User login
With life in the balance, a pediatric palliative care program expands its work to adults
In late March of 2020, when it became clear that hospitals in the greater New York City area would face a capacity crisis in caring for seriously ill patients with COVID-19, members of the leadership team at the Children’s Hospital at Montefiore (CHAM) in the Bronx, N.Y., convened to draft a response plan.
The recommendations put into action that day included moving the hospital’s emergency department from the lower level to the fourth floor, increasing the age limit for patients seen in the ED from 21 years of age to 30 and freeing up an entire hospital floor and a half to accommodate the anticipated surge of patients with COVID-19 admitted to Montefiore’s interconnected adult hospital, according to Sarah E. Norris, MD.
“We made multiple moves all at once,” said Dr. Norris, director of pediatric palliative care at CHAM. “It struck everyone as logical that palliative care had to be expanded, because all of the news we had received as the surge came to New York from around the world was full of death and uncertainty, and would require thoughtful conversations about end-of-life wishes at critical times and how to really respect the person and understand their values.”
When Dr. Norris left the leadership team meeting, she returned to her office, put her face in her hands, and sobbed as she began to process the gravity of what was ahead. “I cried because I knew that so many families were going to suffer a heartbreak, no matter how much we could do,” she said.
Stitching the QUILT
Over the next few days, Dr. Norris began recruiting colleagues from the large Montefiore Health System – most of whom she did not know – who met criteria for work deployment to expand CHAM’s palliative care program of clinician to 27 clinicians consisting of pediatricians, nurse practitioners, and psychologists, to meet the projected needs of COVID-19 patients and their families.
Some candidates for the effort, known as the Quality in Life Team (QUILT), were 65 years of age or older, considered at high risk for developing COVID-19-related complications themselves. Others were immunocompromised or had medical conditions that would not allow them to have direct contact with COVID-19 patients. “There were also clinicians in other parts of our health system whose practice hours were going to be severely reduced,” said Dr. Norris, who is board-certified in general pediatrics and in hospice and palliative care medicine.
Once she assembled QUILT, members participated in a 1-day rapid training webinar covering the basics of palliative care and grief, and readied themselves for one of three roles: physicians to provide face-to-face palliative care in CHAM; supportive callers to provide support to patients with COVID-19 and their families between 12:00-8:00 p.m. each day; and bereavement callers to reach out to families who lost loved ones to COVID-19 and provide grief counseling for 3 weeks.
“This allows families to have at least two contacts a day from the hospital: one from the medical team that’s giving them technical, medical information, and another from members of the QUILT team,” Dr. Norris said. “We provide support for the worry, anxiety, and fear that we know creeps in when you’re separated from your family member, especially during a pandemic when you watch TV and there’s a death count rising.”
During her early meetings with QUILT members via Zoom or on the phone, Dr. Norris encouraged them to stretch their skill sets and mindsets as they shifted from caring for children and adolescents to mostly adults. “Pediatricians are all about family; that’s why we get into this,” she said. “We’re used to treating your kids, but then, suddenly, the parent becomes our patient, like in COVID-19, or the grandparent becomes our patient. We treat you all the same; you’re part of our family. There has been no adult who has died ‘within our house’ that has died alone. There has either been a staff member at their bedside, or when possible, a family member. We are witnessing life until the last breath here.”
‘They have no loved ones with them’
One day, members of CHAM’s medical team contacted Dr. Norris about a patient with COVID-19 who’d been cared for by Montefiore clinicians all of his young life. The boy’s mother, who did not speak English, was at his bedside in the ICU, and the clinicians asked Dr. Norris to speak with her by cell phone while they prepared him for intubation.
“We were looking at each other through a glass window wall in our ICU,” Dr. Norris recalled. “I talked to her the entire time the team worked to put him on the breathing machine, through an interpreter. I asked her to tell me about her son and about her family, and she did. We developed a warm relationship. After that, every day I would see her son through the glass window wall. Every couple of days, I would have the privilege of talking to his mother by phone. At one point, she asked me, ‘Dr. Norris, do you think his lungs will heal?’ I had to tell her no. Almost selfishly, I was relieved we were on the phone, because she cried, and so did I. When he died, she was able to be by his side.”
Frederick J. Kaskel, MD, PhD, joined QUILT as a supportive caller after being asked to go home during his on-call shift on St. Patrick’s Day at CHAM, where he serves as chief emeritus of nephrology. “I was told that I was deemed to be at high risk because of my age,” the 75-year-old said. “The next day, a junior person took over for me, and 2 days later she got sick with COVID-19. She’s fine but she was home for 3 weeks sick as a dog. It was scary.”
In his role as a supportive caller, Dr. Kaskel found himself engaged in his share of detective work, trying to find phone numbers of next of kin for patients hospitalized with COVID-19. “When they come into the ER, they may not have been with a loved one or a family member; they may have been brought in by an EMT,” he said. “Some of them speak little English and others have little documentation with them. It takes a lot of work to get phone numbers.”
Once Dr. Kaskel reaches a loved one by phone, he introduces himself as a member of the QUILT team. “I tell them I’m not calling to update the medical status but just to talk to them about their loved one,” he said. “Then I usually ask, ‘So, how are you doing with this? The stress is enormous, the uncertainties.’ Then they open up and express their fears. I’ve had a lot of people say, ‘we have no money, and I don’t know how we’re going to pay rent for the apartment. We have to line up for food.’ I also ask what they do to alleviate stress. One guy said, ‘I drink a lot, but I’m careful.’ ”
Dr. Kaskel, who is also a past president of the American Society of Pediatric Nephrology, applies that same personable approach in daily conversations with adult patients hospitalized at CHAM with COVID-19, the majority of whom are African Americans in their 30s, 40s, and 50s. “Invariably, they ask, ‘Has my loved one been updated as to my status?’ ” he said. “The second thing they often say is, ‘I’m worried about infecting other people, but I also worry if I’m going to get through this. I’m really afraid I’m going to die.’ I say, ‘You have a wonderful team keeping track of you. They’re seeing you all the time and making changes to your medicines.’ ”
When patients express their fear of dying from the virus, Dr. Kaskel asks them how they’re coping with that fear. Most tell him that they pray.
“If they don’t answer, I ask if they have any hobbies, like ‘Are you watching TV? Are you reading? Do you have your cell phone?’ ” he said. “Then they open up and say things like, ‘I’m listening to music on the cell phone,’ or ‘I’m FaceTiming with my loved ones.’ The use of FaceTime is crucial, because they are in a hospital, critically ill, potentially dying alone with strangers. This really hit me on the first day [of this work]. They have no loved ones with them. They have strangers: the CHAM nurses, the medical residents, the social workers, and the doctors.”
No hospital cheeseburgers
QUILT began its work on April 6, and at one time provided palliative care services for a peak of 92 mostly adult patients with COVID-19. The supportive callers made 249 individual connections with patients and family members by phone from April 6-13, 162 connections from April 13-19, and 130 connections from April 20-26, according to Dr. Norris. As of April 28, the CHAM inpatient census of patients aged 18 years and over with COVID-19 was 42, “and we’re making 130 connections by phone to patients and family members each day,” she said.
QUILT bereavement callers are following 30 families, providing 3 weeks of acute grief counseling from the date of death. “A sad truth is that, here in New York, our entire funeral, burial, cremation system is overwhelmed in volume,” Dr. Norris said. “Only half of the patients we’re following 3 weeks out have been able to have their family member buried or cremated; many are still waiting. What strikes me here is that pediatricians are often partners in care. With time, we’re partners in care in heartbreak, and in the occasional victory. We mourn patients who have died. We’ve had colleagues who died from COVID-19 right here at our hospital. But we stand together like a family.”
Dr. Norris recalled an older woman who came into CHAM’s ICU on a ventilator, critically ill from COVID-19. She called her husband at home every day with updates. “I got to know her husband, and I got to know her through him,” Dr. Norris said. “We talked every single day and she was able to graduate off of the breathing tube and out of the ICU, which was amazing.” The woman was moved to a floor in the adult hospital, but Dr. Norris continues to visit her and to provide her husband with updates, “because I’m devoted to them,” she said.
Recently, physicians in the adult hospital consulted with Dr. Norris about the woman. “They were trying to figure out what to do with her next,” she said. “Could she go home, or did she need rehab? They said, ‘We called you, Dr. Norris, because her husband thinks he can take her home.’ We know that COVID-19 really weakens people, so I went over to see her myself. I thought, ‘No single person could take care of an adult so weak at home.’ So, I called her husband and said, ‘I’m here with your wife, and I have to tell you; if she were my mother, I couldn’t take her home today. I need you to trust me.’ He said, ‘OK. We trust you and know that you have her best interest at heart.’ ”
Dr. Kaskel relayed the story of an older patient who was slowly recovering from COVID-19. During a phone call, he asked the man if there was anything he wanted at that moment.
“He said, ‘I’d love to see my wife and my children and my grandkids. I know I’m going to see them again, but right now, doc, if you could get me a cheeseburger with lettuce and tomato and ketchup and French fries from outside of the hospital, I’d be the happiest man in the world.’
I said, ‘What’s the matter with the cheeseburger made at the hospital?’
He said, ‘No! They can’t make the cheeseburger I want.’
I promised him I’d relay that message to the social worker responsible for the patient. I told her please, if you buy this for him, I’ll pay you back.”
Self-care and the next chapter
Twice each week, QUILT members gather in front of their computer monitors for mandatory Zoom meetings facilitated by two psychologists to share challenges, best practices, and to discuss the difficult work they’re doing. “We meet, because you cannot help someone if you cannot help yourself,” Dr. Norris said. “We have been encouraged each and every meeting to practice self-compassion, and to recognize that things happen during a pandemic – some will be the best you can do.”
She described organizing and serving on QUILT as a grounding experience with important lessons for the delivery of health care after the pandemic subsides and the team members return to their respective practices. “I think we’ve all gained a greater sense of humility, and we understand that the badge I wear every day does not protect me from becoming a patient, or from having my own family fall ill,” she said. “Here, we think about it very simply: ‘I’m going to treat you like you’re part of my own family.’ ”
Dr. Kaskel said that serving on QUILT as a supportive caller is an experience he won’t soon forget.
“The human bond is so accessible if you accept it,” he said. “If someone is an introvert that might not be able to draw out a stranger on the phone, then [he or she] shouldn’t do this [work]. But the fact that you can make a bond with someone that you’re not even seeing in person and know that both sides of this phone call are getting good vibes, that’s a remarkable feeling that I never really knew before, because I’ve never really had to do that before. It brings up feelings like I had after 9/11 – a unified approach to surviving this as people, as a community, the idea that ‘we will get through this,’ even though it’s totally different than anything before. The idea that there’s still hope. Those are things you can’t put a price on.”
An article about how CHAM transformed to provide care to adult COVID-19 patients was published online May 4, 2020, in the Journal of Pediatrics: doi: 10.1016/j.jpeds.2020.04.060.
In late March of 2020, when it became clear that hospitals in the greater New York City area would face a capacity crisis in caring for seriously ill patients with COVID-19, members of the leadership team at the Children’s Hospital at Montefiore (CHAM) in the Bronx, N.Y., convened to draft a response plan.
The recommendations put into action that day included moving the hospital’s emergency department from the lower level to the fourth floor, increasing the age limit for patients seen in the ED from 21 years of age to 30 and freeing up an entire hospital floor and a half to accommodate the anticipated surge of patients with COVID-19 admitted to Montefiore’s interconnected adult hospital, according to Sarah E. Norris, MD.
“We made multiple moves all at once,” said Dr. Norris, director of pediatric palliative care at CHAM. “It struck everyone as logical that palliative care had to be expanded, because all of the news we had received as the surge came to New York from around the world was full of death and uncertainty, and would require thoughtful conversations about end-of-life wishes at critical times and how to really respect the person and understand their values.”
When Dr. Norris left the leadership team meeting, she returned to her office, put her face in her hands, and sobbed as she began to process the gravity of what was ahead. “I cried because I knew that so many families were going to suffer a heartbreak, no matter how much we could do,” she said.
Stitching the QUILT
Over the next few days, Dr. Norris began recruiting colleagues from the large Montefiore Health System – most of whom she did not know – who met criteria for work deployment to expand CHAM’s palliative care program of clinician to 27 clinicians consisting of pediatricians, nurse practitioners, and psychologists, to meet the projected needs of COVID-19 patients and their families.
Some candidates for the effort, known as the Quality in Life Team (QUILT), were 65 years of age or older, considered at high risk for developing COVID-19-related complications themselves. Others were immunocompromised or had medical conditions that would not allow them to have direct contact with COVID-19 patients. “There were also clinicians in other parts of our health system whose practice hours were going to be severely reduced,” said Dr. Norris, who is board-certified in general pediatrics and in hospice and palliative care medicine.
Once she assembled QUILT, members participated in a 1-day rapid training webinar covering the basics of palliative care and grief, and readied themselves for one of three roles: physicians to provide face-to-face palliative care in CHAM; supportive callers to provide support to patients with COVID-19 and their families between 12:00-8:00 p.m. each day; and bereavement callers to reach out to families who lost loved ones to COVID-19 and provide grief counseling for 3 weeks.
“This allows families to have at least two contacts a day from the hospital: one from the medical team that’s giving them technical, medical information, and another from members of the QUILT team,” Dr. Norris said. “We provide support for the worry, anxiety, and fear that we know creeps in when you’re separated from your family member, especially during a pandemic when you watch TV and there’s a death count rising.”
During her early meetings with QUILT members via Zoom or on the phone, Dr. Norris encouraged them to stretch their skill sets and mindsets as they shifted from caring for children and adolescents to mostly adults. “Pediatricians are all about family; that’s why we get into this,” she said. “We’re used to treating your kids, but then, suddenly, the parent becomes our patient, like in COVID-19, or the grandparent becomes our patient. We treat you all the same; you’re part of our family. There has been no adult who has died ‘within our house’ that has died alone. There has either been a staff member at their bedside, or when possible, a family member. We are witnessing life until the last breath here.”
‘They have no loved ones with them’
One day, members of CHAM’s medical team contacted Dr. Norris about a patient with COVID-19 who’d been cared for by Montefiore clinicians all of his young life. The boy’s mother, who did not speak English, was at his bedside in the ICU, and the clinicians asked Dr. Norris to speak with her by cell phone while they prepared him for intubation.
“We were looking at each other through a glass window wall in our ICU,” Dr. Norris recalled. “I talked to her the entire time the team worked to put him on the breathing machine, through an interpreter. I asked her to tell me about her son and about her family, and she did. We developed a warm relationship. After that, every day I would see her son through the glass window wall. Every couple of days, I would have the privilege of talking to his mother by phone. At one point, she asked me, ‘Dr. Norris, do you think his lungs will heal?’ I had to tell her no. Almost selfishly, I was relieved we were on the phone, because she cried, and so did I. When he died, she was able to be by his side.”
Frederick J. Kaskel, MD, PhD, joined QUILT as a supportive caller after being asked to go home during his on-call shift on St. Patrick’s Day at CHAM, where he serves as chief emeritus of nephrology. “I was told that I was deemed to be at high risk because of my age,” the 75-year-old said. “The next day, a junior person took over for me, and 2 days later she got sick with COVID-19. She’s fine but she was home for 3 weeks sick as a dog. It was scary.”
In his role as a supportive caller, Dr. Kaskel found himself engaged in his share of detective work, trying to find phone numbers of next of kin for patients hospitalized with COVID-19. “When they come into the ER, they may not have been with a loved one or a family member; they may have been brought in by an EMT,” he said. “Some of them speak little English and others have little documentation with them. It takes a lot of work to get phone numbers.”
Once Dr. Kaskel reaches a loved one by phone, he introduces himself as a member of the QUILT team. “I tell them I’m not calling to update the medical status but just to talk to them about their loved one,” he said. “Then I usually ask, ‘So, how are you doing with this? The stress is enormous, the uncertainties.’ Then they open up and express their fears. I’ve had a lot of people say, ‘we have no money, and I don’t know how we’re going to pay rent for the apartment. We have to line up for food.’ I also ask what they do to alleviate stress. One guy said, ‘I drink a lot, but I’m careful.’ ”
Dr. Kaskel, who is also a past president of the American Society of Pediatric Nephrology, applies that same personable approach in daily conversations with adult patients hospitalized at CHAM with COVID-19, the majority of whom are African Americans in their 30s, 40s, and 50s. “Invariably, they ask, ‘Has my loved one been updated as to my status?’ ” he said. “The second thing they often say is, ‘I’m worried about infecting other people, but I also worry if I’m going to get through this. I’m really afraid I’m going to die.’ I say, ‘You have a wonderful team keeping track of you. They’re seeing you all the time and making changes to your medicines.’ ”
When patients express their fear of dying from the virus, Dr. Kaskel asks them how they’re coping with that fear. Most tell him that they pray.
“If they don’t answer, I ask if they have any hobbies, like ‘Are you watching TV? Are you reading? Do you have your cell phone?’ ” he said. “Then they open up and say things like, ‘I’m listening to music on the cell phone,’ or ‘I’m FaceTiming with my loved ones.’ The use of FaceTime is crucial, because they are in a hospital, critically ill, potentially dying alone with strangers. This really hit me on the first day [of this work]. They have no loved ones with them. They have strangers: the CHAM nurses, the medical residents, the social workers, and the doctors.”
No hospital cheeseburgers
QUILT began its work on April 6, and at one time provided palliative care services for a peak of 92 mostly adult patients with COVID-19. The supportive callers made 249 individual connections with patients and family members by phone from April 6-13, 162 connections from April 13-19, and 130 connections from April 20-26, according to Dr. Norris. As of April 28, the CHAM inpatient census of patients aged 18 years and over with COVID-19 was 42, “and we’re making 130 connections by phone to patients and family members each day,” she said.
QUILT bereavement callers are following 30 families, providing 3 weeks of acute grief counseling from the date of death. “A sad truth is that, here in New York, our entire funeral, burial, cremation system is overwhelmed in volume,” Dr. Norris said. “Only half of the patients we’re following 3 weeks out have been able to have their family member buried or cremated; many are still waiting. What strikes me here is that pediatricians are often partners in care. With time, we’re partners in care in heartbreak, and in the occasional victory. We mourn patients who have died. We’ve had colleagues who died from COVID-19 right here at our hospital. But we stand together like a family.”
Dr. Norris recalled an older woman who came into CHAM’s ICU on a ventilator, critically ill from COVID-19. She called her husband at home every day with updates. “I got to know her husband, and I got to know her through him,” Dr. Norris said. “We talked every single day and she was able to graduate off of the breathing tube and out of the ICU, which was amazing.” The woman was moved to a floor in the adult hospital, but Dr. Norris continues to visit her and to provide her husband with updates, “because I’m devoted to them,” she said.
Recently, physicians in the adult hospital consulted with Dr. Norris about the woman. “They were trying to figure out what to do with her next,” she said. “Could she go home, or did she need rehab? They said, ‘We called you, Dr. Norris, because her husband thinks he can take her home.’ We know that COVID-19 really weakens people, so I went over to see her myself. I thought, ‘No single person could take care of an adult so weak at home.’ So, I called her husband and said, ‘I’m here with your wife, and I have to tell you; if she were my mother, I couldn’t take her home today. I need you to trust me.’ He said, ‘OK. We trust you and know that you have her best interest at heart.’ ”
Dr. Kaskel relayed the story of an older patient who was slowly recovering from COVID-19. During a phone call, he asked the man if there was anything he wanted at that moment.
“He said, ‘I’d love to see my wife and my children and my grandkids. I know I’m going to see them again, but right now, doc, if you could get me a cheeseburger with lettuce and tomato and ketchup and French fries from outside of the hospital, I’d be the happiest man in the world.’
I said, ‘What’s the matter with the cheeseburger made at the hospital?’
He said, ‘No! They can’t make the cheeseburger I want.’
I promised him I’d relay that message to the social worker responsible for the patient. I told her please, if you buy this for him, I’ll pay you back.”
