User login
Breast cancer history promotes vertebral fracture risk
Women with a history of stage III to stage IV breast cancer had significantly more pathologic vertebral fractures compared to those with stage I and stage II disease, based on data from approximately 5,000 adult women.
Breast cancer remains associated with increased fracture risk in part because of estrogen deficiency, aromatase inhibitors, frailty, and skeletal metastases, wrote Joan C. Lo, MD, of Kaiser Permanente Northern California, Oakland, and colleagues. Fractures associated with these factors have been studied, but many of the existing epidemiologic studies lack detail on fractures related to cancer, they noted. The researchers examined the association between pathologic fractures and major osteoporotic fractures in women with invasive breast cancer who received endocrine therapy.
In a study published in JAMA Network Open (2021 Nov 18. doi: 10.1001/jamanetworkopen.2021.33861), the researchers reviewed data from 5,010 women enrolled in the Pathways Study (3,312 women) or Research Program on Genes, Environment, and Health (RPGEH) study (1,698 women) with newly diagnosed invasive breast cancer who received endocrine therapy. The women were followed for up to 10 years for incident fracture, with a median follow-up period of 6.7 years.
The average age of the women was 60.2 years; 73.3% were non-Hispanic White, 4.9% were Black, 9.4% were Hispanic, and 1.6% were women whose ethnicity was unknown. Approximately 90% of the women were at stage I to stage II at initial diagnosis.
Overall, 340 (6.8%) had incident fractures during the follow-up period. The incident fractures included 46 hip, 104 vertebral, 78 humerus, and 137 wrist fractures. Significantly more women with hip fracture (43.5%) were age 80 years or older, compared with less than 25% of women with vertebral fractures (22.1%), humerus (19.2%), or wrist fracture (15.3%).
Pathologic fractures accounted for 22 of 104 incident vertebral fractures (21.2%) and fewer than 5 of 46 incident hip fractures (8.7%); few wrist and humerus fractures were pathologic. According to tumor stage, 15 of 87 (17.2%) vertebral fractures in women with initial stage I and II were pathologic, compared to 7 of 17 (41.2%) in women with initial stage III to stage IV breast cancer (P < .05).
The results emphasized the need to consider vertebral fracture risk in women with breast cancer, notably advanced stage cancer, as approximately one-third of the incident vertebral fractures in this subset of patients was deemed cancer-related, the researchers noted.
“As the axial skeleton is a common site for breast cancer metastasis and vertebrae a common site for pathologic fracture, primary care physicians should consider the possibility of pathologic fracture in women with higher risk based on advanced-stage cancer history,” the researchers wrote.
The study findings were limited by several factors, including the lack of data on fracture risk factors, treatment, and chemotherapy, and the inclusion only of clinically diagnosed fractures and not asymptomatic vertebral fractures, the researchers noted. However, the results were strengthened by the large sample size and comprehensive fracture assessment, they said. Additional studies to examine nonpathologic fracture risk according to breast cancer treatment, such as the use of aromatase inhibitors versus cytotoxic chemotherapy, may inform which women would benefit from more aggressive osteoporotic fracture prevention, they concluded.
Findings inform shared decision-making
“This study highlights the apparent association between an initial diagnosis of stage III or IV breast cancer and an increased risk for pathologic vertebral fracture,” said Constance Bohon, MD, a gynecologist in private practice in Washington, D.C., in an interview. “Most likely this finding is secondary to breast cancer metastases,” Dr. Bohon noted. However, she questioned whether there is a difference in fracture rates between women who received only aromatase inhibitors, those who received tamoxifen, and those who received both treatments.
“Additional data to determine the age of menopause, exercise frequency, current weight, and family history of osteoporosis may serve to identify those at highest risk for pathologic vertebral fracture,” said Dr. Bohon. “Until further data are available, clinicians should review this study and counsel their patients regarding options to potentially mitigate their apparent increased risk for pathologic vertebral fracture,” she emphasized.
The study was supported by the National Cancer Institute, National Institutes of Health, and the Research Program on Genes, Environment, and Health of Kaiser Permanente Northern California. The researchers had no financial conflicts to disclose. Dr. Bohon had no financial conflicts to disclose but serves on the Editorial Advisory Board of Ob.Gyn. News.
Women with a history of stage III to stage IV breast cancer had significantly more pathologic vertebral fractures compared to those with stage I and stage II disease, based on data from approximately 5,000 adult women.
Breast cancer remains associated with increased fracture risk in part because of estrogen deficiency, aromatase inhibitors, frailty, and skeletal metastases, wrote Joan C. Lo, MD, of Kaiser Permanente Northern California, Oakland, and colleagues. Fractures associated with these factors have been studied, but many of the existing epidemiologic studies lack detail on fractures related to cancer, they noted. The researchers examined the association between pathologic fractures and major osteoporotic fractures in women with invasive breast cancer who received endocrine therapy.
In a study published in JAMA Network Open (2021 Nov 18. doi: 10.1001/jamanetworkopen.2021.33861), the researchers reviewed data from 5,010 women enrolled in the Pathways Study (3,312 women) or Research Program on Genes, Environment, and Health (RPGEH) study (1,698 women) with newly diagnosed invasive breast cancer who received endocrine therapy. The women were followed for up to 10 years for incident fracture, with a median follow-up period of 6.7 years.
The average age of the women was 60.2 years; 73.3% were non-Hispanic White, 4.9% were Black, 9.4% were Hispanic, and 1.6% were women whose ethnicity was unknown. Approximately 90% of the women were at stage I to stage II at initial diagnosis.
Overall, 340 (6.8%) had incident fractures during the follow-up period. The incident fractures included 46 hip, 104 vertebral, 78 humerus, and 137 wrist fractures. Significantly more women with hip fracture (43.5%) were age 80 years or older, compared with less than 25% of women with vertebral fractures (22.1%), humerus (19.2%), or wrist fracture (15.3%).
Pathologic fractures accounted for 22 of 104 incident vertebral fractures (21.2%) and fewer than 5 of 46 incident hip fractures (8.7%); few wrist and humerus fractures were pathologic. According to tumor stage, 15 of 87 (17.2%) vertebral fractures in women with initial stage I and II were pathologic, compared to 7 of 17 (41.2%) in women with initial stage III to stage IV breast cancer (P < .05).
The results emphasized the need to consider vertebral fracture risk in women with breast cancer, notably advanced stage cancer, as approximately one-third of the incident vertebral fractures in this subset of patients was deemed cancer-related, the researchers noted.
“As the axial skeleton is a common site for breast cancer metastasis and vertebrae a common site for pathologic fracture, primary care physicians should consider the possibility of pathologic fracture in women with higher risk based on advanced-stage cancer history,” the researchers wrote.
The study findings were limited by several factors, including the lack of data on fracture risk factors, treatment, and chemotherapy, and the inclusion only of clinically diagnosed fractures and not asymptomatic vertebral fractures, the researchers noted. However, the results were strengthened by the large sample size and comprehensive fracture assessment, they said. Additional studies to examine nonpathologic fracture risk according to breast cancer treatment, such as the use of aromatase inhibitors versus cytotoxic chemotherapy, may inform which women would benefit from more aggressive osteoporotic fracture prevention, they concluded.
Findings inform shared decision-making
“This study highlights the apparent association between an initial diagnosis of stage III or IV breast cancer and an increased risk for pathologic vertebral fracture,” said Constance Bohon, MD, a gynecologist in private practice in Washington, D.C., in an interview. “Most likely this finding is secondary to breast cancer metastases,” Dr. Bohon noted. However, she questioned whether there is a difference in fracture rates between women who received only aromatase inhibitors, those who received tamoxifen, and those who received both treatments.
“Additional data to determine the age of menopause, exercise frequency, current weight, and family history of osteoporosis may serve to identify those at highest risk for pathologic vertebral fracture,” said Dr. Bohon. “Until further data are available, clinicians should review this study and counsel their patients regarding options to potentially mitigate their apparent increased risk for pathologic vertebral fracture,” she emphasized.
The study was supported by the National Cancer Institute, National Institutes of Health, and the Research Program on Genes, Environment, and Health of Kaiser Permanente Northern California. The researchers had no financial conflicts to disclose. Dr. Bohon had no financial conflicts to disclose but serves on the Editorial Advisory Board of Ob.Gyn. News.
Women with a history of stage III to stage IV breast cancer had significantly more pathologic vertebral fractures compared to those with stage I and stage II disease, based on data from approximately 5,000 adult women.
Breast cancer remains associated with increased fracture risk in part because of estrogen deficiency, aromatase inhibitors, frailty, and skeletal metastases, wrote Joan C. Lo, MD, of Kaiser Permanente Northern California, Oakland, and colleagues. Fractures associated with these factors have been studied, but many of the existing epidemiologic studies lack detail on fractures related to cancer, they noted. The researchers examined the association between pathologic fractures and major osteoporotic fractures in women with invasive breast cancer who received endocrine therapy.
In a study published in JAMA Network Open (2021 Nov 18. doi: 10.1001/jamanetworkopen.2021.33861), the researchers reviewed data from 5,010 women enrolled in the Pathways Study (3,312 women) or Research Program on Genes, Environment, and Health (RPGEH) study (1,698 women) with newly diagnosed invasive breast cancer who received endocrine therapy. The women were followed for up to 10 years for incident fracture, with a median follow-up period of 6.7 years.
The average age of the women was 60.2 years; 73.3% were non-Hispanic White, 4.9% were Black, 9.4% were Hispanic, and 1.6% were women whose ethnicity was unknown. Approximately 90% of the women were at stage I to stage II at initial diagnosis.
Overall, 340 (6.8%) had incident fractures during the follow-up period. The incident fractures included 46 hip, 104 vertebral, 78 humerus, and 137 wrist fractures. Significantly more women with hip fracture (43.5%) were age 80 years or older, compared with less than 25% of women with vertebral fractures (22.1%), humerus (19.2%), or wrist fracture (15.3%).
Pathologic fractures accounted for 22 of 104 incident vertebral fractures (21.2%) and fewer than 5 of 46 incident hip fractures (8.7%); few wrist and humerus fractures were pathologic. According to tumor stage, 15 of 87 (17.2%) vertebral fractures in women with initial stage I and II were pathologic, compared to 7 of 17 (41.2%) in women with initial stage III to stage IV breast cancer (P < .05).
The results emphasized the need to consider vertebral fracture risk in women with breast cancer, notably advanced stage cancer, as approximately one-third of the incident vertebral fractures in this subset of patients was deemed cancer-related, the researchers noted.
“As the axial skeleton is a common site for breast cancer metastasis and vertebrae a common site for pathologic fracture, primary care physicians should consider the possibility of pathologic fracture in women with higher risk based on advanced-stage cancer history,” the researchers wrote.
The study findings were limited by several factors, including the lack of data on fracture risk factors, treatment, and chemotherapy, and the inclusion only of clinically diagnosed fractures and not asymptomatic vertebral fractures, the researchers noted. However, the results were strengthened by the large sample size and comprehensive fracture assessment, they said. Additional studies to examine nonpathologic fracture risk according to breast cancer treatment, such as the use of aromatase inhibitors versus cytotoxic chemotherapy, may inform which women would benefit from more aggressive osteoporotic fracture prevention, they concluded.
Findings inform shared decision-making
“This study highlights the apparent association between an initial diagnosis of stage III or IV breast cancer and an increased risk for pathologic vertebral fracture,” said Constance Bohon, MD, a gynecologist in private practice in Washington, D.C., in an interview. “Most likely this finding is secondary to breast cancer metastases,” Dr. Bohon noted. However, she questioned whether there is a difference in fracture rates between women who received only aromatase inhibitors, those who received tamoxifen, and those who received both treatments.
“Additional data to determine the age of menopause, exercise frequency, current weight, and family history of osteoporosis may serve to identify those at highest risk for pathologic vertebral fracture,” said Dr. Bohon. “Until further data are available, clinicians should review this study and counsel their patients regarding options to potentially mitigate their apparent increased risk for pathologic vertebral fracture,” she emphasized.
The study was supported by the National Cancer Institute, National Institutes of Health, and the Research Program on Genes, Environment, and Health of Kaiser Permanente Northern California. The researchers had no financial conflicts to disclose. Dr. Bohon had no financial conflicts to disclose but serves on the Editorial Advisory Board of Ob.Gyn. News.
FROM JAMA NETWORK OPEN
Substantial declines in mortality for most cancers
according to a new analysis.
Researchers found that rates for all cancers combined declined by 27% overall between 1971 and 2019 and decreased significantly for 12 of the 15 top cancer sites analyzed.
The data revealed even greater mortality declines for certain cancers in particular years. For example, mortality from lung cancer was 44% lower in 2019, compared with its peak rate in 1993, whereas it was only 13% lower, compared with morality rates in 1971.
“The cancer mortality rate has reduced considerably since 1971 overall and for most cancer sites because of improvements in prevention, early detection, and treatment,” lead author Ahmedin Jemal, DVM, PhD, American Cancer Society, Kennesaw, Ga., and colleagues wrote.
Advances in surgery, radiotherapy, chemotherapy, precision medicine, and combinations therapies over the past 5 decades have contributed to these significant declines in mortality, Dr. Jemal and colleagues explained. The researchers also credit the “expanded investment” in the National Cancer Institute’s annual budget following the 1971 National Cancer Act, which increased the budget 25-fold from $227 million in 1971 to $6 billion in 2019.
The report, published online Nov. 11, 2021, in JAMA Oncology, analyzed mortality rates for all cancers as well as the top 15 sites using the National Center for Health Statistics.
The researchers found that, overall, deaths declined significantly for all cancers over the study period. Some of the biggest headway since 1971 occurred for stomach and cervical cancers – with 72% and 69% lower mortality rates, respectively – as well as colorectal cancer (56%), oral cavity and pharynx cancer (43%), and ovarian cancer (41%). Mortality rates of female breast cancer and prostate cancer also dropped considerably – both by 39%.
“The decline in mortality for female breast, cervical, colorectal, and prostate cancer in part reflects increased detection (and removal) of premalignant lesions and early-stage cancers,” Dr. Jemal and colleagues noted.
Data suggest that screening likely explains about half of the observed decline in mortality from colorectal cancer between 1975 and 2002. A 2018 study also found that the use of adjuvant chemotherapy was responsible for 63% of the decline in mortality from female breast cancer between 2000 and 2012.
In addition, the authors noted, “the decline in lung, oral cavity and bladder cancers largely reflects reductions in smoking because of enhanced public awareness of the health consequences, implementation of increased cigarette excise taxes, and comprehensive smoke-free laws.”
However, mortality did increase in a few categories. For instance, the mortality rate from pancreatic cancer increased by 3% between 1971 and 2019, and by 8% for both esophageal and brain cancers. Mortality rates from cancer were also greater for 29% of the U.S. counties included in the analysis, mostly those in the South.
The increase in mortality from pancreatic cancer likely reflects the growing rates of obesity in the United States, along with no real advances in pancreatic cancer prevention, early detection, or treatment, the authors suggested. In addition, lack of progress in regions of the south may be related to unequal access to improvements in treatment compared with other parts of the country.
“Improving equity through investment in the social determinants of health and implementation research is critical to furthering the national cancer-control agenda,” the authors concluded.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new analysis.
Researchers found that rates for all cancers combined declined by 27% overall between 1971 and 2019 and decreased significantly for 12 of the 15 top cancer sites analyzed.
The data revealed even greater mortality declines for certain cancers in particular years. For example, mortality from lung cancer was 44% lower in 2019, compared with its peak rate in 1993, whereas it was only 13% lower, compared with morality rates in 1971.
