User login
A New ADC for Lung Cancer: Datopotamab Deruxtecan Now Approved by FDA
This transcript has been edited for clarity.
Hello. It’s Mark Kris, from Memorial Sloan Kettering, talking about a birthday gift I received on June 23 when the FDA approved the indication of datopotamab deruxtecan for people with lung cancers. We have another drug, our third ADC (antibody-drug conjugate) to fight lung cancer, so that’s a gift.
Let’s talk a little bit about that agent. It’s an interesting twist in our practice patterns. What can the drug do? It had a response rate of 45%, which is really important in patients that had EGFR mutations with progression on osimertinib. We really need drugs in that space. The duration of response was about 7 months, which is significant.
One interesting thing in the approval, [was] that the response rate of the blinded folks was greater than that in the investigator-assessed response by about 10%. It’s very interesting. Clearly, we have another drug, and we have it in a space where we need it.
Let’s talk a bit about the toxicity. I’m going to focus more on the paper by Bardia et al that compared datopotamab deruxtecan to various chemo drugs in breast cancer, not in lung cancer. You can take this a little bit with a grain of salt.
First, they saw a whole different array of side effects with datopotamab deruxtecan, things that we don’t normally deal with here. Nausea, stomatitis, alopecia, dry eye, and vomiting. All of those were more than 10% more common in patients that received datopotamab deruxtecan compared to the control. The only things that were more common with the control were neutropenia, leukopenia, and hand-foot syndrome in patients that had capecitabine.
One thing, though, is while you say, “Oh, these weren’t dangerous side effects,” they surely were lifestyle altering. Nobody wants to have these side effects on a daily basis. Again, there’s an increasing awareness about these kinds of lower-grade but still lifestyle-disrupting side effects. When it goes on day after day, you really have to balance that into the benefit you’re going to receive.
I think the second important point is how, when we use this drug, we’re going to have to go to another level to deal with the adverse effects that we are going to see. The first would be nausea and emesis. It is a highly emetogenic regimen based on the NCCN (National Comprehensive Cancer Network) guidelines, so you would need either 3 or 4 antiemetic drugs. That’s number one.
Number two, because of the potential eye problems, you need an eye exam before treatment — and the label says at least annually — with any symptoms. I think it’s very important that you give the patients eyedrops, and in general, the preservative-free eyedrops are the ones that are most effective.
Stomatitis is a very common side effect with that agent. It’s really not seen with the other drugs that even contain the same warhead. There, dexamethasone rinses are important. Now, this is a compounded medicine so you need to be very careful in making sure that you identify pharmacies that will prepare this and will have it available for the patients that need it.
Last, there is the risk of hypersensitivity reactions and there’s a recommendation for premedication for that. As you think about using datopotamab deruxtecan, you need to have all your ducks in a row to treat side effects. You need prophylaxis for hypersensitivity reactions, nausea, and emesis.
The patient will need an eye exam. You need to prepare the patient for possible dry eye and teach them which eyedrops are the best. You also need to ensure the availability of dexamethasone rinses and mouth washes. All that needs to be in place to make sure that the patient can safely use the drug.
I think it’s going to be a useful drug. We don’t yet have a uniformly available way to select patients for its use other than EGFR. I should note that the approval is for EGFR-mutated lung cancers. It doesn’t say which type of mutation, so that would give you some latitude in giving it for exon 20 atypicals as well as for the common sensitizing mutation.
We have another drug. It’s clearly going to be a useful one. It clearly comes with many adverse effects that we don’t normally treat on an everyday basis, we’re used to the diarrhea and skin changes that come on with the EGFR TKIs.
This pattern of side effects is different and requires some additional attention, but with it, the drug can be useful. I’m glad that we have yet another way to fight this disease.
Mark G. Kris, MD, Professor of Medicine, Weill Cornell Medical College; Attending Physician, Department of Medicine, Memorial Sloan Kettering Cancer Center, New York, New York , has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: AstraZeneca; Bristol-Myers Squibb; Merck; Daiichi Sankyo; Received research grant from: National Institute of Health; Received income in an amount equal to or greater than $250 from: AstraZeneca; Bristol-Myers Squibb; Merck; Daiichi Sankyo Others: Editorial support from Genentech
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. It’s Mark Kris, from Memorial Sloan Kettering, talking about a birthday gift I received on June 23 when the FDA approved the indication of datopotamab deruxtecan for people with lung cancers. We have another drug, our third ADC (antibody-drug conjugate) to fight lung cancer, so that’s a gift.
Let’s talk a little bit about that agent. It’s an interesting twist in our practice patterns. What can the drug do? It had a response rate of 45%, which is really important in patients that had EGFR mutations with progression on osimertinib. We really need drugs in that space. The duration of response was about 7 months, which is significant.
One interesting thing in the approval, [was] that the response rate of the blinded folks was greater than that in the investigator-assessed response by about 10%. It’s very interesting. Clearly, we have another drug, and we have it in a space where we need it.
Let’s talk a bit about the toxicity. I’m going to focus more on the paper by Bardia et al that compared datopotamab deruxtecan to various chemo drugs in breast cancer, not in lung cancer. You can take this a little bit with a grain of salt.
First, they saw a whole different array of side effects with datopotamab deruxtecan, things that we don’t normally deal with here. Nausea, stomatitis, alopecia, dry eye, and vomiting. All of those were more than 10% more common in patients that received datopotamab deruxtecan compared to the control. The only things that were more common with the control were neutropenia, leukopenia, and hand-foot syndrome in patients that had capecitabine.
One thing, though, is while you say, “Oh, these weren’t dangerous side effects,” they surely were lifestyle altering. Nobody wants to have these side effects on a daily basis. Again, there’s an increasing awareness about these kinds of lower-grade but still lifestyle-disrupting side effects. When it goes on day after day, you really have to balance that into the benefit you’re going to receive.
I think the second important point is how, when we use this drug, we’re going to have to go to another level to deal with the adverse effects that we are going to see. The first would be nausea and emesis. It is a highly emetogenic regimen based on the NCCN (National Comprehensive Cancer Network) guidelines, so you would need either 3 or 4 antiemetic drugs. That’s number one.
Number two, because of the potential eye problems, you need an eye exam before treatment — and the label says at least annually — with any symptoms. I think it’s very important that you give the patients eyedrops, and in general, the preservative-free eyedrops are the ones that are most effective.
Stomatitis is a very common side effect with that agent. It’s really not seen with the other drugs that even contain the same warhead. There, dexamethasone rinses are important. Now, this is a compounded medicine so you need to be very careful in making sure that you identify pharmacies that will prepare this and will have it available for the patients that need it.
Last, there is the risk of hypersensitivity reactions and there’s a recommendation for premedication for that. As you think about using datopotamab deruxtecan, you need to have all your ducks in a row to treat side effects. You need prophylaxis for hypersensitivity reactions, nausea, and emesis.
The patient will need an eye exam. You need to prepare the patient for possible dry eye and teach them which eyedrops are the best. You also need to ensure the availability of dexamethasone rinses and mouth washes. All that needs to be in place to make sure that the patient can safely use the drug.
I think it’s going to be a useful drug. We don’t yet have a uniformly available way to select patients for its use other than EGFR. I should note that the approval is for EGFR-mutated lung cancers. It doesn’t say which type of mutation, so that would give you some latitude in giving it for exon 20 atypicals as well as for the common sensitizing mutation.
We have another drug. It’s clearly going to be a useful one. It clearly comes with many adverse effects that we don’t normally treat on an everyday basis, we’re used to the diarrhea and skin changes that come on with the EGFR TKIs.
This pattern of side effects is different and requires some additional attention, but with it, the drug can be useful. I’m glad that we have yet another way to fight this disease.
Mark G. Kris, MD, Professor of Medicine, Weill Cornell Medical College; Attending Physician, Department of Medicine, Memorial Sloan Kettering Cancer Center, New York, New York , has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: AstraZeneca; Bristol-Myers Squibb; Merck; Daiichi Sankyo; Received research grant from: National Institute of Health; Received income in an amount equal to or greater than $250 from: AstraZeneca; Bristol-Myers Squibb; Merck; Daiichi Sankyo Others: Editorial support from Genentech
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. It’s Mark Kris, from Memorial Sloan Kettering, talking about a birthday gift I received on June 23 when the FDA approved the indication of datopotamab deruxtecan for people with lung cancers. We have another drug, our third ADC (antibody-drug conjugate) to fight lung cancer, so that’s a gift.
Let’s talk a little bit about that agent. It’s an interesting twist in our practice patterns. What can the drug do? It had a response rate of 45%, which is really important in patients that had EGFR mutations with progression on osimertinib. We really need drugs in that space. The duration of response was about 7 months, which is significant.
One interesting thing in the approval, [was] that the response rate of the blinded folks was greater than that in the investigator-assessed response by about 10%. It’s very interesting. Clearly, we have another drug, and we have it in a space where we need it.
Let’s talk a bit about the toxicity. I’m going to focus more on the paper by Bardia et al that compared datopotamab deruxtecan to various chemo drugs in breast cancer, not in lung cancer. You can take this a little bit with a grain of salt.
First, they saw a whole different array of side effects with datopotamab deruxtecan, things that we don’t normally deal with here. Nausea, stomatitis, alopecia, dry eye, and vomiting. All of those were more than 10% more common in patients that received datopotamab deruxtecan compared to the control. The only things that were more common with the control were neutropenia, leukopenia, and hand-foot syndrome in patients that had capecitabine.
One thing, though, is while you say, “Oh, these weren’t dangerous side effects,” they surely were lifestyle altering. Nobody wants to have these side effects on a daily basis. Again, there’s an increasing awareness about these kinds of lower-grade but still lifestyle-disrupting side effects. When it goes on day after day, you really have to balance that into the benefit you’re going to receive.
I think the second important point is how, when we use this drug, we’re going to have to go to another level to deal with the adverse effects that we are going to see. The first would be nausea and emesis. It is a highly emetogenic regimen based on the NCCN (National Comprehensive Cancer Network) guidelines, so you would need either 3 or 4 antiemetic drugs. That’s number one.
Number two, because of the potential eye problems, you need an eye exam before treatment — and the label says at least annually — with any symptoms. I think it’s very important that you give the patients eyedrops, and in general, the preservative-free eyedrops are the ones that are most effective.
Stomatitis is a very common side effect with that agent. It’s really not seen with the other drugs that even contain the same warhead. There, dexamethasone rinses are important. Now, this is a compounded medicine so you need to be very careful in making sure that you identify pharmacies that will prepare this and will have it available for the patients that need it.
Last, there is the risk of hypersensitivity reactions and there’s a recommendation for premedication for that. As you think about using datopotamab deruxtecan, you need to have all your ducks in a row to treat side effects. You need prophylaxis for hypersensitivity reactions, nausea, and emesis.
The patient will need an eye exam. You need to prepare the patient for possible dry eye and teach them which eyedrops are the best. You also need to ensure the availability of dexamethasone rinses and mouth washes. All that needs to be in place to make sure that the patient can safely use the drug.
I think it’s going to be a useful drug. We don’t yet have a uniformly available way to select patients for its use other than EGFR. I should note that the approval is for EGFR-mutated lung cancers. It doesn’t say which type of mutation, so that would give you some latitude in giving it for exon 20 atypicals as well as for the common sensitizing mutation.
We have another drug. It’s clearly going to be a useful one. It clearly comes with many adverse effects that we don’t normally treat on an everyday basis, we’re used to the diarrhea and skin changes that come on with the EGFR TKIs.
This pattern of side effects is different and requires some additional attention, but with it, the drug can be useful. I’m glad that we have yet another way to fight this disease.
Mark G. Kris, MD, Professor of Medicine, Weill Cornell Medical College; Attending Physician, Department of Medicine, Memorial Sloan Kettering Cancer Center, New York, New York , has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: AstraZeneca; Bristol-Myers Squibb; Merck; Daiichi Sankyo; Received research grant from: National Institute of Health; Received income in an amount equal to or greater than $250 from: AstraZeneca; Bristol-Myers Squibb; Merck; Daiichi Sankyo Others: Editorial support from Genentech
A version of this article first appeared on Medscape.com.
Lung Cancer: Mortality Trends in Veterans and New Treatments
Lung Cancer: Mortality Trends in Veterans and New Treatments
Click to view more from Cancer Data Trends 2025.
- Tehzeeb J, Mahmood F, Gemoets D, Azem A, Mehdi SA. Epidemiology and survival
trends of lung carcinoids in the veteran population. J Clin Oncol. 2023;41:e21049.
doi:10.1200/JCO.2023.41.16_suppl.e21049 - Moghanaki D, Taylor J, Bryant AK, et al. Lung Cancer Survival Trends in the Veterans
Health Administration. Clin Lung Cancer. 2024;25(3):225-232. doi:10.1016/j.
cllc.2024.02.009 - Jalal SI, Guo A, Ahmed S, Kelley MJ. Analysis of actionable genetic alterations in
lung carcinoma from the VA National Precision Oncology Program. Semin Oncol.
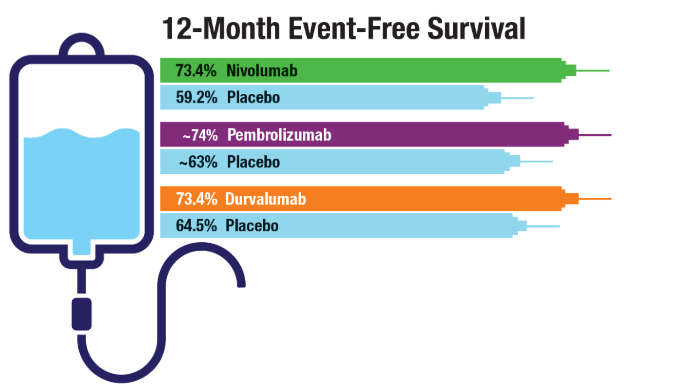
2022;49(3-4):265-274. doi:10.1053/j.seminoncol.2022.06.014 - Cascone T, Awad MM, Spicer JD, et al; for the CheckMate 77T Investigators.
Perioperative Nivolumab in Resectable Lung Cancer. N Engl J Med.
2024;390(19):1756-1769. doi:10.1056/NEJMoa2311926 - Wakelee H, Liberman M, Kato T, et al; for the KEYNOTE-671 Investigators.
Perioperative Pembrolizumab for Early-Stage Non-Small-Cell Lung Cancer. N Engl J
Med. 2023;389(6):491-503. doi:10.1056/NEJMoa2302983 - Heymach JV, Harpole D, Mitsudomi T, et al; for the AEGEAN Investigators.
Perioperative Durvalumab for Resectable Non-Small-Cell Lung Cancer. N Engl J
Med. 2023;389(18):1672-1684. doi:10.1056/NEJMoa2304875 - Duncan FC, Al Nasrallah N, Nephew L, et al. Racial disparities in staging, treatment,
and mortality in non-small cell lung cancer. Transl Lung Cancer Res. 2024;13(1):76-
94. doi:10.21037/tlcr-23-407
Click to view more from Cancer Data Trends 2025.
Click to view more from Cancer Data Trends 2025.
- Tehzeeb J, Mahmood F, Gemoets D, Azem A, Mehdi SA. Epidemiology and survival
trends of lung carcinoids in the veteran population. J Clin Oncol. 2023;41:e21049.
doi:10.1200/JCO.2023.41.16_suppl.e21049 - Moghanaki D, Taylor J, Bryant AK, et al. Lung Cancer Survival Trends in the Veterans
Health Administration. Clin Lung Cancer. 2024;25(3):225-232. doi:10.1016/j.
cllc.2024.02.009 - Jalal SI, Guo A, Ahmed S, Kelley MJ. Analysis of actionable genetic alterations in
lung carcinoma from the VA National Precision Oncology Program. Semin Oncol.
2022;49(3-4):265-274. doi:10.1053/j.seminoncol.2022.06.014 - Cascone T, Awad MM, Spicer JD, et al; for the CheckMate 77T Investigators.
Perioperative Nivolumab in Resectable Lung Cancer. N Engl J Med.
2024;390(19):1756-1769. doi:10.1056/NEJMoa2311926 - Wakelee H, Liberman M, Kato T, et al; for the KEYNOTE-671 Investigators.
Perioperative Pembrolizumab for Early-Stage Non-Small-Cell Lung Cancer. N Engl J
Med. 2023;389(6):491-503. doi:10.1056/NEJMoa2302983 - Heymach JV, Harpole D, Mitsudomi T, et al; for the AEGEAN Investigators.
Perioperative Durvalumab for Resectable Non-Small-Cell Lung Cancer. N Engl J
Med. 2023;389(18):1672-1684. doi:10.1056/NEJMoa2304875 - Duncan FC, Al Nasrallah N, Nephew L, et al. Racial disparities in staging, treatment,
and mortality in non-small cell lung cancer. Transl Lung Cancer Res. 2024;13(1):76-
94. doi:10.21037/tlcr-23-407
- Tehzeeb J, Mahmood F, Gemoets D, Azem A, Mehdi SA. Epidemiology and survival
trends of lung carcinoids in the veteran population. J Clin Oncol. 2023;41:e21049.
doi:10.1200/JCO.2023.41.16_suppl.e21049 - Moghanaki D, Taylor J, Bryant AK, et al. Lung Cancer Survival Trends in the Veterans
Health Administration. Clin Lung Cancer. 2024;25(3):225-232. doi:10.1016/j.
cllc.2024.02.009 - Jalal SI, Guo A, Ahmed S, Kelley MJ. Analysis of actionable genetic alterations in
lung carcinoma from the VA National Precision Oncology Program. Semin Oncol.
2022;49(3-4):265-274. doi:10.1053/j.seminoncol.2022.06.014 - Cascone T, Awad MM, Spicer JD, et al; for the CheckMate 77T Investigators.
Perioperative Nivolumab in Resectable Lung Cancer. N Engl J Med.
2024;390(19):1756-1769. doi:10.1056/NEJMoa2311926 - Wakelee H, Liberman M, Kato T, et al; for the KEYNOTE-671 Investigators.
Perioperative Pembrolizumab for Early-Stage Non-Small-Cell Lung Cancer. N Engl J
Med. 2023;389(6):491-503. doi:10.1056/NEJMoa2302983 - Heymach JV, Harpole D, Mitsudomi T, et al; for the AEGEAN Investigators.
Perioperative Durvalumab for Resectable Non-Small-Cell Lung Cancer. N Engl J
Med. 2023;389(18):1672-1684. doi:10.1056/NEJMoa2304875 - Duncan FC, Al Nasrallah N, Nephew L, et al. Racial disparities in staging, treatment,
and mortality in non-small cell lung cancer. Transl Lung Cancer Res. 2024;13(1):76-
94. doi:10.21037/tlcr-23-407
Lung Cancer: Mortality Trends in Veterans and New Treatments
Lung Cancer: Mortality Trends in Veterans and New Treatments
Lung Cancer Screening Is the Push Smokers Need to Quit
Quitting smoking is challenging, particularly when resources are limited. A recent study in the United States confirmed that an intensive program combining behavioral therapy and medication, linked to a lung cancer screening program, offers the highest success rate. However, its long-term success was similar to that of telephone counseling and drug therapy.
Pulmonologist and experienced smoking cessation specialist from Stuttgart, Germany, Alexander Rupp, MD, emphasized the importance of leveraging routine healthcare interactions to encourage smoking cessation. “Although every doctor-patient contact offers the opportunity to discuss the risks of smoking and the opportunities for smoking cessation, the ‘window of opportunity’ is very wide, especially during lung cancer screening,” he said.
Germany is preparing to launch a lung cancer screening program for high-risk individuals, primarily current smokers and former smokers. Following the establishment of radiation protection regulations for such a program last year, the German Federal Joint Committee is currently working on its design. The initiative could be a game-changer for smoking cessation.
Lung cancer screening has been available for smokers in the United States for some time. Paul M. Cinciripini, PhD, and colleagues from the University of Texas MD Anderson Cancer Center, Houston, examined three smoking cessation strategies with decreasing treatment intensity among screening participants.
Unique Opportunity
Previous studies have shown that participation in a lung cancer screening program — typically offered only to high-risk individuals — significantly increases motivation to quit smoking.
“Repeated contact with doctors, repeated CT scans, and especially the findings that require monitoring all contribute to this effect,” explained Rupp, who regularly offers smoking cessation courses.
It has long been known how smoking cessation works best. “The gold standard is a combination of behavioral therapy support and drug treatment — if there is an addiction and withdrawal symptoms occur after quitting, which is the case for the majority of smokers,” Rupp explained.
The US study reinforced what is already well known: More intensive treatment approaches lead to higher quit rates.
“We know that the more intensively we look after smokers, the higher the quit rate. This applies in both areas: The more therapy sessions we do and the more often we prescribe medication, the more likely the patients are to succeed in remaining abstinent,” Rupp said.
However, resources for intensive smoking cessation programs are limited. A database maintained by the German Cancer Research Center and the German Federal Center for Health Education lists only 455 providers of smoking cessation courses in Germany, “not all of which even work on an evidence-based basis,” Rupp emphasized. Given that there are around 16 million smokers in Germany, there is an urgent need for smoking cessation programs that are less resource-intensive.
Intensity Variations
The US study compared three smoking cessation strategies of varying intensities, integrating behavioral counseling and medication.
Group 1: An integrated program with eight behavioral therapy sessions and 10-12 weeks of nicotine replacement therapy or medication (bupropion or varenicline).
Group 2: Lighter version of the integrated program. It consisted of four telephone consultations, written materials, online support, and 12 weeks of nicotine replacement therapy or medication prescribed by a radiologist.
Group 3: The least intensive approach, with 12 weeks of nicotine replacement therapy alone.
Each strategy was evaluated in 210 lung cancer screening participants aged 55-64 years who smoked an average of 15-20 cigarettes per day.
After 3 months, significantly more participants in the most intensive program (Group 1, 37.1%) had quit smoking than those in the other two groups (Group 2, 27.1%; Group 3, 25.2%).
But after 6 months, the difference between Groups 1 and 2 was not significant. The quit rates were as follows: Group 1, 32.4%; Group 2, 27.6%; and Group 3, 20.5%.
“It can be concluded from these results that the intensity of smoking cessation can be reduced to a certain extent as long as the combination of behavioral counseling and medication is given,” Rupp concluded.
Digital Solutions
Another new possibility, which was not examined in the US study, is digital health applications.
Smoke Free is a digital health application that provides behavioral therapy support for smoking cessation and is available in both German and English. Designed to replicate structured smoking cessation programs and offers an accessible alternative for individuals seeking to quit smoking.
Rupp emphasized the potential of digital tools like Smoke Free to expand access to effective smoking cessation strategies, particularly for those unable to attend in-person programs. While traditional cessation programs are limited in availability, digital apps can increase engagement in and adherence to smoking cessation efforts.
However, the biggest hurdle is smokers’ procrastination: “If you make smokers an offer, they usually do not take action afterward because they are caught in their ambivalence about whether they should quit or not.”
Policy Implications
This makes smoking cessation a mandatory component of lung cancer screening in the future. “It’s about cancer, and patients are really afraid of that,” Rupp advocated.
In a position paper, the German Respiratory Society, supported by multiple medical societies, has called for smoking cessation to be integrated into lung cancer screening protocols, with full coverage of counseling and medication by health insurance.
“Smoking cessation must be a mandatory component. If a participant in the lung cancer screening does not want this, then he or she must actively object,” stressed Rupp, lead author of the position paper. Also, the costs of smoking cessation, including those of withdrawal-inhibiting medication, must be fully covered by statutory health insurance, which has not been the case to date.
“That’s the only thing that makes sense. You can’t deny an addict access to proven treatments, especially when we know that a smoker who quits spontaneously without support has a relapse rate of 95%-97%, and the medication per se increases the quit rate by a factor of two or three,” Rupp concluded.
This story was translated and adapted from Medscape’s German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Quitting smoking is challenging, particularly when resources are limited. A recent study in the United States confirmed that an intensive program combining behavioral therapy and medication, linked to a lung cancer screening program, offers the highest success rate. However, its long-term success was similar to that of telephone counseling and drug therapy.
Pulmonologist and experienced smoking cessation specialist from Stuttgart, Germany, Alexander Rupp, MD, emphasized the importance of leveraging routine healthcare interactions to encourage smoking cessation. “Although every doctor-patient contact offers the opportunity to discuss the risks of smoking and the opportunities for smoking cessation, the ‘window of opportunity’ is very wide, especially during lung cancer screening,” he said.
Germany is preparing to launch a lung cancer screening program for high-risk individuals, primarily current smokers and former smokers. Following the establishment of radiation protection regulations for such a program last year, the German Federal Joint Committee is currently working on its design. The initiative could be a game-changer for smoking cessation.
