User login
Draining Nodule of the Hand
The Diagnosis: Cutaneous Nocardiosis
The wound culture was positive for Nocardia farcinica. The patient received a 5-day course of intravenous sulfamethoxazole-trimethoprim in the hospital and was transitioned to oral sulfamethoxazoletrimethoprim (800 mg/160 mg taken as 1 tablet twice daily) for 6 months. Complete resolution of the infection was noted at 6-month follow-up (Figure).
Nocardia is a gram-positive, aerobic bacterium that typically is found in soil, water, and decaying organic matter.1 There are more than 50 species; N farcinica, Nocardia nova, and Nocardia asteroides are the leading causes of infection in humans and animals. Nocardia asteroides is the most common cause of infection in humans.1,2 Nocardiosis is an uncommon opportunistic infection that usually targets the skin, lungs, and central nervous system.3 Although it mainly affects individuals who are immunocompromised, up to 30% of infections can be seen in immunocompetent hosts who can contract cutaneous nocardiosis after experiencing traumatic injury to the skin.1
Nocardiosis is difficult to diagnose due to its diverse clinical presentations. For example, cutaneous nocardiosis can manifest similar to mycetoma, sporotrichosis, spider bites, nontuberculous mycobacteria such as Mycobacterium marinum, or methicillin-resistant Staphylococcus aureus infections, thus making cutaneous nocardiosis one of the great imitators.1 A culture is required for definitive diagnosis, as Nocardia grows well on nonselective media such as blood or Löwenstein-Jensen agar. It grows as waxy, pigmented, cerebriform colonies 3 to 5 days following incubation.3 The bacterium can be difficult to culture, and it is important to notify the microbiology laboratory if there is a high index of clinical suspicion for infection.
A history of exposure to gardening or handling animals can increase the risk for an individual contracting Nocardia.3 Although nocardiosis can be found across the world, it is native to tropical and subtropical climates such as those found in India, Africa, Latin America, and Southeast Asia.1 Infections mostly are observed in individuals aged 20 to 40 years and tend to affect men more than women. Lesions typically are seen on the lower extremities, but localized infections also can be found on the torso, neck, and upper extremities.1

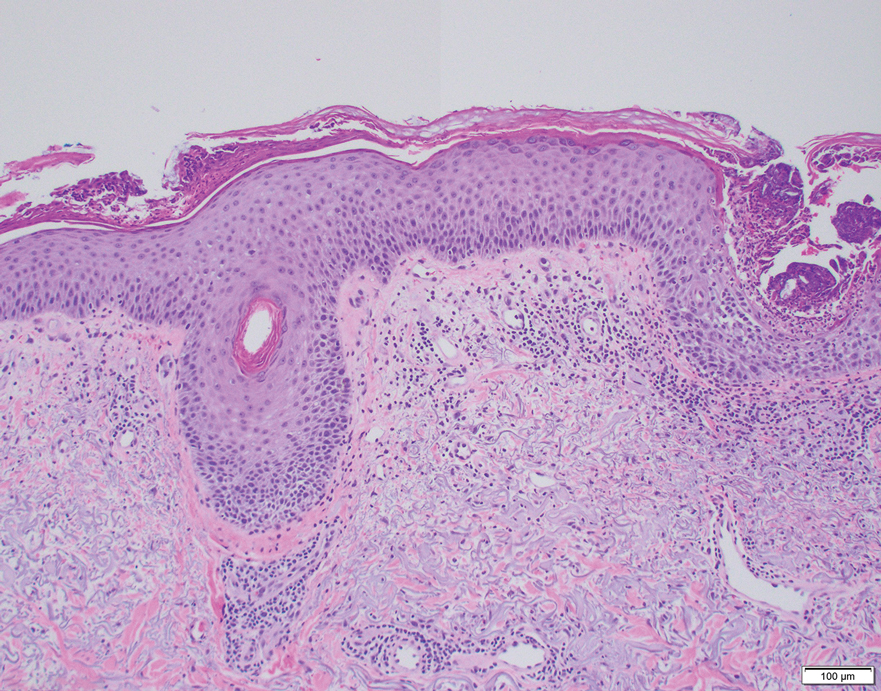
Cutaneous nocardiosis is a granulomatous infection encompassing both cutaneous and subcutaneous tissue, which ultimately can lead to injury of bone and viscera.1 Primary cutaneous nocardiosis can manifest as tumors or nodules that have a sporotrichoid pattern, in which they ascend along the lymphatics. Histopathology of infected tissue frequently shows a subcutaneous dermal infiltrate of neutrophils accompanied with abscess formation, and everlasting lesions may show signs of chronic inflammation and nonspecific granulomas.3
Treatment of nocardiosis should be guided by in vitro susceptibility tests. Sulfamethoxazole-trimethoprim 800 mg/160 mg taken as 1 tablet twice daily is the first-line option. The treatment duration is contingent on the extent, severity, and complications of infection but typically is 3 to 6 months.1
- Yu Q, Song J, Liu Y, et al. Progressive primary cutaneous nocardiosis in an immunocompetent patient. Cutis. 2023;111:E22-E25.
- Gaines RJ, Randall CJ, Ruland RT. Lymphocutaneous nocardiosis from commercially treated lumber: a case report. Cutis. 2006;78:249-251.
- Riswold KJ, Tjarks BJ, Kerkvliet AM. Cutaneous nocardiosis in an immunocompromised patient. Cutis. 2019;104:226-229.
The Diagnosis: Cutaneous Nocardiosis
The wound culture was positive for Nocardia farcinica. The patient received a 5-day course of intravenous sulfamethoxazole-trimethoprim in the hospital and was transitioned to oral sulfamethoxazoletrimethoprim (800 mg/160 mg taken as 1 tablet twice daily) for 6 months. Complete resolution of the infection was noted at 6-month follow-up (Figure).
Nocardia is a gram-positive, aerobic bacterium that typically is found in soil, water, and decaying organic matter.1 There are more than 50 species; N farcinica, Nocardia nova, and Nocardia asteroides are the leading causes of infection in humans and animals. Nocardia asteroides is the most common cause of infection in humans.1,2 Nocardiosis is an uncommon opportunistic infection that usually targets the skin, lungs, and central nervous system.3 Although it mainly affects individuals who are immunocompromised, up to 30% of infections can be seen in immunocompetent hosts who can contract cutaneous nocardiosis after experiencing traumatic injury to the skin.1
Nocardiosis is difficult to diagnose due to its diverse clinical presentations. For example, cutaneous nocardiosis can manifest similar to mycetoma, sporotrichosis, spider bites, nontuberculous mycobacteria such as Mycobacterium marinum, or methicillin-resistant Staphylococcus aureus infections, thus making cutaneous nocardiosis one of the great imitators.1 A culture is required for definitive diagnosis, as Nocardia grows well on nonselective media such as blood or Löwenstein-Jensen agar. It grows as waxy, pigmented, cerebriform colonies 3 to 5 days following incubation.3 The bacterium can be difficult to culture, and it is important to notify the microbiology laboratory if there is a high index of clinical suspicion for infection.
A history of exposure to gardening or handling animals can increase the risk for an individual contracting Nocardia.3 Although nocardiosis can be found across the world, it is native to tropical and subtropical climates such as those found in India, Africa, Latin America, and Southeast Asia.1 Infections mostly are observed in individuals aged 20 to 40 years and tend to affect men more than women. Lesions typically are seen on the lower extremities, but localized infections also can be found on the torso, neck, and upper extremities.1

Cutaneous nocardiosis is a granulomatous infection encompassing both cutaneous and subcutaneous tissue, which ultimately can lead to injury of bone and viscera.1 Primary cutaneous nocardiosis can manifest as tumors or nodules that have a sporotrichoid pattern, in which they ascend along the lymphatics. Histopathology of infected tissue frequently shows a subcutaneous dermal infiltrate of neutrophils accompanied with abscess formation, and everlasting lesions may show signs of chronic inflammation and nonspecific granulomas.3
Treatment of nocardiosis should be guided by in vitro susceptibility tests. Sulfamethoxazole-trimethoprim 800 mg/160 mg taken as 1 tablet twice daily is the first-line option. The treatment duration is contingent on the extent, severity, and complications of infection but typically is 3 to 6 months.1
The Diagnosis: Cutaneous Nocardiosis
The wound culture was positive for Nocardia farcinica. The patient received a 5-day course of intravenous sulfamethoxazole-trimethoprim in the hospital and was transitioned to oral sulfamethoxazoletrimethoprim (800 mg/160 mg taken as 1 tablet twice daily) for 6 months. Complete resolution of the infection was noted at 6-month follow-up (Figure).
Nocardia is a gram-positive, aerobic bacterium that typically is found in soil, water, and decaying organic matter.1 There are more than 50 species; N farcinica, Nocardia nova, and Nocardia asteroides are the leading causes of infection in humans and animals. Nocardia asteroides is the most common cause of infection in humans.1,2 Nocardiosis is an uncommon opportunistic infection that usually targets the skin, lungs, and central nervous system.3 Although it mainly affects individuals who are immunocompromised, up to 30% of infections can be seen in immunocompetent hosts who can contract cutaneous nocardiosis after experiencing traumatic injury to the skin.1
Nocardiosis is difficult to diagnose due to its diverse clinical presentations. For example, cutaneous nocardiosis can manifest similar to mycetoma, sporotrichosis, spider bites, nontuberculous mycobacteria such as Mycobacterium marinum, or methicillin-resistant Staphylococcus aureus infections, thus making cutaneous nocardiosis one of the great imitators.1 A culture is required for definitive diagnosis, as Nocardia grows well on nonselective media such as blood or Löwenstein-Jensen agar. It grows as waxy, pigmented, cerebriform colonies 3 to 5 days following incubation.3 The bacterium can be difficult to culture, and it is important to notify the microbiology laboratory if there is a high index of clinical suspicion for infection.
A history of exposure to gardening or handling animals can increase the risk for an individual contracting Nocardia.3 Although nocardiosis can be found across the world, it is native to tropical and subtropical climates such as those found in India, Africa, Latin America, and Southeast Asia.1 Infections mostly are observed in individuals aged 20 to 40 years and tend to affect men more than women. Lesions typically are seen on the lower extremities, but localized infections also can be found on the torso, neck, and upper extremities.1

Cutaneous nocardiosis is a granulomatous infection encompassing both cutaneous and subcutaneous tissue, which ultimately can lead to injury of bone and viscera.1 Primary cutaneous nocardiosis can manifest as tumors or nodules that have a sporotrichoid pattern, in which they ascend along the lymphatics. Histopathology of infected tissue frequently shows a subcutaneous dermal infiltrate of neutrophils accompanied with abscess formation, and everlasting lesions may show signs of chronic inflammation and nonspecific granulomas.3
Treatment of nocardiosis should be guided by in vitro susceptibility tests. Sulfamethoxazole-trimethoprim 800 mg/160 mg taken as 1 tablet twice daily is the first-line option. The treatment duration is contingent on the extent, severity, and complications of infection but typically is 3 to 6 months.1
- Yu Q, Song J, Liu Y, et al. Progressive primary cutaneous nocardiosis in an immunocompetent patient. Cutis. 2023;111:E22-E25.
- Gaines RJ, Randall CJ, Ruland RT. Lymphocutaneous nocardiosis from commercially treated lumber: a case report. Cutis. 2006;78:249-251.
- Riswold KJ, Tjarks BJ, Kerkvliet AM. Cutaneous nocardiosis in an immunocompromised patient. Cutis. 2019;104:226-229.
- Yu Q, Song J, Liu Y, et al. Progressive primary cutaneous nocardiosis in an immunocompetent patient. Cutis. 2023;111:E22-E25.
- Gaines RJ, Randall CJ, Ruland RT. Lymphocutaneous nocardiosis from commercially treated lumber: a case report. Cutis. 2006;78:249-251.
- Riswold KJ, Tjarks BJ, Kerkvliet AM. Cutaneous nocardiosis in an immunocompromised patient. Cutis. 2019;104:226-229.
A 67-year-old man presented to the emergency department with a draining nodule on the right hand of 4 days’ duration. He reported that the swelling and redness started 1 hour after handling a succulent plant. The following day, the nodule increased in size and exudated yellow pus. He presented with swelling of the thumb and hand, which resulted in a decreased range of motion. He had a history of prediabetes and denied any recent travel, allergies, or animal exposures. Physical examination revealed a draining nodule on the dorsal aspect of the right hand that measured approximately 15×15 mm with surrounding erythema and tenderness. There also was progression of ascending erythema up to the axilla. The patient was admitted to the hospital.

Cold or Flu Virus May Trigger Relapse of Long COVID
researchers have found.
In some cases, they may be experiencing what researchers call viral interference, something also experienced by people with HIV and other infections associated with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
Clinical studies on the issue are limited, but patients, doctors, and researchers report many people who previously had long COVID have developed recurring symptoms after consequent viral infections.
Viral persistence — where bits of virus linger in the body — and viral reactivation remain two of the leading suspects for Yale researchers. Viral activation occurs when the immune system responds to an infection by triggering a dormant virus.
Anecdotally, these flare-ups occur more commonly in patients with long COVID with autonomic dysfunction — severe dizziness when standing up — and other symptoms of ME/CFS, said Alba Azola, MD, a Johns Hopkins Medicine rehabilitation specialist in Baltimore, Maryland, who works with patients with long COVID and other “fatiguing illnesses.”
At last count, about 18% of those surveyed by the Centers for Disease Control and Prevention said they had experienced long COVID. Nearly 60% of those surveyed said they had contracted COVID-19 at least once.
Dr. Azola said that very afternoon she had seen a patient with the flu and a recurrence of previous long COVID symptoms. Not much data exist about cases like this.
“I can’t say there is a specific study looking at this, but anecdotally, we see it all the time,” Dr. Azola said.
She has not seen completely different symptoms; more commonly, she sees a flare-up of previously existing symptoms.
David Putrino, PhD, is director of rehabilitation innovation for the Mount Sinai Health System in New York City. He treats and studies patients with long COVID and echoes what others have seen.
Patients can “recover (or feel recovered) from long COVID until the next immune challenge — another COVID infection, flu infection, pregnancy, food poisoning (all examples we have seen in the clinic) — and experience a significant flare-up of your initial COVID infection,” he said.
“Relapse” is a better term than reinfection, said Jeffrey Parsonnet, MD, an infectious diseases specialist and director of the Dartmouth Hitchcock Post-Acute COVID Syndrome Clinic, Lebanon, New Hampshire.
“We see patients who had COVID-19 followed by long COVID who then get better — either completely or mostly better. Then they’ve gotten COVID again, and this is followed by recurrence of long COVID symptoms,” he said.
“Every patient looks different in terms of what gets better and how quickly. And again, some patients are not better (or even minimally so) after a couple of years,” he said.
Patients Tell Their Stories
On the COVID-19 Long Haulers Support Facebook group, many of the 100,000 followers ask about viral reactivation. Delainne “Laney” Bond, RN, who has battled postinfection chronic illness herself, runs the Facebook group. From what she sees, “each time a person is infected or reinfected with SARS-CoV-2, they have a risk of developing long COVID or experiencing worse long COVID. Multiple infections can lead to progressive health complications.”
The posts on her site include many queries about reinfections. A post from December included nearly 80 comments with people describing the full range of symptoms. Some stories relayed how the reinfection symptoms were short lived. Some report returning to their baseline — not completely symptom free but improved.
Doctors and patients say long COVID comes and goes — relapsing-remitting — and shares many features with other complex multisystem chronic conditions, according to a new National Academy of Sciences report. Those include ME/CFS and the Epstein-Barr virus.
As far as how to treat, Dr. Putrino is one of the clinical researchers testing antivirals. One is Paxlovid; the others are drugs developed for the AIDS virus.
“A plausible mechanism for long COVID is persistence of the SARS-CoV-2 virus in tissue and/or the reactivation of latent pathogens,” according to an explanation of the research on the PolyBio Institute website, which is involved with the research.
In the meantime, “long COVID appears to be a chronic condition with few patients achieving full remission,” according to a new Academy of Sciences report. The report concludes that long COVID recovery can plateau at 6-12 months. They also note that 18%-22% of people who have long COVID symptoms at 5 months are still ill at 1 year.
A version of this article first appeared on Medscape.com.
researchers have found.
In some cases, they may be experiencing what researchers call viral interference, something also experienced by people with HIV and other infections associated with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
Clinical studies on the issue are limited, but patients, doctors, and researchers report many people who previously had long COVID have developed recurring symptoms after consequent viral infections.
Viral persistence — where bits of virus linger in the body — and viral reactivation remain two of the leading suspects for Yale researchers. Viral activation occurs when the immune system responds to an infection by triggering a dormant virus.
Anecdotally, these flare-ups occur more commonly in patients with long COVID with autonomic dysfunction — severe dizziness when standing up — and other symptoms of ME/CFS, said Alba Azola, MD, a Johns Hopkins Medicine rehabilitation specialist in Baltimore, Maryland, who works with patients with long COVID and other “fatiguing illnesses.”
At last count, about 18% of those surveyed by the Centers for Disease Control and Prevention said they had experienced long COVID. Nearly 60% of those surveyed said they had contracted COVID-19 at least once.
Dr. Azola said that very afternoon she had seen a patient with the flu and a recurrence of previous long COVID symptoms. Not much data exist about cases like this.
“I can’t say there is a specific study looking at this, but anecdotally, we see it all the time,” Dr. Azola said.
She has not seen completely different symptoms; more commonly, she sees a flare-up of previously existing symptoms.
David Putrino, PhD, is director of rehabilitation innovation for the Mount Sinai Health System in New York City. He treats and studies patients with long COVID and echoes what others have seen.
Patients can “recover (or feel recovered) from long COVID until the next immune challenge — another COVID infection, flu infection, pregnancy, food poisoning (all examples we have seen in the clinic) — and experience a significant flare-up of your initial COVID infection,” he said.
“Relapse” is a better term than reinfection, said Jeffrey Parsonnet, MD, an infectious diseases specialist and director of the Dartmouth Hitchcock Post-Acute COVID Syndrome Clinic, Lebanon, New Hampshire.
“We see patients who had COVID-19 followed by long COVID who then get better — either completely or mostly better. Then they’ve gotten COVID again, and this is followed by recurrence of long COVID symptoms,” he said.
“Every patient looks different in terms of what gets better and how quickly. And again, some patients are not better (or even minimally so) after a couple of years,” he said.
Patients Tell Their Stories
On the COVID-19 Long Haulers Support Facebook group, many of the 100,000 followers ask about viral reactivation. Delainne “Laney” Bond, RN, who has battled postinfection chronic illness herself, runs the Facebook group. From what she sees, “each time a person is infected or reinfected with SARS-CoV-2, they have a risk of developing long COVID or experiencing worse long COVID. Multiple infections can lead to progressive health complications.”
The posts on her site include many queries about reinfections. A post from December included nearly 80 comments with people describing the full range of symptoms. Some stories relayed how the reinfection symptoms were short lived. Some report returning to their baseline — not completely symptom free but improved.
Doctors and patients say long COVID comes and goes — relapsing-remitting — and shares many features with other complex multisystem chronic conditions, according to a new National Academy of Sciences report. Those include ME/CFS and the Epstein-Barr virus.
As far as how to treat, Dr. Putrino is one of the clinical researchers testing antivirals. One is Paxlovid; the others are drugs developed for the AIDS virus.
“A plausible mechanism for long COVID is persistence of the SARS-CoV-2 virus in tissue and/or the reactivation of latent pathogens,” according to an explanation of the research on the PolyBio Institute website, which is involved with the research.
In the meantime, “long COVID appears to be a chronic condition with few patients achieving full remission,” according to a new Academy of Sciences report. The report concludes that long COVID recovery can plateau at 6-12 months. They also note that 18%-22% of people who have long COVID symptoms at 5 months are still ill at 1 year.
