User login
Factors Associated With Lower-Extremity Amputation in Patients With Diabetic Foot Ulcers
From Northwell Health System, Lake Success, NY.
Abstract
- Objective: To explore factors associated with lower-extremity amputation (LEA) in patients with diabetic foot ulcers using data from the Online Wound Electronic Medical Record Database.
- Design: Retrospective analysis of medical records.
- Setting and participants: Data from 169 individuals with previously diagnosed diabetes mellitus who received wound care for a 6-month period within a span of 2 years was analyzed. A baseline evaluation was obtained and wound(s) were treated, managed, and monitored.
Treatment continued until the patient healed, required an LEA, or phased out of the study, neither healing nor undergoing an amputation. Of the 149 patients who completed the study, 38 had healed ulcers, 14 underwent amputation, and 97 neither healed nor underwent an amputation. All patients were treated under the care of vascular and/or podiatric surgeons. - Measurements: Variables included wound status (healed, amputated, and unhealed/non-amputated); size of wound area; age, gender, race, and ethnicity; white blood cell (WBC) count, hemoglobin A1c (HbA1c), blood glucose, and body mass index (BMI); and presence of osteomyelitis, gangrene, and peripheral vascular disease.
- Results: As compared to the healed and unhealed/non-amputated group, the group of patients who underwent LEA was older and had higher percentages of males, Hispanics, and African Americans; had a higher WBC count, larger wound area, and higher rates of wound infection, osteomyelitis, and neuropathy; and had lower average values of HbA1c, blood glucose, and BMI and a lower rate of peripheral vascular disease.
- Conclusion: The association between HbA1c and LEA highlights a window of relative safety among an at-risk population. By identifying and focusing on factors associated with LEA, health care professionals may be able to decrease the prevalence of LEA in patients with diabetes.
Keywords: diabetic foot ulcer; lower-extremity amputation; risk factors; HbA1c.
An estimated 30.3 million people, or 9.4% of the US population, has diabetes. In 2014, approximately 108,000 amputations were performed on adults with diagnosed diabetes.1 Furthermore, patients with diabetes have a 10-fold increased risk for lower-extremity amputation (LEA), as compared with patients without diabetes.2 The frequency of amputations in the diabetic population is a public health crisis.
Amputation has significant, life-altering consequences. Patients who undergo LEA often face debilitation in their daily activities and must undergo intense rehabilitation to learn basic tasks. Amputations can also impact individuals’ psychological well-being as they come to terms with their altered body and may face challenges in self-perception, confidence, self-esteem, work life, and relationships. In addition, the mortality rate for patients with diabetes 5 years after undergoing LEA is 30%.2 However, public health studies estimate that more than half of LEAs in patients with diabetes are preventable.3
Although studies have explored the relationship between diabetes and LEA, few have sought to identify factors directly correlated with wound care. In the United States, patients with diabetic ulcerations are typically treated in wound care facilities; however, previous studies have concentrated on the conditions that lead to the formation of an ulcer or amputation, viewing amputation and ulcer as 2 separate entities. Our study took into account systemic variables, patient demographics, and specific wound characteristics to explore factors associated with LEA in a high-risk group of patients with diabetes. This study was designed to assess ailments that are prevalent in patients who require a LEA.
Methods
Patients and Setting
A total of 169 patients who were treated at the Comprehensive Wound Healing and Hyperbaric Center (Lake Success, NY), a tertiary facility of the Northwell Health system, participated in this retrospective study. The data for this study were obtained in conjunction with the development of the New York University School of Medicine’s Online Wound Electronic Medical Record to Decrease Limb Amputations in Persons with Diabetes (OWEMR) database. The OWEMR collects individual patient data from satellite locations across the country. Using this database, researchers can analyze similarities and differences between patients who undergo LEA.
This study utilized patient data specific to the Northwell Health facility. All of the patients in our study were enrolled under the criteria of the OWEMR database. In order to be included in the OWEMR database, patients had to be diagnosed with type 1 or type 2 diabetes; have a break in the skin ≥ 0.5 cm2; be 18 years of age or older; and have a measured hemoglobin A1c (HbA1c) value within the past 120 days. Study patients signed an informed consent and committed to being available for follow-up visits to the wound care facility for 6 months after entering the study. Patients were enrolled between 2012 and 2014, and each patient was monitored for a period of 6 months within this time period. Participants were treated with current standards of care using diet, lifestyle, and pharmacologic interventions. This study was approved by the Northwell Health System Institutional Review Board Human Research Protection Program (Manhasset, NY).
Data Collection
On their first visit to the facility, patients were given a physical examination and initial interview regarding their medical history. Clinicians were required to select 1 ulcer that would be examined for the duration of the study. The selection of the ulcer was based on a point system that awarded points for pedal pulses, the ability to be probed to the bone, the location of the ulcer (ie, located on the foot rather than a toe), and the presence of multiple ulcerations. The ulcer with the highest score was selected for the study. If numerous ulcers were evaluated with the same score, the largest and deepest was selected. Wagner classification of the wound was recorded at baseline and taken at each subsequent patient visit. In addition, peripheral sensation was assessed for signs of neuropathy using Semmes-Weinstein monofilament testing.
Once selected, the wound was clinically evaluated, samples for culture were obtained, and blood tests were performed to detect the presence of wound infection. The patient’s blood was drawn for a full laboratory analysis, including white blood cell (WBC) count and measurement of blood glucose and HbA1c levels. Bone biopsy, magnetic resonance imaging, and bone scans were used to detect the presence of osteomyelitis at the discretion of the health care provider. Wounds suspected of infection, underlying osteomyelitis, or gangrene at baseline were excluded. Patients would then return for follow-up visits at least once every 6 weeks, plus or minus 2 weeks, for a maximum of 6 months.
Statistical Analysis
Utilizing SAS version 9.3 (Cary, NC), descriptive statistics (minimum, maximum, mean, median, and SD) were calculated for the following variables: age, WBC count, wound area, HbA1c, blood glucose, and body mass index (BMI). These variables were collected for each patient as per the OWEMR protocol and provided a basis for which to compare patients who underwent amputation and those who did not. Twenty patients were lost to follow-up, and therefore we altered the window of our statistics from 6 months to 3 months to provide the most accurate data, as 6-month follow-up data were limited. The patients were classified into the following categories: healed, amputated, and unhealed/non-amputated. Descriptive statistics were calculated for these 3 groups, analyzing the same variables (age, WBC count, wound area, HbA1c, blood glucose, and BMI). Additional statistical computations were utilized in order to show the prevalence and frequency of our categorical variables: gender, race, ethnicity, osteomyelitis, gangrene, and peripheral vascular disease. The baseline values of WBC count, HbA1c, wound area, and BMI of the 3 groups were analyzed with descriptive statistics for comparison. A multinomial logistic regression was then performed using a 3-level outcome variable: healed, amputated, or unhealed/non-amputated. Each predictor variable was analyzed independently due to the small sample size.
Results
Of the 169 registered patients treated at the Northwell Health facility, all qualified for the OWEMR study and met the study criteria. In the original 169 patients, there were 19 amputations: 6 toe, 6 trans-metatarsal, 6 below knee, and 1 above knee (Table 1). 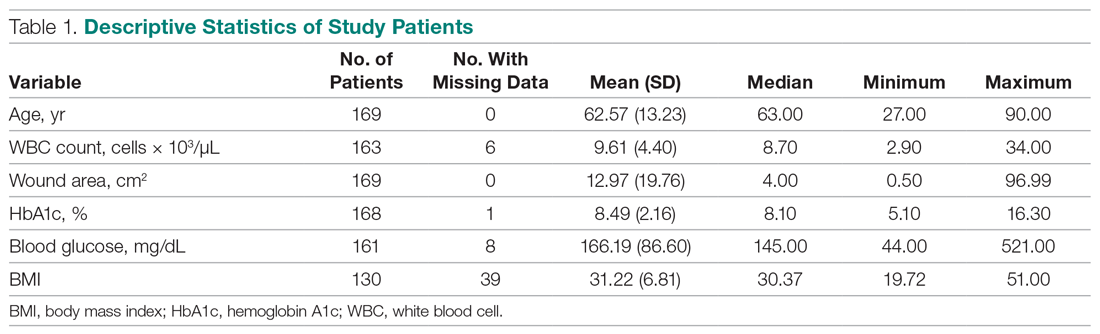
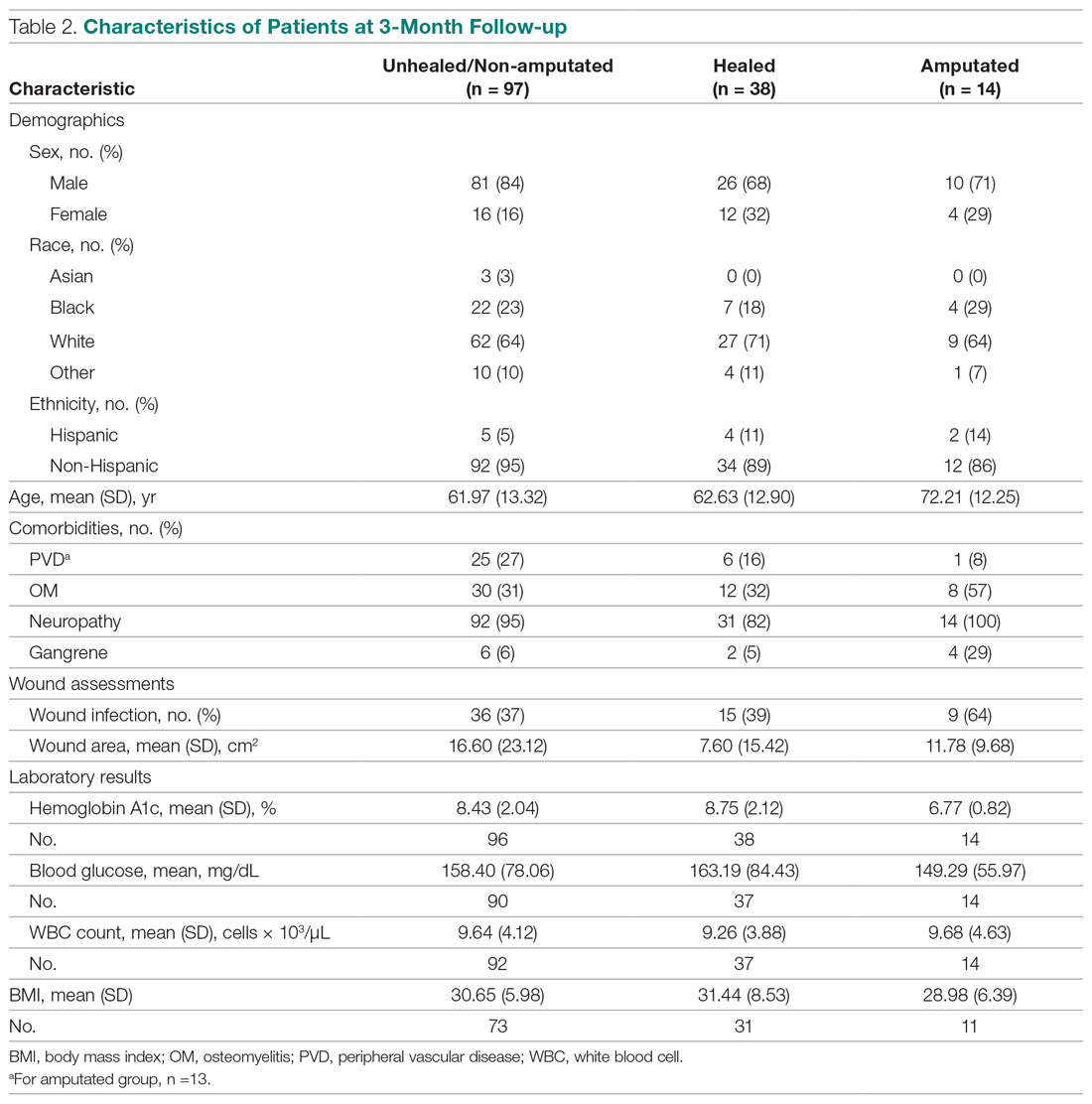
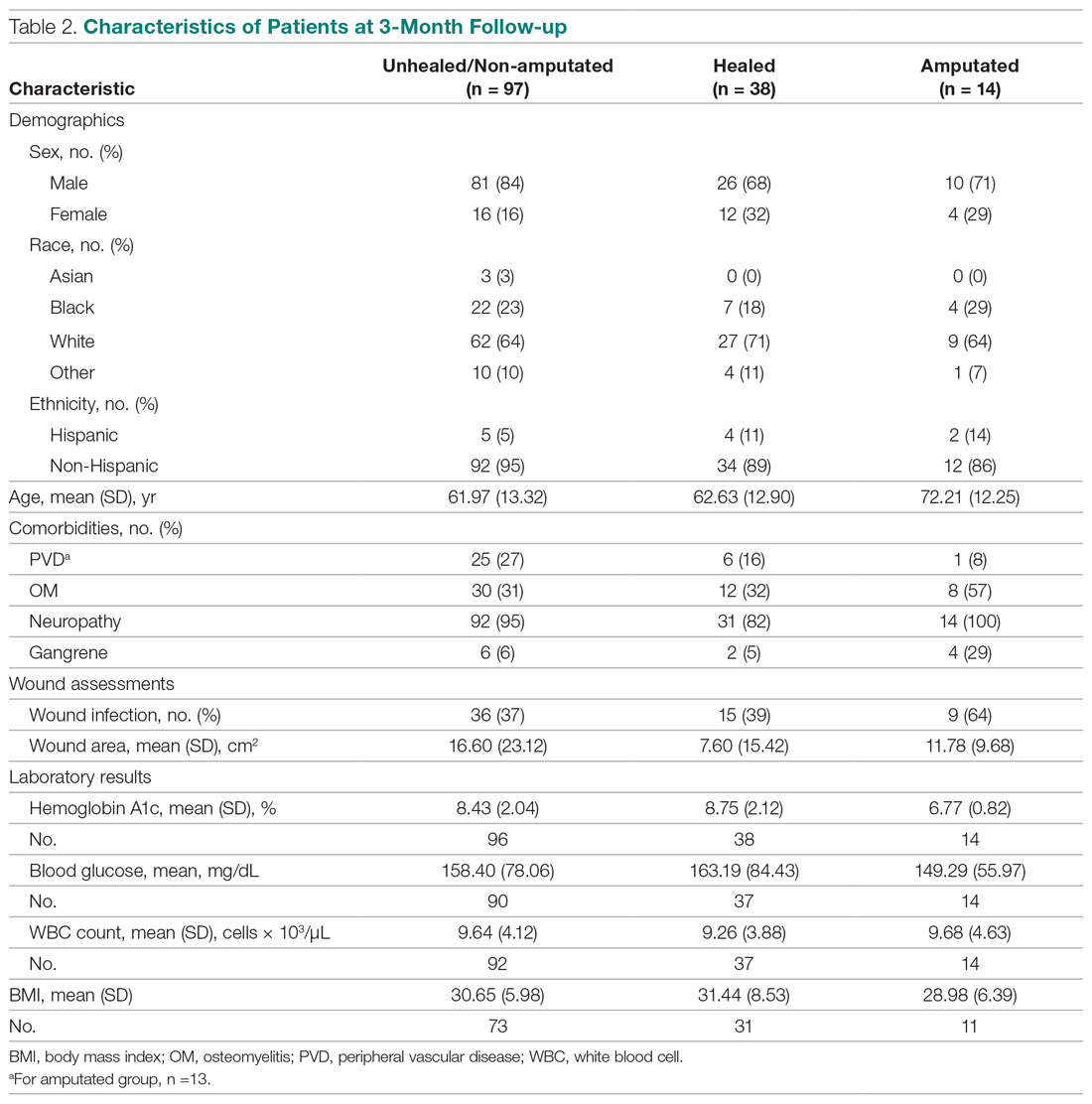
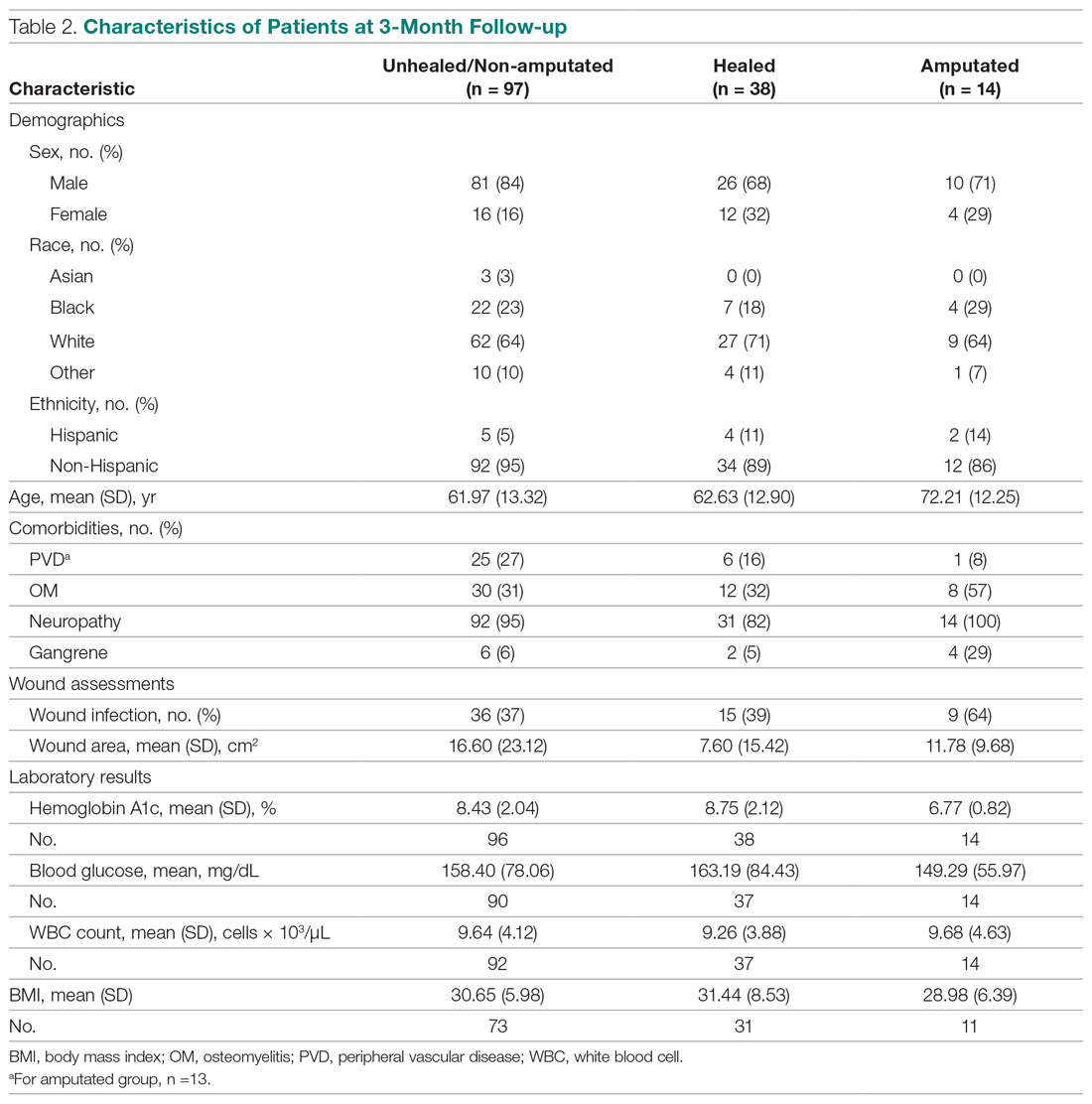
The descriptive statistics of 149 patients grouped into 3 categories (healed, amputated, unhealed/non-amputated) are shown in Table 2.
The results of the logistic regression exploring the differences between the amputation and healed groups and the unhealed/non-amputated group are shown in Table 3. The amputation group had a higher mean age and WBC count and greater wound area. Increased age was determined to be a significant predictor of the odds of amputation (P = 0.0089). For each year increase in age, the odds of amputation increased by 6.5% (odds ratio, 1.07 [95% confidence interval {CI}, 1.02-1.12]). Patients in the amputation group were more likely to be male, Hispanic, and African American and to have wound infections and comorbidities (osteomyelitis, neuropathy, and gangrene).
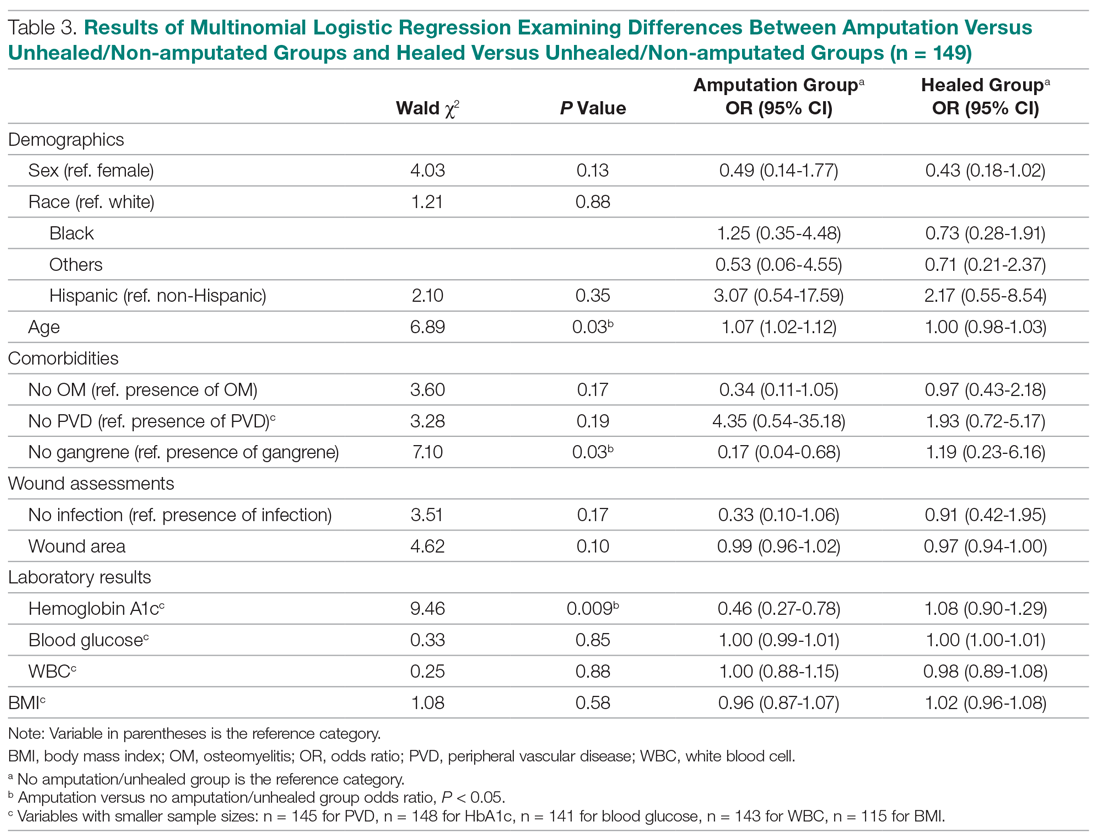
The presence of gangrene was significantly associated with LEA (P = 0.03). Specifically, the odds of patients without gangrene undergoing a LEA were substantially lower compared with their counterparts with gangrene (odds ratio, 0.17; 95% CI, 0.04-0.68; P = 0.0131). However, the presence of gangrene was not associated with the odds of healing compared with the odds of neither healing nor undergoing amputation (P = 0.84; not shown in Table 3).
The amputation group had lower mean values for HbA1c, BMI, and blood glucose levels and a lower rate of peripheral vascular disease. Only the relationship between lower HbA1c and increased odds of amputation versus not healing/non-amputation was found to be statistically significant (95% CI, 0.27-0.78; P = 0.009).
Discussion
This retrospective study was undertaken to evaluate factors associated with LEA in patients with diabetic foot ulcers. Patients with diabetes being treated at a wound care facility often require continuous surgical and metabolic intervention to promote optimal healing: drainage, surgical debridement, irrigation, culturing for infection, and monitoring of blood glucose levels. This treatment requires strict compliance with medical directions and, oftentimes, additional care, such as home-care nursing visits, to maintain a curative environment for the wound. Frequently, wounds on the lower extremity further complicate the healing process by reducing the patient’s mobility and daily life. Due to these factors, many patients progress to LEA. The link between diabetic ulcers and amputation has already been well described in previous studies, with studies showing that history of diabetic foot ulcer significantly predisposes an individual to LEA.4 However, few studies have further investigated demographic factors associated with risk for an amputation. Our study analyzed several categories of patient data taken from a baseline visit. We found that those with highly elevated HbA1c values were less likely to have an amputation than persons with relatively lower levels, a finding that is contrary to previous studies.
