User login
Large scar after multiple procedures
Large scar after multiple procedures
A woman with a history of 3 cesarean deliveries, a tubal ligation reversal, and an abdominoplasty discussed treatment for a large uterine fibroid with her ObGyn. She wanted to avoid a large scar. The ObGyn informed the patient that a laparoscopic hysterectomy could not be promised until her pelvic area was inspected to see if minimally invasive surgery safely could be performed.
During surgery, the ObGyn discovered that pelvic adhesions had distorted the patient’s anatomy; he converted to laparotomy, which left a larger scar.
Two days after surgery, the patient was found to have a bowel injury and underwent additional surgery that included placement of surgical mesh, leaving an enlarged scar.
PATIENT'S CLAIM:
The ObGyn was negligent in injuring the patient’s bowel during hysterectomy and not detecting the injury intraoperatively. Her scars were larger because of the additional repair operation.
PHYSICIAN'S DEFENSE:
Bowel injury is a known complication of the procedure. Many bowel injuries are not detected intraoperatively. The ObGyn made every effort to prevent and check for injury during the procedure.
VERDICT:
An Illinois defense verdict was returned.
Uterus and bowel injured during D&C: $1.5M verdict
A 56-year-old woman underwent hysteroscopy and dilation and curettage (D&C). During the procedure, the gynecologist recognized that he had perforated the uterus and injured the bowel and called in a general surgeon to resect 5 cm of the bowel and repair the uterus.
PATIENT'S CLAIM:
The patient has a large abdominal scar and a chronically distended abdomen. She experienced a year of daily pain and suffering. The D&C was unnecessary and improperly performed: the standard of care is for the gynecologist to operate in a gentle manner; that did not occur.
PHYSICIAN'S DEFENSE:
The D&C was medically necessary. The gynecologist exercised the proper standard of care.
VERDICT:
A $1.5 million New Jersey verdict was returned. The jury found the D&C necessary, but determined that the gynecologist deviated from the accepted standard of care in his performance of the procedure.
Injured ureter allegedly not treated
On December 6, a 42-year-old woman underwent hysterectomy. Postoperatively, she reported increasing dysuria with pain and fever.
On December 13, a computed tomography (CT) scan suggested a partial ureter obstruction. Despite test results, the gynecologist elected to continue to monitor the patient.
The patient’s symptoms continued to worsen and, on December 27, she underwent a second CT scan that identified an obstructed ureter. The gynecologist referred the patient to a urologist, who determined that the patient had sustained a significant ureter injury that required placement of a nephrostomy tube.
PATIENT'S CLAIM:
The gynecologist failed to identify the injury during surgery. The gynecologist was negligent in not consulting a urologist after results of the first CT scan.
PHYSICIAN'S DEFENSE:
Uterine injury is a known complication of the procedure. The gynecologist inspected adjacent organs during surgery but did not find an injury. Postoperative treatment was appropriate.
VERDICT:
The case was presented before a medical review board that concluded that there was no error after the first injury, there was no duty to trace the ureter, and a urology consult was not required after the first CT scan. A Louisiana defense verdict was returned.
Was FHR properly monitored?
After a failed nonstress test, a mother was admitted to triage for blood pressure monitoring. Fetal heart-rate (FHR) monitoring was discontinued at that time. Later that day, FHR monitoring was resumed, fetal distress was detected, and an emergency cesarean delivery was performed. Placental abruption resulted in hypoxia in the baby; she received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The pregnancy was at high risk because of the mother’s hypertension. The ObGyns misread the FHR at admission and discontinued FHR monitoring too early. If continuous FHR monitoring had occurred, fetal distress would have been detected earlier, resulting in a better outcome for the baby.
PHYSICIAN'S DEFENSE:
There were no signs of fetal distress when the FHR monitoring was discontinued. Placental abruption is an acute event that cannot be predicted.
VERDICT:
A Missouri defense verdict was returned.
Should the ObGyn have come to the hospital earlier?
At 39 weeks’ gestation, a mother arrived at the hospital for induction of labor. That evening, the ObGyn, who was not at the hospital, was notified that the mother had an elevated temperature and that the FHR indicated tachycardia. The ObGyn prescribed antibiotics, and the fever subsided. After an hour, the patient was fully dilated and started to push under a nurse’s supervision. Twenty minutes later, the ObGyn was notified that the fetus was experiencing variable decelerations. The ObGyn arrived in 30 minutes and ordered a cesarean delivery. The baby was born 24 minutes later.
The baby began to have seizures 10 hours after birth. He was transferred to another hospital and remained in the neonatal intensive care unit for 15 days. The child received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The ObGyn was negligent in not coming to the hospital when the mother was feverish and the fetus tachycardic. The baby experienced an acute hypoxic ischemic injury; an earlier cesarean delivery would have avoided brain injury.
PHYSICIAN'S DEFENSE:
There was no negligence. The infant did not meet all the criteria for an acute hypoxic ischemic injury. Based on a computed tomography scan taken after the seizures began, the infant’s brain injury most likely occurred hours before birth.
VERDICT:
A Virginia defense verdict was returned.
Large scar after multiple procedures
A woman with a history of 3 cesarean deliveries, a tubal ligation reversal, and an abdominoplasty discussed treatment for a large uterine fibroid with her ObGyn. She wanted to avoid a large scar. The ObGyn informed the patient that a laparoscopic hysterectomy could not be promised until her pelvic area was inspected to see if minimally invasive surgery safely could be performed.
During surgery, the ObGyn discovered that pelvic adhesions had distorted the patient’s anatomy; he converted to laparotomy, which left a larger scar.
Two days after surgery, the patient was found to have a bowel injury and underwent additional surgery that included placement of surgical mesh, leaving an enlarged scar.
PATIENT'S CLAIM:
The ObGyn was negligent in injuring the patient’s bowel during hysterectomy and not detecting the injury intraoperatively. Her scars were larger because of the additional repair operation.
PHYSICIAN'S DEFENSE:
Bowel injury is a known complication of the procedure. Many bowel injuries are not detected intraoperatively. The ObGyn made every effort to prevent and check for injury during the procedure.
VERDICT:
An Illinois defense verdict was returned.
Uterus and bowel injured during D&C: $1.5M verdict
A 56-year-old woman underwent hysteroscopy and dilation and curettage (D&C). During the procedure, the gynecologist recognized that he had perforated the uterus and injured the bowel and called in a general surgeon to resect 5 cm of the bowel and repair the uterus.
PATIENT'S CLAIM:
The patient has a large abdominal scar and a chronically distended abdomen. She experienced a year of daily pain and suffering. The D&C was unnecessary and improperly performed: the standard of care is for the gynecologist to operate in a gentle manner; that did not occur.
PHYSICIAN'S DEFENSE:
The D&C was medically necessary. The gynecologist exercised the proper standard of care.
VERDICT:
A $1.5 million New Jersey verdict was returned. The jury found the D&C necessary, but determined that the gynecologist deviated from the accepted standard of care in his performance of the procedure.
Injured ureter allegedly not treated
On December 6, a 42-year-old woman underwent hysterectomy. Postoperatively, she reported increasing dysuria with pain and fever.
On December 13, a computed tomography (CT) scan suggested a partial ureter obstruction. Despite test results, the gynecologist elected to continue to monitor the patient.
The patient’s symptoms continued to worsen and, on December 27, she underwent a second CT scan that identified an obstructed ureter. The gynecologist referred the patient to a urologist, who determined that the patient had sustained a significant ureter injury that required placement of a nephrostomy tube.
PATIENT'S CLAIM:
The gynecologist failed to identify the injury during surgery. The gynecologist was negligent in not consulting a urologist after results of the first CT scan.
PHYSICIAN'S DEFENSE:
Uterine injury is a known complication of the procedure. The gynecologist inspected adjacent organs during surgery but did not find an injury. Postoperative treatment was appropriate.
VERDICT:
The case was presented before a medical review board that concluded that there was no error after the first injury, there was no duty to trace the ureter, and a urology consult was not required after the first CT scan. A Louisiana defense verdict was returned.
Was FHR properly monitored?
After a failed nonstress test, a mother was admitted to triage for blood pressure monitoring. Fetal heart-rate (FHR) monitoring was discontinued at that time. Later that day, FHR monitoring was resumed, fetal distress was detected, and an emergency cesarean delivery was performed. Placental abruption resulted in hypoxia in the baby; she received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The pregnancy was at high risk because of the mother’s hypertension. The ObGyns misread the FHR at admission and discontinued FHR monitoring too early. If continuous FHR monitoring had occurred, fetal distress would have been detected earlier, resulting in a better outcome for the baby.
PHYSICIAN'S DEFENSE:
There were no signs of fetal distress when the FHR monitoring was discontinued. Placental abruption is an acute event that cannot be predicted.
VERDICT:
A Missouri defense verdict was returned.
Should the ObGyn have come to the hospital earlier?
At 39 weeks’ gestation, a mother arrived at the hospital for induction of labor. That evening, the ObGyn, who was not at the hospital, was notified that the mother had an elevated temperature and that the FHR indicated tachycardia. The ObGyn prescribed antibiotics, and the fever subsided. After an hour, the patient was fully dilated and started to push under a nurse’s supervision. Twenty minutes later, the ObGyn was notified that the fetus was experiencing variable decelerations. The ObGyn arrived in 30 minutes and ordered a cesarean delivery. The baby was born 24 minutes later.
The baby began to have seizures 10 hours after birth. He was transferred to another hospital and remained in the neonatal intensive care unit for 15 days. The child received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The ObGyn was negligent in not coming to the hospital when the mother was feverish and the fetus tachycardic. The baby experienced an acute hypoxic ischemic injury; an earlier cesarean delivery would have avoided brain injury.
PHYSICIAN'S DEFENSE:
There was no negligence. The infant did not meet all the criteria for an acute hypoxic ischemic injury. Based on a computed tomography scan taken after the seizures began, the infant’s brain injury most likely occurred hours before birth.
VERDICT:
A Virginia defense verdict was returned.
Large scar after multiple procedures
A woman with a history of 3 cesarean deliveries, a tubal ligation reversal, and an abdominoplasty discussed treatment for a large uterine fibroid with her ObGyn. She wanted to avoid a large scar. The ObGyn informed the patient that a laparoscopic hysterectomy could not be promised until her pelvic area was inspected to see if minimally invasive surgery safely could be performed.
During surgery, the ObGyn discovered that pelvic adhesions had distorted the patient’s anatomy; he converted to laparotomy, which left a larger scar.
Two days after surgery, the patient was found to have a bowel injury and underwent additional surgery that included placement of surgical mesh, leaving an enlarged scar.
PATIENT'S CLAIM:
The ObGyn was negligent in injuring the patient’s bowel during hysterectomy and not detecting the injury intraoperatively. Her scars were larger because of the additional repair operation.
PHYSICIAN'S DEFENSE:
Bowel injury is a known complication of the procedure. Many bowel injuries are not detected intraoperatively. The ObGyn made every effort to prevent and check for injury during the procedure.
VERDICT:
An Illinois defense verdict was returned.
Uterus and bowel injured during D&C: $1.5M verdict
A 56-year-old woman underwent hysteroscopy and dilation and curettage (D&C). During the procedure, the gynecologist recognized that he had perforated the uterus and injured the bowel and called in a general surgeon to resect 5 cm of the bowel and repair the uterus.
PATIENT'S CLAIM:
The patient has a large abdominal scar and a chronically distended abdomen. She experienced a year of daily pain and suffering. The D&C was unnecessary and improperly performed: the standard of care is for the gynecologist to operate in a gentle manner; that did not occur.
PHYSICIAN'S DEFENSE:
The D&C was medically necessary. The gynecologist exercised the proper standard of care.
VERDICT:
A $1.5 million New Jersey verdict was returned. The jury found the D&C necessary, but determined that the gynecologist deviated from the accepted standard of care in his performance of the procedure.
Injured ureter allegedly not treated
On December 6, a 42-year-old woman underwent hysterectomy. Postoperatively, she reported increasing dysuria with pain and fever.
On December 13, a computed tomography (CT) scan suggested a partial ureter obstruction. Despite test results, the gynecologist elected to continue to monitor the patient.
The patient’s symptoms continued to worsen and, on December 27, she underwent a second CT scan that identified an obstructed ureter. The gynecologist referred the patient to a urologist, who determined that the patient had sustained a significant ureter injury that required placement of a nephrostomy tube.
PATIENT'S CLAIM:
The gynecologist failed to identify the injury during surgery. The gynecologist was negligent in not consulting a urologist after results of the first CT scan.
PHYSICIAN'S DEFENSE:
Uterine injury is a known complication of the procedure. The gynecologist inspected adjacent organs during surgery but did not find an injury. Postoperative treatment was appropriate.
VERDICT:
The case was presented before a medical review board that concluded that there was no error after the first injury, there was no duty to trace the ureter, and a urology consult was not required after the first CT scan. A Louisiana defense verdict was returned.
Was FHR properly monitored?
After a failed nonstress test, a mother was admitted to triage for blood pressure monitoring. Fetal heart-rate (FHR) monitoring was discontinued at that time. Later that day, FHR monitoring was resumed, fetal distress was detected, and an emergency cesarean delivery was performed. Placental abruption resulted in hypoxia in the baby; she received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The pregnancy was at high risk because of the mother’s hypertension. The ObGyns misread the FHR at admission and discontinued FHR monitoring too early. If continuous FHR monitoring had occurred, fetal distress would have been detected earlier, resulting in a better outcome for the baby.
PHYSICIAN'S DEFENSE:
There were no signs of fetal distress when the FHR monitoring was discontinued. Placental abruption is an acute event that cannot be predicted.
VERDICT:
A Missouri defense verdict was returned.
Should the ObGyn have come to the hospital earlier?
At 39 weeks’ gestation, a mother arrived at the hospital for induction of labor. That evening, the ObGyn, who was not at the hospital, was notified that the mother had an elevated temperature and that the FHR indicated tachycardia. The ObGyn prescribed antibiotics, and the fever subsided. After an hour, the patient was fully dilated and started to push under a nurse’s supervision. Twenty minutes later, the ObGyn was notified that the fetus was experiencing variable decelerations. The ObGyn arrived in 30 minutes and ordered a cesarean delivery. The baby was born 24 minutes later.
The baby began to have seizures 10 hours after birth. He was transferred to another hospital and remained in the neonatal intensive care unit for 15 days. The child received a diagnosis of cerebral palsy.
PARENT'S CLAIM:
The ObGyn was negligent in not coming to the hospital when the mother was feverish and the fetus tachycardic. The baby experienced an acute hypoxic ischemic injury; an earlier cesarean delivery would have avoided brain injury.
PHYSICIAN'S DEFENSE:
There was no negligence. The infant did not meet all the criteria for an acute hypoxic ischemic injury. Based on a computed tomography scan taken after the seizures began, the infant’s brain injury most likely occurred hours before birth.
VERDICT:
A Virginia defense verdict was returned.
Letters to the Editor: Alternatives to DEET for pregnant patients; Tissue extraction
“What Insect repellents are safe during pregnancy?”