A version of this article first appeared on Medscape.com.
researchers have found.
In some cases, they may be experiencing what researchers call viral interference, something also experienced by people with HIV and other infections associated with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
Clinical studies on the issue are limited, but patients, doctors, and researchers report many people who previously had long COVID have developed recurring symptoms after consequent viral infections.
Viral persistence — where bits of virus linger in the body — and viral reactivation remain two of the leading suspects for Yale researchers. Viral activation occurs when the immune system responds to an infection by triggering a dormant virus.
Anecdotally, these flare-ups occur more commonly in patients with long COVID with autonomic dysfunction — severe dizziness when standing up — and other symptoms of ME/CFS, said Alba Azola, MD, a Johns Hopkins Medicine rehabilitation specialist in Baltimore, Maryland, who works with patients with long COVID and other “fatiguing illnesses.”
At last count, about 18% of those surveyed by the Centers for Disease Control and Prevention said they had experienced long COVID. Nearly 60% of those surveyed said they had contracted COVID-19 at least once.
Dr. Azola said that very afternoon she had seen a patient with the flu and a recurrence of previous long COVID symptoms. Not much data exist about cases like this.
“I can’t say there is a specific study looking at this, but anecdotally, we see it all the time,” Dr. Azola said.
She has not seen completely different symptoms; more commonly, she sees a flare-up of previously existing symptoms.
David Putrino, PhD, is director of rehabilitation innovation for the Mount Sinai Health System in New York City. He treats and studies patients with long COVID and echoes what others have seen.
Patients can “recover (or feel recovered) from long COVID until the next immune challenge — another COVID infection, flu infection, pregnancy, food poisoning (all examples we have seen in the clinic) — and experience a significant flare-up of your initial COVID infection,” he said.
“Relapse” is a better term than reinfection, said Jeffrey Parsonnet, MD, an infectious diseases specialist and director of the Dartmouth Hitchcock Post-Acute COVID Syndrome Clinic, Lebanon, New Hampshire.
“We see patients who had COVID-19 followed by long COVID who then get better — either completely or mostly better. Then they’ve gotten COVID again, and this is followed by recurrence of long COVID symptoms,” he said.
“Every patient looks different in terms of what gets better and how quickly. And again, some patients are not better (or even minimally so) after a couple of years,” he said.
Patients Tell Their Stories
On the COVID-19 Long Haulers Support Facebook group, many of the 100,000 followers ask about viral reactivation. Delainne “Laney” Bond, RN, who has battled postinfection chronic illness herself, runs the Facebook group. From what she sees, “each time a person is infected or reinfected with SARS-CoV-2, they have a risk of developing long COVID or experiencing worse long COVID. Multiple infections can lead to progressive health complications.”
The posts on her site include many queries about reinfections. A post from December included nearly 80 comments with people describing the full range of symptoms. Some stories relayed how the reinfection symptoms were short lived. Some report returning to their baseline — not completely symptom free but improved.
Doctors and patients say long COVID comes and goes — relapsing-remitting — and shares many features with other complex multisystem chronic conditions, according to a new National Academy of Sciences report. Those include ME/CFS and the Epstein-Barr virus.
As far as how to treat, Dr. Putrino is one of the clinical researchers testing antivirals. One is Paxlovid; the others are drugs developed for the AIDS virus.
“A plausible mechanism for long COVID is persistence of the SARS-CoV-2 virus in tissue and/or the reactivation of latent pathogens,” according to an explanation of the research on the PolyBio Institute website, which is involved with the research.
In the meantime, “long COVID appears to be a chronic condition with few patients achieving full remission,” according to a new Academy of Sciences report. The report concludes that long COVID recovery can plateau at 6-12 months. They also note that 18%-22% of people who have long COVID symptoms at 5 months are still ill at 1 year.
A version of this article first appeared on Medscape.com.
Could Tuberculosis Medication Management Be as Simple as Monitoring Sweat?
Analysis of finger sweat detected isoniazid in adults with tuberculosis (TB) for ≤ 6 hours after administration, based on data from a new pilot study.
Katherine Longman, a PhD student at the University of Surrey, Guildford, England, and colleagues wrote.
Although TB is treatable, “it is well known that insufficient drug dosing leads to treatment failure and drug resistance, and so ensuring that patients have sufficient drug exposure is important,” said corresponding author Melanie J. Bailey, PhD, also of the University of Surrey.
“This can be carried out using blood, but blood is painful to collect and difficult to transport. Finger sweat offers a completely noninvasive way to sample patients,” but its use to determine medication adherence has not been examined, she said.
In a pilot study published in the International Journal of Antimicrobial Agents, the researchers reviewed data from 10 adults with TB who provided finger sweat, blood, and saliva samples at several time points ≤ 6 hours after receiving a controlled dose of isoniazid (median of 300 mg daily). They used liquid chromatography–mass spectrometry to examine the samples.
Overall, “isoniazid and acetyl isoniazid were detected in at least one finger sweat sample from all patients,” with detection rates of 96% and 77%, respectively, the researchers wrote. Given the short half-life of isoniazid, they used a window of 1-6 hours after administration. Isoniazid was consistently detected between 1 and 6 hours after administration, while acetyl isoniazid had a noticeably higher detection rate at 6 hours.
The researchers also examined creatinine to account for variability in volume of sweat samples, and found that finger sweat was significantly correlated to isoniazid concentration. The maximum isoniazid to creatinine ratio in finger sweat occurred mainly in the first hour after drug administration, and the activity of isoniazid in finger sweat over time reflected isoniazid concentration in serum more closely after normalization to creatinine, they said. The Pearson’s correlation coefficient (r) was 0.98 (P < .001; one-tailed), with normalization to creatinine, compared with r = 0.52 without normalization (P = .051).
The study findings were limited by several factors including the lack of knowledge of the last drug dose and lack of confirmation testing with an established method of analysis, the researchers noted. However, the results support the potential of the finger sweat test as a screening tool to indicate patients’ nonadherence or to identify patients at risk of low medication exposure.
“We were surprised that we were able to detect the drug in so many patient samples because the sample volume is so low, and so detection is challenging,” said Dr. Bailey. “We were also surprised that fingerprint and drug levels correlated so well after normalizing to creatinine. This is exciting as it unlocks the possibility to test drug levels, as well as providing a yes/no test.”
In practice, the finger sweat technique could reduce the burden on clinics by offering a completely noninvasive way to test a patient’s medication adherence. Looking ahead, more research is needed to explore whether creatinine normalization is widely applicable, such as whether it works for patients with abnormal kidney function, she added.
Noninvasive Option May Mitigate Treatment Challenges
The current study presents a strategy that might address current limitations in TB management, said Krishna Thavarajah, MD, a pulmonologist and director of the interstitial lung disease program at Henry Ford Hospital, Detroit, Michigan, in an interview.
Both self-administered treatment and directly observed therapy (DOT) for TB therapy have limitations, including adherence as low as 50% for TB regimens, she said. In addition, “DOT availability and efficacy can be limited by cost, personnel availability from an administration perspective, and by distrust of those being treated.”
In the current study, “I was struck by the correlation between the sweat and serum values of [isoniazid] and by the level of sophistication of noninvasive testing, being able to normalize for creatinine to account for different volumes of sweat,” said Dr. Thavarajah. In clinical practice, finger sweat isoniazid could potentially serve as an adjunct or alternative to DOT in patients with TB.
Although adherence to the sampling protocol and possible patient distrust of the process (such as concerns over what else is being collected in their sweat) might be barriers to the use of a finger sweat strategy in the clinical setting, appropriate patient selection, patient training, and encouraging clinicians to incorporate this testing into practice could overcome these barriers, said Dr. Thavarajah.
However, more research is needed to study the finger sweat strategy in larger, real-world samples and to study accuracy and treatment adherence with monitoring in a population undergoing DOT, she said.
The study was supported by the Engineering & Physical Sciences Research Council and by Santander PhD Mobility Awards 2019. The researchers had no financial conflicts to disclose. Dr. Thavarajah had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
Analysis of finger sweat detected isoniazid in adults with tuberculosis (TB) for ≤ 6 hours after administration, based on data from a new pilot study.
Katherine Longman, a PhD student at the University of Surrey, Guildford, England, and colleagues wrote.
Although TB is treatable, “it is well known that insufficient drug dosing leads to treatment failure and drug resistance, and so ensuring that patients have sufficient drug exposure is important,” said corresponding author Melanie J. Bailey, PhD, also of the University of Surrey.
“This can be carried out using blood, but blood is painful to collect and difficult to transport. Finger sweat offers a completely noninvasive way to sample patients,” but its use to determine medication adherence has not been examined, she said.
In a pilot study published in the International Journal of Antimicrobial Agents, the researchers reviewed data from 10 adults with TB who provided finger sweat, blood, and saliva samples at several time points ≤ 6 hours after receiving a controlled dose of isoniazid (median of 300 mg daily). They used liquid chromatography–mass spectrometry to examine the samples.
Overall, “isoniazid and acetyl isoniazid were detected in at least one finger sweat sample from all patients,” with detection rates of 96% and 77%, respectively, the researchers wrote. Given the short half-life of isoniazid, they used a window of 1-6 hours after administration. Isoniazid was consistently detected between 1 and 6 hours after administration, while acetyl isoniazid had a noticeably higher detection rate at 6 hours.
The researchers also examined creatinine to account for variability in volume of sweat samples, and found that finger sweat was significantly correlated to isoniazid concentration. The maximum isoniazid to creatinine ratio in finger sweat occurred mainly in the first hour after drug administration, and the activity of isoniazid in finger sweat over time reflected isoniazid concentration in serum more closely after normalization to creatinine, they said. The Pearson’s correlation coefficient (r) was 0.98 (P < .001; one-tailed), with normalization to creatinine, compared with r = 0.52 without normalization (P = .051).
The study findings were limited by several factors including the lack of knowledge of the last drug dose and lack of confirmation testing with an established method of analysis, the researchers noted. However, the results support the potential of the finger sweat test as a screening tool to indicate patients’ nonadherence or to identify patients at risk of low medication exposure.
“We were surprised that we were able to detect the drug in so many patient samples because the sample volume is so low, and so detection is challenging,” said Dr. Bailey. “We were also surprised that fingerprint and drug levels correlated so well after normalizing to creatinine. This is exciting as it unlocks the possibility to test drug levels, as well as providing a yes/no test.”
In practice, the finger sweat technique could reduce the burden on clinics by offering a completely noninvasive way to test a patient’s medication adherence. Looking ahead, more research is needed to explore whether creatinine normalization is widely applicable, such as whether it works for patients with abnormal kidney function, she added.
Noninvasive Option May Mitigate Treatment Challenges
The current study presents a strategy that might address current limitations in TB management, said Krishna Thavarajah, MD, a pulmonologist and director of the interstitial lung disease program at Henry Ford Hospital, Detroit, Michigan, in an interview.
Both self-administered treatment and directly observed therapy (DOT) for TB therapy have limitations, including adherence as low as 50% for TB regimens, she said. In addition, “DOT availability and efficacy can be limited by cost, personnel availability from an administration perspective, and by distrust of those being treated.”
In the current study, “I was struck by the correlation between the sweat and serum values of [isoniazid] and by the level of sophistication of noninvasive testing, being able to normalize for creatinine to account for different volumes of sweat,” said Dr. Thavarajah. In clinical practice, finger sweat isoniazid could potentially serve as an adjunct or alternative to DOT in patients with TB.
Although adherence to the sampling protocol and possible patient distrust of the process (such as concerns over what else is being collected in their sweat) might be barriers to the use of a finger sweat strategy in the clinical setting, appropriate patient selection, patient training, and encouraging clinicians to incorporate this testing into practice could overcome these barriers, said Dr. Thavarajah.
However, more research is needed to study the finger sweat strategy in larger, real-world samples and to study accuracy and treatment adherence with monitoring in a population undergoing DOT, she said.
The study was supported by the Engineering & Physical Sciences Research Council and by Santander PhD Mobility Awards 2019. The researchers had no financial conflicts to disclose. Dr. Thavarajah had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
Analysis of finger sweat detected isoniazid in adults with tuberculosis (TB) for ≤ 6 hours after administration, based on data from a new pilot study.
Katherine Longman, a PhD student at the University of Surrey, Guildford, England, and colleagues wrote.
Although TB is treatable, “it is well known that insufficient drug dosing leads to treatment failure and drug resistance, and so ensuring that patients have sufficient drug exposure is important,” said corresponding author Melanie J. Bailey, PhD, also of the University of Surrey.
“This can be carried out using blood, but blood is painful to collect and difficult to transport. Finger sweat offers a completely noninvasive way to sample patients,” but its use to determine medication adherence has not been examined, she said.
In a pilot study published in the International Journal of Antimicrobial Agents, the researchers reviewed data from 10 adults with TB who provided finger sweat, blood, and saliva samples at several time points ≤ 6 hours after receiving a controlled dose of isoniazid (median of 300 mg daily). They used liquid chromatography–mass spectrometry to examine the samples.
Overall, “isoniazid and acetyl isoniazid were detected in at least one finger sweat sample from all patients,” with detection rates of 96% and 77%, respectively, the researchers wrote. Given the short half-life of isoniazid, they used a window of 1-6 hours after administration. Isoniazid was consistently detected between 1 and 6 hours after administration, while acetyl isoniazid had a noticeably higher detection rate at 6 hours.
The researchers also examined creatinine to account for variability in volume of sweat samples, and found that finger sweat was significantly correlated to isoniazid concentration. The maximum isoniazid to creatinine ratio in finger sweat occurred mainly in the first hour after drug administration, and the activity of isoniazid in finger sweat over time reflected isoniazid concentration in serum more closely after normalization to creatinine, they said. The Pearson’s correlation coefficient (r) was 0.98 (P < .001; one-tailed), with normalization to creatinine, compared with r = 0.52 without normalization (P = .051).
The study findings were limited by several factors including the lack of knowledge of the last drug dose and lack of confirmation testing with an established method of analysis, the researchers noted. However, the results support the potential of the finger sweat test as a screening tool to indicate patients’ nonadherence or to identify patients at risk of low medication exposure.
“We were surprised that we were able to detect the drug in so many patient samples because the sample volume is so low, and so detection is challenging,” said Dr. Bailey. “We were also surprised that fingerprint and drug levels correlated so well after normalizing to creatinine. This is exciting as it unlocks the possibility to test drug levels, as well as providing a yes/no test.”
In practice, the finger sweat technique could reduce the burden on clinics by offering a completely noninvasive way to test a patient’s medication adherence. Looking ahead, more research is needed to explore whether creatinine normalization is widely applicable, such as whether it works for patients with abnormal kidney function, she added.
Noninvasive Option May Mitigate Treatment Challenges
The current study presents a strategy that might address current limitations in TB management, said Krishna Thavarajah, MD, a pulmonologist and director of the interstitial lung disease program at Henry Ford Hospital, Detroit, Michigan, in an interview.
Both self-administered treatment and directly observed therapy (DOT) for TB therapy have limitations, including adherence as low as 50% for TB regimens, she said. In addition, “DOT availability and efficacy can be limited by cost, personnel availability from an administration perspective, and by distrust of those being treated.”
In the current study, “I was struck by the correlation between the sweat and serum values of [isoniazid] and by the level of sophistication of noninvasive testing, being able to normalize for creatinine to account for different volumes of sweat,” said Dr. Thavarajah. In clinical practice, finger sweat isoniazid could potentially serve as an adjunct or alternative to DOT in patients with TB.
Although adherence to the sampling protocol and possible patient distrust of the process (such as concerns over what else is being collected in their sweat) might be barriers to the use of a finger sweat strategy in the clinical setting, appropriate patient selection, patient training, and encouraging clinicians to incorporate this testing into practice could overcome these barriers, said Dr. Thavarajah.
However, more research is needed to study the finger sweat strategy in larger, real-world samples and to study accuracy and treatment adherence with monitoring in a population undergoing DOT, she said.
The study was supported by the Engineering & Physical Sciences Research Council and by Santander PhD Mobility Awards 2019. The researchers had no financial conflicts to disclose. Dr. Thavarajah had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
FROM THE INTERNATIONAL JOURNAL OF ANTIMICROBIAL AGENTS
Reducing Unnecessary Antibiotics for Conjunctivitis
TOPLINE:
More than two thirds of children with conjunctivitis received antibiotics within a day of their initial ambulatory care visit; however,
METHODOLOGY:
- Researchers evaluated the frequency of topical antibiotic treatment and its association with subsequent health care use among commercially insured children with acute infectious conjunctivitis in the United States.
- This cohort study analyzed data from the 2021 MarketScan Commercial Claims and Encounters Database, including 44,793 children with conjunctivitis (median age, 5 years; 47% girls) and ambulatory care encounters.
- The primary exposure was a topical antibiotic prescription dispensed within 1 day of an ambulatory care visit, with outcomes assessed 2-14 days after the visit.
- The primary outcomes were ambulatory care revisits for conjunctivitis and same-day dispensation of a new topical antibiotic, and secondary outcomes included emergency department revisits and hospitalizations.
TAKEAWAY:
- Topical antibiotics were dispensed within a day of an ambulatory care visit in 69% of the cases; however, they were less frequently dispensed following visits to eye clinics (34%), for children aged 6-11 years (66%), and for those with viral conjunctivitis (28%).
- Ambulatory care revisits for conjunctivitis within 2 weeks occurred in only 3.2% of children who had received antibiotics (adjusted odds ratio [aOR], 1.11; 95% CI, 0.99-1.25).
- Similarly, revisits with same-day dispensation of a new antibiotic were also rare (1.4%), with no significant association between antibiotic treatment and revisits (aOR, 1.10; 95% CI, 0.92-1.33).
- Hospitalizations for conjunctivitis occurred in 0.03% of cases, and emergency department revisits occurred in 0.12%, with no differences between children who received antibiotics and those who did not.
IN PRACTICE:
“Given that antibiotics may not be associated with improved outcomes or change in subsequent health care use and are associated with adverse effects and antibiotic resistance, efforts to reduce overtreatment of acute infectious conjunctivitis are warranted,” the authors wrote.
SOURCE:
The study was led by Daniel J. Shapiro, MD, MPH, of the Department of Emergency Medicine at the University of California, San Francisco, and published online on June 27, 2024, in JAMA Ophthalmology.
LIMITATIONS:
The major limitations of the study included the inability to distinguish scheduled visits from unscheduled revisits, incomplete clinical data such as rare complications of conjunctivitis, and the inability to confirm the accuracy of the coded diagnosis of infectious conjunctivitis, especially in children who did not receive a thorough eye examination.
DISCLOSURES:
This study did not declare receiving funding from any sources. One author reported receiving grants from several sources outside the submitted work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
More than two thirds of children with conjunctivitis received antibiotics within a day of their initial ambulatory care visit; however,
METHODOLOGY:
- Researchers evaluated the frequency of topical antibiotic treatment and its association with subsequent health care use among commercially insured children with acute infectious conjunctivitis in the United States.
- This cohort study analyzed data from the 2021 MarketScan Commercial Claims and Encounters Database, including 44,793 children with conjunctivitis (median age, 5 years; 47% girls) and ambulatory care encounters.
- The primary exposure was a topical antibiotic prescription dispensed within 1 day of an ambulatory care visit, with outcomes assessed 2-14 days after the visit.
- The primary outcomes were ambulatory care revisits for conjunctivitis and same-day dispensation of a new topical antibiotic, and secondary outcomes included emergency department revisits and hospitalizations.
TAKEAWAY:
- Topical antibiotics were dispensed within a day of an ambulatory care visit in 69% of the cases; however, they were less frequently dispensed following visits to eye clinics (34%), for children aged 6-11 years (66%), and for those with viral conjunctivitis (28%).
