User login
Does influenza immunization during pregnancy confer flu protection to newborns?
A recent report on data obtained from the Intermountain Healthcare facilities in Utah and Idaho suggests that maternal influenza vaccination, besides its maternal protective effect, also may benefit the newborn by protecting against influenza. I think that ObGyns generally accept the notion that influenza vaccination has defined maternal benefit. Notably, acceptance of influenza vaccine became much more widespread during and following the H1N1 flu pandemic of 2009. The fact that there may be neonatal and infant benefit as well is certainly not objectionable, especially since flu vaccine is not recommended for infants less than 6 months of age.
Details of the study
Shakib and colleagues’ goal was to compare influenza outcomes in infants younger than 6 months born to women who self-reported receiving or not receiving influenza vaccine during pregnancy. The study cohort included 245,386 women and 249,387 infants who were born between December 2005 and March 2014. The outcomes studied were influenza-like illness (ILI), laboratory-confirmed influenza, and influenza hospitalizations.
Of 866 infants younger than 6 months born to women who had received a flu shot, 32 had 1 or more ILI encounters, compared with 834 born to women who were not immunized (relative risk [RR], 0.36; 95% confidence interval [CI], 0.26–0.52; P<.001). Laboratory-confirmed influenza was identified in 658 infants; of these, 20 were born to women reporting immunization and 638 were born to unimmunized women (RR, 0.30; 95% CI, 0.19–0.46; P<.001). Finally, 151 infants with laboratory-confirmed influenza were hospitalized; 3 were born to immunized women and 148 to women who had not received a flu shot (RR, 0.19; 95% CI, 0.06–0.60; P = .005).
The authors calculated that infants born to women who reported influenza immunization during pregnancy had risk reductions of 64% for ILI, 70% for laboratory-confirmed influenza, and 81% for influenza hospitalizations.
Consider immunization benefits realistically
The authors state in their published report that “Protecting young infants from influenza through maternal immunization during pregnancy is a public health priority.” This may be overstating their case, for the following reasons. First, influenza vaccine has varying degrees of efficacy depending on the particular year and influenza strains that predominate, and it never has been shown to be entirely protective. Second, when looking only at this study’s laboratory-proven cases of influenza in newborns, infants whose mothers were vaccinated had a case rate of 0.84/1,000, while the case rate in newborns born to unvaccinated women was 2.83/1,000. While this shows a difference, the report provides no additional outcome data regarding morbidity or mortality.
In fact, although infant hospitalization rates differed (0.13/1,000 born to vaccinated women versus 0.66/1,000 born to unvaccinated women), there were no influenza-related mortalities in this cohort. The effect seems better when including “influenza-like illness,” but it is unclear why we should think that the influenza vaccine protects against infection that is not caused by influenza.
What this EVIDENCE means for practice
ObGyns should continue to promote influenza vaccination during pregnancy for the maternal protection it imparts. These new data on the potential for newborn protection, although not conclusive, may improve maternal acceptance of vaccination; from that perspective, these data are valuable.
— John T. Repke, MD
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
A recent report on data obtained from the Intermountain Healthcare facilities in Utah and Idaho suggests that maternal influenza vaccination, besides its maternal protective effect, also may benefit the newborn by protecting against influenza. I think that ObGyns generally accept the notion that influenza vaccination has defined maternal benefit. Notably, acceptance of influenza vaccine became much more widespread during and following the H1N1 flu pandemic of 2009. The fact that there may be neonatal and infant benefit as well is certainly not objectionable, especially since flu vaccine is not recommended for infants less than 6 months of age.
Details of the study
Shakib and colleagues’ goal was to compare influenza outcomes in infants younger than 6 months born to women who self-reported receiving or not receiving influenza vaccine during pregnancy. The study cohort included 245,386 women and 249,387 infants who were born between December 2005 and March 2014. The outcomes studied were influenza-like illness (ILI), laboratory-confirmed influenza, and influenza hospitalizations.
Of 866 infants younger than 6 months born to women who had received a flu shot, 32 had 1 or more ILI encounters, compared with 834 born to women who were not immunized (relative risk [RR], 0.36; 95% confidence interval [CI], 0.26–0.52; P<.001). Laboratory-confirmed influenza was identified in 658 infants; of these, 20 were born to women reporting immunization and 638 were born to unimmunized women (RR, 0.30; 95% CI, 0.19–0.46; P<.001). Finally, 151 infants with laboratory-confirmed influenza were hospitalized; 3 were born to immunized women and 148 to women who had not received a flu shot (RR, 0.19; 95% CI, 0.06–0.60; P = .005).
The authors calculated that infants born to women who reported influenza immunization during pregnancy had risk reductions of 64% for ILI, 70% for laboratory-confirmed influenza, and 81% for influenza hospitalizations.
Consider immunization benefits realistically
The authors state in their published report that “Protecting young infants from influenza through maternal immunization during pregnancy is a public health priority.” This may be overstating their case, for the following reasons. First, influenza vaccine has varying degrees of efficacy depending on the particular year and influenza strains that predominate, and it never has been shown to be entirely protective. Second, when looking only at this study’s laboratory-proven cases of influenza in newborns, infants whose mothers were vaccinated had a case rate of 0.84/1,000, while the case rate in newborns born to unvaccinated women was 2.83/1,000. While this shows a difference, the report provides no additional outcome data regarding morbidity or mortality.
In fact, although infant hospitalization rates differed (0.13/1,000 born to vaccinated women versus 0.66/1,000 born to unvaccinated women), there were no influenza-related mortalities in this cohort. The effect seems better when including “influenza-like illness,” but it is unclear why we should think that the influenza vaccine protects against infection that is not caused by influenza.
What this EVIDENCE means for practice
ObGyns should continue to promote influenza vaccination during pregnancy for the maternal protection it imparts. These new data on the potential for newborn protection, although not conclusive, may improve maternal acceptance of vaccination; from that perspective, these data are valuable.
— John T. Repke, MD
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
A recent report on data obtained from the Intermountain Healthcare facilities in Utah and Idaho suggests that maternal influenza vaccination, besides its maternal protective effect, also may benefit the newborn by protecting against influenza. I think that ObGyns generally accept the notion that influenza vaccination has defined maternal benefit. Notably, acceptance of influenza vaccine became much more widespread during and following the H1N1 flu pandemic of 2009. The fact that there may be neonatal and infant benefit as well is certainly not objectionable, especially since flu vaccine is not recommended for infants less than 6 months of age.
Details of the study
Shakib and colleagues’ goal was to compare influenza outcomes in infants younger than 6 months born to women who self-reported receiving or not receiving influenza vaccine during pregnancy. The study cohort included 245,386 women and 249,387 infants who were born between December 2005 and March 2014. The outcomes studied were influenza-like illness (ILI), laboratory-confirmed influenza, and influenza hospitalizations.
Of 866 infants younger than 6 months born to women who had received a flu shot, 32 had 1 or more ILI encounters, compared with 834 born to women who were not immunized (relative risk [RR], 0.36; 95% confidence interval [CI], 0.26–0.52; P<.001). Laboratory-confirmed influenza was identified in 658 infants; of these, 20 were born to women reporting immunization and 638 were born to unimmunized women (RR, 0.30; 95% CI, 0.19–0.46; P<.001). Finally, 151 infants with laboratory-confirmed influenza were hospitalized; 3 were born to immunized women and 148 to women who had not received a flu shot (RR, 0.19; 95% CI, 0.06–0.60; P = .005).
The authors calculated that infants born to women who reported influenza immunization during pregnancy had risk reductions of 64% for ILI, 70% for laboratory-confirmed influenza, and 81% for influenza hospitalizations.
Consider immunization benefits realistically
The authors state in their published report that “Protecting young infants from influenza through maternal immunization during pregnancy is a public health priority.” This may be overstating their case, for the following reasons. First, influenza vaccine has varying degrees of efficacy depending on the particular year and influenza strains that predominate, and it never has been shown to be entirely protective. Second, when looking only at this study’s laboratory-proven cases of influenza in newborns, infants whose mothers were vaccinated had a case rate of 0.84/1,000, while the case rate in newborns born to unvaccinated women was 2.83/1,000. While this shows a difference, the report provides no additional outcome data regarding morbidity or mortality.
In fact, although infant hospitalization rates differed (0.13/1,000 born to vaccinated women versus 0.66/1,000 born to unvaccinated women), there were no influenza-related mortalities in this cohort. The effect seems better when including “influenza-like illness,” but it is unclear why we should think that the influenza vaccine protects against infection that is not caused by influenza.
What this EVIDENCE means for practice
ObGyns should continue to promote influenza vaccination during pregnancy for the maternal protection it imparts. These new data on the potential for newborn protection, although not conclusive, may improve maternal acceptance of vaccination; from that perspective, these data are valuable.
— John T. Repke, MD
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Failure to convert to laparotomy: $6.25M settlement
Failure to convert to laparotomy: $6.25M settlement

A 67-year-old woman with urinary incontinence underwent robot-assisted laparoscopic prolapse surgery and hysterectomy. Complications arose, including an injury to the transverse colon. Postoperatively, the patient developed sepsis and had multiple surgeries. At the time of trial, she used a colostomy bag and had a malabsorption syndrome that required frequent intravenous treatment for dehydration.
Patient's claim:
The gynecologist deviated from the standard of care by failing to convert from a laparoscopic procedure to an open procedure when complications developed.
Defendants' defense:
The procedure was properly performed.
Verdict:
A $6.25 million New Jersey settlement was reached, paid jointly by the gynecologist and the medical center.
Circumcision requires revision
A day after birth, a baby underwent circumcision performed by the mother’s ObGyn. Revision surgery was performed 2.5 years later. When the boy was age 7 years, urethral stricture developed and was treated.
Parents' claim:
Circumcision was improperly performed. Once the child was able to talk, he said that his penis constantly hurt. Pain was only relieved by revision surgery.
Physician's defense:
There was no negligence. Redundant foreskin is often left following a circumcision.
Verdict:
A Michigan defense verdict was returned.
Mother with CP has child with CP
A pregnant woman with cerebral palsy (CP) reported a prior preterm delivery at 24 weeks’ gestation to a high-risk prenatal clinic. At that time, she was offered synthetic progesterone (170HP) injections, but she declined because of the cost. She declined 170HP several times. Nine weeks after her initial visit, she declined 170HP despite ultrasonography (US) showing a shortened cervical length (25 mm) for the gestational age. In 2 weeks, when the cervical length measured 9 mm, she was hospitalized to rule out preterm labor but, before tests began, she left the hospital. Five days later, when her cervical length was 11 mm, she received the first 170HP injection. In the next month she received 4 injections, but she failed to show for the fifth injection and US. The next day, she went to the hospital with cramping. She was given steroids and medication to stop labor. US results indicated that the baby was in breech position. The mother consented to cesarean delivery, but the baby was born vaginally an hour later. The child has mild brain damage, CP, developmental delays, and learning disabilities.
Parents' claim: The mother should have been offered vaginal progesterone, which is cheaper. Given the high risk of preterm birth, steroids administered earlier would have improved fetal development. Cesarean delivery should have been performed.
Defendants' defense: Vaginal progesterone was not available at the time. Starting steroids earlier would not have improved fetal outcome. A cesarean delivery was not possible because the baby was in the birth canal.
Verdict: A $3,500,000 Michigan settlement was reached.
Fallopian tubes grow back, pregnancy
A couple decided they did not want more children and sought counseling from the woman’s ObGyn, who recommended laparoscopic tubal ligation. Several months after surgery, the patient became pregnant and gave birth to a son.
Parents' claim:
The additional child placed an economic hardship on the family, now raising 4 children. The youngest child has language delays and learning disabilities.
Physician's defense:
Regrowth of the fallopian tubes resulting in unwanted pregnancy is a known complication of tubal ligation.
Verdict:
A $397,000 Maryland verdict was returned, including funds for the cost of raising the fourth child and to cope with the child’s special needs.
Challenges in managing labor

At 37 weeks' gestation, a woman was hospitalized in labor. At 1:15 pm, she was dilated 3 cm. At 1:30 pm, she was dilated 4−5 cm with increasing contractions and a reassuring fetal heart rate (FHR). The ObGyn covering for the mother’s ObGyn ordered oxytocin augmentation, which started at 2:45 pm. Shortly thereafter, contractions became more frequent and uterine tachysystole was observed. At 4:12 pm, FHR showed multiple deep decelerations with slow recovery. The baseline dropped to a 90-bpm range and remained that way for 17 minutes. At that point, the ObGyn stopped oxytocin and administered terbutaline; the FHR returned to baseline.
After vaginal delivery, the baby’s Apgar scores were 8 and 9 at 1 and 5 minutes, respectively. Two days later, the baby had seizures and was transferred to the neonatal intensive care unit. An electroencephalogram confirmed seizure activity. Initial imaging results were normal. However, magnetic resonance imaging performed a week after delivery showed bilateral brain damage. The child has spastic displegia, is unable to ambulate, and is blind.
Parents' claim: A suit was filed against the hospital and both ObGyns. The hospital settled before trial. The case was discontinued against the primary ObGyn. The covering ObGyn allegedly made 4 departures from accepted medical practice that caused the child’s injury: ordering and administering oxytocin, failing to closely monitor the FHR, failing to timely administer terbutaline, and failing to timely respond to and correct tachysystole.
Physician's defense: The child’s injury occurred before or after labor. The pregnancy was complicated by multiple kidney infections. A week before delivery, US revealed a blood-flow abnormality. An intranatal hypoxic event did not cause the injury, proven by the fact that, after terbutaline was administered, the FHR promptly normalized.
Verdict: A $3 million New York settlement was reached with the hospital. A $134 million verdict was returned against the covering ObGyn.
Brachial plexus injury during delivery
At 37 weeks' gestation, a mother was admitted to the hospital for induction of labor. Increasing doses of oxytocin were administered. Near midnight, FHR monitoring indicated fetal distress. The ObGyn was called and he ordered cesarean delivery. Once he arrived and examined the mother, he found no fetal concerns and decided to proceed with the original birth plan. At 3:30 am, the patient was fully dilated and in active labor. The ObGyn used a vacuum extractor. Upon delivery of the baby’s head, the ObGyn encountered shoulder dystocia and called for assistance. The child was born with a near-total brachial plexus injury: avulsions of all 5 brachial plexus nerves with trauma to the cervical nerve roots at C5−C8 and T1. The child has undergone multiple nerve grafts and orthopedic operations.
