User login
VTEs tied to immune checkpoint inhibitor cancer treatment
Cancer patients who receive an immune checkpoint inhibitor have more than a doubled rate of venous thromboembolism during the subsequent 2 years, compared with their rate during the 2 years before treatment, according to a retrospective analysis of more than 2,800 patients treated at a single U.S. center.
The study focused on cancer patients treated with an immune checkpoint inhibitor (ICI) at Massachusetts General Hospital in Boston. It showed that during the 2 years prior to treatment with any type of ICI, the incidence of venous thromboembolic events (VTE) was 4.85/100 patient-years that then jumped to 11.75/100 patient-years during the 2 years following treatment. This translated into an incidence rate ratio of 2.43 during posttreatment follow-up, compared with pretreatment, Jingyi Gong, MD, said at the virtual American Heart Association scientific sessions.
The increased VTE rate resulted from rises in both the rate of deep vein thrombosis, which had an IRR of 3.23 during the posttreatment period, and for pulmonary embolism, which showed an IRR of 2.24, said Dr. Gong, a physician at Brigham and Women’s Hospital in Boston. She hypothesized that this effect may result from a procoagulant effect of the immune activation and inflammation triggered by ICIs.
Hypothesis-generating results
Cardiologists cautioned that these findings should only be considered hypothesis generating, but raise an important alert for clinicians to have heightened awareness of the potential for VTE following ICI treatment.
“A clear message is to be aware that there is this signal, and be vigilant for patients who might present with VTE following ICI treatment,” commented Richard J. Kovacs, MD, a cardiologist and professor at Indiana University, Indianapolis. The data that Dr. Gong reported are “moderately convincing,” he added in an interview.
“Awareness that patients who receive ICI may be at increased VTE risk is very important,” agreed Umberto Campia, MD, a cardiologist, vascular specialist, and member of the cardio-oncology group at Brigham and Women’s Hospital, who was not involved in the new study.
The potential impact of ICI treatment on VTE risk is slowly emerging, added Dr. Campia. Until recently, the literature primarily was case reports, but recently another retrospective, single-center study came out that reported a 13% incidence of VTE in cancer patients following ICI treatment. On the other hand, a recently published meta-analysis of more than 20,000 patients from 68 ICI studies failed to find a suggestion of increased VTE incidence following ICI interventions.
Attempting to assess the impact of treatment on VTE risk in cancer patients is challenging because cancer itself boosts the risk. Recommendations on the use of VTE prophylaxis in cancer patients most recently came out in 2014 from the American Society of Clinical Oncology, which said that VTE prophylaxis for ambulatory cancer patients “may be considered for highly select high-risk patients.” The impact of cancer therapy on VTE risk and the need for prophylaxis is usually assessed by applying the Khorana score, Dr. Campia said in an interview.
VTE spikes acutely after ICI treatment
Dr. Gong analyzed VTE incidence rates by time during the total 4-year period studied, and found that the rate gradually and steadily rose with time throughout the 2 years preceding treatment, spiked immediately following ICI treatment, and then gradually and steadily fell back to roughly the rate seen just before treatment, reaching that level about a year after treatment. She ran a sensitivity analysis that excluded patients who died during the first year following their ICI treatment, and in this calculation an acute spike in VTE following ICI treatment still occurred but with reduced magnitude.
She also reported the results of several subgroup analyses. The IRRs remained consistent among women and men, among patients who were aged over or under 65 years, and regardless of cancer type or treatment with corticosteroids. But the subgroup analyses identified two parameters that seemed to clearly split VTE rates.
Among patients on treatment with an anticoagulant agent at the time of their ICI treatment, roughly 10% of the patients, the IRR was 0.56, compared with a ratio of 3.86 among the other patients, suggesting possible protection. A second factor that seemed linked with VTE incidence was the number of ICI treatment cycles a patient received. Those who received more than five cycles had a risk ratio of 3.95, while those who received five or fewer cycles had a RR of 1.66.
Her analysis included 2,842 cancer patients who received treatment with an ICI at Massachusetts General Hospital. Patients averaged 64 years of age, slightly more than half were men, and 13% had a prior history of VTE. Patients received an average of 5 ICI treatment cycles, but a quarter of the patients received more than 10 cycles.
During the 2-year follow-up, 244 patients (9%) developed VTE. The patients who developed VTE were significantly younger than those who did not, with an average age of 63 years, compared with 65. And the patients who eventually developed VTE had a significantly higher prevalence of prior VTE at 18%, compared with 12% among the patients who stayed VTE free.
The cancer types patients had were non–small cell lung, 29%; melanoma, 28%; head and neck, 12%; renal genitourinary, 6%; and other, 25%. ICIs have been available for routine U.S. practice since 2011. The class includes agents such as pembrolizumab (Keytruda) and durvalumab (Imfinzi).
Researchers would need to perform a prospective, randomized study to determine whether anticoagulant prophylaxis is clearly beneficial for patients receiving ICI treatment, Dr. Gong said. But both Dr. Kovacs and Dr. Campia said that more data on this topic are first needed.
“We need to confirm that treatment with ICI is associated with VTEs. Retrospective data are not definitive,” said Dr. Campia. “We would need to prospectively assess the impact of ICI,” which will not be easy, as it’s quickly become a cornerstone for treating many cancers. “We need to become more familiar with the adverse effects of these drugs. We are still learning about their toxicities.”
The study had no commercial funding. Dr. Gong, Dr. Kovacs, and Dr. Campia had no disclosures.
Cancer patients who receive an immune checkpoint inhibitor have more than a doubled rate of venous thromboembolism during the subsequent 2 years, compared with their rate during the 2 years before treatment, according to a retrospective analysis of more than 2,800 patients treated at a single U.S. center.
The study focused on cancer patients treated with an immune checkpoint inhibitor (ICI) at Massachusetts General Hospital in Boston. It showed that during the 2 years prior to treatment with any type of ICI, the incidence of venous thromboembolic events (VTE) was 4.85/100 patient-years that then jumped to 11.75/100 patient-years during the 2 years following treatment. This translated into an incidence rate ratio of 2.43 during posttreatment follow-up, compared with pretreatment, Jingyi Gong, MD, said at the virtual American Heart Association scientific sessions.
The increased VTE rate resulted from rises in both the rate of deep vein thrombosis, which had an IRR of 3.23 during the posttreatment period, and for pulmonary embolism, which showed an IRR of 2.24, said Dr. Gong, a physician at Brigham and Women’s Hospital in Boston. She hypothesized that this effect may result from a procoagulant effect of the immune activation and inflammation triggered by ICIs.
Hypothesis-generating results
Cardiologists cautioned that these findings should only be considered hypothesis generating, but raise an important alert for clinicians to have heightened awareness of the potential for VTE following ICI treatment.
“A clear message is to be aware that there is this signal, and be vigilant for patients who might present with VTE following ICI treatment,” commented Richard J. Kovacs, MD, a cardiologist and professor at Indiana University, Indianapolis. The data that Dr. Gong reported are “moderately convincing,” he added in an interview.
“Awareness that patients who receive ICI may be at increased VTE risk is very important,” agreed Umberto Campia, MD, a cardiologist, vascular specialist, and member of the cardio-oncology group at Brigham and Women’s Hospital, who was not involved in the new study.
The potential impact of ICI treatment on VTE risk is slowly emerging, added Dr. Campia. Until recently, the literature primarily was case reports, but recently another retrospective, single-center study came out that reported a 13% incidence of VTE in cancer patients following ICI treatment. On the other hand, a recently published meta-analysis of more than 20,000 patients from 68 ICI studies failed to find a suggestion of increased VTE incidence following ICI interventions.
Attempting to assess the impact of treatment on VTE risk in cancer patients is challenging because cancer itself boosts the risk. Recommendations on the use of VTE prophylaxis in cancer patients most recently came out in 2014 from the American Society of Clinical Oncology, which said that VTE prophylaxis for ambulatory cancer patients “may be considered for highly select high-risk patients.” The impact of cancer therapy on VTE risk and the need for prophylaxis is usually assessed by applying the Khorana score, Dr. Campia said in an interview.
VTE spikes acutely after ICI treatment
Dr. Gong analyzed VTE incidence rates by time during the total 4-year period studied, and found that the rate gradually and steadily rose with time throughout the 2 years preceding treatment, spiked immediately following ICI treatment, and then gradually and steadily fell back to roughly the rate seen just before treatment, reaching that level about a year after treatment. She ran a sensitivity analysis that excluded patients who died during the first year following their ICI treatment, and in this calculation an acute spike in VTE following ICI treatment still occurred but with reduced magnitude.
She also reported the results of several subgroup analyses. The IRRs remained consistent among women and men, among patients who were aged over or under 65 years, and regardless of cancer type or treatment with corticosteroids. But the subgroup analyses identified two parameters that seemed to clearly split VTE rates.
Among patients on treatment with an anticoagulant agent at the time of their ICI treatment, roughly 10% of the patients, the IRR was 0.56, compared with a ratio of 3.86 among the other patients, suggesting possible protection. A second factor that seemed linked with VTE incidence was the number of ICI treatment cycles a patient received. Those who received more than five cycles had a risk ratio of 3.95, while those who received five or fewer cycles had a RR of 1.66.
Her analysis included 2,842 cancer patients who received treatment with an ICI at Massachusetts General Hospital. Patients averaged 64 years of age, slightly more than half were men, and 13% had a prior history of VTE. Patients received an average of 5 ICI treatment cycles, but a quarter of the patients received more than 10 cycles.
During the 2-year follow-up, 244 patients (9%) developed VTE. The patients who developed VTE were significantly younger than those who did not, with an average age of 63 years, compared with 65. And the patients who eventually developed VTE had a significantly higher prevalence of prior VTE at 18%, compared with 12% among the patients who stayed VTE free.
The cancer types patients had were non–small cell lung, 29%; melanoma, 28%; head and neck, 12%; renal genitourinary, 6%; and other, 25%. ICIs have been available for routine U.S. practice since 2011. The class includes agents such as pembrolizumab (Keytruda) and durvalumab (Imfinzi).
Researchers would need to perform a prospective, randomized study to determine whether anticoagulant prophylaxis is clearly beneficial for patients receiving ICI treatment, Dr. Gong said. But both Dr. Kovacs and Dr. Campia said that more data on this topic are first needed.
“We need to confirm that treatment with ICI is associated with VTEs. Retrospective data are not definitive,” said Dr. Campia. “We would need to prospectively assess the impact of ICI,” which will not be easy, as it’s quickly become a cornerstone for treating many cancers. “We need to become more familiar with the adverse effects of these drugs. We are still learning about their toxicities.”
The study had no commercial funding. Dr. Gong, Dr. Kovacs, and Dr. Campia had no disclosures.
Cancer patients who receive an immune checkpoint inhibitor have more than a doubled rate of venous thromboembolism during the subsequent 2 years, compared with their rate during the 2 years before treatment, according to a retrospective analysis of more than 2,800 patients treated at a single U.S. center.
The study focused on cancer patients treated with an immune checkpoint inhibitor (ICI) at Massachusetts General Hospital in Boston. It showed that during the 2 years prior to treatment with any type of ICI, the incidence of venous thromboembolic events (VTE) was 4.85/100 patient-years that then jumped to 11.75/100 patient-years during the 2 years following treatment. This translated into an incidence rate ratio of 2.43 during posttreatment follow-up, compared with pretreatment, Jingyi Gong, MD, said at the virtual American Heart Association scientific sessions.
The increased VTE rate resulted from rises in both the rate of deep vein thrombosis, which had an IRR of 3.23 during the posttreatment period, and for pulmonary embolism, which showed an IRR of 2.24, said Dr. Gong, a physician at Brigham and Women’s Hospital in Boston. She hypothesized that this effect may result from a procoagulant effect of the immune activation and inflammation triggered by ICIs.
Hypothesis-generating results
Cardiologists cautioned that these findings should only be considered hypothesis generating, but raise an important alert for clinicians to have heightened awareness of the potential for VTE following ICI treatment.
“A clear message is to be aware that there is this signal, and be vigilant for patients who might present with VTE following ICI treatment,” commented Richard J. Kovacs, MD, a cardiologist and professor at Indiana University, Indianapolis. The data that Dr. Gong reported are “moderately convincing,” he added in an interview.
“Awareness that patients who receive ICI may be at increased VTE risk is very important,” agreed Umberto Campia, MD, a cardiologist, vascular specialist, and member of the cardio-oncology group at Brigham and Women’s Hospital, who was not involved in the new study.
The potential impact of ICI treatment on VTE risk is slowly emerging, added Dr. Campia. Until recently, the literature primarily was case reports, but recently another retrospective, single-center study came out that reported a 13% incidence of VTE in cancer patients following ICI treatment. On the other hand, a recently published meta-analysis of more than 20,000 patients from 68 ICI studies failed to find a suggestion of increased VTE incidence following ICI interventions.
Attempting to assess the impact of treatment on VTE risk in cancer patients is challenging because cancer itself boosts the risk. Recommendations on the use of VTE prophylaxis in cancer patients most recently came out in 2014 from the American Society of Clinical Oncology, which said that VTE prophylaxis for ambulatory cancer patients “may be considered for highly select high-risk patients.” The impact of cancer therapy on VTE risk and the need for prophylaxis is usually assessed by applying the Khorana score, Dr. Campia said in an interview.
VTE spikes acutely after ICI treatment
Dr. Gong analyzed VTE incidence rates by time during the total 4-year period studied, and found that the rate gradually and steadily rose with time throughout the 2 years preceding treatment, spiked immediately following ICI treatment, and then gradually and steadily fell back to roughly the rate seen just before treatment, reaching that level about a year after treatment. She ran a sensitivity analysis that excluded patients who died during the first year following their ICI treatment, and in this calculation an acute spike in VTE following ICI treatment still occurred but with reduced magnitude.
She also reported the results of several subgroup analyses. The IRRs remained consistent among women and men, among patients who were aged over or under 65 years, and regardless of cancer type or treatment with corticosteroids. But the subgroup analyses identified two parameters that seemed to clearly split VTE rates.
Among patients on treatment with an anticoagulant agent at the time of their ICI treatment, roughly 10% of the patients, the IRR was 0.56, compared with a ratio of 3.86 among the other patients, suggesting possible protection. A second factor that seemed linked with VTE incidence was the number of ICI treatment cycles a patient received. Those who received more than five cycles had a risk ratio of 3.95, while those who received five or fewer cycles had a RR of 1.66.
Her analysis included 2,842 cancer patients who received treatment with an ICI at Massachusetts General Hospital. Patients averaged 64 years of age, slightly more than half were men, and 13% had a prior history of VTE. Patients received an average of 5 ICI treatment cycles, but a quarter of the patients received more than 10 cycles.
During the 2-year follow-up, 244 patients (9%) developed VTE. The patients who developed VTE were significantly younger than those who did not, with an average age of 63 years, compared with 65. And the patients who eventually developed VTE had a significantly higher prevalence of prior VTE at 18%, compared with 12% among the patients who stayed VTE free.
The cancer types patients had were non–small cell lung, 29%; melanoma, 28%; head and neck, 12%; renal genitourinary, 6%; and other, 25%. ICIs have been available for routine U.S. practice since 2011. The class includes agents such as pembrolizumab (Keytruda) and durvalumab (Imfinzi).
Researchers would need to perform a prospective, randomized study to determine whether anticoagulant prophylaxis is clearly beneficial for patients receiving ICI treatment, Dr. Gong said. But both Dr. Kovacs and Dr. Campia said that more data on this topic are first needed.
“We need to confirm that treatment with ICI is associated with VTEs. Retrospective data are not definitive,” said Dr. Campia. “We would need to prospectively assess the impact of ICI,” which will not be easy, as it’s quickly become a cornerstone for treating many cancers. “We need to become more familiar with the adverse effects of these drugs. We are still learning about their toxicities.”
The study had no commercial funding. Dr. Gong, Dr. Kovacs, and Dr. Campia had no disclosures.
FROM AHA 2020
Using telehealth to deliver palliative care to cancer patients
Traditional delivery of palliative care to outpatients with cancer is associated with many challenges.
Telehealth can eliminate some of these challenges but comes with issues of its own, according to results of the REACH PC trial.
Jennifer S. Temel, MD, of Massachusetts General Hospital in Boston, discussed the use of telemedicine in palliative care, including results from REACH PC, during an educational session at the ASCO Virtual Quality Care Symposium 2020.
Dr. Temel noted that, for cancer patients, an in-person visit with a palliative care specialist can cost time, induce fatigue, and increase financial burden from transportation and parking expenses.
For caregivers and family, an in-person visit may necessitate absence from family and/or work, require complex scheduling to coordinate with other office visits, and result in additional transportation and/or parking expenses.
For health care systems, to have a dedicated palliative care clinic requires precious space and financial expenditures for office personnel and other resources.
These issues make it attractive to consider whether telehealth could be used for palliative care services.
Scarcity of palliative care specialists
In the United States, there is roughly 1 palliative care physician for every 20,000 older adults with a life-limiting illness, according to research published in Annual Review of Public Health in 2014.
