User login
The case for molecular classification of vascular anomalies presented
according to Beth Drolet, MD.
“We now know that 75%-80% of vascular malformations have gene mutations that make the cells either live longer, grow faster, or make them bigger in size,” Dr. Drolet, professor and chair of dermatology at the University of Wisconsin–Madison, said during the Society for Pediatric Dermatology pre-AAD meeting. “The basic binary premise of the current ISSVA [International Society for the Study of Vascular Anomalies] classification dividing vascular anomalies into tumors and malformations is wrong; the biology is not that straightforward. It may be helpful to differentiate between an infantile hemangioma and a capillary malformation during infancy as the hemangioma will grow in the next month, but we now know that patients with capillary malformations also have significant overgrowth of their tissue. We’ve all seen that; it just takes years, not months for us to notice it.”
The change in thinking about the root causes of vascular anomalies, she noted, stems from scientific advances in the understanding of embryonic mosaicism, DNA variation that happens after the zygote is formed, but before birth. “We know that each cell in a zygote will undergo 40 cell divisions before a baby is born,” she said. “Those cell divisions are not as neat as we thought they were. That cell and DNA duplication is actually quite messy, so there are mutations that happen purely because of embryonic cell division.”
Everyone is born with 120 somatic mutations per cell, she continued, “so we have multiple genomes in one human. Not all of those mutations are going to cause disease. Not all of those are going to be functional. About 10% of those mutations will actually be in a coding region of the gene and have the potential to change the function of the protein. If it changes the function of the protein so that the cell can’t survive, that cell dies off, but it gives the cell an advantage. It grows a little bit faster, let’s say. That cell survives, divides, producing a line of cells that can cause disease.”
In 2011, Dr. Drolet and colleagues from the Hemangioma Investigator Group and the Pediatric Dermatology Research Alliance (PeDRA) launched a multisite collaborative group to investigate the role of mosaic genetics in patients with vascular anomalies and discrepancy of growth. To date, 365 patients are enrolled, and the researchers have sequenced 97 of 165 affected tissue samples collected. “What’s nice about the registry is that we enrolled a wide spectrum of diseases: very mild diseases that might be treated by dermatologists to complex, syndromic diseases that might end up in an interdisciplinary vascular anomalies clinic,” she said.
For gene sequencing, the researchers drew from solid tumor biology and used next-generation sequencing with semi-target hybrid capture, “so we’re only looking at a subset of genes,” she said. “Right now, the chip we’re using has 180 cancer-related genes. It sequences the entire exome of the gene with a high depth of coverage, usually over 1,000 X. We use a specific pipeline that can detect very low allele frequency mutation: down to 1%, and robust criteria to determine variant pathogenicity.”
In 75% of tissue samples so far, the researchers have found a gene mutation in one of 13 genes: AKT1, AKT3, BRAF, GNA11, GNAQ, KRAS, MAP2K1, NRAS, PIK3CA, PIK3R1, PTPN11, RASA1, and TEK. According to Dr. Drolet, the common thread in these 13 genes is that they are implicated in cancer and have direct control over the cell cycle. “They’re intracellular proteins that control the cell cycle,” she explained. “These are proteins that are in the cell but interact with transmembrane proteins that receive extracellular messengers of cell growth”.
Understanding and recognizing genetic conditions is complicated, she said, because it involves determining which gene is altered, where in the DNA the gene is altered, how the gene variation will influence the function of the protein, and what tissue expresses that gene. “Then you get your phenotype,” Dr. Drolet said. “If you add mosaicism onto that, you have several additional variables. You need to know: When in embryogenesis did the mutation occur? What region of the body is affected? What cell lineage is affected? That predicts what phenotype you’re going to have.”
While molecular classification efforts continue to be refined, Dr. Drolet incorporates genotyping at every opportunity, like when she counsels parents of a baby born with a vascular stain on its face. “What can we tell them about what else might be wrong? What can we tell them about how this will change over time? What can we tell them about how we can treat it? I think genotyping absolutely helps to clarify that for me,” she said. “I can’t use that alone, but it gives me another piece of evidence to help do a better job in predicting when I need to screen, what I need to screen for, and what might happen in the future. If you combine your genotype with your clinical exam, I really do believe we can start to offer some prognostication for our families, to say, ‘this is the degree of overgrowth we may see over time; these are the complications I predict that you might have.’ ”
Even the vascular stain can give you a clue. “If it’s light and lacey, you probably don’t have a lot of cell cycle activation,” Dr. Drolet said. “If it’s dark and there’s blebs and you’ve got some bleeding at a young age, you’ve got a highly activated mutation, and there’s everything in between.”
Dr. Drolet disclosed that she is a consultant for Venthera and Novartis and is a board member for the Isthmus Project. She also holds intellectual property rights in and is a patent holder for Peds Derm Development Group. Dr. Drolet has also received funding from the Spirit Foundation, Kayleigh’s Crew Endowment, the SPD, PeDRA, and the National Institutes of Health.
according to Beth Drolet, MD.
“We now know that 75%-80% of vascular malformations have gene mutations that make the cells either live longer, grow faster, or make them bigger in size,” Dr. Drolet, professor and chair of dermatology at the University of Wisconsin–Madison, said during the Society for Pediatric Dermatology pre-AAD meeting. “The basic binary premise of the current ISSVA [International Society for the Study of Vascular Anomalies] classification dividing vascular anomalies into tumors and malformations is wrong; the biology is not that straightforward. It may be helpful to differentiate between an infantile hemangioma and a capillary malformation during infancy as the hemangioma will grow in the next month, but we now know that patients with capillary malformations also have significant overgrowth of their tissue. We’ve all seen that; it just takes years, not months for us to notice it.”
The change in thinking about the root causes of vascular anomalies, she noted, stems from scientific advances in the understanding of embryonic mosaicism, DNA variation that happens after the zygote is formed, but before birth. “We know that each cell in a zygote will undergo 40 cell divisions before a baby is born,” she said. “Those cell divisions are not as neat as we thought they were. That cell and DNA duplication is actually quite messy, so there are mutations that happen purely because of embryonic cell division.”
Everyone is born with 120 somatic mutations per cell, she continued, “so we have multiple genomes in one human. Not all of those mutations are going to cause disease. Not all of those are going to be functional. About 10% of those mutations will actually be in a coding region of the gene and have the potential to change the function of the protein. If it changes the function of the protein so that the cell can’t survive, that cell dies off, but it gives the cell an advantage. It grows a little bit faster, let’s say. That cell survives, divides, producing a line of cells that can cause disease.”
In 2011, Dr. Drolet and colleagues from the Hemangioma Investigator Group and the Pediatric Dermatology Research Alliance (PeDRA) launched a multisite collaborative group to investigate the role of mosaic genetics in patients with vascular anomalies and discrepancy of growth. To date, 365 patients are enrolled, and the researchers have sequenced 97 of 165 affected tissue samples collected. “What’s nice about the registry is that we enrolled a wide spectrum of diseases: very mild diseases that might be treated by dermatologists to complex, syndromic diseases that might end up in an interdisciplinary vascular anomalies clinic,” she said.
For gene sequencing, the researchers drew from solid tumor biology and used next-generation sequencing with semi-target hybrid capture, “so we’re only looking at a subset of genes,” she said. “Right now, the chip we’re using has 180 cancer-related genes. It sequences the entire exome of the gene with a high depth of coverage, usually over 1,000 X. We use a specific pipeline that can detect very low allele frequency mutation: down to 1%, and robust criteria to determine variant pathogenicity.”
In 75% of tissue samples so far, the researchers have found a gene mutation in one of 13 genes: AKT1, AKT3, BRAF, GNA11, GNAQ, KRAS, MAP2K1, NRAS, PIK3CA, PIK3R1, PTPN11, RASA1, and TEK. According to Dr. Drolet, the common thread in these 13 genes is that they are implicated in cancer and have direct control over the cell cycle. “They’re intracellular proteins that control the cell cycle,” she explained. “These are proteins that are in the cell but interact with transmembrane proteins that receive extracellular messengers of cell growth”.
Understanding and recognizing genetic conditions is complicated, she said, because it involves determining which gene is altered, where in the DNA the gene is altered, how the gene variation will influence the function of the protein, and what tissue expresses that gene. “Then you get your phenotype,” Dr. Drolet said. “If you add mosaicism onto that, you have several additional variables. You need to know: When in embryogenesis did the mutation occur? What region of the body is affected? What cell lineage is affected? That predicts what phenotype you’re going to have.”
While molecular classification efforts continue to be refined, Dr. Drolet incorporates genotyping at every opportunity, like when she counsels parents of a baby born with a vascular stain on its face. “What can we tell them about what else might be wrong? What can we tell them about how this will change over time? What can we tell them about how we can treat it? I think genotyping absolutely helps to clarify that for me,” she said. “I can’t use that alone, but it gives me another piece of evidence to help do a better job in predicting when I need to screen, what I need to screen for, and what might happen in the future. If you combine your genotype with your clinical exam, I really do believe we can start to offer some prognostication for our families, to say, ‘this is the degree of overgrowth we may see over time; these are the complications I predict that you might have.’ ”
Even the vascular stain can give you a clue. “If it’s light and lacey, you probably don’t have a lot of cell cycle activation,” Dr. Drolet said. “If it’s dark and there’s blebs and you’ve got some bleeding at a young age, you’ve got a highly activated mutation, and there’s everything in between.”
Dr. Drolet disclosed that she is a consultant for Venthera and Novartis and is a board member for the Isthmus Project. She also holds intellectual property rights in and is a patent holder for Peds Derm Development Group. Dr. Drolet has also received funding from the Spirit Foundation, Kayleigh’s Crew Endowment, the SPD, PeDRA, and the National Institutes of Health.
according to Beth Drolet, MD.
“We now know that 75%-80% of vascular malformations have gene mutations that make the cells either live longer, grow faster, or make them bigger in size,” Dr. Drolet, professor and chair of dermatology at the University of Wisconsin–Madison, said during the Society for Pediatric Dermatology pre-AAD meeting. “The basic binary premise of the current ISSVA [International Society for the Study of Vascular Anomalies] classification dividing vascular anomalies into tumors and malformations is wrong; the biology is not that straightforward. It may be helpful to differentiate between an infantile hemangioma and a capillary malformation during infancy as the hemangioma will grow in the next month, but we now know that patients with capillary malformations also have significant overgrowth of their tissue. We’ve all seen that; it just takes years, not months for us to notice it.”
The change in thinking about the root causes of vascular anomalies, she noted, stems from scientific advances in the understanding of embryonic mosaicism, DNA variation that happens after the zygote is formed, but before birth. “We know that each cell in a zygote will undergo 40 cell divisions before a baby is born,” she said. “Those cell divisions are not as neat as we thought they were. That cell and DNA duplication is actually quite messy, so there are mutations that happen purely because of embryonic cell division.”
Everyone is born with 120 somatic mutations per cell, she continued, “so we have multiple genomes in one human. Not all of those mutations are going to cause disease. Not all of those are going to be functional. About 10% of those mutations will actually be in a coding region of the gene and have the potential to change the function of the protein. If it changes the function of the protein so that the cell can’t survive, that cell dies off, but it gives the cell an advantage. It grows a little bit faster, let’s say. That cell survives, divides, producing a line of cells that can cause disease.”
In 2011, Dr. Drolet and colleagues from the Hemangioma Investigator Group and the Pediatric Dermatology Research Alliance (PeDRA) launched a multisite collaborative group to investigate the role of mosaic genetics in patients with vascular anomalies and discrepancy of growth. To date, 365 patients are enrolled, and the researchers have sequenced 97 of 165 affected tissue samples collected. “What’s nice about the registry is that we enrolled a wide spectrum of diseases: very mild diseases that might be treated by dermatologists to complex, syndromic diseases that might end up in an interdisciplinary vascular anomalies clinic,” she said.
For gene sequencing, the researchers drew from solid tumor biology and used next-generation sequencing with semi-target hybrid capture, “so we’re only looking at a subset of genes,” she said. “Right now, the chip we’re using has 180 cancer-related genes. It sequences the entire exome of the gene with a high depth of coverage, usually over 1,000 X. We use a specific pipeline that can detect very low allele frequency mutation: down to 1%, and robust criteria to determine variant pathogenicity.”
In 75% of tissue samples so far, the researchers have found a gene mutation in one of 13 genes: AKT1, AKT3, BRAF, GNA11, GNAQ, KRAS, MAP2K1, NRAS, PIK3CA, PIK3R1, PTPN11, RASA1, and TEK. According to Dr. Drolet, the common thread in these 13 genes is that they are implicated in cancer and have direct control over the cell cycle. “They’re intracellular proteins that control the cell cycle,” she explained. “These are proteins that are in the cell but interact with transmembrane proteins that receive extracellular messengers of cell growth”.
Understanding and recognizing genetic conditions is complicated, she said, because it involves determining which gene is altered, where in the DNA the gene is altered, how the gene variation will influence the function of the protein, and what tissue expresses that gene. “Then you get your phenotype,” Dr. Drolet said. “If you add mosaicism onto that, you have several additional variables. You need to know: When in embryogenesis did the mutation occur? What region of the body is affected? What cell lineage is affected? That predicts what phenotype you’re going to have.”
While molecular classification efforts continue to be refined, Dr. Drolet incorporates genotyping at every opportunity, like when she counsels parents of a baby born with a vascular stain on its face. “What can we tell them about what else might be wrong? What can we tell them about how this will change over time? What can we tell them about how we can treat it? I think genotyping absolutely helps to clarify that for me,” she said. “I can’t use that alone, but it gives me another piece of evidence to help do a better job in predicting when I need to screen, what I need to screen for, and what might happen in the future. If you combine your genotype with your clinical exam, I really do believe we can start to offer some prognostication for our families, to say, ‘this is the degree of overgrowth we may see over time; these are the complications I predict that you might have.’ ”
Even the vascular stain can give you a clue. “If it’s light and lacey, you probably don’t have a lot of cell cycle activation,” Dr. Drolet said. “If it’s dark and there’s blebs and you’ve got some bleeding at a young age, you’ve got a highly activated mutation, and there’s everything in between.”
Dr. Drolet disclosed that she is a consultant for Venthera and Novartis and is a board member for the Isthmus Project. She also holds intellectual property rights in and is a patent holder for Peds Derm Development Group. Dr. Drolet has also received funding from the Spirit Foundation, Kayleigh’s Crew Endowment, the SPD, PeDRA, and the National Institutes of Health.
FROM THE SPD PRE-AAD MEETING
CDC recommends use of Pfizer’s COVID vaccine in 12- to 15-year-olds
The Centers for Disease Control and Prevention’s director Rochelle Walensky, MD, signed off on an advisory panel’s recommendation May 12 endorsing the use of the Pfizer-BioNTech COVID-19 vaccine in adolescents aged 12-15 years.
Earlier in the day the CDC’s Advisory Committee on Immunization Practices voted 14-0 in favor of the safety and effectiveness of the vaccine in younger teens.
Dr. Walensky said in an official statement.
The Food and Drug Administration on May 10 issued an emergency use authorization (EUA) for the Pfizer-BioNTech COVID-19 vaccine for the prevention of COVID-19 in individuals 12-15 years old. The FDA first cleared the Pfizer-BioNTech vaccine through an EUA in December 2020 for those ages 16 and older. Pfizer this month also initiated steps with the FDA toward a full approval of its vaccine.
Dr. Walenksy urged parents to seriously consider vaccinating their children.
“Understandably, some parents want more information before their children receive a vaccine,” she said. “I encourage parents with questions to talk to your child’s healthcare provider or your family doctor to learn more about the vaccine.”
Vaccine “safe and effective”
Separately, the American Academy of Pediatrics issued a statement May 12 in support of vaccinating all children ages 12 and older who are eligible for the federally authorized COVID-19 vaccine.
“As a pediatrician and a parent, I have looked forward to getting my own children and patients vaccinated, and I am thrilled that those ages 12 and older can now be protected,” said AAP President Lee Savio Beers, MD, in a statement. “The data continue to show that this vaccine is safe and effective. I urge all parents to call their pediatrician to learn more about how to get their children and teens vaccinated.”
The expanded clearance for the Pfizer vaccine is seen as a critical step for allowing teens to resume activities on which they missed out during the pandemic.
“We’ve seen the harm done to children’s mental and emotional health as they’ve missed out on so many experiences during the pandemic,” Dr. Beers said. “Vaccinating children will protect them and allow them to fully engage in all of the activities – school, sports, socializing with friends and family – that are so important to their health and development.”
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention’s director Rochelle Walensky, MD, signed off on an advisory panel’s recommendation May 12 endorsing the use of the Pfizer-BioNTech COVID-19 vaccine in adolescents aged 12-15 years.
Earlier in the day the CDC’s Advisory Committee on Immunization Practices voted 14-0 in favor of the safety and effectiveness of the vaccine in younger teens.
Dr. Walensky said in an official statement.
The Food and Drug Administration on May 10 issued an emergency use authorization (EUA) for the Pfizer-BioNTech COVID-19 vaccine for the prevention of COVID-19 in individuals 12-15 years old. The FDA first cleared the Pfizer-BioNTech vaccine through an EUA in December 2020 for those ages 16 and older. Pfizer this month also initiated steps with the FDA toward a full approval of its vaccine.
Dr. Walenksy urged parents to seriously consider vaccinating their children.
“Understandably, some parents want more information before their children receive a vaccine,” she said. “I encourage parents with questions to talk to your child’s healthcare provider or your family doctor to learn more about the vaccine.”
Vaccine “safe and effective”
Separately, the American Academy of Pediatrics issued a statement May 12 in support of vaccinating all children ages 12 and older who are eligible for the federally authorized COVID-19 vaccine.
“As a pediatrician and a parent, I have looked forward to getting my own children and patients vaccinated, and I am thrilled that those ages 12 and older can now be protected,” said AAP President Lee Savio Beers, MD, in a statement. “The data continue to show that this vaccine is safe and effective. I urge all parents to call their pediatrician to learn more about how to get their children and teens vaccinated.”
The expanded clearance for the Pfizer vaccine is seen as a critical step for allowing teens to resume activities on which they missed out during the pandemic.
“We’ve seen the harm done to children’s mental and emotional health as they’ve missed out on so many experiences during the pandemic,” Dr. Beers said. “Vaccinating children will protect them and allow them to fully engage in all of the activities – school, sports, socializing with friends and family – that are so important to their health and development.”
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention’s director Rochelle Walensky, MD, signed off on an advisory panel’s recommendation May 12 endorsing the use of the Pfizer-BioNTech COVID-19 vaccine in adolescents aged 12-15 years.
Earlier in the day the CDC’s Advisory Committee on Immunization Practices voted 14-0 in favor of the safety and effectiveness of the vaccine in younger teens.
Dr. Walensky said in an official statement.
The Food and Drug Administration on May 10 issued an emergency use authorization (EUA) for the Pfizer-BioNTech COVID-19 vaccine for the prevention of COVID-19 in individuals 12-15 years old. The FDA first cleared the Pfizer-BioNTech vaccine through an EUA in December 2020 for those ages 16 and older. Pfizer this month also initiated steps with the FDA toward a full approval of its vaccine.
Dr. Walenksy urged parents to seriously consider vaccinating their children.
“Understandably, some parents want more information before their children receive a vaccine,” she said. “I encourage parents with questions to talk to your child’s healthcare provider or your family doctor to learn more about the vaccine.”
Vaccine “safe and effective”
Separately, the American Academy of Pediatrics issued a statement May 12 in support of vaccinating all children ages 12 and older who are eligible for the federally authorized COVID-19 vaccine.
“As a pediatrician and a parent, I have looked forward to getting my own children and patients vaccinated, and I am thrilled that those ages 12 and older can now be protected,” said AAP President Lee Savio Beers, MD, in a statement. “The data continue to show that this vaccine is safe and effective. I urge all parents to call their pediatrician to learn more about how to get their children and teens vaccinated.”
The expanded clearance for the Pfizer vaccine is seen as a critical step for allowing teens to resume activities on which they missed out during the pandemic.
“We’ve seen the harm done to children’s mental and emotional health as they’ve missed out on so many experiences during the pandemic,” Dr. Beers said. “Vaccinating children will protect them and allow them to fully engage in all of the activities – school, sports, socializing with friends and family – that are so important to their health and development.”
A version of this article first appeared on Medscape.com.
