User login
SPK-8011 AAV-mediated hemophilia A therapy shows stability, durability
SPK-8011, an investigational adeno-associated virus (AAV)–mediated gene therapy for hemophilia A, provides stable and durable factor VIII expression with no major safety concerns, according to findings at least 2 years after a single treatment in patients from a phase 1/2 trial.
The first 5 of 14 adult men with hemophilia A and who had factor VIII (FVIII) activity of 2% or less before treatment with SPK-8011 (at single doses of either 5 × 1011 or 1 × 1012 vg/kg), showed no development of FVIII inhibitors or evidence of FVIII cellular immune response at 106-142 weeks’ follow-up after vector infusion, according to Lindsey A. George, MD, at the International Society of Thrombosis and Haemostasis 2020 virtual congress.
At follow-up, the two who had received a 5 × 1011 vg/kg dose had FVIII activity of 6.9%-8.4%, and the three in the 1 × 1012 vg/kg cohort had FVIII activity of 5.2%-19.8%, said Dr. George, of the Children’s Hospital of Philadelphia.
Overall, 12 of the 14 patients in the study had sustained FVIII expression, including 7 of 9 who received the highest SPK-8011 dose of 2 × 1012 vg/kg. In the 12 with sustained expression, a “remarkable” 91% reduction in the annualized bleeding rate from the year prior to vs. the year after vector infusion was observed, she said.
“Similarly, looking at number of factor infusions before vector infusion relative to the number of factor infusions after vector infusion ... [there was] evidence of remarkable preliminary efficacy,” she added, noting a 96% reduction in factor consumption.
The findings are of note because, while clinical studies of Spark Therapeutic’s SPK-8011 product in hemophilia B and preclinical models in hemophilia A showed promising reductions in bleeds and stable, durable levels of FVIII expression after therapy, the first successful clinical trial of an AAV-mediated gene therapy in hemophilia A – the BioMarin AAV serotype 5 human FVIII-SQ (valoctocogene roxaparvovec) – showed an unexpected decline in FVIII expression at 1, 2, 3, and 4 years.
“This may be particularly relevant in the context of development of multi-serotype AAV neutralizing antibodies (NAb) following AAV vector administration,” Dr. George said, referencing a small study in which she and her colleagues showed long-term persistence of cross-reactive AAV NAb. The findings of that study, which is currently in press in Molecular Therapy, “suggest that repeat AAV vector infusion is unlikely to be possible with current methods.”
Initial results from the SPK-8011 study were presented at the 2018 American Society of Hematology annual meeting. No major safety issues have emerged since those data were presented at ASH; no deaths have occurred, and none of the patients developed FVIII inhibitors.
Treatment-related adverse events were limited to an infusion reaction in one patient, which resolved completely, and liver enzyme elevations in three patients, which also resolved. One serious adverse event – a grade 2 transaminitis that resulted in elective hospitalization for intravenous steroid administration, also resolved.
With respect to vector clearance, there was “no evidence of vector in either saliva, semen, serum, urine, or peripheral blood mononuclear cells by 6 weeks after vector infusion,” Dr. George said.
One-stage assay determination of FVIII activity showed that activity greater than 10% permits an absolute bleeding rate (ABR) of less than 1%, which is consistent with hemophilia natural history studies. Therefore “these data support that FVIII activity that is approximately greater than 10% “may be adequate to either eliminate or achieve an ABR of less than 1,” she said.
“With respect to assay discrepancy, our data at least preliminarily support that the one-stage assay determinant of hepatocyte-derived FVIII correlates with clinical phenotype,” she added.
The findings in the first five patients demonstrate preliminary stability of FVIII expression at follow up between 2 and 3.3 years, she said.
Further, of the nine patients who received the 2 × 1012 vg/kg dose, seven had sustained FVIII expression at about 1.5 years, five of the seven had no bleeds, and two lost FVIII expression and returned to prophylaxis uneventfully, she noted.
“The future directions of this work are ultimately to explore the optimal vector dose and immunosuppression regimens to achieve predictable, safe, efficacious, and durable FVIII expression,” she said.
Asked during a question and answer period about potential reasons for the differences in durability seen with SBK-8011 versus valoctocogene roxaparvovec, Dr. George said they remain unclear but could be related to differences in vector doses and manufacturing platforms.
Emerging data may allow for better comparisons, she added.
Session moderator Sebastien Lacroix-Desmazes, MD, of Centre de Recherche des Cordeliers, Paris, further asked about plans to optimize the immunosuppression regimen.
Plans are indeed in the works to identify the optimal immunosuppression regimen and to optimize immunosuppression in this trial, Dr. George said, noting that Spark Therapeutics “has outlined a plan to further investigate this in phase 1/2 trial before progressing into phase 3 study.”
Spark Therapeutic sponsored the SPK-8011 study. Dr. George disclosed consulting and/or data safety monitoring board activity for Pfizer and AvroBio.
SOURCE: George L et al. 2020 ISTH Congress, Abstract OC 03.5.
SPK-8011, an investigational adeno-associated virus (AAV)–mediated gene therapy for hemophilia A, provides stable and durable factor VIII expression with no major safety concerns, according to findings at least 2 years after a single treatment in patients from a phase 1/2 trial.
The first 5 of 14 adult men with hemophilia A and who had factor VIII (FVIII) activity of 2% or less before treatment with SPK-8011 (at single doses of either 5 × 1011 or 1 × 1012 vg/kg), showed no development of FVIII inhibitors or evidence of FVIII cellular immune response at 106-142 weeks’ follow-up after vector infusion, according to Lindsey A. George, MD, at the International Society of Thrombosis and Haemostasis 2020 virtual congress.
At follow-up, the two who had received a 5 × 1011 vg/kg dose had FVIII activity of 6.9%-8.4%, and the three in the 1 × 1012 vg/kg cohort had FVIII activity of 5.2%-19.8%, said Dr. George, of the Children’s Hospital of Philadelphia.
Overall, 12 of the 14 patients in the study had sustained FVIII expression, including 7 of 9 who received the highest SPK-8011 dose of 2 × 1012 vg/kg. In the 12 with sustained expression, a “remarkable” 91% reduction in the annualized bleeding rate from the year prior to vs. the year after vector infusion was observed, she said.
“Similarly, looking at number of factor infusions before vector infusion relative to the number of factor infusions after vector infusion ... [there was] evidence of remarkable preliminary efficacy,” she added, noting a 96% reduction in factor consumption.
The findings are of note because, while clinical studies of Spark Therapeutic’s SPK-8011 product in hemophilia B and preclinical models in hemophilia A showed promising reductions in bleeds and stable, durable levels of FVIII expression after therapy, the first successful clinical trial of an AAV-mediated gene therapy in hemophilia A – the BioMarin AAV serotype 5 human FVIII-SQ (valoctocogene roxaparvovec) – showed an unexpected decline in FVIII expression at 1, 2, 3, and 4 years.
“This may be particularly relevant in the context of development of multi-serotype AAV neutralizing antibodies (NAb) following AAV vector administration,” Dr. George said, referencing a small study in which she and her colleagues showed long-term persistence of cross-reactive AAV NAb. The findings of that study, which is currently in press in Molecular Therapy, “suggest that repeat AAV vector infusion is unlikely to be possible with current methods.”
Initial results from the SPK-8011 study were presented at the 2018 American Society of Hematology annual meeting. No major safety issues have emerged since those data were presented at ASH; no deaths have occurred, and none of the patients developed FVIII inhibitors.
Treatment-related adverse events were limited to an infusion reaction in one patient, which resolved completely, and liver enzyme elevations in three patients, which also resolved. One serious adverse event – a grade 2 transaminitis that resulted in elective hospitalization for intravenous steroid administration, also resolved.
With respect to vector clearance, there was “no evidence of vector in either saliva, semen, serum, urine, or peripheral blood mononuclear cells by 6 weeks after vector infusion,” Dr. George said.
One-stage assay determination of FVIII activity showed that activity greater than 10% permits an absolute bleeding rate (ABR) of less than 1%, which is consistent with hemophilia natural history studies. Therefore “these data support that FVIII activity that is approximately greater than 10% “may be adequate to either eliminate or achieve an ABR of less than 1,” she said.
“With respect to assay discrepancy, our data at least preliminarily support that the one-stage assay determinant of hepatocyte-derived FVIII correlates with clinical phenotype,” she added.
The findings in the first five patients demonstrate preliminary stability of FVIII expression at follow up between 2 and 3.3 years, she said.
Further, of the nine patients who received the 2 × 1012 vg/kg dose, seven had sustained FVIII expression at about 1.5 years, five of the seven had no bleeds, and two lost FVIII expression and returned to prophylaxis uneventfully, she noted.
“The future directions of this work are ultimately to explore the optimal vector dose and immunosuppression regimens to achieve predictable, safe, efficacious, and durable FVIII expression,” she said.
Asked during a question and answer period about potential reasons for the differences in durability seen with SBK-8011 versus valoctocogene roxaparvovec, Dr. George said they remain unclear but could be related to differences in vector doses and manufacturing platforms.
Emerging data may allow for better comparisons, she added.
Session moderator Sebastien Lacroix-Desmazes, MD, of Centre de Recherche des Cordeliers, Paris, further asked about plans to optimize the immunosuppression regimen.
Plans are indeed in the works to identify the optimal immunosuppression regimen and to optimize immunosuppression in this trial, Dr. George said, noting that Spark Therapeutics “has outlined a plan to further investigate this in phase 1/2 trial before progressing into phase 3 study.”
Spark Therapeutic sponsored the SPK-8011 study. Dr. George disclosed consulting and/or data safety monitoring board activity for Pfizer and AvroBio.
SOURCE: George L et al. 2020 ISTH Congress, Abstract OC 03.5.
SPK-8011, an investigational adeno-associated virus (AAV)–mediated gene therapy for hemophilia A, provides stable and durable factor VIII expression with no major safety concerns, according to findings at least 2 years after a single treatment in patients from a phase 1/2 trial.
The first 5 of 14 adult men with hemophilia A and who had factor VIII (FVIII) activity of 2% or less before treatment with SPK-8011 (at single doses of either 5 × 1011 or 1 × 1012 vg/kg), showed no development of FVIII inhibitors or evidence of FVIII cellular immune response at 106-142 weeks’ follow-up after vector infusion, according to Lindsey A. George, MD, at the International Society of Thrombosis and Haemostasis 2020 virtual congress.
At follow-up, the two who had received a 5 × 1011 vg/kg dose had FVIII activity of 6.9%-8.4%, and the three in the 1 × 1012 vg/kg cohort had FVIII activity of 5.2%-19.8%, said Dr. George, of the Children’s Hospital of Philadelphia.
Overall, 12 of the 14 patients in the study had sustained FVIII expression, including 7 of 9 who received the highest SPK-8011 dose of 2 × 1012 vg/kg. In the 12 with sustained expression, a “remarkable” 91% reduction in the annualized bleeding rate from the year prior to vs. the year after vector infusion was observed, she said.
“Similarly, looking at number of factor infusions before vector infusion relative to the number of factor infusions after vector infusion ... [there was] evidence of remarkable preliminary efficacy,” she added, noting a 96% reduction in factor consumption.
The findings are of note because, while clinical studies of Spark Therapeutic’s SPK-8011 product in hemophilia B and preclinical models in hemophilia A showed promising reductions in bleeds and stable, durable levels of FVIII expression after therapy, the first successful clinical trial of an AAV-mediated gene therapy in hemophilia A – the BioMarin AAV serotype 5 human FVIII-SQ (valoctocogene roxaparvovec) – showed an unexpected decline in FVIII expression at 1, 2, 3, and 4 years.
“This may be particularly relevant in the context of development of multi-serotype AAV neutralizing antibodies (NAb) following AAV vector administration,” Dr. George said, referencing a small study in which she and her colleagues showed long-term persistence of cross-reactive AAV NAb. The findings of that study, which is currently in press in Molecular Therapy, “suggest that repeat AAV vector infusion is unlikely to be possible with current methods.”
Initial results from the SPK-8011 study were presented at the 2018 American Society of Hematology annual meeting. No major safety issues have emerged since those data were presented at ASH; no deaths have occurred, and none of the patients developed FVIII inhibitors.
Treatment-related adverse events were limited to an infusion reaction in one patient, which resolved completely, and liver enzyme elevations in three patients, which also resolved. One serious adverse event – a grade 2 transaminitis that resulted in elective hospitalization for intravenous steroid administration, also resolved.
With respect to vector clearance, there was “no evidence of vector in either saliva, semen, serum, urine, or peripheral blood mononuclear cells by 6 weeks after vector infusion,” Dr. George said.
One-stage assay determination of FVIII activity showed that activity greater than 10% permits an absolute bleeding rate (ABR) of less than 1%, which is consistent with hemophilia natural history studies. Therefore “these data support that FVIII activity that is approximately greater than 10% “may be adequate to either eliminate or achieve an ABR of less than 1,” she said.
“With respect to assay discrepancy, our data at least preliminarily support that the one-stage assay determinant of hepatocyte-derived FVIII correlates with clinical phenotype,” she added.
The findings in the first five patients demonstrate preliminary stability of FVIII expression at follow up between 2 and 3.3 years, she said.
Further, of the nine patients who received the 2 × 1012 vg/kg dose, seven had sustained FVIII expression at about 1.5 years, five of the seven had no bleeds, and two lost FVIII expression and returned to prophylaxis uneventfully, she noted.
“The future directions of this work are ultimately to explore the optimal vector dose and immunosuppression regimens to achieve predictable, safe, efficacious, and durable FVIII expression,” she said.
Asked during a question and answer period about potential reasons for the differences in durability seen with SBK-8011 versus valoctocogene roxaparvovec, Dr. George said they remain unclear but could be related to differences in vector doses and manufacturing platforms.
Emerging data may allow for better comparisons, she added.
Session moderator Sebastien Lacroix-Desmazes, MD, of Centre de Recherche des Cordeliers, Paris, further asked about plans to optimize the immunosuppression regimen.
Plans are indeed in the works to identify the optimal immunosuppression regimen and to optimize immunosuppression in this trial, Dr. George said, noting that Spark Therapeutics “has outlined a plan to further investigate this in phase 1/2 trial before progressing into phase 3 study.”
Spark Therapeutic sponsored the SPK-8011 study. Dr. George disclosed consulting and/or data safety monitoring board activity for Pfizer and AvroBio.
SOURCE: George L et al. 2020 ISTH Congress, Abstract OC 03.5.
FROM THE 2020 ISTH CONGRESS
HSCT or systemic treatment should be offered to HIV+ patients with lymphoma
Systemic or hematopoietic stem cell transplantation (HSCT) treatment of HIV-positive lymphoma patients resulted in improved outcomes, compared with nonsystemic treatment, according to the results of a large database study.
Researchers Thejus T. Jayakrishnan, MD, and colleagues examined patients with lymphoma diagnosed between 2004 and 2015 from the National Cancer Database. Patients were categorized as HIV positive and HIV negative. First-line lymphoma treatment was categorized as no systemic therapy reported, systemic therapy, or HSCT. Multivariate analysis was used to predict treatment and survival, according to Dr. Jayakrishnan, a resident at the department of internal medicine, Allegheny Health Network, Pittsburgh.
A total of 11,160 HIV-positive vs. 349,607 HIV-negative patients were analyzed, including mostly men, with a comorbidity index of 0. The most common lymphoma among HIV-positive patients was diffuse large B-cell lymphoma, according to the report in Clinical Lymphoma, Myeloma & Leukemia.
Among HIV-positive patients, 792 had no systemic treatment, 10,328 underwent systemic treatment, and 40 received HSCT treatment. The results showed that treatment of HIV-positive lymphoma patients resulted in improved outcomes: 3-year overall survival was 43.6% for nonsystemic treatment versus 58.1% for systemic (hazard ratio, 0.56; 95% confidence interval, 0.52-0.61; P < .005) versus 62.2% for HSCT therapy (HR, 0.42; 95% CI, 0.14-1.3; P = .08), the lack of significance in the latter could be caused in part by the small number of patients treated. Outcomes for both treatment regimens were lower, however, compared with non-HIV patients.
“The present study demonstrates improvement in survival outcomes for HIV-positive patients with lymphoma with treatments when feasible, but these outcomes are poor when compared to HIV-negative patients,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Jayakrishnan TT et al. Clin Lymph Myeloma Leuk. 2020 Feb 20. doi: 10.1016/j.clml.2020.06.003.
Systemic or hematopoietic stem cell transplantation (HSCT) treatment of HIV-positive lymphoma patients resulted in improved outcomes, compared with nonsystemic treatment, according to the results of a large database study.
