User login
BAN2401 subanalyses attempt to ease concerns over study design and findings
BARCELONA – Alzheimer’s disease genetic risk status didn’t influence positive findings of the investigational monoclonal antibody, BAN2401, in a post hoc analysis of a phase 2 study’s secondary endpoint, Eisai said in a report released during the Clinical Trials on Alzheimer’s Disease conference.
In fact, according to the new analysis, the positive data presented last summer probably underestimated the molecule’s benefit to homozygous carriers of the apolipoprotein E epsilon-4 (APOE4), Chad Swanson, PhD, said at the meeting.
The new data cut was based on a small fraction of the 856 patients with early Alzheimer’s disease (AD) who were enrolled in Study 201: 10 APOE4 carriers and 69 noncarriers who completed 18 months on infusions of BAN2401 at 10 mg/kg biweekly, the only beneficial dose. The subanalysis determined that carriers benefited much more than did noncarriers on the three clinical measures, said Dr. Swanson, senior director of neurology clinical research at Eisai, and the study’s director:
- The Alzheimer’s Disease Composite Score (ADCOMS), a new measure of subtle cognitive changes in early disease: Carriers, 63% less decline than placebo vs. 7% less in noncarriers.
- Alzheimer’s Disease Assessment Scale-cognitive subscale (ADAS-Cog): Carriers, 84% less decline than placebo vs. 43% less in noncarriers.
- Clinical Dementia Rating-Sum of Boxes (CDR-SB): Carriers, 60% less decline than placebo vs. a 7% worsening in noncarriers.
To strengthen the power of the analysis, Dr. Swanson pooled data from the entire 18 months of both the 10 mg/kg biweekly and the next-highest dose (10 mg/kg monthly). This increased the numbers to 273 carriers and 141 noncarriers who had at least one exposure to the antibody.
He said this corrected the APOE4 imbalance and showed a 25% slowing of ADCOMS decline in carriers, a 6% slowing in noncarriers, and a 21% slowing overall, relative to placebo.
The somewhat counterintuitive findings took even copresenter Jeffrey L. Cummings, MD, by surprise.
“I would have hypothesized a greater effect in noncarriers than carriers, but that’s the great thing about data – they challenge our assumptions,” said Dr. Cummings, director of the Center for Neurodegeneration and Translational Neuroscience and director emeritus of the Cleveland Clinic Lou Ruvo Center for Brain Health in Las Vegas and a consultant for both Eisai and Biogen, the company’s BAN2401 developmental partner. He postulated that APOE4-driven differences in plaque composition could have contributed to the observed benefit. “I think this also points to a very interesting biology that we don’t yet know. The plaque compactness is different, the distribution of diffuse plaques is different. This will bear a lot of additional analysis.”
Study 201 randomized patients with early Alzheimer’s to up to 18 months of treatment with placebo or infusions of BAN2401 at 2.5 mg/kg biweekly, 5 mg/kg monthly, 5 mg/kg biweekly, 10 mg/kg monthly, or 10 mg/kg biweekly. It had two unusual design features. First, patents were allocated to treatment arms by a Bayesian algorithm. The computer program examined results after every 50 enrollees and then allocated new subjects to what were, at that point, the most effective two doses. Additionally, the 18-month study was designed with a potential 12-month exit point, if computer modeling showed that it had at least an 80% probability of reaching at least a 25% cognitive benefit. In December, Eisai announced that the study hit just a 64% probability, missing the primary endpoint. But because Eisai felt the numbers were moving in the right direction, it continued with the additional 6 months of treatment, as allowed for in the study design, and then reanalyzed results with conventional statistics.
Thus, the successes reported at the Alzheimer’s Association International Conference in July and reanalyzed at CTAD, were secondary cognitive and functional outcomes.
Partway through the trial, a European regulatory body became alarmed at the rate of amyloid-related imaging abnormalities (ARIA) in the APOE4 carriers and excluded them from the highest-dose group. This meant that carriers comprised about 70%-80% of every unsuccessful treatment arm but just 29% of the successful one. The unbalanced randomization caused July’s skepticism. The CTAD subanalysis didn’t entirely alleviate it, and several acclaimed Alzheimer’s researchers gave it voice.
“You showed no difference in placebo rates of decline, but an increased benefit in the E4 carriers, which was really interesting,” said Reisa Sperling, MD, of Brigham and Women’s Hospital, Boston. “One difference in the E4 carriers was their rate of ARIA and how long they stayed in the study. How did you account for these issues in this analysis?”
“We didn’t specifically look at that kind of question,” Dr. Swanson said. “I think we feel that we actually see effects in both carriers and noncarriers, and we are still exploring the data and will keep looking through them to see what we can find.”
Gil Rabinovici, MD, also expressed some reservations.
“I agree that the post hoc analyses are encouraging, but I wouldn’t say they alleviate the concern when you have such a dramatic imbalance in a core feature of this disease, like APOE4 between the placebo and the high-dose group,” said Dr. Rabinovici, the Edward Fein and Pearl Landrith Endowed Professor in Memory & Aging at the University of California, San Francisco. “The people on this panel know far more than I do of the pitfalls of these kinds of analyses. We really need to see true randomization to put this issue to rest.”
Biomarkers support subanalysis finding
Dr. Swanson also presented new cerebrospinal fluid biomarker data showing changes in phosphorylated tau, neurogranin, and neurofilament light chain that support the overall 47% slowing of cognitive decline reported last summer. The 10 mg/kg biweekly and monthly groups were again combined to increase the sample size, but it remained quite small, with full data on 16 in the placebo group and 23 in the active group:
- Neurogranin, a synaptic protein that is a marker of neuronal damage, decreased by a median 58 pg/mL (11%), compared with a 13.5-pg/mL increase in the placebo group.
- Phosphorylated tau, a marker of tau pathology in the brain, decreased by a median 12 pg/mL (13%), compared with no change in the placebo group.
- Neurofilament light chain, a neuronal structural scaffold protein that is a marker of axonal degeneration, increased by a median 75 pg/mL in the active group, compared with a 156-pg/mL increase in the placebo group – a 48% difference.
The positive biomarker data bolstered the subanalysis to some extent, researchers felt. But in the end, Study 201 is just a first step for BAN2401, said Laurie Ryan, PhD, chief of the dementias of aging branch in the division of neuroscience at the National Institute on Aging.
“Today’s presentation gave us a new look at the trial data from the summer,” Dr. Ryan said in an interview. “The new analysis supports the findings previously released but is still preliminary. Nothing is definitive in a phase 2 study, so while it appears to suggest a potential positive, beneficial result, it needs further testing.”
Eisai has made its subanalysis presentation slides publicly available.
Dr. Swanson is an employee of Eisai. Dr. Cummings is a consultant for Eisai and Biogen. Dr. Sperling has consulted for numerous pharmaceutical companies. Dr. Rabinovici and Dr. Ryan have no disclosures.
SOURCE: Swanson C et al. CTAD, Symposium 3.
BARCELONA – Alzheimer’s disease genetic risk status didn’t influence positive findings of the investigational monoclonal antibody, BAN2401, in a post hoc analysis of a phase 2 study’s secondary endpoint, Eisai said in a report released during the Clinical Trials on Alzheimer’s Disease conference.
In fact, according to the new analysis, the positive data presented last summer probably underestimated the molecule’s benefit to homozygous carriers of the apolipoprotein E epsilon-4 (APOE4), Chad Swanson, PhD, said at the meeting.
The new data cut was based on a small fraction of the 856 patients with early Alzheimer’s disease (AD) who were enrolled in Study 201: 10 APOE4 carriers and 69 noncarriers who completed 18 months on infusions of BAN2401 at 10 mg/kg biweekly, the only beneficial dose. The subanalysis determined that carriers benefited much more than did noncarriers on the three clinical measures, said Dr. Swanson, senior director of neurology clinical research at Eisai, and the study’s director:
- The Alzheimer’s Disease Composite Score (ADCOMS), a new measure of subtle cognitive changes in early disease: Carriers, 63% less decline than placebo vs. 7% less in noncarriers.
- Alzheimer’s Disease Assessment Scale-cognitive subscale (ADAS-Cog): Carriers, 84% less decline than placebo vs. 43% less in noncarriers.
- Clinical Dementia Rating-Sum of Boxes (CDR-SB): Carriers, 60% less decline than placebo vs. a 7% worsening in noncarriers.
To strengthen the power of the analysis, Dr. Swanson pooled data from the entire 18 months of both the 10 mg/kg biweekly and the next-highest dose (10 mg/kg monthly). This increased the numbers to 273 carriers and 141 noncarriers who had at least one exposure to the antibody.
He said this corrected the APOE4 imbalance and showed a 25% slowing of ADCOMS decline in carriers, a 6% slowing in noncarriers, and a 21% slowing overall, relative to placebo.
The somewhat counterintuitive findings took even copresenter Jeffrey L. Cummings, MD, by surprise.
“I would have hypothesized a greater effect in noncarriers than carriers, but that’s the great thing about data – they challenge our assumptions,” said Dr. Cummings, director of the Center for Neurodegeneration and Translational Neuroscience and director emeritus of the Cleveland Clinic Lou Ruvo Center for Brain Health in Las Vegas and a consultant for both Eisai and Biogen, the company’s BAN2401 developmental partner. He postulated that APOE4-driven differences in plaque composition could have contributed to the observed benefit. “I think this also points to a very interesting biology that we don’t yet know. The plaque compactness is different, the distribution of diffuse plaques is different. This will bear a lot of additional analysis.”
Study 201 randomized patients with early Alzheimer’s to up to 18 months of treatment with placebo or infusions of BAN2401 at 2.5 mg/kg biweekly, 5 mg/kg monthly, 5 mg/kg biweekly, 10 mg/kg monthly, or 10 mg/kg biweekly. It had two unusual design features. First, patents were allocated to treatment arms by a Bayesian algorithm. The computer program examined results after every 50 enrollees and then allocated new subjects to what were, at that point, the most effective two doses. Additionally, the 18-month study was designed with a potential 12-month exit point, if computer modeling showed that it had at least an 80% probability of reaching at least a 25% cognitive benefit. In December, Eisai announced that the study hit just a 64% probability, missing the primary endpoint. But because Eisai felt the numbers were moving in the right direction, it continued with the additional 6 months of treatment, as allowed for in the study design, and then reanalyzed results with conventional statistics.
Thus, the successes reported at the Alzheimer’s Association International Conference in July and reanalyzed at CTAD, were secondary cognitive and functional outcomes.
Partway through the trial, a European regulatory body became alarmed at the rate of amyloid-related imaging abnormalities (ARIA) in the APOE4 carriers and excluded them from the highest-dose group. This meant that carriers comprised about 70%-80% of every unsuccessful treatment arm but just 29% of the successful one. The unbalanced randomization caused July’s skepticism. The CTAD subanalysis didn’t entirely alleviate it, and several acclaimed Alzheimer’s researchers gave it voice.
“You showed no difference in placebo rates of decline, but an increased benefit in the E4 carriers, which was really interesting,” said Reisa Sperling, MD, of Brigham and Women’s Hospital, Boston. “One difference in the E4 carriers was their rate of ARIA and how long they stayed in the study. How did you account for these issues in this analysis?”
“We didn’t specifically look at that kind of question,” Dr. Swanson said. “I think we feel that we actually see effects in both carriers and noncarriers, and we are still exploring the data and will keep looking through them to see what we can find.”
Gil Rabinovici, MD, also expressed some reservations.
