User login
Keep antibiotics unchanged in breakthrough UTIs
Changing the continuous antibiotic prophylactic agent had no significant effect on the risk of a second infection in children with breakthrough urinary tract infections (UTIs), based on data from 62 children treated at a single center.
Continuous antibiotic prophylaxis (CAP) is often used for UTI prevention in children with febrile UTIs or anomalies that predispose them to UTIs, such as vesicoureteral reflux (VUR) or bladder and bowel dysfunction, said Lane M. Shish, MPH, of the University of Washington, Bothell, and colleagues in a poster (#1245) presented at the Pediatric Academic Societies annual meeting.
CAP, once initiated, is used until a planned endpoint or a breakthrough UTI, at which point alternative treatments usually include surgical intervention or a CAP agent change, the researchers said. However, changing the CAP agent is based on consensus without evidence of benefit, they noted.
To evaluate the potential effect of switching or maintaining CAP in cases of breakthrough UTIs, the researchers conducted a retrospective cohort study of all patients younger than 18 years on CAP for UTI prevention enrolled in a pediatric urology registry between January 2013 and August 2020.
All patients experienced a breakthrough UTI while on CAP; CAP was changed for 24 patients and left unchanged for 38 patients.
The primary outcome of second-breakthrough infections occurred in 12 of the changed CAP group and 22 of the unchanged group, with a relative risk of 0.86. The percentage of second breakthrough UTIs resistant to the current CAP was not significantly different between the changed and unchanged CAP groups (75% vs. 77%; P = 0.88).
The researchers also identified a rate ratio of 0.67 for a second breakthrough UTI in the changed CAP group, and found that approximately one-third of these patients (33.3%) developed antibiotic resistance to their initial antibiotic agent and the changed antibiotic agent.
The study findings were limited by several factors, including the retrospective design and small sample size, the researchers noted.
However, the results suggest that changing the CAP after an initial breakthrough UTI in children did not increase the risk of a second breakthrough UTI, and that CAP changing did introduce a risk of developing a second UTI with increased CAP resistance, the researchers noted. The results support leaving a child’s CAP unchanged after an initial breakthrough UTI, although additional research is needed to verify the findings, including studies involving a larger cohort with a multi-institutional prospective evaluation, they concluded.
Manage UTIs to reduce recurrence and resistance
“As we know, avoiding recurrent UTIs is important in preserving renal function in pediatric patients,” said Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, in an interview.
“Avoiding recurrent UTIs is also important to avoid the development and spread of multidrug-resistant organisms,” he said.
Dr. Joos said he was surprised by some of the study findings. “I was surprised that, over the course of this 7-year retrospective review, overall only approximately 50% of patients with a first breakthrough UTI on CAP developed a second breakthrough UTI,” he noted. “Also, the relative risk of a second UTI was not significantly affected by whether the CAP antibiotic was changed after the first infection,” he said. “It would be interesting to see whether these results hold up in a randomized, prospective study,” he added.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose, but serves as a member of the Pediatric News Editorial Advisory Board.
Changing the continuous antibiotic prophylactic agent had no significant effect on the risk of a second infection in children with breakthrough urinary tract infections (UTIs), based on data from 62 children treated at a single center.
Continuous antibiotic prophylaxis (CAP) is often used for UTI prevention in children with febrile UTIs or anomalies that predispose them to UTIs, such as vesicoureteral reflux (VUR) or bladder and bowel dysfunction, said Lane M. Shish, MPH, of the University of Washington, Bothell, and colleagues in a poster (#1245) presented at the Pediatric Academic Societies annual meeting.
CAP, once initiated, is used until a planned endpoint or a breakthrough UTI, at which point alternative treatments usually include surgical intervention or a CAP agent change, the researchers said. However, changing the CAP agent is based on consensus without evidence of benefit, they noted.
To evaluate the potential effect of switching or maintaining CAP in cases of breakthrough UTIs, the researchers conducted a retrospective cohort study of all patients younger than 18 years on CAP for UTI prevention enrolled in a pediatric urology registry between January 2013 and August 2020.
All patients experienced a breakthrough UTI while on CAP; CAP was changed for 24 patients and left unchanged for 38 patients.
The primary outcome of second-breakthrough infections occurred in 12 of the changed CAP group and 22 of the unchanged group, with a relative risk of 0.86. The percentage of second breakthrough UTIs resistant to the current CAP was not significantly different between the changed and unchanged CAP groups (75% vs. 77%; P = 0.88).
The researchers also identified a rate ratio of 0.67 for a second breakthrough UTI in the changed CAP group, and found that approximately one-third of these patients (33.3%) developed antibiotic resistance to their initial antibiotic agent and the changed antibiotic agent.
The study findings were limited by several factors, including the retrospective design and small sample size, the researchers noted.
However, the results suggest that changing the CAP after an initial breakthrough UTI in children did not increase the risk of a second breakthrough UTI, and that CAP changing did introduce a risk of developing a second UTI with increased CAP resistance, the researchers noted. The results support leaving a child’s CAP unchanged after an initial breakthrough UTI, although additional research is needed to verify the findings, including studies involving a larger cohort with a multi-institutional prospective evaluation, they concluded.
Manage UTIs to reduce recurrence and resistance
“As we know, avoiding recurrent UTIs is important in preserving renal function in pediatric patients,” said Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, in an interview.
“Avoiding recurrent UTIs is also important to avoid the development and spread of multidrug-resistant organisms,” he said.
Dr. Joos said he was surprised by some of the study findings. “I was surprised that, over the course of this 7-year retrospective review, overall only approximately 50% of patients with a first breakthrough UTI on CAP developed a second breakthrough UTI,” he noted. “Also, the relative risk of a second UTI was not significantly affected by whether the CAP antibiotic was changed after the first infection,” he said. “It would be interesting to see whether these results hold up in a randomized, prospective study,” he added.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose, but serves as a member of the Pediatric News Editorial Advisory Board.
Changing the continuous antibiotic prophylactic agent had no significant effect on the risk of a second infection in children with breakthrough urinary tract infections (UTIs), based on data from 62 children treated at a single center.
Continuous antibiotic prophylaxis (CAP) is often used for UTI prevention in children with febrile UTIs or anomalies that predispose them to UTIs, such as vesicoureteral reflux (VUR) or bladder and bowel dysfunction, said Lane M. Shish, MPH, of the University of Washington, Bothell, and colleagues in a poster (#1245) presented at the Pediatric Academic Societies annual meeting.
CAP, once initiated, is used until a planned endpoint or a breakthrough UTI, at which point alternative treatments usually include surgical intervention or a CAP agent change, the researchers said. However, changing the CAP agent is based on consensus without evidence of benefit, they noted.
To evaluate the potential effect of switching or maintaining CAP in cases of breakthrough UTIs, the researchers conducted a retrospective cohort study of all patients younger than 18 years on CAP for UTI prevention enrolled in a pediatric urology registry between January 2013 and August 2020.
All patients experienced a breakthrough UTI while on CAP; CAP was changed for 24 patients and left unchanged for 38 patients.
The primary outcome of second-breakthrough infections occurred in 12 of the changed CAP group and 22 of the unchanged group, with a relative risk of 0.86. The percentage of second breakthrough UTIs resistant to the current CAP was not significantly different between the changed and unchanged CAP groups (75% vs. 77%; P = 0.88).
The researchers also identified a rate ratio of 0.67 for a second breakthrough UTI in the changed CAP group, and found that approximately one-third of these patients (33.3%) developed antibiotic resistance to their initial antibiotic agent and the changed antibiotic agent.
The study findings were limited by several factors, including the retrospective design and small sample size, the researchers noted.
However, the results suggest that changing the CAP after an initial breakthrough UTI in children did not increase the risk of a second breakthrough UTI, and that CAP changing did introduce a risk of developing a second UTI with increased CAP resistance, the researchers noted. The results support leaving a child’s CAP unchanged after an initial breakthrough UTI, although additional research is needed to verify the findings, including studies involving a larger cohort with a multi-institutional prospective evaluation, they concluded.
Manage UTIs to reduce recurrence and resistance
“As we know, avoiding recurrent UTIs is important in preserving renal function in pediatric patients,” said Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, in an interview.
“Avoiding recurrent UTIs is also important to avoid the development and spread of multidrug-resistant organisms,” he said.
Dr. Joos said he was surprised by some of the study findings. “I was surprised that, over the course of this 7-year retrospective review, overall only approximately 50% of patients with a first breakthrough UTI on CAP developed a second breakthrough UTI,” he noted. “Also, the relative risk of a second UTI was not significantly affected by whether the CAP antibiotic was changed after the first infection,” he said. “It would be interesting to see whether these results hold up in a randomized, prospective study,” he added.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose, but serves as a member of the Pediatric News Editorial Advisory Board.
FROM PAS 2021
Small increase seen in new COVID-19 cases among children
After 2 consecutive weeks of declines, the number of new COVID-19 cases in children rose slightly, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
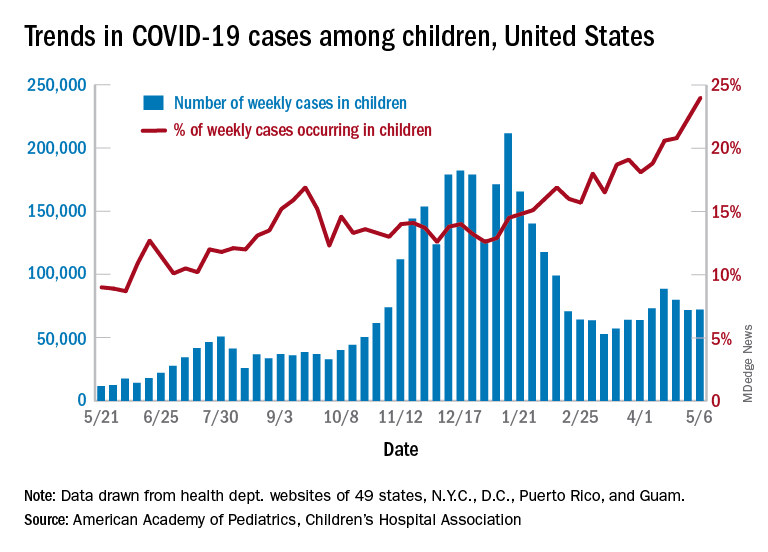
higher than at any other time during the pandemic, the AAP and CHA data show.
It is worth noting, however, that Rhode Island experienced a 30% increase in the last week, adding about 4,900 cases because of data revision and a lag in reporting, the AAP and CHA said in their weekly COVID-19 report.
All the new cases bring the total national count to just over 3.54 million in children, which represents 14.0% of all cases in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. The cumulative case rate as of May 6 was 5,122 per 100,000 children, the two organizations said.
All the new cases that were added to Rhode Island’s total give it the highest cumulative rate in the country: 9,614 cases per 100,000 children. North Dakota is right behind with 9,526 per 100,000, followed by Tennessee (8,898), Connecticut (8,281), and South Carolina (8,274). Vermont has the highest proportion of cases in children at 22.4%, with Alaska next at 20.3% and South Carolina third at 18.7%, according to the AAP and CHA.
Hawaii just reported its first COVID-19–related death in a child, which drops the number of states with zero deaths in children from 10 to 9. Two other new deaths in children from April 30 to May 6 bring the total number to 306 in the 43 states, along with New York City, Puerto Rico, and Guam, that are reporting the age distribution of deaths.
In a separate statement, AAP president Lee Savio Beers acknowledged the Food and Drug Administration’s authorization of the Pfizer-BioNTech vaccine for children aged 12-15 years as “a critically important step in bringing lifesaving vaccines to children and adolescents. ... We look forward to the discussion by the Advisory Committee on Immunization Practices of the CDC, which will make recommendations about the use of this vaccine in adolescents.”
After 2 consecutive weeks of declines, the number of new COVID-19 cases in children rose slightly, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
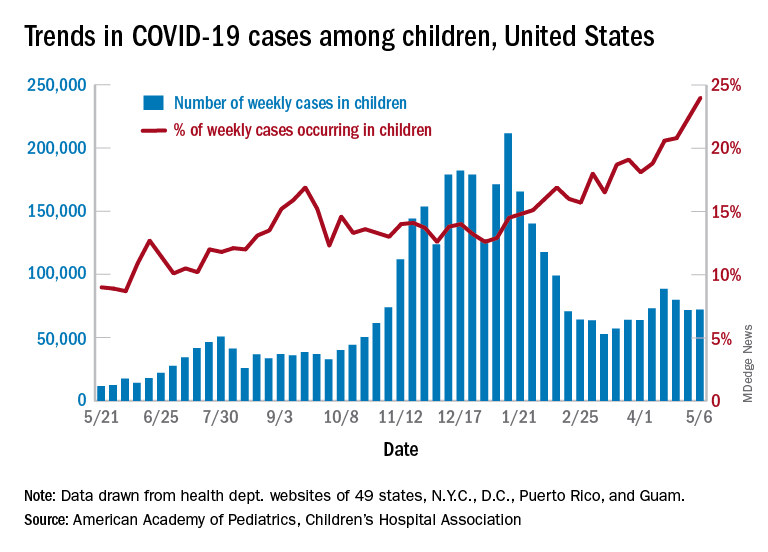
higher than at any other time during the pandemic, the AAP and CHA data show.
It is worth noting, however, that Rhode Island experienced a 30% increase in the last week, adding about 4,900 cases because of data revision and a lag in reporting, the AAP and CHA said in their weekly COVID-19 report.
All the new cases bring the total national count to just over 3.54 million in children, which represents 14.0% of all cases in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. The cumulative case rate as of May 6 was 5,122 per 100,000 children, the two organizations said.
All the new cases that were added to Rhode Island’s total give it the highest cumulative rate in the country: 9,614 cases per 100,000 children. North Dakota is right behind with 9,526 per 100,000, followed by Tennessee (8,898), Connecticut (8,281), and South Carolina (8,274). Vermont has the highest proportion of cases in children at 22.4%, with Alaska next at 20.3% and South Carolina third at 18.7%, according to the AAP and CHA.
Hawaii just reported its first COVID-19–related death in a child, which drops the number of states with zero deaths in children from 10 to 9. Two other new deaths in children from April 30 to May 6 bring the total number to 306 in the 43 states, along with New York City, Puerto Rico, and Guam, that are reporting the age distribution of deaths.
In a separate statement, AAP president Lee Savio Beers acknowledged the Food and Drug Administration’s authorization of the Pfizer-BioNTech vaccine for children aged 12-15 years as “a critically important step in bringing lifesaving vaccines to children and adolescents. ... We look forward to the discussion by the Advisory Committee on Immunization Practices of the CDC, which will make recommendations about the use of this vaccine in adolescents.”