In its 2019 state-by-state report card, the Center to Advance Palliative Care noted that only 72% of U.S. hospitals with 50 or more beds have a palliative care team.
For patients with serious illnesses and those who are socioeconomically or geographically disadvantaged, palliative care is often inaccessible.
Inefficiencies in the current system are an additional impediment. Palliative care specialists frequently see patients during a portion of the patient’s routine visit to subspecialty or primary care clinics. This limits the palliative care specialist’s ability to perform comprehensive assessments and provide patient-centered care efficiently.
Special considerations regarding telehealth for palliative care
As a specialty, palliative care involves interactions that could make the use of telehealth problematic. For example, conveyance of interest, warmth, and touch are challenging or impossible in a video format.
Palliative care specialists engage with patients regarding relatively serious topics such as prognosis and end-of-life preferences. There is uncertainty about how those discussions would be received by patients and their caregivers via video.
Furthermore, there are logistical impediments such as prescribing opioids with video or across state lines.
Despite these concerns, the ENABLE study showed that supplementing usual oncology care with weekly (transitioning to monthly) telephone-based educational palliative care produced higher quality of life and mood than did usual oncology care alone. These results were published in JAMA in 2009.
REACH PC study demonstrates feasibility of telehealth model
Dr. Temel described the ongoing REACH PC trial in which palliative care is delivered via video visits and compared with in-person palliative care for patients with advanced non–small cell lung cancer.
The primary aim of REACH PC is to determine whether telehealth palliative care is equivalent to traditional palliative care in improving quality of life as a supplement to routine oncology care.
Currently, REACH PC has enrolled 581 patients at its 20 sites, spanning a geographically diverse area. Just over half of patients approached about REACH PC agreed to enroll in it. Ultimately, 1,250 enrollees are sought.
Among patients who declined to participate, 7.6% indicated “discomfort with technology” as the reason. Most refusals were due to lack of interest in research (35.1%) and/or palliative care (22.9%).
Older adults were prominent among enrollees. More than 60% were older than 60 years of age, and more than one-third were older than 70 years.
Among patients who began the trial, there were slightly more withdrawals in the telehealth participants, in comparison with in-person participants (13.6% versus 9.1%).
When palliative care clinicians were queried about video visits, 64.3% said there were no challenges. This is comparable to the 65.5% of clinicians who had no challenges with in-person visits.
When problems occurred with video visits, they were most frequently technical (19.1%). Only 1.4% of clinicians reported difficulty addressing topics that felt uncomfortable over video, and 1.5% reported difficulty establishing rapport.
The success rates of video and in-person visits were similar. About 80% of visits accomplished planned goals.
‘Webside’ manner
Strategies such as reflective listening and summarizing what patients say (to verify an accurate understanding of the patient’s perspective) are key to successful palliative care visits, regardless of the setting.
For telehealth visits, Dr. Temel described techniques she defined as “webside manner,” to compensate for the inability of the clinician to touch a patient. These techniques include leaning in toward the camera, nodding, and pausing to be certain the patient has finished speaking before the clinician speaks again.
Is telehealth the future of palliative care?
I include myself among those oncologists who have voiced concern about moving from face-to-face to remote visits for complicated consultations such as those required for palliative care. Nonetheless, from the preliminary results of the REACH PC trial, it appears that telehealth could be a valuable tool.
To minimize differences between in-person and remote delivery of palliative care, practical strategies for ensuring rapport and facilitating a trusting relationship should be defined further and disseminated.
In addition, we need to be vigilant for widening inequities of care from rapid movement to the use of technology (i.e., an equity gap). In their telehealth experience during the COVID-19 pandemic, investigators at Houston Methodist Cancer Center found that patients declining virtual visits tended to be older, lower-income, and less likely to have commercial insurance. These results were recently published in JCO Oncology Practice.
For the foregoing reasons, hybrid systems for palliative care services will probably always be needed.
Going forward, we should heed the advice of Alvin Toffler in his book Future Shock. Mr. Toffler said, “The illiterate of the 21st century will not be those who cannot read and write, but those who cannot learn, unlearn, and relearn.”
The traditional model for delivering palliative care will almost certainly need to be reimagined and relearned.
Dr. Temel disclosed institutional research funding from Pfizer.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Traditional delivery of palliative care to outpatients with cancer is associated with many challenges.
Telehealth can eliminate some of these challenges but comes with issues of its own, according to results of the REACH PC trial.
Jennifer S. Temel, MD, of Massachusetts General Hospital in Boston, discussed the use of telemedicine in palliative care, including results from REACH PC, during an educational session at the ASCO Virtual Quality Care Symposium 2020.
Dr. Temel noted that, for cancer patients, an in-person visit with a palliative care specialist can cost time, induce fatigue, and increase financial burden from transportation and parking expenses.
For caregivers and family, an in-person visit may necessitate absence from family and/or work, require complex scheduling to coordinate with other office visits, and result in additional transportation and/or parking expenses.
For health care systems, to have a dedicated palliative care clinic requires precious space and financial expenditures for office personnel and other resources.
These issues make it attractive to consider whether telehealth could be used for palliative care services.
Scarcity of palliative care specialists
In the United States, there is roughly 1 palliative care physician for every 20,000 older adults with a life-limiting illness, according to research published in Annual Review of Public Health in 2014.
In its 2019 state-by-state report card, the Center to Advance Palliative Care noted that only 72% of U.S. hospitals with 50 or more beds have a palliative care team.
For patients with serious illnesses and those who are socioeconomically or geographically disadvantaged, palliative care is often inaccessible.
Inefficiencies in the current system are an additional impediment. Palliative care specialists frequently see patients during a portion of the patient’s routine visit to subspecialty or primary care clinics. This limits the palliative care specialist’s ability to perform comprehensive assessments and provide patient-centered care efficiently.
Special considerations regarding telehealth for palliative care
As a specialty, palliative care involves interactions that could make the use of telehealth problematic. For example, conveyance of interest, warmth, and touch are challenging or impossible in a video format.
Palliative care specialists engage with patients regarding relatively serious topics such as prognosis and end-of-life preferences. There is uncertainty about how those discussions would be received by patients and their caregivers via video.
Furthermore, there are logistical impediments such as prescribing opioids with video or across state lines.
Despite these concerns, the ENABLE study showed that supplementing usual oncology care with weekly (transitioning to monthly) telephone-based educational palliative care produced higher quality of life and mood than did usual oncology care alone. These results were published in JAMA in 2009.
REACH PC study demonstrates feasibility of telehealth model
Dr. Temel described the ongoing REACH PC trial in which palliative care is delivered via video visits and compared with in-person palliative care for patients with advanced non–small cell lung cancer.
The primary aim of REACH PC is to determine whether telehealth palliative care is equivalent to traditional palliative care in improving quality of life as a supplement to routine oncology care.
Currently, REACH PC has enrolled 581 patients at its 20 sites, spanning a geographically diverse area. Just over half of patients approached about REACH PC agreed to enroll in it. Ultimately, 1,250 enrollees are sought.
Among patients who declined to participate, 7.6% indicated “discomfort with technology” as the reason. Most refusals were due to lack of interest in research (35.1%) and/or palliative care (22.9%).
Older adults were prominent among enrollees. More than 60% were older than 60 years of age, and more than one-third were older than 70 years.
Among patients who began the trial, there were slightly more withdrawals in the telehealth participants, in comparison with in-person participants (13.6% versus 9.1%).
When palliative care clinicians were queried about video visits, 64.3% said there were no challenges. This is comparable to the 65.5% of clinicians who had no challenges with in-person visits.
When problems occurred with video visits, they were most frequently technical (19.1%). Only 1.4% of clinicians reported difficulty addressing topics that felt uncomfortable over video, and 1.5% reported difficulty establishing rapport.
The success rates of video and in-person visits were similar. About 80% of visits accomplished planned goals.
‘Webside’ manner
Strategies such as reflective listening and summarizing what patients say (to verify an accurate understanding of the patient’s perspective) are key to successful palliative care visits, regardless of the setting.
For telehealth visits, Dr. Temel described techniques she defined as “webside manner,” to compensate for the inability of the clinician to touch a patient. These techniques include leaning in toward the camera, nodding, and pausing to be certain the patient has finished speaking before the clinician speaks again.
Is telehealth the future of palliative care?
I include myself among those oncologists who have voiced concern about moving from face-to-face to remote visits for complicated consultations such as those required for palliative care. Nonetheless, from the preliminary results of the REACH PC trial, it appears that telehealth could be a valuable tool.
To minimize differences between in-person and remote delivery of palliative care, practical strategies for ensuring rapport and facilitating a trusting relationship should be defined further and disseminated.
In addition, we need to be vigilant for widening inequities of care from rapid movement to the use of technology (i.e., an equity gap). In their telehealth experience during the COVID-19 pandemic, investigators at Houston Methodist Cancer Center found that patients declining virtual visits tended to be older, lower-income, and less likely to have commercial insurance. These results were recently published in JCO Oncology Practice.
For the foregoing reasons, hybrid systems for palliative care services will probably always be needed.
Going forward, we should heed the advice of Alvin Toffler in his book Future Shock. Mr. Toffler said, “The illiterate of the 21st century will not be those who cannot read and write, but those who cannot learn, unlearn, and relearn.”
The traditional model for delivering palliative care will almost certainly need to be reimagined and relearned.
Dr. Temel disclosed institutional research funding from Pfizer.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Traditional delivery of palliative care to outpatients with cancer is associated with many challenges.
Telehealth can eliminate some of these challenges but comes with issues of its own, according to results of the REACH PC trial.
Jennifer S. Temel, MD, of Massachusetts General Hospital in Boston, discussed the use of telemedicine in palliative care, including results from REACH PC, during an educational session at the ASCO Virtual Quality Care Symposium 2020.
Dr. Temel noted that, for cancer patients, an in-person visit with a palliative care specialist can cost time, induce fatigue, and increase financial burden from transportation and parking expenses.
For caregivers and family, an in-person visit may necessitate absence from family and/or work, require complex scheduling to coordinate with other office visits, and result in additional transportation and/or parking expenses.
For health care systems, to have a dedicated palliative care clinic requires precious space and financial expenditures for office personnel and other resources.
These issues make it attractive to consider whether telehealth could be used for palliative care services.
Scarcity of palliative care specialists
In the United States, there is roughly 1 palliative care physician for every 20,000 older adults with a life-limiting illness, according to research published in Annual Review of Public Health in 2014.
In its 2019 state-by-state report card, the Center to Advance Palliative Care noted that only 72% of U.S. hospitals with 50 or more beds have a palliative care team.
For patients with serious illnesses and those who are socioeconomically or geographically disadvantaged, palliative care is often inaccessible.
Inefficiencies in the current system are an additional impediment. Palliative care specialists frequently see patients during a portion of the patient’s routine visit to subspecialty or primary care clinics. This limits the palliative care specialist’s ability to perform comprehensive assessments and provide patient-centered care efficiently.
Special considerations regarding telehealth for palliative care
As a specialty, palliative care involves interactions that could make the use of telehealth problematic. For example, conveyance of interest, warmth, and touch are challenging or impossible in a video format.
Palliative care specialists engage with patients regarding relatively serious topics such as prognosis and end-of-life preferences. There is uncertainty about how those discussions would be received by patients and their caregivers via video.
Furthermore, there are logistical impediments such as prescribing opioids with video or across state lines.
Despite these concerns, the ENABLE study showed that supplementing usual oncology care with weekly (transitioning to monthly) telephone-based educational palliative care produced higher quality of life and mood than did usual oncology care alone. These results were published in JAMA in 2009.
REACH PC study demonstrates feasibility of telehealth model
Dr. Temel described the ongoing REACH PC trial in which palliative care is delivered via video visits and compared with in-person palliative care for patients with advanced non–small cell lung cancer.
The primary aim of REACH PC is to determine whether telehealth palliative care is equivalent to traditional palliative care in improving quality of life as a supplement to routine oncology care.
Currently, REACH PC has enrolled 581 patients at its 20 sites, spanning a geographically diverse area. Just over half of patients approached about REACH PC agreed to enroll in it. Ultimately, 1,250 enrollees are sought.
Among patients who declined to participate, 7.6% indicated “discomfort with technology” as the reason. Most refusals were due to lack of interest in research (35.1%) and/or palliative care (22.9%).
Older adults were prominent among enrollees. More than 60% were older than 60 years of age, and more than one-third were older than 70 years.
Among patients who began the trial, there were slightly more withdrawals in the telehealth participants, in comparison with in-person participants (13.6% versus 9.1%).
When palliative care clinicians were queried about video visits, 64.3% said there were no challenges. This is comparable to the 65.5% of clinicians who had no challenges with in-person visits.
When problems occurred with video visits, they were most frequently technical (19.1%). Only 1.4% of clinicians reported difficulty addressing topics that felt uncomfortable over video, and 1.5% reported difficulty establishing rapport.
The success rates of video and in-person visits were similar. About 80% of visits accomplished planned goals.
‘Webside’ manner
Strategies such as reflective listening and summarizing what patients say (to verify an accurate understanding of the patient’s perspective) are key to successful palliative care visits, regardless of the setting.
For telehealth visits, Dr. Temel described techniques she defined as “webside manner,” to compensate for the inability of the clinician to touch a patient. These techniques include leaning in toward the camera, nodding, and pausing to be certain the patient has finished speaking before the clinician speaks again.
Is telehealth the future of palliative care?
I include myself among those oncologists who have voiced concern about moving from face-to-face to remote visits for complicated consultations such as those required for palliative care. Nonetheless, from the preliminary results of the REACH PC trial, it appears that telehealth could be a valuable tool.
To minimize differences between in-person and remote delivery of palliative care, practical strategies for ensuring rapport and facilitating a trusting relationship should be defined further and disseminated.
In addition, we need to be vigilant for widening inequities of care from rapid movement to the use of technology (i.e., an equity gap). In their telehealth experience during the COVID-19 pandemic, investigators at Houston Methodist Cancer Center found that patients declining virtual visits tended to be older, lower-income, and less likely to have commercial insurance. These results were recently published in JCO Oncology Practice.
For the foregoing reasons, hybrid systems for palliative care services will probably always be needed.
Going forward, we should heed the advice of Alvin Toffler in his book Future Shock. Mr. Toffler said, “The illiterate of the 21st century will not be those who cannot read and write, but those who cannot learn, unlearn, and relearn.”
The traditional model for delivering palliative care will almost certainly need to be reimagined and relearned.
Dr. Temel disclosed institutional research funding from Pfizer.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
FROM ASCO QUALITY CARE SYMPOSIUM 2020
Home care for bortezomib safe and reduces hospital visits in myeloma patients
Home administration of bortezomib (Velcade), as a once or twice-weekly subcutaneous self-injection is safe in patients with myeloma, significantly reducing hospital visits, and likely improving quality of life, a study shows.
The majority (43 of 52 patients) successfully self-administered bortezomib and completed the course. Also, hospital visits for those on the so-called Homecare programme reduced by 50%, with most visits comprising a fortnightly drug pickup from the drive-through pharmacy.
The work was presented as a poster by lead author and researcher, Kanchana De Abrew, hematology consultant at University Hospital Southampton NHS Foundation Trust, at this year’s virtual British Society of Haematology (BSH) meeting. De Abrew conducted the study while at Queen Alexandra Hospital, Portsmouth.
“We wanted to minimize patient visits to hospital because with travel time and waiting time, patients can easily find a visit takes up a whole morning, so this relates to their quality of life as well as having financial implications for patients,” Dr. De Abrew said in an interview. It also reduced the impact on day units and improved capacity for other services.
Dr. De Abrew noted that the study was conducted in the pre-COVID-19 era, but that the current enhanced threat of infection only served to reinforce the benefits of self-administration at home and avoiding unnecessary hospital visits.
“This project could easily be set up in other hospitals and some other centers have already contacted us about this. It might suit rural areas,” she added.
‘Safe and effective’
Dr. Matthew Jenner, consultant hematologist for University Hospital Southampton NHS Foundation Trust, who was not involved in the study, remarked that the study demonstrated another way to deliver bortezomib outside of hospital in addition to home care services that require trained nurses to administer treatment. “With a modest amount of training of the patient and family, it is both a safe and effective way of delivering treatment. This reduces hospital visits for the patient and frees up much needed capacity for heavily stretched chemotherapy units, creating space for other newer treatments that require hospital attendance.
“It is of benefit all round to both the patients undertaking self-administration and those who benefit from improved capacity,” added Dr. Jenner.
Avoiding hospital visits
Myeloma patients are already immunosuppressed prior to treatment and then this worsens once on treatment. Once they are sitting in a clinic environment they are surrounded by similarly immunosuppressed patients, so their risk is heightened further.
Figures suggest myeloma cases are on the increase. Annually, the United Kingdom sees around 5,800 new cases of myeloma and incidence increased by a significant 32% between the periods of 1993-1995 and 2015-2017. These figures were reflected in the patient numbers at the Queen Alexandra Hospital where the study was carried out. Many patients receive bortezomib, which forms the backbone of four National Institute for Health and Care Excellence (NICE) approved regimens.