- Ambulatory care revisits for conjunctivitis within 2 weeks occurred in only 3.2% of children who had received antibiotics (adjusted odds ratio [aOR], 1.11; 95% CI, 0.99-1.25).
- Similarly, revisits with same-day dispensation of a new antibiotic were also rare (1.4%), with no significant association between antibiotic treatment and revisits (aOR, 1.10; 95% CI, 0.92-1.33).
- Hospitalizations for conjunctivitis occurred in 0.03% of cases, and emergency department revisits occurred in 0.12%, with no differences between children who received antibiotics and those who did not.
IN PRACTICE:
“Given that antibiotics may not be associated with improved outcomes or change in subsequent health care use and are associated with adverse effects and antibiotic resistance, efforts to reduce overtreatment of acute infectious conjunctivitis are warranted,” the authors wrote.
SOURCE:
The study was led by Daniel J. Shapiro, MD, MPH, of the Department of Emergency Medicine at the University of California, San Francisco, and published online on June 27, 2024, in JAMA Ophthalmology.
LIMITATIONS:
The major limitations of the study included the inability to distinguish scheduled visits from unscheduled revisits, incomplete clinical data such as rare complications of conjunctivitis, and the inability to confirm the accuracy of the coded diagnosis of infectious conjunctivitis, especially in children who did not receive a thorough eye examination.
DISCLOSURES:
This study did not declare receiving funding from any sources. One author reported receiving grants from several sources outside the submitted work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
More than two thirds of children with conjunctivitis received antibiotics within a day of their initial ambulatory care visit; however,
METHODOLOGY:
- Researchers evaluated the frequency of topical antibiotic treatment and its association with subsequent health care use among commercially insured children with acute infectious conjunctivitis in the United States.
- This cohort study analyzed data from the 2021 MarketScan Commercial Claims and Encounters Database, including 44,793 children with conjunctivitis (median age, 5 years; 47% girls) and ambulatory care encounters.
- The primary exposure was a topical antibiotic prescription dispensed within 1 day of an ambulatory care visit, with outcomes assessed 2-14 days after the visit.
- The primary outcomes were ambulatory care revisits for conjunctivitis and same-day dispensation of a new topical antibiotic, and secondary outcomes included emergency department revisits and hospitalizations.
TAKEAWAY:
- Topical antibiotics were dispensed within a day of an ambulatory care visit in 69% of the cases; however, they were less frequently dispensed following visits to eye clinics (34%), for children aged 6-11 years (66%), and for those with viral conjunctivitis (28%).
- Ambulatory care revisits for conjunctivitis within 2 weeks occurred in only 3.2% of children who had received antibiotics (adjusted odds ratio [aOR], 1.11; 95% CI, 0.99-1.25).
- Similarly, revisits with same-day dispensation of a new antibiotic were also rare (1.4%), with no significant association between antibiotic treatment and revisits (aOR, 1.10; 95% CI, 0.92-1.33).
- Hospitalizations for conjunctivitis occurred in 0.03% of cases, and emergency department revisits occurred in 0.12%, with no differences between children who received antibiotics and those who did not.
IN PRACTICE:
“Given that antibiotics may not be associated with improved outcomes or change in subsequent health care use and are associated with adverse effects and antibiotic resistance, efforts to reduce overtreatment of acute infectious conjunctivitis are warranted,” the authors wrote.
SOURCE:
The study was led by Daniel J. Shapiro, MD, MPH, of the Department of Emergency Medicine at the University of California, San Francisco, and published online on June 27, 2024, in JAMA Ophthalmology.
LIMITATIONS:
The major limitations of the study included the inability to distinguish scheduled visits from unscheduled revisits, incomplete clinical data such as rare complications of conjunctivitis, and the inability to confirm the accuracy of the coded diagnosis of infectious conjunctivitis, especially in children who did not receive a thorough eye examination.
DISCLOSURES:
This study did not declare receiving funding from any sources. One author reported receiving grants from several sources outside the submitted work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Dengue Surge in US Cases This Year
Federal health officials with the US Centers for Disease Control and Prevention (CDC) have issued an alert, warning health professionals and the public about an increased risk for dengue virus infections in the United States.
The global incidence of dengue in 2024 is the highest on record, reported the agency.
In the United States, Puerto Rico has declared a public health emergency, with 1498 dengue cases reported so far and a “higher-than-expected” number of dengue cases having been identified among US travelers in the first half of this year at 745 cases, according to the alert.
The CDC reports 197 dengue cases in Florida, 134 in New York, 50 in Massachusetts, 40 in California, 14 in Colorado, nine in Arizona, and eight in the District of Columbia, among others.
Transmitted by infected Aedes genus mosquitoes, dengue is the most common arboviral disease globally and is a nationally notifiable disease in the United States.
The six US territories and freely associated states with frequent or continuous dengue transmission are Puerto Rico, American Samoa, the US Virgin Islands, the Federated States of Micronesia, the Republic of the Marshall Islands, and the Republic of Palau.
Monitoring for Dengue
With rising global and domestic cases of dengue, the CDC urges healthcare providers to monitor for dengue:
- Maintain a high index of suspicion in patients with fever who have been in areas with frequent or continuous dengue transmission within 14 days before illness onset.
- Order diagnostic tests for acute dengue infection such as reverse transcription polymerase chain reaction and immunoglobulin M (IgM) antibody tests or nonstructural protein 1 antigen tests and IgM antibody tests.
- Ensure timely reporting of dengue cases to public health authorities.
- Promote mosquito bite prevention measures among people living in or visiting areas with frequent or continuous dengue transmission.
Roughly one in four dengue virus infections are symptomatic and can be mild or severe. Symptoms begin after an incubation period of about 5-7 days.
Symptoms include fever accompanied by nonspecific signs and symptoms such as nausea, vomiting, rash, muscle aches, joint pain, bone pain, pain behind the eyes, headache, or low white blood cell counts.
Disease Progression
Warning signs that may predict progression to severe disease include abdominal pain or tenderness, persistent vomiting, clinical fluid accumulation, mucosal bleeding, lethargy or restlessness, and progressive increase in hematocrit or liver enlargement.
One in 20 people with symptomatic dengue will develop severe disease, with bleeding, shock, or respiratory distress caused by plasma leakage or end-organ impairment.
Infants aged a year or younger, pregnant people, adults aged 65 years or older, people with certain medical conditions, and those with previous dengue infections are at increased risk for severe dengue.
“Healthcare providers should be prepared to recognize, diagnose, manage, and report dengue cases to health authorities; public health partners should investigate cases and disseminate clear prevention messages to the public,” the alert stated.
The CDC is actively implementing several strategies to address the increase in cases of dengue in the United States. In early April, the agency launched a program-led emergency response and is providing monthly situational updates on dengue to partners, stakeholders, and jurisdictions.
The CDC is also expanding laboratory capacity to improve laboratory testing approaches; collaborating with state, tribal, local, and territorial health departments to strengthen dengue surveillance and recommend prevention strategies; and working to educate the public on dengue prevention.
A version of this article first appeared on Medscape.com.
Federal health officials with the US Centers for Disease Control and Prevention (CDC) have issued an alert, warning health professionals and the public about an increased risk for dengue virus infections in the United States.
The global incidence of dengue in 2024 is the highest on record, reported the agency.
In the United States, Puerto Rico has declared a public health emergency, with 1498 dengue cases reported so far and a “higher-than-expected” number of dengue cases having been identified among US travelers in the first half of this year at 745 cases, according to the alert.
The CDC reports 197 dengue cases in Florida, 134 in New York, 50 in Massachusetts, 40 in California, 14 in Colorado, nine in Arizona, and eight in the District of Columbia, among others.
Transmitted by infected Aedes genus mosquitoes, dengue is the most common arboviral disease globally and is a nationally notifiable disease in the United States.
The six US territories and freely associated states with frequent or continuous dengue transmission are Puerto Rico, American Samoa, the US Virgin Islands, the Federated States of Micronesia, the Republic of the Marshall Islands, and the Republic of Palau.
Monitoring for Dengue
With rising global and domestic cases of dengue, the CDC urges healthcare providers to monitor for dengue:
- Maintain a high index of suspicion in patients with fever who have been in areas with frequent or continuous dengue transmission within 14 days before illness onset.
- Order diagnostic tests for acute dengue infection such as reverse transcription polymerase chain reaction and immunoglobulin M (IgM) antibody tests or nonstructural protein 1 antigen tests and IgM antibody tests.
- Ensure timely reporting of dengue cases to public health authorities.
- Promote mosquito bite prevention measures among people living in or visiting areas with frequent or continuous dengue transmission.
Roughly one in four dengue virus infections are symptomatic and can be mild or severe. Symptoms begin after an incubation period of about 5-7 days.
Symptoms include fever accompanied by nonspecific signs and symptoms such as nausea, vomiting, rash, muscle aches, joint pain, bone pain, pain behind the eyes, headache, or low white blood cell counts.
Disease Progression
Warning signs that may predict progression to severe disease include abdominal pain or tenderness, persistent vomiting, clinical fluid accumulation, mucosal bleeding, lethargy or restlessness, and progressive increase in hematocrit or liver enlargement.
One in 20 people with symptomatic dengue will develop severe disease, with bleeding, shock, or respiratory distress caused by plasma leakage or end-organ impairment.
Infants aged a year or younger, pregnant people, adults aged 65 years or older, people with certain medical conditions, and those with previous dengue infections are at increased risk for severe dengue.
“Healthcare providers should be prepared to recognize, diagnose, manage, and report dengue cases to health authorities; public health partners should investigate cases and disseminate clear prevention messages to the public,” the alert stated.
The CDC is actively implementing several strategies to address the increase in cases of dengue in the United States. In early April, the agency launched a program-led emergency response and is providing monthly situational updates on dengue to partners, stakeholders, and jurisdictions.
The CDC is also expanding laboratory capacity to improve laboratory testing approaches; collaborating with state, tribal, local, and territorial health departments to strengthen dengue surveillance and recommend prevention strategies; and working to educate the public on dengue prevention.
A version of this article first appeared on Medscape.com.
Federal health officials with the US Centers for Disease Control and Prevention (CDC) have issued an alert, warning health professionals and the public about an increased risk for dengue virus infections in the United States.
The global incidence of dengue in 2024 is the highest on record, reported the agency.
In the United States, Puerto Rico has declared a public health emergency, with 1498 dengue cases reported so far and a “higher-than-expected” number of dengue cases having been identified among US travelers in the first half of this year at 745 cases, according to the alert.
The CDC reports 197 dengue cases in Florida, 134 in New York, 50 in Massachusetts, 40 in California, 14 in Colorado, nine in Arizona, and eight in the District of Columbia, among others.
Transmitted by infected Aedes genus mosquitoes, dengue is the most common arboviral disease globally and is a nationally notifiable disease in the United States.
The six US territories and freely associated states with frequent or continuous dengue transmission are Puerto Rico, American Samoa, the US Virgin Islands, the Federated States of Micronesia, the Republic of the Marshall Islands, and the Republic of Palau.
Monitoring for Dengue
With rising global and domestic cases of dengue, the CDC urges healthcare providers to monitor for dengue:
- Maintain a high index of suspicion in patients with fever who have been in areas with frequent or continuous dengue transmission within 14 days before illness onset.
- Order diagnostic tests for acute dengue infection such as reverse transcription polymerase chain reaction and immunoglobulin M (IgM) antibody tests or nonstructural protein 1 antigen tests and IgM antibody tests.
- Ensure timely reporting of dengue cases to public health authorities.
- Promote mosquito bite prevention measures among people living in or visiting areas with frequent or continuous dengue transmission.
Roughly one in four dengue virus infections are symptomatic and can be mild or severe. Symptoms begin after an incubation period of about 5-7 days.
Symptoms include fever accompanied by nonspecific signs and symptoms such as nausea, vomiting, rash, muscle aches, joint pain, bone pain, pain behind the eyes, headache, or low white blood cell counts.
Disease Progression
Warning signs that may predict progression to severe disease include abdominal pain or tenderness, persistent vomiting, clinical fluid accumulation, mucosal bleeding, lethargy or restlessness, and progressive increase in hematocrit or liver enlargement.
One in 20 people with symptomatic dengue will develop severe disease, with bleeding, shock, or respiratory distress caused by plasma leakage or end-organ impairment.
Infants aged a year or younger, pregnant people, adults aged 65 years or older, people with certain medical conditions, and those with previous dengue infections are at increased risk for severe dengue.
“Healthcare providers should be prepared to recognize, diagnose, manage, and report dengue cases to health authorities; public health partners should investigate cases and disseminate clear prevention messages to the public,” the alert stated.
The CDC is actively implementing several strategies to address the increase in cases of dengue in the United States. In early April, the agency launched a program-led emergency response and is providing monthly situational updates on dengue to partners, stakeholders, and jurisdictions.
The CDC is also expanding laboratory capacity to improve laboratory testing approaches; collaborating with state, tribal, local, and territorial health departments to strengthen dengue surveillance and recommend prevention strategies; and working to educate the public on dengue prevention.
A version of this article first appeared on Medscape.com.
Extensive Multidrug-Resistant Dermatophytosis From Trichophyton indotineae
To the Editor:
Historically, commonly available antifungal medications have been effective for treating dermatophytosis (tinea). However, recent tinea outbreaks caused by Trichophyton indotineae—a dermatophyte often resistant to terbinafine and sometimes to other antifungals—have been reported in South Asia, Europe, the Middle East, Southeast Asia, and Australia.1-5
Three confirmed cases of T indotineae dermatophytosis in the United States were reported in 2023 in New York3,6; a fourth confirmed case was reported in 2024 in Pennsylvania.7 Post hoc laboratory testing of fungal isolates in New York in 2022 and 2023 identified an additional 11 cases.8 We present a case of extensive multidrug-resistant tinea caused by T indotineae in a man in California.
An otherwise healthy 65-year-old man who had traveled to Europe in the past 3 months presented to his primary care physician with a widespread pruritic rash (Figure 1). He was treated with 2 weeks of oral terbinafine 250 mg/d and topical medicines, including clotrimazole cream 1%, fluocinonide ointment 0.05%, and clobetasol ointment 0.05% without improvement. Subsequently, 2 weeks of oral griseofulvin microsize 500 mg/d also proved ineffective. An antibody test was negative for HIV. His hemoglobin A1c was 6.2% (reference range, ≤5.6%). The patient was referred to dermatology.
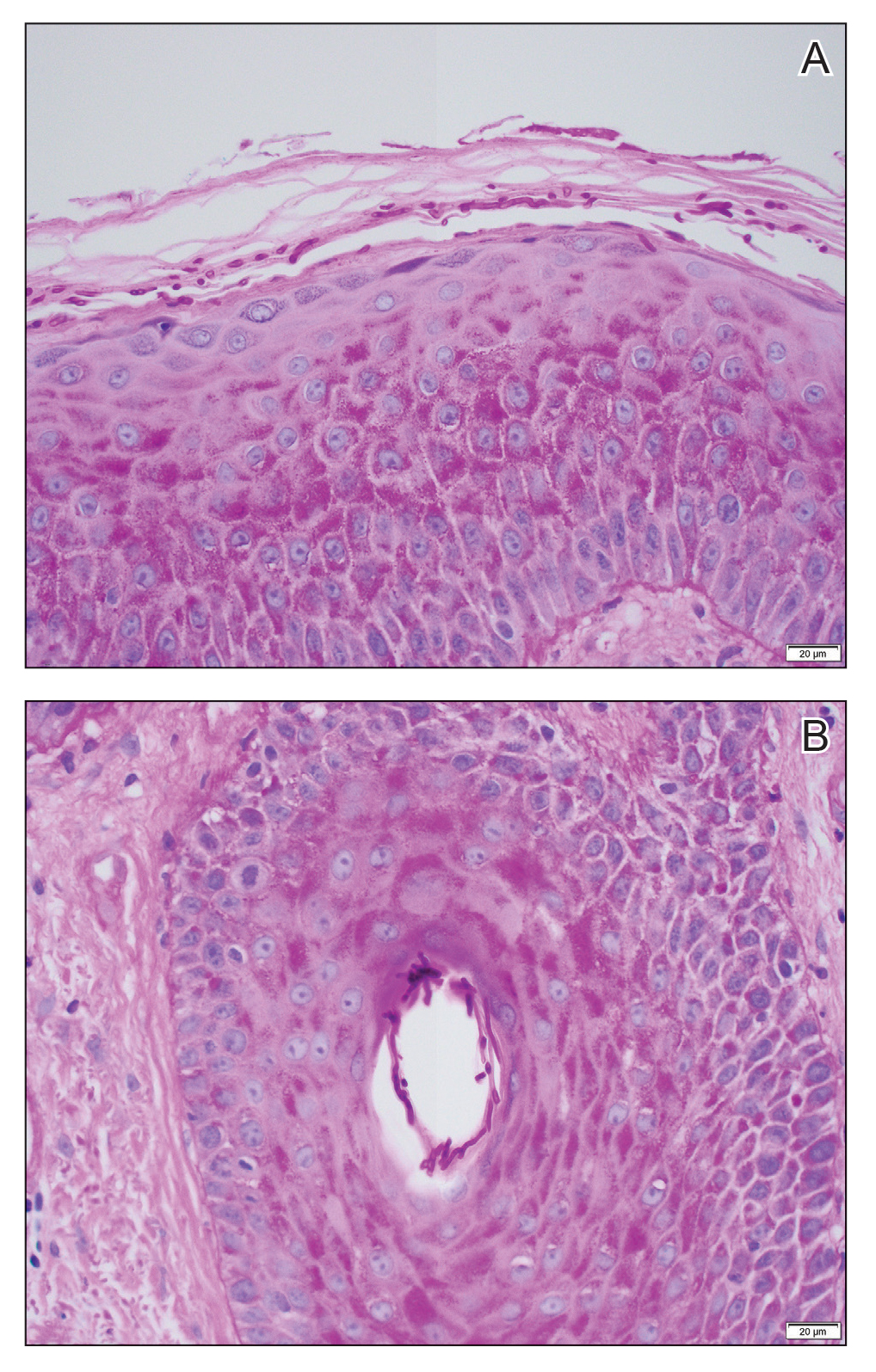
Erythematous plaques—many scaly throughout and some annular with central clearing—were present on the arms, legs, and torso as well as in the groin. Honey crust was present on some plaques on the leg. A potassium hydroxide preparation showed abundant fungal hyphae. Material for fungal and bacterial cultures was collected. The patient was treated again with oral terbinafine 250 mg/d, an oral prednisone taper starting at 60 mg/d for a presumed id reaction, and various oral antihistamines for pruritus; all were ineffective. A bacterial culture showed only mixed skin flora. Oral fluconazole 200 mg/d was prescribed. A skin biopsy specimen showed compact orthokeratosis and parakeratosis of the stratum corneum with few neutrophils and focal pustule formation (Figure 2). Superficial perivascular inflammation, including lymphocytes, histiocytes, and few neutrophils, was present. A periodic acid–Schiff stain showed fungal hyphae in the stratum corneum and a hair follicle (Figure 3). After approximately 2 weeks, mold was identified in the fungal culture. Approximately 2 weeks thereafter, the organism was reported as Trichophyton species.

The rash did not improve; resistance to terbinafine, griseofulvin, and fluconazole was suspected clinically. The fungal isolate was sent to a reference laboratory (University of Texas Health Science Center, San Antonio). Meanwhile, oral itraconazole 200 mg twice daily and ketoconazole cream 2% were prescribed; the rash began to improve. A serum itraconazole trough level obtained 4 days after treatment initiation was 0.5 μg/mL (reference range, ≥0.6 μg/mL). The evening itraconazole dose was increased to 300 mg; a subsequent trough level was 0.8 μg/mL.