“I agree that the post hoc analyses are encouraging, but I wouldn’t say they alleviate the concern when you have such a dramatic imbalance in a core feature of this disease, like APOE4 between the placebo and the high-dose group,” said Dr. Rabinovici, the Edward Fein and Pearl Landrith Endowed Professor in Memory & Aging at the University of California, San Francisco. “The people on this panel know far more than I do of the pitfalls of these kinds of analyses. We really need to see true randomization to put this issue to rest.”
Biomarkers support subanalysis finding
Dr. Swanson also presented new cerebrospinal fluid biomarker data showing changes in phosphorylated tau, neurogranin, and neurofilament light chain that support the overall 47% slowing of cognitive decline reported last summer. The 10 mg/kg biweekly and monthly groups were again combined to increase the sample size, but it remained quite small, with full data on 16 in the placebo group and 23 in the active group:
- Neurogranin, a synaptic protein that is a marker of neuronal damage, decreased by a median 58 pg/mL (11%), compared with a 13.5-pg/mL increase in the placebo group.
- Phosphorylated tau, a marker of tau pathology in the brain, decreased by a median 12 pg/mL (13%), compared with no change in the placebo group.
- Neurofilament light chain, a neuronal structural scaffold protein that is a marker of axonal degeneration, increased by a median 75 pg/mL in the active group, compared with a 156-pg/mL increase in the placebo group – a 48% difference.
The positive biomarker data bolstered the subanalysis to some extent, researchers felt. But in the end, Study 201 is just a first step for BAN2401, said Laurie Ryan, PhD, chief of the dementias of aging branch in the division of neuroscience at the National Institute on Aging.
“Today’s presentation gave us a new look at the trial data from the summer,” Dr. Ryan said in an interview. “The new analysis supports the findings previously released but is still preliminary. Nothing is definitive in a phase 2 study, so while it appears to suggest a potential positive, beneficial result, it needs further testing.”
Eisai has made its subanalysis presentation slides publicly available.
Dr. Swanson is an employee of Eisai. Dr. Cummings is a consultant for Eisai and Biogen. Dr. Sperling has consulted for numerous pharmaceutical companies. Dr. Rabinovici and Dr. Ryan have no disclosures.
SOURCE: Swanson C et al. CTAD, Symposium 3.
BARCELONA – Alzheimer’s disease genetic risk status didn’t influence positive findings of the investigational monoclonal antibody, BAN2401, in a post hoc analysis of a phase 2 study’s secondary endpoint, Eisai said in a report released during the Clinical Trials on Alzheimer’s Disease conference.
In fact, according to the new analysis, the positive data presented last summer probably underestimated the molecule’s benefit to homozygous carriers of the apolipoprotein E epsilon-4 (APOE4), Chad Swanson, PhD, said at the meeting.
The new data cut was based on a small fraction of the 856 patients with early Alzheimer’s disease (AD) who were enrolled in Study 201: 10 APOE4 carriers and 69 noncarriers who completed 18 months on infusions of BAN2401 at 10 mg/kg biweekly, the only beneficial dose. The subanalysis determined that carriers benefited much more than did noncarriers on the three clinical measures, said Dr. Swanson, senior director of neurology clinical research at Eisai, and the study’s director:
- The Alzheimer’s Disease Composite Score (ADCOMS), a new measure of subtle cognitive changes in early disease: Carriers, 63% less decline than placebo vs. 7% less in noncarriers.
- Alzheimer’s Disease Assessment Scale-cognitive subscale (ADAS-Cog): Carriers, 84% less decline than placebo vs. 43% less in noncarriers.
- Clinical Dementia Rating-Sum of Boxes (CDR-SB): Carriers, 60% less decline than placebo vs. a 7% worsening in noncarriers.
To strengthen the power of the analysis, Dr. Swanson pooled data from the entire 18 months of both the 10 mg/kg biweekly and the next-highest dose (10 mg/kg monthly). This increased the numbers to 273 carriers and 141 noncarriers who had at least one exposure to the antibody.
He said this corrected the APOE4 imbalance and showed a 25% slowing of ADCOMS decline in carriers, a 6% slowing in noncarriers, and a 21% slowing overall, relative to placebo.
The somewhat counterintuitive findings took even copresenter Jeffrey L. Cummings, MD, by surprise.
“I would have hypothesized a greater effect in noncarriers than carriers, but that’s the great thing about data – they challenge our assumptions,” said Dr. Cummings, director of the Center for Neurodegeneration and Translational Neuroscience and director emeritus of the Cleveland Clinic Lou Ruvo Center for Brain Health in Las Vegas and a consultant for both Eisai and Biogen, the company’s BAN2401 developmental partner. He postulated that APOE4-driven differences in plaque composition could have contributed to the observed benefit. “I think this also points to a very interesting biology that we don’t yet know. The plaque compactness is different, the distribution of diffuse plaques is different. This will bear a lot of additional analysis.”
Study 201 randomized patients with early Alzheimer’s to up to 18 months of treatment with placebo or infusions of BAN2401 at 2.5 mg/kg biweekly, 5 mg/kg monthly, 5 mg/kg biweekly, 10 mg/kg monthly, or 10 mg/kg biweekly. It had two unusual design features. First, patents were allocated to treatment arms by a Bayesian algorithm. The computer program examined results after every 50 enrollees and then allocated new subjects to what were, at that point, the most effective two doses. Additionally, the 18-month study was designed with a potential 12-month exit point, if computer modeling showed that it had at least an 80% probability of reaching at least a 25% cognitive benefit. In December, Eisai announced that the study hit just a 64% probability, missing the primary endpoint. But because Eisai felt the numbers were moving in the right direction, it continued with the additional 6 months of treatment, as allowed for in the study design, and then reanalyzed results with conventional statistics.
Thus, the successes reported at the Alzheimer’s Association International Conference in July and reanalyzed at CTAD, were secondary cognitive and functional outcomes.
Partway through the trial, a European regulatory body became alarmed at the rate of amyloid-related imaging abnormalities (ARIA) in the APOE4 carriers and excluded them from the highest-dose group. This meant that carriers comprised about 70%-80% of every unsuccessful treatment arm but just 29% of the successful one. The unbalanced randomization caused July’s skepticism. The CTAD subanalysis didn’t entirely alleviate it, and several acclaimed Alzheimer’s researchers gave it voice.
“You showed no difference in placebo rates of decline, but an increased benefit in the E4 carriers, which was really interesting,” said Reisa Sperling, MD, of Brigham and Women’s Hospital, Boston. “One difference in the E4 carriers was their rate of ARIA and how long they stayed in the study. How did you account for these issues in this analysis?”
“We didn’t specifically look at that kind of question,” Dr. Swanson said. “I think we feel that we actually see effects in both carriers and noncarriers, and we are still exploring the data and will keep looking through them to see what we can find.”
Gil Rabinovici, MD, also expressed some reservations.
“I agree that the post hoc analyses are encouraging, but I wouldn’t say they alleviate the concern when you have such a dramatic imbalance in a core feature of this disease, like APOE4 between the placebo and the high-dose group,” said Dr. Rabinovici, the Edward Fein and Pearl Landrith Endowed Professor in Memory & Aging at the University of California, San Francisco. “The people on this panel know far more than I do of the pitfalls of these kinds of analyses. We really need to see true randomization to put this issue to rest.”
Biomarkers support subanalysis finding
Dr. Swanson also presented new cerebrospinal fluid biomarker data showing changes in phosphorylated tau, neurogranin, and neurofilament light chain that support the overall 47% slowing of cognitive decline reported last summer. The 10 mg/kg biweekly and monthly groups were again combined to increase the sample size, but it remained quite small, with full data on 16 in the placebo group and 23 in the active group:
- Neurogranin, a synaptic protein that is a marker of neuronal damage, decreased by a median 58 pg/mL (11%), compared with a 13.5-pg/mL increase in the placebo group.
- Phosphorylated tau, a marker of tau pathology in the brain, decreased by a median 12 pg/mL (13%), compared with no change in the placebo group.
- Neurofilament light chain, a neuronal structural scaffold protein that is a marker of axonal degeneration, increased by a median 75 pg/mL in the active group, compared with a 156-pg/mL increase in the placebo group – a 48% difference.
The positive biomarker data bolstered the subanalysis to some extent, researchers felt. But in the end, Study 201 is just a first step for BAN2401, said Laurie Ryan, PhD, chief of the dementias of aging branch in the division of neuroscience at the National Institute on Aging.
“Today’s presentation gave us a new look at the trial data from the summer,” Dr. Ryan said in an interview. “The new analysis supports the findings previously released but is still preliminary. Nothing is definitive in a phase 2 study, so while it appears to suggest a potential positive, beneficial result, it needs further testing.”
Eisai has made its subanalysis presentation slides publicly available.
Dr. Swanson is an employee of Eisai. Dr. Cummings is a consultant for Eisai and Biogen. Dr. Sperling has consulted for numerous pharmaceutical companies. Dr. Rabinovici and Dr. Ryan have no disclosures.
SOURCE: Swanson C et al. CTAD, Symposium 3.
REPORTING FROM CTAD
Statins cut all-cause mortality in spinal cord injury
ATLANTA – Statin use among a cohort of veterans with traumatic spinal cord injury reduced all-cause mortality, results from a novel observational study showed.
“This is the first clinical study to show that administration of statins irrespective of the lipid levels reduces all-cause mortality, not just cardiovascular mortality,” lead study author Meheroz H. Rabadi, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “This clinical study confirms the impression of several prior studies in animal models with spinal cord injury, which have shown the anti-inflammatory and neuro-protective effects of statins.”
To determine whether statin use in a cohort of patients with traumatic spinal cord injuries (SCI) reduced overall and cause-specific mortality, Dr. Rabadi and his colleagues retrospectively reviewed the medical charts and death records of 163 individuals with SCI who were treated at the Oklahoma City Veterans Administration Medical Center Spinal Cord Injury & Disease, Multiple Sclerosis, and ALS Program, an outpatient clinic, from 2000 to 2014. They collected data on statin use, duration of statin use, and intensity of statin therapy, as well as cause-specific mortality.
Of the 163 subjects studied, 75 (46%) had taken statins for an average of 5.7 years, and had greater cardiovascular risk burdens than those who had not taken statins. The mortality rate for patients on statins, however, was 33.8-49.9 per 1,000 person-years, compared with 47.4-66.8 deaths per 1,000 person-years among those who had not taken statins. Kaplan-Meier survival curves showed a significant difference between the two groups (P less than .0052). Within the statin group, neither duration nor average intensity of statin therapy affected mortality.
“We were surprised to note statins reduced pneumonia-related mortality in patients with SCI,” Dr. Rabadi said. “Since our publication there have been several publications, including a meta-analysis of statins reducing community-acquired pneumonia-related mortality and reducing the need for mechanical ventilation or ICU admission (see CHEST 2015;148:523-32, Clin Med (Lond) 2017;17(5):403-7, and Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2018;40(1):30-40). Another surprise was neither the intensity, duration, or types of statin affected the result.”
He acknowledged certain limitations of the analysis, including its retrospective design, its relatively small sample size, and the fact that most of the subjects were non-Hispanic white men. “Routine prescription of statins in any dose in patients with SCI – even if the lipid profile is normal – is more beneficial than detrimental over the long haul,” concluded Dr. Rabadi, who also directs the Oklahoma VAMC Stroke Program. “Nearly all our patients with SCI continue to be on varying doses of statins.”
Dr. Rabadi reported having no financial disclosures.
[email protected]
SOURCE: Ann Neurol. 2018;84[S22]:S127. Abstract S302.
ATLANTA – Statin use among a cohort of veterans with traumatic spinal cord injury reduced all-cause mortality, results from a novel observational study showed.
“This is the first clinical study to show that administration of statins irrespective of the lipid levels reduces all-cause mortality, not just cardiovascular mortality,” lead study author Meheroz H. Rabadi, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “This clinical study confirms the impression of several prior studies in animal models with spinal cord injury, which have shown the anti-inflammatory and neuro-protective effects of statins.”