ANUSHKA CHELLIAH, MD, AND PATRICK DUFF, MD (JUNE 2016)
Alternatives to DEET
Picaridin is not mentioned in this brief report from Drs. Chelliah and Duff. I suggest reviewing the July 2015 Consumer Reports article on repellents; picaridin is a likely safer alternative to DEET, with the highest efficacy of all those tested, at least in Sawyer Fisherman’s Formula Picaridin Insect Repellent and Natrapel 8 Hour Insect Repellent. Products that have little or no efficacy also were not mentioned, including Avon Skin So Soft, Coleman Naturals Insect Repellent Snap Band, and SuperBand Wristband. In addition, the concentration of products is very important, as is the precise formulation within brands. For example, Off! Deep Woods VIII (with DEET 25%) is very effective versus Off! FamilyCare II Clean Feel (with picaridin 5%), which has very little benefit.
David H. Janowitz, MD
Houston, Texas
Drs. Chelliah and Duff respond
In our short discussion of mosquito repellents, we based our recommendations on publications from the Centers for Disease Control and Prevention (CDC) and the Florida Department of Health. Those publications presented DEET (N,N-diethyl-m-toluamide) at the top of the list for preferred repellents. A recent publication from the Organization of Teratology Information Specialists (MotherToBaby, September 2013) indicated that, in a concentration of 20% to 30%, DEET was safe in pregnancy and was effective in protecting against 90% of all mosquito bites and tick attachments. Increasing the concentration of DEET above 30% does not enhance the product’s effectiveness or prolong its duration of action.
However, Dr. Janowitz is correct in stating that other agents are also highly effective and safe in pregnancy. These agents include picaridin (20%) and oil of lemon/eucalyptus (30%). We thank Dr. Janowitz for directing us to the most recent testing program conducted by Consumer Reports.1 That testing program demonstrated that Sawyer Fisherman’s Formula Picaridin and Natrapel 8 Hour, which each contain 20% picaridin, and Off! Deep Woods VIII, which contains 25% DEET, kept Aedes mosquitoes from biting for approximately 8 hours. The Sawyer product was also effective in preventing bites from the Culex mosquitoes, which carry West Nile virus, and deer ticks, which can transmit Lyme disease. Repel Lemon Eucalyptus (30%) stopped Aedes mosquito bites for 7 hours.
In the Consumer Reports testing program, IR3535 products, which we recommended in our article, did not perform well, nor did repellents that contained only 7% DEET or less than 20% picaridin. Moreover, products made from natural plant oils—such as citronella, lemongrass oil, cedar oil, geraniol, rosemary oil, and cinnamon oil—were not particularly effective. Some did not last for more than 1 hour; some failed immediately.
When applying any of these products, individuals should observe the following guidelines:
- apply insect repellents only to exposed skin or clothing
- do not apply repellents on cuts, wounds, or abraded skin or immediately after shaving
- avoid the eyes and mouth when applying repellent to the face
- after exposure is over, wash the skin with soap and water
- clothing that has been treated with one of these agents or with permethrin should be washed separately before it is worn again.
Reference
- Byrne S. Mosquito repellents that best protect against Zika. Consumer Reports. http://www.consumerreports.org/insect-repellents/mosquito-repellents-that-best-protect-against-zika/. Updated April 16, 2016. Accessed July 25, 2016.
“Tissue extraction: Can the pendulum change direction?”
ARNOLD P. ADVINCULA, MD (JUNE 2016)
We have met the enemy and he is us
While I share the optimism Dr. Advincula expressed in his recent guest editorial regarding a change in the direction of the pendulum that swung away from use of the power morcellator, I feel compelled to express the opinion that this entire fiasco has been nothing other than an outrageous regulatory overreach.
Shortly after the US Food and Drug Administration (FDA) issued its proclamation in April 2014, the Society of Gynecologic Oncology repudiated the bogus statistics that were being used to describe the incidence of leiomyosarcoma and, further, stated that it would not matter how someone’s uterus containing this rare tumor was removed because the outcome would be poor. Similarly, the American Journal of Obstetrics and Gynecology published an article enumerating the expected significant increase in complications and the resulting misery that could be expected for patients whose management was diverted from minimally invasive to open hysterectomy.1 The AAGL also expressed opinions that this was an unnecessary, and counterproductive, policy—all to no avail.
My optimism, however, is tempered by a number of questions: 1) Why did it take more than a year for 36 nationally recognized gynecologic surgeons to write a letter to the FDA denouncing the warning, yet again, and reiterating the errors in analysis used to establish the policy? 2) Why are gynecologic surgeons only now being asked to serve in the FDA’s Network of Experts? Should not that have been the case before the warning was issued? 3) If the perioperative outcomes are similar using a containment bag compared with open morcellation, what is the benefit of using the containment system? I, for one, think that prolonging a procedure another half hour is significant.
The FDA’s egregious policy clearly has had a net negative impact on the welfare of our patients. The gynecologic surgeon community should have pushed back more forcefully and effectively. I hope the next time something like this happens (and it will) we can be better advocates for our patients.
Mark S. Finkelston, DO
Shawnee Mission, Kansas
Reference
- Siedhoff MT, Wheeler SB, Rutstein SE, et al. Laparoscopic hysterectomy with morcellation vs abdominal hysterectomy for presumed fibroid tumors in premenopausal women: a decision analysis. Am J Obstet Gynecol. 2015;212(5):591.e1−e8.
Dr. Advincula responds
I thank Dr. Finkelston for his thoughts regarding my editorial. There is no doubt that the issues surrounding tissue extraction have been heated. Although I do not have definitive answers that explain all of the various reactions, whether immediate or delayed, to the cascade of events surrounding morcellation, I do believe that much of it was a response to N-of-1 policy-making, as very nicely discussed in a New England Journal of Medicine article by Lisa Rosenbaum.1 We must continue to foster constructive dialogues with our regulatory bodies and cultivate the spirit of innovation that has brought so many advances to the field of surgery. Ultimately, going forward, it will be important for clinicians and other health care providers to speak up and not remain silent for fear of being vilified.
Reference
- Rosenbaum L. N-of-1 policymaking—tragedy, trade-offs, and the demise of morcellation. N Engl J Med. 2016;374(10):986−990.
Vaginal hysterectomy solves the tissue morcellation dilemma
Dr. Advincula starts his guest editorial with the statement, “With practical, evidence-based, sound clinical judgement, I believe that it can.”
In fact, what “practical, evidence-based, sound clinical judgement” supports is a return to vaginal hysterectomy with transvaginal extracorporeal morcellation techniques. As Dr. Carl Zimmerman said in a recent debate at the Society of Gynecologic Surgeons (SGS annual meeting), “There is no recorded case of a vaginal hysterectomy with morcellation upgrading a patient with leiomyosarcoma.” In addition, the majority of cases in which Dr. Advincula and others are performing robot-assisted laparoscopic hysterectomy or total laparoscopic hysterectomy have this clinical and demographic profile: average age, 42; average parity, G2; average body mass index, 30; most common diagnosis, abnormal uterine bleeding, fibroids; most common pathology, fibroids; average uterine weight, 165 g. The majority of these can be performed much more safely, quickly, and cost effectively by transvaginal hysterectomy/morcellation. Please see an excellent commentary by Dr. Andrew Walter, immediate past president of SGS, on “Why we should strive for a vaginal hysterectomy rate of 40%.”1
But the main reason Dr. Advincula should not be given a voice on this issue is because he has significant financial conflict of interest with the medical device industry. Should he even be on the OBG <scaps>Management</scaps> board of editors? I do not believe the rest of your editors have anywhere near his level of conflict of interest. Should he not be asked to recuse himself in this debate or abandon his financial connections with the medical device industry? Is this not the whole purpose of the Sunshine Act? Please, should you not be supporting what is in the best interest of our patients and payers?
R. Bruce Councell, MD
Asheville, North Carolina
Reference
- Walter AJ. Why we should strive for a vaginal hysterectomy rate of 40%. ObGyn News. http://www.obgynnews.com/?id=11146&tx_ttnews[tt_news]=505393&cHash=d0dd4348213d571a2dd0f7c6a6873091. Published May 6, 2016. Accessed July 27, 2016.
Dr. Barbieri responds
At OBG Management, we wholeheartedly agree with Dr. Councell that vaginal hysterectomy is an excellent approach to removing the uterus in most women with noncancer indications for surgery. Our recently featured articles focused on vaginal hysterectomy include: “Transforming vaginal hysterectomy: 7 solutions to the most daunting challenges,” “Is energy-based vessel sealing safer than suturing for vaginal hysterectomy?,” Is same-day discharge feasible and safe for women undergoing vaginal hysterectomy?,” and “Can we reduce the use of abdominal hysterectomy and increase the use of vaginal and laparoscopic approaches?” We plan to publish more content on advances in both vaginal and laparoscopic surgery.
We are proud to have Dr. Advincula, an internationally recognized leader in gynecologic surgery, serve on the OBG Management Editorial Board. His expertise and perspective is of great value to our readers. It is true that many leading surgeons, including Dr. Advincula, serve as consultants with manufacturers of surgical devices. Working together, clinical experts and device manufacturers help to advance medical care. In his editorial, Dr. Advincula did disclose these relationships. As a check on the quality and balance in our editorial material, I personally review all content and I have no financial relationships with any pharmaceutical or device manufacturer.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
“What Insect repellents are safe during pregnancy?”
ANUSHKA CHELLIAH, MD, AND PATRICK DUFF, MD (JUNE 2016)
Alternatives to DEET
Picaridin is not mentioned in this brief report from Drs. Chelliah and Duff. I suggest reviewing the July 2015 Consumer Reports article on repellents; picaridin is a likely safer alternative to DEET, with the highest efficacy of all those tested, at least in Sawyer Fisherman’s Formula Picaridin Insect Repellent and Natrapel 8 Hour Insect Repellent. Products that have little or no efficacy also were not mentioned, including Avon Skin So Soft, Coleman Naturals Insect Repellent Snap Band, and SuperBand Wristband. In addition, the concentration of products is very important, as is the precise formulation within brands. For example, Off! Deep Woods VIII (with DEET 25%) is very effective versus Off! FamilyCare II Clean Feel (with picaridin 5%), which has very little benefit.
David H. Janowitz, MD
Houston, Texas
Drs. Chelliah and Duff respond
In our short discussion of mosquito repellents, we based our recommendations on publications from the Centers for Disease Control and Prevention (CDC) and the Florida Department of Health. Those publications presented DEET (N,N-diethyl-m-toluamide) at the top of the list for preferred repellents. A recent publication from the Organization of Teratology Information Specialists (MotherToBaby, September 2013) indicated that, in a concentration of 20% to 30%, DEET was safe in pregnancy and was effective in protecting against 90% of all mosquito bites and tick attachments. Increasing the concentration of DEET above 30% does not enhance the product’s effectiveness or prolong its duration of action.
However, Dr. Janowitz is correct in stating that other agents are also highly effective and safe in pregnancy. These agents include picaridin (20%) and oil of lemon/eucalyptus (30%). We thank Dr. Janowitz for directing us to the most recent testing program conducted by Consumer Reports.1 That testing program demonstrated that Sawyer Fisherman’s Formula Picaridin and Natrapel 8 Hour, which each contain 20% picaridin, and Off! Deep Woods VIII, which contains 25% DEET, kept Aedes mosquitoes from biting for approximately 8 hours. The Sawyer product was also effective in preventing bites from the Culex mosquitoes, which carry West Nile virus, and deer ticks, which can transmit Lyme disease. Repel Lemon Eucalyptus (30%) stopped Aedes mosquito bites for 7 hours.
In the Consumer Reports testing program, IR3535 products, which we recommended in our article, did not perform well, nor did repellents that contained only 7% DEET or less than 20% picaridin. Moreover, products made from natural plant oils—such as citronella, lemongrass oil, cedar oil, geraniol, rosemary oil, and cinnamon oil—were not particularly effective. Some did not last for more than 1 hour; some failed immediately.
When applying any of these products, individuals should observe the following guidelines:
- apply insect repellents only to exposed skin or clothing
- do not apply repellents on cuts, wounds, or abraded skin or immediately after shaving
- avoid the eyes and mouth when applying repellent to the face
- after exposure is over, wash the skin with soap and water
- clothing that has been treated with one of these agents or with permethrin should be washed separately before it is worn again.
Reference
- Byrne S. Mosquito repellents that best protect against Zika. Consumer Reports. http://www.consumerreports.org/insect-repellents/mosquito-repellents-that-best-protect-against-zika/. Updated April 16, 2016. Accessed July 25, 2016.
“Tissue extraction: Can the pendulum change direction?”
ARNOLD P. ADVINCULA, MD (JUNE 2016)
We have met the enemy and he is us
While I share the optimism Dr. Advincula expressed in his recent guest editorial regarding a change in the direction of the pendulum that swung away from use of the power morcellator, I feel compelled to express the opinion that this entire fiasco has been nothing other than an outrageous regulatory overreach.
Shortly after the US Food and Drug Administration (FDA) issued its proclamation in April 2014, the Society of Gynecologic Oncology repudiated the bogus statistics that were being used to describe the incidence of leiomyosarcoma and, further, stated that it would not matter how someone’s uterus containing this rare tumor was removed because the outcome would be poor. Similarly, the American Journal of Obstetrics and Gynecology published an article enumerating the expected significant increase in complications and the resulting misery that could be expected for patients whose management was diverted from minimally invasive to open hysterectomy.1 The AAGL also expressed opinions that this was an unnecessary, and counterproductive, policy—all to no avail.
My optimism, however, is tempered by a number of questions: 1) Why did it take more than a year for 36 nationally recognized gynecologic surgeons to write a letter to the FDA denouncing the warning, yet again, and reiterating the errors in analysis used to establish the policy? 2) Why are gynecologic surgeons only now being asked to serve in the FDA’s Network of Experts? Should not that have been the case before the warning was issued? 3) If the perioperative outcomes are similar using a containment bag compared with open morcellation, what is the benefit of using the containment system? I, for one, think that prolonging a procedure another half hour is significant.
The FDA’s egregious policy clearly has had a net negative impact on the welfare of our patients. The gynecologic surgeon community should have pushed back more forcefully and effectively. I hope the next time something like this happens (and it will) we can be better advocates for our patients.
Mark S. Finkelston, DO
Shawnee Mission, Kansas
Reference
- Siedhoff MT, Wheeler SB, Rutstein SE, et al. Laparoscopic hysterectomy with morcellation vs abdominal hysterectomy for presumed fibroid tumors in premenopausal women: a decision analysis. Am J Obstet Gynecol. 2015;212(5):591.e1−e8.
Dr. Advincula responds
I thank Dr. Finkelston for his thoughts regarding my editorial. There is no doubt that the issues surrounding tissue extraction have been heated. Although I do not have definitive answers that explain all of the various reactions, whether immediate or delayed, to the cascade of events surrounding morcellation, I do believe that much of it was a response to N-of-1 policy-making, as very nicely discussed in a New England Journal of Medicine article by Lisa Rosenbaum.1 We must continue to foster constructive dialogues with our regulatory bodies and cultivate the spirit of innovation that has brought so many advances to the field of surgery. Ultimately, going forward, it will be important for clinicians and other health care providers to speak up and not remain silent for fear of being vilified.