Our study’s findings suggest a higher risk for LEA with increased age. The amputation group was, on average, 7 years older than the other 2 groups. A recent study showed that risk for amputation is directly correlated to patient age, as is the mortality rate after undergoing LEA (2.3%; P < 0.05).5 Our study found that with each increase in age of 1 year, the odds of amputation increased by 6.5%. However, recent evidence on LEA risk and aging suggests that age is of less consequence than the duration of diabetes. One study found that the propensity to develop diabetic foot ulcers increases with the duration of diabetes.6 The same study found that prevalence of ulceration was correlated with age, but the relationship between age and LEA was less significant. A follow-up study for LEA could be done to examine the role of disease duration versus age in LEA.
A consensus among previous studies is that men have a higher risk for LEA.5,7 Men comprised the majority in all 3 groups in our study. In addition, the amputation group in our study had the lowest BMI. Higher BMI generally is associated with an increased risk for health complications. However, a past study conducted in Taiwan reported that obese patients with diabetes were less likely to undergo LEA than those within the normal range for BMI.8 Neither study suggests that obesity is a deterrent for LEA, but both studies may suggest that risk of amputation may approach a maximum frequency at a specific BMI range, and then decrease. This unconfirmed “cyclic” relationship should be evaluated further in a larger sample size.
Most patients in our analysis were Caucasian, followed by African American and South Asian. African Americans were the only racial group with an increased frequency in the amputation group. This finding is supported by a previous study that found that the rate of LEA among patients with diabetes in low-income, predominantly African-American neighborhoods was nearly double that in wealthier, predominantly Caucasian areas.9 A potential problem in the comparison between our data with previous studies is that the studies did not analyze patients with our inclusion criteria. All patients with diabetes in previous investigations were grouped by race, but were not necessarily required to have 1 or more ulcers. Multiple ulcers may predispose an individual to a greater risk for amputation.
Multinomial logistic regression did not suggest an association between initial size of a patient’s wound and the risk of amputation. However, the descriptive data suggests a trend. Patients who did not heal or require an amputation had the largest average wound area. This finding is not surprising in that our study followed individuals for only 3 months. Many wounds require a long course of treatment, especially in patients with diabetes, who may have poor vascularization. However, in comparison to the healed patients, the patients who required an amputation had a larger average wound area. A larger wound requires a plentiful vascular supply for the delivery of clotting factors and nutrients to the damaged area. As wound size increases, an individual’s body must transmit an increased quantity of these factors and nutrients for the regeneration of tissue. In addition, wounds that possess a larger surface area require more debridement and present a greater opportunity for infection. This may also foreshadow a longer, more costly course of treatment. Additionally, individuals coping with large ulcerations are burdened by more elaborate and complex wound dressings.
Elevated levels of HbA1c are associated with increased adverse effects of diabetes, including end-stage renal disease, neuropathy, and infection.10 In a previous study, the risk for amputation was 1.2 times higher in patients with elevated HbA1c.11 In contrast, our study suggested the odds of LEA versus not healing/not undergoing amputation decreased as HbA1c increased. As a patient’s HbA1c level increased by a value of 1, their odds for LEA decreased by 54.3%. This finding contradicts prior studies that have found a positive association between HbA1c and LEA risk, including a study where each percentage increase in HbA1c correlated with a 13% to 15% increased risk of LEA.12 The finding that patients who underwent amputation in our study had lower levels of HbA1c and blood glucose cannot be fully explained. The maximum HbA1c value in the amputated group was 7.9%. The average values for healed patients and those who underwent LEA were 8.75% and 6.77%, respectively.
Blood glucose levels were also found to be the lowest in the amputated group in our study (mean, 149.29 mg/dL vs 163.19 mg/dL in the healed group). Similar results were found in a Brazilian study, in which patients who did not require amputation had higher HbA1c levels. This study also found an association between blood glucose levels above 200 mg/dL and amputations.3 These findings provide interesting opportunities for repeat studies, preferably with a larger number of participants.
Our study is limited by the small sample size. The sample population had to be reduced, as many patients were lost to follow-up. Although this paring down of the sample size can introduce bias, we are confident that our study is representative of the demographic of patients treated in our facility. The loss of patients to follow-up in turn caused the window of analysis to be narrowed, as long-term outcome data were not available. A multisite study observing various population samples can better explore the relationship between HbA1c and risk of amputation.
Conclusion
This retrospective study exploring factors associated with LEA was unique in that all our participants had 1 or more diabetic foot ulcerations, and thus already had an extremely high risk for amputation, in contrast to previous studies that followed persons at risk for developing diabetic foot ulcerations. In contrast to several previous studies, we found that the risk for amputation actually decreased as baseline measurements of HbA1c increased. The results of this study offer many opportunities for future investigations, preferably with a larger sample size. By further isolating and scrutinizing specific factors associated with LEA, researchers can help clinicians focus on providing wound care that promotes limb salvage.
Corresponding author: Alisha Oropallo, MD, MS, Northwell Health Comprehensive Wound Care Healing Center and Hyperbarics, 1999 Marcus Avenue, Suite M6, Lake Success, NY 11042; [email protected].
Financial disclosures: Funding for this research was provided by a multi-institutional AHRQ governmental grant.
1. Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2017. Atlanta, GA: US Department of Health and Human Services; 2017.
2. Uccioli L, Giurato L, Meloni M, et al. Comment on Hoffstad et al. Diabetes, lower-extremity amputation, and death. Diabetes Care. 2015;38:1852-1857.
3. Gamba MA, Gotlieb SLD, Bergamaschi DP, Vianna LAC. Lower extremity amputations in diabetic patients: a case-control study. Rev Saúde Pública. 2004;38:399-404.
4. Martins-Mendes D, Monteiro-Soares M, Boyko EJ, et al. The independent contribution of diabetic foot ulcer on lower extremity amputation and mortality risk. J Diabetes Complications. 2014;28:632-638.
5. Lipsky BA, Weigelt JA, Sun X, et al. Developing and validating a risk score for lower-extremity amputation in patients hospitalized for a diabetic foot infection. Diabetes Care. 2011;34:1695-1700.
6. Al-Rubeaan K, Al Derwish M, Ouizi S, et al. Diabetic foot complications and their risk factors from a large retrospective cohort study. PLoS One. 2015;10:e0124446.
7. Pickwell K, Siersma V, Kars M, et al. Predictors of lower-extremity amputation in patients with an infected diabetic foot ulcer. Diabetes Care. 2015;38:852-857.
8. Lin C, Hsu BR, Tsai J, et al. Effect of limb preservation status and body mass index on the survival of patients with limb-threatening diabetic foot ulcers. J Diabetes Complications. 2017;31:180-185.
9. Stevens CD, Schriger DL, Raffetto B, et al. Geographic clustering of diabetic lower-extremity amputations in low-income regions of California. Health Aff. 2014;33:1383-1390.
10. Liao L, Li C, Liu C, et al. Extreme levels of HbA1c increase incident ESRD risk in Chinese patients with type 2 diabetes: competing risk analysis in national cohort of Taiwan diabetes study. PLoS One. 2015; 10:e0130828.
11. Miyajima S, Shirai A, Yamamoto S, et al. Risk factors for major limb amputations in diabetic foot gangrene patients. Diabetes Res Clin Pract. 2006;71:272-279.
12. Zhao W, Katzmarzyk PT, Horswell R, et al. HbA1c and lower-extremity amputation risk in low-income patients with diabetes. Diabetes Care. 2013;36:3591-3598.
From Northwell Health System, Lake Success, NY.
Abstract
- Objective: To explore factors associated with lower-extremity amputation (LEA) in patients with diabetic foot ulcers using data from the Online Wound Electronic Medical Record Database.
- Design: Retrospective analysis of medical records.
- Setting and participants: Data from 169 individuals with previously diagnosed diabetes mellitus who received wound care for a 6-month period within a span of 2 years was analyzed. A baseline evaluation was obtained and wound(s) were treated, managed, and monitored.
Treatment continued until the patient healed, required an LEA, or phased out of the study, neither healing nor undergoing an amputation. Of the 149 patients who completed the study, 38 had healed ulcers, 14 underwent amputation, and 97 neither healed nor underwent an amputation. All patients were treated under the care of vascular and/or podiatric surgeons. - Measurements: Variables included wound status (healed, amputated, and unhealed/non-amputated); size of wound area; age, gender, race, and ethnicity; white blood cell (WBC) count, hemoglobin A1c (HbA1c), blood glucose, and body mass index (BMI); and presence of osteomyelitis, gangrene, and peripheral vascular disease.
- Results: As compared to the healed and unhealed/non-amputated group, the group of patients who underwent LEA was older and had higher percentages of males, Hispanics, and African Americans; had a higher WBC count, larger wound area, and higher rates of wound infection, osteomyelitis, and neuropathy; and had lower average values of HbA1c, blood glucose, and BMI and a lower rate of peripheral vascular disease.
- Conclusion: The association between HbA1c and LEA highlights a window of relative safety among an at-risk population. By identifying and focusing on factors associated with LEA, health care professionals may be able to decrease the prevalence of LEA in patients with diabetes.
Keywords: diabetic foot ulcer; lower-extremity amputation; risk factors; HbA1c.
An estimated 30.3 million people, or 9.4% of the US population, has diabetes. In 2014, approximately 108,000 amputations were performed on adults with diagnosed diabetes.1 Furthermore, patients with diabetes have a 10-fold increased risk for lower-extremity amputation (LEA), as compared with patients without diabetes.2 The frequency of amputations in the diabetic population is a public health crisis.
Amputation has significant, life-altering consequences. Patients who undergo LEA often face debilitation in their daily activities and must undergo intense rehabilitation to learn basic tasks. Amputations can also impact individuals’ psychological well-being as they come to terms with their altered body and may face challenges in self-perception, confidence, self-esteem, work life, and relationships. In addition, the mortality rate for patients with diabetes 5 years after undergoing LEA is 30%.2 However, public health studies estimate that more than half of LEAs in patients with diabetes are preventable.3
Although studies have explored the relationship between diabetes and LEA, few have sought to identify factors directly correlated with wound care. In the United States, patients with diabetic ulcerations are typically treated in wound care facilities; however, previous studies have concentrated on the conditions that lead to the formation of an ulcer or amputation, viewing amputation and ulcer as 2 separate entities. Our study took into account systemic variables, patient demographics, and specific wound characteristics to explore factors associated with LEA in a high-risk group of patients with diabetes. This study was designed to assess ailments that are prevalent in patients who require a LEA.
Methods
Patients and Setting
A total of 169 patients who were treated at the Comprehensive Wound Healing and Hyperbaric Center (Lake Success, NY), a tertiary facility of the Northwell Health system, participated in this retrospective study. The data for this study were obtained in conjunction with the development of the New York University School of Medicine’s Online Wound Electronic Medical Record to Decrease Limb Amputations in Persons with Diabetes (OWEMR) database. The OWEMR collects individual patient data from satellite locations across the country. Using this database, researchers can analyze similarities and differences between patients who undergo LEA.
This study utilized patient data specific to the Northwell Health facility. All of the patients in our study were enrolled under the criteria of the OWEMR database. In order to be included in the OWEMR database, patients had to be diagnosed with type 1 or type 2 diabetes; have a break in the skin ≥ 0.5 cm2; be 18 years of age or older; and have a measured hemoglobin A1c (HbA1c) value within the past 120 days. Study patients signed an informed consent and committed to being available for follow-up visits to the wound care facility for 6 months after entering the study. Patients were enrolled between 2012 and 2014, and each patient was monitored for a period of 6 months within this time period. Participants were treated with current standards of care using diet, lifestyle, and pharmacologic interventions. This study was approved by the Northwell Health System Institutional Review Board Human Research Protection Program (Manhasset, NY).
Data Collection
On their first visit to the facility, patients were given a physical examination and initial interview regarding their medical history. Clinicians were required to select 1 ulcer that would be examined for the duration of the study. The selection of the ulcer was based on a point system that awarded points for pedal pulses, the ability to be probed to the bone, the location of the ulcer (ie, located on the foot rather than a toe), and the presence of multiple ulcerations. The ulcer with the highest score was selected for the study. If numerous ulcers were evaluated with the same score, the largest and deepest was selected. Wagner classification of the wound was recorded at baseline and taken at each subsequent patient visit. In addition, peripheral sensation was assessed for signs of neuropathy using Semmes-Weinstein monofilament testing.
Once selected, the wound was clinically evaluated, samples for culture were obtained, and blood tests were performed to detect the presence of wound infection. The patient’s blood was drawn for a full laboratory analysis, including white blood cell (WBC) count and measurement of blood glucose and HbA1c levels. Bone biopsy, magnetic resonance imaging, and bone scans were used to detect the presence of osteomyelitis at the discretion of the health care provider. Wounds suspected of infection, underlying osteomyelitis, or gangrene at baseline were excluded. Patients would then return for follow-up visits at least once every 6 weeks, plus or minus 2 weeks, for a maximum of 6 months.
Statistical Analysis
Utilizing SAS version 9.3 (Cary, NC), descriptive statistics (minimum, maximum, mean, median, and SD) were calculated for the following variables: age, WBC count, wound area, HbA1c, blood glucose, and body mass index (BMI). These variables were collected for each patient as per the OWEMR protocol and provided a basis for which to compare patients who underwent amputation and those who did not. Twenty patients were lost to follow-up, and therefore we altered the window of our statistics from 6 months to 3 months to provide the most accurate data, as 6-month follow-up data were limited. The patients were classified into the following categories: healed, amputated, and unhealed/non-amputated. Descriptive statistics were calculated for these 3 groups, analyzing the same variables (age, WBC count, wound area, HbA1c, blood glucose, and BMI). Additional statistical computations were utilized in order to show the prevalence and frequency of our categorical variables: gender, race, ethnicity, osteomyelitis, gangrene, and peripheral vascular disease. The baseline values of WBC count, HbA1c, wound area, and BMI of the 3 groups were analyzed with descriptive statistics for comparison. A multinomial logistic regression was then performed using a 3-level outcome variable: healed, amputated, or unhealed/non-amputated. Each predictor variable was analyzed independently due to the small sample size.
Results
Of the 169 registered patients treated at the Northwell Health facility, all qualified for the OWEMR study and met the study criteria. In the original 169 patients, there were 19 amputations: 6 toe, 6 trans-metatarsal, 6 below knee, and 1 above knee (Table 1). 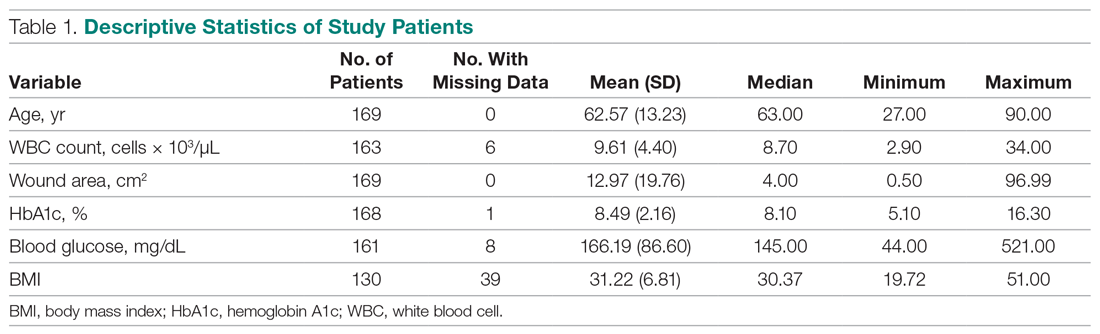
The descriptive statistics of 149 patients grouped into 3 categories (healed, amputated, unhealed/non-amputated) are shown in Table 2.
The results of the logistic regression exploring the differences between the amputation and healed groups and the unhealed/non-amputated group are shown in Table 3. The amputation group had a higher mean age and WBC count and greater wound area. Increased age was determined to be a significant predictor of the odds of amputation (P = 0.0089). For each year increase in age, the odds of amputation increased by 6.5% (odds ratio, 1.07 [95% confidence interval {CI}, 1.02-1.12]). Patients in the amputation group were more likely to be male, Hispanic, and African American and to have wound infections and comorbidities (osteomyelitis, neuropathy, and gangrene).
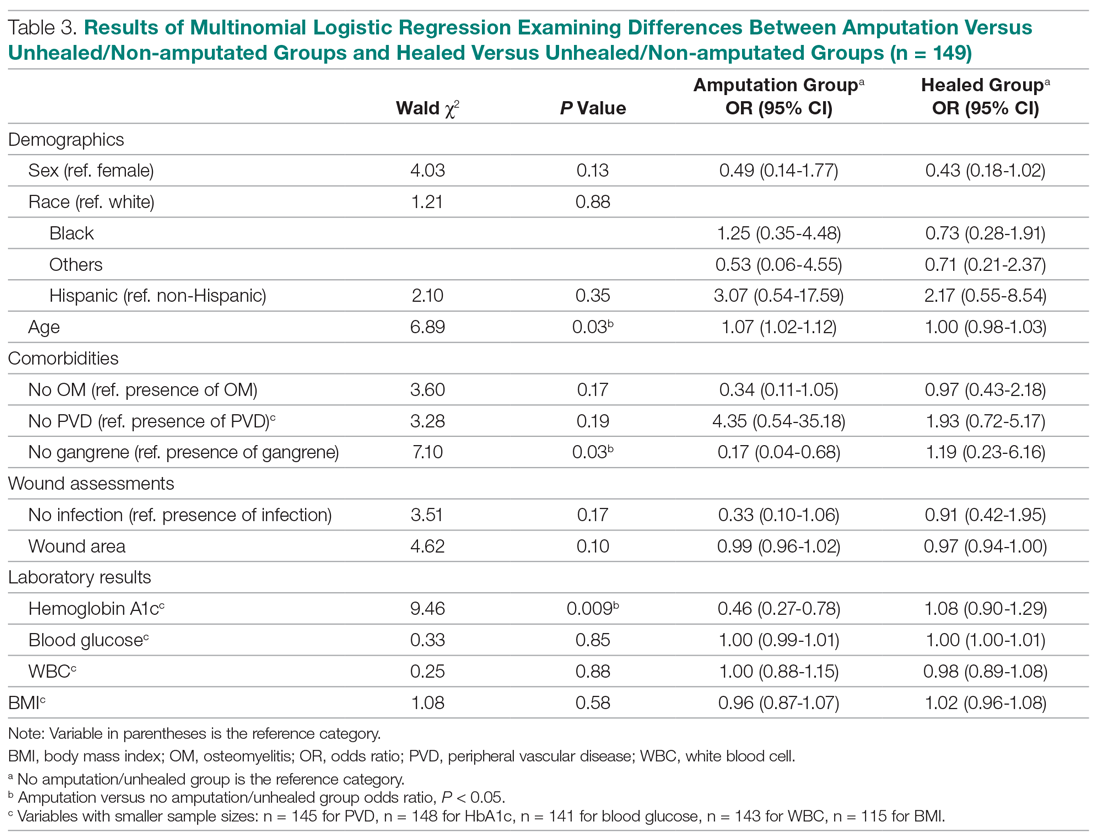
The presence of gangrene was significantly associated with LEA (P = 0.03). Specifically, the odds of patients without gangrene undergoing a LEA were substantially lower compared with their counterparts with gangrene (odds ratio, 0.17; 95% CI, 0.04-0.68; P = 0.0131). However, the presence of gangrene was not associated with the odds of healing compared with the odds of neither healing nor undergoing amputation (P = 0.84; not shown in Table 3).
The amputation group had lower mean values for HbA1c, BMI, and blood glucose levels and a lower rate of peripheral vascular disease. Only the relationship between lower HbA1c and increased odds of amputation versus not healing/non-amputation was found to be statistically significant (95% CI, 0.27-0.78; P = 0.009).
Discussion
This retrospective study was undertaken to evaluate factors associated with LEA in patients with diabetic foot ulcers. Patients with diabetes being treated at a wound care facility often require continuous surgical and metabolic intervention to promote optimal healing: drainage, surgical debridement, irrigation, culturing for infection, and monitoring of blood glucose levels. This treatment requires strict compliance with medical directions and, oftentimes, additional care, such as home-care nursing visits, to maintain a curative environment for the wound. Frequently, wounds on the lower extremity further complicate the healing process by reducing the patient’s mobility and daily life. Due to these factors, many patients progress to LEA. The link between diabetic ulcers and amputation has already been well described in previous studies, with studies showing that history of diabetic foot ulcer significantly predisposes an individual to LEA.4 However, few studies have further investigated demographic factors associated with risk for an amputation. Our study analyzed several categories of patient data taken from a baseline visit. We found that those with highly elevated HbA1c values were less likely to have an amputation than persons with relatively lower levels, a finding that is contrary to previous studies.
Our study’s findings suggest a higher risk for LEA with increased age. The amputation group was, on average, 7 years older than the other 2 groups. A recent study showed that risk for amputation is directly correlated to patient age, as is the mortality rate after undergoing LEA (2.3%; P < 0.05).5 Our study found that with each increase in age of 1 year, the odds of amputation increased by 6.5%. However, recent evidence on LEA risk and aging suggests that age is of less consequence than the duration of diabetes. One study found that the propensity to develop diabetic foot ulcers increases with the duration of diabetes.6 The same study found that prevalence of ulceration was correlated with age, but the relationship between age and LEA was less significant. A follow-up study for LEA could be done to examine the role of disease duration versus age in LEA.
A consensus among previous studies is that men have a higher risk for LEA.5,7 Men comprised the majority in all 3 groups in our study. In addition, the amputation group in our study had the lowest BMI. Higher BMI generally is associated with an increased risk for health complications. However, a past study conducted in Taiwan reported that obese patients with diabetes were less likely to undergo LEA than those within the normal range for BMI.8 Neither study suggests that obesity is a deterrent for LEA, but both studies may suggest that risk of amputation may approach a maximum frequency at a specific BMI range, and then decrease. This unconfirmed “cyclic” relationship should be evaluated further in a larger sample size.
Most patients in our analysis were Caucasian, followed by African American and South Asian. African Americans were the only racial group with an increased frequency in the amputation group. This finding is supported by a previous study that found that the rate of LEA among patients with diabetes in low-income, predominantly African-American neighborhoods was nearly double that in wealthier, predominantly Caucasian areas.9 A potential problem in the comparison between our data with previous studies is that the studies did not analyze patients with our inclusion criteria. All patients with diabetes in previous investigations were grouped by race, but were not necessarily required to have 1 or more ulcers. Multiple ulcers may predispose an individual to a greater risk for amputation.
Multinomial logistic regression did not suggest an association between initial size of a patient’s wound and the risk of amputation. However, the descriptive data suggests a trend. Patients who did not heal or require an amputation had the largest average wound area. This finding is not surprising in that our study followed individuals for only 3 months. Many wounds require a long course of treatment, especially in patients with diabetes, who may have poor vascularization. However, in comparison to the healed patients, the patients who required an amputation had a larger average wound area. A larger wound requires a plentiful vascular supply for the delivery of clotting factors and nutrients to the damaged area. As wound size increases, an individual’s body must transmit an increased quantity of these factors and nutrients for the regeneration of tissue. In addition, wounds that possess a larger surface area require more debridement and present a greater opportunity for infection. This may also foreshadow a longer, more costly course of treatment. Additionally, individuals coping with large ulcerations are burdened by more elaborate and complex wound dressings.
Elevated levels of HbA1c are associated with increased adverse effects of diabetes, including end-stage renal disease, neuropathy, and infection.10 In a previous study, the risk for amputation was 1.2 times higher in patients with elevated HbA1c.11 In contrast, our study suggested the odds of LEA versus not healing/not undergoing amputation decreased as HbA1c increased. As a patient’s HbA1c level increased by a value of 1, their odds for LEA decreased by 54.3%. This finding contradicts prior studies that have found a positive association between HbA1c and LEA risk, including a study where each percentage increase in HbA1c correlated with a 13% to 15% increased risk of LEA.12 The finding that patients who underwent amputation in our study had lower levels of HbA1c and blood glucose cannot be fully explained. The maximum HbA1c value in the amputated group was 7.9%. The average values for healed patients and those who underwent LEA were 8.75% and 6.77%, respectively.
Blood glucose levels were also found to be the lowest in the amputated group in our study (mean, 149.29 mg/dL vs 163.19 mg/dL in the healed group). Similar results were found in a Brazilian study, in which patients who did not require amputation had higher HbA1c levels. This study also found an association between blood glucose levels above 200 mg/dL and amputations.3 These findings provide interesting opportunities for repeat studies, preferably with a larger number of participants.
Our study is limited by the small sample size. The sample population had to be reduced, as many patients were lost to follow-up. Although this paring down of the sample size can introduce bias, we are confident that our study is representative of the demographic of patients treated in our facility. The loss of patients to follow-up in turn caused the window of analysis to be narrowed, as long-term outcome data were not available. A multisite study observing various population samples can better explore the relationship between HbA1c and risk of amputation.