Approximately 1 month after the fungal isolate was sent to the reference laboratory, T indotineae was confirmed based on polymerase chain reaction (PCR) testing of internal transcribed spacer region sequences. Minimum inhibitory concentrations (MICs) obtained through antifungal susceptibility testing (AFST) were reported for fluconazole (8 μg/mL), griseofulvin (2 μg/mL), itraconazole (≤0.03 μg/mL), posaconazole (≤0.03 μg/mL), terbinafine (≥2 μg/mL), and voriconazole (0.125 μg/mL).
Approximately 7 weeks after itraconazole and ketoconazole were started, the rash had completely resolved. Nearly 8 months later (at the time this article was written), the rash had not recurred.
We report a unique case of T indotineae in a patient residing in California. Post hoc laboratory testing of dermatophyte isolates sent to the University of Texas reference laboratory identified terbinafine-resistant T indotineae specimens from the United States and Canada dating to 2017; clinical characteristics of patients from whom those isolates were obtained were unavailable.9
Trichophyton indotineae dermatophytosis typically is more extensive, inflamed, and pruritic, as well as likely more contagious, than tinea caused by other dermatophytes.5 Previously called Trichophyton mentagrophytes genotype VIII when first isolated in 2017, the pathogen was renamed T indotineae in 2020 after important genetic differences were discovered between it and other T mentagrophytes species.5 The emergence of T indotineae has been attributed to concomitant use of topical steroids and antifungals,5,10 inappropriate prescribing of antifungals,5 and nonadherence to antifungal treatment.5
Likely risk factors for T indotineae infection include suboptimal hygiene, overcrowded conditions, hot and humid environments, and tight-fitting synthetic clothing.4 Transmission from family members appears common,5 especially when fomites are shared.4 A case reported in Pennsylvania likely was acquired through sexual contact.7 Travel to South Asia has been associated with acquisition of T indotineae infection,3,5-7 though our patient and some others had not traveled there.3,8 It is not clear whether immunosuppression and diabetes mellitus are associated with T indotineae infection.4,5,8 Trichophyton indotineae also can affect animals,11 though zoonotic transmission has not been reported.4
Not all T indotineae isolates are resistant to one or more antifungals; furthermore, antifungal resistance in other dermatophyte species has been reported.5 Terbinafine resistance in T indotineae is conferred by mutations in the gene encoding squalene epoxidase, which helps synthesize ergosterol—a component of the cell membrane in fungi.2,4,5,12 Although clinical cut-points for MIC obtained by AFST are not well established, T indotineae MICs for terbinafine of 0.5 μg/mL or more correlate with resistance.9 Resistance to azoles has been linked to overexpression of transporter genes, which increase azole efflux from cells, as well as to mutations in the gene encoding lanosterol 14α demethylase.4,12,13
Potassium hydroxide preparations and fungal cultures cannot differentiate T indotineae from other dermatophytes that typically cause tinea.5,14 Histopathologic findings in our case were no different than those of non–T indotineae dermatophytes. Only molecular testing using PCR assays to sequence internal transcribed spacer genes can confirm T indotineae infection. However, PCR assays and AFST are not available in many US laboratories.5 Matrix-assisted laser desorption ionization-time of flight (MALDI-TOF) mass spectrometry has shown promise in distinguishing T indotineae from other dermatophytes, though its clinical use is limited and it cannot assess terbinafine sensitivity.15,16 Clinicians in the United States who want to test specimens from cases suspicious for T indotineae infection should contact their local or state health department or the Centers for Disease Control and Prevention for assistance.3,5
Systemic treatment typically is necessary for T indotineae infection.5 Combinations of oral and topical azoles have been used, as well as topical ciclopirox, amorolfine (not available in the United States), and luliconazole.1,5,17-21
Itraconazole has emerged as the treatment of choice for T indotineae tinea, typically at 200 mg/d and often for courses of more than 3 months.5 Testing for serum itraconazole trough levels, as done for our patient, typically is not recommended. Clinicians should counsel patients to take itraconazole with high-fat foods and an acidic beverage to increase bioavailability.5 Potential adverse effects of itraconazole include heart failure and numerous drug-drug interactions.5,22 Patients with T indotineae dermatophytosis should avoid sharing personal belongings and having skin-to-skin contact of affected areas with others.4
Dermatologists who suspect T indotineae infection should work with public health agencies that can assist with testing and undertake infection surveillance, prevention, and control.5,23 Challenges to diagnosing and managing T indotineae infection include lack of awareness among dermatology providers, the need for specialized laboratory testing to confirm infection, lack of established clinical cut-points for MICs from AFST, the need for longer duration of treatment vs what is needed for typical tinea, and potential challenges with insurance coverage for testing and treatment. Empiric treatment with itraconazole should be considered when terbinafine-resistant dermatophytosis is suspected or when terbinafine-resistant T indotineae infection is confirmed.
Acknowledgments—Jeremy Gold, MD; Dallas J. Smith, PharmD; and Shawn Lockhart, PhD, all of the Centers for Disease Control and Prevention, Mycotic Diseases Branch (Atlanta, Georgia), provided helpful comments to the authors in preparing the manuscript of this article.
- Uhrlaß S, Verma SB, Gräser Y, al. Trichophyton indotineae—an emerging pathogen causing recalcitrant dermatophytoses in India and worldwide—a multidimensional perspective. J Fungi (Basel). 2022;8:757. doi:10.3390/jof8070757
- Jabet A, Brun S, Normand A-C, et al. Extensive dermatophytosis caused by terbinafine-resistant Trichophyton indotineae, France. Emerg Infect Dis. 2022;28:229-233. doi:10.3201/eid2801.210883
- Caplan AS, Chaturvedi S, Zhu Y, et al. Notes from the field. First reported U.S. cases of tinea caused by Trichophyton indotineae—New York City, December 2021-March 2023. MMWR Morb Mortal Wkly Rep. 2023;72:536-537. doi:10.15585/mmwr.mm7219a4
- Jabet A, Normand A-C, Brun S, et al. Trichophyton indotineae, from epidemiology to therapeutic. J Mycol Med. 2023;33:101383. doi:10.1016/j.mycmed.2023.101383
- Hill RC, Caplan AS, Elewski B, et al. Expert panel review of skin and hair dermatophytoses in an era of antifungal resistance. Am J Clin Dermatol. 2024;25:359-389. doi:10.1007/s40257-024-00848-1
- Caplan AS, Zakhem GA, Pomeranz MK. Trichophyton mentagrophytes internal transcribed spacer genotype VIII. JAMA Dermatol. 2023;159:1130. doi:10.1001/jamadermatol.2023.2645
- Spivack S, Gold JAW, Lockhart SR, et al. Potential sexual transmission of antifungal-resistant Trichophyton indotineae. Emerg Infect Dis. 2024;30:807-809. doi:10.3201/eid3004.240115
- Caplan AS, Todd GC, Zhu Y, et al. Clinical course, antifungal susceptibility, and genomic sequencing of Trichophyton indotineae. JAMA Dermatol. Published online May 15, 2024. doi:10.1001/jamadermatol.2024.1126
- Cañete-Gibas CF, Mele J, Patterson HP, et al. Terbinafine-resistant dermatophytes and the presence of Trichophyton indotineae in North America. J Clin Microbiol. 2023;61:e0056223. doi:10.1128/jcm.00562-23
- Gupta AK, Venkataraman M, Hall DC, et al. The emergence of Trichophyton indotineae: implications for clinical practice. Int J Dermatol. 2023;62:857-861.
- Oladzad V, Nasrollahi Omran A, Haghani I, et al. Multi-drug resistance Trichophyton indotineae in a stray dog. Res Vet Sci. 2024;166:105105. doi:10.1016/j.rvsc.2023.105105
- Martinez-Rossi NM, Bitencourt TA, Peres NTA, et al. Dermatophyte resistance to antifungal drugs: mechanisms and prospectus. Front Microbiol. 2018;9:1108. doi:10.3389/fmicb.2018.01108
- Sacheli R, Hayette MP. Antifungal resistance in dermatophytes: genetic considerations, clinical presentations and alternative therapies. J Fungi (Basel). 2021;711:983. doi:10.3390/jof7110983
- Gupta AK, Cooper EA. Dermatophytosis (tinea) and other superficial fungal infections. In: Hospenthal DR, Rinaldi MG, eds. Diagnosis and Treatment of Human Mycoses. Humana Press; 2008:355-381.
- Normand A-C, Moreno-Sabater A, Jabet A, et al. MALDI-TOF mass spectrometry online identification of Trichophyton indotineae using the MSI-2 application. J Fungi (Basel). 2022;8:1103. doi:10.3390/jof8101103
- De Paepe R, Normand A-C, Uhrlaß S, et al. Resistance profile, terbinafine resistance screening and MALDI-TOF MS identification of the emerging pathogen Trichophyton indotineae. Mycopathologia. 2024;189:29. doi:10.1007/s11046-024-00835-4
- Rajagopalan M, Inamadar A, Mittal A, et al. Expert consensus on the management of dermatophytosis in India (ECTODERM India). BMC Dermatol. 2018;18:6. doi:10.1186/s12895-018-0073-1
- Verma SB, Panda S, Nenoff P, et al. The unprecedented epidemic-like scenario of dermatophytosis in India: III. Antifungal resistance and treatment options. Indian J Dermatol Venereol Leprol. 2021;87:468-482. doi:10.25259/IJDVL_303_20
- Shaw D, Singh S, Dogra S, et al. MIC and upper limit of wild-type distribution for 13 antifungal agents against a Trichophyton mentagrophytes–Trichophyton interdigitale complex of Indian origin. Antimicrob Agents Chemother. 2020;64:E01964-19. doi:10.1128/AAC.01964-19
- Burmester A, Hipler U-C, Uhrlaß S, et al. Indian Trichophyton mentagrophytes squalene epoxidase erg1 double mutants show high proportion of combined fluconazole and terbinafine resistance. Mycoses. 2020;63:1175-1180. doi:10.1111/myc.13150
- Khurana A, Agarwal A, Agrawal D, et al. Effect of different itraconazole dosing regimens on cure rates, treatment duration, safety, and relapse rates in adult patients with tinea corporis/cruris: a randomized clinical trial. JAMA Dermatol. 2022;158:1269-1278. doi:10.1001/jamadermatol.2022.3745
- Itraconazole capsule. DailyMed [Internet]. Updated June 3, 2024. Accessed June 19, 2024. https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=2ab38a8a-3708-4b97-9f7f-8e554a15348d
- Bui TS, Katz KA. Resistant Trichophyton indotineae dermatophytosis—an emerging pandemic, now in the US. JAMA Dermatol. Published online May 15, 2024. doi:10.1001/jamadermatol.2024.1125
To the Editor:
Historically, commonly available antifungal medications have been effective for treating dermatophytosis (tinea). However, recent tinea outbreaks caused by Trichophyton indotineae—a dermatophyte often resistant to terbinafine and sometimes to other antifungals—have been reported in South Asia, Europe, the Middle East, Southeast Asia, and Australia.1-5
Three confirmed cases of T indotineae dermatophytosis in the United States were reported in 2023 in New York3,6; a fourth confirmed case was reported in 2024 in Pennsylvania.7 Post hoc laboratory testing of fungal isolates in New York in 2022 and 2023 identified an additional 11 cases.8 We present a case of extensive multidrug-resistant tinea caused by T indotineae in a man in California.
An otherwise healthy 65-year-old man who had traveled to Europe in the past 3 months presented to his primary care physician with a widespread pruritic rash (Figure 1). He was treated with 2 weeks of oral terbinafine 250 mg/d and topical medicines, including clotrimazole cream 1%, fluocinonide ointment 0.05%, and clobetasol ointment 0.05% without improvement. Subsequently, 2 weeks of oral griseofulvin microsize 500 mg/d also proved ineffective. An antibody test was negative for HIV. His hemoglobin A1c was 6.2% (reference range, ≤5.6%). The patient was referred to dermatology.
Erythematous plaques—many scaly throughout and some annular with central clearing—were present on the arms, legs, and torso as well as in the groin. Honey crust was present on some plaques on the leg. A potassium hydroxide preparation showed abundant fungal hyphae. Material for fungal and bacterial cultures was collected. The patient was treated again with oral terbinafine 250 mg/d, an oral prednisone taper starting at 60 mg/d for a presumed id reaction, and various oral antihistamines for pruritus; all were ineffective. A bacterial culture showed only mixed skin flora. Oral fluconazole 200 mg/d was prescribed. A skin biopsy specimen showed compact orthokeratosis and parakeratosis of the stratum corneum with few neutrophils and focal pustule formation (Figure 2). Superficial perivascular inflammation, including lymphocytes, histiocytes, and few neutrophils, was present. A periodic acid–Schiff stain showed fungal hyphae in the stratum corneum and a hair follicle (Figure 3). After approximately 2 weeks, mold was identified in the fungal culture. Approximately 2 weeks thereafter, the organism was reported as Trichophyton species.

The rash did not improve; resistance to terbinafine, griseofulvin, and fluconazole was suspected clinically. The fungal isolate was sent to a reference laboratory (University of Texas Health Science Center, San Antonio). Meanwhile, oral itraconazole 200 mg twice daily and ketoconazole cream 2% were prescribed; the rash began to improve. A serum itraconazole trough level obtained 4 days after treatment initiation was 0.5 μg/mL (reference range, ≥0.6 μg/mL). The evening itraconazole dose was increased to 300 mg; a subsequent trough level was 0.8 μg/mL.
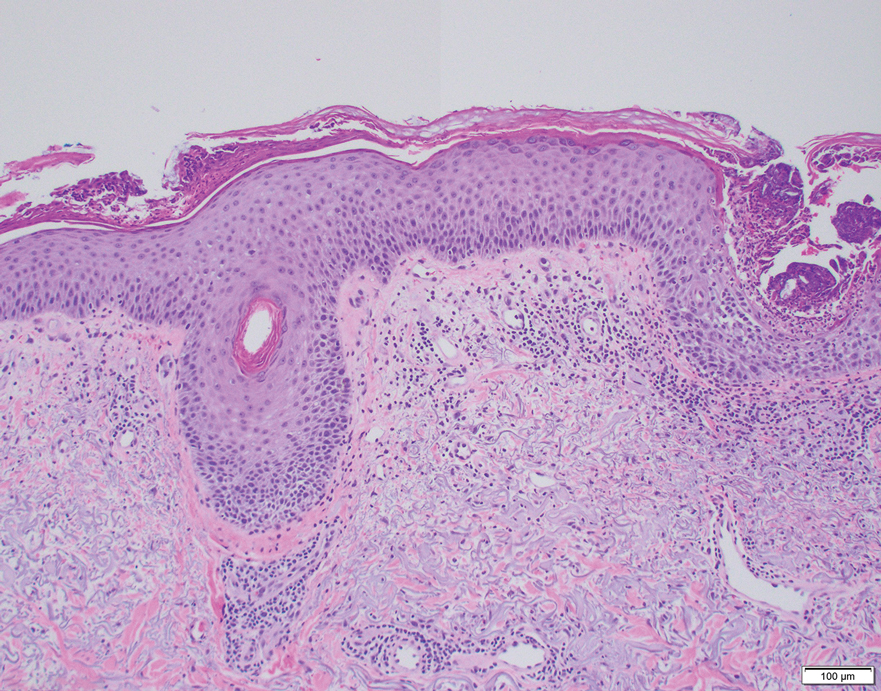
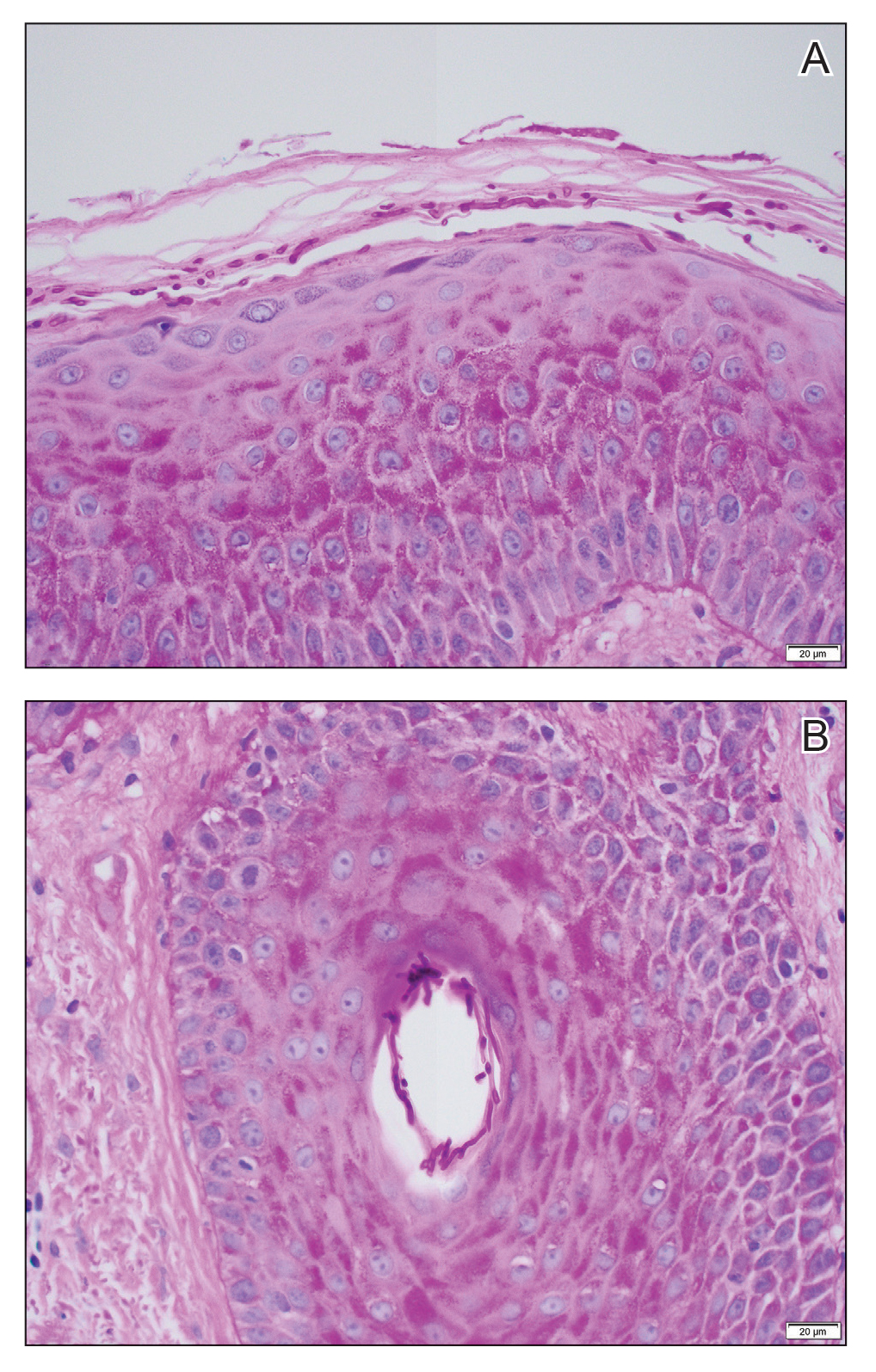
Approximately 1 month after the fungal isolate was sent to the reference laboratory, T indotineae was confirmed based on polymerase chain reaction (PCR) testing of internal transcribed spacer region sequences. Minimum inhibitory concentrations (MICs) obtained through antifungal susceptibility testing (AFST) were reported for fluconazole (8 μg/mL), griseofulvin (2 μg/mL), itraconazole (≤0.03 μg/mL), posaconazole (≤0.03 μg/mL), terbinafine (≥2 μg/mL), and voriconazole (0.125 μg/mL).