Researchers Thejus T. Jayakrishnan, MD, and colleagues examined patients with lymphoma diagnosed between 2004 and 2015 from the National Cancer Database. Patients were categorized as HIV positive and HIV negative. First-line lymphoma treatment was categorized as no systemic therapy reported, systemic therapy, or HSCT. Multivariate analysis was used to predict treatment and survival, according to Dr. Jayakrishnan, a resident at the department of internal medicine, Allegheny Health Network, Pittsburgh.
A total of 11,160 HIV-positive vs. 349,607 HIV-negative patients were analyzed, including mostly men, with a comorbidity index of 0. The most common lymphoma among HIV-positive patients was diffuse large B-cell lymphoma, according to the report in Clinical Lymphoma, Myeloma & Leukemia.
Among HIV-positive patients, 792 had no systemic treatment, 10,328 underwent systemic treatment, and 40 received HSCT treatment. The results showed that treatment of HIV-positive lymphoma patients resulted in improved outcomes: 3-year overall survival was 43.6% for nonsystemic treatment versus 58.1% for systemic (hazard ratio, 0.56; 95% confidence interval, 0.52-0.61; P < .005) versus 62.2% for HSCT therapy (HR, 0.42; 95% CI, 0.14-1.3; P = .08), the lack of significance in the latter could be caused in part by the small number of patients treated. Outcomes for both treatment regimens were lower, however, compared with non-HIV patients.
“The present study demonstrates improvement in survival outcomes for HIV-positive patients with lymphoma with treatments when feasible, but these outcomes are poor when compared to HIV-negative patients,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Jayakrishnan TT et al. Clin Lymph Myeloma Leuk. 2020 Feb 20. doi: 10.1016/j.clml.2020.06.003.
Systemic or hematopoietic stem cell transplantation (HSCT) treatment of HIV-positive lymphoma patients resulted in improved outcomes, compared with nonsystemic treatment, according to the results of a large database study.
Researchers Thejus T. Jayakrishnan, MD, and colleagues examined patients with lymphoma diagnosed between 2004 and 2015 from the National Cancer Database. Patients were categorized as HIV positive and HIV negative. First-line lymphoma treatment was categorized as no systemic therapy reported, systemic therapy, or HSCT. Multivariate analysis was used to predict treatment and survival, according to Dr. Jayakrishnan, a resident at the department of internal medicine, Allegheny Health Network, Pittsburgh.
A total of 11,160 HIV-positive vs. 349,607 HIV-negative patients were analyzed, including mostly men, with a comorbidity index of 0. The most common lymphoma among HIV-positive patients was diffuse large B-cell lymphoma, according to the report in Clinical Lymphoma, Myeloma & Leukemia.
Among HIV-positive patients, 792 had no systemic treatment, 10,328 underwent systemic treatment, and 40 received HSCT treatment. The results showed that treatment of HIV-positive lymphoma patients resulted in improved outcomes: 3-year overall survival was 43.6% for nonsystemic treatment versus 58.1% for systemic (hazard ratio, 0.56; 95% confidence interval, 0.52-0.61; P < .005) versus 62.2% for HSCT therapy (HR, 0.42; 95% CI, 0.14-1.3; P = .08), the lack of significance in the latter could be caused in part by the small number of patients treated. Outcomes for both treatment regimens were lower, however, compared with non-HIV patients.
“The present study demonstrates improvement in survival outcomes for HIV-positive patients with lymphoma with treatments when feasible, but these outcomes are poor when compared to HIV-negative patients,” the researchers concluded.
The authors reported that they had no conflicts of interest.
SOURCE: Jayakrishnan TT et al. Clin Lymph Myeloma Leuk. 2020 Feb 20. doi: 10.1016/j.clml.2020.06.003.
FROM CLINICAL LYMPHOMA, MYELOMA & LEUKEMIA
Heavy menstrual bleeding difficult to control in young patients with inherited platelet disorders
Physician consensus and a broadly effective treatment for heavy menstrual bleeding was not found among young patients with inherited platelet function disorders, according to the results of a retrospective chart review reported in the Journal of Pediatric and Adolescent Gynecology.
Heavy menstrual bleeding (HMB) in girls with inherited platelet function disorders (IPFD) can be difficult to control despite ongoing follow-up and treatment changes, reported Christine M. Pennesi, MD, of the University of Michigan, Ann Arbor, and colleagues.
They assessed 34 young women and girls (ages 9-25 years) diagnosed with IPFDs referred to gynecology and/or hematology at a tertiary care hospital between 2006 and 2018.
Billing codes were used to determine hormonal or nonhormonal treatments, and outcomes over a 1- to 2-year period were collected. The initial treatment was defined as the first treatment prescribed after referral. The primary outcome was treatment failure, defined as a change in treatment method because of continued bleeding.
The majority (56%) of patients failed initial treatment (n = 19); among all 34 individuals followed in the study, an average of 2.7 total treatments were required.
Six patients (18%) remained uncontrolled despite numerous treatment changes (mean treatment changes, four; range, two to seven), and two patients (6%) remained uncontrolled because of noncompliance with treatment.
Overall, the researchers identified a 18% failure rate of successfully treatment of HMB in young women and girls with IPFDs over a 2-year follow-up period.
Of the 26 women who achieved control of HMB within 2-year follow-up, 54% (n = 14) were on hormonal treatments, 27% (n = 7) on nonhormonal treatments, 12% (n = 3) on combined treatments, and 8% (n = 2) on no treatment at time of control, the authors stated.
“The heterogeneity in treatments that were described in this study, clearly demonstrate that, in selecting treatment methods for HMB in young women, other considerations are often in play. This includes patient preference and need for contraception. Some patients or parents may have personal or religious objections to hormonal methods or worry about hormones in this young age group,” the researchers speculated.
“Appropriate counseling in these patients should include that it would not be unexpected for a patient to need more than one treatment before control of bleeding is achieved. This may help to alleviate the fear of teenagers when continued bleeding occurs after starting their initial treatment,” Dr. Pennesi and colleagues concluded.
One of the authors participated in funded trials and received funding from several pharmaceutical companies. The others reported having no disclosures.
SOURCE: Pennesi CM et al. J Pediatr Adolesc Gynecol. 2020 Jun 22. doi: 10.1016/j.jpag.2020.06.019.
Physician consensus and a broadly effective treatment for heavy menstrual bleeding was not found among young patients with inherited platelet function disorders, according to the results of a retrospective chart review reported in the Journal of Pediatric and Adolescent Gynecology.
Heavy menstrual bleeding (HMB) in girls with inherited platelet function disorders (IPFD) can be difficult to control despite ongoing follow-up and treatment changes, reported Christine M. Pennesi, MD, of the University of Michigan, Ann Arbor, and colleagues.
They assessed 34 young women and girls (ages 9-25 years) diagnosed with IPFDs referred to gynecology and/or hematology at a tertiary care hospital between 2006 and 2018.
Billing codes were used to determine hormonal or nonhormonal treatments, and outcomes over a 1- to 2-year period were collected. The initial treatment was defined as the first treatment prescribed after referral. The primary outcome was treatment failure, defined as a change in treatment method because of continued bleeding.
The majority (56%) of patients failed initial treatment (n = 19); among all 34 individuals followed in the study, an average of 2.7 total treatments were required.
Six patients (18%) remained uncontrolled despite numerous treatment changes (mean treatment changes, four; range, two to seven), and two patients (6%) remained uncontrolled because of noncompliance with treatment.
Overall, the researchers identified a 18% failure rate of successfully treatment of HMB in young women and girls with IPFDs over a 2-year follow-up period.
Of the 26 women who achieved control of HMB within 2-year follow-up, 54% (n = 14) were on hormonal treatments, 27% (n = 7) on nonhormonal treatments, 12% (n = 3) on combined treatments, and 8% (n = 2) on no treatment at time of control, the authors stated.
“The heterogeneity in treatments that were described in this study, clearly demonstrate that, in selecting treatment methods for HMB in young women, other considerations are often in play. This includes patient preference and need for contraception. Some patients or parents may have personal or religious objections to hormonal methods or worry about hormones in this young age group,” the researchers speculated.
“Appropriate counseling in these patients should include that it would not be unexpected for a patient to need more than one treatment before control of bleeding is achieved. This may help to alleviate the fear of teenagers when continued bleeding occurs after starting their initial treatment,” Dr. Pennesi and colleagues concluded.
One of the authors participated in funded trials and received funding from several pharmaceutical companies. The others reported having no disclosures.
SOURCE: Pennesi CM et al. J Pediatr Adolesc Gynecol. 2020 Jun 22. doi: 10.1016/j.jpag.2020.06.019.
Physician consensus and a broadly effective treatment for heavy menstrual bleeding was not found among young patients with inherited platelet function disorders, according to the results of a retrospective chart review reported in the Journal of Pediatric and Adolescent Gynecology.
Heavy menstrual bleeding (HMB) in girls with inherited platelet function disorders (IPFD) can be difficult to control despite ongoing follow-up and treatment changes, reported Christine M. Pennesi, MD, of the University of Michigan, Ann Arbor, and colleagues.
They assessed 34 young women and girls (ages 9-25 years) diagnosed with IPFDs referred to gynecology and/or hematology at a tertiary care hospital between 2006 and 2018.
Billing codes were used to determine hormonal or nonhormonal treatments, and outcomes over a 1- to 2-year period were collected. The initial treatment was defined as the first treatment prescribed after referral. The primary outcome was treatment failure, defined as a change in treatment method because of continued bleeding.
The majority (56%) of patients failed initial treatment (n = 19); among all 34 individuals followed in the study, an average of 2.7 total treatments were required.
Six patients (18%) remained uncontrolled despite numerous treatment changes (mean treatment changes, four; range, two to seven), and two patients (6%) remained uncontrolled because of noncompliance with treatment.
Overall, the researchers identified a 18% failure rate of successfully treatment of HMB in young women and girls with IPFDs over a 2-year follow-up period.
Of the 26 women who achieved control of HMB within 2-year follow-up, 54% (n = 14) were on hormonal treatments, 27% (n = 7) on nonhormonal treatments, 12% (n = 3) on combined treatments, and 8% (n = 2) on no treatment at time of control, the authors stated.
“The heterogeneity in treatments that were described in this study, clearly demonstrate that, in selecting treatment methods for HMB in young women, other considerations are often in play. This includes patient preference and need for contraception. Some patients or parents may have personal or religious objections to hormonal methods or worry about hormones in this young age group,” the researchers speculated.
“Appropriate counseling in these patients should include that it would not be unexpected for a patient to need more than one treatment before control of bleeding is achieved. This may help to alleviate the fear of teenagers when continued bleeding occurs after starting their initial treatment,” Dr. Pennesi and colleagues concluded.
One of the authors participated in funded trials and received funding from several pharmaceutical companies. The others reported having no disclosures.
SOURCE: Pennesi CM et al. J Pediatr Adolesc Gynecol. 2020 Jun 22. doi: 10.1016/j.jpag.2020.06.019.
FROM THE JOURNAL OF PEDIATRIC AND ADOLESCENT GYNECOLOGY
Transitioning regimen may prolong proteasome inhibitor–based therapy for MM
Transitioning from parenteral bortezomib-based induction to all-oral ixazomib-lenalidomide-dexamethasone therapy increased proteasome inhibitor (PI)–based treatment adherence and duration, according to early results from a clinical trial designed to include patients representing the real-world U.S. multiple myeloma population.
The US MM-6 study was designed to evaluate a novel in-class therapy (iCT) transitioning approach from intravenous to oral treatment in the community-based setting with the aims of increasing PI-based treatment duration and adherence, maintaining health-related quality of life (HRQoL), and improving outcomes in a representative, real-world, community population of multiple myeloma patients, according to Sudhir Manda, MD, of Arizona Oncology/U.S. Oncology Research, Tucson, and colleagues.
Dr. Manda and colleagues reported on the early results of the US MM-6 trial (NCT03173092), which is a community-based, real-world, open-label, single-arm, phase 4 study of adult multiple myeloma patients who do not meet transplant-eligibility criteria, or for whom transplant would be delayed for 2 years or more, and who are receiving first-line bortezomib-based induction. All patients in the study had no evidence of progressive disease after three treatment cycles.
By the data cutoff for the reported analysis, 84 patients had been treated. The patients had a median age of 73 years; 49% were men; 15% black/African American; 10% Hispanic/Latino. A total of 62% of the patients remain on therapy, with a mean duration of total PI therapy of 10.1 months and of ixazomib-lenalidomide-dexamethasone (ixazomib-Rd) of 7.3 months.
The overall response rate was 62% (complete response, 4%; very good partial response, 25%; partial response, 33%) after bortezomib-based induction and 70% (complete response, 26%; very good partial response, 29%; partial response, 15%) after induction to all-oral ixazomib-Rd.
“The use of this novel iCT approach from parenteral bortezomib-based to oral ixazomib-based therapy facilitates long-term PI-based treatment that is well tolerated in real-world, nontransplant [newly diagnosed multiple myeloma] patients,” according to Dr. Manda and colleagues. In addition, “preliminary findings indicate that the iCT approach results in promising efficacy and high medication adherence, with no adverse impact on patients’ HRQoL or treatment satisfaction.”
The study was sponsored by Millennium Pharmaceuticals. Four of the authors are employees of Millennium Pharmaceuticals and several authors disclosed relationships with various pharmaceutical companies, including Millennium Pharmaceuticals.
SOURCE: Manda S et al. Clin Lymphoma Myeloma Leuk. 2020 Jun 30. doi: 10.1016/j.clml.2020.06.024.
Transitioning from parenteral bortezomib-based induction to all-oral ixazomib-lenalidomide-dexamethasone therapy increased proteasome inhibitor (PI)–based treatment adherence and duration, according to early results from a clinical trial designed to include patients representing the real-world U.S. multiple myeloma population.
The US MM-6 study was designed to evaluate a novel in-class therapy (iCT) transitioning approach from intravenous to oral treatment in the community-based setting with the aims of increasing PI-based treatment duration and adherence, maintaining health-related quality of life (HRQoL), and improving outcomes in a representative, real-world, community population of multiple myeloma patients, according to Sudhir Manda, MD, of Arizona Oncology/U.S. Oncology Research, Tucson, and colleagues.
Dr. Manda and colleagues reported on the early results of the US MM-6 trial (NCT03173092), which is a community-based, real-world, open-label, single-arm, phase 4 study of adult multiple myeloma patients who do not meet transplant-eligibility criteria, or for whom transplant would be delayed for 2 years or more, and who are receiving first-line bortezomib-based induction. All patients in the study had no evidence of progressive disease after three treatment cycles.
By the data cutoff for the reported analysis, 84 patients had been treated. The patients had a median age of 73 years; 49% were men; 15% black/African American; 10% Hispanic/Latino. A total of 62% of the patients remain on therapy, with a mean duration of total PI therapy of 10.1 months and of ixazomib-lenalidomide-dexamethasone (ixazomib-Rd) of 7.3 months.
The overall response rate was 62% (complete response, 4%; very good partial response, 25%; partial response, 33%) after bortezomib-based induction and 70% (complete response, 26%; very good partial response, 29%; partial response, 15%) after induction to all-oral ixazomib-Rd.
“The use of this novel iCT approach from parenteral bortezomib-based to oral ixazomib-based therapy facilitates long-term PI-based treatment that is well tolerated in real-world, nontransplant [newly diagnosed multiple myeloma] patients,” according to Dr. Manda and colleagues. In addition, “preliminary findings indicate that the iCT approach results in promising efficacy and high medication adherence, with no adverse impact on patients’ HRQoL or treatment satisfaction.”
The study was sponsored by Millennium Pharmaceuticals. Four of the authors are employees of Millennium Pharmaceuticals and several authors disclosed relationships with various pharmaceutical companies, including Millennium Pharmaceuticals.
SOURCE: Manda S et al. Clin Lymphoma Myeloma Leuk. 2020 Jun 30. doi: 10.1016/j.clml.2020.06.024.
Transitioning from parenteral bortezomib-based induction to all-oral ixazomib-lenalidomide-dexamethasone therapy increased proteasome inhibitor (PI)–based treatment adherence and duration, according to early results from a clinical trial designed to include patients representing the real-world U.S. multiple myeloma population.
The US MM-6 study was designed to evaluate a novel in-class therapy (iCT) transitioning approach from intravenous to oral treatment in the community-based setting with the aims of increasing PI-based treatment duration and adherence, maintaining health-related quality of life (HRQoL), and improving outcomes in a representative, real-world, community population of multiple myeloma patients, according to Sudhir Manda, MD, of Arizona Oncology/U.S. Oncology Research, Tucson, and colleagues.