After 2 consecutive weeks of declines, the number of new COVID-19 cases in children rose slightly, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
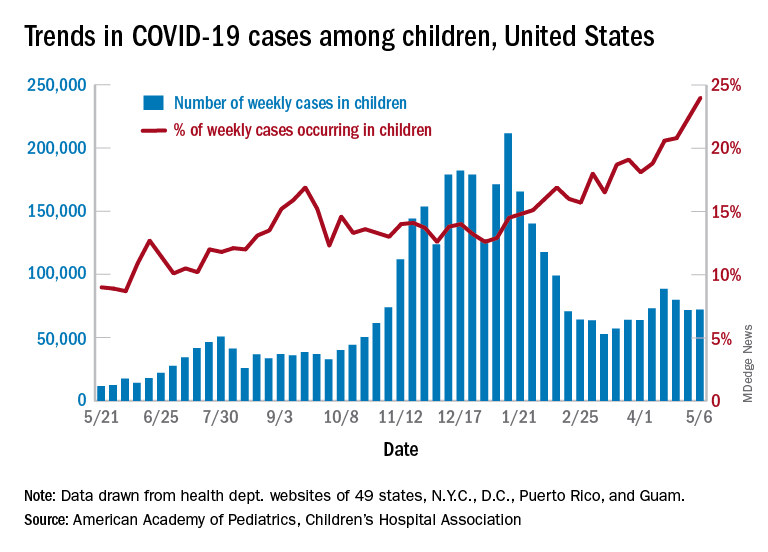
higher than at any other time during the pandemic, the AAP and CHA data show.
It is worth noting, however, that Rhode Island experienced a 30% increase in the last week, adding about 4,900 cases because of data revision and a lag in reporting, the AAP and CHA said in their weekly COVID-19 report.
All the new cases bring the total national count to just over 3.54 million in children, which represents 14.0% of all cases in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. The cumulative case rate as of May 6 was 5,122 per 100,000 children, the two organizations said.
All the new cases that were added to Rhode Island’s total give it the highest cumulative rate in the country: 9,614 cases per 100,000 children. North Dakota is right behind with 9,526 per 100,000, followed by Tennessee (8,898), Connecticut (8,281), and South Carolina (8,274). Vermont has the highest proportion of cases in children at 22.4%, with Alaska next at 20.3% and South Carolina third at 18.7%, according to the AAP and CHA.
Hawaii just reported its first COVID-19–related death in a child, which drops the number of states with zero deaths in children from 10 to 9. Two other new deaths in children from April 30 to May 6 bring the total number to 306 in the 43 states, along with New York City, Puerto Rico, and Guam, that are reporting the age distribution of deaths.
In a separate statement, AAP president Lee Savio Beers acknowledged the Food and Drug Administration’s authorization of the Pfizer-BioNTech vaccine for children aged 12-15 years as “a critically important step in bringing lifesaving vaccines to children and adolescents. ... We look forward to the discussion by the Advisory Committee on Immunization Practices of the CDC, which will make recommendations about the use of this vaccine in adolescents.”
TIPP the scales in managing stress
The past year presented unprecedented challenges for many. In addition, mental health services have also been stretched to capacity. Anecdotally, some hospitals and emergency departments note that more youth have been presenting in mental health crises, and the severity of symptoms has also been higher. Safety planning is important, including working with patients to identify skills they can use in distress. Even those who do not experience suicidal thoughts may struggle with dysregulation or may use coping strategies that may not be the healthiest in the long term.
Within my practice, I see some families who are still waiting for an available therapist, or some may not wish to participate in therapy despite its being recommended. For these families, supporting them in using strategies that they may be willing and able to use in the moment to help them get through the moment of crisis can been helpful:
Case example (identifying details have been changed)
Emily is a 17-year-old girl who has a history of generalized anxiety disorder and obsessive-compulsive disorder. She has had multiple medication trials and a course of cognitive behavioral therapy when younger, with significant improvement in symptoms. She returns to clinic because of increased anxiety related to stressors of the pandemic. She wishes to not return to therapy because of feeling that she received maximal benefit and that further sessions would not be fruitful. However, she struggles with identifying what skills she can use, and her anxiety heightens significantly to near-panic and hyperventilating with even cursory exploration of triggers for her symptoms. Medications are also discussed during this appointment, and it is noted that it may take some time to see therapeutic effect. Of note, she reports no acute safety concerns. She has engaged in skin picking. No reported substance use. As she hyperventilates, she was asked to identify items in the room matching the colors of the rainbow in order. She was able to quickly do this, and then was asked to do it again. Afterward, she noted feeling much less anxious because it distracted her from her thoughts.
Distress tolerance skills can be very helpful to navigate getting through a crisis. When under stress, some may be more likely to engage in behaviors that are not helpful in the long term such as using avoidance; procrastinating; consuming tobacco, alcohol, or other substances; spending too much time on screens; or engaging in self-harm behaviors. While some of these activities may be okay in moderation, others are always harmful. At times, when encouraging patients to use skills with which they may be more familiar, e.g., deep breathing, progressive muscle relaxation, the response may be, “these don’t work!” It can be important to distinguish that the function of these skills is not to make someone feel good or to eliminate the stressor, but to “take some of the edge off” so they are less likely to slide into problematic behaviors. It can be beneficial to have multiple tools at one’s disposal because not all skills will always be effective or available.
TIPP skills (temperature, intense exercise, paced breathing, progressive muscle relaxation) are distress tolerance skills from dialectical behavioral therapy (DBT),1 which was initially developed to treat individuals with borderline personality disorder. More recently, the therapy modality has been applied to individuals who may struggle with emotion regulation for a variety of reasons. TIPP skills work quickly (within seconds to minutes) with the aim to decrease physiological arousal. They do not require a lot of thinking, and many are portable or easy to use. Given the speed of effect, these skills can also be used in lieu of p.r.n. medications or patients can be counseled about trying these instead of turning to substance use. The effect is brief (5-20 minutes), although this may lower the affective temperature sufficiently for someone to get through the intense moment or to be able to then utilize other skills that may require more cognitive reserves.
T – Temperature
Holding one’s breath and placing one’s face in cold water (above 50°) for 10-20 seconds to stimulate the diving response and decrease heart rate. Patients can repeat this up to 3 times. Alternatively, cold compresses or gel eye masks can be used.
I – Intense exercise
Aerobic exercise for 10-20 minutes. This can include running, jumping jacks, dancing to loud music in a way that feels intense. The parasympathetic nervous system (PNS) is activated for approximately 20 minutes after cessation of intense exercise.
P – Paced breathing
Decreasing rate of breathing, with each inhalation/exhalation cycle lasting 10-12 seconds and the exhale being longer than the inhale also activates the PNS.
P – Progressive muscle relaxation (PMR)
Sequentially tensing and relaxing muscles from head to toes. Having at least 5-10 minutes to perform this exercise is preferred.2 Children’s Hospital of Philadelphia offerssample PMR recordings.
Body scans can also be helpful. This practice differs from PMR in that it is a mindfulness practice noting body sensations without trying to change them. The University of Vermont offers some sample exercises.3
These skills were described to Emily. She noted that dunking her face in cold water was effective and it was reassuring knowing she had a tool to help her anxiety. She started to push herself to go outside to exercise. We additionally incorporated other distraction techniques such as identifying items from colors of the rainbow that were around her. She appreciated that she could even do this discreetly while at school. At times she had to do a couple of rounds, but this could help stop her repetitive thoughts so she could use other skills.
Helping patients identify skills that can help in the moment can help them feel supported and gain traction in other areas.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. She has no relevant financial disclosures
References
1. Rathus JH, Miller AL. DBT® Skills manual for adolescents. 2015. Guilford Press.
2. Guided Relaxation Exercises, Children’s Hospital of Philadelphia.
3. Vermont Center for Children, Youth, and Families: Staying Close While Keeping Your Distance.
The past year presented unprecedented challenges for many. In addition, mental health services have also been stretched to capacity. Anecdotally, some hospitals and emergency departments note that more youth have been presenting in mental health crises, and the severity of symptoms has also been higher. Safety planning is important, including working with patients to identify skills they can use in distress. Even those who do not experience suicidal thoughts may struggle with dysregulation or may use coping strategies that may not be the healthiest in the long term.
Within my practice, I see some families who are still waiting for an available therapist, or some may not wish to participate in therapy despite its being recommended. For these families, supporting them in using strategies that they may be willing and able to use in the moment to help them get through the moment of crisis can been helpful:
Case example (identifying details have been changed)
Emily is a 17-year-old girl who has a history of generalized anxiety disorder and obsessive-compulsive disorder. She has had multiple medication trials and a course of cognitive behavioral therapy when younger, with significant improvement in symptoms. She returns to clinic because of increased anxiety related to stressors of the pandemic. She wishes to not return to therapy because of feeling that she received maximal benefit and that further sessions would not be fruitful. However, she struggles with identifying what skills she can use, and her anxiety heightens significantly to near-panic and hyperventilating with even cursory exploration of triggers for her symptoms. Medications are also discussed during this appointment, and it is noted that it may take some time to see therapeutic effect. Of note, she reports no acute safety concerns. She has engaged in skin picking. No reported substance use. As she hyperventilates, she was asked to identify items in the room matching the colors of the rainbow in order. She was able to quickly do this, and then was asked to do it again. Afterward, she noted feeling much less anxious because it distracted her from her thoughts.
Distress tolerance skills can be very helpful to navigate getting through a crisis. When under stress, some may be more likely to engage in behaviors that are not helpful in the long term such as using avoidance; procrastinating; consuming tobacco, alcohol, or other substances; spending too much time on screens; or engaging in self-harm behaviors. While some of these activities may be okay in moderation, others are always harmful. At times, when encouraging patients to use skills with which they may be more familiar, e.g., deep breathing, progressive muscle relaxation, the response may be, “these don’t work!” It can be important to distinguish that the function of these skills is not to make someone feel good or to eliminate the stressor, but to “take some of the edge off” so they are less likely to slide into problematic behaviors. It can be beneficial to have multiple tools at one’s disposal because not all skills will always be effective or available.
TIPP skills (temperature, intense exercise, paced breathing, progressive muscle relaxation) are distress tolerance skills from dialectical behavioral therapy (DBT),1 which was initially developed to treat individuals with borderline personality disorder. More recently, the therapy modality has been applied to individuals who may struggle with emotion regulation for a variety of reasons. TIPP skills work quickly (within seconds to minutes) with the aim to decrease physiological arousal. They do not require a lot of thinking, and many are portable or easy to use. Given the speed of effect, these skills can also be used in lieu of p.r.n. medications or patients can be counseled about trying these instead of turning to substance use. The effect is brief (5-20 minutes), although this may lower the affective temperature sufficiently for someone to get through the intense moment or to be able to then utilize other skills that may require more cognitive reserves.
T – Temperature
Holding one’s breath and placing one’s face in cold water (above 50°) for 10-20 seconds to stimulate the diving response and decrease heart rate. Patients can repeat this up to 3 times. Alternatively, cold compresses or gel eye masks can be used.
I – Intense exercise
Aerobic exercise for 10-20 minutes. This can include running, jumping jacks, dancing to loud music in a way that feels intense. The parasympathetic nervous system (PNS) is activated for approximately 20 minutes after cessation of intense exercise.
P – Paced breathing
Decreasing rate of breathing, with each inhalation/exhalation cycle lasting 10-12 seconds and the exhale being longer than the inhale also activates the PNS.
P – Progressive muscle relaxation (PMR)
Sequentially tensing and relaxing muscles from head to toes. Having at least 5-10 minutes to perform this exercise is preferred.2 Children’s Hospital of Philadelphia offerssample PMR recordings.
Body scans can also be helpful. This practice differs from PMR in that it is a mindfulness practice noting body sensations without trying to change them. The University of Vermont offers some sample exercises.3
These skills were described to Emily. She noted that dunking her face in cold water was effective and it was reassuring knowing she had a tool to help her anxiety. She started to push herself to go outside to exercise. We additionally incorporated other distraction techniques such as identifying items from colors of the rainbow that were around her. She appreciated that she could even do this discreetly while at school. At times she had to do a couple of rounds, but this could help stop her repetitive thoughts so she could use other skills.
Helping patients identify skills that can help in the moment can help them feel supported and gain traction in other areas.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. She has no relevant financial disclosures
References
1. Rathus JH, Miller AL. DBT® Skills manual for adolescents. 2015. Guilford Press.
2. Guided Relaxation Exercises, Children’s Hospital of Philadelphia.
3. Vermont Center for Children, Youth, and Families: Staying Close While Keeping Your Distance.
The past year presented unprecedented challenges for many. In addition, mental health services have also been stretched to capacity. Anecdotally, some hospitals and emergency departments note that more youth have been presenting in mental health crises, and the severity of symptoms has also been higher. Safety planning is important, including working with patients to identify skills they can use in distress. Even those who do not experience suicidal thoughts may struggle with dysregulation or may use coping strategies that may not be the healthiest in the long term.
Within my practice, I see some families who are still waiting for an available therapist, or some may not wish to participate in therapy despite its being recommended. For these families, supporting them in using strategies that they may be willing and able to use in the moment to help them get through the moment of crisis can been helpful:
Case example (identifying details have been changed)
Emily is a 17-year-old girl who has a history of generalized anxiety disorder and obsessive-compulsive disorder. She has had multiple medication trials and a course of cognitive behavioral therapy when younger, with significant improvement in symptoms. She returns to clinic because of increased anxiety related to stressors of the pandemic. She wishes to not return to therapy because of feeling that she received maximal benefit and that further sessions would not be fruitful. However, she struggles with identifying what skills she can use, and her anxiety heightens significantly to near-panic and hyperventilating with even cursory exploration of triggers for her symptoms. Medications are also discussed during this appointment, and it is noted that it may take some time to see therapeutic effect. Of note, she reports no acute safety concerns. She has engaged in skin picking. No reported substance use. As she hyperventilates, she was asked to identify items in the room matching the colors of the rainbow in order. She was able to quickly do this, and then was asked to do it again. Afterward, she noted feeling much less anxious because it distracted her from her thoughts.
Distress tolerance skills can be very helpful to navigate getting through a crisis. When under stress, some may be more likely to engage in behaviors that are not helpful in the long term such as using avoidance; procrastinating; consuming tobacco, alcohol, or other substances; spending too much time on screens; or engaging in self-harm behaviors. While some of these activities may be okay in moderation, others are always harmful. At times, when encouraging patients to use skills with which they may be more familiar, e.g., deep breathing, progressive muscle relaxation, the response may be, “these don’t work!” It can be important to distinguish that the function of these skills is not to make someone feel good or to eliminate the stressor, but to “take some of the edge off” so they are less likely to slide into problematic behaviors. It can be beneficial to have multiple tools at one’s disposal because not all skills will always be effective or available.
