User login
Community Oncology Podcast - Vismodegib for advanced basal cell carcinomas
Community Oncology's podcasts by Editor in Chief Dr. David Henry features an update on vismodegib for advanced basal cell carcinoma and a rapid desensitization regimen for patients with hypersensitivity reactions to platinum compounds and taxanes.
Community Oncology's podcasts by Editor in Chief Dr. David Henry features an update on vismodegib for advanced basal cell carcinoma and a rapid desensitization regimen for patients with hypersensitivity reactions to platinum compounds and taxanes.
Community Oncology's podcasts by Editor in Chief Dr. David Henry features an update on vismodegib for advanced basal cell carcinoma and a rapid desensitization regimen for patients with hypersensitivity reactions to platinum compounds and taxanes.
Vismodegib in advanced basal cell carcinoma
Vismodegib is an oral small-molecule inhibitor of smoothened homologue protein (SMO), a component of the hedgehog signaling pathway that has been shown to have activity in advanced basal cell carcinoma (BCC). In early 2012, vismodegib was approved by the Food and Drug Administration for treatment of adult patients with metastatic BCC (mBCC) who are not candidates for radiation therapy and adult patients with locally advanced BCC that has recurred following surgery or who are not candidates for surgery or radiation therapy1…
*Click on the links to the left of this introduction for a PDF of the full article and an accompanying Commentary.
Vismodegib is an oral small-molecule inhibitor of smoothened homologue protein (SMO), a component of the hedgehog signaling pathway that has been shown to have activity in advanced basal cell carcinoma (BCC). In early 2012, vismodegib was approved by the Food and Drug Administration for treatment of adult patients with metastatic BCC (mBCC) who are not candidates for radiation therapy and adult patients with locally advanced BCC that has recurred following surgery or who are not candidates for surgery or radiation therapy1…
*Click on the links to the left of this introduction for a PDF of the full article and an accompanying Commentary.
Vismodegib is an oral small-molecule inhibitor of smoothened homologue protein (SMO), a component of the hedgehog signaling pathway that has been shown to have activity in advanced basal cell carcinoma (BCC). In early 2012, vismodegib was approved by the Food and Drug Administration for treatment of adult patients with metastatic BCC (mBCC) who are not candidates for radiation therapy and adult patients with locally advanced BCC that has recurred following surgery or who are not candidates for surgery or radiation therapy1…
*Click on the links to the left of this introduction for a PDF of the full article and an accompanying Commentary.
Screening for Melanoma in Aging Patients
Test your knowledge on melanoma screening in aging patients with MD-IQ: the medical intelligence quiz. Click here to answer 5 questions.
Targeted Molecular Therapies in Cutaneous Oncology: Ammunition Not Without Some Backfire [editorial]
In Europe, melanoma is rising in men over 60
MANCHESTER, ENGLAND – Men over the age of 60 years have the highest incidence of malignant melanoma, European data have highlighted.
In the Netherlands, almost 40% of men and 30% of women with newly diagnosed melanoma are over 60 years old, said Dr. Maryska Janssen-Heijnen of VieCuri Medical Centre in Venlo, the Netherlands.
"Future screening campaigns should focus on the elderly, and especially elderly men, because we have seen a very strong increase in incidence," she said at the annual meeting of the International Society of Geriatric Oncology.
A similar situation exists in England, with 30 years’ worth of data from the Office for National Statistics showing a greater proportion of melanoma being diagnosed in people over age 70.
"Older patients tend to present with worse prognostic features – ulceration, high mitotic rate, thicker melanomas, and head and neck distribution being more likely," said Dr. Alistair Ring of Brighton and Sussex Medical School, Brighton, England.
Dr. Ring presented data on all new cases of melanoma reported in England from 1971 to 2010. In 1971, there were 1,094 malignant melanoma registrations – 32% were in men. In 2009, there were 9,771 registrations – 48% were in men.
Looking at incidence by age, the number of registrations in men versus women in 1971 was lower: 33 vs. 64 cases at age 60-64 years, 23 vs. 59 cases at age 65-70, 30 vs. 43 at age 70-74, and 16 vs. 46 at age 75-79 years.
In 2009, however, the number of registrations was higher in men than in women at 60-64 years (637 vs. 592 cases), 65-69 years (580 vs. 460 cases), 70-74 years (562 vs. 429 cases), and 75-79 years (499 vs. 397).
The incidence of melanoma in Holland between 1989 and 2010 was stable for people aged 15-29 years, Dr. Janssen-Heijnen said, with women more likely to be diagnosed than men. The incidence of melanoma has increased among all patients under age 60, but the rate has increased to a greater extent in older patients, particularly in men.
Campaigns to make the public aware about the risk of sun exposure and skin cancer have perhaps helped to encourage screening and reduce melanoma rates in younger people, but the effect appears to have been minimal in the elderly, Dr. Janssen-Heijnen said.
Overall survival also is worse in older than in younger individuals. The poorer survival in elderly might be due to an increased proportion of nodular melanomas in older patients and the development of the disease without early signs and symptoms. Elderly patients also might be less attentive to skin changes and less likely than their younger counterparts to perform self-examinations, she suggested.
The Dutch study found thick (greater than 4 mm) melanomas in 20% of men and 8% of women over age 65 with melanoma. Thick lesions were noted in 16% of men and 5% of women under age 65 with melanoma.
Older patients are also more likely than younger patients to have comorbid conditions, said Dr. Janssen-Heijnen, with 70% of men and 70% of women aged 80 years or older having one or more comorbid conditions at diagnosis of melanoma, versus 28% of men and 23% of women aged 50–64 years.
Recently published data suggest that patients are more likely to die of comorbidity than of their melanoma (Aust. N. Z. J. Public Health 2012;36:441-5).
Dr. Ring also presented data on 454 patients newly diagnosed with melanoma at his institution between 2001 and 2006; almost half (48%) were aged 60 years or older.
"Older patients were more likely to present with more advanced disease," Dr. Ring said. Indeed, 22% of patients aged over 60 years, versus just 8.5% of patients younger than 60 years, were newly diagnosed with stage IIb or stage III disease (P less than .01).
Dr. Ring noted, however, that 67% of patients aged 60 years or older with stage IIb melanoma had no comorbidities (Charlson Comorbidity Index of 0).
"What is important about [these data] is that we’ve got a lot of [older] people with a high risk of recurrence with potentially a low risk of dying from other causes," he commented.
This has implications for enrollment into adjuvant therapy trials, as these patients may represent a population of patients with good potential to respond to recently available targeted agents.
Dr. Janssen-Heijnen and Dr. Ring had no financial disclosures relevant to their presentations.
MANCHESTER, ENGLAND – Men over the age of 60 years have the highest incidence of malignant melanoma, European data have highlighted.
In the Netherlands, almost 40% of men and 30% of women with newly diagnosed melanoma are over 60 years old, said Dr. Maryska Janssen-Heijnen of VieCuri Medical Centre in Venlo, the Netherlands.
"Future screening campaigns should focus on the elderly, and especially elderly men, because we have seen a very strong increase in incidence," she said at the annual meeting of the International Society of Geriatric Oncology.
A similar situation exists in England, with 30 years’ worth of data from the Office for National Statistics showing a greater proportion of melanoma being diagnosed in people over age 70.
"Older patients tend to present with worse prognostic features – ulceration, high mitotic rate, thicker melanomas, and head and neck distribution being more likely," said Dr. Alistair Ring of Brighton and Sussex Medical School, Brighton, England.