Lung cancer screening has been available for smokers in the United States for some time. Paul M. Cinciripini, PhD, and colleagues from the University of Texas MD Anderson Cancer Center, Houston, examined three smoking cessation strategies with decreasing treatment intensity among screening participants.
Unique Opportunity
Previous studies have shown that participation in a lung cancer screening program — typically offered only to high-risk individuals — significantly increases motivation to quit smoking.
“Repeated contact with doctors, repeated CT scans, and especially the findings that require monitoring all contribute to this effect,” explained Rupp, who regularly offers smoking cessation courses.
It has long been known how smoking cessation works best. “The gold standard is a combination of behavioral therapy support and drug treatment — if there is an addiction and withdrawal symptoms occur after quitting, which is the case for the majority of smokers,” Rupp explained.
The US study reinforced what is already well known: More intensive treatment approaches lead to higher quit rates.
“We know that the more intensively we look after smokers, the higher the quit rate. This applies in both areas: The more therapy sessions we do and the more often we prescribe medication, the more likely the patients are to succeed in remaining abstinent,” Rupp said.
However, resources for intensive smoking cessation programs are limited. A database maintained by the German Cancer Research Center and the German Federal Center for Health Education lists only 455 providers of smoking cessation courses in Germany, “not all of which even work on an evidence-based basis,” Rupp emphasized. Given that there are around 16 million smokers in Germany, there is an urgent need for smoking cessation programs that are less resource-intensive.
Intensity Variations
The US study compared three smoking cessation strategies of varying intensities, integrating behavioral counseling and medication.
Group 1: An integrated program with eight behavioral therapy sessions and 10-12 weeks of nicotine replacement therapy or medication (bupropion or varenicline).
Group 2: Lighter version of the integrated program. It consisted of four telephone consultations, written materials, online support, and 12 weeks of nicotine replacement therapy or medication prescribed by a radiologist.
Group 3: The least intensive approach, with 12 weeks of nicotine replacement therapy alone.
Each strategy was evaluated in 210 lung cancer screening participants aged 55-64 years who smoked an average of 15-20 cigarettes per day.
After 3 months, significantly more participants in the most intensive program (Group 1, 37.1%) had quit smoking than those in the other two groups (Group 2, 27.1%; Group 3, 25.2%).
But after 6 months, the difference between Groups 1 and 2 was not significant. The quit rates were as follows: Group 1, 32.4%; Group 2, 27.6%; and Group 3, 20.5%.
“It can be concluded from these results that the intensity of smoking cessation can be reduced to a certain extent as long as the combination of behavioral counseling and medication is given,” Rupp concluded.
Digital Solutions
Another new possibility, which was not examined in the US study, is digital health applications.
Smoke Free is a digital health application that provides behavioral therapy support for smoking cessation and is available in both German and English. Designed to replicate structured smoking cessation programs and offers an accessible alternative for individuals seeking to quit smoking.
Rupp emphasized the potential of digital tools like Smoke Free to expand access to effective smoking cessation strategies, particularly for those unable to attend in-person programs. While traditional cessation programs are limited in availability, digital apps can increase engagement in and adherence to smoking cessation efforts.
However, the biggest hurdle is smokers’ procrastination: “If you make smokers an offer, they usually do not take action afterward because they are caught in their ambivalence about whether they should quit or not.”
Policy Implications
This makes smoking cessation a mandatory component of lung cancer screening in the future. “It’s about cancer, and patients are really afraid of that,” Rupp advocated.
In a position paper, the German Respiratory Society, supported by multiple medical societies, has called for smoking cessation to be integrated into lung cancer screening protocols, with full coverage of counseling and medication by health insurance.
“Smoking cessation must be a mandatory component. If a participant in the lung cancer screening does not want this, then he or she must actively object,” stressed Rupp, lead author of the position paper. Also, the costs of smoking cessation, including those of withdrawal-inhibiting medication, must be fully covered by statutory health insurance, which has not been the case to date.
“That’s the only thing that makes sense. You can’t deny an addict access to proven treatments, especially when we know that a smoker who quits spontaneously without support has a relapse rate of 95%-97%, and the medication per se increases the quit rate by a factor of two or three,” Rupp concluded.
This story was translated and adapted from Medscape’s German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Quitting smoking is challenging, particularly when resources are limited. A recent study in the United States confirmed that an intensive program combining behavioral therapy and medication, linked to a lung cancer screening program, offers the highest success rate. However, its long-term success was similar to that of telephone counseling and drug therapy.
Pulmonologist and experienced smoking cessation specialist from Stuttgart, Germany, Alexander Rupp, MD, emphasized the importance of leveraging routine healthcare interactions to encourage smoking cessation. “Although every doctor-patient contact offers the opportunity to discuss the risks of smoking and the opportunities for smoking cessation, the ‘window of opportunity’ is very wide, especially during lung cancer screening,” he said.
Germany is preparing to launch a lung cancer screening program for high-risk individuals, primarily current smokers and former smokers. Following the establishment of radiation protection regulations for such a program last year, the German Federal Joint Committee is currently working on its design. The initiative could be a game-changer for smoking cessation.
Lung cancer screening has been available for smokers in the United States for some time. Paul M. Cinciripini, PhD, and colleagues from the University of Texas MD Anderson Cancer Center, Houston, examined three smoking cessation strategies with decreasing treatment intensity among screening participants.
Unique Opportunity
Previous studies have shown that participation in a lung cancer screening program — typically offered only to high-risk individuals — significantly increases motivation to quit smoking.
“Repeated contact with doctors, repeated CT scans, and especially the findings that require monitoring all contribute to this effect,” explained Rupp, who regularly offers smoking cessation courses.
It has long been known how smoking cessation works best. “The gold standard is a combination of behavioral therapy support and drug treatment — if there is an addiction and withdrawal symptoms occur after quitting, which is the case for the majority of smokers,” Rupp explained.
The US study reinforced what is already well known: More intensive treatment approaches lead to higher quit rates.
“We know that the more intensively we look after smokers, the higher the quit rate. This applies in both areas: The more therapy sessions we do and the more often we prescribe medication, the more likely the patients are to succeed in remaining abstinent,” Rupp said.
However, resources for intensive smoking cessation programs are limited. A database maintained by the German Cancer Research Center and the German Federal Center for Health Education lists only 455 providers of smoking cessation courses in Germany, “not all of which even work on an evidence-based basis,” Rupp emphasized. Given that there are around 16 million smokers in Germany, there is an urgent need for smoking cessation programs that are less resource-intensive.
Intensity Variations
The US study compared three smoking cessation strategies of varying intensities, integrating behavioral counseling and medication.
Group 1: An integrated program with eight behavioral therapy sessions and 10-12 weeks of nicotine replacement therapy or medication (bupropion or varenicline).
Group 2: Lighter version of the integrated program. It consisted of four telephone consultations, written materials, online support, and 12 weeks of nicotine replacement therapy or medication prescribed by a radiologist.
Group 3: The least intensive approach, with 12 weeks of nicotine replacement therapy alone.
Each strategy was evaluated in 210 lung cancer screening participants aged 55-64 years who smoked an average of 15-20 cigarettes per day.
After 3 months, significantly more participants in the most intensive program (Group 1, 37.1%) had quit smoking than those in the other two groups (Group 2, 27.1%; Group 3, 25.2%).
But after 6 months, the difference between Groups 1 and 2 was not significant. The quit rates were as follows: Group 1, 32.4%; Group 2, 27.6%; and Group 3, 20.5%.
“It can be concluded from these results that the intensity of smoking cessation can be reduced to a certain extent as long as the combination of behavioral counseling and medication is given,” Rupp concluded.
Digital Solutions
Another new possibility, which was not examined in the US study, is digital health applications.
Smoke Free is a digital health application that provides behavioral therapy support for smoking cessation and is available in both German and English. Designed to replicate structured smoking cessation programs and offers an accessible alternative for individuals seeking to quit smoking.
Rupp emphasized the potential of digital tools like Smoke Free to expand access to effective smoking cessation strategies, particularly for those unable to attend in-person programs. While traditional cessation programs are limited in availability, digital apps can increase engagement in and adherence to smoking cessation efforts.
However, the biggest hurdle is smokers’ procrastination: “If you make smokers an offer, they usually do not take action afterward because they are caught in their ambivalence about whether they should quit or not.”
Policy Implications
This makes smoking cessation a mandatory component of lung cancer screening in the future. “It’s about cancer, and patients are really afraid of that,” Rupp advocated.
In a position paper, the German Respiratory Society, supported by multiple medical societies, has called for smoking cessation to be integrated into lung cancer screening protocols, with full coverage of counseling and medication by health insurance.
“Smoking cessation must be a mandatory component. If a participant in the lung cancer screening does not want this, then he or she must actively object,” stressed Rupp, lead author of the position paper. Also, the costs of smoking cessation, including those of withdrawal-inhibiting medication, must be fully covered by statutory health insurance, which has not been the case to date.
“That’s the only thing that makes sense. You can’t deny an addict access to proven treatments, especially when we know that a smoker who quits spontaneously without support has a relapse rate of 95%-97%, and the medication per se increases the quit rate by a factor of two or three,” Rupp concluded.
This story was translated and adapted from Medscape’s German edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
MRI-Invisible Prostate Lesions: Are They Dangerous?
MRI-invisible prostate lesions. It sounds like the stuff of science fiction and fantasy, a creation from the minds of H.G. Wells, who wrote The Invisible Man, or J.K. Rowling, who authored the Harry Potter series.
But MRI-invisible prostate lesions are real. And what these lesions may, or may not, indicate is the subject of intense debate.
MRI plays an increasingly important role in detecting and diagnosing prostate cancer, staging prostate cancer as well as monitoring disease progression. However, on occasion, a puzzling phenomenon arises. Certain prostate lesions that appear when pathologists examine biopsied tissue samples under a microscope are not visible on MRI. The prostate tissue will, instead, appear normal to a radiologist’s eye.
Some experts believe these MRI-invisible lesions are nothing to worry about.
If the clinician can’t see the cancer on MRI, then it simply isn’t a threat, according to Mark Emberton, MD, a pioneer in prostate MRIs and director of interventional oncology at University College London, England.
Laurence Klotz, MD, of the University of Toronto, Ontario, Canada, agreed, noting that “invisible cancers are clinically insignificant and don’t require systematic biopsies.”
Emberton and Klotz compared MRI-invisible lesions to grade group 1 prostate cancer (Gleason score ≤ 6) — the least aggressive category that indicates the cancer that is not likely to spread or kill. For patients on active surveillance, those with MRI-invisible cancers do drastically better than those with visible cancers, Klotz explained.
But other experts in the field are skeptical that MRI-invisible lesions are truly innocuous.
Although statistically an MRI-visible prostate lesion indicates a more aggressive tumor, that is not always the case for every individual, said Brian Helfand, MD, PhD, chief of urology at NorthShore University Health System, Evanston, Illinois.
MRIs can lead to false negatives in about 10%-20% of patients who have clinically significant prostate cancer, though estimates vary.
In one analysis, 16% of men with no suspicious lesions on MRI had clinically significant prostate cancer identified after undergoing a systematic biopsy. Another analysis found that about 35% of MRI-invisible prostate cancers identified via biopsy were clinically significant.
Other studies, however, have indicated that negative MRI results accurately indicate patients at low risk of developing clinically significant cancers. A recent JAMA Oncology analysis, for instance, found that only seven of 233 men (3%) with negative MRI results at baseline who completed 3 years of monitoring were diagnosed with clinically significant prostate cancer.
When a patient has an MRI-invisible prostate tumor, there are a couple of reasons the MRI may not be picking it up, said urologic oncologist Alexander Putnam Cole, MD, assistant professor of surgery, Harvard Medical School, Boston, Massachusetts. “One is that the cancer is aggressive but just very small,” said Cole.
“Another possibility is that the cancer looks very similar to background prostate tissue, which is something that you might expect if you think about more of a low-grade cancer,” he explained.
The experience level of the radiologist interpreting the MRI can also play into the accuracy of the reading.
But Cole agreed that “in general, MRI visibility is associated with molecular and histologic features of progression and aggressiveness and non-visible cancers are less likely to have aggressive features.”
The genomic profiles of MRI-visible and -invisible cancers bear this out.
According to Todd Morgan, MD, chief of urologic oncology at Michigan Medicine, University of Michigan, Ann Arbor, the gene expression in visible disease tends to be linked to more aggressive prostate tumors whereas gene expression in invisible disease does not.
In one analysis, for instance, researchers found that four genes — PHYHD1, CENPF, ALDH2, and GDF15 — associated with worse progression-free survival and metastasis-free survival in prostate cancer also predicted MRI visibility.
“Genes that are associated with visibility are essentially the same genes that are associated with aggressive cancers,” Klotz said.
Next Steps After Negative MRI Result
What do MRI-invisible lesions mean for patient care? If, for instance, a patient has elevated PSA levels but a normal MRI, is a targeted or systematic biopsy warranted?
The overarching message, according to Klotz, is that “you don’t need to find them.” Klotz noted, however, that patients with a negative MRI result should still be followed with periodic repeat imaging.
Several trials support this approach of using MRI to decide who needs a biopsy and delaying a biopsy in men with normal MRIs.
The recent JAMA Oncology analysis found that, among men with negative MRI results, 86% avoided a biopsy over 3 years, with clinically significant prostate cancer detected in only 4% of men across the study period — four in the initial diagnostic phase and seven in the 3-year monitoring phase. However, during the initial diagnostic phase, more than half the men with positive MRI findings had clinically significant prostate cancer detected.
Another recent study found that patients with negative MRI results were much less likely to upgrade to higher Gleason scores over time. Among 522 patients who underwent a systematic and targeted biopsy within 18 months of their grade group 1 designation, 9.2% with negative MRI findings had tumors reclassified as grade group 2 or higher vs 27% with positive MRI findings, and 2.3% with negative MRI findings had tumors reclassified as grade group 3 or higher vs 7.8% with positive MRI findings.
These data suggest that men with grade group 1 cancer and negative MRI result “may be able to avoid confirmatory biopsies until a routine surveillance biopsy in 2-3 years,” according to study author Christian Pavlovich, MD, professor of urologic oncology at the Johns Hopkins University School of Medicine, Baltimore.
Cole used MRI findings to triage who gets a biopsy. When a biopsy is warranted, “I usually recommend adding in some systematic sampling of the other side to assess for nonvisible cancers,” he noted.
Sampling prostate tissue outside the target area “adds maybe 1-2 minutes to the procedure and doesn’t drastically increase the morbidity or risks,” Cole said. It also can help “confirm there is cancer in the MRI target and also confirm there is no cancer in the nonvisible areas.”
According to Klotz, if imaging demonstrates progression, patients should receive a biopsy — in most cases, a targeted biopsy only. And, Klotz noted, skipping routine prostate biopsies in men with negative MRI results can save thousands of men from these procedures, which carry risks for infections and sepsis.
Looking beyond Gleason scores for risk prediction, MRI “visibility is a very powerful risk stratifier,” he said.
A version of this article appeared on Medscape.com.
MRI-invisible prostate lesions. It sounds like the stuff of science fiction and fantasy, a creation from the minds of H.G. Wells, who wrote The Invisible Man, or J.K. Rowling, who authored the Harry Potter series.
But MRI-invisible prostate lesions are real. And what these lesions may, or may not, indicate is the subject of intense debate.
MRI plays an increasingly important role in detecting and diagnosing prostate cancer, staging prostate cancer as well as monitoring disease progression. However, on occasion, a puzzling phenomenon arises. Certain prostate lesions that appear when pathologists examine biopsied tissue samples under a microscope are not visible on MRI. The prostate tissue will, instead, appear normal to a radiologist’s eye.
Some experts believe these MRI-invisible lesions are nothing to worry about.
If the clinician can’t see the cancer on MRI, then it simply isn’t a threat, according to Mark Emberton, MD, a pioneer in prostate MRIs and director of interventional oncology at University College London, England.
Laurence Klotz, MD, of the University of Toronto, Ontario, Canada, agreed, noting that “invisible cancers are clinically insignificant and don’t require systematic biopsies.”
Emberton and Klotz compared MRI-invisible lesions to grade group 1 prostate cancer (Gleason score ≤ 6) — the least aggressive category that indicates the cancer that is not likely to spread or kill. For patients on active surveillance, those with MRI-invisible cancers do drastically better than those with visible cancers, Klotz explained.
But other experts in the field are skeptical that MRI-invisible lesions are truly innocuous.
Although statistically an MRI-visible prostate lesion indicates a more aggressive tumor, that is not always the case for every individual, said Brian Helfand, MD, PhD, chief of urology at NorthShore University Health System, Evanston, Illinois.
MRIs can lead to false negatives in about 10%-20% of patients who have clinically significant prostate cancer, though estimates vary.
In one analysis, 16% of men with no suspicious lesions on MRI had clinically significant prostate cancer identified after undergoing a systematic biopsy. Another analysis found that about 35% of MRI-invisible prostate cancers identified via biopsy were clinically significant.
Other studies, however, have indicated that negative MRI results accurately indicate patients at low risk of developing clinically significant cancers. A recent JAMA Oncology analysis, for instance, found that only seven of 233 men (3%) with negative MRI results at baseline who completed 3 years of monitoring were diagnosed with clinically significant prostate cancer.
When a patient has an MRI-invisible prostate tumor, there are a couple of reasons the MRI may not be picking it up, said urologic oncologist Alexander Putnam Cole, MD, assistant professor of surgery, Harvard Medical School, Boston, Massachusetts. “One is that the cancer is aggressive but just very small,” said Cole.
“Another possibility is that the cancer looks very similar to background prostate tissue, which is something that you might expect if you think about more of a low-grade cancer,” he explained.
The experience level of the radiologist interpreting the MRI can also play into the accuracy of the reading.
But Cole agreed that “in general, MRI visibility is associated with molecular and histologic features of progression and aggressiveness and non-visible cancers are less likely to have aggressive features.”
The genomic profiles of MRI-visible and -invisible cancers bear this out.
According to Todd Morgan, MD, chief of urologic oncology at Michigan Medicine, University of Michigan, Ann Arbor, the gene expression in visible disease tends to be linked to more aggressive prostate tumors whereas gene expression in invisible disease does not.
In one analysis, for instance, researchers found that four genes — PHYHD1, CENPF, ALDH2, and GDF15 — associated with worse progression-free survival and metastasis-free survival in prostate cancer also predicted MRI visibility.
“Genes that are associated with visibility are essentially the same genes that are associated with aggressive cancers,” Klotz said.
Next Steps After Negative MRI Result
What do MRI-invisible lesions mean for patient care? If, for instance, a patient has elevated PSA levels but a normal MRI, is a targeted or systematic biopsy warranted?
The overarching message, according to Klotz, is that “you don’t need to find them.” Klotz noted, however, that patients with a negative MRI result should still be followed with periodic repeat imaging.
Several trials support this approach of using MRI to decide who needs a biopsy and delaying a biopsy in men with normal MRIs.
The recent JAMA Oncology analysis found that, among men with negative MRI results, 86% avoided a biopsy over 3 years, with clinically significant prostate cancer detected in only 4% of men across the study period — four in the initial diagnostic phase and seven in the 3-year monitoring phase. However, during the initial diagnostic phase, more than half the men with positive MRI findings had clinically significant prostate cancer detected.
Another recent study found that patients with negative MRI results were much less likely to upgrade to higher Gleason scores over time. Among 522 patients who underwent a systematic and targeted biopsy within 18 months of their grade group 1 designation, 9.2% with negative MRI findings had tumors reclassified as grade group 2 or higher vs 27% with positive MRI findings, and 2.3% with negative MRI findings had tumors reclassified as grade group 3 or higher vs 7.8% with positive MRI findings.
These data suggest that men with grade group 1 cancer and negative MRI result “may be able to avoid confirmatory biopsies until a routine surveillance biopsy in 2-3 years,” according to study author Christian Pavlovich, MD, professor of urologic oncology at the Johns Hopkins University School of Medicine, Baltimore.
Cole used MRI findings to triage who gets a biopsy. When a biopsy is warranted, “I usually recommend adding in some systematic sampling of the other side to assess for nonvisible cancers,” he noted.
Sampling prostate tissue outside the target area “adds maybe 1-2 minutes to the procedure and doesn’t drastically increase the morbidity or risks,” Cole said. It also can help “confirm there is cancer in the MRI target and also confirm there is no cancer in the nonvisible areas.”
According to Klotz, if imaging demonstrates progression, patients should receive a biopsy — in most cases, a targeted biopsy only. And, Klotz noted, skipping routine prostate biopsies in men with negative MRI results can save thousands of men from these procedures, which carry risks for infections and sepsis.
Looking beyond Gleason scores for risk prediction, MRI “visibility is a very powerful risk stratifier,” he said.
A version of this article appeared on Medscape.com.
MRI-invisible prostate lesions. It sounds like the stuff of science fiction and fantasy, a creation from the minds of H.G. Wells, who wrote The Invisible Man, or J.K. Rowling, who authored the Harry Potter series.
But MRI-invisible prostate lesions are real. And what these lesions may, or may not, indicate is the subject of intense debate.
MRI plays an increasingly important role in detecting and diagnosing prostate cancer, staging prostate cancer as well as monitoring disease progression. However, on occasion, a puzzling phenomenon arises. Certain prostate lesions that appear when pathologists examine biopsied tissue samples under a microscope are not visible on MRI. The prostate tissue will, instead, appear normal to a radiologist’s eye.
Some experts believe these MRI-invisible lesions are nothing to worry about.
If the clinician can’t see the cancer on MRI, then it simply isn’t a threat, according to Mark Emberton, MD, a pioneer in prostate MRIs and director of interventional oncology at University College London, England.
Laurence Klotz, MD, of the University of Toronto, Ontario, Canada, agreed, noting that “invisible cancers are clinically insignificant and don’t require systematic biopsies.”
Emberton and Klotz compared MRI-invisible lesions to grade group 1 prostate cancer (Gleason score ≤ 6) — the least aggressive category that indicates the cancer that is not likely to spread or kill. For patients on active surveillance, those with MRI-invisible cancers do drastically better than those with visible cancers, Klotz explained.
But other experts in the field are skeptical that MRI-invisible lesions are truly innocuous.
Although statistically an MRI-visible prostate lesion indicates a more aggressive tumor, that is not always the case for every individual, said Brian Helfand, MD, PhD, chief of urology at NorthShore University Health System, Evanston, Illinois.
MRIs can lead to false negatives in about 10%-20% of patients who have clinically significant prostate cancer, though estimates vary.
In one analysis, 16% of men with no suspicious lesions on MRI had clinically significant prostate cancer identified after undergoing a systematic biopsy. Another analysis found that about 35% of MRI-invisible prostate cancers identified via biopsy were clinically significant.
Other studies, however, have indicated that negative MRI results accurately indicate patients at low risk of developing clinically significant cancers. A recent JAMA Oncology analysis, for instance, found that only seven of 233 men (3%) with negative MRI results at baseline who completed 3 years of monitoring were diagnosed with clinically significant prostate cancer.
When a patient has an MRI-invisible prostate tumor, there are a couple of reasons the MRI may not be picking it up, said urologic oncologist Alexander Putnam Cole, MD, assistant professor of surgery, Harvard Medical School, Boston, Massachusetts. “One is that the cancer is aggressive but just very small,” said Cole.
“Another possibility is that the cancer looks very similar to background prostate tissue, which is something that you might expect if you think about more of a low-grade cancer,” he explained.
The experience level of the radiologist interpreting the MRI can also play into the accuracy of the reading.
But Cole agreed that “in general, MRI visibility is associated with molecular and histologic features of progression and aggressiveness and non-visible cancers are less likely to have aggressive features.”
The genomic profiles of MRI-visible and -invisible cancers bear this out.
According to Todd Morgan, MD, chief of urologic oncology at Michigan Medicine, University of Michigan, Ann Arbor, the gene expression in visible disease tends to be linked to more aggressive prostate tumors whereas gene expression in invisible disease does not.
In one analysis, for instance, researchers found that four genes — PHYHD1, CENPF, ALDH2, and GDF15 — associated with worse progression-free survival and metastasis-free survival in prostate cancer also predicted MRI visibility.
“Genes that are associated with visibility are essentially the same genes that are associated with aggressive cancers,” Klotz said.
Next Steps After Negative MRI Result
What do MRI-invisible lesions mean for patient care? If, for instance, a patient has elevated PSA levels but a normal MRI, is a targeted or systematic biopsy warranted?
