User login
A Candida Glabrata-Associated Prosthetic Joint Infection: Case Report and Literature Review
A Candida Glabrata-Associated Prosthetic Joint Infection: Case Report and Literature Review
Prosthetic joint infection (PJI) occurs in about 1% to 2% of joint replacements. 1 Risk factors include immunosuppression, diabetes, chronic illnesses, and prolonged operative time.2 Bacterial infections constitute most of these infections, while fungal pathogens account for about 1%. Candida (C.) species, predominantly C. albicans, are responsible for most PJIs.1,3 In contrast, C. glabrata is a rare cause of fungal PJI, with only 18 PJI cases currently reported in the literature.4 C. glabrata PJI occurs more frequently among immunosuppressed patients and is associated with a higher treatment failure rate despite antifungal therapy.5 Treatment of fungal PJI is often complicated, involving multiple surgical debridements, prolonged antifungal therapy, and in some cases, prosthesis removal.6 However, given the rarity of C. glabrata as a PJI pathogen, no standardized treatment guidelines exist, leading to potential delays in diagnosis and tailored treatment.7,8
CASE PRESENTATION
A male Vietnam veteran aged 75 years presented to the emergency department in July 2023 with a fluid collection over his left hip surgical incision site. The patient had a complex medical history that included chronic kidney disease, well-controlled type 2 diabetes, hypertension, and osteoarthritis. His history was further complicated by nonalcoholic steatohepatitis with hepatocellular carcinoma that was treated with transarterial radioembolization and yttrium-90. The patient had undergone a left total hip arthroplasty in 1996 and subsequent open reduction and internal fixation about 9 months prior to his presentation. The patient reported the fluid had been present for about 6 weeks, while he received outpatient monitoring by the orthopedic surgery service. He sought emergency care after noting a moderate amount of purulent discharge on his clothing originating from his hip. In the week prior to admission, the patient observed progressive erythema, warmth, and tenderness over the incision site. Despite these symptoms, the patient remained ambulatory and able to walk long distances with the use of an assistive device.
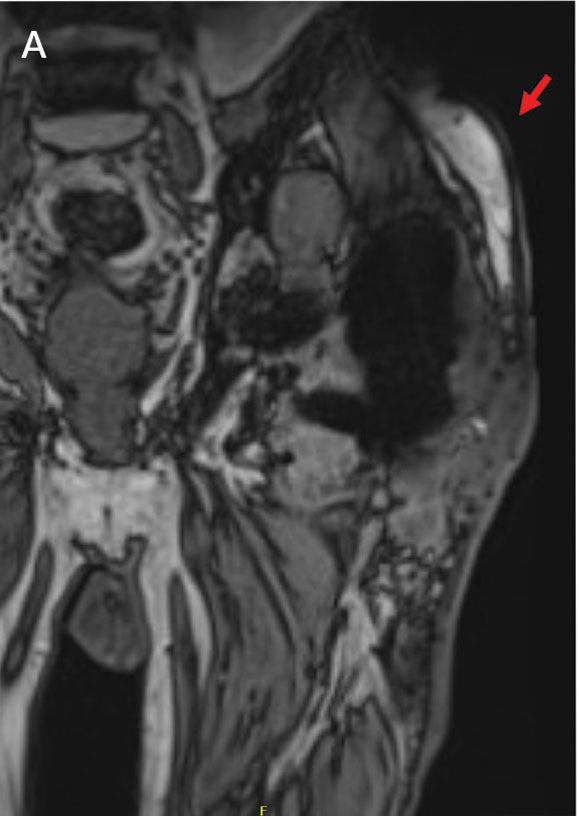
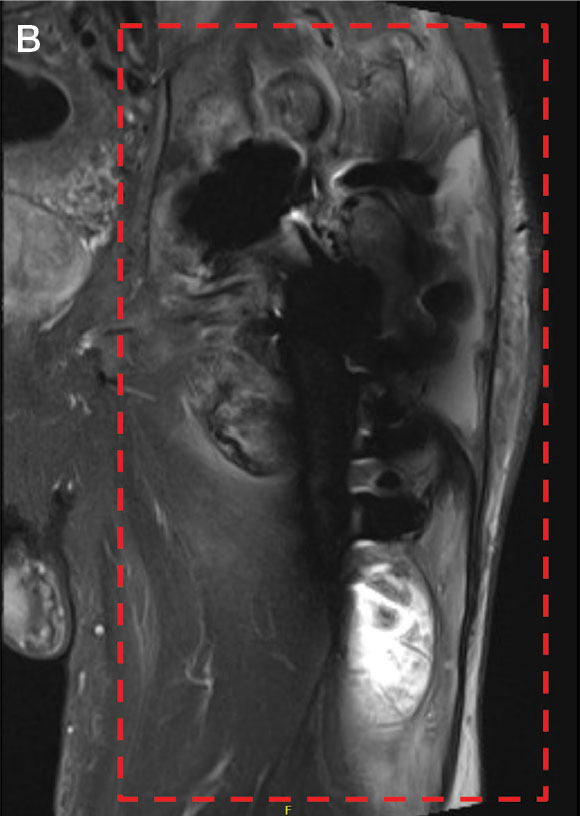
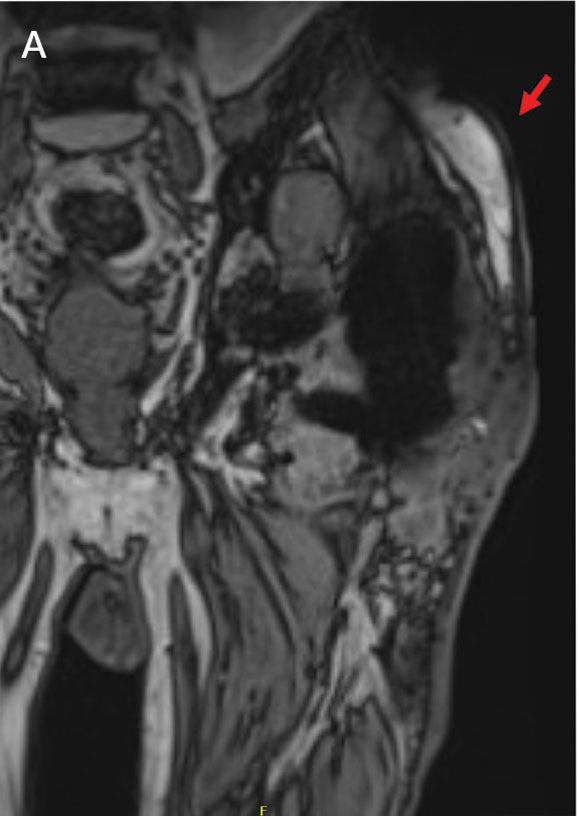
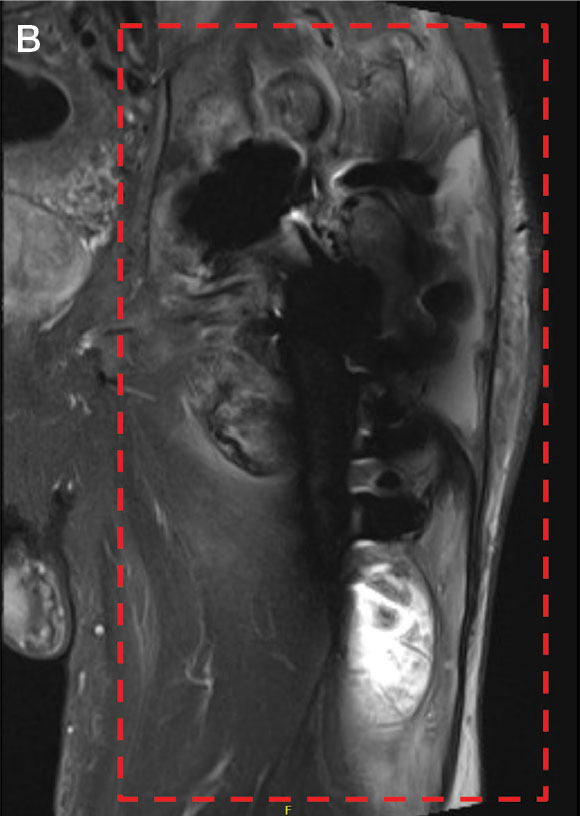
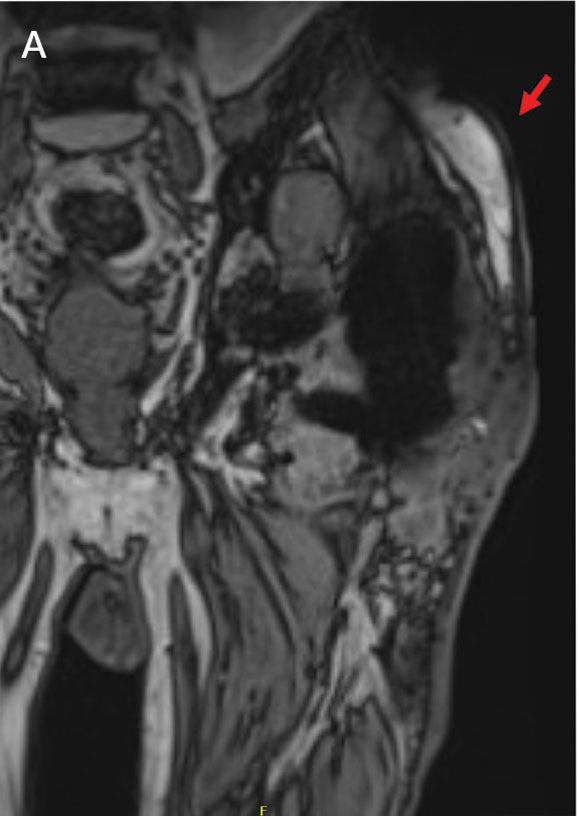
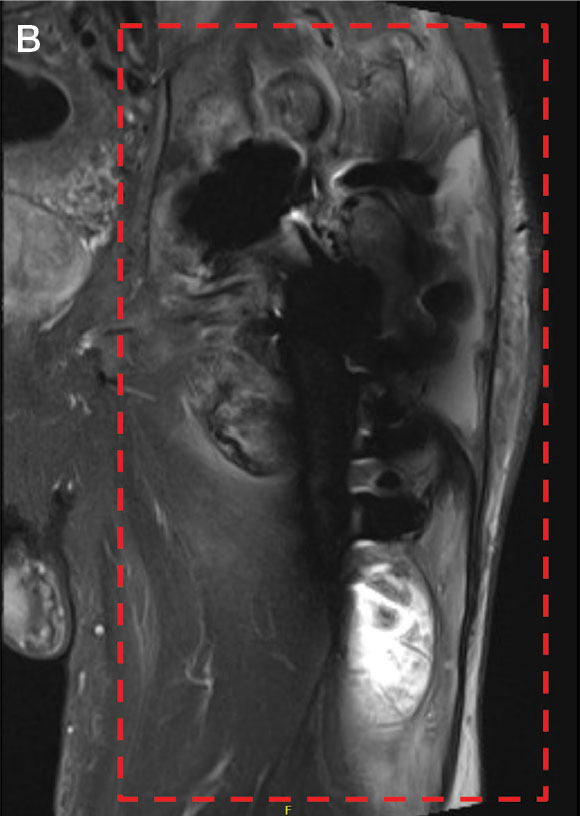
Upon presentation, the patient was afebrile and normotensive. Laboratory testing revealed an elevated erythrocyte sedimentation rate of 77 mm/h (reference range, 0-20 mm/h) and a C-reactive protein of 9.8 mg/L (reference range, 0-2.5 mg/L), suggesting an underlying infectious process. A physical examination revealed a well-healed incision over the left hip with a poorly defined area of fluctuance and evidence of wound dehiscence. The left lower extremity was swollen with 2+ pitting edema, but tenderness was localized to the incision site. Magnetic resonance imaging of the left hip revealed a multiloculated fluid collection abutting the left greater trochanter with extension to the skin surface and inferior extension along the entire length of the surgical fixation hardware (Figure).
Upon admission, orthopedic surgery performed a bedside aspiration of the fluid collection. Samples were sent for analysis, including cell count and bacterial and fungal cultures. Initial blood cultures were sterile. Due to concerns for a bacterial infection, the patient was started on empiric intravenous (IV) ceftriaxone 2 g/day and IV vancomycin 1250 mg/day. Synovial fluid analysis revealed an elevated white blood cell count of 45,000/ìL, but bacterial cultures were negative. Five days after admission, the fungal culture from the left hip wound was notable for presence of C. glabrata, prompting an infectious diseases (ID) consultation. IV micafungin 100 mg/day was initiated as empiric antifungal therapy.
ID and orthopedic surgery teams determined that a combined medical and surgical approach would be best suited for infection control. They proposed 2 main approaches: complete hardware replacement with washout, which carried a higher morbidity risk but a better chance of infection resolution, or partial hardware replacement with washout, which was associated with a lower morbidity risk but a higher risk of infection persistence and recurrence. This decision was particularly challenging for the patient, who prioritized maintaining his functional status, including his ability to continue dancing for pleasure. The patient opted for a more conservative approach, electing to proceed with antifungal therapy and debridement while retaining the prosthetic joint.
After 11 days of hospitalization, the patient was discharged with a peripherally inserted central catheter for long-term antifungal infusions of micafungin 150 mg/day at home. Fungal sensitivity test results several days after discharge confirmed susceptibility to micafungin.
About 2 weeks after discharge, the patient underwent debridement and implant retention (DAIR). Wound cultures were positive for C. glabrata, Enterococcus faecalis, Staphylococcus epidermidis, and Corynebacterium tuberculostearicum. Based on susceptibilities, he completed a 2-month course of IV micafungin 150 mg daily and daptomycin 750 mg daily, followed by an oral suppressive regimen consisting of doxycycline 100 mg twice daily, amoxicillin-clavulanate 2 g twice daily, and fluconazole initially 800 mg daily adjusted to 400 mg daily. The patient continued wound management with twice-daily dressing changes.
Nine months after DAIR, the patient remained on suppressive antifungal and antibacterial therapy. He continued to experience serous drainage from the wound, which greatly affected his quality of life. After discussion with his family and the orthopedic surgery team, he agreed to proceed with a 2-staged revision arthroplasty involving prosthetic explant and antibiotic spacer placement. However, the surgery was postponed due to findings of anemia (hemoglobin, 8.9 g/dL) and thrombocytopenia (platelet count, 73 x 103/λL). At the time of this report, the patient was being monitored closely with his multidisciplinary care team for the planned orthopedic procedure.
DISCUSSION
PJI is the most common cause of primary hip arthroplasty failure; however, fungal species only make up about 1% of PJIs.3,9-11 Patients are typically immunocompromised, undergoing antineoplastic therapies for malignancy, or have other comorbid conditions such as diabetes.12,13 C. glabrata presents a unique diagnostic and therapeutic challenge as it is not only rare but also notorious for its resistance to common antifungal agents. C. glabrata is known to develop multidrug resistance through the rapid accumulation of genomic mutations.14 Its propensity towards forming protective biofilm also arms it with intrinsic resistance to agents like fluconazole.15 Furthermore, based on a review of the available reports in the literature, C. glabrata PJIs are often insidious and present with symptoms closely mimicking those of bacterial PJIs, as it did in the patient in this case.16
Synovial fluid analysis, fungal cultures, and sensitivity testing are paramount for ensuring proper diagnosis for fungal PJI. The patient in this case was empirically treated with micafungin based on recommendations from the ID team. When the sensitivities results were reviewed, the same antifungal therapy was continued. Echinocandins have a favorable toxicity profile in long-term use, as well as efficacy against biofilm-producing organisms like C. glabrata.17,18
While there are a few cases citing DAIR as a feasible surgical strategy for treating fungal PJI, more recent studies have reported greater success with a 2-staged revision arthroplasty involving some combination of debridement, placement of antibiotic-loaded bone cement spacers, and partial or total exchange of the infected prosthetic joint.4,19-23 In this case, complete hardware replacement would have offered the patient the most favorable outlook for eliminating this fungal infection. However, given the patient’s advanced age, significant underlying comorbidities, and functional status, medical management with antifungal therapy and DAIR was favored.
Based on the discussion from the 6-month follow-up visit, the patient was experiencing progressive and persistent wound drainage and frequent dressing changes, highlighting the limitations of medical management for PJI in the setting of retained prosthesis. If the patient ultimately proceeds with a more invasive surgical intervention, another important consideration will be the likelihood of fungal PJI recurrence. At present, fungal PJI recurrence rates following antifungal and surgical treatment have been reported to range between 0% to 50%, which is too imprecise to be considered clinically useful.22-24
Given the ambiguity surrounding management guidelines and limited treatment options, it is crucial to emphasize the timeline of this patient’s clinical presentation and subsequent course of treatment. Upon presentation to the ED in late July, fungal PJI was considered less likely. Initial blood cultures from presentation were negative, which is common with PJIs. It was not until 5 days later that the left hip wound culture showed moderate growth of C. glabrata. Identifying a PJI is clinically challenging due to the lack of standardized diagnostic criteria. However, timely identification and diagnosis of fungal PJI with appropriate antifungal therapy, in patients with limited curative options due to comorbidities, can significantly improve quality of life and overall outcomes.25 Routine fungal and mycobacterial cultures are not currently recommended in PJI guidelines, but this case illustrates it is imperative in immunocompromised hosts.26
This case and the current paucity of similar cases in the literature stress the importance of clinicians publishing their experience in the management of fungal PJI. We strongly recommend that clinicians approach each suspected PJI with careful consideration of the patient’s unique risk factors, comorbidities, and goals of care, when deciding on a curative vs suppressive approach to therapy.
CONCLUSIONS
This case report highlights the importance of considering fungal pathogens for PJIs, especially in high-risk patients, the value of obtaining fungal cultures, the necessity of a multidisciplinary approach, the role of antifungal susceptibility testing, and consideration for the feasibility of a surgical intervention. It underscores the challenges in diagnosis and treatment of C. glabrata-associated PJI, emphasizing the importance of clinician experience-sharing in developing evidence-based management strategies. As the understanding of fungal PJI evolves, continued research and clinical data collection remain crucial for improving patient outcomes in the management of these complex cases.
- Osmon DR, Berbari EF, Berendt AR, et al. Executive summary: diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013;56(1):1-10. doi:10.1093/cid/cis966
- Eka A, Chen AF. Patient-related medical risk factors for periprosthetic joint infection of the hip and knee. Ann Transl Med. 2015;3(16):233. doi:10.3978/j.issn.2305-5839.2015.09.26
- Darouiche RO, Hamill RJ, Musher DM, Young EJ, Harris RL. Periprosthetic candidal infections following arthroplasty. Rev Infect Dis. 1989;11(1):89-96. doi:10.1093/clinids/11.1.89
- Koutserimpas C, Zervakis SG, Maraki S, et al. Non-albicans Candida prosthetic joint infections: a systematic review of treatment. World J Clin Cases. 2019;7(12):1430- 1443. doi:10.12998/wjcc.v7.i12.1430
- Fidel PL Jr, Vazquez JA, Sobel JD. Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans. Clin Microbiol Rev. 1999;12(1):80-96. doi:10.1128/CMR.12.1.80
- Aboltins C, Daffy J, Choong P, Stanley P. Current concepts in the management of prosthetic joint infection. Intern Med J. 2014;44(9):834-840. doi:10.1111/imj.12510
- Lee YR, Kim HJ, Lee EJ, Sohn JW, Kim MJ, Yoon YK. Prosthetic joint infections caused by candida species: a systematic review and a case series. Mycopathologia. 2019;184(1):23-33. doi:10.1007/s11046-018-0286-1
- Herndon CL, Rowe TM, Metcalf RW, et al. Treatment outcomes of fungal periprosthetic joint infection. J Arthroplasty. 2023;38(11):2436-2440.e1. doi:10.1016/j.arth.2023.05.009
- Delaunay C, Hamadouche M, Girard J, Duhamel A; SoFCOT. What are the causes for failures of primary hip arthroplasties in France? Clin Orthop Relat Res. 2013;471(12): 3863-3869. doi:10.1007/s11999-013-2935-5
- Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91(1): 128-133. doi:10.2106/JBJS.H.00155
- Furnes O, Lie SA, Espehaug B, Vollset SE, Engesaeter LB, Havelin LI. Hip disease and the prognosis of total hip replacements. A review of 53,698 primary total hip replacements reported to the Norwegian Arthroplasty Register 1987-99. J Bone Joint Surg Br. 2001;83(4):579-586. doi:10.1302/0301-620x.83b4.11223
- Gonzalez MR, Bedi ADS, Karczewski D, Lozano-Calderon SA. Treatment and outcomes of fungal prosthetic joint infections: a systematic review of 225 cases. J Arthroplasty. 2023;38(11):2464-2471.e1. doi:10.1016/j.arth.2023.05.003
- Gonzalez MR, Pretell-Mazzini J, Lozano-Calderon SA. Risk factors and management of prosthetic joint infections in megaprostheses-a review of the literature. Antibiotics (Basel). 2023;13(1):25. doi:10.3390/antibiotics13010025
- Biswas C, Chen SC, Halliday C, et al. Identification of genetic markers of resistance to echinocandins, azoles and 5-fluorocytosine in Candida glabrata by next-generation sequencing: a feasibility study. Clin Microbiol Infect. 2017;23(9):676.e7-676.e10. doi:10.1016/j.cmi.2017.03.014
- Hassan Y, Chew SY, Than LTL. Candida glabrata: pathogenicity and resistance mechanisms for adaptation and survival. J Fungi (Basel). 2021;7(8):667. doi:10.3390/jof7080667
- Aboltins C, Daffy J, Choong P, Stanley P. Current concepts in the management of prosthetic joint infection. Intern Med J. 2014;44(9):834-840. doi:10.1111/imj.12510
- Pierce CG, Uppuluri P, Tristan AR, et al. A simple and reproducible 96-well plate-based method for the formation of fungal biofilms and its application to antifungal susceptibility testing. Nat Protoc. 2008;3(9):1494-1500. doi:10.1038/nport.2008.141
- Koutserimpas C, Samonis G, Velivassakis E, Iliopoulou- Kosmadaki S, Kontakis G, Kofteridis DP. Candida glabrata prosthetic joint infection, successfully treated with anidulafungin: a case report and review of the literature. Mycoses. 2018;61(4):266-269. doi:10.1111/myc.12736
- Brooks DH, Pupparo F. Successful salvage of a primary total knee arthroplasty infected with Candida parapsilosis. J Arthroplasty. 1998;13(6):707-712. doi:10.1016/s0883-5403(98)80017-x
- Merrer J, Dupont B, Nieszkowska A, De Jonghe B, Outin H. Candida albicans prosthetic arthritis treated with fluconazole alone. J Infect. 2001;42(3):208-209. doi:10.1053/jinf.2001.0819
- Koutserimpas C, Naoum S, Alpantaki K, et al. Fungal prosthetic joint infection in revised knee arthroplasty: an orthopaedic surgeon’s nightmare. Diagnostics (Basel). 2022;12(7):1606. doi:10.3390/diagnostics12071606
- Gao Z, Li X, Du Y, Peng Y, Wu W, Zhou Y. Success rate of fungal peri-prosthetic joint infection treated by 2-stage revision and potential risk factors of treatment failure: a retrospective study. Med Sci Monit. 2018;24:5549-5557. doi:10.12659/MSM.909168
- Hwang BH, Yoon JY, Nam CH, et al. Fungal periprosthetic joint infection after primary total knee replacement. J Bone Joint Surg Br. 2012;94(5):656-659. doi:10.1302/0301-620X.94B5.28125
- Ueng SW, Lee CY, Hu CC, Hsieh PH, Chang Y. What is the success of treatment of hip and knee candidal periprosthetic joint infection? Clin Orthop Relat Res. 2013;471(9):3002-3009. doi:10.1007/s11999-013-3007-6
- Nodzo, Scott R. MD; Bauer, Thomas MD, PhD; Pottinger, et al. Conventional diagnostic challenges in periprosthetic joint infection. J Am Acad Orthop Surg. 2015;23 Suppl:S18-S25. doi:10.5435/JAAOS-D-14-00385
- American Academy of Orthopaedic Surgeons. Diagnosis and prevention of periprosthetic joint infections. March 11, 2019. Accessed February 5, 2025. https://www.aaos.org/pjicpg
Prosthetic joint infection (PJI) occurs in about 1% to 2% of joint replacements. 1 Risk factors include immunosuppression, diabetes, chronic illnesses, and prolonged operative time.2 Bacterial infections constitute most of these infections, while fungal pathogens account for about 1%. Candida (C.) species, predominantly C. albicans, are responsible for most PJIs.1,3 In contrast, C. glabrata is a rare cause of fungal PJI, with only 18 PJI cases currently reported in the literature.4 C. glabrata PJI occurs more frequently among immunosuppressed patients and is associated with a higher treatment failure rate despite antifungal therapy.5 Treatment of fungal PJI is often complicated, involving multiple surgical debridements, prolonged antifungal therapy, and in some cases, prosthesis removal.6 However, given the rarity of C. glabrata as a PJI pathogen, no standardized treatment guidelines exist, leading to potential delays in diagnosis and tailored treatment.7,8
CASE PRESENTATION
A male Vietnam veteran aged 75 years presented to the emergency department in July 2023 with a fluid collection over his left hip surgical incision site. The patient had a complex medical history that included chronic kidney disease, well-controlled type 2 diabetes, hypertension, and osteoarthritis. His history was further complicated by nonalcoholic steatohepatitis with hepatocellular carcinoma that was treated with transarterial radioembolization and yttrium-90. The patient had undergone a left total hip arthroplasty in 1996 and subsequent open reduction and internal fixation about 9 months prior to his presentation. The patient reported the fluid had been present for about 6 weeks, while he received outpatient monitoring by the orthopedic surgery service. He sought emergency care after noting a moderate amount of purulent discharge on his clothing originating from his hip. In the week prior to admission, the patient observed progressive erythema, warmth, and tenderness over the incision site. Despite these symptoms, the patient remained ambulatory and able to walk long distances with the use of an assistive device.