Dr. Ring presented data on all new cases of melanoma reported in England from 1971 to 2010. In 1971, there were 1,094 malignant melanoma registrations – 32% were in men. In 2009, there were 9,771 registrations – 48% were in men.
Looking at incidence by age, the number of registrations in men versus women in 1971 was lower: 33 vs. 64 cases at age 60-64 years, 23 vs. 59 cases at age 65-70, 30 vs. 43 at age 70-74, and 16 vs. 46 at age 75-79 years.
In 2009, however, the number of registrations was higher in men than in women at 60-64 years (637 vs. 592 cases), 65-69 years (580 vs. 460 cases), 70-74 years (562 vs. 429 cases), and 75-79 years (499 vs. 397).
The incidence of melanoma in Holland between 1989 and 2010 was stable for people aged 15-29 years, Dr. Janssen-Heijnen said, with women more likely to be diagnosed than men. The incidence of melanoma has increased among all patients under age 60, but the rate has increased to a greater extent in older patients, particularly in men.
Campaigns to make the public aware about the risk of sun exposure and skin cancer have perhaps helped to encourage screening and reduce melanoma rates in younger people, but the effect appears to have been minimal in the elderly, Dr. Janssen-Heijnen said.
Overall survival also is worse in older than in younger individuals. The poorer survival in elderly might be due to an increased proportion of nodular melanomas in older patients and the development of the disease without early signs and symptoms. Elderly patients also might be less attentive to skin changes and less likely than their younger counterparts to perform self-examinations, she suggested.
The Dutch study found thick (greater than 4 mm) melanomas in 20% of men and 8% of women over age 65 with melanoma. Thick lesions were noted in 16% of men and 5% of women under age 65 with melanoma.
Older patients are also more likely than younger patients to have comorbid conditions, said Dr. Janssen-Heijnen, with 70% of men and 70% of women aged 80 years or older having one or more comorbid conditions at diagnosis of melanoma, versus 28% of men and 23% of women aged 50–64 years.
Recently published data suggest that patients are more likely to die of comorbidity than of their melanoma (Aust. N. Z. J. Public Health 2012;36:441-5).
Dr. Ring also presented data on 454 patients newly diagnosed with melanoma at his institution between 2001 and 2006; almost half (48%) were aged 60 years or older.
"Older patients were more likely to present with more advanced disease," Dr. Ring said. Indeed, 22% of patients aged over 60 years, versus just 8.5% of patients younger than 60 years, were newly diagnosed with stage IIb or stage III disease (P less than .01).
Dr. Ring noted, however, that 67% of patients aged 60 years or older with stage IIb melanoma had no comorbidities (Charlson Comorbidity Index of 0).
"What is important about [these data] is that we’ve got a lot of [older] people with a high risk of recurrence with potentially a low risk of dying from other causes," he commented.
This has implications for enrollment into adjuvant therapy trials, as these patients may represent a population of patients with good potential to respond to recently available targeted agents.
Dr. Janssen-Heijnen and Dr. Ring had no financial disclosures relevant to their presentations.
MANCHESTER, ENGLAND – Men over the age of 60 years have the highest incidence of malignant melanoma, European data have highlighted.
In the Netherlands, almost 40% of men and 30% of women with newly diagnosed melanoma are over 60 years old, said Dr. Maryska Janssen-Heijnen of VieCuri Medical Centre in Venlo, the Netherlands.
"Future screening campaigns should focus on the elderly, and especially elderly men, because we have seen a very strong increase in incidence," she said at the annual meeting of the International Society of Geriatric Oncology.
A similar situation exists in England, with 30 years’ worth of data from the Office for National Statistics showing a greater proportion of melanoma being diagnosed in people over age 70.
"Older patients tend to present with worse prognostic features – ulceration, high mitotic rate, thicker melanomas, and head and neck distribution being more likely," said Dr. Alistair Ring of Brighton and Sussex Medical School, Brighton, England.
Dr. Ring presented data on all new cases of melanoma reported in England from 1971 to 2010. In 1971, there were 1,094 malignant melanoma registrations – 32% were in men. In 2009, there were 9,771 registrations – 48% were in men.
Looking at incidence by age, the number of registrations in men versus women in 1971 was lower: 33 vs. 64 cases at age 60-64 years, 23 vs. 59 cases at age 65-70, 30 vs. 43 at age 70-74, and 16 vs. 46 at age 75-79 years.
In 2009, however, the number of registrations was higher in men than in women at 60-64 years (637 vs. 592 cases), 65-69 years (580 vs. 460 cases), 70-74 years (562 vs. 429 cases), and 75-79 years (499 vs. 397).
The incidence of melanoma in Holland between 1989 and 2010 was stable for people aged 15-29 years, Dr. Janssen-Heijnen said, with women more likely to be diagnosed than men. The incidence of melanoma has increased among all patients under age 60, but the rate has increased to a greater extent in older patients, particularly in men.
Campaigns to make the public aware about the risk of sun exposure and skin cancer have perhaps helped to encourage screening and reduce melanoma rates in younger people, but the effect appears to have been minimal in the elderly, Dr. Janssen-Heijnen said.
Overall survival also is worse in older than in younger individuals. The poorer survival in elderly might be due to an increased proportion of nodular melanomas in older patients and the development of the disease without early signs and symptoms. Elderly patients also might be less attentive to skin changes and less likely than their younger counterparts to perform self-examinations, she suggested.
The Dutch study found thick (greater than 4 mm) melanomas in 20% of men and 8% of women over age 65 with melanoma. Thick lesions were noted in 16% of men and 5% of women under age 65 with melanoma.
Older patients are also more likely than younger patients to have comorbid conditions, said Dr. Janssen-Heijnen, with 70% of men and 70% of women aged 80 years or older having one or more comorbid conditions at diagnosis of melanoma, versus 28% of men and 23% of women aged 50–64 years.
Recently published data suggest that patients are more likely to die of comorbidity than of their melanoma (Aust. N. Z. J. Public Health 2012;36:441-5).
Dr. Ring also presented data on 454 patients newly diagnosed with melanoma at his institution between 2001 and 2006; almost half (48%) were aged 60 years or older.
"Older patients were more likely to present with more advanced disease," Dr. Ring said. Indeed, 22% of patients aged over 60 years, versus just 8.5% of patients younger than 60 years, were newly diagnosed with stage IIb or stage III disease (P less than .01).
Dr. Ring noted, however, that 67% of patients aged 60 years or older with stage IIb melanoma had no comorbidities (Charlson Comorbidity Index of 0).
"What is important about [these data] is that we’ve got a lot of [older] people with a high risk of recurrence with potentially a low risk of dying from other causes," he commented.
This has implications for enrollment into adjuvant therapy trials, as these patients may represent a population of patients with good potential to respond to recently available targeted agents.
Dr. Janssen-Heijnen and Dr. Ring had no financial disclosures relevant to their presentations.
AT THE ANNUAL MEETING OF THE INTERNATIONAL SOCIETY OF GERIATRIC ONCOLOGY
Major Finding: In 1971, 32% of 1,094 malignant melanomas registered in England occurred in men; in 2009, 48% of 9,771 registrations were in men.
Data Source: Two epidemiologic investigations of newly diagnosed melanoma cases in the Netherlands (1989–2010) and England (1971–2009).
Disclosures: Dr. Janssen-Heijnen and Dr. Ring had no financial disclosures relevant to their presentations.
Cancer deaths declined 20% since 1991
Cancer deaths have declined 20% since 1991, which means there were 1.2 million fewer deaths from cancer in 2009, according to the American Cancer Society.