“The cancer mortality rate has reduced considerably since 1971 overall and for most cancer sites because of improvements in prevention, early detection, and treatment,” lead author Ahmedin Jemal, DVM, PhD, American Cancer Society, Kennesaw, Ga., and colleagues wrote.
Advances in surgery, radiotherapy, chemotherapy, precision medicine, and combinations therapies over the past 5 decades have contributed to these significant declines in mortality, Dr. Jemal and colleagues explained. The researchers also credit the “expanded investment” in the National Cancer Institute’s annual budget following the 1971 National Cancer Act, which increased the budget 25-fold from $227 million in 1971 to $6 billion in 2019.
The report, published online Nov. 11, 2021, in JAMA Oncology, analyzed mortality rates for all cancers as well as the top 15 sites using the National Center for Health Statistics.
The researchers found that, overall, deaths declined significantly for all cancers over the study period. Some of the biggest headway since 1971 occurred for stomach and cervical cancers – with 72% and 69% lower mortality rates, respectively – as well as colorectal cancer (56%), oral cavity and pharynx cancer (43%), and ovarian cancer (41%). Mortality rates of female breast cancer and prostate cancer also dropped considerably – both by 39%.
“The decline in mortality for female breast, cervical, colorectal, and prostate cancer in part reflects increased detection (and removal) of premalignant lesions and early-stage cancers,” Dr. Jemal and colleagues noted.
Data suggest that screening likely explains about half of the observed decline in mortality from colorectal cancer between 1975 and 2002. A 2018 study also found that the use of adjuvant chemotherapy was responsible for 63% of the decline in mortality from female breast cancer between 2000 and 2012.
In addition, the authors noted, “the decline in lung, oral cavity and bladder cancers largely reflects reductions in smoking because of enhanced public awareness of the health consequences, implementation of increased cigarette excise taxes, and comprehensive smoke-free laws.”
However, mortality did increase in a few categories. For instance, the mortality rate from pancreatic cancer increased by 3% between 1971 and 2019, and by 8% for both esophageal and brain cancers. Mortality rates from cancer were also greater for 29% of the U.S. counties included in the analysis, mostly those in the South.
The increase in mortality from pancreatic cancer likely reflects the growing rates of obesity in the United States, along with no real advances in pancreatic cancer prevention, early detection, or treatment, the authors suggested. In addition, lack of progress in regions of the south may be related to unequal access to improvements in treatment compared with other parts of the country.
“Improving equity through investment in the social determinants of health and implementation research is critical to furthering the national cancer-control agenda,” the authors concluded.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new analysis.
Researchers found that rates for all cancers combined declined by 27% overall between 1971 and 2019 and decreased significantly for 12 of the 15 top cancer sites analyzed.
The data revealed even greater mortality declines for certain cancers in particular years. For example, mortality from lung cancer was 44% lower in 2019, compared with its peak rate in 1993, whereas it was only 13% lower, compared with morality rates in 1971.
“The cancer mortality rate has reduced considerably since 1971 overall and for most cancer sites because of improvements in prevention, early detection, and treatment,” lead author Ahmedin Jemal, DVM, PhD, American Cancer Society, Kennesaw, Ga., and colleagues wrote.
Advances in surgery, radiotherapy, chemotherapy, precision medicine, and combinations therapies over the past 5 decades have contributed to these significant declines in mortality, Dr. Jemal and colleagues explained. The researchers also credit the “expanded investment” in the National Cancer Institute’s annual budget following the 1971 National Cancer Act, which increased the budget 25-fold from $227 million in 1971 to $6 billion in 2019.
The report, published online Nov. 11, 2021, in JAMA Oncology, analyzed mortality rates for all cancers as well as the top 15 sites using the National Center for Health Statistics.
The researchers found that, overall, deaths declined significantly for all cancers over the study period. Some of the biggest headway since 1971 occurred for stomach and cervical cancers – with 72% and 69% lower mortality rates, respectively – as well as colorectal cancer (56%), oral cavity and pharynx cancer (43%), and ovarian cancer (41%). Mortality rates of female breast cancer and prostate cancer also dropped considerably – both by 39%.
“The decline in mortality for female breast, cervical, colorectal, and prostate cancer in part reflects increased detection (and removal) of premalignant lesions and early-stage cancers,” Dr. Jemal and colleagues noted.
Data suggest that screening likely explains about half of the observed decline in mortality from colorectal cancer between 1975 and 2002. A 2018 study also found that the use of adjuvant chemotherapy was responsible for 63% of the decline in mortality from female breast cancer between 2000 and 2012.
In addition, the authors noted, “the decline in lung, oral cavity and bladder cancers largely reflects reductions in smoking because of enhanced public awareness of the health consequences, implementation of increased cigarette excise taxes, and comprehensive smoke-free laws.”
However, mortality did increase in a few categories. For instance, the mortality rate from pancreatic cancer increased by 3% between 1971 and 2019, and by 8% for both esophageal and brain cancers. Mortality rates from cancer were also greater for 29% of the U.S. counties included in the analysis, mostly those in the South.
The increase in mortality from pancreatic cancer likely reflects the growing rates of obesity in the United States, along with no real advances in pancreatic cancer prevention, early detection, or treatment, the authors suggested. In addition, lack of progress in regions of the south may be related to unequal access to improvements in treatment compared with other parts of the country.
“Improving equity through investment in the social determinants of health and implementation research is critical to furthering the national cancer-control agenda,” the authors concluded.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA ONCOLOGY
Severe COVID two times higher for cancer patients
A new systematic review and meta-analysis finds that unvaccinated cancer patients who contracted COVID-19 last year, were more than two times more likely – than people without cancer – to develop a case of COVID-19 so severe it required hospitalization in an intensive care unit.
“Our study provides the most precise measure to date of the effect of COVID-19 in cancer patients,” wrote researchers who were led by Paolo Boffetta, MD, MPH, a specialist in population science with the Stony Brook Cancer Center in New York.
Dr. Boffetta and colleagues also found that patients with hematologic neoplasms had a higher mortality rate from COVID-19 comparable to that of all cancers combined.
Cancer patients have long been considered to be among those patients who are at high risk of developing COVID-19, and if they contract the disease, they are at high risk of having poor outcomes. Other high-risk patients include those with hypertension, diabetes, chronic kidney disease, or COPD, or the elderly. But how high the risk of developing severe COVID-19 disease is for cancer patients hasn’t yet been documented on a wide scale.
The study, which was made available as a preprint on medRxiv on Oct. 23, is based on an analysis of COVID-19 cases that were documented in 35 reviews, meta-analyses, case reports, and studies indexed in PubMed from authors in North America, Europe, and Asia.
In this study, the pooled odds ratio for mortality for all patients with any cancer was 2.32 (95% confidence interval, 1.82-2.94; 24 studies). For ICU admission, the odds ratio was 2.39 (95% CI, 1.90-3.02; I2 0.0%; 5 studies). And, for disease severity or hospitalization, it was 2.08 (95% CI, 1.60-2.72; I2 92.1%; 15 studies). The pooled mortality odds ratio for hematologic neoplasms was 2.14 (95% CI, 1.87-2.44; I2 20.8%; 8 studies).
Their findings, which have not yet been peer reviewed, confirmed the results of a similar analysis from China published as a preprint in May 2020. The analysis included 181,323 patients (23,736 cancer patients) from 26 studies reported an odds ratio of 2.54 (95% CI, 1.47-4.42). “Cancer patients with COVID-19 have an increased likelihood of death compared to non-cancer COVID-19 patients,” Venkatesulu et al. wrote. And a systematic review and meta-analysis of five studies of 2,619 patients published in October 2020 in Medicine also found a significantly higher risk of death from COVID-19 among cancer patients (odds ratio, 2.63; 95% confidence interval, 1.14-6.06; P = .023; I2 = 26.4%).
Fakih et al., writing in the journal Hematology/Oncology and Stem Cell Therapy conducted a meta-analysis early last year finding a threefold increase for admission to the intensive care unit, an almost fourfold increase for a severe SARS-CoV-2 infection, and a fivefold increase for being intubated.
The three studies show that mortality rates were higher early in the pandemic “when diagnosis and treatment for SARS-CoV-2 might have been delayed, resulting in higher death rate,” Boffetta et al. wrote, adding that their analysis showed only a twofold increase most likely because it was a year-long analysis.
“Future studies will be able to better analyze this association for the different subtypes of cancer. Furthermore, they will eventually be able to evaluate whether the difference among vaccinated population is reduced,” Boffetta et al. wrote.
The authors noted several limitations for the study, including the fact that many of the studies included in the analysis did not include sex, age, comorbidities, and therapy. Nor were the authors able to analyze specific cancers other than hematologic neoplasms.
The authors declared no conflicts of interest.
A new systematic review and meta-analysis finds that unvaccinated cancer patients who contracted COVID-19 last year, were more than two times more likely – than people without cancer – to develop a case of COVID-19 so severe it required hospitalization in an intensive care unit.
“Our study provides the most precise measure to date of the effect of COVID-19 in cancer patients,” wrote researchers who were led by Paolo Boffetta, MD, MPH, a specialist in population science with the Stony Brook Cancer Center in New York.
Dr. Boffetta and colleagues also found that patients with hematologic neoplasms had a higher mortality rate from COVID-19 comparable to that of all cancers combined.
Cancer patients have long been considered to be among those patients who are at high risk of developing COVID-19, and if they contract the disease, they are at high risk of having poor outcomes. Other high-risk patients include those with hypertension, diabetes, chronic kidney disease, or COPD, or the elderly. But how high the risk of developing severe COVID-19 disease is for cancer patients hasn’t yet been documented on a wide scale.
The study, which was made available as a preprint on medRxiv on Oct. 23, is based on an analysis of COVID-19 cases that were documented in 35 reviews, meta-analyses, case reports, and studies indexed in PubMed from authors in North America, Europe, and Asia.
In this study, the pooled odds ratio for mortality for all patients with any cancer was 2.32 (95% confidence interval, 1.82-2.94; 24 studies). For ICU admission, the odds ratio was 2.39 (95% CI, 1.90-3.02; I2 0.0%; 5 studies). And, for disease severity or hospitalization, it was 2.08 (95% CI, 1.60-2.72; I2 92.1%; 15 studies). The pooled mortality odds ratio for hematologic neoplasms was 2.14 (95% CI, 1.87-2.44; I2 20.8%; 8 studies).
Their findings, which have not yet been peer reviewed, confirmed the results of a similar analysis from China published as a preprint in May 2020. The analysis included 181,323 patients (23,736 cancer patients) from 26 studies reported an odds ratio of 2.54 (95% CI, 1.47-4.42). “Cancer patients with COVID-19 have an increased likelihood of death compared to non-cancer COVID-19 patients,” Venkatesulu et al. wrote. And a systematic review and meta-analysis of five studies of 2,619 patients published in October 2020 in Medicine also found a significantly higher risk of death from COVID-19 among cancer patients (odds ratio, 2.63; 95% confidence interval, 1.14-6.06; P = .023; I2 = 26.4%).
Fakih et al., writing in the journal Hematology/Oncology and Stem Cell Therapy conducted a meta-analysis early last year finding a threefold increase for admission to the intensive care unit, an almost fourfold increase for a severe SARS-CoV-2 infection, and a fivefold increase for being intubated.
The three studies show that mortality rates were higher early in the pandemic “when diagnosis and treatment for SARS-CoV-2 might have been delayed, resulting in higher death rate,” Boffetta et al. wrote, adding that their analysis showed only a twofold increase most likely because it was a year-long analysis.
“Future studies will be able to better analyze this association for the different subtypes of cancer. Furthermore, they will eventually be able to evaluate whether the difference among vaccinated population is reduced,” Boffetta et al. wrote.
The authors noted several limitations for the study, including the fact that many of the studies included in the analysis did not include sex, age, comorbidities, and therapy. Nor were the authors able to analyze specific cancers other than hematologic neoplasms.
The authors declared no conflicts of interest.
A new systematic review and meta-analysis finds that unvaccinated cancer patients who contracted COVID-19 last year, were more than two times more likely – than people without cancer – to develop a case of COVID-19 so severe it required hospitalization in an intensive care unit.
“Our study provides the most precise measure to date of the effect of COVID-19 in cancer patients,” wrote researchers who were led by Paolo Boffetta, MD, MPH, a specialist in population science with the Stony Brook Cancer Center in New York.
Dr. Boffetta and colleagues also found that patients with hematologic neoplasms had a higher mortality rate from COVID-19 comparable to that of all cancers combined.
Cancer patients have long been considered to be among those patients who are at high risk of developing COVID-19, and if they contract the disease, they are at high risk of having poor outcomes. Other high-risk patients include those with hypertension, diabetes, chronic kidney disease, or COPD, or the elderly. But how high the risk of developing severe COVID-19 disease is for cancer patients hasn’t yet been documented on a wide scale.
The study, which was made available as a preprint on medRxiv on Oct. 23, is based on an analysis of COVID-19 cases that were documented in 35 reviews, meta-analyses, case reports, and studies indexed in PubMed from authors in North America, Europe, and Asia.
In this study, the pooled odds ratio for mortality for all patients with any cancer was 2.32 (95% confidence interval, 1.82-2.94; 24 studies). For ICU admission, the odds ratio was 2.39 (95% CI, 1.90-3.02; I2 0.0%; 5 studies). And, for disease severity or hospitalization, it was 2.08 (95% CI, 1.60-2.72; I2 92.1%; 15 studies). The pooled mortality odds ratio for hematologic neoplasms was 2.14 (95% CI, 1.87-2.44; I2 20.8%; 8 studies).
Their findings, which have not yet been peer reviewed, confirmed the results of a similar analysis from China published as a preprint in May 2020. The analysis included 181,323 patients (23,736 cancer patients) from 26 studies reported an odds ratio of 2.54 (95% CI, 1.47-4.42). “Cancer patients with COVID-19 have an increased likelihood of death compared to non-cancer COVID-19 patients,” Venkatesulu et al. wrote. And a systematic review and meta-analysis of five studies of 2,619 patients published in October 2020 in Medicine also found a significantly higher risk of death from COVID-19 among cancer patients (odds ratio, 2.63; 95% confidence interval, 1.14-6.06; P = .023; I2 = 26.4%).
Fakih et al., writing in the journal Hematology/Oncology and Stem Cell Therapy conducted a meta-analysis early last year finding a threefold increase for admission to the intensive care unit, an almost fourfold increase for a severe SARS-CoV-2 infection, and a fivefold increase for being intubated.
The three studies show that mortality rates were higher early in the pandemic “when diagnosis and treatment for SARS-CoV-2 might have been delayed, resulting in higher death rate,” Boffetta et al. wrote, adding that their analysis showed only a twofold increase most likely because it was a year-long analysis.
“Future studies will be able to better analyze this association for the different subtypes of cancer. Furthermore, they will eventually be able to evaluate whether the difference among vaccinated population is reduced,” Boffetta et al. wrote.
The authors noted several limitations for the study, including the fact that many of the studies included in the analysis did not include sex, age, comorbidities, and therapy. Nor were the authors able to analyze specific cancers other than hematologic neoplasms.
The authors declared no conflicts of interest.
FROM MEDRXIV
Dogs show potential as medical detectives in breast cancer
Breast cancer screening using urine samples based on the volatile organic compounds (VOCs) sensed by a trained dog is feasible, according to a preliminary study published in the journal Biology June 10.