Parents' claim: Fetal distress should have prompted the ObGyn to perform cesarean delivery. There was no reason to use vacuum extraction. Based on the severity of the outcome, the ObGyn must have applied excessive force and inappropriate traction during delivery maneuvers.
Physician's defense: The standard of care did not require a cesarean delivery. The vacuum extractor did not cause shoulder dystocia. The ObGyn did not apply excessive force or traction to complete the delivery. The extent of the outcome was partially due to a fetal anomaly and hypotonia.
Verdict: An Illinois defense verdict was returned.
HPV-positive pap tests results never reported
A single mother of 4 children underwent Papanicolaou (Pap) tests in 2004, 2005, and 2007 at a federally funded clinic. Each time, she tested positive for oncogenic human papillomaviruses. In 2011, the patient died of cervical cancer.
Estate's claim: The patient was never notified that the results of the 3 Pap tests were abnormal because all correspondence was sent to an outdated address although she had been treated at the same clinic for other issues during that period of time. Cervical dysplasia identified in 2004 progressed to cancer and metastasized, leading to her death 7 years later.
Defendants' defense: The case was settled during trial.
Verdict: A $4,950,000 Illinois settlement was reached.
Failure to convert to laparotomy: $6.25M settlement

A 67-year-old woman with urinary incontinence underwent robot-assisted laparoscopic prolapse surgery and hysterectomy. Complications arose, including an injury to the transverse colon. Postoperatively, the patient developed sepsis and had multiple surgeries. At the time of trial, she used a colostomy bag and had a malabsorption syndrome that required frequent intravenous treatment for dehydration.
Patient's claim:
The gynecologist deviated from the standard of care by failing to convert from a laparoscopic procedure to an open procedure when complications developed.
Defendants' defense:
The procedure was properly performed.
Verdict:
A $6.25 million New Jersey settlement was reached, paid jointly by the gynecologist and the medical center.
Circumcision requires revision
A day after birth, a baby underwent circumcision performed by the mother’s ObGyn. Revision surgery was performed 2.5 years later. When the boy was age 7 years, urethral stricture developed and was treated.
Parents' claim:
Circumcision was improperly performed. Once the child was able to talk, he said that his penis constantly hurt. Pain was only relieved by revision surgery.
Physician's defense:
There was no negligence. Redundant foreskin is often left following a circumcision.
Verdict:
A Michigan defense verdict was returned.
Mother with CP has child with CP
A pregnant woman with cerebral palsy (CP) reported a prior preterm delivery at 24 weeks’ gestation to a high-risk prenatal clinic. At that time, she was offered synthetic progesterone (170HP) injections, but she declined because of the cost. She declined 170HP several times. Nine weeks after her initial visit, she declined 170HP despite ultrasonography (US) showing a shortened cervical length (25 mm) for the gestational age. In 2 weeks, when the cervical length measured 9 mm, she was hospitalized to rule out preterm labor but, before tests began, she left the hospital. Five days later, when her cervical length was 11 mm, she received the first 170HP injection. In the next month she received 4 injections, but she failed to show for the fifth injection and US. The next day, she went to the hospital with cramping. She was given steroids and medication to stop labor. US results indicated that the baby was in breech position. The mother consented to cesarean delivery, but the baby was born vaginally an hour later. The child has mild brain damage, CP, developmental delays, and learning disabilities.
Parents' claim: The mother should have been offered vaginal progesterone, which is cheaper. Given the high risk of preterm birth, steroids administered earlier would have improved fetal development. Cesarean delivery should have been performed.
Defendants' defense: Vaginal progesterone was not available at the time. Starting steroids earlier would not have improved fetal outcome. A cesarean delivery was not possible because the baby was in the birth canal.
Verdict: A $3,500,000 Michigan settlement was reached.
Fallopian tubes grow back, pregnancy
A couple decided they did not want more children and sought counseling from the woman’s ObGyn, who recommended laparoscopic tubal ligation. Several months after surgery, the patient became pregnant and gave birth to a son.
Parents' claim:
The additional child placed an economic hardship on the family, now raising 4 children. The youngest child has language delays and learning disabilities.
Physician's defense:
Regrowth of the fallopian tubes resulting in unwanted pregnancy is a known complication of tubal ligation.
Verdict:
A $397,000 Maryland verdict was returned, including funds for the cost of raising the fourth child and to cope with the child’s special needs.
Challenges in managing labor

At 37 weeks' gestation, a woman was hospitalized in labor. At 1:15 pm, she was dilated 3 cm. At 1:30 pm, she was dilated 4−5 cm with increasing contractions and a reassuring fetal heart rate (FHR). The ObGyn covering for the mother’s ObGyn ordered oxytocin augmentation, which started at 2:45 pm. Shortly thereafter, contractions became more frequent and uterine tachysystole was observed. At 4:12 pm, FHR showed multiple deep decelerations with slow recovery. The baseline dropped to a 90-bpm range and remained that way for 17 minutes. At that point, the ObGyn stopped oxytocin and administered terbutaline; the FHR returned to baseline.
After vaginal delivery, the baby’s Apgar scores were 8 and 9 at 1 and 5 minutes, respectively. Two days later, the baby had seizures and was transferred to the neonatal intensive care unit. An electroencephalogram confirmed seizure activity. Initial imaging results were normal. However, magnetic resonance imaging performed a week after delivery showed bilateral brain damage. The child has spastic displegia, is unable to ambulate, and is blind.
Parents' claim: A suit was filed against the hospital and both ObGyns. The hospital settled before trial. The case was discontinued against the primary ObGyn. The covering ObGyn allegedly made 4 departures from accepted medical practice that caused the child’s injury: ordering and administering oxytocin, failing to closely monitor the FHR, failing to timely administer terbutaline, and failing to timely respond to and correct tachysystole.
Physician's defense: The child’s injury occurred before or after labor. The pregnancy was complicated by multiple kidney infections. A week before delivery, US revealed a blood-flow abnormality. An intranatal hypoxic event did not cause the injury, proven by the fact that, after terbutaline was administered, the FHR promptly normalized.
Verdict: A $3 million New York settlement was reached with the hospital. A $134 million verdict was returned against the covering ObGyn.
Brachial plexus injury during delivery
At 37 weeks' gestation, a mother was admitted to the hospital for induction of labor. Increasing doses of oxytocin were administered. Near midnight, FHR monitoring indicated fetal distress. The ObGyn was called and he ordered cesarean delivery. Once he arrived and examined the mother, he found no fetal concerns and decided to proceed with the original birth plan. At 3:30 am, the patient was fully dilated and in active labor. The ObGyn used a vacuum extractor. Upon delivery of the baby’s head, the ObGyn encountered shoulder dystocia and called for assistance. The child was born with a near-total brachial plexus injury: avulsions of all 5 brachial plexus nerves with trauma to the cervical nerve roots at C5−C8 and T1. The child has undergone multiple nerve grafts and orthopedic operations.
Parents' claim: Fetal distress should have prompted the ObGyn to perform cesarean delivery. There was no reason to use vacuum extraction. Based on the severity of the outcome, the ObGyn must have applied excessive force and inappropriate traction during delivery maneuvers.
Physician's defense: The standard of care did not require a cesarean delivery. The vacuum extractor did not cause shoulder dystocia. The ObGyn did not apply excessive force or traction to complete the delivery. The extent of the outcome was partially due to a fetal anomaly and hypotonia.
Verdict: An Illinois defense verdict was returned.
HPV-positive pap tests results never reported
A single mother of 4 children underwent Papanicolaou (Pap) tests in 2004, 2005, and 2007 at a federally funded clinic. Each time, she tested positive for oncogenic human papillomaviruses. In 2011, the patient died of cervical cancer.
Estate's claim: The patient was never notified that the results of the 3 Pap tests were abnormal because all correspondence was sent to an outdated address although she had been treated at the same clinic for other issues during that period of time. Cervical dysplasia identified in 2004 progressed to cancer and metastasized, leading to her death 7 years later.
Defendants' defense: The case was settled during trial.
Verdict: A $4,950,000 Illinois settlement was reached.
Failure to convert to laparotomy: $6.25M settlement

A 67-year-old woman with urinary incontinence underwent robot-assisted laparoscopic prolapse surgery and hysterectomy. Complications arose, including an injury to the transverse colon. Postoperatively, the patient developed sepsis and had multiple surgeries. At the time of trial, she used a colostomy bag and had a malabsorption syndrome that required frequent intravenous treatment for dehydration.
Patient's claim:
The gynecologist deviated from the standard of care by failing to convert from a laparoscopic procedure to an open procedure when complications developed.
Defendants' defense:
The procedure was properly performed.
Verdict:
A $6.25 million New Jersey settlement was reached, paid jointly by the gynecologist and the medical center.
Circumcision requires revision
A day after birth, a baby underwent circumcision performed by the mother’s ObGyn. Revision surgery was performed 2.5 years later. When the boy was age 7 years, urethral stricture developed and was treated.
Parents' claim:
Circumcision was improperly performed. Once the child was able to talk, he said that his penis constantly hurt. Pain was only relieved by revision surgery.
Physician's defense:
There was no negligence. Redundant foreskin is often left following a circumcision.
Verdict:
A Michigan defense verdict was returned.
Mother with CP has child with CP
A pregnant woman with cerebral palsy (CP) reported a prior preterm delivery at 24 weeks’ gestation to a high-risk prenatal clinic. At that time, she was offered synthetic progesterone (170HP) injections, but she declined because of the cost. She declined 170HP several times. Nine weeks after her initial visit, she declined 170HP despite ultrasonography (US) showing a shortened cervical length (25 mm) for the gestational age. In 2 weeks, when the cervical length measured 9 mm, she was hospitalized to rule out preterm labor but, before tests began, she left the hospital. Five days later, when her cervical length was 11 mm, she received the first 170HP injection. In the next month she received 4 injections, but she failed to show for the fifth injection and US. The next day, she went to the hospital with cramping. She was given steroids and medication to stop labor. US results indicated that the baby was in breech position. The mother consented to cesarean delivery, but the baby was born vaginally an hour later. The child has mild brain damage, CP, developmental delays, and learning disabilities.
Parents' claim: The mother should have been offered vaginal progesterone, which is cheaper. Given the high risk of preterm birth, steroids administered earlier would have improved fetal development. Cesarean delivery should have been performed.
Defendants' defense: Vaginal progesterone was not available at the time. Starting steroids earlier would not have improved fetal outcome. A cesarean delivery was not possible because the baby was in the birth canal.
Verdict: A $3,500,000 Michigan settlement was reached.
Fallopian tubes grow back, pregnancy
A couple decided they did not want more children and sought counseling from the woman’s ObGyn, who recommended laparoscopic tubal ligation. Several months after surgery, the patient became pregnant and gave birth to a son.
Parents' claim:
The additional child placed an economic hardship on the family, now raising 4 children. The youngest child has language delays and learning disabilities.
Physician's defense:
Regrowth of the fallopian tubes resulting in unwanted pregnancy is a known complication of tubal ligation.
Verdict:
A $397,000 Maryland verdict was returned, including funds for the cost of raising the fourth child and to cope with the child’s special needs.
Challenges in managing labor

At 37 weeks' gestation, a woman was hospitalized in labor. At 1:15 pm, she was dilated 3 cm. At 1:30 pm, she was dilated 4−5 cm with increasing contractions and a reassuring fetal heart rate (FHR). The ObGyn covering for the mother’s ObGyn ordered oxytocin augmentation, which started at 2:45 pm. Shortly thereafter, contractions became more frequent and uterine tachysystole was observed. At 4:12 pm, FHR showed multiple deep decelerations with slow recovery. The baseline dropped to a 90-bpm range and remained that way for 17 minutes. At that point, the ObGyn stopped oxytocin and administered terbutaline; the FHR returned to baseline.
After vaginal delivery, the baby’s Apgar scores were 8 and 9 at 1 and 5 minutes, respectively. Two days later, the baby had seizures and was transferred to the neonatal intensive care unit. An electroencephalogram confirmed seizure activity. Initial imaging results were normal. However, magnetic resonance imaging performed a week after delivery showed bilateral brain damage. The child has spastic displegia, is unable to ambulate, and is blind.
Parents' claim: A suit was filed against the hospital and both ObGyns. The hospital settled before trial. The case was discontinued against the primary ObGyn. The covering ObGyn allegedly made 4 departures from accepted medical practice that caused the child’s injury: ordering and administering oxytocin, failing to closely monitor the FHR, failing to timely administer terbutaline, and failing to timely respond to and correct tachysystole.
Physician's defense: The child’s injury occurred before or after labor. The pregnancy was complicated by multiple kidney infections. A week before delivery, US revealed a blood-flow abnormality. An intranatal hypoxic event did not cause the injury, proven by the fact that, after terbutaline was administered, the FHR promptly normalized.
Verdict: A $3 million New York settlement was reached with the hospital. A $134 million verdict was returned against the covering ObGyn.
Brachial plexus injury during delivery
At 37 weeks' gestation, a mother was admitted to the hospital for induction of labor. Increasing doses of oxytocin were administered. Near midnight, FHR monitoring indicated fetal distress. The ObGyn was called and he ordered cesarean delivery. Once he arrived and examined the mother, he found no fetal concerns and decided to proceed with the original birth plan. At 3:30 am, the patient was fully dilated and in active labor. The ObGyn used a vacuum extractor. Upon delivery of the baby’s head, the ObGyn encountered shoulder dystocia and called for assistance. The child was born with a near-total brachial plexus injury: avulsions of all 5 brachial plexus nerves with trauma to the cervical nerve roots at C5−C8 and T1. The child has undergone multiple nerve grafts and orthopedic operations.
Parents' claim: Fetal distress should have prompted the ObGyn to perform cesarean delivery. There was no reason to use vacuum extraction. Based on the severity of the outcome, the ObGyn must have applied excessive force and inappropriate traction during delivery maneuvers.
Physician's defense: The standard of care did not require a cesarean delivery. The vacuum extractor did not cause shoulder dystocia. The ObGyn did not apply excessive force or traction to complete the delivery. The extent of the outcome was partially due to a fetal anomaly and hypotonia.
Verdict: An Illinois defense verdict was returned.
HPV-positive pap tests results never reported
A single mother of 4 children underwent Papanicolaou (Pap) tests in 2004, 2005, and 2007 at a federally funded clinic. Each time, she tested positive for oncogenic human papillomaviruses. In 2011, the patient died of cervical cancer.