TIPP skills (temperature, intense exercise, paced breathing, progressive muscle relaxation) are distress tolerance skills from dialectical behavioral therapy (DBT),1 which was initially developed to treat individuals with borderline personality disorder. More recently, the therapy modality has been applied to individuals who may struggle with emotion regulation for a variety of reasons. TIPP skills work quickly (within seconds to minutes) with the aim to decrease physiological arousal. They do not require a lot of thinking, and many are portable or easy to use. Given the speed of effect, these skills can also be used in lieu of p.r.n. medications or patients can be counseled about trying these instead of turning to substance use. The effect is brief (5-20 minutes), although this may lower the affective temperature sufficiently for someone to get through the intense moment or to be able to then utilize other skills that may require more cognitive reserves.
T – Temperature
Holding one’s breath and placing one’s face in cold water (above 50°) for 10-20 seconds to stimulate the diving response and decrease heart rate. Patients can repeat this up to 3 times. Alternatively, cold compresses or gel eye masks can be used.
I – Intense exercise
Aerobic exercise for 10-20 minutes. This can include running, jumping jacks, dancing to loud music in a way that feels intense. The parasympathetic nervous system (PNS) is activated for approximately 20 minutes after cessation of intense exercise.
P – Paced breathing
Decreasing rate of breathing, with each inhalation/exhalation cycle lasting 10-12 seconds and the exhale being longer than the inhale also activates the PNS.
P – Progressive muscle relaxation (PMR)
Sequentially tensing and relaxing muscles from head to toes. Having at least 5-10 minutes to perform this exercise is preferred.2 Children’s Hospital of Philadelphia offerssample PMR recordings.
Body scans can also be helpful. This practice differs from PMR in that it is a mindfulness practice noting body sensations without trying to change them. The University of Vermont offers some sample exercises.3
These skills were described to Emily. She noted that dunking her face in cold water was effective and it was reassuring knowing she had a tool to help her anxiety. She started to push herself to go outside to exercise. We additionally incorporated other distraction techniques such as identifying items from colors of the rainbow that were around her. She appreciated that she could even do this discreetly while at school. At times she had to do a couple of rounds, but this could help stop her repetitive thoughts so she could use other skills.
Helping patients identify skills that can help in the moment can help them feel supported and gain traction in other areas.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. She has no relevant financial disclosures
References
1. Rathus JH, Miller AL. DBT® Skills manual for adolescents. 2015. Guilford Press.
2. Guided Relaxation Exercises, Children’s Hospital of Philadelphia.
3. Vermont Center for Children, Youth, and Families: Staying Close While Keeping Your Distance.
Focus on youth concerns at well visits
Taking teens’ strengths, values, and dreams, into account through a previsit questionnaire was acceptable to them and may promote discussions with providers, based on data from 91 adolescents.
The American Academy of Pediatrics’ Bright Futures initiative recommends the use of a strength-based approach for adolescent well visits, but the extensive positive psychology inventories to identify teen strengths and values are impractical for the clinical visit setting, wrote Yidan Cao, MPH, of the Child Development through Primary Care at the University of Michigan, Ann Arbor, and colleagues. However, 76% of youth participating in focus groups responded that “using a confidential questionnaire about a teen’s strengths and goals before checkup visits would be a good addition to health care for teens,” the researchers said.
In a study presented in a poster session (#515) at the Pediatric Academic Societies annual meeting, the researchers recruited 91 community youth to participate in 13 focus groups related to teen depression and substance use. The age of the focus group participants ranged from 12 to 18 years, with an average of 15 years, 61.5% were female, and 1.1% identified as transgender. The racial breakdown was 51.6% White, 27.5% African American, 8.8% Asian, 2.2% Native American, 3.3% biracial, and 6.6% unknown.
The participants provided information on potential questionnaire items for an online previsit screening for well visits to assess strengths and identify values, goals, dream jobs, and life wishes.
Suggestions from the participants informed changes to the questionnaire, which included five categories: personal/social goals, goals for academics/training, strengths, values, and dream jobs.
The top endorsed personal goal of “to be happy” was chosen by 13.1% of the participants. The top academic goal was “get good grades” (45.5%). The top endorsed strength was “fitness/coordination/sports/physical activity” (22.9%), while the top value was caring and kindness (25.8%), and the top dream job category was health/medical (30.8%).
Key comments made by the youth participants for improving the previsit questionnaire included adding an option for “I can’t decide,” and allowing for multiple responses to avoid feeling pinned down or judged, the researchers noted.
The researchers highlighted one teen comment: “While I understand the purpose of limiting the participants to two answers, it is incredibly difficult to only choose two. Being limited to two very much restricts your understanding of our values. For example, I would’ve also liked to select ‘to do well in school’ and ‘to make a difference,’ but ‘being happy’ and ‘being loving to all those around me’ had to take precedent.”
The study was limited by not being fully generalizable to all teens, as other teens may hold views and beliefs that differ from those of the focus group participants, the researchers noted.
However, the findings support the value of a strength-based previsit questionnaire for adolescents, they said.
“Structured previsit data could facilitate relationship building and be actionable for assigning strength and resiliency building resources,” they noted. “A final strengths and goals questionnaire is now being piloted in computerized form contributing to decision supports for suggested teleprompters and associated resource options,” and future research may show the value of such previsit data for improved clinical process and outcomes of youth well visits, they concluded.
Recognize the uncertainty of adolescence
“Adolescents are at crossroads of identity, trying to figure out who they are, their goals and values,” said Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, in an interview. “Adolescence is also a critical time when teens have more control and choice over behaviors that impact their health, such as diet, exercise, substance use, and sexual activity. In this critical time period, clinicians can intervene on health-related behaviors and shape the trajectory of a teen’s life. However, to promote teen health, pediatricians need to have their patients’ trust, which can be hard to gain,” she emphasized.
“In my practice, I’ve found that teens often just want to be seen and heard,” said Dr. Curran. “Teens often have many adults in their life who focus on the ‘don’ts’ – don’t use drugs, don’t have sex, for example – and few that praise healthy behaviors or strengths, or seek to understand what is important to them. By listening to teens and understanding what’s important to them, we can then use motivational interviewing techniques to help create meaningful change in health-related behaviors. However, this takes time and investment, which is often in conflict with time pressures in the modern medical system.
“This study is useful because it examined the acceptability of a positive psychology questionnaire to be used at well visits when reviewed by youth, that could be used to streamline this important process,” said Dr. Curran.
“From my practice, I know that understanding a teen’s goals, values, and strengths is important – we do this daily in our practice when working with patients – but it was exciting to see that youth found it acceptable to do this via a previsit survey, which can potentially streamline well visits,” she noted.
The questionnaire is being developed as a pilot program, but more research is needed to determine the direct clinical impact, said Dr. Curran. “It will be important in the future to see if implementation of this questionnaire can be helpful in integrating this information into motivational interviewing and rapport building to help improve teens’ health outcomes.”
The study was supported in part by the National Institute on Drug Abuse and the National Institute of Mental Health. Two coauthors have a financial interest in the CHADIS online reporting program used in the study. Dr. Curran had no financial conflicts to disclose.
Taking teens’ strengths, values, and dreams, into account through a previsit questionnaire was acceptable to them and may promote discussions with providers, based on data from 91 adolescents.
The American Academy of Pediatrics’ Bright Futures initiative recommends the use of a strength-based approach for adolescent well visits, but the extensive positive psychology inventories to identify teen strengths and values are impractical for the clinical visit setting, wrote Yidan Cao, MPH, of the Child Development through Primary Care at the University of Michigan, Ann Arbor, and colleagues. However, 76% of youth participating in focus groups responded that “using a confidential questionnaire about a teen’s strengths and goals before checkup visits would be a good addition to health care for teens,” the researchers said.
In a study presented in a poster session (#515) at the Pediatric Academic Societies annual meeting, the researchers recruited 91 community youth to participate in 13 focus groups related to teen depression and substance use. The age of the focus group participants ranged from 12 to 18 years, with an average of 15 years, 61.5% were female, and 1.1% identified as transgender. The racial breakdown was 51.6% White, 27.5% African American, 8.8% Asian, 2.2% Native American, 3.3% biracial, and 6.6% unknown.
The participants provided information on potential questionnaire items for an online previsit screening for well visits to assess strengths and identify values, goals, dream jobs, and life wishes.
Suggestions from the participants informed changes to the questionnaire, which included five categories: personal/social goals, goals for academics/training, strengths, values, and dream jobs.
The top endorsed personal goal of “to be happy” was chosen by 13.1% of the participants. The top academic goal was “get good grades” (45.5%). The top endorsed strength was “fitness/coordination/sports/physical activity” (22.9%), while the top value was caring and kindness (25.8%), and the top dream job category was health/medical (30.8%).
Key comments made by the youth participants for improving the previsit questionnaire included adding an option for “I can’t decide,” and allowing for multiple responses to avoid feeling pinned down or judged, the researchers noted.
The researchers highlighted one teen comment: “While I understand the purpose of limiting the participants to two answers, it is incredibly difficult to only choose two. Being limited to two very much restricts your understanding of our values. For example, I would’ve also liked to select ‘to do well in school’ and ‘to make a difference,’ but ‘being happy’ and ‘being loving to all those around me’ had to take precedent.”
The study was limited by not being fully generalizable to all teens, as other teens may hold views and beliefs that differ from those of the focus group participants, the researchers noted.
However, the findings support the value of a strength-based previsit questionnaire for adolescents, they said.
“Structured previsit data could facilitate relationship building and be actionable for assigning strength and resiliency building resources,” they noted. “A final strengths and goals questionnaire is now being piloted in computerized form contributing to decision supports for suggested teleprompters and associated resource options,” and future research may show the value of such previsit data for improved clinical process and outcomes of youth well visits, they concluded.
Recognize the uncertainty of adolescence
“Adolescents are at crossroads of identity, trying to figure out who they are, their goals and values,” said Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, in an interview. “Adolescence is also a critical time when teens have more control and choice over behaviors that impact their health, such as diet, exercise, substance use, and sexual activity. In this critical time period, clinicians can intervene on health-related behaviors and shape the trajectory of a teen’s life. However, to promote teen health, pediatricians need to have their patients’ trust, which can be hard to gain,” she emphasized.
“In my practice, I’ve found that teens often just want to be seen and heard,” said Dr. Curran. “Teens often have many adults in their life who focus on the ‘don’ts’ – don’t use drugs, don’t have sex, for example – and few that praise healthy behaviors or strengths, or seek to understand what is important to them. By listening to teens and understanding what’s important to them, we can then use motivational interviewing techniques to help create meaningful change in health-related behaviors. However, this takes time and investment, which is often in conflict with time pressures in the modern medical system.
“This study is useful because it examined the acceptability of a positive psychology questionnaire to be used at well visits when reviewed by youth, that could be used to streamline this important process,” said Dr. Curran.
“From my practice, I know that understanding a teen’s goals, values, and strengths is important – we do this daily in our practice when working with patients – but it was exciting to see that youth found it acceptable to do this via a previsit survey, which can potentially streamline well visits,” she noted.
The questionnaire is being developed as a pilot program, but more research is needed to determine the direct clinical impact, said Dr. Curran. “It will be important in the future to see if implementation of this questionnaire can be helpful in integrating this information into motivational interviewing and rapport building to help improve teens’ health outcomes.”
The study was supported in part by the National Institute on Drug Abuse and the National Institute of Mental Health. Two coauthors have a financial interest in the CHADIS online reporting program used in the study. Dr. Curran had no financial conflicts to disclose.
Taking teens’ strengths, values, and dreams, into account through a previsit questionnaire was acceptable to them and may promote discussions with providers, based on data from 91 adolescents.
The American Academy of Pediatrics’ Bright Futures initiative recommends the use of a strength-based approach for adolescent well visits, but the extensive positive psychology inventories to identify teen strengths and values are impractical for the clinical visit setting, wrote Yidan Cao, MPH, of the Child Development through Primary Care at the University of Michigan, Ann Arbor, and colleagues. However, 76% of youth participating in focus groups responded that “using a confidential questionnaire about a teen’s strengths and goals before checkup visits would be a good addition to health care for teens,” the researchers said.
In a study presented in a poster session (#515) at the Pediatric Academic Societies annual meeting, the researchers recruited 91 community youth to participate in 13 focus groups related to teen depression and substance use. The age of the focus group participants ranged from 12 to 18 years, with an average of 15 years, 61.5% were female, and 1.1% identified as transgender. The racial breakdown was 51.6% White, 27.5% African American, 8.8% Asian, 2.2% Native American, 3.3% biracial, and 6.6% unknown.
The participants provided information on potential questionnaire items for an online previsit screening for well visits to assess strengths and identify values, goals, dream jobs, and life wishes.
Suggestions from the participants informed changes to the questionnaire, which included five categories: personal/social goals, goals for academics/training, strengths, values, and dream jobs.
The top endorsed personal goal of “to be happy” was chosen by 13.1% of the participants. The top academic goal was “get good grades” (45.5%). The top endorsed strength was “fitness/coordination/sports/physical activity” (22.9%), while the top value was caring and kindness (25.8%), and the top dream job category was health/medical (30.8%).
Key comments made by the youth participants for improving the previsit questionnaire included adding an option for “I can’t decide,” and allowing for multiple responses to avoid feeling pinned down or judged, the researchers noted.
The researchers highlighted one teen comment: “While I understand the purpose of limiting the participants to two answers, it is incredibly difficult to only choose two. Being limited to two very much restricts your understanding of our values. For example, I would’ve also liked to select ‘to do well in school’ and ‘to make a difference,’ but ‘being happy’ and ‘being loving to all those around me’ had to take precedent.”
The study was limited by not being fully generalizable to all teens, as other teens may hold views and beliefs that differ from those of the focus group participants, the researchers noted.
However, the findings support the value of a strength-based previsit questionnaire for adolescents, they said.
“Structured previsit data could facilitate relationship building and be actionable for assigning strength and resiliency building resources,” they noted. “A final strengths and goals questionnaire is now being piloted in computerized form contributing to decision supports for suggested teleprompters and associated resource options,” and future research may show the value of such previsit data for improved clinical process and outcomes of youth well visits, they concluded.
Recognize the uncertainty of adolescence
“Adolescents are at crossroads of identity, trying to figure out who they are, their goals and values,” said Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, in an interview. “Adolescence is also a critical time when teens have more control and choice over behaviors that impact their health, such as diet, exercise, substance use, and sexual activity. In this critical time period, clinicians can intervene on health-related behaviors and shape the trajectory of a teen’s life. However, to promote teen health, pediatricians need to have their patients’ trust, which can be hard to gain,” she emphasized.
“In my practice, I’ve found that teens often just want to be seen and heard,” said Dr. Curran. “Teens often have many adults in their life who focus on the ‘don’ts’ – don’t use drugs, don’t have sex, for example – and few that praise healthy behaviors or strengths, or seek to understand what is important to them. By listening to teens and understanding what’s important to them, we can then use motivational interviewing techniques to help create meaningful change in health-related behaviors. However, this takes time and investment, which is often in conflict with time pressures in the modern medical system.