Upon presentation, the patient was afebrile and normotensive. Laboratory testing revealed an elevated erythrocyte sedimentation rate of 77 mm/h (reference range, 0-20 mm/h) and a C-reactive protein of 9.8 mg/L (reference range, 0-2.5 mg/L), suggesting an underlying infectious process. A physical examination revealed a well-healed incision over the left hip with a poorly defined area of fluctuance and evidence of wound dehiscence. The left lower extremity was swollen with 2+ pitting edema, but tenderness was localized to the incision site. Magnetic resonance imaging of the left hip revealed a multiloculated fluid collection abutting the left greater trochanter with extension to the skin surface and inferior extension along the entire length of the surgical fixation hardware (Figure).
Upon admission, orthopedic surgery performed a bedside aspiration of the fluid collection. Samples were sent for analysis, including cell count and bacterial and fungal cultures. Initial blood cultures were sterile. Due to concerns for a bacterial infection, the patient was started on empiric intravenous (IV) ceftriaxone 2 g/day and IV vancomycin 1250 mg/day. Synovial fluid analysis revealed an elevated white blood cell count of 45,000/ìL, but bacterial cultures were negative. Five days after admission, the fungal culture from the left hip wound was notable for presence of C. glabrata, prompting an infectious diseases (ID) consultation. IV micafungin 100 mg/day was initiated as empiric antifungal therapy.
ID and orthopedic surgery teams determined that a combined medical and surgical approach would be best suited for infection control. They proposed 2 main approaches: complete hardware replacement with washout, which carried a higher morbidity risk but a better chance of infection resolution, or partial hardware replacement with washout, which was associated with a lower morbidity risk but a higher risk of infection persistence and recurrence. This decision was particularly challenging for the patient, who prioritized maintaining his functional status, including his ability to continue dancing for pleasure. The patient opted for a more conservative approach, electing to proceed with antifungal therapy and debridement while retaining the prosthetic joint.
After 11 days of hospitalization, the patient was discharged with a peripherally inserted central catheter for long-term antifungal infusions of micafungin 150 mg/day at home. Fungal sensitivity test results several days after discharge confirmed susceptibility to micafungin.
About 2 weeks after discharge, the patient underwent debridement and implant retention (DAIR). Wound cultures were positive for C. glabrata, Enterococcus faecalis, Staphylococcus epidermidis, and Corynebacterium tuberculostearicum. Based on susceptibilities, he completed a 2-month course of IV micafungin 150 mg daily and daptomycin 750 mg daily, followed by an oral suppressive regimen consisting of doxycycline 100 mg twice daily, amoxicillin-clavulanate 2 g twice daily, and fluconazole initially 800 mg daily adjusted to 400 mg daily. The patient continued wound management with twice-daily dressing changes.
Nine months after DAIR, the patient remained on suppressive antifungal and antibacterial therapy. He continued to experience serous drainage from the wound, which greatly affected his quality of life. After discussion with his family and the orthopedic surgery team, he agreed to proceed with a 2-staged revision arthroplasty involving prosthetic explant and antibiotic spacer placement. However, the surgery was postponed due to findings of anemia (hemoglobin, 8.9 g/dL) and thrombocytopenia (platelet count, 73 x 103/λL). At the time of this report, the patient was being monitored closely with his multidisciplinary care team for the planned orthopedic procedure.
DISCUSSION
PJI is the most common cause of primary hip arthroplasty failure; however, fungal species only make up about 1% of PJIs.3,9-11 Patients are typically immunocompromised, undergoing antineoplastic therapies for malignancy, or have other comorbid conditions such as diabetes.12,13 C. glabrata presents a unique diagnostic and therapeutic challenge as it is not only rare but also notorious for its resistance to common antifungal agents. C. glabrata is known to develop multidrug resistance through the rapid accumulation of genomic mutations.14 Its propensity towards forming protective biofilm also arms it with intrinsic resistance to agents like fluconazole.15 Furthermore, based on a review of the available reports in the literature, C. glabrata PJIs are often insidious and present with symptoms closely mimicking those of bacterial PJIs, as it did in the patient in this case.16
Synovial fluid analysis, fungal cultures, and sensitivity testing are paramount for ensuring proper diagnosis for fungal PJI. The patient in this case was empirically treated with micafungin based on recommendations from the ID team. When the sensitivities results were reviewed, the same antifungal therapy was continued. Echinocandins have a favorable toxicity profile in long-term use, as well as efficacy against biofilm-producing organisms like C. glabrata.17,18
While there are a few cases citing DAIR as a feasible surgical strategy for treating fungal PJI, more recent studies have reported greater success with a 2-staged revision arthroplasty involving some combination of debridement, placement of antibiotic-loaded bone cement spacers, and partial or total exchange of the infected prosthetic joint.4,19-23 In this case, complete hardware replacement would have offered the patient the most favorable outlook for eliminating this fungal infection. However, given the patient’s advanced age, significant underlying comorbidities, and functional status, medical management with antifungal therapy and DAIR was favored.
Based on the discussion from the 6-month follow-up visit, the patient was experiencing progressive and persistent wound drainage and frequent dressing changes, highlighting the limitations of medical management for PJI in the setting of retained prosthesis. If the patient ultimately proceeds with a more invasive surgical intervention, another important consideration will be the likelihood of fungal PJI recurrence. At present, fungal PJI recurrence rates following antifungal and surgical treatment have been reported to range between 0% to 50%, which is too imprecise to be considered clinically useful.22-24
Given the ambiguity surrounding management guidelines and limited treatment options, it is crucial to emphasize the timeline of this patient’s clinical presentation and subsequent course of treatment. Upon presentation to the ED in late July, fungal PJI was considered less likely. Initial blood cultures from presentation were negative, which is common with PJIs. It was not until 5 days later that the left hip wound culture showed moderate growth of C. glabrata. Identifying a PJI is clinically challenging due to the lack of standardized diagnostic criteria. However, timely identification and diagnosis of fungal PJI with appropriate antifungal therapy, in patients with limited curative options due to comorbidities, can significantly improve quality of life and overall outcomes.25 Routine fungal and mycobacterial cultures are not currently recommended in PJI guidelines, but this case illustrates it is imperative in immunocompromised hosts.26
This case and the current paucity of similar cases in the literature stress the importance of clinicians publishing their experience in the management of fungal PJI. We strongly recommend that clinicians approach each suspected PJI with careful consideration of the patient’s unique risk factors, comorbidities, and goals of care, when deciding on a curative vs suppressive approach to therapy.
CONCLUSIONS
This case report highlights the importance of considering fungal pathogens for PJIs, especially in high-risk patients, the value of obtaining fungal cultures, the necessity of a multidisciplinary approach, the role of antifungal susceptibility testing, and consideration for the feasibility of a surgical intervention. It underscores the challenges in diagnosis and treatment of C. glabrata-associated PJI, emphasizing the importance of clinician experience-sharing in developing evidence-based management strategies. As the understanding of fungal PJI evolves, continued research and clinical data collection remain crucial for improving patient outcomes in the management of these complex cases.
Prosthetic joint infection (PJI) occurs in about 1% to 2% of joint replacements. 1 Risk factors include immunosuppression, diabetes, chronic illnesses, and prolonged operative time.2 Bacterial infections constitute most of these infections, while fungal pathogens account for about 1%. Candida (C.) species, predominantly C. albicans, are responsible for most PJIs.1,3 In contrast, C. glabrata is a rare cause of fungal PJI, with only 18 PJI cases currently reported in the literature.4 C. glabrata PJI occurs more frequently among immunosuppressed patients and is associated with a higher treatment failure rate despite antifungal therapy.5 Treatment of fungal PJI is often complicated, involving multiple surgical debridements, prolonged antifungal therapy, and in some cases, prosthesis removal.6 However, given the rarity of C. glabrata as a PJI pathogen, no standardized treatment guidelines exist, leading to potential delays in diagnosis and tailored treatment.7,8
CASE PRESENTATION
A male Vietnam veteran aged 75 years presented to the emergency department in July 2023 with a fluid collection over his left hip surgical incision site. The patient had a complex medical history that included chronic kidney disease, well-controlled type 2 diabetes, hypertension, and osteoarthritis. His history was further complicated by nonalcoholic steatohepatitis with hepatocellular carcinoma that was treated with transarterial radioembolization and yttrium-90. The patient had undergone a left total hip arthroplasty in 1996 and subsequent open reduction and internal fixation about 9 months prior to his presentation. The patient reported the fluid had been present for about 6 weeks, while he received outpatient monitoring by the orthopedic surgery service. He sought emergency care after noting a moderate amount of purulent discharge on his clothing originating from his hip. In the week prior to admission, the patient observed progressive erythema, warmth, and tenderness over the incision site. Despite these symptoms, the patient remained ambulatory and able to walk long distances with the use of an assistive device.
Upon presentation, the patient was afebrile and normotensive. Laboratory testing revealed an elevated erythrocyte sedimentation rate of 77 mm/h (reference range, 0-20 mm/h) and a C-reactive protein of 9.8 mg/L (reference range, 0-2.5 mg/L), suggesting an underlying infectious process. A physical examination revealed a well-healed incision over the left hip with a poorly defined area of fluctuance and evidence of wound dehiscence. The left lower extremity was swollen with 2+ pitting edema, but tenderness was localized to the incision site. Magnetic resonance imaging of the left hip revealed a multiloculated fluid collection abutting the left greater trochanter with extension to the skin surface and inferior extension along the entire length of the surgical fixation hardware (Figure).
Upon admission, orthopedic surgery performed a bedside aspiration of the fluid collection. Samples were sent for analysis, including cell count and bacterial and fungal cultures. Initial blood cultures were sterile. Due to concerns for a bacterial infection, the patient was started on empiric intravenous (IV) ceftriaxone 2 g/day and IV vancomycin 1250 mg/day. Synovial fluid analysis revealed an elevated white blood cell count of 45,000/ìL, but bacterial cultures were negative. Five days after admission, the fungal culture from the left hip wound was notable for presence of C. glabrata, prompting an infectious diseases (ID) consultation. IV micafungin 100 mg/day was initiated as empiric antifungal therapy.
ID and orthopedic surgery teams determined that a combined medical and surgical approach would be best suited for infection control. They proposed 2 main approaches: complete hardware replacement with washout, which carried a higher morbidity risk but a better chance of infection resolution, or partial hardware replacement with washout, which was associated with a lower morbidity risk but a higher risk of infection persistence and recurrence. This decision was particularly challenging for the patient, who prioritized maintaining his functional status, including his ability to continue dancing for pleasure. The patient opted for a more conservative approach, electing to proceed with antifungal therapy and debridement while retaining the prosthetic joint.
After 11 days of hospitalization, the patient was discharged with a peripherally inserted central catheter for long-term antifungal infusions of micafungin 150 mg/day at home. Fungal sensitivity test results several days after discharge confirmed susceptibility to micafungin.
About 2 weeks after discharge, the patient underwent debridement and implant retention (DAIR). Wound cultures were positive for C. glabrata, Enterococcus faecalis, Staphylococcus epidermidis, and Corynebacterium tuberculostearicum. Based on susceptibilities, he completed a 2-month course of IV micafungin 150 mg daily and daptomycin 750 mg daily, followed by an oral suppressive regimen consisting of doxycycline 100 mg twice daily, amoxicillin-clavulanate 2 g twice daily, and fluconazole initially 800 mg daily adjusted to 400 mg daily. The patient continued wound management with twice-daily dressing changes.
Nine months after DAIR, the patient remained on suppressive antifungal and antibacterial therapy. He continued to experience serous drainage from the wound, which greatly affected his quality of life. After discussion with his family and the orthopedic surgery team, he agreed to proceed with a 2-staged revision arthroplasty involving prosthetic explant and antibiotic spacer placement. However, the surgery was postponed due to findings of anemia (hemoglobin, 8.9 g/dL) and thrombocytopenia (platelet count, 73 x 103/λL). At the time of this report, the patient was being monitored closely with his multidisciplinary care team for the planned orthopedic procedure.
DISCUSSION
PJI is the most common cause of primary hip arthroplasty failure; however, fungal species only make up about 1% of PJIs.3,9-11 Patients are typically immunocompromised, undergoing antineoplastic therapies for malignancy, or have other comorbid conditions such as diabetes.12,13 C. glabrata presents a unique diagnostic and therapeutic challenge as it is not only rare but also notorious for its resistance to common antifungal agents. C. glabrata is known to develop multidrug resistance through the rapid accumulation of genomic mutations.14 Its propensity towards forming protective biofilm also arms it with intrinsic resistance to agents like fluconazole.15 Furthermore, based on a review of the available reports in the literature, C. glabrata PJIs are often insidious and present with symptoms closely mimicking those of bacterial PJIs, as it did in the patient in this case.16
Synovial fluid analysis, fungal cultures, and sensitivity testing are paramount for ensuring proper diagnosis for fungal PJI. The patient in this case was empirically treated with micafungin based on recommendations from the ID team. When the sensitivities results were reviewed, the same antifungal therapy was continued. Echinocandins have a favorable toxicity profile in long-term use, as well as efficacy against biofilm-producing organisms like C. glabrata.17,18
While there are a few cases citing DAIR as a feasible surgical strategy for treating fungal PJI, more recent studies have reported greater success with a 2-staged revision arthroplasty involving some combination of debridement, placement of antibiotic-loaded bone cement spacers, and partial or total exchange of the infected prosthetic joint.4,19-23 In this case, complete hardware replacement would have offered the patient the most favorable outlook for eliminating this fungal infection. However, given the patient’s advanced age, significant underlying comorbidities, and functional status, medical management with antifungal therapy and DAIR was favored.
Based on the discussion from the 6-month follow-up visit, the patient was experiencing progressive and persistent wound drainage and frequent dressing changes, highlighting the limitations of medical management for PJI in the setting of retained prosthesis. If the patient ultimately proceeds with a more invasive surgical intervention, another important consideration will be the likelihood of fungal PJI recurrence. At present, fungal PJI recurrence rates following antifungal and surgical treatment have been reported to range between 0% to 50%, which is too imprecise to be considered clinically useful.22-24
Given the ambiguity surrounding management guidelines and limited treatment options, it is crucial to emphasize the timeline of this patient’s clinical presentation and subsequent course of treatment. Upon presentation to the ED in late July, fungal PJI was considered less likely. Initial blood cultures from presentation were negative, which is common with PJIs. It was not until 5 days later that the left hip wound culture showed moderate growth of C. glabrata. Identifying a PJI is clinically challenging due to the lack of standardized diagnostic criteria. However, timely identification and diagnosis of fungal PJI with appropriate antifungal therapy, in patients with limited curative options due to comorbidities, can significantly improve quality of life and overall outcomes.25 Routine fungal and mycobacterial cultures are not currently recommended in PJI guidelines, but this case illustrates it is imperative in immunocompromised hosts.26
This case and the current paucity of similar cases in the literature stress the importance of clinicians publishing their experience in the management of fungal PJI. We strongly recommend that clinicians approach each suspected PJI with careful consideration of the patient’s unique risk factors, comorbidities, and goals of care, when deciding on a curative vs suppressive approach to therapy.
CONCLUSIONS
This case report highlights the importance of considering fungal pathogens for PJIs, especially in high-risk patients, the value of obtaining fungal cultures, the necessity of a multidisciplinary approach, the role of antifungal susceptibility testing, and consideration for the feasibility of a surgical intervention. It underscores the challenges in diagnosis and treatment of C. glabrata-associated PJI, emphasizing the importance of clinician experience-sharing in developing evidence-based management strategies. As the understanding of fungal PJI evolves, continued research and clinical data collection remain crucial for improving patient outcomes in the management of these complex cases.
- Osmon DR, Berbari EF, Berendt AR, et al. Executive summary: diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013;56(1):1-10. doi:10.1093/cid/cis966
- Eka A, Chen AF. Patient-related medical risk factors for periprosthetic joint infection of the hip and knee. Ann Transl Med. 2015;3(16):233. doi:10.3978/j.issn.2305-5839.2015.09.26
- Darouiche RO, Hamill RJ, Musher DM, Young EJ, Harris RL. Periprosthetic candidal infections following arthroplasty. Rev Infect Dis. 1989;11(1):89-96. doi:10.1093/clinids/11.1.89
- Koutserimpas C, Zervakis SG, Maraki S, et al. Non-albicans Candida prosthetic joint infections: a systematic review of treatment. World J Clin Cases. 2019;7(12):1430- 1443. doi:10.12998/wjcc.v7.i12.1430
- Fidel PL Jr, Vazquez JA, Sobel JD. Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans. Clin Microbiol Rev. 1999;12(1):80-96. doi:10.1128/CMR.12.1.80
- Aboltins C, Daffy J, Choong P, Stanley P. Current concepts in the management of prosthetic joint infection. Intern Med J. 2014;44(9):834-840. doi:10.1111/imj.12510
- Lee YR, Kim HJ, Lee EJ, Sohn JW, Kim MJ, Yoon YK. Prosthetic joint infections caused by candida species: a systematic review and a case series. Mycopathologia. 2019;184(1):23-33. doi:10.1007/s11046-018-0286-1
- Herndon CL, Rowe TM, Metcalf RW, et al. Treatment outcomes of fungal periprosthetic joint infection. J Arthroplasty. 2023;38(11):2436-2440.e1. doi:10.1016/j.arth.2023.05.009
- Delaunay C, Hamadouche M, Girard J, Duhamel A; SoFCOT. What are the causes for failures of primary hip arthroplasties in France? Clin Orthop Relat Res. 2013;471(12): 3863-3869. doi:10.1007/s11999-013-2935-5
- Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91(1): 128-133. doi:10.2106/JBJS.H.00155
- Furnes O, Lie SA, Espehaug B, Vollset SE, Engesaeter LB, Havelin LI. Hip disease and the prognosis of total hip replacements. A review of 53,698 primary total hip replacements reported to the Norwegian Arthroplasty Register 1987-99. J Bone Joint Surg Br. 2001;83(4):579-586. doi:10.1302/0301-620x.83b4.11223
- Gonzalez MR, Bedi ADS, Karczewski D, Lozano-Calderon SA. Treatment and outcomes of fungal prosthetic joint infections: a systematic review of 225 cases. J Arthroplasty. 2023;38(11):2464-2471.e1. doi:10.1016/j.arth.2023.05.003
- Gonzalez MR, Pretell-Mazzini J, Lozano-Calderon SA. Risk factors and management of prosthetic joint infections in megaprostheses-a review of the literature. Antibiotics (Basel). 2023;13(1):25. doi:10.3390/antibiotics13010025
- Biswas C, Chen SC, Halliday C, et al. Identification of genetic markers of resistance to echinocandins, azoles and 5-fluorocytosine in Candida glabrata by next-generation sequencing: a feasibility study. Clin Microbiol Infect. 2017;23(9):676.e7-676.e10. doi:10.1016/j.cmi.2017.03.014
- Hassan Y, Chew SY, Than LTL. Candida glabrata: pathogenicity and resistance mechanisms for adaptation and survival. J Fungi (Basel). 2021;7(8):667. doi:10.3390/jof7080667
- Aboltins C, Daffy J, Choong P, Stanley P. Current concepts in the management of prosthetic joint infection. Intern Med J. 2014;44(9):834-840. doi:10.1111/imj.12510
- Pierce CG, Uppuluri P, Tristan AR, et al. A simple and reproducible 96-well plate-based method for the formation of fungal biofilms and its application to antifungal susceptibility testing. Nat Protoc. 2008;3(9):1494-1500. doi:10.1038/nport.2008.141
- Koutserimpas C, Samonis G, Velivassakis E, Iliopoulou- Kosmadaki S, Kontakis G, Kofteridis DP. Candida glabrata prosthetic joint infection, successfully treated with anidulafungin: a case report and review of the literature. Mycoses. 2018;61(4):266-269. doi:10.1111/myc.12736
- Brooks DH, Pupparo F. Successful salvage of a primary total knee arthroplasty infected with Candida parapsilosis. J Arthroplasty. 1998;13(6):707-712. doi:10.1016/s0883-5403(98)80017-x
- Merrer J, Dupont B, Nieszkowska A, De Jonghe B, Outin H. Candida albicans prosthetic arthritis treated with fluconazole alone. J Infect. 2001;42(3):208-209. doi:10.1053/jinf.2001.0819
- Koutserimpas C, Naoum S, Alpantaki K, et al. Fungal prosthetic joint infection in revised knee arthroplasty: an orthopaedic surgeon’s nightmare. Diagnostics (Basel). 2022;12(7):1606. doi:10.3390/diagnostics12071606
- Gao Z, Li X, Du Y, Peng Y, Wu W, Zhou Y. Success rate of fungal peri-prosthetic joint infection treated by 2-stage revision and potential risk factors of treatment failure: a retrospective study. Med Sci Monit. 2018;24:5549-5557. doi:10.12659/MSM.909168
- Hwang BH, Yoon JY, Nam CH, et al. Fungal periprosthetic joint infection after primary total knee replacement. J Bone Joint Surg Br. 2012;94(5):656-659. doi:10.1302/0301-620X.94B5.28125
- Ueng SW, Lee CY, Hu CC, Hsieh PH, Chang Y. What is the success of treatment of hip and knee candidal periprosthetic joint infection? Clin Orthop Relat Res. 2013;471(9):3002-3009. doi:10.1007/s11999-013-3007-6
- Nodzo, Scott R. MD; Bauer, Thomas MD, PhD; Pottinger, et al. Conventional diagnostic challenges in periprosthetic joint infection. J Am Acad Orthop Surg. 2015;23 Suppl:S18-S25. doi:10.5435/JAAOS-D-14-00385
- American Academy of Orthopaedic Surgeons. Diagnosis and prevention of periprosthetic joint infections. March 11, 2019. Accessed February 5, 2025. https://www.aaos.org/pjicpg
- Osmon DR, Berbari EF, Berendt AR, et al. Executive summary: diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013;56(1):1-10. doi:10.1093/cid/cis966
- Eka A, Chen AF. Patient-related medical risk factors for periprosthetic joint infection of the hip and knee. Ann Transl Med. 2015;3(16):233. doi:10.3978/j.issn.2305-5839.2015.09.26
- Darouiche RO, Hamill RJ, Musher DM, Young EJ, Harris RL. Periprosthetic candidal infections following arthroplasty. Rev Infect Dis. 1989;11(1):89-96. doi:10.1093/clinids/11.1.89
- Koutserimpas C, Zervakis SG, Maraki S, et al. Non-albicans Candida prosthetic joint infections: a systematic review of treatment. World J Clin Cases. 2019;7(12):1430- 1443. doi:10.12998/wjcc.v7.i12.1430
- Fidel PL Jr, Vazquez JA, Sobel JD. Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans. Clin Microbiol Rev. 1999;12(1):80-96. doi:10.1128/CMR.12.1.80
- Aboltins C, Daffy J, Choong P, Stanley P. Current concepts in the management of prosthetic joint infection. Intern Med J. 2014;44(9):834-840. doi:10.1111/imj.12510
- Lee YR, Kim HJ, Lee EJ, Sohn JW, Kim MJ, Yoon YK. Prosthetic joint infections caused by candida species: a systematic review and a case series. Mycopathologia. 2019;184(1):23-33. doi:10.1007/s11046-018-0286-1
- Herndon CL, Rowe TM, Metcalf RW, et al. Treatment outcomes of fungal periprosthetic joint infection. J Arthroplasty. 2023;38(11):2436-2440.e1. doi:10.1016/j.arth.2023.05.009
- Delaunay C, Hamadouche M, Girard J, Duhamel A; SoFCOT. What are the causes for failures of primary hip arthroplasties in France? Clin Orthop Relat Res. 2013;471(12): 3863-3869. doi:10.1007/s11999-013-2935-5
- Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91(1): 128-133. doi:10.2106/JBJS.H.00155
- Furnes O, Lie SA, Espehaug B, Vollset SE, Engesaeter LB, Havelin LI. Hip disease and the prognosis of total hip replacements. A review of 53,698 primary total hip replacements reported to the Norwegian Arthroplasty Register 1987-99. J Bone Joint Surg Br. 2001;83(4):579-586. doi:10.1302/0301-620x.83b4.11223
- Gonzalez MR, Bedi ADS, Karczewski D, Lozano-Calderon SA. Treatment and outcomes of fungal prosthetic joint infections: a systematic review of 225 cases. J Arthroplasty. 2023;38(11):2464-2471.e1. doi:10.1016/j.arth.2023.05.003
- Gonzalez MR, Pretell-Mazzini J, Lozano-Calderon SA. Risk factors and management of prosthetic joint infections in megaprostheses-a review of the literature. Antibiotics (Basel). 2023;13(1):25. doi:10.3390/antibiotics13010025
- Biswas C, Chen SC, Halliday C, et al. Identification of genetic markers of resistance to echinocandins, azoles and 5-fluorocytosine in Candida glabrata by next-generation sequencing: a feasibility study. Clin Microbiol Infect. 2017;23(9):676.e7-676.e10. doi:10.1016/j.cmi.2017.03.014
- Hassan Y, Chew SY, Than LTL. Candida glabrata: pathogenicity and resistance mechanisms for adaptation and survival. J Fungi (Basel). 2021;7(8):667. doi:10.3390/jof7080667
- Aboltins C, Daffy J, Choong P, Stanley P. Current concepts in the management of prosthetic joint infection. Intern Med J. 2014;44(9):834-840. doi:10.1111/imj.12510
- Pierce CG, Uppuluri P, Tristan AR, et al. A simple and reproducible 96-well plate-based method for the formation of fungal biofilms and its application to antifungal susceptibility testing. Nat Protoc. 2008;3(9):1494-1500. doi:10.1038/nport.2008.141
- Koutserimpas C, Samonis G, Velivassakis E, Iliopoulou- Kosmadaki S, Kontakis G, Kofteridis DP. Candida glabrata prosthetic joint infection, successfully treated with anidulafungin: a case report and review of the literature. Mycoses. 2018;61(4):266-269. doi:10.1111/myc.12736
- Brooks DH, Pupparo F. Successful salvage of a primary total knee arthroplasty infected with Candida parapsilosis. J Arthroplasty. 1998;13(6):707-712. doi:10.1016/s0883-5403(98)80017-x
- Merrer J, Dupont B, Nieszkowska A, De Jonghe B, Outin H. Candida albicans prosthetic arthritis treated with fluconazole alone. J Infect. 2001;42(3):208-209. doi:10.1053/jinf.2001.0819
- Koutserimpas C, Naoum S, Alpantaki K, et al. Fungal prosthetic joint infection in revised knee arthroplasty: an orthopaedic surgeon’s nightmare. Diagnostics (Basel). 2022;12(7):1606. doi:10.3390/diagnostics12071606
- Gao Z, Li X, Du Y, Peng Y, Wu W, Zhou Y. Success rate of fungal peri-prosthetic joint infection treated by 2-stage revision and potential risk factors of treatment failure: a retrospective study. Med Sci Monit. 2018;24:5549-5557. doi:10.12659/MSM.909168
- Hwang BH, Yoon JY, Nam CH, et al. Fungal periprosthetic joint infection after primary total knee replacement. J Bone Joint Surg Br. 2012;94(5):656-659. doi:10.1302/0301-620X.94B5.28125
- Ueng SW, Lee CY, Hu CC, Hsieh PH, Chang Y. What is the success of treatment of hip and knee candidal periprosthetic joint infection? Clin Orthop Relat Res. 2013;471(9):3002-3009. doi:10.1007/s11999-013-3007-6
- Nodzo, Scott R. MD; Bauer, Thomas MD, PhD; Pottinger, et al. Conventional diagnostic challenges in periprosthetic joint infection. J Am Acad Orthop Surg. 2015;23 Suppl:S18-S25. doi:10.5435/JAAOS-D-14-00385
- American Academy of Orthopaedic Surgeons. Diagnosis and prevention of periprosthetic joint infections. March 11, 2019. Accessed February 5, 2025. https://www.aaos.org/pjicpg
A Candida Glabrata-Associated Prosthetic Joint Infection: Case Report and Literature Review
A Candida Glabrata-Associated Prosthetic Joint Infection: Case Report and Literature Review
Total Hip Replacement Superior to Exercise Therapy for Improving Hip Osteoarthritis Pain and Function
For people with severe symptomatic hip osteoarthritis, total hip replacement (THR) alleviates hip pain and improves function much more effectively than a resistance training program supervised by a physiotherapist, according to the results of a randomized controlled clinical trial.