The overarching message, according to Klotz, is that “you don’t need to find them.” Klotz noted, however, that patients with a negative MRI result should still be followed with periodic repeat imaging.
Several trials support this approach of using MRI to decide who needs a biopsy and delaying a biopsy in men with normal MRIs.
The recent JAMA Oncology analysis found that, among men with negative MRI results, 86% avoided a biopsy over 3 years, with clinically significant prostate cancer detected in only 4% of men across the study period — four in the initial diagnostic phase and seven in the 3-year monitoring phase. However, during the initial diagnostic phase, more than half the men with positive MRI findings had clinically significant prostate cancer detected.
Another recent study found that patients with negative MRI results were much less likely to upgrade to higher Gleason scores over time. Among 522 patients who underwent a systematic and targeted biopsy within 18 months of their grade group 1 designation, 9.2% with negative MRI findings had tumors reclassified as grade group 2 or higher vs 27% with positive MRI findings, and 2.3% with negative MRI findings had tumors reclassified as grade group 3 or higher vs 7.8% with positive MRI findings.
These data suggest that men with grade group 1 cancer and negative MRI result “may be able to avoid confirmatory biopsies until a routine surveillance biopsy in 2-3 years,” according to study author Christian Pavlovich, MD, professor of urologic oncology at the Johns Hopkins University School of Medicine, Baltimore.
Cole used MRI findings to triage who gets a biopsy. When a biopsy is warranted, “I usually recommend adding in some systematic sampling of the other side to assess for nonvisible cancers,” he noted.
Sampling prostate tissue outside the target area “adds maybe 1-2 minutes to the procedure and doesn’t drastically increase the morbidity or risks,” Cole said. It also can help “confirm there is cancer in the MRI target and also confirm there is no cancer in the nonvisible areas.”
According to Klotz, if imaging demonstrates progression, patients should receive a biopsy — in most cases, a targeted biopsy only. And, Klotz noted, skipping routine prostate biopsies in men with negative MRI results can save thousands of men from these procedures, which carry risks for infections and sepsis.
Looking beyond Gleason scores for risk prediction, MRI “visibility is a very powerful risk stratifier,” he said.
A version of this article appeared on Medscape.com.
The Evidence Gap: Immunotherapy Timing in Early-Stage NSCLC?
Since October 2023, the US Food and Drug Administration (FDA) has approved three checkpoint inhibitors — pembrolizumab (Keytruda), durvalumab (Imfinzi), and most recently nivolumab (Opdivo) — alongside platinum-containing chemotherapy before surgery and as monotherapy after surgery to treat resectable NSCLC.
But the trials leading to each approval had a major design flaw. The studies failed to distinguish when patients with resectable NSCLC benefited from immunotherapy — before surgery, after surgery, or at both points.
That missing piece has left oncologists without definitive guidance on how best to treat their patients with resectable disease.
Jamie E. Chaft, MD, a thoracic medical oncologist and attending physician at Memorial Sloan Kettering Cancer Center in New York City, was “surprised” that the FDA had approved the three immunotherapy combination regimens without this clarity. Clinicians are now left with studies that can’t evaluate the contribution of the neoadjuvant and adjuvant phases, she said.
But that may soon change.
In July, an FDA advisory committee met to discuss the pending approval of durvalumab.
During this July meeting, the FDA’s Oncologic Drugs Advisory Committee (ODAC) called out issues with AstraZeneca’s design of the trial, expressing concern that AstraZeneca had not followed the agency’s advice to compare patient outcomes with durvalumab in the neoadjuvant and adjuvant phases.
The ODAC panel ultimately voted unanimously in favor of requiring drug companies to demonstrate that patients need immunotherapy both before and after surgery in resectable NSCLC. Several panelists said this requirement should extend beyond NSCLC to other tumor types.
“We need to understand who needs what therapy when,” Daniel Spratt, MD, chairman of the FDA’s ODAC, told Medscape Medical News.
But even if the FDA does require drug companies to assess the benefit of immunotherapy pre- and post-surgery, will oncologists get the answers they need for their patients with resectable NSCLC? Or will the new costly trial design requirements dead-end progress in this space?
Treating Patients Without Clear Evidence
Despite the ODAC’s strong urging to require — not simply request — that drug companies show patients with resectable NSCLC benefit from immunotherapy in both the neoadjuvant and adjuvant settings, the advisory panel did not think durvalumab’s approval should be delayed until the neoadjuvant vs adjuvant question is answered.
A month later, in August, the FDA approved durvalumab for this indication.
Pembrolizumab (Keytruda, Merck) had already been approved 10 months earlier in the neoadjuvant and adjuvant settings in this setting. And most recently, in October, the FDA added nivolumab (Opdivo, Bristol Myers Squibb) to these approvals.
No trial, however, identified when patients benefited from the drug.
Without this understanding, patients may be taking immunotherapy unnecessarily, at significant expense and toxicity risk.
“Toxicities from immunotherapy can occur at any time after initiation,” said Joshua Eric Reuss, MD, a thoracic medical oncologist at Georgetown University’s Lombardi Comprehensive Cancer Center in Washington, DC. And these “risks definitely continue into the adjuvant period.”
So far, the available evidence does suggest that the neoadjuvant phase of immunotherapy confers the greatest benefit, while adjuvant immunotherapy — which can last a year or longer — may expose patients to more costs and toxicities, with no clear benefit.
A 2024 meta-analysis, which included four trials of neoadjuvant-adjuvant immunotherapy and one trial of neoadjuvant immunotherapy in resectable NSCLC, suggested that the addition of adjuvant immunotherapy did not improve event-free survival (hazard ratio [HR], 0.90; P = .59) or overall survival (HR, 1.18; P = .51) compared with neoadjuvant immunotherapy alone.
According to Spratt, “It’s very clear that the neoadjuvant phase is the more important of the two phases.” Given that, “we’re probably overtreating some patients,” said Spratt, also chairman of Radiation Oncology at University Hospitals Seidman Cancer Center and Case Western Reserve University in Cleveland.
Chaft agreed that “there’s very little data that we need the postoperative phase, and what data we do have is post hoc and limited.”
This evidence gap “has created considerable dilemmas” for oncologists and patients who are faced with “the challenge of deciding which therapeutic options or approach are best suited for each individual,” experts wrote in recent consensus recommendations from the International Association for the Study of Lung Cancer.
Clinicians may ultimately be left to make decisions about prescribing postoperative immunotherapy based on their experience and comfort level.
When Chaft’s patients have a pathologic complete response with immunotherapy and chemotherapy in the neoadjuvant phase, “I’m comfortable stopping because the data would suggest they’re almost certainly cured,” she said.
For patients who have viable disease after neoadjuvant therapy, continuing an immunotherapy postoperatively when it didn’t work preoperatively “is not going to make a difference,” Chaft explained. In these cases, Chaft would look to enroll them in a clinical trial evaluating a different regimen because of the risk for relapse.
With patients who did well preoperatively but still have tumor left at the time of surgery, she would discuss continuing the immunotherapy or participating in a trial, she said.
All the FDA-approved regimens are covered by insurance, said Chaft. Clinicians are most comfortable with pembrolizumab because it is the most widely used immunotherapy in advanced NSCLC, she said. But, she added, “there’s really no strong differentiating data between any of the studies; all the results look very comparable.”
When assessing whether a patient may benefit from immunotherapy after surgery, Reuss looks at a range of factors, including disease stage, histology, gene mutations, and pathologic response. Reuss also weighs patient preferences. A patient coming from another country might only want a neoadjuvant regimen, for instance, he said.
That “isn’t exactly the kind of the level one evidence that one likes to see when making treatment decisions,” said Reuss. “Without prospective data, all we can do is cross-trial comparisons and assessment of subgroups.”
If a new regimen comes along that improves outcomes or decision-making, “I think we would pivot to that in a heartbeat,” he said.
But Will FDA Follow ODAC’s Recommendation?
“ODAC has made their point clear,” said Chaft. “Our patients deserve to know that whatever added risk and cost they’re incurring is merited by a clinical outcome.”
Despite the ODAC’s recommendation, it’s not guaranteed that the FDA will follow it.
An FDA spokesperson did not confirm the agency’s decision on the matter but noted that the FDA is “incorporating the panel’s advice.”
Spratt thinks that, going forward, companies will be held to “a higher bar,” but it’s unclear what that bar will look like.
“Whether this is a mandate or a strong recommendation, I think industry is definitely paying attention,” Spratt said. Companies that do not follow the guidance may risk not having their drug approved, “unless it’s just an absolute huge slam dunk of a major benefit to patients.”
In fact, according to Chaft, drug makers seeking approvals of novel entities in this space “won’t have a choice” but to follow any new trial design requirements from the FDA.
Still, getting answers may be a challenge.
Drug companies with immunotherapies already on the market are unlikely to invest the resources to conduct trials comparing the neoadjuvant and adjuvant settings, said Chaft. “It will take too long and cost too much,” she said.
And it remains unclear whether drug companies will decide to stop pursuing novel agents if approvals will ultimately require more expensive and time-consuming trials.
According to Chaft, oncologists have been discussing protocols that could help fill the knowledge gaps. Such trials will be conducted by the National Cancer Institute’s Cooperative Groups, she noted. But it’s early days.
For the time being, with comparative data from phase 3 trials years away, oncologists will have to work with the limited evidence and individual patients in front of them.
Chaft disclosed ties with AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, Genentech/Roche, Guardant Health, Janssen Pharmaceuticals, Eli Lilly, and Merck. Reuss disclosed ties with AstraZeneca, Arcus, AbbVie, Bristol Myers Squibb, CatalYm, Daiichi Sankyo, and Eli Lilly, and that Georgetown has received research funding from Genentech/Roche, Verastem, Nuvalent, LUNGevity Foundation, Exelixis, Arcus, and Revolution Medicines. Spratt disclosed ties with Astellas, AstraZeneca, Bayer, Boston Scientific, Janssen Pharmaceuticals, Novartis, and Pfizer.
A version of this article appeared on Medscape.com.
Since October 2023, the US Food and Drug Administration (FDA) has approved three checkpoint inhibitors — pembrolizumab (Keytruda), durvalumab (Imfinzi), and most recently nivolumab (Opdivo) — alongside platinum-containing chemotherapy before surgery and as monotherapy after surgery to treat resectable NSCLC.
But the trials leading to each approval had a major design flaw. The studies failed to distinguish when patients with resectable NSCLC benefited from immunotherapy — before surgery, after surgery, or at both points.
That missing piece has left oncologists without definitive guidance on how best to treat their patients with resectable disease.
Jamie E. Chaft, MD, a thoracic medical oncologist and attending physician at Memorial Sloan Kettering Cancer Center in New York City, was “surprised” that the FDA had approved the three immunotherapy combination regimens without this clarity. Clinicians are now left with studies that can’t evaluate the contribution of the neoadjuvant and adjuvant phases, she said.
But that may soon change.
In July, an FDA advisory committee met to discuss the pending approval of durvalumab.
During this July meeting, the FDA’s Oncologic Drugs Advisory Committee (ODAC) called out issues with AstraZeneca’s design of the trial, expressing concern that AstraZeneca had not followed the agency’s advice to compare patient outcomes with durvalumab in the neoadjuvant and adjuvant phases.
The ODAC panel ultimately voted unanimously in favor of requiring drug companies to demonstrate that patients need immunotherapy both before and after surgery in resectable NSCLC. Several panelists said this requirement should extend beyond NSCLC to other tumor types.
“We need to understand who needs what therapy when,” Daniel Spratt, MD, chairman of the FDA’s ODAC, told Medscape Medical News.
But even if the FDA does require drug companies to assess the benefit of immunotherapy pre- and post-surgery, will oncologists get the answers they need for their patients with resectable NSCLC? Or will the new costly trial design requirements dead-end progress in this space?
Treating Patients Without Clear Evidence
Despite the ODAC’s strong urging to require — not simply request — that drug companies show patients with resectable NSCLC benefit from immunotherapy in both the neoadjuvant and adjuvant settings, the advisory panel did not think durvalumab’s approval should be delayed until the neoadjuvant vs adjuvant question is answered.
A month later, in August, the FDA approved durvalumab for this indication.
Pembrolizumab (Keytruda, Merck) had already been approved 10 months earlier in the neoadjuvant and adjuvant settings in this setting. And most recently, in October, the FDA added nivolumab (Opdivo, Bristol Myers Squibb) to these approvals.
No trial, however, identified when patients benefited from the drug.
Without this understanding, patients may be taking immunotherapy unnecessarily, at significant expense and toxicity risk.
“Toxicities from immunotherapy can occur at any time after initiation,” said Joshua Eric Reuss, MD, a thoracic medical oncologist at Georgetown University’s Lombardi Comprehensive Cancer Center in Washington, DC. And these “risks definitely continue into the adjuvant period.”
So far, the available evidence does suggest that the neoadjuvant phase of immunotherapy confers the greatest benefit, while adjuvant immunotherapy — which can last a year or longer — may expose patients to more costs and toxicities, with no clear benefit.
A 2024 meta-analysis, which included four trials of neoadjuvant-adjuvant immunotherapy and one trial of neoadjuvant immunotherapy in resectable NSCLC, suggested that the addition of adjuvant immunotherapy did not improve event-free survival (hazard ratio [HR], 0.90; P = .59) or overall survival (HR, 1.18; P = .51) compared with neoadjuvant immunotherapy alone.
According to Spratt, “It’s very clear that the neoadjuvant phase is the more important of the two phases.” Given that, “we’re probably overtreating some patients,” said Spratt, also chairman of Radiation Oncology at University Hospitals Seidman Cancer Center and Case Western Reserve University in Cleveland.
Chaft agreed that “there’s very little data that we need the postoperative phase, and what data we do have is post hoc and limited.”
This evidence gap “has created considerable dilemmas” for oncologists and patients who are faced with “the challenge of deciding which therapeutic options or approach are best suited for each individual,” experts wrote in recent consensus recommendations from the International Association for the Study of Lung Cancer.
Clinicians may ultimately be left to make decisions about prescribing postoperative immunotherapy based on their experience and comfort level.
When Chaft’s patients have a pathologic complete response with immunotherapy and chemotherapy in the neoadjuvant phase, “I’m comfortable stopping because the data would suggest they’re almost certainly cured,” she said.
For patients who have viable disease after neoadjuvant therapy, continuing an immunotherapy postoperatively when it didn’t work preoperatively “is not going to make a difference,” Chaft explained. In these cases, Chaft would look to enroll them in a clinical trial evaluating a different regimen because of the risk for relapse.
With patients who did well preoperatively but still have tumor left at the time of surgery, she would discuss continuing the immunotherapy or participating in a trial, she said.
All the FDA-approved regimens are covered by insurance, said Chaft. Clinicians are most comfortable with pembrolizumab because it is the most widely used immunotherapy in advanced NSCLC, she said. But, she added, “there’s really no strong differentiating data between any of the studies; all the results look very comparable.”
When assessing whether a patient may benefit from immunotherapy after surgery, Reuss looks at a range of factors, including disease stage, histology, gene mutations, and pathologic response. Reuss also weighs patient preferences. A patient coming from another country might only want a neoadjuvant regimen, for instance, he said.
That “isn’t exactly the kind of the level one evidence that one likes to see when making treatment decisions,” said Reuss. “Without prospective data, all we can do is cross-trial comparisons and assessment of subgroups.”
If a new regimen comes along that improves outcomes or decision-making, “I think we would pivot to that in a heartbeat,” he said.
But Will FDA Follow ODAC’s Recommendation?
“ODAC has made their point clear,” said Chaft. “Our patients deserve to know that whatever added risk and cost they’re incurring is merited by a clinical outcome.”
Despite the ODAC’s recommendation, it’s not guaranteed that the FDA will follow it.
An FDA spokesperson did not confirm the agency’s decision on the matter but noted that the FDA is “incorporating the panel’s advice.”
Spratt thinks that, going forward, companies will be held to “a higher bar,” but it’s unclear what that bar will look like.
“Whether this is a mandate or a strong recommendation, I think industry is definitely paying attention,” Spratt said. Companies that do not follow the guidance may risk not having their drug approved, “unless it’s just an absolute huge slam dunk of a major benefit to patients.”
In fact, according to Chaft, drug makers seeking approvals of novel entities in this space “won’t have a choice” but to follow any new trial design requirements from the FDA.
Still, getting answers may be a challenge.
Drug companies with immunotherapies already on the market are unlikely to invest the resources to conduct trials comparing the neoadjuvant and adjuvant settings, said Chaft. “It will take too long and cost too much,” she said.
And it remains unclear whether drug companies will decide to stop pursuing novel agents if approvals will ultimately require more expensive and time-consuming trials.
According to Chaft, oncologists have been discussing protocols that could help fill the knowledge gaps. Such trials will be conducted by the National Cancer Institute’s Cooperative Groups, she noted. But it’s early days.
For the time being, with comparative data from phase 3 trials years away, oncologists will have to work with the limited evidence and individual patients in front of them.
Chaft disclosed ties with AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, Genentech/Roche, Guardant Health, Janssen Pharmaceuticals, Eli Lilly, and Merck. Reuss disclosed ties with AstraZeneca, Arcus, AbbVie, Bristol Myers Squibb, CatalYm, Daiichi Sankyo, and Eli Lilly, and that Georgetown has received research funding from Genentech/Roche, Verastem, Nuvalent, LUNGevity Foundation, Exelixis, Arcus, and Revolution Medicines. Spratt disclosed ties with Astellas, AstraZeneca, Bayer, Boston Scientific, Janssen Pharmaceuticals, Novartis, and Pfizer.
A version of this article appeared on Medscape.com.
Since October 2023, the US Food and Drug Administration (FDA) has approved three checkpoint inhibitors — pembrolizumab (Keytruda), durvalumab (Imfinzi), and most recently nivolumab (Opdivo) — alongside platinum-containing chemotherapy before surgery and as monotherapy after surgery to treat resectable NSCLC.
But the trials leading to each approval had a major design flaw. The studies failed to distinguish when patients with resectable NSCLC benefited from immunotherapy — before surgery, after surgery, or at both points.
That missing piece has left oncologists without definitive guidance on how best to treat their patients with resectable disease.
Jamie E. Chaft, MD, a thoracic medical oncologist and attending physician at Memorial Sloan Kettering Cancer Center in New York City, was “surprised” that the FDA had approved the three immunotherapy combination regimens without this clarity. Clinicians are now left with studies that can’t evaluate the contribution of the neoadjuvant and adjuvant phases, she said.
But that may soon change.
In July, an FDA advisory committee met to discuss the pending approval of durvalumab.
During this July meeting, the FDA’s Oncologic Drugs Advisory Committee (ODAC) called out issues with AstraZeneca’s design of the trial, expressing concern that AstraZeneca had not followed the agency’s advice to compare patient outcomes with durvalumab in the neoadjuvant and adjuvant phases.
The ODAC panel ultimately voted unanimously in favor of requiring drug companies to demonstrate that patients need immunotherapy both before and after surgery in resectable NSCLC. Several panelists said this requirement should extend beyond NSCLC to other tumor types.
“We need to understand who needs what therapy when,” Daniel Spratt, MD, chairman of the FDA’s ODAC, told Medscape Medical News.
But even if the FDA does require drug companies to assess the benefit of immunotherapy pre- and post-surgery, will oncologists get the answers they need for their patients with resectable NSCLC? Or will the new costly trial design requirements dead-end progress in this space?
Treating Patients Without Clear Evidence
Despite the ODAC’s strong urging to require — not simply request — that drug companies show patients with resectable NSCLC benefit from immunotherapy in both the neoadjuvant and adjuvant settings, the advisory panel did not think durvalumab’s approval should be delayed until the neoadjuvant vs adjuvant question is answered.
A month later, in August, the FDA approved durvalumab for this indication.
Pembrolizumab (Keytruda, Merck) had already been approved 10 months earlier in the neoadjuvant and adjuvant settings in this setting. And most recently, in October, the FDA added nivolumab (Opdivo, Bristol Myers Squibb) to these approvals.
No trial, however, identified when patients benefited from the drug.
Without this understanding, patients may be taking immunotherapy unnecessarily, at significant expense and toxicity risk.
“Toxicities from immunotherapy can occur at any time after initiation,” said Joshua Eric Reuss, MD, a thoracic medical oncologist at Georgetown University’s Lombardi Comprehensive Cancer Center in Washington, DC. And these “risks definitely continue into the adjuvant period.”
So far, the available evidence does suggest that the neoadjuvant phase of immunotherapy confers the greatest benefit, while adjuvant immunotherapy — which can last a year or longer — may expose patients to more costs and toxicities, with no clear benefit.
A 2024 meta-analysis, which included four trials of neoadjuvant-adjuvant immunotherapy and one trial of neoadjuvant immunotherapy in resectable NSCLC, suggested that the addition of adjuvant immunotherapy did not improve event-free survival (hazard ratio [HR], 0.90; P = .59) or overall survival (HR, 1.18; P = .51) compared with neoadjuvant immunotherapy alone.
According to Spratt, “It’s very clear that the neoadjuvant phase is the more important of the two phases.” Given that, “we’re probably overtreating some patients,” said Spratt, also chairman of Radiation Oncology at University Hospitals Seidman Cancer Center and Case Western Reserve University in Cleveland.
Chaft agreed that “there’s very little data that we need the postoperative phase, and what data we do have is post hoc and limited.”
This evidence gap “has created considerable dilemmas” for oncologists and patients who are faced with “the challenge of deciding which therapeutic options or approach are best suited for each individual,” experts wrote in recent consensus recommendations from the International Association for the Study of Lung Cancer.
Clinicians may ultimately be left to make decisions about prescribing postoperative immunotherapy based on their experience and comfort level.
When Chaft’s patients have a pathologic complete response with immunotherapy and chemotherapy in the neoadjuvant phase, “I’m comfortable stopping because the data would suggest they’re almost certainly cured,” she said.
For patients who have viable disease after neoadjuvant therapy, continuing an immunotherapy postoperatively when it didn’t work preoperatively “is not going to make a difference,” Chaft explained. In these cases, Chaft would look to enroll them in a clinical trial evaluating a different regimen because of the risk for relapse.
With patients who did well preoperatively but still have tumor left at the time of surgery, she would discuss continuing the immunotherapy or participating in a trial, she said.
All the FDA-approved regimens are covered by insurance, said Chaft. Clinicians are most comfortable with pembrolizumab because it is the most widely used immunotherapy in advanced NSCLC, she said. But, she added, “there’s really no strong differentiating data between any of the studies; all the results look very comparable.”
When assessing whether a patient may benefit from immunotherapy after surgery, Reuss looks at a range of factors, including disease stage, histology, gene mutations, and pathologic response. Reuss also weighs patient preferences. A patient coming from another country might only want a neoadjuvant regimen, for instance, he said.
That “isn’t exactly the kind of the level one evidence that one likes to see when making treatment decisions,” said Reuss. “Without prospective data, all we can do is cross-trial comparisons and assessment of subgroups.”
If a new regimen comes along that improves outcomes or decision-making, “I think we would pivot to that in a heartbeat,” he said.
But Will FDA Follow ODAC’s Recommendation?
“ODAC has made their point clear,” said Chaft. “Our patients deserve to know that whatever added risk and cost they’re incurring is merited by a clinical outcome.”
Despite the ODAC’s recommendation, it’s not guaranteed that the FDA will follow it.
An FDA spokesperson did not confirm the agency’s decision on the matter but noted that the FDA is “incorporating the panel’s advice.”
Spratt thinks that, going forward, companies will be held to “a higher bar,” but it’s unclear what that bar will look like.
“Whether this is a mandate or a strong recommendation, I think industry is definitely paying attention,” Spratt said. Companies that do not follow the guidance may risk not having their drug approved, “unless it’s just an absolute huge slam dunk of a major benefit to patients.”
In fact, according to Chaft, drug makers seeking approvals of novel entities in this space “won’t have a choice” but to follow any new trial design requirements from the FDA.
Still, getting answers may be a challenge.
Drug companies with immunotherapies already on the market are unlikely to invest the resources to conduct trials comparing the neoadjuvant and adjuvant settings, said Chaft. “It will take too long and cost too much,” she said.
And it remains unclear whether drug companies will decide to stop pursuing novel agents if approvals will ultimately require more expensive and time-consuming trials.
According to Chaft, oncologists have been discussing protocols that could help fill the knowledge gaps. Such trials will be conducted by the National Cancer Institute’s Cooperative Groups, she noted. But it’s early days.
For the time being, with comparative data from phase 3 trials years away, oncologists will have to work with the limited evidence and individual patients in front of them.
