User login
EMA gives green light to avapritinib for GIST, acalabrutinib for CLL
The CHMP recommended granting conditional marketing authorization for avapritinib (Ayvakit, Blueprint Medicines) for use in adults with unresectable or metastatic gastrointestinal stromal tumors (GIST) harboring a platelet-derived growth factor receptor alpha (PDGFRA) exon 18 mutation, including PDGFRA D842V mutations. About 6%-10% of GIST tumors harbor this mutation, and avapritinib is a selective and potent inhibitor of KIT and PDGFRA mutant kinases.
The CHMP also adopted a positive opinion for acalabrutinib (Calquence, AstraZeneca) for the treatment of chronic lymphocytic leukemia (CLL) as monotherapy in patients who are treatment-naive or have received at least one prior therapy.
The CHMP opinion on both drugs will be reviewed by the European Commission, which has the authority to grant marketing authorization for medicinal products in the EU.
Detailed recommendations for the use of both drugs will be provided in the summary of product characteristics, which will be published in the European public assessment report and made available in all official EU languages after the products receive marketing authorization by the European Commission.
First targeted therapy for mutation
If approved by the European Commission, avapritinib would be the first treatment in the EU indicated for patients with PDGFRA D842V-mutant GIST.
Avapritinib was approved by the US Food and Drug Administration (FDA) earlier this year for the aforementioned indication. The FDA approval was based on findings from the phase 1 NAVIGATOR trial, which included 43 patients with GIST harboring a PDGFRA exon 18 mutation, including 38 patients with the most common mutation, PDGFRA D842V.
For patients harboring a PDGFRA exon 18 mutation, the overall response rate (ORR) was 84%, with 7% having a complete response and 77% having a partial response. Patients with the PDGFRA D842V mutation achieved an ORR of 89%, with 8% having a complete response and 82% having a partial response.
“GIST harboring a PDGFRA exon 18 mutation do not respond to standard therapies ... Today’s approval provides patients with the first drug specifically approved for GIST harboring this mutation,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence, in a statement at the time of approval.
The most common side effects (≥ 20% of patients) observed in patients taking avapritinib include nausea, fatigue, anemia, periorbital edema, face edema, hyperbilirubinemia, diarrhea, vomiting, peripheral edema, increased lacrimation, decreased appetite, and memory impairment. There may also be a risk of intracranial hemorrhage, in which case the dose should be reduced or the drug should be discontinued.
In the EU, conditional marketing authorization is granted to a medicinal product that fulfills an unmet medical need when the benefit to public health of immediate availability outweighs the risk inherent in the fact that additional data are still required, the CHMP notes on its website.
Avapritinib had received an orphan medicine designation during development, which the EMA will review to determine if the designation can be maintained.
New treatment for CLL
Acalabrutinib is already approved in the United States, Canada, and Australia for the treatment of CLL and small lymphocytic lymphoma. The product was approved at the same time by all three regulatory authorities last year. In the United States, acalabrutinib had previously been approved for use in mantle cell lymphoma.
The CHMP’s positive opinion of acalabrutinib is based on results from two phase 3 trials, ELEVATE TN and ASCEND.
In the ASCEND trial, acalabrutinib was compared with investigator’s choice of idelalisib or bendamustine with rituximab. The trial, which involved 310 patients with relapsed/refractory CLL, showed that acalabrutinib improved progression-free survival (PFS).
At a median follow-up of 16.1 months, the median PFS was not reached with acalabrutinib and was 16.5 months with investigator’s choice of therapy (P < .0001).
The most commonly reported adverse events seen with acalabrutinib were respiratory tract infections, headache, bruising, contusion, diarrhea, nausea, rash, musculoskeletal pain, fatigue, decreased hemoglobin, and decreased platelets.
In the ELEVATE TN trial, acalabrutinib was given alone or combined with obinutuzumab and compared to chlorambucil plus obinutuzumab in patients with previously untreated CLL. There were 535 patients randomized to receive acalabrutinib alone (n = 179), acalabrutinib plus obinutuzumab (n = 179), and chlorambucil plus obinutuzumab (n = 177).
At a median follow-up of 28 months, the median PFS was not reached with acalabrutinib alone or with acalabrutinib plus obinutuzumab, but the median PFS was 22.6 months in the chlorambucil-obinutuzumab arm (P < .0001 for both comparisons).
The most common adverse events in the acalabrutinib arms were headache, diarrhea, neutropenia, and nausea.
A version of this article first appeared on Medscape.com.
The CHMP recommended granting conditional marketing authorization for avapritinib (Ayvakit, Blueprint Medicines) for use in adults with unresectable or metastatic gastrointestinal stromal tumors (GIST) harboring a platelet-derived growth factor receptor alpha (PDGFRA) exon 18 mutation, including PDGFRA D842V mutations. About 6%-10% of GIST tumors harbor this mutation, and avapritinib is a selective and potent inhibitor of KIT and PDGFRA mutant kinases.
The CHMP also adopted a positive opinion for acalabrutinib (Calquence, AstraZeneca) for the treatment of chronic lymphocytic leukemia (CLL) as monotherapy in patients who are treatment-naive or have received at least one prior therapy.
The CHMP opinion on both drugs will be reviewed by the European Commission, which has the authority to grant marketing authorization for medicinal products in the EU.
Detailed recommendations for the use of both drugs will be provided in the summary of product characteristics, which will be published in the European public assessment report and made available in all official EU languages after the products receive marketing authorization by the European Commission.
First targeted therapy for mutation
If approved by the European Commission, avapritinib would be the first treatment in the EU indicated for patients with PDGFRA D842V-mutant GIST.
Avapritinib was approved by the US Food and Drug Administration (FDA) earlier this year for the aforementioned indication. The FDA approval was based on findings from the phase 1 NAVIGATOR trial, which included 43 patients with GIST harboring a PDGFRA exon 18 mutation, including 38 patients with the most common mutation, PDGFRA D842V.
For patients harboring a PDGFRA exon 18 mutation, the overall response rate (ORR) was 84%, with 7% having a complete response and 77% having a partial response. Patients with the PDGFRA D842V mutation achieved an ORR of 89%, with 8% having a complete response and 82% having a partial response.
“GIST harboring a PDGFRA exon 18 mutation do not respond to standard therapies ... Today’s approval provides patients with the first drug specifically approved for GIST harboring this mutation,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence, in a statement at the time of approval.
The most common side effects (≥ 20% of patients) observed in patients taking avapritinib include nausea, fatigue, anemia, periorbital edema, face edema, hyperbilirubinemia, diarrhea, vomiting, peripheral edema, increased lacrimation, decreased appetite, and memory impairment. There may also be a risk of intracranial hemorrhage, in which case the dose should be reduced or the drug should be discontinued.
In the EU, conditional marketing authorization is granted to a medicinal product that fulfills an unmet medical need when the benefit to public health of immediate availability outweighs the risk inherent in the fact that additional data are still required, the CHMP notes on its website.
Avapritinib had received an orphan medicine designation during development, which the EMA will review to determine if the designation can be maintained.
New treatment for CLL
Acalabrutinib is already approved in the United States, Canada, and Australia for the treatment of CLL and small lymphocytic lymphoma. The product was approved at the same time by all three regulatory authorities last year. In the United States, acalabrutinib had previously been approved for use in mantle cell lymphoma.
The CHMP’s positive opinion of acalabrutinib is based on results from two phase 3 trials, ELEVATE TN and ASCEND.
In the ASCEND trial, acalabrutinib was compared with investigator’s choice of idelalisib or bendamustine with rituximab. The trial, which involved 310 patients with relapsed/refractory CLL, showed that acalabrutinib improved progression-free survival (PFS).
At a median follow-up of 16.1 months, the median PFS was not reached with acalabrutinib and was 16.5 months with investigator’s choice of therapy (P < .0001).
The most commonly reported adverse events seen with acalabrutinib were respiratory tract infections, headache, bruising, contusion, diarrhea, nausea, rash, musculoskeletal pain, fatigue, decreased hemoglobin, and decreased platelets.
In the ELEVATE TN trial, acalabrutinib was given alone or combined with obinutuzumab and compared to chlorambucil plus obinutuzumab in patients with previously untreated CLL. There were 535 patients randomized to receive acalabrutinib alone (n = 179), acalabrutinib plus obinutuzumab (n = 179), and chlorambucil plus obinutuzumab (n = 177).
At a median follow-up of 28 months, the median PFS was not reached with acalabrutinib alone or with acalabrutinib plus obinutuzumab, but the median PFS was 22.6 months in the chlorambucil-obinutuzumab arm (P < .0001 for both comparisons).
The most common adverse events in the acalabrutinib arms were headache, diarrhea, neutropenia, and nausea.
A version of this article first appeared on Medscape.com.
The CHMP recommended granting conditional marketing authorization for avapritinib (Ayvakit, Blueprint Medicines) for use in adults with unresectable or metastatic gastrointestinal stromal tumors (GIST) harboring a platelet-derived growth factor receptor alpha (PDGFRA) exon 18 mutation, including PDGFRA D842V mutations. About 6%-10% of GIST tumors harbor this mutation, and avapritinib is a selective and potent inhibitor of KIT and PDGFRA mutant kinases.
The CHMP also adopted a positive opinion for acalabrutinib (Calquence, AstraZeneca) for the treatment of chronic lymphocytic leukemia (CLL) as monotherapy in patients who are treatment-naive or have received at least one prior therapy.
The CHMP opinion on both drugs will be reviewed by the European Commission, which has the authority to grant marketing authorization for medicinal products in the EU.
Detailed recommendations for the use of both drugs will be provided in the summary of product characteristics, which will be published in the European public assessment report and made available in all official EU languages after the products receive marketing authorization by the European Commission.
First targeted therapy for mutation
If approved by the European Commission, avapritinib would be the first treatment in the EU indicated for patients with PDGFRA D842V-mutant GIST.
Avapritinib was approved by the US Food and Drug Administration (FDA) earlier this year for the aforementioned indication. The FDA approval was based on findings from the phase 1 NAVIGATOR trial, which included 43 patients with GIST harboring a PDGFRA exon 18 mutation, including 38 patients with the most common mutation, PDGFRA D842V.
For patients harboring a PDGFRA exon 18 mutation, the overall response rate (ORR) was 84%, with 7% having a complete response and 77% having a partial response. Patients with the PDGFRA D842V mutation achieved an ORR of 89%, with 8% having a complete response and 82% having a partial response.
“GIST harboring a PDGFRA exon 18 mutation do not respond to standard therapies ... Today’s approval provides patients with the first drug specifically approved for GIST harboring this mutation,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence, in a statement at the time of approval.
The most common side effects (≥ 20% of patients) observed in patients taking avapritinib include nausea, fatigue, anemia, periorbital edema, face edema, hyperbilirubinemia, diarrhea, vomiting, peripheral edema, increased lacrimation, decreased appetite, and memory impairment. There may also be a risk of intracranial hemorrhage, in which case the dose should be reduced or the drug should be discontinued.
In the EU, conditional marketing authorization is granted to a medicinal product that fulfills an unmet medical need when the benefit to public health of immediate availability outweighs the risk inherent in the fact that additional data are still required, the CHMP notes on its website.
Avapritinib had received an orphan medicine designation during development, which the EMA will review to determine if the designation can be maintained.
New treatment for CLL
Acalabrutinib is already approved in the United States, Canada, and Australia for the treatment of CLL and small lymphocytic lymphoma. The product was approved at the same time by all three regulatory authorities last year. In the United States, acalabrutinib had previously been approved for use in mantle cell lymphoma.
The CHMP’s positive opinion of acalabrutinib is based on results from two phase 3 trials, ELEVATE TN and ASCEND.
In the ASCEND trial, acalabrutinib was compared with investigator’s choice of idelalisib or bendamustine with rituximab. The trial, which involved 310 patients with relapsed/refractory CLL, showed that acalabrutinib improved progression-free survival (PFS).
At a median follow-up of 16.1 months, the median PFS was not reached with acalabrutinib and was 16.5 months with investigator’s choice of therapy (P < .0001).
The most commonly reported adverse events seen with acalabrutinib were respiratory tract infections, headache, bruising, contusion, diarrhea, nausea, rash, musculoskeletal pain, fatigue, decreased hemoglobin, and decreased platelets.
In the ELEVATE TN trial, acalabrutinib was given alone or combined with obinutuzumab and compared to chlorambucil plus obinutuzumab in patients with previously untreated CLL. There were 535 patients randomized to receive acalabrutinib alone (n = 179), acalabrutinib plus obinutuzumab (n = 179), and chlorambucil plus obinutuzumab (n = 177).
At a median follow-up of 28 months, the median PFS was not reached with acalabrutinib alone or with acalabrutinib plus obinutuzumab, but the median PFS was 22.6 months in the chlorambucil-obinutuzumab arm (P < .0001 for both comparisons).
The most common adverse events in the acalabrutinib arms were headache, diarrhea, neutropenia, and nausea.
A version of this article first appeared on Medscape.com.
FDA okays new CAR T therapy, first for mantle cell lymphoma
The Food and Drug Administration granted accelerated approval to brexucabtagene autoleucel (Tecartus, Kite Pharma), the first approved chimeric antigen receptor (CAR) T cell therapy for the treatment of adult patients with relapsed or refractory mantle cell lymphoma (MCL).
The new agent is the second approved CAR T cell product developed by Kite and follows the 2017 approval of axicabtagene ciloleucel (Yescarta) for diffuse large B-cell lymphoma.
“Despite promising advances, there are still major gaps in treatment for patients with MCL who progress following initial therapy,” investigator Michael Wang, MD, of the University of Texas MD Anderson Cancer Center in Houston, said in a company statement. “Many patients have high-risk disease and are more likely to keep progressing, even after subsequent treatments.”
In the same press statement, Meghan Gutierrez, chief executive officer, Lymphoma Research Foundation, said: “This approval marks the first CAR T cell therapy approved for mantle cell lymphoma patients and represents a new frontier in the treatment of this disease.”
The approval of the single-infusion therapy is based on efficacy and safety data from the ongoing, single-arm ZUMA-2 pivotal trial, which enrolled 74 adult patients. All patients had previously received anthracycline- or bendamustine-containing chemotherapy, an anti-CD20 antibody therapy and a Bruton tyrosine kinase inhibitor (ibrutinib or acalabrutinib).
In the trial, there was an objective response rate, which was the primary outcome measure, of 87% among 60 patients who were evaluable for efficacy analysis; 62% had a complete response.
Among all patients, follow-up was at least 6 months after their first objective disease response. Median duration of response has not yet been reached.
In terms of adverse events, 18% of the 82 patients evaluable for safety experienced > grade 3 cytokine release syndrome and 37% experienced neurologic events, per the company statement. The most common (≥ 10%) grade 3 or higher adverse reactions were anemia, neutropenia, thrombocytopenia, hypotension, hypophosphatemia, encephalopathy, leukopenia, hypoxia, pyrexia, hyponatremia, hypertension, infection-pathogen unspecified, pneumonia, hypocalcemia, and lymphopenia.
Brexucabtagene autoleucel will be manufactured in Kite’s facility in California. In the pivotal trial, there was a 96% manufacturing success rate and a median manufacturing turnaround time of 15 days from leukapheresis to product delivery.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration granted accelerated approval to brexucabtagene autoleucel (Tecartus, Kite Pharma), the first approved chimeric antigen receptor (CAR) T cell therapy for the treatment of adult patients with relapsed or refractory mantle cell lymphoma (MCL).
The new agent is the second approved CAR T cell product developed by Kite and follows the 2017 approval of axicabtagene ciloleucel (Yescarta) for diffuse large B-cell lymphoma.
“Despite promising advances, there are still major gaps in treatment for patients with MCL who progress following initial therapy,” investigator Michael Wang, MD, of the University of Texas MD Anderson Cancer Center in Houston, said in a company statement. “Many patients have high-risk disease and are more likely to keep progressing, even after subsequent treatments.”
In the same press statement, Meghan Gutierrez, chief executive officer, Lymphoma Research Foundation, said: “This approval marks the first CAR T cell therapy approved for mantle cell lymphoma patients and represents a new frontier in the treatment of this disease.”
The approval of the single-infusion therapy is based on efficacy and safety data from the ongoing, single-arm ZUMA-2 pivotal trial, which enrolled 74 adult patients. All patients had previously received anthracycline- or bendamustine-containing chemotherapy, an anti-CD20 antibody therapy and a Bruton tyrosine kinase inhibitor (ibrutinib or acalabrutinib).
In the trial, there was an objective response rate, which was the primary outcome measure, of 87% among 60 patients who were evaluable for efficacy analysis; 62% had a complete response.
Among all patients, follow-up was at least 6 months after their first objective disease response. Median duration of response has not yet been reached.
In terms of adverse events, 18% of the 82 patients evaluable for safety experienced > grade 3 cytokine release syndrome and 37% experienced neurologic events, per the company statement. The most common (≥ 10%) grade 3 or higher adverse reactions were anemia, neutropenia, thrombocytopenia, hypotension, hypophosphatemia, encephalopathy, leukopenia, hypoxia, pyrexia, hyponatremia, hypertension, infection-pathogen unspecified, pneumonia, hypocalcemia, and lymphopenia.