Self-care and the next chapter
Twice each week, QUILT members gather in front of their computer monitors for mandatory Zoom meetings facilitated by two psychologists to share challenges, best practices, and to discuss the difficult work they’re doing. “We meet, because you cannot help someone if you cannot help yourself,” Dr. Norris said. “We have been encouraged each and every meeting to practice self-compassion, and to recognize that things happen during a pandemic – some will be the best you can do.”
She described organizing and serving on QUILT as a grounding experience with important lessons for the delivery of health care after the pandemic subsides and the team members return to their respective practices. “I think we’ve all gained a greater sense of humility, and we understand that the badge I wear every day does not protect me from becoming a patient, or from having my own family fall ill,” she said. “Here, we think about it very simply: ‘I’m going to treat you like you’re part of my own family.’ ”
Dr. Kaskel said that serving on QUILT as a supportive caller is an experience he won’t soon forget.
“The human bond is so accessible if you accept it,” he said. “If someone is an introvert that might not be able to draw out a stranger on the phone, then [he or she] shouldn’t do this [work]. But the fact that you can make a bond with someone that you’re not even seeing in person and know that both sides of this phone call are getting good vibes, that’s a remarkable feeling that I never really knew before, because I’ve never really had to do that before. It brings up feelings like I had after 9/11 – a unified approach to surviving this as people, as a community, the idea that ‘we will get through this,’ even though it’s totally different than anything before. The idea that there’s still hope. Those are things you can’t put a price on.”
An article about how CHAM transformed to provide care to adult COVID-19 patients was published online May 4, 2020, in the Journal of Pediatrics: doi: 10.1016/j.jpeds.2020.04.060.
In late March of 2020, when it became clear that hospitals in the greater New York City area would face a capacity crisis in caring for seriously ill patients with COVID-19, members of the leadership team at the Children’s Hospital at Montefiore (CHAM) in the Bronx, N.Y., convened to draft a response plan.
The recommendations put into action that day included moving the hospital’s emergency department from the lower level to the fourth floor, increasing the age limit for patients seen in the ED from 21 years of age to 30 and freeing up an entire hospital floor and a half to accommodate the anticipated surge of patients with COVID-19 admitted to Montefiore’s interconnected adult hospital, according to Sarah E. Norris, MD.
“We made multiple moves all at once,” said Dr. Norris, director of pediatric palliative care at CHAM. “It struck everyone as logical that palliative care had to be expanded, because all of the news we had received as the surge came to New York from around the world was full of death and uncertainty, and would require thoughtful conversations about end-of-life wishes at critical times and how to really respect the person and understand their values.”
When Dr. Norris left the leadership team meeting, she returned to her office, put her face in her hands, and sobbed as she began to process the gravity of what was ahead. “I cried because I knew that so many families were going to suffer a heartbreak, no matter how much we could do,” she said.
Stitching the QUILT
Over the next few days, Dr. Norris began recruiting colleagues from the large Montefiore Health System – most of whom she did not know – who met criteria for work deployment to expand CHAM’s palliative care program of clinician to 27 clinicians consisting of pediatricians, nurse practitioners, and psychologists, to meet the projected needs of COVID-19 patients and their families.
Some candidates for the effort, known as the Quality in Life Team (QUILT), were 65 years of age or older, considered at high risk for developing COVID-19-related complications themselves. Others were immunocompromised or had medical conditions that would not allow them to have direct contact with COVID-19 patients. “There were also clinicians in other parts of our health system whose practice hours were going to be severely reduced,” said Dr. Norris, who is board-certified in general pediatrics and in hospice and palliative care medicine.
Once she assembled QUILT, members participated in a 1-day rapid training webinar covering the basics of palliative care and grief, and readied themselves for one of three roles: physicians to provide face-to-face palliative care in CHAM; supportive callers to provide support to patients with COVID-19 and their families between 12:00-8:00 p.m. each day; and bereavement callers to reach out to families who lost loved ones to COVID-19 and provide grief counseling for 3 weeks.
“This allows families to have at least two contacts a day from the hospital: one from the medical team that’s giving them technical, medical information, and another from members of the QUILT team,” Dr. Norris said. “We provide support for the worry, anxiety, and fear that we know creeps in when you’re separated from your family member, especially during a pandemic when you watch TV and there’s a death count rising.”
During her early meetings with QUILT members via Zoom or on the phone, Dr. Norris encouraged them to stretch their skill sets and mindsets as they shifted from caring for children and adolescents to mostly adults. “Pediatricians are all about family; that’s why we get into this,” she said. “We’re used to treating your kids, but then, suddenly, the parent becomes our patient, like in COVID-19, or the grandparent becomes our patient. We treat you all the same; you’re part of our family. There has been no adult who has died ‘within our house’ that has died alone. There has either been a staff member at their bedside, or when possible, a family member. We are witnessing life until the last breath here.”
‘They have no loved ones with them’
One day, members of CHAM’s medical team contacted Dr. Norris about a patient with COVID-19 who’d been cared for by Montefiore clinicians all of his young life. The boy’s mother, who did not speak English, was at his bedside in the ICU, and the clinicians asked Dr. Norris to speak with her by cell phone while they prepared him for intubation.
“We were looking at each other through a glass window wall in our ICU,” Dr. Norris recalled. “I talked to her the entire time the team worked to put him on the breathing machine, through an interpreter. I asked her to tell me about her son and about her family, and she did. We developed a warm relationship. After that, every day I would see her son through the glass window wall. Every couple of days, I would have the privilege of talking to his mother by phone. At one point, she asked me, ‘Dr. Norris, do you think his lungs will heal?’ I had to tell her no. Almost selfishly, I was relieved we were on the phone, because she cried, and so did I. When he died, she was able to be by his side.”
Frederick J. Kaskel, MD, PhD, joined QUILT as a supportive caller after being asked to go home during his on-call shift on St. Patrick’s Day at CHAM, where he serves as chief emeritus of nephrology. “I was told that I was deemed to be at high risk because of my age,” the 75-year-old said. “The next day, a junior person took over for me, and 2 days later she got sick with COVID-19. She’s fine but she was home for 3 weeks sick as a dog. It was scary.”
In his role as a supportive caller, Dr. Kaskel found himself engaged in his share of detective work, trying to find phone numbers of next of kin for patients hospitalized with COVID-19. “When they come into the ER, they may not have been with a loved one or a family member; they may have been brought in by an EMT,” he said. “Some of them speak little English and others have little documentation with them. It takes a lot of work to get phone numbers.”
Once Dr. Kaskel reaches a loved one by phone, he introduces himself as a member of the QUILT team. “I tell them I’m not calling to update the medical status but just to talk to them about their loved one,” he said. “Then I usually ask, ‘So, how are you doing with this? The stress is enormous, the uncertainties.’ Then they open up and express their fears. I’ve had a lot of people say, ‘we have no money, and I don’t know how we’re going to pay rent for the apartment. We have to line up for food.’ I also ask what they do to alleviate stress. One guy said, ‘I drink a lot, but I’m careful.’ ”
Dr. Kaskel, who is also a past president of the American Society of Pediatric Nephrology, applies that same personable approach in daily conversations with adult patients hospitalized at CHAM with COVID-19, the majority of whom are African Americans in their 30s, 40s, and 50s. “Invariably, they ask, ‘Has my loved one been updated as to my status?’ ” he said. “The second thing they often say is, ‘I’m worried about infecting other people, but I also worry if I’m going to get through this. I’m really afraid I’m going to die.’ I say, ‘You have a wonderful team keeping track of you. They’re seeing you all the time and making changes to your medicines.’ ”
When patients express their fear of dying from the virus, Dr. Kaskel asks them how they’re coping with that fear. Most tell him that they pray.
“If they don’t answer, I ask if they have any hobbies, like ‘Are you watching TV? Are you reading? Do you have your cell phone?’ ” he said. “Then they open up and say things like, ‘I’m listening to music on the cell phone,’ or ‘I’m FaceTiming with my loved ones.’ The use of FaceTime is crucial, because they are in a hospital, critically ill, potentially dying alone with strangers. This really hit me on the first day [of this work]. They have no loved ones with them. They have strangers: the CHAM nurses, the medical residents, the social workers, and the doctors.”
No hospital cheeseburgers
QUILT began its work on April 6, and at one time provided palliative care services for a peak of 92 mostly adult patients with COVID-19. The supportive callers made 249 individual connections with patients and family members by phone from April 6-13, 162 connections from April 13-19, and 130 connections from April 20-26, according to Dr. Norris. As of April 28, the CHAM inpatient census of patients aged 18 years and over with COVID-19 was 42, “and we’re making 130 connections by phone to patients and family members each day,” she said.
QUILT bereavement callers are following 30 families, providing 3 weeks of acute grief counseling from the date of death. “A sad truth is that, here in New York, our entire funeral, burial, cremation system is overwhelmed in volume,” Dr. Norris said. “Only half of the patients we’re following 3 weeks out have been able to have their family member buried or cremated; many are still waiting. What strikes me here is that pediatricians are often partners in care. With time, we’re partners in care in heartbreak, and in the occasional victory. We mourn patients who have died. We’ve had colleagues who died from COVID-19 right here at our hospital. But we stand together like a family.”
Dr. Norris recalled an older woman who came into CHAM’s ICU on a ventilator, critically ill from COVID-19. She called her husband at home every day with updates. “I got to know her husband, and I got to know her through him,” Dr. Norris said. “We talked every single day and she was able to graduate off of the breathing tube and out of the ICU, which was amazing.” The woman was moved to a floor in the adult hospital, but Dr. Norris continues to visit her and to provide her husband with updates, “because I’m devoted to them,” she said.
Recently, physicians in the adult hospital consulted with Dr. Norris about the woman. “They were trying to figure out what to do with her next,” she said. “Could she go home, or did she need rehab? They said, ‘We called you, Dr. Norris, because her husband thinks he can take her home.’ We know that COVID-19 really weakens people, so I went over to see her myself. I thought, ‘No single person could take care of an adult so weak at home.’ So, I called her husband and said, ‘I’m here with your wife, and I have to tell you; if she were my mother, I couldn’t take her home today. I need you to trust me.’ He said, ‘OK. We trust you and know that you have her best interest at heart.’ ”
Dr. Kaskel relayed the story of an older patient who was slowly recovering from COVID-19. During a phone call, he asked the man if there was anything he wanted at that moment.
“He said, ‘I’d love to see my wife and my children and my grandkids. I know I’m going to see them again, but right now, doc, if you could get me a cheeseburger with lettuce and tomato and ketchup and French fries from outside of the hospital, I’d be the happiest man in the world.’
I said, ‘What’s the matter with the cheeseburger made at the hospital?’
He said, ‘No! They can’t make the cheeseburger I want.’
I promised him I’d relay that message to the social worker responsible for the patient. I told her please, if you buy this for him, I’ll pay you back.”
Self-care and the next chapter
Twice each week, QUILT members gather in front of their computer monitors for mandatory Zoom meetings facilitated by two psychologists to share challenges, best practices, and to discuss the difficult work they’re doing. “We meet, because you cannot help someone if you cannot help yourself,” Dr. Norris said. “We have been encouraged each and every meeting to practice self-compassion, and to recognize that things happen during a pandemic – some will be the best you can do.”
She described organizing and serving on QUILT as a grounding experience with important lessons for the delivery of health care after the pandemic subsides and the team members return to their respective practices. “I think we’ve all gained a greater sense of humility, and we understand that the badge I wear every day does not protect me from becoming a patient, or from having my own family fall ill,” she said. “Here, we think about it very simply: ‘I’m going to treat you like you’re part of my own family.’ ”
Dr. Kaskel said that serving on QUILT as a supportive caller is an experience he won’t soon forget.
“The human bond is so accessible if you accept it,” he said. “If someone is an introvert that might not be able to draw out a stranger on the phone, then [he or she] shouldn’t do this [work]. But the fact that you can make a bond with someone that you’re not even seeing in person and know that both sides of this phone call are getting good vibes, that’s a remarkable feeling that I never really knew before, because I’ve never really had to do that before. It brings up feelings like I had after 9/11 – a unified approach to surviving this as people, as a community, the idea that ‘we will get through this,’ even though it’s totally different than anything before. The idea that there’s still hope. Those are things you can’t put a price on.”
An article about how CHAM transformed to provide care to adult COVID-19 patients was published online May 4, 2020, in the Journal of Pediatrics: doi: 10.1016/j.jpeds.2020.04.060.
Operation Quack Hack: FDA moves to stop fraudulent COVID-19 products
No form of human misery can be allowed to go unexploited, and the pandemic, it seems, is no exception.
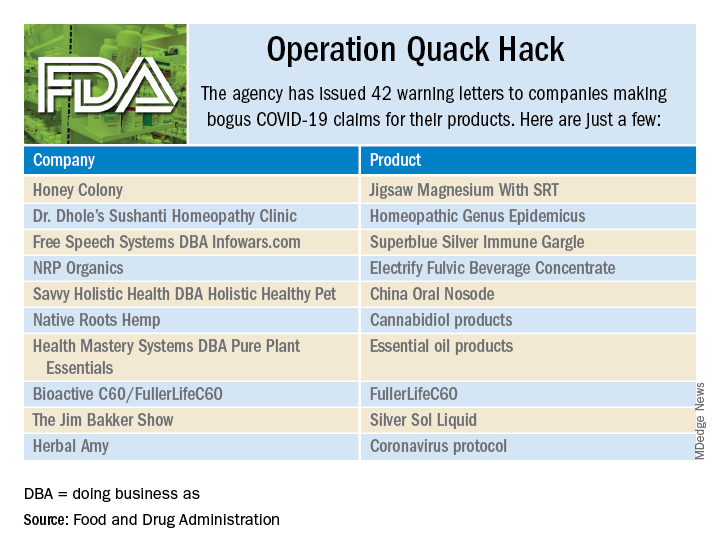
As part of Operation Quack Hack, the Food and Drug Administration has stepped up its investigation and enforcement efforts against companies and individuals that are “taking advantage of widespread fear among consumers during the COVID-19 pandemic” by selling fake products and treatments for coronavirus.
As of May 7, 2020, the agency had issued 42 warning letters to companies that were “selling unapproved products that fraudulently claim to mitigate, prevent, treat, diagnose or cure COVID-19,” the FDA announced in a written statement. Of those 42 products, 29 are no longer being sold with any sort of COVID-19 claim.
Since the beginning of the pandemic, Operation Quack Hack has uncovered hundreds of such products – drugs, testing kits, and personal protective equipment – being sold online, and complaints were sent to domain-name registrars and Internet marketplaces that have, in most cases, removed the postings, the FDA said.
“We will continue to monitor the online ecosystem for fraudulent products peddled by bad actors seeking to profit from this global pandemic. We encourage anyone aware of suspected fraudulent medical products for COVID-19 to report them to the FDA,” the statement said.
No form of human misery can be allowed to go unexploited, and the pandemic, it seems, is no exception.
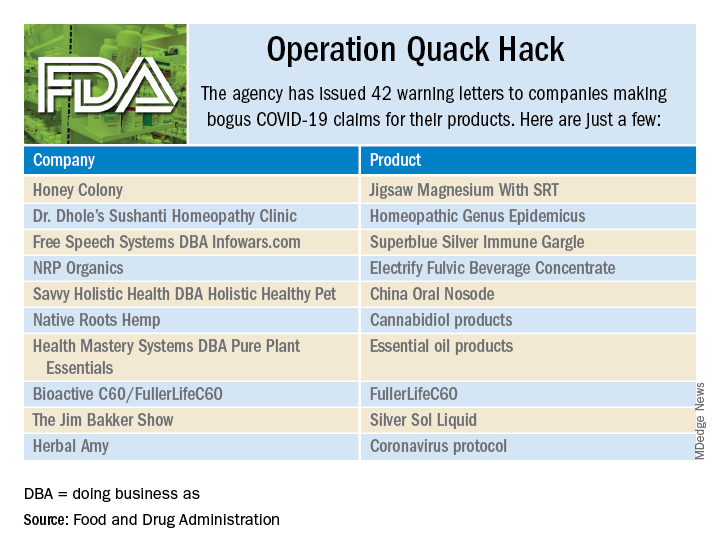
As part of Operation Quack Hack, the Food and Drug Administration has stepped up its investigation and enforcement efforts against companies and individuals that are “taking advantage of widespread fear among consumers during the COVID-19 pandemic” by selling fake products and treatments for coronavirus.
As of May 7, 2020, the agency had issued 42 warning letters to companies that were “selling unapproved products that fraudulently claim to mitigate, prevent, treat, diagnose or cure COVID-19,” the FDA announced in a written statement. Of those 42 products, 29 are no longer being sold with any sort of COVID-19 claim.
Since the beginning of the pandemic, Operation Quack Hack has uncovered hundreds of such products – drugs, testing kits, and personal protective equipment – being sold online, and complaints were sent to domain-name registrars and Internet marketplaces that have, in most cases, removed the postings, the FDA said.
“We will continue to monitor the online ecosystem for fraudulent products peddled by bad actors seeking to profit from this global pandemic. We encourage anyone aware of suspected fraudulent medical products for COVID-19 to report them to the FDA,” the statement said.
No form of human misery can be allowed to go unexploited, and the pandemic, it seems, is no exception.
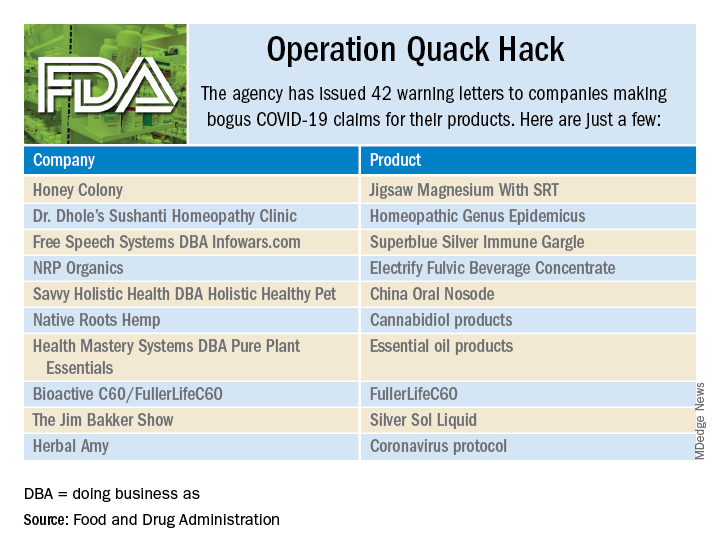
As part of Operation Quack Hack, the Food and Drug Administration has stepped up its investigation and enforcement efforts against companies and individuals that are “taking advantage of widespread fear among consumers during the COVID-19 pandemic” by selling fake products and treatments for coronavirus.
As of May 7, 2020, the agency had issued 42 warning letters to companies that were “selling unapproved products that fraudulently claim to mitigate, prevent, treat, diagnose or cure COVID-19,” the FDA announced in a written statement. Of those 42 products, 29 are no longer being sold with any sort of COVID-19 claim.
Since the beginning of the pandemic, Operation Quack Hack has uncovered hundreds of such products – drugs, testing kits, and personal protective equipment – being sold online, and complaints were sent to domain-name registrars and Internet marketplaces that have, in most cases, removed the postings, the FDA said.
“We will continue to monitor the online ecosystem for fraudulent products peddled by bad actors seeking to profit from this global pandemic. We encourage anyone aware of suspected fraudulent medical products for COVID-19 to report them to the FDA,” the statement said.
U.S. ‘deaths of despair’ from COVID-19 could top 75,000, experts warn
The number of “deaths of despair” could be even higher if the country fails to take bold action to address the mental health toll of unemployment, isolation, and uncertainty, according to the report from the Well Being Trust (WBT) and the Robert Graham Center for Policy Studies in Family Medicine and Primary Care.
“If nothing happens and nothing improves – ie, the worst-case scenario – we could be looking at an additional 150,000 people who died who didn’t have to,” Benjamin Miller, PsyD, WBT chief strategy officer, told Medscape Medical News.
“We can prevent these deaths. We know how and have a bevy of evidence-based solutions. We lack the resources to really stand this up in a way that can most positively impact communities,” Miller added.