Dr. Manda and colleagues reported on the early results of the US MM-6 trial (NCT03173092), which is a community-based, real-world, open-label, single-arm, phase 4 study of adult multiple myeloma patients who do not meet transplant-eligibility criteria, or for whom transplant would be delayed for 2 years or more, and who are receiving first-line bortezomib-based induction. All patients in the study had no evidence of progressive disease after three treatment cycles.
By the data cutoff for the reported analysis, 84 patients had been treated. The patients had a median age of 73 years; 49% were men; 15% black/African American; 10% Hispanic/Latino. A total of 62% of the patients remain on therapy, with a mean duration of total PI therapy of 10.1 months and of ixazomib-lenalidomide-dexamethasone (ixazomib-Rd) of 7.3 months.
The overall response rate was 62% (complete response, 4%; very good partial response, 25%; partial response, 33%) after bortezomib-based induction and 70% (complete response, 26%; very good partial response, 29%; partial response, 15%) after induction to all-oral ixazomib-Rd.
“The use of this novel iCT approach from parenteral bortezomib-based to oral ixazomib-based therapy facilitates long-term PI-based treatment that is well tolerated in real-world, nontransplant [newly diagnosed multiple myeloma] patients,” according to Dr. Manda and colleagues. In addition, “preliminary findings indicate that the iCT approach results in promising efficacy and high medication adherence, with no adverse impact on patients’ HRQoL or treatment satisfaction.”
The study was sponsored by Millennium Pharmaceuticals. Four of the authors are employees of Millennium Pharmaceuticals and several authors disclosed relationships with various pharmaceutical companies, including Millennium Pharmaceuticals.
SOURCE: Manda S et al. Clin Lymphoma Myeloma Leuk. 2020 Jun 30. doi: 10.1016/j.clml.2020.06.024.
FROM CLINICAL LYMPHOMA, MYELOMA AND LEUKEMIA
Endothelial injury may play a major role in COVID-19–associated coagulopathy
A striking clinical feature of illness from SARS-CoV-2 is a marked increase in thrombotic and microvascular complications, or COVID-19–associated coagulopathy (CAC).
A new study suggests endothelial cell injury plays a major role in the pathogenesis of CAC, and blood levels of soluble thrombomodulin correlate with mortality.
George Goshua, MD, of Yale University, New Haven, Conn., presented this study as a late-breaking abstract at the virtual annual congress of the European Hematology Association.
Dr. Goshua cited past research showing CAC to be highly prevalent among hospitalized patients. Venous thromboembolism was found in 17% to 69% of patients, despite thromboprophylaxis.1-4 Arterial thrombosis has been seen in 3.6% to 4.0% of patients,1-3 and autopsy findings have shown microvascular thrombosis in as many as 87% of patients.5-7
For their study, Dr. Goshua and colleagues assessed endothelial cell damage, platelet activation, and hemostatic and fibrinolytic cascade effects of CAC.
The investigators measured markers of endothelial cell injury and platelet activation, plasminogen activation inhibitor 1 (PAI-1), and coagulation factors in stable and critically ill patients hospitalized with COVID-19. In addition, the team sought to identify biomarkers of mortality in hospitalized patients.
Dr. Goshua and colleagues studied 68 adults hospitalized for suspected COVID-19 – 48 in the ICU and 20 outside the ICU. Patients in the ICU received mechanical ventilation, while the non-ICU patients required supplemental oxygen (≤3 L/min per nasal cannula).
There were more men than women (69% vs. 31%) in the ICU population but not in the non-ICU population (40% vs. 60%). There were no statistically significant differences in age or comorbid conditions between the ICU and non-ICU patients.
Results and interpretation
Consistent with augmentation of the coagulation cascade – and as expected – D-dimer and thrombin-antithrombin levels were high in both the ICU and non-ICU populations, but levels were significantly higher (P < .001) among the ICU patients.
Endogenous anticoagulants (antithrombin and proteins C and S) and fibrinolytic enzymes (alpha 2-antiplasmin) were preserved, verifying that CAC is distinct from disseminated intravascular coagulation. Classic fibrinolysis did not occur, as PAI-1 was high in ICU and non-ICU patients, and lysis-30 was normal in nearly all ICU patients (96%).
Von Willebrand factor antigen and activity levels and factor VIII levels were markedly elevated in non-ICU and ICU patients, but they were significantly higher (P < .001) in the ICU cohort. This supports the hypothesis that endothelial cell damage and platelet activation play major roles in CAC.
Similarly, soluble P-selectin, which is shed from endothelial cells and platelets, was dramatically elevated in ICU patients in comparison with controls and non-ICU patients (P < .001 for both comparisons).
Levels of soluble thrombomodulin, which is released from endothelial cells, were not significantly different in ICU patients and controls. However, given thrombomodulin’s significant role in the coagulation cascade, Dr. Goshua and colleagues plotted receiver operating curves to see if soluble thrombomodulin levels were predictive of mortality.
The results showed that soluble thrombomodulin correlated with the probability of survival, both overall and in ICU patients. Soluble thrombomodulin levels greater than 3.26 ng/mL were associated with significantly worse survival in all patients (P = .0087) and ICU patients (P = .0309).
Influence on therapy
Laboratory perturbations were detected in both ICU and non-ICU patients, and otherwise healthy outpatients have exhibited potentially life-threatening CAC, according to Dr. Goshua.
These findings suggest the prothrombotic state occurs early in the pathogenesis of SARS-CoV-2 infection, is driven by platelet activation and endotheliopathy, and becomes more pronounced with worsening severity of infection.
The results of this study prompted a change in how Yale–New Haven Hospital manages COVID-19 patients. Patients without a clinical contraindication now receive aspirin at 81 mg daily in addition to the anticoagulation regimen typically used for all hospitalized COVID-19 patients.
Investigations regarding other medications that can influence platelet-endothelial cell interactions and modulate endothelial cell damage in CAC – such as dipyridamole, defibrotide, and eculizumab – are planned.
Challenges and unanswered questions
Virchow’s triad was described by the eminent German physician, Rudolf Virchow, MD, in the 19th century. It refers to the three broad categories of factors that can predispose patients to thrombosis — circulatory stasis, hypercoagulability, and endothelial injury.
Although all of these elements could be operative in CAC, the current study suggests platelet activation and endothelial cell injury in CAC may be of primary importance.
Because of the limited ability to test critically ill patients and concerns regarding exposure of additional hospital personnel to COVID-19 patients, the current report lacked clarity about the relationship of the detected laboratory abnormalities to confirmed thrombotic events.
It is unknown whether endothelial cells in different organs are damaged uniformly. It is also unclear if the laboratory abnormalities identified in this analysis can be used to monitor response to therapy, to guide follow-up management of discharged patients with CAC, or to identify infected outpatients who should receive prophylactic anticoagulation.
The mechanism by which SARS-CoV-2 injures endothelial cells is not explained by these data. Neutrophil defensins and other prothrombotic peptides or markers of inflammation could play key roles in pathogenesis, assessment of disease severity, or monitoring for therapeutic efficacy.
Today, we have more sophisticated diagnostic tools than Dr. Virchow had. We also have the ability to record and rapidly disseminate information globally. Still, with regard to the COVID-19 pandemic, clinicians face many of the same challenges that confronted Dr. Virchow in his era.
The analysis conducted by Dr. Goshua and colleagues goes a long way toward elucidating some of the mechanisms and therapeutic targets to meet these challenges.
Dr. Goshua disclosed no conflicts of interest.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
SOURCE: Goshua G et al. EHA Congress. Abstract LB2605.
References
1. Klok FA et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res. 2020;191:148-50. doi: 10.1016/j.thromres.2020.04.041.
2. Thomas W et al. Thrombotic complications of patients admitted to intensive care with COVID-19 at a teaching hospital in the United Kingdom. Thromb Res. 2020;191:76-7. doi: 10.1016/j.thromres.2020.04.028
3. Lodigiani C et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9-14. doi: 10.1016/j.thromres.2020.04.024
4. Llitjos JF et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients [published online ahead of print, 2020 Apr 22]. J Thromb Haemost. 2020;10.1111/jth.14869. doi: 10.1111/jth.14869
5. Carsana L et al. Pulmonary post-mortem findings in a large series of COVID-19 cases from Northern Italy. medRxiv 2020.04.19.20054262; doi: 10.1101/2020.04.19.20054262v1.
6. Menter T et al. Post-mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction [published online ahead of print, 2020 May 4]. Histopathology. 2020;10.1111/his.14134. doi: 10.1111/his.14134
7. Lax SF, et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: Results from a prospective, single-center, clinicopathologic case series [published online ahead of print, 2020 May 14]. Ann Intern Med. 2020;M20-2566. doi: 10.7326/M20-2566.
A striking clinical feature of illness from SARS-CoV-2 is a marked increase in thrombotic and microvascular complications, or COVID-19–associated coagulopathy (CAC).
A new study suggests endothelial cell injury plays a major role in the pathogenesis of CAC, and blood levels of soluble thrombomodulin correlate with mortality.
George Goshua, MD, of Yale University, New Haven, Conn., presented this study as a late-breaking abstract at the virtual annual congress of the European Hematology Association.
Dr. Goshua cited past research showing CAC to be highly prevalent among hospitalized patients. Venous thromboembolism was found in 17% to 69% of patients, despite thromboprophylaxis.1-4 Arterial thrombosis has been seen in 3.6% to 4.0% of patients,1-3 and autopsy findings have shown microvascular thrombosis in as many as 87% of patients.5-7
For their study, Dr. Goshua and colleagues assessed endothelial cell damage, platelet activation, and hemostatic and fibrinolytic cascade effects of CAC.
The investigators measured markers of endothelial cell injury and platelet activation, plasminogen activation inhibitor 1 (PAI-1), and coagulation factors in stable and critically ill patients hospitalized with COVID-19. In addition, the team sought to identify biomarkers of mortality in hospitalized patients.
Dr. Goshua and colleagues studied 68 adults hospitalized for suspected COVID-19 – 48 in the ICU and 20 outside the ICU. Patients in the ICU received mechanical ventilation, while the non-ICU patients required supplemental oxygen (≤3 L/min per nasal cannula).
There were more men than women (69% vs. 31%) in the ICU population but not in the non-ICU population (40% vs. 60%). There were no statistically significant differences in age or comorbid conditions between the ICU and non-ICU patients.
Results and interpretation
Consistent with augmentation of the coagulation cascade – and as expected – D-dimer and thrombin-antithrombin levels were high in both the ICU and non-ICU populations, but levels were significantly higher (P < .001) among the ICU patients.
Endogenous anticoagulants (antithrombin and proteins C and S) and fibrinolytic enzymes (alpha 2-antiplasmin) were preserved, verifying that CAC is distinct from disseminated intravascular coagulation. Classic fibrinolysis did not occur, as PAI-1 was high in ICU and non-ICU patients, and lysis-30 was normal in nearly all ICU patients (96%).
Von Willebrand factor antigen and activity levels and factor VIII levels were markedly elevated in non-ICU and ICU patients, but they were significantly higher (P < .001) in the ICU cohort. This supports the hypothesis that endothelial cell damage and platelet activation play major roles in CAC.
Similarly, soluble P-selectin, which is shed from endothelial cells and platelets, was dramatically elevated in ICU patients in comparison with controls and non-ICU patients (P < .001 for both comparisons).
Levels of soluble thrombomodulin, which is released from endothelial cells, were not significantly different in ICU patients and controls. However, given thrombomodulin’s significant role in the coagulation cascade, Dr. Goshua and colleagues plotted receiver operating curves to see if soluble thrombomodulin levels were predictive of mortality.
The results showed that soluble thrombomodulin correlated with the probability of survival, both overall and in ICU patients. Soluble thrombomodulin levels greater than 3.26 ng/mL were associated with significantly worse survival in all patients (P = .0087) and ICU patients (P = .0309).
Influence on therapy
Laboratory perturbations were detected in both ICU and non-ICU patients, and otherwise healthy outpatients have exhibited potentially life-threatening CAC, according to Dr. Goshua.
These findings suggest the prothrombotic state occurs early in the pathogenesis of SARS-CoV-2 infection, is driven by platelet activation and endotheliopathy, and becomes more pronounced with worsening severity of infection.
The results of this study prompted a change in how Yale–New Haven Hospital manages COVID-19 patients. Patients without a clinical contraindication now receive aspirin at 81 mg daily in addition to the anticoagulation regimen typically used for all hospitalized COVID-19 patients.
Investigations regarding other medications that can influence platelet-endothelial cell interactions and modulate endothelial cell damage in CAC – such as dipyridamole, defibrotide, and eculizumab – are planned.
Challenges and unanswered questions
Virchow’s triad was described by the eminent German physician, Rudolf Virchow, MD, in the 19th century. It refers to the three broad categories of factors that can predispose patients to thrombosis — circulatory stasis, hypercoagulability, and endothelial injury.
Although all of these elements could be operative in CAC, the current study suggests platelet activation and endothelial cell injury in CAC may be of primary importance.
Because of the limited ability to test critically ill patients and concerns regarding exposure of additional hospital personnel to COVID-19 patients, the current report lacked clarity about the relationship of the detected laboratory abnormalities to confirmed thrombotic events.
It is unknown whether endothelial cells in different organs are damaged uniformly. It is also unclear if the laboratory abnormalities identified in this analysis can be used to monitor response to therapy, to guide follow-up management of discharged patients with CAC, or to identify infected outpatients who should receive prophylactic anticoagulation.
The mechanism by which SARS-CoV-2 injures endothelial cells is not explained by these data. Neutrophil defensins and other prothrombotic peptides or markers of inflammation could play key roles in pathogenesis, assessment of disease severity, or monitoring for therapeutic efficacy.
Today, we have more sophisticated diagnostic tools than Dr. Virchow had. We also have the ability to record and rapidly disseminate information globally. Still, with regard to the COVID-19 pandemic, clinicians face many of the same challenges that confronted Dr. Virchow in his era.
The analysis conducted by Dr. Goshua and colleagues goes a long way toward elucidating some of the mechanisms and therapeutic targets to meet these challenges.
Dr. Goshua disclosed no conflicts of interest.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
SOURCE: Goshua G et al. EHA Congress. Abstract LB2605.
References
1. Klok FA et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res. 2020;191:148-50. doi: 10.1016/j.thromres.2020.04.041.
2. Thomas W et al. Thrombotic complications of patients admitted to intensive care with COVID-19 at a teaching hospital in the United Kingdom. Thromb Res. 2020;191:76-7. doi: 10.1016/j.thromres.2020.04.028
3. Lodigiani C et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9-14. doi: 10.1016/j.thromres.2020.04.024
4. Llitjos JF et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients [published online ahead of print, 2020 Apr 22]. J Thromb Haemost. 2020;10.1111/jth.14869. doi: 10.1111/jth.14869
5. Carsana L et al. Pulmonary post-mortem findings in a large series of COVID-19 cases from Northern Italy. medRxiv 2020.04.19.20054262; doi: 10.1101/2020.04.19.20054262v1.
6. Menter T et al. Post-mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction [published online ahead of print, 2020 May 4]. Histopathology. 2020;10.1111/his.14134. doi: 10.1111/his.14134
7. Lax SF, et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: Results from a prospective, single-center, clinicopathologic case series [published online ahead of print, 2020 May 14]. Ann Intern Med. 2020;M20-2566. doi: 10.7326/M20-2566.
A striking clinical feature of illness from SARS-CoV-2 is a marked increase in thrombotic and microvascular complications, or COVID-19–associated coagulopathy (CAC).
A new study suggests endothelial cell injury plays a major role in the pathogenesis of CAC, and blood levels of soluble thrombomodulin correlate with mortality.
George Goshua, MD, of Yale University, New Haven, Conn., presented this study as a late-breaking abstract at the virtual annual congress of the European Hematology Association.
Dr. Goshua cited past research showing CAC to be highly prevalent among hospitalized patients. Venous thromboembolism was found in 17% to 69% of patients, despite thromboprophylaxis.1-4 Arterial thrombosis has been seen in 3.6% to 4.0% of patients,1-3 and autopsy findings have shown microvascular thrombosis in as many as 87% of patients.5-7
For their study, Dr. Goshua and colleagues assessed endothelial cell damage, platelet activation, and hemostatic and fibrinolytic cascade effects of CAC.
The investigators measured markers of endothelial cell injury and platelet activation, plasminogen activation inhibitor 1 (PAI-1), and coagulation factors in stable and critically ill patients hospitalized with COVID-19. In addition, the team sought to identify biomarkers of mortality in hospitalized patients.
Dr. Goshua and colleagues studied 68 adults hospitalized for suspected COVID-19 – 48 in the ICU and 20 outside the ICU. Patients in the ICU received mechanical ventilation, while the non-ICU patients required supplemental oxygen (≤3 L/min per nasal cannula).