Brexucabtagene autoleucel will be manufactured in Kite’s facility in California. In the pivotal trial, there was a 96% manufacturing success rate and a median manufacturing turnaround time of 15 days from leukapheresis to product delivery.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration granted accelerated approval to brexucabtagene autoleucel (Tecartus, Kite Pharma), the first approved chimeric antigen receptor (CAR) T cell therapy for the treatment of adult patients with relapsed or refractory mantle cell lymphoma (MCL).
The new agent is the second approved CAR T cell product developed by Kite and follows the 2017 approval of axicabtagene ciloleucel (Yescarta) for diffuse large B-cell lymphoma.
“Despite promising advances, there are still major gaps in treatment for patients with MCL who progress following initial therapy,” investigator Michael Wang, MD, of the University of Texas MD Anderson Cancer Center in Houston, said in a company statement. “Many patients have high-risk disease and are more likely to keep progressing, even after subsequent treatments.”
In the same press statement, Meghan Gutierrez, chief executive officer, Lymphoma Research Foundation, said: “This approval marks the first CAR T cell therapy approved for mantle cell lymphoma patients and represents a new frontier in the treatment of this disease.”
The approval of the single-infusion therapy is based on efficacy and safety data from the ongoing, single-arm ZUMA-2 pivotal trial, which enrolled 74 adult patients. All patients had previously received anthracycline- or bendamustine-containing chemotherapy, an anti-CD20 antibody therapy and a Bruton tyrosine kinase inhibitor (ibrutinib or acalabrutinib).
In the trial, there was an objective response rate, which was the primary outcome measure, of 87% among 60 patients who were evaluable for efficacy analysis; 62% had a complete response.
Among all patients, follow-up was at least 6 months after their first objective disease response. Median duration of response has not yet been reached.
In terms of adverse events, 18% of the 82 patients evaluable for safety experienced > grade 3 cytokine release syndrome and 37% experienced neurologic events, per the company statement. The most common (≥ 10%) grade 3 or higher adverse reactions were anemia, neutropenia, thrombocytopenia, hypotension, hypophosphatemia, encephalopathy, leukopenia, hypoxia, pyrexia, hyponatremia, hypertension, infection-pathogen unspecified, pneumonia, hypocalcemia, and lymphopenia.
Brexucabtagene autoleucel will be manufactured in Kite’s facility in California. In the pivotal trial, there was a 96% manufacturing success rate and a median manufacturing turnaround time of 15 days from leukapheresis to product delivery.
A version of this article originally appeared on Medscape.com.
CCC19, other registries help define COVID/cancer landscape
Initial results from the CCC19 registry were reported as part of the American Society of Clinical Oncology (ASCO) virtual scientific program and published in The Lancet (Lancet. 2020 Jun 20;395[10241]:1907-18).
The latest data were presented at the AACR virtual meeting: COVID-19 and Cancer by Brian I. Rini, MD, of Vanderbilt University, Nashville, Tenn. They were simultaneously published in Cancer Discovery (Cancer Discov. 2020 Jul 22;CD-20-0941).
The CCC19 registry was launched in March by a few institutions as part of “a grassroots idea ... to collect granular data regarding cancer patients and their outcomes with COVID,” Dr. Rini said.
Within a few months of its inception, the registry had partnered with more than 100 institutions worldwide and accrued data from more than 2,000 patients.
The reports in The Lancet and at ASCO included outcomes for the first 928 patients and showed a 13% mortality rate as well as a fivefold increase in the risk of 30-day mortality among patients with COVID-19 and progressing cancer.
The data also showed an increased mortality risk among older patients, men, former smokers, those with poor performance status, those with multiple comorbidities, and those treated with hydroxychloroquine and azithromycin.
The latest data
The CCC19 registry has grown to include 114 sites worldwide, including major comprehensive cancer centers and community sites. As of June 26, there were 2,749 patients enrolled.
Since the last data were reported, the mortality rate increased from 13% to 16% (versus 5% globally). In addition, the increased mortality risk among non-Hispanic black patients and patients with hematologic malignancies reached statistical significance, Dr. Rini said. He noted that the increase in mortality rate was largely attributable to improved follow-up.
Mechanical ventilation was required in 12% of patients, ICU admission was required in 16%, oxygen was required in 45%, and hospitalization was required in 60%. The composite outcome of death, severe illness requiring hospitalization, ICU admission, or mechanical ventilation was reached in 29% of patients, Dr. Rini said.
Mortality rates across cancer types ranged from 3% to 26%, with thyroid and breast cancer patients having the lowest rates (3% and 8%, respectively), and with lymphoma and lung cancer patients having the highest (22% and 26%, respectively), Dr. Rini said.
He noted that the TERAVOLT registry, a COVID-19 registry for patients with thoracic cancers, also showed a very high mortality rate in this subgroup of patients.
Results from TERAVOLT were reported at the AACR virtual meeting I, presented at ASCO, and published in The Lancet (Lancet Oncol. 2020 Jul;21[7]:914-22). The most recent results showed a mortality rate of nearly 36% and reinforce the high mortality rate seen in lung cancer patients in CCC19, Dr. Rini said.
Increased mortality risk
After adjustment for several demographic and disease characteristics, the updated CCC19 data showed a significantly increased risk of mortality among:
- Older patients (adjusted odds ratio [aOR] per decade of age, 1.52).
- Men (aOR, 1.43).
- Current or former smokers vs. never smokers (aOR, 1.28).
- Patients with Eastern Cooperative Oncology Group performance scores of 1 vs. 0 (aOR of 1.80) or 2 vs. 0 (aOR, 4.22).
- Stable cancer vs. remission (aOR, 1.47).
- Progressive cancer vs. remission (aOR, 2.96).
- Non-Hispanic Black vs. White patients (aOR, 1.56).
- Hematologic malignancies vs. solid tumors (aOR, 1.80).
“Importantly, there were some factors that did not reach statistical significance,” Dr. Rini said. These include obesity (aOR, 1.23), recent surgery (aOR, 1.05), receipt of cytotoxic chemotherapy vs. no chemotherapy (aOR, 1.14), and receipt of noncytotoxic chemotherapy vs. no chemotherapy (aOR, 0.75).
“I think this provides some reassurance that cancer care can and should continue for these patients,” Dr. Rini said.
He noted, however, that in TERAVOLT, chemotherapy with or without other treatment was a risk factor for mortality in lung cancer patients when compared with no chemotherapy (OR, 1.71) and when compared with immunotherapy or targeted therapy (OR, 1.64).
NCCAPS and other registries
Dr. Rini discussed a number of registries looking at outcomes in COVID-19 patients with cancer, and he said the findings to date appear to confirm a higher mortality rate among cancer patients, particularly those with lung cancer.
Several factors are emerging that appear to be related to risk, including both cancer-related and non–cancer-related factors, he added.
The ongoing prospective National Cancer Institute COVID-19 in Cancer Patients Study (NCCAPS) “will provide much needed longitudinal data and, importantly, biospecimen collection in a large cohort of patients who have active cancer and are receiving treatment, said Dr. Rini, who is the study’s protocol chair. NCCAPS is a natural history study in that population, he said.
The planned accrual is about 2,000 patients who will be followed for up to 2 years for data collection, imaging scans, and research specimens.
The use of specimens is “a unique and special part of this study,” Dr. Rini said, explaining that the specimens will be used to look for development of antibodies over time, to describe the trajectory of cytokine abnormalities – especially in patients with more acute inpatient courses – to perform DNA-based genome-wide association studies, and to assess coagulation parameters.
NCCAPS is activated at 546 sties, 10 patients were enrolled as of June 21, and rapid accrual is expected over the next several months, he said.
Gypsyamber D’Souza, PhD, session moderator and an infectious disease epidemiologist at Johns Hopkins University in Baltimore, acknowledged the challenge that registry administrators face when trying to balance the need to get data out against the desire to ask the right questions and to have the right comparison groups, stratification, and analyses, especially amid a crisis like the COVID-19 pandemic.
Dr. Rini said it has indeed been a bit of a struggle with CCC19 to determine what information should be published and when, and what constitutes an important update.
“It’s been a learning experience, and frankly, I think we’re still learning,” he said. “This has been such a unique time in terms of a rush to get data out, balanced against making sure that there’s quality data and that you’re actually answering important questions.”
In fact, a number of ongoing registries “should start to produce great data [that will be presented] at upcoming big conferences,” Dr. Rini said. He added that those data “will help piece together different important aspects of this and different hypotheses, and hopefully complement the clinical data that’s starting to come out.”
The CCC19 registry is sponsored by Vanderbilt-Ingram Cancer Center. Dr. Rini disclosed relationships with Pfizer, Merck, Genentech/Roche, Aveo, AstraZeneca, Bristol Myers Squibb, Exelixis, Synthorx, Peloton, Compugen, Corvus, Surface Oncology, 3DMedicines, Aravive, Alkermes, Arrowhead, and PTC Therapeutics. Dr. D’Souza did not disclose any conflicts.
SOURCE: Rini BI. AACR: COVID-19 and Cancer. Abstract IA26.
Initial results from the CCC19 registry were reported as part of the American Society of Clinical Oncology (ASCO) virtual scientific program and published in The Lancet (Lancet. 2020 Jun 20;395[10241]:1907-18).
The latest data were presented at the AACR virtual meeting: COVID-19 and Cancer by Brian I. Rini, MD, of Vanderbilt University, Nashville, Tenn. They were simultaneously published in Cancer Discovery (Cancer Discov. 2020 Jul 22;CD-20-0941).
The CCC19 registry was launched in March by a few institutions as part of “a grassroots idea ... to collect granular data regarding cancer patients and their outcomes with COVID,” Dr. Rini said.
Within a few months of its inception, the registry had partnered with more than 100 institutions worldwide and accrued data from more than 2,000 patients.
The reports in The Lancet and at ASCO included outcomes for the first 928 patients and showed a 13% mortality rate as well as a fivefold increase in the risk of 30-day mortality among patients with COVID-19 and progressing cancer.
The data also showed an increased mortality risk among older patients, men, former smokers, those with poor performance status, those with multiple comorbidities, and those treated with hydroxychloroquine and azithromycin.
The latest data
The CCC19 registry has grown to include 114 sites worldwide, including major comprehensive cancer centers and community sites. As of June 26, there were 2,749 patients enrolled.
Since the last data were reported, the mortality rate increased from 13% to 16% (versus 5% globally). In addition, the increased mortality risk among non-Hispanic black patients and patients with hematologic malignancies reached statistical significance, Dr. Rini said. He noted that the increase in mortality rate was largely attributable to improved follow-up.
Mechanical ventilation was required in 12% of patients, ICU admission was required in 16%, oxygen was required in 45%, and hospitalization was required in 60%. The composite outcome of death, severe illness requiring hospitalization, ICU admission, or mechanical ventilation was reached in 29% of patients, Dr. Rini said.
Mortality rates across cancer types ranged from 3% to 26%, with thyroid and breast cancer patients having the lowest rates (3% and 8%, respectively), and with lymphoma and lung cancer patients having the highest (22% and 26%, respectively), Dr. Rini said.
He noted that the TERAVOLT registry, a COVID-19 registry for patients with thoracic cancers, also showed a very high mortality rate in this subgroup of patients.
Results from TERAVOLT were reported at the AACR virtual meeting I, presented at ASCO, and published in The Lancet (Lancet Oncol. 2020 Jul;21[7]:914-22). The most recent results showed a mortality rate of nearly 36% and reinforce the high mortality rate seen in lung cancer patients in CCC19, Dr. Rini said.
Increased mortality risk
After adjustment for several demographic and disease characteristics, the updated CCC19 data showed a significantly increased risk of mortality among:
- Older patients (adjusted odds ratio [aOR] per decade of age, 1.52).
- Men (aOR, 1.43).
- Current or former smokers vs. never smokers (aOR, 1.28).
- Patients with Eastern Cooperative Oncology Group performance scores of 1 vs. 0 (aOR of 1.80) or 2 vs. 0 (aOR, 4.22).
- Stable cancer vs. remission (aOR, 1.47).
- Progressive cancer vs. remission (aOR, 2.96).
- Non-Hispanic Black vs. White patients (aOR, 1.56).
- Hematologic malignancies vs. solid tumors (aOR, 1.80).
“Importantly, there were some factors that did not reach statistical significance,” Dr. Rini said. These include obesity (aOR, 1.23), recent surgery (aOR, 1.05), receipt of cytotoxic chemotherapy vs. no chemotherapy (aOR, 1.14), and receipt of noncytotoxic chemotherapy vs. no chemotherapy (aOR, 0.75).
“I think this provides some reassurance that cancer care can and should continue for these patients,” Dr. Rini said.
He noted, however, that in TERAVOLT, chemotherapy with or without other treatment was a risk factor for mortality in lung cancer patients when compared with no chemotherapy (OR, 1.71) and when compared with immunotherapy or targeted therapy (OR, 1.64).
NCCAPS and other registries
Dr. Rini discussed a number of registries looking at outcomes in COVID-19 patients with cancer, and he said the findings to date appear to confirm a higher mortality rate among cancer patients, particularly those with lung cancer.
Several factors are emerging that appear to be related to risk, including both cancer-related and non–cancer-related factors, he added.
The ongoing prospective National Cancer Institute COVID-19 in Cancer Patients Study (NCCAPS) “will provide much needed longitudinal data and, importantly, biospecimen collection in a large cohort of patients who have active cancer and are receiving treatment, said Dr. Rini, who is the study’s protocol chair. NCCAPS is a natural history study in that population, he said.
The planned accrual is about 2,000 patients who will be followed for up to 2 years for data collection, imaging scans, and research specimens.
The use of specimens is “a unique and special part of this study,” Dr. Rini said, explaining that the specimens will be used to look for development of antibodies over time, to describe the trajectory of cytokine abnormalities – especially in patients with more acute inpatient courses – to perform DNA-based genome-wide association studies, and to assess coagulation parameters.
NCCAPS is activated at 546 sties, 10 patients were enrolled as of June 21, and rapid accrual is expected over the next several months, he said.
Gypsyamber D’Souza, PhD, session moderator and an infectious disease epidemiologist at Johns Hopkins University in Baltimore, acknowledged the challenge that registry administrators face when trying to balance the need to get data out against the desire to ask the right questions and to have the right comparison groups, stratification, and analyses, especially amid a crisis like the COVID-19 pandemic.
Dr. Rini said it has indeed been a bit of a struggle with CCC19 to determine what information should be published and when, and what constitutes an important update.
“It’s been a learning experience, and frankly, I think we’re still learning,” he said. “This has been such a unique time in terms of a rush to get data out, balanced against making sure that there’s quality data and that you’re actually answering important questions.”
In fact, a number of ongoing registries “should start to produce great data [that will be presented] at upcoming big conferences,” Dr. Rini said. He added that those data “will help piece together different important aspects of this and different hypotheses, and hopefully complement the clinical data that’s starting to come out.”
The CCC19 registry is sponsored by Vanderbilt-Ingram Cancer Center. Dr. Rini disclosed relationships with Pfizer, Merck, Genentech/Roche, Aveo, AstraZeneca, Bristol Myers Squibb, Exelixis, Synthorx, Peloton, Compugen, Corvus, Surface Oncology, 3DMedicines, Aravive, Alkermes, Arrowhead, and PTC Therapeutics. Dr. D’Souza did not disclose any conflicts.
SOURCE: Rini BI. AACR: COVID-19 and Cancer. Abstract IA26.
Initial results from the CCC19 registry were reported as part of the American Society of Clinical Oncology (ASCO) virtual scientific program and published in The Lancet (Lancet. 2020 Jun 20;395[10241]:1907-18).
The latest data were presented at the AACR virtual meeting: COVID-19 and Cancer by Brian I. Rini, MD, of Vanderbilt University, Nashville, Tenn. They were simultaneously published in Cancer Discovery (Cancer Discov. 2020 Jul 22;CD-20-0941).
The CCC19 registry was launched in March by a few institutions as part of “a grassroots idea ... to collect granular data regarding cancer patients and their outcomes with COVID,” Dr. Rini said.
Within a few months of its inception, the registry had partnered with more than 100 institutions worldwide and accrued data from more than 2,000 patients.
The reports in The Lancet and at ASCO included outcomes for the first 928 patients and showed a 13% mortality rate as well as a fivefold increase in the risk of 30-day mortality among patients with COVID-19 and progressing cancer.
The data also showed an increased mortality risk among older patients, men, former smokers, those with poor performance status, those with multiple comorbidities, and those treated with hydroxychloroquine and azithromycin.
The latest data
The CCC19 registry has grown to include 114 sites worldwide, including major comprehensive cancer centers and community sites. As of June 26, there were 2,749 patients enrolled.
Since the last data were reported, the mortality rate increased from 13% to 16% (versus 5% globally). In addition, the increased mortality risk among non-Hispanic black patients and patients with hematologic malignancies reached statistical significance, Dr. Rini said. He noted that the increase in mortality rate was largely attributable to improved follow-up.
Mechanical ventilation was required in 12% of patients, ICU admission was required in 16%, oxygen was required in 45%, and hospitalization was required in 60%. The composite outcome of death, severe illness requiring hospitalization, ICU admission, or mechanical ventilation was reached in 29% of patients, Dr. Rini said.
Mortality rates across cancer types ranged from 3% to 26%, with thyroid and breast cancer patients having the lowest rates (3% and 8%, respectively), and with lymphoma and lung cancer patients having the highest (22% and 26%, respectively), Dr. Rini said.
