
The new consensus report will be jointly endorsed by the ADA, the EASD, the American Association of Clinical Endocrinology, the Diabetes Technology Society, and the Joint British Diabetes Societies for Inpatient Care. The previous consensus statement on the subject was published in 2009 by the ADA alone.
New DKA and HHS definitions reflect emerging trends
The statement will revise the definition of DKA, partly spurred by the increasing occurrence and recognition of euglycemic ketoacidosis arising from the use of sodium-glucose cotransporter 2 (SGLT2) inhibitors. For all patients with hyperglycemic crisis, the hyperglycemia cutoff is now lowered to 200 mg/dL (11.1 mmol/L) from the previous 250 mg/dL.
However, the glucose cutoff has been removed entirely for people with a history of diabetes.
“Both of these changes are recognizing the wide range of glucose levels at the presence of DKA. Approximately 10% of DKA occurs with euglycemia or near-normoglycemia,” noted coauthor Shivani Misra, MD, PhD, senior clinical lecturer and honorary consultant in Metabolic Medicine at Imperial College, London.
For assessing ketosis in DKA, the new statement strongly recommends use of beta-hydroxybutyrate – either via point-of-care test or serum level measured in a laboratory – with a low cutoff of ≥ 3.0 mmol/L. Alternatively, a urine ketone strip value of 2+ or greater can be used.
However, beta-hydroxybutyrate testing is more widely available now than it was in 2009 and is strongly preferred over urine ketone measurement because it’s the predominant ketone during acidosis. Moreover, urine acetoacetate – measured by the strips – paradoxically increases during resolution of DKA, and drug interferences can occur with urine ketone measurement, Dr. Misra noted.
Metabolic acidosis is now defined as a pH < 7.3 and/or a bicarbonate concentration < 18 mmol/L, up from 15 in some prior guidelines including the United Kingdom’s. Also, anion gap has been removed from the main definition but, the document will say, can still be used in settings where ketone testing is unavailable.
As previously, the new statement will classify DKA by mild, moderate, and severe but now for the first time there are recommendations of care for each of those levels, as well as for HHS.
For HHS, the glucose cutoff of ≥ 600 mg/dL will stay the same. But now, the effective serum osmolality has been lowered from > 320 to > 300 mOsml/L to account for the effect of dehydration, along with an alternative criteria of total serum osmolality > 320 mOsm/L. The same two changes as with DKA for both ketones and acidosis have also been included for HHS.
Asked to comment, session audience member and independent diabetes industry consultant Charles Alexander, MD, told this news organization, “I liked the proposal to eliminate the anion gap in decision-making and to focus on measurement of blood ketones, principally beta-hydroxybutyrate, in the diagnosis of DKA and monitoring the effect of treatment.
“If someone is on an SGLT2 inhibitor, there is no need to look at blood glucose levels, which may be normal or near normal in the setting of DKA.”
But Dr. Alexander thinks that they should have eliminated glucose levels entirely as part of the DKA/HHS definition even for people without diabetes.
“The problem is that medical education for many years has taught us that DKA is a condition of high blood glucose, but it may not be. It is good that they said blood glucose levels were not important if the patient had a history of diabetes. However, a glucose of 200mg/dL may not be low enough if someone is on an SGLT2 inhibitor. There needs to be a much lower threshold for measuring blood ketones in anyone with nausea, vomiting, and abdominal pain, regardless of the blood glucose level.”
Acute management: IV fluids, insulin, and potassium
Like the 2009 statement, the new one will include detailed management flowcharts for DKA and HHS, but this time in color. This new statement includes individual algorithms for management with intravenous fluids, insulin, and potassium. Bicarbonate has been removed and relegated to a note at the bottom saying that it should only be considered if pH is < 7.0.
Under fluid treatment, the new statement offers more information about using crystalloids to treat dehydration and a recommendation to add dextrose to IV fluid therapy as a substrate when the glucose drops below 250 mg/dL, in order to prevent hypoglycemia. For euglycemic DKA, the recommendation is to include dextrose and normal saline simultaneously.
And for the first time, subcutaneous rather than IV insulin is considered acceptable for mild, but not moderate or severe, DKA.
Two options are suggested for IV insulin in HHS: The fluid can be given first and low-dose fixed-rate insulin infusion added, or fluids and insulin can be given at the same time.
Criteria for resolution of DKA are a venous pH of ≥ 7.3 or bicarbonate > 18 mmol/L, ketones < 0.6 mmol/L, and glucose ideally < 200 mg/dL (11.0 mmol/L). For HHS, resolution is suggested when the measured or calculated serum osmolality falls to < 300 mosm/kg, blood glucose is < 250mg/dL (13.9 mmol/L), urine output > 0.5 mL/kg/hour, and cognitive status is improved.
The statement also will provide detailed recommended options for transitioning from IV to subcutaneous insulin, but defers to clinical judgment for deciding when the patient can be discharged. The initiation or continuation of SGLT2 inhibitors is not recommended at any time during hospitalization for hyperglycemic crises.
Mitigating complications, preventing recurrence
In addition to listing potential complications of treating hyperglycemic crises, just as the 2009 statement did, the new one will offer mitigation strategies for some of the more common ones. For preventing hypoglycemia, frequent blood glucose monitoring is advised along with adding dextrose to the IV fluids when glucose drops below 250 mg/dL.
For prevention of hypokalemia, which occurs in about half of patients treated for DKA and HHS, the statement recommends potassium monitoring every 4 hours and replacement added to fluids.
Acute kidney injury, also occurring in about half of people treated for DKA and/or HHS, usually resolves with hydration. Daily renal function monitoring is advised.
Preventing recurrence: Many factors beyond clinical
Prevention of recurrence with readmission for DKA and/or HHS, occurring in up to 22% of U.S. patients within 30 days, entails close follow-up within 2-4 weeks after discharge (including via telemedicine), and assessment of possible causes, including mental health disorders and social determinants of health.
Appropriate education should be provided, including “structured education” involving problem-solving, sick day rules, injection techniques, a review of insulin doses, consideration of continuous glucose monitoring (CGM), and home ketone testing.
Patients should be provided with an adequate supply of insulin and durable diabetes equipment, along with contact information for health care professionals who can assist them. Social service professionals can be helpful for patients who lack reliable access.
Dr. Gabbay told this news organization, “The eye-opening thing is we tend to typically think of DKA as how people tend to get diagnosed with diabetes and, yes, that’s true, but that’s only a minority of people. Those might be preventable by early screening, but all these other people and the number of recurrent episodes, that’s an area where it’s really a failure of the system where we can do better in ensuring that doesn’t happen.”
Education is only part of it, he stressed. “It’s not just an intelligence thing. It’s social factors, and there can be complex psychological issues and mental health issues. We need to screen for those things when we see someone coming back the second, third, fifth, or sixth time. We’ve all seen that. Just educating them to take their insulin is not the answer. …You’ve got to ask the questions and engage them to go a little deeper.”
Dr. Gabbay is an employee of the ADA. Dr. Alexander has reported being a nonpaid advisor for diaTribe and a consultant for Kinexum. Dr. Misra has received speaker fees from Sanofi and ABCD and an investigator-initiated research grant from Dexcom, and is a trustee for the Diabetes Research and Wellness Foundation in the United Kingdom.
A version of this article appeared on Medscape.com.
HAMBURG, GERMANY – along with many other updates to the last statement on the topic, published 14 years ago.
Based on extensive literature reviews and observations of current trends, the new document – due to be published soon – will cover diagnosis and management of the two most serious acute hyperglycemic emergencies seen in adults, DKA and hyperosmolar hyperglycemic state (HHS).
New to the 2023 version will be a strong emphasis on the excess morbidity and mortality risks associated with the increasingly common “hybrid” presentation of the two conditions together, now seen in about a third of cases.
The new report will also more strongly urge clinicians to investigate why the person experienced the emergency.
While new-onset diabetes and infection are recognized precipitating causes for DKA, insulin omission related to finances, mental health, and social determinants should be identified, and patients directed to appropriate resources, said experts previewing the upcoming new report at the annual meeting of the European Association for the Study of Diabetes.
“The challenge is, although we were making progress for a long time in terms of those hyperglycemic crises, we’ve really plateaued and there are still people being admitted in large numbers, and when you look more globally even more so,” said American Diabetes Association Chief Science and Medical Officer Robert A. Gabbay, MD, PhD.
The new consensus report will be jointly endorsed by the ADA, the EASD, the American Association of Clinical Endocrinology, the Diabetes Technology Society, and the Joint British Diabetes Societies for Inpatient Care. The previous consensus statement on the subject was published in 2009 by the ADA alone.
New DKA and HHS definitions reflect emerging trends
The statement will revise the definition of DKA, partly spurred by the increasing occurrence and recognition of euglycemic ketoacidosis arising from the use of sodium-glucose cotransporter 2 (SGLT2) inhibitors. For all patients with hyperglycemic crisis, the hyperglycemia cutoff is now lowered to 200 mg/dL (11.1 mmol/L) from the previous 250 mg/dL.
However, the glucose cutoff has been removed entirely for people with a history of diabetes.
“Both of these changes are recognizing the wide range of glucose levels at the presence of DKA. Approximately 10% of DKA occurs with euglycemia or near-normoglycemia,” noted coauthor Shivani Misra, MD, PhD, senior clinical lecturer and honorary consultant in Metabolic Medicine at Imperial College, London.
For assessing ketosis in DKA, the new statement strongly recommends use of beta-hydroxybutyrate – either via point-of-care test or serum level measured in a laboratory – with a low cutoff of ≥ 3.0 mmol/L. Alternatively, a urine ketone strip value of 2+ or greater can be used.
However, beta-hydroxybutyrate testing is more widely available now than it was in 2009 and is strongly preferred over urine ketone measurement because it’s the predominant ketone during acidosis. Moreover, urine acetoacetate – measured by the strips – paradoxically increases during resolution of DKA, and drug interferences can occur with urine ketone measurement, Dr. Misra noted.
Metabolic acidosis is now defined as a pH < 7.3 and/or a bicarbonate concentration < 18 mmol/L, up from 15 in some prior guidelines including the United Kingdom’s. Also, anion gap has been removed from the main definition but, the document will say, can still be used in settings where ketone testing is unavailable.
As previously, the new statement will classify DKA by mild, moderate, and severe but now for the first time there are recommendations of care for each of those levels, as well as for HHS.
For HHS, the glucose cutoff of ≥ 600 mg/dL will stay the same. But now, the effective serum osmolality has been lowered from > 320 to > 300 mOsml/L to account for the effect of dehydration, along with an alternative criteria of total serum osmolality > 320 mOsm/L. The same two changes as with DKA for both ketones and acidosis have also been included for HHS.
Asked to comment, session audience member and independent diabetes industry consultant Charles Alexander, MD, told this news organization, “I liked the proposal to eliminate the anion gap in decision-making and to focus on measurement of blood ketones, principally beta-hydroxybutyrate, in the diagnosis of DKA and monitoring the effect of treatment.
“If someone is on an SGLT2 inhibitor, there is no need to look at blood glucose levels, which may be normal or near normal in the setting of DKA.”
But Dr. Alexander thinks that they should have eliminated glucose levels entirely as part of the DKA/HHS definition even for people without diabetes.
“The problem is that medical education for many years has taught us that DKA is a condition of high blood glucose, but it may not be. It is good that they said blood glucose levels were not important if the patient had a history of diabetes. However, a glucose of 200mg/dL may not be low enough if someone is on an SGLT2 inhibitor. There needs to be a much lower threshold for measuring blood ketones in anyone with nausea, vomiting, and abdominal pain, regardless of the blood glucose level.”
Acute management: IV fluids, insulin, and potassium
Like the 2009 statement, the new one will include detailed management flowcharts for DKA and HHS, but this time in color. This new statement includes individual algorithms for management with intravenous fluids, insulin, and potassium. Bicarbonate has been removed and relegated to a note at the bottom saying that it should only be considered if pH is < 7.0.
Under fluid treatment, the new statement offers more information about using crystalloids to treat dehydration and a recommendation to add dextrose to IV fluid therapy as a substrate when the glucose drops below 250 mg/dL, in order to prevent hypoglycemia. For euglycemic DKA, the recommendation is to include dextrose and normal saline simultaneously.
And for the first time, subcutaneous rather than IV insulin is considered acceptable for mild, but not moderate or severe, DKA.
Two options are suggested for IV insulin in HHS: The fluid can be given first and low-dose fixed-rate insulin infusion added, or fluids and insulin can be given at the same time.
Criteria for resolution of DKA are a venous pH of ≥ 7.3 or bicarbonate > 18 mmol/L, ketones < 0.6 mmol/L, and glucose ideally < 200 mg/dL (11.0 mmol/L). For HHS, resolution is suggested when the measured or calculated serum osmolality falls to < 300 mosm/kg, blood glucose is < 250mg/dL (13.9 mmol/L), urine output > 0.5 mL/kg/hour, and cognitive status is improved.
The statement also will provide detailed recommended options for transitioning from IV to subcutaneous insulin, but defers to clinical judgment for deciding when the patient can be discharged. The initiation or continuation of SGLT2 inhibitors is not recommended at any time during hospitalization for hyperglycemic crises.
Mitigating complications, preventing recurrence
In addition to listing potential complications of treating hyperglycemic crises, just as the 2009 statement did, the new one will offer mitigation strategies for some of the more common ones. For preventing hypoglycemia, frequent blood glucose monitoring is advised along with adding dextrose to the IV fluids when glucose drops below 250 mg/dL.
For prevention of hypokalemia, which occurs in about half of patients treated for DKA and HHS, the statement recommends potassium monitoring every 4 hours and replacement added to fluids.
Acute kidney injury, also occurring in about half of people treated for DKA and/or HHS, usually resolves with hydration. Daily renal function monitoring is advised.
Preventing recurrence: Many factors beyond clinical
Prevention of recurrence with readmission for DKA and/or HHS, occurring in up to 22% of U.S. patients within 30 days, entails close follow-up within 2-4 weeks after discharge (including via telemedicine), and assessment of possible causes, including mental health disorders and social determinants of health.
Appropriate education should be provided, including “structured education” involving problem-solving, sick day rules, injection techniques, a review of insulin doses, consideration of continuous glucose monitoring (CGM), and home ketone testing.
Patients should be provided with an adequate supply of insulin and durable diabetes equipment, along with contact information for health care professionals who can assist them. Social service professionals can be helpful for patients who lack reliable access.
Dr. Gabbay told this news organization, “The eye-opening thing is we tend to typically think of DKA as how people tend to get diagnosed with diabetes and, yes, that’s true, but that’s only a minority of people. Those might be preventable by early screening, but all these other people and the number of recurrent episodes, that’s an area where it’s really a failure of the system where we can do better in ensuring that doesn’t happen.”
Education is only part of it, he stressed. “It’s not just an intelligence thing. It’s social factors, and there can be complex psychological issues and mental health issues. We need to screen for those things when we see someone coming back the second, third, fifth, or sixth time. We’ve all seen that. Just educating them to take their insulin is not the answer. …You’ve got to ask the questions and engage them to go a little deeper.”
Dr. Gabbay is an employee of the ADA. Dr. Alexander has reported being a nonpaid advisor for diaTribe and a consultant for Kinexum. Dr. Misra has received speaker fees from Sanofi and ABCD and an investigator-initiated research grant from Dexcom, and is a trustee for the Diabetes Research and Wellness Foundation in the United Kingdom.
A version of this article appeared on Medscape.com.
AT EASD 2023
Does an elevated TSH value always require therapy?
Thyroxine and L-thyroxine are two of the 10 most frequently prescribed medicinal products. “One large health insurance company ranks thyroid hormone at fourth place in the list of most-sold medications in the United States. It is possibly the second most commonly prescribed preparation,” said Joachim Feldkamp, MD, PhD, director of the University Clinic for General Internal Medicine, Endocrinology, Diabetology, and Infectious Diseases at Central Hospital, Bielefeld, Germany, at the online press conference for the German Society of Endocrinology’s hormone week.
The preparation is prescribed when the thyroid gland produces too little thyroid hormone. The messenger substance thyroid-stimulating hormone (TSH) is used as a screening value to assess thyroid function. An increase in TSH can indicate that too little thyroid hormone is being produced.
“But this does not mean that an underactive thyroid gland is hiding behind every elevated TSH value,” said Dr. Feldkamp. Normally, the TSH value lies between 0.3 and 4.2 mU/L. “Hypothyroidism, as it’s known, is formally present if the TSH value lies above the upper limit of 4.2 mU/L,” said Dr. Feldkamp.