There were more men than women (69% vs. 31%) in the ICU population but not in the non-ICU population (40% vs. 60%). There were no statistically significant differences in age or comorbid conditions between the ICU and non-ICU patients.
Results and interpretation
Consistent with augmentation of the coagulation cascade – and as expected – D-dimer and thrombin-antithrombin levels were high in both the ICU and non-ICU populations, but levels were significantly higher (P < .001) among the ICU patients.
Endogenous anticoagulants (antithrombin and proteins C and S) and fibrinolytic enzymes (alpha 2-antiplasmin) were preserved, verifying that CAC is distinct from disseminated intravascular coagulation. Classic fibrinolysis did not occur, as PAI-1 was high in ICU and non-ICU patients, and lysis-30 was normal in nearly all ICU patients (96%).
Von Willebrand factor antigen and activity levels and factor VIII levels were markedly elevated in non-ICU and ICU patients, but they were significantly higher (P < .001) in the ICU cohort. This supports the hypothesis that endothelial cell damage and platelet activation play major roles in CAC.
Similarly, soluble P-selectin, which is shed from endothelial cells and platelets, was dramatically elevated in ICU patients in comparison with controls and non-ICU patients (P < .001 for both comparisons).
Levels of soluble thrombomodulin, which is released from endothelial cells, were not significantly different in ICU patients and controls. However, given thrombomodulin’s significant role in the coagulation cascade, Dr. Goshua and colleagues plotted receiver operating curves to see if soluble thrombomodulin levels were predictive of mortality.
The results showed that soluble thrombomodulin correlated with the probability of survival, both overall and in ICU patients. Soluble thrombomodulin levels greater than 3.26 ng/mL were associated with significantly worse survival in all patients (P = .0087) and ICU patients (P = .0309).
Influence on therapy
Laboratory perturbations were detected in both ICU and non-ICU patients, and otherwise healthy outpatients have exhibited potentially life-threatening CAC, according to Dr. Goshua.
These findings suggest the prothrombotic state occurs early in the pathogenesis of SARS-CoV-2 infection, is driven by platelet activation and endotheliopathy, and becomes more pronounced with worsening severity of infection.
The results of this study prompted a change in how Yale–New Haven Hospital manages COVID-19 patients. Patients without a clinical contraindication now receive aspirin at 81 mg daily in addition to the anticoagulation regimen typically used for all hospitalized COVID-19 patients.
Investigations regarding other medications that can influence platelet-endothelial cell interactions and modulate endothelial cell damage in CAC – such as dipyridamole, defibrotide, and eculizumab – are planned.
Challenges and unanswered questions
Virchow’s triad was described by the eminent German physician, Rudolf Virchow, MD, in the 19th century. It refers to the three broad categories of factors that can predispose patients to thrombosis — circulatory stasis, hypercoagulability, and endothelial injury.
Although all of these elements could be operative in CAC, the current study suggests platelet activation and endothelial cell injury in CAC may be of primary importance.
Because of the limited ability to test critically ill patients and concerns regarding exposure of additional hospital personnel to COVID-19 patients, the current report lacked clarity about the relationship of the detected laboratory abnormalities to confirmed thrombotic events.
It is unknown whether endothelial cells in different organs are damaged uniformly. It is also unclear if the laboratory abnormalities identified in this analysis can be used to monitor response to therapy, to guide follow-up management of discharged patients with CAC, or to identify infected outpatients who should receive prophylactic anticoagulation.
The mechanism by which SARS-CoV-2 injures endothelial cells is not explained by these data. Neutrophil defensins and other prothrombotic peptides or markers of inflammation could play key roles in pathogenesis, assessment of disease severity, or monitoring for therapeutic efficacy.
Today, we have more sophisticated diagnostic tools than Dr. Virchow had. We also have the ability to record and rapidly disseminate information globally. Still, with regard to the COVID-19 pandemic, clinicians face many of the same challenges that confronted Dr. Virchow in his era.
The analysis conducted by Dr. Goshua and colleagues goes a long way toward elucidating some of the mechanisms and therapeutic targets to meet these challenges.
Dr. Goshua disclosed no conflicts of interest.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
SOURCE: Goshua G et al. EHA Congress. Abstract LB2605.
References
1. Klok FA et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res. 2020;191:148-50. doi: 10.1016/j.thromres.2020.04.041.
2. Thomas W et al. Thrombotic complications of patients admitted to intensive care with COVID-19 at a teaching hospital in the United Kingdom. Thromb Res. 2020;191:76-7. doi: 10.1016/j.thromres.2020.04.028
3. Lodigiani C et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9-14. doi: 10.1016/j.thromres.2020.04.024
4. Llitjos JF et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients [published online ahead of print, 2020 Apr 22]. J Thromb Haemost. 2020;10.1111/jth.14869. doi: 10.1111/jth.14869
5. Carsana L et al. Pulmonary post-mortem findings in a large series of COVID-19 cases from Northern Italy. medRxiv 2020.04.19.20054262; doi: 10.1101/2020.04.19.20054262v1.
6. Menter T et al. Post-mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction [published online ahead of print, 2020 May 4]. Histopathology. 2020;10.1111/his.14134. doi: 10.1111/his.14134
7. Lax SF, et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: Results from a prospective, single-center, clinicopathologic case series [published online ahead of print, 2020 May 14]. Ann Intern Med. 2020;M20-2566. doi: 10.7326/M20-2566.
FROM EHA CONGRESS
Combo drug improves survival in older patients with high-risk/secondary AML
The use of CPX-351, a dual-drug liposomal encapsulation of cytarabine and daunorubicin, was tied to long-term remission and survival in older patients with newly diagnosed high-risk or secondary acute myeloid leukemia (AML), according to final results of a phase 3 study.
As part of the American Society of Clinical Oncology virtual scientific program, Jeffrey E. Lancet, MD, of the Moffitt Cancer Center in Tampa, Fla., presented the 5-year final data from a trial comparing CPX-351 vs. the conventional 7+3 regimen of cytarabine and daunorubicin in more than 300 older adult patients (age 60-75 years) with newly diagnosed high-risk or secondary AML. Early mortality rates for CPX-351 vs. 7+3 were 6% vs. 11% at Day 30 and 14% vs. 21% at day 60, respectively.
The final 5-year follow-up results had a median follow-up of just greater than 60 months, and maintained the improved median overall survival previously observed in the trial with CPX-351 (153 patients), compared with 7+3 (155 patients), Dr. Lancet reported.
Allogeneic hematopoietic stem cell transplant was received by 35% of the patients in the CPX-351 arm and 25% of patients in the 7+3 arm. The median overall survival after transplant was not reached for the CPX-351 arm, compared with 10.3 months with the 7+3 treated patients.
Remission, either complete remission or complete remission with incomplete neutrophil or platelet recovery, was achieved by 48% of patients in the CPX-351 arm and 33% of patients in the 7+3 arm, according to the results of the 5-year follow-up. In addition, among all patients who achieved remission, median overall survival was longer with CPX-351 than with 7+3, and the Kaplan-Meier estimated survival rate was higher for CPX-351 at both 3 years and 5 years.
At 5 years of follow-up, 81% of patients in the CPX-351 arm and 93% of patients in the 7+3 arm had died, with similar causes cited in each arm. Progressive leukemia was the most common primary cause of death in both treatment arms, according to Dr. Lancet.
“The final 5-year follow-up results from this phase 3 study support the prior evidence that CPX-351 has the ability to produce or contribute to long-term remission and survival in older patients with newly diagnosed high-risk or secondary AML,” Dr. Lancet concluded.
CPX-351 (Vyxeos) has been approved by the Food and Drug Administration and the European Medicines Agency for the treatment of adults with newly diagnosed therapy-related AML or AML with myelodysplastic syndrome–related changes.
The study was funded by Jazz Pharmaceuticals. Dr. Lancet disclosed that he has a consulting or advisory role for Agios, Daiichi Sankyo, Jazz Pharmaceuticals, and Pfizer.
SOURCE: Lancet JE et al. ASCO 2020, Abstract 7510.
The use of CPX-351, a dual-drug liposomal encapsulation of cytarabine and daunorubicin, was tied to long-term remission and survival in older patients with newly diagnosed high-risk or secondary acute myeloid leukemia (AML), according to final results of a phase 3 study.
As part of the American Society of Clinical Oncology virtual scientific program, Jeffrey E. Lancet, MD, of the Moffitt Cancer Center in Tampa, Fla., presented the 5-year final data from a trial comparing CPX-351 vs. the conventional 7+3 regimen of cytarabine and daunorubicin in more than 300 older adult patients (age 60-75 years) with newly diagnosed high-risk or secondary AML. Early mortality rates for CPX-351 vs. 7+3 were 6% vs. 11% at Day 30 and 14% vs. 21% at day 60, respectively.
The final 5-year follow-up results had a median follow-up of just greater than 60 months, and maintained the improved median overall survival previously observed in the trial with CPX-351 (153 patients), compared with 7+3 (155 patients), Dr. Lancet reported.
Allogeneic hematopoietic stem cell transplant was received by 35% of the patients in the CPX-351 arm and 25% of patients in the 7+3 arm. The median overall survival after transplant was not reached for the CPX-351 arm, compared with 10.3 months with the 7+3 treated patients.
Remission, either complete remission or complete remission with incomplete neutrophil or platelet recovery, was achieved by 48% of patients in the CPX-351 arm and 33% of patients in the 7+3 arm, according to the results of the 5-year follow-up. In addition, among all patients who achieved remission, median overall survival was longer with CPX-351 than with 7+3, and the Kaplan-Meier estimated survival rate was higher for CPX-351 at both 3 years and 5 years.
At 5 years of follow-up, 81% of patients in the CPX-351 arm and 93% of patients in the 7+3 arm had died, with similar causes cited in each arm. Progressive leukemia was the most common primary cause of death in both treatment arms, according to Dr. Lancet.
“The final 5-year follow-up results from this phase 3 study support the prior evidence that CPX-351 has the ability to produce or contribute to long-term remission and survival in older patients with newly diagnosed high-risk or secondary AML,” Dr. Lancet concluded.
CPX-351 (Vyxeos) has been approved by the Food and Drug Administration and the European Medicines Agency for the treatment of adults with newly diagnosed therapy-related AML or AML with myelodysplastic syndrome–related changes.
The study was funded by Jazz Pharmaceuticals. Dr. Lancet disclosed that he has a consulting or advisory role for Agios, Daiichi Sankyo, Jazz Pharmaceuticals, and Pfizer.
SOURCE: Lancet JE et al. ASCO 2020, Abstract 7510.
The use of CPX-351, a dual-drug liposomal encapsulation of cytarabine and daunorubicin, was tied to long-term remission and survival in older patients with newly diagnosed high-risk or secondary acute myeloid leukemia (AML), according to final results of a phase 3 study.
As part of the American Society of Clinical Oncology virtual scientific program, Jeffrey E. Lancet, MD, of the Moffitt Cancer Center in Tampa, Fla., presented the 5-year final data from a trial comparing CPX-351 vs. the conventional 7+3 regimen of cytarabine and daunorubicin in more than 300 older adult patients (age 60-75 years) with newly diagnosed high-risk or secondary AML. Early mortality rates for CPX-351 vs. 7+3 were 6% vs. 11% at Day 30 and 14% vs. 21% at day 60, respectively.
The final 5-year follow-up results had a median follow-up of just greater than 60 months, and maintained the improved median overall survival previously observed in the trial with CPX-351 (153 patients), compared with 7+3 (155 patients), Dr. Lancet reported.
Allogeneic hematopoietic stem cell transplant was received by 35% of the patients in the CPX-351 arm and 25% of patients in the 7+3 arm. The median overall survival after transplant was not reached for the CPX-351 arm, compared with 10.3 months with the 7+3 treated patients.
Remission, either complete remission or complete remission with incomplete neutrophil or platelet recovery, was achieved by 48% of patients in the CPX-351 arm and 33% of patients in the 7+3 arm, according to the results of the 5-year follow-up. In addition, among all patients who achieved remission, median overall survival was longer with CPX-351 than with 7+3, and the Kaplan-Meier estimated survival rate was higher for CPX-351 at both 3 years and 5 years.
At 5 years of follow-up, 81% of patients in the CPX-351 arm and 93% of patients in the 7+3 arm had died, with similar causes cited in each arm. Progressive leukemia was the most common primary cause of death in both treatment arms, according to Dr. Lancet.
“The final 5-year follow-up results from this phase 3 study support the prior evidence that CPX-351 has the ability to produce or contribute to long-term remission and survival in older patients with newly diagnosed high-risk or secondary AML,” Dr. Lancet concluded.
CPX-351 (Vyxeos) has been approved by the Food and Drug Administration and the European Medicines Agency for the treatment of adults with newly diagnosed therapy-related AML or AML with myelodysplastic syndrome–related changes.
The study was funded by Jazz Pharmaceuticals. Dr. Lancet disclosed that he has a consulting or advisory role for Agios, Daiichi Sankyo, Jazz Pharmaceuticals, and Pfizer.
SOURCE: Lancet JE et al. ASCO 2020, Abstract 7510.
FROM ASCO 2020
Venetoclax plus LDAC tops LDAC alone in AML
At about 18 months’ follow-up in treatment naive acute myelogenous leukemia (AML) patients who were 75 years or older or otherwise unfit for intensive chemotherapy, median overall survival (OS) was 8.4 months when they were randomized to low-dose cytarabine (LDAC) plus the BCL-2 inhibitor venetoclax versus 4.1 months with LDAC plus placebo. The results from the phase 3 trial were reported at the virtual annual congress of the European Hematology Association.
The combination also improved rates of remission, event-free survival, and patient reported outcomes and lessened transfusion requirements. Adverse events were manageable.
The findings position venetoclax add-on with LDAC “as a potential new standard of care” for untreated patients ineligible for intensive chemotherapy, lead investigator Andrew Wei, MD, PhD, an AML researcher at Monash University, Melbourne, said at the meeting.
The study addresses a substantial unmet need. The median age at AML diagnosis is over 68 years old and comorbidities such as heart failure and reduced creatinine clearance are common, which make the risk of toxicity with standard chemotherapy too high. Single-agent alternatives are of limited benefit, so Dr. Wei’s group and others are looking for better options to plug the treatment gap when standard chemotherapy is contraindicated.
Several combinations are under investigation, including LDAC plus venetoclax, which appears to have a synergistic effect greater than either agent on its own, Dr. Wei and colleagues explained in their journal report, which was published online to coincide with his presentation (Blood. 2020 Jun 11;135(24):2137-45).
In a commentary, Bob Lowenberg, Ph, a hematologist with the Erasmus University Medical Center in Rotterdam, and Gerwin Huls, MD, PhD, of the University Medical Center Groningen, both in the Netherlands, said the study “represents a valuable although moderate step forward on the way to a better therapeutic future for the ‘unfit’ patient with AML” (Blood. 2020. Jun 11;135(24): 2114-5).
“A challenging AML population”
In the study, 143 patients were randomized to oral venetoclax 600 mg daily and 68 to placebo in 28-day cycles, on a background of LDAC 20 mg/m2 administered subcutaneously on days 1-10 of each cycle.
“This study enrolled a challenging AML population, with nearly 60% age ≥75 years and a high proportion of patients with secondary disease (38%), prior hypomethylating agent (HMA) treatment (20%), poor cytogenetic risk (32%), and TP53 mutations (15%), which are known factors associated with dismal prognosis in AML,” the investigators noted in their report.
There was a numerical benefit in OS at 12 months – the preplanned primary outcome – but it was not statistically significant. At 18 months, however, and after adjustment for a higher rate of secondary AML in the venetoclax arm and other confounders in a post hoc analysis, survival differences reached significance. The 4.3-month OS benefit with the combination translated into a 30% reduction in the risk of death (hazard ratio, 0.70; 95% confidence interval, 0.50-0.99; P = .04)
Survival outcomes “were particularly promising for patient subgroups with NPM1- (median OS, not reached) and IDH1/2-mutant AML (median OS, 19.4 months),” the team noted.
Complete remission (CR) were 48% in the venetoclax arm, compared with 13% in the placebo group, and 34% of venetoclax patients versus 3% of placebo patients went into remission after their first cycle. Venetoclax subjects also had longer median event free survival (4.7 months vs. 2 months); higher rates of red blood cell and platelet transfusion independence (37% vs. 16%); and higher rates of cytometric minimal residual disease levels below 0.1% (6% vs. 1%).
The findings correlated with “strong improvements” in patient-reported outcomes, including fatigue and quality of life, the investigators reported.