To determine whether statin use in a cohort of patients with traumatic spinal cord injuries (SCI) reduced overall and cause-specific mortality, Dr. Rabadi and his colleagues retrospectively reviewed the medical charts and death records of 163 individuals with SCI who were treated at the Oklahoma City Veterans Administration Medical Center Spinal Cord Injury & Disease, Multiple Sclerosis, and ALS Program, an outpatient clinic, from 2000 to 2014. They collected data on statin use, duration of statin use, and intensity of statin therapy, as well as cause-specific mortality.
Of the 163 subjects studied, 75 (46%) had taken statins for an average of 5.7 years, and had greater cardiovascular risk burdens than those who had not taken statins. The mortality rate for patients on statins, however, was 33.8-49.9 per 1,000 person-years, compared with 47.4-66.8 deaths per 1,000 person-years among those who had not taken statins. Kaplan-Meier survival curves showed a significant difference between the two groups (P less than .0052). Within the statin group, neither duration nor average intensity of statin therapy affected mortality.
“We were surprised to note statins reduced pneumonia-related mortality in patients with SCI,” Dr. Rabadi said. “Since our publication there have been several publications, including a meta-analysis of statins reducing community-acquired pneumonia-related mortality and reducing the need for mechanical ventilation or ICU admission (see CHEST 2015;148:523-32, Clin Med (Lond) 2017;17(5):403-7, and Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2018;40(1):30-40). Another surprise was neither the intensity, duration, or types of statin affected the result.”
He acknowledged certain limitations of the analysis, including its retrospective design, its relatively small sample size, and the fact that most of the subjects were non-Hispanic white men. “Routine prescription of statins in any dose in patients with SCI – even if the lipid profile is normal – is more beneficial than detrimental over the long haul,” concluded Dr. Rabadi, who also directs the Oklahoma VAMC Stroke Program. “Nearly all our patients with SCI continue to be on varying doses of statins.”
Dr. Rabadi reported having no financial disclosures.
[email protected]
SOURCE: Ann Neurol. 2018;84[S22]:S127. Abstract S302.
ATLANTA – Statin use among a cohort of veterans with traumatic spinal cord injury reduced all-cause mortality, results from a novel observational study showed.
“This is the first clinical study to show that administration of statins irrespective of the lipid levels reduces all-cause mortality, not just cardiovascular mortality,” lead study author Meheroz H. Rabadi, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “This clinical study confirms the impression of several prior studies in animal models with spinal cord injury, which have shown the anti-inflammatory and neuro-protective effects of statins.”
To determine whether statin use in a cohort of patients with traumatic spinal cord injuries (SCI) reduced overall and cause-specific mortality, Dr. Rabadi and his colleagues retrospectively reviewed the medical charts and death records of 163 individuals with SCI who were treated at the Oklahoma City Veterans Administration Medical Center Spinal Cord Injury & Disease, Multiple Sclerosis, and ALS Program, an outpatient clinic, from 2000 to 2014. They collected data on statin use, duration of statin use, and intensity of statin therapy, as well as cause-specific mortality.
Of the 163 subjects studied, 75 (46%) had taken statins for an average of 5.7 years, and had greater cardiovascular risk burdens than those who had not taken statins. The mortality rate for patients on statins, however, was 33.8-49.9 per 1,000 person-years, compared with 47.4-66.8 deaths per 1,000 person-years among those who had not taken statins. Kaplan-Meier survival curves showed a significant difference between the two groups (P less than .0052). Within the statin group, neither duration nor average intensity of statin therapy affected mortality.
“We were surprised to note statins reduced pneumonia-related mortality in patients with SCI,” Dr. Rabadi said. “Since our publication there have been several publications, including a meta-analysis of statins reducing community-acquired pneumonia-related mortality and reducing the need for mechanical ventilation or ICU admission (see CHEST 2015;148:523-32, Clin Med (Lond) 2017;17(5):403-7, and Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2018;40(1):30-40). Another surprise was neither the intensity, duration, or types of statin affected the result.”
He acknowledged certain limitations of the analysis, including its retrospective design, its relatively small sample size, and the fact that most of the subjects were non-Hispanic white men. “Routine prescription of statins in any dose in patients with SCI – even if the lipid profile is normal – is more beneficial than detrimental over the long haul,” concluded Dr. Rabadi, who also directs the Oklahoma VAMC Stroke Program. “Nearly all our patients with SCI continue to be on varying doses of statins.”
Dr. Rabadi reported having no financial disclosures.
[email protected]
SOURCE: Ann Neurol. 2018;84[S22]:S127. Abstract S302.
AT ANA 2018
Key clinical point:
Major finding: The mortality rate for patients on statins was 33.8-49.9 per 1,000 person-years, compared with 47.4-66.8 deaths per 1,000 person-years among those who had not taken statins (P less than .0052).
Study details: A retrospective review of 163 individuals with traumatic spinal cord injuries.
Disclosures: Dr. Rabadi reported having no financial disclosures.
Source: Ann Neurol. 2018;84[S22]:S127. Abstract S302.
FDA approves Xyrem to treat children with narcolepsy
The Food and Drug Administration has cleared Xyrem (sodium oxybate) oral solution to treat cataplexy and excessive daytime sleepiness in patients ages 7-17 with narcolepsy.
The central nervous system depressant previously had been approved to treat cataplexy in adults with narcolepsy.
The current approval was granted by the FDA under a Priority Review designation. Xyrem also received the FDA’s Orphan Drug designation, which is intended to encourage the development of drugs for rare diseases.
The agency noted in a press release, however, that the drug would continue to be available only through risk evaluation mitigation strategy (REMS) programs because of “the risk of serious outcomes resulting from inappropriate prescribing, misuse, abuse and diversion.” Xyrem either alone or in combination with other CNS depressants may be associated with reactions including seizure, respiratory depression, decreases in the level of consciousness, coma, and death, the FDA said.
The most common adverse reactions in pediatric patients were enuresis, nausea, headache, vomiting, weight decrease, decreased appetite, and dizziness.
For more information on prescribing Xyrem for pediatric patients, see the revised labeling information on the FDA website.
The Food and Drug Administration has cleared Xyrem (sodium oxybate) oral solution to treat cataplexy and excessive daytime sleepiness in patients ages 7-17 with narcolepsy.
The central nervous system depressant previously had been approved to treat cataplexy in adults with narcolepsy.
The current approval was granted by the FDA under a Priority Review designation. Xyrem also received the FDA’s Orphan Drug designation, which is intended to encourage the development of drugs for rare diseases.
The agency noted in a press release, however, that the drug would continue to be available only through risk evaluation mitigation strategy (REMS) programs because of “the risk of serious outcomes resulting from inappropriate prescribing, misuse, abuse and diversion.” Xyrem either alone or in combination with other CNS depressants may be associated with reactions including seizure, respiratory depression, decreases in the level of consciousness, coma, and death, the FDA said.
The most common adverse reactions in pediatric patients were enuresis, nausea, headache, vomiting, weight decrease, decreased appetite, and dizziness.
For more information on prescribing Xyrem for pediatric patients, see the revised labeling information on the FDA website.
The Food and Drug Administration has cleared Xyrem (sodium oxybate) oral solution to treat cataplexy and excessive daytime sleepiness in patients ages 7-17 with narcolepsy.
The central nervous system depressant previously had been approved to treat cataplexy in adults with narcolepsy.
The current approval was granted by the FDA under a Priority Review designation. Xyrem also received the FDA’s Orphan Drug designation, which is intended to encourage the development of drugs for rare diseases.
The agency noted in a press release, however, that the drug would continue to be available only through risk evaluation mitigation strategy (REMS) programs because of “the risk of serious outcomes resulting from inappropriate prescribing, misuse, abuse and diversion.” Xyrem either alone or in combination with other CNS depressants may be associated with reactions including seizure, respiratory depression, decreases in the level of consciousness, coma, and death, the FDA said.
The most common adverse reactions in pediatric patients were enuresis, nausea, headache, vomiting, weight decrease, decreased appetite, and dizziness.
For more information on prescribing Xyrem for pediatric patients, see the revised labeling information on the FDA website.
Post-mastectomy pain strategy allows for safe, same-day discharge
BOSTON – A multimodal pain regimen allowed for safe and effective same-day discharge of women undergoing mastectomy procedures, a recent study showed.
Women had little need for stronger oral narcotic use in the single center, retrospective study presented at the annual clinical congress of the American College of Surgeons.
The analysis included 72 consecutive mastectomies performed at a single center from November 2015 to July 2017. Most mastectomies were bilateral (61, or 84.7%) while 11 (15.3%) were unilateral.
Patients received a standardized pain regimen including 1 gram of IV acetaminophen interoperatively, combined with 30 mg of IV ketorolac and a 4-level intercostal nerve block with liposomal bupivacaine.
Liposomal bupivacaine has a longer half-life than other anesthetics, according to lead study author Radbeh Torabi, MD, a fifth-year plastic surgery resident at Louisiana State University (LSU) Health Science Center in New Orleans.
“That allows for prolonged pain control, especially during the time when the patient’s going to have the most amount of pain, which is the first day to two days postoperatively,” Dr. Torabi said in an interview.
All 72 patients were discharged home on the same day with just a 1-week prescription for acetaminophen with codeine.
Only 5 patients presented to the emergency room in the 30-day postoperative period, and of those, only 2 (2.8%) required readmission for reasons other than mastectomy-related pain, investigators said. The remaining 3 patients did present with pain, but did not require hospital admission.
Taken together, these findings suggest that this multimodal strategy offers excellent pain control and has the potential to minimize inpatient admissions while decreasing oral narcotic use, investigators said in an interview following their presentation.
“The main takeaway is reducing the amount of prescriptions we give,” Dr. Torabi said.
Study co-author Cameron T. Ward Coker, MD, a fourth-year general surgery resident at LSU, said the multimodal pain strategy used in this study could represent a step toward eliminating the risks associated with opioid prescribing.
“From the feedback we got from our lecture and the other surgeons in the room, it seems like that’s already becoming a widespread phenomenon,” Dr. Coker said.
Patients in the study had an average age of about 57 years and an average BMI of 30, according to the investigators.
Dr. Coker and Dr. Torabi had no disclosures related to the presentation.
SOURCE: Torabi R, et al. Scientific forum abstract at American College of Surgeons Clinical Congress. 2018 Oct 23.
BOSTON – A multimodal pain regimen allowed for safe and effective same-day discharge of women undergoing mastectomy procedures, a recent study showed.
Women had little need for stronger oral narcotic use in the single center, retrospective study presented at the annual clinical congress of the American College of Surgeons.
The analysis included 72 consecutive mastectomies performed at a single center from November 2015 to July 2017. Most mastectomies were bilateral (61, or 84.7%) while 11 (15.3%) were unilateral.
Patients received a standardized pain regimen including 1 gram of IV acetaminophen interoperatively, combined with 30 mg of IV ketorolac and a 4-level intercostal nerve block with liposomal bupivacaine.
Liposomal bupivacaine has a longer half-life than other anesthetics, according to lead study author Radbeh Torabi, MD, a fifth-year plastic surgery resident at Louisiana State University (LSU) Health Science Center in New Orleans.
“That allows for prolonged pain control, especially during the time when the patient’s going to have the most amount of pain, which is the first day to two days postoperatively,” Dr. Torabi said in an interview.
All 72 patients were discharged home on the same day with just a 1-week prescription for acetaminophen with codeine.
Only 5 patients presented to the emergency room in the 30-day postoperative period, and of those, only 2 (2.8%) required readmission for reasons other than mastectomy-related pain, investigators said. The remaining 3 patients did present with pain, but did not require hospital admission.