Conclusion
This retrospective study exploring factors associated with LEA was unique in that all our participants had 1 or more diabetic foot ulcerations, and thus already had an extremely high risk for amputation, in contrast to previous studies that followed persons at risk for developing diabetic foot ulcerations. In contrast to several previous studies, we found that the risk for amputation actually decreased as baseline measurements of HbA1c increased. The results of this study offer many opportunities for future investigations, preferably with a larger sample size. By further isolating and scrutinizing specific factors associated with LEA, researchers can help clinicians focus on providing wound care that promotes limb salvage.
Corresponding author: Alisha Oropallo, MD, MS, Northwell Health Comprehensive Wound Care Healing Center and Hyperbarics, 1999 Marcus Avenue, Suite M6, Lake Success, NY 11042; [email protected].
Financial disclosures: Funding for this research was provided by a multi-institutional AHRQ governmental grant.
From Northwell Health System, Lake Success, NY.
Abstract
- Objective: To explore factors associated with lower-extremity amputation (LEA) in patients with diabetic foot ulcers using data from the Online Wound Electronic Medical Record Database.
- Design: Retrospective analysis of medical records.
- Setting and participants: Data from 169 individuals with previously diagnosed diabetes mellitus who received wound care for a 6-month period within a span of 2 years was analyzed. A baseline evaluation was obtained and wound(s) were treated, managed, and monitored.
Treatment continued until the patient healed, required an LEA, or phased out of the study, neither healing nor undergoing an amputation. Of the 149 patients who completed the study, 38 had healed ulcers, 14 underwent amputation, and 97 neither healed nor underwent an amputation. All patients were treated under the care of vascular and/or podiatric surgeons. - Measurements: Variables included wound status (healed, amputated, and unhealed/non-amputated); size of wound area; age, gender, race, and ethnicity; white blood cell (WBC) count, hemoglobin A1c (HbA1c), blood glucose, and body mass index (BMI); and presence of osteomyelitis, gangrene, and peripheral vascular disease.
- Results: As compared to the healed and unhealed/non-amputated group, the group of patients who underwent LEA was older and had higher percentages of males, Hispanics, and African Americans; had a higher WBC count, larger wound area, and higher rates of wound infection, osteomyelitis, and neuropathy; and had lower average values of HbA1c, blood glucose, and BMI and a lower rate of peripheral vascular disease.
- Conclusion: The association between HbA1c and LEA highlights a window of relative safety among an at-risk population. By identifying and focusing on factors associated with LEA, health care professionals may be able to decrease the prevalence of LEA in patients with diabetes.
Keywords: diabetic foot ulcer; lower-extremity amputation; risk factors; HbA1c.
An estimated 30.3 million people, or 9.4% of the US population, has diabetes. In 2014, approximately 108,000 amputations were performed on adults with diagnosed diabetes.1 Furthermore, patients with diabetes have a 10-fold increased risk for lower-extremity amputation (LEA), as compared with patients without diabetes.2 The frequency of amputations in the diabetic population is a public health crisis.
Amputation has significant, life-altering consequences. Patients who undergo LEA often face debilitation in their daily activities and must undergo intense rehabilitation to learn basic tasks. Amputations can also impact individuals’ psychological well-being as they come to terms with their altered body and may face challenges in self-perception, confidence, self-esteem, work life, and relationships. In addition, the mortality rate for patients with diabetes 5 years after undergoing LEA is 30%.2 However, public health studies estimate that more than half of LEAs in patients with diabetes are preventable.3
Although studies have explored the relationship between diabetes and LEA, few have sought to identify factors directly correlated with wound care. In the United States, patients with diabetic ulcerations are typically treated in wound care facilities; however, previous studies have concentrated on the conditions that lead to the formation of an ulcer or amputation, viewing amputation and ulcer as 2 separate entities. Our study took into account systemic variables, patient demographics, and specific wound characteristics to explore factors associated with LEA in a high-risk group of patients with diabetes. This study was designed to assess ailments that are prevalent in patients who require a LEA.
Methods
Patients and Setting
A total of 169 patients who were treated at the Comprehensive Wound Healing and Hyperbaric Center (Lake Success, NY), a tertiary facility of the Northwell Health system, participated in this retrospective study. The data for this study were obtained in conjunction with the development of the New York University School of Medicine’s Online Wound Electronic Medical Record to Decrease Limb Amputations in Persons with Diabetes (OWEMR) database. The OWEMR collects individual patient data from satellite locations across the country. Using this database, researchers can analyze similarities and differences between patients who undergo LEA.
This study utilized patient data specific to the Northwell Health facility. All of the patients in our study were enrolled under the criteria of the OWEMR database. In order to be included in the OWEMR database, patients had to be diagnosed with type 1 or type 2 diabetes; have a break in the skin ≥ 0.5 cm2; be 18 years of age or older; and have a measured hemoglobin A1c (HbA1c) value within the past 120 days. Study patients signed an informed consent and committed to being available for follow-up visits to the wound care facility for 6 months after entering the study. Patients were enrolled between 2012 and 2014, and each patient was monitored for a period of 6 months within this time period. Participants were treated with current standards of care using diet, lifestyle, and pharmacologic interventions. This study was approved by the Northwell Health System Institutional Review Board Human Research Protection Program (Manhasset, NY).
Data Collection
On their first visit to the facility, patients were given a physical examination and initial interview regarding their medical history. Clinicians were required to select 1 ulcer that would be examined for the duration of the study. The selection of the ulcer was based on a point system that awarded points for pedal pulses, the ability to be probed to the bone, the location of the ulcer (ie, located on the foot rather than a toe), and the presence of multiple ulcerations. The ulcer with the highest score was selected for the study. If numerous ulcers were evaluated with the same score, the largest and deepest was selected. Wagner classification of the wound was recorded at baseline and taken at each subsequent patient visit. In addition, peripheral sensation was assessed for signs of neuropathy using Semmes-Weinstein monofilament testing.
Once selected, the wound was clinically evaluated, samples for culture were obtained, and blood tests were performed to detect the presence of wound infection. The patient’s blood was drawn for a full laboratory analysis, including white blood cell (WBC) count and measurement of blood glucose and HbA1c levels. Bone biopsy, magnetic resonance imaging, and bone scans were used to detect the presence of osteomyelitis at the discretion of the health care provider. Wounds suspected of infection, underlying osteomyelitis, or gangrene at baseline were excluded. Patients would then return for follow-up visits at least once every 6 weeks, plus or minus 2 weeks, for a maximum of 6 months.
Statistical Analysis
Utilizing SAS version 9.3 (Cary, NC), descriptive statistics (minimum, maximum, mean, median, and SD) were calculated for the following variables: age, WBC count, wound area, HbA1c, blood glucose, and body mass index (BMI). These variables were collected for each patient as per the OWEMR protocol and provided a basis for which to compare patients who underwent amputation and those who did not. Twenty patients were lost to follow-up, and therefore we altered the window of our statistics from 6 months to 3 months to provide the most accurate data, as 6-month follow-up data were limited. The patients were classified into the following categories: healed, amputated, and unhealed/non-amputated. Descriptive statistics were calculated for these 3 groups, analyzing the same variables (age, WBC count, wound area, HbA1c, blood glucose, and BMI). Additional statistical computations were utilized in order to show the prevalence and frequency of our categorical variables: gender, race, ethnicity, osteomyelitis, gangrene, and peripheral vascular disease. The baseline values of WBC count, HbA1c, wound area, and BMI of the 3 groups were analyzed with descriptive statistics for comparison. A multinomial logistic regression was then performed using a 3-level outcome variable: healed, amputated, or unhealed/non-amputated. Each predictor variable was analyzed independently due to the small sample size.
Results
Of the 169 registered patients treated at the Northwell Health facility, all qualified for the OWEMR study and met the study criteria. In the original 169 patients, there were 19 amputations: 6 toe, 6 trans-metatarsal, 6 below knee, and 1 above knee (Table 1). 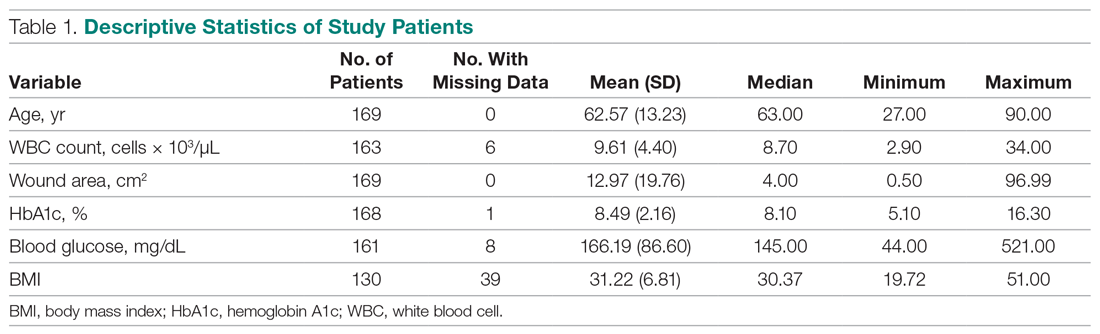
The descriptive statistics of 149 patients grouped into 3 categories (healed, amputated, unhealed/non-amputated) are shown in Table 2.
The results of the logistic regression exploring the differences between the amputation and healed groups and the unhealed/non-amputated group are shown in Table 3. The amputation group had a higher mean age and WBC count and greater wound area. Increased age was determined to be a significant predictor of the odds of amputation (P = 0.0089). For each year increase in age, the odds of amputation increased by 6.5% (odds ratio, 1.07 [95% confidence interval {CI}, 1.02-1.12]). Patients in the amputation group were more likely to be male, Hispanic, and African American and to have wound infections and comorbidities (osteomyelitis, neuropathy, and gangrene).
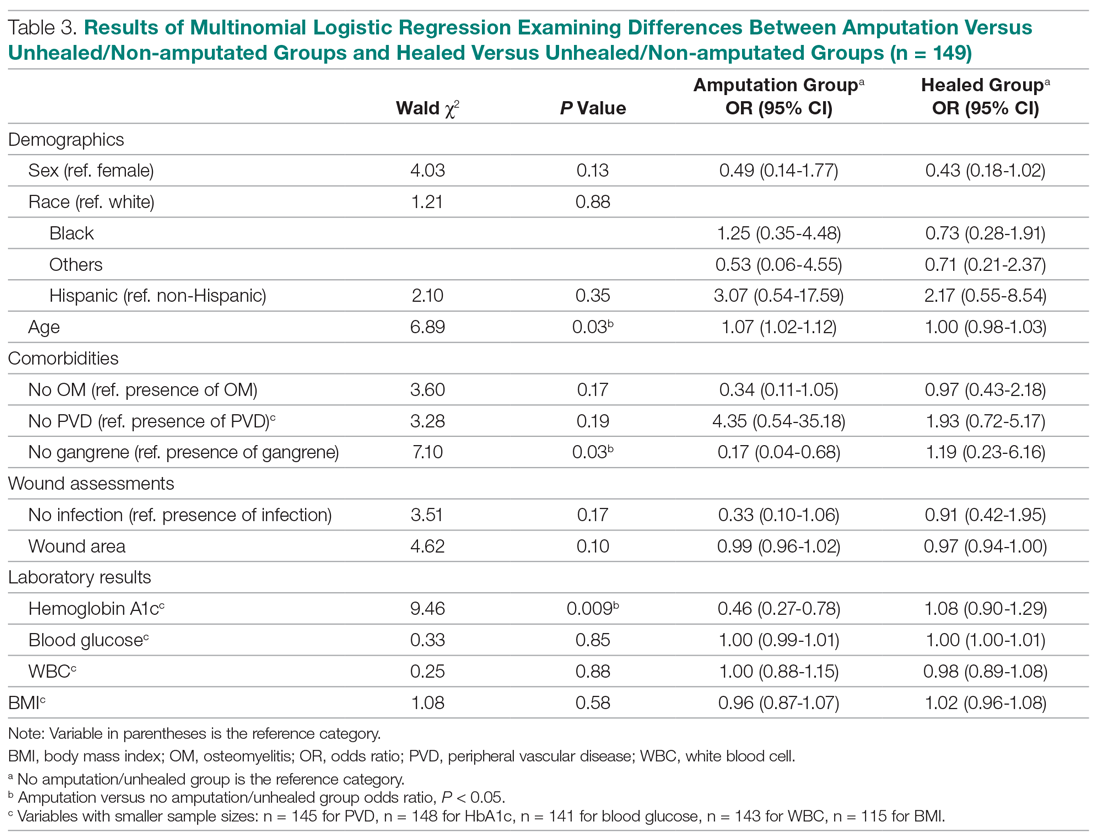
The presence of gangrene was significantly associated with LEA (P = 0.03). Specifically, the odds of patients without gangrene undergoing a LEA were substantially lower compared with their counterparts with gangrene (odds ratio, 0.17; 95% CI, 0.04-0.68; P = 0.0131). However, the presence of gangrene was not associated with the odds of healing compared with the odds of neither healing nor undergoing amputation (P = 0.84; not shown in Table 3).
The amputation group had lower mean values for HbA1c, BMI, and blood glucose levels and a lower rate of peripheral vascular disease. Only the relationship between lower HbA1c and increased odds of amputation versus not healing/non-amputation was found to be statistically significant (95% CI, 0.27-0.78; P = 0.009).
Discussion
This retrospective study was undertaken to evaluate factors associated with LEA in patients with diabetic foot ulcers. Patients with diabetes being treated at a wound care facility often require continuous surgical and metabolic intervention to promote optimal healing: drainage, surgical debridement, irrigation, culturing for infection, and monitoring of blood glucose levels. This treatment requires strict compliance with medical directions and, oftentimes, additional care, such as home-care nursing visits, to maintain a curative environment for the wound. Frequently, wounds on the lower extremity further complicate the healing process by reducing the patient’s mobility and daily life. Due to these factors, many patients progress to LEA. The link between diabetic ulcers and amputation has already been well described in previous studies, with studies showing that history of diabetic foot ulcer significantly predisposes an individual to LEA.4 However, few studies have further investigated demographic factors associated with risk for an amputation. Our study analyzed several categories of patient data taken from a baseline visit. We found that those with highly elevated HbA1c values were less likely to have an amputation than persons with relatively lower levels, a finding that is contrary to previous studies.
Our study’s findings suggest a higher risk for LEA with increased age. The amputation group was, on average, 7 years older than the other 2 groups. A recent study showed that risk for amputation is directly correlated to patient age, as is the mortality rate after undergoing LEA (2.3%; P < 0.05).5 Our study found that with each increase in age of 1 year, the odds of amputation increased by 6.5%. However, recent evidence on LEA risk and aging suggests that age is of less consequence than the duration of diabetes. One study found that the propensity to develop diabetic foot ulcers increases with the duration of diabetes.6 The same study found that prevalence of ulceration was correlated with age, but the relationship between age and LEA was less significant. A follow-up study for LEA could be done to examine the role of disease duration versus age in LEA.
A consensus among previous studies is that men have a higher risk for LEA.5,7 Men comprised the majority in all 3 groups in our study. In addition, the amputation group in our study had the lowest BMI. Higher BMI generally is associated with an increased risk for health complications. However, a past study conducted in Taiwan reported that obese patients with diabetes were less likely to undergo LEA than those within the normal range for BMI.8 Neither study suggests that obesity is a deterrent for LEA, but both studies may suggest that risk of amputation may approach a maximum frequency at a specific BMI range, and then decrease. This unconfirmed “cyclic” relationship should be evaluated further in a larger sample size.
Most patients in our analysis were Caucasian, followed by African American and South Asian. African Americans were the only racial group with an increased frequency in the amputation group. This finding is supported by a previous study that found that the rate of LEA among patients with diabetes in low-income, predominantly African-American neighborhoods was nearly double that in wealthier, predominantly Caucasian areas.9 A potential problem in the comparison between our data with previous studies is that the studies did not analyze patients with our inclusion criteria. All patients with diabetes in previous investigations were grouped by race, but were not necessarily required to have 1 or more ulcers. Multiple ulcers may predispose an individual to a greater risk for amputation.
Multinomial logistic regression did not suggest an association between initial size of a patient’s wound and the risk of amputation. However, the descriptive data suggests a trend. Patients who did not heal or require an amputation had the largest average wound area. This finding is not surprising in that our study followed individuals for only 3 months. Many wounds require a long course of treatment, especially in patients with diabetes, who may have poor vascularization. However, in comparison to the healed patients, the patients who required an amputation had a larger average wound area. A larger wound requires a plentiful vascular supply for the delivery of clotting factors and nutrients to the damaged area. As wound size increases, an individual’s body must transmit an increased quantity of these factors and nutrients for the regeneration of tissue. In addition, wounds that possess a larger surface area require more debridement and present a greater opportunity for infection. This may also foreshadow a longer, more costly course of treatment. Additionally, individuals coping with large ulcerations are burdened by more elaborate and complex wound dressings.
Elevated levels of HbA1c are associated with increased adverse effects of diabetes, including end-stage renal disease, neuropathy, and infection.10 In a previous study, the risk for amputation was 1.2 times higher in patients with elevated HbA1c.11 In contrast, our study suggested the odds of LEA versus not healing/not undergoing amputation decreased as HbA1c increased. As a patient’s HbA1c level increased by a value of 1, their odds for LEA decreased by 54.3%. This finding contradicts prior studies that have found a positive association between HbA1c and LEA risk, including a study where each percentage increase in HbA1c correlated with a 13% to 15% increased risk of LEA.12 The finding that patients who underwent amputation in our study had lower levels of HbA1c and blood glucose cannot be fully explained. The maximum HbA1c value in the amputated group was 7.9%. The average values for healed patients and those who underwent LEA were 8.75% and 6.77%, respectively.
Blood glucose levels were also found to be the lowest in the amputated group in our study (mean, 149.29 mg/dL vs 163.19 mg/dL in the healed group). Similar results were found in a Brazilian study, in which patients who did not require amputation had higher HbA1c levels. This study also found an association between blood glucose levels above 200 mg/dL and amputations.3 These findings provide interesting opportunities for repeat studies, preferably with a larger number of participants.
Our study is limited by the small sample size. The sample population had to be reduced, as many patients were lost to follow-up. Although this paring down of the sample size can introduce bias, we are confident that our study is representative of the demographic of patients treated in our facility. The loss of patients to follow-up in turn caused the window of analysis to be narrowed, as long-term outcome data were not available. A multisite study observing various population samples can better explore the relationship between HbA1c and risk of amputation.
Conclusion
This retrospective study exploring factors associated with LEA was unique in that all our participants had 1 or more diabetic foot ulcerations, and thus already had an extremely high risk for amputation, in contrast to previous studies that followed persons at risk for developing diabetic foot ulcerations. In contrast to several previous studies, we found that the risk for amputation actually decreased as baseline measurements of HbA1c increased. The results of this study offer many opportunities for future investigations, preferably with a larger sample size. By further isolating and scrutinizing specific factors associated with LEA, researchers can help clinicians focus on providing wound care that promotes limb salvage.
Corresponding author: Alisha Oropallo, MD, MS, Northwell Health Comprehensive Wound Care Healing Center and Hyperbarics, 1999 Marcus Avenue, Suite M6, Lake Success, NY 11042; [email protected].
Financial disclosures: Funding for this research was provided by a multi-institutional AHRQ governmental grant.
1. Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2017. Atlanta, GA: US Department of Health and Human Services; 2017.
2. Uccioli L, Giurato L, Meloni M, et al. Comment on Hoffstad et al. Diabetes, lower-extremity amputation, and death. Diabetes Care. 2015;38:1852-1857.
3. Gamba MA, Gotlieb SLD, Bergamaschi DP, Vianna LAC. Lower extremity amputations in diabetic patients: a case-control study. Rev Saúde Pública. 2004;38:399-404.
4. Martins-Mendes D, Monteiro-Soares M, Boyko EJ, et al. The independent contribution of diabetic foot ulcer on lower extremity amputation and mortality risk. J Diabetes Complications. 2014;28:632-638.
5. Lipsky BA, Weigelt JA, Sun X, et al. Developing and validating a risk score for lower-extremity amputation in patients hospitalized for a diabetic foot infection. Diabetes Care. 2011;34:1695-1700.
6. Al-Rubeaan K, Al Derwish M, Ouizi S, et al. Diabetic foot complications and their risk factors from a large retrospective cohort study. PLoS One. 2015;10:e0124446.
7. Pickwell K, Siersma V, Kars M, et al. Predictors of lower-extremity amputation in patients with an infected diabetic foot ulcer. Diabetes Care. 2015;38:852-857.
8. Lin C, Hsu BR, Tsai J, et al. Effect of limb preservation status and body mass index on the survival of patients with limb-threatening diabetic foot ulcers. J Diabetes Complications. 2017;31:180-185.
9. Stevens CD, Schriger DL, Raffetto B, et al. Geographic clustering of diabetic lower-extremity amputations in low-income regions of California. Health Aff. 2014;33:1383-1390.
10. Liao L, Li C, Liu C, et al. Extreme levels of HbA1c increase incident ESRD risk in Chinese patients with type 2 diabetes: competing risk analysis in national cohort of Taiwan diabetes study. PLoS One. 2015; 10:e0130828.
11. Miyajima S, Shirai A, Yamamoto S, et al. Risk factors for major limb amputations in diabetic foot gangrene patients. Diabetes Res Clin Pract. 2006;71:272-279.
12. Zhao W, Katzmarzyk PT, Horswell R, et al. HbA1c and lower-extremity amputation risk in low-income patients with diabetes. Diabetes Care. 2013;36:3591-3598.
1. Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2017. Atlanta, GA: US Department of Health and Human Services; 2017.
2. Uccioli L, Giurato L, Meloni M, et al. Comment on Hoffstad et al. Diabetes, lower-extremity amputation, and death. Diabetes Care. 2015;38:1852-1857.
3. Gamba MA, Gotlieb SLD, Bergamaschi DP, Vianna LAC. Lower extremity amputations in diabetic patients: a case-control study. Rev Saúde Pública. 2004;38:399-404.
4. Martins-Mendes D, Monteiro-Soares M, Boyko EJ, et al. The independent contribution of diabetic foot ulcer on lower extremity amputation and mortality risk. J Diabetes Complications. 2014;28:632-638.
5. Lipsky BA, Weigelt JA, Sun X, et al. Developing and validating a risk score for lower-extremity amputation in patients hospitalized for a diabetic foot infection. Diabetes Care. 2011;34:1695-1700.
6. Al-Rubeaan K, Al Derwish M, Ouizi S, et al. Diabetic foot complications and their risk factors from a large retrospective cohort study. PLoS One. 2015;10:e0124446.
7. Pickwell K, Siersma V, Kars M, et al. Predictors of lower-extremity amputation in patients with an infected diabetic foot ulcer. Diabetes Care. 2015;38:852-857.
8. Lin C, Hsu BR, Tsai J, et al. Effect of limb preservation status and body mass index on the survival of patients with limb-threatening diabetic foot ulcers. J Diabetes Complications. 2017;31:180-185.
9. Stevens CD, Schriger DL, Raffetto B, et al. Geographic clustering of diabetic lower-extremity amputations in low-income regions of California. Health Aff. 2014;33:1383-1390.
10. Liao L, Li C, Liu C, et al. Extreme levels of HbA1c increase incident ESRD risk in Chinese patients with type 2 diabetes: competing risk analysis in national cohort of Taiwan diabetes study. PLoS One. 2015; 10:e0130828.
11. Miyajima S, Shirai A, Yamamoto S, et al. Risk factors for major limb amputations in diabetic foot gangrene patients. Diabetes Res Clin Pract. 2006;71:272-279.
12. Zhao W, Katzmarzyk PT, Horswell R, et al. HbA1c and lower-extremity amputation risk in low-income patients with diabetes. Diabetes Care. 2013;36:3591-3598.
Larger absolute rivaroxaban benefit in diabetes: COMPASS
In the COMPASS trial of patients with stable coronary or peripheral artery disease (PAD), the combination of aspirin plus rivaroxaban, 2.5 mg twice daily, provided a larger absolute benefit on cardiovascular endpoints — including a threefold greater reduction in all-cause mortality — in patients with diabetes compared with the overall population.
The results of the diabetes subset of the COMPASS trial were presented by Deepak Bhatt, MD, Brigham and Women’s Hospital Heart & Vascular Center, Boston, Massachusetts, on March 28 at the “virtual” American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). They were also simultaneously published online in Circulation.
“Use of dual pathway inhibition with low-dose rivaroxaban plus aspirin is particularly attractive in high-risk patients such as those with diabetes,” Bhatt concluded.
The COMPASS trial was first reported in 2017 and showed a new low dose of rivaroxaban (2.5-mg twice-daily; Xarelto, Bayer/Janssen Pharmaceuticals) plus aspirin, 100 mg once daily, was associated with a reduction in ischemic events and mortality and a superior net clinical benefit, balancing ischemic benefit with severe bleeding, compared with aspirin alone for secondary prevention in patients with stable atherosclerotic vascular disease.