Reference
- Rosenbaum L. N-of-1 policymaking—tragedy, trade-offs, and the demise of morcellation. N Engl J Med. 2016;374(10):986−990.
Vaginal hysterectomy solves the tissue morcellation dilemma
Dr. Advincula starts his guest editorial with the statement, “With practical, evidence-based, sound clinical judgement, I believe that it can.”
In fact, what “practical, evidence-based, sound clinical judgement” supports is a return to vaginal hysterectomy with transvaginal extracorporeal morcellation techniques. As Dr. Carl Zimmerman said in a recent debate at the Society of Gynecologic Surgeons (SGS annual meeting), “There is no recorded case of a vaginal hysterectomy with morcellation upgrading a patient with leiomyosarcoma.” In addition, the majority of cases in which Dr. Advincula and others are performing robot-assisted laparoscopic hysterectomy or total laparoscopic hysterectomy have this clinical and demographic profile: average age, 42; average parity, G2; average body mass index, 30; most common diagnosis, abnormal uterine bleeding, fibroids; most common pathology, fibroids; average uterine weight, 165 g. The majority of these can be performed much more safely, quickly, and cost effectively by transvaginal hysterectomy/morcellation. Please see an excellent commentary by Dr. Andrew Walter, immediate past president of SGS, on “Why we should strive for a vaginal hysterectomy rate of 40%.”1
But the main reason Dr. Advincula should not be given a voice on this issue is because he has significant financial conflict of interest with the medical device industry. Should he even be on the OBG <scaps>Management</scaps> board of editors? I do not believe the rest of your editors have anywhere near his level of conflict of interest. Should he not be asked to recuse himself in this debate or abandon his financial connections with the medical device industry? Is this not the whole purpose of the Sunshine Act? Please, should you not be supporting what is in the best interest of our patients and payers?
R. Bruce Councell, MD
Asheville, North Carolina
Reference
- Walter AJ. Why we should strive for a vaginal hysterectomy rate of 40%. ObGyn News. http://www.obgynnews.com/?id=11146&tx_ttnews[tt_news]=505393&cHash=d0dd4348213d571a2dd0f7c6a6873091. Published May 6, 2016. Accessed July 27, 2016.
Dr. Barbieri responds
At OBG Management, we wholeheartedly agree with Dr. Councell that vaginal hysterectomy is an excellent approach to removing the uterus in most women with noncancer indications for surgery. Our recently featured articles focused on vaginal hysterectomy include: “Transforming vaginal hysterectomy: 7 solutions to the most daunting challenges,” “Is energy-based vessel sealing safer than suturing for vaginal hysterectomy?,” Is same-day discharge feasible and safe for women undergoing vaginal hysterectomy?,” and “Can we reduce the use of abdominal hysterectomy and increase the use of vaginal and laparoscopic approaches?” We plan to publish more content on advances in both vaginal and laparoscopic surgery.
We are proud to have Dr. Advincula, an internationally recognized leader in gynecologic surgery, serve on the OBG Management Editorial Board. His expertise and perspective is of great value to our readers. It is true that many leading surgeons, including Dr. Advincula, serve as consultants with manufacturers of surgical devices. Working together, clinical experts and device manufacturers help to advance medical care. In his editorial, Dr. Advincula did disclose these relationships. As a check on the quality and balance in our editorial material, I personally review all content and I have no financial relationships with any pharmaceutical or device manufacturer.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
“What Insect repellents are safe during pregnancy?”
ANUSHKA CHELLIAH, MD, AND PATRICK DUFF, MD (JUNE 2016)
Alternatives to DEET
Picaridin is not mentioned in this brief report from Drs. Chelliah and Duff. I suggest reviewing the July 2015 Consumer Reports article on repellents; picaridin is a likely safer alternative to DEET, with the highest efficacy of all those tested, at least in Sawyer Fisherman’s Formula Picaridin Insect Repellent and Natrapel 8 Hour Insect Repellent. Products that have little or no efficacy also were not mentioned, including Avon Skin So Soft, Coleman Naturals Insect Repellent Snap Band, and SuperBand Wristband. In addition, the concentration of products is very important, as is the precise formulation within brands. For example, Off! Deep Woods VIII (with DEET 25%) is very effective versus Off! FamilyCare II Clean Feel (with picaridin 5%), which has very little benefit.
David H. Janowitz, MD
Houston, Texas
Drs. Chelliah and Duff respond
In our short discussion of mosquito repellents, we based our recommendations on publications from the Centers for Disease Control and Prevention (CDC) and the Florida Department of Health. Those publications presented DEET (N,N-diethyl-m-toluamide) at the top of the list for preferred repellents. A recent publication from the Organization of Teratology Information Specialists (MotherToBaby, September 2013) indicated that, in a concentration of 20% to 30%, DEET was safe in pregnancy and was effective in protecting against 90% of all mosquito bites and tick attachments. Increasing the concentration of DEET above 30% does not enhance the product’s effectiveness or prolong its duration of action.
However, Dr. Janowitz is correct in stating that other agents are also highly effective and safe in pregnancy. These agents include picaridin (20%) and oil of lemon/eucalyptus (30%). We thank Dr. Janowitz for directing us to the most recent testing program conducted by Consumer Reports.1 That testing program demonstrated that Sawyer Fisherman’s Formula Picaridin and Natrapel 8 Hour, which each contain 20% picaridin, and Off! Deep Woods VIII, which contains 25% DEET, kept Aedes mosquitoes from biting for approximately 8 hours. The Sawyer product was also effective in preventing bites from the Culex mosquitoes, which carry West Nile virus, and deer ticks, which can transmit Lyme disease. Repel Lemon Eucalyptus (30%) stopped Aedes mosquito bites for 7 hours.
In the Consumer Reports testing program, IR3535 products, which we recommended in our article, did not perform well, nor did repellents that contained only 7% DEET or less than 20% picaridin. Moreover, products made from natural plant oils—such as citronella, lemongrass oil, cedar oil, geraniol, rosemary oil, and cinnamon oil—were not particularly effective. Some did not last for more than 1 hour; some failed immediately.
When applying any of these products, individuals should observe the following guidelines:
- apply insect repellents only to exposed skin or clothing
- do not apply repellents on cuts, wounds, or abraded skin or immediately after shaving
- avoid the eyes and mouth when applying repellent to the face
- after exposure is over, wash the skin with soap and water
- clothing that has been treated with one of these agents or with permethrin should be washed separately before it is worn again.
Reference
- Byrne S. Mosquito repellents that best protect against Zika. Consumer Reports. http://www.consumerreports.org/insect-repellents/mosquito-repellents-that-best-protect-against-zika/. Updated April 16, 2016. Accessed July 25, 2016.
“Tissue extraction: Can the pendulum change direction?”
ARNOLD P. ADVINCULA, MD (JUNE 2016)
We have met the enemy and he is us
While I share the optimism Dr. Advincula expressed in his recent guest editorial regarding a change in the direction of the pendulum that swung away from use of the power morcellator, I feel compelled to express the opinion that this entire fiasco has been nothing other than an outrageous regulatory overreach.
Shortly after the US Food and Drug Administration (FDA) issued its proclamation in April 2014, the Society of Gynecologic Oncology repudiated the bogus statistics that were being used to describe the incidence of leiomyosarcoma and, further, stated that it would not matter how someone’s uterus containing this rare tumor was removed because the outcome would be poor. Similarly, the American Journal of Obstetrics and Gynecology published an article enumerating the expected significant increase in complications and the resulting misery that could be expected for patients whose management was diverted from minimally invasive to open hysterectomy.1 The AAGL also expressed opinions that this was an unnecessary, and counterproductive, policy—all to no avail.
My optimism, however, is tempered by a number of questions: 1) Why did it take more than a year for 36 nationally recognized gynecologic surgeons to write a letter to the FDA denouncing the warning, yet again, and reiterating the errors in analysis used to establish the policy? 2) Why are gynecologic surgeons only now being asked to serve in the FDA’s Network of Experts? Should not that have been the case before the warning was issued? 3) If the perioperative outcomes are similar using a containment bag compared with open morcellation, what is the benefit of using the containment system? I, for one, think that prolonging a procedure another half hour is significant.
The FDA’s egregious policy clearly has had a net negative impact on the welfare of our patients. The gynecologic surgeon community should have pushed back more forcefully and effectively. I hope the next time something like this happens (and it will) we can be better advocates for our patients.
Mark S. Finkelston, DO
Shawnee Mission, Kansas
Reference
- Siedhoff MT, Wheeler SB, Rutstein SE, et al. Laparoscopic hysterectomy with morcellation vs abdominal hysterectomy for presumed fibroid tumors in premenopausal women: a decision analysis. Am J Obstet Gynecol. 2015;212(5):591.e1−e8.
Dr. Advincula responds
I thank Dr. Finkelston for his thoughts regarding my editorial. There is no doubt that the issues surrounding tissue extraction have been heated. Although I do not have definitive answers that explain all of the various reactions, whether immediate or delayed, to the cascade of events surrounding morcellation, I do believe that much of it was a response to N-of-1 policy-making, as very nicely discussed in a New England Journal of Medicine article by Lisa Rosenbaum.1 We must continue to foster constructive dialogues with our regulatory bodies and cultivate the spirit of innovation that has brought so many advances to the field of surgery. Ultimately, going forward, it will be important for clinicians and other health care providers to speak up and not remain silent for fear of being vilified.
Reference
- Rosenbaum L. N-of-1 policymaking—tragedy, trade-offs, and the demise of morcellation. N Engl J Med. 2016;374(10):986−990.
Vaginal hysterectomy solves the tissue morcellation dilemma
Dr. Advincula starts his guest editorial with the statement, “With practical, evidence-based, sound clinical judgement, I believe that it can.”
In fact, what “practical, evidence-based, sound clinical judgement” supports is a return to vaginal hysterectomy with transvaginal extracorporeal morcellation techniques. As Dr. Carl Zimmerman said in a recent debate at the Society of Gynecologic Surgeons (SGS annual meeting), “There is no recorded case of a vaginal hysterectomy with morcellation upgrading a patient with leiomyosarcoma.” In addition, the majority of cases in which Dr. Advincula and others are performing robot-assisted laparoscopic hysterectomy or total laparoscopic hysterectomy have this clinical and demographic profile: average age, 42; average parity, G2; average body mass index, 30; most common diagnosis, abnormal uterine bleeding, fibroids; most common pathology, fibroids; average uterine weight, 165 g. The majority of these can be performed much more safely, quickly, and cost effectively by transvaginal hysterectomy/morcellation. Please see an excellent commentary by Dr. Andrew Walter, immediate past president of SGS, on “Why we should strive for a vaginal hysterectomy rate of 40%.”1
But the main reason Dr. Advincula should not be given a voice on this issue is because he has significant financial conflict of interest with the medical device industry. Should he even be on the OBG <scaps>Management</scaps> board of editors? I do not believe the rest of your editors have anywhere near his level of conflict of interest. Should he not be asked to recuse himself in this debate or abandon his financial connections with the medical device industry? Is this not the whole purpose of the Sunshine Act? Please, should you not be supporting what is in the best interest of our patients and payers?
R. Bruce Councell, MD
Asheville, North Carolina
Reference
- Walter AJ. Why we should strive for a vaginal hysterectomy rate of 40%. ObGyn News. http://www.obgynnews.com/?id=11146&tx_ttnews[tt_news]=505393&cHash=d0dd4348213d571a2dd0f7c6a6873091. Published May 6, 2016. Accessed July 27, 2016.
Dr. Barbieri responds
At OBG Management, we wholeheartedly agree with Dr. Councell that vaginal hysterectomy is an excellent approach to removing the uterus in most women with noncancer indications for surgery. Our recently featured articles focused on vaginal hysterectomy include: “Transforming vaginal hysterectomy: 7 solutions to the most daunting challenges,” “Is energy-based vessel sealing safer than suturing for vaginal hysterectomy?,” Is same-day discharge feasible and safe for women undergoing vaginal hysterectomy?,” and “Can we reduce the use of abdominal hysterectomy and increase the use of vaginal and laparoscopic approaches?” We plan to publish more content on advances in both vaginal and laparoscopic surgery.
We are proud to have Dr. Advincula, an internationally recognized leader in gynecologic surgery, serve on the OBG Management Editorial Board. His expertise and perspective is of great value to our readers. It is true that many leading surgeons, including Dr. Advincula, serve as consultants with manufacturers of surgical devices. Working together, clinical experts and device manufacturers help to advance medical care. In his editorial, Dr. Advincula did disclose these relationships. As a check on the quality and balance in our editorial material, I personally review all content and I have no financial relationships with any pharmaceutical or device manufacturer.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
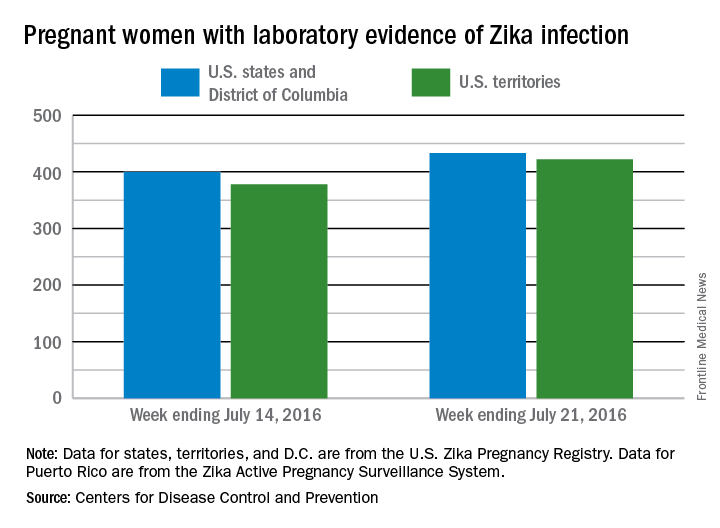
Zika virus RNA detected in serum beyond previously estimated time frame
Zika virus RNA was detected in the serum of five pregnant women beyond previously estimated time frames, according to a new case series study.
“This report adds to the existing evidence that Zika virus RNA in serum may be detected longer than previously expected, an observation now reported among at least eight pregnant women,” reported Dr. Dana Meaney-Delman of the Centers for Disease Control & Prevention, and her colleagues wrote. (Obstet Gynecol. 2016. doi: 10.1097/AOG.0000000000001625).
Five pregnant women who had traveled to or lived in one or more countries with active Zika virus transmission and had prolonged detection of Zika virus RNA in serum were reported to the U.S. Zika Pregnancy Registry, an enhanced surveillance initiative developed by the CDC to collect information on maternal exposure history, clinical presentation, laboratory testing, prenatal imaging, pregnancy screening and complications, fetal and neonatal outcomes, and infant development through the first year of life.