Taken together, these findings suggest that this multimodal strategy offers excellent pain control and has the potential to minimize inpatient admissions while decreasing oral narcotic use, investigators said in an interview following their presentation.
“The main takeaway is reducing the amount of prescriptions we give,” Dr. Torabi said.
Study co-author Cameron T. Ward Coker, MD, a fourth-year general surgery resident at LSU, said the multimodal pain strategy used in this study could represent a step toward eliminating the risks associated with opioid prescribing.
“From the feedback we got from our lecture and the other surgeons in the room, it seems like that’s already becoming a widespread phenomenon,” Dr. Coker said.
Patients in the study had an average age of about 57 years and an average BMI of 30, according to the investigators.
Dr. Coker and Dr. Torabi had no disclosures related to the presentation.
SOURCE: Torabi R, et al. Scientific forum abstract at American College of Surgeons Clinical Congress. 2018 Oct 23.
BOSTON – A multimodal pain regimen allowed for safe and effective same-day discharge of women undergoing mastectomy procedures, a recent study showed.
Women had little need for stronger oral narcotic use in the single center, retrospective study presented at the annual clinical congress of the American College of Surgeons.
The analysis included 72 consecutive mastectomies performed at a single center from November 2015 to July 2017. Most mastectomies were bilateral (61, or 84.7%) while 11 (15.3%) were unilateral.
Patients received a standardized pain regimen including 1 gram of IV acetaminophen interoperatively, combined with 30 mg of IV ketorolac and a 4-level intercostal nerve block with liposomal bupivacaine.
Liposomal bupivacaine has a longer half-life than other anesthetics, according to lead study author Radbeh Torabi, MD, a fifth-year plastic surgery resident at Louisiana State University (LSU) Health Science Center in New Orleans.
“That allows for prolonged pain control, especially during the time when the patient’s going to have the most amount of pain, which is the first day to two days postoperatively,” Dr. Torabi said in an interview.
All 72 patients were discharged home on the same day with just a 1-week prescription for acetaminophen with codeine.
Only 5 patients presented to the emergency room in the 30-day postoperative period, and of those, only 2 (2.8%) required readmission for reasons other than mastectomy-related pain, investigators said. The remaining 3 patients did present with pain, but did not require hospital admission.
Taken together, these findings suggest that this multimodal strategy offers excellent pain control and has the potential to minimize inpatient admissions while decreasing oral narcotic use, investigators said in an interview following their presentation.
“The main takeaway is reducing the amount of prescriptions we give,” Dr. Torabi said.
Study co-author Cameron T. Ward Coker, MD, a fourth-year general surgery resident at LSU, said the multimodal pain strategy used in this study could represent a step toward eliminating the risks associated with opioid prescribing.
“From the feedback we got from our lecture and the other surgeons in the room, it seems like that’s already becoming a widespread phenomenon,” Dr. Coker said.
Patients in the study had an average age of about 57 years and an average BMI of 30, according to the investigators.
Dr. Coker and Dr. Torabi had no disclosures related to the presentation.
SOURCE: Torabi R, et al. Scientific forum abstract at American College of Surgeons Clinical Congress. 2018 Oct 23.
REPORTING FROM THE ACS CLINICAL CONGRESS
Key clinical point:
Major finding: Of 72 women who had same-day discharge after mastectomy, only 3 presented for pain in the 30-day postoperative period.
Study details: A retrospective review of 72 consecutive mastectomies performed at a single surgical center.
Disclosures: The lead author had no disclosures related to the presentation.
Source: Torabi R, et al. Scientific forum abstract at American College of Surgeons Clinical Congress. 2018 Oct 23.
Acute kidney injury linked to later dementia
SAN DIEGO –
That’s according to a new study offering more evidence of a link between kidney disease and neurological problems.
“Clinicians should know that AKI is associated with poor long-term outcomes,” said lead author Jessica B. Kendrick MD, associate professor of medicine at the University of Colorado, Aurora. “We need to identify ways to prevent these long-term consequences.”
The findings were presented at Kidney Week 2018, sponsored by the American Society of Nephrology.
According to Dr. Kendrick, the acute neurological effects of AKI are well known. But no previous studies have examined the potential long-term cerebrovascular complications of AKI.
For the new study, Dr. Kendrick and her colleagues retrospectively analyzed 2,082 hospitalized patients in Utah from 1999 to 2009: 1,041 who completely recovered from AKI by discharge, and 1,041 who did not have AKI.
The average age was 61 years, and the average baseline creatinine was 0.9 ± 0.2 mg/dL. Over a median follow-up of 6 years, 97 patients developed dementia.
Those with AKI were more likely to develop dementia compared with the control group: 7% vs. 2% (hazard ratio, 3.4; 95% confidence interval, 2.14-5.40).
Other studies have linked kidney disease to cognitive impairment.
“There are a lot of theories as to why this is,” nephrologist Daniel Weiner, MD, of Tufts University, Boston, said in an interview. “It is most likely that the presence of kidney disease identifies individuals with a high burden of vascular disease, and that vascular disease, particularly of the small blood vessels, is an important contributor to cognitive impairment and dementia.”
That appears to be most notable in people who have protein in their urine, Dr. Weiner added. “The presence of protein in the urine identifies a severe enough process to affect the blood vessels in the kidney, and there is no reason to think that blood vessels elsewhere in the body, including in the brain, are not similarly affected.”
As for the current study, Dr. Weiner said it could support the vascular disease theory.
“People with vulnerable kidneys to acute injury also have vulnerable brains to acute injury,” he said. “People who get AKI usually have susceptibility to perfusion-related kidney injury. In other words, the small blood vessels that supply the kidney are unable to compensate to maintain sufficient blood flow during a time of low blood pressure or other systemic illness.”
That vulnerability “suggests to me that small blood vessels elsewhere in the body are less likely to be able to respond to challenges like low blood pressure,” Dr. Weiner explained. “If this occurs in the brain, it leads to microvascular disease and greater abnormal white-matter burden. This change in the brain anatomy is highly correlated with cognitive impairment.”
How can physicians put these finding to use? “These patients may require more monitoring,” Dr. Kendrick said. “For example, patients with AKI and complete recovery may not have any follow-up with a nephrologist, and perhaps they should.”
Moving forward, she said, “we are examining the association of AKI with cognitive dysfunction in different patient populations.” Researchers also are planning studies to better understand the mechanisms that are at work, she said.
The National Heart, Lung, and Blood Institute funded the study. The study authors had no disclosures.
SOURCE: Kendrick JB et al. Kidney Week 2018. Abstract TH-OR116.
SAN DIEGO –
That’s according to a new study offering more evidence of a link between kidney disease and neurological problems.
“Clinicians should know that AKI is associated with poor long-term outcomes,” said lead author Jessica B. Kendrick MD, associate professor of medicine at the University of Colorado, Aurora. “We need to identify ways to prevent these long-term consequences.”
The findings were presented at Kidney Week 2018, sponsored by the American Society of Nephrology.
According to Dr. Kendrick, the acute neurological effects of AKI are well known. But no previous studies have examined the potential long-term cerebrovascular complications of AKI.
For the new study, Dr. Kendrick and her colleagues retrospectively analyzed 2,082 hospitalized patients in Utah from 1999 to 2009: 1,041 who completely recovered from AKI by discharge, and 1,041 who did not have AKI.
The average age was 61 years, and the average baseline creatinine was 0.9 ± 0.2 mg/dL. Over a median follow-up of 6 years, 97 patients developed dementia.
Those with AKI were more likely to develop dementia compared with the control group: 7% vs. 2% (hazard ratio, 3.4; 95% confidence interval, 2.14-5.40).
Other studies have linked kidney disease to cognitive impairment.
“There are a lot of theories as to why this is,” nephrologist Daniel Weiner, MD, of Tufts University, Boston, said in an interview. “It is most likely that the presence of kidney disease identifies individuals with a high burden of vascular disease, and that vascular disease, particularly of the small blood vessels, is an important contributor to cognitive impairment and dementia.”
That appears to be most notable in people who have protein in their urine, Dr. Weiner added. “The presence of protein in the urine identifies a severe enough process to affect the blood vessels in the kidney, and there is no reason to think that blood vessels elsewhere in the body, including in the brain, are not similarly affected.”
As for the current study, Dr. Weiner said it could support the vascular disease theory.
“People with vulnerable kidneys to acute injury also have vulnerable brains to acute injury,” he said. “People who get AKI usually have susceptibility to perfusion-related kidney injury. In other words, the small blood vessels that supply the kidney are unable to compensate to maintain sufficient blood flow during a time of low blood pressure or other systemic illness.”
That vulnerability “suggests to me that small blood vessels elsewhere in the body are less likely to be able to respond to challenges like low blood pressure,” Dr. Weiner explained. “If this occurs in the brain, it leads to microvascular disease and greater abnormal white-matter burden. This change in the brain anatomy is highly correlated with cognitive impairment.”
How can physicians put these finding to use? “These patients may require more monitoring,” Dr. Kendrick said. “For example, patients with AKI and complete recovery may not have any follow-up with a nephrologist, and perhaps they should.”
Moving forward, she said, “we are examining the association of AKI with cognitive dysfunction in different patient populations.” Researchers also are planning studies to better understand the mechanisms that are at work, she said.
The National Heart, Lung, and Blood Institute funded the study. The study authors had no disclosures.
SOURCE: Kendrick JB et al. Kidney Week 2018. Abstract TH-OR116.
SAN DIEGO –
That’s according to a new study offering more evidence of a link between kidney disease and neurological problems.
“Clinicians should know that AKI is associated with poor long-term outcomes,” said lead author Jessica B. Kendrick MD, associate professor of medicine at the University of Colorado, Aurora. “We need to identify ways to prevent these long-term consequences.”
The findings were presented at Kidney Week 2018, sponsored by the American Society of Nephrology.
According to Dr. Kendrick, the acute neurological effects of AKI are well known. But no previous studies have examined the potential long-term cerebrovascular complications of AKI.
For the new study, Dr. Kendrick and her colleagues retrospectively analyzed 2,082 hospitalized patients in Utah from 1999 to 2009: 1,041 who completely recovered from AKI by discharge, and 1,041 who did not have AKI.
The average age was 61 years, and the average baseline creatinine was 0.9 ± 0.2 mg/dL. Over a median follow-up of 6 years, 97 patients developed dementia.
Those with AKI were more likely to develop dementia compared with the control group: 7% vs. 2% (hazard ratio, 3.4; 95% confidence interval, 2.14-5.40).
Other studies have linked kidney disease to cognitive impairment.
“There are a lot of theories as to why this is,” nephrologist Daniel Weiner, MD, of Tufts University, Boston, said in an interview. “It is most likely that the presence of kidney disease identifies individuals with a high burden of vascular disease, and that vascular disease, particularly of the small blood vessels, is an important contributor to cognitive impairment and dementia.”
That appears to be most notable in people who have protein in their urine, Dr. Weiner added. “The presence of protein in the urine identifies a severe enough process to affect the blood vessels in the kidney, and there is no reason to think that blood vessels elsewhere in the body, including in the brain, are not similarly affected.”
As for the current study, Dr. Weiner said it could support the vascular disease theory.
“People with vulnerable kidneys to acute injury also have vulnerable brains to acute injury,” he said. “People who get AKI usually have susceptibility to perfusion-related kidney injury. In other words, the small blood vessels that supply the kidney are unable to compensate to maintain sufficient blood flow during a time of low blood pressure or other systemic illness.”