Slow recovery, quick recovery scenarios
For the analysis, Miller and colleagues combined information on the number of deaths from suicide, alcohol, and drugs from 2018 as a baseline (n = 181,686). They projected levels of unemployment from 2020 to 2029 and then used economic modeling to estimate the additional annual number of deaths.
Across nine different scenarios, the number of additional deaths of despair range from 27,644 (quick recovery, smallest impact of unemployment on suicide, alcohol-, and drug-related deaths) to 154,037 (slow recovery, greatest impact of unemployment on these deaths), with 75,000 being the most likely.
The report offers several policy solutions to prevent a surge in “avoidable” deaths. They include finding ways to ameliorate the effects of unemployment and provide meaningful work to those who are out of work. Making access to care easier and fully integrating mental health and addiction care into primary and clinical care as well as community settings are also essential.
These solutions should also serve to prevent drug and alcohol misuse and suicide in normal times, the researchers say.
Miller believes it’s time for the federal government to fully support a framework of excellence in mental health and well-being and to invest in mental health now.
“In the short term, we need at least $48 billion to keep the lights on in the current system,” he said.
“This is because 92.6% of mental health organizations have had to reduce their operations in some capacity, 61.8% have had to completely close at least one program, and 31.0% have had to turn away patients. This scenario is not optimal for people who will need a system to help them right now during a crisis,” he added.
In the long term, $150 billion is needed for a “massive structural redesign” of the US mental health system, Miller said.
“This means bringing mental health fully into all facets of our healthcare system, of our community. It will take robust investment in creating new mechanisms for care ― those that are team-based, create a new type of workforce to deliver that care, and one that is seamless across clinical and community settings,” said Miller.
A version of this article first appeared on Medscape.com.
The number of “deaths of despair” could be even higher if the country fails to take bold action to address the mental health toll of unemployment, isolation, and uncertainty, according to the report from the Well Being Trust (WBT) and the Robert Graham Center for Policy Studies in Family Medicine and Primary Care.
“If nothing happens and nothing improves – ie, the worst-case scenario – we could be looking at an additional 150,000 people who died who didn’t have to,” Benjamin Miller, PsyD, WBT chief strategy officer, told Medscape Medical News.
“We can prevent these deaths. We know how and have a bevy of evidence-based solutions. We lack the resources to really stand this up in a way that can most positively impact communities,” Miller added.
Slow recovery, quick recovery scenarios
For the analysis, Miller and colleagues combined information on the number of deaths from suicide, alcohol, and drugs from 2018 as a baseline (n = 181,686). They projected levels of unemployment from 2020 to 2029 and then used economic modeling to estimate the additional annual number of deaths.
Across nine different scenarios, the number of additional deaths of despair range from 27,644 (quick recovery, smallest impact of unemployment on suicide, alcohol-, and drug-related deaths) to 154,037 (slow recovery, greatest impact of unemployment on these deaths), with 75,000 being the most likely.
The report offers several policy solutions to prevent a surge in “avoidable” deaths. They include finding ways to ameliorate the effects of unemployment and provide meaningful work to those who are out of work. Making access to care easier and fully integrating mental health and addiction care into primary and clinical care as well as community settings are also essential.
These solutions should also serve to prevent drug and alcohol misuse and suicide in normal times, the researchers say.
Miller believes it’s time for the federal government to fully support a framework of excellence in mental health and well-being and to invest in mental health now.
“In the short term, we need at least $48 billion to keep the lights on in the current system,” he said.
“This is because 92.6% of mental health organizations have had to reduce their operations in some capacity, 61.8% have had to completely close at least one program, and 31.0% have had to turn away patients. This scenario is not optimal for people who will need a system to help them right now during a crisis,” he added.
In the long term, $150 billion is needed for a “massive structural redesign” of the US mental health system, Miller said.
“This means bringing mental health fully into all facets of our healthcare system, of our community. It will take robust investment in creating new mechanisms for care ― those that are team-based, create a new type of workforce to deliver that care, and one that is seamless across clinical and community settings,” said Miller.
A version of this article first appeared on Medscape.com.
The number of “deaths of despair” could be even higher if the country fails to take bold action to address the mental health toll of unemployment, isolation, and uncertainty, according to the report from the Well Being Trust (WBT) and the Robert Graham Center for Policy Studies in Family Medicine and Primary Care.
“If nothing happens and nothing improves – ie, the worst-case scenario – we could be looking at an additional 150,000 people who died who didn’t have to,” Benjamin Miller, PsyD, WBT chief strategy officer, told Medscape Medical News.
“We can prevent these deaths. We know how and have a bevy of evidence-based solutions. We lack the resources to really stand this up in a way that can most positively impact communities,” Miller added.
Slow recovery, quick recovery scenarios
For the analysis, Miller and colleagues combined information on the number of deaths from suicide, alcohol, and drugs from 2018 as a baseline (n = 181,686). They projected levels of unemployment from 2020 to 2029 and then used economic modeling to estimate the additional annual number of deaths.
Across nine different scenarios, the number of additional deaths of despair range from 27,644 (quick recovery, smallest impact of unemployment on suicide, alcohol-, and drug-related deaths) to 154,037 (slow recovery, greatest impact of unemployment on these deaths), with 75,000 being the most likely.
The report offers several policy solutions to prevent a surge in “avoidable” deaths. They include finding ways to ameliorate the effects of unemployment and provide meaningful work to those who are out of work. Making access to care easier and fully integrating mental health and addiction care into primary and clinical care as well as community settings are also essential.
These solutions should also serve to prevent drug and alcohol misuse and suicide in normal times, the researchers say.
Miller believes it’s time for the federal government to fully support a framework of excellence in mental health and well-being and to invest in mental health now.
“In the short term, we need at least $48 billion to keep the lights on in the current system,” he said.
“This is because 92.6% of mental health organizations have had to reduce their operations in some capacity, 61.8% have had to completely close at least one program, and 31.0% have had to turn away patients. This scenario is not optimal for people who will need a system to help them right now during a crisis,” he added.
In the long term, $150 billion is needed for a “massive structural redesign” of the US mental health system, Miller said.
“This means bringing mental health fully into all facets of our healthcare system, of our community. It will take robust investment in creating new mechanisms for care ― those that are team-based, create a new type of workforce to deliver that care, and one that is seamless across clinical and community settings,” said Miller.
A version of this article first appeared on Medscape.com.
Fewer than 20% of eligible children received the recommended two doses of flu vaccine
A second booster dose of the influenza vaccine in vaccine-naive children may significantly reduce their likelihood of getting the disease, new research suggests.
Writing for JAMA Pediatrics, researchers reported on a case-control study of 7,533 children presenting to outpatient clinics – all in the U.S. Influenza Vaccine Effectiveness Network – with acute respiratory tract illnesses from 2014 to 2018. The study looked at the effectiveness of vaccination against laboratory-confirmed influenza.
Current U.S. guidelines recommend that children aged 6 months to 8 years receive two doses of the influenza vaccine initially – a priming dose and a booster dose – while those aged 9 years or older are considered to be ‘immunologically primed’ and therefore only require one annual dose.
The study found that 60% of the children had received two doses of the influenza vaccine during their first vaccination season, and 68% were first vaccinated before the current influenza season. Of those who had been vaccinated, 89% had received their first influenza vaccine dose when they were younger than 2 years.
Among the 2,140 children who were unvaccinated before the current influenza season, the 436 children who received two doses of the influenza vaccine had 43% lower odds of influenza compared with the 466 children who received one dose. The overall vaccine effectiveness among this vaccine-naive group aged under 2 years was 38%; for those who received two doses it was 53%, and for those who received one dose it was 23%.
“The higher risk of infection resulting from underdeveloped immune and respiratory tract systems provides a reason to identify vaccination strategies focusing on this vulnerable population of younger children,” wrote Jessie R. Chung, MPH, of the Influenza Division of the Centers for Disease Control and Prevention, and coauthors. “Promoting efforts to improve influenza vaccine coverage—particularly with 2 doses in the first vaccination season – may reduce the burden of influenza illness among young children, who are particularly vulnerable to complications and death from influenza infection.”
Overall 52% of children were unvaccinated for the current influenza season and 9% were partially vaccinated. Of those who were fully vaccinated for the current season, 83% had received one dose in the current season, and 17% had received two doses.
The authors found that full vaccination against any influenza was associated with a 22% lower odds of influenza compared with partial vaccination (95% confidence interval, 0.61-1.01), with partial vaccination defined as anything less than two doses of vaccine in the current season – at least 4 weeks apart – or two or more doses before the current season and one or more doses in the current season. However, even children who were only partially vaccinated still showed statistically significant vaccine effectiveness, except for those who received one dose of vaccine in the current season and were aged under 2 years.
“Compared with older children, young children, even if healthy, are at an elevated risk of influenza infection and influenza-associated complications, such as hospitalization,” the authors wrote. “One recent simulation study reported that even small improvements in either vaccine coverage or VE [vaccine effectiveness], and ideally both, may avert substantial amounts of influenza-associated illnesses, medical visits, and hospitalizations.”
The study also noted that children who had received only a single previous vaccine dose rarely received two doses in the current season.
In an accompanying editorial, Claire Abraham, MD, and Melissa S. Stockwell, MD, of Columbia University Medical Center, New York, wrote that modeling suggested that in the 2017-2018 influenza season, vaccination prevented 1.3 million cases of infection, 895,000 medical visits, 10,500 hospitalizations and 111 deaths in children aged under 5 years.
“This study highlights the importance of administering 2 doses of the influenza vaccine to children younger than 9 years for whom 2 doses are needed, and especially to vaccine naive children younger than 2 years,” they wrote.
But despite many studies showing the impact and importance of influenza vaccination, uptake of this vaccine remained lower than for other pediatric vaccines.
“This present study reemphasizes the need for further research exploring why families who are seemingly willing to vaccinate their children against influenza, as indicated by their receiving the first needed dose of influenza vaccine, find barriers to receiving all of the needed doses, placing their children at higher risk for contracting a potentially devastating virus.”
The U.S. Influenza Vaccine Effectiveness Network is funded by the CDC, and this project also received support from the National Institutes of Health. Eight authors declared grants from the CDC during the conduct of the study, and five declared grants and other funding from private industry outside the study.
SOURCE: Chung J et al. JAMA Pediatrics 2020 May 4. doi: 10.1001/jamapediatrics.2020.0372.
A second booster dose of the influenza vaccine in vaccine-naive children may significantly reduce their likelihood of getting the disease, new research suggests.
Writing for JAMA Pediatrics, researchers reported on a case-control study of 7,533 children presenting to outpatient clinics – all in the U.S. Influenza Vaccine Effectiveness Network – with acute respiratory tract illnesses from 2014 to 2018. The study looked at the effectiveness of vaccination against laboratory-confirmed influenza.
Current U.S. guidelines recommend that children aged 6 months to 8 years receive two doses of the influenza vaccine initially – a priming dose and a booster dose – while those aged 9 years or older are considered to be ‘immunologically primed’ and therefore only require one annual dose.
The study found that 60% of the children had received two doses of the influenza vaccine during their first vaccination season, and 68% were first vaccinated before the current influenza season. Of those who had been vaccinated, 89% had received their first influenza vaccine dose when they were younger than 2 years.
Among the 2,140 children who were unvaccinated before the current influenza season, the 436 children who received two doses of the influenza vaccine had 43% lower odds of influenza compared with the 466 children who received one dose. The overall vaccine effectiveness among this vaccine-naive group aged under 2 years was 38%; for those who received two doses it was 53%, and for those who received one dose it was 23%.
“The higher risk of infection resulting from underdeveloped immune and respiratory tract systems provides a reason to identify vaccination strategies focusing on this vulnerable population of younger children,” wrote Jessie R. Chung, MPH, of the Influenza Division of the Centers for Disease Control and Prevention, and coauthors. “Promoting efforts to improve influenza vaccine coverage—particularly with 2 doses in the first vaccination season – may reduce the burden of influenza illness among young children, who are particularly vulnerable to complications and death from influenza infection.”
Overall 52% of children were unvaccinated for the current influenza season and 9% were partially vaccinated. Of those who were fully vaccinated for the current season, 83% had received one dose in the current season, and 17% had received two doses.
The authors found that full vaccination against any influenza was associated with a 22% lower odds of influenza compared with partial vaccination (95% confidence interval, 0.61-1.01), with partial vaccination defined as anything less than two doses of vaccine in the current season – at least 4 weeks apart – or two or more doses before the current season and one or more doses in the current season. However, even children who were only partially vaccinated still showed statistically significant vaccine effectiveness, except for those who received one dose of vaccine in the current season and were aged under 2 years.
“Compared with older children, young children, even if healthy, are at an elevated risk of influenza infection and influenza-associated complications, such as hospitalization,” the authors wrote. “One recent simulation study reported that even small improvements in either vaccine coverage or VE [vaccine effectiveness], and ideally both, may avert substantial amounts of influenza-associated illnesses, medical visits, and hospitalizations.”
The study also noted that children who had received only a single previous vaccine dose rarely received two doses in the current season.
In an accompanying editorial, Claire Abraham, MD, and Melissa S. Stockwell, MD, of Columbia University Medical Center, New York, wrote that modeling suggested that in the 2017-2018 influenza season, vaccination prevented 1.3 million cases of infection, 895,000 medical visits, 10,500 hospitalizations and 111 deaths in children aged under 5 years.
“This study highlights the importance of administering 2 doses of the influenza vaccine to children younger than 9 years for whom 2 doses are needed, and especially to vaccine naive children younger than 2 years,” they wrote.
But despite many studies showing the impact and importance of influenza vaccination, uptake of this vaccine remained lower than for other pediatric vaccines.
“This present study reemphasizes the need for further research exploring why families who are seemingly willing to vaccinate their children against influenza, as indicated by their receiving the first needed dose of influenza vaccine, find barriers to receiving all of the needed doses, placing their children at higher risk for contracting a potentially devastating virus.”
The U.S. Influenza Vaccine Effectiveness Network is funded by the CDC, and this project also received support from the National Institutes of Health. Eight authors declared grants from the CDC during the conduct of the study, and five declared grants and other funding from private industry outside the study.
SOURCE: Chung J et al. JAMA Pediatrics 2020 May 4. doi: 10.1001/jamapediatrics.2020.0372.
A second booster dose of the influenza vaccine in vaccine-naive children may significantly reduce their likelihood of getting the disease, new research suggests.
Writing for JAMA Pediatrics, researchers reported on a case-control study of 7,533 children presenting to outpatient clinics – all in the U.S. Influenza Vaccine Effectiveness Network – with acute respiratory tract illnesses from 2014 to 2018. The study looked at the effectiveness of vaccination against laboratory-confirmed influenza.
Current U.S. guidelines recommend that children aged 6 months to 8 years receive two doses of the influenza vaccine initially – a priming dose and a booster dose – while those aged 9 years or older are considered to be ‘immunologically primed’ and therefore only require one annual dose.
The study found that 60% of the children had received two doses of the influenza vaccine during their first vaccination season, and 68% were first vaccinated before the current influenza season. Of those who had been vaccinated, 89% had received their first influenza vaccine dose when they were younger than 2 years.
Among the 2,140 children who were unvaccinated before the current influenza season, the 436 children who received two doses of the influenza vaccine had 43% lower odds of influenza compared with the 466 children who received one dose. The overall vaccine effectiveness among this vaccine-naive group aged under 2 years was 38%; for those who received two doses it was 53%, and for those who received one dose it was 23%.
“The higher risk of infection resulting from underdeveloped immune and respiratory tract systems provides a reason to identify vaccination strategies focusing on this vulnerable population of younger children,” wrote Jessie R. Chung, MPH, of the Influenza Division of the Centers for Disease Control and Prevention, and coauthors. “Promoting efforts to improve influenza vaccine coverage—particularly with 2 doses in the first vaccination season – may reduce the burden of influenza illness among young children, who are particularly vulnerable to complications and death from influenza infection.”
Overall 52% of children were unvaccinated for the current influenza season and 9% were partially vaccinated. Of those who were fully vaccinated for the current season, 83% had received one dose in the current season, and 17% had received two doses.
The authors found that full vaccination against any influenza was associated with a 22% lower odds of influenza compared with partial vaccination (95% confidence interval, 0.61-1.01), with partial vaccination defined as anything less than two doses of vaccine in the current season – at least 4 weeks apart – or two or more doses before the current season and one or more doses in the current season. However, even children who were only partially vaccinated still showed statistically significant vaccine effectiveness, except for those who received one dose of vaccine in the current season and were aged under 2 years.
“Compared with older children, young children, even if healthy, are at an elevated risk of influenza infection and influenza-associated complications, such as hospitalization,” the authors wrote. “One recent simulation study reported that even small improvements in either vaccine coverage or VE [vaccine effectiveness], and ideally both, may avert substantial amounts of influenza-associated illnesses, medical visits, and hospitalizations.”
The study also noted that children who had received only a single previous vaccine dose rarely received two doses in the current season.
In an accompanying editorial, Claire Abraham, MD, and Melissa S. Stockwell, MD, of Columbia University Medical Center, New York, wrote that modeling suggested that in the 2017-2018 influenza season, vaccination prevented 1.3 million cases of infection, 895,000 medical visits, 10,500 hospitalizations and 111 deaths in children aged under 5 years.
“This study highlights the importance of administering 2 doses of the influenza vaccine to children younger than 9 years for whom 2 doses are needed, and especially to vaccine naive children younger than 2 years,” they wrote.
But despite many studies showing the impact and importance of influenza vaccination, uptake of this vaccine remained lower than for other pediatric vaccines.
“This present study reemphasizes the need for further research exploring why families who are seemingly willing to vaccinate their children against influenza, as indicated by their receiving the first needed dose of influenza vaccine, find barriers to receiving all of the needed doses, placing their children at higher risk for contracting a potentially devastating virus.”
The U.S. Influenza Vaccine Effectiveness Network is funded by the CDC, and this project also received support from the National Institutes of Health. Eight authors declared grants from the CDC during the conduct of the study, and five declared grants and other funding from private industry outside the study.
SOURCE: Chung J et al. JAMA Pediatrics 2020 May 4. doi: 10.1001/jamapediatrics.2020.0372.
FROM JAMA PEDIATRICS
Novel inflammatory syndrome in children possibly linked to COVID-19
according to reports from National Health Service England, The Lancet, and the New York City health department.
Fifteen children in New York City hospitals have presented with the condition, provisionally called pediatric multisystem inflammatory syndrome, between April 17 and May 1, according to a health alert from New York City health department deputy commissioner Demetre C. Daskalakis, MD, MPH, on May 4. On May 5, the New York state department of health released a health advisory that 64 suspected cases had been reported in children in New York state hospitals, including New York City.
The New York City reports follow a case study published April 7 in Hospital Pediatrics about the presentation. There also was a statement from the U.K.’s Paediatric Intensive Care Society (PICS) on April 27 that noted “blood parameters consistent with severe COVID-19 in children” as well as abdominal pain, gastrointestinal symptoms, and cardiac inflammation.
“Whilst it is too early to say with confidence, features appear to include high CRP [C-reactive protein], high [erythrocyte sedimentation rate] and high ferritin,” the PICS release stated. The cardiac inflammation consists of “myocarditis with raised troponin and [prohormone brain natriuretic peptide],” according to the PICS statement. “Some have an appearance of their coronary arteries in keeping with Kawasaki disease.”
The initial 15 New York City patients reportedly all had “subjective or measured fever, and more than half reported rash, abdominal pain, vomiting, or diarrhea,” but fewer than half had respiratory symptoms.
The case study described a 6-month-old infant who was admitted and diagnosed with classic Kawasaki disease, who also tested positive for COVID-19 with fever and mild respiratory symptoms, reported Veena G. Jones, MD, a pediatric hospitalist in Palo Alto, Calif., and associates.
While many of the U.K. children presenting with the symptoms had a positive polymerase chain reaction tests for infection from SARS-CoV-2, some also had a negative test. Polymerase chain reaction testing in New York City was positive for 4 children and negative for 11 children, but 6 of the those who tested negative had positive serology tests, potentially pointing to postinfection sequelae.