Prolonged detection was defined as the presence of Zika virus RNA detected in serum by real-time reverse transcription-polymerase chain reaction at 14 or more days after symptom onset for symptomatic pregnant women or 21 or more days after last possible exposure to Zika virus for asymptomatic pregnant women. A previous study reported a mean Zika viral RNA duration of 9.9 days, with 14 days being the longest duration of Zika virus RNA detection in a nonpregnant person.
Among the four symptomatic pregnant women, Zika virus RNA was detected in the serum at 17, 23, 44, and 46 days following symptom onset. In the one asymptomatic pregnant woman, Zika virus RNA was detected in serum at 53 days after her travel from an area with active Zika transmission.
Among the five pregnancies, one is ongoing, one was aborted and the fetus tested positive for fetal Zika virus infection, and three resulted in live births of healthy neonates with no reported abnormalities.
“Several questions remain regarding the findings of prolonged detection of Zika virus RNA. Most notably, the duration of Zika virus RNA in serum requires further investigation to determine whether there is a correlation between prolonged viral RNA detection and the presence of infectious virus,” the researchers wrote.
Read the study results here.
On Twitter @jessnicolecraig
Zika virus RNA was detected in the serum of five pregnant women beyond previously estimated time frames, according to a new case series study.
“This report adds to the existing evidence that Zika virus RNA in serum may be detected longer than previously expected, an observation now reported among at least eight pregnant women,” reported Dr. Dana Meaney-Delman of the Centers for Disease Control & Prevention, and her colleagues wrote. (Obstet Gynecol. 2016. doi: 10.1097/AOG.0000000000001625).
Five pregnant women who had traveled to or lived in one or more countries with active Zika virus transmission and had prolonged detection of Zika virus RNA in serum were reported to the U.S. Zika Pregnancy Registry, an enhanced surveillance initiative developed by the CDC to collect information on maternal exposure history, clinical presentation, laboratory testing, prenatal imaging, pregnancy screening and complications, fetal and neonatal outcomes, and infant development through the first year of life.
Prolonged detection was defined as the presence of Zika virus RNA detected in serum by real-time reverse transcription-polymerase chain reaction at 14 or more days after symptom onset for symptomatic pregnant women or 21 or more days after last possible exposure to Zika virus for asymptomatic pregnant women. A previous study reported a mean Zika viral RNA duration of 9.9 days, with 14 days being the longest duration of Zika virus RNA detection in a nonpregnant person.
Among the four symptomatic pregnant women, Zika virus RNA was detected in the serum at 17, 23, 44, and 46 days following symptom onset. In the one asymptomatic pregnant woman, Zika virus RNA was detected in serum at 53 days after her travel from an area with active Zika transmission.
Among the five pregnancies, one is ongoing, one was aborted and the fetus tested positive for fetal Zika virus infection, and three resulted in live births of healthy neonates with no reported abnormalities.
“Several questions remain regarding the findings of prolonged detection of Zika virus RNA. Most notably, the duration of Zika virus RNA in serum requires further investigation to determine whether there is a correlation between prolonged viral RNA detection and the presence of infectious virus,” the researchers wrote.
Read the study results here.
On Twitter @jessnicolecraig
Zika virus RNA was detected in the serum of five pregnant women beyond previously estimated time frames, according to a new case series study.
“This report adds to the existing evidence that Zika virus RNA in serum may be detected longer than previously expected, an observation now reported among at least eight pregnant women,” reported Dr. Dana Meaney-Delman of the Centers for Disease Control & Prevention, and her colleagues wrote. (Obstet Gynecol. 2016. doi: 10.1097/AOG.0000000000001625).
Five pregnant women who had traveled to or lived in one or more countries with active Zika virus transmission and had prolonged detection of Zika virus RNA in serum were reported to the U.S. Zika Pregnancy Registry, an enhanced surveillance initiative developed by the CDC to collect information on maternal exposure history, clinical presentation, laboratory testing, prenatal imaging, pregnancy screening and complications, fetal and neonatal outcomes, and infant development through the first year of life.
Prolonged detection was defined as the presence of Zika virus RNA detected in serum by real-time reverse transcription-polymerase chain reaction at 14 or more days after symptom onset for symptomatic pregnant women or 21 or more days after last possible exposure to Zika virus for asymptomatic pregnant women. A previous study reported a mean Zika viral RNA duration of 9.9 days, with 14 days being the longest duration of Zika virus RNA detection in a nonpregnant person.
Among the four symptomatic pregnant women, Zika virus RNA was detected in the serum at 17, 23, 44, and 46 days following symptom onset. In the one asymptomatic pregnant woman, Zika virus RNA was detected in serum at 53 days after her travel from an area with active Zika transmission.
Among the five pregnancies, one is ongoing, one was aborted and the fetus tested positive for fetal Zika virus infection, and three resulted in live births of healthy neonates with no reported abnormalities.
“Several questions remain regarding the findings of prolonged detection of Zika virus RNA. Most notably, the duration of Zika virus RNA in serum requires further investigation to determine whether there is a correlation between prolonged viral RNA detection and the presence of infectious virus,” the researchers wrote.
Read the study results here.
On Twitter @jessnicolecraig
FROM OBSTETRICS & GYNECOLOGY
CDC warns pregnant women to avoid Miami neighborhood due to Zika risk
Health officials in Florida have identified 10 new cases of locally transmitted Zika virus infections in the neighborhood just north of downtown Miami where four other cases were reported earlier.
Persistent mosquito populations in southern Florida are the leading cause of the disease’s growing incursion into the continental United States, according to Tom Frieden, MD, MPH, director of the Centers for Disease Control and Prevention.
“This suggests that there is a risk of continued, active transmission of Zika in that area,” Dr. Frieden said Aug. 1 during a press call regarding the discovery of new cases by Florida officials.
The CDC is issuing new recommendations for people who either have visited, are currently visiting, or plan to visit this Miami neighborhood at any point after June 15, the earliest known date on which the infected individuals could have been exposed to the virus.
Women who are pregnant or planning to become pregnant are advised to stay away from the neighborhood north of downtown Miami. Women who live in or around Miami, and who either are or plan to become pregnant, should take steps to protect themselves from mosquitoes. Individuals living in Miami should take precautions to prevent transmitting the disease sexually.
Additionally, the CDC is sending an Emergency Response Team to Florida to assist with efforts to quell the mosquito population and spread awareness about Zika virus prevention.
“These experts include individuals with extensive experience in Zika, in addressing pregnancy and birth defects, in mosquito control, in laboratory science, and community engagement,” Dr. Frieden said.
Dr. Frieden reiterated that controlling the local mosquito population is one of the most effective ways to stop ongoing Zika virus transmission. However, current efforts are being hampered by several factors, including small bodies of standing water near which mosquitoes are breeding, the inherent difficulty in killing this species of mosquito, and the possibility that the Aedes aegypti mosquito is resistant to the insecticides being used.
Vector control experts will work with health officials on the ground in Miami to conduct resistance testing on local mosquitoes, in order to confirm whether the insecticides are working. These tests could be done after just 1 week, but may take 3 or more weeks. Further discussion is also ongoing to determine other ways of bringing down the mosquito population.
“What we know about Zika is scary [but] in some ways, what we don’t know about Zika is even more unsettling,” said Dr. Frieden, who added that “at CDC, more than 1,600 of our experts have been working since January to learn more about Zika and protect the health of pregnant women and others.”
Health officials in Florida have identified 10 new cases of locally transmitted Zika virus infections in the neighborhood just north of downtown Miami where four other cases were reported earlier.
Persistent mosquito populations in southern Florida are the leading cause of the disease’s growing incursion into the continental United States, according to Tom Frieden, MD, MPH, director of the Centers for Disease Control and Prevention.
“This suggests that there is a risk of continued, active transmission of Zika in that area,” Dr. Frieden said Aug. 1 during a press call regarding the discovery of new cases by Florida officials.
The CDC is issuing new recommendations for people who either have visited, are currently visiting, or plan to visit this Miami neighborhood at any point after June 15, the earliest known date on which the infected individuals could have been exposed to the virus.
Women who are pregnant or planning to become pregnant are advised to stay away from the neighborhood north of downtown Miami. Women who live in or around Miami, and who either are or plan to become pregnant, should take steps to protect themselves from mosquitoes. Individuals living in Miami should take precautions to prevent transmitting the disease sexually.
Additionally, the CDC is sending an Emergency Response Team to Florida to assist with efforts to quell the mosquito population and spread awareness about Zika virus prevention.
“These experts include individuals with extensive experience in Zika, in addressing pregnancy and birth defects, in mosquito control, in laboratory science, and community engagement,” Dr. Frieden said.
Dr. Frieden reiterated that controlling the local mosquito population is one of the most effective ways to stop ongoing Zika virus transmission. However, current efforts are being hampered by several factors, including small bodies of standing water near which mosquitoes are breeding, the inherent difficulty in killing this species of mosquito, and the possibility that the Aedes aegypti mosquito is resistant to the insecticides being used.
Vector control experts will work with health officials on the ground in Miami to conduct resistance testing on local mosquitoes, in order to confirm whether the insecticides are working. These tests could be done after just 1 week, but may take 3 or more weeks. Further discussion is also ongoing to determine other ways of bringing down the mosquito population.
“What we know about Zika is scary [but] in some ways, what we don’t know about Zika is even more unsettling,” said Dr. Frieden, who added that “at CDC, more than 1,600 of our experts have been working since January to learn more about Zika and protect the health of pregnant women and others.”
Health officials in Florida have identified 10 new cases of locally transmitted Zika virus infections in the neighborhood just north of downtown Miami where four other cases were reported earlier.
Persistent mosquito populations in southern Florida are the leading cause of the disease’s growing incursion into the continental United States, according to Tom Frieden, MD, MPH, director of the Centers for Disease Control and Prevention.
“This suggests that there is a risk of continued, active transmission of Zika in that area,” Dr. Frieden said Aug. 1 during a press call regarding the discovery of new cases by Florida officials.
The CDC is issuing new recommendations for people who either have visited, are currently visiting, or plan to visit this Miami neighborhood at any point after June 15, the earliest known date on which the infected individuals could have been exposed to the virus.
Women who are pregnant or planning to become pregnant are advised to stay away from the neighborhood north of downtown Miami. Women who live in or around Miami, and who either are or plan to become pregnant, should take steps to protect themselves from mosquitoes. Individuals living in Miami should take precautions to prevent transmitting the disease sexually.
Additionally, the CDC is sending an Emergency Response Team to Florida to assist with efforts to quell the mosquito population and spread awareness about Zika virus prevention.
“These experts include individuals with extensive experience in Zika, in addressing pregnancy and birth defects, in mosquito control, in laboratory science, and community engagement,” Dr. Frieden said.
Dr. Frieden reiterated that controlling the local mosquito population is one of the most effective ways to stop ongoing Zika virus transmission. However, current efforts are being hampered by several factors, including small bodies of standing water near which mosquitoes are breeding, the inherent difficulty in killing this species of mosquito, and the possibility that the Aedes aegypti mosquito is resistant to the insecticides being used.
Vector control experts will work with health officials on the ground in Miami to conduct resistance testing on local mosquitoes, in order to confirm whether the insecticides are working. These tests could be done after just 1 week, but may take 3 or more weeks. Further discussion is also ongoing to determine other ways of bringing down the mosquito population.
“What we know about Zika is scary [but] in some ways, what we don’t know about Zika is even more unsettling,” said Dr. Frieden, who added that “at CDC, more than 1,600 of our experts have been working since January to learn more about Zika and protect the health of pregnant women and others.”
2016 Obstetric code changes that could affect your reimbursement (very soon)
By now the upheaval of changing to the new International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) diagnostic coding system has settled. The code freeze that was initiated in 2012 has ended, and the new and revised codes that will go into effect on October 1, 2016, are being revealed. Good documentation will lead to more accurate diagnostic coding, which in turn assists decision makers in their quest to report the health of our population and to make good decisions for resource allocation. You are in the unique position to assist in this process, so keep up the good work.
In this article, I focus on ICD-10 diagnostic coding for obstetric services. I will cover diagnostic coding for gynecologic services in the September issue of OBG Management.
Code revisions for uterine scar and more changes to note
With the upcoming edition of ICD-10, the code Z3A, Weeks’ gestation, will be changed from mandatory reporting to reporting if known. This means that if the patient is no longer pregnant, a Z3A code no longer needs to be reported, and if at the time of service the provider does not know the weeks’ gestation, Z3A would not be required. However, this information should be readily available during the antepartum period and should still be considered important to record and report. And it would still be reported for hospitalization for delivery.
If the code O09.81, Supervision of pregnancy resulting from assisted reproductive technology, is reported, the code Z33.3, Gestational carrier status, may be reported in addition for informational purposes.
When the code O34.29, Maternal care due to uterine scar from other previous surgery, is reported, the tabular index clarifies that this refers to a uterine scar from a transmural uterine incision other than that used for cesarean delivery. This would include incision into the uterine wall to remove fibroids.
The O42 code category, relating to Premature rupture of membranes, should now be interpreted to mean rupture of membranes at or after 37 completed weeks of gestation, rather than after 37 completed weeks.
The code category O99.6, Diseases of the digestive system complicating pregnancy, childbirth, and the puerperium, has been clarified: it does not include hemorrhoids in pregnancy. Therefore, a code from O22.4_ (a final digit of 0 [unspecified], 1, 2, or 3 is required for the trimester) also can be reported if hemorrhoids are present.
A note now clarifies that O99.82, Streptococcus B carrier state complicating pregnancy, childbirth, and the puerperium, cannot be reported with Z22.330, Carrier of streptococcus group B (GBS) in a nonpregnant woman.
New codes for specifying types of ectopic pregnancy
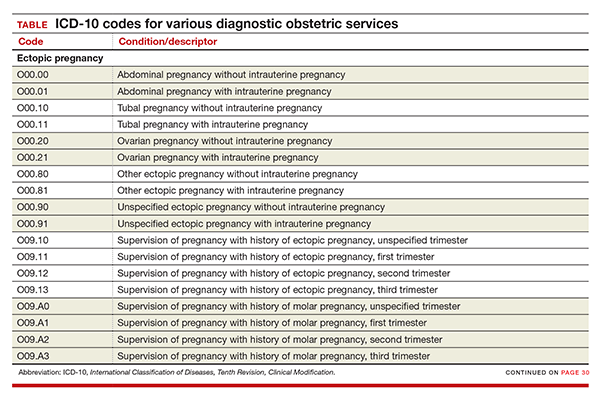
ICD-10 did not initially recognize ectopic pregnancy with and without intrauterine pregnancy, as was the case in ICD-9, but starting in October it will do so. In addition, a history of ectopic or molar pregnancy during a current pregnancy is now reported separately. Each of these codes will require a final digit to indicate the trimester (TABLE).