Estate's claim: The patient was never notified that the results of the 3 Pap tests were abnormal because all correspondence was sent to an outdated address although she had been treated at the same clinic for other issues during that period of time. Cervical dysplasia identified in 2004 progressed to cancer and metastasized, leading to her death 7 years later.
Defendants' defense: The case was settled during trial.
Verdict: A $4,950,000 Illinois settlement was reached.
Additional Medical Verdicts
• Circumcision requires revision
• Mother with CP has child with CP
• Fallopian tubes grow back, pregnancy
• Challenges in managing labor
• Brachial plexus injury during delivery
• HPV-positive Pap tests results never reported
Letters to the Editor: Determining fetal demise; SERMS in menopause; Aspirin for preeclampsia; Treating cesarean scar defect
Determining fetal demise
I appreciate and thank Drs. Esplin and Eller for their discussion of fetal monitoring pitfalls. I agree with their sentiment that this is an inexact science. After 40 years of looking at these strips, I am convinced there must be a better way. I look forward to some innovative approach to better determine fetal well-being in labor. This article raises a question I have asked, and sought the answer to, for years.
On occasion, I have diagnosed intrauterine fetal demise by detecting the maternal heart rate with an internal fetal scalp electrode. On one particular occasion, somewhere between the time of admission, spontaneous rupture of membranes, and applying the fetal scalp electrode, the fetus died. This case was similar to the one you describe in which early efforts with the external Doppler were unsatisfactory and fetal status was suspect. My question: “What is the time interval from the moment of fetal death and loss of fetal electrical activity until the fetus becomes an effective conduit for the conduction of the maternal cardiac signal? Is it minutes, hours, days? Clearly, this would be difficult to evaluate other than on animal models, but I have yet to find an answer.
Edward Hall, MD
Edgewood, Kentucky
Drs. Esplin and Eller respond
We are grateful for your interest in our article. Unfortunately the answer to your question about the timing between fetal demise and the appearance of maternal electrocardiac activity detected by a fetal scalp electrode after transmission through the fetal body is not clear. We are not aware of any data that would conclusively prove the time required for this to occur. It is likely that this type of information would require an animal model to elucidate. However, we are aware of at least 2 clinical cases in which fetal cardiac activity was convincingly documented at admission and for several hours intrapartum with subsequent episodic loss of signal and then delivery of a dead fetus wherein retrospective review confirmed that for a period of time the maternal heart rate was recorded and interpreted to be the fetal heart rate. From these experiences we conclude that this is possible shortly after the fetal demise, likely within minutes to hours.
Despite this uncertainty, we are confident that the information in our article will help clinicians identify and correct those instances when the maternal heart rate is being recorded instead of the fetal heart rate. Fortunately, this rarely involves a situation in which there has been an undiagnosed intrauterine fetal demise.
“SERMs” definition inaccurate
I disagree with Drs. Liu and Collins’ description of selective estrogen receptor modulators (SERMs) on page S18, in which they state, “Estrogens and SERMs are lipid-soluble steroid hormones that bind to 2 specific hormone receptors, estrogen receptor α and estrogen receptor β…” SERMs are not hormones, and they are defined improperly as such.
Gideon G. Panter, MD
New York, New York
Drs. Liu and Collins respond
Thank you for your interest in our article. SERMs are typically synthetic organic compounds that can activate estrogen receptors or modify activity of the estrogen receptor and, thus, can be considered hormones.
Stop aspirin in pregnancy?
Like many colleagues, I had been stopping low-dose aspirin prior to planned or expected delivery. Evidence suggests a bigger risk of rebound hypercoagulability than bleeding after stopping low-dose aspirin, according to an article on aspirin use in the perioperative period.1 Because of lack of benefit and increased risks of stopping aspirin, it may be time to change our practice and continue aspirin to minimize peridelivery thromboembolic risk.
Mark Jacobs, MD
Mill Valley, CA
Reference
- Gerstein NS, Schulman PM, Gerstein WH, Petersen TR, Tawil I. Should more patients continue aspirin therapy perioperatively?: clinical impact of aspirin withdrawal syndrome. Ann Surg. 2012;255:811–819.
Dr. Barbieri responds
I thank Dr. Jacobs for his advice to continue low-dose aspirin throughout pregnancy in women taking aspirin for prevention of preeclampsia. The review he references is focused on elderly patients taking aspirin for existing heart disease, which is a very different population than pregnant women. There are no high-quality data from clinical trials on whether to continue or stop low-dose aspirin in pregnant women as they approach their due date. I think obstetricians can use their best judgment in making the decision of whether to stop low-dose aspirin at 36 or 37 weeks or continue aspirin throughout the pregnancy.
Technique for preventing cesarean scar defect
I read with interest the proposed treatment options that Dr. Nezhat and colleagues suggested for cesarean scar defect. However, nowhere did I see mention of preventing this defect.
For 30 years I have been closing the hysterotomy in a fashion that I believe leaves no presence of an isthmocele and is a superior closure. I overlap the upper flap with the lower flap and, most importantly, close with chromic catgut. A cesarean scar “niche” occurs with involution of the uterus causing the suture line to bunch up. Chromic catgut has a shorter half-life and will “give;” a suture made of polypropylene will not stretch. I use a running interlocking line with sutures about 0.5 inches apart.
Donald M. Werner, MD
Binghamton, New York
Dr. Nezhat and colleagues respond
We thank Dr. Werner for his inquiry regarding the prevention of cesarean scar defects; as we all agree, the best treatment is prevention. As mentioned in our article, there are no definitive results from the studies published to date that show superiority of one surgical technique over another in regard to hysterotomy closure and prevention of cesarean scar defects. Possible risk factors for developing cesarean scar defects include low (cervical) hysterotomy, single-layer uterine wall closure, use of locking sutures, closure of hysterotomy with endometrial-sparing technique, and multiple cesarean deliveries. Although these factors may be associated with increased risk of cesarean scar defects, additional randomized controlled trials need to be performed prior to being able to offer a recommendation on a conclusive preventative measure. For additional information, I would direct you to references 3 and 4 in our article. We thank you for sharing your positive experience and eagerly await additional studies on the topic.
Share your thoughts! Send your Letter to the Editor to [email protected]
Determining fetal demise
I appreciate and thank Drs. Esplin and Eller for their discussion of fetal monitoring pitfalls. I agree with their sentiment that this is an inexact science. After 40 years of looking at these strips, I am convinced there must be a better way. I look forward to some innovative approach to better determine fetal well-being in labor. This article raises a question I have asked, and sought the answer to, for years.
On occasion, I have diagnosed intrauterine fetal demise by detecting the maternal heart rate with an internal fetal scalp electrode. On one particular occasion, somewhere between the time of admission, spontaneous rupture of membranes, and applying the fetal scalp electrode, the fetus died. This case was similar to the one you describe in which early efforts with the external Doppler were unsatisfactory and fetal status was suspect. My question: “What is the time interval from the moment of fetal death and loss of fetal electrical activity until the fetus becomes an effective conduit for the conduction of the maternal cardiac signal? Is it minutes, hours, days? Clearly, this would be difficult to evaluate other than on animal models, but I have yet to find an answer.
Edward Hall, MD
Edgewood, Kentucky
Drs. Esplin and Eller respond
We are grateful for your interest in our article. Unfortunately the answer to your question about the timing between fetal demise and the appearance of maternal electrocardiac activity detected by a fetal scalp electrode after transmission through the fetal body is not clear. We are not aware of any data that would conclusively prove the time required for this to occur. It is likely that this type of information would require an animal model to elucidate. However, we are aware of at least 2 clinical cases in which fetal cardiac activity was convincingly documented at admission and for several hours intrapartum with subsequent episodic loss of signal and then delivery of a dead fetus wherein retrospective review confirmed that for a period of time the maternal heart rate was recorded and interpreted to be the fetal heart rate. From these experiences we conclude that this is possible shortly after the fetal demise, likely within minutes to hours.
Despite this uncertainty, we are confident that the information in our article will help clinicians identify and correct those instances when the maternal heart rate is being recorded instead of the fetal heart rate. Fortunately, this rarely involves a situation in which there has been an undiagnosed intrauterine fetal demise.
“SERMs” definition inaccurate
I disagree with Drs. Liu and Collins’ description of selective estrogen receptor modulators (SERMs) on page S18, in which they state, “Estrogens and SERMs are lipid-soluble steroid hormones that bind to 2 specific hormone receptors, estrogen receptor α and estrogen receptor β…” SERMs are not hormones, and they are defined improperly as such.
Gideon G. Panter, MD
New York, New York
Drs. Liu and Collins respond
Thank you for your interest in our article. SERMs are typically synthetic organic compounds that can activate estrogen receptors or modify activity of the estrogen receptor and, thus, can be considered hormones.
Stop aspirin in pregnancy?
Like many colleagues, I had been stopping low-dose aspirin prior to planned or expected delivery. Evidence suggests a bigger risk of rebound hypercoagulability than bleeding after stopping low-dose aspirin, according to an article on aspirin use in the perioperative period.1 Because of lack of benefit and increased risks of stopping aspirin, it may be time to change our practice and continue aspirin to minimize peridelivery thromboembolic risk.
Mark Jacobs, MD
Mill Valley, CA
Reference
- Gerstein NS, Schulman PM, Gerstein WH, Petersen TR, Tawil I. Should more patients continue aspirin therapy perioperatively?: clinical impact of aspirin withdrawal syndrome. Ann Surg. 2012;255:811–819.
Dr. Barbieri responds
I thank Dr. Jacobs for his advice to continue low-dose aspirin throughout pregnancy in women taking aspirin for prevention of preeclampsia. The review he references is focused on elderly patients taking aspirin for existing heart disease, which is a very different population than pregnant women. There are no high-quality data from clinical trials on whether to continue or stop low-dose aspirin in pregnant women as they approach their due date. I think obstetricians can use their best judgment in making the decision of whether to stop low-dose aspirin at 36 or 37 weeks or continue aspirin throughout the pregnancy.
Technique for preventing cesarean scar defect
I read with interest the proposed treatment options that Dr. Nezhat and colleagues suggested for cesarean scar defect. However, nowhere did I see mention of preventing this defect.
For 30 years I have been closing the hysterotomy in a fashion that I believe leaves no presence of an isthmocele and is a superior closure. I overlap the upper flap with the lower flap and, most importantly, close with chromic catgut. A cesarean scar “niche” occurs with involution of the uterus causing the suture line to bunch up. Chromic catgut has a shorter half-life and will “give;” a suture made of polypropylene will not stretch. I use a running interlocking line with sutures about 0.5 inches apart.
Donald M. Werner, MD
Binghamton, New York
Dr. Nezhat and colleagues respond
We thank Dr. Werner for his inquiry regarding the prevention of cesarean scar defects; as we all agree, the best treatment is prevention. As mentioned in our article, there are no definitive results from the studies published to date that show superiority of one surgical technique over another in regard to hysterotomy closure and prevention of cesarean scar defects. Possible risk factors for developing cesarean scar defects include low (cervical) hysterotomy, single-layer uterine wall closure, use of locking sutures, closure of hysterotomy with endometrial-sparing technique, and multiple cesarean deliveries. Although these factors may be associated with increased risk of cesarean scar defects, additional randomized controlled trials need to be performed prior to being able to offer a recommendation on a conclusive preventative measure. For additional information, I would direct you to references 3 and 4 in our article. We thank you for sharing your positive experience and eagerly await additional studies on the topic.
Share your thoughts! Send your Letter to the Editor to [email protected]
Determining fetal demise
I appreciate and thank Drs. Esplin and Eller for their discussion of fetal monitoring pitfalls. I agree with their sentiment that this is an inexact science. After 40 years of looking at these strips, I am convinced there must be a better way. I look forward to some innovative approach to better determine fetal well-being in labor. This article raises a question I have asked, and sought the answer to, for years.
On occasion, I have diagnosed intrauterine fetal demise by detecting the maternal heart rate with an internal fetal scalp electrode. On one particular occasion, somewhere between the time of admission, spontaneous rupture of membranes, and applying the fetal scalp electrode, the fetus died. This case was similar to the one you describe in which early efforts with the external Doppler were unsatisfactory and fetal status was suspect. My question: “What is the time interval from the moment of fetal death and loss of fetal electrical activity until the fetus becomes an effective conduit for the conduction of the maternal cardiac signal? Is it minutes, hours, days? Clearly, this would be difficult to evaluate other than on animal models, but I have yet to find an answer.
Edward Hall, MD
Edgewood, Kentucky
Drs. Esplin and Eller respond
We are grateful for your interest in our article. Unfortunately the answer to your question about the timing between fetal demise and the appearance of maternal electrocardiac activity detected by a fetal scalp electrode after transmission through the fetal body is not clear. We are not aware of any data that would conclusively prove the time required for this to occur. It is likely that this type of information would require an animal model to elucidate. However, we are aware of at least 2 clinical cases in which fetal cardiac activity was convincingly documented at admission and for several hours intrapartum with subsequent episodic loss of signal and then delivery of a dead fetus wherein retrospective review confirmed that for a period of time the maternal heart rate was recorded and interpreted to be the fetal heart rate. From these experiences we conclude that this is possible shortly after the fetal demise, likely within minutes to hours.
Despite this uncertainty, we are confident that the information in our article will help clinicians identify and correct those instances when the maternal heart rate is being recorded instead of the fetal heart rate. Fortunately, this rarely involves a situation in which there has been an undiagnosed intrauterine fetal demise.
“SERMs” definition inaccurate
I disagree with Drs. Liu and Collins’ description of selective estrogen receptor modulators (SERMs) on page S18, in which they state, “Estrogens and SERMs are lipid-soluble steroid hormones that bind to 2 specific hormone receptors, estrogen receptor α and estrogen receptor β…” SERMs are not hormones, and they are defined improperly as such.
Gideon G. Panter, MD
New York, New York
Drs. Liu and Collins respond
Thank you for your interest in our article. SERMs are typically synthetic organic compounds that can activate estrogen receptors or modify activity of the estrogen receptor and, thus, can be considered hormones.
Stop aspirin in pregnancy?
Like many colleagues, I had been stopping low-dose aspirin prior to planned or expected delivery. Evidence suggests a bigger risk of rebound hypercoagulability than bleeding after stopping low-dose aspirin, according to an article on aspirin use in the perioperative period.1 Because of lack of benefit and increased risks of stopping aspirin, it may be time to change our practice and continue aspirin to minimize peridelivery thromboembolic risk.
