User login
SGLT2 inhibitor ertugliflozin shows no CV death or renal benefit
The sodium-glucose transporter 2 (SGLT-2) inhibitor ertugliflozin broke ranks with the other drugs in its class and failed to produce statistically significant drops in the both the combined incidence of cardiovascular (CV) death or heart failure hospitalization, and the rate of adverse renal outcomes, in the mandated CV outcomes trial run for ertugliflozin with more than 8,200 patients with type 2 diabetes and established CV disease.
Merck, one of the companies that markets the drug, announced the topline results in a quarterly financial report released on April 28, 2020.
According to the report, the results from the ertugliflozin cardiovascular outcomes trial “achieved its primary endpoint of noninferiority for major adverse CV events (MACE), compared to placebo in patients with type 2 diabetes mellitus and established atherosclerotic CV disease,” but “the key secondary endpoints of superiority” of ertugliflozin, compared with placebo, “for time to the composite of CV death or hospitalization for heart failure, CV death alone, and the composite of renal death, dialysis/transplant or doubling of serum creatinine from baseline were not met.”
However, the report added that, “while not a prespecified hypothesis for statistical testing, a reduction in hospitalization for heart failure was observed” with ertugliflozin treatment, and the report further said that the drug’s safety profile in the trial “was consistent with that reported in previous studies.” The statement closed by saying that detailed results from the trial are scheduled to be presented on June 16, 2020, at the virtual American Diabetes Association’s 80th Scientific Sessions.
These results came from the VERTIS CV (Evaluation of Ertugliflozin EffIcacy and Safety Cardiovascular Outcomes) trial, which researchers said in 2018 had administered at least one investigational dose to 8,238 randomized patients at centers in any of 34 countries during two enrollment periods in 2013-2015 and 2016-2017 (Am Heart J. 2018 Dec;206:11-23). The tested agent, ertugliflozin (Steglatro) received Food and Drug Administration marketing approval late in 2017 for the indication of improving glycemic control in patients with type 2 diabetes.
The FDA mandated cardiovascular outcomes trials for new glycemic control drugs in guidance the agency issued in 2008 (the FDA released in March 2020 a draft of updated guidance on this topic).
Other FDA-approved agents from the SGLT2 inhibitor class include canagliflozin (Invokana), dapagliflozin (Farxiga), and empagliflozin (Jardiance), and all three showed evidence for a statistically significant effect on reducing the incidence of CV disease death and heart failure hospitalizations, as well as renal complications (Can J Diabetes. 2020 Feb;44[1]:61-7). The evidence showing that several SGLT2 drugs have important and consistent effects on endpoints like CV death, heart failure hospitalizations, and renal complications has helped propel this class of agents to the forefront of glycemic control treatments. More recently, one agent from this group, dapagliflozin, also significantly cut the rate of heart failure worsening or CV disease death in patients with heart failure with reduced ejection fraction but without diabetes (N Engl J Med. 2019 Nov 21;381[21]:1995-2008). Based on this evidence, the FDA is currently considering adding a new indication for dapagliflozin that would also label it for use in patients with heart failure with reduced ejection fraction but without diabetes.
The sodium-glucose transporter 2 (SGLT-2) inhibitor ertugliflozin broke ranks with the other drugs in its class and failed to produce statistically significant drops in the both the combined incidence of cardiovascular (CV) death or heart failure hospitalization, and the rate of adverse renal outcomes, in the mandated CV outcomes trial run for ertugliflozin with more than 8,200 patients with type 2 diabetes and established CV disease.
Merck, one of the companies that markets the drug, announced the topline results in a quarterly financial report released on April 28, 2020.
According to the report, the results from the ertugliflozin cardiovascular outcomes trial “achieved its primary endpoint of noninferiority for major adverse CV events (MACE), compared to placebo in patients with type 2 diabetes mellitus and established atherosclerotic CV disease,” but “the key secondary endpoints of superiority” of ertugliflozin, compared with placebo, “for time to the composite of CV death or hospitalization for heart failure, CV death alone, and the composite of renal death, dialysis/transplant or doubling of serum creatinine from baseline were not met.”
However, the report added that, “while not a prespecified hypothesis for statistical testing, a reduction in hospitalization for heart failure was observed” with ertugliflozin treatment, and the report further said that the drug’s safety profile in the trial “was consistent with that reported in previous studies.” The statement closed by saying that detailed results from the trial are scheduled to be presented on June 16, 2020, at the virtual American Diabetes Association’s 80th Scientific Sessions.
These results came from the VERTIS CV (Evaluation of Ertugliflozin EffIcacy and Safety Cardiovascular Outcomes) trial, which researchers said in 2018 had administered at least one investigational dose to 8,238 randomized patients at centers in any of 34 countries during two enrollment periods in 2013-2015 and 2016-2017 (Am Heart J. 2018 Dec;206:11-23). The tested agent, ertugliflozin (Steglatro) received Food and Drug Administration marketing approval late in 2017 for the indication of improving glycemic control in patients with type 2 diabetes.
The FDA mandated cardiovascular outcomes trials for new glycemic control drugs in guidance the agency issued in 2008 (the FDA released in March 2020 a draft of updated guidance on this topic).
Other FDA-approved agents from the SGLT2 inhibitor class include canagliflozin (Invokana), dapagliflozin (Farxiga), and empagliflozin (Jardiance), and all three showed evidence for a statistically significant effect on reducing the incidence of CV disease death and heart failure hospitalizations, as well as renal complications (Can J Diabetes. 2020 Feb;44[1]:61-7). The evidence showing that several SGLT2 drugs have important and consistent effects on endpoints like CV death, heart failure hospitalizations, and renal complications has helped propel this class of agents to the forefront of glycemic control treatments. More recently, one agent from this group, dapagliflozin, also significantly cut the rate of heart failure worsening or CV disease death in patients with heart failure with reduced ejection fraction but without diabetes (N Engl J Med. 2019 Nov 21;381[21]:1995-2008). Based on this evidence, the FDA is currently considering adding a new indication for dapagliflozin that would also label it for use in patients with heart failure with reduced ejection fraction but without diabetes.
The sodium-glucose transporter 2 (SGLT-2) inhibitor ertugliflozin broke ranks with the other drugs in its class and failed to produce statistically significant drops in the both the combined incidence of cardiovascular (CV) death or heart failure hospitalization, and the rate of adverse renal outcomes, in the mandated CV outcomes trial run for ertugliflozin with more than 8,200 patients with type 2 diabetes and established CV disease.
Merck, one of the companies that markets the drug, announced the topline results in a quarterly financial report released on April 28, 2020.
According to the report, the results from the ertugliflozin cardiovascular outcomes trial “achieved its primary endpoint of noninferiority for major adverse CV events (MACE), compared to placebo in patients with type 2 diabetes mellitus and established atherosclerotic CV disease,” but “the key secondary endpoints of superiority” of ertugliflozin, compared with placebo, “for time to the composite of CV death or hospitalization for heart failure, CV death alone, and the composite of renal death, dialysis/transplant or doubling of serum creatinine from baseline were not met.”
However, the report added that, “while not a prespecified hypothesis for statistical testing, a reduction in hospitalization for heart failure was observed” with ertugliflozin treatment, and the report further said that the drug’s safety profile in the trial “was consistent with that reported in previous studies.” The statement closed by saying that detailed results from the trial are scheduled to be presented on June 16, 2020, at the virtual American Diabetes Association’s 80th Scientific Sessions.
These results came from the VERTIS CV (Evaluation of Ertugliflozin EffIcacy and Safety Cardiovascular Outcomes) trial, which researchers said in 2018 had administered at least one investigational dose to 8,238 randomized patients at centers in any of 34 countries during two enrollment periods in 2013-2015 and 2016-2017 (Am Heart J. 2018 Dec;206:11-23). The tested agent, ertugliflozin (Steglatro) received Food and Drug Administration marketing approval late in 2017 for the indication of improving glycemic control in patients with type 2 diabetes.
The FDA mandated cardiovascular outcomes trials for new glycemic control drugs in guidance the agency issued in 2008 (the FDA released in March 2020 a draft of updated guidance on this topic).
Other FDA-approved agents from the SGLT2 inhibitor class include canagliflozin (Invokana), dapagliflozin (Farxiga), and empagliflozin (Jardiance), and all three showed evidence for a statistically significant effect on reducing the incidence of CV disease death and heart failure hospitalizations, as well as renal complications (Can J Diabetes. 2020 Feb;44[1]:61-7). The evidence showing that several SGLT2 drugs have important and consistent effects on endpoints like CV death, heart failure hospitalizations, and renal complications has helped propel this class of agents to the forefront of glycemic control treatments. More recently, one agent from this group, dapagliflozin, also significantly cut the rate of heart failure worsening or CV disease death in patients with heart failure with reduced ejection fraction but without diabetes (N Engl J Med. 2019 Nov 21;381[21]:1995-2008). Based on this evidence, the FDA is currently considering adding a new indication for dapagliflozin that would also label it for use in patients with heart failure with reduced ejection fraction but without diabetes.
COVID-19: Defer ‘bread and butter’ procedure for thyroid nodules
With a few notable exceptions, the majority of fine needle aspiration (FNA) biopsies of thyroid nodules should be delayed until the risk of COVID-19, and the burden on resources, has lessened, according to expert consensus.
“Our group recommends that FNA biopsy of most asymptomatic thyroid nodules – taking into account the sonographic characteristics and patients’ clinical picture – be deferred to a later time, when risk of exposure to COVID-19 is more manageable and resource restriction is no longer a concern,” said the endocrinologists, writing in a guest editorial in Clinical Thyroidology.
All elective procedures have been canceled under guidance of the Centers for Disease Control and Prevention, in conjunction with the U.S. surgeon general, in response to the COVID-19 pandemic. However, thyroid nodule FNAs, though elective, fall into the category of being considered medically necessary and potentially prolonging life expectancy
Yet, with approximately 90% of asymptomatic thyroid nodules turning out to be benign and little evidence that early detection and treatment affects disease outcomes, there is a strong argument for deferral in most cases, stressed Ming Lee, MD, and colleagues, of the endocrinology division at Phoenix (Ariz.) Veterans Affairs Health Care System (PVAHCS), who convened a multidisciplinary meeting to address the urgent issue.
Patients should instead be interviewed by an endocrinologist (preferably via telehealth) to collect their clinical history as well as assess their perception of the disease and risk of malignancy, senior author S. Mitchell Harman, MD, chief of PVAHCS, said in an interview.
“The principal guiding factor should be the objectively assessed likelihood of malignancy of the individual patient’s nodule(s),” he said.
“In my opinion, we should also factor in the patient’s level of anxiety, since some patients are more sanguine about risk than others and our goal is to provide relief of anxiety as well as to determine need for, and course of, subsequent treatment,” Dr. Harman added.
Vast majority of malignant thyroid nodules are DTC, which is ‘indolent’
Dr. Lee and colleagues noted that, even of the 10% of thyroid nodules that do prove to be malignant, the vast majority of these (90%) are differentiated thyroid cancers (DTC). In general, patients with DTC “follow an indolent course and have excellent outcomes.”
“There is little evidence that early detection and treatment of DTC significantly alters disease outcomes as the overall mortality rate for DTC has remained low, at around 0.5%,” they wrote.
They also noted that ultrasound features of thyroid nodules can help guide priority for the future timing of an FNA procedure, but should not be the sole basis for deciding on immediate thyroid FNA or surgery.
Exceptions to the rule
Exceptions for considering FNA include more urgent thyroid disease diagnoses, including those that are symptomatic:
Suspected medullary thyroid cancer
“Regarding medullary thyroid cancer (MTC), early diagnosis and surgery do significantly improve outcomes, therefore, delaying FNA of nodules harboring MTC could be potentially injurious,” the authors said.
They suggested, however, measuring calcitonin levels instead, which they noted “is still controversial” in the United States, but “we feel it would be justified in patients with thyroid nodules that would usually be indicated for FNA.”
Those with a family history of MTC, or nodules located in the posterior upper third of lateral lobes (the usual location of MTC), should have calcitonin levels measured.
If calcitonin levels are above 10 pg/mL, “FNA should be offered as early as possible.”
“Significantly elevated serum calcitonin levels (e.g., > 100 pg/mL) should be considered an indication for surgery without cytologic confirmation by FNA,” they added.
Anaplastic thyroid cancer
Anaplastic thyroid cancer, though rare, “is one of the few occasions when thyroid surgery should be performed on an urgent basis, as this condition can worsen very rapidly.
“Patients typically present with a rapidly enlarging thyroid mass that is associated with compressive symptoms, such as dysphagia and dyspnea,” they observed.
In this instance, although FNA is part of the preoperative work-up, it is often nondiagnostic and could require additional sampling.
“At the time of this pandemic, it is reasonable that after a multidisciplinary discussion, such patients with the appropriate clinical scenario be referred for thyroid surgery, with or without prior FNA, based on the team’s judgment,” the authors recommended.
Long-standing thyroid masses
These are usually large and/or closely associated with vital structures, such as the trachea and esophagus, and when such masses cause compressive symptoms, thyroid surgery typically is warranted.
And although prior FNA is helpful to obtain a cytologic diagnosis, as this may change the extent of surgery, it may not always be essential.
Broadly, symptomatic patients with compressive symptoms threatening vital structures can be directly referred to a surgeon, with the timing for surgery jointly decided based on the severity of symptoms, rapidity of disease progression, local COVID-19 status, and available resources.
“During the pandemic, we believe that the vast majority of thyroid FNAs should be considered optional, and extent of surgery can be determined by pathological analysis of frozen sections intraoperatively,” they wrote.
“The value of FNA in these situations is less compelling in the current COVID-19 setting, as the basis of decision for surgery has been already determined,” the authors explained.
If urgent FNA needed, screen patient for COVID-19 and use PPE
Should the need for an urgent thyroid FNA occur, patients should be screened and tested for COVID-19 by a clinician wearing personal protective equipment (PPE), said Dr. Lee and colleagues.
“It is crucial to carefully weigh the risks of COVID-19 exposure, availability of resources, and urgency of these procedures for each patient in our individual practice settings,” they noted.
As restrictions eventually loosen, precautions will still be necessary to some degree, Dr. Harman said.
“I do not consider FNA a ‘high-risk’ procedure in the era of COVID-19, since it does not routinely result in profuse aerosolization of respiratory fluids,” he said in an interview.
“However, patients do sometimes cough or choke due to pressure on the neck and the operator is, of necessity, very close to the patient’s face. Therefore, when we resume FNA, patients will be screened for symptoms of COVID-19 infection and both the operator and the patient will be masked,” Dr. Harman continued.
“We routinely wear gloves, [and] whether the operator will wear a surgical or an N95 mask, disposable gown, etc, will depend on CDC guidance and guidance received from our VA infectious disease experts as it is applied specifically to each patient evaluation.”
The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
With a few notable exceptions, the majority of fine needle aspiration (FNA) biopsies of thyroid nodules should be delayed until the risk of COVID-19, and the burden on resources, has lessened, according to expert consensus.
“Our group recommends that FNA biopsy of most asymptomatic thyroid nodules – taking into account the sonographic characteristics and patients’ clinical picture – be deferred to a later time, when risk of exposure to COVID-19 is more manageable and resource restriction is no longer a concern,” said the endocrinologists, writing in a guest editorial in Clinical Thyroidology.
All elective procedures have been canceled under guidance of the Centers for Disease Control and Prevention, in conjunction with the U.S. surgeon general, in response to the COVID-19 pandemic. However, thyroid nodule FNAs, though elective, fall into the category of being considered medically necessary and potentially prolonging life expectancy
Yet, with approximately 90% of asymptomatic thyroid nodules turning out to be benign and little evidence that early detection and treatment affects disease outcomes, there is a strong argument for deferral in most cases, stressed Ming Lee, MD, and colleagues, of the endocrinology division at Phoenix (Ariz.) Veterans Affairs Health Care System (PVAHCS), who convened a multidisciplinary meeting to address the urgent issue.
Patients should instead be interviewed by an endocrinologist (preferably via telehealth) to collect their clinical history as well as assess their perception of the disease and risk of malignancy, senior author S. Mitchell Harman, MD, chief of PVAHCS, said in an interview.
“The principal guiding factor should be the objectively assessed likelihood of malignancy of the individual patient’s nodule(s),” he said.
“In my opinion, we should also factor in the patient’s level of anxiety, since some patients are more sanguine about risk than others and our goal is to provide relief of anxiety as well as to determine need for, and course of, subsequent treatment,” Dr. Harman added.
Vast majority of malignant thyroid nodules are DTC, which is ‘indolent’
Dr. Lee and colleagues noted that, even of the 10% of thyroid nodules that do prove to be malignant, the vast majority of these (90%) are differentiated thyroid cancers (DTC). In general, patients with DTC “follow an indolent course and have excellent outcomes.”
“There is little evidence that early detection and treatment of DTC significantly alters disease outcomes as the overall mortality rate for DTC has remained low, at around 0.5%,” they wrote.