Codes added for complicating conditions of childbirth and the puerperium
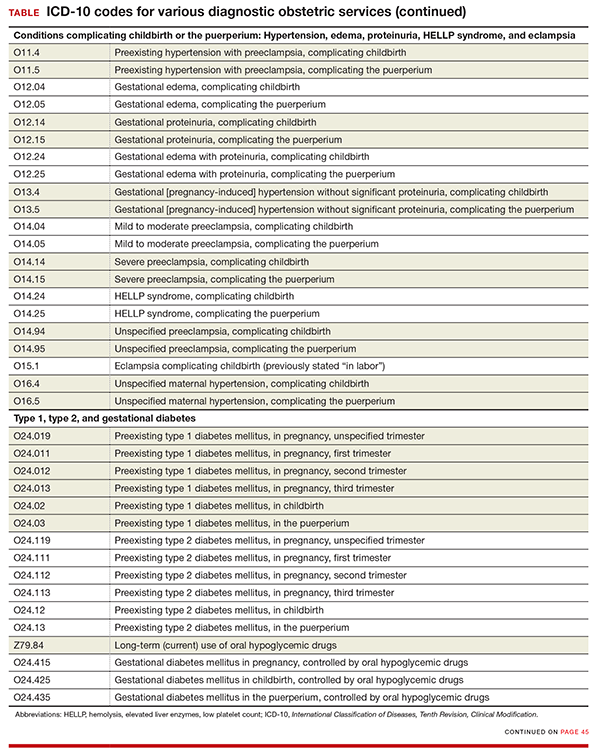
Missing from the ICD-10 lineup last year were codes for conditions related to hypertension, edema, proteinuria, HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome, and eclampsia that were complicating the pregnancy at the time of delivery or after delivery (TABLE).
Note that the “childbirth” code is reported only when a patient delivers at the current episode of care. Once a patient delivers and is discharged, the “puerperium” code should be selected.
Revised descriptions, new reporting instruction for diabetes
The code descriptions for preexisting type 1 and type 2 diabetes were revised, but this change does not impact reporting the codes. However, for type 2 diabetes, the instruction for reporting an additional code has changed. Now, in addition to reporting the code for current use of insulin (Z79.4), when appropriate, report the new added code for use of hypoglycemic agents (Z79.84), such as glyburide or metformin.
For gestational diabetes, new codes have been added for the use of hypoglycemic agents; therefore, no additional code is reported (TABLE).
Disproportion code includes numeric specifier for fetus
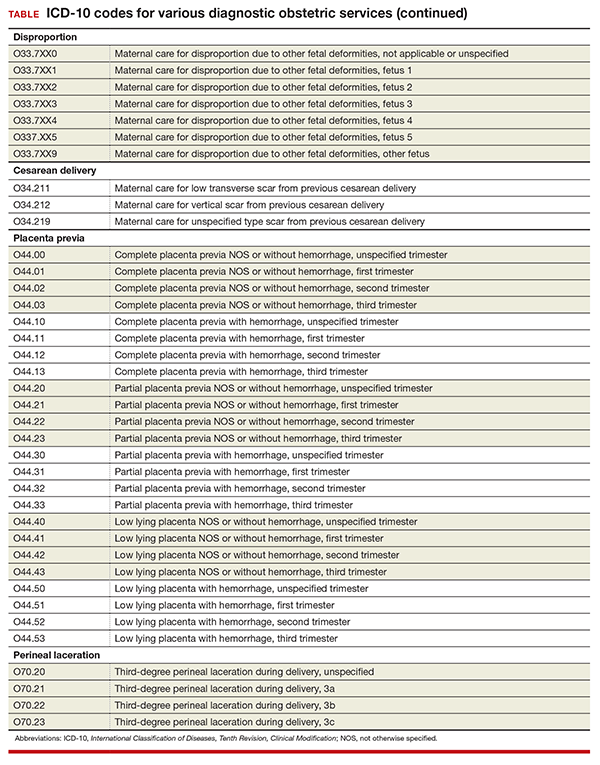
The disproportion code category was expanded to include a final digit for the fetus with the deformity (TABLE). The final digit of the code number denotes which fetus; for example, “0” means a singleton pregnancy, “1” means fetus 1 (number range from 1 to 5), and “9” denotes any fetus after the fifth.
Cesarean delivery scar codes expanded
The code for maternal care for a scar from a previous cesarean delivery has been expanded to 3 different codes (TABLE). Clinicians should make every effort to document and report the location of the previous cesarean as low transverse or vertical. From a coding standpoint, a vertical scar can also be referred to as a classical scar.
Changes to placenta previa codes
The code category for placenta previa has been expanded to capture the degree of previa as complete, partial, or low lying and with or without hemorrhage (TABLE). Going forward, it will be important to carefully document the circumstances so that the most specific code can be reported and tracked. Trimester specification is required as the final digit.
New subclassifications for perineal laceration
The code category for perineal laceration has been expanded with new codes to capture subclassifications for a third-degree laceration that can involve the external and internal anal sphincter (TABLE). Through its collaborative hub, the Women’s Health Registry Alliance (reVITALize) initiative, the American Congress of Obstetricians and Gynecologists (ACOG) worked on the current classification of third- and fourth-degree perineal lacerations, which has been adopted by the Royal College of Obstetricians and Gynaecologists.1
Under this subclassification, a 3a laceration would involve a tear of less than 50% of the external anal sphincter (EAS); 3b would involve a tear of more than 50% of the EAS; and 3c would mean that both the external and internal anal sphincter are torn. ACOG and its collaborative group encourage clinicians to use these subclassifications in documentation to allow for more robust data collection and complete repair information. From a payment standpoint, such information may go a long way to substantiating the severity of a tear, which may require more physician work.
Z code additions
Finally, the ever-popular diagnostic code for Rho(D) immunization is back, and 2 codes have been added for a gestational carrier and 1 for a family history of sudden infant death syndrome. The codes are:
- Z29.13 Encounter for prophylactic Rho(D) immune globulin
- Z31.7 Encounter for procreative management and counseling for gestational carrier
- Z33.3 Pregnant state, gestational carrier
- Z84.82 Family history of sudden infant death syndrome.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee meeting: diagnosis agenda. September 23-24, 2014;38, 39. http://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed July 5, 2016.
By now the upheaval of changing to the new International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) diagnostic coding system has settled. The code freeze that was initiated in 2012 has ended, and the new and revised codes that will go into effect on October 1, 2016, are being revealed. Good documentation will lead to more accurate diagnostic coding, which in turn assists decision makers in their quest to report the health of our population and to make good decisions for resource allocation. You are in the unique position to assist in this process, so keep up the good work.
In this article, I focus on ICD-10 diagnostic coding for obstetric services. I will cover diagnostic coding for gynecologic services in the September issue of OBG Management.
Code revisions for uterine scar and more changes to note
With the upcoming edition of ICD-10, the code Z3A, Weeks’ gestation, will be changed from mandatory reporting to reporting if known. This means that if the patient is no longer pregnant, a Z3A code no longer needs to be reported, and if at the time of service the provider does not know the weeks’ gestation, Z3A would not be required. However, this information should be readily available during the antepartum period and should still be considered important to record and report. And it would still be reported for hospitalization for delivery.
If the code O09.81, Supervision of pregnancy resulting from assisted reproductive technology, is reported, the code Z33.3, Gestational carrier status, may be reported in addition for informational purposes.
When the code O34.29, Maternal care due to uterine scar from other previous surgery, is reported, the tabular index clarifies that this refers to a uterine scar from a transmural uterine incision other than that used for cesarean delivery. This would include incision into the uterine wall to remove fibroids.
The O42 code category, relating to Premature rupture of membranes, should now be interpreted to mean rupture of membranes at or after 37 completed weeks of gestation, rather than after 37 completed weeks.
The code category O99.6, Diseases of the digestive system complicating pregnancy, childbirth, and the puerperium, has been clarified: it does not include hemorrhoids in pregnancy. Therefore, a code from O22.4_ (a final digit of 0 [unspecified], 1, 2, or 3 is required for the trimester) also can be reported if hemorrhoids are present.
A note now clarifies that O99.82, Streptococcus B carrier state complicating pregnancy, childbirth, and the puerperium, cannot be reported with Z22.330, Carrier of streptococcus group B (GBS) in a nonpregnant woman.
New codes for specifying types of ectopic pregnancy
ICD-10 did not initially recognize ectopic pregnancy with and without intrauterine pregnancy, as was the case in ICD-9, but starting in October it will do so. In addition, a history of ectopic or molar pregnancy during a current pregnancy is now reported separately. Each of these codes will require a final digit to indicate the trimester (TABLE).
Codes added for complicating conditions of childbirth and the puerperium
Missing from the ICD-10 lineup last year were codes for conditions related to hypertension, edema, proteinuria, HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome, and eclampsia that were complicating the pregnancy at the time of delivery or after delivery (TABLE).
Note that the “childbirth” code is reported only when a patient delivers at the current episode of care. Once a patient delivers and is discharged, the “puerperium” code should be selected.
Revised descriptions, new reporting instruction for diabetes
The code descriptions for preexisting type 1 and type 2 diabetes were revised, but this change does not impact reporting the codes. However, for type 2 diabetes, the instruction for reporting an additional code has changed. Now, in addition to reporting the code for current use of insulin (Z79.4), when appropriate, report the new added code for use of hypoglycemic agents (Z79.84), such as glyburide or metformin.
For gestational diabetes, new codes have been added for the use of hypoglycemic agents; therefore, no additional code is reported (TABLE).
Disproportion code includes numeric specifier for fetus
The disproportion code category was expanded to include a final digit for the fetus with the deformity (TABLE). The final digit of the code number denotes which fetus; for example, “0” means a singleton pregnancy, “1” means fetus 1 (number range from 1 to 5), and “9” denotes any fetus after the fifth.
Cesarean delivery scar codes expanded
The code for maternal care for a scar from a previous cesarean delivery has been expanded to 3 different codes (TABLE). Clinicians should make every effort to document and report the location of the previous cesarean as low transverse or vertical. From a coding standpoint, a vertical scar can also be referred to as a classical scar.
Changes to placenta previa codes
The code category for placenta previa has been expanded to capture the degree of previa as complete, partial, or low lying and with or without hemorrhage (TABLE). Going forward, it will be important to carefully document the circumstances so that the most specific code can be reported and tracked. Trimester specification is required as the final digit.
New subclassifications for perineal laceration
The code category for perineal laceration has been expanded with new codes to capture subclassifications for a third-degree laceration that can involve the external and internal anal sphincter (TABLE). Through its collaborative hub, the Women’s Health Registry Alliance (reVITALize) initiative, the American Congress of Obstetricians and Gynecologists (ACOG) worked on the current classification of third- and fourth-degree perineal lacerations, which has been adopted by the Royal College of Obstetricians and Gynaecologists.1
Under this subclassification, a 3a laceration would involve a tear of less than 50% of the external anal sphincter (EAS); 3b would involve a tear of more than 50% of the EAS; and 3c would mean that both the external and internal anal sphincter are torn. ACOG and its collaborative group encourage clinicians to use these subclassifications in documentation to allow for more robust data collection and complete repair information. From a payment standpoint, such information may go a long way to substantiating the severity of a tear, which may require more physician work.
Z code additions
Finally, the ever-popular diagnostic code for Rho(D) immunization is back, and 2 codes have been added for a gestational carrier and 1 for a family history of sudden infant death syndrome. The codes are:
- Z29.13 Encounter for prophylactic Rho(D) immune globulin
- Z31.7 Encounter for procreative management and counseling for gestational carrier
- Z33.3 Pregnant state, gestational carrier
- Z84.82 Family history of sudden infant death syndrome.
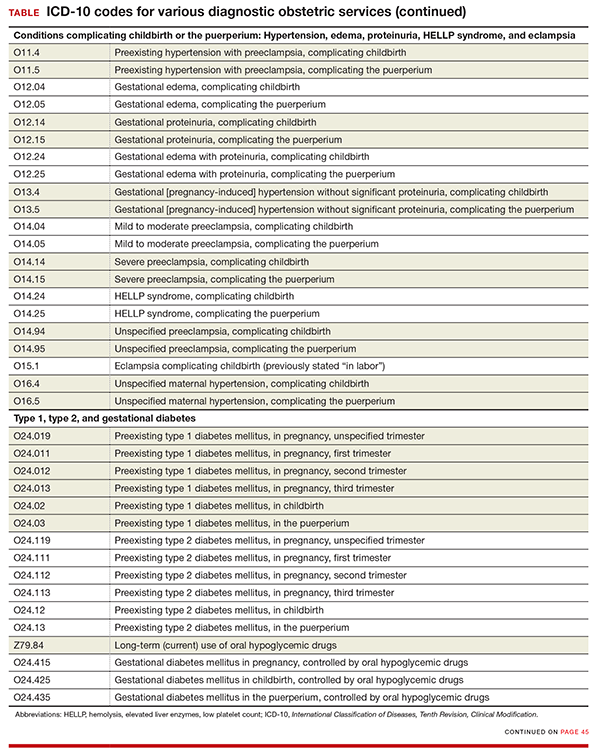
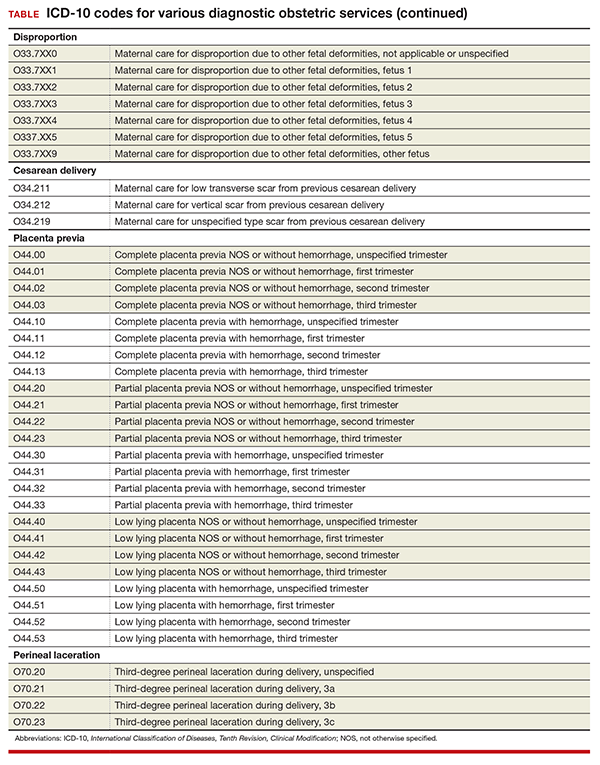
By now the upheaval of changing to the new International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10) diagnostic coding system has settled. The code freeze that was initiated in 2012 has ended, and the new and revised codes that will go into effect on October 1, 2016, are being revealed. Good documentation will lead to more accurate diagnostic coding, which in turn assists decision makers in their quest to report the health of our population and to make good decisions for resource allocation. You are in the unique position to assist in this process, so keep up the good work.
In this article, I focus on ICD-10 diagnostic coding for obstetric services. I will cover diagnostic coding for gynecologic services in the September issue of OBG Management.