Mark Jacobs, MD
Mill Valley, CA
Reference
- Gerstein NS, Schulman PM, Gerstein WH, Petersen TR, Tawil I. Should more patients continue aspirin therapy perioperatively?: clinical impact of aspirin withdrawal syndrome. Ann Surg. 2012;255:811–819.
Dr. Barbieri responds
I thank Dr. Jacobs for his advice to continue low-dose aspirin throughout pregnancy in women taking aspirin for prevention of preeclampsia. The review he references is focused on elderly patients taking aspirin for existing heart disease, which is a very different population than pregnant women. There are no high-quality data from clinical trials on whether to continue or stop low-dose aspirin in pregnant women as they approach their due date. I think obstetricians can use their best judgment in making the decision of whether to stop low-dose aspirin at 36 or 37 weeks or continue aspirin throughout the pregnancy.
Technique for preventing cesarean scar defect
I read with interest the proposed treatment options that Dr. Nezhat and colleagues suggested for cesarean scar defect. However, nowhere did I see mention of preventing this defect.
For 30 years I have been closing the hysterotomy in a fashion that I believe leaves no presence of an isthmocele and is a superior closure. I overlap the upper flap with the lower flap and, most importantly, close with chromic catgut. A cesarean scar “niche” occurs with involution of the uterus causing the suture line to bunch up. Chromic catgut has a shorter half-life and will “give;” a suture made of polypropylene will not stretch. I use a running interlocking line with sutures about 0.5 inches apart.
Donald M. Werner, MD
Binghamton, New York
Dr. Nezhat and colleagues respond
We thank Dr. Werner for his inquiry regarding the prevention of cesarean scar defects; as we all agree, the best treatment is prevention. As mentioned in our article, there are no definitive results from the studies published to date that show superiority of one surgical technique over another in regard to hysterotomy closure and prevention of cesarean scar defects. Possible risk factors for developing cesarean scar defects include low (cervical) hysterotomy, single-layer uterine wall closure, use of locking sutures, closure of hysterotomy with endometrial-sparing technique, and multiple cesarean deliveries. Although these factors may be associated with increased risk of cesarean scar defects, additional randomized controlled trials need to be performed prior to being able to offer a recommendation on a conclusive preventative measure. For additional information, I would direct you to references 3 and 4 in our article. We thank you for sharing your positive experience and eagerly await additional studies on the topic.
Share your thoughts! Send your Letter to the Editor to [email protected]
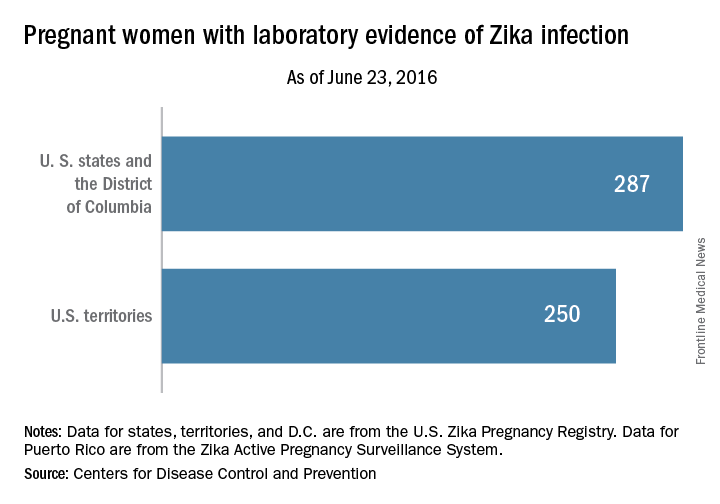
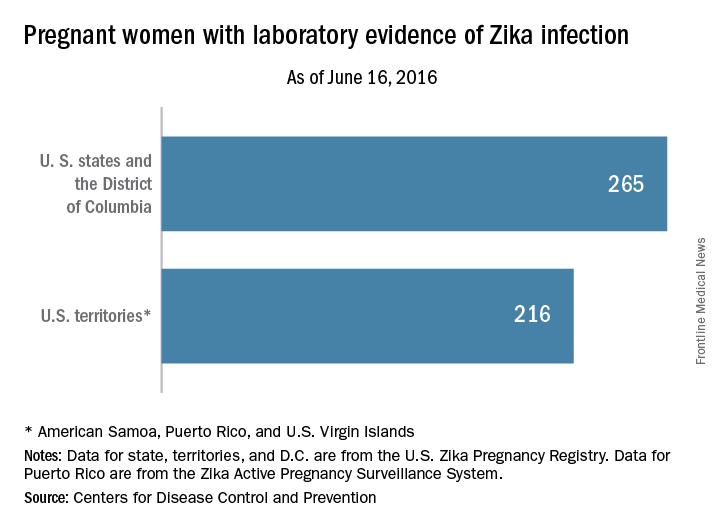
Number of US Zika Cases in Pregnant Women up to 537
During the week ending June 23, 2016, there were three infants born with birth defects and one pregnancy loss among U.S. women who had been infected with Zika virus, according to the Centers for Disease Control and Prevention.
The pregnancy-outcomes data, which were posted June 30, show that a total of seven infants have been born in the United States with Zika-related birth defects and that there have been five pregnancy losses with probable Zika-related birth defects, the CDC reported.
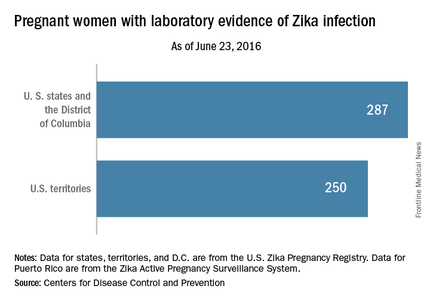
For that same week, there were reports of an additional 22 pregnant women with Zika virus infection in the 50 states and the District of Columbia, bringing the total to 287. Among U.S. territories – American Samoa, Guam, Northern Marianas, Puerto Rico, and the U.S. Virgin Islands – 34 more pregnant women were reported, bringing the territorial number up to 250 and giving the country a total of 537 cases, the CDC said. The CDC is not reporting state- or territorial-level data to protect the privacy of affected women and children.
The figures for states, territories, and the District of Columbia reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System. These are not real-time data and reflect only pregnancy outcomes for women with any laboratory evidence of possible Zika virus infection, although it is not known if Zika virus was the cause of the poor outcomes.
Zika-related birth defects recorded by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
During the week ending June 23, 2016, there were three infants born with birth defects and one pregnancy loss among U.S. women who had been infected with Zika virus, according to the Centers for Disease Control and Prevention.
The pregnancy-outcomes data, which were posted June 30, show that a total of seven infants have been born in the United States with Zika-related birth defects and that there have been five pregnancy losses with probable Zika-related birth defects, the CDC reported.
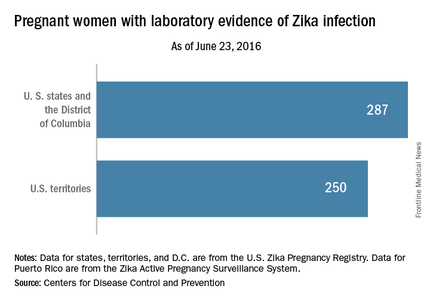
For that same week, there were reports of an additional 22 pregnant women with Zika virus infection in the 50 states and the District of Columbia, bringing the total to 287. Among U.S. territories – American Samoa, Guam, Northern Marianas, Puerto Rico, and the U.S. Virgin Islands – 34 more pregnant women were reported, bringing the territorial number up to 250 and giving the country a total of 537 cases, the CDC said. The CDC is not reporting state- or territorial-level data to protect the privacy of affected women and children.
The figures for states, territories, and the District of Columbia reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System. These are not real-time data and reflect only pregnancy outcomes for women with any laboratory evidence of possible Zika virus infection, although it is not known if Zika virus was the cause of the poor outcomes.
Zika-related birth defects recorded by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
During the week ending June 23, 2016, there were three infants born with birth defects and one pregnancy loss among U.S. women who had been infected with Zika virus, according to the Centers for Disease Control and Prevention.
The pregnancy-outcomes data, which were posted June 30, show that a total of seven infants have been born in the United States with Zika-related birth defects and that there have been five pregnancy losses with probable Zika-related birth defects, the CDC reported.
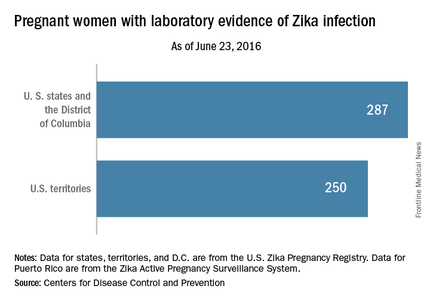
For that same week, there were reports of an additional 22 pregnant women with Zika virus infection in the 50 states and the District of Columbia, bringing the total to 287. Among U.S. territories – American Samoa, Guam, Northern Marianas, Puerto Rico, and the U.S. Virgin Islands – 34 more pregnant women were reported, bringing the territorial number up to 250 and giving the country a total of 537 cases, the CDC said. The CDC is not reporting state- or territorial-level data to protect the privacy of affected women and children.
The figures for states, territories, and the District of Columbia reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System. These are not real-time data and reflect only pregnancy outcomes for women with any laboratory evidence of possible Zika virus infection, although it is not known if Zika virus was the cause of the poor outcomes.
Zika-related birth defects recorded by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
Rash, Microcephaly Not Always Present With Congenital Zika Syndrome
The largest study so far of congenital Zika virus syndrome suggests that microcephaly and maternal rash are not sufficient to detect affected babies.
Writing in the June 29 online edition of The Lancet, researchers report on a case series of 1,501 liveborn infants with suspected congenital Zika virus syndrome reported in Brazil. The study found that one in five definite or probable cases of congenital Zika virus syndrome had a head circumference within the range of normal, and in one third of definite or probable cases, the mother had no history of a rash during pregnancy.
Of the total series, 899 were discarded because they showed no obvious clinical or neuropsychomotor abnormalities such as craniofacial disproportion or neurological symptoms (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736[16]30902-3).
Of the remaining 602 cases, 76 were described as definite cases of congenital Zika virus syndrome because of laboratory evidence of Zika virus infection during pregnancy.
Fifty-four babies were considered highly probable cases of congenital Zika virus syndrome because imaging reports showed features such as brain calcifications and ventricular enlargement suggestive of Zika virus infection and which could not be attributed to other pathogens such as syphilis, cytomegalovirus, or toxoplasmosis.
A further 181 were “moderately probable” – they had similar imaging results to the highly probable group but without test results for other infections – while the 291 somewhat probable cases had imaging results that suggested Zika virus was likely involved.
Among the 391 definitely or probable cases where full information was available, half had both microcephaly and a history of maternal rash, while 87% had at least one of these symptoms.
“There were only two significant differences between the four categories: diagnostic certainty was positively associated with reported rashes and with smaller head circumferences before taking gestational age into account,” wrote Giovanny V. A. França, PhD, of the Secretariat of Health Surveillance, Ministry of Health, Brazil, and coauthors.
Researchers also noted that the discarded cases had larger head circumferences, lower first week mortality, and the mothers were less likely to have a history of rash during pregnancy (20.7% vs 61.4%, 95% confidence interval, 0.27-0.42).
Meanwhile, a second case series in the same edition of The Lancet reported on the pathology of five cases of congenital Zika syndrome, providing further evidence of the link between the virus and congenital abnormalities.
Tissue samples from three fatal cases of the syndrome and two spontaneous abortions found antigens to the Zika virus in the cytoplasm of degenerating and necrotic neurons and glial cells, but no immunohistochemical staining for Zika virus was found outside the central nervous system (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736[16]30883-2).
The five cases all showed signs of brain abnormalities including microcephaly, lissencephaly, cerebellar hypoplasia, and ventriculomegaly, while histopathological studies in the three fatal cases revealed microcalcifications, scattered microglial nodules, cell degeneration, and necrosis.
“The absence of a substantial inflammatory response in the brain and a specific cytopathic viral effect distinguishes Zika virus infection from other important viral infections that are also associated with microcephaly and microcalcifications, such as cytomegalovirus and herpes simplex virus,” wrote Roosecelis Brasil Martines, MD, of the National Center for Emerging and Zoonotic Infectious Diseases, CDC, and coauthors.
There was also a range of other congenital malformations evident in the three fatal cases, including multiple congenital contractures, craniofacial malformations, craniosynostosis, pulmonary hypoplasia, and a wide range of brain abnormalities.
“The mechanism for these deformities in Zika virus infection are not entirely clear, but most probably result from neurotropism of the virus with subsequent damage of the brain and interference in neuromuscular signaling leading to fetal akinesia,” the authors said.
No conflicts of interest were declared for either study.
This study is an important contribution for improving the surveillance system for congenital Zika virus infection but caution should be taken in interpreting results of this case series based on routinely collected data with missing information for many cases and an unknown degree of under-reporting.
For incorporating new information besides microcephaly and rash during pregnancy to detect all affected cases, neurological signs and symptoms could be eligible, but might be difficult to obtain in most settings because of insufficient specialized personnel. The development of an accurate serological test that could be incorporated into routine prenatal care will be essential, and its validation a research priority.
While the current outbreak is a paradigmatic example of how quickly evolving systematic scientific evidence can (and should) change the view on a disease within months, it can be expected that public health authorities, and also the scientific community, will struggle for many years with Zika epidemics and its consequences in Brazil and elsewhere.
Jörg Heukelbach, MD, is from the School of Medicine at the Federal University of Ceará in Brazil, and Guilherme Loureiro Werneck, MD, is from the Social Medicine Institute at the State University of Rio de Janeiro. The comments are excerpted from an accompanying editorial (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736(16)30931-X). No conflicts of interest were declared.
This study is an important contribution for improving the surveillance system for congenital Zika virus infection but caution should be taken in interpreting results of this case series based on routinely collected data with missing information for many cases and an unknown degree of under-reporting.
For incorporating new information besides microcephaly and rash during pregnancy to detect all affected cases, neurological signs and symptoms could be eligible, but might be difficult to obtain in most settings because of insufficient specialized personnel. The development of an accurate serological test that could be incorporated into routine prenatal care will be essential, and its validation a research priority.