In the PROHIP study, the mean increases in Oxford Hip Scores from baseline to 6 months were 15.9 points for THR and 4.5 points for resistance training. The 11.4-point difference in scores was both statistically and clinically significant, the study’s investigators reported in The New England Journal of Medicine.
“Our results are clear: Surgery is superior to exercise in patients who have hip osteoarthritis and indication for surgery, and now we have finally proven that with the highest level of evidence,” corresponding author Thomas Frydendal, PT, PhD, MSc, told this news organization.
Frydendal, who was involved in the study while working on his PhD at University Hospital of Southern Denmark – Lillebaelt Hospital, Vejle, Denmark, the primary center for the trial, is now a postdoctoral researcher at the Department of Clinical Medicine, Aarhus University, and Department of Orthopedic Surgery, Aarhus University Hospital.
“We believe that our findings are pretty robust,” Frydendal added. “I think if someone in the world conducts a trial similar to ours, they will find fairly close or consistent findings, no matter what type of exercise they choose.”
The PROHIP Study
THR is routinely recommended for the management of severe hip osteoarthritis, but since there are no clinical trial data on the effectiveness of this procedure as compared with first-line treatment such as resistance training, the PROHIP study was conceived.
The trial was conducted at four Danish orthopedic centers and designed as a superiority study, the hypothesis being that THR would be better at alleviating self-reported hip pain and improving hip function than resistance training.
Of a possible 1474 individuals with a clinical suspicion of hip osteoarthritis, 791 were deemed eligible for inclusion in the trial. Inclusion criteria were being aged 50 years or older and having an indication for THR based on the presence of hip pain and clinical and radiographic findings.
However, the majority (86%) declined to enter the study, with almost half (43%) deciding to have a THR and enroll in a parallel observational cohort. This meant that only 110 (14%) individuals agreed to participate and underwent randomization, which does limit the study’s generalizability, the PROHIP investigators acknowledged.
Design and Study Population
The change in Oxford Hip Score from baseline to 6 months was selected as the primary outcome measure based on the findings of a prior qualitative study. This 12-item, patient-reported outcome measure gives a score ranging from 0 to 48, with higher scores indicating less hip pain and better hip function. The estimated minimal clinically important difference is a change of 5 points.
After a baseline assessment, 53 of 109 individuals were randomly assigned to undergo THR and 56 to participate in the resistance training program. Overall, the mean age of participants was 67.6 years, and half were women. The average duration of hip pain was a median of 1.7 years.
The median time to receipt of the allocated treatment was 2.8 months in the THR group and 0.5 months in the resistance training group.
Those allocated to the THR group also underwent a “fast track” program that involved patient education, pain management, and early mobilization.
The resistance training group received 12 weeks of exercise supervised by a physiotherapist and then offered 12 weeks of additional exercise conducted on their own. The physiotherapist-supervised exercise sessions were held twice weekly and lasted for 1 hour. These started with a 10-minute warm-up on a stationary bike, followed by a standard set of resistance-based exercises that included a leg press, hip extension, hip flexion, and hip abduction.
‘Reassuring’ Results
In a comment, consultant orthopedic surgeon Antony Palmer, MA, BMBCh, DPhil, said: “It’s reassuring that patients with advanced symptomatic osteoarthritis do well with hip replacements.”
THR does of course come with the potential risk for complications, but “the rate of these is what you’d expect for that procedure,” Palmer said, who works for the Nuffield Orthopaedic Centre, Oxford University Hospital NHS Foundation Trust, and is a senior clinical research fellow at Oxford University in England.
In the THR arm, there was one case of prosthetic joint infection, one hip dislocation, two revision surgeries, one instance of foot drop, and one case of gastroesophageal reflux. Meanwhile, in the resistance training group, there was one hip dislocation, one pelvic fracture, one case of atrial fibrillation, and one urinary tract and renal infection.
Overall, any serious adverse event was reported in six (12%) of 48 patients in the THR arm vs five (9%) of 55 participants in the resistance training group, of which only one, occurring in the resistance training group, resulted in discontinuation of the program.
Resistance Training Role
A notable finding was that, at 6 months, five (9%) people assigned to the THR arm had not undergone surgery, and 12 (21%) people in the resistance training group had undergone a THR.
This could suggest two things, Palmer suggested in the interview. The first is that there could be a small proportion of people assigned to THR who may not need the operation and do well with exercise therapy. And, conversely, there may be those who would do well having the surgery without first going through the intermediate stage of physical therapy.
It’s a suggestion that “maybe we’ve got to refine that a bit better and identify the patients that really do benefit from physiotherapy and who might not need hip replacement as a result,” Palmer said.
Or in other words, “should all patients undergo a program of physiotherapy before considering surgery?” he added.
Authors’ View
The PROHIP investigators conclude: “These results support current recommendations for the management of hip osteoarthritis and may be used to inform and guide shared decision making in clinical practice.”
Moreover, the results “do not oppose the use of resistance training as initial treatment,” says the authors.
Frydendal highlighted in his interview that nearly three out of four of the patients reported not to have undertaken any type of supervised exercise before entry into the study, which is a first-line, guideline-recommended option.
“If a patient tells me, ‘I haven’t done any exercise previously,’ I’d recommend starting with completing a 6- to 12-week exercise program that is tailored to your individual needs and evaluate your symptoms afterward,” he said.
“But we should refer the patient if our first-line treatment does not offer any improvements in the patient’s symptoms, as surgery with total hip replacement is clearly a really good treatment option,” Frydendal said.
The study was funded by the Danish Rheumatism Association, among other independent bodies. Frydendal and Palmer reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
For people with severe symptomatic hip osteoarthritis, total hip replacement (THR) alleviates hip pain and improves function much more effectively than a resistance training program supervised by a physiotherapist, according to the results of a randomized controlled clinical trial.
In the PROHIP study, the mean increases in Oxford Hip Scores from baseline to 6 months were 15.9 points for THR and 4.5 points for resistance training. The 11.4-point difference in scores was both statistically and clinically significant, the study’s investigators reported in The New England Journal of Medicine.
“Our results are clear: Surgery is superior to exercise in patients who have hip osteoarthritis and indication for surgery, and now we have finally proven that with the highest level of evidence,” corresponding author Thomas Frydendal, PT, PhD, MSc, told this news organization.
Frydendal, who was involved in the study while working on his PhD at University Hospital of Southern Denmark – Lillebaelt Hospital, Vejle, Denmark, the primary center for the trial, is now a postdoctoral researcher at the Department of Clinical Medicine, Aarhus University, and Department of Orthopedic Surgery, Aarhus University Hospital.
“We believe that our findings are pretty robust,” Frydendal added. “I think if someone in the world conducts a trial similar to ours, they will find fairly close or consistent findings, no matter what type of exercise they choose.”
The PROHIP Study
THR is routinely recommended for the management of severe hip osteoarthritis, but since there are no clinical trial data on the effectiveness of this procedure as compared with first-line treatment such as resistance training, the PROHIP study was conceived.
The trial was conducted at four Danish orthopedic centers and designed as a superiority study, the hypothesis being that THR would be better at alleviating self-reported hip pain and improving hip function than resistance training.
Of a possible 1474 individuals with a clinical suspicion of hip osteoarthritis, 791 were deemed eligible for inclusion in the trial. Inclusion criteria were being aged 50 years or older and having an indication for THR based on the presence of hip pain and clinical and radiographic findings.
However, the majority (86%) declined to enter the study, with almost half (43%) deciding to have a THR and enroll in a parallel observational cohort. This meant that only 110 (14%) individuals agreed to participate and underwent randomization, which does limit the study’s generalizability, the PROHIP investigators acknowledged.
Design and Study Population
The change in Oxford Hip Score from baseline to 6 months was selected as the primary outcome measure based on the findings of a prior qualitative study. This 12-item, patient-reported outcome measure gives a score ranging from 0 to 48, with higher scores indicating less hip pain and better hip function. The estimated minimal clinically important difference is a change of 5 points.
After a baseline assessment, 53 of 109 individuals were randomly assigned to undergo THR and 56 to participate in the resistance training program. Overall, the mean age of participants was 67.6 years, and half were women. The average duration of hip pain was a median of 1.7 years.
The median time to receipt of the allocated treatment was 2.8 months in the THR group and 0.5 months in the resistance training group.
Those allocated to the THR group also underwent a “fast track” program that involved patient education, pain management, and early mobilization.
The resistance training group received 12 weeks of exercise supervised by a physiotherapist and then offered 12 weeks of additional exercise conducted on their own. The physiotherapist-supervised exercise sessions were held twice weekly and lasted for 1 hour. These started with a 10-minute warm-up on a stationary bike, followed by a standard set of resistance-based exercises that included a leg press, hip extension, hip flexion, and hip abduction.
‘Reassuring’ Results
In a comment, consultant orthopedic surgeon Antony Palmer, MA, BMBCh, DPhil, said: “It’s reassuring that patients with advanced symptomatic osteoarthritis do well with hip replacements.”
THR does of course come with the potential risk for complications, but “the rate of these is what you’d expect for that procedure,” Palmer said, who works for the Nuffield Orthopaedic Centre, Oxford University Hospital NHS Foundation Trust, and is a senior clinical research fellow at Oxford University in England.
In the THR arm, there was one case of prosthetic joint infection, one hip dislocation, two revision surgeries, one instance of foot drop, and one case of gastroesophageal reflux. Meanwhile, in the resistance training group, there was one hip dislocation, one pelvic fracture, one case of atrial fibrillation, and one urinary tract and renal infection.
Overall, any serious adverse event was reported in six (12%) of 48 patients in the THR arm vs five (9%) of 55 participants in the resistance training group, of which only one, occurring in the resistance training group, resulted in discontinuation of the program.
Resistance Training Role
A notable finding was that, at 6 months, five (9%) people assigned to the THR arm had not undergone surgery, and 12 (21%) people in the resistance training group had undergone a THR.
This could suggest two things, Palmer suggested in the interview. The first is that there could be a small proportion of people assigned to THR who may not need the operation and do well with exercise therapy. And, conversely, there may be those who would do well having the surgery without first going through the intermediate stage of physical therapy.
It’s a suggestion that “maybe we’ve got to refine that a bit better and identify the patients that really do benefit from physiotherapy and who might not need hip replacement as a result,” Palmer said.
Or in other words, “should all patients undergo a program of physiotherapy before considering surgery?” he added.
Authors’ View
The PROHIP investigators conclude: “These results support current recommendations for the management of hip osteoarthritis and may be used to inform and guide shared decision making in clinical practice.”
Moreover, the results “do not oppose the use of resistance training as initial treatment,” says the authors.
Frydendal highlighted in his interview that nearly three out of four of the patients reported not to have undertaken any type of supervised exercise before entry into the study, which is a first-line, guideline-recommended option.
“If a patient tells me, ‘I haven’t done any exercise previously,’ I’d recommend starting with completing a 6- to 12-week exercise program that is tailored to your individual needs and evaluate your symptoms afterward,” he said.
“But we should refer the patient if our first-line treatment does not offer any improvements in the patient’s symptoms, as surgery with total hip replacement is clearly a really good treatment option,” Frydendal said.
The study was funded by the Danish Rheumatism Association, among other independent bodies. Frydendal and Palmer reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
For people with severe symptomatic hip osteoarthritis, total hip replacement (THR) alleviates hip pain and improves function much more effectively than a resistance training program supervised by a physiotherapist, according to the results of a randomized controlled clinical trial.
In the PROHIP study, the mean increases in Oxford Hip Scores from baseline to 6 months were 15.9 points for THR and 4.5 points for resistance training. The 11.4-point difference in scores was both statistically and clinically significant, the study’s investigators reported in The New England Journal of Medicine.
“Our results are clear: Surgery is superior to exercise in patients who have hip osteoarthritis and indication for surgery, and now we have finally proven that with the highest level of evidence,” corresponding author Thomas Frydendal, PT, PhD, MSc, told this news organization.
Frydendal, who was involved in the study while working on his PhD at University Hospital of Southern Denmark – Lillebaelt Hospital, Vejle, Denmark, the primary center for the trial, is now a postdoctoral researcher at the Department of Clinical Medicine, Aarhus University, and Department of Orthopedic Surgery, Aarhus University Hospital.
“We believe that our findings are pretty robust,” Frydendal added. “I think if someone in the world conducts a trial similar to ours, they will find fairly close or consistent findings, no matter what type of exercise they choose.”
The PROHIP Study
THR is routinely recommended for the management of severe hip osteoarthritis, but since there are no clinical trial data on the effectiveness of this procedure as compared with first-line treatment such as resistance training, the PROHIP study was conceived.
The trial was conducted at four Danish orthopedic centers and designed as a superiority study, the hypothesis being that THR would be better at alleviating self-reported hip pain and improving hip function than resistance training.
Of a possible 1474 individuals with a clinical suspicion of hip osteoarthritis, 791 were deemed eligible for inclusion in the trial. Inclusion criteria were being aged 50 years or older and having an indication for THR based on the presence of hip pain and clinical and radiographic findings.
However, the majority (86%) declined to enter the study, with almost half (43%) deciding to have a THR and enroll in a parallel observational cohort. This meant that only 110 (14%) individuals agreed to participate and underwent randomization, which does limit the study’s generalizability, the PROHIP investigators acknowledged.
Design and Study Population
The change in Oxford Hip Score from baseline to 6 months was selected as the primary outcome measure based on the findings of a prior qualitative study. This 12-item, patient-reported outcome measure gives a score ranging from 0 to 48, with higher scores indicating less hip pain and better hip function. The estimated minimal clinically important difference is a change of 5 points.
After a baseline assessment, 53 of 109 individuals were randomly assigned to undergo THR and 56 to participate in the resistance training program. Overall, the mean age of participants was 67.6 years, and half were women. The average duration of hip pain was a median of 1.7 years.
The median time to receipt of the allocated treatment was 2.8 months in the THR group and 0.5 months in the resistance training group.
Those allocated to the THR group also underwent a “fast track” program that involved patient education, pain management, and early mobilization.
The resistance training group received 12 weeks of exercise supervised by a physiotherapist and then offered 12 weeks of additional exercise conducted on their own. The physiotherapist-supervised exercise sessions were held twice weekly and lasted for 1 hour. These started with a 10-minute warm-up on a stationary bike, followed by a standard set of resistance-based exercises that included a leg press, hip extension, hip flexion, and hip abduction.
‘Reassuring’ Results
In a comment, consultant orthopedic surgeon Antony Palmer, MA, BMBCh, DPhil, said: “It’s reassuring that patients with advanced symptomatic osteoarthritis do well with hip replacements.”
THR does of course come with the potential risk for complications, but “the rate of these is what you’d expect for that procedure,” Palmer said, who works for the Nuffield Orthopaedic Centre, Oxford University Hospital NHS Foundation Trust, and is a senior clinical research fellow at Oxford University in England.
In the THR arm, there was one case of prosthetic joint infection, one hip dislocation, two revision surgeries, one instance of foot drop, and one case of gastroesophageal reflux. Meanwhile, in the resistance training group, there was one hip dislocation, one pelvic fracture, one case of atrial fibrillation, and one urinary tract and renal infection.
Overall, any serious adverse event was reported in six (12%) of 48 patients in the THR arm vs five (9%) of 55 participants in the resistance training group, of which only one, occurring in the resistance training group, resulted in discontinuation of the program.
Resistance Training Role
A notable finding was that, at 6 months, five (9%) people assigned to the THR arm had not undergone surgery, and 12 (21%) people in the resistance training group had undergone a THR.
This could suggest two things, Palmer suggested in the interview. The first is that there could be a small proportion of people assigned to THR who may not need the operation and do well with exercise therapy. And, conversely, there may be those who would do well having the surgery without first going through the intermediate stage of physical therapy.
It’s a suggestion that “maybe we’ve got to refine that a bit better and identify the patients that really do benefit from physiotherapy and who might not need hip replacement as a result,” Palmer said.
Or in other words, “should all patients undergo a program of physiotherapy before considering surgery?” he added.
Authors’ View
The PROHIP investigators conclude: “These results support current recommendations for the management of hip osteoarthritis and may be used to inform and guide shared decision making in clinical practice.”
Moreover, the results “do not oppose the use of resistance training as initial treatment,” says the authors.
Frydendal highlighted in his interview that nearly three out of four of the patients reported not to have undertaken any type of supervised exercise before entry into the study, which is a first-line, guideline-recommended option.
“If a patient tells me, ‘I haven’t done any exercise previously,’ I’d recommend starting with completing a 6- to 12-week exercise program that is tailored to your individual needs and evaluate your symptoms afterward,” he said.
“But we should refer the patient if our first-line treatment does not offer any improvements in the patient’s symptoms, as surgery with total hip replacement is clearly a really good treatment option,” Frydendal said.
The study was funded by the Danish Rheumatism Association, among other independent bodies. Frydendal and Palmer reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Hip Fractures in Patients With Dementia: To Operate or Not?
In the case of a hip fracture, operating on a patient with dementia can be a difficult decision to make. Indeed, surgery exposes patients with dementia to a higher mortality rate, more delirium and postoperative complications, and a greater loss of mobility than patients of the same age without cognitive impairments. For patients with dementia in institutional settings, survival is better for those who undergo surgery than for those who do not. But what about the prognosis of surgery vs no surgery for patients with dementia who live at home?
To answer this question, researchers in the United States conducted a cohort study using Medicare data. This retrospective study included patients aged 66 years and older with dementia who were living at home and not placed in institutions and who had a hip fracture between January 2017 and June 2018. Patients with incomplete observations, particularly regarding the location and type of residence (home/institution), were excluded from the analysis. Fractures were categorized as (i) fractures of the head and neck, (ii) pertrochanteric, (iii) subtrochanteric, and (iv) multiple/complex. The type and severity (mild, moderate, or severe) of dementia were identified using the diagnostic code list in the International Statistical Classification of Diseases, Tenth Revision.
Examining Mortality
The primary outcome was mortality at 30, 90, and 180 days. Secondary outcomes included hospital delirium; the need for subsequent hospitalization (within 6 months) or home health services (within 10 days); and intensive care interventions such as dialysis, intubation, resuscitation maneuvers, mechanical ventilation, or the insertion of a feeding tube.
Postoperative medical facility admissions were distinguished according to whether there was a plan to return home. To compare the surgery and nonsurgery groups, an inverse propensity score analysis was conducted within subgroups determined by fracture type, comorbidities (using the Elixhauser score), the person or entity responsible for admission (ie, physician, clinic, hospital, etc.), dual eligibility (Medicare and Medicaid), place of residence (ie, urban or rural), race, and sex. Dementia severity was estimated using a frailty index on the basis of evaluation tests that were systematically collected in the Medicare database.
Results Favored Surgery
Among 56,209 patients with dementia who were admitted for a hip fracture (73.0% women; mean age, 86.4 ± 7.0 years), 33,142 (59.0%) underwent surgery and 23,067 (41.0%) did not. Among surgically treated patients, 73.3% had fractures of the head or neck of the femur, and 40.2% had moderate to severe dementia. The nonsurgically treated fractures were 78.5% pertrochanteric. Comorbidities were evenly distributed between the two groups.