They also noted that ultrasound features of thyroid nodules can help guide priority for the future timing of an FNA procedure, but should not be the sole basis for deciding on immediate thyroid FNA or surgery.
Exceptions to the rule
Exceptions for considering FNA include more urgent thyroid disease diagnoses, including those that are symptomatic:
Suspected medullary thyroid cancer
“Regarding medullary thyroid cancer (MTC), early diagnosis and surgery do significantly improve outcomes, therefore, delaying FNA of nodules harboring MTC could be potentially injurious,” the authors said.
They suggested, however, measuring calcitonin levels instead, which they noted “is still controversial” in the United States, but “we feel it would be justified in patients with thyroid nodules that would usually be indicated for FNA.”
Those with a family history of MTC, or nodules located in the posterior upper third of lateral lobes (the usual location of MTC), should have calcitonin levels measured.
If calcitonin levels are above 10 pg/mL, “FNA should be offered as early as possible.”
“Significantly elevated serum calcitonin levels (e.g., > 100 pg/mL) should be considered an indication for surgery without cytologic confirmation by FNA,” they added.
Anaplastic thyroid cancer
Anaplastic thyroid cancer, though rare, “is one of the few occasions when thyroid surgery should be performed on an urgent basis, as this condition can worsen very rapidly.
“Patients typically present with a rapidly enlarging thyroid mass that is associated with compressive symptoms, such as dysphagia and dyspnea,” they observed.
In this instance, although FNA is part of the preoperative work-up, it is often nondiagnostic and could require additional sampling.
“At the time of this pandemic, it is reasonable that after a multidisciplinary discussion, such patients with the appropriate clinical scenario be referred for thyroid surgery, with or without prior FNA, based on the team’s judgment,” the authors recommended.
Long-standing thyroid masses
These are usually large and/or closely associated with vital structures, such as the trachea and esophagus, and when such masses cause compressive symptoms, thyroid surgery typically is warranted.
And although prior FNA is helpful to obtain a cytologic diagnosis, as this may change the extent of surgery, it may not always be essential.
Broadly, symptomatic patients with compressive symptoms threatening vital structures can be directly referred to a surgeon, with the timing for surgery jointly decided based on the severity of symptoms, rapidity of disease progression, local COVID-19 status, and available resources.
“During the pandemic, we believe that the vast majority of thyroid FNAs should be considered optional, and extent of surgery can be determined by pathological analysis of frozen sections intraoperatively,” they wrote.
“The value of FNA in these situations is less compelling in the current COVID-19 setting, as the basis of decision for surgery has been already determined,” the authors explained.
If urgent FNA needed, screen patient for COVID-19 and use PPE
Should the need for an urgent thyroid FNA occur, patients should be screened and tested for COVID-19 by a clinician wearing personal protective equipment (PPE), said Dr. Lee and colleagues.
“It is crucial to carefully weigh the risks of COVID-19 exposure, availability of resources, and urgency of these procedures for each patient in our individual practice settings,” they noted.
As restrictions eventually loosen, precautions will still be necessary to some degree, Dr. Harman said.
“I do not consider FNA a ‘high-risk’ procedure in the era of COVID-19, since it does not routinely result in profuse aerosolization of respiratory fluids,” he said in an interview.
“However, patients do sometimes cough or choke due to pressure on the neck and the operator is, of necessity, very close to the patient’s face. Therefore, when we resume FNA, patients will be screened for symptoms of COVID-19 infection and both the operator and the patient will be masked,” Dr. Harman continued.
“We routinely wear gloves, [and] whether the operator will wear a surgical or an N95 mask, disposable gown, etc, will depend on CDC guidance and guidance received from our VA infectious disease experts as it is applied specifically to each patient evaluation.”
The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
With a few notable exceptions, the majority of fine needle aspiration (FNA) biopsies of thyroid nodules should be delayed until the risk of COVID-19, and the burden on resources, has lessened, according to expert consensus.
“Our group recommends that FNA biopsy of most asymptomatic thyroid nodules – taking into account the sonographic characteristics and patients’ clinical picture – be deferred to a later time, when risk of exposure to COVID-19 is more manageable and resource restriction is no longer a concern,” said the endocrinologists, writing in a guest editorial in Clinical Thyroidology.
All elective procedures have been canceled under guidance of the Centers for Disease Control and Prevention, in conjunction with the U.S. surgeon general, in response to the COVID-19 pandemic. However, thyroid nodule FNAs, though elective, fall into the category of being considered medically necessary and potentially prolonging life expectancy
Yet, with approximately 90% of asymptomatic thyroid nodules turning out to be benign and little evidence that early detection and treatment affects disease outcomes, there is a strong argument for deferral in most cases, stressed Ming Lee, MD, and colleagues, of the endocrinology division at Phoenix (Ariz.) Veterans Affairs Health Care System (PVAHCS), who convened a multidisciplinary meeting to address the urgent issue.
Patients should instead be interviewed by an endocrinologist (preferably via telehealth) to collect their clinical history as well as assess their perception of the disease and risk of malignancy, senior author S. Mitchell Harman, MD, chief of PVAHCS, said in an interview.
“The principal guiding factor should be the objectively assessed likelihood of malignancy of the individual patient’s nodule(s),” he said.
“In my opinion, we should also factor in the patient’s level of anxiety, since some patients are more sanguine about risk than others and our goal is to provide relief of anxiety as well as to determine need for, and course of, subsequent treatment,” Dr. Harman added.
Vast majority of malignant thyroid nodules are DTC, which is ‘indolent’
Dr. Lee and colleagues noted that, even of the 10% of thyroid nodules that do prove to be malignant, the vast majority of these (90%) are differentiated thyroid cancers (DTC). In general, patients with DTC “follow an indolent course and have excellent outcomes.”
“There is little evidence that early detection and treatment of DTC significantly alters disease outcomes as the overall mortality rate for DTC has remained low, at around 0.5%,” they wrote.
They also noted that ultrasound features of thyroid nodules can help guide priority for the future timing of an FNA procedure, but should not be the sole basis for deciding on immediate thyroid FNA or surgery.
Exceptions to the rule
Exceptions for considering FNA include more urgent thyroid disease diagnoses, including those that are symptomatic:
Suspected medullary thyroid cancer
“Regarding medullary thyroid cancer (MTC), early diagnosis and surgery do significantly improve outcomes, therefore, delaying FNA of nodules harboring MTC could be potentially injurious,” the authors said.
They suggested, however, measuring calcitonin levels instead, which they noted “is still controversial” in the United States, but “we feel it would be justified in patients with thyroid nodules that would usually be indicated for FNA.”
Those with a family history of MTC, or nodules located in the posterior upper third of lateral lobes (the usual location of MTC), should have calcitonin levels measured.
If calcitonin levels are above 10 pg/mL, “FNA should be offered as early as possible.”
“Significantly elevated serum calcitonin levels (e.g., > 100 pg/mL) should be considered an indication for surgery without cytologic confirmation by FNA,” they added.
Anaplastic thyroid cancer
Anaplastic thyroid cancer, though rare, “is one of the few occasions when thyroid surgery should be performed on an urgent basis, as this condition can worsen very rapidly.
“Patients typically present with a rapidly enlarging thyroid mass that is associated with compressive symptoms, such as dysphagia and dyspnea,” they observed.
In this instance, although FNA is part of the preoperative work-up, it is often nondiagnostic and could require additional sampling.
“At the time of this pandemic, it is reasonable that after a multidisciplinary discussion, such patients with the appropriate clinical scenario be referred for thyroid surgery, with or without prior FNA, based on the team’s judgment,” the authors recommended.
Long-standing thyroid masses
These are usually large and/or closely associated with vital structures, such as the trachea and esophagus, and when such masses cause compressive symptoms, thyroid surgery typically is warranted.
And although prior FNA is helpful to obtain a cytologic diagnosis, as this may change the extent of surgery, it may not always be essential.
Broadly, symptomatic patients with compressive symptoms threatening vital structures can be directly referred to a surgeon, with the timing for surgery jointly decided based on the severity of symptoms, rapidity of disease progression, local COVID-19 status, and available resources.
“During the pandemic, we believe that the vast majority of thyroid FNAs should be considered optional, and extent of surgery can be determined by pathological analysis of frozen sections intraoperatively,” they wrote.
“The value of FNA in these situations is less compelling in the current COVID-19 setting, as the basis of decision for surgery has been already determined,” the authors explained.
If urgent FNA needed, screen patient for COVID-19 and use PPE
Should the need for an urgent thyroid FNA occur, patients should be screened and tested for COVID-19 by a clinician wearing personal protective equipment (PPE), said Dr. Lee and colleagues.
“It is crucial to carefully weigh the risks of COVID-19 exposure, availability of resources, and urgency of these procedures for each patient in our individual practice settings,” they noted.
As restrictions eventually loosen, precautions will still be necessary to some degree, Dr. Harman said.
“I do not consider FNA a ‘high-risk’ procedure in the era of COVID-19, since it does not routinely result in profuse aerosolization of respiratory fluids,” he said in an interview.
“However, patients do sometimes cough or choke due to pressure on the neck and the operator is, of necessity, very close to the patient’s face. Therefore, when we resume FNA, patients will be screened for symptoms of COVID-19 infection and both the operator and the patient will be masked,” Dr. Harman continued.
“We routinely wear gloves, [and] whether the operator will wear a surgical or an N95 mask, disposable gown, etc, will depend on CDC guidance and guidance received from our VA infectious disease experts as it is applied specifically to each patient evaluation.”
The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Teprotumumab eases thyroid eye disease in all, including smokers
Teprotumumab (Tepezza, Horizon Therapeutics), the first-ever medication approved specifically to treat thyroid eye disease, works in patients regardless of age, gender, and smoking status, new research finds.
The data were presented on March 31 by Raymond S. Douglas, MD, director of the thyroid eye disease program at Cedars-Sinai Medical Center, Los Angeles, during a virtual news conference held by the Endocrine Society. The study had been slated for presentation during ENDO 2020, the society’s annual meeting, which was canceled because of the COVID-19 pandemic.
Thyroid eye disease occurs in up to 50% of people with Graves disease, causing a variety of symptoms, such as eye pain, double vision, light sensitivity or difficulty closing the eye, as well as proptosis, or bulging of the eye, and vision-threatening complications. It affects more women than men, and the symptoms can lead to the progressive inability to perform important daily activities, such as driving or working.
Teprotumumab is a fully human monoclonal antibody inhibitor of the insulin-like growth factor-1 (IGF-1) receptor and was approved by the US Food and Drug Administration in January 2020. Prior to that, therapy typically involved steroids or, in severe cases, surgery.
Blocking the IGF-1 receptor leads to reduced inflammation and reversal of retro-orbital tissue expansion and hyaluronan production in the eye orbit. Teprotumumab is given as an infusion once every 3 weeks for a total of eight infusions.
“Exciting to have an agent” that reduces proptosis to this degree
Previously reported pooled phase 2 and phase 3 data from the randomized, placebo-controlled OPTIC trial involving 171 patients showed significantly greater reductions in proptosis, as well as diplopia, and clinical symptoms of inflammation with teprotumumab versus placebo.
“This has really been unheralded in comparison to other medical therapies previously offered,” Dr. Douglas said during the briefing.
Now, the new analysis shows that the drug works across patient subgroups, he added, highlighting in particular the fact that the agent seems to work equally well in smokers and nonsmokers. Smoking leads to a worse prognosis in thyroid eye disease.
Asked to comment, endocrinologist David C. Lieb, MD, of Eastern Virginia Medical School, Norfolk, said in an interview, “It’s reassuring that this drug appears to have benefits in reducing proptosis across multiple age groups, in both genders, and that there are also benefits seen in patients who smoke and who don’t.”
So far Dr. Lieb has two patients who have been prescribed teprotumumab by their ophthalmologists, but it’s too soon to know how they’ll respond.
“I have no first-hand experience yet, but it’s very exciting to have something to offer patients with active Graves eye disease, which causes a lot of disability for people. It makes work difficult and driving difficult. It’s exciting to have an agent that reduces proptosis to the degree that this one does because we haven’t had anything like this before,” he said.
All patient subgroups benefited in combined analysis
A total of 79 patients completed phase 2 and 76 patients completed phase 3 of the OPTIC trial.
Overall, the proportions achieving proptosis reductions of at least 2 mm without deterioration in the fellow eye at week 24 were 77.4% with teprotumumab versus 14.9% with placebo in the intention-to-treat analysis (P < .001), respectively, and 84.8% versus 17.1% in the per-protocol analysis (P < .001). The number needed to treat was 1.6.
Similar results were achieved across all subgroups of patients: those aged 65 and older versus younger than aged 65 years; male versus female; tobacco user versus nonuser; and U.S. versus E.U. study centers (all P < .001).
Overall, the average decrease in proptosis was 3.1 mm, compared to just 0.4 mm with placebo (P < .001). By subgroup, those reductions ranged from 3.55 mm for those aged 65 and older to 2.93 mm for the U.S. group.
The average proptosis reductions with teprotumumab were 2.99 mm among smokers versus 3.20 mm in nonsmokers, but responses in both groups were significant when compared with placebo.
Smoking contributes to the severity of thyroid eye disease and is associated with more optic neuropathy, poorer response to anti-inflammatory treatment, and worse outcomes, Dr. Douglas said. “Smoking appears to preferentially cause fibroblasts in the orbit to increase proinflammatory cytokines. ... It’s reassuring that this medicine does work in smokers since most other medications are much less effective in reducing inflammatory signs in smoking versus nonsmoking patients.”
Most adverse reactions disappeared after infusion stopped
In the pooled studies overall there were no deaths, but there were seven severe adverse events in the teprotumumab group versus one in the placebo group. Two adverse events in the teprotumumab group – diarrhea and infusion-related reaction – were considered treatment-related and led to drug discontinuation. Another adverse event, Hashimoto’s encephalopathy, was deemed possibly related to the drug and also led to discontinuation.
Treatment-emergent adverse events occurred in 79.8% of patients treated with teprotumumab versus 69.8% with placebo. Those occurring in 5% or more of patients included muscle spasms (25% vs. 7%), nausea (17% vs. 9%), alopecia (13% vs. 8%), and diarrhea (12% vs. 8%). Most were well tolerated and tended to resolve after the infusions ended, Dr. Douglas noted, adding muscle spasms tended to occur at night, improved with massage, and were not accompanied by electrolyte abnormalities.
Antidrug antibodies were detected in two teprotumumab-treated patients, one at study day 1 and another at week 3 during the 24-week treatment period. The patient with antibodies at day 1 also tested positive at week 72. “[Antidrug] antibodies appeared to be very uncommon,” Dr. Douglas noted.
The trial was sponsored by Horizon Therapeutics. Dr. Douglas is a consultant for Horizon Therapeutics and Immunovant. Dr. Lieb has reported no relevant financial relationships. The research will be published in a special supplemental issue of the Journal of the Endocrine Society. In addition to a series of news conferences on March 30-31, the society will host ENDO Online 2020 during June 8-22, which will present programming for clinicians and researchers.
This article first appeared on Medscape.com.
Teprotumumab (Tepezza, Horizon Therapeutics), the first-ever medication approved specifically to treat thyroid eye disease, works in patients regardless of age, gender, and smoking status, new research finds.
The data were presented on March 31 by Raymond S. Douglas, MD, director of the thyroid eye disease program at Cedars-Sinai Medical Center, Los Angeles, during a virtual news conference held by the Endocrine Society. The study had been slated for presentation during ENDO 2020, the society’s annual meeting, which was canceled because of the COVID-19 pandemic.
Thyroid eye disease occurs in up to 50% of people with Graves disease, causing a variety of symptoms, such as eye pain, double vision, light sensitivity or difficulty closing the eye, as well as proptosis, or bulging of the eye, and vision-threatening complications. It affects more women than men, and the symptoms can lead to the progressive inability to perform important daily activities, such as driving or working.
Teprotumumab is a fully human monoclonal antibody inhibitor of the insulin-like growth factor-1 (IGF-1) receptor and was approved by the US Food and Drug Administration in January 2020. Prior to that, therapy typically involved steroids or, in severe cases, surgery.
Blocking the IGF-1 receptor leads to reduced inflammation and reversal of retro-orbital tissue expansion and hyaluronan production in the eye orbit. Teprotumumab is given as an infusion once every 3 weeks for a total of eight infusions.
“Exciting to have an agent” that reduces proptosis to this degree
Previously reported pooled phase 2 and phase 3 data from the randomized, placebo-controlled OPTIC trial involving 171 patients showed significantly greater reductions in proptosis, as well as diplopia, and clinical symptoms of inflammation with teprotumumab versus placebo.
“This has really been unheralded in comparison to other medical therapies previously offered,” Dr. Douglas said during the briefing.
Now, the new analysis shows that the drug works across patient subgroups, he added, highlighting in particular the fact that the agent seems to work equally well in smokers and nonsmokers. Smoking leads to a worse prognosis in thyroid eye disease.