“This study is useful because it examined the acceptability of a positive psychology questionnaire to be used at well visits when reviewed by youth, that could be used to streamline this important process,” said Dr. Curran.
“From my practice, I know that understanding a teen’s goals, values, and strengths is important – we do this daily in our practice when working with patients – but it was exciting to see that youth found it acceptable to do this via a previsit survey, which can potentially streamline well visits,” she noted.
The questionnaire is being developed as a pilot program, but more research is needed to determine the direct clinical impact, said Dr. Curran. “It will be important in the future to see if implementation of this questionnaire can be helpful in integrating this information into motivational interviewing and rapport building to help improve teens’ health outcomes.”
The study was supported in part by the National Institute on Drug Abuse and the National Institute of Mental Health. Two coauthors have a financial interest in the CHADIS online reporting program used in the study. Dr. Curran had no financial conflicts to disclose.
FROM PAS 2021
Genital skin exams in girls: Conduct with care, look for signs of abuse
at the American Academy of Dermatology Virtual Meeting Experience.
“One in four adult women report being childhood victims of sexual abuse, which is just a staggering number. This is an opportunity for us to identify these patients early and give them the terminology to be able to report what is happening to them,” said pediatric dermatologist Kalyani Marathe, MD, MPH, director of the division of dermatology at Cincinnati Children’s Hospital. “We also have the chance to give them a sense of agency over their bodies.”
Dr. Marathe offered the following recommendations when performing a genital skin exam:
- Make sure a “chaperone” is present. “Chaperones are a must when you’re examining children and teens,” she said. “Ask whom they prefer. For prepubertal children, you’re going to usually use the parent who’s there with them. If the parent is their father, they might ask him to step behind the curtain, in which case you can bring over your nurse or medical assistant.” Teens may ask either parent to step out of the room, she said. In that case, a nurse, medical assistant, resident, or trainee can fill in. “If you have male residents or trainees with you and the patient really does not want to be examined by a male, honor their request. Do not force them.”
- Explain why the exam is being performed. Make sure the patient understands why she is being seen, Dr. Marathe advised. For example, say something like “your pediatrician told us that you have an itchy area” or “your mom told us that there’s some loss of color in that area, that you’re having a problem there.” She added that it’s helpful to explain the type of doctor you are, with a comment such as the following: “We’re examining you because we’re doctors who specialize in skin. ... We want to help you feel better and make sure that your skin heals and is healthy.”
- Ask both the child and the parent for permission to perform the exam. While this may seem trivial, “it’s very, very important in setting the right tone for the encounter,” she said. “If the child says yes, we turn to the mom and say: ‘Mom, is it okay for us to do this exam today?’ You can see visible relief on the part of the parent, and as the parent relaxes, the child relaxes. Just saying those few things really makes the encounter so much smoother.” However, “if they say no, you have to honor the response. ... You say: ‘Okay, we’re not going to do the exam today,” and see the patient in a few weeks. If it’s urgent, an exam under anesthesia may be an option, she added.
- Talk to the child about the terms they use for private parts. It can be helpful to ask: “Do you have any terms for your private area?” According to Dr. Marathe, “this is a good chance to educate them on the terms vulva and vagina since they may be using other terminology. Making sure that they have the correct terms will actually help patients identify and report abuse earlier.” Dr. Marathe recalled that a colleague had a patient who’d been calling her private area “pound cake” and had been “reporting to her teacher that someone had been touching her ‘pound cake.’ Her teacher did not know what she meant by that, and this led to a great delay in her childhood abuse being reported.”
- Talk about what will happen during the exam. “I like to show them any instruments that we’re going to be using,” Dr. Marathe said. “If we’re using a flashlight, for example, I like to show them a picture [of a flashlight] or show them that flashlight. If we’re using a camera to do digital photography, show them that. If we’re going to be using a Q-tip or a swab to demonstrate anything or to take a culture, I like to show them that beforehand to make sure that they know what we’re doing.” In regard to photography, “make sure the parent and child know where the photos are going to go, who’s going to see them, what are they going to be used for. If they’re going to be used for educational purposes, make sure they have given explicit permission for that and they know they’ll be deidentified.”
- Make it clear that the exam won’t be painful. It’s important to put both the patient and the parent at ease on this front, Dr. Marathe said. “A lot of parents are concerned that we’re going to do a speculum exam in their prepubertal child. So make sure that it’s clarified ahead of time that we’re not going to be doing a speculum exam.”
Commenting on this topic, Tor Shwayder, MD, a pediatric dermatologist at Henry Ford Health System, Detroit, urged colleagues to take action if they feel suspicious about a possible sign of child abuse, even if they’re far from certain that anything is wrong. “Don’t ignore those feelings in the back of the brain,” he said in an interview.
Most states have child-abuse hotlines for medical professionals, and major hospitals will have child-abuse teams, Dr. Shwayder said. He urged dermatologists to take advantage of these resources when appropriate. “The professionals on the other side of the 800 number or at the hospital will help you. You don’t have to decide immediately whether this is child abuse. You just need to have a suspicion.”
Dr. Marathe and Dr. Shwayder report no disclosures.
at the American Academy of Dermatology Virtual Meeting Experience.
“One in four adult women report being childhood victims of sexual abuse, which is just a staggering number. This is an opportunity for us to identify these patients early and give them the terminology to be able to report what is happening to them,” said pediatric dermatologist Kalyani Marathe, MD, MPH, director of the division of dermatology at Cincinnati Children’s Hospital. “We also have the chance to give them a sense of agency over their bodies.”
Dr. Marathe offered the following recommendations when performing a genital skin exam:
- Make sure a “chaperone” is present. “Chaperones are a must when you’re examining children and teens,” she said. “Ask whom they prefer. For prepubertal children, you’re going to usually use the parent who’s there with them. If the parent is their father, they might ask him to step behind the curtain, in which case you can bring over your nurse or medical assistant.” Teens may ask either parent to step out of the room, she said. In that case, a nurse, medical assistant, resident, or trainee can fill in. “If you have male residents or trainees with you and the patient really does not want to be examined by a male, honor their request. Do not force them.”
- Explain why the exam is being performed. Make sure the patient understands why she is being seen, Dr. Marathe advised. For example, say something like “your pediatrician told us that you have an itchy area” or “your mom told us that there’s some loss of color in that area, that you’re having a problem there.” She added that it’s helpful to explain the type of doctor you are, with a comment such as the following: “We’re examining you because we’re doctors who specialize in skin. ... We want to help you feel better and make sure that your skin heals and is healthy.”
- Ask both the child and the parent for permission to perform the exam. While this may seem trivial, “it’s very, very important in setting the right tone for the encounter,” she said. “If the child says yes, we turn to the mom and say: ‘Mom, is it okay for us to do this exam today?’ You can see visible relief on the part of the parent, and as the parent relaxes, the child relaxes. Just saying those few things really makes the encounter so much smoother.” However, “if they say no, you have to honor the response. ... You say: ‘Okay, we’re not going to do the exam today,” and see the patient in a few weeks. If it’s urgent, an exam under anesthesia may be an option, she added.
- Talk to the child about the terms they use for private parts. It can be helpful to ask: “Do you have any terms for your private area?” According to Dr. Marathe, “this is a good chance to educate them on the terms vulva and vagina since they may be using other terminology. Making sure that they have the correct terms will actually help patients identify and report abuse earlier.” Dr. Marathe recalled that a colleague had a patient who’d been calling her private area “pound cake” and had been “reporting to her teacher that someone had been touching her ‘pound cake.’ Her teacher did not know what she meant by that, and this led to a great delay in her childhood abuse being reported.”
- Talk about what will happen during the exam. “I like to show them any instruments that we’re going to be using,” Dr. Marathe said. “If we’re using a flashlight, for example, I like to show them a picture [of a flashlight] or show them that flashlight. If we’re using a camera to do digital photography, show them that. If we’re going to be using a Q-tip or a swab to demonstrate anything or to take a culture, I like to show them that beforehand to make sure that they know what we’re doing.” In regard to photography, “make sure the parent and child know where the photos are going to go, who’s going to see them, what are they going to be used for. If they’re going to be used for educational purposes, make sure they have given explicit permission for that and they know they’ll be deidentified.”
- Make it clear that the exam won’t be painful. It’s important to put both the patient and the parent at ease on this front, Dr. Marathe said. “A lot of parents are concerned that we’re going to do a speculum exam in their prepubertal child. So make sure that it’s clarified ahead of time that we’re not going to be doing a speculum exam.”
Commenting on this topic, Tor Shwayder, MD, a pediatric dermatologist at Henry Ford Health System, Detroit, urged colleagues to take action if they feel suspicious about a possible sign of child abuse, even if they’re far from certain that anything is wrong. “Don’t ignore those feelings in the back of the brain,” he said in an interview.
Most states have child-abuse hotlines for medical professionals, and major hospitals will have child-abuse teams, Dr. Shwayder said. He urged dermatologists to take advantage of these resources when appropriate. “The professionals on the other side of the 800 number or at the hospital will help you. You don’t have to decide immediately whether this is child abuse. You just need to have a suspicion.”
Dr. Marathe and Dr. Shwayder report no disclosures.
at the American Academy of Dermatology Virtual Meeting Experience.
“One in four adult women report being childhood victims of sexual abuse, which is just a staggering number. This is an opportunity for us to identify these patients early and give them the terminology to be able to report what is happening to them,” said pediatric dermatologist Kalyani Marathe, MD, MPH, director of the division of dermatology at Cincinnati Children’s Hospital. “We also have the chance to give them a sense of agency over their bodies.”
Dr. Marathe offered the following recommendations when performing a genital skin exam:
- Make sure a “chaperone” is present. “Chaperones are a must when you’re examining children and teens,” she said. “Ask whom they prefer. For prepubertal children, you’re going to usually use the parent who’s there with them. If the parent is their father, they might ask him to step behind the curtain, in which case you can bring over your nurse or medical assistant.” Teens may ask either parent to step out of the room, she said. In that case, a nurse, medical assistant, resident, or trainee can fill in. “If you have male residents or trainees with you and the patient really does not want to be examined by a male, honor their request. Do not force them.”
- Explain why the exam is being performed. Make sure the patient understands why she is being seen, Dr. Marathe advised. For example, say something like “your pediatrician told us that you have an itchy area” or “your mom told us that there’s some loss of color in that area, that you’re having a problem there.” She added that it’s helpful to explain the type of doctor you are, with a comment such as the following: “We’re examining you because we’re doctors who specialize in skin. ... We want to help you feel better and make sure that your skin heals and is healthy.”
- Ask both the child and the parent for permission to perform the exam. While this may seem trivial, “it’s very, very important in setting the right tone for the encounter,” she said. “If the child says yes, we turn to the mom and say: ‘Mom, is it okay for us to do this exam today?’ You can see visible relief on the part of the parent, and as the parent relaxes, the child relaxes. Just saying those few things really makes the encounter so much smoother.” However, “if they say no, you have to honor the response. ... You say: ‘Okay, we’re not going to do the exam today,” and see the patient in a few weeks. If it’s urgent, an exam under anesthesia may be an option, she added.
- Talk to the child about the terms they use for private parts. It can be helpful to ask: “Do you have any terms for your private area?” According to Dr. Marathe, “this is a good chance to educate them on the terms vulva and vagina since they may be using other terminology. Making sure that they have the correct terms will actually help patients identify and report abuse earlier.” Dr. Marathe recalled that a colleague had a patient who’d been calling her private area “pound cake” and had been “reporting to her teacher that someone had been touching her ‘pound cake.’ Her teacher did not know what she meant by that, and this led to a great delay in her childhood abuse being reported.”
- Talk about what will happen during the exam. “I like to show them any instruments that we’re going to be using,” Dr. Marathe said. “If we’re using a flashlight, for example, I like to show them a picture [of a flashlight] or show them that flashlight. If we’re using a camera to do digital photography, show them that. If we’re going to be using a Q-tip or a swab to demonstrate anything or to take a culture, I like to show them that beforehand to make sure that they know what we’re doing.” In regard to photography, “make sure the parent and child know where the photos are going to go, who’s going to see them, what are they going to be used for. If they’re going to be used for educational purposes, make sure they have given explicit permission for that and they know they’ll be deidentified.”
- Make it clear that the exam won’t be painful. It’s important to put both the patient and the parent at ease on this front, Dr. Marathe said. “A lot of parents are concerned that we’re going to do a speculum exam in their prepubertal child. So make sure that it’s clarified ahead of time that we’re not going to be doing a speculum exam.”
Commenting on this topic, Tor Shwayder, MD, a pediatric dermatologist at Henry Ford Health System, Detroit, urged colleagues to take action if they feel suspicious about a possible sign of child abuse, even if they’re far from certain that anything is wrong. “Don’t ignore those feelings in the back of the brain,” he said in an interview.
Most states have child-abuse hotlines for medical professionals, and major hospitals will have child-abuse teams, Dr. Shwayder said. He urged dermatologists to take advantage of these resources when appropriate. “The professionals on the other side of the 800 number or at the hospital will help you. You don’t have to decide immediately whether this is child abuse. You just need to have a suspicion.”
Dr. Marathe and Dr. Shwayder report no disclosures.
FROM AAD VMX 2021
How to utilize the updated PHM Core Competencies
Converge 2021 session
Making The Pediatric Hospital Medicine Core Competencies Work for You
Presenters
Erin Fisher, MD, MHM, FAAP; Sandra Gage, MD, PhD, SFHM, FAAP; Jennifer Maniscalco, MD, MPH, MAcM, FAAP; Sofia Teferi, MD, SFHM, FAAP
Session summary
The Pediatric Hospital Medicine (PHM) Core Competencies were originally published in the Journal of Hospital Medicine in 2010, and created a framework for graduate and continuing medical education, reflecting the roles and expectations for all pediatric hospitalists in the United States. Since that time, the field of PHM, scope of practice, and roles of hospitalists has evolved, making a substantial update to this dossier necessary.
The 2020 PHM Core Competencies consist of four sections, including common clinical diagnoses and conditions, specialized services, core skills, and the health care system. The four topics are covered in 66 chapters, which were updated or created for the present version.
The Core Competencies have many practical applications, including teaching or curriculum development, which may be used by trainees as well as PHM providers. The speakers gave real-world examples of the competencies’ application to evaluations, and the continuum of knowledge, skills, attitudes, and system implementation in the development of a trainee from student to practicing hospitalist. Trainees’ knowledge gaps can be identified using the competencies, and utilization of the provided compendium will help identify sources that can aid in teaching.
Professional development is an excellent way to utilize the Core Competencies. Division directors may identify a needed area for improvement and the competencies can serve as a road map for establishing goals, plan development, and analysis of results of the intervention. They are also a great resource for PHM board prep. Although the competencies were not developed specifically for the PHM boards, they do contain all 13 PHM content domains set forth by the American Board of Pediatrics for PHM.