At 180 days, mortality was 31.8% in the surgery group compared with 45.7% in the nonsurgery group, resulting in a significant reduction in the unadjusted relative risk (RR) for death in favor of surgery (RR, 0.67; 95% CI, 0.60-0.76; P < .001). Among patients with mild dementia and a fracture of the head or neck of the femur, mortality at 180 days was 26.5% among surgical patients and 34.9% among nonsurgical patients (RR, 0.67; 95% CI, 0.60-0.76; P < .001). After the investigators adjusted for risk according to propensity score, the benefit of surgery remained significant at 30, 90, and 180 days, regardless of dementia severity. There was no significant difference in mortality for other types of hip fractures between the surgery and nonsurgery groups, however.
The adjusted RR for in-hospital delirium was 1.23 (P = .008), which was significant for the surgery group, but only for those with moderate to severe dementia. There were also fewer permanent placements (P < .001) among the surgically treated patients, and fewer patients with mild dementia required nurse care at home. There was no difference in resuscitation maneuvers between surgery and nonsurgery patients, whether the dementia was mild or not. For patients with a fracture of the head or neck of the femur, there was no difference in the likelihood of rehabilitation admission within 180 days, whether they were operated on or not.
Ethical Considerations
This study can inform discussions among healthcare professionals, patients, and patients’ families about which goals to set and which strategy to choose. The main interest of this study lies in its comparison of outcomes between patients with dementia who were operated on and those who were not, rather than comparing patients with and without dementia. Among patients with dementia living at home with a fracture of the head or neck of the femur, those who underwent surgery had a lower risk for death than those who did not, regardless of the severity of dementia.
It is noteworthy that less than two thirds of patients with dementia underwent surgery, which contradicts recommendations for almost routine surgery for patients with dementia. This observation raises questions about respecting patient wishes and advance directives when known, possible detrimental delays in referrals, and legal-medical issues.
Furthermore, the treatment choices of American surgeons are clearly influenced by the type of hip fracture. Fractures of the head and neck of the femur are typically treated with prosthetic arthroplasty, which simplifies postoperative care, compared with osteosynthesis. The latter procedure is more often used for extra-articular hip fractures but entails higher risks. While survival is an apparently more easily achievable goal through surgery, ethical considerations about other treatment objectives such as pain control, functional recovery, and treatment adequacy cannot be overlooked. It is worth noting that the French National Authority for Health issued recommendations in 2018 regarding the care pathway for patients hospitalized for a hip fracture within an orthogeriatric organization.
This story was translated from JIM, which is part of the Medscape Medical News professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
In the case of a hip fracture, operating on a patient with dementia can be a difficult decision to make. Indeed, surgery exposes patients with dementia to a higher mortality rate, more delirium and postoperative complications, and a greater loss of mobility than patients of the same age without cognitive impairments. For patients with dementia in institutional settings, survival is better for those who undergo surgery than for those who do not. But what about the prognosis of surgery vs no surgery for patients with dementia who live at home?
To answer this question, researchers in the United States conducted a cohort study using Medicare data. This retrospective study included patients aged 66 years and older with dementia who were living at home and not placed in institutions and who had a hip fracture between January 2017 and June 2018. Patients with incomplete observations, particularly regarding the location and type of residence (home/institution), were excluded from the analysis. Fractures were categorized as (i) fractures of the head and neck, (ii) pertrochanteric, (iii) subtrochanteric, and (iv) multiple/complex. The type and severity (mild, moderate, or severe) of dementia were identified using the diagnostic code list in the International Statistical Classification of Diseases, Tenth Revision.
Examining Mortality
The primary outcome was mortality at 30, 90, and 180 days. Secondary outcomes included hospital delirium; the need for subsequent hospitalization (within 6 months) or home health services (within 10 days); and intensive care interventions such as dialysis, intubation, resuscitation maneuvers, mechanical ventilation, or the insertion of a feeding tube.
Postoperative medical facility admissions were distinguished according to whether there was a plan to return home. To compare the surgery and nonsurgery groups, an inverse propensity score analysis was conducted within subgroups determined by fracture type, comorbidities (using the Elixhauser score), the person or entity responsible for admission (ie, physician, clinic, hospital, etc.), dual eligibility (Medicare and Medicaid), place of residence (ie, urban or rural), race, and sex. Dementia severity was estimated using a frailty index on the basis of evaluation tests that were systematically collected in the Medicare database.
Results Favored Surgery
Among 56,209 patients with dementia who were admitted for a hip fracture (73.0% women; mean age, 86.4 ± 7.0 years), 33,142 (59.0%) underwent surgery and 23,067 (41.0%) did not. Among surgically treated patients, 73.3% had fractures of the head or neck of the femur, and 40.2% had moderate to severe dementia. The nonsurgically treated fractures were 78.5% pertrochanteric. Comorbidities were evenly distributed between the two groups.
At 180 days, mortality was 31.8% in the surgery group compared with 45.7% in the nonsurgery group, resulting in a significant reduction in the unadjusted relative risk (RR) for death in favor of surgery (RR, 0.67; 95% CI, 0.60-0.76; P < .001). Among patients with mild dementia and a fracture of the head or neck of the femur, mortality at 180 days was 26.5% among surgical patients and 34.9% among nonsurgical patients (RR, 0.67; 95% CI, 0.60-0.76; P < .001). After the investigators adjusted for risk according to propensity score, the benefit of surgery remained significant at 30, 90, and 180 days, regardless of dementia severity. There was no significant difference in mortality for other types of hip fractures between the surgery and nonsurgery groups, however.
The adjusted RR for in-hospital delirium was 1.23 (P = .008), which was significant for the surgery group, but only for those with moderate to severe dementia. There were also fewer permanent placements (P < .001) among the surgically treated patients, and fewer patients with mild dementia required nurse care at home. There was no difference in resuscitation maneuvers between surgery and nonsurgery patients, whether the dementia was mild or not. For patients with a fracture of the head or neck of the femur, there was no difference in the likelihood of rehabilitation admission within 180 days, whether they were operated on or not.
Ethical Considerations
This study can inform discussions among healthcare professionals, patients, and patients’ families about which goals to set and which strategy to choose. The main interest of this study lies in its comparison of outcomes between patients with dementia who were operated on and those who were not, rather than comparing patients with and without dementia. Among patients with dementia living at home with a fracture of the head or neck of the femur, those who underwent surgery had a lower risk for death than those who did not, regardless of the severity of dementia.
It is noteworthy that less than two thirds of patients with dementia underwent surgery, which contradicts recommendations for almost routine surgery for patients with dementia. This observation raises questions about respecting patient wishes and advance directives when known, possible detrimental delays in referrals, and legal-medical issues.
Furthermore, the treatment choices of American surgeons are clearly influenced by the type of hip fracture. Fractures of the head and neck of the femur are typically treated with prosthetic arthroplasty, which simplifies postoperative care, compared with osteosynthesis. The latter procedure is more often used for extra-articular hip fractures but entails higher risks. While survival is an apparently more easily achievable goal through surgery, ethical considerations about other treatment objectives such as pain control, functional recovery, and treatment adequacy cannot be overlooked. It is worth noting that the French National Authority for Health issued recommendations in 2018 regarding the care pathway for patients hospitalized for a hip fracture within an orthogeriatric organization.
This story was translated from JIM, which is part of the Medscape Medical News professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
In the case of a hip fracture, operating on a patient with dementia can be a difficult decision to make. Indeed, surgery exposes patients with dementia to a higher mortality rate, more delirium and postoperative complications, and a greater loss of mobility than patients of the same age without cognitive impairments. For patients with dementia in institutional settings, survival is better for those who undergo surgery than for those who do not. But what about the prognosis of surgery vs no surgery for patients with dementia who live at home?
To answer this question, researchers in the United States conducted a cohort study using Medicare data. This retrospective study included patients aged 66 years and older with dementia who were living at home and not placed in institutions and who had a hip fracture between January 2017 and June 2018. Patients with incomplete observations, particularly regarding the location and type of residence (home/institution), were excluded from the analysis. Fractures were categorized as (i) fractures of the head and neck, (ii) pertrochanteric, (iii) subtrochanteric, and (iv) multiple/complex. The type and severity (mild, moderate, or severe) of dementia were identified using the diagnostic code list in the International Statistical Classification of Diseases, Tenth Revision.
Examining Mortality
The primary outcome was mortality at 30, 90, and 180 days. Secondary outcomes included hospital delirium; the need for subsequent hospitalization (within 6 months) or home health services (within 10 days); and intensive care interventions such as dialysis, intubation, resuscitation maneuvers, mechanical ventilation, or the insertion of a feeding tube.
Postoperative medical facility admissions were distinguished according to whether there was a plan to return home. To compare the surgery and nonsurgery groups, an inverse propensity score analysis was conducted within subgroups determined by fracture type, comorbidities (using the Elixhauser score), the person or entity responsible for admission (ie, physician, clinic, hospital, etc.), dual eligibility (Medicare and Medicaid), place of residence (ie, urban or rural), race, and sex. Dementia severity was estimated using a frailty index on the basis of evaluation tests that were systematically collected in the Medicare database.
Results Favored Surgery
Among 56,209 patients with dementia who were admitted for a hip fracture (73.0% women; mean age, 86.4 ± 7.0 years), 33,142 (59.0%) underwent surgery and 23,067 (41.0%) did not. Among surgically treated patients, 73.3% had fractures of the head or neck of the femur, and 40.2% had moderate to severe dementia. The nonsurgically treated fractures were 78.5% pertrochanteric. Comorbidities were evenly distributed between the two groups.
At 180 days, mortality was 31.8% in the surgery group compared with 45.7% in the nonsurgery group, resulting in a significant reduction in the unadjusted relative risk (RR) for death in favor of surgery (RR, 0.67; 95% CI, 0.60-0.76; P < .001). Among patients with mild dementia and a fracture of the head or neck of the femur, mortality at 180 days was 26.5% among surgical patients and 34.9% among nonsurgical patients (RR, 0.67; 95% CI, 0.60-0.76; P < .001). After the investigators adjusted for risk according to propensity score, the benefit of surgery remained significant at 30, 90, and 180 days, regardless of dementia severity. There was no significant difference in mortality for other types of hip fractures between the surgery and nonsurgery groups, however.
The adjusted RR for in-hospital delirium was 1.23 (P = .008), which was significant for the surgery group, but only for those with moderate to severe dementia. There were also fewer permanent placements (P < .001) among the surgically treated patients, and fewer patients with mild dementia required nurse care at home. There was no difference in resuscitation maneuvers between surgery and nonsurgery patients, whether the dementia was mild or not. For patients with a fracture of the head or neck of the femur, there was no difference in the likelihood of rehabilitation admission within 180 days, whether they were operated on or not.
Ethical Considerations
This study can inform discussions among healthcare professionals, patients, and patients’ families about which goals to set and which strategy to choose. The main interest of this study lies in its comparison of outcomes between patients with dementia who were operated on and those who were not, rather than comparing patients with and without dementia. Among patients with dementia living at home with a fracture of the head or neck of the femur, those who underwent surgery had a lower risk for death than those who did not, regardless of the severity of dementia.
It is noteworthy that less than two thirds of patients with dementia underwent surgery, which contradicts recommendations for almost routine surgery for patients with dementia. This observation raises questions about respecting patient wishes and advance directives when known, possible detrimental delays in referrals, and legal-medical issues.
Furthermore, the treatment choices of American surgeons are clearly influenced by the type of hip fracture. Fractures of the head and neck of the femur are typically treated with prosthetic arthroplasty, which simplifies postoperative care, compared with osteosynthesis. The latter procedure is more often used for extra-articular hip fractures but entails higher risks. While survival is an apparently more easily achievable goal through surgery, ethical considerations about other treatment objectives such as pain control, functional recovery, and treatment adequacy cannot be overlooked. It is worth noting that the French National Authority for Health issued recommendations in 2018 regarding the care pathway for patients hospitalized for a hip fracture within an orthogeriatric organization.
This story was translated from JIM, which is part of the Medscape Medical News professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Are There Benefits to Taking GLP-1 Receptor Agonists Before Joint Surgery?
Obesity and diabetes increase the risk for complications following joint surgeries like total hip replacement, but can semaglutide and related drugs help?
The question has massive implications. More than 450,000 total hip arthroplasty (THA) procedures are performed annually in the United States, with the number expected to grow to 850,000 by 2030. Obesity is the leading reason for the increase. Semaglutide and other glucagon-like peptide 1 (GLP-1) receptor agonists can lead to dramatic and rapid weight loss, in addition to controlling diabetes, so researchers have wondered if the medications might improve outcomes in patients undergoing joint surgery.
Two studies presented at the 2024 annual meeting of the American Academy of Orthopaedic Surgeons (AAOS) sought to answer the question — but reached different conclusions.
One study of THA patients taking semaglutide found fewer 90-day readmissions for diabetes and fewer prosthetic joint infections at the 2-year mark. Another found similar outcomes on the need for revision surgery, infections, and many other postsurgery metrics in people who took the GLP-1 receptor agonist and those who did not. Neither study had outside funding.
Study: Fewer Infections, Readmissions
For their study, Matthew Magruder, MD, a third-year orthopedic resident at Maimonides Medical Center’s Department of Orthopaedic Surgery and Rehabilitation in New York City, and his colleagues used an administrative claim database (PearlDiver) to identify THA patients who underwent the surgery between January 1, 2020, to October 31, 2021, when semaglutide was approved for the treatment of diabetes but not yet for obesity. The researchers found 9465 patients who had had a primary THA, of whom 1653 had received a prescription for semaglutide.
In total, 84.9% of those on semaglutide had obesity, as did 85.2% of those not on the medication.
Dr. Magruder’s group looked at medical complications such as deep vein thrombosis, myocardial infarction, hypoglycemia, and pulmonary embolism within 90 days of surgery, implant-related complications 2 years after the procedure, rates of readmission within 90 days of the procedure, length of stay in the hospital, and costs of care.
They found that patients taking semaglutide were less likely to be readmitted to the hospital within 90 days of THA (6.2% vs 8.8%; P <.01) and experienced fewer joint infections (1.6% vs 2.9%; P <.01). No significant differences were found in the other outcomes.
Among the potential concerns involving the use of GLP-1 receptor agonists in patients undergoing surgery are their potential to cause hypoglycemia and the risk for aspiration during anesthesia. But those issues did not emerge in the analysis.
“We concluded that this was preliminary evidence that using semaglutide at the time of surgery was safe and potentially effective at reducing complications,” said Dr. Magruder, whose team published their findings in The Journal of Arthroplasty.
Study: Semaglutide Has No Effect on Postop Complications
In another study presented at the AAOS meeting, researchers found that rates of complications after THA were similar in patients with obesity who took semaglutide and those who did not. That information could be helpful for clinicians who have been reluctant to perform THA procedures in patients who also have had bariatric surgery, said Daniel E. Pereira, MD, a resident at Washington University in St. Louis and the first author of the study.
A recent retrospective review found that patients who had bariatric surgery have worse implant survivorship and higher rates of dislocation than do those with a naturally low or high body mass index (BMI).
Pereira and his colleagues used a national database, with deidentified patient records, originally finding 42,410 patients. After matching, they evaluated 616 in each cohort: those who took semaglutide and those who did not. The average age was 62.7 years; average BMI was 35.5.
Both groups had a similar risk for a range of complications including revision surgery, infection of the new joint and surgical site, opioid-related disorders, pulmonary embolism, deep vein thrombosis, and mortality.
“We didn’t observe anything significant [between groups] in terms of the complications,” said David Momtaz, MPH, a fourth-year medical student at the University of Texas Health Science Center at San Antonio, who helped conduct the research.
Dr. Pereira said he hoped the results would end the hesitation he observes, partly due to a lack of research, among some physicians about prescribing semaglutide before THA in appropriate patients. “Our preliminary evidence suggests there is no need to withhold THA in patients who successfully lost weight on semaglutide,” he said.
Expert Perspective: Not Unexpected
Peter Hanson, MD, an orthopedic surgeon and orthopedic medical director at Sharp Grossmont Hospital in La Mesa, California, who specializes in hip and knee replacement, said he was unsurprised by the findings.
The patients he has observed on GLP-1 receptor agonists lose weight, he said, and a few even to the point of not needing a replacement. A recent study found that every 1% decrease in weight was associated with a 2% reduced risk for knee replacement in those with knee osteoarthritis or at risk for it, and every 1% drop in weight was associated with a 3% reduced risk for THA.
“I always advise my overweight patient to lose at least 30 pounds, even if their BMI is less than 40, like many in these studies,” Dr. Hanson said. If a patient’s doctor prescribes semaglutide or another GLP-1 receptor agonist, “I am very supportive, and we postpone surgery until the weight loss is maximized,” he added.
Drs. Magruder, Pereira, Momtaz, and Hanson have no disclosures.
A version of this article appeared on Medscape.com.
Obesity and diabetes increase the risk for complications following joint surgeries like total hip replacement, but can semaglutide and related drugs help?
The question has massive implications. More than 450,000 total hip arthroplasty (THA) procedures are performed annually in the United States, with the number expected to grow to 850,000 by 2030. Obesity is the leading reason for the increase. Semaglutide and other glucagon-like peptide 1 (GLP-1) receptor agonists can lead to dramatic and rapid weight loss, in addition to controlling diabetes, so researchers have wondered if the medications might improve outcomes in patients undergoing joint surgery.
Two studies presented at the 2024 annual meeting of the American Academy of Orthopaedic Surgeons (AAOS) sought to answer the question — but reached different conclusions.
One study of THA patients taking semaglutide found fewer 90-day readmissions for diabetes and fewer prosthetic joint infections at the 2-year mark. Another found similar outcomes on the need for revision surgery, infections, and many other postsurgery metrics in people who took the GLP-1 receptor agonist and those who did not. Neither study had outside funding.
Study: Fewer Infections, Readmissions
For their study, Matthew Magruder, MD, a third-year orthopedic resident at Maimonides Medical Center’s Department of Orthopaedic Surgery and Rehabilitation in New York City, and his colleagues used an administrative claim database (PearlDiver) to identify THA patients who underwent the surgery between January 1, 2020, to October 31, 2021, when semaglutide was approved for the treatment of diabetes but not yet for obesity. The researchers found 9465 patients who had had a primary THA, of whom 1653 had received a prescription for semaglutide.
In total, 84.9% of those on semaglutide had obesity, as did 85.2% of those not on the medication.
Dr. Magruder’s group looked at medical complications such as deep vein thrombosis, myocardial infarction, hypoglycemia, and pulmonary embolism within 90 days of surgery, implant-related complications 2 years after the procedure, rates of readmission within 90 days of the procedure, length of stay in the hospital, and costs of care.
They found that patients taking semaglutide were less likely to be readmitted to the hospital within 90 days of THA (6.2% vs 8.8%; P <.01) and experienced fewer joint infections (1.6% vs 2.9%; P <.01). No significant differences were found in the other outcomes.
Among the potential concerns involving the use of GLP-1 receptor agonists in patients undergoing surgery are their potential to cause hypoglycemia and the risk for aspiration during anesthesia. But those issues did not emerge in the analysis.
“We concluded that this was preliminary evidence that using semaglutide at the time of surgery was safe and potentially effective at reducing complications,” said Dr. Magruder, whose team published their findings in The Journal of Arthroplasty.
Study: Semaglutide Has No Effect on Postop Complications
In another study presented at the AAOS meeting, researchers found that rates of complications after THA were similar in patients with obesity who took semaglutide and those who did not. That information could be helpful for clinicians who have been reluctant to perform THA procedures in patients who also have had bariatric surgery, said Daniel E. Pereira, MD, a resident at Washington University in St. Louis and the first author of the study.
A recent retrospective review found that patients who had bariatric surgery have worse implant survivorship and higher rates of dislocation than do those with a naturally low or high body mass index (BMI).
Pereira and his colleagues used a national database, with deidentified patient records, originally finding 42,410 patients. After matching, they evaluated 616 in each cohort: those who took semaglutide and those who did not. The average age was 62.7 years; average BMI was 35.5.
Both groups had a similar risk for a range of complications including revision surgery, infection of the new joint and surgical site, opioid-related disorders, pulmonary embolism, deep vein thrombosis, and mortality.
“We didn’t observe anything significant [between groups] in terms of the complications,” said David Momtaz, MPH, a fourth-year medical student at the University of Texas Health Science Center at San Antonio, who helped conduct the research.
Dr. Pereira said he hoped the results would end the hesitation he observes, partly due to a lack of research, among some physicians about prescribing semaglutide before THA in appropriate patients. “Our preliminary evidence suggests there is no need to withhold THA in patients who successfully lost weight on semaglutide,” he said.
Expert Perspective: Not Unexpected
Peter Hanson, MD, an orthopedic surgeon and orthopedic medical director at Sharp Grossmont Hospital in La Mesa, California, who specializes in hip and knee replacement, said he was unsurprised by the findings.
The patients he has observed on GLP-1 receptor agonists lose weight, he said, and a few even to the point of not needing a replacement. A recent study found that every 1% decrease in weight was associated with a 2% reduced risk for knee replacement in those with knee osteoarthritis or at risk for it, and every 1% drop in weight was associated with a 3% reduced risk for THA.
“I always advise my overweight patient to lose at least 30 pounds, even if their BMI is less than 40, like many in these studies,” Dr. Hanson said. If a patient’s doctor prescribes semaglutide or another GLP-1 receptor agonist, “I am very supportive, and we postpone surgery until the weight loss is maximized,” he added.
Drs. Magruder, Pereira, Momtaz, and Hanson have no disclosures.
A version of this article appeared on Medscape.com.
Obesity and diabetes increase the risk for complications following joint surgeries like total hip replacement, but can semaglutide and related drugs help?
The question has massive implications. More than 450,000 total hip arthroplasty (THA) procedures are performed annually in the United States, with the number expected to grow to 850,000 by 2030. Obesity is the leading reason for the increase. Semaglutide and other glucagon-like peptide 1 (GLP-1) receptor agonists can lead to dramatic and rapid weight loss, in addition to controlling diabetes, so researchers have wondered if the medications might improve outcomes in patients undergoing joint surgery.
Two studies presented at the 2024 annual meeting of the American Academy of Orthopaedic Surgeons (AAOS) sought to answer the question — but reached different conclusions.
One study of THA patients taking semaglutide found fewer 90-day readmissions for diabetes and fewer prosthetic joint infections at the 2-year mark. Another found similar outcomes on the need for revision surgery, infections, and many other postsurgery metrics in people who took the GLP-1 receptor agonist and those who did not. Neither study had outside funding.
Study: Fewer Infections, Readmissions
For their study, Matthew Magruder, MD, a third-year orthopedic resident at Maimonides Medical Center’s Department of Orthopaedic Surgery and Rehabilitation in New York City, and his colleagues used an administrative claim database (PearlDiver) to identify THA patients who underwent the surgery between January 1, 2020, to October 31, 2021, when semaglutide was approved for the treatment of diabetes but not yet for obesity. The researchers found 9465 patients who had had a primary THA, of whom 1653 had received a prescription for semaglutide.
In total, 84.9% of those on semaglutide had obesity, as did 85.2% of those not on the medication.
Dr. Magruder’s group looked at medical complications such as deep vein thrombosis, myocardial infarction, hypoglycemia, and pulmonary embolism within 90 days of surgery, implant-related complications 2 years after the procedure, rates of readmission within 90 days of the procedure, length of stay in the hospital, and costs of care.
They found that patients taking semaglutide were less likely to be readmitted to the hospital within 90 days of THA (6.2% vs 8.8%; P <.01) and experienced fewer joint infections (1.6% vs 2.9%; P <.01). No significant differences were found in the other outcomes.
Among the potential concerns involving the use of GLP-1 receptor agonists in patients undergoing surgery are their potential to cause hypoglycemia and the risk for aspiration during anesthesia. But those issues did not emerge in the analysis.
“We concluded that this was preliminary evidence that using semaglutide at the time of surgery was safe and potentially effective at reducing complications,” said Dr. Magruder, whose team published their findings in The Journal of Arthroplasty.
Study: Semaglutide Has No Effect on Postop Complications
In another study presented at the AAOS meeting, researchers found that rates of complications after THA were similar in patients with obesity who took semaglutide and those who did not. That information could be helpful for clinicians who have been reluctant to perform THA procedures in patients who also have had bariatric surgery, said Daniel E. Pereira, MD, a resident at Washington University in St. Louis and the first author of the study.
A recent retrospective review found that patients who had bariatric surgery have worse implant survivorship and higher rates of dislocation than do those with a naturally low or high body mass index (BMI).