But clinicians have been slow to prescribe rivaroxaban in this new and very large population.
“It’s been more than 2 years now since main COMPASS results, and there isn’t a sense that this therapy has really caught on,” chair of the current ACC session at which the diabetes subgroup results were presented, Hadley Wilson, MD, Sanger Heart and Vascular Institute, Charlotte, North Carolina, commented:
He asked Bhatt whether the diabetes subgroup may be “the tipping point that will make people aware of rivaroxaban and then that may trickle down to other patients.”
Bhatt said that he hoped that would be the case. “We as a steering committee of this trial could say the results were positive so rivaroxaban should now be used in everyone with stable coronary or peripheral arterial disease, but that is impractical and as you out point out it hasn’t happened,” he replied.
“In PAD/vascular medicine we have embraced this new therapy. In the broader cardiology world there are a lot of patients with stable coronary arterial disease at high ischemic risk who could take rivaroxaban, but its use is bound to be limited by it being a branded drug and the fact that there is a bleeding risk,” Bhatt explained.
“I think we need to identify patients with the highest ischemic risk and focus drugs such as these with a financial cost and a bleeding risk on those who most likely will derive the greatest absolute reduction in risk,” he said. “The PAD subgroup is one group where this is the case, and now we have shown the diabetes subgroup is another. And there is no incremental bleeding risk in this group over the whole population, so they get a much greater benefit without a greater risk. I hope this helps get rivaroxaban at the new lower dose used much more often.”
A total of 18,278 patients were randomly assigned to the combination of rivaroxaban and aspirin or aspirin alone in the COMPASS trial. Of these, 6922 had diabetes mellitus at baseline and 11,356 did not have diabetes.
Results from the current analysis show a consistent and similar relative risk reduction for benefit of rivaroxaban plus aspirin vs placebo plus aspirin in patients both with and without diabetes for the primary efficacy endpoint, a composite of cardiovascular death, myocardial infarction (MI), or stroke, with a hazard ratio of 0.74 for patients with diabetes and 0.77 for those without diabetes, the researchers report.
Because of the higher baseline risk in the diabetes subgroup, these patients had numerically larger absolute risk reductions with rivaroxaban than those without diabetes for the primary efficacy endpoint at 3 years (2.3% vs 1.4%) and for all-cause mortality (1.9% vs 0.6%).
These results translate into a number needed to treat (NNT) with rivaroxaban for 3 years to prevent one CV death, MI, or stroke of 44 for the diabetes group vs 73 for the nondiabetes group; the NNT to prevent one all-cause death was 54 for the diabetes group vs 167 for the nondiabetes group, the authors write.
Because the bleeding hazards were similar among patients with and without diabetes, the absolute net clinical benefit (MI, stroke, cardiovascular death, or bleeding leading to death or symptomatic bleeding into a critical organ) for rivaroxaban was “particularly favorable” in the diabetes group (2.7% fewer events in the diabetes group vs 1.0% fewer events in the nondiabetes group), they add.
Panelist at the ACC Featured Clinical Research session at which these results were presented, Jennifer Robinson, MD, University of Iowa College of Public Health, Iowa City, asked Bhatt how clinicians were supposed to decide which of the many new agents now becoming available for patients with stable coronary artery disease to prescribe first.
“We often forget about rivaroxaban when we’re thinking about what to add next for our secondary prevention patients,” she said. “You also led the REDUCE-IT trial showing benefit of icosapent ethyl, icosapent ethyl icosapent ethyl icosapent ethyl and there is also ezetimibe, PCSK9 inhibitors and SGLT2 inhibitors. For your patients with coronary disease who are already on a high dose statin which one of these would you add next?”
“That is what physicians need to ponder all the time,” Bhatt replied. “And when a patient has several risk factors that are not well controlled, I guess it’s all important. I go through a checklist with my patients and try and figure what they’re not on that could further reduce their risk.”
“In the COMPASS trial there was an overall positive result with rivaroxaban in the whole population. And now we have shown that patients with diabetes had an even greater absolute risk reduction. That pattern has also been seen with other classes of agents including the statins, PCSK9 inhibitors, and icosapent ethyl,” Bhatt noted.
“In patients with diabetes, I will usually target whatever is standing out most at that time. If their glycemic control is completely out of whack, then that is what I would focus on first, and these days often with a SGLT2 inhibitor or GLP-1 agonist. If the LDL was out of control, I would add ezetimibe or a PCSK9 inhibitor. If the triglycerides were high, I would add icosapent ethyl. If multiple things were out of control, I would usually focus on the number most out of kilter first and try not to forget about everything else.”
But Bhatt noted that the challenge with rivaroxaban is that there is no test of thrombosis risk that would prompt the physician to take action. “Basically, the doctor just has to remember to do it. In that regard I would consider whether patients are at low bleeding risk and are they still at high ischemic risk despite controlling other risk factors and, if so, then I would add this low dose of rivaroxaban.”
Another panel member, Sekar Kathiresan, MD, asked Bhatt whether he recommended using available scores to assess the bleeding/thrombosis risk/benefits of adding an antithrombotic.
Bhatt replied: “That’s a terrific question. I guess the right answer is that we should be doing that, but in reality I have to concede that I don’t use these scores. They have shown appropriate C statistics in populations, but they are not fantastic in individual patients.”
“I have to confess that I use the eyeball test. There is nothing as good at predicting future bleeding as past bleeding. So if a patient has had bleeding problems on aspirin alone I wouldn’t add rivaroxaban. But if a patient hasn’t bled before, especially if they had some experience of dual antiplatelet therapy, then they would be good candidates for a low vascular dose of rivaroxaban,” he said.
“It is not as easy as with other drugs as there is always a bleeding trade-off with an antithrombotic. There is no such thing as a free lunch. So patients need careful assessment when considering prescribing rivaroxaban and regular reassessment over time to check if they have had any bleeding,” he added.
The COMPASS study was funded by Bayer. Bhatt reports honoraria from Bayer via the Population Health Research Institute for his role on the COMPASS trial and other research funding from Bayer to the Brigham & Women’s Hospital.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). Abstract 20-LB-20544-ACC. Presented March 28, 2020.
Circulation. Published online March 28, 2020. Full text.
This article first appeared on Medscape.com.
In the COMPASS trial of patients with stable coronary or peripheral artery disease (PAD), the combination of aspirin plus rivaroxaban, 2.5 mg twice daily, provided a larger absolute benefit on cardiovascular endpoints — including a threefold greater reduction in all-cause mortality — in patients with diabetes compared with the overall population.
The results of the diabetes subset of the COMPASS trial were presented by Deepak Bhatt, MD, Brigham and Women’s Hospital Heart & Vascular Center, Boston, Massachusetts, on March 28 at the “virtual” American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). They were also simultaneously published online in Circulation.
“Use of dual pathway inhibition with low-dose rivaroxaban plus aspirin is particularly attractive in high-risk patients such as those with diabetes,” Bhatt concluded.
The COMPASS trial was first reported in 2017 and showed a new low dose of rivaroxaban (2.5-mg twice-daily; Xarelto, Bayer/Janssen Pharmaceuticals) plus aspirin, 100 mg once daily, was associated with a reduction in ischemic events and mortality and a superior net clinical benefit, balancing ischemic benefit with severe bleeding, compared with aspirin alone for secondary prevention in patients with stable atherosclerotic vascular disease.
But clinicians have been slow to prescribe rivaroxaban in this new and very large population.
“It’s been more than 2 years now since main COMPASS results, and there isn’t a sense that this therapy has really caught on,” chair of the current ACC session at which the diabetes subgroup results were presented, Hadley Wilson, MD, Sanger Heart and Vascular Institute, Charlotte, North Carolina, commented:
He asked Bhatt whether the diabetes subgroup may be “the tipping point that will make people aware of rivaroxaban and then that may trickle down to other patients.”
Bhatt said that he hoped that would be the case. “We as a steering committee of this trial could say the results were positive so rivaroxaban should now be used in everyone with stable coronary or peripheral arterial disease, but that is impractical and as you out point out it hasn’t happened,” he replied.
“In PAD/vascular medicine we have embraced this new therapy. In the broader cardiology world there are a lot of patients with stable coronary arterial disease at high ischemic risk who could take rivaroxaban, but its use is bound to be limited by it being a branded drug and the fact that there is a bleeding risk,” Bhatt explained.
“I think we need to identify patients with the highest ischemic risk and focus drugs such as these with a financial cost and a bleeding risk on those who most likely will derive the greatest absolute reduction in risk,” he said. “The PAD subgroup is one group where this is the case, and now we have shown the diabetes subgroup is another. And there is no incremental bleeding risk in this group over the whole population, so they get a much greater benefit without a greater risk. I hope this helps get rivaroxaban at the new lower dose used much more often.”
A total of 18,278 patients were randomly assigned to the combination of rivaroxaban and aspirin or aspirin alone in the COMPASS trial. Of these, 6922 had diabetes mellitus at baseline and 11,356 did not have diabetes.
Results from the current analysis show a consistent and similar relative risk reduction for benefit of rivaroxaban plus aspirin vs placebo plus aspirin in patients both with and without diabetes for the primary efficacy endpoint, a composite of cardiovascular death, myocardial infarction (MI), or stroke, with a hazard ratio of 0.74 for patients with diabetes and 0.77 for those without diabetes, the researchers report.
Because of the higher baseline risk in the diabetes subgroup, these patients had numerically larger absolute risk reductions with rivaroxaban than those without diabetes for the primary efficacy endpoint at 3 years (2.3% vs 1.4%) and for all-cause mortality (1.9% vs 0.6%).
These results translate into a number needed to treat (NNT) with rivaroxaban for 3 years to prevent one CV death, MI, or stroke of 44 for the diabetes group vs 73 for the nondiabetes group; the NNT to prevent one all-cause death was 54 for the diabetes group vs 167 for the nondiabetes group, the authors write.
Because the bleeding hazards were similar among patients with and without diabetes, the absolute net clinical benefit (MI, stroke, cardiovascular death, or bleeding leading to death or symptomatic bleeding into a critical organ) for rivaroxaban was “particularly favorable” in the diabetes group (2.7% fewer events in the diabetes group vs 1.0% fewer events in the nondiabetes group), they add.
Panelist at the ACC Featured Clinical Research session at which these results were presented, Jennifer Robinson, MD, University of Iowa College of Public Health, Iowa City, asked Bhatt how clinicians were supposed to decide which of the many new agents now becoming available for patients with stable coronary artery disease to prescribe first.
“We often forget about rivaroxaban when we’re thinking about what to add next for our secondary prevention patients,” she said. “You also led the REDUCE-IT trial showing benefit of icosapent ethyl, icosapent ethyl icosapent ethyl icosapent ethyl and there is also ezetimibe, PCSK9 inhibitors and SGLT2 inhibitors. For your patients with coronary disease who are already on a high dose statin which one of these would you add next?”
“That is what physicians need to ponder all the time,” Bhatt replied. “And when a patient has several risk factors that are not well controlled, I guess it’s all important. I go through a checklist with my patients and try and figure what they’re not on that could further reduce their risk.”
“In the COMPASS trial there was an overall positive result with rivaroxaban in the whole population. And now we have shown that patients with diabetes had an even greater absolute risk reduction. That pattern has also been seen with other classes of agents including the statins, PCSK9 inhibitors, and icosapent ethyl,” Bhatt noted.
“In patients with diabetes, I will usually target whatever is standing out most at that time. If their glycemic control is completely out of whack, then that is what I would focus on first, and these days often with a SGLT2 inhibitor or GLP-1 agonist. If the LDL was out of control, I would add ezetimibe or a PCSK9 inhibitor. If the triglycerides were high, I would add icosapent ethyl. If multiple things were out of control, I would usually focus on the number most out of kilter first and try not to forget about everything else.”
But Bhatt noted that the challenge with rivaroxaban is that there is no test of thrombosis risk that would prompt the physician to take action. “Basically, the doctor just has to remember to do it. In that regard I would consider whether patients are at low bleeding risk and are they still at high ischemic risk despite controlling other risk factors and, if so, then I would add this low dose of rivaroxaban.”
Another panel member, Sekar Kathiresan, MD, asked Bhatt whether he recommended using available scores to assess the bleeding/thrombosis risk/benefits of adding an antithrombotic.
Bhatt replied: “That’s a terrific question. I guess the right answer is that we should be doing that, but in reality I have to concede that I don’t use these scores. They have shown appropriate C statistics in populations, but they are not fantastic in individual patients.”
“I have to confess that I use the eyeball test. There is nothing as good at predicting future bleeding as past bleeding. So if a patient has had bleeding problems on aspirin alone I wouldn’t add rivaroxaban. But if a patient hasn’t bled before, especially if they had some experience of dual antiplatelet therapy, then they would be good candidates for a low vascular dose of rivaroxaban,” he said.
“It is not as easy as with other drugs as there is always a bleeding trade-off with an antithrombotic. There is no such thing as a free lunch. So patients need careful assessment when considering prescribing rivaroxaban and regular reassessment over time to check if they have had any bleeding,” he added.
The COMPASS study was funded by Bayer. Bhatt reports honoraria from Bayer via the Population Health Research Institute for his role on the COMPASS trial and other research funding from Bayer to the Brigham & Women’s Hospital.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). Abstract 20-LB-20544-ACC. Presented March 28, 2020.
Circulation. Published online March 28, 2020. Full text.
This article first appeared on Medscape.com.
In the COMPASS trial of patients with stable coronary or peripheral artery disease (PAD), the combination of aspirin plus rivaroxaban, 2.5 mg twice daily, provided a larger absolute benefit on cardiovascular endpoints — including a threefold greater reduction in all-cause mortality — in patients with diabetes compared with the overall population.
The results of the diabetes subset of the COMPASS trial were presented by Deepak Bhatt, MD, Brigham and Women’s Hospital Heart & Vascular Center, Boston, Massachusetts, on March 28 at the “virtual” American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). They were also simultaneously published online in Circulation.
“Use of dual pathway inhibition with low-dose rivaroxaban plus aspirin is particularly attractive in high-risk patients such as those with diabetes,” Bhatt concluded.
The COMPASS trial was first reported in 2017 and showed a new low dose of rivaroxaban (2.5-mg twice-daily; Xarelto, Bayer/Janssen Pharmaceuticals) plus aspirin, 100 mg once daily, was associated with a reduction in ischemic events and mortality and a superior net clinical benefit, balancing ischemic benefit with severe bleeding, compared with aspirin alone for secondary prevention in patients with stable atherosclerotic vascular disease.
But clinicians have been slow to prescribe rivaroxaban in this new and very large population.
“It’s been more than 2 years now since main COMPASS results, and there isn’t a sense that this therapy has really caught on,” chair of the current ACC session at which the diabetes subgroup results were presented, Hadley Wilson, MD, Sanger Heart and Vascular Institute, Charlotte, North Carolina, commented:
He asked Bhatt whether the diabetes subgroup may be “the tipping point that will make people aware of rivaroxaban and then that may trickle down to other patients.”
Bhatt said that he hoped that would be the case. “We as a steering committee of this trial could say the results were positive so rivaroxaban should now be used in everyone with stable coronary or peripheral arterial disease, but that is impractical and as you out point out it hasn’t happened,” he replied.
“In PAD/vascular medicine we have embraced this new therapy. In the broader cardiology world there are a lot of patients with stable coronary arterial disease at high ischemic risk who could take rivaroxaban, but its use is bound to be limited by it being a branded drug and the fact that there is a bleeding risk,” Bhatt explained.
“I think we need to identify patients with the highest ischemic risk and focus drugs such as these with a financial cost and a bleeding risk on those who most likely will derive the greatest absolute reduction in risk,” he said. “The PAD subgroup is one group where this is the case, and now we have shown the diabetes subgroup is another. And there is no incremental bleeding risk in this group over the whole population, so they get a much greater benefit without a greater risk. I hope this helps get rivaroxaban at the new lower dose used much more often.”
A total of 18,278 patients were randomly assigned to the combination of rivaroxaban and aspirin or aspirin alone in the COMPASS trial. Of these, 6922 had diabetes mellitus at baseline and 11,356 did not have diabetes.
Results from the current analysis show a consistent and similar relative risk reduction for benefit of rivaroxaban plus aspirin vs placebo plus aspirin in patients both with and without diabetes for the primary efficacy endpoint, a composite of cardiovascular death, myocardial infarction (MI), or stroke, with a hazard ratio of 0.74 for patients with diabetes and 0.77 for those without diabetes, the researchers report.
Because of the higher baseline risk in the diabetes subgroup, these patients had numerically larger absolute risk reductions with rivaroxaban than those without diabetes for the primary efficacy endpoint at 3 years (2.3% vs 1.4%) and for all-cause mortality (1.9% vs 0.6%).
These results translate into a number needed to treat (NNT) with rivaroxaban for 3 years to prevent one CV death, MI, or stroke of 44 for the diabetes group vs 73 for the nondiabetes group; the NNT to prevent one all-cause death was 54 for the diabetes group vs 167 for the nondiabetes group, the authors write.
Because the bleeding hazards were similar among patients with and without diabetes, the absolute net clinical benefit (MI, stroke, cardiovascular death, or bleeding leading to death or symptomatic bleeding into a critical organ) for rivaroxaban was “particularly favorable” in the diabetes group (2.7% fewer events in the diabetes group vs 1.0% fewer events in the nondiabetes group), they add.
Panelist at the ACC Featured Clinical Research session at which these results were presented, Jennifer Robinson, MD, University of Iowa College of Public Health, Iowa City, asked Bhatt how clinicians were supposed to decide which of the many new agents now becoming available for patients with stable coronary artery disease to prescribe first.
“We often forget about rivaroxaban when we’re thinking about what to add next for our secondary prevention patients,” she said. “You also led the REDUCE-IT trial showing benefit of icosapent ethyl, icosapent ethyl icosapent ethyl icosapent ethyl and there is also ezetimibe, PCSK9 inhibitors and SGLT2 inhibitors. For your patients with coronary disease who are already on a high dose statin which one of these would you add next?”
“That is what physicians need to ponder all the time,” Bhatt replied. “And when a patient has several risk factors that are not well controlled, I guess it’s all important. I go through a checklist with my patients and try and figure what they’re not on that could further reduce their risk.”
“In the COMPASS trial there was an overall positive result with rivaroxaban in the whole population. And now we have shown that patients with diabetes had an even greater absolute risk reduction. That pattern has also been seen with other classes of agents including the statins, PCSK9 inhibitors, and icosapent ethyl,” Bhatt noted.
“In patients with diabetes, I will usually target whatever is standing out most at that time. If their glycemic control is completely out of whack, then that is what I would focus on first, and these days often with a SGLT2 inhibitor or GLP-1 agonist. If the LDL was out of control, I would add ezetimibe or a PCSK9 inhibitor. If the triglycerides were high, I would add icosapent ethyl. If multiple things were out of control, I would usually focus on the number most out of kilter first and try not to forget about everything else.”
But Bhatt noted that the challenge with rivaroxaban is that there is no test of thrombosis risk that would prompt the physician to take action. “Basically, the doctor just has to remember to do it. In that regard I would consider whether patients are at low bleeding risk and are they still at high ischemic risk despite controlling other risk factors and, if so, then I would add this low dose of rivaroxaban.”
Another panel member, Sekar Kathiresan, MD, asked Bhatt whether he recommended using available scores to assess the bleeding/thrombosis risk/benefits of adding an antithrombotic.
Bhatt replied: “That’s a terrific question. I guess the right answer is that we should be doing that, but in reality I have to concede that I don’t use these scores. They have shown appropriate C statistics in populations, but they are not fantastic in individual patients.”
“I have to confess that I use the eyeball test. There is nothing as good at predicting future bleeding as past bleeding. So if a patient has had bleeding problems on aspirin alone I wouldn’t add rivaroxaban. But if a patient hasn’t bled before, especially if they had some experience of dual antiplatelet therapy, then they would be good candidates for a low vascular dose of rivaroxaban,” he said.
“It is not as easy as with other drugs as there is always a bleeding trade-off with an antithrombotic. There is no such thing as a free lunch. So patients need careful assessment when considering prescribing rivaroxaban and regular reassessment over time to check if they have had any bleeding,” he added.
The COMPASS study was funded by Bayer. Bhatt reports honoraria from Bayer via the Population Health Research Institute for his role on the COMPASS trial and other research funding from Bayer to the Brigham & Women’s Hospital.
American College of Cardiology 2020 Scientific Session (ACC.20)/World Congress of Cardiology (WCC). Abstract 20-LB-20544-ACC. Presented March 28, 2020.
Circulation. Published online March 28, 2020. Full text.
This article first appeared on Medscape.com.
Keep calm: Under 25s with diabetes aren't being hospitalized for COVID-19
Reports from pediatric endocrinologists in COVID-19 hot spots globally indicate that children, adolescents, and young adults with diabetes have so far not shown a different disease pattern with the virus compared to children and younger people who do not have diabetes.
Indeed, to date [as of March 24]” according to a new statement from the International Society for Pediatric and Adolescent Diabetes (ISPAD), which currently has about 1,300 members around the globe and has instituted a discussion forum about the topic of treating children with both diabetes and COVID-19.
“We find these reports [from colleagues around the world], though anecdotal, to be reassuring,” it notes. However, there are real worries regarding other potentially dangerous effects. ISPAD has expressed concern, for example, that the COVID-19 pandemic will prevent youngsters with existing diabetes who are having diabetic emergencies from seeking hospital care.
Chinese physicians have reported to ISPAD a number of cases of delayed hospital admissions for diabetic ketoacidosis (DKA) in children with known type 1 diabetes because hospital services were closed for non–COVID-19 care.
Andrea Scaramuzza, MD, a pediatric endocrinologist at Ospedale Maggiore di Cremona, Italy, has similarly reported multiple cases of patients presenting to emergency services there with severe DKA.
“These experiences reinforce the importance of continued attentiveness to standard diabetes care to avoid the need for hospitalization and emergency or urgent care visits,” says ISPAD, under the strapline: “Keep calm and mind your diabetes care.”
But it nevertheless stresses that these resources should be used “if needed.”
Worries that new-onset diabetes will be missed during COVID-19
Dr. Scaramuzza said in an interview that there also are concerns regarding delays in diagnoses of new cases of type 1 diabetes “due to the fear families have to go to the emergency department because of COVID-19.”
Indeed, in Italy, a few patients have arrived with very serious DKA, he said. Dr. Scaramuzza noted a colleague from Naples, Dario Iafusco, MD, and colleagues have made a video to keep awareness high regarding new-onset diabetes.
“This coronavirus pandemic can be defeated if you stay at home, but if you know of a child who has excessive thirst, frequent urination, or who starts vomiting,” seek health care advice immediately. “This child could have [type 1] diabetes. Prevent severe DKA, or worse, death,” Dr. Iafusco of the Regional Centre of Paediatric Diabetology G.Stoppoloni Via S. Andrea delle Dame, Naples, said in the video.
Physicians from China have similar observations, reporting to ISPAD several cases of delayed admissions of newly diagnosed type 1 diabetes because hospital services were closed for non–COVID-19 care.
Keep calm and mind your diabetes care; physicians use telemedicine
Meanwhile, last week ISPAD issued guidance for young people with diabetes and their carers about what to do if COVID-19 infection is suspected.
Most advice is the same as for the general public because reports of COVID-19 infection suggest it is much less severe in children and adolescents, and the summary currently serves “as reassurance that youth with diabetes are not more affected by COVID-19 than peers,” it adds.
“Our approach to treating a child with diabetes would be to follow the ISPAD sick-day guidelines, which provide generalized diabetes management in any flu-like illness. We wouldn’t do anything very different right now,” one of the authors, Jamie Wood, MD, associate professor of clinical pediatrics at Case Western Reserve University, Cleveland, said in an interview.
“Any illness makes diabetes more difficult to manage and can increase the risk of DKA,” she emphasized.
“We would reinforce frequent monitoring of blood glucose and ketone levels, to never stop insulin – in fact, when most people are ill, the body is stressed and requires more insulin – and to stay hydrated and treat the underlying symptoms.”
And make sure to “treat the fever,” she stressed. “When patients with type 1 diabetes get fever, they have a tendency to make more ketones, so we recommend aggressive control of fever.”
ISPAD recommends young people aim to keep blood glucose levels between 4 and 10 mmol/L (72-180 mg/dL) and blood ketones below 0.6 mmol/L (10.8 mg/dL) during illness and to never stop insulin.
Guidance is provided on when to seek urgent specialist advice with possible referral to emergency care, for example, in cases in which the patient has DKA symptoms, such as persistent and/or worsened fruity breath odor or vomiting.
Dr. Scaramuzza said in an interview that, in Italy, he and his colleagues have increased their use of telemedicine to keep monitoring their patients with diabetes even from a distance and that it was working very well.
“Technology – such as downloading [records from] insulin pumps, continuous glucose monitoring systems, and the possibility to use Skype or other platforms – really helps,” he noted.