That vulnerability “suggests to me that small blood vessels elsewhere in the body are less likely to be able to respond to challenges like low blood pressure,” Dr. Weiner explained. “If this occurs in the brain, it leads to microvascular disease and greater abnormal white-matter burden. This change in the brain anatomy is highly correlated with cognitive impairment.”
How can physicians put these finding to use? “These patients may require more monitoring,” Dr. Kendrick said. “For example, patients with AKI and complete recovery may not have any follow-up with a nephrologist, and perhaps they should.”
Moving forward, she said, “we are examining the association of AKI with cognitive dysfunction in different patient populations.” Researchers also are planning studies to better understand the mechanisms that are at work, she said.
The National Heart, Lung, and Blood Institute funded the study. The study authors had no disclosures.
SOURCE: Kendrick JB et al. Kidney Week 2018. Abstract TH-OR116.
REPORTING FROM KIDNEY WEEK 2018
Key clinical point: Patients with acute kidney injury seem to face a much higher risk of dementia.
Major finding: Hospitalized patients with AKI were 3.4 times more likely to develop dementia within a median of 6 years, compared with other hospitalized patients.
Study details: A retrospective study of 2,082 propensity-matched hospitalized patients, 1,041 who had AKI and fully recovered, and 1,041 who did not have AKI.
Disclosures: The National Heart, Lung, and Blood Institute funded the study. The authors had no disclosures.
Source: Kendrick JB et al. Kidney Week 2018. Abstract No. TH-OR116.
Challenging Dogma: The banana bag
Necessary, or just another pretty fluid?
The dogma
Patients with alcohol use disorders (AUD) are at risk for nutritional and vitamin deficiencies and may suffer from linked disease states, including Wernicke’s encephalopathy. These conditions may be underrecognized; for instance, an autopsy study suggests that Wernicke’s encephalopathy may have a prevalence rate of 12.5% among alcoholics.1
When patients with AUD are hospitalized, they have often already received a standard IV solution (100 mg of thiamine, 1 mg of folate, 1-2 g of magnesium, and a multivitamin dissolved in saline or dextrose). The practice is common enough that the solution is informally referred to as a “banana bag,” due to the yellow hue imparted by thiamine and multivitamin. These fluids might then be readministered daily during the inpatient stay. But what is the evidence supporting this widespread practice?
The evidence
While the banana bag (or “rally pack”, as it’s also colloquially known) hanging at the patient’s side may look cool, it may not be helping her. Let’s break down the ingredients:
- Folate: Patients with alcohol use disorder are at higher risk for folate deficiency (attributable to poor intake and decreased absorption), but overall rates of folate deficiency are still quite low.2 In addition, most oral and parenteral multivitamins already contain at least 400 mcg folate – the benefit of adding further intravenous folate is not clear.
- Magnesium. Patients with AUD are also at higher risk for magnesium deficiency attributable to increased excretion. While decreased magnesium levels could theoretically increase the risk of alcohol withdrawal symptoms, a Cochrane review found no evidence to support routine supplementation.3
- Multivitamin. Despite theoretical advantages in these (often) malnourished patients, there are no published studies on the benefit or harm of administering a “pan-vitamin” injection. The standard IV formulation is slightly different than an oral vitamin (the IV contains vitamin K, for instance, and lacks calcium), but the bioavailability should be roughly the same, except in rare patients with intestinal malabsorption.4
- IV fluids. Pharmacies typically mix these ingredients in a liter of normal saline or 5% dextrose. Once again, though, individual patients will have different needs. A dehydrated patient would benefit more from normal saline, a patient with alcoholic ketoacidosis would benefit more from dextrose, and a patient with alcohol-related cardiomyopathy likely shouldn’t be getting large volume IV fluids at all.
- Thiamine. Thiamine deficiency is likely the most common and most concerning vitamin deficiency in this patient population. The typical banana bag contains 100 mg of thiamine, which has been the traditional recommended daily amount for Wernicke’s treatment. This dosage, however, was apparently chosen arbitrarily in the 1950s (based on what the authors considered to be a high dose) and current recommendations suggest higher doses given more frequently because of the relatively short half-life of parenteral thiamine.5
Takeaway
The banana bag is a “one-size-fits-all” approach that offers too much of some of its ingredients and not enough of others. It’s better to individualize treatment based on a patient’s needs and consider high-dose thiamine (500 mg one to three times daily) for those at risk for, or showing signs of, Wernicke’s encephalopathy.
Dr. Sehgal and Dr. Hanson are clinical associate professors of medicine in the division of general and hospital medicine at the South Texas Veterans Health Care System and UT-Health San Antonio. Dr. Sehgal (@rtsehgal) is a member of the editorial advisory board for The Hospitalist.
References
1. Torvik A et al. Brain lesions in alcoholics: a neuropathological study with clinical correlation. J Neurol Sci. 1982 Nov;56(2-3):233-48.
2. Schwab RA et al. Prevalence in folate deficiency in emergency department patients with alcohol-related illness or injury. Am J Emerg Med. 1992 May;10(3):203-7.
3. Sarai M et al. Magnesium for alcohol withdrawal. Cochrane Database Syst Rev. 2013 Jun 5;(6):CD008358.
4. Krishel S et al. Intravenous vitamins for alcoholics in the emergency department: a review. J Emerg Med. 1998 May-Jun;16(3):419-24.
5. Donnino MW et al. Myths and misconceptions of Wernicke’s encephalopathy: what every emergency physician should know. Ann Emerg Med. 2007;50(6): 715-21.
Necessary, or just another pretty fluid?
Necessary, or just another pretty fluid?
The dogma
Patients with alcohol use disorders (AUD) are at risk for nutritional and vitamin deficiencies and may suffer from linked disease states, including Wernicke’s encephalopathy. These conditions may be underrecognized; for instance, an autopsy study suggests that Wernicke’s encephalopathy may have a prevalence rate of 12.5% among alcoholics.1
When patients with AUD are hospitalized, they have often already received a standard IV solution (100 mg of thiamine, 1 mg of folate, 1-2 g of magnesium, and a multivitamin dissolved in saline or dextrose). The practice is common enough that the solution is informally referred to as a “banana bag,” due to the yellow hue imparted by thiamine and multivitamin. These fluids might then be readministered daily during the inpatient stay. But what is the evidence supporting this widespread practice?
The evidence
While the banana bag (or “rally pack”, as it’s also colloquially known) hanging at the patient’s side may look cool, it may not be helping her. Let’s break down the ingredients:
- Folate: Patients with alcohol use disorder are at higher risk for folate deficiency (attributable to poor intake and decreased absorption), but overall rates of folate deficiency are still quite low.2 In addition, most oral and parenteral multivitamins already contain at least 400 mcg folate – the benefit of adding further intravenous folate is not clear.
- Magnesium. Patients with AUD are also at higher risk for magnesium deficiency attributable to increased excretion. While decreased magnesium levels could theoretically increase the risk of alcohol withdrawal symptoms, a Cochrane review found no evidence to support routine supplementation.3
- Multivitamin. Despite theoretical advantages in these (often) malnourished patients, there are no published studies on the benefit or harm of administering a “pan-vitamin” injection. The standard IV formulation is slightly different than an oral vitamin (the IV contains vitamin K, for instance, and lacks calcium), but the bioavailability should be roughly the same, except in rare patients with intestinal malabsorption.4
- IV fluids. Pharmacies typically mix these ingredients in a liter of normal saline or 5% dextrose. Once again, though, individual patients will have different needs. A dehydrated patient would benefit more from normal saline, a patient with alcoholic ketoacidosis would benefit more from dextrose, and a patient with alcohol-related cardiomyopathy likely shouldn’t be getting large volume IV fluids at all.
- Thiamine. Thiamine deficiency is likely the most common and most concerning vitamin deficiency in this patient population. The typical banana bag contains 100 mg of thiamine, which has been the traditional recommended daily amount for Wernicke’s treatment. This dosage, however, was apparently chosen arbitrarily in the 1950s (based on what the authors considered to be a high dose) and current recommendations suggest higher doses given more frequently because of the relatively short half-life of parenteral thiamine.5
Takeaway
The banana bag is a “one-size-fits-all” approach that offers too much of some of its ingredients and not enough of others. It’s better to individualize treatment based on a patient’s needs and consider high-dose thiamine (500 mg one to three times daily) for those at risk for, or showing signs of, Wernicke’s encephalopathy.
Dr. Sehgal and Dr. Hanson are clinical associate professors of medicine in the division of general and hospital medicine at the South Texas Veterans Health Care System and UT-Health San Antonio. Dr. Sehgal (@rtsehgal) is a member of the editorial advisory board for The Hospitalist.
References
1. Torvik A et al. Brain lesions in alcoholics: a neuropathological study with clinical correlation. J Neurol Sci. 1982 Nov;56(2-3):233-48.
2. Schwab RA et al. Prevalence in folate deficiency in emergency department patients with alcohol-related illness or injury. Am J Emerg Med. 1992 May;10(3):203-7.
3. Sarai M et al. Magnesium for alcohol withdrawal. Cochrane Database Syst Rev. 2013 Jun 5;(6):CD008358.
4. Krishel S et al. Intravenous vitamins for alcoholics in the emergency department: a review. J Emerg Med. 1998 May-Jun;16(3):419-24.
5. Donnino MW et al. Myths and misconceptions of Wernicke’s encephalopathy: what every emergency physician should know. Ann Emerg Med. 2007;50(6): 715-21.
The dogma
Patients with alcohol use disorders (AUD) are at risk for nutritional and vitamin deficiencies and may suffer from linked disease states, including Wernicke’s encephalopathy. These conditions may be underrecognized; for instance, an autopsy study suggests that Wernicke’s encephalopathy may have a prevalence rate of 12.5% among alcoholics.1
When patients with AUD are hospitalized, they have often already received a standard IV solution (100 mg of thiamine, 1 mg of folate, 1-2 g of magnesium, and a multivitamin dissolved in saline or dextrose). The practice is common enough that the solution is informally referred to as a “banana bag,” due to the yellow hue imparted by thiamine and multivitamin. These fluids might then be readministered daily during the inpatient stay. But what is the evidence supporting this widespread practice?
The evidence
While the banana bag (or “rally pack”, as it’s also colloquially known) hanging at the patient’s side may look cool, it may not be helping her. Let’s break down the ingredients:
- Folate: Patients with alcohol use disorder are at higher risk for folate deficiency (attributable to poor intake and decreased absorption), but overall rates of folate deficiency are still quite low.2 In addition, most oral and parenteral multivitamins already contain at least 400 mcg folate – the benefit of adding further intravenous folate is not clear.
- Magnesium. Patients with AUD are also at higher risk for magnesium deficiency attributable to increased excretion. While decreased magnesium levels could theoretically increase the risk of alcohol withdrawal symptoms, a Cochrane review found no evidence to support routine supplementation.3
- Multivitamin. Despite theoretical advantages in these (often) malnourished patients, there are no published studies on the benefit or harm of administering a “pan-vitamin” injection. The standard IV formulation is slightly different than an oral vitamin (the IV contains vitamin K, for instance, and lacks calcium), but the bioavailability should be roughly the same, except in rare patients with intestinal malabsorption.4
- IV fluids. Pharmacies typically mix these ingredients in a liter of normal saline or 5% dextrose. Once again, though, individual patients will have different needs. A dehydrated patient would benefit more from normal saline, a patient with alcoholic ketoacidosis would benefit more from dextrose, and a patient with alcohol-related cardiomyopathy likely shouldn’t be getting large volume IV fluids at all.