Risk mitigation
Grade 3 or higher adverse events (AEs) included febrile neutropenia (32% in the venetoclax arm versus 29% in the placebo group), neutropenia (47% venetoclax vs. 16% placebo), thrombocytopenia (45% vs. 37%), and anemia (25% vs. 22%). The eight cases of tumor lysis syndrome (TLS) were all in the venetoclax arm. Grade 3 or higher bleeding was higher in the venetoclax arm (11% versus 7%), but the incidence of fatal bleeding was similar between the groups (1.4% venetoclax versus 1.5%).
“Although the venetoclax arm showed modest increases in hematologic AEs, the rate of AEs leading to treatment discontinuation (24% vs. 25%) and the rate of serious AEs such as pneumonia” and sepsis “were nearly identical between” the arms, the team said.
The combination “is more myelosuppressive,” but the effects “were mostly mitigated by venetoclax dose interruptions and reductions.” To mitigate the TLS risk, patients were hospitalized for TLS evaluation and prophylaxis during the 4-day venetoclax ramp-up in the first treatment cycle and for 24 hours after the 600-mg target was reached. “I think this is an extremely important measure to avoid this small but important complication,” Dr. Wei said at the meeting.
A moderate step forward
Dr. Lowenberg and Dr. Huls noted in their commentary that, despite the favorable outcomes, “the results are still sobering with a rapid drop of the survival curves to values of [around] 25% or less within 18 months, and event-free survival rates even falling to considerably lower levels.”
Also, there was a “weak correlation between the relatively wide differences in comparative CR/CRi rates and the much smaller differences in survival,” perhaps “due to a limited depth of the complete responses following venetoclax-LDAC therapy or the early development of therapeutic resistance,” they said.
The commentary also noted another option, adding the hedgehog pathway inhibitor glasdegib, instead of venetoclax, to LDAC. It also improved survival in a similar randomized study in unfit AML and high-risk myelodysplastic syndrome patients, from a median survival of 4.9 months with LDAC alone to 8.8 months with the combination (Leukemia. 2019 Feb;33(2):379-389. doi: 10.1038/s41375-018-0312-9).
Dueling regimens
Another alternative approach – venetoclax plus the HMA agent azacitidine – garnered a lot of attention at the meeting when it was reported that the combination had a median overall survival of 14.7 months, versus 9.6 months with azacitidine alone, in patients ineligible for intensive chemotherapy. CR/CRi rates were 66% with the combination, versus 28%.
“It seems like the results were better with the combination of venetoclax and azacitidine” than venetoclax plus LDAC, said Gunnar Juliusson, MD, PhD, of Lund (Sweden) University, who moderated Dr. Wei’s presentation.
He wanted to know if there was a way to identify patients who would do better on one regimen versus the other and was curious about the fact that the azacitidine study used a dose of 400 mg venetoclax, instead of 600 mg.
Dr. Wei noted the high incidence of poor prognostic factors in his study, including prior HMA treatment in 20%, but also that “we don’t know for sure” if there’s a clinically meaningful benefit with the higher dose.
He also said the optimal number of venetoclax cycles for best response is unknown. For now, treatment is “recommend until either [disease] progression, dose intolerance, or patient or physician preference,” he noted. Venetoclax subjects in his study had a median of four treatment cycles versus two in the placebo group. Combination patients in the azacitidine study had a median of seven cycles versus 4.5 with placebo.
Venetoclax already carries an indication in the United States in combination with azacitidine, decitabine, or LDAC for newly-diagnosed AML in adults 75 years or older or who have comorbidities that preclude use of intensive induction chemotherapy, at a daily dosage of 400 mg with HMAs and 600 mg with LDAC.
Labeling notes that “continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.”
Both venetoclax trials were sponsored by the drug’s maker, AbbVie, which was involved with data interpretation and other matters. Dr. Wei is a consultant for and receives research funding from the company and also receives royalty payments in relation to venetoclax. The commentators did not have any competing financial interests. Disclosures, if any, were not reported for Dr. Juliusson.
SOURCE: Wei AH et al. EHA Congress, Abstract S136.
At about 18 months’ follow-up in treatment naive acute myelogenous leukemia (AML) patients who were 75 years or older or otherwise unfit for intensive chemotherapy, median overall survival (OS) was 8.4 months when they were randomized to low-dose cytarabine (LDAC) plus the BCL-2 inhibitor venetoclax versus 4.1 months with LDAC plus placebo. The results from the phase 3 trial were reported at the virtual annual congress of the European Hematology Association.
The combination also improved rates of remission, event-free survival, and patient reported outcomes and lessened transfusion requirements. Adverse events were manageable.
The findings position venetoclax add-on with LDAC “as a potential new standard of care” for untreated patients ineligible for intensive chemotherapy, lead investigator Andrew Wei, MD, PhD, an AML researcher at Monash University, Melbourne, said at the meeting.
The study addresses a substantial unmet need. The median age at AML diagnosis is over 68 years old and comorbidities such as heart failure and reduced creatinine clearance are common, which make the risk of toxicity with standard chemotherapy too high. Single-agent alternatives are of limited benefit, so Dr. Wei’s group and others are looking for better options to plug the treatment gap when standard chemotherapy is contraindicated.
Several combinations are under investigation, including LDAC plus venetoclax, which appears to have a synergistic effect greater than either agent on its own, Dr. Wei and colleagues explained in their journal report, which was published online to coincide with his presentation (Blood. 2020 Jun 11;135(24):2137-45).
In a commentary, Bob Lowenberg, Ph, a hematologist with the Erasmus University Medical Center in Rotterdam, and Gerwin Huls, MD, PhD, of the University Medical Center Groningen, both in the Netherlands, said the study “represents a valuable although moderate step forward on the way to a better therapeutic future for the ‘unfit’ patient with AML” (Blood. 2020. Jun 11;135(24): 2114-5).
“A challenging AML population”
In the study, 143 patients were randomized to oral venetoclax 600 mg daily and 68 to placebo in 28-day cycles, on a background of LDAC 20 mg/m2 administered subcutaneously on days 1-10 of each cycle.
“This study enrolled a challenging AML population, with nearly 60% age ≥75 years and a high proportion of patients with secondary disease (38%), prior hypomethylating agent (HMA) treatment (20%), poor cytogenetic risk (32%), and TP53 mutations (15%), which are known factors associated with dismal prognosis in AML,” the investigators noted in their report.
There was a numerical benefit in OS at 12 months – the preplanned primary outcome – but it was not statistically significant. At 18 months, however, and after adjustment for a higher rate of secondary AML in the venetoclax arm and other confounders in a post hoc analysis, survival differences reached significance. The 4.3-month OS benefit with the combination translated into a 30% reduction in the risk of death (hazard ratio, 0.70; 95% confidence interval, 0.50-0.99; P = .04)
Survival outcomes “were particularly promising for patient subgroups with NPM1- (median OS, not reached) and IDH1/2-mutant AML (median OS, 19.4 months),” the team noted.
Complete remission (CR) were 48% in the venetoclax arm, compared with 13% in the placebo group, and 34% of venetoclax patients versus 3% of placebo patients went into remission after their first cycle. Venetoclax subjects also had longer median event free survival (4.7 months vs. 2 months); higher rates of red blood cell and platelet transfusion independence (37% vs. 16%); and higher rates of cytometric minimal residual disease levels below 0.1% (6% vs. 1%).
The findings correlated with “strong improvements” in patient-reported outcomes, including fatigue and quality of life, the investigators reported.
Risk mitigation
Grade 3 or higher adverse events (AEs) included febrile neutropenia (32% in the venetoclax arm versus 29% in the placebo group), neutropenia (47% venetoclax vs. 16% placebo), thrombocytopenia (45% vs. 37%), and anemia (25% vs. 22%). The eight cases of tumor lysis syndrome (TLS) were all in the venetoclax arm. Grade 3 or higher bleeding was higher in the venetoclax arm (11% versus 7%), but the incidence of fatal bleeding was similar between the groups (1.4% venetoclax versus 1.5%).
“Although the venetoclax arm showed modest increases in hematologic AEs, the rate of AEs leading to treatment discontinuation (24% vs. 25%) and the rate of serious AEs such as pneumonia” and sepsis “were nearly identical between” the arms, the team said.
The combination “is more myelosuppressive,” but the effects “were mostly mitigated by venetoclax dose interruptions and reductions.” To mitigate the TLS risk, patients were hospitalized for TLS evaluation and prophylaxis during the 4-day venetoclax ramp-up in the first treatment cycle and for 24 hours after the 600-mg target was reached. “I think this is an extremely important measure to avoid this small but important complication,” Dr. Wei said at the meeting.
A moderate step forward
Dr. Lowenberg and Dr. Huls noted in their commentary that, despite the favorable outcomes, “the results are still sobering with a rapid drop of the survival curves to values of [around] 25% or less within 18 months, and event-free survival rates even falling to considerably lower levels.”
Also, there was a “weak correlation between the relatively wide differences in comparative CR/CRi rates and the much smaller differences in survival,” perhaps “due to a limited depth of the complete responses following venetoclax-LDAC therapy or the early development of therapeutic resistance,” they said.
The commentary also noted another option, adding the hedgehog pathway inhibitor glasdegib, instead of venetoclax, to LDAC. It also improved survival in a similar randomized study in unfit AML and high-risk myelodysplastic syndrome patients, from a median survival of 4.9 months with LDAC alone to 8.8 months with the combination (Leukemia. 2019 Feb;33(2):379-389. doi: 10.1038/s41375-018-0312-9).
Dueling regimens
Another alternative approach – venetoclax plus the HMA agent azacitidine – garnered a lot of attention at the meeting when it was reported that the combination had a median overall survival of 14.7 months, versus 9.6 months with azacitidine alone, in patients ineligible for intensive chemotherapy. CR/CRi rates were 66% with the combination, versus 28%.
“It seems like the results were better with the combination of venetoclax and azacitidine” than venetoclax plus LDAC, said Gunnar Juliusson, MD, PhD, of Lund (Sweden) University, who moderated Dr. Wei’s presentation.
He wanted to know if there was a way to identify patients who would do better on one regimen versus the other and was curious about the fact that the azacitidine study used a dose of 400 mg venetoclax, instead of 600 mg.
Dr. Wei noted the high incidence of poor prognostic factors in his study, including prior HMA treatment in 20%, but also that “we don’t know for sure” if there’s a clinically meaningful benefit with the higher dose.
He also said the optimal number of venetoclax cycles for best response is unknown. For now, treatment is “recommend until either [disease] progression, dose intolerance, or patient or physician preference,” he noted. Venetoclax subjects in his study had a median of four treatment cycles versus two in the placebo group. Combination patients in the azacitidine study had a median of seven cycles versus 4.5 with placebo.
Venetoclax already carries an indication in the United States in combination with azacitidine, decitabine, or LDAC for newly-diagnosed AML in adults 75 years or older or who have comorbidities that preclude use of intensive induction chemotherapy, at a daily dosage of 400 mg with HMAs and 600 mg with LDAC.
Labeling notes that “continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.”
Both venetoclax trials were sponsored by the drug’s maker, AbbVie, which was involved with data interpretation and other matters. Dr. Wei is a consultant for and receives research funding from the company and also receives royalty payments in relation to venetoclax. The commentators did not have any competing financial interests. Disclosures, if any, were not reported for Dr. Juliusson.
SOURCE: Wei AH et al. EHA Congress, Abstract S136.
At about 18 months’ follow-up in treatment naive acute myelogenous leukemia (AML) patients who were 75 years or older or otherwise unfit for intensive chemotherapy, median overall survival (OS) was 8.4 months when they were randomized to low-dose cytarabine (LDAC) plus the BCL-2 inhibitor venetoclax versus 4.1 months with LDAC plus placebo. The results from the phase 3 trial were reported at the virtual annual congress of the European Hematology Association.
The combination also improved rates of remission, event-free survival, and patient reported outcomes and lessened transfusion requirements. Adverse events were manageable.
The findings position venetoclax add-on with LDAC “as a potential new standard of care” for untreated patients ineligible for intensive chemotherapy, lead investigator Andrew Wei, MD, PhD, an AML researcher at Monash University, Melbourne, said at the meeting.
The study addresses a substantial unmet need. The median age at AML diagnosis is over 68 years old and comorbidities such as heart failure and reduced creatinine clearance are common, which make the risk of toxicity with standard chemotherapy too high. Single-agent alternatives are of limited benefit, so Dr. Wei’s group and others are looking for better options to plug the treatment gap when standard chemotherapy is contraindicated.
Several combinations are under investigation, including LDAC plus venetoclax, which appears to have a synergistic effect greater than either agent on its own, Dr. Wei and colleagues explained in their journal report, which was published online to coincide with his presentation (Blood. 2020 Jun 11;135(24):2137-45).
In a commentary, Bob Lowenberg, Ph, a hematologist with the Erasmus University Medical Center in Rotterdam, and Gerwin Huls, MD, PhD, of the University Medical Center Groningen, both in the Netherlands, said the study “represents a valuable although moderate step forward on the way to a better therapeutic future for the ‘unfit’ patient with AML” (Blood. 2020. Jun 11;135(24): 2114-5).
“A challenging AML population”
In the study, 143 patients were randomized to oral venetoclax 600 mg daily and 68 to placebo in 28-day cycles, on a background of LDAC 20 mg/m2 administered subcutaneously on days 1-10 of each cycle.
“This study enrolled a challenging AML population, with nearly 60% age ≥75 years and a high proportion of patients with secondary disease (38%), prior hypomethylating agent (HMA) treatment (20%), poor cytogenetic risk (32%), and TP53 mutations (15%), which are known factors associated with dismal prognosis in AML,” the investigators noted in their report.
There was a numerical benefit in OS at 12 months – the preplanned primary outcome – but it was not statistically significant. At 18 months, however, and after adjustment for a higher rate of secondary AML in the venetoclax arm and other confounders in a post hoc analysis, survival differences reached significance. The 4.3-month OS benefit with the combination translated into a 30% reduction in the risk of death (hazard ratio, 0.70; 95% confidence interval, 0.50-0.99; P = .04)
Survival outcomes “were particularly promising for patient subgroups with NPM1- (median OS, not reached) and IDH1/2-mutant AML (median OS, 19.4 months),” the team noted.
Complete remission (CR) were 48% in the venetoclax arm, compared with 13% in the placebo group, and 34% of venetoclax patients versus 3% of placebo patients went into remission after their first cycle. Venetoclax subjects also had longer median event free survival (4.7 months vs. 2 months); higher rates of red blood cell and platelet transfusion independence (37% vs. 16%); and higher rates of cytometric minimal residual disease levels below 0.1% (6% vs. 1%).
The findings correlated with “strong improvements” in patient-reported outcomes, including fatigue and quality of life, the investigators reported.
Risk mitigation
Grade 3 or higher adverse events (AEs) included febrile neutropenia (32% in the venetoclax arm versus 29% in the placebo group), neutropenia (47% venetoclax vs. 16% placebo), thrombocytopenia (45% vs. 37%), and anemia (25% vs. 22%). The eight cases of tumor lysis syndrome (TLS) were all in the venetoclax arm. Grade 3 or higher bleeding was higher in the venetoclax arm (11% versus 7%), but the incidence of fatal bleeding was similar between the groups (1.4% venetoclax versus 1.5%).
“Although the venetoclax arm showed modest increases in hematologic AEs, the rate of AEs leading to treatment discontinuation (24% vs. 25%) and the rate of serious AEs such as pneumonia” and sepsis “were nearly identical between” the arms, the team said.
The combination “is more myelosuppressive,” but the effects “were mostly mitigated by venetoclax dose interruptions and reductions.” To mitigate the TLS risk, patients were hospitalized for TLS evaluation and prophylaxis during the 4-day venetoclax ramp-up in the first treatment cycle and for 24 hours after the 600-mg target was reached. “I think this is an extremely important measure to avoid this small but important complication,” Dr. Wei said at the meeting.
A moderate step forward
Dr. Lowenberg and Dr. Huls noted in their commentary that, despite the favorable outcomes, “the results are still sobering with a rapid drop of the survival curves to values of [around] 25% or less within 18 months, and event-free survival rates even falling to considerably lower levels.”
Also, there was a “weak correlation between the relatively wide differences in comparative CR/CRi rates and the much smaller differences in survival,” perhaps “due to a limited depth of the complete responses following venetoclax-LDAC therapy or the early development of therapeutic resistance,” they said.
The commentary also noted another option, adding the hedgehog pathway inhibitor glasdegib, instead of venetoclax, to LDAC. It also improved survival in a similar randomized study in unfit AML and high-risk myelodysplastic syndrome patients, from a median survival of 4.9 months with LDAC alone to 8.8 months with the combination (Leukemia. 2019 Feb;33(2):379-389. doi: 10.1038/s41375-018-0312-9).