Check again
However, not every elevated TSH value needs to be treated immediately. “From large-scale investigations, we know that TSH values are subject to fluctuations,” said Dr. Feldkamp. Individual measurements must therefore be taken with a grain of salt and almost never justify a therapeutic decision. Therefore, a slightly elevated TSH value should be checked again 2-6 months later, and the patient should be asked if they are experiencing any symptoms. “In 50%-60% of cases, the TSH value normalized at the second checkup without requiring any treatment,” Dr. Feldkamp explained.
The TSH value could be elevated for several reasons:
- Fluctuations depending on the time of day. At night and early in the morning, the TSH value is much higher than in the afternoon. An acute lack of sleep can lead to higher TSH values in the morning.
- Fluctuations depending on the time of year. In winter, TSH values are slightly higher than in the summer owing to adaptation to cooler temperatures. Researchers in the Arctic, for example, have significantly higher TSH values than people who live in warmer regions.
- Age-dependent differences. Children and adolescents have higher TSH values than adults do. The TSH values of adolescents cannot be based on those of adults because this would lead to incorrect treatment. In addition, TSH values increase with age, and slightly elevated values are initially no cause for treatment in people aged 70-80 years. Caution is advised during treatment, because overtreatment can lead to cardiac arrhythmias and a decrease in bone density.
- Sex-specific differences. The TSH values of women are generally a little higher than those in men.
- Obesity. In obesity, TSH increases and often exceeds the normal values usually recorded in persons of normal weight. The elevated values do not reflect a state of hypofunction but rather the body’s adjustment mechanism. If these patients lose weight, the TSH values will drop spontaneously. Slightly elevated TSH values in obese people should not be treated with thyroid hormones.
The nutritional supplement biotin (vitamin H or vitamin B7), which is often taken for skin, hair, and nail growth disorders, can distort measured values. In many of the laboratory methods used, the biotin competes with the test substances used. As a result, it can lead to falsely high and falsely low TSH values. At high doses of biotin (for example, 10 mg), there should be at least a 3-day pause (and ideally a pause of 1 week) before measuring TSH.
Hasty prescriptions
“Sometimes, because of the assumption that every high TSH value is due to sickness-related hypothyroidism, thyroid hormones can be prescribed too quickly,” said Dr. Feldkamp. This is also true for patients with thyroid nodules due to iodine deficiency, who are often still treated with thyroid hormones.
“These days, because we are generally an iodine-deficient nation, iodine would potentially be given in combination with thyroid hormones but not with thyroid hormones alone. There are lots of patients who have been taking thyroid hormones for 30 or 40 years due to thyroid nodules. That should definitely be reviewed,” said Dr. Feldkamp.
When to treat?
Dr. Feldkamp does not believe that standard determination of the TSH value is sensible and advises that clinicians examine patients with newly occurring symptoms, such as excess weight, impaired weight regulation despite reduced appetite, depression, or a high need for sleep.
If there are symptoms, the thyroid function must be clarified further. “This includes determination of free thyroid hormones T3 and T4; detection of antibodies against autologous thyroid tissue such as TPO-Ab [antibody against thyroid peroxidase], TG-Ab [antibody against thyroglobulin], and TRAb [antibody against TSH receptor]; and ultrasound examination of the metabolic organ,” said Dr. Feldkamp. Autoimmune-related hypothyroidism (Hashimoto’s thyroiditis) is the most common cause of an overly high TSH level.
Treatment should take place in the following situations:
- In young patients with TSH values greater than 10 mU/L;
- In young (< 65 years) symptomatic patients with TSH values of 4 to less than 10 mU/L;
- With elevated TSH values that result from thyroid surgery or radioactive iodine therapy;
- In patients with a diffuse enlarged or severely nodular thyroid gland
- In pregnant women with elevated TSH values.
This article was translated from Medscape’s German Edition and a version appeared on Medscape.com.
Thyroxine and L-thyroxine are two of the 10 most frequently prescribed medicinal products. “One large health insurance company ranks thyroid hormone at fourth place in the list of most-sold medications in the United States. It is possibly the second most commonly prescribed preparation,” said Joachim Feldkamp, MD, PhD, director of the University Clinic for General Internal Medicine, Endocrinology, Diabetology, and Infectious Diseases at Central Hospital, Bielefeld, Germany, at the online press conference for the German Society of Endocrinology’s hormone week.
The preparation is prescribed when the thyroid gland produces too little thyroid hormone. The messenger substance thyroid-stimulating hormone (TSH) is used as a screening value to assess thyroid function. An increase in TSH can indicate that too little thyroid hormone is being produced.
“But this does not mean that an underactive thyroid gland is hiding behind every elevated TSH value,” said Dr. Feldkamp. Normally, the TSH value lies between 0.3 and 4.2 mU/L. “Hypothyroidism, as it’s known, is formally present if the TSH value lies above the upper limit of 4.2 mU/L,” said Dr. Feldkamp.
Check again
However, not every elevated TSH value needs to be treated immediately. “From large-scale investigations, we know that TSH values are subject to fluctuations,” said Dr. Feldkamp. Individual measurements must therefore be taken with a grain of salt and almost never justify a therapeutic decision. Therefore, a slightly elevated TSH value should be checked again 2-6 months later, and the patient should be asked if they are experiencing any symptoms. “In 50%-60% of cases, the TSH value normalized at the second checkup without requiring any treatment,” Dr. Feldkamp explained.
The TSH value could be elevated for several reasons:
- Fluctuations depending on the time of day. At night and early in the morning, the TSH value is much higher than in the afternoon. An acute lack of sleep can lead to higher TSH values in the morning.
- Fluctuations depending on the time of year. In winter, TSH values are slightly higher than in the summer owing to adaptation to cooler temperatures. Researchers in the Arctic, for example, have significantly higher TSH values than people who live in warmer regions.
- Age-dependent differences. Children and adolescents have higher TSH values than adults do. The TSH values of adolescents cannot be based on those of adults because this would lead to incorrect treatment. In addition, TSH values increase with age, and slightly elevated values are initially no cause for treatment in people aged 70-80 years. Caution is advised during treatment, because overtreatment can lead to cardiac arrhythmias and a decrease in bone density.
- Sex-specific differences. The TSH values of women are generally a little higher than those in men.
- Obesity. In obesity, TSH increases and often exceeds the normal values usually recorded in persons of normal weight. The elevated values do not reflect a state of hypofunction but rather the body’s adjustment mechanism. If these patients lose weight, the TSH values will drop spontaneously. Slightly elevated TSH values in obese people should not be treated with thyroid hormones.
The nutritional supplement biotin (vitamin H or vitamin B7), which is often taken for skin, hair, and nail growth disorders, can distort measured values. In many of the laboratory methods used, the biotin competes with the test substances used. As a result, it can lead to falsely high and falsely low TSH values. At high doses of biotin (for example, 10 mg), there should be at least a 3-day pause (and ideally a pause of 1 week) before measuring TSH.
Hasty prescriptions
“Sometimes, because of the assumption that every high TSH value is due to sickness-related hypothyroidism, thyroid hormones can be prescribed too quickly,” said Dr. Feldkamp. This is also true for patients with thyroid nodules due to iodine deficiency, who are often still treated with thyroid hormones.
“These days, because we are generally an iodine-deficient nation, iodine would potentially be given in combination with thyroid hormones but not with thyroid hormones alone. There are lots of patients who have been taking thyroid hormones for 30 or 40 years due to thyroid nodules. That should definitely be reviewed,” said Dr. Feldkamp.
When to treat?
Dr. Feldkamp does not believe that standard determination of the TSH value is sensible and advises that clinicians examine patients with newly occurring symptoms, such as excess weight, impaired weight regulation despite reduced appetite, depression, or a high need for sleep.
If there are symptoms, the thyroid function must be clarified further. “This includes determination of free thyroid hormones T3 and T4; detection of antibodies against autologous thyroid tissue such as TPO-Ab [antibody against thyroid peroxidase], TG-Ab [antibody against thyroglobulin], and TRAb [antibody against TSH receptor]; and ultrasound examination of the metabolic organ,” said Dr. Feldkamp. Autoimmune-related hypothyroidism (Hashimoto’s thyroiditis) is the most common cause of an overly high TSH level.
Treatment should take place in the following situations:
- In young patients with TSH values greater than 10 mU/L;
- In young (< 65 years) symptomatic patients with TSH values of 4 to less than 10 mU/L;
- With elevated TSH values that result from thyroid surgery or radioactive iodine therapy;
- In patients with a diffuse enlarged or severely nodular thyroid gland
- In pregnant women with elevated TSH values.
This article was translated from Medscape’s German Edition and a version appeared on Medscape.com.
Thyroxine and L-thyroxine are two of the 10 most frequently prescribed medicinal products. “One large health insurance company ranks thyroid hormone at fourth place in the list of most-sold medications in the United States. It is possibly the second most commonly prescribed preparation,” said Joachim Feldkamp, MD, PhD, director of the University Clinic for General Internal Medicine, Endocrinology, Diabetology, and Infectious Diseases at Central Hospital, Bielefeld, Germany, at the online press conference for the German Society of Endocrinology’s hormone week.
The preparation is prescribed when the thyroid gland produces too little thyroid hormone. The messenger substance thyroid-stimulating hormone (TSH) is used as a screening value to assess thyroid function. An increase in TSH can indicate that too little thyroid hormone is being produced.
“But this does not mean that an underactive thyroid gland is hiding behind every elevated TSH value,” said Dr. Feldkamp. Normally, the TSH value lies between 0.3 and 4.2 mU/L. “Hypothyroidism, as it’s known, is formally present if the TSH value lies above the upper limit of 4.2 mU/L,” said Dr. Feldkamp.
Check again
However, not every elevated TSH value needs to be treated immediately. “From large-scale investigations, we know that TSH values are subject to fluctuations,” said Dr. Feldkamp. Individual measurements must therefore be taken with a grain of salt and almost never justify a therapeutic decision. Therefore, a slightly elevated TSH value should be checked again 2-6 months later, and the patient should be asked if they are experiencing any symptoms. “In 50%-60% of cases, the TSH value normalized at the second checkup without requiring any treatment,” Dr. Feldkamp explained.
The TSH value could be elevated for several reasons:
- Fluctuations depending on the time of day. At night and early in the morning, the TSH value is much higher than in the afternoon. An acute lack of sleep can lead to higher TSH values in the morning.
- Fluctuations depending on the time of year. In winter, TSH values are slightly higher than in the summer owing to adaptation to cooler temperatures. Researchers in the Arctic, for example, have significantly higher TSH values than people who live in warmer regions.
- Age-dependent differences. Children and adolescents have higher TSH values than adults do. The TSH values of adolescents cannot be based on those of adults because this would lead to incorrect treatment. In addition, TSH values increase with age, and slightly elevated values are initially no cause for treatment in people aged 70-80 years. Caution is advised during treatment, because overtreatment can lead to cardiac arrhythmias and a decrease in bone density.
- Sex-specific differences. The TSH values of women are generally a little higher than those in men.
- Obesity. In obesity, TSH increases and often exceeds the normal values usually recorded in persons of normal weight. The elevated values do not reflect a state of hypofunction but rather the body’s adjustment mechanism. If these patients lose weight, the TSH values will drop spontaneously. Slightly elevated TSH values in obese people should not be treated with thyroid hormones.
The nutritional supplement biotin (vitamin H or vitamin B7), which is often taken for skin, hair, and nail growth disorders, can distort measured values. In many of the laboratory methods used, the biotin competes with the test substances used. As a result, it can lead to falsely high and falsely low TSH values. At high doses of biotin (for example, 10 mg), there should be at least a 3-day pause (and ideally a pause of 1 week) before measuring TSH.
Hasty prescriptions
“Sometimes, because of the assumption that every high TSH value is due to sickness-related hypothyroidism, thyroid hormones can be prescribed too quickly,” said Dr. Feldkamp. This is also true for patients with thyroid nodules due to iodine deficiency, who are often still treated with thyroid hormones.
“These days, because we are generally an iodine-deficient nation, iodine would potentially be given in combination with thyroid hormones but not with thyroid hormones alone. There are lots of patients who have been taking thyroid hormones for 30 or 40 years due to thyroid nodules. That should definitely be reviewed,” said Dr. Feldkamp.
When to treat?
Dr. Feldkamp does not believe that standard determination of the TSH value is sensible and advises that clinicians examine patients with newly occurring symptoms, such as excess weight, impaired weight regulation despite reduced appetite, depression, or a high need for sleep.
If there are symptoms, the thyroid function must be clarified further. “This includes determination of free thyroid hormones T3 and T4; detection of antibodies against autologous thyroid tissue such as TPO-Ab [antibody against thyroid peroxidase], TG-Ab [antibody against thyroglobulin], and TRAb [antibody against TSH receptor]; and ultrasound examination of the metabolic organ,” said Dr. Feldkamp. Autoimmune-related hypothyroidism (Hashimoto’s thyroiditis) is the most common cause of an overly high TSH level.
Treatment should take place in the following situations:
- In young patients with TSH values greater than 10 mU/L;
- In young (< 65 years) symptomatic patients with TSH values of 4 to less than 10 mU/L;
- With elevated TSH values that result from thyroid surgery or radioactive iodine therapy;
- In patients with a diffuse enlarged or severely nodular thyroid gland
- In pregnant women with elevated TSH values.
This article was translated from Medscape’s German Edition and a version appeared on Medscape.com.
Thyroid cancer increase observed in transgender female veterans
WASHINGTON – Experts urge a cautious interpretation of these recent study results.
“In our clinic of about 50 transgender women, we noticed that we had two diagnosed cases of thyroid cancer in a year,” first author John Christensen, MD, of UC Davis Health, division of endocrinology, diabetes & metabolism, Sacramento, said in an interivew. He presented their findings at the annual meeting of the American Thyroid Association.
Comparatively, the thyroid cancer prevalence among cisgender male veterans is estimated at about 0.19%; the rate among all those assigned male at birth in the general population is 0.13%, whereas the rate among those assigned female at birth, which has historically been higher for all thyroid cancer subtypes, is 0.44%, according to U.S. cancer statistics for 2020 from the National Cancer Institute.
“About one-third of our [veteran] patients had been receiving estrogen for an average of over 3 years before diagnosis, which could suggest estrogen gender‐affirming hormone therapy [GAHT] may be a potentially important risk factor,” Dr. Christensen said.
Sustained use of external estrogen, especially in cisgender women undergoing fertility treatments, has been linked to an increased risk for thyroid cancer. This is because it can lead to an increase in estrogen receptors in cancerous cells. But experts caution that many other factors also come into play.
“There is definitely an implication that if you give extra estrogen to someone assigned female at birth, you may have an increased risk of thyroid cancer,” Dr. Christensen said. “So, it would stand to reason that even in those who are not assigned female at birth, there may be a risk from exogenous estrogen that may lead to an increased risk of thyroid cancer down the line.”
To investigate the issue in a larger population, Dr. Christensen and colleagues evaluated data from the comprehensive, nationwide Veterans Affairs Informatics and Computing Infrastructure database, including approximately 9 million veterans who had outpatient visits between December 2017 and January 2022.
Of the veterans, 9,988 were determined to likely be transgender women, based on either having an ICD-10 diagnosis code for gender dysphoria or being assigned male at birth and having received an estrogen or estradiol prescription.
Of those patients, 76 had an ICD-10 code indicating thyroid cancer and 34 had verification of the thyroid cancer on chart review, representing a prevalence of 0.34% among transgender female veterans.
The average age at thyroid cancer diagnosis among the veterans was 53.8 years, and 29.4% (10 of 34) of those patients had extrathyroidal disease at the time of their thyroid cancer diagnosis. The median body mass index, available for 26 patients, was 32, which is indicative of obesity.
In terms of the patients’ thyroid cancer subtypes, 22 were papillary cancer, 5 were a follicular variant of papillary cancer, 5 were both papillary and follicular cancer, 4 were follicular cancer, 3 were a Hürthle cell variant of follicular cancer, and one was unknown.
Among 11 (32.3%) of the 34 veterans receiving estrogen GAHT at diagnosis, treatment began an average of 3.38 years prior to diagnosis at variable doses and using various routes of administration.
About half of the patients had a history of smoking; however, Dr. Christensen noted that the role of smoking as being a risk factor in estrogenic cancers has been debated. Though most patients were obese, obesity is both very common and not well established in terms of its quantitative impact on the risk for cancer development.
With the small size of the thyroid cancer cohort and omissions in the medical record among the study’s important limitations, Dr. Christensen urged a cautious interpretation of the findings.