At press time, more cases were reported from the United Kingdom in The Lancet. In London, eight children with hyperinflammatory shock, showing features similar to atypical Kawasaki disease, Kawasaki disease shock syndrome, or toxic shock syndrome, presented within 10 days to Evelina London Children’s Hospital Paediatric ICU, Shelley Riphagen, MBChB, and colleagues revealed.
Clinically, their presentations were similar, with persistent fever, rash, conjunctivitis, peripheral edema, extremity pain, and gastrointestinal symptoms. They all developed warm vasoplegic shock that did not respond to volume resuscitation; noradrenaline and milrinone were administered for hemodynamic support. Seven of the children needed mechanical ventilation for cardiovascular stabilization, although most of them had no significant respiratory involvement.
Of note was development of small pleural, pericardial, and ascitic effusion – “suggestive of a diffuse inflammatory process,” Dr. Riphagen and associates wrote. None of the children initially was positive for SARS-CoV-2; laboratory evidence of infection or inflammation included “elevated concentrations of CRP, procalcitonin, ferritin, triglycerides or d-dimers.”
“A common echocardiographic finding was echobright coronary vessels,” they wrote. “One child developed arrhythmia with refractory shock, requiring extracorporeal life support, and died from a large cerebrovascular infarct.”
As the article went to press, the doctors in that same ICU had seen more than 20 children with similar clinical presentations, Dr. Riphagen and associates reported, and the first 10 tested positive for SARS-CoV-2 antibody, including the 8 described above.
“Most of the children appear to have antibodies to the novel coronavirus, even when they do not have virus detectable in their nose,” said Audrey John, MD, PhD, chief of the division of pediatric infectious diseases at Children’s Hospital of Philadelphia, where clinicians have seen several cases similar to those described by NHS England and the New York City health department. “This suggests that these symptoms are ‘postinfectious,’ likely due to an abnormal immune response that happens after viral infection.”
She noted at the time of her interview, however, that fewer than 100 U.S. pediatric cases appear to have been reported.
“While our understanding is evolving, given the scope of the COVID-19 pandemic, this suggests that this kind of severe disease in children is very rare indeed,” Dr. John said. “Because this syndrome is so newly described, we have to continue to be cautious in attributing this syndrome to COVID-19, as there are many other diseases that look quite similar.”
She advised clinicians to be “wary of attributing fever/rash/shock to this syndrome, as the differential is broad, and we do not want to fail to recognize and treat true toxic shock or tick-borne disease.”
Dawn Nolt, MD, MPH, an associate professor of pediatrics in infectious diseases at Oregon Health & Science University’s Doernbecher Children’s Hospital, Portland, also underscored the need to avoid drawing conclusions too quickly.
“At this time, there is no causality established between SARS-COV-2 and these inflammatory syndromes other than a temporal association,” said Dr. Nolt, whose hospital has not yet seen any of these cases. “If there is a link, then the symptoms may be from a ‘direct hit’ of the virus on tissues, or from an overly exuberant immune response.”
None of the initial 15 New York City children died, although 5 needed mechanical ventilation and over half needed blood pressure support. The one child in London died from a large cerebrovascular infarct.
If the cases are connected to COVID-19, one explanation for the presentation may be related to the leading hypothesis “that SARS-CoV-2 may stimulate the immune system in such a way to promote vasculitis,” Dr. Nolt said in an interview.
“It is unusual that this particular constellation was not reported from the known pediatric cases out of China, where the COVID-19 pandemic originated,” Dr. Nolt said. “If there is a link between SARS-CoV-2 and these inflammatory syndromes, this may have resulted from genetic/host differences, changes in the SARS-CoV-2 virus, or other factors yet to be determined.”
The New York City bulletin recommended that clinicians immediately refer children presenting with the described symptoms to a specialist in pediatric infectious disease, rheumatology, or critical care.
“Early diagnosis and treatment of patients meeting full or partial criteria for Kawasaki disease is critical to preventing end-organ damage and other long-term complications,” the bulletin stated. It recommended aspirin and intravenous immunoglobulin for those who met Kawasaki criteria.
Dr. John said that children with the presentation appear to be responding well to intravenous immunoglobulin and/or steroids. She further emphasized that virtually all pediatric patients recover from COVID-19.
“Physicians should advise families to bring their children and teens back in for evaluation if they develop new fever, rash, or abdominal pain and diarrhea,” Dr. John said. “Families should not be afraid to seek care when their kids are sick. Our pediatric hospitals and EDs are open for business and working hard to protect staff and patients.”
A Kawasaki syndrome diagnosis requires at least 5 days of a fever at 101-104° F or higher along with four of the following five symptoms: rash over the torso; redness and swelling on palms and soles of the feet with later skin peeling; bloodshot, light-sensitive eyes; swollen lymph glands in the neck; and irritation and inflammation of the mouth, lips and throat, sometimes with “strawberry” tongue, according to the American Heart Association.
A press release from the AHA noted that Kawasaki disease is the most common cause of acquired heart disease in developed countries, but the condition remains rare.
Kawasaki disease’s etiology is unknown, but “some evidence suggests an infectious trigger, with winter-spring seasonality of the disease,” wrote the case study authors, noting that past research has linked Kawasaki disease with previous or concurrent infections of rhinovirus/enterovirus, parainfluenza, respiratory syncytial virus, influenza, adenovirus, and the four common human coronavirus strains.
“We have to remember that our experience with this pandemic is less than 12 months,” Dr. Nolt said. “We are still accumulating information, and any additional manifestations, particularly severe ones, adds to our ability to more quickly detect and treat children.”
Dr. Nolt and Dr. John had no disclosures.
SOURCES: Jones VG et al. Hosp Pediatr. 2020 Apr 7. doi: 10.1542/hpeds.2020-0123; Riphagen S et al. Lancet. 2020 May 6. doi: 10.1016/S0140-6736(20)31094-1.
according to reports from National Health Service England, The Lancet, and the New York City health department.
Fifteen children in New York City hospitals have presented with the condition, provisionally called pediatric multisystem inflammatory syndrome, between April 17 and May 1, according to a health alert from New York City health department deputy commissioner Demetre C. Daskalakis, MD, MPH, on May 4. On May 5, the New York state department of health released a health advisory that 64 suspected cases had been reported in children in New York state hospitals, including New York City.
The New York City reports follow a case study published April 7 in Hospital Pediatrics about the presentation. There also was a statement from the U.K.’s Paediatric Intensive Care Society (PICS) on April 27 that noted “blood parameters consistent with severe COVID-19 in children” as well as abdominal pain, gastrointestinal symptoms, and cardiac inflammation.
“Whilst it is too early to say with confidence, features appear to include high CRP [C-reactive protein], high [erythrocyte sedimentation rate] and high ferritin,” the PICS release stated. The cardiac inflammation consists of “myocarditis with raised troponin and [prohormone brain natriuretic peptide],” according to the PICS statement. “Some have an appearance of their coronary arteries in keeping with Kawasaki disease.”
The initial 15 New York City patients reportedly all had “subjective or measured fever, and more than half reported rash, abdominal pain, vomiting, or diarrhea,” but fewer than half had respiratory symptoms.
The case study described a 6-month-old infant who was admitted and diagnosed with classic Kawasaki disease, who also tested positive for COVID-19 with fever and mild respiratory symptoms, reported Veena G. Jones, MD, a pediatric hospitalist in Palo Alto, Calif., and associates.
While many of the U.K. children presenting with the symptoms had a positive polymerase chain reaction tests for infection from SARS-CoV-2, some also had a negative test. Polymerase chain reaction testing in New York City was positive for 4 children and negative for 11 children, but 6 of the those who tested negative had positive serology tests, potentially pointing to postinfection sequelae.
At press time, more cases were reported from the United Kingdom in The Lancet. In London, eight children with hyperinflammatory shock, showing features similar to atypical Kawasaki disease, Kawasaki disease shock syndrome, or toxic shock syndrome, presented within 10 days to Evelina London Children’s Hospital Paediatric ICU, Shelley Riphagen, MBChB, and colleagues revealed.
Clinically, their presentations were similar, with persistent fever, rash, conjunctivitis, peripheral edema, extremity pain, and gastrointestinal symptoms. They all developed warm vasoplegic shock that did not respond to volume resuscitation; noradrenaline and milrinone were administered for hemodynamic support. Seven of the children needed mechanical ventilation for cardiovascular stabilization, although most of them had no significant respiratory involvement.
Of note was development of small pleural, pericardial, and ascitic effusion – “suggestive of a diffuse inflammatory process,” Dr. Riphagen and associates wrote. None of the children initially was positive for SARS-CoV-2; laboratory evidence of infection or inflammation included “elevated concentrations of CRP, procalcitonin, ferritin, triglycerides or d-dimers.”
“A common echocardiographic finding was echobright coronary vessels,” they wrote. “One child developed arrhythmia with refractory shock, requiring extracorporeal life support, and died from a large cerebrovascular infarct.”
As the article went to press, the doctors in that same ICU had seen more than 20 children with similar clinical presentations, Dr. Riphagen and associates reported, and the first 10 tested positive for SARS-CoV-2 antibody, including the 8 described above.
“Most of the children appear to have antibodies to the novel coronavirus, even when they do not have virus detectable in their nose,” said Audrey John, MD, PhD, chief of the division of pediatric infectious diseases at Children’s Hospital of Philadelphia, where clinicians have seen several cases similar to those described by NHS England and the New York City health department. “This suggests that these symptoms are ‘postinfectious,’ likely due to an abnormal immune response that happens after viral infection.”
She noted at the time of her interview, however, that fewer than 100 U.S. pediatric cases appear to have been reported.
“While our understanding is evolving, given the scope of the COVID-19 pandemic, this suggests that this kind of severe disease in children is very rare indeed,” Dr. John said. “Because this syndrome is so newly described, we have to continue to be cautious in attributing this syndrome to COVID-19, as there are many other diseases that look quite similar.”
She advised clinicians to be “wary of attributing fever/rash/shock to this syndrome, as the differential is broad, and we do not want to fail to recognize and treat true toxic shock or tick-borne disease.”
Dawn Nolt, MD, MPH, an associate professor of pediatrics in infectious diseases at Oregon Health & Science University’s Doernbecher Children’s Hospital, Portland, also underscored the need to avoid drawing conclusions too quickly.
“At this time, there is no causality established between SARS-COV-2 and these inflammatory syndromes other than a temporal association,” said Dr. Nolt, whose hospital has not yet seen any of these cases. “If there is a link, then the symptoms may be from a ‘direct hit’ of the virus on tissues, or from an overly exuberant immune response.”
None of the initial 15 New York City children died, although 5 needed mechanical ventilation and over half needed blood pressure support. The one child in London died from a large cerebrovascular infarct.
If the cases are connected to COVID-19, one explanation for the presentation may be related to the leading hypothesis “that SARS-CoV-2 may stimulate the immune system in such a way to promote vasculitis,” Dr. Nolt said in an interview.
“It is unusual that this particular constellation was not reported from the known pediatric cases out of China, where the COVID-19 pandemic originated,” Dr. Nolt said. “If there is a link between SARS-CoV-2 and these inflammatory syndromes, this may have resulted from genetic/host differences, changes in the SARS-CoV-2 virus, or other factors yet to be determined.”
The New York City bulletin recommended that clinicians immediately refer children presenting with the described symptoms to a specialist in pediatric infectious disease, rheumatology, or critical care.
“Early diagnosis and treatment of patients meeting full or partial criteria for Kawasaki disease is critical to preventing end-organ damage and other long-term complications,” the bulletin stated. It recommended aspirin and intravenous immunoglobulin for those who met Kawasaki criteria.
Dr. John said that children with the presentation appear to be responding well to intravenous immunoglobulin and/or steroids. She further emphasized that virtually all pediatric patients recover from COVID-19.
“Physicians should advise families to bring their children and teens back in for evaluation if they develop new fever, rash, or abdominal pain and diarrhea,” Dr. John said. “Families should not be afraid to seek care when their kids are sick. Our pediatric hospitals and EDs are open for business and working hard to protect staff and patients.”
A Kawasaki syndrome diagnosis requires at least 5 days of a fever at 101-104° F or higher along with four of the following five symptoms: rash over the torso; redness and swelling on palms and soles of the feet with later skin peeling; bloodshot, light-sensitive eyes; swollen lymph glands in the neck; and irritation and inflammation of the mouth, lips and throat, sometimes with “strawberry” tongue, according to the American Heart Association.
A press release from the AHA noted that Kawasaki disease is the most common cause of acquired heart disease in developed countries, but the condition remains rare.
Kawasaki disease’s etiology is unknown, but “some evidence suggests an infectious trigger, with winter-spring seasonality of the disease,” wrote the case study authors, noting that past research has linked Kawasaki disease with previous or concurrent infections of rhinovirus/enterovirus, parainfluenza, respiratory syncytial virus, influenza, adenovirus, and the four common human coronavirus strains.
“We have to remember that our experience with this pandemic is less than 12 months,” Dr. Nolt said. “We are still accumulating information, and any additional manifestations, particularly severe ones, adds to our ability to more quickly detect and treat children.”
Dr. Nolt and Dr. John had no disclosures.
SOURCES: Jones VG et al. Hosp Pediatr. 2020 Apr 7. doi: 10.1542/hpeds.2020-0123; Riphagen S et al. Lancet. 2020 May 6. doi: 10.1016/S0140-6736(20)31094-1.
according to reports from National Health Service England, The Lancet, and the New York City health department.
Fifteen children in New York City hospitals have presented with the condition, provisionally called pediatric multisystem inflammatory syndrome, between April 17 and May 1, according to a health alert from New York City health department deputy commissioner Demetre C. Daskalakis, MD, MPH, on May 4. On May 5, the New York state department of health released a health advisory that 64 suspected cases had been reported in children in New York state hospitals, including New York City.
The New York City reports follow a case study published April 7 in Hospital Pediatrics about the presentation. There also was a statement from the U.K.’s Paediatric Intensive Care Society (PICS) on April 27 that noted “blood parameters consistent with severe COVID-19 in children” as well as abdominal pain, gastrointestinal symptoms, and cardiac inflammation.
“Whilst it is too early to say with confidence, features appear to include high CRP [C-reactive protein], high [erythrocyte sedimentation rate] and high ferritin,” the PICS release stated. The cardiac inflammation consists of “myocarditis with raised troponin and [prohormone brain natriuretic peptide],” according to the PICS statement. “Some have an appearance of their coronary arteries in keeping with Kawasaki disease.”
The initial 15 New York City patients reportedly all had “subjective or measured fever, and more than half reported rash, abdominal pain, vomiting, or diarrhea,” but fewer than half had respiratory symptoms.
The case study described a 6-month-old infant who was admitted and diagnosed with classic Kawasaki disease, who also tested positive for COVID-19 with fever and mild respiratory symptoms, reported Veena G. Jones, MD, a pediatric hospitalist in Palo Alto, Calif., and associates.
While many of the U.K. children presenting with the symptoms had a positive polymerase chain reaction tests for infection from SARS-CoV-2, some also had a negative test. Polymerase chain reaction testing in New York City was positive for 4 children and negative for 11 children, but 6 of the those who tested negative had positive serology tests, potentially pointing to postinfection sequelae.
At press time, more cases were reported from the United Kingdom in The Lancet. In London, eight children with hyperinflammatory shock, showing features similar to atypical Kawasaki disease, Kawasaki disease shock syndrome, or toxic shock syndrome, presented within 10 days to Evelina London Children’s Hospital Paediatric ICU, Shelley Riphagen, MBChB, and colleagues revealed.
Clinically, their presentations were similar, with persistent fever, rash, conjunctivitis, peripheral edema, extremity pain, and gastrointestinal symptoms. They all developed warm vasoplegic shock that did not respond to volume resuscitation; noradrenaline and milrinone were administered for hemodynamic support. Seven of the children needed mechanical ventilation for cardiovascular stabilization, although most of them had no significant respiratory involvement.
Of note was development of small pleural, pericardial, and ascitic effusion – “suggestive of a diffuse inflammatory process,” Dr. Riphagen and associates wrote. None of the children initially was positive for SARS-CoV-2; laboratory evidence of infection or inflammation included “elevated concentrations of CRP, procalcitonin, ferritin, triglycerides or d-dimers.”
“A common echocardiographic finding was echobright coronary vessels,” they wrote. “One child developed arrhythmia with refractory shock, requiring extracorporeal life support, and died from a large cerebrovascular infarct.”
As the article went to press, the doctors in that same ICU had seen more than 20 children with similar clinical presentations, Dr. Riphagen and associates reported, and the first 10 tested positive for SARS-CoV-2 antibody, including the 8 described above.
“Most of the children appear to have antibodies to the novel coronavirus, even when they do not have virus detectable in their nose,” said Audrey John, MD, PhD, chief of the division of pediatric infectious diseases at Children’s Hospital of Philadelphia, where clinicians have seen several cases similar to those described by NHS England and the New York City health department. “This suggests that these symptoms are ‘postinfectious,’ likely due to an abnormal immune response that happens after viral infection.”
She noted at the time of her interview, however, that fewer than 100 U.S. pediatric cases appear to have been reported.
“While our understanding is evolving, given the scope of the COVID-19 pandemic, this suggests that this kind of severe disease in children is very rare indeed,” Dr. John said. “Because this syndrome is so newly described, we have to continue to be cautious in attributing this syndrome to COVID-19, as there are many other diseases that look quite similar.”
She advised clinicians to be “wary of attributing fever/rash/shock to this syndrome, as the differential is broad, and we do not want to fail to recognize and treat true toxic shock or tick-borne disease.”
Dawn Nolt, MD, MPH, an associate professor of pediatrics in infectious diseases at Oregon Health & Science University’s Doernbecher Children’s Hospital, Portland, also underscored the need to avoid drawing conclusions too quickly.
“At this time, there is no causality established between SARS-COV-2 and these inflammatory syndromes other than a temporal association,” said Dr. Nolt, whose hospital has not yet seen any of these cases. “If there is a link, then the symptoms may be from a ‘direct hit’ of the virus on tissues, or from an overly exuberant immune response.”
None of the initial 15 New York City children died, although 5 needed mechanical ventilation and over half needed blood pressure support. The one child in London died from a large cerebrovascular infarct.
If the cases are connected to COVID-19, one explanation for the presentation may be related to the leading hypothesis “that SARS-CoV-2 may stimulate the immune system in such a way to promote vasculitis,” Dr. Nolt said in an interview.
“It is unusual that this particular constellation was not reported from the known pediatric cases out of China, where the COVID-19 pandemic originated,” Dr. Nolt said. “If there is a link between SARS-CoV-2 and these inflammatory syndromes, this may have resulted from genetic/host differences, changes in the SARS-CoV-2 virus, or other factors yet to be determined.”
The New York City bulletin recommended that clinicians immediately refer children presenting with the described symptoms to a specialist in pediatric infectious disease, rheumatology, or critical care.
“Early diagnosis and treatment of patients meeting full or partial criteria for Kawasaki disease is critical to preventing end-organ damage and other long-term complications,” the bulletin stated. It recommended aspirin and intravenous immunoglobulin for those who met Kawasaki criteria.
Dr. John said that children with the presentation appear to be responding well to intravenous immunoglobulin and/or steroids. She further emphasized that virtually all pediatric patients recover from COVID-19.
“Physicians should advise families to bring their children and teens back in for evaluation if they develop new fever, rash, or abdominal pain and diarrhea,” Dr. John said. “Families should not be afraid to seek care when their kids are sick. Our pediatric hospitals and EDs are open for business and working hard to protect staff and patients.”
A Kawasaki syndrome diagnosis requires at least 5 days of a fever at 101-104° F or higher along with four of the following five symptoms: rash over the torso; redness and swelling on palms and soles of the feet with later skin peeling; bloodshot, light-sensitive eyes; swollen lymph glands in the neck; and irritation and inflammation of the mouth, lips and throat, sometimes with “strawberry” tongue, according to the American Heart Association.
A press release from the AHA noted that Kawasaki disease is the most common cause of acquired heart disease in developed countries, but the condition remains rare.