The Core Competencies can also be used to justify service line needs and resources in discussions with administration. For instance, if one is a pediatric hospitalist at a community hospital and asked to take over the newborn nursery, the competencies can be used to get buy-in from the group, as a guide for additional training, to provide a framework for development of practice pathways, and to request resources needed.
The Pediatric Core Competencies are a great resource for pediatric hospitalists and group leaders with many uses, from board preparation to education and professional development. They provide a framework for improvement of knowledge, skills, and attitudes within an organization.
Key takeaways
- Given a change in scope of practice of pediatric hospitalists over the past 10 years, the PHM Core Competencies were updated and published in the Journal of Hospital Medicine in 2020.
- The Core Competencies have many practical applications including education, curriculum development, professional development, and PHM board preparation.
- The Core Competencies provide a framework for improvement of knowledge, skills, and attitudes within an organization.
Dr. Schwenk is a pediatric hospitalist at Norton Children’s Hospital in Louisville, Ky., where he serves as a medical director of inpatient services. He is an associate professor of pediatrics at the University of Louisville School of Medicine. He is a Senior Fellow of Hospital Medicine and has served on the executive council of the Pediatrics Special Interest Group and the Annual Meeting Committee for SHM Converge.
Converge 2021 session
Making The Pediatric Hospital Medicine Core Competencies Work for You
Presenters
Erin Fisher, MD, MHM, FAAP; Sandra Gage, MD, PhD, SFHM, FAAP; Jennifer Maniscalco, MD, MPH, MAcM, FAAP; Sofia Teferi, MD, SFHM, FAAP
Session summary
The Pediatric Hospital Medicine (PHM) Core Competencies were originally published in the Journal of Hospital Medicine in 2010, and created a framework for graduate and continuing medical education, reflecting the roles and expectations for all pediatric hospitalists in the United States. Since that time, the field of PHM, scope of practice, and roles of hospitalists has evolved, making a substantial update to this dossier necessary.
The 2020 PHM Core Competencies consist of four sections, including common clinical diagnoses and conditions, specialized services, core skills, and the health care system. The four topics are covered in 66 chapters, which were updated or created for the present version.
The Core Competencies have many practical applications, including teaching or curriculum development, which may be used by trainees as well as PHM providers. The speakers gave real-world examples of the competencies’ application to evaluations, and the continuum of knowledge, skills, attitudes, and system implementation in the development of a trainee from student to practicing hospitalist. Trainees’ knowledge gaps can be identified using the competencies, and utilization of the provided compendium will help identify sources that can aid in teaching.
Professional development is an excellent way to utilize the Core Competencies. Division directors may identify a needed area for improvement and the competencies can serve as a road map for establishing goals, plan development, and analysis of results of the intervention. They are also a great resource for PHM board prep. Although the competencies were not developed specifically for the PHM boards, they do contain all 13 PHM content domains set forth by the American Board of Pediatrics for PHM.
The Core Competencies can also be used to justify service line needs and resources in discussions with administration. For instance, if one is a pediatric hospitalist at a community hospital and asked to take over the newborn nursery, the competencies can be used to get buy-in from the group, as a guide for additional training, to provide a framework for development of practice pathways, and to request resources needed.
The Pediatric Core Competencies are a great resource for pediatric hospitalists and group leaders with many uses, from board preparation to education and professional development. They provide a framework for improvement of knowledge, skills, and attitudes within an organization.
Key takeaways
- Given a change in scope of practice of pediatric hospitalists over the past 10 years, the PHM Core Competencies were updated and published in the Journal of Hospital Medicine in 2020.
- The Core Competencies have many practical applications including education, curriculum development, professional development, and PHM board preparation.
- The Core Competencies provide a framework for improvement of knowledge, skills, and attitudes within an organization.
Dr. Schwenk is a pediatric hospitalist at Norton Children’s Hospital in Louisville, Ky., where he serves as a medical director of inpatient services. He is an associate professor of pediatrics at the University of Louisville School of Medicine. He is a Senior Fellow of Hospital Medicine and has served on the executive council of the Pediatrics Special Interest Group and the Annual Meeting Committee for SHM Converge.
Converge 2021 session
Making The Pediatric Hospital Medicine Core Competencies Work for You
Presenters
Erin Fisher, MD, MHM, FAAP; Sandra Gage, MD, PhD, SFHM, FAAP; Jennifer Maniscalco, MD, MPH, MAcM, FAAP; Sofia Teferi, MD, SFHM, FAAP
Session summary
The Pediatric Hospital Medicine (PHM) Core Competencies were originally published in the Journal of Hospital Medicine in 2010, and created a framework for graduate and continuing medical education, reflecting the roles and expectations for all pediatric hospitalists in the United States. Since that time, the field of PHM, scope of practice, and roles of hospitalists has evolved, making a substantial update to this dossier necessary.
The 2020 PHM Core Competencies consist of four sections, including common clinical diagnoses and conditions, specialized services, core skills, and the health care system. The four topics are covered in 66 chapters, which were updated or created for the present version.
The Core Competencies have many practical applications, including teaching or curriculum development, which may be used by trainees as well as PHM providers. The speakers gave real-world examples of the competencies’ application to evaluations, and the continuum of knowledge, skills, attitudes, and system implementation in the development of a trainee from student to practicing hospitalist. Trainees’ knowledge gaps can be identified using the competencies, and utilization of the provided compendium will help identify sources that can aid in teaching.
Professional development is an excellent way to utilize the Core Competencies. Division directors may identify a needed area for improvement and the competencies can serve as a road map for establishing goals, plan development, and analysis of results of the intervention. They are also a great resource for PHM board prep. Although the competencies were not developed specifically for the PHM boards, they do contain all 13 PHM content domains set forth by the American Board of Pediatrics for PHM.
The Core Competencies can also be used to justify service line needs and resources in discussions with administration. For instance, if one is a pediatric hospitalist at a community hospital and asked to take over the newborn nursery, the competencies can be used to get buy-in from the group, as a guide for additional training, to provide a framework for development of practice pathways, and to request resources needed.
The Pediatric Core Competencies are a great resource for pediatric hospitalists and group leaders with many uses, from board preparation to education and professional development. They provide a framework for improvement of knowledge, skills, and attitudes within an organization.
Key takeaways
- Given a change in scope of practice of pediatric hospitalists over the past 10 years, the PHM Core Competencies were updated and published in the Journal of Hospital Medicine in 2020.
- The Core Competencies have many practical applications including education, curriculum development, professional development, and PHM board preparation.
- The Core Competencies provide a framework for improvement of knowledge, skills, and attitudes within an organization.
Dr. Schwenk is a pediatric hospitalist at Norton Children’s Hospital in Louisville, Ky., where he serves as a medical director of inpatient services. He is an associate professor of pediatrics at the University of Louisville School of Medicine. He is a Senior Fellow of Hospital Medicine and has served on the executive council of the Pediatrics Special Interest Group and the Annual Meeting Committee for SHM Converge.
FROM SHM CONVERGE 2021
High body fat tied to slowed breast maturation in girls with obesity
Girls in late stages of puberty who had elevated levels of body fat showed unusually high levels of several hormones that could contribute to an earlier age of menarche and also slow breast development, according to data from 90 girls who spanned a wide range of body fat in the first longitudinal study to examine links between fat volume, levels of reproductive hormones, and clinical manifestations of hormone action during puberty.
The results showed that girls with greater body fat had higher levels of follicle stimulating hormone, inhibin B, estrone, and certain male-like reproductive hormones, and that this pattern “is specifically tied to body fat,” said Natalie D. Shaw, MD, senior investigator for the study, reported at the annual meeting of the Endocrine Society.
“We found that total body fat is associated with the timing of menarche, as others have reported for body weight,” she noted. The new findings showed that every 1% rise in percent total body fat linked with a significant 3% rise in the likelihood of menarche, menstrual onset. In the new study the average age of menarche was 11.7 years among the overweight or obese girls and 12.8 years among those with normal weights.
But the study’s unique use of an average of about three serial ultrasound breast examinations of each subject during an average 4 years of follow-up also showed that higher levels of body fat linked with slowed breast development in later stages, specifically maturation from stage D to stages D/E and E.
For example, girls with 33% body fat spent an average of 8.2 months in stage D, which stretched to an average of 11.2 months among girls with 38% body fat, reported Madison T. Ortega, a researcher with the Pediatric Endocrinology Group of the National Institute of Environmental Health Sciences in Research Triangle Park, N.C., who presented the report at the meeting.
Ultrasound shows what inspection can’t
Results from “several studies have shown earlier breast development in overweight and obese girls by inspection and palpation,” but the new findings from ultrasound examination provide more nuance about the structural breast changes actually occurring in these adolescents, said Dr. Shaw, who heads the Pediatric Endocrinology Group. The current study “was not designed to capture the onset of breast development,” and “it is possible that increased androgens or insulin resistance in girls with higher body fat interferes with normal breast development,” she explained in an interview.
“The authors showed that the timing and progress of early stages of puberty were not earlier in overweight or obese girls. Luteinizing hormone, the indicator of neuroendocrine pubertal onset, and timing of early stages of breast development were the same in all weight groups. The authors also discovered falsely advanced Turner breast stage designations with ultrasonography in some girls with obesity. This might suggest that prior findings in epidemiologic studies of an earlier start to puberty based mostly on breast development stages identified by self-reported inspection and, rarely, palpation, may have been biased by breast adipose tissue,” said Christine M. Burt Solorzano, MD, a pediatric endocrinologist at the University of Virginia in Charlottesville, who was not involved in the study.
“Development of increased follicle-stimulating hormone in late puberty suggests that pubertal tempo, not onset, may be increased in girls with obesity, and goes along with earlier menarche. Their finding of increased androgen levels during mid to late puberty with obesity are consistent with prior findings,” including work published Dr. Burt Solorzano and her associates, she noted. “Delayed timing of advanced breast morphology was unexpected and may reflect relatively lower levels of progesterone in girls with obesity,” a hormone necessary for later stages of breast maturation.
The findings “reinforce that early breast development in the setting of obesity may in fact reflect adipose tissue and not be a true representation of neuroendocrine precocious puberty,” Dr. Burt Solorzano said in an interview. The findings “also suggest that pubertal initiation may not happen earlier in girls with obesity, as has been thought, but rather the tempo of puberty may be more rapid, leading to earlier menarche.”
A possible step toward PCOS
The long-term clinical consequences of the hormonal state linked with overweight and obesity “are unknown,” said Dr. Shaw. However, she and her coworkers followed a few of their subjects with elevated testosterone levels during midpuberty, and several developed signs of early polycystic ovarian syndrome (PCOS) such as irregular menstrual cycles, acne, and hirsutism. “It may be possible to identify girls at high risk for PCOS before menarche,” she suggested.
Dr. Burt Solorzano agreed that delayed breast development in girls with high levels of body fat may reflect inadequate progesterone production, which when coupled with an obesity-related excess level of androgens could put girls at risk for chronic anovulation and later PCOS.
“Weight management during childhood and early puberty may mitigate the adverse effects of obesity on pubertal progression and avoid some of the lifetime complications related to early menarche,” Dr. Burt Solorzano said.
The Body Weight and Puberty Study enrolled 36 girls who were overweight or obese and 54 girls with normal weight. They averaged 11 years of age, with a range of 8.2-14.7 years. Average percent body fat was 41% among the overweight or obese girls and 27% among those with normal weight. The results reported by Ms. Ortega also appeared in a report published Feb 22, 2021 (J Clin Endocrinol Metab. doi: 10.1210/clinem/dgab092).
Dr. Shaw, Ms. Ortega, and Dr. Burt Solorzano had no disclosures.
Girls in late stages of puberty who had elevated levels of body fat showed unusually high levels of several hormones that could contribute to an earlier age of menarche and also slow breast development, according to data from 90 girls who spanned a wide range of body fat in the first longitudinal study to examine links between fat volume, levels of reproductive hormones, and clinical manifestations of hormone action during puberty.
The results showed that girls with greater body fat had higher levels of follicle stimulating hormone, inhibin B, estrone, and certain male-like reproductive hormones, and that this pattern “is specifically tied to body fat,” said Natalie D. Shaw, MD, senior investigator for the study, reported at the annual meeting of the Endocrine Society.
“We found that total body fat is associated with the timing of menarche, as others have reported for body weight,” she noted. The new findings showed that every 1% rise in percent total body fat linked with a significant 3% rise in the likelihood of menarche, menstrual onset. In the new study the average age of menarche was 11.7 years among the overweight or obese girls and 12.8 years among those with normal weights.
But the study’s unique use of an average of about three serial ultrasound breast examinations of each subject during an average 4 years of follow-up also showed that higher levels of body fat linked with slowed breast development in later stages, specifically maturation from stage D to stages D/E and E.
For example, girls with 33% body fat spent an average of 8.2 months in stage D, which stretched to an average of 11.2 months among girls with 38% body fat, reported Madison T. Ortega, a researcher with the Pediatric Endocrinology Group of the National Institute of Environmental Health Sciences in Research Triangle Park, N.C., who presented the report at the meeting.
Ultrasound shows what inspection can’t
Results from “several studies have shown earlier breast development in overweight and obese girls by inspection and palpation,” but the new findings from ultrasound examination provide more nuance about the structural breast changes actually occurring in these adolescents, said Dr. Shaw, who heads the Pediatric Endocrinology Group. The current study “was not designed to capture the onset of breast development,” and “it is possible that increased androgens or insulin resistance in girls with higher body fat interferes with normal breast development,” she explained in an interview.
“The authors showed that the timing and progress of early stages of puberty were not earlier in overweight or obese girls. Luteinizing hormone, the indicator of neuroendocrine pubertal onset, and timing of early stages of breast development were the same in all weight groups. The authors also discovered falsely advanced Turner breast stage designations with ultrasonography in some girls with obesity. This might suggest that prior findings in epidemiologic studies of an earlier start to puberty based mostly on breast development stages identified by self-reported inspection and, rarely, palpation, may have been biased by breast adipose tissue,” said Christine M. Burt Solorzano, MD, a pediatric endocrinologist at the University of Virginia in Charlottesville, who was not involved in the study.
“Development of increased follicle-stimulating hormone in late puberty suggests that pubertal tempo, not onset, may be increased in girls with obesity, and goes along with earlier menarche. Their finding of increased androgen levels during mid to late puberty with obesity are consistent with prior findings,” including work published Dr. Burt Solorzano and her associates, she noted. “Delayed timing of advanced breast morphology was unexpected and may reflect relatively lower levels of progesterone in girls with obesity,” a hormone necessary for later stages of breast maturation.