Asked to comment, endocrinologist David C. Lieb, MD, of Eastern Virginia Medical School, Norfolk, said in an interview, “It’s reassuring that this drug appears to have benefits in reducing proptosis across multiple age groups, in both genders, and that there are also benefits seen in patients who smoke and who don’t.”
So far Dr. Lieb has two patients who have been prescribed teprotumumab by their ophthalmologists, but it’s too soon to know how they’ll respond.
“I have no first-hand experience yet, but it’s very exciting to have something to offer patients with active Graves eye disease, which causes a lot of disability for people. It makes work difficult and driving difficult. It’s exciting to have an agent that reduces proptosis to the degree that this one does because we haven’t had anything like this before,” he said.
All patient subgroups benefited in combined analysis
A total of 79 patients completed phase 2 and 76 patients completed phase 3 of the OPTIC trial.
Overall, the proportions achieving proptosis reductions of at least 2 mm without deterioration in the fellow eye at week 24 were 77.4% with teprotumumab versus 14.9% with placebo in the intention-to-treat analysis (P < .001), respectively, and 84.8% versus 17.1% in the per-protocol analysis (P < .001). The number needed to treat was 1.6.
Similar results were achieved across all subgroups of patients: those aged 65 and older versus younger than aged 65 years; male versus female; tobacco user versus nonuser; and U.S. versus E.U. study centers (all P < .001).
Overall, the average decrease in proptosis was 3.1 mm, compared to just 0.4 mm with placebo (P < .001). By subgroup, those reductions ranged from 3.55 mm for those aged 65 and older to 2.93 mm for the U.S. group.
The average proptosis reductions with teprotumumab were 2.99 mm among smokers versus 3.20 mm in nonsmokers, but responses in both groups were significant when compared with placebo.
Smoking contributes to the severity of thyroid eye disease and is associated with more optic neuropathy, poorer response to anti-inflammatory treatment, and worse outcomes, Dr. Douglas said. “Smoking appears to preferentially cause fibroblasts in the orbit to increase proinflammatory cytokines. ... It’s reassuring that this medicine does work in smokers since most other medications are much less effective in reducing inflammatory signs in smoking versus nonsmoking patients.”
Most adverse reactions disappeared after infusion stopped
In the pooled studies overall there were no deaths, but there were seven severe adverse events in the teprotumumab group versus one in the placebo group. Two adverse events in the teprotumumab group – diarrhea and infusion-related reaction – were considered treatment-related and led to drug discontinuation. Another adverse event, Hashimoto’s encephalopathy, was deemed possibly related to the drug and also led to discontinuation.
Treatment-emergent adverse events occurred in 79.8% of patients treated with teprotumumab versus 69.8% with placebo. Those occurring in 5% or more of patients included muscle spasms (25% vs. 7%), nausea (17% vs. 9%), alopecia (13% vs. 8%), and diarrhea (12% vs. 8%). Most were well tolerated and tended to resolve after the infusions ended, Dr. Douglas noted, adding muscle spasms tended to occur at night, improved with massage, and were not accompanied by electrolyte abnormalities.
Antidrug antibodies were detected in two teprotumumab-treated patients, one at study day 1 and another at week 3 during the 24-week treatment period. The patient with antibodies at day 1 also tested positive at week 72. “[Antidrug] antibodies appeared to be very uncommon,” Dr. Douglas noted.
The trial was sponsored by Horizon Therapeutics. Dr. Douglas is a consultant for Horizon Therapeutics and Immunovant. Dr. Lieb has reported no relevant financial relationships. The research will be published in a special supplemental issue of the Journal of the Endocrine Society. In addition to a series of news conferences on March 30-31, the society will host ENDO Online 2020 during June 8-22, which will present programming for clinicians and researchers.
This article first appeared on Medscape.com.
Teprotumumab (Tepezza, Horizon Therapeutics), the first-ever medication approved specifically to treat thyroid eye disease, works in patients regardless of age, gender, and smoking status, new research finds.
The data were presented on March 31 by Raymond S. Douglas, MD, director of the thyroid eye disease program at Cedars-Sinai Medical Center, Los Angeles, during a virtual news conference held by the Endocrine Society. The study had been slated for presentation during ENDO 2020, the society’s annual meeting, which was canceled because of the COVID-19 pandemic.
Thyroid eye disease occurs in up to 50% of people with Graves disease, causing a variety of symptoms, such as eye pain, double vision, light sensitivity or difficulty closing the eye, as well as proptosis, or bulging of the eye, and vision-threatening complications. It affects more women than men, and the symptoms can lead to the progressive inability to perform important daily activities, such as driving or working.
Teprotumumab is a fully human monoclonal antibody inhibitor of the insulin-like growth factor-1 (IGF-1) receptor and was approved by the US Food and Drug Administration in January 2020. Prior to that, therapy typically involved steroids or, in severe cases, surgery.
Blocking the IGF-1 receptor leads to reduced inflammation and reversal of retro-orbital tissue expansion and hyaluronan production in the eye orbit. Teprotumumab is given as an infusion once every 3 weeks for a total of eight infusions.
“Exciting to have an agent” that reduces proptosis to this degree
Previously reported pooled phase 2 and phase 3 data from the randomized, placebo-controlled OPTIC trial involving 171 patients showed significantly greater reductions in proptosis, as well as diplopia, and clinical symptoms of inflammation with teprotumumab versus placebo.
“This has really been unheralded in comparison to other medical therapies previously offered,” Dr. Douglas said during the briefing.
Now, the new analysis shows that the drug works across patient subgroups, he added, highlighting in particular the fact that the agent seems to work equally well in smokers and nonsmokers. Smoking leads to a worse prognosis in thyroid eye disease.
Asked to comment, endocrinologist David C. Lieb, MD, of Eastern Virginia Medical School, Norfolk, said in an interview, “It’s reassuring that this drug appears to have benefits in reducing proptosis across multiple age groups, in both genders, and that there are also benefits seen in patients who smoke and who don’t.”
So far Dr. Lieb has two patients who have been prescribed teprotumumab by their ophthalmologists, but it’s too soon to know how they’ll respond.
“I have no first-hand experience yet, but it’s very exciting to have something to offer patients with active Graves eye disease, which causes a lot of disability for people. It makes work difficult and driving difficult. It’s exciting to have an agent that reduces proptosis to the degree that this one does because we haven’t had anything like this before,” he said.
All patient subgroups benefited in combined analysis
A total of 79 patients completed phase 2 and 76 patients completed phase 3 of the OPTIC trial.
Overall, the proportions achieving proptosis reductions of at least 2 mm without deterioration in the fellow eye at week 24 were 77.4% with teprotumumab versus 14.9% with placebo in the intention-to-treat analysis (P < .001), respectively, and 84.8% versus 17.1% in the per-protocol analysis (P < .001). The number needed to treat was 1.6.
Similar results were achieved across all subgroups of patients: those aged 65 and older versus younger than aged 65 years; male versus female; tobacco user versus nonuser; and U.S. versus E.U. study centers (all P < .001).
Overall, the average decrease in proptosis was 3.1 mm, compared to just 0.4 mm with placebo (P < .001). By subgroup, those reductions ranged from 3.55 mm for those aged 65 and older to 2.93 mm for the U.S. group.
The average proptosis reductions with teprotumumab were 2.99 mm among smokers versus 3.20 mm in nonsmokers, but responses in both groups were significant when compared with placebo.
Smoking contributes to the severity of thyroid eye disease and is associated with more optic neuropathy, poorer response to anti-inflammatory treatment, and worse outcomes, Dr. Douglas said. “Smoking appears to preferentially cause fibroblasts in the orbit to increase proinflammatory cytokines. ... It’s reassuring that this medicine does work in smokers since most other medications are much less effective in reducing inflammatory signs in smoking versus nonsmoking patients.”
Most adverse reactions disappeared after infusion stopped
In the pooled studies overall there were no deaths, but there were seven severe adverse events in the teprotumumab group versus one in the placebo group. Two adverse events in the teprotumumab group – diarrhea and infusion-related reaction – were considered treatment-related and led to drug discontinuation. Another adverse event, Hashimoto’s encephalopathy, was deemed possibly related to the drug and also led to discontinuation.
Treatment-emergent adverse events occurred in 79.8% of patients treated with teprotumumab versus 69.8% with placebo. Those occurring in 5% or more of patients included muscle spasms (25% vs. 7%), nausea (17% vs. 9%), alopecia (13% vs. 8%), and diarrhea (12% vs. 8%). Most were well tolerated and tended to resolve after the infusions ended, Dr. Douglas noted, adding muscle spasms tended to occur at night, improved with massage, and were not accompanied by electrolyte abnormalities.
Antidrug antibodies were detected in two teprotumumab-treated patients, one at study day 1 and another at week 3 during the 24-week treatment period. The patient with antibodies at day 1 also tested positive at week 72. “[Antidrug] antibodies appeared to be very uncommon,” Dr. Douglas noted.
The trial was sponsored by Horizon Therapeutics. Dr. Douglas is a consultant for Horizon Therapeutics and Immunovant. Dr. Lieb has reported no relevant financial relationships. The research will be published in a special supplemental issue of the Journal of the Endocrine Society. In addition to a series of news conferences on March 30-31, the society will host ENDO Online 2020 during June 8-22, which will present programming for clinicians and researchers.
This article first appeared on Medscape.com.
New guidelines for testosterone treatment in adult men with age-related low testosterone
Testosterone normally decreases with age in men beginning in their mid-30s, with a rate of decline averaging approximately 1.6% per year. Using a cutoff of a total testosterone less than 325 ng/dL, the incidence of low testosterone is approximately 20% after age 60 years, and 30% after age 70. While the change in labs values has been reasonably validated,
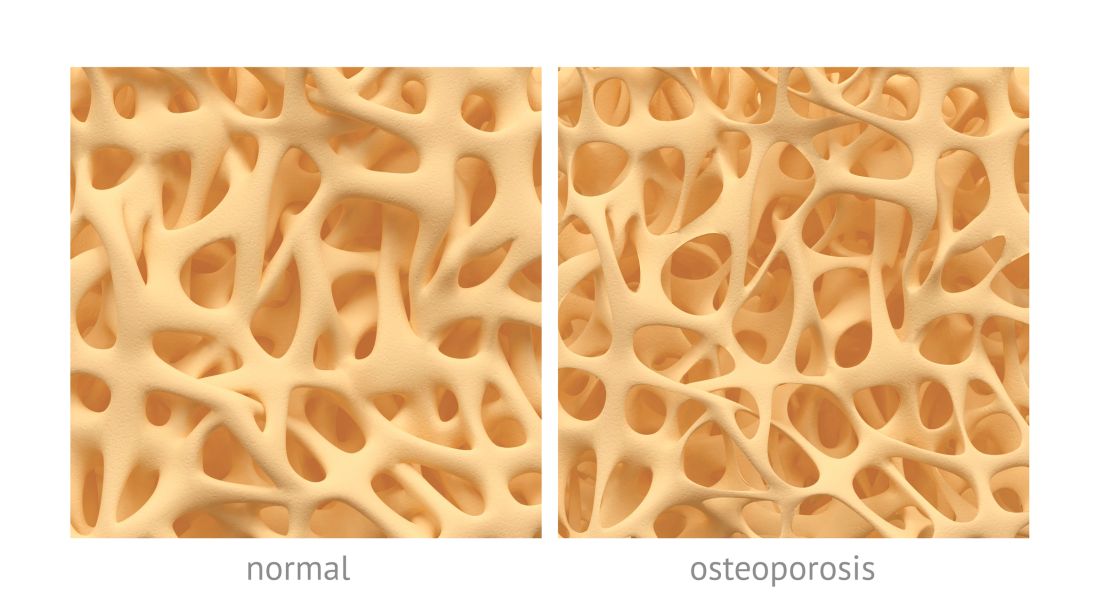
Additional potential symptoms of testosterone deficiency include changes in bone mineral density, decreased libido, depression, erectile dysfunction, loss of hair, and general weakness. Since the symptoms are nonspecific, it is often unclear if someone should be tested or treated for testosterone deficiency. To address this issue, the American College of Physicians commissioned a systematic review of the evidence on testosterone-replacement therapy for age-related testosterone deficiency.1
The evidence review of testosterone replacement in men with age-related low testosterone found the following.
- Low-certainty evidence of improvement in quality of life
- Moderate-certainty evidence of a small improvement in sexual function
- Low-certainty evidence of a small improvement in erectile function
- Low-certainty evidence showing little to no improvement in physical function
- Low-certainty evidence of a small increase to no difference in adverse cardiovascular events
- Moderate-certainty evidence of no increase in the risk for serious adverse events
The trials were not powered to assess mortality, but pool analysis showed fewer deaths among patients treated with testosterone than those who received placebo (odds ratio, 0.47; 95% confidence interval, 0.25-0.89). There were no differences in cognitive function, and the improvement in vitality and fatigue was “less than a small amount.” Evidence from an observational trial showed no increased risk for mortality, cardiovascular events, prostate cancer, or pulmonary embolus or deep vein thrombosis. Of note, most studies excluded men with recent cardiovascular disease.
This evidence review led to the following recommendations.2
Recommendation 1a
Clinicians should have a discussion regarding the potential risk and benefits of treatment with the patients who have documented age-related low testosterone (testosterone levels less than 10.4 nmol/L or 300 ng/dL) and are suffering from sexual dysfunction or have a desire to enhance their sexual function.
This recommendation was based on evidence showing small improvement in sexual function and erectile dysfunction.
Recommendation 1b
For patients who opt for treatment based on recommendation 1a, clinicians should reevaluate the benefit of treatment within 12 months. If a patient is not receiving any benefit in sexual function by 12 months, it is recommended that treatment be stopped at that time.
The ACP recommendation to stop treatment if a patient lacks improvement of sexual function within 12 months stems from low or insufficient evidence regarding potential harm of treatment. If the treatment is not helping the target symptom then the benefit no longer outweighs the potential harm.
Recommendation 1c
For patients who opt for treatment based on recommendation 1a, intramuscular replacement therapy rather than transdermal replacement therapy is recommended because of substantial differences in the cost.
It is important to note that both intramuscular and transdermal testosterone applications have been associated with improvements in sexual function, without any significant differences noted in benefit or harm for the patients. This recommendation is based on a per-person per-year average cost of the intramuscular formulation – $156.32, compared with the transdermal formulation – $2,135.32.
Recommendation 2
The ACP does not endorse the use of testosterone treatment for age-related low testosterone in patients desiring improvement in physical function, mood, energy, or cognitive function.
This clear recommendation is critical, as this might be the most common reason for prescriptions of testosterone – a misplaced belief that testosterone will help general quality of life. The evidence simply does not support this effect of testosterone replacement for age-related testosterone deficiency.
The bottom line
Testosterone levels in men decrease steadily with age, with a great deal of variability. Testosterone replacement therapy may be considered for men with age-related testosterone deficiency and sexual dysfunction. Testosterone replacement therapy is not recommended as a treatment for general fatigue, weakness or with an expectation that it will improve physical function, mood, energy, or cognitive function.
Dr. Hansen is a third-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Hospital–Jefferson Health.
References
1. Diem SJ et al. Efficacy and safety of testosterone treatment in men: An evidence report for a clinical practice guideline by the American College of Physicians. Ann Intern Med. 2020 Jan 21. doi: 10.7326/M19-0830.
2. Qaseem A et al. Testosterone treatment in adult men with age-related low testosterone: A clinical guideline from the American College of Physicians. Ann Intern Med. 2020 Jan 21. doi: 10.7326/M19-0882.
Testosterone normally decreases with age in men beginning in their mid-30s, with a rate of decline averaging approximately 1.6% per year. Using a cutoff of a total testosterone less than 325 ng/dL, the incidence of low testosterone is approximately 20% after age 60 years, and 30% after age 70. While the change in labs values has been reasonably validated,
Additional potential symptoms of testosterone deficiency include changes in bone mineral density, decreased libido, depression, erectile dysfunction, loss of hair, and general weakness. Since the symptoms are nonspecific, it is often unclear if someone should be tested or treated for testosterone deficiency. To address this issue, the American College of Physicians commissioned a systematic review of the evidence on testosterone-replacement therapy for age-related testosterone deficiency.1
The evidence review of testosterone replacement in men with age-related low testosterone found the following.
- Low-certainty evidence of improvement in quality of life
- Moderate-certainty evidence of a small improvement in sexual function
- Low-certainty evidence of a small improvement in erectile function
- Low-certainty evidence showing little to no improvement in physical function
- Low-certainty evidence of a small increase to no difference in adverse cardiovascular events
- Moderate-certainty evidence of no increase in the risk for serious adverse events
The trials were not powered to assess mortality, but pool analysis showed fewer deaths among patients treated with testosterone than those who received placebo (odds ratio, 0.47; 95% confidence interval, 0.25-0.89). There were no differences in cognitive function, and the improvement in vitality and fatigue was “less than a small amount.” Evidence from an observational trial showed no increased risk for mortality, cardiovascular events, prostate cancer, or pulmonary embolus or deep vein thrombosis. Of note, most studies excluded men with recent cardiovascular disease.