Kawasaki disease’s etiology is unknown, but “some evidence suggests an infectious trigger, with winter-spring seasonality of the disease,” wrote the case study authors, noting that past research has linked Kawasaki disease with previous or concurrent infections of rhinovirus/enterovirus, parainfluenza, respiratory syncytial virus, influenza, adenovirus, and the four common human coronavirus strains.
“We have to remember that our experience with this pandemic is less than 12 months,” Dr. Nolt said. “We are still accumulating information, and any additional manifestations, particularly severe ones, adds to our ability to more quickly detect and treat children.”
Dr. Nolt and Dr. John had no disclosures.
SOURCES: Jones VG et al. Hosp Pediatr. 2020 Apr 7. doi: 10.1542/hpeds.2020-0123; Riphagen S et al. Lancet. 2020 May 6. doi: 10.1016/S0140-6736(20)31094-1.
Volunteering during the pandemic: What doctors need to know
A couple of weeks ago, I posted a silly picture of myself with one N95 mask and asked the folks on Twitter what else I might need. In a matter of a few days, I had filled out a form online for volunteering through the Society of Critical Care Medicine, been assigned to work at a hospital in New York City, and booked a hotel and flight.
I was going to volunteer, although I wasn’t sure of exactly what I would be doing. I’m trained as a bariatric surgeon – not obviously suited for critical care, but arguably even less suited for medicine wards.
I undoubtedly would have been less prepared if I hadn’t sought guidance on what to bring with me and generally what to expect. Less than a day after seeking advice, two local women physicians donated N95s, face shields, gowns, bouffants, and coveralls to me. I also received a laminated photo of myself to attach to my gown in the mail from a stranger I met online.
Others suggested I bring goggles, chocolate, protein bars, hand sanitizer, powdered laundry detergent, and alcohol wipes. After running around all over town, I was able find everything but the wipes.
Just as others helped me achieve my goal of volunteering, I hope I can guide those who would like to do similar work by sharing details about my experience and other information I have collected about volunteering.
Below I answer some questions that those considering volunteering might have, including why I went, who I contacted to set this up, who paid for my flight, and what I observed in the hospital.
Motivation and logistics
I am currently serving in a nonclinical role at my institution. So when the pandemic hit the United States, I felt an immense amount of guilt for not being on the front lines caring for patients. I offered my services to local hospitals and registered for the California Health Corps. I live in northern California, which was the first part of the country to shelter in place. Since my home was actually relatively spared, my services weren’t needed.
As the weeks passed, I was slowly getting more and more fit, exercising in my house since there was little else I could do, and the guilt became a cloud gathering over my head.
I decided to volunteer in a place where demands for help were higher – New York. I tried very hard to sign up to volunteer through the state’s registry for health care volunteers, but was unable to do so. Coincidentally, around that same time, I saw on Twitter that Josh Mugele, MD, emergency medicine physician and program director of the emergency medicine residency at Northeast Georgia Medical Center in Gainesville, was on his way to New York. He shared the Society of Critical Care Medicine’s form for volunteering with me, and in less than 48 hours, I was assigned to a hospital in New York City. Five days later I was on a plane from San Francisco to my destination on the opposite side of the country. The airline paid for my flight.
This is not the only path to volunteering. Another volunteer, Sara Pauk, MD, ob.gyn. at the University of Washington, Seattle, found her volunteer role through contacting the New York City Health and Hospitals system directly. Other who have volunteered told me they had contacted specific hospitals or worked with agencies that were placing physicians.
PPE
The Brooklyn hospital where I volunteered provided me with two sets of scrubs and two N95s. Gowns were variably available on our unit, and there was no eye protection. As a colleague of mine, Ben Daxon, MD, anesthesia and critical care physician at the Mayo Clinic in Rochester, Minn., had suggested, anyone volunteering in this context should bring personal protective equipment (PPE) – That includes gowns, bouffants/scrub caps, eye protection, masks, and scrubs.
The “COVID corner”
Once I arrived in New York, I did not feel particularly safe in my hotel, so I moved to another the next day. Then I had to sort out how to keep the whole room from being contaminated. I created a “COVID corner” right by the door where I kept almost everything that had been outside the door.
Every time I walked in the door, I immediately took off my shoes and left them in that corner. I could not find alcohol wipes, even after looking around in the city, so I relied on time to kill the virus, which I presumed was on everything that came from outside.
Groceries stayed by the door for 48-72 hours if possible. After that, I would move them to the “clean” parts of the room. I wore the same outfit to and from the hospital everyday, putting it on right before I left and taking it off immediately after walking into the room (and then proceeding directly to the shower). Those clothes – “my COVID outfit” – lived in the COVID corner. Anything else I wore, including exercise clothes and underwear, got washed right after I wore it.
At the hospital, I would change into scrubs and leave my COVID outfit in a plastic bag inside my handbag. Note: I fully accepted that my handbag was now a COVID handbag. I kept a pair of clogs in the hospital for daily wear. Without alcohol wipes, my room did not feel clean. But I did start to become at peace with my system, even though it was inferior to the system I use in my own home.
Meal time
In addition to bringing snacks from home, I gathered some meal items at a grocery store during my first day in New York. These included water, yogurt, a few protein drinks, fruit, and some mini chocolate croissants. It’s a pandemic – chocolate is encouraged, right?
Neither any of the volunteers I knew nor I had access to a kitchen, so this was about the best I could do.
My first week I worked nights and ate sporadically. A couple of days I bought bagel sandwiches on the way back to the hotel in the morning. Other times, I would eat yogurt or a protein bar.
I had trouble sleeping, so I would wake up early and either do yoga in my room or go for a run in a nearby park. Usually I didn’t plan well enough to eat before I went into the hospital, so I would take yogurt, some fruit, and a croissant with me as I headed out. It was hard eating on the run with a mask on my face.
When I switched to working days, I actually ordered proper dinners from local Thai, Mexican, and Indian restaurants. I paid around $20 a meal.
One night I even had dinner with a coworker who was staying at a hotel close to mine – what a luxury! Prior to all this I had been sheltering in place alone for weeks, so in that sense, this experience was a delight. I interacted with other people, in person, every day!
My commute
My hotel was about 20 minutes from the hospital. Well-meaning folks informed me that Hertz had free car rentals and Uber had discounts for health care workers. When I investigated these options, I found that only employees of certain hospitals were eligible. As a volunteer, I was not eligible.
I ultimately took Uber back and forth, and I was lucky that a few friends had sent me Uber gift cards to defray the costs. Most days, I paid about $20 each way, although 1 day there actually was “surge pricing.” The grand total for the trip was close to $800.
Many of the Uber drivers had put up plastic partitions – reminiscent of the plastic Dexter would use to contain his crime scenes – to increase their separation from their passengers. It was a bit eerie, but also somewhat welcome.
New normal
The actual work at the hospital in Brooklyn where I volunteered was different from usual practice in numerous ways. One of the things I immediately noticed was how difficult it was to get chest x-rays. After placing an emergent chest tube for a tension pneumothorax, it took about 6 hours to get a chest x-ray to assess placement.
Because code medications were needed much more frequently than normal times, these medications were kept in an open supply closet for ease of access. Many of the ventilators looked like they were from the 1970s. (They had been borrowed from the Federal Emergency Management Agency.)
What was most distinct about this work was the sheer volume of deaths and dying patients -- at least one death on our unit occurred every day I was there -- and the way families communicated with their loved ones. Countless times I held my phone over the faces of my unconscious patients to let their family profess their love and beg them to fight. While I have had to deliver bad news over the phone many times in my career, I have never had to intrude on families’ last conversations with their dying loved ones or witness that conversation occurring via a tiny screen.
Reentry
In many ways, I am lucky that I do not do clinical work in my hometown. So while other volunteers were figuring out how many more vacation days they would have to use, or whether they would have to take unpaid leave, and when and how they would get tested, all I had to do was prepare to go back home and quarantine myself for a couple of weeks.
I used up 2 weeks of vacation to volunteer in New York, but luckily, I could resume my normal work the day after I returned home.
Obviously, living in the pandemic is unique to anything we have ever experienced. Recognizing that, I recorded video diaries the whole time I was in New York. I laughed (like when I tried to fit all of my PPE on my tiny head), and I cried – several times. I suppose 1 day I may actually watch them and be reminded of what it was like to have been able to serve in this historic moment. Until then, they will remain locked up on the same phone that served as the only communication vehicle between my patients and their loved ones.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University.
A couple of weeks ago, I posted a silly picture of myself with one N95 mask and asked the folks on Twitter what else I might need. In a matter of a few days, I had filled out a form online for volunteering through the Society of Critical Care Medicine, been assigned to work at a hospital in New York City, and booked a hotel and flight.
I was going to volunteer, although I wasn’t sure of exactly what I would be doing. I’m trained as a bariatric surgeon – not obviously suited for critical care, but arguably even less suited for medicine wards.
I undoubtedly would have been less prepared if I hadn’t sought guidance on what to bring with me and generally what to expect. Less than a day after seeking advice, two local women physicians donated N95s, face shields, gowns, bouffants, and coveralls to me. I also received a laminated photo of myself to attach to my gown in the mail from a stranger I met online.
Others suggested I bring goggles, chocolate, protein bars, hand sanitizer, powdered laundry detergent, and alcohol wipes. After running around all over town, I was able find everything but the wipes.
Just as others helped me achieve my goal of volunteering, I hope I can guide those who would like to do similar work by sharing details about my experience and other information I have collected about volunteering.
Below I answer some questions that those considering volunteering might have, including why I went, who I contacted to set this up, who paid for my flight, and what I observed in the hospital.
Motivation and logistics
I am currently serving in a nonclinical role at my institution. So when the pandemic hit the United States, I felt an immense amount of guilt for not being on the front lines caring for patients. I offered my services to local hospitals and registered for the California Health Corps. I live in northern California, which was the first part of the country to shelter in place. Since my home was actually relatively spared, my services weren’t needed.
As the weeks passed, I was slowly getting more and more fit, exercising in my house since there was little else I could do, and the guilt became a cloud gathering over my head.
I decided to volunteer in a place where demands for help were higher – New York. I tried very hard to sign up to volunteer through the state’s registry for health care volunteers, but was unable to do so. Coincidentally, around that same time, I saw on Twitter that Josh Mugele, MD, emergency medicine physician and program director of the emergency medicine residency at Northeast Georgia Medical Center in Gainesville, was on his way to New York. He shared the Society of Critical Care Medicine’s form for volunteering with me, and in less than 48 hours, I was assigned to a hospital in New York City. Five days later I was on a plane from San Francisco to my destination on the opposite side of the country. The airline paid for my flight.
This is not the only path to volunteering. Another volunteer, Sara Pauk, MD, ob.gyn. at the University of Washington, Seattle, found her volunteer role through contacting the New York City Health and Hospitals system directly. Other who have volunteered told me they had contacted specific hospitals or worked with agencies that were placing physicians.
PPE
The Brooklyn hospital where I volunteered provided me with two sets of scrubs and two N95s. Gowns were variably available on our unit, and there was no eye protection. As a colleague of mine, Ben Daxon, MD, anesthesia and critical care physician at the Mayo Clinic in Rochester, Minn., had suggested, anyone volunteering in this context should bring personal protective equipment (PPE) – That includes gowns, bouffants/scrub caps, eye protection, masks, and scrubs.
The “COVID corner”
Once I arrived in New York, I did not feel particularly safe in my hotel, so I moved to another the next day. Then I had to sort out how to keep the whole room from being contaminated. I created a “COVID corner” right by the door where I kept almost everything that had been outside the door.
Every time I walked in the door, I immediately took off my shoes and left them in that corner. I could not find alcohol wipes, even after looking around in the city, so I relied on time to kill the virus, which I presumed was on everything that came from outside.
Groceries stayed by the door for 48-72 hours if possible. After that, I would move them to the “clean” parts of the room. I wore the same outfit to and from the hospital everyday, putting it on right before I left and taking it off immediately after walking into the room (and then proceeding directly to the shower). Those clothes – “my COVID outfit” – lived in the COVID corner. Anything else I wore, including exercise clothes and underwear, got washed right after I wore it.
At the hospital, I would change into scrubs and leave my COVID outfit in a plastic bag inside my handbag. Note: I fully accepted that my handbag was now a COVID handbag. I kept a pair of clogs in the hospital for daily wear. Without alcohol wipes, my room did not feel clean. But I did start to become at peace with my system, even though it was inferior to the system I use in my own home.
Meal time
In addition to bringing snacks from home, I gathered some meal items at a grocery store during my first day in New York. These included water, yogurt, a few protein drinks, fruit, and some mini chocolate croissants. It’s a pandemic – chocolate is encouraged, right?
Neither any of the volunteers I knew nor I had access to a kitchen, so this was about the best I could do.
My first week I worked nights and ate sporadically. A couple of days I bought bagel sandwiches on the way back to the hotel in the morning. Other times, I would eat yogurt or a protein bar.
I had trouble sleeping, so I would wake up early and either do yoga in my room or go for a run in a nearby park. Usually I didn’t plan well enough to eat before I went into the hospital, so I would take yogurt, some fruit, and a croissant with me as I headed out. It was hard eating on the run with a mask on my face.
When I switched to working days, I actually ordered proper dinners from local Thai, Mexican, and Indian restaurants. I paid around $20 a meal.
One night I even had dinner with a coworker who was staying at a hotel close to mine – what a luxury! Prior to all this I had been sheltering in place alone for weeks, so in that sense, this experience was a delight. I interacted with other people, in person, every day!
My commute
My hotel was about 20 minutes from the hospital. Well-meaning folks informed me that Hertz had free car rentals and Uber had discounts for health care workers. When I investigated these options, I found that only employees of certain hospitals were eligible. As a volunteer, I was not eligible.
I ultimately took Uber back and forth, and I was lucky that a few friends had sent me Uber gift cards to defray the costs. Most days, I paid about $20 each way, although 1 day there actually was “surge pricing.” The grand total for the trip was close to $800.
Many of the Uber drivers had put up plastic partitions – reminiscent of the plastic Dexter would use to contain his crime scenes – to increase their separation from their passengers. It was a bit eerie, but also somewhat welcome.
New normal
The actual work at the hospital in Brooklyn where I volunteered was different from usual practice in numerous ways. One of the things I immediately noticed was how difficult it was to get chest x-rays. After placing an emergent chest tube for a tension pneumothorax, it took about 6 hours to get a chest x-ray to assess placement.
Because code medications were needed much more frequently than normal times, these medications were kept in an open supply closet for ease of access. Many of the ventilators looked like they were from the 1970s. (They had been borrowed from the Federal Emergency Management Agency.)
What was most distinct about this work was the sheer volume of deaths and dying patients -- at least one death on our unit occurred every day I was there -- and the way families communicated with their loved ones. Countless times I held my phone over the faces of my unconscious patients to let their family profess their love and beg them to fight. While I have had to deliver bad news over the phone many times in my career, I have never had to intrude on families’ last conversations with their dying loved ones or witness that conversation occurring via a tiny screen.
Reentry
In many ways, I am lucky that I do not do clinical work in my hometown. So while other volunteers were figuring out how many more vacation days they would have to use, or whether they would have to take unpaid leave, and when and how they would get tested, all I had to do was prepare to go back home and quarantine myself for a couple of weeks.
I used up 2 weeks of vacation to volunteer in New York, but luckily, I could resume my normal work the day after I returned home.
Obviously, living in the pandemic is unique to anything we have ever experienced. Recognizing that, I recorded video diaries the whole time I was in New York. I laughed (like when I tried to fit all of my PPE on my tiny head), and I cried – several times. I suppose 1 day I may actually watch them and be reminded of what it was like to have been able to serve in this historic moment. Until then, they will remain locked up on the same phone that served as the only communication vehicle between my patients and their loved ones.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University.
A couple of weeks ago, I posted a silly picture of myself with one N95 mask and asked the folks on Twitter what else I might need. In a matter of a few days, I had filled out a form online for volunteering through the Society of Critical Care Medicine, been assigned to work at a hospital in New York City, and booked a hotel and flight.
I was going to volunteer, although I wasn’t sure of exactly what I would be doing. I’m trained as a bariatric surgeon – not obviously suited for critical care, but arguably even less suited for medicine wards.
I undoubtedly would have been less prepared if I hadn’t sought guidance on what to bring with me and generally what to expect. Less than a day after seeking advice, two local women physicians donated N95s, face shields, gowns, bouffants, and coveralls to me. I also received a laminated photo of myself to attach to my gown in the mail from a stranger I met online.
Others suggested I bring goggles, chocolate, protein bars, hand sanitizer, powdered laundry detergent, and alcohol wipes. After running around all over town, I was able find everything but the wipes.
Just as others helped me achieve my goal of volunteering, I hope I can guide those who would like to do similar work by sharing details about my experience and other information I have collected about volunteering.
Below I answer some questions that those considering volunteering might have, including why I went, who I contacted to set this up, who paid for my flight, and what I observed in the hospital.
Motivation and logistics
I am currently serving in a nonclinical role at my institution. So when the pandemic hit the United States, I felt an immense amount of guilt for not being on the front lines caring for patients. I offered my services to local hospitals and registered for the California Health Corps. I live in northern California, which was the first part of the country to shelter in place. Since my home was actually relatively spared, my services weren’t needed.
As the weeks passed, I was slowly getting more and more fit, exercising in my house since there was little else I could do, and the guilt became a cloud gathering over my head.
I decided to volunteer in a place where demands for help were higher – New York. I tried very hard to sign up to volunteer through the state’s registry for health care volunteers, but was unable to do so. Coincidentally, around that same time, I saw on Twitter that Josh Mugele, MD, emergency medicine physician and program director of the emergency medicine residency at Northeast Georgia Medical Center in Gainesville, was on his way to New York. He shared the Society of Critical Care Medicine’s form for volunteering with me, and in less than 48 hours, I was assigned to a hospital in New York City. Five days later I was on a plane from San Francisco to my destination on the opposite side of the country. The airline paid for my flight.
This is not the only path to volunteering. Another volunteer, Sara Pauk, MD, ob.gyn. at the University of Washington, Seattle, found her volunteer role through contacting the New York City Health and Hospitals system directly. Other who have volunteered told me they had contacted specific hospitals or worked with agencies that were placing physicians.
PPE
The Brooklyn hospital where I volunteered provided me with two sets of scrubs and two N95s. Gowns were variably available on our unit, and there was no eye protection. As a colleague of mine, Ben Daxon, MD, anesthesia and critical care physician at the Mayo Clinic in Rochester, Minn., had suggested, anyone volunteering in this context should bring personal protective equipment (PPE) – That includes gowns, bouffants/scrub caps, eye protection, masks, and scrubs.
The “COVID corner”
Once I arrived in New York, I did not feel particularly safe in my hotel, so I moved to another the next day. Then I had to sort out how to keep the whole room from being contaminated. I created a “COVID corner” right by the door where I kept almost everything that had been outside the door.
Every time I walked in the door, I immediately took off my shoes and left them in that corner. I could not find alcohol wipes, even after looking around in the city, so I relied on time to kill the virus, which I presumed was on everything that came from outside.
Groceries stayed by the door for 48-72 hours if possible. After that, I would move them to the “clean” parts of the room. I wore the same outfit to and from the hospital everyday, putting it on right before I left and taking it off immediately after walking into the room (and then proceeding directly to the shower). Those clothes – “my COVID outfit” – lived in the COVID corner. Anything else I wore, including exercise clothes and underwear, got washed right after I wore it.
At the hospital, I would change into scrubs and leave my COVID outfit in a plastic bag inside my handbag. Note: I fully accepted that my handbag was now a COVID handbag. I kept a pair of clogs in the hospital for daily wear. Without alcohol wipes, my room did not feel clean. But I did start to become at peace with my system, even though it was inferior to the system I use in my own home.
Meal time
In addition to bringing snacks from home, I gathered some meal items at a grocery store during my first day in New York. These included water, yogurt, a few protein drinks, fruit, and some mini chocolate croissants. It’s a pandemic – chocolate is encouraged, right?
Neither any of the volunteers I knew nor I had access to a kitchen, so this was about the best I could do.
My first week I worked nights and ate sporadically. A couple of days I bought bagel sandwiches on the way back to the hotel in the morning. Other times, I would eat yogurt or a protein bar.