“We are certainly suspicious that GAHT may be associated with an increased risk of thyroid cancer, but I would characterize the trends in our data as being potentially suggestive or hypothesis generating – not conclusive,” he added. “I would hate for any transgender women reading this to stop taking GAHT without talking to their doctors first.”
Commenting on the issue, Maurice Garcia, MD, a clinical associate professor of urology and director of the transgender surgery and health program at Cedars-Sinai Medical Center, Los Angeles, said that any definitive evidence of an increase in cancer risk among transgender people is lacking.
“With an estimated 1.5 [million] to 1.6 million people in the U.S. who are transgender, with many of them receiving GAHT, we haven’t observed a bump or high incidence of any kind of cancer among these people so far,” he said.
“There’s certainly a high potential that hormone therapy, whether it’s feminizing or masculinizing hormone therapy, can affect an individual’s cancer risk,” he added. “But we don’t know of any [definitive evidence] yet of an increase, and, there’s also even the question of whether there could be an opposite effect.”
Regarding the thyroid cancer data, Dr. Garcia agreed that the preliminary nature of the study is a key limitation. “It’s hard to tell if these were comparable groups, or whether those in the transgender group came in with higher risk factors for thyroid cancer.
“Until more statistical analysis is done, I think all that can be said is that it’s speculative.”
Dr. Garcia, who coauthored a review on cancer screening for transgender individuals, underscored that, despite a lack of data suggesting that transgender patients need cancer screening any more than their matched cisgender counterparts, “the point is that we cannot forget to screen them at all.”
Dr. Christensen and Dr. Garcia had no disclosures to report.
A version of this article first appeared on Medscape.com.
WASHINGTON – Experts urge a cautious interpretation of these recent study results.
“In our clinic of about 50 transgender women, we noticed that we had two diagnosed cases of thyroid cancer in a year,” first author John Christensen, MD, of UC Davis Health, division of endocrinology, diabetes & metabolism, Sacramento, said in an interivew. He presented their findings at the annual meeting of the American Thyroid Association.
Comparatively, the thyroid cancer prevalence among cisgender male veterans is estimated at about 0.19%; the rate among all those assigned male at birth in the general population is 0.13%, whereas the rate among those assigned female at birth, which has historically been higher for all thyroid cancer subtypes, is 0.44%, according to U.S. cancer statistics for 2020 from the National Cancer Institute.
“About one-third of our [veteran] patients had been receiving estrogen for an average of over 3 years before diagnosis, which could suggest estrogen gender‐affirming hormone therapy [GAHT] may be a potentially important risk factor,” Dr. Christensen said.
Sustained use of external estrogen, especially in cisgender women undergoing fertility treatments, has been linked to an increased risk for thyroid cancer. This is because it can lead to an increase in estrogen receptors in cancerous cells. But experts caution that many other factors also come into play.
“There is definitely an implication that if you give extra estrogen to someone assigned female at birth, you may have an increased risk of thyroid cancer,” Dr. Christensen said. “So, it would stand to reason that even in those who are not assigned female at birth, there may be a risk from exogenous estrogen that may lead to an increased risk of thyroid cancer down the line.”
To investigate the issue in a larger population, Dr. Christensen and colleagues evaluated data from the comprehensive, nationwide Veterans Affairs Informatics and Computing Infrastructure database, including approximately 9 million veterans who had outpatient visits between December 2017 and January 2022.
Of the veterans, 9,988 were determined to likely be transgender women, based on either having an ICD-10 diagnosis code for gender dysphoria or being assigned male at birth and having received an estrogen or estradiol prescription.
Of those patients, 76 had an ICD-10 code indicating thyroid cancer and 34 had verification of the thyroid cancer on chart review, representing a prevalence of 0.34% among transgender female veterans.
The average age at thyroid cancer diagnosis among the veterans was 53.8 years, and 29.4% (10 of 34) of those patients had extrathyroidal disease at the time of their thyroid cancer diagnosis. The median body mass index, available for 26 patients, was 32, which is indicative of obesity.
In terms of the patients’ thyroid cancer subtypes, 22 were papillary cancer, 5 were a follicular variant of papillary cancer, 5 were both papillary and follicular cancer, 4 were follicular cancer, 3 were a Hürthle cell variant of follicular cancer, and one was unknown.
Among 11 (32.3%) of the 34 veterans receiving estrogen GAHT at diagnosis, treatment began an average of 3.38 years prior to diagnosis at variable doses and using various routes of administration.
About half of the patients had a history of smoking; however, Dr. Christensen noted that the role of smoking as being a risk factor in estrogenic cancers has been debated. Though most patients were obese, obesity is both very common and not well established in terms of its quantitative impact on the risk for cancer development.
With the small size of the thyroid cancer cohort and omissions in the medical record among the study’s important limitations, Dr. Christensen urged a cautious interpretation of the findings.
“We are certainly suspicious that GAHT may be associated with an increased risk of thyroid cancer, but I would characterize the trends in our data as being potentially suggestive or hypothesis generating – not conclusive,” he added. “I would hate for any transgender women reading this to stop taking GAHT without talking to their doctors first.”
Commenting on the issue, Maurice Garcia, MD, a clinical associate professor of urology and director of the transgender surgery and health program at Cedars-Sinai Medical Center, Los Angeles, said that any definitive evidence of an increase in cancer risk among transgender people is lacking.
“With an estimated 1.5 [million] to 1.6 million people in the U.S. who are transgender, with many of them receiving GAHT, we haven’t observed a bump or high incidence of any kind of cancer among these people so far,” he said.
“There’s certainly a high potential that hormone therapy, whether it’s feminizing or masculinizing hormone therapy, can affect an individual’s cancer risk,” he added. “But we don’t know of any [definitive evidence] yet of an increase, and, there’s also even the question of whether there could be an opposite effect.”
Regarding the thyroid cancer data, Dr. Garcia agreed that the preliminary nature of the study is a key limitation. “It’s hard to tell if these were comparable groups, or whether those in the transgender group came in with higher risk factors for thyroid cancer.
“Until more statistical analysis is done, I think all that can be said is that it’s speculative.”
Dr. Garcia, who coauthored a review on cancer screening for transgender individuals, underscored that, despite a lack of data suggesting that transgender patients need cancer screening any more than their matched cisgender counterparts, “the point is that we cannot forget to screen them at all.”
Dr. Christensen and Dr. Garcia had no disclosures to report.
A version of this article first appeared on Medscape.com.
WASHINGTON – Experts urge a cautious interpretation of these recent study results.
“In our clinic of about 50 transgender women, we noticed that we had two diagnosed cases of thyroid cancer in a year,” first author John Christensen, MD, of UC Davis Health, division of endocrinology, diabetes & metabolism, Sacramento, said in an interivew. He presented their findings at the annual meeting of the American Thyroid Association.
Comparatively, the thyroid cancer prevalence among cisgender male veterans is estimated at about 0.19%; the rate among all those assigned male at birth in the general population is 0.13%, whereas the rate among those assigned female at birth, which has historically been higher for all thyroid cancer subtypes, is 0.44%, according to U.S. cancer statistics for 2020 from the National Cancer Institute.
“About one-third of our [veteran] patients had been receiving estrogen for an average of over 3 years before diagnosis, which could suggest estrogen gender‐affirming hormone therapy [GAHT] may be a potentially important risk factor,” Dr. Christensen said.
Sustained use of external estrogen, especially in cisgender women undergoing fertility treatments, has been linked to an increased risk for thyroid cancer. This is because it can lead to an increase in estrogen receptors in cancerous cells. But experts caution that many other factors also come into play.
“There is definitely an implication that if you give extra estrogen to someone assigned female at birth, you may have an increased risk of thyroid cancer,” Dr. Christensen said. “So, it would stand to reason that even in those who are not assigned female at birth, there may be a risk from exogenous estrogen that may lead to an increased risk of thyroid cancer down the line.”
To investigate the issue in a larger population, Dr. Christensen and colleagues evaluated data from the comprehensive, nationwide Veterans Affairs Informatics and Computing Infrastructure database, including approximately 9 million veterans who had outpatient visits between December 2017 and January 2022.
Of the veterans, 9,988 were determined to likely be transgender women, based on either having an ICD-10 diagnosis code for gender dysphoria or being assigned male at birth and having received an estrogen or estradiol prescription.
Of those patients, 76 had an ICD-10 code indicating thyroid cancer and 34 had verification of the thyroid cancer on chart review, representing a prevalence of 0.34% among transgender female veterans.
The average age at thyroid cancer diagnosis among the veterans was 53.8 years, and 29.4% (10 of 34) of those patients had extrathyroidal disease at the time of their thyroid cancer diagnosis. The median body mass index, available for 26 patients, was 32, which is indicative of obesity.
In terms of the patients’ thyroid cancer subtypes, 22 were papillary cancer, 5 were a follicular variant of papillary cancer, 5 were both papillary and follicular cancer, 4 were follicular cancer, 3 were a Hürthle cell variant of follicular cancer, and one was unknown.
Among 11 (32.3%) of the 34 veterans receiving estrogen GAHT at diagnosis, treatment began an average of 3.38 years prior to diagnosis at variable doses and using various routes of administration.
About half of the patients had a history of smoking; however, Dr. Christensen noted that the role of smoking as being a risk factor in estrogenic cancers has been debated. Though most patients were obese, obesity is both very common and not well established in terms of its quantitative impact on the risk for cancer development.
With the small size of the thyroid cancer cohort and omissions in the medical record among the study’s important limitations, Dr. Christensen urged a cautious interpretation of the findings.
“We are certainly suspicious that GAHT may be associated with an increased risk of thyroid cancer, but I would characterize the trends in our data as being potentially suggestive or hypothesis generating – not conclusive,” he added. “I would hate for any transgender women reading this to stop taking GAHT without talking to their doctors first.”
Commenting on the issue, Maurice Garcia, MD, a clinical associate professor of urology and director of the transgender surgery and health program at Cedars-Sinai Medical Center, Los Angeles, said that any definitive evidence of an increase in cancer risk among transgender people is lacking.
“With an estimated 1.5 [million] to 1.6 million people in the U.S. who are transgender, with many of them receiving GAHT, we haven’t observed a bump or high incidence of any kind of cancer among these people so far,” he said.
“There’s certainly a high potential that hormone therapy, whether it’s feminizing or masculinizing hormone therapy, can affect an individual’s cancer risk,” he added. “But we don’t know of any [definitive evidence] yet of an increase, and, there’s also even the question of whether there could be an opposite effect.”
Regarding the thyroid cancer data, Dr. Garcia agreed that the preliminary nature of the study is a key limitation. “It’s hard to tell if these were comparable groups, or whether those in the transgender group came in with higher risk factors for thyroid cancer.
“Until more statistical analysis is done, I think all that can be said is that it’s speculative.”
Dr. Garcia, who coauthored a review on cancer screening for transgender individuals, underscored that, despite a lack of data suggesting that transgender patients need cancer screening any more than their matched cisgender counterparts, “the point is that we cannot forget to screen them at all.”
Dr. Christensen and Dr. Garcia had no disclosures to report.
A version of this article first appeared on Medscape.com.
AT ATA 2023
Hormone therapy less effective in menopausal women with obesity
PHILADELPHIA – , according to a small, retrospective study presented at the annual meeting of the Menopause Society (formerly the North American Menopause Society).
More than 40% of women over age 40 in the United States have obesity, presenter Anita Pershad, MD, an ob.gyn. medical resident at Eastern Virginia Medical School, Norfolk, told attendees. Yet most of the large-scale studies investigating perimenopausal and postmenopausal hormone therapy included participants without major medical comorbidities, so little data exist on how effectively HT works in women with these comorbidities, she said
“The main takeaway of our study is that obesity may worsen a woman’s menopausal symptoms and limit the amount of relief she gets from hormone therapy,” Dr. Pershad said in an interview. “It remains unclear if hormone therapy is less effective in women with obesity overall, or if the expected efficacy can be achieved with alternative design and administration routes. A potential mechanism of action for the observed decreased effect could be due to adipose tissue acting as a heat insulator, promoting the effects of vasomotor symptoms.”
Dr. Pershad and her colleagues conducted a retrospective review of the medical records of 119 patients who presented to a menopause clinic at a Midsouth urban academic medical center between July 2018 and December 2022. Obesity was defined as having a body mass index (BMI) of 30 kg/m2 or greater.
The patients with and without obesity were similar in terms of age, duration of menopause, use of hormone therapy, and therapy acceptance, but patients with obesity were more likely to identify themselves as Black (71% vs. 40%). Women with obesity were also significantly more likely than women without obesity to report vasomotor symptoms (74% vs. 45%, P = .002), genitourinary/vulvovaginal symptoms (60% vs. 21%, P < .001), mood disturbances (11% vs. 0%, P = .18), and decreased libido (29% vs. 11%, P = .017).
There were no significant differences in comorbidities between women with and without obesity, and among women who received systemic or localized HT, the same standard dosing was used for both groups.
Women with obesity were much less likely to see a satisfying reduction in their menopausal symptoms than women without obesity (odds ratio 0.07, 95% confidence interval, 0.01-0.64; P = .006), though the subgroups for each category of HT were small. Among the 20 women receiving systemic hormone therapy, only 1 of the 12 with obesity (8.3%) reported improvement in symptoms, compared with 7 of the 8 women without obesity (88%; P = .0004). Among 33 women using localized hormone therapy, 46% of the 24 women with obesity vs. 89% of the 9 women without obesity experienced symptom improvement (P = .026).
The proportions of women reporting relief from only lifestyle modifications or from nonhormonal medications, such as SSRIs/SNRIs, trazodone, and clonidine, were not statistically different. There were 33 women who relied only on lifestyle modifications, with 31% of the 16 women with obesity and 59% of the 17 women without obesity reporting improvement in their symptoms (P = .112). Similarly, among the 33 women using nonhormonal medications, 75% of the 20 women with obesity and 77% of the 13 women without obesity experienced relief (P = .9).
Women with obesity are undertreated
Dr. Pershad emphasized the need to improve care and counseling for diverse patients seeking treatment for menopausal symptoms.
“More research is needed to examine how women with medical comorbidities are uniquely impacted by menopause and respond to therapies,” Dr. Pershad said in an interview. “This can be achieved by actively including more diverse patient populations in women’s health studies, burdened by the social determinants of health and medical comorbidities such as obesity.”
Stephanie S. Faubion, MD, MBA, director for Mayo Clinic’s Center for Women’s Health, Rochester, Minn., and medical director for The Menopause Society, was not surprised by the findings, particularly given that women with obesity tend to have more hot flashes and night sweats as a result of their extra weight. However, dosage data was not adjusted for BMI in the study and data on hormone levels was unavailable, she said, so it’s difficult to determine from the data whether HT was less effective for women with obesity or whether they were underdosed.
“I think women with obesity are undertreated,” Dr. Faubion said in an interview. “My guess is people are afraid. Women with obesity also may have other comorbidities,” such as hypertension and diabetes, she said, and “the greater the number of cardiovascular risk factors, the higher risk hormone therapy is.” Providers may therefore be leery of prescribing HT or prescribing it at an appropriately high enough dose to treat menopausal symptoms.
Common practice is to start patients at the lowest dose and titrate up according to symptoms, but “if people are afraid of it, they’re going to start the lowest dose” and may not increase it, Dr. Faubion said. She noted that other nonhormonal options are available, though providers should be conscientious about selecting ones whose adverse events do not include weight gain.
Although the study focused on an understudied population within hormone therapy research, the study was limited by its small size, low overall use of hormone therapy, recall bias, and the researchers’ inability to control for other medications the participants may have been taking.
Dr. Pershad said she is continuing research to try to identify the mechanisms underlying the reduced efficacy in women with obesity.
The research did not use any external funding. Dr. Pershad had no industry disclosures, but her colleagues reported honoraria from or speaking for TherapeuticsMD, Astella Pharma, Scynexis, Pharmavite, and Pfizer. Dr. Faubion had no disclosures.
PHILADELPHIA – , according to a small, retrospective study presented at the annual meeting of the Menopause Society (formerly the North American Menopause Society).
More than 40% of women over age 40 in the United States have obesity, presenter Anita Pershad, MD, an ob.gyn. medical resident at Eastern Virginia Medical School, Norfolk, told attendees. Yet most of the large-scale studies investigating perimenopausal and postmenopausal hormone therapy included participants without major medical comorbidities, so little data exist on how effectively HT works in women with these comorbidities, she said
“The main takeaway of our study is that obesity may worsen a woman’s menopausal symptoms and limit the amount of relief she gets from hormone therapy,” Dr. Pershad said in an interview. “It remains unclear if hormone therapy is less effective in women with obesity overall, or if the expected efficacy can be achieved with alternative design and administration routes. A potential mechanism of action for the observed decreased effect could be due to adipose tissue acting as a heat insulator, promoting the effects of vasomotor symptoms.”