Code revisions for uterine scar and more changes to note
With the upcoming edition of ICD-10, the code Z3A, Weeks’ gestation, will be changed from mandatory reporting to reporting if known. This means that if the patient is no longer pregnant, a Z3A code no longer needs to be reported, and if at the time of service the provider does not know the weeks’ gestation, Z3A would not be required. However, this information should be readily available during the antepartum period and should still be considered important to record and report. And it would still be reported for hospitalization for delivery.
If the code O09.81, Supervision of pregnancy resulting from assisted reproductive technology, is reported, the code Z33.3, Gestational carrier status, may be reported in addition for informational purposes.
When the code O34.29, Maternal care due to uterine scar from other previous surgery, is reported, the tabular index clarifies that this refers to a uterine scar from a transmural uterine incision other than that used for cesarean delivery. This would include incision into the uterine wall to remove fibroids.
The O42 code category, relating to Premature rupture of membranes, should now be interpreted to mean rupture of membranes at or after 37 completed weeks of gestation, rather than after 37 completed weeks.
The code category O99.6, Diseases of the digestive system complicating pregnancy, childbirth, and the puerperium, has been clarified: it does not include hemorrhoids in pregnancy. Therefore, a code from O22.4_ (a final digit of 0 [unspecified], 1, 2, or 3 is required for the trimester) also can be reported if hemorrhoids are present.
A note now clarifies that O99.82, Streptococcus B carrier state complicating pregnancy, childbirth, and the puerperium, cannot be reported with Z22.330, Carrier of streptococcus group B (GBS) in a nonpregnant woman.
New codes for specifying types of ectopic pregnancy
ICD-10 did not initially recognize ectopic pregnancy with and without intrauterine pregnancy, as was the case in ICD-9, but starting in October it will do so. In addition, a history of ectopic or molar pregnancy during a current pregnancy is now reported separately. Each of these codes will require a final digit to indicate the trimester (TABLE).
Codes added for complicating conditions of childbirth and the puerperium
Missing from the ICD-10 lineup last year were codes for conditions related to hypertension, edema, proteinuria, HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome, and eclampsia that were complicating the pregnancy at the time of delivery or after delivery (TABLE).
Note that the “childbirth” code is reported only when a patient delivers at the current episode of care. Once a patient delivers and is discharged, the “puerperium” code should be selected.
Revised descriptions, new reporting instruction for diabetes
The code descriptions for preexisting type 1 and type 2 diabetes were revised, but this change does not impact reporting the codes. However, for type 2 diabetes, the instruction for reporting an additional code has changed. Now, in addition to reporting the code for current use of insulin (Z79.4), when appropriate, report the new added code for use of hypoglycemic agents (Z79.84), such as glyburide or metformin.
For gestational diabetes, new codes have been added for the use of hypoglycemic agents; therefore, no additional code is reported (TABLE).
Disproportion code includes numeric specifier for fetus
The disproportion code category was expanded to include a final digit for the fetus with the deformity (TABLE). The final digit of the code number denotes which fetus; for example, “0” means a singleton pregnancy, “1” means fetus 1 (number range from 1 to 5), and “9” denotes any fetus after the fifth.
Cesarean delivery scar codes expanded
The code for maternal care for a scar from a previous cesarean delivery has been expanded to 3 different codes (TABLE). Clinicians should make every effort to document and report the location of the previous cesarean as low transverse or vertical. From a coding standpoint, a vertical scar can also be referred to as a classical scar.
Changes to placenta previa codes
The code category for placenta previa has been expanded to capture the degree of previa as complete, partial, or low lying and with or without hemorrhage (TABLE). Going forward, it will be important to carefully document the circumstances so that the most specific code can be reported and tracked. Trimester specification is required as the final digit.
New subclassifications for perineal laceration
The code category for perineal laceration has been expanded with new codes to capture subclassifications for a third-degree laceration that can involve the external and internal anal sphincter (TABLE). Through its collaborative hub, the Women’s Health Registry Alliance (reVITALize) initiative, the American Congress of Obstetricians and Gynecologists (ACOG) worked on the current classification of third- and fourth-degree perineal lacerations, which has been adopted by the Royal College of Obstetricians and Gynaecologists.1
Under this subclassification, a 3a laceration would involve a tear of less than 50% of the external anal sphincter (EAS); 3b would involve a tear of more than 50% of the EAS; and 3c would mean that both the external and internal anal sphincter are torn. ACOG and its collaborative group encourage clinicians to use these subclassifications in documentation to allow for more robust data collection and complete repair information. From a payment standpoint, such information may go a long way to substantiating the severity of a tear, which may require more physician work.
Z code additions
Finally, the ever-popular diagnostic code for Rho(D) immunization is back, and 2 codes have been added for a gestational carrier and 1 for a family history of sudden infant death syndrome. The codes are:
- Z29.13 Encounter for prophylactic Rho(D) immune globulin
- Z31.7 Encounter for procreative management and counseling for gestational carrier
- Z33.3 Pregnant state, gestational carrier
- Z84.82 Family history of sudden infant death syndrome.
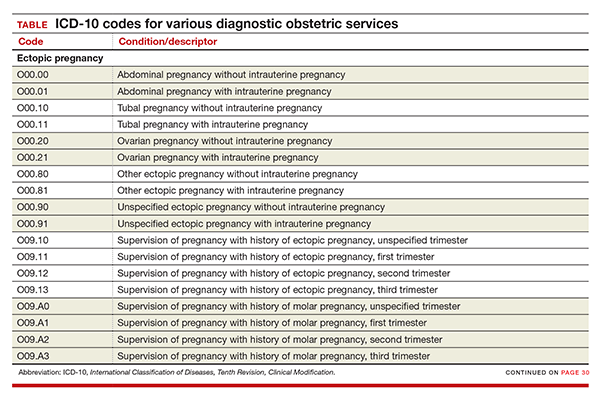
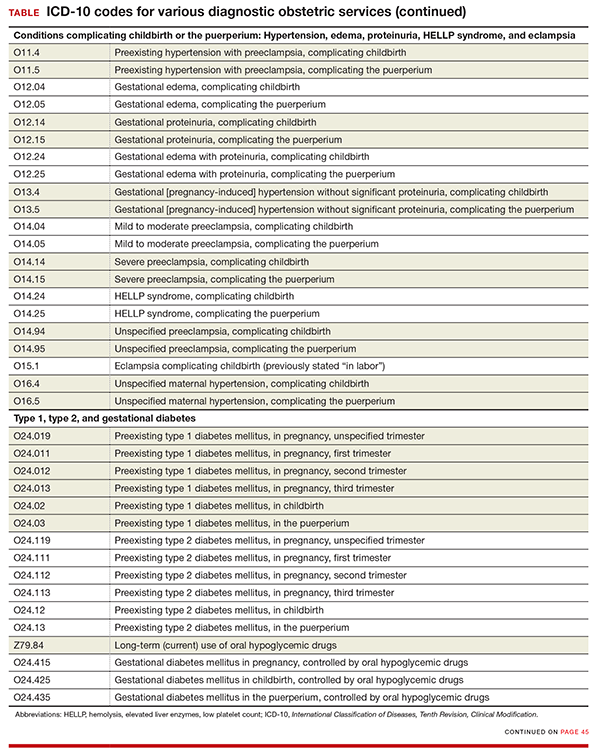
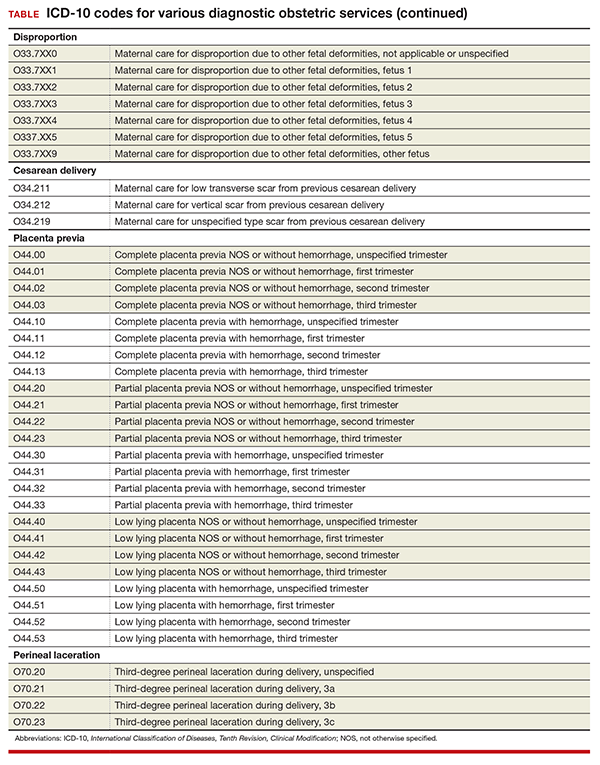
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee meeting: diagnosis agenda. September 23-24, 2014;38, 39. http://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed July 5, 2016.
- Centers for Disease Control and Prevention. ICD-10 Coordination and Maintenance Committee meeting: diagnosis agenda. September 23-24, 2014;38, 39. http://www.cdc.gov/nchs/data/icd/topic_packet_09_23_2012.pdf. Accessed July 5, 2016.
In this Article
- New and expanded codes
- Z code additions
- Table of codes
United States up to 855 cases of Zika in pregnant women
There was one live-born infant with Zika virus–related birth defects and 77 new cases of Zika among pregnant women reported during the week ending July 21, 2016, in the United States, but no additional Zika-related pregnancy losses, according to the Centers for Disease Control and Prevention.
The new cases bring the totals to 13 infants born with birth defects and 855 pregnant women with any laboratory evidence of Zika virus infection. All of the infants with birth defects so far were born in the 50 states and the District of Columbia, which is where six of the seven Zika-related pregnancy losses occurred. There has been only one pregnancy loss in the U.S. territories, but the territories account for almost half (422) of the 855 pregnant women with Zika infection. Of the 77 new infections in pregnant women for the week, 44 occurred in the territories and 33 were in the states, the CDC reported July 28.
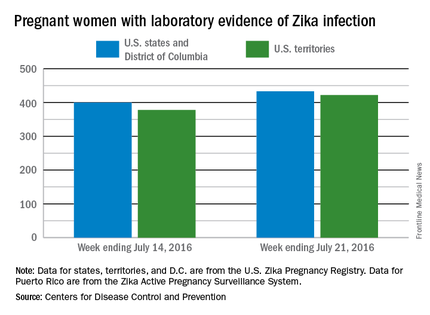
The figures for states, territories, and the District of Columbia reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System.
Zika-related birth defects recorded by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
There was one live-born infant with Zika virus–related birth defects and 77 new cases of Zika among pregnant women reported during the week ending July 21, 2016, in the United States, but no additional Zika-related pregnancy losses, according to the Centers for Disease Control and Prevention.
The new cases bring the totals to 13 infants born with birth defects and 855 pregnant women with any laboratory evidence of Zika virus infection. All of the infants with birth defects so far were born in the 50 states and the District of Columbia, which is where six of the seven Zika-related pregnancy losses occurred. There has been only one pregnancy loss in the U.S. territories, but the territories account for almost half (422) of the 855 pregnant women with Zika infection. Of the 77 new infections in pregnant women for the week, 44 occurred in the territories and 33 were in the states, the CDC reported July 28.
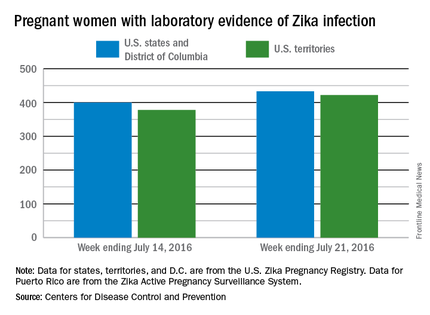
The figures for states, territories, and the District of Columbia reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System.
Zika-related birth defects recorded by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
There was one live-born infant with Zika virus–related birth defects and 77 new cases of Zika among pregnant women reported during the week ending July 21, 2016, in the United States, but no additional Zika-related pregnancy losses, according to the Centers for Disease Control and Prevention.
The new cases bring the totals to 13 infants born with birth defects and 855 pregnant women with any laboratory evidence of Zika virus infection. All of the infants with birth defects so far were born in the 50 states and the District of Columbia, which is where six of the seven Zika-related pregnancy losses occurred. There has been only one pregnancy loss in the U.S. territories, but the territories account for almost half (422) of the 855 pregnant women with Zika infection. Of the 77 new infections in pregnant women for the week, 44 occurred in the territories and 33 were in the states, the CDC reported July 28.
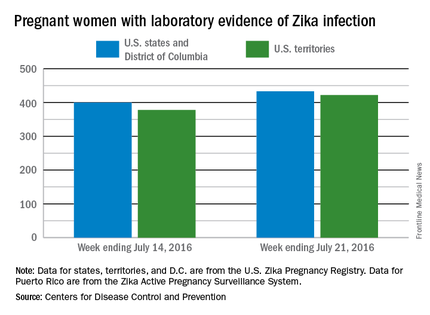
The figures for states, territories, and the District of Columbia reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System.
Zika-related birth defects recorded by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
To cut Zika microcephaly risk, delay pregnancy more than 9 months
Women and couples planning to get pregnant may want to delay that pregnancy more than 9 months if there is an ongoing outbreak of the Zika virus in their area of residence, although that measure alone is not powerful enough to make a significant dent in stopping the Zika virus from spreading.
That is according to a new study in which investigators examined epidemiological data from Colombian Zika virus cases to determine if delaying pregnancies – which has been advised by a number of Central and South American health ministries – would be an effective course of action against the disease and its effects on both pregnant mothers and their fetuses (Ann Intern Med. 2016 Jul 26. doi: 10.7326/M16-0919).
“We developed a data-driven Zika virus transmission model to evaluate the effect of a mass pregnancy delay strategy in which women of reproductive age avoid pregnancy for the recommended duration, at varying degrees of adherence,” wrote Martial L. Ndeffo-Mbah, PhD, of Yale University in New Haven, Conn., and his coauthors.
Cases included were reported to Colombia’s National Institute of Health between Oct. 11, 2015, and May 8, 2016. Investigators classified cases as “suspected cases” of Zika virus infection if the patient presented to a hospital or clinic with “rash, fever (temperature higher than 37.2 degrees C), and at least one of the following symptoms within 5 days of symptom onset that could not be explained by other medical conditions: nonpurulent conjunctivitis or conjunctival hyperemia, arthralgia, myalgia, headache, or malaise.”
Modeling was used to project incidence rates of Zika virus infections, based on a 50% adherence rate to the recommendations.
Among those women who would delay getting pregnant by 6 months or less after possible exposure to Zika virus, prenatal Zika virus infections would decrease by 2%-7%. However, that number would decrease substantially, by 7%-44%, for those who delayed their pregnancy by as much as 9-24 months after exposure.
“Because the incidence peak of the epidemic occurs around 8 months into the outbreak, a strategy to delay pregnancy by more than 9 months, initiated at the onset of the epidemic, would allow women of reproductive age to avoid being pregnant during the incidence peak, when risk for exposure to Zika virus is highest,” Dr. Ndeffo-Mbah and his coauthors noted.