“There has been a rapid increase in telehealth as a way to continue to care for youth with diabetes and decrease risk for infection,” said ISPAD.
“Communication between patients, families, and health care teams is vitally important. Methods to do so that avoid visits to clinics or hospitals can provide needed diabetes advice and reduce risk for COVID-19 transmission.”
A version of this article originally appeared on Medscape.com.
Reports from pediatric endocrinologists in COVID-19 hot spots globally indicate that children, adolescents, and young adults with diabetes have so far not shown a different disease pattern with the virus compared to children and younger people who do not have diabetes.
Indeed, to date [as of March 24]” according to a new statement from the International Society for Pediatric and Adolescent Diabetes (ISPAD), which currently has about 1,300 members around the globe and has instituted a discussion forum about the topic of treating children with both diabetes and COVID-19.
“We find these reports [from colleagues around the world], though anecdotal, to be reassuring,” it notes. However, there are real worries regarding other potentially dangerous effects. ISPAD has expressed concern, for example, that the COVID-19 pandemic will prevent youngsters with existing diabetes who are having diabetic emergencies from seeking hospital care.
Chinese physicians have reported to ISPAD a number of cases of delayed hospital admissions for diabetic ketoacidosis (DKA) in children with known type 1 diabetes because hospital services were closed for non–COVID-19 care.
Andrea Scaramuzza, MD, a pediatric endocrinologist at Ospedale Maggiore di Cremona, Italy, has similarly reported multiple cases of patients presenting to emergency services there with severe DKA.
“These experiences reinforce the importance of continued attentiveness to standard diabetes care to avoid the need for hospitalization and emergency or urgent care visits,” says ISPAD, under the strapline: “Keep calm and mind your diabetes care.”
But it nevertheless stresses that these resources should be used “if needed.”
Worries that new-onset diabetes will be missed during COVID-19
Dr. Scaramuzza said in an interview that there also are concerns regarding delays in diagnoses of new cases of type 1 diabetes “due to the fear families have to go to the emergency department because of COVID-19.”
Indeed, in Italy, a few patients have arrived with very serious DKA, he said. Dr. Scaramuzza noted a colleague from Naples, Dario Iafusco, MD, and colleagues have made a video to keep awareness high regarding new-onset diabetes.
“This coronavirus pandemic can be defeated if you stay at home, but if you know of a child who has excessive thirst, frequent urination, or who starts vomiting,” seek health care advice immediately. “This child could have [type 1] diabetes. Prevent severe DKA, or worse, death,” Dr. Iafusco of the Regional Centre of Paediatric Diabetology G.Stoppoloni Via S. Andrea delle Dame, Naples, said in the video.
Physicians from China have similar observations, reporting to ISPAD several cases of delayed admissions of newly diagnosed type 1 diabetes because hospital services were closed for non–COVID-19 care.
Keep calm and mind your diabetes care; physicians use telemedicine
Meanwhile, last week ISPAD issued guidance for young people with diabetes and their carers about what to do if COVID-19 infection is suspected.
Most advice is the same as for the general public because reports of COVID-19 infection suggest it is much less severe in children and adolescents, and the summary currently serves “as reassurance that youth with diabetes are not more affected by COVID-19 than peers,” it adds.
“Our approach to treating a child with diabetes would be to follow the ISPAD sick-day guidelines, which provide generalized diabetes management in any flu-like illness. We wouldn’t do anything very different right now,” one of the authors, Jamie Wood, MD, associate professor of clinical pediatrics at Case Western Reserve University, Cleveland, said in an interview.
“Any illness makes diabetes more difficult to manage and can increase the risk of DKA,” she emphasized.
“We would reinforce frequent monitoring of blood glucose and ketone levels, to never stop insulin – in fact, when most people are ill, the body is stressed and requires more insulin – and to stay hydrated and treat the underlying symptoms.”
And make sure to “treat the fever,” she stressed. “When patients with type 1 diabetes get fever, they have a tendency to make more ketones, so we recommend aggressive control of fever.”
ISPAD recommends young people aim to keep blood glucose levels between 4 and 10 mmol/L (72-180 mg/dL) and blood ketones below 0.6 mmol/L (10.8 mg/dL) during illness and to never stop insulin.
Guidance is provided on when to seek urgent specialist advice with possible referral to emergency care, for example, in cases in which the patient has DKA symptoms, such as persistent and/or worsened fruity breath odor or vomiting.
Dr. Scaramuzza said in an interview that, in Italy, he and his colleagues have increased their use of telemedicine to keep monitoring their patients with diabetes even from a distance and that it was working very well.
“Technology – such as downloading [records from] insulin pumps, continuous glucose monitoring systems, and the possibility to use Skype or other platforms – really helps,” he noted.
“There has been a rapid increase in telehealth as a way to continue to care for youth with diabetes and decrease risk for infection,” said ISPAD.
“Communication between patients, families, and health care teams is vitally important. Methods to do so that avoid visits to clinics or hospitals can provide needed diabetes advice and reduce risk for COVID-19 transmission.”
A version of this article originally appeared on Medscape.com.
Reports from pediatric endocrinologists in COVID-19 hot spots globally indicate that children, adolescents, and young adults with diabetes have so far not shown a different disease pattern with the virus compared to children and younger people who do not have diabetes.
Indeed, to date [as of March 24]” according to a new statement from the International Society for Pediatric and Adolescent Diabetes (ISPAD), which currently has about 1,300 members around the globe and has instituted a discussion forum about the topic of treating children with both diabetes and COVID-19.
“We find these reports [from colleagues around the world], though anecdotal, to be reassuring,” it notes. However, there are real worries regarding other potentially dangerous effects. ISPAD has expressed concern, for example, that the COVID-19 pandemic will prevent youngsters with existing diabetes who are having diabetic emergencies from seeking hospital care.
Chinese physicians have reported to ISPAD a number of cases of delayed hospital admissions for diabetic ketoacidosis (DKA) in children with known type 1 diabetes because hospital services were closed for non–COVID-19 care.
Andrea Scaramuzza, MD, a pediatric endocrinologist at Ospedale Maggiore di Cremona, Italy, has similarly reported multiple cases of patients presenting to emergency services there with severe DKA.
“These experiences reinforce the importance of continued attentiveness to standard diabetes care to avoid the need for hospitalization and emergency or urgent care visits,” says ISPAD, under the strapline: “Keep calm and mind your diabetes care.”
But it nevertheless stresses that these resources should be used “if needed.”
Worries that new-onset diabetes will be missed during COVID-19
Dr. Scaramuzza said in an interview that there also are concerns regarding delays in diagnoses of new cases of type 1 diabetes “due to the fear families have to go to the emergency department because of COVID-19.”
Indeed, in Italy, a few patients have arrived with very serious DKA, he said. Dr. Scaramuzza noted a colleague from Naples, Dario Iafusco, MD, and colleagues have made a video to keep awareness high regarding new-onset diabetes.
“This coronavirus pandemic can be defeated if you stay at home, but if you know of a child who has excessive thirst, frequent urination, or who starts vomiting,” seek health care advice immediately. “This child could have [type 1] diabetes. Prevent severe DKA, or worse, death,” Dr. Iafusco of the Regional Centre of Paediatric Diabetology G.Stoppoloni Via S. Andrea delle Dame, Naples, said in the video.
Physicians from China have similar observations, reporting to ISPAD several cases of delayed admissions of newly diagnosed type 1 diabetes because hospital services were closed for non–COVID-19 care.
Keep calm and mind your diabetes care; physicians use telemedicine
Meanwhile, last week ISPAD issued guidance for young people with diabetes and their carers about what to do if COVID-19 infection is suspected.
Most advice is the same as for the general public because reports of COVID-19 infection suggest it is much less severe in children and adolescents, and the summary currently serves “as reassurance that youth with diabetes are not more affected by COVID-19 than peers,” it adds.
“Our approach to treating a child with diabetes would be to follow the ISPAD sick-day guidelines, which provide generalized diabetes management in any flu-like illness. We wouldn’t do anything very different right now,” one of the authors, Jamie Wood, MD, associate professor of clinical pediatrics at Case Western Reserve University, Cleveland, said in an interview.
“Any illness makes diabetes more difficult to manage and can increase the risk of DKA,” she emphasized.
“We would reinforce frequent monitoring of blood glucose and ketone levels, to never stop insulin – in fact, when most people are ill, the body is stressed and requires more insulin – and to stay hydrated and treat the underlying symptoms.”
And make sure to “treat the fever,” she stressed. “When patients with type 1 diabetes get fever, they have a tendency to make more ketones, so we recommend aggressive control of fever.”
ISPAD recommends young people aim to keep blood glucose levels between 4 and 10 mmol/L (72-180 mg/dL) and blood ketones below 0.6 mmol/L (10.8 mg/dL) during illness and to never stop insulin.
Guidance is provided on when to seek urgent specialist advice with possible referral to emergency care, for example, in cases in which the patient has DKA symptoms, such as persistent and/or worsened fruity breath odor or vomiting.
Dr. Scaramuzza said in an interview that, in Italy, he and his colleagues have increased their use of telemedicine to keep monitoring their patients with diabetes even from a distance and that it was working very well.
“Technology – such as downloading [records from] insulin pumps, continuous glucose monitoring systems, and the possibility to use Skype or other platforms – really helps,” he noted.
“There has been a rapid increase in telehealth as a way to continue to care for youth with diabetes and decrease risk for infection,” said ISPAD.
“Communication between patients, families, and health care teams is vitally important. Methods to do so that avoid visits to clinics or hospitals can provide needed diabetes advice and reduce risk for COVID-19 transmission.”
A version of this article originally appeared on Medscape.com.
FDA advises stopping SGLT2 inhibitor treatment prior to surgery
The new changes affect canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin, and were made because surgery may put patients being treated with SGLT2 inhibitors at a higher risk of ketoacidosis. Canagliflozin, dapagliflozin, and empagliflozin should be discontinued 3 days before scheduled surgery, and ertugliflozin should be stopped at least 4 days before, the agency noted in a press release. Blood glucose should be monitored after drug discontinuation and appropriately managed before surgery.
“The SGLT2 inhibitor may be restarted once the patient’s oral intake is back to baseline and any other risk factors for ketoacidosis are resolved,” the agency added.
SGLT2 inhibitors lower blood sugar by causing the kidney to remove sugar from the body through urine. Side effects for the drugs vary, but include urinary tract infections and genital mycotic infection. Patients with severe renal impairment or end-stage renal disease, who are on dialysis treatment, or who have a known hypersensitivity to the medication should not take SGLT2 inhibitors, the FDA said.
The new changes affect canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin, and were made because surgery may put patients being treated with SGLT2 inhibitors at a higher risk of ketoacidosis. Canagliflozin, dapagliflozin, and empagliflozin should be discontinued 3 days before scheduled surgery, and ertugliflozin should be stopped at least 4 days before, the agency noted in a press release. Blood glucose should be monitored after drug discontinuation and appropriately managed before surgery.
“The SGLT2 inhibitor may be restarted once the patient’s oral intake is back to baseline and any other risk factors for ketoacidosis are resolved,” the agency added.
SGLT2 inhibitors lower blood sugar by causing the kidney to remove sugar from the body through urine. Side effects for the drugs vary, but include urinary tract infections and genital mycotic infection. Patients with severe renal impairment or end-stage renal disease, who are on dialysis treatment, or who have a known hypersensitivity to the medication should not take SGLT2 inhibitors, the FDA said.
The new changes affect canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin, and were made because surgery may put patients being treated with SGLT2 inhibitors at a higher risk of ketoacidosis. Canagliflozin, dapagliflozin, and empagliflozin should be discontinued 3 days before scheduled surgery, and ertugliflozin should be stopped at least 4 days before, the agency noted in a press release. Blood glucose should be monitored after drug discontinuation and appropriately managed before surgery.
“The SGLT2 inhibitor may be restarted once the patient’s oral intake is back to baseline and any other risk factors for ketoacidosis are resolved,” the agency added.
SGLT2 inhibitors lower blood sugar by causing the kidney to remove sugar from the body through urine. Side effects for the drugs vary, but include urinary tract infections and genital mycotic infection. Patients with severe renal impairment or end-stage renal disease, who are on dialysis treatment, or who have a known hypersensitivity to the medication should not take SGLT2 inhibitors, the FDA said.
Treating COVID-19 in patients with diabetes
Patients with diabetes may be at extra risk for coronavirus disease (COVID-19) mortality, and doctors treating them need to keep up with the latest guidelines and expert advice.
Most health advisories about COVID-19 mention diabetes as one of the high-risk categories for the disease, likely because early data coming out of China, where the disease was first reported, indicated an elevated case-fatality rate for COVID-19 patients who also had diabetes.
In an article published in JAMA, Zunyou Wu, MD, and Jennifer M. McGoogan, PhD, summarized the findings from a February report on 44,672 confirmed cases of the disease from the Chinese Center for Disease Control and Prevention. The overall case-fatality rate (CFR) at that stage was 2.3% (1,023 deaths of the 44,672 confirmed cases). The data indicated that the CFR was elevated among COVID-19 patients with preexisting comorbid conditions, specifically, cardiovascular disease (CFR, 10.5%), diabetes (7.3%), chronic respiratory disease (6.3%), hypertension (6%), and cancer (5.6%).
The data also showed an aged-related trend in the CFR, with patients aged 80 years or older having a CFR of 14.8% and those aged 70-79 years, a rate of 8.0%, while there were no fatal cases reported in patients aged 9 years or younger (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
Those findings have been echoed by the U.S. Centers of Disease Control and Prevention. The American Diabetes Association and the American Association of Clinical Endocrinologists have in turn referenced the CDC in their COVID-19 guidance recommendations for patients with diabetes.
Guidelines were already in place for treatment of infections in patients with diabetes, and
In general, patients with diabetes – especially those whose disease is not controlled, or not well controlled – can be more susceptible to more common infections, such as influenza and pneumonia, possibly because hyperglycemia can subdue immunity by disrupting function of the white blood cells.
Glucose control is key
An important factor in any form of infection control in patients with diabetes seems to be whether or not a patient’s glucose levels are well controlled, according to comments from members of the editorial advisory board for Clinical Endocrinology News. Good glucose control, therefore, could be instrumental in reducing both the risk for and severity of infection.
Paul Jellinger, MD, of the Center for Diabetes & Endocrine Care, Hollywood, Fla., said that, over the years, he had not observed higher infection rates in general in patients with hemoglobin A1c levels below 7, or even higher. However, “a bigger question for me, given the broad category of ‘diabetes’ listed as a risk for serious coronavirus complications by the CDC, has been: Just which individuals with diabetes are really at risk? Are patients with well-controlled diabetes at increased risk as much as those with significant hyperglycemia and uncontrolled diabetes? In my view, not likely.”
Alan Jay Cohen, MD, agreed with Dr. Jellinger. “Many patients have called the office in the last 10 days to ask if there are special precautions they should take because they are reading that they are in the high-risk group because they have diabetes. Many of them are in superb, or at least pretty good, control. I have not seen where they have had a higher incidence of infection than the general population, and I have not seen data with COVID-19 that specifically demonstrates that a person with diabetes in good control has an increased risk,” he said.
“My recommendations to these patients have been the same as those given to the general population,” added Dr. Cohen, medical director at Baptist Medical Group: The Endocrine Clinic, Memphis.
Herbert I. Rettinger, MD, also conceded that poorly controlled blood sugars and confounding illnesses, such as renal and cardiac conditions, are common in patients with long-standing diabetes, but “there is a huge population of patients with type 1 diabetes, and very few seem to be more susceptible to infection. Perhaps I am missing those with poor diet and glucose control.”
Philip Levy, MD, picked up on that latter point, emphasizing that “endocrinologists take care of fewer patients with diabetes than do primary care physicians. Most patients with type 2 diabetes are not seen by us unless the PCP has problems [treating them],” so it could be that PCPs may see a higher number of patients who are at a greater risk for infections.
Ultimately, “good glucose control is very helpful in avoiding infections,” said Dr. Levy, of the Banner University Medical Group Endocrinology & Diabetes, Phoenix.
For sick patients
Guidelines for patients at the Joslin Diabetes Center in Boston advise patients who are feeling sick to continue taking their diabetes medications, unless instructed otherwise by their providers, and to monitor their glucose more frequently because it can spike suddenly.
Patients with type 1 diabetes should check for ketones if their glucose passes 250 mg/dL, according to the guidelines, and patients should remain hydrated at all times and get plenty of rest.
“Sick-day guidelines definitely apply, but patients should be advised to get tested if they have any symptoms they are concerned about,” said Dr. Rettinger, of the Endocrinology Medical Group of Orange County, Orange, Calif.
If patients with diabetes develop COVID-19, then home management may still be possible, according to Ritesh Gupta, MD, of Fortis C-DOC Hospital, New Delhi, and colleagues (Diabetes Metab Syndr. 2020 Mar 10;14[3]:211-2. doi: 10.1016/j.dsx.2020.03.002).
Dr. Rettinger agreed, noting that home management would be feasible as long as “everything is going well, that is, the patient is not experiencing respiratory problems or difficulties in controlling glucose levels. Consider patients with type 1 diabetes who have COVID-19 as you would a nursing home patient – ever vigilant.”
Dr. Gupta and coauthors also recommended basic treatment measures such as maintaining hydration and managing symptoms with acetaminophen and steam inhalation, and home isolation for 14 days or until the symptoms resolve. However, the ADA warns in its guidelines that patients should “be aware that some constant glucose monitoring sensors (Dexcom G5, Medtronic Enlite, and Guardian) are impacted by acetaminophen (Tylenol), and that patients should check with finger sticks to ensure accuracy [if they are taking acetaminophen].”
In the event of hyperglycemia with fever in patients with type 1 diabetes, blood glucose and urinary ketones should be monitored often, the authors wrote, cautioning that “frequent changes in dosage and correctional bolus may be required to maintain normoglycemia.” Dr Rettinger emphasized that “hyperglycemia, as always, is best treated with fluids and insulin and frequent checks of sugars to be sure the treatment regimen is successful.”
In regard to diabetic drug regimens, patients with type 1 or 2 disease should continue on their current medications, advised Yehuda Handelsman, MD. “Some, especially those on insulin, may require more of it. And the patient should increase fluid intake to prevent fluid depletion. We do not reduce antihyperglycemic medication to preserve fluids.
“As for hypoglycemia, we always aim for less to no hypoglycemia,” he continued. “Monitoring glucose and appropriate dosage is the way to go. In other words, do not reduce medications in sick patients who typically need more medication.”
Dr. Handelsman, medical director and principal investigator at Metabolic Institute of America, Tarzana, Calif., added that very sick patients who are hospitalized should be managed with insulin and that oral agents – particularly metformin and sodium-glucose transporter 2 inhibitors – should be stopped.
“Once the patient has recovered and stabilized, you can return to the prior regimen, and, even if the patient is still in hospital, noninsulin therapy can be reintroduced,” he said.
“This is standard procedure in very sick patients, especially those in critical care. Metformin may raise lactic acid levels, and the SGLT2 inhibitors cause volume contraction, fat metabolism, and acidosis,” he explained. “We also stop the glucagon-like peptide receptor–1 analogues, which can cause nausea and vomiting, and pioglitazone because it causes fluid overload.
“Only insulin can be used for acutely sick patients – those with sepsis, for example. The same would apply if they have severe breathing disorders, and definitely, if they are on a ventilator. This is also the time we stop aromatase inhibitor orals and we use insulin.”
Preventive measures
In the interest of maintaining good glucose control, patients also should monitor their glucose levels more frequently so that fluctuations can be detected early and quickly addressed with the appropriate medication adjustments, according to guidelines from the ADA and AACE. They should continue to follow a healthy diet that includes adequate protein and they should exercise regularly.
Patients should ensure that they have enough medication and testing supplies – for at least 14 days, and longer, if costs permit – in case they have to go into quarantine.
General preventive measures, such as frequent hand washing with soap and water, practicing good respiratory hygiene by sneezing or coughing into a facial tissue or bent elbow, also apply for reducing the risk of infection. Touching of the face should be avoided, as should nonessential travel and contact with infected individuals.
Patients with diabetes should always be current with their influenza and pneumonia shots.
Dr. Rettinger said that he always recommends the following preventative measures to his patients and he is using the current health crisis to reinforce them:
- Eat lots of multicolored fruits and vegetables.
- Eat yogurt and take probiotics to keep the intestinal biome strong and functional.
- Be extra vigilant regarding sugars and sugar control to avoid peaks and valleys wherever possible.
- Keep the immune system strong with at least 7-8 hours sleep and reduce stress levels whenever possible.
- Avoid crowds and handshaking.
- Wash hands regularly.
Possible therapies
There are currently no drugs that have been approved specifically for the treatment of COVID-19, although a vaccine against the disease is currently under development.
Dr. Gupta and his colleagues noted in their article that there have been reports of the anecdotal use of antiviral drugs such as lopinavir, ritonavir, interferon-beta, the RNA polymerase inhibitor remdesivir, and chloroquine.
However, Dr. Handelsman said that, as far as he knows, none of these drugs has been shown to be beneficial for COVID-19. “Some [providers] have tried Tamiflu, but with no clear outcomes, and for severely sick patients, they tried medications for anti-HIV, hepatitis C, and malaria, but so far, there has been no breakthrough.”
Dr. Cohen, Dr. Handelsman, Dr. Jellinger, Dr. Levy, and Dr. Rettinger are members of the editorial advisory board of Clinical Endocrinology News. Dr. Gupta and Dr. Wu, and their colleagues, reported no conflicts of interest.
Patients with diabetes may be at extra risk for coronavirus disease (COVID-19) mortality, and doctors treating them need to keep up with the latest guidelines and expert advice.
Most health advisories about COVID-19 mention diabetes as one of the high-risk categories for the disease, likely because early data coming out of China, where the disease was first reported, indicated an elevated case-fatality rate for COVID-19 patients who also had diabetes.
In an article published in JAMA, Zunyou Wu, MD, and Jennifer M. McGoogan, PhD, summarized the findings from a February report on 44,672 confirmed cases of the disease from the Chinese Center for Disease Control and Prevention. The overall case-fatality rate (CFR) at that stage was 2.3% (1,023 deaths of the 44,672 confirmed cases). The data indicated that the CFR was elevated among COVID-19 patients with preexisting comorbid conditions, specifically, cardiovascular disease (CFR, 10.5%), diabetes (7.3%), chronic respiratory disease (6.3%), hypertension (6%), and cancer (5.6%).
The data also showed an aged-related trend in the CFR, with patients aged 80 years or older having a CFR of 14.8% and those aged 70-79 years, a rate of 8.0%, while there were no fatal cases reported in patients aged 9 years or younger (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
Those findings have been echoed by the U.S. Centers of Disease Control and Prevention. The American Diabetes Association and the American Association of Clinical Endocrinologists have in turn referenced the CDC in their COVID-19 guidance recommendations for patients with diabetes.
Guidelines were already in place for treatment of infections in patients with diabetes, and
In general, patients with diabetes – especially those whose disease is not controlled, or not well controlled – can be more susceptible to more common infections, such as influenza and pneumonia, possibly because hyperglycemia can subdue immunity by disrupting function of the white blood cells.
Glucose control is key
An important factor in any form of infection control in patients with diabetes seems to be whether or not a patient’s glucose levels are well controlled, according to comments from members of the editorial advisory board for Clinical Endocrinology News. Good glucose control, therefore, could be instrumental in reducing both the risk for and severity of infection.
Paul Jellinger, MD, of the Center for Diabetes & Endocrine Care, Hollywood, Fla., said that, over the years, he had not observed higher infection rates in general in patients with hemoglobin A1c levels below 7, or even higher. However, “a bigger question for me, given the broad category of ‘diabetes’ listed as a risk for serious coronavirus complications by the CDC, has been: Just which individuals with diabetes are really at risk? Are patients with well-controlled diabetes at increased risk as much as those with significant hyperglycemia and uncontrolled diabetes? In my view, not likely.”
Alan Jay Cohen, MD, agreed with Dr. Jellinger. “Many patients have called the office in the last 10 days to ask if there are special precautions they should take because they are reading that they are in the high-risk group because they have diabetes. Many of them are in superb, or at least pretty good, control. I have not seen where they have had a higher incidence of infection than the general population, and I have not seen data with COVID-19 that specifically demonstrates that a person with diabetes in good control has an increased risk,” he said.
“My recommendations to these patients have been the same as those given to the general population,” added Dr. Cohen, medical director at Baptist Medical Group: The Endocrine Clinic, Memphis.
Herbert I. Rettinger, MD, also conceded that poorly controlled blood sugars and confounding illnesses, such as renal and cardiac conditions, are common in patients with long-standing diabetes, but “there is a huge population of patients with type 1 diabetes, and very few seem to be more susceptible to infection. Perhaps I am missing those with poor diet and glucose control.”