“The extrapolation of our results to widespread implementation is still uncertain,” wrote Shoko Kure, MD, PhD, of Nippon Medical School in Tokyo, and colleagues. “However, even if few dogs could be trained to detect breast cancer, the result may open the door to a robust and inexpensive way to detect breast cancer.” They added that “dog cancer detection is entirely noninvasive, safe and easy for both patients and everyone.”
Early detection of breast cancer, which is the leading cause of death globally, is essential for more efficient treatment. While mammography can detect asymptomatic breast cancer and reduce mortality, it has a poor compliance, is less sensitive in dense breast tissue, detects nonmalignant lesions, and has not been shown to reduce mortality in women younger than 40. VOCs are emitted in the breath, blood, and urine, with different volatile patterns correlated with a variety of diseases including cancers, which dogs can be trained to detect. Breast cancer screening by dog sniffing of the VOCs in urine samples has not been attempted.
Dogs have been used as medical detectives for several cancers and conditions. A study published in 2018 showed that trained dogs who were able to differentiate the specific odor from the metabolic waste of breast cancer in vitro could identify that of colorectal cancer, and vice versa. More recently, research showed that trained dogs could detect advanced prostate cancer in urine samples with high specificity and sensitivity. In this double-blinded pilot study, two dogs were trained to detect Gleason 9 prostate cancer in urine collected from biopsy-confirmed patients. The canine olfaction system was 71% sensitive and as much as 76% specific at detecting Gleason 9 cancer. Along with cancer, trained dogs have been shown to identify people with COVID-19, even those who were asymptomatic. In this study, dogs who sniffed swab samples of armpit sweat could identify which samples came from patients infected with COVID-19 with up to 100% accuracy, while ruling out infection with up to 99% accuracy.
The double-blind study by Dr. Kure aimed to assess the potential of VOCs in urine samples for breast cancer screening by using a single trained sniffer dog – in this case a 9-year-old female Labrador retriever. Urine samples from 40 patients with primary breast cancer and 142 patients with non-breast malignant diseases were included along with samples from 18 healthy volunteers. In 40 times out of 40 runs of the double-blind test, the dog correctly identified urine samples of patients with breast cancer, with 100% sensitivity and 100% specificity.
“The dog in this test successfully differentiated breast cancer from non-breast malignancies and healthy controls,” the authors wrote. “This is the first, preliminary study indicating the feasibility of developing a new breast cancer screening method using urine samples based on VOCs.”
While the authors noted that the study was limited as it relied on one trained dog, they suggested that this method has potential in low-income countries where access to mammography is inadequate.
“Some well-trained sniffing dogs traveling around medically underserved [countries] all over the world could save many lives. Even when a healthy control was indicated by a trained dog, there would be a suspicion of undiagnosed/early-stage cancer, and the person would be advised to undergo medical screening,” the authors wrote.
The authors declared no conflicts of interest.
Breast cancer screening using urine samples based on the volatile organic compounds (VOCs) sensed by a trained dog is feasible, according to a preliminary study published in the journal Biology June 10.
“The extrapolation of our results to widespread implementation is still uncertain,” wrote Shoko Kure, MD, PhD, of Nippon Medical School in Tokyo, and colleagues. “However, even if few dogs could be trained to detect breast cancer, the result may open the door to a robust and inexpensive way to detect breast cancer.” They added that “dog cancer detection is entirely noninvasive, safe and easy for both patients and everyone.”
Early detection of breast cancer, which is the leading cause of death globally, is essential for more efficient treatment. While mammography can detect asymptomatic breast cancer and reduce mortality, it has a poor compliance, is less sensitive in dense breast tissue, detects nonmalignant lesions, and has not been shown to reduce mortality in women younger than 40. VOCs are emitted in the breath, blood, and urine, with different volatile patterns correlated with a variety of diseases including cancers, which dogs can be trained to detect. Breast cancer screening by dog sniffing of the VOCs in urine samples has not been attempted.
Dogs have been used as medical detectives for several cancers and conditions. A study published in 2018 showed that trained dogs who were able to differentiate the specific odor from the metabolic waste of breast cancer in vitro could identify that of colorectal cancer, and vice versa. More recently, research showed that trained dogs could detect advanced prostate cancer in urine samples with high specificity and sensitivity. In this double-blinded pilot study, two dogs were trained to detect Gleason 9 prostate cancer in urine collected from biopsy-confirmed patients. The canine olfaction system was 71% sensitive and as much as 76% specific at detecting Gleason 9 cancer. Along with cancer, trained dogs have been shown to identify people with COVID-19, even those who were asymptomatic. In this study, dogs who sniffed swab samples of armpit sweat could identify which samples came from patients infected with COVID-19 with up to 100% accuracy, while ruling out infection with up to 99% accuracy.
The double-blind study by Dr. Kure aimed to assess the potential of VOCs in urine samples for breast cancer screening by using a single trained sniffer dog – in this case a 9-year-old female Labrador retriever. Urine samples from 40 patients with primary breast cancer and 142 patients with non-breast malignant diseases were included along with samples from 18 healthy volunteers. In 40 times out of 40 runs of the double-blind test, the dog correctly identified urine samples of patients with breast cancer, with 100% sensitivity and 100% specificity.
“The dog in this test successfully differentiated breast cancer from non-breast malignancies and healthy controls,” the authors wrote. “This is the first, preliminary study indicating the feasibility of developing a new breast cancer screening method using urine samples based on VOCs.”
While the authors noted that the study was limited as it relied on one trained dog, they suggested that this method has potential in low-income countries where access to mammography is inadequate.
“Some well-trained sniffing dogs traveling around medically underserved [countries] all over the world could save many lives. Even when a healthy control was indicated by a trained dog, there would be a suspicion of undiagnosed/early-stage cancer, and the person would be advised to undergo medical screening,” the authors wrote.
The authors declared no conflicts of interest.
Breast cancer screening using urine samples based on the volatile organic compounds (VOCs) sensed by a trained dog is feasible, according to a preliminary study published in the journal Biology June 10.
“The extrapolation of our results to widespread implementation is still uncertain,” wrote Shoko Kure, MD, PhD, of Nippon Medical School in Tokyo, and colleagues. “However, even if few dogs could be trained to detect breast cancer, the result may open the door to a robust and inexpensive way to detect breast cancer.” They added that “dog cancer detection is entirely noninvasive, safe and easy for both patients and everyone.”
Early detection of breast cancer, which is the leading cause of death globally, is essential for more efficient treatment. While mammography can detect asymptomatic breast cancer and reduce mortality, it has a poor compliance, is less sensitive in dense breast tissue, detects nonmalignant lesions, and has not been shown to reduce mortality in women younger than 40. VOCs are emitted in the breath, blood, and urine, with different volatile patterns correlated with a variety of diseases including cancers, which dogs can be trained to detect. Breast cancer screening by dog sniffing of the VOCs in urine samples has not been attempted.
Dogs have been used as medical detectives for several cancers and conditions. A study published in 2018 showed that trained dogs who were able to differentiate the specific odor from the metabolic waste of breast cancer in vitro could identify that of colorectal cancer, and vice versa. More recently, research showed that trained dogs could detect advanced prostate cancer in urine samples with high specificity and sensitivity. In this double-blinded pilot study, two dogs were trained to detect Gleason 9 prostate cancer in urine collected from biopsy-confirmed patients. The canine olfaction system was 71% sensitive and as much as 76% specific at detecting Gleason 9 cancer. Along with cancer, trained dogs have been shown to identify people with COVID-19, even those who were asymptomatic. In this study, dogs who sniffed swab samples of armpit sweat could identify which samples came from patients infected with COVID-19 with up to 100% accuracy, while ruling out infection with up to 99% accuracy.
The double-blind study by Dr. Kure aimed to assess the potential of VOCs in urine samples for breast cancer screening by using a single trained sniffer dog – in this case a 9-year-old female Labrador retriever. Urine samples from 40 patients with primary breast cancer and 142 patients with non-breast malignant diseases were included along with samples from 18 healthy volunteers. In 40 times out of 40 runs of the double-blind test, the dog correctly identified urine samples of patients with breast cancer, with 100% sensitivity and 100% specificity.
“The dog in this test successfully differentiated breast cancer from non-breast malignancies and healthy controls,” the authors wrote. “This is the first, preliminary study indicating the feasibility of developing a new breast cancer screening method using urine samples based on VOCs.”
While the authors noted that the study was limited as it relied on one trained dog, they suggested that this method has potential in low-income countries where access to mammography is inadequate.
“Some well-trained sniffing dogs traveling around medically underserved [countries] all over the world could save many lives. Even when a healthy control was indicated by a trained dog, there would be a suspicion of undiagnosed/early-stage cancer, and the person would be advised to undergo medical screening,” the authors wrote.
The authors declared no conflicts of interest.
FROM BIOLOGY
Success of HPV vaccination: ‘Dramatic’ reduction in cervical cancer
Among young women who received the HPV vaccine when they were 12-13 years old (before their sexual debut), cervical cancer rates are 87% lower than among previous nonvaccinated generations.
“It’s been incredible to see the impact of HPV vaccination, and now we can prove it prevented hundreds of women from developing cancer in England,” senior author Peter Sasieni, MD, King’s College London, said in a statement. “To see the real-life impact of the vaccine has been truly rewarding.”
“This study provides the first direct evidence of the impact of the UK HPV vaccination campaign on cervical cancer incidence, showing a large reduction in cervical cancer rates in vaccinated cohorts,” Kate Soldan, MD, U.K. Health Security Agency, London, commented in a statement.
Vanessa Saliba, MD, a consultant epidemiologist for the U.K. Health Security Agency, agreed, saying that “these remarkable findings confirm that the HPV vaccine saves lives by dramatically reducing cervical cancer rates among women.
“This reminds us that vaccines are one of the most important tools we have to help us live longer, healthier lives,” she added.
The study was published online Nov. 3, 2021, in The Lancet.
Approached for comment on the new study, Maurice Markman, MD, president, Medicine and Science Cancer Treatment Centers of America, noted that the results of the English study are very similar to those of a Swedish study of the quadrivalent vaccine alone.
“You can put any superlatives you want in here, but these are stunningly positive results,” Dr. Markman said in an interview. He said that, as an oncologist who has been treating cervical cancer for 40 years, particularly patients with advanced cervical cancer, “I can tell you this is one of the most devastating diseases to women, and the ability to eliminate this cancer with something as simple as a vaccine is the goal of cancer therapy, and it’s been remarkably successful.
“I can only emphasize the critical importance of all parents to see that their children who are eligible for the vaccine receive it. This is a cancer prevention strategy that is unbelievably, remarkably effective and safe,” Dr. Markman added.
National vaccination program
The national HPV vaccination program in England began in 2008. Initially, the bivalent Cervarix vaccine against HPV 16 and 18 was used. HPV 16 and 18 are responsible for 70% to 80% of all cervical cancers in England, the researchers note in their article.
In 2012, the program switched to the quadrivalent HPV vaccine (Gardasil), which is effective against two additional HPV types, HPV 6 and 11. Those strains cause genital warts.
The prevention program originally recommended a three-dose regimen in which both HPV vaccines were used. Currently, two doses are given to girls younger than 15 years. In addition, a single dose of the HPV vaccine provides good protection against persistent infection. The efficacy rate of a single dose is similar to that of three doses, the authors comment.
Population-based registry
The new data come from a population-based cancer registry that shows the incidence of cervical cancer and noninvasive cervical carcinoma (CIN3) in England between January 2006 and June 2019.
The study included seven cohorts of women who were aged 20-64 years at the end of 2019. Three of these cohorts composed the vaccinated population.
The team reports that overall, from January 2006 to June 2019, there were 27,946 cases of cervical cancer and 318,058 cases of CIN3.
In the three vaccinated cohorts, there were around 450 fewer cases of cervical cancer and 17,200 fewer cases of CIN3 than would be expected in a nonvaccinated population.
The three vaccinated cohorts had been eligible to receive Cervarix when they were aged 12-13 years. A catch-up scheme aimed at 14- to 16-year-olds and 16- to 18-year-olds. Most of these persons were vaccinated through a school vaccination program.
The team analyzed the data for each of these cohorts.
Among the cohort eligible for vaccination at 12-13 years of age, 89% received at least one dose of the HPV vaccine; 85% received three shots and were fully vaccinated. Among these persons, the rate of cervical cancer was 87% lower than expected in a nonvaccinated population, and the rate of CIN3 was 97% lower than expected.
For the cohort that was eligible to be vaccinated between the ages of 14 and 16 years, the corresponding reductions were 62% for cervical cancer and 75% for CIN3.
For the cohort eligible for vaccination between the ages of 16 and 18 years (of whom 60% had received at least one dose and 45% were fully vaccinated), the corresponding reduction were 34% for cervical cancer and 39% for CIN3.
The authors acknowledge some limitations with the study, principally that cervical cancer is rare in young women, and these vaccinated populations are still young. The youngest would have been vaccinated at age 12 in 2008 and so would be only 23 years old in 2019, when the follow-up in this current study ended. The authors emphasize that because the vaccinated populations are still young, it is too early to assess the full impact of HPV vaccination on cervical cancer rates.
Editorial commentary
“The relative reductions in cervical cancer, expected as a result of the HPV vaccination program, support the anticipated vaccine effectiveness,” commented two authors of an accompanying editorial, Maggie Cruickshank, MD, University of Aberdeen (Scotland), and Mihaela Grigore, MD, University of Medicine and Pharmacy, Lasi, Romania.
“The scale of the HPV vaccination effect reported by this study should also stimulate vaccination programs in low-income and middle-income countries where the problem of cervical cancer is a far greater public health issue than in those with well established systems of vaccination and screening,” they comment.
“The most important issue, besides the availability of the vaccine ... is the education of the population to accept the vaccination because a high rate of immunization is a key element of success,” they emphasize. “Even in a wealthy country, such as England with free access to HPV immunization, uptake has not reached the 90% vaccination target of girls aged 15 years set by WHO [World Health Organization].”
The authors and editorialists disclosed no relevant financial relationships. Dr. Markman is a regular contributor to Medscape Oncology. He has received income of $250 or more from Genentech, AstraZeneca, Celgene, Clovis, and Amgen.
A version of this article first appeared on Medscape.com.
Among young women who received the HPV vaccine when they were 12-13 years old (before their sexual debut), cervical cancer rates are 87% lower than among previous nonvaccinated generations.
“It’s been incredible to see the impact of HPV vaccination, and now we can prove it prevented hundreds of women from developing cancer in England,” senior author Peter Sasieni, MD, King’s College London, said in a statement. “To see the real-life impact of the vaccine has been truly rewarding.”
“This study provides the first direct evidence of the impact of the UK HPV vaccination campaign on cervical cancer incidence, showing a large reduction in cervical cancer rates in vaccinated cohorts,” Kate Soldan, MD, U.K. Health Security Agency, London, commented in a statement.
Vanessa Saliba, MD, a consultant epidemiologist for the U.K. Health Security Agency, agreed, saying that “these remarkable findings confirm that the HPV vaccine saves lives by dramatically reducing cervical cancer rates among women.
“This reminds us that vaccines are one of the most important tools we have to help us live longer, healthier lives,” she added.
The study was published online Nov. 3, 2021, in The Lancet.
Approached for comment on the new study, Maurice Markman, MD, president, Medicine and Science Cancer Treatment Centers of America, noted that the results of the English study are very similar to those of a Swedish study of the quadrivalent vaccine alone.