A review of the latest USPSTF recommendations
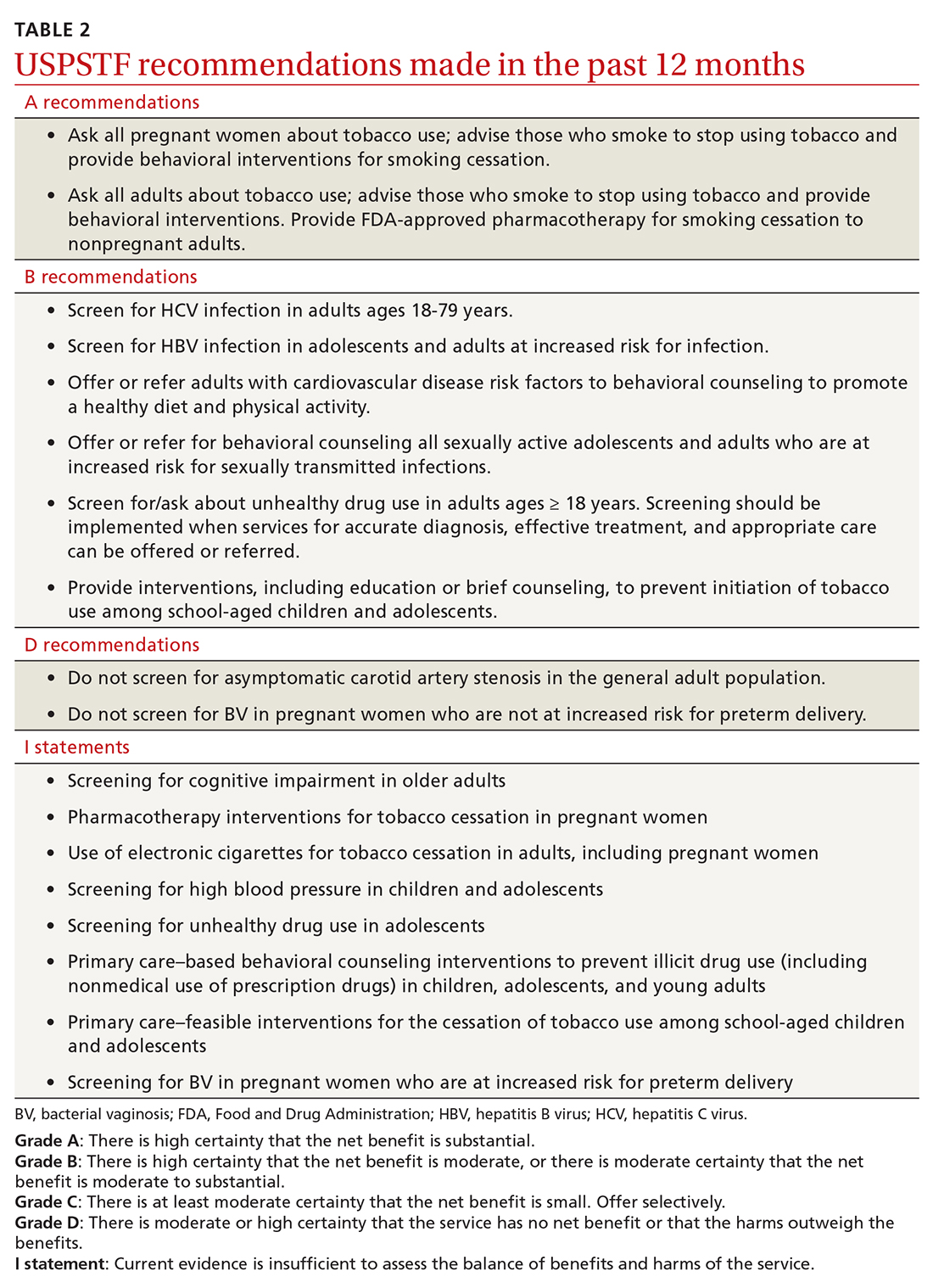
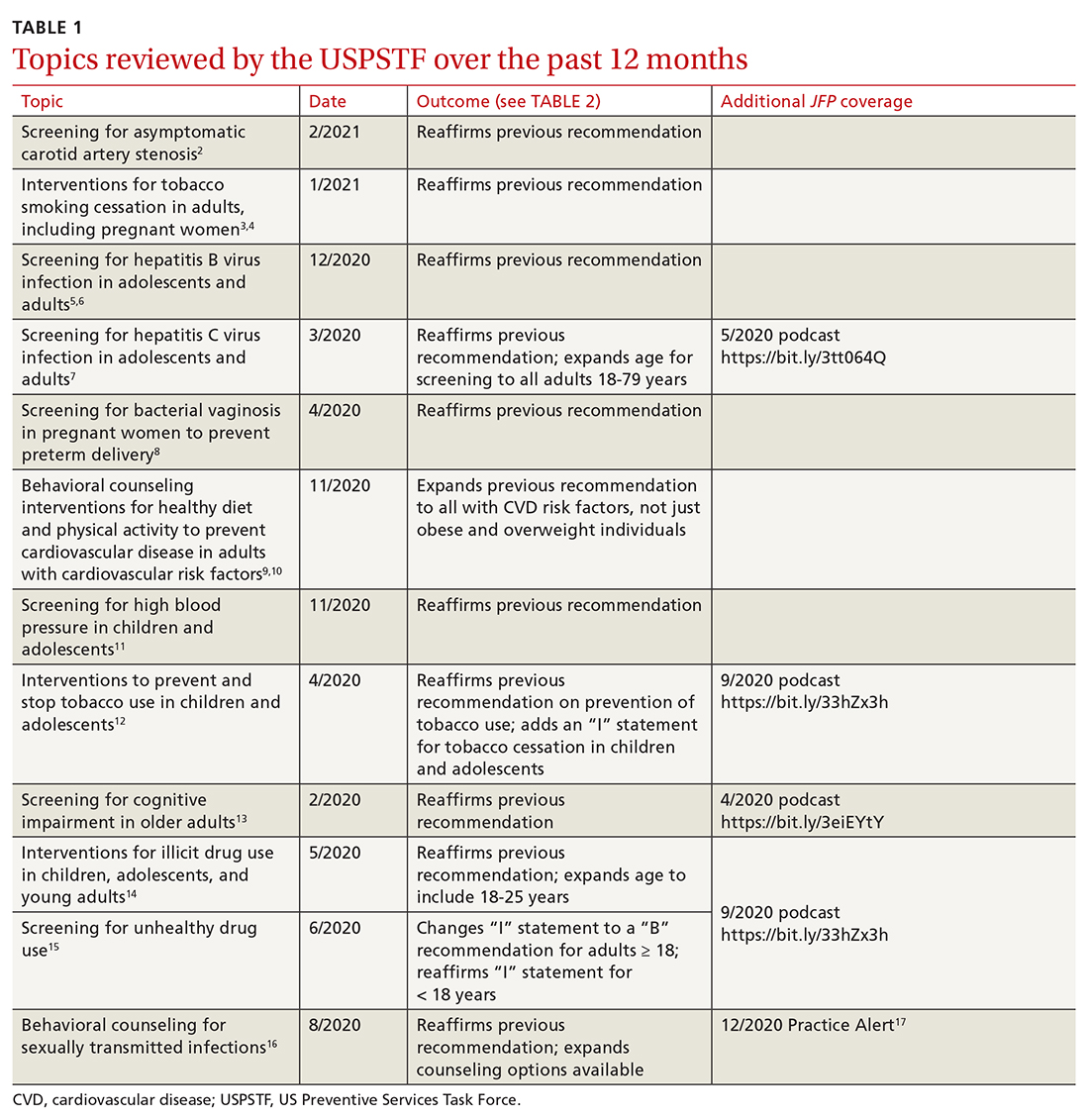
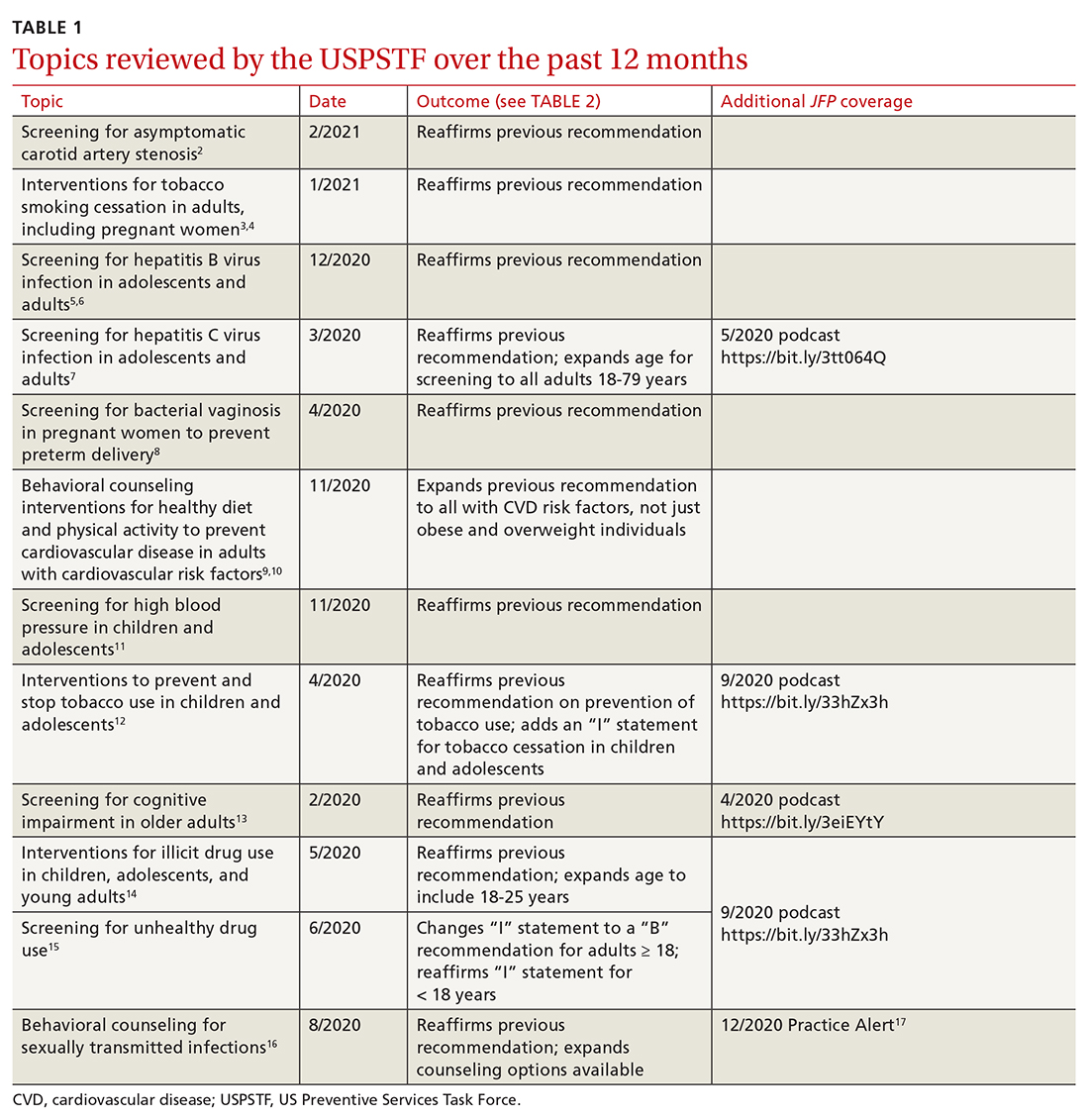
Since the last Practice Alert update on recommendations made by the US Preventive Services Task Force,1 the Task Force has completed work on 12 topics (TABLE 1).2-17 Five of these topics have been discussed in JFP audio recordings, and the links are provided in TABLE 1.
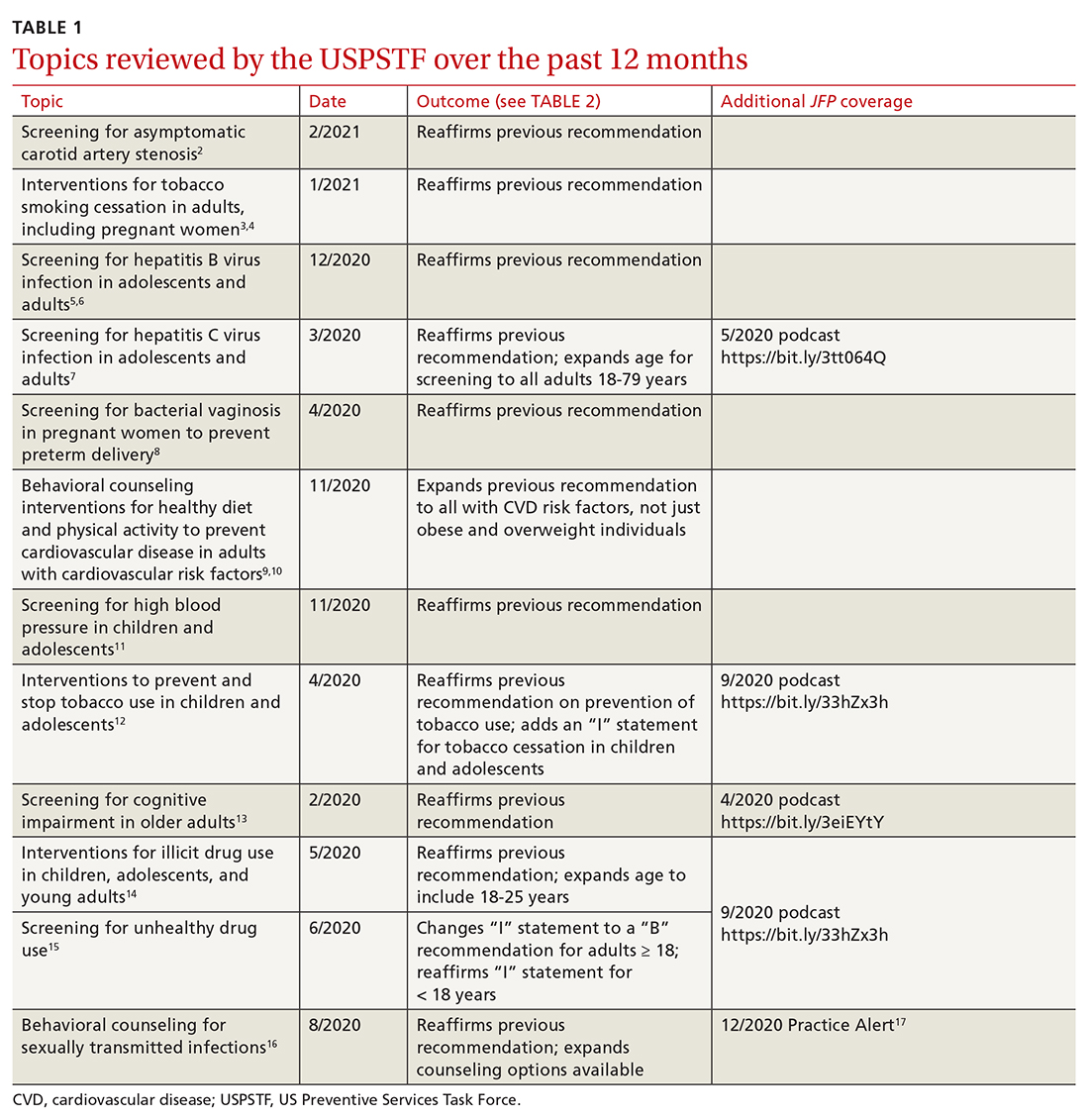
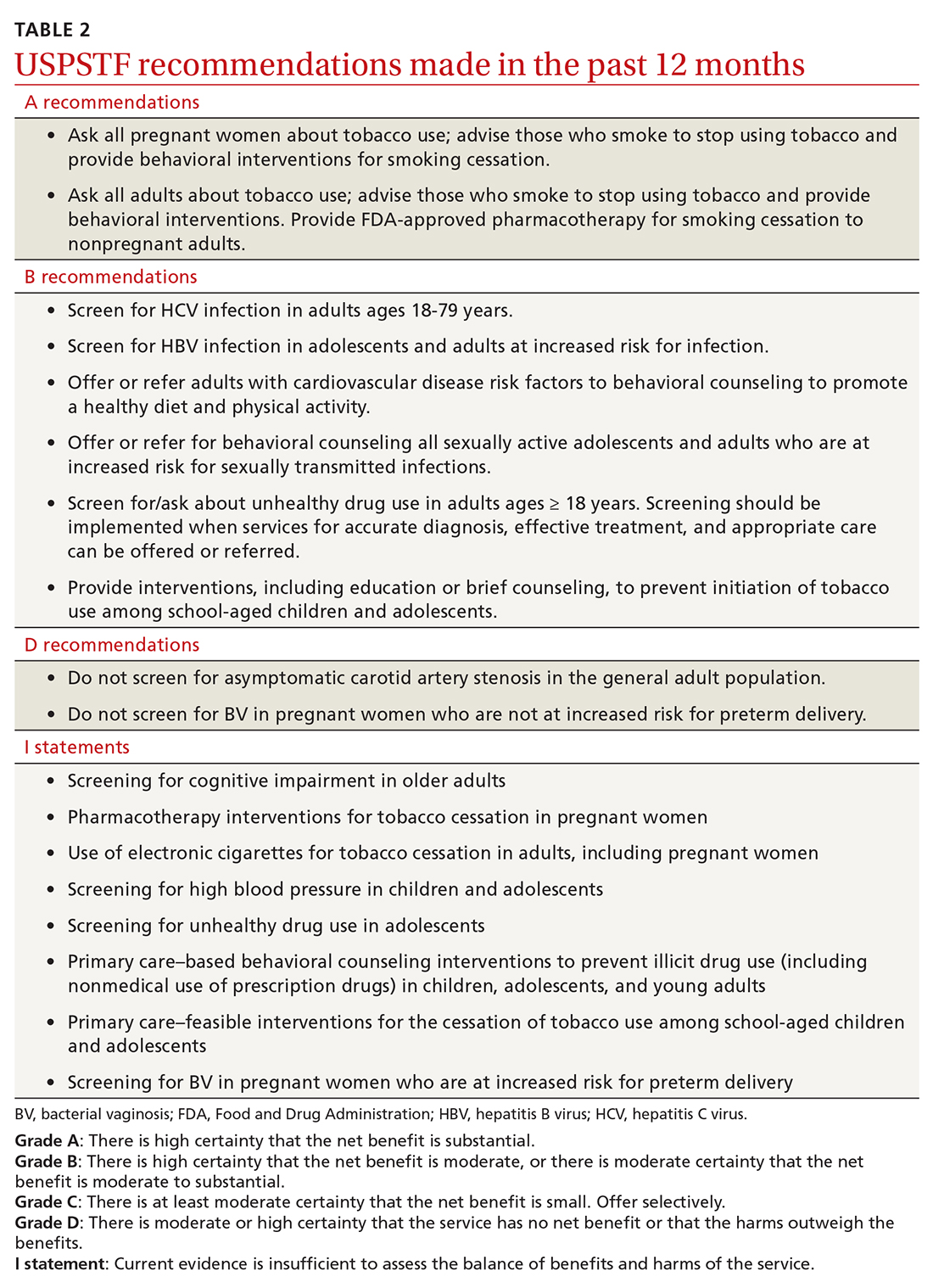
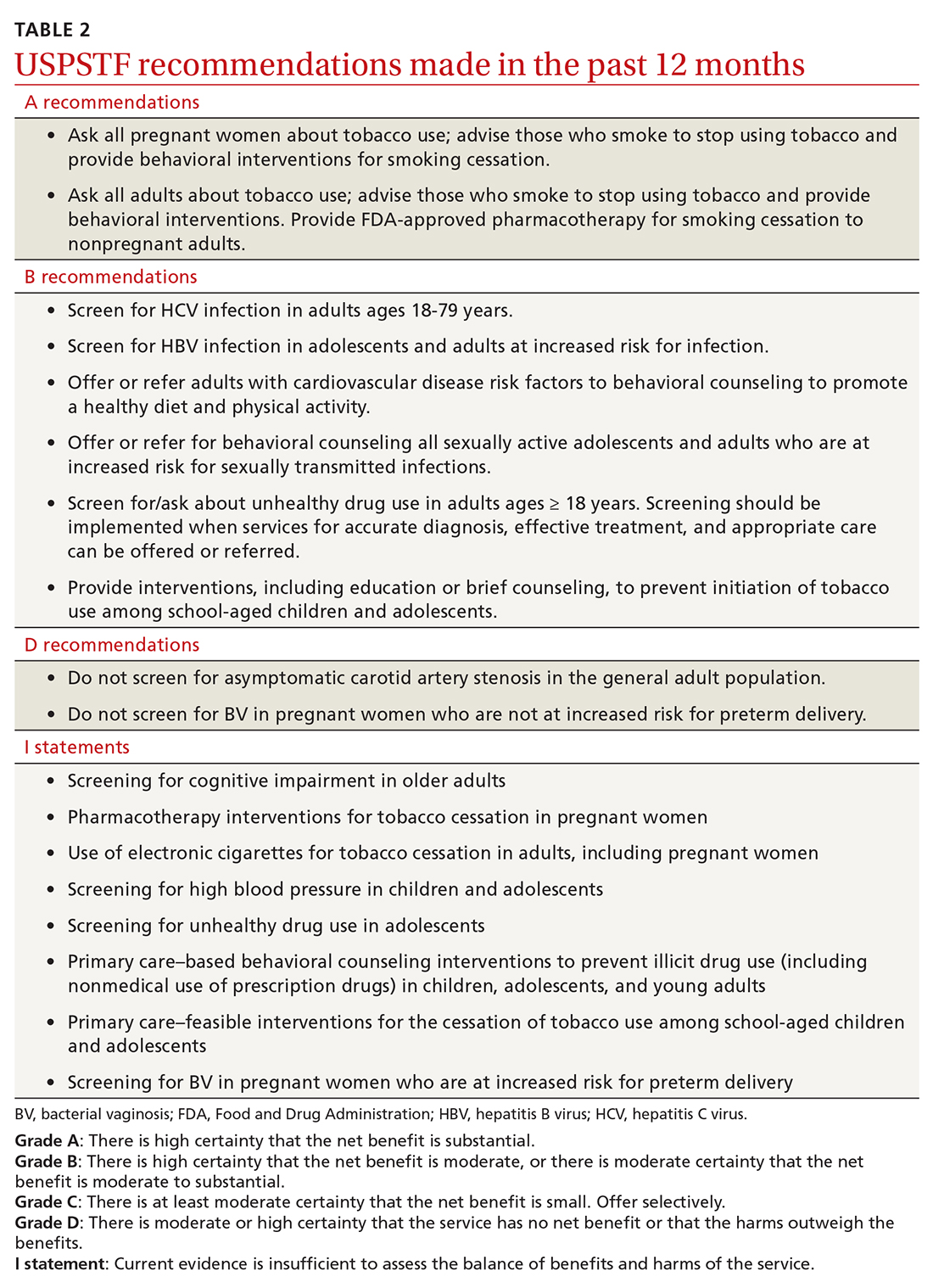
This latest Task Force endeavor resulted in 18 recommendations (TABLE 2), all of which reaffirm previous recommendations on these topics and expand the scope of 2. There were 2 “A” recommendations, 6 “B” recommendations, 2 “D” recommendations, and 8 “I” statements, indicating that there was insufficient evidence to assess effectiveness or harms. The willingness to make “I” statements when there is little or no evidence on the intervention being assessed distinguishes the USPSTF from other clinical guideline committees.
Screening for carotid artery stenosis
One of the “D” recommendations this past year reaffirms the prior recommendation against screening for carotid artery stenosis in asymptomatic adults—ie, those without a history of transient ischemic attack, stroke, or neurologic signs or symptoms that might be caused by carotid artery stenosis.2 The screening tests the Task Force researched included carotid duplex ultrasonography (DUS), magnetic resonance angiography, and computed tomography angiography. The Task Force did not look at the value of auscultation for carotid bruits because it has been proven to be inaccurate and they do not consider it to be a useful screening tool.
The Task Force based its “D” recommendation on a lack of evidence for any benefit in detecting asymptomatic carotid artery stenosis, and on evidence that screening can lead to harms through false-positive tests and potential complications from carotid endarterectomy and carotid artery angioplasty and stenting. In its clinical considerations, the Task Force emphasized the primary prevention of atherosclerotic disease by focusing on the following actions:
- screening for high blood pressure in adults
- encouraging tobacco smoking cessation in adults
- promoting a healthy diet and physical activity in adults with cardiovascular risk factors
- recommending aspirin use to prevent cardiovascular disease and colorectal cancer
- advising statin use for the primary prevention of cardiovascular disease in adults ages 45 to 75 years who have 1 or more risk factors (hyperlipidemia, diabetes, hypertension, smoking) and those with a 10-year risk of a cardiovascular event of 10% or greater.
This “D” recommendation differs from recommendations made by other professional organizations, some of which recommend testing with DUS for asymptomatic patients with a carotid bruit, and others that recommend DUS screening in patients with multiple risk factors for stroke and in those with known peripheral artery disease or other cardiovascular disease.18,19
Smoking cessation in adults
Smoking tobacco is the leading preventable cause of death in the United States, causing about 480,000 deaths annually.3 Smoking during pregnancy increases the risk of complications including miscarriage, congenital anomalies, stillbirth, fetal growth restriction, preterm birth, and placental abruption.
The Task Force published recommendations earlier this year advising all clinicians to ask all adult patients about tobacco use; and, for those who smoke, to provide (or refer them to) smoking cessation behavioral therapy. The Task Force also recommends prescribing pharmacotherapy approved by the Food and Drug Administration (FDA) for smoking cessation for nonpregnant adults. (There is a lack of information to assess the harms and benefits of smoking cessation pharmacotherapy during pregnancy.)
Continue to: FDA-approved medications...
FDA-approved medications for treating tobacco smoking dependence are nicotine replacement therapy (NRT), bupropion hydrochloride, and varenicline.3 NRT is available in transdermal patches, lozenges, gum, inhalers, and nasal sprays.
In addition, the Task Force indicates that there is insufficient evidence to assess the benefits and harms of e-cigarettes when used as a method of achieving smoking cessation: “Few randomized trials have evaluated the effectiveness of e-cigarettes to increase tobacco smoking cessation in nonpregnant adults, and no trials have evaluated e-cigarettes for tobacco smoking cessation in pregnant persons.”4
Hepatitis B infection screening
The Task Force reaffirmed a previous recommendation to screen for hepatitis B virus (HBV) infection only in adults who are at high risk,5 rather than universal screening that it recommends for hepatitis C virus infection (HCV).7 (See: https://bit.ly/3tt064Q). The Task Force has a separate recommendation to screen all pregnant women for hepatitis B at the first prenatal visit.6
Those at high risk for hepatitis B who should be screened include individuals born in countries or regions of the world with a hepatitis B surface antigen (HBsAg) prevalence ≥ 2% and individuals born in the United States who have not received HBV vaccine and whose parents were born in regions with an HBsAg prevalence ≥ 8%.5 (A table listing countries with HBsAg ≥ 8%—as well as those in lower prevalence categories—is included with the recommendation.5)
HBV screening should also be offered to other high-risk groups that have a prevalence of positive HBsAg ≥ 2%: those who have injected drugs in the past or are currently injecting drugs; men who have sex with men; individuals with HIV; and sex partners, needle-sharing contacts, and household contacts of people known to be HBsAg positive.5
Continue to: It is estimated that...