Pereira and his colleagues used a national database, with deidentified patient records, originally finding 42,410 patients. After matching, they evaluated 616 in each cohort: those who took semaglutide and those who did not. The average age was 62.7 years; average BMI was 35.5.
Both groups had a similar risk for a range of complications including revision surgery, infection of the new joint and surgical site, opioid-related disorders, pulmonary embolism, deep vein thrombosis, and mortality.
“We didn’t observe anything significant [between groups] in terms of the complications,” said David Momtaz, MPH, a fourth-year medical student at the University of Texas Health Science Center at San Antonio, who helped conduct the research.
Dr. Pereira said he hoped the results would end the hesitation he observes, partly due to a lack of research, among some physicians about prescribing semaglutide before THA in appropriate patients. “Our preliminary evidence suggests there is no need to withhold THA in patients who successfully lost weight on semaglutide,” he said.
Expert Perspective: Not Unexpected
Peter Hanson, MD, an orthopedic surgeon and orthopedic medical director at Sharp Grossmont Hospital in La Mesa, California, who specializes in hip and knee replacement, said he was unsurprised by the findings.
The patients he has observed on GLP-1 receptor agonists lose weight, he said, and a few even to the point of not needing a replacement. A recent study found that every 1% decrease in weight was associated with a 2% reduced risk for knee replacement in those with knee osteoarthritis or at risk for it, and every 1% drop in weight was associated with a 3% reduced risk for THA.
“I always advise my overweight patient to lose at least 30 pounds, even if their BMI is less than 40, like many in these studies,” Dr. Hanson said. If a patient’s doctor prescribes semaglutide or another GLP-1 receptor agonist, “I am very supportive, and we postpone surgery until the weight loss is maximized,” he added.
Drs. Magruder, Pereira, Momtaz, and Hanson have no disclosures.
A version of this article appeared on Medscape.com.
FROM AAOS 2024
Marathon running does not increase arthritis risk: Survey
Runners who had undergone knee or hip surgery or had a previous hip or knee injury that prevented running were most likely to have arthritis, researchers found. Family history of arthritis, higher body mass index (BMI), and older age were also associated with increased risk of the condition.
The study was presented at the American Academy of Orthopaedic Surgeons 2023 Annual Meeting.
It has generally been thought that running may increase risk of osteoarthritis because it puts more load on joints than walking or standing, noted Grace Hsiao-Wei Lo, MD, an assistant professor of immunology, allergy, and rheumatology at the Baylor College of Medicine, Houston, who was not involved with the work. Research in this area has yielded mixed results: A 2017 analysis of multiple studies found that competitive runners did have higher rates of arthritis than recreational runners, while another study conducted by Dr. Lo found that runners did not have an increased risk of knee osteoarthritis, compared with nonrunners. A 2018 study showed that marathon runners had lower instances of arthritis, compared with the general population.
In this new study, researchers surveyed 3,804 runners who participated in the 2019 or 2021 Chicago Marathon about their running history, average mileage per week, and average running pace. The survey also asked about known risk factors for osteoarthritis, including BMI, family history of arthritis, and past knee and hip injuries that prevented running.
Runners, on average, were about 44 years old and ran 27.9 miles per week. The largest proportion of respondents had completed 2-5 marathons (37.3%), around 21% of respondents had finished 6-10 marathons, and 17% were running their first marathon. Study participants had an average of 15 years of running experience, 1,892 reported a previous hip or knee injury, and 413 had undergone knee or hip surgery. Overall, 36.4% reported experiencing hip or knee pain in the past year, and 7.3% had been diagnosed with arthritis.
Researchers found that there was no association between the risk of osteoarthritis and weekly mileage, years spent running, number of marathons completed, or running pace. Respondents who had undergone knee or hip surgery had the highest risk of osteoarthritis (odds ratio, 5.85; P < .0001), followed by those with a history of knee or hip injuries that prevented running (OR, 5.04; P < .0001). Other identified risk factors were family history of arthritis (OR, 3.47; P < .0001), BMI (OR, 1.10; P < .0001), and older age (OR, 1.08; P < .0001).
The news should be encouraging for runners, said Matthew Hartwell, MD, an orthopedic surgeon at the University of California, San Francisco, who led the research. If someone does not have injuries or surgeries that keep them from running, “you can still continue to run,” he said. “There may not necessarily be this dose-response relationship where the more you run, the more you break down your knee or your hip.”
Still, 24.2% of runners reported that their physician had advised them to reduce their mileage or stop running altogether. Most runners (94.2%) said they planned to run another marathon.
“The results of this study are consistent with the experiences of many lifelong runners and observations of sports medicine professionals that osteoarthritis is not an inevitable consequence of distance running,” said Brett Toresdahl, MD, a sports medicine physician at the Hospital for Special Surgery in New York, who was not involved with the study.
Still, he emphasized that more research is necessary to understand whether running contributes to the risk of developing osteoarthritis. The participants in the study were current marathoners, he noted, so it is likely they have healthy joints that can tolerate running longer distances. “If there is a subset of people who have joints that are negatively affected by running, they wouldn’t likely be registering for a marathon,” he said in an email interview.
Dr. Lo added that comparing these marathoners to a group who did not run would help assess whether running can be harmful to joints. “To be fair, this is a challenging subject to study,” she said. “Osteoarthritis has a long natural history, and so it is difficult to evaluate this kind of question over many years of running and many years of evaluation of arthritis.”
While the research does not answer the question of whether running can lead to osteoarthritis, it helps show the need for long-term research on how running affects joints over time as well as one’s general health, Dr. Toresdahl noted. “I would not be surprised if future longitudinal research will come to the same conclusion that running for the majority of patients is a net benefit for overall health and at least net neutral for joint health when done in moderation,” he said.
Dr. Hartwell, Dr. Lo, and Dr. Toresdahl report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Runners who had undergone knee or hip surgery or had a previous hip or knee injury that prevented running were most likely to have arthritis, researchers found. Family history of arthritis, higher body mass index (BMI), and older age were also associated with increased risk of the condition.
The study was presented at the American Academy of Orthopaedic Surgeons 2023 Annual Meeting.
It has generally been thought that running may increase risk of osteoarthritis because it puts more load on joints than walking or standing, noted Grace Hsiao-Wei Lo, MD, an assistant professor of immunology, allergy, and rheumatology at the Baylor College of Medicine, Houston, who was not involved with the work. Research in this area has yielded mixed results: A 2017 analysis of multiple studies found that competitive runners did have higher rates of arthritis than recreational runners, while another study conducted by Dr. Lo found that runners did not have an increased risk of knee osteoarthritis, compared with nonrunners. A 2018 study showed that marathon runners had lower instances of arthritis, compared with the general population.
In this new study, researchers surveyed 3,804 runners who participated in the 2019 or 2021 Chicago Marathon about their running history, average mileage per week, and average running pace. The survey also asked about known risk factors for osteoarthritis, including BMI, family history of arthritis, and past knee and hip injuries that prevented running.
Runners, on average, were about 44 years old and ran 27.9 miles per week. The largest proportion of respondents had completed 2-5 marathons (37.3%), around 21% of respondents had finished 6-10 marathons, and 17% were running their first marathon. Study participants had an average of 15 years of running experience, 1,892 reported a previous hip or knee injury, and 413 had undergone knee or hip surgery. Overall, 36.4% reported experiencing hip or knee pain in the past year, and 7.3% had been diagnosed with arthritis.
Researchers found that there was no association between the risk of osteoarthritis and weekly mileage, years spent running, number of marathons completed, or running pace. Respondents who had undergone knee or hip surgery had the highest risk of osteoarthritis (odds ratio, 5.85; P < .0001), followed by those with a history of knee or hip injuries that prevented running (OR, 5.04; P < .0001). Other identified risk factors were family history of arthritis (OR, 3.47; P < .0001), BMI (OR, 1.10; P < .0001), and older age (OR, 1.08; P < .0001).
The news should be encouraging for runners, said Matthew Hartwell, MD, an orthopedic surgeon at the University of California, San Francisco, who led the research. If someone does not have injuries or surgeries that keep them from running, “you can still continue to run,” he said. “There may not necessarily be this dose-response relationship where the more you run, the more you break down your knee or your hip.”
Still, 24.2% of runners reported that their physician had advised them to reduce their mileage or stop running altogether. Most runners (94.2%) said they planned to run another marathon.
“The results of this study are consistent with the experiences of many lifelong runners and observations of sports medicine professionals that osteoarthritis is not an inevitable consequence of distance running,” said Brett Toresdahl, MD, a sports medicine physician at the Hospital for Special Surgery in New York, who was not involved with the study.
Still, he emphasized that more research is necessary to understand whether running contributes to the risk of developing osteoarthritis. The participants in the study were current marathoners, he noted, so it is likely they have healthy joints that can tolerate running longer distances. “If there is a subset of people who have joints that are negatively affected by running, they wouldn’t likely be registering for a marathon,” he said in an email interview.
Dr. Lo added that comparing these marathoners to a group who did not run would help assess whether running can be harmful to joints. “To be fair, this is a challenging subject to study,” she said. “Osteoarthritis has a long natural history, and so it is difficult to evaluate this kind of question over many years of running and many years of evaluation of arthritis.”
While the research does not answer the question of whether running can lead to osteoarthritis, it helps show the need for long-term research on how running affects joints over time as well as one’s general health, Dr. Toresdahl noted. “I would not be surprised if future longitudinal research will come to the same conclusion that running for the majority of patients is a net benefit for overall health and at least net neutral for joint health when done in moderation,” he said.
Dr. Hartwell, Dr. Lo, and Dr. Toresdahl report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Runners who had undergone knee or hip surgery or had a previous hip or knee injury that prevented running were most likely to have arthritis, researchers found. Family history of arthritis, higher body mass index (BMI), and older age were also associated with increased risk of the condition.
The study was presented at the American Academy of Orthopaedic Surgeons 2023 Annual Meeting.
It has generally been thought that running may increase risk of osteoarthritis because it puts more load on joints than walking or standing, noted Grace Hsiao-Wei Lo, MD, an assistant professor of immunology, allergy, and rheumatology at the Baylor College of Medicine, Houston, who was not involved with the work. Research in this area has yielded mixed results: A 2017 analysis of multiple studies found that competitive runners did have higher rates of arthritis than recreational runners, while another study conducted by Dr. Lo found that runners did not have an increased risk of knee osteoarthritis, compared with nonrunners. A 2018 study showed that marathon runners had lower instances of arthritis, compared with the general population.
In this new study, researchers surveyed 3,804 runners who participated in the 2019 or 2021 Chicago Marathon about their running history, average mileage per week, and average running pace. The survey also asked about known risk factors for osteoarthritis, including BMI, family history of arthritis, and past knee and hip injuries that prevented running.
Runners, on average, were about 44 years old and ran 27.9 miles per week. The largest proportion of respondents had completed 2-5 marathons (37.3%), around 21% of respondents had finished 6-10 marathons, and 17% were running their first marathon. Study participants had an average of 15 years of running experience, 1,892 reported a previous hip or knee injury, and 413 had undergone knee or hip surgery. Overall, 36.4% reported experiencing hip or knee pain in the past year, and 7.3% had been diagnosed with arthritis.
Researchers found that there was no association between the risk of osteoarthritis and weekly mileage, years spent running, number of marathons completed, or running pace. Respondents who had undergone knee or hip surgery had the highest risk of osteoarthritis (odds ratio, 5.85; P < .0001), followed by those with a history of knee or hip injuries that prevented running (OR, 5.04; P < .0001). Other identified risk factors were family history of arthritis (OR, 3.47; P < .0001), BMI (OR, 1.10; P < .0001), and older age (OR, 1.08; P < .0001).
The news should be encouraging for runners, said Matthew Hartwell, MD, an orthopedic surgeon at the University of California, San Francisco, who led the research. If someone does not have injuries or surgeries that keep them from running, “you can still continue to run,” he said. “There may not necessarily be this dose-response relationship where the more you run, the more you break down your knee or your hip.”
Still, 24.2% of runners reported that their physician had advised them to reduce their mileage or stop running altogether. Most runners (94.2%) said they planned to run another marathon.
“The results of this study are consistent with the experiences of many lifelong runners and observations of sports medicine professionals that osteoarthritis is not an inevitable consequence of distance running,” said Brett Toresdahl, MD, a sports medicine physician at the Hospital for Special Surgery in New York, who was not involved with the study.
Still, he emphasized that more research is necessary to understand whether running contributes to the risk of developing osteoarthritis. The participants in the study were current marathoners, he noted, so it is likely they have healthy joints that can tolerate running longer distances. “If there is a subset of people who have joints that are negatively affected by running, they wouldn’t likely be registering for a marathon,” he said in an email interview.
Dr. Lo added that comparing these marathoners to a group who did not run would help assess whether running can be harmful to joints. “To be fair, this is a challenging subject to study,” she said. “Osteoarthritis has a long natural history, and so it is difficult to evaluate this kind of question over many years of running and many years of evaluation of arthritis.”
While the research does not answer the question of whether running can lead to osteoarthritis, it helps show the need for long-term research on how running affects joints over time as well as one’s general health, Dr. Toresdahl noted. “I would not be surprised if future longitudinal research will come to the same conclusion that running for the majority of patients is a net benefit for overall health and at least net neutral for joint health when done in moderation,” he said.
Dr. Hartwell, Dr. Lo, and Dr. Toresdahl report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM AAOS 2023
Guidelines: Don’t delay total joint arthroplasty for additional nonoperative therapies
Patients with moderate to severe osteoarthritis (OA) or osteonecrosis (ON) eligible for total joint arthroplasty (TJA) who have failed one or more nonoperative therapies should proceed directly to surgery, according to new guidelines from the American College of Rheumatology and the American Association of Hip and Knee Surgeons.
“One of the reasons for creating this guideline was that many patients have been subjected to delays for surgery after completing nonoperative therapy, despite persistent moderate to severe pain, loss of function, and moderate to severe radiographic OA or ON,” said coauthors Susan M. Goodman, MD, a rheumatologist at Hospital for Special Surgery in New York, and Charles Hannon, MD, an orthopedic surgeon at Washington University in St. Louis, in an email interview with this news organization. “This guideline supports surgery being performed in an expeditious fashion after the decision has been made to proceed with surgery by both the physician and patient through a shared decision-making process,” they said.
The guidelines also state that obesity by itself should not be a reason to delay TJA. “We could not find a rationale for a strict cut off for weight/body mass index (BMI). Our literature review revealed that though many adverse events were, in fact, increased in patients with morbid obesity, there is also an increase in adverse events for those who had bariatric surgery prior to their arthroplasty,” they added, noting that patients need to be made aware of the increased risk for adverse events in patients with obesity. Though the guidelines do not pose any BMI cutoffs, they state that weight loss should be “strongly encouraged.” These new recommendations are conditional, and all had a “low” to “very low” certainty of evidence; however, there was high consensus on the recommendations from the expert panel.
The guidelines also recommended:
- Delaying TJA to achieve smoking and nicotine cessation or reduction.
- Delaying TJA to improve glycemic control in patients with diabetes, although the group did not recommend any specific measure or threshold.
- Not delaying TJA in patients with a severe deformity, bone loss, or a neuropathic joint.
The new guidelines formalize what many surgeons have already been doing for the past few years, said Arjun Saxena, MD, MBA, an orthopedic surgeon in Philadelphia who was not involved with the guidelines. “A lot of total joint programs have really focused on patient optimization, including smoking cessation, glycemic control, and weight loss prior to surgery,” he said.
Most importantly, the guidelines put an emphasis on how the decision to proceed with TJA should be a shared decision between a physician and patient, he added. Some insurance companies with prior authorization policies may require a patient to try additional nonoperative therapies before approving surgery, creating barriers to care, he said. “Hopefully [these new recommendations] will help third parties understand that joint replacement is a big decision – most doctors aren’t going to recommend that unless it’s necessary or something that is going to help patients,” he said. “I understand that there is a certain need for preauthorization, but just having strict guidelines isn’t appropriate. You really need to look at the whole picture,” he added.
The full manuscript has been submitted for review and is expected to be jointly published in American College of Rheumatology and the American Association of Hip and Knee Surgeons journals later this year.
Dr. Saxena consults for the orthopedic implant company Corin.
A version of this article originally appeared on Medscape.com.
Patients with moderate to severe osteoarthritis (OA) or osteonecrosis (ON) eligible for total joint arthroplasty (TJA) who have failed one or more nonoperative therapies should proceed directly to surgery, according to new guidelines from the American College of Rheumatology and the American Association of Hip and Knee Surgeons.
“One of the reasons for creating this guideline was that many patients have been subjected to delays for surgery after completing nonoperative therapy, despite persistent moderate to severe pain, loss of function, and moderate to severe radiographic OA or ON,” said coauthors Susan M. Goodman, MD, a rheumatologist at Hospital for Special Surgery in New York, and Charles Hannon, MD, an orthopedic surgeon at Washington University in St. Louis, in an email interview with this news organization. “This guideline supports surgery being performed in an expeditious fashion after the decision has been made to proceed with surgery by both the physician and patient through a shared decision-making process,” they said.
The guidelines also state that obesity by itself should not be a reason to delay TJA. “We could not find a rationale for a strict cut off for weight/body mass index (BMI). Our literature review revealed that though many adverse events were, in fact, increased in patients with morbid obesity, there is also an increase in adverse events for those who had bariatric surgery prior to their arthroplasty,” they added, noting that patients need to be made aware of the increased risk for adverse events in patients with obesity. Though the guidelines do not pose any BMI cutoffs, they state that weight loss should be “strongly encouraged.” These new recommendations are conditional, and all had a “low” to “very low” certainty of evidence; however, there was high consensus on the recommendations from the expert panel.
The guidelines also recommended:
- Delaying TJA to achieve smoking and nicotine cessation or reduction.
- Delaying TJA to improve glycemic control in patients with diabetes, although the group did not recommend any specific measure or threshold.
- Not delaying TJA in patients with a severe deformity, bone loss, or a neuropathic joint.
The new guidelines formalize what many surgeons have already been doing for the past few years, said Arjun Saxena, MD, MBA, an orthopedic surgeon in Philadelphia who was not involved with the guidelines. “A lot of total joint programs have really focused on patient optimization, including smoking cessation, glycemic control, and weight loss prior to surgery,” he said.
Most importantly, the guidelines put an emphasis on how the decision to proceed with TJA should be a shared decision between a physician and patient, he added. Some insurance companies with prior authorization policies may require a patient to try additional nonoperative therapies before approving surgery, creating barriers to care, he said. “Hopefully [these new recommendations] will help third parties understand that joint replacement is a big decision – most doctors aren’t going to recommend that unless it’s necessary or something that is going to help patients,” he said. “I understand that there is a certain need for preauthorization, but just having strict guidelines isn’t appropriate. You really need to look at the whole picture,” he added.
The full manuscript has been submitted for review and is expected to be jointly published in American College of Rheumatology and the American Association of Hip and Knee Surgeons journals later this year.
Dr. Saxena consults for the orthopedic implant company Corin.
A version of this article originally appeared on Medscape.com.
Patients with moderate to severe osteoarthritis (OA) or osteonecrosis (ON) eligible for total joint arthroplasty (TJA) who have failed one or more nonoperative therapies should proceed directly to surgery, according to new guidelines from the American College of Rheumatology and the American Association of Hip and Knee Surgeons.
“One of the reasons for creating this guideline was that many patients have been subjected to delays for surgery after completing nonoperative therapy, despite persistent moderate to severe pain, loss of function, and moderate to severe radiographic OA or ON,” said coauthors Susan M. Goodman, MD, a rheumatologist at Hospital for Special Surgery in New York, and Charles Hannon, MD, an orthopedic surgeon at Washington University in St. Louis, in an email interview with this news organization. “This guideline supports surgery being performed in an expeditious fashion after the decision has been made to proceed with surgery by both the physician and patient through a shared decision-making process,” they said.
The guidelines also state that obesity by itself should not be a reason to delay TJA. “We could not find a rationale for a strict cut off for weight/body mass index (BMI). Our literature review revealed that though many adverse events were, in fact, increased in patients with morbid obesity, there is also an increase in adverse events for those who had bariatric surgery prior to their arthroplasty,” they added, noting that patients need to be made aware of the increased risk for adverse events in patients with obesity. Though the guidelines do not pose any BMI cutoffs, they state that weight loss should be “strongly encouraged.” These new recommendations are conditional, and all had a “low” to “very low” certainty of evidence; however, there was high consensus on the recommendations from the expert panel.
The guidelines also recommended:
- Delaying TJA to achieve smoking and nicotine cessation or reduction.
- Delaying TJA to improve glycemic control in patients with diabetes, although the group did not recommend any specific measure or threshold.
- Not delaying TJA in patients with a severe deformity, bone loss, or a neuropathic joint.
The new guidelines formalize what many surgeons have already been doing for the past few years, said Arjun Saxena, MD, MBA, an orthopedic surgeon in Philadelphia who was not involved with the guidelines. “A lot of total joint programs have really focused on patient optimization, including smoking cessation, glycemic control, and weight loss prior to surgery,” he said.
Most importantly, the guidelines put an emphasis on how the decision to proceed with TJA should be a shared decision between a physician and patient, he added. Some insurance companies with prior authorization policies may require a patient to try additional nonoperative therapies before approving surgery, creating barriers to care, he said. “Hopefully [these new recommendations] will help third parties understand that joint replacement is a big decision – most doctors aren’t going to recommend that unless it’s necessary or something that is going to help patients,” he said. “I understand that there is a certain need for preauthorization, but just having strict guidelines isn’t appropriate. You really need to look at the whole picture,” he added.
The full manuscript has been submitted for review and is expected to be jointly published in American College of Rheumatology and the American Association of Hip and Knee Surgeons journals later this year.
Dr. Saxena consults for the orthopedic implant company Corin.
A version of this article originally appeared on Medscape.com.
New ESC guidelines for cutting CV risk in noncardiac surgery
The European Society of Cardiology guidelines on cardiovascular assessment and management of patients undergoing noncardiac surgery have seen extensive revision since the 2014 version.
They still have the same aim – to prevent surgery-related bleeding complications, perioperative myocardial infarction/injury (PMI), stent thrombosis, acute heart failure, arrhythmias, pulmonary embolism, ischemic stroke, and cardiovascular (CV) death.
Cochairpersons Sigrun Halvorsen, MD, PhD, and Julinda Mehilli, MD, presented highlights from the guidelines at the annual congress of the European Society of Cardiology and the document was simultaneously published online in the European Heart Journal.
The document classifies noncardiac surgery into three levels of 30-day risk of CV death, MI, or stroke. Low (< 1%) risk includes eye or thyroid surgery; intermediate (1%-5%) risk includes knee or hip replacement or renal transplant; and high (> 5%) risk includes aortic aneurysm, lung transplant, or pancreatic or bladder cancer surgery (see more examples below).
It classifies patients as low risk if they are younger than 65 without CV disease or CV risk factors (smoking, hypertension, diabetes, dyslipidemia, family history); intermediate risk if they are 65 or older or have CV risk factors; and high risk if they have CVD.
In an interview, Dr. Halvorsen, professor in cardiology, University of Oslo, zeroed in on three important revisions:
First, recommendations for preoperative ECG and biomarkers are more specific, he noted.
The guidelines advise that before intermediate- or high-risk noncardiac surgery, in patients who have known CVD, CV risk factors (including age 65 or older), or symptoms suggestive of CVD:
- It is recommended to obtain a preoperative 12-lead ECG (class I).
- It is recommended to measure high-sensitivity cardiac troponin T (hs-cTn T) or high-sensitivity cardiac troponin I (hs-cTn I). It is also recommended to measure these biomarkers at 24 hours and 48 hours post surgery (class I).
- It should be considered to measure B-type natriuretic peptide or N-terminal of the prohormone BNP (NT-proBNP).
However, for low-risk patients undergoing low- and intermediate-risk noncardiac surgery, it is not recommended to routinely obtain preoperative ECG, hs-cTn T/I, or BNP/NT-proBNP concentrations (class III).
Troponins have a stronger class I recommendation, compared with the IIA recommendation for BNP, because they are useful for preoperative risk stratification and for diagnosis of PMI, Dr. Halvorsen explained. “Patients receive painkillers after surgery and may have no pain,” she noted, but they may have PMI, which has a bad prognosis.
Second, the guidelines recommend that “all patients should stop smoking 4 weeks before noncardiac surgery [class I],” she noted. Clinicians should also “measure hemoglobin, and if the patient is anemic, treat the anemia.”