He noted that the TERAVOLT registry, a COVID-19 registry for patients with thoracic cancers, also showed a very high mortality rate in this subgroup of patients.
Results from TERAVOLT were reported at the AACR virtual meeting I, presented at ASCO, and published in The Lancet (Lancet Oncol. 2020 Jul;21[7]:914-22). The most recent results showed a mortality rate of nearly 36% and reinforce the high mortality rate seen in lung cancer patients in CCC19, Dr. Rini said.
Increased mortality risk
After adjustment for several demographic and disease characteristics, the updated CCC19 data showed a significantly increased risk of mortality among:
- Older patients (adjusted odds ratio [aOR] per decade of age, 1.52).
- Men (aOR, 1.43).
- Current or former smokers vs. never smokers (aOR, 1.28).
- Patients with Eastern Cooperative Oncology Group performance scores of 1 vs. 0 (aOR of 1.80) or 2 vs. 0 (aOR, 4.22).
- Stable cancer vs. remission (aOR, 1.47).
- Progressive cancer vs. remission (aOR, 2.96).
- Non-Hispanic Black vs. White patients (aOR, 1.56).
- Hematologic malignancies vs. solid tumors (aOR, 1.80).
“Importantly, there were some factors that did not reach statistical significance,” Dr. Rini said. These include obesity (aOR, 1.23), recent surgery (aOR, 1.05), receipt of cytotoxic chemotherapy vs. no chemotherapy (aOR, 1.14), and receipt of noncytotoxic chemotherapy vs. no chemotherapy (aOR, 0.75).
“I think this provides some reassurance that cancer care can and should continue for these patients,” Dr. Rini said.
He noted, however, that in TERAVOLT, chemotherapy with or without other treatment was a risk factor for mortality in lung cancer patients when compared with no chemotherapy (OR, 1.71) and when compared with immunotherapy or targeted therapy (OR, 1.64).
NCCAPS and other registries
Dr. Rini discussed a number of registries looking at outcomes in COVID-19 patients with cancer, and he said the findings to date appear to confirm a higher mortality rate among cancer patients, particularly those with lung cancer.
Several factors are emerging that appear to be related to risk, including both cancer-related and non–cancer-related factors, he added.
The ongoing prospective National Cancer Institute COVID-19 in Cancer Patients Study (NCCAPS) “will provide much needed longitudinal data and, importantly, biospecimen collection in a large cohort of patients who have active cancer and are receiving treatment, said Dr. Rini, who is the study’s protocol chair. NCCAPS is a natural history study in that population, he said.
The planned accrual is about 2,000 patients who will be followed for up to 2 years for data collection, imaging scans, and research specimens.
The use of specimens is “a unique and special part of this study,” Dr. Rini said, explaining that the specimens will be used to look for development of antibodies over time, to describe the trajectory of cytokine abnormalities – especially in patients with more acute inpatient courses – to perform DNA-based genome-wide association studies, and to assess coagulation parameters.
NCCAPS is activated at 546 sties, 10 patients were enrolled as of June 21, and rapid accrual is expected over the next several months, he said.
Gypsyamber D’Souza, PhD, session moderator and an infectious disease epidemiologist at Johns Hopkins University in Baltimore, acknowledged the challenge that registry administrators face when trying to balance the need to get data out against the desire to ask the right questions and to have the right comparison groups, stratification, and analyses, especially amid a crisis like the COVID-19 pandemic.
Dr. Rini said it has indeed been a bit of a struggle with CCC19 to determine what information should be published and when, and what constitutes an important update.
“It’s been a learning experience, and frankly, I think we’re still learning,” he said. “This has been such a unique time in terms of a rush to get data out, balanced against making sure that there’s quality data and that you’re actually answering important questions.”
In fact, a number of ongoing registries “should start to produce great data [that will be presented] at upcoming big conferences,” Dr. Rini said. He added that those data “will help piece together different important aspects of this and different hypotheses, and hopefully complement the clinical data that’s starting to come out.”
The CCC19 registry is sponsored by Vanderbilt-Ingram Cancer Center. Dr. Rini disclosed relationships with Pfizer, Merck, Genentech/Roche, Aveo, AstraZeneca, Bristol Myers Squibb, Exelixis, Synthorx, Peloton, Compugen, Corvus, Surface Oncology, 3DMedicines, Aravive, Alkermes, Arrowhead, and PTC Therapeutics. Dr. D’Souza did not disclose any conflicts.
SOURCE: Rini BI. AACR: COVID-19 and Cancer. Abstract IA26.
FROM AACR: COVID-19 and CANCER
Early screening may halve breast cancer mortality in childhood cancer survivors
Two strategies – annual mammography with MRI and annual MRI alone – at least halved breast cancer mortality when started at the ages of 25 or 30 years.
Jennifer M. Yeh, PhD, of Harvard Medical School in Boston and colleagues reported these results in the Annals of Internal Medicine.
When cost was also considered, 30 years emerged as the preferred starting age, dropping the incremental cost-effectiveness ratio (ICER) below the generally accepted threshold of $100,000 per quality-adjusted life-year gained.
“Our findings underscore the importance of making sure that young women previously treated with chest radiation are informed about their elevated breast cancer risk and the benefits of routine screening. Both primary care providers and oncologists who care for survivors should discuss breast cancer screening with these patients,” Dr. Yeh and colleagues wrote.
“Screening guidelines should emphasize the importance of MRI screening (with or without mammography) among survivors,” the authors recommended. “Our findings also highlight the importance of ensuring that survivors have access to health insurance coverage for MRI screening.”
Implications for awareness, coverage
“My hope is that, by showing the significantly decreased risk of death associated with early breast cancer screening, with harm-benefit ratios considerably lower than benchmarks for average-risk women, this study will help health insurance companies see the benefit in covering early screening for at-risk survivors,” commented Karen E. Effinger, MD, of Emory University, Atlanta, and the Aflac Cancer & Blood Disorders Center at Children’s Healthcare of Atlanta.
“In many survivors, the cost of current screening [as recommended by] guidelines is prohibitive,” added Dr. Effinger, who was not involved in the current study.
The main concern regarding the study’s findings is generalizability to the contemporary era, given the use of a cohort diagnosed and treated decades ago and changes in radiation techniques and dosing since then, she noted in an interview. This limitation was addressed in a sensitivity analysis that halved the women’s base-case lifetime risk of breast cancer and still netted similar results.
“However, it will take many years to determine the true risk reduction of our current treatment strategies,” Dr. Effinger acknowledged.
“It is crucial that we improve our education of both survivors and our colleagues who care for these survivors, especially in regard to risk of subsequent malignancies and the benefits of screening,” Dr. Effinger maintained. “While many people are aware of the risk of breast cancer associated with BRCA mutations, the increased risk in survivors of childhood cancer is not as recognized by nononcologists. This study reinforces that increasing this awareness can save lives.”
In educating their patients about preventive care, health care providers must strike “a fine balance between discussing the risks and benefits of screening without provoking significant anxiety,” she concluded. “It is important for survivors to establish care with a primary care provider in order to develop trust and receive the guidance they need to decrease the risk of early mortality.”
Study details
Dr. Yeh and colleagues developed models to compare outcomes with various screening strategies among women aged 20 years who had received chest radiotherapy for childhood cancer during 1970-1986. The women had been diagnosed with Hodgkin lymphoma (55%), Wilms tumor (12%), non-Hodgkin lymphoma (8%), and other cancers.
The investigators conducted their analysis using data from the Childhood Cancer Survivor Study and other published sources, a lifetime time horizon, and a payer perspective.
The team assessed three strategies: no screening; digital mammography with MRI screening starting at 25 years of age (the current Children’s Oncology Group recommendation), 30 years, or 35 years and continuing to 74 years of age; and MRI only starting at age 25, 30, or 35 years and continuing to age 74 years.
The main study results showed that, without screening, women who had received chest radiation for childhood cancer had a 10%-11% lifetime risk of breast cancer mortality across models.
Relative to no screening, starting at age 25 years, the largest share of deaths was averted with the strategy of annual mammography with MRI – 56.3%-71.2% – or with the strategy of annual MRI alone – 55.7%-62.0%.
These two strategies also yielded the most screening tests, as well as the most false-positive test results and benign biopsy results.
For women who started screening at age 25, there were 4,188-4,879 false-positive test results per 1,000 women for mammography plus MRI and 3,283-3,764 false-positive results per 1,000 women for MRI alone.
For women who started screening at age 25, there were 1,340-1,561 benign biopsy results per 1,000 women for mammography plus MRI and 1,248-1,430 benign results per 1,000 women for MRI alone.
After cost was factored in, beginning screening at age 30 emerged as the preferred strategy to achieve an ICER threshold of less than $100,000 per quality-adjusted life-year gained.
When started at 30 years of age, annual mammography with MRI averted 54.7%-68.8% of breast cancer deaths, with an ICER of $25,400-$113,200 per quality-adjusted life-year gained. Annual MRI alone averted 54.0%-60.0% of breast cancer deaths, with an ICER of $21,800-$50,580 per quality-adjusted life-year gained.
This research was supported by grants from the National Cancer Institute, American Cancer Society, and American Lebanese Syrian Associated Charities. The authors disclosed relationships with GE Healthcare and Biovector. Dr. Effinger disclosed no relevant conflicts of interest.
SOURCE: Yeh JM et al. Ann Intern Med. 2020 Jul 7. doi: 10.7326/M19-3481.
Two strategies – annual mammography with MRI and annual MRI alone – at least halved breast cancer mortality when started at the ages of 25 or 30 years.
Jennifer M. Yeh, PhD, of Harvard Medical School in Boston and colleagues reported these results in the Annals of Internal Medicine.
When cost was also considered, 30 years emerged as the preferred starting age, dropping the incremental cost-effectiveness ratio (ICER) below the generally accepted threshold of $100,000 per quality-adjusted life-year gained.
“Our findings underscore the importance of making sure that young women previously treated with chest radiation are informed about their elevated breast cancer risk and the benefits of routine screening. Both primary care providers and oncologists who care for survivors should discuss breast cancer screening with these patients,” Dr. Yeh and colleagues wrote.
“Screening guidelines should emphasize the importance of MRI screening (with or without mammography) among survivors,” the authors recommended. “Our findings also highlight the importance of ensuring that survivors have access to health insurance coverage for MRI screening.”
Implications for awareness, coverage
“My hope is that, by showing the significantly decreased risk of death associated with early breast cancer screening, with harm-benefit ratios considerably lower than benchmarks for average-risk women, this study will help health insurance companies see the benefit in covering early screening for at-risk survivors,” commented Karen E. Effinger, MD, of Emory University, Atlanta, and the Aflac Cancer & Blood Disorders Center at Children’s Healthcare of Atlanta.
“In many survivors, the cost of current screening [as recommended by] guidelines is prohibitive,” added Dr. Effinger, who was not involved in the current study.
The main concern regarding the study’s findings is generalizability to the contemporary era, given the use of a cohort diagnosed and treated decades ago and changes in radiation techniques and dosing since then, she noted in an interview. This limitation was addressed in a sensitivity analysis that halved the women’s base-case lifetime risk of breast cancer and still netted similar results.
“However, it will take many years to determine the true risk reduction of our current treatment strategies,” Dr. Effinger acknowledged.
“It is crucial that we improve our education of both survivors and our colleagues who care for these survivors, especially in regard to risk of subsequent malignancies and the benefits of screening,” Dr. Effinger maintained. “While many people are aware of the risk of breast cancer associated with BRCA mutations, the increased risk in survivors of childhood cancer is not as recognized by nononcologists. This study reinforces that increasing this awareness can save lives.”
In educating their patients about preventive care, health care providers must strike “a fine balance between discussing the risks and benefits of screening without provoking significant anxiety,” she concluded. “It is important for survivors to establish care with a primary care provider in order to develop trust and receive the guidance they need to decrease the risk of early mortality.”
Study details
Dr. Yeh and colleagues developed models to compare outcomes with various screening strategies among women aged 20 years who had received chest radiotherapy for childhood cancer during 1970-1986. The women had been diagnosed with Hodgkin lymphoma (55%), Wilms tumor (12%), non-Hodgkin lymphoma (8%), and other cancers.
The investigators conducted their analysis using data from the Childhood Cancer Survivor Study and other published sources, a lifetime time horizon, and a payer perspective.
The team assessed three strategies: no screening; digital mammography with MRI screening starting at 25 years of age (the current Children’s Oncology Group recommendation), 30 years, or 35 years and continuing to 74 years of age; and MRI only starting at age 25, 30, or 35 years and continuing to age 74 years.
The main study results showed that, without screening, women who had received chest radiation for childhood cancer had a 10%-11% lifetime risk of breast cancer mortality across models.
Relative to no screening, starting at age 25 years, the largest share of deaths was averted with the strategy of annual mammography with MRI – 56.3%-71.2% – or with the strategy of annual MRI alone – 55.7%-62.0%.
These two strategies also yielded the most screening tests, as well as the most false-positive test results and benign biopsy results.
For women who started screening at age 25, there were 4,188-4,879 false-positive test results per 1,000 women for mammography plus MRI and 3,283-3,764 false-positive results per 1,000 women for MRI alone.
For women who started screening at age 25, there were 1,340-1,561 benign biopsy results per 1,000 women for mammography plus MRI and 1,248-1,430 benign results per 1,000 women for MRI alone.
After cost was factored in, beginning screening at age 30 emerged as the preferred strategy to achieve an ICER threshold of less than $100,000 per quality-adjusted life-year gained.
When started at 30 years of age, annual mammography with MRI averted 54.7%-68.8% of breast cancer deaths, with an ICER of $25,400-$113,200 per quality-adjusted life-year gained. Annual MRI alone averted 54.0%-60.0% of breast cancer deaths, with an ICER of $21,800-$50,580 per quality-adjusted life-year gained.
This research was supported by grants from the National Cancer Institute, American Cancer Society, and American Lebanese Syrian Associated Charities. The authors disclosed relationships with GE Healthcare and Biovector. Dr. Effinger disclosed no relevant conflicts of interest.
SOURCE: Yeh JM et al. Ann Intern Med. 2020 Jul 7. doi: 10.7326/M19-3481.
Two strategies – annual mammography with MRI and annual MRI alone – at least halved breast cancer mortality when started at the ages of 25 or 30 years.
Jennifer M. Yeh, PhD, of Harvard Medical School in Boston and colleagues reported these results in the Annals of Internal Medicine.
When cost was also considered, 30 years emerged as the preferred starting age, dropping the incremental cost-effectiveness ratio (ICER) below the generally accepted threshold of $100,000 per quality-adjusted life-year gained.
“Our findings underscore the importance of making sure that young women previously treated with chest radiation are informed about their elevated breast cancer risk and the benefits of routine screening. Both primary care providers and oncologists who care for survivors should discuss breast cancer screening with these patients,” Dr. Yeh and colleagues wrote.
“Screening guidelines should emphasize the importance of MRI screening (with or without mammography) among survivors,” the authors recommended. “Our findings also highlight the importance of ensuring that survivors have access to health insurance coverage for MRI screening.”
Implications for awareness, coverage
“My hope is that, by showing the significantly decreased risk of death associated with early breast cancer screening, with harm-benefit ratios considerably lower than benchmarks for average-risk women, this study will help health insurance companies see the benefit in covering early screening for at-risk survivors,” commented Karen E. Effinger, MD, of Emory University, Atlanta, and the Aflac Cancer & Blood Disorders Center at Children’s Healthcare of Atlanta.
“In many survivors, the cost of current screening [as recommended by] guidelines is prohibitive,” added Dr. Effinger, who was not involved in the current study.
The main concern regarding the study’s findings is generalizability to the contemporary era, given the use of a cohort diagnosed and treated decades ago and changes in radiation techniques and dosing since then, she noted in an interview. This limitation was addressed in a sensitivity analysis that halved the women’s base-case lifetime risk of breast cancer and still netted similar results.
“However, it will take many years to determine the true risk reduction of our current treatment strategies,” Dr. Effinger acknowledged.
“It is crucial that we improve our education of both survivors and our colleagues who care for these survivors, especially in regard to risk of subsequent malignancies and the benefits of screening,” Dr. Effinger maintained. “While many people are aware of the risk of breast cancer associated with BRCA mutations, the increased risk in survivors of childhood cancer is not as recognized by nononcologists. This study reinforces that increasing this awareness can save lives.”
In educating their patients about preventive care, health care providers must strike “a fine balance between discussing the risks and benefits of screening without provoking significant anxiety,” she concluded. “It is important for survivors to establish care with a primary care provider in order to develop trust and receive the guidance they need to decrease the risk of early mortality.”
Study details
Dr. Yeh and colleagues developed models to compare outcomes with various screening strategies among women aged 20 years who had received chest radiotherapy for childhood cancer during 1970-1986. The women had been diagnosed with Hodgkin lymphoma (55%), Wilms tumor (12%), non-Hodgkin lymphoma (8%), and other cancers.
The investigators conducted their analysis using data from the Childhood Cancer Survivor Study and other published sources, a lifetime time horizon, and a payer perspective.
The team assessed three strategies: no screening; digital mammography with MRI screening starting at 25 years of age (the current Children’s Oncology Group recommendation), 30 years, or 35 years and continuing to 74 years of age; and MRI only starting at age 25, 30, or 35 years and continuing to age 74 years.