Approximately 7 weeks after itraconazole and ketoconazole were started, the rash had completely resolved. Nearly 8 months later (at the time this article was written), the rash had not recurred.
We report a unique case of T indotineae in a patient residing in California. Post hoc laboratory testing of dermatophyte isolates sent to the University of Texas reference laboratory identified terbinafine-resistant T indotineae specimens from the United States and Canada dating to 2017; clinical characteristics of patients from whom those isolates were obtained were unavailable.9
Trichophyton indotineae dermatophytosis typically is more extensive, inflamed, and pruritic, as well as likely more contagious, than tinea caused by other dermatophytes.5 Previously called Trichophyton mentagrophytes genotype VIII when first isolated in 2017, the pathogen was renamed T indotineae in 2020 after important genetic differences were discovered between it and other T mentagrophytes species.5 The emergence of T indotineae has been attributed to concomitant use of topical steroids and antifungals,5,10 inappropriate prescribing of antifungals,5 and nonadherence to antifungal treatment.5
Likely risk factors for T indotineae infection include suboptimal hygiene, overcrowded conditions, hot and humid environments, and tight-fitting synthetic clothing.4 Transmission from family members appears common,5 especially when fomites are shared.4 A case reported in Pennsylvania likely was acquired through sexual contact.7 Travel to South Asia has been associated with acquisition of T indotineae infection,3,5-7 though our patient and some others had not traveled there.3,8 It is not clear whether immunosuppression and diabetes mellitus are associated with T indotineae infection.4,5,8 Trichophyton indotineae also can affect animals,11 though zoonotic transmission has not been reported.4
Not all T indotineae isolates are resistant to one or more antifungals; furthermore, antifungal resistance in other dermatophyte species has been reported.5 Terbinafine resistance in T indotineae is conferred by mutations in the gene encoding squalene epoxidase, which helps synthesize ergosterol—a component of the cell membrane in fungi.2,4,5,12 Although clinical cut-points for MIC obtained by AFST are not well established, T indotineae MICs for terbinafine of 0.5 μg/mL or more correlate with resistance.9 Resistance to azoles has been linked to overexpression of transporter genes, which increase azole efflux from cells, as well as to mutations in the gene encoding lanosterol 14α demethylase.4,12,13
Potassium hydroxide preparations and fungal cultures cannot differentiate T indotineae from other dermatophytes that typically cause tinea.5,14 Histopathologic findings in our case were no different than those of non–T indotineae dermatophytes. Only molecular testing using PCR assays to sequence internal transcribed spacer genes can confirm T indotineae infection. However, PCR assays and AFST are not available in many US laboratories.5 Matrix-assisted laser desorption ionization-time of flight (MALDI-TOF) mass spectrometry has shown promise in distinguishing T indotineae from other dermatophytes, though its clinical use is limited and it cannot assess terbinafine sensitivity.15,16 Clinicians in the United States who want to test specimens from cases suspicious for T indotineae infection should contact their local or state health department or the Centers for Disease Control and Prevention for assistance.3,5
Systemic treatment typically is necessary for T indotineae infection.5 Combinations of oral and topical azoles have been used, as well as topical ciclopirox, amorolfine (not available in the United States), and luliconazole.1,5,17-21
Itraconazole has emerged as the treatment of choice for T indotineae tinea, typically at 200 mg/d and often for courses of more than 3 months.5 Testing for serum itraconazole trough levels, as done for our patient, typically is not recommended. Clinicians should counsel patients to take itraconazole with high-fat foods and an acidic beverage to increase bioavailability.5 Potential adverse effects of itraconazole include heart failure and numerous drug-drug interactions.5,22 Patients with T indotineae dermatophytosis should avoid sharing personal belongings and having skin-to-skin contact of affected areas with others.4
Dermatologists who suspect T indotineae infection should work with public health agencies that can assist with testing and undertake infection surveillance, prevention, and control.5,23 Challenges to diagnosing and managing T indotineae infection include lack of awareness among dermatology providers, the need for specialized laboratory testing to confirm infection, lack of established clinical cut-points for MICs from AFST, the need for longer duration of treatment vs what is needed for typical tinea, and potential challenges with insurance coverage for testing and treatment. Empiric treatment with itraconazole should be considered when terbinafine-resistant dermatophytosis is suspected or when terbinafine-resistant T indotineae infection is confirmed.
Acknowledgments—Jeremy Gold, MD; Dallas J. Smith, PharmD; and Shawn Lockhart, PhD, all of the Centers for Disease Control and Prevention, Mycotic Diseases Branch (Atlanta, Georgia), provided helpful comments to the authors in preparing the manuscript of this article.
To the Editor:
Historically, commonly available antifungal medications have been effective for treating dermatophytosis (tinea). However, recent tinea outbreaks caused by Trichophyton indotineae—a dermatophyte often resistant to terbinafine and sometimes to other antifungals—have been reported in South Asia, Europe, the Middle East, Southeast Asia, and Australia.1-5
Three confirmed cases of T indotineae dermatophytosis in the United States were reported in 2023 in New York3,6; a fourth confirmed case was reported in 2024 in Pennsylvania.7 Post hoc laboratory testing of fungal isolates in New York in 2022 and 2023 identified an additional 11 cases.8 We present a case of extensive multidrug-resistant tinea caused by T indotineae in a man in California.
An otherwise healthy 65-year-old man who had traveled to Europe in the past 3 months presented to his primary care physician with a widespread pruritic rash (Figure 1). He was treated with 2 weeks of oral terbinafine 250 mg/d and topical medicines, including clotrimazole cream 1%, fluocinonide ointment 0.05%, and clobetasol ointment 0.05% without improvement. Subsequently, 2 weeks of oral griseofulvin microsize 500 mg/d also proved ineffective. An antibody test was negative for HIV. His hemoglobin A1c was 6.2% (reference range, ≤5.6%). The patient was referred to dermatology.
Erythematous plaques—many scaly throughout and some annular with central clearing—were present on the arms, legs, and torso as well as in the groin. Honey crust was present on some plaques on the leg. A potassium hydroxide preparation showed abundant fungal hyphae. Material for fungal and bacterial cultures was collected. The patient was treated again with oral terbinafine 250 mg/d, an oral prednisone taper starting at 60 mg/d for a presumed id reaction, and various oral antihistamines for pruritus; all were ineffective. A bacterial culture showed only mixed skin flora. Oral fluconazole 200 mg/d was prescribed. A skin biopsy specimen showed compact orthokeratosis and parakeratosis of the stratum corneum with few neutrophils and focal pustule formation (Figure 2). Superficial perivascular inflammation, including lymphocytes, histiocytes, and few neutrophils, was present. A periodic acid–Schiff stain showed fungal hyphae in the stratum corneum and a hair follicle (Figure 3). After approximately 2 weeks, mold was identified in the fungal culture. Approximately 2 weeks thereafter, the organism was reported as Trichophyton species.

The rash did not improve; resistance to terbinafine, griseofulvin, and fluconazole was suspected clinically. The fungal isolate was sent to a reference laboratory (University of Texas Health Science Center, San Antonio). Meanwhile, oral itraconazole 200 mg twice daily and ketoconazole cream 2% were prescribed; the rash began to improve. A serum itraconazole trough level obtained 4 days after treatment initiation was 0.5 μg/mL (reference range, ≥0.6 μg/mL). The evening itraconazole dose was increased to 300 mg; a subsequent trough level was 0.8 μg/mL.
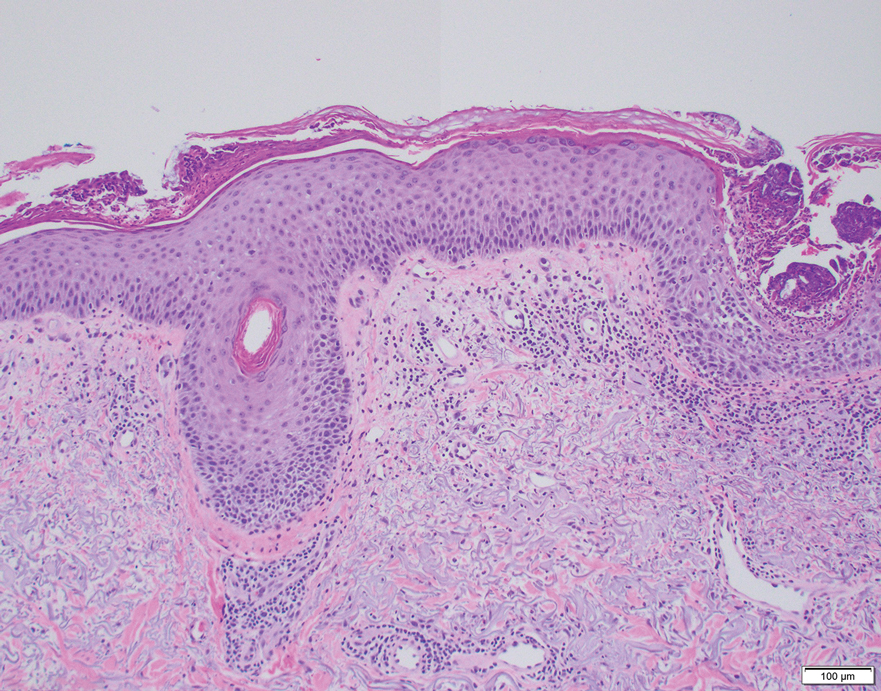
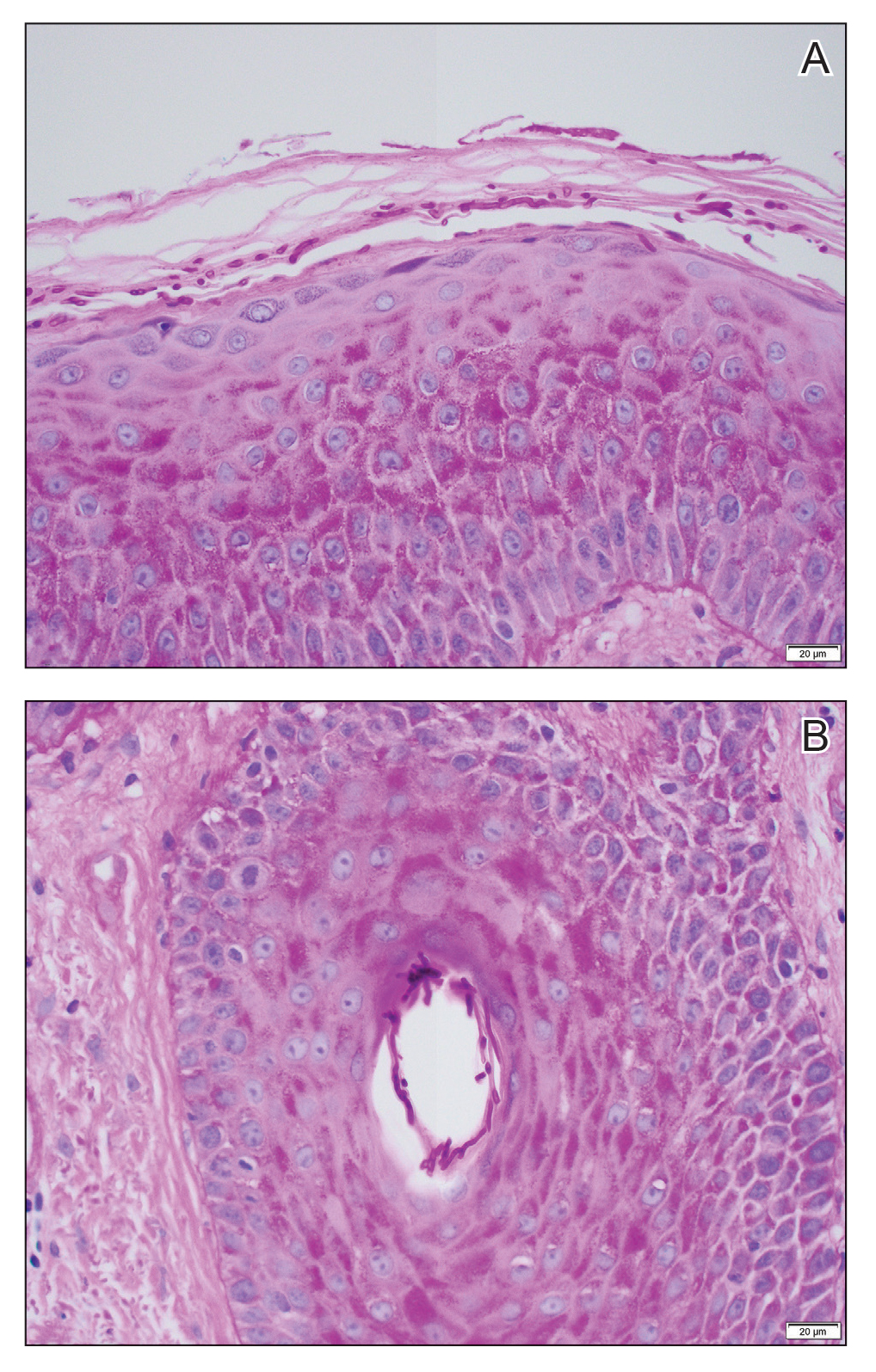
Approximately 1 month after the fungal isolate was sent to the reference laboratory, T indotineae was confirmed based on polymerase chain reaction (PCR) testing of internal transcribed spacer region sequences. Minimum inhibitory concentrations (MICs) obtained through antifungal susceptibility testing (AFST) were reported for fluconazole (8 μg/mL), griseofulvin (2 μg/mL), itraconazole (≤0.03 μg/mL), posaconazole (≤0.03 μg/mL), terbinafine (≥2 μg/mL), and voriconazole (0.125 μg/mL).
Approximately 7 weeks after itraconazole and ketoconazole were started, the rash had completely resolved. Nearly 8 months later (at the time this article was written), the rash had not recurred.
We report a unique case of T indotineae in a patient residing in California. Post hoc laboratory testing of dermatophyte isolates sent to the University of Texas reference laboratory identified terbinafine-resistant T indotineae specimens from the United States and Canada dating to 2017; clinical characteristics of patients from whom those isolates were obtained were unavailable.9
Trichophyton indotineae dermatophytosis typically is more extensive, inflamed, and pruritic, as well as likely more contagious, than tinea caused by other dermatophytes.5 Previously called Trichophyton mentagrophytes genotype VIII when first isolated in 2017, the pathogen was renamed T indotineae in 2020 after important genetic differences were discovered between it and other T mentagrophytes species.5 The emergence of T indotineae has been attributed to concomitant use of topical steroids and antifungals,5,10 inappropriate prescribing of antifungals,5 and nonadherence to antifungal treatment.5
Likely risk factors for T indotineae infection include suboptimal hygiene, overcrowded conditions, hot and humid environments, and tight-fitting synthetic clothing.4 Transmission from family members appears common,5 especially when fomites are shared.4 A case reported in Pennsylvania likely was acquired through sexual contact.7 Travel to South Asia has been associated with acquisition of T indotineae infection,3,5-7 though our patient and some others had not traveled there.3,8 It is not clear whether immunosuppression and diabetes mellitus are associated with T indotineae infection.4,5,8 Trichophyton indotineae also can affect animals,11 though zoonotic transmission has not been reported.4
Not all T indotineae isolates are resistant to one or more antifungals; furthermore, antifungal resistance in other dermatophyte species has been reported.5 Terbinafine resistance in T indotineae is conferred by mutations in the gene encoding squalene epoxidase, which helps synthesize ergosterol—a component of the cell membrane in fungi.2,4,5,12 Although clinical cut-points for MIC obtained by AFST are not well established, T indotineae MICs for terbinafine of 0.5 μg/mL or more correlate with resistance.9 Resistance to azoles has been linked to overexpression of transporter genes, which increase azole efflux from cells, as well as to mutations in the gene encoding lanosterol 14α demethylase.4,12,13
Potassium hydroxide preparations and fungal cultures cannot differentiate T indotineae from other dermatophytes that typically cause tinea.5,14 Histopathologic findings in our case were no different than those of non–T indotineae dermatophytes. Only molecular testing using PCR assays to sequence internal transcribed spacer genes can confirm T indotineae infection. However, PCR assays and AFST are not available in many US laboratories.5 Matrix-assisted laser desorption ionization-time of flight (MALDI-TOF) mass spectrometry has shown promise in distinguishing T indotineae from other dermatophytes, though its clinical use is limited and it cannot assess terbinafine sensitivity.15,16 Clinicians in the United States who want to test specimens from cases suspicious for T indotineae infection should contact their local or state health department or the Centers for Disease Control and Prevention for assistance.3,5
Systemic treatment typically is necessary for T indotineae infection.5 Combinations of oral and topical azoles have been used, as well as topical ciclopirox, amorolfine (not available in the United States), and luliconazole.1,5,17-21
Itraconazole has emerged as the treatment of choice for T indotineae tinea, typically at 200 mg/d and often for courses of more than 3 months.5 Testing for serum itraconazole trough levels, as done for our patient, typically is not recommended. Clinicians should counsel patients to take itraconazole with high-fat foods and an acidic beverage to increase bioavailability.5 Potential adverse effects of itraconazole include heart failure and numerous drug-drug interactions.5,22 Patients with T indotineae dermatophytosis should avoid sharing personal belongings and having skin-to-skin contact of affected areas with others.4
Dermatologists who suspect T indotineae infection should work with public health agencies that can assist with testing and undertake infection surveillance, prevention, and control.5,23 Challenges to diagnosing and managing T indotineae infection include lack of awareness among dermatology providers, the need for specialized laboratory testing to confirm infection, lack of established clinical cut-points for MICs from AFST, the need for longer duration of treatment vs what is needed for typical tinea, and potential challenges with insurance coverage for testing and treatment. Empiric treatment with itraconazole should be considered when terbinafine-resistant dermatophytosis is suspected or when terbinafine-resistant T indotineae infection is confirmed.
Acknowledgments—Jeremy Gold, MD; Dallas J. Smith, PharmD; and Shawn Lockhart, PhD, all of the Centers for Disease Control and Prevention, Mycotic Diseases Branch (Atlanta, Georgia), provided helpful comments to the authors in preparing the manuscript of this article.
- Uhrlaß S, Verma SB, Gräser Y, al. Trichophyton indotineae—an emerging pathogen causing recalcitrant dermatophytoses in India and worldwide—a multidimensional perspective. J Fungi (Basel). 2022;8:757. doi:10.3390/jof8070757
- Jabet A, Brun S, Normand A-C, et al. Extensive dermatophytosis caused by terbinafine-resistant Trichophyton indotineae, France. Emerg Infect Dis. 2022;28:229-233. doi:10.3201/eid2801.210883
- Caplan AS, Chaturvedi S, Zhu Y, et al. Notes from the field. First reported U.S. cases of tinea caused by Trichophyton indotineae—New York City, December 2021-March 2023. MMWR Morb Mortal Wkly Rep. 2023;72:536-537. doi:10.15585/mmwr.mm7219a4
- Jabet A, Normand A-C, Brun S, et al. Trichophyton indotineae, from epidemiology to therapeutic. J Mycol Med. 2023;33:101383. doi:10.1016/j.mycmed.2023.101383
- Hill RC, Caplan AS, Elewski B, et al. Expert panel review of skin and hair dermatophytoses in an era of antifungal resistance. Am J Clin Dermatol. 2024;25:359-389. doi:10.1007/s40257-024-00848-1
- Caplan AS, Zakhem GA, Pomeranz MK. Trichophyton mentagrophytes internal transcribed spacer genotype VIII. JAMA Dermatol. 2023;159:1130. doi:10.1001/jamadermatol.2023.2645
- Spivack S, Gold JAW, Lockhart SR, et al. Potential sexual transmission of antifungal-resistant Trichophyton indotineae. Emerg Infect Dis. 2024;30:807-809. doi:10.3201/eid3004.240115
- Caplan AS, Todd GC, Zhu Y, et al. Clinical course, antifungal susceptibility, and genomic sequencing of Trichophyton indotineae. JAMA Dermatol. Published online May 15, 2024. doi:10.1001/jamadermatol.2024.1126
- Cañete-Gibas CF, Mele J, Patterson HP, et al. Terbinafine-resistant dermatophytes and the presence of Trichophyton indotineae in North America. J Clin Microbiol. 2023;61:e0056223. doi:10.1128/jcm.00562-23
- Gupta AK, Venkataraman M, Hall DC, et al. The emergence of Trichophyton indotineae: implications for clinical practice. Int J Dermatol. 2023;62:857-861.