The overall cancer death rate decreased from 215 per 100,000 in 1991 to 173 per 100,000 in 2009. Death rates declined more sharply for cancers of the lung and prostate in men, for breast cancers in women, and for colon and rectal cancers for men and women. The ACS attributes the drops to decreases in smoking and improvements in early detection and treatment.
The most common causes of cancer death in Americans, accounting for 50% of cancer deaths, are cancers of the lung and bronchus, prostate, and colorectum in men; and cancers of the lung and bronchus, breast, and colorectum in women. This year, there will be 1.6 million cancer cases and 580,350 cancer deaths; lung cancers will account for 25% of cancer deaths in men and women this year, according to estimates from the ACS.
The mortality figures and incidence data are contained in two reports: Cancer Facts & Figures 2013 and Cancer Statistics 2013, both published in CA: A Cancer Journal for Clinicians. (doi:10.3322/caac.21166). The reports were published online on Jan. 18.
Incidence rates are on the decline for most cancers with the exception of melanoma, and liver, thyroid and pancreatic cancer.
Dr. Daniel M. Siegel, president of the American Academy of Dermatology, said in a statement that a rising incidence of melanoma "is particularly concerning because skin cancer can often be easily prevented and detected." Dr. Siegel said that the AAD and its members "are actively working to reduce the incidence of skin cancer and change society’s attitudes and behaviors toward sun exposure and tanning."
Death rates from pancreatic cancer have increased over the last decade, due to what the ACS called "a lack progress in primary prevention, early diagnosis, and treatment of this cancer." The ACS report included a special section devoted to updated information on the occurrence and treatment of pancreatic cancer. Most patients with pancreatic cancer die within a year of diagnosis; the 5-year survival rate is 6%.
The ACS also noted that the disparity in cancer outcomes based on ethnicity and income, "particularly [among] those diagnosed with colorectal or breast cancer where earlier detection and better treatments are credited for the improving trends," said John R. Seffrin, Ph.D., chief executive officer of the ACS, in a statement. "We can and must close this gap so that people are not punished for having the misfortune of being born poor and disadvantaged."
The 5-year survival rate in 2002-2008 for white women with breast cancer, for instance, was 92%, whereas for black women, it was 78%. For colon cancer, the 5-year survival rate was 66% for whites, but 55% for blacks.
On Twitter @aliciaault
Cancer deaths have declined 20% since 1991, which means there were 1.2 million fewer deaths from cancer in 2009, according to the American Cancer Society.
The overall cancer death rate decreased from 215 per 100,000 in 1991 to 173 per 100,000 in 2009. Death rates declined more sharply for cancers of the lung and prostate in men, for breast cancers in women, and for colon and rectal cancers for men and women. The ACS attributes the drops to decreases in smoking and improvements in early detection and treatment.
The most common causes of cancer death in Americans, accounting for 50% of cancer deaths, are cancers of the lung and bronchus, prostate, and colorectum in men; and cancers of the lung and bronchus, breast, and colorectum in women. This year, there will be 1.6 million cancer cases and 580,350 cancer deaths; lung cancers will account for 25% of cancer deaths in men and women this year, according to estimates from the ACS.
The mortality figures and incidence data are contained in two reports: Cancer Facts & Figures 2013 and Cancer Statistics 2013, both published in CA: A Cancer Journal for Clinicians. (doi:10.3322/caac.21166). The reports were published online on Jan. 18.
Incidence rates are on the decline for most cancers with the exception of melanoma, and liver, thyroid and pancreatic cancer.
Dr. Daniel M. Siegel, president of the American Academy of Dermatology, said in a statement that a rising incidence of melanoma "is particularly concerning because skin cancer can often be easily prevented and detected." Dr. Siegel said that the AAD and its members "are actively working to reduce the incidence of skin cancer and change society’s attitudes and behaviors toward sun exposure and tanning."
Death rates from pancreatic cancer have increased over the last decade, due to what the ACS called "a lack progress in primary prevention, early diagnosis, and treatment of this cancer." The ACS report included a special section devoted to updated information on the occurrence and treatment of pancreatic cancer. Most patients with pancreatic cancer die within a year of diagnosis; the 5-year survival rate is 6%.
The ACS also noted that the disparity in cancer outcomes based on ethnicity and income, "particularly [among] those diagnosed with colorectal or breast cancer where earlier detection and better treatments are credited for the improving trends," said John R. Seffrin, Ph.D., chief executive officer of the ACS, in a statement. "We can and must close this gap so that people are not punished for having the misfortune of being born poor and disadvantaged."
The 5-year survival rate in 2002-2008 for white women with breast cancer, for instance, was 92%, whereas for black women, it was 78%. For colon cancer, the 5-year survival rate was 66% for whites, but 55% for blacks.
On Twitter @aliciaault
Cancer deaths have declined 20% since 1991, which means there were 1.2 million fewer deaths from cancer in 2009, according to the American Cancer Society.
The overall cancer death rate decreased from 215 per 100,000 in 1991 to 173 per 100,000 in 2009. Death rates declined more sharply for cancers of the lung and prostate in men, for breast cancers in women, and for colon and rectal cancers for men and women. The ACS attributes the drops to decreases in smoking and improvements in early detection and treatment.
The most common causes of cancer death in Americans, accounting for 50% of cancer deaths, are cancers of the lung and bronchus, prostate, and colorectum in men; and cancers of the lung and bronchus, breast, and colorectum in women. This year, there will be 1.6 million cancer cases and 580,350 cancer deaths; lung cancers will account for 25% of cancer deaths in men and women this year, according to estimates from the ACS.
The mortality figures and incidence data are contained in two reports: Cancer Facts & Figures 2013 and Cancer Statistics 2013, both published in CA: A Cancer Journal for Clinicians. (doi:10.3322/caac.21166). The reports were published online on Jan. 18.
Incidence rates are on the decline for most cancers with the exception of melanoma, and liver, thyroid and pancreatic cancer.
Dr. Daniel M. Siegel, president of the American Academy of Dermatology, said in a statement that a rising incidence of melanoma "is particularly concerning because skin cancer can often be easily prevented and detected." Dr. Siegel said that the AAD and its members "are actively working to reduce the incidence of skin cancer and change society’s attitudes and behaviors toward sun exposure and tanning."
Death rates from pancreatic cancer have increased over the last decade, due to what the ACS called "a lack progress in primary prevention, early diagnosis, and treatment of this cancer." The ACS report included a special section devoted to updated information on the occurrence and treatment of pancreatic cancer. Most patients with pancreatic cancer die within a year of diagnosis; the 5-year survival rate is 6%.
The ACS also noted that the disparity in cancer outcomes based on ethnicity and income, "particularly [among] those diagnosed with colorectal or breast cancer where earlier detection and better treatments are credited for the improving trends," said John R. Seffrin, Ph.D., chief executive officer of the ACS, in a statement. "We can and must close this gap so that people are not punished for having the misfortune of being born poor and disadvantaged."
The 5-year survival rate in 2002-2008 for white women with breast cancer, for instance, was 92%, whereas for black women, it was 78%. For colon cancer, the 5-year survival rate was 66% for whites, but 55% for blacks.
On Twitter @aliciaault
FROM CA: A CANCER JOURNAL FOR CLINICIANS
Don't trust apps to spot skin cancer
Three out of four smartphone applications designed to assess melanoma risk misclassified at least 30% of melanomas as benign in a case-control diagnostic accuracy study.
Although these applications are intended for educational purposes rather than diagnostic purposes, they pose a potential risk to consumers, according to medical student Joel A. Wolf and his colleagues at the University of Pittsburgh.