While the current outbreak is a paradigmatic example of how quickly evolving systematic scientific evidence can (and should) change the view on a disease within months, it can be expected that public health authorities, and also the scientific community, will struggle for many years with Zika epidemics and its consequences in Brazil and elsewhere.
Jörg Heukelbach, MD, is from the School of Medicine at the Federal University of Ceará in Brazil, and Guilherme Loureiro Werneck, MD, is from the Social Medicine Institute at the State University of Rio de Janeiro. The comments are excerpted from an accompanying editorial (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736(16)30931-X). No conflicts of interest were declared.
This study is an important contribution for improving the surveillance system for congenital Zika virus infection but caution should be taken in interpreting results of this case series based on routinely collected data with missing information for many cases and an unknown degree of under-reporting.
For incorporating new information besides microcephaly and rash during pregnancy to detect all affected cases, neurological signs and symptoms could be eligible, but might be difficult to obtain in most settings because of insufficient specialized personnel. The development of an accurate serological test that could be incorporated into routine prenatal care will be essential, and its validation a research priority.
While the current outbreak is a paradigmatic example of how quickly evolving systematic scientific evidence can (and should) change the view on a disease within months, it can be expected that public health authorities, and also the scientific community, will struggle for many years with Zika epidemics and its consequences in Brazil and elsewhere.
Jörg Heukelbach, MD, is from the School of Medicine at the Federal University of Ceará in Brazil, and Guilherme Loureiro Werneck, MD, is from the Social Medicine Institute at the State University of Rio de Janeiro. The comments are excerpted from an accompanying editorial (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736(16)30931-X). No conflicts of interest were declared.
The largest study so far of congenital Zika virus syndrome suggests that microcephaly and maternal rash are not sufficient to detect affected babies.
Writing in the June 29 online edition of The Lancet, researchers report on a case series of 1,501 liveborn infants with suspected congenital Zika virus syndrome reported in Brazil. The study found that one in five definite or probable cases of congenital Zika virus syndrome had a head circumference within the range of normal, and in one third of definite or probable cases, the mother had no history of a rash during pregnancy.
Of the total series, 899 were discarded because they showed no obvious clinical or neuropsychomotor abnormalities such as craniofacial disproportion or neurological symptoms (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736[16]30902-3).
Of the remaining 602 cases, 76 were described as definite cases of congenital Zika virus syndrome because of laboratory evidence of Zika virus infection during pregnancy.
Fifty-four babies were considered highly probable cases of congenital Zika virus syndrome because imaging reports showed features such as brain calcifications and ventricular enlargement suggestive of Zika virus infection and which could not be attributed to other pathogens such as syphilis, cytomegalovirus, or toxoplasmosis.
A further 181 were “moderately probable” – they had similar imaging results to the highly probable group but without test results for other infections – while the 291 somewhat probable cases had imaging results that suggested Zika virus was likely involved.
Among the 391 definitely or probable cases where full information was available, half had both microcephaly and a history of maternal rash, while 87% had at least one of these symptoms.
“There were only two significant differences between the four categories: diagnostic certainty was positively associated with reported rashes and with smaller head circumferences before taking gestational age into account,” wrote Giovanny V. A. França, PhD, of the Secretariat of Health Surveillance, Ministry of Health, Brazil, and coauthors.
Researchers also noted that the discarded cases had larger head circumferences, lower first week mortality, and the mothers were less likely to have a history of rash during pregnancy (20.7% vs 61.4%, 95% confidence interval, 0.27-0.42).
Meanwhile, a second case series in the same edition of The Lancet reported on the pathology of five cases of congenital Zika syndrome, providing further evidence of the link between the virus and congenital abnormalities.
Tissue samples from three fatal cases of the syndrome and two spontaneous abortions found antigens to the Zika virus in the cytoplasm of degenerating and necrotic neurons and glial cells, but no immunohistochemical staining for Zika virus was found outside the central nervous system (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736[16]30883-2).
The five cases all showed signs of brain abnormalities including microcephaly, lissencephaly, cerebellar hypoplasia, and ventriculomegaly, while histopathological studies in the three fatal cases revealed microcalcifications, scattered microglial nodules, cell degeneration, and necrosis.
“The absence of a substantial inflammatory response in the brain and a specific cytopathic viral effect distinguishes Zika virus infection from other important viral infections that are also associated with microcephaly and microcalcifications, such as cytomegalovirus and herpes simplex virus,” wrote Roosecelis Brasil Martines, MD, of the National Center for Emerging and Zoonotic Infectious Diseases, CDC, and coauthors.
There was also a range of other congenital malformations evident in the three fatal cases, including multiple congenital contractures, craniofacial malformations, craniosynostosis, pulmonary hypoplasia, and a wide range of brain abnormalities.
“The mechanism for these deformities in Zika virus infection are not entirely clear, but most probably result from neurotropism of the virus with subsequent damage of the brain and interference in neuromuscular signaling leading to fetal akinesia,” the authors said.
No conflicts of interest were declared for either study.
The largest study so far of congenital Zika virus syndrome suggests that microcephaly and maternal rash are not sufficient to detect affected babies.
Writing in the June 29 online edition of The Lancet, researchers report on a case series of 1,501 liveborn infants with suspected congenital Zika virus syndrome reported in Brazil. The study found that one in five definite or probable cases of congenital Zika virus syndrome had a head circumference within the range of normal, and in one third of definite or probable cases, the mother had no history of a rash during pregnancy.
Of the total series, 899 were discarded because they showed no obvious clinical or neuropsychomotor abnormalities such as craniofacial disproportion or neurological symptoms (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736[16]30902-3).
Of the remaining 602 cases, 76 were described as definite cases of congenital Zika virus syndrome because of laboratory evidence of Zika virus infection during pregnancy.
Fifty-four babies were considered highly probable cases of congenital Zika virus syndrome because imaging reports showed features such as brain calcifications and ventricular enlargement suggestive of Zika virus infection and which could not be attributed to other pathogens such as syphilis, cytomegalovirus, or toxoplasmosis.
A further 181 were “moderately probable” – they had similar imaging results to the highly probable group but without test results for other infections – while the 291 somewhat probable cases had imaging results that suggested Zika virus was likely involved.
Among the 391 definitely or probable cases where full information was available, half had both microcephaly and a history of maternal rash, while 87% had at least one of these symptoms.
“There were only two significant differences between the four categories: diagnostic certainty was positively associated with reported rashes and with smaller head circumferences before taking gestational age into account,” wrote Giovanny V. A. França, PhD, of the Secretariat of Health Surveillance, Ministry of Health, Brazil, and coauthors.
Researchers also noted that the discarded cases had larger head circumferences, lower first week mortality, and the mothers were less likely to have a history of rash during pregnancy (20.7% vs 61.4%, 95% confidence interval, 0.27-0.42).
Meanwhile, a second case series in the same edition of The Lancet reported on the pathology of five cases of congenital Zika syndrome, providing further evidence of the link between the virus and congenital abnormalities.
Tissue samples from three fatal cases of the syndrome and two spontaneous abortions found antigens to the Zika virus in the cytoplasm of degenerating and necrotic neurons and glial cells, but no immunohistochemical staining for Zika virus was found outside the central nervous system (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736[16]30883-2).
The five cases all showed signs of brain abnormalities including microcephaly, lissencephaly, cerebellar hypoplasia, and ventriculomegaly, while histopathological studies in the three fatal cases revealed microcalcifications, scattered microglial nodules, cell degeneration, and necrosis.
“The absence of a substantial inflammatory response in the brain and a specific cytopathic viral effect distinguishes Zika virus infection from other important viral infections that are also associated with microcephaly and microcalcifications, such as cytomegalovirus and herpes simplex virus,” wrote Roosecelis Brasil Martines, MD, of the National Center for Emerging and Zoonotic Infectious Diseases, CDC, and coauthors.
There was also a range of other congenital malformations evident in the three fatal cases, including multiple congenital contractures, craniofacial malformations, craniosynostosis, pulmonary hypoplasia, and a wide range of brain abnormalities.
“The mechanism for these deformities in Zika virus infection are not entirely clear, but most probably result from neurotropism of the virus with subsequent damage of the brain and interference in neuromuscular signaling leading to fetal akinesia,” the authors said.
No conflicts of interest were declared for either study.
FROM THE LANCET
Rash, microcephaly not always present with congenital Zika syndrome
The largest study so far of congenital Zika virus syndrome suggests that microcephaly and maternal rash are not sufficient to detect affected babies.
Writing in the June 29 online edition of The Lancet, researchers report on a case series of 1,501 liveborn infants with suspected congenital Zika virus syndrome reported in Brazil. The study found that one in five definite or probable cases of congenital Zika virus syndrome had a head circumference within the range of normal, and in one third of definite or probable cases, the mother had no history of a rash during pregnancy.
Of the total series, 899 were discarded because they showed no obvious clinical or neuropsychomotor abnormalities such as craniofacial disproportion or neurological symptoms (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736[16]30902-3).
Of the remaining 602 cases, 76 were described as definite cases of congenital Zika virus syndrome because of laboratory evidence of Zika virus infection during pregnancy.
Fifty-four babies were considered highly probable cases of congenital Zika virus syndrome because imaging reports showed features such as brain calcifications and ventricular enlargement suggestive of Zika virus infection and which could not be attributed to other pathogens such as syphilis, cytomegalovirus, or toxoplasmosis.
A further 181 were “moderately probable” – they had similar imaging results to the highly probable group but without test results for other infections – while the 291 somewhat probable cases had imaging results that suggested Zika virus was likely involved.
Among the 391 definitely or probable cases where full information was available, half had both microcephaly and a history of maternal rash, while 87% had at least one of these symptoms.
“There were only two significant differences between the four categories: diagnostic certainty was positively associated with reported rashes and with smaller head circumferences before taking gestational age into account,” wrote Giovanny V. A. França, PhD, of the Secretariat of Health Surveillance, Ministry of Health, Brazil, and coauthors.
Researchers also noted that the discarded cases had larger head circumferences, lower first week mortality, and the mothers were less likely to have a history of rash during pregnancy (20.7% vs 61.4%, 95% confidence interval, 0.27-0.42).
Meanwhile, a second case series in the same edition of The Lancet reported on the pathology of five cases of congenital Zika syndrome, providing further evidence of the link between the virus and congenital abnormalities.
Tissue samples from three fatal cases of the syndrome and two spontaneous abortions found antigens to the Zika virus in the cytoplasm of degenerating and necrotic neurons and glial cells, but no immunohistochemical staining for Zika virus was found outside the central nervous system (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736[16]30883-2).
The five cases all showed signs of brain abnormalities including microcephaly, lissencephaly, cerebellar hypoplasia, and ventriculomegaly, while histopathological studies in the three fatal cases revealed microcalcifications, scattered microglial nodules, cell degeneration, and necrosis.
“The absence of a substantial inflammatory response in the brain and a specific cytopathic viral effect distinguishes Zika virus infection from other important viral infections that are also associated with microcephaly and microcalcifications, such as cytomegalovirus and herpes simplex virus,” wrote Roosecelis Brasil Martines, MD, of the National Center for Emerging and Zoonotic Infectious Diseases, CDC, and coauthors.
There was also a range of other congenital malformations evident in the three fatal cases, including multiple congenital contractures, craniofacial malformations, craniosynostosis, pulmonary hypoplasia, and a wide range of brain abnormalities.
“The mechanism for these deformities in Zika virus infection are not entirely clear, but most probably result from neurotropism of the virus with subsequent damage of the brain and interference in neuromuscular signaling leading to fetal akinesia,” the authors said.
No conflicts of interest were declared for either study.
This study is an important contribution for improving the surveillance system for congenital Zika virus infection but caution should be taken in interpreting results of this case series based on routinely collected data with missing information for many cases and an unknown degree of under-reporting.
For incorporating new information besides microcephaly and rash during pregnancy to detect all affected cases, neurological signs and symptoms could be eligible, but might be difficult to obtain in most settings because of insufficient specialized personnel. The development of an accurate serological test that could be incorporated into routine prenatal care will be essential, and its validation a research priority.
While the current outbreak is a paradigmatic example of how quickly evolving systematic scientific evidence can (and should) change the view on a disease within months, it can be expected that public health authorities, and also the scientific community, will struggle for many years with Zika epidemics and its consequences in Brazil and elsewhere.
Jörg Heukelbach, MD, is from the School of Medicine at the Federal University of Ceará in Brazil, and Guilherme Loureiro Werneck, MD, is from the Social Medicine Institute at the State University of Rio de Janeiro. The comments are excerpted from an accompanying editorial (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736(16)30931-X). No conflicts of interest were declared.
This study is an important contribution for improving the surveillance system for congenital Zika virus infection but caution should be taken in interpreting results of this case series based on routinely collected data with missing information for many cases and an unknown degree of under-reporting.
For incorporating new information besides microcephaly and rash during pregnancy to detect all affected cases, neurological signs and symptoms could be eligible, but might be difficult to obtain in most settings because of insufficient specialized personnel. The development of an accurate serological test that could be incorporated into routine prenatal care will be essential, and its validation a research priority.
While the current outbreak is a paradigmatic example of how quickly evolving systematic scientific evidence can (and should) change the view on a disease within months, it can be expected that public health authorities, and also the scientific community, will struggle for many years with Zika epidemics and its consequences in Brazil and elsewhere.
Jörg Heukelbach, MD, is from the School of Medicine at the Federal University of Ceará in Brazil, and Guilherme Loureiro Werneck, MD, is from the Social Medicine Institute at the State University of Rio de Janeiro. The comments are excerpted from an accompanying editorial (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736(16)30931-X). No conflicts of interest were declared.
This study is an important contribution for improving the surveillance system for congenital Zika virus infection but caution should be taken in interpreting results of this case series based on routinely collected data with missing information for many cases and an unknown degree of under-reporting.
For incorporating new information besides microcephaly and rash during pregnancy to detect all affected cases, neurological signs and symptoms could be eligible, but might be difficult to obtain in most settings because of insufficient specialized personnel. The development of an accurate serological test that could be incorporated into routine prenatal care will be essential, and its validation a research priority.
While the current outbreak is a paradigmatic example of how quickly evolving systematic scientific evidence can (and should) change the view on a disease within months, it can be expected that public health authorities, and also the scientific community, will struggle for many years with Zika epidemics and its consequences in Brazil and elsewhere.