This evidence review led to the following recommendations.2
Recommendation 1a
Clinicians should have a discussion regarding the potential risk and benefits of treatment with the patients who have documented age-related low testosterone (testosterone levels less than 10.4 nmol/L or 300 ng/dL) and are suffering from sexual dysfunction or have a desire to enhance their sexual function.
This recommendation was based on evidence showing small improvement in sexual function and erectile dysfunction.
Recommendation 1b
For patients who opt for treatment based on recommendation 1a, clinicians should reevaluate the benefit of treatment within 12 months. If a patient is not receiving any benefit in sexual function by 12 months, it is recommended that treatment be stopped at that time.
The ACP recommendation to stop treatment if a patient lacks improvement of sexual function within 12 months stems from low or insufficient evidence regarding potential harm of treatment. If the treatment is not helping the target symptom then the benefit no longer outweighs the potential harm.
Recommendation 1c
For patients who opt for treatment based on recommendation 1a, intramuscular replacement therapy rather than transdermal replacement therapy is recommended because of substantial differences in the cost.
It is important to note that both intramuscular and transdermal testosterone applications have been associated with improvements in sexual function, without any significant differences noted in benefit or harm for the patients. This recommendation is based on a per-person per-year average cost of the intramuscular formulation – $156.32, compared with the transdermal formulation – $2,135.32.
Recommendation 2
The ACP does not endorse the use of testosterone treatment for age-related low testosterone in patients desiring improvement in physical function, mood, energy, or cognitive function.
This clear recommendation is critical, as this might be the most common reason for prescriptions of testosterone – a misplaced belief that testosterone will help general quality of life. The evidence simply does not support this effect of testosterone replacement for age-related testosterone deficiency.
The bottom line
Testosterone levels in men decrease steadily with age, with a great deal of variability. Testosterone replacement therapy may be considered for men with age-related testosterone deficiency and sexual dysfunction. Testosterone replacement therapy is not recommended as a treatment for general fatigue, weakness or with an expectation that it will improve physical function, mood, energy, or cognitive function.
Dr. Hansen is a third-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Hospital–Jefferson Health.
References
1. Diem SJ et al. Efficacy and safety of testosterone treatment in men: An evidence report for a clinical practice guideline by the American College of Physicians. Ann Intern Med. 2020 Jan 21. doi: 10.7326/M19-0830.
2. Qaseem A et al. Testosterone treatment in adult men with age-related low testosterone: A clinical guideline from the American College of Physicians. Ann Intern Med. 2020 Jan 21. doi: 10.7326/M19-0882.
Testosterone normally decreases with age in men beginning in their mid-30s, with a rate of decline averaging approximately 1.6% per year. Using a cutoff of a total testosterone less than 325 ng/dL, the incidence of low testosterone is approximately 20% after age 60 years, and 30% after age 70. While the change in labs values has been reasonably validated,
Additional potential symptoms of testosterone deficiency include changes in bone mineral density, decreased libido, depression, erectile dysfunction, loss of hair, and general weakness. Since the symptoms are nonspecific, it is often unclear if someone should be tested or treated for testosterone deficiency. To address this issue, the American College of Physicians commissioned a systematic review of the evidence on testosterone-replacement therapy for age-related testosterone deficiency.1
The evidence review of testosterone replacement in men with age-related low testosterone found the following.
- Low-certainty evidence of improvement in quality of life
- Moderate-certainty evidence of a small improvement in sexual function
- Low-certainty evidence of a small improvement in erectile function
- Low-certainty evidence showing little to no improvement in physical function
- Low-certainty evidence of a small increase to no difference in adverse cardiovascular events
- Moderate-certainty evidence of no increase in the risk for serious adverse events
The trials were not powered to assess mortality, but pool analysis showed fewer deaths among patients treated with testosterone than those who received placebo (odds ratio, 0.47; 95% confidence interval, 0.25-0.89). There were no differences in cognitive function, and the improvement in vitality and fatigue was “less than a small amount.” Evidence from an observational trial showed no increased risk for mortality, cardiovascular events, prostate cancer, or pulmonary embolus or deep vein thrombosis. Of note, most studies excluded men with recent cardiovascular disease.
This evidence review led to the following recommendations.2
Recommendation 1a
Clinicians should have a discussion regarding the potential risk and benefits of treatment with the patients who have documented age-related low testosterone (testosterone levels less than 10.4 nmol/L or 300 ng/dL) and are suffering from sexual dysfunction or have a desire to enhance their sexual function.
This recommendation was based on evidence showing small improvement in sexual function and erectile dysfunction.
Recommendation 1b
For patients who opt for treatment based on recommendation 1a, clinicians should reevaluate the benefit of treatment within 12 months. If a patient is not receiving any benefit in sexual function by 12 months, it is recommended that treatment be stopped at that time.
The ACP recommendation to stop treatment if a patient lacks improvement of sexual function within 12 months stems from low or insufficient evidence regarding potential harm of treatment. If the treatment is not helping the target symptom then the benefit no longer outweighs the potential harm.
Recommendation 1c
For patients who opt for treatment based on recommendation 1a, intramuscular replacement therapy rather than transdermal replacement therapy is recommended because of substantial differences in the cost.
It is important to note that both intramuscular and transdermal testosterone applications have been associated with improvements in sexual function, without any significant differences noted in benefit or harm for the patients. This recommendation is based on a per-person per-year average cost of the intramuscular formulation – $156.32, compared with the transdermal formulation – $2,135.32.
Recommendation 2
The ACP does not endorse the use of testosterone treatment for age-related low testosterone in patients desiring improvement in physical function, mood, energy, or cognitive function.
This clear recommendation is critical, as this might be the most common reason for prescriptions of testosterone – a misplaced belief that testosterone will help general quality of life. The evidence simply does not support this effect of testosterone replacement for age-related testosterone deficiency.
The bottom line
Testosterone levels in men decrease steadily with age, with a great deal of variability. Testosterone replacement therapy may be considered for men with age-related testosterone deficiency and sexual dysfunction. Testosterone replacement therapy is not recommended as a treatment for general fatigue, weakness or with an expectation that it will improve physical function, mood, energy, or cognitive function.
Dr. Hansen is a third-year resident in the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington Hospital–Jefferson Health.
References
1. Diem SJ et al. Efficacy and safety of testosterone treatment in men: An evidence report for a clinical practice guideline by the American College of Physicians. Ann Intern Med. 2020 Jan 21. doi: 10.7326/M19-0830.
2. Qaseem A et al. Testosterone treatment in adult men with age-related low testosterone: A clinical guideline from the American College of Physicians. Ann Intern Med. 2020 Jan 21. doi: 10.7326/M19-0882.
Patients say desiccated thyroid better than standard therapy
new research suggests.
Those were among the findings from qualitative analyses of nearly 700 online posts from three popular online hypothyroidism forums that found that 75% of patients felt they fared better on DTE than the standard therapy of levothyroxine (LT4).
The results were to be presented at the Endocrine Society’s annual meeting in late March, but the meeting was canceled because of the COVID-19 pandemic. They were subsequently published online April 3 in Medicina by Freddy J.K. Toloza, MD, of the University of Arkansas for Medical Sciences, Little Rock, and the Mayo Clinic, Rochester, Minnesota, and colleagues.
Made from desiccated pig thyroid glands, DTE is not approved by the Food and Drug Administration because it predates the agency, but it was grandfathered in and is sold legally by prescription under the names Nature Thyroid, Thyroid USP, and Armour Thyroid.
DTE is currently used by an estimated 10%-29% of patients with hypothyroidism, despite concerns about the risk for hyperthyroidism-associated side effects.
“Current [American Thyroid Association] guidelines strongly suggest the use of levothyroxine over DTE as thyroid replacement therapy. We agree with this recommendation given concerns about DTE’s side effects,” Dr. Toloza said in an interview.
“Nevertheless, additional research should be conducted to understand if this recommendation applies to all hypothyroid patients,” he added, and for those patients who are taking DTE, more research is required to determine who is at risk of side effects and methods to prevent these.
Dr. Toloza said that patients with hypothyroidism who take DTE frequently described a lack of individualized treatments and a feeling of not been listened to as issues that were influencing their choice.
“These findings reinforce the need for patient-centered approaches in current clinical practices. Clinicians need to carefully listen to their patients and consider their individual needs and the context of every patient,” he noted.
A select group of patients do better on combined T4/T3
Asked to comment, endocrinologist Rachel Pessah-Pollack, MD, of New York University Langone Health, said in an interview, “Animal-derived desiccated thyroid hormone contains both T4 and T3. We typically do not recommend using this because it can vary in concentration, meaning that the actual preparation is not physiologic.”
Dr. Pessah-Pollack, a coauthor of the 2012 joint clinical practice guidelines on hypothyroidism by the American Thyroid Association and American Association of Clinical Endocrinologists, added that one of the major concerns about using DTE is the risk for iatrogenic hyperthyroidism, which could potentially lead to atrial fibrillation and fractures.
“That is one of the main factors that drive many professional societies to really use caution regarding DTE. That’s also why major societies recommend against using DTE ... based on the evidence to date,” she said.
The whole issue of “combination therapy” in hypothyroidism is contentious, however. Physicians can also prescribe a “combination” of synthetic levothyroxine (LT4) and triiodothyronine (LT3) treatment; this, along with use of DTE products, has been a subject of debate for many years.
The current (2014) American Thyroid Association guidelines do not specifically rule out use of synthetic LT4/LT3 therapy, rather they “recommend only against the routine use of combination therapy.” And although they don’t expressly endorse use of DTE, they removed a statement saying it “should not be used.”
“There is definitely a select group of patients who do better on combined T4/T3 treatment, and we’re still trying to delineate who that population is,”Dr. Pessah-Pollack said.
“As long as these patients are closely monitored and aware of the risk of hyperthyroidism and have their levels followed to ensure that they’re not hyperthyroid, in select cases this is appropriate.”
“But, first-line is ensuring that a good evaluation occurs. ... Clearly this helps us understand that we do need more studies in this area – well-designed, blinded studies to really help us get to the bottom of this controversy.”
Those taking DTE cite improved symptoms, well-being
Dr. Toloza and colleagues analyzed 673 posts from three online forums, WebMD (Medscape’s parent company), PatientsLikeMe, and Drugs.com, selected from an initial 1,235 posts because they included more complete information.
About half (51%, n = 257) of patients had primary hypothyroidism/Hashimoto’s thyroiditis, 25% (n = 126) had postsurgical hypothyroidism, and 16% (n = 81) had postablation hypothyroidism. Among the 172 posts in which DTE dose information was available, the mean dose was 84.1 mg/day. Treatment duration ranged widely, from 2 weeks to 45 years.
Among the posts describing the source of the DTE prescription, the initial interest was driven mainly by the patient in 54% (n = 88), while 46% (n = 74) said that a clinician drove their interest in trying DTE. (The type of clinician was not reported.)
Among posts mentioning the source of DTE, local pharmacies were the most common (63%, n = 75), followed by pharmacies outside the United States (31%, n = 37), and online (6%, n = 7).
Previous thyroid treatments were mentioned in 300 posts, of which 93% mentioned LT4 monotherapy.
Among the reasons for changing to DTE were no improvement in clinical symptoms (47%, n = 75), development of side effects (24%, n = 38), no change in overall well-being (22%, n = 36), and no changes in laboratory work-up (7%, n = 12).
Perceived benefits of DTE included improvement in clinical symptoms (56%, n = 155), change in overall well-being (34%, n = 94), possibility of reaching previous health status (7%, n = 19), and low cost, compared with previous treatment (3%, n = 8).
Specific symptoms reported to have improved included fatigue (28%, n = 43), weight gain (17%, n = 26), and neurocognitive symptoms (5%, n = 8). The average time to notice benefits with DTE was about 30 days but ranged widely from 2 days to 4 months.
The majority of posts (77%, n = 99) stated that DTE was more effective than their previous therapy, while 13% (n = 17) described it as equally effective, and 10% (n = 13) said it was less effective.
Side effects of DTE were described by 20% (n = 136), including weight loss (15%), fatigue (11%), palpitations (11%), heat intolerance (11%), sleep disturbances (10%), high blood pressure (7%), and hair loss (5%).
“Doctors think they know how u feel”
A qualitative analysis of the posts yielded five major themes: experience with previous therapies before starting DTE, perceived effectiveness and benefits of DTE, DTE side effects, need for individualized therapy for hypothyroidism, and barriers to obtaining DTE.
One patient posted: “Synthroid [levothyroxine] did not help ... and gives me bad side effects. ... My endocrinologist blamed all side effects on everything except the Synthroid.”
Another wrote, “It [Armour] changed my life. ...I’m glad I found a medication that makes me feel normal again. ... All have improved; moods, skin (no itching), no headaches, goiter is down.”
Others cited the lower cost of Armour compared with Synthroid.
However, some expressed negative experiences with DTE, such as, “My doctor expected that this medication would help me with brain fog, energy, and tiredness. I experienced the opposite.”
And some couldn’t obtain it. One wrote, “Doctors think they know how u feel and do not even tell you about Armour. I asked my doctor and was told there was not enough studies on it to show its effectiveness.”
Better evaluation, more data needed
Dr. Pessah-Pollack pointed out that the study data don’t address whether patients’ initially prescribed levothyroxine doses were optimal, and noted that sometimes changes are needed, such as during pregnancy, following weight gain, or if the patient is taking other certain medications.
“It’s unclear from patient-reported symptoms whether or not they actually had an evaluation of their thyroid levels to ensure that their dose of thyroid hormone was correct before switching over to T4/T3 replacement. ... There are many factors that need to be taken into account before we decide that the medication itself isn’t working.”
What’s sorely needed, she said, are “well-designed, blinded studies that look at this controversy.”
“Here, we don’t know why patients are feeling better. ... We need to do additional work including validated symptom questionnaires and comparing thyroid levels of patients who are on Armour thyroid with those on levothyroxine monotherapy.”
Dr. Toloza agrees: “It is not possible to say that DTE is working better for the user due to the limitations and the nature of the data used in our study.”
“However, our findings are in-line with previously published research, which has shown that a subset of patients may prefer DTE to levothyroxine and have higher satisfaction with this treatment. Nevertheless, the reason behind this is still not well understood,” and it should be further investigated.
Dr. Toloza and colleagues reported that they had no conflicts of interests. Dr. Pessah-Pollack has reported being an adviser for Boehringer Ingelheim-Eli Lilly and Radius Health, and a moderator for Sanofi.
This article first appeared on Medscape.com.
new research suggests.
Those were among the findings from qualitative analyses of nearly 700 online posts from three popular online hypothyroidism forums that found that 75% of patients felt they fared better on DTE than the standard therapy of levothyroxine (LT4).
The results were to be presented at the Endocrine Society’s annual meeting in late March, but the meeting was canceled because of the COVID-19 pandemic. They were subsequently published online April 3 in Medicina by Freddy J.K. Toloza, MD, of the University of Arkansas for Medical Sciences, Little Rock, and the Mayo Clinic, Rochester, Minnesota, and colleagues.
Made from desiccated pig thyroid glands, DTE is not approved by the Food and Drug Administration because it predates the agency, but it was grandfathered in and is sold legally by prescription under the names Nature Thyroid, Thyroid USP, and Armour Thyroid.
DTE is currently used by an estimated 10%-29% of patients with hypothyroidism, despite concerns about the risk for hyperthyroidism-associated side effects.
“Current [American Thyroid Association] guidelines strongly suggest the use of levothyroxine over DTE as thyroid replacement therapy. We agree with this recommendation given concerns about DTE’s side effects,” Dr. Toloza said in an interview.
“Nevertheless, additional research should be conducted to understand if this recommendation applies to all hypothyroid patients,” he added, and for those patients who are taking DTE, more research is required to determine who is at risk of side effects and methods to prevent these.
Dr. Toloza said that patients with hypothyroidism who take DTE frequently described a lack of individualized treatments and a feeling of not been listened to as issues that were influencing their choice.
“These findings reinforce the need for patient-centered approaches in current clinical practices. Clinicians need to carefully listen to their patients and consider their individual needs and the context of every patient,” he noted.
A select group of patients do better on combined T4/T3
Asked to comment, endocrinologist Rachel Pessah-Pollack, MD, of New York University Langone Health, said in an interview, “Animal-derived desiccated thyroid hormone contains both T4 and T3. We typically do not recommend using this because it can vary in concentration, meaning that the actual preparation is not physiologic.”
Dr. Pessah-Pollack, a coauthor of the 2012 joint clinical practice guidelines on hypothyroidism by the American Thyroid Association and American Association of Clinical Endocrinologists, added that one of the major concerns about using DTE is the risk for iatrogenic hyperthyroidism, which could potentially lead to atrial fibrillation and fractures.
“That is one of the main factors that drive many professional societies to really use caution regarding DTE. That’s also why major societies recommend against using DTE ... based on the evidence to date,” she said.