“Patients are living longer so in the early 2000s patients had a life expectancy of 2-3 years, whereas now patients live for around 5 years. Also, the scope and lines of treatments have increased a lot. Over 50% of patients are likely to have bortezomib at some point in their management,” explained Dr. De Abrew.
Bortezomib is given once or twice weekly as a subcutaneous injection, and this usually continues for approximately 6-8 months with four to six cycles. Administering the drug in hospital requires around a half-hour slot placing considerable burden on the hematology day unit resources, and this can adversely affect the patient experience with waiting times and the need for frequent hospital visits.
Patient or relatives taught to self-administer at home
In 2017, clinical nurse specialists taught suitable patients to self-administer bortezomib in the Homecare protocol. Patients collected a 2-week supply of the drug. The protocol aimed to improve patient quality of life by reducing hospital visits, and increasing capacity in the hematology day unit. Since the start of the programme in 2017, the majority (71) of myeloma patients at Portsmouth have been treated through the Homecare program.
Dr. De Abrew conducted a retrospective review of patients who received bortezomib between January and October 2019 aimed at determining the effectiveness of the Homecare programme. To this end, she measured the proportion able to commence the Homecare protocol; the proportion successful in completing treatment on the Homecare protocol; the amount of additional clinical nurse specialist time required to support the Homecare protocol; and the number of associated adverse incidents.
A total of 52 bortezomib-treated patients were included in the study. Patients were excluded if they were on a different combination of drugs that required hospital visits, or inpatient care for other reasons. Three patients ceased the drug – two because of toxicity, and one because of rapid progression. The average age of patients was 74 years, and 55.8% were using bortezomib as first-line, 36.5% second-line, and the remainder third-line or more.
The vast majority started the Homecare protocol (45/52), and 25 self-administered and 17 received a relative’s help. A total of 43 completed the self-administration protocol with two reverting to hospital assistance. Bortezomib was given for four to six cycles lasting around 6-8 months.
Clinical nurse specialists trained 38 patients for home care, with an average training time of 43 minutes. Two of these patients were considered unsuitable for self-administration. The remainder were trained by ward nurses or did not require training having received bortezomib previously.
A total of 20 patients required additional clinical nurse specialist time requiring an average of 55 minutes. Of those requiring additional support: Seven needed retraining; two needed the first dose delivered by a nurse specialist; two requested help from the hematology unit; and nine wanted general extra support – for example, help with injection site queries (usually administered to the abdominal area), reassurance during administration, syringe queries, administrative queries, and queries around spillages.
“Importantly, patients always have the phone number of the nurse specialist at hand. But most people managed okay, and even if they needed additional support they still got there,” remarked Dr. De Abrew.
In terms of adverse events, there were six in total. These included three reported spillages (with no harm caused), and three experienced injection site incidents (rash, pain). “We found a low number of reported adverse events,” she said.
Dr. De Abrew added that generally, many more medications were being converted to subcutaneous formulations in myeloma and other hematology conditions. “Perhaps these results could inform self-administration of other drugs. In hematology, we get so many new drugs come through every year, but we don’t get the increased resources to manage this in the day units. Broadening self-administration could really help with capacity as well as improve quality of life for the patients.
“These results show that it can be done!” she said.
Dr. De Abrew declared no relevant conflicts of interest. Dr. Jenner declared receiving honoraria from Janssen, which manufactures branded Velcade (bortezomib).
A version of this story originally appeared on Medscape.com.
Home administration of bortezomib (Velcade), as a once or twice-weekly subcutaneous self-injection is safe in patients with myeloma, significantly reducing hospital visits, and likely improving quality of life, a study shows.
The majority (43 of 52 patients) successfully self-administered bortezomib and completed the course. Also, hospital visits for those on the so-called Homecare programme reduced by 50%, with most visits comprising a fortnightly drug pickup from the drive-through pharmacy.
The work was presented as a poster by lead author and researcher, Kanchana De Abrew, hematology consultant at University Hospital Southampton NHS Foundation Trust, at this year’s virtual British Society of Haematology (BSH) meeting. De Abrew conducted the study while at Queen Alexandra Hospital, Portsmouth.
“We wanted to minimize patient visits to hospital because with travel time and waiting time, patients can easily find a visit takes up a whole morning, so this relates to their quality of life as well as having financial implications for patients,” Dr. De Abrew said in an interview. It also reduced the impact on day units and improved capacity for other services.
Dr. De Abrew noted that the study was conducted in the pre-COVID-19 era, but that the current enhanced threat of infection only served to reinforce the benefits of self-administration at home and avoiding unnecessary hospital visits.
“This project could easily be set up in other hospitals and some other centers have already contacted us about this. It might suit rural areas,” she added.
‘Safe and effective’
Dr. Matthew Jenner, consultant hematologist for University Hospital Southampton NHS Foundation Trust, who was not involved in the study, remarked that the study demonstrated another way to deliver bortezomib outside of hospital in addition to home care services that require trained nurses to administer treatment. “With a modest amount of training of the patient and family, it is both a safe and effective way of delivering treatment. This reduces hospital visits for the patient and frees up much needed capacity for heavily stretched chemotherapy units, creating space for other newer treatments that require hospital attendance.
“It is of benefit all round to both the patients undertaking self-administration and those who benefit from improved capacity,” added Dr. Jenner.
Avoiding hospital visits
Myeloma patients are already immunosuppressed prior to treatment and then this worsens once on treatment. Once they are sitting in a clinic environment they are surrounded by similarly immunosuppressed patients, so their risk is heightened further.
Figures suggest myeloma cases are on the increase. Annually, the United Kingdom sees around 5,800 new cases of myeloma and incidence increased by a significant 32% between the periods of 1993-1995 and 2015-2017. These figures were reflected in the patient numbers at the Queen Alexandra Hospital where the study was carried out. Many patients receive bortezomib, which forms the backbone of four National Institute for Health and Care Excellence (NICE) approved regimens.
“Patients are living longer so in the early 2000s patients had a life expectancy of 2-3 years, whereas now patients live for around 5 years. Also, the scope and lines of treatments have increased a lot. Over 50% of patients are likely to have bortezomib at some point in their management,” explained Dr. De Abrew.
Bortezomib is given once or twice weekly as a subcutaneous injection, and this usually continues for approximately 6-8 months with four to six cycles. Administering the drug in hospital requires around a half-hour slot placing considerable burden on the hematology day unit resources, and this can adversely affect the patient experience with waiting times and the need for frequent hospital visits.
Patient or relatives taught to self-administer at home
In 2017, clinical nurse specialists taught suitable patients to self-administer bortezomib in the Homecare protocol. Patients collected a 2-week supply of the drug. The protocol aimed to improve patient quality of life by reducing hospital visits, and increasing capacity in the hematology day unit. Since the start of the programme in 2017, the majority (71) of myeloma patients at Portsmouth have been treated through the Homecare program.
Dr. De Abrew conducted a retrospective review of patients who received bortezomib between January and October 2019 aimed at determining the effectiveness of the Homecare programme. To this end, she measured the proportion able to commence the Homecare protocol; the proportion successful in completing treatment on the Homecare protocol; the amount of additional clinical nurse specialist time required to support the Homecare protocol; and the number of associated adverse incidents.
A total of 52 bortezomib-treated patients were included in the study. Patients were excluded if they were on a different combination of drugs that required hospital visits, or inpatient care for other reasons. Three patients ceased the drug – two because of toxicity, and one because of rapid progression. The average age of patients was 74 years, and 55.8% were using bortezomib as first-line, 36.5% second-line, and the remainder third-line or more.
The vast majority started the Homecare protocol (45/52), and 25 self-administered and 17 received a relative’s help. A total of 43 completed the self-administration protocol with two reverting to hospital assistance. Bortezomib was given for four to six cycles lasting around 6-8 months.
Clinical nurse specialists trained 38 patients for home care, with an average training time of 43 minutes. Two of these patients were considered unsuitable for self-administration. The remainder were trained by ward nurses or did not require training having received bortezomib previously.
A total of 20 patients required additional clinical nurse specialist time requiring an average of 55 minutes. Of those requiring additional support: Seven needed retraining; two needed the first dose delivered by a nurse specialist; two requested help from the hematology unit; and nine wanted general extra support – for example, help with injection site queries (usually administered to the abdominal area), reassurance during administration, syringe queries, administrative queries, and queries around spillages.
“Importantly, patients always have the phone number of the nurse specialist at hand. But most people managed okay, and even if they needed additional support they still got there,” remarked Dr. De Abrew.
In terms of adverse events, there were six in total. These included three reported spillages (with no harm caused), and three experienced injection site incidents (rash, pain). “We found a low number of reported adverse events,” she said.
Dr. De Abrew added that generally, many more medications were being converted to subcutaneous formulations in myeloma and other hematology conditions. “Perhaps these results could inform self-administration of other drugs. In hematology, we get so many new drugs come through every year, but we don’t get the increased resources to manage this in the day units. Broadening self-administration could really help with capacity as well as improve quality of life for the patients.
“These results show that it can be done!” she said.
Dr. De Abrew declared no relevant conflicts of interest. Dr. Jenner declared receiving honoraria from Janssen, which manufactures branded Velcade (bortezomib).
A version of this story originally appeared on Medscape.com.
Home administration of bortezomib (Velcade), as a once or twice-weekly subcutaneous self-injection is safe in patients with myeloma, significantly reducing hospital visits, and likely improving quality of life, a study shows.
The majority (43 of 52 patients) successfully self-administered bortezomib and completed the course. Also, hospital visits for those on the so-called Homecare programme reduced by 50%, with most visits comprising a fortnightly drug pickup from the drive-through pharmacy.
The work was presented as a poster by lead author and researcher, Kanchana De Abrew, hematology consultant at University Hospital Southampton NHS Foundation Trust, at this year’s virtual British Society of Haematology (BSH) meeting. De Abrew conducted the study while at Queen Alexandra Hospital, Portsmouth.
“We wanted to minimize patient visits to hospital because with travel time and waiting time, patients can easily find a visit takes up a whole morning, so this relates to their quality of life as well as having financial implications for patients,” Dr. De Abrew said in an interview. It also reduced the impact on day units and improved capacity for other services.
Dr. De Abrew noted that the study was conducted in the pre-COVID-19 era, but that the current enhanced threat of infection only served to reinforce the benefits of self-administration at home and avoiding unnecessary hospital visits.
“This project could easily be set up in other hospitals and some other centers have already contacted us about this. It might suit rural areas,” she added.
‘Safe and effective’
Dr. Matthew Jenner, consultant hematologist for University Hospital Southampton NHS Foundation Trust, who was not involved in the study, remarked that the study demonstrated another way to deliver bortezomib outside of hospital in addition to home care services that require trained nurses to administer treatment. “With a modest amount of training of the patient and family, it is both a safe and effective way of delivering treatment. This reduces hospital visits for the patient and frees up much needed capacity for heavily stretched chemotherapy units, creating space for other newer treatments that require hospital attendance.
“It is of benefit all round to both the patients undertaking self-administration and those who benefit from improved capacity,” added Dr. Jenner.
Avoiding hospital visits
Myeloma patients are already immunosuppressed prior to treatment and then this worsens once on treatment. Once they are sitting in a clinic environment they are surrounded by similarly immunosuppressed patients, so their risk is heightened further.
Figures suggest myeloma cases are on the increase. Annually, the United Kingdom sees around 5,800 new cases of myeloma and incidence increased by a significant 32% between the periods of 1993-1995 and 2015-2017. These figures were reflected in the patient numbers at the Queen Alexandra Hospital where the study was carried out. Many patients receive bortezomib, which forms the backbone of four National Institute for Health and Care Excellence (NICE) approved regimens.
“Patients are living longer so in the early 2000s patients had a life expectancy of 2-3 years, whereas now patients live for around 5 years. Also, the scope and lines of treatments have increased a lot. Over 50% of patients are likely to have bortezomib at some point in their management,” explained Dr. De Abrew.
Bortezomib is given once or twice weekly as a subcutaneous injection, and this usually continues for approximately 6-8 months with four to six cycles. Administering the drug in hospital requires around a half-hour slot placing considerable burden on the hematology day unit resources, and this can adversely affect the patient experience with waiting times and the need for frequent hospital visits.
Patient or relatives taught to self-administer at home
In 2017, clinical nurse specialists taught suitable patients to self-administer bortezomib in the Homecare protocol. Patients collected a 2-week supply of the drug. The protocol aimed to improve patient quality of life by reducing hospital visits, and increasing capacity in the hematology day unit. Since the start of the programme in 2017, the majority (71) of myeloma patients at Portsmouth have been treated through the Homecare program.
Dr. De Abrew conducted a retrospective review of patients who received bortezomib between January and October 2019 aimed at determining the effectiveness of the Homecare programme. To this end, she measured the proportion able to commence the Homecare protocol; the proportion successful in completing treatment on the Homecare protocol; the amount of additional clinical nurse specialist time required to support the Homecare protocol; and the number of associated adverse incidents.
A total of 52 bortezomib-treated patients were included in the study. Patients were excluded if they were on a different combination of drugs that required hospital visits, or inpatient care for other reasons. Three patients ceased the drug – two because of toxicity, and one because of rapid progression. The average age of patients was 74 years, and 55.8% were using bortezomib as first-line, 36.5% second-line, and the remainder third-line or more.
The vast majority started the Homecare protocol (45/52), and 25 self-administered and 17 received a relative’s help. A total of 43 completed the self-administration protocol with two reverting to hospital assistance. Bortezomib was given for four to six cycles lasting around 6-8 months.
Clinical nurse specialists trained 38 patients for home care, with an average training time of 43 minutes. Two of these patients were considered unsuitable for self-administration. The remainder were trained by ward nurses or did not require training having received bortezomib previously.
A total of 20 patients required additional clinical nurse specialist time requiring an average of 55 minutes. Of those requiring additional support: Seven needed retraining; two needed the first dose delivered by a nurse specialist; two requested help from the hematology unit; and nine wanted general extra support – for example, help with injection site queries (usually administered to the abdominal area), reassurance during administration, syringe queries, administrative queries, and queries around spillages.
“Importantly, patients always have the phone number of the nurse specialist at hand. But most people managed okay, and even if they needed additional support they still got there,” remarked Dr. De Abrew.
In terms of adverse events, there were six in total. These included three reported spillages (with no harm caused), and three experienced injection site incidents (rash, pain). “We found a low number of reported adverse events,” she said.
Dr. De Abrew added that generally, many more medications were being converted to subcutaneous formulations in myeloma and other hematology conditions. “Perhaps these results could inform self-administration of other drugs. In hematology, we get so many new drugs come through every year, but we don’t get the increased resources to manage this in the day units. Broadening self-administration could really help with capacity as well as improve quality of life for the patients.
“These results show that it can be done!” she said.
Dr. De Abrew declared no relevant conflicts of interest. Dr. Jenner declared receiving honoraria from Janssen, which manufactures branded Velcade (bortezomib).
A version of this story originally appeared on Medscape.com.
Ibrutinib associated with decreased circulating malignant cells and restored T-cell function in CLL patients
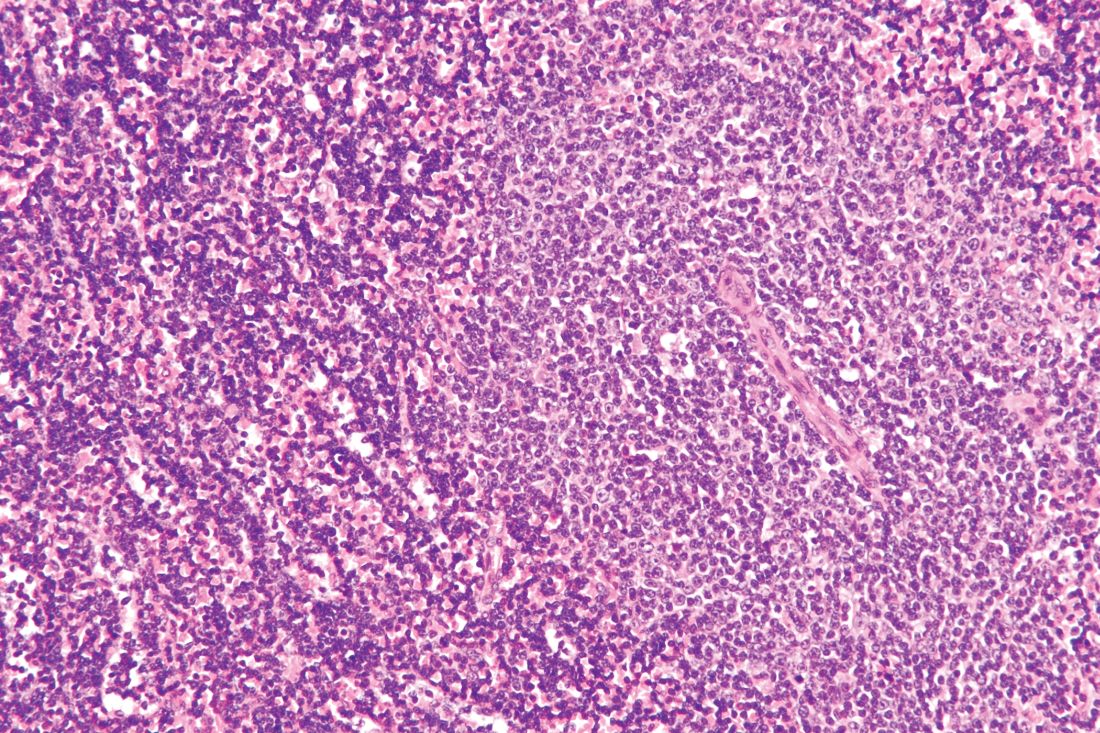
Ibrutinib showed significant impact on circulating malignant and nonmalignant immune cells and was found to restore healthy T-cell function in patients with chronic lymphocytic leukemia (CLL), according to the results of a comparative study of CLL patients and healthy controls.