Dueling regimens
Another alternative approach – venetoclax plus the HMA agent azacitidine – garnered a lot of attention at the meeting when it was reported that the combination had a median overall survival of 14.7 months, versus 9.6 months with azacitidine alone, in patients ineligible for intensive chemotherapy. CR/CRi rates were 66% with the combination, versus 28%.
“It seems like the results were better with the combination of venetoclax and azacitidine” than venetoclax plus LDAC, said Gunnar Juliusson, MD, PhD, of Lund (Sweden) University, who moderated Dr. Wei’s presentation.
He wanted to know if there was a way to identify patients who would do better on one regimen versus the other and was curious about the fact that the azacitidine study used a dose of 400 mg venetoclax, instead of 600 mg.
Dr. Wei noted the high incidence of poor prognostic factors in his study, including prior HMA treatment in 20%, but also that “we don’t know for sure” if there’s a clinically meaningful benefit with the higher dose.
He also said the optimal number of venetoclax cycles for best response is unknown. For now, treatment is “recommend until either [disease] progression, dose intolerance, or patient or physician preference,” he noted. Venetoclax subjects in his study had a median of four treatment cycles versus two in the placebo group. Combination patients in the azacitidine study had a median of seven cycles versus 4.5 with placebo.
Venetoclax already carries an indication in the United States in combination with azacitidine, decitabine, or LDAC for newly-diagnosed AML in adults 75 years or older or who have comorbidities that preclude use of intensive induction chemotherapy, at a daily dosage of 400 mg with HMAs and 600 mg with LDAC.
Labeling notes that “continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.”
Both venetoclax trials were sponsored by the drug’s maker, AbbVie, which was involved with data interpretation and other matters. Dr. Wei is a consultant for and receives research funding from the company and also receives royalty payments in relation to venetoclax. The commentators did not have any competing financial interests. Disclosures, if any, were not reported for Dr. Juliusson.
SOURCE: Wei AH et al. EHA Congress, Abstract S136.
REPORTING FROM EHA CONGRESS
Azacitidine plus enasidenib improves response, but not survival, in mIDH2 AML
Azacitidine plus enasidenib improved complete and overall responses in newly diagnosed acute myelogenous leukemia with isocitrate dehydrogenase 2 gene mutations, compared with azacitidine alone, but it did not improve overall survival in an open-label, phase 2 trial reported at the virtual annual congress of the European Hematology Association.
“Given the very high cost of” enasidenib, and the lack of survival benefit, Gunnar Juliusson, MD, PhD, of Lund University, Sweden, who moderated the study presentation, wondered if it might make more sense to hold enasidenib in reserve until after progression on azacitidine.
“The challenge is going to be exactly” that, “trying to figure out [if] you use both things together” or in sequence. “You can look at it in both ways,” said lead investigator Courtney DiNardo, MD, associate professor in the department of leukemia at the University of Texas MD Anderson Cancer Center, Houston.
“We do know” that with enasidenib monotherapy, there’s “a decrement in the rates of remission and in the duration of response” and overall survival in the salvage setting, so there’s “a clear rationale to give it earlier rather than later,” but “I think this study in some ways provides a few more questions than it really answers,” she said at the meeting.
About 15% of AML patients have leukemogenic isocitrate dehydrogenase 2 (IDH2) mutations; enasidenib, an oral small molecule, inhibits the mutant enzyme. The older AML patients are, the more likely they are to have an IDH2 mutation, so the work “is relevant to our older chemotherapy ineligible population,” Dr. DiNardo said.
The trial was prompted by preclinical indications of synergy with azacitidine; alone, each agent has an overall response rate of about 30% in newly diagnosed AML, and a complete remission (CR) rate of about 20%, she explained.
Her team randomized 68 adults with newly diagnosed AML and an IDH2 mutation to enasidenib 100 mg daily on a 28-day cycle with subcutaneous azacitidine 75 mg/m2 for 7 days during the cycle, and 33 others to just the azacitidine alone.
Their subjects were ineligible for intensive chemotherapy and had intermediate to poor risk cytogenetics. The median age was 75 years, and Eastern Cooperative Oncology Group performance scores were 2 or less.
The overall response rate was 71% with the combination and 42% in the azacitidine alone arm (P = .0064). Fifty-three percent of combination patients, but 12% of azacitidine alone subjects, had complete remissions (P = .0001). The median duration of response with combination therapy was 24.1 months, versus 12.1 months.
Enasidenib plus azacitidine subjects also had greater drops in mutant IDH2 variant allele frequency (median 83.4% versus 17.7%, P < .01) and levels of the downstream oncometabolite 2-hydroxyglutarate (97.8% versus 54.3%; P < .01).
However, median OS was 22 months in both arms (HR 0.99, 95% CI 0.52, 1.87, P = .97). Although median event-free survival favored the combination – 17.2 months versus 10.8 – the results were not statistically significant (HR 0.59, 95% CI 0.30, 1.17, P = .13).
A possible reason for the lack of survival benefit, Dr. DiNardo said, was that seven azacitidine-alone patients (21%) went on to enasidenib after leaving the study, most commonly for disease progression, which occurred in 31% of combination patients versus 52% in the azacitidine-alone arm.
Combination subjects had a median of 10 treatment cycles, vs. 7 in the azacitidine-alone group. Grade 3-4 adverse events included thrombocytopenia (37% combination, 19% azacitidine-alone), neutropenia (35% vs. 22%), anemia (19% vs. 22%), and febrile neutropenia (15% vs. 16%). Grade 3-4 infections were more common with azacitidine monotherapy (31% vs. 18%).
Twelve enasidenib/azacitidine subjects (18%) developed isocitrate dehydrogenase differentiation syndrome, a complication that carries a black box warning in enasidenib’s label.
The work was funded by enasidenib marketer Celgene. Dr. DiNardo is an adviser to, and receives research funding from, the company. Dr. Juliusson’s disclosures, if any, were not reported.
SOURCE: DiNardo CD et al. EHA Congress, abstract S139.
Azacitidine plus enasidenib improved complete and overall responses in newly diagnosed acute myelogenous leukemia with isocitrate dehydrogenase 2 gene mutations, compared with azacitidine alone, but it did not improve overall survival in an open-label, phase 2 trial reported at the virtual annual congress of the European Hematology Association.
“Given the very high cost of” enasidenib, and the lack of survival benefit, Gunnar Juliusson, MD, PhD, of Lund University, Sweden, who moderated the study presentation, wondered if it might make more sense to hold enasidenib in reserve until after progression on azacitidine.
“The challenge is going to be exactly” that, “trying to figure out [if] you use both things together” or in sequence. “You can look at it in both ways,” said lead investigator Courtney DiNardo, MD, associate professor in the department of leukemia at the University of Texas MD Anderson Cancer Center, Houston.
“We do know” that with enasidenib monotherapy, there’s “a decrement in the rates of remission and in the duration of response” and overall survival in the salvage setting, so there’s “a clear rationale to give it earlier rather than later,” but “I think this study in some ways provides a few more questions than it really answers,” she said at the meeting.
About 15% of AML patients have leukemogenic isocitrate dehydrogenase 2 (IDH2) mutations; enasidenib, an oral small molecule, inhibits the mutant enzyme. The older AML patients are, the more likely they are to have an IDH2 mutation, so the work “is relevant to our older chemotherapy ineligible population,” Dr. DiNardo said.
The trial was prompted by preclinical indications of synergy with azacitidine; alone, each agent has an overall response rate of about 30% in newly diagnosed AML, and a complete remission (CR) rate of about 20%, she explained.
Her team randomized 68 adults with newly diagnosed AML and an IDH2 mutation to enasidenib 100 mg daily on a 28-day cycle with subcutaneous azacitidine 75 mg/m2 for 7 days during the cycle, and 33 others to just the azacitidine alone.
Their subjects were ineligible for intensive chemotherapy and had intermediate to poor risk cytogenetics. The median age was 75 years, and Eastern Cooperative Oncology Group performance scores were 2 or less.
The overall response rate was 71% with the combination and 42% in the azacitidine alone arm (P = .0064). Fifty-three percent of combination patients, but 12% of azacitidine alone subjects, had complete remissions (P = .0001). The median duration of response with combination therapy was 24.1 months, versus 12.1 months.
Enasidenib plus azacitidine subjects also had greater drops in mutant IDH2 variant allele frequency (median 83.4% versus 17.7%, P < .01) and levels of the downstream oncometabolite 2-hydroxyglutarate (97.8% versus 54.3%; P < .01).
However, median OS was 22 months in both arms (HR 0.99, 95% CI 0.52, 1.87, P = .97). Although median event-free survival favored the combination – 17.2 months versus 10.8 – the results were not statistically significant (HR 0.59, 95% CI 0.30, 1.17, P = .13).
A possible reason for the lack of survival benefit, Dr. DiNardo said, was that seven azacitidine-alone patients (21%) went on to enasidenib after leaving the study, most commonly for disease progression, which occurred in 31% of combination patients versus 52% in the azacitidine-alone arm.
Combination subjects had a median of 10 treatment cycles, vs. 7 in the azacitidine-alone group. Grade 3-4 adverse events included thrombocytopenia (37% combination, 19% azacitidine-alone), neutropenia (35% vs. 22%), anemia (19% vs. 22%), and febrile neutropenia (15% vs. 16%). Grade 3-4 infections were more common with azacitidine monotherapy (31% vs. 18%).
Twelve enasidenib/azacitidine subjects (18%) developed isocitrate dehydrogenase differentiation syndrome, a complication that carries a black box warning in enasidenib’s label.
The work was funded by enasidenib marketer Celgene. Dr. DiNardo is an adviser to, and receives research funding from, the company. Dr. Juliusson’s disclosures, if any, were not reported.
SOURCE: DiNardo CD et al. EHA Congress, abstract S139.
Azacitidine plus enasidenib improved complete and overall responses in newly diagnosed acute myelogenous leukemia with isocitrate dehydrogenase 2 gene mutations, compared with azacitidine alone, but it did not improve overall survival in an open-label, phase 2 trial reported at the virtual annual congress of the European Hematology Association.
“Given the very high cost of” enasidenib, and the lack of survival benefit, Gunnar Juliusson, MD, PhD, of Lund University, Sweden, who moderated the study presentation, wondered if it might make more sense to hold enasidenib in reserve until after progression on azacitidine.
“The challenge is going to be exactly” that, “trying to figure out [if] you use both things together” or in sequence. “You can look at it in both ways,” said lead investigator Courtney DiNardo, MD, associate professor in the department of leukemia at the University of Texas MD Anderson Cancer Center, Houston.
“We do know” that with enasidenib monotherapy, there’s “a decrement in the rates of remission and in the duration of response” and overall survival in the salvage setting, so there’s “a clear rationale to give it earlier rather than later,” but “I think this study in some ways provides a few more questions than it really answers,” she said at the meeting.
About 15% of AML patients have leukemogenic isocitrate dehydrogenase 2 (IDH2) mutations; enasidenib, an oral small molecule, inhibits the mutant enzyme. The older AML patients are, the more likely they are to have an IDH2 mutation, so the work “is relevant to our older chemotherapy ineligible population,” Dr. DiNardo said.
The trial was prompted by preclinical indications of synergy with azacitidine; alone, each agent has an overall response rate of about 30% in newly diagnosed AML, and a complete remission (CR) rate of about 20%, she explained.
Her team randomized 68 adults with newly diagnosed AML and an IDH2 mutation to enasidenib 100 mg daily on a 28-day cycle with subcutaneous azacitidine 75 mg/m2 for 7 days during the cycle, and 33 others to just the azacitidine alone.
Their subjects were ineligible for intensive chemotherapy and had intermediate to poor risk cytogenetics. The median age was 75 years, and Eastern Cooperative Oncology Group performance scores were 2 or less.
The overall response rate was 71% with the combination and 42% in the azacitidine alone arm (P = .0064). Fifty-three percent of combination patients, but 12% of azacitidine alone subjects, had complete remissions (P = .0001). The median duration of response with combination therapy was 24.1 months, versus 12.1 months.
Enasidenib plus azacitidine subjects also had greater drops in mutant IDH2 variant allele frequency (median 83.4% versus 17.7%, P < .01) and levels of the downstream oncometabolite 2-hydroxyglutarate (97.8% versus 54.3%; P < .01).
However, median OS was 22 months in both arms (HR 0.99, 95% CI 0.52, 1.87, P = .97). Although median event-free survival favored the combination – 17.2 months versus 10.8 – the results were not statistically significant (HR 0.59, 95% CI 0.30, 1.17, P = .13).
A possible reason for the lack of survival benefit, Dr. DiNardo said, was that seven azacitidine-alone patients (21%) went on to enasidenib after leaving the study, most commonly for disease progression, which occurred in 31% of combination patients versus 52% in the azacitidine-alone arm.
Combination subjects had a median of 10 treatment cycles, vs. 7 in the azacitidine-alone group. Grade 3-4 adverse events included thrombocytopenia (37% combination, 19% azacitidine-alone), neutropenia (35% vs. 22%), anemia (19% vs. 22%), and febrile neutropenia (15% vs. 16%). Grade 3-4 infections were more common with azacitidine monotherapy (31% vs. 18%).
Twelve enasidenib/azacitidine subjects (18%) developed isocitrate dehydrogenase differentiation syndrome, a complication that carries a black box warning in enasidenib’s label.
The work was funded by enasidenib marketer Celgene. Dr. DiNardo is an adviser to, and receives research funding from, the company. Dr. Juliusson’s disclosures, if any, were not reported.
SOURCE: DiNardo CD et al. EHA Congress, abstract S139.
FROM EHA CONGRESS
First-in-kind anti-CD47 antibody shows promise for MDS and AML treatment
Magrolimab plus azacitidine (AZA) improved outcomes in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) patients according to the results of a phase 1b study (NCT03248479) presented at the virtual ASCO meeting. The combo especially was promising for the underserved patient population that have the TP53 (p53) mutation.
Magrolimab is a first-in-kind IgG anti-CD47 monoclonal antibody that promotes the elimination of tumor cells through macrophage phagocytosis. CD47 is a “do not eat me” signal on cancer cells that allows the cells to evade macrophages. Its increased expression is predictive of a worse outcome in AML patients, according to David A. Sallman, MD, of the Moffitt Cancer Center, Tampa, Fla., and colleagues.
Dr. Sallman presented the results of a study examining whether magrolimab would provide a synergistic benefit when combined with AZA (which induces other prophagocytic “eat me” signals such as calreticulin on cancer cells). The primary objectives of the study were to examine the safety of magrolimab alone or with AZA, and to assess the efficacy of the magrolimab/AZA combo in 29 untreated AML patients and 39 untreated MDS patients. The majority of both the MDS and AML patients were poor cytogenetic risk at 64% and 72%, respectively. Mutant p53 was present in 13% of the MDS patients and 45% of the AML patients.
No deaths occurred in the first 60 days of the study among either the MDS or AML patients and discontinuation of treatment because of drug-related adverse events was seen in only one of the patients (1.5%) treated with magrolimab/AZA. There was no significant neutropenia or thrombocytopenia caused by the therapy seen, and the majority of the patients improved their neutrophil and platelet counts while on therapy.
Anemia from CD47 blockade was mitigated by the use of a priming dose of magrolimab coupled to a maintenance-dose regimen, resulting in a mild hemoglobin drop on the first dose, which returned to baseline with a majority of patients experiencing significant hemoglobin improvement and a decrease in transfusion frequency over time, according to Dr. Sallman and his colleagues.
The results showed that magrolimab/AZA induced a 91% overall response rate (ORR), with a 42% complete remission (CR) that increased to 56% at 6 months, in the MDS patients. AML patients experienced a 64% ORR (56% CR/CRi [CR with incomplete hematological remission]). These results compare favorably with the CR rate of 6%-17% rate seen for AZA monotherapy, according to Dr. Sallman.
Red blood cell transfusion independence was achieved in 58% of the MDS patients and 64% of the AML patients, and a complete cytogenetic response was seen in 35% and 50% of the MDS and AML patients, respectively.
The combined treatment was especially effective in the patients with p53 mutations, with an overall response rate of 75% for both MDS and AML, and a complete response of 42% and 50%, respectively. During the reported time of the study, the median survival was not reached, which compares favorably with current therapies, according to Dr. Sallman.
“Specifically looking at a very-high-risk p53-mutant subset, complete remissions have been observed in the majority of patients. And again, these have been durable. Based on all of these data, expansion cohorts both in MDS and p53 and AML continue to accrue with registrational studies in progress for MDS and planned for p53-mutant AML,” Dr. Sallman concluded.
The trial was sponsored by Gilead Sciences, and funding was obtained from the California Institute for Regenerative Medicine. Dr. Sallman disclosed that he received research funding from Celgene and has acted in a consulting or advisory role for Agios, argenx, and Celyad. He was also on the speaker’s bureau for a variety of pharmaceutical/biotech companies.