Dr. Pershad and her colleagues conducted a retrospective review of the medical records of 119 patients who presented to a menopause clinic at a Midsouth urban academic medical center between July 2018 and December 2022. Obesity was defined as having a body mass index (BMI) of 30 kg/m2 or greater.
The patients with and without obesity were similar in terms of age, duration of menopause, use of hormone therapy, and therapy acceptance, but patients with obesity were more likely to identify themselves as Black (71% vs. 40%). Women with obesity were also significantly more likely than women without obesity to report vasomotor symptoms (74% vs. 45%, P = .002), genitourinary/vulvovaginal symptoms (60% vs. 21%, P < .001), mood disturbances (11% vs. 0%, P = .18), and decreased libido (29% vs. 11%, P = .017).
There were no significant differences in comorbidities between women with and without obesity, and among women who received systemic or localized HT, the same standard dosing was used for both groups.
Women with obesity were much less likely to see a satisfying reduction in their menopausal symptoms than women without obesity (odds ratio 0.07, 95% confidence interval, 0.01-0.64; P = .006), though the subgroups for each category of HT were small. Among the 20 women receiving systemic hormone therapy, only 1 of the 12 with obesity (8.3%) reported improvement in symptoms, compared with 7 of the 8 women without obesity (88%; P = .0004). Among 33 women using localized hormone therapy, 46% of the 24 women with obesity vs. 89% of the 9 women without obesity experienced symptom improvement (P = .026).
The proportions of women reporting relief from only lifestyle modifications or from nonhormonal medications, such as SSRIs/SNRIs, trazodone, and clonidine, were not statistically different. There were 33 women who relied only on lifestyle modifications, with 31% of the 16 women with obesity and 59% of the 17 women without obesity reporting improvement in their symptoms (P = .112). Similarly, among the 33 women using nonhormonal medications, 75% of the 20 women with obesity and 77% of the 13 women without obesity experienced relief (P = .9).
Women with obesity are undertreated
Dr. Pershad emphasized the need to improve care and counseling for diverse patients seeking treatment for menopausal symptoms.
“More research is needed to examine how women with medical comorbidities are uniquely impacted by menopause and respond to therapies,” Dr. Pershad said in an interview. “This can be achieved by actively including more diverse patient populations in women’s health studies, burdened by the social determinants of health and medical comorbidities such as obesity.”
Stephanie S. Faubion, MD, MBA, director for Mayo Clinic’s Center for Women’s Health, Rochester, Minn., and medical director for The Menopause Society, was not surprised by the findings, particularly given that women with obesity tend to have more hot flashes and night sweats as a result of their extra weight. However, dosage data was not adjusted for BMI in the study and data on hormone levels was unavailable, she said, so it’s difficult to determine from the data whether HT was less effective for women with obesity or whether they were underdosed.
“I think women with obesity are undertreated,” Dr. Faubion said in an interview. “My guess is people are afraid. Women with obesity also may have other comorbidities,” such as hypertension and diabetes, she said, and “the greater the number of cardiovascular risk factors, the higher risk hormone therapy is.” Providers may therefore be leery of prescribing HT or prescribing it at an appropriately high enough dose to treat menopausal symptoms.
Common practice is to start patients at the lowest dose and titrate up according to symptoms, but “if people are afraid of it, they’re going to start the lowest dose” and may not increase it, Dr. Faubion said. She noted that other nonhormonal options are available, though providers should be conscientious about selecting ones whose adverse events do not include weight gain.
Although the study focused on an understudied population within hormone therapy research, the study was limited by its small size, low overall use of hormone therapy, recall bias, and the researchers’ inability to control for other medications the participants may have been taking.
Dr. Pershad said she is continuing research to try to identify the mechanisms underlying the reduced efficacy in women with obesity.
The research did not use any external funding. Dr. Pershad had no industry disclosures, but her colleagues reported honoraria from or speaking for TherapeuticsMD, Astella Pharma, Scynexis, Pharmavite, and Pfizer. Dr. Faubion had no disclosures.
PHILADELPHIA – , according to a small, retrospective study presented at the annual meeting of the Menopause Society (formerly the North American Menopause Society).
More than 40% of women over age 40 in the United States have obesity, presenter Anita Pershad, MD, an ob.gyn. medical resident at Eastern Virginia Medical School, Norfolk, told attendees. Yet most of the large-scale studies investigating perimenopausal and postmenopausal hormone therapy included participants without major medical comorbidities, so little data exist on how effectively HT works in women with these comorbidities, she said
“The main takeaway of our study is that obesity may worsen a woman’s menopausal symptoms and limit the amount of relief she gets from hormone therapy,” Dr. Pershad said in an interview. “It remains unclear if hormone therapy is less effective in women with obesity overall, or if the expected efficacy can be achieved with alternative design and administration routes. A potential mechanism of action for the observed decreased effect could be due to adipose tissue acting as a heat insulator, promoting the effects of vasomotor symptoms.”
Dr. Pershad and her colleagues conducted a retrospective review of the medical records of 119 patients who presented to a menopause clinic at a Midsouth urban academic medical center between July 2018 and December 2022. Obesity was defined as having a body mass index (BMI) of 30 kg/m2 or greater.
The patients with and without obesity were similar in terms of age, duration of menopause, use of hormone therapy, and therapy acceptance, but patients with obesity were more likely to identify themselves as Black (71% vs. 40%). Women with obesity were also significantly more likely than women without obesity to report vasomotor symptoms (74% vs. 45%, P = .002), genitourinary/vulvovaginal symptoms (60% vs. 21%, P < .001), mood disturbances (11% vs. 0%, P = .18), and decreased libido (29% vs. 11%, P = .017).
There were no significant differences in comorbidities between women with and without obesity, and among women who received systemic or localized HT, the same standard dosing was used for both groups.
Women with obesity were much less likely to see a satisfying reduction in their menopausal symptoms than women without obesity (odds ratio 0.07, 95% confidence interval, 0.01-0.64; P = .006), though the subgroups for each category of HT were small. Among the 20 women receiving systemic hormone therapy, only 1 of the 12 with obesity (8.3%) reported improvement in symptoms, compared with 7 of the 8 women without obesity (88%; P = .0004). Among 33 women using localized hormone therapy, 46% of the 24 women with obesity vs. 89% of the 9 women without obesity experienced symptom improvement (P = .026).
The proportions of women reporting relief from only lifestyle modifications or from nonhormonal medications, such as SSRIs/SNRIs, trazodone, and clonidine, were not statistically different. There were 33 women who relied only on lifestyle modifications, with 31% of the 16 women with obesity and 59% of the 17 women without obesity reporting improvement in their symptoms (P = .112). Similarly, among the 33 women using nonhormonal medications, 75% of the 20 women with obesity and 77% of the 13 women without obesity experienced relief (P = .9).
Women with obesity are undertreated
Dr. Pershad emphasized the need to improve care and counseling for diverse patients seeking treatment for menopausal symptoms.
“More research is needed to examine how women with medical comorbidities are uniquely impacted by menopause and respond to therapies,” Dr. Pershad said in an interview. “This can be achieved by actively including more diverse patient populations in women’s health studies, burdened by the social determinants of health and medical comorbidities such as obesity.”
Stephanie S. Faubion, MD, MBA, director for Mayo Clinic’s Center for Women’s Health, Rochester, Minn., and medical director for The Menopause Society, was not surprised by the findings, particularly given that women with obesity tend to have more hot flashes and night sweats as a result of their extra weight. However, dosage data was not adjusted for BMI in the study and data on hormone levels was unavailable, she said, so it’s difficult to determine from the data whether HT was less effective for women with obesity or whether they were underdosed.
“I think women with obesity are undertreated,” Dr. Faubion said in an interview. “My guess is people are afraid. Women with obesity also may have other comorbidities,” such as hypertension and diabetes, she said, and “the greater the number of cardiovascular risk factors, the higher risk hormone therapy is.” Providers may therefore be leery of prescribing HT or prescribing it at an appropriately high enough dose to treat menopausal symptoms.
Common practice is to start patients at the lowest dose and titrate up according to symptoms, but “if people are afraid of it, they’re going to start the lowest dose” and may not increase it, Dr. Faubion said. She noted that other nonhormonal options are available, though providers should be conscientious about selecting ones whose adverse events do not include weight gain.
Although the study focused on an understudied population within hormone therapy research, the study was limited by its small size, low overall use of hormone therapy, recall bias, and the researchers’ inability to control for other medications the participants may have been taking.
Dr. Pershad said she is continuing research to try to identify the mechanisms underlying the reduced efficacy in women with obesity.
The research did not use any external funding. Dr. Pershad had no industry disclosures, but her colleagues reported honoraria from or speaking for TherapeuticsMD, Astella Pharma, Scynexis, Pharmavite, and Pfizer. Dr. Faubion had no disclosures.
AT THE MENOPAUSE SOCIETY ANNUAL MEETING
Hyaluronic acid suppository improves menopause symptoms
TOPLINE:
Among women with genitourinary syndrome of menopause, 12 weeks of treatment with vaginal suppositories containing hyaluronic acid (HLA) reduces vulvovaginal symptoms, according to trial results presented at the annual Menopause Meeting. HLA may be a promising nonhormonal therapy for this condition, the researchers said.
METHODOLOGY:
- Investigators randomly assigned 49 women to receive treatment with a vaginal suppository containing 5 mg of HLA or standard-of-care treatment with vaginal estrogen cream (0.01%).
- The trial was conducted between September 2021 and August 2022.
TAKEAWAY:
- Patients in both treatment arms experienced improvements on the Vulvovaginal Symptom Questionnaire (VSQ), the study’s primary outcome.
- The VSQ assesses vulvovaginal symptoms associated with menopause such as itching, burning, and dryness, as well as the emotional toll of symptoms and their effect on sexual activity.
- Change in VSQ score did not significantly differ between the treatment groups. The measure improved from 5.2 to 1.7 in the group that received estrogen, and from 5.8 to 2.5 in those who received HLA (P = .81).
- No treatment-related severe adverse events were reported.
IN PRACTICE:
“Women often need to decide between different therapies for genitourinary syndrome of menopause,” study author Benjamin Brucker, MD, of New York University said in an interview. “Now we can help counsel them about this formulation of HLA.”
SOURCE:
Poster P-1 was presented at the 2023 meeting of the Menopause Society, held Sept. 27-30 in Philadelphia.
DISCLOSURES:
The study was funded by Bonafide Health, a company that sells supplements to treat menopause symptoms, including vaginal suppositories containing HLA.
A version of this article appeared on Medscape.com.
TOPLINE:
Among women with genitourinary syndrome of menopause, 12 weeks of treatment with vaginal suppositories containing hyaluronic acid (HLA) reduces vulvovaginal symptoms, according to trial results presented at the annual Menopause Meeting. HLA may be a promising nonhormonal therapy for this condition, the researchers said.
METHODOLOGY:
- Investigators randomly assigned 49 women to receive treatment with a vaginal suppository containing 5 mg of HLA or standard-of-care treatment with vaginal estrogen cream (0.01%).
- The trial was conducted between September 2021 and August 2022.
TAKEAWAY:
- Patients in both treatment arms experienced improvements on the Vulvovaginal Symptom Questionnaire (VSQ), the study’s primary outcome.
- The VSQ assesses vulvovaginal symptoms associated with menopause such as itching, burning, and dryness, as well as the emotional toll of symptoms and their effect on sexual activity.
- Change in VSQ score did not significantly differ between the treatment groups. The measure improved from 5.2 to 1.7 in the group that received estrogen, and from 5.8 to 2.5 in those who received HLA (P = .81).
- No treatment-related severe adverse events were reported.
IN PRACTICE:
“Women often need to decide between different therapies for genitourinary syndrome of menopause,” study author Benjamin Brucker, MD, of New York University said in an interview. “Now we can help counsel them about this formulation of HLA.”
SOURCE:
Poster P-1 was presented at the 2023 meeting of the Menopause Society, held Sept. 27-30 in Philadelphia.
DISCLOSURES:
The study was funded by Bonafide Health, a company that sells supplements to treat menopause symptoms, including vaginal suppositories containing HLA.
A version of this article appeared on Medscape.com.
TOPLINE:
Among women with genitourinary syndrome of menopause, 12 weeks of treatment with vaginal suppositories containing hyaluronic acid (HLA) reduces vulvovaginal symptoms, according to trial results presented at the annual Menopause Meeting. HLA may be a promising nonhormonal therapy for this condition, the researchers said.
METHODOLOGY:
- Investigators randomly assigned 49 women to receive treatment with a vaginal suppository containing 5 mg of HLA or standard-of-care treatment with vaginal estrogen cream (0.01%).
- The trial was conducted between September 2021 and August 2022.
TAKEAWAY:
- Patients in both treatment arms experienced improvements on the Vulvovaginal Symptom Questionnaire (VSQ), the study’s primary outcome.
- The VSQ assesses vulvovaginal symptoms associated with menopause such as itching, burning, and dryness, as well as the emotional toll of symptoms and their effect on sexual activity.
- Change in VSQ score did not significantly differ between the treatment groups. The measure improved from 5.2 to 1.7 in the group that received estrogen, and from 5.8 to 2.5 in those who received HLA (P = .81).
- No treatment-related severe adverse events were reported.
IN PRACTICE:
“Women often need to decide between different therapies for genitourinary syndrome of menopause,” study author Benjamin Brucker, MD, of New York University said in an interview. “Now we can help counsel them about this formulation of HLA.”
SOURCE:
Poster P-1 was presented at the 2023 meeting of the Menopause Society, held Sept. 27-30 in Philadelphia.
DISCLOSURES:
The study was funded by Bonafide Health, a company that sells supplements to treat menopause symptoms, including vaginal suppositories containing HLA.
A version of this article appeared on Medscape.com.
Artificial sweeteners in processed foods tied to increased depression risk
new data from the Nurses Health Study II (NHS II) suggest.
Nurses who consumed more than eight servings daily had about a 50% higher risk of developing depression than nurses who consumed four or fewer servings daily.
However, in a secondary analysis, in which the researchers tried to tease out specific foods that may be associated with increased risk, only artificial sweeteners and artificially sweetened beverages were associated with an increased risk of depression.
“Animal studies have shown that artificial sweeteners may trigger the transmission of particular signaling molecules in the brain that are important for mood,” study investigator Andrew T. Chan, MD, MPH, of the clinical and translational epidemiology unit at Massachusetts General Hospital, Boston, said in an interview.
“Given this potential association between ultraprocessed food and multiple adverse health conditions, wherever possible individuals may wish to limit their intake of such foods. This may be a lifestyle change that could have important benefits, particularly for those who struggle with mental health,” Dr. Chan said.
The study was published online in JAMA Network Open.
Multiple potential mechanisms
The findings are based on 31,712 mostly non-Hispanic White women who were free of depression at baseline. The mean age of the patients at baseline was 52 years. As part of the NHS II, the women provided information on diet every 4 years using validated food frequency questionnaires.
Compared with women with low UPF intake, those with high UPF intake had greater body mass index (BMI). In addition, they were apt to smoke and have diabetes, hypertension, and dyslipidemia, and they were less apt to exercise regularly.
During the study period, there were 2,122 incident cases of depression, as determined using a strict definition that required self-reported clinician-diagnosed depression and regular antidepressant use. There were 4,840 incident cases, as determined using a broad definition that required clinical diagnosis and/or antidepressant use.
Compared with women in the lowest quintile of UPF consumption (fewer than four daily servings), those in the highest quintile (more than 8.8 daily servings) had an increased risk of depression.
This was noted for both the strict depression definition (hazard ratio, 1.49; 95% confidence interval, 1.26-1.76; P < .001) and the broad one (HR, 1.34; 95% CI, 1.20-1.50; P < .001).
“Models were not materially altered after inclusion of potential confounders. We did not observe differential associations in subgroups defined by age, BMI, physical activity, or smoking,” the researchers reported.
In secondary analyses, they classified UPF into their components, including ultraprocessed grain foods, sweet snacks, ready-to-eat meals, fats, sauces, ultraprocessed dairy products, savory snacks, processed meat, beverages, and artificial sweeteners.
Comparing the highest with the lowest quintiles, only high intake of artificially sweetened beverages (HR, 1.37; 95% CI, 1.19-1.57; P < .001) and artificial sweeteners (HR, 1.26; 95% CI, 1.10-1.43; P < .001) was associated with greater risk of depression and after multivariable regression.