It is estimated that > 860,000 people in the United States have chronic HBV infection and that close to two-thirds of them are unaware of their infection.5 The screening test for HBV is highly accurate; sensitivity and specificity are both > 98%.5 While there is no direct evidence that screening, detecting, and treating asymptomatic HBV infection reduces morbidity and mortality, the Task Force felt that the evidence for improvement in multiple outcomes in those with HBV when treated with antiviral regimens was sufficient to support the recommendation.
Screening for bacterial vaginosis in pregnancy
While bacterial vaginosis (BV) is associated with a two-fold risk of preterm delivery, treating BV during pregnancy does not seem to reduce this risk, indicating that some other variable is involved.8 In addition, studies that looked at screening for, and treatment of, asymptomatic BV in pregnant women at high risk for preterm delivery (defined primarily as those with a previous preterm delivery) have shown inconsistent results. There is the potential for harm in treating BV in pregnancy, chiefly involving gastrointestinal upset caused by metronidazole or clindamycin.
Given that there are no benefits—and some harms—resulting from treatment, the Task Force recommends against screening for BV in non-high-risk pregnant women. A lack of sufficient information to assess any potential benefits to screening in high-risk pregnancies led the Task Force to an “I” statement on this question.8
Behavioral counseling on healthy diet, exercise for adults with CV risks
Cardiovascular disease (CVD) remains the number one cause of death in the United States. The major risk factors for CVD, which can be modified, are high blood pressure, hyperlipidemia, diabetes, smoking, obesity or overweight, and lack of physical activity.
The Task Force has previously recommended intensive behavioral interventions to improve nutrition and physical activity in those who are overweight/obese and in those with abnormal blood glucose levels,9 and has addressed smoking prevention and cessation.4 This new recommendation applies to those with other CVD risks such as high blood pressure and/or hyperlipidemia and those with an estimated 10-year CVD risk of ≥ 7.5%.10
Continue to: Behavioral interventions...
Behavioral interventions included in the Task Force analysis employed a median of 12 contacts and an estimated 6 hours of contact time over 6 to 18 months.10 Most interventions involved motivational interviewing and instruction on behavioral change methods. These interventions can be provided by primary care clinicians, as well as a wide range of other trained professionals. The Affordable Care Act dictates that all “A” and “B” recommendations must be provided by commercial health plans at no out-of-pocket expense for the patient.
Nutritional advice should include reductions in saturated fats, salt, and sugars and increases in fruits, vegetables, and whole grains. The Mediterranean diet and the Dietary Approaches to Stop Hypertension (DASH) diet are often recommended.10 Physical activity counseling should advocate for 90 to 180 minutes per week of moderate to vigorous activity.
This new recommendation, along with the previous ones pertaining to behavioral interventions for lifestyle changes, make it clear that intensive interventions are needed to achieve meaningful change. Simple advice from a clinician will have little to no effect.
Task Force reviews evidence on HTN, smoking cessation in young people
In 2020 the Task Force completed reviews of evidence relevant to screening for high blood pressure11 and
The 2 “I” statements are in disagreement with recommendations of other professional organizations. The American Academy of Pediatrics (AAP) and the American Heart Association recommend routine screening for high blood pressure starting at age 3 years. And the AAP recommends screening teenagers for tobacco use and offering tobacco dependence treatment, referral, or both (including pharmacotherapy) when indicated. E-cigarettes are not recommended as a treatment for tobacco dependence.20
Continue to: The difference between...
The difference between the methods used by the Task Force and other guideline-producing organizations becomes apparent when it comes to recommendations pertaining to children and adolescents, for whom long-term outcome-oriented studies on prevention issues are rare. The Task Force is unwilling to make recommendations when evidence does not exist. The AAP often makes recommendations based on expert opinion consensus in such situations. One notable part of each Task Force recommendation statement is a discussion of what other organizations recommend on the same topic so that these differences can be openly described.
Better Task Force funding could expand topic coverage
It is worth revisiting 2 issues that were pointed out in last year’s USPSTF summary in this column.1 First, the Task Force methods are robust and evidence based, and recommendations therefore are rarely changed once they are made at an “A”, “B”, or “D” level. Second, Task Force resources are finite, and thus, the group is currently unable to update previous recommendations with greater frequency or to consider many new topics. In the past 2 years, the Task Force has developed recommendations on only 2 completely new topics. Hopefully, its budget can be expanded so that new topics can be added in the future.
1. Campos-Outcalt D. USPSTF roundup. J Fam Pract. 2020;69:201-204.
2. USPSTF. Screening for asymptomatic carotid artery stenosis. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/carotid-artery-stenosis-screening
3. USPSTF. Interventions for tobacco smoking cessation in adults, including pregnant persons. Accessed April 30, 2021. www.uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions
4. USPSTF. Interventions for tobacco smoking cessation in adults, including pregnant persons. JAMA. 2021;325:265-279.
5. USPSTF. Screening for Hepatitis B virus infection in adolescents and adults. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/hepatitis-b-virus-infection-screening
6. USPSTF. Hepatitis B virus infection in pregnant women: screening. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/hepatitis-b-virus-infection-in-pregnant-women-screening
7. USPSTF. Hepatitis C virus infection in adolescents and adults: screening. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/hepatitis-c-screening
8. USPSTF; Owens DK, Davidson KW, Krisk AH, et al. Screening for bacterial vaginosis in pregnant persons to prevent preterm delivery: US Preventive Services Task Force recommendation statement. JAMA. 2020;323:1286-1292.
9. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;161:587-593.
10. USPSTF. Behavioral counseling interventions to promote a healthy and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: US Preventive Services Task Force recommendation statement. JAMA. 2020;324:2069-2075.
11. USPSTF. High blood pressure in children and adolescents: screening. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/blood-pressure-in-children-and-adolescents-hypertension-screening
12. USPSTF. Prevention and cessation of tobacco use in children and adolescents: primary care interventions. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-and-nicotine-use-prevention-in-children-and-adolescents-primary-care-interventions
13. USPSTF. Cognitive impairment in older adults: screening. Accessed March 26, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/cognitive-impairment-in-older-adults-screening
14. USPSTF. Illicit drug use in children, adolescents, and young adults: primary care-based interventions. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/drug-use-illicit-primary-care-interventions-for-children-and-adolescents
15. USPSTF. Unhealthy drug use: screening. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/drug-use-illicit-screening
16. USPSTF. Sexually transmitted infections: behavioral counseling. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/sexually-transmitted-infections-behavioral-counseling.
17. Campos-Outcalt D. USPSTF update on sexually transmitted infections. J Fam Pract. 2020;69:514-517.
18. Brott TG, Halperin JL, Abbara S, et al; ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease. Catheter Cardiovasc Interv. 2013;81:E76-E123.
19. Ricotta JJ, Aburahma A, Ascher E, et al; Society for Vascular Surgery. Updated Society for Vascular Surgery guidelines for management of extracranial carotid disease. J Vasc Surg. 2011;54:e1-e31.
20. Farber HJ, Walley SC, Groner JA, et al; Section on Tobacco Control. Clinical practice policy to protect children from tobacco, nicotine, and tobacco smoke. Pediatrics. 2015;136:1008-1017.
Since the last Practice Alert update on recommendations made by the US Preventive Services Task Force,1 the Task Force has completed work on 12 topics (TABLE 1).2-17 Five of these topics have been discussed in JFP audio recordings, and the links are provided in TABLE 1.
This latest Task Force endeavor resulted in 18 recommendations (TABLE 2), all of which reaffirm previous recommendations on these topics and expand the scope of 2. There were 2 “A” recommendations, 6 “B” recommendations, 2 “D” recommendations, and 8 “I” statements, indicating that there was insufficient evidence to assess effectiveness or harms. The willingness to make “I” statements when there is little or no evidence on the intervention being assessed distinguishes the USPSTF from other clinical guideline committees.
Screening for carotid artery stenosis
One of the “D” recommendations this past year reaffirms the prior recommendation against screening for carotid artery stenosis in asymptomatic adults—ie, those without a history of transient ischemic attack, stroke, or neurologic signs or symptoms that might be caused by carotid artery stenosis.2 The screening tests the Task Force researched included carotid duplex ultrasonography (DUS), magnetic resonance angiography, and computed tomography angiography. The Task Force did not look at the value of auscultation for carotid bruits because it has been proven to be inaccurate and they do not consider it to be a useful screening tool.
The Task Force based its “D” recommendation on a lack of evidence for any benefit in detecting asymptomatic carotid artery stenosis, and on evidence that screening can lead to harms through false-positive tests and potential complications from carotid endarterectomy and carotid artery angioplasty and stenting. In its clinical considerations, the Task Force emphasized the primary prevention of atherosclerotic disease by focusing on the following actions:
- screening for high blood pressure in adults
- encouraging tobacco smoking cessation in adults
- promoting a healthy diet and physical activity in adults with cardiovascular risk factors
- recommending aspirin use to prevent cardiovascular disease and colorectal cancer
- advising statin use for the primary prevention of cardiovascular disease in adults ages 45 to 75 years who have 1 or more risk factors (hyperlipidemia, diabetes, hypertension, smoking) and those with a 10-year risk of a cardiovascular event of 10% or greater.
This “D” recommendation differs from recommendations made by other professional organizations, some of which recommend testing with DUS for asymptomatic patients with a carotid bruit, and others that recommend DUS screening in patients with multiple risk factors for stroke and in those with known peripheral artery disease or other cardiovascular disease.18,19
Smoking cessation in adults
Smoking tobacco is the leading preventable cause of death in the United States, causing about 480,000 deaths annually.3 Smoking during pregnancy increases the risk of complications including miscarriage, congenital anomalies, stillbirth, fetal growth restriction, preterm birth, and placental abruption.
The Task Force published recommendations earlier this year advising all clinicians to ask all adult patients about tobacco use; and, for those who smoke, to provide (or refer them to) smoking cessation behavioral therapy. The Task Force also recommends prescribing pharmacotherapy approved by the Food and Drug Administration (FDA) for smoking cessation for nonpregnant adults. (There is a lack of information to assess the harms and benefits of smoking cessation pharmacotherapy during pregnancy.)
Continue to: FDA-approved medications...
FDA-approved medications for treating tobacco smoking dependence are nicotine replacement therapy (NRT), bupropion hydrochloride, and varenicline.3 NRT is available in transdermal patches, lozenges, gum, inhalers, and nasal sprays.
In addition, the Task Force indicates that there is insufficient evidence to assess the benefits and harms of e-cigarettes when used as a method of achieving smoking cessation: “Few randomized trials have evaluated the effectiveness of e-cigarettes to increase tobacco smoking cessation in nonpregnant adults, and no trials have evaluated e-cigarettes for tobacco smoking cessation in pregnant persons.”4
Hepatitis B infection screening
The Task Force reaffirmed a previous recommendation to screen for hepatitis B virus (HBV) infection only in adults who are at high risk,5 rather than universal screening that it recommends for hepatitis C virus infection (HCV).7 (See: https://bit.ly/3tt064Q). The Task Force has a separate recommendation to screen all pregnant women for hepatitis B at the first prenatal visit.6
Those at high risk for hepatitis B who should be screened include individuals born in countries or regions of the world with a hepatitis B surface antigen (HBsAg) prevalence ≥ 2% and individuals born in the United States who have not received HBV vaccine and whose parents were born in regions with an HBsAg prevalence ≥ 8%.5 (A table listing countries with HBsAg ≥ 8%—as well as those in lower prevalence categories—is included with the recommendation.5)
HBV screening should also be offered to other high-risk groups that have a prevalence of positive HBsAg ≥ 2%: those who have injected drugs in the past or are currently injecting drugs; men who have sex with men; individuals with HIV; and sex partners, needle-sharing contacts, and household contacts of people known to be HBsAg positive.5
Continue to: It is estimated that...
It is estimated that > 860,000 people in the United States have chronic HBV infection and that close to two-thirds of them are unaware of their infection.5 The screening test for HBV is highly accurate; sensitivity and specificity are both > 98%.5 While there is no direct evidence that screening, detecting, and treating asymptomatic HBV infection reduces morbidity and mortality, the Task Force felt that the evidence for improvement in multiple outcomes in those with HBV when treated with antiviral regimens was sufficient to support the recommendation.
Screening for bacterial vaginosis in pregnancy
While bacterial vaginosis (BV) is associated with a two-fold risk of preterm delivery, treating BV during pregnancy does not seem to reduce this risk, indicating that some other variable is involved.8 In addition, studies that looked at screening for, and treatment of, asymptomatic BV in pregnant women at high risk for preterm delivery (defined primarily as those with a previous preterm delivery) have shown inconsistent results. There is the potential for harm in treating BV in pregnancy, chiefly involving gastrointestinal upset caused by metronidazole or clindamycin.
Given that there are no benefits—and some harms—resulting from treatment, the Task Force recommends against screening for BV in non-high-risk pregnant women. A lack of sufficient information to assess any potential benefits to screening in high-risk pregnancies led the Task Force to an “I” statement on this question.8
Behavioral counseling on healthy diet, exercise for adults with CV risks
Cardiovascular disease (CVD) remains the number one cause of death in the United States. The major risk factors for CVD, which can be modified, are high blood pressure, hyperlipidemia, diabetes, smoking, obesity or overweight, and lack of physical activity.
The Task Force has previously recommended intensive behavioral interventions to improve nutrition and physical activity in those who are overweight/obese and in those with abnormal blood glucose levels,9 and has addressed smoking prevention and cessation.4 This new recommendation applies to those with other CVD risks such as high blood pressure and/or hyperlipidemia and those with an estimated 10-year CVD risk of ≥ 7.5%.10
Continue to: Behavioral interventions...
Behavioral interventions included in the Task Force analysis employed a median of 12 contacts and an estimated 6 hours of contact time over 6 to 18 months.10 Most interventions involved motivational interviewing and instruction on behavioral change methods. These interventions can be provided by primary care clinicians, as well as a wide range of other trained professionals. The Affordable Care Act dictates that all “A” and “B” recommendations must be provided by commercial health plans at no out-of-pocket expense for the patient.
Nutritional advice should include reductions in saturated fats, salt, and sugars and increases in fruits, vegetables, and whole grains. The Mediterranean diet and the Dietary Approaches to Stop Hypertension (DASH) diet are often recommended.10 Physical activity counseling should advocate for 90 to 180 minutes per week of moderate to vigorous activity.
This new recommendation, along with the previous ones pertaining to behavioral interventions for lifestyle changes, make it clear that intensive interventions are needed to achieve meaningful change. Simple advice from a clinician will have little to no effect.
Task Force reviews evidence on HTN, smoking cessation in young people
In 2020 the Task Force completed reviews of evidence relevant to screening for high blood pressure11 and
The 2 “I” statements are in disagreement with recommendations of other professional organizations. The American Academy of Pediatrics (AAP) and the American Heart Association recommend routine screening for high blood pressure starting at age 3 years. And the AAP recommends screening teenagers for tobacco use and offering tobacco dependence treatment, referral, or both (including pharmacotherapy) when indicated. E-cigarettes are not recommended as a treatment for tobacco dependence.20
Continue to: The difference between...
The difference between the methods used by the Task Force and other guideline-producing organizations becomes apparent when it comes to recommendations pertaining to children and adolescents, for whom long-term outcome-oriented studies on prevention issues are rare. The Task Force is unwilling to make recommendations when evidence does not exist. The AAP often makes recommendations based on expert opinion consensus in such situations. One notable part of each Task Force recommendation statement is a discussion of what other organizations recommend on the same topic so that these differences can be openly described.
Better Task Force funding could expand topic coverage
It is worth revisiting 2 issues that were pointed out in last year’s USPSTF summary in this column.1 First, the Task Force methods are robust and evidence based, and recommendations therefore are rarely changed once they are made at an “A”, “B”, or “D” level. Second, Task Force resources are finite, and thus, the group is currently unable to update previous recommendations with greater frequency or to consider many new topics. In the past 2 years, the Task Force has developed recommendations on only 2 completely new topics. Hopefully, its budget can be expanded so that new topics can be added in the future.
Since the last Practice Alert update on recommendations made by the US Preventive Services Task Force,1 the Task Force has completed work on 12 topics (TABLE 1).2-17 Five of these topics have been discussed in JFP audio recordings, and the links are provided in TABLE 1.
This latest Task Force endeavor resulted in 18 recommendations (TABLE 2), all of which reaffirm previous recommendations on these topics and expand the scope of 2. There were 2 “A” recommendations, 6 “B” recommendations, 2 “D” recommendations, and 8 “I” statements, indicating that there was insufficient evidence to assess effectiveness or harms. The willingness to make “I” statements when there is little or no evidence on the intervention being assessed distinguishes the USPSTF from other clinical guideline committees.
Screening for carotid artery stenosis
One of the “D” recommendations this past year reaffirms the prior recommendation against screening for carotid artery stenosis in asymptomatic adults—ie, those without a history of transient ischemic attack, stroke, or neurologic signs or symptoms that might be caused by carotid artery stenosis.2 The screening tests the Task Force researched included carotid duplex ultrasonography (DUS), magnetic resonance angiography, and computed tomography angiography. The Task Force did not look at the value of auscultation for carotid bruits because it has been proven to be inaccurate and they do not consider it to be a useful screening tool.
The Task Force based its “D” recommendation on a lack of evidence for any benefit in detecting asymptomatic carotid artery stenosis, and on evidence that screening can lead to harms through false-positive tests and potential complications from carotid endarterectomy and carotid artery angioplasty and stenting. In its clinical considerations, the Task Force emphasized the primary prevention of atherosclerotic disease by focusing on the following actions:
- screening for high blood pressure in adults
- encouraging tobacco smoking cessation in adults
- promoting a healthy diet and physical activity in adults with cardiovascular risk factors
- recommending aspirin use to prevent cardiovascular disease and colorectal cancer
- advising statin use for the primary prevention of cardiovascular disease in adults ages 45 to 75 years who have 1 or more risk factors (hyperlipidemia, diabetes, hypertension, smoking) and those with a 10-year risk of a cardiovascular event of 10% or greater.
This “D” recommendation differs from recommendations made by other professional organizations, some of which recommend testing with DUS for asymptomatic patients with a carotid bruit, and others that recommend DUS screening in patients with multiple risk factors for stroke and in those with known peripheral artery disease or other cardiovascular disease.18,19
Smoking cessation in adults
Smoking tobacco is the leading preventable cause of death in the United States, causing about 480,000 deaths annually.3 Smoking during pregnancy increases the risk of complications including miscarriage, congenital anomalies, stillbirth, fetal growth restriction, preterm birth, and placental abruption.
The Task Force published recommendations earlier this year advising all clinicians to ask all adult patients about tobacco use; and, for those who smoke, to provide (or refer them to) smoking cessation behavioral therapy. The Task Force also recommends prescribing pharmacotherapy approved by the Food and Drug Administration (FDA) for smoking cessation for nonpregnant adults. (There is a lack of information to assess the harms and benefits of smoking cessation pharmacotherapy during pregnancy.)
Continue to: FDA-approved medications...
FDA-approved medications for treating tobacco smoking dependence are nicotine replacement therapy (NRT), bupropion hydrochloride, and varenicline.3 NRT is available in transdermal patches, lozenges, gum, inhalers, and nasal sprays.
In addition, the Task Force indicates that there is insufficient evidence to assess the benefits and harms of e-cigarettes when used as a method of achieving smoking cessation: “Few randomized trials have evaluated the effectiveness of e-cigarettes to increase tobacco smoking cessation in nonpregnant adults, and no trials have evaluated e-cigarettes for tobacco smoking cessation in pregnant persons.”4
Hepatitis B infection screening
The Task Force reaffirmed a previous recommendation to screen for hepatitis B virus (HBV) infection only in adults who are at high risk,5 rather than universal screening that it recommends for hepatitis C virus infection (HCV).7 (See: https://bit.ly/3tt064Q). The Task Force has a separate recommendation to screen all pregnant women for hepatitis B at the first prenatal visit.6
Those at high risk for hepatitis B who should be screened include individuals born in countries or regions of the world with a hepatitis B surface antigen (HBsAg) prevalence ≥ 2% and individuals born in the United States who have not received HBV vaccine and whose parents were born in regions with an HBsAg prevalence ≥ 8%.5 (A table listing countries with HBsAg ≥ 8%—as well as those in lower prevalence categories—is included with the recommendation.5)
HBV screening should also be offered to other high-risk groups that have a prevalence of positive HBsAg ≥ 2%: those who have injected drugs in the past or are currently injecting drugs; men who have sex with men; individuals with HIV; and sex partners, needle-sharing contacts, and household contacts of people known to be HBsAg positive.5
Continue to: It is estimated that...
It is estimated that > 860,000 people in the United States have chronic HBV infection and that close to two-thirds of them are unaware of their infection.5 The screening test for HBV is highly accurate; sensitivity and specificity are both > 98%.5 While there is no direct evidence that screening, detecting, and treating asymptomatic HBV infection reduces morbidity and mortality, the Task Force felt that the evidence for improvement in multiple outcomes in those with HBV when treated with antiviral regimens was sufficient to support the recommendation.
Screening for bacterial vaginosis in pregnancy
While bacterial vaginosis (BV) is associated with a two-fold risk of preterm delivery, treating BV during pregnancy does not seem to reduce this risk, indicating that some other variable is involved.8 In addition, studies that looked at screening for, and treatment of, asymptomatic BV in pregnant women at high risk for preterm delivery (defined primarily as those with a previous preterm delivery) have shown inconsistent results. There is the potential for harm in treating BV in pregnancy, chiefly involving gastrointestinal upset caused by metronidazole or clindamycin.
Given that there are no benefits—and some harms—resulting from treatment, the Task Force recommends against screening for BV in non-high-risk pregnant women. A lack of sufficient information to assess any potential benefits to screening in high-risk pregnancies led the Task Force to an “I” statement on this question.8
Behavioral counseling on healthy diet, exercise for adults with CV risks
Cardiovascular disease (CVD) remains the number one cause of death in the United States. The major risk factors for CVD, which can be modified, are high blood pressure, hyperlipidemia, diabetes, smoking, obesity or overweight, and lack of physical activity.
The Task Force has previously recommended intensive behavioral interventions to improve nutrition and physical activity in those who are overweight/obese and in those with abnormal blood glucose levels,9 and has addressed smoking prevention and cessation.4 This new recommendation applies to those with other CVD risks such as high blood pressure and/or hyperlipidemia and those with an estimated 10-year CVD risk of ≥ 7.5%.10
Continue to: Behavioral interventions...
Behavioral interventions included in the Task Force analysis employed a median of 12 contacts and an estimated 6 hours of contact time over 6 to 18 months.10 Most interventions involved motivational interviewing and instruction on behavioral change methods. These interventions can be provided by primary care clinicians, as well as a wide range of other trained professionals. The Affordable Care Act dictates that all “A” and “B” recommendations must be provided by commercial health plans at no out-of-pocket expense for the patient.
Nutritional advice should include reductions in saturated fats, salt, and sugars and increases in fruits, vegetables, and whole grains. The Mediterranean diet and the Dietary Approaches to Stop Hypertension (DASH) diet are often recommended.10 Physical activity counseling should advocate for 90 to 180 minutes per week of moderate to vigorous activity.
This new recommendation, along with the previous ones pertaining to behavioral interventions for lifestyle changes, make it clear that intensive interventions are needed to achieve meaningful change. Simple advice from a clinician will have little to no effect.
Task Force reviews evidence on HTN, smoking cessation in young people
In 2020 the Task Force completed reviews of evidence relevant to screening for high blood pressure11 and
The 2 “I” statements are in disagreement with recommendations of other professional organizations. The American Academy of Pediatrics (AAP) and the American Heart Association recommend routine screening for high blood pressure starting at age 3 years. And the AAP recommends screening teenagers for tobacco use and offering tobacco dependence treatment, referral, or both (including pharmacotherapy) when indicated. E-cigarettes are not recommended as a treatment for tobacco dependence.20
Continue to: The difference between...
