User login
Safe to skip radiotherapy with negative PET in Hodgkin lymphoma
and can skip the additional radiotherapy that is normally included in the combined modality treatment, say experts reporting the final results from an international phase 3 randomized trial dubbed HD17.
“Most patients with this disease will not need radiotherapy any longer,” concluded first author Peter Borchmann, MD, assistant medical director in the department of hematology/oncology at the University Hospital Cologne (Germany).
Dr. Borchmann was speaking online as part of the virtual edition of the European Hematology Association 25th Annual Congress 2020.
“Importantly, the mortality of patients with early-stage unfavorable Hodgkin lymphoma in the HD17 study did not differ from the normal healthy German population, and this is the first time we have had this finding in one of our studies,” he emphasized.
Dr. Borchmann added that positron emission tomography imaging is key in deciding which patients can skip radiation.
“We conclude from the HD17 trial that the combined modality concept can and should be replaced by a PET-guided omission of radiotherapy for patients with newly diagnosed early-stage unfavorable Hodgkin lymphoma,” he said.
“The vast majority of early-stage unfavorable Hodgkin lymphoma patients can be treated with the brief and highly effective 2+2 chemotherapy alone,” he added.
Therefore, he continued, “PET-guided 2+2 chemotherapy is the new standard of care for the German Hodgkin study group,” which conducted the trial.
The use of both chemotherapy and radiation has long been a standard approach to treatment, and this combined modality treatment is highly effective, Dr. Borchmann explained. But it can cause long-term damage, and the known longer-term negative effects of radiotherapy, such as cardiovascular disease and second malignancies, are a particular concern because patients with early-stage Hodgkin lymphoma are relatively young, with a median age of around 30 years at disease onset.
An expert approached for comment said that the momentum to skip radiotherapy when possible is an ongoing issue, and importantly, this study adds to those efforts.
“The treatment of Hodgkin lymphoma has moved for many years now to less radiation therapy, and this trend will continue with the results of this study,” commented John G. Gribben, MD, director of the Stem Cell Transplantation Program and medical director of the North East London Cancer Research Network Centre at Barts Cancer Center of Excellence and the London School of Medicine.
“We have moved to lower doses and involved fields with the intent of decreasing toxicity, and particularly long-term toxicity from radiotherapy,” he said in an interview.
HD17 study details
For the multicenter, phase 3 HD17 trial, Dr. Borchmann and colleagues turned to PET to identify patients who had and had not responded well to chemotherapy (PET negative and PET positive) and to determine if those who had responded well could safely avoid radiotherapy without compromising efficacy.
“We wanted to determine if we could reduce the treatment intensity by omission of radiotherapy in patients who respond very well to the systemic treatment, so who have a complete metabolic remission after the chemotherapy,” Dr. Borchmann said.
The 2+2 treatment approach includes two cycles of eBEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone) and two subsequent cycles of ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine).
The trial enrolled 1,100 patients with newly diagnosed Hodgkin lymphoma between January 2012 and March 2017. Of these, 979 patients had confirmed PET results, with 651 (66.5%) found to be PET negative, defined as having a Deauville score (DS) of less than 3 (DS3); 238 (24.3%) were DS3, and 90 (9.2%) were DS4.
The study met its primary endpoint of noninferiority in progression-free survival (PFS) at 5 years, with a PFS of 95.1% in the PET-guided group (n = 447), compared with 97.3% in the standard combined-modality treatment group (n = 428), over a median observation time of 45 months, for a difference of 2.2% (P = .12).
“We found that the survival levels were very high, and we can safely conclude the noninferiority of the PET-guided approach in PET-negative patients,” Dr. Borchmann said.
A further analysis showed that the 597 PET-negative patients who did not receive radiotherapy because of their PET status had 5-year PFS that was noninferior to the combined modality group (95.9% vs. 97.7%, respectively; P = .20).
And among 646 patients who received the 2+2 regimen plus radiotherapy, of those confirmed as PET positive (n = 328), the estimated 5-year PFS was significantly lower (94.2%), compared with those determined to be PET negative (n = 318; 97.6%; hazard ratio, 3.03).
A cut-off of DS4 for positivity was associated with a stronger effect, with a lower estimated 5-year PFS of 81.6% vs. 98.8% for DS3 patients and 97.6% for DS less than 3 (P < .0001).
“Only DS4 has a prognostic impact, but not DS3,” Dr. Borchmann said. “DS4 positivity indicates a relevant risk for treatment failure, however, there are few patients in this risk group (9.2% in this trial).”
The 5-year overall survival rates in an intent-to-treat analysis were 98.8% in the standard combined modality group and 98.4% in the PET-guided group.
With a median observation time of 47 months, there have been 10 fatal events in the trial out of 1,100 patients, including two Hodgkin lymphoma-related events and one treatment-related death.
“Overall, Hodgkin lymphoma or treatment-related mortality rates were extremely low,” Dr. Borchmann said.
The study was funded by Deutsche Krebshilfe. Dr. Borchmann and Dr. Gribben have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
and can skip the additional radiotherapy that is normally included in the combined modality treatment, say experts reporting the final results from an international phase 3 randomized trial dubbed HD17.
“Most patients with this disease will not need radiotherapy any longer,” concluded first author Peter Borchmann, MD, assistant medical director in the department of hematology/oncology at the University Hospital Cologne (Germany).
Dr. Borchmann was speaking online as part of the virtual edition of the European Hematology Association 25th Annual Congress 2020.
“Importantly, the mortality of patients with early-stage unfavorable Hodgkin lymphoma in the HD17 study did not differ from the normal healthy German population, and this is the first time we have had this finding in one of our studies,” he emphasized.
Dr. Borchmann added that positron emission tomography imaging is key in deciding which patients can skip radiation.
“We conclude from the HD17 trial that the combined modality concept can and should be replaced by a PET-guided omission of radiotherapy for patients with newly diagnosed early-stage unfavorable Hodgkin lymphoma,” he said.
“The vast majority of early-stage unfavorable Hodgkin lymphoma patients can be treated with the brief and highly effective 2+2 chemotherapy alone,” he added.
Therefore, he continued, “PET-guided 2+2 chemotherapy is the new standard of care for the German Hodgkin study group,” which conducted the trial.
The use of both chemotherapy and radiation has long been a standard approach to treatment, and this combined modality treatment is highly effective, Dr. Borchmann explained. But it can cause long-term damage, and the known longer-term negative effects of radiotherapy, such as cardiovascular disease and second malignancies, are a particular concern because patients with early-stage Hodgkin lymphoma are relatively young, with a median age of around 30 years at disease onset.
An expert approached for comment said that the momentum to skip radiotherapy when possible is an ongoing issue, and importantly, this study adds to those efforts.
“The treatment of Hodgkin lymphoma has moved for many years now to less radiation therapy, and this trend will continue with the results of this study,” commented John G. Gribben, MD, director of the Stem Cell Transplantation Program and medical director of the North East London Cancer Research Network Centre at Barts Cancer Center of Excellence and the London School of Medicine.
“We have moved to lower doses and involved fields with the intent of decreasing toxicity, and particularly long-term toxicity from radiotherapy,” he said in an interview.
HD17 study details
For the multicenter, phase 3 HD17 trial, Dr. Borchmann and colleagues turned to PET to identify patients who had and had not responded well to chemotherapy (PET negative and PET positive) and to determine if those who had responded well could safely avoid radiotherapy without compromising efficacy.
“We wanted to determine if we could reduce the treatment intensity by omission of radiotherapy in patients who respond very well to the systemic treatment, so who have a complete metabolic remission after the chemotherapy,” Dr. Borchmann said.
The 2+2 treatment approach includes two cycles of eBEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone) and two subsequent cycles of ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine).
The trial enrolled 1,100 patients with newly diagnosed Hodgkin lymphoma between January 2012 and March 2017. Of these, 979 patients had confirmed PET results, with 651 (66.5%) found to be PET negative, defined as having a Deauville score (DS) of less than 3 (DS3); 238 (24.3%) were DS3, and 90 (9.2%) were DS4.
The study met its primary endpoint of noninferiority in progression-free survival (PFS) at 5 years, with a PFS of 95.1% in the PET-guided group (n = 447), compared with 97.3% in the standard combined-modality treatment group (n = 428), over a median observation time of 45 months, for a difference of 2.2% (P = .12).
“We found that the survival levels were very high, and we can safely conclude the noninferiority of the PET-guided approach in PET-negative patients,” Dr. Borchmann said.
A further analysis showed that the 597 PET-negative patients who did not receive radiotherapy because of their PET status had 5-year PFS that was noninferior to the combined modality group (95.9% vs. 97.7%, respectively; P = .20).
And among 646 patients who received the 2+2 regimen plus radiotherapy, of those confirmed as PET positive (n = 328), the estimated 5-year PFS was significantly lower (94.2%), compared with those determined to be PET negative (n = 318; 97.6%; hazard ratio, 3.03).
A cut-off of DS4 for positivity was associated with a stronger effect, with a lower estimated 5-year PFS of 81.6% vs. 98.8% for DS3 patients and 97.6% for DS less than 3 (P < .0001).
“Only DS4 has a prognostic impact, but not DS3,” Dr. Borchmann said. “DS4 positivity indicates a relevant risk for treatment failure, however, there are few patients in this risk group (9.2% in this trial).”
The 5-year overall survival rates in an intent-to-treat analysis were 98.8% in the standard combined modality group and 98.4% in the PET-guided group.
With a median observation time of 47 months, there have been 10 fatal events in the trial out of 1,100 patients, including two Hodgkin lymphoma-related events and one treatment-related death.
“Overall, Hodgkin lymphoma or treatment-related mortality rates were extremely low,” Dr. Borchmann said.
The study was funded by Deutsche Krebshilfe. Dr. Borchmann and Dr. Gribben have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
and can skip the additional radiotherapy that is normally included in the combined modality treatment, say experts reporting the final results from an international phase 3 randomized trial dubbed HD17.
“Most patients with this disease will not need radiotherapy any longer,” concluded first author Peter Borchmann, MD, assistant medical director in the department of hematology/oncology at the University Hospital Cologne (Germany).
Dr. Borchmann was speaking online as part of the virtual edition of the European Hematology Association 25th Annual Congress 2020.
“Importantly, the mortality of patients with early-stage unfavorable Hodgkin lymphoma in the HD17 study did not differ from the normal healthy German population, and this is the first time we have had this finding in one of our studies,” he emphasized.
Dr. Borchmann added that positron emission tomography imaging is key in deciding which patients can skip radiation.
“We conclude from the HD17 trial that the combined modality concept can and should be replaced by a PET-guided omission of radiotherapy for patients with newly diagnosed early-stage unfavorable Hodgkin lymphoma,” he said.
“The vast majority of early-stage unfavorable Hodgkin lymphoma patients can be treated with the brief and highly effective 2+2 chemotherapy alone,” he added.
Therefore, he continued, “PET-guided 2+2 chemotherapy is the new standard of care for the German Hodgkin study group,” which conducted the trial.
The use of both chemotherapy and radiation has long been a standard approach to treatment, and this combined modality treatment is highly effective, Dr. Borchmann explained. But it can cause long-term damage, and the known longer-term negative effects of radiotherapy, such as cardiovascular disease and second malignancies, are a particular concern because patients with early-stage Hodgkin lymphoma are relatively young, with a median age of around 30 years at disease onset.
An expert approached for comment said that the momentum to skip radiotherapy when possible is an ongoing issue, and importantly, this study adds to those efforts.
“The treatment of Hodgkin lymphoma has moved for many years now to less radiation therapy, and this trend will continue with the results of this study,” commented John G. Gribben, MD, director of the Stem Cell Transplantation Program and medical director of the North East London Cancer Research Network Centre at Barts Cancer Center of Excellence and the London School of Medicine.
“We have moved to lower doses and involved fields with the intent of decreasing toxicity, and particularly long-term toxicity from radiotherapy,” he said in an interview.
HD17 study details
For the multicenter, phase 3 HD17 trial, Dr. Borchmann and colleagues turned to PET to identify patients who had and had not responded well to chemotherapy (PET negative and PET positive) and to determine if those who had responded well could safely avoid radiotherapy without compromising efficacy.
“We wanted to determine if we could reduce the treatment intensity by omission of radiotherapy in patients who respond very well to the systemic treatment, so who have a complete metabolic remission after the chemotherapy,” Dr. Borchmann said.
The 2+2 treatment approach includes two cycles of eBEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone) and two subsequent cycles of ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine).
The trial enrolled 1,100 patients with newly diagnosed Hodgkin lymphoma between January 2012 and March 2017. Of these, 979 patients had confirmed PET results, with 651 (66.5%) found to be PET negative, defined as having a Deauville score (DS) of less than 3 (DS3); 238 (24.3%) were DS3, and 90 (9.2%) were DS4.
The study met its primary endpoint of noninferiority in progression-free survival (PFS) at 5 years, with a PFS of 95.1% in the PET-guided group (n = 447), compared with 97.3% in the standard combined-modality treatment group (n = 428), over a median observation time of 45 months, for a difference of 2.2% (P = .12).
“We found that the survival levels were very high, and we can safely conclude the noninferiority of the PET-guided approach in PET-negative patients,” Dr. Borchmann said.
A further analysis showed that the 597 PET-negative patients who did not receive radiotherapy because of their PET status had 5-year PFS that was noninferior to the combined modality group (95.9% vs. 97.7%, respectively; P = .20).
And among 646 patients who received the 2+2 regimen plus radiotherapy, of those confirmed as PET positive (n = 328), the estimated 5-year PFS was significantly lower (94.2%), compared with those determined to be PET negative (n = 318; 97.6%; hazard ratio, 3.03).
A cut-off of DS4 for positivity was associated with a stronger effect, with a lower estimated 5-year PFS of 81.6% vs. 98.8% for DS3 patients and 97.6% for DS less than 3 (P < .0001).
“Only DS4 has a prognostic impact, but not DS3,” Dr. Borchmann said. “DS4 positivity indicates a relevant risk for treatment failure, however, there are few patients in this risk group (9.2% in this trial).”
The 5-year overall survival rates in an intent-to-treat analysis were 98.8% in the standard combined modality group and 98.4% in the PET-guided group.
With a median observation time of 47 months, there have been 10 fatal events in the trial out of 1,100 patients, including two Hodgkin lymphoma-related events and one treatment-related death.
“Overall, Hodgkin lymphoma or treatment-related mortality rates were extremely low,” Dr. Borchmann said.
The study was funded by Deutsche Krebshilfe. Dr. Borchmann and Dr. Gribben have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
American Cancer Society update: ‘It is best not to drink alcohol’
In its updated cancer prevention guidelines, the American Cancer Society now recommends that “it is best not to drink alcohol.”
Previously, ACS suggested that, for those who consume alcoholic beverages, intake should be no more than one drink per day for women or two per day for men. That recommendation is still in place, but is now accompanied by this new, stronger directive.
The revised guidelines also place more emphasis on reducing the consumption of processed and red meat and highly processed foods, and on increasing physical activity.
But importantly, there is also a call for action from public, private, and community organizations to work to together to increase access to affordable, nutritious foods and physical activity.
“Making healthy choices can be challenging for many, and there are strategies included in the guidelines that communities can undertake to help reduce barriers to eating well and physical activity,” said Laura Makaroff, DO, American Cancer Society senior vice president. “Individual choice is an important part of a healthy lifestyle, but having the right policies and environmental factors to break down these barriers is also important, and that is something that clinicians can support.”
The guidelines were published in CA: A Cancer Journal for Clinicians.
The link between cancer and lifestyle factors has long been established, and for the past 4 decades, both government and leading nonprofit health organizations, including the ACS and the World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR), have released cancer prevention guidelines and recommendations that focus on managing weight, diet, physical activity, and alcohol consumption.
In 2012, the ACS issued guidelines on diet and physical activity, and their current guideline is largely based on the WCRF/AICR systematic reviews and Continuous Update Project reports, which were last updated in 2018. The ACS guidelines also incorporated systematic reviews conducted by the International Agency on Cancer Research (IARC) and the U.S. Department of Agriculture and the Department of Health and Human Services (USDA/HHS) and other analyses that were published since the WCRF/AICR recommendations were released.
Emphasis on three areas
The differences between the old guidelines and the update do not differ dramatically, but Makaroff highlighted a few areas that have increased emphasis.
Time spent being physically active is critical. The recommendation has changed to encourage adults to engage in 150-300 minutes (2.5-5 hours) of moderate-intensity physical activity, or 75-150 minutes (1.25-2.5 hours) of vigorous-intensity physical activity, or an equivalent combination, per week. Achieving or exceeding the upper limit of 300 minutes is optimal.
“That is more than what we have recommended in the past, along with the continued message that children and adolescents engage in at least 1 hour of moderate- or vigorous-intensity activity each day,” she told Medscape Medical News.
The ACS has also increased emphasis on reducing the consumption of processed and red meat. “This is part of a healthy eating pattern and making sure that people are eating food that is high in nutrients that help achieve and maintain a healthy body weight,” said Makaroff.
A healthy diet should include a variety of dark green, red, and orange vegetables; fiber-rich legumes; and fruits with a variety of colors and whole grains, according to the guidelines. Sugar-sweetened beverages, highly processed foods, and refined grain products should be limited or avoided.
The revised dietary recommendations reflect a shift from a “reductionist or nutrient-centric” approach to one that is more “holistic” and that focuses on dietary patterns. In contrast to a focus on individual nutrients and bioactive compounds, the new approach is more consistent with what and how people actually eat, ACS points out.
The third area that Makaroff highlighted is alcohol, where the recommendation is to avoid or limit consumption. “The current update says not to drink alcohol, which is in line with the scientific evidence, but for those people who choose to drink alcohol, to limit it to one drink per day for women and two drinks per day for men.”
Thus, the change here is that the previous guideline only recommended limiting alcohol consumption, while the update suggests that, optimally, it should be avoided completely.
The ACS has also called for community involvement to help implement these goals: “Public, private, and community organizations should work collaboratively at national, state, and local levels to develop, advocate for, and implement policy and environmental changes that increase access to affordable, nutritious foods; provide safe, enjoyable, and accessible opportunities for physical activity; and limit alcohol for all individuals.”
No smoking guns
Commenting on the guidelines, Steven K. Clinton, MD, PhD, associate director of the Center for Advanced Functional Foods Research and Entrepreneurship at the Ohio State University, Columbus, explained that he didn’t view the change in alcohol as that much of an evolution. “It’s been 8 years since they revised their overall guidelines, and during that time frame, there has been an enormous growth in the evidence that has been used by many organizations,” he said.
Clinton noted that the guidelines are consistent with the whole body of current scientific literature. “It’s very easy to go to the document and look for the ‘smoking gun’ – but the smoking gun is really not one thing,” he said. “It’s a pattern, and what dietitians and nutritionists are telling people is that you need to orchestrate a healthy lifestyle and diet, with a diet that has a foundation of fruits, vegetables, whole grains, and modest intake of refined grains and meat. You are orchestrating an entire pattern to get the maximum benefit.”