Third, the sections on antithrombotic treatment have been significantly revised. “Bridging – stopping an oral antithrombotic drug and switching to a subcutaneous or IV drug – has been common,” Dr. Halvorsen said, “but recently we have new evidence that in most cases that increases the risk of bleeding.”
“We are [now] much more restrictive with respect to bridging” with unfractionated heparin or low-molecular-weight heparin, she said. “We recommend against bridging in patients with low to moderate thrombotic risk,” and bridging should only be considered in patients with mechanical prosthetic heart valves or with very high thrombotic risk.
More preoperative recommendations
In the guideline overview session at the congress, Dr. Halverson highlighted some of the new recommendations for preoperative risk assessment.
If time allows, it is recommended to optimize guideline-recommended treatment of CVD and control of CV risk factors including blood pressure, dyslipidemia, and diabetes, before noncardiac surgery (class I).
Patients commonly have “murmurs, chest pain, dyspnea, and edema that may suggest severe CVD, but may also be caused by noncardiac disease,” she noted. The guidelines state that “for patients with a newly detected murmur and symptoms or signs of CVD, transthoracic echocardiography is recommended before noncardiac surgery (class I).
“Many studies have been performed to try to find out if initiation of specific drugs before surgery could reduce the risk of complications,” Dr. Halvorsen noted. However, few have shown any benefit and “the question of presurgery initiation of beta-blockers has been greatly debated,” she said. “We have again reviewed the literature and concluded ‘Routine initiation of beta-blockers perioperatively is not recommended (class IIIA).’ “
“We adhere to the guidelines on acute and chronic coronary syndrome recommending 6-12 months of dual antiplatelet treatment as a standard before elective surgery,” she said. “However, in case of time-sensitive surgery, the duration of that treatment can be shortened down to a minimum of 1 month after elective PCI and a minimum of 3 months after PCI and ACS.”
Patients with specific types of CVD
Dr. Mehilli, a professor at Landshut-Achdorf (Germany) Hospital, highlighted some new guideline recommendations for patients who have specific types of cardiovascular disease.
Coronary artery disease (CAD). “For chronic coronary syndrome, a cardiac workup is recommended only for patients undergoing intermediate risk or high-risk noncardiac surgery.”
“Stress imaging should be considered before any high risk, noncardiac surgery in asymptomatic patients with poor functional capacity and prior PCI or coronary artery bypass graft (new recommendation, class IIa).”
Mitral valve regurgitation. For patients undergoing scheduled noncardiac surgery, who remain symptomatic despite guideline-directed medical treatment for mitral valve regurgitation (including resynchronization and myocardial revascularization), consider a valve intervention – either transcatheter or surgical – before noncardiac surgery in eligible patients with acceptable procedural risk (new recommendation).
Cardiac implantable electronic devices (CIED). For high-risk patients with CIEDs undergoing noncardiac surgery with high probability of electromagnetic interference, a CIED checkup and necessary reprogramming immediately before the procedure should be considered (new recommendation).
Arrhythmias. “I want only to stress,” Dr. Mehilli said, “in patients with atrial fibrillation with acute or worsening hemodynamic instability undergoing noncardiac surgery, an emergency electrical cardioversion is recommended (class I).”
Peripheral artery disease (PAD) and abdominal aortic aneurysm. For these patients “we do not recommend a routine referral for a cardiac workup. But we recommend it for patients with poor functional capacity or with significant risk factors or symptoms (new recommendations).”
Chronic arterial hypertension. “We have modified the recommendation, recommending avoidance of large perioperative fluctuations in blood pressure, and we do not recommend deferring noncardiac surgery in patients with stage 1 or 2 hypertension,” she said.
Postoperative cardiovascular complications
The most frequent postoperative cardiovascular complication is PMI, Dr. Mehilli noted.
“In the BASEL-PMI registry, the incidence of this complication around intermediate or high-risk noncardiac surgery was up to 15% among patients older than 65 years or with a history of CAD or PAD, which makes this kind of complication really important to prevent, to assess, and to know how to treat.”
“It is recommended to have a high awareness for perioperative cardiovascular complications, combined with surveillance for PMI in patients undergoing intermediate- or high-risk noncardiac surgery” based on serial measurements of high-sensitivity cardiac troponin.
The guidelines define PMI as “an increase in the delta of high-sensitivity troponin more than the upper level of normal,” Dr. Mehilli said. “It’s different from the one used in a rule-in algorithm for non-STEMI acute coronary syndrome.”
Postoperative atrial fibrillation (AFib) is observed in 2%-30% of noncardiac surgery patients in different registries, particularly in patients undergoing intermediate or high-risk noncardiac surgery, she noted.
“We propose an algorithm on how to prevent and treat this complication. I want to highlight that in patients with hemodynamic unstable postoperative AF[ib], an emergency cardioversion is indicated. For the others, a rate control with the target heart rate of less than 110 beats per minute is indicated.”
In patients with postoperative AFib, long-term oral anticoagulation therapy should be considered in all patients at risk for stroke, considering the anticipated net clinical benefit of oral anticoagulation therapy as well as informed patient preference (new recommendations).
Routine use of beta-blockers to prevent postoperative AFib in patients undergoing noncardiac surgery is not recommended.
The document also covers the management of patients with kidney disease, diabetes, cancer, obesity, and COVID-19. In general, elective noncardiac surgery should be postponed after a patient has COVID-19, until he or she recovers completely, and coexisting conditions are optimized.
The guidelines are available from the ESC website in several formats: pocket guidelines, pocket guidelines smartphone app, guidelines slide set, essential messages, and the European Heart Journal article.
Noncardiac surgery risk categories
The guideline includes a table that classifies noncardiac surgeries into three groups, based on the associated 30-day risk of death, MI, or stroke:
- Low (< 1%): breast, dental, eye, thyroid, and minor gynecologic, orthopedic, and urologic surgery.
- Intermediate (1%-5%): carotid surgery, endovascular aortic aneurysm repair, gallbladder surgery, head or neck surgery, hernia repair, peripheral arterial angioplasty, renal transplant, major gynecologic, orthopedic, or neurologic (hip or spine) surgery, or urologic surgery
- High (> 5%): aortic and major vascular surgery (including aortic aneurysm), bladder removal (usually as a result of cancer), limb amputation, lung or liver transplant, pancreatic surgery, or perforated bowel repair.
The guidelines were endorsed by the European Society of Anaesthesiology and Intensive Care. The guideline authors reported numerous disclosures.
A version of this article first appeared on Medscape.com.
The European Society of Cardiology guidelines on cardiovascular assessment and management of patients undergoing noncardiac surgery have seen extensive revision since the 2014 version.
They still have the same aim – to prevent surgery-related bleeding complications, perioperative myocardial infarction/injury (PMI), stent thrombosis, acute heart failure, arrhythmias, pulmonary embolism, ischemic stroke, and cardiovascular (CV) death.
Cochairpersons Sigrun Halvorsen, MD, PhD, and Julinda Mehilli, MD, presented highlights from the guidelines at the annual congress of the European Society of Cardiology and the document was simultaneously published online in the European Heart Journal.
The document classifies noncardiac surgery into three levels of 30-day risk of CV death, MI, or stroke. Low (< 1%) risk includes eye or thyroid surgery; intermediate (1%-5%) risk includes knee or hip replacement or renal transplant; and high (> 5%) risk includes aortic aneurysm, lung transplant, or pancreatic or bladder cancer surgery (see more examples below).
It classifies patients as low risk if they are younger than 65 without CV disease or CV risk factors (smoking, hypertension, diabetes, dyslipidemia, family history); intermediate risk if they are 65 or older or have CV risk factors; and high risk if they have CVD.
In an interview, Dr. Halvorsen, professor in cardiology, University of Oslo, zeroed in on three important revisions:
First, recommendations for preoperative ECG and biomarkers are more specific, he noted.
The guidelines advise that before intermediate- or high-risk noncardiac surgery, in patients who have known CVD, CV risk factors (including age 65 or older), or symptoms suggestive of CVD:
- It is recommended to obtain a preoperative 12-lead ECG (class I).
- It is recommended to measure high-sensitivity cardiac troponin T (hs-cTn T) or high-sensitivity cardiac troponin I (hs-cTn I). It is also recommended to measure these biomarkers at 24 hours and 48 hours post surgery (class I).
- It should be considered to measure B-type natriuretic peptide or N-terminal of the prohormone BNP (NT-proBNP).
However, for low-risk patients undergoing low- and intermediate-risk noncardiac surgery, it is not recommended to routinely obtain preoperative ECG, hs-cTn T/I, or BNP/NT-proBNP concentrations (class III).
Troponins have a stronger class I recommendation, compared with the IIA recommendation for BNP, because they are useful for preoperative risk stratification and for diagnosis of PMI, Dr. Halvorsen explained. “Patients receive painkillers after surgery and may have no pain,” she noted, but they may have PMI, which has a bad prognosis.
Second, the guidelines recommend that “all patients should stop smoking 4 weeks before noncardiac surgery [class I],” she noted. Clinicians should also “measure hemoglobin, and if the patient is anemic, treat the anemia.”
Third, the sections on antithrombotic treatment have been significantly revised. “Bridging – stopping an oral antithrombotic drug and switching to a subcutaneous or IV drug – has been common,” Dr. Halvorsen said, “but recently we have new evidence that in most cases that increases the risk of bleeding.”
“We are [now] much more restrictive with respect to bridging” with unfractionated heparin or low-molecular-weight heparin, she said. “We recommend against bridging in patients with low to moderate thrombotic risk,” and bridging should only be considered in patients with mechanical prosthetic heart valves or with very high thrombotic risk.
More preoperative recommendations
In the guideline overview session at the congress, Dr. Halverson highlighted some of the new recommendations for preoperative risk assessment.
If time allows, it is recommended to optimize guideline-recommended treatment of CVD and control of CV risk factors including blood pressure, dyslipidemia, and diabetes, before noncardiac surgery (class I).
Patients commonly have “murmurs, chest pain, dyspnea, and edema that may suggest severe CVD, but may also be caused by noncardiac disease,” she noted. The guidelines state that “for patients with a newly detected murmur and symptoms or signs of CVD, transthoracic echocardiography is recommended before noncardiac surgery (class I).
“Many studies have been performed to try to find out if initiation of specific drugs before surgery could reduce the risk of complications,” Dr. Halvorsen noted. However, few have shown any benefit and “the question of presurgery initiation of beta-blockers has been greatly debated,” she said. “We have again reviewed the literature and concluded ‘Routine initiation of beta-blockers perioperatively is not recommended (class IIIA).’ “
“We adhere to the guidelines on acute and chronic coronary syndrome recommending 6-12 months of dual antiplatelet treatment as a standard before elective surgery,” she said. “However, in case of time-sensitive surgery, the duration of that treatment can be shortened down to a minimum of 1 month after elective PCI and a minimum of 3 months after PCI and ACS.”
Patients with specific types of CVD
Dr. Mehilli, a professor at Landshut-Achdorf (Germany) Hospital, highlighted some new guideline recommendations for patients who have specific types of cardiovascular disease.
Coronary artery disease (CAD). “For chronic coronary syndrome, a cardiac workup is recommended only for patients undergoing intermediate risk or high-risk noncardiac surgery.”
“Stress imaging should be considered before any high risk, noncardiac surgery in asymptomatic patients with poor functional capacity and prior PCI or coronary artery bypass graft (new recommendation, class IIa).”
Mitral valve regurgitation. For patients undergoing scheduled noncardiac surgery, who remain symptomatic despite guideline-directed medical treatment for mitral valve regurgitation (including resynchronization and myocardial revascularization), consider a valve intervention – either transcatheter or surgical – before noncardiac surgery in eligible patients with acceptable procedural risk (new recommendation).
Cardiac implantable electronic devices (CIED). For high-risk patients with CIEDs undergoing noncardiac surgery with high probability of electromagnetic interference, a CIED checkup and necessary reprogramming immediately before the procedure should be considered (new recommendation).
Arrhythmias. “I want only to stress,” Dr. Mehilli said, “in patients with atrial fibrillation with acute or worsening hemodynamic instability undergoing noncardiac surgery, an emergency electrical cardioversion is recommended (class I).”
Peripheral artery disease (PAD) and abdominal aortic aneurysm. For these patients “we do not recommend a routine referral for a cardiac workup. But we recommend it for patients with poor functional capacity or with significant risk factors or symptoms (new recommendations).”
Chronic arterial hypertension. “We have modified the recommendation, recommending avoidance of large perioperative fluctuations in blood pressure, and we do not recommend deferring noncardiac surgery in patients with stage 1 or 2 hypertension,” she said.
Postoperative cardiovascular complications
The most frequent postoperative cardiovascular complication is PMI, Dr. Mehilli noted.
“In the BASEL-PMI registry, the incidence of this complication around intermediate or high-risk noncardiac surgery was up to 15% among patients older than 65 years or with a history of CAD or PAD, which makes this kind of complication really important to prevent, to assess, and to know how to treat.”
“It is recommended to have a high awareness for perioperative cardiovascular complications, combined with surveillance for PMI in patients undergoing intermediate- or high-risk noncardiac surgery” based on serial measurements of high-sensitivity cardiac troponin.
The guidelines define PMI as “an increase in the delta of high-sensitivity troponin more than the upper level of normal,” Dr. Mehilli said. “It’s different from the one used in a rule-in algorithm for non-STEMI acute coronary syndrome.”
Postoperative atrial fibrillation (AFib) is observed in 2%-30% of noncardiac surgery patients in different registries, particularly in patients undergoing intermediate or high-risk noncardiac surgery, she noted.
“We propose an algorithm on how to prevent and treat this complication. I want to highlight that in patients with hemodynamic unstable postoperative AF[ib], an emergency cardioversion is indicated. For the others, a rate control with the target heart rate of less than 110 beats per minute is indicated.”
In patients with postoperative AFib, long-term oral anticoagulation therapy should be considered in all patients at risk for stroke, considering the anticipated net clinical benefit of oral anticoagulation therapy as well as informed patient preference (new recommendations).
Routine use of beta-blockers to prevent postoperative AFib in patients undergoing noncardiac surgery is not recommended.
The document also covers the management of patients with kidney disease, diabetes, cancer, obesity, and COVID-19. In general, elective noncardiac surgery should be postponed after a patient has COVID-19, until he or she recovers completely, and coexisting conditions are optimized.
The guidelines are available from the ESC website in several formats: pocket guidelines, pocket guidelines smartphone app, guidelines slide set, essential messages, and the European Heart Journal article.
Noncardiac surgery risk categories
The guideline includes a table that classifies noncardiac surgeries into three groups, based on the associated 30-day risk of death, MI, or stroke:
- Low (< 1%): breast, dental, eye, thyroid, and minor gynecologic, orthopedic, and urologic surgery.
- Intermediate (1%-5%): carotid surgery, endovascular aortic aneurysm repair, gallbladder surgery, head or neck surgery, hernia repair, peripheral arterial angioplasty, renal transplant, major gynecologic, orthopedic, or neurologic (hip or spine) surgery, or urologic surgery
- High (> 5%): aortic and major vascular surgery (including aortic aneurysm), bladder removal (usually as a result of cancer), limb amputation, lung or liver transplant, pancreatic surgery, or perforated bowel repair.
The guidelines were endorsed by the European Society of Anaesthesiology and Intensive Care. The guideline authors reported numerous disclosures.
A version of this article first appeared on Medscape.com.
The European Society of Cardiology guidelines on cardiovascular assessment and management of patients undergoing noncardiac surgery have seen extensive revision since the 2014 version.
They still have the same aim – to prevent surgery-related bleeding complications, perioperative myocardial infarction/injury (PMI), stent thrombosis, acute heart failure, arrhythmias, pulmonary embolism, ischemic stroke, and cardiovascular (CV) death.
Cochairpersons Sigrun Halvorsen, MD, PhD, and Julinda Mehilli, MD, presented highlights from the guidelines at the annual congress of the European Society of Cardiology and the document was simultaneously published online in the European Heart Journal.
The document classifies noncardiac surgery into three levels of 30-day risk of CV death, MI, or stroke. Low (< 1%) risk includes eye or thyroid surgery; intermediate (1%-5%) risk includes knee or hip replacement or renal transplant; and high (> 5%) risk includes aortic aneurysm, lung transplant, or pancreatic or bladder cancer surgery (see more examples below).
It classifies patients as low risk if they are younger than 65 without CV disease or CV risk factors (smoking, hypertension, diabetes, dyslipidemia, family history); intermediate risk if they are 65 or older or have CV risk factors; and high risk if they have CVD.
In an interview, Dr. Halvorsen, professor in cardiology, University of Oslo, zeroed in on three important revisions:
First, recommendations for preoperative ECG and biomarkers are more specific, he noted.
The guidelines advise that before intermediate- or high-risk noncardiac surgery, in patients who have known CVD, CV risk factors (including age 65 or older), or symptoms suggestive of CVD:
- It is recommended to obtain a preoperative 12-lead ECG (class I).
- It is recommended to measure high-sensitivity cardiac troponin T (hs-cTn T) or high-sensitivity cardiac troponin I (hs-cTn I). It is also recommended to measure these biomarkers at 24 hours and 48 hours post surgery (class I).
- It should be considered to measure B-type natriuretic peptide or N-terminal of the prohormone BNP (NT-proBNP).
However, for low-risk patients undergoing low- and intermediate-risk noncardiac surgery, it is not recommended to routinely obtain preoperative ECG, hs-cTn T/I, or BNP/NT-proBNP concentrations (class III).
Troponins have a stronger class I recommendation, compared with the IIA recommendation for BNP, because they are useful for preoperative risk stratification and for diagnosis of PMI, Dr. Halvorsen explained. “Patients receive painkillers after surgery and may have no pain,” she noted, but they may have PMI, which has a bad prognosis.
Second, the guidelines recommend that “all patients should stop smoking 4 weeks before noncardiac surgery [class I],” she noted. Clinicians should also “measure hemoglobin, and if the patient is anemic, treat the anemia.”
Third, the sections on antithrombotic treatment have been significantly revised. “Bridging – stopping an oral antithrombotic drug and switching to a subcutaneous or IV drug – has been common,” Dr. Halvorsen said, “but recently we have new evidence that in most cases that increases the risk of bleeding.”
“We are [now] much more restrictive with respect to bridging” with unfractionated heparin or low-molecular-weight heparin, she said. “We recommend against bridging in patients with low to moderate thrombotic risk,” and bridging should only be considered in patients with mechanical prosthetic heart valves or with very high thrombotic risk.
More preoperative recommendations
In the guideline overview session at the congress, Dr. Halverson highlighted some of the new recommendations for preoperative risk assessment.
If time allows, it is recommended to optimize guideline-recommended treatment of CVD and control of CV risk factors including blood pressure, dyslipidemia, and diabetes, before noncardiac surgery (class I).
Patients commonly have “murmurs, chest pain, dyspnea, and edema that may suggest severe CVD, but may also be caused by noncardiac disease,” she noted. The guidelines state that “for patients with a newly detected murmur and symptoms or signs of CVD, transthoracic echocardiography is recommended before noncardiac surgery (class I).
“Many studies have been performed to try to find out if initiation of specific drugs before surgery could reduce the risk of complications,” Dr. Halvorsen noted. However, few have shown any benefit and “the question of presurgery initiation of beta-blockers has been greatly debated,” she said. “We have again reviewed the literature and concluded ‘Routine initiation of beta-blockers perioperatively is not recommended (class IIIA).’ “
“We adhere to the guidelines on acute and chronic coronary syndrome recommending 6-12 months of dual antiplatelet treatment as a standard before elective surgery,” she said. “However, in case of time-sensitive surgery, the duration of that treatment can be shortened down to a minimum of 1 month after elective PCI and a minimum of 3 months after PCI and ACS.”
Patients with specific types of CVD
Dr. Mehilli, a professor at Landshut-Achdorf (Germany) Hospital, highlighted some new guideline recommendations for patients who have specific types of cardiovascular disease.
Coronary artery disease (CAD). “For chronic coronary syndrome, a cardiac workup is recommended only for patients undergoing intermediate risk or high-risk noncardiac surgery.”
“Stress imaging should be considered before any high risk, noncardiac surgery in asymptomatic patients with poor functional capacity and prior PCI or coronary artery bypass graft (new recommendation, class IIa).”
Mitral valve regurgitation. For patients undergoing scheduled noncardiac surgery, who remain symptomatic despite guideline-directed medical treatment for mitral valve regurgitation (including resynchronization and myocardial revascularization), consider a valve intervention – either transcatheter or surgical – before noncardiac surgery in eligible patients with acceptable procedural risk (new recommendation).
Cardiac implantable electronic devices (CIED). For high-risk patients with CIEDs undergoing noncardiac surgery with high probability of electromagnetic interference, a CIED checkup and necessary reprogramming immediately before the procedure should be considered (new recommendation).
Arrhythmias. “I want only to stress,” Dr. Mehilli said, “in patients with atrial fibrillation with acute or worsening hemodynamic instability undergoing noncardiac surgery, an emergency electrical cardioversion is recommended (class I).”
Peripheral artery disease (PAD) and abdominal aortic aneurysm. For these patients “we do not recommend a routine referral for a cardiac workup. But we recommend it for patients with poor functional capacity or with significant risk factors or symptoms (new recommendations).”
Chronic arterial hypertension. “We have modified the recommendation, recommending avoidance of large perioperative fluctuations in blood pressure, and we do not recommend deferring noncardiac surgery in patients with stage 1 or 2 hypertension,” she said.
Postoperative cardiovascular complications
The most frequent postoperative cardiovascular complication is PMI, Dr. Mehilli noted.
“In the BASEL-PMI registry, the incidence of this complication around intermediate or high-risk noncardiac surgery was up to 15% among patients older than 65 years or with a history of CAD or PAD, which makes this kind of complication really important to prevent, to assess, and to know how to treat.”
“It is recommended to have a high awareness for perioperative cardiovascular complications, combined with surveillance for PMI in patients undergoing intermediate- or high-risk noncardiac surgery” based on serial measurements of high-sensitivity cardiac troponin.
The guidelines define PMI as “an increase in the delta of high-sensitivity troponin more than the upper level of normal,” Dr. Mehilli said. “It’s different from the one used in a rule-in algorithm for non-STEMI acute coronary syndrome.”
Postoperative atrial fibrillation (AFib) is observed in 2%-30% of noncardiac surgery patients in different registries, particularly in patients undergoing intermediate or high-risk noncardiac surgery, she noted.
“We propose an algorithm on how to prevent and treat this complication. I want to highlight that in patients with hemodynamic unstable postoperative AF[ib], an emergency cardioversion is indicated. For the others, a rate control with the target heart rate of less than 110 beats per minute is indicated.”
In patients with postoperative AFib, long-term oral anticoagulation therapy should be considered in all patients at risk for stroke, considering the anticipated net clinical benefit of oral anticoagulation therapy as well as informed patient preference (new recommendations).
Routine use of beta-blockers to prevent postoperative AFib in patients undergoing noncardiac surgery is not recommended.
The document also covers the management of patients with kidney disease, diabetes, cancer, obesity, and COVID-19. In general, elective noncardiac surgery should be postponed after a patient has COVID-19, until he or she recovers completely, and coexisting conditions are optimized.
The guidelines are available from the ESC website in several formats: pocket guidelines, pocket guidelines smartphone app, guidelines slide set, essential messages, and the European Heart Journal article.
Noncardiac surgery risk categories
The guideline includes a table that classifies noncardiac surgeries into three groups, based on the associated 30-day risk of death, MI, or stroke:
- Low (< 1%): breast, dental, eye, thyroid, and minor gynecologic, orthopedic, and urologic surgery.
- Intermediate (1%-5%): carotid surgery, endovascular aortic aneurysm repair, gallbladder surgery, head or neck surgery, hernia repair, peripheral arterial angioplasty, renal transplant, major gynecologic, orthopedic, or neurologic (hip or spine) surgery, or urologic surgery
- High (> 5%): aortic and major vascular surgery (including aortic aneurysm), bladder removal (usually as a result of cancer), limb amputation, lung or liver transplant, pancreatic surgery, or perforated bowel repair.
The guidelines were endorsed by the European Society of Anaesthesiology and Intensive Care. The guideline authors reported numerous disclosures.
A version of this article first appeared on Medscape.com.
FROM ESC CONGRESS 2022
Add AFib to noncardiac surgery risk evaluation: New support
Practice has gone back and forth on whether atrial fibrillation (AFib) should be considered in the preoperative cardiovascular risk (CV) evaluation of patients slated for noncardiac surgery, and the Revised Cardiac Risk Index (RCRI), currently widely used as an assessment tool, doesn’t include the arrhythmia.