Chaft disclosed ties with AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, Genentech/Roche, Guardant Health, Janssen Pharmaceuticals, Eli Lilly, and Merck. Reuss disclosed ties with AstraZeneca, Arcus, AbbVie, Bristol Myers Squibb, CatalYm, Daiichi Sankyo, and Eli Lilly, and that Georgetown has received research funding from Genentech/Roche, Verastem, Nuvalent, LUNGevity Foundation, Exelixis, Arcus, and Revolution Medicines. Spratt disclosed ties with Astellas, AstraZeneca, Bayer, Boston Scientific, Janssen Pharmaceuticals, Novartis, and Pfizer.
A version of this article appeared on Medscape.com.
Cellular Therapies for Solid Tumors: The Next Big Thing?
The cutting edge of treating solid tumors with cell therapies got notably sharper in 2024.
First came the US Food and Drug Administration (FDA) approval in February 2024 of the tumor-infiltrating lymphocyte (TIL) therapy lifileucel in unresectable or metastatic melanoma that had progressed on prior immunotherapy, the first cellular therapy for any solid tumor. Then came the August FDA approval of afamitresgene autoleucel in unresectable or metastatic synovial sarcoma with failed chemotherapy, the first engineered T-cell therapy for cancers in soft tissue.
“This was a pipe dream just a decade ago,” Alison Betof Warner, MD, PhD, lead author of a lifileucel study (NCT05640193), said in an interview with Medscape Medical News. “At the start of 2024, we had no approvals of these kinds of products in solid cancers. Now we have two.”
As the director of Solid Tumor Cell Therapy and leader of Stanford Medicine’s Melanoma and Cutaneous Oncology Clinical Research Group, Betof Warner has been at the forefront of developing commercial cell therapy using tumor-infiltrating lymphocytes (TILs).
“The approval of lifileucel increases confidence that we can get these therapies across the regulatory finish line and to patients,” Betof Warner said during the interview. She was not involved in the development of afamitresgene autoleucel.
‘Reverse Engineering’
In addition to her contributions to the work that led to lifileucel’s approval, Betof Warner was the lead author on the first consensus guidelines on management and best practices for tumor-infiltrating lymphocyte cell therapy.
Betof Warner began studying TILs after doing research with her mentors in immuno-oncology, Jedd D. Wolchok and Michael A. Postow. Their investigations — including one that Betof Warner coauthored — into how monoclonal antibodies and checkpoint inhibitors, such as ipilimumab or nivolumab, might extend the lives of people with advanced unresectable or metastatic melanoma inspired her to push further to find ways to minimize treatment while maximizing outcomes for patients. Betof Warner’s interest overall, she said in the interview, is in capitalizing on what can be learned about how the immune system controls cancer.
“What we know is that the immune system has the ability to kill cancer,” Betof Warner said. “Therefore we need to be thinking about how we can increase immune surveillance. How can we enhance that before a patient develops advanced cancer?
Betof Warner said that although TILs are now standard treatment in melanoma, there is about a 30% response rate compared with about a 50% response rate in immunotherapy, and the latter is easier for the patient to withstand.
“Antibodies on the frontline are better than going through a surgery and then waiting weeks to get your therapy,” Betof Warner said in the interview. “You can come into my clinic and get an antibody therapy in 30 minutes and go straight to work. TILs require patients to be in the hospital for weeks at a time and out of work for months at a time.”
In an effort to combine therapies to maximize best outcomes, a phase 3 trial (NCT05727904) is currently recruiting. The TILVANCE-301 trial will compare immunotherapy plus adoptive cell therapy vs immunotherapy alone in untreated unresectable or metastatic melanoma. Betof Warner is not a part of this study.
Cell Therapies Include CAR T Cells and TCRT
In general, adoptive T-cell therapies such as TILs involve the isolation of autologous immune cells that are removed from the body and either expanded or modified to optimize their efficacy in fighting antigens, before their transfer to the patient as a living drug by infusion.
In addition to TILs, adoptive cell therapies for antitumor therapeutics include chimeric antigen receptor (CAR) T cells and engineered T-cell receptor therapy (TCRT).
In CAR T-cell therapy and TCRT, naive T cells are harvested from the patient’s blood then engineered to target a tumor. In TIL therapy, tumor-specific T cells are taken from the patient’s tumor. Once extracted, the respective cells are expanded billions of times and then delivered back to the patient’s body, said Betof Warner.
“The main promise of this approach is to generate responses in what we know as ‘cold’ tumors, or tumors that do not have a lot of endogenous T-cell infiltration or where the T cells are not working well, to bring in tumor targeting T cells and then trigger an immune response,” Betof Warner told an audience at the American Society of Clinical Oncology (ASCO) 2024 annual meeting.
TIL patients also receive interleukin (IL)-2 infusions to further stimulate the cells. In patients being treated with TCRT, they either receive low or no IL-2, Betof Warner said in her ASCO presentation, “Adopting Cutting-Edge Cell Therapies in Melanoma,” part of the session Beyond the Tip of the Iceberg: Next-Generation Cell-Based Therapies.
Decades in the Making
The National Cancer Institute began investigating TILs in the late 1980s, with the current National Cancer Institute (NCI) surgery chief, Steven Rosenberg, MD, PhD, leading the first-ever trials that showed TILs could shrink tumors in people with advanced melanoma.
Since then, NCI staff and others have also investigated TILs beyond melanoma and additional cell therapies based on CAR T cells and TCRT for antitumor therapeutics.
“TCRs are different from CAR Ts because they go after intracellular antigens instead of extracellular antigens,” said Betof Warner. “That has appeal because many of the tumor antigens we’re looking for will be intracellular.”
Because CAR T cells only target extracellular antigens, their utility is somewhat limited. Although several CAR T-cell therapies exist for blood cancers, there currently are no approved CAR T-cell therapies for solid tumors. However, several trials of CAR T cells in gastrointestinal cancers and melanoma are ongoing, said Betof Warner, who is not a part of these studies.
“We are starting to see early-phase efficacy in pediatric gliomas,” Betof Warner said, mentioning a study conducted by colleagues at Stanford who demonstrated potential for anti-GD2 CAR T-cell therapy in deadly pediatric diffuse midline gliomas, tumors on the spine and brain.
In their study, nine out of 11 participants (median age, 15 years) showed benefit from the cell therapy, with one participant’s tumors resolving completely. The results paved the way for the FDA to grant a Regenerative Medicine Advanced Therapy designation for use of anti-GD2 CAR T cells in H3K27M-positive diffuse midline gliomas.
The investigators are now recruiting for a phase 1 trial (NCT04196413). Results of the initial study were published in Nature last month.
Another lesser-known cell therapy expected to advance at some point in the future for solid tumors is use of the body’s natural killer (NK) cells. “They’ve been known about for a long time, but they are more difficult to regulate, which is one reason why it has taken longer to make NK cell therapies,” said Betof Warner, who is not involved in the study of NK cells. “One of their advantages is that, potentially, there could be an ‘off the shelf’ NK product. They don’t necessarily have to be made with autologous cells.”
Risk-Benefit Profiles Depend on Mechanism of Action
If the corresponding TCR sequence of a tumor antigen is known, said Betof Warner, it is possible to use leukapheresis to generate naive circulating lymphocytes. Once infused, the manufactured TCRTs will activate in the body the same as native cells because the signaling is the same.
An advantage to TCRT compared with CAR T-cell therapy is that it targets intracellular proteins, which are significantly present in the tumor, Betof Warner said in her presentation at ASCO 2024. She clarified that tumors will usually be screened for the presence of this antigen before a patient is selected for treatment with that particular therapy, because not all antigens are highly expressed in every tumor.
“Furthermore, the tumor antigen has to be presented by a major histocompatibility complex, meaning there are human leukocyte antigen restrictions, which impacts patient selection,” she said.
A risk with both TCRT and CAR T-cell therapy, according to Betof Warner, is that because there are often shared antigens between tumor and normal tissues, on-target/off-tumor toxicity is a risk.
“TILs are different because they are nonengineered, at least not for antigen recognition. They are polyclonal and go after multiple targets,” Betof Warner said. “TCRs and CARs are engineered to go after one target. So, TILs have much lower rates of on-tumor/off-target effects, vs when you engineer a very high affinity receptor like a TCR or CAR.”
A good example of how this amplification of TCR affinity can lead to poor outcomes is in metastatic melanoma, said Betof Warner.
In investigations (NCI-07-C-0174 and NCI-07-C-0175) of TCRT in metastatic melanoma, for example, the researchers were targeting MART-1 or gp100, which are expressed in melanocytes.
“The problem was that these antigens are also expressed in the eyes and ears, so it caused eye inflammation and hearing loss in a number of patients because it wasn’t specific enough for the tumor,” said Betof Warner. “So, if that target is highly expressed on normal tissue, then you have a high risk.”
Promise of PRAME
Betof Warner said the most promising TCRT at present is the investigational autologous cell therapy IMA203 (NCT03688124), which targets the preferentially expressed antigen (PRAME). Although PRAME is found in many tumors, this testis antigen does not tend to express in normal, healthy adult tissues. Betof Warner is not affiliated with this study.
“It’s maybe the most exciting TCRT cell in melanoma,” Betof Warner told her audience at the ASCO 2024 meeting. Because the expression rate of PRAME in cutaneous and uveal melanoma is at or above 95% and 90%, respectively, she said “it is a really good target in melanoma.”
Phase 1a results reported in late 2023 from a first-in-human trial of IMA203 involving 13 persons with highly advanced melanoma and a median of 5.5 previous treatments showed a 50% objective response rate in the 12 evaluable results. The duration of response ranged between 2.2 and 14.7 months (median follow-up, 14 months).
The safety profile of the treatment was favorable, with no grade 3 adverse events occurring in more than 10% of the cohort, and no grade 5 adverse events at all.
Phase 1b results published in October by maker Immatics showed that in 28 heavily pretreated metastatic melanoma patients, IMA203 had a confirmed objective response rate of 54% with a median duration of response of 12.1 months, while maintaining a favorable tolerability profile.
Accelerated Approvals, Boxed Warnings
The FDA granted accelerated approvals for both lifileucel, the TIL therapy, and afamitresgene autoleucel, the TCRT.
Both were approved with boxed warnings. Lifileucel’s warning is for treatment-related mortality, prolonged severe cytopenia, severe infection, and cardiopulmonary and renal impairment. Afamitresgene autoleucel’s boxed warning is for serious or fatal cytokine release syndrome, which may be severe or life-threatening.
With these approvals, the bar is now raised on TILs and TCRTs, said Betof Warner.
The lifileucel trial studied 73 patients whose melanoma had continued to metastasize despite treatment with a programmed cell death protein (PD-1)/ programmed death-ligand (PD-L1)–targeted immune checkpoint inhibitor and a BRAF inhibitor (if appropriate based on tumor mutation status), and whose lifileucel dose was at least 7.5 billion cells (the approved dose). The cohort also received a median of six IL-2 (aldesleukin) doses.
The objective response rate was 31.5% (95% CI, 21.1-43.4), and median duration of response was not reached (lower bound of 95% CI, 4.1).
In the afamitresgene autoleucel study, 44 of 52 patients with synovial sarcoma received leukapheresis and a single infusion of afamitresgene autoleucel.
The overall response rate was 43.2% (95% CI, 28.4-59.0). The median time to response was 4.9 weeks (95% CI, 4.4-8), and the median duration of response was 6 months (lower bound of 95% CI, 4.6). Among patients who were responsive to the treatment, 45.6% and 39.0% had a duration of response of 6 months or longer and 12 months or longer, respectively.
New Hope for Patients
Betof Warner and her colleagues are now recruiting for an open-label, phase 1/2 investigation of the safety and efficacy of the TIL therapy OBX-115 in adult advanced solid tumors in melanoma or non–small cell lung cancer. The first-in-human results of a previous trial were presented at the ASCO 2024 meeting, and OBX-115 received FDA fast track designation in July.
“I think the results are really promising,” said Betof Warner. “This is an engineered TIL that does not require administering IL-2 to the patient. There were four out of the nine patients who responded to the treatment and there were no dose-limiting toxicities, no cytokine and no intracranial — all of which is excellent.”
For Betof Warner, the possibility that by using their own immune system, patients with advanced and refractory cancers could soon have a one-time treatment with a cell therapy rather than innumerable bouts of chemotherapy pushes her onward.
“The idea that we can treat cancer one time and have it not recur for years — that’s pushing the start of saying there’s a cure of cancer. That a person could move on from cancer like they move on from an infection. That is the potential of this work. We’re not there yet, but that’s where we need to think and dream big,” she said.
Betof Warner disclosed consulting/advisory roles with BluePath Solutions, Bristol-Myers Squibb/Medarex, Immatics, Instil Bio, Iovance Biotherapeutics, Lyell Immunopharma, Merck, Novartis, and Pfizer and research funding and travel expenses from Iovance Biotherapeutics.
A version of this article appeared on Medscape.com.
The cutting edge of treating solid tumors with cell therapies got notably sharper in 2024.
First came the US Food and Drug Administration (FDA) approval in February 2024 of the tumor-infiltrating lymphocyte (TIL) therapy lifileucel in unresectable or metastatic melanoma that had progressed on prior immunotherapy, the first cellular therapy for any solid tumor. Then came the August FDA approval of afamitresgene autoleucel in unresectable or metastatic synovial sarcoma with failed chemotherapy, the first engineered T-cell therapy for cancers in soft tissue.
“This was a pipe dream just a decade ago,” Alison Betof Warner, MD, PhD, lead author of a lifileucel study (NCT05640193), said in an interview with Medscape Medical News. “At the start of 2024, we had no approvals of these kinds of products in solid cancers. Now we have two.”
As the director of Solid Tumor Cell Therapy and leader of Stanford Medicine’s Melanoma and Cutaneous Oncology Clinical Research Group, Betof Warner has been at the forefront of developing commercial cell therapy using tumor-infiltrating lymphocytes (TILs).
“The approval of lifileucel increases confidence that we can get these therapies across the regulatory finish line and to patients,” Betof Warner said during the interview. She was not involved in the development of afamitresgene autoleucel.
‘Reverse Engineering’
In addition to her contributions to the work that led to lifileucel’s approval, Betof Warner was the lead author on the first consensus guidelines on management and best practices for tumor-infiltrating lymphocyte cell therapy.
Betof Warner began studying TILs after doing research with her mentors in immuno-oncology, Jedd D. Wolchok and Michael A. Postow. Their investigations — including one that Betof Warner coauthored — into how monoclonal antibodies and checkpoint inhibitors, such as ipilimumab or nivolumab, might extend the lives of people with advanced unresectable or metastatic melanoma inspired her to push further to find ways to minimize treatment while maximizing outcomes for patients. Betof Warner’s interest overall, she said in the interview, is in capitalizing on what can be learned about how the immune system controls cancer.
“What we know is that the immune system has the ability to kill cancer,” Betof Warner said. “Therefore we need to be thinking about how we can increase immune surveillance. How can we enhance that before a patient develops advanced cancer?
Betof Warner said that although TILs are now standard treatment in melanoma, there is about a 30% response rate compared with about a 50% response rate in immunotherapy, and the latter is easier for the patient to withstand.
“Antibodies on the frontline are better than going through a surgery and then waiting weeks to get your therapy,” Betof Warner said in the interview. “You can come into my clinic and get an antibody therapy in 30 minutes and go straight to work. TILs require patients to be in the hospital for weeks at a time and out of work for months at a time.”
In an effort to combine therapies to maximize best outcomes, a phase 3 trial (NCT05727904) is currently recruiting. The TILVANCE-301 trial will compare immunotherapy plus adoptive cell therapy vs immunotherapy alone in untreated unresectable or metastatic melanoma. Betof Warner is not a part of this study.
Cell Therapies Include CAR T Cells and TCRT
In general, adoptive T-cell therapies such as TILs involve the isolation of autologous immune cells that are removed from the body and either expanded or modified to optimize their efficacy in fighting antigens, before their transfer to the patient as a living drug by infusion.
In addition to TILs, adoptive cell therapies for antitumor therapeutics include chimeric antigen receptor (CAR) T cells and engineered T-cell receptor therapy (TCRT).
In CAR T-cell therapy and TCRT, naive T cells are harvested from the patient’s blood then engineered to target a tumor. In TIL therapy, tumor-specific T cells are taken from the patient’s tumor. Once extracted, the respective cells are expanded billions of times and then delivered back to the patient’s body, said Betof Warner.
“The main promise of this approach is to generate responses in what we know as ‘cold’ tumors, or tumors that do not have a lot of endogenous T-cell infiltration or where the T cells are not working well, to bring in tumor targeting T cells and then trigger an immune response,” Betof Warner told an audience at the American Society of Clinical Oncology (ASCO) 2024 annual meeting.
TIL patients also receive interleukin (IL)-2 infusions to further stimulate the cells. In patients being treated with TCRT, they either receive low or no IL-2, Betof Warner said in her ASCO presentation, “Adopting Cutting-Edge Cell Therapies in Melanoma,” part of the session Beyond the Tip of the Iceberg: Next-Generation Cell-Based Therapies.
Decades in the Making
The National Cancer Institute began investigating TILs in the late 1980s, with the current National Cancer Institute (NCI) surgery chief, Steven Rosenberg, MD, PhD, leading the first-ever trials that showed TILs could shrink tumors in people with advanced melanoma.
Since then, NCI staff and others have also investigated TILs beyond melanoma and additional cell therapies based on CAR T cells and TCRT for antitumor therapeutics.
“TCRs are different from CAR Ts because they go after intracellular antigens instead of extracellular antigens,” said Betof Warner. “That has appeal because many of the tumor antigens we’re looking for will be intracellular.”
Because CAR T cells only target extracellular antigens, their utility is somewhat limited. Although several CAR T-cell therapies exist for blood cancers, there currently are no approved CAR T-cell therapies for solid tumors. However, several trials of CAR T cells in gastrointestinal cancers and melanoma are ongoing, said Betof Warner, who is not a part of these studies.
“We are starting to see early-phase efficacy in pediatric gliomas,” Betof Warner said, mentioning a study conducted by colleagues at Stanford who demonstrated potential for anti-GD2 CAR T-cell therapy in deadly pediatric diffuse midline gliomas, tumors on the spine and brain.
In their study, nine out of 11 participants (median age, 15 years) showed benefit from the cell therapy, with one participant’s tumors resolving completely. The results paved the way for the FDA to grant a Regenerative Medicine Advanced Therapy designation for use of anti-GD2 CAR T cells in H3K27M-positive diffuse midline gliomas.
The investigators are now recruiting for a phase 1 trial (NCT04196413). Results of the initial study were published in Nature last month.
Another lesser-known cell therapy expected to advance at some point in the future for solid tumors is use of the body’s natural killer (NK) cells. “They’ve been known about for a long time, but they are more difficult to regulate, which is one reason why it has taken longer to make NK cell therapies,” said Betof Warner, who is not involved in the study of NK cells. “One of their advantages is that, potentially, there could be an ‘off the shelf’ NK product. They don’t necessarily have to be made with autologous cells.”
Risk-Benefit Profiles Depend on Mechanism of Action
If the corresponding TCR sequence of a tumor antigen is known, said Betof Warner, it is possible to use leukapheresis to generate naive circulating lymphocytes. Once infused, the manufactured TCRTs will activate in the body the same as native cells because the signaling is the same.
An advantage to TCRT compared with CAR T-cell therapy is that it targets intracellular proteins, which are significantly present in the tumor, Betof Warner said in her presentation at ASCO 2024. She clarified that tumors will usually be screened for the presence of this antigen before a patient is selected for treatment with that particular therapy, because not all antigens are highly expressed in every tumor.
“Furthermore, the tumor antigen has to be presented by a major histocompatibility complex, meaning there are human leukocyte antigen restrictions, which impacts patient selection,” she said.
A risk with both TCRT and CAR T-cell therapy, according to Betof Warner, is that because there are often shared antigens between tumor and normal tissues, on-target/off-tumor toxicity is a risk.
“TILs are different because they are nonengineered, at least not for antigen recognition. They are polyclonal and go after multiple targets,” Betof Warner said. “TCRs and CARs are engineered to go after one target. So, TILs have much lower rates of on-tumor/off-target effects, vs when you engineer a very high affinity receptor like a TCR or CAR.”
A good example of how this amplification of TCR affinity can lead to poor outcomes is in metastatic melanoma, said Betof Warner.
In investigations (NCI-07-C-0174 and NCI-07-C-0175) of TCRT in metastatic melanoma, for example, the researchers were targeting MART-1 or gp100, which are expressed in melanocytes.
“The problem was that these antigens are also expressed in the eyes and ears, so it caused eye inflammation and hearing loss in a number of patients because it wasn’t specific enough for the tumor,” said Betof Warner. “So, if that target is highly expressed on normal tissue, then you have a high risk.”
Promise of PRAME
Betof Warner said the most promising TCRT at present is the investigational autologous cell therapy IMA203 (NCT03688124), which targets the preferentially expressed antigen (PRAME). Although PRAME is found in many tumors, this testis antigen does not tend to express in normal, healthy adult tissues. Betof Warner is not affiliated with this study.
“It’s maybe the most exciting TCRT cell in melanoma,” Betof Warner told her audience at the ASCO 2024 meeting. Because the expression rate of PRAME in cutaneous and uveal melanoma is at or above 95% and 90%, respectively, she said “it is a really good target in melanoma.”
Phase 1a results reported in late 2023 from a first-in-human trial of IMA203 involving 13 persons with highly advanced melanoma and a median of 5.5 previous treatments showed a 50% objective response rate in the 12 evaluable results. The duration of response ranged between 2.2 and 14.7 months (median follow-up, 14 months).
The safety profile of the treatment was favorable, with no grade 3 adverse events occurring in more than 10% of the cohort, and no grade 5 adverse events at all.
Phase 1b results published in October by maker Immatics showed that in 28 heavily pretreated metastatic melanoma patients, IMA203 had a confirmed objective response rate of 54% with a median duration of response of 12.1 months, while maintaining a favorable tolerability profile.
Accelerated Approvals, Boxed Warnings
The FDA granted accelerated approvals for both lifileucel, the TIL therapy, and afamitresgene autoleucel, the TCRT.
Both were approved with boxed warnings. Lifileucel’s warning is for treatment-related mortality, prolonged severe cytopenia, severe infection, and cardiopulmonary and renal impairment. Afamitresgene autoleucel’s boxed warning is for serious or fatal cytokine release syndrome, which may be severe or life-threatening.
With these approvals, the bar is now raised on TILs and TCRTs, said Betof Warner.
The lifileucel trial studied 73 patients whose melanoma had continued to metastasize despite treatment with a programmed cell death protein (PD-1)/ programmed death-ligand (PD-L1)–targeted immune checkpoint inhibitor and a BRAF inhibitor (if appropriate based on tumor mutation status), and whose lifileucel dose was at least 7.5 billion cells (the approved dose). The cohort also received a median of six IL-2 (aldesleukin) doses.
The objective response rate was 31.5% (95% CI, 21.1-43.4), and median duration of response was not reached (lower bound of 95% CI, 4.1).
In the afamitresgene autoleucel study, 44 of 52 patients with synovial sarcoma received leukapheresis and a single infusion of afamitresgene autoleucel.
The overall response rate was 43.2% (95% CI, 28.4-59.0). The median time to response was 4.9 weeks (95% CI, 4.4-8), and the median duration of response was 6 months (lower bound of 95% CI, 4.6). Among patients who were responsive to the treatment, 45.6% and 39.0% had a duration of response of 6 months or longer and 12 months or longer, respectively.
New Hope for Patients
Betof Warner and her colleagues are now recruiting for an open-label, phase 1/2 investigation of the safety and efficacy of the TIL therapy OBX-115 in adult advanced solid tumors in melanoma or non–small cell lung cancer. The first-in-human results of a previous trial were presented at the ASCO 2024 meeting, and OBX-115 received FDA fast track designation in July.
“I think the results are really promising,” said Betof Warner. “This is an engineered TIL that does not require administering IL-2 to the patient. There were four out of the nine patients who responded to the treatment and there were no dose-limiting toxicities, no cytokine and no intracranial — all of which is excellent.”
For Betof Warner, the possibility that by using their own immune system, patients with advanced and refractory cancers could soon have a one-time treatment with a cell therapy rather than innumerable bouts of chemotherapy pushes her onward.
“The idea that we can treat cancer one time and have it not recur for years — that’s pushing the start of saying there’s a cure of cancer. That a person could move on from cancer like they move on from an infection. That is the potential of this work. We’re not there yet, but that’s where we need to think and dream big,” she said.