Philip Levy, MD, picked up on that latter point, emphasizing that “endocrinologists take care of fewer patients with diabetes than do primary care physicians. Most patients with type 2 diabetes are not seen by us unless the PCP has problems [treating them],” so it could be that PCPs may see a higher number of patients who are at a greater risk for infections.
Ultimately, “good glucose control is very helpful in avoiding infections,” said Dr. Levy, of the Banner University Medical Group Endocrinology & Diabetes, Phoenix.
For sick patients
Guidelines for patients at the Joslin Diabetes Center in Boston advise patients who are feeling sick to continue taking their diabetes medications, unless instructed otherwise by their providers, and to monitor their glucose more frequently because it can spike suddenly.
Patients with type 1 diabetes should check for ketones if their glucose passes 250 mg/dL, according to the guidelines, and patients should remain hydrated at all times and get plenty of rest.
“Sick-day guidelines definitely apply, but patients should be advised to get tested if they have any symptoms they are concerned about,” said Dr. Rettinger, of the Endocrinology Medical Group of Orange County, Orange, Calif.
If patients with diabetes develop COVID-19, then home management may still be possible, according to Ritesh Gupta, MD, of Fortis C-DOC Hospital, New Delhi, and colleagues (Diabetes Metab Syndr. 2020 Mar 10;14[3]:211-2. doi: 10.1016/j.dsx.2020.03.002).
Dr. Rettinger agreed, noting that home management would be feasible as long as “everything is going well, that is, the patient is not experiencing respiratory problems or difficulties in controlling glucose levels. Consider patients with type 1 diabetes who have COVID-19 as you would a nursing home patient – ever vigilant.”
Dr. Gupta and coauthors also recommended basic treatment measures such as maintaining hydration and managing symptoms with acetaminophen and steam inhalation, and home isolation for 14 days or until the symptoms resolve. However, the ADA warns in its guidelines that patients should “be aware that some constant glucose monitoring sensors (Dexcom G5, Medtronic Enlite, and Guardian) are impacted by acetaminophen (Tylenol), and that patients should check with finger sticks to ensure accuracy [if they are taking acetaminophen].”
In the event of hyperglycemia with fever in patients with type 1 diabetes, blood glucose and urinary ketones should be monitored often, the authors wrote, cautioning that “frequent changes in dosage and correctional bolus may be required to maintain normoglycemia.” Dr Rettinger emphasized that “hyperglycemia, as always, is best treated with fluids and insulin and frequent checks of sugars to be sure the treatment regimen is successful.”
In regard to diabetic drug regimens, patients with type 1 or 2 disease should continue on their current medications, advised Yehuda Handelsman, MD. “Some, especially those on insulin, may require more of it. And the patient should increase fluid intake to prevent fluid depletion. We do not reduce antihyperglycemic medication to preserve fluids.
“As for hypoglycemia, we always aim for less to no hypoglycemia,” he continued. “Monitoring glucose and appropriate dosage is the way to go. In other words, do not reduce medications in sick patients who typically need more medication.”
Dr. Handelsman, medical director and principal investigator at Metabolic Institute of America, Tarzana, Calif., added that very sick patients who are hospitalized should be managed with insulin and that oral agents – particularly metformin and sodium-glucose transporter 2 inhibitors – should be stopped.
“Once the patient has recovered and stabilized, you can return to the prior regimen, and, even if the patient is still in hospital, noninsulin therapy can be reintroduced,” he said.
“This is standard procedure in very sick patients, especially those in critical care. Metformin may raise lactic acid levels, and the SGLT2 inhibitors cause volume contraction, fat metabolism, and acidosis,” he explained. “We also stop the glucagon-like peptide receptor–1 analogues, which can cause nausea and vomiting, and pioglitazone because it causes fluid overload.
“Only insulin can be used for acutely sick patients – those with sepsis, for example. The same would apply if they have severe breathing disorders, and definitely, if they are on a ventilator. This is also the time we stop aromatase inhibitor orals and we use insulin.”
Preventive measures
In the interest of maintaining good glucose control, patients also should monitor their glucose levels more frequently so that fluctuations can be detected early and quickly addressed with the appropriate medication adjustments, according to guidelines from the ADA and AACE. They should continue to follow a healthy diet that includes adequate protein and they should exercise regularly.
Patients should ensure that they have enough medication and testing supplies – for at least 14 days, and longer, if costs permit – in case they have to go into quarantine.
General preventive measures, such as frequent hand washing with soap and water, practicing good respiratory hygiene by sneezing or coughing into a facial tissue or bent elbow, also apply for reducing the risk of infection. Touching of the face should be avoided, as should nonessential travel and contact with infected individuals.
Patients with diabetes should always be current with their influenza and pneumonia shots.
Dr. Rettinger said that he always recommends the following preventative measures to his patients and he is using the current health crisis to reinforce them:
- Eat lots of multicolored fruits and vegetables.
- Eat yogurt and take probiotics to keep the intestinal biome strong and functional.
- Be extra vigilant regarding sugars and sugar control to avoid peaks and valleys wherever possible.
- Keep the immune system strong with at least 7-8 hours sleep and reduce stress levels whenever possible.
- Avoid crowds and handshaking.
- Wash hands regularly.
Possible therapies
There are currently no drugs that have been approved specifically for the treatment of COVID-19, although a vaccine against the disease is currently under development.
Dr. Gupta and his colleagues noted in their article that there have been reports of the anecdotal use of antiviral drugs such as lopinavir, ritonavir, interferon-beta, the RNA polymerase inhibitor remdesivir, and chloroquine.
However, Dr. Handelsman said that, as far as he knows, none of these drugs has been shown to be beneficial for COVID-19. “Some [providers] have tried Tamiflu, but with no clear outcomes, and for severely sick patients, they tried medications for anti-HIV, hepatitis C, and malaria, but so far, there has been no breakthrough.”
Dr. Cohen, Dr. Handelsman, Dr. Jellinger, Dr. Levy, and Dr. Rettinger are members of the editorial advisory board of Clinical Endocrinology News. Dr. Gupta and Dr. Wu, and their colleagues, reported no conflicts of interest.
Patients with diabetes may be at extra risk for coronavirus disease (COVID-19) mortality, and doctors treating them need to keep up with the latest guidelines and expert advice.
Most health advisories about COVID-19 mention diabetes as one of the high-risk categories for the disease, likely because early data coming out of China, where the disease was first reported, indicated an elevated case-fatality rate for COVID-19 patients who also had diabetes.
In an article published in JAMA, Zunyou Wu, MD, and Jennifer M. McGoogan, PhD, summarized the findings from a February report on 44,672 confirmed cases of the disease from the Chinese Center for Disease Control and Prevention. The overall case-fatality rate (CFR) at that stage was 2.3% (1,023 deaths of the 44,672 confirmed cases). The data indicated that the CFR was elevated among COVID-19 patients with preexisting comorbid conditions, specifically, cardiovascular disease (CFR, 10.5%), diabetes (7.3%), chronic respiratory disease (6.3%), hypertension (6%), and cancer (5.6%).
The data also showed an aged-related trend in the CFR, with patients aged 80 years or older having a CFR of 14.8% and those aged 70-79 years, a rate of 8.0%, while there were no fatal cases reported in patients aged 9 years or younger (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
Those findings have been echoed by the U.S. Centers of Disease Control and Prevention. The American Diabetes Association and the American Association of Clinical Endocrinologists have in turn referenced the CDC in their COVID-19 guidance recommendations for patients with diabetes.
Guidelines were already in place for treatment of infections in patients with diabetes, and
In general, patients with diabetes – especially those whose disease is not controlled, or not well controlled – can be more susceptible to more common infections, such as influenza and pneumonia, possibly because hyperglycemia can subdue immunity by disrupting function of the white blood cells.
Glucose control is key
An important factor in any form of infection control in patients with diabetes seems to be whether or not a patient’s glucose levels are well controlled, according to comments from members of the editorial advisory board for Clinical Endocrinology News. Good glucose control, therefore, could be instrumental in reducing both the risk for and severity of infection.
Paul Jellinger, MD, of the Center for Diabetes & Endocrine Care, Hollywood, Fla., said that, over the years, he had not observed higher infection rates in general in patients with hemoglobin A1c levels below 7, or even higher. However, “a bigger question for me, given the broad category of ‘diabetes’ listed as a risk for serious coronavirus complications by the CDC, has been: Just which individuals with diabetes are really at risk? Are patients with well-controlled diabetes at increased risk as much as those with significant hyperglycemia and uncontrolled diabetes? In my view, not likely.”
Alan Jay Cohen, MD, agreed with Dr. Jellinger. “Many patients have called the office in the last 10 days to ask if there are special precautions they should take because they are reading that they are in the high-risk group because they have diabetes. Many of them are in superb, or at least pretty good, control. I have not seen where they have had a higher incidence of infection than the general population, and I have not seen data with COVID-19 that specifically demonstrates that a person with diabetes in good control has an increased risk,” he said.
“My recommendations to these patients have been the same as those given to the general population,” added Dr. Cohen, medical director at Baptist Medical Group: The Endocrine Clinic, Memphis.
Herbert I. Rettinger, MD, also conceded that poorly controlled blood sugars and confounding illnesses, such as renal and cardiac conditions, are common in patients with long-standing diabetes, but “there is a huge population of patients with type 1 diabetes, and very few seem to be more susceptible to infection. Perhaps I am missing those with poor diet and glucose control.”
Philip Levy, MD, picked up on that latter point, emphasizing that “endocrinologists take care of fewer patients with diabetes than do primary care physicians. Most patients with type 2 diabetes are not seen by us unless the PCP has problems [treating them],” so it could be that PCPs may see a higher number of patients who are at a greater risk for infections.
Ultimately, “good glucose control is very helpful in avoiding infections,” said Dr. Levy, of the Banner University Medical Group Endocrinology & Diabetes, Phoenix.
For sick patients
Guidelines for patients at the Joslin Diabetes Center in Boston advise patients who are feeling sick to continue taking their diabetes medications, unless instructed otherwise by their providers, and to monitor their glucose more frequently because it can spike suddenly.
Patients with type 1 diabetes should check for ketones if their glucose passes 250 mg/dL, according to the guidelines, and patients should remain hydrated at all times and get plenty of rest.
“Sick-day guidelines definitely apply, but patients should be advised to get tested if they have any symptoms they are concerned about,” said Dr. Rettinger, of the Endocrinology Medical Group of Orange County, Orange, Calif.
If patients with diabetes develop COVID-19, then home management may still be possible, according to Ritesh Gupta, MD, of Fortis C-DOC Hospital, New Delhi, and colleagues (Diabetes Metab Syndr. 2020 Mar 10;14[3]:211-2. doi: 10.1016/j.dsx.2020.03.002).
Dr. Rettinger agreed, noting that home management would be feasible as long as “everything is going well, that is, the patient is not experiencing respiratory problems or difficulties in controlling glucose levels. Consider patients with type 1 diabetes who have COVID-19 as you would a nursing home patient – ever vigilant.”
Dr. Gupta and coauthors also recommended basic treatment measures such as maintaining hydration and managing symptoms with acetaminophen and steam inhalation, and home isolation for 14 days or until the symptoms resolve. However, the ADA warns in its guidelines that patients should “be aware that some constant glucose monitoring sensors (Dexcom G5, Medtronic Enlite, and Guardian) are impacted by acetaminophen (Tylenol), and that patients should check with finger sticks to ensure accuracy [if they are taking acetaminophen].”
In the event of hyperglycemia with fever in patients with type 1 diabetes, blood glucose and urinary ketones should be monitored often, the authors wrote, cautioning that “frequent changes in dosage and correctional bolus may be required to maintain normoglycemia.” Dr Rettinger emphasized that “hyperglycemia, as always, is best treated with fluids and insulin and frequent checks of sugars to be sure the treatment regimen is successful.”
In regard to diabetic drug regimens, patients with type 1 or 2 disease should continue on their current medications, advised Yehuda Handelsman, MD. “Some, especially those on insulin, may require more of it. And the patient should increase fluid intake to prevent fluid depletion. We do not reduce antihyperglycemic medication to preserve fluids.
“As for hypoglycemia, we always aim for less to no hypoglycemia,” he continued. “Monitoring glucose and appropriate dosage is the way to go. In other words, do not reduce medications in sick patients who typically need more medication.”
Dr. Handelsman, medical director and principal investigator at Metabolic Institute of America, Tarzana, Calif., added that very sick patients who are hospitalized should be managed with insulin and that oral agents – particularly metformin and sodium-glucose transporter 2 inhibitors – should be stopped.
“Once the patient has recovered and stabilized, you can return to the prior regimen, and, even if the patient is still in hospital, noninsulin therapy can be reintroduced,” he said.
“This is standard procedure in very sick patients, especially those in critical care. Metformin may raise lactic acid levels, and the SGLT2 inhibitors cause volume contraction, fat metabolism, and acidosis,” he explained. “We also stop the glucagon-like peptide receptor–1 analogues, which can cause nausea and vomiting, and pioglitazone because it causes fluid overload.
“Only insulin can be used for acutely sick patients – those with sepsis, for example. The same would apply if they have severe breathing disorders, and definitely, if they are on a ventilator. This is also the time we stop aromatase inhibitor orals and we use insulin.”
Preventive measures
In the interest of maintaining good glucose control, patients also should monitor their glucose levels more frequently so that fluctuations can be detected early and quickly addressed with the appropriate medication adjustments, according to guidelines from the ADA and AACE. They should continue to follow a healthy diet that includes adequate protein and they should exercise regularly.
Patients should ensure that they have enough medication and testing supplies – for at least 14 days, and longer, if costs permit – in case they have to go into quarantine.
General preventive measures, such as frequent hand washing with soap and water, practicing good respiratory hygiene by sneezing or coughing into a facial tissue or bent elbow, also apply for reducing the risk of infection. Touching of the face should be avoided, as should nonessential travel and contact with infected individuals.
Patients with diabetes should always be current with their influenza and pneumonia shots.
Dr. Rettinger said that he always recommends the following preventative measures to his patients and he is using the current health crisis to reinforce them:
- Eat lots of multicolored fruits and vegetables.
- Eat yogurt and take probiotics to keep the intestinal biome strong and functional.
- Be extra vigilant regarding sugars and sugar control to avoid peaks and valleys wherever possible.
- Keep the immune system strong with at least 7-8 hours sleep and reduce stress levels whenever possible.
- Avoid crowds and handshaking.
- Wash hands regularly.
Possible therapies
There are currently no drugs that have been approved specifically for the treatment of COVID-19, although a vaccine against the disease is currently under development.
Dr. Gupta and his colleagues noted in their article that there have been reports of the anecdotal use of antiviral drugs such as lopinavir, ritonavir, interferon-beta, the RNA polymerase inhibitor remdesivir, and chloroquine.
However, Dr. Handelsman said that, as far as he knows, none of these drugs has been shown to be beneficial for COVID-19. “Some [providers] have tried Tamiflu, but with no clear outcomes, and for severely sick patients, they tried medications for anti-HIV, hepatitis C, and malaria, but so far, there has been no breakthrough.”
Dr. Cohen, Dr. Handelsman, Dr. Jellinger, Dr. Levy, and Dr. Rettinger are members of the editorial advisory board of Clinical Endocrinology News. Dr. Gupta and Dr. Wu, and their colleagues, reported no conflicts of interest.
COVID-19: Extra caution needed for patients with diabetes
Patients with diabetes may have an increased risk of developing coronavirus infection (COVID-19), along with increased risks of morbidity and mortality, according to researchers writing in Diabetes & Metabolic Syndrome.
Although relevant clinical data remain scarce, patients with diabetes should take extra precautions to avoid infection and, if infected, may require special care, reported Ritesh Gupta, MD, of Fortis C-DOC Hospital, New Delhi, and colleagues.
“The disease severity [with COVID-19] has varied from mild, self-limiting, flu-like illness to fulminant pneumonia, respiratory failure, and death,” the authors wrote.
As of March 16, 2020, the World Health Organization reported 167,515 confirmed cases of COVID-19 and 6,606 deaths from around the world, with a mortality rate of 3.9%. But the actual mortality rate may be lower, the authors suggested, because a study involving more than 1,000 confirmed cases reported a mortality rate of 1.4%.
“Considering that the number of unreported and unconfirmed cases is likely to be much higher than the reported cases, the actual mortality may be less than 1%, which is similar to that of severe seasonal influenza,” the authors said, in reference to an editorial by Anthony S. Fauci, MD, and colleagues in the New England Journal of Medicine. In addition, they noted, mortality rates may vary by region.
The largest study relevant to patients with diabetes, which involved 72,314 cases of COVID-19, showed that patients with diabetes had a threefold higher mortality rate than did those without diabetes (7.3% vs. 2.3%, respectively). These figures were reported by the Chinese Centre for Disease Control and Prevention.
However, data from smaller cohorts with diabetes and COVID-19 have yielded mixed results. For instance, one study, involving 140 patients from Wuhan, suggested that diabetes was not a risk factor for severe disease, and in an analysis of 11 studies reporting on laboratory abnormalities in patients with a diagnosis of COVID-19, raised blood sugar levels or diabetes were not mentioned among the predictors of severe disease.
“Our knowledge about the prevalence of COVID-19 and disease course in people with diabetes will evolve as more detailed analyses are carried out,” the authors wrote. “For now, it is reasonable to assume that people with diabetes are at increased risk of developing infection. Coexisting heart disease, kidney disease, advanced age, and frailty are likely to further increase the severity of disease.”
Prevention first
“It is important that people with diabetes maintain good glycemic control, because it might help in reducing the risk of infection and the severity,” the authors wrote.
In addition to more frequent monitoring of blood glucose levels, they recommended other preventive measures, such as getting adequate nutrition, exercising, and being current with vaccinations for influenza and pneumonia. The latter, they said, may also reduce the risk of secondary bacterial pneumonia after a respiratory viral infection.
In regard to nutrition, adequate protein intake is important and “any deficiencies of minerals and vitamins need to be taken care of,” they advised. Likewise, exercise is known to improve immunity and should continue, but they suggest avoiding gyms and swimming pools.
For patients with coexisting heart and/or kidney disease, they also recommended efforts to stabilize cardiac/renal status.
In addition, the general preventive measures, such as regular and thorough hand washing with soap and water, practicing good respiratory hygiene by sneezing and coughing into a bent elbow or a facial tissue, and avoiding contact with anyone who is infected, should be observed.
As with other patients with chronic diseases that are managed long-term medications, patients with diabetes should always ensure that they have a sufficient supply of their medications and refills, if possible.
After a diagnosis
If patients with diabetes develop COVID-19, then home management may still be possible, wrote the authors, who recommended basic treatment measures such as maintaining hydration and managing symptoms with acetaminophen and steam inhalation, and home isolation for 14 days or until the symptoms resolve.
In the event of hyperglycemia with fever in patients with type 1 diabetes, blood glucose and urinary ketones should be monitored often. “Frequent changes in dosage and correctional bolus may be required to maintain normoglycemia,” they cautioned.
Concerning diabetic drug regimens, they suggest patients avoid antihyperglycemic agents that can cause volume depletion or hypoglycemia and, if necessary, that they reduce oral antidiabetic drugs and follow sick-day guidelines.
For hospitalized patients, the investigators strengthened that statement, advising that oral agents need to be stopped, particularly sodium-glucose cotransporter 2 inhibitors and metformin. “Insulin is the preferred agent for control of hyperglycemia in hospitalized sick patients,” they wrote.
Untested therapies
The authors also discussed a range of untested therapies that may help fight COVID-19, such as antiviral drugs (such as lopinavir and ritonavir), zinc nanoparticles, and vitamin C. Supplementing those recommendations, Dr. Gupta and colleagues provided a concise review of COVID-19 epidemiology and extant data relevant to patients with diabetes.
The investigators reported no conflicts of interest.
SOURCE: Gupta et al. Diabetes Metab Syndr. 2020;14(3):211-12.
Patients with diabetes may have an increased risk of developing coronavirus infection (COVID-19), along with increased risks of morbidity and mortality, according to researchers writing in Diabetes & Metabolic Syndrome.
Although relevant clinical data remain scarce, patients with diabetes should take extra precautions to avoid infection and, if infected, may require special care, reported Ritesh Gupta, MD, of Fortis C-DOC Hospital, New Delhi, and colleagues.
“The disease severity [with COVID-19] has varied from mild, self-limiting, flu-like illness to fulminant pneumonia, respiratory failure, and death,” the authors wrote.
As of March 16, 2020, the World Health Organization reported 167,515 confirmed cases of COVID-19 and 6,606 deaths from around the world, with a mortality rate of 3.9%. But the actual mortality rate may be lower, the authors suggested, because a study involving more than 1,000 confirmed cases reported a mortality rate of 1.4%.
“Considering that the number of unreported and unconfirmed cases is likely to be much higher than the reported cases, the actual mortality may be less than 1%, which is similar to that of severe seasonal influenza,” the authors said, in reference to an editorial by Anthony S. Fauci, MD, and colleagues in the New England Journal of Medicine. In addition, they noted, mortality rates may vary by region.
The largest study relevant to patients with diabetes, which involved 72,314 cases of COVID-19, showed that patients with diabetes had a threefold higher mortality rate than did those without diabetes (7.3% vs. 2.3%, respectively). These figures were reported by the Chinese Centre for Disease Control and Prevention.
However, data from smaller cohorts with diabetes and COVID-19 have yielded mixed results. For instance, one study, involving 140 patients from Wuhan, suggested that diabetes was not a risk factor for severe disease, and in an analysis of 11 studies reporting on laboratory abnormalities in patients with a diagnosis of COVID-19, raised blood sugar levels or diabetes were not mentioned among the predictors of severe disease.
“Our knowledge about the prevalence of COVID-19 and disease course in people with diabetes will evolve as more detailed analyses are carried out,” the authors wrote. “For now, it is reasonable to assume that people with diabetes are at increased risk of developing infection. Coexisting heart disease, kidney disease, advanced age, and frailty are likely to further increase the severity of disease.”
Prevention first
“It is important that people with diabetes maintain good glycemic control, because it might help in reducing the risk of infection and the severity,” the authors wrote.
In addition to more frequent monitoring of blood glucose levels, they recommended other preventive measures, such as getting adequate nutrition, exercising, and being current with vaccinations for influenza and pneumonia. The latter, they said, may also reduce the risk of secondary bacterial pneumonia after a respiratory viral infection.
In regard to nutrition, adequate protein intake is important and “any deficiencies of minerals and vitamins need to be taken care of,” they advised. Likewise, exercise is known to improve immunity and should continue, but they suggest avoiding gyms and swimming pools.
For patients with coexisting heart and/or kidney disease, they also recommended efforts to stabilize cardiac/renal status.
In addition, the general preventive measures, such as regular and thorough hand washing with soap and water, practicing good respiratory hygiene by sneezing and coughing into a bent elbow or a facial tissue, and avoiding contact with anyone who is infected, should be observed.
As with other patients with chronic diseases that are managed long-term medications, patients with diabetes should always ensure that they have a sufficient supply of their medications and refills, if possible.
After a diagnosis
If patients with diabetes develop COVID-19, then home management may still be possible, wrote the authors, who recommended basic treatment measures such as maintaining hydration and managing symptoms with acetaminophen and steam inhalation, and home isolation for 14 days or until the symptoms resolve.
In the event of hyperglycemia with fever in patients with type 1 diabetes, blood glucose and urinary ketones should be monitored often. “Frequent changes in dosage and correctional bolus may be required to maintain normoglycemia,” they cautioned.
Concerning diabetic drug regimens, they suggest patients avoid antihyperglycemic agents that can cause volume depletion or hypoglycemia and, if necessary, that they reduce oral antidiabetic drugs and follow sick-day guidelines.
For hospitalized patients, the investigators strengthened that statement, advising that oral agents need to be stopped, particularly sodium-glucose cotransporter 2 inhibitors and metformin. “Insulin is the preferred agent for control of hyperglycemia in hospitalized sick patients,” they wrote.
Untested therapies
The authors also discussed a range of untested therapies that may help fight COVID-19, such as antiviral drugs (such as lopinavir and ritonavir), zinc nanoparticles, and vitamin C. Supplementing those recommendations, Dr. Gupta and colleagues provided a concise review of COVID-19 epidemiology and extant data relevant to patients with diabetes.
The investigators reported no conflicts of interest.
SOURCE: Gupta et al. Diabetes Metab Syndr. 2020;14(3):211-12.
Patients with diabetes may have an increased risk of developing coronavirus infection (COVID-19), along with increased risks of morbidity and mortality, according to researchers writing in Diabetes & Metabolic Syndrome.
Although relevant clinical data remain scarce, patients with diabetes should take extra precautions to avoid infection and, if infected, may require special care, reported Ritesh Gupta, MD, of Fortis C-DOC Hospital, New Delhi, and colleagues.
“The disease severity [with COVID-19] has varied from mild, self-limiting, flu-like illness to fulminant pneumonia, respiratory failure, and death,” the authors wrote.