The whole issue of “combination therapy” in hypothyroidism is contentious, however. Physicians can also prescribe a “combination” of synthetic levothyroxine (LT4) and triiodothyronine (LT3) treatment; this, along with use of DTE products, has been a subject of debate for many years.
The current (2014) American Thyroid Association guidelines do not specifically rule out use of synthetic LT4/LT3 therapy, rather they “recommend only against the routine use of combination therapy.” And although they don’t expressly endorse use of DTE, they removed a statement saying it “should not be used.”
“There is definitely a select group of patients who do better on combined T4/T3 treatment, and we’re still trying to delineate who that population is,”Dr. Pessah-Pollack said.
“As long as these patients are closely monitored and aware of the risk of hyperthyroidism and have their levels followed to ensure that they’re not hyperthyroid, in select cases this is appropriate.”
“But, first-line is ensuring that a good evaluation occurs. ... Clearly this helps us understand that we do need more studies in this area – well-designed, blinded studies to really help us get to the bottom of this controversy.”
Those taking DTE cite improved symptoms, well-being
Dr. Toloza and colleagues analyzed 673 posts from three online forums, WebMD (Medscape’s parent company), PatientsLikeMe, and Drugs.com, selected from an initial 1,235 posts because they included more complete information.
About half (51%, n = 257) of patients had primary hypothyroidism/Hashimoto’s thyroiditis, 25% (n = 126) had postsurgical hypothyroidism, and 16% (n = 81) had postablation hypothyroidism. Among the 172 posts in which DTE dose information was available, the mean dose was 84.1 mg/day. Treatment duration ranged widely, from 2 weeks to 45 years.
Among the posts describing the source of the DTE prescription, the initial interest was driven mainly by the patient in 54% (n = 88), while 46% (n = 74) said that a clinician drove their interest in trying DTE. (The type of clinician was not reported.)
Among posts mentioning the source of DTE, local pharmacies were the most common (63%, n = 75), followed by pharmacies outside the United States (31%, n = 37), and online (6%, n = 7).
Previous thyroid treatments were mentioned in 300 posts, of which 93% mentioned LT4 monotherapy.
Among the reasons for changing to DTE were no improvement in clinical symptoms (47%, n = 75), development of side effects (24%, n = 38), no change in overall well-being (22%, n = 36), and no changes in laboratory work-up (7%, n = 12).
Perceived benefits of DTE included improvement in clinical symptoms (56%, n = 155), change in overall well-being (34%, n = 94), possibility of reaching previous health status (7%, n = 19), and low cost, compared with previous treatment (3%, n = 8).
Specific symptoms reported to have improved included fatigue (28%, n = 43), weight gain (17%, n = 26), and neurocognitive symptoms (5%, n = 8). The average time to notice benefits with DTE was about 30 days but ranged widely from 2 days to 4 months.
The majority of posts (77%, n = 99) stated that DTE was more effective than their previous therapy, while 13% (n = 17) described it as equally effective, and 10% (n = 13) said it was less effective.
Side effects of DTE were described by 20% (n = 136), including weight loss (15%), fatigue (11%), palpitations (11%), heat intolerance (11%), sleep disturbances (10%), high blood pressure (7%), and hair loss (5%).
“Doctors think they know how u feel”
A qualitative analysis of the posts yielded five major themes: experience with previous therapies before starting DTE, perceived effectiveness and benefits of DTE, DTE side effects, need for individualized therapy for hypothyroidism, and barriers to obtaining DTE.
One patient posted: “Synthroid [levothyroxine] did not help ... and gives me bad side effects. ... My endocrinologist blamed all side effects on everything except the Synthroid.”
Another wrote, “It [Armour] changed my life. ...I’m glad I found a medication that makes me feel normal again. ... All have improved; moods, skin (no itching), no headaches, goiter is down.”
Others cited the lower cost of Armour compared with Synthroid.
However, some expressed negative experiences with DTE, such as, “My doctor expected that this medication would help me with brain fog, energy, and tiredness. I experienced the opposite.”
And some couldn’t obtain it. One wrote, “Doctors think they know how u feel and do not even tell you about Armour. I asked my doctor and was told there was not enough studies on it to show its effectiveness.”
Better evaluation, more data needed
Dr. Pessah-Pollack pointed out that the study data don’t address whether patients’ initially prescribed levothyroxine doses were optimal, and noted that sometimes changes are needed, such as during pregnancy, following weight gain, or if the patient is taking other certain medications.
“It’s unclear from patient-reported symptoms whether or not they actually had an evaluation of their thyroid levels to ensure that their dose of thyroid hormone was correct before switching over to T4/T3 replacement. ... There are many factors that need to be taken into account before we decide that the medication itself isn’t working.”
What’s sorely needed, she said, are “well-designed, blinded studies that look at this controversy.”
“Here, we don’t know why patients are feeling better. ... We need to do additional work including validated symptom questionnaires and comparing thyroid levels of patients who are on Armour thyroid with those on levothyroxine monotherapy.”
Dr. Toloza agrees: “It is not possible to say that DTE is working better for the user due to the limitations and the nature of the data used in our study.”
“However, our findings are in-line with previously published research, which has shown that a subset of patients may prefer DTE to levothyroxine and have higher satisfaction with this treatment. Nevertheless, the reason behind this is still not well understood,” and it should be further investigated.
Dr. Toloza and colleagues reported that they had no conflicts of interests. Dr. Pessah-Pollack has reported being an adviser for Boehringer Ingelheim-Eli Lilly and Radius Health, and a moderator for Sanofi.
This article first appeared on Medscape.com.
new research suggests.
Those were among the findings from qualitative analyses of nearly 700 online posts from three popular online hypothyroidism forums that found that 75% of patients felt they fared better on DTE than the standard therapy of levothyroxine (LT4).
The results were to be presented at the Endocrine Society’s annual meeting in late March, but the meeting was canceled because of the COVID-19 pandemic. They were subsequently published online April 3 in Medicina by Freddy J.K. Toloza, MD, of the University of Arkansas for Medical Sciences, Little Rock, and the Mayo Clinic, Rochester, Minnesota, and colleagues.
Made from desiccated pig thyroid glands, DTE is not approved by the Food and Drug Administration because it predates the agency, but it was grandfathered in and is sold legally by prescription under the names Nature Thyroid, Thyroid USP, and Armour Thyroid.
DTE is currently used by an estimated 10%-29% of patients with hypothyroidism, despite concerns about the risk for hyperthyroidism-associated side effects.
“Current [American Thyroid Association] guidelines strongly suggest the use of levothyroxine over DTE as thyroid replacement therapy. We agree with this recommendation given concerns about DTE’s side effects,” Dr. Toloza said in an interview.
“Nevertheless, additional research should be conducted to understand if this recommendation applies to all hypothyroid patients,” he added, and for those patients who are taking DTE, more research is required to determine who is at risk of side effects and methods to prevent these.
Dr. Toloza said that patients with hypothyroidism who take DTE frequently described a lack of individualized treatments and a feeling of not been listened to as issues that were influencing their choice.
“These findings reinforce the need for patient-centered approaches in current clinical practices. Clinicians need to carefully listen to their patients and consider their individual needs and the context of every patient,” he noted.
A select group of patients do better on combined T4/T3
Asked to comment, endocrinologist Rachel Pessah-Pollack, MD, of New York University Langone Health, said in an interview, “Animal-derived desiccated thyroid hormone contains both T4 and T3. We typically do not recommend using this because it can vary in concentration, meaning that the actual preparation is not physiologic.”
Dr. Pessah-Pollack, a coauthor of the 2012 joint clinical practice guidelines on hypothyroidism by the American Thyroid Association and American Association of Clinical Endocrinologists, added that one of the major concerns about using DTE is the risk for iatrogenic hyperthyroidism, which could potentially lead to atrial fibrillation and fractures.
“That is one of the main factors that drive many professional societies to really use caution regarding DTE. That’s also why major societies recommend against using DTE ... based on the evidence to date,” she said.
The whole issue of “combination therapy” in hypothyroidism is contentious, however. Physicians can also prescribe a “combination” of synthetic levothyroxine (LT4) and triiodothyronine (LT3) treatment; this, along with use of DTE products, has been a subject of debate for many years.
The current (2014) American Thyroid Association guidelines do not specifically rule out use of synthetic LT4/LT3 therapy, rather they “recommend only against the routine use of combination therapy.” And although they don’t expressly endorse use of DTE, they removed a statement saying it “should not be used.”
“There is definitely a select group of patients who do better on combined T4/T3 treatment, and we’re still trying to delineate who that population is,”Dr. Pessah-Pollack said.
“As long as these patients are closely monitored and aware of the risk of hyperthyroidism and have their levels followed to ensure that they’re not hyperthyroid, in select cases this is appropriate.”
“But, first-line is ensuring that a good evaluation occurs. ... Clearly this helps us understand that we do need more studies in this area – well-designed, blinded studies to really help us get to the bottom of this controversy.”
Those taking DTE cite improved symptoms, well-being
Dr. Toloza and colleagues analyzed 673 posts from three online forums, WebMD (Medscape’s parent company), PatientsLikeMe, and Drugs.com, selected from an initial 1,235 posts because they included more complete information.
About half (51%, n = 257) of patients had primary hypothyroidism/Hashimoto’s thyroiditis, 25% (n = 126) had postsurgical hypothyroidism, and 16% (n = 81) had postablation hypothyroidism. Among the 172 posts in which DTE dose information was available, the mean dose was 84.1 mg/day. Treatment duration ranged widely, from 2 weeks to 45 years.
Among the posts describing the source of the DTE prescription, the initial interest was driven mainly by the patient in 54% (n = 88), while 46% (n = 74) said that a clinician drove their interest in trying DTE. (The type of clinician was not reported.)
Among posts mentioning the source of DTE, local pharmacies were the most common (63%, n = 75), followed by pharmacies outside the United States (31%, n = 37), and online (6%, n = 7).
Previous thyroid treatments were mentioned in 300 posts, of which 93% mentioned LT4 monotherapy.
Among the reasons for changing to DTE were no improvement in clinical symptoms (47%, n = 75), development of side effects (24%, n = 38), no change in overall well-being (22%, n = 36), and no changes in laboratory work-up (7%, n = 12).
Perceived benefits of DTE included improvement in clinical symptoms (56%, n = 155), change in overall well-being (34%, n = 94), possibility of reaching previous health status (7%, n = 19), and low cost, compared with previous treatment (3%, n = 8).
Specific symptoms reported to have improved included fatigue (28%, n = 43), weight gain (17%, n = 26), and neurocognitive symptoms (5%, n = 8). The average time to notice benefits with DTE was about 30 days but ranged widely from 2 days to 4 months.
The majority of posts (77%, n = 99) stated that DTE was more effective than their previous therapy, while 13% (n = 17) described it as equally effective, and 10% (n = 13) said it was less effective.
Side effects of DTE were described by 20% (n = 136), including weight loss (15%), fatigue (11%), palpitations (11%), heat intolerance (11%), sleep disturbances (10%), high blood pressure (7%), and hair loss (5%).
“Doctors think they know how u feel”
A qualitative analysis of the posts yielded five major themes: experience with previous therapies before starting DTE, perceived effectiveness and benefits of DTE, DTE side effects, need for individualized therapy for hypothyroidism, and barriers to obtaining DTE.
One patient posted: “Synthroid [levothyroxine] did not help ... and gives me bad side effects. ... My endocrinologist blamed all side effects on everything except the Synthroid.”
Another wrote, “It [Armour] changed my life. ...I’m glad I found a medication that makes me feel normal again. ... All have improved; moods, skin (no itching), no headaches, goiter is down.”
Others cited the lower cost of Armour compared with Synthroid.
However, some expressed negative experiences with DTE, such as, “My doctor expected that this medication would help me with brain fog, energy, and tiredness. I experienced the opposite.”
And some couldn’t obtain it. One wrote, “Doctors think they know how u feel and do not even tell you about Armour. I asked my doctor and was told there was not enough studies on it to show its effectiveness.”
Better evaluation, more data needed
Dr. Pessah-Pollack pointed out that the study data don’t address whether patients’ initially prescribed levothyroxine doses were optimal, and noted that sometimes changes are needed, such as during pregnancy, following weight gain, or if the patient is taking other certain medications.
“It’s unclear from patient-reported symptoms whether or not they actually had an evaluation of their thyroid levels to ensure that their dose of thyroid hormone was correct before switching over to T4/T3 replacement. ... There are many factors that need to be taken into account before we decide that the medication itself isn’t working.”
What’s sorely needed, she said, are “well-designed, blinded studies that look at this controversy.”
“Here, we don’t know why patients are feeling better. ... We need to do additional work including validated symptom questionnaires and comparing thyroid levels of patients who are on Armour thyroid with those on levothyroxine monotherapy.”
Dr. Toloza agrees: “It is not possible to say that DTE is working better for the user due to the limitations and the nature of the data used in our study.”
“However, our findings are in-line with previously published research, which has shown that a subset of patients may prefer DTE to levothyroxine and have higher satisfaction with this treatment. Nevertheless, the reason behind this is still not well understood,” and it should be further investigated.
Dr. Toloza and colleagues reported that they had no conflicts of interests. Dr. Pessah-Pollack has reported being an adviser for Boehringer Ingelheim-Eli Lilly and Radius Health, and a moderator for Sanofi.
This article first appeared on Medscape.com.
Proximal fractures linked to higher mortality
Bone fracture in older adults is associated with greater mortality risk, but the location of the break may be a key factor, according to a new study of outcomes in a Danish database.
Over the follow-up period, those with proximal fractures – breaks in the hip, femur, pelvis, rib, clavicle, and humerus – were more likely to be hospitalized and to die, compared with their matched controls, than were those were with distal fractures in regions like the ankle, forearm, hand, or foot, where the mortality was similar to the matched controls.
“Compared with someone with similar comorbidities without a proximal fracture, there seemed to be an increased hospitalization rate for things like diabetes, heart disease, and lung disease, and then for some of those hospitalizations, there seemed to be an increased mortality, compared with people who hadn’t fractured who were hospitalized,” said Jacqueline Center, MBBS, PhD, of the Garvan Institute of Medical Research, Sydney, in an interview. The study abstract was released online by the Endocrine Society. It had been slated for presentation during ENDO 2020, the society's annual meeting, which was canceled because of the COVID-19 pandemic.*
The study included 212,498 women and 95,372 men aged over 50 years who had a fragility fracture between 2001 and 2014. The researchers excluded high-trauma fractures. They matched each fracture patient with four nonfracture patients, based on sex, age, and comorbidity status. There were 30,677 deaths among women over 384,995 person-years of follow-up, and 19,519 deaths in men over 163,482 person-years of follow-up. Women were a mean age of 72 at the time of fracture, while men were a mean age of 75.
The researchers found that proximal fractures were associated with increased risk of mortality, compared with nonfractured controls, with hazard ratios ranging between 1.5 and 4.0. Distal fractures were not associated with any increased mortality risk.
Comorbidities were common in the study population, with 75% of men and 60% of women having at least one. The risk of mortality increased with increasing numbers of comorbidities in each fracture type, but only proximal fractures were associated with an independent increase in mortality risk over and above comorbidity status.
In the 2 years following fracture, compared with matched controls, proximal fractures were associated with a greater risk of major hospital admission for conditions like cardiovascular disease, cancer, stroke, diabetes, pneumonia, and pulmonary disease. There was no significant difference between controls and those with distal fractures in hospital admission rate. The 2-year mortality risk was higher among subjects with proximal fractures, compared with patients in the no-fracture control group, regardless of whether they were admitted to the hospital, but there was no significant difference in those with distal fractures.
The differing clinical trajectories between those with proximal and distal fractures is a key finding, according to Dr. Center. The cause still isn’t clear, but she suspects that, in those patients who do badly, the fractures are either a signal that something is happening with existing comorbidities of the underlying frailty or that it may exacerbate them. Comorbidity independently and additively contributes to mortality, so that someone with a hip fracture and no comorbidities might have a similar mortality risk as someone with an upper-arm fracture and a couple of comorbidities. “I think it tells us that the person has to be treated as a whole. We need to treat the fracture to treat the underlying osteoporosis, but we also need to look closely at the person with the fracture and treat their comorbidities as well, because they seem to be more vulnerable,” Dr. Center said.
Although patients and clinicians are attuned to the concerns over hip fractures, other fractures should also be noted, according to Nelson Watts, MD, who is director of osteoporosis and bone-health services at Mercy Health in Cincinnati and was not involved in the research. “I think the message for clinicians and patients is that all of these [proximal] fractures need to be taken seriously. The good news is that that we have medications that can cut the risk of further fractures by 50%-70%,” he said in an interview.
Dr. Center has been on an advisory board for Amgen. Dr. Watts has been a speaker for Amgen and Radius and has conducted numerous clinical trials of osteoporosis drugs.
In addition to a series of news conferences, the Endocrine Society is also planning to host ENDO Online 2020 during June 8-22, which will feature on-demand and live programming for clinicians and researchers.
SOURCE: Center J et al. ENDO 2020, Abstract OR13-03.