Betof Warner disclosed consulting/advisory roles with BluePath Solutions, Bristol-Myers Squibb/Medarex, Immatics, Instil Bio, Iovance Biotherapeutics, Lyell Immunopharma, Merck, Novartis, and Pfizer and research funding and travel expenses from Iovance Biotherapeutics.
A version of this article appeared on Medscape.com.
The cutting edge of treating solid tumors with cell therapies got notably sharper in 2024.
First came the US Food and Drug Administration (FDA) approval in February 2024 of the tumor-infiltrating lymphocyte (TIL) therapy lifileucel in unresectable or metastatic melanoma that had progressed on prior immunotherapy, the first cellular therapy for any solid tumor. Then came the August FDA approval of afamitresgene autoleucel in unresectable or metastatic synovial sarcoma with failed chemotherapy, the first engineered T-cell therapy for cancers in soft tissue.
“This was a pipe dream just a decade ago,” Alison Betof Warner, MD, PhD, lead author of a lifileucel study (NCT05640193), said in an interview with Medscape Medical News. “At the start of 2024, we had no approvals of these kinds of products in solid cancers. Now we have two.”
As the director of Solid Tumor Cell Therapy and leader of Stanford Medicine’s Melanoma and Cutaneous Oncology Clinical Research Group, Betof Warner has been at the forefront of developing commercial cell therapy using tumor-infiltrating lymphocytes (TILs).
“The approval of lifileucel increases confidence that we can get these therapies across the regulatory finish line and to patients,” Betof Warner said during the interview. She was not involved in the development of afamitresgene autoleucel.
‘Reverse Engineering’
In addition to her contributions to the work that led to lifileucel’s approval, Betof Warner was the lead author on the first consensus guidelines on management and best practices for tumor-infiltrating lymphocyte cell therapy.
Betof Warner began studying TILs after doing research with her mentors in immuno-oncology, Jedd D. Wolchok and Michael A. Postow. Their investigations — including one that Betof Warner coauthored — into how monoclonal antibodies and checkpoint inhibitors, such as ipilimumab or nivolumab, might extend the lives of people with advanced unresectable or metastatic melanoma inspired her to push further to find ways to minimize treatment while maximizing outcomes for patients. Betof Warner’s interest overall, she said in the interview, is in capitalizing on what can be learned about how the immune system controls cancer.
“What we know is that the immune system has the ability to kill cancer,” Betof Warner said. “Therefore we need to be thinking about how we can increase immune surveillance. How can we enhance that before a patient develops advanced cancer?
Betof Warner said that although TILs are now standard treatment in melanoma, there is about a 30% response rate compared with about a 50% response rate in immunotherapy, and the latter is easier for the patient to withstand.
“Antibodies on the frontline are better than going through a surgery and then waiting weeks to get your therapy,” Betof Warner said in the interview. “You can come into my clinic and get an antibody therapy in 30 minutes and go straight to work. TILs require patients to be in the hospital for weeks at a time and out of work for months at a time.”
In an effort to combine therapies to maximize best outcomes, a phase 3 trial (NCT05727904) is currently recruiting. The TILVANCE-301 trial will compare immunotherapy plus adoptive cell therapy vs immunotherapy alone in untreated unresectable or metastatic melanoma. Betof Warner is not a part of this study.
Cell Therapies Include CAR T Cells and TCRT
In general, adoptive T-cell therapies such as TILs involve the isolation of autologous immune cells that are removed from the body and either expanded or modified to optimize their efficacy in fighting antigens, before their transfer to the patient as a living drug by infusion.
In addition to TILs, adoptive cell therapies for antitumor therapeutics include chimeric antigen receptor (CAR) T cells and engineered T-cell receptor therapy (TCRT).
In CAR T-cell therapy and TCRT, naive T cells are harvested from the patient’s blood then engineered to target a tumor. In TIL therapy, tumor-specific T cells are taken from the patient’s tumor. Once extracted, the respective cells are expanded billions of times and then delivered back to the patient’s body, said Betof Warner.
“The main promise of this approach is to generate responses in what we know as ‘cold’ tumors, or tumors that do not have a lot of endogenous T-cell infiltration or where the T cells are not working well, to bring in tumor targeting T cells and then trigger an immune response,” Betof Warner told an audience at the American Society of Clinical Oncology (ASCO) 2024 annual meeting.
TIL patients also receive interleukin (IL)-2 infusions to further stimulate the cells. In patients being treated with TCRT, they either receive low or no IL-2, Betof Warner said in her ASCO presentation, “Adopting Cutting-Edge Cell Therapies in Melanoma,” part of the session Beyond the Tip of the Iceberg: Next-Generation Cell-Based Therapies.
Decades in the Making
The National Cancer Institute began investigating TILs in the late 1980s, with the current National Cancer Institute (NCI) surgery chief, Steven Rosenberg, MD, PhD, leading the first-ever trials that showed TILs could shrink tumors in people with advanced melanoma.
Since then, NCI staff and others have also investigated TILs beyond melanoma and additional cell therapies based on CAR T cells and TCRT for antitumor therapeutics.
“TCRs are different from CAR Ts because they go after intracellular antigens instead of extracellular antigens,” said Betof Warner. “That has appeal because many of the tumor antigens we’re looking for will be intracellular.”
Because CAR T cells only target extracellular antigens, their utility is somewhat limited. Although several CAR T-cell therapies exist for blood cancers, there currently are no approved CAR T-cell therapies for solid tumors. However, several trials of CAR T cells in gastrointestinal cancers and melanoma are ongoing, said Betof Warner, who is not a part of these studies.
“We are starting to see early-phase efficacy in pediatric gliomas,” Betof Warner said, mentioning a study conducted by colleagues at Stanford who demonstrated potential for anti-GD2 CAR T-cell therapy in deadly pediatric diffuse midline gliomas, tumors on the spine and brain.
In their study, nine out of 11 participants (median age, 15 years) showed benefit from the cell therapy, with one participant’s tumors resolving completely. The results paved the way for the FDA to grant a Regenerative Medicine Advanced Therapy designation for use of anti-GD2 CAR T cells in H3K27M-positive diffuse midline gliomas.
The investigators are now recruiting for a phase 1 trial (NCT04196413). Results of the initial study were published in Nature last month.
Another lesser-known cell therapy expected to advance at some point in the future for solid tumors is use of the body’s natural killer (NK) cells. “They’ve been known about for a long time, but they are more difficult to regulate, which is one reason why it has taken longer to make NK cell therapies,” said Betof Warner, who is not involved in the study of NK cells. “One of their advantages is that, potentially, there could be an ‘off the shelf’ NK product. They don’t necessarily have to be made with autologous cells.”
Risk-Benefit Profiles Depend on Mechanism of Action
If the corresponding TCR sequence of a tumor antigen is known, said Betof Warner, it is possible to use leukapheresis to generate naive circulating lymphocytes. Once infused, the manufactured TCRTs will activate in the body the same as native cells because the signaling is the same.
An advantage to TCRT compared with CAR T-cell therapy is that it targets intracellular proteins, which are significantly present in the tumor, Betof Warner said in her presentation at ASCO 2024. She clarified that tumors will usually be screened for the presence of this antigen before a patient is selected for treatment with that particular therapy, because not all antigens are highly expressed in every tumor.
“Furthermore, the tumor antigen has to be presented by a major histocompatibility complex, meaning there are human leukocyte antigen restrictions, which impacts patient selection,” she said.
A risk with both TCRT and CAR T-cell therapy, according to Betof Warner, is that because there are often shared antigens between tumor and normal tissues, on-target/off-tumor toxicity is a risk.
“TILs are different because they are nonengineered, at least not for antigen recognition. They are polyclonal and go after multiple targets,” Betof Warner said. “TCRs and CARs are engineered to go after one target. So, TILs have much lower rates of on-tumor/off-target effects, vs when you engineer a very high affinity receptor like a TCR or CAR.”
A good example of how this amplification of TCR affinity can lead to poor outcomes is in metastatic melanoma, said Betof Warner.
In investigations (NCI-07-C-0174 and NCI-07-C-0175) of TCRT in metastatic melanoma, for example, the researchers were targeting MART-1 or gp100, which are expressed in melanocytes.
“The problem was that these antigens are also expressed in the eyes and ears, so it caused eye inflammation and hearing loss in a number of patients because it wasn’t specific enough for the tumor,” said Betof Warner. “So, if that target is highly expressed on normal tissue, then you have a high risk.”
Promise of PRAME
Betof Warner said the most promising TCRT at present is the investigational autologous cell therapy IMA203 (NCT03688124), which targets the preferentially expressed antigen (PRAME). Although PRAME is found in many tumors, this testis antigen does not tend to express in normal, healthy adult tissues. Betof Warner is not affiliated with this study.
“It’s maybe the most exciting TCRT cell in melanoma,” Betof Warner told her audience at the ASCO 2024 meeting. Because the expression rate of PRAME in cutaneous and uveal melanoma is at or above 95% and 90%, respectively, she said “it is a really good target in melanoma.”
Phase 1a results reported in late 2023 from a first-in-human trial of IMA203 involving 13 persons with highly advanced melanoma and a median of 5.5 previous treatments showed a 50% objective response rate in the 12 evaluable results. The duration of response ranged between 2.2 and 14.7 months (median follow-up, 14 months).
The safety profile of the treatment was favorable, with no grade 3 adverse events occurring in more than 10% of the cohort, and no grade 5 adverse events at all.
Phase 1b results published in October by maker Immatics showed that in 28 heavily pretreated metastatic melanoma patients, IMA203 had a confirmed objective response rate of 54% with a median duration of response of 12.1 months, while maintaining a favorable tolerability profile.
Accelerated Approvals, Boxed Warnings
The FDA granted accelerated approvals for both lifileucel, the TIL therapy, and afamitresgene autoleucel, the TCRT.
Both were approved with boxed warnings. Lifileucel’s warning is for treatment-related mortality, prolonged severe cytopenia, severe infection, and cardiopulmonary and renal impairment. Afamitresgene autoleucel’s boxed warning is for serious or fatal cytokine release syndrome, which may be severe or life-threatening.
With these approvals, the bar is now raised on TILs and TCRTs, said Betof Warner.
The lifileucel trial studied 73 patients whose melanoma had continued to metastasize despite treatment with a programmed cell death protein (PD-1)/ programmed death-ligand (PD-L1)–targeted immune checkpoint inhibitor and a BRAF inhibitor (if appropriate based on tumor mutation status), and whose lifileucel dose was at least 7.5 billion cells (the approved dose). The cohort also received a median of six IL-2 (aldesleukin) doses.
The objective response rate was 31.5% (95% CI, 21.1-43.4), and median duration of response was not reached (lower bound of 95% CI, 4.1).
In the afamitresgene autoleucel study, 44 of 52 patients with synovial sarcoma received leukapheresis and a single infusion of afamitresgene autoleucel.
The overall response rate was 43.2% (95% CI, 28.4-59.0). The median time to response was 4.9 weeks (95% CI, 4.4-8), and the median duration of response was 6 months (lower bound of 95% CI, 4.6). Among patients who were responsive to the treatment, 45.6% and 39.0% had a duration of response of 6 months or longer and 12 months or longer, respectively.
New Hope for Patients
Betof Warner and her colleagues are now recruiting for an open-label, phase 1/2 investigation of the safety and efficacy of the TIL therapy OBX-115 in adult advanced solid tumors in melanoma or non–small cell lung cancer. The first-in-human results of a previous trial were presented at the ASCO 2024 meeting, and OBX-115 received FDA fast track designation in July.
“I think the results are really promising,” said Betof Warner. “This is an engineered TIL that does not require administering IL-2 to the patient. There were four out of the nine patients who responded to the treatment and there were no dose-limiting toxicities, no cytokine and no intracranial — all of which is excellent.”
For Betof Warner, the possibility that by using their own immune system, patients with advanced and refractory cancers could soon have a one-time treatment with a cell therapy rather than innumerable bouts of chemotherapy pushes her onward.
“The idea that we can treat cancer one time and have it not recur for years — that’s pushing the start of saying there’s a cure of cancer. That a person could move on from cancer like they move on from an infection. That is the potential of this work. We’re not there yet, but that’s where we need to think and dream big,” she said.
Betof Warner disclosed consulting/advisory roles with BluePath Solutions, Bristol-Myers Squibb/Medarex, Immatics, Instil Bio, Iovance Biotherapeutics, Lyell Immunopharma, Merck, Novartis, and Pfizer and research funding and travel expenses from Iovance Biotherapeutics.
A version of this article appeared on Medscape.com.
The Protein Problem: The Unsolved Mystery of AI Drug Dev
The question has been lingering for years in medical science circles. Since 2020, when the artificial intelligence (AI) model AlphaFold made it possible to predict protein structures, would the technology open the drug discovery floodgates?
Short answer: No. At least not yet.
The longer answer goes something like this:
A drug target (such as a mutation) is like a lock. The right drug (a protein designed to bind to the mutation, stopping its activity) is the key. But proteins are fidgety and flexible.
“They’re basically molecular springs,” said Gabriel Monteiro da Silva, PhD, a computational chemistry research scientist at Genesis Therapeutics. “Your key can bend and alter the shape of the lock, and if you don’t account for that, your key might fail.”
This is the protein problem in drug development. Another issue making this challenge so vexing is that proteins don’t act in isolation. Their interactions with other proteins, ribonucleic acid, and DNA can affect how they bind to molecules and the shapes they adopt.
Newer versions of AlphaFold, such as AlphaFold Multimer and AlphaFold 3 (the code for which was recently revealed for academic use), can predict many interactions among proteins and between proteins and other molecules. But these tools still have weak points scientists are trying to overcome or work around.
“Those kinds of dynamics and multiple conformations are still quite challenging for the AI models to predict,” said James Zou, PhD, associate professor of biomedical data science at Stanford University in California.
“We’re finding more and more that the only way we can make these structures useful for drug discovery is if we incorporate dynamics, if we incorporate more physics into the model,” said Monteiro da Silva.
Monteiro da Silva spent 3 years during his PhD at Brown University, Providence, Rhode Island, running physics-based simulations in the lab, trying to understand why proteins carrying certain mutations are drug resistant. His results showed how “the changing landscape of shapes that a protein can take” prevented the drug from binding.
It took him 3 years to model just four mutations.
AI can do better — and the struggle is fascinating. By developing models that build on the predictive power of AlphaFold, scientists are uncovering new details about protein activity — insights that can lead to new therapeutics and reveal why existing ones stop working — much faster than they could with traditional methods or AlphaFold alone.
New Windows into Protein Dynamics
A notable step, “but that’s just the starting point,” said Pedro Beltrao, PhD, an associate professor at Institute of Molecular Systems Biology, ETH Zurich in Switzerland. “It’s still very difficult, given a pocket, to actually design the drug or figure out what the pocket binds.”
Going back to the lock-and-key analogy: While he was at Brown, with a team of researchers in the Rubenstein Group, Monteiro da Silva helped create a model to better understand how mutations affect “the shape and dynamics of the lock.” They manipulated the amino acid sequences of proteins, guiding their evolution. This enabled them to use AlphaFold to predict “protein ensembles” and how frequently those ensembles appear. Each ensemble represents the many different shapes a protein can take under given conditions.
“Essentially, it tries to find the most common shapes that a protein will take over an arbitrary amount of time,” Monteiro da Silva said. “If we can predict these ensembles at scale and fast, then we can screen many mutations that cause resistance and develop drugs that will not be affected by that resistance.”
To evaluate their method, the researchers focused on ABL1, a well-studied kinase that causes leukemia. ABL1 can be drugged – unless it carries or develops a mutation that causes drug resistance. Currently there are no drugs that work against proteins carrying those mutations, according to Monteiro da Silva. The researchers used their hybrid AI-meets-physics method to investigate how drugs bind to different ABL1 mutations, screening 100 mutations in just 1 month.
“It’s not going to be perfect for every one of them. But if we have 100 and we get 20 with good accuracy, that’s better than doing four over 3 years,” Monteiro da Silva said.
A forthcoming paper will make their model publicly available in “an easy-to-use graphical interface” that they hope clinicians and medicinal chemists will try out. It can also complement other AI-based tools that dig into protein dynamics, according to Monteiro da Silva.
Complementary Tools to Speed Up Discovery
Another aspect of the protein problem is scale. One protein can interact with hundreds of other proteins, which in turn may interact with hundreds more, all of which comprise the human interactome.
Feixiong Cheng, PhD, helped build PIONEER, a deep learning model that predicts the three-dimensional (3D) structure of interactions between proteins across the interactome.
Most disease mutations disrupt specific interactions between proteins, making their affinity stronger or weaker, explained Cheng. To treat a disease without causing major side effects, scientists need a precise understanding of those interactions.
“From the drug discovery perspective, we cannot just focus on single proteins. We have to understand the protein environment, in particular how the protein interacts with other proteins,” said Cheng, director of Cleveland Clinic Genome Center, Cleveland.
PIONEER helps by blending AlphaFold’s protein structure predictions with next-generation sequencing, a type of genomic research that identifies mutations in the human genome. The model predicts the 3D structure of the places where proteins interact — the binding sites, or interfaces — across the interactome.
“We tell you not only that a binds b, but where on a and where on b the two proteins interact,” said Haiyuan Yu, PhD, director of the Center for Innovative Proteomics, Cornell University, and co-creator of PIONEER.
This can help scientists understand “why a mutation, protein, or even network is a good target for therapeutic discovery,” Cheng said.
The researchers validated PIONEER’s predictions in the lab, testing the impacts of roughly 3000 mutations on 7000 pairs of interacting proteins. Based on their findings, they plan to develop and test treatments for lung and endometrial cancer.
PIONEER can also help scientists home in on how a mutation causes a disease, such as by showing recurrent mutations.
“If you find cancer mutations hitting an interface again and again and again, it means that this is likely to be driving cancer progression,” said Beltrao.
Beltrao’s lab and others have looked for recurrent mutations by using AlphaFold Multimer and AlphaFold 3 to directly model protein interactions. It’s a much slower approach (Pioneer is more than 5000 faster than AlphaFold Multimer, according to Cheng). But it could allow scientists to model interfaces that are not shown by PIONEER.
“You will need many different things to try to come up with a structural modeling of the interactome, and all these will have limitations,” said Beltrao. “Their method is a very good step forward, and there’ll be other approaches that are complementary, to continue to add details.”
And It Wouldn’t be an AI Mission Without ChatGPT
Large language models, such as ChatGPT, are another way that scientists are adding details to protein structure predictions. Zou used GPT-4 to “fine tune” a protein language model, called evolutionary scale modeling (ESM-2), which predicts protein structures directly from a protein sequence.
First, they trained ChatGPT on thousands of papers and studies containing information about the functions, biophysical properties, and disease relevance of different mutations. Next, they used the trained model to “teach” ESM-2, boosting its ability “to predict which mutations are likely to have larger effects or smaller effects,” Zou said. The same could be done for a model like AlphaFold, according to Zou.
“They are quite complementary in that the large language model contains a lot more information about the functions and the biophysics of different mutations and proteins as captured in text,” he said, whereas “you can’t give AlphaFold a piece of paper.”
Exactly how AlphaFold makes its predictions is another mystery. “It will somehow learn protein dynamics phenomenologically,” said Monteiro da Silva. He and others are trying to understand how that happens, in hopes of creating even more accurate predictive models. But for the time being, AI-based methods still need assistance from physics.
“The dream is that we achieve a state where we rely on just the fast methods, and they’re accurate enough,” he said. “But we’re so far from that.”
A version of this article first appeared on Medscape.com.
The question has been lingering for years in medical science circles. Since 2020, when the artificial intelligence (AI) model AlphaFold made it possible to predict protein structures, would the technology open the drug discovery floodgates?
Short answer: No. At least not yet.
The longer answer goes something like this:
A drug target (such as a mutation) is like a lock. The right drug (a protein designed to bind to the mutation, stopping its activity) is the key. But proteins are fidgety and flexible.
“They’re basically molecular springs,” said Gabriel Monteiro da Silva, PhD, a computational chemistry research scientist at Genesis Therapeutics. “Your key can bend and alter the shape of the lock, and if you don’t account for that, your key might fail.”
This is the protein problem in drug development. Another issue making this challenge so vexing is that proteins don’t act in isolation. Their interactions with other proteins, ribonucleic acid, and DNA can affect how they bind to molecules and the shapes they adopt.
Newer versions of AlphaFold, such as AlphaFold Multimer and AlphaFold 3 (the code for which was recently revealed for academic use), can predict many interactions among proteins and between proteins and other molecules. But these tools still have weak points scientists are trying to overcome or work around.
“Those kinds of dynamics and multiple conformations are still quite challenging for the AI models to predict,” said James Zou, PhD, associate professor of biomedical data science at Stanford University in California.
“We’re finding more and more that the only way we can make these structures useful for drug discovery is if we incorporate dynamics, if we incorporate more physics into the model,” said Monteiro da Silva.
Monteiro da Silva spent 3 years during his PhD at Brown University, Providence, Rhode Island, running physics-based simulations in the lab, trying to understand why proteins carrying certain mutations are drug resistant. His results showed how “the changing landscape of shapes that a protein can take” prevented the drug from binding.
It took him 3 years to model just four mutations.
AI can do better — and the struggle is fascinating. By developing models that build on the predictive power of AlphaFold, scientists are uncovering new details about protein activity — insights that can lead to new therapeutics and reveal why existing ones stop working — much faster than they could with traditional methods or AlphaFold alone.
New Windows into Protein Dynamics
A notable step, “but that’s just the starting point,” said Pedro Beltrao, PhD, an associate professor at Institute of Molecular Systems Biology, ETH Zurich in Switzerland. “It’s still very difficult, given a pocket, to actually design the drug or figure out what the pocket binds.”
Going back to the lock-and-key analogy: While he was at Brown, with a team of researchers in the Rubenstein Group, Monteiro da Silva helped create a model to better understand how mutations affect “the shape and dynamics of the lock.” They manipulated the amino acid sequences of proteins, guiding their evolution. This enabled them to use AlphaFold to predict “protein ensembles” and how frequently those ensembles appear. Each ensemble represents the many different shapes a protein can take under given conditions.
“Essentially, it tries to find the most common shapes that a protein will take over an arbitrary amount of time,” Monteiro da Silva said. “If we can predict these ensembles at scale and fast, then we can screen many mutations that cause resistance and develop drugs that will not be affected by that resistance.”
To evaluate their method, the researchers focused on ABL1, a well-studied kinase that causes leukemia. ABL1 can be drugged – unless it carries or develops a mutation that causes drug resistance. Currently there are no drugs that work against proteins carrying those mutations, according to Monteiro da Silva. The researchers used their hybrid AI-meets-physics method to investigate how drugs bind to different ABL1 mutations, screening 100 mutations in just 1 month.
“It’s not going to be perfect for every one of them. But if we have 100 and we get 20 with good accuracy, that’s better than doing four over 3 years,” Monteiro da Silva said.
A forthcoming paper will make their model publicly available in “an easy-to-use graphical interface” that they hope clinicians and medicinal chemists will try out. It can also complement other AI-based tools that dig into protein dynamics, according to Monteiro da Silva.
Complementary Tools to Speed Up Discovery
Another aspect of the protein problem is scale. One protein can interact with hundreds of other proteins, which in turn may interact with hundreds more, all of which comprise the human interactome.
Feixiong Cheng, PhD, helped build PIONEER, a deep learning model that predicts the three-dimensional (3D) structure of interactions between proteins across the interactome.
Most disease mutations disrupt specific interactions between proteins, making their affinity stronger or weaker, explained Cheng. To treat a disease without causing major side effects, scientists need a precise understanding of those interactions.
“From the drug discovery perspective, we cannot just focus on single proteins. We have to understand the protein environment, in particular how the protein interacts with other proteins,” said Cheng, director of Cleveland Clinic Genome Center, Cleveland.
PIONEER helps by blending AlphaFold’s protein structure predictions with next-generation sequencing, a type of genomic research that identifies mutations in the human genome. The model predicts the 3D structure of the places where proteins interact — the binding sites, or interfaces — across the interactome.
“We tell you not only that a binds b, but where on a and where on b the two proteins interact,” said Haiyuan Yu, PhD, director of the Center for Innovative Proteomics, Cornell University, and co-creator of PIONEER.
This can help scientists understand “why a mutation, protein, or even network is a good target for therapeutic discovery,” Cheng said.
The researchers validated PIONEER’s predictions in the lab, testing the impacts of roughly 3000 mutations on 7000 pairs of interacting proteins. Based on their findings, they plan to develop and test treatments for lung and endometrial cancer.