Jörg Heukelbach, MD, is from the School of Medicine at the Federal University of Ceará in Brazil, and Guilherme Loureiro Werneck, MD, is from the Social Medicine Institute at the State University of Rio de Janeiro. The comments are excerpted from an accompanying editorial (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736(16)30931-X). No conflicts of interest were declared.
The largest study so far of congenital Zika virus syndrome suggests that microcephaly and maternal rash are not sufficient to detect affected babies.
Writing in the June 29 online edition of The Lancet, researchers report on a case series of 1,501 liveborn infants with suspected congenital Zika virus syndrome reported in Brazil. The study found that one in five definite or probable cases of congenital Zika virus syndrome had a head circumference within the range of normal, and in one third of definite or probable cases, the mother had no history of a rash during pregnancy.
Of the total series, 899 were discarded because they showed no obvious clinical or neuropsychomotor abnormalities such as craniofacial disproportion or neurological symptoms (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736[16]30902-3).
Of the remaining 602 cases, 76 were described as definite cases of congenital Zika virus syndrome because of laboratory evidence of Zika virus infection during pregnancy.
Fifty-four babies were considered highly probable cases of congenital Zika virus syndrome because imaging reports showed features such as brain calcifications and ventricular enlargement suggestive of Zika virus infection and which could not be attributed to other pathogens such as syphilis, cytomegalovirus, or toxoplasmosis.
A further 181 were “moderately probable” – they had similar imaging results to the highly probable group but without test results for other infections – while the 291 somewhat probable cases had imaging results that suggested Zika virus was likely involved.
Among the 391 definitely or probable cases where full information was available, half had both microcephaly and a history of maternal rash, while 87% had at least one of these symptoms.
“There were only two significant differences between the four categories: diagnostic certainty was positively associated with reported rashes and with smaller head circumferences before taking gestational age into account,” wrote Giovanny V. A. França, PhD, of the Secretariat of Health Surveillance, Ministry of Health, Brazil, and coauthors.
Researchers also noted that the discarded cases had larger head circumferences, lower first week mortality, and the mothers were less likely to have a history of rash during pregnancy (20.7% vs 61.4%, 95% confidence interval, 0.27-0.42).
Meanwhile, a second case series in the same edition of The Lancet reported on the pathology of five cases of congenital Zika syndrome, providing further evidence of the link between the virus and congenital abnormalities.
Tissue samples from three fatal cases of the syndrome and two spontaneous abortions found antigens to the Zika virus in the cytoplasm of degenerating and necrotic neurons and glial cells, but no immunohistochemical staining for Zika virus was found outside the central nervous system (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736[16]30883-2).
The five cases all showed signs of brain abnormalities including microcephaly, lissencephaly, cerebellar hypoplasia, and ventriculomegaly, while histopathological studies in the three fatal cases revealed microcalcifications, scattered microglial nodules, cell degeneration, and necrosis.
“The absence of a substantial inflammatory response in the brain and a specific cytopathic viral effect distinguishes Zika virus infection from other important viral infections that are also associated with microcephaly and microcalcifications, such as cytomegalovirus and herpes simplex virus,” wrote Roosecelis Brasil Martines, MD, of the National Center for Emerging and Zoonotic Infectious Diseases, CDC, and coauthors.
There was also a range of other congenital malformations evident in the three fatal cases, including multiple congenital contractures, craniofacial malformations, craniosynostosis, pulmonary hypoplasia, and a wide range of brain abnormalities.
“The mechanism for these deformities in Zika virus infection are not entirely clear, but most probably result from neurotropism of the virus with subsequent damage of the brain and interference in neuromuscular signaling leading to fetal akinesia,” the authors said.
No conflicts of interest were declared for either study.
The largest study so far of congenital Zika virus syndrome suggests that microcephaly and maternal rash are not sufficient to detect affected babies.
Writing in the June 29 online edition of The Lancet, researchers report on a case series of 1,501 liveborn infants with suspected congenital Zika virus syndrome reported in Brazil. The study found that one in five definite or probable cases of congenital Zika virus syndrome had a head circumference within the range of normal, and in one third of definite or probable cases, the mother had no history of a rash during pregnancy.
Of the total series, 899 were discarded because they showed no obvious clinical or neuropsychomotor abnormalities such as craniofacial disproportion or neurological symptoms (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736[16]30902-3).
Of the remaining 602 cases, 76 were described as definite cases of congenital Zika virus syndrome because of laboratory evidence of Zika virus infection during pregnancy.
Fifty-four babies were considered highly probable cases of congenital Zika virus syndrome because imaging reports showed features such as brain calcifications and ventricular enlargement suggestive of Zika virus infection and which could not be attributed to other pathogens such as syphilis, cytomegalovirus, or toxoplasmosis.
A further 181 were “moderately probable” – they had similar imaging results to the highly probable group but without test results for other infections – while the 291 somewhat probable cases had imaging results that suggested Zika virus was likely involved.
Among the 391 definitely or probable cases where full information was available, half had both microcephaly and a history of maternal rash, while 87% had at least one of these symptoms.
“There were only two significant differences between the four categories: diagnostic certainty was positively associated with reported rashes and with smaller head circumferences before taking gestational age into account,” wrote Giovanny V. A. França, PhD, of the Secretariat of Health Surveillance, Ministry of Health, Brazil, and coauthors.
Researchers also noted that the discarded cases had larger head circumferences, lower first week mortality, and the mothers were less likely to have a history of rash during pregnancy (20.7% vs 61.4%, 95% confidence interval, 0.27-0.42).
Meanwhile, a second case series in the same edition of The Lancet reported on the pathology of five cases of congenital Zika syndrome, providing further evidence of the link between the virus and congenital abnormalities.
Tissue samples from three fatal cases of the syndrome and two spontaneous abortions found antigens to the Zika virus in the cytoplasm of degenerating and necrotic neurons and glial cells, but no immunohistochemical staining for Zika virus was found outside the central nervous system (Lancet. 2016 Jun 29. doi: 10.1016/S0140-6736[16]30883-2).
The five cases all showed signs of brain abnormalities including microcephaly, lissencephaly, cerebellar hypoplasia, and ventriculomegaly, while histopathological studies in the three fatal cases revealed microcalcifications, scattered microglial nodules, cell degeneration, and necrosis.
“The absence of a substantial inflammatory response in the brain and a specific cytopathic viral effect distinguishes Zika virus infection from other important viral infections that are also associated with microcephaly and microcalcifications, such as cytomegalovirus and herpes simplex virus,” wrote Roosecelis Brasil Martines, MD, of the National Center for Emerging and Zoonotic Infectious Diseases, CDC, and coauthors.
There was also a range of other congenital malformations evident in the three fatal cases, including multiple congenital contractures, craniofacial malformations, craniosynostosis, pulmonary hypoplasia, and a wide range of brain abnormalities.
“The mechanism for these deformities in Zika virus infection are not entirely clear, but most probably result from neurotropism of the virus with subsequent damage of the brain and interference in neuromuscular signaling leading to fetal akinesia,” the authors said.
No conflicts of interest were declared for either study.
FROM THE LANCET
Key clinical point: Microcephaly and maternal rash alone are not sufficient to detect babies affected by congenital Zika virus syndrome.
Major finding: One in five definite or probable cases of congenital Zika virus syndrome had a head circumference within the range of normal, and in one third of definite or probable cases, the mother had no history of a rash during pregnancy.
Data source: Case series of 1,501 liveborn infants with suspected congenital Zika virus syndrome.
Disclosures: No conflicts of interest were declared.
Justices issue ruling on Texas abortion restrictions
The U.S. Supreme Court has ruled that two Texas abortion restrictions are unconstitutional and place a substantial obstacle in the path of women seeking abortions. In a 5-to-3 vote, justices ruled that both provisions of HB 2 create an “undue burden” on abortion access. The court struck down both requirements, reversing a decision by the 5th Circuit.
The majority justices found the requirements – mandating that abortion providers have admitting privileges at a hospital within 30 miles of an abortion clinic in order to provide the service, and that all abortion clinics meet the same requirements as ambulatory surgical centers (ASCs) – are unnecessary and offer little medical advantage to patients.
“The surgical-center requirement provides few, if any, health benefits for women, poses a substantial obstacle to women seeking abortions, and constitutes an ‘undue burden’ on their constitutional right to do so,” wrote Associate Justice Stephen B. Breyer. “Before this requirement was enacted, Texas law required abortion facilities to meet a host of health and safety requirements that were policed by inspections and enforced through administrative, civil, and criminal penalties. Record evidence shows that the new provision imposes a number of additional requirements that are generally unnecessary in the abortion clinic context.”
The majority court added that common sense also suggests that a “physical facility that satisfies a certain physical demand will generally be unable to meet five times that demand without expanding physically or incurring significant costs.” Texas did not provide evidence that such expansions were possible, justices said.
Chief Justice John G. Roberts dissented, along with Associate Justice Samuel Alito Jr. and Associate Justice Clarence Thomas, calling the decision a departure from the court’s obligation to find fairly.
“[The] decision exemplifies the court’s troubling tendency to bend the rules when any effort to limit abortion, or even to speak in opposition to abortion, is at issue,” Associate Justice Thomas wrote in his dissent. “As Justice Alito observes … today’s decision creates an abortion exception to ordinary rules of res judicata, ignores compelling evidence that Texas’ law imposes no unconstitutional burden, and disregards basic principles of the severability doctrine.”
Whole Woman’s Health v. Hellerstedt centered on whether two Texas abortion regulations unconstitutionally restrict women’s access to the procedure. One rule requires abortion providers to have admitting privileges at a hospital within 30 miles and another rule requires abortion clinics to meet the same standards as those of ambulatory surgical centers. The plaintiffs, who are clinics and doctors, argued that both restrictions are unnecessary and limit access to abortion services. The Texas Department of State Health Services argued that the restrictions are reasonable and effective measures that raise the standard of care for abortion patients and ensure health and safety. The 5th U.S. Circuit Court of Appeals sided with the state; the clinics and physicians appealed.
The plaintiffs also asked the Supreme Court to reaffirm prior rulings that outline when a new abortion law imposes an “undue burden” on a patient’s right to end a pregnancy. The standard results from a 1992 Supreme Court decision, Planned Parenthood of Southeastern Pennsylvania v. Casey, in which the justices affirmed abortion rights established in Roe v. Wade.
The plaintiffs also wanted the Supreme Court to instruct lower courts to weigh whether new state restrictions on abortions really serve to protect patient health. The 5th U.S. Circuit Court of Appeals refused to answer this question when it ruled in favor of Texas in 2015, stating that courts must accept that new laws brought before them would serve the public interest.
More than 70 groups and organizations issued friend-of-the-court briefs to the Supreme Court in the case, including 45 briefs in support of the plaintiffs. In its Jan. 4 brief to the Supreme Court, the American College of Obstetricians and Gynecologists argued that the Texas restrictions are inconsistent with accepted medical practice and provide no benefit to patient care.
On Twitter @legal_med
The U.S. Supreme Court has ruled that two Texas abortion restrictions are unconstitutional and place a substantial obstacle in the path of women seeking abortions. In a 5-to-3 vote, justices ruled that both provisions of HB 2 create an “undue burden” on abortion access. The court struck down both requirements, reversing a decision by the 5th Circuit.
The majority justices found the requirements – mandating that abortion providers have admitting privileges at a hospital within 30 miles of an abortion clinic in order to provide the service, and that all abortion clinics meet the same requirements as ambulatory surgical centers (ASCs) – are unnecessary and offer little medical advantage to patients.
“The surgical-center requirement provides few, if any, health benefits for women, poses a substantial obstacle to women seeking abortions, and constitutes an ‘undue burden’ on their constitutional right to do so,” wrote Associate Justice Stephen B. Breyer. “Before this requirement was enacted, Texas law required abortion facilities to meet a host of health and safety requirements that were policed by inspections and enforced through administrative, civil, and criminal penalties. Record evidence shows that the new provision imposes a number of additional requirements that are generally unnecessary in the abortion clinic context.”
The majority court added that common sense also suggests that a “physical facility that satisfies a certain physical demand will generally be unable to meet five times that demand without expanding physically or incurring significant costs.” Texas did not provide evidence that such expansions were possible, justices said.
Chief Justice John G. Roberts dissented, along with Associate Justice Samuel Alito Jr. and Associate Justice Clarence Thomas, calling the decision a departure from the court’s obligation to find fairly.
“[The] decision exemplifies the court’s troubling tendency to bend the rules when any effort to limit abortion, or even to speak in opposition to abortion, is at issue,” Associate Justice Thomas wrote in his dissent. “As Justice Alito observes … today’s decision creates an abortion exception to ordinary rules of res judicata, ignores compelling evidence that Texas’ law imposes no unconstitutional burden, and disregards basic principles of the severability doctrine.”
Whole Woman’s Health v. Hellerstedt centered on whether two Texas abortion regulations unconstitutionally restrict women’s access to the procedure. One rule requires abortion providers to have admitting privileges at a hospital within 30 miles and another rule requires abortion clinics to meet the same standards as those of ambulatory surgical centers. The plaintiffs, who are clinics and doctors, argued that both restrictions are unnecessary and limit access to abortion services. The Texas Department of State Health Services argued that the restrictions are reasonable and effective measures that raise the standard of care for abortion patients and ensure health and safety. The 5th U.S. Circuit Court of Appeals sided with the state; the clinics and physicians appealed.
The plaintiffs also asked the Supreme Court to reaffirm prior rulings that outline when a new abortion law imposes an “undue burden” on a patient’s right to end a pregnancy. The standard results from a 1992 Supreme Court decision, Planned Parenthood of Southeastern Pennsylvania v. Casey, in which the justices affirmed abortion rights established in Roe v. Wade.
The plaintiffs also wanted the Supreme Court to instruct lower courts to weigh whether new state restrictions on abortions really serve to protect patient health. The 5th U.S. Circuit Court of Appeals refused to answer this question when it ruled in favor of Texas in 2015, stating that courts must accept that new laws brought before them would serve the public interest.
More than 70 groups and organizations issued friend-of-the-court briefs to the Supreme Court in the case, including 45 briefs in support of the plaintiffs. In its Jan. 4 brief to the Supreme Court, the American College of Obstetricians and Gynecologists argued that the Texas restrictions are inconsistent with accepted medical practice and provide no benefit to patient care.