SOURCE: Sallman DA et al. ASCO 2020, Abstract 7507.
Magrolimab plus azacitidine (AZA) improved outcomes in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) patients according to the results of a phase 1b study (NCT03248479) presented at the virtual ASCO meeting. The combo especially was promising for the underserved patient population that have the TP53 (p53) mutation.
Magrolimab is a first-in-kind IgG anti-CD47 monoclonal antibody that promotes the elimination of tumor cells through macrophage phagocytosis. CD47 is a “do not eat me” signal on cancer cells that allows the cells to evade macrophages. Its increased expression is predictive of a worse outcome in AML patients, according to David A. Sallman, MD, of the Moffitt Cancer Center, Tampa, Fla., and colleagues.
Dr. Sallman presented the results of a study examining whether magrolimab would provide a synergistic benefit when combined with AZA (which induces other prophagocytic “eat me” signals such as calreticulin on cancer cells). The primary objectives of the study were to examine the safety of magrolimab alone or with AZA, and to assess the efficacy of the magrolimab/AZA combo in 29 untreated AML patients and 39 untreated MDS patients. The majority of both the MDS and AML patients were poor cytogenetic risk at 64% and 72%, respectively. Mutant p53 was present in 13% of the MDS patients and 45% of the AML patients.
No deaths occurred in the first 60 days of the study among either the MDS or AML patients and discontinuation of treatment because of drug-related adverse events was seen in only one of the patients (1.5%) treated with magrolimab/AZA. There was no significant neutropenia or thrombocytopenia caused by the therapy seen, and the majority of the patients improved their neutrophil and platelet counts while on therapy.
Anemia from CD47 blockade was mitigated by the use of a priming dose of magrolimab coupled to a maintenance-dose regimen, resulting in a mild hemoglobin drop on the first dose, which returned to baseline with a majority of patients experiencing significant hemoglobin improvement and a decrease in transfusion frequency over time, according to Dr. Sallman and his colleagues.
The results showed that magrolimab/AZA induced a 91% overall response rate (ORR), with a 42% complete remission (CR) that increased to 56% at 6 months, in the MDS patients. AML patients experienced a 64% ORR (56% CR/CRi [CR with incomplete hematological remission]). These results compare favorably with the CR rate of 6%-17% rate seen for AZA monotherapy, according to Dr. Sallman.
Red blood cell transfusion independence was achieved in 58% of the MDS patients and 64% of the AML patients, and a complete cytogenetic response was seen in 35% and 50% of the MDS and AML patients, respectively.
The combined treatment was especially effective in the patients with p53 mutations, with an overall response rate of 75% for both MDS and AML, and a complete response of 42% and 50%, respectively. During the reported time of the study, the median survival was not reached, which compares favorably with current therapies, according to Dr. Sallman.
“Specifically looking at a very-high-risk p53-mutant subset, complete remissions have been observed in the majority of patients. And again, these have been durable. Based on all of these data, expansion cohorts both in MDS and p53 and AML continue to accrue with registrational studies in progress for MDS and planned for p53-mutant AML,” Dr. Sallman concluded.
The trial was sponsored by Gilead Sciences, and funding was obtained from the California Institute for Regenerative Medicine. Dr. Sallman disclosed that he received research funding from Celgene and has acted in a consulting or advisory role for Agios, argenx, and Celyad. He was also on the speaker’s bureau for a variety of pharmaceutical/biotech companies.
SOURCE: Sallman DA et al. ASCO 2020, Abstract 7507.
Magrolimab plus azacitidine (AZA) improved outcomes in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) patients according to the results of a phase 1b study (NCT03248479) presented at the virtual ASCO meeting. The combo especially was promising for the underserved patient population that have the TP53 (p53) mutation.
Magrolimab is a first-in-kind IgG anti-CD47 monoclonal antibody that promotes the elimination of tumor cells through macrophage phagocytosis. CD47 is a “do not eat me” signal on cancer cells that allows the cells to evade macrophages. Its increased expression is predictive of a worse outcome in AML patients, according to David A. Sallman, MD, of the Moffitt Cancer Center, Tampa, Fla., and colleagues.
Dr. Sallman presented the results of a study examining whether magrolimab would provide a synergistic benefit when combined with AZA (which induces other prophagocytic “eat me” signals such as calreticulin on cancer cells). The primary objectives of the study were to examine the safety of magrolimab alone or with AZA, and to assess the efficacy of the magrolimab/AZA combo in 29 untreated AML patients and 39 untreated MDS patients. The majority of both the MDS and AML patients were poor cytogenetic risk at 64% and 72%, respectively. Mutant p53 was present in 13% of the MDS patients and 45% of the AML patients.
No deaths occurred in the first 60 days of the study among either the MDS or AML patients and discontinuation of treatment because of drug-related adverse events was seen in only one of the patients (1.5%) treated with magrolimab/AZA. There was no significant neutropenia or thrombocytopenia caused by the therapy seen, and the majority of the patients improved their neutrophil and platelet counts while on therapy.
Anemia from CD47 blockade was mitigated by the use of a priming dose of magrolimab coupled to a maintenance-dose regimen, resulting in a mild hemoglobin drop on the first dose, which returned to baseline with a majority of patients experiencing significant hemoglobin improvement and a decrease in transfusion frequency over time, according to Dr. Sallman and his colleagues.
The results showed that magrolimab/AZA induced a 91% overall response rate (ORR), with a 42% complete remission (CR) that increased to 56% at 6 months, in the MDS patients. AML patients experienced a 64% ORR (56% CR/CRi [CR with incomplete hematological remission]). These results compare favorably with the CR rate of 6%-17% rate seen for AZA monotherapy, according to Dr. Sallman.
Red blood cell transfusion independence was achieved in 58% of the MDS patients and 64% of the AML patients, and a complete cytogenetic response was seen in 35% and 50% of the MDS and AML patients, respectively.
The combined treatment was especially effective in the patients with p53 mutations, with an overall response rate of 75% for both MDS and AML, and a complete response of 42% and 50%, respectively. During the reported time of the study, the median survival was not reached, which compares favorably with current therapies, according to Dr. Sallman.
“Specifically looking at a very-high-risk p53-mutant subset, complete remissions have been observed in the majority of patients. And again, these have been durable. Based on all of these data, expansion cohorts both in MDS and p53 and AML continue to accrue with registrational studies in progress for MDS and planned for p53-mutant AML,” Dr. Sallman concluded.
The trial was sponsored by Gilead Sciences, and funding was obtained from the California Institute for Regenerative Medicine. Dr. Sallman disclosed that he received research funding from Celgene and has acted in a consulting or advisory role for Agios, argenx, and Celyad. He was also on the speaker’s bureau for a variety of pharmaceutical/biotech companies.
SOURCE: Sallman DA et al. ASCO 2020, Abstract 7507.
FROM ASCO 2020
New EPOCH for adult patients with Burkitt lymphoma
Adult patients with Burkitt lymphoma can achieve equally sound survival outcomes with dose-adjusted chemotherapy versus high-intensity regimens, but can do so while avoiding the severe toxicities, U.S. study data shows.
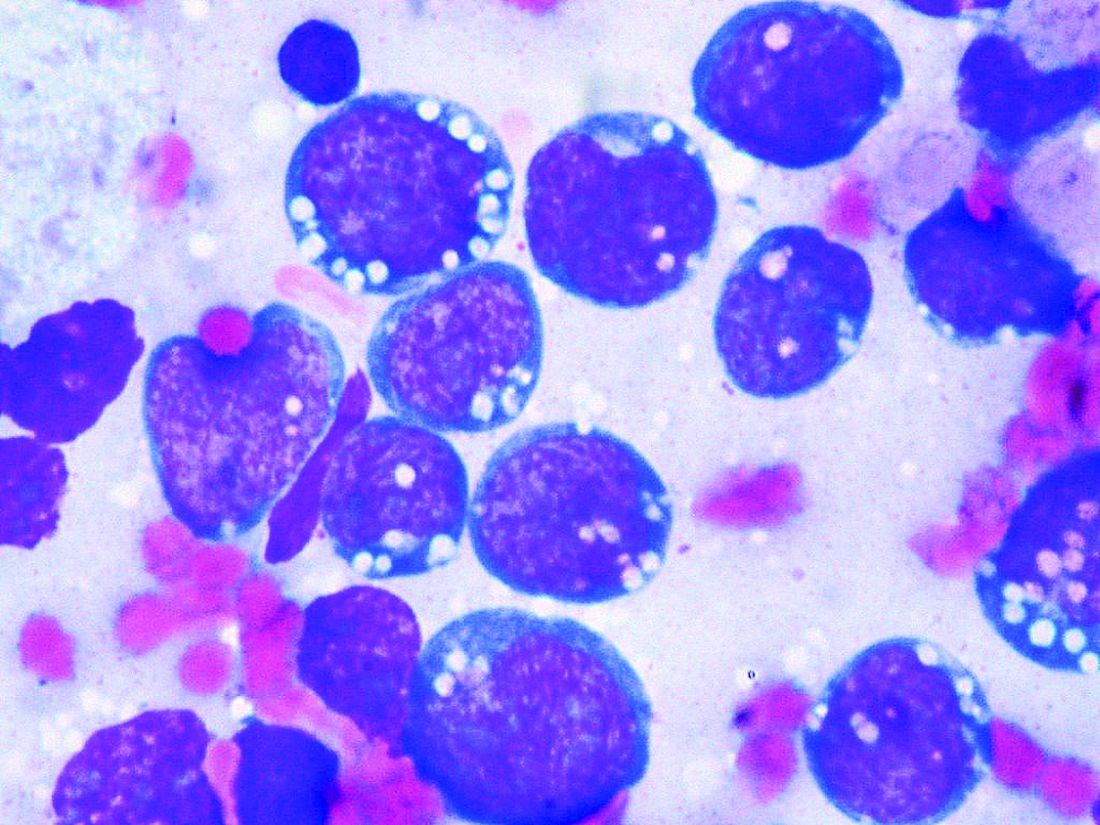
Although Burkitt lymphoma is the most common B-cell non-Hodgkin lymphoma in children, it accounts for only 1% to 2% of adult lymphoma cases.
Highly dose-intensive chemotherapy regimens, developed for children and young adults, have rendered the disease curable. But older patients in particular, and patients with comorbidities such as HIV, can suffer severe adverse effects, as well as late sequelae like second malignancies.
Mark Roschewski, MD, from the lymphoid malignancies branch at the National Cancer Institute in Bethesda, Md., and colleagues therefore examined whether a dose-adjusted regimen would maintain outcomes while reducing toxicities.
Tailoring treatment with etoposide, doxorubicin, and vincristine with prednisone, cyclophosphamide, and rituximab (EPOCH-R) to whether patients had high- or low-risk disease, they achieved 4-year survival rates of higher than 85%.
The research, published by the Journal of Clinical Oncology, also showed that patients taking the regimen, which was well tolerated, had low rates of relapse in the central nervous system.
The team reports that their results with the dose-adjusted regimen “significantly improve on the complexity, cost, and toxicity profile of other regimens,” also highlighting that it is administered on an outpatient basis.
As the outcomes also “compare favorably” with those with high intensity regimens, they say the findings “support our treatment strategies to ameliorate toxicity while maintaining efficacy.”
Importantly, they suggest highly dose-intensive chemotherapy is unnecessary for cure, and carefully defined low-risk patients may be treated with limited chemotherapy.
Dr. Roschewski said in an interview that, in patients aged 40 years and older, dose-adjusted EPOCH-R is “probably the preferred choice,” despite its “weakness” in controlling the disease in patients with active CNS involvement.
However, the “real question” is what to use in younger patients, Dr. Roschewski said, as the “unknown” is whether the additional magnitude of a high-intensity regimen that “gets into the CNS” outweighs the risk of toxicities.
“What was important about our study,” he said, was that patients with CNS involvement “did the worst but it was equally split among patients that died of toxicity and patients that progressed.”
In other words, each choice increases one risk while decreasing another. “So I would have to have that discussion with the patient, and individual patient decisions are typically based on the details,” said Dr. Roschewski.
One issue, however, that could limit the adoption of dose-adjusted EPOCH-R is that, without a randomized study comparing it directly with a high-intensity regimen, clinicians may to stick to what they know.
Dr. Roschewski said that “this is particularly true of more experienced clinicians.”
“They’re less likely, I think, to adopt something else outside of a randomized study because our natural inclination with this disease has always been dose intensity is critical. ... This is a dogma, and to shift from that probably does require a higher level of evidence, at least for some practitioners,” he explained.
Further study details
Following a pilot study of dose-adjusted EPOCH-R in 30 adult patients in which the authors say the regimen showed “high efficacy,” they enrolled 113 patients with untreated Burkitt lymphoma at 22 centers between June 2010 and May 2017.
The patients were divided into low-risk and high-risk categories, with low-risk defined as stage 1 or 2 disease, normal lactate dehydrogenase levels, ECOG performance status ≤ 1, and no tumor mass ≥ 7 cm.
High-risk patients were given six cycles of dose-adjusted EPOCH-R (with rituximab on day 1 only) along with CNS prophylaxis or active therapy with intrathecal methotrexate.
In contrast, low-risk patients were given two cycles of dose-adjusted EPOCH-R, with rituximab on days 1 and 5, followed by positron emission tomography.
If that was negative, the patients had one additional treatment cycle and no CNS prophylaxis, but if it was positive, they were given four additional cycles, plus intrathecal methotrexate.
Of the 113 patients enrolled, 79% were male, median age was 49 years, and 62% were aged at least 40 years, including 26% aged at least 60 years.
The team determined that 13% of the patients were of low risk, 87% were high risk, and 11% had cerebrospinal fluid involvement. One-quarter (24.7%) were HIV positive, with a median CD4+ T-cell count of 268 cells/mm3.
The majority (87%) of low-risk patients received three treatment cycles, and 82% of high-risk patents were administered six treatment cycles.
Over a median follow-up of 58.7 months (4.9 years), the 4-year event-free survival (EFS) rate across the whole cohort was 84.5% and overall survival was 87%.
At the time of analysis, all low-risk patients were in remission; among high-risk patients, the 4-year EFS was 82.1% and overall survival was 84.9%.
The team reports that treatment was equally effective across age groups, and irrespective of HIV status and International Prognostic Index risk group.
Only 2% of high-risk patients with no pretreatment evidence of CNS involvement had relapses in the brain parenchyma. Just over half (55%) of patients with cerebrospinal fluid involvement at presentation experienced disease progression or died.
Five patients died of treatment-related toxicity. Grade 3/4 thrombocytopenia occurred during 17% of cycles, and febrile neutropenia was seen during 16%. Tumor lysis syndrome was rare, occurring in 5% of patients.
Next, the researchers are planning on focusing on CNS disease, looking at EPOCH-R as the backbone and adding intrathecal methotrexate and an additional targeted agent with known CNS penetration.
Dr. Roschewski said that is “a very attractive strategy and ... we will initiate enrollment in that study probably in the next couple of months here at the NCI,” he added, noting that it will be an early phase 1 study.
Another issue he identified that “doesn’t get spoken about quite as much but I do think is important is potentially working on supportive care guidelines for how we manage these patients.” Dr. Roschewski explained, “One of the things you see over and over in these Burkitt lymphoma studies is that some patients don’t make it through therapy because they’re so sick at the beginning, and they have certain risks.
“I think simply improving that type of care, independent of what regimen is used, can potentially improve the outcomes across patient groups.”
The study was funded by the National Cancer Institute, National Institutes of Health, AIDS Malignancy Consortium, and the Cancer Therapy Evaluation Program and Lymphoid Malignancies Branch. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Adult patients with Burkitt lymphoma can achieve equally sound survival outcomes with dose-adjusted chemotherapy versus high-intensity regimens, but can do so while avoiding the severe toxicities, U.S. study data shows.