PIONEER can also help scientists home in on how a mutation causes a disease, such as by showing recurrent mutations.
“If you find cancer mutations hitting an interface again and again and again, it means that this is likely to be driving cancer progression,” said Beltrao.
Beltrao’s lab and others have looked for recurrent mutations by using AlphaFold Multimer and AlphaFold 3 to directly model protein interactions. It’s a much slower approach (Pioneer is more than 5000 faster than AlphaFold Multimer, according to Cheng). But it could allow scientists to model interfaces that are not shown by PIONEER.
“You will need many different things to try to come up with a structural modeling of the interactome, and all these will have limitations,” said Beltrao. “Their method is a very good step forward, and there’ll be other approaches that are complementary, to continue to add details.”
And It Wouldn’t be an AI Mission Without ChatGPT
Large language models, such as ChatGPT, are another way that scientists are adding details to protein structure predictions. Zou used GPT-4 to “fine tune” a protein language model, called evolutionary scale modeling (ESM-2), which predicts protein structures directly from a protein sequence.
First, they trained ChatGPT on thousands of papers and studies containing information about the functions, biophysical properties, and disease relevance of different mutations. Next, they used the trained model to “teach” ESM-2, boosting its ability “to predict which mutations are likely to have larger effects or smaller effects,” Zou said. The same could be done for a model like AlphaFold, according to Zou.
“They are quite complementary in that the large language model contains a lot more information about the functions and the biophysics of different mutations and proteins as captured in text,” he said, whereas “you can’t give AlphaFold a piece of paper.”
Exactly how AlphaFold makes its predictions is another mystery. “It will somehow learn protein dynamics phenomenologically,” said Monteiro da Silva. He and others are trying to understand how that happens, in hopes of creating even more accurate predictive models. But for the time being, AI-based methods still need assistance from physics.
“The dream is that we achieve a state where we rely on just the fast methods, and they’re accurate enough,” he said. “But we’re so far from that.”
A version of this article first appeared on Medscape.com.
The question has been lingering for years in medical science circles. Since 2020, when the artificial intelligence (AI) model AlphaFold made it possible to predict protein structures, would the technology open the drug discovery floodgates?
Short answer: No. At least not yet.
The longer answer goes something like this:
A drug target (such as a mutation) is like a lock. The right drug (a protein designed to bind to the mutation, stopping its activity) is the key. But proteins are fidgety and flexible.
“They’re basically molecular springs,” said Gabriel Monteiro da Silva, PhD, a computational chemistry research scientist at Genesis Therapeutics. “Your key can bend and alter the shape of the lock, and if you don’t account for that, your key might fail.”
This is the protein problem in drug development. Another issue making this challenge so vexing is that proteins don’t act in isolation. Their interactions with other proteins, ribonucleic acid, and DNA can affect how they bind to molecules and the shapes they adopt.
Newer versions of AlphaFold, such as AlphaFold Multimer and AlphaFold 3 (the code for which was recently revealed for academic use), can predict many interactions among proteins and between proteins and other molecules. But these tools still have weak points scientists are trying to overcome or work around.
“Those kinds of dynamics and multiple conformations are still quite challenging for the AI models to predict,” said James Zou, PhD, associate professor of biomedical data science at Stanford University in California.
“We’re finding more and more that the only way we can make these structures useful for drug discovery is if we incorporate dynamics, if we incorporate more physics into the model,” said Monteiro da Silva.
Monteiro da Silva spent 3 years during his PhD at Brown University, Providence, Rhode Island, running physics-based simulations in the lab, trying to understand why proteins carrying certain mutations are drug resistant. His results showed how “the changing landscape of shapes that a protein can take” prevented the drug from binding.
It took him 3 years to model just four mutations.
AI can do better — and the struggle is fascinating. By developing models that build on the predictive power of AlphaFold, scientists are uncovering new details about protein activity — insights that can lead to new therapeutics and reveal why existing ones stop working — much faster than they could with traditional methods or AlphaFold alone.
New Windows into Protein Dynamics
A notable step, “but that’s just the starting point,” said Pedro Beltrao, PhD, an associate professor at Institute of Molecular Systems Biology, ETH Zurich in Switzerland. “It’s still very difficult, given a pocket, to actually design the drug or figure out what the pocket binds.”
Going back to the lock-and-key analogy: While he was at Brown, with a team of researchers in the Rubenstein Group, Monteiro da Silva helped create a model to better understand how mutations affect “the shape and dynamics of the lock.” They manipulated the amino acid sequences of proteins, guiding their evolution. This enabled them to use AlphaFold to predict “protein ensembles” and how frequently those ensembles appear. Each ensemble represents the many different shapes a protein can take under given conditions.
“Essentially, it tries to find the most common shapes that a protein will take over an arbitrary amount of time,” Monteiro da Silva said. “If we can predict these ensembles at scale and fast, then we can screen many mutations that cause resistance and develop drugs that will not be affected by that resistance.”
To evaluate their method, the researchers focused on ABL1, a well-studied kinase that causes leukemia. ABL1 can be drugged – unless it carries or develops a mutation that causes drug resistance. Currently there are no drugs that work against proteins carrying those mutations, according to Monteiro da Silva. The researchers used their hybrid AI-meets-physics method to investigate how drugs bind to different ABL1 mutations, screening 100 mutations in just 1 month.
“It’s not going to be perfect for every one of them. But if we have 100 and we get 20 with good accuracy, that’s better than doing four over 3 years,” Monteiro da Silva said.
A forthcoming paper will make their model publicly available in “an easy-to-use graphical interface” that they hope clinicians and medicinal chemists will try out. It can also complement other AI-based tools that dig into protein dynamics, according to Monteiro da Silva.
Complementary Tools to Speed Up Discovery
Another aspect of the protein problem is scale. One protein can interact with hundreds of other proteins, which in turn may interact with hundreds more, all of which comprise the human interactome.
Feixiong Cheng, PhD, helped build PIONEER, a deep learning model that predicts the three-dimensional (3D) structure of interactions between proteins across the interactome.
Most disease mutations disrupt specific interactions between proteins, making their affinity stronger or weaker, explained Cheng. To treat a disease without causing major side effects, scientists need a precise understanding of those interactions.
“From the drug discovery perspective, we cannot just focus on single proteins. We have to understand the protein environment, in particular how the protein interacts with other proteins,” said Cheng, director of Cleveland Clinic Genome Center, Cleveland.
PIONEER helps by blending AlphaFold’s protein structure predictions with next-generation sequencing, a type of genomic research that identifies mutations in the human genome. The model predicts the 3D structure of the places where proteins interact — the binding sites, or interfaces — across the interactome.
“We tell you not only that a binds b, but where on a and where on b the two proteins interact,” said Haiyuan Yu, PhD, director of the Center for Innovative Proteomics, Cornell University, and co-creator of PIONEER.
This can help scientists understand “why a mutation, protein, or even network is a good target for therapeutic discovery,” Cheng said.
The researchers validated PIONEER’s predictions in the lab, testing the impacts of roughly 3000 mutations on 7000 pairs of interacting proteins. Based on their findings, they plan to develop and test treatments for lung and endometrial cancer.
PIONEER can also help scientists home in on how a mutation causes a disease, such as by showing recurrent mutations.
“If you find cancer mutations hitting an interface again and again and again, it means that this is likely to be driving cancer progression,” said Beltrao.
Beltrao’s lab and others have looked for recurrent mutations by using AlphaFold Multimer and AlphaFold 3 to directly model protein interactions. It’s a much slower approach (Pioneer is more than 5000 faster than AlphaFold Multimer, according to Cheng). But it could allow scientists to model interfaces that are not shown by PIONEER.
“You will need many different things to try to come up with a structural modeling of the interactome, and all these will have limitations,” said Beltrao. “Their method is a very good step forward, and there’ll be other approaches that are complementary, to continue to add details.”
And It Wouldn’t be an AI Mission Without ChatGPT
Large language models, such as ChatGPT, are another way that scientists are adding details to protein structure predictions. Zou used GPT-4 to “fine tune” a protein language model, called evolutionary scale modeling (ESM-2), which predicts protein structures directly from a protein sequence.
First, they trained ChatGPT on thousands of papers and studies containing information about the functions, biophysical properties, and disease relevance of different mutations. Next, they used the trained model to “teach” ESM-2, boosting its ability “to predict which mutations are likely to have larger effects or smaller effects,” Zou said. The same could be done for a model like AlphaFold, according to Zou.
“They are quite complementary in that the large language model contains a lot more information about the functions and the biophysics of different mutations and proteins as captured in text,” he said, whereas “you can’t give AlphaFold a piece of paper.”
Exactly how AlphaFold makes its predictions is another mystery. “It will somehow learn protein dynamics phenomenologically,” said Monteiro da Silva. He and others are trying to understand how that happens, in hopes of creating even more accurate predictive models. But for the time being, AI-based methods still need assistance from physics.
“The dream is that we achieve a state where we rely on just the fast methods, and they’re accurate enough,” he said. “But we’re so far from that.”
A version of this article first appeared on Medscape.com.
Smoking Cessation Offers Benefits at Any Age
This transcript has been edited for clarity.
I would like to briefly talk about a very interesting paper and one that probably has about as much to inform the doctor-patient relationship as any paper you can think of.
The title itself gives you a little bit of that answer before I even discuss the outcome. The paper is “The Benefits of Quitting Smoking at Different Ages,” recently published in The American Journal of Preventive Medicine.
I’m not going to even begin to attempt to explore the statistics of the analysis, but I think the conclusions are both fascinating and important. I will read the first sentence of the results and then just comment on some of the others because there’s just so much data here and I really want to focus on the punchline.
The results section said that, compared with people who never smoked, those who smoke currently, aged 35, 45, 55, 65, or 75, (those were all the groups they looked at), and who have smoked throughout adulthood until that age will lose an average of 9.1, 8.3, 7.3, 5.9, and 4.4 years of life, respectively — obviously, it’s a lot — if they continue to smoke for the rest of their lives.
We know that. It’s terrible. That’s why people should never smoke. Period. End of story. There’s no social value. There’s no health value of smoking. It’s a deadly recreational activity for multiple illnesses, and obviously, cancer is prominent among them.
Here’s the conclusion of the paper that I think is interesting. That doctor, whether it’s a primary care doctor, an oncologist, an ob/gyn, or a family doctor, is seeing Mr Smith or Mrs Jones in the office today, whether they know that patient well or not very well, and they’re still smoking. However, if the person we’re describing here quits smoking at these ages, how much life do they add back, compared with if they continued?
They may say: “Oh, I’ve been smoking all my life. What difference does it make? The die is cast.” Wrong! If you’ve been smoking your whole adult life — so let’s just say that you started at age 18, age 20, age 15, or even age 12 — but you quit smoking at the age of 35, you’re going to add 8 years of life on average. If you quit smoking when you’re 65, having smoked your whole adult life, you will add 1.7 years of life. That’s 1.7 years to be with your family, to be with your grandchildren, and enjoy life. If you ask, “Oh, what difference does it make?” It makes a big difference.
I’ll share another statistic and I’ll be done. I think this is really an interesting one. The chances of gaining at least a year of life among those who quit smoking at the age of 65 was 23.4%. There is a 1 out of 4 chance that you’re going to live an additional year if you stop at age 65. Even if you stop smoking at age 75, you have a 14% chance of living at least an additional year longer than you would have if you didn’t stop smoking.
There is much to think about here, much to consider, and much to discuss potentially with patients.
Dr. Markman is Professor of Medical Oncology and Therapeutics Research, City of Hope Comprehensive Cancer Center; President, Medicine & Science, City of Hope Atlanta, Chicago, Phoenix. He reported conflicts of interest with GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I would like to briefly talk about a very interesting paper and one that probably has about as much to inform the doctor-patient relationship as any paper you can think of.
The title itself gives you a little bit of that answer before I even discuss the outcome. The paper is “The Benefits of Quitting Smoking at Different Ages,” recently published in The American Journal of Preventive Medicine.
I’m not going to even begin to attempt to explore the statistics of the analysis, but I think the conclusions are both fascinating and important. I will read the first sentence of the results and then just comment on some of the others because there’s just so much data here and I really want to focus on the punchline.
The results section said that, compared with people who never smoked, those who smoke currently, aged 35, 45, 55, 65, or 75, (those were all the groups they looked at), and who have smoked throughout adulthood until that age will lose an average of 9.1, 8.3, 7.3, 5.9, and 4.4 years of life, respectively — obviously, it’s a lot — if they continue to smoke for the rest of their lives.
We know that. It’s terrible. That’s why people should never smoke. Period. End of story. There’s no social value. There’s no health value of smoking. It’s a deadly recreational activity for multiple illnesses, and obviously, cancer is prominent among them.
Here’s the conclusion of the paper that I think is interesting. That doctor, whether it’s a primary care doctor, an oncologist, an ob/gyn, or a family doctor, is seeing Mr Smith or Mrs Jones in the office today, whether they know that patient well or not very well, and they’re still smoking. However, if the person we’re describing here quits smoking at these ages, how much life do they add back, compared with if they continued?
They may say: “Oh, I’ve been smoking all my life. What difference does it make? The die is cast.” Wrong! If you’ve been smoking your whole adult life — so let’s just say that you started at age 18, age 20, age 15, or even age 12 — but you quit smoking at the age of 35, you’re going to add 8 years of life on average. If you quit smoking when you’re 65, having smoked your whole adult life, you will add 1.7 years of life. That’s 1.7 years to be with your family, to be with your grandchildren, and enjoy life. If you ask, “Oh, what difference does it make?” It makes a big difference.
I’ll share another statistic and I’ll be done. I think this is really an interesting one. The chances of gaining at least a year of life among those who quit smoking at the age of 65 was 23.4%. There is a 1 out of 4 chance that you’re going to live an additional year if you stop at age 65. Even if you stop smoking at age 75, you have a 14% chance of living at least an additional year longer than you would have if you didn’t stop smoking.
There is much to think about here, much to consider, and much to discuss potentially with patients.
Dr. Markman is Professor of Medical Oncology and Therapeutics Research, City of Hope Comprehensive Cancer Center; President, Medicine & Science, City of Hope Atlanta, Chicago, Phoenix. He reported conflicts of interest with GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I would like to briefly talk about a very interesting paper and one that probably has about as much to inform the doctor-patient relationship as any paper you can think of.
The title itself gives you a little bit of that answer before I even discuss the outcome. The paper is “The Benefits of Quitting Smoking at Different Ages,” recently published in The American Journal of Preventive Medicine.
I’m not going to even begin to attempt to explore the statistics of the analysis, but I think the conclusions are both fascinating and important. I will read the first sentence of the results and then just comment on some of the others because there’s just so much data here and I really want to focus on the punchline.
The results section said that, compared with people who never smoked, those who smoke currently, aged 35, 45, 55, 65, or 75, (those were all the groups they looked at), and who have smoked throughout adulthood until that age will lose an average of 9.1, 8.3, 7.3, 5.9, and 4.4 years of life, respectively — obviously, it’s a lot — if they continue to smoke for the rest of their lives.
We know that. It’s terrible. That’s why people should never smoke. Period. End of story. There’s no social value. There’s no health value of smoking. It’s a deadly recreational activity for multiple illnesses, and obviously, cancer is prominent among them.
Here’s the conclusion of the paper that I think is interesting. That doctor, whether it’s a primary care doctor, an oncologist, an ob/gyn, or a family doctor, is seeing Mr Smith or Mrs Jones in the office today, whether they know that patient well or not very well, and they’re still smoking. However, if the person we’re describing here quits smoking at these ages, how much life do they add back, compared with if they continued?
They may say: “Oh, I’ve been smoking all my life. What difference does it make? The die is cast.” Wrong! If you’ve been smoking your whole adult life — so let’s just say that you started at age 18, age 20, age 15, or even age 12 — but you quit smoking at the age of 35, you’re going to add 8 years of life on average. If you quit smoking when you’re 65, having smoked your whole adult life, you will add 1.7 years of life. That’s 1.7 years to be with your family, to be with your grandchildren, and enjoy life. If you ask, “Oh, what difference does it make?” It makes a big difference.
I’ll share another statistic and I’ll be done. I think this is really an interesting one. The chances of gaining at least a year of life among those who quit smoking at the age of 65 was 23.4%. There is a 1 out of 4 chance that you’re going to live an additional year if you stop at age 65. Even if you stop smoking at age 75, you have a 14% chance of living at least an additional year longer than you would have if you didn’t stop smoking.
There is much to think about here, much to consider, and much to discuss potentially with patients.
Dr. Markman is Professor of Medical Oncology and Therapeutics Research, City of Hope Comprehensive Cancer Center; President, Medicine & Science, City of Hope Atlanta, Chicago, Phoenix. He reported conflicts of interest with GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
Emerging Insights and Therapeutic Strategies for Large Cell Neuroendocrine Carcinoma of the Lung
Emerging Insights and Therapeutic Strategies for Large Cell Neuroendocrine Carcinoma of the Lung
Introduction
Large cell neuroendocrine carcinomas (LCNEC) of the lung are sufficiently rare that large trials to establish a standard of care are impractical. Treatment strategies effective for related malignancies, particularly small-cell lung cancer (SCLC), have been commonly applied to LCNEC of the lung, but it is important to recognize the unique features of LCNEC in order to make a diagnosis and to individualize treatment. As current long-term survival in patients with LCNEC of the lung remains poor, participation in clinical trials should be encouraged. Therapies under investigation include those targeted at the delta-like ligand 3 (DLL3), an antigen highly expressed in neuroendocrine (NE) tumors, and Seneca Valley oncolytic viral (SVV) therapy. Early introduction of palliative care should also be offered to optimize quality of life. High-quality data for LCNEC of the lung and novel breakthrough drugs are much needed.
Background
NE tumors can develop from NE cells in almost any organ.1 After the gastrointestinal tract, the lung is the most common site of NE malignancies. They account for only about 2% of all lung cancers but 25% of NE tumors.2 Criteria for differentiating NE tumors from other tumors in the lung were first proposed in 1991.3 In 2022, the World Health Organization described 5 major subtypes of NE lung malignancies.4 On a spectrum ranging from best to worst outcome among lung cancers, LCNEC has a significantly more aggressive course compared with typical carcinoids (TC) and atypical carcinoids (AC), approaching that of SCLC, which arguably has the worst outcome (Table).5
Table. Comparing NSCLC, SCLC, and LCNEC of the Lung
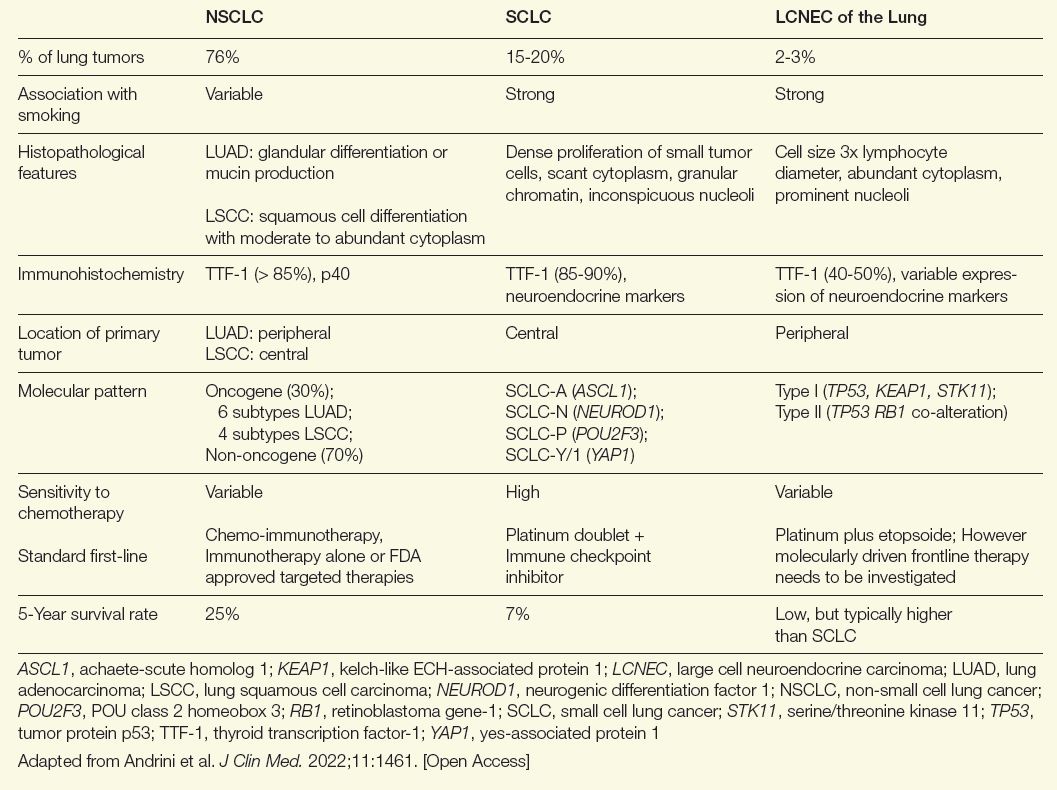
Similarities exist between LCNEC of the lung and other non-small cell lung cancer (NSCLC) types, but there are more parallels with SCLC. Both are more common in male patients and both are associated with a history of smoking.6 They also share a poor prognosis. If diagnosed at an advanced stage, 5-year survival rates for LCNEC of the lung and SCLC have been reported to be as low as 5% to 15%.6
The risk of a delay in establishing the correct diagnosis of LCNEC of the lung, even by experienced pathologists, is considerable. The key diagnostic criteria include expression of at least 1 NE marker, such as chromogranin-A or synaptophysin, a high proliferation rate (> 10 mitoses per high-power field), extensive necrosis, and NE morphology features, such as trabeculae and palisading and rosette formations.7 However, other lung cancers can also express NE markers and some features might be missed without relatively large tissue specimens.7
To improve diagnostic accuracy, additional criteria, such as absence of squamous or adenocarcinoma features or the demonstration of 2 or more NE markers are now being advocated in some reports,8 while others have advocated that terms such as “combined NSCLC/SCLC” should not be accepted as a substitute for differentiating and finalizing a diagnosis of LCNEC of the lung.7 Excisional or resection biopsies, as opposed to needle biopsies, might be required to obtain an adequate tissue sample to reach a definitive diagnosis.
Illustrating the potential for confusion with other lung cancers, LCNEC of the lung can be characterized by 2 subtypes.9 Type 1 is characterized by TP53 and STK11/KEAP1 alternations—similar to adenocarcinomas and squamous cell lung cancers—and it is associated with a higher expression of NE markers, such as ASCL1 and DLL3. Type 2 is typically characterized by inactivation of TP53 and RB1. Ultimately, type I LCNEC of the lung has a mutational pattern similar to NSCLC and type II has a pattern similar to SCLC. While LCNEC is typically located in the periphery of the lung, SCLC is typically centrally located and NSCLC can be found in either location. Complicated further by the fact that a proportion of these tumors have features shared with SCLC and rarer cancers, such as spindle-cell carcinoma and giant cell carcinoma, LCNEC should be considered in the differential diagnosis of any lung cancer with ambiguous features.7
For these reasons, a pathology review should be performed at a high-volume center whenever possible. As part of the diagnostic process, molecular testing should be gathered for all patients whether or not it is required to make or confirm the diagnosis. This information will be informative for guiding treatment, particularly second- and third-line interventions. Rather than being unique and definitive, the individual features of LCNEC of the lung—including the genetic, molecular, histologic, and morphologic characteristics—cumulatively support the diagnosis. After establishing a pathological diagnosis, staging of LCNEC of the lung is paramount. In addition, distinctions between the grades of LCNEC of the lung are relative. For example, tumors with a better relative prognosis typically have fewer gene mutations than tumors with a worse relative prognosis, but mutations are generally found in both.
Bronchoscopy with endobronchial ultrasound can be considered for both diagnosis and staging of locally advanced tumors, but a surgical specimen might still be required for a definitive diagnosis. Differentiating local LCNEC, which has been reported in about 25% of cases, from locally advanced and metastatic disease is critical for planning treatment. Fluorodeoxyglucose F18 (FDG) positron emission tomography (PET) plays an important role in staging LCNEC of the lung. Unlike TC and AC, for LCNEC of the lung there is a very limited role of somatostatin receptor agonist-based imaging or tetraazacyclododecanetetraacetic acid-DPhel-Tyr3-octreotate (DOTATATE) PET during diagnostic workup.