But consideration of preexisting AFib along with the RCRI predicted 30-day mortality more sharply than the RCRI alone in an analysis of data covering several million patients slated for such procedures.
Indeed, AFib emerged as a significant, independent risk factor for a number of bad postoperative outcomes. Mortality within a month of the procedure climbed about 30% for patients with AFib before the noncardiac surgery. Their 30-day risks for stroke and for heart failure hospitalization went up similarly.
The addition of AFib to the RCRI significantly improved its ability to discriminate 30-day postoperative risk levels regardless of age, sex, and type of noncardiac surgery, Amgad Mentias, MD, Cleveland Clinic, told this news organization. And “it was able to correctly up-classify patients to high risk, if AFib was there, and it was able to down-classify some patients to lower risk if it wasn’t there.”
“I think [the findings] are convincing evidence that atrial fib should at least be part of the thought process for the surgical team and the medical team taking care of the patient,” said Dr. Mentias, who is senior author on the study published in the Journal of the American College of Cardiology, with lead author Sameer Prasada, MD, also of the Cleveland Clinic.
The results “call for incorporating AFib as a risk factor in perioperative risk scores for cardiovascular morbidity and mortality,” the published report states.
Supraventricular arrhythmias had been part of the Goldman Risk Index once widely used preoperatively to assess cardiac risk before practice adopted the RCRI in the past decade, observe Anne B. Curtis, MD, and Sai Krishna C. Korada, MD, University at Buffalo, New York, in an accompanying editorial.
The current findings “demonstrate improved prediction of adverse postsurgical outcomes” from supplementing the RCRI with AFib, they write. Given associations between preexisting AFib and serious cardiac events, “it is time to ‘re-revise’ the RCRI and acknowledge the importance of AFib in predicting adverse outcomes” after noncardiac surgery.
The new findings, however, aren’t all straightforward. In one result that remains a bit of a head-scratcher, postoperative risk of myocardial infarction (MI) in patients with preexisting AFib went in the opposite direction of risk for death and other CV outcomes, falling by almost 20%.
That is “hard to explain with the available data,” the report states, but “the use of anticoagulation, whether oral or parenteral (as a bridge therapy in the perioperative period), is a plausible explanation” given the frequent role of thrombosis in triggering MIs.
Consistent with such a mechanism, the group argues, the MI risk reduction was seen primarily among patients with AFib and a CHA2DS2-VASc score of 2 or higher – that is, those at highest risk for stroke and therefore most likely to be on oral anticoagulation. The MI risk reduction wasn’t seen in such patients with a CHA2DS2-VASc score of 0 or 1.
“I think that’s part of the explanation, that anticoagulation can reduce risk of MI. But it’s not the whole explanation,” Dr. Mentias said in an interview. If it were the sole mechanism, he said, then the same oral anticoagulation that protected against MI should have also cut the postoperative stroke risk. Yet that risk climbed 40% among patients with preexisting AFib.
The analysis started with 8.6 million Medicare patients with planned noncardiac surgery, seen from 2015 to 2019, of whom 16.4% had preexisting AFib. Propensity matching for demographics, urgency and type of surgery, CHA2DS2-VASc score, and RCRI index created two cohorts for comparison: 1.13 million patients with and 1.92 million without preexisting AFib.
Preexisting AFib was associated with a higher 30-day risk for death from any cause, the primary endpoint being 8.3% versus 5.8% for those without such AFib (P < .001), for an odds ratio of 1.31 (95% confidence interval, 1.30-1.32).
Corresponding 30-day ORs for other events, all significant at P < .001, were:
- 1.31 (95% CI, 1.30-1.33) for heart failure
- 1.40 (95% CI, 1.37-1.43) for stroke
- 1.59 (95% CI, 1.43-1.75) for systemic embolism
- 1.14 (95% CI, 1.13-1.16) for major bleeding
- 0.81 (95% CI, 0.79-0.82) for MI
Those with preexisting AFib also had longer hospitalizations at a median 5 days, compared with 4 days for those without such AFib (P < .001).
The study has the limitations of most any retrospective cohort analysis. Other limitations, the report notes, include lack of information on any antiarrhythmic meds given during hospitalization or type of AFib.
For example, AFib that is permanent – compared with paroxysmal or persistent – may be associated with more atrial fibrosis, greater atrial dilatation, “and probably higher pressures inside the heart,” Dr. Mentias observed.
“That’s not always the case, but that’s the notion. So presumably people with persistent or permanent atrial fib would have more advanced heart disease, and that could imply more risk. But we did not have that kind of data.”
Dr. Mentias and Dr. Prasada report no relevant financial relationships; disclosures for the other authors are in the report. Dr. Curtis discloses serving on advisory boards for Abbott, Janssen Pharmaceuticals, Sanofi, and Milestone Pharmaceuticals; receiving honoraria for speaking from Medtronic and Zoll; and serving on a data-monitoring board for Medtronic. Dr. Korada reports he has no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Practice has gone back and forth on whether atrial fibrillation (AFib) should be considered in the preoperative cardiovascular risk (CV) evaluation of patients slated for noncardiac surgery, and the Revised Cardiac Risk Index (RCRI), currently widely used as an assessment tool, doesn’t include the arrhythmia.
But consideration of preexisting AFib along with the RCRI predicted 30-day mortality more sharply than the RCRI alone in an analysis of data covering several million patients slated for such procedures.
Indeed, AFib emerged as a significant, independent risk factor for a number of bad postoperative outcomes. Mortality within a month of the procedure climbed about 30% for patients with AFib before the noncardiac surgery. Their 30-day risks for stroke and for heart failure hospitalization went up similarly.
The addition of AFib to the RCRI significantly improved its ability to discriminate 30-day postoperative risk levels regardless of age, sex, and type of noncardiac surgery, Amgad Mentias, MD, Cleveland Clinic, told this news organization. And “it was able to correctly up-classify patients to high risk, if AFib was there, and it was able to down-classify some patients to lower risk if it wasn’t there.”
“I think [the findings] are convincing evidence that atrial fib should at least be part of the thought process for the surgical team and the medical team taking care of the patient,” said Dr. Mentias, who is senior author on the study published in the Journal of the American College of Cardiology, with lead author Sameer Prasada, MD, also of the Cleveland Clinic.
The results “call for incorporating AFib as a risk factor in perioperative risk scores for cardiovascular morbidity and mortality,” the published report states.
Supraventricular arrhythmias had been part of the Goldman Risk Index once widely used preoperatively to assess cardiac risk before practice adopted the RCRI in the past decade, observe Anne B. Curtis, MD, and Sai Krishna C. Korada, MD, University at Buffalo, New York, in an accompanying editorial.
The current findings “demonstrate improved prediction of adverse postsurgical outcomes” from supplementing the RCRI with AFib, they write. Given associations between preexisting AFib and serious cardiac events, “it is time to ‘re-revise’ the RCRI and acknowledge the importance of AFib in predicting adverse outcomes” after noncardiac surgery.
The new findings, however, aren’t all straightforward. In one result that remains a bit of a head-scratcher, postoperative risk of myocardial infarction (MI) in patients with preexisting AFib went in the opposite direction of risk for death and other CV outcomes, falling by almost 20%.
That is “hard to explain with the available data,” the report states, but “the use of anticoagulation, whether oral or parenteral (as a bridge therapy in the perioperative period), is a plausible explanation” given the frequent role of thrombosis in triggering MIs.
Consistent with such a mechanism, the group argues, the MI risk reduction was seen primarily among patients with AFib and a CHA2DS2-VASc score of 2 or higher – that is, those at highest risk for stroke and therefore most likely to be on oral anticoagulation. The MI risk reduction wasn’t seen in such patients with a CHA2DS2-VASc score of 0 or 1.
“I think that’s part of the explanation, that anticoagulation can reduce risk of MI. But it’s not the whole explanation,” Dr. Mentias said in an interview. If it were the sole mechanism, he said, then the same oral anticoagulation that protected against MI should have also cut the postoperative stroke risk. Yet that risk climbed 40% among patients with preexisting AFib.
The analysis started with 8.6 million Medicare patients with planned noncardiac surgery, seen from 2015 to 2019, of whom 16.4% had preexisting AFib. Propensity matching for demographics, urgency and type of surgery, CHA2DS2-VASc score, and RCRI index created two cohorts for comparison: 1.13 million patients with and 1.92 million without preexisting AFib.
Preexisting AFib was associated with a higher 30-day risk for death from any cause, the primary endpoint being 8.3% versus 5.8% for those without such AFib (P < .001), for an odds ratio of 1.31 (95% confidence interval, 1.30-1.32).
Corresponding 30-day ORs for other events, all significant at P < .001, were:
- 1.31 (95% CI, 1.30-1.33) for heart failure
- 1.40 (95% CI, 1.37-1.43) for stroke
- 1.59 (95% CI, 1.43-1.75) for systemic embolism
- 1.14 (95% CI, 1.13-1.16) for major bleeding
- 0.81 (95% CI, 0.79-0.82) for MI
Those with preexisting AFib also had longer hospitalizations at a median 5 days, compared with 4 days for those without such AFib (P < .001).
The study has the limitations of most any retrospective cohort analysis. Other limitations, the report notes, include lack of information on any antiarrhythmic meds given during hospitalization or type of AFib.
For example, AFib that is permanent – compared with paroxysmal or persistent – may be associated with more atrial fibrosis, greater atrial dilatation, “and probably higher pressures inside the heart,” Dr. Mentias observed.
“That’s not always the case, but that’s the notion. So presumably people with persistent or permanent atrial fib would have more advanced heart disease, and that could imply more risk. But we did not have that kind of data.”
Dr. Mentias and Dr. Prasada report no relevant financial relationships; disclosures for the other authors are in the report. Dr. Curtis discloses serving on advisory boards for Abbott, Janssen Pharmaceuticals, Sanofi, and Milestone Pharmaceuticals; receiving honoraria for speaking from Medtronic and Zoll; and serving on a data-monitoring board for Medtronic. Dr. Korada reports he has no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Practice has gone back and forth on whether atrial fibrillation (AFib) should be considered in the preoperative cardiovascular risk (CV) evaluation of patients slated for noncardiac surgery, and the Revised Cardiac Risk Index (RCRI), currently widely used as an assessment tool, doesn’t include the arrhythmia.
But consideration of preexisting AFib along with the RCRI predicted 30-day mortality more sharply than the RCRI alone in an analysis of data covering several million patients slated for such procedures.
Indeed, AFib emerged as a significant, independent risk factor for a number of bad postoperative outcomes. Mortality within a month of the procedure climbed about 30% for patients with AFib before the noncardiac surgery. Their 30-day risks for stroke and for heart failure hospitalization went up similarly.
The addition of AFib to the RCRI significantly improved its ability to discriminate 30-day postoperative risk levels regardless of age, sex, and type of noncardiac surgery, Amgad Mentias, MD, Cleveland Clinic, told this news organization. And “it was able to correctly up-classify patients to high risk, if AFib was there, and it was able to down-classify some patients to lower risk if it wasn’t there.”
“I think [the findings] are convincing evidence that atrial fib should at least be part of the thought process for the surgical team and the medical team taking care of the patient,” said Dr. Mentias, who is senior author on the study published in the Journal of the American College of Cardiology, with lead author Sameer Prasada, MD, also of the Cleveland Clinic.
The results “call for incorporating AFib as a risk factor in perioperative risk scores for cardiovascular morbidity and mortality,” the published report states.
Supraventricular arrhythmias had been part of the Goldman Risk Index once widely used preoperatively to assess cardiac risk before practice adopted the RCRI in the past decade, observe Anne B. Curtis, MD, and Sai Krishna C. Korada, MD, University at Buffalo, New York, in an accompanying editorial.
The current findings “demonstrate improved prediction of adverse postsurgical outcomes” from supplementing the RCRI with AFib, they write. Given associations between preexisting AFib and serious cardiac events, “it is time to ‘re-revise’ the RCRI and acknowledge the importance of AFib in predicting adverse outcomes” after noncardiac surgery.
The new findings, however, aren’t all straightforward. In one result that remains a bit of a head-scratcher, postoperative risk of myocardial infarction (MI) in patients with preexisting AFib went in the opposite direction of risk for death and other CV outcomes, falling by almost 20%.
That is “hard to explain with the available data,” the report states, but “the use of anticoagulation, whether oral or parenteral (as a bridge therapy in the perioperative period), is a plausible explanation” given the frequent role of thrombosis in triggering MIs.
Consistent with such a mechanism, the group argues, the MI risk reduction was seen primarily among patients with AFib and a CHA2DS2-VASc score of 2 or higher – that is, those at highest risk for stroke and therefore most likely to be on oral anticoagulation. The MI risk reduction wasn’t seen in such patients with a CHA2DS2-VASc score of 0 or 1.
“I think that’s part of the explanation, that anticoagulation can reduce risk of MI. But it’s not the whole explanation,” Dr. Mentias said in an interview. If it were the sole mechanism, he said, then the same oral anticoagulation that protected against MI should have also cut the postoperative stroke risk. Yet that risk climbed 40% among patients with preexisting AFib.
The analysis started with 8.6 million Medicare patients with planned noncardiac surgery, seen from 2015 to 2019, of whom 16.4% had preexisting AFib. Propensity matching for demographics, urgency and type of surgery, CHA2DS2-VASc score, and RCRI index created two cohorts for comparison: 1.13 million patients with and 1.92 million without preexisting AFib.
Preexisting AFib was associated with a higher 30-day risk for death from any cause, the primary endpoint being 8.3% versus 5.8% for those without such AFib (P < .001), for an odds ratio of 1.31 (95% confidence interval, 1.30-1.32).
Corresponding 30-day ORs for other events, all significant at P < .001, were:
- 1.31 (95% CI, 1.30-1.33) for heart failure
- 1.40 (95% CI, 1.37-1.43) for stroke
- 1.59 (95% CI, 1.43-1.75) for systemic embolism
- 1.14 (95% CI, 1.13-1.16) for major bleeding
- 0.81 (95% CI, 0.79-0.82) for MI
Those with preexisting AFib also had longer hospitalizations at a median 5 days, compared with 4 days for those without such AFib (P < .001).
The study has the limitations of most any retrospective cohort analysis. Other limitations, the report notes, include lack of information on any antiarrhythmic meds given during hospitalization or type of AFib.
For example, AFib that is permanent – compared with paroxysmal or persistent – may be associated with more atrial fibrosis, greater atrial dilatation, “and probably higher pressures inside the heart,” Dr. Mentias observed.
“That’s not always the case, but that’s the notion. So presumably people with persistent or permanent atrial fib would have more advanced heart disease, and that could imply more risk. But we did not have that kind of data.”
Dr. Mentias and Dr. Prasada report no relevant financial relationships; disclosures for the other authors are in the report. Dr. Curtis discloses serving on advisory boards for Abbott, Janssen Pharmaceuticals, Sanofi, and Milestone Pharmaceuticals; receiving honoraria for speaking from Medtronic and Zoll; and serving on a data-monitoring board for Medtronic. Dr. Korada reports he has no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rapid MRSA and S. aureus decolonization beneficial for emergency hip surgery
LISBON – Screening for Staphylococcus aureus, decolonization, and use of teicoplanin for surgical antimicrobial prophylaxis among patients with methicillin-resistant S. aureus (MRSA) lowered the number of prosthetic joint infections in elderly patients undergoing surgery for fracture of the femur.
The findings were presented in a poster at the 32nd European Congress of Clinical Microbiology & Infectious Diseases (ECCMID) 2022, which was one of the few awarded the accolade of “top-rated poster.”
“We actually found that with our intervention, all prosthetic joint infections decreased, not just the Staphylococcus aureus but those due to MRSA, too,” Natividad Benito, MD, an infectious diseases specialist at Hospital de la Santa Creu i Sant Pau in Barcelona, said in an interview. “We’re pleased with these results because prosthetic joint infections present such a complicated situation for patients and surgeons. This is also a relatively easy intervention to use, and with time, even the PCR [polymerase chain reaction] technology will become cheaper. Now, in our hospital, prosthetic joint infections are rare.”
At Hospital de la Santa Creu i Sant Pau, around 200 hip hemiarthroplasties are performed per year. Preceding the intervention, the hospital recorded 11 prosthetic joint infections, with up to five infections due to S. aureus and up to four due to MRSA.
The intervention was introduced in 2016. After 2 years, there were no cases of prosthetic joint infections due to S. aureus; in 2018 there, was one case of prosthetic joint infection due to MRSA. In 2019, there was one case of prosthetic joint infection, but it was due neither to S. aureus nor MRSA. In 2020 and 2021, there was one infection each year that was due to MRSA.
Jesús Rodríguez Baño, MD, head of the infectious diseases division, Hospital Universitario Virgen Macarena at the University of Seville, Spain, who was not involved in the study, explained that for patients with hip fracture, “the time frame in which colonization can be studied is too short using traditional methods. Prosthetic joint infections in this population have a devastating effect, with not negligible mortality and very important morbidity and health care costs.”
Referring to the significant reduction in the rate of S. aureus prosthetic joint infections in the postintervention period, Dr. Rodríguez Baño said in an interview, “The results are sound, and the important reduction in infection risk invites for the development of a multicenter, randomized trial to confirm these interesting results.
“The authors are commended for measuring the impact of applying a well-justified preventive protocol,” Dr. Rodríguez Baño added. However, the study has some limitations: “It was performed in one center, it was not randomized, and control for potential confounders is needed.”
Decolonization in an emergency femur fracture
This study addressed a particular need in residents of Spain’s long-term care facilities. In 2016, the prevalence of MRSA was high.
Roughly one-third of the general population carry S. aureus in their noses. In care homes, the rate of MRSA is higher than in the general population, at around 30% of those with S. aureus. In Spain, recommendations for patients undergoing elective total joint arthroplasty advise S. aureus decolonization – which can take 5 days – to prevent surgical site infections.
“The problem with the elderly population is not only have they a higher incidence of MRSA but that the surgical prophylaxis is inadequate for MRSA,” Dr. Benito pointed out.
Many patients in long-term care facilities are elderly and frail and are at greater risk of fracture. Unlike elective hip surgery, in which patients are asked to undergo decolonization over the 5 days prior to their operation, with emergent femur fractures, there is insufficient time for such preparation. “These patients with femur fractures need surgery as soon as possible,” said Dr. Benito.
No studies have been conducted to determine the best way to minimize infection risk from S. aureus and MRSA for patients undergoing emergency hip hemiarthroplasty surgery to treat femoral fractures.
In the current study, Dr. Benito and coauthors assessed whether a bundle of measures – including rapid detection of S. aureus nasal carriage by PCR upon arrival in the emergency setting, followed by decolonization of carriers using a topical treatment in the nose and a prescription of surgical antimicrobial prophylaxis (adapted antibiotic prophylaxis for MRSA) – reduces the incidence of prosthetic joint infections after surgery.
The quasi-experimental single-center study included patients admitted to the emergency department at Hospital de la Santa Creu i Sant Pau. The PCR was rapid, with a turnaround of just 1.5 hours. Decolonization of S. aureus carriers was carried out using nasal mupirocin and chlorhexidine gluconate bathing, which was started immediately. It was used for a 5 days and was usually continued throughout and after surgery.
Patients carrying MRSA received teicoplanin as optimal surgical antimicrobial prophylaxis instead of cefazolin. The intervention did not interfere with the timing of surgery. The study’s principal outcomes were overall incidence of prosthetic joint infections and the incidence of those specifically caused by S. aureus and MRSA.
The researchers compared findings regarding these outcomes over 5 consecutive years of the intervention to outcomes during 4 consecutive years prior to the intervention, which started in 2016.
During 2016-2020, from 22% to 31% of the overall number of patients requiring hip hemiarthroplasty were referred from long-term care facilities. From 25% to 29% of these patients tested positive for S. aureus on PCR, and of these, 33%-64% had MRSA.
There were 772 surgical procedures from 2012 to 2015 and 786 from 2017 to 2020.
Prior to the intervention, over the years 2012-2014, S. aureus caused 36%-50% of prosthetic joint infections; 25%-100% of the S. aureus infections were MRSA. This decreased significantly after the intervention.
During 2016-2020, there was an average of 14 prosthetic joint infections (1.5%), compared to 36 (4.7%) in 2012-2015 (P < .001). Similarly, the incidence of prosthetic joint infections due to S. aureus dropped to 0.3% from 1.8% (P < .002). The incidence of MRSA prosthetic joint infections was 0.3% for 2016-2020, versus 1.2% for 2012-2015 (P = .012).
The years 2018, 2020, and 2021 each saw one case of infection due to MRSA. They were most likely due to “the intervention not being performed properly in all cases,” said Dr. Benito.
A prosthetic joint infection is very serious for the patient. “It means reoperating, because antibiotics are not enough to clear the infection. The biofilm and pus of the infection need to be cleaned out, a new prosthesis is needed, after which more antibiotics are needed for around 2 months, which can be hard to tolerate, and even then, the infection might not be eradicated,” explained Dr. Benito. “Many of these people are old and frail, and mortality can be significant. Getting a prosthetic joint infection is catastrophic for these patients.”
Dr. Benito and Dr. Rodríguez-Baño have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
LISBON – Screening for Staphylococcus aureus, decolonization, and use of teicoplanin for surgical antimicrobial prophylaxis among patients with methicillin-resistant S. aureus (MRSA) lowered the number of prosthetic joint infections in elderly patients undergoing surgery for fracture of the femur.
The findings were presented in a poster at the 32nd European Congress of Clinical Microbiology & Infectious Diseases (ECCMID) 2022, which was one of the few awarded the accolade of “top-rated poster.”
“We actually found that with our intervention, all prosthetic joint infections decreased, not just the Staphylococcus aureus but those due to MRSA, too,” Natividad Benito, MD, an infectious diseases specialist at Hospital de la Santa Creu i Sant Pau in Barcelona, said in an interview. “We’re pleased with these results because prosthetic joint infections present such a complicated situation for patients and surgeons. This is also a relatively easy intervention to use, and with time, even the PCR [polymerase chain reaction] technology will become cheaper. Now, in our hospital, prosthetic joint infections are rare.”
At Hospital de la Santa Creu i Sant Pau, around 200 hip hemiarthroplasties are performed per year. Preceding the intervention, the hospital recorded 11 prosthetic joint infections, with up to five infections due to S. aureus and up to four due to MRSA.
The intervention was introduced in 2016. After 2 years, there were no cases of prosthetic joint infections due to S. aureus; in 2018 there, was one case of prosthetic joint infection due to MRSA. In 2019, there was one case of prosthetic joint infection, but it was due neither to S. aureus nor MRSA. In 2020 and 2021, there was one infection each year that was due to MRSA.
Jesús Rodríguez Baño, MD, head of the infectious diseases division, Hospital Universitario Virgen Macarena at the University of Seville, Spain, who was not involved in the study, explained that for patients with hip fracture, “the time frame in which colonization can be studied is too short using traditional methods. Prosthetic joint infections in this population have a devastating effect, with not negligible mortality and very important morbidity and health care costs.”
Referring to the significant reduction in the rate of S. aureus prosthetic joint infections in the postintervention period, Dr. Rodríguez Baño said in an interview, “The results are sound, and the important reduction in infection risk invites for the development of a multicenter, randomized trial to confirm these interesting results.
“The authors are commended for measuring the impact of applying a well-justified preventive protocol,” Dr. Rodríguez Baño added. However, the study has some limitations: “It was performed in one center, it was not randomized, and control for potential confounders is needed.”
Decolonization in an emergency femur fracture
This study addressed a particular need in residents of Spain’s long-term care facilities. In 2016, the prevalence of MRSA was high.
Roughly one-third of the general population carry S. aureus in their noses. In care homes, the rate of MRSA is higher than in the general population, at around 30% of those with S. aureus. In Spain, recommendations for patients undergoing elective total joint arthroplasty advise S. aureus decolonization – which can take 5 days – to prevent surgical site infections.
“The problem with the elderly population is not only have they a higher incidence of MRSA but that the surgical prophylaxis is inadequate for MRSA,” Dr. Benito pointed out.
Many patients in long-term care facilities are elderly and frail and are at greater risk of fracture. Unlike elective hip surgery, in which patients are asked to undergo decolonization over the 5 days prior to their operation, with emergent femur fractures, there is insufficient time for such preparation. “These patients with femur fractures need surgery as soon as possible,” said Dr. Benito.
No studies have been conducted to determine the best way to minimize infection risk from S. aureus and MRSA for patients undergoing emergency hip hemiarthroplasty surgery to treat femoral fractures.