Makaroff is an employee of the ACS. Clinton has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
In its updated cancer prevention guidelines, the American Cancer Society now recommends that “it is best not to drink alcohol.”
Previously, ACS suggested that, for those who consume alcoholic beverages, intake should be no more than one drink per day for women or two per day for men. That recommendation is still in place, but is now accompanied by this new, stronger directive.
The revised guidelines also place more emphasis on reducing the consumption of processed and red meat and highly processed foods, and on increasing physical activity.
But importantly, there is also a call for action from public, private, and community organizations to work to together to increase access to affordable, nutritious foods and physical activity.
“Making healthy choices can be challenging for many, and there are strategies included in the guidelines that communities can undertake to help reduce barriers to eating well and physical activity,” said Laura Makaroff, DO, American Cancer Society senior vice president. “Individual choice is an important part of a healthy lifestyle, but having the right policies and environmental factors to break down these barriers is also important, and that is something that clinicians can support.”
The guidelines were published in CA: A Cancer Journal for Clinicians.
The link between cancer and lifestyle factors has long been established, and for the past 4 decades, both government and leading nonprofit health organizations, including the ACS and the World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR), have released cancer prevention guidelines and recommendations that focus on managing weight, diet, physical activity, and alcohol consumption.
In 2012, the ACS issued guidelines on diet and physical activity, and their current guideline is largely based on the WCRF/AICR systematic reviews and Continuous Update Project reports, which were last updated in 2018. The ACS guidelines also incorporated systematic reviews conducted by the International Agency on Cancer Research (IARC) and the U.S. Department of Agriculture and the Department of Health and Human Services (USDA/HHS) and other analyses that were published since the WCRF/AICR recommendations were released.
Emphasis on three areas
The differences between the old guidelines and the update do not differ dramatically, but Makaroff highlighted a few areas that have increased emphasis.
Time spent being physically active is critical. The recommendation has changed to encourage adults to engage in 150-300 minutes (2.5-5 hours) of moderate-intensity physical activity, or 75-150 minutes (1.25-2.5 hours) of vigorous-intensity physical activity, or an equivalent combination, per week. Achieving or exceeding the upper limit of 300 minutes is optimal.
“That is more than what we have recommended in the past, along with the continued message that children and adolescents engage in at least 1 hour of moderate- or vigorous-intensity activity each day,” she told Medscape Medical News.
The ACS has also increased emphasis on reducing the consumption of processed and red meat. “This is part of a healthy eating pattern and making sure that people are eating food that is high in nutrients that help achieve and maintain a healthy body weight,” said Makaroff.
A healthy diet should include a variety of dark green, red, and orange vegetables; fiber-rich legumes; and fruits with a variety of colors and whole grains, according to the guidelines. Sugar-sweetened beverages, highly processed foods, and refined grain products should be limited or avoided.
The revised dietary recommendations reflect a shift from a “reductionist or nutrient-centric” approach to one that is more “holistic” and that focuses on dietary patterns. In contrast to a focus on individual nutrients and bioactive compounds, the new approach is more consistent with what and how people actually eat, ACS points out.
The third area that Makaroff highlighted is alcohol, where the recommendation is to avoid or limit consumption. “The current update says not to drink alcohol, which is in line with the scientific evidence, but for those people who choose to drink alcohol, to limit it to one drink per day for women and two drinks per day for men.”
Thus, the change here is that the previous guideline only recommended limiting alcohol consumption, while the update suggests that, optimally, it should be avoided completely.
The ACS has also called for community involvement to help implement these goals: “Public, private, and community organizations should work collaboratively at national, state, and local levels to develop, advocate for, and implement policy and environmental changes that increase access to affordable, nutritious foods; provide safe, enjoyable, and accessible opportunities for physical activity; and limit alcohol for all individuals.”
No smoking guns
Commenting on the guidelines, Steven K. Clinton, MD, PhD, associate director of the Center for Advanced Functional Foods Research and Entrepreneurship at the Ohio State University, Columbus, explained that he didn’t view the change in alcohol as that much of an evolution. “It’s been 8 years since they revised their overall guidelines, and during that time frame, there has been an enormous growth in the evidence that has been used by many organizations,” he said.
Clinton noted that the guidelines are consistent with the whole body of current scientific literature. “It’s very easy to go to the document and look for the ‘smoking gun’ – but the smoking gun is really not one thing,” he said. “It’s a pattern, and what dietitians and nutritionists are telling people is that you need to orchestrate a healthy lifestyle and diet, with a diet that has a foundation of fruits, vegetables, whole grains, and modest intake of refined grains and meat. You are orchestrating an entire pattern to get the maximum benefit.”
Makaroff is an employee of the ACS. Clinton has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
In its updated cancer prevention guidelines, the American Cancer Society now recommends that “it is best not to drink alcohol.”
Previously, ACS suggested that, for those who consume alcoholic beverages, intake should be no more than one drink per day for women or two per day for men. That recommendation is still in place, but is now accompanied by this new, stronger directive.
The revised guidelines also place more emphasis on reducing the consumption of processed and red meat and highly processed foods, and on increasing physical activity.
But importantly, there is also a call for action from public, private, and community organizations to work to together to increase access to affordable, nutritious foods and physical activity.
“Making healthy choices can be challenging for many, and there are strategies included in the guidelines that communities can undertake to help reduce barriers to eating well and physical activity,” said Laura Makaroff, DO, American Cancer Society senior vice president. “Individual choice is an important part of a healthy lifestyle, but having the right policies and environmental factors to break down these barriers is also important, and that is something that clinicians can support.”
The guidelines were published in CA: A Cancer Journal for Clinicians.
The link between cancer and lifestyle factors has long been established, and for the past 4 decades, both government and leading nonprofit health organizations, including the ACS and the World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR), have released cancer prevention guidelines and recommendations that focus on managing weight, diet, physical activity, and alcohol consumption.
In 2012, the ACS issued guidelines on diet and physical activity, and their current guideline is largely based on the WCRF/AICR systematic reviews and Continuous Update Project reports, which were last updated in 2018. The ACS guidelines also incorporated systematic reviews conducted by the International Agency on Cancer Research (IARC) and the U.S. Department of Agriculture and the Department of Health and Human Services (USDA/HHS) and other analyses that were published since the WCRF/AICR recommendations were released.
Emphasis on three areas
The differences between the old guidelines and the update do not differ dramatically, but Makaroff highlighted a few areas that have increased emphasis.
Time spent being physically active is critical. The recommendation has changed to encourage adults to engage in 150-300 minutes (2.5-5 hours) of moderate-intensity physical activity, or 75-150 minutes (1.25-2.5 hours) of vigorous-intensity physical activity, or an equivalent combination, per week. Achieving or exceeding the upper limit of 300 minutes is optimal.
“That is more than what we have recommended in the past, along with the continued message that children and adolescents engage in at least 1 hour of moderate- or vigorous-intensity activity each day,” she told Medscape Medical News.
The ACS has also increased emphasis on reducing the consumption of processed and red meat. “This is part of a healthy eating pattern and making sure that people are eating food that is high in nutrients that help achieve and maintain a healthy body weight,” said Makaroff.
A healthy diet should include a variety of dark green, red, and orange vegetables; fiber-rich legumes; and fruits with a variety of colors and whole grains, according to the guidelines. Sugar-sweetened beverages, highly processed foods, and refined grain products should be limited or avoided.
The revised dietary recommendations reflect a shift from a “reductionist or nutrient-centric” approach to one that is more “holistic” and that focuses on dietary patterns. In contrast to a focus on individual nutrients and bioactive compounds, the new approach is more consistent with what and how people actually eat, ACS points out.
The third area that Makaroff highlighted is alcohol, where the recommendation is to avoid or limit consumption. “The current update says not to drink alcohol, which is in line with the scientific evidence, but for those people who choose to drink alcohol, to limit it to one drink per day for women and two drinks per day for men.”
Thus, the change here is that the previous guideline only recommended limiting alcohol consumption, while the update suggests that, optimally, it should be avoided completely.
The ACS has also called for community involvement to help implement these goals: “Public, private, and community organizations should work collaboratively at national, state, and local levels to develop, advocate for, and implement policy and environmental changes that increase access to affordable, nutritious foods; provide safe, enjoyable, and accessible opportunities for physical activity; and limit alcohol for all individuals.”
No smoking guns
Commenting on the guidelines, Steven K. Clinton, MD, PhD, associate director of the Center for Advanced Functional Foods Research and Entrepreneurship at the Ohio State University, Columbus, explained that he didn’t view the change in alcohol as that much of an evolution. “It’s been 8 years since they revised their overall guidelines, and during that time frame, there has been an enormous growth in the evidence that has been used by many organizations,” he said.
Clinton noted that the guidelines are consistent with the whole body of current scientific literature. “It’s very easy to go to the document and look for the ‘smoking gun’ – but the smoking gun is really not one thing,” he said. “It’s a pattern, and what dietitians and nutritionists are telling people is that you need to orchestrate a healthy lifestyle and diet, with a diet that has a foundation of fruits, vegetables, whole grains, and modest intake of refined grains and meat. You are orchestrating an entire pattern to get the maximum benefit.”
Makaroff is an employee of the ACS. Clinton has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Can an app guide cancer treatment decisions during the pandemic?
Deciding which cancer patients need immediate treatment and who can safely wait is an uncomfortable assessment for cancer clinicians during the COVID-19 pandemic.
In early April, as the COVID-19 surge was bearing down on New York City, those treatment decisions were “a juggling act every single day,” Jonathan Yang, MD, PhD, a radiation oncologist from New York’s Memorial Sloan Kettering Cancer Center, told Medscape Medical News.
Eventually, a glut of guidelines, recommendations, and expert opinions aimed at helping oncologists emerged. The tools help navigate the complicated risk-benefit analysis of their patient’s risk of infection by SARS-CoV-2 and delaying therapy.
Now, a new tool, which appears to be the first of its kind, quantifies that risk-benefit analysis. But its presence immediately raises the question: can it help?
Three-Tier Systems Are Not Very Sophisticated
OncCOVID, a free tool that was launched May 26 by the University of Michigan, allows physicians to individualize risk estimates for delaying treatment of up to 25 early- to late-stage cancers. It includes more than 45 patient characteristics, such as age, location, cancer type, cancer stage, treatment plan, underlying medical conditions, and proposed length of delay in care.
Combining these personal details with data from the National Cancer Institute’s SEER (Surveillance, Epidemiology, and End Results) registry and the National Cancer Database, the Michigan app then estimates a patient’s 5- or 10-year survival with immediate vs delayed treatment and weighs that against their risk for COVID-19 using data from the Johns Hopkins Coronavirus Resource Center.
“We thought, isn’t it better to at least provide some evidence-based quantification, rather than a back-of-the-envelope three-tier system that is just sort of ‘made up’?“ explained one of the developers, Daniel Spratt, MD, associate professor of radiation oncology at Michigan Medicine.
Spratt explained that almost every organization, professional society, and government has created something like a three-tier system. Tier 1 represents urgent cases and patients who need immediate treatment. For tier 2, treatment can be delayed weeks or a month, and with tier 3, it can be delayed until the pandemic is over or it’s deemed safe.
“[This system] sounds good at first glance, but in cancer, we’re always talking about personalized medicine, and it’s mind-blowing that these tier systems are only based on urgency and prognosis,” he told Medscape Medical News.
Spratt offered an example. Consider a patient with a very aggressive brain tumor ― that patient is in tier 1 and should undergo treatment immediately. But will the treatment actually help? And how helpful would the procedure be if, say, the patient is 80 years old and, if infected, would have a 30% to 50% chance of dying from the coronavirus?
“If the model says this guy has a 5% harm and this one has 30% harm, you can use that to help prioritize,” summarized Spratt.
The app can generate risk estimates for patients living anywhere in the world and has already been accessed by people from 37 countries. However, Spratt cautions that it is primarily “designed and calibrated for the US.
“The estimates are based on very large US registries, and though it’s probably somewhat similar across much of the world, there’s probably certain cancer types that are more region specific ― especially something like stomach cancer or certain types of head and neck cancer in parts of Asia, for example,” he said.
Although the app’s COVID-19 data are specific to the county level in the United States, elsewhere in the world, it is only country specific.
“We’re using the best data we have for coronavirus, but everyone knows we still have large data gaps,” he acknowledged.
How Accurate?
Asked to comment on the app, Richard Bleicher, MD, leader of the Breast Cancer Program at Fox Chase Cancer Center, Philadelphia, praised the effort and the goal but had some concerns.
“Several questions arise, most important of which is, How accurate is this, and how has this been validated, if at all ― especially as it is too soon to see the outcomes of patients affected in this pandemic?” he told Medscape Medical News.
“We are imposing delays on a broad scale because of the coronavirus, and we are getting continuously changing data as we test more patients. But both situations are novel and may not be accurately represented by the data being pulled, because the datasets use patients from a few years ago, and confounders in these datasets may not apply to this situation,” Bleicher continued.
Although acknowledging the “value in delineating the risk of dying from cancer vs the risk of dying from the SARS-CoV-2 pandemic,” Bleicher urged caution in using the tool to make individual patient decisions.
“We need to remember that the best of modeling ... can be wildly inaccurate and needs to be validated using patients having the circumstances in question. ... This won’t be possible until long after the pandemic is completed, and so the model’s accuracy remains unknown.”
That sentiment was echoed by Giampaolo Bianchini, MD, head of the Breast Cancer Group, Department of Medical Oncology, Ospedale San Raffaele, in Milan, Italy.
“Arbitrarily postponing and modifying treatment strategies including surgery, radiation therapy, and medical therapy without properly balancing the risk/benefit ratio may lead to significantly worse cancer-related outcomes, which largely exceed the actual risks for COVID,” he wrote in an email.
“The OncCOVID app is a remarkable attempt to fill the gap between perception and estimation,” he said. The app provides side by side the COVID-19 risk estimation and the consequences of arbitrary deviation from the standard of care, observed Bianchini.
However, he pointed out weaknesses, including the fact that the “data generated in literature are not always of high quality and do not take into consideration relevant characteristics of the disease and treatment benefit. It should for sure be used, but then also interpreted with caution.”
Another Italian group responded more positively.
“In our opinion, it could be a useful tool for clinicians,” wrote colleagues Alessio Cortelinni and Giampiero Porzio, both medical oncologists at San Salvatore Hospital and the University of L’Aquila, in Italy. “This Web app might assist clinicians in balancing the risk/benefit ratio of being treated and/or access to the outpatient cancer center for each kind of patient (both early and advanced stages), in order to make a more tailored counseling,” they wrote in an email. “Importantly, the Web app might help those clinicians who work ‘alone,’ in peripheral centers, without resources, colleagues, and multidisciplinary tumor boards on whom they can rely.”
Bleicher, who was involved in the COVID-19 Breast Cancer Consortium’s recommendations for prioritizing breast cancer treatment, summarized that the app “may end up being close or accurate, but we won’t know except in hindsight.”
This article first appeared on Medscape.com.
Deciding which cancer patients need immediate treatment and who can safely wait is an uncomfortable assessment for cancer clinicians during the COVID-19 pandemic.
In early April, as the COVID-19 surge was bearing down on New York City, those treatment decisions were “a juggling act every single day,” Jonathan Yang, MD, PhD, a radiation oncologist from New York’s Memorial Sloan Kettering Cancer Center, told Medscape Medical News.
Eventually, a glut of guidelines, recommendations, and expert opinions aimed at helping oncologists emerged. The tools help navigate the complicated risk-benefit analysis of their patient’s risk of infection by SARS-CoV-2 and delaying therapy.
Now, a new tool, which appears to be the first of its kind, quantifies that risk-benefit analysis. But its presence immediately raises the question: can it help?
Three-Tier Systems Are Not Very Sophisticated
OncCOVID, a free tool that was launched May 26 by the University of Michigan, allows physicians to individualize risk estimates for delaying treatment of up to 25 early- to late-stage cancers. It includes more than 45 patient characteristics, such as age, location, cancer type, cancer stage, treatment plan, underlying medical conditions, and proposed length of delay in care.
Combining these personal details with data from the National Cancer Institute’s SEER (Surveillance, Epidemiology, and End Results) registry and the National Cancer Database, the Michigan app then estimates a patient’s 5- or 10-year survival with immediate vs delayed treatment and weighs that against their risk for COVID-19 using data from the Johns Hopkins Coronavirus Resource Center.
“We thought, isn’t it better to at least provide some evidence-based quantification, rather than a back-of-the-envelope three-tier system that is just sort of ‘made up’?“ explained one of the developers, Daniel Spratt, MD, associate professor of radiation oncology at Michigan Medicine.
Spratt explained that almost every organization, professional society, and government has created something like a three-tier system. Tier 1 represents urgent cases and patients who need immediate treatment. For tier 2, treatment can be delayed weeks or a month, and with tier 3, it can be delayed until the pandemic is over or it’s deemed safe.
“[This system] sounds good at first glance, but in cancer, we’re always talking about personalized medicine, and it’s mind-blowing that these tier systems are only based on urgency and prognosis,” he told Medscape Medical News.
Spratt offered an example. Consider a patient with a very aggressive brain tumor ― that patient is in tier 1 and should undergo treatment immediately. But will the treatment actually help? And how helpful would the procedure be if, say, the patient is 80 years old and, if infected, would have a 30% to 50% chance of dying from the coronavirus?
“If the model says this guy has a 5% harm and this one has 30% harm, you can use that to help prioritize,” summarized Spratt.
The app can generate risk estimates for patients living anywhere in the world and has already been accessed by people from 37 countries. However, Spratt cautions that it is primarily “designed and calibrated for the US.
“The estimates are based on very large US registries, and though it’s probably somewhat similar across much of the world, there’s probably certain cancer types that are more region specific ― especially something like stomach cancer or certain types of head and neck cancer in parts of Asia, for example,” he said.
Although the app’s COVID-19 data are specific to the county level in the United States, elsewhere in the world, it is only country specific.
“We’re using the best data we have for coronavirus, but everyone knows we still have large data gaps,” he acknowledged.
How Accurate?
Asked to comment on the app, Richard Bleicher, MD, leader of the Breast Cancer Program at Fox Chase Cancer Center, Philadelphia, praised the effort and the goal but had some concerns.
“Several questions arise, most important of which is, How accurate is this, and how has this been validated, if at all ― especially as it is too soon to see the outcomes of patients affected in this pandemic?” he told Medscape Medical News.
“We are imposing delays on a broad scale because of the coronavirus, and we are getting continuously changing data as we test more patients. But both situations are novel and may not be accurately represented by the data being pulled, because the datasets use patients from a few years ago, and confounders in these datasets may not apply to this situation,” Bleicher continued.
Although acknowledging the “value in delineating the risk of dying from cancer vs the risk of dying from the SARS-CoV-2 pandemic,” Bleicher urged caution in using the tool to make individual patient decisions.
“We need to remember that the best of modeling ... can be wildly inaccurate and needs to be validated using patients having the circumstances in question. ... This won’t be possible until long after the pandemic is completed, and so the model’s accuracy remains unknown.”