Correction, 4/21/20: An earlier version of this article misstated when the interview with Dr. Center took place.
Bone fracture in older adults is associated with greater mortality risk, but the location of the break may be a key factor, according to a new study of outcomes in a Danish database.
Over the follow-up period, those with proximal fractures – breaks in the hip, femur, pelvis, rib, clavicle, and humerus – were more likely to be hospitalized and to die, compared with their matched controls, than were those were with distal fractures in regions like the ankle, forearm, hand, or foot, where the mortality was similar to the matched controls.
“Compared with someone with similar comorbidities without a proximal fracture, there seemed to be an increased hospitalization rate for things like diabetes, heart disease, and lung disease, and then for some of those hospitalizations, there seemed to be an increased mortality, compared with people who hadn’t fractured who were hospitalized,” said Jacqueline Center, MBBS, PhD, of the Garvan Institute of Medical Research, Sydney, in an interview. The study abstract was released online by the Endocrine Society. It had been slated for presentation during ENDO 2020, the society's annual meeting, which was canceled because of the COVID-19 pandemic.*
The study included 212,498 women and 95,372 men aged over 50 years who had a fragility fracture between 2001 and 2014. The researchers excluded high-trauma fractures. They matched each fracture patient with four nonfracture patients, based on sex, age, and comorbidity status. There were 30,677 deaths among women over 384,995 person-years of follow-up, and 19,519 deaths in men over 163,482 person-years of follow-up. Women were a mean age of 72 at the time of fracture, while men were a mean age of 75.
The researchers found that proximal fractures were associated with increased risk of mortality, compared with nonfractured controls, with hazard ratios ranging between 1.5 and 4.0. Distal fractures were not associated with any increased mortality risk.
Comorbidities were common in the study population, with 75% of men and 60% of women having at least one. The risk of mortality increased with increasing numbers of comorbidities in each fracture type, but only proximal fractures were associated with an independent increase in mortality risk over and above comorbidity status.
In the 2 years following fracture, compared with matched controls, proximal fractures were associated with a greater risk of major hospital admission for conditions like cardiovascular disease, cancer, stroke, diabetes, pneumonia, and pulmonary disease. There was no significant difference between controls and those with distal fractures in hospital admission rate. The 2-year mortality risk was higher among subjects with proximal fractures, compared with patients in the no-fracture control group, regardless of whether they were admitted to the hospital, but there was no significant difference in those with distal fractures.
The differing clinical trajectories between those with proximal and distal fractures is a key finding, according to Dr. Center. The cause still isn’t clear, but she suspects that, in those patients who do badly, the fractures are either a signal that something is happening with existing comorbidities of the underlying frailty or that it may exacerbate them. Comorbidity independently and additively contributes to mortality, so that someone with a hip fracture and no comorbidities might have a similar mortality risk as someone with an upper-arm fracture and a couple of comorbidities. “I think it tells us that the person has to be treated as a whole. We need to treat the fracture to treat the underlying osteoporosis, but we also need to look closely at the person with the fracture and treat their comorbidities as well, because they seem to be more vulnerable,” Dr. Center said.
Although patients and clinicians are attuned to the concerns over hip fractures, other fractures should also be noted, according to Nelson Watts, MD, who is director of osteoporosis and bone-health services at Mercy Health in Cincinnati and was not involved in the research. “I think the message for clinicians and patients is that all of these [proximal] fractures need to be taken seriously. The good news is that that we have medications that can cut the risk of further fractures by 50%-70%,” he said in an interview.
Dr. Center has been on an advisory board for Amgen. Dr. Watts has been a speaker for Amgen and Radius and has conducted numerous clinical trials of osteoporosis drugs.
In addition to a series of news conferences, the Endocrine Society is also planning to host ENDO Online 2020 during June 8-22, which will feature on-demand and live programming for clinicians and researchers.
SOURCE: Center J et al. ENDO 2020, Abstract OR13-03.
Correction, 4/21/20: An earlier version of this article misstated when the interview with Dr. Center took place.
Bone fracture in older adults is associated with greater mortality risk, but the location of the break may be a key factor, according to a new study of outcomes in a Danish database.
Over the follow-up period, those with proximal fractures – breaks in the hip, femur, pelvis, rib, clavicle, and humerus – were more likely to be hospitalized and to die, compared with their matched controls, than were those were with distal fractures in regions like the ankle, forearm, hand, or foot, where the mortality was similar to the matched controls.
“Compared with someone with similar comorbidities without a proximal fracture, there seemed to be an increased hospitalization rate for things like diabetes, heart disease, and lung disease, and then for some of those hospitalizations, there seemed to be an increased mortality, compared with people who hadn’t fractured who were hospitalized,” said Jacqueline Center, MBBS, PhD, of the Garvan Institute of Medical Research, Sydney, in an interview. The study abstract was released online by the Endocrine Society. It had been slated for presentation during ENDO 2020, the society's annual meeting, which was canceled because of the COVID-19 pandemic.*
The study included 212,498 women and 95,372 men aged over 50 years who had a fragility fracture between 2001 and 2014. The researchers excluded high-trauma fractures. They matched each fracture patient with four nonfracture patients, based on sex, age, and comorbidity status. There were 30,677 deaths among women over 384,995 person-years of follow-up, and 19,519 deaths in men over 163,482 person-years of follow-up. Women were a mean age of 72 at the time of fracture, while men were a mean age of 75.
The researchers found that proximal fractures were associated with increased risk of mortality, compared with nonfractured controls, with hazard ratios ranging between 1.5 and 4.0. Distal fractures were not associated with any increased mortality risk.
Comorbidities were common in the study population, with 75% of men and 60% of women having at least one. The risk of mortality increased with increasing numbers of comorbidities in each fracture type, but only proximal fractures were associated with an independent increase in mortality risk over and above comorbidity status.
In the 2 years following fracture, compared with matched controls, proximal fractures were associated with a greater risk of major hospital admission for conditions like cardiovascular disease, cancer, stroke, diabetes, pneumonia, and pulmonary disease. There was no significant difference between controls and those with distal fractures in hospital admission rate. The 2-year mortality risk was higher among subjects with proximal fractures, compared with patients in the no-fracture control group, regardless of whether they were admitted to the hospital, but there was no significant difference in those with distal fractures.
The differing clinical trajectories between those with proximal and distal fractures is a key finding, according to Dr. Center. The cause still isn’t clear, but she suspects that, in those patients who do badly, the fractures are either a signal that something is happening with existing comorbidities of the underlying frailty or that it may exacerbate them. Comorbidity independently and additively contributes to mortality, so that someone with a hip fracture and no comorbidities might have a similar mortality risk as someone with an upper-arm fracture and a couple of comorbidities. “I think it tells us that the person has to be treated as a whole. We need to treat the fracture to treat the underlying osteoporosis, but we also need to look closely at the person with the fracture and treat their comorbidities as well, because they seem to be more vulnerable,” Dr. Center said.
Although patients and clinicians are attuned to the concerns over hip fractures, other fractures should also be noted, according to Nelson Watts, MD, who is director of osteoporosis and bone-health services at Mercy Health in Cincinnati and was not involved in the research. “I think the message for clinicians and patients is that all of these [proximal] fractures need to be taken seriously. The good news is that that we have medications that can cut the risk of further fractures by 50%-70%,” he said in an interview.
Dr. Center has been on an advisory board for Amgen. Dr. Watts has been a speaker for Amgen and Radius and has conducted numerous clinical trials of osteoporosis drugs.
In addition to a series of news conferences, the Endocrine Society is also planning to host ENDO Online 2020 during June 8-22, which will feature on-demand and live programming for clinicians and researchers.
SOURCE: Center J et al. ENDO 2020, Abstract OR13-03.
Correction, 4/21/20: An earlier version of this article misstated when the interview with Dr. Center took place.
FROM ENDO 2020
Inflammatory markers may explain COVID-19, diabetes dynamic
COVID-19 infection in patients with type 2 diabetes is associated with a greater increase in inflammatory and coagulation markers, compared with COVID-19 patients without diabetes, according to preliminary findings from a retrospective analysis of COVID-19 patients in Wuhan, China.
The results, though preliminary, could help explain why patients with diabetes and COVID-19 are at greater risk for more severe disease and death.
The results also suggest that more severe disease in patients with diabetes may be the result of a cytokine storm, in which the patient’s immune system overreacts to the virus and inflicts collateral damage on its own organs, according to Herbert I. Rettinger, MD, a clinical endocrinologist in Orange County, Calif., and member of the editorial advisory board for Clinical Endocrinology News. “Understanding the mechanism might help us understand the best way to treat,” COVID-19 in patients with diabetes, he said in an interview.
Dr. Rettinger, who was not involved in the research, noted that the study included only 24 patients with diabetes. Nevertheless, the finding of heightened inflammatory and coagulation markers was “fascinating.”
“This is the first paper I’ve seen [suggesting] that. I don’t know if we can extrapolate [the findings] to other populations, but if biomarkers are elevated in patients with COVID-19 and diabetes, then it’s something worth looking into, and to be aware of and cautious of. We need to pay attention to this,” he commented.
The study was led by Weina Guo and Desheng Hu at Huazhong University of Science and Technology in Wuhan, China, and published in Diabetes/Metabolism Research and Reviews.
The sample included 174 patients with COVID-19, who were treated consecutively during Feb. 10-29, 2020, at a single center. The researchers first assigned the patients to one of two groups – those with comorbid diabetes and those without. They further excluded all other comorbidities, focusing only on 26 patients with no comorbidities and 24 with only diabetes as a comorbidity, to remove all other comorbidities as possible confounding factors. Patients in the diabetes group were significantly older than those without diabetes (61 vs. 41 years, P < .01). The mortality rate was 16.5% in patients with diabetes and 0% in those without (P = .03).
COVID-19 patients with diabetes alone as a comorbidity had a greater risk for severe pneumonia, as evidenced by a higher mean CT score, compared with those without diabetes and no other comorbidities (P = .04). Patients with diabetes also had higher measures of release of tissue injury–related enzymes and were at higher risk of uncontrolled inflammation and hypercoagulable state. In particular, they had higher levels of interleukin-6 (13.7 vs. 4.1 pg/mL, respectively; P < .01), C-reactive protein (76.4 vs. 7.43 mg/L; P < .01), serum ferritin (764.8 vs. 128.9 ng/mL; P < .01), and D-dimer (1.16 vs. 0.25 mcg/mL; P < .01).
“It’s noteworthy that, for diseases that can induce a cytokine storm, IL-6 is a very good predictor of disease severity and prognosis, and its expression time is longer than other cytokines ([tumor necrosis factor] and IL-1). In addition, a significant rise in serum ferritin indicates the activation of the monocyte-macrophage system, which is a crucial part of inflammatory storm. These results indicate that patients with diabetes are susceptible to form an inflammatory storm, which eventually lead to rapid deterioration of COVID-19,” the authors wrote.
They also cited previous findings suggesting that coronavirus might exacerbate, or even cause, diabetes by seriously damaging islets (Acta Diabetol. 2010;47[3]:193-9). “Since viral infection may cause sharp fluctuation of the blood glucose levels of diabetes patients, which adversely affect the recovery of patients, there is reason to suspect that diabetes combined with SARS-CoV-2 pneumonia may form a vicious circle,” they wrote.
That’s one more reason to carefully monitor diabetes patients, said Dr. Rettinger. “Those patients who are able to make insulin might not be able to do so with the infection, and that may last a while, and they may require insulin. You want to keep a watch on things, and if oral agents are not working well, you want to go to insulin as quickly as you can. Probably diabetics should be way more careful and maybe visit the emergency department at earlier than a nondiabetic would.”
Raghavendra Mirmira, MD, PhD, who conducts translational research on diabetes and insulin production, said that the finding was not a complete surprise to him. “With a lot of diseases, having diabetes as a comorbidity can mean worse outcomes, and that’s certainly true of influenza. It was true for the other COVID-like illnesses, such as SARS and MERS,” Dr. Mirmira, who was not involved in the research, said in an interview.
If the findings hold up in larger numbers of patients and across multiple centers, they have the potential to inform patient management, said Dr. Mirmira, director of the Translational Research Center in the department of medicine at the University of Chicago. That will be especially true as data from long-term follow-up of become available. Elevated values in some biomarkers might dictate a patient be sent straight to the ICU or dictate admission to the hospital rather than being sent home, or it could assist patient selection for some of the new therapies that physicians hope will become available.
“The more information we get [about] total outcome, the more informed we’d be about who would benefit from some of the therapies that are in clinical trials now,” he said. Still, it will be a challenge to prove causation, because patients with diabetes have unique clinical characteristics that could also be the source of the difference.
Dr. Mirmira noted that patients with diabetes only were 20 years older on average than those with no comorbidities. “It’s really hard to know if what you’re looking at for the worse outcomes for people with diabetes is because they were older, and we know that older people tend to do much worse with COVID than younger people.” Ideally, patients would also be matched by age, but there are not enough data to do that yet.
The study was funded by
SOURCE: Guo W et al. Diabetes Metab Res Rev. 2020 Mar 31. doi: 10.1002/dmrr.3319.
COVID-19 infection in patients with type 2 diabetes is associated with a greater increase in inflammatory and coagulation markers, compared with COVID-19 patients without diabetes, according to preliminary findings from a retrospective analysis of COVID-19 patients in Wuhan, China.
The results, though preliminary, could help explain why patients with diabetes and COVID-19 are at greater risk for more severe disease and death.
The results also suggest that more severe disease in patients with diabetes may be the result of a cytokine storm, in which the patient’s immune system overreacts to the virus and inflicts collateral damage on its own organs, according to Herbert I. Rettinger, MD, a clinical endocrinologist in Orange County, Calif., and member of the editorial advisory board for Clinical Endocrinology News. “Understanding the mechanism might help us understand the best way to treat,” COVID-19 in patients with diabetes, he said in an interview.
Dr. Rettinger, who was not involved in the research, noted that the study included only 24 patients with diabetes. Nevertheless, the finding of heightened inflammatory and coagulation markers was “fascinating.”
“This is the first paper I’ve seen [suggesting] that. I don’t know if we can extrapolate [the findings] to other populations, but if biomarkers are elevated in patients with COVID-19 and diabetes, then it’s something worth looking into, and to be aware of and cautious of. We need to pay attention to this,” he commented.
The study was led by Weina Guo and Desheng Hu at Huazhong University of Science and Technology in Wuhan, China, and published in Diabetes/Metabolism Research and Reviews.
The sample included 174 patients with COVID-19, who were treated consecutively during Feb. 10-29, 2020, at a single center. The researchers first assigned the patients to one of two groups – those with comorbid diabetes and those without. They further excluded all other comorbidities, focusing only on 26 patients with no comorbidities and 24 with only diabetes as a comorbidity, to remove all other comorbidities as possible confounding factors. Patients in the diabetes group were significantly older than those without diabetes (61 vs. 41 years, P < .01). The mortality rate was 16.5% in patients with diabetes and 0% in those without (P = .03).
COVID-19 patients with diabetes alone as a comorbidity had a greater risk for severe pneumonia, as evidenced by a higher mean CT score, compared with those without diabetes and no other comorbidities (P = .04). Patients with diabetes also had higher measures of release of tissue injury–related enzymes and were at higher risk of uncontrolled inflammation and hypercoagulable state. In particular, they had higher levels of interleukin-6 (13.7 vs. 4.1 pg/mL, respectively; P < .01), C-reactive protein (76.4 vs. 7.43 mg/L; P < .01), serum ferritin (764.8 vs. 128.9 ng/mL; P < .01), and D-dimer (1.16 vs. 0.25 mcg/mL; P < .01).
“It’s noteworthy that, for diseases that can induce a cytokine storm, IL-6 is a very good predictor of disease severity and prognosis, and its expression time is longer than other cytokines ([tumor necrosis factor] and IL-1). In addition, a significant rise in serum ferritin indicates the activation of the monocyte-macrophage system, which is a crucial part of inflammatory storm. These results indicate that patients with diabetes are susceptible to form an inflammatory storm, which eventually lead to rapid deterioration of COVID-19,” the authors wrote.
They also cited previous findings suggesting that coronavirus might exacerbate, or even cause, diabetes by seriously damaging islets (Acta Diabetol. 2010;47[3]:193-9). “Since viral infection may cause sharp fluctuation of the blood glucose levels of diabetes patients, which adversely affect the recovery of patients, there is reason to suspect that diabetes combined with SARS-CoV-2 pneumonia may form a vicious circle,” they wrote.
That’s one more reason to carefully monitor diabetes patients, said Dr. Rettinger. “Those patients who are able to make insulin might not be able to do so with the infection, and that may last a while, and they may require insulin. You want to keep a watch on things, and if oral agents are not working well, you want to go to insulin as quickly as you can. Probably diabetics should be way more careful and maybe visit the emergency department at earlier than a nondiabetic would.”
Raghavendra Mirmira, MD, PhD, who conducts translational research on diabetes and insulin production, said that the finding was not a complete surprise to him. “With a lot of diseases, having diabetes as a comorbidity can mean worse outcomes, and that’s certainly true of influenza. It was true for the other COVID-like illnesses, such as SARS and MERS,” Dr. Mirmira, who was not involved in the research, said in an interview.