The findings “reinforce that early breast development in the setting of obesity may in fact reflect adipose tissue and not be a true representation of neuroendocrine precocious puberty,” Dr. Burt Solorzano said in an interview. The findings “also suggest that pubertal initiation may not happen earlier in girls with obesity, as has been thought, but rather the tempo of puberty may be more rapid, leading to earlier menarche.”
A possible step toward PCOS
The long-term clinical consequences of the hormonal state linked with overweight and obesity “are unknown,” said Dr. Shaw. However, she and her coworkers followed a few of their subjects with elevated testosterone levels during midpuberty, and several developed signs of early polycystic ovarian syndrome (PCOS) such as irregular menstrual cycles, acne, and hirsutism. “It may be possible to identify girls at high risk for PCOS before menarche,” she suggested.
Dr. Burt Solorzano agreed that delayed breast development in girls with high levels of body fat may reflect inadequate progesterone production, which when coupled with an obesity-related excess level of androgens could put girls at risk for chronic anovulation and later PCOS.
“Weight management during childhood and early puberty may mitigate the adverse effects of obesity on pubertal progression and avoid some of the lifetime complications related to early menarche,” Dr. Burt Solorzano said.
The Body Weight and Puberty Study enrolled 36 girls who were overweight or obese and 54 girls with normal weight. They averaged 11 years of age, with a range of 8.2-14.7 years. Average percent body fat was 41% among the overweight or obese girls and 27% among those with normal weight. The results reported by Ms. Ortega also appeared in a report published Feb 22, 2021 (J Clin Endocrinol Metab. doi: 10.1210/clinem/dgab092).
Dr. Shaw, Ms. Ortega, and Dr. Burt Solorzano had no disclosures.
Girls in late stages of puberty who had elevated levels of body fat showed unusually high levels of several hormones that could contribute to an earlier age of menarche and also slow breast development, according to data from 90 girls who spanned a wide range of body fat in the first longitudinal study to examine links between fat volume, levels of reproductive hormones, and clinical manifestations of hormone action during puberty.
The results showed that girls with greater body fat had higher levels of follicle stimulating hormone, inhibin B, estrone, and certain male-like reproductive hormones, and that this pattern “is specifically tied to body fat,” said Natalie D. Shaw, MD, senior investigator for the study, reported at the annual meeting of the Endocrine Society.
“We found that total body fat is associated with the timing of menarche, as others have reported for body weight,” she noted. The new findings showed that every 1% rise in percent total body fat linked with a significant 3% rise in the likelihood of menarche, menstrual onset. In the new study the average age of menarche was 11.7 years among the overweight or obese girls and 12.8 years among those with normal weights.
But the study’s unique use of an average of about three serial ultrasound breast examinations of each subject during an average 4 years of follow-up also showed that higher levels of body fat linked with slowed breast development in later stages, specifically maturation from stage D to stages D/E and E.
For example, girls with 33% body fat spent an average of 8.2 months in stage D, which stretched to an average of 11.2 months among girls with 38% body fat, reported Madison T. Ortega, a researcher with the Pediatric Endocrinology Group of the National Institute of Environmental Health Sciences in Research Triangle Park, N.C., who presented the report at the meeting.
Ultrasound shows what inspection can’t
Results from “several studies have shown earlier breast development in overweight and obese girls by inspection and palpation,” but the new findings from ultrasound examination provide more nuance about the structural breast changes actually occurring in these adolescents, said Dr. Shaw, who heads the Pediatric Endocrinology Group. The current study “was not designed to capture the onset of breast development,” and “it is possible that increased androgens or insulin resistance in girls with higher body fat interferes with normal breast development,” she explained in an interview.
“The authors showed that the timing and progress of early stages of puberty were not earlier in overweight or obese girls. Luteinizing hormone, the indicator of neuroendocrine pubertal onset, and timing of early stages of breast development were the same in all weight groups. The authors also discovered falsely advanced Turner breast stage designations with ultrasonography in some girls with obesity. This might suggest that prior findings in epidemiologic studies of an earlier start to puberty based mostly on breast development stages identified by self-reported inspection and, rarely, palpation, may have been biased by breast adipose tissue,” said Christine M. Burt Solorzano, MD, a pediatric endocrinologist at the University of Virginia in Charlottesville, who was not involved in the study.
“Development of increased follicle-stimulating hormone in late puberty suggests that pubertal tempo, not onset, may be increased in girls with obesity, and goes along with earlier menarche. Their finding of increased androgen levels during mid to late puberty with obesity are consistent with prior findings,” including work published Dr. Burt Solorzano and her associates, she noted. “Delayed timing of advanced breast morphology was unexpected and may reflect relatively lower levels of progesterone in girls with obesity,” a hormone necessary for later stages of breast maturation.
The findings “reinforce that early breast development in the setting of obesity may in fact reflect adipose tissue and not be a true representation of neuroendocrine precocious puberty,” Dr. Burt Solorzano said in an interview. The findings “also suggest that pubertal initiation may not happen earlier in girls with obesity, as has been thought, but rather the tempo of puberty may be more rapid, leading to earlier menarche.”
A possible step toward PCOS
The long-term clinical consequences of the hormonal state linked with overweight and obesity “are unknown,” said Dr. Shaw. However, she and her coworkers followed a few of their subjects with elevated testosterone levels during midpuberty, and several developed signs of early polycystic ovarian syndrome (PCOS) such as irregular menstrual cycles, acne, and hirsutism. “It may be possible to identify girls at high risk for PCOS before menarche,” she suggested.
Dr. Burt Solorzano agreed that delayed breast development in girls with high levels of body fat may reflect inadequate progesterone production, which when coupled with an obesity-related excess level of androgens could put girls at risk for chronic anovulation and later PCOS.
“Weight management during childhood and early puberty may mitigate the adverse effects of obesity on pubertal progression and avoid some of the lifetime complications related to early menarche,” Dr. Burt Solorzano said.
The Body Weight and Puberty Study enrolled 36 girls who were overweight or obese and 54 girls with normal weight. They averaged 11 years of age, with a range of 8.2-14.7 years. Average percent body fat was 41% among the overweight or obese girls and 27% among those with normal weight. The results reported by Ms. Ortega also appeared in a report published Feb 22, 2021 (J Clin Endocrinol Metab. doi: 10.1210/clinem/dgab092).
Dr. Shaw, Ms. Ortega, and Dr. Burt Solorzano had no disclosures.
FROM ENDO 2021
Multidisciplinary approach touted for atopic dermatitis
researchers say.
“I think we really gained insight to how a more holistic approach benefited the patient,” Lawrence Eichenfield, MD, professor of dermatology and pediatrics at the University of California, San Diego, said in an interview.
At the 2021 annual meeting of the International Society of Atopic Dermatitis, he and his colleagues described a pilot program to bring the specialists together at UCSD and Rady Children’s Hospital, San Diego.
Typically, children seeking care for atopic dermatitis see allergists and dermatologists separately for 10- to 15-minute appointments. The specialists sometimes prescribe treatments that conflict or are redundant with each other and may give contradictory instructions.
Instead, Dr. Eichenfield and colleagues designed a program bringing patients in for initial assessments lasting 1-1.5 hours. Patients typically started with visits to a clinical pharmacist, who assessed what medications had been prescribed and how much the patients were actually taking.
The patients then proceeded to separate appointments with an allergist and a dermatologist for evaluations. These specialists then met face to face to develop a treatment plan. At least one of the specialists would then present the plan to the patient and the patient’s family.
“We had a rich set of educational materials that were developed and put online that helped with shared decision-making and increased comfort level with appropriate skin care and medication,” Dr. Eichenfield said.
He and his colleagues assigned a physician assistant trained in both pediatric dermatology and pediatric allergy to coordinate the clinic. They designed combined pediatric dermatology and pediatric allergy fellowships for two fellows. “So, part of this program ended up allowing specially trained individuals who overlapped in fields that traditionally were separate,” said Dr. Eichenfield.
To see how well the approach worked, the researchers followed the progress of 23 patients who were already receiving treatment at one or both of the institutions.
- Eczema Area and Severity Index (EASI) scores decreased from visit 1 to visit 2 by a mean of 15.36 (P < .001), which correlates to a 56.36% average decrease.
- In 20 patients (89.96%), in EASI scores improved 50%.
- Thirteen patients (56.54%) achieved 75% improvement in EASI scores.
- Body surface area scores improved by a mean of 23.21% (P = .002).
- Validated Investigator Global Assessment scores decreased in 56.52% of patients to a clinically significant level.
The study did not include any control group, nor did the researchers report any details on how long the patients had been treated before the multidisciplinary program started or how their prescriptions changed.
Patients benefited from the comprehensive assessment of their symptoms, said Dr. Eichenfield, also chief of pediatric and adolescent dermatology at Rady Children’s Hospital. “Some had significant environmental allergies that might not have been a contributing factor to their atopic dermatitis,” he explained. “The complexities of comorbidities and atopic dermatitis influence the patient, even if one disease state isn’t necessarily directly causative of the other.”
In surveys, patients said they especially appreciated the increased time spent with their specialists. “No one’s ever spent an hour teaching us about eczema,” some commented. The approach motivated patients to take their home treatment more effectively, Dr. Eichenfield believed.
Primary care physicians did not participate in the multidisciplinary program, but the specialists communicated with them and shared electronic medical records with them, he said.
Without a control group, it is hard to say how much difference the multidisciplinary approach made, Jonathan I. Silverberg, MD, PhD, MPH, associate professor of dermatology and director of clinical research and contact dermatitis at George Washington University, Washington, said in an interview.
“What it does show is that there is significant improvement in a variety of endpoints within this multidisciplinary approach,” Dr. Silverberg said in an interview. “And so I have no doubt that this is valid and that a multidisciplinary approach would really improve, holistically, many aspects of patient care.”
Dr. Silverberg ran a multidisciplinary program at Northwestern University, Chicago, which included sleep medicine, endocrinology, gastroenterology, and other specialties as well as dermatology, allergy, and pharmacy.
However, Dr. Silverberg pointed out, a multidisciplinary approach is more expensive than standard care because when specialists spend more time with each patient, they see fewer patients per day. “So many health care systems or academic institutions are not as open as they should be to this kind of interdisciplinary care, which is why it’s so important to have outcome measures showing that this approach actually works.”
Dr. Eichenfield and Dr. Silverberg had no relevant disclosures.
A version of this article first appeared on Medscape.com.
researchers say.
“I think we really gained insight to how a more holistic approach benefited the patient,” Lawrence Eichenfield, MD, professor of dermatology and pediatrics at the University of California, San Diego, said in an interview.
At the 2021 annual meeting of the International Society of Atopic Dermatitis, he and his colleagues described a pilot program to bring the specialists together at UCSD and Rady Children’s Hospital, San Diego.
Typically, children seeking care for atopic dermatitis see allergists and dermatologists separately for 10- to 15-minute appointments. The specialists sometimes prescribe treatments that conflict or are redundant with each other and may give contradictory instructions.
Instead, Dr. Eichenfield and colleagues designed a program bringing patients in for initial assessments lasting 1-1.5 hours. Patients typically started with visits to a clinical pharmacist, who assessed what medications had been prescribed and how much the patients were actually taking.
The patients then proceeded to separate appointments with an allergist and a dermatologist for evaluations. These specialists then met face to face to develop a treatment plan. At least one of the specialists would then present the plan to the patient and the patient’s family.
“We had a rich set of educational materials that were developed and put online that helped with shared decision-making and increased comfort level with appropriate skin care and medication,” Dr. Eichenfield said.
He and his colleagues assigned a physician assistant trained in both pediatric dermatology and pediatric allergy to coordinate the clinic. They designed combined pediatric dermatology and pediatric allergy fellowships for two fellows. “So, part of this program ended up allowing specially trained individuals who overlapped in fields that traditionally were separate,” said Dr. Eichenfield.
To see how well the approach worked, the researchers followed the progress of 23 patients who were already receiving treatment at one or both of the institutions.
- Eczema Area and Severity Index (EASI) scores decreased from visit 1 to visit 2 by a mean of 15.36 (P < .001), which correlates to a 56.36% average decrease.
- In 20 patients (89.96%), in EASI scores improved 50%.
- Thirteen patients (56.54%) achieved 75% improvement in EASI scores.
- Body surface area scores improved by a mean of 23.21% (P = .002).
- Validated Investigator Global Assessment scores decreased in 56.52% of patients to a clinically significant level.
The study did not include any control group, nor did the researchers report any details on how long the patients had been treated before the multidisciplinary program started or how their prescriptions changed.
Patients benefited from the comprehensive assessment of their symptoms, said Dr. Eichenfield, also chief of pediatric and adolescent dermatology at Rady Children’s Hospital. “Some had significant environmental allergies that might not have been a contributing factor to their atopic dermatitis,” he explained. “The complexities of comorbidities and atopic dermatitis influence the patient, even if one disease state isn’t necessarily directly causative of the other.”
In surveys, patients said they especially appreciated the increased time spent with their specialists. “No one’s ever spent an hour teaching us about eczema,” some commented. The approach motivated patients to take their home treatment more effectively, Dr. Eichenfield believed.
Primary care physicians did not participate in the multidisciplinary program, but the specialists communicated with them and shared electronic medical records with them, he said.
Without a control group, it is hard to say how much difference the multidisciplinary approach made, Jonathan I. Silverberg, MD, PhD, MPH, associate professor of dermatology and director of clinical research and contact dermatitis at George Washington University, Washington, said in an interview.
“What it does show is that there is significant improvement in a variety of endpoints within this multidisciplinary approach,” Dr. Silverberg said in an interview. “And so I have no doubt that this is valid and that a multidisciplinary approach would really improve, holistically, many aspects of patient care.”
Dr. Silverberg ran a multidisciplinary program at Northwestern University, Chicago, which included sleep medicine, endocrinology, gastroenterology, and other specialties as well as dermatology, allergy, and pharmacy.
However, Dr. Silverberg pointed out, a multidisciplinary approach is more expensive than standard care because when specialists spend more time with each patient, they see fewer patients per day. “So many health care systems or academic institutions are not as open as they should be to this kind of interdisciplinary care, which is why it’s so important to have outcome measures showing that this approach actually works.”
Dr. Eichenfield and Dr. Silverberg had no relevant disclosures.
A version of this article first appeared on Medscape.com.
researchers say.
“I think we really gained insight to how a more holistic approach benefited the patient,” Lawrence Eichenfield, MD, professor of dermatology and pediatrics at the University of California, San Diego, said in an interview.
At the 2021 annual meeting of the International Society of Atopic Dermatitis, he and his colleagues described a pilot program to bring the specialists together at UCSD and Rady Children’s Hospital, San Diego.
Typically, children seeking care for atopic dermatitis see allergists and dermatologists separately for 10- to 15-minute appointments. The specialists sometimes prescribe treatments that conflict or are redundant with each other and may give contradictory instructions.