- Oladzad V, Nasrollahi Omran A, Haghani I, et al. Multi-drug resistance Trichophyton indotineae in a stray dog. Res Vet Sci. 2024;166:105105. doi:10.1016/j.rvsc.2023.105105
- Martinez-Rossi NM, Bitencourt TA, Peres NTA, et al. Dermatophyte resistance to antifungal drugs: mechanisms and prospectus. Front Microbiol. 2018;9:1108. doi:10.3389/fmicb.2018.01108
- Sacheli R, Hayette MP. Antifungal resistance in dermatophytes: genetic considerations, clinical presentations and alternative therapies. J Fungi (Basel). 2021;711:983. doi:10.3390/jof7110983
- Gupta AK, Cooper EA. Dermatophytosis (tinea) and other superficial fungal infections. In: Hospenthal DR, Rinaldi MG, eds. Diagnosis and Treatment of Human Mycoses. Humana Press; 2008:355-381.
- Normand A-C, Moreno-Sabater A, Jabet A, et al. MALDI-TOF mass spectrometry online identification of Trichophyton indotineae using the MSI-2 application. J Fungi (Basel). 2022;8:1103. doi:10.3390/jof8101103
- De Paepe R, Normand A-C, Uhrlaß S, et al. Resistance profile, terbinafine resistance screening and MALDI-TOF MS identification of the emerging pathogen Trichophyton indotineae. Mycopathologia. 2024;189:29. doi:10.1007/s11046-024-00835-4
- Rajagopalan M, Inamadar A, Mittal A, et al. Expert consensus on the management of dermatophytosis in India (ECTODERM India). BMC Dermatol. 2018;18:6. doi:10.1186/s12895-018-0073-1
- Verma SB, Panda S, Nenoff P, et al. The unprecedented epidemic-like scenario of dermatophytosis in India: III. Antifungal resistance and treatment options. Indian J Dermatol Venereol Leprol. 2021;87:468-482. doi:10.25259/IJDVL_303_20
- Shaw D, Singh S, Dogra S, et al. MIC and upper limit of wild-type distribution for 13 antifungal agents against a Trichophyton mentagrophytes–Trichophyton interdigitale complex of Indian origin. Antimicrob Agents Chemother. 2020;64:E01964-19. doi:10.1128/AAC.01964-19
- Burmester A, Hipler U-C, Uhrlaß S, et al. Indian Trichophyton mentagrophytes squalene epoxidase erg1 double mutants show high proportion of combined fluconazole and terbinafine resistance. Mycoses. 2020;63:1175-1180. doi:10.1111/myc.13150
- Khurana A, Agarwal A, Agrawal D, et al. Effect of different itraconazole dosing regimens on cure rates, treatment duration, safety, and relapse rates in adult patients with tinea corporis/cruris: a randomized clinical trial. JAMA Dermatol. 2022;158:1269-1278. doi:10.1001/jamadermatol.2022.3745
- Itraconazole capsule. DailyMed [Internet]. Updated June 3, 2024. Accessed June 19, 2024. https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=2ab38a8a-3708-4b97-9f7f-8e554a15348d
- Bui TS, Katz KA. Resistant Trichophyton indotineae dermatophytosis—an emerging pandemic, now in the US. JAMA Dermatol. Published online May 15, 2024. doi:10.1001/jamadermatol.2024.1125
- Uhrlaß S, Verma SB, Gräser Y, al. Trichophyton indotineae—an emerging pathogen causing recalcitrant dermatophytoses in India and worldwide—a multidimensional perspective. J Fungi (Basel). 2022;8:757. doi:10.3390/jof8070757
- Jabet A, Brun S, Normand A-C, et al. Extensive dermatophytosis caused by terbinafine-resistant Trichophyton indotineae, France. Emerg Infect Dis. 2022;28:229-233. doi:10.3201/eid2801.210883
- Caplan AS, Chaturvedi S, Zhu Y, et al. Notes from the field. First reported U.S. cases of tinea caused by Trichophyton indotineae—New York City, December 2021-March 2023. MMWR Morb Mortal Wkly Rep. 2023;72:536-537. doi:10.15585/mmwr.mm7219a4
- Jabet A, Normand A-C, Brun S, et al. Trichophyton indotineae, from epidemiology to therapeutic. J Mycol Med. 2023;33:101383. doi:10.1016/j.mycmed.2023.101383
- Hill RC, Caplan AS, Elewski B, et al. Expert panel review of skin and hair dermatophytoses in an era of antifungal resistance. Am J Clin Dermatol. 2024;25:359-389. doi:10.1007/s40257-024-00848-1
- Caplan AS, Zakhem GA, Pomeranz MK. Trichophyton mentagrophytes internal transcribed spacer genotype VIII. JAMA Dermatol. 2023;159:1130. doi:10.1001/jamadermatol.2023.2645
- Spivack S, Gold JAW, Lockhart SR, et al. Potential sexual transmission of antifungal-resistant Trichophyton indotineae. Emerg Infect Dis. 2024;30:807-809. doi:10.3201/eid3004.240115
- Caplan AS, Todd GC, Zhu Y, et al. Clinical course, antifungal susceptibility, and genomic sequencing of Trichophyton indotineae. JAMA Dermatol. Published online May 15, 2024. doi:10.1001/jamadermatol.2024.1126
- Cañete-Gibas CF, Mele J, Patterson HP, et al. Terbinafine-resistant dermatophytes and the presence of Trichophyton indotineae in North America. J Clin Microbiol. 2023;61:e0056223. doi:10.1128/jcm.00562-23
- Gupta AK, Venkataraman M, Hall DC, et al. The emergence of Trichophyton indotineae: implications for clinical practice. Int J Dermatol. 2023;62:857-861.
- Oladzad V, Nasrollahi Omran A, Haghani I, et al. Multi-drug resistance Trichophyton indotineae in a stray dog. Res Vet Sci. 2024;166:105105. doi:10.1016/j.rvsc.2023.105105
- Martinez-Rossi NM, Bitencourt TA, Peres NTA, et al. Dermatophyte resistance to antifungal drugs: mechanisms and prospectus. Front Microbiol. 2018;9:1108. doi:10.3389/fmicb.2018.01108
- Sacheli R, Hayette MP. Antifungal resistance in dermatophytes: genetic considerations, clinical presentations and alternative therapies. J Fungi (Basel). 2021;711:983. doi:10.3390/jof7110983
- Gupta AK, Cooper EA. Dermatophytosis (tinea) and other superficial fungal infections. In: Hospenthal DR, Rinaldi MG, eds. Diagnosis and Treatment of Human Mycoses. Humana Press; 2008:355-381.
- Normand A-C, Moreno-Sabater A, Jabet A, et al. MALDI-TOF mass spectrometry online identification of Trichophyton indotineae using the MSI-2 application. J Fungi (Basel). 2022;8:1103. doi:10.3390/jof8101103
- De Paepe R, Normand A-C, Uhrlaß S, et al. Resistance profile, terbinafine resistance screening and MALDI-TOF MS identification of the emerging pathogen Trichophyton indotineae. Mycopathologia. 2024;189:29. doi:10.1007/s11046-024-00835-4
- Rajagopalan M, Inamadar A, Mittal A, et al. Expert consensus on the management of dermatophytosis in India (ECTODERM India). BMC Dermatol. 2018;18:6. doi:10.1186/s12895-018-0073-1
- Verma SB, Panda S, Nenoff P, et al. The unprecedented epidemic-like scenario of dermatophytosis in India: III. Antifungal resistance and treatment options. Indian J Dermatol Venereol Leprol. 2021;87:468-482. doi:10.25259/IJDVL_303_20
- Shaw D, Singh S, Dogra S, et al. MIC and upper limit of wild-type distribution for 13 antifungal agents against a Trichophyton mentagrophytes–Trichophyton interdigitale complex of Indian origin. Antimicrob Agents Chemother. 2020;64:E01964-19. doi:10.1128/AAC.01964-19
- Burmester A, Hipler U-C, Uhrlaß S, et al. Indian Trichophyton mentagrophytes squalene epoxidase erg1 double mutants show high proportion of combined fluconazole and terbinafine resistance. Mycoses. 2020;63:1175-1180. doi:10.1111/myc.13150
- Khurana A, Agarwal A, Agrawal D, et al. Effect of different itraconazole dosing regimens on cure rates, treatment duration, safety, and relapse rates in adult patients with tinea corporis/cruris: a randomized clinical trial. JAMA Dermatol. 2022;158:1269-1278. doi:10.1001/jamadermatol.2022.3745
- Itraconazole capsule. DailyMed [Internet]. Updated June 3, 2024. Accessed June 19, 2024. https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=2ab38a8a-3708-4b97-9f7f-8e554a15348d
- Bui TS, Katz KA. Resistant Trichophyton indotineae dermatophytosis—an emerging pandemic, now in the US. JAMA Dermatol. Published online May 15, 2024. doi:10.1001/jamadermatol.2024.1125
Practice Points
- Trichophyton indotineae can cause extensive dermatophytosis that often is resistant to terbinafine and in some cases to other antifungals.
- Only molecular testing, which is not widely available, can distinguish T indotineae from other dermatophytes.
- Suspected or confirmed cases of T indotineae dermatophytosis should be reported to public health agencies to provide assistance with testing, as well as surveillance, prevention, and control of infection.
Online Diagnosis of Sexually Transmitted Infections? Ethicist Says We Are Nowhere Close
This transcript has been edited for clarity.
There has been a large amount of news lately about dating online and dating apps. Probably the most common way younger people find potential partners is to go online and see who’s there that they might want to meet.
Online dating is also notorious for being full of scammers. There are all kinds of people out there that you have to be careful of, who are trying to rip you off by saying, “Send me money, I’m in trouble,” or “Now that we have a relationship, will you support my particular entrepreneurial idea?” Certainly, dangers are there.
Another danger we don’t talk much about is meeting people who have sexually transmitted diseases. That’s been a problem before websites and before dating apps. I think the opportunity of meeting more people — strangers, people you don’t really know — who may not tell you the truth about their health, and particularly their sexual health, is really out there.
It’s always good medical advice to tell people to practice safe sex, and that often involves a man wearing a condom. It certainly is the case that we want to attend not just to the prevention of unwanted pregnancy but also to the transmission of diseases. I think it’s very important to tell women of reproductive age to get their HPV shot to try to reduce cancers in their reproductive systems, or sometimes in men — anal cancers, or even being a transmitter of disease.
Even then, certainly one wants to recommend that, in an age where some people are going to meet many partners that they don’t know well or don’t have much background with, it’s wise to try to prevent diseases using the vaccines we’ve got, using the contraceptive methods that will prevent disease transmission, and reminding people to ask about sex life.
I did come across a website that just startled me. It’s called HeHealth, and basically it says to men, if you are conscientious about your sex life, take a picture of your penis, send it to us, and we have doctors — I presume they’re US doctors but I don’t know — who will diagnose venereal diseases based on that picture. I presume women could also say, “Before we have sex, or now that we’re approaching that possibility, I want you to send a picture to this company on this website.”
Now, a couple of reminders. I think we all know this, but just because you’re not manifesting symptoms on your reproductive organs doesn’t mean you don’t have a sexual disease. It’s not a reliable measure. Yes, maybe you could have somebody say: “Oh, that looks nasty. I’m not sure you ought to have sex right now, and maybe you should go get some treatment.” This is going to miss many cases and is not a reliable indicator that your partner is safe in terms of not transmitting diseases to you.
It also isn’t clear what they do with these images. Do they keep them? Who can see them? Could they resell them? What sort of privacy protection have you got if you decide to use this?
There’s another issue here, which is, if they misdiagnose someone and you do catch a sexual disease, who’s liable? Can you go after them for using doctors who weren’t competent or transmitting images that weren’t really adequate because you didn’t know how to take that picture properly when you sent that off to them? There are many unknowns.
The bottom line is that we’re in a different world, I think, of romance. We’re in a world where some people are going to meet more partners. Some people are going to meet more strangers. One approach is to have us take pictures of ourselves, send them off to who knows where, and ask for a green light to go ahead and have sexual relations. I don’t think we’re anywhere close to being able to rely on that as a way to avoid the risks of unprotected sexual behavior.
We do know what to do in dealing with patients who are sexually active. First, we have to ask them. Then we’ve got to recommend available vaccinations to prevent the transmission of some cancers, the HPV vaccine. Then they need that reminder about safe sexual practices not only to protect against unwanted pregnancy, but still, in this day and age, to protect against syphilis, which is on the rise, plus HIV, gonorrhea, chlamydia, and other sexually transmissible diseases.
I’m not going to rely on the penis picture to make the world safe for sex. I think we have to still use the old-fashioned techniques of education and prevention to do the best we can.
Dr. Caplan is director of the Division of Medical Ethics at New York University Langone Medical Center, New York City. He reported conflicts of interest with Johnson & Johnson’s Panel for Compassionate Drug Use and Medscape.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
There has been a large amount of news lately about dating online and dating apps. Probably the most common way younger people find potential partners is to go online and see who’s there that they might want to meet.
Online dating is also notorious for being full of scammers. There are all kinds of people out there that you have to be careful of, who are trying to rip you off by saying, “Send me money, I’m in trouble,” or “Now that we have a relationship, will you support my particular entrepreneurial idea?” Certainly, dangers are there.
Another danger we don’t talk much about is meeting people who have sexually transmitted diseases. That’s been a problem before websites and before dating apps. I think the opportunity of meeting more people — strangers, people you don’t really know — who may not tell you the truth about their health, and particularly their sexual health, is really out there.
It’s always good medical advice to tell people to practice safe sex, and that often involves a man wearing a condom. It certainly is the case that we want to attend not just to the prevention of unwanted pregnancy but also to the transmission of diseases. I think it’s very important to tell women of reproductive age to get their HPV shot to try to reduce cancers in their reproductive systems, or sometimes in men — anal cancers, or even being a transmitter of disease.
Even then, certainly one wants to recommend that, in an age where some people are going to meet many partners that they don’t know well or don’t have much background with, it’s wise to try to prevent diseases using the vaccines we’ve got, using the contraceptive methods that will prevent disease transmission, and reminding people to ask about sex life.
I did come across a website that just startled me. It’s called HeHealth, and basically it says to men, if you are conscientious about your sex life, take a picture of your penis, send it to us, and we have doctors — I presume they’re US doctors but I don’t know — who will diagnose venereal diseases based on that picture. I presume women could also say, “Before we have sex, or now that we’re approaching that possibility, I want you to send a picture to this company on this website.”
Now, a couple of reminders. I think we all know this, but just because you’re not manifesting symptoms on your reproductive organs doesn’t mean you don’t have a sexual disease. It’s not a reliable measure. Yes, maybe you could have somebody say: “Oh, that looks nasty. I’m not sure you ought to have sex right now, and maybe you should go get some treatment.” This is going to miss many cases and is not a reliable indicator that your partner is safe in terms of not transmitting diseases to you.
It also isn’t clear what they do with these images. Do they keep them? Who can see them? Could they resell them? What sort of privacy protection have you got if you decide to use this?
There’s another issue here, which is, if they misdiagnose someone and you do catch a sexual disease, who’s liable? Can you go after them for using doctors who weren’t competent or transmitting images that weren’t really adequate because you didn’t know how to take that picture properly when you sent that off to them? There are many unknowns.
The bottom line is that we’re in a different world, I think, of romance. We’re in a world where some people are going to meet more partners. Some people are going to meet more strangers. One approach is to have us take pictures of ourselves, send them off to who knows where, and ask for a green light to go ahead and have sexual relations. I don’t think we’re anywhere close to being able to rely on that as a way to avoid the risks of unprotected sexual behavior.
We do know what to do in dealing with patients who are sexually active. First, we have to ask them. Then we’ve got to recommend available vaccinations to prevent the transmission of some cancers, the HPV vaccine. Then they need that reminder about safe sexual practices not only to protect against unwanted pregnancy, but still, in this day and age, to protect against syphilis, which is on the rise, plus HIV, gonorrhea, chlamydia, and other sexually transmissible diseases.
I’m not going to rely on the penis picture to make the world safe for sex. I think we have to still use the old-fashioned techniques of education and prevention to do the best we can.
Dr. Caplan is director of the Division of Medical Ethics at New York University Langone Medical Center, New York City. He reported conflicts of interest with Johnson & Johnson’s Panel for Compassionate Drug Use and Medscape.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
There has been a large amount of news lately about dating online and dating apps. Probably the most common way younger people find potential partners is to go online and see who’s there that they might want to meet.
Online dating is also notorious for being full of scammers. There are all kinds of people out there that you have to be careful of, who are trying to rip you off by saying, “Send me money, I’m in trouble,” or “Now that we have a relationship, will you support my particular entrepreneurial idea?” Certainly, dangers are there.
Another danger we don’t talk much about is meeting people who have sexually transmitted diseases. That’s been a problem before websites and before dating apps. I think the opportunity of meeting more people — strangers, people you don’t really know — who may not tell you the truth about their health, and particularly their sexual health, is really out there.
It’s always good medical advice to tell people to practice safe sex, and that often involves a man wearing a condom. It certainly is the case that we want to attend not just to the prevention of unwanted pregnancy but also to the transmission of diseases. I think it’s very important to tell women of reproductive age to get their HPV shot to try to reduce cancers in their reproductive systems, or sometimes in men — anal cancers, or even being a transmitter of disease.
Even then, certainly one wants to recommend that, in an age where some people are going to meet many partners that they don’t know well or don’t have much background with, it’s wise to try to prevent diseases using the vaccines we’ve got, using the contraceptive methods that will prevent disease transmission, and reminding people to ask about sex life.
I did come across a website that just startled me. It’s called HeHealth, and basically it says to men, if you are conscientious about your sex life, take a picture of your penis, send it to us, and we have doctors — I presume they’re US doctors but I don’t know — who will diagnose venereal diseases based on that picture. I presume women could also say, “Before we have sex, or now that we’re approaching that possibility, I want you to send a picture to this company on this website.”
Now, a couple of reminders. I think we all know this, but just because you’re not manifesting symptoms on your reproductive organs doesn’t mean you don’t have a sexual disease. It’s not a reliable measure. Yes, maybe you could have somebody say: “Oh, that looks nasty. I’m not sure you ought to have sex right now, and maybe you should go get some treatment.” This is going to miss many cases and is not a reliable indicator that your partner is safe in terms of not transmitting diseases to you.
It also isn’t clear what they do with these images. Do they keep them? Who can see them? Could they resell them? What sort of privacy protection have you got if you decide to use this?
There’s another issue here, which is, if they misdiagnose someone and you do catch a sexual disease, who’s liable? Can you go after them for using doctors who weren’t competent or transmitting images that weren’t really adequate because you didn’t know how to take that picture properly when you sent that off to them? There are many unknowns.