Therapeutic Strategies
In early stages, resection followed by adjuvant chemotherapy has long been used for LCNEC of the lung. Studies evaluating this approach, such as one that combined cisplatin and etoposide,10 suggest doublet chemotherapy after surgery offers a benefit in LCNEC of the lung comparable to that seen in SCLC. There is limited support for adjunctive radiotherapy in early-stage LCNEC of the lung,5 even if radiotherapy has shown benefit for patients ineligible for surgery.11
In locally advanced and advanced LCNEC (≥ stage III-B) ineligible for resection, chemoradiation has been associated with a survival advantage over chemotherapy alone,12 but due to the high rates of relapse and limited survival, efforts to move to novel therapies have been expanding for both LCNEC of the lung and SCLC. This includes immunotherapies used before or after chemoradiation. Again, much of the interest in immunotherapies has been derived from studies in SCLC, but several small studies have associated checkpoint inhibitors with substantial antitumor activity in patients with LCNEC.13,14 There are no large scale prospective trials to determine the optimal treatment in the first line setting for LCNEC of the lung and most data is extrapolated from treatment of ES-SCLC. In a retrospective study, however, comparing survival of palliative chemotherapy with a SCLC versus a NSCLC regimen, the SCLC regimen was favored.15
Following a pivotal trial of tarlatamab-dlle, that led to an accelerated approval for extensive-stage SCLC in May 2024,16 this drug has also been evaluated in a small group of patients with LCNEC of the lung. The parallels between LCNEC and SCLC have raised hope that this drug, which is a bispecific T-cell engager (BiTE) that binds to the DLL3 ligand and CD3, may provide benefit in LCNEC of the lung that is commensurate with the benefit seen in SCLC. A recently published LCNEC case study supports this potential.17 A high-grade NE-carcinoma-specific oncolytic virus called Seneca Valley virus holds promise. Preclinical data suggest encouraging anticancer activity when SVV is combined with immune checkpoint inhibitor therapy.18 SVV seems to attack cancer cells that express tumor endothelial marker 8 (TEM-8), making it an interesting target in future efforts for screening and tailoring treatment.19 Human studies are in development.
Due to the high frequency of relapse regardless of frontline therapies, there is also growing interest in maintenance strategies to extend disease control. Maintenance regimens that have been evaluated or are being considered include immunotherapies, even if the optimal sequence of treatment modalities remains unknown. The high rate of relapse also encourages early planning of sequential therapies based on molecular testing. Numerous studies of LCNEC of the lung have now identified activating mutations in targetable pathways, such as P13K/AKT/mTOR, KRAS, and FGFR1.18 Patients may also harbor a high tumor mutation burden, a characteristic that might favor treatment with immunotherapy. Each mutation is relevant to only a small proportion of patients with LCNEC. However, when all potentially targetable mutations are considered together, the proportion of patients with LCNEC who would benefit from an individualized therapy is substantial, thus supporting trials of individualized therapy, particularly in the second line.
The high rate of relapse with currently available therapies encourages enrollment in clinical trials, particularly among patients who have already failed a first-line strategy. In the United States, studies are enrolling patients with LCNEC of the lung for checkpoint inhibitors with or without combination chemotherapy, novel BiTE therapies, and novel therapies targeting specific activating pathways. Many of these trials offer enrollment to patients with either SCLC or LCNEC.
Due to poor survival, patients with advancing LCNEC of the lung should be considered for palliative care. Although no guideline protocol exists for palliative care, the American Society of Clinical Oncology recommends palliative care for all individuals with advanced cancer based on evidence of improved quality of life and, in some cases, survival.20
Summary
LCNEC is an uncommon lung malignancy with a poor prognosis in the advanced stages at which it is most often recognized. The risk of overlooking this cancer in the initial diagnosis emphasizes the need for an adequate index of suspicion and familiarity with its distinguishing characteristics. Treatments of LCNEC of the lung have been largely based on those used for SCLC, but there has been an evolution in the understanding of this disease, which includes a greater appreciation for heterogeneity among driving mutations, a growing interest in maintenance therapies to extend the time to relapse, and trials of a growing array of novel therapies, including immunotherapies and BiTEs. Early intervention with these novel therapies and an emphasis on palliative care is needed because LCNEC has such an aggressive course.
Read more from the 2024 Rare Diseases Report: Hematology and Oncology.
- Sultana Q, Kar J, Verma A, et al. A comprehensive review on neuroendocrine neoplasms: presentation, pathophysiology and management. J Clin Med. 2023;12(15):5138. doi:10.3390/jcm12155138
- Gustafsson BI, Kidd M, Chan A, Malfertheiner MV, Modlin IM. Bronchopulmonary neuroendocrine tumors. Cancer. 2008;113(1):5-21. doi:10.1002/cncr.23542
- Travis WD, Linnoila RI, Tsokos MG, et al. Neuroendocrine tumors of the lung with proposed criteria for large-cell neuroendocrine carcinoma. An ultrastructural, immunohistochemical, and flow cytometric study of 35 cases. Am J Surg Pathol. 1991;15(6):529-553. doi:10.1097/00000478-199106000-00003
- Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG. Introduction to the 2015 World Health Organization classification of tumors of the lung, pleura, thymus, and heart. J Thorac Oncol. 2015;10(9):1240-1242. doi:10.1097/JTO.0000000000000663
- Andrini E, Marchese PV, De Biase D, et al. Large cell neuroendocrine carcinoma of the lung: current understanding and challenges. J Clin Med. 2022;11(5):1461. doi:10.3390/jcm11051461
- Lantuejoul S, Fernandez-Cuesta L, Damiola F, Girard N, McLeer A. New molecular classification of large cell neuroendocrine carcinoma and small cell lung carcinoma with potential therapeutic impacts. Transl Lung Cancer Res. 2020;9(5):2233-2244. doi:10.21037/tlcr-20-269
- Lindsay CR, Shaw EC, Moore DA, et al. Large cell neuroendocrine lung carcinoma: consensus statement from The British Thoracic Oncology Group and the Association of Pulmonary Pathologists. Br J Cancer. 2021;125(9):1210-1216. doi:10.1038/s41416-021-01407-9
- Derks JL, Dingemans AC, van Suylen RJ, et al. Is the sum of positive neuroendocrine immunohistochemical stains useful for diagnosis of large cell neuroendocrine carcinoma (LCNEC) on biopsy specimens? Histopathology. 2019;74(4):555-566. doi:10.1111/his.13800
- George J, Walter V, Peifer M, et al. Integrative genomic profiling of large-cell neuroendocrine carcinomas reveals distinct subtypes of high-grade neuroendocrine lung tumors. Nat Commun. 2018;9(1):1048. doi:10.1038/s41467-018-03099-x
- Iyoda A, Hiroshima K, Moriya Y, et al. Prospective study of adjuvant chemotherapy for pulmonary large cell neuroendocrine carcinoma. Ann Thorac Surg. 2006;82(5):1802-1807. doi:10.1016/j.athoracsur.2006.05.109
- Cao L, Wu HF, Zhao L, et al. The role of radiotherapy in pulmonary large cell neuroendocrine carcinoma: propensity score matching analysis. J Radiat Res. 2020;61(4):594-601. doi:10.1093/jrr/rraa036
- Limonnik V, Abel S, Finley GG, Long GS, Wegner RE. Factors associated with treatment receipt and overall survival for patients with locally advanced large cell neuroendocrine carcinoma of the lung: a National Cancer Database analysis. Lung Cancer. 2020;150:107-113. doi:10.1016/j.lungcan.2020.10.001
- Shi Z, Wei J, Xu M, Song Z. Efficacy and safety of immune checkpoint inhibitors in lung large-cell neuroendocrine carcinoma. J Thorac Dis. 2023;15(8):4172-4181. doi:10.21037/jtd-23-348
- Chauhan A, Arnold SM, Kolesar J, Thomas HE, Evers M, Anthony L. Immune checkpoint inhibitors in large cell neuroendocrine carcinoma: current status. Oncotarget. 2018;9(18):14738-14740. doi:10.18632/oncotarget.24553
- Chen H, Ishihara M, Horita N, et al. Effect of adjuvant and palliative chemotherapy in large cell neuroendocrine carcinoma of the lung: a systematic review and metaanalysis. Cancers (Basel). 2021;13(23):5948. doi:10.3390/cancers13235948
- Ahn MJ, Cho BC, Felip E, et al. Tarlatamab for patients with previously treated small-cell lung cancer. N Engl J Med. 2023;389(22):2063-2075. doi:10.1056/NEJMoa2307980
- Patel SA, Whang Y, Medley C, et al. Tartalamab for large-cell neuroendocrine carcinoma in a young adult: a case report. JTO Clin Res Rep. 2024;5(10):100712. doi:10.1016/j.jtocrr.2024.100712
- Corbett V, Hallenbeck P, Rychahou P, Chauhan A. Evolving role of Seneca Valley virus and its biomarker TEM8/ANTXR1 in cancer therapeutics. Front Mol Biosci. 2022;9:930207. doi:10.3389/fmolb.2022.930207
- Kareff SA, Corbett V, Hallenbeck P, Chauhan A. TEM8 in oncogenesis: protein biology, pre-clinical agents, and clinical rationale. Cells. 2023;12(22):2623. doi:10.3390/cells12222623
- Sanders JJ, Temin S, Ghoshal A, et al. Palliative care for patients with cancer: ASCO guideline update. J Clin Oncol. 2024;42(19):2336-2357. doi:10.1200/JCO.24.00542
Introduction
Large cell neuroendocrine carcinomas (LCNEC) of the lung are sufficiently rare that large trials to establish a standard of care are impractical. Treatment strategies effective for related malignancies, particularly small-cell lung cancer (SCLC), have been commonly applied to LCNEC of the lung, but it is important to recognize the unique features of LCNEC in order to make a diagnosis and to individualize treatment. As current long-term survival in patients with LCNEC of the lung remains poor, participation in clinical trials should be encouraged. Therapies under investigation include those targeted at the delta-like ligand 3 (DLL3), an antigen highly expressed in neuroendocrine (NE) tumors, and Seneca Valley oncolytic viral (SVV) therapy. Early introduction of palliative care should also be offered to optimize quality of life. High-quality data for LCNEC of the lung and novel breakthrough drugs are much needed.
Background
NE tumors can develop from NE cells in almost any organ.1 After the gastrointestinal tract, the lung is the most common site of NE malignancies. They account for only about 2% of all lung cancers but 25% of NE tumors.2 Criteria for differentiating NE tumors from other tumors in the lung were first proposed in 1991.3 In 2022, the World Health Organization described 5 major subtypes of NE lung malignancies.4 On a spectrum ranging from best to worst outcome among lung cancers, LCNEC has a significantly more aggressive course compared with typical carcinoids (TC) and atypical carcinoids (AC), approaching that of SCLC, which arguably has the worst outcome (Table).5
Table. Comparing NSCLC, SCLC, and LCNEC of the Lung
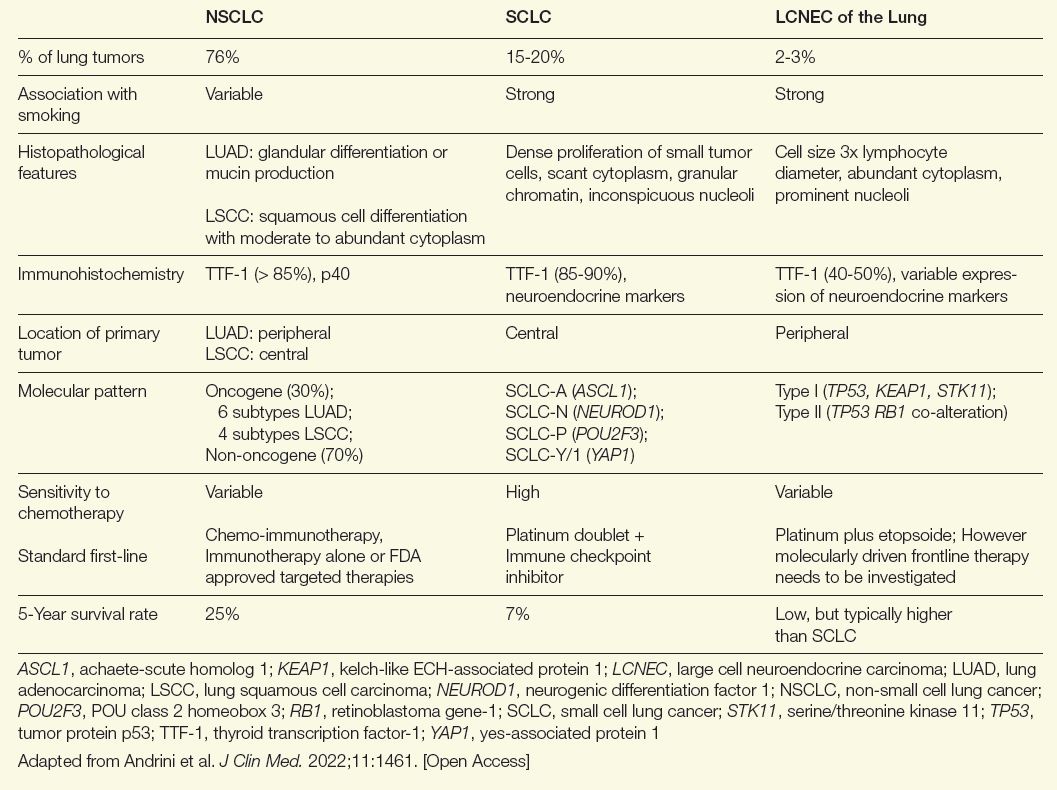
Similarities exist between LCNEC of the lung and other non-small cell lung cancer (NSCLC) types, but there are more parallels with SCLC. Both are more common in male patients and both are associated with a history of smoking.6 They also share a poor prognosis. If diagnosed at an advanced stage, 5-year survival rates for LCNEC of the lung and SCLC have been reported to be as low as 5% to 15%.6
The risk of a delay in establishing the correct diagnosis of LCNEC of the lung, even by experienced pathologists, is considerable. The key diagnostic criteria include expression of at least 1 NE marker, such as chromogranin-A or synaptophysin, a high proliferation rate (> 10 mitoses per high-power field), extensive necrosis, and NE morphology features, such as trabeculae and palisading and rosette formations.7 However, other lung cancers can also express NE markers and some features might be missed without relatively large tissue specimens.7
To improve diagnostic accuracy, additional criteria, such as absence of squamous or adenocarcinoma features or the demonstration of 2 or more NE markers are now being advocated in some reports,8 while others have advocated that terms such as “combined NSCLC/SCLC” should not be accepted as a substitute for differentiating and finalizing a diagnosis of LCNEC of the lung.7 Excisional or resection biopsies, as opposed to needle biopsies, might be required to obtain an adequate tissue sample to reach a definitive diagnosis.
Illustrating the potential for confusion with other lung cancers, LCNEC of the lung can be characterized by 2 subtypes.9 Type 1 is characterized by TP53 and STK11/KEAP1 alternations—similar to adenocarcinomas and squamous cell lung cancers—and it is associated with a higher expression of NE markers, such as ASCL1 and DLL3. Type 2 is typically characterized by inactivation of TP53 and RB1. Ultimately, type I LCNEC of the lung has a mutational pattern similar to NSCLC and type II has a pattern similar to SCLC. While LCNEC is typically located in the periphery of the lung, SCLC is typically centrally located and NSCLC can be found in either location. Complicated further by the fact that a proportion of these tumors have features shared with SCLC and rarer cancers, such as spindle-cell carcinoma and giant cell carcinoma, LCNEC should be considered in the differential diagnosis of any lung cancer with ambiguous features.7
For these reasons, a pathology review should be performed at a high-volume center whenever possible. As part of the diagnostic process, molecular testing should be gathered for all patients whether or not it is required to make or confirm the diagnosis. This information will be informative for guiding treatment, particularly second- and third-line interventions. Rather than being unique and definitive, the individual features of LCNEC of the lung—including the genetic, molecular, histologic, and morphologic characteristics—cumulatively support the diagnosis. After establishing a pathological diagnosis, staging of LCNEC of the lung is paramount. In addition, distinctions between the grades of LCNEC of the lung are relative. For example, tumors with a better relative prognosis typically have fewer gene mutations than tumors with a worse relative prognosis, but mutations are generally found in both.
Bronchoscopy with endobronchial ultrasound can be considered for both diagnosis and staging of locally advanced tumors, but a surgical specimen might still be required for a definitive diagnosis. Differentiating local LCNEC, which has been reported in about 25% of cases, from locally advanced and metastatic disease is critical for planning treatment. Fluorodeoxyglucose F18 (FDG) positron emission tomography (PET) plays an important role in staging LCNEC of the lung. Unlike TC and AC, for LCNEC of the lung there is a very limited role of somatostatin receptor agonist-based imaging or tetraazacyclododecanetetraacetic acid-DPhel-Tyr3-octreotate (DOTATATE) PET during diagnostic workup.
Therapeutic Strategies
In early stages, resection followed by adjuvant chemotherapy has long been used for LCNEC of the lung. Studies evaluating this approach, such as one that combined cisplatin and etoposide,10 suggest doublet chemotherapy after surgery offers a benefit in LCNEC of the lung comparable to that seen in SCLC. There is limited support for adjunctive radiotherapy in early-stage LCNEC of the lung,5 even if radiotherapy has shown benefit for patients ineligible for surgery.11
In locally advanced and advanced LCNEC (≥ stage III-B) ineligible for resection, chemoradiation has been associated with a survival advantage over chemotherapy alone,12 but due to the high rates of relapse and limited survival, efforts to move to novel therapies have been expanding for both LCNEC of the lung and SCLC. This includes immunotherapies used before or after chemoradiation. Again, much of the interest in immunotherapies has been derived from studies in SCLC, but several small studies have associated checkpoint inhibitors with substantial antitumor activity in patients with LCNEC.13,14 There are no large scale prospective trials to determine the optimal treatment in the first line setting for LCNEC of the lung and most data is extrapolated from treatment of ES-SCLC. In a retrospective study, however, comparing survival of palliative chemotherapy with a SCLC versus a NSCLC regimen, the SCLC regimen was favored.15
Following a pivotal trial of tarlatamab-dlle, that led to an accelerated approval for extensive-stage SCLC in May 2024,16 this drug has also been evaluated in a small group of patients with LCNEC of the lung. The parallels between LCNEC and SCLC have raised hope that this drug, which is a bispecific T-cell engager (BiTE) that binds to the DLL3 ligand and CD3, may provide benefit in LCNEC of the lung that is commensurate with the benefit seen in SCLC. A recently published LCNEC case study supports this potential.17 A high-grade NE-carcinoma-specific oncolytic virus called Seneca Valley virus holds promise. Preclinical data suggest encouraging anticancer activity when SVV is combined with immune checkpoint inhibitor therapy.18 SVV seems to attack cancer cells that express tumor endothelial marker 8 (TEM-8), making it an interesting target in future efforts for screening and tailoring treatment.19 Human studies are in development.
Due to the high frequency of relapse regardless of frontline therapies, there is also growing interest in maintenance strategies to extend disease control. Maintenance regimens that have been evaluated or are being considered include immunotherapies, even if the optimal sequence of treatment modalities remains unknown. The high rate of relapse also encourages early planning of sequential therapies based on molecular testing. Numerous studies of LCNEC of the lung have now identified activating mutations in targetable pathways, such as P13K/AKT/mTOR, KRAS, and FGFR1.18 Patients may also harbor a high tumor mutation burden, a characteristic that might favor treatment with immunotherapy. Each mutation is relevant to only a small proportion of patients with LCNEC. However, when all potentially targetable mutations are considered together, the proportion of patients with LCNEC who would benefit from an individualized therapy is substantial, thus supporting trials of individualized therapy, particularly in the second line.
The high rate of relapse with currently available therapies encourages enrollment in clinical trials, particularly among patients who have already failed a first-line strategy. In the United States, studies are enrolling patients with LCNEC of the lung for checkpoint inhibitors with or without combination chemotherapy, novel BiTE therapies, and novel therapies targeting specific activating pathways. Many of these trials offer enrollment to patients with either SCLC or LCNEC.
Due to poor survival, patients with advancing LCNEC of the lung should be considered for palliative care. Although no guideline protocol exists for palliative care, the American Society of Clinical Oncology recommends palliative care for all individuals with advanced cancer based on evidence of improved quality of life and, in some cases, survival.20
Summary
LCNEC is an uncommon lung malignancy with a poor prognosis in the advanced stages at which it is most often recognized. The risk of overlooking this cancer in the initial diagnosis emphasizes the need for an adequate index of suspicion and familiarity with its distinguishing characteristics. Treatments of LCNEC of the lung have been largely based on those used for SCLC, but there has been an evolution in the understanding of this disease, which includes a greater appreciation for heterogeneity among driving mutations, a growing interest in maintenance therapies to extend the time to relapse, and trials of a growing array of novel therapies, including immunotherapies and BiTEs. Early intervention with these novel therapies and an emphasis on palliative care is needed because LCNEC has such an aggressive course.
Read more from the 2024 Rare Diseases Report: Hematology and Oncology.
Introduction
Large cell neuroendocrine carcinomas (LCNEC) of the lung are sufficiently rare that large trials to establish a standard of care are impractical. Treatment strategies effective for related malignancies, particularly small-cell lung cancer (SCLC), have been commonly applied to LCNEC of the lung, but it is important to recognize the unique features of LCNEC in order to make a diagnosis and to individualize treatment. As current long-term survival in patients with LCNEC of the lung remains poor, participation in clinical trials should be encouraged. Therapies under investigation include those targeted at the delta-like ligand 3 (DLL3), an antigen highly expressed in neuroendocrine (NE) tumors, and Seneca Valley oncolytic viral (SVV) therapy. Early introduction of palliative care should also be offered to optimize quality of life. High-quality data for LCNEC of the lung and novel breakthrough drugs are much needed.
Background
NE tumors can develop from NE cells in almost any organ.1 After the gastrointestinal tract, the lung is the most common site of NE malignancies. They account for only about 2% of all lung cancers but 25% of NE tumors.2 Criteria for differentiating NE tumors from other tumors in the lung were first proposed in 1991.3 In 2022, the World Health Organization described 5 major subtypes of NE lung malignancies.4 On a spectrum ranging from best to worst outcome among lung cancers, LCNEC has a significantly more aggressive course compared with typical carcinoids (TC) and atypical carcinoids (AC), approaching that of SCLC, which arguably has the worst outcome (Table).5
Table. Comparing NSCLC, SCLC, and LCNEC of the Lung
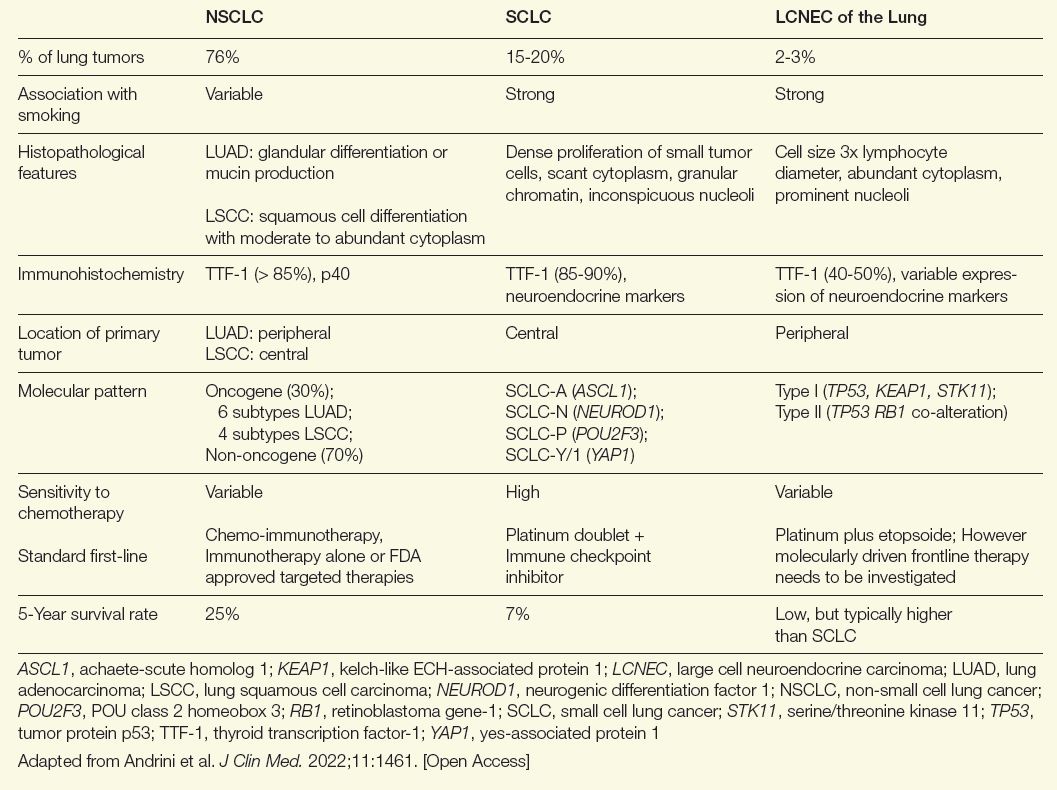
Similarities exist between LCNEC of the lung and other non-small cell lung cancer (NSCLC) types, but there are more parallels with SCLC. Both are more common in male patients and both are associated with a history of smoking.6 They also share a poor prognosis. If diagnosed at an advanced stage, 5-year survival rates for LCNEC of the lung and SCLC have been reported to be as low as 5% to 15%.6
The risk of a delay in establishing the correct diagnosis of LCNEC of the lung, even by experienced pathologists, is considerable. The key diagnostic criteria include expression of at least 1 NE marker, such as chromogranin-A or synaptophysin, a high proliferation rate (> 10 mitoses per high-power field), extensive necrosis, and NE morphology features, such as trabeculae and palisading and rosette formations.7 However, other lung cancers can also express NE markers and some features might be missed without relatively large tissue specimens.7
To improve diagnostic accuracy, additional criteria, such as absence of squamous or adenocarcinoma features or the demonstration of 2 or more NE markers are now being advocated in some reports,8 while others have advocated that terms such as “combined NSCLC/SCLC” should not be accepted as a substitute for differentiating and finalizing a diagnosis of LCNEC of the lung.7 Excisional or resection biopsies, as opposed to needle biopsies, might be required to obtain an adequate tissue sample to reach a definitive diagnosis.