On Twitter @legal_med
The U.S. Supreme Court has ruled that two Texas abortion restrictions are unconstitutional and place a substantial obstacle in the path of women seeking abortions. In a 5-to-3 vote, justices ruled that both provisions of HB 2 create an “undue burden” on abortion access. The court struck down both requirements, reversing a decision by the 5th Circuit.
The majority justices found the requirements – mandating that abortion providers have admitting privileges at a hospital within 30 miles of an abortion clinic in order to provide the service, and that all abortion clinics meet the same requirements as ambulatory surgical centers (ASCs) – are unnecessary and offer little medical advantage to patients.
“The surgical-center requirement provides few, if any, health benefits for women, poses a substantial obstacle to women seeking abortions, and constitutes an ‘undue burden’ on their constitutional right to do so,” wrote Associate Justice Stephen B. Breyer. “Before this requirement was enacted, Texas law required abortion facilities to meet a host of health and safety requirements that were policed by inspections and enforced through administrative, civil, and criminal penalties. Record evidence shows that the new provision imposes a number of additional requirements that are generally unnecessary in the abortion clinic context.”
The majority court added that common sense also suggests that a “physical facility that satisfies a certain physical demand will generally be unable to meet five times that demand without expanding physically or incurring significant costs.” Texas did not provide evidence that such expansions were possible, justices said.
Chief Justice John G. Roberts dissented, along with Associate Justice Samuel Alito Jr. and Associate Justice Clarence Thomas, calling the decision a departure from the court’s obligation to find fairly.
“[The] decision exemplifies the court’s troubling tendency to bend the rules when any effort to limit abortion, or even to speak in opposition to abortion, is at issue,” Associate Justice Thomas wrote in his dissent. “As Justice Alito observes … today’s decision creates an abortion exception to ordinary rules of res judicata, ignores compelling evidence that Texas’ law imposes no unconstitutional burden, and disregards basic principles of the severability doctrine.”
Whole Woman’s Health v. Hellerstedt centered on whether two Texas abortion regulations unconstitutionally restrict women’s access to the procedure. One rule requires abortion providers to have admitting privileges at a hospital within 30 miles and another rule requires abortion clinics to meet the same standards as those of ambulatory surgical centers. The plaintiffs, who are clinics and doctors, argued that both restrictions are unnecessary and limit access to abortion services. The Texas Department of State Health Services argued that the restrictions are reasonable and effective measures that raise the standard of care for abortion patients and ensure health and safety. The 5th U.S. Circuit Court of Appeals sided with the state; the clinics and physicians appealed.
The plaintiffs also asked the Supreme Court to reaffirm prior rulings that outline when a new abortion law imposes an “undue burden” on a patient’s right to end a pregnancy. The standard results from a 1992 Supreme Court decision, Planned Parenthood of Southeastern Pennsylvania v. Casey, in which the justices affirmed abortion rights established in Roe v. Wade.
The plaintiffs also wanted the Supreme Court to instruct lower courts to weigh whether new state restrictions on abortions really serve to protect patient health. The 5th U.S. Circuit Court of Appeals refused to answer this question when it ruled in favor of Texas in 2015, stating that courts must accept that new laws brought before them would serve the public interest.
More than 70 groups and organizations issued friend-of-the-court briefs to the Supreme Court in the case, including 45 briefs in support of the plaintiffs. In its Jan. 4 brief to the Supreme Court, the American College of Obstetricians and Gynecologists argued that the Texas restrictions are inconsistent with accepted medical practice and provide no benefit to patient care.
On Twitter @legal_med
July 2016: Click for Credit
Here are 4 articles in the July issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Pregnancy Alters Pharmacodynamics of Anti-TNF Agents in Women With IBD
To take the posttest, go to: http://bit.ly/1VQFIHf
Expires May 24, 2017
VITALS
Key clinical point: Blood levels of infliximab rose during pregnancy, while adalimumab levels remained stable, even after researchers accounted for changes in albumin, body mass index, and C-reactive protein levels.
Major finding: Median infliximab concentrations rose from 8.5 mcg/mL in the first trimester to a peak of 21 mcg/mL during the middle of the third trimester (P = .04). Median adalimumab levels ranged between 8.6 and 12.2 mcg/mL during pregnancy.
Data source: A prospective study of 25 pregnant women with ulcerative colitis or Crohn's disease.
Disclosures: Dr. Seow disclosed ties with Janssen, AbbVie, Takeda, Shire, and Actavis.
2. Vascular Disease Linked to Sight Loss in Giant Cell Arteritis
To take the posttest, go to: http://bit.ly/1UqLuu5
Expires May 10, 2017
VITALS
Key clinical point: Patients with vascular disease who develop giant cell arteritis may require careful monitoring for sight loss.
Major finding: Overall, 42.9% of patients had some visual disturbance at first clinic review; 7.9% were blind at 6 months.
Data source: Analysis of 433 patients newly diagnosed with GCA participating in the Diagnostic and Classification Criteria in Vasculitis Study (DCVAS).
Disclosures: The DCVAS study is supported by the American College of Rheumatology and is funded by the European League Against Rheumatism and the Vasculitis Foundation. Dr. Yates reported that he had no relevant disclosures.
3. Pediatric and Adolescent Mental Health
Part 1: Diagnoses, drug prescribing vary widely
To take the posttest, go to: http://bit.ly/24FHTxY
Expires April 1, 2017
VITALS
Key clinical point: A lack of psychiatrists only partially accounted for substantial variations in rates of mental illness diagnosis and prescriptions for psychotropic medications given in practices nationwide, a study has shown.
Major finding: Nationwide, 15% of pediatric patients received a mental health diagnosis, and 14% were prescribed psychotropic medications in primary care, regardless of colocated mental health services.
Data source: A retrospective study of electronic health records for 294,748 patients aged 4-18 years.
Disclosures: Dr. Alexander G. Fiks is an investigator for Pfizer; the other researchers said they had no relevant financial disclosures. This study was funded by the National Institutes of Health and the National Institute of Child Health and Human Development under the Best Pharmaceuticals for Children Act.
Part 2: Disorders prevalent in young transgender women
To take the posttest, go to: http://bit.ly/24FCDdq
Expires March 21, 2017
VITALS
Key clinical point: Young transgender women have a high prevalence of psychiatric disorders that is two to four times higher than that in the general population.
Major finding: 41.5% of the study participants had at least one psychiatric disorder, such as major depressive disorder, suicidality, generalized anxiety, PTSD, and alcohol or substance dependence.
Data source: An observational cohort study involving 298 transgender women aged 16-29 years residing in Chicago and Boston.
Disclosures: This study was supported by the National Institute of Mental Health. Dr. Reisner and his associates reported having no relevant financial disclosures.
Here are 4 articles in the July issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Pregnancy Alters Pharmacodynamics of Anti-TNF Agents in Women With IBD
To take the posttest, go to: http://bit.ly/1VQFIHf
Expires May 24, 2017
VITALS
Key clinical point: Blood levels of infliximab rose during pregnancy, while adalimumab levels remained stable, even after researchers accounted for changes in albumin, body mass index, and C-reactive protein levels.
Major finding: Median infliximab concentrations rose from 8.5 mcg/mL in the first trimester to a peak of 21 mcg/mL during the middle of the third trimester (P = .04). Median adalimumab levels ranged between 8.6 and 12.2 mcg/mL during pregnancy.
Data source: A prospective study of 25 pregnant women with ulcerative colitis or Crohn's disease.
Disclosures: Dr. Seow disclosed ties with Janssen, AbbVie, Takeda, Shire, and Actavis.
2. Vascular Disease Linked to Sight Loss in Giant Cell Arteritis
To take the posttest, go to: http://bit.ly/1UqLuu5
Expires May 10, 2017
VITALS
Key clinical point: Patients with vascular disease who develop giant cell arteritis may require careful monitoring for sight loss.
Major finding: Overall, 42.9% of patients had some visual disturbance at first clinic review; 7.9% were blind at 6 months.
Data source: Analysis of 433 patients newly diagnosed with GCA participating in the Diagnostic and Classification Criteria in Vasculitis Study (DCVAS).
Disclosures: The DCVAS study is supported by the American College of Rheumatology and is funded by the European League Against Rheumatism and the Vasculitis Foundation. Dr. Yates reported that he had no relevant disclosures.
3. Pediatric and Adolescent Mental Health
Part 1: Diagnoses, drug prescribing vary widely
To take the posttest, go to: http://bit.ly/24FHTxY
Expires April 1, 2017
VITALS
Key clinical point: A lack of psychiatrists only partially accounted for substantial variations in rates of mental illness diagnosis and prescriptions for psychotropic medications given in practices nationwide, a study has shown.
Major finding: Nationwide, 15% of pediatric patients received a mental health diagnosis, and 14% were prescribed psychotropic medications in primary care, regardless of colocated mental health services.
Data source: A retrospective study of electronic health records for 294,748 patients aged 4-18 years.
Disclosures: Dr. Alexander G. Fiks is an investigator for Pfizer; the other researchers said they had no relevant financial disclosures. This study was funded by the National Institutes of Health and the National Institute of Child Health and Human Development under the Best Pharmaceuticals for Children Act.
Part 2: Disorders prevalent in young transgender women
To take the posttest, go to: http://bit.ly/24FCDdq
Expires March 21, 2017
VITALS
Key clinical point: Young transgender women have a high prevalence of psychiatric disorders that is two to four times higher than that in the general population.
Major finding: 41.5% of the study participants had at least one psychiatric disorder, such as major depressive disorder, suicidality, generalized anxiety, PTSD, and alcohol or substance dependence.
Data source: An observational cohort study involving 298 transgender women aged 16-29 years residing in Chicago and Boston.
Disclosures: This study was supported by the National Institute of Mental Health. Dr. Reisner and his associates reported having no relevant financial disclosures.
Here are 4 articles in the July issue of Clinician Reviews (individual articles are valid for one year from date of publication—expiration dates below):
1. Pregnancy Alters Pharmacodynamics of Anti-TNF Agents in Women With IBD
To take the posttest, go to: http://bit.ly/1VQFIHf
Expires May 24, 2017
VITALS
Key clinical point: Blood levels of infliximab rose during pregnancy, while adalimumab levels remained stable, even after researchers accounted for changes in albumin, body mass index, and C-reactive protein levels.
Major finding: Median infliximab concentrations rose from 8.5 mcg/mL in the first trimester to a peak of 21 mcg/mL during the middle of the third trimester (P = .04). Median adalimumab levels ranged between 8.6 and 12.2 mcg/mL during pregnancy.
Data source: A prospective study of 25 pregnant women with ulcerative colitis or Crohn's disease.
Disclosures: Dr. Seow disclosed ties with Janssen, AbbVie, Takeda, Shire, and Actavis.
2. Vascular Disease Linked to Sight Loss in Giant Cell Arteritis
To take the posttest, go to: http://bit.ly/1UqLuu5
Expires May 10, 2017
VITALS
Key clinical point: Patients with vascular disease who develop giant cell arteritis may require careful monitoring for sight loss.
Major finding: Overall, 42.9% of patients had some visual disturbance at first clinic review; 7.9% were blind at 6 months.
Data source: Analysis of 433 patients newly diagnosed with GCA participating in the Diagnostic and Classification Criteria in Vasculitis Study (DCVAS).
Disclosures: The DCVAS study is supported by the American College of Rheumatology and is funded by the European League Against Rheumatism and the Vasculitis Foundation. Dr. Yates reported that he had no relevant disclosures.
3. Pediatric and Adolescent Mental Health
Part 1: Diagnoses, drug prescribing vary widely
To take the posttest, go to: http://bit.ly/24FHTxY
Expires April 1, 2017
VITALS
Key clinical point: A lack of psychiatrists only partially accounted for substantial variations in rates of mental illness diagnosis and prescriptions for psychotropic medications given in practices nationwide, a study has shown.
Major finding: Nationwide, 15% of pediatric patients received a mental health diagnosis, and 14% were prescribed psychotropic medications in primary care, regardless of colocated mental health services.
Data source: A retrospective study of electronic health records for 294,748 patients aged 4-18 years.
Disclosures: Dr. Alexander G. Fiks is an investigator for Pfizer; the other researchers said they had no relevant financial disclosures. This study was funded by the National Institutes of Health and the National Institute of Child Health and Human Development under the Best Pharmaceuticals for Children Act.
Part 2: Disorders prevalent in young transgender women
To take the posttest, go to: http://bit.ly/24FCDdq
Expires March 21, 2017
VITALS
Key clinical point: Young transgender women have a high prevalence of psychiatric disorders that is two to four times higher than that in the general population.
Major finding: 41.5% of the study participants had at least one psychiatric disorder, such as major depressive disorder, suicidality, generalized anxiety, PTSD, and alcohol or substance dependence.
Data source: An observational cohort study involving 298 transgender women aged 16-29 years residing in Chicago and Boston.
Disclosures: This study was supported by the National Institute of Mental Health. Dr. Reisner and his associates reported having no relevant financial disclosures.
Cases of Zika among pregnant women in U.S. states rise to 265
There was one infant born with birth defects and two pregnancy losses as a result of likely maternal Zika virus infection among U.S. women during the week ending June 16, 2016, according to figures released by the Centers for Disease Control and Prevention.
That brings the Zika-related totals to four infants born with birth defects and five pregnancy losses in the United States, with one of the most recent pregnancy losses occurring in a U.S. territory or Puerto Rico, the CDC reported. The CDC is not reporting state- or territorial-level data to protect the privacy of affected women and children.
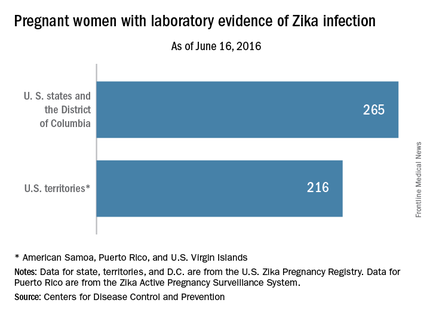
The CDC also said that it has received reports of 265 pregnant women in U.S. states and the District of Columbia and 216 pregnant women in U.S. territories and Puerto Rico who had any laboratory evidence of possible Zika virus infection. This includes women “in whom viral particles have been detected and those with evidence of an immune reaction to a recent virus that is likely to be Zika,” the CDC noted.
The figures for states, territories, and the District of Columbia reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System. These are not real-time data and reflect only pregnancy outcomes for women with any laboratory evidence of possible Zika virus infection, although it is not known if Zika virus was the cause of the poor outcomes. The numbers also do not reflect outcomes among ongoing pregnancies.