The difference between the methods used by the Task Force and other guideline-producing organizations becomes apparent when it comes to recommendations pertaining to children and adolescents, for whom long-term outcome-oriented studies on prevention issues are rare. The Task Force is unwilling to make recommendations when evidence does not exist. The AAP often makes recommendations based on expert opinion consensus in such situations. One notable part of each Task Force recommendation statement is a discussion of what other organizations recommend on the same topic so that these differences can be openly described.
Better Task Force funding could expand topic coverage
It is worth revisiting 2 issues that were pointed out in last year’s USPSTF summary in this column.1 First, the Task Force methods are robust and evidence based, and recommendations therefore are rarely changed once they are made at an “A”, “B”, or “D” level. Second, Task Force resources are finite, and thus, the group is currently unable to update previous recommendations with greater frequency or to consider many new topics. In the past 2 years, the Task Force has developed recommendations on only 2 completely new topics. Hopefully, its budget can be expanded so that new topics can be added in the future.
1. Campos-Outcalt D. USPSTF roundup. J Fam Pract. 2020;69:201-204.
2. USPSTF. Screening for asymptomatic carotid artery stenosis. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/carotid-artery-stenosis-screening
3. USPSTF. Interventions for tobacco smoking cessation in adults, including pregnant persons. Accessed April 30, 2021. www.uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions
4. USPSTF. Interventions for tobacco smoking cessation in adults, including pregnant persons. JAMA. 2021;325:265-279.
5. USPSTF. Screening for Hepatitis B virus infection in adolescents and adults. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/hepatitis-b-virus-infection-screening
6. USPSTF. Hepatitis B virus infection in pregnant women: screening. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/hepatitis-b-virus-infection-in-pregnant-women-screening
7. USPSTF. Hepatitis C virus infection in adolescents and adults: screening. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/hepatitis-c-screening
8. USPSTF; Owens DK, Davidson KW, Krisk AH, et al. Screening for bacterial vaginosis in pregnant persons to prevent preterm delivery: US Preventive Services Task Force recommendation statement. JAMA. 2020;323:1286-1292.
9. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;161:587-593.
10. USPSTF. Behavioral counseling interventions to promote a healthy and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: US Preventive Services Task Force recommendation statement. JAMA. 2020;324:2069-2075.
11. USPSTF. High blood pressure in children and adolescents: screening. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/blood-pressure-in-children-and-adolescents-hypertension-screening
12. USPSTF. Prevention and cessation of tobacco use in children and adolescents: primary care interventions. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-and-nicotine-use-prevention-in-children-and-adolescents-primary-care-interventions
13. USPSTF. Cognitive impairment in older adults: screening. Accessed March 26, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/cognitive-impairment-in-older-adults-screening
14. USPSTF. Illicit drug use in children, adolescents, and young adults: primary care-based interventions. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/drug-use-illicit-primary-care-interventions-for-children-and-adolescents
15. USPSTF. Unhealthy drug use: screening. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/drug-use-illicit-screening
16. USPSTF. Sexually transmitted infections: behavioral counseling. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/sexually-transmitted-infections-behavioral-counseling.
17. Campos-Outcalt D. USPSTF update on sexually transmitted infections. J Fam Pract. 2020;69:514-517.
18. Brott TG, Halperin JL, Abbara S, et al; ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease. Catheter Cardiovasc Interv. 2013;81:E76-E123.
19. Ricotta JJ, Aburahma A, Ascher E, et al; Society for Vascular Surgery. Updated Society for Vascular Surgery guidelines for management of extracranial carotid disease. J Vasc Surg. 2011;54:e1-e31.
20. Farber HJ, Walley SC, Groner JA, et al; Section on Tobacco Control. Clinical practice policy to protect children from tobacco, nicotine, and tobacco smoke. Pediatrics. 2015;136:1008-1017.
1. Campos-Outcalt D. USPSTF roundup. J Fam Pract. 2020;69:201-204.
2. USPSTF. Screening for asymptomatic carotid artery stenosis. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/carotid-artery-stenosis-screening
3. USPSTF. Interventions for tobacco smoking cessation in adults, including pregnant persons. Accessed April 30, 2021. www.uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions
4. USPSTF. Interventions for tobacco smoking cessation in adults, including pregnant persons. JAMA. 2021;325:265-279.
5. USPSTF. Screening for Hepatitis B virus infection in adolescents and adults. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/hepatitis-b-virus-infection-screening
6. USPSTF. Hepatitis B virus infection in pregnant women: screening. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/hepatitis-b-virus-infection-in-pregnant-women-screening
7. USPSTF. Hepatitis C virus infection in adolescents and adults: screening. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/hepatitis-c-screening
8. USPSTF; Owens DK, Davidson KW, Krisk AH, et al. Screening for bacterial vaginosis in pregnant persons to prevent preterm delivery: US Preventive Services Task Force recommendation statement. JAMA. 2020;323:1286-1292.
9. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;161:587-593.
10. USPSTF. Behavioral counseling interventions to promote a healthy and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: US Preventive Services Task Force recommendation statement. JAMA. 2020;324:2069-2075.
11. USPSTF. High blood pressure in children and adolescents: screening. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/blood-pressure-in-children-and-adolescents-hypertension-screening
12. USPSTF. Prevention and cessation of tobacco use in children and adolescents: primary care interventions. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-and-nicotine-use-prevention-in-children-and-adolescents-primary-care-interventions
13. USPSTF. Cognitive impairment in older adults: screening. Accessed March 26, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/cognitive-impairment-in-older-adults-screening
14. USPSTF. Illicit drug use in children, adolescents, and young adults: primary care-based interventions. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/drug-use-illicit-primary-care-interventions-for-children-and-adolescents
15. USPSTF. Unhealthy drug use: screening. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/drug-use-illicit-screening
16. USPSTF. Sexually transmitted infections: behavioral counseling. Accessed April 30, 2021. https://uspreventiveservicestaskforce.org/uspstf/recommendation/sexually-transmitted-infections-behavioral-counseling.
17. Campos-Outcalt D. USPSTF update on sexually transmitted infections. J Fam Pract. 2020;69:514-517.
18. Brott TG, Halperin JL, Abbara S, et al; ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease. Catheter Cardiovasc Interv. 2013;81:E76-E123.
19. Ricotta JJ, Aburahma A, Ascher E, et al; Society for Vascular Surgery. Updated Society for Vascular Surgery guidelines for management of extracranial carotid disease. J Vasc Surg. 2011;54:e1-e31.
20. Farber HJ, Walley SC, Groner JA, et al; Section on Tobacco Control. Clinical practice policy to protect children from tobacco, nicotine, and tobacco smoke. Pediatrics. 2015;136:1008-1017.
High teen BMI linked to stroke risk in young adulthood
High and even high-normal body mass index (BMI) were linked to increased ischemic stroke risk, regardless of whether or not individuals had diabetes.
Overweight and obese adolescent groups in the study had a roughly two- to threefold increased risk of ischemic stroke, which was apparent even before age 30 years in the study that was based on records of Israeli adolescents evaluated prior to mandatory military service.
These findings highlight the importance of treating and preventing high BMI among adolescence, study coauthor Gilad Twig, MD, MPH, PhD, said in a press release.
“Adults who survive stroke earlier in life face poor functional outcomes, which can lead to unemployment, depression and anxiety,” said Dr. Twig, associate professor in the department of military medicine in The Hebrew University in Jerusalem.
The costs of stroke prevention and care, already high, are expected to become even higher as the adolescent obesity prevalence goes up, fueling further increases in stroke rate, Dr. Twig added.
This is believed to be the first study showing that stroke risk is associated with higher BMI values in both men and women, not just men, Dr. Twig and coauthors said in their article, published May 13, 2021 in the journal Stroke. Previous studies assessing the stroke-BMI relationship in adolescents were based on records of Swedish men evaluated during military conscription at age 18.
In the present study, Dr. Twig and coauthors assessed the linkage between adolescent BMI and first stroke event in 1.9 million male and female adolescents in Israel who were evaluated 1 year prior to mandatory military service, between the years of 1985 and 2013.
They cross-referenced that information with stroke events in a national registry to which all hospitals in Israel are required to report.
The adolescents were about 17 years of age on average at the time of evaluation, 58% were male, and 84% were born in Israel. The mean age at the beginning of follow-up for stroke was about 31 years.
Over the follow-up period, investigators identified 1,088 first stroke events, including 921 ischemic and 167 hemorrhagic strokes.
A gradual increase in stroke rate was seen across BMI categories for ischemic strokes, but not so much for hemorrhagic strokes, investigators found.
Hazard ratios for first ischemic stroke event were 1.4 (95% confidence interval, 1.2-1.6) for the high-normal BMI group, 2.0 (95% CI, 1.6-2.4) for the overweight group, and 3.5 (95% CI, 2.8-4.5) for the obese group after adjusting for age and sex at beginning of follow-up, investigators reported.
When the adjusted results were stratified by presence or absence of diabetes, estimates were similar to what was seen in the overall risk model, they added.
Among those young adults who developed ischemic stroke, 43% smoked, 29% had high blood pressure, 17% had diabetes, and 32% had abnormal lipids at the time of diagnosis, the reported data showed.
The clinical and public health implications of these findings could be substantial, since strokes are associated with worse medical and socioeconomic outcomes in younger as compared with older individuals, according to Dr. Twig and coauthors.
Younger individuals with stroke have a higher risk of recurrent stroke, heart attack, long-term care, or death, they said. Moreover, about half of young-adult stroke survivors have poor functional outcomes, and their risk of unemployment and depression/anxiety is higher than in young individuals without stroke.
One limitation of the study is that follow-up BMI data were not available for all participants. As a result, the contribution of obesity to stroke risk over time could not be assessed, and the independent risk of BMI during adolescence could not be determined. In addition, the authors said the study underrepresents orthodox and ultraorthodox Jewish women, as they are not obligated to serve in the Israeli military.
The study authors had no disclosures related to the study, which was supported by a medical corps Israel Defense Forces research grant.
High and even high-normal body mass index (BMI) were linked to increased ischemic stroke risk, regardless of whether or not individuals had diabetes.
Overweight and obese adolescent groups in the study had a roughly two- to threefold increased risk of ischemic stroke, which was apparent even before age 30 years in the study that was based on records of Israeli adolescents evaluated prior to mandatory military service.
These findings highlight the importance of treating and preventing high BMI among adolescence, study coauthor Gilad Twig, MD, MPH, PhD, said in a press release.
“Adults who survive stroke earlier in life face poor functional outcomes, which can lead to unemployment, depression and anxiety,” said Dr. Twig, associate professor in the department of military medicine in The Hebrew University in Jerusalem.
The costs of stroke prevention and care, already high, are expected to become even higher as the adolescent obesity prevalence goes up, fueling further increases in stroke rate, Dr. Twig added.
This is believed to be the first study showing that stroke risk is associated with higher BMI values in both men and women, not just men, Dr. Twig and coauthors said in their article, published May 13, 2021 in the journal Stroke. Previous studies assessing the stroke-BMI relationship in adolescents were based on records of Swedish men evaluated during military conscription at age 18.
In the present study, Dr. Twig and coauthors assessed the linkage between adolescent BMI and first stroke event in 1.9 million male and female adolescents in Israel who were evaluated 1 year prior to mandatory military service, between the years of 1985 and 2013.
They cross-referenced that information with stroke events in a national registry to which all hospitals in Israel are required to report.
The adolescents were about 17 years of age on average at the time of evaluation, 58% were male, and 84% were born in Israel. The mean age at the beginning of follow-up for stroke was about 31 years.
Over the follow-up period, investigators identified 1,088 first stroke events, including 921 ischemic and 167 hemorrhagic strokes.
A gradual increase in stroke rate was seen across BMI categories for ischemic strokes, but not so much for hemorrhagic strokes, investigators found.
Hazard ratios for first ischemic stroke event were 1.4 (95% confidence interval, 1.2-1.6) for the high-normal BMI group, 2.0 (95% CI, 1.6-2.4) for the overweight group, and 3.5 (95% CI, 2.8-4.5) for the obese group after adjusting for age and sex at beginning of follow-up, investigators reported.
When the adjusted results were stratified by presence or absence of diabetes, estimates were similar to what was seen in the overall risk model, they added.
Among those young adults who developed ischemic stroke, 43% smoked, 29% had high blood pressure, 17% had diabetes, and 32% had abnormal lipids at the time of diagnosis, the reported data showed.
The clinical and public health implications of these findings could be substantial, since strokes are associated with worse medical and socioeconomic outcomes in younger as compared with older individuals, according to Dr. Twig and coauthors.
Younger individuals with stroke have a higher risk of recurrent stroke, heart attack, long-term care, or death, they said. Moreover, about half of young-adult stroke survivors have poor functional outcomes, and their risk of unemployment and depression/anxiety is higher than in young individuals without stroke.
One limitation of the study is that follow-up BMI data were not available for all participants. As a result, the contribution of obesity to stroke risk over time could not be assessed, and the independent risk of BMI during adolescence could not be determined. In addition, the authors said the study underrepresents orthodox and ultraorthodox Jewish women, as they are not obligated to serve in the Israeli military.
The study authors had no disclosures related to the study, which was supported by a medical corps Israel Defense Forces research grant.
High and even high-normal body mass index (BMI) were linked to increased ischemic stroke risk, regardless of whether or not individuals had diabetes.
Overweight and obese adolescent groups in the study had a roughly two- to threefold increased risk of ischemic stroke, which was apparent even before age 30 years in the study that was based on records of Israeli adolescents evaluated prior to mandatory military service.
These findings highlight the importance of treating and preventing high BMI among adolescence, study coauthor Gilad Twig, MD, MPH, PhD, said in a press release.
“Adults who survive stroke earlier in life face poor functional outcomes, which can lead to unemployment, depression and anxiety,” said Dr. Twig, associate professor in the department of military medicine in The Hebrew University in Jerusalem.
The costs of stroke prevention and care, already high, are expected to become even higher as the adolescent obesity prevalence goes up, fueling further increases in stroke rate, Dr. Twig added.
This is believed to be the first study showing that stroke risk is associated with higher BMI values in both men and women, not just men, Dr. Twig and coauthors said in their article, published May 13, 2021 in the journal Stroke. Previous studies assessing the stroke-BMI relationship in adolescents were based on records of Swedish men evaluated during military conscription at age 18.
In the present study, Dr. Twig and coauthors assessed the linkage between adolescent BMI and first stroke event in 1.9 million male and female adolescents in Israel who were evaluated 1 year prior to mandatory military service, between the years of 1985 and 2013.
They cross-referenced that information with stroke events in a national registry to which all hospitals in Israel are required to report.
The adolescents were about 17 years of age on average at the time of evaluation, 58% were male, and 84% were born in Israel. The mean age at the beginning of follow-up for stroke was about 31 years.
Over the follow-up period, investigators identified 1,088 first stroke events, including 921 ischemic and 167 hemorrhagic strokes.
A gradual increase in stroke rate was seen across BMI categories for ischemic strokes, but not so much for hemorrhagic strokes, investigators found.
Hazard ratios for first ischemic stroke event were 1.4 (95% confidence interval, 1.2-1.6) for the high-normal BMI group, 2.0 (95% CI, 1.6-2.4) for the overweight group, and 3.5 (95% CI, 2.8-4.5) for the obese group after adjusting for age and sex at beginning of follow-up, investigators reported.
When the adjusted results were stratified by presence or absence of diabetes, estimates were similar to what was seen in the overall risk model, they added.
Among those young adults who developed ischemic stroke, 43% smoked, 29% had high blood pressure, 17% had diabetes, and 32% had abnormal lipids at the time of diagnosis, the reported data showed.
The clinical and public health implications of these findings could be substantial, since strokes are associated with worse medical and socioeconomic outcomes in younger as compared with older individuals, according to Dr. Twig and coauthors.
Younger individuals with stroke have a higher risk of recurrent stroke, heart attack, long-term care, or death, they said. Moreover, about half of young-adult stroke survivors have poor functional outcomes, and their risk of unemployment and depression/anxiety is higher than in young individuals without stroke.
One limitation of the study is that follow-up BMI data were not available for all participants. As a result, the contribution of obesity to stroke risk over time could not be assessed, and the independent risk of BMI during adolescence could not be determined. In addition, the authors said the study underrepresents orthodox and ultraorthodox Jewish women, as they are not obligated to serve in the Israeli military.
The study authors had no disclosures related to the study, which was supported by a medical corps Israel Defense Forces research grant.
FROM STROKE
Late-breaking news on trajectory of ADHD remission headlines world conference
Most patients will not make a full recovery from attention-deficit/hyperactivity disorder in adulthood. This late-breaking finding headlined the World Congress on ADHD – Virtual Event. Held under the specter of SARS-CoV-2, the virtual program delved into the latest research on ADHD pathophysiology, imaging, genetics, and issues on medical and psychiatric comorbidities.
However, one of the conference’s highlights was a piece of unpublished work on remission patterns by Margaret Sibley, PhD, associate professor of psychiatry and behavioral sciences at the University of Washington, Seattle.
Anywhere from 65% to 67% of young adults have desistant ADHD – meaning that they no longer meet criteria. Only up to 23% experience full remission, said Dr. Sibley during a special late-breaking session. All research on remission and most on persistence consider just one endpoint – nothing is known about longitudinal fluctuations in remission status over time.
Her research sought to answer a key question: Do people fully recover from ADHD?
Using data from the Multimodal Treatment of Attention Deficit Hyperactivity Disorder (MTA) Study, Dr. Sibley prospectively followed over 550 children aged 7-9.9 years with DSM-IV combined-type ADHD over 14 years, until 16 years after baseline, using interviews, questionnaires, and rating scales to track symptoms, impairment, and treatment history.
The researchers also came up with a “winning” definition for full remission, which included three or fewer symptoms of inattention and hyperactive impulsivity from all available reporters, negligible ADHD-related impairment based on preestablished impairment rating thresholds, and discontinuation of medication and behavioral treatments for at least a month prior to assessment.
In the longitudinal results, Dr. Sibley and colleagues reported that the majority (63.8%) demonstrated fluctuations between full or partial remission and ADHD recurrence. Only 9.1% sustained full remission over the course of the study. From these findings, ADHD appears to be a fluctuating disorder. While it continues into adulthood for most people, there may also be periods of remission or “good functioning.”
Most desistance from ADHD represents partial, not full remission, said Dr. Sibley. The results also show that recovery by young adulthood is very rare – most patients with remitted ADHD have recurrences.
These are important findings, said Luis Augusto Rohde, MD, PhD, who co-organized the congress’ scientific program committee with Manfred Gerlach, PhD. It shows that a patient’s ADHD may sometimes be more definitive and at other times, no clear phenotype expression emerges.
COVID’s influence
COVID-19 greatly influenced this year’s program’s agenda, said Dr. Rohde. “There’s a lot of evidence that ADHD patients are at greater risk for COVID-19, which is not a surprise,” said Dr. Rohde, professor of child and adolescent psychiatry at the Federal University of Rio Grande do Sul’s department of psychiatry in Porto Alegre, Brazil.
ADHD is a combination of genetic liability and the demands of the environment. “In times like we are living in right now, if you have increasing demands and stress from the environment, you trigger symptoms in those even with lower genetic liability,” he said. ADHD’s pathophysiology involves attention and executive deficit disorder, which means these patients may not follow strategies to avoid infection.
This shows why COVID was so important to the discussion of program topics, he said.
Two experts addressed this subject head on in a point-counterpoint debate, “Residual effects of the 2019 pandemic will mirror the 1918 pandemic: Will we have lots of new ADHD cases?” James Swanson, PhD, professor of pediatrics at the University of California, Irvine, projected that biological coeffects of COVID-19 will lead to ADHD symptoms, generating potentially 5 million new ADHD cases.
David Coghill, MBChB, MD, a professor of child adolescent mental health at the University of Melbourne, countered that not enough data are available yet to back this hypothesis. “Researchers are asking this question, but clinically we don’t know enough.”
While the COVID virus might not directly lead to more cases of ADHD, this could potentially happen indirectly through environmental agents of the pandemic, offered Dr. Rohde. “We’ve clearly seen in our appointments with families and children that they can’t face the amount of schooling and working from home,” he said.
Novel treatments
The conference also addressed new treatments and nonpharmacologic interventions in the pipeline for ADHD. “We had a chance to discuss the possibilities about new medications that address the problems in the current market and to show the potential usefulness of nonpharma interventions such as neuromodulations in ADHD,” said Dr. Rohde. Speakers discussed strategies ranging from family-based mindfulness interventions to oligoantigenic diets in children with ADHD.
Other researchers are looking at novel digital tools to help patients manage and treat ADHD. Adherence is a major problem in chronic disorders like hypertension, diabetes, epilepsy, and ADHD, said Dr. Rohde. “Due to ADHD symptomatology including inattention, novelty-seeking, executive deficits, and difficulties in persistence, it is an even bigger problem in this disorder.”
Speakers at the “ADHD in the digital age – From pitfalls to challenges” session discussed video game strategies to reduce ADHD impairment, and a texting app to improve adherence. Dr. Rohde talked about the FOCUS app, which fosters collaboration between patients, families, and caregivers to efficiently track ADHD symptoms and help customize treatments.
Studies suggest these tools can significantly improve adherence. They’re also well accepted by patients, said Dr. Rohde. While the expectations are high, digital interventions are not a substitute for medication. “More data is needed to include them as part of the clinical interventions for ADHD.”
Dr. Sibley received book royalties from Guilford Press. Dr. Rohde has received grant or research support from, served as a consultant to, and served on the speakers’ bureau of Bial, Medice, Novartis/Sandoz, Pfizer, and Shire/Takeda in the last 3 years. The ADHD and Juvenile Bipolar Disorder Outpatient Programs chaired by Dr. Rohde have received unrestricted educational and research support from the following pharmaceutical companies in the last 3 years: Novartis/Sandoz and Shire/Takeda. Dr. Rohde has received authorship royalties from Oxford Press and ArtMed and travel grants from Shire to take part in the 2018 APA annual meeting. Dr. Swanson has two patents: (PIXA4), which uses a “time-of-flight” camera to measure growth of infants, and a provisional patent on the mechanism of tolerance to stimulant medication (PATSMTA). He has received travel support from Medice and has done legal review for NLS. Dr. Coghill worked for several pharmaceutical companies but had no disclosures relevant to the session debate on the pandemic.
Most patients will not make a full recovery from attention-deficit/hyperactivity disorder in adulthood. This late-breaking finding headlined the World Congress on ADHD – Virtual Event. Held under the specter of SARS-CoV-2, the virtual program delved into the latest research on ADHD pathophysiology, imaging, genetics, and issues on medical and psychiatric comorbidities.
However, one of the conference’s highlights was a piece of unpublished work on remission patterns by Margaret Sibley, PhD, associate professor of psychiatry and behavioral sciences at the University of Washington, Seattle.
Anywhere from 65% to 67% of young adults have desistant ADHD – meaning that they no longer meet criteria. Only up to 23% experience full remission, said Dr. Sibley during a special late-breaking session. All research on remission and most on persistence consider just one endpoint – nothing is known about longitudinal fluctuations in remission status over time.
Her research sought to answer a key question: Do people fully recover from ADHD?
Using data from the Multimodal Treatment of Attention Deficit Hyperactivity Disorder (MTA) Study, Dr. Sibley prospectively followed over 550 children aged 7-9.9 years with DSM-IV combined-type ADHD over 14 years, until 16 years after baseline, using interviews, questionnaires, and rating scales to track symptoms, impairment, and treatment history.
The researchers also came up with a “winning” definition for full remission, which included three or fewer symptoms of inattention and hyperactive impulsivity from all available reporters, negligible ADHD-related impairment based on preestablished impairment rating thresholds, and discontinuation of medication and behavioral treatments for at least a month prior to assessment.