In an exploratory analysis, women who reduced their UPF intake by at least three servings per day were at lower risk of depression (strict definition: HR, 0.84; 95% CI, 0.71-0.99), compared with those with relatively stable intake in each 4-year period.
“Ultraprocessed foods have been associated with several different health outcomes which may reflect an effect on common pathways that underlie chronic conditions,” said Dr. Chan.
For example, UPF intake has been associated with chronic inflammation, which in turns leads to multiple potential adverse health effects, including depression, he explained.
There is also a link between UPF and disruption of the gut microbiome.
“This is an important potential mechanism linking ultraprocessed food to depression since there is emerging evidence that microbes in the gut have been linked with mood through their role in metabolizing and producing proteins that have activity in the brain,” Dr. Chan said.
Association, not causation
Several experts weighed in on the study results in a statement from the U.K. nonprofit organization, Science Media Centre.
Gunter Kuhnle, PhD, professor of nutrition and food science, University of Reading (England), cautioned that the study only offers information on association – not causation.
“It is very possible that people with depression change their diet and might decide to consume foods that are easier to prepare – which would often be foods considered to be ultraprocessed,” Dr. Kuhnle said.
What’s most interesting is that the association between UPF intake and depression was driven by a single factor – artificial sweeteners.
“This supports one of the main criticisms of the UPF concept, that it combines a wide range of different foods and thereby makes it difficult to identify underlying causes,” Dr. Kuhnle added.
“There are currently no data that link artificial sweetener use to mental health, despite most of them having been available for some time. It is also important to note that there are a wide range of different artificial sweeteners that are metabolized very differently and that there might be reverse causality,” Dr. Kuhnle commented.
Paul Keedwell, MBChB, PhD, consultant psychiatrist and fellow of the Royal College of Psychiatrists, said this is an “interesting and important finding, but one that raises more questions. At this stage, we cannot say how big an effect diet has on depression risk compared to other risk factors, like family history of depression, stress levels, and having a supportive social network.”
Dr. Keedwell noted that the investigators carefully excluded the possibility that the effect is mediated by obesity or lack of exercise.
“However, an important consideration is that a diet based on ready meals and artificially sweetened drinks might indicate a hectic lifestyle or one with shift work. In other words, a fast-food diet could be an indirect marker of chronic stress. Prolonged stress probably remains the main risk factor for depression,” Dr. Keedwell said.
Keith Frayn, PhD, professor emeritus of human metabolism, University of Oxford (England), noted that the relationship between artificial sweeteners and depression “stands out clearly” even after adjusting for multiple confounding factors, including BMI, smoking, and exercise.
“This adds to growing concerns about artificial sweeteners and cardiometabolic health. The link with depression needs confirmation and further research to suggest how it might be brought about,” Dr. Frayn cautioned.
The NHS II was funded by a grant from the National Cancer Institute. Dr. Chan reported receiving grants from Bayer and Zoe and personal fees from Boehringer Ingelheim, Pfizer, and Freenome outside this work. Dr. Keedwell and Dr. Kuhnle disclosed no relevant financial relationships. Dr. Frayn is an author of books on nutrition and metabolism.
A version of this article first appeared on Medscape.com.
new data from the Nurses Health Study II (NHS II) suggest.
Nurses who consumed more than eight servings daily had about a 50% higher risk of developing depression than nurses who consumed four or fewer servings daily.
However, in a secondary analysis, in which the researchers tried to tease out specific foods that may be associated with increased risk, only artificial sweeteners and artificially sweetened beverages were associated with an increased risk of depression.
“Animal studies have shown that artificial sweeteners may trigger the transmission of particular signaling molecules in the brain that are important for mood,” study investigator Andrew T. Chan, MD, MPH, of the clinical and translational epidemiology unit at Massachusetts General Hospital, Boston, said in an interview.
“Given this potential association between ultraprocessed food and multiple adverse health conditions, wherever possible individuals may wish to limit their intake of such foods. This may be a lifestyle change that could have important benefits, particularly for those who struggle with mental health,” Dr. Chan said.
The study was published online in JAMA Network Open.
Multiple potential mechanisms
The findings are based on 31,712 mostly non-Hispanic White women who were free of depression at baseline. The mean age of the patients at baseline was 52 years. As part of the NHS II, the women provided information on diet every 4 years using validated food frequency questionnaires.
Compared with women with low UPF intake, those with high UPF intake had greater body mass index (BMI). In addition, they were apt to smoke and have diabetes, hypertension, and dyslipidemia, and they were less apt to exercise regularly.
During the study period, there were 2,122 incident cases of depression, as determined using a strict definition that required self-reported clinician-diagnosed depression and regular antidepressant use. There were 4,840 incident cases, as determined using a broad definition that required clinical diagnosis and/or antidepressant use.
Compared with women in the lowest quintile of UPF consumption (fewer than four daily servings), those in the highest quintile (more than 8.8 daily servings) had an increased risk of depression.
This was noted for both the strict depression definition (hazard ratio, 1.49; 95% confidence interval, 1.26-1.76; P < .001) and the broad one (HR, 1.34; 95% CI, 1.20-1.50; P < .001).
“Models were not materially altered after inclusion of potential confounders. We did not observe differential associations in subgroups defined by age, BMI, physical activity, or smoking,” the researchers reported.
In secondary analyses, they classified UPF into their components, including ultraprocessed grain foods, sweet snacks, ready-to-eat meals, fats, sauces, ultraprocessed dairy products, savory snacks, processed meat, beverages, and artificial sweeteners.
Comparing the highest with the lowest quintiles, only high intake of artificially sweetened beverages (HR, 1.37; 95% CI, 1.19-1.57; P < .001) and artificial sweeteners (HR, 1.26; 95% CI, 1.10-1.43; P < .001) was associated with greater risk of depression and after multivariable regression.
In an exploratory analysis, women who reduced their UPF intake by at least three servings per day were at lower risk of depression (strict definition: HR, 0.84; 95% CI, 0.71-0.99), compared with those with relatively stable intake in each 4-year period.
“Ultraprocessed foods have been associated with several different health outcomes which may reflect an effect on common pathways that underlie chronic conditions,” said Dr. Chan.
For example, UPF intake has been associated with chronic inflammation, which in turns leads to multiple potential adverse health effects, including depression, he explained.
There is also a link between UPF and disruption of the gut microbiome.
“This is an important potential mechanism linking ultraprocessed food to depression since there is emerging evidence that microbes in the gut have been linked with mood through their role in metabolizing and producing proteins that have activity in the brain,” Dr. Chan said.
Association, not causation
Several experts weighed in on the study results in a statement from the U.K. nonprofit organization, Science Media Centre.
Gunter Kuhnle, PhD, professor of nutrition and food science, University of Reading (England), cautioned that the study only offers information on association – not causation.
“It is very possible that people with depression change their diet and might decide to consume foods that are easier to prepare – which would often be foods considered to be ultraprocessed,” Dr. Kuhnle said.
What’s most interesting is that the association between UPF intake and depression was driven by a single factor – artificial sweeteners.
“This supports one of the main criticisms of the UPF concept, that it combines a wide range of different foods and thereby makes it difficult to identify underlying causes,” Dr. Kuhnle added.
“There are currently no data that link artificial sweetener use to mental health, despite most of them having been available for some time. It is also important to note that there are a wide range of different artificial sweeteners that are metabolized very differently and that there might be reverse causality,” Dr. Kuhnle commented.
Paul Keedwell, MBChB, PhD, consultant psychiatrist and fellow of the Royal College of Psychiatrists, said this is an “interesting and important finding, but one that raises more questions. At this stage, we cannot say how big an effect diet has on depression risk compared to other risk factors, like family history of depression, stress levels, and having a supportive social network.”
Dr. Keedwell noted that the investigators carefully excluded the possibility that the effect is mediated by obesity or lack of exercise.
“However, an important consideration is that a diet based on ready meals and artificially sweetened drinks might indicate a hectic lifestyle or one with shift work. In other words, a fast-food diet could be an indirect marker of chronic stress. Prolonged stress probably remains the main risk factor for depression,” Dr. Keedwell said.
Keith Frayn, PhD, professor emeritus of human metabolism, University of Oxford (England), noted that the relationship between artificial sweeteners and depression “stands out clearly” even after adjusting for multiple confounding factors, including BMI, smoking, and exercise.
“This adds to growing concerns about artificial sweeteners and cardiometabolic health. The link with depression needs confirmation and further research to suggest how it might be brought about,” Dr. Frayn cautioned.
The NHS II was funded by a grant from the National Cancer Institute. Dr. Chan reported receiving grants from Bayer and Zoe and personal fees from Boehringer Ingelheim, Pfizer, and Freenome outside this work. Dr. Keedwell and Dr. Kuhnle disclosed no relevant financial relationships. Dr. Frayn is an author of books on nutrition and metabolism.
A version of this article first appeared on Medscape.com.
new data from the Nurses Health Study II (NHS II) suggest.
Nurses who consumed more than eight servings daily had about a 50% higher risk of developing depression than nurses who consumed four or fewer servings daily.
However, in a secondary analysis, in which the researchers tried to tease out specific foods that may be associated with increased risk, only artificial sweeteners and artificially sweetened beverages were associated with an increased risk of depression.
“Animal studies have shown that artificial sweeteners may trigger the transmission of particular signaling molecules in the brain that are important for mood,” study investigator Andrew T. Chan, MD, MPH, of the clinical and translational epidemiology unit at Massachusetts General Hospital, Boston, said in an interview.
“Given this potential association between ultraprocessed food and multiple adverse health conditions, wherever possible individuals may wish to limit their intake of such foods. This may be a lifestyle change that could have important benefits, particularly for those who struggle with mental health,” Dr. Chan said.
The study was published online in JAMA Network Open.
Multiple potential mechanisms
The findings are based on 31,712 mostly non-Hispanic White women who were free of depression at baseline. The mean age of the patients at baseline was 52 years. As part of the NHS II, the women provided information on diet every 4 years using validated food frequency questionnaires.
Compared with women with low UPF intake, those with high UPF intake had greater body mass index (BMI). In addition, they were apt to smoke and have diabetes, hypertension, and dyslipidemia, and they were less apt to exercise regularly.
During the study period, there were 2,122 incident cases of depression, as determined using a strict definition that required self-reported clinician-diagnosed depression and regular antidepressant use. There were 4,840 incident cases, as determined using a broad definition that required clinical diagnosis and/or antidepressant use.
Compared with women in the lowest quintile of UPF consumption (fewer than four daily servings), those in the highest quintile (more than 8.8 daily servings) had an increased risk of depression.
This was noted for both the strict depression definition (hazard ratio, 1.49; 95% confidence interval, 1.26-1.76; P < .001) and the broad one (HR, 1.34; 95% CI, 1.20-1.50; P < .001).
“Models were not materially altered after inclusion of potential confounders. We did not observe differential associations in subgroups defined by age, BMI, physical activity, or smoking,” the researchers reported.
In secondary analyses, they classified UPF into their components, including ultraprocessed grain foods, sweet snacks, ready-to-eat meals, fats, sauces, ultraprocessed dairy products, savory snacks, processed meat, beverages, and artificial sweeteners.
Comparing the highest with the lowest quintiles, only high intake of artificially sweetened beverages (HR, 1.37; 95% CI, 1.19-1.57; P < .001) and artificial sweeteners (HR, 1.26; 95% CI, 1.10-1.43; P < .001) was associated with greater risk of depression and after multivariable regression.
In an exploratory analysis, women who reduced their UPF intake by at least three servings per day were at lower risk of depression (strict definition: HR, 0.84; 95% CI, 0.71-0.99), compared with those with relatively stable intake in each 4-year period.
“Ultraprocessed foods have been associated with several different health outcomes which may reflect an effect on common pathways that underlie chronic conditions,” said Dr. Chan.
For example, UPF intake has been associated with chronic inflammation, which in turns leads to multiple potential adverse health effects, including depression, he explained.
There is also a link between UPF and disruption of the gut microbiome.
“This is an important potential mechanism linking ultraprocessed food to depression since there is emerging evidence that microbes in the gut have been linked with mood through their role in metabolizing and producing proteins that have activity in the brain,” Dr. Chan said.
Association, not causation
Several experts weighed in on the study results in a statement from the U.K. nonprofit organization, Science Media Centre.
Gunter Kuhnle, PhD, professor of nutrition and food science, University of Reading (England), cautioned that the study only offers information on association – not causation.
“It is very possible that people with depression change their diet and might decide to consume foods that are easier to prepare – which would often be foods considered to be ultraprocessed,” Dr. Kuhnle said.
What’s most interesting is that the association between UPF intake and depression was driven by a single factor – artificial sweeteners.
“This supports one of the main criticisms of the UPF concept, that it combines a wide range of different foods and thereby makes it difficult to identify underlying causes,” Dr. Kuhnle added.
“There are currently no data that link artificial sweetener use to mental health, despite most of them having been available for some time. It is also important to note that there are a wide range of different artificial sweeteners that are metabolized very differently and that there might be reverse causality,” Dr. Kuhnle commented.
Paul Keedwell, MBChB, PhD, consultant psychiatrist and fellow of the Royal College of Psychiatrists, said this is an “interesting and important finding, but one that raises more questions. At this stage, we cannot say how big an effect diet has on depression risk compared to other risk factors, like family history of depression, stress levels, and having a supportive social network.”
Dr. Keedwell noted that the investigators carefully excluded the possibility that the effect is mediated by obesity or lack of exercise.
“However, an important consideration is that a diet based on ready meals and artificially sweetened drinks might indicate a hectic lifestyle or one with shift work. In other words, a fast-food diet could be an indirect marker of chronic stress. Prolonged stress probably remains the main risk factor for depression,” Dr. Keedwell said.
Keith Frayn, PhD, professor emeritus of human metabolism, University of Oxford (England), noted that the relationship between artificial sweeteners and depression “stands out clearly” even after adjusting for multiple confounding factors, including BMI, smoking, and exercise.
“This adds to growing concerns about artificial sweeteners and cardiometabolic health. The link with depression needs confirmation and further research to suggest how it might be brought about,” Dr. Frayn cautioned.
The NHS II was funded by a grant from the National Cancer Institute. Dr. Chan reported receiving grants from Bayer and Zoe and personal fees from Boehringer Ingelheim, Pfizer, and Freenome outside this work. Dr. Keedwell and Dr. Kuhnle disclosed no relevant financial relationships. Dr. Frayn is an author of books on nutrition and metabolism.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Night owls have higher risk of developing type 2 diabetes
, compared with their “early bird” counterparts, according to a new study, published in Annals of Internal Medicine.
The work focused on participants’ self-assessed chronotype – an individuals’ circadian preference, or natural preference to sleep and wake up earlier or later, commonly known as being an early bird or a night owl.
Analyzing the self-reported lifestyle behaviors and sleeping habits of more than 60,000 middle-aged female nurses, researchers from Brigham and Women’s Hospital and Harvard Medical School, both in Boston, found that those with a preference for waking up later had a 72% higher risk for diabetes and were 54% more likely to have unhealthy lifestyle behaviors, compared with participants who tended to wake up earlier.
After adjustment for six lifestyle factors – diet, alcohol use, body mass index (BMI), physical activity, smoking status, and sleep duration – the association between diabetes risk and evening chronotype weakened to a 19% higher risk of developing type 2 diabetes.
In a subgroup analysis, this association was stronger among women who either had had no night shifts over the previous 2 years or had worked night shifts for less than 10 years in their careers. For nurses who had worked night shifts recently, the study found no association between evening chronotype and diabetes risk.
The participants, drawn from the Nurses’ Health Study II, were between 45 and 62 years age, with no history of cancer, cardiovascular disease, or diabetes. Researchers followed the group from 2009 until 2017.
Is there a mismatch between natural circadian rhythm and work schedule?
The authors, led by Sina Kianersi, DVM, PhD, of Harvard Medical School, Boston, suggest that their results may be linked to a mismatch between a person’s circadian rhythm and their physical and social environment – for example, if someone lives on a schedule opposite to their circadian preference.
In one 2015 study, female nurses who had worked daytime shifts for more than 10 years but had an evening chronotype had the highest diabetes risk, compared with early chronotypes (51% more likely to develop type 2 diabetes).
In a 2022 study, an evening chronotype was associated with a 30% elevated risk for type 2 diabetes. The authors speculated that circadian misalignment could be to blame – for example, being a night owl but working early morning – which can disrupt glycemic and lipid metabolism.