While delaying pregnancy can significantly reduce the risk of birth defects in infants, the authors noted, it won’t have the same effect on reducing the overall spread of Zika virus in an affected region.
“Our results indicate that delays in pregnancy alone will probably be insufficient to curtail Zika-related birth abnormalities,” the authors concluded. “In the absence of a vaccine or therapeutic drugs for Zika virus infection, a combination of mass and individual pregnancy-delay strategies with effective vector-control measures is needed to curtail the spread and burden of the ongoing outbreak in the Americas.”
The National Institutes of Health funded the study. Dr. Ndeffo-Mbah and his coauthors reported no relevant financial disclosures.
Women and couples planning to get pregnant may want to delay that pregnancy more than 9 months if there is an ongoing outbreak of the Zika virus in their area of residence, although that measure alone is not powerful enough to make a significant dent in stopping the Zika virus from spreading.
That is according to a new study in which investigators examined epidemiological data from Colombian Zika virus cases to determine if delaying pregnancies – which has been advised by a number of Central and South American health ministries – would be an effective course of action against the disease and its effects on both pregnant mothers and their fetuses (Ann Intern Med. 2016 Jul 26. doi: 10.7326/M16-0919).
“We developed a data-driven Zika virus transmission model to evaluate the effect of a mass pregnancy delay strategy in which women of reproductive age avoid pregnancy for the recommended duration, at varying degrees of adherence,” wrote Martial L. Ndeffo-Mbah, PhD, of Yale University in New Haven, Conn., and his coauthors.
Cases included were reported to Colombia’s National Institute of Health between Oct. 11, 2015, and May 8, 2016. Investigators classified cases as “suspected cases” of Zika virus infection if the patient presented to a hospital or clinic with “rash, fever (temperature higher than 37.2 degrees C), and at least one of the following symptoms within 5 days of symptom onset that could not be explained by other medical conditions: nonpurulent conjunctivitis or conjunctival hyperemia, arthralgia, myalgia, headache, or malaise.”
Modeling was used to project incidence rates of Zika virus infections, based on a 50% adherence rate to the recommendations.
Among those women who would delay getting pregnant by 6 months or less after possible exposure to Zika virus, prenatal Zika virus infections would decrease by 2%-7%. However, that number would decrease substantially, by 7%-44%, for those who delayed their pregnancy by as much as 9-24 months after exposure.
“Because the incidence peak of the epidemic occurs around 8 months into the outbreak, a strategy to delay pregnancy by more than 9 months, initiated at the onset of the epidemic, would allow women of reproductive age to avoid being pregnant during the incidence peak, when risk for exposure to Zika virus is highest,” Dr. Ndeffo-Mbah and his coauthors noted.
While delaying pregnancy can significantly reduce the risk of birth defects in infants, the authors noted, it won’t have the same effect on reducing the overall spread of Zika virus in an affected region.
“Our results indicate that delays in pregnancy alone will probably be insufficient to curtail Zika-related birth abnormalities,” the authors concluded. “In the absence of a vaccine or therapeutic drugs for Zika virus infection, a combination of mass and individual pregnancy-delay strategies with effective vector-control measures is needed to curtail the spread and burden of the ongoing outbreak in the Americas.”
The National Institutes of Health funded the study. Dr. Ndeffo-Mbah and his coauthors reported no relevant financial disclosures.
Women and couples planning to get pregnant may want to delay that pregnancy more than 9 months if there is an ongoing outbreak of the Zika virus in their area of residence, although that measure alone is not powerful enough to make a significant dent in stopping the Zika virus from spreading.
That is according to a new study in which investigators examined epidemiological data from Colombian Zika virus cases to determine if delaying pregnancies – which has been advised by a number of Central and South American health ministries – would be an effective course of action against the disease and its effects on both pregnant mothers and their fetuses (Ann Intern Med. 2016 Jul 26. doi: 10.7326/M16-0919).
“We developed a data-driven Zika virus transmission model to evaluate the effect of a mass pregnancy delay strategy in which women of reproductive age avoid pregnancy for the recommended duration, at varying degrees of adherence,” wrote Martial L. Ndeffo-Mbah, PhD, of Yale University in New Haven, Conn., and his coauthors.
Cases included were reported to Colombia’s National Institute of Health between Oct. 11, 2015, and May 8, 2016. Investigators classified cases as “suspected cases” of Zika virus infection if the patient presented to a hospital or clinic with “rash, fever (temperature higher than 37.2 degrees C), and at least one of the following symptoms within 5 days of symptom onset that could not be explained by other medical conditions: nonpurulent conjunctivitis or conjunctival hyperemia, arthralgia, myalgia, headache, or malaise.”
Modeling was used to project incidence rates of Zika virus infections, based on a 50% adherence rate to the recommendations.
Among those women who would delay getting pregnant by 6 months or less after possible exposure to Zika virus, prenatal Zika virus infections would decrease by 2%-7%. However, that number would decrease substantially, by 7%-44%, for those who delayed their pregnancy by as much as 9-24 months after exposure.
“Because the incidence peak of the epidemic occurs around 8 months into the outbreak, a strategy to delay pregnancy by more than 9 months, initiated at the onset of the epidemic, would allow women of reproductive age to avoid being pregnant during the incidence peak, when risk for exposure to Zika virus is highest,” Dr. Ndeffo-Mbah and his coauthors noted.
While delaying pregnancy can significantly reduce the risk of birth defects in infants, the authors noted, it won’t have the same effect on reducing the overall spread of Zika virus in an affected region.
“Our results indicate that delays in pregnancy alone will probably be insufficient to curtail Zika-related birth abnormalities,” the authors concluded. “In the absence of a vaccine or therapeutic drugs for Zika virus infection, a combination of mass and individual pregnancy-delay strategies with effective vector-control measures is needed to curtail the spread and burden of the ongoing outbreak in the Americas.”
The National Institutes of Health funded the study. Dr. Ndeffo-Mbah and his coauthors reported no relevant financial disclosures.
FROM THE ANNALS OF INTERNAL MEDICINE
Key clinical point: Delaying pregnancy after a Zika outbreak can reduce the risk of having a child with microcephaly, but it is only a small part in what must be a larger effort to prevent the spread of Zika virus.
Major finding: Pregnancies delayed by 6 months after a local Zika outbreak could decrease prenatal Zika infections 2%-7%, but delaying pregnancies 9-24 months could decrease infections by 17%-44%.
Data source: A vector-borne Zika virus transmission model of data on Colombian Zika virus infections in 2015-2016.
Disclosures: The National Institutes of Health funded the study. Dr. Ndeffo-Mbah and his coauthors reported no relevant financial disclosures.
Gestational diabetes ups risk for infantile hemangiomas
MINNEAPOLIS – Gestational diabetes and prenatal progesterone use were among the maternal factors associated with increased risk of infantile hemangioma, a benign vascular neoplasm whose incidence has been steadily rising over the past several decades.
Data from a large longitudinal epidemiology study were used to explore the association of a number of maternal risk factors with infantile hemangiomas, said Jennifer Schoch, MD, who presented these findings in a poster session at the annual meeting of the Society for Pediatric Dermatology.
After adjusting for gestational age and multiple gestations, the researchers found that infants born to mothers with gestational diabetes were more likely to have an infantile hemangioma (odds ratio, 1.79; P = .029). Maternal preeclampsia was even more strongly associated with infantile hemangioma (OR, 3.43, P = .017), as was prenatal progesterone use (OR, 2.25; P less than .001). Forceps-assisted vaginal delivery also increased the likelihood of infantile hemangioma (OR, 1.45; P = .035).
Low birth weight, prematurity, and being female and of non-Hispanic white race are some of the infant risk factors known to be associated with infantile hemangioma, but maternal risk factors in the development of infantile hemangioma are less clear, according to the researchers from the Mayo Clinic, Rochester, Minn. Some previous work has suggested that placental abnormalities and invasive procedures carried out during pregnancy, as well as the use of progesterone and corticosteroids during pregnancy, may increase the risk of infantile hemangiomas.
Using a retrospective case-control approach, the researchers used data from the 50-year-old Rochester Epidemiology Project. A chart review identified 869 mother-infant pairs with infantile hemangiomas and 869 age- and sex-matched control maternal-infant pairs whose infants did not have the condition. More than half (65%) of the infants in aggregate were girls (n = 561). Multivariable analysis was used to adjust for gestational age and multiple gestations.
Looking at the trends over time revealed that the rates of gestational diabetes, assisted reproduction techniques, and progesterone use during pregnancy have all increased during the same 35-year period of increased infantile hemangioma incidence, Dr. Schoch said in an interview.
Some earlier work suggests that infantile hemangiomas may arise from fetal placental progenitor cells. Since gestational diabetes can be associated with degradation of the placenta in late pregnancy, Dr. Schoch said that these effects on the placenta may have some connection to the increased risk of infantile hemangiomas in infants whose mothers have gestational diabetes.
Dr. Schoch, who is now professor of dermatology at the University of Florida, Gainesville, also noted that the study, completed during her fellowship at the Mayo Clinic, was limited by the low ethnic diversity of the study population, which draws from several counties in Minnesota and Wisconsin.
The Rochester Epidemiology Project is supported by the National Institutes of Health. The researchers reported having no financial disclosures.
On Twitter @karioakes
MINNEAPOLIS – Gestational diabetes and prenatal progesterone use were among the maternal factors associated with increased risk of infantile hemangioma, a benign vascular neoplasm whose incidence has been steadily rising over the past several decades.
Data from a large longitudinal epidemiology study were used to explore the association of a number of maternal risk factors with infantile hemangiomas, said Jennifer Schoch, MD, who presented these findings in a poster session at the annual meeting of the Society for Pediatric Dermatology.
After adjusting for gestational age and multiple gestations, the researchers found that infants born to mothers with gestational diabetes were more likely to have an infantile hemangioma (odds ratio, 1.79; P = .029). Maternal preeclampsia was even more strongly associated with infantile hemangioma (OR, 3.43, P = .017), as was prenatal progesterone use (OR, 2.25; P less than .001). Forceps-assisted vaginal delivery also increased the likelihood of infantile hemangioma (OR, 1.45; P = .035).
Low birth weight, prematurity, and being female and of non-Hispanic white race are some of the infant risk factors known to be associated with infantile hemangioma, but maternal risk factors in the development of infantile hemangioma are less clear, according to the researchers from the Mayo Clinic, Rochester, Minn. Some previous work has suggested that placental abnormalities and invasive procedures carried out during pregnancy, as well as the use of progesterone and corticosteroids during pregnancy, may increase the risk of infantile hemangiomas.
Using a retrospective case-control approach, the researchers used data from the 50-year-old Rochester Epidemiology Project. A chart review identified 869 mother-infant pairs with infantile hemangiomas and 869 age- and sex-matched control maternal-infant pairs whose infants did not have the condition. More than half (65%) of the infants in aggregate were girls (n = 561). Multivariable analysis was used to adjust for gestational age and multiple gestations.
Looking at the trends over time revealed that the rates of gestational diabetes, assisted reproduction techniques, and progesterone use during pregnancy have all increased during the same 35-year period of increased infantile hemangioma incidence, Dr. Schoch said in an interview.
Some earlier work suggests that infantile hemangiomas may arise from fetal placental progenitor cells. Since gestational diabetes can be associated with degradation of the placenta in late pregnancy, Dr. Schoch said that these effects on the placenta may have some connection to the increased risk of infantile hemangiomas in infants whose mothers have gestational diabetes.
Dr. Schoch, who is now professor of dermatology at the University of Florida, Gainesville, also noted that the study, completed during her fellowship at the Mayo Clinic, was limited by the low ethnic diversity of the study population, which draws from several counties in Minnesota and Wisconsin.
The Rochester Epidemiology Project is supported by the National Institutes of Health. The researchers reported having no financial disclosures.
On Twitter @karioakes
MINNEAPOLIS – Gestational diabetes and prenatal progesterone use were among the maternal factors associated with increased risk of infantile hemangioma, a benign vascular neoplasm whose incidence has been steadily rising over the past several decades.
Data from a large longitudinal epidemiology study were used to explore the association of a number of maternal risk factors with infantile hemangiomas, said Jennifer Schoch, MD, who presented these findings in a poster session at the annual meeting of the Society for Pediatric Dermatology.
After adjusting for gestational age and multiple gestations, the researchers found that infants born to mothers with gestational diabetes were more likely to have an infantile hemangioma (odds ratio, 1.79; P = .029). Maternal preeclampsia was even more strongly associated with infantile hemangioma (OR, 3.43, P = .017), as was prenatal progesterone use (OR, 2.25; P less than .001). Forceps-assisted vaginal delivery also increased the likelihood of infantile hemangioma (OR, 1.45; P = .035).
Low birth weight, prematurity, and being female and of non-Hispanic white race are some of the infant risk factors known to be associated with infantile hemangioma, but maternal risk factors in the development of infantile hemangioma are less clear, according to the researchers from the Mayo Clinic, Rochester, Minn. Some previous work has suggested that placental abnormalities and invasive procedures carried out during pregnancy, as well as the use of progesterone and corticosteroids during pregnancy, may increase the risk of infantile hemangiomas.
Using a retrospective case-control approach, the researchers used data from the 50-year-old Rochester Epidemiology Project. A chart review identified 869 mother-infant pairs with infantile hemangiomas and 869 age- and sex-matched control maternal-infant pairs whose infants did not have the condition. More than half (65%) of the infants in aggregate were girls (n = 561). Multivariable analysis was used to adjust for gestational age and multiple gestations.
Looking at the trends over time revealed that the rates of gestational diabetes, assisted reproduction techniques, and progesterone use during pregnancy have all increased during the same 35-year period of increased infantile hemangioma incidence, Dr. Schoch said in an interview.
Some earlier work suggests that infantile hemangiomas may arise from fetal placental progenitor cells. Since gestational diabetes can be associated with degradation of the placenta in late pregnancy, Dr. Schoch said that these effects on the placenta may have some connection to the increased risk of infantile hemangiomas in infants whose mothers have gestational diabetes.
Dr. Schoch, who is now professor of dermatology at the University of Florida, Gainesville, also noted that the study, completed during her fellowship at the Mayo Clinic, was limited by the low ethnic diversity of the study population, which draws from several counties in Minnesota and Wisconsin.
The Rochester Epidemiology Project is supported by the National Institutes of Health. The researchers reported having no financial disclosures.
On Twitter @karioakes
AT THE SPD ANNUAL MEETING
Key clinical point: Gestational diabetes and other maternal factors may increase the risk for infantile hemangioma.
Major finding: Infants born to mothers with gestational diabetes had an odds ratio of 1.79 for infantile hemangioma (P = .029).
Data source: Retrospective control-matched study of 865 infants with infantile hemangioma.
Disclosures: The researchers reported having no financial disclosures.
Late preterm, early term births declining in United States
Rates of late preterm (34-36 weeks) and early preterm (37-38 weeks) births declined significantly in the United States between 2006 and 2014, according to a report published online July 26 in JAMA.