In the longitudinal results, Dr. Sibley and colleagues reported that the majority (63.8%) demonstrated fluctuations between full or partial remission and ADHD recurrence. Only 9.1% sustained full remission over the course of the study. From these findings, ADHD appears to be a fluctuating disorder. While it continues into adulthood for most people, there may also be periods of remission or “good functioning.”
Most desistance from ADHD represents partial, not full remission, said Dr. Sibley. The results also show that recovery by young adulthood is very rare – most patients with remitted ADHD have recurrences.
These are important findings, said Luis Augusto Rohde, MD, PhD, who co-organized the congress’ scientific program committee with Manfred Gerlach, PhD. It shows that a patient’s ADHD may sometimes be more definitive and at other times, no clear phenotype expression emerges.
COVID’s influence
COVID-19 greatly influenced this year’s program’s agenda, said Dr. Rohde. “There’s a lot of evidence that ADHD patients are at greater risk for COVID-19, which is not a surprise,” said Dr. Rohde, professor of child and adolescent psychiatry at the Federal University of Rio Grande do Sul’s department of psychiatry in Porto Alegre, Brazil.
ADHD is a combination of genetic liability and the demands of the environment. “In times like we are living in right now, if you have increasing demands and stress from the environment, you trigger symptoms in those even with lower genetic liability,” he said. ADHD’s pathophysiology involves attention and executive deficit disorder, which means these patients may not follow strategies to avoid infection.
This shows why COVID was so important to the discussion of program topics, he said.
Two experts addressed this subject head on in a point-counterpoint debate, “Residual effects of the 2019 pandemic will mirror the 1918 pandemic: Will we have lots of new ADHD cases?” James Swanson, PhD, professor of pediatrics at the University of California, Irvine, projected that biological coeffects of COVID-19 will lead to ADHD symptoms, generating potentially 5 million new ADHD cases.
David Coghill, MBChB, MD, a professor of child adolescent mental health at the University of Melbourne, countered that not enough data are available yet to back this hypothesis. “Researchers are asking this question, but clinically we don’t know enough.”
While the COVID virus might not directly lead to more cases of ADHD, this could potentially happen indirectly through environmental agents of the pandemic, offered Dr. Rohde. “We’ve clearly seen in our appointments with families and children that they can’t face the amount of schooling and working from home,” he said.
Novel treatments
The conference also addressed new treatments and nonpharmacologic interventions in the pipeline for ADHD. “We had a chance to discuss the possibilities about new medications that address the problems in the current market and to show the potential usefulness of nonpharma interventions such as neuromodulations in ADHD,” said Dr. Rohde. Speakers discussed strategies ranging from family-based mindfulness interventions to oligoantigenic diets in children with ADHD.
Other researchers are looking at novel digital tools to help patients manage and treat ADHD. Adherence is a major problem in chronic disorders like hypertension, diabetes, epilepsy, and ADHD, said Dr. Rohde. “Due to ADHD symptomatology including inattention, novelty-seeking, executive deficits, and difficulties in persistence, it is an even bigger problem in this disorder.”
Speakers at the “ADHD in the digital age – From pitfalls to challenges” session discussed video game strategies to reduce ADHD impairment, and a texting app to improve adherence. Dr. Rohde talked about the FOCUS app, which fosters collaboration between patients, families, and caregivers to efficiently track ADHD symptoms and help customize treatments.
Studies suggest these tools can significantly improve adherence. They’re also well accepted by patients, said Dr. Rohde. While the expectations are high, digital interventions are not a substitute for medication. “More data is needed to include them as part of the clinical interventions for ADHD.”
Dr. Sibley received book royalties from Guilford Press. Dr. Rohde has received grant or research support from, served as a consultant to, and served on the speakers’ bureau of Bial, Medice, Novartis/Sandoz, Pfizer, and Shire/Takeda in the last 3 years. The ADHD and Juvenile Bipolar Disorder Outpatient Programs chaired by Dr. Rohde have received unrestricted educational and research support from the following pharmaceutical companies in the last 3 years: Novartis/Sandoz and Shire/Takeda. Dr. Rohde has received authorship royalties from Oxford Press and ArtMed and travel grants from Shire to take part in the 2018 APA annual meeting. Dr. Swanson has two patents: (PIXA4), which uses a “time-of-flight” camera to measure growth of infants, and a provisional patent on the mechanism of tolerance to stimulant medication (PATSMTA). He has received travel support from Medice and has done legal review for NLS. Dr. Coghill worked for several pharmaceutical companies but had no disclosures relevant to the session debate on the pandemic.
Most patients will not make a full recovery from attention-deficit/hyperactivity disorder in adulthood. This late-breaking finding headlined the World Congress on ADHD – Virtual Event. Held under the specter of SARS-CoV-2, the virtual program delved into the latest research on ADHD pathophysiology, imaging, genetics, and issues on medical and psychiatric comorbidities.
However, one of the conference’s highlights was a piece of unpublished work on remission patterns by Margaret Sibley, PhD, associate professor of psychiatry and behavioral sciences at the University of Washington, Seattle.
Anywhere from 65% to 67% of young adults have desistant ADHD – meaning that they no longer meet criteria. Only up to 23% experience full remission, said Dr. Sibley during a special late-breaking session. All research on remission and most on persistence consider just one endpoint – nothing is known about longitudinal fluctuations in remission status over time.
Her research sought to answer a key question: Do people fully recover from ADHD?
Using data from the Multimodal Treatment of Attention Deficit Hyperactivity Disorder (MTA) Study, Dr. Sibley prospectively followed over 550 children aged 7-9.9 years with DSM-IV combined-type ADHD over 14 years, until 16 years after baseline, using interviews, questionnaires, and rating scales to track symptoms, impairment, and treatment history.
The researchers also came up with a “winning” definition for full remission, which included three or fewer symptoms of inattention and hyperactive impulsivity from all available reporters, negligible ADHD-related impairment based on preestablished impairment rating thresholds, and discontinuation of medication and behavioral treatments for at least a month prior to assessment.
In the longitudinal results, Dr. Sibley and colleagues reported that the majority (63.8%) demonstrated fluctuations between full or partial remission and ADHD recurrence. Only 9.1% sustained full remission over the course of the study. From these findings, ADHD appears to be a fluctuating disorder. While it continues into adulthood for most people, there may also be periods of remission or “good functioning.”
Most desistance from ADHD represents partial, not full remission, said Dr. Sibley. The results also show that recovery by young adulthood is very rare – most patients with remitted ADHD have recurrences.
These are important findings, said Luis Augusto Rohde, MD, PhD, who co-organized the congress’ scientific program committee with Manfred Gerlach, PhD. It shows that a patient’s ADHD may sometimes be more definitive and at other times, no clear phenotype expression emerges.
COVID’s influence
COVID-19 greatly influenced this year’s program’s agenda, said Dr. Rohde. “There’s a lot of evidence that ADHD patients are at greater risk for COVID-19, which is not a surprise,” said Dr. Rohde, professor of child and adolescent psychiatry at the Federal University of Rio Grande do Sul’s department of psychiatry in Porto Alegre, Brazil.
ADHD is a combination of genetic liability and the demands of the environment. “In times like we are living in right now, if you have increasing demands and stress from the environment, you trigger symptoms in those even with lower genetic liability,” he said. ADHD’s pathophysiology involves attention and executive deficit disorder, which means these patients may not follow strategies to avoid infection.
This shows why COVID was so important to the discussion of program topics, he said.
Two experts addressed this subject head on in a point-counterpoint debate, “Residual effects of the 2019 pandemic will mirror the 1918 pandemic: Will we have lots of new ADHD cases?” James Swanson, PhD, professor of pediatrics at the University of California, Irvine, projected that biological coeffects of COVID-19 will lead to ADHD symptoms, generating potentially 5 million new ADHD cases.
David Coghill, MBChB, MD, a professor of child adolescent mental health at the University of Melbourne, countered that not enough data are available yet to back this hypothesis. “Researchers are asking this question, but clinically we don’t know enough.”
While the COVID virus might not directly lead to more cases of ADHD, this could potentially happen indirectly through environmental agents of the pandemic, offered Dr. Rohde. “We’ve clearly seen in our appointments with families and children that they can’t face the amount of schooling and working from home,” he said.
Novel treatments
The conference also addressed new treatments and nonpharmacologic interventions in the pipeline for ADHD. “We had a chance to discuss the possibilities about new medications that address the problems in the current market and to show the potential usefulness of nonpharma interventions such as neuromodulations in ADHD,” said Dr. Rohde. Speakers discussed strategies ranging from family-based mindfulness interventions to oligoantigenic diets in children with ADHD.
Other researchers are looking at novel digital tools to help patients manage and treat ADHD. Adherence is a major problem in chronic disorders like hypertension, diabetes, epilepsy, and ADHD, said Dr. Rohde. “Due to ADHD symptomatology including inattention, novelty-seeking, executive deficits, and difficulties in persistence, it is an even bigger problem in this disorder.”
Speakers at the “ADHD in the digital age – From pitfalls to challenges” session discussed video game strategies to reduce ADHD impairment, and a texting app to improve adherence. Dr. Rohde talked about the FOCUS app, which fosters collaboration between patients, families, and caregivers to efficiently track ADHD symptoms and help customize treatments.
Studies suggest these tools can significantly improve adherence. They’re also well accepted by patients, said Dr. Rohde. While the expectations are high, digital interventions are not a substitute for medication. “More data is needed to include them as part of the clinical interventions for ADHD.”
Dr. Sibley received book royalties from Guilford Press. Dr. Rohde has received grant or research support from, served as a consultant to, and served on the speakers’ bureau of Bial, Medice, Novartis/Sandoz, Pfizer, and Shire/Takeda in the last 3 years. The ADHD and Juvenile Bipolar Disorder Outpatient Programs chaired by Dr. Rohde have received unrestricted educational and research support from the following pharmaceutical companies in the last 3 years: Novartis/Sandoz and Shire/Takeda. Dr. Rohde has received authorship royalties from Oxford Press and ArtMed and travel grants from Shire to take part in the 2018 APA annual meeting. Dr. Swanson has two patents: (PIXA4), which uses a “time-of-flight” camera to measure growth of infants, and a provisional patent on the mechanism of tolerance to stimulant medication (PATSMTA). He has received travel support from Medice and has done legal review for NLS. Dr. Coghill worked for several pharmaceutical companies but had no disclosures relevant to the session debate on the pandemic.
FROM ADHD 2021
Assessing the cognitive nuances between ADHD and autism
Attention-deficit/hyperactivity disorder and autism spectrum disorder (ASD) often coexist in children and adults, but the range of cognitive abilities can vary widely in these patients. Researchers from around the world are leveraging symptom, cognitive assessment, and neurobiological measures to gain insights on how individuals with ADHD/ASD approach and solve problems.
Several experts discussed the progress of their research during the session, “Overlap and differences of ADHD and autism – new findings of functional imaging and cognition studies” at the World Congress on ADHD – Virtual Event.
“The overlap of these two disorders is a critical issue for our field,” said Sarah Karalunas, PhD, assistant professor of clinical psychology at Purdue University, West Lafayette, Ind., who moderated the session. Clinicians are often asked to make differential diagnoses between these two disorders. Only recently has the DSM-5 allowed their codiagnosis. “There’s increasing recognition that there may be shared cognitive and physiological features that reflect their shared risk and account for the high levels of symptom overlap,” said Dr. Karalunas.
Shared cognitive markers
Under the DSM’s change, “it’s now recognized that an estimated 20%-60% of children with ASD have comorbidities with ADHD, and around 20%-40% of children with ADHD have ASD symptoms,” said Beth Johnson, PhD, a research fellow with the Turner Institute for Brain and Mental Health at Monash University, Melbourne.
The shared overlap on genetic traits and comorbidities such as intellectual disability, anxiety, depression, and oppositional defiant disorder, make it difficult for clinicians to predict clinical outcomes, noted Dr. Johnson.
“We’re now understanding that they’re likely to be multiple autisms and ADHDs, that these symptoms exist on a spectrum of severity or ability,” she said. Dr. Johnson discussed a data-driven subtyping approach based on neurocognitive and symptom profiles in children with ADHD. The aim was to better understand how symptoms are managed across ADHD, ASD and comorbid ASD-ADHD.
As part of this research, her team recruited 295 controls and 117 children with ADHD who underwent clinical phenotyping and also completed working memory tasks, stop signal, and sustained attention tasks.
The researchers divided the children into four stable clusters based on the ADHD rating scale and autism questionnaire data: high ASD/ADHD traits, high ADHD/low ASD, low ADHD/moderate ASD, and low ADHD/ASD. Approximately half of the children with ADHD showed moderate to high ASD symptoms. Looking at neurocognition across the tasks, unsurprisingly, performance was lowest among the high-ASD/ADHD children, with performance on the stop signal being the most pronounced. “Notably, performance on the working memory task worsened with increasing ADHD symptoms,” she reported.
Drift model identifies information processing
Dr. Karalunas has also compared subgroups of ADHD and ASD children. “Our analysis examined whether cognitive impairments in ASD reflect a shared risk mechanism or co-occurring ADHD symptoms and why we see an overlap in these types of impairments,” she said.
Her study included 509 children with ADHD, 97 with ASD, and 301 controls (typical development). All three groups underwent a full cognitive assessment battery that measured attention arousal, basic processing speed, and working memory. Those tasks were collapsed into a series of variables as well as a set of tasks measuring response inhibition, switching, interference control, reward discounting, and measure of reaction time variability.
Four cognitive profiles emerged: a typically developing group, an ADHD group, an ASD group with low levels of ADHD symptoms and an ASD group with high levels of ADHD symptoms.
The ADHD group did worse on many of the tasks than the control group, and the ASD group with low ADHD levels also did poorly relative to the typically developing sample. This shows that autism – even in absence of co-occurring ADHD – demonstrates more cognitive impairment than typically developing kids. The ADHD group with high levels of autism did the most poorly across all of the tasks.
The findings also revealed a symptom severity pattern: the group with fewer symptoms did the best and the group with the most symptoms did the worst. “Overall, this reflects severity of impairment,” said Dr. Karalunas.
To identify measures more specific to either ADHD or autism, Dr. Karalunas and colleagues did a follow-up analysis to characterize cognitive performance. To accomplish this, they applied a drift-diffusion model to the same four cognitive profiles. The model assessed three parameters: drift rate, which relates to the speed or efficiency of information processing, boundary separation or speed accuracy trade-offs (impulsivity), and nondecision time such as motor preparation.
Using the same four cognitive profiles, they found that the ADHD group had slower drift rate relative to the control, although the two groups did not differ on boundary separation, which meant there were no differences on waiting to need to respond. The ADHD group had faster nondecision times. “This is a classic pattern, shown in the literature,” said Dr. Karalunas.
In other results, an interesting pattern began to evolve
Both ASD groups, for example, had much wider boundary separations, which meant they were waiting to be sure before they responded than the ADHD or typically developing groups. In contrast, the two ADHD groups had much faster non-decision times, whereas the two non-ADHD groups had similar nondecisions times.
Unlike the previous analysis, which saw a symptom severity pattern develop, “we’re getting two parameters that seem to track much more specifically to specific symptom domains,” observed Dr. Karalunas.
The results suggest there’s a substantial overlap in cognitive impairments in ADHD/ASD. “But we have pretty strong evidence at this point that these similarities are not accounted for by symptom overlap, especially for things like response and inhibition, working memory and processing speed. These seem to be independently related to ADHD and autism, regardless of the level of comorbid ADHD symptoms in the autism group,” said Dr. Karalunas.
The hope is to expand on these types of analyses to address the interaction of cognition-emotion and social cognition, and empirically define groups based on cognitive performance, she said.
Neurocognitive studies
Researchers have also been studying neural networks to assess ASD and ADHD. Roselyne Chauvin, PhD, a postdoctoral associate at Washington University, St. Louis, discussed the concept of “a task generic connectome,” in which researchers look for a common network between targeted task paradigms to get closer to a common alteration across impairments.
In her research, Dr. Chauvin and colleagues looked at connectivity modulations across three tasks: working memory, reward processing tasks, and stop signal tasks, comparing ADHD patients to siblings and controls. The ADHD group showed reduced sensitivity or a smaller number of connections modulated in the tasks compared with the other groups. Researchers wondered where those missed connections were located.
Dividing the cohorts into task generic and task specific groups, Dr. Chauvin and colleagues found that the ADHD group lacked common processing skills. They were also able to identify reproducible missing circuits in the ADHD participants. Among the cohorts, there was a higher modulation of task-specific edges in the ADHD group.
The ADHD patients seemed to be using more task-tailored alternative strategies that were more challenging and suboptimal.
She also previewed her ongoing work with the EU-AIMS Longitudinal European Autism Project (LEAP) database to study ASD-ADHD comorbidity. In this project, she and her colleagues looked at several tasks: probing emotion processing, inhibitory control, theory of mind, and reward anticipation. Comparing ASD groups with or without ADHD comorbidity or a shared connection, she and her team were able to devise a functional profile predictive of ADHD severity. As an example, “for the connection only used by the ASD with ADHD comorbidity, the more they were using those connections of higher amplitude in the modulation, inside this subset of connection, the higher they would have ADHD severity,” said Dr. Chauvin.
Neural correlates of different behavioral and cognitive profiles haven’t been widely studied, according to Charlotte Tye, PhD, who’s based at the Institute of Psychiatry, Psychology & Neuroscience, King’s College, London. Electroencephalography is a useful technique for understanding the neural correlates of cognitive impairments and teasing apart different models of co-occurrence in ASD and ADHD.
Dr. Tye and colleagues tested this approach in a cohort of boys aged 8-13 years diagnosed with ASD and/or ADHD, measuring EEG while the children did various continuous performance tasks to assess changes in brain activity. Examining P3 amplitude (event-related potential components) they found that children with ADHD or ADHD+ASD showed an attenuated amplitude of the P3, compared with typically developing children and those with ASD.
“This suggests children with an ADHD diagnosis exhibited reduced inhibitory control,” said Dr. Tye. In contrast, children with ASD showed reduced conflict monitoring as indexed by altered N2 amplitude across task conditions.
These, and other studies conducted by Dr. Tye and colleagues indicate that children with ADHD show reduced neural responses during attentional processing, whereas autistic children show typical neural responses, supporting specific profiles.
“Autistic children with a diagnosis of ADHD appear to show the unique patterns of neural responses of autism and ADHD, supporting an additive co-occurrence rather than a distinct condition. This contributes to identification of transdiagnostic subgroups within neurodevelopmental conditions for targeting of personalized intervention, and suggests that children with co-occurring autism and ADHD require support for both conditions,” said Dr. Tye.
An important takeaway from all of these findings is “we can’t look just at how someone does overall on a single test,” said Dr. Karalunas in an interview. “There is a tremendous amount of variability between people who have the same diagnosis, and our research really needs to account for this.”
Attention-deficit/hyperactivity disorder and autism spectrum disorder (ASD) often coexist in children and adults, but the range of cognitive abilities can vary widely in these patients. Researchers from around the world are leveraging symptom, cognitive assessment, and neurobiological measures to gain insights on how individuals with ADHD/ASD approach and solve problems.
Several experts discussed the progress of their research during the session, “Overlap and differences of ADHD and autism – new findings of functional imaging and cognition studies” at the World Congress on ADHD – Virtual Event.
“The overlap of these two disorders is a critical issue for our field,” said Sarah Karalunas, PhD, assistant professor of clinical psychology at Purdue University, West Lafayette, Ind., who moderated the session. Clinicians are often asked to make differential diagnoses between these two disorders. Only recently has the DSM-5 allowed their codiagnosis. “There’s increasing recognition that there may be shared cognitive and physiological features that reflect their shared risk and account for the high levels of symptom overlap,” said Dr. Karalunas.
Shared cognitive markers
Under the DSM’s change, “it’s now recognized that an estimated 20%-60% of children with ASD have comorbidities with ADHD, and around 20%-40% of children with ADHD have ASD symptoms,” said Beth Johnson, PhD, a research fellow with the Turner Institute for Brain and Mental Health at Monash University, Melbourne.
The shared overlap on genetic traits and comorbidities such as intellectual disability, anxiety, depression, and oppositional defiant disorder, make it difficult for clinicians to predict clinical outcomes, noted Dr. Johnson.
“We’re now understanding that they’re likely to be multiple autisms and ADHDs, that these symptoms exist on a spectrum of severity or ability,” she said. Dr. Johnson discussed a data-driven subtyping approach based on neurocognitive and symptom profiles in children with ADHD. The aim was to better understand how symptoms are managed across ADHD, ASD and comorbid ASD-ADHD.
As part of this research, her team recruited 295 controls and 117 children with ADHD who underwent clinical phenotyping and also completed working memory tasks, stop signal, and sustained attention tasks.
The researchers divided the children into four stable clusters based on the ADHD rating scale and autism questionnaire data: high ASD/ADHD traits, high ADHD/low ASD, low ADHD/moderate ASD, and low ADHD/ASD. Approximately half of the children with ADHD showed moderate to high ASD symptoms. Looking at neurocognition across the tasks, unsurprisingly, performance was lowest among the high-ASD/ADHD children, with performance on the stop signal being the most pronounced. “Notably, performance on the working memory task worsened with increasing ADHD symptoms,” she reported.
Drift model identifies information processing
Dr. Karalunas has also compared subgroups of ADHD and ASD children. “Our analysis examined whether cognitive impairments in ASD reflect a shared risk mechanism or co-occurring ADHD symptoms and why we see an overlap in these types of impairments,” she said.
Her study included 509 children with ADHD, 97 with ASD, and 301 controls (typical development). All three groups underwent a full cognitive assessment battery that measured attention arousal, basic processing speed, and working memory. Those tasks were collapsed into a series of variables as well as a set of tasks measuring response inhibition, switching, interference control, reward discounting, and measure of reaction time variability.
Four cognitive profiles emerged: a typically developing group, an ADHD group, an ASD group with low levels of ADHD symptoms and an ASD group with high levels of ADHD symptoms.
The ADHD group did worse on many of the tasks than the control group, and the ASD group with low ADHD levels also did poorly relative to the typically developing sample. This shows that autism – even in absence of co-occurring ADHD – demonstrates more cognitive impairment than typically developing kids. The ADHD group with high levels of autism did the most poorly across all of the tasks.
The findings also revealed a symptom severity pattern: the group with fewer symptoms did the best and the group with the most symptoms did the worst. “Overall, this reflects severity of impairment,” said Dr. Karalunas.
To identify measures more specific to either ADHD or autism, Dr. Karalunas and colleagues did a follow-up analysis to characterize cognitive performance. To accomplish this, they applied a drift-diffusion model to the same four cognitive profiles. The model assessed three parameters: drift rate, which relates to the speed or efficiency of information processing, boundary separation or speed accuracy trade-offs (impulsivity), and nondecision time such as motor preparation.
Using the same four cognitive profiles, they found that the ADHD group had slower drift rate relative to the control, although the two groups did not differ on boundary separation, which meant there were no differences on waiting to need to respond. The ADHD group had faster nondecision times. “This is a classic pattern, shown in the literature,” said Dr. Karalunas.
In other results, an interesting pattern began to evolve
Both ASD groups, for example, had much wider boundary separations, which meant they were waiting to be sure before they responded than the ADHD or typically developing groups. In contrast, the two ADHD groups had much faster non-decision times, whereas the two non-ADHD groups had similar nondecisions times.
Unlike the previous analysis, which saw a symptom severity pattern develop, “we’re getting two parameters that seem to track much more specifically to specific symptom domains,” observed Dr. Karalunas.
The results suggest there’s a substantial overlap in cognitive impairments in ADHD/ASD. “But we have pretty strong evidence at this point that these similarities are not accounted for by symptom overlap, especially for things like response and inhibition, working memory and processing speed. These seem to be independently related to ADHD and autism, regardless of the level of comorbid ADHD symptoms in the autism group,” said Dr. Karalunas.
The hope is to expand on these types of analyses to address the interaction of cognition-emotion and social cognition, and empirically define groups based on cognitive performance, she said.