“You can put any superlatives you want in here, but these are stunningly positive results,” Dr. Markman said in an interview. He said that, as an oncologist who has been treating cervical cancer for 40 years, particularly patients with advanced cervical cancer, “I can tell you this is one of the most devastating diseases to women, and the ability to eliminate this cancer with something as simple as a vaccine is the goal of cancer therapy, and it’s been remarkably successful.
“I can only emphasize the critical importance of all parents to see that their children who are eligible for the vaccine receive it. This is a cancer prevention strategy that is unbelievably, remarkably effective and safe,” Dr. Markman added.
National vaccination program
The national HPV vaccination program in England began in 2008. Initially, the bivalent Cervarix vaccine against HPV 16 and 18 was used. HPV 16 and 18 are responsible for 70% to 80% of all cervical cancers in England, the researchers note in their article.
In 2012, the program switched to the quadrivalent HPV vaccine (Gardasil), which is effective against two additional HPV types, HPV 6 and 11. Those strains cause genital warts.
The prevention program originally recommended a three-dose regimen in which both HPV vaccines were used. Currently, two doses are given to girls younger than 15 years. In addition, a single dose of the HPV vaccine provides good protection against persistent infection. The efficacy rate of a single dose is similar to that of three doses, the authors comment.
Population-based registry
The new data come from a population-based cancer registry that shows the incidence of cervical cancer and noninvasive cervical carcinoma (CIN3) in England between January 2006 and June 2019.
The study included seven cohorts of women who were aged 20-64 years at the end of 2019. Three of these cohorts composed the vaccinated population.
The team reports that overall, from January 2006 to June 2019, there were 27,946 cases of cervical cancer and 318,058 cases of CIN3.
In the three vaccinated cohorts, there were around 450 fewer cases of cervical cancer and 17,200 fewer cases of CIN3 than would be expected in a nonvaccinated population.
The three vaccinated cohorts had been eligible to receive Cervarix when they were aged 12-13 years. A catch-up scheme aimed at 14- to 16-year-olds and 16- to 18-year-olds. Most of these persons were vaccinated through a school vaccination program.
The team analyzed the data for each of these cohorts.
Among the cohort eligible for vaccination at 12-13 years of age, 89% received at least one dose of the HPV vaccine; 85% received three shots and were fully vaccinated. Among these persons, the rate of cervical cancer was 87% lower than expected in a nonvaccinated population, and the rate of CIN3 was 97% lower than expected.
For the cohort that was eligible to be vaccinated between the ages of 14 and 16 years, the corresponding reductions were 62% for cervical cancer and 75% for CIN3.
For the cohort eligible for vaccination between the ages of 16 and 18 years (of whom 60% had received at least one dose and 45% were fully vaccinated), the corresponding reduction were 34% for cervical cancer and 39% for CIN3.
The authors acknowledge some limitations with the study, principally that cervical cancer is rare in young women, and these vaccinated populations are still young. The youngest would have been vaccinated at age 12 in 2008 and so would be only 23 years old in 2019, when the follow-up in this current study ended. The authors emphasize that because the vaccinated populations are still young, it is too early to assess the full impact of HPV vaccination on cervical cancer rates.
Editorial commentary
“The relative reductions in cervical cancer, expected as a result of the HPV vaccination program, support the anticipated vaccine effectiveness,” commented two authors of an accompanying editorial, Maggie Cruickshank, MD, University of Aberdeen (Scotland), and Mihaela Grigore, MD, University of Medicine and Pharmacy, Lasi, Romania.
“The scale of the HPV vaccination effect reported by this study should also stimulate vaccination programs in low-income and middle-income countries where the problem of cervical cancer is a far greater public health issue than in those with well established systems of vaccination and screening,” they comment.
“The most important issue, besides the availability of the vaccine ... is the education of the population to accept the vaccination because a high rate of immunization is a key element of success,” they emphasize. “Even in a wealthy country, such as England with free access to HPV immunization, uptake has not reached the 90% vaccination target of girls aged 15 years set by WHO [World Health Organization].”
The authors and editorialists disclosed no relevant financial relationships. Dr. Markman is a regular contributor to Medscape Oncology. He has received income of $250 or more from Genentech, AstraZeneca, Celgene, Clovis, and Amgen.
A version of this article first appeared on Medscape.com.
Among young women who received the HPV vaccine when they were 12-13 years old (before their sexual debut), cervical cancer rates are 87% lower than among previous nonvaccinated generations.
“It’s been incredible to see the impact of HPV vaccination, and now we can prove it prevented hundreds of women from developing cancer in England,” senior author Peter Sasieni, MD, King’s College London, said in a statement. “To see the real-life impact of the vaccine has been truly rewarding.”
“This study provides the first direct evidence of the impact of the UK HPV vaccination campaign on cervical cancer incidence, showing a large reduction in cervical cancer rates in vaccinated cohorts,” Kate Soldan, MD, U.K. Health Security Agency, London, commented in a statement.
Vanessa Saliba, MD, a consultant epidemiologist for the U.K. Health Security Agency, agreed, saying that “these remarkable findings confirm that the HPV vaccine saves lives by dramatically reducing cervical cancer rates among women.
“This reminds us that vaccines are one of the most important tools we have to help us live longer, healthier lives,” she added.
The study was published online Nov. 3, 2021, in The Lancet.
Approached for comment on the new study, Maurice Markman, MD, president, Medicine and Science Cancer Treatment Centers of America, noted that the results of the English study are very similar to those of a Swedish study of the quadrivalent vaccine alone.
“You can put any superlatives you want in here, but these are stunningly positive results,” Dr. Markman said in an interview. He said that, as an oncologist who has been treating cervical cancer for 40 years, particularly patients with advanced cervical cancer, “I can tell you this is one of the most devastating diseases to women, and the ability to eliminate this cancer with something as simple as a vaccine is the goal of cancer therapy, and it’s been remarkably successful.
“I can only emphasize the critical importance of all parents to see that their children who are eligible for the vaccine receive it. This is a cancer prevention strategy that is unbelievably, remarkably effective and safe,” Dr. Markman added.
National vaccination program
The national HPV vaccination program in England began in 2008. Initially, the bivalent Cervarix vaccine against HPV 16 and 18 was used. HPV 16 and 18 are responsible for 70% to 80% of all cervical cancers in England, the researchers note in their article.
In 2012, the program switched to the quadrivalent HPV vaccine (Gardasil), which is effective against two additional HPV types, HPV 6 and 11. Those strains cause genital warts.
The prevention program originally recommended a three-dose regimen in which both HPV vaccines were used. Currently, two doses are given to girls younger than 15 years. In addition, a single dose of the HPV vaccine provides good protection against persistent infection. The efficacy rate of a single dose is similar to that of three doses, the authors comment.
Population-based registry
The new data come from a population-based cancer registry that shows the incidence of cervical cancer and noninvasive cervical carcinoma (CIN3) in England between January 2006 and June 2019.
The study included seven cohorts of women who were aged 20-64 years at the end of 2019. Three of these cohorts composed the vaccinated population.
The team reports that overall, from January 2006 to June 2019, there were 27,946 cases of cervical cancer and 318,058 cases of CIN3.
In the three vaccinated cohorts, there were around 450 fewer cases of cervical cancer and 17,200 fewer cases of CIN3 than would be expected in a nonvaccinated population.
The three vaccinated cohorts had been eligible to receive Cervarix when they were aged 12-13 years. A catch-up scheme aimed at 14- to 16-year-olds and 16- to 18-year-olds. Most of these persons were vaccinated through a school vaccination program.
The team analyzed the data for each of these cohorts.
Among the cohort eligible for vaccination at 12-13 years of age, 89% received at least one dose of the HPV vaccine; 85% received three shots and were fully vaccinated. Among these persons, the rate of cervical cancer was 87% lower than expected in a nonvaccinated population, and the rate of CIN3 was 97% lower than expected.
For the cohort that was eligible to be vaccinated between the ages of 14 and 16 years, the corresponding reductions were 62% for cervical cancer and 75% for CIN3.
For the cohort eligible for vaccination between the ages of 16 and 18 years (of whom 60% had received at least one dose and 45% were fully vaccinated), the corresponding reduction were 34% for cervical cancer and 39% for CIN3.
The authors acknowledge some limitations with the study, principally that cervical cancer is rare in young women, and these vaccinated populations are still young. The youngest would have been vaccinated at age 12 in 2008 and so would be only 23 years old in 2019, when the follow-up in this current study ended. The authors emphasize that because the vaccinated populations are still young, it is too early to assess the full impact of HPV vaccination on cervical cancer rates.
Editorial commentary
“The relative reductions in cervical cancer, expected as a result of the HPV vaccination program, support the anticipated vaccine effectiveness,” commented two authors of an accompanying editorial, Maggie Cruickshank, MD, University of Aberdeen (Scotland), and Mihaela Grigore, MD, University of Medicine and Pharmacy, Lasi, Romania.
“The scale of the HPV vaccination effect reported by this study should also stimulate vaccination programs in low-income and middle-income countries where the problem of cervical cancer is a far greater public health issue than in those with well established systems of vaccination and screening,” they comment.
“The most important issue, besides the availability of the vaccine ... is the education of the population to accept the vaccination because a high rate of immunization is a key element of success,” they emphasize. “Even in a wealthy country, such as England with free access to HPV immunization, uptake has not reached the 90% vaccination target of girls aged 15 years set by WHO [World Health Organization].”
The authors and editorialists disclosed no relevant financial relationships. Dr. Markman is a regular contributor to Medscape Oncology. He has received income of $250 or more from Genentech, AstraZeneca, Celgene, Clovis, and Amgen.
A version of this article first appeared on Medscape.com.
3D vs 2D mammography for detecting cancer in dense breasts
Text copyright DenseBreast-info.org.
Answer
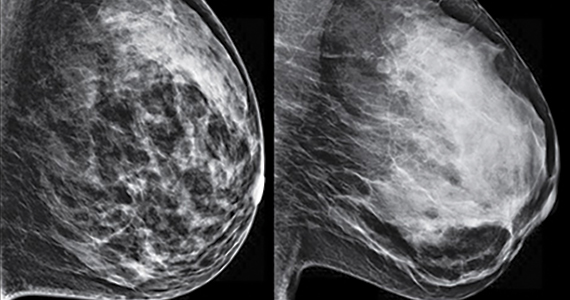
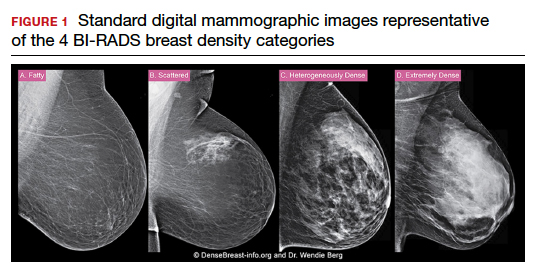
C. Overall, tomosynthesis depicts an additional 1 to 2 cancers per thousand women screened in the first round of screening when added to standard digital mammography;1-3 however, this improvement in cancer detection is only observed in women with fatty breasts (category A), scattered fibroglandular tissue (category B), and heterogeneously dense breasts (category C). Importantly, tomosynthesis does not significantly improve breast cancer detection in women with extremely dense breasts (category D).2,4
Digital breast tomosynthesis, also referred to as “3-dimensional mammography” (3D mammography) or tomosynthesis, uses a dedicated electronic detector system to obtain multiple projection images that are reconstructed by the computer to create thin slices or slabs of multiple slices of the breast. These slices can be individually “scrolled through” by the radiologist to reduce tissue overlap that may obscure breast cancers on a standard mammogram. While tomosynthesis improves breast cancer detection in women with fatty, scattered fibroglandular density, and heterogeneously dense breasts, there is very little soft tissue contrast in extremely dense breasts due to insufficient fat, and some cancers will remain hidden by dense tissue even on sliced images through the breast.
FIGURE 2 shows an example of cancer that was missed on tomosynthesis in a 51-year-old woman with extremely dense breasts and right breast pain. The cancer was masked by extremely dense tissue on standard digital mammography and tomosynthesis; no abnormalities were detected. Ultrasonography showed a 1.6-cm, irregular, hypoechoic mass at the site of pain, and biopsy revealed a grade 3 triple-receptor negative invasive ductal carcinoma.

In women with dense breasts, especially extremely dense breasts, supplemental screening beyond tomosynthesis should be considered. Although tomosynthesis doesn’t improve cancer detection in extremely dense breasts, it does reduce callbacks for additional testing in all breast densities compared with standard digital mammography. Callbacks are reduced from approximately 100‒120 per 1,000 women screened with standard digital mammography alone1,5 to an average of 80 per 1,000 women when tomosynthesis and standard mammography are interpreted together.1-3 ●
For more information, visit medically sourced DenseBreast-info.org. Comprehensive resources include a free CME opportunity, Dense Breasts and Supplemental Screening.
- Conant EF, Zuckerman SP, McDonald ES, et al. Five consecutive years of screening with digital breast tomosynthesis: outcomes by screening year and round. Radiology. 2020;295:285-293.
- Rafferty EA, Durand MA, Conant EF, et al. Breast cancer screening using tomosynthesis and digital mammography in dense and nondense breasts. JAMA. 2016;315:1784-1786.
- Skaane P, Bandos AI, Niklason LT, et al. Digital mammography versus digital mammography plus tomosynthesis in breast cancer screening: the Oslo Tomosynthesis Screening Trial. Radiology. 2019;291:23-30.
- Lowry KP, Coley RY, Miglioretti DL, et al. Screening performance of digital breast tomosynthesis vs digital mammography in community practice by patient age, screening round, and breast density. JAMA Netw Open. 2020;3:e2011792.
- Lee CS, Sengupta D, Bhargavan-Chatfield M, et al. Association of patient age with outcomes of current-era, large-scale screening mammography: analysis of data from the National Mammography Database. JAMA Oncol. 2017;3:1134-1136.
Text copyright DenseBreast-info.org.
Answer
C. Overall, tomosynthesis depicts an additional 1 to 2 cancers per thousand women screened in the first round of screening when added to standard digital mammography;1-3 however, this improvement in cancer detection is only observed in women with fatty breasts (category A), scattered fibroglandular tissue (category B), and heterogeneously dense breasts (category C). Importantly, tomosynthesis does not significantly improve breast cancer detection in women with extremely dense breasts (category D).2,4
Digital breast tomosynthesis, also referred to as “3-dimensional mammography” (3D mammography) or tomosynthesis, uses a dedicated electronic detector system to obtain multiple projection images that are reconstructed by the computer to create thin slices or slabs of multiple slices of the breast. These slices can be individually “scrolled through” by the radiologist to reduce tissue overlap that may obscure breast cancers on a standard mammogram. While tomosynthesis improves breast cancer detection in women with fatty, scattered fibroglandular density, and heterogeneously dense breasts, there is very little soft tissue contrast in extremely dense breasts due to insufficient fat, and some cancers will remain hidden by dense tissue even on sliced images through the breast.
FIGURE 2 shows an example of cancer that was missed on tomosynthesis in a 51-year-old woman with extremely dense breasts and right breast pain. The cancer was masked by extremely dense tissue on standard digital mammography and tomosynthesis; no abnormalities were detected. Ultrasonography showed a 1.6-cm, irregular, hypoechoic mass at the site of pain, and biopsy revealed a grade 3 triple-receptor negative invasive ductal carcinoma.