The main study results showed that, without screening, women who had received chest radiation for childhood cancer had a 10%-11% lifetime risk of breast cancer mortality across models.
Relative to no screening, starting at age 25 years, the largest share of deaths was averted with the strategy of annual mammography with MRI – 56.3%-71.2% – or with the strategy of annual MRI alone – 55.7%-62.0%.
These two strategies also yielded the most screening tests, as well as the most false-positive test results and benign biopsy results.
For women who started screening at age 25, there were 4,188-4,879 false-positive test results per 1,000 women for mammography plus MRI and 3,283-3,764 false-positive results per 1,000 women for MRI alone.
For women who started screening at age 25, there were 1,340-1,561 benign biopsy results per 1,000 women for mammography plus MRI and 1,248-1,430 benign results per 1,000 women for MRI alone.
After cost was factored in, beginning screening at age 30 emerged as the preferred strategy to achieve an ICER threshold of less than $100,000 per quality-adjusted life-year gained.
When started at 30 years of age, annual mammography with MRI averted 54.7%-68.8% of breast cancer deaths, with an ICER of $25,400-$113,200 per quality-adjusted life-year gained. Annual MRI alone averted 54.0%-60.0% of breast cancer deaths, with an ICER of $21,800-$50,580 per quality-adjusted life-year gained.
This research was supported by grants from the National Cancer Institute, American Cancer Society, and American Lebanese Syrian Associated Charities. The authors disclosed relationships with GE Healthcare and Biovector. Dr. Effinger disclosed no relevant conflicts of interest.
SOURCE: Yeh JM et al. Ann Intern Med. 2020 Jul 7. doi: 10.7326/M19-3481.
FROM ANNALS OF INTERNAL MEDICINE
Cancer patient organizations critically affected by pandemic
The COVID-19 pandemic has disrupted every aspect of cancer care, from diagnosis, treatment, and follow-up to participation in clinical trials, according to a new report that collected responses from cancer patient organizations around the world.
The report includes responses from 157 organizations in 56 countries, representing some 350,000 patients with cancer.
“The COVID-19 global pandemic has quite literally wreaked havoc with all of our lives but especially for cancer patients,” said the report’s author, Frances Reid, MBA, program director, World Ovarian Cancer Coalition.
“To those who have the power or influence to ensure that cancer treatment and services are not set back several years, please listen to those organizations who can articulate clearly the impact on patients, work with them, and act on it as soon as you can,” she added.
The new report, entitled “The Impact of COVID-19 on Cancer Patient Organisations,” was released on June 12. The organizations were surveyed from May 11 to May 25.
Cancer diagnosis
Two-thirds of the organizations surveyed said cancer screening programs had been canceled in their country, and 59% indicated they had seen a drop in urgent referrals for suspected cancer.
Some 44% said that access to pathology services had been reduced. One group in Australia reported that “results of pathology tests are taking longer to be returned. Generally a result would be returned within 48 hours. Since COVID-19, results are taking up to 7 days to be returned.”
As for treatment, 68% of organizations reported delays or cancellations of surgery or other treatments; 58% reported there had been a need to modify treatment protocols; and 48% indicated there had been a drop in participation in clinical trials.
Respondents were also concerned about reported increases in stress, anxiety, and isolation among many cancer patients. “Often at increased risk of infection and serious illness themselves ... many have been required to ‘shield’ from others, totally withdrawing from life outside their homes, thus increasing the already high levels of isolation they feel because of their life-limiting conditions,” the report notes.
In addition, some 60% of the organizations said that the pandemic had increased financial hardship among cancer patients. One US group commented: “Unemployment levels in the States similar to depression era. This has been a real challenge as many have lost insurance as well as jobs.”
Only a minority of respondents reported that cancer care was being offered in hospitals with no special arrangements in place to treat concomitant COVID-19 patients.
On the other hand, only 15% of respondents indicated that patients were being treated in a hospital that was not also caring for COVID-19 patients.
“Cancer will not wait for COVID-19 to pass, if it ever will, and the patient organizations are the key to minimizing the devastating impact [COVID-19 is having] on people with cancer,” Reid emphasized.
“More than ever, the patient/support services should be strengthened,” commented a group from France.
Patient services affected
“Almost all organisations (89%) have had to alter their services for people with cancer,” the report notes.
Two thirds of organizations involved in professional educational activities have had to change their services in some way, either by moving them online or stopping programs altogether, at least temporarily. “Some found that doctors and nurses are too busy with the pandemic to participate, and that their appetite for such activity is also diminished,” the report notes.
The volume of phone calls and emails increased in almost 6 of 10 organizations that provide support services for patients. Compared to prepandemic levels, volume increased by an average of 44%.
The most common queries raised by people with cancer (accounting for 85% of all queries) were questions about the risks of contracting COVID-19 and cancer treatments during the pandemic.
Some of the organizations also commented about how they had been affected. One group from Uganda said: “We had a sudden lockdown and we could not access office to give face to face counselling. We stopped research due to national guidelines on research. We continued giving information via phone and social media especially WhatsApp. We created groups for patients and counsellors to continue interacting.”
A group in Costa Rica reported: “We developed a new program of transfers from their homes to the hospital for cancer patients in chemotherapy and radiotherapy. 200 monthly transfers. We created a virtual community instead of our face-to-face support group, we started in April and we have 108 members, virtual sessions are held every two weeks.”
An organization based in the United States reported that it was “totally revamping our educational programs to be delivered in new ways in an online format ― not just replicating the in-person formats, but reaching out to our community and asking them what they would find the most valuable.”
Impact on fundraising
Almost 9 in 10 organizations raise funds to support their activities, the report notes. “A shocking 79% of organisations say they predict a fall in income over the next 12 months, with a further 16% not sure, leaving only 5% confident of their financial stability.”
Every type of fund-raising has been affected by COVID-19, from grants and major donors to community fund-raising events. Sixty percent of organisations said they were trying to find new ways to raise funds.
However, as one organization in Japan noted: “At the moment we can survive and feel it is unethical to ask the public for money when many are facing dire financial personal circumstances.”
A group from Australia commented: “Fundraising has been extremely difficult due to COVID-19 with distancing laws and no group gatherings as well as the economic downturn. Crisis appeals have been unsuccessful and all outdoor events and major events have been cancelled. In Australia we have had to contend with also the fires earlier in the year where a lot of money was donated to leaving other foundations struggling to get donor support.”
A little more than half (55%) of the organizations surveyed have had to cut costs.
Staffing cuts have been made in 1 in 10 of the organizations surveyed. A similar proportion of organizations have furloughed staff. Many if not all staff from numerous organizations are working from home.
A little more than half of those surveyed either provide funding for research or conduct research themselves, but only one quarter of them indicated there had been no change in their research projects. The others have indicated that they had to either reduce the scope of their research, put it on pause, or stop it altogether.
Three quarters of survey respondents noted that they had engaged in advocacy activities prior to the pandemic, and almost two thirds of them said they had to delay these activities.
Several of the organizations expressed thanks to the survey authors.
“COVID-19 is a global pandemic and cancer patients all around the world have similar worries, concerns and questions ― we are a small/medium organisation working in one country but believe in the power of community and coalitions and so this survey is a very welcome part of looking at this from a greater perspective,” commented one British group.
Reid has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The COVID-19 pandemic has disrupted every aspect of cancer care, from diagnosis, treatment, and follow-up to participation in clinical trials, according to a new report that collected responses from cancer patient organizations around the world.
The report includes responses from 157 organizations in 56 countries, representing some 350,000 patients with cancer.
“The COVID-19 global pandemic has quite literally wreaked havoc with all of our lives but especially for cancer patients,” said the report’s author, Frances Reid, MBA, program director, World Ovarian Cancer Coalition.
“To those who have the power or influence to ensure that cancer treatment and services are not set back several years, please listen to those organizations who can articulate clearly the impact on patients, work with them, and act on it as soon as you can,” she added.
The new report, entitled “The Impact of COVID-19 on Cancer Patient Organisations,” was released on June 12. The organizations were surveyed from May 11 to May 25.
Cancer diagnosis
Two-thirds of the organizations surveyed said cancer screening programs had been canceled in their country, and 59% indicated they had seen a drop in urgent referrals for suspected cancer.
Some 44% said that access to pathology services had been reduced. One group in Australia reported that “results of pathology tests are taking longer to be returned. Generally a result would be returned within 48 hours. Since COVID-19, results are taking up to 7 days to be returned.”
As for treatment, 68% of organizations reported delays or cancellations of surgery or other treatments; 58% reported there had been a need to modify treatment protocols; and 48% indicated there had been a drop in participation in clinical trials.
Respondents were also concerned about reported increases in stress, anxiety, and isolation among many cancer patients. “Often at increased risk of infection and serious illness themselves ... many have been required to ‘shield’ from others, totally withdrawing from life outside their homes, thus increasing the already high levels of isolation they feel because of their life-limiting conditions,” the report notes.
In addition, some 60% of the organizations said that the pandemic had increased financial hardship among cancer patients. One US group commented: “Unemployment levels in the States similar to depression era. This has been a real challenge as many have lost insurance as well as jobs.”
Only a minority of respondents reported that cancer care was being offered in hospitals with no special arrangements in place to treat concomitant COVID-19 patients.
On the other hand, only 15% of respondents indicated that patients were being treated in a hospital that was not also caring for COVID-19 patients.
“Cancer will not wait for COVID-19 to pass, if it ever will, and the patient organizations are the key to minimizing the devastating impact [COVID-19 is having] on people with cancer,” Reid emphasized.
“More than ever, the patient/support services should be strengthened,” commented a group from France.
Patient services affected
“Almost all organisations (89%) have had to alter their services for people with cancer,” the report notes.
Two thirds of organizations involved in professional educational activities have had to change their services in some way, either by moving them online or stopping programs altogether, at least temporarily. “Some found that doctors and nurses are too busy with the pandemic to participate, and that their appetite for such activity is also diminished,” the report notes.
The volume of phone calls and emails increased in almost 6 of 10 organizations that provide support services for patients. Compared to prepandemic levels, volume increased by an average of 44%.
The most common queries raised by people with cancer (accounting for 85% of all queries) were questions about the risks of contracting COVID-19 and cancer treatments during the pandemic.
Some of the organizations also commented about how they had been affected. One group from Uganda said: “We had a sudden lockdown and we could not access office to give face to face counselling. We stopped research due to national guidelines on research. We continued giving information via phone and social media especially WhatsApp. We created groups for patients and counsellors to continue interacting.”
A group in Costa Rica reported: “We developed a new program of transfers from their homes to the hospital for cancer patients in chemotherapy and radiotherapy. 200 monthly transfers. We created a virtual community instead of our face-to-face support group, we started in April and we have 108 members, virtual sessions are held every two weeks.”
An organization based in the United States reported that it was “totally revamping our educational programs to be delivered in new ways in an online format ― not just replicating the in-person formats, but reaching out to our community and asking them what they would find the most valuable.”
Impact on fundraising
Almost 9 in 10 organizations raise funds to support their activities, the report notes. “A shocking 79% of organisations say they predict a fall in income over the next 12 months, with a further 16% not sure, leaving only 5% confident of their financial stability.”
Every type of fund-raising has been affected by COVID-19, from grants and major donors to community fund-raising events. Sixty percent of organisations said they were trying to find new ways to raise funds.
However, as one organization in Japan noted: “At the moment we can survive and feel it is unethical to ask the public for money when many are facing dire financial personal circumstances.”
A group from Australia commented: “Fundraising has been extremely difficult due to COVID-19 with distancing laws and no group gatherings as well as the economic downturn. Crisis appeals have been unsuccessful and all outdoor events and major events have been cancelled. In Australia we have had to contend with also the fires earlier in the year where a lot of money was donated to leaving other foundations struggling to get donor support.”
A little more than half (55%) of the organizations surveyed have had to cut costs.
Staffing cuts have been made in 1 in 10 of the organizations surveyed. A similar proportion of organizations have furloughed staff. Many if not all staff from numerous organizations are working from home.
A little more than half of those surveyed either provide funding for research or conduct research themselves, but only one quarter of them indicated there had been no change in their research projects. The others have indicated that they had to either reduce the scope of their research, put it on pause, or stop it altogether.
Three quarters of survey respondents noted that they had engaged in advocacy activities prior to the pandemic, and almost two thirds of them said they had to delay these activities.
Several of the organizations expressed thanks to the survey authors.
“COVID-19 is a global pandemic and cancer patients all around the world have similar worries, concerns and questions ― we are a small/medium organisation working in one country but believe in the power of community and coalitions and so this survey is a very welcome part of looking at this from a greater perspective,” commented one British group.
Reid has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The COVID-19 pandemic has disrupted every aspect of cancer care, from diagnosis, treatment, and follow-up to participation in clinical trials, according to a new report that collected responses from cancer patient organizations around the world.
The report includes responses from 157 organizations in 56 countries, representing some 350,000 patients with cancer.
“The COVID-19 global pandemic has quite literally wreaked havoc with all of our lives but especially for cancer patients,” said the report’s author, Frances Reid, MBA, program director, World Ovarian Cancer Coalition.
“To those who have the power or influence to ensure that cancer treatment and services are not set back several years, please listen to those organizations who can articulate clearly the impact on patients, work with them, and act on it as soon as you can,” she added.
The new report, entitled “The Impact of COVID-19 on Cancer Patient Organisations,” was released on June 12. The organizations were surveyed from May 11 to May 25.
Cancer diagnosis
Two-thirds of the organizations surveyed said cancer screening programs had been canceled in their country, and 59% indicated they had seen a drop in urgent referrals for suspected cancer.
Some 44% said that access to pathology services had been reduced. One group in Australia reported that “results of pathology tests are taking longer to be returned. Generally a result would be returned within 48 hours. Since COVID-19, results are taking up to 7 days to be returned.”
As for treatment, 68% of organizations reported delays or cancellations of surgery or other treatments; 58% reported there had been a need to modify treatment protocols; and 48% indicated there had been a drop in participation in clinical trials.
Respondents were also concerned about reported increases in stress, anxiety, and isolation among many cancer patients. “Often at increased risk of infection and serious illness themselves ... many have been required to ‘shield’ from others, totally withdrawing from life outside their homes, thus increasing the already high levels of isolation they feel because of their life-limiting conditions,” the report notes.
In addition, some 60% of the organizations said that the pandemic had increased financial hardship among cancer patients. One US group commented: “Unemployment levels in the States similar to depression era. This has been a real challenge as many have lost insurance as well as jobs.”
Only a minority of respondents reported that cancer care was being offered in hospitals with no special arrangements in place to treat concomitant COVID-19 patients.
On the other hand, only 15% of respondents indicated that patients were being treated in a hospital that was not also caring for COVID-19 patients.
“Cancer will not wait for COVID-19 to pass, if it ever will, and the patient organizations are the key to minimizing the devastating impact [COVID-19 is having] on people with cancer,” Reid emphasized.
“More than ever, the patient/support services should be strengthened,” commented a group from France.
Patient services affected
“Almost all organisations (89%) have had to alter their services for people with cancer,” the report notes.
Two thirds of organizations involved in professional educational activities have had to change their services in some way, either by moving them online or stopping programs altogether, at least temporarily. “Some found that doctors and nurses are too busy with the pandemic to participate, and that their appetite for such activity is also diminished,” the report notes.
The volume of phone calls and emails increased in almost 6 of 10 organizations that provide support services for patients. Compared to prepandemic levels, volume increased by an average of 44%.
The most common queries raised by people with cancer (accounting for 85% of all queries) were questions about the risks of contracting COVID-19 and cancer treatments during the pandemic.
Some of the organizations also commented about how they had been affected. One group from Uganda said: “We had a sudden lockdown and we could not access office to give face to face counselling. We stopped research due to national guidelines on research. We continued giving information via phone and social media especially WhatsApp. We created groups for patients and counsellors to continue interacting.”
A group in Costa Rica reported: “We developed a new program of transfers from their homes to the hospital for cancer patients in chemotherapy and radiotherapy. 200 monthly transfers. We created a virtual community instead of our face-to-face support group, we started in April and we have 108 members, virtual sessions are held every two weeks.”
An organization based in the United States reported that it was “totally revamping our educational programs to be delivered in new ways in an online format ― not just replicating the in-person formats, but reaching out to our community and asking them what they would find the most valuable.”
Impact on fundraising
Almost 9 in 10 organizations raise funds to support their activities, the report notes. “A shocking 79% of organisations say they predict a fall in income over the next 12 months, with a further 16% not sure, leaving only 5% confident of their financial stability.”
Every type of fund-raising has been affected by COVID-19, from grants and major donors to community fund-raising events. Sixty percent of organisations said they were trying to find new ways to raise funds.
However, as one organization in Japan noted: “At the moment we can survive and feel it is unethical to ask the public for money when many are facing dire financial personal circumstances.”
A group from Australia commented: “Fundraising has been extremely difficult due to COVID-19 with distancing laws and no group gatherings as well as the economic downturn. Crisis appeals have been unsuccessful and all outdoor events and major events have been cancelled. In Australia we have had to contend with also the fires earlier in the year where a lot of money was donated to leaving other foundations struggling to get donor support.”
A little more than half (55%) of the organizations surveyed have had to cut costs.