Instead, Dr. Eichenfield and colleagues designed a program bringing patients in for initial assessments lasting 1-1.5 hours. Patients typically started with visits to a clinical pharmacist, who assessed what medications had been prescribed and how much the patients were actually taking.
The patients then proceeded to separate appointments with an allergist and a dermatologist for evaluations. These specialists then met face to face to develop a treatment plan. At least one of the specialists would then present the plan to the patient and the patient’s family.
“We had a rich set of educational materials that were developed and put online that helped with shared decision-making and increased comfort level with appropriate skin care and medication,” Dr. Eichenfield said.
He and his colleagues assigned a physician assistant trained in both pediatric dermatology and pediatric allergy to coordinate the clinic. They designed combined pediatric dermatology and pediatric allergy fellowships for two fellows. “So, part of this program ended up allowing specially trained individuals who overlapped in fields that traditionally were separate,” said Dr. Eichenfield.
To see how well the approach worked, the researchers followed the progress of 23 patients who were already receiving treatment at one or both of the institutions.
- Eczema Area and Severity Index (EASI) scores decreased from visit 1 to visit 2 by a mean of 15.36 (P < .001), which correlates to a 56.36% average decrease.
- In 20 patients (89.96%), in EASI scores improved 50%.
- Thirteen patients (56.54%) achieved 75% improvement in EASI scores.
- Body surface area scores improved by a mean of 23.21% (P = .002).
- Validated Investigator Global Assessment scores decreased in 56.52% of patients to a clinically significant level.
The study did not include any control group, nor did the researchers report any details on how long the patients had been treated before the multidisciplinary program started or how their prescriptions changed.
Patients benefited from the comprehensive assessment of their symptoms, said Dr. Eichenfield, also chief of pediatric and adolescent dermatology at Rady Children’s Hospital. “Some had significant environmental allergies that might not have been a contributing factor to their atopic dermatitis,” he explained. “The complexities of comorbidities and atopic dermatitis influence the patient, even if one disease state isn’t necessarily directly causative of the other.”
In surveys, patients said they especially appreciated the increased time spent with their specialists. “No one’s ever spent an hour teaching us about eczema,” some commented. The approach motivated patients to take their home treatment more effectively, Dr. Eichenfield believed.
Primary care physicians did not participate in the multidisciplinary program, but the specialists communicated with them and shared electronic medical records with them, he said.
Without a control group, it is hard to say how much difference the multidisciplinary approach made, Jonathan I. Silverberg, MD, PhD, MPH, associate professor of dermatology and director of clinical research and contact dermatitis at George Washington University, Washington, said in an interview.
“What it does show is that there is significant improvement in a variety of endpoints within this multidisciplinary approach,” Dr. Silverberg said in an interview. “And so I have no doubt that this is valid and that a multidisciplinary approach would really improve, holistically, many aspects of patient care.”
Dr. Silverberg ran a multidisciplinary program at Northwestern University, Chicago, which included sleep medicine, endocrinology, gastroenterology, and other specialties as well as dermatology, allergy, and pharmacy.
However, Dr. Silverberg pointed out, a multidisciplinary approach is more expensive than standard care because when specialists spend more time with each patient, they see fewer patients per day. “So many health care systems or academic institutions are not as open as they should be to this kind of interdisciplinary care, which is why it’s so important to have outcome measures showing that this approach actually works.”
Dr. Eichenfield and Dr. Silverberg had no relevant disclosures.
A version of this article first appeared on Medscape.com.
Pediatric cancer survivors at risk for opioid misuse
Survivors of childhood cancers are at increased risk for prescription opioid misuse compared with their peers, a review of a claims database revealed.
Among more than 8,000 patients age 21 or younger who had completed treatment for hematologic, central nervous system, bone, or gonadal cancers, survivors were significantly more likely than were their peers to have an opioid prescription, longer duration of prescription, and higher daily doses of opioids, and to have opioid prescriptions overlapping for a week or more, reported Xu Ji, PhD, of Emory University in Atlanta.
Teenage and young adult patients were at higher risk than were patients younger than 12, and the risk was highest among patients who had been treated for bone malignancies, as well as those who had undergone any hematopoietic stem cell transplant.
“These findings suggest that health care providers who regularly see survivors should explore nonopioid options to help prevent opioid misuse, and screen for potential misuse in those who actually receive opioids,” she said in an oral abstract presented during the annual meeting of the American Society of Pediatric Hematology/Oncology.
“This is a really important topic, and something that’s probably been underinvestigated and underexplored in our patient population,” said session comoderator Sheri Spunt, MD, Endowed Professor of Pediatric Cancer at Stanford (Calif.) University.
Database review
Dr. Ji and colleagues used the IBM MarketScan Commercial Claims and Encounters database from 2009 to 2018 to examine prescription opioid use, potential misuse, and substance use disorders in pediatric cancer survivors in the first year after completion of therapy, and to identify factors associated with risk for misuse or substance use disorders. Specifically, the period of interest was the first year after completion of all treatments, including surgery, chemotherapy, radiation, and stem cell transplant (Abstract 2015).
They looked at deidentified records on any opioid prescription and for treatment of any opioid use or substance use disorder (alcohol, psychotherapeutic drugs, marijuana, or illicit drug use disorders).
They defined indicators of potential misuse as either prescriptions for long-acting or extended-release opioids for acute pain conditions; opioid and benzodiazepine prescriptions overlapping by a week or more; opioid prescriptions overlapping by a week or more; high daily opioid dosage (prescribed daily dose of 100 or greater morphine milligram equivalent [MME]; and/or opioid dose escalation (an increase of at least 50% in mean MMEs per month twice consecutively within 1 year).
They compared outcomes between a total of 8,635 survivors and 44,175 controls, matched on a 1:5 basis with survivors by age, sex, and region, and continuous enrollment during the 1-year posttherapy period.
In each of three age categories – 0 to 11 years, 12 to 17 years, and 18 years and older – survivors were significantly more likely to have received an opioid prescription, at 15% for the youngest survivors vs. 2% of controls, 25% vs. 8% for 12- to 17-year-olds, and 28% vs. 12% for those 18 and older (P < .01 for all three comparisons).
Survivors were also significantly more likely to have any indicator of potential misuse (1.6% vs. 0.1%, 4.6% vs. 0.5%, and 7.4% vs. 1.2%, respectively, P < .001 for all) and both the youngest and oldest groups (but not 12- to 17-year-olds) were significantly more like to have opioid or substance use disorder (0.4% vs. 0% for 0-11 years, 5.76% vs. 4.2% for 18 years and older, P < .001 for both).
Among patients with any opioid prescription, survivors were significantly more likely than were controls of any age to have indicators for potential misuse. For example, 13% of survivors aged 18 years and older had prescriptions for high opioid doses, compared with 5% of controls, and 12% had prescription overlap, vs. 2%.
Compared with patients with leukemia, patients treated for bone malignancies had a 6% greater risk for having any indicator of misuse, while patients with other malignancies were at slightly lower risk for misuse than those who completed leukemia therapy.
Patients who received any stem cell transplant had an 8.4% greater risk for misuse compared with patients who had surgery only.
Opioids pre- and posttreatment?
“Being someone who takes care of a lot of bone cancer patients, I do see patients with these issues,” Dr. Spunt said.
Audience member Jack H. Staddon, MD, PhD, of the Billings (Montana) Clinic, noted the possibility that opioid use during treatment may have been carried on into the posttreatment period, and asked whether use of narcotics during treatment was an independent risk factor for posttreatment narcotic use or misuse.
The researchers plan to investigate this question in future studies, Dr. Ji replied.
They did not report a study funding source. Dr. Ji and coauthors and Dr. Staddon reported no relevant disclosures.
Survivors of childhood cancers are at increased risk for prescription opioid misuse compared with their peers, a review of a claims database revealed.
Among more than 8,000 patients age 21 or younger who had completed treatment for hematologic, central nervous system, bone, or gonadal cancers, survivors were significantly more likely than were their peers to have an opioid prescription, longer duration of prescription, and higher daily doses of opioids, and to have opioid prescriptions overlapping for a week or more, reported Xu Ji, PhD, of Emory University in Atlanta.
Teenage and young adult patients were at higher risk than were patients younger than 12, and the risk was highest among patients who had been treated for bone malignancies, as well as those who had undergone any hematopoietic stem cell transplant.
“These findings suggest that health care providers who regularly see survivors should explore nonopioid options to help prevent opioid misuse, and screen for potential misuse in those who actually receive opioids,” she said in an oral abstract presented during the annual meeting of the American Society of Pediatric Hematology/Oncology.
“This is a really important topic, and something that’s probably been underinvestigated and underexplored in our patient population,” said session comoderator Sheri Spunt, MD, Endowed Professor of Pediatric Cancer at Stanford (Calif.) University.
Database review
Dr. Ji and colleagues used the IBM MarketScan Commercial Claims and Encounters database from 2009 to 2018 to examine prescription opioid use, potential misuse, and substance use disorders in pediatric cancer survivors in the first year after completion of therapy, and to identify factors associated with risk for misuse or substance use disorders. Specifically, the period of interest was the first year after completion of all treatments, including surgery, chemotherapy, radiation, and stem cell transplant (Abstract 2015).
They looked at deidentified records on any opioid prescription and for treatment of any opioid use or substance use disorder (alcohol, psychotherapeutic drugs, marijuana, or illicit drug use disorders).
They defined indicators of potential misuse as either prescriptions for long-acting or extended-release opioids for acute pain conditions; opioid and benzodiazepine prescriptions overlapping by a week or more; opioid prescriptions overlapping by a week or more; high daily opioid dosage (prescribed daily dose of 100 or greater morphine milligram equivalent [MME]; and/or opioid dose escalation (an increase of at least 50% in mean MMEs per month twice consecutively within 1 year).
They compared outcomes between a total of 8,635 survivors and 44,175 controls, matched on a 1:5 basis with survivors by age, sex, and region, and continuous enrollment during the 1-year posttherapy period.
In each of three age categories – 0 to 11 years, 12 to 17 years, and 18 years and older – survivors were significantly more likely to have received an opioid prescription, at 15% for the youngest survivors vs. 2% of controls, 25% vs. 8% for 12- to 17-year-olds, and 28% vs. 12% for those 18 and older (P < .01 for all three comparisons).
Survivors were also significantly more likely to have any indicator of potential misuse (1.6% vs. 0.1%, 4.6% vs. 0.5%, and 7.4% vs. 1.2%, respectively, P < .001 for all) and both the youngest and oldest groups (but not 12- to 17-year-olds) were significantly more like to have opioid or substance use disorder (0.4% vs. 0% for 0-11 years, 5.76% vs. 4.2% for 18 years and older, P < .001 for both).
Among patients with any opioid prescription, survivors were significantly more likely than were controls of any age to have indicators for potential misuse. For example, 13% of survivors aged 18 years and older had prescriptions for high opioid doses, compared with 5% of controls, and 12% had prescription overlap, vs. 2%.
Compared with patients with leukemia, patients treated for bone malignancies had a 6% greater risk for having any indicator of misuse, while patients with other malignancies were at slightly lower risk for misuse than those who completed leukemia therapy.
Patients who received any stem cell transplant had an 8.4% greater risk for misuse compared with patients who had surgery only.
Opioids pre- and posttreatment?
“Being someone who takes care of a lot of bone cancer patients, I do see patients with these issues,” Dr. Spunt said.
Audience member Jack H. Staddon, MD, PhD, of the Billings (Montana) Clinic, noted the possibility that opioid use during treatment may have been carried on into the posttreatment period, and asked whether use of narcotics during treatment was an independent risk factor for posttreatment narcotic use or misuse.
The researchers plan to investigate this question in future studies, Dr. Ji replied.
They did not report a study funding source. Dr. Ji and coauthors and Dr. Staddon reported no relevant disclosures.
Survivors of childhood cancers are at increased risk for prescription opioid misuse compared with their peers, a review of a claims database revealed.
Among more than 8,000 patients age 21 or younger who had completed treatment for hematologic, central nervous system, bone, or gonadal cancers, survivors were significantly more likely than were their peers to have an opioid prescription, longer duration of prescription, and higher daily doses of opioids, and to have opioid prescriptions overlapping for a week or more, reported Xu Ji, PhD, of Emory University in Atlanta.
Teenage and young adult patients were at higher risk than were patients younger than 12, and the risk was highest among patients who had been treated for bone malignancies, as well as those who had undergone any hematopoietic stem cell transplant.
“These findings suggest that health care providers who regularly see survivors should explore nonopioid options to help prevent opioid misuse, and screen for potential misuse in those who actually receive opioids,” she said in an oral abstract presented during the annual meeting of the American Society of Pediatric Hematology/Oncology.
“This is a really important topic, and something that’s probably been underinvestigated and underexplored in our patient population,” said session comoderator Sheri Spunt, MD, Endowed Professor of Pediatric Cancer at Stanford (Calif.) University.
Database review
Dr. Ji and colleagues used the IBM MarketScan Commercial Claims and Encounters database from 2009 to 2018 to examine prescription opioid use, potential misuse, and substance use disorders in pediatric cancer survivors in the first year after completion of therapy, and to identify factors associated with risk for misuse or substance use disorders. Specifically, the period of interest was the first year after completion of all treatments, including surgery, chemotherapy, radiation, and stem cell transplant (Abstract 2015).
They looked at deidentified records on any opioid prescription and for treatment of any opioid use or substance use disorder (alcohol, psychotherapeutic drugs, marijuana, or illicit drug use disorders).
They defined indicators of potential misuse as either prescriptions for long-acting or extended-release opioids for acute pain conditions; opioid and benzodiazepine prescriptions overlapping by a week or more; opioid prescriptions overlapping by a week or more; high daily opioid dosage (prescribed daily dose of 100 or greater morphine milligram equivalent [MME]; and/or opioid dose escalation (an increase of at least 50% in mean MMEs per month twice consecutively within 1 year).
They compared outcomes between a total of 8,635 survivors and 44,175 controls, matched on a 1:5 basis with survivors by age, sex, and region, and continuous enrollment during the 1-year posttherapy period.
In each of three age categories – 0 to 11 years, 12 to 17 years, and 18 years and older – survivors were significantly more likely to have received an opioid prescription, at 15% for the youngest survivors vs. 2% of controls, 25% vs. 8% for 12- to 17-year-olds, and 28% vs. 12% for those 18 and older (P < .01 for all three comparisons).
Survivors were also significantly more likely to have any indicator of potential misuse (1.6% vs. 0.1%, 4.6% vs. 0.5%, and 7.4% vs. 1.2%, respectively, P < .001 for all) and both the youngest and oldest groups (but not 12- to 17-year-olds) were significantly more like to have opioid or substance use disorder (0.4% vs. 0% for 0-11 years, 5.76% vs. 4.2% for 18 years and older, P < .001 for both).