To examine temporal trends in early birth rates, investigators analyzed data in birth registries for six high-income Western countries, including the United States. They focused on singleton live births delivered at 22 or more weeks’ gestation in which the neonates weighed 500 g or more that occurred between 2006 and the most recent year for which data were available for each country. The study included more than 25.7 million U.S. births, 2.4 million in Canada, approximately 306,000 in Denmark, approximately 572,000 in Finland, approximately 469,000 in Norway, and approximately 738,000 in Sweden, Jennifer L. Richards, MPH, of the department of epidemiology, Emory University, Atlanta, and her associates reported.
During the study period, rates of late preterm birth significantly decreased from 6.8% to 5.7% in the United States and from 3.9% to 3.5% in Norway but remained essentially stable in the other countries. Rates of early term birth also decreased significantly from 31.2% to 24.4% in the United States, from 17.6% to 16.8% in Norway, and from 19.5% to 18.5% in Sweden but remained essentially constant in the other countries. The rates were adjusted for mother’s age at delivery and parity (JAMA. 2016;316[4]:410-9. doi:10.1001/jama.2016.9635).
Ms. Richards and her associates attempted to determine whether declining rates in early births correlated with declines in obstetric interventions, specifically labor inductions and prelabor cesarean deliveries, but they found only one such correlation, in the rate of early term births in the United States. Overall, the rates of clinician-initiated obstetric intervention declined from 48.9% in 2006 to 38.7% in 2014 among U.S. early term births. In all other cases, trends in obstetric interventions varied widely over time and from one country to the next. In addition, rates of late preterm and early term births in the United States declined comparably among deliveries in which there were no obstetric interventions, they noted.
The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Paris Descartes University, the Japan Society for the Promotion of Science, and the Japan Ministry of Health, Labour, and Welfare. Ms. Richards reported having no financial disclosures; an associate reported receiving grants from the Uehara Memorial Foundation, the Kanzawa Medical Research Foundation, and the Danone Institute.
Reductions in early term births in the United States have been documented previously, and the investigators found an impressive decline in obstetric interventions among early term births from 48.9% in 2006 to 38.7% in 2014. This reduction may be the result of national and local efforts to reduce nonindicated deliveries prior to 39 weeks. In contrast, the rates of obstetric interventions among late preterm births were relatively constant over the years studied. Although reducing preterm birth is a major goal, sometimes late preterm birth is the best outcome for the mother and/or fetus, and these deliveries would require an obstetric intervention. Thus, the constant rate of obstetric interventions among late preterm births may be associated with a relatively smaller number of nonindicated late preterm births.

|
Dr. Catherine Y. Spong |
Ms. Richards and her colleagues have provided a thoughtful multinational picture of late preterm and early term deliveries and their association with obstetric interventions. More data are needed to better understand the differences between countries and changes over time. Better tools and technologies to date pregnancies are now available, and, as studies continue to demonstrate, it is critical to wait until full term for delivery in uncomplicated pregnancies. Physicians, however, cannot become too devoted to decreasing late preterm and early term birth rates. For pregnancies in which there is a complication and when delivery will optimize the pregnancy outcome, delivery should occur and will require an obstetrical intervention.
Catherine Y. Spong, MD, is at the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Md. She reported having no relevant financial disclosures. These remarks are excerpted from an accompanying editorial (JAMA. 2016;316[4]:395-6).
Reductions in early term births in the United States have been documented previously, and the investigators found an impressive decline in obstetric interventions among early term births from 48.9% in 2006 to 38.7% in 2014. This reduction may be the result of national and local efforts to reduce nonindicated deliveries prior to 39 weeks. In contrast, the rates of obstetric interventions among late preterm births were relatively constant over the years studied. Although reducing preterm birth is a major goal, sometimes late preterm birth is the best outcome for the mother and/or fetus, and these deliveries would require an obstetric intervention. Thus, the constant rate of obstetric interventions among late preterm births may be associated with a relatively smaller number of nonindicated late preterm births.

|
Dr. Catherine Y. Spong |
Ms. Richards and her colleagues have provided a thoughtful multinational picture of late preterm and early term deliveries and their association with obstetric interventions. More data are needed to better understand the differences between countries and changes over time. Better tools and technologies to date pregnancies are now available, and, as studies continue to demonstrate, it is critical to wait until full term for delivery in uncomplicated pregnancies. Physicians, however, cannot become too devoted to decreasing late preterm and early term birth rates. For pregnancies in which there is a complication and when delivery will optimize the pregnancy outcome, delivery should occur and will require an obstetrical intervention.
Catherine Y. Spong, MD, is at the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Md. She reported having no relevant financial disclosures. These remarks are excerpted from an accompanying editorial (JAMA. 2016;316[4]:395-6).
Reductions in early term births in the United States have been documented previously, and the investigators found an impressive decline in obstetric interventions among early term births from 48.9% in 2006 to 38.7% in 2014. This reduction may be the result of national and local efforts to reduce nonindicated deliveries prior to 39 weeks. In contrast, the rates of obstetric interventions among late preterm births were relatively constant over the years studied. Although reducing preterm birth is a major goal, sometimes late preterm birth is the best outcome for the mother and/or fetus, and these deliveries would require an obstetric intervention. Thus, the constant rate of obstetric interventions among late preterm births may be associated with a relatively smaller number of nonindicated late preterm births.

|
Dr. Catherine Y. Spong |
Ms. Richards and her colleagues have provided a thoughtful multinational picture of late preterm and early term deliveries and their association with obstetric interventions. More data are needed to better understand the differences between countries and changes over time. Better tools and technologies to date pregnancies are now available, and, as studies continue to demonstrate, it is critical to wait until full term for delivery in uncomplicated pregnancies. Physicians, however, cannot become too devoted to decreasing late preterm and early term birth rates. For pregnancies in which there is a complication and when delivery will optimize the pregnancy outcome, delivery should occur and will require an obstetrical intervention.
Catherine Y. Spong, MD, is at the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Md. She reported having no relevant financial disclosures. These remarks are excerpted from an accompanying editorial (JAMA. 2016;316[4]:395-6).
Rates of late preterm (34-36 weeks) and early preterm (37-38 weeks) births declined significantly in the United States between 2006 and 2014, according to a report published online July 26 in JAMA.
To examine temporal trends in early birth rates, investigators analyzed data in birth registries for six high-income Western countries, including the United States. They focused on singleton live births delivered at 22 or more weeks’ gestation in which the neonates weighed 500 g or more that occurred between 2006 and the most recent year for which data were available for each country. The study included more than 25.7 million U.S. births, 2.4 million in Canada, approximately 306,000 in Denmark, approximately 572,000 in Finland, approximately 469,000 in Norway, and approximately 738,000 in Sweden, Jennifer L. Richards, MPH, of the department of epidemiology, Emory University, Atlanta, and her associates reported.
During the study period, rates of late preterm birth significantly decreased from 6.8% to 5.7% in the United States and from 3.9% to 3.5% in Norway but remained essentially stable in the other countries. Rates of early term birth also decreased significantly from 31.2% to 24.4% in the United States, from 17.6% to 16.8% in Norway, and from 19.5% to 18.5% in Sweden but remained essentially constant in the other countries. The rates were adjusted for mother’s age at delivery and parity (JAMA. 2016;316[4]:410-9. doi:10.1001/jama.2016.9635).
Ms. Richards and her associates attempted to determine whether declining rates in early births correlated with declines in obstetric interventions, specifically labor inductions and prelabor cesarean deliveries, but they found only one such correlation, in the rate of early term births in the United States. Overall, the rates of clinician-initiated obstetric intervention declined from 48.9% in 2006 to 38.7% in 2014 among U.S. early term births. In all other cases, trends in obstetric interventions varied widely over time and from one country to the next. In addition, rates of late preterm and early term births in the United States declined comparably among deliveries in which there were no obstetric interventions, they noted.
The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Paris Descartes University, the Japan Society for the Promotion of Science, and the Japan Ministry of Health, Labour, and Welfare. Ms. Richards reported having no financial disclosures; an associate reported receiving grants from the Uehara Memorial Foundation, the Kanzawa Medical Research Foundation, and the Danone Institute.
Rates of late preterm (34-36 weeks) and early preterm (37-38 weeks) births declined significantly in the United States between 2006 and 2014, according to a report published online July 26 in JAMA.
To examine temporal trends in early birth rates, investigators analyzed data in birth registries for six high-income Western countries, including the United States. They focused on singleton live births delivered at 22 or more weeks’ gestation in which the neonates weighed 500 g or more that occurred between 2006 and the most recent year for which data were available for each country. The study included more than 25.7 million U.S. births, 2.4 million in Canada, approximately 306,000 in Denmark, approximately 572,000 in Finland, approximately 469,000 in Norway, and approximately 738,000 in Sweden, Jennifer L. Richards, MPH, of the department of epidemiology, Emory University, Atlanta, and her associates reported.
During the study period, rates of late preterm birth significantly decreased from 6.8% to 5.7% in the United States and from 3.9% to 3.5% in Norway but remained essentially stable in the other countries. Rates of early term birth also decreased significantly from 31.2% to 24.4% in the United States, from 17.6% to 16.8% in Norway, and from 19.5% to 18.5% in Sweden but remained essentially constant in the other countries. The rates were adjusted for mother’s age at delivery and parity (JAMA. 2016;316[4]:410-9. doi:10.1001/jama.2016.9635).
Ms. Richards and her associates attempted to determine whether declining rates in early births correlated with declines in obstetric interventions, specifically labor inductions and prelabor cesarean deliveries, but they found only one such correlation, in the rate of early term births in the United States. Overall, the rates of clinician-initiated obstetric intervention declined from 48.9% in 2006 to 38.7% in 2014 among U.S. early term births. In all other cases, trends in obstetric interventions varied widely over time and from one country to the next. In addition, rates of late preterm and early term births in the United States declined comparably among deliveries in which there were no obstetric interventions, they noted.
The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Paris Descartes University, the Japan Society for the Promotion of Science, and the Japan Ministry of Health, Labour, and Welfare. Ms. Richards reported having no financial disclosures; an associate reported receiving grants from the Uehara Memorial Foundation, the Kanzawa Medical Research Foundation, and the Danone Institute.
FROM JAMA
Key clinical point: Late preterm and early term births declined in the United States between 2006 and 2014.
Major finding: Rates of late preterm birth significantly decreased from 6.8% to 5.7% in the United States and from 3.9% to 3.5% in Norway, but remained essentially stable in the other four countries analyzed.
Data source: A descriptive population-based retrospective study of early birth rates in six Western countries.
Disclosures: The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Paris Descartes University, the Japan Society for the Promotion of Science, and the Japan Ministry of Health, Labour, and Welfare. Ms. Richards reported having no financial disclosures; an associate reported receiving grants from the Uehara Memorial Foundation, the Kanzawa Medical Research Foundation, and the Danone Institute.
ACOG: Offer immediate postpartum LARC as option
Use of long-acting reversible contraception immediately post partum can help reduce the risk of unintended and short-interval pregnancy, according to a new policy statement from the American College of Obstetricians and Gynecologists.
“Immediate postpartum LARC should be offered as an effective option for postpartum contraception; there are few contraindications to postpartum IUDs and implants,” according to the statement issued by ACOG’s Committee on Obstetric Practice (Obstet Gynecol. 2016;128:e32-37).
Unintended pregnancies account for approximately 45% of pregnancies in the United States overall, and at least 70% of pregnancies in the first year post partum, the committee noted.
The statement recommends prenatal counseling about the risks and benefits of LARCs, along with alternatives, to help patients make informed decisions. The committee emphasized that health care providers “should counsel women about the convenience and effectiveness of immediate postpartum LARC, as well as the benefits of reducing unintended pregnancy and lengthening pregnancy intervals.”
However, immediate postpartum use of IUDs is contraindicated in women with intrauterine infection at delivery, postpartum hemorrhage, and puerperal sepsis.
The committee called for systems to provide LARC at the comprehensive postpartum visit if necessary, and recommended stocking LARC devices in labor and delivery units for immediate postpartum placement. In addition, coding and reimbursement strategies are needed to support immediate postpartum LARC, according to the statement.
The policy statement was endorsed by the American College of Nurse-Midwives and the Society for Maternal-Fetal Medicine.
Use of long-acting reversible contraception immediately post partum can help reduce the risk of unintended and short-interval pregnancy, according to a new policy statement from the American College of Obstetricians and Gynecologists.
“Immediate postpartum LARC should be offered as an effective option for postpartum contraception; there are few contraindications to postpartum IUDs and implants,” according to the statement issued by ACOG’s Committee on Obstetric Practice (Obstet Gynecol. 2016;128:e32-37).
Unintended pregnancies account for approximately 45% of pregnancies in the United States overall, and at least 70% of pregnancies in the first year post partum, the committee noted.
The statement recommends prenatal counseling about the risks and benefits of LARCs, along with alternatives, to help patients make informed decisions. The committee emphasized that health care providers “should counsel women about the convenience and effectiveness of immediate postpartum LARC, as well as the benefits of reducing unintended pregnancy and lengthening pregnancy intervals.”
However, immediate postpartum use of IUDs is contraindicated in women with intrauterine infection at delivery, postpartum hemorrhage, and puerperal sepsis.
The committee called for systems to provide LARC at the comprehensive postpartum visit if necessary, and recommended stocking LARC devices in labor and delivery units for immediate postpartum placement. In addition, coding and reimbursement strategies are needed to support immediate postpartum LARC, according to the statement.
The policy statement was endorsed by the American College of Nurse-Midwives and the Society for Maternal-Fetal Medicine.
Use of long-acting reversible contraception immediately post partum can help reduce the risk of unintended and short-interval pregnancy, according to a new policy statement from the American College of Obstetricians and Gynecologists.
“Immediate postpartum LARC should be offered as an effective option for postpartum contraception; there are few contraindications to postpartum IUDs and implants,” according to the statement issued by ACOG’s Committee on Obstetric Practice (Obstet Gynecol. 2016;128:e32-37).
Unintended pregnancies account for approximately 45% of pregnancies in the United States overall, and at least 70% of pregnancies in the first year post partum, the committee noted.
The statement recommends prenatal counseling about the risks and benefits of LARCs, along with alternatives, to help patients make informed decisions. The committee emphasized that health care providers “should counsel women about the convenience and effectiveness of immediate postpartum LARC, as well as the benefits of reducing unintended pregnancy and lengthening pregnancy intervals.”
However, immediate postpartum use of IUDs is contraindicated in women with intrauterine infection at delivery, postpartum hemorrhage, and puerperal sepsis.
The committee called for systems to provide LARC at the comprehensive postpartum visit if necessary, and recommended stocking LARC devices in labor and delivery units for immediate postpartum placement. In addition, coding and reimbursement strategies are needed to support immediate postpartum LARC, according to the statement.
The policy statement was endorsed by the American College of Nurse-Midwives and the Society for Maternal-Fetal Medicine.
FROM OBSTETRICS & GYNECOLOGY