The bottom line is that we’re in a different world, I think, of romance. We’re in a world where some people are going to meet more partners. Some people are going to meet more strangers. One approach is to have us take pictures of ourselves, send them off to who knows where, and ask for a green light to go ahead and have sexual relations. I don’t think we’re anywhere close to being able to rely on that as a way to avoid the risks of unprotected sexual behavior.
We do know what to do in dealing with patients who are sexually active. First, we have to ask them. Then we’ve got to recommend available vaccinations to prevent the transmission of some cancers, the HPV vaccine. Then they need that reminder about safe sexual practices not only to protect against unwanted pregnancy, but still, in this day and age, to protect against syphilis, which is on the rise, plus HIV, gonorrhea, chlamydia, and other sexually transmissible diseases.
I’m not going to rely on the penis picture to make the world safe for sex. I think we have to still use the old-fashioned techniques of education and prevention to do the best we can.
Dr. Caplan is director of the Division of Medical Ethics at New York University Langone Medical Center, New York City. He reported conflicts of interest with Johnson & Johnson’s Panel for Compassionate Drug Use and Medscape.
A version of this article first appeared on Medscape.com.
Experts Expect New Human Cases of Avian Flu
With avian influenza spreading quickly around the globe, the virus has more opportunities to mutate and cause problems for people. By some calculations, H5N1 bird flu is still at least two mutations away from widespread human infections, but experts warn that new flu symptoms in individuals at high risk are likely to start turning up in health systems this summer.
“Some of this will not be obvious or at the forefront of our minds.”
Dr. Dugan is leading the team of CDC scientists that is working with partners from the US Department of Agriculture, the US Food and Drug Administration (FDA), and state and local health departments to track and respond to the H5N1 bird flu outbreak currently sweeping through the United States.
Since 2022, avian influenza A viruses have been detected in more than 9300 wild birds in 50 states and territories and in commercial and backyard flocks.
“It’s a bad situation,” said Florian Krammer, PhD, professor of vaccinology at the Icahn School of Medicine at Mount Sinai in New York. “Globally, we’ve seen tons of exposure in cities around the world and even in the birds here in New York City where I am.”
Birds shed the virus in their saliva, mucous, and feces, so people or other animals with close, unprotected contact with infected birds or their contaminated environments can be infected.
And for the first time in March 2024, H5N1 bird flu was reported in dairy cows. The US Department of Agriculture said that at last count, 101 dairy herds in 12 states had been infected, with several cases also found in dairy workers.
From Birds to Cattle and Farm Workers
The National Veterinary Services Laboratories confirmed the infections were highly pathogenic avian influenza H5N1 clade 2.3.4.4b of Eurasian lineage. Also known as the goose, Guangdong clade from China, phylogenetic analysis and epidemiology suggests a single introduction into cows followed by onward transmission.
“I was surprised when H5 was introduced to dairy cattle in this way,” Dr. Dugan said. “Influenza viruses are always surprising us and it reminds me to stay humble and keep an open mind when dealing with them.”
People rarely inhale or get sufficient virus in their eyes or mouth to get sick, Dr. Dugan said, but those in close contact with animals are still at risk for infection, which could lead to upper respiratory tract symptoms such as shortness of breath, cough, sore throat, or runny or stuffy nose.
Like with other viruses, people can also experience muscle or body aches, headache, fatigue, fever or, as was seen in farm workers, conjunctivitis.
But there are less-common symptoms too like diarrhea, nausea, and vomiting — and sometimes, even seizures.
The risk to the general public is still low, Dr. Dugan said, but authorities recommend that people working with animals wash their hands with soap and water and wear personal protective equipment that includes fluid-resistant coveralls, a waterproof apron, a safety-approved respirator, properly fitted goggles or face shield, a head or hair cover, gloves, and boots.
Dr. Dugan said that health care providers often don’t take a history of occupational exposures when a patient presents with flu. But with rising rates of bird flu in new animal hosts, “this will be an important next step.”
Asking Unusual Questions
This approach is not standardized on most electronic health records, so these are questions that clinicians will need to initiate themselves.
“Physicians should ask about work,” said Meghan Davis, PhD, associate professor at the Johns Hopkins Bloomberg School of Public Health in Baltimore. “If it’s not already on the radar, asking about any direct contact with dairy cows, poultry, pigs, wild birds, or wild mammals is important.”
Dr. Davis says she’s worried about a new study tracking risk factors for farm-to-farm transmission because it shows that farms testing positive for avian influenza often have workers with a family member also employed on another farm. “This suggests that we might need to be on the lookout for possible transmission within families,” she said. Now, we have to ask “not just if the person with symptoms has contact with or works on a dairy farm, milk processing plant, or slaughterhouse, but also if any family member does.”
Dr. Davis said that it’s important to bear in mind when taking these histories that there may be younger workers on farms and in slaughter and processing facilities due to exemptions or illegal work.
What is important now is to get the situation under control this season in dairy cattle, Dr. Krammer said. “This will be easier to stop in cows than humans, so this is the time to stop moving dairy cattle and start vaccinating them.”
Spotting New Cases
Since April 2024, there have been three human cases of avian influenza after exposure to dairy cows reported. “And what we don’t want to see this summer is an unusual human cluster of influenza. It’s important we keep a close, watchful eye for this,” Dr. Krammer said.
“Influenza viruses do very interesting things and as we head into fall and winter flu season, we don’t want new human co-infections that could cause major problems for us,” he said.
If people become mixing vessels of a seasonal cocktail of multiple viruses, that could empower H5N1 to mutate again into something more dangerous, sparking a new pandemic.
“It wasn’t all that long ago that we were asking China difficult questions about the steps Chinese authorities took to protect human lives from SARS-CoV-2 in the COVID pandemic. Now, we must ask ourselves many of these questions,” Dr. Krammer said. “We are at a crucial crossroad where we will either elude a new pandemic or see one take off, risking 10 to 20 million lives.”
There is a precedent for safely evading more trouble, Dr. Krammer pointed out. Government agencies have already been working with the poultry industry for a couple of years now. “And here, we have successfully stopped H5N1 with new regulations and policies.”
But moving from poultry farms to cattle has not been an easy transition, Dr. Dugan said. Cattle farms have no experience with bird flu or tactics to contain it with regulations, and officials too are working in new, unfamiliar terrain.
“What we have now isn’t a science problem, it’s a policy issue, and it hasn’t always been clear who is in charge,” Dr. Krammer said.
“Agencies are working together at the state, federal, and global level,” said Dr. Dugan. “We are increasing our transparency and are working to share what we know, when we know it.”
The infrastructure built during the COVID pandemic has helped teams prepare for this new crisis, Dr. Dugan said. Year-round, layered monitoring has clinical labs reporting seasonal influenza and novel cases.
“Laboratories are ready to help with testing,” Dr. Dugan said.
Specimens should be collected as soon as possible from patients with flu symptoms. A nasopharyngeal swab is recommended with a nasal swab combined with an oropharyngeal swab. If a patient has conjunctivitis with or without respiratory symptoms, both a conjunctival swab and a nasopharyngeal swab should be collected.
People with severe respiratory disease should also have lower respiratory tract specimens collected.
Standard, contact, and airborne precautions are recommended for patients presenting for medical care who have illness consistent with influenza and recent exposure to birds or other animals.
Antiviral Drugs
There are four FDA-approved antivirals for influenza: Oseltamivir phosphate (available as a generic drug or by the trade name Tamiflu), zanamivir (Relenza), peramivir (Rapivab) , and baloxavir (Xofluza).
For people with suspected or confirmed avian influenza, treatment is recommended as soon as possible.
There are no clinical trials measuring the outcome of antivirals in people infected with avian influenza. However, data from animal models and human observational studies suggest a benefit.
“We can’t afford to wait this summer,” Dr. Krammer said. “We have an opportunity right now to stop this in cows before we risk infecting more people. I hope we do.”
A version of this article first appeared on Medscape.com.
With avian influenza spreading quickly around the globe, the virus has more opportunities to mutate and cause problems for people. By some calculations, H5N1 bird flu is still at least two mutations away from widespread human infections, but experts warn that new flu symptoms in individuals at high risk are likely to start turning up in health systems this summer.
“Some of this will not be obvious or at the forefront of our minds.”
Dr. Dugan is leading the team of CDC scientists that is working with partners from the US Department of Agriculture, the US Food and Drug Administration (FDA), and state and local health departments to track and respond to the H5N1 bird flu outbreak currently sweeping through the United States.
Since 2022, avian influenza A viruses have been detected in more than 9300 wild birds in 50 states and territories and in commercial and backyard flocks.
“It’s a bad situation,” said Florian Krammer, PhD, professor of vaccinology at the Icahn School of Medicine at Mount Sinai in New York. “Globally, we’ve seen tons of exposure in cities around the world and even in the birds here in New York City where I am.”
Birds shed the virus in their saliva, mucous, and feces, so people or other animals with close, unprotected contact with infected birds or their contaminated environments can be infected.
And for the first time in March 2024, H5N1 bird flu was reported in dairy cows. The US Department of Agriculture said that at last count, 101 dairy herds in 12 states had been infected, with several cases also found in dairy workers.
From Birds to Cattle and Farm Workers
The National Veterinary Services Laboratories confirmed the infections were highly pathogenic avian influenza H5N1 clade 2.3.4.4b of Eurasian lineage. Also known as the goose, Guangdong clade from China, phylogenetic analysis and epidemiology suggests a single introduction into cows followed by onward transmission.
“I was surprised when H5 was introduced to dairy cattle in this way,” Dr. Dugan said. “Influenza viruses are always surprising us and it reminds me to stay humble and keep an open mind when dealing with them.”
People rarely inhale or get sufficient virus in their eyes or mouth to get sick, Dr. Dugan said, but those in close contact with animals are still at risk for infection, which could lead to upper respiratory tract symptoms such as shortness of breath, cough, sore throat, or runny or stuffy nose.
Like with other viruses, people can also experience muscle or body aches, headache, fatigue, fever or, as was seen in farm workers, conjunctivitis.
But there are less-common symptoms too like diarrhea, nausea, and vomiting — and sometimes, even seizures.
The risk to the general public is still low, Dr. Dugan said, but authorities recommend that people working with animals wash their hands with soap and water and wear personal protective equipment that includes fluid-resistant coveralls, a waterproof apron, a safety-approved respirator, properly fitted goggles or face shield, a head or hair cover, gloves, and boots.
Dr. Dugan said that health care providers often don’t take a history of occupational exposures when a patient presents with flu. But with rising rates of bird flu in new animal hosts, “this will be an important next step.”
Asking Unusual Questions
This approach is not standardized on most electronic health records, so these are questions that clinicians will need to initiate themselves.
“Physicians should ask about work,” said Meghan Davis, PhD, associate professor at the Johns Hopkins Bloomberg School of Public Health in Baltimore. “If it’s not already on the radar, asking about any direct contact with dairy cows, poultry, pigs, wild birds, or wild mammals is important.”
Dr. Davis says she’s worried about a new study tracking risk factors for farm-to-farm transmission because it shows that farms testing positive for avian influenza often have workers with a family member also employed on another farm. “This suggests that we might need to be on the lookout for possible transmission within families,” she said. Now, we have to ask “not just if the person with symptoms has contact with or works on a dairy farm, milk processing plant, or slaughterhouse, but also if any family member does.”
Dr. Davis said that it’s important to bear in mind when taking these histories that there may be younger workers on farms and in slaughter and processing facilities due to exemptions or illegal work.
What is important now is to get the situation under control this season in dairy cattle, Dr. Krammer said. “This will be easier to stop in cows than humans, so this is the time to stop moving dairy cattle and start vaccinating them.”
Spotting New Cases
Since April 2024, there have been three human cases of avian influenza after exposure to dairy cows reported. “And what we don’t want to see this summer is an unusual human cluster of influenza. It’s important we keep a close, watchful eye for this,” Dr. Krammer said.
“Influenza viruses do very interesting things and as we head into fall and winter flu season, we don’t want new human co-infections that could cause major problems for us,” he said.
If people become mixing vessels of a seasonal cocktail of multiple viruses, that could empower H5N1 to mutate again into something more dangerous, sparking a new pandemic.
“It wasn’t all that long ago that we were asking China difficult questions about the steps Chinese authorities took to protect human lives from SARS-CoV-2 in the COVID pandemic. Now, we must ask ourselves many of these questions,” Dr. Krammer said. “We are at a crucial crossroad where we will either elude a new pandemic or see one take off, risking 10 to 20 million lives.”
There is a precedent for safely evading more trouble, Dr. Krammer pointed out. Government agencies have already been working with the poultry industry for a couple of years now. “And here, we have successfully stopped H5N1 with new regulations and policies.”
But moving from poultry farms to cattle has not been an easy transition, Dr. Dugan said. Cattle farms have no experience with bird flu or tactics to contain it with regulations, and officials too are working in new, unfamiliar terrain.
“What we have now isn’t a science problem, it’s a policy issue, and it hasn’t always been clear who is in charge,” Dr. Krammer said.
“Agencies are working together at the state, federal, and global level,” said Dr. Dugan. “We are increasing our transparency and are working to share what we know, when we know it.”
The infrastructure built during the COVID pandemic has helped teams prepare for this new crisis, Dr. Dugan said. Year-round, layered monitoring has clinical labs reporting seasonal influenza and novel cases.
“Laboratories are ready to help with testing,” Dr. Dugan said.
Specimens should be collected as soon as possible from patients with flu symptoms. A nasopharyngeal swab is recommended with a nasal swab combined with an oropharyngeal swab. If a patient has conjunctivitis with or without respiratory symptoms, both a conjunctival swab and a nasopharyngeal swab should be collected.
People with severe respiratory disease should also have lower respiratory tract specimens collected.
Standard, contact, and airborne precautions are recommended for patients presenting for medical care who have illness consistent with influenza and recent exposure to birds or other animals.
Antiviral Drugs
There are four FDA-approved antivirals for influenza: Oseltamivir phosphate (available as a generic drug or by the trade name Tamiflu), zanamivir (Relenza), peramivir (Rapivab) , and baloxavir (Xofluza).
For people with suspected or confirmed avian influenza, treatment is recommended as soon as possible.
There are no clinical trials measuring the outcome of antivirals in people infected with avian influenza. However, data from animal models and human observational studies suggest a benefit.
“We can’t afford to wait this summer,” Dr. Krammer said. “We have an opportunity right now to stop this in cows before we risk infecting more people. I hope we do.”
A version of this article first appeared on Medscape.com.
With avian influenza spreading quickly around the globe, the virus has more opportunities to mutate and cause problems for people. By some calculations, H5N1 bird flu is still at least two mutations away from widespread human infections, but experts warn that new flu symptoms in individuals at high risk are likely to start turning up in health systems this summer.
“Some of this will not be obvious or at the forefront of our minds.”
Dr. Dugan is leading the team of CDC scientists that is working with partners from the US Department of Agriculture, the US Food and Drug Administration (FDA), and state and local health departments to track and respond to the H5N1 bird flu outbreak currently sweeping through the United States.
Since 2022, avian influenza A viruses have been detected in more than 9300 wild birds in 50 states and territories and in commercial and backyard flocks.
“It’s a bad situation,” said Florian Krammer, PhD, professor of vaccinology at the Icahn School of Medicine at Mount Sinai in New York. “Globally, we’ve seen tons of exposure in cities around the world and even in the birds here in New York City where I am.”
Birds shed the virus in their saliva, mucous, and feces, so people or other animals with close, unprotected contact with infected birds or their contaminated environments can be infected.
And for the first time in March 2024, H5N1 bird flu was reported in dairy cows. The US Department of Agriculture said that at last count, 101 dairy herds in 12 states had been infected, with several cases also found in dairy workers.
From Birds to Cattle and Farm Workers
The National Veterinary Services Laboratories confirmed the infections were highly pathogenic avian influenza H5N1 clade 2.3.4.4b of Eurasian lineage. Also known as the goose, Guangdong clade from China, phylogenetic analysis and epidemiology suggests a single introduction into cows followed by onward transmission.
“I was surprised when H5 was introduced to dairy cattle in this way,” Dr. Dugan said. “Influenza viruses are always surprising us and it reminds me to stay humble and keep an open mind when dealing with them.”
People rarely inhale or get sufficient virus in their eyes or mouth to get sick, Dr. Dugan said, but those in close contact with animals are still at risk for infection, which could lead to upper respiratory tract symptoms such as shortness of breath, cough, sore throat, or runny or stuffy nose.
Like with other viruses, people can also experience muscle or body aches, headache, fatigue, fever or, as was seen in farm workers, conjunctivitis.
But there are less-common symptoms too like diarrhea, nausea, and vomiting — and sometimes, even seizures.
The risk to the general public is still low, Dr. Dugan said, but authorities recommend that people working with animals wash their hands with soap and water and wear personal protective equipment that includes fluid-resistant coveralls, a waterproof apron, a safety-approved respirator, properly fitted goggles or face shield, a head or hair cover, gloves, and boots.
Dr. Dugan said that health care providers often don’t take a history of occupational exposures when a patient presents with flu. But with rising rates of bird flu in new animal hosts, “this will be an important next step.”
Asking Unusual Questions
This approach is not standardized on most electronic health records, so these are questions that clinicians will need to initiate themselves.
“Physicians should ask about work,” said Meghan Davis, PhD, associate professor at the Johns Hopkins Bloomberg School of Public Health in Baltimore. “If it’s not already on the radar, asking about any direct contact with dairy cows, poultry, pigs, wild birds, or wild mammals is important.”
Dr. Davis says she’s worried about a new study tracking risk factors for farm-to-farm transmission because it shows that farms testing positive for avian influenza often have workers with a family member also employed on another farm. “This suggests that we might need to be on the lookout for possible transmission within families,” she said. Now, we have to ask “not just if the person with symptoms has contact with or works on a dairy farm, milk processing plant, or slaughterhouse, but also if any family member does.”
Dr. Davis said that it’s important to bear in mind when taking these histories that there may be younger workers on farms and in slaughter and processing facilities due to exemptions or illegal work.
What is important now is to get the situation under control this season in dairy cattle, Dr. Krammer said. “This will be easier to stop in cows than humans, so this is the time to stop moving dairy cattle and start vaccinating them.”
Spotting New Cases
Since April 2024, there have been three human cases of avian influenza after exposure to dairy cows reported. “And what we don’t want to see this summer is an unusual human cluster of influenza. It’s important we keep a close, watchful eye for this,” Dr. Krammer said.
“Influenza viruses do very interesting things and as we head into fall and winter flu season, we don’t want new human co-infections that could cause major problems for us,” he said.
If people become mixing vessels of a seasonal cocktail of multiple viruses, that could empower H5N1 to mutate again into something more dangerous, sparking a new pandemic.
“It wasn’t all that long ago that we were asking China difficult questions about the steps Chinese authorities took to protect human lives from SARS-CoV-2 in the COVID pandemic. Now, we must ask ourselves many of these questions,” Dr. Krammer said. “We are at a crucial crossroad where we will either elude a new pandemic or see one take off, risking 10 to 20 million lives.”
There is a precedent for safely evading more trouble, Dr. Krammer pointed out. Government agencies have already been working with the poultry industry for a couple of years now. “And here, we have successfully stopped H5N1 with new regulations and policies.”
But moving from poultry farms to cattle has not been an easy transition, Dr. Dugan said. Cattle farms have no experience with bird flu or tactics to contain it with regulations, and officials too are working in new, unfamiliar terrain.
“What we have now isn’t a science problem, it’s a policy issue, and it hasn’t always been clear who is in charge,” Dr. Krammer said.
“Agencies are working together at the state, federal, and global level,” said Dr. Dugan. “We are increasing our transparency and are working to share what we know, when we know it.”
The infrastructure built during the COVID pandemic has helped teams prepare for this new crisis, Dr. Dugan said. Year-round, layered monitoring has clinical labs reporting seasonal influenza and novel cases.