That sentiment was echoed by Giampaolo Bianchini, MD, head of the Breast Cancer Group, Department of Medical Oncology, Ospedale San Raffaele, in Milan, Italy.
“Arbitrarily postponing and modifying treatment strategies including surgery, radiation therapy, and medical therapy without properly balancing the risk/benefit ratio may lead to significantly worse cancer-related outcomes, which largely exceed the actual risks for COVID,” he wrote in an email.
“The OncCOVID app is a remarkable attempt to fill the gap between perception and estimation,” he said. The app provides side by side the COVID-19 risk estimation and the consequences of arbitrary deviation from the standard of care, observed Bianchini.
However, he pointed out weaknesses, including the fact that the “data generated in literature are not always of high quality and do not take into consideration relevant characteristics of the disease and treatment benefit. It should for sure be used, but then also interpreted with caution.”
Another Italian group responded more positively.
“In our opinion, it could be a useful tool for clinicians,” wrote colleagues Alessio Cortelinni and Giampiero Porzio, both medical oncologists at San Salvatore Hospital and the University of L’Aquila, in Italy. “This Web app might assist clinicians in balancing the risk/benefit ratio of being treated and/or access to the outpatient cancer center for each kind of patient (both early and advanced stages), in order to make a more tailored counseling,” they wrote in an email. “Importantly, the Web app might help those clinicians who work ‘alone,’ in peripheral centers, without resources, colleagues, and multidisciplinary tumor boards on whom they can rely.”
Bleicher, who was involved in the COVID-19 Breast Cancer Consortium’s recommendations for prioritizing breast cancer treatment, summarized that the app “may end up being close or accurate, but we won’t know except in hindsight.”
This article first appeared on Medscape.com.
Deciding which cancer patients need immediate treatment and who can safely wait is an uncomfortable assessment for cancer clinicians during the COVID-19 pandemic.
In early April, as the COVID-19 surge was bearing down on New York City, those treatment decisions were “a juggling act every single day,” Jonathan Yang, MD, PhD, a radiation oncologist from New York’s Memorial Sloan Kettering Cancer Center, told Medscape Medical News.
Eventually, a glut of guidelines, recommendations, and expert opinions aimed at helping oncologists emerged. The tools help navigate the complicated risk-benefit analysis of their patient’s risk of infection by SARS-CoV-2 and delaying therapy.
Now, a new tool, which appears to be the first of its kind, quantifies that risk-benefit analysis. But its presence immediately raises the question: can it help?
Three-Tier Systems Are Not Very Sophisticated
OncCOVID, a free tool that was launched May 26 by the University of Michigan, allows physicians to individualize risk estimates for delaying treatment of up to 25 early- to late-stage cancers. It includes more than 45 patient characteristics, such as age, location, cancer type, cancer stage, treatment plan, underlying medical conditions, and proposed length of delay in care.
Combining these personal details with data from the National Cancer Institute’s SEER (Surveillance, Epidemiology, and End Results) registry and the National Cancer Database, the Michigan app then estimates a patient’s 5- or 10-year survival with immediate vs delayed treatment and weighs that against their risk for COVID-19 using data from the Johns Hopkins Coronavirus Resource Center.
“We thought, isn’t it better to at least provide some evidence-based quantification, rather than a back-of-the-envelope three-tier system that is just sort of ‘made up’?“ explained one of the developers, Daniel Spratt, MD, associate professor of radiation oncology at Michigan Medicine.
Spratt explained that almost every organization, professional society, and government has created something like a three-tier system. Tier 1 represents urgent cases and patients who need immediate treatment. For tier 2, treatment can be delayed weeks or a month, and with tier 3, it can be delayed until the pandemic is over or it’s deemed safe.
“[This system] sounds good at first glance, but in cancer, we’re always talking about personalized medicine, and it’s mind-blowing that these tier systems are only based on urgency and prognosis,” he told Medscape Medical News.
Spratt offered an example. Consider a patient with a very aggressive brain tumor ― that patient is in tier 1 and should undergo treatment immediately. But will the treatment actually help? And how helpful would the procedure be if, say, the patient is 80 years old and, if infected, would have a 30% to 50% chance of dying from the coronavirus?
“If the model says this guy has a 5% harm and this one has 30% harm, you can use that to help prioritize,” summarized Spratt.
The app can generate risk estimates for patients living anywhere in the world and has already been accessed by people from 37 countries. However, Spratt cautions that it is primarily “designed and calibrated for the US.
“The estimates are based on very large US registries, and though it’s probably somewhat similar across much of the world, there’s probably certain cancer types that are more region specific ― especially something like stomach cancer or certain types of head and neck cancer in parts of Asia, for example,” he said.
Although the app’s COVID-19 data are specific to the county level in the United States, elsewhere in the world, it is only country specific.
“We’re using the best data we have for coronavirus, but everyone knows we still have large data gaps,” he acknowledged.
How Accurate?
Asked to comment on the app, Richard Bleicher, MD, leader of the Breast Cancer Program at Fox Chase Cancer Center, Philadelphia, praised the effort and the goal but had some concerns.
“Several questions arise, most important of which is, How accurate is this, and how has this been validated, if at all ― especially as it is too soon to see the outcomes of patients affected in this pandemic?” he told Medscape Medical News.
“We are imposing delays on a broad scale because of the coronavirus, and we are getting continuously changing data as we test more patients. But both situations are novel and may not be accurately represented by the data being pulled, because the datasets use patients from a few years ago, and confounders in these datasets may not apply to this situation,” Bleicher continued.
Although acknowledging the “value in delineating the risk of dying from cancer vs the risk of dying from the SARS-CoV-2 pandemic,” Bleicher urged caution in using the tool to make individual patient decisions.
“We need to remember that the best of modeling ... can be wildly inaccurate and needs to be validated using patients having the circumstances in question. ... This won’t be possible until long after the pandemic is completed, and so the model’s accuracy remains unknown.”
That sentiment was echoed by Giampaolo Bianchini, MD, head of the Breast Cancer Group, Department of Medical Oncology, Ospedale San Raffaele, in Milan, Italy.
“Arbitrarily postponing and modifying treatment strategies including surgery, radiation therapy, and medical therapy without properly balancing the risk/benefit ratio may lead to significantly worse cancer-related outcomes, which largely exceed the actual risks for COVID,” he wrote in an email.
“The OncCOVID app is a remarkable attempt to fill the gap between perception and estimation,” he said. The app provides side by side the COVID-19 risk estimation and the consequences of arbitrary deviation from the standard of care, observed Bianchini.
However, he pointed out weaknesses, including the fact that the “data generated in literature are not always of high quality and do not take into consideration relevant characteristics of the disease and treatment benefit. It should for sure be used, but then also interpreted with caution.”
Another Italian group responded more positively.
“In our opinion, it could be a useful tool for clinicians,” wrote colleagues Alessio Cortelinni and Giampiero Porzio, both medical oncologists at San Salvatore Hospital and the University of L’Aquila, in Italy. “This Web app might assist clinicians in balancing the risk/benefit ratio of being treated and/or access to the outpatient cancer center for each kind of patient (both early and advanced stages), in order to make a more tailored counseling,” they wrote in an email. “Importantly, the Web app might help those clinicians who work ‘alone,’ in peripheral centers, without resources, colleagues, and multidisciplinary tumor boards on whom they can rely.”
Bleicher, who was involved in the COVID-19 Breast Cancer Consortium’s recommendations for prioritizing breast cancer treatment, summarized that the app “may end up being close or accurate, but we won’t know except in hindsight.”
This article first appeared on Medscape.com.
‘A good and peaceful death’: Cancer hospice during the pandemic
Lillie Shockney, RN, MAS, a two-time breast cancer survivor and adjunct professor at Johns Hopkins School of Nursing in Baltimore, Maryland, mourns the many losses that her patients with advanced cancer now face in the midst of the COVID-19 pandemic. But in the void of the usual support networks and treatment plans, she sees the resurgence of something that has recently been crowded out: hospice.
The pandemic has forced patients and their physicians to reassess the risk/benefit balance of continuing or embarking on yet another cancer treatment.
“It’s one of the pearls that we will get out of this nightmare,” said Ms. Shockney, who recently retired as administrative director of the cancer survivorship programs at the Sidney Kimmel Comprehensive Cancer Center.
“Physicians have been taught to treat the disease – so as long as there’s a treatment they give another treatment,” she told Medscape Medical News during a Zoom call from her home. “But for some patients with advanced disease, those treatments were making them very sick, so they were trading longevity over quality of life.”
Of course, longevity has never been a guarantee with cancer treatment, and even less so now, with the risk of COVID-19.
“This is going to bring them to some hard discussions,” says Brenda Nevidjon, RN, MSN, chief executive officer at the Oncology Nursing Society.
“We’ve known for a long time that there are patients who are on third- and fourth-round treatment options that have very little evidence of prolonging life or quality of life,” she told Medscape Medical News. “Do we bring these people out of their home to a setting where there could be a fair number of COVID-positive patients? Do we expose them to that?”
Across the world, these dilemmas are pushing cancer specialists to initiate discussions of hospice sooner with patients who have advanced disease, and with more clarity than before.
One of the reasons such conversations have often been avoided is that the concept of hospice is generally misunderstood, said Ms. Shockney.
“Patients think ‘you’re giving up on me, you’ve abandoned me’, but hospice is all about preserving the remainder of their quality of life and letting them have time with family and time to fulfill those elements of experiencing a good and peaceful death,” she said.
Indeed, hospice is “a benefit meant for somebody with at least a 6-month horizon,” agrees Ms. Nevidjon. Yet the average length of hospice in the United States is just 5 days. “It’s at the very, very end, and yet for some of these patients the 6 months they could get in hospice might be a better quality of life than the 4 months on another whole plan of chemotherapy. I can’t imagine that on the backside of this pandemic we will not have learned and we won’t start to change practices around initiating more of these conversations.”
Silver lining of this pandemic?
It’s too early into the pandemic to have hard data on whether hospice uptake has increased, but “it’s encouraging to hear that hospice is being discussed and offered sooner as an alternative to that third- or fourth-round chemo,” said Lori Bishop, MHA, RN, vice president of palliative and advanced care at the National Hospice and Palliative Care Organization.
“I agree that improving informed-decision discussions and timely access to hospice is a silver lining of the pandemic,” she told Medscape Medical News.
But she points out that today’s hospice looks quite different than it did before the pandemic, with the immediate and very obvious difference being telehealth, which was not widely utilized previously.
In March, the Centers for Medicare & Medicaid Services expanded telehealth options for hospice providers, something that Ms. Bishop and other hospice providers hope will remain in place after the pandemic passes.
“Telehealth visits are offered to replace some in-home visits both to minimize risk of exposure to COVID-19 and reduce the drain on personal protective equipment,” Bishop explained.
“In-patient hospice programs are also finding unique ways to provide support and connect patients to their loved ones: visitors are allowed but limited to one or two. Music and pet therapy are being provided through the window or virtually and devices such as iPads are being used to help patients connect with loved ones,” she said.
Telehealth links patients out of loneliness, but the one thing it cannot do is provide the comfort of touch – an important part of any hospice program.
“Hand-holding ... I miss that a lot,” says Ms. Shockney, her eyes filling with tears. “When you take somebody’s hand, you don’t even have to speak; that connection, and eye contact, is all you need to help that person emotionally heal.”
This article first appeared on Medscape.com.
Lillie Shockney, RN, MAS, a two-time breast cancer survivor and adjunct professor at Johns Hopkins School of Nursing in Baltimore, Maryland, mourns the many losses that her patients with advanced cancer now face in the midst of the COVID-19 pandemic. But in the void of the usual support networks and treatment plans, she sees the resurgence of something that has recently been crowded out: hospice.
The pandemic has forced patients and their physicians to reassess the risk/benefit balance of continuing or embarking on yet another cancer treatment.
“It’s one of the pearls that we will get out of this nightmare,” said Ms. Shockney, who recently retired as administrative director of the cancer survivorship programs at the Sidney Kimmel Comprehensive Cancer Center.
“Physicians have been taught to treat the disease – so as long as there’s a treatment they give another treatment,” she told Medscape Medical News during a Zoom call from her home. “But for some patients with advanced disease, those treatments were making them very sick, so they were trading longevity over quality of life.”
Of course, longevity has never been a guarantee with cancer treatment, and even less so now, with the risk of COVID-19.
“This is going to bring them to some hard discussions,” says Brenda Nevidjon, RN, MSN, chief executive officer at the Oncology Nursing Society.
“We’ve known for a long time that there are patients who are on third- and fourth-round treatment options that have very little evidence of prolonging life or quality of life,” she told Medscape Medical News. “Do we bring these people out of their home to a setting where there could be a fair number of COVID-positive patients? Do we expose them to that?”
Across the world, these dilemmas are pushing cancer specialists to initiate discussions of hospice sooner with patients who have advanced disease, and with more clarity than before.
One of the reasons such conversations have often been avoided is that the concept of hospice is generally misunderstood, said Ms. Shockney.
“Patients think ‘you’re giving up on me, you’ve abandoned me’, but hospice is all about preserving the remainder of their quality of life and letting them have time with family and time to fulfill those elements of experiencing a good and peaceful death,” she said.
Indeed, hospice is “a benefit meant for somebody with at least a 6-month horizon,” agrees Ms. Nevidjon. Yet the average length of hospice in the United States is just 5 days. “It’s at the very, very end, and yet for some of these patients the 6 months they could get in hospice might be a better quality of life than the 4 months on another whole plan of chemotherapy. I can’t imagine that on the backside of this pandemic we will not have learned and we won’t start to change practices around initiating more of these conversations.”
Silver lining of this pandemic?
It’s too early into the pandemic to have hard data on whether hospice uptake has increased, but “it’s encouraging to hear that hospice is being discussed and offered sooner as an alternative to that third- or fourth-round chemo,” said Lori Bishop, MHA, RN, vice president of palliative and advanced care at the National Hospice and Palliative Care Organization.
“I agree that improving informed-decision discussions and timely access to hospice is a silver lining of the pandemic,” she told Medscape Medical News.
But she points out that today’s hospice looks quite different than it did before the pandemic, with the immediate and very obvious difference being telehealth, which was not widely utilized previously.
In March, the Centers for Medicare & Medicaid Services expanded telehealth options for hospice providers, something that Ms. Bishop and other hospice providers hope will remain in place after the pandemic passes.
“Telehealth visits are offered to replace some in-home visits both to minimize risk of exposure to COVID-19 and reduce the drain on personal protective equipment,” Bishop explained.
“In-patient hospice programs are also finding unique ways to provide support and connect patients to their loved ones: visitors are allowed but limited to one or two. Music and pet therapy are being provided through the window or virtually and devices such as iPads are being used to help patients connect with loved ones,” she said.
Telehealth links patients out of loneliness, but the one thing it cannot do is provide the comfort of touch – an important part of any hospice program.
“Hand-holding ... I miss that a lot,” says Ms. Shockney, her eyes filling with tears. “When you take somebody’s hand, you don’t even have to speak; that connection, and eye contact, is all you need to help that person emotionally heal.”
This article first appeared on Medscape.com.
Lillie Shockney, RN, MAS, a two-time breast cancer survivor and adjunct professor at Johns Hopkins School of Nursing in Baltimore, Maryland, mourns the many losses that her patients with advanced cancer now face in the midst of the COVID-19 pandemic. But in the void of the usual support networks and treatment plans, she sees the resurgence of something that has recently been crowded out: hospice.
The pandemic has forced patients and their physicians to reassess the risk/benefit balance of continuing or embarking on yet another cancer treatment.
“It’s one of the pearls that we will get out of this nightmare,” said Ms. Shockney, who recently retired as administrative director of the cancer survivorship programs at the Sidney Kimmel Comprehensive Cancer Center.
“Physicians have been taught to treat the disease – so as long as there’s a treatment they give another treatment,” she told Medscape Medical News during a Zoom call from her home. “But for some patients with advanced disease, those treatments were making them very sick, so they were trading longevity over quality of life.”
Of course, longevity has never been a guarantee with cancer treatment, and even less so now, with the risk of COVID-19.
“This is going to bring them to some hard discussions,” says Brenda Nevidjon, RN, MSN, chief executive officer at the Oncology Nursing Society.
“We’ve known for a long time that there are patients who are on third- and fourth-round treatment options that have very little evidence of prolonging life or quality of life,” she told Medscape Medical News. “Do we bring these people out of their home to a setting where there could be a fair number of COVID-positive patients? Do we expose them to that?”
Across the world, these dilemmas are pushing cancer specialists to initiate discussions of hospice sooner with patients who have advanced disease, and with more clarity than before.
One of the reasons such conversations have often been avoided is that the concept of hospice is generally misunderstood, said Ms. Shockney.
“Patients think ‘you’re giving up on me, you’ve abandoned me’, but hospice is all about preserving the remainder of their quality of life and letting them have time with family and time to fulfill those elements of experiencing a good and peaceful death,” she said.
Indeed, hospice is “a benefit meant for somebody with at least a 6-month horizon,” agrees Ms. Nevidjon. Yet the average length of hospice in the United States is just 5 days. “It’s at the very, very end, and yet for some of these patients the 6 months they could get in hospice might be a better quality of life than the 4 months on another whole plan of chemotherapy. I can’t imagine that on the backside of this pandemic we will not have learned and we won’t start to change practices around initiating more of these conversations.”
Silver lining of this pandemic?
It’s too early into the pandemic to have hard data on whether hospice uptake has increased, but “it’s encouraging to hear that hospice is being discussed and offered sooner as an alternative to that third- or fourth-round chemo,” said Lori Bishop, MHA, RN, vice president of palliative and advanced care at the National Hospice and Palliative Care Organization.
“I agree that improving informed-decision discussions and timely access to hospice is a silver lining of the pandemic,” she told Medscape Medical News.
But she points out that today’s hospice looks quite different than it did before the pandemic, with the immediate and very obvious difference being telehealth, which was not widely utilized previously.
In March, the Centers for Medicare & Medicaid Services expanded telehealth options for hospice providers, something that Ms. Bishop and other hospice providers hope will remain in place after the pandemic passes.
“Telehealth visits are offered to replace some in-home visits both to minimize risk of exposure to COVID-19 and reduce the drain on personal protective equipment,” Bishop explained.
“In-patient hospice programs are also finding unique ways to provide support and connect patients to their loved ones: visitors are allowed but limited to one or two. Music and pet therapy are being provided through the window or virtually and devices such as iPads are being used to help patients connect with loved ones,” she said.
Telehealth links patients out of loneliness, but the one thing it cannot do is provide the comfort of touch – an important part of any hospice program.
“Hand-holding ... I miss that a lot,” says Ms. Shockney, her eyes filling with tears. “When you take somebody’s hand, you don’t even have to speak; that connection, and eye contact, is all you need to help that person emotionally heal.”
This article first appeared on Medscape.com.