Illustrating the potential for confusion with other lung cancers, LCNEC of the lung can be characterized by 2 subtypes.9 Type 1 is characterized by TP53 and STK11/KEAP1 alternations—similar to adenocarcinomas and squamous cell lung cancers—and it is associated with a higher expression of NE markers, such as ASCL1 and DLL3. Type 2 is typically characterized by inactivation of TP53 and RB1. Ultimately, type I LCNEC of the lung has a mutational pattern similar to NSCLC and type II has a pattern similar to SCLC. While LCNEC is typically located in the periphery of the lung, SCLC is typically centrally located and NSCLC can be found in either location. Complicated further by the fact that a proportion of these tumors have features shared with SCLC and rarer cancers, such as spindle-cell carcinoma and giant cell carcinoma, LCNEC should be considered in the differential diagnosis of any lung cancer with ambiguous features.7
For these reasons, a pathology review should be performed at a high-volume center whenever possible. As part of the diagnostic process, molecular testing should be gathered for all patients whether or not it is required to make or confirm the diagnosis. This information will be informative for guiding treatment, particularly second- and third-line interventions. Rather than being unique and definitive, the individual features of LCNEC of the lung—including the genetic, molecular, histologic, and morphologic characteristics—cumulatively support the diagnosis. After establishing a pathological diagnosis, staging of LCNEC of the lung is paramount. In addition, distinctions between the grades of LCNEC of the lung are relative. For example, tumors with a better relative prognosis typically have fewer gene mutations than tumors with a worse relative prognosis, but mutations are generally found in both.
Bronchoscopy with endobronchial ultrasound can be considered for both diagnosis and staging of locally advanced tumors, but a surgical specimen might still be required for a definitive diagnosis. Differentiating local LCNEC, which has been reported in about 25% of cases, from locally advanced and metastatic disease is critical for planning treatment. Fluorodeoxyglucose F18 (FDG) positron emission tomography (PET) plays an important role in staging LCNEC of the lung. Unlike TC and AC, for LCNEC of the lung there is a very limited role of somatostatin receptor agonist-based imaging or tetraazacyclododecanetetraacetic acid-DPhel-Tyr3-octreotate (DOTATATE) PET during diagnostic workup.
Therapeutic Strategies
In early stages, resection followed by adjuvant chemotherapy has long been used for LCNEC of the lung. Studies evaluating this approach, such as one that combined cisplatin and etoposide,10 suggest doublet chemotherapy after surgery offers a benefit in LCNEC of the lung comparable to that seen in SCLC. There is limited support for adjunctive radiotherapy in early-stage LCNEC of the lung,5 even if radiotherapy has shown benefit for patients ineligible for surgery.11
In locally advanced and advanced LCNEC (≥ stage III-B) ineligible for resection, chemoradiation has been associated with a survival advantage over chemotherapy alone,12 but due to the high rates of relapse and limited survival, efforts to move to novel therapies have been expanding for both LCNEC of the lung and SCLC. This includes immunotherapies used before or after chemoradiation. Again, much of the interest in immunotherapies has been derived from studies in SCLC, but several small studies have associated checkpoint inhibitors with substantial antitumor activity in patients with LCNEC.13,14 There are no large scale prospective trials to determine the optimal treatment in the first line setting for LCNEC of the lung and most data is extrapolated from treatment of ES-SCLC. In a retrospective study, however, comparing survival of palliative chemotherapy with a SCLC versus a NSCLC regimen, the SCLC regimen was favored.15
Following a pivotal trial of tarlatamab-dlle, that led to an accelerated approval for extensive-stage SCLC in May 2024,16 this drug has also been evaluated in a small group of patients with LCNEC of the lung. The parallels between LCNEC and SCLC have raised hope that this drug, which is a bispecific T-cell engager (BiTE) that binds to the DLL3 ligand and CD3, may provide benefit in LCNEC of the lung that is commensurate with the benefit seen in SCLC. A recently published LCNEC case study supports this potential.17 A high-grade NE-carcinoma-specific oncolytic virus called Seneca Valley virus holds promise. Preclinical data suggest encouraging anticancer activity when SVV is combined with immune checkpoint inhibitor therapy.18 SVV seems to attack cancer cells that express tumor endothelial marker 8 (TEM-8), making it an interesting target in future efforts for screening and tailoring treatment.19 Human studies are in development.
Due to the high frequency of relapse regardless of frontline therapies, there is also growing interest in maintenance strategies to extend disease control. Maintenance regimens that have been evaluated or are being considered include immunotherapies, even if the optimal sequence of treatment modalities remains unknown. The high rate of relapse also encourages early planning of sequential therapies based on molecular testing. Numerous studies of LCNEC of the lung have now identified activating mutations in targetable pathways, such as P13K/AKT/mTOR, KRAS, and FGFR1.18 Patients may also harbor a high tumor mutation burden, a characteristic that might favor treatment with immunotherapy. Each mutation is relevant to only a small proportion of patients with LCNEC. However, when all potentially targetable mutations are considered together, the proportion of patients with LCNEC who would benefit from an individualized therapy is substantial, thus supporting trials of individualized therapy, particularly in the second line.
The high rate of relapse with currently available therapies encourages enrollment in clinical trials, particularly among patients who have already failed a first-line strategy. In the United States, studies are enrolling patients with LCNEC of the lung for checkpoint inhibitors with or without combination chemotherapy, novel BiTE therapies, and novel therapies targeting specific activating pathways. Many of these trials offer enrollment to patients with either SCLC or LCNEC.
Due to poor survival, patients with advancing LCNEC of the lung should be considered for palliative care. Although no guideline protocol exists for palliative care, the American Society of Clinical Oncology recommends palliative care for all individuals with advanced cancer based on evidence of improved quality of life and, in some cases, survival.20
Summary
LCNEC is an uncommon lung malignancy with a poor prognosis in the advanced stages at which it is most often recognized. The risk of overlooking this cancer in the initial diagnosis emphasizes the need for an adequate index of suspicion and familiarity with its distinguishing characteristics. Treatments of LCNEC of the lung have been largely based on those used for SCLC, but there has been an evolution in the understanding of this disease, which includes a greater appreciation for heterogeneity among driving mutations, a growing interest in maintenance therapies to extend the time to relapse, and trials of a growing array of novel therapies, including immunotherapies and BiTEs. Early intervention with these novel therapies and an emphasis on palliative care is needed because LCNEC has such an aggressive course.
Read more from the 2024 Rare Diseases Report: Hematology and Oncology.
- Sultana Q, Kar J, Verma A, et al. A comprehensive review on neuroendocrine neoplasms: presentation, pathophysiology and management. J Clin Med. 2023;12(15):5138. doi:10.3390/jcm12155138
- Gustafsson BI, Kidd M, Chan A, Malfertheiner MV, Modlin IM. Bronchopulmonary neuroendocrine tumors. Cancer. 2008;113(1):5-21. doi:10.1002/cncr.23542
- Travis WD, Linnoila RI, Tsokos MG, et al. Neuroendocrine tumors of the lung with proposed criteria for large-cell neuroendocrine carcinoma. An ultrastructural, immunohistochemical, and flow cytometric study of 35 cases. Am J Surg Pathol. 1991;15(6):529-553. doi:10.1097/00000478-199106000-00003
- Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG. Introduction to the 2015 World Health Organization classification of tumors of the lung, pleura, thymus, and heart. J Thorac Oncol. 2015;10(9):1240-1242. doi:10.1097/JTO.0000000000000663
- Andrini E, Marchese PV, De Biase D, et al. Large cell neuroendocrine carcinoma of the lung: current understanding and challenges. J Clin Med. 2022;11(5):1461. doi:10.3390/jcm11051461
- Lantuejoul S, Fernandez-Cuesta L, Damiola F, Girard N, McLeer A. New molecular classification of large cell neuroendocrine carcinoma and small cell lung carcinoma with potential therapeutic impacts. Transl Lung Cancer Res. 2020;9(5):2233-2244. doi:10.21037/tlcr-20-269
- Lindsay CR, Shaw EC, Moore DA, et al. Large cell neuroendocrine lung carcinoma: consensus statement from The British Thoracic Oncology Group and the Association of Pulmonary Pathologists. Br J Cancer. 2021;125(9):1210-1216. doi:10.1038/s41416-021-01407-9
- Derks JL, Dingemans AC, van Suylen RJ, et al. Is the sum of positive neuroendocrine immunohistochemical stains useful for diagnosis of large cell neuroendocrine carcinoma (LCNEC) on biopsy specimens? Histopathology. 2019;74(4):555-566. doi:10.1111/his.13800
- George J, Walter V, Peifer M, et al. Integrative genomic profiling of large-cell neuroendocrine carcinomas reveals distinct subtypes of high-grade neuroendocrine lung tumors. Nat Commun. 2018;9(1):1048. doi:10.1038/s41467-018-03099-x
- Iyoda A, Hiroshima K, Moriya Y, et al. Prospective study of adjuvant chemotherapy for pulmonary large cell neuroendocrine carcinoma. Ann Thorac Surg. 2006;82(5):1802-1807. doi:10.1016/j.athoracsur.2006.05.109
- Cao L, Wu HF, Zhao L, et al. The role of radiotherapy in pulmonary large cell neuroendocrine carcinoma: propensity score matching analysis. J Radiat Res. 2020;61(4):594-601. doi:10.1093/jrr/rraa036
- Limonnik V, Abel S, Finley GG, Long GS, Wegner RE. Factors associated with treatment receipt and overall survival for patients with locally advanced large cell neuroendocrine carcinoma of the lung: a National Cancer Database analysis. Lung Cancer. 2020;150:107-113. doi:10.1016/j.lungcan.2020.10.001
- Shi Z, Wei J, Xu M, Song Z. Efficacy and safety of immune checkpoint inhibitors in lung large-cell neuroendocrine carcinoma. J Thorac Dis. 2023;15(8):4172-4181. doi:10.21037/jtd-23-348
- Chauhan A, Arnold SM, Kolesar J, Thomas HE, Evers M, Anthony L. Immune checkpoint inhibitors in large cell neuroendocrine carcinoma: current status. Oncotarget. 2018;9(18):14738-14740. doi:10.18632/oncotarget.24553
- Chen H, Ishihara M, Horita N, et al. Effect of adjuvant and palliative chemotherapy in large cell neuroendocrine carcinoma of the lung: a systematic review and metaanalysis. Cancers (Basel). 2021;13(23):5948. doi:10.3390/cancers13235948
- Ahn MJ, Cho BC, Felip E, et al. Tarlatamab for patients with previously treated small-cell lung cancer. N Engl J Med. 2023;389(22):2063-2075. doi:10.1056/NEJMoa2307980
- Patel SA, Whang Y, Medley C, et al. Tartalamab for large-cell neuroendocrine carcinoma in a young adult: a case report. JTO Clin Res Rep. 2024;5(10):100712. doi:10.1016/j.jtocrr.2024.100712
- Corbett V, Hallenbeck P, Rychahou P, Chauhan A. Evolving role of Seneca Valley virus and its biomarker TEM8/ANTXR1 in cancer therapeutics. Front Mol Biosci. 2022;9:930207. doi:10.3389/fmolb.2022.930207
- Kareff SA, Corbett V, Hallenbeck P, Chauhan A. TEM8 in oncogenesis: protein biology, pre-clinical agents, and clinical rationale. Cells. 2023;12(22):2623. doi:10.3390/cells12222623
- Sanders JJ, Temin S, Ghoshal A, et al. Palliative care for patients with cancer: ASCO guideline update. J Clin Oncol. 2024;42(19):2336-2357. doi:10.1200/JCO.24.00542
- Sultana Q, Kar J, Verma A, et al. A comprehensive review on neuroendocrine neoplasms: presentation, pathophysiology and management. J Clin Med. 2023;12(15):5138. doi:10.3390/jcm12155138
- Gustafsson BI, Kidd M, Chan A, Malfertheiner MV, Modlin IM. Bronchopulmonary neuroendocrine tumors. Cancer. 2008;113(1):5-21. doi:10.1002/cncr.23542
- Travis WD, Linnoila RI, Tsokos MG, et al. Neuroendocrine tumors of the lung with proposed criteria for large-cell neuroendocrine carcinoma. An ultrastructural, immunohistochemical, and flow cytometric study of 35 cases. Am J Surg Pathol. 1991;15(6):529-553. doi:10.1097/00000478-199106000-00003
- Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG. Introduction to the 2015 World Health Organization classification of tumors of the lung, pleura, thymus, and heart. J Thorac Oncol. 2015;10(9):1240-1242. doi:10.1097/JTO.0000000000000663
- Andrini E, Marchese PV, De Biase D, et al. Large cell neuroendocrine carcinoma of the lung: current understanding and challenges. J Clin Med. 2022;11(5):1461. doi:10.3390/jcm11051461
- Lantuejoul S, Fernandez-Cuesta L, Damiola F, Girard N, McLeer A. New molecular classification of large cell neuroendocrine carcinoma and small cell lung carcinoma with potential therapeutic impacts. Transl Lung Cancer Res. 2020;9(5):2233-2244. doi:10.21037/tlcr-20-269
- Lindsay CR, Shaw EC, Moore DA, et al. Large cell neuroendocrine lung carcinoma: consensus statement from The British Thoracic Oncology Group and the Association of Pulmonary Pathologists. Br J Cancer. 2021;125(9):1210-1216. doi:10.1038/s41416-021-01407-9
- Derks JL, Dingemans AC, van Suylen RJ, et al. Is the sum of positive neuroendocrine immunohistochemical stains useful for diagnosis of large cell neuroendocrine carcinoma (LCNEC) on biopsy specimens? Histopathology. 2019;74(4):555-566. doi:10.1111/his.13800
- George J, Walter V, Peifer M, et al. Integrative genomic profiling of large-cell neuroendocrine carcinomas reveals distinct subtypes of high-grade neuroendocrine lung tumors. Nat Commun. 2018;9(1):1048. doi:10.1038/s41467-018-03099-x
- Iyoda A, Hiroshima K, Moriya Y, et al. Prospective study of adjuvant chemotherapy for pulmonary large cell neuroendocrine carcinoma. Ann Thorac Surg. 2006;82(5):1802-1807. doi:10.1016/j.athoracsur.2006.05.109
- Cao L, Wu HF, Zhao L, et al. The role of radiotherapy in pulmonary large cell neuroendocrine carcinoma: propensity score matching analysis. J Radiat Res. 2020;61(4):594-601. doi:10.1093/jrr/rraa036
- Limonnik V, Abel S, Finley GG, Long GS, Wegner RE. Factors associated with treatment receipt and overall survival for patients with locally advanced large cell neuroendocrine carcinoma of the lung: a National Cancer Database analysis. Lung Cancer. 2020;150:107-113. doi:10.1016/j.lungcan.2020.10.001
- Shi Z, Wei J, Xu M, Song Z. Efficacy and safety of immune checkpoint inhibitors in lung large-cell neuroendocrine carcinoma. J Thorac Dis. 2023;15(8):4172-4181. doi:10.21037/jtd-23-348
- Chauhan A, Arnold SM, Kolesar J, Thomas HE, Evers M, Anthony L. Immune checkpoint inhibitors in large cell neuroendocrine carcinoma: current status. Oncotarget. 2018;9(18):14738-14740. doi:10.18632/oncotarget.24553
- Chen H, Ishihara M, Horita N, et al. Effect of adjuvant and palliative chemotherapy in large cell neuroendocrine carcinoma of the lung: a systematic review and metaanalysis. Cancers (Basel). 2021;13(23):5948. doi:10.3390/cancers13235948
- Ahn MJ, Cho BC, Felip E, et al. Tarlatamab for patients with previously treated small-cell lung cancer. N Engl J Med. 2023;389(22):2063-2075. doi:10.1056/NEJMoa2307980
- Patel SA, Whang Y, Medley C, et al. Tartalamab for large-cell neuroendocrine carcinoma in a young adult: a case report. JTO Clin Res Rep. 2024;5(10):100712. doi:10.1016/j.jtocrr.2024.100712
- Corbett V, Hallenbeck P, Rychahou P, Chauhan A. Evolving role of Seneca Valley virus and its biomarker TEM8/ANTXR1 in cancer therapeutics. Front Mol Biosci. 2022;9:930207. doi:10.3389/fmolb.2022.930207
- Kareff SA, Corbett V, Hallenbeck P, Chauhan A. TEM8 in oncogenesis: protein biology, pre-clinical agents, and clinical rationale. Cells. 2023;12(22):2623. doi:10.3390/cells12222623
- Sanders JJ, Temin S, Ghoshal A, et al. Palliative care for patients with cancer: ASCO guideline update. J Clin Oncol. 2024;42(19):2336-2357. doi:10.1200/JCO.24.00542
Emerging Insights and Therapeutic Strategies for Large Cell Neuroendocrine Carcinoma of the Lung
Emerging Insights and Therapeutic Strategies for Large Cell Neuroendocrine Carcinoma of the Lung
2024 Rare Diseases Report: Hematology and Oncology
2024 Rare Diseases Report: Hematology and Oncology
National Organization for Rare Disorders: Strengthening Rare Cancer Advocacy
By Alli Ward
NORD's Rare Cancer Coalition has transformed advocacy and awareness efforts, offering education and fostering research to address the challenges of rare cancers.
Treatment of Glioblastoma: A Potential Shift in Paradigm
By Jeffrey N. Bruce, MD
Immunotherapies and molecular profiling are paving the way for more targeted approaches in treating glioblastoma.
Emerging Insights and Therapeutic Strategies for Large Cell Neuroendocrine Carcinoma of the Lung
By Robert A. Ramirez, DO, FACP, and Aman Chauhan, MD
New diagnostic tools and precision medicine approaches are addressing the unique challenges of this aggressive neuroendocrine cancer.
Advancements in the Treatment of Malignant PEComas with mTOR Inhibitors
By Richard F. Riedel, MD
The use of mTOR inhibitors marks significant progress in managing advanced malignant PEComas, offering new hope for patients.
Cutaneous T-Cell Lymphomas Update: Benefits of a Multidisciplinary Care Approach
By Jina Chung, MD, and Eric Mou, MD
A multidisciplinary care model ensures optimal outcomes for patients with cutaneous T-cell lymphomas, addressing both medical and emotional needs.
Optimizing Myelofibrosis Care in the Age of JAK Inhibitors
By Douglas Tremblay, MD
JAK inhibitors are central to myelofibrosis management, with personalized strategies helping to navigate resistance and improve quality of life.
Current Management and Future Directions in the Treatment of Gallbladder Cancer
By Ghassan K. Abou-Alfa, MD, MBA, JD, FASCO
Molecular profiling and immunotherapy are reshaping the treatment paradigm for gallbladder cancer, improving survival outcomes.
Improving Prognosis in Hepatoblastoma: Evolving Risk Stratification and Treatment Strategies
By Greg M. Tiao, MD
Risk stratification and individualized therapies are driving progress in treating hepatoblastoma, with promising advancements on the horizon.
National Organization for Rare Disorders: Strengthening Rare Cancer Advocacy
By Alli Ward
NORD's Rare Cancer Coalition has transformed advocacy and awareness efforts, offering education and fostering research to address the challenges of rare cancers.
Treatment of Glioblastoma: A Potential Shift in Paradigm
By Jeffrey N. Bruce, MD
Immunotherapies and molecular profiling are paving the way for more targeted approaches in treating glioblastoma.
Emerging Insights and Therapeutic Strategies for Large Cell Neuroendocrine Carcinoma of the Lung
By Robert A. Ramirez, DO, FACP, and Aman Chauhan, MD
New diagnostic tools and precision medicine approaches are addressing the unique challenges of this aggressive neuroendocrine cancer.
Advancements in the Treatment of Malignant PEComas with mTOR Inhibitors
By Richard F. Riedel, MD
The use of mTOR inhibitors marks significant progress in managing advanced malignant PEComas, offering new hope for patients.
Cutaneous T-Cell Lymphomas Update: Benefits of a Multidisciplinary Care Approach
By Jina Chung, MD, and Eric Mou, MD
A multidisciplinary care model ensures optimal outcomes for patients with cutaneous T-cell lymphomas, addressing both medical and emotional needs.
Optimizing Myelofibrosis Care in the Age of JAK Inhibitors
By Douglas Tremblay, MD
JAK inhibitors are central to myelofibrosis management, with personalized strategies helping to navigate resistance and improve quality of life.
Current Management and Future Directions in the Treatment of Gallbladder Cancer
By Ghassan K. Abou-Alfa, MD, MBA, JD, FASCO
Molecular profiling and immunotherapy are reshaping the treatment paradigm for gallbladder cancer, improving survival outcomes.
Improving Prognosis in Hepatoblastoma: Evolving Risk Stratification and Treatment Strategies
By Greg M. Tiao, MD
Risk stratification and individualized therapies are driving progress in treating hepatoblastoma, with promising advancements on the horizon.
National Organization for Rare Disorders: Strengthening Rare Cancer Advocacy
By Alli Ward
NORD's Rare Cancer Coalition has transformed advocacy and awareness efforts, offering education and fostering research to address the challenges of rare cancers.
Treatment of Glioblastoma: A Potential Shift in Paradigm
By Jeffrey N. Bruce, MD
Immunotherapies and molecular profiling are paving the way for more targeted approaches in treating glioblastoma.
Emerging Insights and Therapeutic Strategies for Large Cell Neuroendocrine Carcinoma of the Lung
By Robert A. Ramirez, DO, FACP, and Aman Chauhan, MD
New diagnostic tools and precision medicine approaches are addressing the unique challenges of this aggressive neuroendocrine cancer.
Advancements in the Treatment of Malignant PEComas with mTOR Inhibitors
By Richard F. Riedel, MD
The use of mTOR inhibitors marks significant progress in managing advanced malignant PEComas, offering new hope for patients.
Cutaneous T-Cell Lymphomas Update: Benefits of a Multidisciplinary Care Approach
By Jina Chung, MD, and Eric Mou, MD
A multidisciplinary care model ensures optimal outcomes for patients with cutaneous T-cell lymphomas, addressing both medical and emotional needs.
Optimizing Myelofibrosis Care in the Age of JAK Inhibitors
By Douglas Tremblay, MD
JAK inhibitors are central to myelofibrosis management, with personalized strategies helping to navigate resistance and improve quality of life.
Current Management and Future Directions in the Treatment of Gallbladder Cancer
By Ghassan K. Abou-Alfa, MD, MBA, JD, FASCO
Molecular profiling and immunotherapy are reshaping the treatment paradigm for gallbladder cancer, improving survival outcomes.
Improving Prognosis in Hepatoblastoma: Evolving Risk Stratification and Treatment Strategies
By Greg M. Tiao, MD
Risk stratification and individualized therapies are driving progress in treating hepatoblastoma, with promising advancements on the horizon.
2024 Rare Diseases Report: Hematology and Oncology
2024 Rare Diseases Report: Hematology and Oncology