“Laboratories are ready to help with testing,” Dr. Dugan said.
Specimens should be collected as soon as possible from patients with flu symptoms. A nasopharyngeal swab is recommended with a nasal swab combined with an oropharyngeal swab. If a patient has conjunctivitis with or without respiratory symptoms, both a conjunctival swab and a nasopharyngeal swab should be collected.
People with severe respiratory disease should also have lower respiratory tract specimens collected.
Standard, contact, and airborne precautions are recommended for patients presenting for medical care who have illness consistent with influenza and recent exposure to birds or other animals.
Antiviral Drugs
There are four FDA-approved antivirals for influenza: Oseltamivir phosphate (available as a generic drug or by the trade name Tamiflu), zanamivir (Relenza), peramivir (Rapivab) , and baloxavir (Xofluza).
For people with suspected or confirmed avian influenza, treatment is recommended as soon as possible.
There are no clinical trials measuring the outcome of antivirals in people infected with avian influenza. However, data from animal models and human observational studies suggest a benefit.
“We can’t afford to wait this summer,” Dr. Krammer said. “We have an opportunity right now to stop this in cows before we risk infecting more people. I hope we do.”
A version of this article first appeared on Medscape.com.
FDA Approves New Pneumococcal Vaccine
A new vaccine to prevent invasive pneumococcal disease and pneumococcal pneumonia in adults has been approved by the Food and Drug Administration.
The injectable drug, Capvaxive (Pneumococcal 21-valent Conjugate Vaccine), protects against 22 serotypes that cause invasive pneumococcal disease in adults, the company said in a news release. These strains account for about 84% of invasive pneumococcal disease cases among adults aged 50 years or older and about 85% of these cases in adults aged 65 years or older.
The drug company said about 150,000 adults in the United States are hospitalized annually because of pneumococcal pneumonia.
“Many cases of adult disease are caused by serotypes not included in other approved pneumococcal conjugate vaccines,” Walter Orenstein, MD, a professor emeritus of medicine, epidemiology, global health, and pediatrics at Emory University, Atlanta, Georgia, and a member of Merck’s Scientific Advisory Committee, said in the release.
A draft agenda shows a Centers for Disease Control and Prevention (CDC) advisory panel will meet on June 27 to discuss the vaccine. If the committee votes to approve Capvaxive, the CDC director will decide whether to make it available across the country.
Testing showed that Capvaxive was well tolerated by people it was tested on, with the main reports being pain where they got the shot, fatigue, headaches, and muscle aches, Merck said.
The eight unique serotypes included in CAPVAXIVE will protect against invasive pneumococcal disease and pneumococcal pneumonia, not just pneumonia.
According to Reuters, Merck said Capvaxive has a wholesale acquisition price of $287 per dose, but most people will probably have access to it at no cost if the drug receives a routine CDC recommendation. Capvaxive’s main competition is expected to be Pfizer’s shot, Prevnar 20, which was approved in 2021 for use in adults aged 18 years or older, Reuters reported.
A version of this article appeared on Medscape.com.
A new vaccine to prevent invasive pneumococcal disease and pneumococcal pneumonia in adults has been approved by the Food and Drug Administration.
The injectable drug, Capvaxive (Pneumococcal 21-valent Conjugate Vaccine), protects against 22 serotypes that cause invasive pneumococcal disease in adults, the company said in a news release. These strains account for about 84% of invasive pneumococcal disease cases among adults aged 50 years or older and about 85% of these cases in adults aged 65 years or older.
The drug company said about 150,000 adults in the United States are hospitalized annually because of pneumococcal pneumonia.
“Many cases of adult disease are caused by serotypes not included in other approved pneumococcal conjugate vaccines,” Walter Orenstein, MD, a professor emeritus of medicine, epidemiology, global health, and pediatrics at Emory University, Atlanta, Georgia, and a member of Merck’s Scientific Advisory Committee, said in the release.
A draft agenda shows a Centers for Disease Control and Prevention (CDC) advisory panel will meet on June 27 to discuss the vaccine. If the committee votes to approve Capvaxive, the CDC director will decide whether to make it available across the country.
Testing showed that Capvaxive was well tolerated by people it was tested on, with the main reports being pain where they got the shot, fatigue, headaches, and muscle aches, Merck said.
The eight unique serotypes included in CAPVAXIVE will protect against invasive pneumococcal disease and pneumococcal pneumonia, not just pneumonia.
According to Reuters, Merck said Capvaxive has a wholesale acquisition price of $287 per dose, but most people will probably have access to it at no cost if the drug receives a routine CDC recommendation. Capvaxive’s main competition is expected to be Pfizer’s shot, Prevnar 20, which was approved in 2021 for use in adults aged 18 years or older, Reuters reported.
A version of this article appeared on Medscape.com.
A new vaccine to prevent invasive pneumococcal disease and pneumococcal pneumonia in adults has been approved by the Food and Drug Administration.
The injectable drug, Capvaxive (Pneumococcal 21-valent Conjugate Vaccine), protects against 22 serotypes that cause invasive pneumococcal disease in adults, the company said in a news release. These strains account for about 84% of invasive pneumococcal disease cases among adults aged 50 years or older and about 85% of these cases in adults aged 65 years or older.
The drug company said about 150,000 adults in the United States are hospitalized annually because of pneumococcal pneumonia.
“Many cases of adult disease are caused by serotypes not included in other approved pneumococcal conjugate vaccines,” Walter Orenstein, MD, a professor emeritus of medicine, epidemiology, global health, and pediatrics at Emory University, Atlanta, Georgia, and a member of Merck’s Scientific Advisory Committee, said in the release.
A draft agenda shows a Centers for Disease Control and Prevention (CDC) advisory panel will meet on June 27 to discuss the vaccine. If the committee votes to approve Capvaxive, the CDC director will decide whether to make it available across the country.
Testing showed that Capvaxive was well tolerated by people it was tested on, with the main reports being pain where they got the shot, fatigue, headaches, and muscle aches, Merck said.
The eight unique serotypes included in CAPVAXIVE will protect against invasive pneumococcal disease and pneumococcal pneumonia, not just pneumonia.
According to Reuters, Merck said Capvaxive has a wholesale acquisition price of $287 per dose, but most people will probably have access to it at no cost if the drug receives a routine CDC recommendation. Capvaxive’s main competition is expected to be Pfizer’s shot, Prevnar 20, which was approved in 2021 for use in adults aged 18 years or older, Reuters reported.
A version of this article appeared on Medscape.com.
Acute Sore Throat in Primary Care: When to Reach for the Antibiotics
This transcript has been edited for clarity.
There is a helpful consensus from experts on the best management of patients with acute sore throat. This is a common problem in primary care, and one for which there is a lot of evidence, opinion, and ultimately overprescribing of antibiotics. This consensus presents a pragmatic clinical approach aimed at decreasing overprescribing, yet detecting which patients are likely to benefit from treatment with antibiotics.
Let’s first go over the evidence that forms the basis for the recommendations, then the recommended approach. First, a sore throat can be caused by many different viruses, as well as group A streptococcus (GAS), the group C streptococcus S dysgalactiae, and fusobacterium. We sometimes think of throat cultures as telling us the definitive etiology of a sore throat. In fact, children commonly are colonized with GAS even when not infected — 35% of the time, when GAS is detected on throat swab in a child, GAS is not the cause of the sore throat. Very few adults are colonized with GAS.
Sore throats are usually self-limited, whether they are treated with antibiotics or not, but occasionally complications can occur. Suppurative complications include peritonsillar abscess, sinusitis and sepsis. Nonsuppurative complications are primarily glomerulonephritis and rheumatic fever, which can lead to rheumatic heart disease.
Antibiotics. Antibiotics have three potential benefits in acute sore throat: to reduce the risk of developing rheumatic heart disease, reduce the duration and severity of symptoms, and treat suppurative complications. The risk for rheumatic heart disease has almost vanished in high-income countries, but not in low-income countries. Thus, antibiotic treatment of acute sore throat due to GAS may benefit those in living in, and those who recently emigrated from, low-income countries.
Patients with suppurative complications should be identified because antibiotics are important for this group. Although antibiotics are prescribed primarily to prevent rheumatic fever in this population, they may be mildly helpful in reducing a patient’s symptoms.
Testing. The sensitivity and specificity of high-quality point-of-care tests (POCTs) are on par with those of cultures, with the advantage that the results are available within minutes. Negative tests reduce unneeded antibiotic prescriptions.
Given this evidence, the authors recommend an approach that puts a lot of emphasis on two major things: the risk for rheumatic fever, and clinical assessment. On the basis of these factors, a decision is made about the utility of POCTs and treatment with antibiotics for GAS. The risk for rheumatic fever is based on epidemiology: If the patient is in a low-income country or has recently immigrated from one, then the risk is high, and if not, the risk is low.
Complicated vs uncomplicated? This is determined by clinical assessment of the severity of the patient’s illness, including general appearance. Uncomplicated sore throat means that the patient:
- Is not getting worse after 3 days of illness
- Has a duration of illness ≤ 5 days or is getting better after day 5
- Has mild to moderate symptom severity (bilateral throat pain, the ability to open the mouth fully, and absence of a sandpaper or scarlatiniform rash or strawberry tongue)
For patients with uncomplicated sore throat and low risk for rheumatic fever, the main goals are to reduce antibiotic use and provide symptomatic relief. For these patients, an assessment such as the Centor score can be done. Those with a low Centor score (0-2) can be treated with analgesics and there is no need for a POCT.
In patients with a higher Centor score, the consensus gives two choices: They can either be tested (and treated if the testing is positive), or it is reasonable to forgo testing and use a wait-and-see strategy, with reevaluation if they are getting worse after day 3 or not improving after day 5 days of their illness. Illnesses that last longer than 5 days with sore throat and fatigue should prompt consideration of alternative diagnoses, such as infectious mononucleosis.
For patients with potentially complicated sore throat — including indicators such as worsening symptoms after 3 days or worsening after initiation of antibiotics, inability to open the mouth fully, unilateral neck pain or swelling, or rigors — should undergo a careful evaluation. The need for further testing in these patients, including labs and imaging, should be decided on a case-by-case basis. If the patient appears seriously ill, don’t rely solely on POCT for GAS, but think about other diagnoses.
Rheumatic fever. The approach is very different in patients at high risk for rheumatic fever. POCT for GAS is recommended irrespective of their clinical score, and antibiotics should be prescribed if it’s positive for GAS. If a POCT is unavailable, then the consensus recommends prescribing antibiotics for all high-risk patients who have acute sore throat.
This approach is sensible and puts a lot of emphasis on clinical evaluation, though it should be noted that this approach is considerably different from that in the 2012 Infectious Diseases Society of America guidelines.
Dr. Skolnik, professor, Department of Family Medicine, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director, Department of Family Medicine, Abington Jefferson Health, Abington, Pennsylvania, disclosed ties with AstraZeneca, Teva, Eli Lilly and Company, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, and Bayer.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
There is a helpful consensus from experts on the best management of patients with acute sore throat. This is a common problem in primary care, and one for which there is a lot of evidence, opinion, and ultimately overprescribing of antibiotics. This consensus presents a pragmatic clinical approach aimed at decreasing overprescribing, yet detecting which patients are likely to benefit from treatment with antibiotics.
Let’s first go over the evidence that forms the basis for the recommendations, then the recommended approach. First, a sore throat can be caused by many different viruses, as well as group A streptococcus (GAS), the group C streptococcus S dysgalactiae, and fusobacterium. We sometimes think of throat cultures as telling us the definitive etiology of a sore throat. In fact, children commonly are colonized with GAS even when not infected — 35% of the time, when GAS is detected on throat swab in a child, GAS is not the cause of the sore throat. Very few adults are colonized with GAS.
Sore throats are usually self-limited, whether they are treated with antibiotics or not, but occasionally complications can occur. Suppurative complications include peritonsillar abscess, sinusitis and sepsis. Nonsuppurative complications are primarily glomerulonephritis and rheumatic fever, which can lead to rheumatic heart disease.
Antibiotics. Antibiotics have three potential benefits in acute sore throat: to reduce the risk of developing rheumatic heart disease, reduce the duration and severity of symptoms, and treat suppurative complications. The risk for rheumatic heart disease has almost vanished in high-income countries, but not in low-income countries. Thus, antibiotic treatment of acute sore throat due to GAS may benefit those in living in, and those who recently emigrated from, low-income countries.
Patients with suppurative complications should be identified because antibiotics are important for this group. Although antibiotics are prescribed primarily to prevent rheumatic fever in this population, they may be mildly helpful in reducing a patient’s symptoms.
Testing. The sensitivity and specificity of high-quality point-of-care tests (POCTs) are on par with those of cultures, with the advantage that the results are available within minutes. Negative tests reduce unneeded antibiotic prescriptions.
Given this evidence, the authors recommend an approach that puts a lot of emphasis on two major things: the risk for rheumatic fever, and clinical assessment. On the basis of these factors, a decision is made about the utility of POCTs and treatment with antibiotics for GAS. The risk for rheumatic fever is based on epidemiology: If the patient is in a low-income country or has recently immigrated from one, then the risk is high, and if not, the risk is low.
Complicated vs uncomplicated? This is determined by clinical assessment of the severity of the patient’s illness, including general appearance. Uncomplicated sore throat means that the patient:
- Is not getting worse after 3 days of illness
- Has a duration of illness ≤ 5 days or is getting better after day 5
- Has mild to moderate symptom severity (bilateral throat pain, the ability to open the mouth fully, and absence of a sandpaper or scarlatiniform rash or strawberry tongue)
For patients with uncomplicated sore throat and low risk for rheumatic fever, the main goals are to reduce antibiotic use and provide symptomatic relief. For these patients, an assessment such as the Centor score can be done. Those with a low Centor score (0-2) can be treated with analgesics and there is no need for a POCT.
In patients with a higher Centor score, the consensus gives two choices: They can either be tested (and treated if the testing is positive), or it is reasonable to forgo testing and use a wait-and-see strategy, with reevaluation if they are getting worse after day 3 or not improving after day 5 days of their illness. Illnesses that last longer than 5 days with sore throat and fatigue should prompt consideration of alternative diagnoses, such as infectious mononucleosis.
For patients with potentially complicated sore throat — including indicators such as worsening symptoms after 3 days or worsening after initiation of antibiotics, inability to open the mouth fully, unilateral neck pain or swelling, or rigors — should undergo a careful evaluation. The need for further testing in these patients, including labs and imaging, should be decided on a case-by-case basis. If the patient appears seriously ill, don’t rely solely on POCT for GAS, but think about other diagnoses.
Rheumatic fever. The approach is very different in patients at high risk for rheumatic fever. POCT for GAS is recommended irrespective of their clinical score, and antibiotics should be prescribed if it’s positive for GAS. If a POCT is unavailable, then the consensus recommends prescribing antibiotics for all high-risk patients who have acute sore throat.
This approach is sensible and puts a lot of emphasis on clinical evaluation, though it should be noted that this approach is considerably different from that in the 2012 Infectious Diseases Society of America guidelines.
Dr. Skolnik, professor, Department of Family Medicine, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director, Department of Family Medicine, Abington Jefferson Health, Abington, Pennsylvania, disclosed ties with AstraZeneca, Teva, Eli Lilly and Company, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, and Bayer.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
There is a helpful consensus from experts on the best management of patients with acute sore throat. This is a common problem in primary care, and one for which there is a lot of evidence, opinion, and ultimately overprescribing of antibiotics. This consensus presents a pragmatic clinical approach aimed at decreasing overprescribing, yet detecting which patients are likely to benefit from treatment with antibiotics.
Let’s first go over the evidence that forms the basis for the recommendations, then the recommended approach. First, a sore throat can be caused by many different viruses, as well as group A streptococcus (GAS), the group C streptococcus S dysgalactiae, and fusobacterium. We sometimes think of throat cultures as telling us the definitive etiology of a sore throat. In fact, children commonly are colonized with GAS even when not infected — 35% of the time, when GAS is detected on throat swab in a child, GAS is not the cause of the sore throat. Very few adults are colonized with GAS.
Sore throats are usually self-limited, whether they are treated with antibiotics or not, but occasionally complications can occur. Suppurative complications include peritonsillar abscess, sinusitis and sepsis. Nonsuppurative complications are primarily glomerulonephritis and rheumatic fever, which can lead to rheumatic heart disease.
Antibiotics. Antibiotics have three potential benefits in acute sore throat: to reduce the risk of developing rheumatic heart disease, reduce the duration and severity of symptoms, and treat suppurative complications. The risk for rheumatic heart disease has almost vanished in high-income countries, but not in low-income countries. Thus, antibiotic treatment of acute sore throat due to GAS may benefit those in living in, and those who recently emigrated from, low-income countries.
Patients with suppurative complications should be identified because antibiotics are important for this group. Although antibiotics are prescribed primarily to prevent rheumatic fever in this population, they may be mildly helpful in reducing a patient’s symptoms.
Testing. The sensitivity and specificity of high-quality point-of-care tests (POCTs) are on par with those of cultures, with the advantage that the results are available within minutes. Negative tests reduce unneeded antibiotic prescriptions.
Given this evidence, the authors recommend an approach that puts a lot of emphasis on two major things: the risk for rheumatic fever, and clinical assessment. On the basis of these factors, a decision is made about the utility of POCTs and treatment with antibiotics for GAS. The risk for rheumatic fever is based on epidemiology: If the patient is in a low-income country or has recently immigrated from one, then the risk is high, and if not, the risk is low.
Complicated vs uncomplicated? This is determined by clinical assessment of the severity of the patient’s illness, including general appearance. Uncomplicated sore throat means that the patient:
- Is not getting worse after 3 days of illness
- Has a duration of illness ≤ 5 days or is getting better after day 5
- Has mild to moderate symptom severity (bilateral throat pain, the ability to open the mouth fully, and absence of a sandpaper or scarlatiniform rash or strawberry tongue)
For patients with uncomplicated sore throat and low risk for rheumatic fever, the main goals are to reduce antibiotic use and provide symptomatic relief. For these patients, an assessment such as the Centor score can be done. Those with a low Centor score (0-2) can be treated with analgesics and there is no need for a POCT.
In patients with a higher Centor score, the consensus gives two choices: They can either be tested (and treated if the testing is positive), or it is reasonable to forgo testing and use a wait-and-see strategy, with reevaluation if they are getting worse after day 3 or not improving after day 5 days of their illness. Illnesses that last longer than 5 days with sore throat and fatigue should prompt consideration of alternative diagnoses, such as infectious mononucleosis.
For patients with potentially complicated sore throat — including indicators such as worsening symptoms after 3 days or worsening after initiation of antibiotics, inability to open the mouth fully, unilateral neck pain or swelling, or rigors — should undergo a careful evaluation. The need for further testing in these patients, including labs and imaging, should be decided on a case-by-case basis. If the patient appears seriously ill, don’t rely solely on POCT for GAS, but think about other diagnoses.
Rheumatic fever. The approach is very different in patients at high risk for rheumatic fever. POCT for GAS is recommended irrespective of their clinical score, and antibiotics should be prescribed if it’s positive for GAS. If a POCT is unavailable, then the consensus recommends prescribing antibiotics for all high-risk patients who have acute sore throat.
This approach is sensible and puts a lot of emphasis on clinical evaluation, though it should be noted that this approach is considerably different from that in the 2012 Infectious Diseases Society of America guidelines.
Dr. Skolnik, professor, Department of Family Medicine, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director, Department of Family Medicine, Abington Jefferson Health, Abington, Pennsylvania, disclosed ties with AstraZeneca, Teva, Eli Lilly and Company, Boehringer Ingelheim, Sanofi, Sanofi Pasteur, GlaxoSmithKline, Merck, and Bayer.
A version of this article appeared on Medscape.com.