In women with dense breasts, especially extremely dense breasts, supplemental screening beyond tomosynthesis should be considered. Although tomosynthesis doesn’t improve cancer detection in extremely dense breasts, it does reduce callbacks for additional testing in all breast densities compared with standard digital mammography. Callbacks are reduced from approximately 100‒120 per 1,000 women screened with standard digital mammography alone1,5 to an average of 80 per 1,000 women when tomosynthesis and standard mammography are interpreted together.1-3 ●
For more information, visit medically sourced DenseBreast-info.org. Comprehensive resources include a free CME opportunity, Dense Breasts and Supplemental Screening.
Text copyright DenseBreast-info.org.
Answer
C. Overall, tomosynthesis depicts an additional 1 to 2 cancers per thousand women screened in the first round of screening when added to standard digital mammography;1-3 however, this improvement in cancer detection is only observed in women with fatty breasts (category A), scattered fibroglandular tissue (category B), and heterogeneously dense breasts (category C). Importantly, tomosynthesis does not significantly improve breast cancer detection in women with extremely dense breasts (category D).2,4
Digital breast tomosynthesis, also referred to as “3-dimensional mammography” (3D mammography) or tomosynthesis, uses a dedicated electronic detector system to obtain multiple projection images that are reconstructed by the computer to create thin slices or slabs of multiple slices of the breast. These slices can be individually “scrolled through” by the radiologist to reduce tissue overlap that may obscure breast cancers on a standard mammogram. While tomosynthesis improves breast cancer detection in women with fatty, scattered fibroglandular density, and heterogeneously dense breasts, there is very little soft tissue contrast in extremely dense breasts due to insufficient fat, and some cancers will remain hidden by dense tissue even on sliced images through the breast.
FIGURE 2 shows an example of cancer that was missed on tomosynthesis in a 51-year-old woman with extremely dense breasts and right breast pain. The cancer was masked by extremely dense tissue on standard digital mammography and tomosynthesis; no abnormalities were detected. Ultrasonography showed a 1.6-cm, irregular, hypoechoic mass at the site of pain, and biopsy revealed a grade 3 triple-receptor negative invasive ductal carcinoma.

In women with dense breasts, especially extremely dense breasts, supplemental screening beyond tomosynthesis should be considered. Although tomosynthesis doesn’t improve cancer detection in extremely dense breasts, it does reduce callbacks for additional testing in all breast densities compared with standard digital mammography. Callbacks are reduced from approximately 100‒120 per 1,000 women screened with standard digital mammography alone1,5 to an average of 80 per 1,000 women when tomosynthesis and standard mammography are interpreted together.1-3 ●
For more information, visit medically sourced DenseBreast-info.org. Comprehensive resources include a free CME opportunity, Dense Breasts and Supplemental Screening.
- Conant EF, Zuckerman SP, McDonald ES, et al. Five consecutive years of screening with digital breast tomosynthesis: outcomes by screening year and round. Radiology. 2020;295:285-293.
- Rafferty EA, Durand MA, Conant EF, et al. Breast cancer screening using tomosynthesis and digital mammography in dense and nondense breasts. JAMA. 2016;315:1784-1786.
- Skaane P, Bandos AI, Niklason LT, et al. Digital mammography versus digital mammography plus tomosynthesis in breast cancer screening: the Oslo Tomosynthesis Screening Trial. Radiology. 2019;291:23-30.
- Lowry KP, Coley RY, Miglioretti DL, et al. Screening performance of digital breast tomosynthesis vs digital mammography in community practice by patient age, screening round, and breast density. JAMA Netw Open. 2020;3:e2011792.
- Lee CS, Sengupta D, Bhargavan-Chatfield M, et al. Association of patient age with outcomes of current-era, large-scale screening mammography: analysis of data from the National Mammography Database. JAMA Oncol. 2017;3:1134-1136.
- Conant EF, Zuckerman SP, McDonald ES, et al. Five consecutive years of screening with digital breast tomosynthesis: outcomes by screening year and round. Radiology. 2020;295:285-293.
- Rafferty EA, Durand MA, Conant EF, et al. Breast cancer screening using tomosynthesis and digital mammography in dense and nondense breasts. JAMA. 2016;315:1784-1786.
- Skaane P, Bandos AI, Niklason LT, et al. Digital mammography versus digital mammography plus tomosynthesis in breast cancer screening: the Oslo Tomosynthesis Screening Trial. Radiology. 2019;291:23-30.
- Lowry KP, Coley RY, Miglioretti DL, et al. Screening performance of digital breast tomosynthesis vs digital mammography in community practice by patient age, screening round, and breast density. JAMA Netw Open. 2020;3:e2011792.
- Lee CS, Sengupta D, Bhargavan-Chatfield M, et al. Association of patient age with outcomes of current-era, large-scale screening mammography: analysis of data from the National Mammography Database. JAMA Oncol. 2017;3:1134-1136.
Quiz developed in collaboration with 
FDA posts new websites on accelerated approvals for cancer drugs
, including a public list detailing cases where accelerated approvals have been rescinded for lack of evidence.
On Oct. 29, the Food and Drug Administration posted new websites detailing the status of oncology medicines given these special clearances:
- Ongoing | Cancer Accelerated Approvals
- Verified Clinical Benefit | Cancer Accelerated Approvals
- Withdrawn | Cancer Accelerated Approvals
The FDA’s cancer center also has created a web page called Project Confirm to provide more information on the way it uses accelerated approvals.
There has been increased concern about medicines cleared by accelerated approvals in recent years, culminating in an uproar over the controversial June approval of aducanumab (Aduhelm) for Alzheimer’s disease. This drew more attention to a debate already underway about how much data supports some of the indications for some cancer drugs.
Federal and state officials and advisers are putting more pressure on pharmaceutical companies to prove that medicines that are put on the market through accelerated approval do deliver meaningful benefits for patients.
In addition, earlier this month two of the top health advisers in Barack Obama’s administration proposed a new model through which Medicare could reduce payments for certain cancer drugs cleared through accelerated approvals – and even cut off reimbursements in cases where companies fail to deliver confirmatory evidence for expected benefits.
This “Pay for Drugs That Work Model” was proposed by Richard Frank, PhD, and Ezekiel Emanuel, MD, PhD, in a recent JAMA article. In their view, the FDA’s accelerated drug approval process allows for too many delays in obtaining answers as to whether medicines cleared this way provide expected benefits.
“The proposed Pay for Drugs That Work model could test a modified approach for incentivizing rapid completion of confirmatory trials to inform clinicians and patients about the true risks and benefits of new drugs and improve the value for money of cancer drugs that receive accelerated approval,” they wrote.
Excel files, regular updates
For the FDA, accelerated approvals require balancing an estimated potential benefit for people facing serious diseases (for example, cancer) against serious risks, including potentially exposing patients to costly, toxic drugs that will later be shown not to work for their conditions.
For many years, there has been significant pressure on the FDA to lean toward speedier approvals, with members of Congress, advocacy groups, and drugmakers advocating for broad use of surrogate data in deciding on clearances. The FDA posts biannual reports on its website that highlight how quickly approvals have been granted. But these biannual reports don’t provide much information on the status of accelerated-approval drugs, other than to say if they have been given full approval or withdrawn.
The newly created websites from the FDA’s oncology division appear to reflect growing public interest in knowing what standards the agency sets for confirmatory trials and what deadlines companies face to deliver evidence of significant benefit for their drugs.
The new sortable websites also include details on trials and have links to Excel files which will help researchers and others seeking to track patterns with accelerated approvals. The FDA said in an interview that it intends to update these sites when there are developments with accelerated approvals for cancer drugs, such as new clearances of this type, conversions to regular approvals, and withdrawn approvals.
Julia Beaver, MD, chief of medical oncology at the FDA’s Oncology Center of Excellence, and acting deputy director of the Office of Oncologic Diseases of the FDA’s Center for Drug Evaluation and Research, described the new websites as part of a “commitment to preserve the integrity” of the accelerated approval program.
“These new web pages will make information on our accelerated approvals more transparent,” Dr. Beaver said in an email to this news organization.
The FDA has been able to speed many medicines to market and clear additional uses for drugs already sold through the program, giving people earlier access in many cases to critical medicines, Dr. Beaver said.
More than 165 oncology indications have received accelerated approval, with almost half converted to regular approval in a median of 3 years. Less than 10% of these indications were withdrawn, Dr. Beaver said.
“Of those accelerated approvals that were converted to regular approval, many demonstrated survival advantages to patients with several types of cancer or provided meaningful therapeutic options where none previously existed,” she said.
However, Dr. Beaver also has made public the FDA’s concerns with what she and Richard Pazdur, MD, director of the Oncology Center of Excellence, have described as “dangling” accelerated approvals.
These are cases where the required trials did not end up confirming benefit for a medicine, yet the manufacturer did not move to withdraw an accelerated approval. The FDA’s cancer center has already announced that it is doing an “industry-wide evaluation of accelerated approvals in oncology in which confirmatory trials did not confirm clinical benefit.”
This stems in part from what can be called the FDA’s “growing pains” in its efforts to manage the rapidly changing landscape for these immunotherapy checkpoint inhibitors. This field of medicine has experienced an “unprecedented level of drug development” in recent years, FDA officials said in briefing materials for an Oncologic Drugs Advisory Committee (ODAC) meeting last April on dangling accelerated approvals.
A newly posted chart on withdrawn oncology accelerated approvals, posted by the FDA’s cancer division, makes it clear that the pace of these rescinded clearances has picked up. The chart lists a total 14 withdrawn indications of oncology accelerated approvals.
Six of these withdrawals happened this year.
There were two withdrawals in 2020, including the December withdrawal of nivolumab, (Opdivo) for a form of metastatic lung cancer.
Then there was a significant gap, with no withdrawals going back to 2013 (when there was one). There were two withdrawals in 2012 and three in 2011.
A version of this article first appeared on Medscape.com.
, including a public list detailing cases where accelerated approvals have been rescinded for lack of evidence.
On Oct. 29, the Food and Drug Administration posted new websites detailing the status of oncology medicines given these special clearances:
- Ongoing | Cancer Accelerated Approvals
- Verified Clinical Benefit | Cancer Accelerated Approvals
- Withdrawn | Cancer Accelerated Approvals
The FDA’s cancer center also has created a web page called Project Confirm to provide more information on the way it uses accelerated approvals.
There has been increased concern about medicines cleared by accelerated approvals in recent years, culminating in an uproar over the controversial June approval of aducanumab (Aduhelm) for Alzheimer’s disease. This drew more attention to a debate already underway about how much data supports some of the indications for some cancer drugs.
Federal and state officials and advisers are putting more pressure on pharmaceutical companies to prove that medicines that are put on the market through accelerated approval do deliver meaningful benefits for patients.
In addition, earlier this month two of the top health advisers in Barack Obama’s administration proposed a new model through which Medicare could reduce payments for certain cancer drugs cleared through accelerated approvals – and even cut off reimbursements in cases where companies fail to deliver confirmatory evidence for expected benefits.
This “Pay for Drugs That Work Model” was proposed by Richard Frank, PhD, and Ezekiel Emanuel, MD, PhD, in a recent JAMA article. In their view, the FDA’s accelerated drug approval process allows for too many delays in obtaining answers as to whether medicines cleared this way provide expected benefits.
“The proposed Pay for Drugs That Work model could test a modified approach for incentivizing rapid completion of confirmatory trials to inform clinicians and patients about the true risks and benefits of new drugs and improve the value for money of cancer drugs that receive accelerated approval,” they wrote.
Excel files, regular updates
For the FDA, accelerated approvals require balancing an estimated potential benefit for people facing serious diseases (for example, cancer) against serious risks, including potentially exposing patients to costly, toxic drugs that will later be shown not to work for their conditions.
For many years, there has been significant pressure on the FDA to lean toward speedier approvals, with members of Congress, advocacy groups, and drugmakers advocating for broad use of surrogate data in deciding on clearances. The FDA posts biannual reports on its website that highlight how quickly approvals have been granted. But these biannual reports don’t provide much information on the status of accelerated-approval drugs, other than to say if they have been given full approval or withdrawn.
The newly created websites from the FDA’s oncology division appear to reflect growing public interest in knowing what standards the agency sets for confirmatory trials and what deadlines companies face to deliver evidence of significant benefit for their drugs.
The new sortable websites also include details on trials and have links to Excel files which will help researchers and others seeking to track patterns with accelerated approvals. The FDA said in an interview that it intends to update these sites when there are developments with accelerated approvals for cancer drugs, such as new clearances of this type, conversions to regular approvals, and withdrawn approvals.
Julia Beaver, MD, chief of medical oncology at the FDA’s Oncology Center of Excellence, and acting deputy director of the Office of Oncologic Diseases of the FDA’s Center for Drug Evaluation and Research, described the new websites as part of a “commitment to preserve the integrity” of the accelerated approval program.
“These new web pages will make information on our accelerated approvals more transparent,” Dr. Beaver said in an email to this news organization.
The FDA has been able to speed many medicines to market and clear additional uses for drugs already sold through the program, giving people earlier access in many cases to critical medicines, Dr. Beaver said.
More than 165 oncology indications have received accelerated approval, with almost half converted to regular approval in a median of 3 years. Less than 10% of these indications were withdrawn, Dr. Beaver said.
“Of those accelerated approvals that were converted to regular approval, many demonstrated survival advantages to patients with several types of cancer or provided meaningful therapeutic options where none previously existed,” she said.
However, Dr. Beaver also has made public the FDA’s concerns with what she and Richard Pazdur, MD, director of the Oncology Center of Excellence, have described as “dangling” accelerated approvals.
These are cases where the required trials did not end up confirming benefit for a medicine, yet the manufacturer did not move to withdraw an accelerated approval. The FDA’s cancer center has already announced that it is doing an “industry-wide evaluation of accelerated approvals in oncology in which confirmatory trials did not confirm clinical benefit.”
This stems in part from what can be called the FDA’s “growing pains” in its efforts to manage the rapidly changing landscape for these immunotherapy checkpoint inhibitors. This field of medicine has experienced an “unprecedented level of drug development” in recent years, FDA officials said in briefing materials for an Oncologic Drugs Advisory Committee (ODAC) meeting last April on dangling accelerated approvals.
A newly posted chart on withdrawn oncology accelerated approvals, posted by the FDA’s cancer division, makes it clear that the pace of these rescinded clearances has picked up. The chart lists a total 14 withdrawn indications of oncology accelerated approvals.
Six of these withdrawals happened this year.
There were two withdrawals in 2020, including the December withdrawal of nivolumab, (Opdivo) for a form of metastatic lung cancer.
Then there was a significant gap, with no withdrawals going back to 2013 (when there was one). There were two withdrawals in 2012 and three in 2011.
A version of this article first appeared on Medscape.com.
, including a public list detailing cases where accelerated approvals have been rescinded for lack of evidence.
On Oct. 29, the Food and Drug Administration posted new websites detailing the status of oncology medicines given these special clearances:
- Ongoing | Cancer Accelerated Approvals
- Verified Clinical Benefit | Cancer Accelerated Approvals
- Withdrawn | Cancer Accelerated Approvals
The FDA’s cancer center also has created a web page called Project Confirm to provide more information on the way it uses accelerated approvals.
There has been increased concern about medicines cleared by accelerated approvals in recent years, culminating in an uproar over the controversial June approval of aducanumab (Aduhelm) for Alzheimer’s disease. This drew more attention to a debate already underway about how much data supports some of the indications for some cancer drugs.
Federal and state officials and advisers are putting more pressure on pharmaceutical companies to prove that medicines that are put on the market through accelerated approval do deliver meaningful benefits for patients.