Researchers compared circulating counts of 21 immune blood cell subsets throughout the first year of treatment in 55 patients with relapsed/refractory (R/R) CLL from the RESONATE trial and 50 previously untreated CLL patients from the RESONATE-2 trial with 20 untreated age-matched healthy donors, according to a report published online in Leukemia Research.
In addition, T-cell function was assessed in response to T-cell–receptor stimulation in 21 patients with R/R CLL, compared with 18 age-matched healthy donors, according to Isabelle G. Solman, MS, an employee of Translational Medicine, Pharmacyclics, Sunnyvale, Calif. and colleagues.
Positive indicators
Ibrutinib significantly decreased pathologically high circulating B cells, regulatory T cells, effector/memory CD4+ and CD8+ T cells (including exhausted and chronically activated T cells), natural killer (NK) T cells, and myeloid-derived suppressor cells; preserved naive T cells and NK cells; and increased circulating classical monocytes, according to the researchers.
Ibrutinib also significantly restored T-cell proliferative ability, degranulation, and cytokine secretion. Over the same period, ofatumumab or chlorambucil did not confer the same spectrum of normalization as ibrutinib in multiple immune subsets that were examined, they added.
“These results establish that ibrutinib has a significant and likely positive impact on circulating malignant and nonmalignant immune cells and restores healthy T-cell function,” the researchers indicated.
“Ibrutinib has a significant, progressively positive impact on both malignant and nonmalignant immune cells in CLL. These positive effects on circulating nonmalignant immune cells may contribute to long-term CLL disease control, overall health status, and decreased susceptibility to infection,” they concluded.
The study was funded by Pharmacyclics, an AbbVie Company. Ms. Solman is an employee of Translational Medicine, Pharmacyclics, Sunnyvale, Calif. as were several other authors.
SOURCE: Solman IG et al. Leuk Res. 2020;97. doi: 10.1016/j.leukres.2020.106432.
Ibrutinib showed significant impact on circulating malignant and nonmalignant immune cells and was found to restore healthy T-cell function in patients with chronic lymphocytic leukemia (CLL), according to the results of a comparative study of CLL patients and healthy controls.
Researchers compared circulating counts of 21 immune blood cell subsets throughout the first year of treatment in 55 patients with relapsed/refractory (R/R) CLL from the RESONATE trial and 50 previously untreated CLL patients from the RESONATE-2 trial with 20 untreated age-matched healthy donors, according to a report published online in Leukemia Research.
In addition, T-cell function was assessed in response to T-cell–receptor stimulation in 21 patients with R/R CLL, compared with 18 age-matched healthy donors, according to Isabelle G. Solman, MS, an employee of Translational Medicine, Pharmacyclics, Sunnyvale, Calif. and colleagues.
Positive indicators
Ibrutinib significantly decreased pathologically high circulating B cells, regulatory T cells, effector/memory CD4+ and CD8+ T cells (including exhausted and chronically activated T cells), natural killer (NK) T cells, and myeloid-derived suppressor cells; preserved naive T cells and NK cells; and increased circulating classical monocytes, according to the researchers.
Ibrutinib also significantly restored T-cell proliferative ability, degranulation, and cytokine secretion. Over the same period, ofatumumab or chlorambucil did not confer the same spectrum of normalization as ibrutinib in multiple immune subsets that were examined, they added.
“These results establish that ibrutinib has a significant and likely positive impact on circulating malignant and nonmalignant immune cells and restores healthy T-cell function,” the researchers indicated.
“Ibrutinib has a significant, progressively positive impact on both malignant and nonmalignant immune cells in CLL. These positive effects on circulating nonmalignant immune cells may contribute to long-term CLL disease control, overall health status, and decreased susceptibility to infection,” they concluded.
The study was funded by Pharmacyclics, an AbbVie Company. Ms. Solman is an employee of Translational Medicine, Pharmacyclics, Sunnyvale, Calif. as were several other authors.
SOURCE: Solman IG et al. Leuk Res. 2020;97. doi: 10.1016/j.leukres.2020.106432.
Ibrutinib showed significant impact on circulating malignant and nonmalignant immune cells and was found to restore healthy T-cell function in patients with chronic lymphocytic leukemia (CLL), according to the results of a comparative study of CLL patients and healthy controls.
Researchers compared circulating counts of 21 immune blood cell subsets throughout the first year of treatment in 55 patients with relapsed/refractory (R/R) CLL from the RESONATE trial and 50 previously untreated CLL patients from the RESONATE-2 trial with 20 untreated age-matched healthy donors, according to a report published online in Leukemia Research.
In addition, T-cell function was assessed in response to T-cell–receptor stimulation in 21 patients with R/R CLL, compared with 18 age-matched healthy donors, according to Isabelle G. Solman, MS, an employee of Translational Medicine, Pharmacyclics, Sunnyvale, Calif. and colleagues.
Positive indicators
Ibrutinib significantly decreased pathologically high circulating B cells, regulatory T cells, effector/memory CD4+ and CD8+ T cells (including exhausted and chronically activated T cells), natural killer (NK) T cells, and myeloid-derived suppressor cells; preserved naive T cells and NK cells; and increased circulating classical monocytes, according to the researchers.
Ibrutinib also significantly restored T-cell proliferative ability, degranulation, and cytokine secretion. Over the same period, ofatumumab or chlorambucil did not confer the same spectrum of normalization as ibrutinib in multiple immune subsets that were examined, they added.
“These results establish that ibrutinib has a significant and likely positive impact on circulating malignant and nonmalignant immune cells and restores healthy T-cell function,” the researchers indicated.
“Ibrutinib has a significant, progressively positive impact on both malignant and nonmalignant immune cells in CLL. These positive effects on circulating nonmalignant immune cells may contribute to long-term CLL disease control, overall health status, and decreased susceptibility to infection,” they concluded.
The study was funded by Pharmacyclics, an AbbVie Company. Ms. Solman is an employee of Translational Medicine, Pharmacyclics, Sunnyvale, Calif. as were several other authors.
SOURCE: Solman IG et al. Leuk Res. 2020;97. doi: 10.1016/j.leukres.2020.106432.
FROM LEUKEMIA RESEARCH
Beat AML: Precision medicine strategy feasible, superior to SOC for AML
The 30-day mortality rates were 3.7% versus 20.4% in 224 patients who enrolled in the Beat AML trial precision medicine substudies within 7 days of prospective genomic profiling and 103 who elected SOC chemotherapy, respectively, Amy Burd, PhD, vice president of research strategy for the Leukemia & Lymphoma Society, Rye Brook, N.Y. and her colleagues reported online in Nature Medicine.
Overall survival (OS) at a median of 7.1 months was also significantly longer with precision medicine than with SOC chemotherapy (median, 12.8 vs. 3.9 months), the investigators found.
In an additional 28 patients who selected an investigational therapy rather than a precision medicine strategy or SOC chemotherapy, median OS was not reached, and in 38 who chose palliative care, median OS was 0.6 months, they noted. Care type was unknown in two patients.
The results were similar after controlling for demographic, clinical, and molecular variables and did not change when patients with adverse events of special interest were excluded from the analysis or when only those with survival greater than 2 weeks were included in the analysis.
AML confers an adverse outcome in older adults and therefore is typically treated rapidly after diagnosis. This has precluded consideration of patients’ mutational profile for treatment decisions.
Beat AML, however, sought to prospectively assess the feasibility of quickly ascertaining cytogenetic and mutational data for the purpose of improving outcomes through targeted treatment.
“The study shows that delaying treatment up to 7 days is feasible and safe, and that patients who opted for the precision medicine approach experienced a lower early death rate and superior overall survival, compared with patients who opted for standard of care,” lead study author John C. Byrd, MD, the D. Warren Brown Chair of Leukemia Research of the Ohio State University, Columbus, noted in a press statement from the Leukemia & Lymphoma Society, which conducted the trial. “This patient-centric study shows that we can move away from chemotherapy treatment for patients who won’t respond or can’t withstand the harsh effects of the same chemotherapies we’ve been using for 40 years and match them with a treatment better suited for their individual cases.”
The ongoing Beat AML trial was launched by LLS in 2016 to assess various novel targeted therapies in newly diagnosed AML patients aged 60 years and older. Participants underwent next-generation genomic sequencing, were matched to the appropriate targeted therapy, and were given the option of enrolling on the relevant substudy or selecting an alternate treatment strategy. There are currently 11 substudies assessing novel therapies that have emerged in the wake of “significant progress in understanding the molecular pathogenesis of AML.”
The current findings represent outcomes in patients enrolled between Nov. 2016 and Jan. 2018. The patients had a mean age of 72 years, and those selecting precision medicine vs. SOC had similar demographic and genetic features, the authors noted.
LLS president and chief executive officer Louis J. DeGennaro, PhD, said the findings are practice changing and provide a template for studying precision medicine in other cancers.
“The study is changing significantly the way we look at treating patients with AML, showing that precision medicine ... can improve short- and long-term outcomes for patients with this deadly blood cancer,” he said in the LLS statement. “Further, BEAT AML has proven to be a viable model for other cancer clinical trials to emulate.”
In fact, the model has been applied to the recently launched Beat COVID trial, which looks at acalabrutinib in patients with hematologic cancers and COVID-19 infection, and other trials, including the LLS PedAL global precision medicine trial for children with relapsed acute leukemia, are planned.
“This study sets the path to establish the safety of precision medicine in AML and sets the stage to extend this same approach to younger patients with this disease and other cancers that are urgently treated as a single disease despite recognition of multiple subtypes, the authors concluded.
Dr. Burd is an employee of LLS, which received funding from AbbVie, Agios Pharmaceuticals, Alexion Pharmaceuticals, and a variety of other pharmaceutical and biotechnology companies. Dr. Byrd has received research support from Acerta Pharma, Genentech, Janssen Pharmaceutica, and Pharmacyclics and has served on the advisory board of Syndax Pharmaceuticals.
SOURCE: Burd A et al. Nature Medicine 2020 Oct 26. doi: 10.1038/s41591-020-1089-8.
The 30-day mortality rates were 3.7% versus 20.4% in 224 patients who enrolled in the Beat AML trial precision medicine substudies within 7 days of prospective genomic profiling and 103 who elected SOC chemotherapy, respectively, Amy Burd, PhD, vice president of research strategy for the Leukemia & Lymphoma Society, Rye Brook, N.Y. and her colleagues reported online in Nature Medicine.
Overall survival (OS) at a median of 7.1 months was also significantly longer with precision medicine than with SOC chemotherapy (median, 12.8 vs. 3.9 months), the investigators found.
In an additional 28 patients who selected an investigational therapy rather than a precision medicine strategy or SOC chemotherapy, median OS was not reached, and in 38 who chose palliative care, median OS was 0.6 months, they noted. Care type was unknown in two patients.
The results were similar after controlling for demographic, clinical, and molecular variables and did not change when patients with adverse events of special interest were excluded from the analysis or when only those with survival greater than 2 weeks were included in the analysis.
AML confers an adverse outcome in older adults and therefore is typically treated rapidly after diagnosis. This has precluded consideration of patients’ mutational profile for treatment decisions.
Beat AML, however, sought to prospectively assess the feasibility of quickly ascertaining cytogenetic and mutational data for the purpose of improving outcomes through targeted treatment.
“The study shows that delaying treatment up to 7 days is feasible and safe, and that patients who opted for the precision medicine approach experienced a lower early death rate and superior overall survival, compared with patients who opted for standard of care,” lead study author John C. Byrd, MD, the D. Warren Brown Chair of Leukemia Research of the Ohio State University, Columbus, noted in a press statement from the Leukemia & Lymphoma Society, which conducted the trial. “This patient-centric study shows that we can move away from chemotherapy treatment for patients who won’t respond or can’t withstand the harsh effects of the same chemotherapies we’ve been using for 40 years and match them with a treatment better suited for their individual cases.”
The ongoing Beat AML trial was launched by LLS in 2016 to assess various novel targeted therapies in newly diagnosed AML patients aged 60 years and older. Participants underwent next-generation genomic sequencing, were matched to the appropriate targeted therapy, and were given the option of enrolling on the relevant substudy or selecting an alternate treatment strategy. There are currently 11 substudies assessing novel therapies that have emerged in the wake of “significant progress in understanding the molecular pathogenesis of AML.”
The current findings represent outcomes in patients enrolled between Nov. 2016 and Jan. 2018. The patients had a mean age of 72 years, and those selecting precision medicine vs. SOC had similar demographic and genetic features, the authors noted.
LLS president and chief executive officer Louis J. DeGennaro, PhD, said the findings are practice changing and provide a template for studying precision medicine in other cancers.
“The study is changing significantly the way we look at treating patients with AML, showing that precision medicine ... can improve short- and long-term outcomes for patients with this deadly blood cancer,” he said in the LLS statement. “Further, BEAT AML has proven to be a viable model for other cancer clinical trials to emulate.”
In fact, the model has been applied to the recently launched Beat COVID trial, which looks at acalabrutinib in patients with hematologic cancers and COVID-19 infection, and other trials, including the LLS PedAL global precision medicine trial for children with relapsed acute leukemia, are planned.
“This study sets the path to establish the safety of precision medicine in AML and sets the stage to extend this same approach to younger patients with this disease and other cancers that are urgently treated as a single disease despite recognition of multiple subtypes, the authors concluded.
Dr. Burd is an employee of LLS, which received funding from AbbVie, Agios Pharmaceuticals, Alexion Pharmaceuticals, and a variety of other pharmaceutical and biotechnology companies. Dr. Byrd has received research support from Acerta Pharma, Genentech, Janssen Pharmaceutica, and Pharmacyclics and has served on the advisory board of Syndax Pharmaceuticals.
SOURCE: Burd A et al. Nature Medicine 2020 Oct 26. doi: 10.1038/s41591-020-1089-8.
The 30-day mortality rates were 3.7% versus 20.4% in 224 patients who enrolled in the Beat AML trial precision medicine substudies within 7 days of prospective genomic profiling and 103 who elected SOC chemotherapy, respectively, Amy Burd, PhD, vice president of research strategy for the Leukemia & Lymphoma Society, Rye Brook, N.Y. and her colleagues reported online in Nature Medicine.
Overall survival (OS) at a median of 7.1 months was also significantly longer with precision medicine than with SOC chemotherapy (median, 12.8 vs. 3.9 months), the investigators found.
In an additional 28 patients who selected an investigational therapy rather than a precision medicine strategy or SOC chemotherapy, median OS was not reached, and in 38 who chose palliative care, median OS was 0.6 months, they noted. Care type was unknown in two patients.
The results were similar after controlling for demographic, clinical, and molecular variables and did not change when patients with adverse events of special interest were excluded from the analysis or when only those with survival greater than 2 weeks were included in the analysis.
AML confers an adverse outcome in older adults and therefore is typically treated rapidly after diagnosis. This has precluded consideration of patients’ mutational profile for treatment decisions.
Beat AML, however, sought to prospectively assess the feasibility of quickly ascertaining cytogenetic and mutational data for the purpose of improving outcomes through targeted treatment.
“The study shows that delaying treatment up to 7 days is feasible and safe, and that patients who opted for the precision medicine approach experienced a lower early death rate and superior overall survival, compared with patients who opted for standard of care,” lead study author John C. Byrd, MD, the D. Warren Brown Chair of Leukemia Research of the Ohio State University, Columbus, noted in a press statement from the Leukemia & Lymphoma Society, which conducted the trial. “This patient-centric study shows that we can move away from chemotherapy treatment for patients who won’t respond or can’t withstand the harsh effects of the same chemotherapies we’ve been using for 40 years and match them with a treatment better suited for their individual cases.”
The ongoing Beat AML trial was launched by LLS in 2016 to assess various novel targeted therapies in newly diagnosed AML patients aged 60 years and older. Participants underwent next-generation genomic sequencing, were matched to the appropriate targeted therapy, and were given the option of enrolling on the relevant substudy or selecting an alternate treatment strategy. There are currently 11 substudies assessing novel therapies that have emerged in the wake of “significant progress in understanding the molecular pathogenesis of AML.”
The current findings represent outcomes in patients enrolled between Nov. 2016 and Jan. 2018. The patients had a mean age of 72 years, and those selecting precision medicine vs. SOC had similar demographic and genetic features, the authors noted.
LLS president and chief executive officer Louis J. DeGennaro, PhD, said the findings are practice changing and provide a template for studying precision medicine in other cancers.