Staffing cuts have been made in 1 in 10 of the organizations surveyed. A similar proportion of organizations have furloughed staff. Many if not all staff from numerous organizations are working from home.
A little more than half of those surveyed either provide funding for research or conduct research themselves, but only one quarter of them indicated there had been no change in their research projects. The others have indicated that they had to either reduce the scope of their research, put it on pause, or stop it altogether.
Three quarters of survey respondents noted that they had engaged in advocacy activities prior to the pandemic, and almost two thirds of them said they had to delay these activities.
Several of the organizations expressed thanks to the survey authors.
“COVID-19 is a global pandemic and cancer patients all around the world have similar worries, concerns and questions ― we are a small/medium organisation working in one country but believe in the power of community and coalitions and so this survey is a very welcome part of looking at this from a greater perspective,” commented one British group.
Reid has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Transitioning regimen may prolong proteasome inhibitor–based therapy for MM
Transitioning from parenteral bortezomib-based induction to all-oral ixazomib-lenalidomide-dexamethasone therapy increased proteasome inhibitor (PI)–based treatment adherence and duration, according to early results from a clinical trial designed to include patients representing the real-world U.S. multiple myeloma population.
The US MM-6 study was designed to evaluate a novel in-class therapy (iCT) transitioning approach from intravenous to oral treatment in the community-based setting with the aims of increasing PI-based treatment duration and adherence, maintaining health-related quality of life (HRQoL), and improving outcomes in a representative, real-world, community population of multiple myeloma patients, according to Sudhir Manda, MD, of Arizona Oncology/U.S. Oncology Research, Tucson, and colleagues.
Dr. Manda and colleagues reported on the early results of the US MM-6 trial (NCT03173092), which is a community-based, real-world, open-label, single-arm, phase 4 study of adult multiple myeloma patients who do not meet transplant-eligibility criteria, or for whom transplant would be delayed for 2 years or more, and who are receiving first-line bortezomib-based induction. All patients in the study had no evidence of progressive disease after three treatment cycles.
By the data cutoff for the reported analysis, 84 patients had been treated. The patients had a median age of 73 years; 49% were men; 15% black/African American; 10% Hispanic/Latino. A total of 62% of the patients remain on therapy, with a mean duration of total PI therapy of 10.1 months and of ixazomib-lenalidomide-dexamethasone (ixazomib-Rd) of 7.3 months.
The overall response rate was 62% (complete response, 4%; very good partial response, 25%; partial response, 33%) after bortezomib-based induction and 70% (complete response, 26%; very good partial response, 29%; partial response, 15%) after induction to all-oral ixazomib-Rd.
“The use of this novel iCT approach from parenteral bortezomib-based to oral ixazomib-based therapy facilitates long-term PI-based treatment that is well tolerated in real-world, nontransplant [newly diagnosed multiple myeloma] patients,” according to Dr. Manda and colleagues. In addition, “preliminary findings indicate that the iCT approach results in promising efficacy and high medication adherence, with no adverse impact on patients’ HRQoL or treatment satisfaction.”
The study was sponsored by Millennium Pharmaceuticals. Four of the authors are employees of Millennium Pharmaceuticals and several authors disclosed relationships with various pharmaceutical companies, including Millennium Pharmaceuticals.
SOURCE: Manda S et al. Clin Lymphoma Myeloma Leuk. 2020 Jun 30. doi: 10.1016/j.clml.2020.06.024.
Transitioning from parenteral bortezomib-based induction to all-oral ixazomib-lenalidomide-dexamethasone therapy increased proteasome inhibitor (PI)–based treatment adherence and duration, according to early results from a clinical trial designed to include patients representing the real-world U.S. multiple myeloma population.
The US MM-6 study was designed to evaluate a novel in-class therapy (iCT) transitioning approach from intravenous to oral treatment in the community-based setting with the aims of increasing PI-based treatment duration and adherence, maintaining health-related quality of life (HRQoL), and improving outcomes in a representative, real-world, community population of multiple myeloma patients, according to Sudhir Manda, MD, of Arizona Oncology/U.S. Oncology Research, Tucson, and colleagues.
Dr. Manda and colleagues reported on the early results of the US MM-6 trial (NCT03173092), which is a community-based, real-world, open-label, single-arm, phase 4 study of adult multiple myeloma patients who do not meet transplant-eligibility criteria, or for whom transplant would be delayed for 2 years or more, and who are receiving first-line bortezomib-based induction. All patients in the study had no evidence of progressive disease after three treatment cycles.
By the data cutoff for the reported analysis, 84 patients had been treated. The patients had a median age of 73 years; 49% were men; 15% black/African American; 10% Hispanic/Latino. A total of 62% of the patients remain on therapy, with a mean duration of total PI therapy of 10.1 months and of ixazomib-lenalidomide-dexamethasone (ixazomib-Rd) of 7.3 months.
The overall response rate was 62% (complete response, 4%; very good partial response, 25%; partial response, 33%) after bortezomib-based induction and 70% (complete response, 26%; very good partial response, 29%; partial response, 15%) after induction to all-oral ixazomib-Rd.
“The use of this novel iCT approach from parenteral bortezomib-based to oral ixazomib-based therapy facilitates long-term PI-based treatment that is well tolerated in real-world, nontransplant [newly diagnosed multiple myeloma] patients,” according to Dr. Manda and colleagues. In addition, “preliminary findings indicate that the iCT approach results in promising efficacy and high medication adherence, with no adverse impact on patients’ HRQoL or treatment satisfaction.”
The study was sponsored by Millennium Pharmaceuticals. Four of the authors are employees of Millennium Pharmaceuticals and several authors disclosed relationships with various pharmaceutical companies, including Millennium Pharmaceuticals.
SOURCE: Manda S et al. Clin Lymphoma Myeloma Leuk. 2020 Jun 30. doi: 10.1016/j.clml.2020.06.024.
Transitioning from parenteral bortezomib-based induction to all-oral ixazomib-lenalidomide-dexamethasone therapy increased proteasome inhibitor (PI)–based treatment adherence and duration, according to early results from a clinical trial designed to include patients representing the real-world U.S. multiple myeloma population.
The US MM-6 study was designed to evaluate a novel in-class therapy (iCT) transitioning approach from intravenous to oral treatment in the community-based setting with the aims of increasing PI-based treatment duration and adherence, maintaining health-related quality of life (HRQoL), and improving outcomes in a representative, real-world, community population of multiple myeloma patients, according to Sudhir Manda, MD, of Arizona Oncology/U.S. Oncology Research, Tucson, and colleagues.
Dr. Manda and colleagues reported on the early results of the US MM-6 trial (NCT03173092), which is a community-based, real-world, open-label, single-arm, phase 4 study of adult multiple myeloma patients who do not meet transplant-eligibility criteria, or for whom transplant would be delayed for 2 years or more, and who are receiving first-line bortezomib-based induction. All patients in the study had no evidence of progressive disease after three treatment cycles.
By the data cutoff for the reported analysis, 84 patients had been treated. The patients had a median age of 73 years; 49% were men; 15% black/African American; 10% Hispanic/Latino. A total of 62% of the patients remain on therapy, with a mean duration of total PI therapy of 10.1 months and of ixazomib-lenalidomide-dexamethasone (ixazomib-Rd) of 7.3 months.
The overall response rate was 62% (complete response, 4%; very good partial response, 25%; partial response, 33%) after bortezomib-based induction and 70% (complete response, 26%; very good partial response, 29%; partial response, 15%) after induction to all-oral ixazomib-Rd.
“The use of this novel iCT approach from parenteral bortezomib-based to oral ixazomib-based therapy facilitates long-term PI-based treatment that is well tolerated in real-world, nontransplant [newly diagnosed multiple myeloma] patients,” according to Dr. Manda and colleagues. In addition, “preliminary findings indicate that the iCT approach results in promising efficacy and high medication adherence, with no adverse impact on patients’ HRQoL or treatment satisfaction.”
The study was sponsored by Millennium Pharmaceuticals. Four of the authors are employees of Millennium Pharmaceuticals and several authors disclosed relationships with various pharmaceutical companies, including Millennium Pharmaceuticals.
SOURCE: Manda S et al. Clin Lymphoma Myeloma Leuk. 2020 Jun 30. doi: 10.1016/j.clml.2020.06.024.
FROM CLINICAL LYMPHOMA, MYELOMA AND LEUKEMIA
FDA approves selinexor for relapsed/refractory DLBCL
The Food and Drug Administration has granted accelerated approval of selinexor, a nuclear transport inhibitor, for the treatment of relapsed/refractory diffuse large B-cell lymphoma (DLBCL).
Selinexor (marketed as XPOVIO by Karyopharm Therapeutics) is intended for adult patients with relapsed/refractory DLBCL, not otherwise specified, including DLBCL arising from follicular lymphoma, after at least two lines of systemic therapy, according to the FDA’s announcement.
The FDA granted selinexor accelerated approval for this indication based on the response rate seen in the SADAL trial. Continued approval for this indication “may be contingent upon verification and description of clinical benefit in confirmatory trials,” according to the FDA.
The SADAL trial (NCT02227251) was a phase 2, single-arm, open-label study of patients with DLBCL who had previously received two to five systemic regimens. The patients received selinexor at 60 mg orally on days 1 and 3 of each week.
Results in 134 patients showed an overall response rate of 29% (95% confidence interval: 22-38), with complete responses in 13% of patients. Of 39 patients who achieved a partial or complete response, 38% had a response duration of at least 6 months, and 15% had a response duration of at least 12 months, according to the FDA announcement.
The most common adverse reactions in this trial were fatigue, nausea, diarrhea, appetite decrease, weight decrease, constipation, vomiting, and pyrexia. Grade 3-4 laboratory abnormalities occurred in 15% or more of the patients, and comprised thrombocytopenia, lymphopenia, neutropenia, anemia, and hyponatremia.
Serious adverse reactions occurred in 46% of patients, most often from infection. Gastrointestinal toxicity occurred in 80% of patients, and any-grade hyponatremia occurred in 61%. Central neurological adverse reactions occurred in 25% of patients, including dizziness and mental status changes, according to the announcement.
Warnings and precautions for adverse events – including thrombocytopenia, neutropenia, gastrointestinal toxicity, hyponatremia, serious infection, neurological toxicity, and embryo-fetal toxicity – are provided in the prescribing information.
Selinexor acts through the inhibition of exportin-1 and leads to an accumulation of tumor suppressor proteins, a reduction in oncoproteins, and apoptosis of cancer cells. The drug was previously approved in 2019 for the treatment of relapsed/refractory multiple myeloma.
The SADAL trial was sponsored by Karyopharm Therapeutics.
SOURCE: U.S. Food and Drug Administration. 2020. Approval announcement.
The Food and Drug Administration has granted accelerated approval of selinexor, a nuclear transport inhibitor, for the treatment of relapsed/refractory diffuse large B-cell lymphoma (DLBCL).
Selinexor (marketed as XPOVIO by Karyopharm Therapeutics) is intended for adult patients with relapsed/refractory DLBCL, not otherwise specified, including DLBCL arising from follicular lymphoma, after at least two lines of systemic therapy, according to the FDA’s announcement.
The FDA granted selinexor accelerated approval for this indication based on the response rate seen in the SADAL trial. Continued approval for this indication “may be contingent upon verification and description of clinical benefit in confirmatory trials,” according to the FDA.
The SADAL trial (NCT02227251) was a phase 2, single-arm, open-label study of patients with DLBCL who had previously received two to five systemic regimens. The patients received selinexor at 60 mg orally on days 1 and 3 of each week.
Results in 134 patients showed an overall response rate of 29% (95% confidence interval: 22-38), with complete responses in 13% of patients. Of 39 patients who achieved a partial or complete response, 38% had a response duration of at least 6 months, and 15% had a response duration of at least 12 months, according to the FDA announcement.
The most common adverse reactions in this trial were fatigue, nausea, diarrhea, appetite decrease, weight decrease, constipation, vomiting, and pyrexia. Grade 3-4 laboratory abnormalities occurred in 15% or more of the patients, and comprised thrombocytopenia, lymphopenia, neutropenia, anemia, and hyponatremia.
Serious adverse reactions occurred in 46% of patients, most often from infection. Gastrointestinal toxicity occurred in 80% of patients, and any-grade hyponatremia occurred in 61%. Central neurological adverse reactions occurred in 25% of patients, including dizziness and mental status changes, according to the announcement.
Warnings and precautions for adverse events – including thrombocytopenia, neutropenia, gastrointestinal toxicity, hyponatremia, serious infection, neurological toxicity, and embryo-fetal toxicity – are provided in the prescribing information.
Selinexor acts through the inhibition of exportin-1 and leads to an accumulation of tumor suppressor proteins, a reduction in oncoproteins, and apoptosis of cancer cells. The drug was previously approved in 2019 for the treatment of relapsed/refractory multiple myeloma.
The SADAL trial was sponsored by Karyopharm Therapeutics.
SOURCE: U.S. Food and Drug Administration. 2020. Approval announcement.
The Food and Drug Administration has granted accelerated approval of selinexor, a nuclear transport inhibitor, for the treatment of relapsed/refractory diffuse large B-cell lymphoma (DLBCL).
Selinexor (marketed as XPOVIO by Karyopharm Therapeutics) is intended for adult patients with relapsed/refractory DLBCL, not otherwise specified, including DLBCL arising from follicular lymphoma, after at least two lines of systemic therapy, according to the FDA’s announcement.
The FDA granted selinexor accelerated approval for this indication based on the response rate seen in the SADAL trial. Continued approval for this indication “may be contingent upon verification and description of clinical benefit in confirmatory trials,” according to the FDA.
The SADAL trial (NCT02227251) was a phase 2, single-arm, open-label study of patients with DLBCL who had previously received two to five systemic regimens. The patients received selinexor at 60 mg orally on days 1 and 3 of each week.
Results in 134 patients showed an overall response rate of 29% (95% confidence interval: 22-38), with complete responses in 13% of patients. Of 39 patients who achieved a partial or complete response, 38% had a response duration of at least 6 months, and 15% had a response duration of at least 12 months, according to the FDA announcement.
The most common adverse reactions in this trial were fatigue, nausea, diarrhea, appetite decrease, weight decrease, constipation, vomiting, and pyrexia. Grade 3-4 laboratory abnormalities occurred in 15% or more of the patients, and comprised thrombocytopenia, lymphopenia, neutropenia, anemia, and hyponatremia.
Serious adverse reactions occurred in 46% of patients, most often from infection. Gastrointestinal toxicity occurred in 80% of patients, and any-grade hyponatremia occurred in 61%. Central neurological adverse reactions occurred in 25% of patients, including dizziness and mental status changes, according to the announcement.
Warnings and precautions for adverse events – including thrombocytopenia, neutropenia, gastrointestinal toxicity, hyponatremia, serious infection, neurological toxicity, and embryo-fetal toxicity – are provided in the prescribing information.
Selinexor acts through the inhibition of exportin-1 and leads to an accumulation of tumor suppressor proteins, a reduction in oncoproteins, and apoptosis of cancer cells. The drug was previously approved in 2019 for the treatment of relapsed/refractory multiple myeloma.
The SADAL trial was sponsored by Karyopharm Therapeutics.
SOURCE: U.S. Food and Drug Administration. 2020. Approval announcement.
FROM THE FDA
Ibrutinib-venetoclax produces high MRD-negative rates in CLL/SLL
In patients with previously untreated chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL), a once-daily oral regimen of ibrutinib and venetoclax was associated with deep molecular remissions in both bone marrow and peripheral blood, including in patients with high-risk disease, according to investigators in the phase 2 CAPTIVATE MRD trial.
An intention-to-treat analysis of 164 patients with CLL/SLL treated with the combination of ibrutinib (Imbruvica) and venetoclax (Venclexta) showed a 75% rate of minimal residual disease (MRD) negativity in peripheral blood, and a 68% rate of MRD negativity in bone marrow among patients who received up to 12 cycles of the combination, reported Tanya Siddiqi, MD, of City of Hope National Medical Center, Duarte, Calif., and colleagues.
“This phase 2 study supports synergistic antitumor activity of the combination with notable deep responses across multiple compartments,” she said in an oral presentation during the virtual annual congress of the European Hematology Association.
Not ready to change practice
A hematologist/oncologist who was not involved in the study said that the data from CAPTIVATE MRD look good, but it’s still not known whether concurrent or sequential administration of the agents is optimal, and whether other regimens may be more effective in the first line.
“I think this is promising, but the informative and practice-changing study would be to compare this combination to ibrutinib monotherapy or to venetoclax and obinutuzumab, and that’s actually the subject of the next large German cooperative group study, CLL17,” said Catherine C. Coombs, MD, assistant professor of medicine at the University of North Carolina, and the UNC Lineberger Cancer Center, Chapel Hill.
She noted that the combination of venetoclax and obinutuzumab (Gazyva) is also associated with high rates of MRD negativity in the first-line setting, and that use of this regimen allows clinicians to reserve ibrutinib or acalabrutinib (Calquence) for patients in the relapsed setting.
Prerandomization results
Dr. Siddiqi presented prerandomization results from the MRD cohort of the CAPTIVATE trial (NCT02910583), which is evaluating the combination of ibrutinib and venetoclax for depth of MRD response. Following 12 cycles of the combinations, patients in this cohort are then randomized based on confirmed MRD status, with patients who are MRD negative randomized to maintenance with either ibrutinib or placebo, and patients with residual disease (MRD positive) randomized to maintenance with either ibrutinib alone or with venetoclax.