In addition, earlier this month two of the top health advisers in Barack Obama’s administration proposed a new model through which Medicare could reduce payments for certain cancer drugs cleared through accelerated approvals – and even cut off reimbursements in cases where companies fail to deliver confirmatory evidence for expected benefits.
This “Pay for Drugs That Work Model” was proposed by Richard Frank, PhD, and Ezekiel Emanuel, MD, PhD, in a recent JAMA article. In their view, the FDA’s accelerated drug approval process allows for too many delays in obtaining answers as to whether medicines cleared this way provide expected benefits.
“The proposed Pay for Drugs That Work model could test a modified approach for incentivizing rapid completion of confirmatory trials to inform clinicians and patients about the true risks and benefits of new drugs and improve the value for money of cancer drugs that receive accelerated approval,” they wrote.
Excel files, regular updates
For the FDA, accelerated approvals require balancing an estimated potential benefit for people facing serious diseases (for example, cancer) against serious risks, including potentially exposing patients to costly, toxic drugs that will later be shown not to work for their conditions.
For many years, there has been significant pressure on the FDA to lean toward speedier approvals, with members of Congress, advocacy groups, and drugmakers advocating for broad use of surrogate data in deciding on clearances. The FDA posts biannual reports on its website that highlight how quickly approvals have been granted. But these biannual reports don’t provide much information on the status of accelerated-approval drugs, other than to say if they have been given full approval or withdrawn.
The newly created websites from the FDA’s oncology division appear to reflect growing public interest in knowing what standards the agency sets for confirmatory trials and what deadlines companies face to deliver evidence of significant benefit for their drugs.
The new sortable websites also include details on trials and have links to Excel files which will help researchers and others seeking to track patterns with accelerated approvals. The FDA said in an interview that it intends to update these sites when there are developments with accelerated approvals for cancer drugs, such as new clearances of this type, conversions to regular approvals, and withdrawn approvals.
Julia Beaver, MD, chief of medical oncology at the FDA’s Oncology Center of Excellence, and acting deputy director of the Office of Oncologic Diseases of the FDA’s Center for Drug Evaluation and Research, described the new websites as part of a “commitment to preserve the integrity” of the accelerated approval program.
“These new web pages will make information on our accelerated approvals more transparent,” Dr. Beaver said in an email to this news organization.
The FDA has been able to speed many medicines to market and clear additional uses for drugs already sold through the program, giving people earlier access in many cases to critical medicines, Dr. Beaver said.
More than 165 oncology indications have received accelerated approval, with almost half converted to regular approval in a median of 3 years. Less than 10% of these indications were withdrawn, Dr. Beaver said.
“Of those accelerated approvals that were converted to regular approval, many demonstrated survival advantages to patients with several types of cancer or provided meaningful therapeutic options where none previously existed,” she said.
However, Dr. Beaver also has made public the FDA’s concerns with what she and Richard Pazdur, MD, director of the Oncology Center of Excellence, have described as “dangling” accelerated approvals.
These are cases where the required trials did not end up confirming benefit for a medicine, yet the manufacturer did not move to withdraw an accelerated approval. The FDA’s cancer center has already announced that it is doing an “industry-wide evaluation of accelerated approvals in oncology in which confirmatory trials did not confirm clinical benefit.”
This stems in part from what can be called the FDA’s “growing pains” in its efforts to manage the rapidly changing landscape for these immunotherapy checkpoint inhibitors. This field of medicine has experienced an “unprecedented level of drug development” in recent years, FDA officials said in briefing materials for an Oncologic Drugs Advisory Committee (ODAC) meeting last April on dangling accelerated approvals.
A newly posted chart on withdrawn oncology accelerated approvals, posted by the FDA’s cancer division, makes it clear that the pace of these rescinded clearances has picked up. The chart lists a total 14 withdrawn indications of oncology accelerated approvals.
Six of these withdrawals happened this year.
There were two withdrawals in 2020, including the December withdrawal of nivolumab, (Opdivo) for a form of metastatic lung cancer.
Then there was a significant gap, with no withdrawals going back to 2013 (when there was one). There were two withdrawals in 2012 and three in 2011.
A version of this article first appeared on Medscape.com.
In and out surgeries become the norm during pandemic
Urologist Ronney Abaza, MD, a robotic surgery specialist in Dublin, Ohio, and colleagues, reviewed robotic surgeries at their hospital during COVID-19 restrictions on surgery in Ohio between March 17 and June 5, 2020, and compared them with robotic procedures before COVID-19 and after restrictions were lifted. They published their results in Urology.
Since 2016, the hospital has offered the option of same-day discharge (SDD) to all robotic urologic surgery patients, regardless of procedure or patient-specific factors.
Among patients who had surgery during COVID-19 restrictions, 98% (87/89 patients) opted for SDD versus 52% in the group having surgery before the restrictions (P < .00001). After the COVID-19 surgery restrictions were lifted, the higher rate of SDD remained at 98%.
“There were no differences in 30-day complications or readmissions between SDD and overnight patients,” the authors write.
The right patient, the right motivation for successful surgery
Brian Lane, MD, PhD, a urologic oncologist with Spectrum Health in Grand Rapids, Michigan, told this news organization that, for nephrectomies, uptake of same-day discharge will continue to be slow.
“You have to have the right patient, the right patient motivation, and the surgery has to go smoothly,” he said. “If you start sending everyone home the same day, you will certainly see readmissions,” he said.
Dr. Lane is part of the Michigan Urologic Surgery Improvement Collaborative and he said the group recently looked at same-day discharge outcomes after robotic prostatectomies with SDD as compared with 1-2 nights in the hospital.
The work has not yet been published but, “There was a slight signal that there were increased readmissions with same-day discharge vs. 0-1 day,” he said.
A paper on outcomes of same-day discharge in total knee arthroplasty in the Journal of Bone & Joint Surgery found a higher risk of perioperative complications “including component failure, surgical site infection, knee stiffness, and deep vein thrombosis.” Researchers compared outcomes between 4,391 patients who underwent outpatient TKA and 128,951 patients who underwent inpatient TKA.
But for other many surgeries, same-day discharge numbers are increasing without worsening outcomes.
A paper in the Journal of Robotic Surgery found that same-day discharge following robotic-assisted endometrial cancer staging is “safe and feasible.”
Stephen Bradley, MD, MPH, with the Minneapolis Heart Institute in Minneapolis, and colleagues write in the Journal of the American College of Cardiology: Cardiovascular Interventions that they found a large increase in the use of same-day discharge after elective percutaneous coronary intervention (PCI) was not associated with worse 30-day mortality rates or readmission.
In that study, 114,461 patients were discharged the same day they underwent PCI. The proportion of patients who had a same-day discharge increased from 4.5% in 2009 to 28.6% in the fourth quarter of 2017.
Risk-adjusted 30-day mortality did not change in that time, while risk-adjusted rehospitalization decreased over time and more quickly when patients had same-day discharge.
Deepak L. Bhatt, MD, MPH, and Jonathan G. Sung, MBCHB, both of Brigham and Women’s Hospital Heart & Vascular Center, Harvard Medical School, Boston, wrote in an accompanying article that, “Advances in the devices and techniques of PCI have improved the safety and efficacy of the procedure. In selected patients, same-day discharge has become possible, and overnight in-hospital observation can be avoided. By reducing unnecessary hospital stays, both patients and hospitals could benefit.”
Evan Garden, a medical student at Icahn School of Medicine at Mount Sinai in New York, presented findings at the American Urological Association 2021 annual meeting that show patients selected for same-day discharge after partial or radical nephrectomy did not have increased rates of postoperative complications or readmissions in the immediate postoperative period, compared with standard discharge of 1-3 days.
Case studies in nephrectomy
While several case studies have looked at the feasibility and safety of performing partial and radical nephrectomy with same-day discharge in select cases, “this topic has not been addressed on a national level,” Mr. Garden said.
Few patients who have partial or radical nephrectomies have same-day discharges. The researchers found that fewer than 1% of patients who have either procedure in the sample studied were discharged the same day.
Researchers used the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database, a nationally representative deidentified database that prospectively tracks patient characteristics and 30-day perioperative outcomes for major inpatient and outpatient surgical procedures at more than 700 hospitals.
They extracted all minimally invasive partial and radical nephrectomies from 2012 to 2019 and refined the cohort to 28,140 patients who were theoretically eligible for same-day discharge: Of those, 237 (0.8%) had SSD, and 27,903 (99.2%) had a standard-length discharge (SLD).
The team found that there were no differences in 30-day complications or readmissions between same-day discharge (Clavien-Dindo [CD] I/II, 4.22%; CD III, 0%; CD IV, 1.27%; readmission, 4.64%); and SLD (CD I/II, 4.11%; CD III, 0.95%; CD IV, 0.79%; readmission, 3.90%; all P > .05).
Controlling for demographic and clinical variables, SDD was not associated with greater risk of 30-day complications or readmissions (CD I/II: odds ratio, 1.08; 95% confidence interval, 0.57-2.048; P = .813; CD IV: OR 1.699; 95% CI, 0.537-5.375; P = .367; readmission: OR, 1.254; 95% CI, 0.681-2.31; P = .467).
Mr. Garden and coauthors report no relevant financial relationships.
Dr. Lane reports no relevant financial relationships.
Urologist Ronney Abaza, MD, a robotic surgery specialist in Dublin, Ohio, and colleagues, reviewed robotic surgeries at their hospital during COVID-19 restrictions on surgery in Ohio between March 17 and June 5, 2020, and compared them with robotic procedures before COVID-19 and after restrictions were lifted. They published their results in Urology.
Since 2016, the hospital has offered the option of same-day discharge (SDD) to all robotic urologic surgery patients, regardless of procedure or patient-specific factors.
Among patients who had surgery during COVID-19 restrictions, 98% (87/89 patients) opted for SDD versus 52% in the group having surgery before the restrictions (P < .00001). After the COVID-19 surgery restrictions were lifted, the higher rate of SDD remained at 98%.
“There were no differences in 30-day complications or readmissions between SDD and overnight patients,” the authors write.
The right patient, the right motivation for successful surgery
Brian Lane, MD, PhD, a urologic oncologist with Spectrum Health in Grand Rapids, Michigan, told this news organization that, for nephrectomies, uptake of same-day discharge will continue to be slow.
“You have to have the right patient, the right patient motivation, and the surgery has to go smoothly,” he said. “If you start sending everyone home the same day, you will certainly see readmissions,” he said.
Dr. Lane is part of the Michigan Urologic Surgery Improvement Collaborative and he said the group recently looked at same-day discharge outcomes after robotic prostatectomies with SDD as compared with 1-2 nights in the hospital.
The work has not yet been published but, “There was a slight signal that there were increased readmissions with same-day discharge vs. 0-1 day,” he said.
A paper on outcomes of same-day discharge in total knee arthroplasty in the Journal of Bone & Joint Surgery found a higher risk of perioperative complications “including component failure, surgical site infection, knee stiffness, and deep vein thrombosis.” Researchers compared outcomes between 4,391 patients who underwent outpatient TKA and 128,951 patients who underwent inpatient TKA.
But for other many surgeries, same-day discharge numbers are increasing without worsening outcomes.
A paper in the Journal of Robotic Surgery found that same-day discharge following robotic-assisted endometrial cancer staging is “safe and feasible.”
Stephen Bradley, MD, MPH, with the Minneapolis Heart Institute in Minneapolis, and colleagues write in the Journal of the American College of Cardiology: Cardiovascular Interventions that they found a large increase in the use of same-day discharge after elective percutaneous coronary intervention (PCI) was not associated with worse 30-day mortality rates or readmission.
In that study, 114,461 patients were discharged the same day they underwent PCI. The proportion of patients who had a same-day discharge increased from 4.5% in 2009 to 28.6% in the fourth quarter of 2017.
Risk-adjusted 30-day mortality did not change in that time, while risk-adjusted rehospitalization decreased over time and more quickly when patients had same-day discharge.
Deepak L. Bhatt, MD, MPH, and Jonathan G. Sung, MBCHB, both of Brigham and Women’s Hospital Heart & Vascular Center, Harvard Medical School, Boston, wrote in an accompanying article that, “Advances in the devices and techniques of PCI have improved the safety and efficacy of the procedure. In selected patients, same-day discharge has become possible, and overnight in-hospital observation can be avoided. By reducing unnecessary hospital stays, both patients and hospitals could benefit.”
Evan Garden, a medical student at Icahn School of Medicine at Mount Sinai in New York, presented findings at the American Urological Association 2021 annual meeting that show patients selected for same-day discharge after partial or radical nephrectomy did not have increased rates of postoperative complications or readmissions in the immediate postoperative period, compared with standard discharge of 1-3 days.
Case studies in nephrectomy
While several case studies have looked at the feasibility and safety of performing partial and radical nephrectomy with same-day discharge in select cases, “this topic has not been addressed on a national level,” Mr. Garden said.
Few patients who have partial or radical nephrectomies have same-day discharges. The researchers found that fewer than 1% of patients who have either procedure in the sample studied were discharged the same day.
Researchers used the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database, a nationally representative deidentified database that prospectively tracks patient characteristics and 30-day perioperative outcomes for major inpatient and outpatient surgical procedures at more than 700 hospitals.
They extracted all minimally invasive partial and radical nephrectomies from 2012 to 2019 and refined the cohort to 28,140 patients who were theoretically eligible for same-day discharge: Of those, 237 (0.8%) had SSD, and 27,903 (99.2%) had a standard-length discharge (SLD).
The team found that there were no differences in 30-day complications or readmissions between same-day discharge (Clavien-Dindo [CD] I/II, 4.22%; CD III, 0%; CD IV, 1.27%; readmission, 4.64%); and SLD (CD I/II, 4.11%; CD III, 0.95%; CD IV, 0.79%; readmission, 3.90%; all P > .05).
Controlling for demographic and clinical variables, SDD was not associated with greater risk of 30-day complications or readmissions (CD I/II: odds ratio, 1.08; 95% confidence interval, 0.57-2.048; P = .813; CD IV: OR 1.699; 95% CI, 0.537-5.375; P = .367; readmission: OR, 1.254; 95% CI, 0.681-2.31; P = .467).
Mr. Garden and coauthors report no relevant financial relationships.
Dr. Lane reports no relevant financial relationships.
Urologist Ronney Abaza, MD, a robotic surgery specialist in Dublin, Ohio, and colleagues, reviewed robotic surgeries at their hospital during COVID-19 restrictions on surgery in Ohio between March 17 and June 5, 2020, and compared them with robotic procedures before COVID-19 and after restrictions were lifted. They published their results in Urology.
Since 2016, the hospital has offered the option of same-day discharge (SDD) to all robotic urologic surgery patients, regardless of procedure or patient-specific factors.
Among patients who had surgery during COVID-19 restrictions, 98% (87/89 patients) opted for SDD versus 52% in the group having surgery before the restrictions (P < .00001). After the COVID-19 surgery restrictions were lifted, the higher rate of SDD remained at 98%.
“There were no differences in 30-day complications or readmissions between SDD and overnight patients,” the authors write.
The right patient, the right motivation for successful surgery
Brian Lane, MD, PhD, a urologic oncologist with Spectrum Health in Grand Rapids, Michigan, told this news organization that, for nephrectomies, uptake of same-day discharge will continue to be slow.
“You have to have the right patient, the right patient motivation, and the surgery has to go smoothly,” he said. “If you start sending everyone home the same day, you will certainly see readmissions,” he said.
Dr. Lane is part of the Michigan Urologic Surgery Improvement Collaborative and he said the group recently looked at same-day discharge outcomes after robotic prostatectomies with SDD as compared with 1-2 nights in the hospital.