Previous studies have found that shorter or irregular sleep habits are associated with a higher risk of type 2 diabetes. Other studies have also found that people with an evening chronotype are more likely than early birds to have unhealthy eating habits, have lower levels of physical activity, and smoke and drink.
This new study did not find that an evening chronotype was associated with unhealthy drinking, which the authors defined as having one or more drinks per day.
In an accompanying editorial, two physicians from the Harvard T.H. Chan School of Public Health in Boston caution that the statistical design of the study limits its ability to establish causation.
“Chronotype could change later, which might correlate with lifestyle changes,” write Kehuan Lin, MS, Mingyang Song, MBBS, and Edward Giovannucci, MD. “Experimental trials are required to determine whether chronotype is a marker of unhealthy lifestyle or an independent determinant.”
They also suggest that psychological factors and the type of work being performed by the participants could be potential confounders.
The authors of the study note that their findings might not be generalizable to groups other than middle-aged White female nurses. The study population also had a relatively high level of education and were socioeconomically advantaged.
Self-reporting chronotypes with a single question could also result in misclassification and measurement error, the authors acknowledge.
The findings underscore the value of assessing an individuals’ chronotype for scheduling shift work – for example, assigning night owls to night shifts may improve their metabolic health and sleeping habits, according to the authors of the study.
“Given the importance of lifestyle modification in diabetes prevention, future research is warranted to investigate whether improving lifestyle behaviors could effectively reduce diabetes risk in persons with an evening chronotype,” the authors conclude.
The study was supported by grants from the National Institutes of Health and the European Research Council.
A version of this article first appeared on Medscape.com.
, compared with their “early bird” counterparts, according to a new study, published in Annals of Internal Medicine.
The work focused on participants’ self-assessed chronotype – an individuals’ circadian preference, or natural preference to sleep and wake up earlier or later, commonly known as being an early bird or a night owl.
Analyzing the self-reported lifestyle behaviors and sleeping habits of more than 60,000 middle-aged female nurses, researchers from Brigham and Women’s Hospital and Harvard Medical School, both in Boston, found that those with a preference for waking up later had a 72% higher risk for diabetes and were 54% more likely to have unhealthy lifestyle behaviors, compared with participants who tended to wake up earlier.
After adjustment for six lifestyle factors – diet, alcohol use, body mass index (BMI), physical activity, smoking status, and sleep duration – the association between diabetes risk and evening chronotype weakened to a 19% higher risk of developing type 2 diabetes.
In a subgroup analysis, this association was stronger among women who either had had no night shifts over the previous 2 years or had worked night shifts for less than 10 years in their careers. For nurses who had worked night shifts recently, the study found no association between evening chronotype and diabetes risk.
The participants, drawn from the Nurses’ Health Study II, were between 45 and 62 years age, with no history of cancer, cardiovascular disease, or diabetes. Researchers followed the group from 2009 until 2017.
Is there a mismatch between natural circadian rhythm and work schedule?
The authors, led by Sina Kianersi, DVM, PhD, of Harvard Medical School, Boston, suggest that their results may be linked to a mismatch between a person’s circadian rhythm and their physical and social environment – for example, if someone lives on a schedule opposite to their circadian preference.
In one 2015 study, female nurses who had worked daytime shifts for more than 10 years but had an evening chronotype had the highest diabetes risk, compared with early chronotypes (51% more likely to develop type 2 diabetes).
In a 2022 study, an evening chronotype was associated with a 30% elevated risk for type 2 diabetes. The authors speculated that circadian misalignment could be to blame – for example, being a night owl but working early morning – which can disrupt glycemic and lipid metabolism.
Previous studies have found that shorter or irregular sleep habits are associated with a higher risk of type 2 diabetes. Other studies have also found that people with an evening chronotype are more likely than early birds to have unhealthy eating habits, have lower levels of physical activity, and smoke and drink.
This new study did not find that an evening chronotype was associated with unhealthy drinking, which the authors defined as having one or more drinks per day.
In an accompanying editorial, two physicians from the Harvard T.H. Chan School of Public Health in Boston caution that the statistical design of the study limits its ability to establish causation.
“Chronotype could change later, which might correlate with lifestyle changes,” write Kehuan Lin, MS, Mingyang Song, MBBS, and Edward Giovannucci, MD. “Experimental trials are required to determine whether chronotype is a marker of unhealthy lifestyle or an independent determinant.”
They also suggest that psychological factors and the type of work being performed by the participants could be potential confounders.
The authors of the study note that their findings might not be generalizable to groups other than middle-aged White female nurses. The study population also had a relatively high level of education and were socioeconomically advantaged.
Self-reporting chronotypes with a single question could also result in misclassification and measurement error, the authors acknowledge.
The findings underscore the value of assessing an individuals’ chronotype for scheduling shift work – for example, assigning night owls to night shifts may improve their metabolic health and sleeping habits, according to the authors of the study.
“Given the importance of lifestyle modification in diabetes prevention, future research is warranted to investigate whether improving lifestyle behaviors could effectively reduce diabetes risk in persons with an evening chronotype,” the authors conclude.
The study was supported by grants from the National Institutes of Health and the European Research Council.
A version of this article first appeared on Medscape.com.
, compared with their “early bird” counterparts, according to a new study, published in Annals of Internal Medicine.
The work focused on participants’ self-assessed chronotype – an individuals’ circadian preference, or natural preference to sleep and wake up earlier or later, commonly known as being an early bird or a night owl.
Analyzing the self-reported lifestyle behaviors and sleeping habits of more than 60,000 middle-aged female nurses, researchers from Brigham and Women’s Hospital and Harvard Medical School, both in Boston, found that those with a preference for waking up later had a 72% higher risk for diabetes and were 54% more likely to have unhealthy lifestyle behaviors, compared with participants who tended to wake up earlier.
After adjustment for six lifestyle factors – diet, alcohol use, body mass index (BMI), physical activity, smoking status, and sleep duration – the association between diabetes risk and evening chronotype weakened to a 19% higher risk of developing type 2 diabetes.
In a subgroup analysis, this association was stronger among women who either had had no night shifts over the previous 2 years or had worked night shifts for less than 10 years in their careers. For nurses who had worked night shifts recently, the study found no association between evening chronotype and diabetes risk.
The participants, drawn from the Nurses’ Health Study II, were between 45 and 62 years age, with no history of cancer, cardiovascular disease, or diabetes. Researchers followed the group from 2009 until 2017.
Is there a mismatch between natural circadian rhythm and work schedule?
The authors, led by Sina Kianersi, DVM, PhD, of Harvard Medical School, Boston, suggest that their results may be linked to a mismatch between a person’s circadian rhythm and their physical and social environment – for example, if someone lives on a schedule opposite to their circadian preference.
In one 2015 study, female nurses who had worked daytime shifts for more than 10 years but had an evening chronotype had the highest diabetes risk, compared with early chronotypes (51% more likely to develop type 2 diabetes).
In a 2022 study, an evening chronotype was associated with a 30% elevated risk for type 2 diabetes. The authors speculated that circadian misalignment could be to blame – for example, being a night owl but working early morning – which can disrupt glycemic and lipid metabolism.
Previous studies have found that shorter or irregular sleep habits are associated with a higher risk of type 2 diabetes. Other studies have also found that people with an evening chronotype are more likely than early birds to have unhealthy eating habits, have lower levels of physical activity, and smoke and drink.
This new study did not find that an evening chronotype was associated with unhealthy drinking, which the authors defined as having one or more drinks per day.
In an accompanying editorial, two physicians from the Harvard T.H. Chan School of Public Health in Boston caution that the statistical design of the study limits its ability to establish causation.
“Chronotype could change later, which might correlate with lifestyle changes,” write Kehuan Lin, MS, Mingyang Song, MBBS, and Edward Giovannucci, MD. “Experimental trials are required to determine whether chronotype is a marker of unhealthy lifestyle or an independent determinant.”
They also suggest that psychological factors and the type of work being performed by the participants could be potential confounders.
The authors of the study note that their findings might not be generalizable to groups other than middle-aged White female nurses. The study population also had a relatively high level of education and were socioeconomically advantaged.
Self-reporting chronotypes with a single question could also result in misclassification and measurement error, the authors acknowledge.
The findings underscore the value of assessing an individuals’ chronotype for scheduling shift work – for example, assigning night owls to night shifts may improve their metabolic health and sleeping habits, according to the authors of the study.
“Given the importance of lifestyle modification in diabetes prevention, future research is warranted to investigate whether improving lifestyle behaviors could effectively reduce diabetes risk in persons with an evening chronotype,” the authors conclude.
The study was supported by grants from the National Institutes of Health and the European Research Council.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
Gender-affirming surgeries nearly tripled between 2016 and 2019: Study
a new study published in JAMA Network Open found.
Breast and chest surgeries were the most common procedures performed, and the number of surgical procedures carried out increased with age. The researchers said that, in addition to legal shifts, the established safety of the surgeries and resulting increase in quality of life may also help explain the increase.
“The point of this is to raise awareness and to really document the patterns of care in the United States,” said Jason Wright, MD, an associate professor at Columbia University, New York. “We hope that people understand that these procedures are being performed more commonly and they’re out there.”
A study published in 2022 in JAMA Pediatrics found that the number of chest reconstruction surgeries among U.S. adolescents rose fourfold between 2016 and 2019.
The new study included data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. More than 48,000 patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified. Age ranges were grouped as 12-18 (7.7%), 19-30 (52.3%), and 31-40 (21.8%).
The number of gender-affirming procedures rose from 4,552 in 2016 to a peak of 13,011 in 2019. (A slight decline to 12,818 procedures in 2020 was attributed to the COVID-19 pandemic.) The surgeries were grouped into three categories: breast and chest procedures, which occurred in 56.6% of patients; genital reconstructive surgeries (35.1%), and other facial cosmetic procedures (13.9%).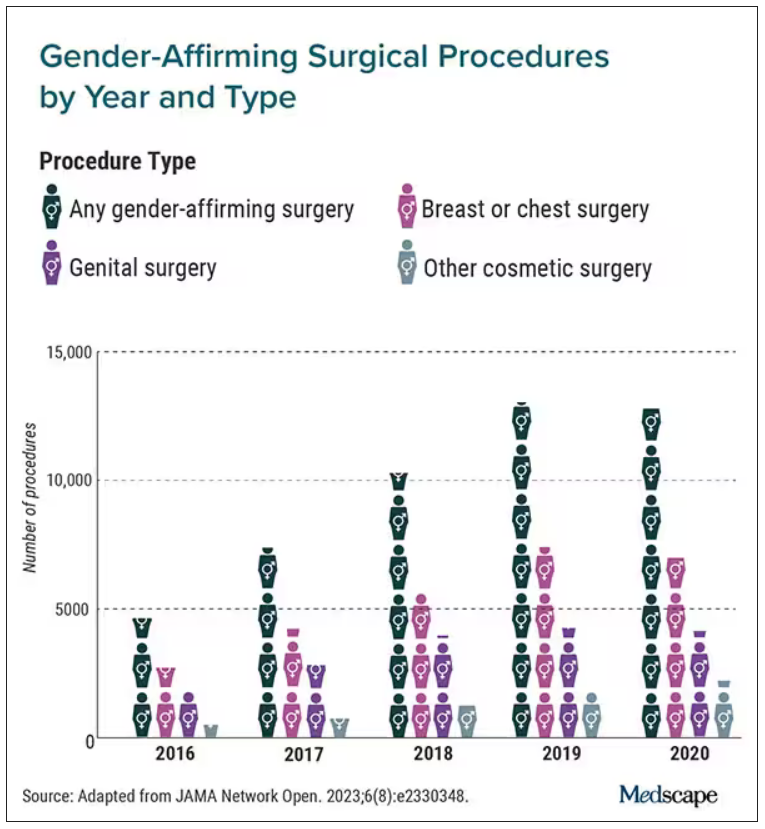
“We really wanted to try to make this as representative as we could,” Dr. Wright said. “I think this is really the best estimates that are available to date.”
Chest and breast procedures made up a higher percentage of surgeries in younger patients, while genital surgical procedures made up a higher percentage in older patients. For example, patients aged 19-30 made up 59.1% of breast or chest surgeries and 44.2% of genital surgeries. However, those aged 31-40 accounted for 26.2% of genital surgeries and 18.1% of breast or chest surgeries. For ages 41-50, the spread was more than double, accounting for 12.8% of genital surgeries and only 6.1% of breast or chest surgeries, according to the researchers.
Undocumented uptick
In addition to more inclusive health insurance, Dr. Wright said the increase in these procedures can also be attributed to studies showing their safety and the long-term association with high patient satisfaction.
Kevin Wang, MD, medical director of Providence–Swedish Health Services’ LGBTQIA+ program in Seattle, agreed that changes in health insurance coverage for gender-affirming surgery likely account in part for their increase. But he added that more clinicians are performing these procedures.
He said gender-affirming surgeries improve quality of life for the people who undergo them. The American Academy of Pediatrics has said it would be conducting a thorough review of the effects of transgender care on youth. A 2018 policy statement from the group said transgender youth should “have access to comprehensive, gender-affirming, and developmentally appropriate health care that is provided in a safe and inclusive clinical space.”
Dr. Wright cited several limitations to his group’s study that may result in the undercapture of transgender individuals and gender-affirming surgery; in particular, while the study captured inpatient and ambulatory surgical procedures in large, nationwide datasets, a small number of the procedures could have been performed in other settings.
Guiding a patient through gender-affirming care and surgical procedures can be an arduous process, including understanding their goals, using hormone therapy, and making referrals to specialists. Dr. Wang said he works to maximize his patients’ physical, mental, and emotional health, and helps them understand the risks.
He cited the double standard of a cisgender woman wanting breast augmentation without justification, but someone who identifies as transgender has many more boxes to check – for example, seeing a behavior health specialist to demonstrate they understand the risks and securing a letter of support from their primary care physician to undergo a similar procedure.
“It’s just interesting how the transgender community has to jump through so many more barriers and hoops for affirming, lifesaving procedures where you have other people who are doing it for aesthetic purposes and do not require any type of authorization,” Dr. Wang said.
Dr. Wright said he hopes the findings call attention to the need for more professionals working in the gender-affirming care field.
“I think for the medical community, it’s important to raise the idea that these procedures are becoming more common,” Dr. Wright said. “We are going to need specialists who have expertise in transgender care and surgeons who have the ability to perform these operations. Hopefully, this sheds light on the resources that are going to be required to care for these patients going forward.”
Dr. Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
a new study published in JAMA Network Open found.
Breast and chest surgeries were the most common procedures performed, and the number of surgical procedures carried out increased with age. The researchers said that, in addition to legal shifts, the established safety of the surgeries and resulting increase in quality of life may also help explain the increase.
“The point of this is to raise awareness and to really document the patterns of care in the United States,” said Jason Wright, MD, an associate professor at Columbia University, New York. “We hope that people understand that these procedures are being performed more commonly and they’re out there.”
A study published in 2022 in JAMA Pediatrics found that the number of chest reconstruction surgeries among U.S. adolescents rose fourfold between 2016 and 2019.
The new study included data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. More than 48,000 patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified. Age ranges were grouped as 12-18 (7.7%), 19-30 (52.3%), and 31-40 (21.8%).
The number of gender-affirming procedures rose from 4,552 in 2016 to a peak of 13,011 in 2019. (A slight decline to 12,818 procedures in 2020 was attributed to the COVID-19 pandemic.) The surgeries were grouped into three categories: breast and chest procedures, which occurred in 56.6% of patients; genital reconstructive surgeries (35.1%), and other facial cosmetic procedures (13.9%).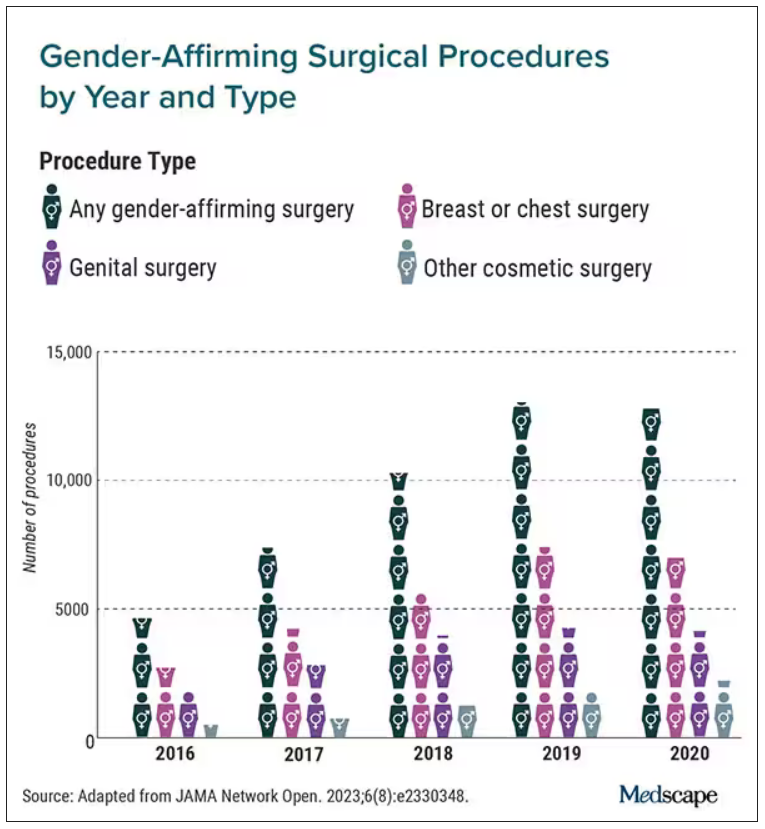
“We really wanted to try to make this as representative as we could,” Dr. Wright said. “I think this is really the best estimates that are available to date.”