Neurocognitive studies
Researchers have also been studying neural networks to assess ASD and ADHD. Roselyne Chauvin, PhD, a postdoctoral associate at Washington University, St. Louis, discussed the concept of “a task generic connectome,” in which researchers look for a common network between targeted task paradigms to get closer to a common alteration across impairments.
In her research, Dr. Chauvin and colleagues looked at connectivity modulations across three tasks: working memory, reward processing tasks, and stop signal tasks, comparing ADHD patients to siblings and controls. The ADHD group showed reduced sensitivity or a smaller number of connections modulated in the tasks compared with the other groups. Researchers wondered where those missed connections were located.
Dividing the cohorts into task generic and task specific groups, Dr. Chauvin and colleagues found that the ADHD group lacked common processing skills. They were also able to identify reproducible missing circuits in the ADHD participants. Among the cohorts, there was a higher modulation of task-specific edges in the ADHD group.
The ADHD patients seemed to be using more task-tailored alternative strategies that were more challenging and suboptimal.
She also previewed her ongoing work with the EU-AIMS Longitudinal European Autism Project (LEAP) database to study ASD-ADHD comorbidity. In this project, she and her colleagues looked at several tasks: probing emotion processing, inhibitory control, theory of mind, and reward anticipation. Comparing ASD groups with or without ADHD comorbidity or a shared connection, she and her team were able to devise a functional profile predictive of ADHD severity. As an example, “for the connection only used by the ASD with ADHD comorbidity, the more they were using those connections of higher amplitude in the modulation, inside this subset of connection, the higher they would have ADHD severity,” said Dr. Chauvin.
Neural correlates of different behavioral and cognitive profiles haven’t been widely studied, according to Charlotte Tye, PhD, who’s based at the Institute of Psychiatry, Psychology & Neuroscience, King’s College, London. Electroencephalography is a useful technique for understanding the neural correlates of cognitive impairments and teasing apart different models of co-occurrence in ASD and ADHD.
Dr. Tye and colleagues tested this approach in a cohort of boys aged 8-13 years diagnosed with ASD and/or ADHD, measuring EEG while the children did various continuous performance tasks to assess changes in brain activity. Examining P3 amplitude (event-related potential components) they found that children with ADHD or ADHD+ASD showed an attenuated amplitude of the P3, compared with typically developing children and those with ASD.
“This suggests children with an ADHD diagnosis exhibited reduced inhibitory control,” said Dr. Tye. In contrast, children with ASD showed reduced conflict monitoring as indexed by altered N2 amplitude across task conditions.
These, and other studies conducted by Dr. Tye and colleagues indicate that children with ADHD show reduced neural responses during attentional processing, whereas autistic children show typical neural responses, supporting specific profiles.
“Autistic children with a diagnosis of ADHD appear to show the unique patterns of neural responses of autism and ADHD, supporting an additive co-occurrence rather than a distinct condition. This contributes to identification of transdiagnostic subgroups within neurodevelopmental conditions for targeting of personalized intervention, and suggests that children with co-occurring autism and ADHD require support for both conditions,” said Dr. Tye.
An important takeaway from all of these findings is “we can’t look just at how someone does overall on a single test,” said Dr. Karalunas in an interview. “There is a tremendous amount of variability between people who have the same diagnosis, and our research really needs to account for this.”
Attention-deficit/hyperactivity disorder and autism spectrum disorder (ASD) often coexist in children and adults, but the range of cognitive abilities can vary widely in these patients. Researchers from around the world are leveraging symptom, cognitive assessment, and neurobiological measures to gain insights on how individuals with ADHD/ASD approach and solve problems.
Several experts discussed the progress of their research during the session, “Overlap and differences of ADHD and autism – new findings of functional imaging and cognition studies” at the World Congress on ADHD – Virtual Event.
“The overlap of these two disorders is a critical issue for our field,” said Sarah Karalunas, PhD, assistant professor of clinical psychology at Purdue University, West Lafayette, Ind., who moderated the session. Clinicians are often asked to make differential diagnoses between these two disorders. Only recently has the DSM-5 allowed their codiagnosis. “There’s increasing recognition that there may be shared cognitive and physiological features that reflect their shared risk and account for the high levels of symptom overlap,” said Dr. Karalunas.
Shared cognitive markers
Under the DSM’s change, “it’s now recognized that an estimated 20%-60% of children with ASD have comorbidities with ADHD, and around 20%-40% of children with ADHD have ASD symptoms,” said Beth Johnson, PhD, a research fellow with the Turner Institute for Brain and Mental Health at Monash University, Melbourne.
The shared overlap on genetic traits and comorbidities such as intellectual disability, anxiety, depression, and oppositional defiant disorder, make it difficult for clinicians to predict clinical outcomes, noted Dr. Johnson.
“We’re now understanding that they’re likely to be multiple autisms and ADHDs, that these symptoms exist on a spectrum of severity or ability,” she said. Dr. Johnson discussed a data-driven subtyping approach based on neurocognitive and symptom profiles in children with ADHD. The aim was to better understand how symptoms are managed across ADHD, ASD and comorbid ASD-ADHD.
As part of this research, her team recruited 295 controls and 117 children with ADHD who underwent clinical phenotyping and also completed working memory tasks, stop signal, and sustained attention tasks.
The researchers divided the children into four stable clusters based on the ADHD rating scale and autism questionnaire data: high ASD/ADHD traits, high ADHD/low ASD, low ADHD/moderate ASD, and low ADHD/ASD. Approximately half of the children with ADHD showed moderate to high ASD symptoms. Looking at neurocognition across the tasks, unsurprisingly, performance was lowest among the high-ASD/ADHD children, with performance on the stop signal being the most pronounced. “Notably, performance on the working memory task worsened with increasing ADHD symptoms,” she reported.
Drift model identifies information processing
Dr. Karalunas has also compared subgroups of ADHD and ASD children. “Our analysis examined whether cognitive impairments in ASD reflect a shared risk mechanism or co-occurring ADHD symptoms and why we see an overlap in these types of impairments,” she said.
Her study included 509 children with ADHD, 97 with ASD, and 301 controls (typical development). All three groups underwent a full cognitive assessment battery that measured attention arousal, basic processing speed, and working memory. Those tasks were collapsed into a series of variables as well as a set of tasks measuring response inhibition, switching, interference control, reward discounting, and measure of reaction time variability.
Four cognitive profiles emerged: a typically developing group, an ADHD group, an ASD group with low levels of ADHD symptoms and an ASD group with high levels of ADHD symptoms.
The ADHD group did worse on many of the tasks than the control group, and the ASD group with low ADHD levels also did poorly relative to the typically developing sample. This shows that autism – even in absence of co-occurring ADHD – demonstrates more cognitive impairment than typically developing kids. The ADHD group with high levels of autism did the most poorly across all of the tasks.
The findings also revealed a symptom severity pattern: the group with fewer symptoms did the best and the group with the most symptoms did the worst. “Overall, this reflects severity of impairment,” said Dr. Karalunas.
To identify measures more specific to either ADHD or autism, Dr. Karalunas and colleagues did a follow-up analysis to characterize cognitive performance. To accomplish this, they applied a drift-diffusion model to the same four cognitive profiles. The model assessed three parameters: drift rate, which relates to the speed or efficiency of information processing, boundary separation or speed accuracy trade-offs (impulsivity), and nondecision time such as motor preparation.
Using the same four cognitive profiles, they found that the ADHD group had slower drift rate relative to the control, although the two groups did not differ on boundary separation, which meant there were no differences on waiting to need to respond. The ADHD group had faster nondecision times. “This is a classic pattern, shown in the literature,” said Dr. Karalunas.
In other results, an interesting pattern began to evolve
Both ASD groups, for example, had much wider boundary separations, which meant they were waiting to be sure before they responded than the ADHD or typically developing groups. In contrast, the two ADHD groups had much faster non-decision times, whereas the two non-ADHD groups had similar nondecisions times.
Unlike the previous analysis, which saw a symptom severity pattern develop, “we’re getting two parameters that seem to track much more specifically to specific symptom domains,” observed Dr. Karalunas.
The results suggest there’s a substantial overlap in cognitive impairments in ADHD/ASD. “But we have pretty strong evidence at this point that these similarities are not accounted for by symptom overlap, especially for things like response and inhibition, working memory and processing speed. These seem to be independently related to ADHD and autism, regardless of the level of comorbid ADHD symptoms in the autism group,” said Dr. Karalunas.
The hope is to expand on these types of analyses to address the interaction of cognition-emotion and social cognition, and empirically define groups based on cognitive performance, she said.
Neurocognitive studies
Researchers have also been studying neural networks to assess ASD and ADHD. Roselyne Chauvin, PhD, a postdoctoral associate at Washington University, St. Louis, discussed the concept of “a task generic connectome,” in which researchers look for a common network between targeted task paradigms to get closer to a common alteration across impairments.
In her research, Dr. Chauvin and colleagues looked at connectivity modulations across three tasks: working memory, reward processing tasks, and stop signal tasks, comparing ADHD patients to siblings and controls. The ADHD group showed reduced sensitivity or a smaller number of connections modulated in the tasks compared with the other groups. Researchers wondered where those missed connections were located.
Dividing the cohorts into task generic and task specific groups, Dr. Chauvin and colleagues found that the ADHD group lacked common processing skills. They were also able to identify reproducible missing circuits in the ADHD participants. Among the cohorts, there was a higher modulation of task-specific edges in the ADHD group.
The ADHD patients seemed to be using more task-tailored alternative strategies that were more challenging and suboptimal.
She also previewed her ongoing work with the EU-AIMS Longitudinal European Autism Project (LEAP) database to study ASD-ADHD comorbidity. In this project, she and her colleagues looked at several tasks: probing emotion processing, inhibitory control, theory of mind, and reward anticipation. Comparing ASD groups with or without ADHD comorbidity or a shared connection, she and her team were able to devise a functional profile predictive of ADHD severity. As an example, “for the connection only used by the ASD with ADHD comorbidity, the more they were using those connections of higher amplitude in the modulation, inside this subset of connection, the higher they would have ADHD severity,” said Dr. Chauvin.
Neural correlates of different behavioral and cognitive profiles haven’t been widely studied, according to Charlotte Tye, PhD, who’s based at the Institute of Psychiatry, Psychology & Neuroscience, King’s College, London. Electroencephalography is a useful technique for understanding the neural correlates of cognitive impairments and teasing apart different models of co-occurrence in ASD and ADHD.
Dr. Tye and colleagues tested this approach in a cohort of boys aged 8-13 years diagnosed with ASD and/or ADHD, measuring EEG while the children did various continuous performance tasks to assess changes in brain activity. Examining P3 amplitude (event-related potential components) they found that children with ADHD or ADHD+ASD showed an attenuated amplitude of the P3, compared with typically developing children and those with ASD.
“This suggests children with an ADHD diagnosis exhibited reduced inhibitory control,” said Dr. Tye. In contrast, children with ASD showed reduced conflict monitoring as indexed by altered N2 amplitude across task conditions.
These, and other studies conducted by Dr. Tye and colleagues indicate that children with ADHD show reduced neural responses during attentional processing, whereas autistic children show typical neural responses, supporting specific profiles.
“Autistic children with a diagnosis of ADHD appear to show the unique patterns of neural responses of autism and ADHD, supporting an additive co-occurrence rather than a distinct condition. This contributes to identification of transdiagnostic subgroups within neurodevelopmental conditions for targeting of personalized intervention, and suggests that children with co-occurring autism and ADHD require support for both conditions,” said Dr. Tye.
An important takeaway from all of these findings is “we can’t look just at how someone does overall on a single test,” said Dr. Karalunas in an interview. “There is a tremendous amount of variability between people who have the same diagnosis, and our research really needs to account for this.”
FROM ADHD 2021
Will COVID-19 result in more ADHD cases? A debate
While it’s possible that residual effects of SARS-CoV-2 could lead to an eruption of attention-deficit/hyperactivity disorder (ADHD) cases, a debate at the World Congress on ADHD – Virtual Event underscored the fact that this is still a hypothesis. The bottom line is there needs to be more data, said Luis Augusto Rohde, MD, PhD, cochair of the congress’ scientific program committee and moderator of the session, “Residual effects of the 2019 pandemic will mirror the 1918 pandemic: Will we have lots of new ADHD cases?”
Considering the current pattern of the pandemic, there is not enough evidence for this to be a concern, Dr. Rohde said in an interview.
James Swanson, PhD, professor of pediatrics at the University of California, Irvine, opined that biological co-effects of COVID-19 are likely to have selective effects in children that may produce symptoms representative of ADHD. Using the 1918 Spanish flu pandemic as a historical reference, he estimated that COVID-19 would produce 5 million individuals with new-onset symptoms related to ADHD. “If these cases meet DSM-5 or ICD-11 criteria, there will be lots of new ADHD cases,” he predicted.
David Coghill, MD, a professor of child adolescent mental health at the University of Melbourne, observed that the sums Dr. Swanson presented “are based on maxing out the potential rather than looking at the sums more realistically.”
Could the 1918 pandemic offer clues?
In a commentary, Dr. Swanson and Nora D. Volkow, MD, wrote about “lessons learned” from the 1918 pandemic, and how residual sequelae in that era led to a condition labeled hyperkinetic syndrome in children. “It may be worthwhile to consider the hypothesis that the COVID-19 pandemic may result in a novel etiologic subtype of ADHD that clinicians may recognize in patients in the future,” wrote the commentators.
In survivors of the 1918 pandemic, brain inflammation or encephalitis sometimes emerged as residual sequelae, said Dr. Swanson. In some adult cases, these symptoms were diagnosed as “encephalitis lethargica” (EL) and were associated with Parkinson’s disease. In 1930, based on patients evaluated after 1918, researchers Franz Kramer and Hans Pollnow at Charité Hospital in Berlin described the behavioral manifestation of EL in children as hyperkinetic syndrome, a condition that was characterized by symptoms similar to the properties of ADHD: lack of concentration, insufficient goal orientation, and increased distractibility. “They even reported on autopsy cases that described brain regions that we now know are associated with ADHD from decades of brain imaging studies,” said Dr. Swanson.
COVID-19 rarely results in severe respiratory problems in children but the absolute number requiring hospitalization has accumulated and is now relatively large, said Dr. Swanson. One study of 1,695 severe COVID-19 cases in children and adolescents used MRI and detected neural effects in specific brain regions such as basal ganglia and frontal lobes that previous research had associated with ADHD. Approximately 22% of these rare but severe cases had documented neurologic involvement, and studies of affected children with mild or none of the initial respiratory symptoms of COVID-19 also detected similar selective effects in these brain regions.
A recent survey of medical records of 80 million people that identified 240,000 COVID cases (mostly adults) revealed that a third had neurological and psychiatric sequelae. Dr. Swanson also mentioned an article he wrote more than a decade ago on environmental as well as genetic factors that resulted in etiologic subtypes of ADHD, which provided a model for the impact of COVID-19 on specific brain regions that are associated with ADHD.
So far, the COVID-19 pandemic has produced 150 million cases worldwide and there are about 100 million survivors, setting an estimate of a maximum number of cases with residual sequelae. “I think that severe COVID-19 will probably be related to severe residual sequelae, and that mild or asymptomatic COVID-19 may be associated with less severe residual sequelae, which may resemble ADHD” said Dr. Swanson. If one-third of the cases manifest in some neurologic or psychiatric systems, this means 27 million would have residual sequelae. If 20% have impaired concentration or brain fog, this could result in about 5 million ADHD cases, he said.
Estimates aren’t evidence
The Swanson/Volkow commentary contains a lot of references to “might, could, and may,” said Dr. Coghill. While it’s true that COVID-19 could produce a novel etiologic subtype of ADHD, “the point here is at the moment, all of this is based on hypotheses,” he said.
The Spanish flu did produce mental health consequences – survivors reported depression, sleep disturbances, mental distraction, dizziness, and difficulties coping at work. In the United States, flu death rates from 1918 to 1920 were directly attributed to suicide rates. Unfortunately, these impacts weren’t widely researched, said Dr. Coghill.
It also seems clear that the 1918 Spanish flu outbreak was associated with significant neurological consequences, said Dr. Coghill. By 1919 and 1920, physicians and researchers in the United Kingdom were reporting increases in a variety of symptoms among some patients recovering from flu, such as neuropathy, neurasthenia, meningitis, degenerative changes in nerve cells, and a decline in visual acuity.
The EL cases Dr. Swanson mentioned did coincide with and reach epidemic proportions alongside the Spanish flu. “But still, a causal relationship is far from proven,” said Dr. Coghill.
Sol Levy, MD, described a “disease of criminals” following the 1918 pandemic, in which patients exhibited a high degree of general hyperkinesis, a difficulty in maintaining quiet attitudes, abruptness and clumsiness, and “explosive motor release of all voluntarily inhibited activities.”
However, these impairments suggest a much broader presentation typically seen in ADHD, noted Dr. Coghill.
Neurological complications occur more commonly than initially thought in severe COVID-19, with estimates ranging from 36% to 84%. But in a systematic review of neuropsychiatric complications of severe coronavirus infection, researchers found few psychiatric sequelae of these infections. While they did mention impaired concentration and difficulties with emotional ability, it’s very important to remember that these conditions “are cardinal symptoms of a wide range of psychiatric disorders,” said Dr. Coghill.
Overall, more neurological and neuropsychiatric symptoms largely confine to those with severe COVID-19, meaning they’re much less likely to occur in children and young adults, he said.
If there are severe effects of COVID-19, Dr. Swanson countered that “they might have more ADHD than the complex residual effects [Dr. Coghill] described. I hope that he’s right, but I do think there will be biological co-effects of COVID-19 that will produce symptoms that are more ADHD than other neurological disorders.”
Epigenetic effects
Researchers are now seeing transgenerational and intergenerational effects of potential infection. “So I certainly back high-quality studies looking at the effects of maternal and paternal infection on offspring,” said Dr. Coghill. Establishing clinical cohort studies to follow up on this population would be essential in understanding the risks of SARS-CoV-2. “That might be one way we’ll see an increase in ADHD,” said Dr. Coghill.
The reality is COVID-19 hasn’t been around for that long, and current knowledge about it is limited, he said. Rapid publications, cross-sectional or retrospective data, and poor methodological quality and rigor make generalizability difficult. In addition, limited testing and detection probably underestimate prevalence of neurological and neuropsychiatric complications.
“If history teaches us anything, it is that we should always be measured in how we glean lessons from the past. So let’s not get ahead of ourselves,” he cautioned.
An informal, post-discussion survey of session participants revealed that a slight majority – 55%-60% – expected residual effects of COVID-19 to lead to more ADHD, compared to 40%-45% who didn’t think this would happen.
Dr. Swanson has two patents: (PIXA4), which uses a “time-of-flight” camera to measure growth on infants, and a provisional patent on the mechanism of tolerance to stimulant medication (PATSMTA). Dr. Coghill worked for several pharmaceutical companies but had no disclosures relevant to this debate.
While it’s possible that residual effects of SARS-CoV-2 could lead to an eruption of attention-deficit/hyperactivity disorder (ADHD) cases, a debate at the World Congress on ADHD – Virtual Event underscored the fact that this is still a hypothesis. The bottom line is there needs to be more data, said Luis Augusto Rohde, MD, PhD, cochair of the congress’ scientific program committee and moderator of the session, “Residual effects of the 2019 pandemic will mirror the 1918 pandemic: Will we have lots of new ADHD cases?”
Considering the current pattern of the pandemic, there is not enough evidence for this to be a concern, Dr. Rohde said in an interview.
James Swanson, PhD, professor of pediatrics at the University of California, Irvine, opined that biological co-effects of COVID-19 are likely to have selective effects in children that may produce symptoms representative of ADHD. Using the 1918 Spanish flu pandemic as a historical reference, he estimated that COVID-19 would produce 5 million individuals with new-onset symptoms related to ADHD. “If these cases meet DSM-5 or ICD-11 criteria, there will be lots of new ADHD cases,” he predicted.
David Coghill, MD, a professor of child adolescent mental health at the University of Melbourne, observed that the sums Dr. Swanson presented “are based on maxing out the potential rather than looking at the sums more realistically.”
Could the 1918 pandemic offer clues?
In a commentary, Dr. Swanson and Nora D. Volkow, MD, wrote about “lessons learned” from the 1918 pandemic, and how residual sequelae in that era led to a condition labeled hyperkinetic syndrome in children. “It may be worthwhile to consider the hypothesis that the COVID-19 pandemic may result in a novel etiologic subtype of ADHD that clinicians may recognize in patients in the future,” wrote the commentators.
In survivors of the 1918 pandemic, brain inflammation or encephalitis sometimes emerged as residual sequelae, said Dr. Swanson. In some adult cases, these symptoms were diagnosed as “encephalitis lethargica” (EL) and were associated with Parkinson’s disease. In 1930, based on patients evaluated after 1918, researchers Franz Kramer and Hans Pollnow at Charité Hospital in Berlin described the behavioral manifestation of EL in children as hyperkinetic syndrome, a condition that was characterized by symptoms similar to the properties of ADHD: lack of concentration, insufficient goal orientation, and increased distractibility. “They even reported on autopsy cases that described brain regions that we now know are associated with ADHD from decades of brain imaging studies,” said Dr. Swanson.
COVID-19 rarely results in severe respiratory problems in children but the absolute number requiring hospitalization has accumulated and is now relatively large, said Dr. Swanson. One study of 1,695 severe COVID-19 cases in children and adolescents used MRI and detected neural effects in specific brain regions such as basal ganglia and frontal lobes that previous research had associated with ADHD. Approximately 22% of these rare but severe cases had documented neurologic involvement, and studies of affected children with mild or none of the initial respiratory symptoms of COVID-19 also detected similar selective effects in these brain regions.
A recent survey of medical records of 80 million people that identified 240,000 COVID cases (mostly adults) revealed that a third had neurological and psychiatric sequelae. Dr. Swanson also mentioned an article he wrote more than a decade ago on environmental as well as genetic factors that resulted in etiologic subtypes of ADHD, which provided a model for the impact of COVID-19 on specific brain regions that are associated with ADHD.
So far, the COVID-19 pandemic has produced 150 million cases worldwide and there are about 100 million survivors, setting an estimate of a maximum number of cases with residual sequelae. “I think that severe COVID-19 will probably be related to severe residual sequelae, and that mild or asymptomatic COVID-19 may be associated with less severe residual sequelae, which may resemble ADHD” said Dr. Swanson. If one-third of the cases manifest in some neurologic or psychiatric systems, this means 27 million would have residual sequelae. If 20% have impaired concentration or brain fog, this could result in about 5 million ADHD cases, he said.
Estimates aren’t evidence
The Swanson/Volkow commentary contains a lot of references to “might, could, and may,” said Dr. Coghill. While it’s true that COVID-19 could produce a novel etiologic subtype of ADHD, “the point here is at the moment, all of this is based on hypotheses,” he said.
The Spanish flu did produce mental health consequences – survivors reported depression, sleep disturbances, mental distraction, dizziness, and difficulties coping at work. In the United States, flu death rates from 1918 to 1920 were directly attributed to suicide rates. Unfortunately, these impacts weren’t widely researched, said Dr. Coghill.
It also seems clear that the 1918 Spanish flu outbreak was associated with significant neurological consequences, said Dr. Coghill. By 1919 and 1920, physicians and researchers in the United Kingdom were reporting increases in a variety of symptoms among some patients recovering from flu, such as neuropathy, neurasthenia, meningitis, degenerative changes in nerve cells, and a decline in visual acuity.
The EL cases Dr. Swanson mentioned did coincide with and reach epidemic proportions alongside the Spanish flu. “But still, a causal relationship is far from proven,” said Dr. Coghill.
Sol Levy, MD, described a “disease of criminals” following the 1918 pandemic, in which patients exhibited a high degree of general hyperkinesis, a difficulty in maintaining quiet attitudes, abruptness and clumsiness, and “explosive motor release of all voluntarily inhibited activities.”