I had trouble sleeping, so I would wake up early and either do yoga in my room or go for a run in a nearby park. Usually I didn’t plan well enough to eat before I went into the hospital, so I would take yogurt, some fruit, and a croissant with me as I headed out. It was hard eating on the run with a mask on my face.
When I switched to working days, I actually ordered proper dinners from local Thai, Mexican, and Indian restaurants. I paid around $20 a meal.
One night I even had dinner with a coworker who was staying at a hotel close to mine – what a luxury! Prior to all this I had been sheltering in place alone for weeks, so in that sense, this experience was a delight. I interacted with other people, in person, every day!
My commute
My hotel was about 20 minutes from the hospital. Well-meaning folks informed me that Hertz had free car rentals and Uber had discounts for health care workers. When I investigated these options, I found that only employees of certain hospitals were eligible. As a volunteer, I was not eligible.
I ultimately took Uber back and forth, and I was lucky that a few friends had sent me Uber gift cards to defray the costs. Most days, I paid about $20 each way, although 1 day there actually was “surge pricing.” The grand total for the trip was close to $800.
Many of the Uber drivers had put up plastic partitions – reminiscent of the plastic Dexter would use to contain his crime scenes – to increase their separation from their passengers. It was a bit eerie, but also somewhat welcome.
New normal
The actual work at the hospital in Brooklyn where I volunteered was different from usual practice in numerous ways. One of the things I immediately noticed was how difficult it was to get chest x-rays. After placing an emergent chest tube for a tension pneumothorax, it took about 6 hours to get a chest x-ray to assess placement.
Because code medications were needed much more frequently than normal times, these medications were kept in an open supply closet for ease of access. Many of the ventilators looked like they were from the 1970s. (They had been borrowed from the Federal Emergency Management Agency.)
What was most distinct about this work was the sheer volume of deaths and dying patients -- at least one death on our unit occurred every day I was there -- and the way families communicated with their loved ones. Countless times I held my phone over the faces of my unconscious patients to let their family profess their love and beg them to fight. While I have had to deliver bad news over the phone many times in my career, I have never had to intrude on families’ last conversations with their dying loved ones or witness that conversation occurring via a tiny screen.
Reentry
In many ways, I am lucky that I do not do clinical work in my hometown. So while other volunteers were figuring out how many more vacation days they would have to use, or whether they would have to take unpaid leave, and when and how they would get tested, all I had to do was prepare to go back home and quarantine myself for a couple of weeks.
I used up 2 weeks of vacation to volunteer in New York, but luckily, I could resume my normal work the day after I returned home.
Obviously, living in the pandemic is unique to anything we have ever experienced. Recognizing that, I recorded video diaries the whole time I was in New York. I laughed (like when I tried to fit all of my PPE on my tiny head), and I cried – several times. I suppose 1 day I may actually watch them and be reminded of what it was like to have been able to serve in this historic moment. Until then, they will remain locked up on the same phone that served as the only communication vehicle between my patients and their loved ones.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University.
Pandemic-related stress rising among ICU clinicians
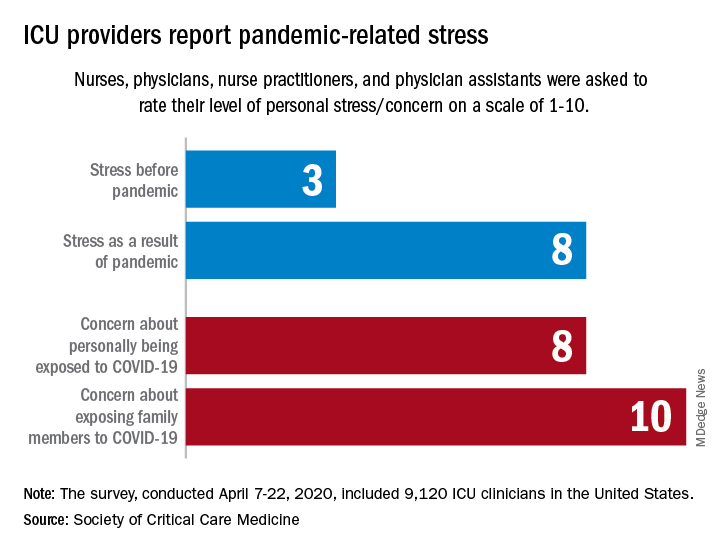
They are worried about getting infected, and they are even more worried about infecting family members, according to the Society for Critical Care Medicine, which surveyed members of four professional organizations – the American Association of Critical-Care Nurses, American College of Chest Physicians, American Thoracic Society, and the SCCM – April 7-22, 2020.
Four items in the survey assessed respondents’ level of stress or concern on a scale of 1-10:
- Personal stress before the COVID-19 pandemic.
- Personal stress as a result of COVID-19 pandemic.
- Concern about personally being exposed to COVID-19.
- Concern about exposing family members to COVID-19.
Personal stress rose from a median of 3 before the pandemic to a current 8, a level that was equaled by personal concerns about being exposed and surpassed (10) by concerns about exposing family members, the SCCM reported in a blog post.
Most of the respondents “are taking special measures to limit the potential spread of the virus to their loved ones, including implementing a decontamination routine before interacting with families,” the SCCM wrote.
The most common strategy, employed by 72% of ICU clinicians, is changing clothes before/after work. Showering before joining family was mentioned by 64% of providers, followed by limiting contact until decontamination (57%) and using hand sanitizer before entering home (51%), the SCCM said.
More extreme measures included self-isolating within their homes (16%) and staying in alternative housing away from their families (12%), the SCCM said, based on data for 9,120 clinicians in the United States.
Most of the respondents (88%) reported having cared for a patient with confirmed or presumed COVID-19. Nurses made up the majority (91%) of the sample, which also included nurse practitioners and physician assistants (4.5%) and physicians (2.9%), as well as smaller numbers of respiratory therapists, pharmacists, and emergency medicine flight personnel.
The results of the survey “underline the personal sacrifices of critical care clinicians during the COVID-19 response and suggest the need to help them proactively manage stress,” the SCCM wrote.
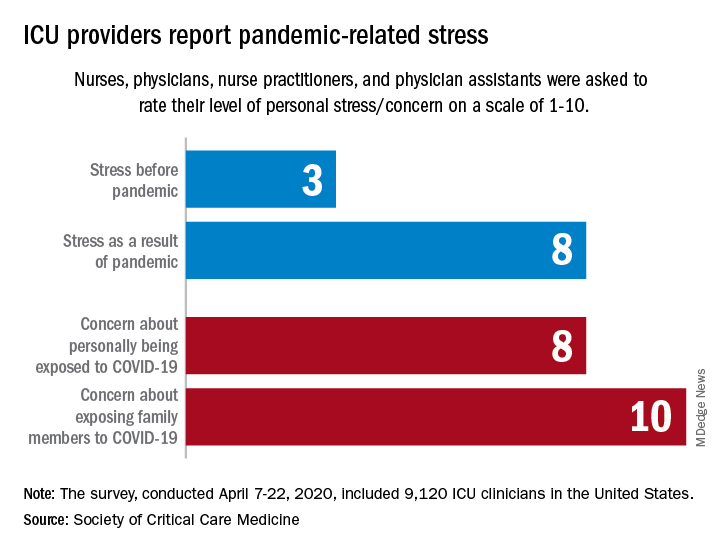
They are worried about getting infected, and they are even more worried about infecting family members, according to the Society for Critical Care Medicine, which surveyed members of four professional organizations – the American Association of Critical-Care Nurses, American College of Chest Physicians, American Thoracic Society, and the SCCM – April 7-22, 2020.
Four items in the survey assessed respondents’ level of stress or concern on a scale of 1-10:
- Personal stress before the COVID-19 pandemic.
- Personal stress as a result of COVID-19 pandemic.
- Concern about personally being exposed to COVID-19.
- Concern about exposing family members to COVID-19.
Personal stress rose from a median of 3 before the pandemic to a current 8, a level that was equaled by personal concerns about being exposed and surpassed (10) by concerns about exposing family members, the SCCM reported in a blog post.
Most of the respondents “are taking special measures to limit the potential spread of the virus to their loved ones, including implementing a decontamination routine before interacting with families,” the SCCM wrote.
The most common strategy, employed by 72% of ICU clinicians, is changing clothes before/after work. Showering before joining family was mentioned by 64% of providers, followed by limiting contact until decontamination (57%) and using hand sanitizer before entering home (51%), the SCCM said.
More extreme measures included self-isolating within their homes (16%) and staying in alternative housing away from their families (12%), the SCCM said, based on data for 9,120 clinicians in the United States.
Most of the respondents (88%) reported having cared for a patient with confirmed or presumed COVID-19. Nurses made up the majority (91%) of the sample, which also included nurse practitioners and physician assistants (4.5%) and physicians (2.9%), as well as smaller numbers of respiratory therapists, pharmacists, and emergency medicine flight personnel.
The results of the survey “underline the personal sacrifices of critical care clinicians during the COVID-19 response and suggest the need to help them proactively manage stress,” the SCCM wrote.
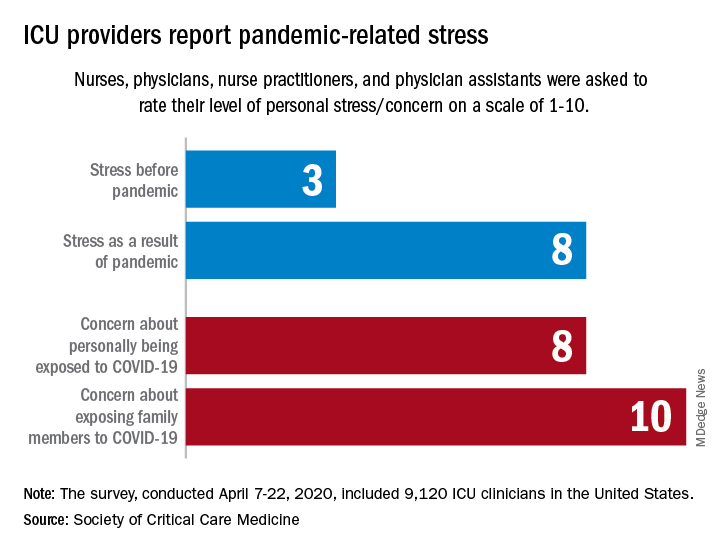
They are worried about getting infected, and they are even more worried about infecting family members, according to the Society for Critical Care Medicine, which surveyed members of four professional organizations – the American Association of Critical-Care Nurses, American College of Chest Physicians, American Thoracic Society, and the SCCM – April 7-22, 2020.
Four items in the survey assessed respondents’ level of stress or concern on a scale of 1-10:
- Personal stress before the COVID-19 pandemic.
- Personal stress as a result of COVID-19 pandemic.
- Concern about personally being exposed to COVID-19.
- Concern about exposing family members to COVID-19.
Personal stress rose from a median of 3 before the pandemic to a current 8, a level that was equaled by personal concerns about being exposed and surpassed (10) by concerns about exposing family members, the SCCM reported in a blog post.
Most of the respondents “are taking special measures to limit the potential spread of the virus to their loved ones, including implementing a decontamination routine before interacting with families,” the SCCM wrote.
The most common strategy, employed by 72% of ICU clinicians, is changing clothes before/after work. Showering before joining family was mentioned by 64% of providers, followed by limiting contact until decontamination (57%) and using hand sanitizer before entering home (51%), the SCCM said.
More extreme measures included self-isolating within their homes (16%) and staying in alternative housing away from their families (12%), the SCCM said, based on data for 9,120 clinicians in the United States.
Most of the respondents (88%) reported having cared for a patient with confirmed or presumed COVID-19. Nurses made up the majority (91%) of the sample, which also included nurse practitioners and physician assistants (4.5%) and physicians (2.9%), as well as smaller numbers of respiratory therapists, pharmacists, and emergency medicine flight personnel.
The results of the survey “underline the personal sacrifices of critical care clinicians during the COVID-19 response and suggest the need to help them proactively manage stress,” the SCCM wrote.
COVID-19: Eight steps for getting ready to see patients again
After COVID-19 hit the Denver area, internist Jean Kutner, MD, and her clinical colleagues drastically reduced the number of patients they saw and kept a minimum number of people in the office. A small team sees patients who still require in-person visits on one side of the clinic; on the other side, another team conducts clinic-based telehealth visits. A rotating schedule allows for social distancing.
The rest of the practice’s physicians are home, conducting more virtual visits.
Dr. Kutner said she is looking forward to reopening her practice completely at some point. She said she realizes that the practice probably won’t be exactly the same as before.
“We have to embrace the fact that the way we practice medicine has fundamentally changed,” said Dr. Kutner, professor of medicine at the University of Colorado at Denver, Aurora, and incoming president of the Society of General Internal Medicine. She anticipates keeping many of these changes in place for the foreseeable future.
Nearly half of 2,600 primary care physicians who responded to a recent national survey said they were struggling to remain open during the crisis. Most have had to limit wellness/chronic-disease management visits, and nearly half reported that physicians or staff were out sick. Layoffs, furloughs, and reduced hours are commonplace; some practices were forced to shut down entirely.
Social distancing helps reduce the rates of hospitalizations and deaths.
For example, remote monitoring capabilities have reduced the need for in-person checks of vital signs, such as respiratory rate oxygenation, blood glucose levels, and heart rate. “We can’t go back,” she said.
Dr. Kutner sees the pandemic as an opportunity to innovate, to think about how primary practices can best utilize their resources, face-to-face time with patients, and when and how to best leverage virtual visits in a way that improves patient health. The goal, of course, is to meet the needs of the patients while keeping everyone safe.
Like many physicians in private practice, Dr. Kutner is concerned about revenue. She hopes the Centers for Medicare & Medicaid Services makes its temporary waivers permanent.
What you need to consider when planning to reopen your office
Physicians say their post-COVID-19 practices will look very different from their prepandemic practices. Many plan to maintain guidelines, such as those from the AAFP, long after the pandemic has peaked.
If you are starting to think about reopening, here are some major considerations.
1. Develop procedures and practices that will keep your patients and staff safe.
“When we return, the first thing we need to do is limit the number of patients in the waiting room,” said Clinton Coleman, MD, who practices internal medicine and nephrology in Teaneck, N.J. “No one is comfortable in a waiting room any longer,” said Dr. Coleman, chief of internal medicine at Holy Name Medical Center in Teaneck.
Careful planning is required to resume in-person care of patients requiring non-COVID-19 care, as well as all aspects of care, according to the CMS. Adequate staff, testing, supplies, and support services, such as pathology services, are just a few considerations. The CMS recommends that physicians “evaluate the necessity of the care based on clinical needs. Providers should prioritize surgical/procedural care and high-complexity chronic disease management; however, select preventive services may also be highly necessary.”
The American Medical Association recently unveiled a checklist for reopening. One key recommendation was for practices to select a date for reopening the office, ideally preceded by a “soft” or incremental reopening to ensure that new procedures are working. The AMA also recommends opening incrementally, continuing telehealth while also inviting patients back into the office.
2. Figure out how to safely see patients, particularly in your waiting areas and common spaces.
Logistic factors, such as managing patient flow, will change. Waiting rooms will be emptier; in some locations, patients may be asked to wait in their cars until an exam room is available.
The AMA also suggests limiting nonpatient visitors by posting the practice’s policy at the entrance and on the practice’s website. If service calls for repairs are needed, have those visitors come outside of normal operating hours.
Commonly shared objects such magazines or toys in pediatric offices will likely disappear. Wipes, hand sanitizers, and the wearing of masks will become even more commonplace. Those who suspect they’re ill or who have respiratory symptoms may be relegated to specific “sick visit” appointment times or taken to designated exam rooms, which will be thoroughly sanitized between patients.
3. Prepare for routine screening of staff and other facility workers.
According to recent CMS guidelines, you and your staff will need to undergo routine screening, as will others who work in the facility (housekeeping, delivery personnel, and anyone else who enters the area). This may mean regularly stocking screening tests and setting guidelines for what to do if one of your staff tests positive.
You may need to hire temporary workers if your staff tests positive. The CDC recommends at the very least understanding the minimum staffing requirements to ensure good patient care and a safe work environment. Consider adjusting staff schedules and rotating clinical personnel to positions that support patient care activities. You may also want to look into cross-training your office staff so that they can fill in or help out with each other’s responsibilities if one or more persons are ill.
Dr. Kutner is on board with these changes. “We don’t want to get rid of social distancing right away, because it will give us a new spike in cases – how do we figure out patient flow while honoring that?”
4. Develop a strategy for triaging and caring for a potential backlog of patients.
“Many of my partners are scared right now because they have no income except for emergencies,” said Andrew Gonzalez, MD, JD, MPH, a vascular surgeon and assistant professor of surgery at Indiana University, Indianapolis. Almost all nonemergency surgery has been put on hold.
“If we don’t operate, the practice makes no money,” he said. He thinks revenue will continue to be a problem as long as patients fear in-person consultations or undergoing surgery for nonacute problems such as hernias.
As restrictions ease, most physicians will face an enormous backlog of patients and will need to find new ways of triaging the most serious cases, he says. Telehealth will help, but Dr. Gonzalez predicts many of his colleagues will be working longer hours and on weekends to catch up. “Physicians are going to have to really think about ways of optimizing their time and workflow to be very efficient, because the backlog is going to prodigious.”
5. Anticipate changes in patient expectations.
This may entail your reconsidering tests and procedures you previously performed and considering developing new sources for some services, phasing some others out, and revising your current approach. It will most likely also mean that you make telemedicine and televisits a greater part of your practice.
Carolyn Kaloostian, MD, a family medicine and geriatric practitioner in Los Angeles, points to increased reliance on community agencies for conducting common office-based procedures, such as performing blood tests and taking ECGs and x-rays. “A lot of patients are using telemedicine or telephone visits and get the lab work or x-rays somewhere that’s less congested,” she said. To become sustainable, many of these changes will hinge on economics – whether and how they are reimbursed.
The pandemic will leave lasting effects in our health care delivery, according to Dr. Kaloostian. She is sure many of her colleagues’ and patients’ current experiences will be infused into future care. “I can’t say we’ll ever be back to normal, necessarily.”
Even if the CMS rolls back its telehealth waivers, some physicians, like Dr. Coleman, plan to continue using the technology extensively. He’s confident about the level of care he’s currently providing patients in his practice. It allows him to better manage many low-income patients who can’t access his office regularly. Not only does splitting his time between the clinic and telehealth allow him to be more available for more patients, he says it also empowers patients to take better care of themselves.
6. Consider a new way to conduct “check-in visits.”
One thing that will likely go by the wayside are “check-in” visits, or so-called “social visits,” those interval appointments that can just as easily be completed virtually. “Patients are going to ask why they need to drive 3 hours so you can tell them their incision looks fine from an operation you did 5 years ago,” Dr. Gonzalez said.
He’s concerned that some people will remain so fearful of the health care system that a formerly busy practice may see the pendulum swing in the opposite direction. If an aneurysm patient skips a visit, that person may also decide not to undergo a CT scan – and something preventable will be missed. “Not everybody has the option to stay away until they feel comfortable. They’re basically playing hot potato. And at some point, the music’s going to stop,” Dr. Gonzalez said.
The pandemic has prompted some very honest conversations with his patients about what truly needs to get done and what may be optional. “Everyone has now become a hyper-rational user of health care,” he said.
7. If you haven’t yet, consider becoming more involved with technology.
In addition to greater use of telehealth, Dr. Kaloostian, assistant professor of clinical family medicine at the University of Southern California, Los Angeles, foresees continued reliance upon technology such as smartphone apps that connect with a user’s smartwatch. This allows for more proactive, remote monitoring.
“For example, any time a patient is having recurrent nighttime trips to the bathroom, I’ll get pinged and know that,” she explained. It means she can reach out and ask about any changes before a fall occurs or a condition worsens. “It provides reassurance to the provider and to the patient that you’re doing all you can to keep an eye on them from afar.”
8. Update or reformulate your business plans.
Some physicians in smaller practices may have to temporarily or permanently rethink their situation. Those who have struggled or who have closed down and are considering reopening need to update their business plans. It may be safer economically to become part of a bigger group that is affiliated with an academic center or join a larger health care system that has more funds or resources.