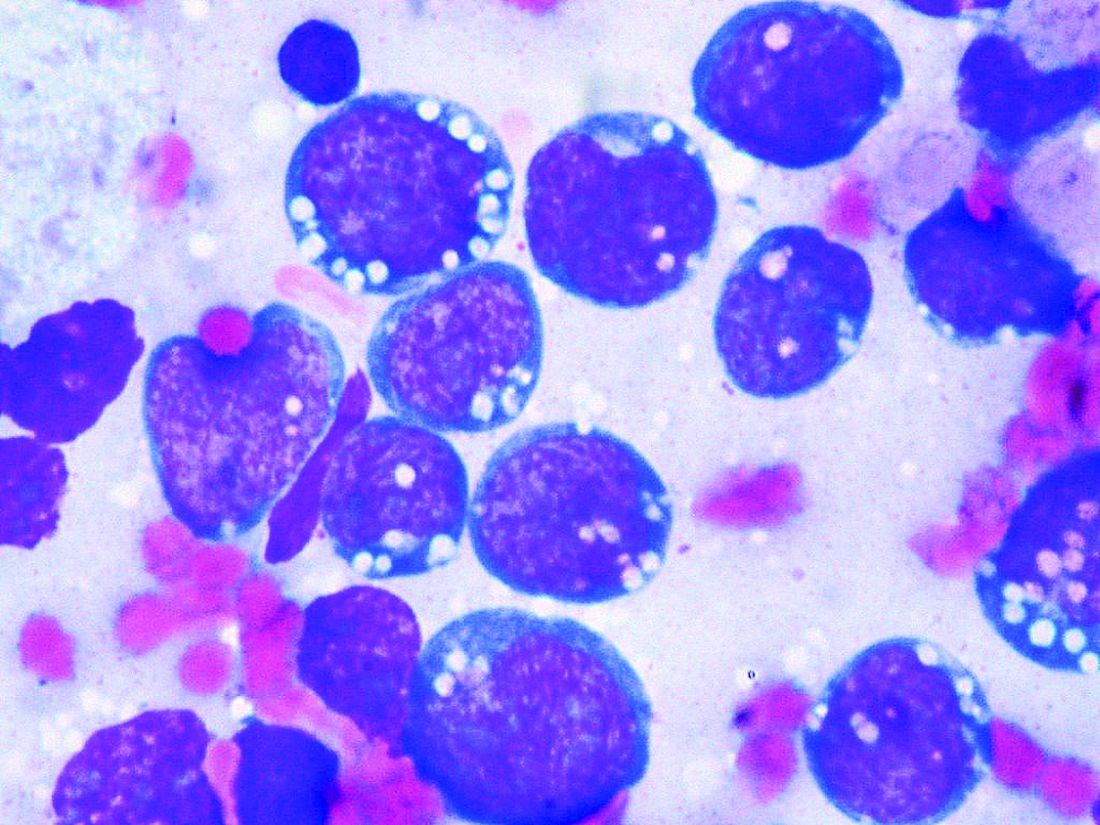
Although Burkitt lymphoma is the most common B-cell non-Hodgkin lymphoma in children, it accounts for only 1% to 2% of adult lymphoma cases.
Highly dose-intensive chemotherapy regimens, developed for children and young adults, have rendered the disease curable. But older patients in particular, and patients with comorbidities such as HIV, can suffer severe adverse effects, as well as late sequelae like second malignancies.
Mark Roschewski, MD, from the lymphoid malignancies branch at the National Cancer Institute in Bethesda, Md., and colleagues therefore examined whether a dose-adjusted regimen would maintain outcomes while reducing toxicities.
Tailoring treatment with etoposide, doxorubicin, and vincristine with prednisone, cyclophosphamide, and rituximab (EPOCH-R) to whether patients had high- or low-risk disease, they achieved 4-year survival rates of higher than 85%.
The research, published by the Journal of Clinical Oncology, also showed that patients taking the regimen, which was well tolerated, had low rates of relapse in the central nervous system.
The team reports that their results with the dose-adjusted regimen “significantly improve on the complexity, cost, and toxicity profile of other regimens,” also highlighting that it is administered on an outpatient basis.
As the outcomes also “compare favorably” with those with high intensity regimens, they say the findings “support our treatment strategies to ameliorate toxicity while maintaining efficacy.”
Importantly, they suggest highly dose-intensive chemotherapy is unnecessary for cure, and carefully defined low-risk patients may be treated with limited chemotherapy.
Dr. Roschewski said in an interview that, in patients aged 40 years and older, dose-adjusted EPOCH-R is “probably the preferred choice,” despite its “weakness” in controlling the disease in patients with active CNS involvement.
However, the “real question” is what to use in younger patients, Dr. Roschewski said, as the “unknown” is whether the additional magnitude of a high-intensity regimen that “gets into the CNS” outweighs the risk of toxicities.
“What was important about our study,” he said, was that patients with CNS involvement “did the worst but it was equally split among patients that died of toxicity and patients that progressed.”
In other words, each choice increases one risk while decreasing another. “So I would have to have that discussion with the patient, and individual patient decisions are typically based on the details,” said Dr. Roschewski.
One issue, however, that could limit the adoption of dose-adjusted EPOCH-R is that, without a randomized study comparing it directly with a high-intensity regimen, clinicians may to stick to what they know.
Dr. Roschewski said that “this is particularly true of more experienced clinicians.”
“They’re less likely, I think, to adopt something else outside of a randomized study because our natural inclination with this disease has always been dose intensity is critical. ... This is a dogma, and to shift from that probably does require a higher level of evidence, at least for some practitioners,” he explained.
Further study details
Following a pilot study of dose-adjusted EPOCH-R in 30 adult patients in which the authors say the regimen showed “high efficacy,” they enrolled 113 patients with untreated Burkitt lymphoma at 22 centers between June 2010 and May 2017.
The patients were divided into low-risk and high-risk categories, with low-risk defined as stage 1 or 2 disease, normal lactate dehydrogenase levels, ECOG performance status ≤ 1, and no tumor mass ≥ 7 cm.
High-risk patients were given six cycles of dose-adjusted EPOCH-R (with rituximab on day 1 only) along with CNS prophylaxis or active therapy with intrathecal methotrexate.
In contrast, low-risk patients were given two cycles of dose-adjusted EPOCH-R, with rituximab on days 1 and 5, followed by positron emission tomography.
If that was negative, the patients had one additional treatment cycle and no CNS prophylaxis, but if it was positive, they were given four additional cycles, plus intrathecal methotrexate.
Of the 113 patients enrolled, 79% were male, median age was 49 years, and 62% were aged at least 40 years, including 26% aged at least 60 years.
The team determined that 13% of the patients were of low risk, 87% were high risk, and 11% had cerebrospinal fluid involvement. One-quarter (24.7%) were HIV positive, with a median CD4+ T-cell count of 268 cells/mm3.
The majority (87%) of low-risk patients received three treatment cycles, and 82% of high-risk patents were administered six treatment cycles.
Over a median follow-up of 58.7 months (4.9 years), the 4-year event-free survival (EFS) rate across the whole cohort was 84.5% and overall survival was 87%.
At the time of analysis, all low-risk patients were in remission; among high-risk patients, the 4-year EFS was 82.1% and overall survival was 84.9%.
The team reports that treatment was equally effective across age groups, and irrespective of HIV status and International Prognostic Index risk group.
Only 2% of high-risk patients with no pretreatment evidence of CNS involvement had relapses in the brain parenchyma. Just over half (55%) of patients with cerebrospinal fluid involvement at presentation experienced disease progression or died.
Five patients died of treatment-related toxicity. Grade 3/4 thrombocytopenia occurred during 17% of cycles, and febrile neutropenia was seen during 16%. Tumor lysis syndrome was rare, occurring in 5% of patients.
Next, the researchers are planning on focusing on CNS disease, looking at EPOCH-R as the backbone and adding intrathecal methotrexate and an additional targeted agent with known CNS penetration.
Dr. Roschewski said that is “a very attractive strategy and ... we will initiate enrollment in that study probably in the next couple of months here at the NCI,” he added, noting that it will be an early phase 1 study.
Another issue he identified that “doesn’t get spoken about quite as much but I do think is important is potentially working on supportive care guidelines for how we manage these patients.” Dr. Roschewski explained, “One of the things you see over and over in these Burkitt lymphoma studies is that some patients don’t make it through therapy because they’re so sick at the beginning, and they have certain risks.
“I think simply improving that type of care, independent of what regimen is used, can potentially improve the outcomes across patient groups.”
The study was funded by the National Cancer Institute, National Institutes of Health, AIDS Malignancy Consortium, and the Cancer Therapy Evaluation Program and Lymphoid Malignancies Branch. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Adult patients with Burkitt lymphoma can achieve equally sound survival outcomes with dose-adjusted chemotherapy versus high-intensity regimens, but can do so while avoiding the severe toxicities, U.S. study data shows.
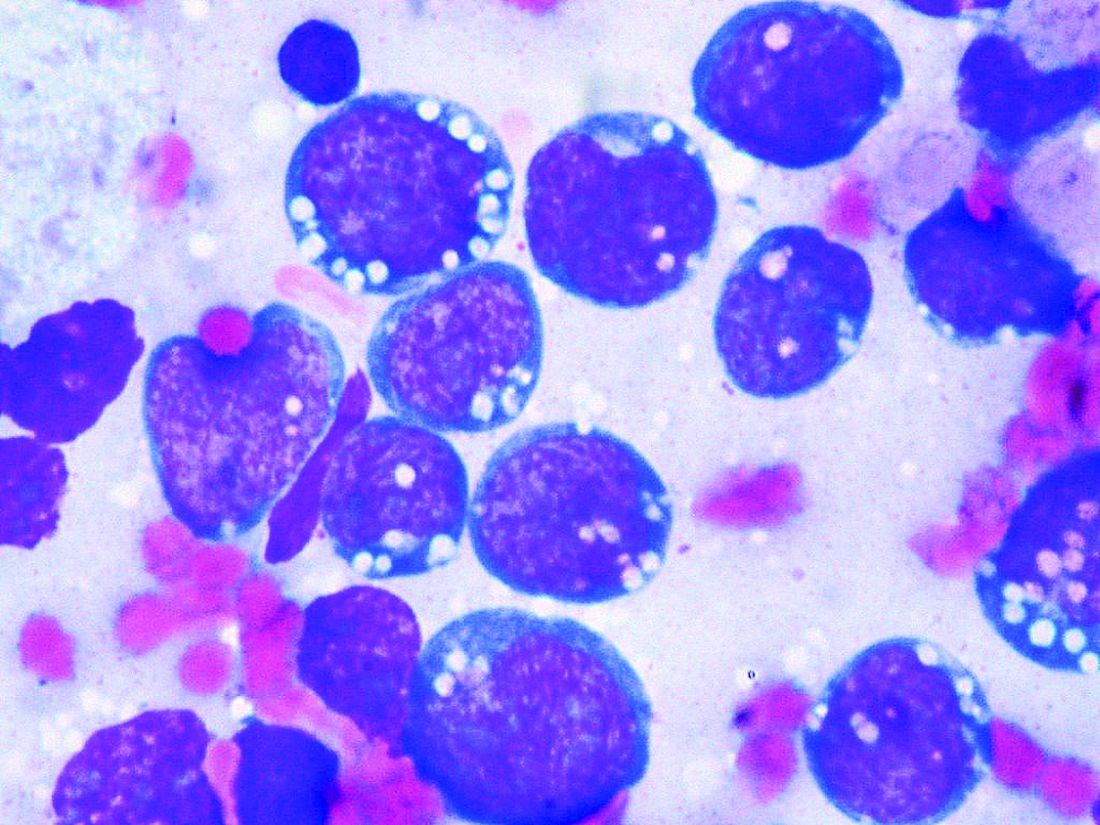
Although Burkitt lymphoma is the most common B-cell non-Hodgkin lymphoma in children, it accounts for only 1% to 2% of adult lymphoma cases.
Highly dose-intensive chemotherapy regimens, developed for children and young adults, have rendered the disease curable. But older patients in particular, and patients with comorbidities such as HIV, can suffer severe adverse effects, as well as late sequelae like second malignancies.
Mark Roschewski, MD, from the lymphoid malignancies branch at the National Cancer Institute in Bethesda, Md., and colleagues therefore examined whether a dose-adjusted regimen would maintain outcomes while reducing toxicities.
Tailoring treatment with etoposide, doxorubicin, and vincristine with prednisone, cyclophosphamide, and rituximab (EPOCH-R) to whether patients had high- or low-risk disease, they achieved 4-year survival rates of higher than 85%.
The research, published by the Journal of Clinical Oncology, also showed that patients taking the regimen, which was well tolerated, had low rates of relapse in the central nervous system.
The team reports that their results with the dose-adjusted regimen “significantly improve on the complexity, cost, and toxicity profile of other regimens,” also highlighting that it is administered on an outpatient basis.
As the outcomes also “compare favorably” with those with high intensity regimens, they say the findings “support our treatment strategies to ameliorate toxicity while maintaining efficacy.”
Importantly, they suggest highly dose-intensive chemotherapy is unnecessary for cure, and carefully defined low-risk patients may be treated with limited chemotherapy.
Dr. Roschewski said in an interview that, in patients aged 40 years and older, dose-adjusted EPOCH-R is “probably the preferred choice,” despite its “weakness” in controlling the disease in patients with active CNS involvement.
However, the “real question” is what to use in younger patients, Dr. Roschewski said, as the “unknown” is whether the additional magnitude of a high-intensity regimen that “gets into the CNS” outweighs the risk of toxicities.
“What was important about our study,” he said, was that patients with CNS involvement “did the worst but it was equally split among patients that died of toxicity and patients that progressed.”
In other words, each choice increases one risk while decreasing another. “So I would have to have that discussion with the patient, and individual patient decisions are typically based on the details,” said Dr. Roschewski.
One issue, however, that could limit the adoption of dose-adjusted EPOCH-R is that, without a randomized study comparing it directly with a high-intensity regimen, clinicians may to stick to what they know.
Dr. Roschewski said that “this is particularly true of more experienced clinicians.”
“They’re less likely, I think, to adopt something else outside of a randomized study because our natural inclination with this disease has always been dose intensity is critical. ... This is a dogma, and to shift from that probably does require a higher level of evidence, at least for some practitioners,” he explained.
Further study details
Following a pilot study of dose-adjusted EPOCH-R in 30 adult patients in which the authors say the regimen showed “high efficacy,” they enrolled 113 patients with untreated Burkitt lymphoma at 22 centers between June 2010 and May 2017.
The patients were divided into low-risk and high-risk categories, with low-risk defined as stage 1 or 2 disease, normal lactate dehydrogenase levels, ECOG performance status ≤ 1, and no tumor mass ≥ 7 cm.
High-risk patients were given six cycles of dose-adjusted EPOCH-R (with rituximab on day 1 only) along with CNS prophylaxis or active therapy with intrathecal methotrexate.
In contrast, low-risk patients were given two cycles of dose-adjusted EPOCH-R, with rituximab on days 1 and 5, followed by positron emission tomography.
If that was negative, the patients had one additional treatment cycle and no CNS prophylaxis, but if it was positive, they were given four additional cycles, plus intrathecal methotrexate.
Of the 113 patients enrolled, 79% were male, median age was 49 years, and 62% were aged at least 40 years, including 26% aged at least 60 years.
The team determined that 13% of the patients were of low risk, 87% were high risk, and 11% had cerebrospinal fluid involvement. One-quarter (24.7%) were HIV positive, with a median CD4+ T-cell count of 268 cells/mm3.
The majority (87%) of low-risk patients received three treatment cycles, and 82% of high-risk patents were administered six treatment cycles.
Over a median follow-up of 58.7 months (4.9 years), the 4-year event-free survival (EFS) rate across the whole cohort was 84.5% and overall survival was 87%.
At the time of analysis, all low-risk patients were in remission; among high-risk patients, the 4-year EFS was 82.1% and overall survival was 84.9%.
The team reports that treatment was equally effective across age groups, and irrespective of HIV status and International Prognostic Index risk group.
Only 2% of high-risk patients with no pretreatment evidence of CNS involvement had relapses in the brain parenchyma. Just over half (55%) of patients with cerebrospinal fluid involvement at presentation experienced disease progression or died.
Five patients died of treatment-related toxicity. Grade 3/4 thrombocytopenia occurred during 17% of cycles, and febrile neutropenia was seen during 16%. Tumor lysis syndrome was rare, occurring in 5% of patients.
Next, the researchers are planning on focusing on CNS disease, looking at EPOCH-R as the backbone and adding intrathecal methotrexate and an additional targeted agent with known CNS penetration.
Dr. Roschewski said that is “a very attractive strategy and ... we will initiate enrollment in that study probably in the next couple of months here at the NCI,” he added, noting that it will be an early phase 1 study.
Another issue he identified that “doesn’t get spoken about quite as much but I do think is important is potentially working on supportive care guidelines for how we manage these patients.” Dr. Roschewski explained, “One of the things you see over and over in these Burkitt lymphoma studies is that some patients don’t make it through therapy because they’re so sick at the beginning, and they have certain risks.
“I think simply improving that type of care, independent of what regimen is used, can potentially improve the outcomes across patient groups.”
The study was funded by the National Cancer Institute, National Institutes of Health, AIDS Malignancy Consortium, and the Cancer Therapy Evaluation Program and Lymphoid Malignancies Branch. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.