If the findings hold up in larger numbers of patients and across multiple centers, they have the potential to inform patient management, said Dr. Mirmira, director of the Translational Research Center in the department of medicine at the University of Chicago. That will be especially true as data from long-term follow-up of become available. Elevated values in some biomarkers might dictate a patient be sent straight to the ICU or dictate admission to the hospital rather than being sent home, or it could assist patient selection for some of the new therapies that physicians hope will become available.
“The more information we get [about] total outcome, the more informed we’d be about who would benefit from some of the therapies that are in clinical trials now,” he said. Still, it will be a challenge to prove causation, because patients with diabetes have unique clinical characteristics that could also be the source of the difference.
Dr. Mirmira noted that patients with diabetes only were 20 years older on average than those with no comorbidities. “It’s really hard to know if what you’re looking at for the worse outcomes for people with diabetes is because they were older, and we know that older people tend to do much worse with COVID than younger people.” Ideally, patients would also be matched by age, but there are not enough data to do that yet.
The study was funded by
SOURCE: Guo W et al. Diabetes Metab Res Rev. 2020 Mar 31. doi: 10.1002/dmrr.3319.
COVID-19 infection in patients with type 2 diabetes is associated with a greater increase in inflammatory and coagulation markers, compared with COVID-19 patients without diabetes, according to preliminary findings from a retrospective analysis of COVID-19 patients in Wuhan, China.
The results, though preliminary, could help explain why patients with diabetes and COVID-19 are at greater risk for more severe disease and death.
The results also suggest that more severe disease in patients with diabetes may be the result of a cytokine storm, in which the patient’s immune system overreacts to the virus and inflicts collateral damage on its own organs, according to Herbert I. Rettinger, MD, a clinical endocrinologist in Orange County, Calif., and member of the editorial advisory board for Clinical Endocrinology News. “Understanding the mechanism might help us understand the best way to treat,” COVID-19 in patients with diabetes, he said in an interview.
Dr. Rettinger, who was not involved in the research, noted that the study included only 24 patients with diabetes. Nevertheless, the finding of heightened inflammatory and coagulation markers was “fascinating.”
“This is the first paper I’ve seen [suggesting] that. I don’t know if we can extrapolate [the findings] to other populations, but if biomarkers are elevated in patients with COVID-19 and diabetes, then it’s something worth looking into, and to be aware of and cautious of. We need to pay attention to this,” he commented.
The study was led by Weina Guo and Desheng Hu at Huazhong University of Science and Technology in Wuhan, China, and published in Diabetes/Metabolism Research and Reviews.
The sample included 174 patients with COVID-19, who were treated consecutively during Feb. 10-29, 2020, at a single center. The researchers first assigned the patients to one of two groups – those with comorbid diabetes and those without. They further excluded all other comorbidities, focusing only on 26 patients with no comorbidities and 24 with only diabetes as a comorbidity, to remove all other comorbidities as possible confounding factors. Patients in the diabetes group were significantly older than those without diabetes (61 vs. 41 years, P < .01). The mortality rate was 16.5% in patients with diabetes and 0% in those without (P = .03).
COVID-19 patients with diabetes alone as a comorbidity had a greater risk for severe pneumonia, as evidenced by a higher mean CT score, compared with those without diabetes and no other comorbidities (P = .04). Patients with diabetes also had higher measures of release of tissue injury–related enzymes and were at higher risk of uncontrolled inflammation and hypercoagulable state. In particular, they had higher levels of interleukin-6 (13.7 vs. 4.1 pg/mL, respectively; P < .01), C-reactive protein (76.4 vs. 7.43 mg/L; P < .01), serum ferritin (764.8 vs. 128.9 ng/mL; P < .01), and D-dimer (1.16 vs. 0.25 mcg/mL; P < .01).
“It’s noteworthy that, for diseases that can induce a cytokine storm, IL-6 is a very good predictor of disease severity and prognosis, and its expression time is longer than other cytokines ([tumor necrosis factor] and IL-1). In addition, a significant rise in serum ferritin indicates the activation of the monocyte-macrophage system, which is a crucial part of inflammatory storm. These results indicate that patients with diabetes are susceptible to form an inflammatory storm, which eventually lead to rapid deterioration of COVID-19,” the authors wrote.
They also cited previous findings suggesting that coronavirus might exacerbate, or even cause, diabetes by seriously damaging islets (Acta Diabetol. 2010;47[3]:193-9). “Since viral infection may cause sharp fluctuation of the blood glucose levels of diabetes patients, which adversely affect the recovery of patients, there is reason to suspect that diabetes combined with SARS-CoV-2 pneumonia may form a vicious circle,” they wrote.
That’s one more reason to carefully monitor diabetes patients, said Dr. Rettinger. “Those patients who are able to make insulin might not be able to do so with the infection, and that may last a while, and they may require insulin. You want to keep a watch on things, and if oral agents are not working well, you want to go to insulin as quickly as you can. Probably diabetics should be way more careful and maybe visit the emergency department at earlier than a nondiabetic would.”
Raghavendra Mirmira, MD, PhD, who conducts translational research on diabetes and insulin production, said that the finding was not a complete surprise to him. “With a lot of diseases, having diabetes as a comorbidity can mean worse outcomes, and that’s certainly true of influenza. It was true for the other COVID-like illnesses, such as SARS and MERS,” Dr. Mirmira, who was not involved in the research, said in an interview.
If the findings hold up in larger numbers of patients and across multiple centers, they have the potential to inform patient management, said Dr. Mirmira, director of the Translational Research Center in the department of medicine at the University of Chicago. That will be especially true as data from long-term follow-up of become available. Elevated values in some biomarkers might dictate a patient be sent straight to the ICU or dictate admission to the hospital rather than being sent home, or it could assist patient selection for some of the new therapies that physicians hope will become available.
“The more information we get [about] total outcome, the more informed we’d be about who would benefit from some of the therapies that are in clinical trials now,” he said. Still, it will be a challenge to prove causation, because patients with diabetes have unique clinical characteristics that could also be the source of the difference.
Dr. Mirmira noted that patients with diabetes only were 20 years older on average than those with no comorbidities. “It’s really hard to know if what you’re looking at for the worse outcomes for people with diabetes is because they were older, and we know that older people tend to do much worse with COVID than younger people.” Ideally, patients would also be matched by age, but there are not enough data to do that yet.
The study was funded by
SOURCE: Guo W et al. Diabetes Metab Res Rev. 2020 Mar 31. doi: 10.1002/dmrr.3319.
FROM DIABETES/METABOLISM RESEARCH AND REVIEWS
High and low trauma yield similar future osteoporotic fracture risk
Average measures of bone mineral density were similar for individuals with high-trauma and low-trauma fractures, and both were significantly distinct from those with no fracture history, based on data from a cohort study of adults aged 40 years and older.
In the past, low-trauma fractures have typically been associated with osteoporosis, wrote William D. Leslie, MD, of the University of Manitoba, Canada, and his colleagues. However, features distinguishing between low- and high-trauma fractures are often arbitrary and “empirical data have questioned whether distinguishing low-trauma from high-trauma fractures is clinically useful for purposes of risk assessment and treatment,” they wrote.
In a study published in Osteoporosis International, the researchers reviewed data from 64,626 individuals with no prior fracture, 858 with high-trauma fractures, and 14,758 with low-trauma fractures. Overall, the average BMD Z-scores for individuals with no previous fracture were slightly positive, while those with either a high-trauma or low-trauma fracture were negative. The scores for individuals with high-trauma fractures or major osteoporotic fractures were similar to those with low-trauma fractures, and significantly lower (P less than .001) than among individuals with no prior fractures.
The study population included adults aged 40 years and older with baseline DXA scans between Jan. 1, 1996, and Mar. 31, 2016. Those with high-trauma fractures were younger than those with low-trauma fractures (65 years vs. 67 years), and fewer individuals with high-trauma fractures were women (77% vs. 87%).
Both high-trauma and low-trauma fractures were similarly and significantly associated with increased risk for incident major osteoporotic fractures (adjusted hazard ratios 1.31 and 1.55, respectively).
The study findings were limited by several factors including incomplete data on external injury codes, the retrospective study design, and the lack of analysis of the time since prior fractures, the researchers noted. However, the results were strengthened by the large sample size, long-term follow-up, and large numbers of incident fractures, they wrote.
The results support data from previous studies and support “the inclusion of high-trauma clinical fractures in clinical assessment for underlying osteoporosis and in the evaluation for intervention to reduce future fracture risk,” they wrote.
In an accompanying editorial, Steven R. Cummings, MD, of California Pacific Medical Center Research Institute, San Francisco, and Richard Eastell, MD, of the University of Sheffield, England, wrote that the practice of rating fractures according to degree of trauma should be eliminated.
“The study adds evidence to the case that it is time to abandon the mistaken beliefs that fractures rated as high trauma are not associated with decreased BMD, indicate no higher risk of subsequent fracture, or are less likely to be prevented by treatments for osteoporosis,” they wrote.
Describing some fractures as due to trauma reinforces the mistaken belief that the fractures are simply due to the trauma, not decreased bone strength, they noted.
“Indeed, we recommend that people stop attempting to rate or record degree of trauma because such ratings are at best inaccurate and would promote the continued neglect of those patients who are misclassified as having fractures that do not warrant evaluation and treatment,” they concluded.
The study received no outside funding. Dr. Leslie, the study’s first author, reported having no financial conflicts to disclose.
Dr. Cummings disclosed consultancy and grant funding from Amgen and Radius. Dr. Eastell disclosed consultancy funding from IDS, Roche Diagnostics, GSK Nutrition, FNIH, Mereo, Lilly, Sandoz, Nittobo, Abbvie, Samsung, and Haoma Medica and grant funding from Nittobo, IDS, Roche, Amgen, and Alexion.
SOURCE: Leslie WD et al. Osteroporos Int. 2020 Mar 16. doi: 10.1007/s00198-019-05274-2.
Average measures of bone mineral density were similar for individuals with high-trauma and low-trauma fractures, and both were significantly distinct from those with no fracture history, based on data from a cohort study of adults aged 40 years and older.
In the past, low-trauma fractures have typically been associated with osteoporosis, wrote William D. Leslie, MD, of the University of Manitoba, Canada, and his colleagues. However, features distinguishing between low- and high-trauma fractures are often arbitrary and “empirical data have questioned whether distinguishing low-trauma from high-trauma fractures is clinically useful for purposes of risk assessment and treatment,” they wrote.
In a study published in Osteoporosis International, the researchers reviewed data from 64,626 individuals with no prior fracture, 858 with high-trauma fractures, and 14,758 with low-trauma fractures. Overall, the average BMD Z-scores for individuals with no previous fracture were slightly positive, while those with either a high-trauma or low-trauma fracture were negative. The scores for individuals with high-trauma fractures or major osteoporotic fractures were similar to those with low-trauma fractures, and significantly lower (P less than .001) than among individuals with no prior fractures.
The study population included adults aged 40 years and older with baseline DXA scans between Jan. 1, 1996, and Mar. 31, 2016. Those with high-trauma fractures were younger than those with low-trauma fractures (65 years vs. 67 years), and fewer individuals with high-trauma fractures were women (77% vs. 87%).
Both high-trauma and low-trauma fractures were similarly and significantly associated with increased risk for incident major osteoporotic fractures (adjusted hazard ratios 1.31 and 1.55, respectively).
The study findings were limited by several factors including incomplete data on external injury codes, the retrospective study design, and the lack of analysis of the time since prior fractures, the researchers noted. However, the results were strengthened by the large sample size, long-term follow-up, and large numbers of incident fractures, they wrote.
The results support data from previous studies and support “the inclusion of high-trauma clinical fractures in clinical assessment for underlying osteoporosis and in the evaluation for intervention to reduce future fracture risk,” they wrote.
In an accompanying editorial, Steven R. Cummings, MD, of California Pacific Medical Center Research Institute, San Francisco, and Richard Eastell, MD, of the University of Sheffield, England, wrote that the practice of rating fractures according to degree of trauma should be eliminated.
“The study adds evidence to the case that it is time to abandon the mistaken beliefs that fractures rated as high trauma are not associated with decreased BMD, indicate no higher risk of subsequent fracture, or are less likely to be prevented by treatments for osteoporosis,” they wrote.
Describing some fractures as due to trauma reinforces the mistaken belief that the fractures are simply due to the trauma, not decreased bone strength, they noted.
“Indeed, we recommend that people stop attempting to rate or record degree of trauma because such ratings are at best inaccurate and would promote the continued neglect of those patients who are misclassified as having fractures that do not warrant evaluation and treatment,” they concluded.
The study received no outside funding. Dr. Leslie, the study’s first author, reported having no financial conflicts to disclose.
Dr. Cummings disclosed consultancy and grant funding from Amgen and Radius. Dr. Eastell disclosed consultancy funding from IDS, Roche Diagnostics, GSK Nutrition, FNIH, Mereo, Lilly, Sandoz, Nittobo, Abbvie, Samsung, and Haoma Medica and grant funding from Nittobo, IDS, Roche, Amgen, and Alexion.
SOURCE: Leslie WD et al. Osteroporos Int. 2020 Mar 16. doi: 10.1007/s00198-019-05274-2.
Average measures of bone mineral density were similar for individuals with high-trauma and low-trauma fractures, and both were significantly distinct from those with no fracture history, based on data from a cohort study of adults aged 40 years and older.
In the past, low-trauma fractures have typically been associated with osteoporosis, wrote William D. Leslie, MD, of the University of Manitoba, Canada, and his colleagues. However, features distinguishing between low- and high-trauma fractures are often arbitrary and “empirical data have questioned whether distinguishing low-trauma from high-trauma fractures is clinically useful for purposes of risk assessment and treatment,” they wrote.
In a study published in Osteoporosis International, the researchers reviewed data from 64,626 individuals with no prior fracture, 858 with high-trauma fractures, and 14,758 with low-trauma fractures. Overall, the average BMD Z-scores for individuals with no previous fracture were slightly positive, while those with either a high-trauma or low-trauma fracture were negative. The scores for individuals with high-trauma fractures or major osteoporotic fractures were similar to those with low-trauma fractures, and significantly lower (P less than .001) than among individuals with no prior fractures.
The study population included adults aged 40 years and older with baseline DXA scans between Jan. 1, 1996, and Mar. 31, 2016. Those with high-trauma fractures were younger than those with low-trauma fractures (65 years vs. 67 years), and fewer individuals with high-trauma fractures were women (77% vs. 87%).
Both high-trauma and low-trauma fractures were similarly and significantly associated with increased risk for incident major osteoporotic fractures (adjusted hazard ratios 1.31 and 1.55, respectively).
The study findings were limited by several factors including incomplete data on external injury codes, the retrospective study design, and the lack of analysis of the time since prior fractures, the researchers noted. However, the results were strengthened by the large sample size, long-term follow-up, and large numbers of incident fractures, they wrote.
The results support data from previous studies and support “the inclusion of high-trauma clinical fractures in clinical assessment for underlying osteoporosis and in the evaluation for intervention to reduce future fracture risk,” they wrote.
In an accompanying editorial, Steven R. Cummings, MD, of California Pacific Medical Center Research Institute, San Francisco, and Richard Eastell, MD, of the University of Sheffield, England, wrote that the practice of rating fractures according to degree of trauma should be eliminated.
“The study adds evidence to the case that it is time to abandon the mistaken beliefs that fractures rated as high trauma are not associated with decreased BMD, indicate no higher risk of subsequent fracture, or are less likely to be prevented by treatments for osteoporosis,” they wrote.
Describing some fractures as due to trauma reinforces the mistaken belief that the fractures are simply due to the trauma, not decreased bone strength, they noted.
“Indeed, we recommend that people stop attempting to rate or record degree of trauma because such ratings are at best inaccurate and would promote the continued neglect of those patients who are misclassified as having fractures that do not warrant evaluation and treatment,” they concluded.
The study received no outside funding. Dr. Leslie, the study’s first author, reported having no financial conflicts to disclose.
Dr. Cummings disclosed consultancy and grant funding from Amgen and Radius. Dr. Eastell disclosed consultancy funding from IDS, Roche Diagnostics, GSK Nutrition, FNIH, Mereo, Lilly, Sandoz, Nittobo, Abbvie, Samsung, and Haoma Medica and grant funding from Nittobo, IDS, Roche, Amgen, and Alexion.
SOURCE: Leslie WD et al. Osteroporos Int. 2020 Mar 16. doi: 10.1007/s00198-019-05274-2.
FROM OSTEOPOROSIS INTERNATIONAL
20% with cancer on checkpoint inhibitors get thyroid dysfunction
new research suggests.
Immune checkpoint inhibitors have revolutionized the treatment of many different types of cancers, but can also trigger a variety of immune-related adverse effects. As these drugs become more widely used, rates of these events appear to be more common in the real-world compared with clinical trial settings.