However, these impairments suggest a much broader presentation typically seen in ADHD, noted Dr. Coghill.
Neurological complications occur more commonly than initially thought in severe COVID-19, with estimates ranging from 36% to 84%. But in a systematic review of neuropsychiatric complications of severe coronavirus infection, researchers found few psychiatric sequelae of these infections. While they did mention impaired concentration and difficulties with emotional ability, it’s very important to remember that these conditions “are cardinal symptoms of a wide range of psychiatric disorders,” said Dr. Coghill.
Overall, more neurological and neuropsychiatric symptoms largely confine to those with severe COVID-19, meaning they’re much less likely to occur in children and young adults, he said.
If there are severe effects of COVID-19, Dr. Swanson countered that “they might have more ADHD than the complex residual effects [Dr. Coghill] described. I hope that he’s right, but I do think there will be biological co-effects of COVID-19 that will produce symptoms that are more ADHD than other neurological disorders.”
Epigenetic effects
Researchers are now seeing transgenerational and intergenerational effects of potential infection. “So I certainly back high-quality studies looking at the effects of maternal and paternal infection on offspring,” said Dr. Coghill. Establishing clinical cohort studies to follow up on this population would be essential in understanding the risks of SARS-CoV-2. “That might be one way we’ll see an increase in ADHD,” said Dr. Coghill.
The reality is COVID-19 hasn’t been around for that long, and current knowledge about it is limited, he said. Rapid publications, cross-sectional or retrospective data, and poor methodological quality and rigor make generalizability difficult. In addition, limited testing and detection probably underestimate prevalence of neurological and neuropsychiatric complications.
“If history teaches us anything, it is that we should always be measured in how we glean lessons from the past. So let’s not get ahead of ourselves,” he cautioned.
An informal, post-discussion survey of session participants revealed that a slight majority – 55%-60% – expected residual effects of COVID-19 to lead to more ADHD, compared to 40%-45% who didn’t think this would happen.
Dr. Swanson has two patents: (PIXA4), which uses a “time-of-flight” camera to measure growth on infants, and a provisional patent on the mechanism of tolerance to stimulant medication (PATSMTA). Dr. Coghill worked for several pharmaceutical companies but had no disclosures relevant to this debate.
While it’s possible that residual effects of SARS-CoV-2 could lead to an eruption of attention-deficit/hyperactivity disorder (ADHD) cases, a debate at the World Congress on ADHD – Virtual Event underscored the fact that this is still a hypothesis. The bottom line is there needs to be more data, said Luis Augusto Rohde, MD, PhD, cochair of the congress’ scientific program committee and moderator of the session, “Residual effects of the 2019 pandemic will mirror the 1918 pandemic: Will we have lots of new ADHD cases?”
Considering the current pattern of the pandemic, there is not enough evidence for this to be a concern, Dr. Rohde said in an interview.
James Swanson, PhD, professor of pediatrics at the University of California, Irvine, opined that biological co-effects of COVID-19 are likely to have selective effects in children that may produce symptoms representative of ADHD. Using the 1918 Spanish flu pandemic as a historical reference, he estimated that COVID-19 would produce 5 million individuals with new-onset symptoms related to ADHD. “If these cases meet DSM-5 or ICD-11 criteria, there will be lots of new ADHD cases,” he predicted.
David Coghill, MD, a professor of child adolescent mental health at the University of Melbourne, observed that the sums Dr. Swanson presented “are based on maxing out the potential rather than looking at the sums more realistically.”
Could the 1918 pandemic offer clues?
In a commentary, Dr. Swanson and Nora D. Volkow, MD, wrote about “lessons learned” from the 1918 pandemic, and how residual sequelae in that era led to a condition labeled hyperkinetic syndrome in children. “It may be worthwhile to consider the hypothesis that the COVID-19 pandemic may result in a novel etiologic subtype of ADHD that clinicians may recognize in patients in the future,” wrote the commentators.
In survivors of the 1918 pandemic, brain inflammation or encephalitis sometimes emerged as residual sequelae, said Dr. Swanson. In some adult cases, these symptoms were diagnosed as “encephalitis lethargica” (EL) and were associated with Parkinson’s disease. In 1930, based on patients evaluated after 1918, researchers Franz Kramer and Hans Pollnow at Charité Hospital in Berlin described the behavioral manifestation of EL in children as hyperkinetic syndrome, a condition that was characterized by symptoms similar to the properties of ADHD: lack of concentration, insufficient goal orientation, and increased distractibility. “They even reported on autopsy cases that described brain regions that we now know are associated with ADHD from decades of brain imaging studies,” said Dr. Swanson.
COVID-19 rarely results in severe respiratory problems in children but the absolute number requiring hospitalization has accumulated and is now relatively large, said Dr. Swanson. One study of 1,695 severe COVID-19 cases in children and adolescents used MRI and detected neural effects in specific brain regions such as basal ganglia and frontal lobes that previous research had associated with ADHD. Approximately 22% of these rare but severe cases had documented neurologic involvement, and studies of affected children with mild or none of the initial respiratory symptoms of COVID-19 also detected similar selective effects in these brain regions.
A recent survey of medical records of 80 million people that identified 240,000 COVID cases (mostly adults) revealed that a third had neurological and psychiatric sequelae. Dr. Swanson also mentioned an article he wrote more than a decade ago on environmental as well as genetic factors that resulted in etiologic subtypes of ADHD, which provided a model for the impact of COVID-19 on specific brain regions that are associated with ADHD.
So far, the COVID-19 pandemic has produced 150 million cases worldwide and there are about 100 million survivors, setting an estimate of a maximum number of cases with residual sequelae. “I think that severe COVID-19 will probably be related to severe residual sequelae, and that mild or asymptomatic COVID-19 may be associated with less severe residual sequelae, which may resemble ADHD” said Dr. Swanson. If one-third of the cases manifest in some neurologic or psychiatric systems, this means 27 million would have residual sequelae. If 20% have impaired concentration or brain fog, this could result in about 5 million ADHD cases, he said.
Estimates aren’t evidence
The Swanson/Volkow commentary contains a lot of references to “might, could, and may,” said Dr. Coghill. While it’s true that COVID-19 could produce a novel etiologic subtype of ADHD, “the point here is at the moment, all of this is based on hypotheses,” he said.
The Spanish flu did produce mental health consequences – survivors reported depression, sleep disturbances, mental distraction, dizziness, and difficulties coping at work. In the United States, flu death rates from 1918 to 1920 were directly attributed to suicide rates. Unfortunately, these impacts weren’t widely researched, said Dr. Coghill.
It also seems clear that the 1918 Spanish flu outbreak was associated with significant neurological consequences, said Dr. Coghill. By 1919 and 1920, physicians and researchers in the United Kingdom were reporting increases in a variety of symptoms among some patients recovering from flu, such as neuropathy, neurasthenia, meningitis, degenerative changes in nerve cells, and a decline in visual acuity.
The EL cases Dr. Swanson mentioned did coincide with and reach epidemic proportions alongside the Spanish flu. “But still, a causal relationship is far from proven,” said Dr. Coghill.
Sol Levy, MD, described a “disease of criminals” following the 1918 pandemic, in which patients exhibited a high degree of general hyperkinesis, a difficulty in maintaining quiet attitudes, abruptness and clumsiness, and “explosive motor release of all voluntarily inhibited activities.”
However, these impairments suggest a much broader presentation typically seen in ADHD, noted Dr. Coghill.
Neurological complications occur more commonly than initially thought in severe COVID-19, with estimates ranging from 36% to 84%. But in a systematic review of neuropsychiatric complications of severe coronavirus infection, researchers found few psychiatric sequelae of these infections. While they did mention impaired concentration and difficulties with emotional ability, it’s very important to remember that these conditions “are cardinal symptoms of a wide range of psychiatric disorders,” said Dr. Coghill.
Overall, more neurological and neuropsychiatric symptoms largely confine to those with severe COVID-19, meaning they’re much less likely to occur in children and young adults, he said.
If there are severe effects of COVID-19, Dr. Swanson countered that “they might have more ADHD than the complex residual effects [Dr. Coghill] described. I hope that he’s right, but I do think there will be biological co-effects of COVID-19 that will produce symptoms that are more ADHD than other neurological disorders.”
Epigenetic effects
Researchers are now seeing transgenerational and intergenerational effects of potential infection. “So I certainly back high-quality studies looking at the effects of maternal and paternal infection on offspring,” said Dr. Coghill. Establishing clinical cohort studies to follow up on this population would be essential in understanding the risks of SARS-CoV-2. “That might be one way we’ll see an increase in ADHD,” said Dr. Coghill.
The reality is COVID-19 hasn’t been around for that long, and current knowledge about it is limited, he said. Rapid publications, cross-sectional or retrospective data, and poor methodological quality and rigor make generalizability difficult. In addition, limited testing and detection probably underestimate prevalence of neurological and neuropsychiatric complications.
“If history teaches us anything, it is that we should always be measured in how we glean lessons from the past. So let’s not get ahead of ourselves,” he cautioned.
An informal, post-discussion survey of session participants revealed that a slight majority – 55%-60% – expected residual effects of COVID-19 to lead to more ADHD, compared to 40%-45% who didn’t think this would happen.
Dr. Swanson has two patents: (PIXA4), which uses a “time-of-flight” camera to measure growth on infants, and a provisional patent on the mechanism of tolerance to stimulant medication (PATSMTA). Dr. Coghill worked for several pharmaceutical companies but had no disclosures relevant to this debate.
FROM ADHD 2021
Taking a drug holiday: Benefits and risks to children with ADHD
For children with attention-deficit/hyperactivity disorder, taking a weekend or summer break from methylphenidate may have some benefits. A drug “holiday” can help assess whether a drug is still useful and possibly help with drug tolerance, weight gain, and growth suppression. But drug holidays are not without their problems, Lily Hechtman, MD, FRCP, professor at the department of psychiatry, McGill University, Montreal, said during a session at the World Congress on ADHD – Virtual Event.
Ceasing a medication can have repercussions from a health and social standpoint, cautioned Dr. Hechtman, a presenter and moderator of the session, “Unsolved mysteries in the treatment of ADHD with psychostimulants.”
The rate of drug holidays is somewhere between 30% and 40% in ADHD patients. Patients have multiple reasons for taking them, said Dr. Hechtman. The American Academy of Child & Adolescent Psychology as well as the National Institute for Health and Clinical Excellence recommend this method to assess whether a medication is still necessary. Parents may opt for a drug holiday because most would prefer their children to take less medication.
A drug holiday can counteract some of the key side effects of stimulant medication such as decreased appetite and weight loss, and the moodiness and irritability that accompanies the medication, as well as sleep problems.
It may also be used to avoid drug tolerance, the need to increase dosage as medication continues. A 2002 study of 166 children and adolescents treated with methylphenidate revealed that 60% had developed drug tolerance. Drug tolerance increases with duration. “So, the longer the child is on medication, the more likely he or she will develop some drug tolerance,” said Dr. Hechtman.
It is hypothesized that a drug holiday results in the resensitization of the neurons in the brain because they aren’t exposed to the stimulation of dopamine release and dopamine exposure.
The minimum time a patient needs a drug holiday to deal with some drug tolerance is about a month. “Even if you have a drug holiday and your drug tolerance has been decreased, it can reoccur with increasing dosages, once medication resumes” after the holiday, said Dr. Hechtman.
The growth factor
A drug holiday can also address concerns about growth suppression. “Some studies show that drug holidays help with growth suppression and others do not,” said Dr. Hechtman.
The Multimodal Treatment of ADHD (MTA) study, which followed children with ADHD from childhood to adolescence into adulthood, offers some key insights on the effects of treatment on growth.
Over a 10-year period, “you could see that the rate of medication use decreased significantly with time” among participants, said Dr. Hechtman, a coauthor of the MTA research. Only 10% who began the study aged 7-9 years were still using stimulants 10 years later. Looking at short-term effects on growth among these children, those who never went on stimulants to begin with had no growth suppression at all, whereas those who underwent early and consistent treatment experienced the greatest growth suppression.
Comparatively, inconsistently medicated participants had less growth suppression than those who remained on medication. “They were pretty close to the controls,” said Dr. Hechtman.
These patterns continued in a 16-year follow-up, as these patients became adults. Based on the results in the inconsistently treated group, this suggests that drug holidays can limit the effects of growth suppression, at least to a certain extent, said Dr. Hechtman.
Other studies have yielded varying results on the impact of drug holidays on height and weight. “The evidence for the utility of drug holidays for medication side effects is there for decreased appetite and weight, but not so much for decreased height,” summarized Dr. Hechtman.
One recent study of 230 children by James Waxmonsky and colleagues that examined drug holidays on weekends and summers showed that drug holidays did increase weight but interestingly, not height. Older studies Dr. Hechtman cited had inconsistent results on height and weight gain and loss. A 2012 study suggested that drug holidays resulted in a slight improvement in appetite for both weekend and school holidays. But only 9% of the children in the sample (n = 51) saw their appetite return to normal levels.
‘Negative things can happen’
The downside of drug holidays is parents may rationalize that their child is doing fine without the medication, and discontinue it. The process of stopping and starting medication can lead to other problems. “Negative things can happen during drug holidays,” said Dr. Hechtman.
The large variability of doses over the weekend can result in rebound and side effects.
A child may go from a full dose, which could be 50-60 mg of stimulant to zero from Friday to Saturday. As a result they have a lot of rebound on that Saturday. Similarly, they go from zero on Sunday to full dose on the Monday, causing lots of side effects. “Also, they will never have a stable effective dose because of the roller-coaster effect of being on and off the drugs,” she noted.
The lack of consistency and accommodation to the side effects can lead to discontinuation of the medication.
Off medication, the child may be more accident prone or have more injuries. “Their behavior off the medication may be such that it leads to social problems,” Dr. Hechtman continued. Weekend activities that require medication such as homework or school projects, family or religious gatherings, or sports and social activities with family and peers may be affected. If the child is behaving poorly off the medication, they may be expelled from such activities. If it’s a summer drug holiday, they may get kicked out of camp or the swimming pool.
If the child’s condition is already worsening, and a drug holiday takes place on top of this, the child may experience a rebound or relapse, in which the condition looks a lot worse than it did with the drugs.
Do drug holidays matter?
Another session speaker, James Swanson, PhD, who noted that the “emergence of tolerance may limit and eventually undermine initial relative benefit” of stimulants, said there may be instances in which drug holidays may be impractical.
Given the poor adherence to ADHD medication, “most treated ADHD cases stop medication anyway and these patients do not have an opportunity for drug holidays,” he said in an interview.
“If tolerance does emerge, then for long-term treatment the concept of drug holiday seems difficult to evaluate to me,” said Dr. Swanson, director of the Child Development Center at the University of California, Irvine.
Planned medication breaks may not be a good way to evaluate efficacy unless it is performed under “double-blind” conditions, he offered. The MTA used an approach of switching between short periods of time, with and without medication. “We did this to compare medication to placebo and to compare doses of medication to optimize the short-term benefit,” said Dr. Swanson, a coauthor of the MTA study.
Dr. Hechtman receives funding from The Canadian Institutes of Health Research. Dr. Swanson has two patents: (PIXA4), which uses a “time-of-flight” camera to measure growth on infants, and a provisional patent on the mechanism of tolerance to stimulant medication (PATSMTA).
For children with attention-deficit/hyperactivity disorder, taking a weekend or summer break from methylphenidate may have some benefits. A drug “holiday” can help assess whether a drug is still useful and possibly help with drug tolerance, weight gain, and growth suppression. But drug holidays are not without their problems, Lily Hechtman, MD, FRCP, professor at the department of psychiatry, McGill University, Montreal, said during a session at the World Congress on ADHD – Virtual Event.
Ceasing a medication can have repercussions from a health and social standpoint, cautioned Dr. Hechtman, a presenter and moderator of the session, “Unsolved mysteries in the treatment of ADHD with psychostimulants.”
The rate of drug holidays is somewhere between 30% and 40% in ADHD patients. Patients have multiple reasons for taking them, said Dr. Hechtman. The American Academy of Child & Adolescent Psychology as well as the National Institute for Health and Clinical Excellence recommend this method to assess whether a medication is still necessary. Parents may opt for a drug holiday because most would prefer their children to take less medication.
A drug holiday can counteract some of the key side effects of stimulant medication such as decreased appetite and weight loss, and the moodiness and irritability that accompanies the medication, as well as sleep problems.
It may also be used to avoid drug tolerance, the need to increase dosage as medication continues. A 2002 study of 166 children and adolescents treated with methylphenidate revealed that 60% had developed drug tolerance. Drug tolerance increases with duration. “So, the longer the child is on medication, the more likely he or she will develop some drug tolerance,” said Dr. Hechtman.
It is hypothesized that a drug holiday results in the resensitization of the neurons in the brain because they aren’t exposed to the stimulation of dopamine release and dopamine exposure.
The minimum time a patient needs a drug holiday to deal with some drug tolerance is about a month. “Even if you have a drug holiday and your drug tolerance has been decreased, it can reoccur with increasing dosages, once medication resumes” after the holiday, said Dr. Hechtman.
The growth factor
A drug holiday can also address concerns about growth suppression. “Some studies show that drug holidays help with growth suppression and others do not,” said Dr. Hechtman.
The Multimodal Treatment of ADHD (MTA) study, which followed children with ADHD from childhood to adolescence into adulthood, offers some key insights on the effects of treatment on growth.
Over a 10-year period, “you could see that the rate of medication use decreased significantly with time” among participants, said Dr. Hechtman, a coauthor of the MTA research. Only 10% who began the study aged 7-9 years were still using stimulants 10 years later. Looking at short-term effects on growth among these children, those who never went on stimulants to begin with had no growth suppression at all, whereas those who underwent early and consistent treatment experienced the greatest growth suppression.
Comparatively, inconsistently medicated participants had less growth suppression than those who remained on medication. “They were pretty close to the controls,” said Dr. Hechtman.
These patterns continued in a 16-year follow-up, as these patients became adults. Based on the results in the inconsistently treated group, this suggests that drug holidays can limit the effects of growth suppression, at least to a certain extent, said Dr. Hechtman.
Other studies have yielded varying results on the impact of drug holidays on height and weight. “The evidence for the utility of drug holidays for medication side effects is there for decreased appetite and weight, but not so much for decreased height,” summarized Dr. Hechtman.
One recent study of 230 children by James Waxmonsky and colleagues that examined drug holidays on weekends and summers showed that drug holidays did increase weight but interestingly, not height. Older studies Dr. Hechtman cited had inconsistent results on height and weight gain and loss. A 2012 study suggested that drug holidays resulted in a slight improvement in appetite for both weekend and school holidays. But only 9% of the children in the sample (n = 51) saw their appetite return to normal levels.
‘Negative things can happen’
The downside of drug holidays is parents may rationalize that their child is doing fine without the medication, and discontinue it. The process of stopping and starting medication can lead to other problems. “Negative things can happen during drug holidays,” said Dr. Hechtman.
The large variability of doses over the weekend can result in rebound and side effects.
A child may go from a full dose, which could be 50-60 mg of stimulant to zero from Friday to Saturday. As a result they have a lot of rebound on that Saturday. Similarly, they go from zero on Sunday to full dose on the Monday, causing lots of side effects. “Also, they will never have a stable effective dose because of the roller-coaster effect of being on and off the drugs,” she noted.
The lack of consistency and accommodation to the side effects can lead to discontinuation of the medication.
Off medication, the child may be more accident prone or have more injuries. “Their behavior off the medication may be such that it leads to social problems,” Dr. Hechtman continued. Weekend activities that require medication such as homework or school projects, family or religious gatherings, or sports and social activities with family and peers may be affected. If the child is behaving poorly off the medication, they may be expelled from such activities. If it’s a summer drug holiday, they may get kicked out of camp or the swimming pool.
If the child’s condition is already worsening, and a drug holiday takes place on top of this, the child may experience a rebound or relapse, in which the condition looks a lot worse than it did with the drugs.
Do drug holidays matter?
Another session speaker, James Swanson, PhD, who noted that the “emergence of tolerance may limit and eventually undermine initial relative benefit” of stimulants, said there may be instances in which drug holidays may be impractical.
Given the poor adherence to ADHD medication, “most treated ADHD cases stop medication anyway and these patients do not have an opportunity for drug holidays,” he said in an interview.
“If tolerance does emerge, then for long-term treatment the concept of drug holiday seems difficult to evaluate to me,” said Dr. Swanson, director of the Child Development Center at the University of California, Irvine.
Planned medication breaks may not be a good way to evaluate efficacy unless it is performed under “double-blind” conditions, he offered. The MTA used an approach of switching between short periods of time, with and without medication. “We did this to compare medication to placebo and to compare doses of medication to optimize the short-term benefit,” said Dr. Swanson, a coauthor of the MTA study.
Dr. Hechtman receives funding from The Canadian Institutes of Health Research. Dr. Swanson has two patents: (PIXA4), which uses a “time-of-flight” camera to measure growth on infants, and a provisional patent on the mechanism of tolerance to stimulant medication (PATSMTA).
For children with attention-deficit/hyperactivity disorder, taking a weekend or summer break from methylphenidate may have some benefits. A drug “holiday” can help assess whether a drug is still useful and possibly help with drug tolerance, weight gain, and growth suppression. But drug holidays are not without their problems, Lily Hechtman, MD, FRCP, professor at the department of psychiatry, McGill University, Montreal, said during a session at the World Congress on ADHD – Virtual Event.
Ceasing a medication can have repercussions from a health and social standpoint, cautioned Dr. Hechtman, a presenter and moderator of the session, “Unsolved mysteries in the treatment of ADHD with psychostimulants.”
The rate of drug holidays is somewhere between 30% and 40% in ADHD patients. Patients have multiple reasons for taking them, said Dr. Hechtman. The American Academy of Child & Adolescent Psychology as well as the National Institute for Health and Clinical Excellence recommend this method to assess whether a medication is still necessary. Parents may opt for a drug holiday because most would prefer their children to take less medication.
A drug holiday can counteract some of the key side effects of stimulant medication such as decreased appetite and weight loss, and the moodiness and irritability that accompanies the medication, as well as sleep problems.
It may also be used to avoid drug tolerance, the need to increase dosage as medication continues. A 2002 study of 166 children and adolescents treated with methylphenidate revealed that 60% had developed drug tolerance. Drug tolerance increases with duration. “So, the longer the child is on medication, the more likely he or she will develop some drug tolerance,” said Dr. Hechtman.
It is hypothesized that a drug holiday results in the resensitization of the neurons in the brain because they aren’t exposed to the stimulation of dopamine release and dopamine exposure.
The minimum time a patient needs a drug holiday to deal with some drug tolerance is about a month. “Even if you have a drug holiday and your drug tolerance has been decreased, it can reoccur with increasing dosages, once medication resumes” after the holiday, said Dr. Hechtman.
The growth factor
A drug holiday can also address concerns about growth suppression. “Some studies show that drug holidays help with growth suppression and others do not,” said Dr. Hechtman.
The Multimodal Treatment of ADHD (MTA) study, which followed children with ADHD from childhood to adolescence into adulthood, offers some key insights on the effects of treatment on growth.
Over a 10-year period, “you could see that the rate of medication use decreased significantly with time” among participants, said Dr. Hechtman, a coauthor of the MTA research. Only 10% who began the study aged 7-9 years were still using stimulants 10 years later. Looking at short-term effects on growth among these children, those who never went on stimulants to begin with had no growth suppression at all, whereas those who underwent early and consistent treatment experienced the greatest growth suppression.
Comparatively, inconsistently medicated participants had less growth suppression than those who remained on medication. “They were pretty close to the controls,” said Dr. Hechtman.
These patterns continued in a 16-year follow-up, as these patients became adults. Based on the results in the inconsistently treated group, this suggests that drug holidays can limit the effects of growth suppression, at least to a certain extent, said Dr. Hechtman.
Other studies have yielded varying results on the impact of drug holidays on height and weight. “The evidence for the utility of drug holidays for medication side effects is there for decreased appetite and weight, but not so much for decreased height,” summarized Dr. Hechtman.