“The study is changing significantly the way we look at treating patients with AML, showing that precision medicine ... can improve short- and long-term outcomes for patients with this deadly blood cancer,” he said in the LLS statement. “Further, BEAT AML has proven to be a viable model for other cancer clinical trials to emulate.”
In fact, the model has been applied to the recently launched Beat COVID trial, which looks at acalabrutinib in patients with hematologic cancers and COVID-19 infection, and other trials, including the LLS PedAL global precision medicine trial for children with relapsed acute leukemia, are planned.
“This study sets the path to establish the safety of precision medicine in AML and sets the stage to extend this same approach to younger patients with this disease and other cancers that are urgently treated as a single disease despite recognition of multiple subtypes, the authors concluded.
Dr. Burd is an employee of LLS, which received funding from AbbVie, Agios Pharmaceuticals, Alexion Pharmaceuticals, and a variety of other pharmaceutical and biotechnology companies. Dr. Byrd has received research support from Acerta Pharma, Genentech, Janssen Pharmaceutica, and Pharmacyclics and has served on the advisory board of Syndax Pharmaceuticals.
SOURCE: Burd A et al. Nature Medicine 2020 Oct 26. doi: 10.1038/s41591-020-1089-8.
FROM NATURE MEDICINE
Novel agents hold promise for frontline AML treatment
Novel therapies are poised to dramatically change frontline therapy for acute myeloid leukemia (AML), and they have the potential to replace chemotherapy, a hematologist/oncologist told colleagues at the virtual Acute Leukemia Forum of Hemedicus.
But more work needs to be done, noted Alexander Perl, MD, MS, associate professor at the University of Pennsylvania, Philadelphia. While advances have transformed AML treatment in the relapsed/refractory setting, “we’re just not seeing that substantive improvement” for newly diagnosed patients, he said. “We need to find the disease-modifying drugs that work in the relapsed/refractory setting and move those frontline. That’s where we’re going to see the transformations.”
Research suggests that low-intensity therapy holds tremendous promise, he said, “with the idea that we could make therapy much more tolerable for the vast majority of patients affected by AML, who, as we know, are older patients.”
Dr. Perl highlighted the 2020 VIALE-A study – venetoclax/azacitidine versus azacitidine/placebo – which reported that “in previously untreated patients who were ineligible for intensive chemotherapy, overall survival was longer and the incidence of remission was higher among patients who received azacitidine plus venetoclax than among those who received azacitidine alone.”
Venetoclax promotes apoptosis in leukemia cells, Dr. Perl said. “To a certain extent, you can think of it as putting the rubber to the road in terms of what actually chemotherapy is designed to do, which is to make leukemic blasts apoptose. It does so without DNA damage and with much less toxicity to the patient. Therefore it can be added to any number of regimens – granted, with mild suppression, but with relatively little extramedullary toxicity.”
Dr. Perl noted that the venetoclax arm “showed a higher response rate than azacitidine in pretty much every subgroup that was looked at, whether patients had de novo leukemia, secondary leukemia, multiple mutational complements, various different karyotypes. The response rates on this study are as high as what we often will see with intensive chemotherapy.” He added that “the winning arm on this trial seems to hold up against any low-intensity therapy, and I would argue against many high-intensity therapies in older patients.”
As for other targeted agents, isocitrate dehydrogenase (IDH) inhibitors “are very promising drugs in the relapsed/refractory setting, which is primarily where these drugs are given. In regard to frontline treatment, “data are coming from a very small study, but they’re very encouraging. It’s hard to entirely say that we’re ready to change practice based on this. But it’s very encouraging – the idea that earlier use of a drug-targeting IDH mutation might lead to substantially better outcomes.”
Moving forward, he said, “we could put all of our eggs in one basket and use many active drugs [at] front line. Or we can perhaps be smart about sequencing these drugs one after another, or using more intensive approaches followed by maintenance approaches followed by more intensive approaches.”
This approach is similar to strategies in myeloma patients “who less and less are relying on an autologous transplant for durable control of their disease, and more and more are using low-intensity biologically targeted drugs,” he said.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
Dr. Perl reported numerous disclosures, including relationships with Daiichi Sankyo, Abbvie, and Astellas.
Novel therapies are poised to dramatically change frontline therapy for acute myeloid leukemia (AML), and they have the potential to replace chemotherapy, a hematologist/oncologist told colleagues at the virtual Acute Leukemia Forum of Hemedicus.
But more work needs to be done, noted Alexander Perl, MD, MS, associate professor at the University of Pennsylvania, Philadelphia. While advances have transformed AML treatment in the relapsed/refractory setting, “we’re just not seeing that substantive improvement” for newly diagnosed patients, he said. “We need to find the disease-modifying drugs that work in the relapsed/refractory setting and move those frontline. That’s where we’re going to see the transformations.”
Research suggests that low-intensity therapy holds tremendous promise, he said, “with the idea that we could make therapy much more tolerable for the vast majority of patients affected by AML, who, as we know, are older patients.”
Dr. Perl highlighted the 2020 VIALE-A study – venetoclax/azacitidine versus azacitidine/placebo – which reported that “in previously untreated patients who were ineligible for intensive chemotherapy, overall survival was longer and the incidence of remission was higher among patients who received azacitidine plus venetoclax than among those who received azacitidine alone.”
Venetoclax promotes apoptosis in leukemia cells, Dr. Perl said. “To a certain extent, you can think of it as putting the rubber to the road in terms of what actually chemotherapy is designed to do, which is to make leukemic blasts apoptose. It does so without DNA damage and with much less toxicity to the patient. Therefore it can be added to any number of regimens – granted, with mild suppression, but with relatively little extramedullary toxicity.”
Dr. Perl noted that the venetoclax arm “showed a higher response rate than azacitidine in pretty much every subgroup that was looked at, whether patients had de novo leukemia, secondary leukemia, multiple mutational complements, various different karyotypes. The response rates on this study are as high as what we often will see with intensive chemotherapy.” He added that “the winning arm on this trial seems to hold up against any low-intensity therapy, and I would argue against many high-intensity therapies in older patients.”
As for other targeted agents, isocitrate dehydrogenase (IDH) inhibitors “are very promising drugs in the relapsed/refractory setting, which is primarily where these drugs are given. In regard to frontline treatment, “data are coming from a very small study, but they’re very encouraging. It’s hard to entirely say that we’re ready to change practice based on this. But it’s very encouraging – the idea that earlier use of a drug-targeting IDH mutation might lead to substantially better outcomes.”
Moving forward, he said, “we could put all of our eggs in one basket and use many active drugs [at] front line. Or we can perhaps be smart about sequencing these drugs one after another, or using more intensive approaches followed by maintenance approaches followed by more intensive approaches.”
This approach is similar to strategies in myeloma patients “who less and less are relying on an autologous transplant for durable control of their disease, and more and more are using low-intensity biologically targeted drugs,” he said.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
Dr. Perl reported numerous disclosures, including relationships with Daiichi Sankyo, Abbvie, and Astellas.
Novel therapies are poised to dramatically change frontline therapy for acute myeloid leukemia (AML), and they have the potential to replace chemotherapy, a hematologist/oncologist told colleagues at the virtual Acute Leukemia Forum of Hemedicus.
But more work needs to be done, noted Alexander Perl, MD, MS, associate professor at the University of Pennsylvania, Philadelphia. While advances have transformed AML treatment in the relapsed/refractory setting, “we’re just not seeing that substantive improvement” for newly diagnosed patients, he said. “We need to find the disease-modifying drugs that work in the relapsed/refractory setting and move those frontline. That’s where we’re going to see the transformations.”
Research suggests that low-intensity therapy holds tremendous promise, he said, “with the idea that we could make therapy much more tolerable for the vast majority of patients affected by AML, who, as we know, are older patients.”
Dr. Perl highlighted the 2020 VIALE-A study – venetoclax/azacitidine versus azacitidine/placebo – which reported that “in previously untreated patients who were ineligible for intensive chemotherapy, overall survival was longer and the incidence of remission was higher among patients who received azacitidine plus venetoclax than among those who received azacitidine alone.”
Venetoclax promotes apoptosis in leukemia cells, Dr. Perl said. “To a certain extent, you can think of it as putting the rubber to the road in terms of what actually chemotherapy is designed to do, which is to make leukemic blasts apoptose. It does so without DNA damage and with much less toxicity to the patient. Therefore it can be added to any number of regimens – granted, with mild suppression, but with relatively little extramedullary toxicity.”
Dr. Perl noted that the venetoclax arm “showed a higher response rate than azacitidine in pretty much every subgroup that was looked at, whether patients had de novo leukemia, secondary leukemia, multiple mutational complements, various different karyotypes. The response rates on this study are as high as what we often will see with intensive chemotherapy.” He added that “the winning arm on this trial seems to hold up against any low-intensity therapy, and I would argue against many high-intensity therapies in older patients.”
As for other targeted agents, isocitrate dehydrogenase (IDH) inhibitors “are very promising drugs in the relapsed/refractory setting, which is primarily where these drugs are given. In regard to frontline treatment, “data are coming from a very small study, but they’re very encouraging. It’s hard to entirely say that we’re ready to change practice based on this. But it’s very encouraging – the idea that earlier use of a drug-targeting IDH mutation might lead to substantially better outcomes.”
Moving forward, he said, “we could put all of our eggs in one basket and use many active drugs [at] front line. Or we can perhaps be smart about sequencing these drugs one after another, or using more intensive approaches followed by maintenance approaches followed by more intensive approaches.”
This approach is similar to strategies in myeloma patients “who less and less are relying on an autologous transplant for durable control of their disease, and more and more are using low-intensity biologically targeted drugs,” he said.
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
Dr. Perl reported numerous disclosures, including relationships with Daiichi Sankyo, Abbvie, and Astellas.
FROM ALF 2020
Novel treatments under study for chronic graft-versus-host disease in allo-HCT
Physicians are gaining a greater understanding of the pathophysiology of chronic graft-versus-host disease (cGVHD) in allo-hematopoietic cell transplantation (allo-HCT), a hematologist/oncologist told colleagues, and novel treatments are being tested.
However, options remain limited. There’s only one Food and Drug Administration–approved therapy for cGVHD that’s failed one or more treatments, and clinical trials remain a crucial option in some cases, said Mary E.D. Flowers, MD, professor of medicine at the University of Washington’s Fred Hutchinson Cancer Research Center, Seattle, in a presentation at the virtual Acute Leukemia Forum of Hemedicus.
According to Dr. Flowers, cGVHD – a product of a graft’s “immunological assault” against the person receiving a transplant – occurs in 40% of patients within a year after allo-HCT. The disorder “is associated with a poor quality of life, disability, and increased mortality after allo-transplantation,” she said. “It’s a syndrome that can be inflammatory and fibrotic. It involves several organs – the skin, the mouth, the eyes, the lungs, the GI tract.”
The median length of treatment after peripheral blood stem cell transplant is 3.5 years, Dr. Flowers said. Seven years after treatment, 10% of those who are alive – and have avoided relapse – will still need treatment. “Corticosteroids remain the first-line [treatment], at 0.5-1.0 [mg/kg], but they do not control at least 40% of the patients with cGVHD.”
In regard to pathophysiology, she highlighted a 2017 report that presented findings about the pathophysiology of cGVHD. The findings, the report authors wrote, “have yielded a raft of potential new therapeutics, centered on naive T-cell depletion, interleukin-17/21 inhibition, kinase inhibition, regulatory T-cell restoration, and CSF-1 inhibition.”
For now, no agents other than corticosteroids have shown benefit in cGVHD as initial therapy, Dr. Flowers said. In fact, several trials closed early from lack of benefit. But trials continue, she said: Results are pending for a completed phase 3 trial of ibrutinib, a Bruton tyrosine kinase inhibitor, plus steroids for initial treatment of cGVHD. Nearly 500 patients were enrolled, she said. And there’s an ongoing phase 2/3 trial of itacitinib, a Janus kinase 1 inhibitor plus steroids as initial treatment.
Dr. Flowers highlighted the case of a patient with moderate cGVHD. The patient was treated with infection prophylaxis, supportive care for oral and eyes manifestations, and prednisone 0.5 mg/kg (at a lower dose because of diabetes) plus a substitution of tacrolimus with sirolimus, a calcineurin inhibitor.
Why sirolimus? At this early point in progression, she said, the patient didn’t necessarily need systemwide chemo-suppression, and calcineurin inhibitors can be “quite effective” in management of inflammation in the liver. “It would be a completely different story once the patient develops severe cGVHR.” In that case, she said, calcineurin inhibitors wouldn’t be appropriate.
The patient’s status deteriorated to severe cGVHD, and sirolimus was replaced with ibrutinib. Other drugs were added to prevent infection and treat bronchiolitis obliterans syndrome.
In general, “the goal of the treatment is get adequate control of clinical manifestations and prevent more severe disease from developing,” Dr. Flowers said.
In response to a question about polypharmacy in patient with advanced disease – “we tend not to peel those drugs off” – Dr. Flowers said she does see new patients who appear to be taking too many medications. “They are on five drugs, and I say, ‘What are we doing?’ ”
Quite often, Dr. Flowers said, she doesn’t add therapies to existing ones but instead looks for substitutes. “A clinical lesson that I feel that I learned over time is: Ask your questions first. What would you like to see in 3 months? Or 6 months? Before you just add another therapy, do you really know what the trajectory of a disease might be?”
Dr. Flowers discloses research support (Pharmacyclics, Incyte), speaker honorarium (Janssen, Johnson & Johnson, Astellas, Mallinckrodt), and consulting relationships (Pharmacyclics, CSL Behring, Fresenius Kabi).
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
Physicians are gaining a greater understanding of the pathophysiology of chronic graft-versus-host disease (cGVHD) in allo-hematopoietic cell transplantation (allo-HCT), a hematologist/oncologist told colleagues, and novel treatments are being tested.
However, options remain limited. There’s only one Food and Drug Administration–approved therapy for cGVHD that’s failed one or more treatments, and clinical trials remain a crucial option in some cases, said Mary E.D. Flowers, MD, professor of medicine at the University of Washington’s Fred Hutchinson Cancer Research Center, Seattle, in a presentation at the virtual Acute Leukemia Forum of Hemedicus.
According to Dr. Flowers, cGVHD – a product of a graft’s “immunological assault” against the person receiving a transplant – occurs in 40% of patients within a year after allo-HCT. The disorder “is associated with a poor quality of life, disability, and increased mortality after allo-transplantation,” she said. “It’s a syndrome that can be inflammatory and fibrotic. It involves several organs – the skin, the mouth, the eyes, the lungs, the GI tract.”
The median length of treatment after peripheral blood stem cell transplant is 3.5 years, Dr. Flowers said. Seven years after treatment, 10% of those who are alive – and have avoided relapse – will still need treatment. “Corticosteroids remain the first-line [treatment], at 0.5-1.0 [mg/kg], but they do not control at least 40% of the patients with cGVHD.”
In regard to pathophysiology, she highlighted a 2017 report that presented findings about the pathophysiology of cGVHD. The findings, the report authors wrote, “have yielded a raft of potential new therapeutics, centered on naive T-cell depletion, interleukin-17/21 inhibition, kinase inhibition, regulatory T-cell restoration, and CSF-1 inhibition.”
For now, no agents other than corticosteroids have shown benefit in cGVHD as initial therapy, Dr. Flowers said. In fact, several trials closed early from lack of benefit. But trials continue, she said: Results are pending for a completed phase 3 trial of ibrutinib, a Bruton tyrosine kinase inhibitor, plus steroids for initial treatment of cGVHD. Nearly 500 patients were enrolled, she said. And there’s an ongoing phase 2/3 trial of itacitinib, a Janus kinase 1 inhibitor plus steroids as initial treatment.
Dr. Flowers highlighted the case of a patient with moderate cGVHD. The patient was treated with infection prophylaxis, supportive care for oral and eyes manifestations, and prednisone 0.5 mg/kg (at a lower dose because of diabetes) plus a substitution of tacrolimus with sirolimus, a calcineurin inhibitor.
Why sirolimus? At this early point in progression, she said, the patient didn’t necessarily need systemwide chemo-suppression, and calcineurin inhibitors can be “quite effective” in management of inflammation in the liver. “It would be a completely different story once the patient develops severe cGVHR.” In that case, she said, calcineurin inhibitors wouldn’t be appropriate.
The patient’s status deteriorated to severe cGVHD, and sirolimus was replaced with ibrutinib. Other drugs were added to prevent infection and treat bronchiolitis obliterans syndrome.
In general, “the goal of the treatment is get adequate control of clinical manifestations and prevent more severe disease from developing,” Dr. Flowers said.
In response to a question about polypharmacy in patient with advanced disease – “we tend not to peel those drugs off” – Dr. Flowers said she does see new patients who appear to be taking too many medications. “They are on five drugs, and I say, ‘What are we doing?’ ”
Quite often, Dr. Flowers said, she doesn’t add therapies to existing ones but instead looks for substitutes. “A clinical lesson that I feel that I learned over time is: Ask your questions first. What would you like to see in 3 months? Or 6 months? Before you just add another therapy, do you really know what the trajectory of a disease might be?”