In addition, Dr. Kaloostian suggests that primary care physicians become more flexible in the short term, perhaps working part time in an urgent care clinic or larger organization to gain additional sources of revenue until their own practice finances pick back up.
For offices that reopen, the AMA recommends contacting medical malpractice insurance carriers to check on possible liability concerns. Congress has provided certain protections for clinicians during this time, but malpractice carriers may have more information and may offer more coverage.
Dr. Coleman said a hybrid model of fewer in-person and more telehealth visits “will allow me to practice in a different way.” If the CMS reimposes prior restrictions, reimbursement may be affected initially, but that will likely change once insurers see the increased cost-effectiveness of this approach. Patients with minor complaints, those who need to have medications refilled, and patients with chronic diseases that need managing won’t have to deal with crowded waiting rooms, and it will help mitigate problems with infection control.
If there’s any upside to the pandemic, it’s an increase in attention given to advanced care planning, said Dr. Kutner. It’s something she hopes continues after everyone stops being in crisis mode. “We’re realizing how important it is to have these conversations and document people’s goals and values and code status,” she said.
Are offices likely to open soon?
An assumption that may or may not be valid is that a practice will remain viable and can return to former capacity. Prior to passage of the CARES Act on March 27, a survey from Kareo, a company in Irvine, California, that makes a technology platform for independent physician practices, found that 9% of respondents reported practice closures. Many more reported concern about potential closures as patient office visits plummet because of stay-at-home orders and other concerns.
By mid-April, a survey from the Primary Care Collaborative and the Larry A. Green Center found that 42% of practices had experienced layoffs and had furloughed staff. Most (85%) have seen dramatic decreases in patient volume.
“Reopening the economy or loosening physical distancing restrictions will be difficult when 20% of primary care practices predict closure within 4 weeks,” the survey concluded.
For the practices and the doctors who make it through this, we’re going to probably be better, stronger, and more efficient, Dr. Gonzalez predicts. This shock has uncovered a lot of weaknesses in the American health care system that doctors have known about and have been complaining about for a long time. It will take an open mind and lots of continued flexibility on the part of physicians, hospitals, health care systems, and the government for these changes to stick.
A version of this article originally appeared on Medscape.com.
After COVID-19 hit the Denver area, internist Jean Kutner, MD, and her clinical colleagues drastically reduced the number of patients they saw and kept a minimum number of people in the office. A small team sees patients who still require in-person visits on one side of the clinic; on the other side, another team conducts clinic-based telehealth visits. A rotating schedule allows for social distancing.
The rest of the practice’s physicians are home, conducting more virtual visits.
Dr. Kutner said she is looking forward to reopening her practice completely at some point. She said she realizes that the practice probably won’t be exactly the same as before.
“We have to embrace the fact that the way we practice medicine has fundamentally changed,” said Dr. Kutner, professor of medicine at the University of Colorado at Denver, Aurora, and incoming president of the Society of General Internal Medicine. She anticipates keeping many of these changes in place for the foreseeable future.
Nearly half of 2,600 primary care physicians who responded to a recent national survey said they were struggling to remain open during the crisis. Most have had to limit wellness/chronic-disease management visits, and nearly half reported that physicians or staff were out sick. Layoffs, furloughs, and reduced hours are commonplace; some practices were forced to shut down entirely.
Social distancing helps reduce the rates of hospitalizations and deaths.
For example, remote monitoring capabilities have reduced the need for in-person checks of vital signs, such as respiratory rate oxygenation, blood glucose levels, and heart rate. “We can’t go back,” she said.
Dr. Kutner sees the pandemic as an opportunity to innovate, to think about how primary practices can best utilize their resources, face-to-face time with patients, and when and how to best leverage virtual visits in a way that improves patient health. The goal, of course, is to meet the needs of the patients while keeping everyone safe.
Like many physicians in private practice, Dr. Kutner is concerned about revenue. She hopes the Centers for Medicare & Medicaid Services makes its temporary waivers permanent.
What you need to consider when planning to reopen your office
Physicians say their post-COVID-19 practices will look very different from their prepandemic practices. Many plan to maintain guidelines, such as those from the AAFP, long after the pandemic has peaked.
If you are starting to think about reopening, here are some major considerations.
1. Develop procedures and practices that will keep your patients and staff safe.
“When we return, the first thing we need to do is limit the number of patients in the waiting room,” said Clinton Coleman, MD, who practices internal medicine and nephrology in Teaneck, N.J. “No one is comfortable in a waiting room any longer,” said Dr. Coleman, chief of internal medicine at Holy Name Medical Center in Teaneck.
Careful planning is required to resume in-person care of patients requiring non-COVID-19 care, as well as all aspects of care, according to the CMS. Adequate staff, testing, supplies, and support services, such as pathology services, are just a few considerations. The CMS recommends that physicians “evaluate the necessity of the care based on clinical needs. Providers should prioritize surgical/procedural care and high-complexity chronic disease management; however, select preventive services may also be highly necessary.”
The American Medical Association recently unveiled a checklist for reopening. One key recommendation was for practices to select a date for reopening the office, ideally preceded by a “soft” or incremental reopening to ensure that new procedures are working. The AMA also recommends opening incrementally, continuing telehealth while also inviting patients back into the office.
2. Figure out how to safely see patients, particularly in your waiting areas and common spaces.
Logistic factors, such as managing patient flow, will change. Waiting rooms will be emptier; in some locations, patients may be asked to wait in their cars until an exam room is available.
The AMA also suggests limiting nonpatient visitors by posting the practice’s policy at the entrance and on the practice’s website. If service calls for repairs are needed, have those visitors come outside of normal operating hours.
Commonly shared objects such magazines or toys in pediatric offices will likely disappear. Wipes, hand sanitizers, and the wearing of masks will become even more commonplace. Those who suspect they’re ill or who have respiratory symptoms may be relegated to specific “sick visit” appointment times or taken to designated exam rooms, which will be thoroughly sanitized between patients.
3. Prepare for routine screening of staff and other facility workers.
According to recent CMS guidelines, you and your staff will need to undergo routine screening, as will others who work in the facility (housekeeping, delivery personnel, and anyone else who enters the area). This may mean regularly stocking screening tests and setting guidelines for what to do if one of your staff tests positive.
You may need to hire temporary workers if your staff tests positive. The CDC recommends at the very least understanding the minimum staffing requirements to ensure good patient care and a safe work environment. Consider adjusting staff schedules and rotating clinical personnel to positions that support patient care activities. You may also want to look into cross-training your office staff so that they can fill in or help out with each other’s responsibilities if one or more persons are ill.
Dr. Kutner is on board with these changes. “We don’t want to get rid of social distancing right away, because it will give us a new spike in cases – how do we figure out patient flow while honoring that?”
4. Develop a strategy for triaging and caring for a potential backlog of patients.
“Many of my partners are scared right now because they have no income except for emergencies,” said Andrew Gonzalez, MD, JD, MPH, a vascular surgeon and assistant professor of surgery at Indiana University, Indianapolis. Almost all nonemergency surgery has been put on hold.
“If we don’t operate, the practice makes no money,” he said. He thinks revenue will continue to be a problem as long as patients fear in-person consultations or undergoing surgery for nonacute problems such as hernias.
As restrictions ease, most physicians will face an enormous backlog of patients and will need to find new ways of triaging the most serious cases, he says. Telehealth will help, but Dr. Gonzalez predicts many of his colleagues will be working longer hours and on weekends to catch up. “Physicians are going to have to really think about ways of optimizing their time and workflow to be very efficient, because the backlog is going to prodigious.”
5. Anticipate changes in patient expectations.
This may entail your reconsidering tests and procedures you previously performed and considering developing new sources for some services, phasing some others out, and revising your current approach. It will most likely also mean that you make telemedicine and televisits a greater part of your practice.
Carolyn Kaloostian, MD, a family medicine and geriatric practitioner in Los Angeles, points to increased reliance on community agencies for conducting common office-based procedures, such as performing blood tests and taking ECGs and x-rays. “A lot of patients are using telemedicine or telephone visits and get the lab work or x-rays somewhere that’s less congested,” she said. To become sustainable, many of these changes will hinge on economics – whether and how they are reimbursed.
The pandemic will leave lasting effects in our health care delivery, according to Dr. Kaloostian. She is sure many of her colleagues’ and patients’ current experiences will be infused into future care. “I can’t say we’ll ever be back to normal, necessarily.”
Even if the CMS rolls back its telehealth waivers, some physicians, like Dr. Coleman, plan to continue using the technology extensively. He’s confident about the level of care he’s currently providing patients in his practice. It allows him to better manage many low-income patients who can’t access his office regularly. Not only does splitting his time between the clinic and telehealth allow him to be more available for more patients, he says it also empowers patients to take better care of themselves.
6. Consider a new way to conduct “check-in visits.”
One thing that will likely go by the wayside are “check-in” visits, or so-called “social visits,” those interval appointments that can just as easily be completed virtually. “Patients are going to ask why they need to drive 3 hours so you can tell them their incision looks fine from an operation you did 5 years ago,” Dr. Gonzalez said.
He’s concerned that some people will remain so fearful of the health care system that a formerly busy practice may see the pendulum swing in the opposite direction. If an aneurysm patient skips a visit, that person may also decide not to undergo a CT scan – and something preventable will be missed. “Not everybody has the option to stay away until they feel comfortable. They’re basically playing hot potato. And at some point, the music’s going to stop,” Dr. Gonzalez said.
The pandemic has prompted some very honest conversations with his patients about what truly needs to get done and what may be optional. “Everyone has now become a hyper-rational user of health care,” he said.
7. If you haven’t yet, consider becoming more involved with technology.
In addition to greater use of telehealth, Dr. Kaloostian, assistant professor of clinical family medicine at the University of Southern California, Los Angeles, foresees continued reliance upon technology such as smartphone apps that connect with a user’s smartwatch. This allows for more proactive, remote monitoring.
“For example, any time a patient is having recurrent nighttime trips to the bathroom, I’ll get pinged and know that,” she explained. It means she can reach out and ask about any changes before a fall occurs or a condition worsens. “It provides reassurance to the provider and to the patient that you’re doing all you can to keep an eye on them from afar.”
8. Update or reformulate your business plans.
Some physicians in smaller practices may have to temporarily or permanently rethink their situation. Those who have struggled or who have closed down and are considering reopening need to update their business plans. It may be safer economically to become part of a bigger group that is affiliated with an academic center or join a larger health care system that has more funds or resources.
In addition, Dr. Kaloostian suggests that primary care physicians become more flexible in the short term, perhaps working part time in an urgent care clinic or larger organization to gain additional sources of revenue until their own practice finances pick back up.
For offices that reopen, the AMA recommends contacting medical malpractice insurance carriers to check on possible liability concerns. Congress has provided certain protections for clinicians during this time, but malpractice carriers may have more information and may offer more coverage.
Dr. Coleman said a hybrid model of fewer in-person and more telehealth visits “will allow me to practice in a different way.” If the CMS reimposes prior restrictions, reimbursement may be affected initially, but that will likely change once insurers see the increased cost-effectiveness of this approach. Patients with minor complaints, those who need to have medications refilled, and patients with chronic diseases that need managing won’t have to deal with crowded waiting rooms, and it will help mitigate problems with infection control.
If there’s any upside to the pandemic, it’s an increase in attention given to advanced care planning, said Dr. Kutner. It’s something she hopes continues after everyone stops being in crisis mode. “We’re realizing how important it is to have these conversations and document people’s goals and values and code status,” she said.
Are offices likely to open soon?
An assumption that may or may not be valid is that a practice will remain viable and can return to former capacity. Prior to passage of the CARES Act on March 27, a survey from Kareo, a company in Irvine, California, that makes a technology platform for independent physician practices, found that 9% of respondents reported practice closures. Many more reported concern about potential closures as patient office visits plummet because of stay-at-home orders and other concerns.
By mid-April, a survey from the Primary Care Collaborative and the Larry A. Green Center found that 42% of practices had experienced layoffs and had furloughed staff. Most (85%) have seen dramatic decreases in patient volume.
“Reopening the economy or loosening physical distancing restrictions will be difficult when 20% of primary care practices predict closure within 4 weeks,” the survey concluded.
For the practices and the doctors who make it through this, we’re going to probably be better, stronger, and more efficient, Dr. Gonzalez predicts. This shock has uncovered a lot of weaknesses in the American health care system that doctors have known about and have been complaining about for a long time. It will take an open mind and lots of continued flexibility on the part of physicians, hospitals, health care systems, and the government for these changes to stick.
A version of this article originally appeared on Medscape.com.
After COVID-19 hit the Denver area, internist Jean Kutner, MD, and her clinical colleagues drastically reduced the number of patients they saw and kept a minimum number of people in the office. A small team sees patients who still require in-person visits on one side of the clinic; on the other side, another team conducts clinic-based telehealth visits. A rotating schedule allows for social distancing.
The rest of the practice’s physicians are home, conducting more virtual visits.
Dr. Kutner said she is looking forward to reopening her practice completely at some point. She said she realizes that the practice probably won’t be exactly the same as before.
“We have to embrace the fact that the way we practice medicine has fundamentally changed,” said Dr. Kutner, professor of medicine at the University of Colorado at Denver, Aurora, and incoming president of the Society of General Internal Medicine. She anticipates keeping many of these changes in place for the foreseeable future.
Nearly half of 2,600 primary care physicians who responded to a recent national survey said they were struggling to remain open during the crisis. Most have had to limit wellness/chronic-disease management visits, and nearly half reported that physicians or staff were out sick. Layoffs, furloughs, and reduced hours are commonplace; some practices were forced to shut down entirely.
Social distancing helps reduce the rates of hospitalizations and deaths.
For example, remote monitoring capabilities have reduced the need for in-person checks of vital signs, such as respiratory rate oxygenation, blood glucose levels, and heart rate. “We can’t go back,” she said.
Dr. Kutner sees the pandemic as an opportunity to innovate, to think about how primary practices can best utilize their resources, face-to-face time with patients, and when and how to best leverage virtual visits in a way that improves patient health. The goal, of course, is to meet the needs of the patients while keeping everyone safe.
Like many physicians in private practice, Dr. Kutner is concerned about revenue. She hopes the Centers for Medicare & Medicaid Services makes its temporary waivers permanent.
What you need to consider when planning to reopen your office
Physicians say their post-COVID-19 practices will look very different from their prepandemic practices. Many plan to maintain guidelines, such as those from the AAFP, long after the pandemic has peaked.
If you are starting to think about reopening, here are some major considerations.
1. Develop procedures and practices that will keep your patients and staff safe.
“When we return, the first thing we need to do is limit the number of patients in the waiting room,” said Clinton Coleman, MD, who practices internal medicine and nephrology in Teaneck, N.J. “No one is comfortable in a waiting room any longer,” said Dr. Coleman, chief of internal medicine at Holy Name Medical Center in Teaneck.
Careful planning is required to resume in-person care of patients requiring non-COVID-19 care, as well as all aspects of care, according to the CMS. Adequate staff, testing, supplies, and support services, such as pathology services, are just a few considerations. The CMS recommends that physicians “evaluate the necessity of the care based on clinical needs. Providers should prioritize surgical/procedural care and high-complexity chronic disease management; however, select preventive services may also be highly necessary.”
The American Medical Association recently unveiled a checklist for reopening. One key recommendation was for practices to select a date for reopening the office, ideally preceded by a “soft” or incremental reopening to ensure that new procedures are working. The AMA also recommends opening incrementally, continuing telehealth while also inviting patients back into the office.
2. Figure out how to safely see patients, particularly in your waiting areas and common spaces.
Logistic factors, such as managing patient flow, will change. Waiting rooms will be emptier; in some locations, patients may be asked to wait in their cars until an exam room is available.
The AMA also suggests limiting nonpatient visitors by posting the practice’s policy at the entrance and on the practice’s website. If service calls for repairs are needed, have those visitors come outside of normal operating hours.
Commonly shared objects such magazines or toys in pediatric offices will likely disappear. Wipes, hand sanitizers, and the wearing of masks will become even more commonplace. Those who suspect they’re ill or who have respiratory symptoms may be relegated to specific “sick visit” appointment times or taken to designated exam rooms, which will be thoroughly sanitized between patients.
3. Prepare for routine screening of staff and other facility workers.
According to recent CMS guidelines, you and your staff will need to undergo routine screening, as will others who work in the facility (housekeeping, delivery personnel, and anyone else who enters the area). This may mean regularly stocking screening tests and setting guidelines for what to do if one of your staff tests positive.
You may need to hire temporary workers if your staff tests positive. The CDC recommends at the very least understanding the minimum staffing requirements to ensure good patient care and a safe work environment. Consider adjusting staff schedules and rotating clinical personnel to positions that support patient care activities. You may also want to look into cross-training your office staff so that they can fill in or help out with each other’s responsibilities if one or more persons are ill.
Dr. Kutner is on board with these changes. “We don’t want to get rid of social distancing right away, because it will give us a new spike in cases – how do we figure out patient flow while honoring that?”
4. Develop a strategy for triaging and caring for a potential backlog of patients.
“Many of my partners are scared right now because they have no income except for emergencies,” said Andrew Gonzalez, MD, JD, MPH, a vascular surgeon and assistant professor of surgery at Indiana University, Indianapolis. Almost all nonemergency surgery has been put on hold.
“If we don’t operate, the practice makes no money,” he said. He thinks revenue will continue to be a problem as long as patients fear in-person consultations or undergoing surgery for nonacute problems such as hernias.
As restrictions ease, most physicians will face an enormous backlog of patients and will need to find new ways of triaging the most serious cases, he says. Telehealth will help, but Dr. Gonzalez predicts many of his colleagues will be working longer hours and on weekends to catch up. “Physicians are going to have to really think about ways of optimizing their time and workflow to be very efficient, because the backlog is going to prodigious.”
5. Anticipate changes in patient expectations.
This may entail your reconsidering tests and procedures you previously performed and considering developing new sources for some services, phasing some others out, and revising your current approach. It will most likely also mean that you make telemedicine and televisits a greater part of your practice.
Carolyn Kaloostian, MD, a family medicine and geriatric practitioner in Los Angeles, points to increased reliance on community agencies for conducting common office-based procedures, such as performing blood tests and taking ECGs and x-rays. “A lot of patients are using telemedicine or telephone visits and get the lab work or x-rays somewhere that’s less congested,” she said. To become sustainable, many of these changes will hinge on economics – whether and how they are reimbursed.
The pandemic will leave lasting effects in our health care delivery, according to Dr. Kaloostian. She is sure many of her colleagues’ and patients’ current experiences will be infused into future care. “I can’t say we’ll ever be back to normal, necessarily.”
Even if the CMS rolls back its telehealth waivers, some physicians, like Dr. Coleman, plan to continue using the technology extensively. He’s confident about the level of care he’s currently providing patients in his practice. It allows him to better manage many low-income patients who can’t access his office regularly. Not only does splitting his time between the clinic and telehealth allow him to be more available for more patients, he says it also empowers patients to take better care of themselves.
6. Consider a new way to conduct “check-in visits.”
One thing that will likely go by the wayside are “check-in” visits, or so-called “social visits,” those interval appointments that can just as easily be completed virtually. “Patients are going to ask why they need to drive 3 hours so you can tell them their incision looks fine from an operation you did 5 years ago,” Dr. Gonzalez said.
He’s concerned that some people will remain so fearful of the health care system that a formerly busy practice may see the pendulum swing in the opposite direction. If an aneurysm patient skips a visit, that person may also decide not to undergo a CT scan – and something preventable will be missed. “Not everybody has the option to stay away until they feel comfortable. They’re basically playing hot potato. And at some point, the music’s going to stop,” Dr. Gonzalez said.
The pandemic has prompted some very honest conversations with his patients about what truly needs to get done and what may be optional. “Everyone has now become a hyper-rational user of health care,” he said.
7. If you haven’t yet, consider becoming more involved with technology.
In addition to greater use of telehealth, Dr. Kaloostian, assistant professor of clinical family medicine at the University of Southern California, Los Angeles, foresees continued reliance upon technology such as smartphone apps that connect with a user’s smartwatch. This allows for more proactive, remote monitoring.