In their new study, Zoe Quandt, MD, of the University of California, San Francisco (UCSF), and colleagues specifically looked at thyroid dysfunction in their own institution’s EHR data and found more than double the rate of hypothyroidism and more than triple the rate of hyperthyroidism, compared with rates in published trials.
Moreover, in contrast to previous studies that have found differences in thyroid dysfunction by checkpoint inhibitor type, Dr. Quandt and colleagues instead found significant differences by cancer type.
Dr. Quandt presented the findings during a virtual press briefing held March 31originally scheduled for ENDO 2020.
“Thyroid dysfunction following checkpoint inhibitor therapy appears to be much more common than was previously reported in clinical trials, and this is one of the first studies to show differences by cancer type rather than by checkpoint inhibitor type,” Dr. Quandt said during the presentation.
However, she also cautioned that there’s “a lot more research to be done to validate case definitions and validate these findings.”
Asked to comment, endocrinologist David C. Lieb, MD, associate professor of medicine at Eastern Virginia Medical School in Norfolk, said in an interview, “These drugs are becoming so much more commonly used, so it’s not surprising that we’re seeing more endocrine complications, especially thyroid disease.”
“Endocrinologists need to work closely with oncologists to make sure patients are being screened and followed appropriately.”
‘A much higher percentage than we were expecting’
Dr. Quandt’s study included 1,146 individuals treated with checkpoint inhibitors at UCSF during 2012-2018 who did not have thyroid cancer or preexisting thyroid dysfunction.
Pembrolizumab (Keytruda) was the most common treatment (45%), followed by nivolumab (Opdivo) (20%). Less than 10% of patients received atezolizumab (Tecentriq), durvalumab (Imfizi), ipilimumab (Yervoy) monotherapy, combined ipilimumab/nivolumab, or other combinations of checkpoint inhibitors.
A total of 19.1% developed thyroid disease, with 13.4% having hypothyroidism and 9.5% hyperthyroidism. These figures far exceed those found in a recent meta-analysis of 38 randomized clinical trials of checkpoint inhibitors that included 7551 patients.
“Using this approach, we found a much higher percentage of patients who developed thyroid dysfunction than we were expecting,” Dr. Quandt said.
In both cases, the two categories – hypothyroidism and hyperthyroidism – aren’t mutually exclusive as hypothyroidism can arise de novo or subsequent to hyperthyroidism.
Dr Lieb commented, “It would be interesting to see what the causes of hyperthyroidism are – thyroiditis or Graves disease.”
Dr. Quandt mentioned a possible reason for the large difference between clinical trial and real-world data.
“Once we’re actually using these drugs outside of clinical trials, some of the restrictions about using them in people with other autoimmune diseases have been lifted, so my guess is that as we give them to a broader population we’re seeing more of these [adverse effects],” she suggested.
Also, “In the initial trials, people weren’t quite as aware of the possibilities of these side effects, so now we’re doing many more labs. Patients get thyroid function tests with every infusion, so I think we’re probably catching more patients who develop disease.”
Differences by cancer type, not checkpoint inhibitor type
And in a new twist, Dr. Quandt found that, in contrast to the differences seen by checkpoint inhibitor type in randomized trials, “surprisingly, we found that this difference did not reach statistical significance.”
“Instead, we saw that cancer type was associated with development of thyroid dysfunction, even after taking checkpoint inhibitor type into account.”
The percentages of patients who developed thyroid dysfunction ranged from 9.7% of those with glioblastoma to 40.0% of those with renal cell carcinoma.
The reason for this is not clear, said Dr. Quandt in an interview.
One possibility relates to other treatments patients with cancer also receive. In renal cell carcinoma, for example, patients also are treated with tyrosine kinase inhibitors, which can also cause thyroid dysfunction, so they may be more susceptible. Or there may be shared antigens activating the immune system.
“That’s definitely one of the questions we’re looking at,” she said.
Dr. Quandt and Dr. Lieb have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests.
Immune checkpoint inhibitors have revolutionized the treatment of many different types of cancers, but can also trigger a variety of immune-related adverse effects. As these drugs become more widely used, rates of these events appear to be more common in the real-world compared with clinical trial settings.
In their new study, Zoe Quandt, MD, of the University of California, San Francisco (UCSF), and colleagues specifically looked at thyroid dysfunction in their own institution’s EHR data and found more than double the rate of hypothyroidism and more than triple the rate of hyperthyroidism, compared with rates in published trials.
Moreover, in contrast to previous studies that have found differences in thyroid dysfunction by checkpoint inhibitor type, Dr. Quandt and colleagues instead found significant differences by cancer type.
Dr. Quandt presented the findings during a virtual press briefing held March 31originally scheduled for ENDO 2020.
“Thyroid dysfunction following checkpoint inhibitor therapy appears to be much more common than was previously reported in clinical trials, and this is one of the first studies to show differences by cancer type rather than by checkpoint inhibitor type,” Dr. Quandt said during the presentation.
However, she also cautioned that there’s “a lot more research to be done to validate case definitions and validate these findings.”
Asked to comment, endocrinologist David C. Lieb, MD, associate professor of medicine at Eastern Virginia Medical School in Norfolk, said in an interview, “These drugs are becoming so much more commonly used, so it’s not surprising that we’re seeing more endocrine complications, especially thyroid disease.”
“Endocrinologists need to work closely with oncologists to make sure patients are being screened and followed appropriately.”
‘A much higher percentage than we were expecting’
Dr. Quandt’s study included 1,146 individuals treated with checkpoint inhibitors at UCSF during 2012-2018 who did not have thyroid cancer or preexisting thyroid dysfunction.
Pembrolizumab (Keytruda) was the most common treatment (45%), followed by nivolumab (Opdivo) (20%). Less than 10% of patients received atezolizumab (Tecentriq), durvalumab (Imfizi), ipilimumab (Yervoy) monotherapy, combined ipilimumab/nivolumab, or other combinations of checkpoint inhibitors.
A total of 19.1% developed thyroid disease, with 13.4% having hypothyroidism and 9.5% hyperthyroidism. These figures far exceed those found in a recent meta-analysis of 38 randomized clinical trials of checkpoint inhibitors that included 7551 patients.
“Using this approach, we found a much higher percentage of patients who developed thyroid dysfunction than we were expecting,” Dr. Quandt said.
In both cases, the two categories – hypothyroidism and hyperthyroidism – aren’t mutually exclusive as hypothyroidism can arise de novo or subsequent to hyperthyroidism.
Dr Lieb commented, “It would be interesting to see what the causes of hyperthyroidism are – thyroiditis or Graves disease.”
Dr. Quandt mentioned a possible reason for the large difference between clinical trial and real-world data.
“Once we’re actually using these drugs outside of clinical trials, some of the restrictions about using them in people with other autoimmune diseases have been lifted, so my guess is that as we give them to a broader population we’re seeing more of these [adverse effects],” she suggested.
Also, “In the initial trials, people weren’t quite as aware of the possibilities of these side effects, so now we’re doing many more labs. Patients get thyroid function tests with every infusion, so I think we’re probably catching more patients who develop disease.”
Differences by cancer type, not checkpoint inhibitor type
And in a new twist, Dr. Quandt found that, in contrast to the differences seen by checkpoint inhibitor type in randomized trials, “surprisingly, we found that this difference did not reach statistical significance.”
“Instead, we saw that cancer type was associated with development of thyroid dysfunction, even after taking checkpoint inhibitor type into account.”
The percentages of patients who developed thyroid dysfunction ranged from 9.7% of those with glioblastoma to 40.0% of those with renal cell carcinoma.
The reason for this is not clear, said Dr. Quandt in an interview.
One possibility relates to other treatments patients with cancer also receive. In renal cell carcinoma, for example, patients also are treated with tyrosine kinase inhibitors, which can also cause thyroid dysfunction, so they may be more susceptible. Or there may be shared antigens activating the immune system.
“That’s definitely one of the questions we’re looking at,” she said.
Dr. Quandt and Dr. Lieb have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests.
Immune checkpoint inhibitors have revolutionized the treatment of many different types of cancers, but can also trigger a variety of immune-related adverse effects. As these drugs become more widely used, rates of these events appear to be more common in the real-world compared with clinical trial settings.
In their new study, Zoe Quandt, MD, of the University of California, San Francisco (UCSF), and colleagues specifically looked at thyroid dysfunction in their own institution’s EHR data and found more than double the rate of hypothyroidism and more than triple the rate of hyperthyroidism, compared with rates in published trials.
Moreover, in contrast to previous studies that have found differences in thyroid dysfunction by checkpoint inhibitor type, Dr. Quandt and colleagues instead found significant differences by cancer type.
Dr. Quandt presented the findings during a virtual press briefing held March 31originally scheduled for ENDO 2020.
“Thyroid dysfunction following checkpoint inhibitor therapy appears to be much more common than was previously reported in clinical trials, and this is one of the first studies to show differences by cancer type rather than by checkpoint inhibitor type,” Dr. Quandt said during the presentation.
However, she also cautioned that there’s “a lot more research to be done to validate case definitions and validate these findings.”
Asked to comment, endocrinologist David C. Lieb, MD, associate professor of medicine at Eastern Virginia Medical School in Norfolk, said in an interview, “These drugs are becoming so much more commonly used, so it’s not surprising that we’re seeing more endocrine complications, especially thyroid disease.”
“Endocrinologists need to work closely with oncologists to make sure patients are being screened and followed appropriately.”
‘A much higher percentage than we were expecting’
Dr. Quandt’s study included 1,146 individuals treated with checkpoint inhibitors at UCSF during 2012-2018 who did not have thyroid cancer or preexisting thyroid dysfunction.
Pembrolizumab (Keytruda) was the most common treatment (45%), followed by nivolumab (Opdivo) (20%). Less than 10% of patients received atezolizumab (Tecentriq), durvalumab (Imfizi), ipilimumab (Yervoy) monotherapy, combined ipilimumab/nivolumab, or other combinations of checkpoint inhibitors.
A total of 19.1% developed thyroid disease, with 13.4% having hypothyroidism and 9.5% hyperthyroidism. These figures far exceed those found in a recent meta-analysis of 38 randomized clinical trials of checkpoint inhibitors that included 7551 patients.
“Using this approach, we found a much higher percentage of patients who developed thyroid dysfunction than we were expecting,” Dr. Quandt said.
In both cases, the two categories – hypothyroidism and hyperthyroidism – aren’t mutually exclusive as hypothyroidism can arise de novo or subsequent to hyperthyroidism.
Dr Lieb commented, “It would be interesting to see what the causes of hyperthyroidism are – thyroiditis or Graves disease.”
Dr. Quandt mentioned a possible reason for the large difference between clinical trial and real-world data.
“Once we’re actually using these drugs outside of clinical trials, some of the restrictions about using them in people with other autoimmune diseases have been lifted, so my guess is that as we give them to a broader population we’re seeing more of these [adverse effects],” she suggested.
Also, “In the initial trials, people weren’t quite as aware of the possibilities of these side effects, so now we’re doing many more labs. Patients get thyroid function tests with every infusion, so I think we’re probably catching more patients who develop disease.”
Differences by cancer type, not checkpoint inhibitor type
And in a new twist, Dr. Quandt found that, in contrast to the differences seen by checkpoint inhibitor type in randomized trials, “surprisingly, we found that this difference did not reach statistical significance.”
“Instead, we saw that cancer type was associated with development of thyroid dysfunction, even after taking checkpoint inhibitor type into account.”
The percentages of patients who developed thyroid dysfunction ranged from 9.7% of those with glioblastoma to 40.0% of those with renal cell carcinoma.
The reason for this is not clear, said Dr. Quandt in an interview.
One possibility relates to other treatments patients with cancer also receive. In renal cell carcinoma, for example, patients also are treated with tyrosine kinase inhibitors, which can also cause thyroid dysfunction, so they may be more susceptible. Or there may be shared antigens activating the immune system.
“That’s definitely one of the questions we’re looking at,” she said.
Dr. Quandt and Dr. Lieb have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Dapagliflozin trial in CKD halted because of high efficacy
AstraZeneca has announced that the phase 3 DAPA-CKD trial for dapagliflozin (Farxiga) in patients with chronic kidney disease has been halted early because of overwhelming efficacy of the drug, at the recommendation of an independent data monitoring committee.
DAPA-CKD is an international, multicenter, randomized, double-blinded trial in 4,245 patients with stage 2-4 chronic kidney disease. Patients received either 10 mg of the dapagliflozin once-daily or a placebo. The primary composite endpoint is worsening of renal function, defined as a composite of an estimated glomerular filtration rate decline of at least 50%, onset of end-stage kidney disease, and death from cardiovascular or renal cause.
The decision to stop the trial came after a routine assessment of efficacy and safety that showed dapagliflozin’s benefits significantly earlier than expected. AstraZeneca will initiate closure of the study, and results will be published and submitted for presentation at a forthcoming medical meeting.
Dapagliflozin is a sodium-glucose transporter 2 inhibitor currently indicated for the treatment type 2 diabetes patients with inadequately controlled type 2 diabetes and for reduction of the risk of hospitalization for heart failure. In August 2019, the drug was granted Fast Track status by the Food and Drug Administration for the treatment of chronic kidney disease. In January 2020, the agency also granted Fast Track status for the reduction of risk of cardiovascular death or worsening of heart failure in adult patients, regardless of diabetes status, with heart failure with reduced ejection fraction.
“Chronic kidney disease patients have limited treatment options, particularly those without type-2 diabetes. We are very pleased the data monitoring committee concluded that patients experienced overwhelming benefit. Farxiga has the potential to change the management of chronic kidney disease for patients around the world,” Mene Pangalos, executive vice president of BioPharmaceuticals R&D, said in the press release.
AstraZeneca has announced that the phase 3 DAPA-CKD trial for dapagliflozin (Farxiga) in patients with chronic kidney disease has been halted early because of overwhelming efficacy of the drug, at the recommendation of an independent data monitoring committee.
DAPA-CKD is an international, multicenter, randomized, double-blinded trial in 4,245 patients with stage 2-4 chronic kidney disease. Patients received either 10 mg of the dapagliflozin once-daily or a placebo. The primary composite endpoint is worsening of renal function, defined as a composite of an estimated glomerular filtration rate decline of at least 50%, onset of end-stage kidney disease, and death from cardiovascular or renal cause.
The decision to stop the trial came after a routine assessment of efficacy and safety that showed dapagliflozin’s benefits significantly earlier than expected. AstraZeneca will initiate closure of the study, and results will be published and submitted for presentation at a forthcoming medical meeting.
Dapagliflozin is a sodium-glucose transporter 2 inhibitor currently indicated for the treatment type 2 diabetes patients with inadequately controlled type 2 diabetes and for reduction of the risk of hospitalization for heart failure. In August 2019, the drug was granted Fast Track status by the Food and Drug Administration for the treatment of chronic kidney disease. In January 2020, the agency also granted Fast Track status for the reduction of risk of cardiovascular death or worsening of heart failure in adult patients, regardless of diabetes status, with heart failure with reduced ejection fraction.
“Chronic kidney disease patients have limited treatment options, particularly those without type-2 diabetes. We are very pleased the data monitoring committee concluded that patients experienced overwhelming benefit. Farxiga has the potential to change the management of chronic kidney disease for patients around the world,” Mene Pangalos, executive vice president of BioPharmaceuticals R&D, said in the press release.
AstraZeneca has announced that the phase 3 DAPA-CKD trial for dapagliflozin (Farxiga) in patients with chronic kidney disease has been halted early because of overwhelming efficacy of the drug, at the recommendation of an independent data monitoring committee.
DAPA-CKD is an international, multicenter, randomized, double-blinded trial in 4,245 patients with stage 2-4 chronic kidney disease. Patients received either 10 mg of the dapagliflozin once-daily or a placebo. The primary composite endpoint is worsening of renal function, defined as a composite of an estimated glomerular filtration rate decline of at least 50%, onset of end-stage kidney disease, and death from cardiovascular or renal cause.
The decision to stop the trial came after a routine assessment of efficacy and safety that showed dapagliflozin’s benefits significantly earlier than expected. AstraZeneca will initiate closure of the study, and results will be published and submitted for presentation at a forthcoming medical meeting.
Dapagliflozin is a sodium-glucose transporter 2 inhibitor currently indicated for the treatment type 2 diabetes patients with inadequately controlled type 2 diabetes and for reduction of the risk of hospitalization for heart failure. In August 2019, the drug was granted Fast Track status by the Food and Drug Administration for the treatment of chronic kidney disease. In January 2020, the agency also granted Fast Track status for the reduction of risk of cardiovascular death or worsening of heart failure in adult patients, regardless of diabetes status, with heart failure with reduced ejection fraction.
“Chronic kidney disease patients have limited treatment options, particularly those without type-2 diabetes. We are very pleased the data monitoring committee concluded that patients experienced overwhelming benefit. Farxiga has the potential to change the management of chronic kidney disease for patients around the world,” Mene Pangalos, executive vice president of BioPharmaceuticals R&D, said in the press release.