Dr. Flowers discloses research support (Pharmacyclics, Incyte), speaker honorarium (Janssen, Johnson & Johnson, Astellas, Mallinckrodt), and consulting relationships (Pharmacyclics, CSL Behring, Fresenius Kabi).
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
Physicians are gaining a greater understanding of the pathophysiology of chronic graft-versus-host disease (cGVHD) in allo-hematopoietic cell transplantation (allo-HCT), a hematologist/oncologist told colleagues, and novel treatments are being tested.
However, options remain limited. There’s only one Food and Drug Administration–approved therapy for cGVHD that’s failed one or more treatments, and clinical trials remain a crucial option in some cases, said Mary E.D. Flowers, MD, professor of medicine at the University of Washington’s Fred Hutchinson Cancer Research Center, Seattle, in a presentation at the virtual Acute Leukemia Forum of Hemedicus.
According to Dr. Flowers, cGVHD – a product of a graft’s “immunological assault” against the person receiving a transplant – occurs in 40% of patients within a year after allo-HCT. The disorder “is associated with a poor quality of life, disability, and increased mortality after allo-transplantation,” she said. “It’s a syndrome that can be inflammatory and fibrotic. It involves several organs – the skin, the mouth, the eyes, the lungs, the GI tract.”
The median length of treatment after peripheral blood stem cell transplant is 3.5 years, Dr. Flowers said. Seven years after treatment, 10% of those who are alive – and have avoided relapse – will still need treatment. “Corticosteroids remain the first-line [treatment], at 0.5-1.0 [mg/kg], but they do not control at least 40% of the patients with cGVHD.”
In regard to pathophysiology, she highlighted a 2017 report that presented findings about the pathophysiology of cGVHD. The findings, the report authors wrote, “have yielded a raft of potential new therapeutics, centered on naive T-cell depletion, interleukin-17/21 inhibition, kinase inhibition, regulatory T-cell restoration, and CSF-1 inhibition.”
For now, no agents other than corticosteroids have shown benefit in cGVHD as initial therapy, Dr. Flowers said. In fact, several trials closed early from lack of benefit. But trials continue, she said: Results are pending for a completed phase 3 trial of ibrutinib, a Bruton tyrosine kinase inhibitor, plus steroids for initial treatment of cGVHD. Nearly 500 patients were enrolled, she said. And there’s an ongoing phase 2/3 trial of itacitinib, a Janus kinase 1 inhibitor plus steroids as initial treatment.
Dr. Flowers highlighted the case of a patient with moderate cGVHD. The patient was treated with infection prophylaxis, supportive care for oral and eyes manifestations, and prednisone 0.5 mg/kg (at a lower dose because of diabetes) plus a substitution of tacrolimus with sirolimus, a calcineurin inhibitor.
Why sirolimus? At this early point in progression, she said, the patient didn’t necessarily need systemwide chemo-suppression, and calcineurin inhibitors can be “quite effective” in management of inflammation in the liver. “It would be a completely different story once the patient develops severe cGVHR.” In that case, she said, calcineurin inhibitors wouldn’t be appropriate.
The patient’s status deteriorated to severe cGVHD, and sirolimus was replaced with ibrutinib. Other drugs were added to prevent infection and treat bronchiolitis obliterans syndrome.
In general, “the goal of the treatment is get adequate control of clinical manifestations and prevent more severe disease from developing,” Dr. Flowers said.
In response to a question about polypharmacy in patient with advanced disease – “we tend not to peel those drugs off” – Dr. Flowers said she does see new patients who appear to be taking too many medications. “They are on five drugs, and I say, ‘What are we doing?’ ”
Quite often, Dr. Flowers said, she doesn’t add therapies to existing ones but instead looks for substitutes. “A clinical lesson that I feel that I learned over time is: Ask your questions first. What would you like to see in 3 months? Or 6 months? Before you just add another therapy, do you really know what the trajectory of a disease might be?”
Dr. Flowers discloses research support (Pharmacyclics, Incyte), speaker honorarium (Janssen, Johnson & Johnson, Astellas, Mallinckrodt), and consulting relationships (Pharmacyclics, CSL Behring, Fresenius Kabi).
The Acute Leukemia Forum is held by Hemedicus, which is owned by the same company as this news organization.
FROM ALF 2020
Final ASCEND study data: Acalabrutinib beat standard of care for r/r CLL
Acalabrutinib, a next-generation Bruton tyrosine kinase inhibitor, provides prolonged progression-free survival and better tolerability, compared with standard-of-care regimens for relapsed or refractory chronic lymphocytic leukemia (CLL), according to final results from the phase 3 ASCEND study.
The estimated 18-month progression-free survival (PFS) at a median of 22 months was 82% in 155 patients treated with acalabrutinib, compared with 48% in 155 treated with investigator’s choice of either idelalisib-rituximab (IdR) or bendamustine-rituximab (BR), which were given in 119 and 36 patients, respectively, Paolo Ghia, MD, PhD, reported at the Society of Hematologic Oncology virtual meeting.
The benefits of acalabrutinib were apparent regardless of high-risk genetic characteristics: Those with and without both del(17p) and TP53 mutations had similarly good PFS outcomes with acalabrutinib versus IdR/BR (HRs, 0.11 and 0.29, respectively), as did those with versus without unmutated IgVH (HRs, 0.28 and 0.30, respectively), said Dr. Ghia, professor of medical oncology at the Università Vita-Salute San Raffaele and IRCCS Ospedale San Raffaele, Milan.
The median overall survival was not reached in either arm, but estimated 18-month OS was 88% in both groups, likely because of the crossover being allowed for nonresponders in the IdR/BR groups, he noted.
Overall responses
The investigator-assessed overall response rates, including partial response or better, were also similar in the groups at 80% and 84%, respectively, and ORR, including partial response with lymphocytosis, was 92% versus 88%.
The duration of response was not reached in the acalabrutinib arm versus 18 months with IdR/BR, and estimated duration of response was 85% versus 49%.
The median drug exposure with acalabrutinib was approximately double that with IdR and about four times that of BR, Dr. Ghia said, noting that the difference between acalabrutinib and BR is explained by the short 6-month duration of treatment with BR, but the difference between acalabrutinib and IdR is because of adverse events (AEs).
Adverse events
AEs were the most common reason for treatment discontinuation in all three groups, but they led to discontinuation in only 16% with acalabrutinib versus 56% with IdR, he added.
The rates of AEs and AEs of clinical interest were generally similar to those reported at the interim analysis as presented in 2019 at the European Hematology Association annual meeting and published in the Journal of Clinical Oncology, despite the additional 6 months of follow up, he said.
Additionally, the incidence of grade 3 or higher AEs, serious AEs, and treatment-related AEs were all greater with IdR than with acalabrutinib or BR. The most common AEs with acalabrutinib were headache, neutropenia, diarrhea, and upper-respiratory infection, which were mostly grade 1 or 2. The most common grade 3 or higher AEs were neutropenia, anemia, and pneumonia, which were reported in 12%, 17%, and 7% of patients.
Confirmatory results
“The final results from the ASCEND study confirm the findings at the interim analysis and support the favorable efficacy and safety of acalabrutinib versus standard-of-care regimens ... in patients with relapsed/refractory CLL,” Dr. Ghia said.
“Overall, these final results from ASCENT support the use of acalabrutinib in patients with relapsed/refractory CLL, including those with high-risk genetic features.”
This study was sponsored by Acerta Pharma. Dr. Ghia reported consulting or advisory roles, grant or research funding, and/or honoraria from Abbvie, BeiGene, Janssen, Gilead Sciences, Sunesis Pharmaceuticals, Juno Therapeutics, ArQule, Adaptive Biotechnologies, Dynamo Therapeutics, MEI Pharma, and Novartis.
SOURCE: Ghia P et al. SOHO 2020, Abstract CLL-091.
Acalabrutinib, a next-generation Bruton tyrosine kinase inhibitor, provides prolonged progression-free survival and better tolerability, compared with standard-of-care regimens for relapsed or refractory chronic lymphocytic leukemia (CLL), according to final results from the phase 3 ASCEND study.
The estimated 18-month progression-free survival (PFS) at a median of 22 months was 82% in 155 patients treated with acalabrutinib, compared with 48% in 155 treated with investigator’s choice of either idelalisib-rituximab (IdR) or bendamustine-rituximab (BR), which were given in 119 and 36 patients, respectively, Paolo Ghia, MD, PhD, reported at the Society of Hematologic Oncology virtual meeting.
The benefits of acalabrutinib were apparent regardless of high-risk genetic characteristics: Those with and without both del(17p) and TP53 mutations had similarly good PFS outcomes with acalabrutinib versus IdR/BR (HRs, 0.11 and 0.29, respectively), as did those with versus without unmutated IgVH (HRs, 0.28 and 0.30, respectively), said Dr. Ghia, professor of medical oncology at the Università Vita-Salute San Raffaele and IRCCS Ospedale San Raffaele, Milan.
The median overall survival was not reached in either arm, but estimated 18-month OS was 88% in both groups, likely because of the crossover being allowed for nonresponders in the IdR/BR groups, he noted.
Overall responses
The investigator-assessed overall response rates, including partial response or better, were also similar in the groups at 80% and 84%, respectively, and ORR, including partial response with lymphocytosis, was 92% versus 88%.
The duration of response was not reached in the acalabrutinib arm versus 18 months with IdR/BR, and estimated duration of response was 85% versus 49%.
The median drug exposure with acalabrutinib was approximately double that with IdR and about four times that of BR, Dr. Ghia said, noting that the difference between acalabrutinib and BR is explained by the short 6-month duration of treatment with BR, but the difference between acalabrutinib and IdR is because of adverse events (AEs).
Adverse events
AEs were the most common reason for treatment discontinuation in all three groups, but they led to discontinuation in only 16% with acalabrutinib versus 56% with IdR, he added.
The rates of AEs and AEs of clinical interest were generally similar to those reported at the interim analysis as presented in 2019 at the European Hematology Association annual meeting and published in the Journal of Clinical Oncology, despite the additional 6 months of follow up, he said.
Additionally, the incidence of grade 3 or higher AEs, serious AEs, and treatment-related AEs were all greater with IdR than with acalabrutinib or BR. The most common AEs with acalabrutinib were headache, neutropenia, diarrhea, and upper-respiratory infection, which were mostly grade 1 or 2. The most common grade 3 or higher AEs were neutropenia, anemia, and pneumonia, which were reported in 12%, 17%, and 7% of patients.
Confirmatory results
“The final results from the ASCEND study confirm the findings at the interim analysis and support the favorable efficacy and safety of acalabrutinib versus standard-of-care regimens ... in patients with relapsed/refractory CLL,” Dr. Ghia said.
“Overall, these final results from ASCENT support the use of acalabrutinib in patients with relapsed/refractory CLL, including those with high-risk genetic features.”
This study was sponsored by Acerta Pharma. Dr. Ghia reported consulting or advisory roles, grant or research funding, and/or honoraria from Abbvie, BeiGene, Janssen, Gilead Sciences, Sunesis Pharmaceuticals, Juno Therapeutics, ArQule, Adaptive Biotechnologies, Dynamo Therapeutics, MEI Pharma, and Novartis.
SOURCE: Ghia P et al. SOHO 2020, Abstract CLL-091.
Acalabrutinib, a next-generation Bruton tyrosine kinase inhibitor, provides prolonged progression-free survival and better tolerability, compared with standard-of-care regimens for relapsed or refractory chronic lymphocytic leukemia (CLL), according to final results from the phase 3 ASCEND study.
The estimated 18-month progression-free survival (PFS) at a median of 22 months was 82% in 155 patients treated with acalabrutinib, compared with 48% in 155 treated with investigator’s choice of either idelalisib-rituximab (IdR) or bendamustine-rituximab (BR), which were given in 119 and 36 patients, respectively, Paolo Ghia, MD, PhD, reported at the Society of Hematologic Oncology virtual meeting.
The benefits of acalabrutinib were apparent regardless of high-risk genetic characteristics: Those with and without both del(17p) and TP53 mutations had similarly good PFS outcomes with acalabrutinib versus IdR/BR (HRs, 0.11 and 0.29, respectively), as did those with versus without unmutated IgVH (HRs, 0.28 and 0.30, respectively), said Dr. Ghia, professor of medical oncology at the Università Vita-Salute San Raffaele and IRCCS Ospedale San Raffaele, Milan.
The median overall survival was not reached in either arm, but estimated 18-month OS was 88% in both groups, likely because of the crossover being allowed for nonresponders in the IdR/BR groups, he noted.
Overall responses
The investigator-assessed overall response rates, including partial response or better, were also similar in the groups at 80% and 84%, respectively, and ORR, including partial response with lymphocytosis, was 92% versus 88%.
The duration of response was not reached in the acalabrutinib arm versus 18 months with IdR/BR, and estimated duration of response was 85% versus 49%.
The median drug exposure with acalabrutinib was approximately double that with IdR and about four times that of BR, Dr. Ghia said, noting that the difference between acalabrutinib and BR is explained by the short 6-month duration of treatment with BR, but the difference between acalabrutinib and IdR is because of adverse events (AEs).
Adverse events
AEs were the most common reason for treatment discontinuation in all three groups, but they led to discontinuation in only 16% with acalabrutinib versus 56% with IdR, he added.
The rates of AEs and AEs of clinical interest were generally similar to those reported at the interim analysis as presented in 2019 at the European Hematology Association annual meeting and published in the Journal of Clinical Oncology, despite the additional 6 months of follow up, he said.
Additionally, the incidence of grade 3 or higher AEs, serious AEs, and treatment-related AEs were all greater with IdR than with acalabrutinib or BR. The most common AEs with acalabrutinib were headache, neutropenia, diarrhea, and upper-respiratory infection, which were mostly grade 1 or 2. The most common grade 3 or higher AEs were neutropenia, anemia, and pneumonia, which were reported in 12%, 17%, and 7% of patients.
Confirmatory results
“The final results from the ASCEND study confirm the findings at the interim analysis and support the favorable efficacy and safety of acalabrutinib versus standard-of-care regimens ... in patients with relapsed/refractory CLL,” Dr. Ghia said.
“Overall, these final results from ASCENT support the use of acalabrutinib in patients with relapsed/refractory CLL, including those with high-risk genetic features.”
This study was sponsored by Acerta Pharma. Dr. Ghia reported consulting or advisory roles, grant or research funding, and/or honoraria from Abbvie, BeiGene, Janssen, Gilead Sciences, Sunesis Pharmaceuticals, Juno Therapeutics, ArQule, Adaptive Biotechnologies, Dynamo Therapeutics, MEI Pharma, and Novartis.
SOURCE: Ghia P et al. SOHO 2020, Abstract CLL-091.
FROM SOHO 2020
Socioeconomic factors affect survival of multiple myeloma patients
Disparities driven by socioeconomic factors have been shown to affect outcomes for patients with a variety of cancer types. Researchers found that this was also true for patients with multiple myeloma, according to a report published in Hematology/Oncology and Stem Cell Therapy.
In particular, survival was affected by a variety of socioeconomic factors.
Researchers conducting the study queried the National Cancer Database for patients diagnosed with multiple myeloma between 2004 and 2016. Only those 56,102 patients who received systemic therapy as the first-line treatment were included, according to Thejus T. Jayakrishnan, MD, of Allegheny Health Network, Pittsburgh, and colleagues.
Enrollment rates for therapy were calculated using receiving systemic therapy as the incident event of interest (numerator) over time to initiation of therapy (denominator). The incident rate ratios were analyzed using Poisson regression. A multivariate Cox proportional hazards model was used for survival analysis of 50,543 patients, and differences were determined as hazard ratios.
Significant differences
The study showed that therapy enrollment was significantly affected by race and sex (P < .005), with the enrollment rate for women and for non-Hispanic Blacks both being lower versus men and non-Hispanic Whites, respectively.
Advanced age, earlier year of diagnosis, lack of insurance or Medicaid, and higher comorbidity were found to be associated with poor survival (HR >1), whereas being a woman or a non-Hispanic Black (who were speculated to have more favorable cytogenetic profiles), having a higher income, and having treatment at an academic center were all associated with improved survival (each category at HR <1).
“Disparities in [multiple myeloma] exist and are caused by a complex interplay of multiple factors, with socioeconomic factors such as insurance and income playing a dominant role. The disparities not only exact high human cost but also negatively impact the economics of health care,” the researchers concluded.
The study was not funded and the authors reported that they had no relevant disclosures.
SOURCE: Jayakrishnan TT et al. Hematol Oncol Stem Cell Ther. 2020 Oct 10. doi: 10.1016/j.hemonc.2020.09.005.
Disparities driven by socioeconomic factors have been shown to affect outcomes for patients with a variety of cancer types. Researchers found that this was also true for patients with multiple myeloma, according to a report published in Hematology/Oncology and Stem Cell Therapy.
In particular, survival was affected by a variety of socioeconomic factors.
Researchers conducting the study queried the National Cancer Database for patients diagnosed with multiple myeloma between 2004 and 2016. Only those 56,102 patients who received systemic therapy as the first-line treatment were included, according to Thejus T. Jayakrishnan, MD, of Allegheny Health Network, Pittsburgh, and colleagues.