"These applications are not subject to any sort of validation or regulatory oversight. Despite disclaimers that these applications are intended for educational purposes, they have the potential to harm users who may believe mistakenly that the evaluation given by such an application is a substitute for medical advice," the investigators wrote. The study was published online Jan. 16 in JAMA Dermatology.
The investigators used the four smartphone applications to evaluate digital images of pigmented cutaneous lesions, including 60 histologically confirmed melanomas and 128 benign control lesions. The applications deemed 85%-98% of the images evaluable.
Based only on the images considered evaluable, the overall sensitivity of the applications ranged from 7% to 98% and the overall specificity ranged from 30% to 94%. Positive predictive value ranged from 33% to 42% and negative predictive value ranged from 65% to 97%.
The highest sensitivity occurred with the only application that sent images to a board-certified dermatologist for analysis within 24 hours; the other three applications relied on automated algorithms for image analysis (JAMA Dermatol. 2013 Jan. 16 [doi:10.1001/jamadermatol.2013.3282]).
"Even the best of these three applications (that used automated algorithms) classified 18 of 60 melanomas (30%) in our study as benign," the investigators said.
The images used for this study were selected from a database of images captured routinely from patients before skin lesion removal. Only close-up images without identifiable features and without equivocal histology were used. The smartphone applications evaluated as part of the study were selected based on their ability to use existing images and on claims or suggestions of "an ability to assist users in determining whether a skin lesion may be malignant," Mr. Wolf and his associates said.
The applications were not identified because the purpose of the study was to determine the accuracy of such applications in general, rather than to make a statement about any particular application, the investigators noted.
Given the ubiquity of smartphone health care applications that are marketed to consumers (13,000 are available in the largest online application store alone, the investigators said), and given that the Food and Drug Administration has announced plans to regulate certain health-related smartphone applications, the findings underscore the need for physicians to be aware of the types of applications available to "aid us in protecting and educating our patients," the investigators noted.
These types of technologies have the potential to improve mortality from melanoma, but extreme care must be taken to prevent potential harm, they added.
"Despite disclaimers presented by each of these applications that they were designed for educational purposes rather than actual diagnosis and that they should not substitute for standard medical care, releasing a tool to the public requires some thought as to how it could be misused. This potential is of particular concern in times of economic hardship, when uninsured and even insured patients, deterred by the cost of copayments for medical visits, may turn to these applications as alternatives to physician evaluation," Mr. Wolf and his associates said.
This study was supported by grants from the National Institutes of Health. Study author Dr. Laura K. Ferris disclosed having served as an investigator and consultant for MELA Sciences Inc. The remaining authors had no disclosures to report.
Three out of four smartphone applications designed to assess melanoma risk misclassified at least 30% of melanomas as benign in a case-control diagnostic accuracy study.
Although these applications are intended for educational purposes rather than diagnostic purposes, they pose a potential risk to consumers, according to medical student Joel A. Wolf and his colleagues at the University of Pittsburgh.
"These applications are not subject to any sort of validation or regulatory oversight. Despite disclaimers that these applications are intended for educational purposes, they have the potential to harm users who may believe mistakenly that the evaluation given by such an application is a substitute for medical advice," the investigators wrote. The study was published online Jan. 16 in JAMA Dermatology.
The investigators used the four smartphone applications to evaluate digital images of pigmented cutaneous lesions, including 60 histologically confirmed melanomas and 128 benign control lesions. The applications deemed 85%-98% of the images evaluable.
Based only on the images considered evaluable, the overall sensitivity of the applications ranged from 7% to 98% and the overall specificity ranged from 30% to 94%. Positive predictive value ranged from 33% to 42% and negative predictive value ranged from 65% to 97%.
The highest sensitivity occurred with the only application that sent images to a board-certified dermatologist for analysis within 24 hours; the other three applications relied on automated algorithms for image analysis (JAMA Dermatol. 2013 Jan. 16 [doi:10.1001/jamadermatol.2013.3282]).
"Even the best of these three applications (that used automated algorithms) classified 18 of 60 melanomas (30%) in our study as benign," the investigators said.
The images used for this study were selected from a database of images captured routinely from patients before skin lesion removal. Only close-up images without identifiable features and without equivocal histology were used. The smartphone applications evaluated as part of the study were selected based on their ability to use existing images and on claims or suggestions of "an ability to assist users in determining whether a skin lesion may be malignant," Mr. Wolf and his associates said.
The applications were not identified because the purpose of the study was to determine the accuracy of such applications in general, rather than to make a statement about any particular application, the investigators noted.
Given the ubiquity of smartphone health care applications that are marketed to consumers (13,000 are available in the largest online application store alone, the investigators said), and given that the Food and Drug Administration has announced plans to regulate certain health-related smartphone applications, the findings underscore the need for physicians to be aware of the types of applications available to "aid us in protecting and educating our patients," the investigators noted.
These types of technologies have the potential to improve mortality from melanoma, but extreme care must be taken to prevent potential harm, they added.
"Despite disclaimers presented by each of these applications that they were designed for educational purposes rather than actual diagnosis and that they should not substitute for standard medical care, releasing a tool to the public requires some thought as to how it could be misused. This potential is of particular concern in times of economic hardship, when uninsured and even insured patients, deterred by the cost of copayments for medical visits, may turn to these applications as alternatives to physician evaluation," Mr. Wolf and his associates said.
This study was supported by grants from the National Institutes of Health. Study author Dr. Laura K. Ferris disclosed having served as an investigator and consultant for MELA Sciences Inc. The remaining authors had no disclosures to report.
Three out of four smartphone applications designed to assess melanoma risk misclassified at least 30% of melanomas as benign in a case-control diagnostic accuracy study.
Although these applications are intended for educational purposes rather than diagnostic purposes, they pose a potential risk to consumers, according to medical student Joel A. Wolf and his colleagues at the University of Pittsburgh.
"These applications are not subject to any sort of validation or regulatory oversight. Despite disclaimers that these applications are intended for educational purposes, they have the potential to harm users who may believe mistakenly that the evaluation given by such an application is a substitute for medical advice," the investigators wrote. The study was published online Jan. 16 in JAMA Dermatology.
The investigators used the four smartphone applications to evaluate digital images of pigmented cutaneous lesions, including 60 histologically confirmed melanomas and 128 benign control lesions. The applications deemed 85%-98% of the images evaluable.
Based only on the images considered evaluable, the overall sensitivity of the applications ranged from 7% to 98% and the overall specificity ranged from 30% to 94%. Positive predictive value ranged from 33% to 42% and negative predictive value ranged from 65% to 97%.
The highest sensitivity occurred with the only application that sent images to a board-certified dermatologist for analysis within 24 hours; the other three applications relied on automated algorithms for image analysis (JAMA Dermatol. 2013 Jan. 16 [doi:10.1001/jamadermatol.2013.3282]).
"Even the best of these three applications (that used automated algorithms) classified 18 of 60 melanomas (30%) in our study as benign," the investigators said.
The images used for this study were selected from a database of images captured routinely from patients before skin lesion removal. Only close-up images without identifiable features and without equivocal histology were used. The smartphone applications evaluated as part of the study were selected based on their ability to use existing images and on claims or suggestions of "an ability to assist users in determining whether a skin lesion may be malignant," Mr. Wolf and his associates said.
The applications were not identified because the purpose of the study was to determine the accuracy of such applications in general, rather than to make a statement about any particular application, the investigators noted.