A total of 164 patients with previously untreated CLL/SLL and active disease requiring treatment who were under age 70 and had good performance status were enrolled. Following an ibrutinib lead-in period with the drug given at 420 mg once daily for three cycles of 28 days, the patients were continued on ibrutinib, and were started on venetoclax with a ramp up to 400 mg once daily, for 12 additional cycles.
As planned, patients were assessed after 15 cycles for tumor lysis syndrome (TLS) risk assessment, MRD, and hematologic, clinical, imaging, and bone marrow exams for response.
The median patient age was 58, with poor-risk features such as deletion 17p seen in 16%, complex karyotype in 19%, and unmutated immunoglobulin heavy chain variable (IGHV) in 59%.
A total of 152 patients (90%) completed all 12 cycles of the combined agents, with a median treatment duration of 14.7 months on ibrutinib and 12 months on venetoclax. Eight patients had adverse events leading to discontinuation, but there were no treatment-related deaths.
A majority of patients had reductions in lymph node burden after the three-cycle ibrutinib lead in. TLS risk also decreased during the lead-in period, with 90% of patients who had a high baseline TLS risk shifting to medium or low-risk categories, and no patients moved into the high-risk category.
“Hospitalization because of this was no longer required in 66% of at-risk patients after three cycles of ibrutinib lead in, and 82% of patients initiated venetoclax ramp up without the need for hospitalization,” Dr. Siddiqi said.
The best response of undetectable MRD was seen in peripheral blood of 75% of 163 evaluable patients, and in bone marrow of 72% of 155 patients. As noted before, the respective rates of MRD negativity in the intention-to-treat population were 75% and 68%. The proportion of patients with undetectable MRD in peripheral blood increased over time, from 57% after six cycles of the combination, she said.
The overall response rate was 97%, including 51% complete responses (CR) or CR with incomplete bone marrow recovery (CRi), and 46% partial (PR) or nodular PR (nPR). Among patients with CR/CRi, 85% had undetectable MRD in peripheral blood and 80% were MRD negative in bone marrow. In patients with PR/nPR, the respective rates were 69% and 59%. The high rates of undetectable MRD were seen irrespective of baseline disease characteristics, including bulky disease, cytogenetic risk category, del(17p) or TP53 mutation, and complex karyotype.
The most common adverse events with the combination were grade 1 or 2 diarrhea, arthralgia, fatigue, headache, and nausea. Grade 3 neutropenia was seen in 17% of patients, and grade 4 neutropenia was seen in 16%. Grade 3 febrile neutropenia and laboratory confirmed TLS occurred in 2 patients each (1%), and there were no grade 4 instances of either adverse event.
Postrandomization follow-up and analyses are currently being conducted, and results will be reported at a future meeting, real or virtual. An analysis of data on a separate cohort of 159 patients treated with the ibrutinib-venetoclax combination for a fixed duration is currently ongoing.
Dr. Siddiqi disclosed research funding and speakers bureau activity for Pharmacyclics, which sponsored the study, and others, as well as consulting/advising for several companies. Dr. Coombs disclosed consulting for AbbVie.
SOURCE: Siddiqi T et al. EHA25. Abstract S158.
In patients with previously untreated chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL), a once-daily oral regimen of ibrutinib and venetoclax was associated with deep molecular remissions in both bone marrow and peripheral blood, including in patients with high-risk disease, according to investigators in the phase 2 CAPTIVATE MRD trial.
An intention-to-treat analysis of 164 patients with CLL/SLL treated with the combination of ibrutinib (Imbruvica) and venetoclax (Venclexta) showed a 75% rate of minimal residual disease (MRD) negativity in peripheral blood, and a 68% rate of MRD negativity in bone marrow among patients who received up to 12 cycles of the combination, reported Tanya Siddiqi, MD, of City of Hope National Medical Center, Duarte, Calif., and colleagues.
“This phase 2 study supports synergistic antitumor activity of the combination with notable deep responses across multiple compartments,” she said in an oral presentation during the virtual annual congress of the European Hematology Association.
Not ready to change practice
A hematologist/oncologist who was not involved in the study said that the data from CAPTIVATE MRD look good, but it’s still not known whether concurrent or sequential administration of the agents is optimal, and whether other regimens may be more effective in the first line.
“I think this is promising, but the informative and practice-changing study would be to compare this combination to ibrutinib monotherapy or to venetoclax and obinutuzumab, and that’s actually the subject of the next large German cooperative group study, CLL17,” said Catherine C. Coombs, MD, assistant professor of medicine at the University of North Carolina, and the UNC Lineberger Cancer Center, Chapel Hill.
She noted that the combination of venetoclax and obinutuzumab (Gazyva) is also associated with high rates of MRD negativity in the first-line setting, and that use of this regimen allows clinicians to reserve ibrutinib or acalabrutinib (Calquence) for patients in the relapsed setting.
Prerandomization results
Dr. Siddiqi presented prerandomization results from the MRD cohort of the CAPTIVATE trial (NCT02910583), which is evaluating the combination of ibrutinib and venetoclax for depth of MRD response. Following 12 cycles of the combinations, patients in this cohort are then randomized based on confirmed MRD status, with patients who are MRD negative randomized to maintenance with either ibrutinib or placebo, and patients with residual disease (MRD positive) randomized to maintenance with either ibrutinib alone or with venetoclax.
A total of 164 patients with previously untreated CLL/SLL and active disease requiring treatment who were under age 70 and had good performance status were enrolled. Following an ibrutinib lead-in period with the drug given at 420 mg once daily for three cycles of 28 days, the patients were continued on ibrutinib, and were started on venetoclax with a ramp up to 400 mg once daily, for 12 additional cycles.
As planned, patients were assessed after 15 cycles for tumor lysis syndrome (TLS) risk assessment, MRD, and hematologic, clinical, imaging, and bone marrow exams for response.
The median patient age was 58, with poor-risk features such as deletion 17p seen in 16%, complex karyotype in 19%, and unmutated immunoglobulin heavy chain variable (IGHV) in 59%.
A total of 152 patients (90%) completed all 12 cycles of the combined agents, with a median treatment duration of 14.7 months on ibrutinib and 12 months on venetoclax. Eight patients had adverse events leading to discontinuation, but there were no treatment-related deaths.
A majority of patients had reductions in lymph node burden after the three-cycle ibrutinib lead in. TLS risk also decreased during the lead-in period, with 90% of patients who had a high baseline TLS risk shifting to medium or low-risk categories, and no patients moved into the high-risk category.
“Hospitalization because of this was no longer required in 66% of at-risk patients after three cycles of ibrutinib lead in, and 82% of patients initiated venetoclax ramp up without the need for hospitalization,” Dr. Siddiqi said.
The best response of undetectable MRD was seen in peripheral blood of 75% of 163 evaluable patients, and in bone marrow of 72% of 155 patients. As noted before, the respective rates of MRD negativity in the intention-to-treat population were 75% and 68%. The proportion of patients with undetectable MRD in peripheral blood increased over time, from 57% after six cycles of the combination, she said.
The overall response rate was 97%, including 51% complete responses (CR) or CR with incomplete bone marrow recovery (CRi), and 46% partial (PR) or nodular PR (nPR). Among patients with CR/CRi, 85% had undetectable MRD in peripheral blood and 80% were MRD negative in bone marrow. In patients with PR/nPR, the respective rates were 69% and 59%. The high rates of undetectable MRD were seen irrespective of baseline disease characteristics, including bulky disease, cytogenetic risk category, del(17p) or TP53 mutation, and complex karyotype.
The most common adverse events with the combination were grade 1 or 2 diarrhea, arthralgia, fatigue, headache, and nausea. Grade 3 neutropenia was seen in 17% of patients, and grade 4 neutropenia was seen in 16%. Grade 3 febrile neutropenia and laboratory confirmed TLS occurred in 2 patients each (1%), and there were no grade 4 instances of either adverse event.
Postrandomization follow-up and analyses are currently being conducted, and results will be reported at a future meeting, real or virtual. An analysis of data on a separate cohort of 159 patients treated with the ibrutinib-venetoclax combination for a fixed duration is currently ongoing.
Dr. Siddiqi disclosed research funding and speakers bureau activity for Pharmacyclics, which sponsored the study, and others, as well as consulting/advising for several companies. Dr. Coombs disclosed consulting for AbbVie.
SOURCE: Siddiqi T et al. EHA25. Abstract S158.
In patients with previously untreated chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL), a once-daily oral regimen of ibrutinib and venetoclax was associated with deep molecular remissions in both bone marrow and peripheral blood, including in patients with high-risk disease, according to investigators in the phase 2 CAPTIVATE MRD trial.
An intention-to-treat analysis of 164 patients with CLL/SLL treated with the combination of ibrutinib (Imbruvica) and venetoclax (Venclexta) showed a 75% rate of minimal residual disease (MRD) negativity in peripheral blood, and a 68% rate of MRD negativity in bone marrow among patients who received up to 12 cycles of the combination, reported Tanya Siddiqi, MD, of City of Hope National Medical Center, Duarte, Calif., and colleagues.
“This phase 2 study supports synergistic antitumor activity of the combination with notable deep responses across multiple compartments,” she said in an oral presentation during the virtual annual congress of the European Hematology Association.
Not ready to change practice
A hematologist/oncologist who was not involved in the study said that the data from CAPTIVATE MRD look good, but it’s still not known whether concurrent or sequential administration of the agents is optimal, and whether other regimens may be more effective in the first line.
“I think this is promising, but the informative and practice-changing study would be to compare this combination to ibrutinib monotherapy or to venetoclax and obinutuzumab, and that’s actually the subject of the next large German cooperative group study, CLL17,” said Catherine C. Coombs, MD, assistant professor of medicine at the University of North Carolina, and the UNC Lineberger Cancer Center, Chapel Hill.
She noted that the combination of venetoclax and obinutuzumab (Gazyva) is also associated with high rates of MRD negativity in the first-line setting, and that use of this regimen allows clinicians to reserve ibrutinib or acalabrutinib (Calquence) for patients in the relapsed setting.
Prerandomization results
Dr. Siddiqi presented prerandomization results from the MRD cohort of the CAPTIVATE trial (NCT02910583), which is evaluating the combination of ibrutinib and venetoclax for depth of MRD response. Following 12 cycles of the combinations, patients in this cohort are then randomized based on confirmed MRD status, with patients who are MRD negative randomized to maintenance with either ibrutinib or placebo, and patients with residual disease (MRD positive) randomized to maintenance with either ibrutinib alone or with venetoclax.
A total of 164 patients with previously untreated CLL/SLL and active disease requiring treatment who were under age 70 and had good performance status were enrolled. Following an ibrutinib lead-in period with the drug given at 420 mg once daily for three cycles of 28 days, the patients were continued on ibrutinib, and were started on venetoclax with a ramp up to 400 mg once daily, for 12 additional cycles.
As planned, patients were assessed after 15 cycles for tumor lysis syndrome (TLS) risk assessment, MRD, and hematologic, clinical, imaging, and bone marrow exams for response.
The median patient age was 58, with poor-risk features such as deletion 17p seen in 16%, complex karyotype in 19%, and unmutated immunoglobulin heavy chain variable (IGHV) in 59%.
A total of 152 patients (90%) completed all 12 cycles of the combined agents, with a median treatment duration of 14.7 months on ibrutinib and 12 months on venetoclax. Eight patients had adverse events leading to discontinuation, but there were no treatment-related deaths.
A majority of patients had reductions in lymph node burden after the three-cycle ibrutinib lead in. TLS risk also decreased during the lead-in period, with 90% of patients who had a high baseline TLS risk shifting to medium or low-risk categories, and no patients moved into the high-risk category.
“Hospitalization because of this was no longer required in 66% of at-risk patients after three cycles of ibrutinib lead in, and 82% of patients initiated venetoclax ramp up without the need for hospitalization,” Dr. Siddiqi said.
The best response of undetectable MRD was seen in peripheral blood of 75% of 163 evaluable patients, and in bone marrow of 72% of 155 patients. As noted before, the respective rates of MRD negativity in the intention-to-treat population were 75% and 68%. The proportion of patients with undetectable MRD in peripheral blood increased over time, from 57% after six cycles of the combination, she said.
The overall response rate was 97%, including 51% complete responses (CR) or CR with incomplete bone marrow recovery (CRi), and 46% partial (PR) or nodular PR (nPR). Among patients with CR/CRi, 85% had undetectable MRD in peripheral blood and 80% were MRD negative in bone marrow. In patients with PR/nPR, the respective rates were 69% and 59%. The high rates of undetectable MRD were seen irrespective of baseline disease characteristics, including bulky disease, cytogenetic risk category, del(17p) or TP53 mutation, and complex karyotype.
The most common adverse events with the combination were grade 1 or 2 diarrhea, arthralgia, fatigue, headache, and nausea. Grade 3 neutropenia was seen in 17% of patients, and grade 4 neutropenia was seen in 16%. Grade 3 febrile neutropenia and laboratory confirmed TLS occurred in 2 patients each (1%), and there were no grade 4 instances of either adverse event.
Postrandomization follow-up and analyses are currently being conducted, and results will be reported at a future meeting, real or virtual. An analysis of data on a separate cohort of 159 patients treated with the ibrutinib-venetoclax combination for a fixed duration is currently ongoing.
Dr. Siddiqi disclosed research funding and speakers bureau activity for Pharmacyclics, which sponsored the study, and others, as well as consulting/advising for several companies. Dr. Coombs disclosed consulting for AbbVie.
SOURCE: Siddiqi T et al. EHA25. Abstract S158.
FROM EHA 2020
FDA gives thumbs up to tazemetostat for follicular lymphoma
The US Food and Drug Administration (FDA) has granted accelerated approval of the EZH2 inhibitor tazemetostat (Tazverik, Epizyme, Inc) for the treatment of relapsed or refractory follicular lymphoma in adult patients with tumors harboring an EZH2 mutation.
Eligible patients must have already received at least two prior systemic therapies and have tumors that are positive for an EZH2 mutation, as detected by an FDA-approved test. The FDA has also approved the cobas EZH2 Mutation Test (Roche Molecular Systems, Inc) as a companion diagnostic test for tazemetostat.
The new indication is also for adult patients with relapsed/refractory follicular lymphoma who have no other satisfactory alternative treatment options.
“In our view, there remains no clear standard of care in the relapsed and/or refractory [follicular lymphoma] population, as not all patients benefit from today’s available therapies,” said Shefali Agarwal, MD, chief medical officer of Epizyme, in a company press release. “Based on this label, physicians will have the ability to use their clinical discretion to prescribe tazemetostat for their relapsed or refractory patients regardless of EZH2 mutational status and without regard to a specific line of treatment where other options are not satisfactory.”
This accelerated approval is based on overall response rate and duration of response. Continued approval for these indications may be contingent upon verification and description of clinical benefit in confirmatory trials, the FDA notes.
Tazemetostat acts as an inhibitor of EZH2 methyltransferase. Earlier this year, the drug was approved for the treatment of metastatic or locally advanced epithelioid sarcoma in cases in which complete resection is not possible. It is the first drug with this mechanism of action and is the first to be indicated for epithelioid sarcoma.
Promising Efficacy in Phase 2 Trial
The new approval for use in follicular lymphoma was based on results from an open-label, single-arm, multicenter phase 2 clinical trial involving patients who had experienced disease progression after being treated with at least two prior systemic regimens. The cohort was divided into two treatment groups: One group consisted of 45 patients with EZH2-activating mutations, the other included 54 patients with wild-type EZH2.
All patients received tazemetostat at 800 mg administered orally twice a day. The primary efficacy outcome measures were overall response rate and duration of response, in accordance with International Working Group Non-Hodgkin Lymphoma criteria.
The median duration of follow-up was 22 months for patients with EZH2-activating mutations and 36 months for those with wild-type tumors.
Among the 45 patients with an EZH2-activating mutation, the median number of lines of prior systemic therapy was 2.0 (range, 1 – 11). In 49% of patients, disease was refractory to rituximab, and in 49%, it was refractory to the patient’s last therapy.
The overall response rate was 69%; 12% of patients achieved a complete response, and 57% achieved a partial response. The median duration of response was 10.9 months and ongoing.
In the cohort of 54 patients with wild-type EZH2, the median number previous therapies was 3.0 (range, 1 – 8); in 59% of patients, disease was refractory to rituximab, and in 41%, it was refractory to the patient’s last therapy.
The overall response rate to tazemetostat treatment was 34%; 4% of patients achieved a complete response, and 30% achieved a partial response. The median duration of response was 13 months.
Serious adverse reactions occurred in 30% of patients. The most common were fatigue, upper respiratory tract infection, musculoskeletal pain, nausea, and abdominal pain. Eight patients (8%) discontinued treatment during the trial because of adverse events. There were no reported deaths. No black box warnings have been published, and there are no contraindications.
“The durable responses observed with this drug are notable in the context of the safety profile and route of oral, at-home administration, and will offer an important new option for physicians as we care for patients with relapsed/refractory follicular lymphoma,” said John Leonard, MD, in a company press release. He is associate dean for clinical research and Richard T. Silver Distinguished Professor of Hematology and Medical Oncology, Meyer Cancer Center, Weill Cornell Medicine and New York–Presbyterian Hospital, New York, and an investigator in the ongoing phase 1b/3 confirmatory trial for tazemetostat.