Among patients with any opioid prescription, survivors were significantly more likely than were controls of any age to have indicators for potential misuse. For example, 13% of survivors aged 18 years and older had prescriptions for high opioid doses, compared with 5% of controls, and 12% had prescription overlap, vs. 2%.
Compared with patients with leukemia, patients treated for bone malignancies had a 6% greater risk for having any indicator of misuse, while patients with other malignancies were at slightly lower risk for misuse than those who completed leukemia therapy.
Patients who received any stem cell transplant had an 8.4% greater risk for misuse compared with patients who had surgery only.
Opioids pre- and posttreatment?
“Being someone who takes care of a lot of bone cancer patients, I do see patients with these issues,” Dr. Spunt said.
Audience member Jack H. Staddon, MD, PhD, of the Billings (Montana) Clinic, noted the possibility that opioid use during treatment may have been carried on into the posttreatment period, and asked whether use of narcotics during treatment was an independent risk factor for posttreatment narcotic use or misuse.
The researchers plan to investigate this question in future studies, Dr. Ji replied.
They did not report a study funding source. Dr. Ji and coauthors and Dr. Staddon reported no relevant disclosures.
FROM 2021 ASPHO CONFERENCE
Genital Primary Herpetic Infection With Concurrent Hepatitis in an Infant
To the Editor:
Cutaneous herpes simplex virus (HSV) infection generally involves mucocutaneous junctions, but virtually any area of the skin can be affected.1 When the genital area of adult patients is affected, the disease usually is sexually transmitted and mainly caused by HSV-2. In infants, genital primary herpetic infection is rare and more commonly is caused by HSV-1 than by HSV-2. We report a rare case of genital primary herpetic infection with concurrent hepatitis in an infant.
An 8-month-old infant with no underlying medical problems, including atopic dermatitis, was referred for erythematous grouped vesicles with erosions on the perianal area of 4 days’ duration (Figure). The skin color appeared normal, not icterus. She also had a fever (temperature, 37.9 °C), and her urination pattern had changed from normal to frequent leakage, possibly owing to pain related to the eroded lesions. Physical examination did not reveal palpable inguinal lymph nodes. The oral mucosa was not involved. The patient’s father had a history of recurrent herpetic infection on both the perioral and perianal areas.

A Tzanck smear revealed giant multinucleated cells with multiple inflammatory cells. Laboratory tests revealed marked leukocytosis, elevated liver enzymes (aspartate aminotransferase, 141 IU/L [reference range, 15 IU/L–60 IU/L]; alanine aminotransferase, 422 IU/L [reference range, 13 IU/L–45 IU/L]), and was positive for herpes simplex viral IgM but negative for herpes simplex viral IgG. A viral culture also demonstrated the growth of HSV. An abdominal ultrasound was normal. Based on the cutaneous and laboratory findings, genital primary herpetic infection with concurrent hepatitis was diagnosed. Intravenous acyclovir 50 mg was administered 3 times daily for 7 days, and a wet dressing with topical mupirocin was employed daily until the skin lesions healed. The fever subsided soon after starting treatment. The liver enzyme counts decreased gradually in serial follow-up (aspartate aminotransferase, 75 IU/L; alanine aminotransferase, 70 IU/L).
Primary herpetic infection usually is asymptomatic, but when symptoms do occur, it is characterized by the sudden onset of painful vesicle clusters over erythematous edematous skin. Lesions can be associated with fever and malaise and may involve the perineum. Urinary symptoms may occur. The average age of onset ranges from 6 months to 4 years. The virus commonly is transmitted by asymptomatic carriers. Autoinoculation from concomitant oral primary herpetic infection or individuals with active herpetic infection is one possible route of transmission. In our patient, we assumed that she acquired the virus from her father during close contact. A diagnosis can be made clinically using direct methods including culture, Tzanck smear, or polymerase chain reaction, or indirect methods such as serologic tests.2
Hepatitis secondary to HSV infection is rare, especially in immunocompetent patients. It occurs during primary infection and rarely during recurrent infection with or without concomitant skin lesions.3 Symptoms include fever, anorexia, nausea, vomiting, abdominal pain, leukopenia, coagulopathy, and marked elevation of serum transaminase levels without jaundice. Based on our patient’s elevated liver enzyme levels and virological evidence of acute primary HSV infection, a lack of evidence of other hepatic viral infections, and the presence of herpes simplex viremia, we concluded that this infant had viral hepatitis as a part of the clinical presentation of primary HSV infection. We did not perform a direct liver biopsy considering her age and accompanying risks.4
Primary herpetic infection usually has a benign course and a short duration. In children, the prognosis depends on underlying immunologic status, not a particular type of HSV. In children with atopic dermatitis, primary herpetic infection tends to occur earlier and is more severe. Early treatment with acyclovir is effective; intravenous treatment is not required unless local complications or systemic involvement are present. Long-term follow-up is recommended because of the possibility of recurrence.
Although the possibility of systemic involvement including hepatitis due to HSV infection is low, awareness among dermatologists about primary herpetic infection and its possible complications would be helpful in the diagnosis and treatment, especially for atypical or extensive cases.
- Jenson HB, Shapiro ED. Primary herpes simplex virus infection of a diaper rash. Pediatr Infect Dis J. 1987;6:1136-1138.
- Batalla A, Flórez A, Dávila P, et al. Genital primary herpes simplexinfection in a 5-month-old infant. Dermatol Online J. 2011;17:8.
- Norvell JP, Blei AT, Jovanovic BD, et al. Herpes simplex virus hepatitis: an analysis of the published literature and institutional cases. Liver Transpl. 2007;13:1428-1434.
- Chen CK, Wu SH, Huang YC. Herpetic gingivostomatitis with severe hepatitis in a previously healthy child. J Microbiol Immunol Infect. 2012;45:324-325.
To the Editor:
Cutaneous herpes simplex virus (HSV) infection generally involves mucocutaneous junctions, but virtually any area of the skin can be affected.1 When the genital area of adult patients is affected, the disease usually is sexually transmitted and mainly caused by HSV-2. In infants, genital primary herpetic infection is rare and more commonly is caused by HSV-1 than by HSV-2. We report a rare case of genital primary herpetic infection with concurrent hepatitis in an infant.
An 8-month-old infant with no underlying medical problems, including atopic dermatitis, was referred for erythematous grouped vesicles with erosions on the perianal area of 4 days’ duration (Figure). The skin color appeared normal, not icterus. She also had a fever (temperature, 37.9 °C), and her urination pattern had changed from normal to frequent leakage, possibly owing to pain related to the eroded lesions. Physical examination did not reveal palpable inguinal lymph nodes. The oral mucosa was not involved. The patient’s father had a history of recurrent herpetic infection on both the perioral and perianal areas.

A Tzanck smear revealed giant multinucleated cells with multiple inflammatory cells. Laboratory tests revealed marked leukocytosis, elevated liver enzymes (aspartate aminotransferase, 141 IU/L [reference range, 15 IU/L–60 IU/L]; alanine aminotransferase, 422 IU/L [reference range, 13 IU/L–45 IU/L]), and was positive for herpes simplex viral IgM but negative for herpes simplex viral IgG. A viral culture also demonstrated the growth of HSV. An abdominal ultrasound was normal. Based on the cutaneous and laboratory findings, genital primary herpetic infection with concurrent hepatitis was diagnosed. Intravenous acyclovir 50 mg was administered 3 times daily for 7 days, and a wet dressing with topical mupirocin was employed daily until the skin lesions healed. The fever subsided soon after starting treatment. The liver enzyme counts decreased gradually in serial follow-up (aspartate aminotransferase, 75 IU/L; alanine aminotransferase, 70 IU/L).
Primary herpetic infection usually is asymptomatic, but when symptoms do occur, it is characterized by the sudden onset of painful vesicle clusters over erythematous edematous skin. Lesions can be associated with fever and malaise and may involve the perineum. Urinary symptoms may occur. The average age of onset ranges from 6 months to 4 years. The virus commonly is transmitted by asymptomatic carriers. Autoinoculation from concomitant oral primary herpetic infection or individuals with active herpetic infection is one possible route of transmission. In our patient, we assumed that she acquired the virus from her father during close contact. A diagnosis can be made clinically using direct methods including culture, Tzanck smear, or polymerase chain reaction, or indirect methods such as serologic tests.2
Hepatitis secondary to HSV infection is rare, especially in immunocompetent patients. It occurs during primary infection and rarely during recurrent infection with or without concomitant skin lesions.3 Symptoms include fever, anorexia, nausea, vomiting, abdominal pain, leukopenia, coagulopathy, and marked elevation of serum transaminase levels without jaundice. Based on our patient’s elevated liver enzyme levels and virological evidence of acute primary HSV infection, a lack of evidence of other hepatic viral infections, and the presence of herpes simplex viremia, we concluded that this infant had viral hepatitis as a part of the clinical presentation of primary HSV infection. We did not perform a direct liver biopsy considering her age and accompanying risks.4
Primary herpetic infection usually has a benign course and a short duration. In children, the prognosis depends on underlying immunologic status, not a particular type of HSV. In children with atopic dermatitis, primary herpetic infection tends to occur earlier and is more severe. Early treatment with acyclovir is effective; intravenous treatment is not required unless local complications or systemic involvement are present. Long-term follow-up is recommended because of the possibility of recurrence.
Although the possibility of systemic involvement including hepatitis due to HSV infection is low, awareness among dermatologists about primary herpetic infection and its possible complications would be helpful in the diagnosis and treatment, especially for atypical or extensive cases.
To the Editor:
Cutaneous herpes simplex virus (HSV) infection generally involves mucocutaneous junctions, but virtually any area of the skin can be affected.1 When the genital area of adult patients is affected, the disease usually is sexually transmitted and mainly caused by HSV-2. In infants, genital primary herpetic infection is rare and more commonly is caused by HSV-1 than by HSV-2. We report a rare case of genital primary herpetic infection with concurrent hepatitis in an infant.
An 8-month-old infant with no underlying medical problems, including atopic dermatitis, was referred for erythematous grouped vesicles with erosions on the perianal area of 4 days’ duration (Figure). The skin color appeared normal, not icterus. She also had a fever (temperature, 37.9 °C), and her urination pattern had changed from normal to frequent leakage, possibly owing to pain related to the eroded lesions. Physical examination did not reveal palpable inguinal lymph nodes. The oral mucosa was not involved. The patient’s father had a history of recurrent herpetic infection on both the perioral and perianal areas.

A Tzanck smear revealed giant multinucleated cells with multiple inflammatory cells. Laboratory tests revealed marked leukocytosis, elevated liver enzymes (aspartate aminotransferase, 141 IU/L [reference range, 15 IU/L–60 IU/L]; alanine aminotransferase, 422 IU/L [reference range, 13 IU/L–45 IU/L]), and was positive for herpes simplex viral IgM but negative for herpes simplex viral IgG. A viral culture also demonstrated the growth of HSV. An abdominal ultrasound was normal. Based on the cutaneous and laboratory findings, genital primary herpetic infection with concurrent hepatitis was diagnosed. Intravenous acyclovir 50 mg was administered 3 times daily for 7 days, and a wet dressing with topical mupirocin was employed daily until the skin lesions healed. The fever subsided soon after starting treatment. The liver enzyme counts decreased gradually in serial follow-up (aspartate aminotransferase, 75 IU/L; alanine aminotransferase, 70 IU/L).
Primary herpetic infection usually is asymptomatic, but when symptoms do occur, it is characterized by the sudden onset of painful vesicle clusters over erythematous edematous skin. Lesions can be associated with fever and malaise and may involve the perineum. Urinary symptoms may occur. The average age of onset ranges from 6 months to 4 years. The virus commonly is transmitted by asymptomatic carriers. Autoinoculation from concomitant oral primary herpetic infection or individuals with active herpetic infection is one possible route of transmission. In our patient, we assumed that she acquired the virus from her father during close contact. A diagnosis can be made clinically using direct methods including culture, Tzanck smear, or polymerase chain reaction, or indirect methods such as serologic tests.2
Hepatitis secondary to HSV infection is rare, especially in immunocompetent patients. It occurs during primary infection and rarely during recurrent infection with or without concomitant skin lesions.3 Symptoms include fever, anorexia, nausea, vomiting, abdominal pain, leukopenia, coagulopathy, and marked elevation of serum transaminase levels without jaundice. Based on our patient’s elevated liver enzyme levels and virological evidence of acute primary HSV infection, a lack of evidence of other hepatic viral infections, and the presence of herpes simplex viremia, we concluded that this infant had viral hepatitis as a part of the clinical presentation of primary HSV infection. We did not perform a direct liver biopsy considering her age and accompanying risks.4
Primary herpetic infection usually has a benign course and a short duration. In children, the prognosis depends on underlying immunologic status, not a particular type of HSV. In children with atopic dermatitis, primary herpetic infection tends to occur earlier and is more severe. Early treatment with acyclovir is effective; intravenous treatment is not required unless local complications or systemic involvement are present. Long-term follow-up is recommended because of the possibility of recurrence.
Although the possibility of systemic involvement including hepatitis due to HSV infection is low, awareness among dermatologists about primary herpetic infection and its possible complications would be helpful in the diagnosis and treatment, especially for atypical or extensive cases.
- Jenson HB, Shapiro ED. Primary herpes simplex virus infection of a diaper rash. Pediatr Infect Dis J. 1987;6:1136-1138.
- Batalla A, Flórez A, Dávila P, et al. Genital primary herpes simplexinfection in a 5-month-old infant. Dermatol Online J. 2011;17:8.
- Norvell JP, Blei AT, Jovanovic BD, et al. Herpes simplex virus hepatitis: an analysis of the published literature and institutional cases. Liver Transpl. 2007;13:1428-1434.
- Chen CK, Wu SH, Huang YC. Herpetic gingivostomatitis with severe hepatitis in a previously healthy child. J Microbiol Immunol Infect. 2012;45:324-325.
- Jenson HB, Shapiro ED. Primary herpes simplex virus infection of a diaper rash. Pediatr Infect Dis J. 1987;6:1136-1138.
- Batalla A, Flórez A, Dávila P, et al. Genital primary herpes simplexinfection in a 5-month-old infant. Dermatol Online J. 2011;17:8.
- Norvell JP, Blei AT, Jovanovic BD, et al. Herpes simplex virus hepatitis: an analysis of the published literature and institutional cases. Liver Transpl. 2007;13:1428-1434.
- Chen CK, Wu SH, Huang YC. Herpetic gingivostomatitis with severe hepatitis in a previously healthy child. J Microbiol Immunol Infect. 2012;45:324-325.
Practice Points
- Parents with a history of herpes simplex virus (HSV) need to be educated before the baby is born to be careful about direct skin contact with the child to prevent the spread of HSV infection.
- Although systemic involvement is not typical, additional tests to rule out internal organ involvement may be required, especially in children.