The work has not yet been published but, “There was a slight signal that there were increased readmissions with same-day discharge vs. 0-1 day,” he said.
A paper on outcomes of same-day discharge in total knee arthroplasty in the Journal of Bone & Joint Surgery found a higher risk of perioperative complications “including component failure, surgical site infection, knee stiffness, and deep vein thrombosis.” Researchers compared outcomes between 4,391 patients who underwent outpatient TKA and 128,951 patients who underwent inpatient TKA.
But for other many surgeries, same-day discharge numbers are increasing without worsening outcomes.
A paper in the Journal of Robotic Surgery found that same-day discharge following robotic-assisted endometrial cancer staging is “safe and feasible.”
Stephen Bradley, MD, MPH, with the Minneapolis Heart Institute in Minneapolis, and colleagues write in the Journal of the American College of Cardiology: Cardiovascular Interventions that they found a large increase in the use of same-day discharge after elective percutaneous coronary intervention (PCI) was not associated with worse 30-day mortality rates or readmission.
In that study, 114,461 patients were discharged the same day they underwent PCI. The proportion of patients who had a same-day discharge increased from 4.5% in 2009 to 28.6% in the fourth quarter of 2017.
Risk-adjusted 30-day mortality did not change in that time, while risk-adjusted rehospitalization decreased over time and more quickly when patients had same-day discharge.
Deepak L. Bhatt, MD, MPH, and Jonathan G. Sung, MBCHB, both of Brigham and Women’s Hospital Heart & Vascular Center, Harvard Medical School, Boston, wrote in an accompanying article that, “Advances in the devices and techniques of PCI have improved the safety and efficacy of the procedure. In selected patients, same-day discharge has become possible, and overnight in-hospital observation can be avoided. By reducing unnecessary hospital stays, both patients and hospitals could benefit.”
Evan Garden, a medical student at Icahn School of Medicine at Mount Sinai in New York, presented findings at the American Urological Association 2021 annual meeting that show patients selected for same-day discharge after partial or radical nephrectomy did not have increased rates of postoperative complications or readmissions in the immediate postoperative period, compared with standard discharge of 1-3 days.
Case studies in nephrectomy
While several case studies have looked at the feasibility and safety of performing partial and radical nephrectomy with same-day discharge in select cases, “this topic has not been addressed on a national level,” Mr. Garden said.
Few patients who have partial or radical nephrectomies have same-day discharges. The researchers found that fewer than 1% of patients who have either procedure in the sample studied were discharged the same day.
Researchers used the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database, a nationally representative deidentified database that prospectively tracks patient characteristics and 30-day perioperative outcomes for major inpatient and outpatient surgical procedures at more than 700 hospitals.
They extracted all minimally invasive partial and radical nephrectomies from 2012 to 2019 and refined the cohort to 28,140 patients who were theoretically eligible for same-day discharge: Of those, 237 (0.8%) had SSD, and 27,903 (99.2%) had a standard-length discharge (SLD).
The team found that there were no differences in 30-day complications or readmissions between same-day discharge (Clavien-Dindo [CD] I/II, 4.22%; CD III, 0%; CD IV, 1.27%; readmission, 4.64%); and SLD (CD I/II, 4.11%; CD III, 0.95%; CD IV, 0.79%; readmission, 3.90%; all P > .05).
Controlling for demographic and clinical variables, SDD was not associated with greater risk of 30-day complications or readmissions (CD I/II: odds ratio, 1.08; 95% confidence interval, 0.57-2.048; P = .813; CD IV: OR 1.699; 95% CI, 0.537-5.375; P = .367; readmission: OR, 1.254; 95% CI, 0.681-2.31; P = .467).
Mr. Garden and coauthors report no relevant financial relationships.
Dr. Lane reports no relevant financial relationships.
Evaluating phantom hCG and low-level hCG elevations in the nonpregnant patient
A human chorionic gonadotropin (hCG) test is commonly ordered by gynecologists prior to surgical procedures, in the workup of bleeding abnormalities, and in the follow-up of ectopic and molar pregnancies, to name a few indications. In doing so, occasionally clinicians will find themselves in the diagnostic dilemma of discovering an inexplicable low-level elevation in hCG, such as in a postmenopausal patient. This clinical picture can be confusing and can be concerning for conditions such as postmolar gestational trophoblastic neoplasia (GTN). However, there can be benign causes of this phenomenon.1 To prevent unnecessary worry, investigation of treatments is important. In fact, misdiagnosis and inappropriate treatment of benign, low-level hCG levels with unnecessary chemotherapy is problematic mismanagement of gestational trophoblastic disease (GTD), and a major cause of litigation.
Human chorionic gonadotropin is a glycoprotein hormone with two subunits (alpha and beta). It can come from multiple sources, including trophoblastic cells, malignant trophoblastic cells, the pituitary gland, and exogenous sources.1 Its alpha-subunit is identical to that of follicle stimulating hormone (FSH), luteinizing hormone (LH), and thyroid-stimulating hormone (TSH). Its beta-subunit is unique, though very similar to that of LH. The free hCG beta subunit can be produced by nontrophoblastic neoplasms. The gene for the beta subunit of hCG is in close proximity to the beta subunit of LH and increases in gonadotropin-releasing hormone (GnRH) in menopause can result in the stimulation of both genes. Understanding the sources of hCG-like glycoproteins and mechanisms for testing is important when considering possible causes for falsely elevated hCG.
Most commercially available serum hCG assays detect normal intact hCG and free beta subunits. They are typically sandwich assays utilizing antibody binding sites in which a solid-phase anti-hCG antibody to a specific hCG target is then mixed with the patient’s serum, trapping or binding the hCG, which is then treated with an indicator antibody. After being washed with the indicator or “capture” antibody, its relative (quantitative) levels can be measured.1
Urine hCG testing (such as urine pregnancy tests) work through capillary action, drawing the patient’s urine across absorbent pads before reaching a pad which contains anti-hCG antibodies (the detection zone) in the test line. These tests are less sensitive than serum tests, but many can detect hCG levels <15-20 mIU/mL.1
When ob.gyns. are asked to consult on or evaluate persistently low-level elevations of hCG in nonpregnant patients they should consider both malignant and nonmalignant etiologies. Malignant causes include GTN or quiescent GTD (e.g., after treatment of a molar pregnancy or GTN), choriocarcinoma (e.g., ovarian germ cell tumors), and nonchoriocarcinoma malignancies (such as cervical, pancreatic, breast, renal). Nonmalignant causes of hCG elevations in nonpregnant patients include pituitary hCG (in postmenopausal patients), exogenous hCG, and phantom hCG.
The first step in diagnostic workup is to perform a urine pregnancy test. Provided that the serum hCG level is > 20 mIU/mL, the urine HCG should be positive unless the cause of elevated levels is “phantom hCG” from heterophilic antibodies. When patients are exposed to animal antigens (such as in vaccines) they can develop antibodies such as human anti-mouse antibody. These antibodies have affinity to the binding antibodies used in many hCG sandwich assays and form a linkage between the solid phase antibody and the detection antibody creating a false-positive result. This false-positive test is only present in serum testing but not urine tests because the patient’s heterophilic antibodies are not excreted by the kidney and thus not available to create a false-positive result. An alternative method to make the diagnosis of phantom hCG is to request that the hCG testing be run at a different lab with a different assay (which may not react with the same affinity to the patient’s anti-animal heterophile antibodies), or to request that the lab perform serial dilutions. If phantom hCG from heterophile antibodies is at play, serial dilutions will result in a nonlinear dilution response.
If the patient’s urine hCG test is positive, then pregnancy should be ruled out with a transvaginal ultrasound. If negative, an ectopic pregnancy should still be considered (unless not medically plausible, such as in postmenopausal women or women who have undergone hysterectomy). In the absence of an intrauterine or ectopic pregnancy, a positive serum and urine pregnancy test could be from exogenous hCG, from malignancy or pituitary hCG. Use of exogenous hCG can be ruled out by taking a thorough history, with particular focus on asking about weight loss medications and muscle building therapies.
If pregnancy and exogenous hCG are ruled out, clinicians should assess for an occult hCG-secreting malignancy. The lab should be asked to measure the proportion of the free beta subunit of hCG, as this is typically what is secreted by malignancies. CT imaging of the chest, abdomen, and pelvis to search for an occult primary tumor should take place. If the patient has been recently treated for molar pregnancy or GTN, and serum hCG levels reside between 100 and 300 mIU/mL, quiescent GTD should be considered the diagnosis. Determination of the proportion of hyperglycosylated hCG to total hCG can help differentiate active choriocarcinoma from quiescent GTD. After restaging imaging has been done to confirm no measurable metastatic foci, observation can follow with monthly hCG measurements. The majority of these cases will eventually resolve without intervention within a year. Quiescent GTD and persistent low-level HCG in the absence of measurable GTN on imaging or symptoms does not require treatment with chemotherapy or hysterectomy, particularly in women who desire future fertility.2
Once occult malignancy has been ruled out, the remaining potential source of hCG is the pituitary gland. As mentioned earlier, hCG shares its morphology with TSH, LH, and FSH. This can result in cross reactivity and false positives. In the menopausal state, GnRH levels increase and thus so do pituitary LH and hCG levels. To confirm that the pituitary is the source of the low-level hCG levels, the provider should prescribe a course of hormonal treatment such as an oral contraceptive pill for a 2- to 3-month period. This should result in suppression of pituitary hCG, and serum hCG levels, as part of a negative feedback loop. Pituitary source of hCG is a benign condition, and, like quiescent GTD, phantom hCG or exogenous hCG does not require intervention.
Getting to the bottom of persistent low-level hCG elevations can be challenging. By following the step-wise algorithm listed here, clinicians can sequentially test for urine hCG, heterophilic antibodies, elevated free beta-subunit, occult malignancy, and pituitary hCG.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest. Email her at [email protected].
References
1. Oyatogun O et al. Ther Adv Reprod Health 2021 Jun 13. doi: 10.1177/2F26334941211016412.
2. Soper JT. Obstet Gynecol. 2021 Feb 1;137(2):355-70.
A human chorionic gonadotropin (hCG) test is commonly ordered by gynecologists prior to surgical procedures, in the workup of bleeding abnormalities, and in the follow-up of ectopic and molar pregnancies, to name a few indications. In doing so, occasionally clinicians will find themselves in the diagnostic dilemma of discovering an inexplicable low-level elevation in hCG, such as in a postmenopausal patient. This clinical picture can be confusing and can be concerning for conditions such as postmolar gestational trophoblastic neoplasia (GTN). However, there can be benign causes of this phenomenon.1 To prevent unnecessary worry, investigation of treatments is important. In fact, misdiagnosis and inappropriate treatment of benign, low-level hCG levels with unnecessary chemotherapy is problematic mismanagement of gestational trophoblastic disease (GTD), and a major cause of litigation.
Human chorionic gonadotropin is a glycoprotein hormone with two subunits (alpha and beta). It can come from multiple sources, including trophoblastic cells, malignant trophoblastic cells, the pituitary gland, and exogenous sources.1 Its alpha-subunit is identical to that of follicle stimulating hormone (FSH), luteinizing hormone (LH), and thyroid-stimulating hormone (TSH). Its beta-subunit is unique, though very similar to that of LH. The free hCG beta subunit can be produced by nontrophoblastic neoplasms. The gene for the beta subunit of hCG is in close proximity to the beta subunit of LH and increases in gonadotropin-releasing hormone (GnRH) in menopause can result in the stimulation of both genes. Understanding the sources of hCG-like glycoproteins and mechanisms for testing is important when considering possible causes for falsely elevated hCG.
Most commercially available serum hCG assays detect normal intact hCG and free beta subunits. They are typically sandwich assays utilizing antibody binding sites in which a solid-phase anti-hCG antibody to a specific hCG target is then mixed with the patient’s serum, trapping or binding the hCG, which is then treated with an indicator antibody. After being washed with the indicator or “capture” antibody, its relative (quantitative) levels can be measured.1
Urine hCG testing (such as urine pregnancy tests) work through capillary action, drawing the patient’s urine across absorbent pads before reaching a pad which contains anti-hCG antibodies (the detection zone) in the test line. These tests are less sensitive than serum tests, but many can detect hCG levels <15-20 mIU/mL.1
When ob.gyns. are asked to consult on or evaluate persistently low-level elevations of hCG in nonpregnant patients they should consider both malignant and nonmalignant etiologies. Malignant causes include GTN or quiescent GTD (e.g., after treatment of a molar pregnancy or GTN), choriocarcinoma (e.g., ovarian germ cell tumors), and nonchoriocarcinoma malignancies (such as cervical, pancreatic, breast, renal). Nonmalignant causes of hCG elevations in nonpregnant patients include pituitary hCG (in postmenopausal patients), exogenous hCG, and phantom hCG.
The first step in diagnostic workup is to perform a urine pregnancy test. Provided that the serum hCG level is > 20 mIU/mL, the urine HCG should be positive unless the cause of elevated levels is “phantom hCG” from heterophilic antibodies. When patients are exposed to animal antigens (such as in vaccines) they can develop antibodies such as human anti-mouse antibody. These antibodies have affinity to the binding antibodies used in many hCG sandwich assays and form a linkage between the solid phase antibody and the detection antibody creating a false-positive result. This false-positive test is only present in serum testing but not urine tests because the patient’s heterophilic antibodies are not excreted by the kidney and thus not available to create a false-positive result. An alternative method to make the diagnosis of phantom hCG is to request that the hCG testing be run at a different lab with a different assay (which may not react with the same affinity to the patient’s anti-animal heterophile antibodies), or to request that the lab perform serial dilutions. If phantom hCG from heterophile antibodies is at play, serial dilutions will result in a nonlinear dilution response.
If the patient’s urine hCG test is positive, then pregnancy should be ruled out with a transvaginal ultrasound. If negative, an ectopic pregnancy should still be considered (unless not medically plausible, such as in postmenopausal women or women who have undergone hysterectomy). In the absence of an intrauterine or ectopic pregnancy, a positive serum and urine pregnancy test could be from exogenous hCG, from malignancy or pituitary hCG. Use of exogenous hCG can be ruled out by taking a thorough history, with particular focus on asking about weight loss medications and muscle building therapies.
If pregnancy and exogenous hCG are ruled out, clinicians should assess for an occult hCG-secreting malignancy. The lab should be asked to measure the proportion of the free beta subunit of hCG, as this is typically what is secreted by malignancies. CT imaging of the chest, abdomen, and pelvis to search for an occult primary tumor should take place. If the patient has been recently treated for molar pregnancy or GTN, and serum hCG levels reside between 100 and 300 mIU/mL, quiescent GTD should be considered the diagnosis. Determination of the proportion of hyperglycosylated hCG to total hCG can help differentiate active choriocarcinoma from quiescent GTD. After restaging imaging has been done to confirm no measurable metastatic foci, observation can follow with monthly hCG measurements. The majority of these cases will eventually resolve without intervention within a year. Quiescent GTD and persistent low-level HCG in the absence of measurable GTN on imaging or symptoms does not require treatment with chemotherapy or hysterectomy, particularly in women who desire future fertility.2
Once occult malignancy has been ruled out, the remaining potential source of hCG is the pituitary gland. As mentioned earlier, hCG shares its morphology with TSH, LH, and FSH. This can result in cross reactivity and false positives. In the menopausal state, GnRH levels increase and thus so do pituitary LH and hCG levels. To confirm that the pituitary is the source of the low-level hCG levels, the provider should prescribe a course of hormonal treatment such as an oral contraceptive pill for a 2- to 3-month period. This should result in suppression of pituitary hCG, and serum hCG levels, as part of a negative feedback loop. Pituitary source of hCG is a benign condition, and, like quiescent GTD, phantom hCG or exogenous hCG does not require intervention.