“Follicular lymphoma remains an incurable disease, and even with the availability of new drugs in recent years, there have remained important unmet needs in the treatment of follicular lymphoma,” he commented.
This article first appeared on Medscape.com.
The US Food and Drug Administration (FDA) has granted accelerated approval of the EZH2 inhibitor tazemetostat (Tazverik, Epizyme, Inc) for the treatment of relapsed or refractory follicular lymphoma in adult patients with tumors harboring an EZH2 mutation.
Eligible patients must have already received at least two prior systemic therapies and have tumors that are positive for an EZH2 mutation, as detected by an FDA-approved test. The FDA has also approved the cobas EZH2 Mutation Test (Roche Molecular Systems, Inc) as a companion diagnostic test for tazemetostat.
The new indication is also for adult patients with relapsed/refractory follicular lymphoma who have no other satisfactory alternative treatment options.
“In our view, there remains no clear standard of care in the relapsed and/or refractory [follicular lymphoma] population, as not all patients benefit from today’s available therapies,” said Shefali Agarwal, MD, chief medical officer of Epizyme, in a company press release. “Based on this label, physicians will have the ability to use their clinical discretion to prescribe tazemetostat for their relapsed or refractory patients regardless of EZH2 mutational status and without regard to a specific line of treatment where other options are not satisfactory.”
This accelerated approval is based on overall response rate and duration of response. Continued approval for these indications may be contingent upon verification and description of clinical benefit in confirmatory trials, the FDA notes.
Tazemetostat acts as an inhibitor of EZH2 methyltransferase. Earlier this year, the drug was approved for the treatment of metastatic or locally advanced epithelioid sarcoma in cases in which complete resection is not possible. It is the first drug with this mechanism of action and is the first to be indicated for epithelioid sarcoma.
Promising Efficacy in Phase 2 Trial
The new approval for use in follicular lymphoma was based on results from an open-label, single-arm, multicenter phase 2 clinical trial involving patients who had experienced disease progression after being treated with at least two prior systemic regimens. The cohort was divided into two treatment groups: One group consisted of 45 patients with EZH2-activating mutations, the other included 54 patients with wild-type EZH2.
All patients received tazemetostat at 800 mg administered orally twice a day. The primary efficacy outcome measures were overall response rate and duration of response, in accordance with International Working Group Non-Hodgkin Lymphoma criteria.
The median duration of follow-up was 22 months for patients with EZH2-activating mutations and 36 months for those with wild-type tumors.
Among the 45 patients with an EZH2-activating mutation, the median number of lines of prior systemic therapy was 2.0 (range, 1 – 11). In 49% of patients, disease was refractory to rituximab, and in 49%, it was refractory to the patient’s last therapy.
The overall response rate was 69%; 12% of patients achieved a complete response, and 57% achieved a partial response. The median duration of response was 10.9 months and ongoing.
In the cohort of 54 patients with wild-type EZH2, the median number previous therapies was 3.0 (range, 1 – 8); in 59% of patients, disease was refractory to rituximab, and in 41%, it was refractory to the patient’s last therapy.
The overall response rate to tazemetostat treatment was 34%; 4% of patients achieved a complete response, and 30% achieved a partial response. The median duration of response was 13 months.
Serious adverse reactions occurred in 30% of patients. The most common were fatigue, upper respiratory tract infection, musculoskeletal pain, nausea, and abdominal pain. Eight patients (8%) discontinued treatment during the trial because of adverse events. There were no reported deaths. No black box warnings have been published, and there are no contraindications.
“The durable responses observed with this drug are notable in the context of the safety profile and route of oral, at-home administration, and will offer an important new option for physicians as we care for patients with relapsed/refractory follicular lymphoma,” said John Leonard, MD, in a company press release. He is associate dean for clinical research and Richard T. Silver Distinguished Professor of Hematology and Medical Oncology, Meyer Cancer Center, Weill Cornell Medicine and New York–Presbyterian Hospital, New York, and an investigator in the ongoing phase 1b/3 confirmatory trial for tazemetostat.
“Follicular lymphoma remains an incurable disease, and even with the availability of new drugs in recent years, there have remained important unmet needs in the treatment of follicular lymphoma,” he commented.
This article first appeared on Medscape.com.
The US Food and Drug Administration (FDA) has granted accelerated approval of the EZH2 inhibitor tazemetostat (Tazverik, Epizyme, Inc) for the treatment of relapsed or refractory follicular lymphoma in adult patients with tumors harboring an EZH2 mutation.
Eligible patients must have already received at least two prior systemic therapies and have tumors that are positive for an EZH2 mutation, as detected by an FDA-approved test. The FDA has also approved the cobas EZH2 Mutation Test (Roche Molecular Systems, Inc) as a companion diagnostic test for tazemetostat.
The new indication is also for adult patients with relapsed/refractory follicular lymphoma who have no other satisfactory alternative treatment options.
“In our view, there remains no clear standard of care in the relapsed and/or refractory [follicular lymphoma] population, as not all patients benefit from today’s available therapies,” said Shefali Agarwal, MD, chief medical officer of Epizyme, in a company press release. “Based on this label, physicians will have the ability to use their clinical discretion to prescribe tazemetostat for their relapsed or refractory patients regardless of EZH2 mutational status and without regard to a specific line of treatment where other options are not satisfactory.”
This accelerated approval is based on overall response rate and duration of response. Continued approval for these indications may be contingent upon verification and description of clinical benefit in confirmatory trials, the FDA notes.
Tazemetostat acts as an inhibitor of EZH2 methyltransferase. Earlier this year, the drug was approved for the treatment of metastatic or locally advanced epithelioid sarcoma in cases in which complete resection is not possible. It is the first drug with this mechanism of action and is the first to be indicated for epithelioid sarcoma.
Promising Efficacy in Phase 2 Trial
The new approval for use in follicular lymphoma was based on results from an open-label, single-arm, multicenter phase 2 clinical trial involving patients who had experienced disease progression after being treated with at least two prior systemic regimens. The cohort was divided into two treatment groups: One group consisted of 45 patients with EZH2-activating mutations, the other included 54 patients with wild-type EZH2.
All patients received tazemetostat at 800 mg administered orally twice a day. The primary efficacy outcome measures were overall response rate and duration of response, in accordance with International Working Group Non-Hodgkin Lymphoma criteria.
The median duration of follow-up was 22 months for patients with EZH2-activating mutations and 36 months for those with wild-type tumors.
Among the 45 patients with an EZH2-activating mutation, the median number of lines of prior systemic therapy was 2.0 (range, 1 – 11). In 49% of patients, disease was refractory to rituximab, and in 49%, it was refractory to the patient’s last therapy.
The overall response rate was 69%; 12% of patients achieved a complete response, and 57% achieved a partial response. The median duration of response was 10.9 months and ongoing.
In the cohort of 54 patients with wild-type EZH2, the median number previous therapies was 3.0 (range, 1 – 8); in 59% of patients, disease was refractory to rituximab, and in 41%, it was refractory to the patient’s last therapy.
The overall response rate to tazemetostat treatment was 34%; 4% of patients achieved a complete response, and 30% achieved a partial response. The median duration of response was 13 months.
Serious adverse reactions occurred in 30% of patients. The most common were fatigue, upper respiratory tract infection, musculoskeletal pain, nausea, and abdominal pain. Eight patients (8%) discontinued treatment during the trial because of adverse events. There were no reported deaths. No black box warnings have been published, and there are no contraindications.
“The durable responses observed with this drug are notable in the context of the safety profile and route of oral, at-home administration, and will offer an important new option for physicians as we care for patients with relapsed/refractory follicular lymphoma,” said John Leonard, MD, in a company press release. He is associate dean for clinical research and Richard T. Silver Distinguished Professor of Hematology and Medical Oncology, Meyer Cancer Center, Weill Cornell Medicine and New York–Presbyterian Hospital, New York, and an investigator in the ongoing phase 1b/3 confirmatory trial for tazemetostat.
“Follicular lymphoma remains an incurable disease, and even with the availability of new drugs in recent years, there have remained important unmet needs in the treatment of follicular lymphoma,” he commented.
This article first appeared on Medscape.com.
New EPOCH for adult patients with Burkitt lymphoma
Adult patients with Burkitt lymphoma can achieve equally sound survival outcomes with dose-adjusted chemotherapy versus high-intensity regimens, but can do so while avoiding the severe toxicities, U.S. study data shows.
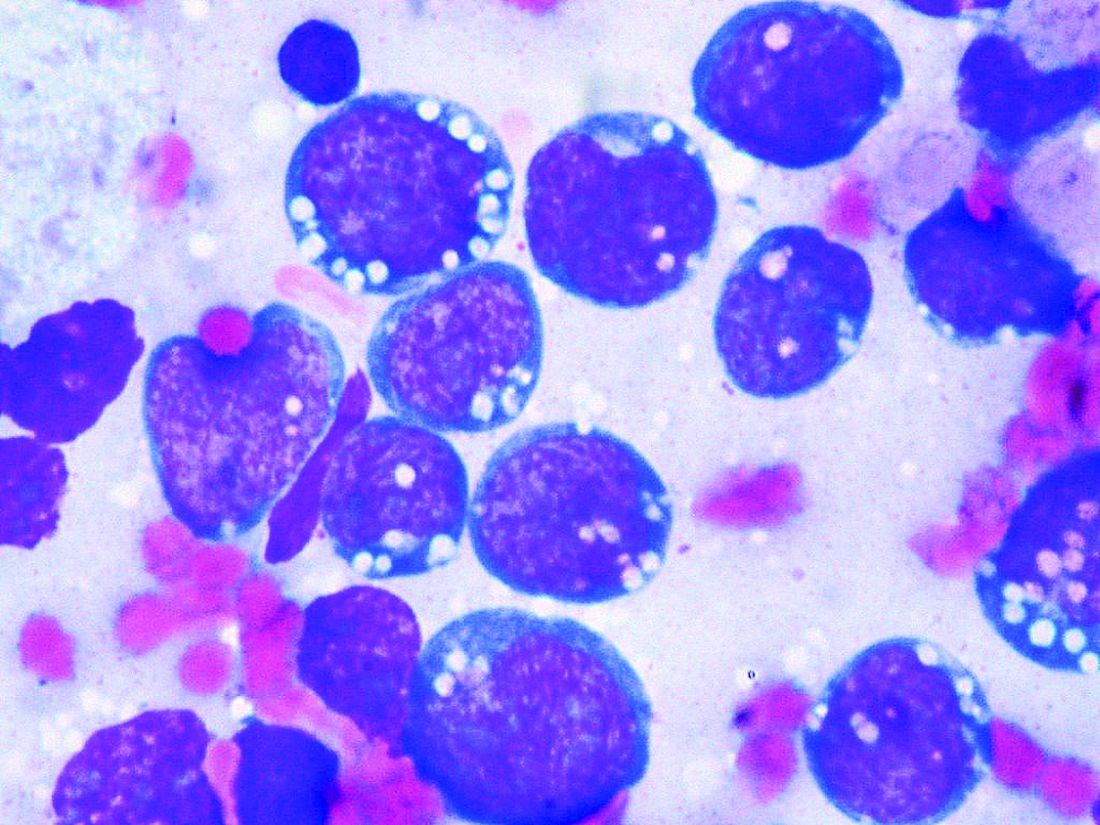
Although Burkitt lymphoma is the most common B-cell non-Hodgkin lymphoma in children, it accounts for only 1% to 2% of adult lymphoma cases.
Highly dose-intensive chemotherapy regimens, developed for children and young adults, have rendered the disease curable. But older patients in particular, and patients with comorbidities such as HIV, can suffer severe adverse effects, as well as late sequelae like second malignancies.
Mark Roschewski, MD, from the lymphoid malignancies branch at the National Cancer Institute in Bethesda, Md., and colleagues therefore examined whether a dose-adjusted regimen would maintain outcomes while reducing toxicities.
Tailoring treatment with etoposide, doxorubicin, and vincristine with prednisone, cyclophosphamide, and rituximab (EPOCH-R) to whether patients had high- or low-risk disease, they achieved 4-year survival rates of higher than 85%.
The research, published by the Journal of Clinical Oncology, also showed that patients taking the regimen, which was well tolerated, had low rates of relapse in the central nervous system.
The team reports that their results with the dose-adjusted regimen “significantly improve on the complexity, cost, and toxicity profile of other regimens,” also highlighting that it is administered on an outpatient basis.
As the outcomes also “compare favorably” with those with high intensity regimens, they say the findings “support our treatment strategies to ameliorate toxicity while maintaining efficacy.”
Importantly, they suggest highly dose-intensive chemotherapy is unnecessary for cure, and carefully defined low-risk patients may be treated with limited chemotherapy.
Dr. Roschewski said in an interview that, in patients aged 40 years and older, dose-adjusted EPOCH-R is “probably the preferred choice,” despite its “weakness” in controlling the disease in patients with active CNS involvement.
However, the “real question” is what to use in younger patients, Dr. Roschewski said, as the “unknown” is whether the additional magnitude of a high-intensity regimen that “gets into the CNS” outweighs the risk of toxicities.
“What was important about our study,” he said, was that patients with CNS involvement “did the worst but it was equally split among patients that died of toxicity and patients that progressed.”
In other words, each choice increases one risk while decreasing another. “So I would have to have that discussion with the patient, and individual patient decisions are typically based on the details,” said Dr. Roschewski.
One issue, however, that could limit the adoption of dose-adjusted EPOCH-R is that, without a randomized study comparing it directly with a high-intensity regimen, clinicians may to stick to what they know.
Dr. Roschewski said that “this is particularly true of more experienced clinicians.”
“They’re less likely, I think, to adopt something else outside of a randomized study because our natural inclination with this disease has always been dose intensity is critical. ... This is a dogma, and to shift from that probably does require a higher level of evidence, at least for some practitioners,” he explained.
Further study details
Following a pilot study of dose-adjusted EPOCH-R in 30 adult patients in which the authors say the regimen showed “high efficacy,” they enrolled 113 patients with untreated Burkitt lymphoma at 22 centers between June 2010 and May 2017.
The patients were divided into low-risk and high-risk categories, with low-risk defined as stage 1 or 2 disease, normal lactate dehydrogenase levels, ECOG performance status ≤ 1, and no tumor mass ≥ 7 cm.
High-risk patients were given six cycles of dose-adjusted EPOCH-R (with rituximab on day 1 only) along with CNS prophylaxis or active therapy with intrathecal methotrexate.
In contrast, low-risk patients were given two cycles of dose-adjusted EPOCH-R, with rituximab on days 1 and 5, followed by positron emission tomography.
If that was negative, the patients had one additional treatment cycle and no CNS prophylaxis, but if it was positive, they were given four additional cycles, plus intrathecal methotrexate.
Of the 113 patients enrolled, 79% were male, median age was 49 years, and 62% were aged at least 40 years, including 26% aged at least 60 years.
The team determined that 13% of the patients were of low risk, 87% were high risk, and 11% had cerebrospinal fluid involvement. One-quarter (24.7%) were HIV positive, with a median CD4+ T-cell count of 268 cells/mm3.
The majority (87%) of low-risk patients received three treatment cycles, and 82% of high-risk patents were administered six treatment cycles.
Over a median follow-up of 58.7 months (4.9 years), the 4-year event-free survival (EFS) rate across the whole cohort was 84.5% and overall survival was 87%.
At the time of analysis, all low-risk patients were in remission; among high-risk patients, the 4-year EFS was 82.1% and overall survival was 84.9%.
The team reports that treatment was equally effective across age groups, and irrespective of HIV status and International Prognostic Index risk group.
Only 2% of high-risk patients with no pretreatment evidence of CNS involvement had relapses in the brain parenchyma. Just over half (55%) of patients with cerebrospinal fluid involvement at presentation experienced disease progression or died.
Five patients died of treatment-related toxicity. Grade 3/4 thrombocytopenia occurred during 17% of cycles, and febrile neutropenia was seen during 16%. Tumor lysis syndrome was rare, occurring in 5% of patients.
Next, the researchers are planning on focusing on CNS disease, looking at EPOCH-R as the backbone and adding intrathecal methotrexate and an additional targeted agent with known CNS penetration.
Dr. Roschewski said that is “a very attractive strategy and ... we will initiate enrollment in that study probably in the next couple of months here at the NCI,” he added, noting that it will be an early phase 1 study.
Another issue he identified that “doesn’t get spoken about quite as much but I do think is important is potentially working on supportive care guidelines for how we manage these patients.” Dr. Roschewski explained, “One of the things you see over and over in these Burkitt lymphoma studies is that some patients don’t make it through therapy because they’re so sick at the beginning, and they have certain risks.
“I think simply improving that type of care, independent of what regimen is used, can potentially improve the outcomes across patient groups.”
The study was funded by the National Cancer Institute, National Institutes of Health, AIDS Malignancy Consortium, and the Cancer Therapy Evaluation Program and Lymphoid Malignancies Branch. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Adult patients with Burkitt lymphoma can achieve equally sound survival outcomes with dose-adjusted chemotherapy versus high-intensity regimens, but can do so while avoiding the severe toxicities, U.S. study data shows.