Zika-related birth defects recorded by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
CDC officials plan to update the pregnancy outcome data every Thursday at www.cdc.gov/zika/geo/pregnancy-outcomes.html.
There was one infant born with birth defects and two pregnancy losses as a result of likely maternal Zika virus infection among U.S. women during the week ending June 16, 2016, according to figures released by the Centers for Disease Control and Prevention.
That brings the Zika-related totals to four infants born with birth defects and five pregnancy losses in the United States, with one of the most recent pregnancy losses occurring in a U.S. territory or Puerto Rico, the CDC reported. The CDC is not reporting state- or territorial-level data to protect the privacy of affected women and children.
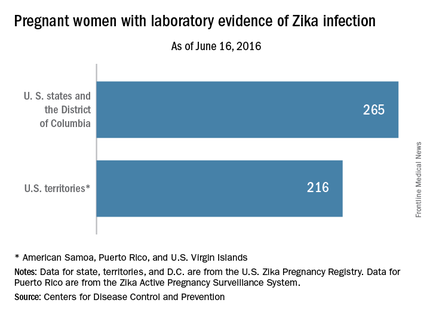
The CDC also said that it has received reports of 265 pregnant women in U.S. states and the District of Columbia and 216 pregnant women in U.S. territories and Puerto Rico who had any laboratory evidence of possible Zika virus infection. This includes women “in whom viral particles have been detected and those with evidence of an immune reaction to a recent virus that is likely to be Zika,” the CDC noted.
The figures for states, territories, and the District of Columbia reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System. These are not real-time data and reflect only pregnancy outcomes for women with any laboratory evidence of possible Zika virus infection, although it is not known if Zika virus was the cause of the poor outcomes. The numbers also do not reflect outcomes among ongoing pregnancies.
Zika-related birth defects recorded by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
CDC officials plan to update the pregnancy outcome data every Thursday at www.cdc.gov/zika/geo/pregnancy-outcomes.html.
There was one infant born with birth defects and two pregnancy losses as a result of likely maternal Zika virus infection among U.S. women during the week ending June 16, 2016, according to figures released by the Centers for Disease Control and Prevention.
That brings the Zika-related totals to four infants born with birth defects and five pregnancy losses in the United States, with one of the most recent pregnancy losses occurring in a U.S. territory or Puerto Rico, the CDC reported. The CDC is not reporting state- or territorial-level data to protect the privacy of affected women and children.
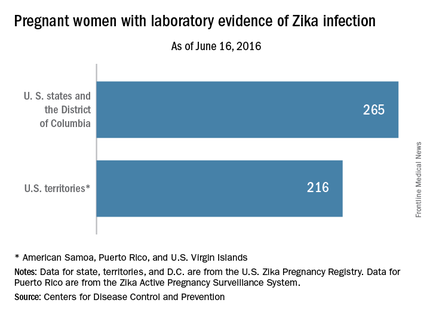
The CDC also said that it has received reports of 265 pregnant women in U.S. states and the District of Columbia and 216 pregnant women in U.S. territories and Puerto Rico who had any laboratory evidence of possible Zika virus infection. This includes women “in whom viral particles have been detected and those with evidence of an immune reaction to a recent virus that is likely to be Zika,” the CDC noted.
The figures for states, territories, and the District of Columbia reflect reporting to the U.S. Zika Pregnancy Registry; data for Puerto Rico are reported to the U.S. Zika Active Pregnancy Surveillance System. These are not real-time data and reflect only pregnancy outcomes for women with any laboratory evidence of possible Zika virus infection, although it is not known if Zika virus was the cause of the poor outcomes. The numbers also do not reflect outcomes among ongoing pregnancies.
Zika-related birth defects recorded by the CDC could include microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from brain damage that affect nerves, muscles, and bones. The pregnancy losses encompass any miscarriage, stillbirth, and termination with evidence of birth defects.
CDC officials plan to update the pregnancy outcome data every Thursday at www.cdc.gov/zika/geo/pregnancy-outcomes.html.
Abortion requests surged in Latin American countries after Zika warnings
Requests for medication abortions have risen significantly in nine Latin American countries since the Pan American Health Organization issued an epidemiologic warning about Zika virus in November 2015.
All of the countries have legal restrictions that make abortions impossible or very difficult to obtain. Nevertheless, women are seeking them in increasing numbers using Women on Web, a nonprofit, international group that supplies information on abortions and facilitates contact with physicians who provide abortifacient medications.
Dr. Abigail Aiken of the University of Texas, Austin, and her colleagues reported the findings June 22 in the New England Journal of Medicine (2016 Jun. doi: 10.1056/NEJMc1605389).
Most of the increased requests occurred in countries that issued a national advisory to pregnant women, the researchers noted. But increases also occurred in two countries with local Zika transmission but no national advisory.
“We cannot definitively attribute the rapid acceleration in requests … to concern about Zika virus exposure,” the researchers wrote in a letter to the editor. However, “In Latin American countries that issued warnings to pregnant women about complications associated with Zika virus infection, requests for abortion through [Women on Web] increased significantly. Our approach may underestimate the effect of the advisories on demand for abortion, since many women may have used an unsafe method, accessed misoprostol from local pharmacies or the black market, or visited local underground providers.”
The authors worked with Women on Web to assess requests for medical abortion consultations from women in 19 Latin American countries between Jan. 1, 2010, and March 2, 2016. They compared these numbers before and after the November 2015 Zika announcement from the Pan American Health Organization.
They divided the data into three groups: countries with local Zika transmission, legally restricted abortion, and a national advisory to pregnant women; countries with no Zika transmission and legally restricted abortion; and countries with local Zika transmission, legally restricted abortion, and no national advisory to pregnant women. The study also included three control countries with no Zika transmission anticipated (Chile, Poland, and Uruguay).
All of the eight countries with local Zika transmission, legally restricted abortion, and a national advisory to pregnant women showed significant increases in Women on Web requests, except Jamaica. The increases were highest in Brazil and Ecuador (108%) and lowest in El Salvador and Costa Rica (36%). The increases reported reflect the relative change between actual and expected requests for abortion medications.
Two of the four countries with no Zika transmission and legally restricted abortion also showed increases: Peru (20.5%) and Argentina (21.8%).
There were no significant increases in requests in any of the seven countries with local Zika transmission, legally restricted abortion, and no national advisory to pregnant women.
The findings suggest a difficult future for many women who desire pregnancy or who conceive in areas of Zika activity, the researchers wrote. “Models that were developed by the World Health Organization predict that 3 million to 4 million persons across the Americas will contract Zika virus infection through 2017, and the virus will inevitably spread to other countries where access to safe abortion is restricted. Official information and advice about potential exposure to the Zika virus should be accompanied by efforts to ensure that all reproductive choices are safe, legal, and accessible.”
Dr. Thomas Gellhaus, president of the American Congress of Obstetricians and Gynecologists (ACOG), said the study “presents alarming insight on how the Zika virus is affecting the lives of pregnant women.”
“ACOG has long recognized that access to reproductive services, including abortion care, is essential for all women,” he said. “All women, must have the legal right to abortion, unconstrained by harassment, unavailability of care, procedure bans, or other legislative or regulatory barriers. The Zika crisis makes it impossible to ignore that women around the world do not have access to this basic health care need.”
ACOG updated its Zika clinical guidelines on June 13.
Two of the researchers are affiliated with Women on Web.
Requests for medication abortions have risen significantly in nine Latin American countries since the Pan American Health Organization issued an epidemiologic warning about Zika virus in November 2015.
All of the countries have legal restrictions that make abortions impossible or very difficult to obtain. Nevertheless, women are seeking them in increasing numbers using Women on Web, a nonprofit, international group that supplies information on abortions and facilitates contact with physicians who provide abortifacient medications.
Dr. Abigail Aiken of the University of Texas, Austin, and her colleagues reported the findings June 22 in the New England Journal of Medicine (2016 Jun. doi: 10.1056/NEJMc1605389).
Most of the increased requests occurred in countries that issued a national advisory to pregnant women, the researchers noted. But increases also occurred in two countries with local Zika transmission but no national advisory.
“We cannot definitively attribute the rapid acceleration in requests … to concern about Zika virus exposure,” the researchers wrote in a letter to the editor. However, “In Latin American countries that issued warnings to pregnant women about complications associated with Zika virus infection, requests for abortion through [Women on Web] increased significantly. Our approach may underestimate the effect of the advisories on demand for abortion, since many women may have used an unsafe method, accessed misoprostol from local pharmacies or the black market, or visited local underground providers.”
The authors worked with Women on Web to assess requests for medical abortion consultations from women in 19 Latin American countries between Jan. 1, 2010, and March 2, 2016. They compared these numbers before and after the November 2015 Zika announcement from the Pan American Health Organization.
They divided the data into three groups: countries with local Zika transmission, legally restricted abortion, and a national advisory to pregnant women; countries with no Zika transmission and legally restricted abortion; and countries with local Zika transmission, legally restricted abortion, and no national advisory to pregnant women. The study also included three control countries with no Zika transmission anticipated (Chile, Poland, and Uruguay).
All of the eight countries with local Zika transmission, legally restricted abortion, and a national advisory to pregnant women showed significant increases in Women on Web requests, except Jamaica. The increases were highest in Brazil and Ecuador (108%) and lowest in El Salvador and Costa Rica (36%). The increases reported reflect the relative change between actual and expected requests for abortion medications.
Two of the four countries with no Zika transmission and legally restricted abortion also showed increases: Peru (20.5%) and Argentina (21.8%).
There were no significant increases in requests in any of the seven countries with local Zika transmission, legally restricted abortion, and no national advisory to pregnant women.
The findings suggest a difficult future for many women who desire pregnancy or who conceive in areas of Zika activity, the researchers wrote. “Models that were developed by the World Health Organization predict that 3 million to 4 million persons across the Americas will contract Zika virus infection through 2017, and the virus will inevitably spread to other countries where access to safe abortion is restricted. Official information and advice about potential exposure to the Zika virus should be accompanied by efforts to ensure that all reproductive choices are safe, legal, and accessible.”
Dr. Thomas Gellhaus, president of the American Congress of Obstetricians and Gynecologists (ACOG), said the study “presents alarming insight on how the Zika virus is affecting the lives of pregnant women.”
“ACOG has long recognized that access to reproductive services, including abortion care, is essential for all women,” he said. “All women, must have the legal right to abortion, unconstrained by harassment, unavailability of care, procedure bans, or other legislative or regulatory barriers. The Zika crisis makes it impossible to ignore that women around the world do not have access to this basic health care need.”
ACOG updated its Zika clinical guidelines on June 13.
Two of the researchers are affiliated with Women on Web.
Requests for medication abortions have risen significantly in nine Latin American countries since the Pan American Health Organization issued an epidemiologic warning about Zika virus in November 2015.
All of the countries have legal restrictions that make abortions impossible or very difficult to obtain. Nevertheless, women are seeking them in increasing numbers using Women on Web, a nonprofit, international group that supplies information on abortions and facilitates contact with physicians who provide abortifacient medications.
Dr. Abigail Aiken of the University of Texas, Austin, and her colleagues reported the findings June 22 in the New England Journal of Medicine (2016 Jun. doi: 10.1056/NEJMc1605389).
Most of the increased requests occurred in countries that issued a national advisory to pregnant women, the researchers noted. But increases also occurred in two countries with local Zika transmission but no national advisory.
“We cannot definitively attribute the rapid acceleration in requests … to concern about Zika virus exposure,” the researchers wrote in a letter to the editor. However, “In Latin American countries that issued warnings to pregnant women about complications associated with Zika virus infection, requests for abortion through [Women on Web] increased significantly. Our approach may underestimate the effect of the advisories on demand for abortion, since many women may have used an unsafe method, accessed misoprostol from local pharmacies or the black market, or visited local underground providers.”
The authors worked with Women on Web to assess requests for medical abortion consultations from women in 19 Latin American countries between Jan. 1, 2010, and March 2, 2016. They compared these numbers before and after the November 2015 Zika announcement from the Pan American Health Organization.
They divided the data into three groups: countries with local Zika transmission, legally restricted abortion, and a national advisory to pregnant women; countries with no Zika transmission and legally restricted abortion; and countries with local Zika transmission, legally restricted abortion, and no national advisory to pregnant women. The study also included three control countries with no Zika transmission anticipated (Chile, Poland, and Uruguay).
All of the eight countries with local Zika transmission, legally restricted abortion, and a national advisory to pregnant women showed significant increases in Women on Web requests, except Jamaica. The increases were highest in Brazil and Ecuador (108%) and lowest in El Salvador and Costa Rica (36%). The increases reported reflect the relative change between actual and expected requests for abortion medications.
Two of the four countries with no Zika transmission and legally restricted abortion also showed increases: Peru (20.5%) and Argentina (21.8%).
There were no significant increases in requests in any of the seven countries with local Zika transmission, legally restricted abortion, and no national advisory to pregnant women.
The findings suggest a difficult future for many women who desire pregnancy or who conceive in areas of Zika activity, the researchers wrote. “Models that were developed by the World Health Organization predict that 3 million to 4 million persons across the Americas will contract Zika virus infection through 2017, and the virus will inevitably spread to other countries where access to safe abortion is restricted. Official information and advice about potential exposure to the Zika virus should be accompanied by efforts to ensure that all reproductive choices are safe, legal, and accessible.”
Dr. Thomas Gellhaus, president of the American Congress of Obstetricians and Gynecologists (ACOG), said the study “presents alarming insight on how the Zika virus is affecting the lives of pregnant women.”
“ACOG has long recognized that access to reproductive services, including abortion care, is essential for all women,” he said. “All women, must have the legal right to abortion, unconstrained by harassment, unavailability of care, procedure bans, or other legislative or regulatory barriers. The Zika crisis makes it impossible to ignore that women around the world do not have access to this basic health care need.”
ACOG updated its Zika clinical guidelines on June 13.
Two of the researchers are affiliated with Women on Web.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Requests for medication abortions have risen in nine Latin American countries since the first Zika warning last November.
Major finding: Requests for abortifacient medications in Brazil and Ecuador rose by about 108%, compared with expected requests.
Data source: The study compared data between Jan. 1, 2010, and March 2, 2016.
Disclosures: Two of the researchers are affiliated with Women on Web, a nonprofit, international group that supplies information on abortions and facilitates contact with physicians who provide abortifacient medications.