Given the ubiquity of smartphone health care applications that are marketed to consumers (13,000 are available in the largest online application store alone, the investigators said), and given that the Food and Drug Administration has announced plans to regulate certain health-related smartphone applications, the findings underscore the need for physicians to be aware of the types of applications available to "aid us in protecting and educating our patients," the investigators noted.
These types of technologies have the potential to improve mortality from melanoma, but extreme care must be taken to prevent potential harm, they added.
"Despite disclaimers presented by each of these applications that they were designed for educational purposes rather than actual diagnosis and that they should not substitute for standard medical care, releasing a tool to the public requires some thought as to how it could be misused. This potential is of particular concern in times of economic hardship, when uninsured and even insured patients, deterred by the cost of copayments for medical visits, may turn to these applications as alternatives to physician evaluation," Mr. Wolf and his associates said.
This study was supported by grants from the National Institutes of Health. Study author Dr. Laura K. Ferris disclosed having served as an investigator and consultant for MELA Sciences Inc. The remaining authors had no disclosures to report.
FROM JAMA DERMATOLOGY
Major Finding: The overall sensitivity of the four smartphone applications ranged from 7% to 98%; overall specificity ranged from 30% to 94%.
Data Source: A case-control diagnostic accuracy study.
Disclosures: This study was supported by grants from the National Institutes of Health. Study author Dr. Laura K. Ferris disclosed having served as an investigator and consultant for MELA Sciences Inc. The remaining authors had no disclosures to report.
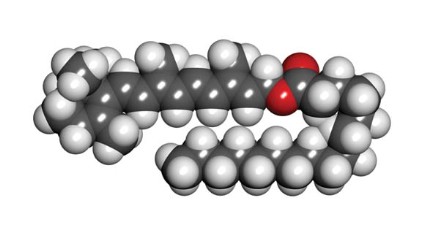
Retinyl palmitate
Retinyl palmitate, a storage and ester form of retinol (vitamin A) and the prevailing type of vitamin A found naturally in the skin (Toxicol. Ind. Health 2005;21:167-75), has become increasingly popular during the past 2 decades. It is widely used in more than 600 skin care products, including cosmetics and sunscreens, and, with FDA approval, over-the-counter and prescription drugs (Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). It was also the subject of a controversial summer 2010 report by the Environmental Working Group (EWG) in which the organization warned of possible photocarcinogenicity associated with retinyl palmitate (RP)-containing sunscreens.
Although vitamin A storage in the epidermis takes the form of retinyl esters and retinols, they act differently when exposed to UV light. The retinols display UVB-resistant and UVB-sensitive characteristics not exhibited by retinyl esters such as RP (Dermatology 1999;199:302-7). The EWG used "vitamin A" and "retinyl palmitate" interchangeably in their criticisms and follow-ups, which is misleading. The vitamin A family of drugs includes retinyl esters, retinol, tretinoin, adapalene, tazarotene, and oral isotretinoin (Accutane), in addition to four carotenoids, including beta-carotene, many of which have been shown to prevent or protect against cancer (Br. J. Cancer 1988;57:428-33; Cancer Epidemiol. Biomarkers Prev. 1997;6:949-56; J. Invest. Dermatol. 1981;76:178-80; Arch. Dermatol. Res. 1981;270:453-62). That does not mean that RP prevents cancer just because oral retinol, beta-carotene, or tretinoin have been shown to do so, for example. In fact, the study that the EWG refers to shows evidence that RP may lead to skin tumors in mice.
In response to the EWG report, Wang et al. acknowledged that of the eight in vitro studies published by the Food and Drug Administration from 2002 to 2009, four revealed that reactive oxygen species were produced by RP after UVA exposure (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67; Toxicol. Ind. Health 2007;23:625-31; Toxicol. Lett. 2006;163:30-43; Int. J. Environ. Res. Public Health 2006;3:185-90; Chem. Res. Toxicol. 2005;18:129-38). However, they questioned the relevance of these results in the context of the convoluted mechanisms of the antioxidant setting in human skin. They also contended that the National Toxicology Program (NTP) study on which the EWG based its report failed to prove that the combination of RP and UV results in photocarcinogenesis and, in fact, was rife with reasons for skepticism (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). The EWG offered its own counterarguments and stood by its report. Rather than wade further into the debate that occurred in 2010 and found its way into the pages of the Journal of the American Academy of Dermatology (2010;63:903-6), let’s review what is known about RP.
What else do we know about RP?
In 1997, Duell et al. showed that unoccluded retinol is more effective at penetrating human skin in vivo than RP or retinoic acid (J. Invest. Dermatol. 1997;109:301-5).
In 2003, Antille et al. used an in vitro model to evaluate the photoprotective activity of RP, and then applied topical RP on the back of hairless mice before exposing them to UVB. They also applied topical RP or a sunscreen on the buttocks of human volunteers before exposing them to four minimal erythema doses of UVB. The investigators found that RP was as efficient in vitro as the commercial filter octylmethoxycinnamate in preventing UVB-induced fluorescence or photobleaching of fluorescent markers. Topical RP also significantly suppressed the formation of thymine dimers in mouse epidermis and human skin. In the volunteers, topical RP was as efficient as an SPF (sun protection factor) 20 sunscreen in preventing sunburn erythema (J. Invest. Dermatol. 2003;121:1163-7).
In 2005, Yan et al. studied the phototoxicity of RP, anhydroretinol (AR), and 5,6-epoxyretinyl palmitate (5,6-epoxy-RP) in human skin Jurkat T cells with and without light irradiation. Irradiation of cells in the absence of a retinoid rendered little damage, but the presence of RP, 5,6-epoxy-RP, or AR (50, 100, 150, and 200 micromol/L) yielded DNA fragmentation, with cell death occurring at retinoid concentrations of 100 micromol/L or greater. The investigators concluded that DNA damage and cytotoxicity are engendered by RP and its photodecomposition products in association with UVA and visible light exposure. They also determined that UVA irradiation of these retinoids produces free radicals that spur DNA strand cleavage (Toxicol. Ind. Health 2005;21:167-75).
RP accounts for most of the retinyl esters endogenously formed in skin. In 2006, Yan et al., noting that exogenous RP accumulates via topically applied cosmetic and skin care formulations, investigated the time course for buildup and disappearance of RP and retinol in the stratified layers of skin from female SKH-1 mice singly or repeatedly dosed with topical creams containing 0.5% or 2% RP. The researchers observed that within 24 hours of application, RP quickly diffused into the stratum corneum and epidermal skin layers. RP and retinol levels were lowest in the dermis, intermediate in the stratum corneum, and highest in the epidermis. In separated skin layers and intact skin, RP and retinol levels declined over time, but for 18 days, RP levels remained higher than control values. The investigators concluded that topically applied RP changed the normal physiological levels of RP and retinol in the skin of mice (Toxicol. Ind. Health 2006;22:181-91).
Having previously shown that irradiation of RP with UVA leads to the formation of photodecomposition products, synthesis of reactive oxygen species, and lipid peroxidation induction, Xia et al. demonstrated comparable results, identifying RP as a photosensitizer following irradiation with UVB light (Int. J. Environ. Res. Public Health 2006;3:185-90).
Recommendations
In light of the controversy swirling around RP and the appropriate concern it has engendered, in addition to the weight of evidence as well as experience from personal observation, I advise patients to avoid daytime use of products with RP high on the ingredient list. I add that it poses real risks while offering minimal benefits. Such patients should be using retinol or tretinoin. I recommend the use of retinoids at night, to avoid the photosensitizing action induced by UVA or UVB on retinoids left on the skin.