Added rituximab was effective in children and adolescents with high-risk B-cell NHL
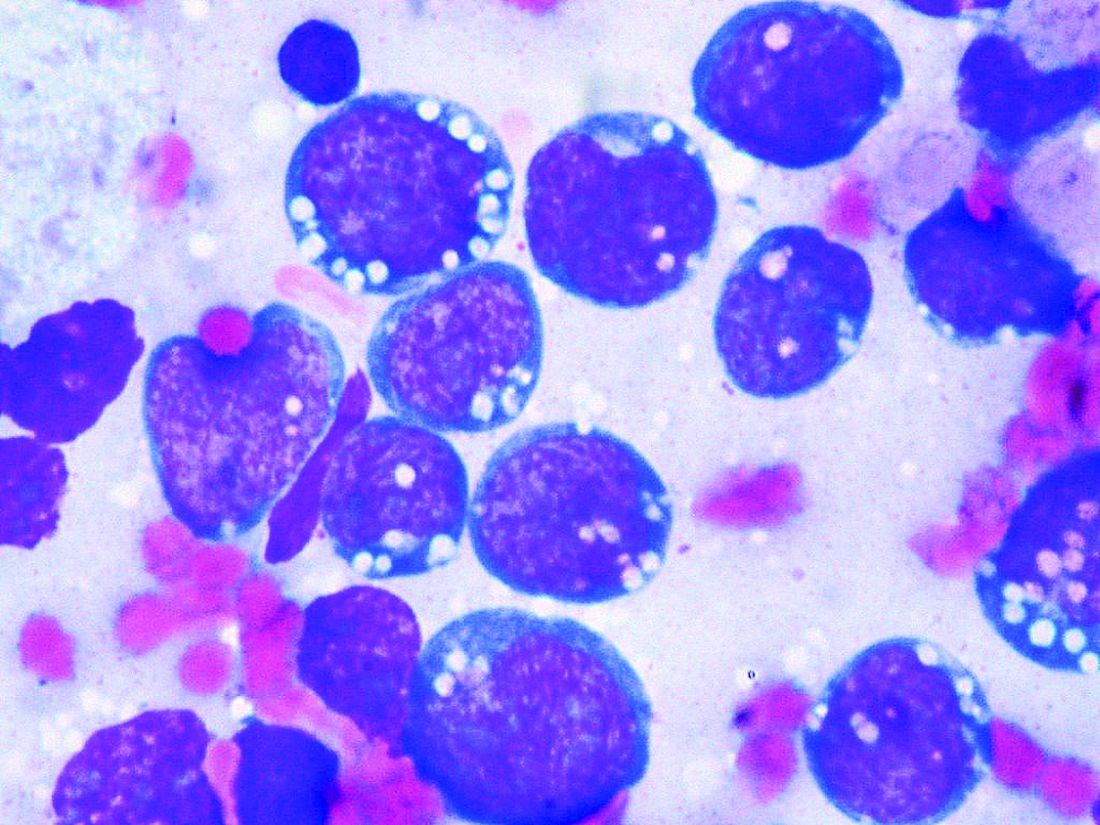
The addition of rituximab to standard chemotherapy was a more effective therapy in children and adolescents with high-risk, high-grade,mature B-cell non-Hodgkin lymphoma than the use of chemotherapy alone, according to a study published in the New England Journal of Medicine. The addition of rituximab resulted in long-term complete remission in the vast majority of patients, reported Veronique Minard-Colin, MD, of the Gustave Roussy Institute, Villejuif Cedex, France, and her colleagues on behalf of the European Intergroup for Childhood Non-Hodgkin Lymphoma and the Children’s Oncology Group.
The researchers performed an open-label, randomized, phase 3 trial of 328 patients younger than 18 years of age with high-risk, mature B-cell non-Hodgkin’s lymphoma (stage III with an elevated lactate dehydrogenase level or stage IV) or acute leukemia to compare the addition of six doses of rituximab to standard lymphomes malins B (LMB) chemotherapy with standard LMB chemotherapy alone. There were 164 patients assigned to each group. The primary end point of the study was event-free survival; overall survival and toxic effects were also followed.
The majority of patients had Burkitt’s lymphoma: 139 (84.8%) in the rituximab-chemotherapy group and 142 (86.6%) in the chemotherapy-alone group, with diffuse large B-cell lymphoma being the second most common cancer: 19 (11.6%) vs. 12 (7.3%), respectively.
Event-free survival at 3 years was 93.9% (95% confidence interval, 89.1-96.7) in the rituximab-chemotherapy group and 82.3% (95% CI, 75.7-87.5) in the chemotherapy group.
Higher 3-year overall survival was also observed (95.1% in the rituximab-chemotherapy group vs. 87.3% in the chemotherapy group; hazard ratio for death, 0.36; 95% CI, 0.16 -0.82).
Eight patients in the rituximab-chemotherapy group died (4 deaths were disease related, 3 were treatment related, and 1 was from a second cancer), as did 20 in the chemotherapy group (17 deaths disease related, and 3 treatment related); HR, 0.36; 95% CI, 0.16-0.82.
The incidence of acute adverse events of grade 4 or higher after prephase treatment was 33.3% in the rituximab-chemotherapy group and 24.2% in the chemotherapy group, a nonsignificant difference (P = .07). However, around twice as many patients in the rituximab-chemotherapy group had a low IgG level at 1 year after trial inclusion, compared with the chemotherapy-alone group, which could indicate the potential for more frequent infections in the long term, the researchers stated.
“An assessment of the long-term effects of combining rituximab with this chemotherapy regimen in children with non-Hodgkin lymphoma, including data on immune status, will be useful,” they added.
The study was funded by the French Ministry of Health, Cancer Research UK, the National Institute for Health Research Clinical Research Network, the Children’s Cancer Foundation Hong Kong, the U.S. National Cancer Institute, and F. Hoffmann–La Roche–Genentech. Several of the authors reported consulting for and institutional and grant funding from F. Hoffmann-LaRoche, which markets rituximab, as well as relationships with other pharmaceutical companies.
SOURCE: Minard-Colin V et al. N Engl J Med. 2020;382:2207-19.
The addition of rituximab to standard chemotherapy was a more effective therapy in children and adolescents with high-risk, high-grade,mature B-cell non-Hodgkin lymphoma than the use of chemotherapy alone, according to a study published in the New England Journal of Medicine. The addition of rituximab resulted in long-term complete remission in the vast majority of patients, reported Veronique Minard-Colin, MD, of the Gustave Roussy Institute, Villejuif Cedex, France, and her colleagues on behalf of the European Intergroup for Childhood Non-Hodgkin Lymphoma and the Children’s Oncology Group.
The researchers performed an open-label, randomized, phase 3 trial of 328 patients younger than 18 years of age with high-risk, mature B-cell non-Hodgkin’s lymphoma (stage III with an elevated lactate dehydrogenase level or stage IV) or acute leukemia to compare the addition of six doses of rituximab to standard lymphomes malins B (LMB) chemotherapy with standard LMB chemotherapy alone. There were 164 patients assigned to each group. The primary end point of the study was event-free survival; overall survival and toxic effects were also followed.
The majority of patients had Burkitt’s lymphoma: 139 (84.8%) in the rituximab-chemotherapy group and 142 (86.6%) in the chemotherapy-alone group, with diffuse large B-cell lymphoma being the second most common cancer: 19 (11.6%) vs. 12 (7.3%), respectively.
Event-free survival at 3 years was 93.9% (95% confidence interval, 89.1-96.7) in the rituximab-chemotherapy group and 82.3% (95% CI, 75.7-87.5) in the chemotherapy group.
Higher 3-year overall survival was also observed (95.1% in the rituximab-chemotherapy group vs. 87.3% in the chemotherapy group; hazard ratio for death, 0.36; 95% CI, 0.16 -0.82).
Eight patients in the rituximab-chemotherapy group died (4 deaths were disease related, 3 were treatment related, and 1 was from a second cancer), as did 20 in the chemotherapy group (17 deaths disease related, and 3 treatment related); HR, 0.36; 95% CI, 0.16-0.82.
The incidence of acute adverse events of grade 4 or higher after prephase treatment was 33.3% in the rituximab-chemotherapy group and 24.2% in the chemotherapy group, a nonsignificant difference (P = .07). However, around twice as many patients in the rituximab-chemotherapy group had a low IgG level at 1 year after trial inclusion, compared with the chemotherapy-alone group, which could indicate the potential for more frequent infections in the long term, the researchers stated.
“An assessment of the long-term effects of combining rituximab with this chemotherapy regimen in children with non-Hodgkin lymphoma, including data on immune status, will be useful,” they added.
The study was funded by the French Ministry of Health, Cancer Research UK, the National Institute for Health Research Clinical Research Network, the Children’s Cancer Foundation Hong Kong, the U.S. National Cancer Institute, and F. Hoffmann–La Roche–Genentech. Several of the authors reported consulting for and institutional and grant funding from F. Hoffmann-LaRoche, which markets rituximab, as well as relationships with other pharmaceutical companies.
SOURCE: Minard-Colin V et al. N Engl J Med. 2020;382:2207-19.
The addition of rituximab to standard chemotherapy was a more effective therapy in children and adolescents with high-risk, high-grade,mature B-cell non-Hodgkin lymphoma than the use of chemotherapy alone, according to a study published in the New England Journal of Medicine. The addition of rituximab resulted in long-term complete remission in the vast majority of patients, reported Veronique Minard-Colin, MD, of the Gustave Roussy Institute, Villejuif Cedex, France, and her colleagues on behalf of the European Intergroup for Childhood Non-Hodgkin Lymphoma and the Children’s Oncology Group.
The researchers performed an open-label, randomized, phase 3 trial of 328 patients younger than 18 years of age with high-risk, mature B-cell non-Hodgkin’s lymphoma (stage III with an elevated lactate dehydrogenase level or stage IV) or acute leukemia to compare the addition of six doses of rituximab to standard lymphomes malins B (LMB) chemotherapy with standard LMB chemotherapy alone. There were 164 patients assigned to each group. The primary end point of the study was event-free survival; overall survival and toxic effects were also followed.
The majority of patients had Burkitt’s lymphoma: 139 (84.8%) in the rituximab-chemotherapy group and 142 (86.6%) in the chemotherapy-alone group, with diffuse large B-cell lymphoma being the second most common cancer: 19 (11.6%) vs. 12 (7.3%), respectively.
Event-free survival at 3 years was 93.9% (95% confidence interval, 89.1-96.7) in the rituximab-chemotherapy group and 82.3% (95% CI, 75.7-87.5) in the chemotherapy group.
Higher 3-year overall survival was also observed (95.1% in the rituximab-chemotherapy group vs. 87.3% in the chemotherapy group; hazard ratio for death, 0.36; 95% CI, 0.16 -0.82).
Eight patients in the rituximab-chemotherapy group died (4 deaths were disease related, 3 were treatment related, and 1 was from a second cancer), as did 20 in the chemotherapy group (17 deaths disease related, and 3 treatment related); HR, 0.36; 95% CI, 0.16-0.82.
The incidence of acute adverse events of grade 4 or higher after prephase treatment was 33.3% in the rituximab-chemotherapy group and 24.2% in the chemotherapy group, a nonsignificant difference (P = .07). However, around twice as many patients in the rituximab-chemotherapy group had a low IgG level at 1 year after trial inclusion, compared with the chemotherapy-alone group, which could indicate the potential for more frequent infections in the long term, the researchers stated.
“An assessment of the long-term effects of combining rituximab with this chemotherapy regimen in children with non-Hodgkin lymphoma, including data on immune status, will be useful,” they added.
The study was funded by the French Ministry of Health, Cancer Research UK, the National Institute for Health Research Clinical Research Network, the Children’s Cancer Foundation Hong Kong, the U.S. National Cancer Institute, and F. Hoffmann–La Roche–Genentech. Several of the authors reported consulting for and institutional and grant funding from F. Hoffmann-LaRoche, which markets rituximab, as well as relationships with other pharmaceutical companies.
SOURCE: Minard-Colin V et al. N Engl J Med. 2020;382:2207-19.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Adding rituximab to chemotherapy was effective in children and adolescents with high-risk, high-grade, mature B-cell non-Hodgkin lymphoma.
Major finding: Higher 3-year overall survival was observed (95.1% in the rituximab-chemotherapy group vs. 87.3% in the chemotherapy group).
Study details: Analysis of 328 patients who underwent randomization to standard chemotherapy vs. chemo plus rituximab (164 patients per group).
Disclosures: The study was funded by the French Ministry of Health, Cancer Research UK, the National Institute for Health Research Clinical Research Network, the Children’s Cancer Foundation Hong Kong, the U.S. National Cancer Institute, and F. Hoffmann–La Roche–Genentech. Several of the authors reported consulting for and institutional and grant funding from F. Hoffmann-LaRoche, which markets rituximab, as well as relationships with other pharmaceutical companies.
Source: Minard-Colin V et al. N Engl J Med. 2020; 382:2207-19.
Pembrolizumab prolonged PFS vs. brentuximab vedotin in r/r Hodgkin lymphoma
Pembrolizumab treatment significantly improved progression-free survival versus brentuximab vedotin in a randomized, phase 3 trial including patients with relapsed or refractory classical Hodgkin lymphoma, an investigator has reported.
Median progression-free survival (PFS) was 13.2 versus 8.3 months in favor of pembrolizumab, according to the report on the KEYNOTE-204 trial, which included patients with classical Hodgkin lymphoma who either had relapsed after autologous stem cell transplant (SCT) or were ineligible for autologous SCT.
of Princess Margaret Cancer Centre in Toronto.
“This PFS benefit extended to key subgroups, including those ineligible for autologous transplant, patients with primary refractory disease, and patients who were brentuximab-vedotin naive,” Dr. Kuruvilla added in his presentation, which was part of the American Society of Clinical Oncology virtual scientific program.
Pneumonitis was more frequent in the pembrolizumab arm, but “appeared in general to be quite well managed” among patients who experienced this adverse event, according to Dr. Kuruvilla, who said that treatment with the programmed death–1 inhibitor should be considered “the preferred treatment option and the new standard of care” for patients with relapsed/refractory classic Hodgkin lymphoma who have relapsed after autologous SCT or are ineligible for it.
Although the pneumonitis findings are important to keep in mind, results of KEYNOTE-204 are indeed “practice defining” and immediately impactful, said Mark J. Roschewski, MD, clinical investigator in the lymphoid malignancies branch at the Center for Cancer Research, part of the National Cancer Institute, Bethesda, Md.
“I would select pembrolizumab over brentuximab for this patient population, particularly those that are refractory to chemotherapy,” he said in a commentary on the study also included in the virtual ASCO proceedings.
“There may be specific patient populations that I’d reconsider, such as those that might be at high risk for lung toxicity,” he added. “They may not be suitable for this, but it’s something to at least to be aware of.”
Although the antibody-drug conjugate brentuximab vedotin has been considered the standard of care for patients with relapse after autologous SCT, there has historically been no standard of care for patients who are ineligible for transplant because of chemorefractory disease, advanced age, or comorbidities, Dr. Kuruvilla said in his presentation.
In the KEYNOTE-204 study, 304 patients with relapsed/refractory classic Hodgkin lymphoma were randomized to receive either pembrolizumab 200 mg or brentuximab at 1.8 mg/kg intravenously every 3 weeks for up to 35 cycles.
The median age of patients was 36 years in the pembrolizumab arm and 35 years in the brentuximab vedotin arm, according to the report. Approximately 37% of the patients had previously undergone autologous SCT. About 40% had been refractory to frontline therapy, while 28% relapsed within 12 months of therapy and 32% relapsed later than 12 months.
Median PFS by blinded independent central review was 13.2 versus 8.3 months in the pembrolizumab and brentuximab arms, respectively (hazard ratio, 0.65; 95% confidence interval, 0.48-0.88; P = .00271), Dr. Kuruvilla reported.
The benefit extended to “key subgroups” in the trial, he added, including those who were ineligible for autologous SCT, those with primary refractory disease, and those who were naive to brentuximab vedotin, with HRs of 0.61, 0.52, and 0.67, respectively.
Pembrolizumab was also associated with more durable responses versus brentuximab vedotin, according to the investigator.
The overall response rate was 65.6% and 54.2%, respectively, for pembrolizumab and brentuximab, although this difference of approximately 11 percentage points did not meet criteria for statistical significance, he said. Duration of response was 20.7 months or pembrolizumab and 13.8 months for brentuximab.
The rate of serious treatment-related adverse events was similar between groups, according to Dr. Kuruvilla, who reported grade 3-5 events occurring in 19.6% and 25.0% of the pembrolizumab and brentuximab arms. Serious treatment-related adverse events were numerically more frequent in the pembrolizumab arm (16.2% vs. 10.5%) and there was one treatment-related death caused by pneumonia, seen in the pembrolizumab arm.
Pneumonitis occurred in 2.6% of the brentuximab-treated patients and in 10.8% of pembrolizumab-treated patients, of which half of cases were grade 3-4, according to the report.
In the pembrolizumab arm, pneumonitis was felt to be drug-related in 15 of 16 cases, according to Dr. Kuruvilla, who added that 15 of 16 patients required corticosteroid therapy. “This has led to the resolution of the pneumonitis in 12 of 16 patients, with ongoing resolution in one further patient.”
Research funding for KEYNOTE-204 came from Merck Sharp & Dohme. Dr. Kuruvilla provided disclosures related to Merck and a variety of other pharmaceutical companies. Dr. Roschewski said he had no relationships to disclose.
SOURCE: Kuruvilla J et al. ASCO 2020, Abstract 8005.
Pembrolizumab treatment significantly improved progression-free survival versus brentuximab vedotin in a randomized, phase 3 trial including patients with relapsed or refractory classical Hodgkin lymphoma, an investigator has reported.
Median progression-free survival (PFS) was 13.2 versus 8.3 months in favor of pembrolizumab, according to the report on the KEYNOTE-204 trial, which included patients with classical Hodgkin lymphoma who either had relapsed after autologous stem cell transplant (SCT) or were ineligible for autologous SCT.
of Princess Margaret Cancer Centre in Toronto.
“This PFS benefit extended to key subgroups, including those ineligible for autologous transplant, patients with primary refractory disease, and patients who were brentuximab-vedotin naive,” Dr. Kuruvilla added in his presentation, which was part of the American Society of Clinical Oncology virtual scientific program.
Pneumonitis was more frequent in the pembrolizumab arm, but “appeared in general to be quite well managed” among patients who experienced this adverse event, according to Dr. Kuruvilla, who said that treatment with the programmed death–1 inhibitor should be considered “the preferred treatment option and the new standard of care” for patients with relapsed/refractory classic Hodgkin lymphoma who have relapsed after autologous SCT or are ineligible for it.
Although the pneumonitis findings are important to keep in mind, results of KEYNOTE-204 are indeed “practice defining” and immediately impactful, said Mark J. Roschewski, MD, clinical investigator in the lymphoid malignancies branch at the Center for Cancer Research, part of the National Cancer Institute, Bethesda, Md.
“I would select pembrolizumab over brentuximab for this patient population, particularly those that are refractory to chemotherapy,” he said in a commentary on the study also included in the virtual ASCO proceedings.