As of March 16, 2020, the World Health Organization reported 167,515 confirmed cases of COVID-19 and 6,606 deaths from around the world, with a mortality rate of 3.9%. But the actual mortality rate may be lower, the authors suggested, because a study involving more than 1,000 confirmed cases reported a mortality rate of 1.4%.
“Considering that the number of unreported and unconfirmed cases is likely to be much higher than the reported cases, the actual mortality may be less than 1%, which is similar to that of severe seasonal influenza,” the authors said, in reference to an editorial by Anthony S. Fauci, MD, and colleagues in the New England Journal of Medicine. In addition, they noted, mortality rates may vary by region.
The largest study relevant to patients with diabetes, which involved 72,314 cases of COVID-19, showed that patients with diabetes had a threefold higher mortality rate than did those without diabetes (7.3% vs. 2.3%, respectively). These figures were reported by the Chinese Centre for Disease Control and Prevention.
However, data from smaller cohorts with diabetes and COVID-19 have yielded mixed results. For instance, one study, involving 140 patients from Wuhan, suggested that diabetes was not a risk factor for severe disease, and in an analysis of 11 studies reporting on laboratory abnormalities in patients with a diagnosis of COVID-19, raised blood sugar levels or diabetes were not mentioned among the predictors of severe disease.
“Our knowledge about the prevalence of COVID-19 and disease course in people with diabetes will evolve as more detailed analyses are carried out,” the authors wrote. “For now, it is reasonable to assume that people with diabetes are at increased risk of developing infection. Coexisting heart disease, kidney disease, advanced age, and frailty are likely to further increase the severity of disease.”
Prevention first
“It is important that people with diabetes maintain good glycemic control, because it might help in reducing the risk of infection and the severity,” the authors wrote.
In addition to more frequent monitoring of blood glucose levels, they recommended other preventive measures, such as getting adequate nutrition, exercising, and being current with vaccinations for influenza and pneumonia. The latter, they said, may also reduce the risk of secondary bacterial pneumonia after a respiratory viral infection.
In regard to nutrition, adequate protein intake is important and “any deficiencies of minerals and vitamins need to be taken care of,” they advised. Likewise, exercise is known to improve immunity and should continue, but they suggest avoiding gyms and swimming pools.
For patients with coexisting heart and/or kidney disease, they also recommended efforts to stabilize cardiac/renal status.
In addition, the general preventive measures, such as regular and thorough hand washing with soap and water, practicing good respiratory hygiene by sneezing and coughing into a bent elbow or a facial tissue, and avoiding contact with anyone who is infected, should be observed.
As with other patients with chronic diseases that are managed long-term medications, patients with diabetes should always ensure that they have a sufficient supply of their medications and refills, if possible.
After a diagnosis
If patients with diabetes develop COVID-19, then home management may still be possible, wrote the authors, who recommended basic treatment measures such as maintaining hydration and managing symptoms with acetaminophen and steam inhalation, and home isolation for 14 days or until the symptoms resolve.
In the event of hyperglycemia with fever in patients with type 1 diabetes, blood glucose and urinary ketones should be monitored often. “Frequent changes in dosage and correctional bolus may be required to maintain normoglycemia,” they cautioned.
Concerning diabetic drug regimens, they suggest patients avoid antihyperglycemic agents that can cause volume depletion or hypoglycemia and, if necessary, that they reduce oral antidiabetic drugs and follow sick-day guidelines.
For hospitalized patients, the investigators strengthened that statement, advising that oral agents need to be stopped, particularly sodium-glucose cotransporter 2 inhibitors and metformin. “Insulin is the preferred agent for control of hyperglycemia in hospitalized sick patients,” they wrote.
Untested therapies
The authors also discussed a range of untested therapies that may help fight COVID-19, such as antiviral drugs (such as lopinavir and ritonavir), zinc nanoparticles, and vitamin C. Supplementing those recommendations, Dr. Gupta and colleagues provided a concise review of COVID-19 epidemiology and extant data relevant to patients with diabetes.
The investigators reported no conflicts of interest.
SOURCE: Gupta et al. Diabetes Metab Syndr. 2020;14(3):211-12.
FROM DIABETES & METABOLIC SYNDROME
Fracture liaison services confer benefit on recurrent fracture risk
Implementation of fracture liaison services (FLS) at two Swedish hospitals was associated with an 18% reduction of recurrent fracture over a median follow-up of 2.2 years, results from an observational cohort study found.
“Patients receiving fracture care within an FLS have higher rates of [bone mineral density] testing, treatment initiation and better adherence,” first author Kristian F. Axelsson, MD, and colleagues wrote in a study published in the Journal of Bone and Mineral Research. “However, the evidence regarding FLS and association to reduced risk of recurrent fracture is insufficient, consisting of smaller studies, studies with short follow-up time, and studies with high risk of various biases.”
Dr. Axelsson, of the department of orthopedic surgery at Skaraborg Hospital, Skövde, Sweden, and colleagues used electronic patient records from four hospitals in Western Sweden to identify all patients aged 50 years or older with a major osteoporotic fracture – defined as a fracture of the wrist, upper arm, hip, vertebra, or pelvis – between 2012 and 2017. The study population consisted of 15,449 patients from two hospitals with FLS and 5,634 patients from two hospitals with no FLS. The researchers used multivariable Cox models to compare all patients with a major osteoporotic fracture during the FLS period with all patients with a major osteoporotic fracture prior to the FLS implementation. The FLS hospitals and non-FLS hospitals were analyzed separately using the same methodology.
The mean age of patients was 74 years, 76% were female, and the most common index fracture site was the wrist (42%). In the hospitals with FLS, the researchers observed 1,247 recurrent fractures during a median follow-up time of 2.2 years. In an unadjusted Cox model, the risk of recurrent fracture was 18% lower in the FLS period, compared with the control period (hazard ratio, 0.82; P = .001). This corresponded to a 3-year number needed to screen of 61, and did not change after adjustment for clinical risk factors. In the non-FLS hospitals, no change in recurrent fracture rate was observed.
Osteoporosis medication treatment rates after fracture did not differ between the FLS and non-FLS hospitals, prior to FLS implementation (14.7% vs. 13.3%, respectively; P = .10). However, following FLS implementation, a larger proportion of fracture patients were treated at the FLS hospitals, compared with those at the non-FLS hospitals (28% vs. 12.9%; P less than .001).
“Our study is the largest yet, including both historic controls and controls at nearby hospitals without implementations of fracture liaison services,” one of the study authors, Mattias Lorentzon, MD, said in an interview. “We were able to rule out temporal trends in refracture risk and show that, [in] patients who had an index fracture at a hospital with an FLS, the refracture rate was lower than for patients who had an index fracture before the FLS was started, indicating that FLS reduce the risk of recurrent fracture. No such trends were observed in hospitals without FLS during the same time period.”
Dr. Lorentzon, head of geriatric medicine at Sahlgrenska University Hospital, Mölndal, Sweden, said that FLS implementation “led to a large increase in the use of osteoporosis medication, which we believe is the reason for the reduction in recurrent fracture risk observed. We believe that our results provide solid evidence that FLS implementation can reduce the rate of recurrent fractures, suggesting that all hospitals treating fracture patients should have fracture liaison services.”
In an interview, Stuart L. Silverman, MD, said that the study adds to compelling data on the efficacy and need for patients with clinical fracture to have case management by a FLS. “We recognize that near term risk is substantial in the year following a fracture,” said Dr. Silverman, who is clinical professor of medicine at Cedars-Sinai Medical Center and the University of California, Los Angeles, and is not affiliated with the Swedish study. “For example, the risk of a subsequent fracture after hip fracture is 8.3%, which is similar to the risk of subsequent acute myocardial infarction after an initial acute MI. However, only 23% of patients receive osteoporosis medication after a hip fracture. Yet a fracture is to osteoporosis what an acute MI is to cardiovascular disease. We recognize that men and women age 65 years and older who have suffered a hip or vertebral fracture should be evaluated for treatment, as this subpopulation is at high risk for a second fracture and evidence supporting treatment efficacy is robust. We need a multidisciplinary clinical system which includes case management such as a fracture liaison service. We know FLS can reduce hip fracture rate in a closed system such as Kaiser by over 40%. This manuscript addresses the utility of a FLS in terms of reducing risk of future fracture.”
The researchers acknowledged certain limitations of the study, including its observational design and the fact that patients prior to the FLS period were fewer and had longer follow-up time, compared with patients during the FLS period.
The study was funded by the Swedish Research Council and by grants from the Sahlgrenska University Hospital. Dr. Axelsson reported that he has received lecture fees from Lilly, Meda/Mylan, and Amgen. Dr. Lorentzon has received lecture fees from Amgen, Lilly, UCB, Radius Health, Meda, GE-Lunar, and Santax Medico/Hologic. The other coauthors reported having no financial disclosures. Dr. Silverman reported that he is a member of the speakers’ bureaus for Amgen and Radius. He is also a consultant for Lilly, Pfizer, and Amgen and has received research grants from Radius and Amgen.
SOURCE: Axelsson K et al. J Bone Min Res. 2020 Feb 25. doi: 10.1002/jbmr.3990.
Implementation of fracture liaison services (FLS) at two Swedish hospitals was associated with an 18% reduction of recurrent fracture over a median follow-up of 2.2 years, results from an observational cohort study found.
“Patients receiving fracture care within an FLS have higher rates of [bone mineral density] testing, treatment initiation and better adherence,” first author Kristian F. Axelsson, MD, and colleagues wrote in a study published in the Journal of Bone and Mineral Research. “However, the evidence regarding FLS and association to reduced risk of recurrent fracture is insufficient, consisting of smaller studies, studies with short follow-up time, and studies with high risk of various biases.”
Dr. Axelsson, of the department of orthopedic surgery at Skaraborg Hospital, Skövde, Sweden, and colleagues used electronic patient records from four hospitals in Western Sweden to identify all patients aged 50 years or older with a major osteoporotic fracture – defined as a fracture of the wrist, upper arm, hip, vertebra, or pelvis – between 2012 and 2017. The study population consisted of 15,449 patients from two hospitals with FLS and 5,634 patients from two hospitals with no FLS. The researchers used multivariable Cox models to compare all patients with a major osteoporotic fracture during the FLS period with all patients with a major osteoporotic fracture prior to the FLS implementation. The FLS hospitals and non-FLS hospitals were analyzed separately using the same methodology.
The mean age of patients was 74 years, 76% were female, and the most common index fracture site was the wrist (42%). In the hospitals with FLS, the researchers observed 1,247 recurrent fractures during a median follow-up time of 2.2 years. In an unadjusted Cox model, the risk of recurrent fracture was 18% lower in the FLS period, compared with the control period (hazard ratio, 0.82; P = .001). This corresponded to a 3-year number needed to screen of 61, and did not change after adjustment for clinical risk factors. In the non-FLS hospitals, no change in recurrent fracture rate was observed.
Osteoporosis medication treatment rates after fracture did not differ between the FLS and non-FLS hospitals, prior to FLS implementation (14.7% vs. 13.3%, respectively; P = .10). However, following FLS implementation, a larger proportion of fracture patients were treated at the FLS hospitals, compared with those at the non-FLS hospitals (28% vs. 12.9%; P less than .001).
“Our study is the largest yet, including both historic controls and controls at nearby hospitals without implementations of fracture liaison services,” one of the study authors, Mattias Lorentzon, MD, said in an interview. “We were able to rule out temporal trends in refracture risk and show that, [in] patients who had an index fracture at a hospital with an FLS, the refracture rate was lower than for patients who had an index fracture before the FLS was started, indicating that FLS reduce the risk of recurrent fracture. No such trends were observed in hospitals without FLS during the same time period.”
Dr. Lorentzon, head of geriatric medicine at Sahlgrenska University Hospital, Mölndal, Sweden, said that FLS implementation “led to a large increase in the use of osteoporosis medication, which we believe is the reason for the reduction in recurrent fracture risk observed. We believe that our results provide solid evidence that FLS implementation can reduce the rate of recurrent fractures, suggesting that all hospitals treating fracture patients should have fracture liaison services.”
In an interview, Stuart L. Silverman, MD, said that the study adds to compelling data on the efficacy and need for patients with clinical fracture to have case management by a FLS. “We recognize that near term risk is substantial in the year following a fracture,” said Dr. Silverman, who is clinical professor of medicine at Cedars-Sinai Medical Center and the University of California, Los Angeles, and is not affiliated with the Swedish study. “For example, the risk of a subsequent fracture after hip fracture is 8.3%, which is similar to the risk of subsequent acute myocardial infarction after an initial acute MI. However, only 23% of patients receive osteoporosis medication after a hip fracture. Yet a fracture is to osteoporosis what an acute MI is to cardiovascular disease. We recognize that men and women age 65 years and older who have suffered a hip or vertebral fracture should be evaluated for treatment, as this subpopulation is at high risk for a second fracture and evidence supporting treatment efficacy is robust. We need a multidisciplinary clinical system which includes case management such as a fracture liaison service. We know FLS can reduce hip fracture rate in a closed system such as Kaiser by over 40%. This manuscript addresses the utility of a FLS in terms of reducing risk of future fracture.”
The researchers acknowledged certain limitations of the study, including its observational design and the fact that patients prior to the FLS period were fewer and had longer follow-up time, compared with patients during the FLS period.
The study was funded by the Swedish Research Council and by grants from the Sahlgrenska University Hospital. Dr. Axelsson reported that he has received lecture fees from Lilly, Meda/Mylan, and Amgen. Dr. Lorentzon has received lecture fees from Amgen, Lilly, UCB, Radius Health, Meda, GE-Lunar, and Santax Medico/Hologic. The other coauthors reported having no financial disclosures. Dr. Silverman reported that he is a member of the speakers’ bureaus for Amgen and Radius. He is also a consultant for Lilly, Pfizer, and Amgen and has received research grants from Radius and Amgen.
SOURCE: Axelsson K et al. J Bone Min Res. 2020 Feb 25. doi: 10.1002/jbmr.3990.
Implementation of fracture liaison services (FLS) at two Swedish hospitals was associated with an 18% reduction of recurrent fracture over a median follow-up of 2.2 years, results from an observational cohort study found.
“Patients receiving fracture care within an FLS have higher rates of [bone mineral density] testing, treatment initiation and better adherence,” first author Kristian F. Axelsson, MD, and colleagues wrote in a study published in the Journal of Bone and Mineral Research. “However, the evidence regarding FLS and association to reduced risk of recurrent fracture is insufficient, consisting of smaller studies, studies with short follow-up time, and studies with high risk of various biases.”
Dr. Axelsson, of the department of orthopedic surgery at Skaraborg Hospital, Skövde, Sweden, and colleagues used electronic patient records from four hospitals in Western Sweden to identify all patients aged 50 years or older with a major osteoporotic fracture – defined as a fracture of the wrist, upper arm, hip, vertebra, or pelvis – between 2012 and 2017. The study population consisted of 15,449 patients from two hospitals with FLS and 5,634 patients from two hospitals with no FLS. The researchers used multivariable Cox models to compare all patients with a major osteoporotic fracture during the FLS period with all patients with a major osteoporotic fracture prior to the FLS implementation. The FLS hospitals and non-FLS hospitals were analyzed separately using the same methodology.
The mean age of patients was 74 years, 76% were female, and the most common index fracture site was the wrist (42%). In the hospitals with FLS, the researchers observed 1,247 recurrent fractures during a median follow-up time of 2.2 years. In an unadjusted Cox model, the risk of recurrent fracture was 18% lower in the FLS period, compared with the control period (hazard ratio, 0.82; P = .001). This corresponded to a 3-year number needed to screen of 61, and did not change after adjustment for clinical risk factors. In the non-FLS hospitals, no change in recurrent fracture rate was observed.
Osteoporosis medication treatment rates after fracture did not differ between the FLS and non-FLS hospitals, prior to FLS implementation (14.7% vs. 13.3%, respectively; P = .10). However, following FLS implementation, a larger proportion of fracture patients were treated at the FLS hospitals, compared with those at the non-FLS hospitals (28% vs. 12.9%; P less than .001).
“Our study is the largest yet, including both historic controls and controls at nearby hospitals without implementations of fracture liaison services,” one of the study authors, Mattias Lorentzon, MD, said in an interview. “We were able to rule out temporal trends in refracture risk and show that, [in] patients who had an index fracture at a hospital with an FLS, the refracture rate was lower than for patients who had an index fracture before the FLS was started, indicating that FLS reduce the risk of recurrent fracture. No such trends were observed in hospitals without FLS during the same time period.”
Dr. Lorentzon, head of geriatric medicine at Sahlgrenska University Hospital, Mölndal, Sweden, said that FLS implementation “led to a large increase in the use of osteoporosis medication, which we believe is the reason for the reduction in recurrent fracture risk observed. We believe that our results provide solid evidence that FLS implementation can reduce the rate of recurrent fractures, suggesting that all hospitals treating fracture patients should have fracture liaison services.”
In an interview, Stuart L. Silverman, MD, said that the study adds to compelling data on the efficacy and need for patients with clinical fracture to have case management by a FLS. “We recognize that near term risk is substantial in the year following a fracture,” said Dr. Silverman, who is clinical professor of medicine at Cedars-Sinai Medical Center and the University of California, Los Angeles, and is not affiliated with the Swedish study. “For example, the risk of a subsequent fracture after hip fracture is 8.3%, which is similar to the risk of subsequent acute myocardial infarction after an initial acute MI. However, only 23% of patients receive osteoporosis medication after a hip fracture. Yet a fracture is to osteoporosis what an acute MI is to cardiovascular disease. We recognize that men and women age 65 years and older who have suffered a hip or vertebral fracture should be evaluated for treatment, as this subpopulation is at high risk for a second fracture and evidence supporting treatment efficacy is robust. We need a multidisciplinary clinical system which includes case management such as a fracture liaison service. We know FLS can reduce hip fracture rate in a closed system such as Kaiser by over 40%. This manuscript addresses the utility of a FLS in terms of reducing risk of future fracture.”
The researchers acknowledged certain limitations of the study, including its observational design and the fact that patients prior to the FLS period were fewer and had longer follow-up time, compared with patients during the FLS period.
The study was funded by the Swedish Research Council and by grants from the Sahlgrenska University Hospital. Dr. Axelsson reported that he has received lecture fees from Lilly, Meda/Mylan, and Amgen. Dr. Lorentzon has received lecture fees from Amgen, Lilly, UCB, Radius Health, Meda, GE-Lunar, and Santax Medico/Hologic. The other coauthors reported having no financial disclosures. Dr. Silverman reported that he is a member of the speakers’ bureaus for Amgen and Radius. He is also a consultant for Lilly, Pfizer, and Amgen and has received research grants from Radius and Amgen.
SOURCE: Axelsson K et al. J Bone Min Res. 2020 Feb 25. doi: 10.1002/jbmr.3990.
FROM THE JOURNAL OF BONE AND MINERAL RESEARCH
Internist reports from COVID-19 front lines near Seattle
KENT, WASHINGTON – The first thing I learned in this outbreak is that my sense of alarm has been deadened by years of medical practice. As a primary care doctor working south of Seattle, in the University of Washington’s Kent neighborhood clinic, I have dealt with long hours, the sometimes-insurmountable problems of the patients I care for, and the constant, gnawing fear of missing something and doing harm. To get through my day, I’ve done my best to rationalize that fear, to explain it away.
I can’t explain how, when I heard the news of the coronavirus epidemic in China, I didn’t think it would affect me. I can’t explain how news of the first patient presenting to an urgent care north of Seattle didn’t cause me, or all health care providers, to think about how we would respond. I can’t explain why so many doctors were dismissive of the very real threat that was about to explode. I can’t explain why it took 6 weeks for the COVID-19 outbreak to seem real to me.
If you work in a doctor’s office, emergency department, hospital, or urgent care center and have not seen a coronavirus case yet, you may have time to think through what is likely to happen in your community. We did not activate a chain of command or decide how information was going to be communicated to the front line and back to leadership. Few of us ran worst-case scenarios.
By March 12, we had 376 confirmed cases, and likely more than a thousand are undetected. The moment of realization of the severity of the outbreak didn’t come to me until Saturday, Feb. 29. In the week prior, several patients had come into the clinic with symptoms and potential exposures, but not meeting the narrow Centers for Disease Control and Prevention testing criteria. They were all advised by the Washington Department of Health to go home. At the time, it seemed like decent advice. Frontline providers didn’t know that there had been two cases of community transmission weeks before, or that one was about to become the first death in Washington state. I still advised patients to quarantine themselves. In the absence of testing, we had to assume everyone was positive and should stay home until 72 hours after their symptoms resolved. Studying the state’s FMLA [Family and Medical Leave Act] intently, I wrote insistent letters to inflexible bosses, explaining that their employees needed to stay home.
I worked that Saturday. Half of my patients had coughs. Our team insisted that they wear masks. One woman refused, and I refused to see her until she did. In a customer service–oriented health care system, I had been schooled to accommodate almost any patient request. But I was not about to put my staff and other patients at risk. Reluctantly, she complied.
On my lunch break, my partner called me to tell me he was at the grocery store. “Why?” I asked, since we usually went together. It became clear he was worried about an outbreak. He had been following the news closely and tried to tell me how deadly this could get and how quickly the disease could spread. I brushed his fears aside, as more evidence of his sweet and overly cautious nature. “It’ll be fine,” I said with misplaced confidence.
Later that day, I heard about the first death and the outbreak at Life Care, a nursing home north of Seattle. I learned that firefighters who had responded to distress calls were under quarantine. I learned through an epidemiologist that there were likely hundreds of undetected cases throughout Washington.
On Monday, our clinic decided to convert all cases with symptoms into telemedicine visits. Luckily, we had been building the capacity to see and treat patients virtually for a while. We have ramped up quickly, but there have been bumps along the way. It’s difficult to convince those who are anxious about their symptoms to allow us to use telemedicine for everyone’s safety. It is unclear how much liability we are taking on as individual providers with this approach or who will speak up for us if something goes wrong.
Patients don’t seem to know where to get their information, and they have been turning to increasingly bizarre sources. For the poorest, who have had so much trouble accessing care, I cannot blame them for not knowing whom to trust. I post what I know on Twitter and Facebook, but I know I’m no match for cynical social media algorithms.
Testing was still not available at my clinic the first week of March, and it remains largely unavailable throughout much of the country. We have lost weeks of opportunity to contain this. Luckily, on March 4, the University of Washington was finally allowed to use their homegrown test and bypass the limited supply from the CDC. But our capacity at UW is still limited, and the test remained unavailable to the majority of those potentially showing symptoms until March 9.
I am used to being less worried than my patients. I am used to reassuring them. But over the first week of March, I had an eerie sense that my alarm far outstripped theirs. I got relatively few questions about coronavirus, even as the number of cases continued to rise. It wasn’t until the end of the week that I noticed a few were truly fearful. Patients started stealing the gloves and the hand sanitizer, and we had to zealously guard them. My hands are raw from washing.
Throughout this time, I have been grateful for a centralized drive with clear protocols. I am grateful for clear messages at the beginning and end of the day from our CEO. I hope that other clinics model this and have daily in-person meetings, because too much cannot be conveyed in an email when the situation changes hourly.
But our health system nationally was already stretched thin before, and providers have sacrificed a lot, especially in the most critical settings, to provide decent patient care. Now we are asked to risk our health and safety, and our family’s, and I worry about the erosion of trust and work conditions for those on the front lines. I also worry our patients won’t believe us when we have allowed the costs of care to continue to rise and ruin their lives. I worry about the millions of people without doctors to call because they have no insurance, and because so many primary care physicians have left unsustainable jobs.
I am grateful that few of my colleagues have been sick and that those that were called out. I am grateful for the new nurse practitioners in our clinic who took the lion’s share of possibly affected patients and triaged hundreds of phone calls, creating note and message templates that we all use. I am grateful that my clinic manager insisted on doing a drill with all the staff members.
I am grateful that we were reminded that we are a team and that if the call center and cleaning crews and front desk are excluded, then our protocols are useless. I am grateful that our registered nurses quickly shifted to triage. I am grateful that I have testing available.
This week, for the first time since I started working, multiple patients asked how I am doing and expressed their thanks. I am most grateful for them.
I can’t tell you what to do or what is going to happen, but I can tell you that you need to prepare now. You need to run drills and catch the holes in your plans before the pandemic reaches you. You need to be creative and honest about the flaws in your organization that this pandemic will inevitably expose. You need to meet with your team every day and remember that we are all going to be stretched even thinner than before.
Most of us will get through this, but many of us won’t. And for those who do, we need to be honest about our successes and failures. We need to build a system that can do better next time. Because this is not the last pandemic we will face.
Dr. Elisabeth Poorman is a general internist at a University of Washington neighborhood clinic in Kent. She completed her residency at Cambridge (Mass.) Health Alliance and specializes in addiction medicine. She also serves on the editorial advisory board of Internal Medicine News.