Chest and breast procedures made up a higher percentage of surgeries in younger patients, while genital surgical procedures made up a higher percentage in older patients. For example, patients aged 19-30 made up 59.1% of breast or chest surgeries and 44.2% of genital surgeries. However, those aged 31-40 accounted for 26.2% of genital surgeries and 18.1% of breast or chest surgeries. For ages 41-50, the spread was more than double, accounting for 12.8% of genital surgeries and only 6.1% of breast or chest surgeries, according to the researchers.
Undocumented uptick
In addition to more inclusive health insurance, Dr. Wright said the increase in these procedures can also be attributed to studies showing their safety and the long-term association with high patient satisfaction.
Kevin Wang, MD, medical director of Providence–Swedish Health Services’ LGBTQIA+ program in Seattle, agreed that changes in health insurance coverage for gender-affirming surgery likely account in part for their increase. But he added that more clinicians are performing these procedures.
He said gender-affirming surgeries improve quality of life for the people who undergo them. The American Academy of Pediatrics has said it would be conducting a thorough review of the effects of transgender care on youth. A 2018 policy statement from the group said transgender youth should “have access to comprehensive, gender-affirming, and developmentally appropriate health care that is provided in a safe and inclusive clinical space.”
Dr. Wright cited several limitations to his group’s study that may result in the undercapture of transgender individuals and gender-affirming surgery; in particular, while the study captured inpatient and ambulatory surgical procedures in large, nationwide datasets, a small number of the procedures could have been performed in other settings.
Guiding a patient through gender-affirming care and surgical procedures can be an arduous process, including understanding their goals, using hormone therapy, and making referrals to specialists. Dr. Wang said he works to maximize his patients’ physical, mental, and emotional health, and helps them understand the risks.
He cited the double standard of a cisgender woman wanting breast augmentation without justification, but someone who identifies as transgender has many more boxes to check – for example, seeing a behavior health specialist to demonstrate they understand the risks and securing a letter of support from their primary care physician to undergo a similar procedure.
“It’s just interesting how the transgender community has to jump through so many more barriers and hoops for affirming, lifesaving procedures where you have other people who are doing it for aesthetic purposes and do not require any type of authorization,” Dr. Wang said.
Dr. Wright said he hopes the findings call attention to the need for more professionals working in the gender-affirming care field.
“I think for the medical community, it’s important to raise the idea that these procedures are becoming more common,” Dr. Wright said. “We are going to need specialists who have expertise in transgender care and surgeons who have the ability to perform these operations. Hopefully, this sheds light on the resources that are going to be required to care for these patients going forward.”
Dr. Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
a new study published in JAMA Network Open found.
Breast and chest surgeries were the most common procedures performed, and the number of surgical procedures carried out increased with age. The researchers said that, in addition to legal shifts, the established safety of the surgeries and resulting increase in quality of life may also help explain the increase.
“The point of this is to raise awareness and to really document the patterns of care in the United States,” said Jason Wright, MD, an associate professor at Columbia University, New York. “We hope that people understand that these procedures are being performed more commonly and they’re out there.”
A study published in 2022 in JAMA Pediatrics found that the number of chest reconstruction surgeries among U.S. adolescents rose fourfold between 2016 and 2019.
The new study included data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. More than 48,000 patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified. Age ranges were grouped as 12-18 (7.7%), 19-30 (52.3%), and 31-40 (21.8%).
The number of gender-affirming procedures rose from 4,552 in 2016 to a peak of 13,011 in 2019. (A slight decline to 12,818 procedures in 2020 was attributed to the COVID-19 pandemic.) The surgeries were grouped into three categories: breast and chest procedures, which occurred in 56.6% of patients; genital reconstructive surgeries (35.1%), and other facial cosmetic procedures (13.9%).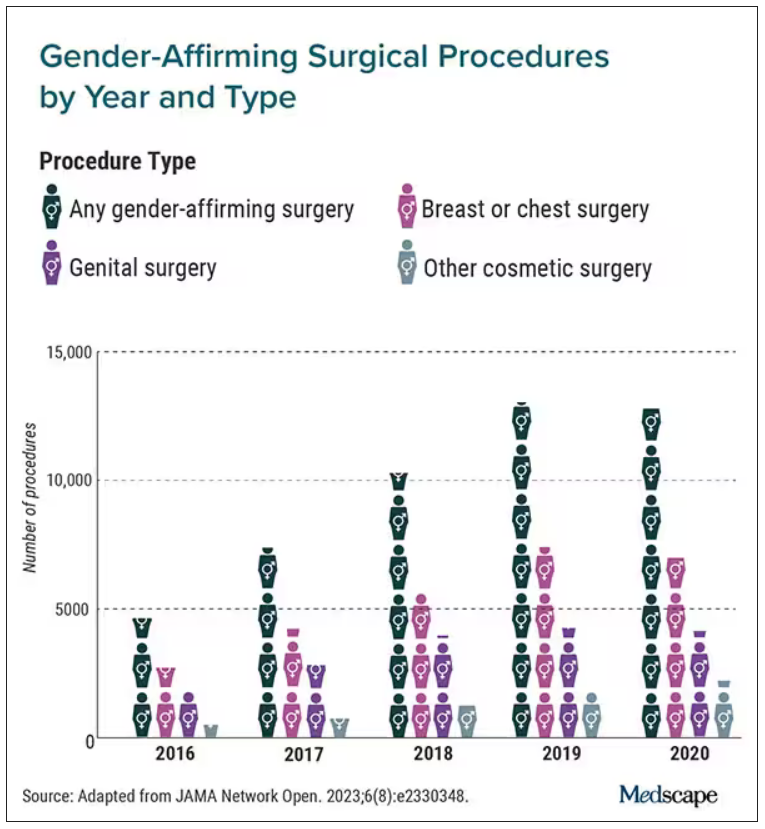
“We really wanted to try to make this as representative as we could,” Dr. Wright said. “I think this is really the best estimates that are available to date.”
Chest and breast procedures made up a higher percentage of surgeries in younger patients, while genital surgical procedures made up a higher percentage in older patients. For example, patients aged 19-30 made up 59.1% of breast or chest surgeries and 44.2% of genital surgeries. However, those aged 31-40 accounted for 26.2% of genital surgeries and 18.1% of breast or chest surgeries. For ages 41-50, the spread was more than double, accounting for 12.8% of genital surgeries and only 6.1% of breast or chest surgeries, according to the researchers.
Undocumented uptick
In addition to more inclusive health insurance, Dr. Wright said the increase in these procedures can also be attributed to studies showing their safety and the long-term association with high patient satisfaction.
Kevin Wang, MD, medical director of Providence–Swedish Health Services’ LGBTQIA+ program in Seattle, agreed that changes in health insurance coverage for gender-affirming surgery likely account in part for their increase. But he added that more clinicians are performing these procedures.
He said gender-affirming surgeries improve quality of life for the people who undergo them. The American Academy of Pediatrics has said it would be conducting a thorough review of the effects of transgender care on youth. A 2018 policy statement from the group said transgender youth should “have access to comprehensive, gender-affirming, and developmentally appropriate health care that is provided in a safe and inclusive clinical space.”
Dr. Wright cited several limitations to his group’s study that may result in the undercapture of transgender individuals and gender-affirming surgery; in particular, while the study captured inpatient and ambulatory surgical procedures in large, nationwide datasets, a small number of the procedures could have been performed in other settings.
Guiding a patient through gender-affirming care and surgical procedures can be an arduous process, including understanding their goals, using hormone therapy, and making referrals to specialists. Dr. Wang said he works to maximize his patients’ physical, mental, and emotional health, and helps them understand the risks.
He cited the double standard of a cisgender woman wanting breast augmentation without justification, but someone who identifies as transgender has many more boxes to check – for example, seeing a behavior health specialist to demonstrate they understand the risks and securing a letter of support from their primary care physician to undergo a similar procedure.
“It’s just interesting how the transgender community has to jump through so many more barriers and hoops for affirming, lifesaving procedures where you have other people who are doing it for aesthetic purposes and do not require any type of authorization,” Dr. Wang said.
Dr. Wright said he hopes the findings call attention to the need for more professionals working in the gender-affirming care field.
“I think for the medical community, it’s important to raise the idea that these procedures are becoming more common,” Dr. Wright said. “We are going to need specialists who have expertise in transgender care and surgeons who have the ability to perform these operations. Hopefully, this sheds light on the resources that are going to be required to care for these patients going forward.”
Dr. Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
FDA okays first-ever new drug for rare bone disorder
Affecting roughly 400 people in the United States and 900 worldwide, FOP is an autosomal dominant condition in which bone develops in soft connective tissue areas of the body where it isn’t normally present (heterotopic ossification), such as the ligaments, tendons, and skeletal muscles. This leads to severe restriction in mobility and function, to the point that people lose the ability to feed or care for themselves. Most are completely disabled by age 30 years and median life expectancy is 56 years, with death often caused by bone formation around the rib cage restricting respiration.
“As a clinician caring for patients with FOP, I personally see the daily challenges and stresses that our patients and their families must contend with ... since the accumulation of heterotopic ossification in FOP is progressive, irreversible, and life altering. This medication is an important treatment option for our FOP community,” said endocrinologist Edward Hsiao, MD, professor of medicine at the University of California, San Francisco, in a statement from Ipsen.
Taken orally, palovarotene selectively targets the gamma subtype of retinoic acid receptors that regulate skeletal development and ectopic bone in the retinoid signaling pathway. The drug mediates interactions between these receptors, growth factors, and proteins within that pathway to reduce new abnormal bone formation.
It is now FDA approved for the treatment of FOP in female patients aged 8 years or older and male patients aged 10 years or older. The recommended dosing is 5 mg daily or weight-based equivalent for pediatric patients under 14 years of age, which can be modified or increased for flare-up symptoms. It is contraindicated during pregnancy.
The FDA approval was based on 18-month data from the phase 3, multicenter, open-label MOVE trial that included 107 adult and pediatric patients, over 10% of the world’s population with FOP. All received oral palovarotene and were compared with untreated individuals from a prior natural history study of the condition. The drug reduced annualized heterotopic ossification volume by 54%.
Side effects were typical of those seen with other systemic retinoid drugs, including mucocutaneous events such as dryness of the skin and mucous membranes, alopecia, drug eruption, rash, and pruritus, and musculoskeletal events, such as arthralgia and premature growth plate closure in growing children.
According to Dr. Hsiao, who was a MOVE investigator, the study “showed that Sohonos can decrease new heterotopic ossification, and that palovarotene can be tolerated by many patients with FOP. Sohonos is not for everyone. As with all medicines there are risks in this case especially for young children who may develop early growth plate closure. In addition, Sohonos has the same side effects as other retinoids.”
The FDA approval of palovarotene follows its rejection for marketing authorization in the European Union in July 2023.
Reached for comment, an Ipsen spokesperson said in an interview: “We reached the end of the regulatory process in the European Union for Sohonos and are disappointed the European Commission decided not to approved palovarotene for people with FOP in Europe.”
The company is developing another drug, fidrisertib, for treating FOP. A pivotal phase 2 trial for that drug is now recruiting patients. Asked where Ipsen might try to market fidrisertib, the spokesperson replied:“At this point, our focus is on the completion of the pivotal trial.”
Meanwhile, in the United States, the FOP community is celebrating the palovarotene approval. In a statement, Michelle Davis, executive director of the International Fibrodysplasia Ossificans Progressiva Association, said: “FOP is life altering to the individuals diagnosed and their families. There’s not a day that goes by where those impacted don’t worry about the debilitating physical pain of muscle that is replaced by bone, another joint locking, or the relentless emotional toll of losing the ability to do an activity they love, or hold a loved one close. ... The first treatment for FOP has been proven to reduce the volume of new abnormal bone growth, which may result in better health outcomes for people living with FOP.”
Ipsen is offering a patient support program to assist with education, coverage, and reimbursement (1-866-435-5677).
A version of this article appeared on Medscape.com.
Affecting roughly 400 people in the United States and 900 worldwide, FOP is an autosomal dominant condition in which bone develops in soft connective tissue areas of the body where it isn’t normally present (heterotopic ossification), such as the ligaments, tendons, and skeletal muscles. This leads to severe restriction in mobility and function, to the point that people lose the ability to feed or care for themselves. Most are completely disabled by age 30 years and median life expectancy is 56 years, with death often caused by bone formation around the rib cage restricting respiration.
“As a clinician caring for patients with FOP, I personally see the daily challenges and stresses that our patients and their families must contend with ... since the accumulation of heterotopic ossification in FOP is progressive, irreversible, and life altering. This medication is an important treatment option for our FOP community,” said endocrinologist Edward Hsiao, MD, professor of medicine at the University of California, San Francisco, in a statement from Ipsen.
Taken orally, palovarotene selectively targets the gamma subtype of retinoic acid receptors that regulate skeletal development and ectopic bone in the retinoid signaling pathway. The drug mediates interactions between these receptors, growth factors, and proteins within that pathway to reduce new abnormal bone formation.
It is now FDA approved for the treatment of FOP in female patients aged 8 years or older and male patients aged 10 years or older. The recommended dosing is 5 mg daily or weight-based equivalent for pediatric patients under 14 years of age, which can be modified or increased for flare-up symptoms. It is contraindicated during pregnancy.
The FDA approval was based on 18-month data from the phase 3, multicenter, open-label MOVE trial that included 107 adult and pediatric patients, over 10% of the world’s population with FOP. All received oral palovarotene and were compared with untreated individuals from a prior natural history study of the condition. The drug reduced annualized heterotopic ossification volume by 54%.
Side effects were typical of those seen with other systemic retinoid drugs, including mucocutaneous events such as dryness of the skin and mucous membranes, alopecia, drug eruption, rash, and pruritus, and musculoskeletal events, such as arthralgia and premature growth plate closure in growing children.
According to Dr. Hsiao, who was a MOVE investigator, the study “showed that Sohonos can decrease new heterotopic ossification, and that palovarotene can be tolerated by many patients with FOP. Sohonos is not for everyone. As with all medicines there are risks in this case especially for young children who may develop early growth plate closure. In addition, Sohonos has the same side effects as other retinoids.”
The FDA approval of palovarotene follows its rejection for marketing authorization in the European Union in July 2023.
Reached for comment, an Ipsen spokesperson said in an interview: “We reached the end of the regulatory process in the European Union for Sohonos and are disappointed the European Commission decided not to approved palovarotene for people with FOP in Europe.”
The company is developing another drug, fidrisertib, for treating FOP. A pivotal phase 2 trial for that drug is now recruiting patients. Asked where Ipsen might try to market fidrisertib, the spokesperson replied:“At this point, our focus is on the completion of the pivotal trial.”
Meanwhile, in the United States, the FOP community is celebrating the palovarotene approval. In a statement, Michelle Davis, executive director of the International Fibrodysplasia Ossificans Progressiva Association, said: “FOP is life altering to the individuals diagnosed and their families. There’s not a day that goes by where those impacted don’t worry about the debilitating physical pain of muscle that is replaced by bone, another joint locking, or the relentless emotional toll of losing the ability to do an activity they love, or hold a loved one close. ... The first treatment for FOP has been proven to reduce the volume of new abnormal bone growth, which may result in better health outcomes for people living with FOP.”
Ipsen is offering a patient support program to assist with education, coverage, and reimbursement (1-866-435-5677).
A version of this article appeared on Medscape.com.