“For example, any time a patient is having recurrent nighttime trips to the bathroom, I’ll get pinged and know that,” she explained. It means she can reach out and ask about any changes before a fall occurs or a condition worsens. “It provides reassurance to the provider and to the patient that you’re doing all you can to keep an eye on them from afar.”
8. Update or reformulate your business plans.
Some physicians in smaller practices may have to temporarily or permanently rethink their situation. Those who have struggled or who have closed down and are considering reopening need to update their business plans. It may be safer economically to become part of a bigger group that is affiliated with an academic center or join a larger health care system that has more funds or resources.
In addition, Dr. Kaloostian suggests that primary care physicians become more flexible in the short term, perhaps working part time in an urgent care clinic or larger organization to gain additional sources of revenue until their own practice finances pick back up.
For offices that reopen, the AMA recommends contacting medical malpractice insurance carriers to check on possible liability concerns. Congress has provided certain protections for clinicians during this time, but malpractice carriers may have more information and may offer more coverage.
Dr. Coleman said a hybrid model of fewer in-person and more telehealth visits “will allow me to practice in a different way.” If the CMS reimposes prior restrictions, reimbursement may be affected initially, but that will likely change once insurers see the increased cost-effectiveness of this approach. Patients with minor complaints, those who need to have medications refilled, and patients with chronic diseases that need managing won’t have to deal with crowded waiting rooms, and it will help mitigate problems with infection control.
If there’s any upside to the pandemic, it’s an increase in attention given to advanced care planning, said Dr. Kutner. It’s something she hopes continues after everyone stops being in crisis mode. “We’re realizing how important it is to have these conversations and document people’s goals and values and code status,” she said.
Are offices likely to open soon?
An assumption that may or may not be valid is that a practice will remain viable and can return to former capacity. Prior to passage of the CARES Act on March 27, a survey from Kareo, a company in Irvine, California, that makes a technology platform for independent physician practices, found that 9% of respondents reported practice closures. Many more reported concern about potential closures as patient office visits plummet because of stay-at-home orders and other concerns.
By mid-April, a survey from the Primary Care Collaborative and the Larry A. Green Center found that 42% of practices had experienced layoffs and had furloughed staff. Most (85%) have seen dramatic decreases in patient volume.
“Reopening the economy or loosening physical distancing restrictions will be difficult when 20% of primary care practices predict closure within 4 weeks,” the survey concluded.
For the practices and the doctors who make it through this, we’re going to probably be better, stronger, and more efficient, Dr. Gonzalez predicts. This shock has uncovered a lot of weaknesses in the American health care system that doctors have known about and have been complaining about for a long time. It will take an open mind and lots of continued flexibility on the part of physicians, hospitals, health care systems, and the government for these changes to stick.
A version of this article originally appeared on Medscape.com.
More guidance on inpatient management of blood glucose in COVID-19
“The glycemic management of many COVID-19–positive patients with diabetes is proving extremely complex, with huge fluctuations in glucose control and the need for very high doses of insulin,” says Diabetes UK’s National Diabetes Inpatient COVID Response Team.
“Intravenous infusion pumps, also required for inotropes, are at a premium and there may be the need to consider the use of subcutaneous or intramuscular insulin protocols,” they note.
Updated as of April 29, all of the information of the National Diabetes Inpatient COVID Response Team is available on the Diabetes UK website.
The new inpatient management graphic adds more detail to the previous “front-door” guidance, as reported by Medscape Medical News.
The document stressed that, as well as identifying patients with known diabetes, it is imperative that all newly admitted patients with COVID-19 are evaluated for diabetes, as the infection is known to cause new-onset diabetes.
Subcutaneous insulin dosing
The new graphic gives extensive details on subcutaneous insulin dosing in place of variable rate intravenous insulin when infusion pumps are not available, and when the patient has a glucose level above 12 mmol/L (216 mg/dL) but does not have DKA or hyperosmolar hyperglycemic state.
However, the advice is not intended for people with COVID-19 causing severe insulin resistance in the intensive care unit.
The other new guidance graphic on managing DKA or hyperosmolar state in people with COVID-19 using subcutaneous insulin is also intended for situations where intravenous infusion isn’t available.
Seek help from specialist diabetes team when needed
This is not to be used for mixed DKA/hyperosmolar state or for patients who are pregnant, have severe metabolic derangement, other significant comorbidity, or impaired consciousness, however.
For those situations, the advice is to seek help from a specialist diabetes team, says Diabetes UK.
Specialist teams will be available to answer diabetes queries, both by signposting to relevant existing local documents and also by providing patient-specific advice.
Indeed, NHS England recommends that such a team be available in every hospital, with a lead consultant designated each day to co-ordinate these services who must be free of other clinical duties when doing so. The role involves co-ordination of the whole service from the emergency department through to liaison with other specialties and managers.
Also newly updated is a page with extensive information for patients, including advice for staying at home, medication use, self-isolating, shielding, hospital and doctor appointments, need for urgent medical advice, and going to the hospital.
It also covers how coronavirus can affect people with diabetes, children and school, pregnancy, work situations, and tips for picking up prescriptions.
Another, shorter document with COVID-19 advice for patients has been posted by the JDRF and Beyond Type 1 Alliance.
It has also been endorsed by the American Diabetes Association, Harvard Medical School, and International Society for Pediatric and Adolescent Diabetes, in partnership with many other professional organizations, including the International Diabetes Federation, American Association of Clinical Endocrinologists, and Association of Diabetes Care & Education Specialists.
The shorter document covers topics such as personal hygiene, distancing, diabetes management, and seeking treatment, as well as links to other resources on what to do when health insurance is lost and legal rights.
This article first appeared on Medscape.com.
“The glycemic management of many COVID-19–positive patients with diabetes is proving extremely complex, with huge fluctuations in glucose control and the need for very high doses of insulin,” says Diabetes UK’s National Diabetes Inpatient COVID Response Team.
“Intravenous infusion pumps, also required for inotropes, are at a premium and there may be the need to consider the use of subcutaneous or intramuscular insulin protocols,” they note.
Updated as of April 29, all of the information of the National Diabetes Inpatient COVID Response Team is available on the Diabetes UK website.
The new inpatient management graphic adds more detail to the previous “front-door” guidance, as reported by Medscape Medical News.
The document stressed that, as well as identifying patients with known diabetes, it is imperative that all newly admitted patients with COVID-19 are evaluated for diabetes, as the infection is known to cause new-onset diabetes.
Subcutaneous insulin dosing
The new graphic gives extensive details on subcutaneous insulin dosing in place of variable rate intravenous insulin when infusion pumps are not available, and when the patient has a glucose level above 12 mmol/L (216 mg/dL) but does not have DKA or hyperosmolar hyperglycemic state.
However, the advice is not intended for people with COVID-19 causing severe insulin resistance in the intensive care unit.
The other new guidance graphic on managing DKA or hyperosmolar state in people with COVID-19 using subcutaneous insulin is also intended for situations where intravenous infusion isn’t available.
Seek help from specialist diabetes team when needed
This is not to be used for mixed DKA/hyperosmolar state or for patients who are pregnant, have severe metabolic derangement, other significant comorbidity, or impaired consciousness, however.
For those situations, the advice is to seek help from a specialist diabetes team, says Diabetes UK.
Specialist teams will be available to answer diabetes queries, both by signposting to relevant existing local documents and also by providing patient-specific advice.
Indeed, NHS England recommends that such a team be available in every hospital, with a lead consultant designated each day to co-ordinate these services who must be free of other clinical duties when doing so. The role involves co-ordination of the whole service from the emergency department through to liaison with other specialties and managers.
Also newly updated is a page with extensive information for patients, including advice for staying at home, medication use, self-isolating, shielding, hospital and doctor appointments, need for urgent medical advice, and going to the hospital.
It also covers how coronavirus can affect people with diabetes, children and school, pregnancy, work situations, and tips for picking up prescriptions.
Another, shorter document with COVID-19 advice for patients has been posted by the JDRF and Beyond Type 1 Alliance.
It has also been endorsed by the American Diabetes Association, Harvard Medical School, and International Society for Pediatric and Adolescent Diabetes, in partnership with many other professional organizations, including the International Diabetes Federation, American Association of Clinical Endocrinologists, and Association of Diabetes Care & Education Specialists.
The shorter document covers topics such as personal hygiene, distancing, diabetes management, and seeking treatment, as well as links to other resources on what to do when health insurance is lost and legal rights.
This article first appeared on Medscape.com.
“The glycemic management of many COVID-19–positive patients with diabetes is proving extremely complex, with huge fluctuations in glucose control and the need for very high doses of insulin,” says Diabetes UK’s National Diabetes Inpatient COVID Response Team.
“Intravenous infusion pumps, also required for inotropes, are at a premium and there may be the need to consider the use of subcutaneous or intramuscular insulin protocols,” they note.
Updated as of April 29, all of the information of the National Diabetes Inpatient COVID Response Team is available on the Diabetes UK website.
The new inpatient management graphic adds more detail to the previous “front-door” guidance, as reported by Medscape Medical News.
The document stressed that, as well as identifying patients with known diabetes, it is imperative that all newly admitted patients with COVID-19 are evaluated for diabetes, as the infection is known to cause new-onset diabetes.
Subcutaneous insulin dosing
The new graphic gives extensive details on subcutaneous insulin dosing in place of variable rate intravenous insulin when infusion pumps are not available, and when the patient has a glucose level above 12 mmol/L (216 mg/dL) but does not have DKA or hyperosmolar hyperglycemic state.
However, the advice is not intended for people with COVID-19 causing severe insulin resistance in the intensive care unit.
The other new guidance graphic on managing DKA or hyperosmolar state in people with COVID-19 using subcutaneous insulin is also intended for situations where intravenous infusion isn’t available.
Seek help from specialist diabetes team when needed
This is not to be used for mixed DKA/hyperosmolar state or for patients who are pregnant, have severe metabolic derangement, other significant comorbidity, or impaired consciousness, however.
For those situations, the advice is to seek help from a specialist diabetes team, says Diabetes UK.
Specialist teams will be available to answer diabetes queries, both by signposting to relevant existing local documents and also by providing patient-specific advice.
Indeed, NHS England recommends that such a team be available in every hospital, with a lead consultant designated each day to co-ordinate these services who must be free of other clinical duties when doing so. The role involves co-ordination of the whole service from the emergency department through to liaison with other specialties and managers.
Also newly updated is a page with extensive information for patients, including advice for staying at home, medication use, self-isolating, shielding, hospital and doctor appointments, need for urgent medical advice, and going to the hospital.
It also covers how coronavirus can affect people with diabetes, children and school, pregnancy, work situations, and tips for picking up prescriptions.
Another, shorter document with COVID-19 advice for patients has been posted by the JDRF and Beyond Type 1 Alliance.
It has also been endorsed by the American Diabetes Association, Harvard Medical School, and International Society for Pediatric and Adolescent Diabetes, in partnership with many other professional organizations, including the International Diabetes Federation, American Association of Clinical Endocrinologists, and Association of Diabetes Care & Education Specialists.
The shorter document covers topics such as personal hygiene, distancing, diabetes management, and seeking treatment, as well as links to other resources on what to do when health insurance is lost and legal rights.
This article first appeared on Medscape.com.
Results from 11 AHA-funded COVID-19 studies expected within months
Work is set to start in June, with findings reported in as few as 6 months. The Cleveland Clinic will coordinate the efforts, collecting and disseminating the findings.
There were more than 750 research proposals in less than a month after the association announced its COVID-19 and Its Cardiovascular Impact Rapid Response Grant initiative.
“We were just blown away and so impressed to see this level of interest and commitment from the teams submitting such thorough proposals so quickly,” AHA President Robert Harrington, MD, chair of the department of medicine at Stanford (Calif.) University, said in a press statement. “There’s so much we don’t know about this unique coronavirus, and we continue to see emerging complications affecting both heart and brain health for which we desperately need answers and we need them quickly.”
The projects include the following:
- A Comprehensive Assessment of Arterial and Venous Thrombotic Complications in Patients with COVID-19, led by Columbia University, New York City.
- Repurposing Drugs for Treatment of Cardiomyopathy Caused by Coronavirus-2 (SARS-CoV-2), led by Brigham and Women’s Hospital and Harvard Medical School, Boston.
- Risk of Severe Morbidity and Mortality of Coronavirus Disease 2019 (COVID-19) Among Patients Taking Antihypertensive Medications, led by Kaiser Permanente Southern California.
- Deep Learning Using Chest Radiographs to Predict COVID-19 Cardiopulmonary Risk, led by Massachusetts General Hospital, Boston.
- Cardiovascular Outcomes and Biomarker Titrated Corticosteroid Dosing for SARS COV-2 (COVID-19): A Randomized Controlled Trial, led by the Mayo Clinic, Rochester Minn.
- Outcomes for Patients With Hypertension, Diabetes, and Heart Disease in the Coronavirus Pandemic: Impact of Angiotensin Converting Enzyme Inhibitors and Angiotensin Receptor Blockers Treatment, led by Stanford University.
- Rapid COVID-19-on-A-Chip to Screen Competitive Targets for SARS-CoV-2 Spike Binding Sites, led by University of California, Los Angeles.
- COVID-19 Infection, African American Women and Cardiovascular Health, led by University of California, San Francisco.
- Myocardial Virus and Gene Expression in SARS CoV-2 Positive Patients with Clinically Important Myocardial Dysfunction, led by the University of Colorado, Aurora.
- The Role of the Platelet in Mediating Cardiovascular Disease in SARS-CoV-2 Infection, led by the University of Massachusetts, Worcester.
- Harnessing Glycomics to Understand Myocardial Injury in COVID-19, led by the University of Nebraska Medical Center, Omaha.
The AHA also awarded $800,000 for short-term projects to members of its new Health Technologies & Innovation Strategically Focused Research Network.
Cincinnati Children’s Hospital will assess the use of ejection fraction to triage COVID-19 patients; Johns Hopkins University, Baltimore, will assess smartphones for “virtual check-in” for stroke symptoms; Stanford will assess digital tracking of COVID-19 patients with cardiovascular complications; and the University of Michigan, Ann Arbor, will assess a system to track physiological and cardiovascular consequences of the infection.
Work is set to start in June, with findings reported in as few as 6 months. The Cleveland Clinic will coordinate the efforts, collecting and disseminating the findings.
There were more than 750 research proposals in less than a month after the association announced its COVID-19 and Its Cardiovascular Impact Rapid Response Grant initiative.
“We were just blown away and so impressed to see this level of interest and commitment from the teams submitting such thorough proposals so quickly,” AHA President Robert Harrington, MD, chair of the department of medicine at Stanford (Calif.) University, said in a press statement. “There’s so much we don’t know about this unique coronavirus, and we continue to see emerging complications affecting both heart and brain health for which we desperately need answers and we need them quickly.”
The projects include the following:
- A Comprehensive Assessment of Arterial and Venous Thrombotic Complications in Patients with COVID-19, led by Columbia University, New York City.
- Repurposing Drugs for Treatment of Cardiomyopathy Caused by Coronavirus-2 (SARS-CoV-2), led by Brigham and Women’s Hospital and Harvard Medical School, Boston.
- Risk of Severe Morbidity and Mortality of Coronavirus Disease 2019 (COVID-19) Among Patients Taking Antihypertensive Medications, led by Kaiser Permanente Southern California.
- Deep Learning Using Chest Radiographs to Predict COVID-19 Cardiopulmonary Risk, led by Massachusetts General Hospital, Boston.
- Cardiovascular Outcomes and Biomarker Titrated Corticosteroid Dosing for SARS COV-2 (COVID-19): A Randomized Controlled Trial, led by the Mayo Clinic, Rochester Minn.
- Outcomes for Patients With Hypertension, Diabetes, and Heart Disease in the Coronavirus Pandemic: Impact of Angiotensin Converting Enzyme Inhibitors and Angiotensin Receptor Blockers Treatment, led by Stanford University.
- Rapid COVID-19-on-A-Chip to Screen Competitive Targets for SARS-CoV-2 Spike Binding Sites, led by University of California, Los Angeles.
- COVID-19 Infection, African American Women and Cardiovascular Health, led by University of California, San Francisco.
- Myocardial Virus and Gene Expression in SARS CoV-2 Positive Patients with Clinically Important Myocardial Dysfunction, led by the University of Colorado, Aurora.
- The Role of the Platelet in Mediating Cardiovascular Disease in SARS-CoV-2 Infection, led by the University of Massachusetts, Worcester.
- Harnessing Glycomics to Understand Myocardial Injury in COVID-19, led by the University of Nebraska Medical Center, Omaha.
The AHA also awarded $800,000 for short-term projects to members of its new Health Technologies & Innovation Strategically Focused Research Network.
Cincinnati Children’s Hospital will assess the use of ejection fraction to triage COVID-19 patients; Johns Hopkins University, Baltimore, will assess smartphones for “virtual check-in” for stroke symptoms; Stanford will assess digital tracking of COVID-19 patients with cardiovascular complications; and the University of Michigan, Ann Arbor, will assess a system to track physiological and cardiovascular consequences of the infection.
Work is set to start in June, with findings reported in as few as 6 months. The Cleveland Clinic will coordinate the efforts, collecting and disseminating the findings.
There were more than 750 research proposals in less than a month after the association announced its COVID-19 and Its Cardiovascular Impact Rapid Response Grant initiative.
“We were just blown away and so impressed to see this level of interest and commitment from the teams submitting such thorough proposals so quickly,” AHA President Robert Harrington, MD, chair of the department of medicine at Stanford (Calif.) University, said in a press statement. “There’s so much we don’t know about this unique coronavirus, and we continue to see emerging complications affecting both heart and brain health for which we desperately need answers and we need them quickly.”
The projects include the following:
- A Comprehensive Assessment of Arterial and Venous Thrombotic Complications in Patients with COVID-19, led by Columbia University, New York City.
- Repurposing Drugs for Treatment of Cardiomyopathy Caused by Coronavirus-2 (SARS-CoV-2), led by Brigham and Women’s Hospital and Harvard Medical School, Boston.
- Risk of Severe Morbidity and Mortality of Coronavirus Disease 2019 (COVID-19) Among Patients Taking Antihypertensive Medications, led by Kaiser Permanente Southern California.
- Deep Learning Using Chest Radiographs to Predict COVID-19 Cardiopulmonary Risk, led by Massachusetts General Hospital, Boston.
- Cardiovascular Outcomes and Biomarker Titrated Corticosteroid Dosing for SARS COV-2 (COVID-19): A Randomized Controlled Trial, led by the Mayo Clinic, Rochester Minn.
- Outcomes for Patients With Hypertension, Diabetes, and Heart Disease in the Coronavirus Pandemic: Impact of Angiotensin Converting Enzyme Inhibitors and Angiotensin Receptor Blockers Treatment, led by Stanford University.
- Rapid COVID-19-on-A-Chip to Screen Competitive Targets for SARS-CoV-2 Spike Binding Sites, led by University of California, Los Angeles.
- COVID-19 Infection, African American Women and Cardiovascular Health, led by University of California, San Francisco.
- Myocardial Virus and Gene Expression in SARS CoV-2 Positive Patients with Clinically Important Myocardial Dysfunction, led by the University of Colorado, Aurora.
- The Role of the Platelet in Mediating Cardiovascular Disease in SARS-CoV-2 Infection, led by the University of Massachusetts, Worcester.
- Harnessing Glycomics to Understand Myocardial Injury in COVID-19, led by the University of Nebraska Medical Center, Omaha.
The AHA also awarded $800,000 for short-term projects to members of its new Health Technologies & Innovation Strategically Focused Research Network.
Cincinnati Children’s Hospital will assess the use of ejection fraction to triage COVID-19 patients; Johns Hopkins University, Baltimore, will assess smartphones for “virtual check-in” for stroke symptoms; Stanford will assess digital tracking of COVID-19 patients with cardiovascular complications; and the University of Michigan, Ann Arbor, will assess a system to track physiological and cardiovascular consequences of the infection.