“There may be specific patient populations that I’d reconsider, such as those that might be at high risk for lung toxicity,” he added. “They may not be suitable for this, but it’s something to at least to be aware of.”
Although the antibody-drug conjugate brentuximab vedotin has been considered the standard of care for patients with relapse after autologous SCT, there has historically been no standard of care for patients who are ineligible for transplant because of chemorefractory disease, advanced age, or comorbidities, Dr. Kuruvilla said in his presentation.
In the KEYNOTE-204 study, 304 patients with relapsed/refractory classic Hodgkin lymphoma were randomized to receive either pembrolizumab 200 mg or brentuximab at 1.8 mg/kg intravenously every 3 weeks for up to 35 cycles.
The median age of patients was 36 years in the pembrolizumab arm and 35 years in the brentuximab vedotin arm, according to the report. Approximately 37% of the patients had previously undergone autologous SCT. About 40% had been refractory to frontline therapy, while 28% relapsed within 12 months of therapy and 32% relapsed later than 12 months.
Median PFS by blinded independent central review was 13.2 versus 8.3 months in the pembrolizumab and brentuximab arms, respectively (hazard ratio, 0.65; 95% confidence interval, 0.48-0.88; P = .00271), Dr. Kuruvilla reported.
The benefit extended to “key subgroups” in the trial, he added, including those who were ineligible for autologous SCT, those with primary refractory disease, and those who were naive to brentuximab vedotin, with HRs of 0.61, 0.52, and 0.67, respectively.
Pembrolizumab was also associated with more durable responses versus brentuximab vedotin, according to the investigator.
The overall response rate was 65.6% and 54.2%, respectively, for pembrolizumab and brentuximab, although this difference of approximately 11 percentage points did not meet criteria for statistical significance, he said. Duration of response was 20.7 months or pembrolizumab and 13.8 months for brentuximab.
The rate of serious treatment-related adverse events was similar between groups, according to Dr. Kuruvilla, who reported grade 3-5 events occurring in 19.6% and 25.0% of the pembrolizumab and brentuximab arms. Serious treatment-related adverse events were numerically more frequent in the pembrolizumab arm (16.2% vs. 10.5%) and there was one treatment-related death caused by pneumonia, seen in the pembrolizumab arm.
Pneumonitis occurred in 2.6% of the brentuximab-treated patients and in 10.8% of pembrolizumab-treated patients, of which half of cases were grade 3-4, according to the report.
In the pembrolizumab arm, pneumonitis was felt to be drug-related in 15 of 16 cases, according to Dr. Kuruvilla, who added that 15 of 16 patients required corticosteroid therapy. “This has led to the resolution of the pneumonitis in 12 of 16 patients, with ongoing resolution in one further patient.”
Research funding for KEYNOTE-204 came from Merck Sharp & Dohme. Dr. Kuruvilla provided disclosures related to Merck and a variety of other pharmaceutical companies. Dr. Roschewski said he had no relationships to disclose.
SOURCE: Kuruvilla J et al. ASCO 2020, Abstract 8005.
Pembrolizumab treatment significantly improved progression-free survival versus brentuximab vedotin in a randomized, phase 3 trial including patients with relapsed or refractory classical Hodgkin lymphoma, an investigator has reported.
Median progression-free survival (PFS) was 13.2 versus 8.3 months in favor of pembrolizumab, according to the report on the KEYNOTE-204 trial, which included patients with classical Hodgkin lymphoma who either had relapsed after autologous stem cell transplant (SCT) or were ineligible for autologous SCT.
of Princess Margaret Cancer Centre in Toronto.
“This PFS benefit extended to key subgroups, including those ineligible for autologous transplant, patients with primary refractory disease, and patients who were brentuximab-vedotin naive,” Dr. Kuruvilla added in his presentation, which was part of the American Society of Clinical Oncology virtual scientific program.
Pneumonitis was more frequent in the pembrolizumab arm, but “appeared in general to be quite well managed” among patients who experienced this adverse event, according to Dr. Kuruvilla, who said that treatment with the programmed death–1 inhibitor should be considered “the preferred treatment option and the new standard of care” for patients with relapsed/refractory classic Hodgkin lymphoma who have relapsed after autologous SCT or are ineligible for it.
Although the pneumonitis findings are important to keep in mind, results of KEYNOTE-204 are indeed “practice defining” and immediately impactful, said Mark J. Roschewski, MD, clinical investigator in the lymphoid malignancies branch at the Center for Cancer Research, part of the National Cancer Institute, Bethesda, Md.
“I would select pembrolizumab over brentuximab for this patient population, particularly those that are refractory to chemotherapy,” he said in a commentary on the study also included in the virtual ASCO proceedings.
“There may be specific patient populations that I’d reconsider, such as those that might be at high risk for lung toxicity,” he added. “They may not be suitable for this, but it’s something to at least to be aware of.”
Although the antibody-drug conjugate brentuximab vedotin has been considered the standard of care for patients with relapse after autologous SCT, there has historically been no standard of care for patients who are ineligible for transplant because of chemorefractory disease, advanced age, or comorbidities, Dr. Kuruvilla said in his presentation.
In the KEYNOTE-204 study, 304 patients with relapsed/refractory classic Hodgkin lymphoma were randomized to receive either pembrolizumab 200 mg or brentuximab at 1.8 mg/kg intravenously every 3 weeks for up to 35 cycles.
The median age of patients was 36 years in the pembrolizumab arm and 35 years in the brentuximab vedotin arm, according to the report. Approximately 37% of the patients had previously undergone autologous SCT. About 40% had been refractory to frontline therapy, while 28% relapsed within 12 months of therapy and 32% relapsed later than 12 months.
Median PFS by blinded independent central review was 13.2 versus 8.3 months in the pembrolizumab and brentuximab arms, respectively (hazard ratio, 0.65; 95% confidence interval, 0.48-0.88; P = .00271), Dr. Kuruvilla reported.
The benefit extended to “key subgroups” in the trial, he added, including those who were ineligible for autologous SCT, those with primary refractory disease, and those who were naive to brentuximab vedotin, with HRs of 0.61, 0.52, and 0.67, respectively.
Pembrolizumab was also associated with more durable responses versus brentuximab vedotin, according to the investigator.
The overall response rate was 65.6% and 54.2%, respectively, for pembrolizumab and brentuximab, although this difference of approximately 11 percentage points did not meet criteria for statistical significance, he said. Duration of response was 20.7 months or pembrolizumab and 13.8 months for brentuximab.
The rate of serious treatment-related adverse events was similar between groups, according to Dr. Kuruvilla, who reported grade 3-5 events occurring in 19.6% and 25.0% of the pembrolizumab and brentuximab arms. Serious treatment-related adverse events were numerically more frequent in the pembrolizumab arm (16.2% vs. 10.5%) and there was one treatment-related death caused by pneumonia, seen in the pembrolizumab arm.
Pneumonitis occurred in 2.6% of the brentuximab-treated patients and in 10.8% of pembrolizumab-treated patients, of which half of cases were grade 3-4, according to the report.
In the pembrolizumab arm, pneumonitis was felt to be drug-related in 15 of 16 cases, according to Dr. Kuruvilla, who added that 15 of 16 patients required corticosteroid therapy. “This has led to the resolution of the pneumonitis in 12 of 16 patients, with ongoing resolution in one further patient.”
Research funding for KEYNOTE-204 came from Merck Sharp & Dohme. Dr. Kuruvilla provided disclosures related to Merck and a variety of other pharmaceutical companies. Dr. Roschewski said he had no relationships to disclose.
SOURCE: Kuruvilla J et al. ASCO 2020, Abstract 8005.
FROM ASCO 2020
Active cancer increases death risk in patients with COVID-19
Patients with COVID-19 and progressing cancer had a fivefold increase in the risk of 30-day mortality, compared with COVID-19–positive cancer patients who were in remission or had no evidence of cancer, according to data from the COVID-19 and Cancer Consortium (CCC19) registry.
Other independent risk factors for death in patients with COVID-19 and cancer were older age, male sex, former smoking, number of comorbidities, Eastern Cooperative Oncology Group (ECOG) performance status of 2 or greater, and treatment with hydroxychloroquine plus azithromycin.
In fact, patients who received hydroxychloroquine and azithromycin had a nearly threefold higher risk of death than did patients who had not received the combination. However, this finding was of “uncertain validity due to a high risk of residual confounding; for example, patients receiving this combination were more likely to have severe disease or more likely to be hospitalized,” said Jeremy L. Warner, MD, of Vanderbilt University Medical Center in Nashville, Tennessee.
Dr. Warner presented these findings in an online press briefing. Additional findings from the CCC19 registry are set to be presented as part of the American Society of Clinical Oncology (ASCO) virtual scientific program. The findings were also published in The Lancet.
‘Severe impact’ in cancer patients
“For people with cancer, the impact of COVID-19 is especially severe, whether they have been exposed to the virus or not. Patients with cancer are typically older adults, often with other underlying conditions, and their immune systems may be suppressed by the cancer, or due to chemotherapy, radiation, or other treatment,” commented ASCO President Howard A. Burris III, MD, who moderated the press briefing but was not involved in the study of CCC19 registry data.
“ASCO members tell us that they have had to delay or modify treatment plans to reduce patients’ risk of infection, and we’re unclear what the impact of these changes will be. Delays in cancer screening and diagnosis are also a major concern,” Dr. Burris continued.
“This does confirm reports that have come out from other centers, including other parts of the world, where they have found that people who have cancer and COVID-19 have a worse outcome,” said Andrew T. Chan, MD, MPH, of Massachusetts General Hospital in Boston, who was not involved in the research.
Dr. Chan’s group has developed a COVID-19 symptom study app with the aim of defining whether people living with cancer are at increased risk for infections, in addition to whether cancer is an independent risk factor for COVID-19 severity or mortality.
“Using data from our app, we were able to show that people who reported living with cancer did have a higher risk of developing COVID and were more likely to be hospitalized related to COVID,” Dr. Chan said in an interview.
Study details
The CCC19 registry collects information from 104 participating institutions in the United States and Canada, as well as anonymous data from individuals in the United States, Argentina, Canada, the European Union, and the United Kingdom.
The sample of 928 patients Dr. Warner presented was evenly balanced by sex. The median age was 66 years, and 30% of patients were aged 75 years or older.
In all, 39% of patients were on active anticancer therapy, and 43% had measurable disease. Breast cancer was the most common diagnosis, followed by prostate cancer, gastrointestinal cancers, lymphomas, and thoracic cancers.
Two-thirds of the patients (68%) had an ECOG performance status of 0 or 1, 8% had a performance status of 2, and 5% a status of 3 or 4. The remaining patients had unknown performance status.
Slightly more than half of patients (52%) were never smokers, 37% were former smokers, and 5% were current smokers. The remaining 6% of patients had unknown smoking status.
At a median follow-up of 21 days, 121 patients (13%) had died. All deaths occurred within 30 days of COVID-19 diagnosis. Among patients who died, 78 were male, 64 were former smokers, 70 were aged 75 years or older, 41 had active stable or responding cancer, 25 had progressing cancer, and 42 had an ECOG performance status of 2 or higher.
In all, 466 patients were hospitalized, and 106 in this group (23%) died. Among the 132 patients admitted to an ICU, 50 (38%) died, including 27 patients aged 75 years or older, and 15 with an ECOG performance status of 2 or greater. Of the 116 patients who required intubation, 50 (43%) died, including 26 who were 75 years or older, and 11 who had a performance status of 2 or greater.
It’s early days yet, and a larger sample size with longer follow-up will be needed to get a more complete picture of how COVID-19 affects specific patient subsets over time, Dr. Warner said.
ASCO has established its own COVID-19 registry to collect both near-term and longitudinal data during the pandemic.
“We’ll be able to learn about both how the pandemic has impacted delivery of cancer care, as well as the longer-term effects of COVID-19 on cancer patients and understand what care approaches are working best,” said Richard L. Schilsky, MD, chief medical officer and executive vice president of ASCO, during the briefing.
The study of CCC19 registry data was supported in part by the National Institutes of Health and the American Cancer Society. Dr. Warner disclosed stock/ownership in HemOnc.org, consulting for IBM and Westat, and travel expenses from IBM. Dr. Burris, Dr. Schilsky, and Dr. Chan reported no disclosures relevant to the study.
SOURCE: Warner J L et al. ASCO 2020, Abstract LBA110.
Patients with COVID-19 and progressing cancer had a fivefold increase in the risk of 30-day mortality, compared with COVID-19–positive cancer patients who were in remission or had no evidence of cancer, according to data from the COVID-19 and Cancer Consortium (CCC19) registry.
Other independent risk factors for death in patients with COVID-19 and cancer were older age, male sex, former smoking, number of comorbidities, Eastern Cooperative Oncology Group (ECOG) performance status of 2 or greater, and treatment with hydroxychloroquine plus azithromycin.
In fact, patients who received hydroxychloroquine and azithromycin had a nearly threefold higher risk of death than did patients who had not received the combination. However, this finding was of “uncertain validity due to a high risk of residual confounding; for example, patients receiving this combination were more likely to have severe disease or more likely to be hospitalized,” said Jeremy L. Warner, MD, of Vanderbilt University Medical Center in Nashville, Tennessee.
Dr. Warner presented these findings in an online press briefing. Additional findings from the CCC19 registry are set to be presented as part of the American Society of Clinical Oncology (ASCO) virtual scientific program. The findings were also published in The Lancet.
‘Severe impact’ in cancer patients
“For people with cancer, the impact of COVID-19 is especially severe, whether they have been exposed to the virus or not. Patients with cancer are typically older adults, often with other underlying conditions, and their immune systems may be suppressed by the cancer, or due to chemotherapy, radiation, or other treatment,” commented ASCO President Howard A. Burris III, MD, who moderated the press briefing but was not involved in the study of CCC19 registry data.
“ASCO members tell us that they have had to delay or modify treatment plans to reduce patients’ risk of infection, and we’re unclear what the impact of these changes will be. Delays in cancer screening and diagnosis are also a major concern,” Dr. Burris continued.
“This does confirm reports that have come out from other centers, including other parts of the world, where they have found that people who have cancer and COVID-19 have a worse outcome,” said Andrew T. Chan, MD, MPH, of Massachusetts General Hospital in Boston, who was not involved in the research.
Dr. Chan’s group has developed a COVID-19 symptom study app with the aim of defining whether people living with cancer are at increased risk for infections, in addition to whether cancer is an independent risk factor for COVID-19 severity or mortality.
“Using data from our app, we were able to show that people who reported living with cancer did have a higher risk of developing COVID and were more likely to be hospitalized related to COVID,” Dr. Chan said in an interview.
Study details
The CCC19 registry collects information from 104 participating institutions in the United States and Canada, as well as anonymous data from individuals in the United States, Argentina, Canada, the European Union, and the United Kingdom.
The sample of 928 patients Dr. Warner presented was evenly balanced by sex. The median age was 66 years, and 30% of patients were aged 75 years or older.
In all, 39% of patients were on active anticancer therapy, and 43% had measurable disease. Breast cancer was the most common diagnosis, followed by prostate cancer, gastrointestinal cancers, lymphomas, and thoracic cancers.
Two-thirds of the patients (68%) had an ECOG performance status of 0 or 1, 8% had a performance status of 2, and 5% a status of 3 or 4. The remaining patients had unknown performance status.
Slightly more than half of patients (52%) were never smokers, 37% were former smokers, and 5% were current smokers. The remaining 6% of patients had unknown smoking status.
At a median follow-up of 21 days, 121 patients (13%) had died. All deaths occurred within 30 days of COVID-19 diagnosis. Among patients who died, 78 were male, 64 were former smokers, 70 were aged 75 years or older, 41 had active stable or responding cancer, 25 had progressing cancer, and 42 had an ECOG performance status of 2 or higher.
In all, 466 patients were hospitalized, and 106 in this group (23%) died. Among the 132 patients admitted to an ICU, 50 (38%) died, including 27 patients aged 75 years or older, and 15 with an ECOG performance status of 2 or greater. Of the 116 patients who required intubation, 50 (43%) died, including 26 who were 75 years or older, and 11 who had a performance status of 2 or greater.
It’s early days yet, and a larger sample size with longer follow-up will be needed to get a more complete picture of how COVID-19 affects specific patient subsets over time, Dr. Warner said.
ASCO has established its own COVID-19 registry to collect both near-term and longitudinal data during the pandemic.
“We’ll be able to learn about both how the pandemic has impacted delivery of cancer care, as well as the longer-term effects of COVID-19 on cancer patients and understand what care approaches are working best,” said Richard L. Schilsky, MD, chief medical officer and executive vice president of ASCO, during the briefing.
The study of CCC19 registry data was supported in part by the National Institutes of Health and the American Cancer Society. Dr. Warner disclosed stock/ownership in HemOnc.org, consulting for IBM and Westat, and travel expenses from IBM. Dr. Burris, Dr. Schilsky, and Dr. Chan reported no disclosures relevant to the study.
SOURCE: Warner J L et al. ASCO 2020, Abstract LBA110.
Patients with COVID-19 and progressing cancer had a fivefold increase in the risk of 30-day mortality, compared with COVID-19–positive cancer patients who were in remission or had no evidence of cancer, according to data from the COVID-19 and Cancer Consortium (CCC19) registry.
Other independent risk factors for death in patients with COVID-19 and cancer were older age, male sex, former smoking, number of comorbidities, Eastern Cooperative Oncology Group (ECOG) performance status of 2 or greater, and treatment with hydroxychloroquine plus azithromycin.
In fact, patients who received hydroxychloroquine and azithromycin had a nearly threefold higher risk of death than did patients who had not received the combination. However, this finding was of “uncertain validity due to a high risk of residual confounding; for example, patients receiving this combination were more likely to have severe disease or more likely to be hospitalized,” said Jeremy L. Warner, MD, of Vanderbilt University Medical Center in Nashville, Tennessee.
Dr. Warner presented these findings in an online press briefing. Additional findings from the CCC19 registry are set to be presented as part of the American Society of Clinical Oncology (ASCO) virtual scientific program. The findings were also published in The Lancet.
‘Severe impact’ in cancer patients
“For people with cancer, the impact of COVID-19 is especially severe, whether they have been exposed to the virus or not. Patients with cancer are typically older adults, often with other underlying conditions, and their immune systems may be suppressed by the cancer, or due to chemotherapy, radiation, or other treatment,” commented ASCO President Howard A. Burris III, MD, who moderated the press briefing but was not involved in the study of CCC19 registry data.
“ASCO members tell us that they have had to delay or modify treatment plans to reduce patients’ risk of infection, and we’re unclear what the impact of these changes will be. Delays in cancer screening and diagnosis are also a major concern,” Dr. Burris continued.
“This does confirm reports that have come out from other centers, including other parts of the world, where they have found that people who have cancer and COVID-19 have a worse outcome,” said Andrew T. Chan, MD, MPH, of Massachusetts General Hospital in Boston, who was not involved in the research.
Dr. Chan’s group has developed a COVID-19 symptom study app with the aim of defining whether people living with cancer are at increased risk for infections, in addition to whether cancer is an independent risk factor for COVID-19 severity or mortality.