Affecting roughly 400 people in the United States and 900 worldwide, FOP is an autosomal dominant condition in which bone develops in soft connective tissue areas of the body where it isn’t normally present (heterotopic ossification), such as the ligaments, tendons, and skeletal muscles. This leads to severe restriction in mobility and function, to the point that people lose the ability to feed or care for themselves. Most are completely disabled by age 30 years and median life expectancy is 56 years, with death often caused by bone formation around the rib cage restricting respiration.
“As a clinician caring for patients with FOP, I personally see the daily challenges and stresses that our patients and their families must contend with ... since the accumulation of heterotopic ossification in FOP is progressive, irreversible, and life altering. This medication is an important treatment option for our FOP community,” said endocrinologist Edward Hsiao, MD, professor of medicine at the University of California, San Francisco, in a statement from Ipsen.
Taken orally, palovarotene selectively targets the gamma subtype of retinoic acid receptors that regulate skeletal development and ectopic bone in the retinoid signaling pathway. The drug mediates interactions between these receptors, growth factors, and proteins within that pathway to reduce new abnormal bone formation.
It is now FDA approved for the treatment of FOP in female patients aged 8 years or older and male patients aged 10 years or older. The recommended dosing is 5 mg daily or weight-based equivalent for pediatric patients under 14 years of age, which can be modified or increased for flare-up symptoms. It is contraindicated during pregnancy.
The FDA approval was based on 18-month data from the phase 3, multicenter, open-label MOVE trial that included 107 adult and pediatric patients, over 10% of the world’s population with FOP. All received oral palovarotene and were compared with untreated individuals from a prior natural history study of the condition. The drug reduced annualized heterotopic ossification volume by 54%.
Side effects were typical of those seen with other systemic retinoid drugs, including mucocutaneous events such as dryness of the skin and mucous membranes, alopecia, drug eruption, rash, and pruritus, and musculoskeletal events, such as arthralgia and premature growth plate closure in growing children.
According to Dr. Hsiao, who was a MOVE investigator, the study “showed that Sohonos can decrease new heterotopic ossification, and that palovarotene can be tolerated by many patients with FOP. Sohonos is not for everyone. As with all medicines there are risks in this case especially for young children who may develop early growth plate closure. In addition, Sohonos has the same side effects as other retinoids.”
The FDA approval of palovarotene follows its rejection for marketing authorization in the European Union in July 2023.
Reached for comment, an Ipsen spokesperson said in an interview: “We reached the end of the regulatory process in the European Union for Sohonos and are disappointed the European Commission decided not to approved palovarotene for people with FOP in Europe.”
The company is developing another drug, fidrisertib, for treating FOP. A pivotal phase 2 trial for that drug is now recruiting patients. Asked where Ipsen might try to market fidrisertib, the spokesperson replied:“At this point, our focus is on the completion of the pivotal trial.”
Meanwhile, in the United States, the FOP community is celebrating the palovarotene approval. In a statement, Michelle Davis, executive director of the International Fibrodysplasia Ossificans Progressiva Association, said: “FOP is life altering to the individuals diagnosed and their families. There’s not a day that goes by where those impacted don’t worry about the debilitating physical pain of muscle that is replaced by bone, another joint locking, or the relentless emotional toll of losing the ability to do an activity they love, or hold a loved one close. ... The first treatment for FOP has been proven to reduce the volume of new abnormal bone growth, which may result in better health outcomes for people living with FOP.”
Ipsen is offering a patient support program to assist with education, coverage, and reimbursement (1-866-435-5677).
A version of this article appeared on Medscape.com.
Skin reactions common at insulin pump infusion sites
new research suggests.
Insulin pump use is increasingly common, but many patients experience infusion-site failure that in some cases leads to discontinuation. In a novel investigation, researchers at the University of Washington, Seattle, used biopsies and noninvasive imaging to compare insulin pump sites with control sites in 30 patients. Several differences were found at pump sites in comparison with control sites, including fibrosis, inflammation, eosinophils, and increased vessel density.
“These findings support allergic sensitization as a potentially common reaction at [insulin pump] sites. The leading candidates causing this include insulin preservatives, plastic materials, and adhesive glue used in device manufacturing,” wrote Andrea Kalus, MD, of the university’s dermatology division, and colleagues. The findings were published recently in Diabetes Care.
The inflammatory response, they wrote, “may result in tissue changes responsible for the infusion-site failures seen frequently in clinical practice.”
Such infusion site problems represent an “Achilles heel” of these otherwise highly beneficial devices, lead author Irl Hirsch, MD, professor of medicine in the division of metabolism, endocrinology, and nutrition, said in a statement. “It doesn’t really matter how good the technology is. We still don’t understand what is happening with the infusion sites, much less to [be able to] fix it.”
Significant differences between pump and nonpump sites
In the cross-sectional study, Dr. Kalus and colleagues used noninvasive optical coherence tomography (OCT) immediately prior to performing punch biopsies at three sites: the site currently in active use, the “recovery site” used 3-5 days prior to the procedures, and control sites never used for pump infusion. Punch biopsies were also performed at those sites.
The mean age of the patients was 48.3 years, the mean diabetes duration was 30.4 years, and the mean duration of pump use was 15.8 years. Nearly all patients (93.3%) reported itchiness at the site, and 76.7% reported skin redness.
Of the 25 patients for whom OCT imaging was successful, statistical analysis showed significant differences in vascular area density and the optical attenuation coefficient, a surrogate for skin inflammation, between the pump and control sites and between recovery sites and current pump sites. The greater vessel density is likely a result of injury and repair related to catheter insertion, the authors said.
In the biopsy samples, both current and recovery sites showed increased fibrosis, fibrin, inflammation, fat necrosis, vascularity, and eosinophils, compared with the control sites, but no significant differences were found between current and recovery sites.
Eosinophils: ‘The most surprising histologic finding’
Eosinophils were found in 73% of skin biopsy specimens from current sites and in 75% of specimens from recovery sites, compared with none from the control sites (for both, P < .01). In all study participants, eosinophils were found in at least one current and/or recovery infusion site deep in the dermis near the interface with fat. The number of eosinophils ranged from 0 to 31 per high-power field, with a median of 4.
The number of eosinophils didn’t vary by type of insulin or brand of pump, but higher counts were seen in those who had used pumps for less than 10 years, compared with more than 20 years (P = .02).
The prevalence and degree of eosinophils were “the most surprising histologic finding,” the authors wrote, adding that “eosinophils are not typically present as a component of resident inflammatory cells in the skin.”
While eosinophils may be present in normal wound healing, “the absolute number and density of eosinophil in these samples support a delayed-type hypersensitivity response, which is typically observed between 2 and 7 days after exposure to an allergen. ... Eosinophils are often correlated with symptoms of itchiness and likely explain the high percentage of participants who reported itchiness in this study,” Dr. Kalus and colleagues wrote.
Correlation found between inflammation and glycemic control
All participants used the Dexcom G6 continuous glucose monitor as part of their usual care. Inflammation scores were positively correlated with insulin dose (P = .009) and were negatively correlated with time in range (P = .01).
No other OCT or biopsy findings differed by duration of pump use, previous use of animal insulin, or type of insulin.
The reason for these findings is unclear, Dr. Hirsch said. “How much was the catheter or the insulin causing the irritation around the sites? How much was it from the preservatives, or is this because of the insulin pump itself? All these questions need to be answered in future studies. ... The real goal of all of this is to minimize skin damage and improve the experience for our patients.”
The study was funded by the Leona M. and Harry B. Helmsley Charitable Trust. Dr. Hirsch reported grants and contracts from Insulet, Medtronic, and Dexcom outside the submitted work; consulting fees from Abbott Diabetes Care, Lifescan, and Hagar outside the submitted work; and honoraria for lectures, presentations, participation on speaker’s bureaus, manuscript writing, or educational events as section editor for UpToDate outside the submitted work. Dr. Kalus has no disclosures.
A version of this article first appeared on Medscape.com.
new research suggests.
Insulin pump use is increasingly common, but many patients experience infusion-site failure that in some cases leads to discontinuation. In a novel investigation, researchers at the University of Washington, Seattle, used biopsies and noninvasive imaging to compare insulin pump sites with control sites in 30 patients. Several differences were found at pump sites in comparison with control sites, including fibrosis, inflammation, eosinophils, and increased vessel density.
“These findings support allergic sensitization as a potentially common reaction at [insulin pump] sites. The leading candidates causing this include insulin preservatives, plastic materials, and adhesive glue used in device manufacturing,” wrote Andrea Kalus, MD, of the university’s dermatology division, and colleagues. The findings were published recently in Diabetes Care.
The inflammatory response, they wrote, “may result in tissue changes responsible for the infusion-site failures seen frequently in clinical practice.”
Such infusion site problems represent an “Achilles heel” of these otherwise highly beneficial devices, lead author Irl Hirsch, MD, professor of medicine in the division of metabolism, endocrinology, and nutrition, said in a statement. “It doesn’t really matter how good the technology is. We still don’t understand what is happening with the infusion sites, much less to [be able to] fix it.”
Significant differences between pump and nonpump sites
In the cross-sectional study, Dr. Kalus and colleagues used noninvasive optical coherence tomography (OCT) immediately prior to performing punch biopsies at three sites: the site currently in active use, the “recovery site” used 3-5 days prior to the procedures, and control sites never used for pump infusion. Punch biopsies were also performed at those sites.
The mean age of the patients was 48.3 years, the mean diabetes duration was 30.4 years, and the mean duration of pump use was 15.8 years. Nearly all patients (93.3%) reported itchiness at the site, and 76.7% reported skin redness.
Of the 25 patients for whom OCT imaging was successful, statistical analysis showed significant differences in vascular area density and the optical attenuation coefficient, a surrogate for skin inflammation, between the pump and control sites and between recovery sites and current pump sites. The greater vessel density is likely a result of injury and repair related to catheter insertion, the authors said.
In the biopsy samples, both current and recovery sites showed increased fibrosis, fibrin, inflammation, fat necrosis, vascularity, and eosinophils, compared with the control sites, but no significant differences were found between current and recovery sites.
Eosinophils: ‘The most surprising histologic finding’
Eosinophils were found in 73% of skin biopsy specimens from current sites and in 75% of specimens from recovery sites, compared with none from the control sites (for both, P < .01). In all study participants, eosinophils were found in at least one current and/or recovery infusion site deep in the dermis near the interface with fat. The number of eosinophils ranged from 0 to 31 per high-power field, with a median of 4.
The number of eosinophils didn’t vary by type of insulin or brand of pump, but higher counts were seen in those who had used pumps for less than 10 years, compared with more than 20 years (P = .02).
The prevalence and degree of eosinophils were “the most surprising histologic finding,” the authors wrote, adding that “eosinophils are not typically present as a component of resident inflammatory cells in the skin.”
While eosinophils may be present in normal wound healing, “the absolute number and density of eosinophil in these samples support a delayed-type hypersensitivity response, which is typically observed between 2 and 7 days after exposure to an allergen. ... Eosinophils are often correlated with symptoms of itchiness and likely explain the high percentage of participants who reported itchiness in this study,” Dr. Kalus and colleagues wrote.
Correlation found between inflammation and glycemic control
All participants used the Dexcom G6 continuous glucose monitor as part of their usual care. Inflammation scores were positively correlated with insulin dose (P = .009) and were negatively correlated with time in range (P = .01).
No other OCT or biopsy findings differed by duration of pump use, previous use of animal insulin, or type of insulin.
The reason for these findings is unclear, Dr. Hirsch said. “How much was the catheter or the insulin causing the irritation around the sites? How much was it from the preservatives, or is this because of the insulin pump itself? All these questions need to be answered in future studies. ... The real goal of all of this is to minimize skin damage and improve the experience for our patients.”
The study was funded by the Leona M. and Harry B. Helmsley Charitable Trust. Dr. Hirsch reported grants and contracts from Insulet, Medtronic, and Dexcom outside the submitted work; consulting fees from Abbott Diabetes Care, Lifescan, and Hagar outside the submitted work; and honoraria for lectures, presentations, participation on speaker’s bureaus, manuscript writing, or educational events as section editor for UpToDate outside the submitted work. Dr. Kalus has no disclosures.
A version of this article first appeared on Medscape.com.
new research suggests.
Insulin pump use is increasingly common, but many patients experience infusion-site failure that in some cases leads to discontinuation. In a novel investigation, researchers at the University of Washington, Seattle, used biopsies and noninvasive imaging to compare insulin pump sites with control sites in 30 patients. Several differences were found at pump sites in comparison with control sites, including fibrosis, inflammation, eosinophils, and increased vessel density.
“These findings support allergic sensitization as a potentially common reaction at [insulin pump] sites. The leading candidates causing this include insulin preservatives, plastic materials, and adhesive glue used in device manufacturing,” wrote Andrea Kalus, MD, of the university’s dermatology division, and colleagues. The findings were published recently in Diabetes Care.
The inflammatory response, they wrote, “may result in tissue changes responsible for the infusion-site failures seen frequently in clinical practice.”
Such infusion site problems represent an “Achilles heel” of these otherwise highly beneficial devices, lead author Irl Hirsch, MD, professor of medicine in the division of metabolism, endocrinology, and nutrition, said in a statement. “It doesn’t really matter how good the technology is. We still don’t understand what is happening with the infusion sites, much less to [be able to] fix it.”
Significant differences between pump and nonpump sites
In the cross-sectional study, Dr. Kalus and colleagues used noninvasive optical coherence tomography (OCT) immediately prior to performing punch biopsies at three sites: the site currently in active use, the “recovery site” used 3-5 days prior to the procedures, and control sites never used for pump infusion. Punch biopsies were also performed at those sites.
The mean age of the patients was 48.3 years, the mean diabetes duration was 30.4 years, and the mean duration of pump use was 15.8 years. Nearly all patients (93.3%) reported itchiness at the site, and 76.7% reported skin redness.
Of the 25 patients for whom OCT imaging was successful, statistical analysis showed significant differences in vascular area density and the optical attenuation coefficient, a surrogate for skin inflammation, between the pump and control sites and between recovery sites and current pump sites. The greater vessel density is likely a result of injury and repair related to catheter insertion, the authors said.
In the biopsy samples, both current and recovery sites showed increased fibrosis, fibrin, inflammation, fat necrosis, vascularity, and eosinophils, compared with the control sites, but no significant differences were found between current and recovery sites.
Eosinophils: ‘The most surprising histologic finding’
Eosinophils were found in 73% of skin biopsy specimens from current sites and in 75% of specimens from recovery sites, compared with none from the control sites (for both, P < .01). In all study participants, eosinophils were found in at least one current and/or recovery infusion site deep in the dermis near the interface with fat. The number of eosinophils ranged from 0 to 31 per high-power field, with a median of 4.
The number of eosinophils didn’t vary by type of insulin or brand of pump, but higher counts were seen in those who had used pumps for less than 10 years, compared with more than 20 years (P = .02).
The prevalence and degree of eosinophils were “the most surprising histologic finding,” the authors wrote, adding that “eosinophils are not typically present as a component of resident inflammatory cells in the skin.”
While eosinophils may be present in normal wound healing, “the absolute number and density of eosinophil in these samples support a delayed-type hypersensitivity response, which is typically observed between 2 and 7 days after exposure to an allergen. ... Eosinophils are often correlated with symptoms of itchiness and likely explain the high percentage of participants who reported itchiness in this study,” Dr. Kalus and colleagues wrote.
Correlation found between inflammation and glycemic control
All participants used the Dexcom G6 continuous glucose monitor as part of their usual care. Inflammation scores were positively correlated with insulin dose (P = .009) and were negatively correlated with time in range (P = .01).
No other OCT or biopsy findings differed by duration of pump use, previous use of animal insulin, or type of insulin.
The reason for these findings is unclear, Dr. Hirsch said. “How much was the catheter or the insulin causing the irritation around the sites? How much was it from the preservatives, or is this because of the insulin pump itself? All these questions need to be answered in future studies. ... The real goal of all of this is to minimize skin damage and improve the experience for our patients.”
The study was funded by the Leona M. and Harry B. Helmsley Charitable Trust. Dr. Hirsch reported grants and contracts from Insulet, Medtronic, and Dexcom outside the submitted work; consulting fees from Abbott Diabetes Care, Lifescan, and Hagar outside the submitted work; and honoraria for lectures, presentations, participation on speaker’s bureaus, manuscript writing, or educational events as section editor for UpToDate outside the submitted work. Dr. Kalus has no disclosures.
A version of this article first appeared on Medscape.com.
FROM DIABETES CARE