Conclusion
Retinyl palmitate does not penetrate very well into the skin. Consequently, for over-the-counter topical formulations, I recommend retinol instead. Because of the slow penetration of RP into the skin, the RP that remains on the skin will undergo photoreaction more than a substance that is rapidly absorbed. When exposed to light, RP on the skin may undergo metabolism and/or photoreaction to generate reactive oxygen species. These reactive oxygen species or free radicals can theoretically lead to increased skin cancer. That said, sufficient evidence to establish a causal link between RP and skin cancer has not been produced. Nor, I’m afraid, are there any good reasons to recommend the use of RP. More research on this subject is needed and will likely emerge in a timely fashion.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected]. This column, "Cosmeceutical Critique," appears regularly in Skin & Allergy News.
Retinyl palmitate, a storage and ester form of retinol (vitamin A) and the prevailing type of vitamin A found naturally in the skin (Toxicol. Ind. Health 2005;21:167-75), has become increasingly popular during the past 2 decades. It is widely used in more than 600 skin care products, including cosmetics and sunscreens, and, with FDA approval, over-the-counter and prescription drugs (Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). It was also the subject of a controversial summer 2010 report by the Environmental Working Group (EWG) in which the organization warned of possible photocarcinogenicity associated with retinyl palmitate (RP)-containing sunscreens.
Although vitamin A storage in the epidermis takes the form of retinyl esters and retinols, they act differently when exposed to UV light. The retinols display UVB-resistant and UVB-sensitive characteristics not exhibited by retinyl esters such as RP (Dermatology 1999;199:302-7). The EWG used "vitamin A" and "retinyl palmitate" interchangeably in their criticisms and follow-ups, which is misleading. The vitamin A family of drugs includes retinyl esters, retinol, tretinoin, adapalene, tazarotene, and oral isotretinoin (Accutane), in addition to four carotenoids, including beta-carotene, many of which have been shown to prevent or protect against cancer (Br. J. Cancer 1988;57:428-33; Cancer Epidemiol. Biomarkers Prev. 1997;6:949-56; J. Invest. Dermatol. 1981;76:178-80; Arch. Dermatol. Res. 1981;270:453-62). That does not mean that RP prevents cancer just because oral retinol, beta-carotene, or tretinoin have been shown to do so, for example. In fact, the study that the EWG refers to shows evidence that RP may lead to skin tumors in mice.
In response to the EWG report, Wang et al. acknowledged that of the eight in vitro studies published by the Food and Drug Administration from 2002 to 2009, four revealed that reactive oxygen species were produced by RP after UVA exposure (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67; Toxicol. Ind. Health 2007;23:625-31; Toxicol. Lett. 2006;163:30-43; Int. J. Environ. Res. Public Health 2006;3:185-90; Chem. Res. Toxicol. 2005;18:129-38). However, they questioned the relevance of these results in the context of the convoluted mechanisms of the antioxidant setting in human skin. They also contended that the National Toxicology Program (NTP) study on which the EWG based its report failed to prove that the combination of RP and UV results in photocarcinogenesis and, in fact, was rife with reasons for skepticism (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). The EWG offered its own counterarguments and stood by its report. Rather than wade further into the debate that occurred in 2010 and found its way into the pages of the Journal of the American Academy of Dermatology (2010;63:903-6), let’s review what is known about RP.
What else do we know about RP?
In 1997, Duell et al. showed that unoccluded retinol is more effective at penetrating human skin in vivo than RP or retinoic acid (J. Invest. Dermatol. 1997;109:301-5).
In 2003, Antille et al. used an in vitro model to evaluate the photoprotective activity of RP, and then applied topical RP on the back of hairless mice before exposing them to UVB. They also applied topical RP or a sunscreen on the buttocks of human volunteers before exposing them to four minimal erythema doses of UVB. The investigators found that RP was as efficient in vitro as the commercial filter octylmethoxycinnamate in preventing UVB-induced fluorescence or photobleaching of fluorescent markers. Topical RP also significantly suppressed the formation of thymine dimers in mouse epidermis and human skin. In the volunteers, topical RP was as efficient as an SPF (sun protection factor) 20 sunscreen in preventing sunburn erythema (J. Invest. Dermatol. 2003;121:1163-7).
In 2005, Yan et al. studied the phototoxicity of RP, anhydroretinol (AR), and 5,6-epoxyretinyl palmitate (5,6-epoxy-RP) in human skin Jurkat T cells with and without light irradiation. Irradiation of cells in the absence of a retinoid rendered little damage, but the presence of RP, 5,6-epoxy-RP, or AR (50, 100, 150, and 200 micromol/L) yielded DNA fragmentation, with cell death occurring at retinoid concentrations of 100 micromol/L or greater. The investigators concluded that DNA damage and cytotoxicity are engendered by RP and its photodecomposition products in association with UVA and visible light exposure. They also determined that UVA irradiation of these retinoids produces free radicals that spur DNA strand cleavage (Toxicol. Ind. Health 2005;21:167-75).
RP accounts for most of the retinyl esters endogenously formed in skin. In 2006, Yan et al., noting that exogenous RP accumulates via topically applied cosmetic and skin care formulations, investigated the time course for buildup and disappearance of RP and retinol in the stratified layers of skin from female SKH-1 mice singly or repeatedly dosed with topical creams containing 0.5% or 2% RP. The researchers observed that within 24 hours of application, RP quickly diffused into the stratum corneum and epidermal skin layers. RP and retinol levels were lowest in the dermis, intermediate in the stratum corneum, and highest in the epidermis. In separated skin layers and intact skin, RP and retinol levels declined over time, but for 18 days, RP levels remained higher than control values. The investigators concluded that topically applied RP changed the normal physiological levels of RP and retinol in the skin of mice (Toxicol. Ind. Health 2006;22:181-91).
Having previously shown that irradiation of RP with UVA leads to the formation of photodecomposition products, synthesis of reactive oxygen species, and lipid peroxidation induction, Xia et al. demonstrated comparable results, identifying RP as a photosensitizer following irradiation with UVB light (Int. J. Environ. Res. Public Health 2006;3:185-90).
Recommendations
In light of the controversy swirling around RP and the appropriate concern it has engendered, in addition to the weight of evidence as well as experience from personal observation, I advise patients to avoid daytime use of products with RP high on the ingredient list. I add that it poses real risks while offering minimal benefits. Such patients should be using retinol or tretinoin. I recommend the use of retinoids at night, to avoid the photosensitizing action induced by UVA or UVB on retinoids left on the skin.
Conclusion
Retinyl palmitate does not penetrate very well into the skin. Consequently, for over-the-counter topical formulations, I recommend retinol instead. Because of the slow penetration of RP into the skin, the RP that remains on the skin will undergo photoreaction more than a substance that is rapidly absorbed. When exposed to light, RP on the skin may undergo metabolism and/or photoreaction to generate reactive oxygen species. These reactive oxygen species or free radicals can theoretically lead to increased skin cancer. That said, sufficient evidence to establish a causal link between RP and skin cancer has not been produced. Nor, I’m afraid, are there any good reasons to recommend the use of RP. More research on this subject is needed and will likely emerge in a timely fashion.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected]. This column, "Cosmeceutical Critique," appears regularly in Skin & Allergy News.
Retinyl palmitate, a storage and ester form of retinol (vitamin A) and the prevailing type of vitamin A found naturally in the skin (Toxicol. Ind. Health 2005;21:167-75), has become increasingly popular during the past 2 decades. It is widely used in more than 600 skin care products, including cosmetics and sunscreens, and, with FDA approval, over-the-counter and prescription drugs (Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). It was also the subject of a controversial summer 2010 report by the Environmental Working Group (EWG) in which the organization warned of possible photocarcinogenicity associated with retinyl palmitate (RP)-containing sunscreens.