“Using data from our app, we were able to show that people who reported living with cancer did have a higher risk of developing COVID and were more likely to be hospitalized related to COVID,” Dr. Chan said in an interview.
Study details
The CCC19 registry collects information from 104 participating institutions in the United States and Canada, as well as anonymous data from individuals in the United States, Argentina, Canada, the European Union, and the United Kingdom.
The sample of 928 patients Dr. Warner presented was evenly balanced by sex. The median age was 66 years, and 30% of patients were aged 75 years or older.
In all, 39% of patients were on active anticancer therapy, and 43% had measurable disease. Breast cancer was the most common diagnosis, followed by prostate cancer, gastrointestinal cancers, lymphomas, and thoracic cancers.
Two-thirds of the patients (68%) had an ECOG performance status of 0 or 1, 8% had a performance status of 2, and 5% a status of 3 or 4. The remaining patients had unknown performance status.
Slightly more than half of patients (52%) were never smokers, 37% were former smokers, and 5% were current smokers. The remaining 6% of patients had unknown smoking status.
At a median follow-up of 21 days, 121 patients (13%) had died. All deaths occurred within 30 days of COVID-19 diagnosis. Among patients who died, 78 were male, 64 were former smokers, 70 were aged 75 years or older, 41 had active stable or responding cancer, 25 had progressing cancer, and 42 had an ECOG performance status of 2 or higher.
In all, 466 patients were hospitalized, and 106 in this group (23%) died. Among the 132 patients admitted to an ICU, 50 (38%) died, including 27 patients aged 75 years or older, and 15 with an ECOG performance status of 2 or greater. Of the 116 patients who required intubation, 50 (43%) died, including 26 who were 75 years or older, and 11 who had a performance status of 2 or greater.
It’s early days yet, and a larger sample size with longer follow-up will be needed to get a more complete picture of how COVID-19 affects specific patient subsets over time, Dr. Warner said.
ASCO has established its own COVID-19 registry to collect both near-term and longitudinal data during the pandemic.
“We’ll be able to learn about both how the pandemic has impacted delivery of cancer care, as well as the longer-term effects of COVID-19 on cancer patients and understand what care approaches are working best,” said Richard L. Schilsky, MD, chief medical officer and executive vice president of ASCO, during the briefing.
The study of CCC19 registry data was supported in part by the National Institutes of Health and the American Cancer Society. Dr. Warner disclosed stock/ownership in HemOnc.org, consulting for IBM and Westat, and travel expenses from IBM. Dr. Burris, Dr. Schilsky, and Dr. Chan reported no disclosures relevant to the study.
SOURCE: Warner J L et al. ASCO 2020, Abstract LBA110.
FROM ASCO 2020
Key clinical point: Patients with progressing cancer and COVID-19 are at an especially high risk of 30-day mortality.
Major finding: Patients with COVID-19 whose cancers were progressing had a fivefold increase in the risk of 30-day mortality, compared with COVID-19–positive cancer patients in remission or with no evidence of cancer.
Study details: Analysis of data on 928 patients enrolled in the COVID-19 and Cancer Consortium (CCC19) registry.
Disclosures: The research was supported, in part, by the National Institutes of Health and the American Cancer Society. Dr. Warner disclosed relationships with HemOnc.org, IBM, and Westat.
Source: Warner J L et al. ASCO 2020, Abstract LBA110.
Patient-focused precautions, testing help blunt pandemic effects on heme-onc unit
Keeping hematologic oncology patients on their treatment regimens and caring for inpatients with hematologic malignancies remained “manageable” during the first 2 months of the COVID-19 pandemic at Levine Cancer Institute in Charlotte, N.C.
That level of manageability has partly been because a surge in cases so far hasn’t arrived at Levine or in most of the surrounding North Carolina and South Carolina communities it serves. As of May 15, 2020, the total number of confirmed and reported COVID-19 cases had reached about 19,000 in North Carolina, and just under 9,000 in South Carolina, out of a total population in the two states of close to 16 million. What’s happened instead at Levine Cancer Institute (LCI) has been a steady but low drumbeat of cases that, by mid-May 2020, totaled fewer than 10 patients with hematologic malignancies diagnosed with COVID-19.
“For a large system with multiple sites throughout North and South Carolina that saw 17,200 new patients in 2019 – including solid tumor, benign hematology, and malignant hematology patients – with 198,000 total patient visits, it is safe to say that we are off to a good start. However, we remain in the early throes of the pandemic and we will need to remain vigilant going forward,” said Peter Voorhees, MD, professor of medicine and director of Medical Operations and Outreach Services in LCI’s Department of Hematologic Oncology and Blood Disorders.
The limited effects to date of COVID-19 at LCI has been thanks to a regimen of great caution for preventing infections that’s been consistently conveyed to LCI patients from before the pandemic’s onset, liberal testing that started early, a proactive plan to defer and temporarily replace infusion care when medically appropriate, a novel staffing approach designed to minimize and contain potential staff outbreaks, and an early pivot to virtual patient contact when feasible.
COVID-19 has had limited penetration into the LCI case load because patients have, in general, “been very careful,” said Dr. Voorhees.
“My impression is that the incidence has been low partly because our patients, especially those with hematologic malignancies including those on active chemotherapy, were already getting warned to be cautious even before the coronavirus using distancing, masking, and meticulous hand hygiene,” he said in an interview that reviewed the steps LCI took starting in March to confront and manage the effects of the then-nascent pandemic. “Since we started screening asymptomatic patients in the inpatient and outpatient settings we have identified only one patient with COVID-19 infection, which supports the low rate of infection in our patient population thus far.”
Another key step was the launch of “robust” testing for the COVID-19 virus starting on March 9, using an in-house assay from LCI’s parent health system, Atrium Health, that delivered results within 24 hours. Testing became available at LCI “earlier than at many other health systems.” At first, testing was limited to patients or staff presenting with symptoms, but in the following weeks, it expanded to more patients, including those without symptoms who were scheduled for treatment at the apheresis center, cell donors and cell recipients, patients arriving for inpatient chemotherapy or cellular therapy, patients arriving from a skilled nursing facility or similar environments, and more recently, outpatient chemotherapy patients. “We’re now doing a lot of screening,” Dr. Voorhees said. “In general, screening has been well received because patients recognize that it’s for their own safety.”
Another piece of COVID-19 preparedness was a move toward technology as an alternative to face-to-face encounters between patients and staff. “We adopted virtual technology early.” When medically appropriate, they provided either video consultations with more tech-savvy patients or telephone-based virtual visits for patients who preferred a more familiar interface. As LCI starts the process of reentry for patients whose face-to-face encounters were deferred, virtual visits will remain an important facet of maintaining care while limiting exposure for appropriate patients and facilitating adequate space for social distancing in the clinics and infusion centers.
Atrium Health also launched a “virtual hospital” geared to intensified remote management of COVID-19 patients who aren’t sick enough for hospitalization. “People who test positive automatically enter the virtual hospital and have regular interactions with their team of providers,” with LCI providing additional support for their patients who get infected. Patients receive an equipment kit that lets them monitor and transmit their vital signs. The virtual hospital program also helps expedite personal needs like delivery of prescriptions and food. “It helps patients manage at home, and has been incredibly useful,” said Dr. Voorhees.
Perhaps the most challenging step LCI clinicians took to preclude a potential COVID-19 case surge was to review all patients receiving infusional therapy or planned cellular therapy and triage those who could potentially tolerate a temporary change to either an oral, at-home regimen or to a brief hold on their treatment. Some patients on maintenance, outpatient infusion-therapy regimens “expressed concern about coming to the clinic. We looked at the patients scheduled to come for infusions and decided which visits were essential and which were deferrable without disrupting care by briefly using a noninfusional approach,” said Dr. Voorhees. The number of patients who had their regimens modified or held was “relatively small,” and with the recent recognition that a surge of infections has not occurred, “we’re now rolling out cautious reentry of those patients back to their originally prescribed chemotherapy.”
In addition to concerns of exposure at infusion clinics, there are concerns about the heightened susceptibility of immunosuppressed hematologic oncology patients to COVID-19 and their risk for more severe infection. “Our view is that, if patients tested positive, continuing immunosuppressive treatment would likely be detrimental,” so when possible treatment is temporarily suspended and then resumed when the infection has cleared. “When patients test positive for a prolonged period, a decision to resume treatment must be in the best interests of the patient and weigh the benefits of resuming therapy against the risks of incurring a more severe infection by restarting potentially immunosuppressive therapy,” Dr. Voorhees said.
The enhanced risk that cancer patients face if they develop COVID-19 was documented in a recent review of 218 cancer patients hospitalized for COVID-19 during parts of March and April in a large New York health system. The results showed an overall mortality rate of 28%, including a 37% rate among 54 patients with hematologic malignancies and a 25% rate among 164 patients with solid tumors. The mortality rate “may not be quite as high as they reported because that depends on how many patients you test, but there is no question that patients with more comorbidities are at higher risk. Patients with active cancer on chemotherapy are a particularly vulnerable population, and many have expressed concerns about their vulnerability,” he observed.
For the few LCI patients who developed COVID-19 infection, the medical staff has had several therapeutic options they could match to each patient’s needs, with help from the Atrium Health infectious disease team. LCI and Atrium Health are participating in several COVID-19 clinical treatment trials, including an investigational convalescent plasma protocol spearheaded by the Mayo Clinic. They have also opened a randomized, phase 2 trial evaluating the safety and efficacy of selinexor (Xpovio), an oral drug that’s Food and Drug Administration approved for patients with multiple myeloma, for treatment of moderate or severe COVID-19 infection. Additional studies evaluating blockade of granulocyte-macrophage colony-stimulating factor, as well as inhaled antiviral therapy, have recently launched, and several additional studies are poised to open in the coming weeks.
The LCI and Atrium Health team also has a supply of the antiviral agent remdesivir as part of the FDA’s expanded access protocol and emergency use authorization. They also have a supply of and experience administering the interleukin-6 receptor inhibitor tocilizumab (Actemra), which showed some suggestion of efficacy in limited experience treating patients with severe or critical COVID-19 infections. Clinicians at LCI have not used the investigational and unproven agents hydroxychloroquine, chloroquine, and azithromycin to either prevent or treat COVID-19.
LCI also instituted measures to try to minimize the risk that staff members could become infected and transmit the virus while asymptomatic. Following conversations held early on with COVID-19–experienced health authorities in China and Italy, the patient-facing LCI staff split into two teams starting on March 23 that alternated responsibility for direct patient interactions every 2 weeks. When one of these teams was off from direct patient contact they continued to care for patients remotely through virtual technologies. The concept was that, if a staffer became infected while remaining asymptomatic during their contact with patients, their status would either become diagnosable or resolve during their 2 weeks away from seeing any patients. Perhaps in part because of this approach infections among staff members “have not been a big issue. We’ve had an incredibly low infection rate among the LCI staff,” Dr. Voorhees noted.
By mid-May, with the imminent threat of a sudden CODIV-19 surge moderated, heme-onc operations at LCI began to cautiously revert to more normal operations. “We’re continuing patient screening for signs and symptoms of COVID-19 infection, testing for asymptomatic infections, and requiring masking and social distancing in the clinics and hospitals, but we’re starting to slowly restore the number of patients at our clinics [virtual and face to face[ and infusion centers,” and the staff’s division into two teams ended. “The idea was to get past a surge and make sure our system was not overwhelmed. We anticipated a local surge in late April, but then it kept getting pushed back. Current projections are for the infection rate among LCI patients to remain low provided that community spread remains stable or, ideally, decreases.” The LCI infectious disease staff is closely monitoring infection rates for early recognition of an outbreak, with plans to follow any new cases with contact tracing. So far, the COVID-19 pandemic at LCI “has been very manageable,” Dr. Voorhees concluded.
“We’re now better positioned to deal with a case surge if it were to happen. We could resume the two-team approach, hospital-wide plans are now in place for a future surge, and we are now up and running with robust testing and inpatient and outpatient virtual technology. The first time, we were all learning on the fly.”
The LCI biostatistics team has been prospectively collecting the Institutes’s COVID-19 patient data, with plans to report their findings.
Dr. Voorhees has had financial relationships with Bristol-Myers Squibb/Celgene, Janssen, Novartis, and Oncopeptides, none of which are relevant to this article.
Keeping hematologic oncology patients on their treatment regimens and caring for inpatients with hematologic malignancies remained “manageable” during the first 2 months of the COVID-19 pandemic at Levine Cancer Institute in Charlotte, N.C.
That level of manageability has partly been because a surge in cases so far hasn’t arrived at Levine or in most of the surrounding North Carolina and South Carolina communities it serves. As of May 15, 2020, the total number of confirmed and reported COVID-19 cases had reached about 19,000 in North Carolina, and just under 9,000 in South Carolina, out of a total population in the two states of close to 16 million. What’s happened instead at Levine Cancer Institute (LCI) has been a steady but low drumbeat of cases that, by mid-May 2020, totaled fewer than 10 patients with hematologic malignancies diagnosed with COVID-19.
“For a large system with multiple sites throughout North and South Carolina that saw 17,200 new patients in 2019 – including solid tumor, benign hematology, and malignant hematology patients – with 198,000 total patient visits, it is safe to say that we are off to a good start. However, we remain in the early throes of the pandemic and we will need to remain vigilant going forward,” said Peter Voorhees, MD, professor of medicine and director of Medical Operations and Outreach Services in LCI’s Department of Hematologic Oncology and Blood Disorders.
The limited effects to date of COVID-19 at LCI has been thanks to a regimen of great caution for preventing infections that’s been consistently conveyed to LCI patients from before the pandemic’s onset, liberal testing that started early, a proactive plan to defer and temporarily replace infusion care when medically appropriate, a novel staffing approach designed to minimize and contain potential staff outbreaks, and an early pivot to virtual patient contact when feasible.
COVID-19 has had limited penetration into the LCI case load because patients have, in general, “been very careful,” said Dr. Voorhees.
“My impression is that the incidence has been low partly because our patients, especially those with hematologic malignancies including those on active chemotherapy, were already getting warned to be cautious even before the coronavirus using distancing, masking, and meticulous hand hygiene,” he said in an interview that reviewed the steps LCI took starting in March to confront and manage the effects of the then-nascent pandemic. “Since we started screening asymptomatic patients in the inpatient and outpatient settings we have identified only one patient with COVID-19 infection, which supports the low rate of infection in our patient population thus far.”
Another key step was the launch of “robust” testing for the COVID-19 virus starting on March 9, using an in-house assay from LCI’s parent health system, Atrium Health, that delivered results within 24 hours. Testing became available at LCI “earlier than at many other health systems.” At first, testing was limited to patients or staff presenting with symptoms, but in the following weeks, it expanded to more patients, including those without symptoms who were scheduled for treatment at the apheresis center, cell donors and cell recipients, patients arriving for inpatient chemotherapy or cellular therapy, patients arriving from a skilled nursing facility or similar environments, and more recently, outpatient chemotherapy patients. “We’re now doing a lot of screening,” Dr. Voorhees said. “In general, screening has been well received because patients recognize that it’s for their own safety.”
Another piece of COVID-19 preparedness was a move toward technology as an alternative to face-to-face encounters between patients and staff. “We adopted virtual technology early.” When medically appropriate, they provided either video consultations with more tech-savvy patients or telephone-based virtual visits for patients who preferred a more familiar interface. As LCI starts the process of reentry for patients whose face-to-face encounters were deferred, virtual visits will remain an important facet of maintaining care while limiting exposure for appropriate patients and facilitating adequate space for social distancing in the clinics and infusion centers.
Atrium Health also launched a “virtual hospital” geared to intensified remote management of COVID-19 patients who aren’t sick enough for hospitalization. “People who test positive automatically enter the virtual hospital and have regular interactions with their team of providers,” with LCI providing additional support for their patients who get infected. Patients receive an equipment kit that lets them monitor and transmit their vital signs. The virtual hospital program also helps expedite personal needs like delivery of prescriptions and food. “It helps patients manage at home, and has been incredibly useful,” said Dr. Voorhees.
Perhaps the most challenging step LCI clinicians took to preclude a potential COVID-19 case surge was to review all patients receiving infusional therapy or planned cellular therapy and triage those who could potentially tolerate a temporary change to either an oral, at-home regimen or to a brief hold on their treatment. Some patients on maintenance, outpatient infusion-therapy regimens “expressed concern about coming to the clinic. We looked at the patients scheduled to come for infusions and decided which visits were essential and which were deferrable without disrupting care by briefly using a noninfusional approach,” said Dr. Voorhees. The number of patients who had their regimens modified or held was “relatively small,” and with the recent recognition that a surge of infections has not occurred, “we’re now rolling out cautious reentry of those patients back to their originally prescribed chemotherapy.”
In addition to concerns of exposure at infusion clinics, there are concerns about the heightened susceptibility of immunosuppressed hematologic oncology patients to COVID-19 and their risk for more severe infection. “Our view is that, if patients tested positive, continuing immunosuppressive treatment would likely be detrimental,” so when possible treatment is temporarily suspended and then resumed when the infection has cleared. “When patients test positive for a prolonged period, a decision to resume treatment must be in the best interests of the patient and weigh the benefits of resuming therapy against the risks of incurring a more severe infection by restarting potentially immunosuppressive therapy,” Dr. Voorhees said.
The enhanced risk that cancer patients face if they develop COVID-19 was documented in a recent review of 218 cancer patients hospitalized for COVID-19 during parts of March and April in a large New York health system. The results showed an overall mortality rate of 28%, including a 37% rate among 54 patients with hematologic malignancies and a 25% rate among 164 patients with solid tumors. The mortality rate “may not be quite as high as they reported because that depends on how many patients you test, but there is no question that patients with more comorbidities are at higher risk. Patients with active cancer on chemotherapy are a particularly vulnerable population, and many have expressed concerns about their vulnerability,” he observed.
For the few LCI patients who developed COVID-19 infection, the medical staff has had several therapeutic options they could match to each patient’s needs, with help from the Atrium Health infectious disease team. LCI and Atrium Health are participating in several COVID-19 clinical treatment trials, including an investigational convalescent plasma protocol spearheaded by the Mayo Clinic. They have also opened a randomized, phase 2 trial evaluating the safety and efficacy of selinexor (Xpovio), an oral drug that’s Food and Drug Administration approved for patients with multiple myeloma, for treatment of moderate or severe COVID-19 infection. Additional studies evaluating blockade of granulocyte-macrophage colony-stimulating factor, as well as inhaled antiviral therapy, have recently launched, and several additional studies are poised to open in the coming weeks.
The LCI and Atrium Health team also has a supply of the antiviral agent remdesivir as part of the FDA’s expanded access protocol and emergency use authorization. They also have a supply of and experience administering the interleukin-6 receptor inhibitor tocilizumab (Actemra), which showed some suggestion of efficacy in limited experience treating patients with severe or critical COVID-19 infections. Clinicians at LCI have not used the investigational and unproven agents hydroxychloroquine, chloroquine, and azithromycin to either prevent or treat COVID-19.