- Thiamine. Thiamine deficiency is likely the most common and most concerning vitamin deficiency in this patient population. The typical banana bag contains 100 mg of thiamine, which has been the traditional recommended daily amount for Wernicke’s treatment. This dosage, however, was apparently chosen arbitrarily in the 1950s (based on what the authors considered to be a high dose) and current recommendations suggest higher doses given more frequently because of the relatively short half-life of parenteral thiamine.5
Takeaway
The banana bag is a “one-size-fits-all” approach that offers too much of some of its ingredients and not enough of others. It’s better to individualize treatment based on a patient’s needs and consider high-dose thiamine (500 mg one to three times daily) for those at risk for, or showing signs of, Wernicke’s encephalopathy.
Dr. Sehgal and Dr. Hanson are clinical associate professors of medicine in the division of general and hospital medicine at the South Texas Veterans Health Care System and UT-Health San Antonio. Dr. Sehgal (@rtsehgal) is a member of the editorial advisory board for The Hospitalist.
References
1. Torvik A et al. Brain lesions in alcoholics: a neuropathological study with clinical correlation. J Neurol Sci. 1982 Nov;56(2-3):233-48.
2. Schwab RA et al. Prevalence in folate deficiency in emergency department patients with alcohol-related illness or injury. Am J Emerg Med. 1992 May;10(3):203-7.
3. Sarai M et al. Magnesium for alcohol withdrawal. Cochrane Database Syst Rev. 2013 Jun 5;(6):CD008358.
4. Krishel S et al. Intravenous vitamins for alcoholics in the emergency department: a review. J Emerg Med. 1998 May-Jun;16(3):419-24.
5. Donnino MW et al. Myths and misconceptions of Wernicke’s encephalopathy: what every emergency physician should know. Ann Emerg Med. 2007;50(6): 715-21.
IDEAS study meets first aim of changing 3-month clinical management, health outcomes
BARCELONA – Amyloid PET brain imaging changed clinical management in 60% of patients with a diagnosis of mild cognitive impairment or dementia and confirmed a presumptive Alzheimer’s diagnosis in 95% of those with positive scans.
But the scans also benefited amyloid-negative patients, Gil Rabinovici, MD, said at the Clinical Trials on Alzheimer’s Disease conference. Before the test, 71% carried an Alzheimer’s disease (AD) diagnosis; after the test, just 10% did, opening the way for an accurate diagnosis and more effective treatment.
“These patients were saved from unnecessary treatment for Alzheimer’s,” said Dr. Rabinovici, the Edward Fein and Pearl Landrith Endowed Professor in Memory & Aging at the University of California, San Francisco. They received more suitable care plans because of the confirmation.
He presented final results of aim one of the IDEAS (Imaging Dementia–Evidence for Amyloid Scanning) study, which seeks to prove that amyloid imaging changes clinical management and improves health outcomes in Medicare beneficiaries who have been diagnosed with mild cognitive impairment (MCI) or dementia of uncertain cause. Its two aims are to show that amyloid PET imaging affects a patient’s care plan within 3 months of the scan and that this impacts major medical outcomes 12 months later. In diagnostically uncertain cases, investigators theorized, amyloid PET imaging would lead to significant changes in patient management, which would then translate into improved medical outcomes.
Ultimately, investigators hope the U.S.-wide, open-label study will prove the clinical value of amyloid PET scanning and convince the Centers for Medicare & Medicaid Services to make the test a fully covered service.
So far, IDEAS has accrued data on 11,409 patients and is quickly closing in on the 18,000-patient target. The patients reported on at CTAD were aged a mean of 75 years and were largely white; only 4% were black and 4% Hispanic. The mean Mini-Mental Scale Exam score was 26. AD was the leading suspect pathology in 73% of the 6,905 with MCI and in 83% of those with dementia of uncertain etiology. Overall, 44% were taking AD medications at baseline.
Scans were positive in 55% of those with MCI and in 70% of those with dementia. Overall, the scans changed clinical management in 61% (7,018), including 60% of those with MCI and 63% of those with dementia.
“We also asked physicians how much the scan results contributed to these changes, and 86.7% replied that they ‘contributed significantly,’ ” Dr. Rabinovici said.
Most changes involved adjustments to medication. AD drugs were started in 44% of MCI patients and in 45% of dementia patients, and non-AD drugs started in 22% and 25%, respectively. About a fifth of the patients received counseling in wake of the scan results.
Medication adjustments also varied by scan result. Among amyloid-positive MCI patients, AD drug use increased from 40% before imaging to 81% after; among amyloid-negative MCI patients, drug use decreased slightly from 27% to 24%. Among amyloid-positive dementia patients, AD drug use increased from 63% to 91%, and among amyloid-negative patients, it dropped from 50% to 44%. All these changes were statistically significant.
The primary diagnosis changed from AD to non-AD in 25%, and from non-AD to AD in 10%. Among amyloid-positive patients, the diagnosis prevalence jumped from 80.0% to 95.5%; among amyloid-negative patients, it dropped from 71% to just 10%.
“IDEAS now provides the strongest data we have supporting the beneficial impact of amyloid PET on patient management,” said Dr. Rabinovici. “Aim two, which is the 12-month health outcomes, we expect to be completed by the end of next year.”
The IDEAS team is also looking at a furthering the investigation with a study called, aptly, “NEW IDEAS.” That would reach out to recruit the minorities that were so underrepresented in the main study and include patients with early-onset MCI or dementia. Building up a library of DNA and blood plasma samples might also fit into the new project.
IDEAS is a funding collaboration of the CMS, the Alzheimer’s Association, Avid Radiopharmaceuticals/Eli Lilly, General Electric Healthcare, Piramal Imaging, and the American College of Radiology. Dr. Rabinovici had no financial disclosures.
BARCELONA – Amyloid PET brain imaging changed clinical management in 60% of patients with a diagnosis of mild cognitive impairment or dementia and confirmed a presumptive Alzheimer’s diagnosis in 95% of those with positive scans.
But the scans also benefited amyloid-negative patients, Gil Rabinovici, MD, said at the Clinical Trials on Alzheimer’s Disease conference. Before the test, 71% carried an Alzheimer’s disease (AD) diagnosis; after the test, just 10% did, opening the way for an accurate diagnosis and more effective treatment.
“These patients were saved from unnecessary treatment for Alzheimer’s,” said Dr. Rabinovici, the Edward Fein and Pearl Landrith Endowed Professor in Memory & Aging at the University of California, San Francisco. They received more suitable care plans because of the confirmation.
He presented final results of aim one of the IDEAS (Imaging Dementia–Evidence for Amyloid Scanning) study, which seeks to prove that amyloid imaging changes clinical management and improves health outcomes in Medicare beneficiaries who have been diagnosed with mild cognitive impairment (MCI) or dementia of uncertain cause. Its two aims are to show that amyloid PET imaging affects a patient’s care plan within 3 months of the scan and that this impacts major medical outcomes 12 months later. In diagnostically uncertain cases, investigators theorized, amyloid PET imaging would lead to significant changes in patient management, which would then translate into improved medical outcomes.
Ultimately, investigators hope the U.S.-wide, open-label study will prove the clinical value of amyloid PET scanning and convince the Centers for Medicare & Medicaid Services to make the test a fully covered service.
So far, IDEAS has accrued data on 11,409 patients and is quickly closing in on the 18,000-patient target. The patients reported on at CTAD were aged a mean of 75 years and were largely white; only 4% were black and 4% Hispanic. The mean Mini-Mental Scale Exam score was 26. AD was the leading suspect pathology in 73% of the 6,905 with MCI and in 83% of those with dementia of uncertain etiology. Overall, 44% were taking AD medications at baseline.
Scans were positive in 55% of those with MCI and in 70% of those with dementia. Overall, the scans changed clinical management in 61% (7,018), including 60% of those with MCI and 63% of those with dementia.
“We also asked physicians how much the scan results contributed to these changes, and 86.7% replied that they ‘contributed significantly,’ ” Dr. Rabinovici said.
Most changes involved adjustments to medication. AD drugs were started in 44% of MCI patients and in 45% of dementia patients, and non-AD drugs started in 22% and 25%, respectively. About a fifth of the patients received counseling in wake of the scan results.
Medication adjustments also varied by scan result. Among amyloid-positive MCI patients, AD drug use increased from 40% before imaging to 81% after; among amyloid-negative MCI patients, drug use decreased slightly from 27% to 24%. Among amyloid-positive dementia patients, AD drug use increased from 63% to 91%, and among amyloid-negative patients, it dropped from 50% to 44%. All these changes were statistically significant.
The primary diagnosis changed from AD to non-AD in 25%, and from non-AD to AD in 10%. Among amyloid-positive patients, the diagnosis prevalence jumped from 80.0% to 95.5%; among amyloid-negative patients, it dropped from 71% to just 10%.
“IDEAS now provides the strongest data we have supporting the beneficial impact of amyloid PET on patient management,” said Dr. Rabinovici. “Aim two, which is the 12-month health outcomes, we expect to be completed by the end of next year.”
The IDEAS team is also looking at a furthering the investigation with a study called, aptly, “NEW IDEAS.” That would reach out to recruit the minorities that were so underrepresented in the main study and include patients with early-onset MCI or dementia. Building up a library of DNA and blood plasma samples might also fit into the new project.
IDEAS is a funding collaboration of the CMS, the Alzheimer’s Association, Avid Radiopharmaceuticals/Eli Lilly, General Electric Healthcare, Piramal Imaging, and the American College of Radiology. Dr. Rabinovici had no financial disclosures.
BARCELONA – Amyloid PET brain imaging changed clinical management in 60% of patients with a diagnosis of mild cognitive impairment or dementia and confirmed a presumptive Alzheimer’s diagnosis in 95% of those with positive scans.
But the scans also benefited amyloid-negative patients, Gil Rabinovici, MD, said at the Clinical Trials on Alzheimer’s Disease conference. Before the test, 71% carried an Alzheimer’s disease (AD) diagnosis; after the test, just 10% did, opening the way for an accurate diagnosis and more effective treatment.
“These patients were saved from unnecessary treatment for Alzheimer’s,” said Dr. Rabinovici, the Edward Fein and Pearl Landrith Endowed Professor in Memory & Aging at the University of California, San Francisco. They received more suitable care plans because of the confirmation.
He presented final results of aim one of the IDEAS (Imaging Dementia–Evidence for Amyloid Scanning) study, which seeks to prove that amyloid imaging changes clinical management and improves health outcomes in Medicare beneficiaries who have been diagnosed with mild cognitive impairment (MCI) or dementia of uncertain cause. Its two aims are to show that amyloid PET imaging affects a patient’s care plan within 3 months of the scan and that this impacts major medical outcomes 12 months later. In diagnostically uncertain cases, investigators theorized, amyloid PET imaging would lead to significant changes in patient management, which would then translate into improved medical outcomes.
Ultimately, investigators hope the U.S.-wide, open-label study will prove the clinical value of amyloid PET scanning and convince the Centers for Medicare & Medicaid Services to make the test a fully covered service.
So far, IDEAS has accrued data on 11,409 patients and is quickly closing in on the 18,000-patient target. The patients reported on at CTAD were aged a mean of 75 years and were largely white; only 4% were black and 4% Hispanic. The mean Mini-Mental Scale Exam score was 26. AD was the leading suspect pathology in 73% of the 6,905 with MCI and in 83% of those with dementia of uncertain etiology. Overall, 44% were taking AD medications at baseline.
Scans were positive in 55% of those with MCI and in 70% of those with dementia. Overall, the scans changed clinical management in 61% (7,018), including 60% of those with MCI and 63% of those with dementia.
“We also asked physicians how much the scan results contributed to these changes, and 86.7% replied that they ‘contributed significantly,’ ” Dr. Rabinovici said.
Most changes involved adjustments to medication. AD drugs were started in 44% of MCI patients and in 45% of dementia patients, and non-AD drugs started in 22% and 25%, respectively. About a fifth of the patients received counseling in wake of the scan results.