Enrollment rates for therapy were calculated using receiving systemic therapy as the incident event of interest (numerator) over time to initiation of therapy (denominator). The incident rate ratios were analyzed using Poisson regression. A multivariate Cox proportional hazards model was used for survival analysis of 50,543 patients, and differences were determined as hazard ratios.
Significant differences
The study showed that therapy enrollment was significantly affected by race and sex (P < .005), with the enrollment rate for women and for non-Hispanic Blacks both being lower versus men and non-Hispanic Whites, respectively.
Advanced age, earlier year of diagnosis, lack of insurance or Medicaid, and higher comorbidity were found to be associated with poor survival (HR >1), whereas being a woman or a non-Hispanic Black (who were speculated to have more favorable cytogenetic profiles), having a higher income, and having treatment at an academic center were all associated with improved survival (each category at HR <1).
“Disparities in [multiple myeloma] exist and are caused by a complex interplay of multiple factors, with socioeconomic factors such as insurance and income playing a dominant role. The disparities not only exact high human cost but also negatively impact the economics of health care,” the researchers concluded.
The study was not funded and the authors reported that they had no relevant disclosures.
SOURCE: Jayakrishnan TT et al. Hematol Oncol Stem Cell Ther. 2020 Oct 10. doi: 10.1016/j.hemonc.2020.09.005.
Disparities driven by socioeconomic factors have been shown to affect outcomes for patients with a variety of cancer types. Researchers found that this was also true for patients with multiple myeloma, according to a report published in Hematology/Oncology and Stem Cell Therapy.
In particular, survival was affected by a variety of socioeconomic factors.
Researchers conducting the study queried the National Cancer Database for patients diagnosed with multiple myeloma between 2004 and 2016. Only those 56,102 patients who received systemic therapy as the first-line treatment were included, according to Thejus T. Jayakrishnan, MD, of Allegheny Health Network, Pittsburgh, and colleagues.
Enrollment rates for therapy were calculated using receiving systemic therapy as the incident event of interest (numerator) over time to initiation of therapy (denominator). The incident rate ratios were analyzed using Poisson regression. A multivariate Cox proportional hazards model was used for survival analysis of 50,543 patients, and differences were determined as hazard ratios.
Significant differences
The study showed that therapy enrollment was significantly affected by race and sex (P < .005), with the enrollment rate for women and for non-Hispanic Blacks both being lower versus men and non-Hispanic Whites, respectively.
Advanced age, earlier year of diagnosis, lack of insurance or Medicaid, and higher comorbidity were found to be associated with poor survival (HR >1), whereas being a woman or a non-Hispanic Black (who were speculated to have more favorable cytogenetic profiles), having a higher income, and having treatment at an academic center were all associated with improved survival (each category at HR <1).
“Disparities in [multiple myeloma] exist and are caused by a complex interplay of multiple factors, with socioeconomic factors such as insurance and income playing a dominant role. The disparities not only exact high human cost but also negatively impact the economics of health care,” the researchers concluded.
The study was not funded and the authors reported that they had no relevant disclosures.
SOURCE: Jayakrishnan TT et al. Hematol Oncol Stem Cell Ther. 2020 Oct 10. doi: 10.1016/j.hemonc.2020.09.005.
FROM HEMATOLOGY/ONCOLOGY AND STEM CELL THERAPY
Are oncologists ready to confront a second wave of COVID-19?
Canceled appointments, postponed surgeries, and delayed cancer diagnoses – all are a recipe for exhaustion for oncologists around the world, struggling to reach and treat their patients during the pandemic. Physicians and their teams felt the pain as COVID-19 took its initial march around the globe.
“We saw the distress of people with cancer who could no longer get to anyone on the phone. Their medical visit was usually canceled. Their radiotherapy session was postponed or modified, and chemotherapy postponed,” says Axel Kahn, MD, chairman of the board of directors of La Ligue Nationale Contre le Cancer (National League Against Cancer). “In the vast majority of cases, cancer treatment can be postponed or readjusted, without affecting the patient’s chances of survival, but there has been a lot of anxiety because the patients do not know that.”
The stay-at-home factor was one that played out across many months during the first wave.
“I believe that the ‘stay-home’ message that we transmitted was rigorously followed by patients who should have come to the emergency room much earlier and who, therefore, were admitted with a much more deteriorated general condition than in non-COVID-19 times,” says Benjamín Domingo Arrué, MD, from the department of medical oncology at Hospital Universitari i Politècnic La Fe in Valencia, Spain.
And in Brazil, some of the impact from the initial hit of COVID-19 on oncology is only now being felt, according to Laura Testa, MD, head of breast medical oncology, Instituto do Câncer do Estado de São Paulo.
“We are starting to see a lot of cancer cases that didn’t show up at the beginning of the pandemic, but now they are arriving to us already in advanced stages,” she said. “These patients need hospital care. If the situation worsens and goes back to what we saw at the peak of the curve, I fear the public system won’t be able to treat properly the oncology patients that need hospital care and the patients with cancer who also have COVID-19.”
But even as health care worker fatigue and concerns linger, oncologists say that what they have learned in the last 6 months has helped them prepare as COVID-19 cases increase and a second global wave kicks up.
Lessons from the first wave
In the United States, COVID-19 hit different regions at different times and to different degrees. One of the areas hit first was Seattle.
“We jumped on top of this, we were evidence based, we put things in place very, very quickly,” said Julie Gralow, MD, professor at the University of Washington and the Fred Hutchinson Cancer Research Center, both in Seattle.
“We did a really good job keeping COVID out of our cancer centers,” Dr. Gralow said. “We learned how to be super safe, and to keep symptomatic people out of the building, and to limit the extra people they could bring with them. It’s all about the number of contacts you have.”
The story was different, though, for oncologists in several other countries, and sometimes it varied immensely within each nation.
“We treated fewer patients with cancer during the first wave,” says Dirk Arnold, MD, medical director of the Asklepios Tumor Center Hamburg (Germany), in an interview. “In part, this was because staff were quarantined and because we had a completely different infrastructure in all of the hospitals. But also fewer patients with cancer came to the clinic at all. A lot of resources were directed toward COVID-19.”
In Spain, telemedicine helped keep up with visits, but other areas felt the effect of COVID-19 patient loads.
“At least in the oncology department of our center, we have practically maintained 100% of visits, mostly by telephone,” says Dr. Arrué, “but the reality is that our country has not yet been prepared for telemedicine.”
Laura Mezquita, MD, of the department of medical oncology at Hospital Clinic de Barcelona, describes a more dramatic situation: “We have seen how some of our patients, especially with metastatic disease, have been dismissed for intensive care and life-support treatments, as well as specific treatments against COVID-19 (tocilizumab, remdesivir, etc.) due to the general health collapse of the former wave,” she said. She adds that specific oncologic populations, such as those with thoracic tumors, have been more affected.
Distress among oncologists
Many oncologists are still feeling stressed and fatigued after the first wave, just as a second string of outbreaks is on its way.
A survey presented at last month’s ESMO 2020 Congress found that, in July-August, moral distress was reported by one-third of the oncologists who responded, and more than half reported a feeling of exhaustion.
“The tiredness and team exhaustion is noticeable,” said Dr. Arnold. “We recently had a task force discussion about what will happen when we have a second wave and how the department and our services will adapt. It was clear that those who were at the very front in the first wave had only a limited desire to do that again in the second wave.”
Another concern: COVID-19’s effect on staffing levels.
“We have a population of young caregivers who are affected by the COVID-19 disease with an absenteeism rate that is quite unprecedented,” said Sophie Beaupère, general delegate of Unicancer since January.
She said that, in general, the absenteeism rate in the cancer centers averages 5%-6%, depending on the year. But that rate is now skyrocketing.
Stop-start cycle for surgery
As caregivers quarantined around the world, more than 10% of patients with cancer had treatment canceled or delayed during the first wave of the pandemic, according to another survey from ESMO, involving 109 oncologists from 18 countries.
Difficulties were reported for surgeries by 34% of the centers, but also difficulties with delivering chemotherapy (22% of centers), radiotherapy (13.7%), and therapy with checkpoint inhibitors (9.1%), monoclonal antibodies (9%), and oral targeted therapy (3.7%).
Stopping surgery is a real concern in France, noted Dr. Kahn, the National League Against Cancer chair. He says that in regions that were badly hit by COVID-19, “it was not possible to have access to the operating room for people who absolutely needed surgery; for example, patients with lung cancer that was still operable. Most of the recovery rooms were mobilized for resuscitation.”
There may be some solutions, suggested Thierry Breton, director general of the National Institute of Cancer in France. “We are getting prepared, with the health ministry, for a possible increase in hospital tension, which would lead to a situation where we would have to reschedule operations. Nationally, regionally, and locally, we are seeing how we can resume and prioritize surgeries that have not been done.”
Delays in cancer diagnosis
While COVID-19 affected treatment, many oncologists say the major impact of the first wave was a delay in diagnosing cancer. Some of this was a result of the suspension of cancer screening programs, but there was also fear among the general public about visiting clinics and hospitals during a pandemic.
“We didn’t do so well with cancer during the first wave here in the U.K.,” said Karol Sikora, PhD, MBBChir, professor of cancer medicine and founding dean at the University of Buckingham Medical School, London. “Cancer diagnostic pathways virtually stalled partly because patients didn’t seek help, but getting scans and biopsies was also very difficult. Even patients referred urgently under the ‘2-weeks-wait’ rule were turned down.”
In France, “the delay in diagnosis is indisputable,” said Dr. Kahn. “About 50% of the cancer diagnoses one would expect during this period were missed.”
“I am worried that there remains a major traffic jam that has not been caught up with, and, in the meantime, the health crisis is worsening,” he added.
In Seattle, Dr. Gralow said the first COVID-19 wave had little impact on treatment for breast cancer, but it was in screening for breast cancer “where things really got messed up.”
“Even though we’ve been fully ramped up again,” she said, concerns remain. To ensure that screening mammography is maintained, “we have spaced out the visits to keep our waiting rooms less populated, with a longer time between using the machine so we can clean it. To do this, we have extended operating hours and are now opening on Saturday.
“So we’re actually at 100% of our capacity, but I’m really nervous, though, that a lot of people put off their screening mammogram and aren’t going to come in and get it.
“Not only did people get the message to stay home and not do nonessential things, but I think a lot of people lost their health insurance when they lost their jobs,” she said, and without health insurance, they are not covered for cancer screening.
Looking ahead, with a plan
Many oncologists agree that access to care can and must be improved – and there were some positive moves.
“Some regimens changed during the first months of the pandemic, and I don’t see them going back to the way they were anytime soon,” said Dr. Testa. “The changes/adaptations that were made to minimize the chance of SARS-CoV-2 infection are still in place and will go on for a while. In this context, telemedicine helped a lot. The pandemic forced the stakeholders to step up and put it in place in March. And now it’s here to stay.”
The experience gained in the last several months has driven preparation for the next wave.
“We are not going to see the disorganization that we saw during the first wave,” said Florence Joly, MD, PhD, head of medical oncology at the Centre François Baclesse in Caen, France. “The difference between now and earlier this year is that COVID diagnostic tests are available. That was one of the problems in the first wave. We had no way to diagnose.”
On the East Coast of the United States, medical oncologist Charu Aggarwal, MD, MPH, is also optimistic: “I think we’re at a place where we can manage.”
“I believe if there was going to be a new wave of COVID-19 cases we would be: better psychologically prepared and better organized,” said Dr. Aggarwal, assistant professor of medicine in the hematology-oncology division at the University of Pennsylvania, Philadelphia. “We already have experience with all of the tools, we have telemedicine available, we have screening protocols available, we have testing, we are already universally masking, everyone’s hand-washing, so I do think that means we would be okay.”
Dr. Arnold agreed that “we are much better prepared than for the first wave, but … we have immense tasks in the area of patient management, the digitization of patient care, the clear allocation of resources when there is a second or third wave. In many areas of preparation, I believe, unfortunately, we are not as well positioned as we had actually hoped.”
The first wave of COVID hit cancer services in the United Kingdom particularly hard: One modeling study suggested that delays in cancer referrals will lead to thousands of additional deaths and tens of thousands of life-years lost.
“Cancer services are working at near normal levels now, but they are still fragile and could be severely compromised again if the NHS [National Health Service] gets flooded by COVID patients,” said Dr. Sikora.
The second wave may be different. “Although the number of infections has increased, the hospitalizations have only risen a little. Let’s see what happens,” he said in an interview. Since then, however, infections have continued to rise, and there has been an increase in hospitalizations. New social distancing measures in the United Kingdom were put into place on Oct. 12, with the aim of protecting the NHS from overload.
Dr. Arrué describes it this way: “The reality is that the ‘second wave’ has left behind the initial grief and shock that both patients and health professionals experienced when faced with something that, until now, we had only seen in the movies.” The second wave has led to new restrictions – including a partial lockdown since the beginning of October.
Dr. Aggarwal says her department recently had a conference with Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, about the impact of COVID-19 on oncology.
“I asked him what advice he’d give oncologists, and he said to go back to as much screening as you were doing previously as quickly as possible. That’s what must be relayed to our oncologists in the community – and also to primary care physicians – because they are often the ones who are ordering and championing the screening efforts.”
This article was originated by Aude Lecrubier, Medscape French edition, and developed by Zosia Chustecka, Medscape Oncology. With additional reporting by Kate Johnson, freelance medical journalist, Claudia Gottschling for Medscape Germany, Leoleli Schwartz for Medscape em português, Tim Locke for Medscape United Kingdom, and Carla Nieto Martínez, freelance medical journalist for Medscape Spanish edition.
This article first appeared on Medscape.com.
Canceled appointments, postponed surgeries, and delayed cancer diagnoses – all are a recipe for exhaustion for oncologists around the world, struggling to reach and treat their patients during the pandemic. Physicians and their teams felt the pain as COVID-19 took its initial march around the globe.
“We saw the distress of people with cancer who could no longer get to anyone on the phone. Their medical visit was usually canceled. Their radiotherapy session was postponed or modified, and chemotherapy postponed,” says Axel Kahn, MD, chairman of the board of directors of La Ligue Nationale Contre le Cancer (National League Against Cancer). “In the vast majority of cases, cancer treatment can be postponed or readjusted, without affecting the patient’s chances of survival, but there has been a lot of anxiety because the patients do not know that.”
The stay-at-home factor was one that played out across many months during the first wave.
“I believe that the ‘stay-home’ message that we transmitted was rigorously followed by patients who should have come to the emergency room much earlier and who, therefore, were admitted with a much more deteriorated general condition than in non-COVID-19 times,” says Benjamín Domingo Arrué, MD, from the department of medical oncology at Hospital Universitari i Politècnic La Fe in Valencia, Spain.
And in Brazil, some of the impact from the initial hit of COVID-19 on oncology is only now being felt, according to Laura Testa, MD, head of breast medical oncology, Instituto do Câncer do Estado de São Paulo.
“We are starting to see a lot of cancer cases that didn’t show up at the beginning of the pandemic, but now they are arriving to us already in advanced stages,” she said. “These patients need hospital care. If the situation worsens and goes back to what we saw at the peak of the curve, I fear the public system won’t be able to treat properly the oncology patients that need hospital care and the patients with cancer who also have COVID-19.”
But even as health care worker fatigue and concerns linger, oncologists say that what they have learned in the last 6 months has helped them prepare as COVID-19 cases increase and a second global wave kicks up.
Lessons from the first wave
In the United States, COVID-19 hit different regions at different times and to different degrees. One of the areas hit first was Seattle.
“We jumped on top of this, we were evidence based, we put things in place very, very quickly,” said Julie Gralow, MD, professor at the University of Washington and the Fred Hutchinson Cancer Research Center, both in Seattle.
“We did a really good job keeping COVID out of our cancer centers,” Dr. Gralow said. “We learned how to be super safe, and to keep symptomatic people out of the building, and to limit the extra people they could bring with them. It’s all about the number of contacts you have.”
The story was different, though, for oncologists in several other countries, and sometimes it varied immensely within each nation.
“We treated fewer patients with cancer during the first wave,” says Dirk Arnold, MD, medical director of the Asklepios Tumor Center Hamburg (Germany), in an interview. “In part, this was because staff were quarantined and because we had a completely different infrastructure in all of the hospitals. But also fewer patients with cancer came to the clinic at all. A lot of resources were directed toward COVID-19.”
In Spain, telemedicine helped keep up with visits, but other areas felt the effect of COVID-19 patient loads.
“At least in the oncology department of our center, we have practically maintained 100% of visits, mostly by telephone,” says Dr. Arrué, “but the reality is that our country has not yet been prepared for telemedicine.”
Laura Mezquita, MD, of the department of medical oncology at Hospital Clinic de Barcelona, describes a more dramatic situation: “We have seen how some of our patients, especially with metastatic disease, have been dismissed for intensive care and life-support treatments, as well as specific treatments against COVID-19 (tocilizumab, remdesivir, etc.) due to the general health collapse of the former wave,” she said. She adds that specific oncologic populations, such as those with thoracic tumors, have been more affected.