LCI also instituted measures to try to minimize the risk that staff members could become infected and transmit the virus while asymptomatic. Following conversations held early on with COVID-19–experienced health authorities in China and Italy, the patient-facing LCI staff split into two teams starting on March 23 that alternated responsibility for direct patient interactions every 2 weeks. When one of these teams was off from direct patient contact they continued to care for patients remotely through virtual technologies. The concept was that, if a staffer became infected while remaining asymptomatic during their contact with patients, their status would either become diagnosable or resolve during their 2 weeks away from seeing any patients. Perhaps in part because of this approach infections among staff members “have not been a big issue. We’ve had an incredibly low infection rate among the LCI staff,” Dr. Voorhees noted.
By mid-May, with the imminent threat of a sudden CODIV-19 surge moderated, heme-onc operations at LCI began to cautiously revert to more normal operations. “We’re continuing patient screening for signs and symptoms of COVID-19 infection, testing for asymptomatic infections, and requiring masking and social distancing in the clinics and hospitals, but we’re starting to slowly restore the number of patients at our clinics [virtual and face to face[ and infusion centers,” and the staff’s division into two teams ended. “The idea was to get past a surge and make sure our system was not overwhelmed. We anticipated a local surge in late April, but then it kept getting pushed back. Current projections are for the infection rate among LCI patients to remain low provided that community spread remains stable or, ideally, decreases.” The LCI infectious disease staff is closely monitoring infection rates for early recognition of an outbreak, with plans to follow any new cases with contact tracing. So far, the COVID-19 pandemic at LCI “has been very manageable,” Dr. Voorhees concluded.
“We’re now better positioned to deal with a case surge if it were to happen. We could resume the two-team approach, hospital-wide plans are now in place for a future surge, and we are now up and running with robust testing and inpatient and outpatient virtual technology. The first time, we were all learning on the fly.”
The LCI biostatistics team has been prospectively collecting the Institutes’s COVID-19 patient data, with plans to report their findings.
Dr. Voorhees has had financial relationships with Bristol-Myers Squibb/Celgene, Janssen, Novartis, and Oncopeptides, none of which are relevant to this article.
Keeping hematologic oncology patients on their treatment regimens and caring for inpatients with hematologic malignancies remained “manageable” during the first 2 months of the COVID-19 pandemic at Levine Cancer Institute in Charlotte, N.C.
That level of manageability has partly been because a surge in cases so far hasn’t arrived at Levine or in most of the surrounding North Carolina and South Carolina communities it serves. As of May 15, 2020, the total number of confirmed and reported COVID-19 cases had reached about 19,000 in North Carolina, and just under 9,000 in South Carolina, out of a total population in the two states of close to 16 million. What’s happened instead at Levine Cancer Institute (LCI) has been a steady but low drumbeat of cases that, by mid-May 2020, totaled fewer than 10 patients with hematologic malignancies diagnosed with COVID-19.
“For a large system with multiple sites throughout North and South Carolina that saw 17,200 new patients in 2019 – including solid tumor, benign hematology, and malignant hematology patients – with 198,000 total patient visits, it is safe to say that we are off to a good start. However, we remain in the early throes of the pandemic and we will need to remain vigilant going forward,” said Peter Voorhees, MD, professor of medicine and director of Medical Operations and Outreach Services in LCI’s Department of Hematologic Oncology and Blood Disorders.
The limited effects to date of COVID-19 at LCI has been thanks to a regimen of great caution for preventing infections that’s been consistently conveyed to LCI patients from before the pandemic’s onset, liberal testing that started early, a proactive plan to defer and temporarily replace infusion care when medically appropriate, a novel staffing approach designed to minimize and contain potential staff outbreaks, and an early pivot to virtual patient contact when feasible.
COVID-19 has had limited penetration into the LCI case load because patients have, in general, “been very careful,” said Dr. Voorhees.
“My impression is that the incidence has been low partly because our patients, especially those with hematologic malignancies including those on active chemotherapy, were already getting warned to be cautious even before the coronavirus using distancing, masking, and meticulous hand hygiene,” he said in an interview that reviewed the steps LCI took starting in March to confront and manage the effects of the then-nascent pandemic. “Since we started screening asymptomatic patients in the inpatient and outpatient settings we have identified only one patient with COVID-19 infection, which supports the low rate of infection in our patient population thus far.”
Another key step was the launch of “robust” testing for the COVID-19 virus starting on March 9, using an in-house assay from LCI’s parent health system, Atrium Health, that delivered results within 24 hours. Testing became available at LCI “earlier than at many other health systems.” At first, testing was limited to patients or staff presenting with symptoms, but in the following weeks, it expanded to more patients, including those without symptoms who were scheduled for treatment at the apheresis center, cell donors and cell recipients, patients arriving for inpatient chemotherapy or cellular therapy, patients arriving from a skilled nursing facility or similar environments, and more recently, outpatient chemotherapy patients. “We’re now doing a lot of screening,” Dr. Voorhees said. “In general, screening has been well received because patients recognize that it’s for their own safety.”
Another piece of COVID-19 preparedness was a move toward technology as an alternative to face-to-face encounters between patients and staff. “We adopted virtual technology early.” When medically appropriate, they provided either video consultations with more tech-savvy patients or telephone-based virtual visits for patients who preferred a more familiar interface. As LCI starts the process of reentry for patients whose face-to-face encounters were deferred, virtual visits will remain an important facet of maintaining care while limiting exposure for appropriate patients and facilitating adequate space for social distancing in the clinics and infusion centers.
Atrium Health also launched a “virtual hospital” geared to intensified remote management of COVID-19 patients who aren’t sick enough for hospitalization. “People who test positive automatically enter the virtual hospital and have regular interactions with their team of providers,” with LCI providing additional support for their patients who get infected. Patients receive an equipment kit that lets them monitor and transmit their vital signs. The virtual hospital program also helps expedite personal needs like delivery of prescriptions and food. “It helps patients manage at home, and has been incredibly useful,” said Dr. Voorhees.
Perhaps the most challenging step LCI clinicians took to preclude a potential COVID-19 case surge was to review all patients receiving infusional therapy or planned cellular therapy and triage those who could potentially tolerate a temporary change to either an oral, at-home regimen or to a brief hold on their treatment. Some patients on maintenance, outpatient infusion-therapy regimens “expressed concern about coming to the clinic. We looked at the patients scheduled to come for infusions and decided which visits were essential and which were deferrable without disrupting care by briefly using a noninfusional approach,” said Dr. Voorhees. The number of patients who had their regimens modified or held was “relatively small,” and with the recent recognition that a surge of infections has not occurred, “we’re now rolling out cautious reentry of those patients back to their originally prescribed chemotherapy.”
In addition to concerns of exposure at infusion clinics, there are concerns about the heightened susceptibility of immunosuppressed hematologic oncology patients to COVID-19 and their risk for more severe infection. “Our view is that, if patients tested positive, continuing immunosuppressive treatment would likely be detrimental,” so when possible treatment is temporarily suspended and then resumed when the infection has cleared. “When patients test positive for a prolonged period, a decision to resume treatment must be in the best interests of the patient and weigh the benefits of resuming therapy against the risks of incurring a more severe infection by restarting potentially immunosuppressive therapy,” Dr. Voorhees said.
The enhanced risk that cancer patients face if they develop COVID-19 was documented in a recent review of 218 cancer patients hospitalized for COVID-19 during parts of March and April in a large New York health system. The results showed an overall mortality rate of 28%, including a 37% rate among 54 patients with hematologic malignancies and a 25% rate among 164 patients with solid tumors. The mortality rate “may not be quite as high as they reported because that depends on how many patients you test, but there is no question that patients with more comorbidities are at higher risk. Patients with active cancer on chemotherapy are a particularly vulnerable population, and many have expressed concerns about their vulnerability,” he observed.
For the few LCI patients who developed COVID-19 infection, the medical staff has had several therapeutic options they could match to each patient’s needs, with help from the Atrium Health infectious disease team. LCI and Atrium Health are participating in several COVID-19 clinical treatment trials, including an investigational convalescent plasma protocol spearheaded by the Mayo Clinic. They have also opened a randomized, phase 2 trial evaluating the safety and efficacy of selinexor (Xpovio), an oral drug that’s Food and Drug Administration approved for patients with multiple myeloma, for treatment of moderate or severe COVID-19 infection. Additional studies evaluating blockade of granulocyte-macrophage colony-stimulating factor, as well as inhaled antiviral therapy, have recently launched, and several additional studies are poised to open in the coming weeks.
The LCI and Atrium Health team also has a supply of the antiviral agent remdesivir as part of the FDA’s expanded access protocol and emergency use authorization. They also have a supply of and experience administering the interleukin-6 receptor inhibitor tocilizumab (Actemra), which showed some suggestion of efficacy in limited experience treating patients with severe or critical COVID-19 infections. Clinicians at LCI have not used the investigational and unproven agents hydroxychloroquine, chloroquine, and azithromycin to either prevent or treat COVID-19.
LCI also instituted measures to try to minimize the risk that staff members could become infected and transmit the virus while asymptomatic. Following conversations held early on with COVID-19–experienced health authorities in China and Italy, the patient-facing LCI staff split into two teams starting on March 23 that alternated responsibility for direct patient interactions every 2 weeks. When one of these teams was off from direct patient contact they continued to care for patients remotely through virtual technologies. The concept was that, if a staffer became infected while remaining asymptomatic during their contact with patients, their status would either become diagnosable or resolve during their 2 weeks away from seeing any patients. Perhaps in part because of this approach infections among staff members “have not been a big issue. We’ve had an incredibly low infection rate among the LCI staff,” Dr. Voorhees noted.
By mid-May, with the imminent threat of a sudden CODIV-19 surge moderated, heme-onc operations at LCI began to cautiously revert to more normal operations. “We’re continuing patient screening for signs and symptoms of COVID-19 infection, testing for asymptomatic infections, and requiring masking and social distancing in the clinics and hospitals, but we’re starting to slowly restore the number of patients at our clinics [virtual and face to face[ and infusion centers,” and the staff’s division into two teams ended. “The idea was to get past a surge and make sure our system was not overwhelmed. We anticipated a local surge in late April, but then it kept getting pushed back. Current projections are for the infection rate among LCI patients to remain low provided that community spread remains stable or, ideally, decreases.” The LCI infectious disease staff is closely monitoring infection rates for early recognition of an outbreak, with plans to follow any new cases with contact tracing. So far, the COVID-19 pandemic at LCI “has been very manageable,” Dr. Voorhees concluded.
“We’re now better positioned to deal with a case surge if it were to happen. We could resume the two-team approach, hospital-wide plans are now in place for a future surge, and we are now up and running with robust testing and inpatient and outpatient virtual technology. The first time, we were all learning on the fly.”
The LCI biostatistics team has been prospectively collecting the Institutes’s COVID-19 patient data, with plans to report their findings.
Dr. Voorhees has had financial relationships with Bristol-Myers Squibb/Celgene, Janssen, Novartis, and Oncopeptides, none of which are relevant to this article.
Oncologists’ income and satisfaction are up
Oncologists continue to rank above the middle range for all specialties in annual compensation for physicians, according to findings from the newly released Medscape Oncologist Compensation Report 2020.
The average earnings for oncologists who participated in the survey was $377,000, which was a 5% increase from the $359,000 reported for 2018.
Just over two-thirds (67%) of oncologists reported that they felt that they were fairly compensated, which is quite a jump from 53% last year.
In addition, oncologists appear to be very satisfied with their profession. Similar to last year’s findings, 84% said they would choose medicine again, and 96% said they would choose the specialty of oncology again.
Earning in top third of all specialties
The average annual earnings reported by oncologists put this specialty in eleventh place among 29 specialties. Orthopedic specialists remain at the head of the list, with estimated earnings of $511,000, followed by plastic surgeons ($479,000), otolaryngologists ($455,000), and cardiologists ($438,000), according to Medscape’s compensation report, which included responses from 17,461 physicians in over 30 specialties.

At the bottom of the estimated earnings list were public health and preventive medicine doctors and pediatricians. For both specialties, the reported annual earnings was $232,000. Family medicine specialists were only marginally higher at $234,000.
Radiologists ($427,000), gastroenterologists ($419,000), and urologists ($417,000) all reported higher earnings than oncologists, whereas neurologists, at $280,000, rheumatologists, at $262,000, and internal medicine physicians, at $251,000, earned less.
The report also found that gender disparities in income persist, with male oncologists earning 17% more than their female colleagues. The gender gap in oncology is somewhat less than that seen for all specialties combined, in which men earned 31% more than women, similar to last year’s figure of 33%.
Male oncologists reported spending 38.8 hours per week seeing patients, compared with 34.9 hours reported by female oncologists. This could be a factor contributing to the gender pay disparity. Overall, the average amount of time seeing patients was 37.9 hours per week.
Frustrations with paperwork and denied claims
Surveyed oncologists cited some of the frustrations they are facing, such as spending nearly 17 hours a week on paperwork and administrative tasks. They reported that 16% of claims are denied or have to be resubmitted. As for the most challenging part of the job, oncologists (22%), similar to physicians overall (26%), found that having so many rules and regulations takes first place, followed by working with electronic health record systems (20%), difficulties getting fair reimbursement (19%), having to work long hours (12%), and dealing with difficult patients (8%). Few oncologists were concerned about lawsuits (4%), and 4% reported that there were no challenges.
Oncologists reported that the most rewarding part of their job was gratitude/relationships with patients (31%), followed by knowing that they are making the world a better place (27%). After that, oncologists agreed with statements about being very good at what they do/finding answers/diagnoses (22%), having pride in being a doctor (9%), and making good money at a job they like (8%).
Other key findings
Other key findings from the Medscape Oncologist Compensation Report 2020 included the following:
- Regarding payment models, 80% take insurance, 41% are in fee-for-service arrangements, and 18% are in accountable care organizations (21%). Only 3% are in direct primary care, and 1% are cash-only practices or have a concierge practice.
- 65% of oncologists state that they will continue taking new and current Medicare/Medicaid patients. None said that they would not take on new Medicare/Medicaid patients, and 35% remain undecided. These numbers differed from physicians overall; 73% of all physicians surveyed said they would continue taking new/current Medicare/Medicaid patients, 6% said that will not take on new Medicare patients, and 4% said they will not take new Medicaid patients. In addition, 3% and 2% said that they would stop treating some or all of their Medicare and Medicaid patients, respectively.
- About half (51%) of oncologists use nurse practitioners, about a third (34%) use physician assistants, and 37% use neither. This was about the same as physicians overall.
- A larger percentage of oncologists (38%) expect to participate in MIPS (merit-based incentive payment system), and only 8% expect to participate in APMs (alternative payment models). This was similar to the findings for physicians overall, with more than one-third (37%) expecting to participate in MIPS and 9% planning to take part in APMs.
Impact of COVID-19 pandemic
The Medscape compensation reports also gives a glimpse of the impact the COVID-19 pandemic is having on physician compensation.
Since the beginning of the pandemic, practices have reported a 55% decrease in revenue and a 60% drop in patient volume. Physician practices and hospitals have laid off or furloughed personnel and have cut pay, and 9% of practices have closed their doors, at least for the time being.
A total of 43,000 health care workers were laid off in March, the report notes.
The findings tie in with those reported elsewhere. For example, a survey conducted by the Medical Group Management Association, which was reported by Medscape Medical News, found that 97% of physician practices have experienced negative financial effects directly or indirectly related to COVID-19.
Specialties were hard hit, especially those that rely on elective procedures, such as dermatology and cardiology. Oncology care has also been disrupted. For example, a survey conducted by the American Cancer Society Cancer Action Network found that half of the cancer patients and survivors who responded reported changes, delays, or disruptions to the care they were receiving.
This article first appeared on Medscape.com.
Oncologists continue to rank above the middle range for all specialties in annual compensation for physicians, according to findings from the newly released Medscape Oncologist Compensation Report 2020.
The average earnings for oncologists who participated in the survey was $377,000, which was a 5% increase from the $359,000 reported for 2018.
Just over two-thirds (67%) of oncologists reported that they felt that they were fairly compensated, which is quite a jump from 53% last year.
In addition, oncologists appear to be very satisfied with their profession. Similar to last year’s findings, 84% said they would choose medicine again, and 96% said they would choose the specialty of oncology again.
Earning in top third of all specialties
The average annual earnings reported by oncologists put this specialty in eleventh place among 29 specialties. Orthopedic specialists remain at the head of the list, with estimated earnings of $511,000, followed by plastic surgeons ($479,000), otolaryngologists ($455,000), and cardiologists ($438,000), according to Medscape’s compensation report, which included responses from 17,461 physicians in over 30 specialties.

At the bottom of the estimated earnings list were public health and preventive medicine doctors and pediatricians. For both specialties, the reported annual earnings was $232,000. Family medicine specialists were only marginally higher at $234,000.
Radiologists ($427,000), gastroenterologists ($419,000), and urologists ($417,000) all reported higher earnings than oncologists, whereas neurologists, at $280,000, rheumatologists, at $262,000, and internal medicine physicians, at $251,000, earned less.
The report also found that gender disparities in income persist, with male oncologists earning 17% more than their female colleagues. The gender gap in oncology is somewhat less than that seen for all specialties combined, in which men earned 31% more than women, similar to last year’s figure of 33%.
Male oncologists reported spending 38.8 hours per week seeing patients, compared with 34.9 hours reported by female oncologists. This could be a factor contributing to the gender pay disparity. Overall, the average amount of time seeing patients was 37.9 hours per week.
Frustrations with paperwork and denied claims
Surveyed oncologists cited some of the frustrations they are facing, such as spending nearly 17 hours a week on paperwork and administrative tasks. They reported that 16% of claims are denied or have to be resubmitted. As for the most challenging part of the job, oncologists (22%), similar to physicians overall (26%), found that having so many rules and regulations takes first place, followed by working with electronic health record systems (20%), difficulties getting fair reimbursement (19%), having to work long hours (12%), and dealing with difficult patients (8%). Few oncologists were concerned about lawsuits (4%), and 4% reported that there were no challenges.
Oncologists reported that the most rewarding part of their job was gratitude/relationships with patients (31%), followed by knowing that they are making the world a better place (27%). After that, oncologists agreed with statements about being very good at what they do/finding answers/diagnoses (22%), having pride in being a doctor (9%), and making good money at a job they like (8%).
Other key findings
Other key findings from the Medscape Oncologist Compensation Report 2020 included the following:
- Regarding payment models, 80% take insurance, 41% are in fee-for-service arrangements, and 18% are in accountable care organizations (21%). Only 3% are in direct primary care, and 1% are cash-only practices or have a concierge practice.
- 65% of oncologists state that they will continue taking new and current Medicare/Medicaid patients. None said that they would not take on new Medicare/Medicaid patients, and 35% remain undecided. These numbers differed from physicians overall; 73% of all physicians surveyed said they would continue taking new/current Medicare/Medicaid patients, 6% said that will not take on new Medicare patients, and 4% said they will not take new Medicaid patients. In addition, 3% and 2% said that they would stop treating some or all of their Medicare and Medicaid patients, respectively.