Although vitamin A storage in the epidermis takes the form of retinyl esters and retinols, they act differently when exposed to UV light. The retinols display UVB-resistant and UVB-sensitive characteristics not exhibited by retinyl esters such as RP (Dermatology 1999;199:302-7). The EWG used "vitamin A" and "retinyl palmitate" interchangeably in their criticisms and follow-ups, which is misleading. The vitamin A family of drugs includes retinyl esters, retinol, tretinoin, adapalene, tazarotene, and oral isotretinoin (Accutane), in addition to four carotenoids, including beta-carotene, many of which have been shown to prevent or protect against cancer (Br. J. Cancer 1988;57:428-33; Cancer Epidemiol. Biomarkers Prev. 1997;6:949-56; J. Invest. Dermatol. 1981;76:178-80; Arch. Dermatol. Res. 1981;270:453-62). That does not mean that RP prevents cancer just because oral retinol, beta-carotene, or tretinoin have been shown to do so, for example. In fact, the study that the EWG refers to shows evidence that RP may lead to skin tumors in mice.
In response to the EWG report, Wang et al. acknowledged that of the eight in vitro studies published by the Food and Drug Administration from 2002 to 2009, four revealed that reactive oxygen species were produced by RP after UVA exposure (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67; Toxicol. Ind. Health 2007;23:625-31; Toxicol. Lett. 2006;163:30-43; Int. J. Environ. Res. Public Health 2006;3:185-90; Chem. Res. Toxicol. 2005;18:129-38). However, they questioned the relevance of these results in the context of the convoluted mechanisms of the antioxidant setting in human skin. They also contended that the National Toxicology Program (NTP) study on which the EWG based its report failed to prove that the combination of RP and UV results in photocarcinogenesis and, in fact, was rife with reasons for skepticism (J. Am. Acad. Dermatol. 2010;63:903-6; Photodermatol. Photoimmunol. Photomed. 2011;27:58-67). The EWG offered its own counterarguments and stood by its report. Rather than wade further into the debate that occurred in 2010 and found its way into the pages of the Journal of the American Academy of Dermatology (2010;63:903-6), let’s review what is known about RP.
What else do we know about RP?
In 1997, Duell et al. showed that unoccluded retinol is more effective at penetrating human skin in vivo than RP or retinoic acid (J. Invest. Dermatol. 1997;109:301-5).
In 2003, Antille et al. used an in vitro model to evaluate the photoprotective activity of RP, and then applied topical RP on the back of hairless mice before exposing them to UVB. They also applied topical RP or a sunscreen on the buttocks of human volunteers before exposing them to four minimal erythema doses of UVB. The investigators found that RP was as efficient in vitro as the commercial filter octylmethoxycinnamate in preventing UVB-induced fluorescence or photobleaching of fluorescent markers. Topical RP also significantly suppressed the formation of thymine dimers in mouse epidermis and human skin. In the volunteers, topical RP was as efficient as an SPF (sun protection factor) 20 sunscreen in preventing sunburn erythema (J. Invest. Dermatol. 2003;121:1163-7).
In 2005, Yan et al. studied the phototoxicity of RP, anhydroretinol (AR), and 5,6-epoxyretinyl palmitate (5,6-epoxy-RP) in human skin Jurkat T cells with and without light irradiation. Irradiation of cells in the absence of a retinoid rendered little damage, but the presence of RP, 5,6-epoxy-RP, or AR (50, 100, 150, and 200 micromol/L) yielded DNA fragmentation, with cell death occurring at retinoid concentrations of 100 micromol/L or greater. The investigators concluded that DNA damage and cytotoxicity are engendered by RP and its photodecomposition products in association with UVA and visible light exposure. They also determined that UVA irradiation of these retinoids produces free radicals that spur DNA strand cleavage (Toxicol. Ind. Health 2005;21:167-75).
RP accounts for most of the retinyl esters endogenously formed in skin. In 2006, Yan et al., noting that exogenous RP accumulates via topically applied cosmetic and skin care formulations, investigated the time course for buildup and disappearance of RP and retinol in the stratified layers of skin from female SKH-1 mice singly or repeatedly dosed with topical creams containing 0.5% or 2% RP. The researchers observed that within 24 hours of application, RP quickly diffused into the stratum corneum and epidermal skin layers. RP and retinol levels were lowest in the dermis, intermediate in the stratum corneum, and highest in the epidermis. In separated skin layers and intact skin, RP and retinol levels declined over time, but for 18 days, RP levels remained higher than control values. The investigators concluded that topically applied RP changed the normal physiological levels of RP and retinol in the skin of mice (Toxicol. Ind. Health 2006;22:181-91).
Having previously shown that irradiation of RP with UVA leads to the formation of photodecomposition products, synthesis of reactive oxygen species, and lipid peroxidation induction, Xia et al. demonstrated comparable results, identifying RP as a photosensitizer following irradiation with UVB light (Int. J. Environ. Res. Public Health 2006;3:185-90).
Recommendations
In light of the controversy swirling around RP and the appropriate concern it has engendered, in addition to the weight of evidence as well as experience from personal observation, I advise patients to avoid daytime use of products with RP high on the ingredient list. I add that it poses real risks while offering minimal benefits. Such patients should be using retinol or tretinoin. I recommend the use of retinoids at night, to avoid the photosensitizing action induced by UVA or UVB on retinoids left on the skin.
Conclusion
Retinyl palmitate does not penetrate very well into the skin. Consequently, for over-the-counter topical formulations, I recommend retinol instead. Because of the slow penetration of RP into the skin, the RP that remains on the skin will undergo photoreaction more than a substance that is rapidly absorbed. When exposed to light, RP on the skin may undergo metabolism and/or photoreaction to generate reactive oxygen species. These reactive oxygen species or free radicals can theoretically lead to increased skin cancer. That said, sufficient evidence to establish a causal link between RP and skin cancer has not been produced. Nor, I’m afraid, are there any good reasons to recommend the use of RP. More research on this subject is needed and will likely emerge in a timely fashion.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected]. This column, "Cosmeceutical Critique," appears regularly in Skin & Allergy News.
Community Oncology Podcast - Everolimus for tuberous sclerosis
Everolimus for tuberous sclerosis-associated tumors, BRCA testing in underserved women, and thoughts on cancer care site of service are the topics for the December 2012 Community Oncology podcast by Editor in Chief Dr. David Henry.
Everolimus for tuberous sclerosis-associated tumors, BRCA testing in underserved women, and thoughts on cancer care site of service are the topics for the December 2012 Community Oncology podcast by Editor in Chief Dr. David Henry.
Everolimus for tuberous sclerosis-associated tumors, BRCA testing in underserved women, and thoughts on cancer care site of service are the topics for the December 2012 Community Oncology podcast by Editor in Chief Dr. David Henry.
CAT-STARTS mnemonic guides Mohs wound closure
SAN DIEGO – Before he proceeds to close a wound following Mohs surgery, Dr. Howard Steinman employs the mnemonic CAT-STARTS to help him select the repair.
A modification of STARTS, Dr. Steinman uses CAT-STARTS to represent the following factors he considers prior to carrying out the repair: first assess the Cosmetic units, Areas of available skin, and Textures of available skin. Then consider closure options: Second intention and Simple (linear) repairs, Transposition flaps, Advancement flaps, Rotation flaps, Tissue interpolation flaps, and Skin grafts.