Distress among oncologists
Many oncologists are still feeling stressed and fatigued after the first wave, just as a second string of outbreaks is on its way.
A survey presented at last month’s ESMO 2020 Congress found that, in July-August, moral distress was reported by one-third of the oncologists who responded, and more than half reported a feeling of exhaustion.
“The tiredness and team exhaustion is noticeable,” said Dr. Arnold. “We recently had a task force discussion about what will happen when we have a second wave and how the department and our services will adapt. It was clear that those who were at the very front in the first wave had only a limited desire to do that again in the second wave.”
Another concern: COVID-19’s effect on staffing levels.
“We have a population of young caregivers who are affected by the COVID-19 disease with an absenteeism rate that is quite unprecedented,” said Sophie Beaupère, general delegate of Unicancer since January.
She said that, in general, the absenteeism rate in the cancer centers averages 5%-6%, depending on the year. But that rate is now skyrocketing.
Stop-start cycle for surgery
As caregivers quarantined around the world, more than 10% of patients with cancer had treatment canceled or delayed during the first wave of the pandemic, according to another survey from ESMO, involving 109 oncologists from 18 countries.
Difficulties were reported for surgeries by 34% of the centers, but also difficulties with delivering chemotherapy (22% of centers), radiotherapy (13.7%), and therapy with checkpoint inhibitors (9.1%), monoclonal antibodies (9%), and oral targeted therapy (3.7%).
Stopping surgery is a real concern in France, noted Dr. Kahn, the National League Against Cancer chair. He says that in regions that were badly hit by COVID-19, “it was not possible to have access to the operating room for people who absolutely needed surgery; for example, patients with lung cancer that was still operable. Most of the recovery rooms were mobilized for resuscitation.”
There may be some solutions, suggested Thierry Breton, director general of the National Institute of Cancer in France. “We are getting prepared, with the health ministry, for a possible increase in hospital tension, which would lead to a situation where we would have to reschedule operations. Nationally, regionally, and locally, we are seeing how we can resume and prioritize surgeries that have not been done.”
Delays in cancer diagnosis
While COVID-19 affected treatment, many oncologists say the major impact of the first wave was a delay in diagnosing cancer. Some of this was a result of the suspension of cancer screening programs, but there was also fear among the general public about visiting clinics and hospitals during a pandemic.
“We didn’t do so well with cancer during the first wave here in the U.K.,” said Karol Sikora, PhD, MBBChir, professor of cancer medicine and founding dean at the University of Buckingham Medical School, London. “Cancer diagnostic pathways virtually stalled partly because patients didn’t seek help, but getting scans and biopsies was also very difficult. Even patients referred urgently under the ‘2-weeks-wait’ rule were turned down.”
In France, “the delay in diagnosis is indisputable,” said Dr. Kahn. “About 50% of the cancer diagnoses one would expect during this period were missed.”
“I am worried that there remains a major traffic jam that has not been caught up with, and, in the meantime, the health crisis is worsening,” he added.
In Seattle, Dr. Gralow said the first COVID-19 wave had little impact on treatment for breast cancer, but it was in screening for breast cancer “where things really got messed up.”
“Even though we’ve been fully ramped up again,” she said, concerns remain. To ensure that screening mammography is maintained, “we have spaced out the visits to keep our waiting rooms less populated, with a longer time between using the machine so we can clean it. To do this, we have extended operating hours and are now opening on Saturday.
“So we’re actually at 100% of our capacity, but I’m really nervous, though, that a lot of people put off their screening mammogram and aren’t going to come in and get it.
“Not only did people get the message to stay home and not do nonessential things, but I think a lot of people lost their health insurance when they lost their jobs,” she said, and without health insurance, they are not covered for cancer screening.
Looking ahead, with a plan
Many oncologists agree that access to care can and must be improved – and there were some positive moves.
“Some regimens changed during the first months of the pandemic, and I don’t see them going back to the way they were anytime soon,” said Dr. Testa. “The changes/adaptations that were made to minimize the chance of SARS-CoV-2 infection are still in place and will go on for a while. In this context, telemedicine helped a lot. The pandemic forced the stakeholders to step up and put it in place in March. And now it’s here to stay.”
The experience gained in the last several months has driven preparation for the next wave.
“We are not going to see the disorganization that we saw during the first wave,” said Florence Joly, MD, PhD, head of medical oncology at the Centre François Baclesse in Caen, France. “The difference between now and earlier this year is that COVID diagnostic tests are available. That was one of the problems in the first wave. We had no way to diagnose.”
On the East Coast of the United States, medical oncologist Charu Aggarwal, MD, MPH, is also optimistic: “I think we’re at a place where we can manage.”
“I believe if there was going to be a new wave of COVID-19 cases we would be: better psychologically prepared and better organized,” said Dr. Aggarwal, assistant professor of medicine in the hematology-oncology division at the University of Pennsylvania, Philadelphia. “We already have experience with all of the tools, we have telemedicine available, we have screening protocols available, we have testing, we are already universally masking, everyone’s hand-washing, so I do think that means we would be okay.”
Dr. Arnold agreed that “we are much better prepared than for the first wave, but … we have immense tasks in the area of patient management, the digitization of patient care, the clear allocation of resources when there is a second or third wave. In many areas of preparation, I believe, unfortunately, we are not as well positioned as we had actually hoped.”
The first wave of COVID hit cancer services in the United Kingdom particularly hard: One modeling study suggested that delays in cancer referrals will lead to thousands of additional deaths and tens of thousands of life-years lost.
“Cancer services are working at near normal levels now, but they are still fragile and could be severely compromised again if the NHS [National Health Service] gets flooded by COVID patients,” said Dr. Sikora.
The second wave may be different. “Although the number of infections has increased, the hospitalizations have only risen a little. Let’s see what happens,” he said in an interview. Since then, however, infections have continued to rise, and there has been an increase in hospitalizations. New social distancing measures in the United Kingdom were put into place on Oct. 12, with the aim of protecting the NHS from overload.
Dr. Arrué describes it this way: “The reality is that the ‘second wave’ has left behind the initial grief and shock that both patients and health professionals experienced when faced with something that, until now, we had only seen in the movies.” The second wave has led to new restrictions – including a partial lockdown since the beginning of October.
Dr. Aggarwal says her department recently had a conference with Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, about the impact of COVID-19 on oncology.
“I asked him what advice he’d give oncologists, and he said to go back to as much screening as you were doing previously as quickly as possible. That’s what must be relayed to our oncologists in the community – and also to primary care physicians – because they are often the ones who are ordering and championing the screening efforts.”
This article was originated by Aude Lecrubier, Medscape French edition, and developed by Zosia Chustecka, Medscape Oncology. With additional reporting by Kate Johnson, freelance medical journalist, Claudia Gottschling for Medscape Germany, Leoleli Schwartz for Medscape em português, Tim Locke for Medscape United Kingdom, and Carla Nieto Martínez, freelance medical journalist for Medscape Spanish edition.
This article first appeared on Medscape.com.
Canceled appointments, postponed surgeries, and delayed cancer diagnoses – all are a recipe for exhaustion for oncologists around the world, struggling to reach and treat their patients during the pandemic. Physicians and their teams felt the pain as COVID-19 took its initial march around the globe.
“We saw the distress of people with cancer who could no longer get to anyone on the phone. Their medical visit was usually canceled. Their radiotherapy session was postponed or modified, and chemotherapy postponed,” says Axel Kahn, MD, chairman of the board of directors of La Ligue Nationale Contre le Cancer (National League Against Cancer). “In the vast majority of cases, cancer treatment can be postponed or readjusted, without affecting the patient’s chances of survival, but there has been a lot of anxiety because the patients do not know that.”
The stay-at-home factor was one that played out across many months during the first wave.
“I believe that the ‘stay-home’ message that we transmitted was rigorously followed by patients who should have come to the emergency room much earlier and who, therefore, were admitted with a much more deteriorated general condition than in non-COVID-19 times,” says Benjamín Domingo Arrué, MD, from the department of medical oncology at Hospital Universitari i Politècnic La Fe in Valencia, Spain.
And in Brazil, some of the impact from the initial hit of COVID-19 on oncology is only now being felt, according to Laura Testa, MD, head of breast medical oncology, Instituto do Câncer do Estado de São Paulo.
“We are starting to see a lot of cancer cases that didn’t show up at the beginning of the pandemic, but now they are arriving to us already in advanced stages,” she said. “These patients need hospital care. If the situation worsens and goes back to what we saw at the peak of the curve, I fear the public system won’t be able to treat properly the oncology patients that need hospital care and the patients with cancer who also have COVID-19.”
But even as health care worker fatigue and concerns linger, oncologists say that what they have learned in the last 6 months has helped them prepare as COVID-19 cases increase and a second global wave kicks up.
Lessons from the first wave
In the United States, COVID-19 hit different regions at different times and to different degrees. One of the areas hit first was Seattle.
“We jumped on top of this, we were evidence based, we put things in place very, very quickly,” said Julie Gralow, MD, professor at the University of Washington and the Fred Hutchinson Cancer Research Center, both in Seattle.
“We did a really good job keeping COVID out of our cancer centers,” Dr. Gralow said. “We learned how to be super safe, and to keep symptomatic people out of the building, and to limit the extra people they could bring with them. It’s all about the number of contacts you have.”
The story was different, though, for oncologists in several other countries, and sometimes it varied immensely within each nation.
“We treated fewer patients with cancer during the first wave,” says Dirk Arnold, MD, medical director of the Asklepios Tumor Center Hamburg (Germany), in an interview. “In part, this was because staff were quarantined and because we had a completely different infrastructure in all of the hospitals. But also fewer patients with cancer came to the clinic at all. A lot of resources were directed toward COVID-19.”
In Spain, telemedicine helped keep up with visits, but other areas felt the effect of COVID-19 patient loads.
“At least in the oncology department of our center, we have practically maintained 100% of visits, mostly by telephone,” says Dr. Arrué, “but the reality is that our country has not yet been prepared for telemedicine.”
Laura Mezquita, MD, of the department of medical oncology at Hospital Clinic de Barcelona, describes a more dramatic situation: “We have seen how some of our patients, especially with metastatic disease, have been dismissed for intensive care and life-support treatments, as well as specific treatments against COVID-19 (tocilizumab, remdesivir, etc.) due to the general health collapse of the former wave,” she said. She adds that specific oncologic populations, such as those with thoracic tumors, have been more affected.
Distress among oncologists
Many oncologists are still feeling stressed and fatigued after the first wave, just as a second string of outbreaks is on its way.
A survey presented at last month’s ESMO 2020 Congress found that, in July-August, moral distress was reported by one-third of the oncologists who responded, and more than half reported a feeling of exhaustion.
“The tiredness and team exhaustion is noticeable,” said Dr. Arnold. “We recently had a task force discussion about what will happen when we have a second wave and how the department and our services will adapt. It was clear that those who were at the very front in the first wave had only a limited desire to do that again in the second wave.”
Another concern: COVID-19’s effect on staffing levels.
“We have a population of young caregivers who are affected by the COVID-19 disease with an absenteeism rate that is quite unprecedented,” said Sophie Beaupère, general delegate of Unicancer since January.
She said that, in general, the absenteeism rate in the cancer centers averages 5%-6%, depending on the year. But that rate is now skyrocketing.
Stop-start cycle for surgery
As caregivers quarantined around the world, more than 10% of patients with cancer had treatment canceled or delayed during the first wave of the pandemic, according to another survey from ESMO, involving 109 oncologists from 18 countries.
Difficulties were reported for surgeries by 34% of the centers, but also difficulties with delivering chemotherapy (22% of centers), radiotherapy (13.7%), and therapy with checkpoint inhibitors (9.1%), monoclonal antibodies (9%), and oral targeted therapy (3.7%).
Stopping surgery is a real concern in France, noted Dr. Kahn, the National League Against Cancer chair. He says that in regions that were badly hit by COVID-19, “it was not possible to have access to the operating room for people who absolutely needed surgery; for example, patients with lung cancer that was still operable. Most of the recovery rooms were mobilized for resuscitation.”
There may be some solutions, suggested Thierry Breton, director general of the National Institute of Cancer in France. “We are getting prepared, with the health ministry, for a possible increase in hospital tension, which would lead to a situation where we would have to reschedule operations. Nationally, regionally, and locally, we are seeing how we can resume and prioritize surgeries that have not been done.”
Delays in cancer diagnosis
While COVID-19 affected treatment, many oncologists say the major impact of the first wave was a delay in diagnosing cancer. Some of this was a result of the suspension of cancer screening programs, but there was also fear among the general public about visiting clinics and hospitals during a pandemic.
“We didn’t do so well with cancer during the first wave here in the U.K.,” said Karol Sikora, PhD, MBBChir, professor of cancer medicine and founding dean at the University of Buckingham Medical School, London. “Cancer diagnostic pathways virtually stalled partly because patients didn’t seek help, but getting scans and biopsies was also very difficult. Even patients referred urgently under the ‘2-weeks-wait’ rule were turned down.”
In France, “the delay in diagnosis is indisputable,” said Dr. Kahn. “About 50% of the cancer diagnoses one would expect during this period were missed.”
“I am worried that there remains a major traffic jam that has not been caught up with, and, in the meantime, the health crisis is worsening,” he added.
In Seattle, Dr. Gralow said the first COVID-19 wave had little impact on treatment for breast cancer, but it was in screening for breast cancer “where things really got messed up.”
“Even though we’ve been fully ramped up again,” she said, concerns remain. To ensure that screening mammography is maintained, “we have spaced out the visits to keep our waiting rooms less populated, with a longer time between using the machine so we can clean it. To do this, we have extended operating hours and are now opening on Saturday.
“So we’re actually at 100% of our capacity, but I’m really nervous, though, that a lot of people put off their screening mammogram and aren’t going to come in and get it.
“Not only did people get the message to stay home and not do nonessential things, but I think a lot of people lost their health insurance when they lost their jobs,” she said, and without health insurance, they are not covered for cancer screening.
Looking ahead, with a plan
Many oncologists agree that access to care can and must be improved – and there were some positive moves.
“Some regimens changed during the first months of the pandemic, and I don’t see them going back to the way they were anytime soon,” said Dr. Testa. “The changes/adaptations that were made to minimize the chance of SARS-CoV-2 infection are still in place and will go on for a while. In this context, telemedicine helped a lot. The pandemic forced the stakeholders to step up and put it in place in March. And now it’s here to stay.”
The experience gained in the last several months has driven preparation for the next wave.
“We are not going to see the disorganization that we saw during the first wave,” said Florence Joly, MD, PhD, head of medical oncology at the Centre François Baclesse in Caen, France. “The difference between now and earlier this year is that COVID diagnostic tests are available. That was one of the problems in the first wave. We had no way to diagnose.”
On the East Coast of the United States, medical oncologist Charu Aggarwal, MD, MPH, is also optimistic: “I think we’re at a place where we can manage.”
“I believe if there was going to be a new wave of COVID-19 cases we would be: better psychologically prepared and better organized,” said Dr. Aggarwal, assistant professor of medicine in the hematology-oncology division at the University of Pennsylvania, Philadelphia. “We already have experience with all of the tools, we have telemedicine available, we have screening protocols available, we have testing, we are already universally masking, everyone’s hand-washing, so I do think that means we would be okay.”
Dr. Arnold agreed that “we are much better prepared than for the first wave, but … we have immense tasks in the area of patient management, the digitization of patient care, the clear allocation of resources when there is a second or third wave. In many areas of preparation, I believe, unfortunately, we are not as well positioned as we had actually hoped.”
The first wave of COVID hit cancer services in the United Kingdom particularly hard: One modeling study suggested that delays in cancer referrals will lead to thousands of additional deaths and tens of thousands of life-years lost.
“Cancer services are working at near normal levels now, but they are still fragile and could be severely compromised again if the NHS [National Health Service] gets flooded by COVID patients,” said Dr. Sikora.
The second wave may be different. “Although the number of infections has increased, the hospitalizations have only risen a little. Let’s see what happens,” he said in an interview. Since then, however, infections have continued to rise, and there has been an increase in hospitalizations. New social distancing measures in the United Kingdom were put into place on Oct. 12, with the aim of protecting the NHS from overload.
Dr. Arrué describes it this way: “The reality is that the ‘second wave’ has left behind the initial grief and shock that both patients and health professionals experienced when faced with something that, until now, we had only seen in the movies.” The second wave has led to new restrictions – including a partial lockdown since the beginning of October.
Dr. Aggarwal says her department recently had a conference with Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, about the impact of COVID-19 on oncology.
“I asked him what advice he’d give oncologists, and he said to go back to as much screening as you were doing previously as quickly as possible. That’s what must be relayed to our oncologists in the community – and also to primary care physicians – because they are often the ones who are ordering and championing the screening efforts.”
This article was originated by Aude Lecrubier, Medscape French edition, and developed by Zosia Chustecka, Medscape Oncology. With additional reporting by Kate Johnson, freelance medical journalist, Claudia Gottschling for Medscape Germany, Leoleli Schwartz for Medscape em português, Tim Locke for Medscape United Kingdom, and Carla Nieto Martínez, freelance medical journalist for Medscape Spanish edition.
This article first appeared on Medscape.com.