One recent study of 230 children by James Waxmonsky and colleagues that examined drug holidays on weekends and summers showed that drug holidays did increase weight but interestingly, not height. Older studies Dr. Hechtman cited had inconsistent results on height and weight gain and loss. A 2012 study suggested that drug holidays resulted in a slight improvement in appetite for both weekend and school holidays. But only 9% of the children in the sample (n = 51) saw their appetite return to normal levels.
‘Negative things can happen’
The downside of drug holidays is parents may rationalize that their child is doing fine without the medication, and discontinue it. The process of stopping and starting medication can lead to other problems. “Negative things can happen during drug holidays,” said Dr. Hechtman.
The large variability of doses over the weekend can result in rebound and side effects.
A child may go from a full dose, which could be 50-60 mg of stimulant to zero from Friday to Saturday. As a result they have a lot of rebound on that Saturday. Similarly, they go from zero on Sunday to full dose on the Monday, causing lots of side effects. “Also, they will never have a stable effective dose because of the roller-coaster effect of being on and off the drugs,” she noted.
The lack of consistency and accommodation to the side effects can lead to discontinuation of the medication.
Off medication, the child may be more accident prone or have more injuries. “Their behavior off the medication may be such that it leads to social problems,” Dr. Hechtman continued. Weekend activities that require medication such as homework or school projects, family or religious gatherings, or sports and social activities with family and peers may be affected. If the child is behaving poorly off the medication, they may be expelled from such activities. If it’s a summer drug holiday, they may get kicked out of camp or the swimming pool.
If the child’s condition is already worsening, and a drug holiday takes place on top of this, the child may experience a rebound or relapse, in which the condition looks a lot worse than it did with the drugs.
Do drug holidays matter?
Another session speaker, James Swanson, PhD, who noted that the “emergence of tolerance may limit and eventually undermine initial relative benefit” of stimulants, said there may be instances in which drug holidays may be impractical.
Given the poor adherence to ADHD medication, “most treated ADHD cases stop medication anyway and these patients do not have an opportunity for drug holidays,” he said in an interview.
“If tolerance does emerge, then for long-term treatment the concept of drug holiday seems difficult to evaluate to me,” said Dr. Swanson, director of the Child Development Center at the University of California, Irvine.
Planned medication breaks may not be a good way to evaluate efficacy unless it is performed under “double-blind” conditions, he offered. The MTA used an approach of switching between short periods of time, with and without medication. “We did this to compare medication to placebo and to compare doses of medication to optimize the short-term benefit,” said Dr. Swanson, a coauthor of the MTA study.
Dr. Hechtman receives funding from The Canadian Institutes of Health Research. Dr. Swanson has two patents: (PIXA4), which uses a “time-of-flight” camera to measure growth on infants, and a provisional patent on the mechanism of tolerance to stimulant medication (PATSMTA).
FROM ADHD 2021
States ready plans to get Pfizer COVID vaccine to younger teens
after the Food and Drug Administration authorized its use in this age group May 10.
Some states hope to start the vaccinations as early as May 13, officials said at an Association of State and Territorial Health Officials news conference.
There are, however, two more steps before shots can reach younger arms. On May 12, the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices is expected to recommend use of the vaccine in this age group. Then CDC Director Rochelle Walensky, MD, must make a final decision to begin vaccinating 12- to 15-year-olds.
Some hoping to start this week
Both the CDC panel and Dr. Walensky are expected to sign off on the vaccine’s use. States have been making plans on how to tailor the vaccination message not just to the patient this time, but to parents and guardians as well, some of whom are hesitant to consent.
Some schools, assuming approval May 12, are ready to start vaccinating in cafeterias and gyms.
Anne Zink, MD, president-elect of the Association of State and Territorial Health Officials and Alaska chief medical officer, told reporters that many of her state’s boroughs and districts have booked in-person vaccines for their schools May 12 as the state has dismissal for summer as early as this week.
Maine is readying four types of distribution sites for the vaccines: primary care offices, Walgreen’s and CVS pharmacies, mass vaccination sites, and schools, said Nirav Shah, MD, current ASTHO president and director of the Maine Center for Disease Control and Prevention.
Starting later this week, he said, the state hopes to host large vaccination clinics for people age 12 and over.
Eliminating barriers
States are working to break down barriers through education and improving access.
In Alaska, many of the drive-through evening vaccination sites are being changed to Pfizer sites so parents just getting off work can take their kids.
It’s also important to get young people to speak to their peers about the importance of vaccines, she said. Some teen groups in Alaska are hosting Zoom calls where they share with children and families why they chose to get vaccinated.
In Maine, Dr. Shah said, “the notion of informed consent applies with equal force to adults as it does with adolescents.” But at least in Maine, it is not required that a parent be on site and present during the vaccination itself.
A parent could sign a form allowing the child to be vaccinated in a school-based clinic. Maine also allows verbal consent so a parent can give consent over the phone, Dr. Shah said.
Dividing vaccine trays
Vaccines going to pediatrician and family medicine offices presents a challenge in that smaller numbers of doses are needed for those venues than at large vaccination sites that get trays of 1,170 Pfizer doses each.
Dr. Shah says states have been talking with federal authorities on the need for smaller packaging.
“Breaking the trays up into smaller lot sizes takes a fair amount of effort,” Dr. Shah said. “We understand that later this month the lot size will be going down to 450.”
But even that will be too much for small offices, he said.
Similarly, an effort is being made in Maine to make sure doctors’ offices are not limited by their refrigeration capabilities. The Pfizer vaccine must be kept at ultra-cold temperatures that many primary care doctors’ offices may not have.
“If they need a cool cube with dry ice, we can furnish that to them,” Dr. Shah said.
Should they be mandated?
Dr. Zink said Alaska generally has high acceptance for recommendations around COVID-19 and has no plans to mandate the COVID-19 vaccines for children.
Umair A. Shah, MD, secretary of health at the Washington State Department of Health, said, “Our number one ability to get people vaccinated is for them to be encouraged to do so, to be incentivized to do so, to do everything we can to make the vaccine choice the easy choice,” including eliminating language, cultural and access barriers.
However, he said, “in higher education, University of Washington and Washington State University have indicated they are going to require COVID vaccines for kids to come back to school. I do think that is something that is increasingly being looked at.”
Though the messages will be tailored differently across the states the bottom line will be the same, Dr. Shah said: The vaccines work and they are safe.
But most critically, “Vaccines are our pathway to moving forward and once and for all ending this pandemic,” he said.
A version of this article first appeared on Medscape.com.
after the Food and Drug Administration authorized its use in this age group May 10.
Some states hope to start the vaccinations as early as May 13, officials said at an Association of State and Territorial Health Officials news conference.
There are, however, two more steps before shots can reach younger arms. On May 12, the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices is expected to recommend use of the vaccine in this age group. Then CDC Director Rochelle Walensky, MD, must make a final decision to begin vaccinating 12- to 15-year-olds.
Some hoping to start this week
Both the CDC panel and Dr. Walensky are expected to sign off on the vaccine’s use. States have been making plans on how to tailor the vaccination message not just to the patient this time, but to parents and guardians as well, some of whom are hesitant to consent.
Some schools, assuming approval May 12, are ready to start vaccinating in cafeterias and gyms.
Anne Zink, MD, president-elect of the Association of State and Territorial Health Officials and Alaska chief medical officer, told reporters that many of her state’s boroughs and districts have booked in-person vaccines for their schools May 12 as the state has dismissal for summer as early as this week.
Maine is readying four types of distribution sites for the vaccines: primary care offices, Walgreen’s and CVS pharmacies, mass vaccination sites, and schools, said Nirav Shah, MD, current ASTHO president and director of the Maine Center for Disease Control and Prevention.
Starting later this week, he said, the state hopes to host large vaccination clinics for people age 12 and over.
Eliminating barriers
States are working to break down barriers through education and improving access.
In Alaska, many of the drive-through evening vaccination sites are being changed to Pfizer sites so parents just getting off work can take their kids.
It’s also important to get young people to speak to their peers about the importance of vaccines, she said. Some teen groups in Alaska are hosting Zoom calls where they share with children and families why they chose to get vaccinated.
In Maine, Dr. Shah said, “the notion of informed consent applies with equal force to adults as it does with adolescents.” But at least in Maine, it is not required that a parent be on site and present during the vaccination itself.
A parent could sign a form allowing the child to be vaccinated in a school-based clinic. Maine also allows verbal consent so a parent can give consent over the phone, Dr. Shah said.
Dividing vaccine trays
Vaccines going to pediatrician and family medicine offices presents a challenge in that smaller numbers of doses are needed for those venues than at large vaccination sites that get trays of 1,170 Pfizer doses each.
Dr. Shah says states have been talking with federal authorities on the need for smaller packaging.
“Breaking the trays up into smaller lot sizes takes a fair amount of effort,” Dr. Shah said. “We understand that later this month the lot size will be going down to 450.”
But even that will be too much for small offices, he said.
Similarly, an effort is being made in Maine to make sure doctors’ offices are not limited by their refrigeration capabilities. The Pfizer vaccine must be kept at ultra-cold temperatures that many primary care doctors’ offices may not have.
“If they need a cool cube with dry ice, we can furnish that to them,” Dr. Shah said.
Should they be mandated?
Dr. Zink said Alaska generally has high acceptance for recommendations around COVID-19 and has no plans to mandate the COVID-19 vaccines for children.
Umair A. Shah, MD, secretary of health at the Washington State Department of Health, said, “Our number one ability to get people vaccinated is for them to be encouraged to do so, to be incentivized to do so, to do everything we can to make the vaccine choice the easy choice,” including eliminating language, cultural and access barriers.
However, he said, “in higher education, University of Washington and Washington State University have indicated they are going to require COVID vaccines for kids to come back to school. I do think that is something that is increasingly being looked at.”
Though the messages will be tailored differently across the states the bottom line will be the same, Dr. Shah said: The vaccines work and they are safe.
But most critically, “Vaccines are our pathway to moving forward and once and for all ending this pandemic,” he said.
A version of this article first appeared on Medscape.com.
after the Food and Drug Administration authorized its use in this age group May 10.
Some states hope to start the vaccinations as early as May 13, officials said at an Association of State and Territorial Health Officials news conference.
There are, however, two more steps before shots can reach younger arms. On May 12, the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices is expected to recommend use of the vaccine in this age group. Then CDC Director Rochelle Walensky, MD, must make a final decision to begin vaccinating 12- to 15-year-olds.
Some hoping to start this week
Both the CDC panel and Dr. Walensky are expected to sign off on the vaccine’s use. States have been making plans on how to tailor the vaccination message not just to the patient this time, but to parents and guardians as well, some of whom are hesitant to consent.
Some schools, assuming approval May 12, are ready to start vaccinating in cafeterias and gyms.
Anne Zink, MD, president-elect of the Association of State and Territorial Health Officials and Alaska chief medical officer, told reporters that many of her state’s boroughs and districts have booked in-person vaccines for their schools May 12 as the state has dismissal for summer as early as this week.
Maine is readying four types of distribution sites for the vaccines: primary care offices, Walgreen’s and CVS pharmacies, mass vaccination sites, and schools, said Nirav Shah, MD, current ASTHO president and director of the Maine Center for Disease Control and Prevention.
Starting later this week, he said, the state hopes to host large vaccination clinics for people age 12 and over.
Eliminating barriers
States are working to break down barriers through education and improving access.
In Alaska, many of the drive-through evening vaccination sites are being changed to Pfizer sites so parents just getting off work can take their kids.
It’s also important to get young people to speak to their peers about the importance of vaccines, she said. Some teen groups in Alaska are hosting Zoom calls where they share with children and families why they chose to get vaccinated.
In Maine, Dr. Shah said, “the notion of informed consent applies with equal force to adults as it does with adolescents.” But at least in Maine, it is not required that a parent be on site and present during the vaccination itself.
A parent could sign a form allowing the child to be vaccinated in a school-based clinic. Maine also allows verbal consent so a parent can give consent over the phone, Dr. Shah said.
Dividing vaccine trays
Vaccines going to pediatrician and family medicine offices presents a challenge in that smaller numbers of doses are needed for those venues than at large vaccination sites that get trays of 1,170 Pfizer doses each.
Dr. Shah says states have been talking with federal authorities on the need for smaller packaging.
“Breaking the trays up into smaller lot sizes takes a fair amount of effort,” Dr. Shah said. “We understand that later this month the lot size will be going down to 450.”
But even that will be too much for small offices, he said.
Similarly, an effort is being made in Maine to make sure doctors’ offices are not limited by their refrigeration capabilities. The Pfizer vaccine must be kept at ultra-cold temperatures that many primary care doctors’ offices may not have.
“If they need a cool cube with dry ice, we can furnish that to them,” Dr. Shah said.
Should they be mandated?
Dr. Zink said Alaska generally has high acceptance for recommendations around COVID-19 and has no plans to mandate the COVID-19 vaccines for children.
Umair A. Shah, MD, secretary of health at the Washington State Department of Health, said, “Our number one ability to get people vaccinated is for them to be encouraged to do so, to be incentivized to do so, to do everything we can to make the vaccine choice the easy choice,” including eliminating language, cultural and access barriers.
However, he said, “in higher education, University of Washington and Washington State University have indicated they are going to require COVID vaccines for kids to come back to school. I do think that is something that is increasingly being looked at.”
Though the messages will be tailored differently across the states the bottom line will be the same, Dr. Shah said: The vaccines work and they are safe.
But most critically, “Vaccines are our pathway to moving forward and once and for all ending this pandemic,” he said.
A version of this article first appeared on Medscape.com.
ADHD in preschool kids: Adrenergic agonists may be a better fit
A new study finds that alpha2-adrenergic agonists may be of benefit and have fewer side effects than stimulant medications for the treatment of attention-deficit/hyperactivity disorder in preschool-age children.
The study was published online May 4 in JAMA.
As part of a retrospective analysis, Elizabeth Harstad, MD, MPH, of Boston Children’s Hospital and colleagues evaluated health record data from 497 preschool-age children with ADHD across seven developmental-behavioral pediatric practices in the United States. Children included in the evaluation were younger than 6 years and were treated for ADHD between Jan. 1, 2013, and July 1, 2017, with either an alpha2-adrenergic agonist or a stimulant.
Overall, 175 children (35%) were prescribed an alpha2-adrenergic agonist (most often guanfacine) as first-line ADHD medication, and 322 children (65%) were prescribed a stimulant (most often a methylphenidate-based preparation). Before any medication regimens were initiated, 62% of children received behavioral therapy.
“These findings suggest that for some children there may be a concern about either how well a stimulant will work or how well a stimulant will be tolerated that is leading clinicians to instead prescribe an alpha2-adrenergic agonist as the first medication tried,” Dr. Harstad said in an interview.
Clinical improvement was noted in 66% of children treated with alpha2-adrenergic agonists (95% confidence interval, 57.5%-73.9%) and in 78% of children treated with stimulants (95% CI, 72.4%-83.4%).
Most adverse effects were more common among children who received stimulants than among those who received alpha2-adrenergic agonists. These adverse effects included difficulty falling asleep (21% vs. 11%), decreased appetite (38% vs. 7%), increased stomachaches (13% vs. 5%), and increased skin picking/repetitive behaviors (11% vs. 5%). Only daytime sleepiness was more frequent among children who received an alpha2-adrenergic agonist rather than a stimulant (38% vs. 3%).
“We also found that for the youngest children (<4 years old), those initiated on alpha2-adrenergic agonists stayed on these medications longer than those initiated on stimulants, which may indicate that they are better tolerated, although more research is needed to confirm this,” Dr. Harstad said.
“While our study focused on how well medications work and how well they are tolerated when used to treat preschool-age children with ADHD, it is important to remember that behavioral therapy is recommended as first-line treatment for ADHD in preschool-age children, not medication,” Dr. Harstad added.
Mark Wolraich, MD, of the University of Oklahoma, echoed that sentiment. “The article mentions that behavioral interventions, in the form of parent training in behavior management, is an effective first-line treatment” and, per the American Academy of Pediatrics guidelines, “is the first line of treatment recommended for preschool-age children before medication should be considered.”
Dr. Wolraich also noted that “neither drug has official FDA [U.S. Food and Drug Administration] approval in this age group” but that “methylphenidate comes the closest to having met the FDA requirements for approval in this age group, which is why the AAP guidelines recommended its use if parent training in behavior management is not sufficient.”
Although Dr. Harstad and colleagues note that the study included a large and diverse sample size from across the United States, they acknowledge that “further research, including from randomized clinical trials, is needed to assess comparative effectiveness of alpha2-adrenergic agonists versus stimulants.”
Funding for the study was provided through a cooperative agreement with the Maternal and Child Health Bureau, the Health Resources and Services Administration, and the U.S. Department of Health & Human Services. Dr. Harstad has reported receiving reported receiving compensation for serving as a medical reviewer for Understood.org and grant funding from the Palmer Family Fund for Autism Research to conduct research related to autism spectrum disorder at Boston Children’s Hospital. Disclosures for the other authors are listed in the original article. Dr. Wolraich has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study finds that alpha2-adrenergic agonists may be of benefit and have fewer side effects than stimulant medications for the treatment of attention-deficit/hyperactivity disorder in preschool-age children.
The study was published online May 4 in JAMA.
As part of a retrospective analysis, Elizabeth Harstad, MD, MPH, of Boston Children’s Hospital and colleagues evaluated health record data from 497 preschool-age children with ADHD across seven developmental-behavioral pediatric practices in the United States. Children included in the evaluation were younger than 6 years and were treated for ADHD between Jan. 1, 2013, and July 1, 2017, with either an alpha2-adrenergic agonist or a stimulant.
Overall, 175 children (35%) were prescribed an alpha2-adrenergic agonist (most often guanfacine) as first-line ADHD medication, and 322 children (65%) were prescribed a stimulant (most often a methylphenidate-based preparation). Before any medication regimens were initiated, 62% of children received behavioral therapy.
“These findings suggest that for some children there may be a concern about either how well a stimulant will work or how well a stimulant will be tolerated that is leading clinicians to instead prescribe an alpha2-adrenergic agonist as the first medication tried,” Dr. Harstad said in an interview.
Clinical improvement was noted in 66% of children treated with alpha2-adrenergic agonists (95% confidence interval, 57.5%-73.9%) and in 78% of children treated with stimulants (95% CI, 72.4%-83.4%).
Most adverse effects were more common among children who received stimulants than among those who received alpha2-adrenergic agonists. These adverse effects included difficulty falling asleep (21% vs. 11%), decreased appetite (38% vs. 7%), increased stomachaches (13% vs. 5%), and increased skin picking/repetitive behaviors (11% vs. 5%). Only daytime sleepiness was more frequent among children who received an alpha2-adrenergic agonist rather than a stimulant (38% vs. 3%).
“We also found that for the youngest children (<4 years old), those initiated on alpha2-adrenergic agonists stayed on these medications longer than those initiated on stimulants, which may indicate that they are better tolerated, although more research is needed to confirm this,” Dr. Harstad said.
“While our study focused on how well medications work and how well they are tolerated when used to treat preschool-age children with ADHD, it is important to remember that behavioral therapy is recommended as first-line treatment for ADHD in preschool-age children, not medication,” Dr. Harstad added.
Mark Wolraich, MD, of the University of Oklahoma, echoed that sentiment. “The article mentions that behavioral interventions, in the form of parent training in behavior management, is an effective first-line treatment” and, per the American Academy of Pediatrics guidelines, “is the first line of treatment recommended for preschool-age children before medication should be considered.”
Dr. Wolraich also noted that “neither drug has official FDA [U.S. Food and Drug Administration] approval in this age group” but that “methylphenidate comes the closest to having met the FDA requirements for approval in this age group, which is why the AAP guidelines recommended its use if parent training in behavior management is not sufficient.”
Although Dr. Harstad and colleagues note that the study included a large and diverse sample size from across the United States, they acknowledge that “further research, including from randomized clinical trials, is needed to assess comparative effectiveness of alpha2-adrenergic agonists versus stimulants.”
Funding for the study was provided through a cooperative agreement with the Maternal and Child Health Bureau, the Health Resources and Services Administration, and the U.S. Department of Health & Human Services. Dr. Harstad has reported receiving reported receiving compensation for serving as a medical reviewer for Understood.org and grant funding from the Palmer Family Fund for Autism Research to conduct research related to autism spectrum disorder at Boston Children’s Hospital. Disclosures for the other authors are listed in the original article. Dr. Wolraich has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study finds that alpha2-adrenergic agonists may be of benefit and have fewer side effects than stimulant medications for the treatment of attention-deficit/hyperactivity disorder in preschool-age children.
The study was published online May 4 in JAMA.
As part of a retrospective analysis, Elizabeth Harstad, MD, MPH, of Boston Children’s Hospital and colleagues evaluated health record data from 497 preschool-age children with ADHD across seven developmental-behavioral pediatric practices in the United States. Children included in the evaluation were younger than 6 years and were treated for ADHD between Jan. 1, 2013, and July 1, 2017, with either an alpha2-adrenergic agonist or a stimulant.
Overall, 175 children (35%) were prescribed an alpha2-adrenergic agonist (most often guanfacine) as first-line ADHD medication, and 322 children (65%) were prescribed a stimulant (most often a methylphenidate-based preparation). Before any medication regimens were initiated, 62% of children received behavioral therapy.
“These findings suggest that for some children there may be a concern about either how well a stimulant will work or how well a stimulant will be tolerated that is leading clinicians to instead prescribe an alpha2-adrenergic agonist as the first medication tried,” Dr. Harstad said in an interview.
Clinical improvement was noted in 66% of children treated with alpha2-adrenergic agonists (95% confidence interval, 57.5%-73.9%) and in 78% of children treated with stimulants (95% CI, 72.4%-83.4%).
Most adverse effects were more common among children who received stimulants than among those who received alpha2-adrenergic agonists. These adverse effects included difficulty falling asleep (21% vs. 11%), decreased appetite (38% vs. 7%), increased stomachaches (13% vs. 5%), and increased skin picking/repetitive behaviors (11% vs. 5%). Only daytime sleepiness was more frequent among children who received an alpha2-adrenergic agonist rather than a stimulant (38% vs. 3%).
“We also found that for the youngest children (<4 years old), those initiated on alpha2-adrenergic agonists stayed on these medications longer than those initiated on stimulants, which may indicate that they are better tolerated, although more research is needed to confirm this,” Dr. Harstad said.
“While our study focused on how well medications work and how well they are tolerated when used to treat preschool-age children with ADHD, it is important to remember that behavioral therapy is recommended as first-line treatment for ADHD in preschool-age children, not medication,” Dr. Harstad added.
Mark Wolraich, MD, of the University of Oklahoma, echoed that sentiment. “The article mentions that behavioral interventions, in the form of parent training in behavior management, is an effective first-line treatment” and, per the American Academy of Pediatrics guidelines, “is the first line of treatment recommended for preschool-age children before medication should be considered.”
Dr. Wolraich also noted that “neither drug has official FDA [U.S. Food and Drug Administration] approval in this age group” but that “methylphenidate comes the closest to having met the FDA requirements for approval in this age group, which is why the AAP guidelines recommended its use if parent training in behavior management is not sufficient.”
Although Dr. Harstad and colleagues note that the study included a large and diverse sample size from across the United States, they acknowledge that “further research, including from randomized clinical trials, is needed to assess comparative effectiveness of alpha2-adrenergic agonists versus stimulants.”
Funding for the study was provided through a cooperative agreement with the Maternal and Child Health Bureau, the Health Resources and Services Administration, and the U.S. Department of Health & Human Services. Dr. Harstad has reported receiving reported receiving compensation for serving as a medical reviewer for Understood.org and grant funding from the Palmer Family Fund for Autism Research to conduct research related to autism spectrum disorder at Boston Children’s Hospital. Disclosures for the other authors are listed in the original article. Dr. Wolraich has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.