In the current study, Dr. Benito and coauthors assessed whether a bundle of measures – including rapid detection of S. aureus nasal carriage by PCR upon arrival in the emergency setting, followed by decolonization of carriers using a topical treatment in the nose and a prescription of surgical antimicrobial prophylaxis (adapted antibiotic prophylaxis for MRSA) – reduces the incidence of prosthetic joint infections after surgery.
The quasi-experimental single-center study included patients admitted to the emergency department at Hospital de la Santa Creu i Sant Pau. The PCR was rapid, with a turnaround of just 1.5 hours. Decolonization of S. aureus carriers was carried out using nasal mupirocin and chlorhexidine gluconate bathing, which was started immediately. It was used for a 5 days and was usually continued throughout and after surgery.
Patients carrying MRSA received teicoplanin as optimal surgical antimicrobial prophylaxis instead of cefazolin. The intervention did not interfere with the timing of surgery. The study’s principal outcomes were overall incidence of prosthetic joint infections and the incidence of those specifically caused by S. aureus and MRSA.
The researchers compared findings regarding these outcomes over 5 consecutive years of the intervention to outcomes during 4 consecutive years prior to the intervention, which started in 2016.
During 2016-2020, from 22% to 31% of the overall number of patients requiring hip hemiarthroplasty were referred from long-term care facilities. From 25% to 29% of these patients tested positive for S. aureus on PCR, and of these, 33%-64% had MRSA.
There were 772 surgical procedures from 2012 to 2015 and 786 from 2017 to 2020.
Prior to the intervention, over the years 2012-2014, S. aureus caused 36%-50% of prosthetic joint infections; 25%-100% of the S. aureus infections were MRSA. This decreased significantly after the intervention.
During 2016-2020, there was an average of 14 prosthetic joint infections (1.5%), compared to 36 (4.7%) in 2012-2015 (P < .001). Similarly, the incidence of prosthetic joint infections due to S. aureus dropped to 0.3% from 1.8% (P < .002). The incidence of MRSA prosthetic joint infections was 0.3% for 2016-2020, versus 1.2% for 2012-2015 (P = .012).
The years 2018, 2020, and 2021 each saw one case of infection due to MRSA. They were most likely due to “the intervention not being performed properly in all cases,” said Dr. Benito.
A prosthetic joint infection is very serious for the patient. “It means reoperating, because antibiotics are not enough to clear the infection. The biofilm and pus of the infection need to be cleaned out, a new prosthesis is needed, after which more antibiotics are needed for around 2 months, which can be hard to tolerate, and even then, the infection might not be eradicated,” explained Dr. Benito. “Many of these people are old and frail, and mortality can be significant. Getting a prosthetic joint infection is catastrophic for these patients.”
Dr. Benito and Dr. Rodríguez-Baño have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
LISBON – Screening for Staphylococcus aureus, decolonization, and use of teicoplanin for surgical antimicrobial prophylaxis among patients with methicillin-resistant S. aureus (MRSA) lowered the number of prosthetic joint infections in elderly patients undergoing surgery for fracture of the femur.
The findings were presented in a poster at the 32nd European Congress of Clinical Microbiology & Infectious Diseases (ECCMID) 2022, which was one of the few awarded the accolade of “top-rated poster.”
“We actually found that with our intervention, all prosthetic joint infections decreased, not just the Staphylococcus aureus but those due to MRSA, too,” Natividad Benito, MD, an infectious diseases specialist at Hospital de la Santa Creu i Sant Pau in Barcelona, said in an interview. “We’re pleased with these results because prosthetic joint infections present such a complicated situation for patients and surgeons. This is also a relatively easy intervention to use, and with time, even the PCR [polymerase chain reaction] technology will become cheaper. Now, in our hospital, prosthetic joint infections are rare.”
At Hospital de la Santa Creu i Sant Pau, around 200 hip hemiarthroplasties are performed per year. Preceding the intervention, the hospital recorded 11 prosthetic joint infections, with up to five infections due to S. aureus and up to four due to MRSA.
The intervention was introduced in 2016. After 2 years, there were no cases of prosthetic joint infections due to S. aureus; in 2018 there, was one case of prosthetic joint infection due to MRSA. In 2019, there was one case of prosthetic joint infection, but it was due neither to S. aureus nor MRSA. In 2020 and 2021, there was one infection each year that was due to MRSA.
Jesús Rodríguez Baño, MD, head of the infectious diseases division, Hospital Universitario Virgen Macarena at the University of Seville, Spain, who was not involved in the study, explained that for patients with hip fracture, “the time frame in which colonization can be studied is too short using traditional methods. Prosthetic joint infections in this population have a devastating effect, with not negligible mortality and very important morbidity and health care costs.”
Referring to the significant reduction in the rate of S. aureus prosthetic joint infections in the postintervention period, Dr. Rodríguez Baño said in an interview, “The results are sound, and the important reduction in infection risk invites for the development of a multicenter, randomized trial to confirm these interesting results.
“The authors are commended for measuring the impact of applying a well-justified preventive protocol,” Dr. Rodríguez Baño added. However, the study has some limitations: “It was performed in one center, it was not randomized, and control for potential confounders is needed.”
Decolonization in an emergency femur fracture
This study addressed a particular need in residents of Spain’s long-term care facilities. In 2016, the prevalence of MRSA was high.
Roughly one-third of the general population carry S. aureus in their noses. In care homes, the rate of MRSA is higher than in the general population, at around 30% of those with S. aureus. In Spain, recommendations for patients undergoing elective total joint arthroplasty advise S. aureus decolonization – which can take 5 days – to prevent surgical site infections.
“The problem with the elderly population is not only have they a higher incidence of MRSA but that the surgical prophylaxis is inadequate for MRSA,” Dr. Benito pointed out.
Many patients in long-term care facilities are elderly and frail and are at greater risk of fracture. Unlike elective hip surgery, in which patients are asked to undergo decolonization over the 5 days prior to their operation, with emergent femur fractures, there is insufficient time for such preparation. “These patients with femur fractures need surgery as soon as possible,” said Dr. Benito.
No studies have been conducted to determine the best way to minimize infection risk from S. aureus and MRSA for patients undergoing emergency hip hemiarthroplasty surgery to treat femoral fractures.
In the current study, Dr. Benito and coauthors assessed whether a bundle of measures – including rapid detection of S. aureus nasal carriage by PCR upon arrival in the emergency setting, followed by decolonization of carriers using a topical treatment in the nose and a prescription of surgical antimicrobial prophylaxis (adapted antibiotic prophylaxis for MRSA) – reduces the incidence of prosthetic joint infections after surgery.
The quasi-experimental single-center study included patients admitted to the emergency department at Hospital de la Santa Creu i Sant Pau. The PCR was rapid, with a turnaround of just 1.5 hours. Decolonization of S. aureus carriers was carried out using nasal mupirocin and chlorhexidine gluconate bathing, which was started immediately. It was used for a 5 days and was usually continued throughout and after surgery.
Patients carrying MRSA received teicoplanin as optimal surgical antimicrobial prophylaxis instead of cefazolin. The intervention did not interfere with the timing of surgery. The study’s principal outcomes were overall incidence of prosthetic joint infections and the incidence of those specifically caused by S. aureus and MRSA.
The researchers compared findings regarding these outcomes over 5 consecutive years of the intervention to outcomes during 4 consecutive years prior to the intervention, which started in 2016.
During 2016-2020, from 22% to 31% of the overall number of patients requiring hip hemiarthroplasty were referred from long-term care facilities. From 25% to 29% of these patients tested positive for S. aureus on PCR, and of these, 33%-64% had MRSA.
There were 772 surgical procedures from 2012 to 2015 and 786 from 2017 to 2020.
Prior to the intervention, over the years 2012-2014, S. aureus caused 36%-50% of prosthetic joint infections; 25%-100% of the S. aureus infections were MRSA. This decreased significantly after the intervention.
During 2016-2020, there was an average of 14 prosthetic joint infections (1.5%), compared to 36 (4.7%) in 2012-2015 (P < .001). Similarly, the incidence of prosthetic joint infections due to S. aureus dropped to 0.3% from 1.8% (P < .002). The incidence of MRSA prosthetic joint infections was 0.3% for 2016-2020, versus 1.2% for 2012-2015 (P = .012).
The years 2018, 2020, and 2021 each saw one case of infection due to MRSA. They were most likely due to “the intervention not being performed properly in all cases,” said Dr. Benito.
A prosthetic joint infection is very serious for the patient. “It means reoperating, because antibiotics are not enough to clear the infection. The biofilm and pus of the infection need to be cleaned out, a new prosthesis is needed, after which more antibiotics are needed for around 2 months, which can be hard to tolerate, and even then, the infection might not be eradicated,” explained Dr. Benito. “Many of these people are old and frail, and mortality can be significant. Getting a prosthetic joint infection is catastrophic for these patients.”
Dr. Benito and Dr. Rodríguez-Baño have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ECCMID 2022
Inadequate pain relief in OA, high opioid use before TKA
Inadequate pain relief was recorded in 68.8% of a sample of people with hip or knee OA who participated in the population-based EpiReumaPt study, researchers reported at the OARSI 2022 World Congress.
“This can be explained by a lack of effectiveness of current management strategies, low uptake of recommended interventions by health care professionals, and also by low adherence by patients to medication and lifestyle interventions,” said Daniela Sofia Albino Costa, MSc, a PhD student at NOVA University Lisbon.
In addition to looking at the prevalence of inadequate pain relief – defined as a score of 5 or higher on the Numeric Pain Rating Scale (NPRS) – the study she presented at the congress, which was sponsored by the Osteoarthritis Research Society International, looked at the predictors for inadequate pain control.
It was found that being female, obesity, and having multimorbidity doubled the risk of inadequate versus adequate pain control, with respective odds ratios of 2.32 (P < .001), 2.26 (P = .006), and 2.07 (P = .001). Overweight was also associated with an increased odds ratio for poor pain control (OR, 1.84; P = .0035).
“We found that patients with inadequate pain relief also have a low performance on activities of daily living and a low quality of life,” Ms. Costa said.
Nearly one-third (29%) of patients in the inadequate pain relief group (n = 765) took medication, versus 15% of patients in the adequate pain relief group (n = 270). This was mostly NSAIDs, but also included analgesics and antipyretics, and in a few cases (4.8% vs. 1.3%), simple opioids.
“We know that current care is not concordant with recommendations,” said Ms. Costa, noting that medication being used as first-line treatment and core nonpharmacologic interventions are being offered to less than half of patients who are eligible.
In addition, the rate for total joint replacement has increased globally, and pain is an important predictor for this.
“So, we need to evaluate pain control and current management offered to people with hip or knee arthritis to identify to identify areas for improvement,” Ms. Costa said.
High rates of prescription opioid use before TKA
In a separate study also presented at the congress, Daniel Rhon, DPT, DSc, director of musculoskeletal research in primary care at Brooke Army Medical Center in San Antonio, gave a worrying glimpse of high rates of opioid use in the 4 years before total knee arthroplasty (TKA).
Using data from the U.S. Military Health System, the records of all individuals who had a knee replacement procedure between January 2017 and December 2018 were studied, to identify and characterize the use of prescription opioids.
Of the 46,362 individuals, 52.9% had prior opioid use, despite the fact that “opioids are not recommended for the management of knee OA,” said Dr. Rhon.
He also reported that as many as 40% of those who had at least one prescription for opioids had received a high-potency drug, such as fentanyl or oxycodone. The mean age of participants overall was 65 years, with a higher mean for those receiving opioids than those who did not (68 vs. 61.5 years). Data on sex and ethnicity were not available in time for presentation at the congress.
“Most of these individuals are getting these opioid prescriptions probably within 6 months, which maybe aligns with escalation of pain and maybe the decision to have that knee replacement,” Dr. Rhon said. Individuals that used opioids filled their most recent prescription a median of 146 days before TKA to surgery, with a mean of 317 days.
“You can’t always link the reason for the opioid prescription, that’s not really clear in the database,” he admitted; however, an analysis was performed to check if other surgeries had been performed that may have warranted the opioid treatment. The results revealed that very few of the opioid users (4%-7%) had undergone another type of surgical procedure.
“So, we feel a little bit better, that these findings weren’t for other surgical procedures,” said Dr. Rhon. He added that future qualitative research was needed to understand why health care professionals were prescribing opioids, and why patients felt like they needed them.
“That’s bad,” Haxby Abbott, PhD, DPT, a research professor at the University of Otago, Dunedin, New Zealand, commented on Twitter.
Dr. Abbott, who was not involved in the study, added: “We’ve done a similar study of the whole NZ population [currently under review] – similar to Australia and not nearly as bad as you found. That needs urgent attention.”
Sharp rise in opioid use 2 years before TKA
Lower rates of opioid use before TKA were seen in two European cohorts, at 43% in England and 33% in Sweden, as reported by Clara Hellberg, PhD, MD, of Lund (Sweden) University. However, rates had increased over a 10-year study period from a respective 23% and 16%, with a sharp increase in use in the 2 years before knee replacement.
The analysis was based on 49,043 patients from the English national database Clinical Practice Research Datalink, and 5,955 patients from the Swedish Skåne Healthcare register who had undergone total knee replacement between 2015 and 2019 and were matched by age, sex and general practice to individuals not undergoing knee replacement.
The prevalence ratio for using opioids over a 10-year period increased from 1.6 to 2.7 in England, and from 1.6 to 2.6 in Sweden.
“While the overall prevalence of opioid use was higher in England, the majority of both cases and controls were using weak opioids,” Dr. Hellberg said.
“Codeine was classified as a weak opioid, whereas morphine was classified as a strong opioid,” she added.
In contrast, the proportion of people using strong opioids in Sweden was greater than in England, she said.
The high opioid use found in the study highlights “the need for better opioid stewardship, and the availability of acceptable, effective alternatives,” Dr. Hellberg and associates concluded in their abstract.
The study presented by Ms. Costa was funded by the Portuguese national funding agency for science, research and technology and by an independent research grant from Pfizer. Dr. Rhon acknowledged grant funding from the National Institutes of Health and the U.S. Department of Defense. Dr. Hellberg had no conflicts of interest to disclose.
Inadequate pain relief was recorded in 68.8% of a sample of people with hip or knee OA who participated in the population-based EpiReumaPt study, researchers reported at the OARSI 2022 World Congress.
“This can be explained by a lack of effectiveness of current management strategies, low uptake of recommended interventions by health care professionals, and also by low adherence by patients to medication and lifestyle interventions,” said Daniela Sofia Albino Costa, MSc, a PhD student at NOVA University Lisbon.
In addition to looking at the prevalence of inadequate pain relief – defined as a score of 5 or higher on the Numeric Pain Rating Scale (NPRS) – the study she presented at the congress, which was sponsored by the Osteoarthritis Research Society International, looked at the predictors for inadequate pain control.
It was found that being female, obesity, and having multimorbidity doubled the risk of inadequate versus adequate pain control, with respective odds ratios of 2.32 (P < .001), 2.26 (P = .006), and 2.07 (P = .001). Overweight was also associated with an increased odds ratio for poor pain control (OR, 1.84; P = .0035).
“We found that patients with inadequate pain relief also have a low performance on activities of daily living and a low quality of life,” Ms. Costa said.
Nearly one-third (29%) of patients in the inadequate pain relief group (n = 765) took medication, versus 15% of patients in the adequate pain relief group (n = 270). This was mostly NSAIDs, but also included analgesics and antipyretics, and in a few cases (4.8% vs. 1.3%), simple opioids.
“We know that current care is not concordant with recommendations,” said Ms. Costa, noting that medication being used as first-line treatment and core nonpharmacologic interventions are being offered to less than half of patients who are eligible.
In addition, the rate for total joint replacement has increased globally, and pain is an important predictor for this.
“So, we need to evaluate pain control and current management offered to people with hip or knee arthritis to identify to identify areas for improvement,” Ms. Costa said.
High rates of prescription opioid use before TKA
In a separate study also presented at the congress, Daniel Rhon, DPT, DSc, director of musculoskeletal research in primary care at Brooke Army Medical Center in San Antonio, gave a worrying glimpse of high rates of opioid use in the 4 years before total knee arthroplasty (TKA).
Using data from the U.S. Military Health System, the records of all individuals who had a knee replacement procedure between January 2017 and December 2018 were studied, to identify and characterize the use of prescription opioids.
Of the 46,362 individuals, 52.9% had prior opioid use, despite the fact that “opioids are not recommended for the management of knee OA,” said Dr. Rhon.
He also reported that as many as 40% of those who had at least one prescription for opioids had received a high-potency drug, such as fentanyl or oxycodone. The mean age of participants overall was 65 years, with a higher mean for those receiving opioids than those who did not (68 vs. 61.5 years). Data on sex and ethnicity were not available in time for presentation at the congress.
“Most of these individuals are getting these opioid prescriptions probably within 6 months, which maybe aligns with escalation of pain and maybe the decision to have that knee replacement,” Dr. Rhon said. Individuals that used opioids filled their most recent prescription a median of 146 days before TKA to surgery, with a mean of 317 days.
“You can’t always link the reason for the opioid prescription, that’s not really clear in the database,” he admitted; however, an analysis was performed to check if other surgeries had been performed that may have warranted the opioid treatment. The results revealed that very few of the opioid users (4%-7%) had undergone another type of surgical procedure.
“So, we feel a little bit better, that these findings weren’t for other surgical procedures,” said Dr. Rhon. He added that future qualitative research was needed to understand why health care professionals were prescribing opioids, and why patients felt like they needed them.
“That’s bad,” Haxby Abbott, PhD, DPT, a research professor at the University of Otago, Dunedin, New Zealand, commented on Twitter.
Dr. Abbott, who was not involved in the study, added: “We’ve done a similar study of the whole NZ population [currently under review] – similar to Australia and not nearly as bad as you found. That needs urgent attention.”
Sharp rise in opioid use 2 years before TKA
Lower rates of opioid use before TKA were seen in two European cohorts, at 43% in England and 33% in Sweden, as reported by Clara Hellberg, PhD, MD, of Lund (Sweden) University. However, rates had increased over a 10-year study period from a respective 23% and 16%, with a sharp increase in use in the 2 years before knee replacement.
The analysis was based on 49,043 patients from the English national database Clinical Practice Research Datalink, and 5,955 patients from the Swedish Skåne Healthcare register who had undergone total knee replacement between 2015 and 2019 and were matched by age, sex and general practice to individuals not undergoing knee replacement.
The prevalence ratio for using opioids over a 10-year period increased from 1.6 to 2.7 in England, and from 1.6 to 2.6 in Sweden.
“While the overall prevalence of opioid use was higher in England, the majority of both cases and controls were using weak opioids,” Dr. Hellberg said.
“Codeine was classified as a weak opioid, whereas morphine was classified as a strong opioid,” she added.
In contrast, the proportion of people using strong opioids in Sweden was greater than in England, she said.
The high opioid use found in the study highlights “the need for better opioid stewardship, and the availability of acceptable, effective alternatives,” Dr. Hellberg and associates concluded in their abstract.
The study presented by Ms. Costa was funded by the Portuguese national funding agency for science, research and technology and by an independent research grant from Pfizer. Dr. Rhon acknowledged grant funding from the National Institutes of Health and the U.S. Department of Defense. Dr. Hellberg had no conflicts of interest to disclose.
Inadequate pain relief was recorded in 68.8% of a sample of people with hip or knee OA who participated in the population-based EpiReumaPt study, researchers reported at the OARSI 2022 World Congress.
“This can be explained by a lack of effectiveness of current management strategies, low uptake of recommended interventions by health care professionals, and also by low adherence by patients to medication and lifestyle interventions,” said Daniela Sofia Albino Costa, MSc, a PhD student at NOVA University Lisbon.
In addition to looking at the prevalence of inadequate pain relief – defined as a score of 5 or higher on the Numeric Pain Rating Scale (NPRS) – the study she presented at the congress, which was sponsored by the Osteoarthritis Research Society International, looked at the predictors for inadequate pain control.
It was found that being female, obesity, and having multimorbidity doubled the risk of inadequate versus adequate pain control, with respective odds ratios of 2.32 (P < .001), 2.26 (P = .006), and 2.07 (P = .001). Overweight was also associated with an increased odds ratio for poor pain control (OR, 1.84; P = .0035).
“We found that patients with inadequate pain relief also have a low performance on activities of daily living and a low quality of life,” Ms. Costa said.
Nearly one-third (29%) of patients in the inadequate pain relief group (n = 765) took medication, versus 15% of patients in the adequate pain relief group (n = 270). This was mostly NSAIDs, but also included analgesics and antipyretics, and in a few cases (4.8% vs. 1.3%), simple opioids.
“We know that current care is not concordant with recommendations,” said Ms. Costa, noting that medication being used as first-line treatment and core nonpharmacologic interventions are being offered to less than half of patients who are eligible.
In addition, the rate for total joint replacement has increased globally, and pain is an important predictor for this.
“So, we need to evaluate pain control and current management offered to people with hip or knee arthritis to identify to identify areas for improvement,” Ms. Costa said.
High rates of prescription opioid use before TKA
In a separate study also presented at the congress, Daniel Rhon, DPT, DSc, director of musculoskeletal research in primary care at Brooke Army Medical Center in San Antonio, gave a worrying glimpse of high rates of opioid use in the 4 years before total knee arthroplasty (TKA).
Using data from the U.S. Military Health System, the records of all individuals who had a knee replacement procedure between January 2017 and December 2018 were studied, to identify and characterize the use of prescription opioids.
Of the 46,362 individuals, 52.9% had prior opioid use, despite the fact that “opioids are not recommended for the management of knee OA,” said Dr. Rhon.
He also reported that as many as 40% of those who had at least one prescription for opioids had received a high-potency drug, such as fentanyl or oxycodone. The mean age of participants overall was 65 years, with a higher mean for those receiving opioids than those who did not (68 vs. 61.5 years). Data on sex and ethnicity were not available in time for presentation at the congress.
“Most of these individuals are getting these opioid prescriptions probably within 6 months, which maybe aligns with escalation of pain and maybe the decision to have that knee replacement,” Dr. Rhon said. Individuals that used opioids filled their most recent prescription a median of 146 days before TKA to surgery, with a mean of 317 days.
“You can’t always link the reason for the opioid prescription, that’s not really clear in the database,” he admitted; however, an analysis was performed to check if other surgeries had been performed that may have warranted the opioid treatment. The results revealed that very few of the opioid users (4%-7%) had undergone another type of surgical procedure.
“So, we feel a little bit better, that these findings weren’t for other surgical procedures,” said Dr. Rhon. He added that future qualitative research was needed to understand why health care professionals were prescribing opioids, and why patients felt like they needed them.
“That’s bad,” Haxby Abbott, PhD, DPT, a research professor at the University of Otago, Dunedin, New Zealand, commented on Twitter.
Dr. Abbott, who was not involved in the study, added: “We’ve done a similar study of the whole NZ population [currently under review] – similar to Australia and not nearly as bad as you found. That needs urgent attention.”
Sharp rise in opioid use 2 years before TKA
Lower rates of opioid use before TKA were seen in two European cohorts, at 43% in England and 33% in Sweden, as reported by Clara Hellberg, PhD, MD, of Lund (Sweden) University. However, rates had increased over a 10-year study period from a respective 23% and 16%, with a sharp increase in use in the 2 years before knee replacement.
The analysis was based on 49,043 patients from the English national database Clinical Practice Research Datalink, and 5,955 patients from the Swedish Skåne Healthcare register who had undergone total knee replacement between 2015 and 2019 and were matched by age, sex and general practice to individuals not undergoing knee replacement.
The prevalence ratio for using opioids over a 10-year period increased from 1.6 to 2.7 in England, and from 1.6 to 2.6 in Sweden.
“While the overall prevalence of opioid use was higher in England, the majority of both cases and controls were using weak opioids,” Dr. Hellberg said.
“Codeine was classified as a weak opioid, whereas morphine was classified as a strong opioid,” she added.
In contrast, the proportion of people using strong opioids in Sweden was greater than in England, she said.
The high opioid use found in the study highlights “the need for better opioid stewardship, and the availability of acceptable, effective alternatives,” Dr. Hellberg and associates concluded in their abstract.
The study presented by Ms. Costa was funded by the Portuguese national funding agency for science, research and technology and by an independent research grant from Pfizer. Dr. Rhon acknowledged grant funding from the National Institutes of Health and the U.S. Department of Defense. Dr. Hellberg had no conflicts of interest to disclose.
FROM OARSI 2022