- About half (51%) of oncologists use nurse practitioners, about a third (34%) use physician assistants, and 37% use neither. This was about the same as physicians overall.
- A larger percentage of oncologists (38%) expect to participate in MIPS (merit-based incentive payment system), and only 8% expect to participate in APMs (alternative payment models). This was similar to the findings for physicians overall, with more than one-third (37%) expecting to participate in MIPS and 9% planning to take part in APMs.
Impact of COVID-19 pandemic
The Medscape compensation reports also gives a glimpse of the impact the COVID-19 pandemic is having on physician compensation.
Since the beginning of the pandemic, practices have reported a 55% decrease in revenue and a 60% drop in patient volume. Physician practices and hospitals have laid off or furloughed personnel and have cut pay, and 9% of practices have closed their doors, at least for the time being.
A total of 43,000 health care workers were laid off in March, the report notes.
The findings tie in with those reported elsewhere. For example, a survey conducted by the Medical Group Management Association, which was reported by Medscape Medical News, found that 97% of physician practices have experienced negative financial effects directly or indirectly related to COVID-19.
Specialties were hard hit, especially those that rely on elective procedures, such as dermatology and cardiology. Oncology care has also been disrupted. For example, a survey conducted by the American Cancer Society Cancer Action Network found that half of the cancer patients and survivors who responded reported changes, delays, or disruptions to the care they were receiving.
This article first appeared on Medscape.com.
Oncologists continue to rank above the middle range for all specialties in annual compensation for physicians, according to findings from the newly released Medscape Oncologist Compensation Report 2020.
The average earnings for oncologists who participated in the survey was $377,000, which was a 5% increase from the $359,000 reported for 2018.
Just over two-thirds (67%) of oncologists reported that they felt that they were fairly compensated, which is quite a jump from 53% last year.
In addition, oncologists appear to be very satisfied with their profession. Similar to last year’s findings, 84% said they would choose medicine again, and 96% said they would choose the specialty of oncology again.
Earning in top third of all specialties
The average annual earnings reported by oncologists put this specialty in eleventh place among 29 specialties. Orthopedic specialists remain at the head of the list, with estimated earnings of $511,000, followed by plastic surgeons ($479,000), otolaryngologists ($455,000), and cardiologists ($438,000), according to Medscape’s compensation report, which included responses from 17,461 physicians in over 30 specialties.

At the bottom of the estimated earnings list were public health and preventive medicine doctors and pediatricians. For both specialties, the reported annual earnings was $232,000. Family medicine specialists were only marginally higher at $234,000.
Radiologists ($427,000), gastroenterologists ($419,000), and urologists ($417,000) all reported higher earnings than oncologists, whereas neurologists, at $280,000, rheumatologists, at $262,000, and internal medicine physicians, at $251,000, earned less.
The report also found that gender disparities in income persist, with male oncologists earning 17% more than their female colleagues. The gender gap in oncology is somewhat less than that seen for all specialties combined, in which men earned 31% more than women, similar to last year’s figure of 33%.
Male oncologists reported spending 38.8 hours per week seeing patients, compared with 34.9 hours reported by female oncologists. This could be a factor contributing to the gender pay disparity. Overall, the average amount of time seeing patients was 37.9 hours per week.
Frustrations with paperwork and denied claims
Surveyed oncologists cited some of the frustrations they are facing, such as spending nearly 17 hours a week on paperwork and administrative tasks. They reported that 16% of claims are denied or have to be resubmitted. As for the most challenging part of the job, oncologists (22%), similar to physicians overall (26%), found that having so many rules and regulations takes first place, followed by working with electronic health record systems (20%), difficulties getting fair reimbursement (19%), having to work long hours (12%), and dealing with difficult patients (8%). Few oncologists were concerned about lawsuits (4%), and 4% reported that there were no challenges.
Oncologists reported that the most rewarding part of their job was gratitude/relationships with patients (31%), followed by knowing that they are making the world a better place (27%). After that, oncologists agreed with statements about being very good at what they do/finding answers/diagnoses (22%), having pride in being a doctor (9%), and making good money at a job they like (8%).
Other key findings
Other key findings from the Medscape Oncologist Compensation Report 2020 included the following:
- Regarding payment models, 80% take insurance, 41% are in fee-for-service arrangements, and 18% are in accountable care organizations (21%). Only 3% are in direct primary care, and 1% are cash-only practices or have a concierge practice.
- 65% of oncologists state that they will continue taking new and current Medicare/Medicaid patients. None said that they would not take on new Medicare/Medicaid patients, and 35% remain undecided. These numbers differed from physicians overall; 73% of all physicians surveyed said they would continue taking new/current Medicare/Medicaid patients, 6% said that will not take on new Medicare patients, and 4% said they will not take new Medicaid patients. In addition, 3% and 2% said that they would stop treating some or all of their Medicare and Medicaid patients, respectively.
- About half (51%) of oncologists use nurse practitioners, about a third (34%) use physician assistants, and 37% use neither. This was about the same as physicians overall.
- A larger percentage of oncologists (38%) expect to participate in MIPS (merit-based incentive payment system), and only 8% expect to participate in APMs (alternative payment models). This was similar to the findings for physicians overall, with more than one-third (37%) expecting to participate in MIPS and 9% planning to take part in APMs.
Impact of COVID-19 pandemic
The Medscape compensation reports also gives a glimpse of the impact the COVID-19 pandemic is having on physician compensation.
Since the beginning of the pandemic, practices have reported a 55% decrease in revenue and a 60% drop in patient volume. Physician practices and hospitals have laid off or furloughed personnel and have cut pay, and 9% of practices have closed their doors, at least for the time being.
A total of 43,000 health care workers were laid off in March, the report notes.
The findings tie in with those reported elsewhere. For example, a survey conducted by the Medical Group Management Association, which was reported by Medscape Medical News, found that 97% of physician practices have experienced negative financial effects directly or indirectly related to COVID-19.
Specialties were hard hit, especially those that rely on elective procedures, such as dermatology and cardiology. Oncology care has also been disrupted. For example, a survey conducted by the American Cancer Society Cancer Action Network found that half of the cancer patients and survivors who responded reported changes, delays, or disruptions to the care they were receiving.
This article first appeared on Medscape.com.
Video coaching may relieve anxiety and distress for long-distance cancer caregivers
Anxiety and distress related to caring for a cancer patient who lives far away may be alleviated through an intervention that includes video-based coaching sessions with a nurse practitioner or social worker, a randomized study suggests.
About 20% of long-distance caregivers had a significant reduction in anxiety and 25% had a significant reduction in distress when they received video coaching sessions, attended oncologist visits via video, and had access to a website specifically designed for their needs.
Adding the caregiver to oncologist office visits made the patients feel better supported and didn’t add a significant amount of time to the encounter, said Sara L. Douglas, PhD, RN, of Case Western Reserve University, Cleveland.
Taken together, these results suggest that fairly simple technologies can be leveraged to help caregivers cope with psychological strains related to supporting a patient who doesn’t live nearby, Dr. Douglas said.
Distance caregivers, defined as those who live an hour or more away from the patient, can experience high rates of distress and anxiety because they lack first-hand information or may have uncertainty about the patient’s current condition, according to Dr. Douglas and colleagues.
“Caregivers’ high rates of anxiety and distress have been found to have a negative impact not only upon their own health but upon their ability to provide high quality care to the patient,” Dr. Douglas said.
With this in mind, she and her colleagues conducted a 4-month study of distance caregivers. Dr. Douglas presented results from the study at the American Society of Clinical Oncology virtual scientific program during a press briefing in advance of the meeting. This year, ASCO’s annual meeting is split into two parts. The virtual scientific program will be presented online on May 29-31, and the virtual education program will be available Aug. 8-10.
Study details
The study enrolled 441 distance caregivers of cancer patients, and Dr. Douglas presented results in 311 of those caregivers. (Data in the presentation differ from the abstract.) The caregivers were, on average, 47 years of age. Most were female (72%), white (67%), the child of the patient (63%), currently employed (81%), and new to the distance caregiver role (89%).
The caregivers were randomized to one of three study arms.
One arm received the full intervention, which consisted of four video-coaching sessions with an advanced practice nurse or social worker, videoconference office visits with the physician and patient, and access to a website with information for cancer distance caregivers. A second arm received no video coaching but had access to the website and participated in video visits with the physician and patient. The third arm, which only received access to the website, served as the study’s control group.
Results
Dr. Douglas said that the full intervention had the biggest impact on caregivers’ distress and anxiety.
Among distance caregivers who received the full intervention, 19.2% had a significant reduction in anxiety (P = .03), as measured in online surveys before and after the intervention using the PROMIS Anxiety instrument. Furthermore, 24.8% of these caregivers had a significant reduction in distress (P = .02) from preintervention to post intervention, as measured by the National Comprehensive Cancer Network Distress Thermometer. Overall, distress and anxiety scores decreased in this arm.
Distance caregivers who only had physician-patient video visits and website access had a “moderate” reduction in distress and anxiety, Dr. Douglas said. Among these caregivers, 17.3% had an improvement in anxiety from baseline, and 19.8% had an improvement in distress. Overall, distress scores decreased, but anxiety scores increased slightly in this arm.
In the control arm, 13.1% of caregivers had an improvement in anxiety from baseline, and 18% had an improvement in distress. Overall, both anxiety and distress scores increased in this arm.
“While the full intervention yielded the best results for distance caregivers, we recognize that not all health care systems have the resources to provide individualized coaching sessions to distance caregivers,” Dr. Douglas said. “Therefore, it is worth noting that videoconference office visits alone are found to be of some benefit in improving distress and anxiety in this group of cancer caregivers.”
The study results suggest videoconferencing interventions can improve the emotional well-being of remote caregivers who provide “critical support” for cancer patients, said ASCO President Howard A. “Skip” Burris III, MD.
“As COVID-19 forces separation from loved ones and increases anxiety for people with cancer and their caregivers, providing emotional support virtually is more important than ever,” Dr. Burris said in a news release highlighting the study.
This study was funded by the National Institutes of Health and Case Comprehensive Cancer Center. Dr. Douglas reported having no disclosures. Other researchers involved in the study disclosed relationships with BridgeBio Pharma, Cardinal Health, Apexigen, Roche/Genentech, Seattle Genetics, Tesaro, Array BioPharma, Abbvie, Bristol-Myers Squibb, and Celgene. A full list of Dr. Burris’s financial disclosures is available on the ASCO website.
SOURCE: Douglas SL et al. ASCO 2020, Abstract 12123.
Anxiety and distress related to caring for a cancer patient who lives far away may be alleviated through an intervention that includes video-based coaching sessions with a nurse practitioner or social worker, a randomized study suggests.
About 20% of long-distance caregivers had a significant reduction in anxiety and 25% had a significant reduction in distress when they received video coaching sessions, attended oncologist visits via video, and had access to a website specifically designed for their needs.
Adding the caregiver to oncologist office visits made the patients feel better supported and didn’t add a significant amount of time to the encounter, said Sara L. Douglas, PhD, RN, of Case Western Reserve University, Cleveland.
Taken together, these results suggest that fairly simple technologies can be leveraged to help caregivers cope with psychological strains related to supporting a patient who doesn’t live nearby, Dr. Douglas said.
Distance caregivers, defined as those who live an hour or more away from the patient, can experience high rates of distress and anxiety because they lack first-hand information or may have uncertainty about the patient’s current condition, according to Dr. Douglas and colleagues.
“Caregivers’ high rates of anxiety and distress have been found to have a negative impact not only upon their own health but upon their ability to provide high quality care to the patient,” Dr. Douglas said.
With this in mind, she and her colleagues conducted a 4-month study of distance caregivers. Dr. Douglas presented results from the study at the American Society of Clinical Oncology virtual scientific program during a press briefing in advance of the meeting. This year, ASCO’s annual meeting is split into two parts. The virtual scientific program will be presented online on May 29-31, and the virtual education program will be available Aug. 8-10.
Study details
The study enrolled 441 distance caregivers of cancer patients, and Dr. Douglas presented results in 311 of those caregivers. (Data in the presentation differ from the abstract.) The caregivers were, on average, 47 years of age. Most were female (72%), white (67%), the child of the patient (63%), currently employed (81%), and new to the distance caregiver role (89%).
The caregivers were randomized to one of three study arms.
One arm received the full intervention, which consisted of four video-coaching sessions with an advanced practice nurse or social worker, videoconference office visits with the physician and patient, and access to a website with information for cancer distance caregivers. A second arm received no video coaching but had access to the website and participated in video visits with the physician and patient. The third arm, which only received access to the website, served as the study’s control group.
Results
Dr. Douglas said that the full intervention had the biggest impact on caregivers’ distress and anxiety.
Among distance caregivers who received the full intervention, 19.2% had a significant reduction in anxiety (P = .03), as measured in online surveys before and after the intervention using the PROMIS Anxiety instrument. Furthermore, 24.8% of these caregivers had a significant reduction in distress (P = .02) from preintervention to post intervention, as measured by the National Comprehensive Cancer Network Distress Thermometer. Overall, distress and anxiety scores decreased in this arm.
Distance caregivers who only had physician-patient video visits and website access had a “moderate” reduction in distress and anxiety, Dr. Douglas said. Among these caregivers, 17.3% had an improvement in anxiety from baseline, and 19.8% had an improvement in distress. Overall, distress scores decreased, but anxiety scores increased slightly in this arm.
In the control arm, 13.1% of caregivers had an improvement in anxiety from baseline, and 18% had an improvement in distress. Overall, both anxiety and distress scores increased in this arm.
“While the full intervention yielded the best results for distance caregivers, we recognize that not all health care systems have the resources to provide individualized coaching sessions to distance caregivers,” Dr. Douglas said. “Therefore, it is worth noting that videoconference office visits alone are found to be of some benefit in improving distress and anxiety in this group of cancer caregivers.”
The study results suggest videoconferencing interventions can improve the emotional well-being of remote caregivers who provide “critical support” for cancer patients, said ASCO President Howard A. “Skip” Burris III, MD.
“As COVID-19 forces separation from loved ones and increases anxiety for people with cancer and their caregivers, providing emotional support virtually is more important than ever,” Dr. Burris said in a news release highlighting the study.
This study was funded by the National Institutes of Health and Case Comprehensive Cancer Center. Dr. Douglas reported having no disclosures. Other researchers involved in the study disclosed relationships with BridgeBio Pharma, Cardinal Health, Apexigen, Roche/Genentech, Seattle Genetics, Tesaro, Array BioPharma, Abbvie, Bristol-Myers Squibb, and Celgene. A full list of Dr. Burris’s financial disclosures is available on the ASCO website.
SOURCE: Douglas SL et al. ASCO 2020, Abstract 12123.
Anxiety and distress related to caring for a cancer patient who lives far away may be alleviated through an intervention that includes video-based coaching sessions with a nurse practitioner or social worker, a randomized study suggests.
About 20% of long-distance caregivers had a significant reduction in anxiety and 25% had a significant reduction in distress when they received video coaching sessions, attended oncologist visits via video, and had access to a website specifically designed for their needs.
Adding the caregiver to oncologist office visits made the patients feel better supported and didn’t add a significant amount of time to the encounter, said Sara L. Douglas, PhD, RN, of Case Western Reserve University, Cleveland.
Taken together, these results suggest that fairly simple technologies can be leveraged to help caregivers cope with psychological strains related to supporting a patient who doesn’t live nearby, Dr. Douglas said.
Distance caregivers, defined as those who live an hour or more away from the patient, can experience high rates of distress and anxiety because they lack first-hand information or may have uncertainty about the patient’s current condition, according to Dr. Douglas and colleagues.
“Caregivers’ high rates of anxiety and distress have been found to have a negative impact not only upon their own health but upon their ability to provide high quality care to the patient,” Dr. Douglas said.
With this in mind, she and her colleagues conducted a 4-month study of distance caregivers. Dr. Douglas presented results from the study at the American Society of Clinical Oncology virtual scientific program during a press briefing in advance of the meeting. This year, ASCO’s annual meeting is split into two parts. The virtual scientific program will be presented online on May 29-31, and the virtual education program will be available Aug. 8-10.
Study details
The study enrolled 441 distance caregivers of cancer patients, and Dr. Douglas presented results in 311 of those caregivers. (Data in the presentation differ from the abstract.) The caregivers were, on average, 47 years of age. Most were female (72%), white (67%), the child of the patient (63%), currently employed (81%), and new to the distance caregiver role (89%).
The caregivers were randomized to one of three study arms.
One arm received the full intervention, which consisted of four video-coaching sessions with an advanced practice nurse or social worker, videoconference office visits with the physician and patient, and access to a website with information for cancer distance caregivers. A second arm received no video coaching but had access to the website and participated in video visits with the physician and patient. The third arm, which only received access to the website, served as the study’s control group.
Results
Dr. Douglas said that the full intervention had the biggest impact on caregivers’ distress and anxiety.
Among distance caregivers who received the full intervention, 19.2% had a significant reduction in anxiety (P = .03), as measured in online surveys before and after the intervention using the PROMIS Anxiety instrument. Furthermore, 24.8% of these caregivers had a significant reduction in distress (P = .02) from preintervention to post intervention, as measured by the National Comprehensive Cancer Network Distress Thermometer. Overall, distress and anxiety scores decreased in this arm.
Distance caregivers who only had physician-patient video visits and website access had a “moderate” reduction in distress and anxiety, Dr. Douglas said. Among these caregivers, 17.3% had an improvement in anxiety from baseline, and 19.8% had an improvement in distress. Overall, distress scores decreased, but anxiety scores increased slightly in this arm.
In the control arm, 13.1% of caregivers had an improvement in anxiety from baseline, and 18% had an improvement in distress. Overall, both anxiety and distress scores increased in this arm.
“While the full intervention yielded the best results for distance caregivers, we recognize that not all health care systems have the resources to provide individualized coaching sessions to distance caregivers,” Dr. Douglas said. “Therefore, it is worth noting that videoconference office visits alone are found to be of some benefit in improving distress and anxiety in this group of cancer caregivers.”
The study results suggest videoconferencing interventions can improve the emotional well-being of remote caregivers who provide “critical support” for cancer patients, said ASCO President Howard A. “Skip” Burris III, MD.
“As COVID-19 forces separation from loved ones and increases anxiety for people with cancer and their caregivers, providing emotional support virtually is more important than ever,” Dr. Burris said in a news release highlighting the study.
This study was funded by the National Institutes of Health and Case Comprehensive Cancer Center. Dr. Douglas reported having no disclosures. Other researchers involved in the study disclosed relationships with BridgeBio Pharma, Cardinal Health, Apexigen, Roche/Genentech, Seattle Genetics, Tesaro, Array BioPharma, Abbvie, Bristol-Myers Squibb, and Celgene. A full list of Dr. Burris’s financial disclosures is available on the ASCO website.
SOURCE: Douglas SL et al. ASCO 2020, Abstract 12123.
FROM ASCO 2020