KENT, WASHINGTON – The first thing I learned in this outbreak is that my sense of alarm has been deadened by years of medical practice. As a primary care doctor working south of Seattle, in the University of Washington’s Kent neighborhood clinic, I have dealt with long hours, the sometimes-insurmountable problems of the patients I care for, and the constant, gnawing fear of missing something and doing harm. To get through my day, I’ve done my best to rationalize that fear, to explain it away.
I can’t explain how, when I heard the news of the coronavirus epidemic in China, I didn’t think it would affect me. I can’t explain how news of the first patient presenting to an urgent care north of Seattle didn’t cause me, or all health care providers, to think about how we would respond. I can’t explain why so many doctors were dismissive of the very real threat that was about to explode. I can’t explain why it took 6 weeks for the COVID-19 outbreak to seem real to me.
If you work in a doctor’s office, emergency department, hospital, or urgent care center and have not seen a coronavirus case yet, you may have time to think through what is likely to happen in your community. We did not activate a chain of command or decide how information was going to be communicated to the front line and back to leadership. Few of us ran worst-case scenarios.
By March 12, we had 376 confirmed cases, and likely more than a thousand are undetected. The moment of realization of the severity of the outbreak didn’t come to me until Saturday, Feb. 29. In the week prior, several patients had come into the clinic with symptoms and potential exposures, but not meeting the narrow Centers for Disease Control and Prevention testing criteria. They were all advised by the Washington Department of Health to go home. At the time, it seemed like decent advice. Frontline providers didn’t know that there had been two cases of community transmission weeks before, or that one was about to become the first death in Washington state. I still advised patients to quarantine themselves. In the absence of testing, we had to assume everyone was positive and should stay home until 72 hours after their symptoms resolved. Studying the state’s FMLA [Family and Medical Leave Act] intently, I wrote insistent letters to inflexible bosses, explaining that their employees needed to stay home.
I worked that Saturday. Half of my patients had coughs. Our team insisted that they wear masks. One woman refused, and I refused to see her until she did. In a customer service–oriented health care system, I had been schooled to accommodate almost any patient request. But I was not about to put my staff and other patients at risk. Reluctantly, she complied.
On my lunch break, my partner called me to tell me he was at the grocery store. “Why?” I asked, since we usually went together. It became clear he was worried about an outbreak. He had been following the news closely and tried to tell me how deadly this could get and how quickly the disease could spread. I brushed his fears aside, as more evidence of his sweet and overly cautious nature. “It’ll be fine,” I said with misplaced confidence.
Later that day, I heard about the first death and the outbreak at Life Care, a nursing home north of Seattle. I learned that firefighters who had responded to distress calls were under quarantine. I learned through an epidemiologist that there were likely hundreds of undetected cases throughout Washington.
On Monday, our clinic decided to convert all cases with symptoms into telemedicine visits. Luckily, we had been building the capacity to see and treat patients virtually for a while. We have ramped up quickly, but there have been bumps along the way. It’s difficult to convince those who are anxious about their symptoms to allow us to use telemedicine for everyone’s safety. It is unclear how much liability we are taking on as individual providers with this approach or who will speak up for us if something goes wrong.
Patients don’t seem to know where to get their information, and they have been turning to increasingly bizarre sources. For the poorest, who have had so much trouble accessing care, I cannot blame them for not knowing whom to trust. I post what I know on Twitter and Facebook, but I know I’m no match for cynical social media algorithms.
Testing was still not available at my clinic the first week of March, and it remains largely unavailable throughout much of the country. We have lost weeks of opportunity to contain this. Luckily, on March 4, the University of Washington was finally allowed to use their homegrown test and bypass the limited supply from the CDC. But our capacity at UW is still limited, and the test remained unavailable to the majority of those potentially showing symptoms until March 9.
I am used to being less worried than my patients. I am used to reassuring them. But over the first week of March, I had an eerie sense that my alarm far outstripped theirs. I got relatively few questions about coronavirus, even as the number of cases continued to rise. It wasn’t until the end of the week that I noticed a few were truly fearful. Patients started stealing the gloves and the hand sanitizer, and we had to zealously guard them. My hands are raw from washing.
Throughout this time, I have been grateful for a centralized drive with clear protocols. I am grateful for clear messages at the beginning and end of the day from our CEO. I hope that other clinics model this and have daily in-person meetings, because too much cannot be conveyed in an email when the situation changes hourly.
But our health system nationally was already stretched thin before, and providers have sacrificed a lot, especially in the most critical settings, to provide decent patient care. Now we are asked to risk our health and safety, and our family’s, and I worry about the erosion of trust and work conditions for those on the front lines. I also worry our patients won’t believe us when we have allowed the costs of care to continue to rise and ruin their lives. I worry about the millions of people without doctors to call because they have no insurance, and because so many primary care physicians have left unsustainable jobs.
I am grateful that few of my colleagues have been sick and that those that were called out. I am grateful for the new nurse practitioners in our clinic who took the lion’s share of possibly affected patients and triaged hundreds of phone calls, creating note and message templates that we all use. I am grateful that my clinic manager insisted on doing a drill with all the staff members.
I am grateful that we were reminded that we are a team and that if the call center and cleaning crews and front desk are excluded, then our protocols are useless. I am grateful that our registered nurses quickly shifted to triage. I am grateful that I have testing available.
This week, for the first time since I started working, multiple patients asked how I am doing and expressed their thanks. I am most grateful for them.
I can’t tell you what to do or what is going to happen, but I can tell you that you need to prepare now. You need to run drills and catch the holes in your plans before the pandemic reaches you. You need to be creative and honest about the flaws in your organization that this pandemic will inevitably expose. You need to meet with your team every day and remember that we are all going to be stretched even thinner than before.
Most of us will get through this, but many of us won’t. And for those who do, we need to be honest about our successes and failures. We need to build a system that can do better next time. Because this is not the last pandemic we will face.
Dr. Elisabeth Poorman is a general internist at a University of Washington neighborhood clinic in Kent. She completed her residency at Cambridge (Mass.) Health Alliance and specializes in addiction medicine. She also serves on the editorial advisory board of Internal Medicine News.
KENT, WASHINGTON – The first thing I learned in this outbreak is that my sense of alarm has been deadened by years of medical practice. As a primary care doctor working south of Seattle, in the University of Washington’s Kent neighborhood clinic, I have dealt with long hours, the sometimes-insurmountable problems of the patients I care for, and the constant, gnawing fear of missing something and doing harm. To get through my day, I’ve done my best to rationalize that fear, to explain it away.
I can’t explain how, when I heard the news of the coronavirus epidemic in China, I didn’t think it would affect me. I can’t explain how news of the first patient presenting to an urgent care north of Seattle didn’t cause me, or all health care providers, to think about how we would respond. I can’t explain why so many doctors were dismissive of the very real threat that was about to explode. I can’t explain why it took 6 weeks for the COVID-19 outbreak to seem real to me.
If you work in a doctor’s office, emergency department, hospital, or urgent care center and have not seen a coronavirus case yet, you may have time to think through what is likely to happen in your community. We did not activate a chain of command or decide how information was going to be communicated to the front line and back to leadership. Few of us ran worst-case scenarios.
By March 12, we had 376 confirmed cases, and likely more than a thousand are undetected. The moment of realization of the severity of the outbreak didn’t come to me until Saturday, Feb. 29. In the week prior, several patients had come into the clinic with symptoms and potential exposures, but not meeting the narrow Centers for Disease Control and Prevention testing criteria. They were all advised by the Washington Department of Health to go home. At the time, it seemed like decent advice. Frontline providers didn’t know that there had been two cases of community transmission weeks before, or that one was about to become the first death in Washington state. I still advised patients to quarantine themselves. In the absence of testing, we had to assume everyone was positive and should stay home until 72 hours after their symptoms resolved. Studying the state’s FMLA [Family and Medical Leave Act] intently, I wrote insistent letters to inflexible bosses, explaining that their employees needed to stay home.
I worked that Saturday. Half of my patients had coughs. Our team insisted that they wear masks. One woman refused, and I refused to see her until she did. In a customer service–oriented health care system, I had been schooled to accommodate almost any patient request. But I was not about to put my staff and other patients at risk. Reluctantly, she complied.
On my lunch break, my partner called me to tell me he was at the grocery store. “Why?” I asked, since we usually went together. It became clear he was worried about an outbreak. He had been following the news closely and tried to tell me how deadly this could get and how quickly the disease could spread. I brushed his fears aside, as more evidence of his sweet and overly cautious nature. “It’ll be fine,” I said with misplaced confidence.
Later that day, I heard about the first death and the outbreak at Life Care, a nursing home north of Seattle. I learned that firefighters who had responded to distress calls were under quarantine. I learned through an epidemiologist that there were likely hundreds of undetected cases throughout Washington.
On Monday, our clinic decided to convert all cases with symptoms into telemedicine visits. Luckily, we had been building the capacity to see and treat patients virtually for a while. We have ramped up quickly, but there have been bumps along the way. It’s difficult to convince those who are anxious about their symptoms to allow us to use telemedicine for everyone’s safety. It is unclear how much liability we are taking on as individual providers with this approach or who will speak up for us if something goes wrong.
Patients don’t seem to know where to get their information, and they have been turning to increasingly bizarre sources. For the poorest, who have had so much trouble accessing care, I cannot blame them for not knowing whom to trust. I post what I know on Twitter and Facebook, but I know I’m no match for cynical social media algorithms.
Testing was still not available at my clinic the first week of March, and it remains largely unavailable throughout much of the country. We have lost weeks of opportunity to contain this. Luckily, on March 4, the University of Washington was finally allowed to use their homegrown test and bypass the limited supply from the CDC. But our capacity at UW is still limited, and the test remained unavailable to the majority of those potentially showing symptoms until March 9.
I am used to being less worried than my patients. I am used to reassuring them. But over the first week of March, I had an eerie sense that my alarm far outstripped theirs. I got relatively few questions about coronavirus, even as the number of cases continued to rise. It wasn’t until the end of the week that I noticed a few were truly fearful. Patients started stealing the gloves and the hand sanitizer, and we had to zealously guard them. My hands are raw from washing.
Throughout this time, I have been grateful for a centralized drive with clear protocols. I am grateful for clear messages at the beginning and end of the day from our CEO. I hope that other clinics model this and have daily in-person meetings, because too much cannot be conveyed in an email when the situation changes hourly.
But our health system nationally was already stretched thin before, and providers have sacrificed a lot, especially in the most critical settings, to provide decent patient care. Now we are asked to risk our health and safety, and our family’s, and I worry about the erosion of trust and work conditions for those on the front lines. I also worry our patients won’t believe us when we have allowed the costs of care to continue to rise and ruin their lives. I worry about the millions of people without doctors to call because they have no insurance, and because so many primary care physicians have left unsustainable jobs.
I am grateful that few of my colleagues have been sick and that those that were called out. I am grateful for the new nurse practitioners in our clinic who took the lion’s share of possibly affected patients and triaged hundreds of phone calls, creating note and message templates that we all use. I am grateful that my clinic manager insisted on doing a drill with all the staff members.
I am grateful that we were reminded that we are a team and that if the call center and cleaning crews and front desk are excluded, then our protocols are useless. I am grateful that our registered nurses quickly shifted to triage. I am grateful that I have testing available.
This week, for the first time since I started working, multiple patients asked how I am doing and expressed their thanks. I am most grateful for them.
I can’t tell you what to do or what is going to happen, but I can tell you that you need to prepare now. You need to run drills and catch the holes in your plans before the pandemic reaches you. You need to be creative and honest about the flaws in your organization that this pandemic will inevitably expose. You need to meet with your team every day and remember that we are all going to be stretched even thinner than before.
Most of us will get through this, but many of us won’t. And for those who do, we need to be honest about our successes and failures. We need to build a system that can do better next time. Because this is not the last pandemic we will face.
Dr. Elisabeth Poorman is a general internist at a University of Washington neighborhood clinic in Kent. She completed her residency at Cambridge (Mass.) Health Alliance and specializes in addiction medicine. She also serves on the editorial advisory board of Internal Medicine News.
FDA to revise safety evaluation of type 2 diabetes drugs
The US Food and Drug Administration (FDA) has issued new draft guidance for industry on evaluating the safety of new drugs for type 2 diabetes and removed the “outdated” 12-year-old requirement for standardized cardiovascular outcomes trials (CVOTs).
The new draft guidance, “Type 2 Diabetes Mellitus: Evaluating the Safety of New Drugs for Improving Glycemic Control,” will replace the December 2008 requirement that manufacturers conduct CVOTs to rule out unacceptable cardiovascular safety risk. That move followed concerns raised at the time about the thiazolidinedione class of glucose-lowering drugs.
Since then, “FDA has reviewed the results of several [CVOTs] conducted to meet the December 2008 guidance recommendations. None of the CVOTs to date have identified an increased risk of ischemic cardiovascular events; some of the CVOTs have instead demonstrated a reduced risk for cardiovascular events,” according to the federal register announcement.
In October 2018, the FDA’s Endocrinologic and Metabolic Drugs Advisory Committee narrowly voted (10 to 9) to continue requiring CVOTs, but most panel members also recommended some changes to them, including requirements for safety data beyond cardiovascular events.
Based on the CVOT results over the years and the panel’s recommendations, “FDA is revisiting the recommendations of the December 2008 guidance and is now proposing an updated approach to evaluating the safety of new drugs and biologics to improve glycemic control.”
“The new draft guidance does not contain the recommendation that sponsors of all new therapies for type 2 diabetes uniformly rule out a specific degree of risk for ischemic cardiovascular adverse outcomes,” the FDA said.
Instead, the draft calls for at least 4000 patient-years of exposure to the new drug in phase 3 trials and inclusion of study participants with comorbid conditions and/or diabetes complications, including at least 500 with stage 3-4 chronic kidney disease, 600 with established cardiovascular disease, and at least 600 over the age of 65 years.
The FDA is soliciting stakeholder input on these and other issues, including study duration, subject demographics, specific safety concerns, and event adjudication.
In a statement, Lisa Yanoff, MD, acting director of the Division for Metabolism and Endocrinology Products in the FDA’s Center for Drug Evaluation and Research, said: “By following previous FDA recommendations, sponsors have shown that new type 2 diabetes drugs do not have excess ischemic cardiovascular risk, which has provided reassuring cardiovascular safety information for millions of diabetes patients. Now, with this proposed approach, we will have broader, valuable safety information for these medications.”
The draft is open for comments for 90 days after March 9, 2020. It is available online, along with a link for submitting comments.
This article first appeared on Medscape.com.
The US Food and Drug Administration (FDA) has issued new draft guidance for industry on evaluating the safety of new drugs for type 2 diabetes and removed the “outdated” 12-year-old requirement for standardized cardiovascular outcomes trials (CVOTs).
The new draft guidance, “Type 2 Diabetes Mellitus: Evaluating the Safety of New Drugs for Improving Glycemic Control,” will replace the December 2008 requirement that manufacturers conduct CVOTs to rule out unacceptable cardiovascular safety risk. That move followed concerns raised at the time about the thiazolidinedione class of glucose-lowering drugs.
Since then, “FDA has reviewed the results of several [CVOTs] conducted to meet the December 2008 guidance recommendations. None of the CVOTs to date have identified an increased risk of ischemic cardiovascular events; some of the CVOTs have instead demonstrated a reduced risk for cardiovascular events,” according to the federal register announcement.
In October 2018, the FDA’s Endocrinologic and Metabolic Drugs Advisory Committee narrowly voted (10 to 9) to continue requiring CVOTs, but most panel members also recommended some changes to them, including requirements for safety data beyond cardiovascular events.
Based on the CVOT results over the years and the panel’s recommendations, “FDA is revisiting the recommendations of the December 2008 guidance and is now proposing an updated approach to evaluating the safety of new drugs and biologics to improve glycemic control.”
“The new draft guidance does not contain the recommendation that sponsors of all new therapies for type 2 diabetes uniformly rule out a specific degree of risk for ischemic cardiovascular adverse outcomes,” the FDA said.
Instead, the draft calls for at least 4000 patient-years of exposure to the new drug in phase 3 trials and inclusion of study participants with comorbid conditions and/or diabetes complications, including at least 500 with stage 3-4 chronic kidney disease, 600 with established cardiovascular disease, and at least 600 over the age of 65 years.
The FDA is soliciting stakeholder input on these and other issues, including study duration, subject demographics, specific safety concerns, and event adjudication.
In a statement, Lisa Yanoff, MD, acting director of the Division for Metabolism and Endocrinology Products in the FDA’s Center for Drug Evaluation and Research, said: “By following previous FDA recommendations, sponsors have shown that new type 2 diabetes drugs do not have excess ischemic cardiovascular risk, which has provided reassuring cardiovascular safety information for millions of diabetes patients. Now, with this proposed approach, we will have broader, valuable safety information for these medications.”
The draft is open for comments for 90 days after March 9, 2020. It is available online, along with a link for submitting comments.
This article first appeared on Medscape.com.
The US Food and Drug Administration (FDA) has issued new draft guidance for industry on evaluating the safety of new drugs for type 2 diabetes and removed the “outdated” 12-year-old requirement for standardized cardiovascular outcomes trials (CVOTs).
The new draft guidance, “Type 2 Diabetes Mellitus: Evaluating the Safety of New Drugs for Improving Glycemic Control,” will replace the December 2008 requirement that manufacturers conduct CVOTs to rule out unacceptable cardiovascular safety risk. That move followed concerns raised at the time about the thiazolidinedione class of glucose-lowering drugs.
Since then, “FDA has reviewed the results of several [CVOTs] conducted to meet the December 2008 guidance recommendations. None of the CVOTs to date have identified an increased risk of ischemic cardiovascular events; some of the CVOTs have instead demonstrated a reduced risk for cardiovascular events,” according to the federal register announcement.
In October 2018, the FDA’s Endocrinologic and Metabolic Drugs Advisory Committee narrowly voted (10 to 9) to continue requiring CVOTs, but most panel members also recommended some changes to them, including requirements for safety data beyond cardiovascular events.
Based on the CVOT results over the years and the panel’s recommendations, “FDA is revisiting the recommendations of the December 2008 guidance and is now proposing an updated approach to evaluating the safety of new drugs and biologics to improve glycemic control.”
“The new draft guidance does not contain the recommendation that sponsors of all new therapies for type 2 diabetes uniformly rule out a specific degree of risk for ischemic cardiovascular adverse outcomes,” the FDA said.
Instead, the draft calls for at least 4000 patient-years of exposure to the new drug in phase 3 trials and inclusion of study participants with comorbid conditions and/or diabetes complications, including at least 500 with stage 3-4 chronic kidney disease, 600 with established cardiovascular disease, and at least 600 over the age of 65 years.
The FDA is soliciting stakeholder input on these and other issues, including study duration, subject demographics, specific safety concerns, and event adjudication.
In a statement, Lisa Yanoff, MD, acting director of the Division for Metabolism and Endocrinology Products in the FDA’s Center for Drug Evaluation and Research, said: “By following previous FDA recommendations, sponsors have shown that new type 2 diabetes drugs do not have excess ischemic cardiovascular risk, which has provided reassuring cardiovascular safety information for millions of diabetes patients. Now, with this proposed approach, we will have broader, valuable safety information for these medications.”
The draft is open for comments for 90 days after March 9, 2020. It is available online, along with a link for submitting comments.
This article first appeared on Medscape.com.
Osilodrostat gets FDA go-ahead for Cushing’s disease in adults
who either are not good candidates for pituitary gland surgery – the recommended first-line therapy – or in whom the disease persists after surgery.
Cushing’s disease is a rare condition caused when a pituitary tumor releases too much of the hormone adrenocorticotropin, which in turn, triggers the adrenal gland to overproduce cortisol. The condition is associated with serious health complications, including high blood pressure, obesity, type 2 diabetes, and compromised immunity.
Osilodrostat is the first therapy approved by the FDA to tackle the overproduction of cortisol, which it does by blocking the 11-beta-hydroxylase enzyme and thus preventing cortisol synthesis, the agency said in a press release.
In November 2019, the European Medicines Agency recommended the granting of a marketing authorization for osilodrostat, also for treating adults with Cushing’s disease.
The U.S. approval was based on outcomes from a study that evaluated the drug’s safety and efficacy in 137 adults with Cushing’s disease who had undergone pituitary surgery but were not cured, or who were not surgical candidates, according the release. About three-quarters of the patients were women, and the mean age was 41 years.
All of the patients started a 24-week, single-arm, open-label period at a dose of 2 mg of osilodrostat twice daily that could be increased every 2 weeks to 30 mg twice daily.
By week 24, cortisol levels in roughly half the patients were within the normal range, and 71 patients who did not need any more dose increases and who tolerated the drug were randomized to either osilodrostat or placebo for an 8-week withdrawal study. At the end of that time, 86% of the osilodrostat patients maintained their normal-range cortisol levels, compared with 30% of those taking placebo.
Osilodrostat is taken as an oral tablet twice a day, in the morning and evening. Among the common side effects reported in the study were adrenal insufficiency, headache, vomiting, nausea, fatigue, and edema, although hypocortisolism, QTc prolongation, and elevations in adrenal hormone precursors, and androgens may also occur, according to the release.
The drug had been given an Orphan Drug Designation in recognition of its intended use in the treatment of a rare disease. The approval was granted to Novartis.
who either are not good candidates for pituitary gland surgery – the recommended first-line therapy – or in whom the disease persists after surgery.
Cushing’s disease is a rare condition caused when a pituitary tumor releases too much of the hormone adrenocorticotropin, which in turn, triggers the adrenal gland to overproduce cortisol. The condition is associated with serious health complications, including high blood pressure, obesity, type 2 diabetes, and compromised immunity.
Osilodrostat is the first therapy approved by the FDA to tackle the overproduction of cortisol, which it does by blocking the 11-beta-hydroxylase enzyme and thus preventing cortisol synthesis, the agency said in a press release.
In November 2019, the European Medicines Agency recommended the granting of a marketing authorization for osilodrostat, also for treating adults with Cushing’s disease.
The U.S. approval was based on outcomes from a study that evaluated the drug’s safety and efficacy in 137 adults with Cushing’s disease who had undergone pituitary surgery but were not cured, or who were not surgical candidates, according the release. About three-quarters of the patients were women, and the mean age was 41 years.
All of the patients started a 24-week, single-arm, open-label period at a dose of 2 mg of osilodrostat twice daily that could be increased every 2 weeks to 30 mg twice daily.
By week 24, cortisol levels in roughly half the patients were within the normal range, and 71 patients who did not need any more dose increases and who tolerated the drug were randomized to either osilodrostat or placebo for an 8-week withdrawal study. At the end of that time, 86% of the osilodrostat patients maintained their normal-range cortisol levels, compared with 30% of those taking placebo.
Osilodrostat is taken as an oral tablet twice a day, in the morning and evening. Among the common side effects reported in the study were adrenal insufficiency, headache, vomiting, nausea, fatigue, and edema, although hypocortisolism, QTc prolongation, and elevations in adrenal hormone precursors, and androgens may also occur, according to the release.
The drug had been given an Orphan Drug Designation in recognition of its intended use in the treatment of a rare disease. The approval was granted to Novartis.
who either are not good candidates for pituitary gland surgery – the recommended first-line therapy – or in whom the disease persists after surgery.
Cushing’s disease is a rare condition caused when a pituitary tumor releases too much of the hormone adrenocorticotropin, which in turn, triggers the adrenal gland to overproduce cortisol. The condition is associated with serious health complications, including high blood pressure, obesity, type 2 diabetes, and compromised immunity.
Osilodrostat is the first therapy approved by the FDA to tackle the overproduction of cortisol, which it does by blocking the 11-beta-hydroxylase enzyme and thus preventing cortisol synthesis, the agency said in a press release.
In November 2019, the European Medicines Agency recommended the granting of a marketing authorization for osilodrostat, also for treating adults with Cushing’s disease.
The U.S. approval was based on outcomes from a study that evaluated the drug’s safety and efficacy in 137 adults with Cushing’s disease who had undergone pituitary surgery but were not cured, or who were not surgical candidates, according the release. About three-quarters of the patients were women, and the mean age was 41 years.
All of the patients started a 24-week, single-arm, open-label period at a dose of 2 mg of osilodrostat twice daily that could be increased every 2 weeks to 30 mg twice daily.
By week 24, cortisol levels in roughly half the patients were within the normal range, and 71 patients who did not need any more dose increases and who tolerated the drug were randomized to either osilodrostat or placebo for an 8-week withdrawal study. At the end of that time, 86% of the osilodrostat patients maintained their normal-range cortisol levels, compared with 30% of those taking placebo.
Osilodrostat is taken as an oral tablet twice a day, in the morning and evening. Among the common side effects reported in the study were adrenal insufficiency, headache, vomiting, nausea, fatigue, and edema, although hypocortisolism, QTc prolongation, and elevations in adrenal hormone precursors, and androgens may also occur, according to the release.
The drug had been given an Orphan Drug Designation in recognition of its intended use in the treatment of a rare disease. The approval was granted to Novartis.