"Prior to closing, I draw in the surrounding cosmetic units of the face. Once you’ve done that, you should pay attention to the relaxed skin tension lines," Dr. Steinman said at a meeting sponsored by the American Society for Mohs Surgery.
To illustrate, he showed attendees a digital image of a patient’s nasal lesion prior to repair. "I draw in the midline, the side of the nasal dorsum and nasal-jugal lines, and the alar fold," he explained. "Then I look at the skin texture. This case had a mix of sebaceous skin and smooth skin, so I factored that consideration in to my repair."
Candidate wounds for second-intention healing "are small, shallow wounds, usually less than 1 cm in diameter," said Dr. Steinman, who practices dermatology and Mohs surgery in Irving, Tex. "They’re usually less than a half centimeter deep. Second-intention healing is often especially effective for the alar fold and the medial canthus and less effective for the cheeks, chin, and around the lips."
If healing by second intention is not an option, "you want to consider your repair choices, from the simplest to the most complex," he said. Thus, consider simple (linear) repairs. Thereafter, his suggested order of complexity begins with transposition flaps, followed by advancement flaps, rotation flaps, tissue interpolation flaps, and skin grafts.
"The midline of the nose and the midline of the forehead are two of the best places to do linear repairs, as is the cheek and forehead," Dr. Steinman commented. "One thing to remember about straight line repairs is that they cause significant secondary motion perpendicular to the axis of closure. You need to respect that when doing linear repairs near free margins," he added.
If you unable to close a wound in a side-to-side fashion, "a transition flap may be your best option," he continued. "Because rotation flaps require longer, broad incisions, in my view you should often think about an advancement flap as your next choice after transposition flaps in terms of complexity."
Tissue interpolation flaps are reserved "for instances where no local skin flap is a better choice," he said. "The midline forehead flap is excellent for distal nasal defects because you have a broad area of skin and it’s based on a vascular pedicle. Interpolation flaps are two-stage procedures."
He views skin grafts to be a last choice for most wound repairs. "If you do them well and, when needed, laser or abrade them, they often look acceptable, but in my opinion they are the last option for many locations," he said.
Dr. Steinman said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Before he proceeds to close a wound following Mohs surgery, Dr. Howard Steinman employs the mnemonic CAT-STARTS to help him select the repair.
A modification of STARTS, Dr. Steinman uses CAT-STARTS to represent the following factors he considers prior to carrying out the repair: first assess the Cosmetic units, Areas of available skin, and Textures of available skin. Then consider closure options: Second intention and Simple (linear) repairs, Transposition flaps, Advancement flaps, Rotation flaps, Tissue interpolation flaps, and Skin grafts.
"Prior to closing, I draw in the surrounding cosmetic units of the face. Once you’ve done that, you should pay attention to the relaxed skin tension lines," Dr. Steinman said at a meeting sponsored by the American Society for Mohs Surgery.
To illustrate, he showed attendees a digital image of a patient’s nasal lesion prior to repair. "I draw in the midline, the side of the nasal dorsum and nasal-jugal lines, and the alar fold," he explained. "Then I look at the skin texture. This case had a mix of sebaceous skin and smooth skin, so I factored that consideration in to my repair."
Candidate wounds for second-intention healing "are small, shallow wounds, usually less than 1 cm in diameter," said Dr. Steinman, who practices dermatology and Mohs surgery in Irving, Tex. "They’re usually less than a half centimeter deep. Second-intention healing is often especially effective for the alar fold and the medial canthus and less effective for the cheeks, chin, and around the lips."
If healing by second intention is not an option, "you want to consider your repair choices, from the simplest to the most complex," he said. Thus, consider simple (linear) repairs. Thereafter, his suggested order of complexity begins with transposition flaps, followed by advancement flaps, rotation flaps, tissue interpolation flaps, and skin grafts.
"The midline of the nose and the midline of the forehead are two of the best places to do linear repairs, as is the cheek and forehead," Dr. Steinman commented. "One thing to remember about straight line repairs is that they cause significant secondary motion perpendicular to the axis of closure. You need to respect that when doing linear repairs near free margins," he added.
If you unable to close a wound in a side-to-side fashion, "a transition flap may be your best option," he continued. "Because rotation flaps require longer, broad incisions, in my view you should often think about an advancement flap as your next choice after transposition flaps in terms of complexity."
Tissue interpolation flaps are reserved "for instances where no local skin flap is a better choice," he said. "The midline forehead flap is excellent for distal nasal defects because you have a broad area of skin and it’s based on a vascular pedicle. Interpolation flaps are two-stage procedures."
He views skin grafts to be a last choice for most wound repairs. "If you do them well and, when needed, laser or abrade them, they often look acceptable, but in my opinion they are the last option for many locations," he said.
Dr. Steinman said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Before he proceeds to close a wound following Mohs surgery, Dr. Howard Steinman employs the mnemonic CAT-STARTS to help him select the repair.
A modification of STARTS, Dr. Steinman uses CAT-STARTS to represent the following factors he considers prior to carrying out the repair: first assess the Cosmetic units, Areas of available skin, and Textures of available skin. Then consider closure options: Second intention and Simple (linear) repairs, Transposition flaps, Advancement flaps, Rotation flaps, Tissue interpolation flaps, and Skin grafts.
"Prior to closing, I draw in the surrounding cosmetic units of the face. Once you’ve done that, you should pay attention to the relaxed skin tension lines," Dr. Steinman said at a meeting sponsored by the American Society for Mohs Surgery.
To illustrate, he showed attendees a digital image of a patient’s nasal lesion prior to repair. "I draw in the midline, the side of the nasal dorsum and nasal-jugal lines, and the alar fold," he explained. "Then I look at the skin texture. This case had a mix of sebaceous skin and smooth skin, so I factored that consideration in to my repair."
Candidate wounds for second-intention healing "are small, shallow wounds, usually less than 1 cm in diameter," said Dr. Steinman, who practices dermatology and Mohs surgery in Irving, Tex. "They’re usually less than a half centimeter deep. Second-intention healing is often especially effective for the alar fold and the medial canthus and less effective for the cheeks, chin, and around the lips."
If healing by second intention is not an option, "you want to consider your repair choices, from the simplest to the most complex," he said. Thus, consider simple (linear) repairs. Thereafter, his suggested order of complexity begins with transposition flaps, followed by advancement flaps, rotation flaps, tissue interpolation flaps, and skin grafts.
"The midline of the nose and the midline of the forehead are two of the best places to do linear repairs, as is the cheek and forehead," Dr. Steinman commented. "One thing to remember about straight line repairs is that they cause significant secondary motion perpendicular to the axis of closure. You need to respect that when doing linear repairs near free margins," he added.
If you unable to close a wound in a side-to-side fashion, "a transition flap may be your best option," he continued. "Because rotation flaps require longer, broad incisions, in my view you should often think about an advancement flap as your next choice after transposition flaps in terms of complexity."
Tissue interpolation flaps are reserved "for instances where no local skin flap is a better choice," he said. "The midline forehead flap is excellent for distal nasal defects because you have a broad area of skin and it’s based on a vascular pedicle. Interpolation flaps are two-stage procedures."
He views skin grafts to be a last choice for most wound repairs. "If you do them well and, when needed, laser or abrade them, they often look acceptable, but in my opinion they are the last option for many locations," he said.
Dr. Steinman said that he had no relevant financial conflicts to disclose.
EXPERT ANALYSIS FROM A MEETING SPONSORED BY THE AMERICAN SOCIETY FOR MOHS SURGERY