Medication adjustments also varied by scan result. Among amyloid-positive MCI patients, AD drug use increased from 40% before imaging to 81% after; among amyloid-negative MCI patients, drug use decreased slightly from 27% to 24%. Among amyloid-positive dementia patients, AD drug use increased from 63% to 91%, and among amyloid-negative patients, it dropped from 50% to 44%. All these changes were statistically significant.
The primary diagnosis changed from AD to non-AD in 25%, and from non-AD to AD in 10%. Among amyloid-positive patients, the diagnosis prevalence jumped from 80.0% to 95.5%; among amyloid-negative patients, it dropped from 71% to just 10%.
“IDEAS now provides the strongest data we have supporting the beneficial impact of amyloid PET on patient management,” said Dr. Rabinovici. “Aim two, which is the 12-month health outcomes, we expect to be completed by the end of next year.”
The IDEAS team is also looking at a furthering the investigation with a study called, aptly, “NEW IDEAS.” That would reach out to recruit the minorities that were so underrepresented in the main study and include patients with early-onset MCI or dementia. Building up a library of DNA and blood plasma samples might also fit into the new project.
IDEAS is a funding collaboration of the CMS, the Alzheimer’s Association, Avid Radiopharmaceuticals/Eli Lilly, General Electric Healthcare, Piramal Imaging, and the American College of Radiology. Dr. Rabinovici had no financial disclosures.
REPORTING FROM CTAD
Key clinical point: Amyloid PET imaging can refine equivocal dementia diagnoses.
Major finding:
Study details: The IDEAS study has thus far accrued data on 11,409 subjects.
Disclosures: IDEAS is a funding collaboration of the Centers for Medicare & Medicaid Services, the Alzheimer’s Association, Avid Radiopharmaceuticals/Eli Lilly, General Electric Healthcare, Piramal Imaging, and the American College of Radiology. Dr. Rabinovici had no financial disclosures.
Stroke risk in elderly following AMI extends to 12 weeks
ATLANTA – Acute myocardial infarction is associated with a risk of stroke that extends beyond the 1-month time window currently considered the at-risk period, according to an analysis of Medicare data.
“The results of our study may allow clinicians to more accurately counsel patients regarding their stroke etiology and may allow refinement of stroke etiology classification systems and clinical trial selection criteria,” lead study author Alexander E. Merkler, MD, said in an interview in advance of the annual meeting of the American Neurological Association.
In an effort to better understand the duration of heightened stroke risk after acute myocardial infarction, Dr. Merkler, a neurologist at New York–based Weill Cornell Medicine, and his colleagues conducted a retrospective cohort study using inpatient and outpatient claims during 2008-2015 from a nationally representative 5% sample of Medicare beneficiaries who were at least 66 years old. They used previously validated ICD-9-CM diagnosis codes to ascertain the exposure variable of acute MI and the outcome of ischemic stroke but excluded strokes that occurred during an acute MI hospitalization.
Patients were censored at the time of ischemic stroke, death, end of Medicare coverage, or by Sept. 30, 2015. The researchers fit Cox regression models separately for the groups with and without acute MI to examine its association with ischemic stroke after adjusting for demographics, stroke risk factors, and Charlson comorbidities. Next, they used the corresponding survival probabilities to compute the hazard ratio (HR) in each 4-week interval after discharge, up to week 12. They also conducted a subgroup analysis to evaluate the duration of heightened ischemic stroke risk by MI type: ST-segment elevation MI (STEMI) versus non-STEMI (NSTEMI).
Dr. Merkler and his colleagues drew from data on 1.7 million eligible beneficiaries. Of these, 46,182 were hospitalized for acute MI and 80,466 for ischemic stroke. After they adjusted for demographics, stroke risk factors, and Charlson comorbidities, the researchers found that the risk of ischemic stroke was highest in the first 4 weeks after discharge from the MI hospitalization (HR, 2.7), yet remained elevated during weeks 5-8 (HR, 2.0) and weeks 9-12 (HR, 1.6). It was no longer significantly elevated afterward. The prolonged period of heightened ischemic stroke risk was evident in patients with both STEMI and NSTEMI.
“We were surprised by how long the risk of stroke lasts after MI,” Dr. Merkler said. He acknowledged certain limitations of the analysis, including the fact that patients were all over the age of 65 years. “In addition, we lack granular detail such as severity of MI [and] the extent of stroke work-up,” he said.
Dr. Merkler disclosed that he is supported by a grant from the National Institutes of Health and by the Leon Levy Foundation in Neuroscience. Most of his coauthors are also supported by NIH grants.
[email protected]
Source: Ann Neurol. 2018;84[S22]:S146-7, Abstract M122.
ATLANTA – Acute myocardial infarction is associated with a risk of stroke that extends beyond the 1-month time window currently considered the at-risk period, according to an analysis of Medicare data.
“The results of our study may allow clinicians to more accurately counsel patients regarding their stroke etiology and may allow refinement of stroke etiology classification systems and clinical trial selection criteria,” lead study author Alexander E. Merkler, MD, said in an interview in advance of the annual meeting of the American Neurological Association.
In an effort to better understand the duration of heightened stroke risk after acute myocardial infarction, Dr. Merkler, a neurologist at New York–based Weill Cornell Medicine, and his colleagues conducted a retrospective cohort study using inpatient and outpatient claims during 2008-2015 from a nationally representative 5% sample of Medicare beneficiaries who were at least 66 years old. They used previously validated ICD-9-CM diagnosis codes to ascertain the exposure variable of acute MI and the outcome of ischemic stroke but excluded strokes that occurred during an acute MI hospitalization.
Patients were censored at the time of ischemic stroke, death, end of Medicare coverage, or by Sept. 30, 2015. The researchers fit Cox regression models separately for the groups with and without acute MI to examine its association with ischemic stroke after adjusting for demographics, stroke risk factors, and Charlson comorbidities. Next, they used the corresponding survival probabilities to compute the hazard ratio (HR) in each 4-week interval after discharge, up to week 12. They also conducted a subgroup analysis to evaluate the duration of heightened ischemic stroke risk by MI type: ST-segment elevation MI (STEMI) versus non-STEMI (NSTEMI).
Dr. Merkler and his colleagues drew from data on 1.7 million eligible beneficiaries. Of these, 46,182 were hospitalized for acute MI and 80,466 for ischemic stroke. After they adjusted for demographics, stroke risk factors, and Charlson comorbidities, the researchers found that the risk of ischemic stroke was highest in the first 4 weeks after discharge from the MI hospitalization (HR, 2.7), yet remained elevated during weeks 5-8 (HR, 2.0) and weeks 9-12 (HR, 1.6). It was no longer significantly elevated afterward. The prolonged period of heightened ischemic stroke risk was evident in patients with both STEMI and NSTEMI.
“We were surprised by how long the risk of stroke lasts after MI,” Dr. Merkler said. He acknowledged certain limitations of the analysis, including the fact that patients were all over the age of 65 years. “In addition, we lack granular detail such as severity of MI [and] the extent of stroke work-up,” he said.
Dr. Merkler disclosed that he is supported by a grant from the National Institutes of Health and by the Leon Levy Foundation in Neuroscience. Most of his coauthors are also supported by NIH grants.
[email protected]
Source: Ann Neurol. 2018;84[S22]:S146-7, Abstract M122.
ATLANTA – Acute myocardial infarction is associated with a risk of stroke that extends beyond the 1-month time window currently considered the at-risk period, according to an analysis of Medicare data.
“The results of our study may allow clinicians to more accurately counsel patients regarding their stroke etiology and may allow refinement of stroke etiology classification systems and clinical trial selection criteria,” lead study author Alexander E. Merkler, MD, said in an interview in advance of the annual meeting of the American Neurological Association.
In an effort to better understand the duration of heightened stroke risk after acute myocardial infarction, Dr. Merkler, a neurologist at New York–based Weill Cornell Medicine, and his colleagues conducted a retrospective cohort study using inpatient and outpatient claims during 2008-2015 from a nationally representative 5% sample of Medicare beneficiaries who were at least 66 years old. They used previously validated ICD-9-CM diagnosis codes to ascertain the exposure variable of acute MI and the outcome of ischemic stroke but excluded strokes that occurred during an acute MI hospitalization.
Patients were censored at the time of ischemic stroke, death, end of Medicare coverage, or by Sept. 30, 2015. The researchers fit Cox regression models separately for the groups with and without acute MI to examine its association with ischemic stroke after adjusting for demographics, stroke risk factors, and Charlson comorbidities. Next, they used the corresponding survival probabilities to compute the hazard ratio (HR) in each 4-week interval after discharge, up to week 12. They also conducted a subgroup analysis to evaluate the duration of heightened ischemic stroke risk by MI type: ST-segment elevation MI (STEMI) versus non-STEMI (NSTEMI).
Dr. Merkler and his colleagues drew from data on 1.7 million eligible beneficiaries. Of these, 46,182 were hospitalized for acute MI and 80,466 for ischemic stroke. After they adjusted for demographics, stroke risk factors, and Charlson comorbidities, the researchers found that the risk of ischemic stroke was highest in the first 4 weeks after discharge from the MI hospitalization (HR, 2.7), yet remained elevated during weeks 5-8 (HR, 2.0) and weeks 9-12 (HR, 1.6). It was no longer significantly elevated afterward. The prolonged period of heightened ischemic stroke risk was evident in patients with both STEMI and NSTEMI.
“We were surprised by how long the risk of stroke lasts after MI,” Dr. Merkler said. He acknowledged certain limitations of the analysis, including the fact that patients were all over the age of 65 years. “In addition, we lack granular detail such as severity of MI [and] the extent of stroke work-up,” he said.
Dr. Merkler disclosed that he is supported by a grant from the National Institutes of Health and by the Leon Levy Foundation in Neuroscience. Most of his coauthors are also supported by NIH grants.
[email protected]
Source: Ann Neurol. 2018;84[S22]:S146-7, Abstract M122.
AT ANA 2018
Key clinical point: .
Major finding: The risk of ischemic stroke was highest in the first 4 weeks after discharge from the MI hospitalization (HR, 2.7), yet remained elevated during weeks 5-8 (HR, 2.0) and weeks 9-12 (HR, 1.6).
Study details: An analysis of 46,182 Medicare beneficiaries who were hospitalized for acute MI and 80,466 who were hospitalized for ischemic stroke.
Disclosures: Dr. Merkler disclosed that he is supported by a grant from the National Institutes of Health and by the Leon Levy Foundation in Neuroscience. Most of his coauthors are also supported by NIH grants.
Source: Ann Neurol. 2018;84[S22]:S146-7, Abstract M122.
New Registry Offers Insight Into Opsoclonus-Myoclonus Syndrome
WASHINGTON – a rare disease affecting only 1 in 5,000,000 individuals, mostly aged 1-5 years, based on data from a new patient registry.
In partnership with the National Organization of Rare Disorders (NORD) the nonprofit OMSLife Foundation has created a patient registry to better understand the disease experience in patients, wrote Mike Michaelis, chairman of OMSLife, and his colleagues. Early data from 275 enrolled patients were presented in a poster at the NORD Rare Summit, held by the National Organization for Rare Disorders.
The registry patients were mainly born in the United States (86%) and white (74%); approximately half were female. Of 150 patients who indicated symptoms at onset, 87% reported ataxia. Additional symptoms at onset were myoclonus (61%), opsoclonus (59%), tremors (46%), sleep disturbances (45%), temper tantrums (38%), vomiting (27%), fever (13%), headache (9%) and other symptoms (13%).