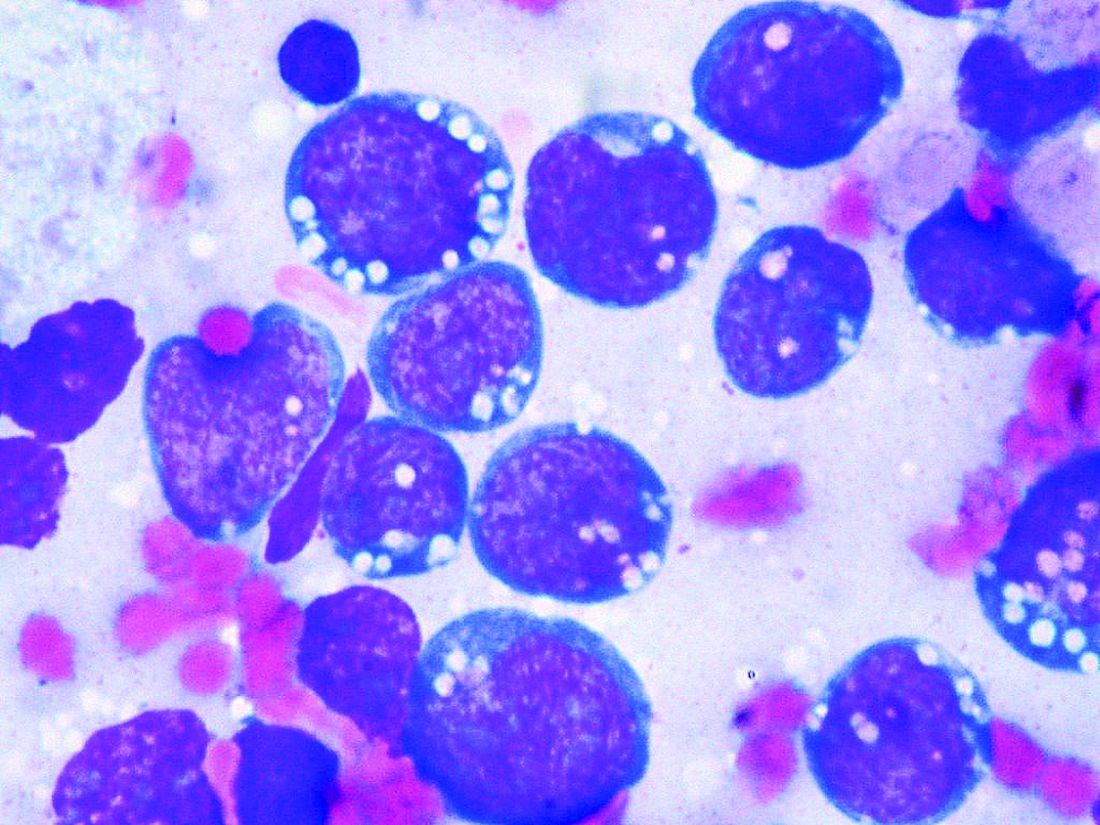
Although Burkitt lymphoma is the most common B-cell non-Hodgkin lymphoma in children, it accounts for only 1% to 2% of adult lymphoma cases.
Highly dose-intensive chemotherapy regimens, developed for children and young adults, have rendered the disease curable. But older patients in particular, and patients with comorbidities such as HIV, can suffer severe adverse effects, as well as late sequelae like second malignancies.
Mark Roschewski, MD, from the lymphoid malignancies branch at the National Cancer Institute in Bethesda, Md., and colleagues therefore examined whether a dose-adjusted regimen would maintain outcomes while reducing toxicities.
Tailoring treatment with etoposide, doxorubicin, and vincristine with prednisone, cyclophosphamide, and rituximab (EPOCH-R) to whether patients had high- or low-risk disease, they achieved 4-year survival rates of higher than 85%.
The research, published by the Journal of Clinical Oncology, also showed that patients taking the regimen, which was well tolerated, had low rates of relapse in the central nervous system.
The team reports that their results with the dose-adjusted regimen “significantly improve on the complexity, cost, and toxicity profile of other regimens,” also highlighting that it is administered on an outpatient basis.
As the outcomes also “compare favorably” with those with high intensity regimens, they say the findings “support our treatment strategies to ameliorate toxicity while maintaining efficacy.”
Importantly, they suggest highly dose-intensive chemotherapy is unnecessary for cure, and carefully defined low-risk patients may be treated with limited chemotherapy.
Dr. Roschewski said in an interview that, in patients aged 40 years and older, dose-adjusted EPOCH-R is “probably the preferred choice,” despite its “weakness” in controlling the disease in patients with active CNS involvement.
However, the “real question” is what to use in younger patients, Dr. Roschewski said, as the “unknown” is whether the additional magnitude of a high-intensity regimen that “gets into the CNS” outweighs the risk of toxicities.
“What was important about our study,” he said, was that patients with CNS involvement “did the worst but it was equally split among patients that died of toxicity and patients that progressed.”
In other words, each choice increases one risk while decreasing another. “So I would have to have that discussion with the patient, and individual patient decisions are typically based on the details,” said Dr. Roschewski.
One issue, however, that could limit the adoption of dose-adjusted EPOCH-R is that, without a randomized study comparing it directly with a high-intensity regimen, clinicians may to stick to what they know.
Dr. Roschewski said that “this is particularly true of more experienced clinicians.”
“They’re less likely, I think, to adopt something else outside of a randomized study because our natural inclination with this disease has always been dose intensity is critical. ... This is a dogma, and to shift from that probably does require a higher level of evidence, at least for some practitioners,” he explained.
Further study details
Following a pilot study of dose-adjusted EPOCH-R in 30 adult patients in which the authors say the regimen showed “high efficacy,” they enrolled 113 patients with untreated Burkitt lymphoma at 22 centers between June 2010 and May 2017.
The patients were divided into low-risk and high-risk categories, with low-risk defined as stage 1 or 2 disease, normal lactate dehydrogenase levels, ECOG performance status ≤ 1, and no tumor mass ≥ 7 cm.
High-risk patients were given six cycles of dose-adjusted EPOCH-R (with rituximab on day 1 only) along with CNS prophylaxis or active therapy with intrathecal methotrexate.
In contrast, low-risk patients were given two cycles of dose-adjusted EPOCH-R, with rituximab on days 1 and 5, followed by positron emission tomography.
If that was negative, the patients had one additional treatment cycle and no CNS prophylaxis, but if it was positive, they were given four additional cycles, plus intrathecal methotrexate.
Of the 113 patients enrolled, 79% were male, median age was 49 years, and 62% were aged at least 40 years, including 26% aged at least 60 years.
The team determined that 13% of the patients were of low risk, 87% were high risk, and 11% had cerebrospinal fluid involvement. One-quarter (24.7%) were HIV positive, with a median CD4+ T-cell count of 268 cells/mm3.
The majority (87%) of low-risk patients received three treatment cycles, and 82% of high-risk patents were administered six treatment cycles.
Over a median follow-up of 58.7 months (4.9 years), the 4-year event-free survival (EFS) rate across the whole cohort was 84.5% and overall survival was 87%.
At the time of analysis, all low-risk patients were in remission; among high-risk patients, the 4-year EFS was 82.1% and overall survival was 84.9%.
The team reports that treatment was equally effective across age groups, and irrespective of HIV status and International Prognostic Index risk group.
Only 2% of high-risk patients with no pretreatment evidence of CNS involvement had relapses in the brain parenchyma. Just over half (55%) of patients with cerebrospinal fluid involvement at presentation experienced disease progression or died.
Five patients died of treatment-related toxicity. Grade 3/4 thrombocytopenia occurred during 17% of cycles, and febrile neutropenia was seen during 16%. Tumor lysis syndrome was rare, occurring in 5% of patients.
Next, the researchers are planning on focusing on CNS disease, looking at EPOCH-R as the backbone and adding intrathecal methotrexate and an additional targeted agent with known CNS penetration.
Dr. Roschewski said that is “a very attractive strategy and ... we will initiate enrollment in that study probably in the next couple of months here at the NCI,” he added, noting that it will be an early phase 1 study.
Another issue he identified that “doesn’t get spoken about quite as much but I do think is important is potentially working on supportive care guidelines for how we manage these patients.” Dr. Roschewski explained, “One of the things you see over and over in these Burkitt lymphoma studies is that some patients don’t make it through therapy because they’re so sick at the beginning, and they have certain risks.
“I think simply improving that type of care, independent of what regimen is used, can potentially improve the outcomes across patient groups.”
The study was funded by the National Cancer Institute, National Institutes of Health, AIDS Malignancy Consortium, and the Cancer Therapy Evaluation Program and Lymphoid Malignancies Branch. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Adult patients with Burkitt lymphoma can achieve equally sound survival outcomes with dose-adjusted chemotherapy versus high-intensity regimens, but can do so while avoiding the severe toxicities, U.S. study data shows.
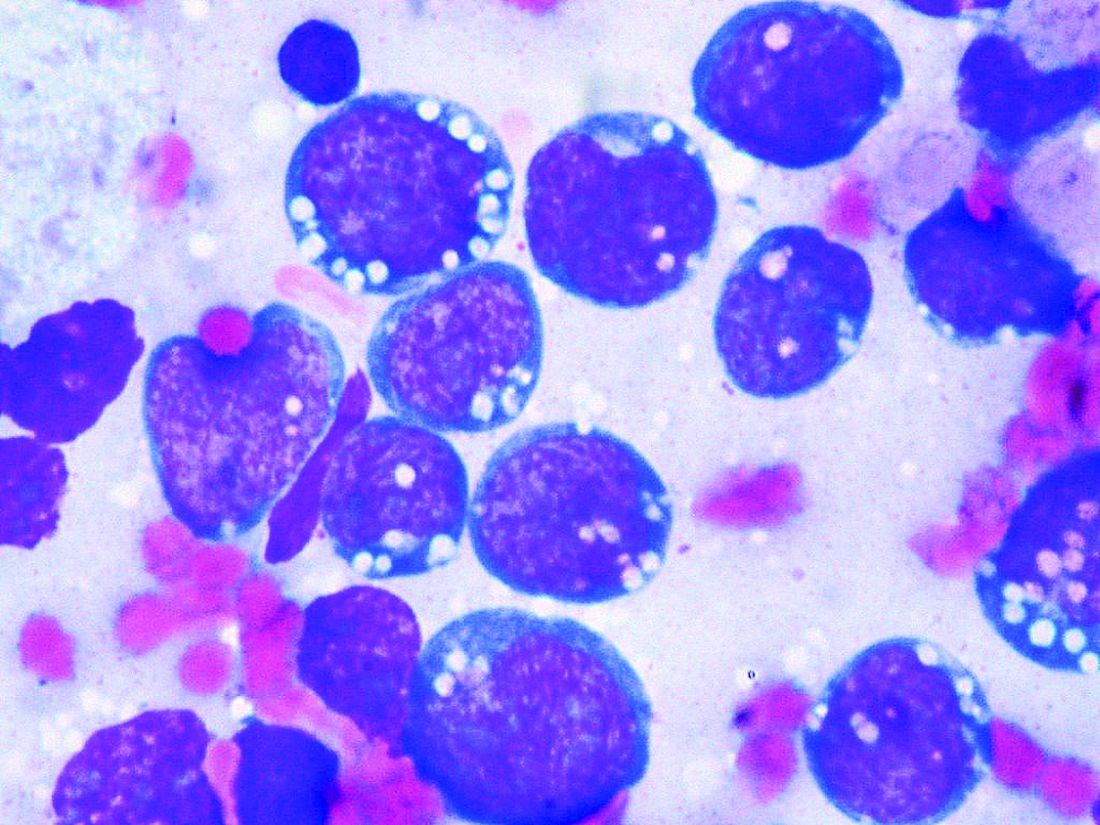
Although Burkitt lymphoma is the most common B-cell non-Hodgkin lymphoma in children, it accounts for only 1% to 2% of adult lymphoma cases.
Highly dose-intensive chemotherapy regimens, developed for children and young adults, have rendered the disease curable. But older patients in particular, and patients with comorbidities such as HIV, can suffer severe adverse effects, as well as late sequelae like second malignancies.
Mark Roschewski, MD, from the lymphoid malignancies branch at the National Cancer Institute in Bethesda, Md., and colleagues therefore examined whether a dose-adjusted regimen would maintain outcomes while reducing toxicities.
Tailoring treatment with etoposide, doxorubicin, and vincristine with prednisone, cyclophosphamide, and rituximab (EPOCH-R) to whether patients had high- or low-risk disease, they achieved 4-year survival rates of higher than 85%.
The research, published by the Journal of Clinical Oncology, also showed that patients taking the regimen, which was well tolerated, had low rates of relapse in the central nervous system.
The team reports that their results with the dose-adjusted regimen “significantly improve on the complexity, cost, and toxicity profile of other regimens,” also highlighting that it is administered on an outpatient basis.
As the outcomes also “compare favorably” with those with high intensity regimens, they say the findings “support our treatment strategies to ameliorate toxicity while maintaining efficacy.”
Importantly, they suggest highly dose-intensive chemotherapy is unnecessary for cure, and carefully defined low-risk patients may be treated with limited chemotherapy.
Dr. Roschewski said in an interview that, in patients aged 40 years and older, dose-adjusted EPOCH-R is “probably the preferred choice,” despite its “weakness” in controlling the disease in patients with active CNS involvement.
However, the “real question” is what to use in younger patients, Dr. Roschewski said, as the “unknown” is whether the additional magnitude of a high-intensity regimen that “gets into the CNS” outweighs the risk of toxicities.
“What was important about our study,” he said, was that patients with CNS involvement “did the worst but it was equally split among patients that died of toxicity and patients that progressed.”
In other words, each choice increases one risk while decreasing another. “So I would have to have that discussion with the patient, and individual patient decisions are typically based on the details,” said Dr. Roschewski.
One issue, however, that could limit the adoption of dose-adjusted EPOCH-R is that, without a randomized study comparing it directly with a high-intensity regimen, clinicians may to stick to what they know.
Dr. Roschewski said that “this is particularly true of more experienced clinicians.”
“They’re less likely, I think, to adopt something else outside of a randomized study because our natural inclination with this disease has always been dose intensity is critical. ... This is a dogma, and to shift from that probably does require a higher level of evidence, at least for some practitioners,” he explained.
Further study details
Following a pilot study of dose-adjusted EPOCH-R in 30 adult patients in which the authors say the regimen showed “high efficacy,” they enrolled 113 patients with untreated Burkitt lymphoma at 22 centers between June 2010 and May 2017.
The patients were divided into low-risk and high-risk categories, with low-risk defined as stage 1 or 2 disease, normal lactate dehydrogenase levels, ECOG performance status ≤ 1, and no tumor mass ≥ 7 cm.
High-risk patients were given six cycles of dose-adjusted EPOCH-R (with rituximab on day 1 only) along with CNS prophylaxis or active therapy with intrathecal methotrexate.
In contrast, low-risk patients were given two cycles of dose-adjusted EPOCH-R, with rituximab on days 1 and 5, followed by positron emission tomography.
If that was negative, the patients had one additional treatment cycle and no CNS prophylaxis, but if it was positive, they were given four additional cycles, plus intrathecal methotrexate.
Of the 113 patients enrolled, 79% were male, median age was 49 years, and 62% were aged at least 40 years, including 26% aged at least 60 years.
The team determined that 13% of the patients were of low risk, 87% were high risk, and 11% had cerebrospinal fluid involvement. One-quarter (24.7%) were HIV positive, with a median CD4+ T-cell count of 268 cells/mm3.
The majority (87%) of low-risk patients received three treatment cycles, and 82% of high-risk patents were administered six treatment cycles.
Over a median follow-up of 58.7 months (4.9 years), the 4-year event-free survival (EFS) rate across the whole cohort was 84.5% and overall survival was 87%.
At the time of analysis, all low-risk patients were in remission; among high-risk patients, the 4-year EFS was 82.1% and overall survival was 84.9%.
The team reports that treatment was equally effective across age groups, and irrespective of HIV status and International Prognostic Index risk group.
Only 2% of high-risk patients with no pretreatment evidence of CNS involvement had relapses in the brain parenchyma. Just over half (55%) of patients with cerebrospinal fluid involvement at presentation experienced disease progression or died.
Five patients died of treatment-related toxicity. Grade 3/4 thrombocytopenia occurred during 17% of cycles, and febrile neutropenia was seen during 16%. Tumor lysis syndrome was rare, occurring in 5% of patients.
Next, the researchers are planning on focusing on CNS disease, looking at EPOCH-R as the backbone and adding intrathecal methotrexate and an additional targeted agent with known CNS penetration.
Dr. Roschewski said that is “a very attractive strategy and ... we will initiate enrollment in that study probably in the next couple of months here at the NCI,” he added, noting that it will be an early phase 1 study.
Another issue he identified that “doesn’t get spoken about quite as much but I do think is important is potentially working on supportive care guidelines for how we manage these patients.” Dr. Roschewski explained, “One of the things you see over and over in these Burkitt lymphoma studies is that some patients don’t make it through therapy because they’re so sick at the beginning, and they have certain risks.
“I think simply improving that type of care, independent of what regimen is used, can potentially improve the outcomes across patient groups.”
The study was funded by the National Cancer Institute, National Institutes of Health, AIDS Malignancy Consortium, and the Cancer Therapy Evaluation Program and Lymphoid Malignancies Branch. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.