Getting to the bottom of persistent low-level hCG elevations can be challenging. By following the step-wise algorithm listed here, clinicians can sequentially test for urine hCG, heterophilic antibodies, elevated free beta-subunit, occult malignancy, and pituitary hCG.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest. Email her at [email protected].
References
1. Oyatogun O et al. Ther Adv Reprod Health 2021 Jun 13. doi: 10.1177/2F26334941211016412.
2. Soper JT. Obstet Gynecol. 2021 Feb 1;137(2):355-70.
A human chorionic gonadotropin (hCG) test is commonly ordered by gynecologists prior to surgical procedures, in the workup of bleeding abnormalities, and in the follow-up of ectopic and molar pregnancies, to name a few indications. In doing so, occasionally clinicians will find themselves in the diagnostic dilemma of discovering an inexplicable low-level elevation in hCG, such as in a postmenopausal patient. This clinical picture can be confusing and can be concerning for conditions such as postmolar gestational trophoblastic neoplasia (GTN). However, there can be benign causes of this phenomenon.1 To prevent unnecessary worry, investigation of treatments is important. In fact, misdiagnosis and inappropriate treatment of benign, low-level hCG levels with unnecessary chemotherapy is problematic mismanagement of gestational trophoblastic disease (GTD), and a major cause of litigation.
Human chorionic gonadotropin is a glycoprotein hormone with two subunits (alpha and beta). It can come from multiple sources, including trophoblastic cells, malignant trophoblastic cells, the pituitary gland, and exogenous sources.1 Its alpha-subunit is identical to that of follicle stimulating hormone (FSH), luteinizing hormone (LH), and thyroid-stimulating hormone (TSH). Its beta-subunit is unique, though very similar to that of LH. The free hCG beta subunit can be produced by nontrophoblastic neoplasms. The gene for the beta subunit of hCG is in close proximity to the beta subunit of LH and increases in gonadotropin-releasing hormone (GnRH) in menopause can result in the stimulation of both genes. Understanding the sources of hCG-like glycoproteins and mechanisms for testing is important when considering possible causes for falsely elevated hCG.
Most commercially available serum hCG assays detect normal intact hCG and free beta subunits. They are typically sandwich assays utilizing antibody binding sites in which a solid-phase anti-hCG antibody to a specific hCG target is then mixed with the patient’s serum, trapping or binding the hCG, which is then treated with an indicator antibody. After being washed with the indicator or “capture” antibody, its relative (quantitative) levels can be measured.1
Urine hCG testing (such as urine pregnancy tests) work through capillary action, drawing the patient’s urine across absorbent pads before reaching a pad which contains anti-hCG antibodies (the detection zone) in the test line. These tests are less sensitive than serum tests, but many can detect hCG levels <15-20 mIU/mL.1
When ob.gyns. are asked to consult on or evaluate persistently low-level elevations of hCG in nonpregnant patients they should consider both malignant and nonmalignant etiologies. Malignant causes include GTN or quiescent GTD (e.g., after treatment of a molar pregnancy or GTN), choriocarcinoma (e.g., ovarian germ cell tumors), and nonchoriocarcinoma malignancies (such as cervical, pancreatic, breast, renal). Nonmalignant causes of hCG elevations in nonpregnant patients include pituitary hCG (in postmenopausal patients), exogenous hCG, and phantom hCG.
The first step in diagnostic workup is to perform a urine pregnancy test. Provided that the serum hCG level is > 20 mIU/mL, the urine HCG should be positive unless the cause of elevated levels is “phantom hCG” from heterophilic antibodies. When patients are exposed to animal antigens (such as in vaccines) they can develop antibodies such as human anti-mouse antibody. These antibodies have affinity to the binding antibodies used in many hCG sandwich assays and form a linkage between the solid phase antibody and the detection antibody creating a false-positive result. This false-positive test is only present in serum testing but not urine tests because the patient’s heterophilic antibodies are not excreted by the kidney and thus not available to create a false-positive result. An alternative method to make the diagnosis of phantom hCG is to request that the hCG testing be run at a different lab with a different assay (which may not react with the same affinity to the patient’s anti-animal heterophile antibodies), or to request that the lab perform serial dilutions. If phantom hCG from heterophile antibodies is at play, serial dilutions will result in a nonlinear dilution response.
If the patient’s urine hCG test is positive, then pregnancy should be ruled out with a transvaginal ultrasound. If negative, an ectopic pregnancy should still be considered (unless not medically plausible, such as in postmenopausal women or women who have undergone hysterectomy). In the absence of an intrauterine or ectopic pregnancy, a positive serum and urine pregnancy test could be from exogenous hCG, from malignancy or pituitary hCG. Use of exogenous hCG can be ruled out by taking a thorough history, with particular focus on asking about weight loss medications and muscle building therapies.
If pregnancy and exogenous hCG are ruled out, clinicians should assess for an occult hCG-secreting malignancy. The lab should be asked to measure the proportion of the free beta subunit of hCG, as this is typically what is secreted by malignancies. CT imaging of the chest, abdomen, and pelvis to search for an occult primary tumor should take place. If the patient has been recently treated for molar pregnancy or GTN, and serum hCG levels reside between 100 and 300 mIU/mL, quiescent GTD should be considered the diagnosis. Determination of the proportion of hyperglycosylated hCG to total hCG can help differentiate active choriocarcinoma from quiescent GTD. After restaging imaging has been done to confirm no measurable metastatic foci, observation can follow with monthly hCG measurements. The majority of these cases will eventually resolve without intervention within a year. Quiescent GTD and persistent low-level HCG in the absence of measurable GTN on imaging or symptoms does not require treatment with chemotherapy or hysterectomy, particularly in women who desire future fertility.2
Once occult malignancy has been ruled out, the remaining potential source of hCG is the pituitary gland. As mentioned earlier, hCG shares its morphology with TSH, LH, and FSH. This can result in cross reactivity and false positives. In the menopausal state, GnRH levels increase and thus so do pituitary LH and hCG levels. To confirm that the pituitary is the source of the low-level hCG levels, the provider should prescribe a course of hormonal treatment such as an oral contraceptive pill for a 2- to 3-month period. This should result in suppression of pituitary hCG, and serum hCG levels, as part of a negative feedback loop. Pituitary source of hCG is a benign condition, and, like quiescent GTD, phantom hCG or exogenous hCG does not require intervention.
Getting to the bottom of persistent low-level hCG elevations can be challenging. By following the step-wise algorithm listed here, clinicians can sequentially test for urine hCG, heterophilic antibodies, elevated free beta-subunit, occult malignancy, and pituitary hCG.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest. Email her at [email protected].
References
1. Oyatogun O et al. Ther Adv Reprod Health 2021 Jun 13. doi: 10.1177/2F26334941211016412.
2. Soper JT. Obstet Gynecol. 2021 Feb 1;137(2):355-70.
Antibiotic and glucocorticoid use before cancer therapy could have detrimental effect on outcomes
“Our results confirm the detrimental impact on oncological outcomes of antibiotics and glucocorticoids at a dosage ≥10 mg/day when given within 1 month before or after ICI onset,” Marie Kostine, MD, of Bordeaux (France) University Hospital, and colleagues wrote in the European Journal of Cancer. “Moreover, we show that other comedications may significantly alter the antitumoral response of ICI, such as proton pump inhibitors, psychotropic drugs, morphine, aspirin, and insulin, whereas others seem to have no impact.”
While immune checkpoint inhibitors are transforming the treatment of advanced cancers, gut microbiota composition is an important determinant of response to ICIs. Antibiotic treatments are known to alter the gut microbiota. Other drugs, such as proton pump inhibitors, antidiabetic agents, aspirin, NSAIDs, glucocorticoids, immunomodulators, psychotropic drugs, and analgesics, have been associated with changes in microbiome composition. Since many patients with advanced cancer are exposed to such drugs, this study looked at the possible influence of these comedications on the antitumor effect and safety of ICIs.
The observational study included 635 patients with advanced cancer treated with ICIs between May 2015 and September 2017. Comedications given within 1 month before or 1 month after the first administration of an ICI were reviewed from medical records. Psychotropic drugs, proton pump inhibitors, ACE inhibitors and/or angiotensin II receptor blockers (ARBs), glucocorticoids, antibiotics, statins, and morphine were the most prescribed comedications.
Baseline use of antibiotics, glucocorticoids greater than 10 mg/day, proton pump inhibitors, psychotropic drugs, morphine, and insulin was associated with decreased overall survival and tumor response. However, the coadministration of statins, ACE inhibitors and/or ARBs, NSAIDs, aspirin, and oral diabetes drugs did not impact patient outcomes. Additionally, treatments that altered the response to ICIs were associated with a decreased incidence of immune-related adverse events.
“These results suggest some practical advice in a patient candidate to ICIs,” the authors wrote. “First, antibiotic treatment should be limited to documented infections,” and “withdrawal of proton pump inhibitors and psychotropic drugs should be considered.
“Regarding baseline glucocorticoids use, the cutoff of 10 mg/day should be respected, considering the deleterious effect of higher dosage. Moreover, because of the lack of impact of inhaled or topical glucocorticoids, local routes should be preferred,” the authors wrote. “Conversely, our study brings reassuring data regarding the use of glucocorticoids for the management of immune-related adverse events, which did not alter ICI efficacy, confirming previous reports.”
The authors noted that the observational nature of the study does not allow any causal conclusion, adding that it remains unknown whether the effect of comedications “on cancer outcomes is thoroughly mediated by changes in microbiota or other immunomodulatory properties.”
Along with the retrospective design, study limitations included reporting bias and missing data on baseline comedications, specific prognostic factors and cancer outcomes.
The authors noted no conflicts of interest.
“Our results confirm the detrimental impact on oncological outcomes of antibiotics and glucocorticoids at a dosage ≥10 mg/day when given within 1 month before or after ICI onset,” Marie Kostine, MD, of Bordeaux (France) University Hospital, and colleagues wrote in the European Journal of Cancer. “Moreover, we show that other comedications may significantly alter the antitumoral response of ICI, such as proton pump inhibitors, psychotropic drugs, morphine, aspirin, and insulin, whereas others seem to have no impact.”
While immune checkpoint inhibitors are transforming the treatment of advanced cancers, gut microbiota composition is an important determinant of response to ICIs. Antibiotic treatments are known to alter the gut microbiota. Other drugs, such as proton pump inhibitors, antidiabetic agents, aspirin, NSAIDs, glucocorticoids, immunomodulators, psychotropic drugs, and analgesics, have been associated with changes in microbiome composition. Since many patients with advanced cancer are exposed to such drugs, this study looked at the possible influence of these comedications on the antitumor effect and safety of ICIs.
The observational study included 635 patients with advanced cancer treated with ICIs between May 2015 and September 2017. Comedications given within 1 month before or 1 month after the first administration of an ICI were reviewed from medical records. Psychotropic drugs, proton pump inhibitors, ACE inhibitors and/or angiotensin II receptor blockers (ARBs), glucocorticoids, antibiotics, statins, and morphine were the most prescribed comedications.
Baseline use of antibiotics, glucocorticoids greater than 10 mg/day, proton pump inhibitors, psychotropic drugs, morphine, and insulin was associated with decreased overall survival and tumor response. However, the coadministration of statins, ACE inhibitors and/or ARBs, NSAIDs, aspirin, and oral diabetes drugs did not impact patient outcomes. Additionally, treatments that altered the response to ICIs were associated with a decreased incidence of immune-related adverse events.
“These results suggest some practical advice in a patient candidate to ICIs,” the authors wrote. “First, antibiotic treatment should be limited to documented infections,” and “withdrawal of proton pump inhibitors and psychotropic drugs should be considered.
“Regarding baseline glucocorticoids use, the cutoff of 10 mg/day should be respected, considering the deleterious effect of higher dosage. Moreover, because of the lack of impact of inhaled or topical glucocorticoids, local routes should be preferred,” the authors wrote. “Conversely, our study brings reassuring data regarding the use of glucocorticoids for the management of immune-related adverse events, which did not alter ICI efficacy, confirming previous reports.”
The authors noted that the observational nature of the study does not allow any causal conclusion, adding that it remains unknown whether the effect of comedications “on cancer outcomes is thoroughly mediated by changes in microbiota or other immunomodulatory properties.”
Along with the retrospective design, study limitations included reporting bias and missing data on baseline comedications, specific prognostic factors and cancer outcomes.
The authors noted no conflicts of interest.
“Our results confirm the detrimental impact on oncological outcomes of antibiotics and glucocorticoids at a dosage ≥10 mg/day when given within 1 month before or after ICI onset,” Marie Kostine, MD, of Bordeaux (France) University Hospital, and colleagues wrote in the European Journal of Cancer. “Moreover, we show that other comedications may significantly alter the antitumoral response of ICI, such as proton pump inhibitors, psychotropic drugs, morphine, aspirin, and insulin, whereas others seem to have no impact.”
While immune checkpoint inhibitors are transforming the treatment of advanced cancers, gut microbiota composition is an important determinant of response to ICIs. Antibiotic treatments are known to alter the gut microbiota. Other drugs, such as proton pump inhibitors, antidiabetic agents, aspirin, NSAIDs, glucocorticoids, immunomodulators, psychotropic drugs, and analgesics, have been associated with changes in microbiome composition. Since many patients with advanced cancer are exposed to such drugs, this study looked at the possible influence of these comedications on the antitumor effect and safety of ICIs.
The observational study included 635 patients with advanced cancer treated with ICIs between May 2015 and September 2017. Comedications given within 1 month before or 1 month after the first administration of an ICI were reviewed from medical records. Psychotropic drugs, proton pump inhibitors, ACE inhibitors and/or angiotensin II receptor blockers (ARBs), glucocorticoids, antibiotics, statins, and morphine were the most prescribed comedications.
Baseline use of antibiotics, glucocorticoids greater than 10 mg/day, proton pump inhibitors, psychotropic drugs, morphine, and insulin was associated with decreased overall survival and tumor response. However, the coadministration of statins, ACE inhibitors and/or ARBs, NSAIDs, aspirin, and oral diabetes drugs did not impact patient outcomes. Additionally, treatments that altered the response to ICIs were associated with a decreased incidence of immune-related adverse events.
“These results suggest some practical advice in a patient candidate to ICIs,” the authors wrote. “First, antibiotic treatment should be limited to documented infections,” and “withdrawal of proton pump inhibitors and psychotropic drugs should be considered.
“Regarding baseline glucocorticoids use, the cutoff of 10 mg/day should be respected, considering the deleterious effect of higher dosage. Moreover, because of the lack of impact of inhaled or topical glucocorticoids, local routes should be preferred,” the authors wrote. “Conversely, our study brings reassuring data regarding the use of glucocorticoids for the management of immune-related adverse events, which did not alter ICI efficacy, confirming previous reports.”
The authors noted that the observational nature of the study does not allow any causal conclusion, adding that it remains unknown whether the effect of comedications “on cancer outcomes is thoroughly mediated by changes in microbiota or other immunomodulatory properties.”
Along with the retrospective design, study limitations included reporting bias and missing data on baseline comedications, specific prognostic factors and cancer outcomes.
The authors noted no conflicts of interest.
FROM THE EUROPEAN JOURNAL OF CANCER