The researchers reviewed associations of symptoms at onset to determine the frequency of other symptoms for each individual symptom. Ataxia was present with 89% or higher instances of the other reported symptoms. Of note, some symptoms occurred more frequently than expected, such as temper tantrums and tremors in approximately 70% of patients with sleep disturbances. Myoclonus and opsoclonus, as well as fever and vomiting, also were significantly associated with the presence of other symptoms.
Two-thirds of the registry patients (69%) were diagnosed within 3 months of symptom onset, and 83% of these were diagnosed by a neurologist. Based on the Mitchell-Pike OMS severity scale, 59% of the patients met criteria for severe disease, 34% were classified as moderate, and 7% were mild. The registry is ongoing, but the current data provide insight on the clinical picture and common symptoms of OMS, the researchers said.
OMS Life was established in 2012 to support patients, caregivers, and researchers in raising awareness of opsoclonus-myoclonus syndrome as well as funds for research.
The study was supported by the OMSLife Foundation, NORD, and Trio Health Analytics. The researchers are employed by these organizations.
WASHINGTON – a rare disease affecting only 1 in 5,000,000 individuals, mostly aged 1-5 years, based on data from a new patient registry.
In partnership with the National Organization of Rare Disorders (NORD) the nonprofit OMSLife Foundation has created a patient registry to better understand the disease experience in patients, wrote Mike Michaelis, chairman of OMSLife, and his colleagues. Early data from 275 enrolled patients were presented in a poster at the NORD Rare Summit, held by the National Organization for Rare Disorders.
The registry patients were mainly born in the United States (86%) and white (74%); approximately half were female. Of 150 patients who indicated symptoms at onset, 87% reported ataxia. Additional symptoms at onset were myoclonus (61%), opsoclonus (59%), tremors (46%), sleep disturbances (45%), temper tantrums (38%), vomiting (27%), fever (13%), headache (9%) and other symptoms (13%).
The researchers reviewed associations of symptoms at onset to determine the frequency of other symptoms for each individual symptom. Ataxia was present with 89% or higher instances of the other reported symptoms. Of note, some symptoms occurred more frequently than expected, such as temper tantrums and tremors in approximately 70% of patients with sleep disturbances. Myoclonus and opsoclonus, as well as fever and vomiting, also were significantly associated with the presence of other symptoms.
Two-thirds of the registry patients (69%) were diagnosed within 3 months of symptom onset, and 83% of these were diagnosed by a neurologist. Based on the Mitchell-Pike OMS severity scale, 59% of the patients met criteria for severe disease, 34% were classified as moderate, and 7% were mild. The registry is ongoing, but the current data provide insight on the clinical picture and common symptoms of OMS, the researchers said.
OMS Life was established in 2012 to support patients, caregivers, and researchers in raising awareness of opsoclonus-myoclonus syndrome as well as funds for research.
The study was supported by the OMSLife Foundation, NORD, and Trio Health Analytics. The researchers are employed by these organizations.
WASHINGTON – a rare disease affecting only 1 in 5,000,000 individuals, mostly aged 1-5 years, based on data from a new patient registry.
In partnership with the National Organization of Rare Disorders (NORD) the nonprofit OMSLife Foundation has created a patient registry to better understand the disease experience in patients, wrote Mike Michaelis, chairman of OMSLife, and his colleagues. Early data from 275 enrolled patients were presented in a poster at the NORD Rare Summit, held by the National Organization for Rare Disorders.
The registry patients were mainly born in the United States (86%) and white (74%); approximately half were female. Of 150 patients who indicated symptoms at onset, 87% reported ataxia. Additional symptoms at onset were myoclonus (61%), opsoclonus (59%), tremors (46%), sleep disturbances (45%), temper tantrums (38%), vomiting (27%), fever (13%), headache (9%) and other symptoms (13%).
The researchers reviewed associations of symptoms at onset to determine the frequency of other symptoms for each individual symptom. Ataxia was present with 89% or higher instances of the other reported symptoms. Of note, some symptoms occurred more frequently than expected, such as temper tantrums and tremors in approximately 70% of patients with sleep disturbances. Myoclonus and opsoclonus, as well as fever and vomiting, also were significantly associated with the presence of other symptoms.
Two-thirds of the registry patients (69%) were diagnosed within 3 months of symptom onset, and 83% of these were diagnosed by a neurologist. Based on the Mitchell-Pike OMS severity scale, 59% of the patients met criteria for severe disease, 34% were classified as moderate, and 7% were mild. The registry is ongoing, but the current data provide insight on the clinical picture and common symptoms of OMS, the researchers said.
OMS Life was established in 2012 to support patients, caregivers, and researchers in raising awareness of opsoclonus-myoclonus syndrome as well as funds for research.
The study was supported by the OMSLife Foundation, NORD, and Trio Health Analytics. The researchers are employed by these organizations.
REPORTING FROM NORD SUMMIT 2018
Key clinical point: Most patients with OMS experienced multiple symptoms at disease onset; ataxia was the most common.
Major finding: Approximately 87% of patients with OMS reported ataxia at disease onset and 59% experienced severe disease.
Study details: The data come from a registry including 275 OMS patients.
Disclosures: The study was supported by the OMSLife Foundation, NORD, and Trio Health Analytics. The researchers are employed by these organizations.
Drug overdose deaths down since late 2017
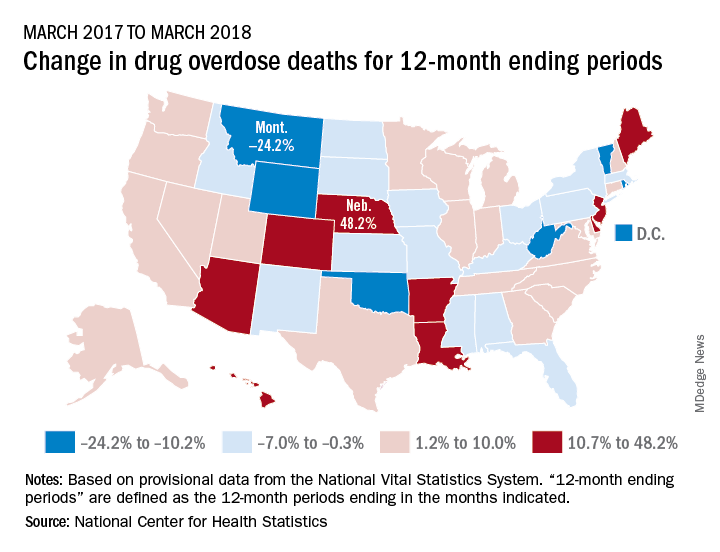
Longer-term data, however, show an increase over the year from March 2017 to March 2018, as the short-term decrease was not enough to overcome the previous year’s increase. The provisional 12-month ending count – deaths during the 12-month period ending in the month indicated – went from 66,859 in March 2017 to 68,690 in March 2018, an increase of 2.7%, the NCHS reported.
That year-long increase was not spread evenly among the states. Nebraska’s 12-month ending count jumped over 48% from March 2017 to March 2018, more than twice as much as second-place Hawaii’s 20.9%. Montana had the largest drop over that year, –24.2%, with Wyoming next at –20.7% and the District of Columbia third at –14.8%, data from the National Vital Statistics System show.
“Provisional drug overdose death data are often incomplete,” the NCHS noted, “and the degree of completeness varies by jurisdiction and 12-month ending period. Consequently, the numbers of drug overdose deaths are underestimated, based on provisional data relative to final data and are subject to random variation.”
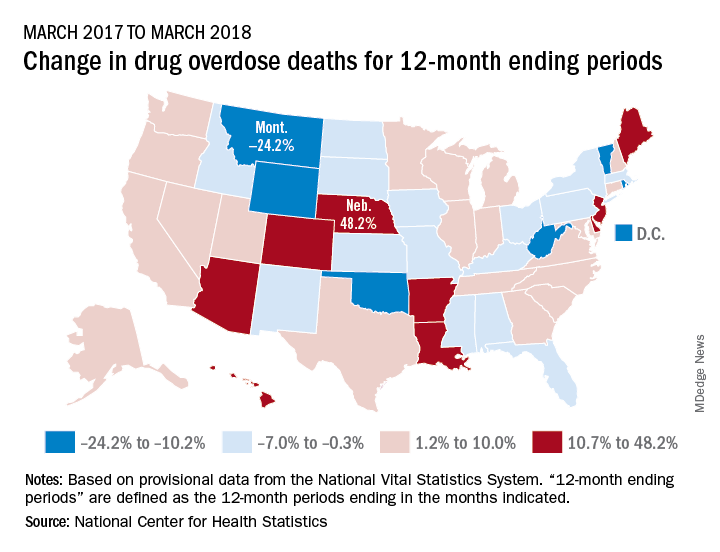
Longer-term data, however, show an increase over the year from March 2017 to March 2018, as the short-term decrease was not enough to overcome the previous year’s increase. The provisional 12-month ending count – deaths during the 12-month period ending in the month indicated – went from 66,859 in March 2017 to 68,690 in March 2018, an increase of 2.7%, the NCHS reported.
That year-long increase was not spread evenly among the states. Nebraska’s 12-month ending count jumped over 48% from March 2017 to March 2018, more than twice as much as second-place Hawaii’s 20.9%. Montana had the largest drop over that year, –24.2%, with Wyoming next at –20.7% and the District of Columbia third at –14.8%, data from the National Vital Statistics System show.
“Provisional drug overdose death data are often incomplete,” the NCHS noted, “and the degree of completeness varies by jurisdiction and 12-month ending period. Consequently, the numbers of drug overdose deaths are underestimated, based on provisional data relative to final data and are subject to random variation.”
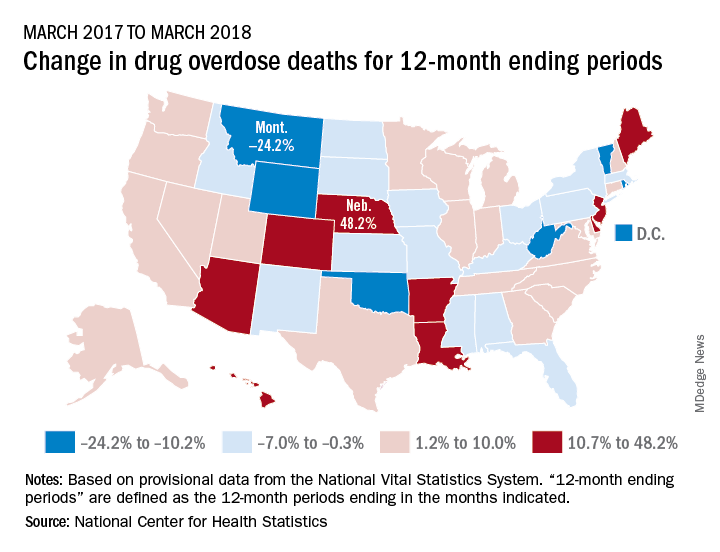
Longer-term data, however, show an increase over the year from March 2017 to March 2018, as the short-term decrease was not enough to overcome the previous year’s increase. The provisional 12-month ending count – deaths during the 12-month period ending in the month indicated – went from 66,859 in March 2017 to 68,690 in March 2018, an increase of 2.7%, the NCHS reported.
That year-long increase was not spread evenly among the states. Nebraska’s 12-month ending count jumped over 48% from March 2017 to March 2018, more than twice as much as second-place Hawaii’s 20.9%. Montana had the largest drop over that year, –24.2%, with Wyoming next at –20.7% and the District of Columbia third at –14.8%, data from the National Vital Statistics System show.
“Provisional drug overdose death data are often incomplete,” the NCHS noted, “and the degree of completeness varies by jurisdiction and 12-month ending period. Consequently, the numbers of drug overdose deaths are underestimated, based on provisional data relative to final data and are subject to random variation.”